Your Account
Manage your account, subscriptions and profile.
MyKomen Health
ShareForCures
In Your Community
In Your Community
View resources and events in your local community.
Change your location:

Susan G. Komen®
One moment can change everything.

Susan G. Komen Blog
Stories about breast cancer that can inspire and inform.
Blog | Newsroom
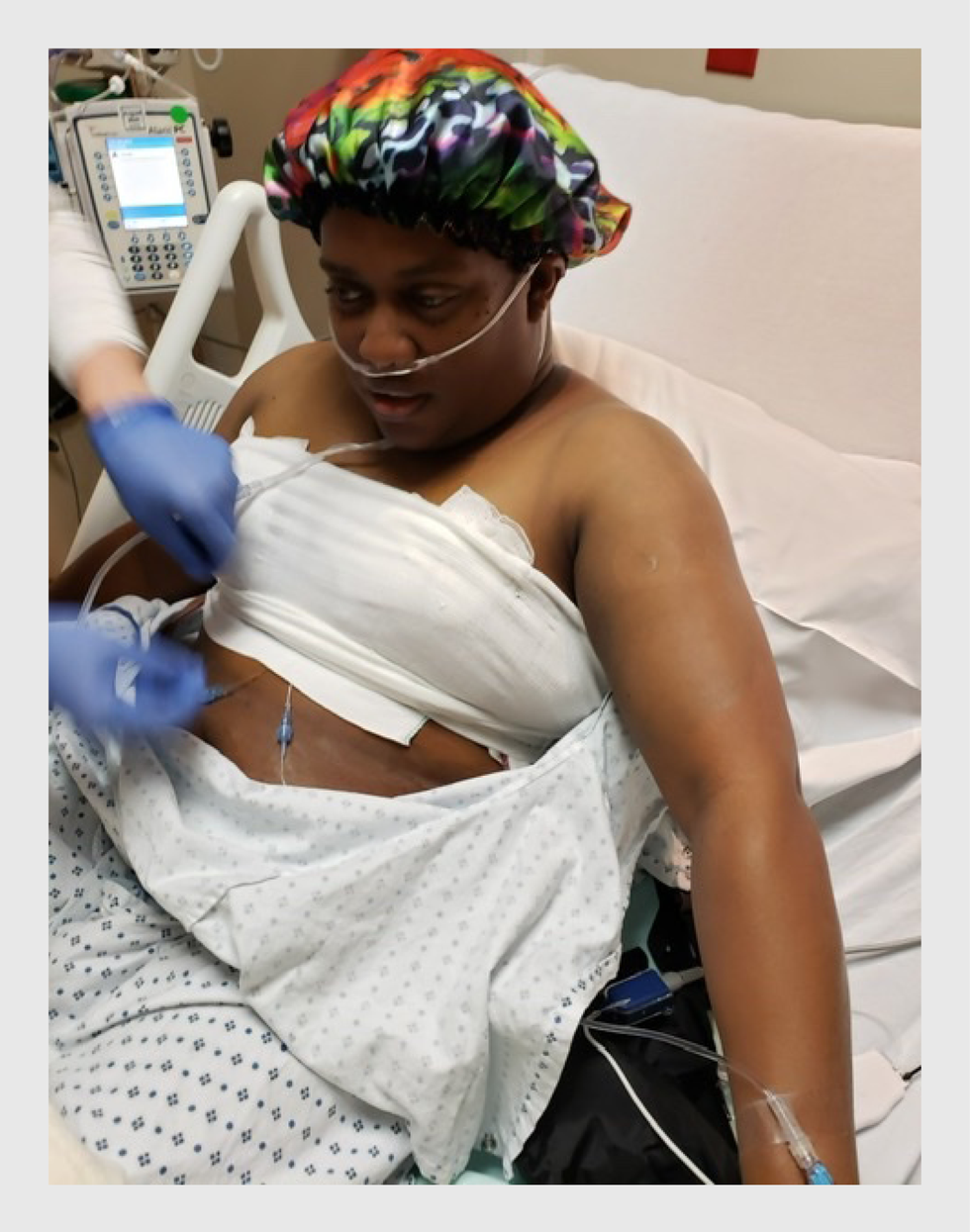
Alecia’s Story: I Am a Breast Cancer Survivor

Because of a family history of breast cancer, Alecia Robinson underwent twice yearly breast MRIs. In April 2022, Alecia was diagnosed with stage 1A invasive ductal carcinoma ER, PR+, HER2+ . This is her story in her own words.
I felt no particular sense of anxiety when I left my breast MR I appointment in April 2022 because, at that time, those appointments had been part of my regular routine for the past year and a half and, fortunately, each time the results had come back with no concerning changes.
On that day’s checklist, I ticked off my MRI. Then I headed to the mall to buy clothes for an upcoming vacation. I was supposed to leave in five days to visit family in the Virginia/Maryland area.
But less than two hours after my MRI, as I am happily sorting through racks of clothing, my phone rings, and it is the doctor who has my MRI results. “Ms. Robinson, we see something on this MRI that was not there on your last one, and we need you to come in to have an ultrasound ,” the doctor said. “If we see the same concerning spot on your ultrasound, we will do a biopsy right then and there. Are you available to come in tomorrow?”
The next day, I have the ultrasound and the doctor sees the same spot. I have a biopsy that same day. Two days later, while at work, I get another call, “Ms. Robinson, unfortunately, it is breast cancer.”
My medical history, my experience walking the breast cancer treatment journey alongside my aunt who had breast cancer, and my work in the area of medical education case simulation meant that I knew many of the questions to ask my doctors. I had some idea of what to expect as I moved forward in treatment and yet my journey through breast cancer almost emotionally broke me…almost.
Within the two weeks after my diagnosis, I had an MRI, an ultrasound, a mammogram and two biopsies. I also met with my breast surgeon . Things were moving fast – major treatment decisions, lifechanging decisions were having to be made and even me, a woman who had ridden all of those bucking bulls in all of those other major health issue rodeos, was struggling to hold on, stay calm and figure out what were the right decisions to make.

According to all of the tests and imaging, I had a small tumor in my left breast and no indication it had spread to my lymph nodes . My surgeon said that I was most likely looking at stage 1 cancer, however, that could not be confirmed until after my surgery and pathology reports were in. Based on the information that we had, I was a good candidate for a lumpectomy . Going the lumpectomy route, I would also need to have chemotherapy and radiation .
My other option was to have a mastectomy followed by chemotherapy, but no radiation. I wanted to make the decision right then as I wanted to get the surgery scheduled as soon as possible. After being given some time, right there in the surgeon’s office to think about it and discuss it with my sister, I made the decision to have a lumpectomy. It was scheduled for a couple of weeks later and would take place about a month after my diagnosis. My sister and I left the surgeon’s office, and in the hours that followed, though the surgery had been scheduled and everything had been set, I still felt unsettled about my decision.
After a conversation with another of my medical specialty doctors and after giving it some more serious thought, I came to the conclusion that for both personal and medical reasons, I really did not want to go through radiation. I determined a mastectomy would be best for me. The only question now was whether I would have only the affected breast removed or would I have both breasts removed. Although none of us can assuredly predict the future, at that moment, all I could hear was my inner voice emphatically saying, “Go ahead. Take both of them because you can’t do this again.” I ultimately decided to have a double mastectomy.
What energy I had after surgery was used just trying to get through each day, each week and each month of chemotherapy. I was too weak to work and as an independent contractor, I did not have the benefit of sick pay from a job. There were still bills that had to be paid and costs for supplements that I took to ease the chemotherapy side effects.
I knew that there were organizations that offered financial assistance to breast cancer patients, including Komen, who I reached out to. What I remember about the exchange I had with the Komen representative who was on the phone with me was her warmth and her eagerness to share how the Komen Financial Assistance Program could possibly help me. Later, I would think about how important that comforting energy was to me as I explained my needs to her. For those patients who might feel hesitant or self-conscious about asking for financial help, her reassuring energy was calming. She told me about the fairly simple process to apply.
I completed the short application, got the necessary documentation from my oncologist and within a few weeks, the Komen financial assistance money was deposited into my checking account. I was struck by how easy Komen made the process to apply for help.
That an organization like Komen can step in and help those who are fighting for their health and their lives is a true gift. Komen lifts some of the burden. With great support from family, friends and Komen, I pushed on through treatment, rang the bell on July 3, 2023, and now, three months shy of two years after diagnosis, here I am gratefully claiming that I am a breast cancer survivor.
Statements and opinions expressed are that of the individual and do not express the views or opinions of Susan G. Komen. This information is being provided for educational purposes only and is not to be construed as medical advice. Persons with breast cancer should consult their healthcare provider with specific questions or concerns about their treatment.
Related Stories

‘I’m A Breast Cancer Survivor And A Proud ‘Flattie.’ Here’s Why I Said No To Reconstructive Surgery’
“You don’t need implants to feel beautiful.”

Christina Miner, 46, had both breasts removed during a double mastectomy in May 2020. She opted to forgo reconstructive surgery and is now a proud “flattie.”
One August morning in 2019, after church, I finally did the thing I’d been terrified to do because I was afraid of what I might find. I gently leaned over the bed to cuff under my left breast, which had been swollen and painful for months. I didn’t have to press hard—there was already a lump in my palm. I screamed for my husband. That night, I lay curled up next to him, crying and praying.
Ductal carcinoma in-situ, Stage 0, ER/PR+, Grade 3, to be exact. My doctor explained that Grade 3 meant the cancer was growing fast, and Stage 0 meant it was still localized in my ducts. The surgery had to happen soon.
This wasn’t the start of my breast cancer story—that began decades ago—but it was the start of my journey to becoming a proud, double mastectomy, flat-chested , breast cancer survivor.
My breasts were removed during a double mastectomy on January 6, 2020.
The surgeon put in two expanders (little balloons of saline that stretch the skin for an eventual implant) in preparation for reconstruction surgery. I was scheduled to come back in April to get my implants.
That was the plan: mastectomy, implants, nipple tattoos. I thought that might bring back some normalcy. But as the world ground to a halt in March of 2020 as the COVID-19 pandemic set in, everything went on hold. It turned out to be a blessing in disguise.
After surgery, I never stopped hurting. I started having intense headaches, extreme fatigue, gastrointestinal issues, difficulty walking, and heaviness in my chest. I was losing weight. I remember trying to scoop ice cream, and I just fell apart in the kitchen, crying because I wasn’t able to do even that simple task. I had to take everything one second at a time.
During my telehealth appointments, I tried to explain that something was off.
But it was hard for doctors to see what was going on over a screen. By the end of April, I was placed first in line for the surgery to take the expanders out.
Two weeks before surgery, my health got worse. The skin around my left breast became leathery, tightening and hardening. Then, the skin began twisting. I could feel fluid swishing around. It felt like the implant was coming out of my chest, and I didn’t know how much longer I could withstand it.
By the time I walked into the hospital for surgery on May 6, my doctor had decided that I had breast implant illness and capsular contracture, which is when the scar tissue capsule that forms around the implant tightens and squeezes the implant. While there’s no official medical diagnosis for breast implant illness aside from a collection of symptoms, my doctor listened to me.
“This is making you sick,” she said.
I spent nearly two decades struggling with breast pain before my cancer diagnosis.
From 2005 to 2015, I brought up my symptoms at every doctor’s appointment. But I was told “that happens sometimes,” or that I had dense breasts, fibrocystic breast tissue, and another condition causing benign lesions. So, I lived with the pain —which is so often the case for Black women, whose discomfort has historically been pushed aside and ignored. It feels as if society doesn’t hear us, especially when it comes to pain. Then came the cancer.
Before the expander removal surgery, I told the doctor that I would do anything to feel better and asked her to do whatever was best for my health. But the damage, scarring, and inflammation in my body made the decision easy for both of us.
“I will never put another implant in your chest,” she told me when I woke up. Instead, my doctor left "angel wings," or "dog ears," which are little flaps of skin on the side of my chest in case I wanted reconstruction with my own body tissue later. Everything else was gone.
My surgeon took me flat, but it’s not quite an aesthetic flat closure (AFC), where a surgeon removes extra skin, pockets of fat, and excess tissue and tightens and smooths out the remaining tissue to create a flat chest wall. I’ll have a revision if I want true AFC, but for now, I’m happy with my healthy chest and angel wings.

At first, I had a really hard time feeling like a woman after going flat.
My breasts had been trying to kill me, but they were still part of my identity. This was how God made me, and that was stripped away. I had struggled with low confidence and self-esteem in the past, and this felt like the ultimate test.
My new routine started when I was first diagnosed with breast cancer. First thing in the morning, I would just sit still and breathe—even if it was only for five minutes. Then, I’d go out for my daily walk. As I walked, I’d pray. Other times, I just enjoyed nature. And through the beauty of it all, and through the darkness of it all, I discovered who I was.
As my body began to recover, I started healing mentally and spiritually , too. There was no big moment of acceptance. It took a lot of work. But I had to be okay with myself.
These days, I’m cancer free. I’m working with a trainer, dietitian, and wellness coach to regain strength and stay healthy. I'm a different person.
But there are still times, especially when I’m buying clothes, when it can be discouraging. There’s not a lot for us “flatties” out there. V-necks fall really low on the neckline and other shirts bunch up. I look for swimsuits with a distracting pattern up top. Initially, intimacy with my husband was hard.
While I did a lot of big healing work on my own, social media became a place where I could tell my story, and find answers and community, especially with other “flat” survivors. I’m now an ambassador for Stand Tall AFC , a campaign to de-stigmatize the loss of breasts to cancer treatment and normalize going flat, as well as a co-facilitator of the "Newly Diagnosed Group" for a group called Here for The Girls , an organization for breast cancer patients under the age of 51.
I’m not just a survivor, I’m a victor.
Eventually, I learned to ignore the voice in my head asking what people think of my flat chest and scars. It took a lot of loss to discover how resilient and beautiful and confident I really am.
When I got my diagnosis, I knew this was no longer just about me. I share my story because hearing about other people’s journeys helped me keep moving. And maybe something in my story will help you go forward, too.
For the women going flat, know your breasts do not define you. You have choices and options. It’s your right to advocate for yourself and to be heard. You don’t have to go back to “normal,” because there is no normal after breast cancer. And you don't have to have implants to feel beautiful.
Right now, I feel the strongest, most beautiful and the most confident—on the inside and outside—in my life. I never used to take photos of myself in sports bras. Now, I’m the Sports Bra Queen on Instagram, sharing my story. I’ve never shown photos of my bare chest before today. But I’m sharing my scars because they’re beautiful, and because they speak a message. They speak of resilience, life, and freedom. And I want them to speak for those who can’t.

