- Introduction to Genomics
- Educational Resources
- Policy Issues in Genomics
- The Human Genome Project
- Funding Opportunities
- Funded Programs & Projects
- Division and Program Directors
- Scientific Program Analysts
- Contact by Research Area
- News & Events
- Research Areas
- Research investigators
- Research Projects
- Clinical Research
- Data Tools & Resources
- Genomics & Medicine
- Family Health History
- For Patients & Families
- For Health Professionals
- Jobs at NHGRI
- Training at NHGRI
- Funding for Research Training
- Professional Development Programs
- NHGRI Culture
- Social Media
- Broadcast Media
- Image Gallery
- Press Resources
- Organization
- NHGRI Director
- Mission & Vision
- Policies & Guidance
- Institute Advisors
- Strategic Vision
- Leadership Initiatives
- Diversity, Equity, and Inclusion
- Partner with NHGRI
- Staff Search

Genetic Disorders
Many human diseases have a genetic component. Some of these conditions are under investigation by researchers at or associated with the National Human Genome Research Institute (NHGRI).
A genetic disorder is a disease caused in whole or in part by a change in the DNA sequence away from the normal sequence. Genetic disorders can be caused by a mutation in one gene (monogenic disorder), by mutations in multiple genes (multifactorial inheritance disorder), by a combination of gene mutations and environmental factors, or by damage to chromosomes (changes in the number or structure of entire chromosomes, the structures that carry genes). As we unlock the secrets of the human genome (the complete set of human genes), we are learning that nearly all diseases have a genetic component. Some diseases are caused by mutations that are inherited from the parents and are present in an individual at birth, like sickle cell disease. Other diseases are caused by acquired mutations in a gene or group of genes that occur during a person's life. Such mutations are not inherited from a parent, but occur either randomly or due to some environmental exposure (such as cigarette smoke). These include many cancers, as well as some forms of neurofibromatosis.
List of Genetic Disorders
This list of genetic, orphan and rare diseases is provided for informational purposes only and is by no means comprehensive.

Featured Content
Last updated: May 18, 2018
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Genetic Disorders of Bone or Osteodystrophies of Jaws-A Review
Affiliations.
- 1 Private Practitioner, Oral Medicine and Radiology, Vishakapatnam, Andhra Pradesh, India.
- 2 Department of Oral Medicine and Radiology, Tirumala Institute of Dental Sciences, Nizamabad, Telangana, India.
- 3 Department of Prosthodontics, Kamineni Institute of Dental Sciences, Narketpally, Telangana, India.
- 4 Department of Oral Medicine and Radiology, Kamineni Institute of Dental Sciences, Narketpally, Telangana, India.
- 5 Department of Pedodontics and Preventive Dentistry, JSS Dental College, Mysore, Karnataka, India.
- 6 Department of Orthodontics, Kamineni Institute of Dental Sciences, Narketpally, Telangana, India.
- 7 Private Practitioner, MDS in Oral Pathology, Hyderabad, Telangana, India.
- 8 Department of Oral Pathology, Tirumala Institute of Dental Sciences, Nizamabad, Telangana, India.
- PMID: 33987622
- PMCID: PMC8110367
- DOI: 10.1055/s-0041-1724105
Bone is a specialized form of connective tissue, which is mineralized and made up of approximately 28% type I collagen and 5% noncollagenous matrix proteins. The properties of bone are very remarkable, because it is a dynamic tissue, undergoing constant renewal in response to mechanical, nutritional, and hormonal influences. In 1978, "The International Nomenclature of Constitutional Diseases of Bone" divided bone disorders into two broad groups: osteochondrodysplasias and dysostoses. The osteochondrodysplasia group is further subdivided into two categories: dysplasias (abnormalities of bone and/or cartilage growth) and osteodystrophies (abnormalities of bone and/or cartilage texture). The dysplasias form the largest group of bone disorders, hence the loose term "skeletal dysplasia" that is often incorrectly used when referring to a condition that is in reality an osteodystrophy or dysostosis. The word "dystrophy" implies any condition of abnormal development. "Osteodystrophies," as their name implies, are disturbances in the growth of bone. It is also known as osteodystrophia. It includes bone diseases that are neither inflammatory nor neoplastic but may be genetic, metabolic, or of unknown origin. Recent studies have shown that bone influences the activity of other organs, and the bone is also influenced by other organs and systems of the body, providing new insights and evidencing the complexity and dynamic nature of bone tissue. The 1,25-dihydroxyvitamin D3, or simply vitamin D, in association with other hormones and minerals, is responsible for mediating the intestinal absorption of calcium, which influences plasma calcium levels and bone metabolism. Diagnosis of the specific osteodystrophy type is a rather complex process and various biochemical markers and radiographic findings are used, so as to facilitate this condition. For diagnosis, we must consider the possibility of lesions related to bone metabolism altered by chronic renal failure (CRI), such as the different types of osteodystrophies, and differentiate from other possible neoplastic and/or inflammatory pathologies. It is important that the dentist must be aware of patients medical history, suffering from any systemic diseases, and identify the interference of the drugs and treatments to control them, so that we can able to perform the correct diagnosis and propose the most adequate treatment and outcomes of the individuals with bone lesions.
Keywords: CRI—Chronic renal failure; FGFR3—Fibroblast growth factor receptor; M-CSF—Macrophage colony stimulating factor; PTH—Parathyroid hormone; RANKL—Receptor activator of NF-B ligand; TGF—Transforming growth factor.
The Author(s). This is an open access article published by Thieme under the terms of the Creative Commons Attribution License, permitting unrestricted use, distribution, and reproduction so long as the original work is properly cited. ( https://creativecommons.org/licenses/by/4.0/ ).
PubMed Disclaimer
Conflict of interest statement
Conflict of Interest None declared.
Similar articles
- Osteodystrophies of jaws. Santana N, Mehazabin S, Sangeetha K, Kumari M. Santana N, et al. J Oral Maxillofac Pathol. 2020 May-Aug;24(2):405. doi: 10.4103/jomfp.JOMFP_225_19. Epub 2020 Sep 9. J Oral Maxillofac Pathol. 2020. PMID: 33456267 Free PMC article. Review.
- Skeletal Dysplasias: An Overview. Offiah AC. Offiah AC. Endocr Dev. 2015;28:259-276. doi: 10.1159/000381051. Epub 2015 Jun 12. Endocr Dev. 2015. PMID: 26138847 Review.
- 1alpha(OH)D3 One-alpha-hydroxy-cholecalciferol--an active vitamin D analog. Clinical studies on prophylaxis and treatment of secondary hyperparathyroidism in uremic patients on chronic dialysis. Brandi L. Brandi L. Dan Med Bull. 2008 Nov;55(4):186-210. Dan Med Bull. 2008. PMID: 19232159 Review.
- [Changes in mineral metabolism in stage 3, 4, and 5 chronic kidney disease (not on dialysis)]. Lorenzo Sellares V, Torregrosa V. Lorenzo Sellares V, et al. Nefrologia. 2008;28 Suppl 3:67-78. Nefrologia. 2008. PMID: 19018742 Spanish.
- Minimizing bone abnormalities in children with renal failure. Ziólkowska H. Ziólkowska H. Paediatr Drugs. 2006;8(4):205-22. doi: 10.2165/00148581-200608040-00001. Paediatr Drugs. 2006. PMID: 16898852 Review.
- Cancellous bone-like tissue replacement from calcinosis in patients with systemic sclerosis with multiple external root resorption. Memida T, Matsuda S, Nakamoto T, Ouhara K, Kajiya M, Hirata S, Sugiyama E, Kakimoto N, Mizuno N. Memida T, et al. Bone Rep. 2022 Jan 8;16:101165. doi: 10.1016/j.bonr.2021.101165. eCollection 2022 Jun. Bone Rep. 2022. PMID: 35059476 Free PMC article.
- Clarke B. Normal bone anatomy and physiology. Clin J Am Soc Nephrol. 2008;3(03) 03:S131–S139. - PMC - PubMed
- Downey P A, Siegel M I. Bone biology and the clinical implications for osteoporosis. Phys Ther. 2006;86(01):77–91. - PubMed
- Ralston S H. Bone structure and metabolism. Medicine. 2013;41(10):581–585.
- Matsuo K, Irie N. Osteoclast-osteoblast communication. Arch Biochem Biophys. 2008;473(02):201–209. - PubMed
- Shafer W G, Hine M K, Levy B M. 4th ed. Philadelphia: Saunders; 2000. A Textbook of Oral Pathology; pp. 678–680.
Publication types
- Search in MeSH
LinkOut - more resources
Full text sources.
- Europe PubMed Central
- Georg Thieme Verlag Stuttgart, New York
- PubMed Central
Other Literature Sources
- scite Smart Citations
Research Materials
- NCI CPTC Antibody Characterization Program

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- - Google Chrome
Intended for healthcare professionals
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Etiology and clinical...
Etiology and clinical presentation of birth defects: population based study
- Related content
- Peer review
- Marcia L Feldkamp , associate professor 1 ,
- John C Carey , professor 1 ,
- Janice L B Byrne , professor 1 2 ,
- Sergey Krikov , bioinformaticist 1 ,
- Lorenzo D Botto , professor 1
- 1 Division of Medical Genetics, Department of Pediatrics, 295 Chipeta Way, Suite 2S010, University of Utah School of Medicine, Salt Lake City, UT, USA,
- 2 Division of Maternal-Fetal Medicine, Department of Obstetrics and Gynecology, University of Utah School of Medicine, Salt Lake City, UT, USA
- Correspondence to: M L Feldkamp marcia.feldkamp{at}hsc.utah.edu
- Accepted 3 May 2017
Objective To assess causation and clinical presentation of major birth defects.
Design Population based case cohort.
Setting Cases of birth defects in children born 2005-09 to resident women, ascertained through Utah’s population based surveillance system. All records underwent clinical re-review.
Participants 5504 cases among 270 878 births (prevalence 2.03%), excluding mild isolated conditions (such as muscular ventricular septal defects, distal hypospadias).
Main outcome measures The primary outcomes were the proportion of birth defects with a known etiology (chromosomal, genetic, human teratogen, twinning) or unknown etiology, by morphology (isolated, multiple, minors only), and by pathogenesis (sequence, developmental field defect, or known pattern of birth defects).
Results Definite cause was assigned in 20.2% (n=1114) of cases: chromosomal or genetic conditions accounted for 94.4% (n=1052), teratogens for 4.1% (n=46, mostly poorly controlled pregestational diabetes), and twinning for 1.4% (n=16, conjoined or acardiac). The 79.8% (n=4390) remaining were classified as unknown etiology; of these 88.2% (n=3874) were isolated birth defects. Family history (similarly affected first degree relative) was documented in 4.8% (n=266). In this cohort, 92.1% (5067/5504) were live born infants (isolated and non-isolated birth defects): 75.3% (4147/5504) were classified as having an isolated birth defect (unknown or known etiology).
Conclusions These findings underscore the gaps in our knowledge regarding the causes of birth defects. For the causes that are known, such as smoking or diabetes, assigning causation in individual cases remains challenging. Nevertheless, the ongoing impact of these exposures on fetal development highlights the urgency and benefits of population based preventive interventions. For the causes that are still unknown, better strategies are needed. These can include greater integration of the key elements of etiology, morphology, and pathogenesis into epidemiologic studies; greater collaboration between researchers (such as developmental biologists), clinicians (such as medical geneticists), and epidemiologists; and better ways to objectively measure fetal exposures (beyond maternal self reports) and closer (prenatally) to the critical period of organogenesis.
Introduction
Birth defects are inborn errors of development. Broadly defined, they include any structural or functional anomaly with measureable effects on physical, intellectual, and social wellbeing. 1 Birth defects represent a considerable and increasing clinical and public health challenge because of their worldwide impact on population health.
Major birth defects are common, costly, and critical. Collectively, they occur in one in 33 births, 2 which in 2006 translated into an estimated 7.9 million babies worldwide. 3 In the US alone, the cost of care during a single year (2004) was estimated at $2.6bn (£2bn, €2.4bn). 4 This estimate does not account for the considerable indirect and lifelong personal and societal costs. Finally, many birth defects critically affect survival. In the US, birth defects are the leading cause of infant mortality 5 and in 2013 were associated with 4778 deaths, one in every five deaths in the first year of life.
The temporal trends are even more concerning. The occurrence of birth defects, with few localized exceptions (such as neural tube defects in countries that implemented folic acid fortification), has not decreased for many decades. Birth defects might indeed increase worldwide, with the alarming increase of known risk factors such as maternal diabetes and obesity. New threats such as the Zika epidemic are emerging. Unless progress is made in identifying and preventing the root causes of birth defects, these conditions will continue to have draining effects on the survival and health of individuals, families, and countries.
Progress in detecting and characterizing risk factors for birth defects has come mainly from epidemiologic studies. In fact, such studies have produced many associations between risk factors and groups of birth defects. Translating these associations to actual causes, however, has been difficult. As a first step in filling this gap, we evaluated the clinical and etiologic profile of birth defects in a well characterized population based case cohort through systematic review by clinicians, using a multidimensional assessment tool that incorporates etiology, morphology, and pathogenesis.
Study population
The data source for this study was Utah’s statewide population based public health surveillance system (Utah Birth Defect Network, UBDN), housed at the Utah Department of Health. There is no patient involvement or contact as part of this surveillance system. The network monitors birth defects among all pregnancy outcomes (live births, stillbirths, pregnancy terminations) among Utah residents. If a termination occurred, existing medical records were ascertained and reviewed to determine eligibility. To identify potential cases, the program uses multiple reporting sources, both prenatal and postnatal. All reporting sources are mandated to regularly submit any potential diagnosis in infants aged up to 24 months and are legally protected to report if a diagnosis is made after 24 months. The detailed clinical information for each case is based on the abstracted prenatal and postnatal clinical records by trained data abstractors. The presence of a prenatal diagnosis without autopsy or postnatal confirmation is not sufficient for inclusion in the system, with few exceptions, the main one being anencephaly if well described by a perinatologist. For example, hydronephrosis based on only prenatal diagnosis was not eligible for inclusion unless it was confirmed postnatally. Some birth defects have not ever been eligible for inclusion in the surveillance system because it is more challenging to identify and ascertain all cases or they are not considered a birth defect—for example, isolated muscular ventricular septal defects, patent foramen ovale, patent ductus arteriosus, talipes equinovarus, congenital hip dysplasia/dislocation, congenital pulmonary airway malformation, and cryptorchidism. Cases of fetal alcohol syndrome were included only if a major birth defect was diagnosed. Further details of the system’s case ascertainment and medical record abstraction have been published elsewhere. 6 7
Clinical case review
A team of clinicians with training in medical genetics (LDB, JCC, JLBB) reviewed case records, including inpatient and outpatient records, laboratory reports (such as genomic microarray), diagnostic evaluations (such as ultrasound images and echocardiograms), operative notes, and autopsy reports. Once a case was deemed eligible, the clinician generated a list of the major and minor defects and the timing of first diagnosis (prenatal or postnatal). Each defect was coded with the World Health Organization international classification of diseases (version 9) with British Paediatric Association extensions (ICD-9 BPA). In addition, the clinician provided three additional classifications for each case: known etiology (yes, no); isolated versus multiple (unrelated) birth defect versus syndromic (that is, known etiology: genetic or environmental); and whether the case was familial (yes, no). A case was considered familial if a first degree relative (parent or sib) had a concordant phenotype.
Multidimensional etiologic classification
To systematically capture the clinical presentation and etiology in the study cohort we developed and implemented a multidimensional classification with three axes: etiology (known, unknown), morphology (isolated, multiple majors, minors only), and pathogenesis (sequence, developmental field, or pattern). Table 1 ⇓ summarizes the system and definitions. Briefly:
Classification groups and definitions for etiologic classification of all cases of birth defects in Utah, 2005-09
- View inline
Known etiology was assigned based on specific and conservative criteria and could be either genetic, environmental (teratogenic), or due to twinning:
Genetic—cases were classified as having a known genetic etiology if there was documentation of abnormal chromosomal number (trisomy) or structure (insertion, deletion) or a single gene condition (such as Noonan syndrome)
Environmental—this required documentation of exposure to a recognized human teratogen 8 (for example, medication, such as valproic acid, or pregestational diabetes with abnormal hemoglobin A 1c concentration during the periconceptional period or early pregnancy). Among mothers noted to have diabetes (pregestational or gestational), we reviewed their timing of diagnosis before or during pregnancy, medication use for control of blood sugar, and if listed, the hemoglobin A 1c testing date and concentration. Women listed as having gestational diabetes with a diagnosis in the first trimester were reclassified as having pregestational diabetes if their hemoglobin A 1c was >5.6. To assign diabetes as a cause, the mother had to have evidence of poorly controlled pregestational diabetes and an infant with selected birth defects that, based on the published literature, were indicative of diabetic embryopathy 9 10 11 : heterotaxy, holoprosencephaly, multiple vertebral defects, bilateral renal defects, or caudal dysgenesis. Conversely, pregestational diabetes in cases of isolated defects such as anencephaly or a congenital heart defect, or a major with minor defect was not considered as a known cause for those particular infants
Twinning—abnormalities in twinning included either acardiac or conjoined twins.
Morphology: a case with a single major birth defect (with or without a minor birth defect) was considered isolated. This definition includes isolated sequences. Infants without a major birth defect were included if they had a chromosomal anomaly (such as trisomy 21 with no reported major birth defect, normal echocardiogram, and none of the selected list of objective minor defects) or eligible genetic condition (such as skeletal dysplasia). Only a selected list of minor defects was classified and analyzed; these were selected because they can be considered as objective findings with limited variation in reporting and classification (table 1 ⇑ ). This list included mainly discontinuous traits such as preauricular tags or single umbilical artery, rather than continuous traits such as hypertelorism, which require careful measurements and chart based decision criteria
Pathogenesis: three groups were created and defined by mechanism based on embryology, not ICD-9 BPA codes (sequence, developmental field defect, or known pattern of birth defects, table 1 ⇑ ). An example of a “known pattern” is the VATER/VACTERL association. This association was operationally defined as the presence of three or more VACTERL defects (vertebral defects, anal atresia, cardiac anomaly, esophageal atresia or tracheoesophageal (TE) fistula, renal malformation, radial limb malformation) with at least one being either esophageal atresia/TE fistula or anal atresia. 12 To further promote consistency, the same clinical geneticist (JCC) reviewed and classified all cases of potential VACTERL association
Implementation of multidimensional classification
For this study, the clinicians together developed a systematic process for the re-review of all cases. In general, each case was reviewed by one clinician, and the accuracy of the classification was further enhanced by assigning certain phenotypes to the clinician with the greatest expertise in that specialty. We re-reviewed the complete population based resident cohort for five consecutive birth years (1 January 2005 to 31 December 2009). We elected to assess this five year birth cohort because some genetic tests can be ordered well after infancy, changing the classification status. Case classification can also change as knowledge progresses. For example, cases of CHARGE association (coloboma, heart defect, choanal atresia, growth/developmental retardation, genital and ear abnormalities) were changed from “multiple congenital anomaly” to “syndrome/genetic” after mutations in the CHD7 gene were established as a cause in 2004 13 —in this situation, cases that met the established clinical criteria for CHARGE (with or without CHD7 mutation testing) were reclassified as “genetic.” The classification was supported by an Access database module that captured both the classifications and comments from the clinical reviewers.
The cohort included 6547 confirmed cases. We excluded 834 cases of isolated birth defect: twin related (n=2); pelviectasis or hydronephrosis without evidence of obstruction (n=47); small (<4 mm) secundum atrial septal defects (n=200); and distal (first degree) or megameatus type hypospadias (n=585). We also excluded spontaneous abortions occurring at <20 weeks’ gestation (n=209). After exclusions, the final study cohort included 5504 cases.
Statistical analyses were done with SAS Enterprise Guide version 6.1 software (SAS Institute, Cary, NC, 2013).
Patient involvement
No patients were involved in setting the research question or the outcome measures, nor were they involved in the design and implementation of the study. There are no plans to involve patients in the dissemination of results.
The population based study cohort included 5504 infants with major birth defects among 270 878 total births (live births and stillbirths), giving a prevalence of 2.03%. In this cohort, 92.1% (5067/5504) of cases (isolated and non-isolated) occurred in liveborn infants: 75.3% (4147/5504) had an isolated defect (unknown and known etiology combined) (table 2, ⇓ fig 1 ⇓ ). A positive family history (having a similarly affected first degree relative) was documented in 4.8% cases overall (266/5504). Compared with the underlying birth cohort (births in Utah, 2005-09), the affected cohort included more boys (57.7%, P<0.001), even after we excluded cases known to be sex limited anomalies (such as hypospadias, 47,XXY/XYY/XXX, 45,X).
Number of cases of birth defects, percentage, and prevalence (per 1000 births) stratified by morphology (isolated and non-isolated) and pregnancy outcome in Utah, 2005-09
Fig 1 Known and unknown etiology of birth defects
- Download figure
- Open in new tab
- Download powerpoint
Unknown etiology
Overall, 79.8% of cases (n=4390) were classified as unknown etiology (table 3 ⇓ ), 3.6% were known to be familial (isolated 3.7%; multiple 2.7%). Boys were over-represented in both isolated (59.5%, P<0.001) and multiple (55.4%, P=0.02) case groups.
Etiologic classification of birth defects stratified by morphology and pregnancy outcome in Utah, 2005-09. Figures are numbers (percentage)
Among the unknown etiology case group, 344 (7.8% of 4390) were further classified as a sequence (n=242, 70.3%), a developmental field defect (n=71, 20.6%), or a known pattern (n=31, 9.0%) (table 4 ⇓ ). Isolated defects accounted for most cases classified as a sequence (n=187, 77.3%) or developmental field defect (n=50, 70.4%), whereas cases classified as a pattern were more likely to have multiple birth defects (n=30, 96.8%). Eighteen of 20 infants with birth defects consistent with VATER/VACTERL association (known pattern) were classified as unknown etiology.
Pathogenesis of 344 cases of birth defects with unknown etiology, stratified by morphology and pregnancy outcome in Utah, 2005-09. Figures are numbers (percentage)
Known etiology
A fifth (20.2%, n=1114) of cases were assigned a known etiology (table 3 ⇑ ). As shown in figure 2 ⇓ , 90.4% of the cases with a known etiology were represented by the three common trisomies (21, 18, 13), Turner syndrome, structural chromosomal abnormalities, and single gene disorders.
Fig 2 Number and cumulative percent of cases of birth defects with a known etiology, Utah 2005-09. TBSS=tract based spatial statistics
For the known etiology case group, 57 (5.1% of 1114) were further classified as a sequence (n=35, 61.4%), a developmental field defect (n=13, 22.8%), or a known pattern (n=10, 17.5%) (data not shown). Of the remaining two cases with VATER/VACTERL association (known pattern), one case occurred with pregestational diabetes (teratogen) and another with partial trisomy (7q11.21 duplication) (chromosomal-structure).
In this five year population based birth defect case cohort, systematic clinical review identified known etiology in only one in five—specific etiology could not be conclusively assigned in most (79.8%) cases. We considered the etiology known if there was conclusive evidence of one of four factors: chromosomal abnormalities (structure or number), genetic conditions, twinning, or an established human teratogen. Methods to determine if an environmental exposure is a human teratogen were recently reviewed and applied to the birth defects associated with the Zika virus. 14
Based on current science, our study revises and updates the historical findings from two well known hospital based studies of infants with birth defects. 15 16 The overall conclusion remains that a specific cause cannot yet be determined for most birth defects, underscoring the current gaps in knowledge and the challenge of primary prevention.
Comparison with other studies
We focused on major birth defects (excluding some common defects), for a prevalence of 2%. If we extrapolate from this conservative estimate, we estimate that each year a minimum of 78 000 infants are born in the US with a serious birth defect. In 63 000, there would be no identifiable etiology. These figures are intended as minimum estimates. With different criteria for inclusion, investigators have reported a prevalence of 2.24% among infants with a birth defect diagnosed before discharge from the maternity ward or before the age of 5 days at Boston Hospital for Women 16 and 5.5% 17 from the Texas Birth Defects Monitoring Program.
Our estimate of a known etiology in just over 20% is conservative. As genetic technology advances and more discoveries made on the genetic causes of birth defects, the proportion with a known cause will increase. For example, estimates of the genetic contribution to congenital heart disease (the most common birth defect) has increased, based on recent data suggesting that copy number variants and de novo mutations together could account for 15% of all cases. 18 19 20 Also, for some well known risk factors, attribution of an exposure to a birth defect in an individual case remains challenging. The epidemiologic metric of attributable fraction (that is, the proportion of birth defects attributable to the exposure when cause is known) is applicable to populations, not individual cases. In this study, it was not possible to determine if a woman’s history of smoking directly resulted in her infant’s oral facial cleft as the modest odds ratio of about 1.3 predicts that many children do not have an oral cleft because of that exposure. For pregestational diabetes, however, we used data on the estimates and attributable fraction of 70% for isolated and 90% for multiple defects 10 to select certain birth defects as related to diabetes.
Determination of etiology is critically important to focus research efforts for reduction of risk or prevention of occurrence (such as preconception folic acid supplementation and neural tube defects). Few studies have tried to directly assess the proportion of birth defects with or without a known etiology. Higurashi and colleagues re-examined infants each month for the first year to identify those with malformation syndromes not diagnosed at birth but did not mention the proportion without a known etiology. 21 Two hospital based cohorts used different methods (such as inclusion criteria and diagnosis within days after birth) to generate estimates of those infants without a known etiology. 15 16 Nelson and Holmes estimated 43.2% of their infants with birth defects born in a single hospital did not have a known etiology. 16 Infants were included if they received a diagnosis on or before the fifth day of life. Notably, cases considered to be familial (14.5%) or “multifactorial” (23%) were considered to be of known etiology; however, definitions were not provided and the inclusion especially of the “multifactorial” conditions is debatable. In contrast, in our study, we defined familial cases only as infants with an affected first degree relative (4.8% overall, 3.6% unknown etiology). Moreover, because of the difficulty in defining and proving multifactorial inheritance, we did not have such a category. Of note, if we add the cases classified by Nelson and Holmes 16 as multifactorial inheritance (23%) and familial (14.5%) to those that they classified originally as unknown (43.2%), the total adds to 80.7%, similar to our finding.
The causes of birth defects currently without known etiology are probably complex and could include interactions between the genetic profiles of parents and embryo and the environmental milieu during preconception and early gestation. For some birth defects, some progress has been made over the past decades, such as the contribution of microdeletions (such as deletion 22q11 in cases of heart defects and cleft palate 22 23 24 25 ) and novel single gene mutations (such as CHD7 mutations in CHARGE syndrome 13 ). While these genetic causes are relatively straightforward, however, it is likely that further research will discover more complex networks accounting for genetic and environmental contributions to birth defects etiology. Accumulating evidence is uncovering developmental networks that when disrupted can cause birth defect syndromes. 26 Some of these networks could also be influenced by environmental exposures, such as the midline patterning network related to the sonic hedgehog gene, which directly involves cholesterol metabolism. For example, the risk for holoprosencephaly could be increased not only by mutations in sonic hedgehog but potentially also by environmental influences (yet undiscovered) that alter the embryonic cholesterol biosynthesis, perhaps interacting with sonic hedgehog variants. 26
Birth defects know no geographic boundary and occur in every country of the world. Because many countries do not have the capacity to monitor birth defects that occur among all pregnancy outcomes, it is difficult to estimate their true worldwide prevalence and global burden. Based on the findings of this study, however, if we count only those infants live born with an isolated birth defect, 25% of the cases will be missed. The resulting underestimation of the burden of disease can have serious policy implications and hinder the investments in research and interventions to better prevent and treat these major threats to childhood survival and lifelong health.
Research to understand birth defect etiology requires a well defined and clinically characterized case group. Cases with known etiology must be carefully identified and excluded to maximize the chance of discovery. 27 While commonly used birth defect classification schemes (such as ICD-9 or ICD-10) are valuable for general purposes such as studies on morbidity and mortality, they are not ideal in the evaluation of etiologies or trends 28 and could overestimate prevalence. 29 30 31 32 These coding systems are typically organized by anatomy or function rather than cause or embryologic process. Few studies have applied classifications specific to birth defects to population based cohorts. One of these, the National Birth Defects Prevention Study, has leveraged the collaboration of clinical geneticists and epidemiologists to pursue discovery of modifiable causes of birth defects. 33 34 35 Continued progress will require the combined effort and a multidisciplinary approach that incorporates not only the clinical evaluation by dysmorphologists/clinical geneticists and the methodological expertise of epidemiologists but also includes experts in developmental biology, pharmacology, infectious diseases, immunology, and bioinformatics, in addition to a more objective assessment of periconceptional exposures that improve on the typical maternal self reports. Finally, it would be helpful to integrate etiology, morphology, and pathogenesis assessment into the basic framework of epidemiologic studies. Such integration will improve precision and assist researchers to focus research initiatives and investigate common pathways among birth defects.
Limitations
This study has potential limitations. The birth prevalence of 2.03% reported in this study is lower than the 2.24-5.5% reported elsewhere. 2 16 17 Such lower prevalence estimates could relate to the eligibility criteria of the Utah surveillance system, which exclude some common mostly milder conditions that are variably defined and ascertained (such as muscular ventricular septal defects, clubfoot, cryptorchidism). Also, because cases were classified based on data abstracted from mother and infant medical records, there is a possibility that critical information for appropriate classification was unavailable at the time of medical record abstraction. In addition, we could have underestimated the proportion caused by a teratogen if an exposure (such as maternal pregestational diabetes) was not noted in the medical record or not queried by the physician of record. The information in these medical records comes from different specialists, often including perinatologists, genetic counselors, neonatologists, and/or pediatric geneticists. Whereas some level of etiologic under-ascertainment cannot be excluded, it is unlikely that an established environmental cause of birth defects would be missed by everyone involved in the care of the mother and the child. For a genetic investigation, the laboratory evaluation (such as karyotype, microarray) was determined by the clinician(s) caring for the infant and was tailored to the clinical presentation. We would expect some variation within the practice of medicine.
Conclusion and public health implications
Understanding the etiology of birth defects should be both a public health and research priority. Our findings underscore the large gaps in current knowledge of the causes of birth defects. These gaps in turn represent opportunities for both basic and translational researchers. Such research can be particularly powerful and efficient if done in collaboration with population based birth defect surveillance programs enhanced with clinical expertise and meaningful case classification. 36 Advances in the knowledge of the causal pathway leading to birth defects can be the basis for better primary prevention interventions, resulting in longer and better lives. For clinicians and parents, it is important to understand what can be done today to prevent birth defects, in particular the role of preconception care focusing on optimal women’s health (including screening/treating chronic illnesses, attaining folic acid sufficiency, etc). In addition, investigation of potential causes of a birth defect at the time of diagnosis (such as whether a genetic condition is present) can help to better plan management and appropriately counsel families, including the relief of anxiety related to unfounded information and guilt.
What is already known on this topic
Birth defects are common, costly, and critical
Two hospital based studies have tried to directly assess the proportion of birth defects with or without a known etiology
What this study adds
In this population based birth defect case cohort, the cause was established in only one in every five infants
The inability to understand etiology in four of five cases highlights the urgent need for better basic and translational research as a basis for primary prevention and care
In addition, many birth defects are associated with fetal loss: estimates of the global burden of birth defects that consider only liveborn infants with isolated conditions will underestimate this burden by at least 25%, and even more for selected conditions
Contributors: MLF, JCC, JLBB, and LDB conceived and designed the project. SK and MLF cleaned and conducted the analysis for the project. All authors interpreted the data, drafted the manuscript, and assisted with manuscript revisions. MLF is guarantor.
Funding: This publication was supported by a cooperative agreement (No U01DD000490) from the Centers for Disease Control and Prevention. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention. Data were provided by the Utah Birth Defect Network, a program within the Utah Department of Health. This project is supported by the Health Resources and Services Administration (HRSA) of the US Department of Health and Human Services (HHS) under grant No B04MC25374. This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, the US Government, or the Utah Department of Health.
Competing interests: All authors have completed the ICMJE uniform disclosure form and declare no support from any organization for the submitted work, no financial relationships with any organizations that might have an interest in the submitted work in the previous three years, and no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: Not required.
Data sharing: No additional data available.
Transparency: The lead author (the manuscript’s guarantor) affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
- ↵ World Health Organization (WHO). Sixty-third World Health Assembly. Birth Defects. Report by the Secretariat. A63/10. April 2010.
- ↵ Centers for Disease Control and Prevention (CDC). Update on overall prevalence of major birth defects--Atlanta, Georgia, 1978-2005. MMWR Morb Mortal Wkly Rep 2008 ; 357 : 1 - 5 . pmid:18185492 . OpenUrl
- ↵ Christianson A, Howson CP, Modell B. March of Dimes Global Report on Birth Defects. The Hidden Toll of Dying and Disabled Children. March of Dimes Birth Defects Foundation, 2006 .
- ↵ Russo CA, Elixhauser A. Hospitalizations for Birth Defects, 2004. HCUP Statistical Brief #24. U.S. Agency for Healthcare Research and Quality, 2007 .
- ↵ Mathews TJ, MacDorman MF, Thoma ME. Infant mortality statistics from the 2013 period linked birth/infant death data set. National vital statistics reports; National Center for Health Statistics; 2015;64(9).
- ↵ Feldkamp M, Macleod L, Young L, Lecheminant K, Carey JC. The methodology of the Utah Birth Defect Network: congenital heart defects as an illustration. Birth Defects Res A Clin Mol Teratol 2005 ; 357 : 693 - 9 . doi:10.1002/bdra.20212 pmid:16240379 . OpenUrl
- ↵ Stevenson DA, Carey JC, Byrne JLB, Srisukhumbowornchai S, Feldkamp ML. Analysis of skeletal dysplasias in the Utah population. Am J Med Genet A 2012 ; 357 : 1046 - 54 . doi:10.1002/ajmg.a.35327 pmid:22461456 . OpenUrl
- ↵ Stevenson RE. Human Malformations and related anomalies. In: Stevenson RE, Hall JG, Everman DB, Solomon BD, eds. Human Malformations and Related Anomalies. 3rd ed . Oxford University Press, 2016 : 1 - 35 .
- ↵ Mills JL. Malformations in infants of diabetic mothers. Teratology 25:385-94. 1982. Birth Defects Res A Clin Mol Teratol 2010 ; 357 : 769 - 78 . pmid:20973049 . OpenUrl
- ↵ Correa A, Gilboa SM, Besser LM, et al. Diabetes mellitus and birth defects. Am J Obstet Gynecol 2008 ; 357 : 237.e1 - 9 . doi:10.1016/j.ajog.2008.06.028 pmid:18674752 . OpenUrl
- ↵ Gilbert-Barness E. Teratogenic causes of malformations. Ann Clin Lab Sci 2010 ; 357 : 99 - 114 . pmid:20421621 . OpenUrl
- ↵ Botto LD, Khoury MJ, Mastroiacovo P, et al. The spectrum of congenital anomalies of the VATER association: an international study. Am J Med Genet 1997 ; 357 : 8 - 15 . doi:10.1002/(SICI)1096-8628(19970711)71:1<8::AID-AJMG2>3.0.CO;2-V pmid:9215761 . OpenUrl
- ↵ Vissers LE, van Ravenswaaij CM, Admiraal R, et al. Mutations in a new member of the chromodomain gene family cause CHARGE syndrome. Nat Genet 2004 ; 357 : 955 - 7 . doi:10.1038/ng1407 pmid:15300250 . OpenUrl
- ↵ Rasmussen SA, Jamieson DJ, Honein MA, Petersen LR. Zika virus and birth defects – reviewing the evidence for causality. N Engl J Med 2016 ; 357 : 1981 - 7 . doi:10.1056/NEJMsr1604338 pmid:27074377 . OpenUrl
- ↵ Martínez-Frías ML, Bermejo E, Frías JL. Pathogenetic classification of a series of 27,145 consecutive infants with congenital defects. Am J Med Genet 2000 ; 357 : 246 - 9 . doi:10.1002/(SICI)1096-8628(20000131)90:3<246::AID-AJMG12>3.0.CO;2-Q pmid:10678664 . OpenUrl
- ↵ Nelson K, Holmes LB. Malformations due to presumed spontaneous mutations in newborn infants. N Engl J Med 1989 ; 357 : 19 - 23 . doi:10.1056/NEJM198901053200104 pmid:2909875 . OpenUrl
- ↵ Texas Department of State Health Services (TDSHS). Texas Birth Defects Registry’s Report of Birth Defects among 1999-2011 Deliveries: Summary and Key Findings. 2015. http://www.dshs.state.tx.us/birthdefects/data/BD_Data_99-11/Report-of-Birth-Defects-Among-1999-2011-Deliveries.aspx .
- ↵ Yuan S, Zaidi S, Brueckner M. Congenital heart disease: emerging themes linking genetics and development. Curr Opin Genet Dev 2013 ; 357 : 352 - 9 . doi:10.1016/j.gde.2013.05.004 pmid:23790954 . OpenUrl
- ↵ Al Turki S, Manickaraj AK, Mercer CL, et al. UK10K Consortium. Rare variants in NR2F2 cause congenital heart defects in humans. Am J Hum Genet 2014 ; 357 : 574 - 85 . doi:10.1016/j.ajhg.2014.03.007 pmid:24702954 . OpenUrl
- ↵ Warburton D, Ronemus M, Kline J, et al. The contribution of de novo and rare inherited copy number changes to congenital heart disease in an unselected sample of children with conotruncal defects or hypoplastic left heart disease. Hum Genet 2014 ; 357 : 11 - 27 . doi:10.1007/s00439-013-1353-9 pmid:23979609 . OpenUrl
- ↵ Higurashi M, Iijima K, Sugimoto Y, et al. The birth prevalence of malformation syndromes in Tokyo infants: a survey of 14,430 newborn infants. Am J Med Genet 1980 ; 357 : 189 - 94 . doi:10.1002/ajmg.1320060303 pmid:7424972 . OpenUrl
- ↵ de la Chapelle A, Herva R, Koivisto M, Aula P. A deletion in chromosome 22 can cause DiGeorge syndrome. Hum Genet 1981 ; 357 : 253 - 6 . doi:10.1007/BF00278938 pmid:7250965 . OpenUrl
- ↵ Kelley RI, Zackai EH, Emanuel BS, Kistenmacher M, Greenberg F, Punnett HH. The association of the DiGeorge anomalad with partial monosomy of chromosome 22. J Pediatr 1982 ; 357 : 197 - 200 . doi:10.1016/S0022-3476(82)80116-9 pmid:7097410 . OpenUrl
- ↵ Amati F, Mari A, Digilio MC, et al. 22q11 deletions in isolated and syndromic patients with tetralogy of Fallot. Hum Genet 1995 ; 357 : 479 - 82 . doi:10.1007/BF00223856 pmid:7759065 . OpenUrl
- ↵ Takahashi K, Kido S, Hoshino K, Ogawa K, Ohashi H, Fukushima Y. Frequency of a 22q11 deletion in patients with conotruncal cardiac malformations: a prospective study. Eur J Pediatr 1995 ; 357 : 878 - 81 . doi:10.1007/BF01957496 pmid:8582397 . OpenUrl
- ↵ Jorde LB, Carey JC, Bamshad MJ. Developmental genes. In: Jorde LB, Carey JC, Bamshad MJ, eds. Medical Genetics. 4th ed . Mosby Elsevier, 2016 : 193 - 211 .
- ↵ Rasmussen SA, Olney RS, Holmes LB, Lin AE, Keppler-Noreuil KM, Moore CA. National Birth Defects Prevention Study. Guidelines for case classification for the National Birth Defects Prevention Study. Birth Defects Res A Clin Mol Teratol 2003 ; 357 : 193 - 201 . doi:10.1002/bdra.10012 pmid:12797461 . OpenUrl
- ↵ Rasmussen SA, Moore CA. Effective coding in birth defects surveillance. Teratology 2001 ; 357 ( Suppl 1 ): S3 - 7 . doi:10.1002/tera.1077 pmid:11745837 . OpenUrl
- ↵ Källén B, Hay S, Klingberg M. Birth defects monitoring systems: accomplishments and goals. In: Kalter H, ed. Issues and Reviews in Teratology. Plenum Publishing Corporation, 1984 : 1 - 22 doi:10.1007/978-1-4615-7314-2_1 .
- ↵ Cunniff C, Kirby RS, Senner JW, et al. Deaths associated with renal agenesis: a population-based study of birth prevalence, case ascertainment, and etiologic heterogeneity. Teratology 1994 ; 357 : 200 - 4 . doi:10.1002/tera.1420500305 pmid:7871484 . OpenUrl
- ↵ De Wals P, Trochet C, Pinsonneault L. Prevalence of neural tube defects in the province of Quebec, 1992. Can J Public Health 1999 ; 357 : 237 - 9 . pmid:10489719 . OpenUrl
- ↵ Reefhuis J, de Walle HE, Cornel MC. Artefactual increasing frequency of omphaloceles in the Northern Netherlands: lessons for systematic analysis of apparent epidemics. Int J Epidemiol 1999 ; 357 : 258 - 62 . doi:10.1093/ije/28.2.258 pmid:10342688 . OpenUrl
- ↵ Browne ML, Van Zutphen AR, Botto LD, Louik C, Richardson S, Druschel CM. Maternal butalbital use and selected defects in the national birth defects prevention study. Headache 2014 ; 357 : 54 - 66 . doi:10.1111/head.12203 pmid:24001268 . OpenUrl
- ↵ Reefhuis J, Devine O, Friedman JM, Louik C, Honein MA. National Birth Defects Prevention Study. Specific SSRIs and birth defects: Bayesian analysis to interpret new data in the context of previous reports. BMJ 2015 ; 357 : h3190 . doi:10.1136/bmj.h3190 pmid:26156519 . OpenUrl
- ↵ Botto LD, Krikov S, Carmichael SL, Munger RG, Shaw GM, Feldkamp ML. National Birth Defects Prevention Study. Lower rate of selected congenital heart defects with better maternal diet quality: a population-based study. Arch Dis Child Fetal Neonatal Ed 2016 ; 357 : F43 - 9 . doi:10.1136/archdischild-2014-308013 pmid:26304461 . OpenUrl
- ↵ Moore CA, McCabe ERB. Editorial utility of population-based birth defects surveillance for monitoring the health of infants and as a foundation for etiologic research. Birth Defects Res A Clin Mol Teratol 2015 ; 357 : 895 - 8 . doi:10.1002/bdra.23421 pmid:26458078 . OpenUrl
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- PubMed/Medline
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Hereditary metabolic bone diseases: a review of pathogenesis, diagnosis and management.

