12 Ways to Show Compassion in Nursing (With Examples)

It is not uncommon to face difficult, often heartbreaking, situations as a nurse. Knowing what to say or how to respond is not always easy. Even the most experienced nurses can struggle at times. What happens when you don't know what to say to a patient or how to act when a loved one is given bad news? How can nurses show compassion in nursing practice while still maintaining composure and professionalism? Is that even possible? The good news is even though some days are easier than others, it is possible to learn ways to be more compassionate as a nurse. In this article, I will share why compassion in nursing is essential and offer 12 ways to show compassion in nursing practice.

What Does Compassion in Nursing Practice Exactly Mean?
Why is compassion important in nursing practice, 1. patients are more comfortable., 2. compassionate nursing practices improve patient outcomes., 3. compassion in nursing practice extends beyond patient care, affecting interprofessional relationships., 4. compassionate nursing helps strengthen nurse-patient relationships., 6 key skills a nurse must-have for delivering compassionate care, 1. resilience:, 2. excellent communication:, 3. emotional intelligence:, 4. confidence:, 5. cultural awareness:, 6. critical thinking:, how can nurses show compassion in nursing practice, 1. listen to what your patients and their loved ones say (and what they do not say)., for example:, 2. show genuine interest., 3. learn to express empathy when appropriate., 4. acknowledge your patient’s feelings., 5. be patient., 6. respect your patient’s need for privacy., 7. take the time to explain treatment plans and answer questions., 8. get to know your patients., 9. be present., 10. be aware of moments that require high levels of compassion., 11. even if you can’t empathize with your patient, you can sympathize., 12. take care of yourself., what causes compassion fatigue in nursing practice, 5 tips to prevent compassion fatigue in nursing practice, 1. set emotional boundaries., 2. practice self-awareness., 3. establish a healthy work-life balance., 4. implement active coping mechanisms., 5. develop a support system., useful resources to develop compassion in nursing practice, youtube videos, my final thoughts.

- Debate article
- Open access
- Published: 11 July 2016
Reflections about experiences of compassionate care from award winning undergraduate nurses – What, so what … now what?
- Stephen Smith 1 ,
- Asha James 3 ,
- Allison Brogan 2 ,
- Elizabeth Adamson 1 &
- Mandy Gentleman 1
Journal of Compassionate Health Care volume 3 , Article number: 6 ( 2016 ) Cite this article
65k Accesses
3 Citations
3 Altmetric
Metrics details
From 2007 until 2012 Edinburgh Napier University’s School of Nursing Midwifery and Social Care in conjunction with NHS Lothian, collaborated on a programme of action research entitled, the Leadership in Compassionate Care Programme. One strand of this research focused on learning and teaching about compassionate care within the undergraduate curriculum. This debate article focuses on the care issues raised by two award winning nursing students who reflected on the development of their compassionate caring skills during their three year Bachelor of Nursing programme.
The reflective accounts debate the following issues related to compassionate care; Personal drivers supporting the provision of compassionate care, Challenging and influencing care practices, Providing relationship centred care and, Living with what can’t be achieved. Throughout the debate a model of compassionate care developed from the Leadership in Compassionate Care Programme is used to reflect on key practice issues and provide a framework for practice development.
The care issues presented in this paper identify a need to support students in healthcare to; Develop strategies in questioning care practices which do not meet expectations of compassionate care; undertake focussed reflective activities where each student can explore personal drivers, values and perspectives of compassion; actively connect learning in practice with theory in university, enable development in compassionate caring and strategies that support self-compassion; facilitate an understanding and development of emotional intelligence supporting development of resilience.
Implications for healthcare staff are to; Collectively seek, hear and respond to feedback about their service; activate caring conversations within the healthcare team; consider how the model of compassionate care presented in this paper, can be used to reflect on practice and provide a framework for development; consider how we maximise the experience of care during brief moments of contact with patients/families; activate leadership that promotes a culture of openness facilitating the development of compassionate care.
From 2007 until 2012 Edinburgh Napier University’s School of Nursing Midwifery and Social Care in conjunction with NHS Lothian, collaborated on a programme entitled, the Leadership in Compassionate Care Programme (LCCP) [ 1 ]. NHS Lothian provides a comprehensive range of primary, community-based and acute hospital services for the second largest residential population in Scotland - circa 800,000 people, it employs approximately 24,000 staff. The School of Nursing, Midwifery and Social Care at Edinburgh Napier University provides undergraduate and post graduate education to nurses, midwives and multidisciplinary staff involved in health and social care. There are approximately 1600 students in the school.
The LCCP utilised an action research approach with the aim of embedding compassionate care in NHS healthcare practice and within undergraduate nursing and midwifery education. The LCCP encompassed four key strands of work: developing compassionate clinical practice; supporting newly qualified practitioners; leadership development and undergraduate nurse education. This action research programme was funded by a private benefactor. A key outcome of this action research identified a model for compassionate care in practice which incorporates six components, see Fig. 1 . This model relates to activities undertaken between care providers, service users and their families/important others, for example caring conversations should take place between care providers as well as between staff and service users. Debating, challenging and celebrating care provision is an important activity to be undertaken amongst staff. The LCCP action research identified that this was a key activity if compassionate care is to flourish in a care setting. Throughout this article reference will be made to this model and how the reflections presented highlight its key components.
Model for compassionate care in practice [ 14 ]
This debate article focuses on the care issues raised by two nursing students (adult field) who reflected on development of compassionate caring skills during their three year Bachelor of Nursing programme. These reflections were written as part of their successful submission for the Simon Pullin award. The Simon Pullin award is given to students who have shown excellence in the development of person centred, compassionate caring skills during their programmes of study. The award is dedicated to the memory of Simon Pullin, who was a Senior Nurse on the Leadership in Compassionate Care Programme from its commencement in December 2007 until his death in July 2011. This award highlights the fundamental importance of compassionate care as part of contemporary Nursing and Midwifery practice. The award winners Alison Brogan and Asha James have contributed their reflections and analysis of compassionate care in the planning and writing of this paper and they have agreed to be identified within this writing. The key issues related to the provision of compassionate nursing care debated in this article are as follows:
Personal drivers supporting the provision of compassionate care
Challenging and influencing care practices, providing relationship centred care, living with what can’t be achieved.
This article incorporates the What, So what and Now what [ 2 ] reflective model as a way of reflecting on experiences of compassionate care.
Borton’s model asks individual’s to consider three questions: “What?”, “So what?” and “Now what?” The first question asks a person to consider what has happened, the second question is to allow the person to try and make sense of what has happened and evaluate events and the last question is to consider a way forward and think about what could happen in the future [ 3 ].
The LCCP identified that discussions about care ‘caring conversations’ and working with feedback are key activities enabling compassionate care to thrive. The use of a reflective model acts as a as a springboard supporting such discussions in practice (Table 1 ).
‘I was a child carer from a very young age for my mum, who suffered with alcohol dependency. Life was far from easy, but I always understood that my mum did not choose to live like this and what she had was an illness. However it appeared that many healthcare professionals did not share this understanding and their lack of compassion, respect and dignity often left my mum feeling judged, embarrassed and worthless. This caused a lot of distress for my mum and for the family. This was the beginning of my dream of becoming a nurse… if I was a nurse I would be kind to my patients and care for everyone the way I would have liked my mum to be cared for…. The negative attitudes we experienced as a family by healthcare professionals have enforced my passion for person centred, compassionate care.’ Asha
It is evident from this reflection that past negative experiences of healthcare had provided a strong personal driver to enter the nursing profession but moreover to develop a future focus on care that is compassionate and directed towards the person, their needs and their context. The negative elements of this account point to feelings of injustice, frustration and are a consequence of care experiences resulting in emotional distress for a vulnerable person and their family. It is indeed commendable on a personal level that despite these significant negative experiences this generated a desire for Asha to become a nurse and ultimately lead to successful completion of a nursing degree and recognition of excellence in the development of her compassionate caring skills.
This reflection triggers questions about how health and social care educators can support students to learn from their life experiences and consider their individual values and how this may support developments of caring and compassionate attributes in practice. In Asha’s reflective account, development in compassionate caring arose from her previous negative experiences of healthcare and this appears to have been integral to her approach to care and her values. It is necessary to support each student within their own context and personal experience. When considering Asha’s experience of caring for her mother, the complexity of this situation and the impact on Asha’s own health and wellbeing are key factors to consider.
‘ Like many children in my situation, I was exposed to domestic violence and parental mental health illness, as a result my functioning was adversely affected. School in general was a struggle and I left with practically no qualifications. I had no confidence and low self-esteem. When I was twenty four, my mum died, she had Cirrhosis of the liver. This was a devastating time for myself and my family. I went to counselling and gradually started to turn my life around. It’s taken many years and with the support of my husband, who has always believed in me, I started college to gain the qualifications I needed to get me into nursing. I could not ask for more. I am confident and happy in what I am doing today.’ Asha
It is clear from this candid reflection that considerable work and energy from Asha herself, her family and professionals have enabled a sense of wellbeing and healing to emerge. This in turn enables her to practice with emotional intelligence and to raise a challenge with colleagues when care standards are not achieved. It is critical to consider how colleagues, teams and organisations support this maintenance of functioning over time.
Questions are therefore raised as to how we support learners who have less clear articulation of past experiences of care, their personal values and where this leads in the development of caring skills. Indeed how does this issue play out for learners who have directly experienced abuse or life contexts where experiences of compassion would be deemed less than positive? There appears something fundamentally crucial about mirroring a compassionate, person centred learning experience for our students whilst we encourage them to explore their values and approach to care. This in turn raises questions about academic staff modelling attributes of care and compassion within their professional practice.
As we have discussed when students embark on their programme of study they bring with them their own life experience, values and beliefs, and some of these will be challenged as they experience healthcare practice. One way that students can be encouraged to reflect on the experiences of those who give and receive care is through listening to and reflecting on stories gathered within clinical practice and relating this to their own experiences of giving care ([ 4 – 6 , 1 ]). Nursing students often make reference to their own personal care encounters, episodes that have been deemed less than compassionate can present a strong driver for student nurses to achieve more positive experiences for others. Teasing out learning from stories provides a student centred approach to considering issues of care and compassion. What do I make of the care experience? What would I have done in this situation and why would I respond in this way? What possibilities of compassionate caring are evident in this story/context? Reviewing stories in a group learning context facilitates the student to further explore varied perceptions and approaches to care and compassion. This form of group learning requires careful facilitation enabling students to safely question practice and approaches to care, then consider possibilities for their future practice.
The intertwining of practice learning experiences with the students’ life experiences and values provides a potentially provocative opportunity for development. There are some thorny practical issues here that require deliberation if we are to maximise this practice learning. How do we support students and mentors to capture these learning stories from practice and how do we integrate these within theoretical learning about compassionate care within the university context? If personal stories and narratives are a key component of learning about compassionate care we need to activate the integration of this learning between theory and practice.
Caring is fundamental to nursing and therefore must be an integral part of nurse education. Concerns about poor care and lack of compassion are frequently reported in the media, those responsible for nurse education are acutely aware of this as they develop curricula and focus on preparing students for the profession. Whether compassionate care can actually be taught has been debated [ 7 ]. McLean [ 8 ] makes a case for a values based curriculum that encourages self-awareness through a values based enquiry model which encourages the student to challenge existing beliefs and values and develop the character they require to be providers of care and compassion. Nurse Educators can teach the theory of compassionate care but application in practice can be challenging as demonstrated in the reflective accounts in this paper. Curtis [ 9 ] found that student nurses wanted to provide compassionate care but felt unsure of their capacity to do this and sustain it in practice. Others suggest that students’ ideals of care, though already present as a strong motivator when they commence their studies, increased as they grew in knowledge and competence [ 10 ]. They also found that when students experience moral distress when these ideals are challenged through witnessing poor care, these ideals are upheld. These emotionally challenging situations can however become a vehicle for personal and professional growth when students find the courage to uphold their ideals and increase their ability to provide care that is more compassionate [ 10 ].
While nurses are focused on caring for others, it has been argued that practitioners require to be compassionate with themselves [ 11 ], and this is associated with the development of emotional intelligence [ 12 ]. The emotionally intelligent nurse is said to be one” that can work in harmony with thoughts and feelings” ([ 13 ], p. 94) therefore is able to respond to both when working directly with patients and their families. This form of emotional intelligence provides the potential of understanding and connecting with those being cared for whilst recognising and responding to personal strengths and vulnerabilities. Research evidence suggest a connection between emotional intelligence and cultural intelligence (Moon, [ 14 ]) and this is evident in the reflections of care shared by Asha and Allison. Cultural intelligence relates a person’s capacity to function successfully in culturally diverse situations (Ang, Dyne & Koh [ 15 ]). In the account of a clinical placement experience overseas, Asha expressed astonishment and concern at the discriminatory custom and practice she encountered. The cultural approach to care for indigenous people was in direct conflict with her ideals of compassionate person centred care and she felt unable to act in the way directed. Instead she engaged in building a trusting relationship with the family and was rewarded with expressions of gratitude. Not only did it take courage as a student to challenge the practice of a registered nurse but particular resolve and determination to do this in a different culture. By demonstrating how a person centred accepting approach could be not only successful but welcome by a patient and their family she challenged her colleague.
Whether compassionate care can actually be taught has been debated [ 7 ]. McLean [ 8 ] makes a case for a values based curriculum that encourages self-awareness through a values based enquiry model which encourages the student to challenge existing beliefs and values and develop the character they require to be providers of care and compassion.
In addition it has been argued that unless a healthcare practitioner is compassionate to themselves they cannot provide compassionate care for others [ 11 ], and this is associated with the development of emotional intelligence [ 12 ]. The emotionally intelligent nurse is said to be one” that can work in harmony with thoughts and feelings” ([ 13 ], p. 94) therefore is able to respond to both when working directly with patients and their families. This form of emotional intelligence provides the potential of understanding and connecting with those being cared for whilst recognising and responding to personal strengths and vulnerabilities. Research evidence suggest a connection between emotional intelligence and cultural intelligence (Moon, [ 14 ]) and this is evident in the reflections of care shared by these students.
Considering the model of compassionate care identified by the LCCP [ 1 ] it would seem appropriate that Caring conversations and Feedback would be critical components of the model to concentrate on. Observing and participating in caring conversations in practice will provide opportunities to hear debates and have discussions about how to care, and develop understanding of the real dilemmas of care. In addition receiving feedback about their own caring and compassionate skills from practice mentors will complement the potential for students to develop caring skills and reflexive practice. All of these activities will provide opportunities to both challenge and construct learning based on their own drivers and values.
Both of our students incorporated the issue of challenging and influencing compassionate care practices within their reflective accounts. They took different approaches to influence staff. It is recognised that for students and NHS staff raising concerns about practice with mentors and practice staff can be a daunting experience [ 16 ].
‘Encouragingly I recognised that as a third year student I was starting to feel confident in being able to influence colleagues. Whilst in the community setting I cared for a patient who could be rude and verbally aggressive. He was abrupt with me during my first solo visit and referred to me as student. He had COPD and leg wounds, he was very particular about everything and was quite obsessive. I realised that this man had little control over anything in his life and I suspected this is what drove his behaviour. By my third visit I had worked out exactly how he liked things done and instead of letting him get anxious and out of breath telling me what to do, I gently took control of the situation. I did things in the order he liked….. this didn’t take any more time – in fact it saved time. By the end of my fourth visit he asked my name. I was able to relay this during handover with my community colleagues and I explained that I thought his behaviour had been driven by fear and loss of control. With this understanding and consideration of what was driving his aggressive behaviour his relationships with the nursing team improved significantly. He seemed more content during nursing visits and so did some of the nursing staff.’ Allison
This reflective account highlights a particular approach to a challenging caring situation, namely approaching it with eyes wide open, thinking what is happening here and what could my contribution be? It is evident behaviours were observed with a view to understanding them and importantly considering how this guided practice. It is evident that emotional intelligence was key in considering and moderating practice behaviour in this context. ‘ Theoretical and editorial literature confirms emotional intelligence concepts are central to nursing practice. Emotional intelligence needs to be explicit within nursing education as emotional intelligence might impact the quality of student learning, ethical decision-making, critical thinking, evidence and knowledge use in practice’ [ 17 ]. The challenge to her community colleagues was to adapt their practice in the light of an enhanced understanding of the person’s situation. Talking about this openly with colleagues as part of a formal forum facilitated an enhanced change of communication style and active recognition of the reasons behind the patient’s irritable behaviour. In turn this gave an opportunity to consider action/practices which would enhance the care experience for both the patient and the nursing staff? Smith et al [ 18 ] highlighted the importance of reflective forums when considering an understanding of compassionate care in the workplace, findings from this action research identified three key themes; leadership, culture, professional and personal development. It is evident that these findings and key themes have congruence with Alison’s reflective account and the outcomes for the community team.
The influence and challenge here was based on Alison’s perceptions and experience of care provision. She used her own observations and positive practice experience to influence colleagues asking, can we learn from what I have done? This approach differs to asking the question what can we do about this? This way of influencing appeared natural and real, focusing on an approach which had been successful in practice ensured relevance for staff and additionally provided tangible possibilities for development.
Allison also identified,
‘The nurse manager in this setting was a role model to the team and often openly reflected on her experiences both positive and negative. This encouraged the nursing team to mirror this practice….. The team got together twice daily to discuss patient care. The nurse manager would often make a point of asking what went well and what would you improve. Change was not something to be feared rather it was embraced.’
With this insight Alison was able to utilise this team’s strengths to influence a development in care, further evidence of active emotional intelligence impacting upon practice.
Asha’s influence on care practices adopted a different approach.
‘I was fortunate to undertake a student placement in Western Australia, I was placed in a medical ward in one of Australia’s public hospitals where many of the patients lived in relative poverty. This was a fantastic learning opportunity for me…… There were a lot of aboriginal people attending the hospital and I witnessed some discrimination from Australian healthcare professionals which really surprised me. I was given three patients to care for, one was aboriginal. The nurse I was working with said to me that when caring for this particular patient I had to leave the room once I had done what I was supposed to do. I was not to make eye contact with the patient or the family and not to engage in conversation other than health related topics. I could not believe that I was hearing this from a healthcare professional, this goes against my own values and everything I have been taught. I challenged the nurse about her behaviour…… I was told that this is just how it is and aboriginal people take it as a threat if you make eye contact. I explained I cannot provide care like this and thought it was only fair to treat people as individuals. The next time we worked together she was surprised at how quickly I had built good trusting relationships with the patient and family. I spent time demonstrating empathy, kindness, dignity and respect I got to know everyone…… The family expressed how grateful they were to me for my care which made it all worthwhile!’ Asha
In this reflection the challenge to practice was forthright and highlighted concerns about the provision of compassionate, person centred care. It would appear that a growing awareness of discriminatory care in this clinical context triggered this response to the mentor. It is evident that Asha demonstrated commitment to the quality of care she wanted to provide, moreover she was able to articulate this clearly and challenge current practice with her mentor. This confidence is admirable given she was working in an unfamiliar setting where a culture of discrimination had been identified and working with unfamiliar staff. This brief scenario demonstrates a student nurse whose values, life experience, academic development and clinical practice enabled this way of challenging practice. Clinical confidence, commitment to quality of care and influence is demonstrated and indicates that this can be achieved by student nurses towards the conclusion of their studies.
Asha stated, ‘ when you are a student it is quite easy to feel unsure of yourself or your skills as a nurse, especially when faced with a new situation. Challenging my mentor was not something that came easy to me, however, being firm in my belief by speaking up I feel certain I have helped and cared. I continually set goals to push myself to have the confidence to speak up if I felt it was important to me. You are always going to meet people in life with negative attitudes, but it is important to me not to let them influence my thoughts and actions in any way. I found it difficult relating to the nurse who I reacted to as I felt that she stereotyped this patient and her family. I have no doubt that my own personal experience motivated my decision to question her practice. Having a bit of knowledge also gave me confidence to speak up. I had done a little research about communicating with Aboriginal people prior to visiting Australia, and I was aware that some (but not all) Aboriginal people are uncomfortable with direct eye contact. I felt that I was mature enough to make my own judgements on how to communicate effectively to overcome any barriers.’
Within recent public failures of NHS care, an inability to speak up and raise concerns about practice were highlighted as a factor in the general lowering of care standards, recommendations aimed at addressing this culture and behaviour were identified, ‘Ensure openness, transparency and candour throughout the system about matters of concern’ [ 19 ]. It is therefore critical that caring conversations are healthy and can positively influence the behaviour and care provided by practitioners and the culture of the caring environment. There is evidence of a need to talk about our healthcare organisations with positive values and a clear vision of how compassionate organisation should function [ 20 ].
It is evident that feedback from the patient, their family and the mentor indicated that the care experience provided by Asha was very positive. Unfortunately from this brief reflection we do not have evidence of influence on the mentors practice in this area of care other than her surprise at the positive level of therapeutic relationship developed. There is evidence however that the care provided to this patient and family was influenced and became consistent with Asha’s standards of compassion and person centeredness.
