

Personal Stories
We want to hear your story.
Tell us how mental illness has affected your life.
Share Your Story
Find Your Local NAMI
Call the NAMI Helpline at
800-950-6264
Or text "HelpLine" to 62640
My Depression in My Life
Depression is something that shows itself differently for everyone. There is no one person, or one story, or one experience that can make someone universally understand truly how depression alters the lives of those of us who suffer from it. I can’t make anyone understand how it is for everyone, but I can tell you how it alters my life, and maybe that will help people understand how all-encompassing it really is.
For me there are two main ways that my depression manifests itself when it breaks through the barriers I have set with the help of years of therapy and medication. There is the gut wrenching loneliness and near constant anxiety and then there is the checking out, the feeling nothing at all, the numbness. Sometimes I don’t know which is worse, but I will try to explain both.
The Loneliness and Anxiety:
In some ways I consider this step one of when my depression spikes because it always seems to come first. But I don’t consider it step one in levels of horribleness. Like I said above I really think that both ways my depression hits me are pretty awful and I couldn’t say which is worse.
You know that feeling you have in your gut when you are about to and/or really need to cry. While that is what it is like. All the time. I could be laughing and having a great time with my friends, which I often am because my friends are great, and yet in the back of my mind I feel more alone than ever and I just want to curl up into fetal position and cry. But I never can. I can’t go home and cry and then feel better, because it’s not like there is something to cry about, or really anything to be sad about. And it isn’t really sadness. It is complete solitude. It’s when my brain tells me that I am alone, that I can’t be loved, that no one really wants me around, and worst of all that no one will understand me.
That is worst of all because at the place I am in my life, no matter what I have been through in the past, or what my depression tries to make me believe I know that I can be loved, that I’m not alone and that I am wanted. And I know that because of the hard work I have done to get to that place in my life, and because of some of the amazing people in my life who make sure that I know that they are there for me, that they love me, and that they want to spend time with me.
But the idea that no one will ever truly understand who I am, or any of that. That is a little harder to dissuade myself from believing. Because as much as I can tell people what I went, and still go through and what goes through my mind, who can really understand me other than me. And that isn’t necessarily a bad thing, but the way my depression tells me it, it is a bad thing.
So there I am surrounded by people, very possibly having some of the best experiences of my life, feeling like I need to bawl, completely unable to, and nearly having an anxiety attack because I just want it to end.
And it is here where two things happen. It is here where I wish for and welcome the numbness because I don’t want to feel the all-encompassing loneliness and anxiety. It is also where I think about cutting.
I have not cut myself in three and a half years. And I know that it doesn’t solve my problems. I know that I shouldn’t and I don’t want to. Even when I want to I don’t want to.
But here, when I am feeling the all-encompassing loneliness which is the very last thing that I want to feel, I think about cutting because it lets me feel something else.
The physical act of cutting gives me something to think about and focus on, something other than that loneliness. And when I am not physically cutting, instead of thinking about how lonely I am and how that feeling will never end I think about the next time I can cut, or the most recent time I did.
And Then The Numbness:
I don’t really know how to explain this numbness. It is simply a period of time where I feel literally nothing. I fake happiness/normal emotion around friends, not always very well, and when I am alone I just don’t care about anything.
This is when my grades often fall because I don’t care about anything, including school, and therefore school work.
And then, sometimes I just want to feel something, anything, and so that is when I think about cutting. I think about cutting because it gives me something to feel, something I can control, but still feel.
The numbness comes because I can’t handle what I’m thinking and feeling, because it is too much for me to deal with, so I shut everything off so I don’t have to feel it.
In some ways, cutting transitions me back into feeling. But again, cutting, NOT A SOLUTION, NOT HEALTHY.
And something that I no longer do.
Now, for the past three and a half years, whenever I think of cutting, which I still do. It is still my first thought in either of these situations, I instead do one of the many things that I have come to know to help me cope.
For example, I force myself to spend more time with my friends, because I know that the loneliness will pass and I can talk myself out of feeling lonely when I am not physically alone.
I read/watch anything romantic. I pretend that I am one of the characters, and then I feel what they feel instead of what I am feeling (or preventing myself from feeling).
I belt along to old school Taylor Swift. Because what is more beautiful than a summer romance in a small country town with Chevy trucks and Tim McGraw?
And though my schoolwork does still sometimes fall through the cracks, I always make myself do some work.
Basically I force myself to live my life, because well, it is my life, and I refuse to live it feeling alone when I’m not, and numb when I could be great.
So even though I do feel those things far more often than I would like it is something that I live with, because I have depression.
Because depression is a disease, and I will always have it.
Because my depression is a part of who I am.
And most of all, because I only have one life, and I want to live it. Because even though when my depression spikes it makes me want to not live sometimes, I refuse.
Because I am the author of my own life and I choose to put a semicolon instead of a period at every point that my depression tells me otherwise.
So that is how my depression affects my life. That is how I deal with it. Like it or not I always will.
Essays About Depression: Top 8 Examples Plus Prompts
Many people deal with mental health issues throughout their lives; if you are writing essays about depression, you can read essay examples to get started.
An occasional feeling of sadness is something that everyone experiences from time to time. Still, a persistent loss of interest, depressed mood, changes in energy levels, and sleeping problems can indicate mental illness. Thankfully, antidepressant medications, therapy, and other types of treatment can be largely helpful for people living with depression.
People suffering from depression or other mood disorders must work closely with a mental health professional to get the support they need to recover. While family members and other loved ones can help move forward after a depressive episode, it’s also important that people who have suffered from major depressive disorder work with a medical professional to get treatment for both the mental and physical problems that can accompany depression.
If you are writing an essay about depression, here are 8 essay examples to help you write an insightful essay. For help with your essays, check out our round-up of the best essay checkers .
- 1. My Best Friend Saved Me When I Attempted Suicide, But I Didn’t Save Her by Drusilla Moorhouse
- 2. How can I complain? by James Blake
- 3. What it’s like living with depression: A personal essay by Nadine Dirks
- 4. I Have Depression, and I’m Proof that You Never Know the Battle Someone is Waging Inside by Jac Gochoco
- 5. Essay: How I Survived Depression by Cameron Stout
- 6. I Can’t Get Out of My Sweat Pants: An Essay on Depression by Marisa McPeck-Stringham
- 7. This is what depression feels like by Courtenay Harris Bond
8. Opening Up About My Struggle with Recurring Depression by Nora Super
1. what is depression, 2. how is depression diagnosed, 3. causes of depression, 4. different types of depression, 5. who is at risk of depression, 6. can social media cause depression, 7. can anyone experience depression, the final word on essays about depression, is depression common, what are the most effective treatments for depression, top 8 examples, 1. my best friend saved me when i attempted suicide, but i didn’t save her by drusilla moorhouse.
“Just three months earlier, I had been a patient in another medical facility: a mental hospital. My best friend, Denise, had killed herself on Christmas, and days after the funeral, I told my mom that I wanted to die. I couldn’t forgive myself for the role I’d played in Denise’s death: Not only did I fail to save her, but I’m fairly certain I gave her the idea.”
Moorhouse makes painstaking personal confessions throughout this essay on depression, taking the reader along on the roller coaster of ups and downs that come with suicide attempts, dealing with the death of a loved one, and the difficulty of making it through major depressive disorder.
2. How can I complain? by James Blake
“I wanted people to know how I felt, but I didn’t have the vocabulary to tell them. I have gone into a bit of detail here not to make anyone feel sorry for me but to show how a privileged, relatively rich-and-famous-enough-for-zero-pity white man could become depressed against all societal expectations and allowances. If I can be writing this, clearly it isn’t only oppression that causes depression; for me it was largely repression.”
Musician James Blake shares his experience with depression and talks about his struggles with trying to grow up while dealing with existential crises just as he began to hit the peak of his fame. Blake talks about how he experienced guilt and shame around the idea that he had it all on the outside—and so many people deal with issues that he felt were larger than his.
3. What it’s like living with depression: A personal essay by Nadine Dirks
“In my early adulthood, I started to feel withdrawn, down, unmotivated, and constantly sad. What initially seemed like an off-day turned into weeks of painful feelings that seemed they would never let up. It was difficult to enjoy life with other people my age. Depression made typical, everyday tasks—like brushing my teeth—seem monumental. It felt like an invisible chain, keeping me in bed.”
Dirks shares her experience with depression and the struggle she faced to find treatment for mental health issues as a Black woman. Dirks discusses how even though she knew something about her mental health wasn’t quite right, she still struggled to get the diagnosis she needed to move forward and receive proper medical and psychological care.
4. I Have Depression, and I’m Proof that You Never Know the Battle Someone is Waging Inside by Jac Gochoco
“A few years later, at the age of 20, my smile had fallen, and I had given up. The thought of waking up the next morning was too much for me to handle. I was no longer anxious or sad; instead, I felt numb, and that’s when things took a turn for the worse. I called my dad, who lived across the country, and for the first time in my life, I told him everything. It was too late, though. I was not calling for help. I was calling to say goodbye.”
Gochoco describes the war that so many people with depression go through—trying to put on a brave face and a positive public persona while battling demons on the inside. The Olympic weightlifting coach and yoga instructor now work to share the importance of mental health with others.
5. Essay: How I Survived Depression by Cameron Stout
“In 1993, I saw a psychiatrist who prescribed an antidepressant. Within two months, the medication slowly gained traction. As the gray sludge of sadness and apathy washed away, I emerged from a spiral of impending tragedy. I helped raise two wonderful children, built a successful securities-litigation practice, and became an accomplished cyclist. I began to take my mental wellness for granted. “
Princeton alum Cameron Stout shared his experience with depression with his fellow Tigers in Princeton’s alumni magazine, proving that even the most brilliant and successful among us can be rendered powerless by a chemical imbalance. Stout shares his experience with treatment and how working with mental health professionals helped him to come out on the other side of depression.
6. I Can’t Get Out of My Sweat Pants: An Essay on Depression by Marisa McPeck-Stringham
“Sometimes, when the depression got really bad in junior high, I would come straight home from school and change into my pajamas. My dad caught on, and he said something to me at dinner time about being in my pajamas several days in a row way before bedtime. I learned it was better not to change into my pajamas until bedtime. People who are depressed like to hide their problematic behaviors because they are so ashamed of the way they feel. I was very ashamed and yet I didn’t have the words or life experience to voice what I was going through.”
McPeck-Stringham discusses her experience with depression and an eating disorder at a young age; both brought on by struggles to adjust to major life changes. The author experienced depression again in her adult life, and thankfully, she was able to fight through the illness using tried-and-true methods until she regained her mental health.
7. This is what depression feels like by Courtenay Harris Bond
“The smallest tasks seem insurmountable: paying a cell phone bill, lining up a household repair. Sometimes just taking a shower or arranging a play date feels like more than I can manage. My children’s squabbles make me want to scratch the walls. I want to claw out of my own skin. I feel like the light at the end of the tunnel is a solitary candle about to blow out at any moment. At the same time, I feel like the pain will never end.”
Bond does an excellent job of helping readers understand just how difficult depression can be, even for people who have never been through the difficulty of mental illness. Bond states that no matter what people believe the cause to be—chemical imbalance, childhood issues, a combination of the two—depression can make it nearly impossible to function.
“Once again, I spiraled downward. I couldn’t get out of bed. I couldn’t work. I had thoughts of harming myself. This time, my husband urged me to start ECT much sooner in the cycle, and once again, it worked. Within a matter of weeks I was back at work, pretending nothing had happened. I kept pushing myself harder to show everyone that I was “normal.” I thought I had a pattern: I would function at a high level for many years, and then my depression would be triggered by a significant event. I thought I’d be healthy for another ten years.”
Super shares her experience with electroconvulsive therapy and how her depression recurred with a major life event despite several years of solid mental health. Thankfully, Super was able to recognize her symptoms and get help sooner rather than later.
7 Writing Prompts on Essays About Depression
When writing essays on depression, it can be challenging to think of essay ideas and questions. Here are six essay topics about depression that you can use in your essay.

Depression can be difficult to define and understand. Discuss the definition of depression, and delve into the signs, symptoms, and possible causes of this mental illness. Depression can result from trauma or personal circumstances, but it can also be a health condition due to genetics. In your essay, look at how depression can be spotted and how it can affect your day-to-day life.
Depression diagnosis can be complicated; this essay topic will be interesting as you can look at the different aspects considered in a diagnosis. While a certain lab test can be conducted, depression can also be diagnosed by a psychiatrist. Research the different ways depression can be diagnosed and discuss the benefits of receiving a diagnosis in this essay.
There are many possible causes of depression; this essay discusses how depression can occur. Possible causes of depression can include trauma, grief, anxiety disorders, and some physical health conditions. Look at each cause and discuss how they can manifest as depression.

There are many different types of depression. This essay topic will investigate each type of depression and its symptoms and causes. Depression symptoms can vary in severity, depending on what is causing it. For example, depression can be linked to medical conditions such as bipolar disorder. This is a different type of depression than depression caused by grief. Discuss the details of the different types of depression and draw comparisons and similarities between them.
Certain genetic traits, socio-economic circumstances, or age can make people more prone to experiencing symptoms of depression. Depression is becoming more and more common amongst young adults and teenagers. Discuss the different groups at risk of experiencing depression and how their circumstances contribute to this risk.
Social media poses many challenges to today’s youth, such as unrealistic beauty standards, cyber-bullying, and only seeing the “highlights” of someone’s life. Can social media cause depression in teens? Delve into the negative impacts of social media when writing this essay. You could compare the positive and negative sides of social media and discuss whether social media causes mental health issues amongst young adults and teenagers.
This essay question poses the question, “can anyone experience depression?” Although those in lower-income households may be prone to experiencing depression, can the rich and famous also experience depression? This essay discusses whether the privileged and wealthy can experience their possible causes. This is a great argumentative essay topic, discuss both sides of this question and draw a conclusion with your final thoughts.
When writing about depression, it is important to study examples of essays to make a compelling essay. You can also use your own research by conducting interviews or pulling information from other sources. As this is a sensitive topic, it is important to approach it with care; you can also write about your own experiences with mental health issues.
Tip: If writing an essay sounds like a lot of work, simplify it. Write a simple 5 paragraph essay instead.
FAQs On Essays About Depression
According to the World Health Organization, about 5% of people under 60 live with depression. The rate is slightly higher—around 6%—for people over 60. Depression can strike at any age, and it’s important that people who are experiencing symptoms of depression receive treatment, no matter their age.
Suppose you’re living with depression or are experiencing some of the symptoms of depression. In that case, it’s important to work closely with your doctor or another healthcare professional to develop a treatment plan that works for you. A combination of antidepressant medication and cognitive behavioral therapy is a good fit for many people, but this isn’t necessarily the case for everyone who suffers from depression. Be sure to check in with your doctor regularly to ensure that you’re making progress toward improving your mental health.
If you’re still stuck, check out our general resource of essay writing topics .