MS Diagnoses Are Rising—And Doctors Don’t Know Why

Kourtney Kardashian's Urgent Fetal Surgery
New FLiRT COVID-19 Variants: Symptoms, Treatment

Kim Kardashian's Waist At The Met Gala Shocks

The 'Slow Morning' Wellness Trend, Explained

10 Ways To Make Yourself Cry When You Can't

The AI Health Revolution Is Here

Kelly Osbourne Didn't Use Ozempic For Weight Loss

Why You Feel Guilty For Staying In On A Sunny Day

7 Best Essential Oils Diffusers Of 2024

Kate Beckinsale Health & Hospitalization Timeline
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
What It Means to Be a Breast Cancer Survivor
Living well after breast cancer looks different for everyone
- Survivorship
- Survival Rates
- Lifestyle Tips
Risk of Recurrence
- Ongoing Care
Frequently Asked Questions
Breast cancer impacts a person long after treatment and recovery, and being a breast cancer survivor looks different for everyone. Regardless of how a person defines survivorship , there are long-term risks and concerns to consider as a survivor.
This article will discuss breast cancer survival, present survival rates by cancer stage, offer tips on living well, and provide information about the risk of recurrence and ongoing follow-up needs.
Jon Vallejo / Getty Images
Different Takes on Breast Cancer Survivorship
Being a breast cancer survivor means different things to different people. Some people may call themselves a survivor during treatment , others may not use the word "survivor" until the cancer is in remission , and others may not want to call themselves a survivor until many cancer-free years have passed.
Regardless of a person's cancer stage , breast cancer typically has a high survival rate. Therefore, adopting a healthy lifestyle can protect against the cancer returning, new cancers developing, further complications forming, and treatment side effects persisting.
Breast Cancer Survival Rates
Breast cancer generally has a high survival rate , with over 90% of people fully recovering after five years. These rates change, however, based on different factors, such as race, location of the cancer, and lifestyle.
Localized, Regional, and Distant Breast Cancer
Breast cancer survival rates are tracked by whether the cancer is localized, regional, or distant. Localized cancer is contained within the breast. Those with localized breast cancer have a 99% five-year survival rate.
Regional cancer is found in nearby lymph nodes outside of the breast . Those with regional breast cancer have an 86% five-year survival rate.
Distant cancer has spread to other parts of the body. Those with distant breast cancer have a 29% five-year survival rate.
Other Factors
Beyond cancer location in the body, other factors impacting survivorship include race, age, overall health, response to treatment, the speed at which the tumor spreads , and other factors.
Lifestyle Tips for Living Well After Breast Cancer
Breast cancer can impact your life long after you've recovered. Adopting a lifestyle that promotes physical and mental health will help support overall well-being as a cancer survivor. Here are some ways to live well as a breast cancer survivor:
- Schedule regular follow-up medical care.
- Recognize mental health disorder symptoms and follow up with a mental health provider if you're experiencing signs of mental illness, such as depression or anxiety .
- Maintain regular exercise to help with the long-term effects of treatment, including fatigue and bone loss.
- Don't smoke.
- Limit alcohol use.
- Work with your healthcare provider or nutritionist to ensure you are getting sufficient vitamins and nutrients.
- Work with a pain specialist for chronic pain and neuropathy (nerve damage).
- Use nonhormonal, water-based lubricants for sexual dysfunction concerns.
Breast Cancer Survivors and Mental Illness
The prevalence of depression and anxiety is around 22% in breast cancer survivors; this is higher than the rate for general cancer. Getting regular screenings and recognizing symptoms is an important way to prevent mental health disorders when recovering from breast cancer.
Adjusting Once Treatment Ends
Some people experience ongoing physical and mental health challenges even after treatment ends. These can include:
- Ongoing anxiety and depression
- Sleep issues
- Continuing pain
- Lymphedema (swelling in the skin)
- Vasomotor symptoms (hot flashes and night sweats)
- Infertility
These ongoing concerns can make it difficult to readjust to life socially, professionally, in relationships, and in other aspects of life.
Recurrence is dangerous and is the leading cause of death from breast cancer, mainly due to cancer metastasizing (spreading) to other body parts, such as distant organs or bones. Breast cancer recurrence happens when cancer that was determined to be in remission returns. This differs from a new cancer forming.
Recurrence can occur within the first five years of being diagnosed with breast cancer or much later, after 10 or even 15 years from the initial diagnosis. Ongoing screenings and check-ins with a healthcare provider can help detect cancer recurrence early.
Breast Cancer Recurrence and Healthy Lifestyles
Some research suggests that physical exercise, maintaining a healthy diet, and other psychosocial factors protect against breast cancer recurrence.
Ongoing Follow-Up Care
Follow-up care will likely continue for many years following a breast cancer diagnosis, even after the cancer is in remission. Expected follow-up care includes:
- Regular physicals with a primary healthcare provider
- Ongoing screenings for cancer recurrence or new cancer and education for screening at home
- Regular mammograms
- Ongoing endocrine therapy treatment
- Conversations with medical professionals about body image concerns, cognitive impairment from treatment, cardiotoxicity (treatment-related heart problems), and mental health concerns like depression, anxiety, and post-traumatic stress
- Treatment for inflammation and pain management
- Treatment of premature menopause symptoms, if applicable
Being a survivor of breast cancer means different things to different people. For many, it's part of their lifelong identity. Breast cancer has a high survivorship rate of 90% after five years; that rate varies depending on whether the cancer has spread and the person's race, age, and lifestyle factors.
Regardless of how long you've been a breast cancer survivor, you can improve your lifestyle to reduce the risk of cancer recurrence. Some examples include receiving regular follow-up care, recognizing mental health symptoms if they arise, exercising, limiting alcohol use, not smoking, and eating a healthy diet.
Even with lifestyle adjustments, it is common to experience long-term side effects from cancer treatment, including mental health condition, sleep issues, fatigue, and continuing pain. Working with a medical and mental healthcare team can help make life after breast cancer more manageable.
A Word From Verywell
As a breast cancer survivor, it's common for your identity, relationships, and sense of self to change over time. As you navigate what it means to be a survivor, pay close attention to your mental and physical well-being. Check in with your healthcare provider, mental health provider, and other breast cancer survivors to stay healthy in recovery.
After cancer is in remission, ongoing medical and follow-up care is still needed. There is a continued risk for cancer recurrence and other physical and mental health symptoms to arise even 10 or 15 years after breast cancer remission. Attending ongoing medical follow-up appointments can help detect and prevent future complications from breast cancer.
Yes. Breast cancer is one of the most treatable types of cancer. It has an overall survival rate of 90%. Factors affecting survival rates include the spread of cancer, race, age, and lifestyle.
Having breast cancer can slightly increase your risk of developing other cancers. Still, most people develop another breast cancer rather than other cancers after breast cancer remission.
Runowicz CD, Leach CR, Henry NL, et al. American cancer society/american society of clinical oncology breast cancer survivorship care guideline . JCO . 2016;34(6):611-635. doi:10.3322/caac.21319
American Cancer Society. Survival rates for breast cancer .
Iqbal J, Ginsburg O, Rochon PA, et al. Differences in breast cancer stage at diagnosis and cancer-specific survival by race and ethnicity in the united states . JAMA. 2015;313(2):165-173. doi:10.1001/jama.2014.17322
Carreira H, Williams R, Müller M, et al. Associations between breast cancer survivorship and adverse mental health outcomes: a systematic review . JNCI. 2018;110(12):1311–1327. doi:10.1093/jnci/djy177
Ahmad A. Pathways to breast cancer recurrence . International Scholarly Research Notices . 2013;2013:e290568. doi:10.1155/2013/290568
Loprinzi PD. Physical activity and the risk of breast cancer recurrence: a literature review . Oncology Nursing Society . 2012;5600;39(3):269-274. doi:10.1188/12.ONF.269-274
American Cancer Society. Second Cancers After Breast Cancer .
By Melissa Porrey LPC, NCC Porrey is a licensed professional counselor and writer based in DC. She is a nationally board-certified counselor.
- Conditionally
- Newsletter Signup
Health Conditions Chevron
Cancer Chevron
Breast Cancer Chevron
I’m a Black Woman Who Survived Breast Cancer. Here’s What I Want Other Women of Color to Know.
By Allison Tsai

On May 1, 2020, just as the world was shutting down due to COVID-19, Jamelle Singleton’s world was closing in for a different reason: breast cancer. As devastating as the diagnosis was to Singleton, who is now 35, it’s one that almost didn’t happen. Despite her symptoms, which initially included an achy pain in her left breast, her doctor told her that it was very unlikely she had breast cancer because she was young and healthy. As a Black woman, Singleton felt like her concerns were too easily dismissed, and it wasn’t until she advocated for herself that she received the life-altering diagnosis. But once she finally had an answer, she also found a new purpose.
This is her story as told to SELF’s associate health director Allison Tsai.
I’m not your “typical” breast cancer patient. Unlike a majority of people 1 with the disease, I never felt that telltale, panic-inducing lump . But I did feel like something wasn’t quite right with my body. My first symptom, a dull pain in my left breast, felt like a muscle ache. But I had never felt pain like this before in that area, so I went to see my ob-gyn , just to be safe. She didn’t seem to take my discomfort as seriously as I did and told me I probably just pulled a muscle from holding my daughter, London, who was 2 years old at the time. She also didn’t order a mammogram to further investigate what was going on, and I just kind of accepted that answer.
But just one month later, my symptoms only progressed. One day, I looked down and noticed blood leaking from my nipple . This definitely wasn’t normal, so I went back to my ob-gyn and insisted on a mammogram this time. I told her I would really feel more comfortable if we took a closer look at what was going on. A screening, a biopsy, and a flurry of doctor’s appointments later, I finally had an answer: It was breast cancer—stage III, HER2-positive 2 invasive ductal carcinoma, to be exact. Invasive ductal carcinoma is the most common type of breast cancer 3 , and mine had spread to the lymph nodes in my armpit.
Looking back, I get the sense that my doctor wasn’t aware that breast cancer disproportionately affects young Black women 4,5. Otherwise, I have to believe she would have ordered the mammogram right away. Knowing what I know now, I wish I would have questioned my doctor more and advocated for myself earlier. It’s not easy as a woman of color. You may feel a little intimidated from speaking up, especially if you feel like you have to push through a doctor’s biases.
Once I finally got my diagnosis, I immediately started chemotherapy. I did six intensive rounds and a total of 17 antibody treatments. Not only did I feel like I had the flu every day, but I was in isolation because of the pandemic. My husband had to solo parent our daughter while I was at the hospital. I endured these grueling treatments for four months, losing all of my hair, eyebrows and eyelashes included, in the process. This was one of my biggest fears, so when it did happen, I took it pretty hard.

By Katie Camero

By Julia Sullivan

By Jenna Ryu
It was a deeply emotional time for me. I’d just lost my mother to Paget’s disease 6 , a rare form of cancer, a few months before. My diagnosis simultaneously opened those wounds and created new ones. Mostly, I just felt scared and sad because the life I once knew—as a healthy wife and mom—was changing drastically.
In some ways, though, my mom’s journey with cancer prepared me for the long fight ahead. A month after I completed chemo, I had a double mastectomy per my doctor’s advice. I knew that after the surgery I wasn’t going to be able to pick up London for a while, and it was really tough having that talk with her. Even saying goodbye to her before my surgery was really difficult, because I didn’t want her to see me like that. I was already bald and sick because of the chemo, and then I had to go to surgery. When I came out, I had two surgical drains on my sides. Even though she didn’t totally understand, she knew something was different. It was such a hard recovery, and I was essentially immobile for two months.
Then, a couple months after that, I started radiation therapy. Since I had stage III cancer and it had spread to my lymph nodes, radiation was a way to make sure there were no lingering microscopic cancer cells. Just trying to survive was like a part-time job. For five weeks, I got up at 7 a.m., Monday through Friday, to go to my treatments. These appointments often lasted hours. Afterward, I would come home and just rest.
On April 28, 2021, a year after I first felt that unusual ache in my breast, I was officially declared cancer-free and done with treatment. That’s the date I plan to celebrate my “cancer-versary.” But I still feel the mental and physical weight of chemotherapy every day. I struggle with overwhelming fatigue. Sometimes, “chemo brain” strikes mid-conversation, and I can’t remember what I was saying. Thankfully, though, my hair is growing back, and I’m strong enough to pick up my daughter again. I’m just happy I’m still around to thank my family, who helped me so much through my treatment and recovery.
Now, I’m deciding whether or not I want to have reconstructive breast surgery. It was my personal decision to go flat—I didn’t want to put my body through any more at the time. I’m comfortable with my new body type and having fun trying on clothes and figuring out what works for me, at least for now. Whatever happens in the future, it is my decision—one thing that I finally have power over. The last year was a whirlwind of treatments and doctors making decisions about my body. It’s nice to have some control back.
Cancer has taken a lot away from me, but it’s also helped me find a new meaning in life. During my chemotherapy treatments, I would sit alone in the hospital for half a day. It gave me a chance to practice self-care in new ways—something I had a hard time prioritizing before my diagnosis. That’s when I started journaling. Taking pen to paper awoke a deep passion for writing in me, which I then started doing on Instagram . I’ve shared everything about my journey with breast cancer and all the feelings that go with it. I want newly diagnosed people to use it as a guide, and more importantly, to know they’re not alone.
That’s how I caught the attention of the Young Survival Coalition , who offered me a part-time job as a community content coordinator. It’s changed my life in ways I didn’t realize were possible. Now, I can reach out to other breast cancer patients who went through similar experiences that I did and help them tell their stories too.
Sharing my pain now has a purpose. Spreading the word about breast cancer , especially in women of color, has become one of my passions. When I was first diagnosed, other survivors (we call them Pink Sisters) helped me make sense of the journey. They answered all of my nitty-gritty questions, like what to expect from chemotherapy and what I need to have at home after surgery. So I want to pay it forward.
Now that I’m a part of this resilient community, I’ve found there are so many women of color who are dealing with breast cancer at a young age. I try to show them there is hope on the other side, and that having a voice is extremely important. My message is twofold: First, finding a support system, even virtually, will be your foundation. It’s what gets you through. Second, self-advocacy is necessary for women of color. Find your voice and don’t be afraid to use it.
When you are put in a situation as devastating as this one, you realize nobody else is going to speak up for you if you don’t—especially if you’re a Black woman. We don’t look like what people think of as the average breast cancer patient, so it might take a bit more effort to make your concerns heard. It’s imperative that you do speak up, though, because Black women are 40% more likely to die from breast cancer than white women. 7
Remember, this is your body. This is how you are feeling. Advocating for yourself can literally be the difference between life and death. Continue to speak up until someone listens. Keep asking questions until you get the answers you deserve. Surviving breast cancer switched something in me. I am better, stronger. Because when you have no choice but to be strong, that’s what you become.
- Cancer epidermiol, Typical and atypical presenting symptoms of breast cancer and their associations with diagnostic intervals: Evidence from a national audit of cancer diagnosis
- Mayo Clinic, HER2-positive breast cancer: What is it?
- American Cancer Society, Types of breast cancer
- Journal of Breast Imaging , Breast cancer screening recommendations: African American women are at a disadvantage
- NIH *Seer Explorer, Breast recent trends in SEER age-adjusted incidence rates, 2000-2018
- American Cancer Society, Paget disease of the breast
- American Cancer Society, Breast cancer facts & figures 2019-2020
- 8 Questions to Ask Your Doctor If You’re Diagnosed With Triple Negative Breast Cancer
- This Is What It’s Like to Find Out You Have Triple Negative Breast Cancer
- How I’m Managing My Cancer Care During the Coronavirus Pandemic

SELF does not provide medical advice, diagnosis, or treatment. Any information published on this website or by this brand is not intended as a substitute for medical advice, and you should not take any action before consulting with a healthcare professional.