As discussed above Asha made earlier reference within her reflective account to personal experience early in her own life where she experienced discrimination as a consequence of family circumstances, and which enabled her to empathise with the indigenous family who may have felt isolated and misunderstood. Determination to provide compassionate care and challenge established practice took courage, confidence and commitment all of which are identified as fundamental values of care [ 21 ]. This emphasises the need to actively engage with each student throughout their period of study exploring their values, attitudes and caring behaviours.
Cultural sensitively is clearly an element of compassionate person centred care as demonstrated in this example and there is growing awareness that this should be taught within nursing education [ 22 ]. For some time nursing curricula has focused on fitness for practice and clinical competence and this is vital for patient safety but nursing is more than this. Nurses education is increasingly challenged to ensure that graduates are equipped with a spectrum of knowledge, skills and ability where compassionate, person centred care is consistent with safe and effective care. This requires acknowledgement that the students who enter our programmes of study come from a variety of life experiences and cultural backgrounds and as educators we too must meet the challenge to provide a learning experience that addresses and meets the needs of a diverse group of students. This raises the question of how this can be done and how can we ensure that nursing graduates are ready to meet the needs of the people in their care, can also care for themselves, and be able to grow with an ever changing healthcare system?
In relation to the LCCP model of compassionate care the examples provided above in relation to challenging and influencing care highlight the themes; Person centred risk taking and Involving valuing and transparency. Both reflections highlight practices that were focussed on adapting practice to individual need, for example following the instructions of the patient in order to develop trust and reduce anxiety whilst understanding their need for control. Similarly having an awareness of cultural practices but focusing and responding to the patient as an individual. Risks taken here related to deliberately doing things differently from colleagues and experiencing potential negativity as a consequence. Also taking a different approach may not be accepted by colleagues in the long run.
‘I will never forget one of the patients I cared for. After ten weeks she shared that she had outlived all her relatives ….. she said she didn’t know what she had done to deserve this and was so lonely she had no one to cuddle her, then she asked me for a hug. I will never forget the solitary tear drop running down her face when she gave me a hug. I wonder how long it had been since that woman had been hugged? This is one defining moment of my training which makes me strive to build appropriate compassionate therapeutic relationships at every opportunity.’ Allison
This example from practice highlights that personal connection is important in the delivery of compassionate care and that although the patient’s overall care was not being criticised, the emotional aspect of her being had somehow been forgotten. The question, what was important to that individual at that particular time had not been asked. This example also shows that relationships can take time to foster and develop. After 10 weeks of contact with Alison, this woman shared her feelings and vulnerability allowing Alison to respond to her needs in a simple but profound way. There is much debate in the nursing literature focused on terms such as relationship centred care, person centred care and compassionate care [ 23 ]. Following a pragmatic stance they each point to an approach to care that focuses on enhancing the experience of care itself, however relationship centred care provides a balance to this approach whereby the experience of the care giver and care receiver must equally be acknowledged to achieve an overall enriched environment of care [ 24 ].
This care experience emphasises the importance of touch, specifically the request for a hug when feeling isolated and lonely. Perhaps focusing on the appropriate use of touch within a caring relationship can support staff to maximise the caring experience when brief moments are all that are available to staff within busy clinical settings. Touch is not comforting or appropriate for everyone but the questions is, how can we maximise the appropriate use and effectiveness of touch when we have minimal time to care?
‘Many nurses hold the opinion that building relationships and honing communication skills are key to excellent patient care…. During my first year at university I observed that building therapeutic relationships and adapting communication style both saved time and improved patient care. I observed a colleague waking a patient abruptly in keeping with ward routine. The patient who had dementia did not take kindly to being rushed out of bed. She became tearful and ultimately aggressive. This resulted in two members of staff having to assist in calming the situation. In contrast, I witnessed another nurse gently rouse the patient in the morning. She held her hand and physically brought herself down to her level. This nurses’ tone and demeanour was gentle and patient centred, this initial interaction did take longer, however overall it saved time as the patient was happy to allow staff to assist her with her daily care. Inconsistency within the nursing team on this particular ward was very evident.’ Allison
How do we share and provide an opportunity to maximise good practice such as described in this account, and what is the role of a leader in promoting and sustaining compassionate care such as this? Role modelling has been celebrated in an earlier reflection by Allison. The intent and behaviours of leaders are important when establishing a culture of openness and transparency where feedback is viewed as “the norm”. This form of culture facilitates the possibility of sharing and maximising positive practice as well as giving consideration to practice situations which are challenging and fraught. In essence this is working directly with local feedback from patients and staff and holding a persistent focus on caring conversations.
‘What factors drive poor behaviours like this where there appears to be inconsistent approaches to patient care? Notably, the nurse manager on this ward was rarely available. The lack of direct leadership resulted in poor team work and communication within the team. How can we create environments where all patients are given this type of individualised care? Is this primarily driven by influential leadership? I believe a strong inspirational leadership style is a key factor in driving culture change? I believe cultures can be changed when staff are empowered to suggest improvement and champion change.’ Allison
This reflective account highlights the key theme of ‘Creating spaces that work’. What would it take to develop consistency of practice within the care team? Allison’s focus rests on leadership but moreover the need for the team to share, debate and consider how care can be enhanced, in essence work with ’Caring conversations’.
It is considered that most nurses will experience what is commonly termed Compassion fatigue. This concept has been debated widely within the nursing arena. Coetzee and Klopper [ 25 ] conclude that this this develops gradually and is a cumulative process. It is thought that this occurs when one is consistently subject to intense, acute interactions with patients and families. Compassion fatigue can be described as feeling negative emotions as a result of feeling unable to fulfil their moral role as nurses. Have more experienced healthcare providers become burnt out? In tandem with compassionate skills should we should also teach nurses to avoid becoming fatigued. This would allow compassion to be preserved rather than eroded. If this is the case how do we go about safeguarding ourselves and others from the effects of compassion fatigue? Indeed, what makes one person more adept at sustaining their compassion whilst working in highly charged emotionally draining environments? Can resilience be taught or nurtured? Gentry [ 26 ] highlighted that a healthcare providers ability to “self-care” seemed to have a positive influence on their ability to deal with the effects of compassion fatigue.
Self-care was identified primarily as anxiety management and included practices such as speaking to colleagues, exercise and meditation. During the three year nursing programme at Edinburgh Napier University students are given ample opportunity to reflect in peer groups there are also sessions teaching mindfulness. During one module nursing students were invited to organise aerobic exercise classes. Is the UK nursing workplace ready or able to uphold and commit to providing organisational strategies to combat the effects of compassion fatigue? There has been little research into techniques on how to reduce fatigue in healthcare professionals and the resulting effect this would have on standards of care, this is an area which would benefit from further research.
‘Within one clinical setting where I worked a colleague experienced the loss of her spouse. She was regularly involved with palliative patients and was given the option to move to a different role within the team. This role did not involve palliative care and is allowing an experienced and dedicated member of staff to better deal with her grief. It also means she is still effectively contributing to the workplace. What makes it possible for one clinical area to offer this type of support where as other areas do not? How can this become the norm as opposed to the exception?’ Allison
The example of good practice above highlights that relationship centred care is critical to staff relationships. This provides a practical but considered example of the theme Knowing you knowing me. Understanding a staff members context and vulnerability and responding to this may enhance the ability to care in practice and sends a message to staff that they are of value and matter.
As a student nurse, the relationship between myself the patient and their family is vital. Holistic care and having excellent verbal and non-verbal communication skills are essential in order to understand the needs of each patient and their loved ones whilst they are receiving healthcare…. I have learned how a person’s body language can say a completely different thing as to what they are telling you, thereby taking the time to listen and by doing the little things can not only make the patient feel cared for but actually cared about.’ Asha
The authors of this paper would acknowledge that courage can be required to pick up on non-verbal behaviours and then comment or respond to them [ 21 ]. These forms of interaction may take longer than originally anticipated but aim to get at the heart of what matters. In addition recognising the needs of the family/carers in the provision of care to promote a sense of caring for all involved is also important.
‘For the first time I felt inadequate in terms of providing compassionate care. It was my first exposure to an emergency medicine environment. During one shift I was very conscious of a daughter sitting with her mother. The mother was having an acute breathlessness problem and her daughter was crying. I was dealing with a patient who had a gastric bleed. On my way to get some clean linen for this patient, the only thing I could offer this distressed daughter was a tissue and a few words which seemed very inadequate…. I really felt I was letting someone down…. My thoughts were interrupted when my patient said you are so gentle thank you for being so gentle. I realised I was doing my best and providing care to the patient with the greatest need…. The lesson learned here is that in the demanding role of nursing I will have to prioritise and make decisions such as these.’ Allison
This reflection highlights the dilemma experienced by care providers when they identify distress and are unable to respond in a manner that meets their aspirations of care. A feeling of inadequacy related to compassionate care provision was acknowledged, this did not relate to an absence of compassion or a failure to respond, rather it points to a busy clinical context where priorities need to lie with those who have the most acute needs. A compassionate response was evident in the provision of a tissue and a few words and this is commendable practice amidst a busy clinical setting. It is interesting to note however that this intervention was deemed inadequate.
This reflection raises a number of key questions about the context and environment of care and the impact these factors have upon staff experience.
Was this area short staffed or experiencing an acutely busy period and feeling stretched at this time? What is the norm of practice here, do other members of the team feel similarly and where are these experiences and feelings discussed and debated as a team?
How would other members of the team manage this situation and how can staff retain their awareness and desire to be compassionate when the busyness of the area necessitates a focus on clinical priorities?
A further question relates to the resilience of staff, how do staff stay resilient and work with potential compromises to the compassionate care they aspire to deliver?
Brown [ 27 ] debates these issues concluding that, ‘in organisations there needs to be clear intention, leadership and determination for compassionate care to become central in all healthcare practice’. His conclusions focus on small group experiential reflection and learning by healthcare workers as the most effective way to consolidate compassionate care values in practice. Indeed within the LCCP [ 1 ] staff coming together to debate and discuss what compassionate care looks like in their service was a key activity in negotiating a definition for practice; moving the potentially nebulous concept of compassionate care into a more tangible approach for local practice. Principles of compassionate care were most usefully derived from hearing and understanding experiences of patients, relatives and staff and initiating responsive action [ 28 ].
Paley [ 29 ] argues that organisational and situational factors directly impact upon care delivery and that this results in care providers being too busy or focused on other organisationally directed issues to recognise or address compassionate care. It is argued that the blame for a compassion deficit therefore rests with the organisation. In a related issue Timmins and De Vries [ 30 ] also point to organisational factors that determine outcomes of poor care. These authors focus on cognitive dissonance as experienced by care providers; the aim is to provide good care however due to organisational pressures which dominate the context this form of care is not achievable. In order to rationalise this dissonance between care aspirations and the actual, less positive, care experience, standards of care are revised to a lower level thereby managing the dissonance experienced. In the reflection provided above neither of these two phenomenon were evident. Frustration was expressed due to the busyness of the practice area and a need to focus on clinical priorities but distress was identified and a compassionate response elicited.
It is interesting however that this student was dissatisfied with her compassionate response in this busy context, this response raises questions about how staff are supported and able to work through these situations when optimal care has not been possible. There is a wealth of evidence available testifying to the significant challenges facing healthcare professionals in contemporary practice (Iles, & Vaughan Smith [ 31 ] therefore it is important to consider how staff develop resilience and self-compassion as a counter to this situational and cultural context as well as responding to physical and organisational factors impacting upon compassionate caring.
The following practice example from Allison demonstrates tensions in achieving her desired standards of care and how she has been developing strategies to address these.
‘I have been a qualified nurse for a year now and often miss being a student. There was certainly more time to spend with patients. Instead of supporting an upset patient with post-operative nausea and vomiting it is my first priority to organise the administration of an anti-emetic. There is often no extra time to spend with the patient following this as I could have another patient returning from theatre. How do we make these shortened interactions count and make our patients feel cared for as an individual? Is it about tone and communication style? Is it about delegation and recognising that other members of the team can help. I have certainly asked student nurses or care assistants to comfort patients when I have been unable to fulfil this role due to time restraints.’ Allison
The challenge raised of maximising the positive impact for patients of brief interactions when a brief moment is all that is available, seems an important focus for learning. It is unreasonable for staff to experience a sense of guilt regarding care experiences such as those described above when staffing and situational variables dominate practice and are out with a nurses’ sphere of control or influence. What would help nurses and other care staff discuss their experiences, learning, and the positive strategies employed which would enable the possibility of working towards a shared understanding and improvement?
In regard to the LCCP model of care the key themes related to the reflections above could relate to Feedback and Creating spaces that work. It would have been fascinating to hear directly from the patients described in the reflections detailed above. What was their perception of the care and compassion they received? Did a tissue and a few words, or the provision of an anti-emetic meet their needs? Patients can be acutely aware of the busyness of clinical areas and consequently try to minimize the work load of staff as a response. Without seeking feedback directly from these people and their experience of care, we are left with assumptions and possibilities. There is the possibility that care staff can be unduly critical of their practice when deficits are perceived in the care provided, however such deficits may or may not be the experience of those we care for. Actively seeking, hearing and responding to feedback within the local context can provide a reality check and focus for both celebrating excellent care and genuinely understanding care deficits. Considering, Creating spaces that work, would focus reflections on issues connected to the physical environment, culture and ways of working. A group discussion may reassure the team that they are doing all they can, it may raise possibilities for change or connecting with the broader organisation for direct support and development.
Summary - Now what?
The student nurse reflections discussed within this paper prompt us to pause and be encouraged as we glimpse examples of excellent care and celebrate what can be achieved. They also remind us that provision of compassionate care is indeed possible, it does take place on a day to day basis and often hinges on the little things that make a massive difference to those receiving and providing care. However personal drivers, values and perspectives of quality care are critical aspects of providing compassionate care. These elements though are not little things to articulate and develop for individuals, teams and indeed organisations engaged in the provision of contemporary healthcare.
To support the development of compassionate care this article focused on key issues identified from the reflective accounts of two award winning student nurses. These included supporting students in healthcare to;
Develop strategies in questioning care practices which do not meet their expectation of compassionate care
Undertake regular focussed reflective activities where each student can explore personal drivers, values and perspectives of compassionate caring.
Actively connect learning in practice with theory and reflective activities within university, enabling consistent development in compassionate caring.
Facilitate an understanding of emotional intelligence, leading to strategies for self-compassion and the development of resilience
It is necessary to consider the implications of these reflections in terms of supporting healthcare staff to;
Collectively seek, hear and respond to feedback about their service
Activate caring conversations within the healthcare team, celebrate what works well and understand the reasons for this, considering what can be done differently and better and how can we learn and support one another.
Consider how the model of compassionate care, presented in this paper, can be used to reflect on practice and indeed provide a framework and focus for local practice development.
Consider how we maximise the experience of care during brief moments of contact with patients/families.
Activate leadership that strives for a culture of openness which facilitates the development of compassionate care.
Abbreviations
LCCP, Leadership in Compassionate Care Programme
Edinburgh Napier and NHS Lothian. Leadership in Compassionate Care Programme, Final Report. Edinburgh: Edinburgh Napier University; 2012.
Google Scholar
Borton T. Reach, Touch and Teach. London: Hutchinson; 1970.
Jasper, M. Beginning reflective practice. Nelson Thorne: Cheltenham; 2003.
Adamson E, Dewar B. Compassionate Care: Student nurses' learning through reflection and the use of story. Nurse Educ Pract. 2015;15(3):155–61.
Article PubMed Google Scholar
Adamson E, Dewar B. Compassion in the nursing curriculum: making it more explicit. J Holist Healthc. 2011;8(3):42–5.
Adamson E, Smith S (2014) Can Compassionate Care be Taught? Experiences from the Leadership in Compassionate Care Programme, Edinburgh Napier University & NHS Lothian IN Shea, S., Wynyard, R., Lionis, C. (2015) Providing compassionate healthcare: challenges in policy and practice. Routledge Oxon.
Bradshaw A. Measuring nursing care and compassion: the McDonaldised nurse? J Med Ethics. 2009;35:465–8.
Article CAS PubMed Google Scholar
Mclean C. The yellow brick road: a values based curriculum model. Nurse Educ Pract. 2012;12(3):159–63.
Curtis K, Horton K, Smith P. Student nurse socialisation in compassionate practice: a grounded theory study. Nurse Educ Today. 2012;32(7):790–5.
Pedersen, Birgith, and Kerstin Sivonen. "The impact of clinical encounters on student nurses’ ethical caring." Nursing ethics 19.6 (2012): 838–848.
Neff, K. Self Compassion. 2015. Available from: http://self-compassion.org/ .
Heffernan M, Quinn M, McNulty R, Fitzpatrick J. Self-compassion and emotional intelligence in nurses. Int J Nurs Pract. 2010;16:366–73.
Freshwater D, Stickley T. The heart of the art: emotional intelligence in nurse education. Nurs Inq. 2004;11(2):91–8.
Moon T. Emotional intelligence correlates of the four-factor model of cultural intelligence. J Manag Psychol. 2010;25(8):866–10
Ang S, Dyne L Van, Koh S K. Personality correlates of the four factor model of cultural intelligence. Group and organization management. 2006;31:100–123.
Article Google Scholar
Royal College of Nursing. Raising concerns: a guide for RCN members. 2015. Available at: http://www.rcn.org.uk/support/raising_concerns .
Bulmer Smith K, Profetto-McGrath J, Cummings G. Emotional intelligence and nursing: an integrative literature review. Int J Nurs Stud. 2009;46(12):1624–36.
Smith S, Gentleman M, Loads D, Pullin S. An exploration of a restorative space: a creative approach to reflection for nurse lecturer's focused on experiences of compassion in the workplace. Nurse Educ Today. 2014;34:1225–31.
Francis R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry Executive Summary. London: The Stationary Office; 2013.
Ballat J, Campling P. Intelligent Kindness Reforming the culture of healthcare. London: Royal College of Psychiatrists Publications; 2011.
Department of Health. Compassion in Practice: Nursing, Midwifery and Care Staff Our Vision and Strategy. 2012. Available form, http://www.england.nhs.uk/wpcontent/uploads/2012/12/compassion-in-practice.pdf .
Hugues K, Hood L. Teaching methods and an outcome tool for measuring cultural sensitivity in undergraduate nursing students. J Transcult Nurs. 2007;18(1):57–62.
Nolan M, Davies S, Brown J, Keady J, Nolan J. Beyond 'person-centred' care: a new vision for gerontological nursing. J Clin Nurs. 2004;13(1):45–53.
Nolan M, Davies S, Brown J, Nolan J, Keady J. The Senses Framework: Improving Care for Older People Through a Relationship-Centred Approach, Getting Research Into Practice Series. Sheffield: University of Sheffield; 2006.
Coetzee S, Klopper H. Compassion fatigue within nursing practice: a concept analysis. Nurs Health Sci. 2010;12:235–43.
Gentry J. Compassion fatigue: a crucible of transformation. J Trauma Pract. 2002;1(3/4):37–61.
Brown C. Experiential learning and compassionate care. In: Shea S, Wynyard R, Lionis C, editors. Providing compassionate healthcare: Challenges in policy and practice. Oxon: Routledge; 2014. p. 54–67.
Smith S, Dewar B, Pullin S, Tocher R. Relationship centred outcomes focused on compassionate care for older people within in-patient care settings. Int J Older People Nursing. 2010;5:128–36. doi: 10.1111/j.1748-3743.2010.00224.x .
Paley J. Social psychology and the compassion deficit. Nurse Educ Today. 2013;33:1451–2.
Timmins F, de Vries M. Nurses are not bystanders: a response to Paley. Nurse Educ Today. 2014;34(10):1269–71.
Iles V, Vaughan Smith J. Working in health care could be one of the most satisfying jobs in the world – why doesn’t it feel like that? Paper from the ‘Take it to the Limit’ Learning Set. 2009. Available at: http://www.reallylearning.com/Current_Projects/Learning_Sets/take-it-to-the-limit-report2.pdf .
Download references
Acknowledgements
This paper does not present material from funded research.
Availability of data and materials
The data on which the conclusions of the manuscript rely are presented in the main paper.
Authors’ contributions
All authors have contributed to the writing of this paper in accordance with the International Committee of Medical Journal Editors (ICMJE) guidelines.
Competing interests
There are no competing interests identified related to the writing and publication of this paper.
Consent for publication
Consent has been sought from participants whose accounts have been included in this paper.
Ethics approval and consent to participate
The information presented in this debate article does not originate from original research but from material presented by undergraduate nursing students as part of an award portfolio submission. As this paper does not represent research no ethical approval was sought.
