- Faye Abdellah: 21 Nursing Problems Theory

Faye Abdellah is a celebrated nurse theorist, military nurse, and leader in nursing research. Get to know the major concepts of her “ 21 Nursing Problems ” nursing theory, its application, and its impact on nursing.

Table of Contents
Early life of faye abdellah, as an educator, as a researcher, established nursing standards, military nursing service, abdellah’s typology of 21 nursing problems, awards and honors, assumptions, nursing problems, problem solving, basic needs, sustenal care needs, remedial care needs, restorative care needs, patient-centered approaches to nursing, 21 nursing problems and the nursing process, recommended resources, external links, biography of faye glenn abdellah.
Faye Glenn Abdellah (March 13, 1919 – present) is a nursing research pioneer who developed the “Twenty-One Nursing Problems.” Her nursing model was progressive for the time in that it refers to a nursing diagnosis during a time in which nurses were taught that diagnoses were not part of their role in health care.
She was the first nurse officer to rank a two-star rear admiral, the first nurse, and the first woman to serve as a Deputy Surgeon General.
On March 13, 1919, Faye Abdellah was born in New York to a father of Algerian heritage and a Scottish mother. Her family subsequently moved to New Jersey, where she attended high school.
Years later, on May 6, 1937, the German hydrogen-fueled airship Hindenburg exploded over Lakehurst.

Abdellah and her brother witnessed the explosion, destruction, and fire after the ignited hydrogen killed many people. That incident became the turning point in Abdellah’s life. It was that time when she realized that she would never again be powerless to assist when people were in such a dire need of assistance. It was at that moment she vowed that she would learn to nurse and become a professional nurse.
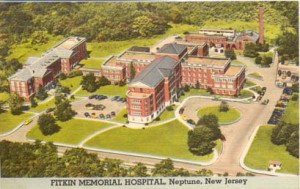
Faye Abdellah earned a nursing diploma from Fitkin Memorial Hospital’s School of Nursing, now known as Ann May School of Nursing.
It was sufficient to practice nursing during her time in the 1940s, but she believed that nursing care should be based on research, not hours of care.
Abdellah went on to earn three degrees from Columbia University: a bachelor of science degree in nursing in 1945, a master of arts degree in physiology in 1947, and a doctor of education degree in 1955.

With her advanced education, Abdellah could have chosen to become a doctor. However, as she explained in one of her interviews that she wanted to be an M.D. because she could do all she wanted to do in nursing, which is a caring profession.
Career and Appointments
In her early twenties, Faye Abdellah worked as a health nurse at a private school, and her first administrative position was on the faculty of Yale University from 1945-1949. At that time, she was required to teach a class called “120 Principles of Nursing Practice,” using a standard nursing textbook published by the National League for Nursing. The book included guidelines that had no scientific basis, which challenged Abdellah to explain everything she called the “brilliant” students.

After a year, Abdellah became so frustrated that she gathered her colleagues in the Yale courtyard and burned the textbooks. The next morning the school’s dean told her she would have to pay for the destroyed texts. It took a year for Abdellah to settle the debt, but she never regretted her actions because it started her on the long road to pursue the scientific basis of the nursing practice .
In 1949, she met Lucile Petry Leone, the first Nurse Officer, and decided to join the Public Health Service. Her first assignment was with the division of nursing that focused on research and studies. They performed studies with numerous hospitals to improve nursing practice .
Abdellah was an advocate of degree programs for nursing. Diploma programs, she believes, were never meant to prepare nurses at the professional level. Nursing education, she argued, should be based on research; she herself became among the first in her role as an educator to focus on theory and research. Her first studies were qualitative; they simply described situations. As her career progressed, her research evolved to include physiology, chemistry, and behavioral sciences.
In 1957, Abdellah spearheaded a research team in Manchester, Connecticut, that established the groundwork for what became known as progressive patient care . In this framework, critical care patients were treated in an intensive care unit, followed by a transition to immediate care and then home care. The first two segments of the care program proved very popular within the caregiver profession. Abdellah is also credited with developing the first nationally tested coronary care unit as an outgrowth of her work in Manchester.

Home care, which is the third phase of the progressive patient care equation, was not widely accepted in the mid-twentieth century. Abdellah explained that people at the time kept saying home care would mean having a maid or a nurse in everyone’s home. They could not figure out that home care with nurses teaching self-care would help patients regain independent function. Forty years later, home care had become an essential part of long-term health care.
In another innovation within her field, Abdellah developed the Patient Assessment of Care Evaluation (PACE), a system of standards used to measure the relative quality of individual health-care facilities that were still used in the healthcare industry into the 21st century. She was also one of the first people in the healthcare industry to develop a classification system for patient care and patient-oriented records.

Classification systems have evolved in different ways within the health-care industry, and Abdellah’s work was foundational in developing the most widely used form: Diagnostic related groups, or DRGs. DRGs, which became the standard coding system used by Medicare, categorize patients according to particular primary and secondary diagnoses. This system keeps health-care costs down because each DRG code includes the maximum amount Medicare will payout for a specific diagnosis or procedure while also taking into account patient age and length of stay in a healthcare facility. Providers are given an incentive to keep costs down because they only realize a profit if costs are less than the amount specified by the relevant DRG category.

During her 40-year career as a Commissioned Officer in the U.S. Public Health Service from 1949 to 1989, Abdellah was assigned to work with the Korean people during the Korean War. As a senior officer, she was alternatively assigned to Japan, China , Russia, Australia, and the Scandinavian countries to identify the Public Health Service’s role in dealing with various health problems. She was able to assist and initiate, in an advisory role, numerous studies in those countries.
She served as Chief Nurse Officer from 1970 to 1987 and was the first nurse to achieve the rank of a two-star Flag Officer named by U.S. Surgeon General C. Everett Koop as the first woman and nurse Deputy Surgeon General from 1982 to 1989. After retirement, Abdellah founded and served as the first dean in the Graduate School of Nursing, GSN, Uniformed Services University of the Health Sciences (USUHS).
Faye Abdellah is well known for developing the “Twenty-One Nursing Problems Theory” that has interrelated the concepts of health, nursing problems, and problem-solving.
She views nursing as an art and a science that molds the attitude, intellectual competencies, and technical skills of the individual nurse into the desire and ability to help individuals cope with their health needs, whether they are ill or well.
She used Henderson’s 14 basic human needs and nursing research to establish the classification of nursing problems.
Faye Abdellah’s theory is further discussed below.
As a consultant and educator, Faye Abdellah shared her nursing theories with caregivers around the world. She led seminars in France, Portugal, Israel, Japan, China, New Zealand, Australia, and the former Soviet Union. She also served as a research consultant to the World Health Organization. From her global perspective, Abdellah learned to appreciate nontraditional and complementary medical treatments and developed the belief such non-Western treatments deserved scientific research.

Also, she has been active in professional nursing associations and is a prolific author, with more than 150 publications. Her publications include Better Nursing Care Through Nursing Research and Patient-Centered Approaches to Nursing . She also developed educational materials in many areas of public health, including AIDS , hospice care , and drug addiction.
Abdellah considers her greatest accomplishment being able to “play a role in establishing a foundation for nursing research as a science.” Her book, Patient-Centered Approaches to Nursing , emphasizes nursing science and has elicited changes throughout nursing curricula. Her work, which is based on the problem-solving method, serves as a vehicle for delineating nursing (patient) problems as the patient moves toward a healthy outcome.

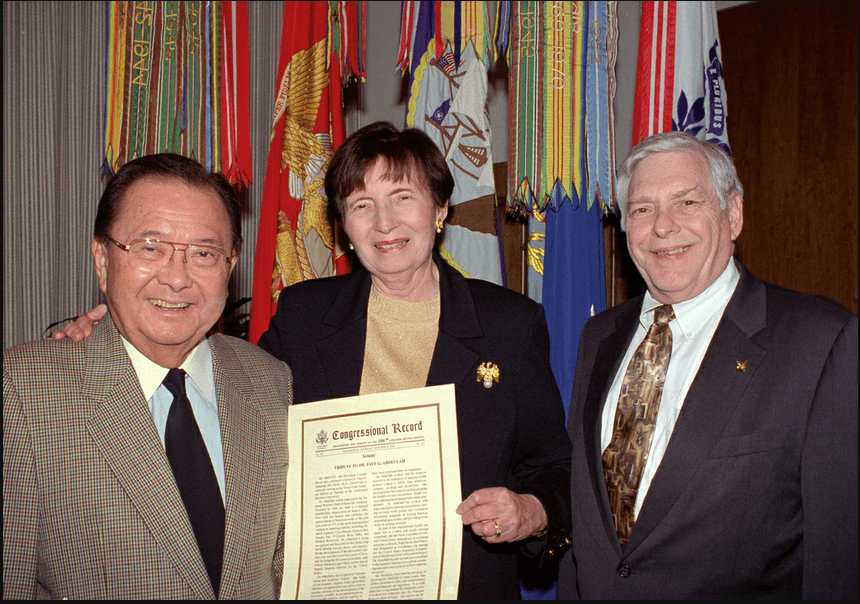
Faye Abdellah is recognized as a leader in nursing research and nursing as a profession within the Public Health Service (PHS) and as an international expert on health problems. She was named a “living legend” by the American Academy of Nursing in 1994 and was inducted into the National Women’s Hall of Fame in 2000 for a lifetime spent establishing and leading essential health care programs for the United States. In 2012, Abdellah was inducted into the American Nurses Association Hall of Fame for a lifetime of contributions to nursing.
Her contributions to nursing and public health have been recognized with almost 90 professional and academic honors, such as the Allied Signal Achievement Award for pioneering research in aging and Sigma Theta Tau’s Lifetime Achievement Award.
Abdellah’s leadership , her publications, and her lifelong contributions have set a new standard for nursing and health care. Her legacy of more than 60 years of extraordinary accomplishments lives nationally and globally.
Aside from being the first nurse and the first woman to serve as a Deputy Surgeon General, Faye Glenn Abdellah also made a name in the nursing profession to formulate her “21 Nursing Problems Theory.” Her theory changed the focus of nursing from disease-centered to patient-centered and began to include the care of families and the elderly in nursing care. The Patient Assessment of Care Evaluation developed by Abdellah is now the standard used in the United States.
Abdellah’s 21 Nursing Problems Theory
According to Faye Glenn Abdellah’s theory, “Nursing is based on an art and science that molds the attitudes, intellectual competencies, and technical skills of the individual nurse into the desire and ability to help people, sick or well, cope with their health needs.”
The patient-centered approach to nursing was developed from Abdellah’s practice, and the theory is considered a human needs theory. It was formulated to be an instrument for nursing education , so it most suitable and useful in that field. The nursing model is intended to guide care in hospital institutions but can also be applied to community health nursing, as well.
The assumptions Abdellah’s “21 Nursing Problems Theory” relate to change and anticipated changes that affect nursing; the need to appreciate the interconnectedness of social enterprises and social problems; the impact of problems such as poverty, racism, pollution, education, and so forth on health and health care delivery; changing nursing education ; continuing education for professional nurses; and development of nursing leaders from underserved groups.
- Learn to know the patient.
- Sort out relevant and significant data.
- Make generalizations about available data concerning similar nursing problems presented by other patients.
- Identify the therapeutic plan.
- Test generalizations with the patient and make additional generalizations.
- Validate the patient’s conclusions about his nursing problems.
- Continue to observe and evaluate the patient over a period of time to identify any attitudes and clues affecting this behavior.
- Explore the patient’s and family’s reaction to the therapeutic plan and involve them in the plan.
- Identify how the nurse feels about the patient’s nursing problems.
- Discuss and develop a comprehensive nursing care plan .
Major Concepts of 21 Nursing Problems Theory
The model has interrelated concepts of health and nursing problems and problem-solving, which is inherently logical in nature.
She describes nursing recipients as individuals (and families), although she does not delineate her beliefs or assumptions about the nature of human beings.
Health, or the achieving of it, is the purpose of nursing services. Although Abdellah does not define health, she speaks to “total health needs” and “a healthy state of mind and body.”
Health may be defined as the dynamic pattern of functioning whereby there is a continued interaction with internal and external forces that results in the optimal use of necessary resources to minimize vulnerabilities.
Society is included in “ planning for optimum health on local, state, and international levels.” However, as Abdellah further delineates her ideas, the focus of nursing service is clearly the individual.
The client’s health needs can be viewed as problems, overt as an apparent condition, or covert as a hidden or concealed one.
Because covert problems can be emotional, sociological, and interpersonal in nature, they are often missed or misunderstood. Yet, in many instances, solving the covert problems may solve the overt problems as well.
Quality professional nursing care requires that nurses be able to identify and solve overt and covert nursing problems. The problem-solving process can meet these requirements by identifying the problem, selecting pertinent data, formulating hypotheses, testing hypotheses through collecting data, and revising hypotheses when necessary based on conclusions obtained from the data.
Subconcepts
The following are the subconcepts of Faye Abdellah’s “21 Nursing Problems” theory and their definitions.
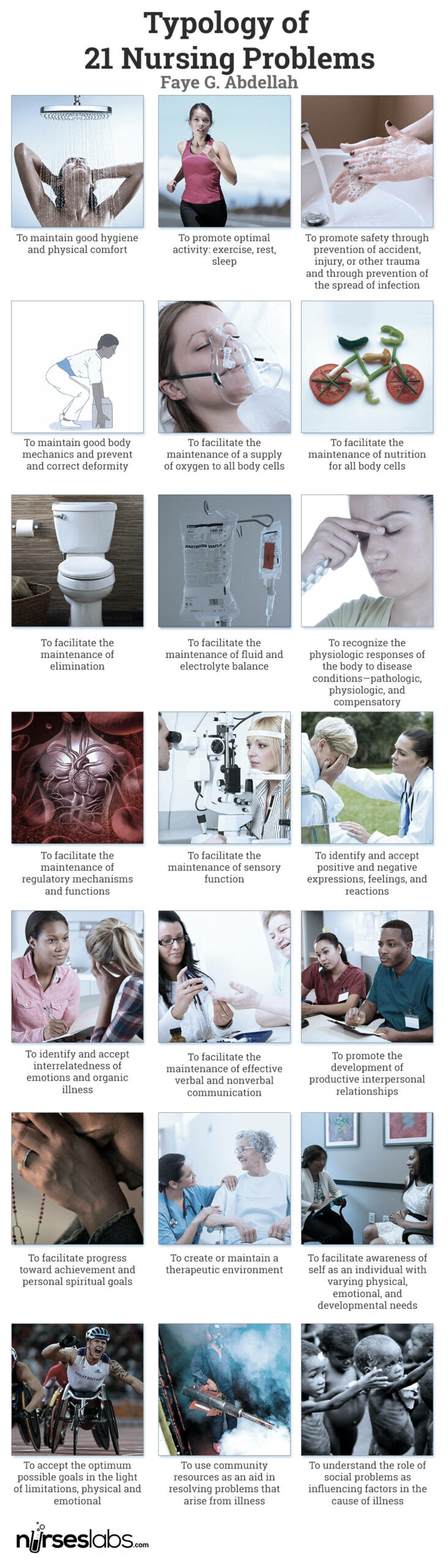
The 21 nursing problems fall into three categories: physical, sociological, and emotional needs of patients; types of interpersonal relationships between the patient and nurse; and common elements of patient care . She used Henderson’s 14 basic human needs and nursing research to establish the classification of nursing problems. Abdellah’s 21 Nursing Problems are the following:
- To maintain good hygiene and physical comfort .
- To promote optimal activity: exercise, rest, sleep
- To promote safety by preventing accidents, injuries, or other trauma and preventing the spread of infection .
- To maintain good body mechanics and prevent and correct the deformity.
- To facilitate the maintenance of a supply of oxygen to all body cells.
- To facilitate the maintenance of nutrition for all body cells.
- To facilitate the maintenance of elimination.
- To facilitate the maintenance of fluid and electrolyte balance.
- To recognize the physiologic responses of the body to disease conditions—pathologic, physiologic, and compensatory.
- To facilitate the maintenance of regulatory mechanisms and functions.
- To facilitate the maintenance of sensory function.
- To identify and accept positive and negative expressions, feelings, and reactions.
- To identify and accept interrelatedness of emotions and organic illness.
- To facilitate the maintenance of effective verbal and nonverbal communication .
- To promote the development of productive interpersonal relationships.
- To facilitate progress toward achievement and personal spiritual goals.
- To create or maintain a therapeutic environment.
- To facilitate awareness of self as an individual with varying physical, emotional, and developmental needs.
- To accept the optimum possible goals in the light of limitations, physical and emotional.
- To use community resources as an aid in resolving problems that arise from an illness.
- To understand the role of social problems as influencing factors in the cause of illness.
Moreover, patients’ needs are further divided into four categories: basic to all patients , sustenance care needs , remedial care needs , and restorative care needs .
The basic needs of an individual patient are to maintain good hygiene and physical comfort ; promote optimal health through healthy activities, such as exercise, rest, and sleep ; promote safety through the prevention of health hazards like accidents, injury , or other trauma and the prevention of the spread of infection; and maintain good body mechanics and prevent or correct deformity.
Sustenal care needs to facilitate the maintenance of a supply of oxygen to all body cells; facilitate the maintenance of nutrition of all body cells; facilitate the maintenance of elimination; facilitate the maintenance of fluid and electrolyte balance; recognize the physiological responses of the body to disease conditions; facilitate the maintenance of regulatory mechanisms and functions, and facilitate the maintenance of sensory function.
Remedial care needs to identify and accept positive and negative expressions, feelings, and reactions; identify and accept the interrelatedness of emotions and organic illness; facilitate the maintenance of effective verbal and non- verbal communication ; promote the development of productive interpersonal relationships; facilitate progress toward achievement of personal spiritual goals; create and maintain a therapeutic environment; and facilitate awareness of the self as an individual with varying physical, emotional, and developmental needs.
Restorative care needs include the acceptance of the optimum possible goals in light of limitations, both physical and emotional; the use of community resources as an aid to resolving problems that arise from an illness; and the understanding of the role of social problems as influential factors in the case of illness.
Abdellah’s work, based on the problem-solving method, serves as a vehicle for delineating nursing (patient) problems as the patient moves toward a healthy outcome. The theory identifies ten steps to identify the patient’s problem and 11 nursing skills to develop a treatment typology.

The ten steps are:
- Validate the patient’s conclusions about his nursing problems.
- Continue to observe and evaluate the patient over a period of time to identify any attitudes and clues affecting his or her behavior.
- Explore the patient and their family’s reactions to the therapeutic plan and involve them in the plan.
- Identify how the nurses feel about the patient’s nursing problems.
The 11 nursing skills are:
- observation of health status
- skills of communication
- application of knowledge
- the teaching of patients and families
- planning and organization of work
- use of resource materials
- use of personnel resources
- problem-solving
- the direction of work of others
- therapeutic uses of the self
- nursing procedure
Abdellah also explained nursing as a comprehensive service, which includes:
- Recognizing the nursing problems of the patient
- Deciding the appropriate course of action to take in terms of relevant nursing principles
- Providing continuous care of the individual’s total needs
- Providing continuous care to relieve pain and discomfort and provide immediate security for the individual
- Adjusting the total nursing care plan to meet the patient’s individual needs
- Helping the individual to become more self- directing in attaining or maintaining a healthy state of body and mind
- Instructing nursing personnel and family to help the individual do for himself that which he can within his limitations
- Helping the individual to adjust to his limitations and emotional problems
- Working with allied health professions in planning for optimum health on local, state, national, and international levels
- Carrying out continuous evaluation and research to improve nursing techniques and to develop new techniques to meet people’s health needs
Faye Abdellah’s work is a set of problems formulated in terms of nursing-centered services used to determine the patient’s needs. The nursing-centered orientation to client care appears to be contradicting the client-centered approach that Abdellah professes to support. This can be observed by her desire to move away from a disease-centered orientation.
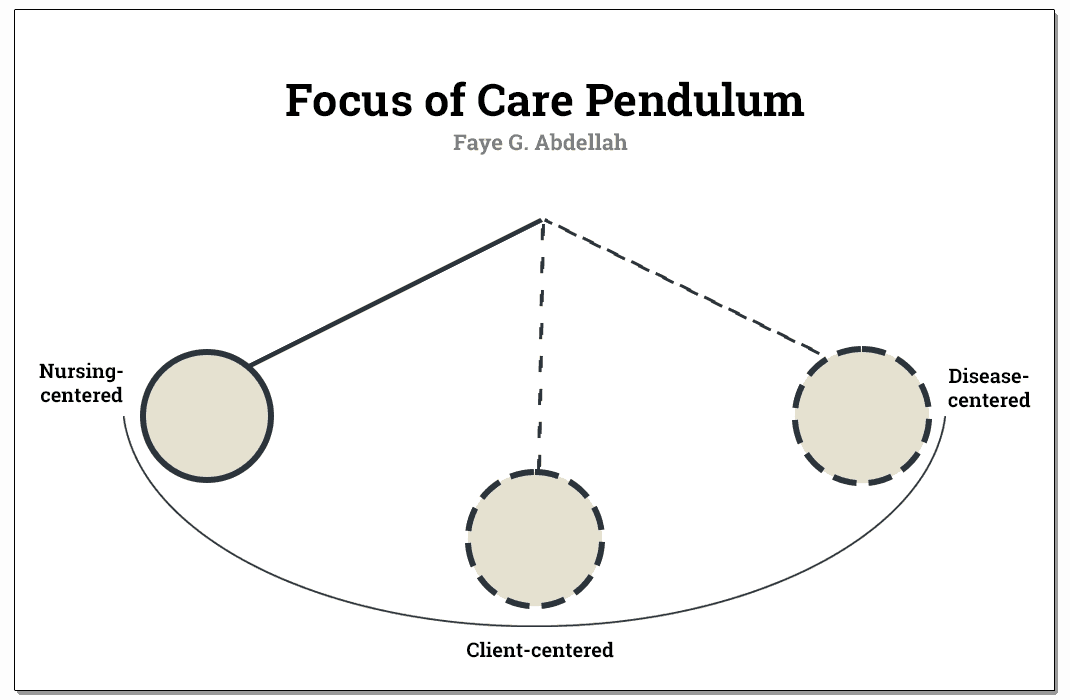
In her attempt to bring the nursing practice to its proper relationship with restorative and preventive measures for meeting total client needs, she seems to swing the pendulum to the opposite pole, from the disease orientation to nursing orientation, while leaving the client somewhere in the middle.
The nursing process in Abdellah’s theory includes assessment , nursing diagnosis , planning, implementation , and evaluation.
In the assessment phase , the nursing problems implement a standard procedure for data collection . A principle underlying the problem-solving approach is that for each identified problem, pertinent data is collected. The overt or covert nature of problems necessitates a direct or indirect approach, respectively.
The outcome of the collection of data in the first phase concludes the patient’s possible problems, which can be grouped under one or more of the broader nursing problems. This will further lead to the nursing diagnosis .
After formulating the diagnosis, a nursing care plan is developed, and appropriate nursing interventions are determined. The nurse now sets those interventions in action, which complete the implementation phase of the nursing process .
The evaluation takes place after the interventions have been carried out. The most convenient evaluation would be the nurse’s progress or lack of progress toward achieving the goals established in the planning phase.
With Faye Abdellah’s aim in formulating a clear categorization of patient’s problems as health needs, she rather conceptualized nurses’ actions in nursing care, which is contrary to her aim. Nurses’ roles were defined to alleviate the problems assessed through the proposed problem-solving approach.
The problem-solving approach introduced by Abdellah has the advantage of increasing the nurse’s critical and analytical thinking skills since the care to be provided would be based on sound assessment and validation of findings.
One can identify that the framework is strongly applied to individuals as the focus of nursing care. The inclusion of an aggregate of people such as the community or society would make the theory of Abdellah more generalizable since nurses do not only provide one-person service, especially now that the community healthcare level is sought to have higher importance than curative efforts in the hospital.
The following are the strengths of Faye Abdellah’s “21 Nursing Problems” theory.
- The problem-solving approach is readily generalizable to the client with specific health needs and specific nursing problems.
- With the model’s nature, healthcare providers and practitioners can use Abdellah’s problem-solving approach to guide various activities within the clinical setting. This is true when considering a nursing practice that deals with clients with specific needs and specific nursing problems.
- The language of Faye Abdellah’s framework is simple and easy to comprehend.
- The theoretical statement greatly focuses on problem-solving, an activity that is inherently logical in nature.
The following are the limitations of Faye Abdellah’s “21 Nursing Problems” theory.
- The major limitation to Abdellah’s theory and the 21 nursing problems is their robust nurse-centered orientation. She rather conceptualized nurses’ actions in nursing care which is contrary to her aim.
- Another point is the lack of emphasis on what the client is to achieve was given in client care.
- The framework seems to focus quite heavily on nursing practice and individuals. This somewhat limits the generalizing ability, although the problem-solving approach is readily generalizable to clients with specific health needs and specific nursing.
- Also, Abdellah’s framework is inconsistent with the concept of holism. The nature of the 21 nursing problems attests to this. As a result, the client may be diagnosed with numerous problems leading to fractionalized care efforts. Potential problems might be overlooked because the client is not deemed to be in a particular illness stage.
Abdellah’s typology of 21 nursing problems is a conceptual model mainly concerned with patient’s needs and nurses’ role in problem identification using a problem analysis approach.
According to the model, patients are described as having physical, emotional, and sociological needs. People are also the only justification for the existence of nursing. Without people, nursing would not be a profession since they are the recipients of nursing.
Patient-centered approaches to nursing health are described as a state mutually exclusive of illness. Abdellah does not define health but speaks to “total health needs” and “a healthy state of mind and body” in her nursing description.
However, Abdellah rather conceptualized nurses’ actions in nursing care, contrary to her aim of formulating a clear categorization of patients’ problems as health needs. Nurses’ roles were defined to alleviate the problems assessed through the proposed problem-solving approach.
As a whole, the theory is intended to guide care not just in the hospital setting but can also be applied to community nursing, as well. The model has interrelated concepts of health and nursing problems and problem-solving, which is inherently logical in nature.
Furthermore, the 21 nursing problems progressed to a second-generation development referred to as patient problems and patient outcomes . Abdellah educated the public on AIDS , drug addiction, violence, smoking, and alcoholism. Her work is a problem-centered approach or philosophy of nursing.
Recommended books and resources to learn more about nursing theory:
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. For more information, check out our privacy policy .
- Nursing Theorists and Their Work (10th Edition) by Alligood Nursing Theorists and Their Work, 10th Edition provides a clear, in-depth look at nursing theories of historical and international significance. Each chapter presents a key nursing theory or philosophy, showing how systematic theoretical evidence can enhance decision making, professionalism, and quality of care.
- Knowledge Development in Nursing: Theory and Process (11th Edition) Use the five patterns of knowing to help you develop sound clinical judgment. This edition reflects the latest thinking in nursing knowledge development and adds emphasis to real-world application. The content in this edition aligns with the new 2021 AACN Essentials for Nursing Education.
- Nursing Knowledge and Theory Innovation, Second Edition: Advancing the Science of Practice (2nd Edition) This text for graduate-level nursing students focuses on the science and philosophy of nursing knowledge development. It is distinguished by its focus on practical applications of theory for scholarly, evidence-based approaches. The second edition features important updates and a reorganization of information to better highlight the roles of theory and major philosophical perspectives.
- Nursing Theories and Nursing Practice (5th Edition) The only nursing research and theory book with primary works by the original theorists. Explore the historical and contemporary theories that are the foundation of nursing practice today. The 5th Edition, continues to meet the needs of today’s students with an expanded focus on the middle range theories and practice models.
- Strategies for Theory Construction in Nursing (6th Edition) The clearest, most useful introduction to theory development methods. Reflecting vast changes in nursing practice, it covers advances both in theory development and in strategies for concept, statement, and theory development. It also builds further connections between nursing theory and evidence-based practice.
- Middle Range Theory for Nursing (4th Edition) This nursing book’s ability to break down complex ideas is part of what made this book a three-time recipient of the AJN Book of the Year award. This edition includes five completely new chapters of content essential for nursing books. New exemplars linking middle range theory to advanced nursing practice make it even more useful and expand the content to make it better.
- Nursing Research: Methods and Critical Appraisal for Evidence-Based Practice This book offers balanced coverage of both qualitative and quantitative research methodologies. This edition features new content on trending topics, including the Next-Generation NCLEX® Exam (NGN).
- Nursing Research (11th Edition) AJN award-winning authors Denise Polit and Cheryl Beck detail the latest methodologic innovations in nursing, medicine, and the social sciences. The updated 11th Edition adds two new chapters designed to help students ensure the accuracy and effectiveness of research methods. Extensively revised content throughout strengthens students’ ability to locate and rank clinical evidence.
Recommended site resources related to nursing theory:
- Nursing Theories and Theorists: The Definitive Guide for Nurses MUST READ! In this guide for nursing theories, we aim to help you understand what comprises a nursing theory and its importance, purpose, history, types or classifications, and give you an overview through summaries of selected nursing theories.
Other resources related to nursing theory:
- Betty Neuman: Neuman Systems Model
- Dorothea Orem: Self-Care Deficit Theory
- Dorothy Johnson: Behavioral System Model
- Florence Nightingale: Environmental Theory
- Hildegard Peplau: Interpersonal Relations Theory
- Ida Jean Orlando: Deliberative Nursing Process Theory
- Imogene King: Theory of Goal Attainment
- Jean Watson: Theory of Human Caring
- Lydia Hall: Care, Cure, Core Nursing Theory
- Madeleine Leininger: Transcultural Nursing Theory
- Martha Rogers: Science of Unitary Human Beings
- Myra Estrin Levine: The Conservation Model of Nursing
- Nola Pender: Health Promotion Model
- Sister Callista Roy: Adaptation Model of Nursing
- Virginia Henderson: Nursing Need Theory
- Abdellah, F.G. The federal role in nursing education. Nursing outlook. 1987, 35(5),224-225.
- Abdellah, F.G. Public policy impacting on nursing care of older adults. In E.M. Baines (Ed.), perspectives on gerontological nursing. Newbury, CA: Sage publications. 1991.
- Abdellah, F.G., & Levine, E. Preparing nursing research for the 21st century. New York: Springer. 1994.
- Abdellah, F.G., Beland, I.L., Martin, A., & Matheney, R.V. Patient-centered approaches to nursing (2nd ed.). New York: Mac Millan. 1968.
- Abdellah, F.G. Evolution of nursing as a profession: perspective on manpower development. International Nursing Review, 1972); 19, 3..
- Abdellah, F.G.). The nature of nursing science. In L.H. Nicholl (Ed.), perspectives on nursing theory. Boston: Little, Brown, 1986.
- Craddock, J. (2013). Encyclopedia of world biography supplement. Detroit, Mich.: Gale. https://www.encyclopedia.com/doc/1G2-3435000010.html
- Better Patient Care Through Nursing Research
- Preparing Nursing Research for the 21st Century: Evolution, Methodologies, Challenges
With contributions by Wayne, G. (for Biography), Vera, M.
6 thoughts on “Faye Abdellah: 21 Nursing Problems Theory”
Thank you for sharing Angelo
I mean no disrespect to RADM Abdellah’s service to our nation, but the USPHS is not part of the military. It is part of the Uniformed Services, but not in the Dept of Defense.
Oh! Good to know! Thanks for clarifying :)
An insightful information 👌
I was a brand new lieutenant US Army and just graduated from college to become a nurse. I had used Faye Abdellah’s Theories as the rationale for nursing care plans in school papers, so I was very familiar. A big professional regret was I had the opportunity to meet Faye at a nursing conference in Germany. I was a timid young nurse and somewhat shy and saw her in one of the conference sessions sitting by herself. I wish I introduced myself and talked to her. I really respected her as a pioneer in nursing theory.
thanks for sharing.
Leave a Comment Cancel reply

ANA Nursing Resources Hub
Search Resources Hub

Critical Thinking in Nursing: Tips to Develop the Skill
4 min read • February, 09 2024
Critical thinking in nursing helps caregivers make decisions that lead to optimal patient care. In school, educators and clinical instructors introduced you to critical-thinking examples in nursing. These educators encouraged using learning tools for assessment, diagnosis, planning, implementation, and evaluation.
Nurturing these invaluable skills continues once you begin practicing. Critical thinking is essential to providing quality patient care and should continue to grow throughout your nursing career until it becomes second nature.
What Is Critical Thinking in Nursing?
Critical thinking in nursing involves identifying a problem, determining the best solution, and implementing an effective method to resolve the issue using clinical decision-making skills.
Reflection comes next. Carefully consider whether your actions led to the right solution or if there may have been a better course of action.
Remember, there's no one-size-fits-all treatment method — you must determine what's best for each patient.
How Is Critical Thinking Important for Nurses?
As a patient's primary contact, a nurse is typically the first to notice changes in their status. One example of critical thinking in nursing is interpreting these changes with an open mind. Make impartial decisions based on evidence rather than opinions. By applying critical-thinking skills to anticipate and understand your patients' needs, you can positively impact their quality of care and outcomes.
Elements of Critical Thinking in Nursing
To assess situations and make informed decisions, nurses must integrate these specific elements into their practice:
- Clinical judgment. Prioritize a patient's care needs and make adjustments as changes occur. Gather the necessary information and determine what nursing intervention is needed. Keep in mind that there may be multiple options. Use your critical-thinking skills to interpret and understand the importance of test results and the patient’s clinical presentation, including their vital signs. Then prioritize interventions and anticipate potential complications.
- Patient safety. Recognize deviations from the norm and take action to prevent harm to the patient. Suppose you don't think a change in a patient's medication is appropriate for their treatment. Before giving the medication, question the physician's rationale for the modification to avoid a potential error.
- Communication and collaboration. Ask relevant questions and actively listen to others while avoiding judgment. Promoting a collaborative environment may lead to improved patient outcomes and interdisciplinary communication.
- Problem-solving skills. Practicing your problem-solving skills can improve your critical-thinking skills. Analyze the problem, consider alternate solutions, and implement the most appropriate one. Besides assessing patient conditions, you can apply these skills to other challenges, such as staffing issues .