Select "Patients / Caregivers / Public" or "Researchers / Professionals" to filter your results. To further refine your search, toggle appropriate sections on or off.
Cancer Research Catalyst The Official Blog of the American Association for Cancer Research

Home > Cancer Research Catalyst > Cancer Survivors: In Their Words
Cancer Survivors: In Their Words
This year alone, an estimated 1.8 million people will hear their doctor say they have cancer. The individual impact of each person can be clouded in the vast statistics. In honor of National Cancer Survivor Month, Cancer Today would like to highlight several personal essays we’ve published from cancer survivors at different stages of their treatment.

In this essay , psychiatrist Adam P. Stern’s cerebral processing of his metastatic kidney cancer diagnosis gives rise to piercing questions. When he drops off his 3-year-old son to daycare, he ponders a simple exchange: his son’s request for a routine morning hug before he turns to leave. “Will he remember me, only a little, just enough to mythologize me as a giant who used to carry him up the stairs? As my health declines, will he have to learn to adjust to a dad who used to be like all the other dads but then wasn’t?” he questions.

In another essay from a parent with a young child, Amanda Rose Ferraro describes the abrupt change from healthy to not healthy after being diagnosed with acute myeloid leukemia in May 2017. After a 33-day hospital stay, followed by weeklong chemotherapy treatments, Ferraro’s cancer went into remission, but a recurrence required more chemotherapy and a stem cell transplant. Ferraro describes harrowing guilt over being separated from her 3-year-old son, who at one point wanted nothing to do with her. “Giving up control is hard, but not living up to what I thought a mother should be was harder. I had to put myself first, and it was the hardest thing I had ever done,” she writes.
In January 1995, 37-year-old Melvin Mann was diagnosed with chronic myelogenous leukemia, which would eventually mean he would need to take a chance on a phase I clinical trial that tested an experimental drug called imatinib—a treatment that would go on to receive U.S. Food and Drug Administration approval under the brand name Gleevec. It would also mean trusting a system with a documented history of negligence and abuse of Black people like him: “Many patients, especially some African Americans, are afraid they will be taken advantage of because of past unethical experiments like the infamous Tuskegee syphilis study,” Mann writes, before describing changes that make current trials safer. Mann’s been on imatinib ever since and has enjoyed watching his daughter become a physician and celebrating 35 years of marriage.

In another essay , Carly Flumer addresses the absurdity of hearing doctors reassure her that she had a good cancer after she was diagnosed with stage I papillary thyroid cancer in 2017. “What I did hear repeatedly from various physicians was that I had the ‘good cancer,’ and that ‘if you were to have a cancer, thyroid would be the one to get,’” she writes.
In another piece for Cancer Today , Flumer shares how being diagnosed with cancer just four months after starting a graduate program shaped her education and future career path.
For Liza Bernstein, her breast cancer diagnosis created a paradox as she both acknowledged and denied the disease the opportunity to define who she was. “In the privacy of my own mind, I refused to accept that cancer was part of my identity, even though it was affecting it as surely as erosion transforms the landscape,” she writes . “Out in the world, I’d blurt out, ‘I have cancer,’ because I took questions from acquaintances like ‘How are you, what’s new?’ literally. Answering casual questions with the unvarnished truth wasn’t claiming cancer as my identity. It was an attempt to dismiss the magnitude of it, like saying ‘I have a cold.’” By her third primary breast cancer diagnosis, Bernstein reassesses and moves closer to acceptance as she discovers her role as advocate.

As part of the staff of Cancer Today , a magazine and online resource for cancer patients, survivors and caregivers, we often refer to a succinct tagline to sum up our mission: “Practical knowledge. Real hope.” Part of providing information is also listening closely to cancer survivors’ experiences. As we celebrate National Cancer Survivor Month, we elevate these voices, and all patients and survivors in their journeys.
Cancer Today is a magazine and online resource for cancer patients, survivors, and caregivers published by the American Association for Cancer Research. Subscriptions to the magazine are free to cancer patients, survivors and caregivers who live in the U.S.
- About This Blog
- Blog Policies
- Tips for Contributors

New AACR-Novocure Funding Initiatives Support Tumor Treating Fields Research
Can We Treat Colorectal Cancer With Immunotherapy?

Researchers Head to Washington for AACR Early-career Hill Day
Cancel reply
Your email address will not be published. Required fields are marked *
Join the Discussion (max: 750 characters)...
This site uses Akismet to reduce spam. Learn how your comment data is processed .
- Share Your Story
- National Cancer Research Month
- National Cancer Survivor Month
Advertisement
Psychosocial experiences of breast cancer survivors: a meta-review
- Open access
- Published: 01 March 2023
- Volume 18 , pages 84–123, ( 2024 )
Cite this article
You have full access to this open access article

- King R. 1 ,
- Stafford L. 1 ,
- Butow P. 2 ,
- Giunta S. 2 &
- Laidsaar-Powell R. 2
4111 Accesses
3 Citations
14 Altmetric
Explore all metrics
Advances in breast cancer care have led to a high rate of survivorship. This meta-review (systematic review of reviews) assesses and synthesises the voluminous qualitative survivorship evidence-base, providing a comprehensive overview of the main themes regarding breast cancer survivorship experiences, and areas requiring further investigation.
Sixteen breast cancer reviews identified by a previous mixed cancer survivorship meta-review were included, with additional reviews published between 1998 and 2020, and primary papers published after the last comprehensive systematic review between 2018 and 2020, identified via database searches (MEDLINE, Embase, CINAHL, PsycINFO). Quality was assessed using the Joanna Briggs Institute Critical Appraisal Checklist for Systematic Reviews and the CASP (Critical Appraisal Skills Programme Qualitative) checklist for primary studies. A meta-ethnographic approach was used to synthesise data.
Of 1673 review titles retrieved, 9 additional reviews were eligible (25 reviews included in total). Additionally, 76 individual papers were eligible from 2273 unique papers. Reviews and studies commonly focused on specific survivorship groups (including those from ethnic minorities, younger/older, or with metastatic/advanced disease), and topics (including return to work). Eight themes emerged: (1) Ongoing impact and search for normalcy, (2) Uncertainty, (3) Identity: Loss and change, (4) Isolation and being misunderstood, (5) Posttraumatic growth, (6) Return to work, (7) Quality of care, and (8) Support needs and coping strategies.
Conclusions
Breast cancer survivors continue to face challenges and require interventions to address these.
Implications for Cancer Survivors.
Breast cancer survivors may need to prepare for ongoing psychosocial challenges in survivorship and proactively seek support to overcome these.
Similar content being viewed by others
A meta-review of qualitative research on adult cancer survivors: current strengths and evidence gaps
Post-traumatic growth after cancer: a scoping review of qualitative research

