Case Study: Managing Severe Asthma in an Adult
—he follows his treatment plan, but this 40-year-old male athlete has asthma that is not well-controlled. what’s the next step.
By Kirstin Bass, MD, PhD Reviewed by Michael E. Wechsler, MD, MMSc
This case presents a patient with poorly controlled asthma that remains refractory to treatment despite use of standard-of-care therapeutic options. For patients such as this, one needs to embark on an extensive work-up to confirm the diagnosis, assess for comorbidities, and finally, to consider different therapeutic options.

Case presentation and patient history
Mr. T is a 40-year-old recreational athlete with a medical history significant for asthma, for which he has been using an albuterol rescue inhaler approximately 3 times per week for the past year. During this time, he has also been waking up with asthma symptoms approximately twice a month, and has had three unscheduled asthma visits for mild flares. Based on the National Asthma Education and Prevention Program guidelines , Mr. T has asthma that is not well controlled. 1
As a result of these symptoms, spirometry was performed revealing a forced expiratory volume in the first second (FEV1) of 78% predicted. Mr. T then was prescribed treatment with a low-dose corticosteroid, fluticasone 44 mcg at two puffs twice per day. However, he remained symptomatic and continued to use his rescue inhaler 3 times per week. Therefore, he was switched to a combination inhaled steroid and long-acting beta-agonist (LABA) (fluticasone propionate 250 mcg and salmeterol 50 mcg, one puff twice a day) by his primary care doctor.
Initial pulmonary assessment Even with this step up in his medication, Mr. T continued to be symptomatic and require rescue inhaler use. Therefore, he was referred to a pulmonologist, who performed the initial work-up shown here:
- Spirometry, pre-albuterol: FEV1 79%, post-albuterol: 12% improvement
- Methacholine challenge: PC 20 : 1.0 mg/mL
- Chest X-ray: Within normal limits
Continued pulmonary assessment His dose of inhaled corticosteroid (ICS) and LABA was increased to fluticasone 500 mcg/salmeterol 50 mcg, one puff twice daily. However, he continued to have symptoms and returned to the pulmonologist for further work-up, shown here:
- Chest computed tomography (CT): Normal lung parenchyma with no scarring or bronchiectasis
- Sinus CT: Mild mucosal thickening
- Complete blood count (CBC): Within normal limits, white blood cells (WBC) 10.0 K/mcL, 3% eosinophils
- Immunoglobulin E (IgE): 25 IU/mL
- Allergy-skin test: Positive for dust, trees
- Exhaled NO: Fractional exhaled nitric oxide (FeNO) 53 parts per billion (pbb)
Assessment for comorbidities contributing to asthma symptoms After this work-up, tiotropium was added to his medication regimen. However, he remained symptomatic and had two more flares over the next 3 months. He was assessed for comorbid conditions that might be affecting his symptoms, and results showed:
- Esophagram/barium swallow: Negative
- Esophageal manometry: Negative
- Esophageal impedance: Within normal limits
- ECG: Within normal limits
- Genetic testing: Negative for cystic fibrosis, alpha1 anti-trypsin deficiency
The ear, nose, and throat specialist to whom he was referred recommended only nasal inhaled steroids for his mild sinus disease and noted that he had a normal vocal cord evaluation.
Following this extensive work-up that transpired over the course of a year, Mr. T continued to have symptoms. He returned to the pulmonologist to discuss further treatment options for his refractory asthma.
Diagnosis Mr. T has refractory asthma. Work-up for this condition should include consideration of other causes for the symptoms, including allergies, gastroesophageal reflux disease, cardiac disease, sinus disease, vocal cord dysfunction, or genetic diseases, such as cystic fibrosis or alpha1 antitrypsin deficiency, as was performed for Mr. T by his pulmonary team.
Treatment options When a patient has refractory asthma, treatment options to consider include anticholinergics (tiotropium, aclidinium), leukotriene modifiers (montelukast, zafirlukast), theophylline, anti-immunoglobulin E (IgE) antibody therapy with omalizumab, antibiotics, bronchial thermoplasty, or enrollment in a clinical trial evaluating the use of agents that modulate the cell signaling and immunologic responses seen in asthma.
Treatment outcome Mr. T underwent bronchial thermoplasty for his asthma. One year after the procedure, he reports feeling great. He has not taken systemic steroids for the past year, and his asthma remains controlled on a moderate dose of ICS and a LABA. He has also been able to resume exercising on a regular basis.
Approximately 10% to 15% of asthma patients have severe asthma refractory to the commonly available medications. 2 One key aspect of care for this patient population is a careful workup to exclude other comorbidities that could be contributing to their symptoms. Following this, there are several treatment options to consider, as in recent years there have been several advances in the development of asthma therapeutics. 2
Treatment options for refractory asthma There are a number of currently approved therapies for severe, refractory asthma. In addition to therapy with ICS or combination therapies with ICS and LABAs, leukotriene antagonists have good efficacy in asthma, especially in patients with prominent allergic or exercise symptoms. 2 The anticholinergics, such as tiotropium, which was approved for asthma in 2015, enhance bronchodilation and are useful adjuncts to ICS. 3-5 Omalizumab is a monoclonal antibody against IgE recommended for use in severe treatment-refractory allergic asthma in patients with atopy. 2 A nonmedication therapeutic option to consider is bronchial thermoplasty, a bronchoscopic procedure that uses thermal energy to disrupt bronchial smooth muscle. 6,7
Personalizing treatment for each patient It is important to personalize treatment based on individual characteristics or phenotypes that predict the patient's likely response to treatment, as well as the patient's preferences and practical issues, such as adherence and cost. 8
In this case, tiotropium had already been added to Mr. T's medications and his symptoms continued. Although addition of a leukotriene modifier was an option for him, he did not wish to add another medication to his care regimen. Omalizumab was not added partly for this reason, and also because of his low IgE level. As his bronchoscopy was negative, it was determined that a course of antibiotics would not be an effective treatment option for this patient. While vitamin D insufficiency has been associated with adverse outcomes in asthma, T's vitamin D level was tested and found to be sufficient.
We discussed the possibility of Mr. T's enrollment in a clinical trial. However, because this did not guarantee placement within a treatment arm and thus there was the possibility of receiving placebo, he opted to undergo bronchial thermoplasty.
Bronchial thermoplasty Bronchial thermoplasty is effective for many patients with severe persistent asthma, such as Mr. T. This procedure may provide additional benefits to, but does not replace, standard asthma medications. During the procedure, thermal energy is delivered to the airways via a bronchoscope to reduce excess airway smooth muscle and limit its ability to constrict the airways. It is an outpatient procedure performed over three sessions by a trained physician. 9
The effects of bronchial thermoplasty have been studied in several trials. The first large-scale multicenter randomized controlled study was the Asthma Intervention Research (AIR) Trial , which enrolled patients with moderate to severe asthma. 10 In this trial, patients who underwent the procedure had a significant improvement in asthma symptoms as measured by symptom-free days and scores on asthma control and quality of life questionnaires, as well as reductions in mild exacerbations and increases in morning peak expiratory flow. 10 Shortly after the AIR trial, the Research in Severe Asthma (RISA) trial was conducted to evaluate bronchial thermoplasty in patients with more severe, symptomatic asthma. 11 In this population, bronchial thermoplasty resulted in a transient worsening of asthma symptoms, with a higher rate of hospitalizations during the treatment period. 11 Hospitalization rate equalized between the treatment and control groups in the posttreatment period, however, and the treatment group showed significant improvements in rescue medication use, prebronchodilator forced expiratory volume in the first second (FEV1) % predicted, and asthma control questionnaire scores. 11
The AIR-2 trial followed, which was a multicenter, randomized, double-blind, sham-controlled study of 288 patients with severe asthma. 6 Similar to the RISA trial, patients in the treatment arm of this trial experienced an increase in adverse respiratory effects during the treatment period, the most common being airway irritation (including wheezing, chest discomfort, cough, and chest pain) and upper respiratory tract infections. 6
The majority of adverse effects occurred within 1 day of the procedure and resolved within 7 days. 6 In this study, bronchial thermoplasty was found to significantly improve quality of life, as well as reduce the rate of severe exacerbations by 32%. 6 Patients who underwent the procedure also reported fewer adverse respiratory effects, fewer days lost from work, school, or other activities due to asthma, and an 84% risk reduction in emergency department visits. 6
Long-term (5-year) follow-up studies have been conducted for patients in both the AIR and the AIR-2 trials. In patients who underwent bronchial thermoplasty in either study, the rate of adverse respiratory effects remained stable in years 2 to 5 following the procedure, with no increase in hospitalizations or emergency department visits. 7,12 Additionally, FEV1 remained stable throughout the 5-year follow-up period. 7,12 This finding was maintained in patients enrolled in the AIR-2 trial despite decreased use of daily ICS. 7
Bronchial thermoplasty is an important addition to the asthma treatment armamentarium. 7 This treatment is currently approved for individuals with severe persistent asthma who remain uncontrolled despite the use of an ICS and LABA. Several clinical trials with long-term follow-up have now demonstrated its safety and ability to improve quality of life in patients with severe asthma, such as Mr. T.
Severe asthma can be a challenge to manage. Patients with this condition require an extensive workup, but there are several treatments currently available to help manage these patients, and new treatments are continuing to emerge. Managing severe asthma thus requires knowledge of the options available as well as consideration of a patient's personal situation-both in terms of disease phenotype and individual preference. In this case, the patient expressed a strong desire to not add any additional medications to his asthma regimen, which explained the rationale for choosing to treat with bronchial thermoplasty. Personalized treatment necessitates exploring which of the available or emerging options is best for each individual patient.
Published: April 16, 2018
- 1. National Asthma Education and Prevention Program: Asthma Care Quick Reference.
- 2. Olin JT, Wechsler ME. Asthma: pathogenesis and novel drugs for treatment. BMJ . 2014;349:g5517.
- 3. Boehringer Ingelheim. Asthma: U.S. FDA approves new indication for SPIRIVA Respimat [press release]. September 16, 2015.
- 4. Peters SP, Kunselman SJ, Icitovic N, et al. Tiotropium bromide step-up therapy for adults with uncontrolled asthma. N Engl J Med . 2010;363:1715-1726.
- 5. Kerstjens HA, Engel M, Dahl R. Tiotropium in asthma poorly controlled with standard combination therapy. N Engl J Med . 2012;367:1198-1207.
- 6. Castro M, Rubin AS, Laviolette M, et al. Effectiveness and safety of bronchial thermoplasty in the treatment of severe asthma: a multicenter, randomized, double-blind, sham-controlled clinical trial. Am J Respir Crit Care Med . 2010;181:116-124.
- 7. Wechsler ME, Laviolette M, Rubin AS, et al. Bronchial thermoplasty: long-term safety and effectiveness in patients with severe persistent asthma. J Allergy Clin Immunol . 2013;132:1295-1302.
- 8. Global Initiative for Asthma: Pocket Guide for Asthma Management and Prevention (for Adults and Children Older than 5 Years).
- 10. Cox G, Thomson NC, Rubin AS, et al. Asthma control during the year after bronchial thermoplasty. N Engl J Med . 2007;356:1327-1337.
- 11. Pavord ID, Cox G, Thomson NC, et al. Safety and efficacy of bronchial thermoplasty in symptomatic, severe asthma. Am J Respir Crit Care Med . 2007;176:1185-1191.
- 12. Thomson NC, Rubin AS, Niven RM, et al. Long-term (5 year) safety of bronchial thermoplasty: Asthma Intervention Research (AIR) trial. BMC Pulm Med . 2011;11:8.

