How to conduct qualitative interviews (tips and best practices)
Last updated
18 May 2023
Reviewed by
Miroslav Damyanov
However, conducting qualitative interviews can be challenging, even for seasoned researchers. Poorly conducted interviews can lead to inaccurate or incomplete data, significantly compromising the validity and reliability of your research findings.
When planning to conduct qualitative interviews, you must adequately prepare yourself to get the most out of your data. Fortunately, there are specific tips and best practices that can help you conduct qualitative interviews effectively.
- What is a qualitative interview?
A qualitative interview is a research technique used to gather in-depth information about people's experiences, attitudes, beliefs, and perceptions. Unlike a structured questionnaire or survey, a qualitative interview is a flexible, conversational approach that allows the interviewer to delve into the interviewee's responses and explore their insights and experiences.
In a qualitative interview, the researcher typically develops a set of open-ended questions that provide a framework for the conversation. However, the interviewer can also adapt to the interviewee's responses and ask follow-up questions to understand their experiences and views better.
- How to conduct interviews in qualitative research
Conducting interviews involves a well-planned and deliberate process to collect accurate and valid data.
Here’s a step-by-step guide on how to conduct interviews in qualitative research, broken down into three stages:

1. Before the interview
The first step in conducting a qualitative interview is determining your research question . This will help you identify the type of participants you need to recruit. Once you have your research question, you can start recruiting participants by identifying potential candidates and contacting them to gauge their interest in participating in the study.
After that, it's time to develop your interview questions. These should be open-ended questions that will elicit detailed responses from participants. You'll also need to get consent from the participants, ideally in writing, to ensure that they understand the purpose of the study and their rights as participants. Finally, choose a comfortable and private location to conduct the interview and prepare the interview guide.
2. During the interview
Start by introducing yourself and explaining the purpose of the study. Establish a rapport by putting the participants at ease and making them feel comfortable. Use the interview guide to ask the questions, but be flexible and ask follow-up questions to gain more insight into the participants' responses.
Take notes during the interview, and ask permission to record the interview for transcription purposes. Be mindful of the time, and cover all the questions in the interview guide.
3. After the interview
Once the interview is over, transcribe the interview if you recorded it. If you took notes, review and organize them to make sure you capture all the important information. Then, analyze the data you collected by identifying common themes and patterns. Use the findings to answer your research question.
Finally, debrief with the participants to thank them for their time, provide feedback on the study, and answer any questions they may have.
- What kinds of questions should you ask in a qualitative interview?
Qualitative interviews involve asking questions that encourage participants to share their experiences, opinions, and perspectives on a particular topic. These questions are designed to elicit detailed and nuanced responses rather than simple yes or no answers.
Effective questions in a qualitative interview are generally open-ended and non-leading. They avoid presuppositions or assumptions about the participant's experience and allow them to share their views in their own words.
In customer research , you might ask questions such as:
What motivated you to choose our product/service over our competitors?
How did you first learn about our product/service?
Can you walk me through your experience with our product/service?
What improvements or changes would you suggest for our product/service?
Have you recommended our product/service to others, and if so, why?
The key is to ask questions relevant to the research topic and allow participants to share their experiences meaningfully and informally.
- How to determine the right qualitative interview participants
Choosing the right participants for a qualitative interview is a crucial step in ensuring the success and validity of the research . You need to consider several factors to determine the right participants for a qualitative interview. These may include:
Relevant experiences : Participants should have experiences related to the research topic that can provide valuable insights.
Diversity : Aim to include diverse participants to ensure the study's findings are representative and inclusive.
Access : Identify participants who are accessible and willing to participate in the study.
Informed consent : Participants should be fully informed about the study's purpose, methods, and potential risks and benefits and be allowed to provide informed consent.
You can use various recruitment methods, such as posting ads in relevant forums, contacting community organizations or social media groups, or using purposive sampling to identify participants who meet specific criteria.
- How to make qualitative interview subjects comfortable
Making participants comfortable during a qualitative interview is essential to obtain rich, detailed data. Participants are more likely to share their experiences openly when they feel at ease and not judged.
Here are some ways to make interview subjects comfortable:
Explain the purpose of the study
Start the interview by explaining the research topic and its importance. The goal is to give participants a sense of what to expect.
Create a comfortable environment
Conduct the interview in a quiet, private space where the participant feels comfortable. Turn off any unnecessary electronics that can create distractions. Ensure your equipment works well ahead of time. Arrive at the interview on time. If you conduct a remote interview, turn on your camera and mute all notetakers and observers.
Build rapport
Greet the participant warmly and introduce yourself. Show interest in their responses and thank them for their time.
Use open-ended questions
Ask questions that encourage participants to elaborate on their thoughts and experiences.
Listen attentively
Resist the urge to multitask . Pay attention to the participant's responses, nod your head, or make supportive comments to show you’re interested in their answers. Avoid interrupting them.
Avoid judgment
Show respect and don't judge the participant's views or experiences. Allow the participant to speak freely without feeling judged or ridiculed.
Offer breaks
If needed, offer breaks during the interview, especially if the topic is sensitive or emotional.
Creating a comfortable environment and establishing rapport with the participant fosters an atmosphere of trust and encourages open communication. This helps participants feel at ease and willing to share their experiences.
- How to analyze a qualitative interview
Analyzing a qualitative interview involves a systematic process of examining the data collected to identify patterns, themes, and meanings that emerge from the responses.
Here are some steps on how to analyze a qualitative interview:
1. Transcription
The first step is transcribing the interview into text format to have a written record of the conversation. This step is essential to ensure that you can refer back to the interview data and identify the important aspects of the interview.
2. Data reduction
Once you’ve transcribed the interview, read through it to identify key themes, patterns, and phrases emerging from the data. This process involves reducing the data into more manageable pieces you can easily analyze.
The next step is to code the data by labeling sections of the text with descriptive words or phrases that reflect the data's content. Coding helps identify key themes and patterns from the interview data.
4. Categorization
After coding, you should group the codes into categories based on their similarities. This process helps to identify overarching themes or sub-themes that emerge from the data.
5. Interpretation
You should then interpret the themes and sub-themes by identifying relationships, contradictions, and meanings that emerge from the data. Interpretation involves analyzing the themes in the context of the research question.
6. Comparison
The next step is comparing the data across participants or groups to identify similarities and differences. This step helps to ensure that the findings aren’t just specific to one participant but can be generalized to the wider population.
7. Triangulation
To ensure the findings are valid and reliable, you should use triangulation by comparing the findings with other sources, such as observations or interview data.
8. Synthesis
The final step is synthesizing the findings by summarizing the key themes and presenting them clearly and concisely. This step involves writing a report that presents the findings in a way that is easy to understand, using quotes and examples from the interview data to illustrate the themes.
- Tips for transcribing a qualitative interview
Transcribing a qualitative interview is a crucial step in the research process. It involves converting the audio or video recording of the interview into written text.
Here are some tips for transcribing a qualitative interview:
Use transcription software
Transcription software can save time and increase accuracy by automatically transcribing audio or video recordings.
Listen carefully
When manually transcribing, listen carefully to the recording to ensure clarity. Pause and rewind the recording as necessary.
Use appropriate formatting
Use a consistent format for transcribing, such as marking pauses, overlaps, and interruptions. Indicate non-verbal cues such as laughter, sighs, or changes in tone.
Edit for clarity
Edit the transcription to ensure clarity and readability. Use standard grammar and punctuation, correct misspellings, and remove filler words like "um" and "ah."
Proofread and edit
Verify the accuracy of the transcription by listening to the recording again and reviewing the notes taken during the interview.
Use timestamps
Add timestamps to the transcription to reference specific interview sections.
Transcribing a qualitative interview can be time-consuming, but it’s essential to ensure the accuracy of the data collected. Following these tips can produce high-quality transcriptions useful for analysis and reporting.
- Why are interview techniques in qualitative research effective?
Unlike quantitative research methods, which rely on numerical data, qualitative research seeks to understand the richness and complexity of human experiences and perspectives.
Interview techniques involve asking open-ended questions that allow participants to express their views and share their stories in their own words. This approach can help researchers to uncover unexpected or surprising insights that may not have been discovered through other research methods.
Interview techniques also allow researchers to establish rapport with participants, creating a comfortable and safe space for them to share their experiences. This can lead to a deeper level of trust and candor, leading to more honest and authentic responses.
- What are the weaknesses of qualitative interviews?
Qualitative interviews are an excellent research approach when used properly, but they have their drawbacks.
The weaknesses of qualitative interviews include the following:
Subjectivity and personal biases
Qualitative interviews rely on the researcher's interpretation of the interviewee's responses. The researcher's biases or preconceptions can affect how the questions are framed and how the responses are interpreted, which can influence results.
Small sample size
The sample size in qualitative interviews is often small, which can limit the generalizability of the results to the larger population.
Data quality
The quality of data collected during interviews can be affected by various factors, such as the interviewee's mood, the setting of the interview, and the interviewer's skills and experience.
Socially desirable responses
Interviewees may provide responses that they believe are socially acceptable rather than truthful or genuine.
Conducting qualitative interviews can be expensive, especially if the researcher must travel to different locations to conduct the interviews.
Time-consuming
The data analysis process can be time-consuming and labor-intensive, as researchers need to transcribe and analyze the data manually.
Despite these weaknesses, qualitative interviews remain a valuable research tool. You can take steps to mitigate the impact of these weaknesses by incorporating the perspectives of other researchers or participants in the analysis process, using multiple data sources , and critically analyzing your biases and assumptions.
Mastering the art of qualitative interviews is an essential skill for businesses looking to gain deep insights into their customers' needs, preferences, and behaviors. By following the tips and best practices outlined in this article, you can conduct interviews that provide you with rich data that you can use to make informed decisions about your products, services, and marketing strategies.
Remember that effective communication, active listening, and proper analysis are critical components of successful qualitative interviews. By incorporating these practices into your customer research, you can gain a competitive edge and build stronger customer relationships.
Get started today
Go from raw data to valuable insights with a flexible research platform
Editor’s picks
Last updated: 21 December 2023
Last updated: 16 December 2023
Last updated: 6 October 2023
Last updated: 5 March 2024
Last updated: 25 November 2023
Last updated: 15 February 2024
Last updated: 11 March 2024
Last updated: 12 December 2023
Last updated: 6 March 2024
Last updated: 10 April 2023
Last updated: 20 December 2023
Latest articles
Related topics, log in or sign up.
Get started for free
Root out friction in every digital experience, super-charge conversion rates, and optimize digital self-service
Uncover insights from any interaction, deliver AI-powered agent coaching, and reduce cost to serve
Increase revenue and loyalty with real-time insights and recommendations delivered to teams on the ground
Know how your people feel and empower managers to improve employee engagement, productivity, and retention
Take action in the moments that matter most along the employee journey and drive bottom line growth
Whatever they’re are saying, wherever they’re saying it, know exactly what’s going on with your people
Get faster, richer insights with qual and quant tools that make powerful market research available to everyone
Run concept tests, pricing studies, prototyping + more with fast, powerful studies designed by UX research experts
Track your brand performance 24/7 and act quickly to respond to opportunities and challenges in your market
Explore the platform powering Experience Management
- Free Account
- For Digital
- For Customer Care
- For Human Resources
- For Researchers
- Financial Services
- All Industries
Popular Use Cases
- Customer Experience
- Employee Experience
- Employee Exit Interviews
- Net Promoter Score
- Voice of Customer
- Customer Success Hub
- Product Documentation
- Training & Certification
- XM Institute
- Popular Resources
- Customer Stories
Market Research
- Artificial Intelligence
- Partnerships
- Marketplace
The annual gathering of the experience leaders at the world’s iconic brands building breakthrough business results, live in Salt Lake City.
- English/AU & NZ
- Español/Europa
- Español/América Latina
- Português Brasileiro
- REQUEST DEMO
- Experience Management
- Qualitative Research Interviews
Try Qualtrics for free
How to carry out great interviews in qualitative research.
11 min read An interview is one of the most versatile methods used in qualitative research. Here’s what you need to know about conducting great qualitative interviews.
What is a qualitative research interview?
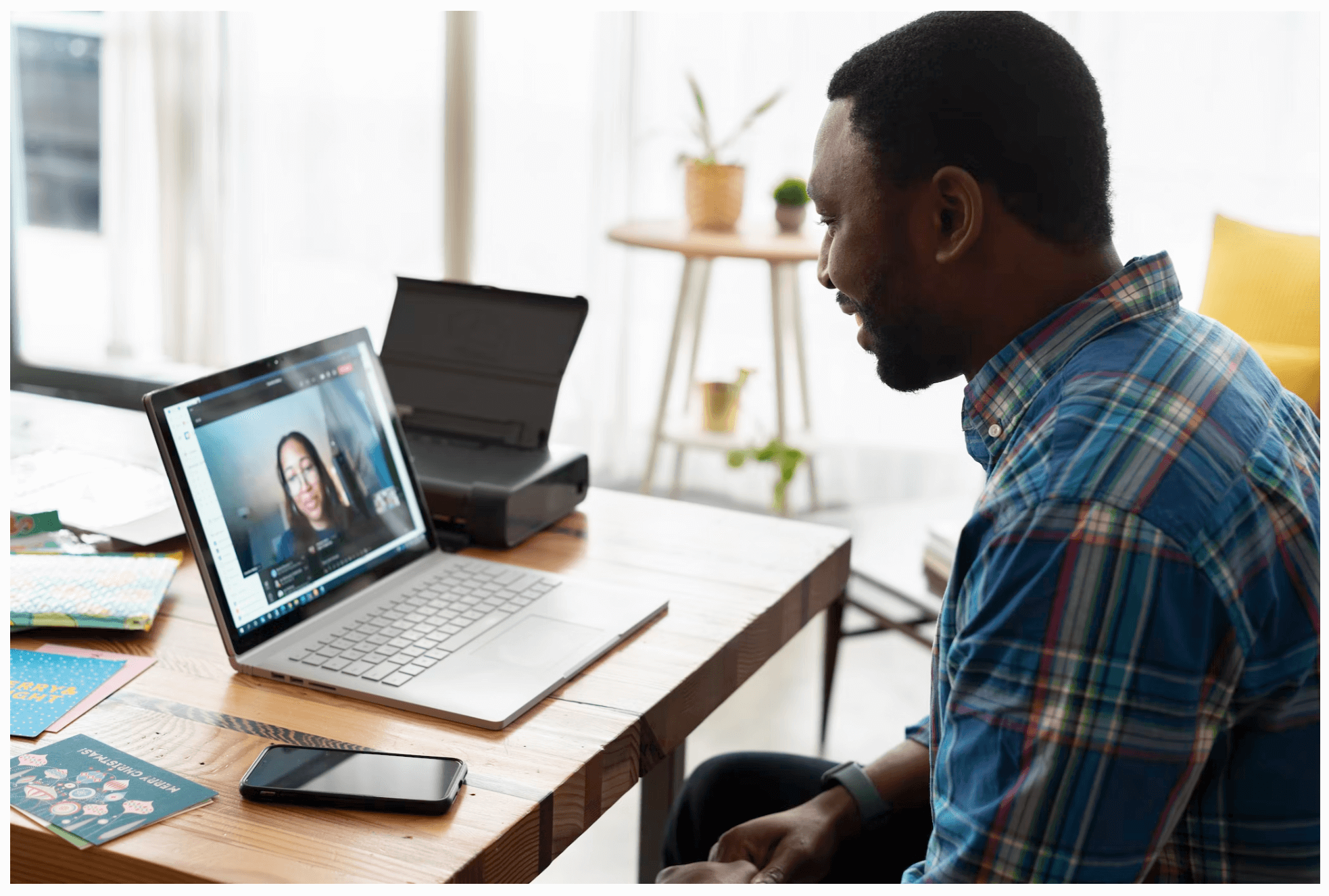
Qualitative research interviews are a mainstay among q ualitative research techniques, and have been in use for decades either as a primary data collection method or as an adjunct to a wider research process. A qualitative research interview is a one-to-one data collection session between a researcher and a participant. Interviews may be carried out face-to-face, over the phone or via video call using a service like Skype or Zoom.
There are three main types of qualitative research interview – structured, unstructured or semi-structured.
- Structured interviews Structured interviews are based around a schedule of predetermined questions and talking points that the researcher has developed. At their most rigid, structured interviews may have a precise wording and question order, meaning that they can be replicated across many different interviewers and participants with relatively consistent results.
- Unstructured interviews Unstructured interviews have no predetermined format, although that doesn’t mean they’re ad hoc or unplanned. An unstructured interview may outwardly resemble a normal conversation, but the interviewer will in fact be working carefully to make sure the right topics are addressed during the interaction while putting the participant at ease with a natural manner.
- Semi-structured interviews Semi-structured interviews are the most common type of qualitative research interview, combining the informality and rapport of an unstructured interview with the consistency and replicability of a structured interview. The researcher will come prepared with questions and topics, but will not need to stick to precise wording. This blended approach can work well for in-depth interviews.
Free eBook: The qualitative research design handbook
What are the pros and cons of interviews in qualitative research?
As a qualitative research method interviewing is hard to beat, with applications in social research, market research, and even basic and clinical pharmacy. But like any aspect of the research process, it’s not without its limitations. Before choosing qualitative interviewing as your research method, it’s worth weighing up the pros and cons.
Pros of qualitative interviews:
- provide in-depth information and context
- can be used effectively when their are low numbers of participants
- provide an opportunity to discuss and explain questions
- useful for complex topics
- rich in data – in the case of in-person or video interviews , the researcher can observe body language and facial expression as well as the answers to questions
Cons of qualitative interviews:
- can be time-consuming to carry out
- costly when compared to some other research methods
- because of time and cost constraints, they often limit you to a small number of participants
- difficult to standardize your data across different researchers and participants unless the interviews are very tightly structured
- As the Open University of Hong Kong notes, qualitative interviews may take an emotional toll on interviewers
Qualitative interview guides
Semi-structured interviews are based on a qualitative interview guide, which acts as a road map for the researcher. While conducting interviews, the researcher can use the interview guide to help them stay focused on their research questions and make sure they cover all the topics they intend to.
An interview guide may include a list of questions written out in full, or it may be a set of bullet points grouped around particular topics. It can prompt the interviewer to dig deeper and ask probing questions during the interview if appropriate.
Consider writing out the project’s research question at the top of your interview guide, ahead of the interview questions. This may help you steer the interview in the right direction if it threatens to head off on a tangent.
Avoid bias in qualitative research interviews
According to Duke University , bias can create significant problems in your qualitative interview.
- Acquiescence bias is common to many qualitative methods, including focus groups. It occurs when the participant feels obliged to say what they think the researcher wants to hear. This can be especially problematic when there is a perceived power imbalance between participant and interviewer. To counteract this, Duke University’s experts recommend emphasizing the participant’s expertise in the subject being discussed, and the value of their contributions.
- Interviewer bias is when the interviewer’s own feelings about the topic come to light through hand gestures, facial expressions or turns of phrase. Duke’s recommendation is to stick to scripted phrases where this is an issue, and to make sure researchers become very familiar with the interview guide or script before conducting interviews, so that they can hone their delivery.
What kinds of questions should you ask in a qualitative interview?
The interview questions you ask need to be carefully considered both before and during the data collection process. As well as considering the topics you’ll cover, you will need to think carefully about the way you ask questions.
Open-ended interview questions – which cannot be answered with a ‘yes’ ‘no’ or ‘maybe’ – are recommended by many researchers as a way to pursue in depth information.
An example of an open-ended question is “What made you want to move to the East Coast?” This will prompt the participant to consider different factors and select at least one. Having thought about it carefully, they may give you more detailed information about their reasoning.
A closed-ended question , such as “Would you recommend your neighborhood to a friend?” can be answered without too much deliberation, and without giving much information about personal thoughts, opinions and feelings.
Follow-up questions can be used to delve deeper into the research topic and to get more detail from open-ended questions. Examples of follow-up questions include:
- What makes you say that?
- What do you mean by that?
- Can you tell me more about X?
- What did/does that mean to you?
As well as avoiding closed-ended questions, be wary of leading questions. As with other qualitative research techniques such as surveys or focus groups, these can introduce bias in your data. Leading questions presume a certain point of view shared by the interviewer and participant, and may even suggest a foregone conclusion.
An example of a leading question might be: “You moved to New York in 1990, didn’t you?” In answering the question, the participant is much more likely to agree than disagree. This may be down to acquiescence bias or a belief that the interviewer has checked the information and already knows the correct answer.
Other leading questions involve adjectival phrases or other wording that introduces negative or positive connotations about a particular topic. An example of this kind of leading question is: “Many employees dislike wearing masks to work. How do you feel about this?” It presumes a positive opinion and the participant may be swayed by it, or not want to contradict the interviewer.
Harvard University’s guidelines for qualitative interview research add that you shouldn’t be afraid to ask embarrassing questions – “if you don’t ask, they won’t tell.” Bear in mind though that too much probing around sensitive topics may cause the interview participant to withdraw. The Harvard guidelines recommend leaving sensitive questions til the later stages of the interview when a rapport has been established.
More tips for conducting qualitative interviews
Observing a participant’s body language can give you important data about their thoughts and feelings. It can also help you decide when to broach a topic, and whether to use a follow-up question or return to the subject later in the interview.
Be conscious that the participant may regard you as the expert, not themselves. In order to make sure they express their opinions openly, use active listening skills like verbal encouragement and paraphrasing and clarifying their meaning to show how much you value what they are saying.
Remember that part of the goal is to leave the interview participant feeling good about volunteering their time and their thought process to your research. Aim to make them feel empowered , respected and heard.
Unstructured interviews can demand a lot of a researcher, both cognitively and emotionally. Be sure to leave time in between in-depth interviews when scheduling your data collection to make sure you maintain the quality of your data, as well as your own well-being .
Recording and transcribing interviews
Historically, recording qualitative research interviews and then transcribing the conversation manually would have represented a significant part of the cost and time involved in research projects that collect qualitative data.
Fortunately, researchers now have access to digital recording tools, and even speech-to-text technology that can automatically transcribe interview data using AI and machine learning. This type of tool can also be used to capture qualitative data from qualitative research (focus groups,ect.) making this kind of social research or market research much less time consuming.
Data analysis
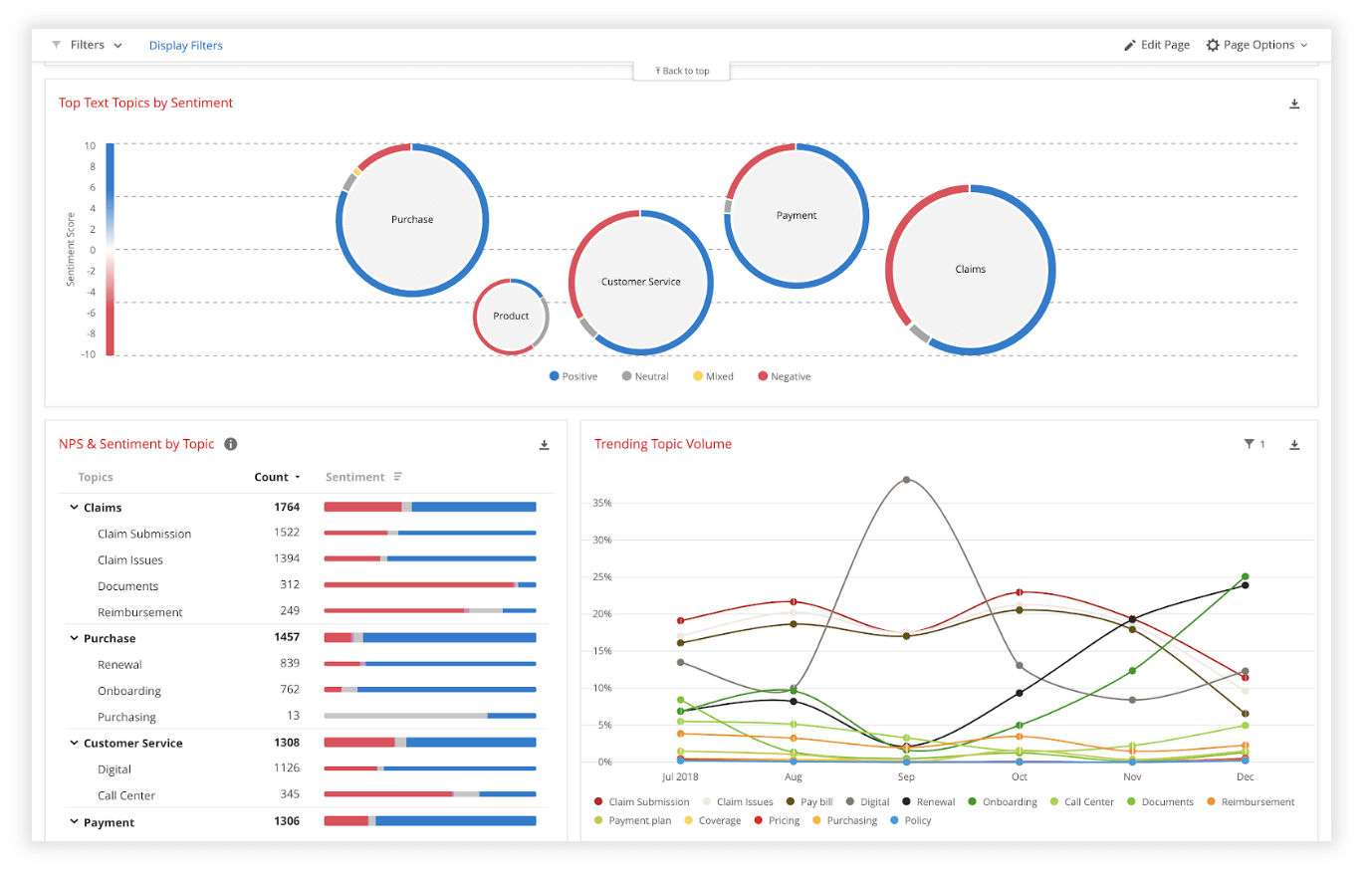
Qualitative interview data is unstructured, rich in content and difficult to analyze without the appropriate tools. Fortunately, machine learning and AI can once again make things faster and easier when you use qualitative methods like the research interview.
Text analysis tools and natural language processing software can ‘read’ your transcripts and voice data and identify patterns and trends across large volumes of text or speech. They can also perform khttps://www.qualtrics.com/experience-management/research/sentiment-analysis/
which assesses overall trends in opinion and provides an unbiased overall summary of how participants are feeling.
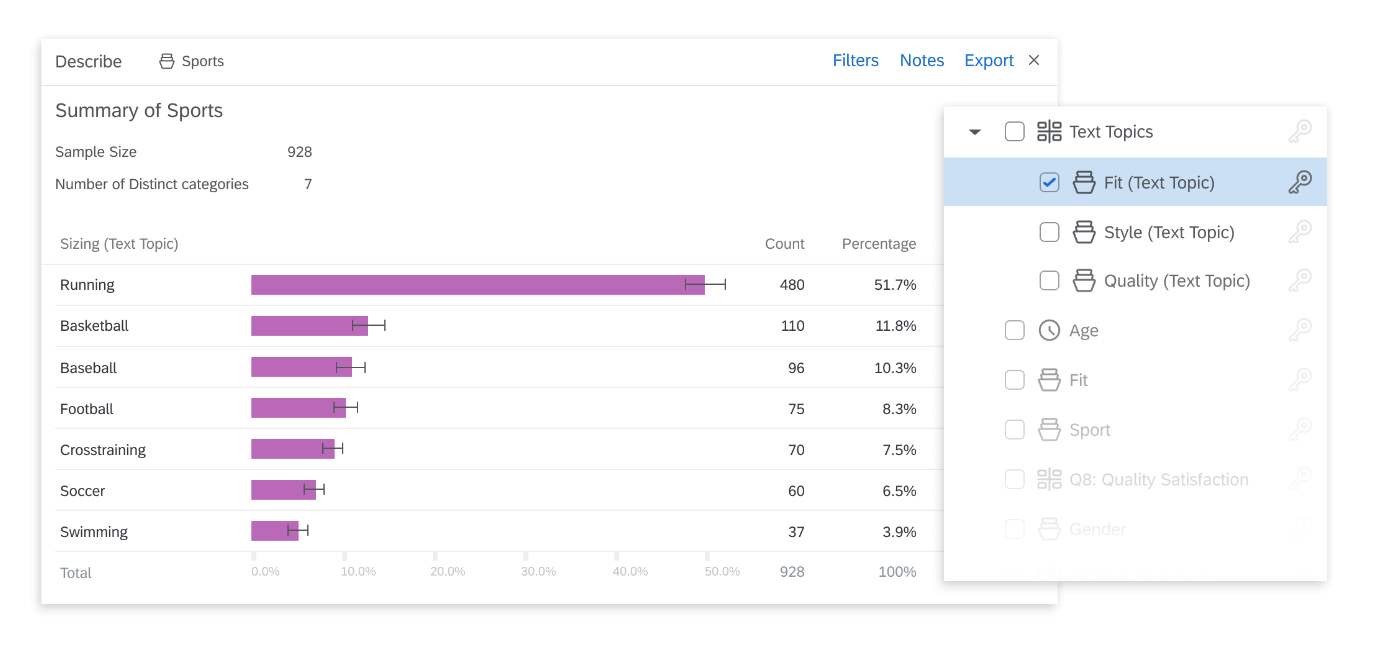
Another feature of text analysis tools is their ability to categorize information by topic, sorting it into groupings that help you organize your data according to the topic discussed.
All in all, interviews are a valuable technique for qualitative research in business, yielding rich and detailed unstructured data. Historically, they have only been limited by the human capacity to interpret and communicate results and conclusions, which demands considerable time and skill.
When you combine this data with AI tools that can interpret it quickly and automatically, it becomes easy to analyze and structure, dovetailing perfectly with your other business data. An additional benefit of natural language analysis tools is that they are free of subjective biases, and can replicate the same approach across as much data as you choose. By combining human research skills with machine analysis, qualitative research methods such as interviews are more valuable than ever to your business.
Related resources
Market intelligence 10 min read, marketing insights 11 min read, ethnographic research 11 min read, qualitative vs quantitative research 13 min read, qualitative research questions 11 min read, qualitative research design 12 min read, primary vs secondary research 14 min read, request demo.
Ready to learn more about Qualtrics?
How to Conduct Interviews in Qualitative Research: Interview Guidelines for Qualitative Research
Rev › Blog › Market Research › How to Conduct Interviews in Qualitative Research: Interview Guidelines for Qualitative Research
Qualitative research interviews are depth interviews. They elicit detailed feedback from your leads and customers. Unstructured interviews reveal why people react in a certain way or make certain decisions. According to The Hartford , qualitative research provides an anecdotal look into your business. That provides an important form of data.
Why Your Business Should Use a Qualitative Interview Process
Qualitative research helps business owners:
- Identify customer needs
- Clarify marketing messages
- Generate ideas for improvements of a product
- Decide to extend a line or brand
- Gain perspective on how a product fits into a customer’s lifestyle
How Is Conducting Qualitative Research & Quantitative Research Different?
Quantitative research concerns measurable quantities and numbers. It involves close-ended questions. Answer possibilities include yes or no, true or false, or various set choices. Qualitative research is descriptive and concerned with understanding behavior. It invites people to tell their stories in their own words.
Examples of Qualitative Research
Qualitative research helps researchers understand the social reality of individuals, groups and cultures. Qualitative research for businesses involves understanding consumer behavior. It can involve ethnographic techniques, including participant observation and field research. It also includes phenomenology, understanding life experiences using written or recorded narratives. Qualitative research also includes in-depth interviews.
What Is a Qualitative Interview?
A qualitative interview is a more personal form of research compared to questionnaires. The interviewer can probe or ask follow-up research questions of the interview participant. In some cases, subjects may start to interview the interviewer. This fosters deep discussion of the interview topic.
Why Are Interview Techniques in Qualitative Research Effective?
Qualitative research interviews help you explain, understand and explore opinions, behavior and experiences. Qualitative research can provide insights into a phenomenon. Qualitative research discoveries can be further researched and analyzed to influence business decisions.
How Are Interviews in Qualitative Research Formatted?
Qualitative research interviews may take place one-on-one or in focus groups. Learn how to run a successful focus group . Interviews span around 30 to 90 minutes. The interview can take place in person, over the phone or through video chat. The interviewer collects information about opinions, behavior, attitudes, feelings, preferences and knowledge.
How to Conduct Interviews in Qualitative Research
1. determine your goal., 2. target people to interview., 3. design interview questions., 4. prep the interview., 5. conduct the interview., 6. transcribe and analyze the interview., 7. optimize and evolve your interview guide., the first step in qualitative research: determine your goal.
Determine what you want to study:
- A current or potential product, service or brand positioning
- Strengths and weaknesses in products
- Purchasing decisions
- Reactions to advertising or marketing campaigns
- Usability of a website or other interactive services
- Perceptions about the company, brand or product
- Reactions to packaging and design
How Can You Decide a Goal for a Qualitative Interview?
Have your business team ask the following questions:
- What information do you want to get?
- Why do you want to pursue in-depth information about this research topic?
- Why is a qualitative interview process the best solution for this research?
- How will you use qualitative data to improve your business?
How to Determine the Right Interview Participants
When looking for people to talk to for a qualitative interview, consider your goal. If you want to expand a product line, interview existing customers about their needs. If you’re researching marketing, ask new customers how they found your business. Match interview subjects with the goal of the interview.
How to Design Interview Questions for Qualitative Research
When you’re creating an interview guide, it’s a good idea to:
- Plan structured interviews with open ended questions.
- Avoid leading questions.
- Create interview questions that are clear and easy to understand.
- Make research questions focused but flexible.
- Design questions that align with data collection and data analysis goals.
Tips for Preparing a Qualitative Research Interview
Preparation improves interview effectiveness. Tips to prepare include:
- Create an interview guide. The guide should include questions, question intent and answer-based paths to take.
- Choose a setting where the subject feels comfortable.
- Build rapport with interview participants.
- Have a reliable way to record the interview.
- Rehearse the interview first.
Environmental Concerns for Qualitative Interviews
The setting of a qualitative interview also affects the quality of the interview. Consider the needs of the subject. For example, if you’re interviewing a teenager, a formal boardroom may not be the best setting. Some cultures may not value direct eye contact. An interview that’s non-face-to-face may be better.
How to Make Qualitative Interview Subjects Comfortable
For long interviews, offer water and breaks to participants. Be polite and respectful when interacting with interview subjects. Let interview participants know the purpose of the research. Explain exactly how you’ll use their answers. Address terms of confidentiality if necessary. Thank participants after the interview and let them know what to expect next.
What Are Interview Techniques in Qualitative Research?
Qualitative research techniques include:
- Start interviews with “get-to-know-you” questions to put the interview participant at ease.
- Pay attention.
- Use active listening techniques.
- Watch for body language cues.
- Pivot questions as needed.
- Acknowledge emotions.
- Avoid interrogation.
- Ending interviews, ask subjects if they have anything to add.
What Is Active Listening in Interviews in Qualitative Research?
Active listening techniques include:
- Make eye contact.
- Lean in and use body language to show you’re listening.
- Don’t get distracted by devices.
- Use verbal affirmation.
- Paraphrase answers for reflection.
- Reference earlier answers.
- Avoid interrupting.
- Embrace pauses.
- Ask for clarification.
- Pay attention in the moment.
Tips for Transcribing a Qualitative Interview
It’s best to transcribe and analyze a qualitative research interview right away. This helps you optimize future interviews. Transcribe the interview word for word. Note non-verbal interactions in your transcription. Interactions like pauses and laughter can provide deeper insights into responses.
How to Analyze a Qualitative Interview
Analyze your qualitative research data early. That way, you can identify emerging themes to shape future interviews. Consider adding these to each interview report:
- The goal of the interview
- Details about the interview participant
- Questions asked, summarized responses and key findings
- Recommendations
Relate the analysis to the goal of the qualitative research interview.
Optimize the Interview Guide for Qualitative Research
Each interview can help you improve the efficiency and effectiveness of future ones. Adjust your interview guide based on insights from each previous interview. Keep all versions of your transcriptions and interview guides with notes on them. You can reference these for future qualitative research.
Get Reliable Transcription Services for Qualitative Research Interviews
As mentioned, you should transcribe qualitative research interviews as soon as possible. There are several reasons for this.
- You can gain insights that help you shape your interview guide. You might identify questions to add or questions to clarify.
- Your interview participants may not be appropriate for this type of qualitative research. Finding more targeted interview subjects may be better.
- Answers may evolve the qualitative research goal and/or data analysis.
At Rev, we understand the need for fast transcription for accurate market research. We provide a turnaround time of as few as 12 hours, no matter how big your project is. We guarantee 99%+ accuracy. Learn about Rev’s market research transcription . We can help make your qualitative research project a success.
Download our FREE Qualitative Research Interview Checklist
Everybody’s favorite speech-to-text blog.
We combine AI and a huge community of freelancers to make speech-to-text greatness every day. Wanna hear more about it?
Twelve tips for conducting qualitative research interviews
Affiliations.
- 1 Department of Learning, Informatics, Management and Ethics, Karolinska Institutet , Stockholm , Sweden.
- 2 Department of Education, Stockholm University , Stockholm , Sweden.
- 3 Primary Health Care Unit, Institute of Medicine, The Sahlgrenska Academy, University of Gothenburg , Gothenburg , Sweden.
- PMID: 30261797
- DOI: 10.1080/0142159X.2018.1497149
The qualitative research interview is an important data collection tool for a variety of methods used within the broad spectrum of medical education research. However, many medical teachers and life science researchers undergo a steep learning curve when they first encounter qualitative interviews, both in terms of new theory but also regarding new methods of inquiry and data collection. This article introduces the concept of qualitative research interviews for novice researchers within medical education, providing 12 tips for conducting qualitative research interviews.
- Data Collection / methods
- Interviews as Topic*
- Qualitative Research*
- Research Design*
- Skip to main content
- Skip to primary sidebar
- Skip to footer
- QuestionPro