Disclosures
Students who win the Simon Pullin Award receive £250.00 prize money and an award letter from the university. The application process involves submitting a portfolio which contains the following: a reflective account written by the student identifying their experience of learning and development in compassionate caring during their undergraduate studies; accounts of feedback about compassionate care development from practice mentors, service users and university academic staff, usually the students’ personal development tutor. The portfolios are reviewed by a panel of academic staff and service users.
Author information
Authors and affiliations.
School of Nursing Midwifery and Social Care, Sighthill Campus Edinburgh Napier University, Room 4B29, Sighthill Court, Edinburgh, EH11 4BN, Scotland
Stephen Smith, Elizabeth Adamson & Mandy Gentleman
Distict Nursing Team, NHS Lothian, Edinburgh, Scotland
Allison Brogan
St John of God Hospital, Perth, Western Australia, Australia
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Stephen Smith .
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Smith, S., James, A., Brogan, A. et al. Reflections about experiences of compassionate care from award winning undergraduate nurses – What, so what … now what?. J of Compassionate Health Care 3 , 6 (2016). https://doi.org/10.1186/s40639-016-0023-x
Download citation
Received : 09 January 2016
Accepted : 01 June 2016
Published : 11 July 2016
DOI : https://doi.org/10.1186/s40639-016-0023-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Relationships
- Person-centred
- Action research
- Undergraduate curriculum
- Healthcare students
Journal of Compassionate Health Care
ISSN: 2053-2393
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Olivia's Site
"nurse: just another word to describe a person strong enough to tolerate anything and soft enough to understand anyone.", empathy and compassionate care essay by: olivia gagne, december 4, 2019 ogagne.
One important thing I have learned in clinical is that I have the power to make a difference in patients lives, one patient at a time. To do so, a nurse must remember to not only use empathy, but compassion as well. One story that I always remember is the star fish story. It’s about a five year old girl on a beach in Florida after a hurricane had destroyed their land. There were thousands of star fish washed up on the shore. The little girl was throwing starfish back into the ocean, one starfish at a time. When her father saw her, he said “why are you even bothering? You will never be able to save them all”. As the little girl looked at her father, she picked one up and threw it back into the ocean. She then said, “I saved that one”. This is a story my high school guidance councilor told me. It has always stuck with me and has made me realize one important lesson in nursing. It’s not about how many lives you saved, its about making a difference one person at a time.
From the hallway of the hospital I heard my patient moaning. When I walked in for the first time, they reached for my hand but spoke no words. They squeezed my hand, very tight, and immediately calmed down. As I introduced myself, they intimately looked at me and moaned “hi”. At that moment I realized a few things. They could hear and understand me, but they cannot talk due to the accident the patient was in. Secondly, they needed human touch. No student nurse had taken care of this patient prior to when I had arrived that day. The nurses said the patient has been agitated and emotional since the morning. But as I held the patients’ hand, they were relaxed and showed their half dropping smile.
Throughout my clinical I took care of this patient. In the beginning, I immediately had empathy. I put myself in the patients’ shoes and started to picture how scared I would be if I was waking up from a coma. I pictured what it would feel like if I couldn’t talk or communicate the way I wanted to. But during this time, I learned that communication isn’t always through speaking, but can also be from hand squeezing for yes, or shaking their head for no. I could tell they were scared when they moaned after trying to speak to their PT instructor. Later in the night, it was time to give the patient a bed bath. After washing my patients’ body with a warm wet cloth, I asked the patient if they wanted lotion and a foot massage. Immediately they squeezed my hand for yes. When we massaged my patients’ feet, once again, their whole body relaxed. At the end of the night, I realized that it’s important to focus on the small things for each individual patient. Although some wouldn’t know how to comfort this patient, I slowly figured it out over my seven-hour clinical. You need to have patience, and to focus on going above and beyond to make your patient feel cared for. As a good nurse, you need to use compassionate care, and focus on the small actions throughout your shift. During this shift I started to realize what compassionate care was. It’s not about going into the patients; room, taking their vitals and leaving. It’s about using empathy to feel what they feel and putting to action what you think would make them feel better; such as a foot massage with lotion and holding their hand when they reach out.
As a future nurse, in order to use empathy and compassion in my future practice, it’s important to understand what they mean and how they intertwine with nursing. Empathy is being able to feel what the patient is going through while putting yourself in their shoes. How would you feel if this was you? It’s important for nurses to use empathy. By putting ourselves in the patients’ shoes, we are only then able to further understand what they are feeling, and what they are going through. Jean Watson, a nurse herself, put together ten carative factors that help to support empathy in nursing. She stated that it’s important to “create a healing environment for the physical and spiritual self, while respecting human dignity” (Watson, 2018). While respecting the patient and creating an environment of healing, this encompasses empathy in nursing. By trying to understand how they feel and what they are going through, the nurse then can move on to compassionate nursing.
Compassionate nursing is using kindness, empathy, and love to ultimately care for the patient. It’s being able to focus on the patients’ needs and to help relieve their suffering. Jean Watson’s carative factor one focuses on “the formation of a humanistic-altruistic system of values” (Gonzalo, 2019). This refers to using love and kindness in your care of practice. For example, this could be as simple as holding your patients’ hand while they are crying. It’s holding back their hair while they throw up and giving them an ice pack when the medications haven’t relieved their pain. Compassionate care is going above and beyond what one needs to do. It’s not only providing physical healing, but as said in carative factor eight, it’s the “provision of support, and corrective mental, physical, societal, and spiritual” help for the patient (Gonzalo, 2019).
A nurse who demonstrates compassionate care is able to “understand a deeper meaning of (the patients) healthcare situation”, as demonstrated throughout Jeans ten carative factors (Watson, 2018). Both empathy and compassion are found throughout Jean Watsons Carative factors. By using both, it truly changes the patients’ outcomes. Carative factor four states the importance of the “development of a helping-trusting, human caring relation” (Gonzalo, 2019). Therefore, by using empathy and compassion, the patient trusts the nurse more, and builds a stronger foundation of hope, care, and love between both the nurse and the patient. This increases patient healing far past only physical healing, and truly benefits the clients outcomes. Both compassionate care and empathy help to demonstrate the amazing power of a compassionate nurse in healing the patient not only physically, but mentally.
My role for the patient talked about above was wanting to help them feel loved and cared for. By holding their hand when they reached out, and focusing on the small things the patient needs, I was able to build a stronger patient nurse relationship. I also met the patients’ spouse multiple times, and learned more about what they patient did before the accident. In my future, I want to remember this patients impact on me, and my impact on the patient. The patient made me realize that they aren’t only patients. They are a mother, father, aunt, uncle, daughter, cousin, and friend. They might be a couch, teacher, firefighter, singer, gymnast, or swimmer. In my future, I want to improve in remembering that each patient has a different identity than what the nurse knows them as. They are more than just a patient. They are human. They need touch just like we need touch, they need love and kindness, and ultimately they need understanding and care.
In my future I will have more patients, more documentation, and more priorities. But I need to remember this one special thing I have learned. In my future, I want to remember why I joined nursing. This includes something I learned from the starfish story. It truly does not matter the amount of patients you helped compared to how many your co-worker helped. It comes back to providing compassionate care for one patient at a time and being the best nurse you can be for that individual patient. This includes helping people heal not only physically, but socially, emotionally, and mentally. My goal is to improve on focusing on each patient for who they are and helping to provide the patient with what they need. I will incorporate this into my everyday life as a future nurse by coming back to the core of nursing. This includes being kind, loving, caring and compassionate. By remembering a nurses’ core values, I will be able to focus on the little things every day to make a small difference one patient at a time.
Gonzalo, A. (2019, September 12). Jean Watson: Theory of Human Caring. Retrieved November 12,
2019, from https://nurseslabs.com/jean-watsons-philosophy-theory-transpersonal-caring/ .
Watson, J. (2018, October 7). Jean Watson Theorist Presentation. Retrieved November 12, 2019, from https://www.youtube.com/watch?time_continue=313&v=o1EN0VH9xCE&feature=emb_logo
One thought on “ Empathy And Compassionate Care Essay By: Olivia Gagne ”
Great site and very well done!
Comments are closed.
Compassionate Care Concept
As an essential principle of person-centered care, compassionate care refers to the way nurses relate to others as human beings and involves “noticing another person’s vulnerability, experiencing an emotional reaction to this, and acting in some way with them in a way that is meaningful for people.” Compassionate care is interrelated with other concepts such as caring, empathy, and respect and is also closely associated with patient satisfaction.
View Tool Kit Resources

ESSAY SAUCE
FOR STUDENTS : ALL THE INGREDIENTS OF A GOOD ESSAY
Essay: Compassionate care in nursing
Essay details and download:.
- Subject area(s): Nursing essays
- Reading time: 8 minutes
- Price: Free download
- Published: 15 September 2019*
- File format: Text
- Words: 2,154 (approx)
- Number of pages: 9 (approx)
Text preview of this essay:
This page of the essay has 2,154 words. Download the full version above.
This essay, will be explore and discuss why ensuring compassionate care in nursing is important and how it relates to the NHS (National Health Service) values. Compassion can be described as, feeling sympathy for someone else’s misfortune (WordReference, 2015, cited in Perez-Bret et al., 2016). There is no correct definition for compassionate care as it is mainly demonstrated through the unique bond formed between the patient and nurse. It can be characterised by actions taken by the nurse to care and show an understanding for the patients’ needs and their suffering (Baughan & Smith, 2013). This essay will cover the different legislations which require nurses to provide compassionate, humanistic care to patients, theoretical frameworks and evidence-based practices which express the significance of compassionate care and therapeutic relationships. Additionally, how nurses implement techniques to form relationships with patients and relatives to provide patient-centred care.
Care and compassion being two of the 6 C’s express the importance of compassionate care and its importance to nursing. Being caring and compassionate is the minimum expectation of nurses, and it is endlessly stated by the NMC that care should be given effectively, without delays; this represents the significance of a caring nurse as they are the main aspects of nursing (NMC, 2015). Compassion is also stated in the NMC Code of Conduct (2015), it proclaims, compassionately is the way to respond to the needs to patients especially those who are in the last few days and hours of life. Compassion is fundamental, building trust between patients and nurses, also indicating patients are being treated as people rather than procedures. Bramley and Matiti (2014) held a study in compassion and what it means to patients; majority of patients stated, compassion is when nurses give them time and portray a caring attitude. This study also retrieved that patients find a striking link between care and compassion thus they would substitute care for compassion and vice versa. One of the patients in the study described compassion as “… a caring attitude to people as people and not things (Participant 5, ward D: L 4)” (Bramley and Matiti, 2014, p. 2794). Bramley and Matiti (2014) found that patients express nurses demonstrating caring and compassionate attributes through giving them time, talking to them as people, nurses placing themselves in the situation of patients and caring about their feelings. This study helps nurses as knowledge of patients understanding of compassionate care can help them improve on attributes patients anticipate when being cared for.
The NHS constitution establishes the principles and values of NHS England. The purpose of this is to clarify the right entitlements for service users, the public and also staff. NHS values are also included, these have been inspired by patients, the public and staff, making sure nothing is missed. A few of the values are; respect and dignity, commitment to quality of care, compassion, improving lives and everyone counts (Department of Health & Social Care, 2015). These values are to ensure patients are the centre of attention and they are delivered humanistic, person-centred care. NHS values explain the significance of compassion as it is a key value that is naturally expected from nurses and other health care staff. The Royal College of Nursing (2018) developed eight principles with the help of the Department of Health and the NMC (Nursing and Midwifery Council), the public and health care staff were also a part of the progression process. The principles are there for nurses and student nurses to apply when caring for patients. One of the eight principles are, nurses and nursing staff treat everyone with care ensuring dignity and humanity is maintained throughout – nurses should understand the patients’ needs and requirements and are to show compassion and sensitivity, overall nurses should provide care in a way in which everyone is respected and treated equally (Royal College of Nursing, 2018).
Professionalism in nursing is the autonomous decision-making of a group of medical professionals who share similar values (NMC, 2017). Nurses providing good healthcare through excellent, professional practice and behaviour upholds the expected nursing standards. The NMC focuses nurses on professionalism to guarantee safe and effective, person-centred care (Glasper, 2017). Professionalism being a vital attribute to nurses is to prevent publicised scandals such as the ‘Mid-Staffordshire Inquiry’. Partnership is recognised in healthcare guidelines therefore is an attribute for nurses to either develop improve on (Baillie, 2016). Nurses working in partnership with their patients allows patients to make decisions about their own treatment, also this leads to improved communication skills between a nurse and service user (Baillie, 2016). A scenario of working in partnership with patients can be, a patient at a&e is suicidal and overdosed on paracetamol. The nurse is responsible for taking care and explaining the effects and treatments for overdose. While explaining to the patients the effects, the nurse is able to build a therapeutic relationship with the patient over time as partnership means the service user can ask questions. On the other hand, if the patient refuses treatment and disregards the recommendations of the nurse, it could lead to conflict.
Conflict can occur when a nurse tries to build a relationship/partnership with the service user. However, conflict can also arise between healthcare professionals due to poor leadership and change, plus issues with interpersonal relationships (McKibben, 2017). This type of conflict can affect the quality of care patients receive, therefore the NMC has highlighted, nurses must communicate and work cooperatively in partnership to resolve any conflict within healthcare teams (NMC, 2015). There are many different reasons of why conflict can arise between nurses and patients, reasons like disagreements in decision-making, conflicting medical and religious beliefs additionally, conflicting opinions. Through conflict, nursing standards can rise. Oglethorpe and Oglethorpe (2009) stated, nursing conflict can result in critical thinking leading to well thought-out/quality decision-making by nurses, resorting in enhanced care quality received by patients.
A therapeutic relationship is when nurses and patients communicate effectively, whether it is regarding treatment or general conversations asking how they are. Through communication, nurses can provide exceptional medical care. Good communication and interpersonal skills allow nurses to communicate with patient’s relatives as well as other health professionals. A therapeutic relationship is called ‘therapeutic’ because it helps nurses to meet the needs of patients through a shared agreement (McQueen, 2000). Therapeutic relationships are fundamental as they signify compassionate care since it shows there is good nurse-patient interaction, which aid nurses with smoother care plan administration as patients are more trusting of nurses.
Marsham (2012) explored learning disability nurses therapeutic role and found that it is a big focus when it comes to interventions raising standards in nursing. This is because patient-nurse relationships reflect a more humanistic approach to nursing which can also be referred to as compassionate care since nurses take time to build a rapport with patients to provide unique patient centred care. Therapeutic relationships are all the more important as they are seen as the “… heart of care” (Marsham, 2012, p. 237). To build a relationship with patients, it can be easy for nurses to start using jargon without realising, also it is very easy for them to dominate treatment as nurses are the professionals and the patients are not. Therefore, the NMC stated “work in partnership with patients to make sure you deliver care effectively” (NMC, 2015, p. 4). Nurses are to make sure their patients understand their treatment and care plans. To help explain procedures to patients and build a relationship, there are a few key attributes nurses should acquire. Being sensitive, showing empathy, being approachable, a good listener and also being receptive to the patient. Callery and Milnes (2012) undertook a study of communication between nurses, patients and their parents. The study showed that there is a ‘triadic’ relationship formed when communicating with 3 people. In their study, the child was known as the ‘dyad’ who observed the conversations between the nurse and parent. Overall evidence from this study showed, communication is imperative with everyone including children (Callery and Milnes, 2012). Callery and Milnes study links to clinical practice as communication helps provide effective nursing care, in addition to improvement in patient mental health.
To provide person-centred care, the main focus for a nurse should be, is the patient happy. Carl Rogers, a humanistic psychologist believed patient health improves better once they improve their psychological state of mind (McLeod, 2014). This theory links to clinical practice as nurses are not just helping patients medically but also mentally. Hence, nurses tend to focus on encouraging elderly patients to focus on something or someone instead of an unconscious motive. McLeod (2014) stated, Carl Rogers’ humanistic approach to therapy is to ensure patients are benefitting by feelings of greater self-worth. Nurses are able to use Rogers’ person-centred approach to build therapeutic relationships with service users by taking time to ask them ‘how are you’. The main emphasis on a therapeutic relationship with patients is to increase the care and compassion received by the service users. Bettering nurses on attributes alike care and compassion improves quality of care; as stated by Glasper (2017); professionalism enhances and guarantees safe and effective patient-centred care, therefore professionalism is the leading attribute which nurses should possess and is repeatedly stated in the NMC: Code of Conduct. Rogers (1975, cited in McLeod, 2014) stated, showing empathy to patients means the nurse is able to understand the patients’ feelings, in return this slowly allows the patient to open up to the nurse. The best way to form a therapeutic relationship with patients is to show sensitivity, receptiveness and empathy towards patients. Contrariwise, showing sympathy can be demeaning for patients (Rogers, 1975, cited in McLeod, 2014).
With nursing comes a great deal of legal issues. With healthcare involving many laws and legislations, it means there is a bigger spotlight on the performance of health professionals, more importantly, nurses. The NMC: Code of Conduct incorporates many different laws to ensure nurses perform safe clinical practice. Nurses have a duty of care, to protect patient’s rights to privacy and confidentiality (NMC, 2015). The ‘duty of care’ nurses have is to provide humanistic care as it is their human right, and to prevent any neglect and poor, unsafe practice. The Nursing and Midwifery Council has set Codes of Conducts for nurses to follow when practicing their profession; nursing without being registered on the NMC register is a crime (NMC, 2015). An example of failed duty of care is the Mid-Staffordshire Inquiry of which’s findings were, poor leadership within healthcare teams and inadequate staff policies leading to extremely low standards of care (Hughes, 2013). Dimond (2015) states the accountability and expectations of nurses to the public also how nurses can be liable whether or not they are aware of the laws which are imposed in the nursing profession. An example of this could be, if there is a road traffic accident, if there is a nurse present (not on shift), they are expected to help and in some circumstances can be morally responsible if they refuse to assist, even if there is no legal obligation to volunteer nursing services (Dimond, 2015). To prevent any scandals like the Mid-Staffordshire inquiry, nurses should have knowledge of the laws they are to follow and aim to care for patients compassionately, with patient needs having the most attention.
Compassionate care is having the patients best interest at heart. Ethics are a fundamental in nursing; respect for autonomy, beneficence, non-maleficence and justice are the four principles of biomedical ethics (UK Clinical Ethics Network, 2001). In the Mid-Staffordshire inquiry, findings showed patients autonomy was not respected and were faced with maleficence as the Francis Report (2013) highlighted, patients were ‘so dehydrated they resorted to drinking water from vases’ (Hughes, 2013). Autonomy can be demonstrated by treating patients as autonomous individuals. An example of this is, although dementia patients do not have capacity, it is still the nurses’ responsibility and duty of care to treat them as an autonomous individual by being caring and compassionate and having a ‘holistic’ view (Skår, 2010). Correspondingly, attempting to get to know the patient no matter their capacity demonstrates autonomy; nurses carry out autonomous practice when they show courage and competence while taking dominating situations they are responsible for (Skår, 2010). Compassion and care are basic attribute to when providing ‘humanistic’ care. Humanistic care is to be received by all patients, majorly palliative patients as providing humanistic care for patients is to promote consolation and protect patient dignity in their last stages of their life (Wu & Volker, 2012).
To conclude, care and compassion are the most important attributes nurses should possess to provide exceptional patient-centred care. Building therapeutic relationships/partnerships with patients and relatives can help provide adequate tailored care as patients can make decisions concerning their treatment, leaving both patient and nurse in mutual agreement (McQueen, 2000). Conflict can arise between patients if therapeutic relationships are not formed. Conflict develops between healthcare professionals also due to changes in leadership. Nurses should follow laws and legislations when caring for patients, demonstrating professionalism and also as the NMC incorporates professionalism numerous time in the NMC: Code of Conduct. Overall, compassionate care can be demonstrated through excellent implementation of laws and the Code of Conduct in clinical practice.
...(download the rest of the essay above)
About this essay:
If you use part of this page in your own work, you need to provide a citation, as follows:
Essay Sauce, Compassionate care in nursing . Available from:<https://www.essaysauce.com/nursing-essays/2018-5-3-1525376612/> [Accessed 01-04-24].
These Nursing essays have been submitted to us by students in order to help you with your studies.
* This essay may have been previously published on Essay.uk.com at an earlier date.