Treatable traits and future exacerbation risk in severe asthma, baker’s asthma, the long-term trajectory of mild asthma, age, gender, & systemic corticosteroid comorbidities, ask the expert: william busse, md, challenges the current definition of the atopic march, considering the curveballs in asthma treatment, do mucus plugs play a bigger role in chronic severe asthma than previously thought, an emerging subtype of copd is associated with early respiratory disease.

A Case Study of a Patient with Bronchial Asthma
Jul 13, 2014
2.66k likes | 20.38k Views
A Case Study of a Patient with Bronchial Asthma. Prepared by: Airen L. Jamago LTI - Male Department. I. DEMOGRAPHIC DATA. Name: Patient X Age: 47 years old Sex: Male Nationality: Saudi Date of Admission: Dec. 7, 2011. II. PHYSICAL ASSESSMENT.
Share Presentation
- chronic inflammation
- metered dose inhaler
- jamago lti male department
- interventions
- administer oxygen

Presentation Transcript
A Case Study of a Patientwith Bronchial Asthma Prepared by: Airen L. Jamago LTI- Male Department
I. DEMOGRAPHIC DATA Name: Patient X Age: 47 years old Sex: Male Nationality: Saudi Date of Admission: Dec. 7, 2011
II. PHYSICAL ASSESSMENT • SKIN - warm, slightly dry, hair evenly distributed • HEAD - symmetric skull, no flaking of scalp, no lesions and tenderness • EYES - no redness and discharges, sclera white and clear, pupils reactive to light and accommodation • NOSE AND SINUSES - nasal septum straight, not perforated, no discharged, NGT present
MOUTH - dry lips, no gum bleeding, tongue and uvula in midline position, oral cavity slightly pale, no ulcers, no swelling and palpable masses NECK - no palpable lymph nodes, trachea on midline position, Tracheostomy tube present BREAST - nipples at the same level, no palpable masses and discharge
THORAX AND LUNGS - thorax is symmetric, chest expansion is decrease due to muscle weakness, bony prominences are marked, there is loss of subcutaneous tissue, no tenderness, wheezes audible upon auscultation • UPPER EXTREMITIES - decorticate position, arms are unable to abduct and adduct • NAILS - convex in curvature, rough, with slightly delayed capillary refill
ABDOMEN - not distended, ( + ) bowel sounds LOWER EXTREMITIES - unable to flex, abduct and adduct GENITALIA - skin of the glans penis is smooth, no ulceration, urethral meatus located ventrally on the end of the penis, no discharge and palpable masses
III. PATIENT HISTORY
A. Past Medical History
B. Present Medical History
IV. TOPIC PRESENTATION
V. ANATOMY AND PHYSIOLOGY
V. ETIOLOGY inflammation Asthma symptoms
VI. ETIOLOGY
VII. Signs and Symptoms Common Symptoms: Coughing, especially at night Wheezing Shortness of breath Chest tightness, pain, or pressure
Signs of Pending Asthma Attack • Frequent cough, especially at night • Losing your breath easily or shortness of breath • Feeling very tired or weak when exercising • Wheezing or coughing after exercise • Feeling tired, easily upset, grouchy, or moody • Decreases or changes in lung function as measured on a peak flow meter • Signs of a cold or allergies (sneezing, runny nose, cough, nasal congestion, sore throat, and headache) • Trouble sleeping
Symptoms of Asthma Attack • Severe wheezing when breathing both in and out • Coughing that won't stop • Very rapid breathing • Chest pain or pressure • Tightened neck and chest muscles, called retractions • Difficulty talking • Feelings of anxiety or panic • Pale, sweaty face • Blue lips or fingernails
VIII. INTERVENTIONS The four parts of continually managing asthma are: Identify and minimize contact with asthma triggers. Understand and take medications as prescribed. Monitor asthma to recognize signs when it is getting worse. Know what to do when asthma gets worse.
Nursing Interventions Maintain respiratory function and relieve broncho-constriction while allowing mucus plug expulsion. Control exercise-induced asthma by having the patient sit down, rest, and use diaphragmatic and pulse-lip breathing until shortness of breath subsides. Supervise the patient’s drug regimen.
Demonstrate the proper use of metered dose inhaler properly. Reassure the patient during an asthma attack and stay with him. Place the patient in semi-fowler’s position and encourage diaphragmatic breathing
Assist him to relax as much as possible. • Administer oxygen via nasal cannula to ease breathing and to increase arterial oxygen saturation during an acute asthma attack. • Adjust oxygen according to the patient’s vital functions and ABG measurements. • Administer drugs and I.V. fluids as ordered.
Combat dehydration with I.V. fluids until the patient can tolerate oral fluids, which will help loosen secretions. Encourage the patient to express his fears and concerns about his illness. Encourage the patient to identify and comply with care measures and activities that promote relaxation.
IX. TREATMENT Good asthma control will: Prevent chronic and troublesome symptoms, such as coughingand shortness of breath Reduce your need for quick-relief medicines Help you maintain good lung function Let you maintain your normal activity level and sleep through the night Prevent asthma attacks that could result in an emergency room visit or hospital stay
Long-Term Control Medicines Inhaled corticosteroids Cromolyn Omalizumab Inhaled long-acting beta2 agonists Leukotriene modifiers Theophylline
Quick-Relief Medicines Proventil Ventolin Xopenex
X. COMPLICATIONS • Decreased ability to exercise and take part in other activities • Lack of sleep due to night time symptoms • Permanent changes in the function of the lungs • Persistent cough • Trouble breathing that requires breathing assistance (ventilator) • DEATH
XI. PRIORITIZATION OF NURSING PROBLEMS Ineffective airway clearance related to mucus accumulation. Impaired Gas Exchange related to altered oxygen supply, obstruction of airways by secretions, bronchospasm. Ineffective breathing pattern related to decreased lung expansion. Hyperthermia related to underlying infection in the lungs. Impaired nutrition less than body requirements related to inadequate intake.
NURSING CARE PLAN NO. 1
NURSING CARE PLAN 2
NURSING CARE PLAN 3
XIV. CONCLUSION • Asthma is a chronic inflammation of the bronchial tubes (airways) that causes swelling and narrowing (constriction) of the airways. • The bronchial narrowing is usually either totally or at least partially reversible with treatments. • The most common chronic illness in children, affecting one in every 15. • It involves only the bronchial tubes and usually does not affect the air sacs or the lung tissue. • The narrowing that occurs in asthma is caused by three major factors: inflammation, bronchospasm, and hyperreactivity.
Allergy can play a role in some, but not all, asthma patients. Many factors can precipitate asthma attacks and they are classified as either allergens or irritants. • Symptoms include shortness of breath, wheezing, cough, and chest tightness.It is usually diagnosed based on the presence of wheezing and confirmed with breathing tests. • Chest X-rays are usually normal in asthma patients. • Avoiding precipitating factors is important in the management of asthma. • Medications can be used to reverse or prevent bronchospasm in patients with asthma.
XV. BIBLIOGRAPHY nursingfile.com/.../nursing-interventions-for-asthma.htm www.nhlbi.nih.gov/health/prof/lung/asthma/nurs_gde.pdf www.webmd.com/asthma/guide/asthma-symptoms www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001196 www.medicinenet.com/asthma/article.htm Murray, J. and J. Nadel. Textbook of Respiratory Medicine. Third edition. Philadelphia: W.B. Saunders Company, 2000.Peters, et al. "Tiotropium Bromide Step-Up Therapy for Adults With Uncontrolled Asthma." NEJM363 (2010): 1715-1726. Medically reviewed by: Ellen Reich, MD, Board Certified in Allergy and Immunology, Board Certified in Pediatrics
- More by User
Bronchial asthma
. Asthma:human killer!. Background of asthma. Prevalence :in the world: 1.6 hundred million in China: 1~3 % in Shenyang: 1.24 %(1999) GINA: Global Initiative for Asthma(1994) WHO/HLBI Bronchial asthmatic diagnosis guideline (1997) Chinese Medical Academ
1.59k views • 41 slides
A CASE OF BRONCHIAL ASTHMA
A CASE OF BRONCHIAL ASTHMA. By Dr. Jawahar Shah M.D.(Hom). NOTE: To protect the patient’s identity, we have used a model’s picture or photographs for the purpose of presentation. Case 4 A CASE OF ASTHMA. Mrs. H.M
926 views • 17 slides
Case of Bronchial asthma with acne
Case of Bronchial asthma with acne. Hawk and other birds of prey. Non-verbal language. Four Hand Gestures constantly Of strangulation for freedom and opp of strangulation, tied up Moving up (Circular movement of hand)
946 views • 69 slides
A case study of a patient with diabetes mellitus
A case study of a patient with diabetes mellitus. Prepared by: Josmy Joseph LTIM-Department. I. Demographic data. Name: Patient X Age: 56 yrs.old Nationality: Saudi Date of Admission: July 9,2012. ii. Physical ASSESSMENT.
4.48k views • 30 slides
BRONCHIAL ASTHMA
BRONCHIAL ASTHMA. Introduction to Primary Care: a course of the Center of Post Graduate Studies i n FM. PO Box 27121 – Riyadh 11417 Tel: 4912326 – Fax: 4970847. 1. Objectives. To describe how to make the diagnosis of asthma utilizing the Saudi Asthma Guidelines.
1.28k views • 47 slides
Bronchial Asthma
Bronchial Asthma. Mohammed Bahkali Mohammed Al- Obayli. 2012. WHAT IS ASTHMA ?.
2.93k views • 82 slides

Bronchial Asthma. Rucci Copian Clar Coronado Kayson Credo. Objectives . Identify pertinent findings from the history and physical examination that would contribute to the diagnosis of asthma Provide an approach in diagnosing patients with ashtma Learn how to manage patients with ashtma.
1.01k views • 59 slides
Bronchial asthma. L de Man Dept of Physiotherapy UFS 2012. Definition. Asthma is a disease characterised by a wide variety of resistance to airflow
873 views • 19 slides
BRONCHIAL ASTHMA. Definition of Asthma. Clinically - Widespread airway narrowing which changes in severity over short periods of time, either spontaneously or in response to treatment Physiologically - Bronchial Hyperresponsiveness Pathologically - Airway inflammation. ASTHMA PATHOLOGY.
2.08k views • 112 slides
bronchial asthma
bronchial asthma. Introduction.
1.46k views • 48 slides
BRONCHIAL ASTHMA. prof . Mohammad Ali Khan MB, DCH , MRCP(UK) Head of paediatric department SIMS/Services Hospital, Lahore. BRONCHIAL ASTHMA. Definition Reversible Bronchospasm Hyper-reactivity Variability Allergic Disorder Chronic Inflammatory Disorder
1.75k views • 25 slides
Bronchial Asthma. Alena Vlachová. Definition. Chronic inflammatory disease with inflammation due to complex interaction between inflammatory cells,mediastors and airways cells
634 views • 31 slides
Bronchial asthma. By: Nur Izzatul Ashikin Harun Moderator: Dr Nik Azman Nik Adib. Outline. Definition Diagnosis Management and prevention 1 Develop patient-doctor relationship 2 Identify and reduce exposure to risk factor 3 Assess , treat and monitor asthma
1.2k views • 51 slides
A CASE OF BRONCHIAL ASTHMA. By Dr. Jawahar Shah M.D.(Hom). NOTE: To protect the patient’s identity, we have used a model’s picture or photographs for the purpose of presentation. Mr. B.D.N., aged 67, a well known social worker with a strong inclination to help people.
737 views • 36 slides
BRONCHIAL ASTHMA. Hülya ERCAN SARIÇOBAN,MD. Bronchial Asthma-Definition. Asthma is a chronic inflammatory condition of the lung airways resulting in episodic airflow obstruction. Etiology.
1.03k views • 44 slides
Bronchial Asthma. Nathir M Obeidat. Bronchial Asthma Definition. Bronchial asthma is a clinical syndrome characterised by recurrent episodes of airway obstruction , which resolve spontaneously or as a result of treatment.
790 views • 54 slides