How to Develop and Apply Critical-Thinking Skills in Nursing
Critical-thinking skills develop as you gain experience and advance in your career. The ability to predict and respond to nursing challenges increases as you expand your knowledge and encounter real-life patient care scenarios outside of what you learned from a textbook.
Here are five ways to nurture your critical-thinking skills:
- Be a lifelong learner. Continuous learning through educational courses and professional development lets you stay current with evidence-based practice . That knowledge helps you make informed decisions in stressful moments.
- Practice reflection. Allow time each day to reflect on successes and areas for improvement. This self-awareness can help identify your strengths, weaknesses, and personal biases to guide your decision-making.
- Open your mind. Don't assume you're right. Ask for opinions and consider the viewpoints of other nurses, mentors , and interdisciplinary team members.
- Use critical-thinking tools. Structure your thinking by incorporating nursing process steps or a SWOT analysis (strengths, weaknesses, opportunities, and threats) to organize information, evaluate options, and identify underlying issues.
- Be curious. Challenge assumptions by asking questions to ensure current care methods are valid, relevant, and supported by evidence-based practice .
Critical thinking in nursing is invaluable for safe, effective, patient-centered care. You can successfully navigate challenges in the ever-changing health care environment by continually developing and applying these skills.
Images sourced from Getty Images
Related Resources

Item(s) added to cart

How To Improve Critical Thinking Skills In Nursing? 24 Strategies With Examples
Last updated on August 19th, 2023
Nurses play a critical role in making critical decisions that directly impact patient outcomes in the dynamic field of healthcare. Developing strong critical thinking skills is essential for success in this role.
In this article, we present a comprehensive list of 23 nursing-specific strategies aimed at improving critical thinking and improve the quality of patient care.
24 Strategies to improve critical thinking skills in nursing
You may also want to check out: 15 Attitudes of Critical Thinking in Nursing (Explained W/ Examples)
1. Reflective Journaling: Delving into Deeper Understanding
Reflective journaling is a potent tool for nurses to explore their experiences, actions, and decisions.
By regularly pondering over situations and analyzing their thought processes, nurses can identify strengths and areas for improvement.
This practice encourages the conscious development of critical thinking by comparing past experiences with current knowledge and exploring alternative solutions.
After a particularly challenging case, a nurse reflects on their decision-making process, exploring what worked well and what could have been done differently.
2. Meeting with Colleagues: Collaborative Learning for Critical Thinking
Regular interactions with colleagues foster a collaborative learning environment. Sharing experiences, discussing diverse viewpoints, and providing constructive feedback enhance critical thinking skills .
Colleagues’ insights can challenge assumptions and broaden perspectives, ultimately leading to more well-rounded clinical judgments.
A nursing team gathers to discuss a recent complex case, sharing their perspectives, insights, and lessons learned to collectively improve patient care strategies.
3. Concept Mapping: Visualizing Complexity
Concept mapping is an excellent technique to synthesize intricate patient information. By creating visual representations of patient problems and interventions, nurses can identify relationships and patterns that might not be apparent otherwise.
This strategy aids in comprehensive care planning and encourages nurses to think holistically about patient care.
Creating a concept map to connect patient symptoms, diagnostics, and interventions reveals patterns that help the nurse formulate a comprehensive care plan.
4. Socratic Questioning: Digging Deeper into Situations
The art of Socratic questioning involves asking probing questions that lead to deeper understanding.
Applying this technique allows nurses to uncover assumptions, examine inconsistencies, and explore multiple viewpoints.
This approach is especially valuable when reviewing patient history, discussing conditions, and planning care strategies.
When assessing a patient’s deteriorating condition, a nurse asks probing questions to uncover potential underlying causes and prioritize appropriate interventions.
5. Inductive and Deductive Reasoning: From Specifics to Generalizations
Developing skills in both inductive and deductive reasoning equips nurses to analyze situations from different angles.
Inductive reasoning involves drawing conclusions from specific observations, while deductive reasoning starts with general premises to arrive at specific conclusions.
Proficient use of these methods enhances nurses’ ability to make accurate clinical judgments.
When encountering a series of patients with similar symptoms, a nurse uses inductive reasoning to identify a common pattern and deduce potential causes.
6. Distinguishing Statements: Fact, Inference, Judgment, and Opinion
Clear thinking demands the ability to differentiate between statements of fact, inference, judgment, and opinion.
Nurses must critically evaluate information sources, ensuring they rely on evidence-based practice.
This skill safeguards against misinformation and supports informed decision-making.
While reviewing a patient’s history, a nurse differentiates factual medical information from inferences and subjective judgments made by different healthcare professionals.
7. Clarifying Assumptions: Promoting Effective Communication
Recognizing assumptions and clarifying their underlying principles is vital for effective communication. Nurses often hold differing assumptions, which can impact patient care.
By acknowledging these assumptions and encouraging open discussions, nursing teams can collaboratively create care plans that align with patients’ best interests.
Before suggesting a treatment plan, a nurse engages in a conversation with a patient to understand their cultural beliefs and preferences, ensuring assumptions are not made.
8. Clinical Simulations: Learning through Virtual Scenarios
Clinical simulations provide nurses with a risk-free environment to practice decision-making and problem-solving skills.
These virtual scenarios mimic real-life patient situations and allow nurses to test different approaches, assess outcomes, and reflect on their choices.
By engaging in simulations, nurses can refine their critical thinking abilities, learn from mistakes, and gain confidence in their clinical judgment.
Engaging in a simulated scenario where a patient’s condition rapidly changes challenges a nurse’s decision-making skills in a controlled environment.
9. Case Studies and Grand Rounds: Analyzing Complex Cases
Engaging in case studies and participating in grand rounds exposes nurses to complex patient cases that require in-depth analysis.
Working through these scenarios encourages nurses to consider various factors, potential interventions, and their rationale.
Discussing these cases with colleagues and experts fosters collaborative critical thinking and widens the spectrum of possible solutions.
Nurses participate in grand rounds, discussing a challenging case involving multiple medical specialties, encouraging a holistic approach to patient care.
10. Continuing Education and Lifelong Learning: Expanding Knowledge
Staying up-to-date with the latest advancements in nursing and healthcare is crucial for effective critical thinking.
Pursuing continuing education opportunities, attending conferences, and engaging in self-directed learning keeps nurses informed about new research, technologies, and best practices.
This continuous learning enriches their knowledge base, enabling them to approach patient care with a well-rounded perspective.
Attending a nursing conference on the latest advancements in wound care equips a nurse with evidence-based techniques to improve patient outcomes.
11. Debates and Discussions: Encouraging Thoughtful Dialogue
Organizing debates or participating in structured discussions on healthcare topics stimulates critical thinking.
Engaging in debates requires researching and presenting evidence-based arguments, promoting the evaluation of different perspectives.
Nurses can exchange insights, challenge assumptions, and refine their ability to defend their viewpoints logically.
Engaging in a debate on the pros and cons of a new treatment method encourages nurses to critically analyze different viewpoints and strengthen their own understanding.
12. Multidisciplinary Collaboration: Gaining Insights from Various Disciplines
Collaborating with professionals from diverse healthcare disciplines enriches nurses’ critical thinking.
Interacting with doctors, pharmacists, therapists, and other experts allows nurses to benefit from different viewpoints and approaches.
This cross-disciplinary collaboration broadens their understanding and encourages innovative problem-solving.
Collaborating with physical therapists, nutritionists, and pharmacists helps a nurse develop a holistic care plan that addresses all aspects of a patient’s recovery.
13. Ethical Dilemma Analysis: Balancing Patient Autonomy and Best Practice
Ethical dilemmas are common in nursing practice. Analyzing these situations requires nurses to weigh the principles of beneficence, non-maleficence, autonomy, and justice.
By critically examining ethical scenarios, nurses develop the capacity to navigate morally complex situations, prioritize patient welfare, and make ethically sound decisions.
When faced with a patient’s refusal of treatment due to religious beliefs, a nurse evaluates the ethical considerations, respects autonomy, and seeks alternatives.
14. Root Cause Analysis: Investigating Adverse Events
When adverse events occur, performing a root cause analysis helps identify the underlying causes and contributing factors.
Nurses engage in a systematic process of analyzing events, exploring the “5 Whys” technique , and developing strategies to prevent similar occurrences in the future.
This approach cultivates a thorough and analytical approach to problem-solving.
After a medication error, a nurse leads a root cause analysis to identify system failures and implement preventive measures to enhance patient safety.
15. Creative Thinking Exercises: Expanding Solution Repertoire
Encouraging creative thinking through brainstorming sessions or scenario-based exercises widens the range of possible solutions nurses consider.
By thinking outside the box and exploring innovative approaches, nurses develop adaptable problem-solving skills that can be applied to complex patient care challenges.
Brainstorming creative approaches to comfort a distressed pediatric patient empowers a nurse to find innovative methods beyond routine interventions.
16. Journal Clubs: Fostering Evidence-Based Discussion
Participating in journal clubs involves healthcare professionals coming together to dissect recent research articles.
This practice ignites critical thinking by allowing nurses to evaluate study methodologies, scrutinize findings, and consider the implications for their practice.
Engaging in evidence-based discussions not only cultivates a culture of critical inquiry but also reinforces continuous learning.
At the monthly journal club meeting, Nurse Mark engages in a discussion on a recent research article focusing on pain management strategies for post-operative patients.
The group analyzes the study design, scrutinizes the findings, and considers the potential implications for their practice.
During the discussion, Mark raises thought-provoking questions about the study’s methodology and suggests potential applications in their hospital’s patient care protocols.
This active participation in journal clubs not only refines Mark’s critical thinking but also instills evidence-based practices into his nursing approach.
17. Critical Reflection Groups: Collaborative Learning and Analysis
Similarly, establishing critical reflection groups, where nurses meet regularly to discuss experiences, cases, and challenges, fosters collective learning.
These sessions encourage the exchange of diverse perspectives, enriching the analysis process and ultimately enhancing patient care strategies.
Through shared insights and discussions, nurses can refine their clinical reasoning and broaden their problem-solving capabilities.
Nurse Emma actively participates in critical reflection groups in order to broaden her clinical knowledge. During a recent meeting, the group tackled a difficult patient case with complicated symptomatology.
Emma suggests alternative diagnostic pathways based on her own experiences. Emma’s critical thinking skills are honed as a result of the group’s dynamic interaction, which also emphasizes the importance of collaborative decision-making in complex scenarios.
18. Mindfulness and Reflection Practices: Enhancing Self-Awareness
Mindfulness techniques, such as meditation and deep breathing, encourage self-awareness and a clear mind.
Engaging in these practices helps nurses become more attuned to their thoughts and emotions, leading to better self-regulation and improved decision-making during high-pressure situations.
Engaging in mindfulness exercises before a demanding shift helps a nurse maintain focus, manage stress, and make clear-headed decisions.
19. Problem-Based Learning: Applying Knowledge in Real Scenarios
Problem-based learning involves presenting nurses with real-world patient cases and encouraging them to collaboratively solve the problems.
This approach bridges the gap between theoretical knowledge and practical application, fostering critical thinking through active problem-solving.
Working through a simulated patient case challenges nurses to apply theoretical knowledge to practical situations, refining their clinical reasoning.
20. Self-Assessment and Feedback: Evaluating Decision-Making Skills
Regularly assessing one’s own decision-making process and seeking feedback from peers and mentors is essential for improvement.
Reflecting on past decisions, considering alternative approaches, and understanding the rationale behind them contribute to the refinement of critical thinking skills.
A nurse evaluates their performance after a patient’s unexpected complication, seeking feedback from peers and mentors to identify areas for improvement.
21. Cultural Competence Training: Navigating Diverse Perspectives
Cultural competence training enhances critical thinking by enabling nurses to understand the diverse cultural beliefs and practices of patients.
This knowledge is vital for providing patient-centered care, as it encourages nurses to think critically about the unique needs of each individual.
A nurse attends cultural competence training to understand the dietary preferences of a diverse patient population, ensuring respectful and patient-centered care.
22. Active Listening and Empathetic Communication: Gathering Insights
Active listening and empathetic communication with patients and their families enable nurses to gather comprehensive information about their conditions, concerns, and preferences.
This data forms the basis for critical analysis and informed decision-making in patient care.
Through attentive listening, a nurse uncovers a patient’s underlying concerns, leading to an informed care plan that addresses both medical needs and emotional well-being.
23. Mentorship and Preceptorship: Learning from Experienced Professionals
Having a mentor or preceptor provides novice nurses with the opportunity to learn from experienced professionals.
Mentors guide critical thinking by sharing their insights, challenging assumptions, and offering guidance in complex situations. This relationship fosters growth and expertise development.
A novice nurse gains valuable insight from a mentor, who guides them through complex cases, offering real-world wisdom and refining critical thinking skills.
24. Self-Assessment and Feedback: Evaluating Decision-Making Skills
Reflecting on past decisions, considering alternative approaches, and understanding the rationale behind them contribute to the refinement of critical thinking skills .
Nurse Sarah regularly takes time to assess her decision-making skills by reviewing past patient cases. After a challenging case involving conflicting symptoms, she reflects on her initial approach, the outcomes, and what she could have done differently.
She seeks feedback from her senior colleague, who provides insights on alternative diagnostic paths. Sarah’s self-assessment and feedback-seeking process enable her to identify areas for improvement and refine her critical thinking in similar situations.
- Clinical Reasoning In Nursing (Explained W/ Example)
- 8 Stages Of The Clinical Reasoning Cycle
- What is Critical Thinking in Nursing? (Explained W/ Examples)
Enhancing critical thinking skills is an ongoing journey that transforms nursing practice.
Reflective journaling, collaborative learning, concept mapping, Socratic questioning , reasoning techniques, distinguishing statements, and clarifying assumptions all play integral roles in nurturing these skills.
By incorporating these strategies into their daily routines, nurses can improve their critical thinking skills.
Additionally, this will help nurses in navigating the complexities of the healthcare field with confidence, expertise, and the ability to make well-informed decisions that improve patient outcomes.
Comments are closed.
Medical & Legal Disclaimer
All the contents on this site are for entertainment, informational, educational, and example purposes ONLY. These contents are not intended to be used as a substitute for professional medical advice or practice guidelines. However, we aim to publish precise and current information. By using any content on this website, you agree never to hold us legally liable for damages, harm, loss, or misinformation. Read the privacy policy and terms and conditions.
Privacy Policy
Terms & Conditions
© 2024 nurseship.com. All rights reserved.
Account Management
Log in to manage your policy, generate a certificate of insurance (COI), make a payment, and more.
Log in to your account to update your information or manage your policy.
Download a Certificate of Insurance (COI) to provide to your employer.
Make a Payment
Make a one-time payment, set up autopay, or update your payment information.
Submit a notice of an incident or claim in just minutes.
Topics on this page:
Why Critical Thinking in Nursing Is Important
8 examples of critical thinking in nursing, improving the quality of patient care, the importance of critical thinking in nursing.
Jul 24, 2024
While not every decision is an immediate life-and-death situation, there are hundreds of decisions nurses must make every day that impact patient care in ways small and large.
“Being able to assess situations and make decisions can lead to life-or-death situations,” said nurse anesthetist Aisha Allen . “Critical thinking is a crucial and essential skill for nurses.”
The National League for Nursing Accreditation Commission (NLNAC) defines critical thinking in nursing this way: “the deliberate nonlinear process of collecting, interpreting, analyzing, drawing conclusions about, presenting, and evaluating information that is both factually and belief-based. This is demonstrated in nursing by clinical judgment, which includes ethical, diagnostic, and therapeutic dimensions and research.”
An eight-year study by Johns Hopkins reports that 10% of deaths in the U.S. are due to medical error — the third-highest cause of death in the country.
“Diagnostic errors, medical mistakes, and the absence of safety nets could result in someone’s death,” wrote Dr. Martin Makary , professor of surgery at Johns Hopkins University School of Medicine.
Everyone makes mistakes — even doctors. Nurses applying critical thinking skills can help reduce errors.
“Question everything,” said pediatric nurse practitioner Ersilia Pompilio RN, MSN, PNP . “Especially doctor’s orders.” Nurses often spend more time with patients than doctors and may notice slight changes in conditions that may not be obvious. Resolving these observations with treatment plans can help lead to better care.
Key Nursing Critical Thinking Skills
Some of the most important critical thinking skills nurses use daily include interpretation, analysis, evaluation, inference, explanation, and self-regulation.
- Interpretation: Understanding the meaning of information or events.
- Analysis: Investigating a course of action based on objective and subjective data.
- Evaluation: Assessing the value of information and its credibility.
- Inference: Making logical deductions about the impact of care decisions.
- Explanation: Translating complicated and often complex medical information to patients and families in a way they can understand to make decisions about patient care.
- Self-Regulation: Avoiding the impact of unconscious bias with cognitive awareness.
These skills are used in conjunction with clinical reasoning. Based on training and experience, nurses use these skills and then have to make decisions affecting care.
It’s the ultimate test of a nurse’s ability to gather reliable data and solve complex problems. However, critical thinking goes beyond just solving problems. Critical thinking incorporates questioning and critiquing solutions to find the most effective one. For example, treating immediate symptoms may temporarily solve a problem, but determining the underlying cause of the symptoms is the key to effective long-term health.
Here are some real-life examples of how nurses apply critical thinking on the job every day, as told by nurses themselves.
Example #1: Patient Assessments
“Doing a thorough assessment on your patient can help you detect that something is wrong, even if you’re not quite sure what it is,” said Shantay Carter , registered nurse and co-founder of Women of Integrity . “When you notice the change, you have to use your critical thinking skills to decide what’s the next step. Critical thinking allows you to provide the best and safest care possible.”
Example #2: First Line of Defense
Often, nurses are the first line of defense for patients.
“One example would be a patient that had an accelerated heart rate,” said nurse educator and adult critical care nurse Dr. Jenna Liphart Rhoads . “As a nurse, it was my job to investigate the cause of the heart rate and implement nursing actions to help decrease the heart rate prior to calling the primary care provider.”
Nurses with poor critical thinking skills may fail to detect a patient in stress or deteriorating condition. This can result in what’s called a “ failure to rescue ,” or FTR, which can lead to adverse conditions following a complication that leads to mortality.
Example #3: Patient Interactions
Nurses are the ones taking initial reports or discussing care with patients.
“We maintain relationships with patients between office visits,” said registered nurse, care coordinator, and ambulatory case manager Amelia Roberts . “So, when there is a concern, we are the first name that comes to mind (and get the call).”
“Several times, a parent called after the child had a high temperature, and the call came in after hours,” Roberts said. “Doing a nursing assessment over the phone is a special skill, yet based on the information gathered related to the child’s behavior (and) fluid intake, there were several recommendations I could make.”
Deciding whether it was OK to wait until the morning, page the primary care doctor, or go to the emergency room to be evaluated takes critical thinking.
Example #4: Using Detective Skills
Nurses have to use acute listening skills to discern what patients are really telling them (or not telling them) and whether they are getting the whole story.
“I once had a 5-year-old patient who came in for asthma exacerbation on repeated occasions into my clinic,” said Pompilio. “The mother swore she was giving her child all her medications, but the asthma just kept getting worse.”
Pompilio asked the parent to keep a medication diary.
“It turned out that after a day or so of medication and alleviation in some symptoms, the mother thought the child was getting better and stopped all medications,” she said.
Example #5: Prioritizing
“Critical thinking is present in almost all aspects of nursing, even those that are not in direct action with the patient,” said Rhoads. “During report, nurses decide which patient to see first based on the information gathered, and from there they must prioritize their actions when in a patient’s room. Nurses must be able to scrutinize which medications can be taken together, and which modality would be best to help a patient move from the bed to the chair.”
A critical thinking skill in prioritization is cognitive stacking. Cognitive stacking helps create smooth workflow management to set priorities and help nurses manage their time. It helps establish routines for care while leaving room within schedules for the unplanned events that will inevitably occur. Even experienced nurses can struggle with juggling today’s significant workload, prioritizing responsibilities, and delegating appropriately.
Example #6: Medication & Care Coordination
Another aspect that often falls to nurses is care coordination. A nurse may be the first to notice that a patient is having an issue with medications.
“Based on a report of illness in a patient who has autoimmune challenges, we might recommend that a dose of medicine that interferes with immune response be held until we communicate with their specialty provider,” said Roberts.
Nurses applying critical skills can also help ease treatment concerns for patients.
“We might recommend a patient who gets infusions come in earlier in the day to get routine labs drawn before the infusion to minimize needle sticks and trauma,” Robert said.
Example #7: Critical Decisions
During the middle of an operation, the anesthesia breathing machine Allen was using malfunctioned.
“I had to critically think about whether or not I could fix this machine or abandon that mode of delivering nursing anesthesia care safely,” she said. “I chose to disconnect my patient from the malfunctioning machine and retrieve tools and medications to resume medication administration so that the surgery could go on.”
Nurses are also called on to do rapid assessments of patient conditions and make split-second decisions in the operating room.
“When blood pressure drops, it is my responsibility to decide which medication and how much medication will fix the issue,” Allen said. “I must work alongside the surgeons and the operating room team to determine the best plan of care for that patient’s surgery.”
“On some days, it seems like you are in the movie ‘The Matrix,’” said Pompilio. “There’s lots of chaos happening around you. Your patient might be decompensating. You have to literally stop time and take yourself out of the situation and make a decision.”
Example #8: Fast & Flexible Decisions
Allen said she thinks electronics are great, but she can remember a time when technology failed her.
“The hospital monitor that gives us vitals stopped correlating with real-time values,” she said. “So I had to rely on basic nursing skills to make sure my patient was safe. (Pulse check, visual assessments, etc.)”
In such cases, there may not be enough time to think through every possible outcome. Critical thinking combined with experience gives nurses the ability to think quickly and make the right decisions.
Nurses who think critically are in a position to significantly increase the quality of patient care and avoid adverse outcomes.
“Critical thinking allows you to ensure patient safety,” said Carter. “It’s essential to being a good nurse.”
Nurses must be able to recognize a change in a patient’s condition, conduct independent interventions, anticipate patients and provider needs, and prioritize. Such actions require critical thinking ability and advanced problem-solving skills.
“Nurses are the eyes and ears for patients, and critical thinking allows us to be their advocates,” said Allen.
Image courtesy of iStock.com/ davidf
Last updated on Jul 24, 2024. Originally published on Aug 25, 2021.
- Career Growth
The views expressed in this article are those of the author and do not necessarily reflect those of Berxi™ or Berkshire Hathaway Specialty Insurance Company. This article (subject to change without notice) is for informational purposes only, and does not constitute professional advice. Click here to read our full disclaimer
The product descriptions provided here are only brief summaries and may be changed without notice. The full coverage terms and details, including limitations and exclusions, are contained in the insurance policy. If you have questions about coverage available under our plans, please review the policy or contact us at 833-242-3794 or [email protected] . “20% savings” is based on industry pricing averages.
Berxi™ is a part of Berkshire Hathaway Specialty Insurance ( BHSI ). Insurance products are distributed through Berkshire Hathaway Global Insurance Services, California License # 0K09397. BHSI is part of Berkshire Hathaway’s National Indemnity group of insurance companies, consisting of National Indemnity and its affiliates, which hold financial strength ratings of A++ from AM Best and AA+ from Standard & Poor’s. The rating scales can be found at www.ambest.com and www.standardandpoors.com , respectively.
No warranty, guarantee, or representation, either expressed or implied, is made as to the correctness, accuracy, completeness, adequacy, or sufficiency of any representation or information. Any opinions expressed herein are subject to change without notice.
The information on this web site is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment, and does not purport to establish a standard of care under any circumstances. All content, including text, graphics, images and information, contained on or available through this web site is for general information purposes only based upon the information available at the time of presentation, and does not constitute medical, legal, regulatory, compliance, financial, professional, or any other advice.
BHSI makes no representation and assumes no responsibility or liability for the accuracy of information contained on or available through this web site, and such information is subject to change without notice. You are encouraged to consider and confirm any information obtained from or through this web site with other sources, and review all information regarding any medical condition or treatment with your physician or medical care provider. NEVER DISREGARD PROFESSIONAL MEDICAL ADVICE OR DELAY SEEKING MEDICAL TREATMENT BECAUSE OF SOMETHING THAT YOU HAVE READ ON OR ACCESSED THROUGH THIS WEB SITE.
BHSI is not a medical organization, and does not recommend, endorse or make any representation about the efficacy, appropriateness or suitability of any specific tests, products, procedures, treatments, services, opinions, health care providers or other information contained on or available through this web site. BHSI IS NOT RESPONSIBLE FOR, AND EXPRESSLY DISCLAIMS ALL LIABILITY FOR, ANY ADVICE, COURSE OF TREATMENT, DIAGNOSIS OR ANY OTHER SERVICES OR PRODUCTS THAT YOU OBTAIN AFTER REVIEWING THIS WEB SITE.
Want Berxi articles delivered straight to your inbox? Sign up for our monthly newsletter below!
" * " indicates required fields
How we use your email address Berxi will not sell or rent your email address to third parties unless otherwise notified. Other than where necessary to administer your insurance policy or where required by law, Berxi will not disclose your email address to third parties. Your email address is required to identify you for access to the Berxi website. You may also receive newsletters, product updates, and communications about quotes and policies.
Paul Dughi is a contributing writer for Berxi, as well as a journalist and freelance writer. He has held executive management positions in the media industry for the past 25 years.
Related Articles

Breaking Bad News to Patients: A Nurse’s Guide to SPIKES
Michael Walton Jul 24, 2024

Delegation in Nursing: Steps, Skills, & Solutions for Creating Balance at Work
Kristy Snyder Jul 24, 2024

The 7 Most Common Nursing Mistakes (And What You Can Do If You Make One)
Paul Dughi Jul 24, 2024
- LOGIN / FREE TRIAL