Do cancer patients use the term resilience? A systematic review of qualitative studies
Avoid common mistakes on your manuscript.
Introduction
Breast cancer (BC), while highly prevalent globally (highest incidence cancer among women in 159/185 countries) [ 1 ], has a high survival rateThe average five-year survival rate in Australia for BC from 2013 to 2017 was 91.5%, compared to 69.7% for all cancer types combined [ 2 ]. Cancer survivors are defined as individuals diagnosed with cancer who have completed their initial cancer treatment [ 3 ], including those considered cured and those living with ‘advanced’ disease (including locally advanced and metastatic cancer), receiving ongoing care.
BC survivors may experience significant long-term psychosocial effects that impact their quality of life, including fatigue, pain, difficulty sleeping, cognitive challenges, sexual dysfunction, depression, anxiety and fear of recurrence or progression [ 4 , 5 , 6 , 7 ]. Women with advanced BC may additionally experience feelings of abandonment, isolation, existential distress and a loss of control [ 4 , 8 , 9 ]. Thus, BC survivors may benefit from tailored support and care [ 4 , 8 ].
To inform development of BC survivorship services, a comprehensive understanding of women’s experiences and needs is required. Qualitative research, which captures women’s lived experiences, is well placed to provide that understanding [ 10 ]. The number of qualitative studies focusing on BC survivorship has steadily increased since the late 1990s (see Fig. 1 ). Systematic reviews which aim to critically appraise and summarise the findings of these primary studies have also increased. While systematic reviews provide a high level of evidence to inform research and policy [ 11 , 12 ], many BC survivorship systematic reviews focus on specific topics (for example, return to work [ 13 ]) or populations (for example, women from a particular ethnicity [ 14 ]). To provide a more complete picture of the evidence base and identify areas of research density/paucity, a meta-review (systematic review of systematic reviews) is required. Meta-reviews can synthesise entire fields of research and are particularly beneficial when there is a large evidence base on a topic [ 12 ]. Such an overview is required firstly to ensure that new research investigates areas where data are lacking, and secondly to guide BC health professionals in their provision of care, particularly within survivorship centres which focus on this phase of the disease.
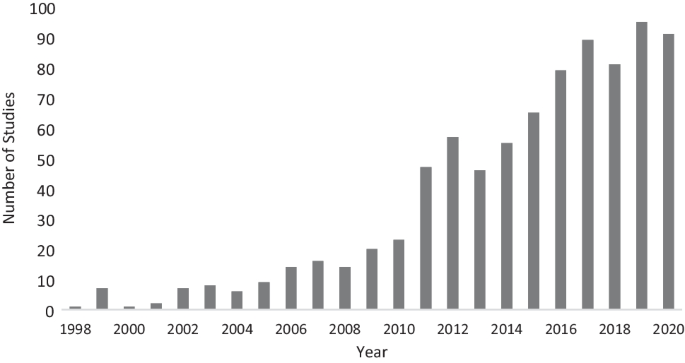
PubMed search results by year for BC survivorship qualitative studies. Articles on PubMed for the search terms (breast cancer) AND (survivor*) AND (qualitative)
To date, one meta-review of qualitative cancer survivorship studies has been conducted [ 15 ]. Laidsaar-Powell et al.’s [ 15 ] meta-review of 60 qualitative systematic reviews conducted between 1998 and 2018 included 19 reviews addressing BC survivorship. However, due to its wide scope, no specific detail was provided about BC survivorship, and systematic reviews focused on advanced BC were not included. Furthermore, new systematic reviews and primary qualitative studies focused on BC survivorship have been published since 2018. Thus, the current study aimed to conduct an extensivemeta-review of qualitative BC systematic reviews supplemented by a systematic review of primary qualitative studies conducted since the last SR search-date. This BC meta-review aims to provide the first truly comprehensive and exhaustive summary of qualitative evidence focusing on survivorship experiences of women with BC, across both early and advanced stage disease.
Search strategy
This meta-review and systematic review followed Smith et al.’s [ 12 ] meta-review guidelines, and adhered to a predefined protocol registered on the International Prospective Register of Systematic Reviews (PROSPERO; registration #CRD42021258728, https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021258728 ). BC survivorship reviews identified in Laidsaar-Powell et al.’s [ 15 ] original meta-review ( n = 19) were examined for eligibility. Three literature searches were conducted via electronic databases (MEDLINE, Embase, CINAHL, PsycINFO). Search 1 identified systematic reviews published between May 2018 (the latest date searched by Laidsaar-Powell et al. [ 15 ]) and August 2020 (the date of this search), used the keywords: (breast cancer) AND (survivor* OR post-treatment) AND (qualitative OR experience OR thematic analysis OR interviews OR focus groups) AND (review OR synthesis OR summary). Search 2 conducted in October 2020, identified systematic reviews focusing on advanced BC survivorship. This search did not restrict publication date. It used the same search terms, replacing the keywords: (survivor* OR post-treatment) with (advanced OR metastatic OR late stage). Search 3 conducted in February 2021, focused on primary papers published since the last search conducted for an eligible comprehensive systematic review (January 2018), using the same search terms, but omitting the terms (review OR synthesis OR summary). Search results were imported into Covidence reviewsoftware [ 16 ], with duplicates deleted. Study selection, data extraction and bias assessment were undertaken by one author (RK), with 20% independently reviewed by a second reviewer to check accuracy; disagreements were resolved through consensus and discussion with the wider research team.
Eligibility criteria and study selection
Systematic reviews/papers were included if they were published in English in peer-reviewed journals, and reported qualitative findings relating to BC survivorship experiences. Letters to the editor, conference abstracts, commentaries, and case studies were excluded. Reviews /papers focused on end-of-life/palliative care, caregivers, practitioners, paediatrics/adolescents (i.e. under 18 years of age), or patients currently undergoing or yet to undergo initial treatment, or which focused on service provision, interventions or treatment evaluations, were excluded. Reviews/papers reporting both qualitative and quantitative results or multiple populations (e.g. survivors and patients) were included provided qualitative survivorship findings were reported separately and in sufficient detail to be extracted. Initially, titles and abstracts, then eligible or potentially eligible full-texts, were reviewed for evaluation against eligibility criteria.
Data extraction and bias assessment
Data were extracted onto a study-designed form (see Tables 1 and 2 ). The Joanna Briggs Institute Critical Appraisal Checklist for Systematic Reviews and Research Synthesis [ 11 ] and the Qualitative Critical Appraisal Skills Programme (CASP) [ 17 ] were used for bias assessment (see Supplementary Table 1 and 2 for checklist items). One item for systematic reviews (‘was the likelihood of publication bias assessed?’) was excluded, as it primarily relates to quantitative findings. Each review/paper received a score out of 10 derived from the 10 applicable items (scored as 1 = yes or not applicable, and 0 = no or unclear), with higher scores indicating better quality.
Data synthesis and interpretation
Thematic synthesis was conducted by RK, in consultation with the broader research team, whereby iterative revisions of themes and categories were discussed until consensus was reached. A meta-ethnographic approach [ 18 ] was used, including (1) extraction of findings from included reviews/papers, with an accompanying quote; (2) development of categories for findings where there are at least two examples; and (3) development of higher order categories. Categorisation involved repeated, detailed examination of assembled findings for similarity in meaning.
Figure 2 describes the study selection process guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [ 19 ]. Three of the 19 Laidsaar-Powell et al. [ 15 ] BC reviews were excluded as they contained very limited qualitative BC findings. After deletion of duplicates and eligibility screening, 25 systematic reviews were included in this meta-review (including 7 from Search 1 and 2 from Search 2), with an additional 76 primary papers.
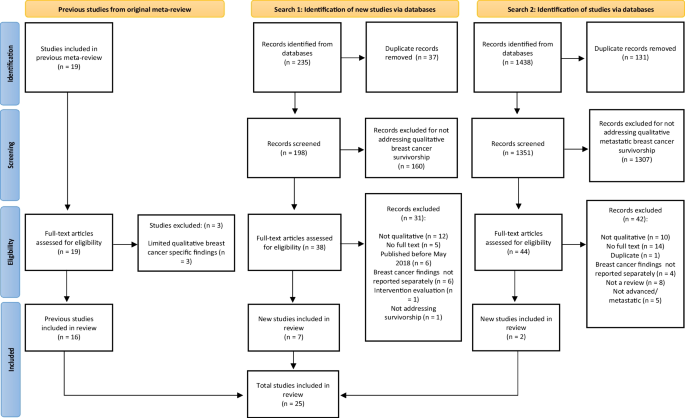
PRISMA flow chart for the meta-review literature search
Study characteristics
Eight systematic reviews included qualitative studies only and 17 included mixed methods studies. Fourteen (56%) reviews were published in the past five years (2016–2020), reflecting the recent increase in BC survivorship research (see Fig. 3 ). Of the papers, only three were mixed methods.
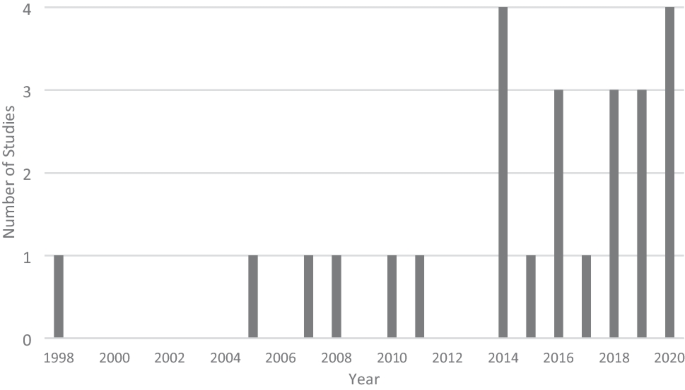
Number of systematic reviews included by year published
Three systematic reviews focused completely or partially on metastatic/advanced BC [ 5 , 20 , 21 ]. Five reviews focused on ethnic minorities including African American [ 14 , 22 , 23 ], Asian American [ 24 ], and Korean American [ 25 ] women. Two reviews focused on rural BC survivors [ 26 , 27 ] and three focused completely or partially on age (i.e. younger and older BC survivors) [ 28 , 29 , 30 ]. Some reviews had a broad focus on BC survivorship and psychosocial needs, while others covered specific topics including return to work [ 13 , 31 , 32 , 33 , 34 ], cognitive difficulties [ 34 , 35 ], adherence to adjuvant endocrine therapy [ 36 ], pain [ 37 ], spirituality [ 20 ], parenthood [ 38 ], and sexual functioning [ 29 ].
Seven papers focused on metastatic BC [ 39 , 40 , 41 , 42 , 43 , 44 , 45 ]. Five focused on African American survivors [ 46 , 47 , 48 , 49 , 50 ], eleven on ‘younger’ survivors (e.g. under 50 years) [ 41 , 43 , 49 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 ], nine on return to work [ 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 ], two on cognitive difficulties [ 68 , 69 ], four on lymphoedema [ 65 , 70 , 71 , 72 ], four on cancer-related fatigue [ 73 , 74 , 75 , 76 ], five on sexual and/or reproductive health [ 51 , 58 , 77 , 78 , 79 ], and four on healthy lifestyle factors (i.e. nutrition and exercise) [ 45 , 54 , 80 , 81 ]. Other populations/topics explored included low SES survivors [ 39 , 82 ], sexuality and gender diverse survivors [ 83 ], infant feeding [ 84 ], healthcare experience [ 85 , 86 , 87 ], economic burden [ 71 ], parenthood [ 88 ], posttraumatic growth [ 89 ], fear of recurrence [ 90 , 91 , 92 ], adjuvant endocrine therapy persistence/management [ 93 , 94 ], and religion/spirituality [ 94 ]. Other papers had a wider scope, exploring BC survivors’ experiences and psychosocial needs.
Quality assessment
See Tables 1 and 2 for an overview of the methodological quality of included reviews/papers. Six systematic reviews received a score of 10/10, indicating high methodological quality. Most reviews (12) scored in the moderate quality range (7–9/10). Seven SRs scored 5–6/10, indicating limited methodological quality. Items F (‘was critical appraisal conducted by two or more reviewers independently?’) and G (‘were there methods to minimise errors in data extraction?’) were the two most unmet items.
Fourteen papers received a score of 10/10. Most papers (60) scored in the moderate quality range (7–9/10). Two papers scored 4–6/10, indicating limited methodological quality. Item F (‘has the relationship between researcher and participants been adequately considered?’) was the most unmet item.
Thematic analysis
From the included reviews/papers, 8 over-arching themes were identified: (1) Ongoing impact and search for normalcy, (2) Uncertainty, (3) Identity: Loss and change, (4) Isolation and being misunderstood, (5) Posttraumatic growth, (6) Return to work, (7) Quality of care, and (8) Support needs and coping strategies. These themes are presented with subthemes and participant quotes selected from systematic reviews (reviews) and primary papers (papers), where appropriate.
Theme 1: Ongoing impact and search for normalcy
“am i healthy or am i not”.
The ongoing impact of BC and its treatment came as a shock to many women as they transitioned into survivorship [ 36 ]. Many systematic reviews examined the impact of ongoing symptoms on survivorship, including persistent pain, fatigue and weakness, feeling unwell, sleeping difficulties, lymphoedema, impaired cognition (including ‘chemobrain’), skin conditions, menopausal symptoms, sexual problems, and fertility issues [ 5 , 13 , 21 , 22 , 29 , 33 , 34 , 35 , 36 , 37 ], as did primary papers (PPs) [ 41 , 44 , 49 , 51 , 52 , 55 , 68 , 69 , 70 , 73 , 74 , 75 , 76 , 79 , 84 , 85 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 ]. These ongoing side-effects challenged expectations that after treatment, BC survivors would return to their premorbid level of health. Instead, survivors found themselves in a space between illness and health [Review: [ 37 ]].
Now I've finished my treatment but am stuck in a period where I sit and think ‘am I healthy or am I not?’ It's like something in between [Review: [ 37 ]] You kind of think, you’ll have your surgery…and then life will go back to normal, but it doesn't [PP: [ 85 ]]
Physical and cognitive symptoms led to significant limitations that impacted daily life (e.g. inability to clean or drive), as well as impairing social, occupational, and physical activities [Reviews: [ 5 , 13 , 21 , 33 , 34 , 36 , 37 ]; Papers [ 44 , 70 , 95 , 96 ]].
I can't ride a scooter, I can't raise my arms… I can't lift a pack of milk, it's too painful [Review: [ 37 ] ] Less able to play with grandkids or do simple chores requiring strength or lifting [Paper: [ 70 ]]
Some survivors reported feelings of desperation and fatalism that their symptoms would never improve [Review: [ 37 ]].
Sometimes when I wake up I think ‘will the pain be like this every day, always, always…’ that's hard to manage sometimes [Review: [ 37 ]]
Due to the significant impact of persistent side-effects, some survivors began to value their quality of life (QOL) (i.e. symptom management) over length of life [Review: [ 36 ]]. For example, some BC survivors chose to cease adjuvant treatment designed to prevent recurrence and prolong life, to reduce debilitating side-effects and increase quality of life [Review: [ 36 ]; Paper: [ 93 ]].
I said, I’ve had tamoxifen, and I’ve had breast cancer. I would rather have breast cancer [Review: [ 36 ] ] I chose a lesser time left. I said at my age, does it matter if the cancer comes back one way or another… I like my home and I like being involved in the community, going to the club and that. Coming off the tablet has given me back that quality of life [Review: [ 36 ]].
Psychological impact
BC survivors also experienced psychological problems due to enduring side-effects, ongoing uncertainty and concern about the future. They expressed feelings of sadness, shock, guilt, insecurity, worry, anger, fear, disappointment, distress, and grief [Reviews: [ 5 , 21 , 28 , 29 , 33 ]; Papers: [ 41 , 49 , 52 , 55 , 57 , 68 , 70 , 74 , 75 , 79 , 96 , 97 , 98 , 99 , 102 , 103 , 104 ]], especially those experiencing recurrence [Review [ 5 ]:].
It [BC recurrence] was such a dreadful disappointment that I got a feeling that it didn’t matter what I did. That little devil who has sunk his claws into me isn’t going to let go… the disappointment was enormous [Review [ 5 ]:]