1. Introduction
2. sclerosing disorders, 2.1. osteopetrosis, 2.1.1. overview and pathogenesis, 2.1.2. clinical, biochemical and radiographic presentation, 2.1.3. treatment, 2.2. progressive diaphyseal dysplasia, 2.2.1. overview and pathogenesis, 2.2.2. clinical, biochemical and radiographic presentation, 2.2.3. treatment, 2.3. melorheostosis, 2.3.1. overview and pathogenesis, 2.3.2. clinical, biochemical and radiographic presentation, 2.3.3. treatment, 2.4. pyknodysostosis, 2.4.1. overview and pathogenesis, 2.4.2. clinical, biochemical and radiographic presentation, 2.4.3. treatment, 2.5. high bone mass associated with lrp5 and lrp6 mutations, 2.5.1. overview and pathogenesis, 2.5.2. clinical presentation, 2.5.3. treatment, 2.6. pyle disease, 2.6.1. overview and pathogenesis, 2.6.2. clinical and radiographic presentation, 2.6.3. treatment, 2.7. hyperostosis corticalis generalisata, 2.7.1. overview and pathogenesis, 2.7.2. clinical and biochemical presentation, 2.7.3. treatment, 2.8. sclerosteosis, 2.8.1. overview and pathogenesis, 2.8.2. clinical presentation, 2.8.3. treatment, 2.9. juvenile paget’s disease, 2.9.1. overview and pathogenesis, 2.9.2. clinical, biochemical and radiographic presentation, 2.9.3. treatment, 2.10. paget’s disease, 2.10.1. overview and pathogenesis, 2.10.2. clinical, biochemical and radiographic presentation, 2.10.3. treatment, 2.11. osteopathia striata, 2.11.1. overview and pathogenesis, 2.11.2. clinical and radiographic presentation, 2.11.3. treatment, 2.12. osteopoikilosis, 2.12.1. overview and pathogenesis, 2.12.2. clinical and radiographic presentation, 2.12.3. treatment, 3. disorders of defective bone mineralization, 3.1. hypophosphatasia, 3.1.1. overview and pathogenesis, 3.1.2. clinical and biochemical presentation, 3.1.3. treatment, 3.2. hypophosphatemic rickets, 3.2.1. overview and pathogenesis, 3.2.2. clinical and biochemical presentation, 3.2.3. treatment, 3.3. vitamin d-dependent rickets, 3.3.1. overview and pathogenesis, 3.3.2. clinical and biochemical presentation, 3.3.3. treatment, 3.4. axial osteomalacia, 3.4.1. overview and pathogenesis, 3.4.2. clinical and biochemical presentation, 3.4.3. treatment, 4. disorders of bone matrix and cartilage formation, 4.1. achondroplasia, 4.1.1. overview and pathogenesis, 4.1.2. clinical presentation, 4.1.3. treatment, 4.2. multiple exostoses, 4.2.1. overview and pathogenesis, 4.2.2. clinical and radiographic presentation, 4.2.3. treatment, 4.3. patchydermoperiostosis, 4.3.1. overview and pathogenesis, 4.3.2. clinical presentation, 4.3.3. treatment, 4.4. osteoporosis-pseudoglioma syndrome, 4.4.1. overview and pathogenesis, 4.4.2. clinical presentation, 4.4.3. treatment, 4.5. osteogenesis imperfecta, 4.5.1. overview and pathogenesis, 4.5.2. clinical presentation, 4.5.3. treatment, 4.6. other hereditary connective tissue disorders including ehlers-danlos syndrome, marfan syndrome and loeys-dietz syndrome, 4.6.1. overview and pathogenesis, 4.6.2. clinical presentation and diagnosis, 4.6.3. treatment, 5. conclusions, author contributions, institutional review board statement, informed consent statement, data availability statement, conflicts of interest.
- El Sayed, S.A.; Nezwek, T.A.; Varacallo, M. Physiology, Bone. In StatPearls ; StatPearls Publishing: Treasure Island, FL, USA, 2022. [ Google Scholar ]
- Florencio-Silva, R.; Sasso, G.R.d.S.; Sasso-Cerri, E.; Simões, M.J.; Cerri, P.S. Biology of Bone Tissue: Structure, Function, and Factors That Influence Bone Cells. Biomed. Res. Int. 2015 , 2015 , 421746. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Shahi, M.; Peymani, A.; Sahmani, M. Regulation of Bone Metabolism. Rep. Biochem. Mol. Biol. 2017 , 5 , 73–82. [ Google Scholar ]
- Guntur, A.R.; Rosen, C.J. Bone as an endocrine organ. Endocr. Pract. 2012 , 18 , 758–762. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Wu, C.C.; Econs, M.J.; DiMeglio, L.A.; Insogna, K.L.; Levine, M.A.; Orchard, P.J.; Miller, W.P.; Petryk, A.; Rush, E.T.; Shoback, D.M.; et al. Diagnosis and Management of Osteopetrosis: Consensus Guidelines From the Osteopetrosis Working Group. J. Clin. Endocrinol. Metab. 2017 , 102 , 3111–3123. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Sobacchi, C.; Schulz, A.; Coxon, F.P.; Villa, A.; Helfrich, M.H. Osteopetrosis: Genetics, treatment and new insights into osteoclast function. Nat. Rev. Endocrinol. 2013 , 9 , 522–536. [ Google Scholar ] [ CrossRef ]
- Stark, Z.; Savarirayan, R. Osteopetrosis. Orphanet J. Rare Dis. 2009 , 4 , 5. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Palagano, E.; Menale, C.; Sobacchi, C.; Villa, A. Genetics of Osteopetrosis. Curr. Osteoporos. Rep. 2018 , 16 , 13–25. [ Google Scholar ] [ CrossRef ]
- Penna, S.; Capo, V.; Palagano, E.; Sobacchi, C.; Villa, A. One Disease, Many Genes: Implications for the Treatment of Osteopetroses. Front. Endocrinol. 2019 , 10 , 85. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Nagai, R.; Kooh, S.W.; Balfe, J.W.; Fenton, T.; Halperin, M.L. Renal tubular acidosis and osteopetrosis with carbonic anhydrase II deficiency: Pathogenesis of impaired acidification. Pediatr. Nephrol. 1997 , 11 , 633–636. [ Google Scholar ] [ CrossRef ]
- Dupuis-Girod, S.; Corradini, N.g.; Hadj-Rabia, S.; Fournet, J.-C.; Faivre, L.; Le Deist, F.o.; Durand, P.; Doffinger, R.; Smahi, A.; Israel, A.; et al. Osteopetrosis, Lymphedema, Anhidrotic Ectodermal Dysplasia, and Immunodeficiency in a Boy and Incontinentia Pigmenti in His Mother. Pediatrics 2002 , 109 , e97. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Helfrich, M.H.; Aronson, D.C.; Everts, V.; Mieremet, R.H.P.; Gerritsen, E.J.A.; Eckhardt, P.G.; Groot, C.G.; Scherft, J.P. Morphologic features of bone in human osteopetrosis. Bone 1991 , 12 , 411–419. [ Google Scholar ] [ CrossRef ]
- Charoenngam, N.; Cevik, M.B.; Holick, M.F. Diagnosis and management of pediatric metabolic bone diseases associated with skeletal fragility. Curr. Opin Pediatr. 2020 , 32 , 560–573. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Zheng, L.-C.; OuYang, X.-L.; Liu, G.-C.; Zhang, W.-J.; Zhang, X.-M. 99Tcm-MDP Imaging of Osteopetrosis: Case Report. Medicine 2015 , 94 , e929. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hamdan, A.-L.H.; Nabulsi, M.M.; Farhat, F.T.; Haidar, R.K.; Fuleihan, N.S. When bone becomes marble: Head and neck manifestations of osteopetrosis. Paediatr. Child Health 2006 , 11 , 37–40. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Steward, C.G. Neurological aspects of osteopetrosis. Neuropathol. Appl. Neurobiol. 2003 , 29 , 87–97. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Capulli, M.; Maurizi, A.; Ventura, L.; Rucci, N.; Teti, A. Effective Small Interfering RNA Therapy to Treat CLCN7-dependent Autosomal Dominant Osteopetrosis Type 2. Mol. Ther. Nucleic Acids 2015 , 4 , e248. [ Google Scholar ] [ CrossRef ]
- Kinoshita, A. Camurati-Engelmann disease. Nihon Rinsho 2015 , 73 , 2149–2159. [ Google Scholar ]
- Kinoshita, A.; Fukumaki, Y.; Shirahama, S.; Miyahara, A.; Nishimura, G.; Haga, N.; Namba, A.; Ueda, H.; Hayashi, H.; Ikegawa, S.; et al. TGFB1 mutations in four new families with Camurati-Engelmann disease: Confirmation of independently arising LAP-domain-specific mutations. Am. J. Med. Genet. A 2004 , 127 , 104–107. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Van Hul, W.; Boudin, E.; Vanhoenacker, F.M.; Mortier, G. Camurati–Engelmann Disease. Calcif. Tissue Int. 2019 , 104 , 554–560. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sparkes, R.S.; Graham, C.B. Camurati-Engelmann disease. Genetics and clinical manifestations with a review of the literature. J. Med. Genet. 1972 , 9 , 73. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Janssens, K.; Vanhoenacker, F.; Bonduelle, M.; Verbruggen, L.; Van Maldergem, L.; Ralston, S.; Guañabens, N.; Migone, N.; Wientroub, S.; Divizia, M.T.; et al. Camurati-Engelmann disease: Review of the clinical, radiological, and molecular data of 24 families and implications for diagnosis and treatment. J. Med. Genet. 2006 , 43 , 1. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Naveh, Y.; Alon, U.; Kaftori, J.K.; Berant, M. Progressive diaphyseal dysplasia: Evaluation of corticosteroid therapy. Pediatrics 1985 , 75 , 321–323. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Agarwal, K.; Rajan, R.; Paul, J.; Cherian, K.E.; Kapoor, N.; Paul, T.V. Losartan as a Steroid-Sparing Adjunct in a Patient With Features of Refractory Camurati-Engelmann Disease. AACE Clin. Case Rep. 2022 , 8 , 54–57. [ Google Scholar ] [ CrossRef ]
- Abdulla, M. Camurati-Engelmann disease with good treatment response to Losartan. Indian J. Nucl. Med. 2019 , 34 , 223–225. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Akhurst, R.J. Targeting TGF-β Signaling for Therapeutic Gain. Cold Spring Harb. Perspect Biol. 2017 , 9 , a022301. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Rossi, M.; Battafarano, G.; De Martino, V.; Scillitani, A.; Minisola, S.; Del Fattore, A. Looking for new anabolic treatment from rare diseases of bone formation. J. Endocrinol. 2021 , 248 , R29–R40. [ Google Scholar ] [ CrossRef ]
- Wordsworth, P.; Chan, M. Melorheostosis and Osteopoikilosis: A Review of Clinical Features and Pathogenesis. Calcif. Tissue Int. 2019 , 104 , 530–543. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Kotwal, A.; Clarke, B.L. Melorheostosis: A Rare Sclerosing Bone Dysplasia. Curr. Osteoporos. Rep. 2017 , 15 , 335–342. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Couto, A.R.; Bruges-Armas, J.; Peach, C.A.; Chapman, K.; Brown, M.A.; Wordsworth, B.P.; Zhang, Y. A Novel LEMD3 Mutation Common to Patients with Osteopoikilosis With and Without Melorheostosis. Calcif. Tissue Int. 2007 , 81 , 81–84. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kang, H.; Jha, S.; Deng, Z.; Fratzl-Zelman, N.; Cabral, W.A.; Ivovic, A.; Meylan, F.; Hanson, E.P.; Lange, E.; Katz, J.; et al. Somatic activating mutations in MAP2K1 cause melorheostosis. Nat. Commun. 2018 , 9 , 1390. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Gnoli, M.; Staals, E.L.; Campanacci, L.; Bedeschi, M.F.; Faletra, F.; Gallone, S.; Gaudio, A.; Mattina, T.; Gurrieri, F.; Percesepe, A.; et al. Melorheostosis and Osteopoikilosis Clinical and Molecular Description of an Italian Case Series. Calcif. Tissue Int. 2019 , 105 , 215–221. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Fick, C.N.; Fratzl-Zelman, N.; Roschger, P.; Klaushofer, K.; Jha, S.; Marini, J.C.; Bhattacharyya, T. Melorheostosis: A Clinical, Pathologic, and Radiologic Case Series. Am. J. Surg. Pathol. 2019 , 43 , 1554. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Gagliardi, G.G.; Mahan, K.T. Melorheostosis: A Literature Review and Case Report with Surgical Considerations. J. Foot Ankle Surg. 2010 , 49 , 80–85. [ Google Scholar ] [ CrossRef ]
- Suresh, S.; Muthukumar, T.; Saifuddin, A. Classical and unusual imaging appearances of melorheostosis. Clin. Radiol. 2010 , 65 , 593–600. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Whyte, M.P.; Murphy, W.A.; Siegel, B.A. 99mTc-Pyrophosphate Bone Imaging in Osteopoikilosis, Osteopathia Striata, and Melorheostosis. Radiology 1978 , 127 , 439–443. [ Google Scholar ] [ CrossRef ]
- Schmidt, G.S.; Schacht, J.P.; Knee, T.S.; Shakir, M.K.M.; Hoang, T.D. Pyknodysostosis (Osteopetrosis Acro-Osteolytica). AACE Clin. Case Rep. 2020 , 6 , e257–e261. [ Google Scholar ] [ CrossRef ]
- LeBlanc, S.; Savarirayan, R. Pycnodysostosis. In GeneReviews((R)) ; Adam, M.P., Ardinger, H.H., Pagon, R.A., Wallace, S.E., Bean, L.J.H., Gripp, K.W., Mirzaa, G.M., Amemiya, A., Eds.; University of Washington: Seattle, WA, USA, 1993. [ Google Scholar ]
- Fratzl-Zelman, N.; Valenta, A.; Roschger, P.; Nader, A.; Gelb, B.D.; Fratzl, P.; Klaushofer, K. Decreased Bone Turnover and Deterioration of Bone Structure in Two Cases of Pycnodysostosis. J. Clin. Endocrinol. Metab. 2004 , 89 , 1538–1547. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ramaiah, K.K.K.; George, G.B.; Padiyath, S.; Sethuraman, R.; Cherian, B. Pyknodysostosis: Report of a rare case with review of literature. Imaging Sci. Dent. 2011 , 41 , 177–181. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Omer Sulaiman, H.; Thalange, N.K.S. Pycnodysostosis: A Growth Hormone Responsive Skeletal Dysplasia. AACE Clin. Case Rep. 2021 , 7 , 231–235. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Soliman, A.T.; Ramadan, M.A.F.; Sherif, A.; Aziz Bedair, E.-S.M.; Rizk, M.M. Pycnodysostosis: Clinical, radiologic, and endocrine evaluation and linear growth after growth hormone therapy. Metab.—Clin. Exp. 2001 , 50 , 905–911. [ Google Scholar ] [ CrossRef ]
- Testani, E.; Scarano, E.; Leoni, C.; Dittoni, S.; Losurdo, A.; Colicchio, S.; Gnoni, V.; Vollono, C.; Zampino, G.; Paludetti, G.; et al. Upper airway surgery of obstructive sleep apnea in pycnodysostosis: Case report and literature review. Am. J. Med. Genet. Part A 2014 , 164 , 2029–2035. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Vieira Ortegosa, M.; Romeo Bertola, D.; Aguena, M.; Passos-Bueno, M.R.; Ae Kim, C.; Justamante De Faria, M.E. Challenges in the Orthodontic Treatment of a Patient with Pycnodysostosis. Cleft Palate-Craniofacial J. 2014 , 51 , 735–739. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Cui, Y.; Niziolek, P.J.; MacDonald, B.T.; Zylstra, C.R.; Alenina, N.; Robinson, D.R.; Zhong, Z.; Matthes, S.; Jacobsen, C.M.; Conlon, R.A.; et al. Lrp5 functions in bone to regulate bone mass. Nat. Med. 2011 , 17 , 684–691. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Boyden, L.M.; Mao, J.; Belsky, J.; Mitzner, L.; Farhi, A.; Mitnick, M.A.; Wu, D.; Insogna, K.; Lifton, R.P. High Bone Density Due to a Mutation in LDL-Receptor–Related Protein 5. N. Engl. J. Med. 2002 , 346 , 1513–1521. [ Google Scholar ] [ CrossRef ]
- Gregson, C.L.; Wheeler, L.; Hardcastle, S.A.; Appleton, L.H.; Addison, K.A.; Brugmans, M.; Clark, G.R.; Ward, K.A.; Paggiosi, M.; Stone, M.; et al. Mutations in Known Monogenic High Bone Mass Loci Only Explain a Small Proportion of High Bone Mass Cases. J. Bone Miner. Res. 2016 , 31 , 640–649. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Kwee, M.L.; Balemans, W.; Cleiren, E.; Gille, J.J.P.; Van Der Blij, F.; Sepers, J.M.; Van Hul, W. An Autosomal Dominant High Bone Mass Phenotype in Association With Craniosynostosis in an Extended Family Is Caused by an LRP5 Missense Mutation. J. Bone Miner. Res. 2005 , 20 , 1254–1260. [ Google Scholar ] [ CrossRef ]
- Whyte, M.P.; McAlister, W.H.; Zhang, F.; Bijanki, V.N.; Nenninger, A.; Gottesman, G.S.; Lin, E.L.; Huskey, M.; Duan, S.; Dahir, K.; et al. New explanation for autosomal dominant high bone mass: Mutation of low-density lipoprotein receptor-related protein 6. Bone 2019 , 127 , 228–243. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Brance, M.L.; Brun, L.R.; Cóccaro, N.M.; Aravena, A.; Duan, S.; Mumm, S.; Whyte, M.P. High bone mass from mutation of low-density lipoprotein receptor-related protein 6 (LRP6). Bone 2020 , 141 , 115550. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Pyle, E. A Case of Unusual Bone Development. JBJS 1931 , 13 , 874–876. [ Google Scholar ]
- Houschyar, K.S.; Tapking, C.; Borrelli, M.R.; Popp, D.; Duscher, D.; Maan, Z.N.; Chelliah, M.P.; Li, J.; Harati, K.; Wallner, C.; et al. Wnt Pathway in Bone Repair and Regeneration—What Do We Know So Far. Front. Cell Dev. Biol. 2019 , 6 , 170. [ Google Scholar ] [ CrossRef ]
- Beighton, P. Pyle disease (metaphyseal dysplasia). J. Med. Genet. 1987 , 24 , 321–324. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Faden, M.A.; Krakow, D.; Ezgu, F.; Rimoin, D.L.; Lachman, R.S. The Erlenmeyer flask bone deformity in the skeletal dysplasias. Am. J. Med. Genet. A 2009 , 149 , 1334–1345. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Soares, D.X.; Almeida, A.M.; Barreto, A.R.F.; Alencar, E.; Silva, I.J.; de Castro, J.D.V.; Magalhães Pinto, F.J.; Dias, D.A.; Aguiar, L.B. Pyle disease (metaphyseal dysplasia) presenting in two adult sisters. Radiol. Case Rep. 2016 , 11 , 405–410. [ Google Scholar ] [ CrossRef ]
- van Lierop, A.H.; Hamdy, N.A.T.; van Egmond, M.E.; Bakker, E.; Dikkers, F.G.; Papapoulos, S.E. Van Buchem disease: Clinical, biochemical, and densitometric features of patients and disease carriers. J. Bone Miner. Res. 2013 , 28 , 848–854. [ Google Scholar ] [ CrossRef ]
- Nassar, K.; Rachidi, W.; Janani, S.; Mkinsi, O. Van Buchem’s Disease. Jt. Bone Spine 2016 , 83 , 737–738. [ Google Scholar ] [ CrossRef ]
- Van Hul, W.; Balemans, W.; Van Hul, E.; Dikkers, F.G.; Obee, H.; Stokroos, R.J.; Hildering, P.; Vanhoenacker, F.; Van Camp, G.; Willems, P.J. Van Buchem disease (hyperostosis corticalis generalisata) maps to chromosome 17q12-q21. Am. J. Hum. Genet. 1998 , 62 , 391–399. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Sebastian, A.; Loots, G.G. Genetics of Sost/SOST in sclerosteosis and van Buchem disease animal models. Metabolism 2018 , 80 , 38–47. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- van Lierop, A.H.; Hamdy, N.A.T.; Hamersma, H.; van Bezooijen, R.L.; Power, J.; Loveridge, N.; Papapoulos, S.E. Patients with sclerosteosis and disease carriers: Human models of the effect of sclerostin on bone turnover. J. Bone Miner. Res. 2011 , 26 , 2804–2811. [ Google Scholar ] [ CrossRef ]
- Balemans, W.; Ebeling, M.; Patel, N.; Van Hul, E.; Olson, P.; Dioszegi, M.; Lacza, C.; Wuyts, W.; Van Den Ende, J.; Willems, P.; et al. Increased bone density in sclerosteosis is due to the deficiency of a novel secreted protein (SOST). Hum. Mol. Genet. 2001 , 10 , 537–544. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Bhadada, S.K.; Rastogi, A.; Steenackers, E.; Boudin, E.; Arya, A.; Dhiman, V.; Bhansali, A.; Van Hul, W. Novel SOST gene mutation in a sclerosteosis patient and her parents. Bone 2013 , 52 , 707–710. [ Google Scholar ] [ CrossRef ]
- Fijalkowski, I.; Geets, E.; Steenackers, E.; Van Hoof, V.; Ramos, F.J.; Mortier, G.; Fortuna, A.M.; Van Hul, W.; Boudin, E. A Novel Domain-Specific Mutation in a Sclerosteosis Patient Suggests a Role of LRP4 as an Anchor for Sclerostin in Human Bone. J. Bone Miner. Res. 2016 , 31 , 874–881. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Bukowska-Olech, E.; Sowińska-Seidler, A.; Szczałuba, K.; Jamsheer, A. A novel biallelic splice-site variant in the LRP4 gene causes sclerosteosis 2. Birth Defects Res. 2020 , 112 , 652–659. [ Google Scholar ] [ CrossRef ]
- Beighton, P.; Durr, L.; Hamersma, H. The Clinical Features of Sclerosteosis. Ann. Intern. Med. 1976 , 84 , 393–397. [ Google Scholar ] [ CrossRef ]
- Beighton, P.; Barnard, A.; Hamersma, H.; Wouden, A.v.d. The syndromic status of sclerosteosis and van Buchem disease. Clin. Genet. 1984 , 25 , 175–181. [ Google Scholar ] [ CrossRef ]
- Polyzos, S.A.; Cundy, T.; Mantzoros, C.S. Juvenile Paget disease. Metab.—Clin. Exp. 2018 , 80 , 15–26. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Michou, L.; Collet, C.; Laplanche, J.-L.; Orcel, P.; Cornélis, F. Genetics of Paget’s disease of bone. Jt. Bone Spine 2006 , 73 , 243–248. [ Google Scholar ] [ CrossRef ]
- Osteoprotegerin Deficiency and Juvenile Paget’s Disease. N. Engl. J. Med. 2002 , 347 , 1622–1623. [ CrossRef ] [ PubMed ]
- Kerr, N.M.; Cassinelli, H.R.; DiMeglio, L.A.; Tau, C.; Tüysüz, B.; Cundy, T.; Vincent, A.L. Ocular Manifestations of Juvenile Paget Disease. Arch. Ophthalmol. 2010 , 128 , 698–703. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Naot, D.; Choi, A.; Musson, D.S.; Simsek Kiper, P.Ö.; Utine, G.E.; Boduroglu, K.; Peacock, M.; DiMeglio, L.A.; Cundy, T. Novel homozygous mutations in the osteoprotegerin gene TNFRSF11B in two unrelated patients with juvenile Paget’s disease. Bone 2014 , 68 , 6–10. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Polyzos, S.A.; Makras, P.; Anastasilakis, A.D.; Mintziori, G.; Kita, M.; Papatheodorou, A.; Kokkoris, P.; Terpos, E. Periostin and sclerostin levels in juvenile Paget’s disease. Clin. Cases Miner. Bone Metab. 2017 , 14 , 269–271. [ Google Scholar ] [ CrossRef ]
- Polyzos, S.A.; Anastasilakis, A.D.; Litsas, I.; Efstathiadou, Z.; Kita, M.; Arsos, G.; Moralidis, E.; Papatheodorou, A.; Terpos, E. Profound hypocalcemia following effective response to zoledronic acid treatment in a patient with juvenile Paget’s disease. J. Bone Miner. Metab. 2010 , 28 , 706–712. [ Google Scholar ] [ CrossRef ]
- Tüysüz, B.; Mercimek, S.; Üngür, S.; Deniz, M. Calcitonin treatment in osteoectasia with hyperphosphatasia (juvenile Paget’s disease): Radiographic changes after treatment. Pediatr. Radiol. 1999 , 29 , 838–841. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Polyzos, S.A.; Singhellakis, P.N.; Naot, D.; Adamidou, F.; Malandrinou, F.C.; Anastasilakis, A.D.; Polymerou, V.; Kita, M. Denosumab Treatment for Juvenile Paget’s Disease: Results From Two Adult Patients With Osteoprotegerin Deficiency (“Balkan” Mutation in the TNFRSF11B Gene). J. Clin. Endocrinol. Metab. 2014 , 99 , 703–707. [ Google Scholar ] [ CrossRef ]
- Cundy, T.; Davidson, J.; Rutland, M.D.; Stewart, C.; DePaoli, A.M. Recombinant Osteoprotegerin for Juvenile Paget’s Disease. N. Engl. J. Med. 2005 , 353 , 918–923. [ Google Scholar ] [ CrossRef ]
- Tan, A.; Ralston, S.H. Paget’s disease of bone. QJM Int. J. Med. 2014 , 107 , 865–869. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Cook, S.; Wall, C. Paget’s disease of bone: A clinical update. Aust. J. Gen. Pract. 2021 , 50 , 23–29. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Mirra, J.M. Pathogenesis of Paget’s disease based on viral etiology. Clin. Orthop. Relat. Res. 1987 , 217 , 162–170. [ Google Scholar ] [ CrossRef ]
- Hocking, L.; Slee, F.; Haslam, S.I.; Cundy, T.; Nicholson, G.; van Hul, W.; Ralston, S.H. Familial Paget’s disease of bone: Patterns of inheritance and frequency of linkage to chromosome 18q. Bone 2000 , 26 , 577–580. [ Google Scholar ] [ CrossRef ]
- Alonso, N.; Calero-Paniagua, I.; Del Pino-Montes, J. Clinical and Genetic Advances in Paget’s Disease of Bone: A Review. Clin. Rev. Bone Miner. Metab. 2017 , 15 , 37–48. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Gianfrancesco, F.; Rendina, D.; Di Stefano, M.; Mingione, A.; Esposito, T.; Merlotti, D.; Gallone, S.; Magliocca, S.; Goode, A.; Formicola, D.; et al. A nonsynonymous TNFRSF11A variation increases NFκB activity and the severity of Paget’s disease. J. Bone Miner. Res. 2012 , 27 , 443–452. [ Google Scholar ] [ CrossRef ]
- Makaram, N.S.; Ralston, S.H. Genetic Determinants of Paget’s Disease of Bone. Curr. Osteoporos. Rep. 2021 , 19 , 327–337. [ Google Scholar ] [ CrossRef ]
- Beyens, G.; Daroszewska, A.; de Freitas, F.; Fransen, E.; Vanhoenacker, F.; Verbruggen, L.; Zmierczak, H.-G.; Westhovens, R.; Van Offel, J.; Ralston, S.H.; et al. Identification of Sex-Specific Associations Between Polymorphisms of the Osteoprotegerin Gene, TNFRSF11B, and Paget’s Disease of Bone. J. Bone Miner. Res. 2007 , 22 , 1062–1071. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Rabjohns, E.M.; Hurst, K.; Ghosh, A.; Cuellar, M.C.; Rampersad, R.R.; Tarrant, T.K. Paget’s Disease of Bone: Osteoimmunology and Osteoclast Pathology. Curr. Allergy Asthma Rep. 2021 , 21 , 23. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Winn, N.; Lalam, R.; Cassar-Pullicino, V. Imaging of Paget’s disease of bone. Wien. Med. Wochenschr. 2017 , 167 , 9–17. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hosking, D.; Lyles, K.; Brown, J.P.; Fraser, W.D.; Miller, P.; Curiel, M.D.; Devogelaer, J.-P.; Hooper, M.; Su, G.; Zelenakas, K.; et al. Long-Term Control of Bone Turnover in Paget’s Disease With Zoledronic Acid and Risedronate. J. Bone Miner. Res. 2007 , 22 , 142–148. [ Google Scholar ] [ CrossRef ]
- Reid, I.R.; Sharma, S.; Kalluru, R.; Eagleton, C. Treatment of Paget’s Disease of Bone with Denosumab: Case Report and Literature Review. Calcif. Tissue Int. 2016 , 99 , 322–325. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Perdu, B.; Freitas, F.d.; Frints, S.G.M.; Schouten, M.; Schrander-Stumpel, C.; Barbosa, M.; Pinto-Basto, J.; Reis-Lima, M.; Vernejoul, M.-C.d.; Becker, K.; et al. Osteopathia striata with cranial sclerosis owing to WTX gene defect. J. Bone Miner. Res. 2010 , 25 , 82–90. [ Google Scholar ] [ CrossRef ]
- Holman, S.K.; Morgan, T.; Baujat, G.; Cormier-Daire, V.; Cho, T.J.; Lees, M.; Samanich, J.; Tapon, D.; Hove, H.D.; Hing, A.; et al. Osteopathia striata congenita with cranial sclerosis and intellectual disability due to contiguous gene deletions involving the WTX locus. Clin. Genet. 2013 , 83 , 251–256. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ward, L.M.; Rauch, F.; Travers, R.; Roy, M.; Montes, J.; Chabot, G.; Glorieux, F.H. Osteopathia striata with cranial sclerosis: Clinical, radiological, and bone histological findings in an adolescent girl. Am. J. Med. Genet. Part A 2004 , 129 , 8–12. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Gear, R.; Savarirayan, R. Osteopathia Striata with Cranial Sclerosis. In GeneReviews((R)) ; Adam, M.P., Ardinger, H.H., Pagon, R.A., Wallace, S.E., Bean, L.J.H., Gripp, K.W., Mirzaa, G.M., Amemiya, A., Eds.; University of Washington: Seattle, WA, USA, 1993. [ Google Scholar ]
- Sultana, A.; Sjöström, M. Orthognathic surgery in a patient with osteopathia striata combined with cranial sclerosis: A case report. Oral Maxillofac. Surg. Cases 2020 , 6 , 100194. [ Google Scholar ] [ CrossRef ]
- Zhang, Q.; Mo, Z.H.; Dong, C.S.; Yang, F.; Xie, Y.H.; Jin, P. Identification of a novel LEMD3 Y871X mutation in a three-generation family with osteopoikilosis and review of the literature. J. Endocrinol. Investig. 2016 , 39 , 679–685. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Woyciechowsky, T.G.; Monticielo, M.R.; Keiserman, B.; Monticielo, O.A. Osteopoikilosis: What does the rheumatologist must know about it? Clin. Rheumatol. 2012 , 31 , 745–748. [ Google Scholar ] [ CrossRef ]
- Krishnappa, R.; Kumar, N.; Alva, K.; Shetty, P.; Dang, M.; Mohamed, S. Plasma cell myeloma with unusual presentations. J. Orthop. Traumatol. Rehabil. 2013 , 6 , 84–86. [ Google Scholar ]
- Ozdemirel, A.E.; Cakit, B.D.; Erdem, H.R.; Koc, B. A rare benign disorder mimicking metastasis on radiographic examination: A case report of osteopoikilosis. Rheumatol. Int. 2011 , 31 , 1113–1116. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Tuncel, M.; Caner, B. Osteopoikilosis: A major diagnostic problem solved by bone scintigraphy. Rev. Española Med. Nucl. Imagen Mol. 2012 , 31 , 93–96. [ Google Scholar ] [ CrossRef ]
- Ellanti, P.; Clarke, B.; Gray, J. Osteopoikilosis. Ir. J. Med. Sci. 2010 , 179 , 615–616. [ Google Scholar ] [ CrossRef ]
- Khan, A.A.; Josse, R.; Kannu, P.; Villeneuve, J.; Paul, T.; Van Uum, S.; Greenberg, C.R. Hypophosphatasia: Canadian update on diagnosis and management. Osteoporos. Int. 2019 , 30 , 1713–1722. [ Google Scholar ] [ CrossRef ]
- Mornet, E. Hypophosphatasia. Orphanet J. Rare Dis. 2007 , 2 , 40. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Whyte, M.P. Hypophosphatasia: Enzyme Replacement Therapy Brings New Opportunities and New Challenges. J. Bone Miner. Res. 2017 , 32 , 667–675. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Whyte, M.P. Hypophosphatasia—Aetiology, nosology, pathogenesis, diagnosis and treatment. Nat. Rev. Endocrinol. 2016 , 12 , 233–246. [ Google Scholar ] [ CrossRef ]
- Mornet, E. Hypophosphatasia. Metab. —Clin. Exp. 2018 , 82 , 142–155. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Beck, C.; Morbach, H.; Richl, P.; Stenzel, M.; Girschick, H.J. How can calcium pyrophosphate crystals induce inflammation in hypophosphatasia or chronic inflammatory joint diseases? Rheumatol. Int. 2009 , 29 , 229–238. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Lahorgue Nunes, M.; Mugnol, F.; Bica, I.; Machado Fiori, R. Pyridoxine-Dependent Seizures Associated With Hypophosphatasia in a Newborn. J. Child Neurol. 2002 , 17 , 222–224. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Zhang, Q.; Qin, Z.; Yi, S.; Wei, H.; Zhou, X.z.; Shen, F. Case Report: Variations in the ALPL Gene in Chinese Patients With Hypophosphatasia. Front. Genet. 2021 , 12 , 732621. [ Google Scholar ] [ CrossRef ]
- Millán, J.L.; Whyte, M.P. Alkaline Phosphatase and Hypophosphatasia. Calcif. Tissue Int. 2016 , 98 , 398–416. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Chodirker, B.N.; Coburn, S.P.; Seargeant, L.E.; Whyte, M.P.; Greenberg, C.R. Increased plasma pyridoxal-5′-phosphate levels before and after pyridoxine loading in carriers of perinatal/infantile hypophosphatasia. J. Inherit. Metab. Dis. 1990 , 13 , 891–896. [ Google Scholar ] [ CrossRef ]
- Conti, F.; Ciullini, L.; Pugliese, G. Hypophosphatasia: Clinical manifestation and burden of disease in adult patients. Clin. Cases Miner. Bone Metab. Off. J. Ital. Soc. Osteoporos. Miner. Metab. Skelet. Dis. 2017 , 14 , 230–234. [ Google Scholar ] [ CrossRef ]
- Fraser, D. Hypophosphatasia. Am. J. Med. 1957 , 22 , 730–746. [ Google Scholar ] [ CrossRef ]
- Whyte, M.P. Hypophosphatasia: An overview For 2017. Bone 2017 , 102 , 15–25. [ Google Scholar ] [ CrossRef ]
- Whyte, M.P.; Wenkert, D.; Zhang, F. Hypophosphatasia: Natural history study of 101 affected children investigated at one research center. Bone 2016 , 93 , 125–138. [ Google Scholar ] [ CrossRef ]
- Bowden, S.A.; Foster, B.L. Profile of asfotase alfa in the treatment of hypophosphatasia: Design, development, and place in therapy. Drug Des. Dev. Ther. 2018 , 12 , 3147–3161. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Whyte, M.P.; Greenberg, C.R.; Salman, N.J.; Bober, M.B.; McAlister, W.H.; Wenkert, D.; Van Sickle, B.J.; Simmons, J.H.; Edgar, T.S.; Bauer, M.L.; et al. Enzyme-replacement therapy in life-threatening hypophosphatasia. New Engl. J. Med. 2012 , 366 , 904–913. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Simon, S.; Resch, H.; Klaushofer, K.; Roschger, P.; Zwerina, J.; Kocijan, R. Hypophosphatasia: From Diagnosis to Treatment. Curr. Rheumatol. Rep. 2018 , 20 , 69. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Baumgartner-Sigl, S.; Haberlandt, E.; Mumm, S.; Scholl-Bürgi, S.; Sergi, C.; Ryan, L.; Ericson, K.L.; Whyte, M.P.; Högler, W. Pyridoxine-responsive seizures as the first symptom of infantile hypophosphatasia caused by two novel missense mutations (c.677T>C, p.M226T; c.1112C>T, p.T371I) of the tissue-nonspecific alkaline phosphatase gene. Bone 2007 , 40 , 1655–1661. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Beck-Nielsen, S.S.; Mughal, Z.; Haffner, D.; Nilsson, O.; Levtchenko, E.; Ariceta, G.; de Lucas Collantes, C.; Schnabel, D.; Jandhyala, R.; Mäkitie, O. FGF23 and its role in X-linked hypophosphatemia-related morbidity. Orphanet J. Rare Dis. 2019 , 14 , 58. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Prié, D.; Friedlander, G. Reciprocal Control of 1,25-Dihydroxyvitamin D and FGF23 Formation Involving the FGF23/Klotho System. Clin. J. Am. Soc. Nephrol. 2010 , 5 , 1717. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Endo, I.; Fukumoto, S.; Ozono, K.; Namba, N.; Inoue, D.; Okazaki, R.; Yamauchi, M.; Sugimoto, T.; Minagawa, M.; Michigami, T.; et al. Nationwide survey of fibroblast growth factor 23 (FGF23)-related hypophosphatemic diseases in Japan: Prevalence, biochemical data and treatment. Endocr. J. 2015 , 62 , 811–816. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Beck-Nielsen, S.S.; Brock-Jacobsen, B.; Gram, J.; Brixen, K.; Jensen, T.K. Incidence and prevalence of nutritional and hereditary rickets in southern Denmark. Eur. J. Endocrinol. 2009 , 160 , 491–497. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Rafaelsen, S.; Johansson, S.; Ræder, H.; Bjerknes, R. Hereditary hypophosphatemia in Norway: A retrospective population-based study of genotypes, phenotypes, and treatment complications. Eur. J. Endocrinol. 2016 , 174 , 125–136. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Dixon, P.H.; Christie, P.T.; Wooding, C.; Trump, D.; Grieff, M.; Holm, I.; Gertner, J.M.; Schmidtke, J.; Shah, B.; Shaw, N.; et al. Mutational Analysis of PHEX Gene in X-Linked Hypophosphatemia1. J. Clin. Endocrinol. Metab. 1998 , 83 , 3615–3623. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- White, K.E.; Evans, W.E.; O’Riordan, J.L.H.; Speer, M.C.; Econs, M.J.; Lorenz-Depiereux, B.; Grabowski, M.; Meitinger, T.; Strom, T.M. Autosomal dominant hypophosphataemic rickets is associated with mutations in FGF23. Nat. Genet. 2000 , 26 , 345–348. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Levy-Litan, V.; Hershkovitz, E.; Avizov, L.; Leventhal, N.; Bercovich, D.; Chalifa-Caspi, V.; Manor, E.; Buriakovsky, S.; Hadad, Y.; Goding, J.; et al. Autosomal-recessive hypophosphatemic rickets is associated with an inactivation mutation in the ENPP1 gene. Am. J. Hum. Genet. 2010 , 86 , 273–278. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Farrow, E.G.; Davis, S.I.; Ward, L.M.; Summers, L.J.; Bubbear, J.S.; Keen, R.; Stamp, T.C.B.; Baker, L.R.I.; Bonewald, L.F.; White, K.E. Molecular analysis of DMP1 mutants causing autosomal recessive hypophosphatemic rickets. Bone 2009 , 44 , 287–294. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Carpenter, T.O.; Imel, E.A.; Holm, I.A.; Jan de Beur, S.M.; Insogna, K.L. A clinician’s guide to X-linked hypophosphatemia. J. Bone Miner. Res. Off. J. Am. Soc. Bone Miner. Res. 2011 , 26 , 1381–1388. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Petje, G.; Meizer, R.; Radler, C.; Aigner, N.; Grill, F. Deformity correction in children with hereditary hypophosphatemic rickets. Clin. Orthop. Relat. Res. 2008 , 466 , 3078–3085. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Linglart, A.; Biosse-Duplan, M.; Briot, K.; Chaussain, C.; Esterle, L.; Guillaume-Czitrom, S.; Kamenicky, P.; Nevoux, J.; Prié, D.; Rothenbuhler, A.; et al. Therapeutic management of hypophosphatemic rickets from infancy to adulthood. Endocr. Connect. 2014 , 3 , R13–R30. [ Google Scholar ] [ CrossRef ]
- Haffner, D.; Emma, F.; Eastwood, D.M.; Duplan, M.B.; Bacchetta, J.; Schnabel, D.; Wicart, P.; Bockenhauer, D.; Santos, F.; Levtchenko, E.; et al. Clinical practice recommendations for the diagnosis and management of X-linked hypophosphataemia. Nat. Rev. Nephrol. 2019 , 15 , 435–455. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Baroncelli, G.I.; Toschi, B.; Bertelloni, S. Hypophosphatemic rickets. Curr. Opin. Endocrinol. Diabetes Obes. 2012 , 19 , 460–467. [ Google Scholar ] [ CrossRef ]
- Choy, M. Pharmaceutical Approval Update. P T A Peer-Rev. J. Formul. Manag. 2018 , 43 , 326–327. [ Google Scholar ]
- Carpenter, T.O.; Whyte, M.P.; Imel, E.A.; Boot, A.M.; Högler, W.; Linglart, A.; Padidela, R.; van’t Hoff, W.; Mao, M.; Chen, C.-Y.; et al. Burosumab Therapy in Children with X-Linked Hypophosphatemia. New Engl. J. Med. 2018 , 378 , 1987–1998. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Imel, E.A.; Glorieux, F.H.; Whyte, M.P.; Munns, C.F.; Ward, L.M.; Nilsson, O.; Simmons, J.H.; Padidela, R.; Namba, N.; Cheong, H.I.; et al. Burosumab versus conventional therapy in children with X-linked hypophosphataemia: A randomised, active-controlled, open-label, phase 3 trial. Lancet 2019 , 393 , 2416–2427. [ Google Scholar ] [ CrossRef ]
- Mäkitie, O.; Doria, A.; Kooh, S.W.; Cole, W.G.; Daneman, A.; Sochett, E. Early treatment improves growth and biochemical and radiographic outcome in X-linked hypophosphatemic rickets. J. Clin. Endocrinol. Metab. 2003 , 88 , 3591–3597. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Quinlan, C.; Guegan, K.; Offiah, A.; Neill, R.O.; Hiorns, M.P.; Ellard, S.; Bockenhauer, D.; Hoff, W.V.t.; Waters, A.M. Growth in PHEX-associated X-linked hypophosphatemic rickets: The importance of early treatment. Pediatr. Nephrol. 2012 , 27 , 581–588. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Wacker, M.; Holick, M.F. Sunlight and Vitamin D: A global perspective for health. Dermatoendocrinol 2013 , 5 , 51–108. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Holick, M.F. Vitamin D deficiency. N. Engl. J. Med. 2007 , 357 , 266–281. [ Google Scholar ] [ CrossRef ]
- Charoenngam, N.; Shirvani, A.; Holick, M.F. Vitamin D for skeletal and non-skeletal health: What we should know. J. Clin. Orthop. Trauma 2019 , 10 , 1082–1093. [ Google Scholar ] [ CrossRef ]
- Holick, M.F. Resurrection of vitamin D deficiency and rickets. J. Clin. Invest. 2006 , 116 , 2062–2072. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Levine, M.A. Diagnosis and Management of Vitamin D Dependent Rickets. Front. Pediatr. 2020 , 8 , 315. [ Google Scholar ] [ CrossRef ]
- Chen, H.; Hewison, M.; Hu, B.; Adams, J.S. Heterogeneous nuclear ribonucleoprotein (hnRNP) binding to hormone response elements: A cause of vitamin D resistance. Proc. Natl. Acad. Sci. USA 2003 , 100 , 6109–6114. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Roizen, J.D.; Li, D.; O’Lear, L.; Javaid, M.K.; Shaw, N.J.; Ebeling, P.R.; Nguyen, H.H.; Rodda, C.P.; Thummel, K.E.; Thacher, T.D.; et al. CYP3A4 mutation causes vitamin D-dependent rickets type 3. J. Clin. Investig. 2018 , 128 , 1913–1918. [ Google Scholar ] [ CrossRef ]
- Balsan, S.; Garabédian, M.; Larchet, M.; Gorski, A.M.; Cournot, G.; Tau, C.; Bourdeau, A.; Silve, C.; Ricour, C. Long-term nocturnal calcium infusions can cure rickets and promote normal mineralization in hereditary resistance to 1,25-dihydroxyvitamin D. J. Clin. Investig. 1986 , 77 , 1661–1667. [ Google Scholar ] [ CrossRef ]
- Whyte, M.P.; Fallon, M.D.; Murphy, W.A.; Teitelbaum, S.L. Axial osteomalacia: Clinical, laboratory and genetic investigation of an affected mother and son. Am. J. Med. 1981 , 71 , 1041–1049. [ Google Scholar ] [ CrossRef ]
- Nelson, A.M.; Riggs, B.L.; Jowsey, J.O. Atypical axial osteomalacia. report of four cases with two having features of ankylosing spondylitis. Arthritis Rheum. 1978 , 21 , 715–722. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Vajo, Z.; Francomano, C.A.; Wilkin, D.J. The Molecular and Genetic Basis of Fibroblast Growth Factor Receptor 3 Disorders: The Achondroplasia Family of Skeletal Dysplasias, Muenke Craniosynostosis, and Crouzon Syndrome with Acanthosis Nigricans. Endocr. Rev. 2000 , 21 , 23–39. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Ornitz, D.M.; Legeai-Mallet, L. Achondroplasia: Development, pathogenesis, and therapy. Dev. Dyn. Off. Publ. Am. Assoc. Anat. 2017 , 246 , 291–309. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Pauli, R.M. Achondroplasia: A comprehensive clinical review. Orphanet J. Rare Dis. 2019 , 14 , 1. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Tavormina, P.L.; Shiang, R.; Thompson, L.M.; Zhu, Y.-Z.; Wilkin, D.J.; Lachman, R.S.; Wilcox, W.R.; Rimoin, D.L.; Cohn, D.H.; Wasmuth, J.J. Thanatophoric dysplasia (types I and II) caused by distinct mutations in fibroblast growth factor receptor 3. Nat. Genet. 1995 , 9 , 321–328. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Chang, T.K.; Wang, Y.; Liu, A.M.; Tung, J.C. Thanatophoric dysplasia type I. Acta Paediatr. Taiwan 2001 , 42 , 39–41. [ Google Scholar ] [ PubMed ]
- Yolanda, N.; Yulianto, F.; Arina, S.; Edwin, J. A full-term infant with type II thanatophoric dysplasia. Case Rep. Perinat. Med. 2019 , 8 . [ Google Scholar ] [ CrossRef ]
- Bober, M.B.; Bellus, G.A.; Nikkel, S.M.; Tiller, G.E. Hypochondroplasia. In GeneReviews((R)) ; Adam, M.P., Ardinger, H.H., Pagon, R.A., Wallace, S.E., Bean, L.J.H., Gripp, K.W., Mirzaa, G.M., Amemiya, A., Eds.; University of Washington: Seattle, WA, USA, 1993. [ Google Scholar ]
- Yamashita, A.; Morioka, M.; Kishi, H.; Kimura, T.; Yahara, Y.; Okada, M.; Fujita, K.; Sawai, H.; Ikegawa, S.; Tsumaki, N. Statin treatment rescues FGFR3 skeletal dysplasia phenotypes. Nature 2014 , 513 , 507–511. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- McCormick, C.; Duncan, G.; Goutsos, K.T.; Tufaro, F. The putative tumor suppressors EXT1 and EXT2 form a stable complex that accumulates in the Golgi apparatus and catalyzes the synthesis of heparan sulfate. Proc. Natl. Acad. Sci. USA 2000 , 97 , 668–673. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Pacifici, M. The pathogenic roles of heparan sulfate deficiency in hereditary multiple exostoses. Matrix Biol. J. Int. Soc. Matrix Biol. 2018 , 71–72 , 28–39. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Beltrami, G.; Ristori, G.; Scoccianti, G.; Tamburini, A.; Capanna, R. Hereditary Multiple Exostoses: A review of clinical appearance and metabolic pattern. Clin. Cases Miner. Bone Metab. Off. J. Ital. Soc. Osteoporos. Miner. Metab. Skelet. Dis. 2016 , 13 , 110–118. [ Google Scholar ] [ CrossRef ]
- Kose, O.; Ertas, A.; Celiktas, M.; Kisin, B. Fracture of an osteochondroma treated successfully with total excision: Two case reports. Cases J. 2009 , 2 , 8062. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Errani, C.; Vanel, D.; Donati, D.; Picci, P.; Faldini, C. Spontaneous healing of an osteochondroma fracture. Diagn. Interv. Imaging 2015 , 96 , 283–285. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Robbins, M.M.; Kuo, S.; Epstein, R. Non-Traumatic Fracture of an Osteochondroma Mimicking Malignant Degeneration in an Adult with Hereditary Multiple Exostoses. Radiol. Case Rep. 2015 , 3 , 99. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Deng, Q.; Li, P.; Che, M.; Liu, J.; Biswas, S.; Ma, G.; He, L.; Wei, Z.; Zhang, Z.; Yang, Y.; et al. Activation of hedgehog signaling in mesenchymal stem cells induces cartilage and bone tumor formation via Wnt/β-Catenin. eLife 2019 , 8 , e50208. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Pacifici, M. Hereditary multiple exostoses: Are there new plausible treatment strategies? Expert Opin. Orphan Drugs 2018 , 6 , 385–391. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Abdullah, N.R.A.; Jason, W.L.C.; Nasruddin, A.B. Pachydermoperiostosis: A rare mimicker of acromegaly. Endocrinol. Diabetes Metab. Case Rep. 2017 , 2017 , 17-0029. [ Google Scholar ] [ CrossRef ]
- Mittal, A.; Gupta, N.; Soneja, M. Touraine-Solente-Gole syndrome. BMJ Case Rep. 2019 , 12 , e232238. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Akaranuchat, N.; Limsuvan, P. Touraine–Solente–Gole syndrome: Clinical manifestation with bilateral true eyelid ptosis. JPRAS Open 2019 , 21 , 6–13. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Joshi, A.; Nepal, G.; Shing, Y.K.; Panthi, H.P.; Baral, S. Pachydermoperiostosis (Touraine-Solente-Gole syndrome): A case report. J. Med. Case Rep. 2019 , 13 , 39. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Zhang, Z.; He, J.-W.; Fu, W.-Z.; Zhang, C.-Q.; Zhang, Z.-L. Mutations in the SLCO2A1 Gene and Primary Hypertrophic Osteoarthropathy: A Clinical and Biochemical Characterization. J. Clin. Endocrinol. Metab. 2013 , 98 , E923–E933. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Li, Y.; Dong, R.; Wang, G.; Zhang, H.; Yang, X.; Li, Z.; Guan, J.; Gai, Z.; Liu, Y. Establishment of a novel human iPSC line (SDQLCHi032-A) derived from a patient with primary hypertrophic osteoarthropathy caused by HPGD homozygous mutation. Stem Cell Res. 2021 , 52 , 102217. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Uppal, S.; Diggle, C.P.; Carr, I.M.; Fishwick, C.W.G.; Ahmed, M.; Ibrahim, G.H.; Helliwell, P.S.; Latos-Bieleńska, A.; Phillips, S.E.V.; Markham, A.F.; et al. Mutations in 15-hydroxyprostaglandin dehydrogenase cause primary hypertrophic osteoarthropathy. Nat. Genet. 2008 , 40 , 789–793. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Zhang, H.; Yang, B. Successful treatment of pachydermoperiostosis patients with etoricoxib, aescin, and arthroscopic synovectomy: Two case reports. Medicine 2017 , 96 , e8865. [ Google Scholar ] [ CrossRef ]
- Flayell, G. Reversal of pulmonary hypertrophic osteoarthropathy by vagotomy. Lancet 1956 , 267 , 260–262. [ Google Scholar ] [ CrossRef ]
- Bingol, U.A.; Cinar, C. Pachydermoperiostosis: Aesthetic Treatment of Prematurely Aging Face With Facelift and Botulinum Toxin A. J. Craniofacial Surg. 2014 , 25 , e563–e564. [ Google Scholar ] [ CrossRef ]
- Ai, M.; Heeger, S.; Bartels, C.F.; Schelling, D.K.; Osteoporosis-Pseudoglioma Collaborative, G. Clinical and molecular findings in osteoporosis-pseudoglioma syndrome. Am. J. Hum. Genet. 2005 , 77 , 741–753. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Kondo, H. Complex genetics of familial exudative vitreoretinopathy and related pediatric retinal detachments. Taiwan J. Ophthalmol. 2015 , 5 , 56–62. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Chen, J.; Stahl, A.; Krah, N.M.; Seaward, M.R.; Joyal, J.-S.; Juan, A.M.; Hatton, C.J.; Aderman, C.M.; Dennison, R.J.; Willett, K.L.; et al. Retinal Expression of Wnt-Pathway Mediated Genes in Low-Density Lipoprotein Receptor-Related Protein 5 (Lrp5) Knockout Mice. PLoS ONE 2012 , 7 , e30203. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Toomes, C.; Bottomley, H.M.; Jackson, R.M.; Towns, K.V.; Scott, S.; Mackey, D.A.; Craig, J.E.; Jiang, L.; Yang, Z.; Trembath, R.; et al. Mutations in LRP5 or FZD4 underlie the common familial exudative vitreoretinopathy locus on chromosome 11q. Am. J. Hum. Genet. 2004 , 74 , 721–730. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Wilson, G.; Moore, A.; Allgrove, J. Bilateral retinal detachments at birth: The osteoporosis pseudoglioma syndrome. Br. J. Ophthalmol. 2001 , 85 , 1139. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Gowda, V.K.; Vegda, H.; Shivappa, S.K.; Benakappa, N. Osteoporosis Pseudoglioma Syndrome. J. Pediatr. Neurosci. 2020 , 15 , 334–335. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Streeten, E.A.; McBride, D.; Puffenberger, E.; Hoffman, M.E.; Pollin, T.I.; Donnelly, P.; Sack, P.; Morton, H. Osteoporosis-pseudoglioma syndrome: Description of 9 new cases and beneficial response to bisphosphonates. Bone 2008 , 43 , 584–590. [ Google Scholar ] [ CrossRef ]
- Miyazawa, S.; Nakamura, Y.; Kosho, T.; Kawame, H.; Narumi, S.; Hasegawa, T.; Suzuki, T.; Kato, H. Efficacy of denosumab therapy for osteoporosis-pseudoglioma syndrome with osteoporosis: A case report. Mod. Rheumatol. Case Rep. 2019 , 3 , 45–48. [ Google Scholar ] [ CrossRef ]
- Homaei, A.; Chegini, V.; Saffari, F. Clinical Response to Treatment with Teriparatide in an Adolescent with Osteoporosis-Pseudoglioma Syndrome (OPPG): A Case Report. Int. J. Endocrinol. Metab. 2022 , 20 , e121031. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Tosi, L.L.; Oetgen, M.E.; Floor, M.K.; Huber, M.B.; Kennelly, A.M.; McCarter, R.J.; Rak, M.F.; Simmonds, B.J.; Simpson, M.D.; Tucker, C.A.; et al. Initial report of the osteogenesis imperfecta adult natural history initiative. Orphanet J. Rare Dis. 2015 , 10 , 146. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Basel, D.; Steiner, R.D. Osteogenesis imperfecta: Recent findings shed new light on this once well-understood condition. Genet. Med. 2009 , 11 , 375–385. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Tournis, S.; Dede, A.D. Osteogenesis imperfecta—A clinical update. Metab.—Clin. Exp. 2018 , 80 , 27–37. [ Google Scholar ] [ CrossRef ]
- Dubail, J.; Brunelle, P.; Baujat, G.; Huber, C.; Doyard, M.; Michot, C.; Chavassieux, P.; Khairouni, A.; Topouchian, V.; Monnot, S.; et al. Homozygous Loss-of-Function Mutations in CCDC134 Are Responsible for a Severe Form of Osteogenesis Imperfecta. J. Bone Miner. Res. 2020 , 35 , 1470–1480. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Lindahl, K.; Langdahl, B.; Ljunggren, Ö.; Kindmark, A. THERAPY OF ENDOCRINE DISEASE: Treatment of osteogenesis imperfecta in adults. Eur. J. Endocrinol. 2014 , 171 , R79–R90. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Subramanian, S.; Viswanathan, V.K. Osteogenesis Imperfecta. In StatPearls ; StatPearls Publishing: Treasure Island, FL, USA, 2022. [ Google Scholar ]
- Marini, J.C.; Forlino, A.; Bächinger, H.P.; Bishop, N.J.; Byers, P.H.; Paepe, A.D.; Fassier, F.; Fratzl-Zelman, N.; Kozloff, K.M.; Krakow, D.; et al. Osteogenesis imperfecta. Nat. Rev. Dis. Prim. 2017 , 3 , 17052. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Thomas, I.H.; DiMeglio, L.A. Advances in the Classification and Treatment of Osteogenesis Imperfecta. Curr. Osteoporos. Rep. 2016 , 14 , 1–9. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Palomo, T.; Fassier, F.; Ouellet, J.; Sato, A.; Montpetit, K.; Glorieux, F.H.; Rauch, F. Intravenous Bisphosphonate Therapy of Young Children With Osteogenesis Imperfecta: Skeletal Findings During Follow Up Throughout the Growing Years. J. Bone Miner. Res. 2015 , 30 , 2150–2157. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hennedige, A.A.; Jayasinghe, J.; Khajeh, J.; Macfarlane, T.V. Systematic review on the incidence of bisphosphonate related osteonecrosis of the jaw in children diagnosed with osteogenesis imperfecta. J. Oral Maxillofac. Res. 2014 , 4 , e1. [ Google Scholar ] [ CrossRef ]
- Hoyer-Kuhn, H.; Franklin, J.; Allo, G.; Kron, M.; Netzer, C.; Eysel, P.; Hero, B.; Schoenau, E.; Semler, O. Safety and efficacy of denosumab in children with osteogenesis imperfect--a first prospective trial. J. Musculoskelet. Neuronal Interact. 2016 , 16 , 24–32. [ Google Scholar ]
- Trifirò, G.; Mora, S.; Marelli, S.; Luzi, L.; Pini, A. Increased fracture rate in children and adolescents with Marfan syndrome. Bone 2020 , 135 , 115333. [ Google Scholar ] [ CrossRef ]
- Carter, N.; Duncan, E.; Wordsworth, P. Bone mineral density in adults with Marfan syndrome. Rheumatology 2000 , 39 , 307–309. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Rolfes, M.C.; Deyle, D.R.; King, K.S.; Hand, J.L.; Graff, A.H.; Derauf, C. Fracture incidence in Ehlers-Danlos syndrome—A population-based case-control study. Child Abus. Negl. 2019 , 91 , 95–101. [ Google Scholar ] [ CrossRef ]
- Banica, T.; Coussens, M.; Verroken, C.; Calders, P.; De Wandele, I.; Malfait, F.; Zmierczak, H.G.; Goemaere, S.; Lapauw, B.; Rombaut, L. Higher fracture prevalence and smaller bone size in patients with hEDS/HSD—A prospective cohort study. Osteoporos. Int. 2020 , 31 , 849–856. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Tan, E.W.; Offoha, R.U.; Oswald, G.L.; Skolasky, R.L.; Dewan, A.K.; Zhen, G.; Shapiro, J.R.; Dietz, H.C.; Cao, X.; Sponseller, P.D. Increased fracture risk and low bone mineral density in patients with loeys–dietz syndrome. Am. J. Med. Genet. Part A 2013 , 161 , 1910–1914. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Malfait, F.; Francomano, C.; Byers, P.; Belmont, J.; Berglund, B.; Black, J.; Bloom, L.; Bowen, J.M.; Brady, A.F.; Burrows, N.P.; et al. The 2017 international classification of the Ehlers–Danlos syndromes. Am. J. Med. Genet. Part C: Semin. Med. Genet. 2017 , 175 , 8–26. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Robinson, P.N.; Godfrey, M. The molecular genetics of Marfan syndrome and related microfibrillopathies. J. Med. Genet. 2000 , 37 , 9. [ Google Scholar ] [ CrossRef ]
- Mizuguchi, T.; Collod-Beroud, G.; Akiyama, T.; Abifadel, M.; Harada, N.; Morisaki, T.; Allard, D.; Varret, M.; Claustres, M.; Morisaki, H.; et al. Heterozygous TGFBR2 mutations in Marfan syndrome. Nat. Genet. 2004 , 36 , 855–860. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- MacCarrick, G.; Black, J.H., 3rd; Bowdin, S.; El-Hamamsy, I.; Frischmeyer-Guerrerio, P.A.; Guerrerio, A.L.; Sponseller, P.D.; Loeys, B.; Dietz, H.C., 3rd. Loeys-Dietz syndrome: A primer for diagnosis and management. Genet. Med. Off. J. Am. Coll. Med. Genet. 2014 , 16 , 576–587. [ Google Scholar ] [ CrossRef ]
- Hussein, D.; Olsson, C.; Lagerstedt-Robinson, K.; Moreira, T. Novel Mutation of the TGF-β 3 Protein (Loeys-Dietz Type 5) Associated With Aortic and Carotid Dissections. Neurol. Genet. 2021 , 7 , e625. [ Google Scholar ] [ CrossRef ]
- Beighton, P.; Paepe, A.D.; Steinmann, B.; Tsipouras, P.; Wenstrup, R.J. Ehlers-Danlos syndromes: Revised nosology, Villefranche, 1997. Am. J. Med. Genet. 1998 , 77 , 31–37. [ Google Scholar ] [ CrossRef ]
- von Kodolitsch, Y.; De Backer, J.; Schüler, H.; Bannas, P.; Behzadi, C.; Bernhardt, A.M.; Hillebrand, M.; Fuisting, B.; Sheikhzadeh, S.; Rybczynski, M.; et al. Perspectives on the revised Ghent criteria for the diagnosis of Marfan syndrome. Appl. Clin. Genet. 2015 , 8 , 137–155. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Carbone, L.; Tylavsky, F.A.; Bush, A.J.; Koo, W.; Orwoll, E.; Cheng, S. Bone Density in Ehlers-Danlos Syndrome. Osteoporos. Int. 2000 , 11 , 388–392. [ Google Scholar ] [ CrossRef ]
- Dolan, A.L.; Arden, N.K.; Grahame, R.; Spector, T.D. Assessment of bone in Ehlers Danlos syndrome by ultrasound and densitometry. Ann. Rheum. Dis. 1998 , 57 , 630. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Moura, B.; Tubach, F.; Sulpice, M.; Boileau, C.; Jondeau, G.; Muti, C.; Chevallier, B.; Ounnoughene, Y.; Le Parc, J.-M. Bone mineral density in Marfan syndrome. A large case-control study. Jt. Bone Spine 2006 , 73 , 733–735. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Holick, M.F.; Hossein-Nezhad, A.; Tabatabaei, F. Multiple fractures in infants who have Ehlers-Danlos/hypermobility syndrome and or vitamin D deficiency: A case series of 72 infants whose parents were accused of child abuse and neglect. Dermato-Endocrinology 2017 , 9 , e1279768. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Holick, M.F.; Shirvani, A.; Charoenngam, N. Fetal Fractures in an Infant with Maternal Ehlers-Danlos Syndrome, CCDC134 Pathogenic Mutation and a Negative Genetic Test for Osteogenesis Imperfecta. Children 2021 , 8 , 512. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- OSTEOGENESIS IMPERFECTA, TYPE XXII.; OI22. Available online: https://www.omim.org/entry/619795 (accessed on 6 April 2022).
- Morris, J.A.; Kemp, J.P.; Youlten, S.E.; Laurent, L.; Logan, J.G.; Chai, R.C.; Vulpescu, N.A.; Forgetta, V.; Kleinman, A.; Mohanty, S.T.; et al. An atlas of genetic influences on osteoporosis in humans and mice. Nat. Genet. 2019 , 51 , 258–266. [ Google Scholar ] [ CrossRef ] [ PubMed ]
Click here to enlarge figure
| Disorder | Clinical Manifestations | Causative Genetic Variations |
|---|---|---|
| Sclerosing disorders | ||
| Autosomal dominant osteopetrosis | Increased BMD, bony sclerosis, bone fragility, metaphyseal deformity, osteomyelitis, tooth eruption defects, dental caries, moderate bone marrow failure, cranial nerves impingement (II, VII, VIII) | mutation mutation |
| Classic autosomal recessive osteopetrosis | Increased BMD, bony sclerosis, bone fragility, metaphyseal deformity, osteomyelitis, tooth eruption defects, dental caries, hydrocephalus, hypocalcemia, severe bone marrow failure, extramedullary hematopoiesis, hepatosplenomegaly, cranial nerves impingement (II, VII, VIII) | , CLCN7, OSTM1, SNX10, or PLEKHM1 mutation (encoding RANKL) or TNFRSF11A (encoding RANK) mutation |
| X-linked osteopetrosis, lymphedema, anhidrotic ectodermal dysplasia and immunodeficiency | Increased BMD, bony sclerosis, bone fragility, metaphyseal deformity, osteomyelitis, tooth eruption defects, dental caries, anhidrotic ectodermal dysplasia, lymphedema, immunodeficiency | stop codon mutation |
| Autosomal recessive osteopetrosis with renal tubular acidosis | Increased BMD, bony sclerosis, bone fragility, metaphyseal deformity, osteomyelitis, tooth eruption defects, dental caries, renal tubular acidosis, developmental delay, intracranial calcification, cranial nerves impingement, bone marrow failure (rare) | mutation |
| Progressive Diaphyseal Dysplasia | Symmetric periosteal/endosteal thickening of long bone diaphysis (primarily femur and tibia), increased BMD, leg pain, muscle weakness, fatigue, slim limbs, tender bones, cranial enlargement, prominent forehead, cranial nerve palsy, hydrocephalus, hypocalciuria, hypocalcemia | mutation |
| Melorheostosis | Bone resembles dripping wax from a melting candle (affecting appendicular skeleton and adjacent soft tissue), dense hyperostosis of periosteal/endosteal surfaces, pain, bony swelling, joint and limb deformities, limited motion, numbness, weakness | mutation |
| Juvenile Paget’s Disease | Rapid bone turnover in children, bone deformities and fractures, short stature, elevated bone alkaline phosphatase, hearing loss, retinopathy, vascular calcification, internal carotid artery aneurysm | mutation (encoding OPG) |
| Paget’s disease | Bone pain, fractures and deformity, headache, hearing loss, nerve compression, spinal stenosis, high-output cardiac failure | mutation (encoding RANK) mutation (encoding OPG) |
| High bone mass associated with LRP5 mutation | Extremely high BMD, increased calvarial thickness, craniosynostosis, striking square jaw, torus palatinus, thickened cortices of long bone | mutation |
| High bone mass associated with LRP6 mutation | Extremely high BMD, absence of adult maxillary incisors, broad jaw, torus palatinus, thickening of the skull, optic nerve dilatation, narrowing of optic and autidory canals | mutation |
| Pyle disease | Genu valgum, “Erlenmeyer flask” deformity, metaphyseal fracture, dental abnormalities, prognathism | mutation |
| Hyperostosis Corticalis Generalista | Endosteal hyperostosis of the mandible, skull, ribs, clavicles, and diaphysis of long bones, facial nerve palsy, hearing loss, optic atrophy | mutation (encoding sclerostin) |
| Sclerosteosis | Generalized bone overgrowth, jaw enlargement, facial abnormality, cranial nerve impingement, increased intracranial pressure, syndactyly, tall stature | mutation |
| Pyknodysostosis | short-limbed, short stature, dysmorphic facial features (small jaw, obtuse mandibular angle, and convex nasal ridge), osteosclerosis, bone fragility and fractures, dental and nail abnormalities, kyphoscoliosis, chest deformity, high arched palate, proptosis, blue sclera | mutation (encoding cathepsin K) |
| Osteopathia Striata | Linear striations within the metaphyseal areas of long bones, macrocephaly, characteristic facial features (frontal bossing, hypertelorism, depressed nasal bridge, prominent mandible, and epicanthal folds), hearing loss, orofacial clefting, mild developmental delay In males: congenital, musculoskeletal defects (in mild cases). Multiple-malformation syndrome (in severe cases) | mutation |
| Osteopoikilosis | Numerous bone islands that typically affect the appendicular skeleton, usually free of any major symptoms | mutation |
| Demineralization disorders | ||
| Hypophosphatasia | ||
| Odonto hypophosphatasia | Premature loss of primary teeth | mutation |
| Adult hypophosphatasia | Bone pain, pseudogout, calcium pyrophosphate dihydrate crystal deposition in ligaments, and soft tissues. | |
| Childhood hypophosphatasia | Premature loss of primary teeth, bone pain, craniosynostosis, rachitic rosary, flaring of metaphysis, bowed legs, waddling gait | |
| Infantile hypophosphatasia | Skeletal rachitic deformities, brachycephaly, hypertelorism, increased intracranial pressure, tracheomalacia, chest wall deformity, recurrent pneumonia, hypercalcemia, hypercalciuria, pyridoxine-dependent seizure | |
| Perinatal hypophosphatasia | In utero limb deformities, cardiopulmonary failure, brain hemorrhage, myelophthisic anemia | |
| Hypophosphatemic rickets | Proximal muscle weakness, waddling gait, short stature, defective limb growth with preserved trunk growth, delayed tooth eruption, increased risk of dental abscesses, frontal bossing, parietal flattening, craniosynostosis, genu valgum/varum, intoeing or extoeing leg deformities, thickening of costochondral junctions | mutation mutation mutation mutation mutation |
| Vitamin D-dependent rickets | Proximal muscle weakness, waddling gait, short stature, sweating, delayed tooth eruption, sweating, craniotabes, frontal bossing, widened fontanelles, rachitic rosary, sternal protrusion, ribs deformities, flattened pelvic bones, bowing deformities of arms and legs, genu valgum/varum, flattened pelvic bones, hypocalcemic tetany, seizures, laryngospasm, cardiomyopathy, alopecia (for vitamin D-dependent rickets type II) | mutation mutation |
| Axial osteomalacia | Bone pain along the axial skeleton, findings resembling ankylosing spondylosis | |
| Disorders of bone matrix and cartilage formation | ||
| Achondroplasia | Short statue, prominent abdomen and buttocks, macrocephaly, frontal bossing, depressed nasal bridge, short extremities, limited range of motion at the elbows | mutation |
| Hypochondroplasia | Short stature without macrocephaly, short appendicular bone (less pronounced than achondroplasia) | |
| Thanatophoric dysplasia | Short extremities, redundant skin on the arms and legs, respiratory failure, flattened spine and curved femurs (type 1), straight femur and cloverleaf skull (type 2) | |
| Multiple exostosis | Multiple osteochondroma causing impingement of nerves and muscle tendons, nontraumatic fractures of osteochondroma | or EXT2 mutation |
| Patchydermoperiostosis | Clubbing of the fingers and toes, furrowing and thickening of the facial skin and the scalp, cylindrical enlargement of upper and lower extremities, hyperhydrosis, arthalgia | or SLCO2A1 mutation |
| Osteoporosis-pseudoglioma syndrome | Juvenile-onset osteoporosis, fragility fractures, scoliosis, short stature, limb deformities, craniotabes, visual impairment, intellectual disability, hypotonia, joint hypermobility, seizures | mutation |
| Osteogenesis imperfecta | ||
| OI type I | Mild, normal or short stature, blue sclerae, late-onset hearing loss | or COL1A2 mutation mutation |
| OI type II | Perinatally lethal, minimal calvarial mineralization | , COL1A2, CRTAP, LEPRE1, PPIB or BMP1 mutation |
| OI type III | Severe, progressively deforming bones | , COL1A2, CRTAP, LEPRE1, PPIB, FKBP10, SERPINH1, SERINF1 or WNT1 mutation |
| OI type IV | More severe than type I, lesser severe than type II and type III, short stature, bone deformity | , COL1A2, CRTAP, FKBP10, SP7, SERPINF1, WNT1 or TMEM38B mutation |
| OI type V | Normal-to-severe skeletal deformity, hyperplastic callus formation, intraosseous membrane ossifications | mutation |
| OI type VI | Presence of osteoid, fish-scale appearance of the lamellar bone pattern | mutation |
| OI type VII | Severe to lethal, rhizomelia | mutation |
| OI type VIII | Severe to lethal, rhizomelia, coxa vara, popcorn metaphyses | mutation |
| OI type IX | Short bowed femurs with anterior, bowing of the tibiae, grey sclerae | mutation |
| OI type X | Severe skeletal deformity, blue sclerae, dentinogenesis imperfecta, skin abnormalities, inguinal hernia | mutation |
| OI type XI | Joint contractures (distorted lamellar, structure and a fish scale-like pattern), normal to grey sclerae | mutation |
| OI type XII | Fractures, mild bone deformations, generalized osteoporosis, delayed teeth eruption, progressive hearing loss, no dentinogenesis imperfecta, white sclerae | mutation |
| OI type XIII | Severe skeletal deformity, delayed tooth eruption, facial hypoplasia | mutation |
| OI type XIV | Severe bone deformity, normal-to-blue sclerae | mutation |
| OI type XV | Fractures, bone deformities, short stature, blue sclerae | mutation |
| OI type XVI | Prenatal onset of multiple fractures of ribs and long bones, blue sclerae, decreased ossification of the skull, and severe demineralization. | mutation |
| OI type XVII | Fractures, motor delay, muscle hypotonia, lower extremity weakness, decreased calf muscle mass, joint hyperlaxity, and soft skin | mutation |
| OI type XVIII | Congenital bowing of the long bones, wormian bones, blue sclerae, vertebral collapse, multiple fractures | mutation |
| OI type XIX | Moderate short stature, blue sclerae, pectus carinatum, bowing of lower extremity long bones, multiple fractures | mutation |
| OI type XX | Osteopenia, skeletal deformity, multiple fractures, respiratory failure | mutation |
| OI type XXI | Short stature, failure to thrive, wormian bones, bowed limbs, chest deformity, hypotonia, joint hypermobility, dysmorphic facies, blue sclerae, dentinogenesis imperfecta, scoliosis, fractures, platyspondyly. | mutation |
| OI type XXII | Intrauterine growth retardation, short stature, multiple fractures, decreased thoracic size, short limbs, blue sclerae | mutation |
| Ehlers-Danlos syndrome | ||
| Classical EDS, types I and II | Joint hypermobility, hyperextensible skin, easy bruisability, doughy-velvety skin, atrophic scars | , COL5A2 or COL1A1 (rarely) mutation |
| Classical-like EDS | Hyperextensible skin, doughy-velvety skin texture, atropic scars, easy bruisability, joint hypermobility | mutation |
| Hypermobile EDS, type III | Joint hypermobility, joint dislocations-subluxations including temporal mandibular joint, hyperextensible skin, doughy-velvety skin, hernias, gastroparesis, high palate with dental crowding, bone fractures, vascular fragility, mast cell hyperactivity, postural orthostatic tachycardia syndrome, atrophic and hypertrophic scarring, poor wound healing, pieziogenic blisters on heels | |
| Vascular EDS, type IV | Arterial rupture (aorta, mesenteric, cerebrovascular, splenic, renal arteries), organ rupture (colon, uterus), easy bruising, translucent skin | or COL1A1 (rarely) mutation |
| Cardiac-valvular type EDS | Progressive weakening of heart valves, hyperextensible skin, atrophic scars, easy bruisability, joint hypermobility | mutation |
| Kyphoscoliotic EDS, type VI | Joint hypermobility, kyphoscoliosis, osteopenia, hypotonia at birth, blue sclerae, Marfanoid habitus | or FKBP14 mutation |
| Arthrochalasia EDS, types VIIA and VIIB | Congenital hip dislocations, recurrent subluxations, joint hypermobility, hyperextensible skin, muscle hypotonia, osteopenia | or COL1A2 mutation |
| Dermatosparaxis EDS, type VIIC | Severe bruisability, blue sclerae, severe skin fragility, sagging skin, visceral fragility, growth retardation | mutation |
| Periodontal EDS, type VIII | Early onset severe periodontitis, unattached gingiva, pretibial plaques, hyperextensible skin, Marfanoid features, joint hypermobility | mutation |
| Spondylodysplastic EDS | Short stature, delayed eruption of teeth, hypodontia, limb bowing, joint laxity, osteopenia, hyperextensible, thin skin, delayed wound healing with atrophic scars | , B3GALT5 or SLC39A13 mutation |
| Musculocontractural EDS | Congenital contractures (thumb, finger, club feet), severe kyphoscoliosis, recurrent dislocations, easy bruisability, craniofacial features (broad forehead, small mouth, micrognathia, protruding jaw), hyperextensible fragile skin, atrophic scars | or DSE mutation |
| Brittle cornea syndrome | Thin cornea, retinal detachment, globe rupture, blue sclerae, keratoconus, high myopia | or PRDM6 mutation |
| Myopathic EDS | Congenital hypotonia, proximal joint contractures, distal joint hypermobility, atrophic scars | mutation |
| Marfan’s syndrome | Aortic disease: aortic root disease, leading to aneurysmal dilatation, aortic regurgitation and dissection; Cardiac disease: mitral valve prolapse; Skeletal findings: arachnodactyly, pectus carinatum, pectus excavatum, abnormal upper/lower segments and arm span/height, scoliosis, kyphosis, malar hypoplasia, retrognathia; Ocular abnormalities: ectopia lentis, flat cornea, miosis, retinal detachment, glaucoma. Dural ectasia, emphysematous, pneumothorax, skin striae, arm span to height ratio >1.5 | mutation mutation |
| Loeys-Dietz syndrome | Craniosynostosis, scoliosis, pectus excavatum/carinatum, clubfoot, pes planus, elongated limbs, joint instability/contracture, dural ectasia, bruising, abnormal scar, striae, skin translucency, spontaneous pneumothorax, hernias, hypertelorism, strabismus, bifid uvula, cleft palate, increased risk of immune disorders (i.e., allergies, asthma, eczema, inflammatory bowel disease) | mutation mutation mutation mutation mutation |
| MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
Share and Cite
Charoenngam, N.; Nasr, A.; Shirvani, A.; Holick, M.F. Hereditary Metabolic Bone Diseases: A Review of Pathogenesis, Diagnosis and Management. Genes 2022 , 13 , 1880. https://doi.org/10.3390/genes13101880
Charoenngam N, Nasr A, Shirvani A, Holick MF. Hereditary Metabolic Bone Diseases: A Review of Pathogenesis, Diagnosis and Management. Genes . 2022; 13(10):1880. https://doi.org/10.3390/genes13101880
Charoenngam, Nipith, Aryan Nasr, Arash Shirvani, and Michael F. Holick. 2022. "Hereditary Metabolic Bone Diseases: A Review of Pathogenesis, Diagnosis and Management" Genes 13, no. 10: 1880. https://doi.org/10.3390/genes13101880
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
- Share full article
Advertisement
Supported by
A Family’s Shared Defect Sheds Light on the Human Genome