Amanda has an M.S.Ed degree from the University of Pennsylvania in School and Mental Health Counseling and is a National Academy of Sports Medicine Certified Personal Trainer. She has experience writing magazine articles, newspaper articles, SEO-friendly web copy, and blog posts.
View all posts
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- Winter 2024 | VOL. 36, NO. 1 CURRENT ISSUE pp.A5-81
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
The Links Between Stress and Depression: Psychoneuroendocrinological, Genetic, and Environmental Interactions
- Gustavo E. Tafet , M.D., Ph.D. ,
- Charles B. Nemeroff , M.D., Ph.D.
Search for more papers by this author
The role of stress in the origin and development of depression may be conceived as the result of multiple converging factors, including the chronic effect of environmental stressors and the long-lasting effects of stressful experiences during childhood, all of which may induce persistent hyperactivity of the hypothalamic-pituitary-adrenal axis. These changes, including increased availability of corticotropin-releasing factor and cortisol, are also associated with hyperactivity of the amygdala, hypoactivity of the hippocampus, and decreased serotonergic neurotransmission, which together result in increased vulnerability to stress. The role of other monoaminergic neurotransmitters, genetic polymorphisms, epigenetic mechanisms, inflammatory processes, and altered cognitive processing has also been considered in the development of a comprehensive model of the interactions between different factors of vulnerability. Further understanding of the underlying mechanisms that link these factors may contribute significantly to the development of more effective treatments and preventive strategies in the interface between stress and mood disorders.
The link between stressful life events and the origin and development of depression has been widely investigated, providing an increasing body of evidence supporting this association. 1 – 3 Environmental factors likely affect individuals in somewhat different manners, therefore triggering an adaptive response to stress, which depends on both psychological and biological aspects in the interaction between stressors and individual resources. Psychological aspects include all of the cognitive processing related to incoming information; the subjective appraisal of different features related to stressors, such as magnitude and chronicity, predictability, and controllability; and potential resources to cope with them. Biological mediators include the activation of different neural structures underlying information processing, including sensory pathways, which convey environmental input to the CNS, and the resulting activation of neural and neuroendocrine cascades of molecular events, mediated by the subsequent activation of the sympathetic division of the autonomic nervous system and the hypothalamic-pituitary-adrenal (HPA) axis. 4 The efficacy of an adaptive response implies that it may be rapidly activated, to allow reacting in a successful and effective manner during stressful situations, and it should be efficiently controlled and concluded afterward. If it continues in a prolonged and excessive manner (e.g., during chronic stressful situations), it may lead to maladaptive changes, which in turn may contribute to the development of pathological conditions such as anxiety and mood disorders, including depression, particularly in individuals with increased genetic vulnerability. In this regard, various polymorphisms have been investigated as candidate genes, which are known to participate in important molecular pathways involved in the origin of depression. The presence of these genetic variations appears to be involved in the development of depression in response to stressful events, including adverse experiences during childhood and environmental stressors during adulthood. 5 – 10 Moreover, various studies have focused on the role of gene–environment interactions, including the search for these polymorphic variants and the role of transcriptional regulation by epigenetic mechanisms. 6 , 11 – 13 In addition, inflammatory processes associated with adaptive responses to stressful situations, with the consequent synthesis and release of proinflammatory cytokines, may lead to further maladaptive changes of neural and neuroendocrine systems, therefore contributing to the development of depressive symptoms, particularly in chronically stressed individuals.
This article aims to review the evidence for the role played by stress, associated with different converging factors, including a genetic diathesis, a history of adverse early life events, hyperactivity of the HPA axis, decreased monoamines, increased proinflammatory cytokines, and epigenetic mechanisms, such as those observed in response to environmental stressful conditions, and their potential interactions in the etiology of depression. An increased understanding of these factors and their potential interactions may lead to more effective strategies for the treatment of this disorder.
Processing of Environmental Stressors in the Brain
Environmental stressors are perceived and transmitted through sensory pathways to different structures in the CNS, such as the thalamus, which convey projections to the amygdala, and to sensory and association cortices, which in turn also project to different areas of the prefrontal cortex (PFC), including the orbitofrontal cortex, the medial PFC, and the anterior cingulate cortex (ACC). 4 , 7 Direct projections from the thalamus to the amygdala contribute to activate arousal and early alarm reactions, with the subsequent activation of the autonomic nervous system and the HPA axis, whereas indirect projections may reach the amygdala from sensory and association cortices as well as from transition cortices. The latter areas, including the entorhinal, perirhinal, and parahippocampal cortices, in turn project to the hippocampus, where sensory input is integrated with contextual cues, to convey more elaborated information to the amygdala. 14
The amygdala plays a critical role in emotional processing, including the assessment of the emotional relevance of environmental stimuli as well as internal stressors. It plays a key role in the regulation of autonomic and neuroendocrine responses, through projections to the lateral hypothalamus, which mediate the activation of the sympathetic branch of the autonomic nervous system; through direct projections to the paraventricular nucleus of the hypothalamus; or indirectly through the bed nucleus of the stria terminalis, which is involved in activation of the HPA axis. 14 In addition, the amygdala shares important connections with the orbitofrontal cortex and the medial PFC, 15 including Brodmann areas 10 and 32, and the subgenual ACC (Brodmann area 25). 16 The orbitofrontal cortex (Brodmann areas 11–14) has been associated with integration of multimodal sensory stimuli and primary appraisal of their positive or negative value, therefore participating in their affective assessment. 17 The medial PFC overlaps with the ACC, particularly in the subgenual ACC, 17 which regulates emotional responses generated by the amygdala. 18 These structures are in turn connected with the dorsolateral PFC (Brodmann areas 9 and 46) and the ventrolateral PFC (Brodmann areas 45 and 47), which participate in cognitive control and voluntary regulation of emotion. The dorsolateral PFC, which has been associated with executive aspects of cognitive processing 19 (most notably with conscious processing and working memory), receives input from the amygdala through the orbitofrontal cortex and ACC. 15 , 17 The dorsolateral PFC reciprocally projects back to limbic structures, mostly through indirect connections to the ventromedial PFC (Brodmann area 32), which projects to the subgenual ACC. 19 It has been proposed that projections from the ventromedial PFC and the subgenual ACC exert a modulatory effect on the amygdala, 19 , 20 which in turn sends excitatory output to the hypothalamus, 17 – 19 therefore regulating the activity of the HPA axis.
Decreased volume of the subgenual ACC has been described, together with hyperactivity of the amygdala, in individuals with mood disorders, 16 , 21 which has been associated with the role of the subgenual ACC in the top-down regulatory pathway between the dorsolateral PFC and the amygdala, allowing conscious down-regulation of negative emotions. These corticolimbic pathways may be dysfunctional in patients with depression, in which the dorsolateral PFC, dorsomedial PFC, orbitofrontal cortex, and ACC appear to be dysfunctional, particularly during cognitive-emotional tasks, with the consequent disruption of their top-down inhibitory effect expressed in the impaired cognitive modulation of emotions. 20 , 21 Recovery of conscious regulation of negative emotions has been associated with clinical recovery. In addition, decreased hippocampal volume has also been observed, along with increased activity of the amygdala and reduced activity of the dorsolateral PFC. 21 More recently, we documented changes in cortical thickness in patients exposed to child abuse and neglect, with the findings specific to the nature of the abuse. 22
Figure 1 illustrates the network of functional connections among different neural structures involved in adaptive responses to stress, including the processing of environmental stimuli through cortical and subcortical structures, and the activation of the HPA axis.
FIGURE 1. Schematic Representation of Neural Structures Involved in the Stress Response a
a Stressors are perceived by sensory receptors, which convey information to the thalamus, primary sensory cortices, association cortices, transition cortices, the hippocampus, and the amygdala. The amygdala also receives direct input from the thalamus. The orbitofrontal cortex and the medial prefrontal cortex are reciprocally connected and, together with the anterior cingulate cortex, convey information from sensory cortices and association cortices to subcortical structures, including direct connections to the hypothalamus and reciprocal connections with the amygdala. The amygdala participates in the activation of the HPA axis through stimulatory projections to the paraventricular nucleus of the hypothalamus, with consequent synthesis and release of CRF, which stimulates the release of ACTH from the pituitary. In turn, this stimulates the release of glucocorticoids from the adrenals, particularly cortisol. Cortisol exerts negative feedback at the level of the hypothalamus and the pituitary, as well as through the hippocampus, which exerts an inhibitory effect on the HPA axis. Activation of the HPA axis is also regulated by norepinephrine, through projections from the locus coeruleus, and serotonin, and through projections from the raphe nuclei. Both aminergic systems participate in regulation of the stress response through connections with the amygdala and the hippocampus, therefore exerting regulatory effects on both limbic structures. The amygdala is also involved in the activation of the autonomic component of the stress response through CRF inputs to the locus coeruleus. Solid lines indicate stimulatory inputs, whereas dotted lines indicate inhibitory inputs. ACC, anterior cingulate cortex; ACTH, adrenocorticotropin; CRF, corticotropin-releasing factor; DLPFC, dorsolateral prefrontal cortex; HPA, hypothalamic-pituitary-adrenal; MPFC, medial prefrontal cortex; OFC, orbitofrontal cortex.
Role of the HPA Axis
Activation of the HPA axis is initiated in limbic structures, including direct projections from the central nucleus of the amygdala, or indirectly through the bed nucleus of the stria terminalis, which projects to the hypothalamic paraventricular nucleus, where corticotropin-releasing factor (CRF) is synthesized in parvocellular neurons and released to reach the anterior pituitary. There, CRF regulates the transcription of the proopiomelanocortin gene (a common precursor for adrenocorticotropin, β-endorphin, and related peptides) and stimulates the release of adrenocorticotropin into the systemic circulation. Adrenocorticotropin acts upon the adrenal cortex to stimulate the biosynthesis and release of glucocorticoids, particularly cortisol. 23
At the molecular level, cortisol binds to mineralocorticoid receptors (type I) and glucocorticoid receptors (GRs; type II), constituting a hormone-receptor complex, which in turn undergoes conformational changes to allow its recognition and binding to a glucocorticoid response element, in the promoter region of many target genes. 24 Cortisol regulates the activity of the HPA axis through multiple negative feedback loops, which require its binding to GRs located in the paraventricular nucleus and the pituitary, where it down-regulates the synthesis and release of CRF and adrenocorticotropin, respectively, and GRs in the hippocampus, which in turn activates GABAergic projections to the paraventricular nucleus that inhibit HPA axis activity. Hence, many of the effects of cortisol may be understood as a result of transcriptional regulation of various genes, including those involved in the negative feedback loops responsible for the regulation of the HPA axis. 24
In response to short-term exposure to environmental stressors, the amygdala stimulates the HPA axis with the consequent synthesis and release of cortisol, 14 which is self-regulated by negative feedback mechanisms mediated by the glucocorticoid. In addition, the HPA system interacts with CRF neurons in the amygdala, activating a positive feedback loop involved in fear and anger reactions; the HPA also activates catecholaminergic neurons, stimulating arousal and improving cognitive functions. Hence, upon exposure to acute or short-term stressors, cortisol is expected to exert widespread metabolic effects, which is mostly necessary to maintain or restore homeostasis. 25 Cortisol is actively involved in the mobilization of energetic resources, including the stimulation of gluconeogenesis with the resulting increased levels of circulating glucose, and the down-regulation of inflammatory processes, therefore contributing to coping with the stressful situation.
Chronic and persistent activation of the HPA system may disrupt physiological mechanisms, including negative feedback loops, resulting in persistent activation of the system. Circadian rhythms normally characterized by wide variations, with morning zeniths and evening nadirs, are markedly altered during chronic stress, with the consequent increase in plasma cortisol levels and blunted circadian rhythm, mostly due to increased levels of cortisol during the evening and mild changes in the morning. 25 Prolonged exposure to increased levels of cortisol may induce detrimental effects on hippocampal neurons, reducing dendritic branching and inhibiting neurogenesis. 26 Moreover, hypersecretion of CRF and cortisol was also associated with decreased hippocampal volume, particularly in individuals exposed to childhood trauma. 27 Because the hippocampus is involved in the regulation of the HPA axis, it is conceivable that patients with major depression and early life trauma who exhibit reduced hippocampal volume 28 , 29 may also exhibit decreased hippocampal function, therefore resulting in further sensitization of stress responses. 5 These observations support previous reports that associated the origin of depressive symptoms with decreased expression of GRs at the hypothalamic and hippocampal levels, 24 with the resulting hypercortisolism. Hence, an increasing body of evidence supports the association between chronic stress and depression at the molecular level, where hyperactivity of the HPA axis, with the consequent increase of cortisol, represents one of the most consistent findings in both syndromal mood and certain anxiety disorders. 23 , 26
Various studies have focused on genes involved in the regulation of the HPA system, including both the mineralocorticoid receptor and GR genes, resulting in the identification of different single-nucleotide polymorphisms (SNPs). Among these, two different SNPs in the GR gene (BclI and Asp363Ser) have been associated with increased vulnerability for depression in the general population, probably through increased glucocorticoid sensitivity. 30 More recently, various studies have focused on the FK506-binding protein FKBP5, a cochaperone of hsp-90 involved in the regulation of GR sensitivity, 31 which is also involved in HPA axis responsivity. This protein is a component of the GR heterocomplex, which, upon binding of cortisol, is replaced by FKBP4, which in turn facilitates the nuclear translocation of the hormone-receptor complex and its transcriptional activity. 32 Altered GR function may lead to impaired feedback regulation, with the resulting HPA hyperactivation commonly observed in chronic stress and depression. Therefore, various SNPs have been identified in the FKBP5 gene, some of them associated with increased FKBP5 protein expression, which in turn may lead to changes in GR, with the resulting effect on HPA axis regulation. 32 Increased FKBP5 protein expression may reduce hormone-binding affinity and may interfere with the translocation of the hormone-receptor complex. It is noteworthy that glucocorticoids may induce increased expression of this cochaperone, constituting an intracellular negative feedback loop to regulate GR activity. 33 One of the SNPs of the FBPP5 gene, defined as the substitution of a cytosine (C) by a thymine (T) and therefore identified as the high-induction allele T, was associated with increased FKBP5 protein expression and altered HPA response. Upon exposure to stressful stimuli, carriers of the T allele exhibited slower recovery of the cortisol response and homozygous carriers of the allele who experienced severe abuse during childhood presented increased vulnerability for the development of depression during adulthood, 34 which may also be associated with having an increased number of depressive episodes. 32
Role of CRF
CRF-containing circuits in the CNS play a critical role in the coordination of the stress response, both as a neuroendocrine factor regulating the HPA axis and through its function as a neurotransmitter, mediating behavioral, immune, and autonomic responses to stress. 35 CRF neurons are localized throughout different cortical areas, participating in neural pathways involved in cognitive responses, and limbic areas such as the central nucleus of the amygdala and the bed nucleus of the stria terminalis, where it participates in the regulation of emotional responses. 23 CRF projections from the amygdala have been shown to reach the hypothalamic paraventricular nucleus (therefore enhancing the activation of the HPA axis in response to stress) and the monoaminergic nuclei in the brainstem, including the locus coeruleus (LC) and the raphe nuclei (RN). 3 Moreover, CRF stimulates norepinephrine release in the LC, 36 with the consequent noradrenergic activation of the autonomic nervous system and the HPA axis, while mainly inhibiting serotonergic neurons in the RN, 37 which in turn may affect other structures through serotonergic projections to the amygdala, hippocampus, and paraventricular nucleus. 3 Therefore, through the regulation of these monoaminergic systems, CRF participates in neurobiological processes underlying mood and anxiety disorders, producing anxiogenic and depressogenic effects. 35 Increased CSF concentrations of CRF have consistently been reported in depressed and suicidal patients. 38 In addition, CRF may also be involved in anxiety and the encoding of emotional memories, 23 , 35 playing a critical role in the stress response not only during adulthood but also in mediation of the long-lasting effects of trauma and other early life stressful experiences. Moreover, increased levels of CRF may also be involved in neuroplastic changes induced by chronic stress, 39 and this effect may also be enhanced by glucocorticoids as a component of the stress response. 40
Various studies have focused on CRF, CRF-binding protein, and CRF type 1 receptor (CRHR1) genes, resulting in several important findings. 41 Indeed, several SNPs in the CRHR1 and haplotypes formed by certain SNPs involved in mediating the effects of early adverse experiences on the risk for adult depression have been identified. 42 Upon binding to CRF, this receptor participates in the activation of the HPA axis and plays a critical role in emotional and cognitive functions mediated by CRF in extrahypothalamic brain regions, including the amygdala and the LC, 35 therefore influencing arousal, attention, conscious perception of emotional experiences, and memory consolidation. Two haplotypes formed by different SNPs in the CRHR1 gene were associated with reduced symptoms of depression in subjects exposed to early stressful experiences. Because CRHR1 may be critically involved in the consolidation of emotionally charged memories, such as those produced by childhood aversive experiences, it was proposed that carriers of two copies of these haplotypes, which also exhibited overrepresentation of the protective alleles of the studied SNPs, 42 may have altered activation of memory consolidation processes. This may lead to decreased emotional influence in the cognitive processing of these memories, therefore protecting the individual from his or her potentially depressogenic and anxiogenic effects. 43
Role of Serotonin
The serotonergic hypothesis of depression posits deficient serotonergic activity in the CNS with increased vulnerability for the development of depression. The main groups of serotonergic neurons in the CNS are located within the boundaries of the RN, where an array of ascending projections arise from the dorsal RN (B6 and B7) and the medial RN (B8). The dorsal RN–forebrain tract projects to the PFC, amygdala, nucleus accumbens, and ventral hippocampus, among other forebrain structures, 44 and it participates in the state of anticipatory anxiety and thus plays an adaptive role during stressful situations. 45 The dorsal RN–forebrain tract has been associated with activation of the limbic structures (e.g., the amygdala) in the presence of environmental stressors associated with unpleasant experiences, and it is also involved in the regulation of potential emotional reactions. Alterations of this system, particularly involving dorsal RN–amygdala projections, may be associated with symptoms of anxiety. 45 The medial RN–forebrain tract projects to the dorsal hippocampus and hypothalamus, among other neural structures, 44 , 45 and it participates in conferring tolerance to unpleasant, unavoidable, and persistent aversive stimuli such as those perceived during chronic stressful situations. The medial RN–forebrain tract is also associated with adaptive control on negative emotional experiences. Therefore, alterations of this system, particularly involving medial RN–hippocampal projections, may be associated with decreased tolerance to aversive stimuli, learned helplessness, and subsequent depression. 45 , 46 Serotonergic neurons in the RN are also interconnected and are physiologically integrated with other monoaminergic systems in the brainstem, including noradrenergic and dopaminergic circuits. 47 It has been shown that both the dorsal RN and the medial RN receive noradrenergic projections, 48 which appear to be excitatory. The LC receives serotonergic projections from the RN reciprocally, 48 which appear to exert an indirect modulatory effect by inhibiting glutamatergic activation of the LC. The dorsal RN also modulates dopaminergic activity through projections to the ventral tegmental area, which appear to be excitatory, 49 and dopaminergic projections to the dorsal RN reciprocally exert an indirect inhibitory effect by increasing the activity of somatodendritic 5-hydroxytryptamine (serotonin [5-HT]) autoreceptors. 44
Figure 2 illustrates the network of functional connections between different neurotransmitter systems in the CNS, as well as their respective connections with different cortical and limbic structures involved in the stress response.
FIGURE 2. Schematic Representation of Neurotransmitter Systems Involved in the Stress Response and Regulation of Emotional and Cognitive Functions a
a The raphe nuclei send serotonergic projections from their medial component to the hippocampus and from their dorsal component to the amygdala and the DLPFC. The locus coeruleus sends noradrenergic projections to the hippocampus and the amygdala. The ventral tegmental area sends dopaminergic projections to the nucleus accumbens and the DLPFC. The nucleus accumbens is reciprocally connected with the amygdala and the OFC, which in turn is reciprocally connected with the medial prefrontal cortex and the ACC. All of these are reciprocally connected with the amygdala and with the DLPFC. Reciprocal connections between the raphe nuclei, the locus coeruleus, and the ventral tegmental area are also represented. ACC, anterior cingulate cortex; D, dorsal; DLPFC, dorsolateral prefrontal cortex; M, medial; OFC, orbitofrontal cortex.
At the molecular level, 5-HT is released into the synaptic cleft, where it binds to both presynaptic and postsynaptic receptors. A growing number of 5-HT receptors have been identified, including 14 different types, classified in seven families with various subtypes each. Each of the serotonin receptor subtypes exhibits a unique regional neuroanatomic distribution, conferring specificity on the effects of activation of this widespread and diffuse serotonergic innervation. Synaptic concentrations of 5-HT are regulated by the serotonin transporter (5-HTT), which is responsible for its reuptake, therefore regulating its availability to bind and activate specific 5-HT receptors. 47 The 5-HTT is believed to be the primary molecular target of selective serotonin reuptake inhibitors antidepressants. Hence, 5-HTT blockade by selective serotonin reuptake inhibitors is translated into higher 5-HT concentrations in the synaptic cleft, allowing increased activation of 5-HT receptors. 46 , 47 The clinical efficacy of antidepressants is not directly associated with this acute mechanism; instead, it is linked to more adaptive changes. Continuous administration of selective serotonin reuptake inhibitors leads to desensitization or down-regulation of somatodendritic 5-HT 1A autoreceptors in the RN after several days (which are known to moderate the release of 5-HT into the synaptic cleft) and up-regulation of postsynaptic 5-HT 1A and desensitization of 5-HT 2A receptors. 50
In addition to serotonergic projections directly involved in cognitive and emotional functions, projections from the RN have been shown to innervate CRF-containing neurons in the paraventricular nucleus. 51 There is evidence that these projections stimulate the HPA axis and the autonomic nervous system; glucocorticoids and catecholamines may reciprocally affect the serotonergic system during stressful situations. 46 Various studies have shown that postsynaptic 5-HT 1A receptors in different limbic structures may be down-regulated or desensitized by glucocorticoids or exposure to chronic stress. 52 , 53 In addition, it has been shown that cortisol may increase 5-HT uptake in vitro, an effect attributed to increased expression of the 5-HTT gene by the glucocorticoid, 54 therefore providing further support for the reciprocal regulation of the HPA and 5-HT systems and their potential interplay in the interface between stress and depression. 46
Various studies have also focused on the structure of the 5-HTT gene, in which a polymorphism was identified in its promoter region. 55 The promoter activity is regulated by sequence elements located in the upstream regulatory region, known as the 5-HTT gene-linked polymorphic region (5-HTTLPR), where a short (S) and a long (L) allele have been identified. 6 Hence, the short promoter variant (5-HTTLPR-S) was associated with decreased transcriptional efficiency compared with the long allele (5-HTTLPR-L), resulting in decreased expression of the 5-HTT gene, 55 which may affect the modulation of serotonergic activity in response to stress. This notion has been supported by multiple clinical and preclinical studies, 56 including evidence observed in functional brain imaging studies, in which carriers of the S allele (homozygous or heterozygous for the short allele) exhibited increased amygdala reactivity to fearful and threatening stressors compared with those homozygous for the L allele, 57 which suggests that variations in the 5-HTT gene may be involved in psychological responses to stress. 6 Although various studies have shown increasing evidence that this polymorphism moderates the relationship between stress and depression, 56 there are still other studies suggesting certain controversy around this hypothesis.
The amygdala participates in the regulation of emotional reactions to stressful events, and its increased reactivity was associated with anxiety and altered mood regulation. 14 Hence, a potential association between 5-HTT gene polymorphism and increased reactivity of the amygdala in response to negative stressors 58 may contribute to a better understanding of the potential effect of the molecular mechanisms underlying this association. Moreover, the amygdala also plays a critical role in the activation of the HPA axis, and hyperactivation of the amygdala may also lead to increased plasma levels of cortisol. Indeed, carriers of the S allele exhibit increased activation of the amygdala and elevated cortisol levels in response to a laboratory stressor. 11 The association between the 5-HTTLPR-S variation and a potentially decreased expression of the 5-HTT gene may appear paradoxical, considering the potential vulnerability attributed to 5-HTTLPR-S carriers. Therefore, it is conceivable that alterations in 5-HTT gene regulation (and consequent effects on synaptic 5-HT levels) may differ, with the former expressed as a result of constitutive conditions and the latter triggered by environmental factors. It has been proposed that 5-HTTLPR-S carriers may exhibit “essentially” increased concentrations of 5-HT, which may result in down-regulation of postsynaptic 5-HT receptors. This may lead to a relative desensitization of the serotonergic system, 58 providing a potential explanation for the vulnerability exhibited by 5-HTTLPR-S carriers. By contrast, up-regulation of the 5-HTT gene, associated with the effect of environmental stressors and the resulting hyperactivation of the HPA axis and hypercortisolism, may lead to increased 5-HT reuptake and decreased concentrations of 5-HT in the synaptic cleft, 54 which has been widely associated with the development of mood disorders.
Role of Dopamine
Dopamine has also been implicated in the neural mechanisms of stress responses, including stress-related regulation of the HPA axis, as well as in the pathophysiology of depression. 59 , 60 The main groups of dopaminergic neurons in the CNS comprise the retro-rubro field (A8), the substantia nigra pars compacta (A9), and the ventral tegmental area (A10), where the mesolimbic and mesocortical pathways arise. The mesolimbic pathway projects mainly to the nucleus accumbens and other limbic structures, including the amygdala, hippocampus, bed nucleus of the stria terminalis, and septum. This pathway is implicated in the processing and reinforcement of rewarding stimuli, motivation, and the subjective experience of pleasure. 59 The mesocortical pathway projects mainly to the PFC, ACC, and entorhinal cortex and is critically involved in cognitive functions such as concentration and working memory. 59
Environmental stressors provoke increased activity in the amygdala, which in turn may increase the concentrations of dopamine in the mesocortical pathway (particularly in the PFC), therefore conferring exaggerated salience to relatively mild negative stimuli 60 and contributing to the resulting negative bias in cognitive processing. Regarding the mesolimbic pathway, it has been shown that stressful events may induce opposite responses, depending on the potential controllability of the stimuli, 61 and the consequent subjective assessment. Therefore, exposure to acute and controllable stressors was associated with increased dopamine release in the ventral striatum, whereas exposure to chronic and uncontrollable stressful stimuli was associated with decreased dopaminergic activity 61 with resulting anhedonia. Moreover, it has been shown that unavoidable or uncontrollable stressors may lead to decreased dopamine release in the nucleus accumbens and impaired response to environmental stimuli, which may result in the expression and exacerbation of depressive symptoms induced by stress. 62 The inability to experience pleasure, associated with loss of interest and motivation in usual activities, constitutes the pathognomonic anhedonia exhibited by patients with depression, 59 , 60 and it has been shown that impaired dopaminergic function is critically involved in altered reward processing underlying anhedonia. 63 , 64 Moreover, the mesolimbic dopaminergic pathway, particularly the nucleus accumbens, participates in the processing of rewarding and hedonic experiences in association with the orbitofrontal cortex, which may be involved in the subjective assessments of hedonic and rewarding value. 65 The orbitofrontal cortex is connected with the ACC and dorsolateral PFC, where this emotional input participates in cognitive processes; by contrast, the nucleus accumbens receives dopaminergic projections from the ventral tegmental area, which may be enhanced by glutamatergic stimulation from the amygdala, to increase motivation. 65 Substantial interaction has also been described between the ventral tegmental area and the RN, 59 which may be critically involved in emotional processing.
Because increased dopamine release in the mesolimbic pathway has been observed not only in response to rewarding stimuli but also in the presence of aversive situations (particularly when these are perceived as controllable and escapable 61 ), it has been suggested that dopamine plays an adaptive role associated with motivation, increased arousal, and behavioral control in response to stress, including both appetitive and aversive conditions. 66
Role of Norepinephrine
Catecholamines (and more specifically norepinephrine) have long been posited to play a major role in the pathophysiology of affective disorders, forming the catecholamine hypothesis of depression. The main group of norepinephrine-containing neurons in the CNS is located within the LC (A6), where various projections arise to widely innervate cortical and subcortical areas, 48 including the amygdala, the hippocampus, and the paraventricular nucleus of the hypothalamus. 36 Projections from the LC to the ventral tegmental area have been described, in which norepinephrine has been shown to potentiate dopamine release. Projections from the LC to the RN have also been described, in which norepinephrine exerts regulatory effects on 5-HT release. 48 There is also evidence of reciprocal regulation between norepinephrine and 5-HT, not only through connections between both aminergic systems but also through limbic structures such as the hippocampus. 67 In addition, reciprocal connections between norepinephrine - and CRF-containing neurons suggest a critical role of the LC in the regulation of neural and neuroendocrine responses to stress. 36
In response to acute stressors, norepinephrine is released throughout different structures in the CNS, resulting in enhanced arousal and hypervigilance, in the context of adaptive responses to stress. Moreover, activation of the LC has been associated with subsequent stimulation of the lateral hypothalamus, which in turn participates in the activation of the sympathetic branch of the autonomic nervous system, therefore complementing the adaptive response to stress. 36 A potential dysfunction of the LC has been observed during chronic stress (particularly upon exposure to unavoidable or uncontrollable stressors), leading to altered norepinephrine release, which was associated with some features of learned helplessness as well as problems in cognitive functions such as attention and memory, which are frequently observed in depression. In addition, dysregulation of the norepinephrine system has also been described in altered states of arousal, 48 which is commonly observed in anxiety disorders as well as in depression.
Neuroplasticity and Neurogenesis: Role of Neurotrophic Factors
Several studies have focused on the potential role of neurotrophic factors in critical neural processes, with particular attention on the neurotrophin family, which is composed of nerve growth factor, brain-derived neurotrophic factor (BDNF), neurotrophin-3, neurotrophin-4/5, and neurotrophin-6. Among these neurotrophins, a growing body of research has focused on the role of BDNF in the regulation of brain development, neuroplasticity, and neurogenesis. 68 Various studies strongly suggest that decreased levels of BDNF may lead to depressive symptoms, whereas up-regulation of BDNF is associated with clinical recovery. 69 In vitro studies have demonstrated that BDNF may decrease 5-HT uptake, suggesting a potential role of the neurotrophin in regulation of 5-HTT. 70 Chronic stress, with the resulting activation of the HPA axis, may damage neurons in certain CNS structures (particularly in the hippocampus, where high levels of GRs have been found) and these changes have been associated with decreased availability of neurotrophic factors such as BDNF. 71 Moreover, it has been shown that increased levels of glucocorticoids, at least partially, may be involved in down-regulation of BDNF. 72 By contrast, it has been demonstrated that various antidepressants increase the expression of BDNF in the hippocampus 69 in a dose-dependent and time-dependent manner, which is consistent with the time dependency of therapeutic effects of antidepressants, therefore suggesting a role for BDNF in their mechanism of action. 73 The potential association between successful pharmacotherapy and the observed up-regulation of BDNF in the hippocampus suggests that BDNF may be involved in the long-lasting effects of antidepressants through neuroplastic changes in certain neural structures such as the hippocampus, amygdala, and PFC. 69 Moreover, it has been shown that BDNF and 5-HT may induce hippocampal neurogenesis. 74
Most neurons in the CNS are generated during early periods of development, although more recent studies have demonstrated that some neural structures, such as the dentate gyrus of the hippocampus, actually continue generating neurons later in life. 75 Therefore, neurogenesis in the adult CNS may be stimulated by special conditions, particularly those related to enhanced hippocampal activity and increased levels of 5-HT, 76 , 77 but it may be inhibited by stressful situations and increased levels of glucocorticoids. 78 Under chronic stress conditions, with increased activation of the HPA axis, inhibition of hippocampal neurogenesis may interfere with the formation of new cognitions, therefore contributing to provoking and sustaining ongoing depressogenic conditions. According to this hypothesis, successful therapeutic interventions may require recovery of the normal rate of hippocampal neurogenesis. This recovery may be associated with a direct effect of antidepressants through increasing levels of 5-HT 75 or indirectly through modulation of the HPA axis and increasing levels of BDNF, which was associated with up-regulation of neuroplasticity and increasing neurogenesis. This hypothesis remains quite controversial because of failure to confirm the increase in neurogenesis after long-term antidepressant treatment. 79
Various studies have focused on BDNF gene regulation and variations potentially involved in mood disorders, resulting in the identification of different SNPs. Among these, an SNP has been identified at nucleotide position 196 in the coding region of the BDNF gene, where a guanine (G) is replaced by an adenine (A), resulting in the substitution of valine (Val) by methionine (Met) at codon 66, which is thus termed Val66Met. This is where the presence of a Met allele has been associated with a functional alteration (i.e., abnormal intracellular trafficking and decreased secretion of BDNF). 73 , 76 Studies on carriers of the Met-BDNF allele revealed relatively smaller hippocampal volumes compared with those individuals who were homozygous for the Val-BDNF allele. 73 This was also associated with reduced hippocampal activation and deficient cognitive performance, 12 , 73 which have also been associated with lower emotional stability and increased vulnerability for the development of depressive symptoms.
Inflammatory Processes: Role of Cytokines
It has been demonstrated that acute and chronic psychosocial stress may activate inflammatory responses. 80 Increased blood concentrations of proinflammatory cytokines, such as interleukin-1, interleukin-6, and tumor necrosis factor-alpha, have been associated with the effect of diverse environmental stimuli, including psychosocial stress, 81 and this immune activation has also been observed in major depression. 82 Moreover, major depression may induce increased inflammatory responses to stress, and this has been observed mostly in patients exposed to adverse early life events, therefore suggesting a link between these and increased inflammatory responses to stress later in life. 80 To understand the role of proinflammatory cytokines in chronic stress and the subsequent development of depression, various studies have focused on their potential mechanisms of action. Environmental stressors activate the sympathetic branch of the autonomic nervous system, with the resulting release of catecholamines, which in turn activates their receptors on immune cells and thus stimulates the release of proinflammatory cytokines. 83 Chronic inflammatory responses in the CNS may result in excessive release of proinflammatory cytokines, which in turn may lead to decreased concentrations of neurotrophins (including BDNF), leading to impaired neuroplasticity 83 and decreased neurogenesis (particularly in the hippocampus 82 ), which have been associated with the origin of cognitive impairment and mood disorders. Proinflammatory cytokines have also been involved in regulation of the HPA axis, stimulating release of CRF with resulting hypercortisolism, 83 which has been associated with reduced sensitivity of GRs and glucocorticoid resistance. 81 , 83 Increased levels of cortisol, such as those observed during chronic stress, may lead to decreased synthesis of 5-HT due to reduced activity of the rate-limiting enzyme tryptophan hydroxylase. Hypercortisolism has been also associated with increased activity of tryptophan dioxygenase (indoleamine-pyrrole 2,3-dioxygenase), which is responsible for the degradation of tryptophan to kynurenine, with the resulting decreased synthesis and release of 5-HT. 83 Proinflammatory cytokines such as interferon have also been involved in the modulation of this pathway, stimulating indoleamine-pyrrole 2,3-dioxygenase and thus leading to reduced synthesis of 5-HT and increased synthesis of kynurenine. 84 Degradation of kynurenine leads to the formation of 3-hydroxykynurenine, which produces free radical species involved in oxidative stress, and kynurenic acid and quinolinic acid, which activate the glutamatergic system. This leads to neurotoxicity and neuronal apoptosis, which are also involved in the pathophysiology of depression. 83 , 84 In addition, certain proinflammatory cytokines, such as interleukin-1 and tumor necrosis factor, have been shown to affect serotonergic neurotransmission by stimulating the 5-HTT and thus reducing intersynaptic concentrations of 5-HT in the CNS. 83 , 85
Understanding the molecular mechanisms underlying neuroinflammatory processes in the CNS, particularly the role played by proinflammatory cytokines in mood disorders, has inspired various studies aimed at improving depressive symptoms by attenuating these processes. Preclinical studies have demonstrated the efficacy of certain anti-inflammatory cytokines to block the depressive-like state induced by proinflammatory cytokines in rodents. 83 Other studies have also approached the consequences of proinflammatory cytokines, antagonizing the activity of the glutamatergic system, activated by the kynurenine pathway. 81
Stress, Appraisal, and Coping: Role of Psychological Vulnerability
Psychological vulnerability depends on various features related to stressful life events (including strength, intensity, and length of the impact) and the availability of personal resources to cope with them. More remarkably, however, it may depend on cognitive appraisal, particularly the balance between stressors and individual resources, and the resulting coping strategies. 86 Chronic exposure to unavoidable and uncontrollable stressors may lead to decreasing cognitive and behavioral coping strategies to handle environmental events, mostly as a result of cognitive appraisals that personal resources are not enough, which has been associated with increasing feelings of helplessness. 86 According to the cognitive model of depression, 87 early life experiences provide the background to develop cognitive schemas, which in turn represent the basis to transform simple data into cognitions that are learned and stored in long-term memory. Adverse early life events, including childhood sexual or physical abuse 88 and peer victimization 89 (also known as bullying), may contribute to the formation of particular cognitive schemas. These schemas may be inactive during long periods and reactivated by new experiences at a later time, particularly those with strong emotional valence. In response to stressful situations in adulthood, activated dysfunctional schemas may induce negative biases during information processing, with consequent dysfunctional effects, including cognitive processing, emotional reactions, and behavioral responses, constituting the essential core of cognitive vulnerability. 87 Therefore, dysfunctional schemas shaped during childhood, with systematic negative biases, may lead to negatively biased appraisals, with consequent limitations in further processing of the resulting cognitions, therefore leading to feelings of helplessness and subsequent depression.
Epigenetics: Role of Gene–Environment Interactions
The term epigenetics refers to heritable characteristics that are not determined by structural changes in the underlying genetic sequence. At the molecular level, epigenetic mechanisms involve biochemical changes of nucleotides, without altering the DNA sequence, and the associated histone proteins, which constitute chromatin. Changes in the structure of chromatin may affect gene expression by allowing transcription factors to gain access to gene regulatory elements. Hence, environmental factors may induce changes in the chromatin state, which in turn may improve exposure of genes to the impact of different transcription factors, therefore increasing or decreasing gene expression while the original DNA sequence remains unaltered. 90 Potential changes include DNA methylation, which has been associated with down-regulation of gene expression; histone acetylation, which may induce up-regulation of gene expression; and histone methylation and phosphorylation, both of which may lead to activation or repression of transcriptional events. 90 Recent research has contributed to identifying epigenetic mechanisms in the context of stressful situations, which may induce long-lasting changes in gene expression in different neural structures. In turn, such changes have been associated with the development of stress-related conditions such as anxiety disorders and depression. Preclinical studies have revealed that chronic stress may regulate histone acetylation in the hippocampus, inducing transient increases and subsequent decreases; transient increases have also been observed in the amygdala. 91
In addition, preclinical studies also revealed that increased levels of CRF, observed during chronic stress conditions, have been associated with decreased DNA methylation at the promoter region of the CRF gene. 92 Moreover, a history of early adverse experiences has been associated with changes in histone markers and DNA methylation of the GR gene, particularly in the hippocampus, and changes in DNA methylation have also been observed in the GR and BDNF genes. 41 Therefore, chronic stress, including early stressful experiences, may induce diverse epigenetic changes in different neural structures, with a subsequent effect on their respective functions. This, in turn, may predispose individuals to increased vulnerability to stress and to the development of diverse clinical conditions such as depression.
Childhood Trauma: Role of Early Adverse Experiences
Early life stress, defined as adverse conditions and traumatic events experienced during childhood, represents a major factor of vulnerability in the origin and development of depression and bipolar disorder. 3 , 5 , 27 The association between a history of adverse and traumatic experiences during childhood and the development of mood disorders later in life has been observed particularly after additional stressful events during adulthood. 5 It has been shown that adverse early life events (including abuse, neglect, or loss) contribute to the formation of dysfunctional cognitive schemas, which may induce negative biases in response to stressful situations at a later time, therefore contributing to generating cognitive vulnerability. 56 This mechanism was also recently described in victims of bullying. 89 Moreover, it has been proposed that certain early life events, such as neglect, may lead to the formation of dysfunctional attitudes; this has also been associated with long-term hyperactivity of the HPA axis. 93 The effect of adverse early life events has been conclusively demonstrated to induce long-lasting changes in neural and neuroendocrine systems involved in adaptive responses to stress, particularly in CRF neurotransmission. 23 This, in turn, may be translated into persistent sensitization and increased responsiveness to stress. 3 , 5 Increased levels of CRF may lead to hyperactivity of the HPA axis and hypercortisolism, which may induce morphologic changes such as reduced hippocampal volume. 72 In this regard, various studies have focused on the role of hippocampal GRs, and increased levels of cortisol (in a sustained and prolonged manner) have been shown to induce down-regulation of GRs in certain areas of the hippocampus. 94 Moreover, additional research has suggested that the availability and efficacy of hippocampal GRs may be permanently affected as a result of early stressful experiences, 88 therefore contributing to glucocorticoid resistance and the consequent hyperreactivity of the HPA axis observed in response to additional stressful situations. In addition, increased concentrations of cortisol and decreased GR availability, induced by stressful situations during childhood, have been associated with decreased hippocampal volume and neural activity in adulthood as well as increased reactivity of the HPA axis, with the consequent functional alterations observed in adulthood. 88 , 95 A history of early life adverse experiences was also associated with hyperreactivity of neural and neuroendocrine responses to stress, which is reflected through increased CRF activity, hypercortisolism, and glucocorticoid resistance. 27 , 96
Klengel et al. 97 reported that a polymorphism in the FKBP5 gene increases the risk for the development of stress-related psychiatric disorders in adults by an allelic-specific, child abuse/neglect–dependent DNA demethylation in functional glucocorticoid response elements of FKBP5. Thus, activation of a sensitized system in the presence of additional stressful situations later in life may result in an exaggerated and maladaptive activation of the stress response, therefore generating increased vulnerability to the development of depressive symptoms upon exposure to additional stressors in adulthood. 42 , 98
Conclusions
The role of stressful life events in the origin and development of depression may be conceptualized as the result of multiple interactions between the effect of environmental stressors and individual factors of vulnerability. Figure 3 illustrates the role of these factors and their potential interactions at the interface between chronic stress and depression. Genetic factors, including SNPs, may be associated with functional and structural alterations in certain neural structures, including increased reactivity of the amygdala and decreased function of the hippocampus. Adverse early life events have been shown to engender biological changes in the developing CNS, as well as psychological changes reflected in the formation of dysfunctional cognitive schemas, 99 with the resulting biased cognitive processing of environmental stimuli, which may be translated into cognitive and emotional vulnerability. 87 These may be further activated in response to stress in adulthood, contributing to increased vulnerability to depression. 27
FIGURE 3. Schematic Representation of Different Factors Involved in the Stress Response and Their Potential Role in Stress and Depression a
a Genetic polymorphisms (represented as genetic vulnerability) participate in the development of the CNS and, together with the influence of early environmental factors (represented by early life stress) and chronic stress, result in a particular CNS phenotype. Early life stress may also induce certain cognitive vulnerability, which in turn may result in emotional vulnerability. Upon the impact of traumatic events or chronic stress, a predisposed CNS responds with increased levels of CRF, hyperactivation of the HPA axis, and increased levels of cortisol, which may lead to molecular changes in different circuits (represented by molecular vulnerability), as well as altered cognitive and emotional responses (represented by emotional vulnerability). This, in turn, may result in increased vulnerability for the development of symptoms of anxiety and depression. CRF, corticotropin-releasing factor; HPA, hypothalamic-pituitary-adrenal.
The impact of abuse and neglect during childhood clearly leads to persistent changes in neural and neuroendocrine systems involved in the regulation of adaptive responses. Functional or structural alterations in the CNS, particularly in the cerebrocortical regions as well as in the amygdala and the hippocampus, along with cognitive biases, may induce biological changes such as increased levels of CRF. Upon exposure to environmental stressors, this mechanism may be translated into hyperactivity of the HPA system, with increased levels of CRF and cortisol, which in turn may lead to transcriptional events. Such molecular changes affecting different aminergic systems, particularly on the regulation of 5-HT together with altered cognitive processing, may result in emotional changes, thereby predisposing to symptoms of anxiety and depression. Therefore, multiple vulnerability factors (including psychological, biological, cognitive, genetic, and epigenetic factors) converge on different aspects of HPA regulation. This complex set of pathways likely links vulnerability to stress with the pathogenesis of depression. In addition, environmental stress has also been associated with inflammatory responses in the CNS with excessive release of proinflammatory cytokines, which may lead to further stimulation of the HPA axis, with resulting hypercortisolism and impaired 5-HT neurotransmission. Proinflammatory cytokines have also been associated with decreased neurotrophins, with resulting decreases in neuroplasticity and neurogenesis. Therefore, a better understanding of the molecular mechanisms underlying these processes may allow novel strategies aimed at improving depressive symptoms by attenuating neuroinflammation.
The observation that some individuals may exhibit stronger vulnerability to environmental stressors but others may be less sensitive, more resistant, or even resilient to similar experiences highlights the importance of further investigation of the nature of different risk factors. Future research should focus on further understanding the neurobiological background underlying these factors and should identify potential windows of intervention, including neural and molecular mechanisms involved in the interface between cognitive processing of environmental stressors and their potential effects in epigenetic processes. This may lead to the development of more successful treatments aimed at not only restoring altered neural and neuroendocrine mechanisms but also preventing the development of anxiety and mood disorders in vulnerable individuals.
This may be achieved either by identifying different vulnerability factors, which in turn may become targets for novel therapeutic interventions, or by increasing and promoting protective resources in individuals exposed to stressful conditions, particularly those exposed to traumatic events or adverse conditions during childhood.
Dr. Nemeroff has in the last 3 years consulted to Takeda, Xhale, Mitsubishi, Clintara, Taisho, Prismic, and Gerson Lehrman, has received grants/research support from NIH and the Agency for Healthcare Research and Quality, has served on the scientific advisory boards for Xhale, AFSP, the Brain and Behavior Research Foundation, Clintara, and the Anxiety and Depression Association of America, and holds stock in Celgene, Seattle Genetics, Abbvie, Titan, OPKO, and Xhale. Dr. Tafet reports no financial relationships with commercial interests.
1 Gold PW : The organization of the stress system and its dysregulation in depressive illness . Mol Psychiatry 2015 ; 20:32–47 Crossref , Medline , Google Scholar
2 Nemeroff CB : The preeminent role of early untoward experience on vulnerability to major psychiatric disorders: the nature-nurture controversy revisited and soon to be resolved . Mol Psychiatry 1999 ; 4:106–108 Crossref , Medline , Google Scholar
3 Heim C, Nemeroff CB : The role of childhood trauma in the neurobiology of mood and anxiety disorders: preclinical and clinical studies . Biol Psychiatry 2001 ; 49:1023–1039 Crossref , Medline , Google Scholar
4 López JF, Akil H, Watson SJ : Neural circuits mediating stress . Biol Psychiatry 1999 ; 46:1461–1471 Crossref , Medline , Google Scholar
5 Heim C, Newport DJ, Mletzko T, et al. : The link between childhood trauma and depression: insights from HPA axis studies in humans . Psychoneuroendocrinology 2008 ; 33:693–710 Crossref , Medline , Google Scholar
6 Caspi A, Sugden K, Moffitt TE, et al. : Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene . Science 2003 ; 301:386–389 Crossref , Medline , Google Scholar
7 Kaufman J, Plotsky PM, Nemeroff CB, et al. : Effects of early adverse experiences on brain structure and function: clinical implications . Biol Psychiatry 2000 ; 48:778–790 Crossref , Medline , Google Scholar
8 Kaufman J, Yang BZ, Douglas-Palumberi H, et al. : Brain-derived neurotrophic factor-5-HTTLPR gene interactions and environmental modifiers of depression in children . Biol Psychiatry 2006 ; 59:673–680 Crossref , Medline , Google Scholar
9 Bradley RG, Binder EB, Epstein MP, et al. : Influence of child abuse on adult depression: moderation by the corticotropin-releasing hormone receptor gene . Arch Gen Psychiatry 2008 ; 65:190–200 Crossref , Medline , Google Scholar
10 Nemeroff CB, Seligman F : The pervasive and persistent neurobiological and clinical aftermath of child abuse and neglect . J Clin Psychiatry 2013 ; 74:999–1001 Crossref , Medline , Google Scholar
11 Gotlib IH, Joormann J, Minor KL, et al. : HPA axis reactivity: a mechanism underlying the associations among 5-HTTLPR, stress, and depression . Biol Psychiatry 2008 ; 63:847–851 Crossref , Medline , Google Scholar
12 Gatt JM, Nemeroff CB, Dobson-Stone C, et al. : Interactions between BDNF Val66Met polymorphism and early life stress predict brain and arousal pathways to syndromal depression and anxiety . Mol Psychiatry 2009 ; 14:681–695 Crossref , Medline , Google Scholar
13 Binder EB, Owens MJ, Liu W, et al. : Association of polymorphisms in genes regulating the corticotropin-releasing factor system with antidepressant treatment response . Arch Gen Psychiatry 2010 ; 67:369–379 Crossref , Medline , Google Scholar
14 LeDoux JE : Brain mechanisms of emotion and emotional learning . Curr Opin Neurobiol 1992 ; 2:191–197 Crossref , Medline , Google Scholar
15 Ghashghaei HT, Hilgetag CC, Barbas H : Sequence of information processing for emotions based on the anatomic dialogue between prefrontal cortex and amygdala . Neuroimage 2007 ; 34:905–923 Crossref , Medline , Google Scholar
16 Drevets WC, Savitz J, Trimble M : The subgenual anterior cingulate cortex in mood disorders . CNS Spectr 2008 ; 13:663–681 Crossref , Medline , Google Scholar
17 Price JL, Drevets WC : Neural circuits underlying the pathophysiology of mood disorders . Trends Cogn Sci 2012 ; 16:61–71 Crossref , Medline , Google Scholar
18 Etkin A, Egner T, Kalisch R : Emotional processing in anterior cingulate and medial prefrontal cortex . Trends Cogn Sci 2011 ; 15:85–93 Crossref , Medline , Google Scholar
19 Ray RD, Zald DH : Anatomical insights into the interaction of emotion and cognition in the prefrontal cortex . Neurosci Biobehav Rev 2012 ; 36:479–501 Crossref , Medline , Google Scholar
20 Motzkin JC, Philippi CL, Wolf RC, et al. : Ventromedial prefrontal cortex is critical for the regulation of amygdala activity in humans . Biol Psychiatry 2015 ; 77:276–284 Crossref , Medline , Google Scholar
21 Zhong M, Wang X, Xiao J, et al. : Amygdala hyperactivation and prefrontal hypoactivation in subjects with cognitive vulnerability to depression . Biol Psychol 2011 ; 88:233–242 Crossref , Medline , Google Scholar
22 Heim CM, Mayberg HS, Mletzko T, et al. : Decreased cortical representation of genital somatosensory field after childhood sexual abuse . Am J Psychiatry 2013 ; 170:616–623 Crossref , Medline , Google Scholar
23 Arborelius L, Owens MJ, Plotsky PM, et al. : The role of corticotropin-releasing factor in depression and anxiety disorders . J Endocrinol 1999 ; 160:1–12 Crossref , Medline , Google Scholar
24 Holsboer F : The corticosteroid receptor hypothesis of depression . Neuropsychopharmacology 2000 ; 23:477–501 Crossref , Medline , Google Scholar
25 Chrousos GP : Stress and disorders of the stress system . Nat Rev Endocrinol 2009 ; 5:374–381 Crossref , Medline , Google Scholar
26 Baumeister D, Lightman SL, Pariante CM : The interface of stress and the HPA axis in behavioural phenotypes of mental illness . Curr Top Behav Neurosci 2014 ; 18:13–24 Crossref , Medline , Google Scholar
27 Nemeroff CB, Binder E : The preeminent role of childhood abuse and neglect in vulnerability to major psychiatric disorders: toward elucidating the underlying neurobiological mechanisms . J Am Acad Child Adolesc Psychiatry 2014 ; 53:395–397 Crossref , Medline , Google Scholar
28 Bremner JD, Narayan M, Anderson ER, et al. : Hippocampal volume reduction in major depression . Am J Psychiatry 2000 ; 157:115–118 Link , Google Scholar
29 Vythilingam M, Heim C, Newport J, et al. : Childhood trauma associated with smaller hippocampal volume in women with major depression . Am J Psychiatry 2002 ; 159:2072–2080 Crossref , Medline , Google Scholar
30 DeRijk RH, Schaaf M, de Kloet ER : Glucocorticoid receptor variants: clinical implications . J Steroid Biochem Mol Biol 2002 ; 81:103–122 Crossref , Medline , Google Scholar
31 Horstmann S, Lucae S, Menke A, et al. : Polymorphisms in GRIK4, HTR2A, and FKBP5 show interactive effects in predicting remission to antidepressant treatment . Neuropsychopharmacology 2010 ; 35:727–740 Crossref , Medline , Google Scholar
32 Binder EB, Salyakina D, Lichtner P, et al. : Polymorphisms in FKBP5 are associated with increased recurrence of depressive episodes and rapid response to antidepressant treatment . Nat Genet 2004 ; 36:1319–1325 Crossref , Medline , Google Scholar
33 Vermeer H, Hendriks-Stegeman BI, van der Burg B, et al. : Glucocorticoid-induced increase in lymphocytic FKBP51 messenger ribonucleic acid expression: a potential marker for glucocorticoid sensitivity, potency, and bioavailability . J Clin Endocrinol Metab 2003 ; 88:277–284 Crossref , Medline , Google Scholar
34 Appel K, Schwahn C, Mahler J, et al. : Moderation of adult depression by a polymorphism in the FKBP5 gene and childhood physical abuse in the general population . Neuropsychopharmacology 2011 ; 36:1982–1991 Crossref , Medline , Google Scholar
35 Nemeroff CB : Neurobiological consequences of childhood trauma . J Clin Psychiatry 2004 ; 65(Suppl 1):18–28 Medline , Google Scholar
36 Valentino RJ, Foote SL, Page ME : The locus coeruleus as a site for integrating corticotropin-releasing factor and noradrenergic mediation of stress responses . Ann N Y Acad Sci 1993 ; 697:173–188 Crossref , Medline , Google Scholar
37 Kirby LG, Rice KC, Valentino RJ : Effects of corticotropin-releasing factor on neuronal activity in the serotonergic dorsal raphe nucleus . Neuropsychopharmacology 2000 ; 22:148–162 Crossref , Medline , Google Scholar
38 Nemeroff CB, Widerlöv E, Bissette G, et al. : Elevated concentrations of CSF corticotropin-releasing factor-like immunoreactivity in depressed patients . Science 1984 ; 226:1342–1344 Crossref , Medline , Google Scholar
39 Regev L, Baram TZ : Corticotropin releasing factor in neuroplasticity . Front Neuroendocrinol 2014 ; 35:171–179 Crossref , Medline , Google Scholar
40 Timmermans W, Xiong H, Hoogenraad CC, et al. : Stress and excitatory synapses: from health to disease . Neuroscience 2013 ; 248:626–636 Crossref , Medline , Google Scholar
41 McEwen BS, Eiland L, Hunter RG, et al. : Stress and anxiety: structural plasticity and epigenetic regulation as a consequence of stress . Neuropharmacology 2012 ; 62:3–12 Crossref , Medline , Google Scholar
42 Kendler KS, Kuhn JW, Prescott CA : Childhood sexual abuse, stressful life events and risk for major depression in women . Psychol Med 2004 ; 34:1475–1482 Crossref , Medline , Google Scholar
43 Polanczyk G, Caspi A, Williams B, et al. : Protective effect of CRHR1 gene variants on the development of adult depression following childhood maltreatment: replication and extension . Arch Gen Psychiatry 2009 ; 66:978–985 Crossref , Medline , Google Scholar
44 Hensler JG : Serotonergic modulation of the limbic system . Neurosci Biobehav Rev 2006 ; 30:203–214 Crossref , Medline , Google Scholar
45 Deakin JF, Graeff FG : 5-HT and mechanisms of defence . J Psychopharmacol 1991 ; 5:305–315 Crossref , Medline , Google Scholar
46 Tafet GE, Bernardini R : Psychoneuroendocrinological links between chronic stress and depression . Prog Neuropsychopharmacol Biol Psychiatry 2003 ; 27:893–903 Crossref , Medline , Google Scholar
47 Hamon M, Blier P : Monoamine neurocircuitry in depression and strategies for new treatments . Prog Neuropsychopharmacol Biol Psychiatry 2013 ; 45:54–63 Crossref , Medline , Google Scholar
48 Ressler KJ, Nemeroff CB : Role of norepinephrine in the pathophysiology and treatment of mood disorders . Biol Psychiatry 1999 ; 46:1219–1233 Crossref , Medline , Google Scholar
49 Kranz GS, Kasper S, Lanzenberger R : Reward and the serotonergic system . Neuroscience 2010 ; 166:1023–1035 Crossref , Medline , Google Scholar
50 Gray NA, Milak MS, DeLorenzo C, et al. : Antidepressant treatment reduces serotonin-1A autoreceptor binding in major depressive disorder . Biol Psychiatry 2013 ; 74:26–31 Crossref , Medline , Google Scholar
51 Lesch KP, Gutknecht L : Focus on The 5-HT1A receptor: emerging role of a gene regulatory variant in psychopathology and pharmacogenetics . Int J Neuropsychopharmacol 2004 ; 7:381–385 Crossref , Medline , Google Scholar
52 López JF, Chalmers DT, Little KY, et al. : A.E. Bennett Research Award. Regulation of serotonin1A, glucocorticoid, and mineralocorticoid receptor in rat and human hippocampus: implications for the neurobiology of depression . Biol Psychiatry 1998 ; 43:547–573 Crossref , Medline , Google Scholar
53 van Riel E, van Gemert NG, Meijer OC, et al. : Effect of early life stress on serotonin responses in the hippocampus of young adult rats . Synapse 2004 ; 53:11–19 Crossref , Medline , Google Scholar
54 Tafet GE, Toister-Achituv M, Shinitzky M : Enhancement of serotonin uptake by cortisol: a possible link between stress and depression . Cogn Affect Behav Neurosci 2001 ; 1:96–104 Crossref , Medline , Google Scholar
55 Lesch KP, Bengel D, Heils A, et al. : Association of anxiety-related traits with a polymorphism in the serotonin transporter gene regulatory region . Science 1996 ; 274:1527–1531 Crossref , Medline , Google Scholar
56 Karg K, Burmeister M, Shedden K, et al. : The serotonin transporter promoter variant (5-HTTLPR), stress, and depression meta-analysis revisited: evidence of genetic moderation . Arch Gen Psychiatry 2011 ; 68:444–454 Crossref , Medline , Google Scholar
57 Hariri AR, Mattay VS, Tessitore A, et al. : Serotonin transporter genetic variation and the response of the human amygdala . Science 2002 ; 297:400–403 Crossref , Medline , Google Scholar
58 Hariri AR, Drabant EM, Munoz KE, et al. : A susceptibility gene for affective disorders and the response of the human amygdala . Arch Gen Psychiatry 2005 ; 62:146–152 Crossref , Medline , Google Scholar
59 Dunlop BW, Nemeroff CB : The role of dopamine in the pathophysiology of depression . Arch Gen Psychiatry 2007 ; 64:327–337 Crossref , Medline , Google Scholar
60 Nestler EJ, Carlezon WA Jr : The mesolimbic dopamine reward circuit in depression . Biol Psychiatry 2006 ; 59:1151–1159 Crossref , Medline , Google Scholar
61 Suridjan I, Boileau I, Bagby M, et al. : Dopamine response to psychosocial stress in humans and its relationship to individual differences in personality traits . J Psychiatr Res 2012 ; 46:890–897 Crossref , Medline , Google Scholar
62 Cabib S, Puglisi-Allegra S : The mesoaccumbens dopamine in coping with stress . Neurosci Biobehav Rev 2012 ; 36:79–89 Crossref , Medline , Google Scholar
63 Krishnan V, Nestler EJ : Linking molecules to mood: new insight into the biology of depression . Am J Psychiatry 2010 ; 167:1305–1320 Crossref , Medline , Google Scholar
64 Bogdan R, Nikolova YS, Pizzagalli DA : Neurogenetics of depression: a focus on reward processing and stress sensitivity . Neurobiol Dis 2013 ; 52:12–23 Crossref , Medline , Google Scholar
65 Der-Avakian A, Markou A : The neurobiology of anhedonia and other reward-related deficits . Trends Neurosci 2012 ; 35:68–77 Crossref , Medline , Google Scholar
66 Pruessner JC, Champagne F, Meaney MJ, et al. : Dopamine release in response to a psychological stress in humans and its relationship to early life maternal care: a positron emission tomography study using [11C]raclopride . J Neurosci 2004 ; 24:2825–2831 Crossref , Medline , Google Scholar
67 Mongeau R, Blier P, de Montigny C : The serotonergic and noradrenergic systems of the hippocampus: their interactions and the effects of antidepressant treatments . Brain Res Brain Res Rev 1997 ; 23:145–195 Crossref , Medline , Google Scholar
68 Mitchelmore C, Gede L : Brain derived neurotrophic factor: epigenetic regulation in psychiatric disorders . Brain Res 2014 ; 1586:162–172 Crossref , Medline , Google Scholar
69 Duman RS, Monteggia LM : A neurotrophic model for stress-related mood disorders . Biol Psychiatry 2006 ; 59:1116–1127 Crossref , Medline , Google Scholar
70 Mössner R, Daniel S, Albert D, et al. : Serotonin transporter function is modulated by brain-derived neurotrophic factor (BDNF) but not nerve growth factor (NGF) . Neurochem Int 2000 ; 36:197–202 Crossref , Medline , Google Scholar
71 Ota KT, Duman RS : Environmental and pharmacological modulations of cellular plasticity: role in the pathophysiology and treatment of depression . Neurobiol Dis 2013 ; 57:28–37 Crossref , Medline , Google Scholar
72 Suri D, Vaidya VA : Glucocorticoid regulation of brain-derived neurotrophic factor: relevance to hippocampal structural and functional plasticity . Neuroscience 2013 ; 239:196–213 Crossref , Medline , Google Scholar
73 Duman RS : Role of neurotrophic factors in the etiology and treatment of mood disorders . Neuromolecular Med 2004 ; 5:11–25 Crossref , Medline , Google Scholar
74 Mahar I, Bambico FR, Mechawar N, et al. : Stress, serotonin, and hippocampal neurogenesis in relation to depression and antidepressant effects . Neurosci Biobehav Rev 2014 ; 38:173–192 Crossref , Medline , Google Scholar
75 Jacobs BL, van Praag H, Gage FH : Adult brain neurogenesis and psychiatry: a novel theory of depression . Mol Psychiatry 2000 ; 5:262–269 Crossref , Medline , Google Scholar
76 Malberg JE, Eisch AJ, Nestler EJ, et al. : Chronic antidepressant treatment increases neurogenesis in adult rat hippocampus . J Neurosci 2000 ; 20:9104–9110 Crossref , Medline , Google Scholar
77 Alenina N, Klempin F : The role of serotonin in adult hippocampal neurogenesis . Behav Brain Res 2015 ; 277:49–57 Crossref , Medline , Google Scholar
78 Krugers HJ, Lucassen PJ, Karst H, et al. : Chronic stress effects on hippocampal structure and synaptic function: relevance for depression and normalization by anti-glucocorticoid treatment . Front Synaptic Neurosci 2010 ; 2:24 Medline , Google Scholar
79 Hanson ND, Nemeroff CB, Owens MJ : Lithium, but not fluoxetine or the corticotropin-releasing factor receptor 1 receptor antagonist R121919, increases cell proliferation in the adult dentate gyrus . J Pharmacol Exp Ther 2011 ; 337:180–186 Crossref , Medline , Google Scholar
80 Haroon E, Raison CL, Miller AH : Psychoneuroimmunology meets neuropsychopharmacology: translational implications of the impact of inflammation on behavior . Neuropsychopharmacology 2012 ; 37:137–162 Crossref , Medline , Google Scholar
81 Capuron L, Miller AH : Immune system to brain signaling: neuropsychopharmacological implications . Pharmacol Ther 2011 ; 130:226–238 Crossref , Medline , Google Scholar
82 Cattaneo A, Macchi F, Plazzotta G, et al. : Inflammation and neuronal plasticity: a link between childhood trauma and depression pathogenesis . Front Cell Neurosci 2015 ; 9:40 Crossref , Medline , Google Scholar
83 Leonard BE : The concept of depression as a dysfunction of the immune system . Curr Immunol Rev 2010 ; 6:205–212 Crossref , Medline , Google Scholar
84 Loftis JM, Huckans M, Morasco BJ : Neuroimmune mechanisms of cytokine-induced depression: current theories and novel treatment strategies . Neurobiol Dis 2010 ; 37:519–533 Crossref , Medline , Google Scholar
85 Zhu CB, Blakely RD, Hewlett WA : The proinflammatory cytokines interleukin-1beta and tumor necrosis factor-alpha activate serotonin transporters . Neuropsychopharmacology 2006 ; 31:2121–2131 Crossref , Medline , Google Scholar
86 Folkman S, Lazarus RS : The relationship between coping and emotion: implications for theory and research . Soc Sci Med 1988 ; 26:309–317 Crossref , Medline , Google Scholar
87 Beck AT : The evolution of the cognitive model of depression and its neurobiological correlates . Am J Psychiatry 2008 ; 165:969–977 Crossref , Medline , Google Scholar
88 Heim C, Binder EB : Current research trends in early life stress and depression: review of human studies on sensitive periods, gene-environment interactions, and epigenetics . Exp Neurol 2012 ; 233:102–111 Crossref , Medline , Google Scholar
89 Gibb BE, Abramson LY, Alloy LB : Emotional maltreatment from parents, verbal peer victimization, and cognitive vulnerability to depression . Cogn Ther Res 2004 ; 28:1–21 Crossref , Google Scholar
90 Stankiewicz AM, Swiergiel AH, Lisowski P : Epigenetics of stress adaptations in the brain . Brain Res Bull 2013 ; 98:76–92 Crossref , Medline , Google Scholar
91 Peña CJ, Bagot RC, Labonté B, et al. : Epigenetic signaling in psychiatric disorders . J Mol Biol 2014 ; 426:3389–3412 Crossref , Medline , Google Scholar
92 Elliott E, Ezra-Nevo G, Regev L, et al. : Resilience to social stress coincides with functional DNA methylation of the Crf gene in adult mice . Nat Neurosci 2010 ; 13:1351–1353 Crossref , Medline , Google Scholar
93 Peng H, Long Y, Li J, et al. : Hypothalamic-pituitary-adrenal axis functioning and dysfunctional attitude in depressed patients with and without childhood neglect . BMC Psychiatry 2014 ; 14:45 Crossref , Medline , Google Scholar
94 Sapolsky RM, Krey LC, McEwen BS : Stress down-regulates corticosterone receptors in a site-specific manner in the brain . Endocrinology 1984 ; 114:287–292 Crossref , Medline , Google Scholar
95 Korosi A, Naninck EF, Oomen CA, et al. : Early-life stress mediated modulation of adult neurogenesis and behavior . Behav Brain Res 2012 ; 227:400–409 Crossref , Medline , Google Scholar
96 Meaney MJ, Szyf M : Environmental programming of stress responses through DNA methylation: life at the interface between a dynamic environment and a fixed genome . Dialogues Clin Neurosci 2005 ; 7:103–123 Medline , Google Scholar
97 Klengel T, Mehta D, Anacker C, et al. : Allele-specific FKBP5 DNA demethylation mediates gene-childhood trauma interactions . Nat Neurosci 2013 ; 16:33–41 Crossref , Medline , Google Scholar
98 Hammen C, Henry R, Daley SE : Depression and sensitization to stressors among young women as a function of childhood adversity . J Consult Clin Psychol 2000 ; 68:782–787 Crossref , Medline , Google Scholar
99 Gould F, Clarke J, Heim C, et al. : The effects of child abuse and neglect on cognitive functioning in adulthood . J Psychiatr Res 2012 ; 46:500–506 Crossref , Medline , Google Scholar
- How inflammation influences psychiatric disease 19 March 2024 | World Journal of Psychiatry, Vol. 14, No. 3
- The relationship between neuroticism and the acute psychological stress response: Evidence from the autonomic nervous system 18 March 2024 | Current Psychology, Vol. 92
- Fermented mixed grain ameliorates chronic stress-induced depression-like behavior and memory deficit 27 July 2023 | Food Science and Biotechnology, Vol. 33, No. 4
- Virtual Reality Breathing Interventions for Mental Health: A Systematic Review and Meta-Analysis of Randomized Controlled Trials 18 January 2024 | Applied Psychophysiology and Biofeedback, Vol. 49, No. 1
- Unraveling the associations between unhealthy lifestyle behaviors and mental health in the general adult Chinese population: A cross-sectional study Journal of Affective Disorders, Vol. 349
- Stress exposure, perceived stress severity, and their effects on health 1 April 2024 | Sociology: Theory, Methods, Marketing, Vol. 49, No. 1
- Evaluation of the anxiolytic activity of ethanolic extract of Ziziphus mauritiana Lam. in Swiss albino mice Pharmacological Research - Modern Chinese Medicine, Vol. 10
- The Role of Lysophosphatidic Acid in Neuropsychiatric and Neurodegenerative Disorders 4 March 2024 | Future Pharmacology, Vol. 4, No. 1
- Value of serum brain-derived neurotrophic factor and glial fibrillary acidic protein for detecting depression in patients with Helicobacter pylori infection Neuroscience Letters, Vol. 825
- A soy protein enzymatic digest mitigates Nrf2-related oxidative stress and attenuates depression-like behavior in a mouse model of sub-chronic restraint stress Heliyon, Vol. 10, No. 6
- Alleviating Stress in Parkinson’s Disease: Symptomatic Treatment, Disease Modification, or Both? Journal of Parkinson's Disease, Vol. 9
- Life Stressors and Mental Well-Being: Experiences of African American Women Navigating Perinatal Loss and Pregnancy Subsequent to Loss 6 February 2024 | Journal of Black Psychology, Vol. 2
- Behavioural characteristics and sex differences of a treatment-resistant depression model: Chronic mild stress in the Wistar-Kyoto rat Behavioural Brain Research, Vol. 457
- A mouse model of oral contraceptive exposure: Depression, motivation, and the stress response Hormones and Behavior, Vol. 158
- Effects of relaxation interventions during pregnancy on maternal mental health, and pregnancy and newborn outcomes: A systematic review and meta-analysis 25 January 2024 | PLOS ONE, Vol. 19, No. 1
- Histone 3 Trimethylation Patterns are Associated with Resilience or Stress Susceptibility in a Rat Model of Major Depression Disorder 16 January 2024 | Molecular Neurobiology, Vol. 13
- Diet Quality Mediates the Relationship Between Chronic Stress and Inflammation in Patients With Metabolic Syndrome 9 January 2024 | Journal of Cardiovascular Nursing, Vol. 14
- Socioecological Model of a Military Family’s Health and Well-Being: Inside a Slovenian Military Family 24 August 2022 | Armed Forces & Society, Vol. 50, No. 1
- Association between inflammatory bowel disease and subsequent depression or anxiety disorders - A retrospective cohort study of 31,728 outpatients Journal of Psychiatric Research, Vol. 169
- Clotrimazole ameliorates chronic mild stress-induced depressive-like behavior in rats; crosstalk between the HPA, NLRP3 inflammasome, and Wnt/β-catenin pathways International Immunopharmacology, Vol. 127
- Assessing the Effectiveness of STAPP@Work, a Self-Management Mobile App, in Reducing Work Stress and Preventing Burnout: Single-Case Experimental Design Study 29 February 2024 | Journal of Medical Internet Research, Vol. 26
- Depression in Final-Year Medical Students in Ho Chi Minh City, Vietnam: The Role of Career-Choice Motivation 18 March 2024 | Journal of Medical Education and Curricular Development, Vol. 11
- A neuronal coping mechanism linking stress-induced anxiety to motivation for reward Science Advances, Vol. 9, No. 49
- Effect of breathwork on stress and mental health: A meta-analysis of randomised-controlled trials 9 January 2023 | Scientific Reports, Vol. 13, No. 1
- Chronic social defeat alters brain vascular-associated cell gene expression patterns leading to vascular dysfunction and immune system activation 28 June 2023 | Journal of Neuroinflammation, Vol. 20, No. 1
- Wistar-Kyoto rats and chronically stressed Wistar rats present similar depression- and anxiety-like behaviors but different corticosterone and endocannabinoid system modulation Progress in Neuro-Psychopharmacology and Biological Psychiatry, Vol. 127
- Investigating the potential effects of α-synuclein aggregation on susceptibility to chronic stress in a mouse Parkinson’s disease model 19 September 2023 | Pharmacological Reports, Vol. 75, No. 6
- A comparative analysis of depressive-like behavior: Exploring sex-related differences and insights 29 November 2023 | PLOS ONE, Vol. 18, No. 11
- Effect of consumption of blue maize tortilla on anxiety-like behaviour, learning, memory and hippocampal BDNF expression in a chronic stress model in rats 29 September 2022 | Nutritional Neuroscience, Vol. 26, No. 11
- Lactobacillus reuteri ATG-F4 Alleviates Chronic Stress-induced Anhedonia by Modulating the Prefrontal Serotonergic System Experimental Neurobiology, Vol. 32, No. 5
- The presentation of anxiety and depression among children and youth diagnosed with hidradenitis suppurativa: A review 10 October 2023 | Pediatric Dermatology, Vol. 63
- Psychological, behavioural and biological factors associated with gastrointestinal symptoms in autistic adults and adults with autistic traits 16 February 2023 | Autism, Vol. 27, No. 7
- Effects of Online Pilates and Face-to-Face Pilates Intervention on Body Composition, Muscle Mechanical Properties, Cardiometabolic Parameters, Mental Health, and Physical Fitness in Middle-Aged Women with Obesity 19 October 2023 | Healthcare, Vol. 11, No. 20
- Antidepressant effects of coumarins and their derivatives: A critical analysis of research advances European Journal of Pharmacology, Vol. 956
- Adverse Childhood Experiences, Intimate Partner Violence, and Mental Well-Being Among Mothers of Toddlers in Tirana, Albania: A Cross-Sectional Mediation Analysis 29 September 2023 | Violence Against Women, Vol. 9
- Emphasizing the Crosstalk Between Inflammatory and Neural Signaling in Post-traumatic Stress Disorder (PTSD) 25 April 2023 | Journal of Neuroimmune Pharmacology, Vol. 18, No. 3
- Stress-mediated dysregulation of the Rap1 small GTPase impairs hippocampal structure and function iScience, Vol. 26, No. 9
- Exploring Novel Therapeutic Approaches for Depressive Disorders: The Role of Allopregnanolone Agonists Cureus, Vol. 291
- Nervous-System-Wise Functional Estimation of Directed Brain–Heart Interplay Through Microstate Occurrences IEEE Transactions on Biomedical Engineering, Vol. 70, No. 8
- Stress in the social context: a behavioural and eco-evolutionary perspective 2 August 2023 | Journal of Experimental Biology, Vol. 226, No. 15
- Pathways to Psychopathology Among Autistic Adults 28 June 2023 | Current Psychiatry Reports, Vol. 25, No. 8
- Stress-Activated Protein Kinase JNK Modulates Depression-like Behaviors in Mice 18 January 2023 | Molecular Neurobiology, Vol. 60, No. 5
- Chronic oral ketamine prevents anhedonia and alters neuronal activation in the lateral habenula and nucleus accumbens in rats under chronic unpredictable mild stress Neuropharmacology, Vol. 228
- Dietary tryptophan-rich protein hydrolysate can acutely impact physiological and psychological measures of mood and stress in healthy adults 28 March 2022 | Nutritional Neuroscience, Vol. 26, No. 4
- Mental health as part of the integrative palliative care in all levels of care in urooncology 23 April 2022 | Aging & Mental Health, Vol. 27, No. 4
- Antidepressant and Neuroprotective Effects of 3-Hydroxy Paroxetine, an Analog of Paroxetine in Rats 26 November 2022 | International Journal of Neuropsychopharmacology, Vol. 26, No. 3
- Cortisol Biosensors: From Sensing Principles to Applications 15 March 2023 | World Scientific Annual Review of Functional Materials
- Elevated Hippocampal CRMP5 Mediates Chronic Stress-Induced Cognitive Deficits by Disrupting Synaptic Plasticity, Hindering AMPAR Trafficking, and Triggering Cytokine Release 3 March 2023 | International Journal of Molecular Sciences, Vol. 24, No. 5
- Can a single session of noninvasive brain stimulation applied over the prefrontal cortex prevent stress-induced cortisol release? Progress in Neuro-Psychopharmacology and Biological Psychiatry, Vol. 121
- Psychoneuro-oncology: How chronic stress grows cancer Clinics in Dermatology, Vol. 54
- Peripheral brain-derived neurotrophic factor (BDNF) and salivary cortisol levels in college students with different levels of academic stress. Study protocol 22 February 2023 | PLOS ONE, Vol. 18, No. 2
- The Role of Genetics in the Development and Pharmacotherapy of Depression and Its Impact on Drug Discovery 2 February 2023 | International Journal of Molecular Sciences, Vol. 24, No. 3
- Role of group II metabotropic glutamate receptors in ketamine's antidepressant actions Pharmacology Biochemistry and Behavior, Vol. 223
- Relating parental stress with sleep disorders in parents and children 25 January 2023 | PLOS ONE, Vol. 18, No. 1
- Anxiety, depression, and academic stress among medical students during the COVID-19 pandemic 11 January 2023 | Frontiers in Psychology, Vol. 13
- Associations Between Demographic, Clinical, and Symptom Characteristics and Stress in Oncology Patients Receiving Chemotherapy 4 March 2022 | Cancer Nursing, Vol. 46, No. 1
- Prevalence of Common Alleles of Some Stress Resilience Genes among Adolescents Born in Different Periods Relative to the Socioeconomic Crisis of the 1990s in Russia 21 December 2022 | Current Issues in Molecular Biology, Vol. 45, No. 1
- Introducing a depression-like syndrome for translational neuropsychiatry: a plea for taxonomical validity and improved comparability between humans and mice 14 September 2022 | Molecular Psychiatry, Vol. 28, No. 1
- Targeting the Arginine Vasopressin V1b Receptor System and Stress Response in Depression and Other Neuropsychiatric Disorders 1 April 2023 | Neuropsychiatric Disease and Treatment, Vol. Volume 19
- Efficacy and Anti-Inflammatory Activity of Ashwagandha Sustained-Release Formulation on Depression and Anxiety Induced by Chronic Unpredictable Stress: in vivo and in vitro Studies 1 July 2023 | Journal of Experimental Pharmacology, Vol. Volume 15
- Gender Differences in Older Adults’ Muscle Strength and Depressive Symptoms: A Relationship Mediated Through Perceived Stress 27 September 2023 | Research in Community and Public Health Nursing, Vol. 34
- Increased academic stress is associated with decreased plasma BDNF in Chilean college students 3 November 2023 | PeerJ, Vol. 11
- Interaction effect between childhood abuse and interleukin-1β levels on suicidality in depressed patients 25 April 2022 | European Archives of Psychiatry and Clinical Neuroscience, Vol. 272, No. 8
- Prevalence, associated factors and perinatal outcomes of antepartum depression in Ibadan Nigeria 18 March 2022 | BMC Pregnancy and Childbirth, Vol. 22, No. 1
- Stress, mental disorder and ketamine as a novel, rapid acting treatment European Neuropsychopharmacology, Vol. 65
- Neighbourhood crime and major depression in Sweden: A national cohort study Health & Place, Vol. 78
- Preschool Depression and Hippocampal Volume: The Moderating Role of Family Income Journal of the American Academy of Child & Adolescent Psychiatry, Vol. 61, No. 11
- HPA Axis Responsiveness Associates with Central Serotonin Transporter Availability in Human Obesity and Non-Obesity Controls 25 October 2022 | Brain Sciences, Vol. 12, No. 11
- Restraint Stress and Repeated Corticosterone Administration Differentially Affect Neuronal Excitability, Synaptic Transmission and 5-HT7 Receptor Reactivity in the Dorsal Raphe Nucleus of Young Adult Male Rats 18 November 2022 | International Journal of Molecular Sciences, Vol. 23, No. 22
- Sleep disorders mediate the link between childhood trauma and depression severity in children and adolescents with depression 28 October 2022 | Frontiers in Psychiatry, Vol. 13
- The cumulative effect of chronic stress and depressive symptoms affects heart rate in a working population 13 October 2022 | Frontiers in Psychiatry, Vol. 13
- Depression among people with dyspepsia and H. pylori infection: A community based cross-sectional study in Ethiopia 6 October 2022 | PLOS ONE, Vol. 17, No. 10
- Cross-Sectional Analysis of Mental Health among University Students: Do Sex and Academic Level Matter? 3 October 2022 | International Journal of Environmental Research and Public Health, Vol. 19, No. 19
- Hormonal contraceptives, stress, and the brain: The critical need for animal models Frontiers in Neuroendocrinology, Vol. 67
- Olfactory loss is a predisposing factor for depression, while olfactory enrichment is an effective treatment for depression 28 September 2022 | Frontiers in Neuroscience, Vol. 16
- Understanding the basis of major depressive disorder in oncological patients: Biological links, clinical management, challenges, and lifestyle medicine 16 September 2022 | Frontiers in Oncology, Vol. 12
- The Lived Experiences of Depression in Huntington’s Disease: A Qualitative Study Journal of Huntington's Disease, Vol. 11, No. 3
- Exaggerated amygdala response to threat and association with immune hyperactivity in depression Brain, Behavior, and Immunity, Vol. 104
- Causal Symbolic Information Transfer for the Assessment of functional Brain-Heart Interplay through EEG Microstates Occurrences: a proof-of-concept study
- Mental Health Conditions According to Stress and Sleep Disorders 29 June 2022 | International Journal of Environmental Research and Public Health, Vol. 19, No. 13
- Different Areas of Chronic Stress and Their Associations with Depression 19 July 2022 | International Journal of Environmental Research and Public Health, Vol. 19, No. 14
- Vestibular Disability/Handicap in Fibromyalgia: A Questionnaire Study 11 July 2022 | Journal of Clinical Medicine, Vol. 11, No. 14
- Perceived stress and E-cigarette use during emerging adulthood: A longitudinal examination of initiation, progression, and continuation Preventive Medicine, Vol. 160
- Efficacy of Withania somnifera supplementation on adult’s cognition and mood Journal of Ayurveda and Integrative Medicine, Vol. 13, No. 2
- CCR2 monocytes repair cerebrovascular damage caused by chronic social defeat stress Brain, Behavior, and Immunity, Vol. 101
- The interplay between self-esteem, expectancy, cognitive control, rumination, and the experience of stress: A network analysis 14 February 2022 | Current Psychology, Vol. 79
- The Cortisol Assessment List (CoAL) A tool to systematically document and evaluate cortisol assessment in blood, urine and saliva Comprehensive Psychoneuroendocrinology, Vol. 9
- Introduction to the Study of Stress 17 May 2022
- Neurobiological Approach to Stress 17 May 2022
- Clinical Approach to Stress 17 May 2022
- Medical Comorbidities of Hispanics with Mental Health Problems 2 December 2022
- Specific and cumulative lifetime stressors in the aetiology of major depression: A longitudinal community-based population study 26 January 2022 | Epidemiology and Psychiatric Sciences, Vol. 31
- Associations of state-level and county-level hate crimes with individual-level cardiovascular risk factors in a prospective cohort study of middle-aged Americans: the National Longitudinal Survey of Youths 1979 19 January 2022 | BMJ Open, Vol. 12, No. 1
- The role of pre-pandemic depression for changes in depression, anxiety, and loneliness during the COVID-19 pandemic: Results from a longitudinal probability sample of adults from Germany 3 November 2022 | European Psychiatry, Vol. 65, No. 1
- Interleukin-6 expression and its modulation by diacerein in a rat model of chronic stress induced cardiac dysfunction Heliyon, Vol. 7, No. 12
- Psychometric properties and correlates of Chinese version of Perceived Stress Scale (CPSS-10) in people with common mental disorders with different employment Statuses 4 August 2021 | Hong Kong Journal of Occupational Therapy, Vol. 34, No. 2
- Association between the expression of lncRNA BASP-AS1 and volume of right hippocampal tail moderated by episode duration in major depressive disorder: a CAN-BIND 1 report 8 September 2021 | Translational Psychiatry, Vol. 11, No. 1
- Psychoneuroimmunology in the context of perinatal depression - Tools for improved clinical practice Brain, Behavior, & Immunity - Health, Vol. 17
- MicroRNAs as Critical Biomarkers of Major Depressive Disorder: A Comprehensive Perspective 10 November 2021 | Biomedicines, Vol. 9, No. 11
- Treadmill exercise sex-dependently alters susceptibility to depression-like behaviour, cytokines and BDNF in the hippocampus and prefrontal cortex of rats with sporadic Alzheimer-like disease Physiology & Behavior, Vol. 241
- Childhood trauma and depression in college students: Mediating and moderating effects of psychological resilience Asian Journal of Psychiatry, Vol. 65
- Back to nature: herbal treatment, environmental enrichment, and social play can protect against unpredictable chronic stress in Long-Evans rats (Rattus norvegicus) 1 August 2021 | Psychopharmacology, Vol. 238, No. 10
- Maternal chewing improves prenatal stress-induced cognitive deficit and anxiety-like behavior associated with alterations of the apoptotic response and serotonin pathway in mouse offspring Archives of Oral Biology, Vol. 130
- HPA Axis in the Pathomechanism of Depression and Schizophrenia: New Therapeutic Strategies Based on Its Participation 30 September 2021 | Brain Sciences, Vol. 11, No. 10
- Roles of fibroblast growth factor 21 in the control of depression‐like behaviours after social defeat stress in male rodents 1 September 2021 | Journal of Neuroendocrinology, Vol. 33, No. 10
- Weak and uneven associations of home, neighborhood, and school environments with stress hormone output across multiple timescales 4 May 2020 | Molecular Psychiatry, Vol. 26, No. 9
- Impact of depression and stress on placental DNA methylation in ethnically diverse pregnant women Epigenomics, Vol. 13, No. 18
- Stress and Western diets increase vulnerability to neuropsychiatric disorders: A common mechanism 16 September 2019 | Nutritional Neuroscience, Vol. 24, No. 8
- Associations of job strain and family strain with risk of major depressive episode: A prospective cohort study in U.S. working men and women Journal of Psychosomatic Research, Vol. 147
- Prolonged Maternal Separation Induces the Depression-Like Behavior Susceptibility to Chronic Unpredictable Mild Stress Exposure in Mice BioMed Research International, Vol. 2021
- Endometriosis and related pelvic pain: association with stress, anxiety and depressive symptoms Minerva Obstetrics and Gynecology, Vol. 73, No. 3
- Title: “Labels Matter: Is it stress or is it Trauma?” 10 July 2021 | Translational Psychiatry, Vol. 11, No. 1
- Depression, anxiety, and the COVID-19 pandemic: Severity of symptoms and associated factors among university students after the end of the movement lockdown 27 May 2021 | PLOS ONE, Vol. 16, No. 5
- Traditional Chinese Medicine Body Constitutions and Psychological Determinants of Depression among University Students in Malaysia: A Pilot Study 18 May 2021 | International Journal of Environmental Research and Public Health, Vol. 18, No. 10
- A pioneering FreeSurfer volumetric study of a series of patients with mesial temporal lobe epilepsy and hippocampal sclerosis with comorbid depression Psychiatry Research: Neuroimaging, Vol. 311
- Increased Stress Resistance and Lifespan in Chaenorhabditis elegans Wildtype and Knockout Mutants—Implications for Depression Treatment by Medicinal Herbs 24 March 2021 | Molecules, Vol. 26, No. 7
- Activation of PPG neurons following acute stressors differentially involves hindbrain serotonin in male rats Neuropharmacology, Vol. 187
- Comorbid anxiety-like behavior in a rat model of colitis is mediated by an upregulation of corticolimbic fatty acid amide hydrolase 15 January 2021 | Neuropsychopharmacology, Vol. 46, No. 5
- Prenatal Alcohol Exposure and Hypothalamic-Pituitary-Adrenal Axis Activity of the Offspring in Humans: a Systematic Review 5 January 2021 | Current Addiction Reports, Vol. 8, No. 1
- Depression and anxiety in the Malaysian urban population and their association with demographic characteristics, quality of life, and the emergence of the COVID-19 pandemic 19 February 2021 | Current Psychology, Vol. 16
- Hypothalamic Inflammation as a Potential Pathophysiologic Basis for the Heterogeneity of Clinical, Hormonal, and Metabolic Presentation in PCOS 5 February 2021 | Nutrients, Vol. 13, No. 2
- Potential Interactions Between Environmental and Psychoneurobiological Factors in the Interface Between Stress and Depression: A Road Map to Resilience 24 January 2021
- The 2020 Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for mood disorders 22 December 2020 | Australian & New Zealand Journal of Psychiatry, Vol. 55, No. 1
- Effects of an African Circle Dance Programme on Internally Displaced Persons with Depressive Symptoms: A Quasi-Experimental Study 19 January 2021 | International Journal of Environmental Research and Public Health, Vol. 18, No. 2
- Yoga and Lifestyle Factors in Heart Disease
- Association between depression, anxiety, stress and perceived quality of life in a Malaysian B40 urban community during the COVID-19 lockdown: A cross-sectional study 29 July 2021 | F1000Research, Vol. 10
- Fluoxetine increases hippocampal neural survival by improving axonal transport in stress-induced model of depression male rats Physiology & Behavior, Vol. 227
- A Systematic Review of the Association Between Psychological Stress and Dementia Risk in Humans Journal of Alzheimer's Disease, Vol. 78, No. 1
- A Gut Feeling: The Importance of the Intestinal Microbiota in Psychiatric Disorders 19 October 2020 | Frontiers in Immunology, Vol. 11
- Efficacy of probiotics on stress in healthy volunteers: A systematic review and meta‐analysis based on randomized controlled trials 14 July 2020 | Brain and Behavior, Vol. 10, No. 9
- The influence of the duration of chronic unpredictable mild stress on the behavioural responses of C57BL/6J mice 18 May 2020 | Behavioural Pharmacology, Vol. 31, No. 6
- Corticosterone Induced the Increase of proBDNF in Primary Hippocampal Neurons Via Endoplasmic Reticulum Stress 6 May 2020 | Neurotoxicity Research, Vol. 38, No. 2
- Monoaminergic balances predict non-depression-like phenotype in Learned Helplessness Paradigm Neuroscience, Vol. 440
- Abnormal functional connectivity as neural biological substrate of trait and state characteristics in major depressive disorder Progress in Neuro-Psychopharmacology and Biological Psychiatry, Vol. 102
- Chronic stress and endothelial dysfunction: mechanisms, experimental challenges, and the way ahead American Journal of Physiology-Heart and Circulatory Physiology, Vol. 319, No. 2
- Heart Rate Variability as an Index of Differential Brain Dynamics at Rest and After Acute Stress Induction 2 July 2020 | Frontiers in Neuroscience, Vol. 14
- Early life stress and glutamate neurotransmission in major depressive disorder European Neuropsychopharmacology, Vol. 35
- Prevalence of and factors associated with depression among hill tribe individuals aged 30 years and over in Thailand Heliyon, Vol. 6, No. 6
- State-of-the-Art: Inflammatory and Metabolic Markers in Mood Disorders 6 June 2020 | Life, Vol. 10, No. 6
- Pharmacological Treatment of Anxiety Disorders: The Role of the HPA Axis 15 May 2020 | Frontiers in Psychiatry, Vol. 11
- Neuroinflammation and depressive disorder: The role of the hypothalamus Journal of Clinical Neuroscience, Vol. 75
- From Work Well-Being to Burnout: A Hypothetical Phase Model 30 April 2020 | Frontiers in Neuroscience, Vol. 14
- Finding intestinal fortitude: Integrating the microbiome into a holistic view of depression mechanisms, treatment, and resilience Neurobiology of Disease, Vol. 135
- Role of glucocorticoid- and monoamine-metabolizing enzymes in stress-related psychopathological processes 19 July 2019 | Stress, Vol. 23, No. 1
- Is Stress a Cause or a Consequence of Endometriosis? 6 January 2020 | Reproductive Sciences, Vol. 27, No. 1
- Hypothalamic–pituitary–adrenal axis and stress
- Immune response to stress induction as a predictor of cognitive-behavioral therapy outcomes in adolescent mood disorders: A pilot study Journal of Psychiatric Research, Vol. 120
- Enduring and Sex-specific Changes in Hippocampal Gene Expression after a Subchronic Immune Challenge Neuroscience, Vol. 428
- Childhood maltreatment and risk for suicide attempts in major depression: a sex-specific approach 7 May 2019 | European Journal of Psychotraumatology, Vol. 10, No. 1
- How Do Couples Cope With Unemployment: Examining Relationships Among Support, Undermining, and Depression 10 March 2019 | The Family Journal, Vol. 27, No. 3
- REM sleep’s unique associations with corticosterone regulation, apoptotic pathways, and behavior in chronic stress in mice 25 January 2019 | Proceedings of the National Academy of Sciences, Vol. 116, No. 7
- Subclinical Lipopolysaccharide from Salmonella Enteritidis Induces Dysregulation of Bioactive Substances from Selected Brain Sections and Glands of Neuroendocrine Axes 2 February 2019 | Toxins, Vol. 11, No. 2
- Advance in Stress for Depressive Disorder 30 November 2019
- Antidepressant and anxiolytic effects of the proprietary Chinese medicine Shexiang Baoxin pill in mice with chronic unpredictable mild stress Journal of Food and Drug Analysis, Vol. 27, No. 1
- Frontiers in Neuroscience, Vol. 13
- A gene–gene interaction between the vascular endothelial growth factor a and brain-derived neurotrophic factor genes is associated with psychological distress in the Taiwanese population Taiwanese Journal of Psychiatry, Vol. 33, No. 3
- An investigation into the stress-relieving and pharmacological actions of an ashwagandha (Withania somnifera) extract 1 September 2019 | Medicine, Vol. 98, No. 37
- Cortisol and alpha-amylase assessment in psychotherapeutic intervention studies: A systematic review Neuroscience & Biobehavioral Reviews, Vol. 95
- Neighborhood disorder, exposure to violence, and perceived discrimination in relation to symptoms in midlife women 19 October 2018 | Women's Midlife Health, Vol. 4, No. 1
- Potassium 2-(1-hydroxypentyl)-benzoate improves depressive-like behaviors in rat model Acta Pharmaceutica Sinica B, Vol. 8, No. 6
- Emotional stress regulation: The role of relative frontal alpha asymmetry in shaping the stress response Biological Psychology, Vol. 138
- Late chronotype is associated with enhanced amygdala reactivity and reduced fronto-limbic functional connectivity to fearful versus happy facial expressions NeuroImage, Vol. 171
- Behavioral and structural adaptations to stress Frontiers in Neuroendocrinology, Vol. 49
- The Neurochemistry of Stress: the Chemistry of the Stress Response and Stress Vulnerability 30 June 2018 | Neurochemical Journal, Vol. 12, No. 2
- Hair cortisol and the relationship with chronic pain and quality of life in endometriosis patients Psychoneuroendocrinology, Vol. 89
- miRNAs As Critical Epigenetic Players in Determining Neurobiological Correlates of Major Depressive Disorder 25 October 2017
- Hepatology International, Vol. 12, No. 4
- Neuropsychopharmacology, Vol. 43, No. 5
- Bibliographie
- Medical Yoga Therapy 10 February 2017 | Children, Vol. 4, No. 2
- Psihijatrija danas, Vol. 49, No. 1
- Hippocampal volume and integrity as predictors of cognitive decline in intact elderly NeuroReport, Vol. 27, No. 11
- Psychosocial stress based on public speech in humans: is there a real life/laboratory setting cross-adaptation? 4 July 2016 | Stress, Vol. 19, No. 4
- Share full article
Advertisement
Supported by
Personal Health
The Devastating Ways Depression and Anxiety Impact the Body
Mind and body form a two-way street.