‘I have been appalled at the violence taking place over recent days’
STEVE FORD, EDITOR
- You are here: Archive
Thinking your way to successful problem-solving
13 September, 2001 By NT Contributor
VOL: 97, ISSUE: 37, PAGE NO: 36
Jacqueline Wheeler, DMS, MSc, RGN, is a lecturer at Buckinghamshire Chilterns University College
Problems - some people like them, some do not think they have any, while others shy away from them as if they were the plague. Opportunities, in the form of problems, are part of your life.
The most difficult decision is deciding to tackle a problem and implement a solution, especially as it is sometimes easier to ignore its existence. Problem-solving takes time and effort, but once a problem has been addressed the nurse can feel satisfied that the issue has been resolved and is therefore less likely to re-emerge.
Nurses make clinical decisions using two different approaches. The first is the rationalist approach, which involves an analysis of a situation so that subsequent actions are rational, logical and based on knowledge and judgement. The second approach is based on a phenomenological perspective, where a fluid, flexible and dynamic approach to decision-making is required, such as when dealing with an acutely ill patient.
Types of problems
Problems come in different guises and the solver can perceive them either as a challenge or a threat. One of the most common types of problem is when the unexpected happens. As a nurse you plan and implement care for a patient based on your knowledge and experience, only to find that the patient’s reaction is totally different from that expected but without any apparent reason.
Another type of problem is an assignment where others set a goal or task. Throughout your working life you will be required to undertake duties on behalf of other people. For some this is difficult as they feel unable to control their workload. Others see it as an opportunity to develop new skills or take on additional responsibilities. Opportunities can be perceived as problems by those who fear failure.
A third type of problem is when a dilemma arises. This is when it is difficult to choose the best solution to a problem because the nurse is confronted with something that challenges his or her personal and/or professional values.
Diagnosing problems
The sooner a problem is identified and solutions devised, the better for all involved. So try to anticipate or identify problems when they occur through continuously monitoring staff performance and patient outcomes.
Listening to and observing junior staff will help you to detect work or organisational concerns, because when there are problems staff are likely to behave in an unusual or inconsistent manner.
Initial analysis
Remember that people view things differently, so what you perceive as a problem may not be one to anyone else. So before you begin thinking about what to do - whether to keep it under surveillance, contain it or find a solution - you should undertake an initial analysis. This will help you to understand the problem more clearly.
An analysis will also enable you to prioritise its importance in relation to other problems as problems do not occur one at a time.
Routine problems often need little clarification, so an initial analysis is recommended for non-routine problems only. Even then, not all problems justify the same degree of analysis. But where it is appropriate, an initial analysis will provide a basis from which to generate solutions.
Perception is also important when dealing with patients’ problems. For example, if a patient gives up reading because he or she cannot hold the book (objective), the nurse may assume it is because the patient has lost interest (subjective, one’s own view).
Generating solutions
It is essential for the problem-solver to remember that, where possible, solutions must come from those connected with the problem. If it is to be resolved, agreement must be owned by those involved as they are probably the best and only people who can resolve their differences. The manager should never feel that he or she must be on hand to deal with all disputes.
To solve a problem you need to generate solutions. However, the obvious solution may not necessarily be the best. To generate solutions, a mixture of creative and analytical thinking is needed (Bransford, 1993).
Creativity is about escaping from preconceived ideas that block the way to finding an innovative solution to a problem. An effective tool for assisting in this process is the technique of lateral thinking, which is based largely on the work of Edward de Bono, who regards thinking as a skill.
There are several ways to encourage creative decision-making. One method that works best for specific or simple problems is brainstorming. If the ground rules of confidentiality and being non-judgemental are applied, it will produce a free flow of ideas generated without fear of criticism (Rawlinson, 1986).
Time constraints and staff availability may make it difficult for all those involved in a problem to meet. In such cases an adaptation of brainstorming - where a blank piece of paper is given to those involved and each writes down four solutions to the problem - may be the answer. A similar technique is the collective notebook, where people are asked to record their thoughts and ideas about a problem for a specified period.
An alternative is where one person writes down a list of solutions in order of priority, which is then added to by others. This helps to prioritise the ideas generated. All these methods produce data that can then be analysed by the problem-solver.
When the problem affects people in different geographical areas, solutions can be generated by obtaining the opinion of experts through the use of a questionnaire, which is known as the Delphi technique (McKenna, 1994).
When an apparently insurmountable problem presents itself, it is often useful to divide it into smaller pieces. This is known as convergent thinking. Using divergent thinking - where you consider a problem in different ways to expand your view - may also help.
A final alternative is the stepladder technique, which is time-consuming but effective if the issue is stirring up strong feelings. This requires the people involved in the problem to be organised into groups. First, two people try to solve the problem, then a third member is drawn in, to whom the solution reached by the first two is presented. All three then try to agree a solution. More people are added to the group, if necessary, in a similar way, until there is agreement of all involved. Provided the individuals are motivated to solve the problem, this technique creates ownership and commitment to implementing the agreed solution.
Analytical thinking, which follows a logical process of eliminating ideas, will enable you to narrow the range down to one feasible solution.
Although someone has to make the ultimate decision on which solution to implement, there are advantages to group decision-making: a greater number of possible solutions are generated and conflicts are resolved, resulting in decisions being reached through rational discussion.
This does, however, require the group to be functioning well or the individuals involved may feel inhibited in contributing to the decision-making. One individual may dominate the group or competition between individuals may result in the need to win taking precedence over deciding on an agreed practical solution.
As nursing becomes less bureaucratic individuals are being encouraged to put forward their own ideas, but social pressures to conform may inhibit the group. We do not solve problems and make decisions in isolation, but are influenced by the environment in which we work and the role we fulfil in that environment. If group members lack commitment and/or motivation, they may accept the first solution and pay little attention to other solutions offered.
Making a decision
There are three types of decision-making environments: certain, risk and uncertain. The certain environment, where we have sufficient information to allow us to select the best solution, is the most comfortable within which to make a decision, but it is the least often encountered.
We usually encounter the risk environment, where we lack complete certainty about the outcomes of various courses of action.
Finally, the uncertain environment is the least comfortable within which to make decisions as we are almost forced to do this blind. We are unable to forecast the possible outcomes of alternative courses of action and, therefore, have to rely heavily on creative intuition and the educated guess.
Taking this into consideration, you should not contemplate making a decision until you have all the information needed. Before you make your decision, remind yourself of the objective, reassess the priorities, consider the options and weigh up the strengths, weaknesses, opportunities and threats of each solution.
An alternative is to use the method that Thomas Edison used to solve the problem of the electric light bulb. Simply focus on your problem as you drift off to sleep, and when you wake up your subconscious mind will have presented you with the answer. But bear in mind that this is not a scientific way of solving problems - your subconscious can be unreliable.
If you are not sure about your decision, test the solution out on others who do not own the problem but may have encountered a similar dilemma. Once you have made your choice stick to it, or you may find it difficult to implement because those involved will never be sure which solution is current. They will also be reluctant to become involved in any future decision-making because of your uncertainty.
The next step is to ensure that all the people involved know what decision has been made. Where possible, brief the group and follow this up with written communication to ensure everyone knows what is expected of them. You may need to sell the decision to some, especially if they were not involved in the decision-making process or the solution chosen is not theirs.
Implementing the solution
Finally, to ensure the solution is implemented, check that the people involved know who is to do what, by when and that it has happened. Review the results of implementing your solution (see Box) and praise and thank all those involved.
- Part 1 of this series was published in last week’s issue: Wheeler, J. (2001) How to delegate your way to a better working life. Nursing Times; 97: 36, 34-35.
Next week. Part three: a step-by-step guide to effective report writing.
- Add to Bookmarks
Related articles
Christmas prize gave winner a head start in her studies
As we announce the winner of the Nursing Times Christmas Competition for 2017, we…
Competition winner goes the extra mile to put patients at ease
In December, Nursing Times invited readers to nominate a nurse who makes a real…

Inter-professional education: if we are working together, shouldn’t we be learning together?
As nurses, no matter what our field of practice, we always work…

Special recognition for nurses who treated terror attack victims
Nurses from the hospital trusts that treated the victims of this year’s…
Have your say
Sign in or Register a new account to join the discussion.
Fastest Nurse Insight Engine
- MEDICAL ASSISSTANT
- Abdominal Key
- Anesthesia Key
- Basicmedical Key
- Otolaryngology & Ophthalmology
- Musculoskeletal Key
- Obstetric, Gynecology and Pediatric
- Oncology & Hematology
- Plastic Surgery & Dermatology
- Clinical Dentistry
- Radiology Key
- Thoracic Key
- Veterinary Medicine
- Gold Membership
Critical Thinking and Decision-Making Skills
Chapter 4 Critical Thinking and Decision-Making Skills Betsy Frank http://evolve.elsevier.com/Huber/leadership/ In an era of changing reimbursements, value based purchasing, and expanded roles for nursing in the health care delivery system, critical thinking and decision making are important skills for nurses caring for patients and for nurse leaders and managers. Both the American Nurses Association’s (2009) and American Association of Nurse Executives’ (2005) standards for practice for nurse administrators and executives support the fact that in a fast-paced health care delivery environment, staff nurses, leaders, and managers must be able to analyze and synthesize a large array of information, use critical thinking and decision making skills to deliver effective day to day patient care, and solve complex problems that occur in complex health care delivery systems (see Figure 4-1 ). Furthermore, the Magnet Hospital initiative and the Institute of Medicine’s ( Committee on the Robert Wood Johnson Foundation, 2011 ) Future of Nursing report highlight the need for nurses to be able to be fully involved and even take the lead in decision making from the unit level to the larger health care delivery system. FIGURE 4-1 Differences and interactions among critical thinking, problem solving, and decision making. Nurses are a cadre of knowledge workers within the health care system. As such, they need information, resources, and support from their environment. In fact, the nurse manager’s expertise in critical thinking and shared decision making are essential for creating healthy work environments where quality and effective care can be delivered ( Kramer et al., 2010 ; Zori et al., 2010 ). Critical thinking and decision-making competences include analytical skills as well as intuition. Just as intuition is part of expert clinical practice ( Benner, 1984 ), intuition plays an important role in developing managerial and leadership expertise (Shirey, 2007). DEFINITIONS Critical thinking can be defined as a set of cognitive skills including “interpretation, analysis, evaluation, inference, explanation, and self-regulation” ( Facione, 2007 , p. 1). Using these skills, nurses in direct patient care and leaders and managers can reflect analytically, reconceptualize events, and avoid the tendency to make decisions and problem solve hastily or on the basis of inadequate information. Facione also pointed out that critical thinking is not only a skill but also a disposition that is grounded in a strong ethical component. Critical thinking in nursing can be defined as “purposeful, informed, outcomes focused thinking…[that] applies logic, intuition, creativity and is grounded in specific knowledge, skills, and experience” ( Alfaro-LeFevre, 2009 , p. 7). Alfaro-LeFevre noted that outcomes-focused thinking helps to prevent, control, and solve problems. Tanner (2000) noted that critical thinking is much more than just the five steps of the nursing process. Problem solving involves moving from an undesirable to a desirable state ( Chambers, 2009 ). Problem solving occurs in a variety of nursing contexts, including direct client care, team-level leadership, and systems-level leadership. Nurses and nurse managers are challenged to move from step-by-step problem-solving techniques to incorporating creative thinking, which involves considering the context when meeting current and future challenges in health care delivery ( Chambers, 2009 ; Rubenfeld & Scheffer, 2006 ). Decision making is the process of making choices that will provide maximum benefit ( Drummond, 2001 ). Decision making can also be defined as a behavior exhibited in selecting and implementing a course of action from alternative courses of action for dealing with a situation or problem. It may or may not be the result of an immediate problem. Critical thinking and effective decision making are the foundation of effective problem solving. If problems require urgent action, then decisions must be made rapidly; if solutions do not need to be identified immediately, decision making can occur in a more deliberative way. Because problems change over time, decisions made at one point in time may need to be changed ( Choo, 2006 ). For example, decisions about how to staff a unit when a nurse calls in sick have to be made immediately. However, if a unit is chronically short-staffed, a decision regarding long-term solutions will have to be made. The process of selecting one course of action from alternatives forms the basic core of the definition of decision making. Choo (2006) noted that all decisions are bounded by cognitive and mental limits, how much information is processed, and values and assumptions. In other words, no matter the decision-making process, all decisions are limited by a variety of known and unknown factors. In a chaotic health care delivery environment, where regulations and standards of care are always changing, any decision may cause an unanticipated future problem. BACKGROUND Critical Thinking Critical thinking is both an attitude toward handling issues and a reasoning process. Critical thinking is not synonymous with problem solving and decision making ( Figure 4-1 ), but it is the foundation for effective decision making that helps to solve problems ( Fioratou et al., 2011 ). Figure 4-2 illustrates the way obstacles such as poor judgment or biased thinking create detours to good judgment and effective decision making. Critical thinking helps overcome these obstacles. Critical thinking skills may not come naturally. The nurse who is a critical thinker has to be open-minded and have the ability to reflect on present and past actions and to analyze complex information. Nurses who are critical thinkers also have a keen awareness of their surroundings ( Fioratou et al., 2011 ). FIGURE 4-2 Decision-making maze. Critical thinking is a skill that is developed for clarity of thought and improvement in decision-making effectiveness. The roots of the concept of critical thinking can be traced to Socrates, who developed a method of questioning as a way of thinking more clearly and with greater logical consistency. He demonstrated that people often cannot rationally justify confident claims to knowledge. Confused meanings, inadequate evidence, or self-contradictory beliefs may lie below the surface of rhetoric. Therefore it is important to ask deep questions and probe into thinking sequences, seek evidence, closely examine reasoning and assumptions, analyze basic concepts, and trace out implications. Other thinkers, such as Plato, Aristotle, Thomas Aquinas, Francis Bacon, and Descartes, emphasized the importance of systematic critical thinking and the need for a systematic disciplining of the mind to guide it in clarity and precision of thinking. In the early 1900s, Dewey equated critical thinking with reflective thought ( The Critical Thinking Community, 2008 ). Critical thinking, then, is characterized by thinking that has a purpose, is systematic, considers alternative viewpoints, occurs within a frame of reference, and is grounded in information ( The Critical Thinking Community, 2008 ). Questioning is implicit in the critical thinking process. The following are some of the questions to be asked when thinking critically about a problem or issue ( Elder & Paul, n.d. ): • What is the question being asked? • Is this the right question? • Is there another question that must be answered first? • What information is needed? • Given the information, what conclusions are justified? • Are there alternative viewpoints? No matter what questions are asked, critical thinkers need to know the “why” of the thinking, the mode of reasoning (inductive or deductive), what the source and accuracy of the information is, what the underlying assumptions and concepts are, and what might be the outcome of the thinking ( The Critical Thinking Community, 2008 ). Critical Thinking in Nursing Nurses in clinical practice continually make judgments and decisions based on the assessment and diagnosis of client needs and practice problems or situations. Clinical judgment is a complex skill grounded in critical thinking. Clinical judgment results in nursing actions directed toward achieving health outcomes ( Alfaro-LeFevre, 2009 ). Scheffer and Rubenfeld (2000) have stated that habits of the mind that are characteristic of critical thinking by nurses include confidence, contextual perspective, creativity, flexibility, inquisitiveness, intellectual integrity, open-mindedness, perseverance, and reflection. Emphasizing the value of expert experience and holistic judgment ability, Benner (2003) cautioned that clinical judgments must not rely too heavily on technology and that the economic incentives to use technology must not come at the expense of human critical thinking and reasoning in individual cases. Critical thinkers have been distinguished from traditional thinkers in nursing. A traditional thinker, thought to be the norm in nursing, preserves status quo. Critical thinkers go beyond the step-by-step processes outlined in the nursing process and traditional problem solving. A critical thinker challenges and questions the norm and considers in the context of decision making potential unintended consequences. Unlike traditional thinkers, critical thinkers are creative in their thinking and anticipate the consequences of their thinking ( Rubenfeld & Scheffer, 2006 ). Creativity is necessary to deal with the complex twenty-first century health care delivery environment. Nurse leaders and managers have an obligation to create care delivery climates that promote critical thinking, which leads to innovative solutions to problems within the system of care ( Committee on the Robert Wood Johnson Foundation Initiative on the Future of Nursing, at the Institute of Medicine; Institute of Medicine, 2011 ; Porter-O’Grady, 2011 ). Such a climate encourages deep reflection, especially so that nurses feel safe to learn from mistakes, and encourages nurses to ask questions and consider a variety of viewpoints and alternative solutions to problems. What specific strategies can be used to promote a climate in which critical thinking is fostered? First and foremost, the nurse manager/leader, in the role of mentor, coach, or preceptor, should encourage questions such as “Is what you are doing or proposing based on sound evidence?” ( Ignatavicius, 2008 ). However, Snowden and Boone (2007) cautioned that “best practice, by definition is past practice” (p. 71). Therefore use of best practices needs to be examined carefully in order to use them appropriately. Staff nurses and managers must use critical thinking skills in order to determine the appropriateness of implementing recommended practice protocols. As managers, allowing staff and self “think time” is essential for reflection and is a key component of critical thinking ( Zori & Morrison, 2009 ). Nurse managers’ critical thinking abilities promotes a positive practice environment which can lead to better patient outcomes ( Zori, Nosek, & Musil, 2010 ). Coaching new and experienced nurses to develop expertise in clinical judgment is critically important. Many new nurses, in particular, need to further develop their critical thinking skills ( Fero et al., 2008 ; Forneris & Peden-McAlpine, 2009 ). In addition to having preceptors and others ask questions of new nurses, nurse managers and leaders can use other strategies to enhance critical thinking in nursing staff. Developing concept maps is another useful strategy to promote critical thinking. Although typically used in prelicensure programs ( Ellermann et al., 2006 ), nurse managers can encourage their preceptors to use concept maps with orientees ( Toofany, 2008 ). Developing concept maps in concert with others further develops a nurse’s critical thinking through the process of dialogue. Simulations also promote critical thinking or “thinking like a nurse” ( Tanner, 2006 ). According to Tanner, simulations can promote clinical reasoning, which leads to making conclusions in the form of clinical judgments and, thus, effective problem solving. The use of human patient simulators is well known in educational settings. Simulators may also be useful in orienting new graduates to the acute care setting ( Leigh, 2011 ). Pulman and colleagues (2009) have reported on the use of simulators to promote critical thinking role development in inter-professional environments. Decision Making Decision making is the essence of leadership and management. It is what leaders and managers are expected to do ( Keynes, 2008 ). Thus decisions are visible outcomes of the leadership and management process. The effectiveness of decision making is one criterion for evaluating a leader or manager. Yet staff nurses and nurse managers and leaders must make decisions in uncertain and complex environments ( Clancy & Delaney, 2005 ). Within a climate of uncertainty and complexity, nurse managers and leaders must also understand that all decision making involves high-stakes risk taking ( Clancy & Delaney, 2005 ; Keynes, 2008 ). If poor decisions are made, progress can be impeded, resources wasted, harm caused, and a career adversely affected. The results of poor decisions may be subtle and not appear until years later. Take, for instance, a decision to reduce expenses by decreasing the ratio of registered nurses to nurses’ aides. There may be a short-term cost savings, but if not implemented appropriately, this tactic may result in the gradual erosion of patient care over time (Kane et al., 2007). Unintended effects may include higher turnover of experienced nurses, increased adverse events such as medication errors, decreased staff morale, and lower patient satisfaction scores. The long-term outcome of this decision may actually result in increased expenses not reduced expenses. Thus it is vital for nurses to understand decision making and explore styles and strategies to enhance decision-making skills. Decision making, like traditional problem solving, has been traditionally thought of as a process with identifiable steps yet influenced by the context and by whether there is an intuitive grasp of the situation. However, Effken and colleagues (2010) stated that decision making is much more. Expert decision making is a constructive process in which the outcomes are not preplanned or simply pulled out of a memory bank. Instead, expert decision-making activities are creative, innovative, and adapted to uncertainty and the context of the current problem, using learning from prior experience (p. 189). Nurses make decisions in personal, clinical, and organizational situations and under conditions of certainty, uncertainty, and risk. Various decision-making models and strategies exist. Nurses’ control over decision making may vary as to amount of control and where in the process they can influence decisions. Although decision-making is more than a step-by-step process as noted by Effken and colleagues (2010) , awareness of the components, process, and strategies of decision making contributes to effectiveness in nursing leadership and management decision making. The basic elements of decision making, which enhances day to day activities, contributes to strategic planning and solves problems can be summarized into the following two parts: (1) identifying the goal for decision-making, and (2) making the decision. According to Guo (2008, p. 120) , the steps of the decision-making process can be illustrated as follows, using DECIDE: • D efine the problem and determine why anything should be done about it and explore what could be happening. • E stablish desirable criteria for what you want to accomplish. What should stay the same and what can be done to avoid future problems? • C onsider all possible alternative choices that will accomplish the desired goal or criteria for problem solution. • I dentify the best choice or alternative based on experience, intuition, experimentation. • D evelop and implement an action plan for problem solution. • E valuate decision through monitoring, troubleshooting, and feedback. Notice how these steps are analogous to the traditional problem-solving process or nursing process well-known by nurses and nurse managers. Thus decision making is used to solve problems. However, decision making is more than just problem solving. Decision making may also be the result of opportunities, challenges, or more long-term leadership initiatives as opposed to being triggered by an immediate problem. In any case, the processes are virtually the same, but their purposes may be slightly different. Nurse managers use decision making in managing resources and the environment of care delivery. Decision making involves an evaluation of the effectiveness of the outcomes that result from the decision-making process itself. Whether nurse managers are the sole decision makers or facilitate group decision making, all the factors that influence the problem-solving process also impact how decisions are made: who owns the problem that will result in a decision, what is the context of the decision to be made, and what lenses or perspectives influence the decision to be made? For example, the chief executive officer may frame issues as a competitive struggle not unlike a sports event. The marketing staff may interpret problems as military battles that need to be won. Nurse executives may view concerns from a care or family frame that emphasizes collaboration and working together. Learning and understanding which analogies and perspectives offer the best view of a problem or issue are vital to effective decision making. It may be necessary for nurse managers to expand their frame of reference and be willing to consider even the most outlandish ideas. Obviously, it is important to begin the goal definition phase with staff members who are closest to the issue. That includes staff nurses in concert with their managers. Often, decisions can originate within the confines of the shared governance system that may be in place within an organization ( Dunbar et al., 2007 ). It is wise, also, to consider adding individuals who have no connection with the issue whatsoever. Often it is these “unconnected” staff members who bring new decision frames to the meeting and have the most unbiased view of the problem. One of the core competencies for all health professionals is working in interprofessional teams ( Interprofessional Education Collaborative Expert Panel, 2011 ). Therefore using interprofessional teams for problem solving and decision making can be assumed to be more effective than working in disciplinary silos. No matter who is involved in the decision-making process, the basic steps to arrive at a decision to resolve problems remain the same. One critical aspect to note, however, is that in making decisions, nurse managers must have situational awareness ( Sharma & Ivancevic, 2010 ). That is, decision makers must always consider the context in which the outcome of the decision is to occur. A decision that leads to a desired outcome on one patient care unit may lead to undesirable outcomes on another unit because the patient care environment and personnel are different. DECISION OUTCOMES When looking at outcomes, one critical aspect of decision making is to determine the desired outcome. The desired outcome may vary, according to Guo (2008) , from an ideal or short-term resolution to covering up a situation. What is desired may be (1) for a problem to go away forever, (2) to make sure that all involved in this problem are satisfied with the solution and gain some benefit from it, or (3) to obtain an ideal solution. Sometimes a quick decision is desired, and researching different aspects of the problem or allowing for participation in decision making is not appropriate. For example, in disaster management, the nurse leader will use predetermined procedures for determining roles of the various personnel involved (Coyle et al., 2007). Desired decisions can be categorized into two end points: minimal and optimal. A minimal decision results in an outcome that is sufficient, satisfies basic requirements, and minimally meets desired objectives. This is sometimes called a “satisficing” decision . An optimizing decision includes comparing all possible solutions with desired objectives and then selecting the optimal solution that best meets objectives ( Choo, 2006 ; Guo, 2008 ). In addition to these two strategies, Layman (2011) drawing from Etzioni (1986) , discussed two other strategies: mixed scanning and incrementalism. Incrementalism is slow progress toward an optimal course of action. Mixed scanning combines the stringent rationalism of optimizing with the “muddling through” approach of incrementalism to form substrategies. Optimizing has the goal of selecting the course of action with the highest payoff (maximization). Limitations of time, money, or people may prevent the decision maker from selecting the more deliberative and slower process of optimizing. Still, the decision maker needs to focus on techniques that will enhance effectiveness in decision-making situations. Barriers to effective decision making exist and, once identified, can lead to going back through the decision-making process. Flaws in thinking can create hidden traps in decision making. These are common psychological tendencies that create barriers or biases in cognitive reflection and appraisal. Six common distortions are as follows ( Hammond et al., 1998 ; 2006 ): 1. Anchoring trap: When a decision is being considered, the mind gives a disproportionate weight to the first information it receives. Past events, trends, and numbers outweigh current and future realities. All individuals have preconceived notions and biases that influence decisions in a variety of ways. For instance the Institute of Medicine (IOM, 2001) endorsed the use of c omputerized p hysician o rder e ntry (CPOE) as one solution to reduce medication errors. Furthermore, The Centers for Medicare and Medicaid Services has set forth meaningful use criteria for implementation of CPOE as well as electronic health records (EHR). Despite incentive payments for implementing EHR ( HFMA P & P Board, 2012 ), the financial costs involved, human-factor errors and work-flow issues can hamper successful implementation ( Campbell et al., 2006 ). 2. Status-quo trap: Decision makers display a strong bias toward alternatives that perpetuate the status quo. In the face or rapid change in the environment, past practices that exhibit any sense of permanence provide managers with a feeling of security. 3. Sunk-cost trap: Past decisions become sunk costs, and new choices are often made in a way that justifies past choices. This may result in becoming trapped by an escalation of commitment. Because of rapid, ongoing advances in medical technology, managers are frequently pressured to replace existing equipment before it is fully depreciated. If the new equipment provides a higher level of quality at a lower cost, the sunk cost of the existing equipment is irrelevant to the decision-making process. However, managers may delay purchasing new equipment and forgo subsequent savings because the equipment has yet to reach the end of its useful life. 4. Confirming-evidence trap: Kahneman and colleagues (2011) noted that decision makers also fall into the trap of confirmation bias where contradictory data are ignored. This bias leads people to seek out information that supports an existing instinct or point of view while avoiding contradictory evidence. A typical example is favoring new technology over less glamorous alternatives. A decision maker may become so enamored by technological solutions (and slick vendor demonstrations) that he or she may unconsciously decide in favor of these systems even though strong evidence supports implementing less costly solutions first. 5. Framing trap: The way a problem is initially framed profoundly influences the choices made. Different framing of the same problem can lead to different decision responses. A decision frame can be viewed as a window into the varied reasons a problem exists. As implied by the word frame , individuals may perceive problems only within the boundaries of their own frame. The human resources director may perceive a staffing shortage as a compensation problem, the chief financial officer as an insurance reimbursement issue, the director of education as a training issue, and the chief nursing officer as a work environment problem. Obviously all these issues may contribute, in part, to the problem; however, each person, in looking through his or her individual frame, sees only that portion with which he or she is most familiar ( Layman, 2011 ). 6. Estimating and forecasting traps: People make estimates or forecasts about uncertain events, but their minds are not calibrated for making estimates in the face of uncertainty. The notion that experience is the parent of wisdom suggests that mature managers, over the course of their careers, learn from their mistakes. It is reasonable to assume that the knowledge gained from a manager’s failed projects would be applied to future decisions. Whether right or wrong, humans tend to take credit for successful projects and find ways to blame external factors on failed ones. Unfortunately, this form of overconfidence often results in overly optimistic projections in project planning. This optimism is usually buried in the analysis done before ranking alternatives and recommendations. Conversely, excessive cautiousness or prudence may also result in faulty decisions. This is called aversion bias ( Kahneman et al., 2011 ). Dramatic events may overly influence decisions because of recall and memory, exaggerating the probability of rare but catastrophic occurrences. It is important that managers objectively examine project planning assumptions in the decision-making process to ensure accurate projections. Because misperceptions, biases, and flaws in thinking can influence choices, actions related to awareness, testing, and mental discipline can be employed to ferret out errors in thinking before the stage of decision making ( Hammond et al., 1998 ). Data-driven decision making is important ( Dexter et al., 2011 ; Lamont, 2010 ; Mick, 2011 ). The electronic health record can be mined for valuable data, upon which fiscal, human resource, and patient care decisions can be made. However, the data derived can be overwhelming and cause decision makers to make less than optimal decisions. Shared decision making can help ameliorate decision traps ( Kahneman et al., 2011 ) because dissent within the group may help those accountable for the decision to prevent errors that are “motivated by self-interest” (p. 54). More alternatives can be generated by a group and more data can be gathered upon which to base the decision, rather than just using data that is more readily apparent. DECISION-MAKING SITUATIONS The situations in which decisions are made may be personal, clinical, or organizational ( Figure 4-3 ). Personal decision making is a familiar part of everyday life. Personal decisions range from multiple small daily choices to time management and career or life choices. FIGURE 4-3 Decision-making situations. Clinical decision making in nursing relates to quality of care and competency issues. According to Tanner (2006) , decision making in the clinical arena is called clinical judgment . In nursing, as with all health professions, clinical judgments should be patient-centered, use available evidence from research and other sources, and use available informatics tools (IOM, 2003). These crucial judgments should take place within the context of interprofessional collaboration. Within a hospital or other health care agency, a social network forms that is interprofessional ( Tan et al., 2005 ). This social network has to collaborate for positive change within the organization and to make clinical decisions of the highest quality. Nurses manage care and make decisions under conditions of certainty, uncertainty, and risk. For example, if research has shown that, under prescribed conditions, the selection of a specific nursing intervention is highly likely to produce a certain outcome, then the nurse in that situation faces a condition of relative certainty. An example would be the prevention of decubitus ulcers by frequent repositioning. If little knowledge is available or if the specific situation is more complex or variant from the usual, then the nurse faces uncertainty. Risk situations occur when a threat of harm to patients exists. Conditions of risk occur commonly relative to the administration of medications, crisis events, infection control, invasive procedures, and the use of technology in nursing practice. Furthermore, these conditions also apply to the administration of nursing care delivery, in which decision making is a critical function. Conditions of uncertainty and complexity are common in nursing care management. Over time, the complexity of health care processes has increased as a natural outgrowth of innovation and new technology. With computerized integration of billing, physician ordering, results of diagnostic tests, information about medications and their actions and side effects, and critical pathways and computerized charting, complexity increases more. Trying to integrate so many data points in care delivery can overwhelm the care provider who is making clinical judgments. As a result, subtle failures in any part of the information system can go unnoticed and have catastrophic outcomes. For example, if the computer system in the emergency room cannot “talk” to the system in the operating room, then errors in care management, such as giving cephalexin to patient who has an allergy can occur. If a provider fails to input critical information, such as a medication that a patient is taking, a fatal drug interaction could occur when another provider prescribes a new medication. Ready access to the Internet and online library sources can further create complexity in the decision-making process as care providers have access to more information upon which to make decisions. Readily accessible information related to evidence-based practice and information gleaned from human resources records and clinical systems can overwhelm nurse managers and leaders. Nurse leaders are coming to understand that innovation and new technology are the driving forces behind the discovery of new knowledge and improvements in patient care. Overlapping, unclear, and changing roles for nurses as a result of new technology and services create complex decision-making situations and impact the quality of care delivered (IOM, 2003). In addition, workflow interruptions can inhibit critical thinking, particularly in a chaotic environment ( Cornell et al., 2011 ; Sitterding et al., 2012 ). ADMINISTRATIVE AND ORGANIZATIONAL DECISION MAKING According to Choo (2006) , organizations use information to “make decisions that commit resources and capabilities to purposeful action” (p. 1). Nurse managers, for example, make staffing decisions and thus commit financial resources for the purpose of delivering patient care. Hospital administrators may decide to add additional services to keep up with external forces. These decisions subsequently have financial implications related to reimbursement, staffing, and the like. Etzioni (1989) noted that the traditional model for business decisions was rationalism. However, he further asserted that as information flow became more complex and faster-paced, a new decision-making model based on the use of partial information that has not been fully analyzed had begun to evolve. He called this model “humble decision making.” This approach arises in response to the need to make a decision when the amount of data exceeds the time available to analyze it. For instance, predicting the outcome of clinical and administrative decisions in health care is problematic because such processes are collectively defined as c omplex a daptive s ystems (CASs). A CAS is characterized by groups of individuals who act in unpredictable, nonlinear (not cause and effect) ways, such that one person’s actions affect all the others ( Holden, 2005 ). In CASs, humans do behave in unpredictable ways ( Tan et al., 2005 ). Critical thinking can help all health care personnel to examine these complex systems, wherein groups solve problems through complex, continually altering interactions between the environment and all involved in the decision making ( Fioratou et al., 2011 ). Situations within the environment constantly change and decision makers need to reframe their thinking as they broaden their awareness of the context of their decisions ( Sharma & Ivancevic, 2010 ). Having situation awareness is a must ( Fioratou et al., 2011 ; Sitterding et al., 2012 ). Decision makers need to make every effort to forecast unanticipated consequences of their decisions. For example if staffing is cut, what adverse events might occur (Kane et al., 2007)? Decision making is also influenced by the manager’s leadership style. A democratic/collaborative style of leadership and decision making works best in a complex adaptive system, such as a hospital, which is characterized by a large array of social relationships that can have an economic impact on an organization. Staff nurses who are not engaged in shared decision making may experience less job satisfaction and subsequently may leave an organization, leading to loss of expertise in patient care ( Gromley, 2011 ). However, the full array of leadership styles may at some time be used in the decision-making process. Vroom and Yetton (1973) proposed a classic managerial decision-making model that identified five managerial decision styles on a continuum from minimal subordinate involvement to delegation. Their model uses a contingency approach, which assumes that situational variables and personal attributes of the leader influence leader behavior and thus can affect organizational effectiveness. To diagnose the situation, the decision maker examines the following seven problem attributes: 1. The importance of the quality of the decision 2. Whether there is sufficient information/expertise 3. The amount of structure to the problem 4. The extent to which acceptance/commitment of followers is critical to implementation 5. The probability that an autocratic decision will be accepted 6. The motivation of followers to achieve organizational goals 7. The extent to which conflict over preferred solutions is likely
Share this:
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
Related posts:
- Legal and Ethical Issues
- Change and Innovation
- Data Management and Clinical Informatics
- Power and Conflict
Stay updated, free articles. Join our Telegram channel
Comments are closed for this page.