- Solutions Industries Gaming Automotive Sports and events Education Government Travel & Hospitality Financial Services Healthcare Cannabis Technology Use Case NPS+ Communities Audience Contactless surveys Mobile LivePolls Member Experience GDPR Positive People Science 360 Feedback Surveys
- Resources Blog eBooks Survey Templates Case Studies Training Help center
Home Market Research Research Tools and Apps
Qualitative Interview: What it is & How to conduct one

A qualitative interview is commonly used in research projects involving new products, brand positioning, purchase dynamics, market research, social research, behavioral analysis, exploring market segments, etc. Recent data also suggests that it is highly effective when used in employee engagement initiatives.
It has also proven to be extremely helpful when it comes to problem definition as well as developing an approach to a particular problem.
What is a Qualitative Interview?
A qualitative Interview is a research approach used in a qualitative study where more personal interaction is required and detailed in depth information is gathered from the participant. Qualitative interviews usually involve follow-up questions and are conducted in a conversation or discussion format.
A qualitative interview is a more personal form of research agenda compared to general questionnaires or focused group studies. Such formats often include open-ended and follow-up questions .
LEARN ABOUT: Behavioral Research
How to conduct a Qualitative Interview?
Conducting a qualitative interview requires careful planning and implementation to ensure that you gather meaningful and rich data. Here are some steps to consider when conducting a qualitative research interview:
Clearly define the purpose of your qualitative interview and the specific research method questions you want to address. It will help you design appropriate research interview questions and interview guides for your data analysis.
Identify the target population or specific individuals who can provide valuable insights related to your research questions. Consider criteria such as demographics, expertise, or experiences that align with your research methods and objectives. Use appropriate methods, such as purposive sampling of data collection, to recruit participants who can offer diverse perspectives.
Before conducting the interview, ensure that participants understand the purpose, procedures, and potential risks or benefits of their involvement. Obtain their informed consent, clearly explaining their rights as participants, including confidentiality and their ability to withdraw from the study at any time.
Prepare a flexible in depth interviews guide that includes a set of open-ended interview questions for an interview participant. The guide should be designed to elicit participants’ perspectives, experiences, and insights related to your research objectives for conducting interviews. Consider using probing techniques to encourage participants to elaborate on their responses and explore different dimensions of the topic.
Select a suitable location for the in depth interviews that is comfortable, private, and free from distractions for an interview participant. Create a relaxed and welcoming atmosphere to help participants feel at ease and encourage open communication for qualitative interviewing. Establish rapport and build trust with participants by introducing yourself, explaining the purpose of conducting interviews, and actively listening to their responses.
Start by asking introductory questions to establish a rapport with the participant. Follow the qualitative interview guide, but remain flexible and responsive to participants’ responses. Allow participants to speak freely and provide detailed answers, using probing techniques to delve deeper into their experiences, emotions, and perspectives. Take notes or record the interview (with participants’ consent) to capture accurate and detailed information.
Show respect for their experiences and perspectives, even if they differ from yours. Avoid making judgments or imposing your own beliefs during the interview. Create a non-judgmental and inclusive environment that encourages participants to share their thoughts and feelings honestly.
Transcribe the interview recordings or review your notes promptly after each interview while the details remain fresh. Analyze the qualitative data using appropriate methods, such as thematic data analysis, to identify patterns, themes, and insights. Ensure that the data is anonymized and handled following ethical guidelines.
By following these steps, you can conduct a qualitative research interview that facilitates rich and meaningful discussions, resulting in valuable data analysis for your research process.
LEARN ABOUT: Research Process Steps
Types of Qualitative Interviews
The interview itself can be conducted over multiple formats. Qualitative researchers can employ several types of qualitative interviews based on their research objectives and the nature of the study. Here are some popular types of qualitative interviews:

Structured interviews involve a predetermined set of questions that are asked in the same order and manner to each participant. The questions of structured interviews are typically closed-ended or have limited response options. This type of interview is proper when researchers aim to collect specific information in a standardized way, allowing for easier comparison and analysis of responses across participants.
Semi-structured interviews combine predetermined questions with flexibility for additional probing and follow-up questions. Researchers have a set of core questions to guide the interview but can adapt the interview data collection process based on participants’ responses. This type of approach allows for a deeper exploration of participants’ experiences, thoughts, and perspectives while maintaining some standardization level.
Unstructured interviews involve open-ended questions and a free-flowing conversation between the interviewer and the participant. The interviewer may have a general topic or area of interest but allows the conversation to evolve naturally. Unstructured interviews provide a high degree of flexibility and allow participants to express themselves more freely, often leading to rich and nuanced data.
Each qualitative interview type has its strengths and is suited for different research purposes. Researchers or a research team should carefully select the appropriate type of research interview that aligns with their research objectives, the nature of the phenomenon under investigation, and the population being studied.
LEARN ABOUT: Structured Question
Advantages of Using Qualitative Interviews
Qualitative interview techniques offer several advantages as a research method. Here are some of the key advantages:
A qualitative interview allows researchers to delve deeply into participants’ experiences, perspectives, and opinions. Using open-ended questions and probing techniques, researchers can uncover rich and detailed information beyond mere surface-level responses. This in-depth exploration provides a comprehensive understanding of the research topic.
Qualitative interviews offer flexibility in adapting the interview data collection process to the specific needs of each participant. Researchers can tailor their questions, follow-up probes, and overall approach based on the participant’s responses, allowing for a more personalized and engaging research experience. This flexibility enhances the quality and richness of the data collection.
Qualitative interview prioritizes the voices and perspectives of participants. Through interactive and conversational exchanges, participants can express their thoughts, emotions, and beliefs in their own words. This approach ensures that the research captures individuals’ nuanced and diverse experiences, offering insights that may not be obtained through other methods.
A qualitative research interview provides a holistic understanding of the social and cultural context surrounding participants’ experiences. Researchers can explore the factors influencing participants’ perspectives, such as cultural norms, societal expectations, or personal histories. This contextual understanding enhances the interpretation and analysis of the data, providing a comprehensive view of the research topic.
Qualitative interviews are particularly effective when studying sensitive or complex topics. It allows participants to share their experiences and emotions in a safe and confidential environment, facilitating a deeper exploration of potentially challenging subjects. This method also enables researchers to capture these topics’ nuances, contradictions, and subtleties, contributing to a more comprehensive understanding.
Qualitative research interviews can empower participants by giving them a voice and acknowledging the value of their experiences. By actively listening and engaging in meaningful dialogue, researchers validate participants’ contributions and foster a sense of ownership over their narratives. This empowerment can positively affect participants’ self-esteem, self-reflection, and personal growth.
Overall, qualitative interview provides researchers with a powerful tool to explore complex phenomena, gain in-depth insights, and understand the subjective experiences of individuals. By capitalizing on the advantages of this method, researchers can generate valuable and nuanced data that contributes to the advancement of knowledge in their respective fields.
Learn more by reading our guide: Types of Interviews .
Disadvantages of a Qualitative Interview
While a qualitative interview has many advantages, it is essential to acknowledge their potential limitations. Here are some of the disadvantages associated with qualitative interviews:
Qualitative interviews involve interaction between the researcher and participants, which introduces the possibility of subjective interpretations and biases. Researchers may unintentionally influence participants’ responses through questioning techniques, non-verbal cues, or personal beliefs. Researchers must be aware of their biases and take steps to minimize their impact on data collection and analysis.
The findings from qualitative research interviews are typically based on small sample size and specific context, making it difficult to generalize the results to a larger population. While qualitative research aims to provide an in-depth understanding, it may need more statistical representativeness than quantitative research methods offer. Therefore, when applying qualitative interview findings to broader populations or contexts, caution must be exercised.
Qualitative interviews can be time-consuming and require substantial resources. Conducting in depth interviews, transcribing data, and analyzing the qualitative data are labor-intensive tasks that require significant time and effort. Researchers must be prepared for qualitative interviews of a detailed and time-consuming nature, especially when working with large or diverse participant samples.
Ensuring the validity and reliability of qualitative research interviews can be challenging. Validity refers to the extent to which the interview data accurately represent participants’ experiences and perspectives, while reliability relates to the consistency and replicability of the findings. Factors such as interviewer bias, participant recall, and social desirability may compromise the validity and reliability of the data. Researchers must employ rigorous methodologies, triangulate data from multiple sources, and establish trustworthiness to enhance the credibility of their findings.
Qualitative interviews capture participants’ experiences and perspectives at a specific time and within a particular context. However, these experiences may evolve or change over time or in different contexts. Researchers must be mindful of the limitations of capturing participants’ experiences, recognizing that their findings may only partially represent the dynamic nature of human behavior and perceptions.
Despite these disadvantages, qualitative interviews remain a valuable research method that offers unique insights into individuals’ experiences and perspectives.
Learn About: Steps in qualitative Research
Qualitative interviews are valuable for gaining in-depth insights into individuals’ experiences, perspectives, and behaviors. They offer a unique opportunity to explore complex phenomena, uncover rich narratives, and understand the underlying meanings and interpretations that individuals assign to their experiences.
To summarize, Qualitative Research can either be a valuable tool to discover problems or help elevate any research programs with subjective data or leave researchers with amorphous and contradictory data. The key is to use the approach in combination with other qualitative and quantitative research techniques to enhance the depth of the data gathered.
CREATE FREE ACCOUNT
Authors : Harpal Singh & Shabeen Shareef
MORE LIKE THIS

AI Question Generator: Create Easy + Accurate Tests and Surveys
Apr 6, 2024

Top 17 UX Research Software for UX Design in 2024
Apr 5, 2024

Healthcare Staff Burnout: What it Is + How To Manage It
Apr 4, 2024
Top 15 Employee Retention Software in 2024
Other categories.
- Academic Research
- Artificial Intelligence
- Assessments
- Brand Awareness
- Case Studies
- Communities
- Consumer Insights
- Customer effort score
- Customer Engagement
- Customer Experience
- Customer Loyalty
- Customer Research
- Customer Satisfaction
- Employee Benefits
- Employee Engagement
- Employee Retention
- Friday Five
- General Data Protection Regulation
- Insights Hub
- Life@QuestionPro
- Market Research
- Mobile diaries
- Mobile Surveys
- New Features
- Online Communities
- Question Types
- Questionnaire
- QuestionPro Products
- Release Notes
- Research Tools and Apps
- Revenue at Risk
- Survey Templates
- Training Tips
- Uncategorized
- Video Learning Series
- What’s Coming Up
- Workforce Intelligence
Qualitative Research 101: Interviewing
5 Common Mistakes To Avoid When Undertaking Interviews
By: David Phair (PhD) and Kerryn Warren (PhD) | March 2022
Undertaking interviews is potentially the most important step in the qualitative research process. If you don’t collect useful, useable data in your interviews, you’ll struggle through the rest of your dissertation or thesis. Having helped numerous students with their research over the years, we’ve noticed some common interviewing mistakes that first-time researchers make. In this post, we’ll discuss five costly interview-related mistakes and outline useful strategies to avoid making these.
Overview: 5 Interviewing Mistakes
- Not having a clear interview strategy /plan
- Not having good interview techniques /skills
- Not securing a suitable location and equipment
- Not having a basic risk management plan
- Not keeping your “ golden thread ” front of mind
1. Not having a clear interview strategy
The first common mistake that we’ll look at is that of starting the interviewing process without having first come up with a clear interview strategy or plan of action. While it’s natural to be keen to get started engaging with your interviewees, a lack of planning can result in a mess of data and inconsistency between interviews.
There are several design choices to decide on and plan for before you start interviewing anyone. Some of the most important questions you need to ask yourself before conducting interviews include:
- What are the guiding research aims and research questions of my study?
- Will I use a structured, semi-structured or unstructured interview approach?
- How will I record the interviews (audio or video)?
- Who will be interviewed and by whom ?
- What ethics and data law considerations do I need to adhere to?
- How will I analyze my data?
Let’s take a quick look at some of these.
The core objective of the interviewing process is to generate useful data that will help you address your overall research aims. Therefore, your interviews need to be conducted in a way that directly links to your research aims, objectives and research questions (i.e. your “golden thread”). This means that you need to carefully consider the questions you’ll ask to ensure that they align with and feed into your golden thread. If any question doesn’t align with this, you may want to consider scrapping it.
Another important design choice is whether you’ll use an unstructured, semi-structured or structured interview approach . For semi-structured interviews, you will have a list of questions that you plan to ask and these questions will be open-ended in nature. You’ll also allow the discussion to digress from the core question set if something interesting comes up. This means that the type of information generated might differ a fair amount between interviews.
Contrasted to this, a structured approach to interviews is more rigid, where a specific set of closed questions is developed and asked for each interviewee in exactly the same order. Closed questions have a limited set of answers, that are often single-word answers. Therefore, you need to think about what you’re trying to achieve with your research project (i.e. your research aims) and decided on which approach would be best suited in your case.
It is also important to plan ahead with regards to who will be interviewed and how. You need to think about how you will approach the possible interviewees to get their cooperation, who will conduct the interviews, when to conduct the interviews and how to record the interviews. For each of these decisions, it’s also essential to make sure that all ethical considerations and data protection laws are taken into account.
Finally, you should think through how you plan to analyze the data (i.e., your qualitative analysis method) generated by the interviews. Different types of analysis rely on different types of data, so you need to ensure you’re asking the right types of questions and correctly guiding your respondents.
Simply put, you need to have a plan of action regarding the specifics of your interview approach before you start collecting data. If not, you’ll end up drifting in your approach from interview to interview, which will result in inconsistent, unusable data.

2. Not having good interview technique
While you’re generally not expected to become you to be an expert interviewer for a dissertation or thesis, it is important to practice good interview technique and develop basic interviewing skills .
Let’s go through some basics that will help the process along.
Firstly, before the interview , make sure you know your interview questions well and have a clear idea of what you want from the interview. Naturally, the specificity of your questions will depend on whether you’re taking a structured, semi-structured or unstructured approach, but you still need a consistent starting point . Ideally, you should develop an interview guide beforehand (more on this later) that details your core question and links these to the research aims, objectives and research questions.
Before you undertake any interviews, it’s a good idea to do a few mock interviews with friends or family members. This will help you get comfortable with the interviewer role, prepare for potentially unexpected answers and give you a good idea of how long the interview will take to conduct. In the interviewing process, you’re likely to encounter two kinds of challenging interviewees ; the two-word respondent and the respondent who meanders and babbles. Therefore, you should prepare yourself for both and come up with a plan to respond to each in a way that will allow the interview to continue productively.
To begin the formal interview , provide the person you are interviewing with an overview of your research. This will help to calm their nerves (and yours) and contextualize the interaction. Ultimately, you want the interviewee to feel comfortable and be willing to be open and honest with you, so it’s useful to start in a more casual, relaxed fashion and allow them to ask any questions they may have. From there, you can ease them into the rest of the questions.
As the interview progresses , avoid asking leading questions (i.e., questions that assume something about the interviewee or their response). Make sure that you speak clearly and slowly , using plain language and being ready to paraphrase questions if the person you are interviewing misunderstands. Be particularly careful with interviewing English second language speakers to ensure that you’re both on the same page.
Engage with the interviewee by listening to them carefully and acknowledging that you are listening to them by smiling or nodding. Show them that you’re interested in what they’re saying and thank them for their openness as appropriate. This will also encourage your interviewee to respond openly.
Need a helping hand?
3. Not securing a suitable location and quality equipment
Where you conduct your interviews and the equipment you use to record them both play an important role in how the process unfolds. Therefore, you need to think carefully about each of these variables before you start interviewing.
Poor location: A bad location can result in the quality of your interviews being compromised, interrupted, or cancelled. If you are conducting physical interviews, you’ll need a location that is quiet, safe, and welcoming . It’s very important that your location of choice is not prone to interruptions (the workplace office is generally problematic, for example) and has suitable facilities (such as water, a bathroom, and snacks).
If you are conducting online interviews , you need to consider a few other factors. Importantly, you need to make sure that both you and your respondent have access to a good, stable internet connection and electricity. Always check before the time that both of you know how to use the relevant software and it’s accessible (sometimes meeting platforms are blocked by workplace policies or firewalls). It’s also good to have alternatives in place (such as WhatsApp, Zoom, or Teams) to cater for these types of issues.
Poor equipment: Using poor-quality recording equipment or using equipment incorrectly means that you will have trouble transcribing, coding, and analyzing your interviews. This can be a major issue , as some of your interview data may go completely to waste if not recorded well. So, make sure that you use good-quality recording equipment and that you know how to use it correctly.
To avoid issues, you should always conduct test recordings before every interview to ensure that you can use the relevant equipment properly. It’s also a good idea to spot check each recording afterwards, just to make sure it was recorded as planned. If your equipment uses batteries, be sure to always carry a spare set.

4. Not having a basic risk management plan
Many possible issues can arise during the interview process. Not planning for these issues can mean that you are left with compromised data that might not be useful to you. Therefore, it’s important to map out some sort of risk management plan ahead of time, considering the potential risks, how you’ll minimize their probability and how you’ll manage them if they materialize.
Common potential issues related to the actual interview include cancellations (people pulling out), delays (such as getting stuck in traffic), language and accent differences (especially in the case of poor internet connections), issues with internet connections and power supply. Other issues can also occur in the interview itself. For example, the interviewee could drift off-topic, or you might encounter an interviewee who does not say much at all.
You can prepare for these potential issues by considering possible worst-case scenarios and preparing a response for each scenario. For instance, it is important to plan a backup date just in case your interviewee cannot make it to the first meeting you scheduled with them. It’s also a good idea to factor in a 30-minute gap between your interviews for the instances where someone might be late, or an interview runs overtime for other reasons. Make sure that you also plan backup questions that could be used to bring a respondent back on topic if they start rambling, or questions to encourage those who are saying too little.
In general, it’s best practice to plan to conduct more interviews than you think you need (this is called oversampling ). Doing so will allow you some room for error if there are interviews that don’t go as planned, or if some interviewees withdraw. If you need 10 interviews, it is a good idea to plan for 15. Likely, a few will cancel , delay, or not produce useful data.

5. Not keeping your golden thread front of mind
We touched on this a little earlier, but it is a key point that should be central to your entire research process. You don’t want to end up with pages and pages of data after conducting your interviews and realize that it is not useful to your research aims . Your research aims, objectives and research questions – i.e., your golden thread – should influence every design decision and should guide the interview process at all times.
A useful way to avoid this mistake is by developing an interview guide before you begin interviewing your respondents. An interview guide is a document that contains all of your questions with notes on how each of the interview questions is linked to the research question(s) of your study. You can also include your research aims and objectives here for a more comprehensive linkage.
You can easily create an interview guide by drawing up a table with one column containing your core interview questions . Then add another column with your research questions , another with expectations that you may have in light of the relevant literature and another with backup or follow-up questions . As mentioned, you can also bring in your research aims and objectives to help you connect them all together. If you’d like, you can download a copy of our free interview guide here .
Recap: Qualitative Interview Mistakes
In this post, we’ve discussed 5 common costly mistakes that are easy to make in the process of planning and conducting qualitative interviews.
To recap, these include:
If you have any questions about these interviewing mistakes, drop a comment below. Alternatively, if you’re interested in getting 1-on-1 help with your thesis or dissertation , check out our dissertation coaching service or book a free initial consultation with one of our friendly Grad Coaches.
Psst… there’s more (for free)
This post is part of our dissertation mini-course, which covers everything you need to get started with your dissertation, thesis or research project.
You Might Also Like:

Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Print Friendly

What We Offer
With a comprehensive suite of qualitative and quantitative capabilities and 55 years of experience in the industry, Sago powers insights through adaptive solutions.
- Recruitment
- Communities
- Methodify® Automated research
- QualBoard® Digital Discussions
- QualMeeting® Digital Interviews
- Global Qualitative
- Global Quantitative
- In-Person Facilities
- Research Consulting
- Europe Solutions
- Neuromarketing Tools
- Trial & Jury Consulting
Who We Serve
Form deeper customer connections and make the process of answering your business questions easier. Sago delivers unparalleled access to the audiences you need through adaptive solutions and a consultative approach.
- Consumer Packaged Goods
- Financial Services
- Media Technology
- Medical Device Manufacturing
- Marketing Research
With a 55-year legacy of impact, Sago has proven we have what it takes to be a long-standing industry leader and partner. We continually advance our range of expertise to provide our clients with the highest level of confidence.
- Global Offices
- Partnerships & Certifications
- News & Media
- Researcher Events

Sago Launches AI Video Summaries on QualBoard to Streamline Data Synthesis

Sago Executive Chairman Steve Schlesinger to Receive Quirk’s Lifetime Achievement Award

16 Ways to Prepare for the Next Holiday Campaign
Drop into your new favorite insights rabbit hole and explore content created by the leading minds in market research.
- Case Studies
- Knowledge Kit

The Swing Voter Project Wisconsin: March 2024

The Deciders February 2024: African American voters in North Carolina
- Get in touch

- Account Logins

A Step-by-Step Guide for a Successful Qualitative Interview
- Resources , Blog

Key Takeaways:
- Qualitative interviews provide in-depth insights from individual respondents, and are useful when follow-up or clarification is needed
- Clarity of objectives and audience is essential to gathering actionable insights from your qualitative research project
- Build a strong researcher-respondent relationship to elicit honest and engaged responses
Qualitative research uses in-depth interviews to gain rich non-numerical data from individuals. This data helps researchers understand concepts, opinions, and personal experiences. Interviews are an excellent method to discover the “why” behind people’s preferences or behaviors, but they require a thoughtful approach.
Continue reading as we explore use cases and define the steps to follow for a successful qualitative interview.
In this Article:
When Should I Use Qualitative Interviews? Conducting a Successful Qualitative Interview – Step by Step Guide
1. Determine Your Objective 2. Understand Your Audience 3. Design Appropriate Questions 4. Organize and Prepare for the Interview 5. Conduct the Interview 6. Transcribe and Analyze Responses 7. Learn, Adapt, and Evolve Your Interviews
Start Conducting Qualitative Interviews with Sago
Ready to conduct your qualitative interviews.
Book a consultation with our team for help with recruitment, facilities, and more.
Book a consultation
When Should I Use Qualitative Interviews?
Qualitative research is used to obtain context and describe underlying factors. It describes “how” and “why.”
Perhaps a business wants to understand what product features are most or least important to each target segment. They could ask:
“Between product A and product B, how would the features in each product influence your buying decision?”
This creates an opportunity for the respondent to reveal what features are personally important and unimportant for them. In an interview setting, researchers can go deeper into why these features are important, and how important each feature is in comparison to others.
Qualitative interviews are best when:
- You need in-depth insights
- You want answers to a range of follow-up questions, building on prior responses
- Your questions require significant explanation and reasoning
- You explore complex and confusing topics with respondents
- You want to understand what drives consumer decisions
- You want to hear the unique voice of your audience first-hand
Conducting a Successful Qualitative Interview – Step by Step Guide
Knowing when to use a qualitative interview is a great first step, but now you need to understand how best to conduct one. Our experts share a range of steps to follow as you embark on a qualitative interview and best practices for each.
1. Determine Your Objective
What are you trying to understand? The answer to this is critical in guiding your qualitative research process.
Some common examples:
- Understand consumer perceptions of products, services, or brand
- Reveal strengths and weaknesses in product or service portfolios
- Understand consumer buying behaviors
- Test the usability of a website or digital service
- Emotional reactions to packaging design and marketing assets
2. Understand Your Audience
Who is your target audience for this project? Have a clear understanding of who you need to hear from to meet your research objective.
Here are some examples of objectives, and the sample that is most suited to each:
- If you want to understand how existing customers perceive the quality of your products, you need a sample of existing customers.
- If you want to understand why consumers choose competitor products over yours, you need a sample of non-customers who buy products from your primary competitor.
- If you want to understand how the average person perceives your brand, you need a combination of existing customers, non-customers with awareness of your brand, and unaware non-customers.
3. Design Appropriate Questions
The questions you ask must align with the objectives of your research without being leading or introducing bias.
Here are some best practices when designing research questions:
- Keep questions open-ended. This increases the depth of insight obtained.
- Follow a structure. For instance, a tree diagram where every question has pre-determined follow-up questions based on anticipated answers. A planned structure increases the quality and validity of responses and reduces distractions.
- Design questions that simplify data collection and analysis. Format the responses collected to be compatible with your tools during data ingestion.
- Keep it simple. Focus on clarity when designing research questions to improve respondent understanding and engagement.
4. Organize and Prepare for the Interview
Relationships are essential to the interview process. Preparation beforehand helps build the respondent-researcher relationship. This relationship creates trust and elicits more honest and in-depth answers from participants. Here are some ways to prepare for an interview:
- Give respondents as much information as possible—such as question lists and question intent. Put this into an interview handbook to improve engagement and effectiveness.
- Conduct the interview in a suitable environment with minimal distractions and stressors.
- Have the necessary materials to record information.
- Interview yourself to identify and fix problems before you start interviewing others.
5. Conduct the Interview
With a structure in place, researchers have a clear plan of action throughout the interview.
During the interview, stay attuned to emotional reactions and body language with the following techniques:
- Create a relaxed atmosphere. Ask respondents about their lives, work, and passions to establish a connection.
- Give respondents your full attention. An engaged researcher encourages an engaged respondent. Plus, they gave up their personal time to help you out.
- Read body language. Is the respondent crossing their arms, looking down to the floor, or not making eye contact? These reactions may signal discomfort or anxiety, offering an opportunity to build rapport.
- Follow the questions but be flexible when listening. Deviations from the script may lead to unexpected and valuable insights.
6. Transcribe and Analyze Responses
Convert recorded audio responses to text. Decide early which tool or solution will work best for your needs.
Similarly, researchers may need to annotate video responses to describe behaviors and surrounding context before analysis; e.g., this person gritted their teeth during that response, that person’s vocal tone was anxious and uncertain, etc.
Transcribe responses into a format ready for analysis upon ingestion into your business intelligence tools.
7. Learn, Adapt, and Evolve Your Interviews
Each interview is an opportunity to improve the process. Take time after a project to evaluate how it went.
What did you learn about the process? Was it easy or confusing? Was the respondent comfortable or on edge? Did you get the responses you needed?
Scrutinize your interview approach. Look for ways to improve and innovate the process for better outcomes next time.
Now, you should have a good idea of when to use and how to approach qualitative interviews.
Sago has decades of experience across both quantitative and qualitative research. Our experts find interviews ideal for in-depth qualitative insights that guide new product and service development or improve market positioning for existing offerings. We offer both in-person facilities and online spaces to conduct qualitative interviews.
If you still have questions, get in touch with Sago for help with your next research project.

Building Trust Through Inclusive Healthcare Research Recruitment

OnDemand: Moderator Minutes: Maximizing Efficient with QualBoard – Streamline Your Projects with Support & AI

2024 Trends in Research: Fact or Fiction?

The Swing Voter Project in Michigan – February 2024

OnDemand: 5 Steps to High-Quality Data: Mitigating the Challenges of Data Quality in Quantitative Research

How Leading Brands Use Insights to Win Market Share

The Deciders January 2024: Trump-Voting Women Who Oppose Dobbs

The State of New Year’s Resolutions: A Closer Look at Mindsets and Habits

It’s Time to Change the Way We Write Screeners
Take a deep dive into your favorite market research topics

How can we help support you and your research needs?

BEFORE YOU GO
Have you considered how to harness AI in your research process? Check out our on-demand webinar for everything you need to know

Five Tips for Conducting Effective Qualitative Interviews

An interviewer conducts household survey in rural El Salvador for a Center for Health Policy and Inequalities Research study. Photo by Hy V. Huynh.
Published March 12, 2018 under Research News
In qualitative research, in-depth interviews can be an immensely helpful investigative tool. However, the nuances of one-on-one interviewing can sometimes make it difficult to obtain useful results. Rae Jean Proeschold-Bell , associate research professor and founding director of the Evidence Lab at the Duke Global Health Institute, frequently integrates qualitative interviews into her research. In this article, she shares five interviewing tips that have served her well.
1. Convey Intent
Proeschold-Bell says it’s important for the interviewer to know the intent behind each question so that it can be clearly conveyed to the interviewee. Understanding the intent of a question, she’s found, helps interviewers decide whether or not the participant has fully answered the question. This way, they can ask follow-up questions and not leave gaps at the time of data collection. Proeschold-Bell recommends writing the intent of each question below it in italics on the interview script.
Proeschold-Bell also suggests a few more subtle techniques for helping interviewees understand what is really being asked and soliciting pertinent and thorough responses. Asking the question in several different ways can help clarify its meaning. Follow-up prompts such as “That’s really helpful; tell me more about that,” or “Can you describe what was unpleasant about it?” can also give interviewees helpful guidance in crafting their responses.
“You can also convey intent by explaining more broadly why you’re doing the research, so interviewees will be more likely to give you relevant information,” Proeschold-Bell said.
2. Don’t Sway the Participants
Acquiescence bias, which occurs when interviewees agree with what they think the interviewer wants to hear instead of giving their unbiased answer, can often prevent interviewees from sharing all relevant information. Research from Focus Groups: A Practical Guide for Applied Research shows that when power dynamics are present in an interview, it may be especially difficult for an interviewee to give an honest answer.
To minimize acquiescence bias, interviewers can emphasize that the participant is the expert in the subject matter of the interview. For example, they can start the interview by saying, “I’ve asked you to talk with me today because you are an expert in what it’s like to be a patient in Eldoret.”
Interviewers should also avoid nodding or other body language that expresses agreement with the participant. Instead, interviewers should say, “That’s very helpful,” or “Thank you for those thoughts.” Otherwise, participants might elaborate on a point that isn’t actually very important to them just because the interviewer seemed to agree.
Proeschold-Bell also recommends that interviewers pay attention to—and record—interviewees’ non-verbal responses, which often communicate feelings and attitudes that the verbal response doesn’t capture.
3. Eliminate Interviewer Bias
Proeschold-Bell says it’s critically important to eliminate interviewer bias through the interview process. Knowing the interview guide extremely well helps an interviewer pace the interview to avoid running out of time, and adhering to the scripted wording for each question helps maintain unbiased prompting across all interviews. Additionally, if an interviewee starts answering a question that is going to be asked later, the interviewer can ask them to wait.
It’s best to ask interview questions in a specific order because covering certain questions first may influence how interviewees think during later questions. Finally, she recommends, “Ask all questions of all respondents, even if you think you know what they’ll say. They will surprise you sometimes!”
4. Consider a “Test Run” Period
Proeschold-Bell sees her first several interviews for a study as pilots. Learning from these first few test runs and improving questions and interview techniques for future interviews can have a significant impact on the quality of the study. This means that data quality from the first few interviews may not be as strong since some of the questions change, but the data from the interviews later on will be more useful. Proeschold-Bell recommends numbering interviews chronologically to link interviews to the phase of development in which they were conducted.
5. Make Time for Post-Interview Reflection
After an interview, Proeschold-Bell recommends immediately reviewing the data. “This helps capture good ideas that may otherwise be forgotten,” she says. In fact, she suggests creating a review form with a few open-ended questions that can help capture strong reactions and flag questions that didn’t work well or questions that should be added.
It’s also helpful, she says, to note responses that were different from those given in previous interviews. Doing this may generate ideas to analyze more carefully later on.
Looking for more research design tools? Check out Proeschold-Bell’s recent article, “ Five Tips for Designing an Effective Survey .”
Proeschold-Bell recommends that interviewers pay attention to—and record—interviewees’ non-verbal responses, which often communicate feelings and attitudes that the verbal response doesn’t capture.
- Rae Jean Proeschold-Bell
Related News

Around DGHI
Understanding COVID Failures Isn’t About Pointing Fingers
April 5, 2024