Bronchial Asthma. Chronic inflammatory disorder of the airway, which characterized by hyper-responsiveness, mucosal edema, mucus production Inflammation obstruction from mucosal edema reducing the airway diameter & contraction of bronchial smooth muscle
459 views • 8 slides
A CASE OF BRONCHIAL ASTHMA. By Dr. Jawahar Shah M.D.(Hom). NOTE: To protect the patient’s identity, we have used a model’s picture or photographs for the purpose of presentation. Case of Breathlessness. A young female patient 2 yrs old reports with breathlessness.
229 views • 12 slides
A CASE OF BRONCHIAL ASTHMA. By Dr. Jawahar Shah M.D.(Hom). NOTE: To protect the patient’s identity, we have used a model’s picture or photographs for the purpose of presentation. Case 7 Case of bronchial asthma.
234 views • 13 slides
A CASE OF BRONCHIAL ASTHMA. By Dr. Jawahar Shah M.D.(Hom). NOTE: To protect the patient’s identity, we have used a model’s picture or photographs for the purpose of presentation. A CASE BRONCHIAL ASTHMA. 12 Years old boy was brought on 27th July 1986, suffering from Bronchial Asthma.
311 views • 17 slides
A CASE OF BRONCHIAL ASTHMA. By Dr. Jawahar Shah M.D.(Hom). NOTE: To protect the patient’s identity, we have used a model’s picture or photographs for the purpose of presentation. CASE OF ASTHMA.
604 views • 26 slides
A CASE OF BRONCHIAL ASTHMA. By Dr. Jawahar Shah M.D.(Hom). NOTE: To protect the patient’s identity, we have used a model’s picture or photographs for the purpose of presentation. A Muslim lady – 40 years having 5 children was brought to me with very bad asthma since last 12 years.
687 views • 15 slides

- My presentations
Auth with social network:
Download presentation
We think you have liked this presentation. If you wish to download it, please recommend it to your friends in any social system. Share buttons are a little bit lower. Thank you!
Presentation is loading. Please wait.
To view this video please enable JavaScript, and consider upgrading to a web browser that supports HTML5 video
A Case Study of a Patient with Bronchial Asthma
Published by Marion Gardner Modified over 9 years ago
Similar presentations
Presentation on theme: "A Case Study of a Patient with Bronchial Asthma"— Presentation transcript:
RESPIRATORY EMERGENCIES
RESPIRATORY EMERGENCIES. Nose/mouth – pharynx/oropharynx – Larynx – Trachea – Bronchi – Bronchioles – Lungs- Alveoli.
What You Need to Know About Asthma Going for the 3 Increases: Increase in Health, Increase in Happiness & Increase in Energy Strategies for Success in.

Melissa Lewis, RN Allied Health Sciences I 4th Block
Respiratory Tract Conditions
Respiratory Teresa V. Hurley, MSN, RN. Anatomy of the Lungs Main organs of respiration Main organs of respiration Extend from the base of diaphragm to.

Chronic obstructive pulmonary disease (COPD) Dr. Walaa Nasr Lecturer of Adult Nursing Second year.
4.5 Lung disease – fibrosis, asthma and emphysema.
The RESPIRATORY System Unit 3 Transportation Systems.
Dr. Maha Al-Sedik. Why do we study respiratory emergency? Respiratory Calls are some of the most Common calls you will see. Respiratory care is.
Disorders of the respiratory system. Respiratory structures such as the airways, alveoli and pleural membranes may all be affected by various disease.
Management of Patients With Chronic Pulmonary Disease.
Respiratory system. The primary function of the respiratory system is the supply of oxygen to the blood and the removal of carbon dioxide.
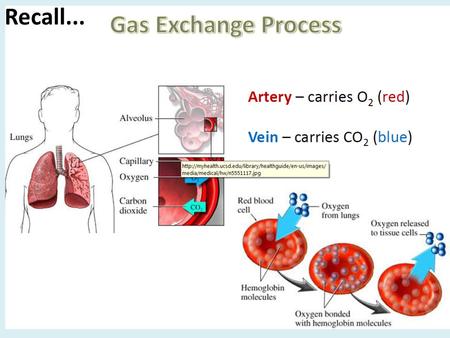
Recall.... Why is diffusion important? - Gas exchange b/w a living cell & the environment always takes place by diffusion across a moist surface. - The.
6 th Grade. Asthma is a chronic lung disease that can be life threatening. The exact cause is unknown. However, once an individual has asthma, his or.
Lisa Nave Nursing Platt College. Asthma is a chronic inflammatory disease of the lungs characterized by narrowing of the airways in the lungs causing.
Asthma is a chronic inflammatory disease of the airways, characterized by coughing, wheezing, chest tightness, and difficult breathing.
Diseases and Abnormal Conditions of The Respiratory System
By: Carter Paquette, Ethan Eldridge, Brendan Marusiak, Nik Brading.
About project
© 2024 SlidePlayer.com Inc. All rights reserved.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Perspective
- Open access
- Published: 16 October 2014
A woman with asthma: a whole systems approach to supporting self-management
- Hilary Pinnock 1 ,
- Elisabeth Ehrlich 1 ,
- Gaylor Hoskins 2 &
- Ron Tomlins 3
npj Primary Care Respiratory Medicine volume 24 , Article number: 14063 ( 2014 ) Cite this article
16k Accesses
2 Citations
6 Altmetric
Metrics details
- Health care
A 35-year-old lady attends for review of her asthma following an acute exacerbation. There is an extensive evidence base for supported self-management for people living with asthma, and international and national guidelines emphasise the importance of providing a written asthma action plan. Effective implementation of this recommendation for the lady in this case study is considered from the perspective of a patient, healthcare professional, and the organisation. The patient emphasises the importance of developing a partnership based on honesty and trust, the need for adherence to monitoring and regular treatment, and involvement of family support. The professional considers the provision of asthma self-management in the context of a structured review, with a focus on a self-management discussion which elicits the patient’s goals and preferences. The organisation has a crucial role in promoting, enabling and providing resources to support professionals to provide self-management. The patient’s asthma control was assessed and management optimised in two structured reviews. Her goal was to avoid disruption to her work and her personalised action plan focused on achieving that goal.
Similar content being viewed by others

Psilocybin microdosers demonstrate greater observed improvements in mood and mental health at one month relative to non-microdosing controls

An overview of clinical decision support systems: benefits, risks, and strategies for success