“Things will never be normal, and that’s awful”
Many survivors sought normalcy after treatment: a return to pre-cancer health and ability [Reviews: [ 5 , 13 , 21 , 22 , 28 , 36 ]; Papers: [ 95 , 97 , 100 , 105 , 106 ]]. Re-establishing normalcy involved adjusting daily activities to match limitations, focusing on relationships, and not focusing on the BC [Review: [ 21 ]; Paper: [ 69 ]]. Additionally, women attempted to rebuild their pre-treatment lives (and identity) to re-establish normalcy, including returning to work [Review: [ 13 ]]. For some, a return to normalcy was perceived as impossible. Significant changes to the body (e.g. scarring, menopausal symptoms, physical and cognitive impairment) and to lives (e.g. career and relational disruptions) made the life that women once had, or imagined for their future, impossible to reach [Review: [ 28 ]; Papers: [ 70 , 107 ]. Recurrence exacerbated this sense of loss [Review: [ 5 ]].
I feel so terribly sad that things will never be normal again. Things will never be normal, and that's awful [Review [ 5 ]:] This [BC related lymphoedema] will affect my life forever [Paper: [ 70 ]]
Theme 2: Uncertainty
Patient to survivor.
BC survivors underwent a transition from undergoing primary treatment (being a patient) to life post-treatment (survivorship) and this transition was characterised by uncertainty regarding future quality and length of life [Reviews: [ 28 , 37 , 108 ]; Papers: [ 91 , 96 , 109 , 110 ]]. This uncertainty was exacerbated by decreased support from and contact with health providers and other patients, as women shifted to self-management while losing the hospital ‘safety net’ [Reviews: [ 14 , 37 , 108 ]; Papers [ 60 , 85 , 96 , 100 ]:].
The problems start after that [end of treatment]: whom do you turn to when you have pain in your hip like I do? [Review: [ 37 ]]
Uncertainty of symptoms
BC survivors experienced uncertainty and worry related to ongoing symptoms and need for further treatment (e.g. ongoing adjuvant treatment) [Reviews: [ 34 , 36 , 108 ]; Papers: [ 48 , 109 ]]. One review noted survivors were unsure about the likely duration of ongoing cognitive impairment, which was compounded by a lack of information about their symptoms [Review: [ 34 ]].
Fear of recurrence and death anxiety
The transition into survivorship and loss of regular contact with the treatment team heightened many women’s fears of cancer recurrence (FCR) [Review: [ 14 ]]. FCR, recently defined as “fear, worry or concern relating to the possibility that cancer will come back or progress” (p. 3266)[ 111 ], was a common and significant issue for survivors [Reviews: [ 28 , 30 , 36 , 37 , 38 , 108 ]; Papers: [ 52 , 55 , 56 , 57 , 82 , 90 , 91 , 92 , 99 , 101 , 109 , 110 , 112 ]]. FCR focused women on the uncertainty of their future [Review: [ 5 ]].
One of my biggest fears is the 5-year waiting period, to find out if we are going to survive or not. That creates suspense, fear, and negative emotions… I feel like I’m standing on a balance just waiting to see which way it is going to go [Review: [ 5 ]]. The furthest I can think is the coming weeks and months. I don't make long-term plans [Review: [ 5 ]]
FCR can lead to excessive vigilance regarding symptoms. While some degree of symptom monitoring is required for early detection of recurrence if it occurs, hypervigilance can lead to ongoing and exacerbated fears and anxiety. Many women had difficulty determining what is ‘normal’ and what may be a sign of recurrence [Reviews: [ 37 , 108 ]; Paper: [ 52 ]].
You really listen to your body in quite a different way now. Every little thing you feel in your body could be signs of something abnormal [Review: [ 37 ]]
Women with metastatic BC were particularly hyper-vigilant while monitoring for signs of disease progression [Reviews: [ 5 , 21 ]]. The need for symptom monitoring and the possibility of recurrence meant the survivorship period had no certain endpoint [Review: [ 108 ]].
“My time’s running out”
Reviews found a preoccupation with death in BC survivors [Reviews: [ 28 , 37 ]], particularly in survivors with advanced BC [Reviews: [ 5 , 20 , 21 ]]. For some women, this led to a sense of urgency to live life to the full, leaving them out of step with friends and family [Review: [ 37 ]; Paper: [ 41 ]].
It felt like everyone was driving too slowly and I didn't have the time to sit there and wait… I felt like ‘you have all the time in the world, but my time's running out’ [Review: [ 37 ]].
Younger women coped with thoughts of death by attempting to have some control over the process through communicating their dying wishes, while mothers coped by making plans to ensure their children would be well cared for [Review: [ 28 ]]. However, not everyone feared death, as was found for some survivors with advanced BC [Review: [ 5 ]].
I've kind of come to terms with these fears, and I'm not really afraid of dying [Review: [ 5 ]]
Theme 3: Identity: loss and change
“i’m different… i’m imperfect”.
Bodily changes due to BC and its treatment (including loss of hair and one or both breasts), meant that many women were persistently reminded of their cancer due to an altered body image. Some felt a loss of control and alienated from their bodies, disfigured and undesirable, with a changed identity [Reviews: [ 5 , 14 , 21 , 22 , 28 , 29 , 113 ]; Papers: [ 48 , 51 , 53 , 70 , 78 , 95 , 98 , 99 , 101 , 103 , 104 , 110 , 112 , 114 ]]. However, some survivors did not experience body image disturbances or were able to adapt to changes over time [Papers: [ 53 , 110 ]], even viewing their scars as positive signs they were disease-free [Review: [ 113 ]].
Each time I passed a mirror I jumped back because I didn't recognise myself [Review: [ 5 ]] I'm different from those who are normal… For myself, I'm imperfect. I had the surgery and lost one side [of the breast] [Review: [ 113 ]] I saw myself and I felt bad they had taken my breast. But then, I said, `No. Thank God. Because it was taken, I live.' Then I was assimilating, and now it's normal for me, that I don't have my chest [Paper: [ 53 ]].
For some women, losing a breast led to changes in their sense of femininity and womanhood [Review: [ 113 ] ].
… you started discovering that you were now just half a woman ‐ my femininity disappeared… [Review: [ 113 ]]
In reviews focusing on African American BC survivors, hair loss from treatment (and changes to hair texture and colour), as well as body altering surgeries, left women feeling damaged and less feminine and this was amplified by a desire to appear strong and to look well [Reviews: [ 14 , 22 ]].
Sexuality and relationships: “I felt something was missing”
The impact of BC treatment on women’s bodies also affected sexuality and intimate relationships [Reviews: [ 5 , 21 , 22 , 29 , 113 ]; Papers: [ 53 , 58 , 76 , 77 , 78 , 79 , 95 , 96 , 97 ]]. Insecurities after mastectomy reduced women’s sense of sexual desirability [Reviews: [ 5 , 22 , 113 ]; Paper: [ 77 ]].
The majority of us feel degraded as women as we see ourselves in the mirror and wonder, ‘If we cannot accept ourselves, how can our husbands or partners?’ [Review: [ 5 ]]
Other treatment side-effects impacting sexual activity and intimacy included early menopause, pain, vaginal dryness, and reduced sexual desire/libido [Reviews: [ 22 , 29 ]]. Some women felt rejected by partners due to changes in their relationship [Review: [ 22 ]].
Fertility and infertility
Reviews/papers examined association between identity and fertility and how BC and treatments posed a threat to this part of women’s lives [Reviews: [ 28 , 29 , 38 ]; Papers: [ 52 , 53 , 88 , 96 ]]. For some women, especially pre-menopausal women, loss and grief related to infertility was significant and served as an emotional reminder of BC [Review: [ 28 ]]. For other survivors, a pregnancy post-cancer was considered restorative and normalising [Paper: [ 84 ]].
To have something grow inside you on purpose in contrast to this cancer that grew unwelcome… you’re trusting in your body again…It felt just so normal [Paper: [ 84 ]]
Fertility, for others, was viewed as secondary to survival and preventing recurrence [Review: [ 38 ]]. While some women desired children in the future, others decided against children due to FCR, genetic risk and the health of the baby [Review: [ 38 ]].
Changing and maintaining roles
For many survivors, there was a significant shift in roles and relationships, from providing to receiving care [Reviews: [ 22 , 25 , 28 , 108 ]; Paper: [ 76 ]]. There was also a desire (and sometimes expectation from others) to maintain identity and normalcy by fulfilling former roles, such as upholding the role of homemaker [Review: [ 34 ]], returning to work [Review: [ 13 ]], or caregiving [Reviews: [ 25 , 28 ]; Papers: [ 39 , 43 , 114 ]]. For some women, however, this expectation to fulfil their pre-diagnosis role was a challenge and burden [Review: [ 25 ]].
Even after getting chemo, I still had to take care of my children, so that was hard [Review: [ 25 ]]
Theme 4: Isolation and being misunderstood
Limitations and stigmatisation meant some survivors isolated themselves or felt unable to fully participate in social life, consequently reducing the social support available to them [Reviews: [ 21 , 113 ]; Papers: [ 44 , 48 , 72 , 74 , 90 , 103 ]]. Some survivors, especially older survivors, reported not wanting to burden those around them [Reviews: [ 25 , 28 ]; Paper: [ 90 ]]. Many also felt misunderstood by others (including family, community and co-workers) as they struggled with ongoing challenges from their diagnosis and treatment. Survivors described an unrealistic expectation from those around them that they would fully recover and be symptom-free after primary treatment [Reviews: [ 13 , 14 , 25 , 32 , 34 , 37 ]; Papers: [ 56 , 107 ]], especially when they may appear physically well to others [Paper: [ 43 ]].
Families don’t understand. They say they understand, but they expect us to be the same people as before the disease [Review: [ 25 ]] That’s one of the things that people don’t understand about having stage IV cancer. I think a lot of people think [your] appearance should be bald and super thin and kind of sickly looking. When I tell people, “I’ll always have stage IV cancer,” they look at me. “No, you don’t.” I’m like, “I look normal, I know.” You can look normal. People don’t realise that [Paper: [ 43 ]].
Theme 5: Posttraumatic growth
“to grow from it, to heal from it”.
Many reviews/papers identified posttraumatic growth alongside the negative impacts of BC and its treatment [Reviews: [ 5 , 13 , 21 , 28 , 32 , 34 , 113 ]; Papers: [ 39 , 48 , 55 , 56 , 57 , 89 , 102 , 104 , 105 , 109 , 110 , 114 ]]. Some women were able to embrace and accept their new bodies [Reviews: [ 5 , 113 ]; Paper: [ 114 ]].
[Cancer] definitely changed my life… for the better. It gave me more of a clarity about myself… to take it and grow from it, and heal from it, and achieve from it [Paper [ 39 ]:] I like my body better now… I've accepted it so I like my body… it's part of life you know and you just get on with it… [Review: [ 113 ]] ‘Wakeup call’
Some survivors also reported a greater appreciation for life and a sense of gratitude, viewing their cancer experience as a turning point and making the most of their lives now [Reviews: [ 5 , 21 , 28 , 34 , 113 ]; Papers: [ 39 , 57 , 102 ]].
Little things now mean a lot to me. I don't take life for granted any more [Review: [ 5 ]] [Cancer] definitely changed my life, but it changed it for the better. It gave me more of a clarity about myself [Paper [ 39 ]:]
For some, the shift to focusing on appreciating life included a re-evaluation of their work/life balance, [Reviews: [ 13 , 32 ]; Paper: [ 55 ]], working towards personal goals and values, prioritising relationships, and contributing to the community [Reviews: [ 21 , 34 ]; Papers: [ 48 , 89 , 109 ]]. This included a sense of empowerment through focusing on healthy lifestyle changes and self-management [Papers: [ 48 , 105 , 109 ]]. Finding meaning in the BC experience was realised by connecting with (and supporting) others diagnosed with BC and advocating for increased BC awareness [Reviews: [ 5 , 20 , 21 , 28 ]; Papers: [ 48 , 55 , 109 , 110 ]].
Theme 6: Return to work
Four reviews specifically focused on the return-to-work experience for BC survivors [Reviews: [ 13 , 31 , 32 , 33 ]], while one review discussed return to work in the context of cognitive changes [Review: [ 34 ]]. Employment was also discussed in many primary papers [Papers: [ 53 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 95 , 99 ]]. Returning to work was important to many survivors as a way of regaining a sense of normalcy, meaning, identity, support and connection [Reviews: [ 13 , 32 , 34 ]; Paper: [ 95 ]]. However, some survivors found the work environment unsupportive, with some even facing discrimination [Reviews: [ 31 , 32 ]; Papers: [ 53 , 63 ]]. Privacy regarding disclosure of illness was an issue; some survivors found that employers did not keep their health status confidential [Review: [ 32 ]]. Treatment side effects and body insecurities led to challenges and loss of confidence at work [Reviews: [ 13 , 31 , 33 ]; Papers: [ 63 , 64 ]].
I had to lean down to do anything on the bottom, lower shelf or even for bags to pack them, I was like this [covered her chest] all the time, holding it together… every minute of my working day you’re thinking of it [Review: [ 33 ]].
Some survivors reported cognitive impairments such as problems with concentration, executive function, memory, and speed of processing [Review: [ 33 , 34 ]; Papers: [ 63 , 68 ]].
With this memory thing, I was very frustrated at work and so I thought that I can’t go on like this. It was a chore now going to work than a joy [Review: [ 33 ]]
Many survivors experienced anxiety and frustration around their capacity to return to work [Reviews: [ 13 , 31 , 32 , 33 ]]. This was further complicated by employers expecting survivors to be as capable post-treatment as they were pre-diagnosis and survivors not wanting to disappoint or mislead them [Reviews: [ 13 , 31 , 32 ]]. Survivors also described financial pressure to return to work [Reviews: [ 13 , 32 ]].
Theme 7: Quality of care
Health care experiences.
Many reviews focused on experience of the health care system as a cancer survivor. While many women reported positive healthcare experiences, some reported negative interactions. AlOmeir et al. [ 36 ] reviewed factors influencing survivors’ adherence to adjuvant treatment, finding that the decision to accept or delay treatment was influenced by trust in health care providers as well as concerns, expectations and knowledge of the treatment. Selamat et al.’s [ 34 ] review, focused on experience of cognitive changes, found survivors experienced a lack of information about cognitive deficits and felt invalidated and dismissed by health professionals. Some survivors with metastatic BC reported that their needs were not met if care focused on physical symptoms to the exclusion of psychosocial needs [Review: [ 21 ]].
Feeling alone; lack of information and support
Survivors noted a need for information about the reality of survivorship and disease management, especially about ongoing side-effects [Reviews: [ 22 , 28 , 30 , 31 , 34 , 36 , 37 ]; Papers: [ 60 , 87 , 95 , 98 , 99 , 100 , 109 ]].