By Natalie Angier
- Jan. 9, 2017
They said it was their family curse: a rare congenital deformity called syndactyly, in which the thumb and index finger are fused together on one or both hands. Ten members of the extended clan were affected, and with each new birth, they told Stefan Mundlos of the Max Planck Institute for Molecular Genetics, the first question was always: “How are the baby’s hands? Are they normal?”
Afflicted relatives described feeling like outcasts in their village, convinced that their “strange fingers” repulsed everybody they knew — including their unaffected kin. “One woman told me that she never received a hug from her father,” Dr. Mundlos said. “He avoided her.”
The family, under promise of anonymity, is taking part in a study by Dr. Mundlos and his colleagues of the origin and development of limb malformations. And while the researchers cannot yet offer a way to prevent syndactyly, or to entirely correct it through surgery, Dr. Mundlos has sought to replace the notion of a family curse with “a rational answer for their condition,” he said — and maybe a touch of pioneers’ pride.
The scientists have traced the family’s limb anomaly to a novel class of genetic defects unlike any seen before, a finding with profound implications for understanding a raft of heretofore mysterious diseases.
The mutations affect a newly discovered design feature of the DNA molecule called topologically associating domains, or TADs. It turns out that the vast informational expanse of the genome is divvied up into a series of manageable, parochial and law-abiding neighborhoods with strict nucleic partitions between them — each one a TAD.
Breach a TAD barrier, and you end up with the molecular equivalent of that famous final scene in Mel Brooks’s comedy, “Blazing Saddles,” when the cowboy actors from one movie set burst through a wall and onto the rehearsal stage of a campy Fred Astaire-style musical. Soon fists, top hats and cream pies are flying.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .
Advertisement
Genetic Hair Disorders: A Review
- Open access
- Published: 22 July 2019
- Volume 9 , pages 421–448, ( 2019 )
Cite this article
You have full access to this open access article

- Azhar Ahmed 1 , 3 ,
- Hind Almohanna 2 ,
- Jacob Griggs 3 &
- Antonella Tosti 3
31k Accesses
28 Citations
154 Altmetric
42 Mentions
Explore all metrics
Hair loss in early childhood represents a broad differential diagnosis which can be a diagnostic and therapeutic challenge for a physician. It is important to consider the diagnosis of a genetic hair disorder. Genetic hair disorders are a large group of inherited disorders, many of which are rare. Genetic hair abnormalities in children can be an isolated phenomenon or part of genetic syndromes. Hair changes may be a significant finding or even the initial presentation of a syndrome giving a clue to the diagnosis, such as Netherton syndrome and trichothiodystrophy. Detailed history including family history and physical examination of hair and other ectodermal structures such as nails, sweat glands, and sebaceous glands with the use of dermoscopic devices and biopsy all provide important clues to establish the correct diagnosis. Understanding the pathophysiology of genetic hair defects will allow for better comprehension of their treatment and prognosis. For example, in patients with an isolated hair defect, the main problem is aesthetic. In contrast, when the hair defect is associated with a syndrome, the prognosis will depend mainly on the associated condition. Treatment of many genetic hair disorders is focused on treating the primary cause and minimizing trauma to the hair.
Similar content being viewed by others

Leukonychia: What Can White Nails Tell Us?