Full access? Get Clinical Tree

- Subscribe to journal Subscribe
- Get new issue alerts Get alerts
Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
Nurse leaders as problem-solvers
Addressing lateral and horizontal violence.
Anthony, Michelle R. PhD, RN; Brett, Anne Liners PhD, RN
Michelle R. Anthony is a program coordinator at Columbia (S.C.) VA Health Care System. Anne Liners Brett is doctoral faculty at the University of Phoenix in Tempe, Ariz.
Acknowledgment: The authors acknowledge the support of the University of Phoenix Center for Educational and Instructional Technology Research.
The contents of this article do not represent the views of the US Department of Veterans Affairs or the United States Government.
The authors and planners have disclosed no potential conflicts of interest, financial or otherwise.
For more than 126 additional continuing-education articles related to management topics, go to NursingCenter.com/CE .
Earn CE credit online: Go to http://nursing.ceconnection.com and receive a certificate within minutes .
Read about a qualitative, grounded theory study that looked to gain a deeper understanding of nurse leaders' perceptions of their role in addressing lateral and horizontal violence, and the substantive theory developed from the results.

The issue of lateral and horizontal violence (LHV) has plagued the nursing profession for more than 3 decades, yet solutions remain elusive. The significance of LHV isn't lost on nurse leaders because it creates an unhealthy work environment. Research literature worldwide has continued to report the prevalence of disruptive behaviors experienced by nursing students, novice nurses, and seasoned nurses in the workforce. The World Health Organization, International Council of Nurses, and Public Services International have recognized this issue as a major global public health priority. 1
LHV, also called nurse-on-nurse aggression, disruptive behavior, or incivility, undermines a culture of safety and negatively impacts patient care. 2,3 This experience, known to nurses as “eating their young,” isn't only intimidating and disruptive, it's also costly and demoralizing to the nursing profession and healthcare organizations. 4,5 Although the impact of LHV can be dreadful for both the institution and its staff, little is known about the reasons for these behaviors among nursing professionals. 2
LHV encompasses all acts of meanness, hostility, disruption, discourtesy, backbiting, divisiveness, criticism, lack of unison, verbal or mental abuse, and scapegoating. 6 The sole intent of bullying behaviors is to purposefully humiliate and demean victims. Bullying behaviors also taint healthcare organizations; cause irreparable harm to workplace culture; breakdown team communication; and severely impact the quality of the care provided, thereby jeopardizing patient safety. 7,8 Researchers have reported that acts of LHV are used to demonstrate power, domination, or aggression; for retribution; to control others; and to enhance self-image. 9-12
Previous studies have shown that the frequency of LHV in healthcare organizations is quite severe, with about 90% of new nurses surveyed reporting acts of incivility by their coworkers. 13 Sixty-five percent of nurses in one survey reported witnessing incidents of despicable acts, whereas another 46% of coworkers in the same survey reported the issue as “very serious” and “somewhat serious.” 13
LHV poses a significant challenge for nurse leaders who are legally and morally responsible for providing a safe working environment. 2,6 The purpose of this qualitative, grounded theory study was to gain a deeper understanding of nurse leaders' perceptions of their role in addressing LHV and develop a substantive theory from the results.
Literature review
A paucity of evidence exists in the literature regarding how nurse leaders perceive their role in addressing LHV. 14 Studies have shown that this phenomenon is attributed to heavy workloads, a stressful work environment, and lack of workgroup cohesiveness, as well as organizational factors such as misuse of authority and the lack of organizational policies and procedures for addressing LHV behaviors. 15
In one study, one-third of the nurses reported that they had observed emotional abuse during several of their work shifts. 16 Another study indicated that 30% of survey respondents (n = 2,100) stated LHV occurs weekly. 17 A third study revealed that 25% of participants noted LHV happened monthly, and a fourth study of ED nurses reported that about 27.3% of the nurses had experienced LHV perpetrated by nursing leadership (managers, supervisors, charge nurses, and directors), physicians, or peers in the last 6 months. 18
In a survey completed by members of the Washington State Emergency Nurses Association, 27% of respondents experienced acts of bullying in the past 6 months. 19 Another study reported that 27% to 85% of nurse respondents had experienced some form of uncivil behavior. 20 Other data have shown that those more vulnerable to violent, disruptive, and intimidating behaviors are newly licensed nurses beginning their careers. 21
Although nurse leaders can be perpetrators of LHV, they play an essential role in addressing LHV behaviors and creating a safe work environment. 22 The literature suggests that, in many cases, a lack of awareness and response by nurse leaders adds to the prevalence of LHV. 23 This may be due, in part, to nurse leaders being aligned with the perpetrators who are creating the toxic work environment. 6 The literature suggests that an environment where staff members feel safe to practice results in a culture that decreases burnout and promotes nurse retention and quality outcomes. 24,25
This qualitative, grounded theory study focused on nurse leaders' perception of their role in breaking the cycle of LHV for staff members whom they supervise. Two research questions guided the study: 1. How do nurse leaders perceive their role in addressing LHV among nursing staff members under their supervision? 2. What substantive theory may emerge from the data collected during interviews with nurse leaders?
A grounded theory methodology was used to explore the nurse leader's role in addressing LHV with the intent of developing a substantive theory through the meaningful organization of data themes to provide a framework to address the phenomenon of LHV. Purposive sampling was used to recruit a total of 14 participants for this study from a large healthcare system in the Southeastern US. The participants were chosen because of their experience with LHV and their ability to discuss and reflect on those experiences. Informed consent was obtained before the start of the study, which included explaining the reason for the study and what to expect. In addition, permission was obtained from the Institutional Review Board.
Data collection and analysis
Demographic data collected to describe the sample included gender, age range, number of years holding a management position, supervisory responsibility, and highest degree obtained. (See Table 1 .)

Semistructured, in-depth interviews were the primary mode of data collection. The recorded interviews were conducted face-to-face and lasted about 60 minutes. Data collection continued until saturation was achieved. Data saturation occurred when no new descriptive codes, categories, or themes were emerging from the analyzed data. The interviews were transcribed verbatim and verified through a member check process.
During the data analysis process, themes and patterns were identified. Data from each participant's interview were examined to determine if the responses were aligned with the identified themes. Analysis of the data included coding at increasingly abstract levels and constant comparison. Qualitative software assisted in coding the information and uncovering subtle trends.
Four themes emerged from core categories developed during the qualitative data coding process.
Theme 1: Understanding/addressing LHV . In question one, participants were asked to describe their understanding of LHV. Five subthemes emerged from the data collected with this question. (See Table 2 .)

Theme 2: Experience addressing LHV . In the second question, participants were asked about their experience with addressing incidents of LHV. Six subthemes were identified. (See Table 3 .)

Theme 3: Role perception in addressing LHV . In the third question, participants were asked what they perceive their role to be in addressing LHV. Six subthemes resulted from this question. (See Table 4 .)

Theme 4: Organizational impediment to addressing LHV . In question four, participants were asked to describe the factors within the organization that influence or impede their role in addressing LHV. This question yielded nine subthemes. (See Table 5 .)

Substantive theory
As a result of the themes that emerged from the data, a substantive theory was developed. This is especially important for the nursing profession to develop as a scientifically based practice. Theories help guide research and provide the expansion, generation, and validation of the science of nursing knowledge. 26 The substantive theory will help nurse leaders become more cognizant of the role that effective leadership plays in preventing or intervening in incidents of LHV in the workplace. The analysis revealed that nurse leaders are aware that the quality of patient care and staff well-being can be adversely affected by the impact of LHV.
Data themes were used to formulate the following theory: Nurse leaders address LHV affecting their staff members by solving problems, creating a safe work environment, and reducing institutional barriers that impede addressing LHV in a timely fashion. Nurse leaders perceive their role as a problem-solver, which is a necessary step in advocacy. 27 Problem-solving is a process that contains the elements of decision-making and critical thinking. 28
The theory that emerged from the core categories explicitly focused on the central phenomenon of LHV in the nursing work environment. Figure 1 shows the interrelatedness of the themes to the resultant substantive theory.

Discussion and implications
The study results have several implications for both the nursing profession and nurse leaders. The nursing profession requires decisive and robust leadership, and the role of the nurse leader is to be a combination of nurturer, investigator, and judge to examine incidents of LHV. 26,29-32 Nurse leaders are responsible for setting the tone and expectations for a safe work environment. This includes modeling the expected ethical behaviors; for example, doing the right things for the right reasons, being collegial toward each other, and being respectful of other's differences. One participant remarked, “This is a different world based on how I was raised. I was raised to be respectful to people.”
In addition, nurse leaders are responsible for enforcing policies created to address disruptive behaviors and working with the administration as soon as an incident occurs. Past research indicates that a healthy and collaborative work environment fosters nurse engagement and patient safety. 25,30 Staff members and patients need a leader to protect them when necessary; thus, the nurse leader needs to “walk the walk” in providing a safe environment for all. Nurse leaders engaged in these kinds of behaviors are providing strong leadership and practicing strong decision-making, thus ensuring the continued robustness of their organizations.
Recommendations and limitations
Future research could replicate this study in a different geographic region to explore the causes of LHV by soliciting the views of nursing students, new graduate nurses, and nurse educators from unionized and nonunionized hospital systems and comparing the results to further understand this phenomenon. Additionally, developing a tool to test the substantive theory could substantiate the nurse leader's role as a problem-solver to address incidence of LHV in the workplace.
The decision to conduct this study in one type of healthcare organization limits the ability to compare the interviewed nurse leaders' experiences with nurse leaders in other healthcare organizations. The experiences of nurses in other healthcare organizations may be different; thus, overall generalizability of the study may be limited.
Say “no” to the status quo
The results of this study support the findings of previous researchers. 23,31,33,34 Accepting the status quo is unacceptable and can cause irreparable harm to organizational well-being if LHV isn't addressed. Collaboration between nurse leaders and administrators is essential to successfully reduce institutional obstacles that prevent the timely handling of LHV incidents. The role of the nurse leader as a problem-solver should be clear, defined, and well supported to seek resolutions to toxic behaviors that are hurting the work environment. But we must remember that creating a policy doesn't equal change. Every employee from the lowest level in the organization to the highest ranks of administration must model civil behaviors.
INSTRUCTIONS Nurse leaders as problem-solvers: Addressing lateral and horizontal violence
Test instructions.
- Read the article. The test for this CE activity is to be taken online at http://nursing.ceconnection.com .
- You'll need to create (it's free!) and login to your personal CE Planner account before taking online tests. Your planner will keep track of all your Lippincott Professional Development online CE activities for you.
- There's only one correct answer for each question. A passing score for this test is 14 correct answers. If you pass, you can print your certificate of earned contact hours and access the answer key. If you fail, you have the option of taking the test again at no additional cost.
- For questions, contact Lippincott Professional Development: 1-800-787-8985 .
- Registration deadline is June 3, 2022 .
PROVIDER ACCREDITATION
Lippincott Professional Development will award 1.5 contact hours for this continuing nursing education activity.
Lippincott Professional Development is accredited as a provider of continuing nursing education by the American Nurses Credentialing Center's Commission on Accreditation.
This activity is also provider approved by the California Board of Registered Nursing, Provider Number CEP 11749 for 1.5 contact hours, and the District of Columbia, Georgia, and Florida CE Broker #50-1223.
Payment: The registration fee for this test is $17.95.
- + Favorites
- View in Gallery
Readers Of this Article Also Read
Leadership strategies to promote frontline nursing staff engagement, nurse leader competencies: a toolkit for success, keeping the peace: conflict management strategies for nurse managers, principles for sustaining shared/professional governance in nursing, workplace incivility: nurse leaders as change agents.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Healthcare (Basel)

Factors Influencing Problem-Solving Competence of Nursing Students: A Cross-Sectional Study
Eunhee choi.
1 Department of Nursing, Korean Bible University, 32 Dongil-ro(st) 214-gil, Nowon-gu, Seoul 01757, Korea; moc.revan@1029iohci
Jaehee Jeon
2 Department of Nursing, Gangneung-Wonju National University, Gangneung-si 26403, Korea
Associated Data
Not applicable.
Problem-solving ability is an important competency for nursing students to enable them to solve various problems that occur in dynamic clinical settings. The purpose of this cross-sectional study was to identify the factors that affect the problem-solving ability of nursing students. The subjects of this study were 192 nursing college students in their second year or beyond. The research tool consisted of an online questionnaire, with a total of 91 items regarding general characteristics, metacognition, and communication competence. Data collection was conducted from 10 to 30 March 2022. An online survey link was uploaded to the student group of a social network service from two nursing colleges that permitted data collection. Subjects who agreed to participate directly accessed and responded to the online survey. The collected data were analyzed using descriptive statistics, and the factors associated with the problem-solving ability of nursing students were examined using hierarchical multiple regression analysis. The subjects’ mean problem-solving ability score was 3.63 out of 5. Factors affecting problem-solving ability were age, communication competence, and metacognition, among which metacognition had the greatest influence. These variables explained 51.2% of the problem-solving ability of nursing students. Thus, it is necessary to provide guidance to improve metacognition and to develop educational methods to improve communication competence in curricular and non-curricular courses to improve the problem-solving ability of nursing students.
1. Introduction
Nurses must have the ability to develop individual problem-solving methods to satisfy their patients’ diverse and high-level health needs [ 1 ]. However, the medical field is characterized by uncertainty, instability, and unpredictability; thus, it is not easy for nurses to apply or utilize the knowledge learned within controlled situations in schools, and therefore, it is often difficult for nurses to address the health needs of patients [ 2 ]. The problem-solving ability required in such situations is an essential skill that college students majoring in nursing must have in order to effectively perform their assigned nursing tasks after graduation, while successfully adapting in order to practice in a rapidly changing medical field [ 3 ]. Therefore, strategies to improve the problem-solving ability of nursing students should be applied in their education.
This study aimed to examine the relationship between metacognition, communication competency, and the problem-solving ability of nursing students, and to identify factors that affect nursing students’ problem-solving ability. The results represent basic data that could help inform the development of educational strategies to improve the communication skills of nursing students.
Problem solving involves recognizing the difference between the problem solver’s current state and the goal state to be reached, and resolving the obstacles that prevent them from achieving the goal [ 4 ]. Acquiring problem-solving ability based on judgment and critical thinking is an important element of nursing education [ 5 ]. Furthermore, the use of effective problem-solving strategies based on professional knowledge is a competency that a professional nurse should possess [ 3 ].
Recently, metacognition has been recognized in psychology and pedagogy as a central element of the understanding, self-learning, communication, and problem-solving processes. Metacognition is the ability to think about one’s own thinking [ 6 ], as expressed by the individual knowing and controlling their thought processes and applying previously acquired knowledge, skills, and experiences using appropriate strategies [ 7 ]. In particular, metacognition is an important variable for learning and problem-solving. It is the knowledge related to the selection of an appropriate strategy for the task; the establishment, selection, and application of problem-solving measures; evaluation of the effectiveness of the applied measures; and checking and adjusting the performance process [ 6 , 7 ]. Accordingly, interest in metacognition is increasing in the field of nursing, with emphasis on the problem-solving ability of nursing students [ 8 ].
Metacognition affects problem solving by cultivating the learner’s active attitude, linking existing knowledge with new knowledge, and fostering the development of practical cognitive strategies that can be used for problem solving [ 7 ]. Previous studies on learners’ metacognition have observed that a higher level of metacognition leads to an improvement in the problem-solving process, as metacognition has a significant effect on goal setting and problem-solving performance [ 9 ]. Thus, metacognition and problem-solving ability are closely related; furthermore, metacognition is a key strategic aspect in the problem-solving process [ 10 ]. Although metacognition is a powerful predictor of learning outcomes and problem-solving success, it is not clear how metacognition works regarding cognitive strategies and learning outcomes [ 11 ]. A study of adolescent metacognition-related cognition (learning strategies and problem-solving strategies) and how metacognition affects various types of learning performance confirmed that problem solving is the only mediator between general metacognition and learning performance [ 11 ]. Metacognition plays a major role in improving learning and work ability, and the appropriate use of metacognition when performing nursing tasks can improve the personal lives of nurses [ 12 ]. Therefore, it is necessary to assess the influence of metacognition and problem-solving ability on nursing education.
Communication competence is a major factor that affects problem-solving ability [ 13 ]. It is essential for smoothly maintaining professional relationships with medical personnel, patients, and guardians in diverse and complex medical environments [ 14 ]. Since communication competence is an important aspect of problem solving, it can affect the quality of nursing and the satisfaction of the patient [ 15 ]. There is an urgent need to improve communication competence, as various issues that arise during the clinical process can be solved through communication between medical staff and patients, and nurses are responsible for much of the continuous communication with patients and their guardians [ 16 ]. However, a lack of communication competence among nurses may lead to miscommunication, and thereby, poor outcomes, even if nurses possess good problem-solving methods [ 13 ].
While previous studies have revealed the relationship between communication competence and the problem-solving ability of nursing students [ 13 , 17 ], there is a lack of research regarding the relationship between metacognition, communication competence, and problem-solving ability. Through this research, we confirmed the relationship between the metacognition and problem-solving ability of nursing college students, the relationship between communication ability and problem-solving ability, and finally, examined the factors that affect variables associated with problem-solving ability, including metacognition.
2. Materials and Methods
2.1. design.
This study used quantitative methods to investigate the relationship between the metacognition, communication ability, and problem-solving ability of nursing students and to identify factors that affect problem-solving ability.
2.2. Participants and Procedures
The subjects of this study were nursing students enrolled in two nursing colleges in the same city and region. Since data collection was conducted in March, second-year, third-year, and fourth-year students, with college life experience, were targeted. The required number of study subjects was calculated using the G-Power 3.1.9.7 program, which determined a significance level of 0.05, an effect size of 0.15, a power of 0.90, and 11 predictors, for multiple regression analysis. The minimum sample size was 152. In consideration of the dropout rate, 170 was set as the target number of subjects.
Data collection was conducted from 10 to 30 March 2022. The survey was conducted online. Consent for participation in the study was obtained by the individual reading the explanation of the purpose of the study and checking a consent box, which was displayed on the first screen of the online survey. The study subjects were redirected to the questionnaire completion page after providing their consent. It required approximately 10 min to complete the questionnaire. A total of 200 participants accessed and completed the questionnaire; 192 questionnaires were used for analysis after excluding 8 questionnaires that were determined to have been completedinccurately.
2.3. Instruments
The tools of this study consisted of a total of 91 items, including 9 items regarding general characteristics, 20 metacognition items, 15 items dealing with communication competencies, and 45 regarding problem-solving skills.
The items regarding the general characteristics of the subjects included age, sex, academic level, interpersonal relationships, satisfaction with major, problem based learning (PBL) experience, number of related experiences, clinical practice experience (yes or no), and number of weeks of clinical practice experience.
Metacognition was assessed using the state metacognitive inventory developed by O’Neil Jr et al. [ 18 ], as modified and supplemented by Joo [ 19 ]. It consists of a total of 20 items that assess the four sub-factors of metacognition: cognition, cognitive strategy, plan, and monitoring, using a 5-point Likert scale ranging from 1 point, for ‘not at all’, to 5 points, for ‘strongly agree’. The Cronbach’s α measure of the reliability of the tool was 0.86 at the time of development and 0.89 in the study of Joo [ 19 ]. The value in the current study was 0.91.
Communication competence was measured using a comprehensive interpersonal communication competence scale developed by Rubin [ 20 ], as modified and supplemented by Hur [ 21 ] to fit Korean culture. This tool consists of 15 items related to communication, such as self-exposure, cross-exposure, social tension relief, assertiveness, and concentration. Each item is assessed on a 5-point Likert scale ranging from 1 point, for ‘not at all’, to 5 points, for ‘strongly agree’. The Cronbach’ α reliability measure at the time of development was 0.72, and the value in this study was 0.84.
Problem-solving ability was assessed via a life-skills measurement tool developed by the Korea Educational Development Institute [ 22 ]. This tool considers 5 problem factors (clarification, cause analysis, alternative development, plan and implementation, and performance evaluation) and 9 sub-factors (problem recognition, information collection, analysis ability, divergent thinking, decision making, planning ability, execution and risk taking, evaluation, and feedback), and thus consists of 45 items in total. Each item is assessed on a 5-point Likert scale ranging from 1 point, for ‘very rarely’, to 5 points, for ‘very often’, with higher scores indicating better problem-solving skills. The reliability at the time of tool development was indicated by a Cronbach’s α value of 0.95, whereas in this study, the Cronbach’s α value was 0.90.