Key recommendations for primary care from the 2022 Global Initiative for Asthma (GINA) update
A 35-year-old sales representative attends the practice for an asthma review. Her medical record notes that she has had asthma since childhood, and although for many months of the year her asthma is well controlled (when she often reduces or stops her inhaled steroids), she experiences one or two exacerbations a year requiring oral steroids. These are usually triggered by a viral upper respiratory infection, though last summer when the pollen count was particularly high she became tight chested and wheezy for a couple of weeks.
Her regular prescription is for fluticasone 100 mcg twice a day, and salbutamol as required. She has a young family and a busy lifestyle so does not often manage to find time to attend the asthma clinic. A few weeks previously, an asthma attack had interfered with some important work-related travel, and she has attended the clinic on this occasion to ask about how this can be managed better in the future. There is no record of her having been given an asthma action plan.
What do we know about asthma self-management? The academic perspective
Supported self-management reduces asthma morbidity.
The lady in this case study is struggling to maintain control of her asthma within the context of her busy professional and domestic life. The recent unfortunate experience which triggered this consultation offers a rare opportunity to engage with her and discuss how she can manage her asthma better. It behoves the clinician whom she is seeing (regardless of whether this is in a dedicated asthma clinic or an appointment in a routine general practice surgery) to grasp the opportunity and discuss self-management and provide her with a (written) personalised asthma action plan (PAAP).
The healthcare professional advising the lady is likely to be aware that international and national guidelines emphasise the importance of supporting self-management. 1 – 4 There is an extensive evidence base for asthma self-management: a recent synthesis identified 22 systematic reviews summarising data from 260 randomised controlled trials encompassing a broad range of demographic, clinical and healthcare contexts, which concluded that asthma self-management reduces emergency use of healthcare resources, including emergency department visits, hospital admissions and unscheduled consultations and improves markers of asthma control, including reduced symptoms and days off work, and improves quality of life. 1 , 2 , 5 – 12 Health economic analysis suggests that it is not only clinically effective, but also a cost-effective intervention. 13
Personalised asthma action plans
Key features of effective self-management approaches are:
Self-management education should be reinforced by provision of a (written) PAAP which reminds patients of their regular treatment, how to monitor and recognise that control is deteriorating and the action they should take. 14 – 16 As an adult, our patient can choose whether she wishes to monitor her control with symptoms or by recording peak flows (or a combination of both). 6 , 8 , 9 , 14 Symptom-based monitoring is generally better in children. 15 , 16
Plans should have between two and three action points including emergency doses of reliever medication; increasing low dose (or recommencing) inhaled steroids; or starting a course of oral steroids according to severity of the exacerbation. 14
Personalisation of the action plan is crucial. Focussing specifically on what actions she could take to prevent a repetition of the recent attack is likely to engage her interest. Not all patients will wish to start oral steroids without advice from a healthcare professional, though with her busy lifestyle and travel our patient is likely to be keen to have an emergency supply of prednisolone. Mobile technology has the potential to support self-management, 17 , 18 though a recent systematic review concluded that none of the currently available smart phone ‘apps’ were fit for purpose. 19
Identification and avoidance of her triggers is important. As pollen seems to be a trigger, management of allergic rhinitis needs to be discussed (and included in her action plan): she may benefit from regular use of a nasal steroid spray during the season. 20
Self-management as recommended by guidelines, 1 , 2 focuses narrowly on adherence to medication/monitoring and the early recognition/remediation of exacerbations, summarised in (written) PAAPs. Patients, however, may want to discuss how to reduce the impact of asthma on their life more generally, 21 including non-pharmacological approaches.
Supported self-management
The impact is greater if self-management education is delivered within a comprehensive programme of accessible, proactive asthma care, 22 and needs to be supported by ongoing regular review. 6 With her busy lifestyle, our patient may be reluctant to attend follow-up appointments, and once her asthma is controlled it may be possible to make convenient arrangements for professional review perhaps by telephone, 23 , 24 or e-mail. Flexible access to professional advice (e.g., utilising diverse modes of consultation) is an important component of supporting self-management. 25
The challenge of implementation
Implementation of self-management, however, remains poor in routine clinical practice. A recent Asthma UK web-survey estimated that only 24% of people with asthma in the UK currently have a PAAP, 26 with similar figures from Sweden 27 and Australia. 28 The general practitioner may feel that they do not have time to discuss self-management in a routine surgery appointment, or may not have a supply of paper-based PAAPs readily available. 29 However, as our patient rarely finds time to attend the practice, inviting her to make an appointment for a future clinic is likely to be unsuccessful and the opportunity to provide the help she needs will be missed.
The solution will need a whole systems approach
A systematic meta-review of implementing supported self-management in long-term conditions (including asthma) concluded that effective implementation was multifaceted and multidisciplinary; engaging patients, training and motivating professionals within the context of an organisation which actively supported self-management. 5 This whole systems approach considers that although patient education, professional training and organisational support are all essential components of successful support, they are rarely effective in isolation. 30 A systematic review of interventions that promote provision/use of PAAPs highlighted the importance of organisational systems (e.g., sending blank PAAPs with recall reminders). 31 A patient offers her perspective ( Box 1 ), a healthcare professional considers the clinical challenge, and the challenges are discussed from an organisational perspective.
Box 1: What self-management help should this lady expect from her general practitioner or asthma nurse? The patient’s perspective
The first priority is that the patient is reassured that her condition can be managed successfully both in the short and the long term. A good working relationship with the health professional is essential to achieve this outcome. Developing trust between patient and healthcare professional is more likely to lead to the patient following the PAAP on a long-term basis.
A review of all medication and possible alternative treatments should be discussed. The patient needs to understand why any changes are being made and when she can expect to see improvements in her condition. Be honest, as sometimes it will be necessary to adjust dosages before benefits are experienced. Be positive. ‘There are a number of things we can do to try to reduce the impact of asthma on your daily life’. ‘Preventer treatment can protect against the effect of pollen in the hay fever season’. If possible, the same healthcare professional should see the patient at all follow-up appointments as this builds trust and a feeling of working together to achieve the aim of better self-management.
Is the healthcare professional sure that the patient knows how to take her medication and that it is taken at the same time each day? The patient needs to understand the benefit of such a routine. Medication taken regularly at the same time each day is part of any self-management regime. If the patient is unused to taking medication at the same time each day then keeping a record on paper or with an electronic device could help. Possibly the patient could be encouraged to set up a system of reminders by text or smartphone.
Some people find having a peak flow meter useful. Knowing one's usual reading means that any fall can act as an early warning to put the PAAP into action. Patients need to be proactive here and take responsibility.
Ongoing support is essential for this patient to ensure that she takes her medication appropriately. Someone needs to be available to answer questions and provide encouragement. This could be a doctor or a nurse or a pharmacist. Again, this is an example of the partnership needed to achieve good asthma control.
It would also be useful at a future appointment to discuss the patient’s lifestyle and work with her to reduce her stress. Feeling better would allow her to take simple steps such as taking exercise. It would also be helpful if all members of her family understood how to help her. Even young children can do this.
From personal experience some people know how beneficial it is to feel they are in a partnership with their local practice and pharmacy. Being proactive produces dividends in asthma control.
What are the clinical challenges for the healthcare professional in providing self-management support?
Due to the variable nature of asthma, a long-standing history may mean that the frequency and severity of symptoms, as well as what triggers them, may have changed over time. 32 Exacerbations requiring oral steroids, interrupting periods of ‘stability’, indicate the need for re-assessment of the patient’s clinical as well as educational needs. The patient’s perception of stability may be at odds with the clinical definition 1 , 33 —a check on the number of short-acting bronchodilator inhalers the patient has used over a specific period of time is a good indication of control. 34 Assessment of asthma control should be carried out using objective tools such as the Asthma Control Test or the Royal College of Physicians three questions. 35 , 36 However, it is important to remember that these assessment tools are not an end in themselves but should be a springboard for further discussion on the nature and pattern of symptoms. Balancing work with family can often make it difficult to find the time to attend a review of asthma particularly when the patient feels well. The practice should consider utilising other means of communication to maintain contact with patients, encouraging them to come in when a problem is highlighted. 37 , 38 Asthma guidelines advocate a structured approach to ensure the patient is reviewed regularly and recommend a detailed assessment to enable development of an appropriate patient-centred (self)management strategy. 1 – 4
Although self-management plans have been shown to be successful for reducing the impact of asthma, 21 , 39 the complexity of managing such a fluctuating disease on a day-to-day basis is challenging. During an asthma review, there is an opportunity to work with the patient to try to identify what triggers their symptoms and any actions that may help improve or maintain control. 38 An integral part of personalised self-management education is the written PAAP, which gives the patient the knowledge to respond to the changes in symptoms and ensures they maintain control of their asthma within predetermined parameters. 9 , 40 The PAAP should include details on how to monitor asthma, recognise symptoms, how to alter medication and what to do if the symptoms do not improve. The plan should include details on the treatment to be taken when asthma is well controlled, and how to adjust it when the symptoms are mild, moderate or severe. These action plans need to be developed between the doctor, nurse or asthma educator and the patient during the review and should be frequently reviewed and updated in partnership (see Box 1). Patient preference as well as clinical features such as whether she under- or over-perceives her symptoms should be taken into account when deciding whether the action plan is peak flow or symptom-driven. Our patient has a lot to gain from having an action plan. She has poorly controlled asthma and her lifestyle means that she will probably see different doctors (depending who is available) when she needs help. Being empowered to self-manage could make a big difference to her asthma control and the impact it has on her life.
The practice should have protocols in place, underpinned by specific training to support asthma self-management. As well as ensuring that healthcare professionals have appropriate skills, this should include training for reception staff so that they know what action to take if a patient telephones to say they are having an asthma attack.
However, focusing solely on symptom management strategies (actions) to follow in the presence of deteriorating symptoms fails to incorporate the patients’ wider views of asthma, its management within the context of her/his life, and their personal asthma management strategies. 41 This may result in a failure to use plans to maximise their health potential. 21 , 42 A self-management strategy leading to improved outcomes requires a high level of patient self-efficacy, 43 a meaningful partnership between the patient and the supporting health professional, 42 , 44 and a focused self-management discussion. 14
Central to both the effectiveness and personalisation of action plans, 43 , 45 in particular the likelihood that the plan will lead to changes in patients’ day-to-day self-management behaviours, 45 is the identification of goals. Goals are more likely to be achieved when they are specific, important to patients, collaboratively set and there is a belief that these can be achieved. Success depends on motivation 44 , 46 to engage in a specific behaviour to achieve a valued outcome (goal) and the ability to translate the behavioural intention into action. 47 Action and coping planning increases the likelihood that patient behaviour will actually change. 44 , 46 , 47 Our patient has a goal: she wants to avoid having her work disrupted by her asthma. Her personalised action plan needs to explicitly focus on achieving that goal.
As providers of self-management support, health professionals must work with patients to identify goals (valued outcomes) that are important to patients, that may be achievable and with which they can engage. The identification of specific, personalised goals and associated feasible behaviours is a prerequisite for the creation of asthma self-management plans. Divergent perceptions of asthma and how to manage it, and a mismatch between what patients want/need from these plans and what is provided by professionals are barriers to success. 41 , 42
What are the challenges for the healthcare organisation in providing self-management support?
A number of studies have demonstrated the challenges for primary care physicians in providing ongoing support for people with asthma. 31 , 48 , 49 In some countries, nurses and other allied health professionals have been trained as asthma educators and monitor people with stable asthma. These resources are not always available. In addition, some primary care services are delivered in constrained systems where only a few minutes are available to the practitioner in a consultation, or where only a limited range of asthma medicines are available or affordable. 50
There is recognition that the delivery of quality care depends on the competence of the doctor (and supporting health professionals), the relationship between the care providers and care recipients, and the quality of the environment in which care is delivered. 51 This includes societal expectations, health literacy and financial drivers.
In 2001, the Australian Government adopted a programme developed by the General Practitioner Asthma Group of the National Asthma Council Australia that provided a structured approach to the implementation of asthma management guidelines in a primary care setting. 52 Patients with moderate-to-severe asthma were eligible to participate. The 3+ visit plan required confirmation of asthma diagnosis, spirometry if appropriate, assessment of trigger factors, consideration of medication and patient self-management education including provision of a written PAAP. These elements, including regular medical review, were delivered over three visits. Evaluation demonstrated that the programme was beneficial but that it was difficult to complete the third visit in the programme. 53 – 55 Accordingly, the programme, renamed the Asthma Cycle of Care, was modified to incorporate two visits. 56 Financial incentives are provided to practices for each patient who receives this service each year.