Essay Categories:
- Accounting essays
- Architecture essays
- Business essays
- Computer science essays
- Criminology essays
- Economics essays
- Education essays
- Engineering essays
- English language essays
- Environmental studies essays
- Essay examples
- Finance essays
- Geography essays
- Health essays
- History essays
- Hospitality and tourism essays
- Human rights essays
- Information technology essays
- International relations
- Leadership essays
- Linguistics essays
- Literature essays
- Management essays
- Marketing essays
- Mathematics essays
- Media essays
- Medicine essays
- Military essays
- Miscellaneous essays
- Music Essays
- Nursing essays
- Philosophy essays
- Photography and arts essays
- Politics essays
- Project management essays
- Psychology essays
- Religious studies and theology essays
- Sample essays
- Science essays
- Social work essays
- Sociology essays
- Sports essays
- Types of essay
- Zoology essays
- Open access
- Published: 18 May 2022
Compassion in healthcare: an updated scoping review of the literature
- Sydney Malenfant 1 , 2 ,
- Priya Jaggi 1 , 3 ,
- K. Alix Hayden 4 &
- Shane Sinclair 1 , 3 , 5
BMC Palliative Care volume 21 , Article number: 80 ( 2022 ) Cite this article
14k Accesses
32 Citations
15 Altmetric
Metrics details
A previous review on compassion in healthcare (1988-2014) identified several empirical studies and their limitations. Given the large influx and the disparate nature of the topic within the healthcare literature over the past 5 years, the objective of this study was to provide an update to our original scoping review to provide a current and comprehensive map of the literature to guide future research and to identify gaps and limitations that remain unaddressed.
Eight electronic databases along with the grey literature were searched to identify empirical studies published between 2015 and 2020. Of focus were studies that aimed to explore compassion within the clinical setting, or interventions or educational programs for improving compassion, sampling clinicians and/or patient populations. Following title and abstract review, two reviewers independently screened full-text articles, and performed data extraction. Utilizing a narrative synthesis approach, data were mapped onto the categories, themes, and subthemes that were identified in the original review. Newly identified categories were discussed among the team until consensus was achieved.
Of the 14,166 number of records identified, 5263 remained after removal of duplicates, and 50 articles were included in the final review. Studies were predominantly conducted in the UK and were qualitative in design. In contrast to the original review, a larger number of studies sampled solely patients ( n = 12), and the remainder focused on clinicians ( n = 27) or a mix of clinicians and other (e.g. patients and/or family members) ( n = 11). Forty-six studies explored perspectives on the nature of compassion or compassionate behaviours, traversing six themes: nature of compassion, development of compassion, interpersonal factors related to compassion, action and practical compassion, barriers and enablers of compassion, and outcomes of compassion. Four studies reported on the category of educational or clinical interventions, a notable decrease compared to the 10 studies identified in the original review.
Conclusions
Since the original scoping review on compassion in healthcare, while a greater number of studies incorporated patient perspectives, clinical or educational interventions appeared to be limited. More efficacious and evidence-based interventions or training programs tailored towards improving compassion for patients in healthcare is required.
Peer Review reports
Compassion in healthcare has continued to receive growing interest over the past decade [ 1 ] from researchers, educators, clinicians, policy makers, patients, and families alike, with patients strongly emphasizing its importance to their overall quality of care [ 2 , 3 , 4 , 5 ]. Compassion has been associated with a positive impact on the patient experience and a variety of patient-reported outcomes – specifically, reduced patient symptom burden [ 6 , 7 , 8 ], improved quality of life [ 6 , 9 , 10 , 11 ], and even an enhancement in quality-of-care ratings [ 5 , 6 , 12 , 13 , 14 , 15 , 16 ]. While compassion is recognized as a standard of care and a core component of patients’ healthcare experience, it is also been found to be lacking in terms of its provision [ 3 , 5 , 6 , 12 , 17 , 18 , 19 , 20 , 21 , 22 , 23 ] and in much need for improvement [ 24 , 25 , 26 , 27 , 28 ]. A lack of compassion has been associated to increased patient/family complaints, healthcare costs, and adverse medical events [ 19 , 24 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 ]. Both the Canadian and American Medical Associations list compassion as one of their core virtues exemplified by the ethical physician [ 37 , 38 ], with the Canadian Medical Association (CMA) stating that “a compassionate physician recognizes suffering and vulnerability, seeks to understand the unique circumstances of each patient, attempts to alleviate the patient’s suffering, and accompanies the suffering and vulnerable patient” (p.2) [ 37 ]. Furthermore, researchers agree that while compassion is vital across healthcare settings, it is a central goal and tenant of quality palliative care where multifactorial suffering is prevalent, requiring future research, including how it can be sustained in palliative care providers [ 39 , 40 , 41 , 42 ]. However, it was only recently that compassion was delineated from a related construct, empathy (i.e. the ability to resonate with another’s positive or negative feelings) [ 43 , 44 ], highlighting action as one of its additional, yet paramount components [ 6 , 44 , 45 ]. The necessity of action within conceptualizations of compassion was independently affirmed by both palliative care patients' and palliative care providers' definitions of compassion, with patients defining compassion as “ a virtuous response that seeks to address the suffering and needs of a person through relational understanding and action ” [ 6 ], and healthcare providers (HCPs) defining compassion as: “a virtuous and intentional response to know a person, discern their needs and ameliorate their suffering through relational understanding and action” [ 45 ]. With the emergence of empirical models and definitions of compassion [ 6 , 45 ], and a valid and reliable patient-reported compassion measure for research and clinical use [ 15 ], studies have now shifted towards determining whether compassion can be trained or cultivated in practicing clinicians, while nurturing and sustaining the innate qualities related to compassion that these individuals already possess [ 8 , 46 , 47 , 48 , 49 ]. Recent studies suggest that while compassion is largely inherent, it can be influenced by life experiences and can fluctuate over time [ 50 , 51 ]. Educational leaders within healthcare settings have also emphasized the need to incorporate compassion training into their curriculum [ 52 ]. A systematic review found that implementing various curriculum strategies could result in practicing clinicians enhancing their overall levels of compassion and empathy, as perceived by the physician participants themselves, patients, standardized patients, or third-party observers, using a variety of measurement tools [ 52 ]. While recent reviews have identified the current landscape of compassion training programs [ 53 , 54 ], (i.e. those with the goal of cultivating compassion in others), studies identified in these reviews still present significant limitations such as: an absence of training to develop HCP skills within the interpersonal domains of compassion; lack of multi-modal training programs for practicing HCPs; reliance on self-reported assessments of learning outcomes as opposed to patient-reported outcomes; and a lack of Randomized Controlled Trials (RCTs) and longitudinal studies determining the retention and integration of skills into clinical practice [ 54 ]. As such, developing compassion training that is empirically based, clinically relevant and addresses these limitations is required and necessary in evidence-based, patient-centred healthcare delivery [ 54 ].
Despite remarkable efforts towards enhancing compassion in healthcare and a burgeoning knowledge base on the topic, the academic literature on compassion in healthcare remains deficient, specifically in regard to how compassion is perceived by patients themselves – the ultimate beneficiaries [ 1 , 55 ]. This lack of patient perspectives was a key limitation identified in a previous scoping review by Sinclair et al. (2016), a study which undertook a synthesis of the existing literature within a 25-year period (1988-2014) in order to determine what is known about compassion in healthcare. This original scoping review demonstrated an array of study types, settings, participant types (i.e. clinicians and patients), operational definitions and cultivation techniques, while also affirming the interpersonal nature of compassion, its predication on action, and associated barriers and facilitators in both education and practice [ 1 ]. Interestingly, patients themselves were widely underrepresented throughout the identified studies, with only 30% of them including patients, largely in a limited fashion, and the remainder focusing on clinicians, and/or students, and/or caregivers. Studies also failed to include patient-derived definitions of compassion, and studies that exclusively sampled patients and/or outcomes related to patients’ health and quality of life were also lacking [ 1 ]. Further, of the compassion interventions that were identified in this original review, only two were randomized controlled trials evaluating clinical interventions, and eight were educational interventions, of which only two of the interventions used validated tools to measure compassion – one of which used a tool measuring empathy [ 1 ]. The absence of a comprehensive knowledge base and an ambiguous understanding of how compassion is conceptualized by patients and HCPs in various healthcare contexts, makes operationalizing and improving its delivery to patients an extremely daunting and challenging task.
Despite considerable advancement in the field of compassion in healthcare over the past 30 years, including the identification of associated research gaps and recommendations to guide research [ 1 ], there has been a rapid influx of disparate studies over the past 5 years (Fig. 1 ) that require a further mapping of the literature to determine if previously identified limitations have been addressed and if any new domains of compassion research have emerged. Therefore, in keeping with the iterative nature of scoping reviews [ 56 , 57 ], the objective of this scoping review was to provide an update to our original review [ 1 ] to include contributions to the healthcare literature over the past 5 years. The review question was: What is currently known about compassion in healthcare? In addition to an overview of how the field of compassion in healthcare has evolved, readers of this review will gain evidence-based knowledge in four specific areas: 1) the nature of compassion and how it is conceptualized in the healthcare literature; 2) the feasibility and reputed impact of clinical and educational compassion interventions; 3) challenges and enablers to integrating compassion in contemporary healthcare; and 4) whether compassion can be meaningfully and rigorously measured.
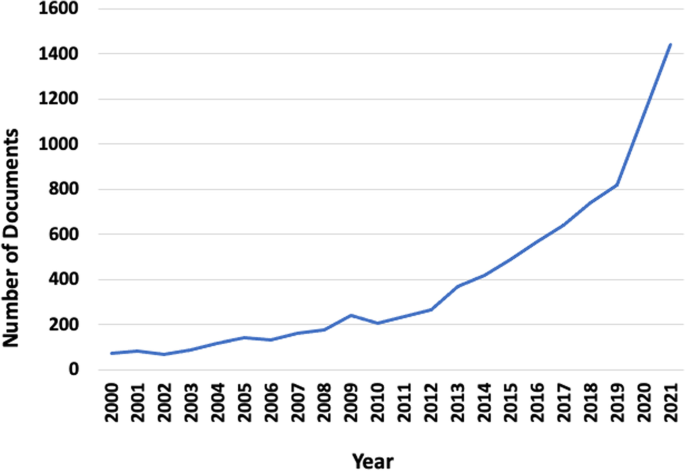
Number of documents from 2000 to 2021 (Scopus search: Compassion in healthcare)
Search strategy
Through consultation with a research librarian (KAH), a search for existing knowledge synthesis reviews on compassion in healthcare was performed using MEDLINE, Google Scholar, and Prospero. Apart from the original scoping review [ 1 ] and a more recent review targeting compassion in the pediatric population [ 58 ], no other completed knowledge synthesis reviews were identified on this topic.
The current scoping review is an update of the original scoping review published in 2016 [ 1 ]. A study protocol was written a priori to guide this current review, which is reported in accordance with the PRISMA-ScR reporting guidelines [ 59 ]. The included studies from the original review ( n = 44) were first analyzed for keywords and subject headings by KAH. The search in the original review was intentionally broad and included terms such as “delivery of healthcare, healthcare, palliative, palliative care, end-of-life, terminal, end-of-life care, terminal care, terminally ill patient, euthanasia, cancer, neoplasm, carcinoma, tumor, religion, spirituality” (p.2) [ 1 ]. These terms, however, did not show up consistently in the 44 included studies of the original review and as such, were not included into the refined updated search strategy. This initial analysis determined that two concepts were constant across the 44 studies: compassion and HCPs, becoming the focus of the refined search for the current review. For each concept, both keywords and subject headings were utilized, where keywords were the same for all databases, and subject headings were defined by each database’s controlled vocabulary. The draft search strategies were tested to ensure all the original included studies were captured. Once the search strategy was finalized, it was limited to English and date limits of January 1, 2015 – November 2020. The original review included studies published up to December 31, 2014. The final searches were run between November 16 and November 27, 2020, and results uploaded into Covidence, with each upload automatically deduplicated.
Congruent with our original review, the following databases were searched: MEDLINE(R) and Epub Ahead of Print, In-Process & Other Non-Indexed Citations and Daily 1946 to November 16, 2020 (OVID), Embase 1974 to 2020 November 25 (OVID), EBM Reviews - Cochrane Central Register of Controlled Trials October 2020 (OVID), APA PsycInfo 1806 to November Week 32,020 (OVID), CINAHL Plus with Full Text (Ebsco), Academic Search Complete (Ebsco), and Scopus (Elsevier). Additional file 1 provides the search strategies for each database.
Eligibility criteria
Studies that sampled inpatients or outpatients, and/or qualified clinicians (e.g. physicians, nurses, healthcare aides) were included in the final analysis. Studies were excluded if they sampled healthy non-clinical populations exclusively, as our focus was on clinicians or patients—individuals within society who have had significant experiences of suffering. While the original study [ 1 ] and search strategy herein did not exclude students, in keeping with the iterative nature of scoping reviews [ 56 ], the search criteria was refined at the title and abstract screening phase to exclude studies that sampled students exclusively (i.e. nursing students, residents, medical students, etc.), for the sake of feasibility and in recognition that barriers and facilitators to compassion in healthcare primarily occur in ongoing clinical practice [ 60 , 61 ]. We were interested in studies that had a primary aim to explore compassion towards others within the clinical setting or those that focused on interventions or educational programs aimed at improving compassion in clinical care. As such, studies that focused on other related concepts such as compassion fatigue, compassion satisfaction, empathy, or intervention studies aimed at fostering self-compassion (i.e. mindfulness-based stress reduction or compassion-focused therapies) were excluded. Congruent with the original scoping review [ 1 ], we retained a broad interest on categories of studies exploring compassion in healthcare such as perspectives, clinical outcomes, knowledge, skills, or attitudes on the topic [ 1 ]. Only primary and secondary studies using qualitative, quantitative, or mixed method designs were included. As such, systematic reviews, books, chapters, letters, commentaries, editorials, dissertations/theses, conference abstracts, and case studies were excluded [ 1 ].
Study selection
At the title and abstract screening (level 1), a calibration exercise of a random sample of articles ( n = 50) was conducted by two independent reviewers (SM and SS), to test the screening tool to ensure a standardized application of the selection criteria. At level 1, a minimum threshold of 80% agreement (number of agreements/number of agreements + disagreements) [ 62 , 63 ] was utilized to guide screening of the remaining titles and abstracts. Congruence in the calibration exercise of the 50 articles was 90%, after which one reviewer (SM) proceeded with screening the remaining titles and abstracts [ 64 ]. Following the title and abstract screening, two independent reviewers (SM and PJ) conducted a full-text review (level 2) of a random sample of included studies ( n = 10) to determine whether they would either be included or excluded for data extraction. Congruence in Level 2 screening was initially 70%, with all disagreements being resolved through clarification of the selection criteria and discussion between reviewers until consensus was reached, refining the inclusion/exclusion criteria in an iterative manner, prior to conducting an independent review of the remaining articles that would then proceed to the data extraction phase [ 65 ].
Data items and extraction process
Two reviewers (SM and PJ) independently reviewed each study meeting the criteria for a full-text review to identify eligible studies for data extraction. As an additional measure of rigour and quality assurance, the data extraction form was initially tested between the reviewers for 10 articles, with modification incorporated thereafter [ 65 ]. The review team (SM and PJ) met bi-weekly to review the extracted data from each study, resolve any identified discrepancies, and ensure completion and accuracy of the extracted data. A standardized data extraction sheet in excel was used to extract the following variables: study title, author, year published, journal, country of origin, study background and purpose, study setting, design, sample, participant information, data collection methods, analysis methods, results, conclusions, and limitations (both author and reviewer-identified). The manner in which the topic of compassion was conceptualized was also documented for each study.
Data synthesis
A narrative synthesis of the data was performed given the heterogeneity of studies, in accordance with the original review [ 1 ]. Each study was initially grouped by study participants (i.e. HCPs/students or HCPs/patients or patients/students or HCPs/patients/students) and study type (compassion interventions or perspectives of compassion and compassionate behavior). Frequencies for each of these groupings were tabulated. For the narrative synthesis [ 66 ], any quantitative data were initially translated to qualitative descriptions. The previously identified categories, themes, and subthemes (Table 1 ) [ 1 ] that emerged from the data in the original scoping review were utilized as a template, allowing us to map the current results onto these pre-existing categories, themes, and subthemes. Any new potential categories, themes, and/or subthemes that emerged were documented and discussed through a consensus process (SM, PJ, SS). Data were analyzed by three members of the research team (SM, PJ and SS), by reviewing the extracted data, resolving any inconsistencies or answering any queries that arose. A decision-making trail was compiled for the placement of the data into their respective categories, themes, and subthemes.
Search flow and study characteristics
Our search strategy resulted in a total of 14,166 records identified from the eight databases (Fig. 2 ). Removal of duplicates resulted in 5263 records remaining. After title and abstract screening, 133 potentially relevant reports underwent a full text review, after which 84 studies were excluded. A total of 49 articles underwent data extraction and synthesis of results (Table 2 ) (Fig. 2 ). One article [ 67 ] contained two separate eligible studies and has been reported herein as two separate studies [ 67 , 68 ]. Thus, for sake of clarity, this narrative synthesis consists of 50 studies. Overall, we found that the studies fell within two overarching categories: perspectives or behaviours of compassion, and compassion interventions (Table 1 ) [ 1 ]. Studies that fell within each of these categories were organized as per their themes and subthemes, according to those that were identified in the original scoping review (Table 3 ). No new themes or subthemes were identified from the updated search.
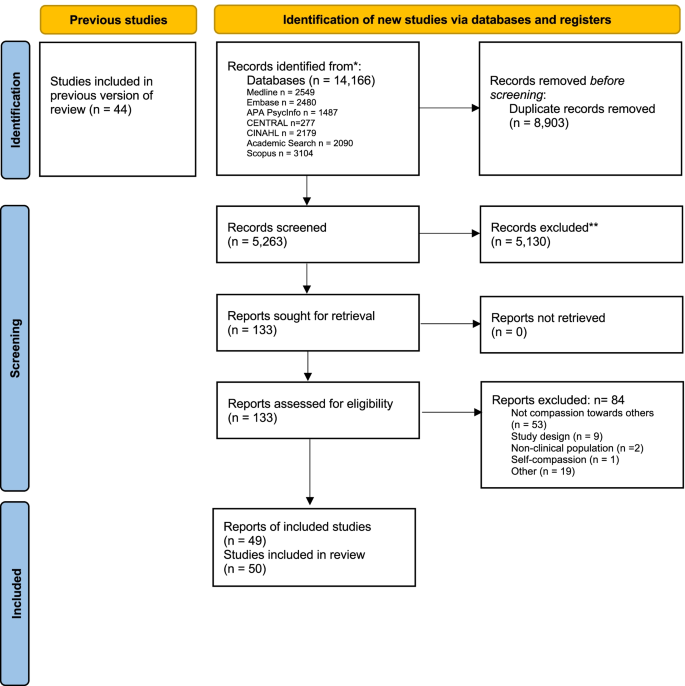
PRISMA 2020 flow diagram for updated systematic reviews which included searches of databases and registers only
Studies were predominantly qualitative in nature, with some quantitative and mixed-methods study designs. Two studies were randomized controlled trials (quantitative design). Most of the studies were conducted in the United Kingdom (Table 2 ), followed by Canada and the United States. Two studies collected data from 15 different countries (Table 2 ), with two other secondary studies utilizing this larger dataset to report exclusively on the results from Greece and Cyprus, and the USA exclusively. Twelve studies sampled patients, and the remainder focused on HCP participants or a mix of HCP, students, patients, and/or family caregivers (Tables 2 and 3 ).
Category: perspectives on compassion and compassionate behaviours in healthcare
Forty-six studies explored perspectives on the nature of compassion or compassionate behaviours (Table 3 ). Similar to the previous scoping review [ 1 ], perspectives on compassion were presented from either patients or HCPs, or a combination of participants (i.e. HCPs and/or patients along with students, family caregivers or even the public) (Table 3 ). The majority of these studies presenting perspectives on compassion were qualitative in design ( n = 35), followed by mixed methods ( n = 5) and cross-sectional survey studies ( n = 5). Two were quantitative randomized clinical trials. Twenty-three studies on perspectives of compassion sampled HCP participants exclusively (Table 3 ).
Theme: the nature of compassion in healthcare
Twenty-seven studies reported participants’ perspectives on the nature of compassion, which included the conceptualization of compassion and/or its temporal aspects (Table 3 ).