2.4. Statistical Analysis
Statistical analyses were performed using SPSS (ver. 25) statistical software (IBM). The subjects’ general characteristics, metacognition, communication competence, and problem-solving ability were analyzed by number and percentage, as well as mean and standard deviation. To test the normality of all variables, skewness and kurtosis were assessed. In general, when the absolute value of skewness is less than 2 or the absolute value of kurtosis is less than 7, there are no problems associated with deviations in the variable distributions from normality [ 23 ]. In this study, skewness ranged between −0.002 and 0.435, with absolute values less than 2, and kurtosis ranged between −0.204 to 1.580, with absolute values less than 7, thus indicating that the variables satisfied the assumption of univariate normality. Differences in metacognition, communication competence, and problem-solving ability according to the general characteristics of the subjects were analyzed by mean, standard deviation, independent t-test, and one-way ANOVA, followed by Scheffé’s post hoc analysis. The correlation between metacognition, communication competence, and problem-solving ability of the participants was analyzed using Pearson’s correlation coefficient. Factors affecting the subject’s problem-solving ability were analyzed using hierarchical multiple regression.
2.5. Ethical Considerations
Before the study was conducted, the research proposal and questionnaire were approved by the Institutional Review Board of Gangneung–Wonju National University (No: GWNUIRB-2022-1). The tools used in the study were used after obtaining the consent of the original author. When explaining the purpose of the study, it was emphasized that the participants had the right to withdraw from the study at any time, that the anonymity and confidentiality of the survey results were guaranteed, and that the study results would not be used for other purposes. Participants were provided with a small gift to motivate participation.
3.1. General Characteristics
Table 1 illustrates that the participants’ mean age was 21.56 ± 1.99. Most participants were women (81.3%).
General Characteristics of Participants (N = 192).
| Variable | Categories | N | % |
|---|---|---|---|
| Sex | Male | 36 | 18.7 |
| Female | 156 | 81.3 | |
| Age (years) | <21 | 62 | 32.3 |
| 21~<23 | 84 | 43.8 | |
| ≥23 | 46 | 24.0 | |
| Mean ± SD | 21.56 ± 1.99 | ||
| Academic level | Sophomore | 63 | 32.8 |
| Junior | 64 | 33.3 | |
| Senior | 65 | 33.9 | |
| Interpersonal relationships | Very good | 29 | 15.1 |
| Good | 118 | 61.5 | |
| Moderate | 45 | 23.4 | |
| Satisfaction with major | Very satisfied | 30 | 15.6 |
| Satisfied | 100 | 52.1 | |
| Moderately satisfied | 47 | 24.5 | |
| Dissatisfied | 15 | 7.8 | |
| PBL experience | Yes | 130 | 68.2 |
| No | 62 | 31.8 | |
| Number of PBL experiences | 0 | 62 | 32.3 |
| 1~2 | 29 | 15.1 | |
| 3~6 | 55 | 28.6 | |
| ≥7 | 46 | 24.0 | |
| Clinical practice experience | Yes | 104 | 50.2 |
| No | 88 | 46.8 | |
| Weeks of clinical practice experience | 0 | 88 | 45.9 |
| 1~6 | 54 | 28.1 | |
| ≥7 | 50 | 26.0 |
† SD, standard deviation; ‡ PBL, problem-based learning.
3.2. Scores for Metacognition, Communication Competence, and Problem-Solving Ability
Table 2 illustrates that the average score of the subjects’ metacognition was 3.86 ± 0.47 (out of 5). Among the sub-domains, cognitive strategy showed the highest score of 4.03 ± 0.45, followed by monitoring, with 3.90 ± 0.59. The average for communication competence was 3.92 ± 0.42 points (out of 5 points). The average for problem-solving ability was 3.63 ± 0.35 (out of 5), and among the sub-domains, problem clarification was the highest at 3.83 ± 0.52, and cause analysis was the lowest at 3.28 ± 0.36.
Scores for metacognition, communication competence, and problem-solving ability. (N = 192).
| Variables | Categories | M ± SD | Range | Min | Max | Skewness | Kurtosis |
|---|---|---|---|---|---|---|---|
| Cognition | 3.87 ± 0.54 | 1–5 | 2.00 | 5.00 | −0.405 | 0.616 | |
| Cognitive strategy | 4.03 ± 0.45 | 1–5 | 2.80 | 5.00 | −0.002 | −0.204 | |
| Planning | 3.66 ± 0.59 | 1–5 | 2.00 | 5.00 | −0.234 | 0.449 | |
| Monitoring | 3.90 ± 0.59 | 1–5 | 2.20 | 5.00 | −0.366 | 0.364 | |
| 3.86 ± 0.47 | 1–5 | 2.35 | 5.00 | −0.214 | 0.607 | ||
| 3.92 ± 0.42 | 1–5 | 2.60 | 4.93 | 0.025 | 0.582 | ||
| Problem clarification | 3.83 ± 0.52 | 1–5 | 1.80 | 5.00 | −0.508 | 1.288 | |
| Cause analysis | 3.28 ± 0.36 | 1–5 | 2.50 | 5.00 | 0.435 | 1.171 | |
| Alternative development | 3.64 ± 0.47 | 1–5 | 2.20 | 5.00 | 0.285 | 0.989 | |
| Planning/implementation | 3.63 ± 0.51 | 1–5 | 1.50 | 5.00 | −0.203 | 1.580 | |
| Performance evaluation | 3.65 ± 0.39 | 1–5 | 2.60 | 5.00 | 0.351 | 1.205 | |
| 3.63 ± 0.35 | 1–5 | 2.53 | 4.64 | 0.243 | 1.253 | ||
3.3. Differences in Problem-Solving Ability According to General Characteristics
The problem-solving ability according to the general characteristics of the subjects was as follows ( Table 3 ): age (F = 4.32, p = 0.015), academic level (F = 10.17, p < 0.001), interpersonal relationships (F = 9.47, p < 0.001), satisfaction with major (F = 3.73, p = 0.012), PBL experience (F = 3.73, p = 0.012), number of PBL experiences (F = 3.20, p = 0.025), and practical experience (F = 2.74, p = 0.007). There was a significant difference in problem-solving ability accorfing to the number of training weeks (F = 4.46, p = 0.013). Scheffé’s post hoc analysis indicated that participants older than 23 years old and younger than 20 years old, as well as fourth-year students, were more dissatisfied than were second-year students. In other cases, interpersonal relationships were very good. Additionally, satisfaction with the major was more than satisfactory. Problem-solving ability was statistically significantly higher for those with more than 7 weeks of practice, and there was no case of not having more than 7 weeks of practice.
Differences in metacognition, communication competence, and problem-solving ability according to nursing students’ general characteristics (N = 192).
| M ± SD | t/F( ) | M ± SD | t/F( ) | M ± SD | t/F( ) | ||
| Age (years) | <21 | 3.75 ± 0.48 | 2.83 (0.061) | 3.87 ± 0.38 | 0.84 (0.433) | 3.54 ± 0.32 | 4.32 (0.015) a < c |
| 21–<23 | 3.92 ± 0.47 | 3.95 ± 0.42 | 3.64 ± 0.37 | ||||
| ≥23 | 3.92 ± 0.44 | 3.96 ± 0.47 | 3.73 ± 0.31 | ||||
| Sex | Male | 3.92 ± 0.42 | 0.68 (0.409) | 3.95 ± 0.41 | 0.30 (0.584) | 3.70 ± 0.35 | 1.81 (0.181) |
| Female | 3.85 ± 0.49 | 3.92 ± 0.42 | 3.61 ± 0.34 | ||||
| Academic level | Sophomore | 3.72 ± 0.59 | 5.59 (0.004) a < c | 3.80 ± 0.43 | 4.58 (0.011) a < c | 3.51 ± 0.29 | 10.17 (<0.001) a < c |
| Junior | 3.89 ± 0.47 | 3.96 ± 0.35 | 3.60 ± 0.32 | ||||
| Senior | 3.99 ± 0.45 | 4.01 ± 0.44 | 3.77 ± 0.37 | ||||
| Interpersonal relationships | Very good | 4.07 ± 0.54 | 5.79 (0.004) a > c | 4.38 ± 0.40 | 40.71 (<0.001) c < b < a | 3.78 ± 0.48 | 9.47 (<0.001) b, c < a |
| Good | 3.88 ± 0.44 | 3.92 ± 0.32 | 3.66 ± 0.29 | ||||
| Moderate | 3.70 ± 0.48 | 3.63 ± 0.39 | 3.46 ± 0.33 | ||||
| Satisfaction with major | Very satisfied | 4.09 ± 0.43 | 7.21 (<0.001) d < b, c < a | 4.19 ± 0.48 | 7.70 (<0.001) c, d < a | 3.76 ± 0.38 | 3.73 (0.012) d < a, b |
| Satisfied | 3.92 ± 0.45 | 3.94 ± 0.38 | 3.66 ± 0.33 | ||||
| Moderately satisfied | 3.71 ± 0.50 | 3.77 ± 0.40 | 3.53 ± 0.35 | ||||
| Dissatisfied | 3.55 ± 0.37 | 3.77 ± 0.31 | 3.52 ± 0.23 | ||||
| PBL experience | Yes | 3.93 ± 0.47 | 2.92 (0.004) | 3.98 ± 0.40 | 2.74 (0.007) | 3.68 ± 0.36 | 3.06 (0.003) |
| No | 3.72 ± 0.47 | 3.81 ± 0.43 | 3.52 ± 0.28 | ||||
| Number of PBL experiences | 0 | 3.72 ± 0.47 | 2.87 (0.038) | 3.81 ± 0.43 | 2.47 (0.063) | 3.52 ± 0.28 | 3.20 (0.025) |
| 1~2 | 3.92 ± 0.51 | 3.97 ± 0.47 | 3.66 ± 0.42 | ||||
| 3~6 | 3.95 ± 0.47 | 3.98 ± 0.38 | 3.70 ± 0.36 | ||||
| ≥7 | 3.91 ± 0.44 | 3.98 ± 0.38 | 3.68 ± 0.32 | ||||
| Clinical practice experience | Yes | 3.93 ± 0.42 | 2.40 (0.019) | 3.97 ± 0.38 | 1.58 (0.115) | 3.69 ± 0.32 | 2.74 (0.007) |
| No | 3.78 ± 0.52 | 3.91 ± 0.44 | 3.56 ± 0.36 | ||||
| Weeks of clinical practice experience | 0 | 3.78 ± 0.52 | 3.02 (0.051) | 3.87 ± 0.46 | 1.58 (0.208) | 3.56 ± 0.36 | 4.46 (0.013) a < c |
| 1~6 | 3.96 ± 0.40 | 3.93 ± 0.35 | 3.66 ± 0.29 | ||||
| ≥7 | 3.91 ± 0.44 | 4.00 ± 0.41 | 3.73 ± 0.35 | ||||
† Scheffé test; ‡ PBL, problem based learning.
3.4. Relationship beetween Metacognition, Communication Competence, and Problem-Solving Ability
There was a strong, significantly positive correlation between metacognition and problem-solving ability (r = 0.672, p < 0.001), and communication competence and problem-solving ability (r = 0.542, p < 0.001). There was also a strong, significantly positive correlation between metacognition and communication competence (r = 0.557, p < 0.001; Table 4 ).
Relationships between metacognition, communication competence, and problem-solving ability (N = 192).
| Variables | Metacognition | Communication Competence | Problem-Solving Ability |
|---|---|---|---|
| r ( ) | r ( ) | r ( ) | |
| Metacognition | 1 | ||
| Communication competence | 0.557 (<0.001) | 1 | |
| Problem-solving ability | 0.672 (<0.001) | 0.542 (<0.001) | 1 |
3.5. Factors Influencing Problem-Solving Ability
Among general characteristics, variables were converted into dummy variables as needed to confirm their effect on the problem-solving ability of nursing students (e.g., age, 23 years or older = 1; academic level, third year = 1; interpersonal relationships, very good = 1; satisfaction with major, more than satisfied = 1; the number of PBL experiences, 3–6 times = 1; and the number of training weeks, 7 weeks or more = 1). A hierarchical stepwise multiple regression analysis was then performed, inputting communication ability followed by metacognition, which were significantly correlated.
The Durbin–Watson value was 1.96 (close to 2), which confirmed that there was no autocorrelation between the independent variables. The variance inflation factor was 1.013 to 4.999; as all value were less than 10, there were no problems with multicollinearity between independent variables.
General characteristics that showed a significant difference with problem-solving ability in univariate analyses were first input to Model 1, namely age, academic level, interpersonal relationships, and satisfaction with major. This model explained 8.1% of the variance in problem-solving ability. When PBL experience and frequency, clinical practice, and number of weeks were added to Model 1 (Model 2), the variance explained was 12.5%, namely an increased of 4.4% compared to Model 1. When communication competence and metacognition were additionally added to Model 2 (Model 3), the variance explained was 51.2%, which is an increase of 38.7% compared to Model 2. Finally, age (β = 0.11, p = 0.048), communication competence (β = 0.24, p = 0.001), and metacognition (β = 0.52, p = 0.023) were significantly related to problem-solving ability. These variables exhibited an explanatory power of 51.2% (F = 21.01, p < 0.001) regarding job satisfaction; the most influential variable was metacognition ( Table 5 ).
Factors influencing problem-solving ability (N = 192).
| Variables | Model 1 | Model 2 | Model 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| B | β | t | B | β | t | B | β | t | |
| Age (R = ≥23) | 0.13 | 0.16 | 2.29 * | 0.10 | 0.13 | 1.77 | 0.09 | 0.11 | 1.99 * |
| Academic level (R = Junior) | −0.06 | −0.09 | −1.22 | −0.23 | −0.31 | −2.71 * | −0.12 | −0.17 | 1.91 |
| Interpersonal relationships (R = Very good) | 0.16 | 0.17 | 2.41 * | 0.14 | 0.15 | 2.11 * | −0.19 | −0.02 | −0.33 |
| Satisfaction with major (R = Satisfied) | 0.13 | 0.17 | 2.40 * | 0.11 | 0.15 | 2.10 * | −0.01 | −0.02 | −0.35 |
| PBL experience | −0.25 | −0.34 | −2.25 * | −0.09 | −0.11 | −1.01 | |||
| Number of PBL experiences (R = 3–6) | 0.14 | 0.19 | 1.66 | 0.14 | 0.18 | 2.13 * | |||
| Clinical practice experience | 0.11 | 0.16 | 1.16 | 0.11 | 0.16 | 1.16 | |||
| Weeks of clinical practice experience (R = ≥7) | −0.00 | −0.004 | −0.03 | 0.09 | 0.12 | −0.03 | |||
| Communication competence | 0.19 | 0.24 | 3.42 * | ||||||
| Metacognition | 0.38 | 0.52 | 8.22 * | ||||||
| Adj R = 0.081, F = 5.20, = 0.001 | Adj R = 0.125, F = 4.42, < 0.001 | Adj R = 0.512, F = 21.01, < 0.001 | |||||||
† Dummy variables; ‡ Reference; ¶ PBL, problem-based learning; * p < 0.05.
4. Discussion
In this study, the mean problem-solving ability score of nursing students was 3.63 out of 5, which is similar to the 3.56 points reported in a study targeting third- and fourth- year students in the department of nursing [ 24 ]. However, the current value is higher than the 3.44 points reported in a study targeting first- and second-year students [ 13 ]. Participants in these studies were nursing students in the second, third, and fourth years of study in this paper, in the third and fourth years in the study done by Kim et al. [ 24 ]; and in the first and second grades in the study by Ji et al. [ 13 ]. Problem-solving ability can be developed under the influence of various factors; those identified in previous studies include communication ability [ 13 ], critical thinking ability [ 12 , 25 ], metacognition [ 11 ], and self-directed learning [ 2 ]. These factors are continuously improved through various interpersonal relationships formed while learning and studying liberal arts and other major subjects, rather than existing as innate abilities [ 26 ]. Therefore, the degree of problem-solving ability was rather high in the study targeting the upper grades. Problem-solving ability in various unexpected situations is essential for working as a nurse [ 27 ]. In the current study, the problem-solving ability score of nursing students approximated the 72.6 percentile of the full 100-point scale. Although this score is relatively high, it is nevertheless necessary to improve problem-solving ability; given the nature of the nurse’s job, this ability represents a very important competency. Therefore, it is necessary to improve the problem-solving ability level of nursing students in Korea. The results of this study showed that factors affecting nursing students’ problem-solving ability were metacognition, communication competence, and age. It is necessary to establish a strategy that considers these factors to improve the problem-solving ability of nursing students.
The participants’ average metacognitive score was 3.86 out of 5, which was slightly higher than the 3.61 observed in a study conducted using the same tools for second-year nursing students [ 12 ]. While direct comparison using other tools is difficult, the metacognitive level of 72.3 obtained by Kim [ 28 ] for all grades in the nursing department was lower than the 77.2 points (out of 100 points) obtained in this study. According to Sternberg and Sternberg [ 29 ], the problem-solving phase includes problem identification, problem expression, strategy formulation, information construction, resource allocation, supervision, and evaluation. For health science students, metacognitive instruction has been shown to have a positive effect on students’ problem-solving ability and in improving academic achievement [ 30 ]. That is, metacognition is a key factor in predicting learning outcomes in the problem-solving domain [ 31 ]. These results were replicated in this study, which showed that a higher metacognitive level of nursing students indicated a significantly higher problem-solving ability. The subjects of this study were second-, third-, and fourth-year nursing students, and it is thought that their metacognitive level was improved compared to students in earlier phases of education, as a result of the curriculum of the nursing department. Educational programs and strategies to improve metacognition will be needed to improve the problem-solving ability of nursing students. The components of metacognition are thinking deeply in the planning stage, establishing possible strategies, undertaking regulating and monitoring activities to carry out the strategy, and revising and regulating to ensure that the solution is progressing in an appropriate direction to achieve the goal [ 32 ]. Therefore, a professor who instructs and checks nursing students is necessary to enable them to set their own goals in the curricular and non-curricular programs as they advance through the course, plan and implement strategies to achieve their goals through deep thinking, and conduct their own monitoring and control processes.
The average communication competence score of the subjects was 3.92 out of 5. Previous studies targeting students in various years of the course at the department of nursing found that the communication competence of nursing students also improved as they progressed through the course, with values reported of 3.58 points [ 33 ] and 3.56 points [ 34 ].
In previous studies, communication competence was a factor affecting nursing students’ problem-solving ability [ 13 ]. However, the current study is valuable because it additionally revealed that the level of problem-solving ability significantly increased according to the level of communication competence. Case-based education is suggested as a strategy to simultaneously improve communication competence and problem-solving skills in nursing student education [ 17 ]. This is because it is difficult to solve problems through integrative thinking and effective communication in a clinical environment, such as a hospital, with only theoretical knowledge of nursing subjects. Thus, the PBL method is applied to theoretical education in nursing colleges [ 35 , 36 ]. The results of this study showed that the presence or absence of PBL education had a significant effect on the problem-solving ability of nursing students; this ability improved when the PBL factor was added to Model 2. Therefore, it is necessary for nursing professors to practice and improve the communication competence of their students through case-based education in various subjects beginning in the first year to improve the problem-solving abilities of the students.
Additionally, the age of the subjects was also a factor influencing the problem-solving ability. Stewart, Cooper, and Moulding [ 37 ] reported that metacognitive levels increase with age. The study revealed that the communication competence of nursing students improved through various experiences [ 38 ]. Age may have had a similar influence.
Previous studies identified critical thinking disposition, empathy, nursing professional intuition, self-leadership [ 24 ], learning motivation [ 17 ], and communication competence [ 13 ] as examples of factors that affect nursing students’ problem-solving ability. However, this study demonstrated that metacognition also significantly affects the problem-solving ability of nursing students. In particular, metacognition and communication competence are considered key concepts, as they explained 51.2% of nursing students’ problem-solving ability. Therefore, it is necessary to consider and continuously apply educational strategies to improve metacognition and communication competence in the education of nursing students in the future.
This study is limited by the small number of nursing colleges that were included in the sampling, as this hinders the generalizability of the results.
5. Conclusions
This was a descriptive research study that identified the degree of and correlations between metacognition, communication competence, and problem-solving ability of nursing students, and identified factors that affect problem-solving ability. The results demonstrated that age, communication competence, and metacognition were the factors that most significantly affected the problem-solving ability of nursing students. Among these factors, metacognition had the greatest influence. Therefore, to improve the problem-solving ability of nursing students, an educational strategy is needed to improve communication competence through case-based learning in the curriculum, and development and application of activities such as PBL. In addition, the guidance of professors is needed to enable nursing students to improve their metacognition.
Since this study revealed that metacognition is a factor that influences the problem-solving ability of nursing students, we recommend conducting a study to check whether it affects actual problem-solving by developing and applying a metacognitive improvement curriculum in the future.
Acknowledgments
We would like to thank the nursing students who participated in the study.
Funding Statement
This study was supported by the research fund of Korean Bible University in 2021.
Author Contributions
Conceptualization, E.C. and J.J.; methodology, E.C. and J.J.; validation, E.C.; formal analysis, E.C.; investigation, E.C. and J.J.; resources, E.C. and J.J.; data curation, E.C.; writing—original draft preparation, E.C.; writing—review and editing, J.J.; supervision, E.C.; project administration, E.C. and J.J.; funding acquisition, E.C. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of Gangneung–Wonju National University (No. GWNUIRB-2022-1).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Conflicts of interest.
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.

You are here
Strategies for using a problem solving approach to solution.
A. Identify Problem
- Ask the client to describe what is happening. Who are the other people involved?
- Help the client break down the problem to focus on the immediate issue (priority).
- What are the triggers and patterns of possible self-destructive acts?
- Assist the client to self-monitor through the use of diaries to recall and detail relationships, moods, triggers, and patterns of self-harm behaviour.
B. Explore Past Attempts to Address Issue
- Help the client identify what has worked in the past.
- Help the client identify supports/resources/personal strengths.
C. Explore Alternatives/Challenges to Determine Solutions
- Identify small steps that will provide change and some control.
- Examine the role of medications to reduce anxiety (APA, 2003).
- Explore safe alternatives, such as breathing and relaxation (Frazier et al., 2003).
D. Choose Solutions
- Focus on helping the client identify small steps, coping strategies, stress reduction, problem-solving and self-examination of results.
E. Implement Process
- Identify when patient will “stop and think” and use collaboratively agreed upon action.
- Journaling successes, emotions, and learning is helpful (Fontaine, 2003).
- Provide time limited therapeutic sessions to assist the client in resolving current interpersonal problems (Gaynes, West, Ford, Frame, Klein & Lohr, 2004).
F. Evaluate Outcomes
- Promote realistic self-appraisal through discussing with the client their abilities and limitations. Help the client reflect outcomes of purposeful tasks.
- Encourage – point out small successes and reinforce the client’s ability to appraise themselves (Fontaine, 2003).
The 5 Nursing Process Steps – (Learn Each Step in Detail)