They (the doctors) said in a year you'll be back to your regular everyday life, and I'm not. It's a disappointment [Review: [ 37 ]] We feel lost, really. There is a lot of information missing—information about knowing what to do, where to call [Paper: [ 60 ]]
Survivors also noted a need for relevant information, empathy and support from health services, otherwise they felt dismissed, unsupported and alone [Reviews: [ 36 , 37 ]; Papers: [ 40 , 46 , 51 , 68 , 72 , 82 , 84 , 85 , 90 , 91 , 97 , 105 ]].
I wished that my pain at home was followed up much more [Review: [ 37 ]]
Reviews identified barriers for survivors to access health services. For rural BC survivors, location and transport needs were a barrier to care [Review: [ 26 ]]. For some low SES and/or ethnically diverse BC survivors, there were concerns about the quality of care they had access to [Paper: [ 39 ]].
It’s a county hospital, so it’s an overly stressed system … They don’t have resources … I was told that in a private institute, you were assigned a nutritionist, a social worker and a binder that had everything broken down … I wish we had a universal medical system and when you get cancer this is what you get [Paper: [ 39 ]].
Several primary papers highlighted the ongoing financial burden/barrier associated with BC due to healthcare cost and productivity loss [Papers: [ 82 , 99 , 103 , 105 , 112 ]], including BC survivors with lymphoedema [Paper: [ 71 ]].
I lost my job ‘cause I got diagnosed with breast cancer so financially it was very difficult … I was out of work for almost a year … with the chemo… I was really sick and then I went back against the doctor’s orders ‘cause I needed to make money… When I came back to work that’s when they expected me to resume all of the duties… full force and…I got fired… [Paper: [ 71 ]].
Language can also pose a significant challenge when seeking information and support. Wen et al. [Review: [ 24 ]] found for Asian American women, communication with health professionals was sometimes challenging. Similarly, survivors struggled to find support groups in their community when there was a language barrier or perceived cultural differences [Review: [ 25 ]].
Americans don’t seem to share their emotions with immigrants like us. They don’t try to talk to us first… [Review: [ 25 ]]
Theme 8: Support needs and coping strategies
Social support.
BC survivors reported needing practical and emotional support from family, partners, friends, community groups, co-workers, other BC survivors and health providers [Reviews: [ 5 , 14 , 21 , 22 , 23 , 25 , 26 , 27 , 28 , 29 , 34 , 36 , 115 ]; Papers: [ 39 , 43 , 47 , 48 , 49 , 53 , 54 , 55 , 68 , 69 , 74 , 78 , 82 , 84 , 95 , 97 , 99 , 105 , 109 , 112 , 114 , 116 ]]. These supports helped survivors to engage in activities, contribute to community, talk about their experiences, and cope with distress [Reviews: [ 21 , 34 ]]. Support from other survivors was important due to shared experiences [Reviews: [ 21 , 22 ]; Papers: [ 69 , 73 , 84 ]].
My kids are my all and being with them keeps me going. Even through what I’m going through now.. They’re like my sun. I see them, and I light up [Paper: [ 39 ]] Yeah when I met fellow survivors at BCF (Breast Cancer Foundation) … yeah … I thought, they also experienced what I have experienced. So it’s OK. It’s not too bad and we laughed about it [Paper: [ 69 ]].
Spirituality
Spirituality was important to many survivors in coping with their BC and its ongoing impact on their lives [Reviews: [ 5 , 14 , 20 , 21 , 22 , 23 , 24 , 27 , 29 , 115 ]; Papers: [ 39 , 41 , 47 , 48 , 49 , 50 , 78 , 94 , 97 , 102 , 103 , 109 , 114 ]], as it helped them to cope with uncertainty and accept their condition [Reviews: [ 5 , 20 , 21 ]].
He's chosen me to survive this cancer journey. It's really helpful to me to have a higher power that I choose to call God and to believe that I have a purpose in this world [Review: [ 5 ]].
My spirituality and belief in God are so strong and my faith keeps me strong [Paper: [ 39 ]]
“We must learn to live with it”
Besides social support and spirituality, women found other ways to cope, including adapting daily activities to accommodate limitations, accepting side-effects and integrating the disease into current life [Reviews: [ 27 , 37 , 115 ]].
I learned to change some of my movements. I learned movements that relieve. Instead of wringing the kitchen glove like that, now I wring it like this, against the side of the sink [Review: [ 37 ]].
Others, especially women with advanced BC [Reviews: [ 5 , 21 , 22 ]], and rural BC survivors [Review: [ 27 ]], coped through avoidance or denial of their disease, such as trying to forget about their condition [Paper: [ 90 ]].
Thinking positively and hopefully, as well as having a ‘fighting spirit’ towards the disease and its ongoing impact, was important for some [Reviews: [ 5 , 21 , 22 , 23 , 115 ]; Paperss: [ 41 , 47 , 107 ]].
I believe that a person should be satisfied and not embittered…. Constant anger will cause more disease [Review: [ 5 ]]
Many older survivors coped by not having the expectation they would return to full health, as they had already begun to accept declining health as part of aging [Review: [ 28 ]]. These survivors focused on their present experience rather than focusing on the past or future [Review: [ 28 ]].
This meta-review identified and synthesised 25 systematic reviews, and an additional 76 primary papers to describe the psychosocial experience of BC survivors. Overall, the quality of included reviews and papers was mixed, with the majority of studies classified as of moderate quality, suggesting that future research could be improved by following recommended methodological procedures [ 11 ]. Some of the included reviews/papers focused on specific groups of BC survivors, including younger/older, rural, ethnic minorities, and survivors with metastatic BC. Return to work was well covered, as was quality of care. Ongoing symptoms (e.g. physical, cognitive, psychological and sexual) was an area of saturation within the included systematic reviews.
Eight of the included systematic reviews were published after the Laidsaar-Powell et al. [ 15 ] meta-review and focused on adherence to adjuvant endocrine treatment, rural BC survivors, pain, return to work, sexual problems, metastatic BC, transitioning from patient to survivor, and survivorship characteristics of different BC stages (post-treatment to recurrence and metastatic BC). More recent reviews emphasised ongoing physical and psychological impacts, changes to identity and roles, as well as the transition from patient to survivor. In recent papers, similar topics were covered with many papers focusing on specific populations (e.g. metastatic BC, BC survivors with lymphoedema, low SES, African-American, sexual and gender diverse, young BC survivors) and/or topics (e.g. sexual and reproductive health, cognitive impairment, return to work, posttraumatic growth, cancer-related fatigue).
After combining all of the reviews/papers, the meta-review synthesis resulted in eight overarching themes. A key thread across many of these themes was the challenging transition from patient to survivor; characterised by searching for normalcy, ongoing treatment and side effect impacts, feelings of uncertainty, FCR, lack of information, feeling misunderstood, and changing roles and identity. For many women, this transition was complicated by unmet expectations that once treatment was completed women would return to their healthy premorbid life, which was not a reality for many. Instead, they faced ongoing symptoms and limitations, which in turn led to a sense of being misunderstood by family members and employers. For those women who belonged to an ethnic minority group, challenges could be further exacerbated by difficulties communicating with health professionals and accessing support from within their own communities [ 24 , 25 ].
These themes reflect the findings of a scoping review by Maheu et al. [ 117 ] which focused on uncertainty and FCR in BC survivors. The authors found that the experience of uncertainty was characterised by doubt, liminality, a sense of insecurity, and an inability to meet expectations. Uncertainty was also found to be a cause of FCR. Lack of information and lost connection to health professionals were found to exacerbate both uncertainty and fear of recurrence [ 117 ], as was noted in the current study.
While most research reported in this review focused on the ongoing challenges faced by BC survivors, within some reviews women also reported positive aspects of their survivorship experience, including greater appreciation of life. Positive outcomes have been previously identified in survivorship research, emphasising the resilience demonstrated by many cancer survivors [ 118 ]. Posttraumatic growth refers to the positive change (or growth) that occurs in individuals after a significant stressor [ 119 , 120 ]. Reflecting these domains, many cancer survivors report appreciation for the value of life, more self-confidence and self-esteem, positive social interactions and stronger interpersonal relationships, reprioritisation of personal values, as well as strengthened religious faith and spirituality [ 118 , 119 ] after BC.
Clinical implications
Due to the long-lasting impacts that BC survivors face during their survivorship, highlighted in this review, these women require ongoing support to manage their symptoms and improve both quality of life and metastatic BC survival outcomes [ 4 , 121 ]. BC survivorship research can inform psychosocial interventions and these should ideally be embedded into established patient care [ 122 ]. Interventions may include individualised support, with regular assessment of ongoing challenges and survivorship needs, as well as addressing healthy lifestyle changes, treatment adherence, and symptoms where needed [ 123 ]. Support during survivorship should be sustained and more than a one-off consultation [ 123 ]. For rural BC survivors, scheduling all appointments on one day and providing support and information via various sources (e.g. social media, internet resources) are suggested ways of improving their health care experience [ 26 ].
One important strategy to address the long-term needs of BC survivors is the use of survivorship care plans (SCPs) which are designed to provide support and information during the transition into survivorship [ 124 ]. Individualised SCPs created by the oncology treatment team [ 124 ] can provide information regarding quality of life and concerns for BC survivors, as well as including plans for follow-up and disease recurrence surveillance [ 124 ]. SCPs aim to provide BC survivors with a realistic understanding of what to expect as they transition into survivorship, normalising their feelings of uncertainty. Kozul et al. [ 125 ] noted that SCPs can promote discussion of varied survivorship issues, including side effects, FCR, medication adherence, psychosocial/mental health, bone health, difficulties with relationships, exercise, and fertility, and prompt referral to appropriate health professionals for help with these issues.
Interventions aimed specifically at body image, sexuality, and identity may also help women struggling with the impact of BC on their bodies (e.g. after mastectomy) and function (e.g. inability to return to work/care). Morales-Sánchez et al. [ 126 ] systematically reviewed eight studies of interventions aimed at improving body image and self-esteem, finding varied effectiveness. Of the interventions, group therapies (e.g. cognitive behavioural therapy groups) were found to demonstrate the most positive results. Other interventions, such as psychosexual counselling and intimacy enhancement (couple-based) interventions, have also been found to improve sexuality and intimacy concerns [ 127 , 128 ].
An important consideration for all interventions is cultural appropriateness. As highlighted in our findings, many women prefer to access support that includes others like them, conforms with their values and beliefs, and which can help them with specific issues such as challenges with language and communication.
Further research
While the current review highlights the large body of evidence examining BC survivorship, several gaps in the evidence base are noted, including BC survivors with BRCA 1/2 gene mutations, women receiving tailored treatments (including emerging treatments such as immunotherapy/targeted therapies), those of low socioeconomic status, and the unique experiences of BC survivors with multimorbidity and complex health care needs. While the included reviews discussed the impact of various long-term side-effects of BC and its treatment (e.g. sexual dysfunction, cognitive impairment, psychological distress, loss of fertility, sleep impairment, body image concerns, lymphoedema, ongoing pain, and fatigue), some late effects (emerging months or years after treatment completion) were not covered, including cardiotoxicity and osteoporosis [ 123 , 129 ]. Lifestyle changes are recommended to reduce risk of cardiotoxicity and osteoporosis including addressing tobacco and alcohol use, managing weight, and increasing exercise [ 123 , 129 ]. These lifestyle changes may also decrease the risk of recurrence and are therefore commonly part of BC survivorship care [ 121 , 123 , 124 , 129 ]. Despite the importance of lifestyle changes in survivorship, this was rarely discussed in the included reviews/papers.
Experiences of gender and sexually diverse BC survivors were also largely missing from the included reviews/papers, reflecting a paucity of research within this area. A recent PP from Brown and McElroy [ 83 ] that focused on the unmet needs of sexual and gender minority BC survivors found that these survivors experienced a lack of appropriate support from health care systems and BC survivor organisations.
Strengths and limitations
This study has several limitations. Searches were limited to reviews published in English and, therefore non-English reviews may not have been included. Systematic reviews may be limited by the interpretation provided by these reviews and their choice of quotations, and this review only included primary papers published after the last search made by a systematic review. Therefore, some detail may be missing. Additionally, it is likely that some included reviews drew upon the findings of the same primary papers; therefore, some duplication of results across reviews is possible.
By focusing on qualitative and non-intervention studies, this meta-review may be missing valuable information about the BC survivorship experience. Future studies could incorporate a wider range of research types. Nevertheless, this meta-review is the first to synthesise the available qualitative evidence of BC survivorship and provides the most comprehensive overview of BC survivor experiences to date.