Concurrently, other programmes were implemented which support practice-based care. Since 2002, the National Asthma Council has provided best-practice asthma and respiratory management education to health professionals, 57 and this programme will be continuing to 2017. The general practitioner and allied health professional trainers travel the country to provide asthma and COPD updates to groups of doctors, nurses and community pharmacists. A number of online modules are also provided. The PACE (Physician Asthma Care Education) programme developed by Noreen Clark has also been adapted to the Australian healthcare system. 58 In addition, a pharmacy-based intervention has been trialled and implemented. 59
To support these programmes, the National Asthma Council ( www.nationalasthma.org.au ) has developed resources for use in practices. A strong emphasis has been on the availability of a range of PAAPs (including plans for using adjustable maintenance dosing with ICS/LABA combination inhalers), plans for indigenous Australians, paediatric plans and plans translated into nine languages. PAAPs embedded in practice computer systems are readily available in consultations, and there are easily accessible online paediatric PAAPs ( http://digitalmedia.sahealth.sa.gov.au/public/asthma/ ). A software package, developed in the UK, can be downloaded and used to generate a pictorial PAAP within the consultation. 60
One of the strongest drivers towards the provision of written asthma action plans in Australia has been the Asthma Friendly Schools programme. 61 , 62 Established with Australian Government funding and the co-operation of Education Departments of each state, the Asthma Friendly Schools programme engages schools to address and satisfy a set of criteria that establishes an asthma-friendly environment. As part of accreditation, the school requires that each child with asthma should have a written PAAP prepared by their doctor to assist (trained) staff in managing a child with asthma at school.
The case study continues...
The initial presentation some weeks ago was during an exacerbation of asthma, which may not be the best time to educate a patient. It is, however, a splendid time to build on their motivation to feel better. She agreed to return after her asthma had settled to look more closely at her asthma control, and an appointment was made for a routine review.
At this follow-up consultation, the patient’s diagnosis was reviewed and confirmed and her trigger factors discussed. For this lady, respiratory tract infections are the usual trigger but allergic factors during times of high pollen count may also be relevant. Assessment of her nasal airway suggested that she would benefit from better control of allergic rhinitis. Other factors were discussed, as many patients are unaware that changes in air temperature, exercise and pets can also trigger asthma exacerbations. In addition, use of the Asthma Control Test was useful as an objective assessment of control as well as helping her realise what her life could be like! Many people with long-term asthma live their life within the constraints of their illness, accepting that is all that they can do.
After assessing the level of asthma control, a discussion about management options—trigger avoidance, exercise and medicines—led to the development of a written PAAP. Asthma can affect the whole family, and ways were explored that could help her family understand why it is important that she finds time in the busy domestic schedules to take her regular medication. Family and friends can also help by understanding what triggers her asthma so that they can avoid exposing her to perfumes, pollens or pets that risk triggering her symptoms. Information from the national patient organisation was provided to reinforce the messages.
The patient agreed to return in a couple of weeks, and a recall reminder was set up. At the second consultation, the level of control since the last visit will be explored including repeat spirometry, if appropriate. Further education about the pathophysiology of asthma and how to recognise early warning signs of loss of control can be given. Device use will be reassessed and the PAAP reviewed. Our patient’s goal is to avoid disruption to her work and her PAAP will focus on achieving that goal. Finally, agreement will be reached with the patient about future routine reviews, which, now that she has a written PAAP, could be scheduled by telephone if all is well, or face-to-face if a change in her clinical condition necessitates a more comprehensive review.
Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention, 2012. Available from: http://www.ginasthma.org (accessed July 2013).
British Thoracic Society/Scottish Intercollegiate Guideline Network British Guideline on the Management of Asthma. Thorax 2008; 63 (Suppl 4 iv1–121, updated version available from: http://www.sign.ac.uk (accessed January 2014).
Article Google Scholar
National Asthma Council Australia. Australian Asthma Handbook. Available from: http://www.nationalasthma.org.au/handbook (accessed May 2014).
National Asthma Education and Prevention Program (NAEPP) Coordinating Committee. Expert Panel Report 3 (EPR3): Guidelines for the Diagnosis and Management of Asthma. Available from: https://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm (accessed May 2014).
Taylor SJC, Pinnock H, Epiphaniou E, Pearce G, Parke H . A rapid synthesis of the evidence on interventions supporting self-management for people with long-term conditions. (PRISMS Practical Systematic Review of Self-Management Support for long-term conditions). Health Serv Deliv Res (in press).
Gibson PG, Powell H, Wilson A, Abramson MJ, Haywood P, Bauman A et al. Self-management education and regular practitioner review for adults with asthma. Cochrane Database Syst Rev 2002: (Issue 3) Art No. CD001117.
Tapp S, Lasserson TJ, Rowe BH . Education interventions for adults who attend the emergency room for acute asthma. Cochrane Database Syst Rev 2007: (Issue 3) Art No. CD003000.
Powell H, Gibson PG . Options for self-management education for adults with asthma. Cochrane Database Syst Rev 2002: (Issue 3) Art No: CD004107.
Toelle B, Ram FSF . Written individualised management plans for asthma in children and adults. Cochrane Database Syst Rev 2004: (Issue 1) Art No. CD002171.
Lefevre F, Piper M, Weiss K, Mark D, Clark N, Aronson N . Do written action plans improve patient outcomes in asthma? An evidence-based analysis. J Fam Pract 2002; 51 : 842–848.
PubMed Google Scholar
Boyd M, Lasserson TJ, McKean MC, Gibson PG, Ducharme FM, Haby M . Interventions for educating children who are at risk of asthma-related emergency department attendance. Cochrane Database Syst Rev 2009: (Issue 2) Art No.CD001290.
Bravata DM, Gienger AL, Holty JE, Sundaram V, Khazeni N, Wise PH et al. Quality improvement strategies for children with asthma: a systematic review. Arch Pediatr Adolesc Med 2009; 163 : 572–581.
Bower P, Murray E, Kennedy A, Newman S, Richardson G, Rogers A . Self-management support interventions to reduce health care utilisation without compromising outcomes: a rapid synthesis of the evidence. Available from: http://www.nets.nihr.ac.uk/projects/hsdr/11101406 (accessed April 2014).
Gibson PG, Powell H . Written action plans for asthma: an evidence-based review of the key components. Thorax 2004; 59 : 94–99.
Article CAS Google Scholar
Bhogal SK, Zemek RL, Ducharme F . Written action plans for asthma in children. Cochrane Database Syst Rev 2006: (Issue 3) Art No. CD005306.
Zemek RL, Bhogal SK, Ducharme FM . Systematic review of randomized controlled trials examining written action plans in children: what is the plan?. Arch Pediatr Adolesc Med 2008; 162 : 157–163.
Pinnock H, Slack R, Pagliari C, Price D, Sheikh A . Understanding the potential role of mobile phone based monitoring on asthma self-management: qualitative study. Clin Exp Allergy 2007; 37 : 794–802.
de Jongh T, Gurol-Urganci I, Vodopivec-Jamsek V, Car J, Atun R . Mobile phone messaging for facilitating self-management of long-term illnesses. Cochrane Database Syst Rev 2012: (Issue 12) Art No. CD007459.
Huckvale K, Car M, Morrison C, Car J . Apps for asthma self-management: a systematic assessment of content and tools. BMC Med 2012; 10 : 144.
Allergic Rhinitis and its Impact on Asthma. Management of Allergic Rhinitis and its Impact on Asthma: Pocket Guide. ARIA 2008. Available from: http://www.whiar.org (accessed May 2014).
Ring N, Jepson R, Hoskins G, Wilson C, Pinnock H, Sheikh A et al. Understanding what helps or hinders asthma action plan use: a systematic review and synthesis of the qualitative literature. Patient Educ Couns 2011; 85 : e131–e143.
Moullec G, Gour-Provencal G, Bacon SL, Campbell TS, Lavoie KL . Efficacy of interventions to improve adherence to inhaled corticosteroids in adult asthmatics: Impact of using components of the chronic care model. Respir Med 2012; 106 : 1211–1225.
Pinnock H, Bawden R, Proctor S, Wolfe S, Scullion J, Price D et al. Accessibility, acceptability and effectiveness of telephone reviews for asthma in primary care: randomised controlled trial. BMJ 2003; 326 : 477–479.
Pinnock H, Adlem L, Gaskin S, Harris J, Snellgrove C, Sheikh A . Accessibility, clinical effectiveness and practice costs of providing a telephone option for routine asthma reviews: phase IV controlled implementation study. Br J Gen Pract 2007; 57 : 714–722.
PubMed PubMed Central Google Scholar
Kielmann T, Huby G, Powell A, Sheikh A, Price D, Williams S et al. From support to boundary: a qualitative study of the border between self care and professional care. Patient Educ Couns 2010; 79 : 55–61.
Asthma UK . Compare your care report. Asthma UK, 2013. Available from: http://www.asthma.org.uk (accessed January 2014).
Stallberg B, Lisspers K, Hasselgren M, Janson C, Johansson G, Svardsudd K . Asthma control in primary care in Sweden: a comparison between 2001 and 2005. Prim Care Respir J 2009; 18 : 279–286.
Reddel H, Peters M, Everett P, Flood P, Sawyer S . Ownership of written asthma action plans in a large Australian survey. Eur Respir J 2013; 42 . Abstract 2011.
Wiener-Ogilvie S, Pinnock H, Huby G, Sheikh A, Partridge MR, Gillies J . Do practices comply with key recommendations of the British Asthma Guideline? If not, why not? Prim Care Respir J 2007; 16 : 369–377.
Kennedy A, Rogers A, Bower P . Support for self care for patients with chronic disease. BMJ 2007; 335 : 968–970.
Ring N, Malcolm C, Wyke S, Macgillivray S, Dixon D, Hoskins G et al. Promoting the Use of Personal Asthma Action Plans: A Systematic Review. Prim Care Respir J 2007; 16 : 271–283.
Taylor DR, Bateman ED, Boulet LP, Boushey HA, Busse WW, Casale TB et al. A new perspective on concepts of asthma severity and control. Eur Respir J 2008; 32 : 545–554.
Horne R . Compliance, adherence, and concordance: implications for asthma treatment. Chest 2006; 130 (suppl): 65S–72S.
Reddel HK, Taylor DR, Bateman ED, Boulet L-P, Boushey HA, Busse WW et al. An official American Thoracic Society/European Respiratory Society statement: asthma control and exacerbations standardizing endpoints for clinical asthma trials and clinical practice. Am J Respir Crit Care Med 2009; 180 : 59–99.
Thomas M, Kay S, Pike J, Rosenzweig JR, Hillyer EV, Price D . The Asthma Control Test (ACT) as a predictor of GINA guideline-defined asthma control: analysis of a multinational cross-sectional survey. Prim Care Respir J 2009; 18 : 41–49.
Hoskins G, Williams B, Jackson C, Norman P, Donnan P . Assessing asthma control in UK primary care: use of routinely collected prospective observational consultation data to determine appropriateness of a variety of control assessment models. BMC Fam Pract 2011; 12 : 105.
Pinnock H, Fletcher M, Holmes S, Keeley D, Leyshon J, Price D et al. Setting the standard for routine asthma consultations: a discussion of the aims, process and outcomes of reviewing people with asthma in primary care. Prim Care Respir J 2010; 19 : 75–83.
McKinstry B, Hammersley V, Burton C, Pinnock H, Elton RA, Dowell J et al. The quality, safety and content of telephone and face-to-face consultations: a comparative study. Qual Saf Health Care 2010; 19 : 298–303.
Gordon C, Galloway T . Review of Findings on Chronic Disease Self-Management Program (CDSMP) Outcomes: Physical, Emotional & Health-Related Quality of Life, Healthcare Utilization and Costs . Centers for Disease Control and Prevention and National Council on Aging: Atlanta, GA, USA, 2008.
Beasley R, Crane J . Reducing asthma mortality with the self-management plan system of care. Am J Respir Crit Care Med 2001; 163 : 3–4.
Ring N, Jepson R, Pinnock H, Wilson C, Hoskins G, Sheikh A et al. Encouraging the promotion and use of asthma action plans: a cross study synthesis of qualitative and quantitative evidence. Trials 2012; 13 : 21.
Jones A, Pill R, Adams S . Qualitative study of views of health professionals and patients on guided self-management plans for asthma. BMJ 2000; 321 : 1507–1510.
Bandura A . Self-efficacy: toward a unifying theory of behavioural change. Psychol Rev 1977; 84 : 191–215.
Gollwitzer PM, Sheeran P . Implementation intentions and goal achievement: a meta-analysis of effects and processes. Adv Exp Soc Psychol 2006; 38 : 69–119.
Google Scholar
Hardeman W, Johnston M, Johnston DW, Bonetti D, Wareham NJ, Kinmonth AL . Application of the theory of planned behaviour change interventions: a systematic review. Psychol Health 2002; 17 : 123–158.
Schwarzer R . Modeling health behavior change: how to predict and modify the adoption and maintenance of health behaviors. Appl Psychol 2008; 57 : 1–29.
Sniehotta F . Towards a theory of intentional behaviour change: plans, planning, and self-regulation. Br J Health Psychol 2009; 14 : 261–273.
Okelo SO, Butz AM, Sharma R, Diette GB, Pitts SI, King TM et al. Interventions to modify health care provider adherence to asthma guidelines: a systematic review. Pediatrics 2013; 132 : 517–534.
Grol R, Grimshaw RJ . From best evidence to best practice: effective implementation of change in patients care. Lancet 2003; 362 : 1225–1230.
Jusef L, Hsieh C-T, Abad L, Chaiyote W, Chin WS, Choi Y-J et al. Primary care challenges in treating paediatric asthma in the Asia-Pacific region. Prim Care Respir J 2013; 22 : 360–362.
Donabedian A . Evaluating the quality of medical care. Milbank Q 2005; 83 : 691–729.
Fardy HJ . Moving towards organized care of chronic disease. The 3+ visit plan. Aust Fam Physician 2001; 30 : 121–125.
CAS PubMed Google Scholar
Glasgow NJ, Ponsonby AL, Yates R, Beilby J, Dugdale P . Proactive asthma care in childhood: general practice based randomised controlled trial. BMJ 2003; 327 : 659.
Douglass JA, Goemann DP, Abramson MJ . Asthma 3+ visit plan: a qualitative evaluation. Intern Med J 2005; 35 : 457–462.
Beilby J, Holton C . Chronic disease management in Australia; evidence and policy mismatch, with asthma as an example. Chronic Illn 2005; 1 : 73–80.
The Department of Health. Asthma Cycle of Care. Accessed on 14 May 2014 at http://www.health.gov.au/internet/main/publishing.nsf/Content/asthma-cycle .
National Asthma Council Australia. Asthma and Respiratory Education Program. Accessed on 14 May 2014 at http://www.nationalasthma.org.au/health-professionals/education-training/asthma-respiratory-education-program .
Patel MR, Shah S, Cabana MD, Sawyer SM, Toelle B, Mellis C et al. Translation of an evidence-based asthma intervention: Physician Asthma Care Education (PACE) in the United States and Australia. Prim Care Respir J 2013; 22 : 29–34.
Armour C, Bosnic-Anticevich S, Brilliant M, Burton D, Emmerton L, Krass I et al. Pharmacy Asthma Care Program (PACP) improves outcomes for patients in the community. Thorax 2007; 62 : 496–502.
Roberts NJ, Mohamed Z, Wong PS, Johnson M, Loh LC, Partridge MR . The development and comprehensibility of a pictorial asthma action plan. Patient Educ Couns 2009; 74 : 12–18.
Henry RL, Gibson PG, Vimpani GV, Francis JL, Hazell J . Randomised controlled trial of a teacher-led asthma education program. Pediatr Pulmonol 2004; 38 : 434–442.
National Asthma Council Australia. Asthma Friendly Schools program. Accessed on 14 May 2014 at http://www.asthmaaustralia.org.au/Asthma-Friendly-Schools.aspx .
Download references
Author information
Authors and affiliations.
Asthma UK Centre for Applied Research, Centre for Population Health Sciences, The University of Edinburgh, Edinburgh, UK,
Hilary Pinnock & Elisabeth Ehrlich
NMAHP-RU, University of Stirling, Stirling, UK,
Gaylor Hoskins
Discipline of General Practice, University of Sydney, Sydney, NSW, Australia
Ron Tomlins
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Hilary Pinnock .
Ethics declarations
Competing interests.
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
Reprints and permissions
About this article
Cite this article.
Pinnock, H., Ehrlich, E., Hoskins, G. et al. A woman with asthma: a whole systems approach to supporting self-management. npj Prim Care Resp Med 24 , 14063 (2014). https://doi.org/10.1038/npjpcrm.2014.63
Download citation
Received : 23 June 2014
Revised : 15 July 2014
Accepted : 15 July 2014
Published : 16 October 2014
DOI : https://doi.org/10.1038/npjpcrm.2014.63
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative

Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Join our Mailing List
Working locally in primary care and collaborating globally to improve respiratory health
Clinical case study - asthma, clinical case study - asthma, resource information.
- Disease management
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center
BRONCHIAL ASTHMA: A REVIEW OF SYMPTOMS AND EMERGENCY CONDUCTS (Atena Editora)

2024, BRONCHIAL ASTHMA: A REVIEW OF SYMPTOMS AND EMERGENCY CONDUCTS (Atena Editora)
Introduction: Bronchial asthma is a medical condition marked by chronic inflammation of the airways and variable restriction of expiratory flow, which can be partially or completely reversible, naturally or with the use of medication. Objective: To analyze the symptoms that indicate asthma and the essential emergency therapeutic approaches to effectively manage this clinical condition. Methodology: This study is a systematic literature review, carried out in 2024. Trials, meta-analyses and systematic reviews published in the last 12 months, in the PubMed database, were selected and eligible. The terms “Asthma” AND “Treatment” AND “Symptom” were used. Results: A total of 38 studies were found, including 3 clinical trials, no meta-analysis and 5 systematic reviews. After analysis, it is concluded that the symptoms are characterized by shortness of breath, a feeling of tightness in the chest and wheezing when breathing. The cough, both dry and productive, is more evident at night. Bronchial reactivity increases the sensitivity of the airways to allergens, irritants and exercise, which can lead to acute attacks that require urgent medical attention. For the treatment of asthma in acute crisis situations, emergency therapeutic interventions are essential. Prompt use of short-acting bronchodilators relieves airway constriction. Systemic corticosteroids help reduce inflammation, while oxygen therapy is administered to ensure adequate oxygenation. In extreme cases, epinephrine may be used to improve respiratory function. Continuous monitoring of vital signs is crucial, and hospitalization may be necessary in more serious situations. Having a personalized and fundamental action plan and seeking immediate medical assistance is crucial in the face of severe and persistent symptoms. Conclusions: Therefore, bronchial asthma is a complex condition that requires a multifaceted approach for its effective management. The characteristic symptoms, such as shortness of breath, wheezing and coughing, may indicate an imminent crisis, requiring emergency therapeutic interventions, including bronchodilators, corticosteroids and oxygen therapy. Early recognition of signs of deterioration and prompt intervention are crucial to avoid serious complications and hospitalizations. A personalized action plan and the search for immediate medical assistance are essential to ensure adequate control of the condition and a better quality of life for asthmatic patients.
Related Papers
Asthma is the leading chronic disease among children in most industrialized countries. However, the evidence base on specific aspects of pediatric asthma, including therapeutic strategies, is limited and no recent international guidelines have focused exclusively on pediatric asthma. As a result, the European Academy of Allergy and Clinical Immunology and the American Academy of Allergy, Asthma and Immunology nominated expert teams to find a consensus to serve as a guideline for clinical practice in Europe as well as in North America. This consensus report recommends strategies that include pharmacological treatment, allergen and trigger avoidance and asthma education. The report is part of the PRACTALL initiative**, which is endorsed by both academies.
ASTHMA IN PRIMARY CARE: THE ROLE OF BASIC HEALTH UNITS IN THE PREVENTION OF EXACERBATIONS (Atena Editora)
Atena Editora
Asthma is a chronic, inflammatory lung disease characterized by a hyperresponsiveness of the airways that limits the respiratory flow, mainly triggered by environmental exposure and inadequate management of the disease. This disease affects about 300 million people worldwide and a good part of the Brazilian population. Its epidemiological characteristic is the generation of extensive expenses for the federal governments and for the SUS, having as the basis of its pharmacological treatment the use of corticosteroids and bronchodilators of short and long duration, using inhalation devices as essential equipment and more modern according to new studies to avoid its most important complication: exacerbation (with its main symptoms of hypoxemia, dyspnea and lowered level of consciousness). The objective of this work is to understand the role of health professionals in Primary Care and how to prevent these exacerbations and effectively reduce morbidity and mortality and reduce costs. A search was carried out in review articles, in order to understand the best ways to approach the patient in primary care, based on 3 main pillars: environmental control for the asthmatic patient; the correct use of inhaler devices and the initial management of an asthma attack. It is concluded that, with this review article, the role of professionals in Primary Health Care and Basic Health Units are essential for better asthma control, reducing possible crises and improving the patient's quality of life.
Applied Sciences
Carmen Rondón
Respiratory diseases are pathological conditions that affect airways, hampering breathing and causing high mortality. In particular, asthma and allergic rhinitis (AR) are two of the most common airway diseases that affect millions of people and have a high prevalence in childhood and adulthood. Asthma is a heterogeneous chronic inflammatory disease characterized by wheezing, chest tightness, shortness of breath, and cough. AR occurs with rhinorrhea, nasal congestion, and sneezing. Indeed, these pathologies share common physiopathological mechanisms such as airway hyperresponsiveness and similar immunopathology such as tissue eosinophilia and T-helper type 2 inflammation. Moreover, AR can be an important risk factor for suffering asthma. Thus, early diagnosis and effective treatment are crucial to improving the health and quality of life of these patients. Classical drugs such as corticosteroids have been used; however, in the last decades, efforts to improve treatments have increase...
FACTORS ASSOCIATED WITH CONTROLLED ASTHMA IN CHILDREN AND ADOLESCENTS IN THE MUNICIPALITY OF PRIMAVERA DO LESTE MATO GROSSO IN 2016 (Atena Editora)
Introduction: Asthma is a very prevalent disease in childhood and is usually associated with various environmental and household exposure factors, personal history and family history. It is a condition that affects the quality of life of individuals. Goal: It is to analyze the influence of sociodemographic and economic factors, birth and childhood conditions, paternal and maternal pathological history, intra-household exposure and, mainly, exposure to pesticides on controlled asthma in children and adolescents. Methodology: Case-control study with primary data collected through the International Study of Asthma and Allergies in Childhood (ISAAC) questionnaire in children and adolescents in the city of Primavera do Leste – MT. The sample obtained by randomization is 452 individuals, 226 cases and 226 controls. Results: In logistic regression, low birth weight (OR = 2.04), attendance at daycare (OR = 1.78), household activity that uses pesticides (OR = 2.74) remained factors favorable to the development of controlled asthma. Breastfeeding (OR = 0.04) as a protective factor against asthma. Conclusion: The association of several sociodemographic factors, the child's physiological history, household exposure and exposure to pesticides with controlled asthma was observed. Therefore, prevention and health promotion actions must start from primary health care, with education of the population about the need for the correct use of Personal Protective Equipment, as well as the cautious use of pesticides in or near the home.
TOMOGRAPHIC PATTERNS IN THE DIAGNOSTIC APPROACH TO COVID 19 (Atena Editora)
Introduction: Computed axial tomography is a diagnostic imaging study in the field of medicine, it is expressed in images that show the interior of the human body structurally, through millimeter cross-sections using radiation. Objective: To identify the radiological findings in the chest computed tomography for the diagnosis of COVID - 19, through a systematic review of evidence-based medicine. Methodology: Non-experimental descriptive study, through a systematic review of scientific articles from the main evidence-based medicine repositories and databases, through a search prism (Pubmed, Cochrane, Elseiver, Google Scholar). It is a logical deductive method, through the literature search, the radiological parameters of computed tomography in patients diagnosed with COVID - 19 are analyzed and described. Conclusion: Lung computed tomography can fully show its distribution, results of changes in shape and density and dynamic changes in patients with COVID-19 in the course of the disease and important clinical manifestations. The combination of the patient's laboratory indicators can help guide early clinical diagnosis, early isolation and early rehabilitation of coronavirus, and can be used as a basis for evaluating treatment-induced adverse reactions and the time in which symptoms linked to the radiological study appear.
Annals of Thoracic Medicine
Hassan S . Alorainy
Nikolai Khaltaev
World Journal of Clinical Cases
Seval Kendirli
David Carmona
Mahsa Akbari
Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
RELATED PAPERS
Turkish Archives of Otorhinolaryngology
vural fidan
Laura Larrea Mantilla
palani sami
Allergologia et Immunopathologia
Busquets Monge
European Respiratory Journal
Emílio Pizzichini
Respiration; international review of thoracic diseases
Thomas Rothe
Asian Pacific Journal of Allergy and Immunology
Nittha Oer-areemitr
mercedes rodriguez
Journal of Clinical and Nursing Research
Efficacy and safety of immunotherapy for allergic rhinitis in the induction phase (Atena Editora)
Respiratory care
Caroline Bibi Trunk-Black Juel
ASSOCIATION BETWEEN RHINOVIRUS AND RESPIRATORY SYNCYTIAL VIRUS (RSV) LINKED TO ASTHMA EXACERBATION IN PEDIATRIC PATIENTS (Atena Editora)
Pediatric Pulmonology
Heather Zar
Kenneth Bautista
South African medical journal = Suid-Afrikaanse tydskrif vir geneeskunde
Ahmed Manjra
Majdym Idrees
Expert Opinion on Pharmacotherapy
Timothy Albertson
Snezana Zivanovic
CHARACTERISTICS AND CLINICAL MANAGEMENT OF NEONATES WITH COVID-19 – AN INTEGRATIVE LITERATURE REVIEW (Atena Editora)
Rinda Aulia Utami
Journal of investigational allergology & clinical immunology: official organ of the International Association of Asthmology (INTERASMA) and Sociedad Latinoamericana de Alergia e Inmunología
Alessandro Massolo
ISRN Allergy
giuliano molinari
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024