Subtheme: conceptualizing compassion in healthcare
Compassion was conceptualized through patient perspectives ( n = 12 studies), in which participants were asked about what compassion meant to them in reflecting on their personal experiences with their HCPs [ 6 , 45 , 98 , 101 , 102 , 103 , 106 , 107 , 109 , 110 , 111 , 112 ]. Several features that patients recognized as signifying compassion included: kindness, authenticity, attentiveness, forming a relational connection, displaying presence and warmth, acceptance, understanding, listening, helping, communicating effectively, being involved, and being gentle and caring [ 6 , 44 , 98 , 101 , 102 , 103 , 106 , 107 , 109 , 110 , 111 , 112 ]. Sinclair et al. (2016; 2018) conceptualized and validated an empirical model of compassion from both the patient and HCP perspective, further defining compassion as “a virtuous response that seeks to address the suffering and needs of a person through relational understanding and action” [ 6 , 45 ]. Menage et al. (2020) also conceptualized compassion in midwifery care through a model, highlighting its key components as “being with me”, “relationship with me”, and “empowering me” [ 109 ]. International, online survey studies conducted with a total of 1323 nurses, nurse educators, and nurse managers representing 15 different countries (Table 3 ) used a pre-imposed dictionary definition of compassion “a deep awareness of the suffering of others and a wish to alleviate it” [ 77 , 82 , 87 , 88 ]. Interestingly, while this survey defined compassion a priori [ 77 , 82 , 87 , 88 ], some participants provided their own definitions, with some participants from Spain identifying this definition as problematic, noting that the term compassion itself was problematic in being associated with religious beliefs, and as such, diminishing the evidence-based approach of nursing care within the Spanish context [ 77 ]. One study aimed to investigate compassion in a specific cultural context focusing particularly on South Asian patients [ 111 ]. While South Asians perceived compassion in a similar vein to other patient groups (i.e. compassion being composed of HCP embedded qualities, relational connection, and an action-orientated nature) [ 6 , 110 ] and as a universal concept that extends across humanity regardless of cultural differences, they also highlighted the importance of compassionate HCPs possessing cultural sensitivity, and accepting cultural beliefs and practices in a non-judgemental manner [ 111 ]. In another study, patient participants felt that compassion was demonstrated through HCPs’ ability to demonstrate intuition, provide evidence-based care, and be proficient in managing time in their clinical practice [ 99 ]. Similarly, Dalvandi et al. (2019) reported that patients perceived compassion to be associated with a capable HCP [ 107 ]. In fact, the authors reported that HCPs’ caring attributes or ability to meaningfully connect with his/her patients was seen as less desirable compared to their overall clinical competence [ 107 ].
Eighteen studies highlighted HCP conceptualizations of compassion and compassionate behaviours [ 45 , 77 , 79 , 81 , 82 , 83 , 84 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 95 , 98 , 101 , 102 ]. Similar to patients, HCPs recognized compassion as involving an inner desire to want to relieve one’s suffering [ 45 , 79 , 87 ] and as a response based on sensitivity to patients’ preferences [ 90 ]. Sinclair et al. (2018) generated a HCP model of compassion, in which HCPs defined compassion as a “virtuous and intentional response to know a person, to discern their needs and ameliorate their suffering through relational understanding and action” (p. 5) [ 45 ]. Additionally, in a study by Tierney et al. (2017), HCPs defined compassion in the workplace as “professional compassion,” which encompassed traits such as being a good communicator, being cognizant of patients’ needs, and through providing small acts of kindness [ 84 ]. This study also described the concept of professional compassion as involving some degree of “tough love” or through providing “scare tactics” (i.e. emphasizing to patients their medical conditions that may result in their mortality), which was driven from practitioners’ desire to help prevent future medical complications in patients – an approach to care that was further emphasized in relation to compassion sometimes requiring a more conscious effort as opposed to it occurring spontaneously [ 84 ]. In studies involving physicians from palliative care and medical oncology contexts [ 81 , 89 ], while compassion was thought to consist of both intangible and tangible skills (i.e. being present, holding a patient’s hand, and supportive touch) to address patients’ emotional needs [ 81 ], having standardized end-of-life conversations with patients and their family caregivers was integral to ensuring that their needs were adequately addressed and to educating them about their disease trajectory [ 81 , 89 ].
Subtheme: temporal aspects of compassion in healthcare
Patient and HCP participants alike perceived time as one of the components related to the nature of compassion, describing compassion as being fluid and dynamic in nature, something that can be developed over time, while also being influenced by the availability of time (i.e. taking time to listen to patients) [ 6 , 81 , 83 , 87 , 94 , 95 , 110 ]. Although compassion has been reported as developing over time, it has also been recognized as something that can be attained by HCPs in instances where there is a limited amount of time, through thoughtfully connecting with patients in the moment, acknowledging the difficulties that they’re facing, using humor, physical gestures conveying comfort, and relating to patients’ social concerns [ 81 , 94 ]. Compassion was recognized as adaptable to the situation and clinical setting [ 83 , 90 ] and something that patients may better appreciate and become more aware of overtime during their care journey [ 90 ]. Interestingly, nurse participants in the rehabilitation setting thought that providing compassion should not be obligatory given its situational nature and should instead be delivered with discretion or tempered [ 90 ]. As such, the provision of compassion depended on the individual nurse’s own personal values balanced with their duty of care [ 90 ]. Compassion was also perceived as requiring HCPs to “slow down” [ 83 , 89 ], particularly in the palliative care context where creating a space for dying was characterized by ‘slowness’ [ 89 ].
Theme: the development of compassion in healthcare
Thirty studies explored the development of compassion, which included both its innate nature and external factors that could equip clinicians with the necessary skills to further enact compassion in their clinical care.
Subtheme: antecedents of compassion
Patients and HCPs both recognized the intrinsic qualities or virtues of individual HCPs to be integral to providing compassion, some of which included virtues of love, kindness, genuineness, consideration, understanding, and wisdom [ 6 , 44 , 45 , 50 , 68 , 73 , 77 , 79 , 80 , 82 , 84 , 85 , 88 , 90 , 94 , 95 , 98 , 101 , 102 , 106 , 109 , 110 , 111 , 112 ] (Table 3 ). While various participants in a study by Kneafsey et al. (2015) described compassion as an innate emotion and a part of one’s personality at birth [ 94 , 95 ], other studies recognized that past experiences also shape one’s ability to be compassionate [ 76 , 80 , 85 ]. For example, nurses described their own psychological empowerment to contribute to their ability to provide more compassion, as driven by their length of experience working within the field of healthcare [ 85 ]. Patients and clinicians also perceived compassion to be motivated by their own personal experiences of suffering, having had to provide care to ill family members, or to be developed through family upbringing, role modelling, self-reflection and life experiences [ 6 , 76 , 80 , 110 ]. Religion, spirituality or culture, and an appreciation for a recognition of the shared humanity between oneself, patients, family, and colleagues were also perceived as external factors that could facilitate or motivate one to provide compassion [ 80 , 90 , 110 , 111 ]. Furthermore, various HCP participants in a study by Taylor et al. (2020) indicated that their own cultural values must denote they are person-centred, caring, and open, and hold intent to be compassionate [ 98 ]. Additionally, a HCP’s attitude was found to be a forerunner of compassion, influencing their behaviour and practices towards their patients [ 98 , 102 ]. In a few studies, HCP participants felt that compassion should be a prerequisite to pursuing a career in healthcare [ 79 , 80 , 84 , 94 ]. In one study, HCP participants felt that a personal interest in compassion must be vested in, dismissing the notion of any external motivations or conditions compelling one to being compassionate (i.e. from the healthcare organization itself) [ 80 ]. In other studies, participants described compassion as a predisposition or a driver through which they chose to pursue a career in healthcare and a core value that draws many physicians and nurses into healthcare professions [ 84 , 94 ].
Subtheme: cultivating compassion
Several studies reported that compassion can be taught and that HCPs can be equipped with tangible knowledge and skills for improving compassion in their professional practice [ 50 , 82 , 88 , 94 , 95 , 101 , 106 ]. Both HCP and patient participants emphasized clinical role-modeling, by compassionate HCPs, as being a salient means for improving compassion [ 50 , 72 , 80 , 83 , 100 , 106 ]. While role models in the form of teachers or peers were seen as imperative for motivating physicians and nurses (especially newly graduated clinicians) to be compassionate [ 80 , 94 ], it was also suggested that uncompassionate behaviours (i.e. answering to patients indifferently, ambivalence, and disregard) were equally transferrable to HCP colleagues [ 100 ]. A supportive environment that is conducive to learning was another factor that patients thought to be advantageous in compassion training [ 50 ]. Patients receiving palliative care believed that HCPs might increase their capacity for compassion by adopting a more reflective practice – through contemplating their own beliefs and reflecting on what their patients may be experiencing [ 50 ] – an experiential approach that was further supported by patient and HCP participants in a study by Smith-MacDonald et al. (2019) [ 101 ].
Reynolds et al. (2019) explored the effectiveness of “compassion-inducing” images to combat clinical scenarios that were thought to challenge medical students’ and health professionals’ (physicians, nurses, other) ability to be compassionate in dealing with patients presenting with “disgusting symptoms” and/or those who were thought to be responsible for their own health problems [ 93 ]. The authors reported that while patients presenting with “disgusting symptoms” (i.e. more challenging, more likely to wear a mask) influenced medical students more than the qualified HCPs, the use of compassion-inducing images mitigated group differences [ 93 ]. Similarly, Ling et al. (2020) tested the impact of “common humanity scenarios” on one’s ability to provide compassion and found that study participants (nursing, medicine, social work, occupational therapists, pastoral care practitioners, etc.), reported enhanced levels of compassion after being exposed to scenarios reflecting common humanity, further identifying common humanity as a prerequisite for providing compassion [ 75 ].
Theme: interpersonal factors associated with compassion in the clinical setting
Both relational and clinical communication were the predominant interpersonal dimensions associated with compassion, identified in studies involving both HCP and patient participants.

Subtheme: relational factors
The ability of HCPs to interact with patients, to deeply connect and share in their experience through an outward expression of their innate virtues, along with creating a relational space to do so, was seen as paramount to the provision of compassion in healthcare. This space was commonly described by patients as extending beyond a clinical relationship to one in which HCPs would actively engage in the patients’ suffering through awareness and engaged caregiving [ 6 , 44 , 45 , 73 , 91 , 101 , 110 , 111 ]. This entailed not only being physically present with the patient and addressing their medical needs, but seeking to understand their unique needs (e.g. emotional) and appreciate the patient as a person [ 6 , 44 , 45 , 73 , 79 , 89 , 99 , 101 , 110 , 111 ]. An inability to understand the emotional state of the patient or leaving patients feeling worried or vulnerable was felt to be associated with uncompassionate HCPs [ 91 , 94 , 99 , 102 ]. Skills such as being able to express affection, kindness, tenderness, being able to actively listen [ 77 , 78 , 88 , 89 , 94 ], showing understanding, and being supportive were perceived to be more effective expressions of compassion than routine, task-oriented care [ 99 ]. The ability to relationally understand patients was further highlighted as a distinct feature from sympathy, in which a shallow and superficial emotional response from HCPs can leave patients feeling demoralized, depressed, and feeling pity for themselves [ 44 ]. Getting to know the patient and going through a process of knowing through recurrent interactions and building rapport was important to both patients and HCPs alike [ 84 , 87 , 98 , 112 ]. Study participants indicated that encounters which lack connection renders HCPs as ingenuine and as having a lack of compassionate intent [ 98 ]. HCPs highlighted relational challenges such as receptivity, proximity, fragmentation, and lack of shared understanding between and within the healthcare team(s) and patients as potential hinderance to compassion [ 72 ]. On the contrary, being able to build rapport and connect with or relate to patients and their family was perceived as essential [ 76 ]. As such, relational aspects of compassion were found to be multidirectional, expressed between two or more people including patients, families, and HCPs [ 83 ]. Inside the workplace, supportive inter- and intra-disciplinary relationships helped to enhance the unity of the care team and thus aid in the development of more concise care plans which led to more consistency in patient care [ 76 , 102 ]. A few studies noted some subtle differences in the expressed relational needs of females versus males, which may impact compassion. For example, female participants emphasized their emotional needs requiring more attention in comparison to men [ 107 ] and thus, reflecting the need for female nurse HCPs to be able to better relate to them and subsequently personalize their care more effectively [ 108 , 109 ].
Subtheme: clinical communication
Both patient and HCP participants identified clinical communication to be a prominent component of compassion in healthcare. An integral domain of the Patient Compassion Model [ 6 , 110 ] was relational communication, referring to the verbal and non-verbal displays of compassion within the clinical context that seeks to establish a deeper understanding of a person as an individual – an aspect of compassion that was also identified in other studies [ 6 , 45 , 101 , 110 ]. Facets of relational communication included HCPs demeanor, affect (emotional resonance), engagement and behaviour [ 6 , 45 , 101 , 110 ]. It was also stated in one study that through relational communication, actively listening, involved listening to the subtext of what is not said (i.e., being attuned to the non-verbal cues, using silence, and paying attention to tone of voice), can help uncover patients’ concealed suffering [ 45 ]. Taylor et al. (2020) further differentiate that indicative communication is different from traditional communication, such that body language must be accompanied with tone of voice to demonstrate a compassionate intent [ 98 ].
Other studies have also highlighted notable components of verbal and non-verbal communication in which HCPs can convey compassion to their patients, such as tone of voice, personalization, attentiveness, actively listening, body language (i.e. smiling, eye contact) and even touch [ 79 , 87 , 88 , 89 , 91 , 94 , 95 , 99 , 109 ]. While communicating relevant information in a timely manner was seen as paramount to providing compassion for patients undergoing withdrawal of life-sustaining treatment [ 86 ], it was also found that HCPs’ display of emotion could help further humanize the interaction with patients, as long as it was exhibited in ways that were not too burdensome to the patient’s family [ 86 ]. Patients’ perception of compassion may also depend largely on the content that is being delivered [ 72 , 104 , 105 ]. For example, using the Physician Compassion Questionnaire to rate clinicians on five dimensions of warm-cold; pleasant-unpleasant; compassionate-distant; sensitive-insensitive; and caring-uncaring [ 104 ], advanced cancer patients in a randomized clinical trial considered physicians who provided a more optimistic prognosis to be significantly more compassionate compared to physicians who delivered less optimistic prognostic information [ 104 , 105 ]. Similarly in another study, HCP participants felt that despite a HCP’s intention, more emotionally challenging conversations involving goals of care or prognostication may be perceived by patients as being less compassionate [ 72 ]. Various studies suggest that communicating information through plain and simple language for patients to understand, delivered in a sensitive manner, was crucial in demonstrating compassion [ 6 , 95 , 103 , 110 ]. Also, women participants who received midwifery care during their pregnancy perceived midwives as more compassionate when they “communicate as an equal” – i.e. without any implied professional superiority [ 109 ].
In two cross sectional survey studies, in addition to other modes of non-verbal communication such as listening and connecting with patients, nurse participants particularly highlighted “touching” (i.e. holding a patient’s hand, giving a back rub, placing a hand on the patient, healing touch, or human touch) to be paramount to relieving one’s suffering and offering a sense of healing and comfort [ 87 , 88 ]. Along with having HCPs identify with patients by trying to understand their situation, patients and HCPs in various studies emphasized supportive touch to be an important aspect of HCPs connecting with the patients [ 45 , 50 , 83 , 101 , 103 ].
Theme: action and practical compassion in healthcare
Patients and HCPs stipulated action-based components of compassion as quintessential, particularly those directed at proactively alleviating patient suffering and addressing their needs through tangible means [ 6 , 44 , 45 , 50 , 73 , 81 , 95 , 101 , 110 , 111 ], whilst considering sensitivity to the patients’ condition [ 6 , 45 , 103 ]. Participants referred to the importance of “small acts of kindness” across a few studies [ 6 , 44 , 45 , 72 , 83 , 84 , 103 , 110 ], such as providing comfort [ 86 , 87 , 103 ] and performing actions that were supererogatory in nature or going above and beyond without expectation of receiving anything in return, as key features of actions associated with compassion [ 6 , 77 , 81 , 87 , 110 ]. For nurses in palliative care, action was evident in being proactive in planning the palliative pathway with the patients and families before the patient had reached their terminal phase [ 89 ]. In some cases, the technical and physical aspects of compassion compared to other humanistic approaches were more desirable to patients, particularly those in hospital surgery wards, where the alleviation of pain is more critical to their overall health quality [ 107 ], or when looking for compassion in the task-based features of having to undergo diagnostic tests, such as radiography [ 112 ]. In contrast, clinicians in a study conducted by Roze des Ordons et al. (2020) felt that an overly biomedical approach could contribute to the over medicalization of an illness which in turn can lead to more patient suffering and even missed opportunities for integrating patients’ goals and values into their care plans, which is paramount in improving quality of life [ 72 ]. Similarly, nurses in one study felt that to be compassionate, there is a strong need for competency in relieving pain through both pharmacological and non-pharmacological means [ 87 ], including but not limited to, providing emotional comfort. Finally, in addition to utilizing a proactive action-based approach to care, patients receiving midwifery care felt that a midwife’s ability to teach and coach mothers by providing them with necessary information about their condition was considered an act of practical compassion [ 109 ].
Theme: challenges and enablers of compassion in healthcare
More than half of the studies ( n = 30; 60%) identified various educational and/or practice-setting challenges and enablers to compassion (Table 3 ), with 11 studies specifically identifying the exploration of barriers and facilitators to compassion in hospital, critical care, palliative care, intensive care, mental health, acute care, long-term care, and medical-surgical contexts as a primary study aim [ 67 , 68 , 72 , 73 , 74 , 76 , 84 , 92 , 100 , 101 , 102 ].
Subtheme: educational challenges and enablers
Four studies identified educational challenges and barriers to providing compassion [ 50 , 74 , 83 , 107 ]. HCP participants identified feeling particularly challenged in providing compassion within clinical practice, when there was a perceived incongruence between their theoretical knowledge of compassion and their ability to apply it [ 72 , 74 ]—a phenomena conceptualized as compassion distress [ 44 ]. Similarly, while clinicians acknowledged that they could learn compassion vicariously through their colleague role models (i.e. enablers to compassion), not having those role models routinely available impeded HCPs’ ability to grow in their capacity for compassion [ 72 ]. Patients, on the contrary, felt that a supportive teaching environment was necessary to allow HCPs to safely reflect on their innate qualities, such as their virtuous, past life experiences, and vocational motivators to further nourish their abilities to provide compassion [ 50 ]. Patients in this study also felt that experiential methods of learning compassion would likely be more beneficial to HCPs over traditional didactic approaches [ 50 ]. Interestingly, in contrast to HCP education in providing compassion, a survey conducted with 300 hospitalized patients that aimed to determine the importance and extent of providing compassion in nursing care revealed that patients level of education influenced how compassion was experienced – i.e. patients with an academic-level of education were more aware of system issues, had better communication skills and a higher expectation to participate in the treatment process, and as such perceived HCPs as being less compassionate than those who had lower than a diploma level of education [ 107 ].
Subtheme: practice setting challenges and enablers
Numerous studies ( n = 29) identified specific challenges and enablers impacting the provision of compassion within the healthcare setting, with challenges being identified disproportionally in comparison to enablers. The most commonly identified challenges were time constraints [ 72 , 73 , 74 , 77 , 79 , 81 , 84 , 88 , 91 , 92 , 95 , 96 , 101 , 106 , 112 ], organizational culture (i.e. excessive workload and inadequate staffing) [ 72 , 73 , 77 , 79 , 84 , 88 , 90 , 92 , 94 , 96 , 100 , 106 , 109 , 112 ], lack of resources [ 79 , 100 ], and the clinical environment/culture itself [ 72 , 74 , 79 , 89 , 90 , 92 , 94 , 95 , 98 , 100 , 101 , 106 , 112 ]. Some studies commented on how advancing technology in the clinical setting can serve as a barrier to HCPs’ ability to provide compassion [ 72 , 106 ]. For example, HCPs in critical and palliative care settings perceived technology as distracting them from attending to their patients’ emotional needs, requiring them instead to focus more on physical aspects of care [ 72 ]. HCP and patient participants in other studies felt that the need for HCPs to juggle daily administrative or organizational requirements contributed to a myopic focus of care that centred on tasks or checking off “ticky boxes” rather than on providing high-quality, compassion [ 77 , 109 ]. One study identified organizational threats (i.e. daily organizational demands and workplace stresses) as inhibitors to compassion [ 67 ], where increased perceived organizational threats led to a decreased ability for HCPs to provide compassion to patients [ 67 ]. Sims et al. (2020) further examined “intentional rounding”, a structured process that involves nurses performing periodic checks of their patients’ fundamental care needs using a standardised protocol and documentation, and its contribution to the delivery of compassionate nursing care. Ironically, this care strategy was actually perceived by participants to be more of a barrier to providing compassion, as nurses were left to prioritize their documentation over direct patient care [ 96 ].
Another practice setting barrier to providing compassion was the lack of managerial engagement or support [ 74 , 101 ], which can contribute to fragmented teams, lack of unity [ 76 , 101 ], resulting in less compassion to patients in settings were collaboration between nurses was lacking [ 89 ]. Additionally, nurses in hospital settings felt muted in their ability to provide compassion when their managers failed to support them in its delivery [ 74 ]. HCPs also felt that after the death of a patient, their grief and mourning affected their ability to provide compassion to their patients, highlighting the need for managerial support and compassion towards themselves from their colleagues or managers as they worked through their own mourning [ 98 ]. In the acute care context, care was thought to be susceptible to fragmentation given the various division of HCP roles, multiple team members, shiftwork, and sequential transitions, all leading to varying intensity and duration of patient interactions [ 72 ]. On the other hand, support networks amongst HCPs were also seen as enablers to compassion within various practice settings [ 68 , 76 , 78 , 79 , 91 , 98 ]. For example, the need for HCPs to engage in a team dynamic to support the delivery of compassion to patients was highlighted by Murray et al. (2020), specifically with respect to maintaining good communication, encouraging and listening to one another, being present, and open-minded [ 78 ]. Findings from Brennan et al. (2019) concur with this notion of the importance of HCPs fostering strong connections with their colleagues to enhance the delivery of compassion within their organizational settings [ 79 ].