One of the most important tools a nurse can use in practice is the nursing process. Although nursing schools teach first-year students about the nursing process, some nurses fail to grasp the impact its proper use can have on patient care. In this article, I will share information about the nursing process, its history, its purpose, its main characteristics, and the 5 steps involved in carrying out the nursing process. After reading this article, you will be able to answer the question, “what is the nursing process” and understand what is involved in each of the 5 steps of the nursing process. Additionally, throughout this article, after discussing a step of the nursing process, I will share an example of how the nurse would proceed with that step. For this article’s purposes, we will use information about the following patient: Mr. Collie, a fifty-four-year-old white male being admitted to the Medical-Surgical floor for acute congestive heart failure.
What is the Nursing Process in Simple Words?
When was the nursing process developed, who developed the nursing process, what is the purpose of the nursing process, what are the 7 main characteristics of the nursing process, 1. within the legal scope of practice, 2. based on sound knowledge, 4. client-centered, 5. goal-directed, 6. prioritized, 7. dynamic and cyclical, how many steps are there in the nursing process, what are the 5 steps of the nursing process, step #1: assessment phase.
| The first phase of the nursing process is the assessment phase. In this phase, the nurse collects and organizes data related to the patient. Data includes information about the patient, family, caregivers, or the patient's community or environment as it is relevant to his health and well-being. |
| All phases of the nursing process are essential. The following are a few reasons why the assessment phase is important for nurses to provide care. In the assessment phase of the nursing process steps, the nurse gathers all pertinent information that will be used to establish a care plan. Every other step of the nursing process builds upon the previous. Without a thorough assessment, the other steps of nursing care may be negatively impacted, resulting in unfavorable outcomes. When assessments are performed correctly, they help reduce risks to patient safety which could occur when symptoms or other factors are not considered. |
| The assessment phase of the nursing process involves gathering information about the patient which is used to guide planning care, setting goals for recovery, and evaluating patient progress. Nurses can obtain information about the patient by implementing the following objectives. The patient is the nurse’s main source of information. Therefore, it is essential to establish rapport with them as soon as possible. with the patient's family or caregivers when appropriate. Family members, friends, or other caregivers often offer insight into what is going on with the patient. It is important for nurses to listen to the patient’s support people and gather any information available. When the patient feels comfortable, it makes it easier to get the necessary information that will be used to establish a plan of care. The patient interview is one of the main sources of information used to plan patient care. Any information that is measurable or observable such as vital signs and test results is considered objective data. Subjective data is information gathered from the patient. |
| Assessments are vital to the nursing process. The information gathered in the assessment phase impacts every component of patient care. Nurses must demonstrate excellent verbal and written communication skills, strong attention to detail, and possess an in-depth understanding of body systems. The most frequently used clinical skills for patient assessment are inspection, percussion, palpation, and auscultation. |
| The assessment phase is a critical component of the nursing process. Information gathered in this phase is used to establish a foundation upon which all patient care moving forward is established. Remember, it is normal for patients to feel nervous or fearful when they are sick and in an unfamiliar place, like a hospital. Therefore, the nurse needs to establish an environment conducive to patient comfort. The assessment may include but is not limited to, the following aspects: environmental, physical, cultural, psychological, safety, and psychosocial assessments. The following is a guideline of what should happen during the assessment phase. During the assessment phase, the nurse collects objective and subjective data using proven methods to assess the patient. The most common methods for collecting data are the patient interview, physical examination, and observation. The patient interview is a deliberate or intended communication or conversation with the patient. It is used to obtain information, identify problems that concern the patient and/or the nurse, evaluate changes, provide support, and educate the patient and family/caregivers. The nurse will also conduct a head-to-toe nursing assessment addressing each body system and noting any abnormalities, complaints, or concerns. Observation requires the nurse to use all their senses (sight, touch, smell, hearing) to learn about the patient. After collecting data, the nurse must organize and validate data and document about the patient's health status. Validation is the process of verifying data to be sure it is factual and accurate. Nurses must be careful to not come to conclusions without adequate data to support their conclusion. It is also necessary to understand the difference between inferences and cues. Cues are signals the patient uses to alert the nurse about a concern or question or objective data the nurse can observe or measure. Inferences are the nurse's conclusion or interpretation based on cues. For example, the patient may complain about a painful incision two days post-operatively, and the nurse may observe the incision site is red and feels hot. These are cues. The nurse then makes an inference that the operative incision is infected. After data from the assessment is collected, organized, and validated, it must be recorded. One thing I always tell nursing students and cannot stress enough to any nurse is, "If you didn't document it, you didn't do it." While that may seem harsh, from a legal standpoint, if a nurse is asked to verify care or treatment and there is no supporting documentation, there is no way to prove the care occurred. Thorough documentation is one of the best ways for everyone involved in patient care to be aware of changes in the patient's status, and it helps promote effective collaboration within the interdisciplinary team. |
| While all the nursing process steps are essential, without a thorough assessment, the other steps of the nursing process are not as easy to follow through. Nurses must recognize barriers that could impede the assessment phase and find ways to overcome them. The following are five common challenges you may face during the assessment phase and some suggestions on how to overcome them. Limited Time There are days when nurses feel as though there aren’t enough hours to accomplish all the work that needs to be done. When you are short-staffed or have several patients waiting for a nursing assessment before you can initiate care, it can feel a bit overwhelming. Even on the busiest of days, it is important for nurses to perform thorough nursing assessments for all patients assigned to them. That means it is necessary to learn to manage time efficiently. The first step in overcoming limited time is to be familiar with the format or forms your employer uses to record assessments. For example, the Health Information Technology for Economic and Clinical Health Act of 2009 advanced the adoption and use of electronic health records. Nearly one hundred percent of hospitals use some type of EHR. Electronic health records have helped improve workflow by eliminating time spent pulling physical charts or documenting in paper charts. Interruptions It is not uncommon for interruptions to occur when nurses are performing assessments. While some interruptions may be necessary, all are not. Interruptions during patient assessments can delay care and could result in errors or omissions. The best way to overcome the challenge of interruptions during the assessment step of the nursing process is to provide for privacy before you begin the assessment. Whether you are working in triage, assessing a patient newly admitted to your floor, or in a busy emergency room, it is possible to reduce interruption. Pull the privacy curtain closed if you are in an area with more than one patient or several staff close by. Some facilities use "Do Not Disturb" or "Room in Use" signs to provide privacy for nurses and patients. Inexperience Every nurse knows the importance of a good nursing assessment. Newly graduated nurses are less experienced than other nurses and may feel uneasy about performing a nursing assessment alone. Additionally, if your facility changes its documentation format or implements a new program for charting, and you've not yet used the program, your inexperience could pose a challenge when doing an assessment. The only way to overcome inexperience is to become experienced. Nursing assessments are typically classified as either a Complete Health Assessment or a Problem-Focused Assessment. Know which type of assessment you need to perform. Gather basic equipment: gloves, thermometer, blood pressure cuff, stethoscope, penlight, and watch. Establish a sense of trust and respect between the patient and yourself. No matter which type of assessment you perform, it should be systematic, making sure you cover each body system. If you assess each body system and make notes about what is normal/abnormal, you decrease the chances of omissions in documentation. Remember, take your time, trust your instincts, and if you need help, ask for it. Patient Anxiety Patient anxiety can create a significant challenge for nurses during a patient assessment. Anxiety can hinder communication making it difficult to gather all the necessary data. If anxiety is bad enough, it can cause changes in vital signs, which could be misinterpreted as something more than an anxious reaction. Before beginning an assessment, take the time to make your patient comfortable. While you may not have time for a long conversation or "get to know you" session, you can ease your patient's anxiety by being calm and friendly. Some questions may make patients feel uncomfortable, especially teenagers. Allow them time to answer your questions without feeling rushed. Verify their understanding by asking if they can explain what you've discussed in their own words. Remember, everyone gets nervous or anxious at times, and when we are sick, it can be worse. It's nothing personal against you or your skills. Make everything about the patient. Patients Not Being Forthcoming About Symptoms Whether it is fear of the unknown, embarrassment, or another reason, there are times when patients may be apprehensive about sharing personal information. Lack of information or omission of details that the patient may think is irrelevant may negatively impact the process of care planning. Therefore, while it is easy to understand a patient's apprehension, it is crucial for nurses to gather as much information as possible when performing a nursing assessment. It can be easy to feel frustrated if a patient is not forthcoming about symptoms during an assessment. Keep in mind, being sick and needing medical care can be frightening. The best way to get patients to talk to you is to be accepting of them, no matter what. Be sure to tell your patient you are there for them and will work with them to help them get better. When you say things like you will "work with them," it lets your patient know you are going to do your part, but you expect them to do theirs as well. If you feel like your patient is withholding information, instead of making an accusation, try to rephrase the question. Make your questions clear so the patient knows what information you need. |
| The format for recording nursing assessment data may vary from one facility to another. However, the information gathered for the assessment is relatively similar. The following are examples of content the nurse should include in the initial nursing assessment phase of the nursing process. 04/19/22 13.30 J. Mock, LPN 54 yrs. 2 mos. M 6’2” 268lbs 4oz Dr. Michael Coulvan 03/04/1968 CHF, acute Temp 98.8, Resp. 20, Pulse 76, BP 136/80 NKDA, no food allergies Jerold R. Collie 123 Blakely Lane, Clayton, MO. 1234 (318) 555-1234 Alert & Oriented x3; PERRLA, Unaided hearing; Bilateral hand grips equal; Bilateral foot push equal; no evidence of tremors; denies tingling, burning, loss of consciousness, hallucinations, disorientation, visual disturbances, or hx/o brain injury or stroke. Pulses present, regular, and strong: x2 upper extremities (Radial); present X2 lower extremities (Pedal); heart rate regular, strong; capillary refill <3 second upper and lower extremities Respirations even, labored; Dyspnea on exertion; Lungs: Bilateral rales in lung bases; Cough: Nonproductive; Oxygen: 2L per NC Reports 10 lb weight gain in last two weeks. Continent of bowel; Last BM 4/19/22; Laxatives: No, Enemas: No; Hx of Constipation: No Continent of bladder; Uses urinal prn; urinal emptied of approximately 200 cc clear, amber urine Skin is pink, warm, and dry; Mucous membranes pink and moist Reports pain and stiffness in joints of hands mostly in the a.m.; denies history of gout, arthritis, bursitis, or fractures; Negative paralysis; Negative contractures, No congenital anomalies; No prosthetic devices; Able to carry out most ADLs with minimal assist but may require periods of rest r/t dyspnea with exertion; Uses walker for ambulation. Headache Constant, throbbing 5 Full weight-bearing; Ambulatory with 1 person assist; Client uses walker occasionally; No supportive devices Client is alert, friendly, and answers questions readily; Comprehension: rapid. Divorced; Client lives alone in his own home; Has two adult children who live nearby and visit frequently; Client reports he has several close friends who call or visit often. History of hypertension; Denies any other medical issues prior to this admission. Client reports previous substance abuse, methamphetamine was his drug of choice. Client states he has been substance and alcohol-free for three years. Paternal hx/o CHF, HTN, and Lung Ca. Maternal hx/o DM, and HTN. *In addition to the information the nurse will gather during her assessment, the assessment phase of the nursing process includes gathering objective data such as copies of laboratory or diagnostic testing. If the facility uses electronic health records, as most do, this information will probably already be uploaded to the patient’s electronic chart. It is, however, the nurse’s responsibility to gather and verify all data is available. |
| The assessment phase of the nursing process lays the foundation upon which all other nursing process steps build. The information gathered during the nursing assessment tells the nurse about the patient’s history, current complaints, medications, and any other pertinent information that may impact care planning. Without a thorough, proper patient assessment, it is impossible to develop a patient-specific care plan. Nurses collect data during the assessment phase by communicating with the patient, spouse, and caregivers, reading patient records, nursing observation, and collecting measurable data such as vital signs. Subjective data is any information the nurse collects through communication. A few examples of subjective data include the reason for the patient’s visit to the doctor, patient or family medical history, medications the patient is taking, and any symptoms such as chills, aches, or pain. Objective data is any measurable information obtained from sources other than the patient. For example, the patient’s height, weight, vital signs, and laboratory or diagnostic test results are objective data collected during a patient assessment. Nurses collect verbal data by talking to patients, their family members (when appropriate), and other members of the healthcare team. Subjective matter is usually often the result of verbal communication during the patient interview. Nonverbal data is collected during the assessment phase of the nursing process by observing the patient's body language, reading patient charts, or medical test results. For example, the patient may not offer a verbal report of pain, but the nurse may observe him clutching or guarding his side, which could indicate pain. The nurse can use the nonverbal data to form assessment questions as a way of following up with what she has observed or read. The primary source of data collection during the nursing assessment is the patient. Other sources include family, friends, caregivers, and other members of the healthcare team. Data are also collected from laboratory or diagnostic reports, the patient’s medical records, and the nurse’s observations. Tertiary data are data gathered from sources such as the patient's chart, lab, or x-ray reports. Nurses may also use tertiary sources such as diagnostic manuals or textbooks to verify or compare information. Nurses can use a few methods to verify the accuracy of data collected during the assessment phase of the nursing process. A few ways to verify data is to clarify information with the patient by asking additional questions, compare objective and subjective data to see if there are any discrepancies, recheck data by repeating the assessment, and verifying data with another nurse or healthcare team member. One example of verifying data is to perform repeat vital sign check. For instance, if Mr. Jones has a blood pressure reading of 220/100 but has no history of hypertension, the nurse should retake his blood pressure to validate its accuracy. If the nurse feels it is necessary, they may use different equipment or ask someone else to perform the vital sign check to check for accuracy. The primary methods nurses use to collect data are observation, patient interviews, and head-to-toe assessments. Nurses use various tools and equipment to help gather data about patients. A few examples of tools and equipment nurses use include a stethoscope, blood pressure cuff, thermometer, pulse oximeter, and scales. You may need a glucometer and lancets to check blood sugar, as well. |
Step #2: Diagnosis Phase
| Diagnosis is the second phase of the nursing process. It is also designated by the American Nurses Association as the second Standard of Practice. The standard is defined by the ANA stating, "The registered nurse’s analysis of assessment data to determine actual or potential diagnoses, problems, and issues.” The nursing diagnosis reflects the nurse’s clinical judgment about a patient’s response to potential or actual health issues or needs. |
| Before a plan of care can be established, nurses must determine which nursing diagnosis/diagnoses apply to their patients. The following are a few reasons why the diagnosis phase of the nursing process is important. The diagnosis phase of the nursing process helps nurses view the patient from a holistic perspective. Using a nursing diagnosis can lead to higher quality nursing care and improved patient safety, as care is based upon the needs outlined in the diagnosis. The diagnosis phase helps increase the nurse’s awareness and can strengthen their professional role. |
| In the diagnosis phase, the nurse follows a set of objectives that end with developing the nursing diagnosis/diagnoses used to establish patient care. These are the main objectives of the diagnosis phase: The nurse must identify what problem the patient is experiencing related to the medical diagnosis. Any situation or problem that could result because of the patient’s medical diagnosis is a risk factor for a nursing diagnosis and must be addressed. All data gathered during the assessment phase of the nursing process must be compiled, validated, and analyzed to support an appropriate nursing diagnosis. Nursing theories involve an organized framework of concepts and purposes that guide nursing practices. A nurse’s theory is their unique perspective about the patient’s status and measures needed to improve the patient’s outcome. After identifying problems and risk factors, analyzing data, and developing a nursing theory, the nurse can then establish a nursing diagnosis or diagnoses which is used to establish a nursing care plan. |
| Nurses will utilize several skills in the diagnosis phase of the nursing process steps. Critical thinking, problem-solving, and communication skills are necessary to work in this phase. Nurses must also demonstrate the ability to prioritize patient needs. |
| The diagnosis phase of the nursing process involves three main steps: data analysis, identification of the patient’s health problems, risks, and strengths, and formation of diagnostic statements. Data Analysis involves the nurse clustering cues, comparing patient data against standards, and identifying inconsistencies or gaps in the data. After data analysis, the nurse will work with the client to identify actual, risk, and possible diagnoses. In this step, the nurse will determine if an identified problem classifies as a nursing diagnosis, medical diagnosis, or collaborative diagnosis/problem. It is important to involve the patient in this step whenever possible, to identify the client's resources, coping abilities, and strengths. The last step of the diagnosis phase involves creating a nursing diagnosis. The nursing diagnosis may have up to three components: a NANDA-I approved , a which defines the cause of the diagnosis, and an as that uses patient-specific data to justify the diagnosis and diagnostic statement. |
| The nursing diagnosis is different from a medical diagnosis. It requires careful consideration of the patient’s individual problems, situation, and needs to develop appropriate nursing diagnoses. Here are a few examples of challenges that may occur during the diagnosis phase of the nursing process and some suggestions on how to overcome them. Creating a Nursing Diagnosis Is Often a Complex Process Although there are resources and guidelines to help nurses develop nursing diagnoses, the process can be complex. Before nurses can create a nursing diagnosis, they must interview and assess the patient and review data, which can be time-consuming. While you may not overcome the complexities of creating nursing diagnoses, it is possible to make the process easier. For example, be sure to review all objective data, including baseline vitals, laboratory or diagnostic test results, and subjective data. Make sure the patient's medical history is accurate and find answers to any questions not yet answered. The more information you have to work with, the easier it becomes to develop diagnoses based on that data. Nurses May Interpret Data Differently Some data are taken at face value, such as laboratory or diagnostic test results or vital signs, which are measurable. Subjective data is data reported by the patient. It is information given to the nurse by the patient based on the patient’s perception of what he is feeling. Despite efforts to appreciate the patient’s perception, nurses sometimes interpret data differently. When this happens, it can create a challenge when developing nursing diagnoses for the nursing care plan. It is essential for nurses to have a clear understanding of which data is objective or subjective. Once the differences in data are realized, nurses must be careful to not rely upon only one piece of data or their own perception of data to create a nursing diagnosis. Instead, establishing nursing diagnoses should be a collaborative effort among the nursing care team. Nurses assigned to a patient’s care should discuss their perception of data and make informed decisions based on all data. Insufficient Data to Support a Nursing Diagnosis Nurses must review all available data, including but not limited to subjective and objective findings, lab and diagnostic test results, and narrative notes from the patient interview before a nursing diagnosis can be made. If the nurse does not obtain enough data during the assessment, it will be difficult to establish appropriate nursing diagnoses. The best way to overcome the challenge of insufficient data is to perform a thorough assessment, patient and/or family interview, and make sure all results from any tests are readily available for review. If you have reached the diagnosis phase of the nursing process and find you do not have enough data, go back to the sources of information and gather data. You may find that you need to reassess the patient or ask additional questions. Lack of Communication Between Nursing Staff Although patients are assigned a primary nurse, nursing is a team effort that requires collaboration. When there is a lack of communication between nursing team members, information may be inadvertently omitted from notes or reports. This failure in communication makes getting a complete view of the patient's status difficult, resulting in challenges in developing appropriate nursing diagnoses. Nurses must be alert and responsive to patients and one another. End of shift report is an excellent way for nurses to communicate changes in a patient's status. Nurses should make notes of anything pertinent before handing off care to the next shift nurse and clearly communicate concerns about the patient's progress or lack thereof. When the lack of communication is resolved, nurses can compare information to use when establishing nursing diagnoses, ensuring the patient gets the best care possible. Deciding the Type of Nursing Diagnose to Use There are four main types of nursing diagnoses: Problem-focused, Risk, Health Promotion, and Syndrome. When nurses get to the diagnosis phase of the nursing process, they must determine which type or types of diagnoses are relevant to their patients. While experienced nurses may find it easier to decide which type of diagnosis to use, new or less experienced nurses may find it challenging. Additionally, some healthcare facilities prefer nurses to use a specific type of diagnosis, which can be frustrating, especially if the nurse feels a different type of nursing diagnosis is more appropriate. Overcoming the challenge of choosing the right type of nursing diagnosis requires understanding when each type is most appropriate. If the nurse has sufficient data from the assessment phase, they can then identify potential diagnoses and determine which type of diagnosis to use. The following are the four types of nursing diagnoses and examples of each. focus on a specific problem the patient is experiencing. This type of diagnosis has three components: a nursing diagnosis, related factors or diagnosis statement, and defining characteristics or the as evidenced by statement. For example, the patient with chronic obstructive pulmonary disease (COPD) could have a problem-focused nursing diagnosis of "Ineffective Breathing Pattern related to decreased lung expansion as evidenced by dyspnea and ineffective cough." identify potential problems or risks the patient may experience because of his medical diagnosis. A risk nursing diagnosis typically has two components, the diagnosis, and risk factors. The patient with COPD may have a risk diagnosis of "Risk for Ineffective Airway Clearance related to decreased lung capacity." (a.k.a. Wellness Nursing Diagnosis) is based on the nurse's clinical judgment about the patient's desire and motivation to increase his well-being. These diagnoses focus on the client's transition from one level of wellness to a higher level of wellness. Health promotion nursing diagnoses are usually one-part statements or include only a diagnostic statement. The COPD patient's Health Promotion Nursing Diagnosis may state "Readiness for Enhanced Wellness." are clinical judgments related to a cluster of risk nursing diagnoses predicted to occur because of a particular event or situation. The syndrome nursing diagnosis is also written as a one-part statement. For example, the COPD patient may have a syndrome diagnosis of “Ineffective Airway Clearance, Impaired Gas Exchange, Ineffective Breathing Pattern.” |
| After reviewing the data collected in the assessment phase of the nursing process, the nurse determines which type of diagnosis is appropriate and moves to the planning phase. In the case of Mr. Collie, the nurse chooses a problem-focused nursing diagnosis and a risk nursing diagnosis. • Decreased Cardiac Output r/t impaired contractility and increased preload and afterload AEB irregular heartrate of 118, fatigue, and dyspnea on exertion (Problem-focused) • Risk for Impaired Skin Integrity r/t edema, decreased tissue perfusion, and decreased activity. (Risk) |
| Although they share similarities, nursing and medical diagnoses are different. The nursing diagnosis is used by a nurse to identify a patient’s actual or potential risk(s), wellness, or responses to a health problem, condition, or state. A medical diagnosis is used by physicians to determine or identify a specific condition, disease, or pathologic state. NANDA-I stands for North American Nursing Diagnosis Association International. NANDA-I is a professional organization that researches, develops, disseminates, and refines nursing diagnosis terminology. The organization was formed as NANDA in 1982, it was renamed NANDA-I in 2002 because of its increased worldwide membership. Each nursing diagnosis is made up of four main components: problem and its definition, etiology, risk factors, and defining characteristics. The primary purpose of establishing a nursing diagnosis is to communicate the healthcare needs of the patient among members of the healthcare team and within the delivery system. The nursing diagnosis allows nurses to facilitate individualized care for the patient and family and strengthens the profession. The nursing diagnosis serves as the basis for selecting nursing interventions, which have a significant impact on patient outcomes. If an accurate nursing diagnosis is not chosen, the plan of care and subsequent nursing interventions may not address the patient’s issues appropriately resulting in negative patient outcomes. Nursing diagnoses are ranked in order of importance. Immediate life-threatening problems or issues related to survival are given the highest priority. Nursing diagnoses focus on the patient’s response to health conditions, and patients often respond differently. Therefore, it is not uncommon for patients with the same medical diagnosis to have different nursing diagnoses. |
Step #3: Planning Phase
| The planning phase of the nursing process is the stage where nursing care plans that outline goals and outcomes are created. The goals and outcomes formulated during this phase directly impact patient care and are based on evidence-based nursing practices. |
| The planning phase of the nursing process is essential in promoting high-quality patient care. It is considered the framework upon which scientific nursing practice is based. The following are three of the top reasons why the planning phase is so important. Care planning provides direction for personalized patient care based on the client's unique needs. The planning phase enhances communication between patients, nurses, and other members of the healthcare team. Planning encourages continuity of care across the healthcare continuum and promotes positive patient outcomes. |
| The American Nurses Association's Standards of Clinical Nursing Practice identifies planning as one of the essential principles for promoting the delivery of competent nursing care. The planning phase of the nursing process has five main objectives, all of which focus on nursing interventions to promote positive patient outcomes. The following are the main objectives of the planning phase. The nurse reviews the nursing diagnoses and prioritizes them according to physiological and psychological importance. This step helps the nurse organize the patient’s nursing diagnoses into a format that promotes effective planning. This objective of the planning phase of the nursing process involves setting goals related to each diagnosis. Goal setting helps to provide guidelines for nursing interventions and establishes criteria by which the care plan's effectiveness is evaluated. Remember the acronym SMART when developing goals. SMART goals are Specific, Measurable, Relevant, and Time-bound. After goals are established, the nurse can identify expected outcomes based on each goal. Outcomes should be realistic, mutually desired by the patient and nurse, and attainable within a designated amount of time. After goals are agreed upon and established, the nurse then implements decision-making skills to select nursing interventions that are relevant to the nursing diagnoses. Interventions are prioritized in order of planned implementation. After priorities, goals, outcomes, and interventions are established, the nurse must document the care plan. Documentation of the care plan includes nursing orders which communicate the interventions the nursing staff will implement for the client. Nursing orders must be well-written and should include the order date, which action will be performed, a detailed description, the time frame in which the intervention will be performed, and the nurse's signature. |
| Nurses utilize many of the same skills for each of the nursing process steps. In the planning phase, nurses must have strong communication skills, time management and organizational skills, and a willingness to work collaboratively with the patient and interdisciplinary team. Nurses must have strong critical thinking skills, as they must weigh the risks and consequences of each intervention. |
| The planning phase of the nursing process is when nurses formulate goals and outcomes that impact patient care. This step involves prioritizing patient needs, identifying expected outcomes, establishing nursing interventions, and identifying patient-centered goals. In the planning phase, nurses identify goals and outcomes for patient care based on evidence-based practice guidelines. Once objectives of planning are met, the nurse creates a written plan of care, or care plan. The care plan is a written guide organizing data about the patient's care into a formal statement of strategies or interventions the nurse will enact to help the patient achieve optimal outcomes. |
| It is normal to face challenges, no matter which phase of patient care you are involved with. The planning phase can feel a bit tricky because nurses need to be careful to develop plans considering the individuality of the patient. The following are a few examples of challenges you could phase when you begin planning patient care. Not Knowing How to Format the Care Plan There are different formats for creating a care plan. If nurses do not know the format their facility uses, it can be easy to overlook components of the plan, which may impact the delivery of care and patient outcomes. Not knowing how to format a care plan is probably one of the easiest challenges to overcome in the planning phase. With the implementation of electronic health records and programs that help nurses choose nursing diagnoses and interventions, creating care plans has become easier. As a nurse creating a care plan, your job is to make sure all relevant information is included in the plan. The nursing diagnosis, interventions and expected outcomes, time frames in which outcomes should be accomplished, and a place to document evaluations should all be included. Not Establishing Goals and Expected Outcomes Have you ever heard the saying, "Failure to plan is planning to fail"? That principle applies to everything in life, including patient care. No care plan is complete without clear goals and outcome identification. If there are no goals or an insufficient number of goals relevant to the nursing diagnoses, deciding on interventions is impossible. The nursing care plan should always be patient-centered and individualized. Goals and outcomes should be tailored to meet each patient's needs and should be considerate of the patient's cultural beliefs and values. Nurses use the nursing care plan as a road map that all members of the nursing team use to help the patient reach goals. It is vital that nurses establish goals that are attainable and relevant to the patient's specific needs. In the planning phase of the nursing process, the nurse should establish short-term and long-term goals and determine the outcome associated with achieving those goals. Establishing goals and outcomes is vital to this step in the nursing process. Therefore, nurses should take the time to consider each goal and outcome carefully and discuss the plan with the patient and healthcare team. Unrealistic Goals While it is okay to be optimistic about a patient’s ability to achieve goals, it is essential for nurses to be realistic about what their patients can or cannot do. If goals are unrealistic, patients can quickly become frustrated. Frustration often leads to noncompliance, which can negatively affect patient outcomes. After carefully determining nursing diagnoses, the nurse must determine which goals the patient can achieve realistically. Realistic goals are specific and well-defined, measurable, achievable, relevant to the patient's status and needs, and achievable within a specific timeframe. To overcome the challenge of unrealistic goals, identify what is essential in helping the patient achieve optimal outcomes. Discuss goals with the patient, family, care providers, and nurse manager. Once realistic goals are identified, offer support and encouragement to the patient. The nurse should continually monitor and assess the patient's progress toward meeting goals. Limited Patient Input Although nurses can create nursing care plans independent of patient input, excluding patients from plans about their care may lead to distrust or confusion. If a patient feels he cannot communicate with nurses or his opinion is not valued, it can result in noncompliance with the care plan and negatively impact the patient’s outcome. When patients are involved in their care, the processes of planning and implementation seem to flow easier. Nurses can overcome the challenge of limited patient output by promoting a comfortable, trusting nurse-patient relationship which encourages patient participation. Ask the patient about their health goals and what limits they feel may affect their ability to reach goals. Offer suggestions about desired goals and expected outcomes and explain why they are relevant to the patient's health and long-term well-being. Being Unsure of Appropriate Time Frames to Meet Expected Outcomes/Goals It is possible for nurses to create realistic goals and expected outcomes in the care plan but to set unrealistic time frames in which the patient is expected to meet those goals. One reason this challenge occurs is nurses sometimes fail to plan care based on an individual patient’s abilities. Instead, they establish goals based on their perception of what any patient with the same diagnosis may be capable of achieving. When working through the planning phase of the nursing process, nurses must consider patients as individuals with specific needs and abilities. The nurse should specify a time frame for achieving goals that is reasonable and that does not create undue stress or worry for the patient. When discussing the care plan with the patient, it is important to explain each goal to the patient. Include education about why there is an anticipated time for accomplishing goals and what each person's responsibilities are to help make achieving the goals possible. |
| Once the nursing diagnosis or diagnoses are established, the nurse completes the planning phase of the nursing process by determining patient goals and expected outcomes and establishing which nursing interventions to initiate. The following are goals and expected outcomes for Mr. Collie based on the nursing diagnoses of Decreased Cardiac Output and Risk for Impaired Skin Integrity. The client will verbalize understanding of activities and lifestyle changes focused on reducing cardiac workload. The client will demonstrate adequate cardiac output AEB vital signs within normal limits. The client will report decreased episodes of dyspnea. Monitor vital signs. Palpate peripheral pulses. Assess for signs of edema. Monitor for signs of pallor or cyanosis. Maintain skin integrity. The client will verbalize understanding of techniques/behaviors to prevent skin breakdown by end of shift. Inspect skin, noting areas of altered circulation, bony prominences, and/or signs of emaciation. Encourage frequent position changes Provide alternating pressure mattress, heel protectors, and elbow protectors |
| There are four main components of a nursing care plan: Client Assessment, including medical and diagnostic reports, Nursing Diagnosis, Desired Outcomes/Goals, Nursing Interventions with evidence-based rationale, and Evaluation. The best way to write a nursing care plan is to include information associated with the nursing process steps. Review all relevant data, medical history, vital signs and assessment data, physical, emotional, spiritual, ad psychosocial needs, identify areas where improvement is needed, and establish risk factors. A nursing diagnosis is an actual or potential health problem that nurses can address without physician intervention. A few examples include risk for falls, risk for compromised skin integrity, and risk for dehydration. Setting goals requires establishing desired outcomes and identifying measures by which the patient will achieve them. Although there may be situations where it is not possible, it is ideal to set goals with the patient when they are able. Nursing interventions are actions taken by the nurse to help patients achieve goals and meet desired outcomes. Nursing interventions include initiating fall precautions, administering medications, and assessing the patient’s pain level. of the plan and change or update, as needed or indicated. The next two FAQs about the planning phase are related to setting goals. Goals are statements of purpose describing an objective to be accomplished. All goals in the nursing care plan should be client-centered and measurable. Each goal should focus on the problem, measures to resolve the problem, and rehabilitation. The time frame given to accomplish goals in the care plan varies, depending on the setting where patient care is provided. A tip I always share with students is, if you are not sure how to write a goal, try converting the nursing diagnosis into a positive statement of action. A short-term goal in nursing care plans is a goal focused on demonstrating a change in behavior. Short-term goals can be completed in as little as a few minutes or up to a few days. The nurse should consider what behavior the patient can most easily exhibit or identify to show understanding of goals and attempts to achieve goals. For example, let’s consider the following nursing diagnosis and determine a short-term goal. Long-term goals are the desired outcome related to accomplishing one or more short-term goals for an extended period. In some cases, long-term goals can take weeks, months, or even years, to achieve. Planning occurs in three stages: initial, ongoing, and discharge. Initial planning occurs when the nurse performing the admission assessment develops a preliminary plan of care. Ongoing planning is the process of updating the patient’s plan of care as new information is collected and evaluated. Discharge planning begins at admission and involves the anticipation of the client’s needs and plans to meet those needs after discharge from care. When possible, the patient should be included in all phases of the nursing process. The patient is the best source of data, the person being treated, and usually the most reliable source of information used to determine the patient’s strengths, weaknesses, and likelihood of compliance with a plan of care. |
Step #4: Implementation Phase
| The fourth phase of the nursing process is the implementation phase. This phase is when nurses initiate the interventions established during the planning phase. |
| After the nursing assessment is performed, nursing diagnoses are established, and a care plan is developed, the plan must be initiated. All phases of the nursing process are essential. The following are three of the top reasons why the implementation phase is so important. Implementation of the nursing process is significant because it involves action on the nurse's part to promote positive patient outcomes. Conversely, if the care plan is not implemented, there is a lack of nursing care, negatively impacting patient outcomes. When the nursing care plan is implemented (implementation phase), nurses can begin to gauge patient responses to interventions. Implementation supports continuity of care. Care begins from the first patient encounter and continues until discharge. |
| The implementation phase of the nursing process is an ongoing process in patient care. From the time a plan is established, the implementation process continues in a cycle which includes the five objectives below. The nursing care plan is developed based on data from the initial nursing assessment. However, because a patient's condition can change quickly or nurses may obtain new data, ongoing assessments are necessary to validate the need for proposed interventions. Ongoing observations and assessments provide information supporting adaptations of the nursing care plan to promote improved, individualized care. Utilizing data from initial and going assessments, the nurse then establishes priorities for implementing care. Prioritization is based upon which problems are considered most important by the nurse, patient, family/significant others, previously scheduled tests/treatments (diagnostic tests, surgery, therapy), and available resources. Before implementing nursing interventions, the nurse must review proposed interventions and determine the skills and knowledge level required to safely and effectively implement them. For example, the nurse will consider if the patient can independently perform an activity, if a family member may assist, or if the activity requires assistance from a healthcare professional. Although some interventions require the skills and knowledge of a registered nurse, others are less complex and may be delegated to licensed practical/vocational nurses or assistive personnel. The nurse allocates personnel resources by determining the needs of the client, the type of personnel who are available, and facility protocol for care. After verifying priorities and determining resources, the nurse can initiate nursing interventions. Interventions are determined by the cause of the problem and often vary among patients with similar nursing diagnoses depending on expected outcomes for each patient. When initiating nursing interventions, the patient's preference and developmental level should be considered. Additionally, nurses must review the physician's orders which may impact nursing interventions by imposing restrictions on specific factors such as the patient's allowed activity level or diet. Nurses are legally obligated to document all interventions and any observations concerning the patient's response to those interventions. Documentation may be done on checklists, flow sheets, or in narrative form. Any verbal communication between the patient and nurse or among the healthcare team related to interventions and patient responses should be recorded, as well. |
| Like the other nursing process steps, the implementation phase requires broad clinical knowledge, critical thinking and analysis skills, and strong judgment. Whether a nurse is caring for one patient, or several patients, careful planning and time management skills are essential in this phase. Nurses must have psychomotor, interpersonal, and cognitive skills as these serve as competencies through which high-quality nursing care is delivered. Psychomotor skills are necessary to safely perform nursing activities such as handling medical equipment competently. Interpersonal skills help nurses establish therapeutic nurse-patient relationships and promote interdisciplinary collaboration. Cognitive skills are necessary to help the nurse understand the rationale for proposed interventions and make appropriate observations. |
| Implementation involves a focus on accomplishing predetermined goals and continuous progress toward achieving desired outcomes. This phase of the nursing process involves prioritizing nursing interventions, assessing patient safety during nursing interventions, delegating interventions when appropriate, and documenting all interventions performed. |
| Nursing interventions vary depending on the patient and the setting where care is provided. The following are examples of common challenges nurses face during the implementation phase of the nursing process and suggestions for how to overcome them. Lack of Clinical Experience Even when goals and desired outcomes are clearly defined, inexperienced nurses may find implementing nursing interventions challenging. Inexperience may occur because the nurse is newly graduated or if a nurse is transferred to a department where they have never worked. While the most effective way to overcome a lack of clinical experience is to work as much as you can and gain experience, patient care cannot wait for us to feel comfortable performing unfamiliar tasks. When nurses face challenges implementing patient care because of inexperience, the best way to overcome it is to speak up and ask for help. As a nursing instructor, I always encouraged my students to ask questions about everything. The only bad question is the one you do not ask. Nurse leaders, supervisors, and administrators appreciate nurses who readily admit when they need help or guidance. Patient Noncompliance Noncompliance is recognized by NANDA-I as a nursing diagnosis. It is defined as “the behavior of a patient or caregiver that does not correspond with the therapeutic plan agreed upon by the individual, family or guardian, and healthcare provider.” Noncompliance can negatively impact patient outcomes, reduce the patient’s quality of life, and result in increased healthcare costs. One of the best ways to prevent or stop patient noncompliance is to involve the patient in all aspects of care planning. Nurses should ensure the patient is educated about their illness, plans to manage the illness, and expected outcomes of therapies. Education should also include information about how noncompliance may negatively affect the patient's outcome. The patient's understanding of all education should be verified, and if the nurse is unsure the patient clearly understands, teaching should be repeated. Psychosocial Factors Psychosocial factors can impact all aspects of patient care. For example, if there is a presence of domestic abuse or violence, the patient may be afraid to discuss important issues related to care, which could result in misunderstanding established goals. Psychosocial factors may seem a little tricky to navigate. However, if they become a factor affecting the implementation of the nursing process steps, nurses must find a way to try and address the issues. For instance, if the nurse suspects a patient is afraid to discuss certain issues in the presence of others, the nurse should ask for privacy while talking to the patient. By doing so, the nurse offers the patient the opportunity to speak openly without fear of retaliation by an abuser. Then the nurse can discuss options for care with the patient and how to proceed moving forward. Nursing Care Plan Does Not Reflect Appropriate Care for the Nursing Diagnoses Every step of the nursing process builds upon the previous step. Nurses must perform a thorough assessment and collect sufficient data before making nursing diagnoses. After a nursing diagnosis is established, interventions are planned to help resolve the issue(s) the patient is experiencing. If the planned interventions do not align appropriately with the care expected for a nursing diagnosis, implementing the care plan properly cannot occur. It is vital for nurses to handle each phase of the nursing process with deliberate care and appropriate actions. Nursing care plans should be evaluated by the nursing team to ensure that the patient’s needs are addressed, and planned interventions are relevant to the nursing diagnosis/diagnoses. Nursing Shortage The World Health Organization estimates a shortage of more than four million nurses in the United States. No matter how well-written a nursing care plan is, if there is not enough staff to carry out the nursing interventions, the plan cannot be successfully implemented. While it is understandable that one nurse cannot remedy the nursing shortage, there are things all nurses can do to help relieve the impact the shortage causes. |
| Implementation of the nursing care plan involves educating the patient and helping him achieve goals and expected outcomes. It also involves putting the planned nursing interventions into action. To implement the care plan, the nurse will establish priorities, delegate tasks to appropriate staff, initiate interventions, and document interventions and the patient’s response. Nursing documentation should be accurate and relevant to the patient. Use appropriate nursing language and facility-approved abbreviations. In the case of Mr. Collie, the nurse's documentation may look like the following narrative. 04/19/22 @ 1430: Discussed plan of care with client and son who was present in the room, including educating about goals and expected outcomes. The client verbalizes understanding of the importance of lifestyle and activity changes to reduce cardiac workload, the need for vital signs to be within normal limits, and measures to decrease episodes of dyspnea, and safety precautions. The client also verbalizes understanding of the risk for impaired skin integrity and verbally recalls skin integrity is at risk due to "bad circulation and swelling." The client voices understanding that frequent position changes and keeping the skin clean and dry will decrease the likelihood of skin breakdown. Assessed peripheral pulses, which are present and strong bilaterally in upper and lower extremities X2, 2+ pitting edema noted in bilateral lower extremities. Skin remains intact, pink, warm, and dry, no signs of redness or pallor. Heel and elbow protectors applied. Alternating pressure mattress in place and operational. ------------D. Leonard, RN |
| The first step in the process of implementing a nursing care plan is to determine what, how, and when an intervention should be performed. Once you know the what, how, and when, you can determine if the task can be delegated and to whom. The three types of interventions implemented in the nursing process are independent, dependent, and interdependent. are actions nurses can perform on their own and do not require assistance from other team members. For example, routine tasks such as monitoring vital signs or assessing the patient's pain level are independent nursing interventions. require instructions or input from the physician. For instance, if the patient needs a new medication, the physician must prescribe the medication and order the amount and frequency. Dependent nursing interventions are interventions the nurse may not initiate on her own. are also known as collaborative interventions. These interventions involve all members of the interdisciplinary team. For example, if a patient had a total knee replacement, his recovery plan may include a prescription medication from the doctor, assistance with dressing from the nurse or unlicensed assistive personnel, and physical or occupational therapy by the physical therapist or occupational therapist. While many sources use the words interchangeably, intervention and implementation are defined somewhat differently. Interventions are planned nursing activities performed on a patient's behalf. They include assessment, adherence to medication therapy, and problem-solving. Implementation is . Strategies to prioritize patient care typically include the use of nursing diagnoses combined with Maslow’s Hierarchy of Needs Theory. Any nursing diagnosis that suggests a risk or threat to the patient’s survival should be the nurse’s first priority. Remember your ABCs: Airway, Breathing, Circulation. Other physiological needs necessary for survival are considered. Psychosocial needs are then addressed. Psychological needs including a sense of love or belonging, self-esteem, and self-actualization are prioritized last. Medication administration is part of the implementation phase of the nursing process steps. The nursing interventions outlined in the planning phase should include information about medication administration. When the nurse initiates the action of administering the medication, she is implementing the plan of care. All members of the nursing team have roles related to implementing the care plan. In the planning phase of the nursing process, the Registered Nurse determines which tasks may be delegated to Licensed Practical/Vocational Nurses, Nursing Assistants, or other members of the healthcare team. It is essential to remember that, even if a task is delegated, the RN in charge of the patient’s care is accountable for making sure all tasks are completed. |
Step #5: Evaluation Phase
| Evaluation is the final phase of the nursing process. Although evaluation is considered the last of the nursing process steps, it does not indicate an end to the nursing process. Instead, evaluation should be an ongoing process carried out in daily nursing activities that ensures quality nursing interventions and the effectiveness of those interventions. |
| The evaluation phase of the nursing process is important because it fulfills several purposes. The following are the top three reasons why this phase is essential in the nursing process. The primary purpose of an evaluation is to determine the patient’s progress toward achieving established goals and outcomes. Through evaluation, it is possible to determine a healthcare agency’s ability to provide safe and effective healthcare services. Evaluation provides a mechanism to help nurses define, explain, and measure the results of nursing interventions. |
| The Standards of Clinical Nursing Practice established by the American Nurses Association designates evaluation as a fundamental component of the nursing process. This phase of the nursing process has the following objectives. The effectiveness of nursing interventions is determined by evaluating goals and expected outcomes to determine if they provide direction for patient care. It is essential to evaluate nursing interventions because they serve as standards by which patient progress is measured. The evaluation phase is not meant to make nurses feel as if their work is being critiqued or judged. Evaluation allows nurses to verify if the care they are providing meets the standard of care for the patient’s needs. Evaluation involves reviewing all aspects of the patient’s care and determining its effectiveness in helping the patient recover. Because nurses work collaboratively with one another and other members of the healthcare team, the evaluation phase promotes the nurses’ sense of accountability to their patients and to one another. In the evaluation phase of the nursing process, nurses compare and analyze data from the time the patient was admitted to care and determine if positive or negative trends are occurring. This data is helpful in deciding the next course of action to take in patient care. Although the evaluation phase is the fifth and last step in the nursing process, nurses constantly evaluate patient progress. Evaluation allows nurses to establish a pattern of continuous care and attention, which helps promote positive patient outcomes. |
| The evaluation phase of the nursing process is primarily based on the nurse's accurate and efficient use of observation, critical thinking, and communication skills. Some changes in a patient's status may be subtle, requiring sharp observational skills. The ability to analyze reassessment data and use critical thinking are necessary to determine if outcomes have been met or decide if changes in the care plan are needed. As in other phases of patient care, the nurse must demonstrate strong communication skills, as evaluation includes the patient and all members of the healthcare team. |
| During the evaluation phase of the nursing process, nurses determine the patient’s response to interventions and whether goals have been met. The evaluation process consists of seven steps, as follows. Standards and goals are established during the planning phase of the nursing process steps and carried out in the implementation phase. Nurses use evaluation to determine the presence of changes in the patient's status relevant to the established standards. The nurse uses assessment skills early in the nursing process to gather data used to establish goals and expected outcomes. Those same skills are vital for comprehensive, effective evaluation to occur. Nurses gather data to help determine the success of nursing interventions. The data collected during the evaluation phase must answer the question, “Did the patient achieve the treatment goals and expected outcomes outlined in the care plan?” Nurses validate goal achievement by analyzing the patient’s response to nursing interventions outlined in the nursing care plan. Effective nursing interventions address relevant patient needs. If the nursing intervention is efficient, it can be a primary factor related to helping clients resolve actual or potential problems or risk factors. During the evaluation phase, the nurse must use critical thinking skills to determine which nursing actions contributed to improved patient outcomes and to what degree they were effective. This step in the evaluation process allows the nurse to analyze the patient's response to interventions, determine the benefits of those interventions, and identify opportunities or needs for change. In the evaluation phase of the nursing process, the nurse uses observation and assessment skills to reevaluate the patient's status. In this step, the nurse compares baseline data collected in the initial nursing assessment with the patient's current health status. If the evaluation determines a lack of progress toward established goals, the nursing care plan is revised or modified. At this point, revisions are developed by beginning the nursing process anew. The client is reassessed (Assessment), more appropriate nursing diagnoses are established (Diagnosis), new or revised goals and outcomes are developed (Planning), new nursing interventions are implemented, or previous interventions are repeated to maximize effectiveness (Implementation). Then the patient's response is reevaluated (Evaluation). |
| The evaluation phase of the nursing process is the point where nurses and patients hope to see measurable improvement. The following are a few challenges nurses may face when in the evaluation phase. Incomplete Documentation Every nurse is responsible for documenting patient progress and other pertinent information. If one nurse fails to document and report patient changes or progress, or to record laboratory or diagnostic test results, it can lead to challenges when it is time for the evaluation phase. The most effective way to overcome this challenge is to avoid it happening altogether. Be sure to document information about your patients during each shift. Any change in status, progress or lack of progress, subjective and objective findings, or other relevant information should be readily available for any nurse caring for that patient. Patient Frustration In a perfect world, patients would be admitted to care, nursing interventions would be implemented, and we would see positive results. Unfortunately, it doesn’t always work that way. One of the challenges nurses face in the evaluation phase is frustration related to slow progress or failing to meet goals. Overcoming the challenges that occur when patients become frustrated takes patience and understanding. If you find yourself in the evaluation phase of the nursing process steps and faced with this situation, take the time to talk to your patient. Assure them that progress does not always happen as quickly as we would like and encourage them to keep pressing forward. Let your patient know that you are there to support and help them and that your priority is to see them improve. Sometimes all it takes to calm a patient and help them regain focus is an assuring word and calming presence. Patients Withholding Information It is not uncommon for patients to try and mask symptoms or deny concerns when nurses evaluate their progress. This is especially common when a patient has been hospitalized or in a care facility for an extended period and wants to return home. In situations like this, a strong nurse-patient relationship and good communication skills are necessary. If you feel your patient is not being forthcoming about their progress, or perhaps new symptoms have emerged that they do not want to discuss, ask direct questions. Explain the importance of transparency when reporting progress, problems, or concerns. Family Denial of the Patient’s Need for Continued Care As nurses, we naturally hope that interventions positively impact our patients and that we can see improvement when evaluating them. Family members hope to see their loved ones recover and return to normal, as well. A significant challenge nurses can face when evaluating patient progress occurs when the patient's status declines or there is little improvement and family members deny the reality of the patient's situation. Many times, the fear of the unknown or lack of understanding is what causes family denial. If family members struggle with accepting the idea of continued care or changes in the plan of care, the nurse should acknowledge their concerns and offer support. When appropriate, talk with the patient and family together and discuss the previous plan of care and any suggestions for alterations or changes and the rationale for them. Patient Wishing to Terminate Care Before Discharge Goals Are Met Nurses understand that patients respond differently to care with some progressing faster than others, and the evaluation process helps to identify those patients who need extra time or updated care plans. Unfortunately, because patients do not always understand the complexities of interventions and expected outcomes, it can lead to feelings of despair. If patients slowly progress or fail to meet goals and expected outcomes, their frustration sometimes leads them to give up or desire to seek care elsewhere. When faced with this challenge, it is crucial for nurses to approach the patient with an attitude of empathy and attempt to discuss the patient's concerns. Depending on the patient's status and ability to understand, it may take some time and reinforced teaching to help them understand that slow progress is not failure. Explain your view of your patient's current status compared to his status on admission. Encourage the patient by assuring him that even slow progress is progress. Offer ideas of ways you think the care plan can be amended to suit his needs and ask for input. Remember, despite your best efforts, there may be times when patients decide to terminate care. Unless the patient has been deemed incapable of making informed decisions, you may not interfere with his choice to leave your care. It is necessary to document everything you discuss with the patient and his response to your instructions and education. If the patient decides to leave your facility's care, there is appropriate paperwork to be signed, called an A.M.A. (Against Medical Advice) discharge. The charge nurse or physician is usually responsible for having the patient sign this form and submitting it to administration. |
| In the evaluation phase, the nurse reassesses the patient and determines if goals and outcomes are being met or if the care plan needs to be modified. Observations are recorded in the patient’s chart. 04/20/22 @ 1500: After twenty-four hours of nursing intervention, the client demonstrates adequate cardiac output as evidenced by decreased blood pressure of 130/78 and pulse rate of 72. The client states his breathing is less labored and that if he begins to feel short of breath, he lies still to rest. O2 per NC @ 2L continuous. Observed 500 cc clear, amber urine in the urinal. The patient continues to have 2+ pitting edema in bilateral lower extremities. MD notified, awaiting response/order. The client has turned/repositioned q2h to decrease the risk of impaired skin integrity. No signs of compromised skin integrity noted at this time. -------D. Leonard, RN |
| The primary purpose of evaluation in the nursing process steps is to determine if patient goals and expected outcomes have been met or if the nursing care plan needs to be modified. The steps of evaluation in the nursing process include collecting data, comparing data with desired goals and expected outcomes, analyzing the patient’s response to nursing interventions, identifying factors impacting the success or failure of the nursing care plan, continuing, modifying, or terminating the care plan, and planning future nursing care. Although the nursing process is focused on nursing diagnoses and interventions, each member of the patient’s healthcare team has a role and the actions they take in patient care can impact the effectiveness of the nursing care plan. Therefore, the most effective way of improving evaluation in the nursing process, is to include the patient, family (when appropriate), and all members of the interdisciplinary team in the process. Although healthcare facilities and organizations have minimum guidelines for the frequency of nurse evaluations, it should be an ongoing process involved in patient care. The patient’s status and the effectiveness of nursing interventions should be continuously evaluated, and the care plan should be modified, when necessary. In the evaluation phase, nurses gather much of the same type of information as what is gathered during the assessment. During this phase, nurses review current vital signs and laboratory or diagnostic test results. They use information entered into the patient’s chart, such as nurses’ notes, flow sheets, and other pertinent information. Additionally, during the evaluation, nurses reinterview the patient and look for both subjective and objective data to determine if the plan of care was effective. The registered nurse assigned to the patient’s care is the primary person responsible for the evaluation phase of the nursing process. The RN evaluates all information necessary to determine if the goals and expected outcomes were met or if alterations in the plan are needed. Keep in mind, however, every member of the nursing care team plays a vital role in the RN's ability to conduct a thorough evaluation because each person is responsible for documenting their work and the patient’s response. |
Useful Resources to Gain More Information About the Nursing Process
Blogs/websites, youtube videos, my final thoughts, frequently asked questions answered by our expert, 1. how is nursing process different from the scientific method, 2. do all nurses use the nursing process, 3. do doctors also use the nursing process, 4. what does adpie stand for, 5. is it always necessary for a nurse to follow all steps of the nursing process, 6. how does critical thinking impact the nursing process, 7. how does a health information system affect the nursing process, 8. how to use maslow hierarchy in the nursing process, 9. which nursing process step includes tasks that can be delegated, 10. which nursing process step includes tasks that cannot be delegated, 11. how does the nursing process apply to pharmacology.