By Jane E. Brody
It’s no surprise that when a person gets a diagnosis of heart disease, cancer or some other life-limiting or life-threatening physical ailment, they become anxious or depressed. But the reverse can also be true: Undue anxiety or depression can foster the development of a serious physical disease, and even impede the ability to withstand or recover from one. The potential consequences are particularly timely, as the ongoing stress and disruptions of the pandemic continue to take a toll on mental health .
The human organism does not recognize the medical profession’s artificial separation of mental and physical ills. Rather, mind and body form a two-way street. What happens inside a person’s head can have damaging effects throughout the body, as well as the other way around. An untreated mental illness can significantly increase the risk of becoming physically ill, and physical disorders may result in behaviors that make mental conditions worse.
In studies that tracked how patients with breast cancer fared, for example, Dr. David Spiegel and his colleagues at Stanford University School of Medicine showed decades ago that women whose depression was easing lived longer than those whose depression was getting worse. His research and other studies have clearly shown that “the brain is intimately connected to the body and the body to the brain,” Dr. Spiegel said in an interview. “The body tends to react to mental stress as if it was a physical stress.”
Despite such evidence, he and other experts say, chronic emotional distress is too often overlooked by doctors. Commonly, a physician will prescribe a therapy for physical ailments like heart disease or diabetes, only to wonder why some patients get worse instead of better.
Many people are reluctant to seek treatment for emotional ills. Some people with anxiety or depression may fear being stigmatized, even if they recognize they have a serious psychological problem. Many attempt to self-treat their emotional distress by adopting behaviors like drinking too much or abusing drugs, which only adds insult to their pre-existing injury.
And sometimes, family and friends inadvertently reinforce a person’s denial of mental distress by labeling it as “that’s just the way he is” and do nothing to encourage them to seek professional help.
How common are anxiety and depression?
Anxiety disorders affect nearly 20 percent of American adults . That means millions are beset by an overabundance of the fight-or-flight response that primes the body for action. When you’re stressed, the brain responds by prompting the release of cortisol, nature’s built-in alarm system. It evolved to help animals facing physical threats by increasing respiration, raising the heart rate and redirecting blood flow from abdominal organs to muscles that assist in confronting or escaping danger.
These protective actions stem from the neurotransmitters epinephrine and norepinephrine, which stimulate the sympathetic nervous system and put the body on high alert. But when they are invoked too often and indiscriminately, the chronic overstimulation can result in all manner of physical ills, including digestive symptoms like indigestion, cramps, diarrhea or constipation, and an increased risk of heart attack or stroke.
Depression, while less common than chronic anxiety, can have even more devastating effects on physical health. While it’s normal to feel depressed from time to time, more than 6 percent of adults have such persistent feelings of depression that it disrupts personal relationships, interferes with work and play, and impairs their ability to cope with the challenges of daily life. Persistent depression can also exacerbate a person’s perception of pain and increase their chances of developing chronic pain.
“Depression diminishes a person’s capacity to analyze and respond rationally to stress,” Dr. Spiegel said. “They end up on a vicious cycle with limited capacity to get out of a negative mental state.”
Potentially making matters worse, undue anxiety and depression often coexist, leaving people vulnerable to a panoply of physical ailments and an inability to adopt and stick with needed therapy.
A study of 1,204 elderly Korean men and women initially evaluated for depression and anxiety found that two years later, these emotional disorders increased their risk of physical disorders and disability. Anxiety alone was linked with heart disease, depression alone was linked with asthma, and the two together were linked with eyesight problems, persistent cough, asthma, hypertension, heart disease and gastrointestinal problems.
Treatment can counter emotional tolls
Although persistent anxiety and depression are highly treatable with medications, cognitive behavioral therapy and talk therapy, without treatment these conditions tend to get worse. According to Dr. John Frownfelter, treatment for any condition works better when doctors understand “the pressures patients face that affect their behavior and result in clinical harm.”
Dr. Frownfelter is an internist and chief medical officer of a start-up called Jvion. The organization uses artificial intelligence to identify not just medical factors but psychological, social and behavioral ones as well that can impact the effectiveness of treatment on patients’ health. Its aim is to foster more holistic approaches to treatment that address the whole patient, body and mind combined.
The analyses used by Jvion, a Hindi word meaning life-giving, could alert a doctor when underlying depression might be hindering the effectiveness of prescribed treatments for another condition. For example, patients being treated for diabetes who are feeling hopeless may fail to improve because they take their prescribed medication only sporadically and don’t follow a proper diet, Dr. Frownfelter said.
“We often talk about depression as a complication of chronic illness,” Dr. Frownfelter wrote in Medpage Today in July . “But what we don’t talk about enough is how depression can lead to chronic disease. Patients with depression may not have the motivation to exercise regularly or cook healthy meals. Many also have trouble getting adequate sleep.”
Some changes to medical care during the pandemic have greatly increased patient access to depression and anxiety treatment. The expansion of telehealth has enabled patients to access treatment by psychotherapists who may be as far as a continent away.
Patients may also be able to treat themselves without the direct help of a therapist. For example, Dr. Spiegel and his co-workers created an app called Reveri that teaches people self-hypnosis techniques designed to help reduce stress and anxiety, improve sleep, reduce pain and suppress or quit smoking.
Improving sleep is especially helpful, Dr. Spiegel said, because “it enhances a person’s ability to regulate the stress response system and not get stuck in a mental rut.” Data demonstrating the effectiveness of the Reveri app has been collected but not yet published, he said.
Jane Brody is the Personal Health columnist, a position she has held since 1976. She has written more than a dozen books including the best sellers “Jane Brody’s Nutrition Book” and “Jane Brody’s Good Food Book.” More about Jane E. Brody
Jane Brody’s Personal Health Advice
After joining the new york times in 1965, she was its personal health columnist from 1976 to 2022. revisit some of her most memorable writing:.
Brody’s first column, on jogging , ran on Nov. 10, 1976. Her last, on Feb. 21. In it, she highlighted the evolution of health advice throughout her career.
Personal Health has often offered useful advice and a refreshing perspective. Declutter? This is why you must . Cup of coffee? Yes, please.
As a columnist, she has never been afraid to try out, and write about, new things — from intermittent fasting to knitting groups .
How do you put into words the pain of losing a spouse of 43 years? It is “nothing like losing a parent,” she wrote of her own experience with grieving .
Need advice on aging? She has explored how to do it gracefully , building muscle strength and knee replacements .
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- March 01, 2024 | VOL. 181, NO. 3 CURRENT ISSUE pp.171-254
- February 01, 2024 | VOL. 181, NO. 2 pp.83-170
- January 01, 2024 | VOL. 181, NO. 1 pp.1-82
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
The Critical Relationship Between Anxiety and Depression
- Ned H. Kalin , M.D.
Search for more papers by this author
Anxiety and depressive disorders are among the most common psychiatric illnesses; they are highly comorbid with each other, and together they are considered to belong to the broader category of internalizing disorders. Based on statistics from the Substance Abuse and Mental Health Services Administration, the 12-month prevalence of major depressive disorder in 2017 was estimated to be 7.1% for adults and 13.3% for adolescents ( 1 ). Data for anxiety disorders are less current, but in 2001–2003, their 12-month prevalence was estimated to be 19.1% in adults, and 2001–2004 data estimated that the lifetime prevalence in adolescents was 31.9% ( 2 , 3 ). Both anxiety and depressive disorders are more prevalent in women, with an approximate 2:1 ratio in women compared with men during women’s reproductive years ( 1 , 2 ).
Across all psychiatric disorders, comorbidity is the rule ( 4 ), which is definitely the case for anxiety and depressive disorders, as well as their symptoms. With respect to major depression, a worldwide survey reported that 45.7% of individuals with lifetime major depressive disorder had a lifetime history of one or more anxiety disorder ( 5 ). These disorders also commonly coexist during the same time frame, as 41.6% of individuals with 12-month major depression also had one or more anxiety disorder over the same 12-month period. From the perspective of anxiety disorders, the lifetime comorbidity with depression is estimated to range from 20% to 70% for patients with social anxiety disorder ( 6 ), 50% for patients with panic disorder ( 6 ), 48% for patients with posttraumatic stress disorder (PTSD) ( 7 ), and 43% for patients with generalized anxiety disorder ( 8 ). Data from the well-known Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study demonstrate comorbidity at the symptom level, as 53% of the patients with major depression had significant anxiety and were considered to have an anxious depression ( 9 ).
Anxiety and depressive disorders are moderately heritable (approximately 40%), and evidence suggests shared genetic risk across the internalizing disorders ( 10 ). Among internalizing disorders, the highest level of shared genetic risk appears to be between major depressive disorder and generalized anxiety disorder. Neuroticism is a personality trait or temperamental characteristic that is associated with the development of both anxiety and depression, and the genetic risk for developing neuroticism also appears to be shared with that of the internalizing disorders ( 11 ). Common nongenetic risk factors associated with the development of anxiety and depression include earlier life adversity, such as trauma or neglect, as well as parenting style and current stress exposure. At the level of neural circuits, alterations in prefrontal-limbic pathways that mediate emotion regulatory processes are common to anxiety and depressive disorders ( 12 , 13 ). These findings are consistent with meta-analyses that reveal shared structural and functional brain alterations across various psychiatric illnesses, including anxiety and major depression, in circuits involving emotion regulation ( 13 ), executive function ( 14 ), and cognitive control ( 15 ).
Anxiety disorders and major depression occur during development, with anxiety disorders commonly beginning during preadolescence and early adolescence and major depression tending to emerge during adolescence and early to mid-adulthood ( 16 – 18 ). In relation to the evolution of their comorbidity, studies demonstrate that anxiety disorders generally precede the presentation of major depressive disorder ( 17 ). A European community-based study revealed, beginning at age 15, the developmental relation between comorbid anxiety and major depression by specifically focusing on social phobia (based on DSM-IV criteria) and then asking the question regarding concurrent major depressive disorder ( 18 ). The findings revealed a 19% concurrent comorbidity between these disorders, and in 65% of the cases, social phobia preceded major depressive disorder by at least 2 years. In addition, initial presentation with social phobia was associated with a 5.7-fold increased risk of developing major depressive disorder. These associations between anxiety and depression can be traced back even earlier in life. For example, childhood behavioral inhibition in response to novelty or strangers, or an extreme anxious temperament, is associated with a three- to fourfold increase in the likelihood of developing social anxiety disorder, which in turn is associated with an increased risk to develop major depressive disorder and substance abuse ( 19 ).
It is important to emphasize that the presence of comor‐bid anxiety symptoms and disorders matters in relation to treatment. Across psychiatric disorders, the presence of significant anxiety symptoms generally predicts worse outcomes, and this has been well demonstrated for depression. In the STAR*D study, patients with anxious major depressive disorder were more likely to be severely depressed and to have more suicidal ideation ( 9 ). This is consistent with the study by Kessler and colleagues ( 5 ), in which patients with anxious major depressive disorder, compared with patients with nonanxious major depressive disorder, were found to have more severe role impairment and more suicidal ideation. Data from level 1 of the STAR*D study (citalopram treatment) nicely illustrate the impact of comorbid anxiety symptoms on treatment. Compared with patients with nonanxious major depressive disorder, those 53% of patients with an anxious depression were less likely to remit and also had a greater side effect burden ( 20 ). Other data examining patients with major depressive disorder and comorbid anxiety disorders support the greater difficulty and challenge in treating patients with these comorbidities ( 21 ).
This issue of the Journal presents new findings relevant to the issues discussed above in relation to understanding and treating anxiety and depressive disorders. Drs. Conor Liston and Timothy Spellman, from Weill Cornell Medicine, provide an overview for this issue ( 22 ) that is focused on understanding mechanisms at the neural circuit level that underlie the pathophysiology of depression. Their piece nicely integrates human neuroimaging studies with complementary data from animal models that allow for the manipulation of selective circuits to test hypotheses generated from the human data. Also included in this issue is a review of the data addressing the reemergence of the use of psychedelic drugs in psychiatry, particularly for the treatment of depression, anxiety, and PTSD ( 23 ). This timely piece, authored by Dr. Collin Reiff along with a subgroup from the APA Council of Research, provides the current state of evidence supporting the further exploration of these interventions. Dr. Alan Schatzberg, from Stanford University, contributes an editorial in which he comments on where the field is in relation to clinical trials with psychedelics and to some of the difficulties, such as adequate blinding, in reliably studying the efficacy of these drugs ( 24 ).
In an article by McTeague et al. ( 25 ), the authors use meta-analytic strategies to understand the neural alterations that are related to aberrant emotion processing that are shared across psychiatric disorders. Findings support alterations in the salience, reward, and lateral orbital nonreward networks as common across disorders, including anxiety and depressive disorders. These findings add to the growing body of work that supports the concept that there are common underlying factors across all types of psychopathology that include internalizing, externalizing, and thought disorder dimensions ( 26 ). Dr. Deanna Barch, from Washington University in St. Louis, writes an editorial commenting on these findings and, importantly, discusses criteria that should be met when we consider whether the findings are actually transdiagnostic ( 27 ).
Another article, from Gray and colleagues ( 28 ), addresses whether there is a convergence of findings, specifically in major depression, when examining data from different structural and functional neuroimaging modalities. The authors report that, consistent with what we know about regions involved in emotion processing, the subgenual anterior cingulate cortex, hippocampus, and amygdala were among the regions that showed convergence across multimodal imaging modalities.
In relation to treatment and building on our understanding of neural circuit alterations, Siddiqi et al. ( 29 ) present data suggesting that transcranial magnetic stimulation (TMS) targeting can be linked to symptom-specific treatments. Their findings identify different TMS targets in the left dorsolateral prefrontal cortex that modulate different downstream networks. The modulation of these different networks appears to be associated with a reduction in different types of symptoms. In an editorial, Drs. Sean Nestor and Daniel Blumberger, from the University of Toronto ( 30 ), comment on the novel approach used in this study to link the TMS-related engagement of circuits with symptom improvement. They also provide a perspective on how we can view these and other circuit-based findings in relation to conceptualizing personalized treatment approaches.
Kendler et al. ( 31 ), in this issue, contribute an article that demonstrates the important role of the rearing environment in the risk to develop major depression. Using a unique design from a Swedish sample, the analytic strategy involves comparing outcomes from high-risk full sibships and high-risk half sibships where at least one of the siblings was home reared and one was adopted out of the home. The findings support the importance of the quality of the rearing environment as well as the presence of parental depression in mitigating or enhancing the likelihood of developing major depression. In an accompanying editorial ( 32 ), Dr. Myrna Weissman, from Columbia University, reviews the methods and findings of the Kendler et al. article and also emphasizes the critical significance of the early nurturing environment in relation to general health.
This issue concludes with an intriguing article on anxiety disorders, by Gold and colleagues ( 33 ), that demonstrates neural alterations during extinction recall that differ in children relative to adults. With increasing age, and in relation to fear and safety cues, nonanxious adults demonstrated greater connectivity between the amygdala and the ventromedial prefrontal cortex compared with anxious adults, as the cues were being perceived as safer. In contrast, neural differences between anxious and nonanxious youths were more robust when rating the memory of faces that were associated with threat. Specifically, these differences were observed in the activation of the inferior temporal cortex. In their editorial ( 34 ), Dr. Dylan Gee and Sahana Kribakaran, from Yale University, emphasize the importance of developmental work in relation to understanding anxiety disorders, place these findings into the context of other work, and suggest the possibility that these and other data point to neuroscientifically informed age-specific interventions.
Taken together, the papers in this issue of the Journal present new findings that shed light onto alterations in neural function that underlie major depressive disorder and anxiety disorders. It is important to remember that these disorders are highly comorbid and that their symptoms are frequently not separable. The papers in this issue also provide a developmental perspective emphasizing the importance of early rearing in the risk to develop depression and age-related findings important for understanding threat processing in patients with anxiety disorders. From a treatment perspective, the papers introduce data supporting more selective prefrontal cortical TMS targeting in relation to different symptoms, address the potential and drawbacks for considering the future use of psychedelics in our treatments, and present new ideas supporting age-specific interventions for youths and adults with anxiety disorders.
Disclosures of Editors’ financial relationships appear in the April 2020 issue of the Journal .
1 Substance Abuse and Mental Health Services Administration (SAMHSA): Key substance use and mental health indicators in the United States: results from the 2017 National Survey on Drug Use and Health (HHS Publication No. SMA 18-5068, NSDUH Series H-53). Rockville, Md, Center for Behavioral Health Statistics and Quality, SAMHSA, 2018. https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHFFR2017/NSDUHFFR2017.htm Google Scholar
2 Kessler RC, Chiu WT, Demler O, et al. : Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication . Arch Gen Psychiatry 2005 ; 62:617–627, correction, 62:709 Crossref , Medline , Google Scholar
3 Merikangas KR, He JP, Burstein M, et al. : Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A) . J Am Acad Child Adolesc Psychiatry 2010 ; 49:980–989 Crossref , Medline , Google Scholar
4 Kessler RC, McGonagle KA, Zhao S, et al. : Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey . Arch Gen Psychiatry 1994 ; 51:8–19 Crossref , Medline , Google Scholar
5 Kessler RC, Sampson NA, Berglund P, et al. : Anxious and non-anxious major depressive disorder in the World Health Organization World Mental Health Surveys . Epidemiol Psychiatr Sci 2015 ; 24:210–226 Crossref , Medline , Google Scholar
6 Dunner DL : Management of anxiety disorders: the added challenge of comorbidity . Depress Anxiety 2001 ; 13:57–71 Crossref , Medline , Google Scholar
7 Kessler RC, Sonnega A, Bromet E, et al. : Posttraumatic stress disorder in the National Comorbidity Survey . Arch Gen Psychiatry 1995 ; 52:1048–1060 Crossref , Medline , Google Scholar
8 Brawman-Mintzer O, Lydiard RB, Emmanuel N, et al. : Psychiatric comorbidity in patients with generalized anxiety disorder . Am J Psychiatry 1993 ; 150:1216–1218 Link , Google Scholar
9 Fava M, Alpert JE, Carmin CN, et al. : Clinical correlates and symptom patterns of anxious depression among patients with major depressive disorder in STAR*D . Psychol Med 2004 ; 34:1299–1308 Crossref , Medline , Google Scholar
10 Hettema JM : What is the genetic relationship between anxiety and depression? Am J Med Genet C Semin Med Genet 2008 ; 148C:140–146 Crossref , Medline , Google Scholar
11 Hettema JM, Neale MC, Myers JM, et al. : A population-based twin study of the relationship between neuroticism and internalizing disorders . Am J Psychiatry 2006 ; 163:857–864 Link , Google Scholar
12 Kovner R, Oler JA, Kalin NH : Cortico-limbic interactions mediate adaptive and maladaptive responses relevant to psychopathology . Am J Psychiatry 2019 ; 176:987–999 Link , Google Scholar
13 Etkin A, Schatzberg AF : Common abnormalities and disorder-specific compensation during implicit regulation of emotional processing in generalized anxiety and major depressive disorders . Am J Psychiatry 2011 ; 168:968–978 Link , Google Scholar
14 Goodkind M, Eickhoff SB, Oathes DJ, et al. : Identification of a common neurobiological substrate for mental illness . JAMA Psychiatry 2015 ; 72:305–315 Crossref , Medline , Google Scholar
15 McTeague LM, Huemer J, Carreon DM, et al. : Identification of common neural circuit disruptions in cognitive control across psychiatric disorders . Am J Psychiatry 2017 ; 174:676–685 Link , Google Scholar
16 Beesdo K, Knappe S, Pine DS : Anxiety and anxiety disorders in children and adolescents: developmental issues and implications for DSM-V . Psychiatr Clin North Am 2009 ; 32:483–524 Crossref , Medline , Google Scholar
17 Kessler RC, Wang PS : The descriptive epidemiology of commonly occurring mental disorders in the United States . Annu Rev Public Health 2008 ; 29:115–129 Crossref , Medline , Google Scholar
18 Ohayon MM, Schatzberg AF : Social phobia and depression: prevalence and comorbidity . J Psychosom Res 2010 ; 68:235–243 Crossref , Medline , Google Scholar
19 Clauss JA, Blackford JU : Behavioral inhibition and risk for developing social anxiety disorder: a meta-analytic study . J Am Acad Child Adolesc Psychiatry 2012 ; 51:1066–1075 Crossref , Medline , Google Scholar
20 Fava M, Rush AJ, Alpert JE, et al. : Difference in treatment outcome in outpatients with anxious versus nonanxious depression: a STAR*D report . Am J Psychiatry 2008 ; 165:342–351 Link , Google Scholar
21 Dold M, Bartova L, Souery D, et al. : Clinical characteristics and treatment outcomes of patients with major depressive disorder and comorbid anxiety disorders: results from a European multicenter study . J Psychiatr Res 2017 ; 91:1–13 Crossref , Medline , Google Scholar
22 Spellman T, Liston C : Toward circuit mechanisms of pathophysiology in depression . Am J Psychiatry 2020 ; 177:381–390 Link , Google Scholar
23 Reiff CM, Richman EE, Nemeroff CB, et al. : Psychedelics and psychedelic-assisted psychotherapy . Am J Psychiatry 2020 ; 177:391–410 Link , Google Scholar
24 Schatzberg AF : Some comments on psychedelic research (editorial). Am J Psychiatry 2020 ; 177:368–369 Link , Google Scholar
25 McTeague LM, Rosenberg BM, Lopez JW, et al. : Identification of common neural circuit disruptions in emotional processing across psychiatric disorders . Am J Psychiatry 2020 ; 177:411–421 Link , Google Scholar
26 Caspi A, Moffitt TE : All for one and one for all: mental disorders in one dimension . Am J Psychiatry 2018 ; 175:831–844 Link , Google Scholar
27 Barch DM : What does it mean to be transdiagnostic and how would we know? (editorial). Am J Psychiatry 2020 ; 177:370–372 Abstract , Google Scholar
28 Gray JP, Müller VI, Eickhoff SB, et al. : Multimodal abnormalities of brain structure and function in major depressive disorder: a meta-analysis of neuroimaging studies . Am J Psychiatry 2020 ; 177:422–434 Link , Google Scholar
29 Siddiqi SH, Taylor SF, Cooke D, et al. : Distinct symptom-specific treatment targets for circuit-based neuromodulation . Am J Psychiatry 2020 ; 177:435–446 Link , Google Scholar
30 Nestor SM, Blumberger DM : Mapping symptom clusters to circuits: toward personalizing TMS targets to improve treatment outcomes in depression (editorial). Am J Psychiatry 2020 ; 177:373–375 Abstract , Google Scholar
31 Kendler KS, Ohlsson H, Sundquist J, et al. : The rearing environment and risk for major depression: a Swedish national high-risk home-reared and adopted-away co-sibling control study . Am J Psychiatry 2020 ; 177:447–453 Abstract , Google Scholar
32 Weissman MM : Is depression nature or nurture? Yes (editorial). Am J Psychiatry 2020 ; 177:376–377 Abstract , Google Scholar
33 Gold AL, Abend R, Britton JC, et al. : Age differences in the neural correlates of anxiety disorders: an fMRI study of response to learned threat . Am J Psychiatry 2020 ; 177:454–463 Link , Google Scholar
34 Gee DG, Kribakaran S : Developmental differences in neural responding to threat and safety: implications for treating youths with anxiety (editorial). Am J Psychiatry 2020 ; 177:378–380 Abstract , Google Scholar
- Cited by None
- Neuroanatomy
- Neurochemistry
- Neuroendocrinology
- Other Research Areas
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Psychiatry
Family and Academic Stress and Their Impact on Students' Depression Level and Academic Performance
1 School of Mechatronics Engineering, Daqing Normal University, Daqing, China
2 School of Marxism, Heilongjiang University, Harbin, China
Jacob Cherian
3 College of Business, Abu Dhabi University, Abu Dhabi, United Arab Emirates
Noor Un Nisa Khan
4 Faculty of Business Administration, Iqra University Karachi Pakistan, Karachi, Pakistan
Kalpina Kumari
5 Faculty of Department of Business Administration, Greenwich University Karachi, Karachi, Pakistan
Muhammad Safdar Sial
6 Department of Management Sciences, COMSATS University Islamabad (CUI), Islamabad, Pakistan
Ubaldo Comite
7 Department of Business Sciences, University Giustino Fortunato, Benevento, Italy
Beata Gavurova
8 Faculty of Mining, Ecology, Process Control and Geotechnologies, Technical University of Kosice, Kosice, Slovakia
József Popp
9 Hungarian National Bank–Research Center, John von Neumann University, Kecskemét, Hungary
10 College of Business and Economics, University of Johannesburg, Johannesburg, South Africa
Associated Data
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Current research examines the impact of academic and familial stress on students' depression levels and the subsequent impact on their academic performance based on Lazarus' cognitive appraisal theory of stress. The non-probability convenience sampling technique has been used to collect data from undergraduate and postgraduate students using a modified questionnaire with a five-point Likert scale. This study used the SEM method to examine the link between stress, depression, and academic performance. It was confirmed that academic and family stress leads to depression among students, negatively affecting their academic performance and learning outcomes. This research provides valuable information to parents, educators, and other stakeholders concerned about their childrens' education and performance.
Introduction
Higher education institutions (HEIs) are believed to be one of the strongest pillars in the growth of any nation ( 1 ). Being the principal stakeholder, the performance of HEIs mainly relies on the success of its students ( 2 ). To successfully compete in the prevailing dynamic industrial environment, students are not only supposed to develop their knowledge but are also expected to have imperative skills and abilities ( 3 ). In the current highly competitive academic environment, students' performance is largely affected by several factors, such as social media, academic quality, family and social bonding, etc. ( 4 ). Aafreen et al. ( 2 ) stated that students continuously experience pressure from different sources during academic life, which ultimately causes stress among students.
Stress is a common factor that largely diminishes individual morale ( 5 ). It develops when a person cannot handle their inner and outer feelings. When the stress becomes chronic or exceeds a certain level, it affects an individual's mental health and may lead to different psychological disorders, such as depression ( 6 ). Depression is a worldwide illness marked by feelings of sadness and the inability to feel happy or satisfied ( 7 ). Nowadays, it is a common disorder, increasing day by day. According to the World Health Organization ( 8 , 9 ), depression was ranked third among the global burden of disease and predicted to take over first place by 2030.
Depression leads to decreased energy, difficulty thinking, concentrating, and making career decisions ( 6 ). Students are a pillar of the future in building an educated society. For them, academic achievement is a big goal of life and can severely be affected if the students fall prey to depression ( 10 , 11 ). There can be several reasons for this: family issues, exposure to a new lifestyle in colleges and universities, poor academic grades, favoritism by teachers, etc. Never-ending stress or academic pressure of studies can also be a chief reason leading to depression in students ( 12 ). There is a high occurrence of depression in emerging countries, and low mental health literacy has been theorized as one of the key causes of escalating rates of mental illness ( 13 ).
Several researchers, such as ( 6 , 14 , 15 ) have studied stress and depression elements from a performance perspective and reported that stress and depression negatively affect the academic performance of students. However, Aafreen et al. ( 2 ) reported contradictory results and stated that stress sharpens the individual's mind and reflexes and enables workers to perform better in taxing situations. Ardalan ( 16 ) conducted a study in the United States (US). They reported that depression is a common issue among students in the US, and 20 percent of them may have a depressive disorder spanning 12 months or more. It affects students' mental and physical health and limits their social relationships and professional career.
However, the current literature provides mixed results on the relationship between stress and performance. Therefore, the current research investigates stress among students from family and academic perspectives using Lazaru's theory which describes stress as a relation between an individual and his environment and examines how it impacts students' depression level, leading to their academic performance. Most of the available studies on stress and depression are from industrial perspectives, and limited attention is paid to stress from family and institutional perspectives and examines its impact on students' depression level, leading to their academic performance, particularly in Pakistan, the place of the study. Besides, the present study follows a multivariate statistical technique, followed by structural equation modeling (SEM) to examine the relationship between stated variables which is also a study's uniqueness.
This paper is divided into five main sections. The current section provided introduction, theoretical perspective, and background of the study. In the second section, a theoretical framework, a detailed literature review and research hypotheses of the underlying relationships are being proposed. In the third and fourth section, methodology and analysis have been discussed. Finally, in the last section, the conclusion, limitations, implications, and recommendations for future research have been proposed.
Theory and Literature
The idea of cognitive appraisal theory was presented in 1966 by psychologist Richard Lazarus in Psychological Stress and Coping Process. According to this theory, appraisal and coping are two concepts that are central to any psychological stress theory. Both are interrelated. According to the theory, stress is the disparity between stipulations placed on the individuals and their coping resources ( 17 ). Since its first introduction as a comprehensive theory ( 18 ), a few modifications have been experienced in theory later. The recent adaptation states that stress is not defined as a specific incitement or psychological, behavioral, or subjective response. Rather, stress is seen as a relation between an individual and his environment ( 19 ). Individuals appraise the environment as significant for their well-being and try to cope with the exceeding demands and challenges.
Cognitive appraisal is a model based on the idea that stress and other emotional processes depend on a person's expectancies regarding the significance and outcome of an event, encounter, or function. This explains why there are differences in intensity, duration, and quality of emotions elicited in people in response to the environment, which objectively, are equal for all ( 18 ). These appraisals may be influenced by various factors, including a person's goals, values, motivations, etc., and are divided into primary and secondary appraisals, specific patterns of which lead to different kinds of stress ( 20 ). On the other hand, coping is defined as the efforts made by a person to minimize, tolerate, or master the internal and external demands placed on them, a concept intimately related to cognitive appraisal and, therefore, to the stress-relevant person-environment transactions.
Individuals experience different mental and physiological changes when encountering pressure, such as stress ( 21 , 22 ). The feelings of stress can be either due to factors in the external environment or subjective emotions of individuals, which can even lead to psychological disorders such as anxiety and depression. Excess stress can cause health problems. A particularly negative impact has been seen in students due to the high level of stress they endure, affecting their learning outcomes. Various methods are used to tackle stress. One of the methods is trying to pinpoint the causes of stress, which leads us to different terms such as family stress and academic stress. The two factors, stress and depression, have greatly impacted the students' academic performances. This research follows the Lazarus theory based on stress to examine the variables. See the conceptual framework of the study in Figure 1 .