Alumni Stories
Alumni Spotlight: Nour Hammad MS’22
March 29, 2024

Education News
Palmquist, Green Named to Director Roles for DGHI Education Programs
March 27, 2024
- Harvard Library
- Research Guides
- Faculty of Arts & Sciences Libraries
Library Support for Qualitative Research
- Interview Research
- Resources for Methodology
- Remote Research & Virtual Fieldwork
Resources for Research Interviewing
Nih-funded qualitative research.
- Oral History
- Data Management & Repositories
- Campus Access
Types of Interviews
- Engaging Participants
Interview Questions
- Conducting Interviews
- Transcription
- Coding and Analysis
- Managing & Finding Interview Data
- UX & Market Research Interviews
Textbooks, Guidebooks, and Handbooks
- The Ethnographic Interview by James P. Spradley “Spradley wrote this book for the professional and student who have never done ethnographic fieldwork (p. 231) and for the professional ethnographer who is interested in adapting the author’s procedures (p. iv). Part 1 outlines in 3 chapters Spradley’s version of ethnographic research, and it provides the background for Part 2 which consists of 12 guided steps (chapters) ranging from locating and interviewing an informant to writing an ethnography. Most of the examples come from the author’s own fieldwork among U.S. subcultures . . . Steps 6 and 8 explain lucidly how to construct a domain and a taxonomic analysis” (excerpted from book review by James D. Sexton, 1980).
- Fundamentals of Qualitative Research by Johnny Saldana (Series edited by Patricia Leavy) Provides a soup-to-nuts overview of the qualitative data collection process, including interviewing, participant observation, and other methods.
- InterViews by Steinar Kvale Interviewing is an essential tool in qualitative research and this introduction to interviewing outlines both the theoretical underpinnings and the practical aspects of the process. After examining the role of the interview in the research process, Steinar Kvale considers some of the key philosophical issues relating to interviewing: the interview as conversation, hermeneutics, phenomenology, concerns about ethics as well as validity, and postmodernism. Having established this framework, the author then analyzes the seven stages of the interview process - from designing a study to writing it up.
- Practical Evaluation by Michael Quinn Patton Surveys different interviewing strategies, from, a) informal/conversational, to b) interview guide approach, to c) standardized and open-ended, to d) closed/quantitative. Also discusses strategies for wording questions that are open-ended, clear, sensitive, and neutral, while supporting the speaker. Provides suggestions for probing and maintaining control of the interview process, as well as suggestions for recording and transcription.
- The SAGE Handbook of Interview Research by Amir B. Marvasti (Editor); James A. Holstein (Editor); Jaber F. Gubrium (Editor); Karyn D. McKinney (Editor) The new edition of this landmark volume emphasizes the dynamic, interactional, and reflexive dimensions of the research interview. Contributors highlight the myriad dimensions of complexity that are emerging as researchers increasingly frame the interview as a communicative opportunity as much as a data-gathering format. The book begins with the history and conceptual transformations of the interview, which is followed by chapters that discuss the main components of interview practice. Taken together, the contributions to The SAGE Handbook of Interview Research: The Complexity of the Craft encourage readers simultaneously to learn the frameworks and technologies of interviewing and to reflect on the epistemological foundations of the interview craft.
- The SAGE Handbook of Online Research Methods by Nigel G. Fielding, Raymond M. Lee and Grant Blank (Editors) Bringing together the leading names in both qualitative and quantitative online research, this new edition is organised into nine sections: 1. Online Research Methods 2. Designing Online Research 3. Online Data Capture and Data Collection 4. The Online Survey 5. Digital Quantitative Analysis 6. Digital Text Analysis 7. Virtual Ethnography 8. Online Secondary Analysis: Resources and Methods 9. The Future of Online Social Research
ONLINE RESOURCES, COMMUNITIES, AND DATABASES
- Interviews as a Method for Qualitative Research (video) This short video summarizes why interviews can serve as useful data in qualitative research.
- Companion website to Bloomberg and Volpe's Completing Your Qualitative Dissertation: A Road Map from Beginning to End, 4th ed Provides helpful templates and appendices featured in the book, as well as links to other useful dissertation resources.
- International Congress of Qualitative Inquiry Annual conference hosted by the International Center for Qualitative Inquiry at the University of Illinois at Urbana-Champaign, which aims to facilitate the development of qualitative research methods across a wide variety of academic disciplines, among other initiatives.
- METHODSPACE An online home of the research methods community, where practicing researchers share how to make research easier.
- SAGE researchmethods Researchers can explore methods concepts to help them design research projects, understand particular methods or identify a new method, conduct their research, and write up their findings. A "methods map" facilitates finding content on methods.
The decision to conduct interviews, and the type of interviewing to use, should flow from, or align with, the methodological paradigm chosen for your study, whether that paradigm is interpretivist, critical, positivist, or participative in nature (or a combination of these).
Structured:
- Structured Interview. Entry in The SAGE Encyclopedia of Social Science Research Methodsby Floyd J. Fowler Jr., Editors: Michael S. Lewis-Beck; Alan E. Bryman; Tim Futing Liao (Editor) A concise article noting standards, procedures, and recommendations for developing and testing structured interviews. For an example of structured interview questions, you may view the Current Population Survey, May 2008: Public Participation in the Arts Supplement (ICPSR 29641), Apr 15, 2011 at https://doi.org/10.3886/ICPSR29641.v1 (To see the survey questions, preview the user guide, which can be found under the "Data and Documentation" tab. Then, look for page 177 (attachment 8).
Semi-Structured:
- Semi-Structured Interview. Entry in The SAGE Encyclopedia of Qualitative Research Methodsby Lioness Ayres; Editor: Lisa M. Given The semi-structured interview is a qualitative data collection strategy in which the researcher asks informants a series of predetermined but open-ended questions. The researcher has more control over the topics of the interview than in unstructured interviews, but in contrast to structured interviews or questionnaires that use closed questions, there is no fixed range of responses to each question.
Unstructured:
- Unstructured Interview. Entry in The SAGE Encyclopedia of Qualitative Research Methodsby Michael W. Firmin; Editor: Lisa M. Given Unstructured interviews in qualitative research involve asking relatively open-ended questions of research participants in order to discover their percepts on the topic of interest. Interviews, in general, are a foundational means of collecting data when using qualitative research methods. They are designed to draw from the interviewee constructs embedded in his or her thinking and rationale for decision making. The researcher uses an inductive method in data gathering, regardless of whether the interview method is open, structured, or semi-structured. That is, the researcher does not wish to superimpose his or her own viewpoints onto the person being interviewed. Rather, inductively, the researcher wishes to understand the participant's perceptions, helping him or her to articulate percepts such that they will be understood clearly by the journal reader.
Genres and Uses
Focus groups:.
- "Focus Groups." Annual Review of Sociology 22 (1996): 129-1524.by David L. Morgan Discusses the use of focus groups and group interviews as methods for gathering qualitative data used by sociologists and other academic and applied researchers. Focus groups are recommended for giving voice to marginalized groups and revealing the group effect on opinion formation.
- Qualitative Research Methods: A Data Collector's Field Guide (See Module 4: "Focus Groups")by Mack, N., et al. This field guide is based on an approach to doing team-based, collaborative qualitative research that has repeatedly proven successful in research projects sponsored by Family Health International (FHI) throughout the developing world. With its straightforward delivery of information on the main qualitative methods being used in public health research today, the guide speaks to the need for simple yet effective instruction on how to do systematic and ethically sound qualitative research. The aim of the guide is thus practical. In bypassing extensive discussion on the theoretical underpinnings of qualitative research, it distinguishes itself as a how-to guide to be used in the field.
In-Depth (typically One-on-One):
- A Practical Introduction to in-Depth Interviewingby Alan Morris Are you new to qualitative research or a bit rusty and in need of some inspiration? Are you doing a research project involving in-depth interviews? Are you nervous about carrying out your interviews? This book will help you complete your qualitative research project by providing a nuts and bolts introduction to interviewing. With coverage of ethics, preparation strategies and advice for handling the unexpected in the field, this handy guide will help you get to grips with the basics of interviewing before embarking on your research. While recognising that your research question and the context of your research will drive your approach to interviewing, this book provides practical advice often skipped in traditional methods textbooks.
- Qualitative Research Methods: A Data Collector's Field Guide (See Module 3: "In-Depth Interviews")by Mack, N., et al. This field guide is based on an approach to doing team-based, collaborative qualitative research that has repeatedly proven successful in research projects sponsored by Family Health International (FHI) throughout the developing world. With its straightforward delivery of information on the main qualitative methods being used in public health research today, the guide speaks to the need for simple yet effective instruction on how to do systematic and ethically sound qualitative research. The aim of the guide is thus practical. In bypassing extensive discussion on the theoretical underpinnings of qualitative research, it distinguishes itself as a how-to guide to be used in the field.
Folklore Research and Oral Histories:
In addition to the following resource, see the Oral History page of this guide for helpful resources on Oral History interviewing.
American Folklife Center at the Library of Congress. Folklife and Fieldwork: A Layman’s Introduction to Field Techniques Interviews gathered for purposes of folklore research are similar to standard social science interviews in some ways, but also have a good deal in common with oral history approaches to interviewing. The focus in a folklore research interview is on documenting and trying to understand the interviewee's way of life relative to a culture or subculture you are studying. This guide includes helpful advice and tips for conducting fieldwork in folklore, such as tips for planning, conducting, recording, and archiving interviews.
An interdisciplinary scientific program within the Institute for Quantitative Social Science which encourages and facilitates research and instruction in the theory and practice of survey research. The primary mission of PSR is to provide survey research resources to enhance the quality of teaching and research at Harvard.
- Internet, Phone, Mail, and Mixed-Mode Surveysby Don A. Dillman; Jolene D. Smyth; Leah Melani Christian The classic survey design reference, updated for the digital age. The new edition is thoroughly updated and revised, and covers all aspects of survey research. It features expanded coverage of mobile phones, tablets, and the use of do-it-yourself surveys, and Dillman's unique Tailored Design Method is also thoroughly explained. This new edition is complemented by copious examples within the text and accompanying website. It includes: Strategies and tactics for determining the needs of a given survey, how to design it, and how to effectively administer it. How and when to use mail, telephone, and Internet surveys to maximum advantage. Proven techniques to increase response rates. Guidance on how to obtain high-quality feedback from mail, electronic, and other self-administered surveys. Direction on how to construct effective questionnaires, including considerations of layout. The effects of sponsorship on the response rates of surveys. Use of capabilities provided by newly mass-used media: interactivity, presentation of aural and visual stimuli. The Fourth Edition reintroduces the telephone--including coordinating land and mobile.
User Experience (UX) and Marketing:
- See the "UX & Market Research Interviews" tab on this guide, above. May include Focus Groups, above.
Screening for Research Site Selection:
- Research interviews are used not only to furnish research data for theoretical analysis in the social sciences, but also to plan other kinds of studies. For example, interviews may allow researchers to screen appropriate research sites to conduct empirical studies (such as randomized controlled trials) in a variety of fields, from medicine to law. In contrast to interviews conducted in the course of social research, such interviews do not typically serve as the data for final analysis and publication.
ENGAGING PARTICIPANTS
Research ethics .
- Human Subjects (IRB) The Committee on the Use of Human Subjects (CUHS) serves as the Institutional Review Board for the University area which includes the Cambridge and Allston campuses at Harvard. Find your IRB contact person , or learn about required ethics training. You may also find the IRB Lifecycle Guide helpful. This is the preferred IRB portal for Harvard graduate students and other researchers. IRB forms can be downloaded via the ESTR Library (click on the "Templates and Forms" tab, then navigate to pages 2 and 3 to find the documents labelled with “HUA” for the Harvard University Area IRB. Nota bene: You may use these forms only if you submit your study to the Harvard University IRB). The IRB office can be reached through email at [email protected] or by telephone at (617) 496-2847.
- Undergraduate Research Training Program (URTP) Portal The URTP at Harvard University is a comprehensive platform to create better prepared undergraduate researchers. The URTP is comprised of research ethics training sessions, a student-focused curriculum, and an online decision form that will assist students in determining whether their project requires IRB review. Students should examine the URTP's guide for student researchers: Introduction to Human Subjects Research Protection.
- Ethics reports From the Association of Internet Researchers (AoIR)
- Respect, Beneficence, and Justice: QDR General Guidance for Human Participants If you are hoping to share your qualitative interview data in a repository after it has been collected, you will need to plan accordingly via informed consent, careful de-identification procedures, and data access controls. Consider consulting with the Qualitative Research Support Group at Harvard Library and consulting with Harvard's Dataverse contacts to help you think through all of the contingencies and processes.
- "Conducting a Qualitative Child Interview: Methodological Considerations." Journal of Advanced Nursing 42/5 (2003): 434-441 by Kortesluoma, R., et al. The purpose of this article is to illustrate the theoretical premises of child interviewing, as well as to describe some practical methodological solutions used during interviews. Factors that influence data gathered from children and strategies for taking these factors into consideration during the interview are also described.
- "Crossing Cultural Barriers in Research Interviewing." Qualitative Social Work 63/3 (2007): 353-372 by Sands, R., et al. This article critically examines a qualitative research interview in which cultural barriers between a white non-Muslim female interviewer and an African American Muslim interviewee, both from the USA, became evident and were overcome within the same interview.
- Decolonizing Methodologies: Research and Indigenous Peoples by Linda Tuhiwai Smith This essential volume explores intersections of imperialism and research - specifically, the ways in which imperialism is embedded in disciplines of knowledge and tradition as 'regimes of truth.' Concepts such as 'discovery' and 'claiming' are discussed and an argument presented that the decolonization of research methods will help to reclaim control over indigenous ways of knowing and being. The text includes case-studies and examples, and sections on new indigenous literature and the role of research in indigenous struggles for social justice.
This resource, sponsored by University of Oregon Libraries, exemplifies the use of interviewing methodologies in research that foregrounds traditional knowledge. The methodology page summarizes the approach.
- Ethics: The Need to Tread Carefully. Chapter in A Practical Introduction to in-Depth Interviewing by Alan Morris Pay special attention to the sections in chapter 2 on "How to prevent and respond to ethical issues arising in the course of the interview," "Ethics in the writing up of your interviews," and "The Ethics of Care."
- Handbook on Ethical Issues in Anthropology by Joan Cassell (Editor); Sue-Ellen Jacobs (Editor) This publication of the American Anthropological Association presents and discusses issues and sources on ethics in anthropology, as well as realistic case studies of ethical dilemmas. It is meant to help social science faculty introduce discussions of ethics in their courses. Some of the topics are relevant to interviews, or at least to studies of which interviews are a part. See chapters 3 and 4 for cases, with solutions and commentary, respectively.
- Research Ethics from the Chanie Wenjack School for Indigenous Studies, Trent University (Open Access) An overview of Indigenous research ethics and protocols from the across the globe.
- Resources for Equity in Research Consult these resources for guidance on creating and incorporating equitable materials into public health research studies that entail community engagement.
The SAGE Handbook of Qualitative Research Ethics by Ron Iphofen (Editor); Martin Tolich (Editor) This handbook is a much-needed and in-depth review of the distinctive set of ethical considerations which accompanies qualitative research. This is particularly crucial given the emergent, dynamic and interactional nature of most qualitative research, which too often allows little time for reflection on the important ethical responsibilities and obligations. Contributions from leading international researchers have been carefully organized into six key thematic sections: Part One: Thick Descriptions Of Qualitative Research Ethics; Part Two: Qualitative Research Ethics By Technique; Part Three: Ethics As Politics; Part Four: Qualitative Research Ethics With Vulnerable Groups; Part Five: Relational Research Ethics; Part Six: Researching Digitally. This Handbook is a one-stop resource on qualitative research ethics across the social sciences that draws on the lessons learned and the successful methods for surmounting problems - the tried and true, and the new.
RESEARCH COMPLIANCE AND PRIVACY LAWS
Research Compliance Program for FAS/SEAS at Harvard : The Faculty of Arts and Sciences (FAS), including the School of Engineering and Applied Sciences (SEAS), and the Office of the Vice Provost for Research (OVPR) have established a shared Research Compliance Program (RCP). An area of common concern for interview studies is international projects and collaboration . RCP is a resource to provide guidance on which international activities may be impacted by US sanctions on countries, individuals, or entities and whether licenses or other disclosure are required to ship or otherwise share items, technology, or data with foreign collaborators.
- Harvard Global Support Services (GSS) is for students, faculty, staff, and researchers who are studying, researching, or working abroad. Their services span safety and security, health, culture, outbound immigration, employment, financial and legal matters, and research center operations. These include travel briefings and registration, emergency response, guidance on international projects, and managing in-country operations.
Generative AI: Harvard-affiliated researchers should not enter data classified as confidential ( Level 2 and above ), including non-public research data, into publicly-available generative AI tools, in accordance with the University’s Information Security Policy. Information shared with generative AI tools using default settings is not private and could expose proprietary or sensitive information to unauthorized parties.
Privacy Laws: Be mindful of any potential privacy laws that may apply wherever you conduct your interviews. The General Data Protection Regulation is a high-profile example (see below):
- General Data Protection Regulation (GDPR) This Regulation lays down rules relating to the protection of natural persons with regard to the processing of personal data and rules relating to the free movement of personal data. It protects fundamental rights and freedoms of natural persons and in particular their right to the protection of personal data. The free movement of personal data within the Union shall be neither restricted nor prohibited for reasons connected with the protection of natural persons with regard to the processing of personal data. For a nice summary of what the GDPR requires, check out the GDPR "crash course" here .
SEEKING CONSENT
If you would like to see examples of consent forms, ask your local IRB, or take a look at these resources:
- Model consent forms for oral history, suggested by the Centre for Oral History and Digital Storytelling at Concordia University
- For NIH-funded research, see this resource for developing informed consent language in research studies where data and/or biospecimens will be stored and shared for future use.
POPULATION SAMPLING
If you wish to assemble resources to aid in sampling, such as the USPS Delivery Sequence File, telephone books, or directories of organizations and listservs, please contact our data librarian or write to [email protected] .
- Research Randomizer A free web-based service that permits instant random sampling and random assignment. It also contains an interactive tutorial perfect for students taking courses in research methods.
- Practical Tools for Designing and Weighting Survey Samples by Richard Valliant; Jill A. Dever; Frauke Kreuter Survey sampling is fundamentally an applied field. The goal in this book is to put an array of tools at the fingertips of practitioners by explaining approaches long used by survey statisticians, illustrating how existing software can be used to solve survey problems, and developing some specialized software where needed. This book serves at least three audiences: (1) Students seeking a more in-depth understanding of applied sampling either through a second semester-long course or by way of a supplementary reference; (2) Survey statisticians searching for practical guidance on how to apply concepts learned in theoretical or applied sampling courses; and (3) Social scientists and other survey practitioners who desire insight into the statistical thinking and steps taken to design, select, and weight random survey samples. Several survey data sets are used to illustrate how to design samples, to make estimates from complex surveys for use in optimizing the sample allocation, and to calculate weights. Realistic survey projects are used to demonstrate the challenges and provide a context for the solutions. The book covers several topics that either are not included or are dealt with in a limited way in other texts. These areas include: sample size computations for multistage designs; power calculations related to surveys; mathematical programming for sample allocation in a multi-criteria optimization setting; nuts and bolts of area probability sampling; multiphase designs; quality control of survey operations; and statistical software for survey sampling and estimation. An associated R package, PracTools, contains a number of specialized functions for sample size and other calculations. The data sets used in the book are also available in PracTools, so that the reader may replicate the examples or perform further analyses.
- Sampling: Design and Analysis by Sharon L. Lohr Provides a modern introduction to the field of sampling. With a multitude of applications from a variety of disciplines, the book concentrates on the statistical aspects of taking and analyzing a sample. Overall, the book gives guidance on how to tell when a sample is valid or not, and how to design and analyze many different forms of sample surveys.
- Sampling Techniques by William G. Cochran Clearly demonstrates a wide range of sampling methods now in use by governments, in business, market and operations research, social science, medicine, public health, agriculture, and accounting. Gives proofs of all the theoretical results used in modern sampling practice. New topics in this edition include the approximate methods developed for the problem of attaching standard errors or confidence limits to nonlinear estimates made from the results of surveys with complex plans.
- "Understanding the Process of Qualitative Data Collection" in Chapter 13 (pp. 103–1162) of 30 Essential Skills for the Qualitative Researcher by John W. Creswell Provides practical "how-to" information for beginning researchers in the social, behavioral, and health sciences with many applied examples from research design, qualitative inquiry, and mixed methods.The skills presented in this book are crucial for a new qualitative researcher starting a qualitative project.
- Survey Methodology by Robert M. Groves; Floyd J. Fowler; Mick P. Couper; James M. Lepkowski; Eleanor Singer; Roger Tourangeau; Floyd J. Fowler coverage includes sampling frame evaluation, sample design, development of questionnaires, evaluation of questions, alternative modes of data collection, interviewing, nonresponse, post-collection processing of survey data, and practices for maintaining scientific integrity.
The way a qualitative researcher constructs and approaches interview questions should flow from, or align with, the methodological paradigm chosen for the study, whether that paradigm is interpretivist, critical, positivist, or participative in nature (or a combination of these).
Constructing Your Questions
Helpful texts:.
- "Developing Questions" in Chapter 4 (pp. 98–108) of Becoming Qualitative Researchers by Corrine Glesne Ideal for introducing the novice researcher to the theory and practice of qualitative research, this text opens students to the diverse possibilities within this inquiry approach, while helping them understand how to design and implement specific research methods.
- "Learning to Interview in the Social Sciences" Qualitative Inquiry, 9(4) 2003, 643–668 by Roulston, K., deMarrais, K., & Lewis, J. B. See especially the section on "Phrasing and Negotiating Questions" on pages 653-655 and common problems with framing questions noted on pages 659 - 660.
- Qualitative Research Interviewing: Biographic Narrative and Semi-Structured Methods (See sections on “Lightly and Heavily Structured Depth Interviewing: Theory-Questions and Interviewer-Questions” and “Preparing for any Interviewing Sequence") by Tom Wengraf Unique in its conceptual coherence and the level of practical detail, this book provides a comprehensive resource for those concerned with the practice of semi-structured interviewing, the most commonly used interview approach in social research, and in particular for in-depth, biographic narrative interviewing. It covers the full range of practices from the identification of topics through to strategies for writing up research findings in diverse ways.
- "Scripting a Qualitative Purpose Statement and Research Questions" in Chapter 12 (pp. 93–102) of 30 Essential Skills for the Qualitative Researcher by John W. Creswell Provides practical "how-to" information for beginning researchers in the social, behavioral, and health sciences with many applied examples from research design, qualitative inquiry, and mixed methods.The skills presented in this book are crucial for a new qualitative researcher starting a qualitative project.
- Some Strategies for Developing Interview Guides for Qualitative Interviews by Sociology Department, Harvard University Includes general advice for conducting qualitative interviews, pros and cons of recording and transcription, guidelines for success, and tips for developing and phrasing effective interview questions.
- Tip Sheet on Question Wording by Harvard University Program on Survey Research

Let Theory Guide You:
The quality of your questions depends on how you situate them within a wider body of knowledge. Consider the following advice:
A good literature review has many obvious virtues. It enables the investigator to define problems and assess data. It provides the concepts on which percepts depend. But the literature review has a special importance for the qualitative researcher. This consists of its ability to sharpen his or her capacity for surprise (Lazarsfeld, 1972b). The investigator who is well versed in the literature now has a set of expectations the data can defy. Counterexpectational data are conspicuous, readable, and highly provocative data. They signal the existence of unfulfilled theoretical assumptions, and these are, as Kuhn (1962) has noted, the very origins of intellectual innovation. A thorough review of the literature is, to this extent, a way to manufacture distance. It is a way to let the data of one's research project take issue with the theory of one's field.
McCracken, G. (1988), The Long Interview, Sage: Newbury Park, CA, p. 31
When drafting your interview questions, remember that everything follows from your central research question. Also, on the way to writing your "operationalized" interview questions, it's helpful to draft broader, intermediate questions, couched in theory. Nota bene: While it is important to know the literature well before conducting your interview(s), be careful not to present yourself to your research participant(s) as "the expert," which would be presumptuous and could be intimidating. Rather, the purpose of your knowledge is to make you a better, keener listener.
If you'd like to supplement what you learned about relevant theories through your coursework and literature review, try these sources:
- Annual Reviews Review articles sum up the latest research in many fields, including social sciences, biomedicine, life sciences, and physical sciences. These are timely collections of critical reviews written by leading scientists.
- HOLLIS - search for resources on theories in your field Modify this example search by entering the name of your field in place of "your discipline," then hit search.
- Oxford Bibliographies Written and reviewed by academic experts, every article in this database is an authoritative guide to the current scholarship in a variety of fields, containing original commentary and annotations.
- ProQuest Dissertations & Theses (PQDT) Indexes dissertations and masters' theses from most North American graduate schools as well as some European universities. Provides full text for most indexed dissertations from 1990-present.
- Very Short Introductions Launched by Oxford University Press in 1995, Very Short Introductions offer concise introductions to a diverse range of subjects from Climate to Consciousness, Game Theory to Ancient Warfare, Privacy to Islamic History, Economics to Literary Theory.
CONDUCTING INTERVIEWS
Equipment and software: .
- Lamont Library loans microphones and podcast starter kits, which will allow you to capture audio (and you may record with software, such as Garage Band).
- Cabot Library loans digital recording devices, as well as USB microphones.
If you prefer to use your own device, you may purchase a small handheld audio recorder, or use your cell phone.
- Audio Capture Basics (PDF) - Helpful instructions, courtesy of the Lamont Library Multimedia Lab.
- Getting Started with Podcasting/Audio: Guidelines from Harvard Library's Virtual Media Lab for preparing your interviewee for a web-based recording (e.g., podcast, interview)
- Camtasia Screen Recorder and Video Editor
- Zoom: Video Conferencing, Web Conferencing
- Visit the Multimedia Production Resources guide! Consult it to find and learn how to use audiovisual production tools, including: cameras, microphones, studio spaces, and other equipment at Cabot Science Library and Lamont Library.
- Try the virtual office hours offered by the Lamont Multimedia Lab!
TIPS FOR CONDUCTING INTERVIEWS
Quick handout: .
- Research Interviewing Tips (Courtesy of Dr. Suzanne Spreadbury)
Remote Interviews:
- For Online or Distant Interviews, See "Remote Research & Virtual Fieldwork" on this guide .
- Deborah Lupton's Bibliography: Doing Fieldwork in a Pandemic
Seeking Consent:
Books and articles: .
- "App-Based Textual Interviews: Interacting With Younger Generations in a Digitalized Social Reallity."International Journal of Social Research Methodology (12 June 2022). Discusses the use of texting platforms as a means to reach young people. Recommends useful question formulations for this medium.
- "Learning to Interview in the Social Sciences." Qualitative Inquiry, 9(4) 2003, 643–668 by Roulston, K., deMarrais, K., & Lewis, J. B. See especially the section on "Phrasing and Negotiating Questions" on pages 653-655 and common problems with framing questions noted on pages 659-660.
- "Slowing Down and Digging Deep: Teaching Students to Examine Interview Interaction in Depth." LEARNing Landscapes, Spring 2021 14(1) 153-169 by Herron, Brigette A. and Kathryn Roulston. Suggests analysis of videorecorded interviews as a precursor to formulating one's own questions. Includes helpful types of probes.
- Using Interviews in a Research Project by Nigel Joseph Mathers; Nicholas J Fox; Amanda Hunn; Trent Focus Group. A work pack to guide researchers in developing interviews in the healthcare field. Describes interview structures, compares face-to-face and telephone interviews. Outlines the ways in which different types of interview data can be analysed.
- “Working through Challenges in Doing Interview Research.” International Journal of Qualitative Methods, (December 2011), 348–66 by Roulston, Kathryn. The article explores (1) how problematic interactions identified in the analysis of focus group data can lead to modifications in research design, (2) an approach to dealing with reported data in representations of findings, and (3) how data analysis can inform question formulation in successive rounds of data generation. Findings from these types of examinations of interview data generation and analysis are valuable for informing both interview practice as well as research design.
Videos:

The way a qualitative researcher transcribes interviews should flow from, or align with, the methodological paradigm chosen for the study, whether that paradigm is interpretivist, critical, positivist, or participative in nature (or a combination of these).
TRANSCRIPTION
Before embarking on a transcription project, it's worthwhile to invest in the time and effort necessary to capture good audio, which will make the transcription process much easier. If you haven't already done so, check out the audio capture guidelines from Harvard Library's Virtual Media Lab , or contact a media staff member for customized recommendations. First and foremost, be mindful of common pitfalls by watching this short video that identifies the most common errors to avoid!
SOFTWARE:
- Adobe Premiere Pro Speech-To-Text automatically generates transcripts and adds captions to your videos. Harvard affiliates can download Adobe Premiere in the Creative Cloud Suite.
- GoTranscript provides cost-effective human-generated transcriptions.
- pyTranscriber is an app for generating automatic transcription and/or subtitles for audio and video files. It uses the Google Cloud Speech-to-Text service, has a friendly graphical user interface, and is purported to work nicely with Chinese.
- Otter provides a new way to capture, store, search and share voice conversations, lectures, presentations, meetings, and interviews. The startup is based in Silicon Valley with a team of experienced Ph.Ds and engineers from Google, Facebook, Yahoo and Nuance (à la Dragon). Free accounts available. This is the software that Zoom uses to generate automated transcripts, so if you have access to a Zoom subscription, you have access to Otter transcriptions with it (applicable in several languages ). As with any automated approach, be prepared to correct any errors after the fact, by hand.
- Panopto is available to Harvard affiliates and generates ASR (automated speech recognition) captions . You may upload compatible audio files into it. As with any automatically generated transcription, you will need to make manual revisions. ASR captioning is available in several languages . Panopto maintains robust security practices, including strong authentication measures and end-to-end encryption, ensuring your content remains private and protected.
- REV.Com allows you to record and transcribe any calls on the iPhone, both outgoing and incoming. It may be useful for recording phone interviews. Rev lets you choose whether you want an AI- or human-generated transcription, with a fast turnaround. Rev has Service Organization Controls Type II (SOC2) certification (a SOC2 cert looks at and verifies an organization’s processing integrity, privacy practices, and security safeguards).
- Scribie Audio/Video Transcription provides automated or manual transcriptions for a small fee. As with any transcription service, some revisions will be necessary after the fact, particularly for its automated transcripts.
- Sonix automatically transcribes, translates, and helps to organize audio and video files in over 40 languages. It's fast and affordable, with good accuracy. The free trial includes 30 minutes of free transcription.
- TranscriptionWing uses a human touch process to clean up machine-generated transcripts so that the content will far more accurately reflect your audio recording.
- Whisper is a tool from OpenAI that facilitates transcription of sensitive audiovisual recordings (e.g., of research interviews) on your own device. Installation and use depends on your operating system and which version you install. Important Note: The Whisper API, where audio is sent to OpenAI to be processed by them and then sent back (usually through a programming language like Python) is NOT appropriate for sensitive data. The model should be downloaded with tools such as those described in this FAQ , so that audio is kept to your local machine. For assistance, contact James Capobianco .
EQUIPMENT:
- Transcription pedals are in circulation and available to borrow from the Circulation desk at Lamont, or use at Lamont Library's Media Lab on level B. For hand-transcribing your interviews, they work in conjunction with software such as Express Scribe , which is loaded on Media Lab computers, or you may download for free on your own machine (Mac or PC versions; scroll down the downloads page for the latter). The pedals are plug-and-play USB, allow a wide range of playback speeds, and have 3 programmable buttons, which are typically set to rewind/play/fast-forward. Instructions are included in the bag that covers installation and set-up of the software, and basic use of the pedals.
NEED HELP?
- Try the virtual office hours offered by the Lamont Multimedia Lab!
- If you're creating podcasts, login to Canvas and check out the Podcasting/Audio guide .
Helpful Texts:
- "Transcription as a Crucial Step of Data Analysis" in Chapter 5 of The SAGE Handbook of Qualitative Data Analysisby Uwe Flick (Editor) Covers basic terminology for transcription, shares caveats for transcribers, and identifies components of vocal behavior. Provides notation systems for transcription, suggestions for transcribing turn-taking, and discusses new technologies and perspectives. Includes a bibliography for further reading.
- "Transcribing the Oral Interview: Part Art, Part Science " on p. 10 of the Centre for Community Knowledge (CCK) newsletter: TIMESTAMPby Mishika Chauhan and Saransh Srivastav
QUALITATIVE DATA ANALYSIS
Software .
- Free download available for Harvard Faculty of Arts and Sciences (FAS) affiliates
- Desktop access at Lamont Library Media Lab, 3rd floor
- Desktop access at Harvard Kennedy School Library (with HKS ID)
- Remote desktop access for Harvard affiliates from IQSS Computer Labs . Email them at [email protected] and ask for a new lab account and remote desktop access to NVivo.
- Virtual Desktop Infrastructure (VDI) access available to Harvard T.H. Chan School of Public Health affiliates
CODING AND THEMEING YOUR DATA
Data analysis methods should flow from, or align with, the methodological paradigm chosen for your study, whether that paradigm is interpretivist, critical, positivist, or participative in nature (or a combination of these). Some established methods include Content Analysis, Critical Analysis, Discourse Analysis, Gestalt Analysis, Grounded Theory Analysis, Interpretive Analysis, Narrative Analysis, Normative Analysis, Phenomenological Analysis, Rhetorical Analysis, and Semiotic Analysis, among others. The following resources should help you navigate your methodological options and put into practice methods for coding, themeing, interpreting, and presenting your data.
- Users can browse content by topic, discipline, or format type (reference works, book chapters, definitions, etc.). SRM offers several research tools as well: a methods map, user-created reading lists, a project planner, and advice on choosing statistical tests.
- Abductive Coding: Theory Building and Qualitative (Re)Analysis by Vila-Henninger, et al. The authors recommend an abductive approach to guide qualitative researchers who are oriented towards theory-building. They outline a set of tactics for abductive analysis, including the generation of an abductive codebook, abductive data reduction through code equations, and in-depth abductive qualitative analysis.
- Analyzing and Interpreting Qualitative Research: After the Interview by Charles F. Vanover, Paul A. Mihas, and Johnny Saldana (Editors) Providing insight into the wide range of approaches available to the qualitative researcher and covering all steps in the research process, the authors utilize a consistent chapter structure that provides novice and seasoned researchers with pragmatic, "how-to" strategies. Each chapter author introduces the method, uses one of their own research projects as a case study of the method described, shows how the specific analytic method can be used in other types of studies, and concludes with three questions/activities to prompt class discussion or personal study.
- "Analyzing Qualitative Data." Theory Into Practice 39, no. 3 (2000): 146-54 by Margaret D. LeCompte This article walks readers though rules for unbiased data analysis and provides guidance for getting organized, finding items, creating stable sets of items, creating patterns, assembling structures, and conducting data validity checks.
- "Coding is Not a Dirty Word" in Chapter 1 (pp. 1–30) of Enhancing Qualitative and Mixed Methods Research with Technology by Shalin Hai-Jew (Editor) Current discourses in qualitative research, especially those situated in postmodernism, represent coding and the technology that assists with coding as reductive, lacking complexity, and detached from theory. In this chapter, the author presents a counter-narrative to this dominant discourse in qualitative research. The author argues that coding is not necessarily devoid of theory, nor does the use of software for data management and analysis automatically render scholarship theoretically lightweight or barren. A lack of deep analytical insight is a consequence not of software but of epistemology. Using examples informed by interpretive and critical approaches, the author demonstrates how NVivo can provide an effective tool for data management and analysis. The author also highlights ideas for critical and deconstructive approaches in qualitative inquiry while using NVivo. By troubling the positivist discourse of coding, the author seeks to create dialogic spaces that integrate theory with technology-driven data management and analysis, while maintaining the depth and rigor of qualitative research.
- The Coding Manual for Qualitative Researchers by Johnny Saldana An in-depth guide to the multiple approaches available for coding qualitative data. Clear, practical and authoritative, the book profiles 32 coding methods that can be applied to a range of research genres from grounded theory to phenomenology to narrative inquiry. For each approach, Saldaña discusses the methods, origins, a description of the method, practical applications, and a clearly illustrated example with analytic follow-up. Essential reading across the social sciences.
- Flexible Coding of In-depth Interviews: A Twenty-first-century Approach by Nicole M. Deterding and Mary C. Waters The authors suggest steps in data organization and analysis to better utilize qualitative data analysis technologies and support rigorous, transparent, and flexible analysis of in-depth interview data.
- From the Editors: What Grounded Theory is Not by Roy Suddaby Walks readers through common misconceptions that hinder grounded theory studies, reinforcing the two key concepts of the grounded theory approach: (1) constant comparison of data gathered throughout the data collection process and (2) the determination of which kinds of data to sample in succession based on emergent themes (i.e., "theoretical sampling").
- “Good enough” methods for life-story analysis, by Wendy Luttrell. In Quinn N. (Ed.), Finding culture in talk (pp. 243–268). Demonstrates for researchers of culture and consciousness who use narrative how to concretely document reflexive processes in terms of where, how and why particular decisions are made at particular stages of the research process.
- Presentation slides on coding and themeing your data, derived from Saldana, Spradley, and LeCompte Click to request access.
- Qualitative Data Analysis by Matthew B. Miles; A. Michael Huberman A practical sourcebook for researchers who make use of qualitative data, presenting the current state of the craft in the design, testing, and use of qualitative analysis methods. Strong emphasis is placed on data displays matrices and networks that go beyond ordinary narrative text. Each method of data display and analysis is described and illustrated.
- "A Survey of Qualitative Data Analytic Methods" in Chapter 4 (pp. 89–138) of Fundamentals of Qualitative Research by Johnny Saldana Provides an in-depth introduction to coding as a heuristic, particularly focusing on process coding, in vivo coding, descriptive coding, values coding, dramaturgical coding, and versus coding. Includes advice on writing analytic memos, developing categories, and themeing data.
- "Thematic Networks: An Analytic Tool for Qualitative Research." Qualitative Research : QR, 1(3), 385–405 by Jennifer Attride-Stirling Details a technique for conducting thematic analysis of qualitative material, presenting a step-by-step guide of the analytic process, with the aid of an empirical example. The analytic method presented employs established, well-known techniques; the article proposes that thematic analyses can be usefully aided by and presented as thematic networks.
- Using Thematic Analysis in Psychology by Virginia Braun and Victoria Clark Walks readers through the process of reflexive thematic analysis, step by step. The method may be adapted in fields outside of psychology as relevant. Pair this with One Size Fits All? What Counts as Quality Practice in Reflexive Thematic Analysis? by Virginia Braun and Victoria Clark
TESTING OR GENERATING THEORIES
The quality of your data analysis depends on how you situate what you learn within a wider body of knowledge. Consider the following advice:
Once you have coalesced around a theory, realize that a theory should reveal rather than color your discoveries. Allow your data to guide you to what's most suitable. Grounded theory researchers may develop their own theory where current theories fail to provide insight. This guide on Theoretical Models from Alfaisal University Library provides a helpful overview on using theory.
MANAGING & FINDING INTERVIEW DATA
Managing your elicited interview data, general guidance: .
- Research Data Management @ Harvard A reference guide with information and resources to help you manage your research data. See also: Harvard Research Data Security Policy , on the Harvard University Research Data Management website.
- Data Management For Researchers: Organize, Maintain and Share Your Data for Research Success by Kristin Briney. A comprehensive guide for scientific researchers providing everything they need to know about data management and how to organize, document, use and reuse their data.
- Open Science Framework (OSF) An open-source project management tool that makes it easy to collaborate within and beyond Harvard throughout a project's lifecycle. With OSF you can manage, store, and share documents, datasets, and other information with your research team. You can also publish your work to share it with a wider audience. Although data can be stored privately, because this platform is hosted on the Internet and designed with open access in mind, it is not a good choice for highly sensitive data.
- Free cloud storage solutions for Harvard affiliates to consider include: Google Drive , DropBox , or OneDrive ( up to DSL3 )
Data Confidentiality and Secure Handling:
- Data Security Levels at Harvard - Research Data Examples This resource provided by Harvard Data Security helps you determine what level of access is appropriate for your data. Determine whether it should be made available for public use, limited to the Harvard community, or be protected as either "confidential and sensitive," "high risk," or "extremely sensitive." See also: Harvard Data Classification Table
- Harvard's Best Practices for Protecting Privacy and Harvard Information Security Collaboration Tools Matrix Follow the nuts-and-bolts advice for privacy best practices at Harvard. The latter resource reveals the level of security that can be relied upon for a large number of technological tools and platforms used at Harvard to conduct business, such as email, Slack, Accellion Kiteworks, OneDrive/SharePoint, etc.
- “Protecting Participant Privacy While Maintaining Content and Context: Challenges in Qualitative Data De‐identification and Sharing.” Proceedings of the ASIST Annual Meeting 57 (1) (2020): e415-420 by Myers, Long, and Polasek Presents an informed and tested protocol, based on the De-Identification guidelines published by the Qualitative Data Repository (QDR) at Syracuse University. Qualitative researchers may consult it to guide their data de-identification efforts.
- QDS Qualitative Data Sharing Toolkit The Qualitative Data Sharing (QDS) project and its toolkit was funded by the NIH National Human Genome Research Institute (R01HG009351). It provides tools and resources to help researchers, especially those in the health sciences, share qualitative research data while protecting privacy and confidentiality. It offers guidance on preparing data for sharing through de-identification and access control. These health sciences research datasets in ICPSR's Qualitative Data Sharing (QDS) Project Series were de-identified using the QuaDS Software and the project’s QDS guidelines.
- Table of De-Identification Techniques
- Generative AI Harvard-affiliated researchers should not enter data classified as confidential ( Level 2 and above ), including non-public research data, into publicly-available generative AI tools, in accordance with the University’s Information Security Policy. Information shared with generative AI tools using default settings is not private and could expose proprietary or sensitive information to unauthorized parties.
- Harvard Information Security Quick Reference Guide Storage guidelines, based on the data's security classification level (according to its IRB classification) is displayed on page 2, under "handling."
- Email Encryption Harvard Microsoft 365 users can now send encrypted messages and files directly from the Outlook web or desktop apps. Encrypting an email adds an extra layer of security to the message and its attachments (up to 150MB), and means only the intended recipient (and their inbox delegates with full access) can view it. Message encryption in Outlook is approved for sending high risk ( level 4 ) data and below.
Sharing Qualitative Data:
- Repositories for Qualitative Data If you have cleared this intention with your IRB, secured consent from participants, and properly de-identified your data, consider sharing your interviews in one of the data repositories included in the link above. Depending on the nature of your research and the level of risk it may present to participants, sharing your interview data may not be appropriate. If there is any chance that sharing such data will be desirable, you will be much better off if you build this expectation into your plans from the beginning.
- Guide for Sharing Qualitative Data at ICPSR The Inter-university Consortium for Political and Social Research (ICPSR) has created this resource for investigators planning to share qualitative data at ICPSR. This guide provides an overview of elements and considerations for archiving qualitative data, identifies steps for investigators to follow during the research life cycle to ensure that others can share and reuse qualitative data, and provides information about exemplars of qualitative data
International Projects:
- Research Compliance Program for FAS/SEAS at Harvard The Faculty of Arts and Sciences (FAS), including the School of Engineering and Applied Sciences (SEAS), and the Office of the Vice Provost for Research (OVPR) have established a shared Research Compliance Program (RCP). An area of common concern for interview studies is international projects and collaboration . RCP is a resource to provide guidance on which international activities may be impacted by US sanctions on countries, individuals, or entities and whether licenses or other disclosure are required to ship or otherwise share items, technology, or data with foreign collaborators.
Finding Extant Interview Data
Finding journalistic interviews: .
- Academic Search Premier This all-purpose database is great for finding articles from magazines and newspapers. In the Advanced Search, it allows you to specify "Document Type": Interview.
- Guide to Newspapers and Newspaper Indexes Use this guide created to Harvard Librarians to identify newspapers collections you'd like to search. To locate interviews, try adding the term "interview" to your search, or explore a database's search interface for options to limit your search to interviews. Nexis Uni and Factiva are the two main databases for current news.
- Listen Notes Search for podcast episodes at this podcast aggregator, and look for podcasts that include interviews. Make sure to vet the podcaster for accuracy and quality! (Listen Notes does not do much vetting.)
- NPR and ProPublica are two sites that offer high-quality long-form reporting, including journalistic interviews, for free.
Finding Oral History and Social Research Interviews:
- To find oral histories, see the Oral History page of this guide for helpful resources on Oral History interviewing.
- Repositories for Qualitative Data It has not been a customary practice among qualitative researchers in the social sciences to share raw interview data, but some have made this data available in repositories, such as the ones listed on the page linked above. You may find published data from structured interview surveys (e.g., questionnaire-based computer-assisted telephone interview data), as well as some semi-structured and unstructured interviews.
- If you are merely interested in studies interpreting data collected using interviews, rather than finding raw interview data, try databases like PsycInfo , Sociological Abstracts , or Anthropology Plus , among others.
Finding Interviews in Archival Collections at Harvard Library:
In addition to the databases and search strategies mentioned under the "Finding Oral History and Social Research Interviews" category above, you may search for interviews and oral histories (whether in textual or audiovisual formats) held in archival collections at Harvard Library.
- HOLLIS searches all documented collections at Harvard, whereas HOLLIS for Archival Discovery searches only those with finding aids. Although HOLLIS for Archival Discovery covers less material, you may find it easier to parse your search results, especially when you wish to view results at the item level (within collections). Try these approaches:
Search in HOLLIS :
- To retrieve items available online, do an Advanced Search for interview* OR "oral histor*" (in Subject), with Resource Type "Archives/Manuscripts," then refine your search by selecting "Online" under "Show Only" on the right of your initial result list. Revise the search above by adding your topic in the Keywords or Subject field (for example: African Americans ) and resubmitting the search.
- To enlarge your results set, you may also leave out the "Online" refinement; if you'd like to limit your search to a specific repository, try the technique of searching for Code: Library + Collection on the "Advanced Search" page .
Search in HOLLIS for Archival Discovery :
- To retrieve items available online, search for interview* OR "oral histor*" limited to digital materials . Revise the search above by adding your topic (for example: artist* ) in the second search box (if you don't see the box, click +).
- To preview results by collection, search for interview* OR "oral histor*" limited to collections . Revise the search above by adding your topic (for example: artist* ) in the second search box (if you don't see the box, click +). Although this method does not allow you to isolate digitized content, you may find the refinement options on the right side of the screen (refine by repository, subject or names) helpful. Once your select a given collection, you may search within it (e.g., for your topic or the term interview).
UX & MARKET RESEARCH INTERVIEWS
Ux at harvard library .
- User Experience and Market Research interviews can inform the design of tangible products and services through responsive, outcome-driven insights. The User Research Center at Harvard Library specializes in this kind of user-centered design, digital accessibility, and testing. They also offer guidance and resources to members of the Harvard Community who are interested in learning more about UX methods. Contact [email protected] or consult the URC website for more information.
Websites
- User Interviews: The Beginner’s Guide (Chris Mears)
- Interviewing Users (Jakob Nielsen)
Books
- Interviewing Users: How to Uncover Compelling Insights by Steve Portigal; Grant McCracken (Foreword by) Interviewing is a foundational user research tool that people assume they already possess. Everyone can ask questions, right? Unfortunately, that's not the case. Interviewing Users provides invaluable interviewing techniques and tools that enable you to conduct informative interviews with anyone. You'll move from simply gathering data to uncovering powerful insights about people.
- Rapid Contextual Design by Jessamyn Wendell; Karen Holtzblatt; Shelley Wood This handbook introduces Rapid CD, a fast-paced, adaptive form of Contextual Design. Rapid CD is a hands-on guide for anyone who needs practical guidance on how to use the Contextual Design process and adapt it to tactical projects with tight timelines and resources. Rapid Contextual Design provides detailed suggestions on structuring the project and customer interviews, conducting interviews, and running interpretation sessions. The handbook walks you step-by-step through organizing the data so you can see your key issues, along with visioning new solutions, storyboarding to work out the details, and paper prototype interviewing to iterate the design all with as little as a two-person team with only a few weeks to spare *Includes real project examples with actual customer data that illustrate how a CD project actually works.
Videos