Global Initiative for Asthma - GINA
GINA Slide Set
Updated august 2023.
What’s New in 2023 — Slide Set
PowerPoint slide set summarizing GINA’s objectives, documents, and management recommendations from the 2023 update of the GINA Report, with background information about asthma and the burden of this disease.
GINA documents are protected by copyright. A single copy of this document may be downloaded for your own educational use, but copies may not be made for distribution or posted on a website without authorization from GINA. No additions or changes may be made to slides. Use of the slide set or of individual slides for commercial or promotional purposes requires approval from GINA.
ADDITIONAL SLIDE SETS:
2022 GINA Difficult-to-treat & Severe Asthma Guide — Slide Set COVID-19 — Slide Set
What is known about asthma?
Asthma is a common and potentially serious chronic disease that imposes a substantial burden on patients, their families and the community. It causes respiratory symptoms, limitation of activity, and flare-ups (attacks) that sometimes require urgent health care and may be fatal.
Fortunately… asthma can be effectively treated and most patients can achieve good control of their asthma. When asthma is under good control, patients can:
- Avoid troublesome symptoms during day and night
- Need little or no reliever medication
- Have productive, physically active lives
- Have normal or near normal lung function
- Avoid serious asthma flare-ups (exacerbations, or attacks)
What is asthma? Asthma causes symptoms such as wheezing, shortness of breath, chest tightness, and cough that vary over time in their occurrence, frequency and intensity.
These symptoms are associated with variable expiratory airflow, i.e., difficulty breathing air out of the lungs due to bronchoconstriction (airway narrowing), airway wall thickening, and increased mucus. Some variation in airflow can also occur in people without asthma, but it is greater in asthma.
Factors that may trigger or worsen asthma symptoms include viral infections, domestic or occupational allergens (e.g., house dust mite, pollens, cockroach), tobacco smoke, exercise and stress. These responses are more likely when asthma is uncontrolled. Some drugs can induce or trigger asthma, e.g., beta-blockers, and (in some patients) aspirin or other NSAIDs.
Asthma flare-ups (also called exacerbations or attacks) may occur, even in people taking asthma treatment. When asthma is uncontrolled, or in some high-risk patients, these episodes are more frequent and more severe, and may be fatal.
A stepwise approach to treatment takes into account the effectiveness of available medications, their safety, and their cost to the payer or patient.
Regular controller treatment , particularly with inhaled corticosteroid (ICS)-containing medications, markedly reduces the frequency and severity of asthma symptoms and the risk of having a flare-up.
Asthma is a common condition, affecting all levels of society. Olympic athletes, famous leaders and celebrities, and ordinary people live successful and active lives with asthma .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.16(5); 2024 May
- PMC11183517

Subglottic Adenoid Cystic Carcinoma Mimicking Bronchial Asthma: A Case Report
1 Internal Medicine, Sri Devaraj Urs Academy of Higher Education and Research, Kolar, IND
Guruprasad T J
2 Respiratory Medicine, Sri Devaraj Urs Medical College, Kolar, IND
Spurthy Padmanabha
3 Pulmonology, Sri Devaraj Urs Academy of Higher Education and Research, Kolar, IND
Harshitha K R
Adenoid cystic carcinoma (ACC) is a rare type of tumor that usually originates from minor salivary glands in the oral cavity. ACC of the larynx is even rare. This case study describes a 36-year-old non-smoking male farmer who initially presented with dyspnea and was misdiagnosed with bronchial asthma. Spirometry revealed fixed airway obstruction. Further evaluation revealed a pedunculated mass obstructing the airway, which was diagnosed as ACC by histopathological examination of the biopsy specimen. The patient was treated with radiation therapy, resulting in clinical improvement after six weeks. ACC is highly invasive and slow-growing, with perineural extension and a higher risk of recurrence. Metastasis in the lungs is common. Adequate preoperative staging, including imaging with computed tomography (CT) and magnetic resonance imaging, is important for planning treatment. The role of radiation therapy with concurrent chemotherapy is still under trial.
Introduction
Laryngeal carcinoma is the second most prevalent malignancy of the upper aero-digestive tract with over 13,000 cases documented yearly in the United States solely [ 1 ]. Despite squamous cell carcinoma (SCC) contributing to the majority (~90%) of malignant laryngeal tumors, the larynx is susceptible to a wide range of malignancies with different histologic characteristics [ 2 ]. ACC is a relatively slow-growing tumor that most frequently arises from minor salivary glands of the oral cavity, paranasal sinuses, pharynx, and larynx [ 3 ]. Adenoid cystic carcinomas (ACC) predominantly affect salivary glands of the oral cavity. ACC of the larynx is one of the rarest variants accounting for <1% of laryngeal tumors, originating along the mucosa of the laryngo-tracheal tract, as there are few salivary glands [ 4 , 5 ]. The available research estimates that there have only been less than 100 case reports on ACC published globally [ 6 ]. In contrast to SCC, ACC of the larynx is not related to a history of smoking or no distinct predisposing risk factors to this malignancy [ 4 , 5 ]. Hoarseness and dyspnea are frequently the predominant symptoms, while local-regional metastases are extremely rare, at least for cancers that start in the subglottic region [ 6 , 7 ]. The median survival period is about eight years [ 7 ]. Although the clinical behavior of extra laryngeal ACC is well known, currently only limited case series are available for laryngeal ACCs. Here, we describe a case of ACC of the larynx with an atypical presentation that was initially misdiagnosed as asthma. However, the following discussion details how further evaluation helped in arriving at an accurate diagnosis.
Case presentation
A 36-year-old Indian farmer, a non-smoker male, presented with a history of dyspnea for five months, which aggravated on exertion, for which he was treated for bronchial asthma with bronchodilators in a local hospital. His dyspnea had worsened for half a month and was associated with noisy breathing for five days. The patient also complained of a cough for one week associated with yellow mucoid, non-foul smelling, and occasionally blood-tinged sputum. He complained of hoarseness of voice for five days. He denied a history of chest pain, palpitations, orthopnea, facial puffiness, upper limb swelling, difficulty in swallowing, fever, loss of weight, and loss of appetite. The patient had no known comorbidities. He gave the history of a road traffic accident 12 years ago with blunt trauma chest and rib fractures.
Physical examination on presentation revealed a temperature of 36.9°C, pulse of 91 bpm, blood pressure of 124/80 mmHg, respiratory rate of 23 cycles/minute, and oxygen saturation of 96% on room air. Stidor was present. Respiratory system examination revealed no abnormality on inspection, palpation, and percussion. Bilateral vesicular breath sounds of reduced intensity were heard in all areas of auscultation associated with inspiratory rhonchi.
On further evaluation, a posterior-anterior (PA) view chest radiograph revealed hyperinflated lung fields, with normal mediastinum (Figure (Figure1A). 1A ). Spirometry was suggestive of fixed upper airway obstruction (Figure (Figure1B). 1B ). Routine blood investigations were within normal limits.

PA, posterior-anterior
The patient underwent a check bronchoscopy for evaluation of upper airway obstruction, which revealed a pedunculated mass arising from the right posterolateral subglottic area causing near-total airway obstruction (Figure (Figure2 2 ).

A contrast-enhanced CT of the neck and thorax revealed a round to oval well-defined soft tissue density mass lesion arising from the posterolateral aspect of the trachea in the region of subglottis with posterior extension causing near-total obstruction of the tracheal lumen. The study did not reveal any significant involvement of mediastinal or cervical lymph nodes. The tumor mass showed no infiltration into surrounding structures, vessels, or nerves (Figure 3 ).

CECT, contrast-enhanced computed tomography
The patient underwent elective tracheostomy followed by microlaryngeal surgery. Intraoperative findings revealed edematous left aryepiglottic fold, edematous false cords, and fibrous subglottic stenosis. A biopsy was taken. Grossly, the specimen was described as a gray-white soft tissue. Microscopy revealed basaloid cells arranged in a cribriform pattern (Figure (Figure4) 4 ) and lobules with abundant hyaline globules (Figure (Figure5), 5 ), with focal areas showing necrosis and hemorrhage. Histopathological examination was suggestive of ACC. Immunohistochemistry of ACC cells revealed positive for S100 and negative for P63, which suggested that the tumor consisted of myoepithelial cells.

Based on histopathology and CECT head and neck, the patient was diagnosed with carcinoma subglottis cT1 N0 M0 stage I (AJCC) ACC. The patient was advised for laryngectomy with modified radical neck dissection but the patient was unwilling for surgery, hence the patient was treated with radical radiotherapy (RT) via IMRT with neck irradiation. The primary tumor was irradiated with 70 Gy in 35 fractions, 2 Gy/fraction, and 5 fractions/week. During follow-up after six weeks post-RT, the patient had improved clinically.
ACC is a rare malignancy of the larynx, with a mean age of presentation between the fifth and sixth decade of life, lacking a distinct gender predominance [ 8 - 10 ]. The youngest age of ACC presentation is 12 years as reported by Javadi et al. [ 10 ]. ACC originates from mixed seromucinous glands of the larynx. Although these glands diminish in number from supraglottis to subglottis, subglottis remains the most commonly affected location. Nearly two-thirds of ACC originates from the subglottic region, and the remaining one-third of cases arise from the supraglottic region, leaving the glottic region an extremely uncommon site for ACC [ 8 , 9 ]. The etiology of ACC is still unclear. ACC of the larynx is a highly invasive and slow-growing tumor with perineural extension with an increased rate of recurrence after initial treatment [ 10 ].
The initial presentation of laryngeal ACC varies with the anatomical site and size of the tumor. Tumors arising from supraglottis present with dysphagia and pharyngeal paresthesia. Hoarseness of voice or dyspnea indicates involvement of the glottis. The presence of airway obstruction and stridor implicates the presence of a subglottic tumor [ 11 , 12 ]. Laryngeal ACC remains asymptomatic in the beginning stages, with submucosal non-ulcerated mass, leading to a delay in the diagnosis giving a chance for ACC to spread deeply before a diagnosis is made [ 11 , 13 ]. In this case, the growth was arising from the subglottic area obliterating the trachea and causing dyspnea associated with stridor.
Despite the rarity of cervical lymph node metastasis in ACC accounting for nearly 10-15% of head and neck cases, nodal metastasis poses as one of the commonest reasons for therapy failure [ 10 , 14 ]. However, neck dissection is performed in all the patients with ACC with evidence of nodal metastasis evidenced by physical examination and imaging modalities [ 14 ].
ACC has demonstrated a high rate of perineural invasion even in the early stages of the tumor leading to treatment failure and early recurrence. Distant metastasis can occur even in the absence of local recurrence. The most frequent location of distant metastases in ACC is the lungs, with vertebral metastasis contributing to poor survival [ 10 , 12 ]. However, few authors have described lesser survival in tumors originating from minor salivary glands suspecting that they might have originated secondary to an increased rate of distant metastasis [ 12 ].
Histopathological evaluation is necessary as the clinical presentation of ACC mimics laryngeal SCC. Based on histology, the World Health Organization classification of tumors, there are three subtypes of ACC namely cribriform, tubular, and solid. The tubular subtype (well differentiated/grade I) has the best prognosis, cribriform (moderately differentiated/grade II) is the commonest variety, and the least common subtype, which is the solid variant (poorly differentiated/grade III), exhibits the worst prognosis. The cells in each of these categories have a mucinous or hyaline matrix. Although basaloid SCC is a well-known entity in the larynx and the prognosis for ACC is significantly better than that of basaloid SCC, it is still necessary to distinguish the basaloid variant of SCC from ACC despite the etiological and histological distinctions between laryngeal SCC and ACC [ 15 ]. Often these ACCs demonstrate mixed histological growth patterns hence classified according to the predominant pattern.
Adequate preoperative workup for staging is necessary. Contrast-enhanced computed tomography (CECT) scan of the head and neck is the preferred imaging modality in ACC to assess the location of the primary tumor, extra luminal extension, regional and distant metastasis, and to stage the primary tumor. In our case, the CECT neck and thorax showed a submucosal mass in the subglottic area without any extension to the extra laryngeal soft tissues or regional metastasis, correlating with the histopathological findings. MRI is the modality of choice to evaluate soft tissue and perineural spread of tumors with a sensitivity of 95% [ 16 ].
Management of ACC is still a controversy. The primary modality in the treatment of ACC is radical surgery with neck dissection. Post-operative radiotherapy is advised in cases with residual lesions or involved margins. Patients will have benefit in terms of locoregional control. Postoperatively, a dose of 60 Gy-66 Gy can be given based on the presence of positive margin/perineural invasion [ 17 ]. Neck node stations can be irradiated based on lymph node involvement as per standard protocol. In settings where RT is used definitely, gross tumors and nerves with tumor involvement can be irradiated to a dose of 70 Gy with irradiation of the neck to standard dose and elective volumes using the same principles of rest of head and neck tumors. Overall survival benefit is 26.5 to 87% and locoregional recurrence rate is 24 to 57% with definitive radiotherapy [ 18 ]. The role of RT with concurrent chemotherapy in ACC is ongoing [ 19 ].
Conclusions
ACC of the larynx is a rare and invasive tumor with varied clinical presentations. Accurate diagnosis is crucial for appropriate treatment planning. While surgery is the primary treatment, radiation therapy plays a significant role, especially in cases of residual disease or involvement of margins. Further research is needed to better understand this rare malignancy and optimize treatment strategies.
The authors have declared that no competing interests exist.
Author Contributions
Acquisition, analysis, or interpretation of data: Spurthy Padmanabha, K K Athish, Guruprasad T J, Harshitha K R
Critical review of the manuscript for important intellectual content: Spurthy Padmanabha, Guruprasad T J, Harshitha K R
Supervision: Spurthy Padmanabha, Guruprasad T J
Drafting of the manuscript: K K Athish, Guruprasad T J
Concept and design: Guruprasad T J
Human Ethics
Consent was obtained or waived by all participants in this study
Got any suggestions?
We want to hear from you! Send us a message and help improve Slidesgo
Top searches
Trending searches