In general, literature on clinical challenges and enablers from the patient perspective appeared to be lacking. Ironically, the majority of studies focused on HCPs perspectives on patient factors (personality, behaviours, communication issues, etc.) effecting HCPs ability to provide compassion in clinical care, with little discussion of HCP factors (personality, behaviours, communication issues, etc.). Studies that did include patients’ perspectives, identified language barriers as a significant challenge to experiencing compassion from their HCPs [ 72 , 100 , 102 , 111 ], reportedly undermining HCPs’ motivation or aptitude for providing compassion in the process [ 100 , 111 ]. However, a study by Singh et al. (2020), acknowledged that language barriers could be overcome by having interpreters readily available and by being cognizant of patients, particularly female patients, preferences related to the sex and gender of their HCPs [ 111 ]. Interestingly, in a qualitative study of nurses, family members and patients, sex was also a predictor of compassion, with women being perceived as being more innately compassionate than men [ 100 ].
Theme: outcomes of compassionate care
Three studies identified the impact of compassion on patient health outcomes exclusively from the patient perspective [ 6 , 44 , 111 ], and one from the perspectives of both family physicians and inpatient/outpatient residents [ 94 ]. Patients felt that compassion alleviated their suffering, enhanced overall well-being, and positively augmented the quality of care they received from their HCPs by allaying distress and enhancing their relationship with their HCPs [ 6 , 44 , 111 ]. On the contrary, those patients who recoined healthcare interactions lacking in compassion reported negative outcomes such as frustration, being overwhelmed, and a lack of dignity and hope [ 6 ]. In a separate study, patients felt that compassionate physicians achieve a better understanding of their patients’ issues and concerns, facilitating more open communication, which in turn helps to strengthen the level of trust in the patient-physician relationship [ 94 ]. Compassion was also felt to have assisted physicians in constructing more supportive and caring treatment plans for their patients, which ultimately facilitated patient compliance [ 94 ]. Lastly, a compassionate approach was perceived to help enable physicians to better cope with more challenging patient scenarios, such as those patients presenting with more psychosocial or emotional distress [ 94 ].
Category: compassion interventions
Four studies focused on compassion interventions for HCPs (i.e. clinicians, policy makers, and managers) and patients (Table 4 ). These interventions studies traversed the themes of clinical and educational interventions (Table 3 ).
Theme: clinical interventions
Gould et al. (2017) conducted a quantitative (baseline and 4 months post) intervention with clinicians (ward managers, healthcare assistants, staff nurses and charge nurses) and patients [ 97 ]. This study sought to evaluate the “Creating Learning Environments for Compassionate Care (CLECC)” program that aimed to enhance clinicians’ capacity for providing compassion by embedding ward-based manager and team practices including dialogue, reflective learning, and mutual support [ 97 ]. As indicated by patient-reported evaluations of emotional care using the Patient Evaluation of Emotional Care during Hospitalisation (PEECH) tool, higher scores post-intervention indicated better patient-reported experiences. However, staff self-reported empathy, using the Jefferson Empathy Scale, did not show any significant difference in scores between baseline and follow-up. Overall, the CLECC program was favorable towards reducing negative staff-patient interactions and was anecdotally felt to offer potential benefit in reducing patients’ experiences of lack of emotional connection with the healthcare team [ 97 ].
Theme: educational interventions
Three studies were thematized as educational interventions, each of which were components of the Leaders for Compassionate Care Programme (LCCP) [ 69 , 70 , 71 ], which aims to empower leaders while supporting their teams in delivering high-quality and compassionate patient-centred care [ 69 , 70 ]. These studies varied in design – one being a quantitative cross-sectional survey [ 69 ], and two being qualitative and mixed-methods longitudinal designs [ 70 , 71 ]. Two studies explored the impact of the LCCP on participants’ personal development, learning experience, service and care delivery, and overall satisfaction with the program; one of these studies identified factors that can embed compassionate care in healthcare environments [ 69 , 70 ]. In one study, there were reported improvements in participants’ perceived ability to show respect and empathy in their interactions with patients [ 69 ]. The study authors also reported that the program was felt to increase motivation and confidence in leading the delivery of compassionate care [ 69 ]. A conceptual model was offered by MacArthur et al. (2017), centering on ‘compassionate care’ where the needs of patients, relatives and staff are viewed as being distinct, and on the other hand, inter-related, in which sustainability requires a focus on relationship-centred care mediated through relational practice and relational inquiry, and a need for investment in infrastructure and leadership at both the strategic and local levels [ 70 ].
The LCCP also influenced ways of working and specific practice development techniques – particularly, staff receiving regular feedback from patients on how their delivery of compassion influenced their communication with their patients [ 70 ]. Smith et al. (2017) evaluated how the LCCP impacted participants’ ability to listen, learn, and respond to patient feedback – a practice that reportedly improved compassion [ 71 ], with staff finding value in the experiences of sharing and learning from feedback.
State of the science: the ongoing monotony, persistent gaps, and incremental progress of compassion research in healthcare
This scoping review provides an updated synthesis of the current literature on the topic of compassion in healthcare over the past 5 years (2015-2020), in keeping with the methodology of the original scoping review that was conducted by members of the Compassion Research Lab [ 1 ]. Since the publication of the original scoping review, studies presenting exclusively on patient conceptualizations of compassion have increased (nine studies in total compared to only two that were identified previously), addressing a previously identified limitation—the underrepresentation of the recipients of compassion – patients themselves. This updated review also revealed that HCP and patient perspectives on compassion and compassionate behaviours traversed the themes and subthemes that were previously identified (Table 1 ), including but not limited to temporal aspects of compassion (i.e. situational in nature, with an ebb and a flow), interpersonal features (i.e. relational care and clinical communication), action, and practicality. While HCPs and patients also identified numerous barriers and enablers to compassion, adaptive behaviours to overcome challenges to compassion were reported in numerous studies coinciding with a general aversion by participants – the notion of absolute barriers to dynamic nature and robustness of compassion. This suggests that in relation to compassion, barriers need to be reconceptualized as challenges—challenges that can be overcome.
The nature and conflation of compassion: the need for conceptual specificity
In regards to the nature of compassion, while a lack of conceptual specificity persists, additional research focused on the construct of compassion in healthcare over the last 5 years, including the establishment of empirical models of compassion, has produced a growing consensus that compassion is inherently relational, consisting of acknowledging, engaging and proactively attending to another person’s suffering that stems from the innate qualities and good intentions of a fellow human being [ 6 , 45 , 79 , 82 , 87 , 88 , 101 ]. The centrality and willingness to proactively address multifactorial suffering, is not only the central aim of palliative care [ 40 , 41 , 42 ], but is a defining feature of a compassionate relationship in comparison to other forms of relationships, including empathetic and caring relationships [ 44 ]. HCP participants in multiple studies were clear that compassion was other-orientated, was predicated in suffering, and required action aimed at alleviating it [ 6 , 82 , 87 ]. While conceptual clarity and consensus has grown since our original study, additional research over this period also identified some slight cultural variances in relation to compassion, specifically in how it is both expressed and experienced. For example, while there were similarities in how Greek and Cyprus participants perceived compassion, differences also persisted in their definitions, with more than half of the Cyprus participants defining compassion as “empathy and kindness”, whereas Greek participants were more likely to define it as “a deep awareness of the suffering of others and a wish to alleviate it” [ 88 ]. However, caution should be exercised in attributing these results strictly to ‘cultural difference’, as is evident in further interpretation of these study results that one plausible reason for these differences is the fact that the Greek participants were practicing registered nurses, whereas those from Cyprus were nursing students who had less clinical experience and exposure to patient suffering. Further, although patients have clearly delineated compassion from empathy and sympathy [ 44 ], a couple of included studies utilized definitions of compassion that embedded the term or aspects of empathy [ 77 , 103 ]. Despite established differences between these terms, one study argued that compassion and empathy are in fact interdependent [ 98 ], while participants in another study, concluded that empathy was subsumed within compassion, with compassion enhancing components of empathy while adding action [ 95 ]. Despite this lack of conceptual clarity, the attributes or skills comprising compassion were recognized across most of the studies, including the dynamic, responsive, and proactive nature of compassionate action, in comparison to a more static, reactionary, and passive nature of empathy, sympathy, and routine care [ 44 , 50 , 86 , 92 , 99 , 107 ].
Clinical and educational compassion interventions: can compassion be taught?
The notion of whether one can be trained to become compassionate remains the topic of ongoing debate within the literature, although this debate has dissipated since the previous review. Antecedents, in the form of inherent virtues or personal qualities, and previous personal experiences of suffering and receiving compassion have been previously identified as facilitators of compassion [ 1 , 6 , 45 , 101 , 110 , 111 ]. Studies within this current review have extended what previously was a largely dichotomous (nature vs. nurture) approach to this issue to a more intersectional understanding, comprised of various factors [ 80 , 94 ]. This complex relationship between intrapersonal factors embedded within individual HCPs and interpersonal factors embedded in the relational and clinical space, was advanced by Uygur in their Compassion Trichotomy [ 94 ], which highlights the importance and interdependence of motivation (personal reflection and values), capacity (awareness and regulation of energy, emotion, and cognition), and connection (sustained patient–physician relationship) which influences physicians’ level of compassion [ 94 ]. Other studies also highlighted intrinsic altruistic motivators (e.g. personal attitudes, virtues) as catalysts, but not preconditions to providing or enhancing compassion [ 45 , 76 , 80 , 98 , 106 ]. While there is ongoing debate on whether virtues themselves can be cultivated, we have reported elsewhere that virtues can be cultivated, however the outcomes of this training will vary based on the innate virtues that trainees possess at baseline [ 50 ].
Clinical and educational compassion interventions: how do we teach compassion?
An equally compelling question related to compassion training, arising from studies in this updated review, is how and what are the best methods for cultivating compassion amongst practicing clinicians. While studies suggested that compassion could be cultivated [ 82 , 88 , 95 ] and broad educational approaches such as personal development practices were proposed [ 95 ], the intricacies of how and what would be required in a training program remained largely unexplored. While participants in other studies, provided suggestions for teaching methods associated with compassion training [ 50 , 94 , 101 , 106 ], including the use of compassion-inducing imagery, sharing heartfelt stories or narratives [ 75 , 93 ], being exposed to compassionate role models and leadership [ 50 , 106 ], and through using an experiential approach to learning involving mentorship and self-reflection [ 50 , 79 , 101 ], these recommendations lacked augmentation with educational studies investigating these issues specifically. While one study aimed to investigate the impact of common humanity scenarios on cultivating compassion [ 75 ], results from this study were largely predicated on the relational features of compassion and failed to include its action component [ 75 ]. Although this study and others focus exclusively on enhancing elements of affective compassion in HCPs [ 75 , 93 ], viewing common humanity scenarios and interventions focused on perspective-taking of HCPs towards patients, fails to address the multiple domains that comprise compassion and the potential benefit of interventions aimed at enhancing patient perspective-taking towards HCPs [ 6 , 45 , 61 ]. Regardless of these shortcomings, the need to develop, enhance, and sustain a culture of compassion in complex healthcare systems is well-recognized [ 24 , 25 , 26 , 27 , 28 , 113 , 114 ]. A recent realist review [ 54 ] and environmental scan [ 52 ] on compassion education literature revealed the intricacies of compassion education programs, describing what works for whom and in what context, which could ultimately inform the development of a comprehensive, evidence-based, clinically-informed compassion training program for HCPs. An imperative, and neglected, factor to cultivating and sustaining compassion in healthcare identified in this recent realist review, was the role of healthcare system and organizational leaders in creating the conditions, educational resources, and policies to ensure that compassion is not only embedded across the healthcare system, but is considered a shared responsibility, and not simply the onus of HCPs [ 54 ]. A recent systematic review of predictors of physician compassion revealed similar findings, namely that research on the barriers and facilitators to compassion in healthcare remains disproportionately practitioner-centric, requiring greater research on the both the patient perspective and the influence of broader organizational and system factors [ 61 ].
Clinical and educational compassion interventions: can we measure compassion?
Surprisingly in this updated review, only four of the studies pertained to evaluating compassion educational or clinical interventions – a notable decrease from the 10 interventions identified in the previous review [ 1 ]. While one intervention study’s primary aim was to evaluate the Creating Learning Environments for Compassionate Care (CLECC), an educational programme focused on developing managerial and team practices at a group level to enhance team capacity to provide compassionate care for patients (Table 4 ), researchers utilized the Jefferson Scale of Empathy (JSE) to obtain a nurse-reported measure of empathy at baseline and follow-up [ 97 ], rather than using a valid and reliable measure of compassion—the construct of interest. It is interesting to note that the rational for using the JSE in this intervention study was attributed to the fact that the authors were unable to identify a sufficiently psychometrically robust, valid, and reliable measure for compassion, affirming the findings of a previous systematic review of existing compassion measures [ 55 ]. The lack of a sufficiently robust compassion measure in this and other intervention studies has been a significant impediment in the advancement of the field and the validity of these compassion interventions, further conflating the concepts of compassion and empathy in the process. The inherent limitations of previous compassion measures were recently addressed in the development of the Sinclair Compassion Questionnaire (SCQ) [ 15 , 55 ] – a psychometrically rigorous and robust patient-reported compassion measure. The other three intervention studies identified were educational interventions conducted in the UK, aimed towards HCPs, which analyzed the Leaders for Compassionate Care Program (LCCP) within the hospital settings, none of which included patient outcomes [ 69 , 70 , 71 ]. Additionally, while the results of these studies focused heavily on participants’ overall satisfaction with the LCCP programme itself, whether it actually improved compassion to patients and families was precariously not assessed.
Challenges and enablers to compassion
With respect to the literature on challenges and enablers of compassion within practice settings, time constraints, workloads, and staff shortages, remained a prevalent issue in this updated review, as was the case in our original review [ 72 , 73 , 74 , 77 , 79 , 81 , 84 , 92 , 94 , 95 , 100 , 101 , 106 , 112 ]. Despite this persistent challenge, both HCP and patient participants felt that forging a compassionate connection between patients and HCPs could be established in the moment, through ones’ demeanor, the tenor of care, intention, and presence within even the shortest of interactions [ 6 , 45 , 73 ].
Limitations
There are a few limitations to this updated review . First , despite applying a robust methodology to identify eligible studies, it is possible that relevant studies could have been inadvertently missed. Secondly, since only English publications were included, we recognize that numerous non-English studies on compassion were excluded, thus limiting generalizability to other non-English speaking settings. Thirdly, in utilizing the previously identified thematic framework generated from the original review in synthesizing the studies within this current review, there is a possibility that this hindered the emergence of additional themes. This decision was purposeful on the part of the review authors in order to remain methodologically congruent with our original review, a decision that we nonetheless were cognisant of in allowing new categories to emerge from the results through a consensus process, thereby avoiding the force fitting of current studies into a predetermined framework. Fourth, while the evidence that self-compassion improves compassion is lacking [ 115 ], in excluding intervention studies that focused on improving self-compassion as a means to create more compassionate HCPs, there is a remote possibility that pertinent results were missed. Lastly, despite their inclusion in the original study, studies focusing solely on medical students, trainees, or residents were excluded (except when combined with HCP participants), for the sake of feasibility and because our primary focus was practicing HCPs– who are frequently exposed to patient suffering in a healthcare system were compassion is challenged.
Implications
An empirically-based, clinically-relevant, patient orientated definition of compassion, that reflects the dynamic nature and multiple domains of the construct of interest is imperative to the fidelity and advancement of educational and clinical interventions designed to improve it. In our original review, there was a notable paucity of studies that conceptualized compassion from not only the perspectives of those who receive it, but also those who strive to provide it—where compassion and suffering reside [ 1 ]. Since our original review, targeted efforts to establish the conceptual foundation of compassion were undertaken in various studies identified herein, including but not limited to the development of models of compassion from the perspectives of both patients and clinicians alike. These models of compassion further provide an empirical blueprint depicting the nature, components, flow, facilitators, and inhibitors of compassion for use in research, education, and practice. While these recent studies addressed a conceptual gap identified in the original review, a growing theory-practice gap has emerged in its place over the last 5 years between researchers and HCPs’ knowledge of compassion and their ability to adequately assess it in research and address in clinical practice. While the recent development of a psychometrically rigorous and robust patient-reported compassion measure has partially addressed this issue, there is now a critical need to further address this theory-practice gap through the development of evidence-based educational training programs that equip practicing HCP with the attitudes, knowledge, skills, and behaviours that comprehensively traverse each of the domains of compassion. Similarly, there is a pressing need for RCTs, including future 3-arm RCTs that compare the compassion intervention group to not only standard care, but other related educational interventions such as empathy training. Furthermore, since cultural and gender differences pertaining to how compassion is both expressed and experienced were alluded to within the studies reviewed herein, these individuals and differences must evolve from the realm of platitudes and good intentions to the realm of research priorities and action. While compassion was affirmed as a universal concept in this review, compassion also seeks to understand the uniqueness of the person and their individual needs—whether those individuals are patients or practicing HCPs. Future studies on the topic of compassion need to investigate and honour these differences, whether in the form of validating existing definitions, measures, and interventions of compassion within various cultures, genders, or individuals who experience systemic inequities in care and in society more broadly. Lastly, while assessing the transferability of recently developed valid and reliable patient compassion measures is needed, the existence and further development of valid and reliable research tools offers the ability to begin to meaningfully assess these differences, and provides the means to assess and deliver personalized compassion.
Since the publication of original scoping review 6 years ago, research on the topic of compassion in healthcare while seeing considerable advances, remains largely theoretical in nature, with limited educational and clinical intervention studies. Despite these limitations, compassion has received increasing attention from researchers, policy makers, educators, HCPs, and particularly patients who consistently identify compassion as a central feature of their overall experience of healthcare. With a firm conceptual foundation of compassion now established with the perspectives of patients embedded therein, greater attention needs to focus on addressing the growing theory-practice gap between what is empirically known and implemented into training and practice. Additional research is needed on developing compassion training programs that honour and are tailored to individuals—including but not limited to their gender identity and cultural background.
Availability of data and materials
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Healthcare Providers
Randomized Controlled Trials
Creating Learning Environments for Compassionate Care
Leaders for Compassionate Care Program
Sinclair S, Norris JM, McConnell S, Chochinov HM, Hack TH, Hagen NA, et al. Compassion: a scoping review of the healthcare literature. BMC Palliative Care. 2016;15(6):1–16. https://doi.org/10.1186/s12904-016-0080-0 .
Article Google Scholar
Cherlin E, Schulman-Green D, McCorkle R, Johnson-Hurzeler R, Bradley E. Family perceptions of clinicians' outstanding practices in end-of-life care. J Palliat Care. 2004;20(2):113–6.
Heyland DK, Dodek P, Rocker G, Groll D, Gafni A, Pichora D, et al. Canadian researchers end-of-life network (CARENET). What matters most in end-of-life care: perceptions of seriously ill patients and their family members. CMAJ. 2006;174(5):627–33. https://doi.org/10.1503/cmaj.050626 .
Article PubMed PubMed Central Google Scholar
Heyland DK, Cook DJ, Rocker GM, Dodek PM, Kutsogiannis DJ, et al. Canadian researchers at the end of life network (CARENET). Defining priorities for improving end-of-life care in Canada. CMAJ. 2010;182(16):E747–52. https://doi.org/10.1503/cmaj.100131 .
McDonagh JR, Elliott TB, Engelberg RA, Treece PD, Shannon SE, et al. Family satisfaction with family conferences about end-of-life care in the intensive care unit: increased proportion of family speech is associated with increased satisfaction. Crit Care Med. 2004;32(7):1484–8. https://doi.org/10.1097/01.ccm.0000127262.16690.65 .
Article PubMed Google Scholar
Sinclair S, McClement S, Raffin-Bouchal S, Hack TF, Hagen NA, McConnell S, et al. Compassion in health care: an empirical model. J Pain Symptom Manag. 2016;51(2):193–203. https://doi.org/10.1016/j.jpainsymman.2015.10.009 .
Fogarty LA, Curbow BA, Wingard JR, McDonnell K, Somerfield MR. Can 40 seconds of compassion reduce patient anxiety? J Clin Oncol. 1999;17(1):371–9. https://doi.org/10.1200/JCO.1999.17.1.371 .
Article CAS PubMed Google Scholar
Vivino BL, Thompson BJ, Hill CE, Ladany N. Compassion in psychotherapy: the perspective of therapists nominated as compassionate. Psychother Res. 2009;19(2):157–71.