This meta-review synthesised the qualitative BC survivorship evidence base and found that BC survivorship is characterised by many ongoing physical and psychosocial impacts, as well as posttraumatic growth in some women. The quality of research within this meta-review was moderate, and future studies should make use of methodological quality guidelines when conducting systematic reviews and primary research. The findings suggest that BC survivors experience significant uncertainty and changes in identity, along with ongoing physical and psychosocial challenges. It is therefore important to provide timely and accessible support to these women, such as through the use of individualised SCPs. Specialised information about and support for ongoing effects and interventions aimed at body image, sexuality, and identity may be beneficial. To address gaps in the BC research, future studies should include BC survivors with BRCA 1/2 gene mutations, women receiving tailored treatments, women from low socioeconomic backgrounds, BC survivors with multimorbidity and complex health care needs, late effects, as well as interventions targeting gender and sexually diverse BC survivors.
Data availability
Data are available within an institutional repository.
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: Globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49. https://doi.org/10.3322/caac.21660 .
Article PubMed Google Scholar
Australian Institute of Health and Welfare (AIHW). Cancer in Australia 2021. https://aihw.gov.au . Accessed 21/12/2022.
Clinical Oncology Society of Australia (COSA). Survivorship care. Critical components of cancer survivorship care in Australia position statement. 2016. https://cosa.org.au .
Fallowfield L, Jenkins V. Psychosocial/survivorship issues in breast cancer: are we doing better? J Natl Cancer Inst. 2015;107(1):335. https://doi.org/10.1093/jnci/dju335 .
Smit A, Coetzee BJ, Roomaney R, Bradshaw M, Swartz L. Women’s stories of living with breast cancer: a systematic review and meta-synthesis of qualitative evidence. Soc Sci Med. 2019;222:231–45. https://doi.org/10.1016/j.socscimed.2019.01.020 .
Carreira H, Williams R, Muller M, Harewood R, Stanway S, Bhaskaran K. Associations between breast cancer survivorship and adverse mental health outcomes: a systematic review. J Natl Cancer Inst. 2018;110(12):1311–27. https://doi.org/10.1093/jnci/djy177 .
Article PubMed PubMed Central Google Scholar
Schmidt ME, Wiskemann J, Steindorf K. Quality of life, problems, and needs of disease-free breast cancer survivors 5 years after diagnosis. Qual Life Res. 2018;27(8):2077–86. https://doi.org/10.1007/s11136-018-1866-8 .
Mayer M. Lessons learned from the metastatic breast cancer community. Semin Oncol Nurs. 2010;26(3):195–202. https://doi.org/10.1016/j.soncn.2010.05.004 .
Mosher CE, Johnson C, Dickler M, Norton L, Massie MJ, DuHamel K. Living with metastatic breast cancer: a qualitative analysis of physical, psychological, and social sequelae. Breast J. 2013;19(3):285–92. https://doi.org/10.1111/tbj.12107 .
Holloway I, Galvin K. Qualitative research in nursing and healthcare. Chichester, UK: John Wiley & Sons; 2016.
Google Scholar
Aromataris E, Fernandez R, Godfrey CM, Holly C, Khalil H, Tungpunkom P. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. Int J Evid Based Healthc. 2015;13(3):132–40. https://doi.org/10.1097/XEB.0000000000000055 .
Smith V, Devane D, Begley CM, Clarke M. Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Med Res Methodol. 2011;11(1):15. https://doi.org/10.1186/1471-2288-11-15 .
Banning M. Employment and breast cancer: a meta-ethnography. Eur J Cancer Care (Engl). 2011;20(6):708–19. https://doi.org/10.1111/j.1365-2354.2011.01291.x .
Article CAS PubMed Google Scholar
Mollica M, Newman SD. Breast cancer in african americans: from patient to survivor. J Transcult Nurs. 2014;25(4):334–40. https://doi.org/10.1177/1043659614524248 .
Laidsaar-Powell R, Konings S, Rankin N, Koczwara B, Kemp E, Mazariego C, et al. A meta-review of qualitative research on adult cancer survivors: current strengths and evidence gaps. J Cancer Surviv. 2019;13(6):852–89. https://doi.org/10.1007/s11764-019-00803-8 .
Innovation VH. Covidence systematic review software . www.covidence.org .
Programme CAS. Casp qualitative . 2018; Available from: https://casp-uk.net/wp-content/uploads/2018/01/CASP-Qualitative-Checklist-2018.pdf .
Noblit GW, Hare RD. Meta-ethnography: synthesising qualitative studies. Newbury Park, CA: Sage; 1988.
Book Google Scholar
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: The prisma statement. BMJ. 2009;339(jul21 1):2535–2535. https://doi.org/10.1136/bmj.b2535 .
Article Google Scholar
Flanigan M, Wyatt G, Lehto R. Spiritual perspectives on pain in advanced breast cancer: a scoping review. Pain Manag Nurs. 2019;20(5):432–43. https://doi.org/10.1016/j.pmn.2019.04.002 .
Willis K, Lewis S, Ng F, Wilson L. The experience of living with metastatic breast cancer–a review of the literature. Health Care Women Int. 2015;36(5):514–42. https://doi.org/10.1080/07399332.2014.896364 .
Nolan TS, Frank J, Gisiger-Camata S, Meneses K. An integrative review of psychosocial concerns among young african american breast cancer survivors. Cancer Nurs. 2018;41(2):139–55. https://doi.org/10.1097/NCC.0000000000000477 .
Russell KM, Von Ah DM, Giesler RB, Storniolo AM, Haase JE. Quality of life of african american breast cancer survivors: how much do we know? Cancer Nurs. 2008;31(6):E36-45. https://doi.org/10.1097/01.NCC.0000339254.68324.d7 .
Wen KY, Fang CY, Ma GX. Breast cancer experience and survivorship among asian americans: a systematic review. J Cancer Surviv. 2014;8(1):94–107. https://doi.org/10.1007/s11764-013-0320-8 .
Yoon H, Chatters L, Kao TS, Saint-Arnault D, Northouse L. Factors affecting quality of life for korean american cancer survivors: an integrative review. Oncol Nurs Forum. 2016;43(3):E132–42. https://doi.org/10.1188/16.ONF.E132-E142 .
Anbari AB, Wanchai A, Graves R. Breast cancer survivorship in rural settings: a systematic review. Support Care Cancer. 2020;28(8):3517–31. https://doi.org/10.1007/s00520-020-05308-0 .
Bettencourt BA, Schlegel RJ, Talley AE, Molix LA. The breast cancer experience of rural women: a literature review. Psychooncol. 2007;16(10):875–87. https://doi.org/10.1002/pon.1235 .
Campbell-Enns HJ, Woodgate RL. The psychosocial experiences of women with breast cancer across the lifespan: a systematic review. Psychooncol. 2017;26(11):1711–21. https://doi.org/10.1002/pon.4281 .
Chang YC, Chang SR, Chiu SC. Sexual problems of patients with breast cancer after treatment: a systematic review. Cancer Nurs. 2019;42(5):418–25. https://doi.org/10.1097/NCC.0000000000000592 .
Vivar CG, McQueen A. Informational and emotional needs of long-term survivors of breast cancer. J Adv Nurs. 2005;51(5):520–8. https://doi.org/10.1111/j.1365-2648.2005.03524.x .
Zomkowski K, Cruz de Souza B, Pinheiro da Silva F, Moreira GM, de Souza Cunha N, Sperandio FF. Physical symptoms and working performance in female breast cancer survivors: a systematic review. Disabil Rehabil. 2017;40(13):1485–93. https://doi.org/10.1080/09638288.2017.1300950 .
Tiedtke C, de Rijk A, Dierckx de Casterle B, Christiaens MR, Donceel P. Experiences and concerns about “returning to work” for women breast cancer survivors: a literature review. Psychooncol. 2019;19(7):677–83. https://doi.org/10.1002/pon.1633 .
Bijker R, Duijts SFA, Smith SN, de Wildt-Liesveld R, Anema JR, Regeer BJ. Functional impairments and work-related outcomes in breast cancer survivors: a systematic review. J Occup Rehabil. 2018;28(3):429–51. https://doi.org/10.1007/s10926-017-9736-8 .
Selamat MH, Loh SY, Mackenzie L, Vardy J. Chemobrain experienced by breast cancer survivors: a meta-ethnography study investigating research and care implications. PLoS One. 2014;9(9):e108002. https://doi.org/10.1371/journal.pone.0108002 .
Article CAS PubMed PubMed Central Google Scholar
Henneghan A. Modifiable factors and cognitive dysfunction in breast cancer survivors: a mixed-method systematic review. Support Care Cancer. 2016;24(1):481–97. https://doi.org/10.1007/s00520-015-2927-y .
AlOmeir O, Patel N, Donyai P. Adherence to adjuvant endocrine therapy among breast cancer survivors: a systematic review and meta-synthesis of the qualitative literature using grounded theory. Support Care Cancer. 2020;28(11):5075–84. https://doi.org/10.1007/s00520-020-05585-9 .
Armoogum J, Harcourt D, Foster C, Llewellyn A, McCabe CS. The experience of persistent pain in adult cancer survivors: a qualitative evidence synthesis. Eur J Cancer Care (Engl). 2020;29(1):e13192. https://doi.org/10.1111/ecc.13192 .
Goncalves V, Sehovic I, Quinn G. Childbearing attitudes and decisions of young breast cancer survivors: a systematic review. Hum Reprod Update. 2014;20(2):279–92. https://doi.org/10.1093/humupd/dmt039 .
Adler SR, Coulter YZ, Stone K, Glaser J, Duerr M, Enochty S. End-of-life concerns and experiences of living with advanced breast cancer among medically underserved women. J Pain Symptom Manage. 2019;58(6):959–67. https://doi.org/10.1016/j.jpainsymman.2019.08.006 .
Alfieri S, Brunelli C, Capri G, Caraceni A, Bianchi GV, Borreani C. A qualitative study on the needs of women with metastatic breast cancer. J Cancer Educ. 2021. https://doi.org/10.1007/s13187-020-01954-4 .
Ginter AC. “The day you lose your hope is the day you start to die”: quality of life measured by young women with metastatic breast cancer. J Psychosoc Oncol. 2020;38(4):418–34. https://doi.org/10.1080/07347332.2020.1715523 .
Lee Mortensen G, Madsen IB, Krogsgaard R, Ejlertsen B. Quality of life and care needs in women with estrogen positive metastatic breast cancer: a qualitative study. Acta Oncol. 2018;57(1):146–51. https://doi.org/10.1080/0284186X.2017.1406141 .
Lundquist DM, Berry DL, Boltz M, DeSanto-Madeya SA, Grace PJ. Wearing the mask of wellness: the experience of young women living with advanced breast cancer. Oncol Nurs Forum. 2019;46(3):329–37. https://doi.org/10.1188/19.ONF.329-337 .
Mosher CE, Daily S, Tometich D, Matthias MS, Outcalt SD, Hirsh A, et al. Factors underlying metastatic breast cancer patients' perceptions of symptom importance: a qualitative analysis. Eur J Cancer Care (Engl). 2018;27. https://doi.org/10.1111/ecc.12540
Oostra DL, Burse NR, Wolf LJ, Schleicher E, Mama SK, Bluethmann S, et al. Understanding nutritional problems of metastatic breast cancer patients: Opportunities for supportive care through ehealth. Cancer Nurs. 2020;44(2):154–62. https://doi.org/10.1097/NCC.0000000000000788 .
Ceballos RM, Hohl SD, Molina Y, Hempstead B, Thompson-Dodd J, Weatherby S, et al. Oncology provider and african-american breast cancer survivor perceptions of the emotional experience of transitioning to survivorship. J Psychosoc Oncol. 2021;39(1):35–53. https://doi.org/10.1080/07347332.2020.1752880 .
Davis CM, Nyamathi AM, Abuatiq A, Fike GC, Wilson AM. Understanding supportive care factors among african american breast cancer survivors. J Transcult Nurs. 2018;29(1):21–9. https://doi.org/10.1177/1043659616670713 .
Ford YR. Stories of african-american breast cancer survivors. J Natl Black Nurses Assoc. 2019;30(2):26–33.
PubMed Google Scholar
Nolan TS, Ivankova N, Carson TL, Spaulding AM, Dunovan S, Davies S, et al. Life after breast cancer: “being” a young African American survivor. Ethn Health. 2019. https://doi.org/10.1080/13557858.2019.1682524 .
Yan AF, Stevens P, Holt C, Walker A, Ng A, McManus P, et al. Culture, identity, strength and spirituality: a qualitative study to understand experiences of african american women breast cancer survivors and recommendations for intervention development. Eur J Cancer Care (Engl). 2019;28(3):e13013. https://doi.org/10.1111/ecc.13013 .
Black KZ, Eng E, Schaal JC, Johnson LS, Nichols HB, Ellis KR, et al. The other side of through: young breast cancer survivors’ spectrum of sexual and reproductive health needs. Qual Health Res. 2020;30(13):2019–32. https://doi.org/10.1177/1049732320929649 .
Henneghan A, Phillips C, Courtney A. We are different: young adult survivors’ experience of breast cancer. Breast J. 2018;24(6):1126–8. https://doi.org/10.1111/tbj.13128 .
Hubbeling HG, Rosenberg SM, Gonzalez-Robledo MC, Cohn JG, Villarreal-Garza C, Partridge AH, et al. Psychosocial needs of young breast cancer survivors in mexico city, mexico. PLoS One. 2018;13(5):e0197931. https://doi.org/10.1371/journal.pone.0197931 .
Milosevic E, Brunet J, Campbell KL. Exploring tensions within young breast cancer survivors’ physical activity, nutrition and weight management beliefs and practices. Disabil Rehabil. 2020;42(5):685–91. https://doi.org/10.1080/09638288.2018.1506512 .
Raque-Bogdan TL, Hoffman MA, Joseph EC, Ginter AC, White R, Schexnayder K, et al. Everything is more critical: a qualitative study of the experiences of young breast cancer survivors. Couns Values. 2018;63(2):210–31. https://doi.org/10.1002/cvj.12089 .
Rees S. A qualitative exploration of the meaning of the term “survivor” to young women living with a history of breast cancer. Eur J Cancer Care (Engl). 2018;27(3):e12847. https://doi.org/10.1111/ecc.12847 .
Wilson E. Social work, cancer survivorship and liminality: meeting the needs of young women diagnosed with early stage breast cancer. J Soc Work Pract. 2020;34(1):95–111. https://doi.org/10.1080/02650533.2019.1604497 .
Gorman JR, Smith E, Drizin JH, Lyons KS, Harvey SM. Navigating sexual health in cancer survivorship: a dyadic perspective. Support Care Cancer. 2020;28(11):5429–39. https://doi.org/10.1007/s00520-020-05396-y .
Bilodeau K, Tremblay D, Durand MJ. Return to work after breast cancer treatments: Rebuilding everything despite feeling “in-between.” Eur J Oncol Nurs. 2019;41(165):165–72. https://doi.org/10.1016/j.ejon.2019.06.004 .
Bilodeau K, Tremblay D, Durand MJ. Gaps and delays in survivorship care in the return-to-work pathway for survivors of breast cancer-a qualitative study. Curr Oncol. 2019;26(3):e414–7. https://doi.org/10.3747/co.26.4787 .
Caron M, Durand MJ, Tremblay D. Perceptions of breast cancer survivors on the supporting practices of their supervisors in the return-to-work process: a qualitative descriptive study. J Occup Rehabil. 2018;28(1):89–96. https://doi.org/10.1007/s10926-017-9698-x .
Fassier JB, Lamort-Bouche M, Broc G, Guittard L, Peron J, Rouat S, et al. Developing a return to work intervention for breast cancer survivors with the intervention mapping protocol: challenges and opportunities of the needs assessment. Front Publ Health. 2018;6:35. https://doi.org/10.3389/fpubh.2018.00035 .
Luo SX, Liu JE, Cheng ASK, Xiao SQ, Su YL, Feuerstein M. Breast cancer survivors report similar concerns related to return to work in developed and developing nations. J Occup Rehabil. 2019;29(1):42–51. https://doi.org/10.1007/s10926-018-9762-1 .
Sengun Inan F, Gunusen N, Ozkul B, Akturk N. A dimension in recovery: return to working life after breast cancer. Cancer Nurs. 2020;43(6):E328–34. https://doi.org/10.1097/NCC.0000000000000757 .
Sun Y, Shigaki CL, Armer JM. The influence of breast cancer related lymphedema on women’s return-to-work. Womens Health (Lond). 2020;16:1745506520905720. https://doi.org/10.1177/1745506520905720 .
van Maarschalkerweerd PEA, Schaapveld M, Paalman CH, Aaronson NK, Duijts SFA. Changes in employment status, barriers to, and facilitators of (return to) work in breast cancer survivors 5–10 years after diagnosis. Disabil Rehabil. 2020;42(21):3052–8. https://doi.org/10.1080/09638288.2019.1583779 .