Conceptual framework.
Academic Stress
Academic issues are thought to be the most prevalent source of stress for college students ( 23 ). For example, according to Yang et al. ( 24 ), students claimed that academic-related pressures such as ongoing study, writing papers, preparing for tests, and boring professors were the most important daily problems. Exams and test preparation, grade level competitiveness, and gaining a big quantity of knowledge in a short period of time all contribute to academic pressure. Perceived stress refers to a condition of physical or psychological arousal in reaction to stressors ( 25 , 26 ). When college students face excessive or negative stress, they suffer physical and psychological consequences. Excessive stress can cause health difficulties such as fatigue, loss of appetite, headaches, and gastrointestinal issues. Academic stress has been linked to a variety of negative effects, including ill health, anxiety, depression, and poor academic performance. Travis et al. ( 27 ), in particular, discovered strong links between academic stress and psychological and physical health.
Family Stress
Parental participation and learning effect how parents treat their children, as well as how they handle their children's habits and cognitive processes ( 28 ). This, in turn, shapes their children's performance and behaviors toward them. As a result, the parent-child relationship is dependent on the parents' attitudes, understanding, and perspectives. When parents have positive views, the relationship between them and their children will be considerably better than when they have negative attitudes. Parents respond to unpleasant emotions in a variety of ways, which can be classified as supportive or non-supportive ( 29 ). Parents' supportive reactions encourage children to explore their emotions by encouraging them to express them or by assisting them in understanding and coping with an emotion-eliciting scenario. Non-supportive behaviors, such as downplaying the kid's emotional experience, disciplining the child, or getting concerned by the child's display, transmit the child the message that expressing unpleasant emotions is inappropriate and unacceptable. Supportive parental reactions to unpleasant emotions in children have been linked to dimensions of emotional and social competence, such as emotion comprehension and friendship quality. Non-supportive or repressive parental reactions, on the other hand, have been connected to a child's stored negative affect and disordered behaviors during emotion-evoking events, probably due to an inability or unwillingness to communicate unpleasant sentiments ( 30 , 31 ).
Academic Stress and Students' Depression Levels
Generally, it is believed that mental health improves as we enter into adulthood, and depression disorder starts to decline between the age of 18 and 25. On the other hand, excessive depression rates are the highest pervasiveness during this evolution ( 15 ), and many university students in the particular screen above clinical cut-off scores for huge depression ( 14 , 32 ). Afreen et al. ( 2 ) stated that 30% of high school students experience depression from different perspectives. This means a major chunk of fresh high school graduates are more likely to confront depression or are more vulnerable to encountering depression while enrolling in the university. As the students promote to a higher level of education, there are many factors while calculating the stress like, for example, the syllabus is tough to comprehend, assignments are quite challenging with unrealistic deadlines, and accommodation problems for the students who are shifted from other cities, etc. ( 33 ). Experiences related to university can also contribute while studying depression. The important thing to consider is depression symptoms vary from time to time throughout the academic years ( 34 ); subjective and objective experiences are directly connected to the depression disorder ( 6 ), stress inherent in the university situation likely donates to the difference in university students' depressing experiences.
Stress negatively impacts students' mental peace, and 42.3% of students of Canadian university respondents testified devastating levels of anxiety and stress ( 35 , 36 ). Moreover, there were (58.1%) students who stated academic projects are too tough to handle for them. In Germany, Bulgaria, and Poland, a huge sample of respondents consider assignments a burden on their lives that cannot stand compared to relationships or any other concern in life ( 14 ).
In several countries, university students were studied concerning stress, and results show that depression disorder and apparent anxiety are correlated to educational needs and demands ( 37 ). In their cross-sectional study conducted on a sample of 900 Canadian students, Lörz et al. ( 38 ) concluded that strain confronted due to academic workload relatively has high bleak symptoms even after controlling 13 different risk affecting factors for depression (e.g., demographic features, abusive past, intellectual way, and personality, currently experienced stressful trials in life, societal support). Few have exhibited that students who are tired of educational workload or the students who name them traumatic tend to have more depressing disorders ( 15 ).
These relations can be described by examining the stress and coping behaviors that highlight the role of positive judgments in the stress times ( 39 ), containing the Pancer and colleagues' university modification framework ( 40 , 41 ). The evaluation concept includes examining the circumstances against the available resources, for instance, the effectiveness of coping behavior and societal support. As per these frameworks, if demand is considered unapproachable and resources are lacking, confronted stress and interrelated adverse effects will be high, conceivably giving birth to difficulties in an adjustment like mental instability. Stress triggering situations and the resources in the educational area led to excessive workload, abilities, and study and enhanced time managing skills.
Sketching the overall evaluation frameworks, Pancer et al. ( 40 ) established their framework to exhibit the constructive and damaging adjustment results for the university students dealing with the academic challenges. They stated that while students enroll in the university, they evaluate all the stress-related factors that students confront. They consider them manageable as long as they have sufficient resources. On the other hand, if the available resources do not match the stress factors, it will surely result in a negative relationship, which will lead students to experience depression for sure. Based on the given arguments, the researcher formulates the following hypothesis:
- H1: Increased academic stress results in increased depression levels in students.
Family Stress and Students' Depression Levels
According to Topuzoglu et al. ( 42 ), 3% to 16.9% of individuals are affected by depression worldwide. There are fewer chances for general people to confront depression than university students ( 43 , 44 ). In Mirza et al.'s ( 45 ) study, 1/3 of students encounter stress and depression (a subjective mean occurrence of 30.6%) of all participant students, which suggests students have a 9% higher rate of experiencing depression than general people. Depression can destroy life; it greatly impacts living a balanced life. It can impact students' personal and social relationships, educational efficiency, quality of life, affecting their social and family relationships, academic productivity, and bodily operations ( 46 , 47 ). This declines their abilities, and they get demotivated to learn new things, resulting in unsatisfactory performances, and it can even result in university dropouts ( 48 ). Depression is a continuous substantial risk aspect for committing suicide for university students ( 49 ); thus, it is obliged to discover the factors that can give rise to students' depression.
Seventy-five percentage of students in China of an intermediate school are lucky enough to enroll in higher education. The more students pursue higher education, the more they upsurge for depression (in 2002, the depression rate was 5 to 10%, 2011 it rises 24 to 38%) ( 5 ). Generally, University students' age range is late teens to early twenties, i.e., 18–23 years. Abbas ( 50 ) named the era of university students as “post-adolescence. Risk factors for teenage depression have several and complicated problems of individual characteristics and family and educational life ( 51 ). Amongst the huge depression factors, relationship building with family demands a major chunk of attention and time since factors like parenting and family building play an important role in children's development ( 52 , 53 ). Halonen et al. ( 54 ) concluded that factors like family binding play a major role in development, preservation, and driving adolescent depression. Generally speaking, depressed teenagers tend to have a weaker family relationship with their parents than non-depressed teenagers.
There are two types of family risk factors, soft and hard. Hard factors are encountered in families with a weak family building structure, parents are little to no educated at all, and of course, the family status (economically). Several studies have proved that students of hard risk factors are more likely to encounter depression. Firstly, students from broken families have low confidence in every aspect of life, and they are weak at handling emotional breakdowns compared to students from complete and happy families ( 55 – 57 ). Secondly, the university students born in educated families, especially mothers (at least a college degree or higher degree), are less likely to confront depression than the university students born in families with little to no educated families. Secondly, children born with educated mothers or mothers who at least have a college degree tend to be less depressive than the children of less-educated mothers ( 58 ). However, Parker et al. and Mahmood et al. ( 59 , 60 ) stated a strong relationship between depression and mothers with low literacy levels.
On the other hand, Chang et al. ( 46 ) couldn't prove the authentication of this relationship in university students. Thirdly, university students who belong to lower class families tend to have more unstable mental states and are more likely to witness depression than middle or upper-class families ( 61 ). Jadoon et al. and Abbas et al. ( 62 , 63 ) said that there is no link between depression and economic status. Their irrelevance can be because medical students often come from educated and wealthy families and know their jobs are guaranteed as soon as they graduate. Therefore, the relationship between the hard family environment and depression can be known by targeting a huge audience, and there are several factors to consider while gauging this relationship.
The soft family environment is divided into clear factors (parenting style example, family guidelines, rules, the parent with academic knowledge, etc.) and implied factors (family norm, parent-child relationship, communication within the family, etc.). The soft factor is the key factor within the family that cannot be neglected while studying the teenagers' mental state or depression. Families make microsystems within the families, and families are the reason to build and maintain dysfunctional behavior by multiple functional procedures ( 64 ). Amongst the soft family environmental factors, consistency and struggles can be helpful while forecasting the mental health of teenagers. The youth of broken families, family conflict, weak family relationships, and marital issues, especially unhappy married life, are major factors for youth depression ( 65 ). Ruchkin et al. ( 66 ) stated that African Americans usually have weak family bonding, and their teenagers suffer from depression even when controlling for source bias. Whereas, few researchers have stated, family unity is the most serious factor while foreseeing teenagers' depression. Eaton noted that extreme broken family expressions might hurt emotionality and emotional regulation ( 67 , 68 ).
Social circle is also considered while studying depression in teenagers ( 69 – 71 ). The traditional Pakistani culture emphasizes collectivism and peace and focuses on blood relations and sensitive sentiments. Adolescents with this type of culture opt to get inspired by family, but students who live in hostels or share the room with other students lose this family inspiration. This transformation can be a big risk to encounter depression ( 72 ). Furthermore, in Pakistan securing employment is a big concern for university students. If they want a good job in the future, they have to score good grades and maintain GPA from the beginning. They have to face different challenges all at once, like aggressive educational competition, relationships with peers and family, and of course the biggest employment stress all alone. The only source for coping with these pressures is the family that can be helpful for fundings. If the students do not get ample support the chances are of extreme depression. The following hypothesis is suggested:
- H2: Increased family stress level results in increased depression levels in students.
Students' Depression Levels and Students' Academic Performance
University students denote many people experiencing a crucial conversion from teenagers to adulthood: a time that is generally considered the most traumatic time in one's ( 73 ). This then gets accumulated with other challenges like changes in social circle and exams tension, which possibly puts students' mental health at stake. It has been concluded that one-third of students experience moderate to severe depression in their entire student life ( 74 ). This is the rate that can be increased compared to the general people ( 75 , 76 ). Students with limited social-class resources tend to be more helpless. Additionally, depressed students in attainable-focused environments (for instance, higher academic institutes) are likely to score lower grades with a sense of failure and more insufficient self-assurance because they consider themselves failures, find the world unfair, and have future uncertainties. Furthermore, students with low self-esteem are rigid to take on challenging assignments and projects, hence they are damaging their educational career ( 77 ).
Depression can be defined as a blend of physical, mental, bodily processes, and benightedness which can make themselves obvious by symptoms like, for example, poor sleep schedule, lack of concentration, ill thoughts, and state of remorse ( 78 , 79 ). But, even after such a huge number of depressions in students and the poor academic system, research has not explored the effect of depression on educational performance. A study has shown that the relationship between emotional stability and academic performance in university students and financial status directly results in poor exam performance. As the study further concluded, it was verified depression is an independent factor ( 80 ). Likewise, students suffering from depression score poor grades, but this relationship vanished if their depression got treated. Apart from confidence breaking, depression is a big failure for their academic life. Students with depression symptoms bunk more classes, assessments, and assignments. They drop courses if they find them challenging than non-depressed peers, and they are more likely to drop out of university completely ( 81 ). Students suffering from depression can become ruthless, ultimately affecting their educational performance and making them moody ( 82 ).
However, it has been stated that the association between anxiety and educational performance is even worse and ambiguous. At the same time, some comprehensive research has noted that the greater the anxiousness, the greater the student's performance. On the other hand, few types of research have shown results where there is no apparent relationship between anxiety and poorer academic grades ( 83 ). Ironically, few studies have proposed that a higher anxiety level may improve academic performance ( 84 , 85 ). Current research by Khan et al. ( 86 ) on the undergraduate medical students stated that even though the high occurrence of huge depression between the students, the students GPA is unharmed. Therefore, based on given differences in various research findings, this research is supposed to find a more specific and clear answer to the shared relationship between students' depression levels and academic performance. Based on the given arguments, the researcher formulates the following hypothesis:
- H3: Students' depression level has a significant negative effect on their academic performance.
Methodology
Target population and sampling procedure.
The target audience of this study contains all male and female students studying in the public, private, or semi-government higher education institutions located in Rawalpindi/Islamabad. The researchers collected data from undergraduate and postgraduate students from the management sciences, engineering, and computer science departments. The sampling technique which has been used is the non-probability sampling technique. A questionnaire was given to the students, and they were requested to fill it and give their opinion independently. The questionnaire is based on five points Likert scale.
However, stress and depression are the most common issue among the students, which affects their learning outcomes adversely. A non-probability sampling technique gathered the data from February 2020 to May 2020. The total questionnaires distributed among students were 220, and 186 responses were useful. Of which 119 respondents were females, 66 males, and 1 preferred not to disclose. See Table 1 for detailed demographic information of respondents.
Respondent's demographic profile.
Measurement Scales
We have divided this instrument into two portions. In the first section, there is demographic information of respondents. The second section includes 14 items based on family stress, academic stress, students' depression levels, and students' academic performance. Academic and family stress were measured by 3 item scale for each construct, and students' depression level and academic performance were measured by 4 item scale for each separate construct. The five-point Likert scale is used to measure the items, in which one signifies strongly disagree (S.D), second signifies disagree (D.A), third signifies neither agree nor disagree (N), fourth signifies agree (A.G), and the fifth signifies strongly agree (S.A). The questionnaire has been taken from Gold Berg ( 87 ), which is modified and used in the given questionnaire.
Data Analysis and Results
The researchers used the SEM technique to determine the correlation between stress, depression, and academic performance. According to Prajogo and Cooper ( 88 ), it can remove biased effects triggered by the measurement faults and shape a hierarchy of latent constructs. SPSS v.23 and AMOS v.23 have been used to analyze the collected data. Kaiser-Meyer-Olkin test is used to test the competence of the sample. The value obtained is 0.868, which fulfills the Kaiser et al. ( 89 ), a minimum requirement of 0.6. The multicollinearity factor was analyzed through the variance inflation factor (VIF). It shows the value of 3.648 and meets the requirement of Hair et al. ( 90 ), which is < 4. It also indicates the absence of multicollinearity. According to Schwarz et al. ( 91 ), common method bias (CMB) is quite complex in quantitative studies. Harman's test of a single factor has been used to analyze CMB. The result obtained for the single factor is 38.63%. As stated by Podsakoff et al. ( 92 ), if any of the factors gives value < 50% of the total variance, it is adequate and does not influence the CMB. Therefore, we can say that there is no issue with CMB. Considering the above results are adequate among the measurement and structural model, we ensure that the data is valued enough to analyze the relation.
Assessment of the Measurement and Structural Model
The association between the manifest factors and their elements is examined by measuring model and verified by the Confirmatory Factor Analysis (CFA). CFA guarantees legitimacy and the unidimensional of the measurement model ( 93 ). Peterson ( 94 ) stated that the least required, i.e., 0.8 for the measurement model, fully complies with its Cronbach's alpha value, i.e., 0.802. Therefore, it can confidently be deduced that this measurement model holds satisfactory reliability. As for the psychological legitimacy can be analyzed through factor loading, where the ideal loading is above 0.6 for already established items ( 95 ). Also, according to the recommendation of Molina et al. ( 96 ), the minimum value of the average variance extracted (AVE) for all results is supposed to be >0.5. Table 2 gives detail of the variables and their quantity of things, factor loading, merged consistency, and AVE values.
Instrument reliability and validity.
A discriminant validity test was performed to ensure the empirical difference of all constructs. For this, it was proposed by Fornell and Larcker ( 97 ) that the variance of the results is supposed to be greater than other constructs. The second indicator of discriminant validity is that the square root values of AVE have a greater correlation between the two indicators. Hair et al. ( 90 ) suggested that the correlation between the pair of predictor variables should not be higher than 0.9. Table 3 shows that discriminant validity recommended by Hair et al. ( 90 ) and Fornell and Larcker ( 97 ) was proved clearly that both conditions are fulfilled and indicates that the constructs have adequate discriminant validity.
Discriminant validity analysis.
Acd. Strs, Academic Stress; Fam. Strs, Family Stress; Std. Dep. Lev, Student's Depression Level; Std. Acd. Perf, Student's Academic Performance .
Kaynak ( 98 ) described seven indicators that ensure that the measurement model fits correctly. These indicators include standardized root mean squared residual (SRMR), root means a square error of approximation (RMSEA), comparative fit index (CFI), normative fit index (NFI), adjusted goodness of fit index (AGFI), the goodness of fit index (GFI) and chi-square to a degree of freedom (x 2 /DF). Tucker-Lewis's index (TLI) is also included to ensure the measurement and structural model's fitness. In the measurement model, the obtained result shows that the value of x 2 /DF is 1.898, which should be lower than 2 suggested by Byrne ( 99 ), and this value also meets the requirement of Bagozzi and Yi ( 100 ), i.e., <3. The RMSEA has the value 0.049, which fully meets the requirement of 0.08, as stated by Browne and Cudeck ( 101 ). Furthermore, the SRMR acquired value is 0.0596, which assemble with the required need of < 0.1 by Hu and Bentler ( 102 ). Moreover, according to Bentler and Bonett ( 103 ), McDonald and Marsh ( 104 ), and Bagozzi and Yi ( 100 ), the ideal value is 0.9, and the values obtained from NFI, GFI, AGFI, CFI, and TLI are above the ideal value.
Afterward, the structural model was analyzed and achieved the findings, which give the value of x 2 /DF 1.986. According to Browne and Cudeck ( 101 ), the RMSEA value should not be greater than 0.08, and the obtained value of RMSEA is 0.052, which meets the requirement perfectly. The minimum requirement of Hu and Bentler ( 102 ) should be <0.1, for the structural model fully complies with the SRMR value 0.0616. According to a recommendation of McDonald and Marsh ( 104 ) and Bagozzi and Yi ( 100 ), the ideal value must be up to 0.9, and Table 4 also shows that the values of NFI, GFI, AGFI, CFI, and TLI, which are above than the ideal value and meets the requirement. The above results show that both the measurement and structural models are ideally satisfied with the requirements and the collected data fits correctly.
Analysis of measurement and structural model.
Testing of Hypotheses
The SEM technique is used to examine the hypotheses. Each structural parameter goes along with the hypothesis. The academic stress (Acd. Strs) with the value β = 0.293 while the p -value is 0.003. These outcomes show a significant positive relationship between academic stress (Acd. Strs) and students' depression levels (Std. Dep. Lev). With the β = 0.358 and p = 0.001 values, the data analysis discloses that the family stress (Fam. Strs) has a significant positive effect on the students' depression level (Std. Dep. Lev). However, the student's depression level (Std. Dep. Lev) also has a significant negative effect on their academic performance (Std. Acd. Perf) with the values of β = −0.319 and p = 0.001. Therefore, the results supported the following hypotheses H 1 , H 2 , and H 3 . The sub-hypotheses analysis shows that the results are statistically significant and accepted. In Table 5 , the details of the sub-hypotheses and the principals are explained precisely. Please see Table 6 to review items with their mean and standard deviation values. Moreover, Figure 2 represents the structural model.
Examining the hypotheses.
Description of items, mean, and standard deviation.