Soler-Gonzalez J, San-Martin M, Delgado-Bolton R, Vivanco L. Human connections and their roles in the occupational well-being of healthcare professionals: a study on loneliness and empathy. Front Psychol. 2017;8:1475. https://doi.org/10.3389/fpsyg.2017.01475 .
Riggs JS, Woodby LL, Burgio KL, Bailey FA, Williams BR. "Don't get weak in your compassion": bereaved next of kin's suggestions for improving end-of-life care in veterans affairs medical centers. J Am Geriatr Soc. 2014;62(4):642–8.
Lown BA, Dunne H, Muncer SJ, Chadwick R. How important is compassionate healthcare to you? A comparison of the perceptions of people in the United States and Ireland. J Res Nurs. 2017;22:60–9.
Flocke SA, Miller WL, Crabtree BF. Relationships between physician practice style, patient satisfaction, and attributes of primary care. J Fam Pract. 2002;51(10):835–40.
PubMed Google Scholar
Doohan I, Saveman BI. Need for compassion in prehospital and emergency care: a qualitative study on bus crash survivors' experiences. Int Emerg Nurs. 2015;23:115–9.
Ross AJ, Anderson JE, Kodate N, et al. Simulation training for improving the quality of care for older people: an independent evaluation of an innovative programme for interprofessional education. BMJ Qual Saf. 2013;22:495–505.
Sinclair S, Hack TF, MacInnis C, Jaggi P, Boss H, McClement S, et al. The development and validation of the Sinclair compassion questionnaire (SCQ). BMJ Open. 2021;11(6):e045988. https://doi.org/10.1136/bmjopen-2020-045988 .
Papadopoulos I, Ali S. Measuring compassion in nurses and other healthcare professionals: an integrative review. Nurse Educ Pract. 2016;16(1):133–9.
The Beryl Institute. Consumer study on patient experience. 2018. Accessed on December 16th, 2019 from https://www.theberylinstitute.org/page/PXCONSUMERSTUDY .
Crowther J, Wilson KC, Horton S, Lloyd-Williams M. Compassion in healthcare - lessons from a qualitative study of the end of life care of people with dementia. J R Soc Med. 2013;106(12):492–7.
Lown BA, Rosen J, Marttila J. An agenda for improving compassionate care: a survey shows about half of patients say such care is missing. Health Aff. 2011;30:1772–8.
Foreward YR, Shea S, Wynyard R, Lionis C, editors. Compassionate healthcare: challenges in policy and practice. London, UK: Routledge; 2014:xix-xxiii.
Google Scholar
Crawford P, Brown B, Kvangarsnes M, Gilbert P. The design of compassionate care. J Clin Nurs. 2014;23(23-24):3589–99. https://doi.org/10.1111/jocn.12632 .
Brown B, Crawford P, Gilbert P, et al. Practical compassions: repertoires of practice and compassion talk in acute mental healthcare. Sociol Health Ill. 2014;36(3):383–99.
Tarberg AS, Kvangarsnes M, Hole T, Thronæs M, Madssen TS, Landstad BJ. Silent voices: family caregivers’ narratives of involvement in palliative care. Nurs Open. 2019;6(4):1446–54.
Francis R. Report of the mid Staffordshire NHS Foundation trust public inquiry. London, England: The Stationary Office; 2013.
Paterson R. Can we mandate compassion? Hast Cent Rep. 2011;41(2):20–3.
Department of Health. Confidence in caring: a framework for best practice. London, England: Department of Health; 2008.
Department of Health and Social Care (UK). Report on the use and experience of the Liverpool care pathway. 2013. Accessed on February 19th, 2020 from https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/212450/Liverpool_Care_Pathway.pdf .
NHS Commissioning Board. Compassion in practice: nursing, midwifery and care staff–our vision and strategy. Leeds, England: NHS Commissioning Board; 2012.
Trzeciak S, Roberts BW, Mazzarelli AJ. Compassionomics: hypothesis and experimental approach. Med Hypotheses. 2017;107:92–7.
Epstein RM, Franks P, Shields CG, et al. Patient-centered communication and diagnostic testing. Ann Fam Med. 2005;3:415–21.
Attree M. Patients' and relatives' experiences and perspectives of 'Good' and 'Not so Good' quality care. J Adv Nurs. 2001;33(4):456–66. https://doi.org/10.1046/j.1365-2648.2001.01689.x .
Stewart M, Brown JB, Donner A, McWhinney IR, Oates J, Weston WW, et al. The impact of patient-centered care on outcomes. J Fam Pract. 2000;49(9):796–804.
CAS PubMed Google Scholar
Reader TW, Gillespie A, Roberts J. Patient complaints in healthcare systems: a systematic review and coding taxonomy. BMJ Qual Saf. 2014;23(8):678–89. https://doi.org/10.1136/bmjqs-2013-002437 .
Schwartz A, Weiner SJ, Weaver F, Yudkowsky R, Sharma G, Binns-Calvey A, et al. Uncharted territory: measuring costs of diagnostic errors outside the medical record. BMJ Qual Saf. 2012;21(11):918–24. https://doi.org/10.1136/bmjqs-2012-000832 .
West CP, Huschka MM, Novotny PJ, Sloan JA, Kolars JC, Habermann TM, et al. Association of perceived medical errors with resident distress and empathy: a prospective longitudinal study. JAMA. 2006;296(9):1071–8. https://doi.org/10.1001/jama.296.9.1071 .
Lloyd M, Carson A. Making compassion count: equal recognition and authentic involvement in mental health care. Int J Consum Stud. 2011;35(6):616–21.
Canadian Medical Association, code of Ethics. 2004. Accessed on August 19, 2021 from https://policybase.cma.ca/en/viewer?file=%2fdocuments%2fPolicyPDF%2fPD19-03.pdf#phrase=false
American Medical Association. Code of Medical Ethics: Principle 1. 2001; Accessed on August 19, 2021 from https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/principles-of-medical-ethics.pdf
Brito-Pons G, Librada-Flores S. Compassion in palliative care: a review. Curr Opin Support Palliat Care. 2018;(4):472–9. https://doi.org/10.1097/SPC.0000000000000393 PMID: 30300152.
Mills J, Wand T, Fraser JA. Palliative care professionals' care and compassion for self and others: a narrative review. Int J Palliat Nurs. 2017;23(5):219–29. https://doi.org/10.12968/ijpn.2017.23.5.219 PMID: 28548918.
World Health Organization. Definition of palliative care. Geneva: World Health Organization; 2020.
World Health Organization. Planning and implementing palliative care services: a guide for programme managers. Geneva: World Health Organization; 2016.
Singer T, Klimecki OM. Empathy and compassion. Curr Biol. 2014;24:R875–8.
Article CAS Google Scholar
Sinclair S, Beamer K, Hack TF, McClement S, Raffin Bouchal S, Chochinov HM, et al. Sympathy, empathy and compassion: palliative care patients’ understandings. Experiences and Preferences Palliat Med. 2016;31(5):437–47. https://doi.org/10.1177/0269216316663499 .
Sinclair S, Hack TF, Raffin S, McClement S, Stajduhar K, Singh P, et al. What are healthcare providers understanding and experiences of compassion: the healthcare compassion model. BMJ Open. 2018;18(8):e019701. https://doi.org/10.1136/bmjopen-2017-019701 .
Bray L, O'Brien MR, Kirton J, Zubairu K, Christiansen A. The role of professional education in developing compassionate practitioners: a mixed methods study exploring the perceptions of health professionals and pre-registration students. Nurse Educ Today. 2014;34(3):480–6. https://doi.org/10.1016/j.nedt.2013.06.017 .
Wear D, Zarconi J. Can compassion be taught? Let’s ask our students. J Gen Intern Med. 2008;23:948–53.
Dewar B, Mackay R. Appreciating and developing compassionate care in an acute hospital setting caring for older people. Int J Older People Nursing. 2010;5(4):299–308. https://doi.org/10.1111/j.1748-3743.2010.00251.x .
Bond C, Stacey G, Field-Richards S, Callaghan P, Keeley P, Lymn J, et al. The concept of compassion within UK media-generated discourse: a corpus-informed analysis. J Clin Nurs. 2018;27(15-16):3081–90. https://doi.org/10.1111/jocn.14496 .
Sinclair S, Torres M, Raffin-Bouchal S, Hack TF, McClement S, Hagen N, et al. Compassion training in healthcare: what are patients’ perspectives on training healthcare providers? BMC Med Educ. 2016;16(169). https://doi.org/10.1186/s12909-016-0695-0 .
Sinclair S, Kondejewski J, Jaggi P, Dennett L, Roze des Ordons AL, Hack TF. What is the state of compassion education? A systematic review of compassion training in health care. Acad Med. 2021;96(7):1057–70. https://doi.org/10.1097/ACM.0000000000004114 .
Sinclair S, Harris D, Kondejewski J, Roze des Ordons AL, Jaggi P, Hack TF. Program Leaders' and Educators' Perspectives on the Factors Impacting the Implementation and Sustainment of Compassion Training Programs: A Qualitative Study. Teach Learn Med. 2022:1-16. https://doi.org/10.1080/10401334.2021.2017941 .
Patel S, Pelletier-Bui A, Smith S, Roberts MB, Kilgannon H, Trzeciak S, et al. Curricula for empathy and compassion training in medical education: a systematic review. PLoS One. 2019;14(8):e0221412. https://doi.org/10.1371/journal.pone.0221412 .
Article CAS PubMed PubMed Central Google Scholar
Sinclair S, Kondejewski J, Jaggi P, Roze des Ordons AL, Kassam A, Hayden KA, et al. What works for whom in compassion training programs offered to practicing healthcare providers: a realist review. BMC Med Educ. 2021;21(1):455. https://doi.org/10.1186/s12909-021-02863-w .
Sinclair S, Russell LB, Hack TF, Kondejewski J, Sawatzky R. Measuring compassion in healthcare: a comprehensive and critical review. Patient. 2017;10(4):389–405. https://doi.org/10.1007/s40271-016-0209-5 .
Arksey H, Malley O, L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(143):1–7. https://doi.org/10.1186/s12874-018-0611-x .
Sinclair S, Kondejewski J, Schulte F, Letourneau N, Kuhn S, Raffin-Bouchal S, et al. Compassion in pediatric healthcare: a scoping review. J Pediatr Nurs. 2020;51:57–66. https://doi.org/10.1016/j.pedn.2019.12.009 .
Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73. https://doi.org/10.7326/M18-0850 .
Fernando AT, Consedine NS. Development and initial psychometric properties of the barriers to physician compassion questionnaire. Postgrad Med J. 2014;90(1065):388–95. https://doi.org/10.1136/postgradmedj-2013-132127 .
Pavlova A, Wang CXY, Boggiss AL, O'Callaghan A, Consedine NS. Predictors of physician compassion, empathy, and related constructs: a systematic review. J Gen Intern Med. 2021;20:1–12. https://doi.org/10.1007/s11606-021-07055-2 Epub ahead of print.
McAlister AM, Lee D, Ehlert K, Kajfez R, Faber CJ, Kennedy M. Qualitative coding: an approach to assess inter-rater reliability. Ohio: Paper presented at the 2017 American Society for Engineering Education Annual Conference & Exposition Columbus; 2017. [cited 2020 February 19]. Available from https://www.researchgate.net/publication/323343316_Qualitative_Coding_An_Approach_to_Assess_Inter-Rater_Reliability
McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb). 2012;22(3):276–82.
Lefebvre C, Glanville J, Briscoe S, Littlewood A MC, Metzendorf M-I, et al. JPT H, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Chapter 4: Searching for and selecting studies. Cochrane: Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021). p. 2021. Available from www.training.cochrane.org/handbook
Aromataris E, Munn Z. JBI Manual for Evidence Synthesis. 11.2.7. In: Data Extraction: JBI; 2020. Available from https://wiki.jbi.global/display/MANUAL/11.2.7+Data+extraction .
Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Guidance on the conduct of narrative synthesis in systematic reviews: a product from the ESRC methods Programme. 2006.
Henshall LE, Alexander T, Molyneux P, Gardiner E, McLellan A. Study 1. The relationship between perceived organisational threat and compassion for others: implications for the NHS. Study 2. Clin Psychol Psychother. 2018;25:231–49. https://doi.org/10.1002/cpp.2157 .
Henshall LE, Alexander T, Molyneux P, Gardiner E, McLellan A. The relationship between perceived organisational threat and compassion for others: implications for the NHS. Study 2. Clin Psychol Psychother. 2018;25:231–49. https://doi.org/10.1002/cpp.2157 .
Saab MM, Drennan J, Cornally N, Landers M, Hegarty J, Savage E, et al. Impact of a compassionate care leadership programme. Br J Nurs. 2019;28(11):708–14. https://doi.org/10.12968/bjon.2019.28.11.708 .
MacArthur J, Wilkinson H, Gray MA, Matthews-Smith G. Embedding compassionate care in local NHS practice: developing a conceptual model through realistic evaluation. J Res Nurs. 2017;22(1-2):130–47. https://doi.org/10.1177/1744987116678901 .
Smith S, Gentleman M, Conway L, Sloan S. Valuing feedback: an evaluation of a National Health Service programme to support compassionate care practice through hearing and responding to feedback. J Res Nurs. 2017;22(1-2, 112):–127. https://doi.org/10.1177/1744987116685913 .
Ordons AL R d, MacIsaac L, Hui J, Everson J, Ellaway RH. Compassion in the clinical context: constrained, distributed, and adaptive. J Gen Intern Med. 2020;35(1):198–206. https://doi.org/10.1007/s11606-019-05467-9 .
Singh P, Raffin-Bouchal S, McClement S, Hack TF, Stajduhar K, Hagen NA, et al. Healthcare providers' perspectives on perceived barriers and facilitators of compassion: results from a grounded theory study. J Clin Nurs. 2018;27(9-10):2083–97. https://doi.org/10.1111/jocn.14357 .
Valizadeh L, Zamanzadeh V, Dewar B, Rahmani A, Ghafourifard M. Nurse's perceptions of organisational barriers to delivering compassionate care: a qualitative study. Nurs Ethics. 2018;25(5):580–90. https://doi.org/10.1177/0969733016660881 .
Ling D, Olver J, Petrakis M. Investigating how viewing common humanity scenarios impacts compassion: a novel approach. Br J Soc Work. 2020;50:1724–42. https://doi.org/10.1093/bjsw/bcz124 .
Jones J, Winch S, Strube P, Mitchell M, Henderson A. Delivering compassionate care in intensive care units: nurses' perceptions of enablers and barriers. J Adv Nurs. 2016;72(12):3137–46. https://doi.org/10.1111/jan.13064 .
Papadopoulos I, Taylor G, Ali S, Aagard M, Akman O, Alpers LM, et al. Exploring Nurses' meaning and experiences of compassion: an international online survey involving 15 countries. J Transcult Nurs. 2017;28(3):286–95. https://doi.org/10.1177/1043659615624740 .
Murray SJ, Tuqiri KA. The heart of caring – understanding compassionate care through storytelling. IPDJ. 2020;10(1):1–13.
Brennan H, Westbrook J, Parry S. An understanding, a way of life: an exploration of learning disability professionals’ experiences of compassion. Br J Learn Disabil. 2020;48:348–55. https://doi.org/10.1111/bld.12311 .
Zamanzadeh V, Valizadeh L, Rahmani A, van der Cingel M, Ghafourifard M. Factors facilitating nurses to deliver compassionate care: a qualitative study. Scand J Caring Sci. 2018;32(1):92–7. https://doi.org/10.1111/scs.12434 .
Bessen S, Jain RH, Brooks WB, Mishra M. "sharing in hopes and worries"-a qualitative analysis of the delivery of compassionate care in palliative care and oncology at end of life. Int J Qual Stud Health Well-being. 2019;14(1):1622355. https://doi.org/10.1080/17482631.2019.1622355 .
Papadopoulos I, Zorba A, Koulouglioti C, Ali S, Aagard M, Akman O, et al. International study on nurses' views and experiences of compassion. Int Nurs Rev. 2016;63(3):395–405. https://doi.org/10.1111/inr.12298 .
Roze des Ordons AL, MacIsaac L, Everson J, Ellaway RH. A pattern language of compassion in intensive care and palliative care contexts. BMC Palliat Care. 2019;18(15):1–9. https://doi.org/10.1186/s12904-019-0402-0 .
Tierney S, Seers K, Tutton E, Reeve J. Enabling the flow of compassionate care: a grounded theory study. BMC Health Serv Res. 2017;17(174):1–12. https://doi.org/10.1186/s12913-017-2120-8 .
Ledoux K, Forchuk C, Higgins C, Rudnick A. The effect of organizational and personal variables on the ability to practice compassionately. Appl Nurs Res. 2018;41:15–20. https://doi.org/10.1016/j.apnr.2018.03.001 .
Efstathiou N, Ives J. Compassionate care during withdrawal of treatment: a secondary analysis of ICU nurses' experiences. Nurs Ethics. 2018;25(8):1075–86. https://doi.org/10.1177/0969733016687159 .
Aagard M, Papadopoulos I, Biles J. Exploring compassion in U.S. nurses: results from an international research study. OJIN. 2018;23(1). https://doi.org/10.3912/OJIN.Vol23No01PPT44 .
Papadopoulos I, Kouta C, Malliarou M, Shea S, Apostolara P, Vasiliou M. Exploring the cultural aspects of compassion in nursing care: a comparative study of Greece and Cyprus. Int J Caring Sci. 2016;9(2):471–80.
Skorpen Tarberg A, Landstad BJ, Hole T, Thronæs M, Kvangarsnes M. Nurses’ experiences of compassionate care in the palliative pathway. J Clin Nurs. 2020;29:4818–26. https://doi.org/10.1111/jocn.15528 .
Burridge L, Foster M. Compassion in rehabilitation nurses who provide direct patient care: principles to pragmatics. JARNA. 2019;22(1):7–15. https://doi.org/10.33235/jarna.22.1.7-15 .
Ferraz SL, O'Connor M, Mazzucchelli TG. Exploring compassion from the perspective of health care professionals working in palliative care. J Palliat Med. 2020;23(11):1478–84. https://doi.org/10.1089/jpm.2019.0682 .
Christiansen A, O'Brien MR, Kirton JA, Zubairu K, Bray L. Delivering compassionate care: the enablers and barriers. Br J Nurs. 2015;10-23;24(16):833–7. https://doi.org/10.12968/bjon.2015.24.16.833 .
Reynolds L, Powell P, Sing Lin Y, Ravi K, Chung C, Consedine NS. Fighting the flinch: experimentally induced compassion makes a difference in health care providers. Br J Health Psychol. 2019;24:982–98. https://doi.org/10.1111/bjhp.12390 .
Uygur J, Brown JB, Herbert C. Understanding compassion in family medicine: a qualitative study. Br J Gen Pract. 2019;69(680):e208–16. https://doi.org/10.3399/bjgp19X701285 .
Kneafsey R, Brown S, Sein K, Chamley C, Parsons J. A qualitative study of key stakeholders' perspectives on compassion in healthcare and the development of a framework for compassionate interpersonal relations. J Clin Nurs. 2016;25(1-2):70–9. https://doi.org/10.1111/jocn.12964 .
Sims S, Leamy M, Levenson R, Brearley S, Ross F, Harris R. The delivery of compassionate nursing care in a tick-box culture: qualitative perspectives from a realist evaluation of intentional rounding. Int J Nurs Stud. 2020;107:103580. https://doi.org/10.1016/j.ijnurstu.2020.103580 .
Gould LJ, Griffiths P, Barker HR, Libberton P, Mesa-Eguiagaray I, Pickering RM, et al. Compassionate care intervention for hospital nursing teams caring for older people: a pilot cluster randomised controlled trial. BMJ Open. 2018;8:e018563. https://doi.org/10.1136/bmjopen-2017-018563 .
Taylor A, Hodgson D. The Behavioural display of compassion in radiation therapy: purpose, meaning and interpretation. J Med Imaging Radiat Sci. 2020;51(4S):S59–71. https://doi.org/10.1016/j.jmir.2020.08.003 .
Tehranineshat B, Rakhshan M, Torabizadeh C, Fararouei M. Nurses', patients', and family caregivers' perceptions of compassionate nursing care. Nurs Ethics. 2019;26(6):1707–20. https://doi.org/10.1177/0969733018777884 .
Babaei S, Taleghani F. Compassionate care challenges and barriers in clinical nurses: a qualitative study. Iran J Nurs Midwifery Res. 2019;24(3):213–9. https://doi.org/10.4103/ijnmr IJNMR_100_18.
Smith-MacDonald L, Venturato L, Hunter P, Kaasalainen S, Sussman S, McCleary L, et al. Perspectives and experiences of compassion in long-term care facilities within Canada: a qualitative study of patients, family members and health care providers. BMC Geriatr. 2019;19(128):1–12. https://doi.org/10.1186/s12877-019-1135-x .