Instructional Presentations on Interview Skills
- Interview/Oral History Research for RSRA 298B: Master's Thesis Reading and Research (Spring 2023) Slideshow covers: Why Interviews?, Getting Context, Engaging Participants, Conducting the Interview, The Interview Guide, Note Taking, Transcription, File management, and Data Analysis.
- Interview Skills From an online class on February 13, 2023: Get set up for interview research. You will leave prepared to choose among the three types of interviewing methods, equipped to develop an interview schedule, aware of data management options and their ethical implications, and knowledgeable of technologies you can use to record and transcribe your interviews. This workshop complements Intro to NVivo, a qualitative data analysis tool useful for coding interview data.
NIH Data Management & Sharing Policy (DMSP) This policy, effective January 25, 2023, applies to all research, funded or conducted in whole or in part by NIH, that results in the generation of scientific data , including NIH-funded qualitative research. Click here to see some examples of how the DMSP policy has been applied in qualitative research studies featured in the 2021 Qualitative Data Management Plan (DMP) Competition . As a resource for the community, NIH has developed a resource for developing informed consent language in research studies where data and/or biospecimens will be stored and shared for future use. It is important to note that the DMS Policy does NOT require that informed consent obtained from research participants must allow for broad sharing and the future use of data (either with or without identifiable private information). See the FAQ for more information.
- << Previous: Remote Research & Virtual Fieldwork
- Next: Oral History >>
Except where otherwise noted, this work is subject to a Creative Commons Attribution 4.0 International License , which allows anyone to share and adapt our material as long as proper attribution is given. For details and exceptions, see the Harvard Library Copyright Policy ©2021 Presidents and Fellows of Harvard College.
- University Libraries
- Research Guides
- Topic Guides
- Research Methods Guide
- Interview Research
Research Methods Guide: Interview Research
- Introduction
- Research Design & Method
- Survey Research
- Data Analysis
- Resources & Consultation
Tutorial Videos: Interview Method
Interview as a Method for Qualitative Research

Goals of Interview Research
- Preferences
- They help you explain, better understand, and explore research subjects' opinions, behavior, experiences, phenomenon, etc.
- Interview questions are usually open-ended questions so that in-depth information will be collected.
Mode of Data Collection
There are several types of interviews, including:
- Face-to-Face
- Online (e.g. Skype, Googlehangout, etc)
FAQ: Conducting Interview Research
What are the important steps involved in interviews?
- Think about who you will interview
- Think about what kind of information you want to obtain from interviews
- Think about why you want to pursue in-depth information around your research topic
- Introduce yourself and explain the aim of the interview
- Devise your questions so interviewees can help answer your research question
- Have a sequence to your questions / topics by grouping them in themes
- Make sure you can easily move back and forth between questions / topics
- Make sure your questions are clear and easy to understand
- Do not ask leading questions
- Do you want to bring a second interviewer with you?
- Do you want to bring a notetaker?
- Do you want to record interviews? If so, do you have time to transcribe interview recordings?
- Where will you interview people? Where is the setting with the least distraction?
- How long will each interview take?
- Do you need to address terms of confidentiality?
Do I have to choose either a survey or interviewing method?
No. In fact, many researchers use a mixed method - interviews can be useful as follow-up to certain respondents to surveys, e.g., to further investigate their responses.
Is training an interviewer important?
Yes, since the interviewer can control the quality of the result, training the interviewer becomes crucial. If more than one interviewers are involved in your study, it is important to have every interviewer understand the interviewing procedure and rehearse the interviewing process before beginning the formal study.
- << Previous: Survey Research
- Next: Data Analysis >>
- Last Updated: Aug 21, 2023 10:42 AM
Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
Methodology
- What Is Qualitative Research? | Methods & Examples
What Is Qualitative Research? | Methods & Examples
Published on June 19, 2020 by Pritha Bhandari . Revised on June 22, 2023.
Qualitative research involves collecting and analyzing non-numerical data (e.g., text, video, or audio) to understand concepts, opinions, or experiences. It can be used to gather in-depth insights into a problem or generate new ideas for research.
Qualitative research is the opposite of quantitative research , which involves collecting and analyzing numerical data for statistical analysis.
Qualitative research is commonly used in the humanities and social sciences, in subjects such as anthropology, sociology, education, health sciences, history, etc.
- How does social media shape body image in teenagers?
- How do children and adults interpret healthy eating in the UK?
- What factors influence employee retention in a large organization?
- How is anxiety experienced around the world?
- How can teachers integrate social issues into science curriculums?
Table of contents
Approaches to qualitative research, qualitative research methods, qualitative data analysis, advantages of qualitative research, disadvantages of qualitative research, other interesting articles, frequently asked questions about qualitative research.
Qualitative research is used to understand how people experience the world. While there are many approaches to qualitative research, they tend to be flexible and focus on retaining rich meaning when interpreting data.
Common approaches include grounded theory, ethnography , action research , phenomenological research, and narrative research. They share some similarities, but emphasize different aims and perspectives.
Note that qualitative research is at risk for certain research biases including the Hawthorne effect , observer bias , recall bias , and social desirability bias . While not always totally avoidable, awareness of potential biases as you collect and analyze your data can prevent them from impacting your work too much.
Receive feedback on language, structure, and formatting
Professional editors proofread and edit your paper by focusing on:
- Academic style
- Vague sentences
- Style consistency
See an example

Each of the research approaches involve using one or more data collection methods . These are some of the most common qualitative methods:
- Observations: recording what you have seen, heard, or encountered in detailed field notes.
- Interviews: personally asking people questions in one-on-one conversations.
- Focus groups: asking questions and generating discussion among a group of people.
- Surveys : distributing questionnaires with open-ended questions.
- Secondary research: collecting existing data in the form of texts, images, audio or video recordings, etc.
- You take field notes with observations and reflect on your own experiences of the company culture.
- You distribute open-ended surveys to employees across all the company’s offices by email to find out if the culture varies across locations.
- You conduct in-depth interviews with employees in your office to learn about their experiences and perspectives in greater detail.
Qualitative researchers often consider themselves “instruments” in research because all observations, interpretations and analyses are filtered through their own personal lens.
For this reason, when writing up your methodology for qualitative research, it’s important to reflect on your approach and to thoroughly explain the choices you made in collecting and analyzing the data.
Qualitative data can take the form of texts, photos, videos and audio. For example, you might be working with interview transcripts, survey responses, fieldnotes, or recordings from natural settings.
Most types of qualitative data analysis share the same five steps:
- Prepare and organize your data. This may mean transcribing interviews or typing up fieldnotes.
- Review and explore your data. Examine the data for patterns or repeated ideas that emerge.
- Develop a data coding system. Based on your initial ideas, establish a set of codes that you can apply to categorize your data.
- Assign codes to the data. For example, in qualitative survey analysis, this may mean going through each participant’s responses and tagging them with codes in a spreadsheet. As you go through your data, you can create new codes to add to your system if necessary.
- Identify recurring themes. Link codes together into cohesive, overarching themes.
There are several specific approaches to analyzing qualitative data. Although these methods share similar processes, they emphasize different concepts.
Qualitative research often tries to preserve the voice and perspective of participants and can be adjusted as new research questions arise. Qualitative research is good for:
- Flexibility
The data collection and analysis process can be adapted as new ideas or patterns emerge. They are not rigidly decided beforehand.
- Natural settings
Data collection occurs in real-world contexts or in naturalistic ways.
- Meaningful insights
Detailed descriptions of people’s experiences, feelings and perceptions can be used in designing, testing or improving systems or products.
- Generation of new ideas
Open-ended responses mean that researchers can uncover novel problems or opportunities that they wouldn’t have thought of otherwise.
Here's why students love Scribbr's proofreading services
Discover proofreading & editing
Researchers must consider practical and theoretical limitations in analyzing and interpreting their data. Qualitative research suffers from:
- Unreliability
The real-world setting often makes qualitative research unreliable because of uncontrolled factors that affect the data.
- Subjectivity
Due to the researcher’s primary role in analyzing and interpreting data, qualitative research cannot be replicated . The researcher decides what is important and what is irrelevant in data analysis, so interpretations of the same data can vary greatly.
- Limited generalizability
Small samples are often used to gather detailed data about specific contexts. Despite rigorous analysis procedures, it is difficult to draw generalizable conclusions because the data may be biased and unrepresentative of the wider population .
- Labor-intensive
Although software can be used to manage and record large amounts of text, data analysis often has to be checked or performed manually.
If you want to know more about statistics , methodology , or research bias , make sure to check out some of our other articles with explanations and examples.
- Chi square goodness of fit test
- Degrees of freedom
- Null hypothesis
- Discourse analysis
- Control groups
- Mixed methods research
- Non-probability sampling
- Quantitative research
- Inclusion and exclusion criteria
Research bias
- Rosenthal effect
- Implicit bias
- Cognitive bias
- Selection bias
- Negativity bias
- Status quo bias
Quantitative research deals with numbers and statistics, while qualitative research deals with words and meanings.
Quantitative methods allow you to systematically measure variables and test hypotheses . Qualitative methods allow you to explore concepts and experiences in more detail.
There are five common approaches to qualitative research :
- Grounded theory involves collecting data in order to develop new theories.
- Ethnography involves immersing yourself in a group or organization to understand its culture.
- Narrative research involves interpreting stories to understand how people make sense of their experiences and perceptions.
- Phenomenological research involves investigating phenomena through people’s lived experiences.
- Action research links theory and practice in several cycles to drive innovative changes.
Data collection is the systematic process by which observations or measurements are gathered in research. It is used in many different contexts by academics, governments, businesses, and other organizations.
There are various approaches to qualitative data analysis , but they all share five steps in common:
- Prepare and organize your data.
- Review and explore your data.
- Develop a data coding system.
- Assign codes to the data.
- Identify recurring themes.
The specifics of each step depend on the focus of the analysis. Some common approaches include textual analysis , thematic analysis , and discourse analysis .
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
Bhandari, P. (2023, June 22). What Is Qualitative Research? | Methods & Examples. Scribbr. Retrieved April 8, 2024, from https://www.scribbr.com/methodology/qualitative-research/
Is this article helpful?

Pritha Bhandari
Other students also liked, qualitative vs. quantitative research | differences, examples & methods, how to do thematic analysis | step-by-step guide & examples, unlimited academic ai-proofreading.
✔ Document error-free in 5minutes ✔ Unlimited document corrections ✔ Specialized in correcting academic texts
- All services
- Transcriptions samples
- Captions and subtitles samples
- Multi-languages
We Trust in Human Precision
20,000+ Professional Language Experts Ready to Help. Expertise in a variety of Niches.
- API Pricing
- Cost estimate
- Customer loyalty program
- Educational Discount
- Non-Profit Discount
- Green Initiative Discount1
Value-Driven Pricing
Unmatched expertise at affordable rates tailored for your needs. Our services empower you to boost your productivity.
- Special Discounts
- Enterprise transcription solutions
- Enterprise translation solutions
- Transcription/Caption API
- AI Transcription Proofreading API
Trusted by Global Leaders
GoTranscript is the chosen service for top media organizations, universities, and Fortune 50 companies.
- API solutions
GoTranscript
One of the Largest Online Transcription and Translation Agencies in the World. Founded in 2005.