education technology
239 templates
computer technology
306 templates

ai technology
186 templates

cyber security
10 templates

meet the teacher
30 templates

first day of school
70 templates
Asthma Clinical Case
It seems that you like this template, asthma clinical case presentation, free google slides theme, powerpoint template, and canva presentation template.
Asthma is a condition in which breathing becomes laborious. Wheezing, coughing, chest tightness, and shortness of breath are common when one undergoes this disease. Get to know a little bit more about asthma studying some clinical cases with our futuristic template!
The structure of this theme is based on a clinical case. The purple background contains geometric shapes with gradients that look like computer glitches. This makes the design very futuristic. We have added a few pictures of people using inhalers and grotesque sans serif typefaces, which are very visually appealing and perfect of a clinical case!
Features of this template
- A futuristic template with gradients and transparencies
- 100% editable and easy to modify
- 28 different slides to impress your audience
- Contains easy-to-edit graphics, maps and mockups
- Includes 500+ icons and Flaticon’s extension for customizing your slides
- Designed to be used in Google Slides, Canva, and Microsoft PowerPoint
- 16:9 widescreen format suitable for all types of screens
- Includes information about fonts, colors, and credits of the free resources used
How can I use the template?
Am I free to use the templates?
How to attribute?
Attribution required If you are a free user, you must attribute Slidesgo by keeping the slide where the credits appear. How to attribute?
Related posts on our blog.

How to Add, Duplicate, Move, Delete or Hide Slides in Google Slides

How to Change Layouts in PowerPoint

How to Change the Slide Size in Google Slides
Related presentations.
Premium template
Unlock this template and gain unlimited access


Provide details on what you need help with along with a budget and time limit. Questions are posted anonymously and can be made 100% private.

Studypool matches you to the best tutor to help you with your question. Our tutors are highly qualified and vetted.

Your matched tutor provides personalized help according to your question details. Payment is made only after you have completed your 1-on-1 session and are satisfied with your session.

- Homework Q&A
- Become a Tutor
All Subjects
Mathematics
Programming
Health & Medical
Engineering
Computer Science
Foreign Languages
Access over 35 million academic & study documents
Case presentation: bronchial asthma.
Sign up to view the full document!

24/7 Study Help
Stuck on a study question? Our verified tutors can answer all questions, from basic math to advanced rocket science !

Similar Documents
working on a study question?
Studypool is powered by Microtutoring TM
Copyright © 2024. Studypool Inc.
Studypool is not sponsored or endorsed by any college or university.
Ongoing Conversations

Access over 35 million study documents through the notebank
Get on-demand Q&A study help from verified tutors
Read 1000s of rich book guides covering popular titles

Sign up with Google
Sign up with Facebook
Already have an account? Login
Login with Google
Login with Facebook
Don't have an account? Sign Up

IMAGES
VIDEO
COMMENTS
A case study on bronchial asthma. A 48-year old female patient presented with breathlessness, chest tightness, and cough with expectoration for one day. Her medical history noted these symptoms for 7 days. On examination, she had an elevated pulse, respiratory rate, hemoglobin, red blood cell count, white blood cell count, and eosinophils.
Case on bronchial asthma. - The patient, an 82-year-old female, presented with fever, shortness of breath, and cough. She has a history of hypertension, heart valve surgery, and coronary artery bypass grafting. - She was diagnosed with bronchial asthma exacerbated by a lower respiratory tract infection. Her treatment included nebulizers ...
28 likes • 15,412 views. G. Gerlin George. Case presentation on bronchial asthma, respiratory disorder, Introduction-Definition-History collection-Physical examination-lab diagnosis- nursing diagnosis of asthma, treatment of asthma. Health & Medicine. 1 of 51. Case presentation on bronchial asthma - Download as a PDF or view online for free.
Apr 27, 2024 • Download as PPTX, PDF •. 0 likes • 17 views. B. BibikaMalla. case study. Health & Medicine. 1 of 107. Download now. Bronchial asthma.pptx, A clinical case study - Download as a PDF or view online for free.
Asthma Case Presentation. Asthma is a chronic disease characterized by recurrent attacks of breathlessness and wheezing that vary in severity. The main cause is airway hyper-reactivity, an exaggerated response of the airways to stimuli. Common contributing factors include allergen exposure, dietary deficiencies, drugs, exercise, and infections.
This document provides information on bronchial asthma including its definition, classification, pathophysiology, and treatment approaches. It discusses the different types of asthma such as atopic, non-atopic, and drug-induced asthma. It describes the cells and mediators involved in asthma inflammation. It covers the mechanisms and classes of ...
It defines bronchial asthma as a chronic inflammatory disease of the airways and discusses allergies as the strongest predisposing factor. The document outlines objectives, assessments, treatments, and teaching points for managing patients with asthma or asthma exacerbations like status asthmaticus. Read more. Health & Medicine. 1 of 53.
The majority of adverse effects occurred within 1 day of the procedure and resolved within 7 days. 6. In this study, bronchial thermoplasty was found to significantly improve quality of life, as ...
A CASE OF BRONCHIAL ASTHMA. A CASE OF BRONCHIAL ASTHMA. By Dr. Jawahar Shah M.D.(Hom). NOTE: To protect the patient's identity, we have used a model's picture or photographs for the purpose of presentation. A CASE BRONCHIAL ASTHMA. 12 Years old boy was brought on 27th July 1986, suffering from Bronchial Asthma. 306 views • 17 slides
NEJM363 (2010): Medically reviewed by: Ellen Reich, MD, Board Certified in Allergy and Immunology, Board Certified in Pediatrics. Download ppt "A Case Study of a Patient with Bronchial Asthma". Name: Patient X Age: 47 years old Sex: Male Nationality: Saudi I. DEMOGRAPHIC DATA Name: Patient X Age: 47 years old Sex: Male Nationality: Saudi Date ...
I discussed in this powerpoint video about bronchial asthma and everything related to it like symptoms, types, causes, treatment, diagnosis and also for the ...
Results/Discussion. Bronchial asthma is a chronic inflammatory disease of the airways characterized by bronchial hyperreactivity and a variable degree of airway obstruction. It is diagnosed on the basis of the clinical history, physical examination, and pulmonary function tests, including reversibility testing and measurement of bronchial ...
A number of studies have demonstrated the challenges for primary care physicians in providing ongoing support for people with asthma. 31,48,49 In some countries, nurses and other allied health ...
Clinical case study - asthma . 2019 . Clinical Case Study - Asthma. pdf. Clinical Case Study - Asthma. 6.34 MB. Resource information. Respiratory conditions. Asthma; Respiratory topics. Disease management; Diagnosis; Type of resource. Presentation . Author(s) Jaime Correia de Sousa Ioanna Tsiligianni Miguel Román Rodriguez
At the end of this presentation students will be able to: Give a definition of asthma. Discuss what could cause asthma. Identify four triggers of asthma. Describe symptoms of an asthma flare-up. Explain three asthma treatment strategies. Develop an interprofessional plan of care for an asthma sufferer.
Clinical presentation (recurrent, episodic attacks of wheezing, cough, dyspnea, itchy red eyes, nasal discharge, stuffiness, and chest tightness), and PFT findings (FEV1/FVC of 0.65, FEV1 is 60% of predictive and post-bronchodilator therapy the FEV1 increases to 74% of predictive) are consistent with the diagnosis of asthma.
Methodology: Case-control study with primary data collected through the International Study of Asthma and Allergies in Childhood (ISAAC) questionnaire in children and adolescents in the city of Primavera do Leste - MT. The sample obtained by randomization is 452 individuals, 226 cases and 226 controls.
What's New in 2023 — Slide Set. PowerPoint slide set summarizing GINA's objectives, documents, and management recommendations from the 2023 update of the GINA Report, with background information about asthma and the burden of this disease. GINA documents are protected by copyright. A single copy of this document may be downloaded for your ...
This case study describes a 36-year-old non-smoking male farmer who initially presented with dyspnea and was misdiagnosed with bronchial asthma. Spirometry revealed fixed airway obstruction. Further evaluation revealed a pedunculated mass obstructing the airway, which was diagnosed as ACC by histopathological examination of the biopsy specimen.
Background:Bronchial asthma is a non-communicable disease demanding long-term adherence to medical treatment and self-management. The effectiveness of a Nurse-Led Clinic for the management of long-...
Free Google Slides theme, PowerPoint template, and Canva presentation template. Asthma is a condition in which breathing becomes laborious. Wheezing, coughing, chest tightness, and shortness of breath are common when one undergoes this disease. Get to know a little bit more about asthma studying some clinical cases with our futuristic template ...
Background: The use of biologic agents for severe asthma has transformed management, decreasing asthma exacerbations, improving lung function, reducing corticosteroid use, and decreasing ...
Asthma is a chronic disease of the airways that causes airway hyperresponsiveness, mucosal edema and mucus production. This inflammation, ultimately leads to recurrent episodes of asthma symptoms: cough, chest tightness, wheezing and dyspnea. Post a Question. Provide details on what you need help with along with a budget and time limit. ...