Common Skin Condition in Black Skin

Cutaneous Disorders of the Breast
Avoid common mistakes on your manuscript.
Introduction
Hair is a skin appendage that shares a common developmental pathway with other ectodermal tissue [ 1 ]. Human hair is a key phenotypic indicator of possible underlying metabolic or genetic syndromes.
Genetic hair disorders can cause severe alopecia in both adults and children and may occasionally present as part of a multisystem syndrome. So, the diagnosis of these genetic disorders is important not only for the initiation of proper therapy but also for the detection of other associated ectodermal anomalies and for appropriate genetic counselling. Affected children and their parents are usually psychologically impacted by such conditions.
In this review we summarize the main genetic hair disorders and discuss the clinical features, known associated genetic abnormalities, and current treatment modalities. The review will focus on hypotrichosis, hair shaft disorders (with and without increased fragility), and ectodermal dysplasia. Table 1 summarize the gene defect, clinical presentation, and treatment tried for each genetic hair disorder.
We searched keywords using PubMed and Medline to identify all relevant publications. The terms “Hair loss,” “Alopecia,” “Hypotrichosis,” “Trichorrhexis nodosa,” “Trichorrhexis invaginate,” “Bamboo hair,” “Pili torti,” “Trichothiodystrophy,” “Monilethrix,” “Pili annulati,” “Woolly hair,” “Uncombable hair syndrome,” “Pili trianguli et canaliculi,” “Ectodermal dysplasias,” “Trichorhinophalangeal syndrome,” “pediatric,” “congenital,” “genetic,” and “children” were included as a search terms to identify all relevant publications.
Three independent researchers performed a literature search to identify all relevant studies. Only published articles written in English were chosen. A total of 159 articles within the last 50 years were selected to be included in this review.
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964, as revised in 2013. This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors. Tables/figures are original and have been produced by the authors for this particular publication. The authors have consent from the patients for using their images in this publication.
- Hypotrichosis
In hypotrichosis, sparse hair is the result of a hair regeneration defect, caused by impairment in hair cycling and anchoring of the hair shaft in the skin [ 2 ]. Mutations in different genes have been associated with non-syndromic as well as syndromic forms [ 3 ], including hypotrichosis simplex, hypotrichosis with juvenile macular dystrophy (HJMD), Marie Unna hypotrichosis (MUH), and autosomal recessive woolly hair/hypotrichosis simplex.
Hypotrichosis Simplex
Hypotrichosis simplex (HS) (Mendelian Inheritance in Man (MIM) 146520, MIM 278150, MIM 146550, MIM 613981, and MIM 605389) [ 4 ] is a descriptive term for the clinical manifestations related to diffuse hair thinning without any morphological abnormalities of the hair shaft. Several hereditary hypotrichosis simplex (HHS) pedigrees have been published showing autosomal dominant inheritance, while others show autosomal recessive inheritance. Clinical variability can be observed on the basis of patient’s age of onset, as well as eyebrow and eyelash involvement [ 5 ]. Mutations in six genes have been identified for isolated HS, and mutations in three of them— CDSN (MIM 602593), APCDD1 (MIM 607479), and RPL21 (MIM 603636)—are responsible for autosomal dominant forms [ 4 ].
When the hypotrichosis simplex is only limited to the scalp, it is called hereditary hypotrichosis simplex of the scalp (HHSS) (MIM 146520), which is a rare non-syndromic autosomal dominant condition characterized by exclusively scalp hair loss, sparing other ectodermal structures and with no systemic abnormalities [ 6 ]. It is caused by nonsense mutations in the corneodesmosin gene ( CDSN ) which leads to expression of a truncated protein probably toxic to hair growth [ 7 ].
Patients present with normal hair at birth, then a gradually progressive scalp hair loss begins in the middle of the first decade ending with almost complete hair loss by the third decade. Eyebrows, eyelashes, and other body hair beside teeth and nails are completely normal. Developmental and intellectual development are normal [ 8 ]. Hypotrichosis simplex of the scalp was first described by Toribio and Quinones [ 9 ]. Males and females are affected equally [ 9 ].
Marine Unna Hypotrichosis
Marie Unna hypotrichosis, also known as Marie Unna hereditary hypotrichosis (MUHH) (OMIM ID #146550) is a rare autosomal dominant condition characterized by scalp hair that is sparse or absent at birth [ 10 ], with variable coarse, wiry hair regrowth in childhood, and potential loss again at puberty causing non-scarring alopecia [ 11 ]. It was first described by Marie-Unna in a German family, where individuals over seven generations were affected by a previously unreported type of congenital hypotrichosis. The exact mechanism of hair loss is not yet known, and genetic factors may play a role. There are hypotheses that might contribute to the pathogenesis including decreased number of functional follicles, altered hair shaft morphology, and abnormal follicle cycling [ 12 ]. Mutation of the U2HR gene, located in chromosome 8p21 is responsible for MUH. Several mutations in the U2HR gene that have been reported in the literature [ 10 , 13 , 14 ].
Patients have normal to adequate hair at birth and develop pattern alopecia resembling severe androgenetic alopecia at puberty [ 15 ]. Eyelashes, eyebrows, body hair, and secondary sexual hair are sparse or absent. Loss of eyebrows and presence of wiry, twisted scalp hair, resembling pili torti, is important for diagnosis [ 16 ]. Nails, teeth, and sweat glands are normal. Milia-like facial lesions can occur [ 17 ].
The hair shaft shows irregular twisting at odd angles and diameter variability along its length on light microscopy. Peeling of the cuticle and longitudinal grooves are noticeable on scanning electron microscopy [ 15 ]. Histologically, the number of hair follicles is decreased and there is a mild to moderate inflammatory infiltrate, but no fibrosis and scarring. The distinctive pattern of hair loss and twisted hair shaft provides a clue to the diagnosis of MUH. Unfortunately, there is no effective treatment available [ 17 ].
Autosomal Recessive Wooly Hair/Hypotrichosis Simplex (ARWH/H) or Familial Woolly Hair (WFH)
Autosomal recessive woolly hair/hypotrichosis simplex (ARWH/H) (OMIM ID #604379) is rare disorder characterized by tightly curled hair with variable light color (woolly hair) since infancy and variable degree of hypotrichosis [ 18 ]. It is caused by a mutation in P2RY5 or lipase membrane H gene ( LIPH ) [ 18 ]. LIPH encodes PA-PLA1a, a phospholipase A1 family member that produces lysophosphatidic acid (LPA) from phosphatidic acid, and plays a crucial role in hair growth in humans. LPA is an extracellular mediator that has many biological functions [ 19 ]. A mutation in P2RY5 gene (which is expressed in both Henle’s and Huxley’s layers of the inner root sheath of the hair follicle) had been identified in six consanguineous Pakistani families [ 20 ]. Patients have sparse, coarse, dry, and tightly curled hair, usually blond or lighter than other family members [ 21 , 22 ] (Fig. 1 ).

Autosomal recessive woolly hair/hypotrichosis. Note sparse blond curled hair
Hypotrichosis with Juvenile Macular Dystrophy
Congenital hypotrichosis associated with juvenile macular dystrophy (MIM 601553) is a rare autosomal recessive disorder characterized by early hair loss, heralding progressive degeneration of the retinal macula leading to early blindness during the second to third decade of life [ 23 , 24 ]. HJMD prevalence is unknown and has only been reported in approximately 30 patients [ 25 , 26 , 27 , 28 , 29 , 30 ].
Sprecher et al. [ 23 ] used mapping in four consanguineous families to localize the gene defective in HJMD to 16q22.1. This region contains CDH3 , encoding P-cadherin, which is expressed in the hair follicles and retinal pigment epithelium. Mutation analysis shows in all families a common homozygous deletion in exon 8 of CDH3 . These findings establish for the first time the molecular etiology of HJMD and link a cadherin molecule in the pathogenesis of this hair and retinal disorder [ 23 ]. Furthermore, Indelman et al. reported another four members of a consanguineous family with HJMD. Light and scanning electron microscopy of the hair shaft revealed pili torti. Fundus examination of the eyes showed marked degeneration of the macular pigment epithelium. DNA analysis of the entire coding sequence of CDH3 revealed, in all affected individuals, a homozygous missense mutation resulting in a single amino acid substitution at position 503 of P-cadherin sequence (R503H). This is considered the first missense mutation reported in CDH3 and second mutation found to underlie HJMD [ 31 ].
Additionally, Indelman and his colleagues assessed nine patients belonging to five families to further characterize the CDH3 mutation spectrum and delineate possible phenotype–genotype correlations. Significant inter- and intrafamilial differences in hair morphology were found, as well as differences in associated skin findings, severity, and age of onset of visual disability [ 32 ]. It has been recommended that all patients with congenital hypotrichosis should undergo a thorough fundus examination [ 26 , 27 , 33 , 33 ]. A therapeutic window for gene augmentation therapy to preserve visual acuity was suggested. More novel mutations in the CDH3 gene in HJMD have been reported afterwards [ 25 , 28 , 29 , 30 , 35 , 36 , 37 , 38 , 39 , 40 ].
Therapy for Hypotrichosis
The treatment of this type of alopecia is unsatisfactory. Topical minoxidil can improve the hair density and texture but for most patients wearing a wig is the best option [ 7 ].
Hair Shaft Disorders
Hair shaft disorders with increased fragility, trichorrhexis nodosa.
Trichorrhexis nodosa (TN) refers to the light microscopic appearance of a fracture with splaying out of individual cortical cells from the main body of the hair shaft, producing an appearance suggestive of two brushes pushed together [ 41 ]. The condition can be classified into three variants: primary congenital form, trichorrhexis nodosa as part of other syndromes, and acquired trichorrhexis nodosa [ 42 ]. The acquired form of trichorrhexis nodosa is due to repeated trauma to the hair shaft, and it is beyond the scope of this review.
The primary genetic form of TN (congenital trichorrhexis nodosa) is inherited in an autosomal dominant pattern. The hair is usually normal at birth, then it is replaced with fragile hair a few months later. This condition may improve with time [ 41 ].
The forms of TN as part of syndromes include argininosuccinic aciduria, citrullinemia, and trichohepatoenteric syndrome [ 43 ]. TN can occurs in association with monilethrix, trichothiodystrophy, Netherton syndrome, and Menkes syndrome as a response to injury of otherwise damaged hair shaft [ 41 ].
Argininosuccinic aciduria and citrullinemia are a group of urea cycle disorders caused by a deficiency of enzymes required to convert toxic ammonia into urea. Clinical manifestations of these diseases are mostly due to hyperammonemia, which affects the central nervous system. Affected individuals may also develop hepatic dysfunction [ 44 ].
Argininosuccinic aciduria is an inborn error of urea synthesis. It is due to deficiency of argininosuccinic lyase. If untreated, it may present with failure to thrive and mental retardation. The hair finding of TN is an important diagnostic clue in this syndrome. These patients have normal hair at birth but then develop TN when they are 1–2 years of age [ 45 ].
Citrullinemia is also a rare genetic error of the urea cycle. There is a deficiency of argininosuccinate synthetase, resulting in increased blood ammonia, citrullinemia, and decreased arginine level [ 46 ]. Patients with this syndrome have abnormally fragile hair with TN [ 46 ].
Treatment of TN is challenging in its genetic form and it is dependent mainly on managing the underlying disorder. Zinc sulfate 45 mg/day and 50 mg/day was given to two children with TN for 2 years. They had associated alopecia and dry scaly skin. The treatment enhanced the hair growth, despite persistence of TN microscopically. One of them had normal zinc level at initiation of the therapy [ 47 ].
Trichorrhexis Invaginata
In trichorrhexis invaginata (TI), also known as Bamboo hair, the hair shaft invaginates at several point along its length (Fig. 2 ). Low magnification trichoscopy shows multiple small nodules spaced at irregular intervals. With high magnification trichoscopy, it is possible to see invagination of the distal part of the shaft into its proximal part, forming a ball in a cup appearance. Sometimes the proximal cupped end may be seen after the distal end has fractured (golf tee sign) [ 48 ] (Fig. 3 ).
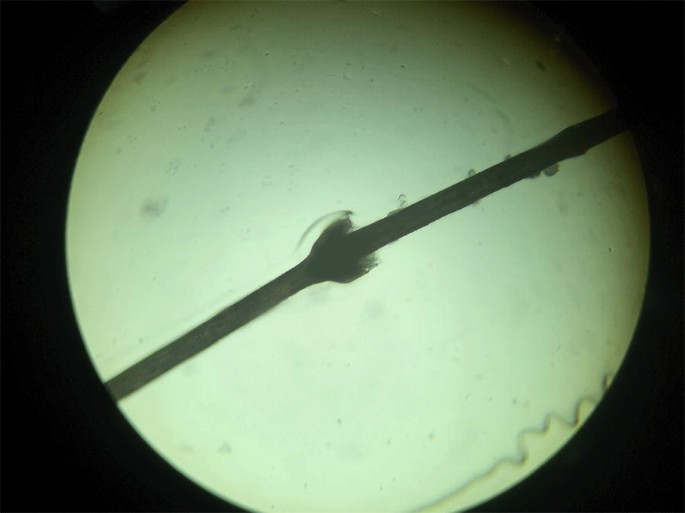
Trichorrhexis invaginate under microscopy. Invagination of the distal part of the hair shaft into its proximal part forming a ball in a cup appearance
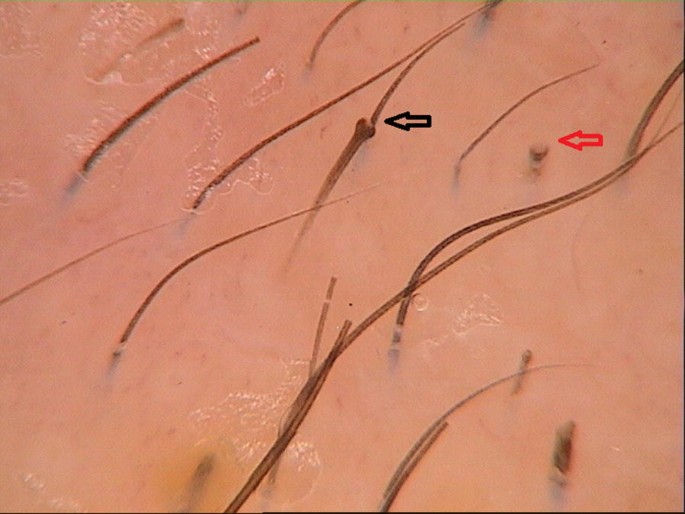
Trichoscopic finding in trichorrhexis invaginate. Note the invagination of the distal part of the shaft into its proximal part forming a ball in a cup appearance (black arrow). Proximal cupped end also seen after the distal end has fractured (golf tee sign) (red arrow)
TI is a pathognomonic finding of Netherton syndrome, a rare autosomal recessive condition caused by mutations in the SPINK5 gene. Netherton syndrome is characterized by a triad of congenital ichthyosiform erythroderma (CIE) or ichthyosis linearis circumflexa (ILC), atopic diathesis (elevated serum IgE), and short sparse fragile hair with trichorrhexis invaginata [ 49 ].
Hair improves with aging, but the eyebrows usually exhibit some hairs with the abnormality and should be checked for diagnosis [ 50 ]. Trichoscopy allows fast diagnosis of this condition as the affected hairs might be difficult to detect, as only 20–50% of hair is affected [ 49 ]. Other hair findings in patients with Netherton syndrome may resemble pili torti-like, trichorrhexis nodosa-like, and helical hairs [ 51 ].
Treatment aims to deal with the skin findings of Netherton syndrome more than the hair abnormality, and may include low dose oral steroids, etretinate [ 52 ], psoralen ultraviolet A therapy, topical tacrolimus [ 53 ], and lactate lotion 12% [ 54 ].
Monilethrix
Monilethrix (beaded hair) comes from monile (necklace, in Latin) and thrix (hair, in Greek). It is most commonly transmitted as an autosomal dominant disease [ 55 ], with high penetrance and variable severity [ 56 ].
Three genes have been associated with monilethrix ( KRT81 , KRT83 , and KRT86 , coding for the type II hair keratins Hb1, Hb3, and Hb6) [ 57 ]. An autosomal recessive form has been described, caused by a mutation in the DSG4 gene, encoding for desmoglein 4 protein [ 58 ].
The scalp hair is usually normal at birth. Within a few weeks to months, the hair is then replaced by dull, dry, and brittle hair which break easily, leaving a stubble-like appearance. The hair on the nape of the neck and occipital area are the most commonly affected areas and is usually accompanied by follicular keratosis [ 59 ] (Fig. 4 ). Lanugo hair is normal in the neonatal period, and clinical signs of monilethrix appear when the terminal hair begins to form [ 60 ]. In most cases, hair growth will be a maximum of 8 cm in length, but mild cases with hair of almost normal length can occur [ 41 ]. Eyebrows, eyelashes, and body hair can be affected, too [ 61 ]. The condition can be associated with keratosis pilaris, koilonychia, retarded growth, and juvenile cataract [ 62 ].

Clinical picture of monilethrix. Alopecia is more severe in the occipital region that also presents keratotic follicular papules
Trichoscopy will show normal medullated nodes of hair, along with non-medullated internodal thin hair at regular intervals (Fig. 5 ). The internode represents the diseased abnormal hair where it can be easily fractured [ 63 ]. Light microscopy shows typical beaded or moniliform appearance of the hair.

Trichoscopic finding in monilethrix. Typical beaded or moniliform appearance of the hair
Monilethrix usually persists into adulthood but may improve at puberty, pregnancy, or with an oral contraceptive [ 64 ]. Variable results have been obtained from systemic retinoid therapy where etretinate at 0.5 mg/kg/day and acitretin 0.5 mg/kg/day were tried with satisfactory results, but relapse occurred after discontinuation of these medications [ 65 , 66 ].
Daily topical minoxidil 2% 1 mL for 1 year showed a good response in four patients [ 67 ]. Low dose of oral minoxidil was tried on two women with good treatment response after 6 months [ 68 ]. Gentle hair care may diminish weathering and improve the condition [ 68 ].
Pili torti (PT) is a hair shaft disorder characterized by a flattened hair shaft that irregularly twists over its own axis. This finding can be seen via light microscopy and trichoscopy [ 69 ] (Fig. 6 ). Although a few pili torti hairs are commonly seen in association with other hair shaft disorders, there are rare conditions where pili torti is the exclusive finding [ 41 ]. In classic early onset pili torti, it can be associated with other, usually minor, ectodermal abnormalities. Both autosomal dominant and recessive forms have been reported. Females are most commonly affected, where they are born with abnormal hair or normal hair that is replaced with fragile, spangled, easily broken hair at different levels. The hair color is usually lighter than the unaffected relative’s hair color. Eyebrows and eyelashes can be affected. This condition improves with puberty [ 70 ].

Trichoscopic feature of pili torti. Note the flattened hair shaft that twists over its own axis
Late onset (Beare) pili torti is an autosomal dominant condition in which the eyebrows and eyelashes are broken off with an early age of onset, then the scalp hair after puberty becomes coarse, stiff, and jet black [ 71 ].
Pili torti can be part of other syndromes:
Bjornstad syndrome: Autosomal recessive condition. The patient will have both pili torti and sensorineural hearing loss. It is caused by mutations in the BCS1L gene [ 72 ].
Crandall syndrome: Autosomal recessive condition. The patient will have pituitary hormones dysfunction, hypogonadism, pili torti, and deafness [ 73 ].
Menkes syndrome: X-linked recessive condition. It is due to a mutation in the X-linked ATP7A gene, which encodes a copper-transporting ATPase. In this syndrome there is a maldistribution of the body’s copper leading to dysfunctions of all processes that need this element. The patient will have sparse, pale, lightly pigmented hair with a steel wool appearance. Eyebrows are affected, too. The skin is pale and doughy with a bowed upper lip. There will be associated vascular, neurological, and skeletal dysfunction due to decrease in activity of copper-dependent enzymes [ 74 ].
Bazex–Dupré–Christol syndrome (BDC syndrome) is a rare X-liked dominant disorder. It is characterized by triad of (1) follicular atrophoderma, especially on the dorsum of hands and feet, (2) multiple basal cell carcinomas on the face, occurring mainly during the second decade of life, and (3) congenital generalized hypotrichosis with associated hair shaft abnormalities (pili torti, trichorrhexis nodosa) [ 75 ]. The expression of these main features may vary [ 76 ]. Common associated symptoms are milia and hypohidrosis [ 77 ].
Trichothiodystrophy
Trichothiodystrophy (TTD) is an autosomal recessive condition characterized by low sulfur or cysteine levels on the hair. Varying degrees of clinical presentations from isolated hair shaft abnormality to a more severe developmental delay, intellectual disability, recurrent infections, and even death at early childhood [ 78 ]. The PIBIDS acronym refer to photosensitivity, ichthyosis, brittle hair, intellectual impairment, decrease fertility, and short stature [ 79 ].
About half of the cases with TTD have photosensitivity. Light microscopy will show trichoschisis (transverse fracture through the hair shaft) with or without trichorrhexisis nodosa [ 80 ]. Both trichoschisis and alternating light and dark bands (tiger tail) are visible under polarized light [ 81 ].
Trichothiodystrophy is caused by several functionally related genetic defects involving the transcription factor TFIIH/XPD-XPB complex. Current thinking is that transcription factor IIH has a dual function—transcription and DNA repair [ 82 ].
Hair Shaft Disorders Without Hair Fragility
Pili annulati.
Pili annulati (PA) is sporadic or autosomal dominant, and clinically presents as speckled-appearing or shiny spangled scalp hair. The PA locus has been mapped to chromosome 12q24.32–24.33, and recombination events define a critical region of 2.9 Mb containing 36 genes [ 83 ]. The hair shaft presents alternating light and dark bands. Trichoscopy features include bright bands caused by light scattered from clusters of air-filled cavities in the hair [ 84 ] (Fig. 7 ). These air-filled cavities appear dark on light microscopy [ 85 ]. Usually PA is not associated with hair fragility; however, a few cases associated with severe hair fragility have been reported [ 86 , 87 ].

Trichoscopic feature of pili annulati with bright band along the hair shaft
Furthermore, two patients were described in the literature with pili annulati in whom fragility of hair developed in a causal relationship with the onset of androgenetic alopecia [ 88 ]. There are a few diseases that have been reported to be associated with PA including autoimmune thyroid disease and primary immunoglobulin A deficiency [ 85 ].
PA carries excellent prognosis and treatment is usually unnecessary [ 89 ]. Cases of PA in association with alopecia areata have been reported even though the association is possibly coincidental. In a case treatment with topical minoxidil 2% solution twice daily, hair growth was induced after 2 months and the new hair lacked the ringed appearance [ 90 ].
Woolly Hair
Woolly hair (WH) is a group of hair shaft disorders characterized by short, kinked, tightly curled hair [ 91 ] (Fig. 1 ). Trichoscopic examination reveals that the hair shafts have waves at short intervals [ 69 ]. WH has three different subtypes: hereditary woolly hair (HWH), familial woolly hair (FWH), and woolly hair nevus (WHN) [ 92 ]. HWH is an autosomal dominant form with a variable degree of tight curling. It presents in hairs all over the scalp. Usually the hair density is normal in HWH and hair color is variable. A missense mutation within the helix initiation motif of the keratin K71 gene causes the dominant form [ 91 ]. Moreover, the dominant form has been described with disruption of keratin 74 [ 93 ].
FWH is an autosomal recessive type which is known as autosomal recessive woolly hair/hypotrichosis simplex (ARWH/H) and presents with tightly curled, sparse, thin, short white or blond hair since birth [ 94 , 95 ]. This disease was discussed in detail under the “ Hypotrichosis ” section. WHN is considered the isolated or localized type of WH and characterized by a well-demarcated area that is lighter than the normal hair and has a smaller diameter [ 92 ].
When WH is accompanied by palmoplantar keratoderma, it may be associated with fatal cardiomyopathy like Carvajal syndrome or Naxos syndrome [ 96 ], and hence this condition should alert the physician to a cardiac disease [ 97 , 98 , 99 ].
Carvajal syndrome is an autosomal recessive disorder due to a desmoplakin gene mutation. It is characterized by wooly hair at birth, striate palmoplantar keratoderma which develops after infancy, and left-sided ventricular cardiomyopathy. Other features include follicular keratoses on face, elbows, abdomen, and lower limbs, in addition to finger clubbing, psoriasiform keratosis, and transient pruritic blisters. The main cause of death is heart failure which can occur in adolescence. Early cardiac intervention can decrease mortality and improve prognosis [ 100 ].
Naxos syndrome is an autosomal recessive disorder due to a plakoglobin gene mutation. The clinical features include wooly hair at birth, diffuse palmoplantar keratosis developing during the first year of life, and arrhythmogenic right ventricular cardiomyopathy. The last of these presents by adolescence with arrhythmia and automatic implantable cardioverter defibrillator is usually indicated which may prevent sudden death [ 101 ].
WH may be an isolated finding or associated with additional clinical symptoms. WH has been reported with keratosis pilaris [ 69 ], congenital ichthyosis [ 99 ], Noonan syndrome, cardiofaciocutaneous syndrome [ 102 ], osteoma cutis [ 103 ], nail dystrophy [ 104 ], and severe neurologic disorders [ 105 ].
WH is most evident during childhood; the appearances can become less severe in adulthood since the manageability improves with age [ 106 ]. However, some individuals do not improve with age [ 107 ]. Treatment with nonablative fractional lasers stimulated normal hair growth in three adult men with autosomal recessive WH [ 108 ].
Pili Trianguli et Canaliculi, “Uncombable Hair Syndrome” or “Spun Glass Hair Syndrome”
Pili trianguli et canaliculi most often presents in infancy or early childhood, with spun-glass-appearing scalp hairs that are dry, curly, blond, and totally resist all efforts of styling [ 109 ]. Hair is not fragile and grows normally [ 110 ]. Most reported cases are sporadic, but autosomal dominant and autosomal recessive inheritance has been described [ 111 ]. Mutations are located in three genes involving PADI3 (peptidylarginine deiminase 3), TGM3 (transglutaminase 3), and TCHH (trichohyalin) [ 112 ]. Electron microscopy reveals irregularly shaped triangular shafts on cross section, which are areas of the internal root sheath that have been abnormally keratinized. Several conditions have been reported in association with uncombable hair, such as ectodermal dysplasia, retinal dysplasia/pigmentary dystrophy, juvenile cataract, tooth enamel anomalies, oligodontia, digit abnormalities, and phalangoepiphyseal dysplasia [ 109 ].
In most cases of uncombable hair syndrome, the hair texture and manageability improve with ageing [ 111 ].
Ectodermal Dysplasias
Ectodermal dysplasias include a big group of disorders characterized by isolated or associated abnormalities in the teeth, hair, nails, and sweating function [ 113 ]. These disorders may also include abnormalities in other ectoderm-derived structures such as the meibomian glands, mammary glands, branchial arch cartilages, and pigment cells, anterior pituitary, thymus, and melanocytes [ 114 , 115 ].
Hair is the most frequent appendage affected by ectodermal dysplasias [ 115 ], with manifestations of alopecia and hypotrichosis. Common trichoscopic findings in ectodermal dysplasia include follicular units with a single hair, abnormalities in hair shaft pigmentation, pili torti, trichoschisis, pili canaliculi, trichorrhexis nodosa, and pseudomonilethrix [ 116 ].
Hypohidrotic Ectodermal Dysplasia (Christ–Siemens–Touraine Syndrome)
Hypohidrotic ectodermal dysplasia (HED) is an ectodermal dysplasia which principally causes sparse hair, the inability to sweat, and abnormal or missing teeth (Fig. 8 ). The X-linked form is the most common, occurring in approximately 1 in 17,000 live births [ 117 ]. Males are disproportionately affected by the X-linked HED; however, approximately one-third of cases are inherited in either an autosomal recessive or autosomal dominant pattern, of which males and females are affected equally [ 114 ]. Approximately 90% of cases are due to mutations in the EDA1 , EDAR , EDARADD , or WNT10A genes [ 118 ]. These genes encode for proteins utilized in the tumor necrosis factor α (TNFα) signaling pathway [ 117 ]. These mutations disrupt communication between surface epithelial cells and the underlying mesenchyme during embryonic development, thereby impairing the development of skin appendages [ 119 ].

Hypohidrotic ectodermal dysplasia. Scalp hair is thin, sparse, slow-growing, and lightly pigmented. Note the flat nasal bridge
Hypohidrosis due to hypoplasia of sweat glands leads to fevers as a child and heat intolerance throughout life, especially during exercise [ 120 ]. Hypodontia is seen with an average of nine permanent teeth in patients with HED, which are frequently smaller than normal and with altered shape [ 121 ]. Patients with HED exhibit a typical facies with prominent forehead, thick lips, and a flattened nasal bridge [ 122 ].
Scalp hair is thin, sparse, slow-growing, and lightly pigmented, though secondary sexual hair can be normal [ 122 ]. In microscopic hair analysis of 22 patients with HED, investigators found an increased incidence of variable shaft thickness, trichorrhexis nodosa, and pili torti compared to normal controls [ 123 ]. Phototrichogram analysis in a control-matched group of 12 patients with HED showed significantly decreased number of terminal hairs, decreased number of follicular units, decreased number of hairs per follicular unit, decreased terminal hair width, and decreased hair growth rate [ 124 ].
No specific guidelines for diagnosing HED have been published. Individuals are typically diagnosed during infancy as a result of the characteristic features of hypotrichosis, hypohidrosis, and hypodontia and typical facies [ 122 ]. Hypohidrosis can be confirmed with the starch–iodine test.
Biopsy is not routinely performed; however, horizontally sectioned 4-mm punch biopsy specimens of the scalp or palms that lack eccrine structures are diagnostic of HED; scalp biopsy is much more sensitive than palmar biopsy [ 123 ].
Genetic testing for mutations in the EDAR , EDARADD , or WNT10A genes can be done to confirm diagnosis.
There is currently no cure for HED, so treatment is focused on managing symptoms. It is important for HED patients to control their exposure to heat in light of their hypohidrosis. During hot weather, they should have access to a cool environment and plenty of water. A dentist can help treat the patient’s dental symptoms.
There is some promising data regarding EDA-A1 replacement protein that binds to the EDA-A1 receptor (EDAR) called EDI200 developed by Edimer Pharmaceuticals. EDI200 is a targeted therapy that has been shown to be effective in preventing manifestation of the disease when administered to newborn X-linked HED dog and mouse animal models [ 125 ]. These benefits persisted through adulthood in these animals. However, a phase II clinical trial (ClinicalTrials.gov Identifier NCT01775462) showed inconclusive results in humans [ 122 ].
Management of hair symptoms is discussed below.
Hidrotic Ectodermal Dysplasia (Clouston Syndrome)
Hidrotic ectodermal dysplasia (Clouston syndrome) is a rare autosomal dominant disorder characterized by nail thickening/shortening, palmoplantar keratoderma, and short, thin sparse hair. It is caused by different missense mutations in the gap junction β6 gene ( GJB6 ), which encodes for connexin-30 [ 126 ]. The disease is most frequently associated with those of French–Canadian descent [ 127 ], but has been seen in other ethnicities. Unlike hypohidrotic ectodermal dysplasia, patients with Clouston syndrome have the ability to sweat and have normal dentition.
Patients with Clouston exhibit pale-colored, patchy, wiry, and brittle scalp hair during infancy, with progressive hair loss typically leading to total alopecia by puberty. Eyebrows, axillary, and pubic hair are sparse or absent, and eyelashes are short and sparse [ 128 ]. Hair abnormalities under light microscopy include trichorrhexis nodosa, trichoptilosis, pili bifurcati, variable diameter, damaged cuticles, and irregular helical twists [ 129 , 130 ]. Electron microscopy of the abnormal hair shows a square shape in transverse section and longitudinal grooving [ 131 ].
Clouston syndrome should be suspected in individuals with nail dystrophy, hypotrichosis, and palmoplantar hyperkeratosis starting early in life [ 128 ]. The diagnosis can be confirmed by genetic analysis. The best initial genetic test is targeted analysis for the four known GJB6 pathogenic variants, and if initial testing is inconclusive, sequence analysis can be done [ 126 ].
There is no cure for Clouston disease; its treatment involves management of symptoms. Artificial nails may be used to improve appearance of nails. Skin emollients may improve palmoplantar hyperkeratosis [ 128 ].
AEC Syndrome/Rapp–Hodgkin Syndrome
AEC syndrome is an ectodermal dysplasia characterized by ankyloblepharon (partial or complete fusion of the eyelids), ectodermal defects, and cleft lip/palate. Rapp–Hodgkin syndrome is distinguished from AEC syndrome by the absence of ankyloblepharon [ 132 ]. Once thought to be separate disorders, the two diseases are now considered to be varying presentations of the same genetic disease [ 132 , 133 , 134 , 135 ]. AEC syndrome is due to a mutation in the TP63 gene, coding for the p63 protein, which is involved in epidermal differentiation [ 136 ]. The disease has an autosomal dominant pattern of inheritance, though approximately 70% of mutations arise de novo [ 137 ]. Additional symptoms include dental hypoplasia, nail dysplasia, decreased sweating, and hair symptoms described below [ 137 ].
Virtually 100% of newborns with AEC syndrome have skin erosions of the scalp of varying severity, with severe erosions leading to scarring alopecia and hypotrichosis (Fig. 9 ) [ 137 ]. In a review of 72 cases of Rapp–Hodgkin syndrome, 82% of cases exhibited hair described as dry, wiry, and sparse; 36% showed pili torti et canaliculi, 24% had hypopigmented hair, 21% had scalp dermatitis, and 18% had a prominent forehead or high frontal hairline [ 138 ]. Scalp hair loss frequently begins at puberty and continues through the 20s and 30s, and typically affects the frontal hairline to the crown, with relative sparing of the occipital and temporal regions, but often leads to almost complete hair loss [ 138 ]. Absence or thinning of eyebrows and eyelashes is common, and body hair is usually sparse. Varying severity of Rapp–Hodgkin syndrome can manifest with different degrees of hair symptoms.