Learning Materials
- Business Studies
- Combined Science
- Computer Science
- Engineering
- English Literature
- Environmental Science
- Human Geography
- Macroeconomics
- Microeconomics
- Problem Solving in Nursing Management
Dive deep into the multifaceted world of nursing management with a special focus on problem-solving. This comprehensive guide presents a detailed look at the process, importance, and challenges of problem-solving in nursing management. By highlighting essential skills, neurologically based frameworks, and the relationship with decision-making, it offers both theoretical understanding and practical solutions. Explore real-life case studies, leadership's role, and the link with critical thinking. This is an enriching journey towards developing strategic competencies and achieving effective problem-solving in a vital healthcare sector.
Create learning materials about Problem Solving in Nursing Management with our free learning app!
- Instand access to millions of learning materials
- Flashcards, notes, mock-exams and more
- Everything you need to ace your exams
Millions of flashcards designed to help you ace your studies
- Cell Biology
What do the algorithm-based and intuition-driven approaches to problem-solving in nursing management entail?
What is the first stage of problem solving in nursing practice?
What is problem solving in nursing management and how is it different from decision making?
What is the relationship between critical thinking and problem solving in nursing?
What is the final stage of problem solving in nursing practice?
What is the significance of problem-solving in nursing management?
What are the key skills required for effective problem-solving in nursing management?
How can critical thinking skills be enhanced for effective problem solving in nursing management?
What are the key steps involved in the problem-solving process in nursing management?
What does the neurological framework in nursing management involve?
What is decision making in nursing management?
- Clinical Placement
- Human Anatomy
- Intensive Care Nursing
- Mental Health Nursing
- Nursing Management
- Antimicrobial Stewardship
- Audit Compliance Nursing
- Billing Practices for Hospitals
- Biohazard Management
- Budget Management
- Budget Planning
- Capital Resources
- Care Evaluation
- Clinical Pathways
- Communication Skills
- Crisis Management
- Customer Service in Nursing
- Delegation of Nurses
- Disinfection Techniques
- Emergency Drills
- Emergency Preparedness
- Expense Management
- Financial Management in Nursing
- Fiscal Responsibility
- HIPAA Compliance
- Hazard Identification
- Healthcare Technology
- Hospital Asset Management
- Hospital Contract Negotiation
- Hospital Funding Sources
- Hospital Revenue Cycle
- Hygiene Protocols
- Insurance Relations Hospitals
- Interdisciplinary Team
- Labor Relations
- Nurse Staff Training
- Nursing Data Analysis
- Nursing Grant Writing
- Nursing Scheduling
- Operational Efficiency
- Patient Flow
- Patient Loyalty
- Reimbursement Strategies
- Retention Strategies
- Revenue Generation
- Sanitation Practices
- Staff Development
- Staffing Models
- Staffing in Nursing
- Stakeholder Engagement
- Strategic Planning in Nursing
- Time Management
- Waste Disposal in Hospital
- Worker Safety
- Workforce Planning
- Workplace Harmony
- Nursing Theories
- Types of Nursing
Understanding Problem Solving in Nursing Management
Problem solving in nursing management is a crucial process that you need to grasp as a prospective or current nurse. This involves using a logical, systematic approach to resolving issues encountered in a nursing environment, focusing on maintaining quality patient care .
Problem Solving: This is identifying and overcoming obstacles to achieving a goal. In nursing, this generally revolves around improving patient health outcomes and ensuring efficient healthcare facility operations.
Importance of Problem Solving in Nursing Management
Nursing professionals are constantly faced with intricate issues that require decisive and effective solutions. The ability to implement problem-solving is crucial in maintaining optimal patient care , operational efficiency , and fostering team collaboration.
For instance, suppose a sudden shortage of resources like catheters or syringes is experienced in a healthcare facility. In such a case, the nursing manager will need to swiftly solve the problem either by reallocating resources, timely ordering supplies, or finding a temporary alternative, ensuring the patients' needs are continually met.
Key Skills Required for Problem Solving in Nursing Management
Effective problem-solving in nursing management is anchored on a set of key skills. These abilities equip you to navigate complex situations and formulate impactful solutions. They include:
- Critical Thinking: This is your ability to analyse situations in detail and understand their implications.
- Decisiveness: The readiness to make important decisions swiftly and confidently.
- Communication: Sharing and receiving information clearly and effectively.
- Collaboration: Working effectively as part of a team.
These skills are interconnected. For example, your ability to think critically informs your decisiveness. Your decisions are then made clear to your team through effective communication, and together, through collaboration, the problem is solved.
Common Challenges in Problem Solving in Nursing Management
In your nursing management journey, you will come across multiple challenges when attempting to solve problems. These obstacles might occur due to several factors, such as resource limitations, personnel issues, and complex patient needs .
| Resource Constraints | Shortage of essential medical supplies or understaffing. |
| Personnel Issues | Conflicts among team members or unforeseen absence of staff. |
| Complex | Patients with rare medical conditions that require specialized care. |
While these challenges can be daunting, equipping yourself with robust problem-solving skills will help you navigate these complications and maintain high standards of patient care.
Scrutinising the Problem Solving Process in Nursing Management
Delving deeper into the problem-solving process in nursing management, you get to navigate its intricacies and mechanisms. This exploration can bolster your abilities to resolve complex situations in your nursing career.
Steps involved in the Problem Solving Process
Problem-solving in nursing management is a multifaceted task that often involves several steps. To understand how to tackle issues expertly, you will need a clear understanding of each stage.
Problem-Solving Process: A systematic approach used to address complications and make decisions. In nursing, it’s composed of several steps, each essential to the resolution of issues.
Here are the key steps:
- Identification: In this stage, you recognise the existence of a problem. It is essential to understand the barriers to your goals and spotlight areas that require improvement.
- Definition: You clearly articulate the problem. By understanding its nuances, magnitude, and implications, you can efficiently tailor a solution.
- Analysis: This involves examining the problem closely from different perspectives, which includes understanding the cause and effect, stakeholders involved, and potential impacts.
- Development of Solutions: Here you brainstorm possible solutions. It's essential to contemplate multiple alternatives to ensure the most effective resolution is chosen.
- Decision Making: In this step, you select the best solution based on the gathered information and analysis. Considerations may include effectiveness, resources needed, and potential side effects.
- Implementation: You put the chosen solution into action, carefully monitoring its effectiveness and making necessary adjustments.
- Evaluation: Finally, you assess the outcome. This helps to determine the effectiveness of your solution and informs future problem-solving efforts.
Neurological Framework for Problem Solving in Nursing Management
Many problem-solving methods exist, but one valuable perspective is through understanding the neurological framework in nursing management. This biological approach delves into how your brain processes information and develops solutions.
Neurological Framework: A biological perspective that explains how a nurse's brain processes, analyses, and responds to problems encountered in the nursing environment.
This framework refers to cognitive processes which involve:
- Critical thinking: This involves actively and skillfully conceptualising, applying, analysing, and evaluating information gathered from observation, experience, reflection, or communication.
- Decision making: This is the cognitive process of selecting a course of action from multiple possibilities. It's based on both intuition and logical reasoning.
- Problem-solving: This involves overcoming hurdles and finding a conclusion, and it usually includes decision-making. It involves creativity and critical thinking to arrive at effective solutions.
Role of Creativity in the Problem Solving Process
Nursing management often involves complex and unique problems. To effectively tackle these challenges, it's crucial to breed creativity in the problem-solving process.
Imagine there's a sudden surge in patient intake due to a local health crisis, resulting in a bed shortage. A creative solution might be to convert other non-critical spaces such as conference rooms temporarily into patient monitoring units, thereby managing the surge effectively.
Importance of Team Collaboration in the Problem Solving Process
In a nursing environment, you are not working in isolation. Collaboration is a critical aspect of problem-solving in nursing management, as diverse insights can lead to innovative and effective solutions.
Consider a scenario where there's a need to implement a new system for managing patient records. To effectively solve potential issues in system implementation, you might need input from various team members including nursing staff, IT specialists, and data management experts. Each member's contribution, based on their expertise and perspective, is crucial in charting a comprehensive problem-solving strategy, ensuring the successful implementation and integration of the new system.
Decision Making and Problem Solving in Nursing Management
Decision making and problem-solving are two interconnected aspects in the realm of nursing management. Understanding their correlation and distinctiveness is key to effectively managing issues and improving patient outcomes in a healthcare setting.
The Interplay between Decision Making and Problem Solving
The connection between decision making and problem solving in nursing management is truly significant. In almost every situation where a problem arises, decision making is an inseparable component of the problem-solving process.
Decision Making in Nursing: This involves selecting a course of action from different alternatives. It is the bridge connecting problem analysis with implementing solutions, and it requires evaluation of information, predicaments, and possible outcomes.
Once you have identified and defined a problem, analysed it, and developed potential solutions, the next step involves decision making. This is where you select the most suitable solution among the alternatives.
For instance, if you are dealing with a bed shortage problem in your healthcare facility, some possible solutions could be outsourcing to other healthcare facilities, using other spaces such as conference rooms as makeshift wards, or deploying portable hospital beds.
Each of these solutions has its pros and cons, and it's here that decision-making skills come into play. You'll need to compare and contrast each option, considering factors like cost, time, resources available, and the overall impact on patient care. The chosen solution is then implemented, and the effects are evaluated for future reference.
Distinguishing Decision Making from Problem Solving in Nursing Management
Though inherently connected, problem solving and decision making are distinct processes within nursing management. Where problem-solving is a comprehensive process that entails identifying, analysing, and solving issues, decision making is a component nested within this process, acting as the transition point from analysis to action.
Problem Solving in Nursing: This is a broader process involving the identification of an issue or obstacle, systematic analysis to understand it, devising potential solutions, choosing the most suitable through decision making, implementing it, and finally reviewing the effectiveness of the implemented solution.
Consider a real-life scenario such as medication errors. If these errors are occurring frequently in your healthcare setup, the problem-solving process will involve identifying the issue (increased medication errors), defining and analysing it (finding the root causes, such as miscommunication or system glitches). This would then lead to brainstorming potential solutions, like improved communication systems or enhanced employee training. The decision-making process would then come into play when choosing the best solution to implement.
Techniques for Effective Decision Making in Problem Solving Scenarios
Effective decision making underpins successful problem solving in nursing management. Implementing the right techniques can enhance your decision-making process, thus leading to more effective problem resolution.
Some proven techniques include:
- Pros and Cons Analysis: List the advantages and disadvantages of each solution to help you visualise the impacts of each decision.
- Decision Matrix: Establish criteria and rate potential solutions. The choice with the highest score is then considered the best decision.
- Cost-Benefit Analysis: Determine the financial implication of each decision and compare it to the benefits. Solutions with a high benefit-cost ratio are preferred.
Working collaboratively to brainstorm and analyse solutions promotes critical thinking and creativity, ensuring that the chosen solution maximises the use of resources and improves patient outcomes .
In unavoidable circumstances where decisions have to be made rapidly and with limited information, using intuition, a nurse's experience, and insights combined with analytical thinking can be beneficial. This is where the balanced blend of clinical expertise and effective risk-taking come into play.
Decision making is never static in nursing management. The cyclic nature of the decision-making process, where outcomes of decisions are continually assessed and feedback is used to improve future decision making, showcases its dynamic and iterative nature. This reinforces the vital role decision making plays in the problem-solving process.
Unpacking Examples of Problem Solving in Nursing Management
By exploring various examples and case studies, you gain a practical view of problem-solving in nursing management. These insights can better equip you to tackle real-life challenges in a healthcare setting.
Case Study Analysis of Problem Solving Scenarios
Case studies provide a thorough view of how problem-solving strategies are applied in various nursing management scenarios. Analysing such cases exposes you to diverse methods and solutions and encourages you to think critically and innovatively.
Case Study Analysis: A detailed examination of a particular instance or event to draw conclusions, develop solutions, or learn from the situation.
Let's investigate a case concerning patient waiting times. In a healthcare facility, it is observed that patients often have to wait for prolonged periods to receive care, leading to dissatisfaction and affecting the overall quality of service. The problem-solving steps might look like this:
- Identification and Definition: The problem is identified as long patient waiting times. It is defined as patients waiting more than 45 minutes to receive care.
- Analysis: The cause of the problem is found to be a shortage of nursing staff during peak hours.
- Development of Solutions: Several possible solutions emerge, such as recruiting additional staff, offering overtime to existing staff, or streamlining operational processes to reduce inefficiencies.
- Decision Making: After careful analysis, it is decided to hire additional part-time staff to handle peak hours.
- Implementation: The recruitment process is initiated and new members integrated into the team.
- Evaluation: After a few months, waiting times are reassessed. A significant reduction is observed, confirming the effectiveness of the solution.
Case study analysis provides a rich source of knowledge and transferable insights that can be helpful in similar or entirely different scenarios. Drawing parallels from varying contexts and understanding how solutions are adapted to unique situations helps bolster your problem-solving skills and adaptability in nursing management.
Varied Approaches to Problem Solving in Different Nursing Scenarios
Different nursing scenarios call for diverse problem-solving strategies. Understanding the varying approaches, from algorithm-based to intuition-driven, equips you to manage multidimensional and intricate issues effectively.
Algorithm-based Approach: This involves following a clearly defined set of rules or procedures to solve a problem. It can be applicable in situations with defined parameters and scope, such as diagnosing a health condition based on a specific set of symptoms.
Intuition-driven Approach: This combines a nurse's experience, knowledge, and instinct to solve a problem. It applies to ambiguous scenarios where conventional rules may not be applicable, such as managing a patient's fear or anxiety.
Problem-solving in nursing management is all about adapting to the environment and the situation. The right approach may vary, calling for flexibility, creativity, critical thinking, and a deep understanding of the issue for successful resolution.
Real Life Applications of Problem Solving Strategies in Nursing Management
The real world of nursing is complex and dynamic, and various problem-solving strategies can apply on any given day. To navigate smoothly, you need to understand how the various approaches can be adapted to specific situations.
Consider solving a recurrent communication issue within your nursing team. The algorithmic approach might involve establishing clear communication protocols or using digital tools to streamline interaction. However, the intuition-driven approach might involve informal team-building meetings to foster better personal connections. In this situation, the best solution might be a blend of the two approaches to ensure both procedural clarity and improved team relationships.
The key takeaway here is that there is no "one-size-fits-all" solution in nursing management. Problem-solving requires flexibility, openness, and the ability to judge which strategy will perform best in a particular scenario.
Exploring Nursing Management Problem-Solving Strategies
Problem-solving strategies in nursing management form the backbone of effective healthcare services. By ensuring that nursing personnel can tackle issues with aplomb and proficiency, these strategies contribute significantly to patient satisfaction and positive outcomes.
Development of Strategic Problem-Solving Competencies
The first step towards demystifying problem-solving processes in nursing management is the development of strategic problem-solving competencies. The journey from novice to expert involves honing these skills and integrating them into your practical work.
Strategic Problem-Solving Competencies: These are a set of core skills that facilitate effective problem-solving in nursing management, including critical thinking, innovative thinking, collaboration, adaptability, leadership, and decision-making.
Acquiring these skills involves both academic learning and practical experiences. Gaining theoretical knowledge lays the foundation, while integrating this knowledge within a clinical context enriches and refines these competencies.
- Critical Thinking: This involves analysing situations from multiple perspectives, evaluating different solutions, and making informed decisions.
- Innovative Thinking: Innovative thinking pertains to thinking outside the box, especially when conventional solutions are inadequate.
- Collaboration: In nursing, effective problem-solving often requires collaborative efforts, valuing diverse ideas and working towards common goals.
- Adaptability: Healthcare settings are continually changing, and the ability to swiftly adapt to new situations is crucial.
- Leadership: Good leadership skills facilitate effective management of teams and ensuring that everyone is following the established problem-solving process.
- Decision Making: Ability to implement effective decisions is vital for successful problem solving.
Role of Leadership in Implementing Problem Solving Strategies
The role of leadership in implementing problem-solving strategies must not be understated. Effective leadership not only guides teams through problem-solving processes but also fosters a supportive environment where team members feel safe to contribute ideas and question assumptions.
Leadership in Nursing: This involves guiding, motivating, and supporting nursing staff to deliver quality healthcare services. Also, it encompasses enhancing team cooperation, improving communication, and fostering a culture of continuous learning.
Leadership employs a variety of approaches in implementing problem-solving strategies. Different leadership styles can be applied based on the nature of the problem and the team dynamics. Transformational leadership, for instance, inspires others to exceed their personal goals and work for a collective purpose. On the other hand, participative leadership encourages open discussions and collective decision-making, promoting a more inclusive and democratic problem-solving process.
Leadership is also instrumental in creating an environment that encourages the sharing of problems openly, without fear of judgment, hence facilitating early identification and efficient resolution of issues. By also ensuring that learning opportunities are provided to enhance team problem-solving capabilities, leadership positively influences problem-solving outcomes.
Use of Resources in Problem Solving Strategies
Effective resource utilization is a critical component of successful problem-solving strategies in nursing management. The term 'resources' in this context includes human resources such as nursing staff and doctors, as well as material resources like medical supplies, equipment, and facilities.
Resource Utilisation: This refers to the efficient and effective use of available resources to achieve desired outcomes. In nursing, it involves ensuring that staff, equipment, and supplies are optimally used to deliver quality healthcare services and solve arising problems.
Problem-solving often necessitates the optimal use of available resources. For example, if there is an issue of high patient-to-nurse ratio, one of the possible solutions could be redistributing nursing staff according to workload and patient needs, or hiring additional staff if finances permit.
Every solution should be weighed based on its resource implications. The best solution is often the one that optimally utilises available resources to provide the maximum benefit. For example, while hiring additional staff might solve the problem, it might not be the best solution if the budget is very limited. In such a case, reallocation of existing staff may be a more practical solution.
Similarly, if there is a shortage of a particular supply, then alternatives may need to be sought, or rationing implemented. A critical analysis of such situations is necessary to ensure that the solutions proposed and implemented do not create other problems related to resource allocation and use.
It's also important to remember to continuously evaluate the impact of your solutions on resource utilisation. This will not only help you ensure sustainable use of resources but also contribute to continuous improvement in problem-solving strategies.
Understanding the stages of problem-solving in nursing practice is fundamental to addressing various challenges that arise in the healthcare sector. These problem-solving stages enable you to identify issues, create and implement solutions, and review the outcomes for improvement purposes.
Initial Assessment and Identification: The First Stage of Problem Solving
The initial phase of problem-solving in nursing management involves the assessment and identification of the issue at hand. This stage is critical as the correct identification of the problem lays the foundation for effective solution design and implementation.
Initial Assessment: This is the preliminary evaluation of the situation, leading to the recognition of existing problems. This stage involves observation, questioning, and data gathering to understand the issue better.
This initial step requires keen observation skills and critical thinking. While observation helps in gathering relevant details, critical thinking enables you to scrutinize this information and identify potential problems. You could also use feedback from your team and other relevant stakeholders to gain a comprehensive understanding of the issue.
For instance, suppose you discover unusually high levels of patient discomfort during specific hours. The initial assessment might involve examining patient records during these hours, observing nursing practices in these time frames, and seeking feedback from both patients and nursing staff. This comprehensive approach could potentially reveal the issue, like a shortage of staff during peak hours, leading to delayed or inefficient care.
Formulating Actionable Solutions: The Mid Stages of the Problem-solving Process
Once the problem is identified, the next phase is generating actionable solutions. The validity and effectiveness of these solutions significantly influence the problem-solving process's success, thus necessitating careful deliberation and thorough evaluation.
Actionable Solution: A practical, feasible strategy that can be implemented to resolve the problem. It's typically developed through brainstorming, analysis, and evaluation of various alternatives.
The process of formulating actionable solutions involves brainstorming potential remedies, evaluating these against a set criteria, and choosing the most viable option. Ideally, this should be a collaborative effort involving all relevant stakeholders. Collaborative problem-solving encourages diversity in ideas and promotes inclusivity.
| Careful Analysis | Evaluation Against Set Criteria | Choosing Viable Option |
| Gather as many potential solutions as possible through brainstorming sessions | Evaluate potential solutions based on criteria such as feasibility, efficiency, and impact | The most suitable solution is chosen after careful evaluation |
Innovation is a key driver in formulating actionable solutions. Traditional problem-solving methods might fail in the face of complex or unique problems, necessitating innovative ideas. Remember, the most effective solutions often result from 'thinking outside the box'.
Evaluation and Reflection: The Final Stage of Problem Solving
The final stage of problem-solving is evaluation and reflection. After implementing the chosen solution, it is essential to assess its effectiveness in solving the identified problem. This stage offers an opportunity to learn from the implemented action and make necessary adjustments for future improvement.
Evaluation and Reflection: This stage involves reviewing the implemented solution to assess its effectiveness. Reflection involves learning from the process and experiences to ensure continuous improvement.
To achieve meaningful evaluation and reflection, a systematic approach must be adopted. Begin with the assessment of the effect of the solution on the original problem. Have the waiting times reduced following the staff adjustments? Is there an improved level of patient comfort? These are the kind of questions you need to address.
Following the evaluation, it's crucial to reflect on the entire process. Consider what worked well and what didn't. Reflecting on these experiences offers valuable insights that can be used to improve future problem-solving processes.
Take the earlier example of high levels of patient discomfort due to staff shortage during peak hours. Suppose, after implementing the solution of adjusting staff schedules, you find that there's a significant improvement in patient comfort levels. This shows that your solution worked. However, during reflection, you realise that the process took more time than necessary due to delayed decision-making. For future improvement, you could consider setting specific timelines for each stage of the problem-solving process.
In conclusion, problem-solving is a cyclical process. It doesn't end with implementing a solution; instead, it opens doors for continuous learning and improvement. Adapting to this cycle is key to honing your problem-solving proficiency in nursing management.
Critical Thinking and Problem Solving in Nursing
Problem solving in nursing management is underpinned by the practice of critical thinking. An understanding of the delicate interplay between these two capabilities is central to the enhancement of nursing management and the ultimate delivery of efficient patient care.
The Connection Between Critical Thinking and Problem Solving in Nursing
There is a strong relationship between critical thinking and problem solving in nursing, evidenced by the significant role each plays in the healthcare sector. Critical thinking provides the foundation upon which problem-solving strategies are built.
Critical Thinking: This is the disciplined process of analysing, interpreting, evaluating, and drawing conclusions from varying levels of data, information or experiences. It involves a deeper level of thinking to understand, evaluate and resolve complex issues or situations.
The process of problem-solving often begins with an evaluation of the situation, gathering data, appraising the data, and coming with strategic solutions. By applying critical thinking, you can get a clear understanding of the problem, which helps devise more effective solutions.
For example, in implementing new protocols in a nursing unit, critical thinking may involve evaluating the necessity of the change, the potential effect on the nursing staff’s workflow, and patient care. The ability to think critically facilitates well-informed decisions, thereby enhancing the problem-solving process.
Beyond problem identification and solution generation, critical thinking is also instrumental in the review phase of the problem-solving process. It allows you to reflect on the effectiveness of implemented solutions, the overall process, and areas that could be improved. Therefore, the integration of critical thinking not only enriches problem-solving but also contributes to continuous learning and improvement in nursing management.
Enhancing Critical Thinking for Effective Problem Solving in Nursing Management
Enhancing critical thinking skills in the nursing workforce enriches problem-solving efforts and ultimately results in improved patient outcomes and service delivery. This strengthening could be achieved through several strategies.
Enhancing Critical Thinking: The process of improving critical thinking skills to enhance one's ability to evaluate complex situations effectively and make informed decisions.
Firstly, continuous learning and professional development activities such as workshops, seminars, and online courses can provide essential tools for sharpening critical thinking skills.
Secondly, fostering a culture of open communication and collaborative problem-solving offers great benefits. These platforms facilitate the sharing of diverse perspectives, promoting deep analyses, and enriching the problem-solving process.
Lastly, reflective practice can also positively impact critical thinking abilities. Regular reflection on your practice, experiences, and learnings enables you to identify gaps in your thinking and areas of improvement. It encourages a deeper level of thinking that enriches the problem-solving process.
- Continuous learning and participation in professional development activities.
- Fostering a culture of open communication and collaborative problem-solving.
- Engaging in reflective practice regularly.
Examples of Critical Thinking Leading to Effective Problem Solving
The application of critical thinking skills often results in improved problem-solving outcomes in nursing management. Several instances illustrate this relationship.
For instance, consider a situation where a nursing unit has seen a significant increase in medication errors. The nursing manager applies critical thinking to evaluate the situation, identify potential causes, and devise solutions. Through an in-depth review of pharmaceutical administration procedures, team collaboration, discussion, and data evaluation, the nursing manager identifies the root cause - an overly complicated method of logging medication.
Armed with this information, they innovate a simpler, more effective system. By cutting down on needless complexity, the nursing unit sees a drastic decrease in medication errors. This example shows how the application of critical thinking streamlined a complex process, providing an effective solution to the problem at hand.
Another instance could be changing patient demographics, with more elderly patients requiring care. A nursing manager applies critical thinking to understand the unique needs of these patients and the potential challenges that might arise in catering to these needs. As a result, they develop tailored care plans and training programmes for the nursing staff to better care for elderly patients, resulting in improved patient satisfaction.
These examples highlight how critical thinking can lead to effective problem solving in nursing management, ultimately resulting in better service delivery and patient care. Therefore, enhancing critical thinking should be seen as a vital strategy for improving problem-solving proficiency in nursing management.
Problem Solving in Nursing Management - Key takeaways
- Problem Solving in Nursing Management: It is a thorough process involving the identification, analysis, and (de)cision-making to solve issues in nursing management. It also includes implementation and review of the effectiveness of the solutions.
- Decision Making Techniques: Different techniques such as Pros and Cons Analysis, Decision Matrix, and Cost-Benefit Analysis can enhance the decision-making process in problem-solving scenarios.
- Case Study Analysis: It involves the detailed examination of various scenarios to inform problem-solving strategies and practice.
- Approaches to Problem-Solving: Different approaches may apply in different nursing scenarios, such as the algorithm-based approach for well-defined scenarios and the intuition-driven approach for ambiguous situations.
- Strategic Problem-Solving Competencies: These are essential skills including critical thinking, innovative thinking, collaboration, adaptability, leadership, and decision-making, crucial in effective problem-solving.
- Leadership in Nursing: Leadership plays a key role in guiding, motivating, and supporting nursing staff. It influences the successful implementation of problem-solving strategies.
- Resource Utilisation: Efficient and effective use of available resources, such as nursing staff, equipment, and supplies, is vital in problem-solving in nursing management.
- Stages of Problem Solving in Nursing Practice: The stages include the identification, analysis, and resolution of problems, which are crucial in responding to challenges in the healthcare sector.
Flashcards in Problem Solving in Nursing Management 14
The algorithm-based approach involves following a clear set of rules or procedures to solve a problem, often with defined parameters. The intuition-driven approach combines a nurse's experience, knowledge, and instinct to solve a problem, especially in ambiguous scenarios.
The first stage of problem solving in nursing practice is initial assessment and identification, which involves the evaluation of the situation to recognise existing problems. This stage requires observation, questioning, and data gathering.
Problem solving is a broader process involving the identification of an issue, systematic analysis to understand it, devising potential solutions, choosing the most suitable through decision making, implementing it, and finally reviewing the effectiveness of the implemented solution. Decision making, on the other hand, is a component nested within this process.
Critical thinking provides the foundation for problem-solving strategies in nursing. It involves the disciplined process of analysing, evaluating, and interpreting data, which allows for a clear understanding of the problem and thus the generation of effective solutions. Critical thinking also enriches the problem-solving process by facilitating review and continuous improvement.
The final stage of problem solving in nursing practice is evaluation and reflection, where the effectiveness of the implemented solution is assessed, and learnings are drawn from the process for future improvement.
Problem-solving in nursing management is crucial in maintaining optimal patient care, operational efficiency, and fostering team collaboration by resolving intricate issues with decisive and effective solutions.
Learn with 14 Problem Solving in Nursing Management flashcards in the free StudySmarter app
We have 14,000 flashcards about Dynamic Landscapes.
Already have an account? Log in
Frequently Asked Questions about Problem Solving in Nursing Management
Test your knowledge with multiple choice flashcards.
Join the StudySmarter App and learn efficiently with millions of flashcards and more!
Keep learning, you are doing great.
Discover learning materials with the free StudySmarter app