Structural model.
Discussion and Conclusion
These findings add to our knowledge of how teenage depression is predicted by academic and familial stress, leading to poor academic performance, and they have practical implications for preventative and intervention programs to safeguard adolescents' mental health in the school context. The outcomes imply that extended academic stress positively impacts students' depression levels with a β of 0.293 and a p -value sof 0.003. However, according to Wang et al. ( 5 ), a higher level of academic stress is linked to a larger level of school burnout, which leads to a higher degree of depression. Satinsky et al. ( 105 ) also claimed that university officials and mental health specialists have expressed worry about depression and anxiety among Ph.D. students, and that his research indicated that depression and anxiety are quite common among Ph.D. students. Deb et al. ( 106 ) found the same results and concluded that depression, anxiety, behavioral difficulties, irritability, and other issues are common among students who are under a lot of academic stress. Similarly, Kokou-Kpolou et al. ( 107 ) revealed that depressive symptoms are common among university students in France. They also demonstrate that socioeconomic and demographic characteristics have a role.
However, Wang et al. ( 5 ) asserted that a higher level of academic stress is associated with a higher level of school burnout, which in return, leads to a higher level of depression. Furthermore, Satinsky et al. ( 105 ) also reported that university administrators and mental health clinicians have raised concerns about depression and anxiety and concluded in his research that depression and anxiety are highly prevalent among Ph.D. students. Deb et al. ( 106 ) also reported the same results and concluded that Depression, anxiety, behavioral problems, irritability, etc. are few of the many problems reported in students with high academic stress. Similary, Kokou-Kpolou et al. ( 107 ) confirmed that university students in France have a high prevalence of depressive symptoms. They also confirm that socio-demographic factors and perceived stress play a predictive role in depressive symptoms among university students. As a result, academic stress has spread across all countries, civilizations, and ethnic groups. Academic stress continues to be a serious problem impacting a student's mental health and well-being, according to the findings of this study.
With the β= 0.358 and p = 0.001 values, the data analysis discloses that the family stress (Fam. Strs) has a significant positive effect on the students' depression level (Std. Dep. Lev). Aleksic ( 108 ) observed similar findings and concluded that many and complicated concerns of personal traits, as well as both home and school contexts, are risk factors for teenage depression. Similarly, Wang et al. ( 109 ) indicated that, among the possible risk factors for depression, family relationships need special consideration since elements like parenting styles and family dynamics influence how children grow. Family variables influence the onset, maintenance, and course of juvenile depression, according to another study ( 110 ). Depressed adolescents are more likely than normal teenagers to have bad family and parent–child connections.
Conversely, students' depression level has a significantly negative impact on their academic performance with β and p -values of −0.319 and 0.001. According ( 111 ), anxiety and melancholy have a negative influence on a student's academic performance. Adolescents and young adults suffer from depression, which is a common and dangerous mental illness. It's linked to an increase in family issues, school failure, especially among teenagers, suicide, drug addiction, and absenteeism. While the transition to adulthood is a high-risk period for depression in general ( 5 ), young people starting college may face extra social and intellectual challenges that increase their risk of melancholy, anxiety, and stress ( 112 ). Students' high rates of depression, anxiety, and stress have serious consequences. Not only may psychological morbidity have a negative impact on a student's academic performance and quality of life, but it may also disturb family and institutional life ( 107 ). Therefore, long-term untreated depression, anxiety, or stress can have a negative influence on people's ability to operate and produce, posing a public health risk ( 113 ).
Theoretical Implications
The current study makes various contributions to the existing literature on servant leadership. Firstly, it enriches the limited literature on the role of family and academic stress and their impact on students' depression levels. Although, a few studies have investigated stress and depression and its impact on Students' academic performance ( 14 , 114 ), however, their background i.e., family and institutions are largely ignored.
Secondly, it explains how the depression level impacts students' academic learning, specifically in the Asian developing countries region. Though a substantial body of empirical research has been produced in the last decade on the relationship between students' depression levels and its impact on their academic achievements, however, the studies conducted in the Pakistani context are scarce ( 111 , 115 ). Thus, this study adds further evidence to prior studies conducted in different cultural contexts and validates the assumption that family and academic stress are key sources depression and anxiety among students which can lead toward their low academic grades and their overall performance.
This argument is in line with our proposed theory in the current research i.e., cognitive appraisal theory which was presented in 1966 by psychologist Richard Lazarus. Lazarus's theory is called the appraisal theory of stress, or the transactional theory of stress because the way a person appraises the situation affects how they feel about it and consequently it's going to affect his overall quality of life. In line with the theory, it suggests that events are not good or bad, but the way we think about them is positive or negative, and therefore has an impact on our stress levels.
Practical Implications
According to the findings of this study, high levels of depressive symptoms among college students should be brought to the attention of relevant departments. To prevent college student depression, relevant departments should improve the study and life environment for students, try to reduce the generation of negative life events, provide adequate social support for students, and improve their cognitive and coping capacities to improve their mental qualities.
Stress and depression, on the other hand, may be managed with good therapy, teacher direction, and family support. The outcomes of this study provide an opportunity for academic institutions to address students' psychological well-being and requirements. Emotional well-being support services for students at Pakistan's higher education institutions are lacking in many of these institutions, which place a low priority on the psychological requirements of these students. As a result, initiatives that consistently monitor and enhance kids' mental health are critical. Furthermore, stress-reduction treatments such as biofeedback, yoga, life-skills training, mindfulness meditation, and psychotherapy have been demonstrated to be useful among students. Professionals in the sector would be able to adapt interventions for pupils by understanding the sources from many spheres.
Counseling clinics should be established at colleges to teach students about stress and sadness. Counselors should instill in pupils the importance of positive conduct and decision-making. The administration of the school should work to create a good and safe atmosphere. Furthermore, teachers should assume responsibility for assisting and guiding sad pupils, since this will aid in their learning and performance. Support from family members might also help you get through difficult times.
Furthermore, these findings support the importance of the home environment as a source of depression risk factors among university students, implying that family-based treatments and improvements are critical in reducing depression among university students.