Clinical picture of AEC syndrome with scalp erosions leading to scarring alopecia and hypotrichosis
Diagnosis can be suspected owing to the characteristic clinical features described above, and can be confirmed with sequence analysis of the TP63 gene [ 137 ].
Treatment focuses on management of symptoms. Neonatal scalp skin erosions should be treatment with dilute bleach soaks in order to prevent secondary infection [ 137 ], perhaps decreasing incidence of scarring alopecia after healing. Cleft lip and palate can be corrected by surgery, and ankyloblepharon typically resolves on its own but may be corrected by an ophthalmologist if necessary [ 137 ].
Managing Hair Symptoms of Ectodermal Dysplasias
The use of topical minoxidil has been proposed and its effectiveness in certain types of epidermal dysplasia is supported by isolated case reports, used either on its own [ 139 ] or in combination with topical tretinoin [ 140 ]. Using only topical minoxidil is probably the safer option due to possibility of side effects when used in combination with tretinoin, such as eruptive pyogenic granuloma [ 141 ]. The cases supporting the effectiveness of minoxidil involved HED and Clouston syndrome [ 142 ]; it is unknown whether minoxidil’s effectiveness is generalizable to other forms of ectodermal dysplasia.
Some surgical techniques have been used with success. Patients are generally poor candidates for hair transplant because of lack of sufficient donor sites [ 143 ]. However, autologous hair transplantation has been used to replace eyebrows in a patient with ectodermal dysplasia [ 144 ]. Tissue expansion surgery has been successfully used to correct areas of alopecia in a patient with hypohidrotic ectodermal dysplasia [ 145 ].
Patients may opt for use of a wig. A great resource for education and support meant for patients with ectodermal dysplasia is The National Foundation for Ectodermal Dysplasias ( http://www.NFED.org ).
Trichorhinophalangeal Syndrome (TRPS)
Trichorhinophalangeal syndrome (TRPS) is a group of two autosomal dominant genetic diseases (TRPS I and TRPS II) characterized by skeletal abnormalities, distinct facial features, and ectodermal features. TRPS I is caused by a pathogenic variant of the TRPS1 gene, and TRPS II is caused by a continuous 8q23.3–q24.11 deletion including the TRPS1 , RAD21 , and EXT1 genes. Clinical features include a large pear-shaped nose, thick and broad eyebrows, prominent ears, short stature, short digits, cone-shaped epiphyses, dystrophic nails, and fine, sparse hair. TRPS II may be accompanied by mild to moderate intellectual disability [ 146 ].
The hair of patients with TRPS is typically fine, sparse, slow-growing, and not very pigmented [ 146 ]. The pathologic change and pattern of hair loss is similar to that seen in male pattern baldness, with recession of the frontotemporal hairline and thinning of hair diameter [ 147 ]. Approximately one-third of males go nearly or completely bald within a few years after puberty, while women typically keep most of their hair but have a high frontal hairline [ 148 ]. Patients may have sparse lateral eyebrows and eyelashes [ 149 ].
Scanning electron microscopy of the hair shaft may be normal or show changes in cuticular pattern and hair shaft structure [ 150 ]. Light microscopy may show thinning of the distal end of the hair shaft, trichorrhexis nodosa, and trichoptilosis [ 149 , 151 ].
In mice, the TRPS1 gene has been shown to be involved in the Wnt signaling pathway, involved in follicle morphogenesis. In humans with TRPS, two keratin-related genes ( KRT6C and KRTAP3-1 ) were found to be downregulated in balding areas of the scalp as compared to nonbalding areas. TRPS1 protein expression has been shown to be regulated by androgens [ 152 ], providing a possible mechanism for why hair loss seen in TRPS can mimic male pattern baldness.
Diagnosis can typically be made clinically on the basis of typical findings. Many cases, especially in TRPS II, arise de novo and thus family history is not necessary to make a diagnosis. Sequence analysis can typically confirm the diagnosis of TRPS I, and chromosomal microarray analysis can be used to diagnose TRPS II.
Despite similarities in appearance to male pattern baldness, topical minoxidil and oral finasteride have not been shown to be effective in patients with TRPS. Hair transplant has been shown to be a viable option in these patients, with favorable results seen at 3-year follow-up [ 147 ]. In patients for whom hair transplant is not an option, the use of wigs can be considered if desired [ 146 ].
Atrichia with Papular Lesions
Atrichia with papular lesions (APL) is a rare autosomal recessive disease with irreversible alopecia of the scalp, eyebrows, axillary, and pubic hair, which starts a few months after birth and is associated with development keratin cysts over the body [ 153 ].
It is due to mutation in the zinc finger domain of human hairless gene (HL) on chromosome region 8p12 [ 154 ]. The hair matrix cells in APL undergo premature apoptosis associated with loss of neural cell adhesion molecule positivity and disconnection from overlying epithelial sheath. This results in loss of messages between dermal papillae and the bulge’s stem cells leading to disruption in hair growth [ 155 ]. Lanugo hairs are present at birth, but the alopecia is complete within the first year of life as the catagen follicles are unable to re-enter the anagen phase. Progressive keratin retention into follicular structures results in cyst formation, clinically evident as papules [ 156 ].
Histology of this disorder shows the infundibular part of the hair follicle with replacement of the middle and lower part by keratinizing cysts. Differential diagnosis includes vitamin D-resistant rickets type II, which also causes total alopecia in early life. It is due to a mutation of vitamin D receptor (VDR), suggesting that VDR and HL gene, both of which are zinc finger proteins, may be involved in the same genetic pathway of hair follicle control [ 157 ].
Another clinical differential diagnosis of APL is alopecia universalis (AU), so AU should be excluded to avoid the need for systemic steroid and immunosuppressive medication [ 158 ].
Diagnostic criteria of this disorder were revised by Yip et al. (Tables 1 , 2 ) [ 159 ].
Cui C-Y, Schlessinger D. EDA signaling and skin appendage development. Cell Cycle. 2006;5(21):2477–83. https://doi.org/10.4161/cc.5.21.3403 .
Article CAS PubMed Google Scholar
Basel-Vanagaite L, Pasmanik-Chor M, Lurie R, Yeheskel A, Kjaer KW. CDH3-related syndromes: report on a new mutation and overview of the genotype-phenotype correlations. Mol Syndromol. 2010;1(5):223–30. https://doi.org/10.1159/000327156 .
Duverger O, Morasso MI. To grow or not to grow: hair morphogenesis and human genetic hair disorders. Semin Cell Dev Biol. 2014;25–26:22–33. https://doi.org/10.1016/j.semcdb.2013.12.006 .
Article PubMed Google Scholar
Pasternack SM, Refke M, Paknia E, et al. Mutations in SNRPE, which encodes a core protein of the spliceosome, cause autosomal-dominant hypotrichosis simplex. Am J Hum Genet. 2013;92(1):81–7. https://doi.org/10.1016/j.ajhg.2012.10.022 .
Article CAS PubMed PubMed Central Google Scholar
Xu C, Zhang L, Chen N, et al. A new locus for hereditary hypotrichosis simplex maps to chromosome 13q12.12 approximately 12.3 in a Chinese family. J Cutan Pathol. 2010;37(7):758–63. https://doi.org/10.1111/j.1600-0560.2009.01415.x .
Cambiaghi S, Barbareschi M. A sporadic case of congenital hypotrichosis simplex of the scalp: difficulties in diagnosis and classification. Pediatr Dermatol. 16(4):301–4. http://www.ncbi.nlm.nih.gov/pubmed/10469417 . Accessed 21 Nov 2018.
Betz RC. Alopezien und Hypotrichosen im Kindesalter. Der Hautarzt. 2014;65(6):520–6. https://doi.org/10.1007/s00105-013-2714-y .
Article CAS Google Scholar
Betz RC, Lee YA, Bygum A, et al. A gene for hypotrichosis simplex of the scalp maps to chromosome 6p21.3. Am J Hum Genet. 2000;66(6):1979–83. https://doi.org/10.1086/302934 .
Toribio J, Quinones PA. Hereditary hypotrichosis simplex of the scalp. Br J Dermatol. 1974;91(6):687–96. https://doi.org/10.1111/j.1365-2133.1974.tb12455.x .
Mende B, Kreysel HW. [Hypotrichosis congenita hereditaria Marie Unna with Ehlers-Danlos syndrome and atopy]. Hautarzt. 1987;38(9):532–5. http://www.ncbi.nlm.nih.gov/pubmed/3692855 . Accessed 20 Nov 2018.
Yan KL, He PP, Yang S, et al. Marie Unna hereditary hypotrichosis: report of a Chinese family and evidence for genetic heterogeneity. Clin Exp Dermatol. 2004;29(5):460–3. https://doi.org/10.1111/j.1365-2230.2004.01570.x .
Podjasek JO, Hand JL. Marie-Unna hereditary hypotrichosis: case report and review of the literature. Pediatr Dermatol. 2011;28(2):202–4. https://doi.org/10.1111/j.1525-1470.2011.01387.x .
Yun S-K, Cho Y-G, Song KH, et al. Identification of a novel U2HR mutation in a Korean woman with Marie Unna hereditary hypotrichosis. Int J Dermatol. 2014;53(11):1358–61. https://doi.org/10.1111/ijd.12545 .
Yoshida K, Hayashi R, Shimomura Y, Niizeki H. Novel heterozygous mutation, c.74C>G (p.Pro25Arg), in the U2HR gene underlies Marie Unna hereditary hypotrichosis in a Japanese family. J Dermatol. 2017;44(8):e184–5. https://doi.org/10.1111/1346-8138.13868 .
Roberts JL, Whiting DA, Henry D, Basler G, Woolf L. Marie Unna congenital hypotrichosis: clinical description, histopathology, scanning electron microscopy of a previously unreported large pedigree. J Investig Dermatol Symp Proc. 1999;4(3):261–7. http://www.ncbi.nlm.nih.gov/pubmed/10674378 . Accessed 20 Nov 2018.
Mansur AT, Elcioglu NH, Redler S, et al. Marie Unna hereditary hypotrichosis: a Turkish family with loss of eyebrows and a U2HR mutation. Am J Med Genet A. 2010;152A(10):2628–33. https://doi.org/10.1002/ajmg.a.33649 .
Srinivas SM, Hiremagalore R. Marie-Unna hereditary hypotrichosis. Int J Trichol. 2014;6(4):182–4. https://doi.org/10.4103/0974-7753.142873 .
Article Google Scholar
Horev L, Tosti A, Rosen I, et al. Mutations in lipase H cause autosomal recessive hypotrichosis simplex with woolly hair. J Am Acad Dermatol. 2009;61(5):813–8. https://doi.org/10.1016/j.jaad.2009.04.020 .
Shinkuma S, Akiyama M, Inoue A, et al. Prevalent LIPH founder mutations lead to loss of P2Y5 activation ability of PA-PLA1alpha in autosomal recessive hypotrichosis. Hum Mutat. 2010;31(5):602–10. https://doi.org/10.1002/humu.21235 .
Shimomura Y, Wajid M, Ishii Y, et al. Disruption of P2RY5, an orphan G protein-coupled receptor, underlies autosomal recessive woolly hair. Nat Genet. 2008;40(3):335–9. https://doi.org/10.1038/ng.100 .
Salamon T. On a family with the recessive trait of woolly hair, hypotrichosis and other anomalies. Hautarzt. 1963;14:540–4. http://www.ncbi.nlm.nih.gov/pubmed/14113527 . Accessed 20 Nov 2018.
Itoh E, Nakahara T, Furumura M, Furue M, Shimomura Y. Case of autosomal recessive woolly hair/hypotrichosis with atopic dermatitis. J Dermatol. 2017;44(10):1185–6. https://doi.org/10.1111/1346-8138.13660 .
Sprecher E, Bergman R, Richard G, et al. Hypotrichosis with juvenile macular dystrophy is caused by a mutation in CDH3, encoding P-cadherin. Nat Genet. 2001;29(2):134–6. https://doi.org/10.1038/ng716 .
Wagner H. Makulaaffektion vergesellschaftet mit Haarabnormalitat von anugotypus, beide vielleicht angeboren bei zwei Geschwistern. Graefes Arch Klin Exp Ophthalmol. 1935;134:71.
Karti O, Abali S, Ayhan Z, et al. CDH3 gene related hypotrichosis and juvenile macular dystrophy—a case with a novel mutation. Am J Ophthalmol Case Rep. 2017;7:129–33. https://doi.org/10.1016/j.ajoc.2017.06.007 .
Article PubMed PubMed Central Google Scholar
Khan AO, Bolz HJ. Phenotypic observations in “hypotrichosis with juvenile macular dystrophy” (recessive CDH3 mutations). Ophthalmic Genet. 2016;37(3):301–6. https://doi.org/10.3109/13816810.2015.1071411 .
Elfatoiki FZ, Cordoliani F, Pascal Regane P, Afforitit-Demoge A. Hypotrichosis with juvenile macular dystrophy: Portuguese case. Dermatol Online J. 2016;22(5). http://www.ncbi.nlm.nih.gov/pubmed/27617529 . Accessed 20 Nov 2018.
Indelman M, Eason J, Hummel M, et al. Novel CDH3 mutations in hypotrichosis with juvenile macular dystrophy. Clin Exp Dermatol. 2007;32(2):191–6. http://www.ncbi.nlm.nih.gov/pubmed/17342797 . Accessed 20 Nov 2018.
Jelani M, Salman Chishti M, Ahmad W. A novel splice-site mutation in the CDH3 gene in hypotrichosis with juvenile macular dystrophy. Clin Exp Dermatol. 2009;34(1):68–73. https://doi.org/10.1111/j.1365-2230.2008.02933.x .
Kamran-ul-Hassan Naqvi S, Azeem Z, Ali G, Ahmad W. A novel splice-acceptor site mutation in CDH3 gene in a consanguineous family exhibiting hypotrichosis with juvenile macular dystrophy. Arch Dermatol Res. 2010;302(9):701–3. https://doi.org/10.1007/s00403-010-1035-6 .
Indelman M, Bergman R, Lurie R, et al. A missense mutation in CDH3, encoding P-cadherin, causes hypotrichosis with juvenile macular dystrophy. J Investig Dermatol. 2002;119(5):1210–3. https://doi.org/10.1046/j.1523-1747.2002.19528.x .
Indelman M, Hamel CP, Bergman R, et al. Phenotypic diversity and mutation spectrum in hypotrichosis with juvenile macular dystrophy. J Investig Dermatol. 2003;121(5):1217–20. https://doi.org/10.1046/j.1523-1747.2003.12550_1.x .
Indelman M, Leibu R, Jammal A, Bergman R, Sprecher E. Molecular basis of hypotrichosis with juvenile macular dystrophy in two siblings. Br J Dermatol. 2005;153(3):635–8. https://doi.org/10.1111/j.1365-2133.2005.06734.x .
Mason JO, Patel SA. A case of hypotrichosis with juvenile macular dystrophy. Retin Cases Brief Rep. 2015;9(2):164–7. https://doi.org/10.1097/ICB.0000000000000127 .
Shimomura Y, Wajid M, Kurban M, Christiano AM. Splice site mutations in the P-cadherin gene underlie hypotrichosis with juvenile macular dystrophy. Dermatology. 2010;220(3):208–12. https://doi.org/10.1159/000275673 .
Avitan-Hersh E, Indelman M, Khamaysi Z, Leibu R, Bergman R. A novel nonsense CDH3 mutation in hypotrichosis with juvenile macular dystrophy. Int J Dermatol. 2012;51(3):325–7. https://doi.org/10.1111/j.1365-4632.2011.04973.x .
Halford S, Holt R, Németh AH, Downes SM. Homozygous deletion in CDH3 and hypotrichosis with juvenile macular dystrophy. Arch Ophthalmol. 2012;130(11):1490–2. https://doi.org/10.1001/archophthalmol.2012.708 .
Ahmad F, Ali RH, Muhammad D, et al. Novel homozygous sequence variants in the CDH3 gene encoding P-cadherin underlying hypotrichosis with juvenile macular dystrophy in consanguineous families. Eur J Dermatol. 2016;26(6):610–2. https://doi.org/10.1684/ejd.2016.2848 .
Blanco-Kelly F, Rodrigues-Jacy da Silva L, Sanchez-Navarro I, et al. New CDH3 mutation in the first Spanish case of hypotrichosis with juvenile macular dystrophy, a case report. BMC Med Genet. 2017;18(1):1. https://doi.org/10.1186/s12881-016-0364-5 .
Vicente LP, Finzi S, Susanna R, Young TL. Hypotrichosis with juvenile macular dystrophy: a case report with molecular study. Arq Bras Oftalmol. 2017;80(1):49–51. https://doi.org/10.5935/0004-2749.20170013 .
Rogers M. Hair shaft abnormalities: part I. Australas J Dermatol. 1995;36(4):179–84. http://www.ncbi.nlm.nih.gov/pubmed/8593104 . Accessed 13 Nov 2018 (quiz 185–6).
Martin AM, Sugathan P. Localised acquired trichorrhexis nodosa of the scalp hair induced by a specific comb and combing habit—a report of three cases. Int J Trichol. 2011;3(1):34–7. https://doi.org/10.4103/0974-7753.82138 .
Hwang ST, Park BC. Trichorrhexis nodosa after hair transplantation: dermoscopic, pathologic and electron microscopy analyses. Dermatol Surg. 2013;39(11):1721–4. https://doi.org/10.1111/dsu.12325 .
Summar ML, Dobbelaere D, Brusilow S, Lee B. Diagnosis, symptoms, frequency and mortality of 260 patients with urea cycle disorders from a 21-year, multicentre study of acute hyperammonaemic episodes. Acta Paediatr. 2008;97(10):1420–5. https://doi.org/10.1111/j.1651-2227.2008.00952.x .
Urea Cycle Disorders Conference group. Consensus statement from a conference for the management of patients with urea cycle disorders. J Pediatr. 2001;138(1 Suppl):S1–5. http://www.ncbi.nlm.nih.gov/pubmed/11148543 . Accessed 13 Nov 2018.
Patel HP, Unis ME. Pili torti in association with citrullinemia. J Am Acad Dermatol. 1985;12(1 Pt 2):203–6. http://www.ncbi.nlm.nih.gov/pubmed/3973120 . Accessed 8 Feb 2019.
Slonim AE, Sadick N, Pugliese M, Meyers-Seifer CH. Clinical response of alopecia, trichorrhexis nodosa, and dry, scaly skin to zinc supplementation. J Pediatr. 1992;121(6):890–5. http://www.ncbi.nlm.nih.gov/pubmed/1447651 . Accessed 13 Nov 2018.
Rudnicka L, Rakowska A, Kurzeja M, Olszewska M. Hair shafts in trichoscopy. Dermatol Clin. 2013;31(4):695–708. https://doi.org/10.1016/j.det.2013.06.007 .
Saleem HMK, Shahid MF, Shahbaz A, Sohail A, Shahid MA, Sachmechi I. Netherton syndrome: a case report and review of literature. Cureus. 2018;10(7):e3070. https://doi.org/10.7759/cureus.3070 .
Powell J, Dawber RP, Ferguson DJ, Griffiths WA. Netherton’s syndrome: increased likelihood of diagnosis by examining eyebrow hairs. Br J Dermatol. 1999;141(3):544–6. http://www.ncbi.nlm.nih.gov/pubmed/10583065 . Accessed 13 Nov 2018.
Ito M, Ito K, Hashimoto K. Pathogenesis in trichorrhexis invaginata (bamboo hair). J Investig Dermatol. 1984;83(1):1–6. http://www.ncbi.nlm.nih.gov/pubmed/6547464 . Accessed 14 Nov 2018.
Caputo R, Vanotti P, Bertani E. Netherton’s syndrome in two adult brothers. Arch Dermatol. 1984;120(2):220–2. http://www.ncbi.nlm.nih.gov/pubmed/6696474 . Accessed 14 Nov 2018.
Suga Y, Tsuboi R, Hashimoto Y, Yoshiike T, Ogawa H. A case of ichthyosis linearis circumflexa successfully treated with topical tacrolimus. J Am Acad Dermatol. 2000;42(3):520–2. http://www.ncbi.nlm.nih.gov/pubmed/10688732 . Accessed 14 Nov 2018.
Wehr RF, Hickman J, Krochmal L. Effective treatment of Netherton’s syndrome with 12% lactate lotion. J Am Acad Dermatol. 1988;19(1 Pt 1):140–2. http://www.ncbi.nlm.nih.gov/pubmed/3403739 . Accessed 14 Nov 2018.
de Oliveira EF, de Araripe ALCA. Monilethrix: a typical case report with microscopic and dermatoscopic findings. An Bras Dermatol. 2015;90(1):126–7. https://doi.org/10.1590/abd1806-4841.20153357 .
Amichai B, Metzker A. Hair loss in a 6-month-old child. Monilethrix. Arch Dermatol. 1996;132(5):574–5, 577–8. http://www.ncbi.nlm.nih.gov/pubmed/8624158 . Accessed 8 Feb 2019.
van Steensel M, Vreeburg M, Urbina MT, López P, Morice-Picard F, van Geel M. Novel KRT83 and KRT86 mutations associated with monilethrix. Exp Dermatol. 2015;24(3):222–4. https://doi.org/10.1111/exd.12624 .
Ullah A, Raza SI, Ali RH, et al. A novel deletion mutation in the DSG4 gene underlies autosomal recessive hypotrichosis with variable phenotype in two unrelated consanguineous families. Clin Exp Dermatol. 2015;40(1):78–84. https://doi.org/10.1111/ced.12457 .
Narmatha GR, Chithra S, Balasubramanian N. Monilethrix. Indian J Dermatol Venereol Leprol. 68(4):220–1. http://www.ncbi.nlm.nih.gov/pubmed/17656942 . Accessed 8 Feb 2019.
Singh G, Siddalingappa K, Nischal KC, Naik LC, Lokanatha K. Monilethrix in three generations. Indian J Dermatol. 2008;53(2):99–100. https://doi.org/10.4103/0019-5154.41660 .
Ferrando J, Galve J, Torres-Puente M, Santillán S, Nogués S, Grimalt R. Monilethrix: a new family with the novel mutation in KRT81 gene. Int J Trichol. 2012;4(1):53–5. https://doi.org/10.4103/0974-7753.96105 .
Shah V, Tharini GK, Manoharan K. Monilethrix with Holt-Oram syndrome: case report of a rare association. Int J Trichol. 2015;7(1):33–5. https://doi.org/10.4103/0974-7753.153455 .
Bentley-Phillips B, Bayles MA. A previously undescribed hereditary hair anomaly (pseudo-monilethrix). Br J Dermatol. 1973;89(2):159–67. http://www.ncbi.nlm.nih.gov/pubmed/4726892 . Accessed 14 Nov 2018.
Mirmirani P, Huang KP, Price VH. A practical, algorithmic approach to diagnosing hair shaft disorders. Int J Dermatol. 2011;50(1):1–12. https://doi.org/10.1111/j.1365-4632.2010.04768.x .
de Berker D, Dawber RP. Monilethrix treated with oral retinoids. Clin Exp Dermatol. 1991;16(3):226–8. http://www.ncbi.nlm.nih.gov/pubmed/1934581 . Accessed 20 Nov 2018.
Karincaoglu Y, Coskun BK, Seyhan ME, Bayram N. Monilethrix: improvement with acitretin. Am J Clin Dermatol. 2005;6(6):407–10. https://doi.org/10.2165/00128071-200506060-00008 .
Rossi A, Iorio A, Scali E, et al. Monilethrix treated with minoxidil. Int J Immunopathol Pharmacol. 2011;24(1):239–42. https://doi.org/10.1177/039463201102400129 .
Sinclair R. Treatment of monilethrix with oral minoxidil. JAAD Case Rep. 2016;2(3):212–5. https://doi.org/10.1016/j.jdcr.2016.02.011 .
Rudnicka L, Rakowska A, Kerzeja M, Olszewska M. Hair shafts in trichoscopy: clues for diagnosis of hair and scalp diseases. Dermatol Clin. 2013;31(4):695–708. https://doi.org/10.1016/j.det.2013.06.007 .
Choudhary S, Tarafdar P, Jawade S, Singh A. A point to note in pili torti. Int J Trichol. 2018;10(2):95. https://doi.org/10.4103/ijt.ijt_111_16 .
Martin-Scott I. Congenital pilar defect showing features of pili torti. Br J Dermatol. 1953;65(1):35–6. http://www.ncbi.nlm.nih.gov/pubmed/13019001 . Accessed 20 Nov 2018.
Marubashi Y, Yanagishita T, Muto J, et al. Morphological analyses in fragility of pili torti with Björnstad syndrome. J Dermatol. 2017;44(4):455–8. https://doi.org/10.1111/1346-8138.13700 .
Crandall BF, Samec L, Sparkes RS, Wright SW. A familial syndrome of deafness, alopecia, and hypogonadism. J Pediatr. 1973;82(3):461–5. http://www.ncbi.nlm.nih.gov/pubmed/4698933 . Accessed 20 Nov 2018.
Cosimo QC, Daniela L, Elsa B, Carlo D-V, Giuseppe F. Kinky hair, kinky vessels, and bladder diverticula in Menkes disease. J Neuroimaging. 2011;21(2):e114–6. https://doi.org/10.1111/j.1552-6569.2010.00476.x .
Yung A, Newton-Bishop JA. A case of Bazex–Dupré–Christol syndrome associated with multiple genital trichoepitheliomas. Br J Dermatol. 2005;153(3):682–4. https://doi.org/10.1111/j.1365-2133.2005.06819.x .
Yesenia Arévalo N, Buján MM, Cervini AB, Pierini AM. Bazex–Dupré–Christol syndrome: case series. Arch Argent Pediatr. 2015;113(5):e256–9. https://doi.org/10.5546/aap.2015.e256 .
Herges A, Stieler W, Stadler R. [Bazex-Dupré-Christol syndrome. Follicular atrophoderma, multiple basal cell carcinomas and hypotrichosis]. Hautarzt. 1993;44(6):385–91. http://www.ncbi.nlm.nih.gov/pubmed/8335462 . Accessed 8 Feb 2019.
Singh G, Miteva M. Prognosis and management of congenital hair shaft disorders with fragility-part I. Pediatr Dermatol. 2016;33(5):473–80. https://doi.org/10.1111/pde.12894 .
Lambert WC, Gagna CE, Lambert MW. Trichothiodystrophy: photosensitive, TTD-P, TTD, Tay syndrome. Adv Exp Med Biol. 2010;685:106–10. http://www.ncbi.nlm.nih.gov/pubmed/20687499 . Accessed 26 Nov 2018.
Hashimoto S, Egly JM. Trichothiodystrophy view from the molecular basis of DNA repair/transcription factor TFIIH. Hum Mol Genet. 2009;18(R2):R224–30. https://doi.org/10.1093/hmg/ddp390 .
Yang YW, Yarbrough K, Mitkov M, Russi D, Price HN, Swanson DL. Polarized transilluminating dermoscopy: bedside trichoscopic diagnosis of trichothiodystrophy. Pediatr Dermatol. 2018;35(1):147–9. https://doi.org/10.1111/pde.13290 .
Theil AF, Mandemaker IK, van den Akker E, et al. Trichothiodystrophy causative TFIIEβ mutation affects transcription in highly differentiated tissue. Hum Mol Genet. 2017;26(23):4689–98. https://doi.org/10.1093/hmg/ddx351 .
Giehl KA, Eckstein GN, Benet-Pagès A, et al. A gene locus responsible for the familial hair shaft abnormality pili annulati maps to chromosome 12q24.32–24.33. J Investig Dermatol. 2004;123(6):1073–7. https://doi.org/10.1111/j.0022-202x.2004.23423.x .
Akoglu G, Emre S, Metin A, et al. Pili annulati with fragility: electron microscopic findings of a case. Int J Trichol. 2012;4(2):89–92. https://doi.org/10.4103/0974-7753.96909 .
Castelli E, Fiorella S, Caputo V. Pili annulati coincident with alopecia areata, autoimmune thyroid disease, and primary IgA deficiency: case report and considerations on the literature. Case Rep Dermatol. 2012;4(3):250–5. https://doi.org/10.1159/000345469 .
Werner K, St-Surin-Lord S, Sperling LC. Pili annulati associated with hair fragility: cause or coincidence? Cutis. 2013;91(1):36–8. http://www.ncbi.nlm.nih.gov/pubmed/23461057 . Accessed 21 Nov 2018.
Gonzalez AM, Borda LJ, Tosti A. Pili annulati with severe trichorrhexis nodosa: a case report and review of the literature. Skin Appendage Disord. 2019;5(2):114–6. https://doi.org/10.1159/000491910 .
Hofbauer GF, Tsambaos D, Spycher MA, Trüeb RM. Acquired hair fragility in pili anulati: causal relationship with androgenetic alopecia. Dermatology. 2001;203(1):60–2. https://doi.org/10.1159/000051706 .
Berk DR, Bayliss SJ, Giehl KA. Pili annulati: a report of 2 American families. Cutis. 2013;91(5):254–57. http://www.ncbi.nlm.nih.gov/pubmed/23772432 . Accessed 21 Nov 2018.
Smith SR, Kirkpatrick RC, Kerr JH, Mezebich D. Alopecia areata in a patient with pili annulati. J Am Acad Dermatol. 1995;32(5 Pt 1):816–8. http://www.ncbi.nlm.nih.gov/pubmed/7722034 . Accessed 21 Nov 2018.
Fujimoto A, Farooq M, Fujikawa H, et al. A missense mutation within the helix initiation motif of the keratin K71 gene underlies autosomal dominant woolly hair/hypotrichosis. J Investig Dermatol. 2012;132(10):2342–9. https://doi.org/10.1038/jid.2012.154 .
Hutchinson PE, Cairns RJ, Wells RS. Woolly hair. Clinical and general aspects. Trans St Johns Hosp Dermatol Soc. 1974;60(2):160–77. http://www.ncbi.nlm.nih.gov/pubmed/4467886 . Accessed 20 Nov 2018.
Shimomura Y, Wajid M, Petukhova L, Kurban M, Christiano AM. Autosomal-dominant woolly hair resulting from disruption of keratin 74 (KRT74), a potential determinant of human hair texture. Am J Hum Genet. 2010;86(4):632–8. https://doi.org/10.1016/j.ajhg.2010.02.025 .
Nakamura M, Tokura Y. Congenital woolly hair without P2RY5 mutation. Dermatoendocrinol. 2009;1(1):58–9. http://www.ncbi.nlm.nih.gov/pubmed/20046591 . Accessed 21 Nov 2018.
Hayashi R, Inoue A, Suga Y, Aoki J, Shimomura Y. Analysis of unique mutations in the LPAR6 gene identified in a Japanese family with autosomal recessive woolly hair/hypotrichosis: establishment of a useful assay system for LPA6. J Dermatol Sci. 2015;78(3):197–205. https://doi.org/10.1016/j.jdermsci.2015.03.006 .
Baykan A, Olgar Ş, Argun M, et al. Different clinical presentations of Naxos disease and Carvajal syndrome: case series from a single tertiary center and review of the literature. Anatol J Cardiol. 2015;15(5):404–8. https://doi.org/10.5152/akd.2014.5413 .
Ramot Y, Zlotogorski A. The twisting tale of woolly hair: a trait with many causes. J Med Genet. 2015;52(4):217–23. https://doi.org/10.1136/jmedgenet-2014-102630 .
Polivka L, Bodemer C, Hadj-Rabia S. Combination of palmoplantar keratoderma and hair shaft anomalies, the warning signal of severe arrhythmogenic cardiomyopathy: a systematic review on genetic desmosomal diseases. J Med Genet. 2016;53(5):289–95. https://doi.org/10.1136/jmedgenet-2015-103403 .
Tursen U, Kaya TI, Ikizoglu G, Aktekin M, Aras N. Genetic syndrome with ichthyosis: congenital ichthyosis, follicular atrophoderma, hypotrichosis, and woolly hair; second report. Br J Dermatol. 2002;147(3):604–6. http://www.ncbi.nlm.nih.gov/pubmed/12207612 . Accessed 21 Nov 2018.
Srinivas SM, Kumar P, Basavaraja GV. Carvajal syndrome. Int J Trichol. 2016;8(1):53–5. https://doi.org/10.4103/0974-7753.179400 .
Islam AM, Rahman MT, Chowdhury AH. Cardiocutaneous syndrome (Naxos disease) in a Bangladeshi boy. Cardiovasc Diagn Ther. 2016;6(5):462–5. https://doi.org/10.21037/cdt.2016.03.07 .
Venugopal V, Karthikeyan S, Gnanaraj P, Narasimhan M. Woolly hair nevus: a rare entity. Int J Trichol. 2012;4(1):42–3. https://doi.org/10.4103/0974-7753.96090 .
Ruggieri M, Pavone V, Smilari P, Rizzo R, Sorge G. Primary osteoma cutis—multiple café-au-lait spots and woolly hair anomaly. Pediatr Radiol. 1995;25(1):34–6. http://www.ncbi.nlm.nih.gov/pubmed/7761159 . Accessed 21 Nov 2018.
Vasudevan B, Verma R, Pragasam V, Badad A. A rare case of woolly hair with unusual associations. Indian Dermatol Online J. 2013;4(3):222–4. https://doi.org/10.4103/2229-5178.115524 .
Pavone P, Falsaperla R, Barbagallo M, Polizzi A, Praticò AD, Ruggieri M. Clinical spectrum of woolly hair: indications for cerebral involvement. Ital J Pediatr. 2017;43(1):99. https://doi.org/10.1186/s13052-017-0417-1 .
Tanahashi K, Sugiura K, Takeichi T, et al. Prevalent founder mutation c.736T>A of LIPH in autosomal recessive woolly hair of Japanese leads to variable severity of hypotrichosis in adulthood. J Eur Acad Dermatol Venereol. 2013;27(9):1182–4. https://doi.org/10.1111/j.1468-3083.2012.04526.x .
Gonzalez FCG, Hernandez REG, Galilea ON. Woolly hair nevus in a toddler. Int J Trichol. 2014;6(4):187–8. https://doi.org/10.4103/0974-7753.142890 .
Cho S, Choi MJ, Zheng Z, Goo B, Kim D-Y, Cho SB. Clinical effects of non-ablative and ablative fractional lasers on various hair disorders: a case series of 17 patients. J Cosmet Laser Ther. 2013;15(2):74–9. https://doi.org/10.3109/14764172.2013.764436 .
Hicks J, Metry DW, Barrish J, Levy M. Uncombable hair (cheveux incoiffables, pili trianguli et canaliculi) syndrome: brief review and role of scanning electron microscopy in diagnosis. Ultrastruct Pathol. 25(2):99–103. http://www.ncbi.nlm.nih.gov/pubmed/11407534 . Accessed 21 Nov 2018.
Garty B, Metzker A, Mimouni M, Varsano I. Uncombable hair: a condition with autosomal dominant inheritance. Arch Dis Child. 1982;57(9):710–2. http://www.ncbi.nlm.nih.gov/pubmed/7125692 . Accessed 21 Nov 2018.
Hebert AA, Charrow J, Esterly NB, Fretzin DF, Opitz JM, Reynolds JF. Uncombable hair (pili trianguli et canaliculi): evidence for dominant inheritance with complete penetrance based on scanning electron microscopy. Am J Med Genet. 1987;28(1):185–93. https://doi.org/10.1002/ajmg.1320280126 .
Basmanav FBÜ, Cau L, Tafazzoli A, et al. Mutations in three genes encoding proteins involved in hair shaft formation cause uncombable hair syndrome. Am J Hum Genet. 2016;99(6):1292–304. https://doi.org/10.1016/j.ajhg.2016.10.004 .
Itin PH. Etiology and pathogenesis of ectodermal dysplasias. Am J Med Genet Part A. 2014;164(10):2472–7. https://doi.org/10.1002/ajmg.a.36550 .
Fete TJ, Grange DK. Ectodermal dysplasias. In: Hand JL, Corona R, editors. UpToDate. UpToDate, Waltham, MA. Accessed 22 Oct 2018.
Visinoni ÁF, Lisboa-Costa T, Pagnan NAB, Chautard-Freire-Maia EA. Ectodermal dysplasias: clinical and molecular review. Am J Med Genet Part A. 2009;149A(9):1980–2002. https://doi.org/10.1002/ajmg.a.32864 .
Rakowska A, Górska R, Rudnicka L, Zadurska M. Trichoscopic hair evaluation in patients with ectodermal dysplasia. J Pediatr. 2015;167(1):193–5. https://doi.org/10.1016/j.jpeds.2015.04.002 .
Trzeciak WH, Koczorowski R. Molecular basis of hypohidrotic ectodermal dysplasia: an update. J Appl Genet. 2016;57(1):51–61. https://doi.org/10.1007/s13353-015-0307-4 .
Cluzeau C, Hadj-Rabia S, Jambou M, et al. Only four genes (EDA1, EDAR, EDARADD, and WNT10A) account for 90% of hypohidrotic/anhidrotic ectodermal dysplasia cases. Hum Mutat. 2011;32(1):70–2. https://doi.org/10.1002/humu.21384 .
Schmidt-Ullrich R, Paus R. Molecular principles of hair follicle induction and morphogenesis. Bioessays. 2005;27(3):247–61. https://doi.org/10.1002/bies.20184 .
Hammersen JE, Neukam V, NüSken K-D, Schneider H. Systematic evaluation of exertional hyperthermia in children and adolescents with hypohidrotic ectodermal dysplasia: an observational study. Pediatr Res. 2011;70(3):297–301. https://doi.org/10.1203/PDR.0b013e318227503b .
Lexner MO, Bardow A, Hertz JM, Nielsen LA, Kreiborg S. Anomalies of tooth formation in hypohidrotic ectodermal dysplasia. Int J Paediatr Dent. 2007;17(1):10–8. https://doi.org/10.1111/j.1365-263X.2006.00801.x .
Wright JT, Grange DK, Fete M. Hypohidrotic ectodermal dysplasia. 2003 Apr 28 [Updated 2017 Jun 1]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews ® [Internet]. Seattle: University of Washington; 1993–2018.
Rouse C, Siegfried E, Breer W, Nahass G. Hair and sweat glands in families with hypohidrotic ectodermal dysplasia. Arch Dermatol. 2004;140(7):850–5. https://doi.org/10.1001/archderm.140.7.850 .
Jones KB, Goodwin AF, Landan M, et al. Characterization of X-linked hypohidrotic ectodermal dysplasia (XL-HED) hair and sweat gland phenotypes using phototrichogram analysis and live confocal imaging. Am J Med Genet A. 2013;161A(7):1585–93. https://doi.org/10.1002/ajmg.a.35959 .
Huttner K. Future developments in XLHED treatment approaches. Am J Med Genet Part A. 2014;164(10):2433–6. https://doi.org/10.1002/ajmg.a.36499 .
Lamartine J, Munhoz Essenfelder G, Kibar Z, et al. Mutations in GJB6 cause hidrotic ectodermal dysplasia. Nat Genet. 2000;26(2):142–4. https://doi.org/10.1038/79851 .
Clouston HR. A hereditary ectodermal dystrophy. Can Med Assoc J. 1929;21(1):18–31.
CAS PubMed PubMed Central Google Scholar
Der Kaloustian VM. Hidrotic ectodermal dysplasia 2. 2005 Apr 25 [Updated 2015 Jan 22]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews ® [Internet]. Seattle: University of Washington; 1993–2018.
Hirano SA, Mason AR, Salkey K, Williams JV, Pariser DM. Light microscopic hair shaft analysis in ectodermal dysplasia syndromes. Pediatr Dermatol. 2012;29(4):414–20. https://doi.org/10.1111/j.1525-1470.2011.01606.x .
Sanches S, Rebellato PRO, Fabre AB, de Campos GLM. Do you know this syndrome? Clouston syndrome. An Bras Dermatol. 2017;92(3):417–8. https://doi.org/10.1590/abd1806-4841.20175716 .
Escobar V, Goldblatt LI, Bixler D, Weaver D. Clouston syndrome: an ultrastructural study. Clin Genet. 1983;24(2):140–6.
Kannu P, Savarirayan R, Ozoemena L, White SM, McGrath JA. Rapp-Hodgkin ectodermal dysplasia syndrome: the clinical and molecular overlap with Hay–Wells syndrome. Am J Med Genet Part A. 2006;140A(8):887–91. https://doi.org/10.1002/ajmg.a.31187 .
Clements SE, Techanukul T, Holden ST, et al. Rapp–Hodgkin and Hay–Wells ectodermal dysplasia syndromes represent a variable spectrum of the same genetic disorder. Br J Dermatol. 2010;163(3):624–9. https://doi.org/10.1111/j.1365-2133.2010.09859.x .
Cambiaghi S, Tadini G, Barbareschi M, Menni S, Caputo R. Rapp–Hodgkin syndrome and AEC syndrome: are they the same entity? Br J Dermatol. 1994;130(1):97–101.
Bertola DR, Kim CA, Albano LMJ, Scheffer H, Meijer R, van Bokhoven H. Molecular evidence that AEC syndrome and Rapp–Hodgkin syndrome are variable expression of a single genetic disorder. Clin Genet. 2004;66(1):79–80. https://doi.org/10.1111/j.0009-9163.2004.00278.x .
Zarnegar BJ, Webster DE, Lopez-Pajares V, et al. Genomic profiling of a human organotypic model of AEC syndrome reveals ZNF750 as an essential downstream target of mutant TP63. Am J Hum Genet. 2012;91(3):435–43. https://doi.org/10.1016/j.ajhg.2012.07.007 .
Sutton VR, van Bokhoven H. TP63-related disorders. 2010 Jun 8 [Updated 2015 Aug 6]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews ® . Seattle: University of Washington; 1993–2018.
Park S-W, Yong SL, Martinka M, Shapiro J. Rapp-Hodgkin syndrome: a review of the aspects of hair and hair color. J Am Acad Dermatol. 2005;53(4):729–35. https://doi.org/10.1016/j.jaad.2005.05.038 .
Lee H-E, Chang I-K, Im M, Seo Y-J, Lee J-H, Lee Y. Topical minoxidil treatment for congenital alopecia in hypohidrotic ectodermal dysplasia. J Am Acad Dermatol. 2013;68(4):e139–40. https://doi.org/10.1016/j.jaad.2012.10.019 .
Melkote S, Dhurat RS, Palav A, Jerajani HR. Alopecia in congenital hidrotic ectodermal dysplasia responding to treatment with a combination of topical minoxidil and tretinoin. Int J Dermatol. 2009;48(2):184–5. https://doi.org/10.1111/j.1365-4632.2009.03907.x .
Baran R. Explosive eruption of pyogenic granuloma on the scalp due to topical combination therapy of minoxidil and retinoic acid. Dermatologica. 1989;179(2):76–8.
Article MathSciNet CAS PubMed Google Scholar
Harrison S, Sinclair R. Hypotrichosis and nail dysplasia: a novel hidrotic ectodermal dysplasia. Australas J Dermatol. 2004;45(2):103–5. https://doi.org/10.1111/j.1440-0960.2004.00055.x .
National Foundation for Ectodermal Dysplasias. Treating hair problems in ectodermal dysplasias. 2016. https://juyhw1n8m4a3a6yng24eww91-wpengine.netdna-ssl.com/wp-content/uploads/2016/06/Treating-Hair-Problems-in-Ectodermal-Dysplasias.pdf . Accessed 22 Oct 2018.
Nilforoushzadeh MA, Adibi N, Mirbagher L. A novel treatment strategy for eyebrow transplantation in an ectodermal dysplasia patient. J Res Med Sci. 2012;17(4):407–11.
PubMed PubMed Central Google Scholar
Mitsukawa N, Omori N, Tominaga M, et al. Tissue expansion for correction of alopecia in a child with hypohidrotic ectodermal dysplasia. J Dermatol. 2016;43(11):1382–4. https://doi.org/10.1111/1346-8138.13415 .
Maas S, Shaw A, Bikker H, Hennekam RC. Trichorhinophalangeal syndrome. 2017 Apr 20. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews ® [Internet]. Seattle (WA): University of Washington; 1993–2018.
Choi MS, Park MJ, Park M, et al. Treatment of hair loss in the trichorhinophalangeal syndrome. Ann Dermatol. 2018;30(3):382. https://doi.org/10.5021/ad.2018.30.3.382 .
Rudnicka L, Olszewska M, Waśkiel A, Rakowska A. Trichoscopy in hair shaft disorders. Dermatol Clin. 2018;36(4):421–30. https://doi.org/10.1016/j.det.2018.05.009 .
Seitz CS, Lüdecke H-J, Wagner N, Bröcker E-B, Hamm H. Trichorhinophalangeal syndrome type I. Arch Dermatol. 2001;137(11):1437–42. https://doi.org/10.1001/archderm.137.11.1437 .
Oh C, Jeon J, Kim J. Trichorhinophalangeal syndrome type I—clinical, microscopic, and molecular features. Indian J Dermatol Venereol Leprol. 2014;80(1):54. https://doi.org/10.4103/0378-6323.125515 .
Lalević-Vasić BM, Nikolić MM, Polić DJ. Study of hair in type I tricho-rhino-phalangeal syndrome. Ann Dermatol Venereol. 1994;121(9):618–22.
PubMed Google Scholar
Chang GTG, Jhamai M, van Weerden WM, Jenster G, Brinkmann AO. The TRPS1 transcription factor: androgenic regulation in prostate cancer and high expression in breast cancer. Endocr Relat Cancer. 2004;11(4):815–22. https://doi.org/10.1677/erc.1.00853 .
Bansal M, Manchanda K, Lamba S, Pandey S. Atrichia with papular lesions. Int J Trichol. 2011;3(2):112–4. https://doi.org/10.4103/0974-7753.90827 .
Thomas M, Daniel S. Atrichia congenita with papular lesions. Indian J Dermatol Venereol Leprol. 2011;77(1):70–2. https://doi.org/10.4103/0378-6323.74994 .
Verma R, Vasudevan B, Pragasam V, Badad A, Mitra D, Neema S. Congenital atrichia with papular lesions. Indian J Paediatr Dermatology. 2014;15(2):94–4. http://go.galegroup.com.access.library.miami.edu/ps/retrieve.do?tabID=T002&resultListType=RESULT_LIST&searchResultsType=SingleTab&searchType=AdvancedSearchForm¤tPosition=1&docId=GALE%7CA381469477&docType=Case+study&sort=RELEVANCE&contentSegment=&prodId=AONE&contentSet=GALE%7CA381469477&searchId=R1&userGroupName=miami_richter&inPS=true . Accessed 21 Nov 2018.
Rocha VB, Michalany N, Valente NYS, Pereira LB, Donati A. Atrichia with papular lesions: importance of histology at an early disease stage. Ski Appendage Disord. 2018;4(3):129–30. https://doi.org/10.1159/000480519 .
Miller J, Djabali K, Chen T, et al. Atrichia caused by mutations in the vitamin D receptor gene is a phenocopy of generalized atrichia caused by mutations in the hairless gene. J Investig Dermatol. 2001;117(3):612–7. https://doi.org/10.1046/j.0022-202x.2001.01438.x .
Zlotogorski A, Panteleyev AA, Aita VM, Christiano AM. Clinical and molecular diagnostic criteria of congenital atrichia with papular lesions. J Investig Dermatol. 2001;117(6):1662–5. https://doi.org/10.1046/j.0022-202x.2001.01618.x .
Yip L, Horev L, Sinclair R, Zlotogorski A. Atrichia with papular lesions: a report of three novel human hairless gene mutations and a revision of diagnostic criteria. Acta Derm Venereol. 2008;88(4):346–9. https://doi.org/10.2340/00015555-0466 .
Download references
Acknowledgements
Special thanks to the staff of the clinics at the University of Miami Hospital for their help and support.
No funding or sponsorship was received for this study or publication of this article.
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Dr. Antonella Tosti: Consultant P&G, DS Laboratories, Monat, PI: Incyte, Pfeizer, Aclaris, Nutrifol. Azhar Ahmed, Hind Almohanna and Jacob Griggs have nothing to disclose. Dr. Antonella Tosti is a member of the journals Editorial Board.
Compliance with Ethics Guidelines
Data availability.
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Author information
Authors and affiliations.
Department of Dermatology, King Fahad General Hospital, Medina, Saudi Arabia
Azhar Ahmed
Department of Dermatology and Dermatologic Surgery, Prince Sultan Military Medical City, Riyadh, Saudi Arabia
Hind Almohanna
Department of Dermatology and Cutaneous Surgery, University of Miami Miller School of Medicine, University of Miami Hospital, Miami, FL, USA
Azhar Ahmed, Jacob Griggs & Antonella Tosti
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Azhar Ahmed .
Additional information
Enhanced digital features.
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.8578415 .
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License ( http://creativecommons.org/licenses/by-nc/4.0/ ), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Reprints and permissions
About this article
Ahmed, A., Almohanna, H., Griggs, J. et al. Genetic Hair Disorders: A Review. Dermatol Ther (Heidelb) 9 , 421–448 (2019). https://doi.org/10.1007/s13555-019-0313-2
Download citation
Received : 01 April 2019
Published : 22 July 2019
Issue Date : 01 September 2019
DOI : https://doi.org/10.1007/s13555-019-0313-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Ectodermal dysplasias
- Genetic hair disorders
- Hair shaft disorders
- Find a journal
- Publish with us
- Track your research

Write a research paper about a hereditary condition or deformity.

you are probably not ugly you might be clingy or annoying. it depends on what gender you are. i can flirt well but can you? ya need to reach out to others and be kind to them and dont be like sex sex sex okay.
then, government officials implement the solution
Another question on Advanced Placement (AP)

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- SAGE Open Med
- PMC10757446
Hereditary spastic paraplegia: Novel insights into the pathogenesis and management
Wireko andrew awuah.
1 Sumy State University, Sumy, Ukraine
Joecelyn Kirani Tan
2 Faculty of Medicine, University of St. Andrews, St. Andrews, Scotland, UK
Anastasiia D Shkodina
3 Department of Neurological Diseases, Poltava State Medical University, Poltava, Ukraine

Tomas Ferreira
4 Department of Clinical Neurosciences, School of Clinical Medicine, University of Cambridge, Cambridge, UK
Favour Tope Adebusoye
Adele mazzoleni.
5 Barts and the London School of Medicine and Dentistry, London, UK
Jack Wellington
6 Cardiff University School of Medicine, Cardiff University, Wales, UK
7 Norwich Medical School, University of East Anglia, Norwich, UK
Ellie Chilcott
Helen huang.
8 Royal College of Surgeons in Ireland, University of Medicine and Health Sciences, Dublin, Ireland
Toufik Abdul-Rahman
Vallabh shet.
9 Faculty of Medicine, Bangalore Medical College and Research Institute, Karnataka, India
Oday Atallah
10 Department of Neurosurgery, Hannover Medical School, Hannover, Germany
Jacob Kalmanovich
11 Drexel University College of Medicine, Philadelphia, PA, USA
Riaz Jiffry
Divine elizabeth madhu, kateryna sikora, oleksii kmyta, mykhailo yu delva.
Hereditary spastic paraplegia is a genetically heterogeneous neurodegenerative disorder characterised primarily by muscle stiffness in the lower limbs. Neurodegenerative disorders are conditions that result from cellular and metabolic abnormalities, many of which have strong genetic ties. While ageing is a known contributor to these changes, certain neurodegenerative disorders can manifest early in life, progressively affecting a person’s quality of life. Hereditary spastic paraplegia is one such condition that can appear in individuals of any age. In hereditary spastic paraplegia, a distinctive feature is the degeneration of long nerve fibres in the corticospinal tract of the lower limbs. This degeneration is linked to various cellular and metabolic processes, including mitochondrial dysfunction, remodelling of the endoplasmic reticulum membrane, autophagy, abnormal myelination processes and alterations in lipid metabolism. Additionally, hereditary spastic paraplegia affects processes like endosome membrane trafficking, oxidative stress and mitochondrial DNA polymorphisms. Disease-causing genetic loci and associated genes influence the progression and severity of hereditary spastic paraplegia, potentially affecting various cellular and metabolic functions. Although hereditary spastic paraplegia does not reduce a person’s lifespan, it significantly impairs their quality of life as they age, particularly with more severe symptoms. Regrettably, there are currently no treatments available to halt or reverse the pathological progression of hereditary spastic paraplegia. This review aims to explore the metabolic mechanisms underlying the pathophysiology of hereditary spastic paraplegia, emphasising the interactions of various genes identified in recent network studies. By comprehending these associations, targeted molecular therapies that address these biochemical processes can be developed to enhance treatment strategies for hereditary spastic paraplegia and guide clinical practice effectively.
Graphical abstract

Introduction
Hereditary spastic paraplegia (HSP) constitutes a diverse group of rare neurological disorders, typically arising from single-gene defects, with a global incidence rate of 3.6 per 100,000 individuals. 1 HSP is characterised by spasticity and paralysis in the lower limbs, resulting from developmental and neurodegenerative abnormalities in lower limb neurons. 2 Approximately 80 genes have been associated with HSP, including SPG3A , SPG4 and SPG11 , which are prominent spastic paraplegia genes. 2 , 3
Among the dominant HSP types (AD-HSP), SPG4 is identified as the most prevalent, accounting for 40%–45% of familial cases. 3 The second most common form of AD-HSP, SPG3A , is caused by mutations in the ATL1 , estimated to contribute to about 7% of AD-HSP cases. 4 The autosomal recessive HSP type SPG11 is prevalent, affecting 18% of HSP patients globally, with the majority of cases found in Northern Africa and Western Asia. 1 Nevertheless, there is geographical variation in the prevalence of different HSP types, with SPG4 being the dominant form in German ethnic groups. 5
The pathogenesis of HSP involves a complex network of physiological processes, including membrane transport, endoplasmic reticulum (ER) shaping, mitochondrial functionality, DNA repair, autophagy, lipid metabolism and myelination. 1 Recent studies have also highlighted the potential roles of mitochondrial DNA (mtDNA) polymorphisms and abnormalities in endosome membrane trafficking and oxidative stress in the onset of the disease. HSP symptoms can manifest at any age, from infancy to late adulthood, with varying rates of progression and impairment. 1 , 2 The most common genetic mutations and pathogenic pathways are illustrated in Figure 1 .