About StudySmarter
StudySmarter is a globally recognized educational technology company, offering a holistic learning platform designed for students of all ages and educational levels. Our platform provides learning support for a wide range of subjects, including STEM, Social Sciences, and Languages and also helps students to successfully master various tests and exams worldwide, such as GCSE, A Level, SAT, ACT, Abitur, and more. We offer an extensive library of learning materials, including interactive flashcards, comprehensive textbook solutions, and detailed explanations. The cutting-edge technology and tools we provide help students create their own learning materials. StudySmarter’s content is not only expert-verified but also regularly updated to ensure accuracy and relevance.

StudySmarter Editorial Team
Team Nursing Teachers
- 25 minutes reading time
- Checked by StudySmarter Editorial Team
Study anywhere. Anytime.Across all devices.
Create a free account to save this explanation..
Save explanations to your personalised space and access them anytime, anywhere!
By signing up, you agree to the Terms and Conditions and the Privacy Policy of StudySmarter.
Sign up to highlight and take notes. It’s 100% free.
Join over 22 million students in learning with our StudySmarter App
The first learning app that truly has everything you need to ace your exams in one place
- Flashcards & Quizzes
- AI Study Assistant
- Study Planner
- Smart Note-Taking

Get unlimited access with a free StudySmarter account.
- Instant access to millions of learning materials.
- Flashcards, notes, mock-exams, AI tools and more.
- Everything you need to ace your exams.

- Registered Nurse to Master of Science in Nursing in Administrative Leadership in Nursing
- Registered Nurse to Master of Science in Nursing in Nursing Education
- Registered Nurse to Master of Science in Nursing in Nursing Informatics
- Master of Science in Nursing in Administrative Leadership in Nursing
- Master of Science in Nursing in Nursing Education
- Master of Science in Nursing in Nursing Informatics
- Graduate Nursing Certificate in Administrative Leadership
- Graduate Nursing Certificate in Nursing Education
- Graduate Nursing Certificate in Nursing Informatics
- Accreditations, Accolades & Quick Facts
- Faculty Profiles
- Student Services
Welcome to our website! How did you hear about us? Take Survey »
Home » Degrees » RN to MSN » Registered Nurse to Master of Science in Nursing in Administrative Leadership in Nursing » How Leaders Approach Problem-Solving
How Leaders Approach Problem-Solving
- Published On: July 12, 2022
No environment is free from problems. But, some require more creative solutions than others.
Healthcare, in particular, presents almost unlimited opportunities for things to go wrong — both in terms of patient care and inter-staff/intra-staff relationships. The problems present within healthcare settings are often a matter of life and death.
It takes effective leadership to keep all issues to a minimum and patient safety remains a priority.
What Makes a Great Leader?
If we think about the great leaders throughout time, they share a few common characteristics. Specific to nurse leaders, Indeed.com lists the following as core qualities for leaders:
- compassion/empathy
- critical thinking
- dedication to excellence
- communication
- collaboration/team building
- open-mindedness
- forward-thinking
- accessibility
Another valuable quality in leadership is being proactive in problem-solving. Good leaders handle issues as they arrive. They are capable of “putting out fires,” and that’s important. Yet, great leaders anticipate problems before they come to a head.
Core Skills Nurse Leaders Need to Possess
While some of the above resonates as more intuitive, emotional intelligence — as opposed to procedural — can be learned. Of course, there are practical skills nurse leaders need to develop as well.
Examples of these skills are healthcare finance and economics. Mastering budgets and efficiently allocating resources is important for nurse leaders. Nurses also need to know how to communicate financial demands to upper administration.
The online Registered Nurse (RN) to Master of Science in Nursing (MSN) in Administrative Leadership program from Northeastern State University (NSU) dedicates a course to heightening nurses’ skills and knowledge surrounding this responsibility.
NSU’s program also includes a course titled Organizational and Systems Management in Nursing. The course description states that nurses will learn about “contemporary influences, theories, principles, and functional strategies related to management/administration and organizational systems at the micro, meso, and macrosystem levels.”
Leadership’s Role in Addressing Lateral and Horizontal Violence (LHV)
While nurse leaders don’t necessarily need to be experts in human resources, it’s a substantial knowledge base. Human resources knowledge is especially relevant given the persistence of lateral and horizontal violence (LHV) within the nursing profession. The World Health Organization (WHO), International Council of Nurses and Public Services International have recognized this issue as a significant global public health priority.
Just how dangerous is LHV to nursing? A study published by Nurse Management describes LHV as: “all acts of meanness, hostility, disruption, discourtesy, backbiting, divisiveness, criticism, lack of unison, verbal or mental abuse, and scapegoating. [These] behaviors taint healthcare organizations; cause irreparable harm to workplace culture; breakdown team communication; and severely impact the quality of the care provided, thereby jeopardizing patient safety.”
With a solid leadership foundation, nurses can handle toxic behaviors that damage the work environment. In doing so, they change the workplace culture and guiding others to follow in their footsteps.
Empowerment Sets Everyone Up for Success
Perhaps the greatest responsibility of a nurse leader is to empower those in their charge. John Quincy Adams said, “If your actions inspire others to dream more, learn more, do more and become more, you are a leader.”
Northeastern State University recognizes empowerment as an essential skill. In the Leadership Development for the Advanced Nursing Professional course, students learn to “effectively manage change, empower others, and influence political processes.”
What Type of Leader Do You Aspire to Be?
It takes much more than “putting in your time” to become an effective leader. Nurses might rise through the ranks based on experience, but are they actually effecting change in the nursing profession? Unless they possess a robust leadership skill set, the answer is likely no. So, what kind of leader do you want to be?
Learn more about Northeastern State University’s online RN to MSN in Administrative Leadership program .
Related Articles
Our commitment to content publishing accuracy.
Articles that appear on this website are for information purposes only. The nature of the information in all of the articles is intended to provide accurate and authoritative information in regard to the subject matter covered.
The information contained within this site has been sourced and presented with reasonable care. If there are errors, please contact us by completing the form below.
Timeliness: Note that most articles published on this website remain on the website indefinitely. Only those articles that have been published within the most recent months may be considered timely. We do not remove articles regardless of the date of publication, as many, but not all, of our earlier articles may still have important relevance to some of our visitors. Use appropriate caution in acting on the information of any article.
Report inaccurate article content:
- Email Address *
REQUEST INFORMATION
Submit this form, and an Enrollment Specialist will contact you to answer any questions.
*All fields required.
- Program of Interest * Program of Interest* Graduate Nursing Certificate in Administrative Leadership Graduate Nursing Certificate in Nursing Education Graduate Nursing Certificate in Nursing Informatics MSN in Administrative Leadership in Nursing MSN in Nursing Education MSN in Nursing Informatics RN to BSN RN to MSN in Administrative Leadership RN to MSN in Nursing Education RN to MSN in Nursing Informatics
- First Name *
- Last Name *
- How did you hear about us? * How did you hear about us?* Coworker Email Employer Family/Friend Information Session Magazine/Newspaper Online Professional Organization Radio/TV
- Phone This field is for validation purposes and should be left unchanged.
Or call 844-351-6656
By submitting this form, I am providing my digital signature agreeing that Northeastern State University (NSU) and its agent, Risepoint, may email me or contact me regarding educational services by telephone and/or text message utilizing automated technology or a pre-recorded message at the telephone number(s) provided above. I understand this consent is not a condition to attend NSU or to purchase any other goods or services. Privacy Policy . SMS Terms .

Begin Application Process
for help with any questions you have.

- Social Media
- Direct mail
- Search Engine
- Event/Conference
- This is my first time
- Within the last 30 days
- 1-2 months ago
- 3+ months ago
Request Information
- Email This field is for validation purposes and should be left unchanged.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Problem solving in nursing practice: application, process, skill acquisition and measurement
Affiliation.
- 1 King's College, University of London, England.
- PMID: 8320382
- DOI: 10.1046/j.1365-2648.1993.18060886.x
This paper analyses the role of problem solving in nursing practice including the process, acquisition and measurement of problem-solving skills. It is argued that while problem-solving ability is acknowledged as critical if today's nurse practitioner is to maintain effective clinical practice, to date it retains a marginal place in nurse education curricula. Further, it has attracted limited empirical study. Such an omission, it is argued, requires urgent redress if the nursing profession is to meet effectively the challenges of the next decade and beyond.
PubMed Disclaimer
Similar articles
- The perceived problem-solving ability of nurse managers. Terzioglu F. Terzioglu F. J Nurs Manag. 2006 Jul;14(5):340-7. doi: 10.1111/j.1365-2934.2006.00551.x. J Nurs Manag. 2006. PMID: 16787468
- Problem-solving skills of senior student nurses: an exploratory study using simulation. Roberts JD. Roberts JD. Int J Nurs Stud. 2000 Apr;37(2):135-43. doi: 10.1016/s0020-7489(99)00064-4. Int J Nurs Stud. 2000. PMID: 10684955
- Clinical problem-solving in nursing: insights from the literature. Taylor C. Taylor C. J Adv Nurs. 2000 Apr;31(4):842-9. doi: 10.1046/j.1365-2648.2000.01342.x. J Adv Nurs. 2000. PMID: 10759980 Review.
- Knowledge-driven problem-solving models in nursing education. Chowlowski KM, Chan LK. Chowlowski KM, et al. J Nurs Educ. 1995 Apr;34(4):148-54. doi: 10.3928/0148-4834-19950401-04. J Nurs Educ. 1995. PMID: 7782881 Review.
- Responsible education for today's professional nurses. Bartels JE. Bartels JE. J Prof Nurs. 1997 Jan-Feb;13(1):4. doi: 10.1016/s8755-7223(97)80018-x. J Prof Nurs. 1997. PMID: 9183104 No abstract available.
Publication types
- Search in MeSH
LinkOut - more resources
Full text sources.

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Soft skills
- What is a credential?
- Why do a credential?
- How do credentials work?
- Selecting your level
- How will I be assessed?
- Benefits for professionals
- Benefits for organisations
- Benefits for postgraduates
Problem solving techniques: Steps and methods

Posted on May 29, 2019
Constant disruption has become a hallmark of the modern workforce and organisations want problem solving skills to combat this. Employers need people who can respond to change – be that evolving technology, new competitors, different models for doing business, or any of the other transformations that have taken place in recent years.
In addition, problem solving techniques encompass many of the other top skills employers seek . For example, LinkedIn’s list of the most in-demand soft skills of 2019 includes creativity, collaboration and adaptability, all of which fall under the problem-solving umbrella.
Despite its importance, many employees misunderstand what the problem solving method really involves.
What constitutes effective problem solving?
Effective problem solving doesn’t mean going away and coming up with an answer immediately. In fact, this isn’t good problem solving at all, because you’ll be running with the first solution that comes into your mind, which often isn’t the best.
Instead, you should look at problem solving more as a process with several steps involved that will help you reach the best outcome. Those steps are:
- Define the problem
- List all the possible solutions
- Evaluate the options
- Select the best solution
- Create an implementation plan
- Communicate your solution
Let’s look at each step in a little more detail.

1. Define the problem
The first step to solving a problem is defining what the problem actually is – sounds simple, right? Well no. An effective problem solver will take the thoughts of everyone involved into account, but different people might have different ideas on what the root cause of the issue really is. It’s up to you to actively listen to everyone without bringing any of your own preconceived notions to the conversation. Learning to differentiate facts from opinion is an essential part of this process.
An effective problem solver will take the opinions of everyone involved into account
The same can be said of data. Depending on what the problem is, there will be varying amounts of information available that will help you work out what’s gone wrong. There should be at least some data involved in any problem, and it’s up to you to gather as much as possible and analyse it objectively.
2. List all the possible solutions
Once you’ve identified what the real issue is, it’s time to think of solutions. Brainstorming as many solutions as possible will help you arrive at the best answer because you’ll be considering all potential options and scenarios. You should take everyone’s thoughts into account when you’re brainstorming these ideas, as well as all the insights you’ve gleaned from your data analysis. It also helps to seek input from others at this stage, as they may come up with solutions you haven’t thought of.
Depending on the type of problem, it can be useful to think of both short-term and long-term solutions, as some of your options may take a while to implement.

3. Evaluate the options
Each option will have pros and cons, and it’s important you list all of these, as well as how each solution could impact key stakeholders. Once you’ve narrowed down your options to three or four, it’s often a good idea to go to other employees for feedback just in case you’ve missed something. You should also work out how each option ties in with the broader goals of the business.
There may be a way to merge two options together in order to satisfy more people.
4. Select an option
Only now should you choose which solution you’re going to go with. What you decide should be whatever solves the problem most effectively while also taking the interests of everyone involved into account. There may be a way to merge two options together in order to satisfy more people.
5. Create an implementation plan
At this point you might be thinking it’s time to sit back and relax – problem solved, right? There are actually two more steps involved if you want your problem solving method to be truly effective. The first is to create an implementation plan. After all, if you don’t carry out your solution effectively, you’re not really solving the problem at all.
Create an implementation plan on how you will put your solution into practice. One problem solving technique that many use here is to introduce a testing and feedback phase just to make sure the option you’ve selected really is the most viable. You’ll also want to include any changes to your solution that may occur in your implementation plan, as well as how you’ll monitor compliance and success.
6. Communicate your solution
There’s one last step to consider as part of the problem solving methodology, and that’s communicating your solution . Without this crucial part of the process, how is anyone going to know what you’ve decided? Make sure you communicate your decision to all the people who might be impacted by it. Not everyone is going to be 100 per cent happy with it, so when you communicate you must give them context. Explain exactly why you’ve made that decision and how the pros mean it’s better than any of the other options you came up with.
Prove your problem solving skills with Deakin
Employers are increasingly seeking soft skills, but unfortunately, while you can show that you’ve got a degree in a subject, it’s much harder to prove you’ve got proficiency in things like problem solving skills. But this is changing thanks to Deakin’s micro-credentials. These are university-level micro-credentials that provide an authoritative and third-party assessment of your capabilities in a range of areas, including problem solving. Reach out today for more information .

- Liberty University
- Jerry Falwell Library
- Special Collections
- < Previous
Home > ETD > Doctoral > 5866
Doctoral Dissertations and Projects
Exploring student perceptions of problem-based learning and clinical field experiences: a phenomenological study.
Ashley Michelle Boles , Liberty University Follow
School of Education
Doctor of Philosophy in Education (PhD)
Mary Strickland
problem-based learning, medical education, higher-order thinking and processing, critical thinking, clinical reasoning, problem-solving, clinical field experiences
Disciplines
Education | Medicine and Health Sciences
Recommended Citation
Boles, Ashley Michelle, "Exploring Student Perceptions of Problem-Based Learning and Clinical Field Experiences: A Phenomenological Study" (2024). Doctoral Dissertations and Projects . 5866. https://digitalcommons.liberty.edu/doctoral/5866
The purpose of this phenomenological study is to understand the experiences of participating in a physical therapy course primarily taught using problem-based learning teaching methods for Doctor of Physical Therapy students at a university in the mid-western United States. This study aimed to understand student perception of PBL and its effects on clinical field experiences (CFEs), specifically related to higher-order processing skills. The theory guiding this study was the social constructivism theory as it explains how knowledge acquisition and learning occurs through social interactions during problem-based learning activities. The central research question this study attempted to answer was: What were the experiences of DPT students who participate in a PBL education? This study design was a qualitative, hermeneutic phenomenological study. Convenience sampling was done from a pool of DPT students at a university in the midwestern United States. Data collection methods included journal prompts, individual interviews, and focus groups. Data analysis was based on van Manen’s data analysis methods. Findings reveal DPT students preferred PBL over traditional teaching methods and felt the use of PBL improved their higher-order thinking and processing skills. Participants felt that PBL teaching methods were conducive to their learning as the method allowed for real-time feedback and a perception of better content retention. DPT students also felt that using PBL teaching methods improved their ability to prioritize and funnel information to organize information in a way conducive to developing a solution to the problem. Participants felt that the problem-solving, critical thinking, and clinical reasoning they developed during the therapeutic exercise course did carry over into their ability to apply these higher-order thinking and processing skills during CFEs.
Since August 09, 2024
Included in
Education Commons , Medicine and Health Sciences Commons
- Collections
- Faculty Expert Gallery
- Theses and Dissertations
- Conferences and Events
- Open Educational Resources (OER)
- Explore Disciplines
Advanced Search
- Notify me via email or RSS .
Faculty Authors
- Submit Research
- Expert Gallery Login
Student Authors
- Undergraduate Submissions
- Graduate Submissions
- Honors Submissions
Home | About | FAQ | My Account | Accessibility Statement
Privacy Copyright

IMAGES
COMMENTS
Problem-solving in nursing is the vital foundation that makes up a nurse's clinical judgment and critical thinking skills. Having a strong problem-solving skillset is pertinent to possessing the ability and means to provide safe, quality care to a variety of patients. Nurses must rely on their clinical judgment and critical thinking skills to ...
Nurses can implement the original nursing process to guide patient care for problem solving in nursing. These steps include: Assessment. Use critical thinking skills to brainstorm and gather information. Diagnosis. Identify the problem and any triggers or obstacles. Planning. Collaborate to formulate the desired outcome based on proven methods ...
A free flow of ideas is essential to problem-solving and decision-making because it helps prevent preconceived ideas from controlling the process. Many decisions in healthcare are arrived at by group or teams rather than by the individual, and this type of decision-making requires special skills. General steps to all decision making include:
Abdellah's work, based on the problem-solving method, serves as a vehicle for delineating nursing (patient) problems as the patient moves toward a healthy outcome. The theory identifies ten steps to identify the patient's problem and 11 nursing skills to develop a treatment typology.
Problem-solving skills. Practicing your problem-solving skills can improve your critical-thinking skills. Analyze the problem, consider alternate solutions, and implement the most appropriate one. ... Structure your thinking by incorporating nursing process steps or a SWOT analysis (strengths, weaknesses, opportunities, and threats) ...
The following are examples of attributes of excellent critical thinking skills in nursing. 1. The ability to interpret information: In nursing, the interpretation of patient data is an essential part of critical thinking. Nurses must determine the significance of vital signs, lab values, and data associated with physical assessment.
Step 2: Analyze the Problem. Break down the problem to get an understanding of the problem. Determine how the problem developed. Determine the impact of the problem. Step 3: Develop Solutions. Brainstorm and list all possible solutions that focus on resolving the identified problem. Do not eliminate any possible solutions at this stage.
2. Meeting with Colleagues: Collaborative Learning for Critical Thinking. Regular interactions with colleagues foster a collaborative learning environment. Sharing experiences, discussing diverse viewpoints, and providing constructive feedback enhance critical thinking skills. Colleagues' insights can challenge assumptions and broaden ...
This paper analyses the role of problem solving in nursing practice including the process, acquisition and measurement of problem-solving skills It is argued that while problem-solving ability is acknowledged as critical if today's nurse practitioner is to maintain effective clinical practice, to date it retains a marginal place in nurse education curricula Further, it has attracted limited ...
Some of the most important critical thinking skills nurses use daily include interpretation, analysis, evaluation, inference, explanation, and self-regulation. Interpretation: Understanding the meaning of information or events. Analysis: Investigating a course of action based on objective and subjective data. Evaluation: Assessing the value of ...
To solve a problem you need to generate solutions. However, the obvious solution may not necessarily be the best. To generate solutions, a mixture of creative and analytical thinking is needed (Bransford, 1993). Creativity is about escaping from preconceived ideas that block the way to finding an innovative solution to a problem.
Problem solving occurs in a variety of nursing contexts, including direct client care, team-level leadership, and systems-level leadership. Nurses and nurse managers are challenged to move from step-by-step problem-solving techniques to incorporating creative thinking, which involves considering the context when meeting current and future ...
Nurse leaders perceive their role as a problem-solver, which is a necessary step in advocacy. 27 Problem-solving is a process that contains the elements of decision-making and critical thinking. 28. The theory that emerged from the core categories explicitly focused on the central phenomenon of LHV in the nursing work environment.
Background. Problem solving involves recognizing the difference between the problem solver's current state and the goal state to be reached, and resolving the obstacles that prevent them from achieving the goal [].Acquiring problem-solving ability based on judgment and critical thinking is an important element of nursing education [].Furthermore, the use of effective problem-solving ...
D. Choose Solutions. Focus on helping the client identify small steps, coping strategies, stress reduction, problem-solving and self-examination of results. E. Implement Process. Identify when patient will "stop and think" and use collaboratively agreed upon action. Journaling successes, emotions, and learning is helpful (Fontaine, 2003).
Critical thinking, problem-solving, and communication skills are necessary to work in this phase. Nurses must also demonstrate the ability to prioritize patient needs. ... Nurses utilize many of the same skills for each of the nursing process steps. In the planning phase, nurses must have strong communication skills, time management and ...
The problem-solving steps might look like this: Identification and Definition: The problem is identified as long patient waiting times. It is defined as patients waiting more than 45 minutes to receive care. ... Essential problem-solving skills in nursing management include critical thinking, decision-making, effective communication, leadership ...
Problem solving in clinical nursing practice is the essence of good care delivery. This paper gives an overview of a research study which identified the cognitive problem solving process nurses use while delivering care. The study was conducted in the clinical setting and used a qualitative research methodology of observation, followed by in ...
mentorship. delegation. open-mindedness. forward-thinking. accessibility. Another valuable quality in leadership is being proactive in problem-solving. Good leaders handle issues as they arrive. They are capable of "putting out fires," and that's important. Yet, great leaders anticipate problems before they come to a head.
Abstract. This paper analyses the role of problem solving in nursing practice including the process, acquisition and measurement of problem-solving skills. It is argued that while problem-solving ability is acknowledged as critical if today's nurse practitioner is to maintain effective clinical practice, to date it retains a marginal place in ...
1. Define the problem. Diagnose the situation so that your focus is on the problem, not just its symptoms. Helpful problem-solving techniques include using flowcharts to identify the expected steps of a process and cause-and-effect diagrams to define and analyze root causes.. The sections below help explain key problem-solving steps.
Evaluate the options. Select the best solution. Create an implementation plan. Communicate your solution. Let's look at each step in a little more detail. The first solution you come up with won't always be the best - taking the time to consider your options is an essential problem solving technique. 1.
The purpose of this phenomenological study is to understand the experiences of participating in a physical therapy course primarily taught using problem-based learning teaching methods for Doctor of Physical Therapy students at a university in the mid-western United States. This study aimed to understand student perception of PBL and its effects on clinical field experiences (CFEs ...