Limitations and Future Research Implications
The current study has a few limitations. The researcher gathered data from the higher education level of university students studying in Islamabad and Rawalpindi institutions. In the future, researchers are required to widen their region and gather information from other cities of Pakistan, for instance, Lahore, Karachi, etc. Another weakness of the study is that it is cross-sectional in nature. We need to do longitudinal research in the future to authoritatively assert the cause-and-effect link between academic and familial stress and their effects on students' academic performance since cross-sectional studies cannot establish significant cause and effect relationships. Finally, the study's relatively small sample size is a significant weakness. Due to time and budget constraints, it appears that the capacity to perform in-depth research of all firms in Pakistan's pharmaceutical business has been limited. Even though the findings are substantial and meaningful, the small sample size is predicted to limit generalizability and statistical power. This problem can be properly solved by increasing the size of the sample by the researchers, in future researches.
Data Availability Statement
Ethics statement.
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
All authors contributed to conceptualization, formal analysis, investigation, methodology, writing and editing of the original draft, and read and agreed to the published version of the manuscript.
This work was funded by the 2020 Heilongjiang Province Philosophy and Social Science Research Planning Project on Civic and Political Science in Universities (Grant No. 20SZB01). This work is supported by the Scientific Grant Agency of the Ministry of Education, Science, Research, and Sport of the Slovak Republic and the Slovak Academy Sciences as part of the research project VEGA 1/0797/20: Quantification of Environmental Burden Impacts of the Slovak Regions on Health, Social and Economic System of the Slovak Republic.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
Authors would like to thank all persons who directly or indirectly participated in the completion of this manuscript.
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Verywell Mind Insights
- 2023 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
7 Depression Research Paper Topic Ideas
Nancy Schimelpfening, MS is the administrator for the non-profit depression support group Depression Sanctuary. Nancy has a lifetime of experience with depression, experiencing firsthand how devastating this illness can be.
Cara Lustik is a fact-checker and copywriter.
:max_bytes(150000):strip_icc():format(webp)/Cara-Lustik-1000-77abe13cf6c14a34a58c2a0ffb7297da.jpg)
In psychology classes, it's common for students to write a depression research paper. Researching depression may be beneficial if you have a personal interest in this topic and want to learn more, or if you're simply passionate about this mental health issue. However, since depression is a very complex subject, it offers many possible topics to focus on, which may leave you wondering where to begin.
If this is how you feel, here are a few research titles about depression to help inspire your topic choice. You can use these suggestions as actual research titles about depression, or you can use them to lead you to other more in-depth topics that you can look into further for your depression research paper.
What Is Depression?
Everyone experiences times when they feel a little bit blue or sad. This is a normal part of being human. Depression, however, is a medical condition that is quite different from everyday moodiness.
Your depression research paper may explore the basics, or it might delve deeper into the definition of clinical depression or the difference between clinical depression and sadness .
What Research Says About the Psychology of Depression
Studies suggest that there are biological, psychological, and social aspects to depression, giving you many different areas to consider for your research title about depression.
Types of Depression
There are several different types of depression that are dependent on how an individual's depression symptoms manifest themselves. Depression symptoms may vary in severity or in what is causing them. For instance, major depressive disorder (MDD) may have no identifiable cause, while postpartum depression is typically linked to pregnancy and childbirth.
Depressive symptoms may also be part of an illness called bipolar disorder. This includes fluctuations between depressive episodes and a state of extreme elation called mania. Bipolar disorder is a topic that offers many research opportunities, from its definition and its causes to associated risks, symptoms, and treatment.
Causes of Depression
The possible causes of depression are many and not yet well understood. However, it most likely results from an interplay of genetic vulnerability and environmental factors. Your depression research paper could explore one or more of these causes and reference the latest research on the topic.
For instance, how does an imbalance in brain chemistry or poor nutrition relate to depression? Is there a relationship between the stressful, busier lives of today's society and the rise of depression? How can grief or a major medical condition lead to overwhelming sadness and depression?
Who Is at Risk for Depression?
This is a good research question about depression as certain risk factors may make a person more prone to developing this mental health condition, such as a family history of depression, adverse childhood experiences, stress , illness, and gender . This is not a complete list of all risk factors, however, it's a good place to start.
The growing rate of depression in children, teenagers, and young adults is an interesting subtopic you can focus on as well. Whether you dive into the reasons behind the increase in rates of depression or discuss the treatment options that are safe for young people, there is a lot of research available in this area and many unanswered questions to consider.
Depression Signs and Symptoms
The signs of depression are those outward manifestations of the illness that a doctor can observe when they examine a patient. For example, a lack of emotional responsiveness is a visible sign. On the other hand, symptoms are subjective things about the illness that only the patient can observe, such as feelings of guilt or sadness.
An illness such as depression is often invisible to the outside observer. That is why it is very important for patients to make an accurate accounting of all of their symptoms so their doctor can diagnose them properly. In your depression research paper, you may explore these "invisible" symptoms of depression in adults or explore how depression symptoms can be different in children .
How Is Depression Diagnosed?
This is another good depression research topic because, in some ways, the diagnosis of depression is more of an art than a science. Doctors must generally rely upon the patient's set of symptoms and what they can observe about them during their examination to make a diagnosis.
While there are certain laboratory tests that can be performed to rule out other medical illnesses as a cause of depression, there is not yet a definitive test for depression itself.
If you'd like to pursue this topic, you may want to start with the Diagnostic and Statistical Manual of Mental Disorders (DSM). The fifth edition, known as DSM-5, offers a very detailed explanation that guides doctors to a diagnosis. You can also compare the current model of diagnosing depression to historical methods of diagnosis—how have these updates improved the way depression is treated?
Treatment Options for Depression
The first choice for depression treatment is generally an antidepressant medication. Selective serotonin reuptake inhibitors (SSRIs) are the most popular choice because they can be quite effective and tend to have fewer side effects than other types of antidepressants.
Psychotherapy, or talk therapy, is another effective and common choice. It is especially efficacious when combined with antidepressant therapy. Certain other treatments, such as electroconvulsive therapy (ECT) or vagus nerve stimulation (VNS), are most commonly used for patients who do not respond to more common forms of treatment.
Focusing on one of these treatments is an option for your depression research paper. Comparing and contrasting several different types of treatment can also make a good research title about depression.
A Word From Verywell
The topic of depression really can take you down many different roads. When making your final decision on which to pursue in your depression research paper, it's often helpful to start by listing a few areas that pique your interest.
From there, consider doing a little preliminary research. You may come across something that grabs your attention like a new study, a controversial topic you didn't know about, or something that hits a personal note. This will help you narrow your focus, giving you your final research title about depression.
Remes O, Mendes JF, Templeton P. Biological, psychological, and social determinants of depression: A review of recent literature . Brain Sci . 2021;11(12):1633. doi:10.3390/brainsci11121633
National Institute of Mental Health. Depression .
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition . American Psychiatric Association.
National Institute of Mental Health. Mental health medications .
Ferri, F. F. (2019). Ferri's Clinical Advisor 2020 E-Book: 5 Books in 1 . Netherlands: Elsevier Health Sciences.
By Nancy Schimelpfening Nancy Schimelpfening, MS is the administrator for the non-profit depression support group Depression Sanctuary. Nancy has a lifetime of experience with depression, experiencing firsthand how devastating this illness can be.
Home — Essay Samples — Nursing & Health — Mental Health — My Struggle with Anxiety and Depression
My Struggle with Anxiety and Depression
- Categories: College Students Mental Health
About this sample

Words: 751 |
Published: Mar 16, 2024
Words: 751 | Pages: 2 | 4 min read
Table of contents
Personal experience, impact on college students, factors contributing to anxiety and depression in college students, seeking support and treatment.