How To Conduct Interviews in Qualitative Research

Qualitative research interviews are in-depth interviews that aim to answer detailed questions from customers or leads. It’s a more personal form of research that seeks to probe deep into the minds of the interview participant. This also elicits a better and more valuable discussion of the topic.
What is the difference between qualitative and quantitative interviews?
While quantitative interviews usually measure data, qualitative focus on the ideas, beliefs, and mindsets of people. Most research interviews give business insights into how their consumer react or make decisions about their product or service.
Business owners benefit from qualitative research interviews by identifying their customer needs. Through qualitative research, businesses can gain perspective on how their service or product benefits their customer’s lifestyles. It also helps them clarify important marketing messages to generate ideas for improvement for their product or brand.
Qualitative research interviews include open-ended questions that invite people to their stories using their own words. The following are some things qualitative research can give insight about:
- Consumer behavior for improving business decisions
- The social reality of people in a group or culture
Formatting of Qualitative Research Interviews
Qualitative research interviews are usually done one-on-one or in focus groups. The interview often revolves around the interviewee’s opinion, knowledge, and feelings about the subject. Most qualitative research interviews are in person, but there are also interviews that are made over the phone or through video chat. They usually span around 30 to 90 minutes.
Conducting Qualitative Research Interviews
Qualitative interviews are similar to deep conversations. The interviewer and interviewee have a conversation about a topic with the goal of gathering information and insight from the respondent. The questions are open-ended and often require participants to use their own words and phrases.
Step 1: Identifying Your Objective
Before performing any interview, the interviewer must first have goals for the project. The goals or objectives will often be based on questions that should be answered. Here are examples of questions to find your objectives for the interview:
- Who is your target respondent?
- What is it that you’d like to learn?
- How would you use the results?
The first step is simply the preparation stage that will help guide your future steps. But it will dictate the success of the next steps.
Step 2: Listing Your Target Respondents
Once you’ve defined your objectives, the next step is to determine your respondents. Research interviews with clients or customers are the easiest as most companies already have a database list of their customers’ email, names, and phone numbers. If you wish to interview strangers or non-customers, the process will take more time and will be more costly since you have no prior relationship with the people you want to interview.
Step 3: Prepare Yourself Before the Interview
Preparation is important for every interview. Successful planning and consideration of everyone involved is key to having informative and valuable results. If you’re interviewing someone and you’ll have to discuss a subject, a deep reading about the topic will help you develop great questions that will improve the overall experience of your interview.
If you’re conducting a qualitative interview, you should test your equipment such as your recording tools and other gadgets that will be used. The important thing to remember is that the location, time, and tools used shouldn’t affect data collection.
Step 4: Do a Test Run
Have a few test interviews to help you improve your questions and interview techniques. If you’re doing a study, this will be helpful in improving the quality of the research. Data from test interviews are often discarded since they aren’t very useful. It’s important to have a few test interviews to create a better and less biased result later on.
Step 5: Build rapport with your interviewees
Building rapport with your respondents is very important before and after the interview. The reason many interviews fail is that the respondent doesn’t trust the interviewer that much to reveal information. If it’s an interview with a single person that will be publicized, it helps if you draft a short summary of your questions to inform the person what you’ll be talking about in the interview.
Step 6: Be prepared to listen
When you’re interviewing someone you have to show that you respect them and remain interested in what they have to say. Active listening is something many people have struggled with, unfortunately, even interviewers. There are many novice interviewers who often talk a lot during conversations. This can be caused by nervousness or lack of experience.
To actively listen is to respect your respondent. It helps them think more about their answers which can then help you gain open and honest interview results.
Other Important Research Interview Tips
- Make sure all questions given are understandable and clear. Review all questions you have before the interview itself. Always carry a list of questions that you have to ask during the interview.
- Let the respondents know the purpose of the interview. The respondents have the right to know the nature of the interview and what the results are going to be used for.
- Ask to clarify and repeat answers if you don’t understand them. Never assume answers from the people you interview.
- Avoid irrelevant discussions. It’s okay to stray away from the topic, but always try to inform your respondent that the interview should be focused on a certain topic.
- Keep it short. Make interviews short, just around an hour or two.
- Summarize the interview. After the interview, do a short summary of the points you’ve covered and asked for during the course of the interview.
How To Analyze Qualitative Interview Data
Most analysis of qualitative interview data begins with reviewing transcripts of the interviews. Transcripts can be obtained by taking notes during the interview or recording the interview with a digital device and transcribing it afterward. Transcripts give you a written copy of the interview word for word. Transcripts also include non-verbal gestures and tone of voice that allow the interview to be reviewed more accurately later on.
- Open access
- Published: 05 April 2024
Challenges to conducting research on oral health with older adults living in long-term care facilities
- Thayse Mayra Chaves Ramos 1 ,
- Álvaro Augusto da Silva Alves 1 ,
- Thais Andrade Apolinário 1 ,
- Flávia Fonseca de Toledo 1 ,
- Viviane Elisângela Gomes 1 ,
- Kevan Guilherme Nóbrega Barbosa 1 ,
- Aline Araújo Sampaio 2 &
- Raquel Conceição Ferreira 1
BMC Oral Health volume 24 , Article number: 422 ( 2024 ) Cite this article
12 Accesses
1 Altmetric
Metrics details
The challenges to conducting oral health studies involving older people in long-term care facilities (LTCFs) must be debated.
This study aimed to investigate researchers’ perceptions and experiences while conducting an epidemiological survey on oral health among older individuals residing in LTCFs.
A qualitative study was conducted involving six researchers who utilized field diaries to record their impressions during data collection through interviews (older individuals (or their proxies), caregivers, and LTCF coordinators) and oral examinations of the older people participants. Additionally, researchers responded to open-ended questions about their experiences. The collected material was subjected to content analysis by two researchers.
The themes that emerged from the analysis were institutional context, aspects affecting the operationalization of the study, and data collection oriented by the clinical-functional profile of the older people. According to the researchers’ perceptions, LTCF coordinators demonstrated concern for the study’s benefits for older adults and the preservation of institutional routines during the research process. Caregivers emerged as vital sources of information, guiding researchers in navigating the challenges posed by the physical and mental complexities of the older people participants, necessitating empathy, sensitivity, and attentive listening from the researchers. The organization of materials and a streamlined data collection process proved essential for optimizing time efficiency and reducing stress for participants and researchers.
The researchers recognized the important role played by LTCF coordinators and formal caregivers, underscoring the significance of empathetic methodologies and streamlined data collection processes in mitigating the challenges inherent to research conducted within LTCFs.
Peer Review reports
Population aging is a global phenomenon presenting significant challenges to healthcare systems worldwide due to the burden of chronic age-related conditions [ 1 ]. The aging process often leads to frailty and increased functional dependence, resulting in a notable rise in institutionalization [ 2 ]. In Brazil, as observed in other countries like the United States, France, and China, the age pyramid has undergone an inversion, contributing to a higher prevalence of chronic diseases and functional dependence among older individuals. Consequently, the population residing in long-term care facilities (LTCFs) has grown substantially [ 3 , 4 , 5 ].
Older adults living in LTCFs generally depend more on daily activities than their non-institutionalized counterparts, and oral health is a prominent concern [ 6 , 7 ]. Institutionalization can negatively impact older individuals eating habits, cognition, and overall functioning, resulting in deteriorating health conditions [ 6 , 8 ]. Furthermore, significant barriers to oral health care exist within nursing home settings [ 9 , 10 ]. The oral health of this group is characterized by severe tooth loss, oral diseases, and biofilm accumulation [ 11 , 12 , 13 ]. These conditions have been associated with adverse outcomes in terms of general health, quality of life, and mortality [ 14 ]. In Brazil, the operations of LTCFs are regulated by the National Vigilance Agency. However, despite the recognized need to improve oral health care provision in these institutions, the regulations do not explicitly address oral health. Therefore, research in LTCFs is imperative to generate robust scientific evidence concerning the oral health needs of older individuals. Such evidence is essential for enhancing standards of care and making informed decisions that prioritize the overall health and well-being of older populations. A recent review analyzing barriers to translating research into oral healthcare policy and practice for older adults stressed the need for increased efforts to undertake research involving older adults, including frail older adults living in residential care, to develop an evidence-informed paradigm for oral health care and expand policies and care practices for this age group [ 15 ].
However, conducting studies involving older people in LTCFs poses numerous challenges, demanding meticulous planning, considerable time, and ample resources to overcome these obstacles [ 16 ]. Nevertheless, there is a lack of research discussing these challenges [ 17 , 18 , 19 ], particularly strategies to include older individuals with dementia in studies [ 20 , 21 ]. Although health research may share similar challenges, none of these studies have discussed research experiences, including oral health assessment. The previously reported challenges were related to obtaining consent, conducting interviews, engaging caregivers and family members, maintaining privacy, addressing participant attrition, obtaining sufficient sample sizes, accounting for intra-institution cluster effects, dealing with incomplete data, and navigating rigid LTCF practices and routines [ 16 , 17 , 18 , 19 , 20 , 21 ]. For older individuals with dementia, researchers emphasize the need for inclusive strategies, considering their communication difficulties, memory loss, diminished autonomy in decision-making, and emotional disposition [ 20 ]. The only identified systematic review on methods for involving older people in health-related studies highlights the viability of studies involving older adults, emphasizing the importance of clear communication, building good relationships, and employing flexible approaches [ 22 ].
This study aimed to investigate researchers’ perceptions and experiences while conducting an epidemiological survey of oral health among older individuals residing in LTCFs. The findings of this study can provide a valuable understanding of the challenges faced during the study and identify effective strategies to improve the quality and efficiency of future research in this context. Furthermore, understanding researchers’ perspectives makes it possible to develop specific recommendations to enhance research methods for this vulnerable population. By addressing these challenges and designing effective strategies, this research can improve the quality of studies focusing on older populations living in LTCFs and promote evidence-informed oral healthcare policies and practices for this age group.
This study employed a qualitative method with a phenomenological approach to explore the experiences of researchers during data collection with older individuals residing in LTCFs and their perceptions of the execution of this work. The phenomenological approach, centered on language, seeks to capture the essence of the lived experience and the emergent meanings from that experience. Previous knowledge of the phenomenon is disregarded to explore how the subjects experience events [ 23 , 24 ]. Field diaries and an online form with open-ended questions were used to explore the researchers’ experiences.
Context of study
The research was conducted at philanthropic LTCFs in Belo Horizonte, Brazil, during a cross-sectional study between August 2022 and March 2023. In 2022, there were 28 philanthropic LTCFs in the city. The sample planning aimed to include all older individuals residing in these facilities, irrespective of their cognitive status. The study participants were coordinators of the LTCFs, formal caregivers of older people, and individuals aged 60 years or older residing in these facilities. The formal caregivers of the older adults were remunerated professionals with employment ties in the LTCFs, having received specific training as elderly caregivers or being nursing technicians. During data collection, they assisted and cared for the older adults. Epidemiological data were collected through interviews with the coordinators, formal caregivers, and older individuals or their proxies (caregivers). The collected variables followed the model of the International Classification of Functioning, Disability, and Health (Fig. 1 ), which included anthropometric measures and physical and oral examinations conducted at the LTCFs.
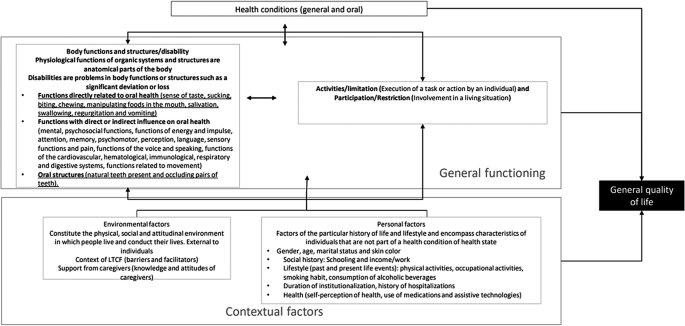
Model adapted from International Classification of Functioning, Disability and Health
The six researchers involved in the study had undergone prior training for conducting interviews, and four of them received calibration exercises for the oral examinations. All six researchers participated in the data collection process for the epidemiological research. These researchers consisted of both undergraduate dental students and master’s degree graduate students, who formed pairs to serve as interviewers, examiners, and/or assistants (annotators).
A pilot study was carried out at one of the LTCFs participating in the research to ensure the smooth execution of the study. This pilot study allowed for testing the digital data recording tools and refining the sequence and dynamics for conducting interviews and examinations. The pilot study served as a preparatory phase, ensuring the research procedures were well-coordinated and optimized before the main data collection phase.
Procedure and participants
The research utilized a field diary as the primary method to record informal conversations, observations of the behavior of older people and formal caregivers during data collection, reflections on the examination process and methods employed, as well as the researchers’ impressions regarding the data collection process within the LTCF setting [ 25 , 26 ]. Researchers independently and freely made digital-format entries in their respective field diaries.
All six researchers independently and freely made digital-format entries in their respective field diaries. Criterion sampling was the method utilized for selecting this sample, which encompassed all researchers who have shared an experience, yet exhibit variations in characteristics and individual experiences [ 27 ]. In addition to the field diary, an online form with open-ended questions was employed to collect individual feedback from each researcher about their feelings and experiences as a researcher during the fieldwork. The form included the following guiding questions: (1) How was your experience collecting data at the LTCFs, considering the older people, caregivers, and LTCF context? (2) What was the most striking aspect during the days you collected data at the LTCFs? (3) If you were to advise a researcher about beginning data collection at a long-term care facility through interviews with older people, what observations would you share to ensure their success? (4) what is the main aspect that should be considered for satisfactory data collection with older people similar to those encountered at the LTCFs? The responses to these questions contributed to the researchers’ reflections and perspectives. They were considered part of the corpus of analysis for the study.
Data analysis
The contents of the field diaries and open-ended questions were independently submitted to exhaustive readings by two researchers with experience in qualitative studies for a more in-depth capturing of the information. Subsequently, the data underwent content analysis, following the approach proposed by Graneheim and Lundman [ 28 ]. The researchers identified units of meaning within the records and extracted the essence of each unit, resulting in the creation of condensed units of meaning. Through this process, categories and themes that emerged from the analyzed content were identified. Reliability was ensured through continual discussion of the data with the team. Consensus meetings were held to ensure agreement on the themes that emerged. In the final analysis, codes such as R1, R2, and so forth were used to represent each of the interviewees, allowing for a systematic and organized representation of the participants’ contributions.
Ethical aspects
This study received approval from the Human Research Ethics Committee of the Universidade Federal de Minas Gerais. The participants signed a statement of informed consent.
Results and discussion
The data collection for the epidemiological study on oral health assessment in 14 LTCFs, 311 older people, and 164 formal caregivers involved six researchers. They recorded their observations in field diaries and responded to open-ended questions. Through content analysis of the field diaries and open-ended questions, three main themes emerged: (1) institutional context, (2) aspects affecting the operationalization of the study, and (3) data collection oriented by the clinical-functional profile of the older people. The categories under each theme are presented in Table 1 .
Institutional context
Results regarding the institutional context are presented in Table 2 , showcasing the units of meaning that illustrate the categories within this theme. The researchers recognized the crucial social role played by LTCFs in reintegrating older people, particularly those who have experienced neglect or loneliness, perceiving these institutions as mandated by Brazilian legislation to care for and support older individuals [ 29 ]. Regarding the ambience of LTCFs , the study revealed a wide variation in the activities and services offered to residents across different institutions. As stipulated by the Brazilian Resolution, LTCFs should provide a welcoming environment that upholds older people’s human rights and dignity, including aspects such as identity, freedom of beliefs, freedom to come and go, privacy, and respect [ 30 ]. The ambience also encompasses fostering family and community involvement in caregiving, the coexistence of residents with different degrees of dependence, supporting residents’ autonomy, promoting leisure opportunities, and preventing violence or discrimination against residents [ 29 ]. The Brazilian regulation also standardizes structural aspects of the LTCFs, human resources, health care, nutrition, washing, processing, and storage of clothing, and cleaning facilities [ 29 ]. The researchers’ perceptions indicated the importance of establishing systematized assessment processes to reveal the different levels of quality of the LTCFs, indicating the need for policies that favor achieving the principles of ambience and the well-being of the older people who reside in these facilities.
The profile of the older people living in the LTCFs , as recorded by the researchers, was characterized by high frequencies of cognitive impairment, clinical-functional frailty, mental and behavioral disorders, and dependence in performing basic and instrumental activities of daily living. These characteristics posed challenges during the data collection process, as many participants exhibited refusal, resistance, and low levels of cooperation with the study due to their health conditions. This clinical-functional profile is similar to that described for older people living in long-term care facilities worldwide [ 8 , 14 ]. The researchers also observed rapid functional decline among the older people during the data collection period when the same individuals were visited on different occasions from one week to the next. As a cross-sectional study, the researchers sought to conclude data collection in the first and only approach to older people, whenever possible.
Moreover, fluctuating interest in participation necessitated additional attempts to secure their involvement due to emotional and health-related fluctuations. A previous study involving older people with dementia found that verbal communication varied between weeks, from one day to another, and even within the same day [ 20 ]. Another challenge was dealing with the losses of individuals. Data collection began with mapping all residents at the institution by consulting the records. When seeking older people for interviews, there were cases of death – either recent or longer ago. In the latter case, it was perceived that the LTCFs did not perform regular updating and the separation of records.
Regarding oral health , the researchers identified a precarious situation among older people, with a high frequency of tooth loss, caries, and periodontal disease in the remaining teeth, along with unsatisfactory dental prostheses and accumulation of biofilm and dental calculus. This oral health profile aligns with previous studies in different countries, highlighting the substantial burden of oral diseases among institutionalized older individuals [ 13 , 31 , 32 ]. This researchers perception reflects the oral health profile of older people living in LTCFs in Belo Horizonte for more than a decade and a half [ 12 ], demonstrating that this population is a special needs group requiring oral care improvements [ 11 , 31 ].
The researchers recorded the difficulty of older people accessing routine oral care, as many depend on caregivers who have an excessive workload, have little time available to perform oral hygiene, do not prioritize it, or are unaware of its importance. A daily routine of oral hygiene during bathing was often observed, as reported in a previous study, in which nurses reported that the teeth of the majority of residents were brushed at least once a day [ 13 ]. The researchers’ findings underscore the pressing need for improved oral care for this special needs population, emphasizing the importance of incorporating oral hygiene into routine healthcare practices, promoting oral care initiatives, and providing training for caregivers [ 13 , 33 ].
Aspects affecting the operationalization of the study
The researchers encountered various challenges related to the operationalization of the study, particularly in gaining the acceptance and cooperation of LTCFs. Results regarding the operationalization of the study are presented in Table 3 . The signing of informed consent by the LTCF coordinators proved to be a complex process, with many expressing resistance and skepticism about the study’s potential impact and benefits for the older residents. Some questioned the importance of a study involving individuals at the end of life. The researchers faced concerns about interrupting institutional routines and potential risks to the residents without any direct return. Similar challenges have been observed in studies conducted in the United Kingdom, where the presence of researchers was perceived as intrusive [ 17 ]. In compliance with Brazilian legislation on research involving human beings, participation must be consented to clearly and voluntarily with no financial compensation. As experienced by other researchers, flexibility and creativity were needed to justify the importance of the project to generate evidence that reinforces the importance of oral health for this group. It was also essential to emphasize the low risk associated with the participation of older individuals [ 17 ]. Establishing a trusting relationship with the coordinators of the LTCFs proved vital for their willingness to participate in the study. The researchers tried to showcase the study’s potential in generating valuable knowledge, organizing academic extension activities tailored to this specific population, and the potential benefits it could bring to enhance resident care. The presence of researchers might have encountered increased resistance during the pandemic, leading to visit cancellations due to concerns about the higher risk of mortality and morbidity from the coronavirus among older people [ 34 ].
The study planning at LTCFs should include the time spent on recruitment and the need for different approaches for contact: repeated telephone calls, personal visits, the presentation of documents/written projects, and the joint determination of a data collection timeframe. Researchers should also be prepared to deal with refusals, as occurred in this study when coordinators vehemently refused to participate, stating that they did not have the authorization or that the LTCF was part of a network that did not permit study participation. This challenge shows that building collaborative relationships with LTCFs is essential to understand research concerns clearly and to plan a project involving vulnerable adults jointly [ 15 ]. In contrast, the researchers also recorded situations in which the coordinators were receptive to the study, recognizing that it is important to demonstrate the needs of this population, which could result in programs and policies for older people who reside in LTCFs.
The process of obtaining informed consent from the older residents themselves was also challenging, especially for those with severe cognitive impairment. In such cases, consent was given by caregivers or LTCF coordinators acting as guardians of the older people. The issue of consent by proxy and the ability of the proxy to represent the wishes of cognitively impaired adults has been a subject of debate [ 15 ]. Several researchers have highlighted the challenges of obtaining informed consent and respecting the autonomy of individuals with dementia [ 16 , 17 , 18 , 19 , 20 , 21 , 35 ]. Hubbard and Maas emphasized the importance of continually monitoring the individual’s desire to participate, even when a proxy provides consent through the interpretation of verbal and nonverbal signs. They asserted that consent is an ongoing process rather than an a priori one-time event, as Crossan & McColgan (1999) mentioned. We encountered similar situations where residents could not provide direct consent. In such cases, the researchers took great care to explain the study and obtain their assent while interpreting their facial expressions and behavior to respect their autonomy and wishes. Despite these efforts, 15 invited older people chose not to participate.
The institutional routines of LTCFs significantly impacted the study execution. Researchers had to consider and respect the schedules and activities of the older residents, leading to adjustments in the data collection timeframe. Additionally, finding suitable times for interviews and examinations was challenging due to the residents’ mobility problems and caregivers’ availability. The researchers had to collaborate with LTCF coordinators to find mutually agreeable time slots while ensuring minimal disruption to the institution and its residents. Finding suitable time slots to conduct interviews was also a significant challenge, as observed in a previous study exploring the perception of dignity among older people residing in LTCFs [ 19 ]. The authors of that study emphasized the need to avoid peak activity times, such as meals or regular visits by physicians, and to avoid conducting interviews immediately after an activity, such as lunch, as participants often displayed weariness and lethargy during such periods [ 19 ]. To overcome this challenge, the research team collaborated with the LTCF coordinators to agree on appropriate data collection times that did not disrupt the institution’s routines or inconvenience the residents. This required a significant consideration of each location’s availability and the staff’s workload. Other researchers have noted these challenges [ 17 , 19 , 20 , 21 , 35 ], especially considering that caregivers are crucial as proxies for older people. Researchers also had to contend with the unavailability of caregivers to answer questions due to their multifaceted responsibilities in caring for many residents. Introducing the study could thus be an additional burden for them, which many might perceive as unwanted.
In addition to respecting the institutional dynamics, the execution of data collection required careful organization by the researchers regarding the selection of data collection location and methods . Many residents faced mobility issues, making moving from one place to another challenging. In some instances, caregivers were unavailable to assist in this task, requiring additional time to reach the most suitable location for the interview or oral examination. Factors such as lighting, privacy, and participant comfort had to be considered during this process. Adapting the data collection process to the specific situation encountered at each LTCF was necessary. Some facilities had designated spaces for the study, while others lacked appropriate areas, leading to examinations being conducted wherever possible, such as in TV armchairs or beds. Previous studies have discussed the need for such adaptations [ 17 , 20 ]. According to Hall, Longhurst and Higginson, these field situations also posed challenges to maintaining privacy during data collection, which became especially sensitive during oral examinations [ 19 ]. The proximity required for oral examinations could generate discomfort, mainly when conducted in the presence of colleagues and staff. Efforts were made to ensure privacy in such situations. Consequently, conducting studies in this context demanded considerable flexibility and reciprocity, considering the limitations and demands of the LTCFs [ 19 ]. The researchers were also concerned about biosafety and cross-infection prevention [ 36 ], mainly due to the vulnerability of older people to the COVID-19 pandemic. Adhering to strict protocols and protective measures during data collection became essential to safeguard the health of both residents and researchers.
Various measures can be employed to ensure standardization and successful data collection. Providing proper training and ongoing supervision for the researchers is essential. This training should cover all aspects of the data collection process, including interview techniques, oral examination protocols, and ethical considerations. Additionally, it is crucial to ensure that the researchers have access to the minimum necessary resources required for data collection, such as sterilized clinical kits, personal protective equipment, and appropriate data recording tools. A comprehensive manual of norms and standard procedures should be prepared to maintain consistency and adherence to established protocols. This manual should outline step-by-step instructions for each stage of the data collection process, from participant recruitment to data recording and analysis. Regular reference to this manual will help researchers follow standardized procedures and minimize the risk of errors or deviations during the study [ 37 ].
The high proportion of older people with cognitive impairment created additional complexities. Variables related to subjective aspects, such as quality of life and self-perception of health, posed challenges since some residents had limited discursive capacity. The researchers utilized validated instruments designed for older adults with adequate cognitive levels but recognized the need for more context-specific tools for individuals with dementia. Challenges to assessing subjective aspects of the lives of older people with dementia have been discussed, considering the lack of validated instruments for this population. There is a debate in the literature on whether data collected from individuals with dementia are reliable due to cognitive impairment [ 38 ]. However, more recently, there has been growing recognition that such individuals can express perceptions, needs, and concerns [ 38 , 39 ], and their subjective experiences should be considered and investigated in studies [ 20 , 39 ]. Approaches such as structured observation focused on nonverbal communication (facial expressions and body language) and nonstructured observation within the ethnographic tradition have been employed in previous studies to understand the social world of older people [ 20 ]. A study assessing quality of life among older people with dementia combined observation with interviews using open-ended questions, and older people were included based on their capacity to communicate verbally in a conversation rather than based on the diagnosis of dementia [ 20 ]. The literature describes the need to use multiple (qualitative and quantitative) methods in studies involving individuals with dementia with different levels of verbal communication skills to promote a contextualized, multidimensional assessment [ 39 ]. Such approaches should also be considered strategies to understand the quality of life in the context of oral health assessments in future studies and to guide care strategies considering the experiences and wishes of individuals with dementia.
Data collection oriented by the clinical-functional profile of the older people
The researchers revealed that the clinical-functional profile of older people requires differentiated approaches for data collection, particularly the use of relational skills, such as empathy, active listening, patience, sensitivity, and flexibility to deal with different behaviors – ranging from cooperative to resistant individuals. Results regarding the data collection oriented by the clinical-functional profile of the older people are presented in Table 4 . Cognitive impairment and levels of cooperation were identified as obstacles to the data collection process, with frequent resistance to the study. The progression of cognitive decline leads to a deterioration of cognitive functions and behavior and mood disorders, including depression, irritability, and aggressiveness [ 40 , 41 , 42 ].
This profile of the older people also required communication strategies on the part of the researchers, who needed to be direct and clear, often involving the participation of the caregivers. The researchers manifested insecurity, feeling unprepared to understand and deal with older people in some situations. Hubbard, Downs, and Tester [ 20 ] suggest that researchers dealing with dementia should be trained as skilled verbal and nonverbal communicators, sensitive to how dementia impacts memory, decision-making capacity, and emotions. Developing strategies tailored to each participant’s unique experiences and listening to their voice is essential. Hall, Longhurst, and Higginson [ 19 ] add that researchers must be particularly patient, and the extra time and training for this must be built into the research design. Establishing set protocols for handling various responses ensures uniformity and consistency [ 19 ]. Researchers also had to contend with parallel conversations,” where older people spoke about other subjects and extended the conversation. This required employing different communication strategies and striking a balance between listening to the older person and returning to the assessment without causing discomfort [ 16 , 20 ].
Sensory impairments, such as low visual and hearing acuity, also compromise communication. Hearing impairment is common among older people [ 43 ], and there are also high proportions of blindness and vision impairment among residents of LTCFs [ 44 , 45 ]. Interviews involving older people with hearing impairment were found to be draining, as the researchers needed to raise their voices and repeat questions. This limitation can negatively impact the quality of dialogue and create discomfort for the older person [ 20 ].
The researchers highlighted the caregivers’ knowledge in guiding the data collection process according to the clinical-functional profile of the participants. Being familiar with older people and their physical and mental status, caregivers served as valuable mediators, offering insights into effective communication and strategies for dealing with each case. Caregivers of older people perform the functions of accompaniment and care, offering emotional support as well as support in their social interactions, assisting and accompanying routines of personal and environmental hygiene, nutrition, preventive health care, the administration of medications and other health procedures, and assisting and accompanying the mobility of older people in activities of education, culture, recreation, and leisure [ 46 ]. Moreover, caregivers also acted as a proxy for older adults with cognitive impairment, providing information about health and daily activities. The researchers recognized caregivers as a source of support during data collection, contributing to a more efficient and enjoyable data collection process by helping identify older people and guiding them to data collection locations.
The research techniques proved suitable and valuable for understanding the researchers’ experiences. The records of these experiences revealed various challenges and strategies in conducting studies involving older people residing in LTCFs, considering the diversity of residents’ profiles and the institutional context. Table 5 presents a synthesis of the main challenges and the strategies employed to deal with them during the data collection process. Additionally, practical aspects have been listed as recommendations for future studies involving this population.
The main limitation of this study was to have restricted the researchers’ records to field diaries and a form with open-ended questions. Verbal manifestations during the interviews could have revealed new or different perceptions from what was recorded. However, all material obtained was analyzed. The information on the forms at the end of the data collection period had similar content to that recorded during the process but was more synthesized and systematized. Thus, these were complementary methods that demonstrated consistency in the perceptions of the researchers’ experiences.
The researchers recognized the important role played by LTCF coordinators and formal caregivers, underscoring the significance of empathetic methodologies and streamlined data collection processes in mitigating the challenges inherent to research conducted within LTCFs. The institutional context significantly influences the planning and execution of research involving older adults residing in LTCFs, particularly those with clinical-functional profiles that necessitate specific tailored approaches. Respecting older adults’ autonomy and establishing effective and respectful communication are fundamental for building trust. Recognizing the caregivers’ knowledge provides valuable understanding for the data collection process. The LTCF willingness to participate in the research reflects their commitment to advancing knowledge in the field while upholding institutional routines and residents’ well-being. Beyond methodological considerations, such as selecting appropriate variables, defining the sample, and employing valid measures, social and cultural aspects of the LTCFs can impact costs, required human resources, and the execution timeline. In conclusion, conducting studies in LTCFs demands careful planning, effective communication, and flexibility to address institutional and residents’ diverse profiles. Collaborating closely with LTCF staff and caregivers is essential for successful data collection and ultimately benefiting this vulnerable population.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
WHO. World health statistics 2020: monitoring health for the SDGs, sustainable development goals. 2020. https://digitalcommons.fiu.edu/cgi/viewcontent.cgi?article=1547&context=srhreports . Acesso em 5 de agosto de 2023.
Hajek A, Brettschneider C, Lange C, et al. Longitudinal predictors of institutionalization in Old Age. PLoS ONE. 2015;10(12):e0144203. https://doi.org/10.1371/journal.pone.0144203 .
Article CAS PubMed PubMed Central Google Scholar
China. Ministry Civil Affairs People’s Republic China. China civil affairs statistical yearbook. China Statistical Publishing House.; 2013. http://www.stats.gov.cn/sj/ndsj/2013/indexeh.htm . Acesso em 5 de agosto de 2023.
Peng R, Wu B. Changes of Health Status and Institutionalization among older adults in China. J Aging Health. 2015;27(7):1223–46. https://doi.org/10.1177/0898264315577779 .
Article PubMed Google Scholar
de Laffon C, Morley JE, Levy C, et al. Prevention of Functional decline by reframing the role of nursing homes? J Am Med Dir Assoc. 2017;18(2):105–10. https://doi.org/10.1016/j.jamda.2016.11.019 .
Article Google Scholar
Farias I, Sousa SA, Almeida LFD, Santiago BM, Pereira AC, Cavalcanti YW. Does non-institutionalized elders have a better oral health status compared to institutionalized ones? A systematic review and meta-analysis. Cien Saude Colet. 2020;25(6):2177–92. https://doi.org/10.1590/1413-81232020256.18252018 .
Benksim A, Ait Addi R, Khalloufi E, Habibi A, Cherkaoui M. Self-reported morbidities, nutritional characteristics, and associated factors in institutionalized and non-institutionalized older adults. BMC Geriatr. 2021;21(1):136. https://doi.org/10.1186/s12877-021-02067-3 .
Article PubMed PubMed Central Google Scholar
de Medeiros MMD, Carletti TM, Magno MB, Maia LC, Cavalcanti YW, Rodrigues-Garcia RCM. Does the institutionalization influence elderly’s quality of life? A systematic review and meta-analysis. BMC Geriatr. 2020;20(1):44–44. https://doi.org/10.1186/s12877-020-1452-0 .
Czwikla J, Herzberg A, Kapp S, et al. Home care recipients have poorer oral health than nursing home residents: results from two German studies. Article J Dentistry. 2021;107103607. https://doi.org/10.1016/j.jdent.2021.103607 .
Ferreira RC, Wolff CS, Silami CMd, Nogueira AM. Atenção odontológica E práticas de higiene bucal em instituições de longa permanência geriátricas. Cien Saude Colet. 2011;16. https://doi.org/10.1590/S1413-81232011000400032 .
Ferreira RC, Magalhães CS, Rocha ES, Schwambach CW, Moreira AN. Oral health among institutionalized elderly in Belo Horizonte, Minas Gerais State. Brazil Cad Saude Publica. 2009;25(11). https://doi.org/10.1590/s0102-311x2009001100008 .
Ferreira RC, De Magalhães CS, Moreira AN. Tooth loss, denture wearing and associated factors among an elderly institutionalized Brazilian population. Gerodontology. 2008;25(3):168–78. https://doi.org/10.1111/j.1741-2358.2008.00214.x .
Saarela RKT, Hiltunen K, Kautiainen H, Roitto HM, Mäntylä P, Pitkälä KH. Oral hygiene and health-related quality of life in institutionalized older people. Eur Geriatr Med. 2022;13(1):213–20. https://doi.org/10.1007/s41999-021-00547-8 .
Wong FMF, Ng YTY, Leung WK. Oral health and its Associated factors among older institutionalized Residents-A systematic review. Int J Environ Res Public Health. 2019;16(21):4132. https://doi.org/10.3390/ijerph16214132 .
Allen F, Tsakos G. Challenges in oral health research for older adults. Gerodontology. 2023;00:1–7. https://doi.org/10.1111/ger.12681 .
Zermansky AG, Alldred DP, Petty DR, Raynor DK. Striving to recruit: the difficulties of conducting clinical research on elderly care home residents. J R Soc Med. 2007;100(6):258–61. https://doi.org/10.1177/014107680710000608 .
Jenkins C, Smythe A, Galant-Miecznikowska M, Bentham P, Oyebode J. Overcoming challenges of conducting research in nursing homes. Nurs Older People. 2016;28(5):16–23. https://doi.org/10.7748/nop.28.5.16.s24 .
Maas ML, Kelley LS, Park M, Specht JP. Issues in conducting research in nursing homes. West J Nurs Res. 2002;24(4):373–89. https://doi.org/10.1177/01945902024004006 .
Hall S, Longhurst S, Higginson IJ. Challenges to conducting research with older people living in nursing homes. BMC Geriatr. 2009;9:38. https://doi.org/10.1186/1471-2318-9-38 .
Hubbard G, Downs MG, Tester S. Including older people with dementia in research: challenges and strategies. Aging Ment Health. 2003;7(5):351–62. https://doi.org/10.1080/1360786031000150685 .
Article CAS PubMed Google Scholar
Goodman C, Baron NL, Machen I, et al. Culture, consent, costs and care homes: enabling older people with dementia to participate in research. Aging Ment Health. 2011;15(4):475–81. https://doi.org/10.1080/13607863.2010.543659 .
Schilling I, Gerhardus A. Methods for Involving Older People in Health Research-A Review of the literature. Int J Environ Res Public Health. 2017;14(12). https://doi.org/10.3390/ijerph14121476 .
van Manen M. Phenomenology in its original sense. Qual Health Res. 2017;27(6):810–25. https://doi.org/10.1177/1049732317699381 .
Silva RV. Oliveira WFd. O método fenomenológico nas pesquisas em saúde no Brasil: Uma análise de produção científica. Trab Educ Saúde. 2018;16(3):1421–41.
Bartlett R, Milligan C. The development of diary techniques for research. In What is Diary Method? 2015(pp. 1–12). https://doi.org/10.5040/9781472572578.ch-001 .
Snowden M. Use of diaries in research. Nurs Stand. 2015;29(44):36–41. https://doi.org/10.7748/ns.29.44.36.e9251 .
Albine M, Irene Korstjens. Series: practical guidance to qualitative research. Part 3: Sampling, data collection and analysis. Eur J Gen Pract. 2018;24(1):9–18. https://doi.org/10.1080/13814788.2017.1375091 .
Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–12. https://doi.org/10.1016/j.nedt.2003.10.001 .
Brasil, DE 27 DE MAIO DE. Agência Nacional de Vigilância Sanitária. Resolução da Diretoria Colegiada - RDC nº 502, 2021. Dispõe sobre o funcionamento de Instituição de Longa Permanência para Idosos, de caráter residencial. http://bibliotecadigital.anvisa.ibict.br/jspui/bitstream/anvisa/423/1/RDCn531_04 . 08.2021_publicada06.08.2021_versão%20web.pd. Acesso em 5 de agosto de 2023.
Brasil. Política nacional de assistência social. Ministério do Desenvolvimento Social e Combate à Fome. 2004. http://blog.mds.gov.br/redesuas/wp-content/uploads/2019/07/PNAS_2004.pdf . Acesso em 5 de agosto de 2023.
Yoon MN, Ickert C, Slaughter SE, Lengyel C, Carrier N, Keller H. Oral health status of long-term care residents in Canada: results of a national cross-sectional study. Gerodontology. 2018;35(4):359–64. https://doi.org/10.1111/ger.12356 .
De Visschere L, Janssens B, De Reu G, Duyck J, Vanobbergen J. An oral health survey of vulnerable older people in Belgium. Clin Oral Investig. 2016;20(8):1903–12. https://doi.org/10.1007/s00784-015-1652-8 .
Volk L, Spock M, Sloane PD, Zimmerman S. Improving evidence-based oral health of nursing home residents through coaching by Dental hygienists. J Am Med Dir Assoc. 2020;21(2):281–3. https://doi.org/10.1016/j.jamda.2019.09.022 .
Brito AACd, Silva JdVe, Holanda JMF, Souza RRMNd L. TCdOMKC. Vulnerability of institutionalized older people and social support in the perspective of the COVID-19 pandemic. Rev. bras. geriatr. gerontol. 2022;25(6):e220051. https://doi.org/10.1590/1981-22562022025.220051 .
Shepherd V. Advances and challenges in conducting ethical trials involving populations lacking capacity to consent: a decade in review. Contemp Clin Trials. 2020;95:106054. https://doi.org/10.1016/j.cct.2020.106054 .
Lee YA, Salahuddin M, Gibson-Young L, Oliver GD. Assessing personal protective equipment needs for healthcare workers. Health Sci Rep. 2021;4(3):e370. https://doi.org/10.1002/hsr2.370 .
Organização Pan-Americana da Saúde. Módulos de Princípios de Epidemiologia para o Controle de Enfermidades. Módulo 4: vigilância em saúde pública / Organização Pan-Americana da Saúde. Brasília: Organização Pan-Americana da Saúde; Ministério da Saúde, 2010. 52 p.: il. 7 volumes. ISBN 978-85-7967-022-0.
Kitwood T. The experience of dementia. Aging Ment Health. 1997;1(1):13–22. https://doi.org/10.1080/13607869757344 .
de Boer ME, Hertogh CM, Dröes RM, Riphagen II, Jonker C, Eefsting JA. Suffering from dementia - the patient’s perspective: a review of the literature. Int Psychogeriatr. 2007;19(6):1021–39. https://doi.org/10.1017/s1041610207005765 .
Margari F, Sicolo M, Spinelli L, et al. Aggressive behavior, cognitive impairment, and depressive symptoms in elderly subjects. Neuropsychiatr Dis Treat. 2012;8:347–53. https://doi.org/10.2147/ndt.s33745 .
McKhann GM, Knopman DS, Chertkow H, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):263–9. https://doi.org/10.1016/j.jalz.2011.03.005 .
Rodrigo-Claverol M, Malla-Clua B, Marquilles-Bonet C, et al. Animal-assisted therapy improves communication and mobility among Institutionalized people with cognitive impairment. Int J Environ Res Public Health. 2020;17(16):5899. https://doi.org/10.3390/ijerph17165899 .
Gènova-Maleras R, Álvarez-Martín E, Catalá-López F, NFd L-B, Morant-Ginestar C. Aproximación a la carga de enfermedad de las personas mayores en España. Gac Sanit. 2011;25:47–50. https://doi.org/10.1016/j.gaceta.2011.09.018 .
Gioffrè-Florio M, Murabito LM, Visalli C, Pergolizzi FP, Famà F. Trauma in elderly patients: a study of prevalence, comorbidities and gender differences. G Chir. 2018;39(1):35–40. https://doi.org/10.11138/gchir/2018.39.1.035 .
Larsen PP, Thiele S, Krohne TU, et al. Visual impairment and blindness in institutionalized elderly in Germany. Graefes Arch Clin Exp Ophthalmol. 2019;257(2):363–70. https://doi.org/10.1007/s00417-018-4196-1 .
Brasil. Câmara dos Deputados. Projeto de Lei nº 4.702, de 12 de novembro de 2012, aguardando parecer. 2012. http://www.camara.gov.br/proposicoesWeb/fichadetramitacao?idProposicao=559429 . Acesso em 5 de agosto de 2023.
Download references
Acknowledgements
Not applicable.
This research was supported by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (001), Fundação de Amparo à Pesquisa do Estado de Minas Gerais (PPM-00603-18), and Conselho Nacional de Desenvolvimento Científico Tecnológico (CNPq: 310938/2022-8).
Author information
Authors and affiliations.
Department of Community and Preventive Dentistry, School of Dentistry, Universidade Federal de Minas Gerais, Belo Horizonte, Brazil
Thayse Mayra Chaves Ramos, Álvaro Augusto da Silva Alves, Thais Andrade Apolinário, Flávia Fonseca de Toledo, Viviane Elisângela Gomes, Kevan Guilherme Nóbrega Barbosa & Raquel Conceição Ferreira
Department of Clinical, Pathology and Surgical Dentistry, School of Dentistry, Universidade Federal de Minas Gerais, Belo Horizonte, Brazil
Aline Araújo Sampaio
You can also search for this author in PubMed Google Scholar
Contributions
The authors contributions were: Conceptualization, RCF and TMCR; Acquisition of data or analysis and interpretation of data, TMCR, AASA, TAA, FFT, RCF, AAS, VEG; Supervision, RCF, AAS; Writing – original draft, TMCR; Writing – review & editing, TMCR, RCF, AAS, VEG, KGNB; All authors read and approved the final manuscript.
Corresponding authors
Correspondence to Thayse Mayra Chaves Ramos or Raquel Conceição Ferreira .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ramos, T.M.C., da Silva Alves, Á.A., Apolinário, T.A. et al. Challenges to conducting research on oral health with older adults living in long-term care facilities. BMC Oral Health 24 , 422 (2024). https://doi.org/10.1186/s12903-024-04204-x
Download citation
Received : 03 November 2023
Accepted : 29 March 2024
Published : 05 April 2024
DOI : https://doi.org/10.1186/s12903-024-04204-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Oral health
- Data collection
- Nursing homes
BMC Oral Health
ISSN: 1472-6831
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- West Africa
- Microdata Portal
POST-DOCTORAL RESEARCH SCIENTIST IN QUALITATIVE IMPACT EVALUATION (IE)
The African Population and Health Research Center (APHRC) is an African-led and Africa-based international research institution committed to conducting high-quality and policy-relevant multidisciplinary research. Our goal is to generate evidence for meaningful action, engage with policymakers in the region to disseminate our research findings, influence policy decisions, and improve the quality of life in Africa. APHRC’s Data Synergy Unit supports all Program Units across the Center in the application and utility of monitoring and IE approaches to inform the implementation and assess the performance of the projects aligned to the different research priorities at subnational and national levels across Africa.
To this end, APHRC seeks to recruit one (1) Post-Doctoral Research Scientist in Qualitative IE to support the qualitative IE activities at the center in the following research thematic areas:
- Human development with focusing on inclusive policies and practices for early childhood development, education, and youth empowerment systems in Africa;
- Health and Wellbeing with focusing on effective interventions/ or strategies and policies to promote equitable health and well-being of all people in Africa; and,
- Population Dynamics and Urbanization focusing on the generation of evidence in the areas of urbanization, fertility, and aging and their implications for developing sustainable and resilient cities in Africa.
As a Postdoctoral Research Scientist in Qualitative IE, the successful candidate will support all four thematic areas, working collaboratively with APHRC researchers.
The position will be based at the Center’s Head Office in Nairobi, Kenya; and may include some travels to conduct qualitative IE (IE) activities in other Anglophone and Francophone African countries. As a Qualitative IE Specialist , the Postdoctoral Research Scientist will be primarily responsible for the management of IE projects and supporting researchers at the Center on appropriate qualitative IE designs for different undertakings in the designated research thematic areas. The expected specific duties and responsibilities include the following:
Technical leadership and support
- Leading the design and implementation of development-related qualitative IEs and research studies;
- Support researchers at the Center in the adoption of qualitative IE designs in research studies including complex IEs based on modern practices such as appreciative inquiry, participatory approaches, most significant change, outcome harvesting, contribution analysis, comparative case studies, and process tracing among others .;
- Develop and deepen innovative approaches to IE for example, through training of researchers at the center in IE methodology, developing and writing papers that utilize IE methodologies in peer-reviewed journals, engaging with IE communities of practice to strengthen the Center’s visibility in IE practice, etc.
Fundraising for IE sustainability
- Contribute to the resource mobilization for IE projects to ensure that the Center sustains its IE mandate to the foreseeable future;
- Support IE proposal writing and other fundraising activities – including designing qualitative IE approaches geared towards leveraging funds to broaden the current mandate of the Data Synergy and Evaluations (DSE) Unit;
- Actively collaborate with and contribute to the work of other Program Areas at APHRC to strengthen the IE mandate;
Management of IE Projects
- Establish, monitor, and update work plans and budgets for IE projects;
- Oversee mobilization of IE teams, including organizing and managing team planning meetings and overseeing all necessary logistical preparations for field data collection;
- Identify, recruit, and train research assistants; support teams technically; assist in orienting consultant team members to procedures for working with APHRC;
- Assure high-quality deliverables and evaluation reports;
- Support development of IE including background and supporting research for ongoing/upcoming IE and oversight of survey development: interview and focus group discussion guides, and observation checklists among others;
- Manage qualitative IE datasets (audio recordings and transcripts) throughout the IE life-cycle from coordination of local data collection partners to data management including transcriptions cleaning and coding to preliminary and final analyses;
- Serve as a responsive point of contact for clients, ensure contract compliance, and support contract reporting requirements;
- Support the IE team to develop, review, and finalize IE analysis plans, and evaluation frameworks, and contribute to the drafting of work plans, data collection tools, and field monitoring tools for each IE activity;
- Work with the Project Evaluation Team to provide timely updates and reports on evaluation activities as needed;
- Participate and/or support the dissemination of IE findings at local, national, and international fora through abstract presentations, roundtable discussions, publications, blogs, policy briefs, and working papers among others;
- Carry out any other functions that may be assigned to you from time to time by the Senior Management Team at the Center;
Key Competencies, qualifications, and experience
- Ph.D. in Social Sciences, Sociology, Medical Anthropology, Public Health, International Health, Social Work and Social Administration, Public Policy, and other related disciplines, with specialization and significant demonstrated experience in Qualitative IE of development projects, preferably public health;
- Advanced skills in qualitative IE designs, data collection approaches, and rigorous data analysis;
- Strong qualitative research skills, and ability to conduct and work with large qualitative datasets using computer assisted qualitative data analysis (CAQDAs) software programs (RQDA, Dedoose, Nvivo, MAXQDA, and ATLAS.ti);
- At least 3 years of work experience in project evaluation and impact analysis is essential;
- Demonstrated experience in in-depth qualitative impact analysis methods, including mixed-methods IE;
- Experience designing and implementing one or more of the following: implementation research, formative evaluation, process evaluations, process monitoring, summative evaluation, and IE;
- At least five (5) publications or technical reports (or a doctoral research thesis) that utilized qualitative IE methodologies/approaches, with 3 or more first-author publications .
- Excellent qualitative scientific writing, presentation, and communication skills including the ability to present arguments and analysis in a structured and succinct manner;
- Sound causal reasoning, and good knowledge of the theory of change, evaluation criteria, causal attribution, and limitations of qualitative IEs;
- Ability to work independently; self-starter and highly motivated;
- Strong theoretical and applied qualitative knowledge; fluency in French is highly desirable
- Knowledge of economic evaluation and quantitative IE methods will be an added advantage;
- Proficiency in the English language is a must;
- Working knowledge of East, Southern, Northern, and West African regions is desirable.
Interested candidates are invited to submit their applications as one PDF document in English through this link by Monday, April 15, 2024 and include:
- A letter of application not exceeding 1-page, highlighting your qualifications and experience relevant to the terms of reference, and the thematic areas ;
- A statement of research interests and goals (1 page) about the position;
- A detailed CV (5 pages max.) with contact information for three professional references.
Non-adherence to these requirements will lead to your application not being reviewed. Applications will be reviewed on a rolling basis and incomplete applications will not be considered . Only shortlisted candidates will be contacted.
Special Notice
APHRC is an equal opportunity employer that is committed to creating a diverse and inclusive workplace. All employment decisions are made on the basis of qualifications and organizational needs. Reasonable accommodation may be provided to applicants with disabilities upon request, to support their participation in the recruitment process.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- JNMA J Nepal Med Assoc
- v.58(232); 2020 Dec