Common genetic mutations and pathogenesis pathways in HSP. The diagram depicts the most common genetic mutations associated with HSP, as well as the pathogenesis pathways that contribute to the disease. The genetic loci for HSP are classified based on the mode of inheritance, and the figure highlights the common pathways that lead to HSP.
Clinically, HSP is categorised into two distinct groups: pure and complicated HSP, distinguished by the symptoms exhibited by patients. 6 Pure HSP typically presents with lower limb stiffness and urinary urgency, whereas complicated HSP is associated with a broader spectrum of symptoms, including signs of both upper and lower motor neuron dysfunction, such as fasciculations and increased spasticity. 1
In addition to primary neurological manifestations, HSP can lead to various secondary symptoms, encompassing paraesthesia, rigidity, scoliosis, malaise and muscle cramps and extending to cognitive dysfunction, ataxia and peripheral neuropathy. 1 The clinical picture is further complicated by the variability in symptom severity and age-related exacerbations that impact mobility and, consequently, the quality of life of affected individuals.
Recent advancements in artificial intelligence and machine learning have provided the means to utilise network analysis tools for the stratifying disease features in HSP, offering novel approaches to enhance our understanding of HSP subtypes. 7 By employing bioinformatics tools alongside molecular studies, this approach has revealed shared biological processes among clusters of HSP patients. Although further research is required to replicate and validate these findings, they suggest that patients can be grouped into distinct aetiological categories, based on molecular features that characterising HSP in each case. This implies that there may be more molecular interactions at play in the initiation and development of HSP than currently known. 7 By categorising patients with common molecular processes and comprehending all the mechanisms contributing to HSP development, this approach may pave the way for the development of precision medicine tools to improve patients’ quality of life.
Nevertheless, therapeutic options for HSP are presently limited, with no available disease-modifying interventions capable of reversing or slowing down disease progression. This review aims to explore the genetic basis of HSP, investigating the intricate relationships within interactome networks to unveil the metabolic mechanisms crucial to its pathophysiology. Understanding these associations may pave the way for targeted molecular therapy of various metabolic pathways, enabling the development of more effective HSP treatment algorithms and guiding valuable therapeutic strategies in clinical practice.
Methodology
This narrative review on the pathogenesis and management of HSP employed a rigorous methodology to ensure a comprehensive exploration of the topic. The inclusion criteria encompassed studies of various designs, including observational studies, case–control investigations, cohort studies and randomised controlled trials. Furthermore, the review considered studies involving both paediatric and adult populations, as well as those addressing all types of HSP. There was no set time frame for study inclusions, although we prioritised recently published papers to reflect on current advances on the topic. The literature search was conducted through prominent databases, including Scopus, MEDLINE, EMBASE and the Cochrane Library. The search was characterised by the use of precise search terms, such as ‘HSP’, ‘management’, ‘treatment’ and ‘pathogenesis’. Additionally, a manual search was performed to identify references from recently published reviews. It is important to note that stand-alone abstracts and unpublished studies were excluded from the review.
Through this comprehensive and methodical approach, the review aspires to offer a high-quality academic assessment, presenting novel insights into the pathogenesis and management of HSP. This will facilitate a thorough synthesis of pertinent findings and contribute to a deeper understanding of this complex condition. A summary of the methodology is provided in Table 1 for reference.
Summary of methodology for pathogenesis and management of HSP.
| Methodology steps | Description |
|---|---|
| Literature search | Scopus, MEDLINE, EMBASE and the Cochrane Library |
| Inclusion criteria | Full-text articles published in the English language were selected, with no specific time frame |
| A diverse range of study designs, comprising observational studies, case–control investigations, cohort studies, cross-sectional analyses and randomised controlled trials | |
| Studies involving paediatric and adult populations | |
| Studies addressing all subtypes of HSP | |
| Exclusion criteria | Stand-alone abstracts and unpublished studies |
| Search terms | Precise terms such as ‘Hereditary spastic paraplegia’, ‘management’, ‘treatment’ and ‘pathogenesis’ were employed |
| Additional search | A manual search was systematically undertaken to identify references pertaining to recently published reviews |
| Sample size requirement | No strict sample size requirement |
Comprehensive overview of HSP pathophysiology
Oxidative stress and mitochondrial dysfunction.
Oxidative stress and mitochondrial dysfunction are central to the pathogenesis of HSP. Neurons have a high energy demand to maintain their resting membrane potential and support axonal transport, especially in long axons. Therefore, the proper functioning and organised distribution of mitochondria within neurons are crucial. 8
One key aetiological element in HSP pathogenesis is the absence of the paraplegin/ AFG3L2 complex in the inner mitochondrial membrane. This complex not only prevents neuronal degeneration but also sustains the oxidative phosphorylation pathway, responsible for generating adenosine triphosphate (ATP). 9 In SPG7 patients with loss-of-function mutations in this complex, cells become more vulnerable to oxidative stress, leading to increased sensitivity to reactive oxygen species and reduced mitochondrial ATP production. 9 , 10 This can further impair neuronal function and contribute to the onset of HSP.
Disruption of mitochondrial fission–fusion dynamics can lead to morphological, mobility, and spatial distribution changes in mitochondria. 8 This results in impaired mitochondrial axonal transport, leading to deficiencies in oxidative phosphorylation, apoptosis, deletion mutations in mtDNA, and ultimately axonal degeneration. 8 Several HSP subtypes, including SPG15, SPG48 and SPG31 , have been linked to impaired mitochondrial dynamics. 11 , 12 Meanwhile, SPG7 and SPG61 are associated with mitochondrial morphology and network disruptions. 13 Notably, the SPG7 gene encoding paraplegin, a protein found in the inner mitochondrial membrane, and the SPG13 gene encoding heat shock protein-60, a mitochondrial chaperone, are both related to mitochondrial dysfunction and spastic paraplegia. 14 Mutations in mitochondrial fusion–fission genes have also been reported in various HSP types, including dynamin-related protein 1 ( DRP1 ), optic atrophy gene 1 and mitofusin-1 and -2 ( Mfn1 and Mfn2 ). 15 , 16
Mitophagy is another crucial process in the regulation of mitochondrial dynamics and function within axons. 17 Disruption of mitophagy can lead to the formation of abnormal mitochondrial networks and subsequent axonal degeneration. 17 HSP subtypes such as SPG11 , SPG15 and SPG48 result from autosomal recessive mutations in the genes SPG11 , ZFYVE26 and AP5Z1 , encoding spatacsin, SPASTIZIN and AP5Z1, respectively. 18 These genes hold promise for the discovery of new therapeutic targets for these HSP subtypes. Recent research has shown that inhibiting the overexpression of DRP1 , a mediator of mitochondrial fission, can reverse axonal defects observed in neurons of SPG15 and SPG48 -HSP subtypes. 8
Finally, the accumulation of mitochondria within axons, lack of ATP and disruption of the neuronal cytoskeleton can result in axonal swelling, leading to various neurological disorders, including HSP. 11 , 12
Metabolic processes influencing HSP
Disturbed er function and hsp.
Disrupted ER function is a significant contributor to the pathogenesis of HSP. The ER is essential for proper lipid synthesis and metabolism and facilitates intracellular communication by generating microdomains in plasma membranes. 19 Neurodegenerative processes have been linked to ER and lysosomal malfunction, where sphingolipids are produced and degraded. Sphingolipids are crucial for normal neuronal structure and functionality. 19 Patients with a missense mutation in fatty acid-2-hydroxylase, the enzyme responsible for sphingolipid production, are at risk of developing complex HSP. 20 Additionally, deficiencies in proteins like Receptor Expression-Enhancing Protein 1 (REEP1), which play a vital role in shaping the tubular ER network, can lead to shorter corticospinal axons and rapid declines in motor function tests, indicative of early onset HSP. 21
The spastin gene, typically involved in conventional microtubule production and cellular stability, has a strong association with HSP development. 22 Recent research has shown that spastin dysfunction leads to the accumulation of lipid droplets (LDs) within neuronal cells. 22 While more research is needed to fully understand these novel findings, it is plausible to hypothesise that HSP pathogenesis may involve an alternative mechanism of abnormal LD accumulation and metabolism in addition to the well-known spastin gene dysfunction. 23
Moreover, three distinct mutations – frameshift, whole-gene deletion and single missense mutations – within the reticulon 2 (RTN2) gene have been associated with aberrant ER morphogenesis in SPG12 . 24 RTN2 encodes a member of the reticulon family, which serves as prototypic ER-shaping proteins in families afflicted by SPG12 . The truncated RTN2 protein is believed to act through a haploinsufficiency mechanism, although the possibility of a toxic gain of function in the cytosol or nucleus remains. 24 The interaction between RTN2 and spastin is contingent on a hydrophobic region within spastin, a region involved in ER localisation and projected to form a curvature-inducing/sensing hairpin loop domain. 24 These findings collectively suggest the involvement of a reticulon protein in axonopathy as part of a network of interactions among HSP proteins engaged in ER shaping. This supports the prevailing hypothesis that ER dysfunction constitutes a pathogenic mechanism in HSP.
Ornithine metabolism and HSP
The ornithine and HSP genes are illustrative instances of metabolic pathways that exhibit multiple links with lipid metabolism. 25 Ornithine, a non-essential amino acid found in the urea cycle, is recognised for its pivotal role in various metabolic processes. Dysregulation of ornithine metabolism has been associated with several diseases, including leukaemia, hyperammonemia, neuroblastoma and neurodegenerative syndromes like HSP. 25
Mutations in the ALDH18A1 gene, which participates in the ornithine pathway, have been correlated with the pathogenesis of HSP. 25 The ALDH18A1 gene encodes the P5CS enzyme, which catalyses the initial step in the biosynthesis of proline and ornithine. 25 , 26 This enzyme converts gamma-glutamyl phosphate into gamma-glutamyl semialdehyde, which subsequently undergoes spontaneous degradation to P5C. Located in the inner mitochondrial membrane, P5C can then be further metabolised into proline or, through the urea cycle, into ornithine, citrulline and ultimately arginine, with the assistance of the P5C reductase ( PYCR1 ) enzyme ( Figure 2 ). 25 , 26 Consequently, low levels of plasma ornithine are a matter of concern for individuals with HSP.

The ornithine metabolic cycle and its association with lipid metabolism in relation to HSP.
P5C: pyrroline-5-carboxylate; OAT: ornithine aminotransferase; OTCA: ornithine transcarbamylase; AS: argininosuccinate.
HSP resulting from ALDH18A1 gene mutations can manifest as either a simple autosomal recessive or complex autosomal dominant condition. Patients from autosomal dominant families consistently exhibit low to extremely low plasma citrulline levels, along with less consistently reduced plasma levels of ornithine, arginine and proline, regardless of the specific protein domain affected by the mutation. 25 Notably, patients with autosomal dominant HSP linked to ALDH18A1 mutations may derive substantial benefits from long-term citrulline supplementation, a therapeutic approach that has demonstrated success in patients with inborn metabolic disorders affecting the urea cycle, either directly or indirectly, such as ornithine transcarbamylase deficiency or lysinuric protein intolerance.
Lesser known mechanisms in HSP
Spastic paralysis is a frequently observed phenotype in various rare mutations affecting interconnected pathways related to glutamate and urea cycle metabolism, as well as mitochondrial degeneration. 27 Notable examples of such mutations involve PYCR1 and NMNAT1 genes, which are associated with cutis laxa and the nicotinamide adenine dinucleotide (NAD) biosynthetic network, respectively. 27 A comprehensive examination of the underlying pathology associated with these mutations can provide valuable insights into our comprehension of HSP ( Figure 3 ).

Lesser known mechanisms in HSP.
Source: Created with Biorender.com .
PYCR1 mutations
PYCR1 mutations have been implicated in an autosomal recessive neurocutaneous syndrome associated with a range of clinical manifestations, including mental retardation, cutis laxa, joint hyperlaxity, progeroid dysmorphia, growth retardation, microcephaly and corpus callosum dysgenesis. These mutations are also believed to play a role in neurodegeneration within the mitochondria. 28
The PYCR1 gene encodes the enzyme P5C reductase, which is responsible for the final step in proline biosynthesis, converting P5C into L-proline. 28 Notably, although proline plasma levels remain normal in individuals with PYCR1 mutations, they exhibit mitochondrial abnormalities characterised by increased apoptosis during oxidative stress, resulting in the development of cutis laxa with progeroid changes. 28
It is worth noting that mutations in the PYCR1 gene, as well as P5CS deficiency associated with the ornithine cycle, share common features, including connective tissue defects and developmental delays. Both enzymes are situated in the inner membrane of mitochondria. 27 , 28
NMNAT1 mutations
The Nicotinamide mononucleotide adenylyltransferase enzyme plays a crucial role as a co-substrate for a group of enzymes within the NAD biosynthetic network. Recent evidence from whole-exome sequencing indicates a potential link between a variant in NMNAT1 and HSP. 29 This association was observed in two affected siblings diagnosed with HSP, where a homozygous variant (Glu257Lys) in NMNAT1 , the most prevalent variant in patients with LCA9 , displayed clinical manifestations completely consistent with pure HSP. 29 Notably, this study represents the first report of NMNAT1 mutations contributing to neurological disorders by disrupting the regulation of physiological NAD homeostasis. To validate this hypothesis, further rigorous and large-scale clinical trials are imperative.
Cellular transport mechanisms and HSP
Malfunction in axonal transport represent an additional pathophysiological process associated with specific subtypes of HSP. 12 Axonal transport plays a vital role in various essential functions, encompassing the regulation of axon composition, the preservation of axonal function, and the support of neurogenesis. 12 This process relies on motor proteins, including kinesin for anterograde transport, which facilitates the movement of ribonucleic acids (RNAs), proteins, lipids and mitochondria towards axon terminals and growth cones. In contrast, retrograde transport is orchestrated by dynein motor proteins, responsible for transporting trophic factors and misfolded proteins back to the soma for degradation. 30
Kinesin heavy chain 5A ( KHC5A ) is a pivotal anterograde motor protein belonging to the kinesin family that is responsible for transporting neurofilaments and vesicles to growth cones and synapses. 31 It also plays a regulatory role in cargo transport within dendrites and is involved in processes such as exocytosis and endocytosis. The KHC5A protein is encoded by the KIF5A gene, which has been found to be mutated not only in SPG10 but also in other neurodegenerative diseases, including Charcot–Marie–Tooth (CMT) disease Type 2 and amyotrophic lateral sclerosis (ALS). 31 These mutations predominantly manifest as missense changes and tend to cluster in the gene’s N-terminal motor domain, as indicated by comprehensive genome-wide analyses. A similar anterograde protein, the Kinesin Family Member 1A protein ( KIF1A ), encoded by the KIF1A gene, is responsible for the transport of membranous organelles along the axon. 31 Notably, Klebe et al. 32 employed targeted next-generation sequencing to establish that mutations in the KIF1A gene underlie the development of SPG30 .
KIF1A gene mutations have also been associated with other neurological conditions, including hereditary sensory neuropathy type IIC and nonsyndromic intellectual disability. 33 On the other hand, the SPAST gene, mutated in the most prevalent form of autosomal dominant HSP, SPG4 , encodes for spastin, a protein pivotal in regulating microtubule dynamics and arrays. 34 , 35 As the normal functioning of kinesin and dynein motor proteins relies heavily on microtubule activity, any dysregulation stemming from mutant spastin proteins can lead to defective axonal transport. 36 Another analogous protein, Spartin, encoded by the SPART gene, is also associated with microtubule dynamics, in addition to its involvement in endosomal trafficking, and has been implicated in SPG20 , also known as Troyer syndrome. 37
Distinctively, SPG33 is a subtype of HSP resulting from mutations in the ZFYVE27 gene, which encodes for protrudin. Protrudin is a protein localised to the ER and plays a role in the outgrowth of neurites. 18 SPG33 stands out as its causative protein, protrudin, interacts with proteins associated with several other spastic paraplegias. It forms connections with both SPG4 and atlastin-1 ( SPG3A ), while also interacting with the KIF5 proteins ( SPG10 ). 18
Membrane trafficking in ER networks
HSP-associated genes have been identified to play pivotal roles as modifiers and regulators of the ER network, impacting protein secretion and calcium sequestration. 38 The ER, a membrane-bound organelle, participates in a multitude of cellular processes and, most notably, plays a critical role in expanding axonal membranes to facilitate postsynaptic signalling pathways. 38 Mutations that disrupt ER shaping and function contribute not only to the phenotypic spectrum of HSP but also to various other neurodegenerative conditions, including Alzheimer’s disease (AD), CMT, Parkinson’s disease (PD) and ALS. 38
Genetically, HSP can be inherited in different modes, including autosomal dominant, autosomal recessive, X-linked or mitochondrial. However, the most prevalent form of HSP is autosomal dominant HSP, affecting 75%–80% of HSP patients. 39 Dysregulation in the tubular ER network can largely be attributed to three main genes: SPG3A/ATL1, SPG4/SPAST and SPG31/REEP1 , accounting for approximately 50% of HSP cases. 40 Heterozygous mutations in the ATL1 gene result in SPG3A AD-HSP. ATL1 encodes the GTPase atlastin, which interacts with spastin. 41 Atlastin-1 is instrumental in shaping the ER morphology by catalysing the fusion of membrane tubules, forming three-way junctions. 42 Mutations in this gene culminate in the abnormal morphogenesis of the ER and Golgi, thereby impacting axon development and maintenance, ultimately contributing to HSP. 43 The SPAST gene encodes for spastin, which is part of the ATPases Associated with the diverse cellular Activities (AAA) family. Spastin plays a crucial role in mediating microtubule stability, and its loss has been shown to result in defective synaptic growth and neurotransmission in vivo in Drosophila. 44 , 45 This highlights spastin as a potential therapeutic target for HSP treatment.
Mutations in the REEP1 gene are another well-recognised cause of SPG31 AD-HSP. 46 Previous studies yielded conflicting data regarding the localisation of REEP1 , with both the ER and mitochondria being suggested. However, an in vitro study clarified that REEP1 is localised in the ER-mitochondria interface. Pathological REEP1 mutations disrupt ER-mitochondria interactions, leading to growth defects and neuronal degeneration, which can be attributed to the inability to maintain healthy long axons in HSP. 47 Within the ER, REEP1 forms protein complexes with both atlastin-1 and spastin, necessitating the presence of hydrophobic hairpin domains in these proteins. 47 Further in vitro research highlighted the role of REEP proteins, particularly those with extended C-terminal domains (REEP1–4), in ER shaping and their involvement in interactions between ER tubules and the microtubule cytoskeleton. 47 Notably, an SPG31 mutation in REEP1 without a C-terminal domain was found to fail to interact with the ER membrane in corticospinal neurons, potentially contributing to the pathogenesis of HSP. 47
The BSCL2 gene, also known as the Berardinelli–Seip congenital lipodystrophy gene, encodes the ER protein seipin. Mutant seipins in BSCL2 -associated HSP have been found to accumulate in the ER, triggering the upregulation of ER-stress-mediated molecules, which, in turn, induce apoptosis. This mechanism provides insight into the degeneration observed in HSP. 48
The ER is co-localised by protrudin, a membrane protein involved in polarised vesicular trafficking in neurons. 49 In vitro studies demonstrated that the forced expression of protrudin promotes the formation and stabilisation of the ER tubular network. Conversely, mutant protrudin cells exhibited greater susceptibility to ER stress, potentially contributing to the pathogenesis of HSP. 49
Vesicular trafficking of lysosomes
Lysosomes are dynamic organelles enclosed by a single membrane, displaying significant heterogeneity in terms of size, location, shape, enzyme composition and substrates within cells. These organelles house a multitude of integral and peripheral membrane proteins, including transporters and ion channels. 50 – 52 The acidic environment of the lysosomal lumen, with a pH typically ranging from 4.5 to 5.5, is primarily maintained by the lysosomal multi-subunit V-ATPase. In this low-pH setting, over 50 intralysosomal hydrolases become activated, enabling the breakdown of macromolecules like proteins, nucleic acids, lipids and carbohydrates. 52 – 54
Lysosomes play a crucial role in importing and degrading various substances, including endocytic materials like small molecules and cell surface proteins, phagocytosis of larger particles such as inflammatory cells and exogenous bacteria, and autophagy of cytoplasmic components like damaged mitochondria, ER and other lysosomes. 52 – 54 These organelles act as cellular waste disposal sites, recycling the by-products of lysosomal digestion for cellular maintenance.
Lysosomal dysfunction is clinically implicated in various human disorders, including lysosomal storage diseases such as Tay–Sachs disease and neurodegenerative diseases like ALS and HSP. 55 , 56 In HSP, genes like the kinesin family member 5A gene ( KIF5A ) and protrudin play essential roles in vesicular trafficking and ER-lysosome interactions, respectively, contributing to the pathogenesis of the disease. 57 , 58 Additionally, lysosomal proteins such as VPS35 (vacuolar protein sorting 35 orthologs), a component of the Retromer complex that sorts endosomal products, have been associated with HSP. 59
The absence of components of the Wiskott–Aldrich syndrome protein and SCAR homologue 1 (WASH-1) complex, which interacts with endosomes, as well as the absence of FAM21 and actin-capping proteins responsible for regulating actin dynamics, can result in increased tubulation of early endosomes. This change may be due to the lack of actin-mediated forces needed for the separation of tubular transport intermediates from endosomes. This alteration affects the transport of early endosomal compartments and is particularly relevant in the case of corticospinal neurons, which have exceptionally long axons and are more susceptible to reductions in functional WASH. This susceptibility could be a contributing factor in HSP. 60
Furthermore, endosomal membrane trafficking in HSP is associated with specific proteins, including KIAA0415 ( SPG48 ), spatacsin ( SPG11 ) and spastizin/FYVE-CENT ( SPG15 ). Clinical similarities between SPG11 and SPG15 are noted, including their presentation as juvenile parkinsonism and a connection with the thin corpus callosum. The interaction of spastizin and spatacsin with the SPG48 protein KIAA0415 suggests a link between HSP and DNA repair. 61
Macro-autophagy
Autophagy is a fundamental cellular process that enables cells to respond effectively to potential disruptions, safeguarding the cellular environment from organelles and misfolded proteins that could compromise internal balance. 62 Macro-autophagy, a central aspect of autophagy, involves the sequestration of cytoplasmic components into double-membrane vesicles known as autophagosomes, which subsequently merge with lysosomes to form autolysosomes. 62 This pivotal cellular process is indispensable for normal cell function, and any defects in autophagy have far-reaching implications, particularly in the context of neurodegenerative conditions like HSP. 63 The malfunction of the autophagic pathway, in conjunction with endolysosomal processes, has been associated with 24 gene mutations linked to HSP, signifying its pivotal role in the pathogenesis of HSP ( Figure 4 ). 63

Macro-autophagy.
The autophagosome
In the process of autophagosome biogenesis, malfunctioning proteins serve as attractants for autophagy-related (ATG) proteins, initiating the creation of phagophore assembly site (PAS) and ultimately giving rise to the formation of a phagophore. 64 This sequence is then succeeded by nucleation and elongation phases, culminating in the generation of an autophagosome that encapsulates intracellular material.
Within this process, ATG protein 9A ( ATG9A ) plays a crucial role. ATG9A , a transmembrane protein, is indispensable for the assembly of autophagosomes. During autophagy, ATG9A is transported to the PAS by vesicle transport mechanisms and takes on the pivotal role of overseeing the regulation and elongation of the phagophore ( Figure 4 ). 64
Adaptor protein deficiency syndromes, the Kinesin family and autosome-lysosome fusion in HSP
Adaptor Protein Complex 4 (AP-4) is a complex predominantly associated with the trans-Golgi network (TGN). Depletion of this complex has been linked to HSP and has direct consequences on ATG9A , including its mislocalisation and retention at the TGN rather than reaching the PAS). 65 Mutations in AP-4 have been identified in severe neurodevelopmental forms of HSP, specifically SPG47, SPG50, SPG51 and SPG52 , collectively known as AP-4 deficiency syndromes. 66
Another pivotal player in the ATG9A trafficking process is KIF1A , a member of the Kinesin-3 family. ATG9A is typically located at the PAS and axon terminals. 32 Pathological variations in KIF1A have been associated with impaired transport of ATG-9 to neurites and are linked to both autosomal recessive and dominant forms of HSP, including SGP30 . 32
Furthermore, several other genes in the Kinesin family have been implicated in HSP. Mutations in KIF5A , which encodes the heavy chain of kinesin-1, are known to disrupt axonal transport, particularly affecting neuronal microtubule motors. This disruption is associated with SPG10- HSP. 67 These kinesin motors play essential roles in the fusion of autophagosomes with lysosomes, and their differential intracellular locations necessitate trafficking. 67 Another protein involved in the union of autophagosomes and lysosomes is Light Chain 3 (LC3), a member of the ATG8 protein family, which recruits interacting partners to initiate transport, tethering, and fusion, including the Homotypic Fusion and Vacuole Protein Sorting Tethering Complex (HOPS). 68
Additionally, the Tectonin Beta-Propeller Repeat Containing 2 ( TECPR2 ) protein is associated with pathways involving ATG8 and the HOPS complex family. Mutations in the TECPR2 gene have been linked to SPG49 -HSP. A study examining fibroblasts from an HSP patient revealed defects in autophagy associated with TECPR2 mutations. 69 It is suggested that TECPR2 regulates autophagosome-lysosome tethering and fusion by interacting with LC3 and HOPS ( Figure 4 ). 70
Impaired lysosomal storage and HSP
ATP13A2 is an enzyme closely associated with lysosomal transport and SPG78- HSP. This enzyme belongs to the P5-type transport ATPase family and plays a pivotal role in lysosomal function. Individuals with ATP13A2 mutations often exhibit an abnormal accumulation of lysosomal and autophagosome structures, resulting in impaired lysosomal storage. This disruption leads to a defect in the clearance of damaged mitochondria and hinders the degradation of intracellular protein aggregates. 70
Once autophagosomes have tethered to lysosomes to form autolysosomes, the internal materials contained within are subjected to degradation. The final step in autophagic pathways is the recycling of lysosomal components, which facilitates the formation of new lysosomes during reformation. 70
Multiple proteins linked to HSP are known to play roles in the process of lysosomal reformation, including spatacsin ( SPG11 ), spastizin ( SPG15 ), AP5Z1 ( SPG48 ) and the AP-4 complex. AP5Z1 is a part of the adaptor protein complex 5 (AP-5) and is closely associated with both spatacsin and spastizin. 71 Mutations in AP5Z1 can result in the loss of AP-5 protein function, leading to abnormal storage of lysosomal materials ( Figure 4 ). 72
Myelination disruptions and HSP
The PLP1 gene encodes proteolipid protein 1. Mutations in the PLP1 gene itself or in its distal enhancers have been identified as contributing factors to HSP and specifically as causative factors for with SPG2 being one of the specific manifestations linked to these mutations. 73 – 75 Notably, a microdeletion at the Xq22.2 region, which contains one of the distal enhancers of the PLP1 gene, has been found to lead to SPG2 -HSP. 73 When these distal enhancers are absent or impaired, the transcription of PLP1 in oligodendrocytes can be suppressed. This transcriptional suppression can limit the ability of the gene to maintain myelin, contributing to the development of the SPG2 phenotype. 73
The L1CAM gene is responsible for encoding myelin proteins, which play a crucial role as they are expressed on oligodendrocytes that provide vital support to motor neurons. 76 When mutations occur in the L1CAM gene, it results in a deficiency of myelin proteins in neurons. 76 Notably, in the axons of neurons expressing the Trk-fused gene (TFG) mutation (p.R106C), there is a reduction in the levels of cell surface L1CAM when compared to controls. This observation supports the idea that the transport of L1CAM to the cell surface is compromised in these conditions. 77 , 78 These findings underscore the significance of effective membrane trafficking in the early secretory pathway, especially in the context of the long corticospinal motor neurons that degenerate in cases of HSPs. Such efficient trafficking is essential for maintaining neuronal homeostasis. 77
Intersecting genes and metabolic pathways in diseases related to HSP
Familial als.
Familial ALS (fALS) is a rapidly progressing neurodegenerative disease that leads to paralysis. 79 Multiple genes, including BSCL2, ERLIN1, ERLIN2, SPG11 and more, are thought to contribute to fALS. Differentiating between HSP and fALS can be challenging as each of these genes interacts with the metabolic pathways associated with both conditions. 80
Seipin is a protein encoded by the BSCL2 gene. Seipin is highly prevalent in the brain, particularly in spinal motor neurons and cortical neurons in the frontal lobes. It is a membrane protein found in the ER of various cell types and is believed to be involved in the formation of LDs. 81 In fALS, this gene and its variants, such as P.N88S , P.S90L and P.S90W , 82 exhibit a harmful gain-of-function mutation. This mutation results in the misfolding of Seipin protein, leading to its accumulation in the ER, causing neurotoxicity and ultimately resulting in neurodegeneration. Studies suggest that BSCL2 mutations can lead to a wide range of manifestations involving both upper and lower motor neurons, as well as peripheral motor axons. Patients with the P.N88S mutation may have a shorter disease course than patients with the P.S90L mutation. 81
The ERLIN1 gene codes for an ER protein known as ER lipid raft-associated protein 1. ERLIN1 forms a ring-shaped complex with ERLIN 2 to create the ERLIN1-2 complex. This complex is involved in the ER-associated degradation (ERAD) pathway, which is activated when the ER is under stress. The ERAD pathway identifies misfolded proteins, ubiquitinates them and transports them for degradation via a proteasome or autophagosome. Although limited to case series analyses, ERLIN1 mutations have been shown to correlate with SPG62 , a pure subtype of HSP that specifically impairs upper motor neurons and causes focal deficits. 83 Given that ERLIN2 participates in the ERAD pathway of inositol 1,4,5-triphosphate (IP3), which is important for ubiquitination and the control of cellular cholesterol homeostasis, 84 further investigation into this connection is warranted, as the genetic spectrum of the disease may be broader than initially reported.
The SPG11 gene, responsible for the development of spastic paraplegia and the most prevalent subtype of HSP, is inherited in an autosomal recessive manner. It codes for a protein called Spastacsin, whose exact function is yet to be fully understood. 85 This genetic mutation typically results in progressive spasticity, neuropathy, cognitive impairment and a thin corpus callosum observed on MRI. The role of Spastacsin may also be involved in weight gain and management, but its complete range of functions remains unclear. 85 Exome sequencing has shown that heterozygous deletions may lead to missense and nonsense mutations, with premature stop codons in the SPG11 gene. Such mutations are prominently expressed across various brain regions, leading to nonsense, insertional and deletional mutations, resulting in frame shifts and loss of functionality. 86 This is particularly relevant because it has been associated with corpus callosum thinning, dementia symptoms and overall grey matter impoverishment. 85 Additionally, reduced volumetric size has been reported in various brain regions, such as the thalamus, accumbens nucleus, substantia nigra, amygdala and red nucleus. 85 Notably, clinical studies have shown that the spectrum attributed to SPG11 mutations is broader than previously documented, with patients afflicted by autosomal recessive juvenile ALS (ARJALS) exhibiting extended periods of survival. 87 Therefore, conducting a comprehensive analysis of SPG11 mutations in additional families with motor neuron disorders showing similar clinical manifestations is essential. 87 Consequently, further research into the mechanisms causing neurodegeneration associated with SPG11 functionality is warranted. 86
Monogenic PD/parkinsonism
Parkinsonism represents a group of neurological disorders characterised by symptoms such as rigidity, tremors and slowed movement. 88 A significant study of SPG11 , one of the largest cohort studies on the subject, revealed that 60% of participants responded to levodopa (L-Dopa) treatment, and one in six SPG11 individuals exhibited parkinsonian features, suggesting a strong connection between parkinsonism and SPG11 . 89 Research in this area has shed light on the crucial role of SPG11 in the existence and functionality of neurons. 89 Specific SPG11 mutations have been shown to harm dopaminergic neurons, suggesting that these mutations might lead to early-onset parkinsonism. 90 Furthermore, the analysis of HSP patients presenting with parkinsonism-like symptoms has revealed various additional variants in genes such as SPG7, FA2H and the ZFYVE26 / SPG15 complex HSP genes. 90 Patients with SPG7 often exhibit symptoms of Parkinsonism. 91 Regardless of the number of mutant alleles, the type of variation, or the status of patient or carrier, pathogenic variants of SPG7 impact mtDNA homeostasis. Consequently, SPG7 plays a role in promoting mtDNA maintenance, and variations in this gene may result in parkinsonism due to anomalies in mtDNA. 91 Intriguingly, the study mentioned found that a genetic cause of parkinsonism was not identified in more than half of the included patients, hinting at the possible involvement of as-yet-unidentified genes in this condition. 90
The ATP13A2 gene encodes a P5-type transport ATPase protein found in lysosomes. 92 While its specific binding partners are not yet known, ATP13A2 expression has been associated with neuronal protection by preventing the accumulation of manganese. 70 , 92 Loss of ATP13A2 function can lead to mitochondrial and lysosomal dysfunction in neuronal groups, contributing to the development of neurological diseases such as HSP and parkinsonism. 70 Whole-exome sequencing and homozygosity mapping have revealed a homozygous p.Thr512Ile (c.1535C 4T) mutation in ATP13A2 , which has been associated with Kufor–Rakeb syndrome, an autosomal recessive form of juvenile-onset parkinsonism. This research underscores the connection between ATP13A2 , parkinsonism and HSP. 70 Routine screening of patients with complex HSP for ATP13A2 mutations may prove beneficial in clinical practice.
The UCHL1 gene, also known as the PARK5 gene, codes for ubiquitin carboxyl-terminal esterase L1, which is a deubiquitinating enzyme involved in hydrolysing ubiquitin in the ubiquitin-proteasome pathway. UCHL1 is highly expressed in neuronal, neuroendocrine and podocyte cells, where it helps maintain ubiquitin stability, a crucial factor in brain functionality. 93 Meta-analyses of the UCHL1S18Y variant and its association with PD have demonstrated a significantly increased risk of sporadic PD in individuals with the AA genotype of this gene variant. 94
Hereditary neuropathy
Hereditary neuropathies encompass a class of inherited diseases affecting the peripheral nervous system. One such condition is CMT, characterised by symptoms such as symmetrical, length-dependent motor neuropathy, muscle weakness, paraesthesia and foot deformities. Typically, CMT manifests in childhood and progresses slowly. There are clinical and genetic similarities between CMT and other distal hereditary motor neuropathies (dHMNs). 92 Genes associated with dHMNs, including the COQ7 variant, have also been linked to HSP. 95
CMT type 2 is primarily caused by mutations in the BSCL2 gene. Exome sequencing studies have identified BSCL2 mutations in individuals clinically suspected of having CMT type 2. For example, among 47 Japanese CMT patients, 5 had heterozygous BSCL2 mutations. Notably, p.N88T and p.S141A mutations were observed in three cases. Patients with p.N88T exhibited a severe clinical presentation that began at an early age (1.5 years) and included vocal cord paralysis, distinguishing it from previous findings. 96 P.S141A is considered a unique and uncommon variation associated with CMT demyelinating neuropathy. 96 However, further cases are needed to confirm the pathogenic significance of p.S141A and p.N88T in CMT. In another study, three of 206 Chinese patients with CMT had BSCL2 mutations ( p.S154W , p.S154L , p.A437P and p.A282V ). Variants of the BSCL2 gene have also been implicated in dHMNs. In Taiwan, 76 CMT type 2 patients with dHMNs were found to carry two BSCL2 variants: p.S90L (in a CMT family) and p.R96H (in a sporadic dHMN case). 97
Methionyl-tRNA synthetase, also known as MARS1 , is an enzyme responsible for charging tRNAs with their corresponding amino acids, a crucial step in protein synthesis. 97 , 98 Mutations in MARS1 have been linked to the aberrant production of neurofilaments within axons. 99 Although MARS1 has been suggested as a potential gene associated with a subtype of CMT disease, the evidence is limited to exome sequencing analysis of a single family with CMT, necessitating further investigation into the potential role of MARS1 mutations, particularly in cases of axonal CMT. 100 , 101
REEP1, encoded by the REEP1 gene, is a protein expressed in neurons throughout the brain and spinal cord, localised in both the ER and mitochondria. It is believed to play a role in developing the tubular network structure of the ER, regulating its size and protein processing capacity, and enhancing G-protein coupled receptor (GPCR) activity. 102 The HSP phenotype has been associated with REEP1 . Interestingly, intellectual disability and behavioural problems have been linked to factors outside of REEP1 in HSP patients, such as SPAST -HSP missense mutations. 102 , 103 Additionally, the SPG31 gene has been correlated with REEP1 , with REEP1 recently identified as the causative gene for dHMN type 5. 104
The ALS5/SPG11/KIAA1840 gene has emerged as the causative factor behind a diverse array of clinical presentations, encompassing autosomal recessive HSP, ARJALS and autosomal recessive axonal CMT2 (ARCMT2). Notably, no significant large deletions or duplications have been associated with the ALS5/SPG11/KIAA1840 gene, and haematological and biochemical profiles appear unremarkable. 105 However, it is linked to the loss of myelinated fibres, resulting in motor and sensory axonal neuropathy, with a more pronounced impact on the lower limbs and characterised by low amplitudes of compound motor and sensory nerve action potentials. 105 As such, it is imperative to consider genetic screening of the ALS5/SPG11/KIAA1840 gene not only in patients exhibiting symptoms of autosomal recessive HSP with thin corpus callosum and ARJALS but also in cases of ARCMT2. 105
Given the intricate and heterogeneous nature of these neurodegenerative conditions, next-generation sequencing techniques stand as the most effective diagnostic tools for identifying the genetic underpinnings in patients presenting with myelopathy or neuropathy, whether through targeted sequencing panel approaches or whole-genome sequencing. 105
Cerebellar ataxia
Ataxia is a clinical manifestation characterised by issues such as speech difficulties, abnormal gait, loss of voluntary muscle control and uncoordinated ocular movements. Cerebellar ataxia patients often exhibit symptoms like tremors, overshooting movements, impaired articulation and poor balance. Importantly, these ataxia-related features share common pathogenic mechanisms with HSP. 106
The Calpain-1 ( CAPN1) gene encodes calcium-activated neutral proteases known as calpains. CAPN1 is believed to contribute to essential neural processes and functional pathways that are common to both the corticospinal and cerebellar tracts. 107 Its involvement has been associated with SPG76 , a condition characterised by cerebellar ataxia, further underscoring the connection between cerebellar ataxia and HSP. 107 , 108
The KIF1A gene codes for a motor protein responsible for transporting membrane-bound organelles along axonal microtubules. Mutations in KIF1A have been linked to autosomal recessive SPG30 and, in some cases, are associated with cerebellar ataxia. Additionally, hereditary sensory neuropathy and mental retardation type 9 (autosomal dominant) have been observed in connection with KIF1A mutations. 109 , 110 Notably, an estimated number of 61 KIF1A mutations have been reported, and certain missense variants have been associated with cerebellar atrophy and ataxia. 110 , 111
Spastic ataxia of Charlevoix–Saguenay
Spastic Ataxia of Charlevoix–Saguenay (SACS), also known as Sacsin, encodes the sacsin protein highly expressed in the central nervous system. It plays a crucial role in recruiting Hsp70 chaperone proteins that help regulate the effects of ataxia-related proteins, such as amazon-1. 112 , 113 Whole-exome sequencing studies have identified various SACS variants and their associations with changes in protein function and resultant phenotypes. For instance, gene variants p.Y508C and L.456V have been linked to infantile-onset spinocerebellar ataxia. 114
Vacuolar Protein Sorting 13 Homolog D ( VPS13D ) codes for a protein involved in lipid transport between organelle membranes and is thought to play a role in mitochondrial clearance, contributing to overall cell health, mitochondrial size and homeostasis. 115 Dysfunctions in the VPS13D gene have been reported in patients with autosomal recessive cerebellar ataxia. In some cases, individuals with VPS13D mutations have displayed adult-onset cerebellar ataxia, macrosaccadic intrusions, pyramidal tract signs and neuropathy. 116 In other instances, VPS13D mutations were found in individuals with pure HSP or complex HSP, with variations in the age of onset and symptom complexity associated with the nature of the mutations. 117 , 118
ERAD pathway
The ER plays a pivotal role in the regulation of cellular calcium levels. Two distinct classes of calcium release channels, inositol IP3 and ryanodine receptors, are instrumental in mediating this regulation. GPCRs on the plasma membrane activate IP3 receptors located in the ER membrane, leading to the efflux of calcium from the ER into the cytoplasm. 119 Dysregulation of this mechanism has been implicated in the pathophysiology of several neurodegenerative diseases, including HSP, spinocerebellar ataxias and Huntington’s disease. The ERAD pathway is responsible for the degradation of active IP3 receptors. Compromised functioning of the ERAD pathway may also contribute to the development of neurodegenerative disorders. 119
The intersecting genes and metabolic pathways in diseases related to HSP have been summarised in Table 2 .
Summary of intersecting genes and metabolic pathways in diseases related to hereditary spastic paraplegia.
| Diseases related to HSP | Intersecting genes and metabolic pathways |
|---|---|
| Familial amyotrophic lateral sclerosis. – | (P.N88S, P.S90L and P.S90W variants), genes interact with the metabolic pathways associated with both HSP and fALS |
| Monogenic Parkinson’s disease/parkinsonism – | Strong link between -HSP, and parkinsonism Probable link between -HSP and parkinsonism, through anomalies in mitochondrial DNA due to dysfunction in , which promotes mitochondrial DNA maintenance Probable link between gene and HSP and Parkinsonism variant increases the risk of sporadic Parkinson’s disease |
| Hereditary neuropathy , – , – | gene variant, which is related to dHMNs, is associated with HSP (p.N88S, and p.S141A variants) Probable link between CMT and mutation, leading to aberrant production of neurofilaments intrinsic to axons Link between gene, -HSP and dHMN type 5 genes are causative for HSP, ARJALS and ARCMT2 |
| Cerebellar ataxia – , , , – | Intersecting genes between cerebellar ataxia and HSP include gene, gene, gene and gene Compromised ERAD pathway, and dysregulation in the mechanism involving IP3, ryanodine receptors |
HSP: hereditary spastic paraplegia; fALS: familial amyotrophic lateral sclerosis; SPG: spastic paraplegia; dHMN: distal hereditary motor neuropathy; DNA: deoxyribonucleic acid; CMT: Charcot–Marie–Tooth disease; ARJALS: autosomal recessive juvenile amyotrophic lateral sclerosis; ARCMT2 : autosomal recessive axonal Charcot–Marie–Tooth disease type 2; ERAD: ER-associated degradation; IP3: 1,4,5-triphosphate.
Current and emerging therapeutic targets and management strategies
This review covers both pharmacological therapies and non-pharmacological therapies for HSP management.
Pharmacological therapies
Intrathecal baclofen therapy.
Baclofen if a selective GABA-B receptor agonist and is frequently used for the treatment of spasticity. 120 It can be administered orally or intrathecally by the surgical implantation of a specialised pump. A more recent retrospective investigation of intrathecal baclofen (ITB) device implantation in seven patients with HSP revealed significant improvements in the Reflex Scale and spasticity according to the modified Ashworth Scale, as well as improvements in the modified Rankin Scale. 120 Long-term implantation observed improvement in spasticity for 2–3 years, followed by a stable phase of ambulatory and other mobility functions for 4–5 years. Additionally, there was no reported adverse events ( Table 3 ). 120
Summary table of the effects of pharmacological treatments on hereditary spastic paraplegia.
| Author (s), year | Drug | Action | Studied effect in HSP |
|---|---|---|---|
| Pucks-Faes et al. | Intrathecal baclofen injections | Agonist of the beta subunit of the GABA receptors is administered intrathecally through surgical implantation of a specialised pump | Significant improvements in the Reflex Scale and spasticity according to the modified Ashworth Scale. Improvements in the modified Rankin Scale. Improvement in spasticity for 2–3 years, followed by a stable phase of ambulatory and other mobility functions for 4–5 years. No reported adverse events |
| Faber et al. | L-Dopa | Amino acid precursor to dopamine | RCT demonstrated no significant improvement for SP11 HSP-related parkinsonism |
| Diniz de Lima et al. | Botulinum toxin type A injection | Inhibits neuromuscular function by binding presynaptically to cholinergic nerve terminals and lowering acetylcholine release | Reduction in the adductor tone, with transient and tolerable adverse events. No functional improvement observed |
| Bellofatto et al. | Dalfampridine (4- aminopyridine) | Targets the nervous system directly, and blocks the voltage-gated potassium channels to improve action potential conduction in demyelinated axons | General improvement in motor function as measured by gait analysis, TWT, the 6 MWT. Decreased weariness on the MFIS. Perceived improvement in emotional stability. Greater concentration when doing specified activities |
| Marelli et al. | Cholesterol-lowering drugs (atorvastatin) | Reduction in plasma 27-OHC | Significant reduction in total serum bile acids associated with a relative decrease of ursodeoxycholic and lithocholic acids compared to deoxycholic acid., for -related HSP |
| Sardina et al. | Pharmacological interventions inhibiting neddylation-mediated degradation in neurons | Inhibits neddylation-mediated degradation in neurons | Inhibition of neddylation processes effectively restores spastin levels and subsequently rescue neurite cells in spastin mouse model of HSP and patient-derived cells. Promising potential as a therapeutic target for addressing -HSP |
HSP: hereditary spastic paraplegia; GABA: Gamma-aminobutyric acid; SPG: spastic paraplegia; MAS: MAS modified Ashworth scale; SPRS: spastic paraplegia rating scale, MFIS: modified fatigue impact scale, 6 MWT: 6-meter walk test; CYP7B1 : oxysterol-7-hydroxylase; L-Dopa: Levodopa; MSWS-12: 12-item multiple sclerosis walking scale; TWT: time up and go test; 27-OHC: 27-hydroxycholesterol.
L-Dopa, an amino acid precursor to dopamine commonly used to manage PD symptoms, has been explored for its potential in HSP treatment. Historically, the evidence for L-Dopa in HSP has been largely based on case studies, offering limited-quality data. 121 , 122 Although case studies have reported positive outcomes with L-Dopa treatment in HSP patients, an RCT conducted on individuals with SPG11 HSP-related parkinsonism did not show significant improvements in the cohort. 89 This disparity highlights the need for more comprehensive research to unravel the complex mechanisms underlying parkinsonism in HSP. For instance, the ineffectiveness of L-Dopa treatment might be attributed to extreme postsynaptic disruption, suggesting that further studies are warranted ( Table 3 ).
Botulinum toxin injection
Botulinum toxin functions by inhibiting neuromuscular activity, binding to cholinergic nerve terminals, and reducing acetylcholine release. In a double-blind, randomised, placebo-controlled crossover trial (SPASTOX Trial), 55 HSP patients received either botulinum toxin type A (BoNT-A) injections or saline injections. 123 The results indicated that BoNT-A effectively reduced adductor tone, with transient and tolerable adverse events. However, it did not lead to significant functional improvements ( Table 3 ). 123
Dalfampridine (4-aminopyridine)
Dalfampridine, an oral medication given at a dose of 10 mg twice daily for 15 days, yielded significant results in trials. It is a voltage-dependent potassium channel blocker designed to enhance walking ability in patients. 121 A study involving six patients showed a general improvement in motor function, as assessed through gait analysis, the time up and go test (TWT), the 6-meter walk test (6 MWT) and reduced fatigue based on the Modified Fatigue Impact Scale (MFIS). Patients also reported enhanced concentration during specific activities and perceived improvements in emotional stability. 121 Nevertheless, since these studies were uncontrolled, further controlled research is essential to provide stronger evidence regarding the safety and efficacy of dalfampridine for HSP patients ( Table 3 ).
Cholesterol-lowering drugs
SPG5- HSP is caused by recessive mutations in the gene for oxysterol-7-hydroxylase ( CYP7B1 ), resulting in the accumulation of neurotoxic oxysterols. 124 Cholesterol-lowering drugs, such as atorvastatin, have shown some potential in managing this subtype of HSP. A study involving 14 HSP patients revealed that treatment with atorvastatin led to a moderate reduction in plasma 27-hydroxycholesterol (27-OHC) levels, along with a significant decrease in total serum bile acids. This was associated with a relative decrease in ursodeoxycholic and lithocholic acids when compared to deoxycholic acid levels ( Table 3 ). 124
Drugs inhibiting neddylation process
As previously elucidated, the diminished function of spastin has been associated with the pathogenesis of HSP. Investigations conducted in a spastin mouse model of HSP and utilising patient-derived cells have unveiled that the overexpression of Homeodomain Interacting Protein Kinase 2 ( HIPK2 ) or inhibition of neddylation processes can effectively restores spastin levels and subsequently rescue neurite cells. 125 These insightful observations present the intriguing prospect of employing pharmacological interventions to inhibit neddylation-mediated degradation in neurons, thereby unearthing a novel and promising therapeutic target for addressing SPG4- HSP ( Table 3 ). 125
Non-pharmacological therapies
Transcranial and direct current stimulation.
Research into transcranial and direct current stimulation as potential treatments for HSP has been undertaken to alleviate symptoms and enhance patients' quality of life. Repetitive transcranial magnetic stimulation (rTMS) is a non-invasive technique that involves modulating neural networks by applying magnetic pulses. 126 Two RCTs have explored the use of rTMS. Although one trial, involving eight patients, showed improvements in lower limb spasticity, secondary outcomes such as lower limb motor function and short-term quality of life improvements did not significantly differ between treatment and control groups. 127 In the other trial, leg muscle strength improved, but spasticity in distal leg muscles did not significantly change. 126 Although there was speculation that rTMS could be paired with gait training to achieve greater functional improvements, an RCT on gait-adaptability training for HSP patients did not show significant benefits. 128 Notably, an RCT on transcutaneous spinal direct current stimulation (tsDCS), a non-invasive method for modulating spinal cord function, demonstrated reductions in spasticity and is proposed as a complementary strategy for patients not responding to alternative treatments ( Table 4 ). 129
Summary table of the effects of non-pharmacological interventions on hereditary spastic paraplegia.
| Author, Year | Intervention | Action | Studied effect in HSP |
|---|---|---|---|
| Bastani et al. , Antczac et al. | Repetitive transcranial magnetic stimulation | Non-invasive modulation of the neural network by the application of magnetic pulses | Limited improvements in lower limb spasticity and leg muscles strength |
| Ardolino et al. | Spinal direct current stimulation | Non-invasive modulation of spinal cord function, possibly through modulating GABA(a)ergic intracortical networks and interhemispheric balance | Improvement in spasticity levels of participants, and proposed as a complementary treatment option |
| Park et al. | Selective dorsal rhizotomy | Surgical intervention entails the selective severing of sensory nerve fibres, typically those contributing to the induction of spasticity | Almost 90% of the patients experienced successful removal of spasticity and ability to regain independence. 16% of the patients experienced improvement in ambulatory function and regained independence in walking. Complications, although rate, include spinal fluid leak, mild lower limb numbness and functional decline requiring wheelchair |
| Hauser et al. | mRNA injection | Injections containing mRNA facilitates the conversion of 25- and 27-hydroxycholesterol and mitigates the accumulation of neurotoxic lipids | Positive results in animal studies of HSP, in particular, leading to lowered 25- and 27-hydroxycholester levels in mice liver and brain |
| Costamagna et al. | Human NMJ generated from patient-derived iPSC | The NMJ model was created to produce lower motor neurons and myotubes, thereby preserving the genetic characteristics of the HSP patient donors | Promising potential in the exploration of novel treatment options for rescuing axonal defects and diverse cellular processes, including membrane trafficking intracellular motility and protein degradation in HSP |
HSP: hereditary spastic paraplegia; SPG: spastic paraplegia, MAS: MAS modified Ashworth scale; SPRS: spastic paraplegia rating scale; MFIS: modified fatigue impact scale; 6 MWT: 6-meter walk test; CYP7B1 : oxysterol-7-hydroxylase; iPSC: induced pluripotent stem cells; NMJ: neuromuscular junction.
Selective dorsal rhizotomy
Selective dorsal rhizotomy (SDR) is a surgical procedure commonly used to manage spastic cerebral palsy, aiming to reduce spasticity and enhance ambulatory function. It has also been explored for HSP patients. 130 In a study by Park et al., 130 37 HSP patients, with SPG4 and SPG3A being the most common genetic mutations, underwent SDR. The procedure successfully eliminated spasticity in almost 90% of the patients, enabling them to regain independence. Approximately 16% of the patients experienced an improvement in ambulatory function, regaining their ability to walk independently. Although complications are rare, they can include spinal fluid leaks, mild lower limb numbness, and functional decline necessitating the use of a wheelchair ( Table 4 ). 130
Disease modifying therapies and biomarkers
Currently, there are no available disease modifying therapies (DMTs) for HSP. However, certain subtypes may present opportunities for the development of interventions. For example, SPG5 , characterised by a loss-of-function mutation leading to the accumulation of 25- and 27-hydroxycholesterol, which can cross the blood–brain barrier and disrupt neurons, has been a focus of study. The injection of CYP7B1 mRNA has been explored as a potential treatment option. 131 This strategy has demonstrated a reduction in the accumulation of neurotoxic agents in mouse liver and brain. Given the potential for targeting this enzyme through lipid-lowering therapies, 132 it is conceivable that DMTs may be identified along this route in the future ( Table 4 ). 131
Novel stem cells
The use of patient-derived induced pluripotent stem cells (iPSCs) has been investigated for various neurological and motor disorders, including spinal muscular dystrophy and ALS. However, HSP, characterised by more widespread axonal degeneration that extends beyond the corticospinal tract, may limit the potential application of iPSCs, as described in the literature. 133 Human neuromuscular junctions (NMJs) generated from iPSCs obtained from five HSP patients have shown promise. These NMJs create lower motor neurons and myotubes while maintaining the genetic background of HSP patient donors. 134 The NMJ model has displayed potential in exploring novel treatment options for addressing axonal defects and various cellular processes, including membrane trafficking, intracellular motility and protein degradation in HSP ( Table 4 ). 134
Limitations of study
This comprehensive review employs a methodologically rigorous approach to elucidate various facets of HSP, offering valuable insights into its underlying mechanisms, genetic determinants and the current landscape of treatment options, including those under active investigation. Nevertheless, it is essential to acknowledge certain inherent limitations.
Firstly, the literature search strategy encompassed a diverse array of reputable databases, including Scopus, MEDLINE, EMBASE and the Cochrane Library. Despite the diligence in this process, it is possible that some pertinent studies on the subject may have inadvertently been omitted, as no search methodology can claim absolute exhaustiveness. Secondly, a notable limitation lies in the review’s exclusive focus on English-language literature. While this approach ensured the inclusion of a substantial body of relevant research, it may have unintentionally excluded valuable insights presented in non-English publications. This linguistic bias introduced by the language restriction warrants consideration, as it may have implications for the comprehensiveness of the review. Furthermore, the review process itself may introduce certain biases. For instance, the selection of specific keywords for the search query may inadvertently exclude relevant literature that employs differing terminology, thereby potentially affecting the scope of the review. Interpretive bias, stemming from the subjective judgement involved in synthesising and analysing the selected literature, is an additional limitation. Lastly, it is worth noting that some studies are small-scale with limited sample sizes, limiting the generalisability of the findings across the population.
Conclusion and prospects
Due to the heterogeneous clinical nature of HSP, early diagnoses and subsequent management becomes challenging. Although genetics-based management has shown progress for some neurological disorders, HSP lags behind due to its genetic diversity, complex disease processes, range of subtypes and slower disease onset. Moreover, screening and scoring systems, such as the 6- and 10-min walk test alongside the TWT used to assess fatigue and quality of life, may be beneficial in HSP. To advance our understanding and treatment of this neuromuscular condition, extensive research is required, which should involve international collaboration and RCTs conducted on substantial population cohorts. These efforts are particularly critical when considering the administration of combination medications. Furthermore, there is a pressing need for the identification of biomarkers and distinctive mechanisms that can differentiate HSP from other neurological disorders presenting similar clinical symptoms. Additionally, research should focus on the development of promising pharmacological and non-pharmacological treatments, striving to strike a balance between treatment efficacy and the mitigation of adverse effects when addressing HSP symptoms.
Acknowledgments
We acknowledge Icormed Research Collaborative and Toufik’s World Medical Association for their research facilitation.
Author contributions: Conceptualisation: W.A.A. and H.H. Data Curation: W.A.A., J.K.T., A.D.S., T.F., F.T.A., A.M., J.W., L.D., E.C. and H.H. Writing – Original draft: W.A.A., J.K.T., A.D.S., T.F., F.T.A., A.M., J.W., L.D., E.C., H.H., T.A.R., V.S., O.A., J.K., R.J. and D.E.M. Writing – Second draft: W.A.A., J.K.T., A.D.S., T.F., F.T.A., A.M., J.W., L.D., E.C., H.H., T.A.R., V.S., O.A., J.K., R.J., D.E.M., K.S., O.K. and M.Y.D. Review and Editing: W.A.A., J.K.T., A.D.S., H.H., O.A. and M.Y.D. Visualisation: V.S. and A.D.S. Approval of final manuscript: All authors.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Ethical approval: Not applicable.
Informed consent: Not applicable.