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Prof. Kifaru
Verified writer
- Expert in: Education Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
1 pages / 670 words
3 pages / 1405 words
5 pages / 2111 words
2 pages / 978 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Mental Health
However, psychology also uses behavior along with the mapping to the DSM from the checklist survey to separate genuine from faked mental illness and this epistemological problem can be solved using the proven to be successful [...]
Easterlin, M., Chung, P., & Leng, M. (2023). Association of Team Sports Participation With Long-term Mental Health Outcomes Among Individuals Exposed to Adverse Childhood Experiences. JAMA Pediatrics.National Public Radio (NPR). [...]
Mental health stigma is a pervasive issue that has long hindered individuals from seeking the help they need and perpetuated damaging stereotypes and misconceptions. In this comprehensive essay, we will delve deeply into the [...]
Mental illness within the criminal justice system is a complex and pressing issue that intersects legal, medical, and ethical considerations. This essay examines the challenges posed by mental illness among individuals in the [...]
J.D. is an 8 year-old male student at Central Philadelphia elementary school whom is diagnosed with Attention-Deficit Hyperactivity Disorder. J.D. was referred by his physician to receive psychiatric inpatient treatment [...]
Arnekrans et al. (2018) state that childhood trauma is also known as developmental trauma and this refers to numerous amounts of stressful experiences in child development. Many of these stressful experiences consist of divorce, [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Depression Facts and Statistics: What You Need to Know
- Overview and Facts
- Commonality
- By Age, Gender, Ethnicity
- Causes and Risk Factors
- Diagnosis, and Treatment
Depression and Suicide
Depression —also called clinical depression or major depressive disorder (MDD)—is a debilitating mental illness that impacts between 200 and 300 million people worldwide, regardless of age. Depression can look and feel different for each person, and many people may not even show any outward signs of depression.
This article will provide an overview of facts, information, and statistics about depression.
Georgijevic / Getty Images
Depression Overview and Quick Facts
People with depression often experience similar feelings. Though depression can look and feel different for each person, there are several common symptoms. These include:
- Deep sadness
- Hopelessness
Understanding depression can help you cope or support a loved one living with the condition. Here are some quick facts about depression:
- Depression is common : Depression is the primary cause of disability around the world, and the number of people with depression has increased steadily in recent times.
- Different people experience different symptoms : While the experience differs for each person, it's common for people to lose interest in things they once enjoyed and experience ongoing fatigue.
- Depression occurs at different intensities : Depression can be mild, moderate, or severe and can affect people differently depending on their symptoms, coping abilities, and resources.
- Depression can increase the risk of death for some people : In severe and untreated cases, depression can lead to increased mortality in some people, usually due to suicide.
If you are having suicidal thoughts, contact the 988 Suicide & Crisis Lifeline at 988 for support and assistance from a trained counselor. If you or a loved one are in immediate danger, call 911.
For more mental health resources, see our National Helpline Database .
How Common Is Depression?
Depression is one of the most common mental illnesses worldwide. Though its prevalence varies by country, depression is the leading cause of death in many places. Statistics include:
- Depression affects between 200 and 300 million people worldwide : The rate of depression is around 17% in the United States and ranges from 8% to 12% in most countries.
- The pandemic impacted rates of depression : A 2023 report found that since the onset of the COVID-19 pandemic, depression and anxiety rates went up by 25% worldwide.
- Depression also impacts children : Research shows that around 3% of children under 13 years old and 5.6% of teens suffer from depression.
Depression by Age, Gender, and Ethnicity
Though depression can impact anyone, depression is more common in certain populations. Characteristics such as age, gender, and ethnicity are not risk factors, but people within certain groups are more susceptible to depression due to external circumstances such as discrimination, bias, and cultural norms around mental health, as follows:
- Depression is one of the most common illnesses in children and adolescents : Depression is the leading cause of disease and disability in children, and adolescents with depression are at high risk of suicide. Depression in early childhood may increase the risk of depression and difficulty concentrating later in life, which can negatively impact a person's development.
- LGBTQ youth are disproportionately affected by depression : A 2022 survey by The Trevor Project—a youth LGBTQ suicide-prevention organization—found that 58% of LGBTQ youth experienced depression symptoms, and 45% had seriously considered suicide in the last year.
- Women are more likely to have depression than men : Women's risk of depression is about twice that of men's ; however, they are less likely to complete suicide.
Depression Causes and Risk Factors
Several risk factors can lead to depression. These include:
- Genetics : Depression has a heritability rate of around 38%. This means that in someone with depression, there's a 38% chance that their depression is due to genetics.
- Other mental illnesses : The most common mental illnesses in which depression is also present are bipolar disorder and anxiety, and 60% of people with depression also have or have had anxiety. People with anxiety or bipolar disorder may be at risk of developing depression, and vice versa.
- Stressful life events : Experiencing a stressful life event, such as childhood trauma or recent difficulties like the death of a loved one, can contribute to depression.
- Income level : Depression rates generally increase as family income level decreases. Those who live below the poverty line are at the highest risk of depression.
Screening, Early Depression Diagnosis, and Treatment
Depression is a treatable illness, but most people do not seek treatment to manage their symptoms. With screening tools and early symptom detection, such as the following: depression can be diagnosed and effectively treated in most people:
- Your medical or mental health provider can provide assessments to diagnose depression : There are simple, quick assessments available to measure depression symptoms. An example is the Patient Health Questionnaire-9 (PHQ-9).
- Receiving a diagnosis leads to appropriate treatment : Treatment for depression can include a combination of self-care techniques, social support, and clinical treatment such as medication and therapy.
- Having an accurate diagnosis can be empowering : Understanding why you experience specific symptoms makes you better equipped to seek effective treatments.
- For many people, treatment can be short-term : One of the most effective treatment methods for depression—cognitive behavioral therapy (CBT)—can be provided in six to 10 sessions. With appropriate symptom management, long-term and ongoing treatment may not be needed for everyone.
Along with therapy, medications such as selective serotonin reuptake inhibitors (SSRIs) can also help manage depression symptoms.
Severe Depression
Some people have severe depression symptoms and may experience ongoing distress, self-neglect, or self-harming behavior. Those with severe depression should seek immediate treatment from a licensed mental health provider.
In some people with severe cases, depression can lead to suicide. Here are some facts about suicide and depression:
- Suicidal thoughts and attempts are associated with depression : The rate of suicide for people with depression is around 15%.
- Suicide is more than an attempt to harm or kill oneself : Suicidal behaviors include thinking about suicide, threatening to kill oneself, planning for suicide, attempting suicide, and completing suicide. All behaviors related to suicidal thinking and action should be taken seriously.
- Suicide is complex and connected to multiple factors : There isn't one reason or one situation that causes a person to die by suicide. Suicidal thoughts and behaviors come about for several complex reasons, which can include genetics, difficult or stressful life situations, and mental illness.
- Although connected, suicidal thoughts and depression are not always part of a causal relationship : Suicidal thoughts and behaviors are frequently connected, but one doesn't necessarily mean the other. A person with depression is not necessarily going to be suicidal, and a person who has suicidal thoughts may not have depression.
A mental health professional can help provide an accurate diagnosis and treatment plan for anyone experiencing symptoms of depression or suicidality.
Depression is a common mental illness affecting millions of people worldwide. Though anyone can have depression, it is more commonly reported in women than men, teens than young children, and non-Hispanic Black men than those of other ethnic groups.
People with co-occurring mental illnesses, inadequate income, and having family members with depression are at higher risk. Depression is also linked to suicide, and anyone thinking or talking about suicide should be taken seriously.
Flint J, Kendler KS. The genetics of major depression [published correction appears in Neuron. 2014;81(5):1214]. Neuron . 2014;81(3):484-503. doi:10.1016/j.neuron.2014.01.027
DeRubeis RJ, Strunk DR. The Oxford Handbook of Mood Disorders. Oxford University Press; 2017.
Stringaris A. Editorial: what is depression? . J Child Psychol Psychiatry . 2017;58(12):1287-1289. doi:10.1111/jcpp.12844
Patel V. Talking sensibly about depression . PLoS Med . 2017;14(4):e1002257. doi:10.1371/journal.pmed.1002257
Wegner M, Amatriain-Fernández S, Kaulitzky A, Murillo-Rodriguez E, Machado S, Budde H. Systematic review of meta-analyses: exercise effects on depression in children and adolescents . Front Psychiatry . 2020;11:81. doi:10.3389/fpsyt.2020.00081
Lim GY, Tam WW, Lu Y, Ho CS, Zhang MW, Ho RC. Prevalence of depression in the community from 30 countries between 1994 and 2014 [published correction appears in Sci Rep. 2022 Sep 1;12(1):14856]. Sci Rep . 2018;8(1):2861. doi:10.1038/s41598-018-21243-x
Kupcova I, Danisovic L, Klein M, Harsanyi S. Effects of the COVID-19 pandemic on mental health, anxiety, and depression . BMC Psychol . 2023;11(1):108. doi:10.1186/s40359-023-01130-5.
The Trevor Project. The Trevor Project: 2022 national survey on LGBTQ youth mental health .
Brody DJ, Pratt LA, Hughes JP. Prevalence of depression among adults aged 20 and over: United States, 2013-2016 . NCHS Data Brief . 2018;(303):1-8.
Orsolini L, Latini R, Pompili M, et al. Understanding the complex of suicide in depression: from research to clinics . Psychiatry Investig . 2020;17(3):207-221. doi:10.30773/pi.2019.0171
Find anything you save across the site in your account
By Lauren Oyler

In her short story “Five Signs of Disturbance,” Lydia Davis writes of a woman who is “frightened”:
She cannot always decide whether what seems to her a sign of disturbance should be counted as such, since it is fairly normal for her, such as talking aloud to herself or eating too much, or whether it should be counted because to someone else it might seem at least somewhat abnormal, and so, after thinking of ten or eleven signs, she wavers between counting five and seven signs as real signs of disturbance and finally settles on five, partly because she cannot accept the idea that there could be as many as seven.
I would have thought it’s normal to be weird about a few things, but being confronted with such a perspective always makes me doubt myself. I, too, wonder constantly if the things I do and experience are normal. But I have many more signs of disturbance than ten or eleven. I think.
I could say I’m sleeping badly, but it’s worse than that—I’m sleeping incorrectly. When I lie down, I don’t actually rest my head on the pillow; instead, I hold it slightly aloft, so that it touches the pillow but, instead of sinking into the soft material, remains hovering above it. To an observer I would seem to be lying down normally. I tell myself to relax—among other issues, I’m worried I’ll develop a thick neck. When I do, I’m shocked at how much I had just moments before been not relaxing. This is sleep , I think. This is what going to sleep actually feels like . But soon I find my head has risen above the pillow again, and I must admit to myself that I don’t know what going to sleep actually feels like.
From this you’d think I have trouble falling asleep; not so. I’m usually exhausted. But I almost always wake up too soon. Sometimes for no reason; sometimes by a tingling in my ring and pinky fingers, which I experience because I hold my arms tense in sleep, often with my hands in fists so tight that they leave marks from my nails on my palm. I learned the tingling is caused by the ulnar nerve, from a masseuse who observed my posture; she also intuited that I had been born via C-section and was thus likely dealing with an original sense of having been forcibly removed from a place of safety. The clenching, broadly, leads me to grind my teeth, which I have done for at least ten years, and the grinding, probably, leads to the tinnitus, which is relatively new. One of these things might also be at fault for what’s known as exploding head syndrome: at night, I sometimes see flashes of light behind my closed eyes, as if there are fireworks outside my window, and hear mechanical sounds that aren’t there. Despite its spectacular name, the condition is “prognostically benign,” accompanied by no pain or immediate threat to health. The fear I experience along with these hallucinations inspires a series of logical justifications: it’s all in my head, which is, of course, exactly the problem.
Trouble sleeping is certainly normal, but it doesn’t help the project of being awake. While socializing, I am cheerful, gossipy, and quite fun until I’m sleepy, but sometimes I catch myself doing artistic things with my hands and posture—fidgeting, wringing, clenching—even as I engage charmingly (I hope) with my interlocutors. Other times, I will look down from a conversation and notice, Oh, the fist again; because I can laugh at myself, I hold it up to show my friend, as if it contains a surprise. I do not pick or bite my nails, but in groups or alone, at home or out, I cannot keep my shoulders down. (Large deltoids—almost as bad as a thick neck.) Twice now, at parties, men have come up behind me and attempted to physically correct my posture, followed by a little lecture. Never mind the cell-phone addiction, the laptop that sits on the table so that I must look down on it, the ambient tension of contemporary life, when I must be on guard against men who randomly correct my posture. The slouch, they say, is the result of my failure to accept myself as a tall woman.
I honestly don’t think that’s it, but should you really take my word for it? I sometimes feel strange pains in various parts of my body, just fleeting ones, which I then waste a lot of time thinking about. I have occasionally fainted for no reason, and more than once broken out in hives. I get sweaty, feel anxious about being sweaty—about the sweat becoming visible to others, disgusting them—and get sweatier. After I go in the sun, I experience what I call a sunburn neurosis, my skin burning and tingling, though I remain, owing to anxious sunscreen application, as white as a Victorian ghost; I haven’t had a sunburn since I was a teen-ager. Acid reflux can last for weeks. I often find it difficult to eat because I am nauseated due to stress.
I don’t have any phobias, but I do feel afraid. When I’m particularly stressed, I sense movement out of the corner of my eye and jump, like an animal preparing to fend off attack; there’s nothing there. I hold my breath, make little noises, sing little songs, shake. Sometimes I perform feats of what might look from the outside like symptoms of very mild obsessive-compulsive disorder: checking more than twice that the front door is locked; changing the combination on a locker at the gym or a museum multiple times, because I am afraid someone saw me set it. I am hesitant to even mention this one, knowing, because of my years-long Internet addiction—which I would attribute to, among other things, an attempt to escape my anxious, spiralling thoughts, or maybe to externalize them—that if someone claims they “are O.C.D.” about facts of life, such as cleaning the kitchen, people get mad: perfectionism, neuroticism, and thoroughness are not O.C.D. In my defense, I never clean the kitchen.
My work suffers, of course. How could it not? I’m sadly not a perfectionist but, rather, an avoider and a regretter. There are periods when I will respond to e-mails at a reasonable pace, and then there’s the e-mail about a potentially lucrative project that I ignored for months. I haven’t even opened it; I don’t know what it says. Since childhood, I’ve had versions of “the packing dream,” in which I am surrounded by clothes strewn chaotically around the room, and I cannot choose what to bring on a trip. I may have enough time to finish packing, or I may already be too late. Whatever the scenario, it’s never one of those dreams about physical impediments, in which you try to move but can’t; the obstacle is always only my own mind, my own incapability, and that is the torment—that I’ve done this to myself. (I have never actually missed a flight.) As for work, I always manage to “get it done,” though I don’t know how. It’s probably a reasonable enough fear of failure—or fear of failing to achieve the impossibly ambitious vision in my mind—that is my obstacle. Even worse is the possibility, floated by sanguine meditators and accepters of things-as-they-are, that I may need the anxiety, and the promise of eventual relief from it, to do anything at all.
What about panic attacks? I’ve never had the kind of panic attack that people mistake for a medical emergency, but sometimes I become very still, sort of unable to move, for, I don’t know, ten to twenty minutes to an hour, and my muscles are sore the next day. There are the usual racing thoughts: love, squandered potential, unlikely vanities, loss of income. Injustices committed against me; chores. Will I get cancer? Knowing that everyone worries they have cancer helps only a little bit. My ultimate anxiety is not that a certain fear will come true. Rather, I experience panic as mostly meta: the horror of being trapped, in this mind-set, for the rest of my life.
Naturally, I am not merely anxious; I am also very sad. The two are, for me, inextricable: I get anxious that I’ll get sad and sad that I’m so anxious. It’s harder to describe the depression, and the fear of it, because fewer physical symptoms are involved. Weeping, that telltale sign of sadness, is usually cathartic, a response to a specific buildup of identifiable issues, and thus not involved in what I can’t help but think of as the true suffering, which recedes and returns, recedes and returns. People often talk about being unable to get out of bed in the morning. What if you can get out of bed—after about an hour and a half of lying awake in it, thinking about how you should get out of bed? What if you can get out of bed but find it beckons you back throughout the day? What if you are, owing to your difficulty sleeping, just tired? Which comes first, exhaustion or depression? Does it matter?
Even knowing that “normal” is a nefarious construct, used to shame and control, there’s something about these symptoms that makes me want to know how many people have them; they mean nothing to me alone because none of them is so unusual as to cause alarm, or even merit comment, and so they might mean anything. Is it really such a big deal? I don’t know where to put the emphasis, how to tell it, and this is particularly disturbing because knowing where to put the emphasis is my vocation, which is also bound up with, I’ll admit, my “sense of self.” “You don’t seem anxious,” friends will say, surprised at my competent narration. This is not the response I want. How competent could it be if no one believes what I’m telling them?
I can shift the blame. As with anything that matters, the language we use to describe “mental illness” is all wrong. Mental illness is “real,” as real as a tumor, but not the same kind of real as a tumor. Its effects are measurable, in blood pressure or hours slept, or noticeable, in weird hand gestures or an erratic mode of speaking, but mental illness has no shape or volume; its size cannot be conveyed through comparisons to fruits and vegetables. It becomes real in the description of its effects, in the naming of everything around it, rather than in attempts to define it, though we have many words and phrases that approach the task. “Disturbance” is funny, and accurate, because it refers both to the internal condition and what it produces: behavior that might unsettle oneself or others. I become “nervous” in small-stakes situations of short or predetermined time frames; “nervousness” no longer describes the anxious disposition, as it did in the past, but the feeling of being anxious about a specific thing that is usually imminent. I’m “neurotic” because I know the basics of psychoanalysis and am a fast-talking big-city professional; I’m “neurasthenic” because I know the word. My mother used to call herself, as well as me, a “worrywart”; to “worry” is to fidget with something in the mind. “Panic” is acute, “attack” is very acute, and a “fit” is a cute version of a “panic attack”; “throwing a fit” is what children do and what adults do when they are “freaking out” while simultaneously making childish demands. Like “freaking out,” “going insane” is applicable as a joke in retrospect, though it became too popular on the Internet and lost its edge, particularly because the sort of people who said it were just the sort who ought to be arguing that the usage stigmatizes people with mental illnesses. I still indulge in “crazy,” which is classic, and permitted, I think, because I am. “Distressed” is the joke version of nervous, though someone “in distress” is being euphemized, as is someone “behaving erratically.” A “crisis” is both intense and prolonged; a “spiral” is a crisis about one issue, characterized by repetitive and catastrophic thinking, and “spiralling” may feature prominently in crises, but in a slightly funny way. I fear having a true “breakdown,” which suggests, to me, among other things, a failure of speech, but I also fantasize about having a true breakdown for the same reason. I am rarely, if ever, “hysterical”; that’s sexist. “Mentally ill” is, of course, insufficient, though when I have seen other people “in crisis” I have thought I actually understand the term. The concept of “mental health,” did you know, comes from Plato, who said that it could be cultivated through the elimination of passion by reason. Today, good mental health means something like the elimination of both passion and reason.
Unless I’m about to appear onstage, in which case I am “nervous,” I describe myself as “anxious” so that people know I’m serious: this is not a passing worry but a constant state, and if I were to seek a medical diagnosis I would get one, handily. The question “Why don’t you?” naturally arises. The answer is that I do not feel it would help, and might even create more problems than it solves. In medicine, the problem of language is a problem of classification; I do not seek a diagnosis, probably, because I do not want to be trapped in a single term. (I hate being trapped, you might have noticed.) Like everyone else’s, my mind dabbles in an array of mental illnesses to create a bespoke product, and I find all the terms I know either ludicrously broad or ludicrously specific. I learned from Scott Stossel’s upsettingly thorough 2014 book, “ My Age of Anxiety: Fear, Hope, Dread, and the Search for Peace of Mind ,” that the term “generalized anxiety disorder” was conceived at a dinner party, in the nineteen-seventies, held among members of a task force working on the DSM-III . According to David Sheehan, a psychiatrist who was there, they were all drunk, wondering how to classify a colleague who “didn’t suffer from panic attacks but who worried all the time . . . just sort of generally anxious.” “For the next thirty years,” Sheehan continues, “the world collected data” on the group’s drunken musing. The point of this anecdote, Stossel establishes, is not to say that generalized anxiety disorder isn’t real but to demonstrate how somewhat arbitrary decisions made by powerful people can shape how we see ourselves. I also don’t mean to suggest that the ideas that we have while drunk are bad—more that drunkenness can give us an admirable economy and frankness, and encourage us to just pick something and go with it, something that some of us, sober, really struggle to do.
An essay like this is supposed to have a narrative. Where does my anxiety come from? Famously, it’s overdetermined. First, my parents: they passed down bad genes, and then they might not have raised me right. To go further I’d have to discuss the ways that they might not have been raised right, and then discuss the ways that they might not have raised me right. Although, like everyone, I have a list of these in the Notes app on my phone, and I update it every few days when a new injustice committed against my past innocence reveals itself, I am hesitant to go down this path, which narrows to a tunnel, which is eventually pitch-dark. The packing dream, a desire to escape my humble origins; the sunburn neurosis, from my mother’s warnings. I am the way I am because my father did this, or my mother didn’t do that. Not a very satisfying conclusion.
What about society? That’s what’s fucked up. In the early two-thousands, a group of academics in Chicago formed a collective called the Feel Tank—an alternative to the think tank, though of course they also opposed “the facile splitting of thinking and feeling.” According to their manifesto, they sought “to understand the economic and the nervous system of contemporary life” by being “interested in the potential for ‘bad feelings’ like hopelessness, apathy, anxiety, fear, numbness, despair and ambivalence to constitute and be constituted as forms of resistance.” One of their early slogans was “Depressed? . . . It might be political.”
Here the concept of normality truly collapses: what is normal—financial precarity, an inability to plan for the future, war—is not good at all. Feel Tank Chicago was established as part of the “affective turn” in the academic humanities, which began in the nineties; this approach to understanding emotions as shaped by power structures has become wildly influential, though it’s not new. For example: the concept of Americanitis, popularized by William James at the end of the nineteenth century, described “the high-strung, nervous, active temperament of the American people,” according to an 1898 issue of the Journal of the American Medical Association . The causes—advances in technology and accompanying pressures of capitalism—were much the same as they are today. Wherever the contemporary occurs, anxiety and depression are seen as natural reactions to it, and performances of profound mental discord in response to the news will be familiar to anyone on social media.
If conventional understandings of mental illness tend to make it about you—the chemicals in your brain or the particular contours of your childhood—this conception wonders if you can harness its power to make things better for everyone. Nice. But there’s something a little simplistic about the way one can attribute all feelings of negativity, disconnection, or anxiety to what amounts to a higher power, as anyone who’s read those social-media laments will know. Doesn’t this encourage more bad feelings: solipsism, nihilism, futility? Looking for something to blame may feel better than beating oneself up, but it doesn’t feel good . In her 2012 book, “ Depression: A Public Feeling ,” Ann Cvetkovich describes the Public Feelings Project—Feel Tank Chicago described themselves as a “cell” of this larger group—as an attempt to “depathologize negative feelings so that they can be seen as a possible resource for political action,” but without suggesting “that depression is thereby converted into a positive experience.”
Indeed, the encouragement to understand our suffering as determined by external conditions does not seem to ease it. The comfort of believing you are normal is that you have company in misery and that your condition seems less likely to become worse. But if “normal” is, by definition, something that is getting worse all the time, then your condition is a form of solidarity—not necessarily a source of solace. (And if you derive solace from the solidarity, do you really want to sacrifice the quality that grants you access to it?) For my purposes—which are, I suppose, to understand whether and how I am abnormal without annoying the reader—stories that foreground their protagonists’ participation in public feeling tend to be unsatisfying. If my suffering has nothing do with me, if it’s the expression of social and political conditions, why should the reader, or well-meaning friend, care? This is why narratives that compete directly with the idea of collective feeling and collective resistance, conservative tales of bootstrapping and hard work, are so compelling: they make a lot more sense.
Until the revolution that would be our relief comes, we must “do the work” to get better ourselves. “Have you tried talking to someone?” people ask, when I mention my various issues. Are you that somebody? No: they mean that, in addition to the natural sleep aids, the regular exercise, the healthy diet, the cultivation of hobbies, the having of friends, the practicing of meditation, and the occasional massage, I should go to therapy.
I have tried talking to someone; it’s fine. The responses I get when I utter the magic words “my therapist” are more thought-provoking than any of the personal revelations I’ve uncovered with him so far, though the idea is that you need to do it for years for the benefits to accrue. “I’m proud of you,” friends say. As if it is so difficult to think seriously about myself for hours a day—as if that weren’t what I was doing with my anxiety anyway. These friends will talk about my problems with me endlessly, as long as I am “in therapy.” If I am not, or if I express my doubts about the possibility of transcending the workings of my own mind by paying someone to guide me through the process, the response is unanimous: I must find a new therapist, someone who is “right” for me. They wonder, gently, gently: Is it possible that I, so high-achieving, am unconsciously telling the therapist what I think he wants to hear—deceiving him by being adequately emotional, apparently reflective, in order to give true self-knowledge the slip? Should I not find someone meaner, nicer, female, more intellectual, less intellectual, someone who will not fall for my tricks?
Or: I must try a different therapeutic approach. A bit of research quickly reveals an expanse of options: somatic-experiencing therapy, cognitive behavioral therapy, dialectical behavioral therapy, integrative therapy, gestalt therapy, humanistic therapy, psychodynamic therapy, exposure therapy, shock therapy, biofeedback, counselling, coaching, one of the innumerable schools of psychoanalysis. At a wedding, I was strongly recommended E.M.D.R., or “eye-movement desensitization and reprocessing” therapy, in which eye movement is stimulated in an attempt to retrain the brain to respond to trauma. Some of these styles of therapy are more or less the same thing, just with different names, but, given the nature of the enterprise, you have to assume that the selection of one name or another, or a combination of names, indicates subtle differences in method that surely multiply to create different outcomes. Whether you’re supposed to think about outcomes is a key differentiating factor in therapeutic approaches.
A psychiatrist might prescribe medication, a fraught topic. It’s hard to write about medication without having taken it oneself, which I have so far resisted. I’ve tried a couple of popular pharmaceuticals recreationally and find I am more afraid of them than I am of illegal club drugs; they really work. While I have no idea what it’s like to be on psychiatric medication long term, no one else can say what it’s like, either; the medications famously interact with each person differently, so there is no way to understand them as an experience except through trial and error. The possible side effects are sometimes just as bad as the symptoms they’re supposed to alleviate. The process of stopping these medications, which many patients want to do , is criminally under-studied and requires a painful period of weaning that comes with prohibitively bad side effects, too. (To start antidepressants is to sign up for some future moment when you won’t want to take them anymore, and to have to decide whether you want to experience “brain zaps” in order to stop.)
At the same time, they often help. Criticize what you believe to be the craven overprescription of psychiatric medication in the United States and someone on the Internet will take personal offense: Wellbutrin saved my life! At the end of Sheila Heti’s 2018 novel, “ Motherhood ,” the narrator begins taking antidepressants, and all her problems—primarily her vacillation about the question of whether to have a child, which constitutes the entire novel, along with a debilitating, weeping sadness around her period—are suddenly solved, with what the critic Willa Paskin called a “lexapro-ex-machina.” The abruptness of the ironic conclusion is itself a comment on the role that psychiatric medication plays in North American life, but this plot point, one of the book’s very few, also demonstrates the way philosophical searching ceases when the anguish that propels it is no longer there. Medication allows Heti’s narrator to ignore the upsetting reality that she could go on trying to decide, or regretting, forever. There is no arc, nor character development, nor point, without anticlimactic intervention.
I once attended a session of what I called jaw yoga, hoping to “manage” my bruxism. It was conducted by a Greek woman named Angela who described herself as a dancer, choreographer, and yoga coach; she was also, incredibly, an actual dentist. At the union of these disparate interests was a passionate belief that the jaw had been neglected in the world of dance and that the rest of the body had been neglected in the world of dentistry. “Once you are grinding and pressing the teeth, your cranium and shoulders, hips, knees and feet are reacting to this pressure,” her course description read, beneath a photo of her lying on her stomach, cupping her jaw in her hands. “Once the skeleton is affected, also the organs are reacting. A chain reaction of organs and emotions is put in motion.” She told us how to identify the various parts of the jaw and ended the class by singing along to a recording of “All You Need Is Love.” As we left, she passed out business cards that read “You are the point.”
It didn’t work, though maybe I should have attended more sessions. A resistance to helping oneself is often a simple denial of reality: I don’t want it to be true that I need help, not because I would like to imagine myself as strong and never in need—a common explanation—but because I do not want to have these problems that are notoriously difficult to solve, about which there is no professional agreement. I do not want to embark on a years-long project dedicated to my own mind. I have other things to think about.
A final worry: Am I being confessional? The great trick of declaring outsized anguish, of being publicly and clinically wrecked by one’s feelings, is that once you do it your feelings set the limits, and no one wants to hurt them. The confession is a simple form of writing. It does not contextualize, illuminate, or complicate. Its main purpose is not the creation of aesthetic beauty out of the materials at hand (life, pain) but selfishness: relieving the confessor’s desire to confess. The form travels in one direction, from me to you, offering no path to analysis, critique, or, God forbid, argument. If the feelings are unique, the confession is justified; if they’re normal, it is, too. One yearns for the breakthrough, the epiphany, the point, that will make sense of it all, and thus cure it. But catharsis for me is boring for you. ♦
This is drawn from “ No Judgment .”
New Yorker Favorites
The repressive, authoritarian soul of “ Thomas the Tank Engine .”
Why the last snow on Earth may be red .
Harper Lee’s abandoned true-crime novel .
How the super-rich are preparing for doomsday .
What if a pill could give you all the benefits of a workout ?
A photographer’s college classmates, back then and now .
Sign up for our daily newsletter to receive the best stories from The New Yorker .
By signing up, you agree to our User Agreement and Privacy Policy & Cookie Statement . This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.

By Katy Waldman
By Dennis Zhou
By José Antonio Rodríguez
By Rebecca Mead
Essay: Stress, depression and the holidays — how to cope this season

Everyone feels blue or sad sometimes, especially these days with the weather getting colder and darker and the stress of the holidays right around the corner.
These feelings can be short-lived and pass within a couple of days. Unfortunately, due to the increased isolation and financial pressures, many of us are facing more serious mental health issues such as depression.
Depression can interfere with daily life and causes pain for both you and those who care about you. Depression is a common but serious illness. People often give you advice to “just get over it” or “pull yourself up by your bootstraps.”
There are several types of depression. Seasonal affective disorder, a type of depression, is most common in areas of the country that do not get a lot of sunlight during parts of the year.
Adjustment disorder with depressive symptoms is also quite common now as a result of people struggling with the changes brought about by COVID-19 and its impact on our daily living.
There are many people with a depressive illness that do not seek help but most people with depression can get better with treatment.
Medications, psychotherapies and other methods can effectively treat people with depression. If you are experiencing any symptoms of depression such as trouble sleeping, trouble eating, extreme sadness, loss of interest in things, feeling hopeless or helpless and you would like help, there are many places to turn. You can talk to your primary care provider about how you are feeling and he or she can help you negotiate getting the services that will help.
Mental health clinics typically house providers, such as psychiatrists, psychologists, social workers or mental health counselors. There are also private mental health practitioners and clinics as well as employee assistance programs that can be accessed through your place of employment. Often the first few visits to an employee assistance program is free of charge.
Sylvan Beach: Essay - Why we are betting on Sylvan Beach
Sometimes people experiencing depression and other mental illnesses feel there is no place to turn and begin to look at harming themselves as an option. If you are thinking about harming yourself, or know someone who is, tell someone who can help immediately.
Do not leave your friend or relative alone, and do not isolate yourself.
Call your doctor.
Call 911 or go to a hospital emergency room to get immediate help, or ask a friend or family member to help you do these things.
Call the toll-free, 24-hour hotline of the National Suicide Prevention Lifeline at 1-800-273-TALK (1-800-273-8255); TTY: 1-800-799-4TTY (4889) to talk to a trained counselor. suicidepreventionlifeline.org
Call the Mobile Crisis Assessment Team 315-732-MCAT (6228).
When you face a stressful event or major life change, you can take some steps to care for your emotional well-being.
Do what works for you. For example, you can:
• Talk things over with supports (family and friends)
• Try to keep eating a healthy diet
• Stick to a regular sleep routine
• Get regular physical activity
• Engage in a hobby you enjoy
• Find a support group geared toward your situation
• Find support from a faith community
If you use these kinds of self-care steps but they don't seem to be helping, be sure to talk to your doctor.
Most people find treatment helpful, and they often require treatment only briefly. However, others may benefit from longer treatment.
For additional resources visit: nimh.nih.gov
Jodi Kapes is the director of behavioral health at Mohawk Valley Health System in Utica.