Conducting Qualitative Interviews using Virtual Communication Tools amid COVID-19 Pandemic: A Learning Opportunity for Future Research
Lalita kumari sah.
1 Faculty of Medicine Health and Social Care, Canterbury Christ Church University, Kent, United Kingdom
Devendra Raj Singh
2 Department of Public Health, Asian College for Advance Studies, Purbanchal University, Satdobato, Lalitpur, Nepal
Rajeeb Kumar Sah
The COVID-19 pandemic has threatened the health and wellbeing of the global citizens which has led to a significant change in attitude, lifestyle and behaviour of people from diverse professions, including academics and researchers. Doctoral students and funded researchers with the time limit to their research project have experienced stress and anxiety due to the struggle of negotiating and managing timeline to complete the fieldwork for their research. In the current circumstances, increasing number of researchers are looking for alternative methods to conduct the fieldwork and complete the data collection. In this context, the aim of this viewpoint is to provide reflections on the challenges and opportunities experienced by the authors while conducting qualitative research fieldwork during the COVID-19 pandemic.
INTRODUCTION
The COVID-19 pandemic has contributed to the wider structural changes in our society that has affected people's daily lives. For example, working from home is becoming normal and has possibly blurred the lines between personal and professional settings; travel restrictions has limited the movement of people around the world; national and local lockdowns have affected in-person individual or group meetings and social gatherings; and planning indoor and outdoor activities have become precarious and challenging. From researcher perspectives, this has constrained the planned and ongoing research activities both within and outside the health sectors. 1 In this context, the viewpoint discusses the challenges and opportunities to use virtual communication tools while conducting qualitative research fieldwork during and beyond the pandemic.
CHALLENGES TO QUALITATIVE RESEARCH FIELDWORK DURING COVID-19
Doctoral students and funded researchers with the time limit to their research project have experienced stress and anxiety due to the struggle of negotiating and managing timeline to complete the fieldwork for their research. 2 Health related research where participants are recruited from the community or hospital settings faces extra obstacles due to the risk of community transmissions which is highly likely to be higher in such settings. Despite social distancing and other safety measures to protect participants and general public from the virus, the fear of the pandemic still exists within the community. Evidence suggests that many people who are COVID-19 positive may not show any symptoms but can still transmit the virus. 3 In such situation, participants as well as researchers are hesitant to meet face-to-face or spend extended period of time in the field for the purpose of research interviews. Even if participants agree to take part in face-to-face interviews, they are likely to be anxious due to the fear of COVID-19 and may rush to end the interview sooner as they are likely to feel uncomfortable due to the current COVID-19 situation. Therefore, in the current circumstances, increasing number of researchers are looking for alternative methods to conduct the fieldwork and complete the data collection.
National and local lockdowns, social distancing and travel restrictions have forced universities and research institutions around the world to rethink their research strategy, especially in relation to the fieldwork, to safeguard and support both researchers and participants from COVID-19. Some institutions are encouraging researchers to complete the data collection using virtual communication tools while others argue that it may not be the best option to do so because of the challenges and disadvantages associated with the virtual interviewing. Doctoral students and funded researchers with the time limit to their research project are at the crossroads of taking quick decisions about the fieldwork for their project. Although many UK institutions and funding organisations have extended the deadline by 3 to 6 months with financial support, 4 , 5 the anxiety of the researchers have not diminished as the pandemic continues. The decision-making for researchers who are required to travel to other countries or within the country to complete their fieldwork is further complicated as we continue to live and work under local and national restrictions. Moreover, the increase in travel costs, lack of regular flights and the requirements of self-isolation, in many cases on both sides, have presented additional challenges for such researchers. As a result, researchers experience issues of financial burden, time constraints, and other psychological concerns related to the fear of COVID-19 infection, possibility of lack of productivity and time management in the fieldwork. The experience of second wave of COVID-19 and uncertainties about returning to normal routine demands an immediate action to look for alternative methods to complete the fieldwork rather than the postponement of research projects any further. As the pandemic continues, institutions have taken a flexible approach to support their researchers and have advised to explore alternative methodology and methods to complete the research project and, where possible, explore virtual communication tools and use them to collect data for their research project. However, these virtual methods of data collection come up with its own challenges and opportunities which we have discussed below.
USING VIRTUAL COMMUNICATION TOOLS FOR QUALITATIVE INTERVIEWS
The use of virtual technology is increasingly embedded in teaching and learning activities of students and has been widely used and appreciated by educators, technologists and students in every fields of the study for many years. 6 – 8 Likewise, the use of virtual communication tools for data collection is not a new technique and it has been used for several decades while conducting survey. 9 Sedgwick and Spiers has recommended that video conferencing is the most viable and cost-effective alternative to face-to-face in-depth interviewing to overcome geographical barriers and time constraints. 10 Many researchers have commonly used Skype interviewing as data collection methods before, 11 however researchers largely preferred face-to-face interviews before the pandemic. The restriction imposed due to COVID-19 has compelled researchers to explore virtual communication tools further and have provided an opportunity to grow knowledge and understanding about using information technology effectively in the research fieldwork. The popularity of Zoom, Microsoft Teams and Google Hangouts has become the saviour for the virtual conferences, research dissemination and networking during COVID-19. Similarly, the accessibility of voice/video calls through social media such as Facebook and WhatsApp have brought the connectivity to the masses, which is important if we want to use these virtual communication tools for qualitative interviews.
The use of virtual communication tools such as Zoom, Microsoft Teams, Google Hangouts, Facebook and WhatsApp have provided good alternatives for researchers to advance and progress with the data collection process to support their fieldwork. Our experiences of conducting interviews from research participants in both community settings and institutional settings of Nepal during COVID-19 pandemic showed that most participants were excited and felt safe to participate in virtual interviews. Also, it was easier to mutually agree a convenient time to conduct interviews and it has saved the time researchers would have spent travelling to conduct the fieldwork.
The first author, who is an international researcher doing her PhD at the UK university, was faced with the challenges of travelling to Nepal to collect the data for her research. In the current situation, where there are increasing number of COVID-19 cases in both Nepal and the UK, travelling was not an easy option and face-to-face interviews would have presented its own challenges as discussed earlier in this paper. Traditionally, if the researchers are not able to collect data themselves then they recruit research assistant(s), who is trained and managed by the researcher in line with the ethical guidelines, to facilitate the data collection process. 12 , 13 However, the use of virtual communication tools has made it possible for the researchers to conduct the interviews themselves without recruiting research assistant(s), which is an advantage for the early career researchers in terms of gaining first-hand experience of interviewing participants. This enhance researchers experience of conducting fieldwork and provide opportunities to develop skills in conducting interviews.
The use of virtual communication tools has also allowed researchers to connect to the gatekeepers and equip them with ethical guidelines of autonomy, anonymity and confidentiality for the research during an initial preparation for the virtual data collection. Gatekeepers invariably play an important role in facilitating researchers' access to the participants 14 and can play a crucial role in acting as a reliable person to provide post-interview safeguarding for the participants. However, researchers must make sure that the gatekeepers are not playing the role of research assistants and are not present during the interviews with the participants. There should be a clear understanding about the role and limitations of the gatekeepers among the researchers and those who are playing role of the gatekeepers.
OVERCOMING CHALLENGES WHILE USING VIRTUAL COMMUNICATION TOOLS
Researchers have raised concerns that online interviews may limit the participation of people who do not have access to the internet connection or where the participants are going to incur charge for using the internet to participate in the interviews. In developing countries such as Nepal, it is important that the researcher do not expect the participants to incur any charge or costs for participating in the research. One way to tackle this issue is to provide the facility such as phone/tablet to the gatekeeper that can be kept at the interview site and can be used by all the participants. If the interview site is in a hospital, the internet connection can be freely accessible from the hospital WiFi network or the researcher should arrange the purchase of the internet data package to address this issue. Also, the researcher can purposefully plan to consider the location of the sampling unit where diverse participants are present for example, a hospital that covers a large number of people from different geographical location, wider sociocultural and economic background in the region. This strategy can address the issue of limitation of wider participation in the research. Lack of skills to use the technology in developing countries is still a challenge in the 21 st century. 15 This means majority of people find it difficult to take part in virtual media interviews, and again it may limit the chances of approaching a wide range of participants in the research in the community settings. Therefore, the researcher must have an arrangement to address the issue and one of the options could be training the gatekeeper who can facilitate the technology. However, the researcher needs to make sure that the gatekeeper is not interfering or taking part in the interview process.
Many researchers are not convinced with the idea of virtual interviews, as PhD students and early career researchers would have the limitations to gain first-hand experience of the fieldwork for data collections and field observation. However, some researchers may argue that conducting a virtual fieldwork is much more challenging and provides the skills for future research, as the use of technology in the research is likely to increase post pandemic. The other challenges are when the research deals with sensitive topics or with vulnerable participants. For example, pregnant woman as a research participant may feel upset while sharing their experiences about mental health issues. However, it is important to highlight that video conferencing allows researcher to see the participants' facial expressions and body language, which allows researchers to make use of reflexivity in difficult circumstances.
For example, if the participant becomes uncomfortable during the interview, the researcher can give time and space that will help the participant to compose themselves. 11 In addition, a reliable person such as gatekeepers, must be present or accessible at the interview site, but not in the same room for confidentiality purposes, to provide emotional support to the participants or signposting them to the available support and services upon the guidance of the researcher.
In our research fieldwork, we took a pre-determined 3-steps approach to the virtual conversations with the research participants i.e. rapport building, interview conversation and closing the conversation. Although this was not an in-person interviews, it was important for us to build rapport with the participant before discussing interview questions. This allowed us to neutralise the environment where participants felt more comfortable about discussing their life stories in relations to their health and wellbeing, which is important for any health related qualitative research. Following the interviews, it was important for us not to abruptly end the conversation, but to provide support by continuing with general conversations to protect the participant from vulnerability. Therefore, ending the conversation with information and message of support ensured that the participants left the conversation feeling strong and protected.
WAYS FORWARD
In these unprecedented times of the COVID-19 pandemic, researchers should have a realistic plan for their research project rather than being too ambitious. As the pandemic continues, it is important that researchers are prepared with alternative methods for data collection. As the use of technology in learning and teaching has increase significantly, it is likely that this trend will be followed in the research fieldwork and dissemination process. Looking at the advantages of using virtual communication tools for conducting qualitative interviews, many researchers are likely to adopt this technique during and after the pandemic to overcome the time constraints and financial burden of the research process. If the challenges of the virtual communication tools are addressed appropriately, the virtual interviewing methods are likely to become a preferred choice rather than an alternate option.
Conflict of Interest
- Open access
- Published: 28 March 2024
Nurses’ perceptions of how their professional autonomy influences the moral dimension of end-of-life care to nursing home residents– a qualitative study
- Rachel Gilbert 1 &
- Daniela Lillekroken ORCID: orcid.org/0000-0002-7463-8977 1
BMC Nursing volume 23 , Article number: 216 ( 2024 ) Cite this article
244 Accesses
Metrics details
Over the years, caring has been explained in various ways, thus presenting various meanings to different people. Caring is central to nursing discipline and care ethics have always had an important place in nursing ethics discussions. In the literature, Joan Tronto’s theory of ethics of care is mostly discussed at the personal level, but there are still a few studies that address its influence on caring within the nursing context, especially during the provision of end-of-life care. This study aims to explore nurses’ perceptions of how their professional autonomy influences the moral dimension of end-of-life care provided to nursing home residents.
This study has a qualitative descriptive design. Data were collected by conducting five individual interviews and one focus group during a seven-month period between April 2022 and September 2022. Nine nurses employed at four Norwegian nursing homes were the participants in this study. Data were analysed by employing a qualitative deductive content analysis method.
The content analysis generated five categories that were labelled similar to Tronto’s five phases of the care process: (i) caring about, (ii) caring for, (iii) care giving, (iv) care receiving and (v) caring with. The findings revealed that nurses’ autonomy more or less influences the decision-making care process at all five phases, demonstrating that the Tronto’s theory contributes to greater reflectiveness around what may constitute ‘good’ end-of-life care.
Conclusions
Tronto’s care ethics is useful for understanding end-of-life care practice in nursing homes. Tronto’s care ethics provides a framework for an in-depth analysis of the asymmetric relationships that may or may not exist between nurses and nursing home residents and their next-of-kin. This can help nurses see and understand the moral dimension of end-of-life care provided to nursing home residents during their final days. Moreover, it helps handle moral responsibility around end-of-life care issues, providing a more complex picture of what ‘good’ end-of-life care should be.
Peer Review reports
In recent decades, improving end-of-life care has become a global priority [ 1 ]. The proportion of older residents dying in nursing homes is rising across the world [ 2 ], resulting in a significant need to improve the quality of end-of-life care provided to residents. Therefore, throughout the world, nursing homes are becoming increasingly important as end-of-life care facilities [ 3 ]. As the largest professional group in healthcare [ 4 ], nurses primarily engage in direct care activities [ 5 ] and patient communication [ 6 ] positioning them in close proximity to patients. This proximity affords them the opportunity to serve as information brokers and mediators in end-of-life decision-making [ 7 ]. They also develop trusting relationships with residents and their next-of-kin, relationships that may be beneficial for the assessment of residents and their next-of-kin’s needs [ 8 ]. Moreover, nurses have the opportunity to gain a unique perspective that allows them to become aware of if and when a resident is not responding to a treatment [ 9 ].
When caring for residents in their critical end-of-life stage, nurses form a direct and intense bond with the resident’s next-of-kin, hence nurses become central to end-of-life care provision and decision-making in nursing homes [ 10 ]. The degree of residents and their next-of-kin involvement in the decision-making process in practice remains a question [ 11 ]. Results from a study conducted in six European countries [ 12 ], demonstrate that, in long-term care facilities, too many care providers are often involved, resulting in difficulties in reaching a consensus in care. Although nurses believe that their involvement is beneficial to residents and families, there is a need for more empirical evidence of these benefits at the end-of-life stage. However, the question of who should be responsible for making decisions is still difficult to answer [ 13 ]. One study exploring nurse’s involvement in end-of-life decisions revealed that nurses experience ethical problems and uncertainty about the end-of-life care needs of residents [ 14 ]. Another study [ 10 ] reported patients being hesitant to discuss end-of‐life issues with their next-of-kin, resulting in nurses taking over; thus, discussing end-of-life issues became their responsibility. A study conducted in several nursing homes from the UK demonstrated that ethical issues associated with palliative care occurred most frequently during decision-making, causing greater distress among care providers [ 15 ].
Previous research has revealed that there are some conflicts over end-of-life care that consume nurses’ time and attention at the resident’s end-of-life period [ 16 ]. The findings from a meta-synthesis presenting nurses’ perspectives dealing with ethical dilemmas and ethical problems in end-of-life care revealed that nurses are deeply involved with patients as human beings and display an inner responsibility to fight for their best interests and wishes in end-of-life care [ 17 ].
Within the Norwegian context, several studies have explored nurses’ experiences with ethical dilemmas when providing end-of-life care in nursing homes. One study describing nurses’ ethical dilemmas concerning limitation of life-prolonging treatment suggested that there are several disagreements between the next-of-kin’s wishes and what the resident may want or between the wishes of the next-of-kin and what the staff consider to be right [ 18 ]. Another study revealed that nurses provide ‘more of everything’ and ‘are left to dealing with everything on their own’ during the end-of-life care process [ 19 ] (p.13) . Several studies aiming to explore end-of-life decision-making in nursing homes revealed that nurses experience challenges in protecting the patient’s autonomy regarding issues of life-prolonging treatment, hydration, nutrition and hospitalisation [ 20 , 21 , 22 ]. Other studies conducted in the same context have described that nurses perceive ethical problems as a burden and as barriers to decision-making in end-of-life care [ 8 , 23 ].
Nursing, as a practice, is fundamentally grounded in moral values. The nurse-patient relationship, central to nursing care provision, holds ethical importance and significance. It is crucial to recognise that the context within which nurses practice can both shape and be shaped by nursing’s moral values. These values collectively constitute what can be termed the ethical dimension of nursing [ 24 ]. Nursing ethos and practices are rooted in ethical values and principles; therefore, one of the position statements of the International Council of Nurses [ 25 ] refers to nurses’ role in providing care to dying patients and their families as an inherent part of the International Classification for Nursing Practice [ 26 ] (e.g., dignity, autonomy, privacy and dignified dying). Furthermore, ethical competence is recognised as an essential element of nursing practice [ 27 ], and it should be considered from the following viewpoints: ethical decision-making, ethical sensitivity, ethical knowledge and ethical reflection.
The term ‘end-of-life care’ is often used interchangeably with various terms such as terminal care, hospice care, or palliative care. End-of life care is defined as care ‘to assist persons who are facing imminent or distant death to have the best quality of life possible till the end of their life regardless of their medical diagnosis, health conditions, or ages’ [ 28 ] (p.613) . From this perspective, professional autonomy is an important feature of nurses’ professionalism [ 29 ]. Professional autonomy can be defined based on two elements: independence in decision-making and the ability to use competence, which is underpinned by three themes: shared leadership, professional skills, inter- and intraprofessional collaboration and a healthy work environment [ 30 ].
As presented earlier, research studies have reported that nurses experience a range of difficulties or shortcomings during the decision-making process; therefore, autonomous practice is essential for safe and quality care [ 31 ]. Moreover, autonomous practice is particularly important for the moral dimension in end-of-life care, where nurses may need to assume more responsibility in the sense of defining and giving support to matters that are at risk of not respecting ethical principles or fulfilling their ethical, legal and professional duties towards the residents they care for.
To the best of the researchers’ knowledge, little is known about nurses’ perceptions of how their professional autonomy influences the moral dimension of end-of-life care provided to nursing home residents; therefore, the aim of this study is to explore nurses’ perceptions of how their professional autonomy influences the moral dimension of end-of-life care provided to nursing home residents.
Theoretical framework
Joan Tronto is an American political philosopher and one of the most influential care ethicists. Her theory of the ethics of care [ 32 , 33 , 34 ] has been chosen as the present study’s theoretical framework. The ethics of care is a feminist-based ethical theory, focusing on caring as a moral attitude and a sensitive and supportive response of the nurse to the situation and circumstances of a vulnerable human being who is in need of help [ 33 , 34 , 35 ]. In this sense, nurses’ caring behaviour has the character of a means—helping to reach the goal of nursing practice—which here entails providing competent end-of-life care.
Thinking about the process of care, in her early works [ 32 , 33 , 34 ], Tronto proposes four different phases of caring and four elements of care. Although the phases may be interchangeable and often overlap with each other, the elements of care are fundamental to demonstrate caring. The phases of caring involve cognitive, emotional and action strategies.
The first phase of caring is caring about , which involves the nurse’s recognition of being in need of care and includes concern, worry about someone or something. In this phase, the element of care is attentiveness, which entails the detection of the patient and/or family need.
The second phase is caring for , which implies nurses taking responsibility for the caring process. In this phase, responsibility is the element of care and requires nurses to take responsibility to meet a need that has been identified.
The third phase is care giving , which encompasses the actual physical work of providing care and requires direct engagement with care. The element of care in this phase is competence, which involves nurses having the knowledge, skills and values necessary to meet the goals of care.
The fourth phase is care receiving , which involves an evaluation of how well the care giving meets the caring needs. In this phase, responsiveness is the element of care and requires the nurse to assess whether the care provided has met the patient/next-of-kin care needs. This phase helps preserve the patient–nurse relationship, which is a distinctive aspect of the ethics of care [ 36 ].
In 2013, Tronto [ 35 ] updated the ethics of care by adding a fifth phase of caring— caring with —which is the common thread weaving among the four phases. When care is responded to through care receiving and new needs are identified, nurses return to the first phase and begin again. The care elements in this phase are trust and solidarity. Within a healthcare context, trust builds as patients and nurses realise that they can rely on each other to participate in their care and care activities. Solidarity occurs when patients, next-of-kin, nurses and others (i.e., ward leaders, institutional management) engage in these processes of care together rather than alone.
To the best of our knowledge, these five phases of caring and their elements of caring have never been interpreted within the context of end-of-life care. The ethics of care framework offers a context-specific way of understanding how nurses’ professional autonomy influences the moral dimension of end-of-life care provided to nursing home residents, revealing similarities with Tronto’s five phases, which has motivated choosing her theory.
Aim of the study
The present study aims to explore nurses’ perceptions of how their professional autonomy influences the moral dimension of end-of-life care provided to nursing home residents.
The current study has a qualitative descriptive design using five individual interviews and one focus group to explore nurses’ perceptions of how their professional autonomy influences the moral dimension of end-of-life care provided to nursing home residents.
Setting and participants
The setting for the study was four nursing homes located in different municipalities from the South-Eastern region of Norway. Nursing homes in Norway are usually public assisted living facilities and offer all-inclusive accommodation to dependent individuals on a temporary or permanent basis [ 37 ]. The provision of care in the Norwegian nursing homes is regulated by the ‘Regulation of Quality of Care’ [ 38 ], aiming to improve nursing home residents’ quality of life by offering quality care that meets residents’ fundamental physiological and psychosocial needs and to support their individual autonomy through the provision of daily nursing care and activities tailored to their specific needs, and, when the time comes, a dignified end-of-life care in safe milieu.
End-of-life care is usually planned and provided by nurses having a post graduate diploma in either palliative nursing or oncology nursing– often holding an expert role, hence ensuring that the provision of end-of-life care meets the quality criteria and the resident’s needs and preferences [ 39 ].
To obtain rich information to answer the research question, it was important to involve participants familiar with the topic of study and who had experience working in nursing homes and providing end-of-life care to residents; therefore, a purposive sample was chosen. In this study, a heterogeneous sampling was employed, which involved including participants from different nursing homes with varying lengths of employment and diverse experiences in providing end-of-life care to residents. This approach was chosen to gather data rich in information [ 40 ]. Furthermore, when recruiting participants, the first author was guided by Malterud et al.’s [ 41 ] pragmatic principle, suggesting that the more ‘information power’ the participants provided, the smaller the sample size needed to be, and vice versa. Therefore, the sample size was not determined by saturation but instead by the number of participants who agreed to participate. However, participants were chosen because they had particular characteristics such as experience and roles which would enable understanding how their professional autonomy influences the moral dimension of end-of-life care provided to nursing home residents.
The inclusion criteria for the participants were as follows: (i) to be a registered nurse, (ii) had a minimum work experience of two years employed at a nursing home, and (iii) had clinical experience with end-of-life/palliative care. To recruit participants, the first author sent a formal application with information about the study to four nursing homes. After approval had been given, the participants were asked and recruited by the leadership from each nursing home. The participants were then contacted by the first author by e-mail and scheduled a time for meeting and conducting the interviews.
Ten nurses from four different nursing homes were invited to participate, but only nine agreed. The participants were all women, aged between 27 and 65 and their work experience ranged from 4 to 21 years. Two participants had specialist education in palliative care, and one was currently engaged in a master’s degree in nursing science. Characteristics of the participants are presented in Table 1 :
Data collection methods
Data were collected through five semistructured individual and one focus group interviews. Both authors conducted the interviews together. The study was carried out between April and September 2022. Due to the insecurity related to the situation caused by the post-SARS-CoV-2 virus pandemic and concerns about potential new social distancing regulations imposed by the Norwegian government, four participants from the same nursing home opted for a focus group interview format. This decision was motivated by a desire to mitigate the potential negative impact that distancing regulations might have on data collection. The interviews were guided by an interview guide developed after reviewing relevant literature on end-of-life care and ethical dilemmas. The development of the interview guide consisted of five phases: (i) identifying the prerequisites for using semi-structured interviews; (ii) retrieving and using previous knowledge; (iii) formulating the preliminary semi-structured interview guide; (iv) pilot testing the interview guide; and (v) presenting the complete semistructured interview guide [ 42 ]. The interview guide was developed by both authors prior to the onset of the project and consisted of two demographic questions and eight main open-ended questions. The interview guide underwent initial testing with a colleague employed at the same nursing home as the first author. After the pilot phase in phase four, minor language revisions were made to specific questions to bolster the credibility of the interview process and ensure the collection of comprehensive and accurate data. The same interview guide was used to conduct individual interviews and focus group (Table 2 ).
The interviews were all conducted in a quiet room at a nursing home. Each interview lasted between 30 and 60 min and were digitally recorded. The individual interviews were transcribed verbatim by the first author. The focus group interview was transcribed by the second author.
Ethical perspectives
Prior to the onset of the data collection, ethical approval and permission to conduct the study were sought from the Norwegian Agency for Shared Services in Education and Research (Sikt/Ref. number 360,657) and from each leader of the nursing home. The study was conducted in accordance with the principles of the Declaration of Helsinki of the World Medical Association [ 43 ]: informed consent, consequences and confidentiality. The participants received written information about the aim of the study, how the researcher would ensure their confidentiality and, if they chose to withdraw from the study, their withdrawal would not have any negative consequences for their employment at nursing homes. Data were anonymised, and the digital records of the interviews were stored safely on a password-protected personal computer. The transcripts were stored in a locked cabinet in accordance with the existing rules and regulations for research data storage at Oslo Metropolitan University. The participants did not receive any financial or other benefits from participating in the study. Written consent was obtained prior to data collection, but verbal consent was also provided before each interview. None of the participants withdrew from the study.
Data analysis
The data were analysed by employing a qualitative deductive content analysis, as described by Kyngäs and Kaakinen [ 44 ]. Both researchers independently conducted the data analysis manually. The empirical data consisted of 63 pages (34,727 words) of transcripts from both individual and focus group interviews. The deductive content analysis was performed in three steps: (i) preparation, (ii) organisation and (iii) reporting of the results.
During the first step—preparation—each researcher, individually, read the transcripts several times to get an overview of the data and select units of analysis by searching for recurring codes and meanings and to carefully compare the similarities and differences between coded data. These codes were labelled independently by both researchers and placed into an analysis matrix.
During the next step—organisation—the researchers met and discussed and then compared and revised the labels several times until they agreed about the preliminary findings. During the interpretative process towards developing an understanding of the empirical data, the content of the labels referred to nurses’ perceptions about how their professional autonomy influences the moral dimension of end-of-life care provided to nursing home residents, revealing similarities with the five phases of Tronto’s theory of ethics of care [ 32 , 33 ], thus assigning them to the five phases of the theory. Following this final refinement, one main category and five categories, each supported by several subcategories, were identified, as presented in Table 3 .
Reporting the results was the last step in the analysis. To enhance the understanding of the study’s findings, the findings are presented with supporting excerpts from the participants.
In qualitative studies, trustworthiness is the main parameter for appraising the rigour of the study [ 45 ]. To enhance the trustworthiness of the study, four criteria—credibility, transferability, dependability and confirmability, as described by Lincoln and Guba [ 46 ]—were applied.
To support credibility, a detailed description of the sample and the sampling process was provided. Furthermore, the interview guide and the questions that the participants were asked during the interviews are made available to the readers. Moreover, although the data were collected from five individual interviews and one focus group, triangulation of two data collection methods allowed researchers to ensure that the study is based on diverse perceptions and experiences, strengthening the credibility and impact of the study’s findings [ 47 ].
Detailed information about the sample and setting supports the assessment of the transferability of the findings. In this way, the readers can recognise and evaluate whether the findings would be applicable to similar contexts with a similar sample. Quotes from the participants’ statements are given to support the findings. Each quote ends with a number representing the code that each nurse was given before conducting the interviews (i.e., Participant in interview 1, PI1 or participant 6 in focus group interview, P6FG).
To increase dependability, the same interview guide was used to ask all participants the same questions. Dependability was also increased by the researchers reading and analysing the interviews independently and then checking the consistency of the data analysis technique with each other and discussing the analytical process until a consensus was reached.
To enhance confirmability, excerpts from the participants’ statements were included when presenting the findings, thus verifying the concordance of findings with the raw data. This demonstrates that the data were not based on preconceived notions.
Trustworthiness was also supported by member checking, meaning that the researchers sent the participants the transcripts of the interviews immediately after data collection; then, the interviews were transcribed. The participants were asked to review the transcripts and check the accuracy of the data; hence, they had the opportunity to add, remove or clarify their statements. Only one participant answered this request, stating that the transcripts were accurate, and she did not have any further comments. Despite encountering a suboptimal response from participants, the authors remain confident in the trustworthiness of the study. Rich data, derived from a combination of individual and focus group interviews, yielded diverse and nuanced responses from participants, reinforcing the credibility of the findings.
Reflexivity is the researcher’s reflection on their position during the research process [ 48 ]. Both researchers have clinical experience in providing end-of-life care to nursing home residents. Therefore, it was critical to be aware of the impact that their clinical backgrounds might have on the research process from information seeking during the analysis of data and discussion of the findings. To avoid early interpretation of the data, the researchers were aware of their preunderstanding and tried to put it on hold. Both authors engaged in discussions regarding apprehensions and reflections, actively participating in the triangulation process throughout the study to prevent potential bias during data collection, analysis, and interpretation. The theoretical framework was brought in the end of the analysis process, which helped label the emerged findings.
The analysis of the empirical data combined with an ethical reflection helped researchers to identify and understand the moral dimension of nurses’ experiences with end-of-life care provided to nursing home residents. During the analysis, an overarching category emerged– ‘The moral dimension of the provision of end-of life care’– describing nurses’ perceptions about how their professional autonomy influences the moral dimension of end-of-life care provided to nursing home residents. The participants agreed that end-of-life care is a care process that undergoes several phases, with each phase having its own ethical quality or its own element of care, here according to Tronto’s moral qualities [ 34 ]. In the following section, the findings are described using Tronto’s identified moral qualities for each of the five phases of the care process [ 32 , 33 , 34 , 35 ].
Caring about—being attentive
For the participants, being autonomous was perceived as a feature that increased their awareness of the resident’s caring needs during their last days of life. The participants agreed that the caring process involves paying attention, listening and recognising residents’ unspoken needs. Moreover, it implies nurses being able to make autonomous decisions when deciding which needs to care about at one particular moment.
The participants agreed that the core values of providing end-of-life care were to alleviate suffering, maintain dignity and provide comfort care. The participants perceived caring about as having sufficient knowledge, along with the experience and autonomy in practice, as well as providing comprehensive end-of-life care for residents. For the participants, caring about during the end-of-life process means them being present and dedicated. This implies nurses carefully observing, autonomously acting, and making decisions based on their judgements, and thus, they can decide and choose their course of action promptly based on resident’s condition or side effects. Moreover, caring about involved participants being attentive to perceiving the residents’ needs when the residents could no longer articulate themselves. The participants expressed their worries about resident’s bodily deterioration, leading them to lose their ability to express needs, as shown by the following quote:
There is not much communication when residents go into their last stage of life. Well… some of them are consciously until their death, but most are sedated; therefore, it is necessary to use your knowledge and experience to assess not only their needs for food and liquids or bodily hygiene, but also, we have to monitor their response to pain killers and other medication, and if it’s too much or too little, we need to do what’s needed to reduce or increase the medication and not let them suffer (PI3).
Some of the participants expressed that attentiveness to the residents’ care needs was a skill based on their clinical gaze developed during their careers. Other participants discussed that building a close relationship with the residents while they still could walk and talk was a precondition that helped them develop a clinical gaze, hence facilitating the nurses’ being attentive. Attentiveness allowed the participants to do what was needed when knowing the residents’ needs during the provision of end-of-life care. This may be interpreted as the moral or ethical quality of caring about during the end-of-life caring process, as demonstrated by the following statement:
We have time to know the resident before their health condition worsens… We previously knew what they wanted and how they wanted… their stay at nursing home gives us the opportunity to know their preferences and needs. Morally, we are obliged to provide the same quality of care they received when they could express themselves (PI4).
Caring for—taking responsibility
According to several participants, another phase within the end-of-life caring process was taking responsibility to care for. The participants agreed that monitoring the residents in their last days implies assuming responsibility. Assuming responsibility was perceived as an autonomous caring activity. They also discussed taking this responsibility seriously, which is a moral dimension of the end-of-life caring process and, ultimately, of the nursing profession. Usually, this responsibility was taken by a nurse, but it also involved other healthcare personnel or even next-of-kin. Among these responsibilities, the participants mentioned that the end-of-life caring process included not only caring for the resident’s physiological and psychosocial needs, but also assigning permanent healthcare personnel to continuously monitor the resident. Although the participants were aware that they share responsibilities for the caring process, ‘who does what…’, they ultimately had the overall responsibility for the whole end-of-life caring process.
Another responsibility included communication, which included listening, providing information, and supporting the residents’ next-of-kin. One of the participants expressed this as follows:
When I observe that the resident’s health worsens, I inform the next-of-kin and invite the spouse or the children to a meeting together with the responsible doctor and I, and we inform the next-of-kin what they might expect. The end-of-life care is not only about the resident and their last days, but also is to care for their next-of-kin to meet their needs and to overcome guilt feelings, anger or sadness.… (PI1).
Another way to care for patients was to deliberately increase opportunities to exercise autonomy during the caring process. For instance, the focus group participants discussed issues around advanced life support during the resident’s last days of life. Being prepared and having knowledge were the preconditions that gave them the authority to identify and make decisions about residents’ needs in here-and-now moments, hence exercising their autonomy. Some participants shared their experiences with controversies between next-of-kins’ and nurses’ assessments of what is the best care for the residents during their last days of life. Therefore, the importance of taking the initiative to discuss and clarify the resident’s needs and preferences was emphasised during the focus group interview, as shown in the following quote:
Some next-of-kins express wishes for advance life support and hospitalisation for their loved ones… and sometimes, to meet their needs, we try this, but the resident is suffering. The resident comes back to us after one or two days… To avoid this, clear guidelines, and a dialogue between the resident, their next-of-kin and us at the very beginning [when the resident enters the nursing home] is important… I think that minimalising the occurrence of difficult or conflictual situations and relieving the sufferance is care for both resident and their next-of-kin (P8FG).
Care giving—knowing what, why, how and when
During the interviews, the participants also discussed the caregiving process and provided concrete examples of what their caregiving encompassed. Spending extra time with the resident, choosing to be in the room and holding their hand to maintain physical contact was perceived as an autonomous caring act and a deliberate choice. One participant described this as follows:
For me, it is important that the dying person feels or hears that I am here with him or her… how he or she feels in these moments matters to me. I do it because I want to do it.… (PI5).
Other participants said that being autonomous when they actually provided caregiving to residents helped them make continuous assessments based on knowledge about what , how , how much , when and why to care. Knowledge and skills were decisive factors in providing competent care and making autonomous decisions during the caregiving phase; hence, competence was perceived as a moral dimension of caregiving. One of the participants said the following:
Caregiving at end-of-life is not only about giving morphine according to the doctor’s prescription… it involves all the judgements you have to make, all the skills you have… from preventing the occurrence of bedsores to knowing when to stop feeding but preventing thirst… think about all this knowledge and experience you must have to be able to make autonomous bedside judgements about when , why and so on.… (PI2).
Care giving at the end-of-life was described as all the necessary activities a nurse does to provide comfort and compassionate care to a dying resident. Among these activities, providing fundamental care and keeping residents comfortable and free of pain were seen as parts of the caregiving process. Moreover, adequate pain relief and symptom management were described as the moral dimension of care giving at this stage of end-of-life care, as one of the participants from the focus group interview said:
You cannot be passive when you see that the resident is suffering. I cannot go home and think that I should have done one or the other. It is against the nurses’ code of ethics and my personal moral and ethical principles. You have to act… I have to do what is needed… first thing first… pain relief and then personal hygiene! (P9FG)
Some of the participants mentioned some challenges they encountered during the care giving process. They said that care giving implies also standing in demanding situations. The lack of healthcare personnel with necessary knowledge or formal palliative care education or handling ethical dilemmas was seen as demanding situations that influenced the provision of care giving. Most of the participants felt that they were alone during the decision-making processes, which increased their awareness of their professional autonomy:
Sometimes, during weekends or evenings, I am the only nurse among the healthcare staff, and I have an overall responsibility for all nursing home residents. I have to prioritise who gets my attention and who needs me the most. Things can happen, regardless of whether it is Friday evening or weekend. I have to make a decision and do what is needed: to be with the dying resident and to support his or her next-of-kin in that moment. (PI5)
Care receiving—assessing caregiving