Data availability statement: No data available.
- Open access
- Published: 29 July 2016
A genetic assessment of the English bulldog
- Niels C. Pedersen 1 ,
- Ashley S. Pooch 2 &
- Hongwei Liu 1
Canine Genetics and Epidemiology volume 3 , Article number: 6 ( 2016 ) Cite this article
68k Accesses
24 Citations
2264 Altmetric
Metrics details
This study examines genetic diversity among 102 registered English Bulldogs used for breeding based on maternal and paternal haplotypes, allele frequencies in 33 highly polymorphic short tandem repeat (STR) loci on 25 chromosomes, STR-linked dog leukocyte antigen (DLA) class I and II haplotypes, and the number and size of genome-wide runs of homozygosity (ROH) determined from high density SNP arrays. The objective was to assess whether the breed retains enough genetic diversity to correct the genotypic and phenotypic abnormalities associated with poor health, to allow for the elimination of deleterious recessive mutations, or to make further phenotypic changes in body structure or coat. An additional 37 English bulldogs presented to the UC Davis Veterinary Clinical Services for health problems were also genetically compared with the 102 registered dogs based on the perception that sickly English bulldogs are products of commercial breeders or puppy-mills and genetically different and inferior.
Four paternal haplotypes, with one occurring in 93 % of dogs, were identified using six Y-short tandem repeat (STR) markers. Three major and two minor matrilines were identified by mitochondrial D-loop sequencing. Heterozygosity was determined from allele frequencies at genomic loci; the average number of alleles per locus was 6.45, with only 2.7 accounting for a majority of the diversity. However, observed and expected heterozygosity values were nearly identical, indicating that the population as a whole was in Hardy-Weinberg equilibrium (HWE). However, internal relatedness (IR) and adjusted IR (IRVD) values demonstrated that a number of individuals were the offspring of parents that were either more inbred or outbred than the population as a whole. The diversity of DLA class I and II haplotypes was low, with only 11 identified DLA class I and nine class II haplotypes. Forty one percent of the breed shared a single DLA class I and 62 % a single class II haplotype. Nineteen percent of the dogs were homozygous for the dominant DLA class I haplotype and 42 % for the dominant DLA class II haplotype. The extensive loss of genetic diversity is most likely the result of a small founder population and artificial genetic bottlenecks occurring in the past. The prominent phenotypic changes characteristic of the breed have also resulted in numerous large runs of homozygosity (ROH) throughout the genome compared to Standard Poodles, which were phenotypically more similar to indigenous-type dogs.
Conclusions
English bulldogs have very low genetic diversity resulting from a small founder population and artificial genetic bottlenecks. Although some phenotypic and genotypic diversity still exists within the breed, whether it is sufficient to use reverse selection to improve health, select against simple recessive deleterious traits, and/or to accommodate further genotypic/phenotypic manipulations without further decreasing existing genetic diversity is questionable.
Plain English Summary
The English bulldog is one of the most popular breeds in the world because of its child-like appearance and demeanor. The alterations in body type and behavior needed to create the breed have required physical changes well beyond its village dog ancestors. These changes have occurred over hundreds of years but have become particularly rapid over the last decades. Unfortunately, popularity does not equate to health and there have been increasing pressures on breeders to moderate the extreme physical changes that now affect the breed and its health. Improving health through genetic manipulations presumes that enough diversity still exists to improve the breed from within, and if not, to add diversity by outcrossing to other breeds. The present study was an assessment of genetic diversity that still exists in a representative number of individual English bulldogs using DNA rather than pedigrees. The results confirm that the breed has lost considerable genetic diversity through such things as small founder population and artificial genetic bottlenecks resulting from highly focused selection for specific desired physical traits. This is manifested by a narrowing of allele diversity in many parts of the genome, and the creation of numerous large regions of the genome that are essentially identical within the breed, which are significantly different from other dogs. Loss of genetic diversity is also pronounced in the region of the genome that contains many of the genes that regulate normal immune responses. The loss of genetic diversity and extreme changes in various regions of the genome will make it very difficult to improve breed health from within the existing gene pool. Loss of present genetic diversity is further threatened by rapid integration of new coat color mutations, increased wrinkling of the coat, and attempts to create a more compact body type. Contrary to current beliefs, brachycephaly and the resulting breathing problems in the breed are the result of complex changes in head structure, and cannot be corrected by merely lengthening the face. Furthermore, other issues in English bulldogs need to be addressed, including many serious health problems that are not associated with brachycephaly, but are intrinsic to inbreeding.
The first mention of what might be a contemporary type bulldog was reported in 1632 [ 1 ]. The “bull” refers to the breed’s use in the sport of bull baiting in England. Bull baiting, which had its beginning even centuries earlier with the Egyptians, Greeks and Romans, became a national sport in England from the 13 th to 18 th centuries [ 1 ]. The objective was for the dog to latch onto the bull’s nose and force it to the ground, with the first dog to do so the victor. These original bulldogs had stockier bodies, larger heads and stronger jaws, and a more ferocious and aggressive temperament than the common indigenous dogs of the period. Therefore, their ancestors were presumably mastiff-type dogs originally bred in Asia for their strength and aggressiveness. Controversy exists as to whether these Mastiffs were crossed with breeds such as the Pug to make them more effective at bull baiting [ 1 ]. The first description of a Bulldog as a distinct entity from the Mastiff was in 1631 in a letter written from Mr. Eaton in Spain to a friend in England [ 1 ]. The bulldog was further genetically altered over the 500 year period of bull baiting by “selection of the fittest,” with emphasis on increasing agility and putting more power and weight into the head and front end to minimize spinal damage when they were shaken by the bulls [ 1 ].
Attempts to legislate against bull baiting began in the UK in 1802 and the sport was finally abolished by an Act of Parliament in 1835, which led the breed to the brink of extinction [ 1 ]. The Bulldog endured by the efforts of a small group of aficionados and the breed underwent even more change in size and temperament after 1835 to ultimately make them into the shorter-faced, squatter and more affable companion dog that we know today. Footnote 1 The first Bulldogs appeared in show rings in the UK in 1860, and the Bulldog was first recognized by the American Kennel Club in 1886. Footnote 2
A number of modern breeds use “bull” or “bulldog” in their names and all have evolved from the original Bulldogs and Mastiff-type dogs [ 1 , 2 ]. Some of these breeds are of more ancient origin, while others are reconstructions of breeds that no longer exist. The modern Olde English Bulldogge is a reconstruction of the original bulldog based on crosses between English bulldog, American bulldog, American Pit Bull Terrier and Mastiff. Footnote 3 The Miniature bulldogs, French bulldog and American bulldog are also constructed breeds that nonetheless trace some of their ancestry to the original English bulldog. Although there are several “bulldogs,” the ideal English bulldog is easily differentiated by its huge head with wedge-shaped body, short and folded ears; stocky build with deep furrows of the skin, especially of the face; short or corkscrew tail; short thick legs with equally broad paws; and a gentle, child-like appearance and disposition [ 2 ].
The outward appearance of many dog breeds change with time, and this is also true of the English bulldog. Footnote 4 , Footnote 5 Photographs of English bulldogs from the nineteenth century depict dogs with less pronounced brachycephaly, less chondrodystrophic skeletal structure, a long tail, and without excessive skin folds on their face or body. Footnote 6 A picture of an English bulldog from 1935 can be found on an orange crate label advertising California oranges (Fig. 1 ) and this dog was already differing in appearance from its ancestors pictured a century earlier and from contemporary English bulldogs. However, photographs of modern English bulldogs still demonstrate a range of phenotypic diversity, with some dogs being smaller and squatter or larger and longer-legged, some with smooth rather than wrinkled coats, some with less brachycephalic and furrowed faces, some with longer and less chondrodystrophic limbs, some more prognathous than others, some with intact tails, and others with different shaped remnants of tails. Footnote 7 , Footnote 8
A drawing of an English bulldog from 1935 copied from a California Orange Crate Label of the Rudolph Marketing Company.
Although much has been said about the ill-health of contemporary English Bulldogs, the English bulldog of the late 19 th century also had its share of health problems and critics. 5 Therefore, the English bulldog was not initially popular in the UK, although its popularity has greatly increased over the last decades in many affluent countries [ 3 ]. English bulldog owners love their baby-like appearance and demeanor and the breed has been cited as one of the prime examples of exuberant anthropomorphism [ 4 ]. Health problems of the breed have not decreased its popularity and deviations from the original standard based on changing perceptions of “champion form” have led to even more conformational changes that have further affected breed health. 5
The health problems of the English bulldog have been well documented and start with conception, fetal development and parturition. Severe conformational changes have necessitated a high rate of artificial insemination and Caesarean sections and litter sizes tend to be small. 5, Footnote 9 The breed ranks second in congenital disease and associated puppy mortality [ 5 ], due mainly to birth defects such as flat chests with splayed legs; anasarca (water babies) and cleft palate [ 6 ]. Footnote 10 , Footnote 11 Although some English bulldogs enjoy reasonable health, their longevity is definitely affected by the degree of conformational change and inbreeding, which is reflected by lifespan estimates ranging from 3.2 to 11.3 years with a median of 8.4 years [ 7 ]. Individuals requiring extensive veterinary care at a young age rarely live beyond 5–6 years of age, leading to a bimodal mortality curve for the breed. 11
The brachycephalic syndrome is a leading cause of ill-health and death in the breed. However, the syndrome is not caused by brachycephaly per se, as brachycephalic breeds such as the boxer do not suffer the syndrome to the same degree. The bulldog tongue is excessively large at the base, the palate is large and easily obstructed by the base of the tongue, the lower jaw is pushed forward (prognathous), and the nares are frequently stenotic and the trachea hypoplastic. This leads to loud panting during physical exercise, stridor during rest and slobbering; sleep apnea, hypercapnia and hypochloremia/hypomagnesemia; exercise intolerance, cyanosis and collapse; and choking fits manifested by gagging, retching, vomiting, aerophagia/flatulence and aspiration pneumonia [ 8 – 12 ]. The breathing difficulties of English bulldogs also make them very sensitive to overheating and heat stroke.
Chondrodysplasia, a heritable skeletal disorder that has been incorporated into the phenotype of many dog breeds [ 13 ], predisposes English bulldogs to skeletal disorders such as hip dysplasia, elbow dysplasia, luxating patella and shoulders, intervertebral disk disease, cruciate ligament rupture, hemivertebra, torsional pelvic deformity and problems with normal copulation and parturition [ 14 , 15 ]. Prognathism predisposes to dental disease, while excessive folding of the skin, especially on the face, is associated with skin fold dermatitis, muzzle acne, folliculitis, furunculosis, and eye conditions such as entropion, ectropion, and eversion of the third eyelid. The cork-screw tail can result in tail fold dermatitis. Other heritable conditions that are related to loss of genetic diversity and inbreeding include cataract, various heart valve defects including pulmonic stenosis, hydrocephalus, cysteine urolithiasis, and hiatal hernias; immunologic disorders that include a propensity for severe demodectic mange indicative of immunodeficiency, allergies associated with atopic dermatitis and ear infections, and autoimmune diseases such as hypothyroidism; and cancers including glioblastoma, mast cell sarcoma and lymphoma [ 15 , 16 ]. Although the bond and affection between English bulldogs and their owners is strong, the cost of treating health problems is often prohibitive and many of them end up in shelters or euthanized.
Severe health problems in English bulldogs in the USA and the UK have prompted articles [ 16 ] such as “Can the Bulldog be saved?” The article documented the short lives of University of Georgia mascots and re-kindled the humane issues of knowingly breeding dogs destined to lives of serious ill-health. An earlier broadcast on the BBC spawned three independent reports identifying the English bulldog as a breed in need of genetic intervention, presumably to breed away from the extremes of brachycephaly and chondrodysplasia and increase genetic diversity. The British Kennel Club responded to these criticisms by revising the English bulldog standard to select against obvious breathing difficulties and avoid extreme facial wrinkling. Footnote 12 However, bulldog breeders in the UK argue that “what you’ll get is a completely different dog, not a British bulldog” 12 , a strange argument given the continuous phenotypic changes that have occurred within the breed over many decades. 6,7,8 Groups in The Netherlands have called for a ban on English bulldogs based on a belief that the breed can no longer be returned to a health, while supporters believe that the breed can be returned to health from within and are petitioning the government against the ban. Footnote 13 American breeders of English bulldogs have avoided the issue and even deny that the breed is unhealthy, pointing to its popularity as proof [ 3 ]. However, the bulldog has been banned from plane travel in the cargo hold by many domestic and international airlines due to a high incidence of deaths. Footnote 14
English bulldogs have risen from 5 th to 4 th in popularity between 2013 and 2015 in AKC registrations [ 3 ], proving that the public is more enamored with the dog than concerned about its health. Assuming that this attitude will change and steps taken to improve the breed’s health, how can this best be accomplished? Diehard breeders would argue that this should involve genetic change from within existing bloodlines. The question then becomes whether there is enough residual phenotypic and genotypic diversity to significantly improve the health of the breed using the existing stock. Although there is still phenotypic variability in the breed based on photographs 6,7,8 , bulldogs that reproduce without assistance, move freely, walk or run for long distances, and breathe normally even at rest are the exception.
Efforts are underway in the UK to improve the health of bulldogs from within the breed by making modest changes on what is acceptable in a show dog. However, there is very little knowledge about the actual genetic status of the breed and whether enough genetic and phenotypic diversity still exists to significantly improve health without further reducing existing genetic diversity or relying on outcrossing. Breeders still rely heavily on pedigrees and coefficients of inbreeding (COI). The problem is that pedigrees emphasize ancestors and inheritance by descent but not actual genetic makeup. They are also subject to parentage errors and COIs based on a few recent generations are of limited value in a breed that started with few founders subjected to numerous artificial bottlenecks that occurred decades and even centuries earlier. Therefore, we endeavored to conduct a broad-based genetic assessment of the breed using DNA rather than pedigrees. The findings of this study indicate that English bulldogs may have insufficient genetic diversity to significantly improve gross physical abnormalities associated with poor health, to eliminate simple recessive deleterious traits, or to use inbreeding to rapidly integrate new coat colors and to breed for a smaller and more compact shape without further decreasing genetic diversity in individuals and adding to their health problems.
Sample acquisition and DNA extraction
The Veterinary Genetics Laboratory (VGL) (UC Davis School of Veterinary Medicine, Davis, CA, USA) provided DNA samples of 102 registered English Bulldogs; 87 of the dogs were from the USA, six from Finland, three each from Canada and Austria, and one each from Czechoslovakia, Hungary, and Argentina. DNA from these dogs was submitted mainly for coat color or hyperuricosuria mutation testing and used in breeding programs. As such, they were presumed to be of adequate health and therefore listed as “controls”. Thirty-seven DNA samples were collected from whole blood of English bulldogs submitted for various diagnostic tests at the UC Davis Veterinary Medical Teaching Hospital (VMTH). These dogs were seen for a variety of health problems ranging from breathing problems, eye problems, skin disorders, orthopedic problems, or cancer and were therefore listed as “case”. DNA was extracted using established procedures [ 17 ].
Determination of maternal and paternal haplotypes
Maternal haplotypes were determined by sequencing 655 bp of the mitochondrial D-loop (nucleotide 15453–16107) in 48 English Bulldogs as described [ 18 ]. Dogs were as unrelated as possible based on genomic STR markers. Sequences were analyzed using Geneious software [ 19 ]. Final sequences were compared to the National Center for Biotechnology Information (NCBI) database using nucleotide Basic Local Alignment Search Tool (BLAST) [ 20 ]. Paternal haplotypes were determined from the 44 male dogs in the group based upon a panel of six Y-STR markers, including 650.79.2 , 990.35.4 , MS34A , MS34B , MS41A , and MS41B [ 21 , 22 ].
Genomic STR markers and DLA class I and II STR markers
Thirty-three STR loci across 25 chromosomes were used to assess genomic diversity, while four STR loci were used to determine DLA class I haplotypes and three STR loci were used for DLA class II haplotypes. The primer sequences, dye markers, conditions for amplification and analysis of these STR markers have been published [ 23 ].
The use of allele frequencies for standard genetic assessments
A genetic assessment using allele frequencies was conducted using GenAlEx 6.5 software [ 24 ]. The population statistics used in this study included Aa, Ae, Ho, He, and the inbreeding coefficient F. Aa represented the average number of alleles at each locus; Ae represented the average effective number of alleles at each locus; Ho is observed heterozygosity, while He is the expected heterozygosity if the population was randomly breeding. The value F is an inbreeding coefficient derived by [1-(Ho/He)]. An F value of 0 indicates that the population as a whole is in Hardy-Weinberg equilibrium (HWE), i.e., randomly breeding. A negative F value of −1.0 indicates that that every member of the population is genetically distinct, while a F value of +1.0 indicates that all members were genetically identical. Principal coordinate analysis (PCoA) was performed in Excel using the XLSTAT software.
Internal relatedness (IR) is a statistical estimate of how closely an individual dog’s parents were related to each other [ 23 ]. It also uses allele frequency data, but unlike Ho and He, it gives more weight to uncommon alleles. An IR value of −1.0 means both parents were totally unrelated, while a value of +1.0 means the parents were genetically identical. Internal relatedness values can also be used to plot the population as a whole and estimate the amount of genetic diversity lost as a result of breed creation [ 23 ]. The latter estimate is made by adjusting the frequencies of alleles found at each genomic STR locus to the frequency of the same allele in a large population of random breeding village dogs, thus yielding IR-village dog (IRVD). These village dogs breed randomly and have genetic links with most modern breeds, and they are one of the largest single reservoirs of ancestral diversity inherited by descent [ 22 , 25 , 26 ]. The IR and IRVD were graphed using the software R [ 27 ].
Analysis of GWAS data for runs of homozygosity
Illumina 170 K CanineHD datasets for English bulldog and Standard poodle were obtained from other GWAS studies [ 28 , 29 ] and filtered for minor allele frequency (<0.05) and genotype (>90 %). Ten English bulldogs and 10 Standard Poodles were randomly selected and their SNP arrays interrogated for runs of homozygosity (ROH) using PLINK [ 30 ]. Runs of homozygosity with allele sharing across all individuals were identified by applying the option –homozyg-group . The analysis yielded the number, size range of ROH, and the portion of ROH that was shared (consensus ROH) by all individuals interrogated. This information was extended by looking for the consensus ROH that were shared by 6–9 of the 10 individuals tested.
- Paternal haplotypes
Paternal haplotypes were determined for 44 male English Bulldogs in the study population using six Y-specific STRS. Haplotype 1 was dominant in 93.1 % of the dogs, while haplotype 2–4 were observed in 2.3 % of dogs each (Table 1 ). Paternal haplotypes three and four were closely related to the dominant haplotype 1 and appeared to arise from a single mutation in the MS41B STR locus, changing K to J or L, respectively. Test data from the UC Davis Veterinary Genetics Laboratory has also found the dominant haplotype 1 of the English bulldog in the French bulldog, Bull Terrier, Bull mastiff, Miniature bull terrier, Staffordshire bull terrier, Wire-haired fox terrier, Beagle, and Coton de Tulear.
- Maternal haplotypes
Five maternal haplotypes were identified in the control population based on mitochondrial sequences. The sequences of the haplotypes observed in English bulldogs corresponded to GenBank Accession numbers as follows: EBU-A (GenBank:KP665923), EBU-C (GenBank:KP665928), EBU-J (GenBank:KP665924), EBU-K (GenBank:KP665914), and EBU-7 (GenBank:KP665930). Maternal haplotype frequencies and variations of base pair positions are listed in Table 2 . Three of the five haplotypes were found in 90.9 % of the dogs. The five maternal haplotypes identified in English bulldogs have been found among a number of common dog breeds, with the three most common matrilines (EBU-C, −J and –K) also found in mastiff- and brachycephalic-type breeds (Table 3 ).
Genetic assessment of healthy and unhealthy English bulldogs using 33 genomic STR loci
A genetic assessment of 102 control English bulldogs based on the alleles and their frequencies at each of the 33 genomic STR loci was conducted and the population statistics were evaluated with GenAlex 6.51 software (Tables 4 and 5 ). The highest number of individual alleles found for a single autosomal STR locus was eleven ( VGL1165 ), and the lowest was three ( INRA21 ). Most of the loci had one or two alleles that dominated in frequency. Nineteen of 33 loci had single alleles with a frequency ≥ 50 %, which are highlighted in Table 4 . Six of the STRs had one allele with a frequency of 70 % or greater, and allele 202 at locus REN162C04 was virtually fixed with a frequency of 0.99 amongst the 102 dogs studied (Table 4 ). The average number of alleles per locus was 6.46, of which an average of 2.77 alleles per locus contributed disproportionately to overall diversity (Table 5 ). The observed and expected heterozygosity (Ho and He) were essentially the same, yielding an inbreeding coefficient (F) close to zero. The Ho, He and F values indicated that this population of 102 dogs was in HWE.
Results from a genetic assessment of 37 unhealthy case dogs were compared to that of the 102 presumably healthy controls (Table 5 ). The two populations were essentially identical by all of the genetic parameters, with the exception of the average alleles per locus for case dogs, which was a lower in case dogs (Table 5 ). However, this difference was due to variation in sample size, because Aa was similar (5.182 vs 5.364) when the 37 case dogs were compared to 37 control dogs randomly selected from the larger population by Excel (data not shown). Observed and expected heterozygosity did not differ between case and control dogs and the values for F were near zero for both groups. No differences were detected between case and control populations by principal coordinate analysis (Fig. 2 ).
PCoA plot of 102 healthy English bulldogs (control) and 37 English bulldogs admitted to the VMTH for a variety of health problems (case)
Internal relatedness and adjusted internal relatedness
The mean IR value for the 102 English Bulldogs was 0.007, with individuals ranging from−0.234 (most outbred) to +0.304 (most inbred) (Fig. 3 , Table 6 ). This suggested that there were highly inbred individuals in the population, which were balanced by an equal portion of outbred dogs, giving the impression that the population as a whole was a product of random breeding.
Internal relatedness (IR, solid line ) and internal relatedness relative to village dogs (IRVD, dash line ) of 102 English Bulldogs
The adjusted IR value (IR-village dog or IRVD) for the population gave a more accurate measure of just how inbred the parents of modern English bulldogs were compared to village- or landrace- type dogs from which the breed evolved. IRVD values ranged from 0.043 to 0.64 with a mean of 0.335 (Fig. 3 , Table 6 ]. Therefore, 78/102 bulldogs (77 %) had IRVD values >0.25 and were more closely related to each other than offspring of full sibling parents from a random breeding village dog population. Values >0.25 would occur only if full sibling parents were offspring of inbred parents; the more inbred the parents the higher the IRVD score.
The IR and IRVD values for English bulldogs were further compared with the Standard Poodle (Fig. 4 , Table 6 ). Standard Poodles like the English bulldog, are very popular and a sub-population has been extensively inbred for a uniform and desirable appearance [ 23 ]. A comparison of minimum and maximum IR values for the two breeds show parents of individual Standard Poodles to be both more unrelated (−0.306 vs−0.234) and related (0.304 vs 0.528) than parents of individual English bulldogs (Table 6 ). The differences are even more apparent when comparing IRVD values (Table 6 ). This comparison demonstrated that many Standard Poodles were offspring of parents that were even more inbred than parents of the most inbred English bulldogs. Although both breeds appear to be highly inbred, Standard Poodles have retained much more genetic diversity across the breed [ 23 ].
Internal relatedness (IR, solid line ) and internal relatedness relative to village dogs (IRVD, dash line ) of 664 American Standard Poodle
Frequency of STR-associated DLA Class I and II haplotypes
Eleven DLA class I and nine class II haplotypes were identified among the 102 English bulldogs tested (Table 7 ). The dominant class I haplotype was observed in 40.7 % of the dogs, while the three most common haplotypes together accounted for nearly 80 % of all class I haplotypes. The dominant class II haplotype was found in 62.3 % of English bulldogs, while the two most common were present in 86 % of individuals. The three most common DLA class I and two most common class II haplotypes were homozygous in 24.5 and 50 % of dogs, respectively (Table 7 ).
Individual alleles within the 7 STR loci that defined the DLA class I and II regions were assessed for heterozygosity. Each of seven loci was defined by one dominant and one semi-dominant allele and several minor alleles (Table 8 ). The most common alleles were usually found in the most prevalent DLA class I and II haplotypes.
Although the DLA is in strong linkage disequilibrium compared to other regions of the genome, there are recombination hotspots within the DLA and fixation indices using allele frequencies at the seven class I and II STR loci is of some value (Table 9 ). The average DLA class I/II associated alleles per STR loci was 5.43, but only 2.16 (40 %) were contributing to most of the genetic diversity (Table 9 ). This was a reflection of the imbalance in the frequency and homozygosity of certain founding DLA class I and II haplotypes, although the observed and expected heterozygosity were similar and F was near zero. The neutral F value indicated that the imbalance in DLA classes I/II haplotypes was not a recent occurrence but resulted from small number of ancestral founders or artificial genetic bottlenecks much earlier in breed evolution. Periods of inbreeding associated with genetic bottlenecks such as popular sire effects are often followed by a return to random breeding, although the outcome may be a permanent reduction in founder size [ 23 ].
Runs of homozygosity (ROH) in genomes of English bulldogs and Standard Poodles
The English bulldog is very different in outward appearance to breeds such as the Standard Poodle, which still resembles its Middle Eastern/SE Asian village dog and their European Landrace relatives in most aspects. Therefore, variations within genomes of the English bulldogs were compared with those of the Standard Poodle. The implication was that variations within the genome would be much greater in the English bulldog because the extreme conformational changes would require much more intense positive selection within specific parts of the genome. GWAS data from 10 randomly selected English bulldogs and Standard Poodles was obtained from previous studies [ 23 , 29 ]. The level of inbreeding based on the proportion of SNPs that were homozygous in canine 170 K arrays was virtually identical in the two breeds; 0.65 ± 0.03 in English bulldogs and 0.63 ± 0.03 in Standard Poodles. The results of IR and IRVD comparisons also showed that highly inbred individuals existed in both breeds. Therefore, it can be assumed that variations in the genomes of English bulldogs and Standard Poodles were not associated with inbreeding per se, but to strong positive selection pressures in various regions of the genome related to comparative breed specific traits and to an associated loss of genetic diversity. The GWAS data was then used to estimate the number and size of ROH in the two breeds.
The largest consensus ROH was determined for all 10 dogs of each breed (Table 10 ). As expected, the number of large consensus ROH shared by 100 % of the population is low because different proportions of individuals will possess one or more heterozygous SNP that create variable sized runs of overlapping homozygosity within these larger ROH. The effect of this small amount of heterozygosity can be offset by identifying the largest consensus ROH shared by at least 9, 8, 7 or 6 out of 10 individuals in the population (Table 10 ).
Two consensus ROH 4.71 Mb and 2.65 Mb in size were identified on different chromosomes in 100 % of English bulldogs tested. The largest autosomal ROH in a single English bulldog was 58.24 Mb on CFA20. The largest consensus ROH on the X-chromosome (CFA39) was 51.35 Mb on five of the six male dogs in the group. The number of consensus ROH that were detected on autosomes increased as the number of dogs that shared larger consensus ROH decreased. Nine of ten of the dogs shared eight additional ROH compared to 10/10 dogs; 8/10 dogs an additional 16 ROH compared to 10/10 and 9/10 dogs; 7/10 dogs had 39 more ROH compared to 8/10, 9/10 and 10/10 dogs; and 6/10 dogs had 53 more ROH than 7/10, 8/10, 9/10 and 10/10 dogs (Table 10 ). In total, 118 consensus ROH ranging from 1.31 to 3.68 Mb on 31 different autosomes were shared by at least 6 of the 10 dogs studied (Table 10 ).
The number and size of ROH were much lower in Standard Poodles than English bulldogs (Table 10 ). No consensus ROH was shared among all 10 of the Standard Poodles and only one ROH of 0.11 Mb was shared by 9/10 of individuals. Twenty-one ROH on 16 chromosomes with consensus sizes of 1.33 ± 0.83 M were shared by at least 6/10 of the dogs. The largest ROH of a single Standard Poodle was 59.16 Mb on CFA11. The largest consensus ROH was 3.66 Mb on CFA30 shared by 8/10 Standard Poodles. A total of 30 consensus ROH on 19 chromosomes and 0.11–1.96 MB in size were shared by at least 6/10 Standard Poodles in the population tested. Therefore, ROH of English bulldogs were larger, more variable in size between individuals, more numerous, and involved many more chromosomes than those of Standard Poodles.
This study examined genetic diversity among contemporary English bulldogs used for breeding purposes from the USA ( n = 87) and several other countries ( n = 15). Thirty-seven pet English bulldogs seen for health problems at UC Davis Veterinary Clinical Services were also included in the study. The populations that were tested evolved from one major and three minor paternal haplotypes and three major and two minor maternal haplotypes. One paternal haplotype, which was found only in a one dog, appeared to be distinct. The two remaining minor paternal haplotypes, also in single dogs, differed from the dominant paternal haplotype by a simple mutation. This pattern of a single dominant paternal haplotype and a small number of maternal haplotypes has been observed in most pure breeds and is therefore not unique to English bulldogs [ 21 , 25 ].
The paternal and maternal haplotypes identified in these English bulldogs provides a window into the breed’s ancestry. The dominant paternal haplotype occurs as expected in several bracycephalic breeds that include “bull” in their breed names, as well as breeds such as the Beagle, Coton de Tulear, and Wire-haired fox terrier. The minor unrelated haplotype has been found in a related genetic form in Akita and Beagles. The two minor mutant haplotypes have not been seen in any other breed suggesting that these have arisen by mutations within the breed. The major maternal haplotype EBU-J occurs in several of the brachycephalic breeds (Boxer, Pug, Boston Terrier) as well as small Mastiff-type dogs (Bull Mastiff, English Bull Terrier, American Pit Bull Terrier), while EBU-K has been found in Asian Mastiffs such as the Shiba Inu and Shikoku. Therefore, the maternal haplotypes seen in English bulldogs support the general belief that English bulldogs evolved from Mastiff-type dogs crossed with brachycephalic breeds such as the Pug [ 1 ]. It is tempting to associate paternal rather than maternal introgressions from smaller and much less aggressive non-brachycephalic breeds were used to make English bulldogs more acceptable as household pets.
Evidence obtained from the 33 genomic STR loci provides additional evidence for the small founder population and artificial genetic bottlenecks that led to the modern English bulldog. The average number of alleles per locus was similar to other pure breeds that have been diversity tested. Footnote 15 However, an examination of the average effective alleles per locus indicates that only one or two alleles are actually contributing to the overall genotype and phenotype diversity of the breed. Six of 33 loci had an allele with frequency >70 %, and allele 202 at locus REN162C04 was homozygous in 101/102 dogs studied. Loss of genetic diversity as a result of pure-breeding, especially when those breeds undergo selection for conformation, is well documented [ 25 ]. The various conformational changes used in creating breed-specific phenotypes often results in large regions of extended homozygosity across the genome [ 31 – 35 ]. The larger and more numerous these regions, the more often they will be associated with an STR and the more likely that certain STR alleles will be at higher frequency and also exist in a homozygous state.
Measurements of observed and expected heterozygosity (Ho and He) and the inbreeding coefficient F are also useful in looking at the genetic makeup of a population. Observed and expected heterozygosity were similar for the English bulldogs tested, yielding an inbreeding coefficient F that was close to zero (0.001). This indicated that the population as a whole was in HWE despite a limited gene pool and that English bulldog breeders were doing a reasonable job of identifying more distantly related dogs for mating. However, IR values indicated that He, Ho and F values were misleading, as many individual dogs in the study were actually products of parents that were much more related to each other than assumed from the population-wide fixation indices.
Internal relatedness has been widely used as an indicator of population fitness [ 36 – 42 ], implying that closely related parents reflect a loss of genetic diversity in the total population under study. The average IR value is 0.25 for a litter of puppies born to full sibling parents from a genetically diverse and randomly bred population. The average IR value for English bulldogs was around 0.007, however there were a number of individuals with IR values around 0.20. However, IR does not take into account the degree of genetic diversity that has been lost as a result of breed development. Virtually all of modern pure-breeds can trace their origins to village-type dogs that proliferated during the Neolithic era in the Middle East and SE Asia and populated other regions of the world [ 22 , 26 ]. Allele and allele frequencies found in pure breeds can be adjusted to the frequencies of those same alleles found in village dog populations and used to re-calculate or adjust IR values to approximate the expected diversity if no founder effects or artificial bottlenecks occurred during a breed’s evolution. When IR values were adjusted using allele frequencies in village dogs, the mean IRVD value for English bulldogs rose to 0.34, with 50 % of dogs having even greater values. A mean value of 0.34 indicates that the average English bulldog is genetically equivalent to offspring of full sibling parents that came from a highly inbred subpopulation of village-type progenitors. This shift to the right of the IRVD compared to IR curve was also seen in Standard Poodles, but to a much less degree, reflecting the greater amount of initial or retained genetic diversity in Standard Poodles.
The low number of different DLA class I and II haplotypes in English bulldogs was associated with an imbalance in the relative frequency of each haplotype. Four of 11 class I and 3/9 class II haplotypes were found in over 90 % of the individual English bulldogs tested. Moreover, there was a high level of homozygosity among the dominant DLA class I (19 %) and II (42 %) haplotypes. Although not balanced in frequency, genetic assessment of the seven STR alleles associated with the DLA class I and II regions showed them to be randomly segregating at this time. This indicated that the over-representation of certain haplotypes occurred at the onset of breed creation as a result of small founder numbers, and/or that it was associated with artificial genetic bottlenecks that were subsequently masked by a return to random selection. Although the DLA region is only a small part of the genome, the importance of these haplotype imbalances, small haplotype numbers, and increased homozygosity should not be underestimated [ 23 , 42 ]. The breed suffers greatly from allergies, immunodeficiency, and a number of autoimmune disorders, which may be a reflection of loss of balanced selection and heterozygote advantage in the DLA region.
In order to gauge the extent to which humans shaped the phenotype of English bulldogs from typical dogs, we decided to compare the English bulldog with a breed that was similarly inbred based on the number of homozygous SNPs identified by Illumina 170 K canine SNP arrays and IR scores, but outwardly similar in appearance to the ancestral dog. The Standard Poodle, which has been similarly studied [ 23 ], met the desired criteria. One hundred nineteen ROH with consensus sizes ranging from 1.31 to 3.68 Mb and shared by at least 6/10 dogs tested were identified on 30 of the 38 autosomes. This was compared to 31 ROH with consensus sizes ranging from 0.11 to 1.96 MB on 19 chromosomes for the Standard Poodle. Although a proportion of the ROH observed in both English bulldog and Standard Poodle can be attributed to natural selection pressures occurring over thousands of years [ 33 , 34 ], the differences in ROH size and number are better explained by the comparative changes in outward appearance. The physical traits of English bulldogs, such as extreme brachycephaly, chondrodysplasia, skin furrowing, differences in tail structure, size and behavior, are extreme compared to the physical changes seen in Standard Poodles. These specific and extreme phenotypic traits required strong positive selection (strong sweeps) in specific regions of the genome [ 43 ], while ROH required for the Standard Poodle phenotype were not nearly as strong or widespread. The variation in ROH observed in the genome of English bulldogs and Standard Poodles were in line with the findings of others. Vaysse and colleagues [ 32 ] identified 44 genomic regions among 49 pure breeds that had undergone intense selection and 22 blocks of SNPs in certain breeds that extended over one million bases. Lindblad-Toh and a large group of investigators [ 31 ] compared the haplotype structure of the genome of the Boxer and 10 other breeds and found regions of linkage disequilibrium extending over several megabases within a breed and tens of kilobases between breeds.
We did not associate runs of homozygosity in English bulldogs with characteristic phenotypic traits but are confident based on previous studies that the greater genomic variation in English bulldogs compared to Standard Poodles reflected stronger human-directed selection in the former breed than in the latter. Pollinger and colleagues [ 44 ] also concluded that strong artificial selection for breed-defining traits have reduced variation within many regions of the genome. Associations between ROH and species/breed traits such as those found in English bulldogs have been demonstrated for human-directed selection in many pure breeds [29, 32, 33, 45, 46]. Brachycephaly is a prominent phenotypic trait in the English bulldog and not a naturally selected phenotype of ancestral village- or landrace-type dogs. A ROH around 500 kb on CFA1 was associated with brachycephaly in a study that compared a number of brachycephalic breeds [ 29 ]. A more recent study confirmed the existence of the brachycephaly-associated region on CFA1 in boxers, but also identified a >8 Mb ROH on CFA26 [ 44 ]. Variation in CFA10 has been linked to ear morphology and body mass in a number of breeds [ 45 ]. Genomic regions of positive selection in dog breeds have also been associated with adaption to a diet richer in starch [ 35 ]. Vaysse and colleagues [ 32 ] also identified runs of homozygosity associated with breed-defining characteristics such as chondrodysplasia in Dachshund [590 Kb] and wrinkled skin in Sharpei [1.4 Mb], characteristics of English bulldogs but not Standard Poodles. They also concluded that artificial selection in domestic animals targeted different functional categories than natural selection. Pollinger et al., [ 44 ] identified a 40 Mb selective sweep on CFA11 associated with black coat color in Large Munsterlander and a 10 MB region on CFA3 in Dachshund containing FGFR3 , which is responsible for achondroplasia in humans and presumably linked with related genes responsible for canine chondrodysplasia.
It can be assumed from this and other studies that the small founder population of the English bulldog, estimated at 68 individuals, Footnote 16 coupled with human created artificial genetic bottlenecks have greatly diminished genetic diversity and fostered a wide range of health problems. Small founder numbers and artificial bottlenecks are a much more powerful cause of lost genetic diversity than inbreeding [ 33 ]. Some bulldog breeders from the UK have already realized that the artificial selection process had gone too far, either on their own or bowed by public pressure, and have revised breed standards that discourage physical features “that might prevent a dog breathing, walking and seeing freely” [ 46 ]. However, the brachycephalic syndrome in English bulldogs is much more complex than a “shortened head.” Breeds such as the Boxer are similarly brachycephalic but do not suffer to the same degree. In the case of the English bulldog, the nostrils are narrow, the base of the tongue is large and broad, the palate elongated and thickened, thus allowing for blockage of the pharynx especially during sleep [ 8 – 11 ]. The tracheas are usually hypoplastic (narrow), further compromising normal ventilation [ 47 ]. The constant pressures on the upper airways created by these obstructions may also damage and weaken the laryngeal muscles, cause eversion of the lateral ventricles, and further decrease pharyngeal patency [ 48 ]. The laryngeal collapse is in turn associated with bronchial collapse [ 49 ]. Therefore, the breathing problems in the English bulldogs go beyond mere shortening of the face and require specific changes in the nares, rostral skull, tongue, oropharynx and trachea. Concentrating on the brachycephalic syndrome also ignores other serious problems in the breed, such as inability to breed and deliver normally, poor mothering, high puppy mortality, the accumulation of simple recessive deleterious traits, a number of orthopedic problems, certain cancers, allergies, immunodeficiency, and autoimmune disorders. The authors would agree with O’Neill and colleagues [ 50 ] that breeding reforms should target commonly-diagnosed complex disorders that are amenable to genetic improvement and should place special focus on at-risk breeds. Unfortunately, in the case of English bulldogs, this list is very long, but it may still be possible to target the most serious of these disorders for genetic correction.
Assuming that there is a will to improve the overall health of English bulldogs, the question raised by this study is whether or not there is sufficient genotypic diversity remaining in the breed to allow “reverse genetics” to correct phenotypic abnormalities that have major impacts on health. There are certainly phenotypic differences that still exist between various lines of English bulldogs and among individuals, and many English bulldogs enjoy much better health than others. The regions flanking consensus ROH vary greatly in size in individual English bulldogs, suggesting that some of these regions may contain “hidden” genetic diversity that may prove critical for reversing the degree of brachycephaly or chondrodysplasia. The existence of phenotypic variation within the breed is evident from photographs of modern English bulldogs. 7,8 The one region of the genome of English bulldogs that is least amenable to reverse genetics may be the DLA, which has very low diversity based on DLA class I and II haplotypes and a high level of homozygosity. The nine DLA class II haplotypes recognized in this group of English bull dogs were only a fraction of the 88 haplotypes that were reported for dogs in 2007 [ 51 ]. Genes within the DLA are important in regulating self/non-self recognition and immune responses and play a role in autoimmune disorders, allergies, and immun.
Populations that have lost genetic diversity through small founder numbers and artificial genetic bottlenecks are more likely to accumulate deleterious traits [ 33 , 52 ]. A lack of genetic diversity also makes it harder to eliminate deleterious traits from a population once they are recognized. The mutation responsible for hyperuricosuria is carried by 25.5 % of English bulldogs and 3.1 % of the breed are homozygous and excrete uric acid [ 53 ]. Elimination of this recessive mutation from the breed could lead to a significant loss of breed-wide genetic diversity.
A low level of breed-wide genetic diversity also limits the ability to rapidly introduce desired traits, usually in the form of simple recessive mutations. There is increased demand for smaller and more compact English bulldogs, dogs with wrinkled coats and rare coat colors. Such refinements in the breed create popular sire effects and yet more artificial genetic bottlenecks that will cause the loss of more genetic diversity if not properly managed. The negative effects of the rapid introduction of new genetic traits on the health have been best documented in the “The Rare Color Bulldog Craze”. Footnote 17 Indeed, English bulldog breeders appear to be more interested in adding recessive coat color mutations to increase puppy value than eliminating known deleterious mutations. English bulldog breeders around the world ordered 2482 tests from VGL UC Davis involving coat color between 2012 and 2016 compared to 62 tests for the hyperuricosuria mutation. Footnote 18
In conclusion, English bulldog breeders differ widely on their perception of health problems in their breed and what do about them. Some breeders blame disreputable or backyard “commercial” breeders for the unhealthy dogs that are being sold. Footnote 19 , Footnote 20 However, genetic differences were not observed between pet English bulldogs seen at the UC Davis Veterinary Clinical Services and presumably healthy breeding dogs being genetically tested for certain traits. Healthy and unhealthy bulldogs shared the same alleles at genomic STR loci and the allele frequencies are virtually identical. The same was true for DLA class I and II haplotypes. Other English bulldog breeders believe that the health of the breed can be improved by breeding from within existing bloodlines, although there has been little movement by breeders to embrace this concept. This is fueled by purists that vigorously argue that any deviation from the original standards is no longer a British (English) bulldog [ 47 ], even though the breed has continued to evolve in appearance over centuries and even the last few decades. Still others believe that health cannot be restored from within the breed without resorting to outcrossing. 12,13
The feelings of individual English bulldog breeders about the health of their breed and what if anything should be done about it may ultimately be taken out of their hands. English bulldog breeders across the world must take seriously constitutional amendments on the rights of animals. The European Union has recently updated their rules on animal welfare in 2015. Footnote 21 Although it was written specifically for farm animals; it holds that “animals” have rights of ‘freedom from discomfort” and ‘freedom from pain, injury and disease.” The EU rules on animal welfare have been restated in much greater detail by a 2013 constitutional amendment in Switzerland, which extended such rights to all animals [ 54 ]. Although it has not been uniformly enforced, many Swiss breeders have proactively begun outcrossing English bulldogs with the Olde English Bulldogge to create what is known as the “Continental Bulldog”, Footnote 22 which will help bring the breed into compliance.
Breeding of the English bulldog for extremes of brachycephaly, chondrodysplasia, skin folding and child-like appearance and personality has required a level of human-directed positive selection that has made the English bulldog both one of the most popular and unhealthiest of dog breeds. A DNA-based assessment of the breed along a number of parameters has confirmed that the breed is greatly lacking in genetic diversity, which may preclude or minimize the ability of breeders to recreate healthier phenotypes from existing genetic stock, to eliminate deleterious mutations, and to add in new phenotypic traits.
Abbreviations
AKC, American Kennel Club; DLA, dog Leukocyte antigen; IR, internal relatedness; STR, short tandem repeat; VGL, veterinary genetics laboratory, UC Davis
Breed Information Centre. Bulldog. http://www.thekennelclub.org.uk/services/public/breed/display.aspx?id=4084 , accessed 08/02/2016.
The American Kennel Club: Get To Know The Bulldog. http://www.akc.org/dog-breeds/bulldog/ , accessed on 26/06/2016.
Olde English Bulldogge, https://en.wikipedia.org/wiki/Olde_English_Bulldogge , accessed 26/06/2016.
Images of English Bulldogs through history, https://www.google.com/search?q=images+of+english+bulldogs+through+history&biw=1539&bih=703&tbm=isch&tbo=u&source=univ&sa=X&ved=0ahUKEwiX28n6-YTNAhVGLmMKHfGSAuQQsAQIGw , accessed 26/06/2016.
English bulldogs have been screwed for a long time. http://retrieverman.net/2012/04/26/english-bulldogs-have-been-screwed-for-a-long-time/ , accessed 26/06/2016.
Images for English bulldogs from 19th century. https://www.google.com/#q=pictures+of+English+bulldogs+from+19th+century , accessed 26/06/2016.
Images of English bulldogs. https://www.google.com/search?q=images+of+english+bulldogs&biw=1559&bih=744&tbm=isch&tbo=u&source=univ&sa=X&sqi=2&ved=0ahUKEwiMz_KorunKAhVM6GMKHVdOD9IQsAQIGw&dpr=1 , accessed 26/06/2016.
https://www.google.com/search?q=english+bulldogs+in+switzerland&biw=1920&bih=940&site=webhp&tbm=isch&tbo=u&source=univ&sa=X&ved=0ahUKEwjEkf6PzcjMAhUP42MKHR2QAYgQsAQINw , accessed 26/06/2016.
Why are bulldog puppies so expensive? braselsbulldogs.tripod.com/id38.htm, accessed 08/02/2016.
Dog Breed Info Center. Water (Walrus) Puppies (Anasarca puppies). www.dogbreedinfo.com/whelpingwaterpuppies.htm , accessed 26/06/2016.
Report from the Kennel Club/British Small Animal Veterinary Association Scientific Committee. Summary results of the purebred dog health survey for British bulldogs. http://www.thekennelclub.org.uk/media/16342/british%20bulldog.pdf , accessed 26/06/2016.
Britain’s Kennel Club announces sweeping reforms. http://latimesblogs.latimes.com/unleashed/2009/01/britains-kennel.html , accessed 27/06/2016.
A petition from the campaign to Save the English Bulldog Breed. Sign the Petition to: Department of Agriculture The Netherlands, Secretary of State: Dijksma. https://www.causes.com/actions/1742598-save-the-english-bulldog-breed , accessed 27/06/2016.
Airlines Ban Bulldogs, Snub-Nosed Breeds From Flying Because Of Health Risks To Dogs. http://www.huffingtonpost.com/2011/10/10/bulldogs-banned-airlines-health-risks_n_1003495.html , accessed 27/06/2016.
Canine genetic diversity. https://www.vgl.ucdavis.edu/services/dog.php , accessed 27/06/2016.
Bulldog (English bulldog). http://www.dogbreedhealth.com/bulldog/ , accessed 27/06/2016.
The Rare Color BullDog Craze. https://www.musclebully.com/general/the-rare-color-bulldog-craze/ , accessed 27/06/2016.
Veterinary Genetics Laboratory, UC Davis. The records of this laboratory show that English bulldog owners ordered 2482 tests involving coat color between 2012 and 2016 compared to 62 tests involving the hyperuricosuria mutation.
Why purchase a bulldog puppy from a reputable breeder? http://www.bulldogsworld.com/puppy/why-purchase-bulldog-puppy-reputable-breeder , accessed 27/06/2016.
How to breed English bulldogs. http://www.wikihow.com/Breed-English-Bulldogs , accessed 27/06/2016.
Animal welfare. http://ec.europa.eu/food/animals/welfare/index_en.htm , accessed 27/06/2016.
Continental bulldog. https://en.wikipedia.org/wiki/Continental_bulldog , accessed 27/06/2016.
Marien-de Luca C. History of the English Bulldog. http://www.bulldoginformation.com/english-bulldog-history.html . Accessed 26 June 2016.
Fogle B, Morgan T. The new encyclopedia of the dog. New York: Dorling Kindersley; 2000. p. 381. ISBN 0-7894-6130-7.
Google Scholar
Smith, S. AKC News. 2015. Most popular breeds in America. www.akc.org/news/the-most-popular-dog-breeds-in-america/ . Accessed 26 June 2016.
Serpell J. People in disguise. Anthropomorphism and the human-pet relationship. In: Daston L, Mitman G, editors. Thinking with animals: new perspectives on anthropomorphism. New York: Columbia University Press; 2005. p. 129.
Fleming JM, Creevy KE, Promislow DE. Mortality in North American dogs from 1984 to 2004: an investigation into age-, size-, and breed-related causes of death. J Vet Intern Med. 2011;25(2):187–8.
Article CAS PubMed Google Scholar
Nganvongpanit K, Yano T. Prevalence of Swimming Puppy Syndrome in 2,443 Puppies during the Years 2006–2012 in Thailand. Vet. Med. Intnl. 2013. doi: 10.1155/2013/617803
O’Neill DG, Church DB, McGreevy PD, Thomson PC, Brodbelt DC. Longevity and mortality of owned dogs in England. Vet J. 2013;198(3):638–43.
Article PubMed Google Scholar
Roedler FS, Pohl S, Oechtering GU. How does severe brachycephaly affect dog’s lives? Results of a structured preoperative owner questionnaire. Vet J. 2013;198(3):606–10.
Hoareau GL, Mellema MS, Silverstein DC. Indication, management, and outcome of brachycephalic dogs requiring mechanical ventilation. J Vet Emerg Crit Care. 2011;21(3):226–35.
Article Google Scholar
Hoareau GL, Jourdan G, Mellema M, Verwaerde P. Evaluation of arterial blood gases and arterial blood pressures in brachycephalic dogs. J Vet Intern Med. 2012;26(4):897–904.
O’Neill DG, Jackson C, Guy JH, Church DB, McGreevy PD, Thomson PC, Brodbelt DC. Epidemiological associations between brachycephaly and upper respiratory tract disorders in dogs attending veterinary practices in England. Canine Genet Epidem. 2015;2:10. doi: 10.1186/s40575-015-0023-8 .
Mellema MS, Hoareau GL. Hypomagnesemia in brachycephalic dogs. J Vet Intern Med. 2014;28(5):1418–23.
Article CAS PubMed PubMed Central Google Scholar
Linden E, Craig K, Dittmer KE, Thompson KG. Bones and Joints. In: Maxie G (Ed.) Jubb, Kennedy & Palmer’s Pathology of Domestic Animals: Volume 1, 6th Edition, Philadelphia, PA, USA: Saunders Ltd. Philadelphia; 2015. p.37.
Volta A, Gnudi G, Morgan JP, Bonazzi M, Manfredi S, Bottarelli E, et al. Radiographic features of pelvis and hip joint development of English Bulldogs. Vet Comp Orthop Traumatol. 2010;23(1):19–27.
CAS PubMed Google Scholar
Marien, C. The Bulldog Information Library: A Guide to inherited and congenital diseases In Bulldogs, including genetic predisposition to Diseases. http://www.bulldoginformation.com/bulldogs-hereditary-defects.html . Accessed 26 June 2016.
Densiet-Lewis B. 2011. Can the bulldog be saved? www.nytimes.com/2011/11/27/magazine/can-the-bulldog-be-saved.html?_r=0 . Accessed 26 June 2016.
Irion DN, Schaffer AL, Famula TR, Eggleston ML, Hughes SS, Pedersen NC. Analysis of genetic variation in 28 dog breed populations with 100 microsatellite markers. J Hered. 2003;94(1):81–7.
Vilá C, Maldonado J, Wayne RK. Phylogenetic relationships, evolution, and genetic diversity of the domestic dog. J Hered. 1999;90(1):71–7.
Kearse M, Roir R, Wilson A, Stones-Havas S, Cheung M, Sturrock S, et al. Geneious basic: an integrated and extendable desktop software platform for the organization and analysis of sequence data. Bioinformatics. 2012;28(12):1647–9.
Article PubMed PubMed Central Google Scholar
Altschul SF, Gish W, Miller W, Myers EW, Lipman DJ. Basic local alignment search tool. J Mol Biol. 1990;215(3):403–10.
Bannasch DL, Bannasch MJ, Ryun JR, Famula TR, Pedersen NC. Y chromosome haplotype analysis in purebred dogs. Mamm Genome. 2005;16(4):273–80.
Brown SK, Pedersen NC, Jafarishorijeh S, Bannasch DL, Ahrens KD, Wu JT, Okon M, Sacks BN. Phylogenetic distinctiveness of middle eastern and Southeast Asian village dog Y chromosomes illuminates dog origins. PLoS ONE 2011;6(12): doi: 10.1371/journal.pone.0028496
Pedersen NC, Brucker L, Tessier NG, Liu H, Penedo MC, Hughes S, Oberbauer A. The effect of genetic bottlenecks and inbreeding on the incidence of two major autoimmune diseases in standard poodles, sebaceous adenitis and Addison’s disease. Canine Genet Epidemiol. 2015;27(2):14. doi: 10.1186/s40575-015-0026-5 .
Peakall R, Smouse PE. GenAlEx 6.5: genetic analysis in Excel. Population genetic software for teaching and research – an update. Bioinformatics. 2012;28(19):2537–39.
Pedersen NC, Liu H, Theilen G, Sacks BN. The effects of dog breed development on genetic diversity and the relative influences of performance and conformation breeding. J Anim Breed Genet. 2013;130:236–48.
Pilot M, Malewski T, Moura AE, Grzybowski T, Oleński K, Ruść A, Kamiński S, Ruiz Fadel F, Mills DS, Alagaili AN, Mohammed OB, Kłys G, Okhlopkov IM, Suchecka E, Bogdanowicz W. On the origin of mongrels: evolutionary history of free-breeding dogs in Eurasia. Proc Biol Sci. 2015; 282(1820): doi: 10.1098/rspb.2015.2189
R Development Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2008. http://www.R-project.org . Accessed 26 June 2016. ISBN 3-900051-07-0.
Pedersen NC, Liu H, McLaughlin B, Sacks BN. Genetic characterization of healthy and sebaceous adenitis affected standard poodles from the United States and the United Kingdom. Tissue Antigens. 2012;80(1):46–57.
Bannasch D, Young A, Myers J, Dickinson P, Gregg J, Davis R, Bongcam-Rudloff E, Webster MT, Lindblad-Toh K, Pedersen N. Localization of Canine Brachycephaly Using an Across Breed Mapping Approach. PLoS ONE, 2010. doi: 10.1371/journal.pone.0009632
Purcell S, Neale B, Todd-Brown K, Thomas L, Ferreira MAR, Bender D, Maller J, Sklar P, de Bakker PIW, Daly MJ, Sham PC. PLINK: a toolset for whole-genome association and population-based linkage analysis. Am J Hum Genet. 2007;81(3):559–75.
Lindblad-Toh K, Wade CM, Mikkelsen TS, Karlsson EK, Jaffe DB, Kamal M, et al. Genome sequence, comparative analysis and haplotype structure of the domestic dog. Nature. 2005;438(7069):803–1.
Vaysse A, Ratnakumar A, Derrien T, Axelsson E, Rosengren Pielberg G, Sigurdsson S, et al. Identification of genomic regions associated with phenotypic variation between dog breeds using selection mapping. PLoS Genet 2011;7: doi: 10.1371/journal.pgen.1002316
Marsden CD, Ortega-Del Vecchyo D, O’Brien DP, Taylor JF, Ramirez O, Vilà C, Marques-Bonet T, Schnabel RD, Wayne RK, Lohmueller KE. Bottlenecks and selective sweeps during domestication have increased deleterious genetic variation in dogs. Proc Natl Acad Sci U S A. 2016;113(1):152–7.
Cagan A, Blass T. Identification of genomic variants putatively targeted by selection during dog domestication. BMC Evol Biol. 2016;16:10. doi: 10.1186/s12862-015-0579-7 .
Axelsson E, Ratnakumar A, Arendt ML, Maqbool K, Webster MT, Perloski M, Liberg O, Arnemo JM, Hedhammar A, Lindblad-Toh K. The genomic signature of dog domestication reveals adaptation to a starch-rich diet. Nature. 2013;495(7441):360–4.
Amos W, Wilmer JW, Fullard K, Burg TM, Croxall JP, Bloch D, et al. The influence of parental relatedness on reproductive success. Proc R Soc Lond B. 2001;268(1480):2021–7.
Article CAS Google Scholar
California sea lions. Inbreeding influences the response of these animals to different pathogens in the wild. Nature. 2003;422(6927):35.
Hoffman JI, Boyd IL, Amos W. Exploring the relationship between parental relatedness and male reproductive success in the antarctic fur seal arctocephalus gazella. Evolution. 2004;58(9):2087–99.
Bean K, Amos W, Pomeroy PP, Twiss SD, Coulson TN, Boyd IL. Patterns of parental relatedness and pup survival in the grey seal ( Halichoerus grypus ). Mol Ecol. 2004;13(8):2365–70.
Banks SC, Dubach J, Viggers KL, Lindenmayer DB. Adult survival and microsatellite diversity in possums: effects of major histocompatibility complex-linked microsatellite diversity but not multilocus inbreeding estimators. Oecologia. 2009;162(2):359–70.
Forstmeier W, Schielzeth H, Mueller JC, Ellegren H, Kempenaers B. Heterozygosity–fitness correlations in zebra finches: microsatellite markers can be better than their reputation. Mol Ecol. 2012;21(13):3237–49.
Pedersen NC, Liu H, Leonard A, Griffioen L. A search for genetic diversity among Italian Greyhounds from Continental Europe and the USA and the effect of inbreeding on susceptibility to autoimmune disease. Canine Genet Epidemiol. 2015;2:17. doi: 10.1186/s40575-015-0030-9 .
Quilez J, Short AD, Martínez V, Kennedy LJ, Ollier W, Sanchez A, Altet L, Francino O. A selective sweep of >8 Mb on chromosome 26 in the Boxer genome. BMC Genomics. 2011. doi: 10.1186/1471-2164-12-339
Pollinger JP, Bustamante CD, Fledel-Alon A, Schmutz S, Gray MM, Wayne RK. Selective sweep mapping of genes with large phenotypic effects. Genome Res. 2005;15(12):1809–19.
Webster MT, Kamgari N, Perloski M, Hoeppner MP, Axelsson E, Hedhammar Å, Pielberg G, Lindblad-Toh K. Linked genetic variants on chromosome 10 control ear morphology and body mass among dog breeds. BMC Genomics. 2015;16:474. doi: 10.1186/s12864-015-1702-2 .
Bates, D. Iconic British bulldog to be scrapped as kennel club overhauls breeding rules. http://www.dailymail.co.uk/news/article-1114766/Iconic-British-bulldog-scrapped-Kennel-Club-overhauls-breeding-rules.html . Accessed 26 June 2016.
Harvey CE, Fink EA. Tracheal diameter: analysis of radiographic measurements in brachycephalic and nonbrachycephalic dogs. J Am Anim Hosp Assoc. 1982;18:570–6.
Petrof BJ, Pack AI, Kelly AM, Eby J, Hendricks JC. Pharyngeal myopathy of loaded upper airway in dogs with sleep apnea. J Appl Physiol. 1994;76(4):1746–52.
De Lorenzi D, Bertoncello D, Drigo M. Bronchial abnormalities found in a consecutive series of 40 brachycephalic dogs. J Am Vet Med Assoc. 2009;235(7):835–40.
O Neill DG, Church DB, McGreevy PD, Thomson PC, Brodbelt DC. Prevalence of disorders recorded in dogs attending primary-care veterinary practices in England. PLoS One. 2014;9(3): doi: 10.1371/journal.pone.0090501 .
Kennedy LJ, Barnes A, Short A, Brown JJ, Lester S, Seddon J, Fleeman L, Francino O, Brkljacic M, Knyazev S, Happ GM, Ollier WE. Canine DLA diversity: 1. New alleles and haplotypes. Tissue Antigens. 2007;69 Suppl 1:272–88.
Farrell LL, Schoenebeck JJ, Wiener P, Clements DN, Summers KM. The challenges of pedigree dog health: approaches to combating inherited disease, Canine Genet Epidemiol. 2015; 2: (3): doi: 10.1186/s40575-015-0014-9
Karmi N, Safra N, Young A, Bannasch DL. Validation of a urine test and characterization of the putative genetic mutation for hyperuricosuria in Bulldogs and Black Russian Terriers. Am J Vet Res. 2010;71(8):909–14.
Gerritsen V. Animal welfare in Switzerland- constitutional aim, social commitment, and a major challenge. Global Journal Animal Law, 2013, 1: http://www.tierimrecht.org/de/PDF_Files_gesammelt/GJAL_Gerritsen2013.pdf . Accessed 26 June 2016.
Download references
Acknowledgements
Funding to support this study was obtained from the Center for Companion Animal Health, UC Davis. We would also like to thank the Veterinary Genetics Laboratory at the UC Davis School of Veterinary Medicine for providing DNA samples, advice on sample testing, providing tests at no cost, and assisting with data collection. We are grateful for Merial for encouraging veterinary students to obtain research experience through the STAR program. We thank Dr. Danika Bannasch, UC Davis, for contributing GWAS data from English bulldogs.
ASP received a Student Training Advanced Research (STAR) summer award from the Merial Veterinary Scholars Program. The authors would like to acknowledge and thank the Center for Companion Animal Health and the Veterinary Genetics Laboratory at UC Davis School for providing the necessary funds and no-cost testing for this project.
Availability of data and materials
The authors will make freely available upon request reproducible datasets and details on software applications, reagents and test procedures used in this study. Confidential information will be excluded.
Authors’ contributions
NCP: project conception, project design, analysis, and manuscript preparation. ASP: data collection, data extraction, analysis, preparation of initial draft and poster for scientific presentation. HL: data collection, data extraction, analysis. DLB: provided GWAS data on English bulldogs. All authors read and approved the final manuscript.
Authors’ information
NCP, D.V.M., Ph.D., is an emeritus distinguished Professor and former director of the Center for Companion Animal Health and the Veterinary Genetics laboratory, UC Davis. ASP, B.S., is a third year student pursuing a D.V.M. at UC Davis. HL, M.S., is a staff research associate IV and laboratory manager for NCP.
Competing interests
The authors declare that they have no competing interests.
Ethics approval and consent to participate
Experiments were done with DNA samples that were on file and no live animals were directly involved. Therefore, no institutional animal use and care committee approval was required.
Author information
Authors and affiliations.
Center for Companion Animal Health, School of Veterinary Medicine, University of California, One Shields Avenue, Davis, CA, 95616, USA
Niels C. Pedersen & Hongwei Liu
School of Veterinary Medicine, University of California, One Shields Avenue, Davis, CA, 95616, USA
Ashley S. Pooch
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Niels C. Pedersen .
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Pedersen, N.C., Pooch, A.S. & Liu, H. A genetic assessment of the English bulldog. Canine Genet Epidemiol 3 , 6 (2016). https://doi.org/10.1186/s40575-016-0036-y
Download citation
Received : 23 March 2016
Accepted : 10 June 2016
Published : 29 July 2016
DOI : https://doi.org/10.1186/s40575-016-0036-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- English bulldog
- Genetic assessment
- Short tandem repeats (STRs)
- Internal relatedness (IR)
- Dog leukocyte antigen (DLA)
- DLA class I and II
- Runs of homozygosity (ROH)
Canine Medicine and Genetics
ISSN: 2662-9380
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 03 November 1870
Hereditary Deformities
- WILLIAM FIELD 1
Nature volume 3 , page 7 ( 1870 ) Cite this article
146 Accesses
Metrics details
THE alleged instances hereditary deformity produced by your correspondent in NATURE for Oct. 20 do not seem at all satisfactory. They may all be referred either to an hereditary disease of the part affected, as in the suppuration of the cow's horn; or to coincidence, accompanied by a slight stretch of imagination on the part of the first narrator, as in the cases of the scar on the forehead and the crooked finger.
Article PDF
Author information, authors and affiliations.
Faversham, Rent
WILLIAM FIELD
You can also search for this author in PubMed Google Scholar
Rights and permissions
Reprints and permissions
About this article
Cite this article.
FIELD, W. Hereditary Deformities. Nature 3 , 7 (1870). https://doi.org/10.1038/003007f0
Download citation
Issue Date : 03 November 1870
DOI : https://doi.org/10.1038/003007f0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