Babaei S, Taleghani F, Keyvanara M. Contextual facilitators and maintaining of compassion-based care: an ethnographic study. Iran J Nurs Midwifery Res. 2017;22(2):91–6. https://doi.org/10.4103/ijnmr IJNMR_79_16.
Fernando A, Rea C, Malpas P. Compassion from a palliative care perspective. N Z Med J. 2018;131(1468):25–32.
Tanco K, Rhondali W, Perez-Cruz P, Tanzi S, Chisholm GB, Baile W, et al. Patient perception of physician compassion after a more optimistic vs a less optimistic message: a randomized clinical trial. JAMA Oncol. 2015;1(2):176–83. https://doi.org/10.1001/jamaoncol.2014.297 .
Tanco K, Azhar A, Rhondali W, Rodriguez-Nunez A, Liu D, Wu J, et al. The effect of message content and clinical outcome on Patients' perception of physician compassion: a randomized controlled trial. Oncologist. 2018;23(3):375–82. https://doi.org/10.1634/theoncologist.2017-0326 .
Straughair C, Clarke A, Machin A. A constructivist grounded theory study to explore compassion through the perceptions of individuals who have experienced nursing care. J Adv Nurs. 2019;75(7):1527–38. https://doi.org/10.1111/jan.13987 .
Dalvandi A, Vaisi-Raygani A, Nourozi K, Ebadi A, Rahgozar M. The importance and extent of providing compassionate nursing care from the viewpoint of patients hospitalized in educational hospitals in Kermanshah - Iran 2017. Open Access Maced J Med Sci. 2019;7(6):1047–52. https://doi.org/10.3889/oamjms.2019.204 .
Wittkowski A, Hare DJ, Gillham R. Using the repertory grid technique to explore the experience of compassion by mothers in a mother and baby unit. Midwifery. 2019;75:24–32. https://doi.org/10.1016/j.midw.2019.04.003 .
Menage D, Bailey E, Lees S, Coad J. Women's lived experience of compassionate midwifery: human and professional. Midwifery. 2020;85:102662. https://doi.org/10.1016/j.midw.2020.102662 .
Sinclair S, Jaggi P, Hack TF, McClement S, Raffin Bouchal S, Singh P. Assessing the credibility and transferability of the patient compassion model in non-cancer palliative populations. BMC Palliat Care. 2018;17:108. https://doi.org/10.1186/s12904-018-0358-5 .
Singh P, King-Shier K, Sinclair S. South Asian patients' perceptions and experiences of compassion in healthcare. Ethn Health. 2020;25(4):606–24. https://doi.org/10.1080/13557858.2020.1722068 .
Bleiker J, Knapp K, Morgan-Trimmer S, Hopkins S. What medical imaging professionals talk about when they talk about compassion. J Med Imaging Radiat Sci. 2020;51(4S):S44–52. https://doi.org/10.1016/j.jmir.2020.08.009 .
Maclean R. The Vale of Leven hospital inquiry. Edinburgh: APS Group Scotland; 2014.
Willis L. Raising the bar: the shape of caring review. London: Health Education England; 2015.
Sinclair S, Kondejewski J, Raffin Bouchal S, King-Shier K, Singh P. Can self-compassion promote healthcare provider wellbeing and compassionate care to others? Results of a systematic review. Appl Psychol Health Well-being. 2017;9(2):168–206. https://doi.org/10.1111/aphw.12086 .
Download references
Acknowledgements
Not applicable.
Author information
Authors and affiliations.
Compassion Research Lab, University of Calgary, 2500 University Drive NW, Calgary, Alberta, T2N 1N4, Canada
Sydney Malenfant, Priya Jaggi & Shane Sinclair
Section of Palliative Care, Department of Family Medicine, Alberta Health Services, Zone, Calgary, Canada
Sydney Malenfant
Faculty of Nursing, University of Calgary, 2500 University Drive NW, Calgary, Alberta, T2N 1N4, Canada
Priya Jaggi & Shane Sinclair
Libraries and Cultural Resources, University of Calgary, Calgary, Alberta, Canada
K. Alix Hayden
Division of Palliative Medicine Department of Oncology, Cumming School of Medicine, University of Calgary, 2500 University Drive NW, Calgary, Alberta, T2N 1N4, Canada
Shane Sinclair
You can also search for this author in PubMed Google Scholar
Contributions
SM conceptualized the study, developed the search strategy, screened the articles, performed data extraction and analysis, and provided interpretation of the data, and contributed to the writing of the manuscript. PJ coordinated the entire study, conceptualized the study, developed the search strategy, screened the articles, performed data extraction and analysis, and provided interpretation of the data, and contributed to the writing of the manuscript. KAH provided methodological expertise, developed the search strategy, and contributed to the writing of the manuscript. SS oversaw the entire study, conceptualized the study, developed the search strategy, screened titles and abstracts, provided guidance on data extraction, performed data analysis and provided interpretation of the data, and contributed to the writing of the manuscript. All authors have read and approved the manuscript.
Corresponding author
Correspondence to Shane Sinclair .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Malenfant, S., Jaggi, P., Hayden, K.A. et al. Compassion in healthcare: an updated scoping review of the literature. BMC Palliat Care 21 , 80 (2022). https://doi.org/10.1186/s12904-022-00942-3
Download citation
Received : 02 September 2021
Accepted : 05 April 2022
Published : 18 May 2022
DOI : https://doi.org/10.1186/s12904-022-00942-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Healthcare providers
- Scoping review
- Intervention
BMC Palliative Care
ISSN: 1472-684X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Caring, compassion and competence in healthcare
Nompumelelo ntshingila.
1 Department of Nursing, Faculty of Health Sciences, University of Johannesburg, Johannesburg, South Africa
The theme for this section focused on caring, compassion and competence in healthcare. Caring as a phenomenon and as a science is about human beings (Karlsson & Pennbrant 2020 ). As stated by Watson ( 2022 ), caring as a science is grounded in nursing scholarship and is also relevant to other disciplines in the academia, such as feminist studies, peace studies, education, ethics and human service fields, for example, social work and healthcare professions generally.
Various authors have termed compassion as the fundamental concept in healthcare (Papadopoulos & Ali 2016 ; Pehlivan & Güner 2020 ). Following a systematic literature review conducted by Perez-Bret, Altisent and Rocafort ( 2016 ), compassion is defined as ‘the sensitivity shown to understand another person’s suffering, combined with a willingness to help and to promote the wellbeing of that person and to find a solution to their situation’. To be compassionate requires understanding the pain and experiences of others. The concept of compassion comprises respect and awareness of others. Bradshaw ( 2011 ) confirms that compassionate care as a concept dates back to the time of Florence Nightingale and is associated mainly with nursing as a profession. Compassionate care is instead expressed in actions rather than words. The actions needed are firm touch, gentle, courteous manner and kindness (Bradshaw 2011 ). Furthermore, compassionate care is said to entail a set of four attributes: wisdom, humanity, love and empathy (Su et al. 2020 ).
Core competence in healthcare is for the healthcare provider to practice skills that meet the needs of the patients using logical thinking (Fukada 2018 ). Healthcare professionals must be competent providers of compassionate care. Pehlivan and Güner ( 2020 ) highlight the benefits and challenges of providing compassionate care in various healthcare environments. The benefits are improving understanding of involving patients and families in care, determining patients’ and families’ needs, using appropriate approaches and improving patient outcomes. The challenges are work environment challenges and individual factors. Babaei and Taleghani ( 2019 ) further included sociocultural barriers such as gender and lack of mutual language as barriers to compassionate care.
For the 2022 Health SA Gesondheid special collection, several manuscripts were submitted under the theme of caring, compassionate care and competence. This theme had the most submissions. The manuscripts reviewed under this theme ranged from qualitative, quantitative and systematic reviews. The issues addressed pertained to the challenges of providing competent, compassionate care across the healthcare context. These were challenges related to patients, healthcare providers and students. The manuscripts addressed current issues of coronavirus disease 2019 (COVID-19), gender-based violence, post-exposure prophylaxis and mental health challenges in the healthcare context. The studies’ settings were urban and rural contexts in South Africa and Namibia.
It is evident from the submissions that compassionate care and competence is a theme that will generate conversations in the healthcare context and seems to be of significant interest. I am positive that the articles that are published on the theme of caring, compassion and competence will provide an opportunity for further evidence-based research.
How to cite this article: Ntshingila, N., 2022, ‘Caring, compassion and competence in healthcare’, Health SA Gesondheid 27(0), a2133. https://doi.org/10.4102/hsag.v27i0.2133
- Babaei, S. & Taleghani, F., 2019, ‘ Compassionate care challenges and barriers in clinical nurses: A qualitative study ’, Iranian Journal of Nursing and Midwifery Research 24 ( 3 ), 213–219. 10.4103/ijnmr.IJNMR_100_18 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bradshaw, A., 2011, ‘ Compassion: What history teaches us ’, Nursing Times 107 ( 19–20 ), 12–14. [ PubMed ] [ Google Scholar ]
- Fukada, M., 2018, ‘ Nursing competency: Definition, structure and development ’, Yonago Acta Medica 61 ( 1 ), 1–7. 10.33160/yam.2018.03.001 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Karlsson, M. & Pennbrant, S., 2020, ‘ Ideas of caring in nursing practice ’, Nursing Philosophy 21 , e12325. 10.1111/nup.12325 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Papadopoulos, I. & Ali, S., 2016, ‘ Measuring compassion in nurses and other healthcare professionals: An integrative review ’, Nurse Education Practice 16 ( 1 ), 133–139. 10.1016/j.nepr.2015.08.001 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pehlivan, T. & Güner, P., 2020, ‘ Compassionate care: Can it be defined, provided, and measured? ’, Journal of Psychiatric Nursing 11 ( 1 ), 64–69. 10.14744/phd.2019.20082 [ CrossRef ] [ Google Scholar ]
- Perez-Bret, E., Altisent, R. & Rocafort, J., 2016, ‘ Definition of compassion in healthcare: A systematic literature review ’, International Journal of Palliative Nursing 22 ( 12 ), 599–606. 10.12968/ijpn.2016.22.12.599 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Su, J.J., Masika, G.M., Paguio, J.T. & Redding, S.R., 2020, ‘ Defining compassionate nursing care ’, Nursing Ethics 27 ( 2 ), 480–493. 10.1177/0969733019851546 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Watson, J., 2022, Watson’s caring science & human caring theory , viewed 15 August 2022, from https://www.watsoncaringscience.org/jean-bio/caring-science-theory/ . [ Google Scholar ]
- Cancer Nursing Practice
- Emergency Nurse
- Evidence-Based Nursing
- Learning Disability Practice
- Mental Health Practice
- Nurse Researcher
- Nursing Children and Young People
- Nursing Management
- Nursing Older People
- Nursing Standard
- Primary Health Care
- RCN Nursing Awards
- Nursing Live
- Nursing Careers and Job Fairs
- CPD webinars on-demand
- --> Advanced -->

- Clinical articles
- CPD articles
- CPD Quizzes
- Expert advice
- Clinical placements
- Study skills
- Clinical skills
- University life
- Person-centred care
- Career advice
- Revalidation
CPD Previous
Developing and maintaining compassionate care in nursing, amanda henderson nursing director, princess alexandra hospital, metro south health, queensland, australia, jenny jones ethicist, princess alexandra hospital, metro south health, queensland, australia.
Compassionate care is a fundamental aspect of nursing, and is an important value that is embedded in nurses’ professional standards and codes of practice. However, nurses may experience several challenges in their practice that can impede their ability to provide compassionate care. This article aims to support and guide nurses in developing their capacity to be compassionate. It explores concepts related to compassion, including compassion satisfaction, fatigue, literacy and self-compassion, and outlines strategies that nurses can implement to promote compassionate care. This article encourages nurses to identify their personal and professional values, to understand how these can influence their attitudes and behaviours. By raising awareness of these concepts, as well as the challenges and changing nature of compassion, it is hoped that nurses’ capacity to provide compassionate care will be enhanced.
Nursing Standard . 32, 4, 60-69. doi: 10.7748/ns.2017.e10895
This article has been subject to external double-blind peer review and checked for plagiarism using automated software
None declared
Received: 12 May 2017
Accepted: 26 July 2017
compassion - compassion fatigue - compassion satisfaction - compassionate care - person-centred care - self-compassion
User not found
Want to read more?
Already have access log in, 3-month trial offer for £5.25/month.
- Unlimited access to all 10 RCNi Journals
- RCNi Learning featuring over 175 modules to easily earn CPD time
- NMC-compliant RCNi Revalidation Portfolio to stay on track with your progress
- Personalised newsletters tailored to your interests
- A customisable dashboard with over 200 topics
Alternatively, you can purchase access to this article for the next seven days. Buy now
Are you a student? Our student subscription has content especially for you. Find out more

20 September 2017 / Vol 32 issue 4
TABLE OF CONTENTS
DIGITAL EDITION
- LATEST ISSUE
- SIGN UP FOR E-ALERT
- WRITE FOR US
- PERMISSIONS
Share article: Developing and maintaining compassionate care in nursing
We use cookies on this site to enhance your user experience.
By clicking any link on this page you are giving your consent for us to set cookies.
Home — Essay Samples — Life — Compassion — Compassion – One of the Most Important Values
Compassion – One of The Most Important Values
- Categories: Compassion Personal Philosophy
About this sample

Words: 505 |
Published: Sep 1, 2020
Words: 505 | Page: 1 | 3 min read

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Verified writer
- Expert in: Life Philosophy

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
1 pages / 579 words
2 pages / 873 words
4 pages / 1989 words
4.5 pages / 2031 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Compassion
Charity, with its far-reaching impact, stands as a beacon of hope in a world facing multifaceted challenges. This essay delves into the profound importance of charity in fostering positive social change, emphasizing its role in [...]
Mother Teresa, a name that resonates with compassion, selflessness, and tireless dedication to serving the poorest of the poor. Born on August 26, 1910, in Skopje, now the capital of North Macedonia, Mother Teresa's life [...]
Receiving is often regarded as an essential aspect of human interactions, yet it stands in the shadow of the more celebrated act of giving. This essay delves into the dynamics of giving and receiving, examining the emotional, [...]
In the grand symphony of life, pediatrics stands as a testament to the power of compassion, growth, advocacy, teamwork, and discovery. As I embark on this noble journey, I am steadfast in my commitment to becoming a pediatrician [...]
When it involves education, reading, writing, and arithmetic, accustomed take center stage and were the quality menu of what was instructed to students beginning in school. In today’s world of education, wherever students area [...]
“On Compassion” is an essay written by Barbara Lazear Ascher. The main argument of Ascher's piece deals with acts of compassion, as well as the motives behind them. Ascher utilizes a somber tone, being a third party observer. [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free

IMAGES
VIDEO
COMMENTS
Compassionate Nursing Care and Its Perception Essay. Exclusively available on IvyPanda. Updated: Jan 20th, 2024. The idea of compassion is essential to nursing practice, and it is regarded as the cornerstone of the industry's ethical standards. In their daily work, nurses everywhere deal with moral dilemmas involving compassion.
3. Emotional Intelligence: Nurses with high emotional intelligence typically find it easier to handle interpersonal relationships with patients and coworkers. When you develop an awareness of your emotions and the emotions of others, you can provide more compassionate nursing care. 4.
Introduction. Compassion is one of the most important virtues in medicine, expected from medical professionals and anticipated by patients (Frampton et al., 2013; Fernando and Consedine, 2014a).Despite evidence of its centrality to effective clinical care, most research has focused on compassion fatigue and burnout (Fernando and Consedine, 2014a, b), neglecting the study of compassion itself ...
1. INTRODUCTION. Compassion is fundamental to palliative care and can create an environment of safety for patients and family caregivers. Compassionate care is built on trust and good relationships between the patient, the family and healthcare personnel (Brito‐Pons & Librada‐Flores, 2018; Larkin, 2016). There are various definitions of compassionate care (Crawford et al., 2014; Feo et al ...
Background From 2007 until 2012 Edinburgh Napier University's School of Nursing Midwifery and Social Care in conjunction with NHS Lothian, collaborated on a programme of action research entitled, the Leadership in Compassionate Care Programme. One strand of this research focused on learning and teaching about compassionate care within the undergraduate curriculum. This debate article focuses ...
A nurse who demonstrates compassionate care is able to "understand a deeper meaning of (the patients) healthcare situation", as demonstrated throughout Jeans ten carative factors (Watson, 2018). Both empathy and compassion are found throughout Jean Watsons Carative factors. By using both, it truly changes the patients' outcomes.
Compassionate Care Concept. As an essential principle of person-centered care, compassionate care refers to the way nurses relate to others as human beings and involves "noticing another person's vulnerability, experiencing an emotional reaction to this, and acting in some way with them in a way that is meaningful for people.".
Abstract. The Institute of Medicine defines patient-centered care as "providing care that is respectful of, and responsive to, individual patient preferences, needs and values, and ensuring that patient values guide all clinical decisions.". What is missing in this definition is an explicit emphasis on compassion.
Introduction. Compassion is a virtue and a necessary trait of nursing and being a nurse [].It is a feeling evoked by witnessing others pain that leads to taking measures to help them [].Compassion is the human and moral part of care, and according to many nursing literatures, compassion is the philosophical foundation and centrepiece of the nursing profession.
Compassionate care is composed of two major characteristics; being able to realize the factors that make up an individual while also being able to empathize with their situation and condition. Nurses perform routine procedures and skills throughout their shift. The first hallmark of compassionate care is context.
This page of the essay has 2,154 words. Download the full version above. This essay, will be explore and discuss why ensuring compassionate care in nursing is important and how it relates to the NHS (National Health Service) values. Compassion can be described as, feeling sympathy for someone else's misfortune (WordReference, 2015, cited in ...
Compassionate care is crucial in the realm of healthcare; it has the power to improve the quality of the patient experience and treatment outcomes. Results from the present study support the notion that patient healthcare satisfaction varies greatly depending on whether they feel that they have received compassionate care from their HCPs ...
Compassion in healthcare has continued to receive growing interest over the past decade [] from researchers, educators, clinicians, policy makers, patients, and families alike, with patients strongly emphasizing its importance to their overall quality of care [2,3,4,5].Compassion has been associated with a positive impact on the patient experience and a variety of patient-reported outcomes ...
The actions needed are firm touch, gentle, courteous manner and kindness (Bradshaw 2011 ). Furthermore, compassionate care is said to entail a set of four attributes: wisdom, humanity, love and empathy (Su et al. 2020 ). Core competence in healthcare is for the healthcare provider to practice skills that meet the needs of the patients using ...
Compassionate care is a fundamental aspect of nursing, and is an important value that is embedded in nurses' professional standards and codes of practice. However, nurses may experience several challenges in their practice that can impede their ability to provide compassionate care. This article aims to support and guide nurses in developing ...
Essay about Compassionate Care. Good Essays. 2083 Words. 9 Pages. Open Document. The purpose of this essay is to look at barriers of compassion and what nurses could do overcome these barriers. Three sub topics will be looked at over the course of this essay and a conclusion will be made to evaluate these essays findings and to provide some ...
Leadership in health care is recognized as a necessity to ensure high-quality care, embody support for staff, and establish working environments that prioritize people over rules, regulations, and hierarchies (West et al., 2015).It is argued that compassionate leadership has a positive impact on "patient experience, staff engagement and organisational performance" (Bolden et al., 2019, p. 2).
The significance of compassion to the professional behaviour in nurses will be discussed here. As indicated by the definition of nursing, the basis of nursing lie on compassion, care and respect for the frail and sufferers. Hence compassion is described as the moral obligation imposed on nurses as a result of vulnerability and their dependency ...
Compassionate Care Through Intentional Rounding Every day, individuals are admitted to hospitals experiencing uncertainty, fear, and anxiety. At its very core, the profession of nursing is centered around compassion, and providing meaningful care for patients. Intentional rounding is a variable system that has been created in order for nurses ...
Essay about Compassionate Care The definition of compassion in the oxford dictionary is ''sympathetic pity and concern for the suffering or misfortunes of others''. Oxford dictionary (2013) However senior lecturer Penny Harrison says there is no accurate definition for compassion as it is a word that can be understood in different ways.
From the exploration of many investigations and vast amounts of research, it has been discovered that nurses can deliver compassionate care in innumerable ways. Compassionate care is a top priority in the nursing profession (Dewer, 2012). Compassionate care is "witnessing another person's suffering and experiencing a subsequent desire to ...
Compassion is not only about how we care to our fellow human. Compassion is also about our nature and our country. Our nature needs our care. ... "On Compassion" is an essay written by Barbara Lazear Ascher. The main argument of Ascher's piece deals with acts of compassion, as well as the motives behind them. Ascher utilizes a somber tone ...
Essay On Compassionate Care, Put Marine Corps Resume, Social Media Essay 1000 Words, Easy Essay On My Class Room, Do My Esl Best Essay On Hillary, Custom Cv Ghostwriters Service Uk, Ap English Poetry Essay Sample Some FAQs related to our essay writer service