Several participants stated that, during the care-giving process, it was important to assess how the resident receive the care provided at the end-of-life stage. This was possible by monitoring the resident’s state of being but to also assess the outcomes of their care giving activities. They also reflected on their assessments and how they subsequently dealt with those assessments.
All the participants were confident in their knowledge and with their care giving at the end-of-life stage. They were aware that their care activities had consequences for the residents’ physiological and psychosocial needs. The assessment of the resident’s state of being was made by nurses listening, observing and interpreting resident’s response to care giving as signs of comfort or discomfort. One of the participants explained this as follows:
When providing personal care, if the resident presents any signs that can be interpreted as discomfort, I think that priority number one is me not causing more pain or suffering. However, I also understand that this person needs more pain killers, so I have to make sure that this person receives adequate medicine. (PI5)
Some participants also discussed the importance of assessing their care giving activities. They mentioned the importance of their assessments of the benefits of all care giving against the burden of all interventions and treatments. Their professional autonomy allowed them to make decisions about how to eschew care giving that was inappropriately and burdensome and choose the best comforting care for the resident. The participants stated that knowledge and experience were important in making such decisions, and their professional autonomy facilitated making choices of the best and less burdensome care giving. One of the participants said the following:
We have to assess whether the care giving provided meets the resident’s needs or not, whether the care comforts or perceives it as a burden and how the resident responds to this provision of care. (PI4)
During the interviews, some of the participants revealed a feeling of guilt when assessing that care giving altered the resident’s state of being, thus leading to new needs for care. They also discussed that the moral obligation and intention to relieve the suffering of the resident should override the foreseen but unintended harmful effects of care giving, including medication or other care interventions. One of the participants shared her experience as follows:
I still remember the attitude some of us had for a while ago… too much or too often morphine depresses the respiration and leads to death… I was struggling with feelings of guilt and even moral distress when I observed residents were still suffering because the medication they received had little or maybe no effect. I called the doctor and explained the situation… usually, the experienced doctors listen to us… and he [the doctor] prescribed more morphine.… (PI3).
Documentation of the response to care giving was also an issue discussed during the interviews. Some participants emphasised the importance of keeping detailed reports for a proper assessment of the care giving and medication and its outcomes. All reports were digitally written. Informal discussions between nurses and next-of-kin were also documented, especially when next-of-kin evaluated the care their loved ones received. The participants indicated that the more written information there was, the better. One participant acknowledged the following:
There is no such thing as ‘too much information’… being open about the morphine’s side effects and what to expect in the next hours or days is important for them [next-of-kin]. It helps them understand that end-of-life care is a process, not a quick fix procedure. (PI5)
Caring with—It is a teamwork process
During the interviews, most of the participants reflected upon the end-of-life caring process and its occurrence within the context of care in nursing home. The participants discussed that end-of-life care is not only about the responsibilities nurses have towards residents and their next-of-kin, but also the responsibilities of others who may influence the caring process. They perceived the caring process as an interplay between residents, next-of-kin, and themselves, along with how they relate to each other, which influences the caring process. However, as several participants asserted, this process did not occur in a vacuum: it occurred within an organisational context, which then influenced the caring process from the very beginning. One participant emphasised the importance of stable healthcare personnel within a caring organisation:
High staff turnover does not facilitate good end-of-life caregiving. Both residents and their next-of-kin need continuity and predictability in caring for and among healthcare personnel. They need somebody they know and trust… being exposed to new people every day increases their stress levels. (PI1)
Other participants discussed the importance of the leadership style and how the leader’s support influenced the culture of end-of-life care at the ward. The participants revealed that, within a caring context where their natural potential was enhanced through an enabling leadership style, they felt that they could provide competent and compassionate end-of-life care. One of the participants from the focus group stated that a positive leadership style supports nurses’ professional autonomy, thus helping them control the caring process, to have independence and to increase their ability to make clinical decisions and competent judgements regarding resident’s end-of-life care. One participant shared her experience as follows:
My leader gives me the freedom to make decisions when it comes to deciding what is best for the resident… She [the leader] enables me to be autonomous during the caring process, and this makes me aware of what and how to care.… (PI2).
The participants from the focus group interview also discussed how the nursing home’s caring culture influences care practice. They perceived the nursing home’s caring culture as positive, enabling good end-of-life care but also defective and an obstacle to care. They emphasised the importance of providing dignifying end-of-life care for residents. During the focus group interview, two of the participants engaged in a dialogue:
End-of-life care is providing care to the most vulnerable people, and it should be dignified… To do so, I have to provide care in a ‘caring room’ filled with dignity. (P7FG) Although next-of-kin and I have different perspectives of what good end-of-life care might be, we care together, we are a caring team which ensures in our own way that the resident receives competent care.… Yes, you [P7] mentioned this ‘caring room’… maybe we should open the door more often into this room and invite next-of-kin. (P6FG)
The aim of the present study was to explore nurses’ perceptions of how their professional autonomy influences the moral dimension of end-of-life care provided to nursing home residents. In the following, we discuss these perceptions in relation to Tronto’s [ 32 , 35 ] ethics of care framework and other supporting literature. To identify the moral dimension of these perceptions, we have related them to the moral qualities corresponding to each phase of the care process, as described by Tronto [ 33 , 35 ].
In the first phase of the care process—caring about—the participants discussed the importance of being attentive to which type of care needs to be provided, which is the moral quality of the first phase of care. Similar to findings from another study [ 49 ], findings from the present study revealed that some participants perceived autonomous practice as carrying out actions based on their decisions. Caring about entails detecting the resident’s needs, hence obliging nurses to ‘do something’ [ 50 ]. This particular skill was seen as an autonomous caring activity, that is, the nurses’ deliberate choice of putting on hold their self-interest and/or agenda and ‘a capacity genuinely to understand the perspective of the other in need’ [ 35 ] (p.34) , here nursing home resident.
In Tronto’s view [ 33 ], nurses’ attentiveness contributes to building up a caring relationship with a patient. The findings from the current study reveal that nurses perceived the provision of competent and compassionate end-of-life care as a result of their clinical gaze developed through certain activities, attitudes and knowledge of the patient, and through mutual relationships between the residents, next-of-kin and them. These results are supported by findings from previous studies that emphasise the importance of the nurse’s past experiences with the resident [ 51 ] and the significance of developing a good relationship with the resident and their next-of-kin [ 8 , 23 , 52 , 53 , 54 ] to provide adequate care. Moreover, similar to findings from other studies [ 55 , 56 ], the present study reveal that, to respond to the resident’s end-of-life care needs, nurses must bring not only their professional knowledge, clinical experience and ability to work autonomously but even ethical sensitivity. These findings enforce Gastman’s [ 50 ] view on caring, in which caring should respond to the patient’s care needs. This involves nurses having empathy, capacity of judgement and the ability to see what is required in a specific situation (here, end-of-life care), which, according to Gastmans [ 50 ], is inherent in the moral dimension of nursing practice.
The second phase of care—caring for—refers to nurses taking on the burden of meeting the needs identified in the first phase, that is, caring about. There was no ambiguity, and the participants had no doubts regarding who had the responsibility for the provision of end-of-life care to nursing home residents. The nurses’ responsibility was seen as a moral dimension of care. In line with Pursio et al.’s study [ 30 ], the present findings indicate that the freedom to make patient care decisions and work independently has a positive impact on the moral dimension of end-of-life care for nursing home residents. However, nurses’ work was not only about meeting residents’ needs, but also to create a safe milieu, a communicative space together with each other and with the resident’s next-of-kin, thus sharing power and control over the care process. Similar findings are displayed in an integrative literature review [ 53 ], demonstrating that a positive culture of collaborative and reciprocal relationships, a willingness to engage and become engaged and nurses communicating with intent to share and support rather than inform all lead to facilitating decision-making in nursing homes. According to Tronto [ 35 ], to facilitate end-of-life decision-making, nurses must take the initiative to allocate responsibilities; otherwise, the nurses withdraw themselves from their responsibility. By exercising their professional autonomy to assign responsibilities, nurses strive to mitigate the power imbalance among residents, their next-of-kin, and themselves, thereby preventing the occurrence of potential power struggles in their relationships [ 34 ]. This proactive approach helps prevent the emergence of end-of-life care dilemmas that could undermine the moral dimension of end-of-life care.
The third phase of care—care giving—requires, according to Tronto [ 35 ], the moral quality of nurses’ competence, meaning nurses directly engaging with care. The findings revealed that the nurses provided end-of-life care, and to do so, they needed to have competence, which implies the nurses having the knowledge, skills and values necessary to know what, why, how and when to provide end-of-life adequately. In addition, good end-of-life care requires the competence to individualise care—to provide competent care based on the resident’s physical, psychological, cultural and spiritual needs [ 57 ] while considering the resident’s context of care. Nurses’ competence is crucial for their autonomy; however, to effectively utilize their competence, nurses must be capable of assessing care needs and responding promptly [ 30 ]. Otherwise, delays in assessing residents’ care needs could undermine the moral dimension of end-of-life care. To provide individualised competent care, it is necessary that nurses make continuous assessments. As the findings reveal, the nurses were concerned with providing competent care, that is, adequate pain management. If the care provided was incompetent and led to more pain for the resident, the nurses perceived psychological distress—a state of being that resulted in response to a variety of moral events—leading to the nurses feeling anger, frustration, guilt, powerlessness and stress [ 58 ]. According to Tronto [ 34 ] (p.17) , ‘incompetent care is not only a technical problem, but a moral one’; however, as the findings reveal, the provision of competent care also depends on the nurses’ ability to prioritise decision-making when standing alone. Although nurses’ professional autonomy enabled them to make decisions and choose the right what , how , how much , when , and why , the lack of adequately educated healthcare personnel make the decision-making process a technical problem, which could weaken the moral dimension of end-of -life care.
The fourth phase—care receiving—involves the moral quality responsiveness. This means nurses being responsive to the reaction of the nursing home residents to end-of-life care process. As the findings have revealed, nursing home residents are vulnerable to nurses’ act of care or lack of care. According to Gastmans [ 59 ], care is a reciprocal practice that occurs within the framework of a relationship between the care provider (nurse) and care receiver (resident). The reciprocity consists of nurses assessing that the care provided actually meets the resident’s needs for pain management and other physiological and spiritual needs. The nurses had to make autonomous end-of-life care decisions to meet the resident’s needs. This involved the nurse’s attention to care giving to not be perceived as power abuse, which could have negative consequences for the moral dimension of end-of-life care provision.
According to Tronto [ 33 ], vulnerability may lead to unequal relationships where power abuse may occur. Nursing home residents are in a vulnerable position because they rely on nurses’ competence and ability to alleviate suffering and assess and reassess the residents’ responsiveness to pain management. To avoid an unequal relationship between resident and nurse, nurses must assess whether the care provided is competent or incompetent. Besides assessing and documenting the care provided and its outcomes, informal discussions between the resident’s next-of-kin and nurses were also assessed as important for next-of-kin perceiving a balanced power and equal position within the relationship. However, because each end-of-life act of care may alter the resident’s state of being, responsiveness requires more attentiveness [ 34 ]. Nurses must therefore meet the resident’s new needs for care with compassion and a commitment to maintaining the highest quality of life throughout the evolving stages of the resident’s end-of-life journey.
The final phase of care—caring with—requires that solidarity and trust are the foundation of all care giving to meet caring needs [ 35 ]. The moral quality of this caring phase is solidarity. The findings from the present study suggest that the nurses felt solidarity with both the residents and their leaders. The nurses felt that they were given the support and freedom to act autonomously when making decisions regarding end-of-life care, but similar to findings from a previous study [ 22 ], they also recognised the impact that organisational factors, such as leadership and care culture, may have on the justice and equality of the care provided when they prioritise care to whom needed it the most. Similar to findings from another study [ 49 ], participants in the present study described autonomy as the ability to make independent decisions and prioritise care for those who needed it most. However, according to Tronto [ 35 ], all nurses have a responsibility to help determine how care activities and responsibilities should be allocated. Residents, their next-of-kin and other healthcare personnel may have different views on how they may perceive appropriate, compassionate and dignified end-of-life care [ 20 , 21 ].Therefore, it is important to have transparency in nurse–resident–next-of-kin relations if the element of power within the relationship should be replaced by trust. Otherwise, the nurses’ autonomy may negatively influence the moral dimension of end-of-life care provided to nursing home residents. By opening the door of the “caring room” and inviting next-of-kin to participate in the care process, nurses may contribute to a greater reflectiveness around what may constitute ‘good’ end-of-life care.
Strengths and limitations
One of the strengths of the study is the use of Joan Tronto’s theory of the ethics of care [ 32 , 34 , 35 ] and its five phases and elements of care to discuss the study’s findings. This allows a deeper understanding of how nurses’ professional autonomy influences the moral dimension of end-of-life care provided to nursing home residents. Another strength lies in the utilisation of two distinct methods of data collection: individual and focus group interviews. These approaches provided diverse datasets that shed light on various aspects of how nurses’ professional autonomy impacts the moral dimension of end-of-life care. Furthermore, the inclusion of participants with varying work experiences from four nursing homes enhances the richness and depth of the data generated from the interviews, further strengthening the quality of the study. Member checking ensures that the researcher’s interpretations accurately reflect the participants’ experiences and perspectives, thereby enhancing the validity of the study. This practice can be considered one of the methodological strengths of the study.
The current study has also some limitations that need to be considered. First, a limitation may be related to the size of the participant sample. The sample consisted of only nine nurses, a number that may be seen as a limitation in data collection. To challenge this limitation, the researchers posed follow-up questions during the interviews, thus offering the participants the opportunity to provide rich descriptions of their experiences with end-of-life care. Even though the sample consisted of only nine nurses, these participants reflected on and described their everyday work experiences. The participants’ rich descriptions were evaluated as possessing sufficient information power [ 41 ], thereby enhancing the overall quality of dialogues during interviews– a notable strength.
Second, the findings are limited to these nine participants and their personal work experiences in four different Norwegian nursing homes. This means that the sample is small and context dependent, which may limit the transferability and generalisability of the findings.
A third limitation pertains to the potential influence of the chosen theoretical framework on researchers’ preunderstanding during data analysis. To avoid bias, the theoretical framework was introduced at the end of the data analyses and after the coding process was conducted. The theoretical framework contributed to situating the knowledge from the empirical data into theoretical knowledge and vice versa. However, to be certain about interpretations and knowing that the qualitative nature of the study cannot completely exclude the impact of the preunderstanding on the analysis of the data, both researchers were aware of their theoretical preunderstanding and tried not to make conclusions beforehand.
The ethics of care framework provides opportunities for nurses to analyse their own caring activities during the provision of end-of-life care to nursing home residents. The exploration of the moral dimension of the provision of end-of-life care, utilising Tronto’s theory, revealed that moral qualities, such as attentiveness, responsibility, competence, responsiveness, and solidarity are influenced to a certain extent by nurses’ autonomy. What is crucial for the provision of competent end-of-life care is the nurses’ awareness of acting properly in accordance with the moral qualities to each of the phases of caring. Therefore, to provide competent end-of-life care nurses must be attentive to residents’ care needs, take on the responsibility for the care provided to ensure that residents’ needs are met, provide competent care based on knowledge, skills and values and assess how residents respond to the care provided. In other words, this is the basic nursing process in action, and this problem-solving approach is needed for the provision of competent end-of-life care.
Data availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request. Data are located in controlled access data storage at Oslo Metropolitan University.
Abbreviations
Participant in interview [number of the individual interview
Participant [number] in Focus Group interview
World Health Organization. Palliative Care. Key Facts. 2020. https://www.who.int/palliativecare/en/ . Accessed 13 February 2023.
Broad JB, Gott M, Kim H, Boyd M, Chen H, Connolly MJ. Where do people die? An international comparison of the percentage of deaths occurring in hospital and residential aged care settings in 45 populations, using published and available statistics. Int J Public Health. 2013;58(2):257–67.
Article PubMed Google Scholar
Hoben M, Chamberlain SA, Knopp-Sihota JA, Poss JW, Thompson GN, Estabrooks CA. Impact of symptoms and Care practices on nursing home residents at the end of life: a rating by front-line Care Providers. JAMDA. 2016;17(2):155–61.
PubMed Google Scholar
World Health Organization. Nursing and midwifery. Key Facts. 2022. https://www.who.int/news-room/fact-sheets/detail/nursing-and-midwifery . Accessed 22 February 2023.
Westbrook JI, Ampt A. Design, application and testing of the Work Observation Method by activity timing (WOMBAT) to measure clinicians’ patterns of work and communication. Int J Med Inf. 2009;78(Suppl 1):S25–33.
Article Google Scholar
Munyisia EN, Yu P, Hailey D. How nursing staff spend their time on activities in a nursing home: an observational study. J Adv Nurs. 2011;67(9):1908–17.
Hernández-Marrero P, Fradique E, Pereira SM. Palliative care nursing involvement in end-of-life decision-making: qualitative secondary analysis. Nurs Ethics. 2019;26(6):1680–95.
Bollig G, Gjengedal E, Rosland JH. They know!-Do they? A qualitative study of residents and relatives views on advance care planning, end-of-life care, and decision-making in nursing homes. Palliat Med. 2016;30(5):456–70.
Dillworth J, Dickson VV, Mueller A, Shuluk J, Yoon HW, Capezuti E. Nurses’ perspectives: hospitalized older patients and end-of-life decision-making. Nurs Crit Care. 2016;21(2):e1–11.
Shimada C, Hirayama R, Wakui T, Nakazato K, Obuchi S, Ishizaki T, Takahashi R. Reconsidering long-term care in the end-of-life context in Japan. Geriatr Geront Int. 2016;16(S1):132–9.
Low LPL. Decision-making experiences and patterns in Residential Care homes for older residents, Family members and Care Providers. In: Grazia DO, Antonio G, Daniele S, editors. Gerontology. Rijeka: IntechOpen; 2018.
Google Scholar
ten Koppel M, Pasman HRW, van der Steen JT, van Hout HPJ, Kylänen M, Van den Block L, et al. Consensus on treatment for residents in long-term care facilities: perspectives from relatives and care staff in the PACE cross-sectional study in 6 European countries. BMC Palliat Care. 2019;18(1):73.
Article PubMed PubMed Central Google Scholar
Paganini MC, Bousso RS. Nurses’ autonomy in end-of-life situations in intensive care units. Nurs Ethics. 2015;22(7):803–14.
Odachi R, Tamaki T, Ito M, Okita T, Kitamura Y, Sobue T. Nurses’ experiences of End-of-life care in Long-Term Care hospitals in Japan: balancing improving the quality of life and sustaining the lives of patients dying at hospitals. Asian Nurs Res (Korean Soc Nurs Sci). 2017;11(3):207–15.
Muldrew Née Preshaw DH, McLaughlin D, Brazil K. Ethical issues experienced during palliative care provision in nursing homes. Nurs Ethics. 2019;26(6):1848–60.
Munn JC, Dobbs D, Meier A, Williams CS, Biola H, Zimmerman S. The end-of-life experience in long-term care: five themes identified from focus groups with residents, family members, and staff. Gerontologist. 2008;48(4):485–94.
Karlsson M, Berggren I, Kasén A, Söderlund M. A qualitative Metasynthesis from nurses’ perspective when dealing with ethical dilemmas and ethical problems in end-of-Life Care. Int J Hum Caring. 2015;19(1):40–8.
Gjerberg E, Førde R, Pedersen R, Bollig G. Ethical challenges in the provision of end-of-life care in Norwegian nursing homes. Soc Sci Med. 2010;71(4):677–84.
Svendsen SJ, Landmark BT. Dying patients in nursing homes: nurses provide more of everything and are left to deal with everything on their own. Sykepleien Forskning. 2017;12:e63396.
Dreyer A, Forde R, Nortvedt P. Autonomy at the end of life: life-prolonging treatment in nursing homes—relatives’ role in the decision-making process. J Med Ethics. 2009;35(11):672.
Article CAS PubMed Google Scholar
Dreyer A, Førde R, Nortvedt P. Life-prolonging treatment in nursing homes: how do physicians and nurses describe and justify their own practice? J Med Ethics. 2010;36(7):396.
Dreyer A, Førde R, Nortvedt P. Ethical decision-making in nursing homes: influence of organizational factors. Nurs Ethics. 2011;18(4):514–25.
Bollig G, Schmidt G, Rosland JH, Heller A. Ethical challenges in nursing homes–staff’s opinions and experiences with systematic ethics meetings with participation of residents’ relatives. Scand J Caring Sci. 2015;29(4):810–23.
Scott PA. Nursing and the ethical dimension of practice. In: Scott PA, editor. Key concepts and issues in nursing Ethics. Cham: Springer International Publishing; 2018.
2021; Code of Ethics for Nurses. International Council of Nurses (ICN), Geneva. https://www.icn.ch/sites/default/files/2023-04/ICN_Code-of-Ethics_EN_Web_0_0.pdf . Accessed 5 March 2023.
2017; International Classification for Nursing Practice (ICNP), Geneva. https://www.icn.ch/sites/default/files/inline-files/Palliative_Care.pdf .
Poikkeus T, Numminen O, Suhonen R, Leino-Kilpi H. A mixed-method systematic review: support for ethical competence of nurses. J Adv Nurs. 2014;70(2):256–71.
Izumi S, Nagae H, Sakurai C, Imamura E. Defining end-of-life care from perspectives of nursing ethics. Nurs Ethics. 2012;19(5):608–18.
Ohnsorge K, Keller HR, Widdershoven GA, Rehmann-Sutter C. Ambivalence’ at the end of life: how to understand patients’ wishes ethically. Nurs Ethics. 2012;19(5):629–41.
Pursio K, Kankkunen P, Sanner-Stiehr E, Kvist T. Professional autonomy in nursing: an integrative review. J Nurs Manag. 2021;29(6):1565–77.
Kramer M, Schmalenberg C. The practice of clinical autonomy in hospitals: 20 000 nurses tell their story. Crit Care Nurse. 2008;28(6):58–71.
Fisher B, Tronto JC. Towards a Feminist Theory of Care. In: Abel E, Nelson M, editors. Circles of care. Albany, NY: SUNNY; 1990.
Tronto JC. Moral boundaries: a political argument for an Ethic of Care. 1st ed. New York: Routledge; 1993.
Tronto JC. An Ethic of Care. Generations: J Am Soc Aging. 1998;22(3):15–20.
CAS Google Scholar
Tronto JC. Caring democracy: markets, Equality, and Justice. NYU; 2013.
Edwards SD. Is there a distinctive care ethics? Nurs Ethics. 2011;18(2):184–91.
Jacobsen FF, Mekki TE. Health and the Changing Welfare State in Norway: a Focus on Municipal Health Care for Elderly Sick. Ageing Int. 2012;37:125–42.
Norwegian Ministry of Health and Care Services. Forskrift om kvalitet i pleie - og omsorgstjenestene (Regulation on quality of care). 2003. [In Norwegian]. https://lovdata.no/dokument/SF/forskrift/2003-06-27-792 . Accessed 20 February 2023.
Mæhre KS, Bergdahl E, Hemberg J. Patients’, relatives’ and nurses’ experiences of palliative care on an advanced care ward in a nursing home setting in Norway. Nurs Open. 2023;10(4):2464–76.
Polit DF, Beck CT. Nursing research: generating and assessing evidence for nursing practice. 11th ed. Philadelphia: Wolters Kluwer; 2021.
Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by Information Power. Qual Health Res. 2016;26(13):1753–60.
Kallio H, Pietilä A-M, Johnson M, Kangasniemi M. Systematic methodological review: developing a framework for a qualitative semi-structured interview guide. J Adv Nurs. 2016;72(12):2954–65.
World Medical Association Declaration of Helsinki. Ethical principles for Medical Research Involving human subjects. JAMA. 2013;310(20):2191–4.
Kyngäs H, Kaakinen P. Deductive content analysis. In: Kyngäs H, Mikkonen K, Kääriäinen M, editors. The application of content analysis in Nursing Science Research. Cham: Springer International Publishing; 2020.
Chapter Google Scholar
Kyngäs H, Kääriäinen M, Elo S. The trustworthiness of Content Analysis. In: Kyngäs H, Mikkonen K, Kääriäinen M, editors. The application of content analysis in Nursing Science Research. Cham: Springer Nature Switzerland AG; 2020.
Lincoln YS, Guba EG. Naturalistic inquiry. Beverly Hills, Calif.: Sage; 1985.
Book Google Scholar
Helen N, Roberta H. Triangulation in research, with examples. Evid Based Nurs. 2019;22(3):67.
Berger R. Now I see it, now I don’t: researcher’s position and reflexivity in qualitative research. Qual Res. 2015;15(2):219–34.
Oshodi TO, Bruneau B, Crockett R, Kinchington F, Nayar S, West E. Registered nurses’ perceptions and experiences of autonomy: a descriptive phenomenological study. BMC Nurs. 2019;18(1):51.
Gastmans C. Care as a moral attitude in nursing. Nurs Ethics. 1999;6(3):214–23.
Lachman VD. Applying the ethics of care to your nursing practice. Medsurg Nurs. 2012;21(2):112.
Roberts AR, Ishler KJ. Family involvement in the nursing home and Perceived Resident Quality of Life. Gerontologist. 2017;58(6):1033–43.
Lynch B, Ryan AA, O’Neill M, Penney S. The factors that influence care home residents’ and families’ engagement with decision-making about their care and support: an integrative review of the literature. BMC Geriatr. 2022;22(1):873.
Hedman M, Häggström E, Mamhidir AG, Pöder U. Caring in nursing homes to promote autonomy and participation. Nurs Ethics. 2019;26(1):280–92.
Alshammari F, Sim J, Lapkin S, Stephens M. Registered nurses’ knowledge, attitudes and beliefs about end-of-life care in non-specialist palliative care settings: a mixed studies review. Nurse Educ Pract. 2022;59:103294.
Ghaemizade Shushtari SS, Molavynejad S, Adineh M, Savaie M, Sharhani A. Effect of end-of-life nursing education on the knowledge and performance of nurses in the intensive care unit: a quasi-experimental study. BMC Nurs. 2022;21(1):102.
Vanlaere L, Gastmans C. A personalist approach to care ethics. Nurs Ethics. 2011;18(2):161–73.
Morley G, Bradbury-Jones C, Ives J. What is ‘moral distress’ in nursing? A feminist empirical bioethics study. Nurs Ethics. 2020;27(5):1297–314.
Gastmans C. The care perspective in healthcare ethics. In: Davis AJ, Tschudin V, de Raeve L, editors. Essentials of teaching and learning in nursing ethics. New York: Churchill Livingstone Elsevier; 2006.
Download references
Acknowledgements
We would like to express gratitude to the nurses who participated in this study, thereby contributing to the data collection. Additionally, we extend our thanks to the Oslo Metropolitan University Library for granting approval and for their support in covering the publication fee of this article.
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and affiliations.
Department of Nursing and Health Promotion, Oslo Metropolitan University, PB 4, St. Olavs Plass, N-0130, Oslo, Norway
Rachel Gilbert & Daniela Lillekroken
You can also search for this author in PubMed Google Scholar
Contributions
D.L. contributed to the study conception, data collection, and analysis, and wrote the main manuscript text. R.G. was involved in data collection, analysis, reflection, and manuscript writing. D.L. was responsible for administrative work related to journal submission and was also involved in reviewing and editing the manuscript. R.G. and D.L. have read and approved the manuscript before submission.
Corresponding author
Correspondence to Daniela Lillekroken .
Ethics declarations
Ethics approval and consent to participate.
The Norwegian Agency for Shared Services in Education and Research approved the study protocol (Sikt/Ref. number 360657) and concluded that the study was not subject to the Norwegian Health Research Act (LOV-2008-06-20-44; https://lovdata.no/dokument/NL/lov/2008-06-20-44 ). An English version of the Norwegian Health Research Act can be found at: https://www.uib.no/en/med/81598/norwegian-health-research-act . This study does not aim to get insight into participants’ health status, sexuality, ethnicity, and political affiliation (sensitive information), therefore, no additional approval from a local ethics committee or institutional review board (IRB) was necessary to be obtained to conduct the study. This study was performed according to principles outlined in the Declaration of Helsinki, and in accordance with Oslo Metropolitan University’s guidelines and regulations. Data were kept confidential and used only for this research purpose. The researchers provided verbal and written information about the study. Informed consent was obtained from all participants prior data collection.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Gilbert, R., Lillekroken, D. Nurses’ perceptions of how their professional autonomy influences the moral dimension of end-of-life care to nursing home residents– a qualitative study. BMC Nurs 23 , 216 (2024). https://doi.org/10.1186/s12912-024-01865-5
Download citation
Received : 06 December 2023
Accepted : 13 March 2024
Published : 28 March 2024
DOI : https://doi.org/10.1186/s12912-024-01865-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- End-of-life
- Moral qualities
- Moral dimension
- Nursing homes
- Professional autonomy
- Qualitative study
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
- Open access
- Published: 05 April 2024
Barriers and facilitators to guideline for the management of pediatric off-label use of drugs in China: a qualitative descriptive study
- Min Meng 1 , 2 , 3 , 4 na1 ,
- Jiale Hu 5 na1 ,
- Xiao Liu 6 ,
- Min Tian 4 ,
- Wenjuan Lei 4 ,
- Enmei Liu 2 , 3 ,
- Zhu Han 7 ,
- Qiu Li 2 , 3 , 8 &
- Yaolong Chen 1 , 2 , 3 , 9 , 10 , 11
BMC Health Services Research volume 24 , Article number: 435 ( 2024 ) Cite this article
Metrics details
Despite being a global public health concern, there is a research gap in analyzing implementation strategies for managing off-label drug use in children. This study aims to understand professional health managers’ perspectives on implementing the Guideline in hospitals and determine the Guideline’s implementation facilitators and barriers.
Pediatric directors, pharmacy directors, and medical department directors from secondary and tertiary hospitals across the country were recruited for online interviews. The interviews were performed between June 27 and August 25, 2022. The Consolidated Framework for Implementation Research (CFIR) was adopted for data collection, data analysis, and findings interpretation to implement interventions across healthcare settings.
Individual interviews were conducted with 28 healthcare professionals from all over the Chinese mainland. Key stakeholders in implementing the Guideline for the Management of Pediatric Off-Label Use of Drugs in China (2021) were interviewed to identify 57 influencing factors, including 27 facilitators, 29 barriers, and one neutral factor, based on the CFIR framework. The study revealed the complexity of the factors influencing managing children’s off-label medication use. A lack of policy incentives was the key obstacle in external settings. The communication barrier between pharmacists and physicians was the most critical internal barrier.
To our knowledge, this study significantly reduces the implementation gap in managing children’s off-label drug use. We provided a reference for the standardized management of children’s off-label use of drugs.
Peer Review reports
Introduction
Off-label drug use in pediatrics is a global public health issue [ 1 ], particularly in China [ 2 , 3 ]. According to a systematic review, pediatric off-label medicine prescription rates ranged from 22.7% to 51.2% in outpatient settings and 40.48% to 78.96% in hospitalized children in China [ 4 ]. However, there are numerous unreasonable examples of off-label drug use in children, posing significant risks to children’s safety [ 5 , 6 ]. As a result, the Guideline for the Management of Pediatric Off-label Use of Drugs in China (i.e., the Guideline) was developed in 2021 by the Chinese Society of Pediatric Clinical Pharmacology, the Chinese Medical Association, and the National Clinical Research Center for Child Health and Disorders (Children’s Hospital of Chongqing Medical University), in collaboration with the Chinese GRADE Center [ 7 ].
However, translating evidence from clinical practice guidelines (i.e., CPG) into practice, also known as implementation [ 8 , 9 ], is a complex process influenced by various factors such as political and social, the health organizational system, the CPG context, healthcare professionals, and patients [ 10 ]. For example, only about half of Chinese healthcare professionals follow the recommendations and understand the clinical practice guidelines, which range from 3 to 86% [ 9 ].
To enhance guideline adherence among healthcare professionals, it is necessary to identify the facilitators and barriers to guideline implementation [ 11 ]. In addition, theory-based guideline implementation research can assist implementers in avoiding potential pitfalls that may hinder their effectiveness [ 12 ]. Consequently, identifying factors that influence the implementation of recommendations, that is, implementation barriers and facilitators [ 10 ], is essential for the early clinical translation of guidelines to implement strategies tailored to anticipated barriers [ 13 ] and to optimize the implementation of interventions [ 14 ].
Off-label use of drugs in children is a complex aspect of clinical practice [ 15 ]. Only a small number of studies have demonstrated that the following are obstacles to the management of pediatric off-label use in China: lack of time to offer sources of information and evidence of off-label use, no available expert panel on off-label use, no adverse drug reaction monitoring system, no database of off-label drugs, no ethics council or pharmacy administration committee, difficulties in gaining written agreement from parents or guardians, and absence of a unified regulatory framework [ 16 , 17 , 18 ]. In addition, doctors’ awareness prescription of off-label drugs [ 19 , 20 , 21 , 22 ], their fear of legal repercussions [ 23 ], and they are less of informing parents about off-label drugs [ 21 , 24 ] were obstacles to managing children’s off-label drug use. However, none of the present research is theoretically based on guideline implementation studies and hence may lack systematicity in identifying factors influencing off-label drug use management in children. In addition, implementation strategies for managing pediatric off-label drug use are understudied.
Implementation strategies tailed based on the implementation contextual factors can promote adherence among healthcare professionals [ 25 ]. The Consolidated Framework for Implementation Research (CFIR), a well-known implementation science framework, has been extensively used as a framework in recent research on strategies for implementing guidelines, and it has successfully identified the influencing factors for guidelines’ implementation [ 26 , 27 , 28 , 29 , 30 , 31 ].Therefore, this study used CFIR for guiding data collection, data analysis, and findings interpretation to implement interventions across healthcare settings and aimed to understand professional health managers’ perspectives on implementing the Guideline in hospitals and determine the Guideline’s implementation facilitators and barriers. Also, the suggestions for implementing the Guideline were created by mapping the identified barriers to the Expert Recommendations for Implementing Change (ERIC) and selecting the appropriate strategies for implementation [ 26 , 32 ].
Research design
A qualitative descriptive study design was used in this study to understand professional health managers’ perceived barriers and facilitators to implementing the Guideline in hospitals [ 33 ]. In the previous study, 896 healthcare professionals from mainland China were invited to complete a questionnaire to rate the urgency and difficulty of implementing each of the 21 recommendations in the Guideline, ranking the recommendations according to combined scores, and selecting the top five of them (See Table 1 ).
Setting and sample
The study was conducted collaboratively by the Clinical Pharmacology Group of the Pediatric Society of the Chinese Medical Association and the National Clinical Research Center for Child Health (Children’s Hospital of Chongqing Medical University). Pediatric directors, pharmacy directors, and medical department directors from secondary and tertiary hospitals across the country were recruited voluntarily through the members’ units for online interviews via Tencent Meeting ( https://meeting.tencent.com ).
Reading available studies and performing some initial research helped create an interview framework [ 16 , 17 , 34 , 35 , 36 ]. Before the formal interviews started, a pharmacy director was recruited to participate in the pretest, and the interview plan was modified to consider the pretest results. The formal interviews were performed between June 27 and August 25, 2022, and participants were recruited using the convenience sampling approach. All the professionals with at least one year of management experience in pediatric off-label drug use were included. All experts invited to present were encouraged to participate and were given comprehensive information on the study via WeChat. They were instructed to read the Guideline in detail and ask the guideline developers to explain any questions accordingly [ 7 ]. Detailed interview times and locations were negotiated after signing an electronic informed consent. The sample size for this investigation was determined based on data coding, data saturation, and study feasibility [ 37 ].
Data collection
A semi-structured interview outline was created, with all questions revolving around the CFIR. The conversation will focus on potential contributing elements and obstacles to the Guideline’s implementation (See Supplementary Material 2 ). The CFIR framework and pre-interview were used to determine the validity of a structured interview in this qualitative research.
Data collection and analysis were repeated to discover new insights from early interviews that would guide later interviews and data collection [ 33 ]. We used Tencent Conferences ( https://meeting.tencent.com ) for audio recording and Xunfeitingjian Software ( https://www.iflyrec.com/ ) for transcriptions. Each interview was recorded with a particular interviewer label and then transcribed verbatim. All interviewees had the chance to examine the interview recordings to increase credibility and reliability.
Data analysis
The facilitators and barriers of the Guideline were investigated explicitly in the qualitative content analysis of expert interview data [ 38 ]. Both inductive and deductive methods were used to identify facilitators, barriers, and neutral factors [ 39 ]. A neutral influence has no positive or negative consequences or both positive and negative consequences but is overall neutral [ 40 ]. Meaningful text units, such as sentences, paragraphs, and words, were inductively extracted into coding and then subjected to CFIR framework analysis. These codes were then classified into subcategories and generic categories for further evaluation [ 41 ]. Information extraction and coding in Chinese were carried out independently by two researchers (MM and LX), and any discrepancies were resolved through discussion. The final findings were translated into English and further discussed by the research team to enable researcher triangulation and to reach a consensus on the results [ 42 ].
Role of the funding sources
The funder provided support for expert consultation fees and research publication costs. The study’s design and execution were not influenced by the research funding.
Characteristics of participants
Individual interviews were conducted with 28 healthcare professionals. The interviews ranged from 21 to 56 min. Half of the participants had a bachelor’s degree, and 60.7% were male. Among the participants, pediatric directors, pharmacy directors, and medical department director were ten, nine, and nine, correspondingly. About 40% of participants had more than 20 years of experience, 27 were in senior positions, and one was in an intermediate position. There were 15 from tertiary hospitals and 13 from secondary hospitals, respectively. Twenty of the professionals interviewed were dissatisfied with the current management of off-label drug use in children. Participants came from all across the Chinese mainland (see Table 2 ).
Identified influencing factors
According to the findings of the interviews, there are 57 factors influencing the implementation of the Guideline in China, including 27 facilitators, 29 barriers, and one neutral factor. These contributing factors were spread throughout 29 constructs in the four CFIR domains studied for the guidelines (see Table 3 and Supplementary Material 1 ). The most influential factors were found in the internal setting, and the fewest influences were found in the intervention characteristics, which was 24 and ten, respectively. Following the CFIR framework, including intervention characteristics, external setting, internal setting and individual characteristics, we will present the following descriptions of all influential factors.
Intervention characteristics
In seven of the eight constructs in the CFIR domain of intervention characteristics, three facilitators and seven barriers were identified (see Table 3 and Supplementary Material 1 ). Many experts supported the implementation of the Guideline and praised the quality and strength of the evidence in terms of facilitators. The Guideline’s key relative strengths were the Guideline developed by a pediatric specialty hospital, which was in charge of developing pharmaceuticals for pediatrics, including national interdisciplinary specialists with more impact. It is more advantageous than comparable existing guidelines in China.
The barriers included a lack of practicality, unnecessary clinical practice, a need for context-specific adaptation, poor trialability in non-children’s hospitals, poor feasibility in primary hospitals, some complicated recommendations, and a need for some cost. The participant said, “With or without this guideline, it has little impact on clinical practice; it is just an additional option to consider.” which showed the Guideline is not particularly meaningful. The absence of emergency response capacity, the shortage of pediatricians, and the inability to accurately estimate adverse drug reactions are the key barriers to implementation in primary care facilities. The adaptations to the guidelines that are required to fit the implementing setting include suiting the primary level, renaming off-label drug use to expanded drug use, managing pediatric population subgroups differently (neonates, infants, children, and adolescents), improving process management, and simplifying clinical practice. The management of off-label use of drugs should be implemented for all patients while managing the pediatric population, according to the broad view of non-children’s hospital managers who believe that the pediatric population is too small. Costs that need to be considered include the cost of purchasing, maintaining, and updating the database, the cost of recruiting assessment experts, the cost of legislation, training, and dissemination, as well as the time clinicians must spend managing off-label drugs.
External setting
In the four constructs of the external setting, a total of 12 influencing factors were included, with five facilitating factors, six barrier factors, and one neutral factor (see Table 3 and Supplementary Material 1 ). In terms of facilitating factors, the Guideline can meet children’s treatment needs, pharmaceutical companies participate in and promote clinical trials, the Physicians Law of the People’s Republic of China encourages the management of off-label drug use in children, the occurrence of off-label drug use disputes in children raises concerns in this area, and unique improvement campaigns. Neutral influences include the Guangdong Pharmaceutical Society, the Shandong Pharmaceutical Society, and similar guidelines from other countries.
The barriers included a lack of patient understanding, pharmaceutical industry off-label promotion, too many choices, non-reimbursement by health insurance, risk of legal conflicts, and a lack of administrative or policy promotion. Although clinicians may have some authority, they will still have to deal with the problem and risk of off-label use of drugs because patients frequently lack comprehension of their use. " Well-known professionals collect a variety of evidence and then inform the patient of any potential adverse effects,, the parents will claim, ‘I signed the informed permission, but I do not know the medicine and saw the instructions did not include this use. You are a doctor, and you know whether to use it.' if the accident occurs.” In China, the health insurance reimbursement system has a direct impact on clinicians’ treatment behavior, and “there is a big problem with not being reimbursed for any medications that are used off-label. " In addition, the possibility of legal disputes arising from the off-label use of medications in children worries many doctors. A participant said,” After all, there is no particular legislation, and while the Physician Law specifies that off-label drug use is subject to standards and guidelines, there are still risks in practice. " Furthermore, the lack of administrative or policy impetus for the guideline is an essential barrier, “Regarding the current context of hospital medication use in China, the power of professionals is constantly pushed by the force of administration or policy. “