How much stress is too much? A psychiatrist explains the links between toxic stress and poor health − and how to get help
Professor of Psychiatry and Family Medicine, University of Cincinnati
Disclosure statement
Lawson R. Wulsin received funding in 2010 from the Veterans Administration support a secondary analysis of data from the Framingham Heart Study, which was published and contributed in part to the substance of this article.
View all partners
COVID-19 taught most people that the line between tolerable and toxic stress – defined as persistent demands that lead to disease – varies widely. But some people will age faster and die younger from toxic stressors than others.
So how much stress is too much, and what can you do about it?
I’m a psychiatrist specializing in psychosomatic medicine , which is the study and treatment of people who have physical and mental illnesses. My research is focused on people who have psychological conditions and medical illnesses as well as those whose stress exacerbates their health issues.
I’ve spent my career studying mind-body questions and training physicians to treat mental illness in primary care settings. My forthcoming book is titled “Toxic Stress: How Stress is Killing Us and What We Can Do About It.”
A 2023 study of stress and aging over the life span – one of the first studies to confirm this piece of common wisdom – found that four measures of stress all speed up the pace of biological aging in midlife. It also found that persistent high stress ages people in a comparable way to the effects of smoking and low socioeconomic status , two well-established risk factors for accelerated aging.
The difference between good stress and the toxic kind
Good stress – a demand or challenge you readily cope with – is good for your health. In fact, the rhythm of these daily challenges, including feeding yourself, cleaning up messes, communicating with one another and carrying out your job, helps to regulate your stress response system and keep you fit.
Toxic stress, on the other hand, wears down your stress response system in ways that have lasting effects, as psychiatrist and trauma expert Bessel van der Kolk explains in his bestselling book “ The Body Keeps the Score .”
The earliest effects of toxic stress are often persistent symptoms such as headache, fatigue or abdominal pain that interfere with overall functioning. After months of initial symptoms, a full-blown illness with a life of its own – such as migraine headaches, asthma, diabetes or ulcerative colitis – may surface.
When we are healthy, our stress response systems are like an orchestra of organs that miraculously tune themselves and play in unison without our conscious effort – a process called self-regulation. But when we are sick, some parts of this orchestra struggle to regulate themselves, which causes a cascade of stress-related dysregulation that contributes to other conditions.
For instance, in the case of diabetes, the hormonal system struggles to regulate sugar. With obesity, the metabolic system has a difficult time regulating energy intake and consumption. With depression, the central nervous system develops an imbalance in its circuits and neurotransmitters that makes it difficult to regulate mood, thoughts and behaviors.
‘Treating’ stress
Though stress neuroscience in recent years has given researchers like me new ways to measure and understand stress , you may have noticed that in your doctor’s office, the management of stress isn’t typically part of your treatment plan.
Most doctors don’t assess the contribution of stress to a patient’s common chronic diseases such as diabetes, heart disease and obesity, partly because stress is complicated to measure and partly because it is difficult to treat. In general, doctors don’t treat what they can’t measure.
Stress neuroscience and epidemiology have also taught researchers recently that the chances of developing serious mental and physical illnesses in midlife rise dramatically when people are exposed to trauma or adverse events, especially during vulnerable periods such as childhood .
Over the past 40 years in the U.S., the alarming rise in rates of diabetes , obesity , depression, PTSD, suicide and addictions points to one contributing factor that these different illnesses share: toxic stress.
Toxic stress increases the risk for the onset, progression, complications or early death from these illnesses.
Suffering from toxic stress
Because the definition of toxic stress varies from one person to another, it’s hard to know how many people struggle with it. One starting point is the fact that about 16% of adults report having been exposed to four or more adverse events in childhood . This is the threshold for higher risk for illnesses in adulthood.
Research dating back to before the COVID-19 pandemic also shows that about 19% of adults in the U.S. have four or more chronic illnesses . If you have even one chronic illness, you can imagine how stressful four must be.
And about 12% of the U.S. population lives in poverty , the epitome of a life in which demands exceed resources every day. For instance, if a person doesn’t know how they will get to work each day, or doesn’t have a way to fix a leaking water pipe or resolve a conflict with their partner, their stress response system can never rest. One or any combination of threats may keep them on high alert or shut them down in a way that prevents them from trying to cope at all.
Add to these overlapping groups all those who struggle with harassing relationships, homelessness, captivity, severe loneliness, living in high-crime neighborhoods or working in or around noise or air pollution. It seems conservative to estimate that about 20% of people in the U.S. live with the effects of toxic stress.
Recognizing and managing stress and its associated conditions
The first step to managing stress is to recognize it and talk to your primary care clinician about it. The clinician may do an assessment involving a self-reported measure of stress .
The next step is treatment. Research shows that it is possible to retrain a dysregulated stress response system. This approach, called “lifestyle medicine ,” focuses on improving health outcomes through changing high-risk health behaviors and adopting daily habits that help the stress response system self-regulate.
Adopting these lifestyle changes is not quick or easy, but it works.
The National Diabetes Prevention Program , the Ornish “UnDo” heart disease program and the U.S. Department of Veterans Affairs PTSD program , for example, all achieve a slowing or reversal of stress-related chronic conditions through weekly support groups and guided daily practice over six to nine months. These programs help teach people how to practice personal regimens of stress management, diet and exercise in ways that build and sustain their new habits.
There is now strong evidence that it is possible to treat toxic stress in ways that improve health outcomes for people with stress-related conditions. The next steps include finding ways to expand the recognition of toxic stress and, for those affected, to expand access to these new and effective approaches to treatment.
- Neuroscience
- Chronic stress
- Adverse childhood experiences
- Adverse childhood events

Deputy Editor - Technology

Sydney Horizon Educators (Identified)

Assistant Grants Officer

Deputy Vice-Chancellor (Academic and Student Life)

Visiting Professor - 2024-25 Australia-Korea Chair in Australian Studies at Seoul National University

Ask This Question to Reduce Your Anxiety and Depression
A personal perspective: one tool to find relief from anxiety and depression..
Updated March 11, 2024 | Reviewed by Jessica Schrader
- What Is Depression?
- Find counselling to overcome depression
- Anxiety and depression can be driven by avoidance behaviors.
- This simple question can be a powerful wellness tool: “What I am avoiding?”
- It can also help to create a “Fun, Soothe, and Avoid List.”

I have feelings about my feelings. When I get anxious, I start to feel anxious about my anxiety ; when I start to feel depressed, I get more depressed about being depressed. And when I start to feel those feelings, I get more anxious and I manically scramble to fix it, which only worsens the whole situation. What I've discovered is that self-care and self-soothing all are good and fine to calm and support myself. But there's a missing element that I was overlooking. A question that may reduce my anxiety and depression .
Self-care involves taking care of my physical self by eating well, sleeping , and exercising enough. Self-soothing might involve finding things that calm me down like deep breathing or feeling the softness of my housecoat. But there's an entirely different tool that my therapist brought to my attention : avoidance. I can be the driver of depression and anxiety. Not always, but sometimes. For those of you who haven't heard about her and would like to know more about her, you can read about her in this post .
The Connection Between Avoidance and Feeling Bad
I often look for the origins of my struggling in past trauma , my attachment style issues, and my emotional baggage. They've certainly contributed, but there's a more practical and concrete cause. Avoidance may be the culprit creating my nail-biting, dark-space emotions. Not always but sometimes.
I then ask myself this question: What I am avoiding?
I may find I've been getting things done but I haven't been getting the right things done. When I avoid important to-dos my anxiety intensifies; I feel bad about myself and the more depressed I can get.
Now that I recognize the connection, I look at my to-do list, reflect on my personal responsibilities, and see where, if at all, I’ve been procrastinating. I break the task down to its tiniest components. Set a timer for 10 minutes and take a step toward completion. When I do this, I feel relief, a little hope, and start to feel better about myself. Lo and behold, my depression or anxiety, or maybe both, slowly lessen. The pressure is off. Like how a ball held under water rises ever so slightly when the hand that’s holding it back reduces the resistance.
The simple question " What am I avoiding?" has become a powerful wellness tool.
The Fun, Soothe, and Avoid List
Andie made another suggestion: create a Fun, Soothe, and Avoid List. It’s on my fridge where I can see it every day. It has two columns. On the left are fun and/or soothing activities; on the right are things I tend to avoid.
Under the left column: dancing in the kitchen to music; listening to my favorite radio station (yes, I am that old-school); winter swimming with my best friend; texting goofy GIFs. Under the avoidance column: bookkeeping (not surprising); starting work projects; doing laundry; folding said laundry. I’m always adding to the list.
Anxiety and depression narrow my focus. I fixate on how scared and depressed I feel, which tricks me into thinking I can’t accomplish anything which perpetuates the avoidance.
When I see I’m doing the two-step avoidance dance, the key is to not turn on myself, which would only fuel the fires of anxiety and depression. Instead, as best I can, I embrace my perfect imperfection, my wonderful messy humanness, and take one teeny-weeny step towards that task. Sometimes all I can manage is to list the first two steps of said task. I said tiny, right? Anywhere along the line, if my anxiety or depression starts to rise, I step back, pause, and breathe. Once my nervous system calms, I continue with the task.
Anxiety and depression can be driven by avoidance behaviors. Gently asking the question "What am I avoiding?" can equal forward motion and as a result reduced anxiety and depression.
Managing my mental health is a process of compassionately embracing my humanness and taking one small step at a time toward healing.
"What Am I Avoiding?" Wellness Tool
Before you begin, create your list of fun and soothing activities and tasks you avoid. Put it in a place you’ll see daily. When you notice feelings of anxiety and/or depression, try the following steps:
- Ask yourself "What am I avoiding?"
- Scan your to-do list and your avoid column and identify what you’ve been putting off.
- Bring forward the most self-compassion you can.
- Set a timer for five to 10 minutes and start on the tiniest step towards completing the task.
- If anxiety or depression increases, be gentle, pause, and take a breath.
- Return to the task when you feel a tiny easing of the stress .

Victoria Maxwell is a playwright, actor, and lecturer on her 'lived' experiences of bipolar disorder, anxiety, psychosis and recovery.
- Find a Therapist
- Find a Treatment Center
- Find a Support Group
- International
- New Zealand
- South Africa
- Switzerland
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience
Anxiety and Depression Among College Students Essay
Education is expected to have appositive importance on the student’s life by enhancing their capability to think and improving their competency. However, it often acts as a source of stress that affects students’ mental health adversely. This causation of academic stress often emanates from the need to have high grades, the requirement to change attitude for success, and even pressures put by various school assignments. These pressures introduced by education can make the student undergo a series of anxiety, depression, and stress trying to conform to the forces. The causes of academic stress are well-researched but there is still no explanation why the rate of strain increases despite some measures being implemented to curb student stress. This research explores this niche by using 100 participants who study at my college.
Introduction
Nowadays there are many reasons that cause stress among growing number of students who might not know they are going through the condition most of the time. Hence, undiscovered discouragement or uneasiness can cause understudies to feel that they are continually passing up unique open doors. It prompts substance misuse; self-destruction is the second most typical reason for death among undergrads. The main hypothesis of this article is that college and university students have higher depression rates.
Problem Statement
This proposal undercovers how the problem of anxiety and depression is progressing if not addressed. With such countless youngsters experiencing undiscovered tension, it may be challenging for them to appreciate school. Understudies’ emotional well-being is risked when pressure and trouble go unnoticed, which can prompt social and educational issues (Nelson & Liebel, 2018). Educators might battle to perceive uneasiness since these circumstances manifest themselves contrastingly in different people.
Anxiety and depression are complicated disorders with numerous elements that impact people differently. Teachers and staff must be well trained to deal with these unforeseen events. Understudies coming to college come from various financial foundations, which can prompt an assortment of psychological wellness chances (Li et al., 2021). Additionally, current works will be evaluated to differentiate the risk factors associated with stress among university undergraduates worldwide.
There are various reasons which might cause the onset of anxiety and depression. It can be absence of rest, terrible dietary patterns, and lack of activity add to the gloom in undergrads (Ghrouz et al., 2019). Scholarly pressure, which incorporates monetary worries, strain to track down a decent profession after graduation, and bombed connections, is sufficient to drive a few understudies to exit school or more awful.
Numerous parts of school life add to despondency risk factors. For example, understudies today are owing debtors while having fewer work prospects than prior. Discouraged kids are bound to foster the problems like substance misuse (Lattie et al., 2019). For adaptation to close-to-home trouble, discouraged understudies are more inclined than their non-discouraged companions to knock back the firewater, drink pot, and participate in unsafe sexual practices.
Hypothesis on the Topic
The central hypothesis for this study is that college students have a higher rate of anxiety and depression. The study will integrate various methodologies to prove the hypothesis of nullifying it. High rates of anxiety and depression can lead to substance misuse, behavioral challenges, and suicide (Lipson et al., 2018). Anxiety is one of the most critical indicators of academic success, it shows how students’ attitudes change, reflecting on their overall performance.
Methods Section
Participants.
The study will use college students who are joining and those already in college. The research period is planned to last six months; college students are between the ages of 18 and 21 and life is changing rapidly at this age (Spillebout et al., 2019). This demography will come from the college where I study. The participants will be chosen randomly, the total number will be 100, both female and male, and from all races.
Apparatus/ Materials/ Instruments
Some of the materials to be used in the study will include pencils, papers, and tests. Paper and pencil are typical supplies that students are familiar with, so using them will not cause additional stress. It will be used during the interview with the students and throughout the study will be in effect (Huang et al., 2018). These have been applied in various studies before, and, hence, they will be instrumental in this study.
The study will follow a step-wise procedure to get the required results. First, the students’ pre-depression testing results would be researched and recorded. Second, the students would undergo standardized testing in the same groups. Scholarly accomplishment is impacted by past intellectual performance and standardized testing (Chang et al., 2020). Third, the students’ levels of depression and anxiety would be monitored along with their test results.
The study will use a descriptive, cross-sectional design with categorical and continuous data. The sample demographic characteristics were described using descriptive statistics. Pearson’s proportion of skewness values and common mistake of skewness was utilized to test the ordinariness of the persistent factors. The distinctions in mean scores between sociodemographic variables and stress will be examined using Tests (Lipson et al., 2018). The independent variable will be essential because it will provide the basis of measurement.
The 100 participants had different anxiety levels, as seen from the Test taken and the various evaluations. Forty-five of the participants had high levels, 23 had medium levels, while the remaining 32 had low levels (Lipson et al., 2018). The correlation and ANOVA, which had a degree of era margin of 0.05, were allowed (Lipson et al., 2018). This finding aligns intending to have clear and comprehensive outcomes.
Significance of the Study
If the results would be not significant, it means that students are not subjected to more pressure on average. If the study results in significant outcomes, this would mean that there is much that needs to be done to reduce student’s anxiety. The idea that scholarly accomplishment is indispensable to progress is built up in higher instructive conditions (Nelson & Liebel, 2018). Many colleges devote money to tutoring, extra instruction, and other support services to help students succeed.
APA Ethical Guidelines
The study will have to follow the APA ethical guidelines because it involves experimenting with humans. Some of the policies include having consent from the participant, debriefing the participant on the study’s nature, and getting IRB permission (Nelson & Liebel, 2018). Ethical guidelines should comply with proficient, institutional, and government rules. They habitually administer understudies whom they likewise instruct to give some examples of obligations.
Limitations
The study also had some limitations, making it hard to get the desired outcomes. It was not easy to detect the population-level connections, but not causality. This case hardened the aspect of confounding and getting the relevant random assignment needed for the study had to access (Nelson & Liebel, 2018). For the right individuals for the investigation to be identified, the sampling was not easy.
This study would be essential as it will create a platform for future studies. The result that was gotten shows that many college students are undergoing the problem of anxiety and depression without knowing that it is happening. Educators will have awareness on what aspects of academics they need to modify to ensure their students are not experiencing mental health challenges. Hence, it makes it possible for future researchers to conduct studies to provide possible solutions.
Chang, J., Yuan, Y., & Wang, D. (2020). Mental health status and its influencing factors among college students during the epidemic of COVID-19. Journal of Southern Medical University , 40(2), 171-176.
Ghrouz, A. K., Noohu, M. M., Manzar, D., Warren Spence, D., BaHammam, A. S., & Pandi-Perumal, S. R. (2019). Physical activity and sleep quality in relation to mental health among college students. Sleep and Breathing Journal , 23(2), 627-634.
Huang, J., Nigatu, Y. T., Smail-Crevier, R., Zhang, X., & Wang, J. (2018). Interventions for common mental health problems among university and college students: A systematic review and meta-analysis of randomized controlled trials. Journal of Psychiatric Research , 107, 1-10.
Lattie, E. G., Adkins, E. C., Winquist, N., Stiles-Shields, C., Wafford, Q. E., & Graham, A. K. (2019). Digital mental health interventions for depression, anxiety, and enhancement of psychological well-being among college students: A systematic review. Journal of Medical Internet Research , 21(7), e12869.
Li, Y., Zhao, J., Ma, Z., McReynolds, L. S., Lin, D., Chen, Z.,… & Liu, X. (2021). Mental health among college students during the COVID-19 pandemic in China: A 2-wave longitudinal survey. Journal of Affective Disorders , 281, 597-604.
Lipson, S. K., Kern, A., Eisenberg, D., & Breland-Noble, A. M. (2018). Mental health disparities among college students of color. Journal of Adolescent Health , 63(3), 348-356.
Nelson, J. M., & Liebel, S. W. (2018). Anxiety and depression among college students with attention-deficit/hyperactivity disorder (ADHD): Cross-informant, sex, and subtype differences. Journal of American College Health , 66(2), 123-132.
Spillebout, A., Dechelotte, P., Ladner, J., & Tavolacci, M. P. (2019). Mental health among university students with eating disorders and irritable bowel syndrome in France. Journal of Affective Disorders , 67(5), 295-301.
The following table shows the significant issues that affect the mental health state of most college students. Based on Huang et al.’s research, the biggest concern for most students included stress about their loved ones. Additionally, the authors found that worrying about one’s academics and schooling was the second depressing experience among most college students.
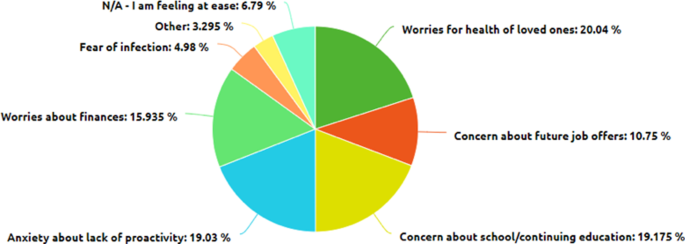
The following figure shows how on top of the current stressors for students, COVID-19 affects their mental health. Li et al.’s research demonstrates that COVID-19 placed more financial burden than before, especially on students with part-time jobs who often face anxiety and stress due to lack of tuition fees (Li et al., 2021). Generally, the research shows that the financial consequences of coronavirus affect the mental state of most college students.
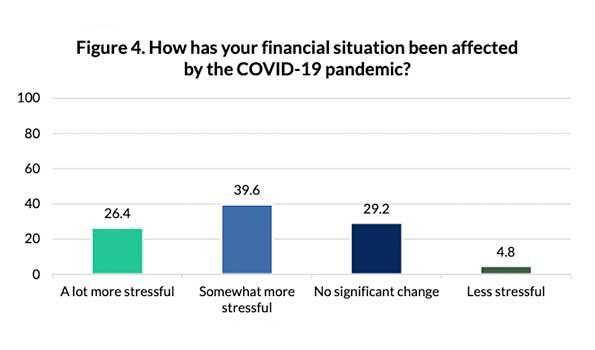
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2023, April 10). Anxiety and Depression Among College Students. https://ivypanda.com/essays/anxiety-and-depression-among-college-students/
"Anxiety and Depression Among College Students." IvyPanda , 10 Apr. 2023, ivypanda.com/essays/anxiety-and-depression-among-college-students/.
IvyPanda . (2023) 'Anxiety and Depression Among College Students'. 10 April.
IvyPanda . 2023. "Anxiety and Depression Among College Students." April 10, 2023. https://ivypanda.com/essays/anxiety-and-depression-among-college-students/.
1. IvyPanda . "Anxiety and Depression Among College Students." April 10, 2023. https://ivypanda.com/essays/anxiety-and-depression-among-college-students/.
Bibliography
IvyPanda . "Anxiety and Depression Among College Students." April 10, 2023. https://ivypanda.com/essays/anxiety-and-depression-among-college-students/.
- Incorporating Technology in Science Curriculum
- The Targeting Market of the Sustainable Coffee Shop
- Academic Writing: Flipped Classroom Method
- Racism: Healthcare Crisis and the Nurses Role
- The African American Women Leadership in Higher Education
- Undiscovered Killers: The Ineffectiveness of Zero-Tolerance Policies
- Fear associated with sexuality issues in society
- Mean-Variance Skewness Portfolio Performance Gauging
- Medication and Preventive Systems
- How Cognitive Behavioral Therapy Benefits Children
- Defense Mechanisms and Brain Structure
- Coping with Stress and Physical Health Problems
- Quality of Life With Schizophrenia
- Schizophrenia: The Etiology Analysis
- Schizophrenia as a Chronic Mental Disorder
Prevalence and Correlates of Probable Depression and Post-Traumatic Stress Disorder Among Female Sex Workers in Lilongwe, Malawi
Add to collection, downloadable content.
- Affiliation: School of Medicine, UNC Project-Malawi
- Affiliation: School of Medicine
- Affiliation: Gillings School of Global Public Health, Department of Epidemiology
- Affiliation: School of Medicine, Department of Psychiatry
- Other Affiliation: The Ohio State University
- Globally, female sex workers (FSW) experience a high prevalence of mental health disorders, but in sub-Saharan Africa, these are rarely identified. If left untreated, mental health disorders may place FSW and their partners at risk for HIV/sexually transmitted infections (STIs). We assessed the prevalence and correlates of probable depression, post-traumatic stress disorder (PTSD), and suicidal ideation (SI) in a cohort of 200 FSW in Lilongwe, Malawi. FSW completed the Patient Health Questionnaire-9 and the PTSD Check List—Civilian Version. The prevalence of depression was 8%, as was the prevalence of PTSD. Nearly half (49%) of FSW were experiencing mild depression. FSW were more likely to have probable depression if they completed primary school or initiated sex work before 18 years. They were more likely to have probable PTSD if they had ≥ 20 clients per week or initiated sex work before 18 years. Interventions are needed to diagnose mental health disorders among FSW at great risk for HIV/STIs.
- Sub-Saharan Africa
- Mental health
- https://doi.org/10.17615/f03z-bz96
- https://doi.org/10.1007/s11469-017-9829-9
- In Copyright
- International Journal of Mental Health and Addiction
- Fogarty International Center, FIC
- National Heart, Lung, and Blood Institute, NHLBI: T32 AI0700
- National Cancer Institute, NCI
- National Institutes of Health, NIH: R25 TW009340
- Center for AIDS Research, University of North Carolina at Chapel Hill, UNC CFAR: P30 AI50410
- NIH Office of the Director, OD
- Office of Research on Women's Health, ORWH
- Springer New York LLC
This work has no parents.
Select type of work
Master's papers.
Deposit your masters paper, project or other capstone work. Theses will be sent to the CDR automatically via ProQuest and do not need to be deposited.
Scholarly Articles and Book Chapters
Deposit a peer-reviewed article or book chapter. If you would like to deposit a poster, presentation, conference paper or white paper, use the “Scholarly Works” deposit form.
Undergraduate Honors Theses
Deposit your senior honors thesis.
Scholarly Journal, Newsletter or Book
Deposit a complete issue of a scholarly journal, newsletter or book. If you would like to deposit an article or book chapter, use the “Scholarly Articles and Book Chapters” deposit option.
Deposit your dataset. Datasets may be associated with an article or deposited separately.
Deposit your 3D objects, audio, images or video.
Poster, Presentation, Protocol or Paper
Deposit scholarly works such as posters, presentations, research protocols, conference papers or white papers. If you would like to deposit a peer-reviewed article or book chapter, use the “Scholarly Articles and Book Chapters” deposit option.

IMAGES
VIDEO
COMMENTS
Research reveals that a wayward stress system attack on the brain can lead to depression. The legacy of our evolutionary and biological stress responses is a significant burden for humans today ...
Depression is a disorder characterized by prolonged periods of sadness and loss of interest in life. The symptoms include irritability, insomnia, anxiety, and trouble concentrating. This disorder can produce physical problems, self-esteem issues, and general stress in a person's life. Difficult life events and trauma are typical causes of ...
Depression and anxiety occur at a similar time. Anxiety is caused due to an overwhelming fear of an expected occurrence of an event that is unclear to a person. More than 25 million people globally are affected by anxiety disorders. People feel anxious in moments such as when making important decisions, before facing an interview panel, and ...
Share your story, message, poem, quote, photo or video of hope, struggle or recovery. By sharing your experience, you can let others know that they are not alone. NAMI HelpLine is available M-F 10 am - 10 pm, ET. Connect by phone 800-950-6264 or text "Helpline". to 62640, or chat. In a crisis call or text 988.*.
PSYCHOLOGICAL STRESS. Psychological stress has been increasingly featured in scientific works as well as in popular media such as internet, newspapers and TV due to terrorism, war [], divorce and unemployment [].Psychological stress which is an adaptation to the fight-or-flight response during evolution, can induce a constellation of physiological responses (including nervous, endocrine and ...
Research the different ways depression can be diagnosed and discuss the benefits of receiving a diagnosis in this essay. 3. Causes of Depression. There are many possible causes of depression; this essay discusses how depression can occur. Possible causes of depression can include trauma, grief, anxiety disorders, and some physical health ...
Chronic stress can have negative effects on your body and mind and create a multitude of unpleasant physical and psychological symptoms. For example, it can cause tension, leading to muscle pain ...
The link between stressful life events and the origin and development of depression has been widely investigated, providing an increasing body of evidence supporting this association. 1-3 Environmental factors likely affect individuals in somewhat different manners, therefore triggering an adaptive response to stress, which depends on both psychological and biological aspects in the ...
Anxiety disorders affect nearly 20 percent of American adults. That means millions are beset by an overabundance of the fight-or-flight response that primes the body for action. When you're ...
In addition, initial presentation with social phobia was associated with a 5.7-fold increased risk of developing major depressive disorder. These associations between anxiety and depression can be traced back even earlier in life. For example, childhood behavioral inhibition in response to novelty or strangers, or an extreme anxious temperament ...
Essay grade: Good. 2 pages / 821 words. This may be one of the largest silent epidemics the world has ever had. Students and teenagers everywhere are depressed. Up to one in five children show signs of depression or some other mental disorder every year. The worst part is, nearly 80% of the...
Depression is a mood-affective disorder that causes a persistent feeling of sadness, loneliness, and starting loss of interest in things. A major depressive disorder or clinical depression is that which affects feeling, thinking, and behavior and can lead to a variety of emotional and physical problems. Depression causes feelings of sadness and ...
Maladaptive response to stress results in various physical, psychological, and behavioral negative effects. Negative effects of stress on physical health include increased heart rates, sweating, high blood pressure, and long-term development of the cardiac condition. Psychological effects include the development of anxiety, depression, and ...
Therefore, long-term untreated depression, anxiety, or stress can have a negative influence on people's ability to operate and produce, posing a public health risk . Theoretical Implications The current study makes various contributions to the existing literature on servant leadership.
The possible causes of depression are many and not yet well understood. However, it most likely results from an interplay of genetic vulnerability and environmental factors. Your depression research paper could explore one or more of these causes and reference the latest research on the topic. For instance, how does an imbalance in brain ...
Anxiety and depression are two of the most common mental health disorders that affect millions of people worldwide. These disorders can have a profound impact on an individual's overall well-being, leading to a range of physical, emotional, and cognitive symptoms that can interfere with daily functioning and quality of life.
Depression can cause a range of psychological and physical symptoms, including: persistent depressed mood. loss of interest or pleasure in hobbies and activities. changes in appetite and body ...
This essay has been submitted by a student. This essay is based on the case study of Tracy 42 years old mother of two who has experienced a difficult upbringing and has been diagnosed with Depression and Anxiety. Depression is a mood disorder that causes a persistent feeling of sadness, low self-esteem, and loss of interest in daily activities .
According to Joyce et al. (2016), "depression and anxiety disorders are the leading cause of sickness absence and long-term work incapacity in most developed countries" (p. 683). In addition, The Canadian Mental Health Association (2017) argues that "mental illnesses cost canadian employers billions of dollars in absenteeism or sick days ...
Depression affects between 200 and 300 million people worldwide: The rate of depression is around 17% in the United States and ranges from 8% to 12% in most countries.; The pandemic impacted rates of depression: A 2023 report found that since the onset of the COVID-19 pandemic, depression and anxiety rates went up by 25% worldwide.; Depression also impacts children: Research shows that around ...
Wherever the contemporary occurs, anxiety and depression are seen as natural reactions to it, and performances of profound mental discord in response to the news will be familiar to anyone on ...
The Present Definition of a Depressive Disorder. Depression can be defined as a disorder that affects a person's mental health, resulting in a dampened emotional state for an extended time. It is an exhausting mental condition that affects people's daily lives by influencing them towards adopting negative patterns of behavior (Lu, Li, Li ...
When you face a stressful event or major life change, you can take some steps to care for your emotional well-being. Do what works for you. For example, you can: • Talk things over with supports ...
Over the past 40 years in the U.S., the alarming rise in rates of diabetes, obesity, depression, PTSD, suicide and addictions points to one contributing factor that these different illnesses share ...
Anxiety is the overwhelming feeling of worryness and nervousness in the thought of an questionable outcome. Depression is the overwhelming feeling of sadness which can lead to heavy demoralization. Thoughts of doubt and nervous behavior are the drives of these disorders and the reason why they are paired together very oftenly.
Lo and behold, my depression or anxiety, or maybe both, slowly lessen. The pressure is off. Like how a ball held under water rises ever so slightly when the hand that's holding it back reduces ...
Anxiety and depression are complicated disorders with numerous elements that impact people differently. Teachers and staff must be well trained to deal with these unforeseen events. Understudies coming to college come from various financial foundations, which can prompt an assortment of psychological wellness chances (Li et al., 2021).
We assessed the prevalence and correlates of probable depression, post-traumatic stress disorder (PTSD), and suicidal ideation (SI) in a cohort of 200 FSW in Lilongwe, Malawi. FSW completed the Patient Health Questionnaire-9 and the PTSD Check List—Civilian Version. The prevalence of depression was 8%, as was the prevalence of PTSD.