IMAGES
VIDEO
COMMENTS
Idiopathic scoliosis (AIS) is the most common pediatric spinal deformity, affecting ~3% of children worldwide. AIS significantly impacts national health in the U. S. alone, creating disfigurement and disability for over 10% of patients and costing billions of dollars annually for treatment. Despite many investigations, the underlying etiology ...
Rare genetic diseases are the result of a continuous forward genetic screen that nature is conducting on humans. Here, we present epistemological and systems biology arguments highlighting the importance of studying these rare genetic diseases. We contend that the expanding catalog of mutations in ∼4,000 genes, which cause ∼6,500 diseases ...
AnkitaSi. Because they can be passed from parents to their children, genetic diseases are frequently referred to as hereditary. Some malignancies are examples of hereditary diseases. elevated cholesterol; cystic fibrosis condition. A human being may receive the "brown-eye trait" from one of their parents, which is an example of an inherited ...
Genetic disorders are of different types i.e. single-gene. disorders, chromosomal disorders, complex disorder s. This paper intends to be as an introductory paper for the project "Human genetic ...
Introduction. Genetic skeletal diseases, often called skeletal dysplasias, are a heterogeneous group of heritable conditions with generalized bone and cartilage impairment caused by pathogenic variants in genes primarily affecting skeletogenesis and/or bone homeostasis (1, 2).Although the overall incidence of genetic skeletal diseases is around one in 5000 births (), some conditions are ...
Variations in our DNA and differences in how that DNA functions (alone or in combinations), alongside the environment (which encompasses lifestyle), contribute to disease processes. This review explores the genetic basis of human disease, including single gene disorders, chromosomal imbalances, epigenetics, cancer and complex disorders, and ...
A genetic disorder is a disease caused in whole or in part by a change in the DNA sequence away from the normal sequence. Genetic disorders can be caused by a mutation in one gene (monogenic disorder), by mutations in multiple genes (multifactorial inheritance disorder), by a combination of gene mutations and environmental factors, or by damage to chromosomes (changes in the number or ...
nce a person's chances of developing a genetic conditio. . One import. nt factor is how the condition is inherited. For example:Autosomal dominant inheritance: A person affected by an autosomal dominant disorder (image on page 12) has a 50. percent chance of passing the mutated gene to each child. The chance that a c.
It is also known as osteodystrophia. It includes bone diseases that are neither inflammatory nor neoplastic but may be genetic, metabolic, or of unknown origin. Recent studies have shown that bone influences the activity of other organs, and the bone is also influenced by other organs and systems of the body, providing new insights and ...
Objective To assess causation and clinical presentation of major birth defects. Design Population based case cohort. Setting Cases of birth defects in children born 2005-09 to resident women, ascertained through Utah's population based surveillance system. All records underwent clinical re-review. Participants 5504 cases among 270 878 births (prevalence 2.03%), excluding mild isolated ...
Abstract. Syndromic genetic conditions, in aggregate, affect 8% of the population 1. Many syndromes have recognizable facial features 2 that are highly informative to clinical geneticists 3, 4, 5 ...
Definition. Mutations in DNA can result in genetic disorders. Genetic disorders are conditions that occur as a result of changes to or mutations in DNA within the body's cells. Most cells in the ...
The head is anatomically the most sophisticated part of the body and its evolution was fundamental to the origin of vertebrates; understanding its development is a formidable problem in biology. A ...
Hereditary metabolic bone diseases are characterized by genetic abnormalities in skeletal homeostasis and encompass one of the most diverse groups among rare diseases. In this review, we examine 25 selected hereditary metabolic bone diseases and recognized genetic variations of 78 genes that represent each of the three groups, including sclerosing bone disorders, disorders of defective bone ...
34 Alberts, 2015. 35 Alberts, 2015. The Inheritance of Traits: From Genetics to Heredity. ical energy t hrough cellular res piration to be used by the plant as an. energy source. Th is process is ...
By Natalie Angier. Jan. 9, 2017. They said it was their family curse: a rare congenital deformity called syndactyly, in which the thumb and index finger are fused together on one or both hands ...
Hair loss in early childhood represents a broad differential diagnosis which can be a diagnostic and therapeutic challenge for a physician. It is important to consider the diagnosis of a genetic hair disorder. Genetic hair disorders are a large group of inherited disorders, many of which are rare. Genetic hair abnormalities in children can be an isolated phenomenon or part of genetic syndromes ...
Answer: 2 📌📌📌 question Write a research paper about a hereditary condition or deformity. - the answers to estudyassistant.com
Hereditary spastic paraplegia is a genetically heterogeneous neurodegenerative disorder characterised primarily by muscle stiffness in the lower limbs. Neurodegenerative disorders are conditions that result from cellular and metabolic abnormalities, many of which have strong genetic ties. While ageing is a known contributor to these changes ...
Background This study examines genetic diversity among 102 registered English Bulldogs used for breeding based on maternal and paternal haplotypes, allele frequencies in 33 highly polymorphic short tandem repeat (STR) loci on 25 chromosomes, STR-linked dog leukocyte antigen (DLA) class I and II haplotypes, and the number and size of genome-wide runs of homozygosity (ROH) determined from high ...
IN the lessons in Ethnology in "Cassell's Popular Educator," it is stated, on the authority of Dr. Theodor Waitz, and the Secretary of the Anthropological Society, that "an officer, whose ...
THE alleged instances hereditary deformity produced by your correspondent in NATURE for Oct. 20 do not seem at all satisfactory. They may all be referred either to an hereditary disease of the ...