Internal setting
The 14 structures of the internal setting in CFIR contained the most influencing elements, with 15 facilitators and nine barriers (see Table 3 and Supplementary Material 1 ). The facilitators included graded management, a dedicated person to drive, the addition of prescription review rules, promotion by societies or associations, promotion by medical associations, cultural alignment with the hospital, high urgency, fitting firmly with the hospital’s management, availability of punishments, alignment with hospital management goals, a better learning environment, proper off-label drug coverage by the hospital, a team of off-label drug management, a database, and clinical pharmacists’ support of off-label drug use. Off-label drugs are not reimbursed by Medicare but are covered by some hospitals. " The hospital will pay for reasonable off-label drugs that are approved by the hospital but are not paid for by health insurance.” Furthermore, many hospitals are prepared to implement off-label management in children, and interview experts believe that clinical pharmacist support can help manage the off-label use of drugs. A participant said, “Our clinical pharmacists are our most important resource for explaining off-label drug use. The combination of clinicians and clinical pharmacists coming together to assess the safety and efficacy of the drugs is particularly good.”
The barriers included the low priority of pediatrics in non-children’s hospitals, the unfavorable social environment, the conflict between clinicians and patients, the lack of communication between pharmacists and clinicians, a lack of priority in comparison to other daily work, a lack of personal gain, low-level physician compliance, complex management procedures, a lack of attention from hospital leadership, and a lack of specialized training. According to many experts, managing pediatric off-label drug use does not prioritize daily work since it is only a small component of rational medication management or daily diagnosis and treatment. A participant said, " Off-label drugs for children are just a minor part of clinical treatment. In the arduous clinical work, I must always prioritize the patient, making off-label drugs impossible to focus on”. Additionally, especially in primary hospitals, there is a lack of specialized training in using off-label medications in children.
Individual characteristics
In the four constructs of the individual characteristics, a total of 11 influencing factors were included, with four facilitating factors and seven barrier factors (see Table 3 and Supplementary Material 1 ). The facilitators included an alignment with personal beliefs, physician confidence, a willingness to promote, and a high degree of professional restraint and self-defense of pediatric doctors. The transmission and promotion of guidelines with coworkers, classmates, and some network contacts were mentioned by experts as methods. Furthermore, some interviewers considered pediatricians more self-aware and disciplined than adult physicians.
The barriers included a lack of understanding of the Benefit and Risk Assessment framework, low titles, a lack of passion and innovation on the part of pharmacists, a wide range of technical competence, a few physicians’ poor ethical principles, an ignorance of physicians’ management of off-label use drugs, and a physicians’ empiricism with drug use. Recommendation 4.1’s benefit and risk assessment framework confused many medical professionals. They offered some solutions, such as “I hope to use it as a quantitative adjustment of a scale,” “make it a scoring system,” “make its voice recognizable,” or “make it as intelligent standard operating procedures.” The more considerable barriers are physicians’ empirical use of drugs and a lack of awareness about off-label drug management. “Clinically, there isn’t a clear line between right and wrong, and I think that after the recommendations are put into place, there will be a lot of resistance to changing doctors’ habits if they need to.”
Role differences
Conflicting views exist among experts on the interaction between clinical pharmacists and physicians. A pharmacist said, “The most challenging component of communicating with clinicians is clinical department chiefs, in particular. Some medical professionals will collect books, manuals, guidelines, and other information to prove their point to you. We must explain that any use not listed in the drug manual is considered off-label, but it may not be irrational. Additionally, you must carefully and exhaustively offer evidence when introducing each form of an off-label drug one at a time. With the medical department, communication is still quite simple.” In contrast, doctors contended that “prescriptions are frequently evaluated by the hospital’s pharmacy department, for example, in the case of incorrect dosage. Then a deduction is required, and much work and time must be spent on fighting and appealing each time.” Clinicians expect pharmacists to devote their time and energy as the driving force behind the off-label use of drugs for children, even though the varied feedback from the roles for communication may be related to the various goals of the different roles for managing off-label drugs for children. A participant said, “Pharmacy is expected by medical departments to offer a catalog or to advance scientific management, but their primary goal is self-preservation and minimizing dangers to clinicians during treatment. Clinicians are also extremely hopeful that pharmacies will become more clinically friendly through constant appeal and standardization, some actions to support the development of a reliable system, and a social environment. However, clinicians might not invest much time or effort in this area.”
Conflicting influential factors
Some interview experts viewed clinical pharmacists as facilitators, but some believed that they made managing children’s off-label drug use more difficult. “It is appropriate for clinical pharmacists to direct the clinical use of medications because they are more knowledgeable about drug toxicology and adverse effects. But the current situation of over-centralization of clinical pharmacist rights and restriction of clinical use of medications to clinicians, as well as the lack of personal competence of clinical pharmacists, may hinder the rational clinical use of medications, including off-label use in children,” one medical director stated.
Many experts regarded the Law on Doctors of the People's Republic of China as a facilitating factor, but some experts still think there are legal concerns involved in putting the Guidelines into practice. An expert said, “The Physicians’ Law contains 67 items, including four on the use of off-label drugs, which is considerable progress for the management of off-label use of drugs. However, there is no targeted legislation. Clinicians are at higher risk of experiencing adverse side effects from using off-label drugs.” The experts regard the guidelines’ implementation as urgent but not a priority. An interviewer said, “As a result of our current inadequate drug supply and the urgent demand for pediatric medications, experts stressed the urgent necessity to address the issue of off-label prescriptions for children.” However, according to experts, it is not given the highest priority for implementation, primarily due to the busy and complex clinical work and the concern about off-label use of drugs making up a tiny portion of daily work. Additionally, managing children’s off-label drug use is also not a standard component of hospital assessments, and medical staff typically puts the hospital’s assessment requirement first.
According to our knowledge, this is the first study conducted by Chinese guideline developers to tailor the implementation strategy of the guidelines. Key stakeholders in the implementation of the Guideline for the management of pediatric off-label use of drugs in China (2021) were interviewed to identify 57 influencing factors, including 27 facilitators, 29 barriers, and one neutral factor, based on the implementation science CFIR framework and using one-on-one expert in-depth interviews. Based on mapping the critical barriers to the CFIR-ERIC [ 26 , 32 ], recommendations for implementation strategies were made, such as tailoring strategies, encouraging adaptability, inquiring of national health administrations to promote recommendations, and establishing networks for communication between clinicians and pharmacists. The study revealed the complexity of the factors influencing managing children’s off-label medication use. We will update the Guideline to address the lack of patient awareness, and a lack of policy incentives (non-reimbursement by health insurance and a lack of administrative or policy promotion) were the key obstacles in external settings. The communication barriers between pharmacists and physicians were found to be the most critical internal barriers. Regarding individual characteristics, the main barriers were pharmacists’ varying technical competence and physicians’ empiricism with medication use. Additionally, this study discovered that even though the PRC Physicians Law’s enforcement helped implement and promote the Guideline, it still needs to relieve the issue of legal dangers for medical staff completely. The difference in the barriers to implementing the Guideline for different roles of medical staff is the communication barrier between pharmacists and physicians.
According to this qualitative study, the Guideline was viewed as having less applicability for primary hospitals by many experts. The findings were consistent with a 2017 study on managing children’s off-label drug use, which also found a significant difference between the management of children’s off-label drug use in secondary and tertiary hospitals [ 17 ]. In China, each hospital grade has a unique set of medical duties, and the higher the grade, the greater the capacity for treatment [ 43 , 44 ]. As map CFIR-ERIC suggests, we should tailor strategies [ 26 , 32 ]. It is advised that guideline developers should take into account the creation of implementation strategies for various hospital grades [ 14 ]. Additionally, many experts feel that the Benefit and Risk Assessment Framework in recommendation 4.1 is difficult to comprehend and would like to quantify and improve the framework’s operability to help physicians make speedy and accurate decision-making. Intelligent assisted decision-making technologies have been created globally and deployed in clinical practice [ 45 , 46 , 47 ]. Artificial intelligence-based and scientifically sound assisted decision-making systems for children’s off-label drug use to have some shortcomings [ 45 ]. As map CFIR-ERIC suggests, we should promote adaptability and suggest researchers should develop a more practical framework for monitoring the use of off-label drugs in children or a scientifically validated off-label medication-assisted decision-making system to make it easy to follow [ 26 , 32 ].
As our findings show, in China, the lack of policy incentives and Medicare not covering off-label medicine costs are severe barriers to managing off-label drug use in children [ 48 , 49 ], Belgium [ 50 ], the Czech Republic [ 51 ], Germany [ 52 ], Italy [ 53 ], Switzerland [ 53 ], the United States [ 54 , 55 ], Slovakia [ 55 ], Greece [ 5 ], and Poland [ 56 ], were currently capable of paying for certain off-label drugs by general health insurance. As a result, it is proposed that China’s health insurance department consider establishing a national essential specified reimbursement catalog for off-label drugs based on the relevant experience of the countries mentioned above. Also, we find that a lack of administrative & policy promotion is a barrier. Policies are the most influential drivers of medical practice improvement in China. For example, the Chinese Special Rectification Activity on Clinical Antibiotic Use (CSRA), launched in 2011, has been implemented by hospitals and promoted by policy. Numerous studies have demonstrated its rapid and long-term implementation effect [ 57 , 58 , 59 ]. Alter incentive/allowance structures, involve executive boards, and build a coalition were mapped by CFIR-ERIC [ 26 , 32 ]; consequently, the national health administration is called upon to promote implementing off-label drug use management in children.
Although the Law on Doctors of the People's Republic of China was a reasonable basis for off-label use, physicians and hospitals face potential legal risks in practice, according to our research, which may be because of its implementation challenges [ 59 ]. According to Chinese Physicians Law, “in special cases where effective therapies are not yet available, a physician may, after obtaining the patient’s explicit informed consent, use a drug that is not stated in the drug’s instructions but has evidence to support its use,” which indicates that there are two conditions for using drugs off-label. First, obtain the patient’s informed consent. Second, there is evidence supported. Clinical challenges exist in obtaining informed permission from parents of children, primarily because of their lack of comprehension of the concept of off-label use of drugs [ 19 , 60 ] and an increased risk of adverse reaction [ 60 ], which is further worsened by the crisis in doctor-patient trust crisis [ 61 ]. Additionally, the current inaccessibility of evidence, mainly because of the shortage of locally evidence-based data for pediatrics [ 62 , 63 ], the shortage of evidence-based specialists [ 64 ], and the ignorance of “evidence-based medicine” and its critical databases among doctors both domestically and internationally [ 65 ]. As a result, the following two suggestions are recommended: On the one hand, information sharing and disease-specific education [ 66 ] can help doctors and patients communicate more effectively. The Guideline’s developers should create patient and public versions of the Guidelines [ 67 , 68 ] to “translate” the rationale and recommendations into a format that patients and the general public can understand and use, as well as to assist parents of children in understanding the meaning and necessity of off-label drugs in a friendly manner. Parents will have a better grasp of why off-label drug use is necessary. On the other hand, the authors of the recommendations should invite evidence-based specialists to regularly update the “list of common types of pediatric off-label use of drugs, evidence levels, and recommendations” in Recommendation 1.2, making it easy for clinicians to access the evidence-based information regarding the use of drugs off-label in children.
Clinical pharmacists actively contribute to managing off-label drugs in children, as the experts indicated in their interviews [ 69 , 70 , 71 , 72 ]. However, the study identified communication barriers between pharmacists and physicians, which is consistent with the findings [ 73 ]. On the one hand, the idea of the doctor as a leader is ingrained in the medical profession. The power gap between doctors and pharmacists makes doctors seem unapproachable to pharmacists [ 74 , 75 ]. On the other, most clinical pharmacists in China originally trained as ordinary pharmacists and went on to finish a year of continuing clinical pharmacy education [ 76 , 77 ]. A need for more clarity of duty and role conflict among clinical pharmacists is frequently the result of shorter training programs and quick duty transitions [ 76 ]. The wide range mainly demonstrates this in clinical pharmacist competence [ 78 ], which has caused physicians to need more faith in their expertise [ 73 ]. In order to improve the communication effectiveness of pediatric off-label use of drug management, it is suggested to investigate appropriate communication strategies and establish networks for communication between doctors and pharmacists according to the CFIR-ERIC map [ 26 , 32 ]. For instance, physician-pharmacist-patient communication has become more effective and satisfying thanks to the situation-background-assessment-recommendation (SBAR) standardized communication model [ 79 , 80 ].
To our knowledge, this study significantly reduces the implementation gap in managing children’s off-label drug use. We systematically identified and analyzed the “Guideline for the Management of Pediatric Off-Label Use of Drugs in China” implementation challenges using the CFIR framework and gave suggestions for implementing the Guideline. In this study, we investigated the perspectives of healthcare professionals in various hospital roles on the management of children’s off-label drug use. We provided a reference for the standardized management of children’s off-label use of drugs.
Limitations
The study also has some limitations. Firstly, only the key stakeholders in the Guideline—the head of pediatrics, the head of the pharmacy, and the medical department director were included in the study, whichmeans that not all influencing factors were identified. Still, since all participants have rich experience in the field and experience managing off-label drug use in children, we believe they are more representative. Second, quotations with codes were translated into English from the expert interviews and data analysis done in Chinese. Although no researchers of the international collaborative team had read the original transcripts, a consensus was reached through an iterative process and triangulation to ensure the objectivity of the data collection and analysis.
Implications for further research and clinical practice
Planning the implementation of guidelines, including a good fit between implementation strategies, relevant interventions, and contexts, is more complicated and demanding [ 81 ]. The findings of this study indicate that future complex interventions for the Guideline will be necessary because of several influencing factors. It is advised that future intervention studies be designed using the new framework for complex interventions, which includes intervention development or identification, feasibility, assessment, and implementation [ 82 ]. Partnership, target population-centered, evidence, and theory-based, implementation-based, efficiency-based, stepped or phased, intervention-specific, and combination are currently recommended intervention development and design methodologies [ 83 ]. Combining the Chinese implementation settings will be possible concerning numerous implementation strategies, such as workflow and regulation optimization, assessment tool development, resource input, or multidisciplinary collaboration [ 84 ]. Consequently, complex interventions may be established to encourage the implementation of guidelines at various levels of the hospital setting. In addition, appropriate process evaluation methods should be adopted to comprehend and better understand the causal mechanisms and contextual factors associated with outcome change [ 85 , 86 ].
Despite being a global public health concern, there is a research gap in analyzing implementation strategies for managing off-label drug use in children. In the future, the Guideline will be updated based on facilitators and barriers, and interventions will be created in various settings to advance guidelines’ implementation by guideline developers. Additionally, the findings in this study are regarded as a baseline for comparison with the barriers and facilitators evaluated during and after implementing an intervention to improve the use of off-label drug management strategies.
Data availability
To preserve the anonymity of interviewees, the transcribed interviews are not available for sharing. The remaining data generated or analysed during this study are included in this published article and its supplementary information file.
Frattarelli DA, Galinkin JL, Green TP, Johnson TD, Neville KA, Paul IM, Van Den Anker JN. Off-label use of drugs in children. Pediatrics. 2014;133(3):563–7.
Article PubMed Google Scholar
Allen HC, Garbe MC, Lees J, Aziz N, Chaaban H, Miller JL, Johnson P, DeLeon S. Off-label medication use in children, more common than we think: a systematic review of the literature. J Okla State Med Assoc. 2018;111(8):776–83.
PubMed PubMed Central Google Scholar
Balan S, Hassali MAA, Mak VSL. Two decades of off-label prescribing in children: a literature review. World J Pediatrics: WJP. 2018;14(6):528–40.
Li Y, Jia L, Teng L. A systematic review of off-label drug use at home and abroad for pediatrics. Chin J Hosp Pharm. 2016;36(23):2114–9.
CAS Google Scholar
Schrier L, Hadjipanayis A, Stiris T, Ross-Russell RI, Valiulis A, Turner MA, Zhao W, De Cock P, de Wildt SN, Allegaert K, et al. Off-label use of medicines in neonates, infants, children, and adolescents: a joint policy statement by the European Academy of Paediatrics and the European society for Developmental Perinatal and Pediatric Pharmacology. Eur J Pediatrics. 2020;179(5):839–47.
Article Google Scholar
Cui J, Zhao L, Liu X, Liu M, Zhong L. Analysis of the potential inappropriate use of medications in pediatric outpatients in China. BMC Health Serv Res. 2021;21(1):1273.
Article PubMed PubMed Central Google Scholar
Meng M, Liu E, Zhang B, Lu Q, Zhang X, Ge B, Wu Y, Wang L, Wang M, Luo Z et al. Guideline for the management of pediatric off-label use of drugs in China (2021). BMC Pediatr. 2022;22(1):442.
Rabin BA, Brownson RC, Haire-Joshu D, Kreuter MW, Weaver NL. A glossary for dissemination and implementation research in health. J Public Health Manag Pract. 2008;14(2):117–23.
Liu M, Zhang C, Zha Q, Yang W, Yuwen Y, Zhong L, Bian Z, Han X, Lu A. A national survey of Chinese medicine doctors and clinical practice guidelines in China. BMC Complement Altern Med. 2017;17(1):451.
Correa VC, Lugo-Agudelo LH, Aguirre-Acevedo DC, Contreras JAP, Borrero AMP, Patiño-Lugo DF, Valencia DAC. Individual, health system, and contextual barriers and facilitators for the implementation of clinical practice guidelines: a systematic metareview. Health Res Policy Syst. 2020;18(1):74.
Houghton C, Meskell P, Delaney H, Smalle M, Glenton C, Booth A, Chan XHS, Devane D, Biesty LM. Barriers and facilitators to healthcare workers’ adherence with infection prevention and control (IPC) guidelines for respiratory infectious diseases: a rapid qualitative evidence synthesis. Cochrane Database Syst Rev. 2020;4(4):CD013582.
PubMed Google Scholar
McArthur C, Bai Y, Hewston P, Giangregorio L, Straus S, Papaioannou A. Barriers and facilitators to implementing evidence-based guidelines in long-term care: a qualitative evidence synthesis. Implement Sci. 2021;16(1):70.
Fischer F, Lange K, Klose K, Greiner W, Kraemer A. Barriers and strategies in Guideline Implementation-A scoping review. Healthc (Basel Switzerland). 2016;4(3):36.
Baker R, Camosso-Stefinovic J, Gillies C, Shaw EJ, Cheater F, Flottorp S, Robertson N, Wensing M, Fiander M, Eccles MP et al. Tailored interventions to address determinants of practice. Cochrane Database Syst Rev. 2015;2015(4):CD005470.
Rusz C-M, Ősz B-E, Jîtcă G, Miklos A, Bătrînu M-G, Imre S. Off-Label Medication: From a Simple Concept to Complex Practical Aspects. Int J Environ Res Public Health. 2021;18(19).
Mei M, Wang L, Liu E, Li Z, Guo Z, Zhang X, Xu H. Current practice, management and awareness of pediatric off-label drug use in China-A questionnaire based cross-sectional survey. Chin J Evid Based Pediatr. 2017;12(04):289–94.
Google Scholar
Mei M, Xu H, Wang L, Huang G, Gui Y, Zhang X. Current practice and awareness of pediatric off-label drug use in Shanghai, China -a questionnaire-based study. BMC Pediatr. 2019;19(1):281.
Zhang L, Li Y, Liu Y, Zeng L, Hu D, Huang L, Chen M, Lv J, Yang C. Pediatric off-label drug use in China: risk factors and management strategies. J Evid Based Med. 2013;6(1):4-18..
Balan S, Hassali MA, Mak VSL. Awareness, knowledge and views of off-label prescribing in children: a systematic review. Br J Clin Pharmacol. 2015;80(6):1269–80.
Article CAS PubMed PubMed Central Google Scholar
Balan S, Ahmad Hassali MA, Mak VSL. Attitudes, knowledge and views on off-label prescribing in children among healthcare professionals in Malaysia. Int J Clin Pharm. 2019;41(4):1074–84.
AbuAlsaud Z, Alshayban D, Joseph R, Pottoo FH. Off-label medications use in the Eastern Province of Saudi Arabia: the views of General practitioners, pediatricians, and other specialists. Hosp Pharm. 2020;55(1):37–43.
Pérez RP, Antorán M, Solá CA, Riechmann ER, Pea MJM. [Results from the 2012–2013 paediatric national survey on off-label drug use in children in Spain (OL-PED study)]. Anales De Pediatría. 2014;81(1):16-21.
Wittich CM, Burkle CM, Lanier WL. Ten common questions (and their answers) about off-label drug use. Mayo Clin Proc. 2012;87(10):982–90.
Joret-Descout P, Bataille J, Brion F, Bourdon O, Hartmann JF, Prot-Labarthe S. [Attitudes and experiences of off-label prescribing among paediatricians in a French university teaching hospital]. Ann Pharm Fr. 2016;74(3):222–31.
Article CAS PubMed Google Scholar
Flodgren G, Hall AM, Goulding L, Eccles MP, Grimshaw JM, Leng GC, Shepperd S. Tools developed and disseminated by guideline producers to promote the uptake of their guidelines. Cochrane Database Syst Rev. 2016;2016(8):CD010669.
Waltz TJ, Powell BJ, Fernández ME, Abadie B, Damschroder LJ. Choosing implementation strategies to address contextual barriers: diversity in recommendations and future directions. Implement Sci. 2019;14(1):42.
Breimaier HE, Halfens RJ, Lohrmann C. Effectiveness of multifaceted and tailored strategies to implement a fall-prevention guideline into acute care nursing practice: a before-and-after, mixed-method study using a participatory action research approach. BMC Nurs. 2015;14:18.
McManus K, Cheetham A, Riney L, Brailsford J, Fishe JN. Implementing oral systemic corticosteroids for Pediatric Asthma into EMS Treatment guidelines: a qualitative study. Prehosp Emerg Care. 2023;27(7):886-892.
VanDevanter N, Kumar P, Nguyen N, Nguyen L, Nguyen T, Stillman F, Weiner B, Shelley D. Application of the Consolidated Framework for Implementation Research to assess factors that may influence implementation of tobacco use treatment guidelines in the Viet Nam public health care delivery system. Implement Sci. 2017;12(1):27.
Breimaier HE, Heckemann B, Halfens RJ, Lohrmann C. The Consolidated Framework for Implementation Research (CFIR): a useful theoretical framework for guiding and evaluating a guideline implementation process in a hospital-based nursing practice. BMC Nurs. 2015;14:43.
Hu J, Ruan H, Li Q, Gifford W, Zhou Y, Yu L, Harrison D. Barriers and facilitators to Effective Procedural Pain treatments for Pediatric patients in the Chinese context: a qualitative descriptive study. J Pediatr Nurs. 2020;54:78–85.
Powell BJ, Waltz TJ, Chinman MJ, Damschroder LJ, Smith JL, Matthieu MM, Proctor EK, Kirchner JE. A refined compilation of implementation strategies: results from the Expert recommendations for Implementing Change (ERIC) project. Implement Sci. 2015;10:21.
Moser A, Korstjens I. Series: practical guidance to qualitative research. Part 3: Sampling, data collection and analysis. Eur J Gen Pract.2018;24(1):9-18..
Stewart D, Rouf A, Snaith A, Elliott K, Helms PJ, McLay JS. Attitudes and experiences of community pharmacists towards paediatric off-label prescribing: a prospective survey. Br J Clin Pharmacol. 2007;64(1):90–5.
Mukattash T, Hawwa AF, Trew K, McElnay JC. Healthcare professional experiences and attitudes on unlicensed/off-label paediatric prescribing and paediatric clinical trials. Eur J Clin Pharmacol. 2011;67(5):449–61.
Zhang Qiuwen P, Dong H, Jiale, et al.:.Interpretation of the components of the Comprehensive Framework for Implementation Research (CFIR). Chin J Evidence-Based Med. 2021;21(03):355–60.
Hennink MM, Kaiser BN, Marconi VC. Code saturation versus meaning saturation: how many interviews are Enough? Qual Health Res. 2017;27(4):591–608.
Goodman LA. Snowball Sampling. Annals Math Stat. 1961;32(1):148–70.
Sacks D, Baxter B, Campbell BCV, Carpenter JS, Cognard C, Dippel D, Eesa M, Fischer U, Hausegger K, Hirsch JA, et al. Multisociety Consensus Quality Improvement revised Consensus Statement for Endovascular Therapy of Acute ischemic stroke. Int J Stroke. 2018;13(6):612–32.
Damschroder LJ, Lowery JC. Evaluation of a large-scale weight management program using the consolidated framework for implementation research (CFIR). Implement Sci. 2013;8(1):51.
Keith RE, Crosson JC, O’Malley AS, Cromp D, Taylor EF. Using the Consolidated Framework for Implementation Research (CFIR) to produce actionable findings: a rapid-cycle evaluation approach to improving implementation. Implement Sci. 2017;12(1):15.
Vermeulen J, Beeckman K, Turcksin R, Van Winkel L, Gucciardo L, Laubach M, Peersman W, Swinnen E. The experiences of last-year student midwives with high-fidelity Perinatal Simulation training: a qualitative descriptive study. Women Birth. 2017;30(3):253–61.
Ji S, Wang W, Zhang P, Zeng C, Li L, Yu F, Zhou X. Research on the rationality of hospital human resources allocation under the background of graded diagnosis and treatment. Chin J Evidence-Based Med. 2020;20(9):1004–11.
Wu C, Xie G. Differences in perceived professionalism of medical workers in different levels of hospitals and insights. Med Manage;2018;36):184–6.
Sharma M, Savage C, Nair M, Larsson I, Svedberg P, Nygren JM. Artificial Intelligence Applications in Health Care Practice: scoping review. J Med Internet Res. 2022;24(10):e40238.
Liao P, Hsu P, Chu W, Chu W. Applying artificial intelligence technology to support decision-making in nursing: a case study in Taiwan. Health Inf J. 2015;21(2):137–48.
Wu J, Gou F, Tan Y. A Staging Auxiliary Diagnosis Model for Nonsmall Cell Lung Cancer Based on the Intelligent Medical System. Comput Math Methods Med.2021;2021:6654946.
Zuo W, Sun Y, Liu R, Du L, Yang N, Sun W, Wang P, Tang X, Liu Y, Ma Y, et al. Management guideline for the off-label use of medicine in China. Expert Rev Clin Pharmacol. 2021;2022:1–16.
Liu R, Niu Z, Zuo W, Hu Y, Zhang B. Atitude and medical insurance coverage for of label use in various countries. Chin Hosptial Manage. 2021;37(10):838–41.
Dooms M, Cassiman D, Simoens S. Off-label use of orphan medicinal products: a Belgian qualitative study. Orphanet J Rare Dis. 2016;11(1):144.
Vostalová L, Mazelová J, Samek J, Vocelka M. Health Technology Assessment in Evaluation of Pharmaceuticals in the Czech Republic. Int J Technol Assess Health Care. 2017;33(3):339–44.
Seidenschnur KEK, Dressler C, Weller K, Nast A, Werner RN. Off-label prescriptions and decisions on reimbursement requests in Germany - a retrospective analysis. J Dtsch Dermatol Ges. 2017;15(11):1103–9.
Pauwels K, Huys I, Casteels M, De Nys K, Simoens S. Market access of cancer drugs in European countries: improving resource allocation. Target Oncol. 2014;9(2):95-110..
Teagarden JR, Dreitlein WB, Kourlas H, Nichols L. Influence of pharmacy benefit practices on off-label dispensing of drugs in the United States. Clin Pharmacol Ther. 2012;91(5):943–5.
Löblová O, Csanádi M, Ozierański P, Kaló Z, King L, McKee M. Patterns of alternative access: unpacking the Slovak extraordinary drug reimbursement regime 2012–2016. Health Policy. 2019;123(8):713–20.
Badora K, Caban A, Rémuzat C, Dussart C, Toumi M. Proposed changes to the reimbursement of pharmaceuticals and medical devices in Poland and their impact on market access and the pharmaceutical industry. J Mark Access Health Policy. 2017;5(1):1381544.
Wu X, Chen Y, Xu J. Effect of special rectification of antibiotics. Chin J Nosocomiology. 2014;24(22):5540–2.
Huang J, Wang D, Li J. Effect of special rectification on use intensity of before and after strict policy on use intensity of antimicrobial. Chin J Nosocomiology. 2014;24(1):99–101.
Qian X, Pan Y, Su D, Gong J, Xu S, Lin Y, Li X. Trends of Antibiotic Use and Expenditure after an intensified antimicrobial stewardship policy at a 2,200-Bed Teaching Hospital in China. Front Public Health. 2021;9:729778.
Guidi B, Parziale A, Nocco L, Maiese A, La Russa R, Di Paolo M, Turillazzi E. Regulating pediatric off-label uses of medicines in the EU and USA: challenges and potential solutions: comparative regulation framework of off label prescriptions in pediatrics: a review. Int J Clin Pharm. 2022;44(1):264–9.
Zhou M, Zhao L, Campy KS, Wang S. Changing of China׳s health policy and doctor–patient relationship: 1949–2016. Health Policy Technol. 2017;6(3):358–67.
Li J, Yan K, Kong Y, Ye X, Ge M, Zhang C. A cross-sectional study of children clinical trials registration in the world based on ClinicalTrials.gov establishment. Chin J Evidence-Based Pediatr. 2016;11(1):3–7.
Jiang J, Shen J, Li C, Qi L, Ni S. Development of pediatric clinical trials at home and abroad. J Clin Pediatr. 2020;39(8):636–40.
Li B, Yan Y, Lv M, Zhao G, Li Z, Feng S, Hu J, Zhang Y, Yu X, Zhang J, et al. Clinical epidemiology in China series. Paper 1: evidence-based medicine in China: an oral history study. J Clin Epidemiol. 2021;140:165–71.
Barzkar F, Baradaran HR, Koohpayehzadeh J. Knowledge, attitudes and practice of physicians toward evidence-based medicine: a systematic review. J Evid Based Med. 2018;11(4):246–51.
Georgopoulou S, Prothero L, D’Cruz DP. Physician-patient communication in rheumatology: a systematic review. Rheumatol Int. 2018;38(5):763–75.
Wang X, Chen Y, Akl EA, Tokalić R, Marušić A, Qaseem A, Falck-Ytter Y, Lee MS, Siedler M, Barber SL, et al. The reporting checklist for public versions of guidelines: RIGHT-PVG. Implement Sci. 2021;16(1):10.
About the G-I-N. PUBLIC Toolkit: patient and public involvement in guidelines [ https://g-i-n.net/toolkit ].
Zheng Z, Zeng Y, Huang H. Pharmacists’ role in off-label drug use in China. Eur J Hosp Pharm. 2018;25(2):116.
Deng T, Lin M, Zhang S, Yang X. Thinking and practice of clinical pharmacists participating in the treatment of Infectious diseases. Chin J Pharmacoepidemiology. 2022;31(3):178–83.
Li W, Zheng L, Luo X. Clinical pharmacist interventions in obstetrics and gynecology: off-label use of drugs. Herald Med. 2021;40(10):1435–8.
Li Y, Cai J, Jia M, Jia W, Liu J. Analysis of off-label use of anti-tumor drugs and clinical pharmaceutical intervention in a third-grade hospital in Xinjiang. Chin J Clin Ration Drug Use. 2019;14(9):1–4.
Cai F, Zhang J. Investigation and analysis of how to promote the clinical reasonable medication from doctors, clinical pharmacists and patients. China Med Pharm. 2015;5(4):122–46.
Thomas J, Kumar K, Chur-Hansen A. How pharmacy and medicine students experience the power differential between professions: even if the pharmacist knows better, the doctor’s decision goes. PLoS ONE. 2021;16(8):e0256776.
Baker L, Egan-Lee E, Martimianakis MAT, Reeves S. Relationships of power: implications for interprofessional education. J Interprof Care. 2011;25(2):98-104..
Li W, Lin G, Xu A, Huang Y, Xi X. Role ambiguity and role conflict and their influence on responsibility of clinical pharmacists in China. Int J Clin Pharm. 2020;42(3):879–86.
Zhao J, Zhou Y, Ma L, Sheng X, Cui Y. Current situation and enlightenment of clinical pharmacists training in Peking University First Hospital. Clin Medication J. 2017;15(3):86–8.
Tu D, Zhao L, Wang L, Huang Z. Thinking on improving pharmacists’clinical Pharmaceu⁃ Tical Care under the Transformation of pharmacists. Sci Educ Article Collects 2021(7):116–8.
Zhang J, Wang Y, Shi X, Bao Q, Shen G. Clinical practice for PIVAS pharmacists based upon SBAR communication model. Chin J Hosp Pharm. 2021;41(3):309–13.
Lo L, Rotteau L, Shojania K. Can SBAR be implemented with high fidelity and does it improve communication between healthcare workers? A systematic review. BMJ Open. 2021;11(12):e055247.
Schultes M-T, Albers B, Caci L, Nyantakyi E, Clack L. A modified implementation mapping methodology for evaluating and learning from existing implementation. Front Public Health. 2022;10:836552.
Rutter H, Savona N, Glonti K, Bibby J, Cummins S, Finegood DT, Greaves F, Harper L, Hawe P, Moore L, et al. The need for a complex systems model of evidence for public health. Lancet. 2017;390(10112):2602–4.
O’Cathain A, Croot L, Sworn K, Duncan E, Rousseau N, Turner K, Yardley L, Hoddinott P. Taxonomy of approaches to developing interventions to improve health: a systematic methods overview. Pilot Feasibility Stud. 2019;5:41.
Zhao J, Bai W, Zhang Q, Su Y, Wang J, Du X, Zhou Y, Kong C, Qing Y, Gong S, et al. Evidence-based practice implementation in healthcare in China: a living scoping review. Lancet Reg Health West Pac. 2022;20:100355.
Quasdorf T, Clack L, Laporte Uribe F, Holle D, Berwig M, Purwins D, Schultes M-T, Roes M. Theoretical approaches to process evaluations of complex interventions in health care: a systematic scoping review protocol. Syst Rev. 2021;10(1):268.
Brown CH, Curran G, Palinkas LA, Aarons GA, Wells KB, Jones L, Collins LM, Duan N, Mittman BS, Wallace A et al. An overview of research and evaluation designs for dissemination and implementation. Annu Rev Public Health. 2017;38:1-22.
Download references
Acknowledgements
Thanks to Professor Fei Yin of Xiangya Hospital Central South University for his help in recruiting experts for the interviews.
This research was funded by the Chevidence Lab Child & Adolescent Health of Chongqing Medical University’s Children’s Hospital’s Key Project in 2022 (LY03007).
Author information
Min Meng and Jiale Hu contribute equally.
Authors and Affiliations
Chevidence Lab of Child & Adolescent Health, Children’s Hospital of Chongqing Medical University, Chongqing, China
Min Meng & Yaolong Chen
National Clinical Research Center for Child Health and Disorders, Ministry of Education Key Laboratory of Child Development and Disorders, International Science and Technology Cooperation Base of Child Development and Critical Disorders, Children’s Hospital of Chongqing Medical University, Chongqing, China
Min Meng, Enmei Liu, Qiu Li & Yaolong Chen
Chongqing Key Laboratory of Pediatrics, Chongqing, China
Department of Pharmacy, Gansu Provincial Hospital, Lanzhou, China
Min Meng, Min Tian & Wenjuan Lei
Department of Nurse Anesthesia, Virginia Commonwealth University, Richmond, USA
School of Public Health, Lanzhou University, Lanzhou, China
College of Pharmacy, Gansu University of Chinese Medicine, Lanzhou, China
Department of Nephrology, Children’s Hospital of Chongqing Medical University, Chongqing, China
Research Unit of Evidence-Based Evaluation and Guidelines, Chinese Academy of Medical Sciences(2021RU017), School of Basic Medical Sciences, Lanzhou University, Lanzhou, China
Yaolong Chen
WHO Collaborating Centre for Guideline Implementation and Knowledge Translation, Lanzhou, China
Lanzhou University GRADE Center, Lanzhou, China
You can also search for this author in PubMed Google Scholar
Contributions
MM and JH are joint first authors. YC and QL designed the study. MM organized all expert interviews with the help of JH and requested experts to examine the interview recordings. XL and MM extracted information and coded in Chinese.WL and XL analyzed the data. MT and ZH translated interview. MM and JH drafted the manuscript. YC and QL revised the article. All authors have read and approved the final manuscript.
Corresponding authors
Correspondence to Qiu Li or Yaolong Chen .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the Research Ethics Committees at Gansu Provincial People’s Hospital (approval number: 2022 − 152). All participants signed the informed consent form. All interviews were conducted anonymously, and all transcripts and other records were kept private. Participants were informed that they could start, refuse, or withdraw from the study without negative consequences.The study was performed in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Meng, M., Hu, J., Liu, X. et al. Barriers and facilitators to guideline for the management of pediatric off-label use of drugs in China: a qualitative descriptive study. BMC Health Serv Res 24 , 435 (2024). https://doi.org/10.1186/s12913-024-10860-0
Download citation
Received : 06 May 2023
Accepted : 12 March 2024
Published : 05 April 2024
DOI : https://doi.org/10.1186/s12913-024-10860-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Off-label use
- Qualitative research
- Implementation science
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Conducting interviews involves a well-planned and deliberate process to collect accurate and valid data. Here's a step-by-step guide on how to conduct interviews in qualitative research, broken down into three stages: 1. Before the interview. The first step in conducting a qualitative interview is determining your research question. This will ...
A qualitative research interview is a one-to-one data collection session between a researcher and a participant. Interviews may be carried out face-to-face, over the phone or via video call using a service like Skype or Zoom. There are three main types of qualitative research interview - structured, unstructured or semi-structured.
Qualitative research interviews are depth interviews. They elicit detailed feedback from your leads and customers. Unstructured interviews reveal why people react in a certain way or make certain decisions. According to The Hartford, qualitative research provides an anecdotal look into your business. That provides an important form of data.
Summary. The qualitative research interview is a powerful data-collection tool which affords researchers in medical education opportunities to explore unknown areas of education and practice within medicine. This paper articulates 12 tips for consideration when conducting qualitative research interviews, and outlines the qualitative research ...
Abstract. The qualitative research interview is an important data collection tool for a variety of methods used within the broad spectrum of medical education research. However, many medical teachers and life science researchers undergo a steep learning curve when they first encounter qualitative interviews, both in terms of new theory but also ...
Designing and structuring the interview Qualitative interviews can range from highly exploratory to addressing specific hypotheses. As a result, the structure of interviews can range from loose conversations to structured exchanges in which all interviewees are asked the exact same set of questions. Your choice of interview
An interview is a qualitative research method that relies on asking questions in order to collect data. Interviews involve two or more people, one of whom is the interviewer asking the questions. ... Depending on the type of interview you are conducting, your questions will differ in style, phrasing, and intention. Structured interview ...
Qualitative interviews usually involve follow-up questions and are conducted in a conversation or discussion format. A qualitative interview is a more personal form of research agenda compared to general questionnaires or focused group studies. Such formats often include open-ended and follow-up questions. LEARN ABOUT: Behavioral Research.
5. Not keeping your golden thread front of mind. We touched on this a little earlier, but it is a key point that should be central to your entire research process. You don't want to end up with pages and pages of data after conducting your interviews and realize that it is not useful to your research aims.
It is the most widely used method in qualitative research. It is flexible, inexpensive, and does not inter-fere with the researcher's life the way that ethnography does. This chapter looks at qualitative interviewing and how it compares to other types of collect-ing evidence in research, particularly structured interviewing and ethnography.
Sago has decades of experience across both quantitative and qualitative research. Our experts find interviews ideal for in-depth qualitative insights that guide new product and service development or improve market positioning for existing offerings. We offer both in-person facilities and online spaces to conduct qualitative interviews.
Interviewing. This is the most common format of data collection in qualitative research. According to Oakley, qualitative interview is a type of framework in which the practices and standards be not only recorded, but also achieved, challenged and as well as reinforced.[] As no research interview lacks structure[] most of the qualitative research interviews are either semi-structured, lightly ...
Interviews provide a rich and dynamic method of collecting data in qualitative research that can provide thoughtful insight into the study question. We have described a step‐by‐step process for conducting interviews that may be useful for those who are conducting qualitative medical education research.
We also demonstrate how, when conducting qualitative research, qualitative researchers are continually making decisions and those decision-making processes are informed by the preceding steps in the research process. ... For interviews, researchers should conduct unstructured in-depth phenomenological one-on-one interviews with only the people ...
In this article, she shares five interviewing tips that have served her well. 1. Convey Intent. Proeschold-Bell says it's important for the interviewer to know the intent behind each question so that it can be clearly conveyed to the interviewee. Understanding the intent of a question, she's found, helps interviewers decide whether or not ...
Abstract. This paper aims to provide an overview of the use and assessment of qualitative research methods in the health sciences. Qualitative research can be defined as the study of the nature of phenomena and is especially appropriate for answering questions of why something is (not) observed, assessing complex multi-component interventions ...
InterViews by Steinar Kvale Interviewing is an essential tool in qualitative research and this introduction to interviewing outlines both the theoretical underpinnings and the practical aspects of the process. After examining the role of the interview in the research process, Steinar Kvale considers some of the key philosophical issues relating ...
Introduce yourself and explain the aim of the interview. Devise your questions so interviewees can help answer your research question. Have a sequence to your questions / topics by grouping them in themes. Make sure you can easily move back and forth between questions / topics. Make sure your questions are clear and easy to understand.
Qualitative research is increasing in popularity in health services research as is evidenced by the number of commentaries espousing the value of qualitative research, 6, 7 as well as guidelines that outline the best approach to reporting qualitative research. 8 This research methodology also makes a regular appearance in many pharmacy research ...
Qualitative research methods. Each of the research approaches involve using one or more data collection methods.These are some of the most common qualitative methods: Observations: recording what you have seen, heard, or encountered in detailed field notes. Interviews: personally asking people questions in one-on-one conversations. Focus groups: asking questions and generating discussion among ...
Conducting Qualitative Research Interviews . Qualitative interviews are similar to deep conversations. The interviewer and interviewee have a conversation about a topic with the goal of gathering information and insight from the respondent. The questions are open-ended and often require participants to use their own words and phrases.
How do we determine whether a book featuring qualitative research is empirically sound and not just a lovely, interesting read? ... A Guide to Evaluating Ethnographic and Interview Research by Mario Luis Small and Jessica McCrory Calarco Oakland, CA, University of California Press, 2022, 240 pp., $85.00 (hardcover), $24.95 (paperback), ISBN ...
The challenges to conducting oral health studies involving older people in long-term care facilities (LTCFs) must be debated. This study aimed to investigate researchers' perceptions and experiences while conducting an epidemiological survey on oral health among older individuals residing in LTCFs. A qualitative study was conducted involving six researchers who utilized field diaries to ...
As a Postdoctoral Research Scientist in Qualitative IE, the successful candidate will support all four thematic areas, working collaboratively with APHRC researchers. The position will be based at the Center's Head Office in Nairobi, Kenya; and may include some travels to conduct qualitative IE (IE) activities in other Anglophone and ...
From researcher perspectives, this has constrained the planned and ongoing research activities both within and outside the health sectors. 1 In this context, the viewpoint discusses the challenges and opportunities to use virtual communication tools while conducting qualitative research fieldwork during and beyond the pandemic.
Data were collected by conducting five individual interviews and one focus group during a seven-month period between April 2022 and September 2022. Nine nurses employed at four Norwegian nursing homes were the participants in this study. Data were analysed by employing a qualitative deductive content analysis method.
To answer our research question, we adopted a qualitative inductive research design. This research design is consistent with studies that took a similar perspective on how technologies can create business value [].In conducting our structured literature review, we followed the approach of Webster and Watson [] and included recommendations of Wolfswinkel et al. [] when considering the inclusion ...
Research design. A qualitative descriptive study design was used in this study to understand professional health managers' perceived barriers and facilitators to implementing the Guideline in hospitals [].In the previous study, 896 healthcare professionals from mainland China were invited to complete a questionnaire to rate the urgency and difficulty of implementing each of the 21 ...