Zomkowski K, Cruz de Souza B, Moreira GM, Volkmer C, Da Silva Honorio GJ, Moraes Santos G, et al. Qualitative study of return to work following breast cancer treatment. Occup Med (Lond). 2019;69(3):189–94. https://doi.org/10.1093/occmed/kqz024 .
Bolton G, Isaacs A. Women’s experiences of cancer-related cognitive impairment, its impact on daily life and care received for it following treatment for breast cancer. Psychol Health Med. 2018;23(10):1261–74. https://doi.org/10.1080/13548506.2018.1500023 .
Henderson FM, Cross AJ, Baraniak AR. “A new normal with chemobrain”: experiences of the impact of chemotherapy-related cognitive deficits in long-term breast cancer survivors. Health Psychol Open. 2019;6(1):2055102919832234. https://doi.org/10.1177/2055102919832234 .
Anbari AB, Wanchai A, Armer JM. Breast cancer-related lymphedema and quality of life: a qualitative analysis over years of survivorship. Chronic Illn. 2019;17(3):1–12. https://doi.org/10.1177/1742395319872796 .
Dean LT, Moss SL, Ransome Y, Frasso-Jaramillo L, Zhang Y, Visvanathan K, et al. “It still affects our economic situation”: long-term economic burden of breast cancer and lymphedema. Support Care Cancer. 2019;27(5):1697–708. https://doi.org/10.1007/s00520-018-4418-4 .
Ostby PL, Armer JM, Smith K, Stewart BR. Patient perceptions of barriers to self-management of breast cancer-related lymphedema. West J Nurs Res. 2018;40(12):1800–17. https://doi.org/10.1177/0193945917744351 .
Kim S, Han J, Lee MY, Jang MK. The experience of cancer-related fatigue, exercise and exercise adherence among women breast cancer survivors: insights from focus group interviews. J Clin Nurs. 2020;29(5–6):758–69. https://doi.org/10.1111/jocn.15114 .
Levkovich I, Cohen M, Karkabi K. The experience of fatigue in breast cancer patients 1–12 month post-chemotherapy: a qualitative study. Behav Med. 2019;45(1):7–18. https://doi.org/10.1080/08964289.2017.1399100 .
Penner C, Zimmerman C, Conboy L, Kaptchuk T, Kerr C. “Honorable toward your whole self”: experiences of the body in fatigued breast cancer survivors. Front Psychol. 2020;11:1502. https://doi.org/10.3389/fpsyg.2020.01502 .
Haeng-Mi S, Park EY, Eun-Jeong K. Cancer-related fatigue of breast cancer survivors: qualitative research. Asian Oncol Nurs. 2020;20(4):141–9. https://doi.org/10.5388/aon.2020.20.4.141 .
Canzona MR, Fisher CL, Ledford CJW. Perpetuating the cycle of silence: The intersection of uncertainty and sexual health communication among couples after breast cancer treatment. Support Care Cancer. 2019;27(2):659–68. https://doi.org/10.1007/s00520-018-4369-9 .
Fouladi N, Pourfarzi F, Dolattorkpour N, Alimohammadi S, Mehrara E. Sexual life after mastectomy in breast cancer survivors: a qualitative study. Psychooncol. 2018;27(2):434–41. https://doi.org/10.1002/pon.4479 .
Tat S, Doan T, Yoo GJ, Levine EG. Qualitative exploration of sexual health among diverse breast cancer survivors. J Cancer Educ. 2018;33(2):477–84. https://doi.org/10.1007/s13187-016-1090-6 .
Stalsberg R, Eikemo TA, Lundgren S, Reidunsdatter RJ. Physical activity in long-term breast cancer survivors - a mixed-methods approach. Breast. 2019;46:126–35. https://doi.org/10.1016/j.breast.2019.05.014 .
Chumdaeng SSH, Chontawan R, Soivong P. Health behavior changes among survivors of breast cancer after treatment completion. Pacific Rim Int J Nurs Res. 2020;24(4):472–84.
Enzler CJ, Torres S, Jabson J, Ahlum Hanson A, Bowen DJ. Comparing provider and patient views of issues for low-resourced breast cancer patients. Psychooncol. 2019;28(5):1018–24. https://doi.org/10.1002/pon.5035 .
Brown MT, McElroy JA. Unmet support needs of sexual and gender minority breast cancer survivors. Support Care Cancer. 2018;26(4):1189–96. https://doi.org/10.1007/s00520-017-3941-z .
Azulay Chertok IR, Wolf JH, Beigelman S, Warner E. Infant feeding among women with a history of breast cancer. J Cancer Surviv. 2020;14(3):356–62. https://doi.org/10.1007/s11764-019-00852-z .
Brennan L, Kessie T, Caulfield B. Patient experiences of rehabilitation and the potential for an mhealth system with biofeedback after breast cancer surgery: qualitative study. JMIR Mhealth Uhealth. 2020;8(7):e19721. https://doi.org/10.2196/19721 .
Cherif E, Martin-Verdier E, Rochette C. Investigating the healthcare pathway through patients’ experience and profiles: implications for breast cancer healthcare providers. BMC Health Serv Res. 2020;20(1):735. https://doi.org/10.1186/s12913-020-05569-9 .
Rafn BS, Midtgaard J, Camp PG, Campbell KL. Shared concern with current breast cancer rehabilitation services: a focus group study of survivors’ and professionals’ experiences and preferences for rehabilitation care delivery. BMJ Open. 2020;10(7):e037280. https://doi.org/10.1136/bmjopen-2020-037280 .
Faccio F, Mascheroni E, Ionio C, Pravettoni G, Alessandro Peccatori F, Pisoni C, et al. Motherhood during or after breast cancer diagnosis: a qualitative study. Eur J Cancer Care (Engl). 2020;29(2):e13214. https://doi.org/10.1111/ecc.13214 .
Inan FS, Ustun B. Post-traumatic growth in the early survival phase: from turkish breast cancer survivors’ perspective. Eur J Breast Health. 2020;16(1):66–71. https://doi.org/10.5152/ejbh.2019.5006 .
Lai WS, Shu BC, Hou WL. A qualitative exploration of the fear of recurrence among taiwanese breast cancer survivors. Eur J Cancer Care (Engl). 2019;28(5):e13113. https://doi.org/10.1111/ecc.13113 .
Maheu C, Hebert M, Louli J, Yao TR, Lambert S, Cooke A, et al. Revision of the fear of cancer recurrence cognitive and emotional model by lee-jones et al with women with breast cancer. Cancer Rep (Hoboken). 2019;2(4):e1172. https://doi.org/10.1002/cnr2.1172 .
Sengun Inan F, Ustun B. Fear of recurrence in turkish breast cancer survivors: a qualitative study. J Transcult Nurs. 2019;30(2):146–53. https://doi.org/10.1177/1043659618771142 .
Lambert LK, Balneaves LG, Howard AF, Chia SK, Gotay CC. Understanding adjuvant endocrine therapy persistence in breast cancer survivors. BMC Cancer. 2018;18(1):732. https://doi.org/10.1186/s12885-018-4644-7 .
Toledo G, Ochoa CY, Farias AJ. Religion and spirituality: their role in the psychosocial adjustment to breast cancer and subsequent symptom management of adjuvant endocrine therapy. Support Care Cancer. 2021;29(6):3017–24. https://doi.org/10.1007/s00520-020-05722-4 .
Jakobsen K, Magnus E, Lundgren S, Reidunsdatter RJ. Everyday life in breast cancer survivors experiencing challenges: a qualitative study. Scand J Occup Ther. 2018;25(4):298–307. https://doi.org/10.1080/11038128.2017.1335777 .
Keesing S, Rosenwax L, McNamara B. The implications of women’s activity limitations and role disruptions during breast cancer survivorship. Womens Health (Lond). 2018;14:1745505718756381. https://doi.org/10.1177/1745505718756381 .
Keesing S, Rosenwax L, McNamara B. A call to action: The need for improved service coordination during early survivorship for women with breast cancer and partners. Women Health. 2019;59(4):406–19. https://doi.org/10.1080/03630242.2018.1478362 .
Kim SH, Park S, Kim SJ, Hur MH, Lee BG, Han MS. Self-management needs of breast cancer survivors after treatment: results from a focus group interview. Cancer Nurs. 2020;43(1):78–85. https://doi.org/10.1097/NCC.0000000000000641 .
Knaul FM, Doubova SV, Gonzalez Robledo MC, Durstine A, Pages GS, Casanova F, et al. Self-identity, lived experiences, and challenges of breast, cervical, and prostate cancer survivorship in mexico: a qualitative study. BMC Cancer. 2020;20(1):577. https://doi.org/10.1186/s12885-020-07076-w .
Liska A, Lamontagne A, Sambrooke K, Snowdon A, Mitchell F. A patient’s perspective: Bridging the transition following radiation therapy for patients with breast cancer. J Med Imaging Radiat Sci. 2020;51(4S):S72–7. https://doi.org/10.1016/j.jmir.2020.08.008 .
Pembroke M, Bradley J, Nemeth LS. Breast cancer survivors’ unmet needs after completion of radiation therapy treatment. Oncol Nurs Forum. 2020;47(4):436–45. https://doi.org/10.1188/20.ONF.436-445 .
Pintado S. Breast cancer patients’ search for meaning. Health Care Women Int. 2018;39(7):771–83. https://doi.org/10.1080/07399332.2018.1465427 .
Dsouza SM, Vyas N, Narayanan P, Parsekar SS, Gore M, Sharan K. A qualitative study on experiences and needs of breast cancer survivors in Karnataka India. Clin Epidemiol Global Health. 2018;6:69–74. https://doi.org/10.1016/j.cegh.2017.08.001 .
Rashidi E, Morda R, Karnilowicz W. “I will not be defined by this. I’m not going to live like a victim; it is not going to define my life”: exploring breast cancer survivors’ experiences and sense of self. Qual Health Res. 2021;31(2):349–60. https://doi.org/10.1177/1049732320968069 .
Cheng KKF, Cheng HL, Wong WH, Koh C. A mixed-methods study to explore the supportive care needs of breast cancer survivors. Psychooncol. 2018;27(1):265–71. https://doi.org/10.1002/pon.4503 .
Article CAS Google Scholar
Chen SQ, Sun N, Ge W, Su JE, Li QR. The development process of self-acceptance among chinese women with breast cancer. Jpn J Nurs Sci. 2020;17(2):e12308. https://doi.org/10.1111/jjns.12308 .
Drageset S, Lindstrom TC, Ellingsen S. “I have both lost and gained” Norwegian survivors’ experiences of coping 9 years after primary breast cancer surgery. Cancer Nurs. 2020;43(1):E30–7. https://doi.org/10.1097/NCC.0000000000000656 .
Chao YH, Wang SY, Sheu SJ. Integrative review of breast cancer survivors’ transition experience and transitional care: dialog with transition theory perspectives. Breast Cancer. 2020;27(5):810–8. https://doi.org/10.1007/s12282-020-01097-w .
Rapport F, Khanom A, Doel MA, Hutchings HA, Bierbaum M, Hogden A, et al. Women’s perceptions of journeying toward an unknown future with breast cancer: the “lives at risk study.” Qual Health Res. 2018;28(1):30–46. https://doi.org/10.1177/1049732317730569 .
Schwartz NA, von Glascoe CA. The body in the mirror: breast cancer, liminality and borderlands. Med Anthropol. 2021;40(1):64–78. https://doi.org/10.1080/01459740.2020.1775220 .
Lebel S, Ozakinci G, Humphris G, Mutsaers B, Thewes B, Prins J, et al. From normal response to clinical problem: definition and clinical features of fear of cancer recurrence. Support Care Cancer. 2016;24(8):3265–8. https://doi.org/10.1007/s00520-016-3272-5 .
BinshaPappachan C, D’Silva F, Safeekh AT. Life beyond the diagnosis of breast cancer: a qualitative study on the lived experiences of breast cancer survivors. Indian J Publ Health Res Dev. 2020;11(3):73–7. https://doi.org/10.37506/ijphrd.v11i3.688 .
Sun L, Ang E, Ang WHD, Lopez V. Losing the breast: a meta-synthesis of the impact in women breast cancer survivors. Psychooncol. 2018;27(2):376–85. https://doi.org/10.1002/pon.4460 .
Chuang LY, Hsu YY, Yin SY, Shu BC. Staring at my body: the experience of body reconstruction in breast cancer long-term survivors. Cancer Nurs. 2018;41(3):E56–61. https://doi.org/10.1097/NCC.0000000000000507 .
Gotay CC, Muraoka MY. Quality of life in long-term survivors of adult-onset cancers. J Natl Cancer Inst. 1998;90(9):656–67. https://doi.org/10.1093/jnci/90.9.656 .
Llewellyn A, Howard C, McCabe C. An exploration of the experiences of women treated with radiotherapy for breast cancer: learning from recent and historical cohorts to identify enduring needs. Eur J Oncol Nurs. 2019;39:47–54. https://doi.org/10.1016/j.ejon.2019.01.002 .
Maheu C, Singh M, Tock WL, Eyrenci A, Galica J, Hebert M, et al. Fear of cancer recurrence, health anxiety, worry, and uncertainty: a scoping review about their conceptualization and measurement within breast cancer survivorship research. Front Psychol. 2021;12:644932. https://doi.org/10.3389/fpsyg.2021.644932 .
Alfano CM, Rowland JH. Recovery issues in cancer survivorship: a new challenge for supportive care. Cancer J. 2006;12(5):432–43. https://doi.org/10.1097/00130404-200609000-00012 .
Stanton AL, Bower JE, Low CA. Posttraumatic growth after cancer. In: Tedeschi LCR, editor. Handbook of posttraumatic growth: Research and practic. Place: Published; 2014. p. 152–89.
Tedeschi RG, Calhoun LG. The posttraumatic growth inventory: measuring the positive legacy of trauma. J Trauma Stress. 1996;9(3):455–71. https://doi.org/10.1007/BF02103658 .
Zdenkowski N, Tesson S, Lombard J, Lovell M, Hayes S, Francis PA, et al. Supportive care of women with breast cancer: key concerns and practical solutions. Med J Aust. 2016;205(10):471–5. https://doi.org/10.5694/mja16.00947 .
Jacobsen PB, Wagner LI. A new quality standard: the integration of psychosocial care into routine cancer care. J Clin Oncol. 2012;30(11):1154–9. https://doi.org/10.1200/JCO.2011.39.5046 .
Moore HCF. Breast cancer survivorship. Semin Oncol. 2020;47(4):222–8. https://doi.org/10.1053/j.seminoncol.2020.05.004 .
Post KE, Moy B, Furlani C, Strand E, Flanagan J, Peppercorn JM. Survivorship model of care: development and implementation of a nurse practitioner-led intervention for patients with breast cancer. Clin J Oncol Nurs. 2017;21(4):E99–105. https://doi.org/10.1188/17.CJON.E99-E105 .
Kozul C, Stafford L, Little R, Bousman C, Park A, Shanahan K, et al. Breast cancer survivor symptoms: a comparison of physicians’ consultation records and nurse-led survivorship care plans. Clin J Oncol Nurs. 2020;24(3):E34–42. https://doi.org/10.1188/20.CJON.E34-E42 .
Morales-Sanchez L, Luque-Ribelles V, Gil-Olarte P, Ruiz-Gonzalez P, Guil R. Enhancing self-esteem and body image of breast cancer women through interventions: a systematic review. Int J Environ Res Public Health. 2021;18(4):1640. https://doi.org/10.3390/ijerph18041640 .
Fatehi S, Maasoumi R, Atashsokhan G, Hamidzadeh A, Janbabaei G, Mirrezaie SM. The effects of psychosexual counseling on sexual quality of life and function in iranian breast cancer survivors: a randomized controlled trial. Breast Cancer Res Treat. 2019;175(1):171–9. https://doi.org/10.1007/s10549-019-05140-z .
Reese JB, Smith KC, Handorf E, Sorice K, Bober SL, Bantug ET, et al. A randomized pilot trial of a couple-based intervention addressing sexual concerns for breast cancer survivors. J Psychosoc Oncol. 2019;37(2):242–63. https://doi.org/10.1080/07347332.2018.1510869 .
Nardin S, Mora E, Varughese FM, D’Avanzo F, Vachanaram AR, Rossi V, et al. Breast cancer survivorship, quality of life, and late toxicities. Front Oncol. 2020;10:864. https://doi.org/10.3389/fonc.2020.00864 .
ALmegewly W, Gould D, Anstey S. Hidden voices: an interpretative phenomenological analysis of the experience of surviving breast cancer in saudi arabia. J Res Nurs. 2019;24(1–2):122–32. https://doi.org/10.1177/1744987118809482 .
Currin-McCulloch J, Stanton A, Boyd R, Neaves M ,Jones B. Understanding breast cancer survivors' information-seeking behaviours and overall experiences: a comparison of themes derived from social media posts and focus groups. Psychol Health. 2020. https://doi.org/10.1080/08870446.2020.1792903
Download references
Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and affiliations.
Melbourne School of Psychological Sciences, The University of Melbourne, Melbourne, Australia
King R. & Stafford L.
Centre for Medical Psychology and Evidence-Based Decision-Making, School of Psychology, The University of Sydney, Sydney, Australia
Butow P., Giunta S. & Laidsaar-Powell R.
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the study conception and design, material preparation, data collection and analysis. The first draft of the manuscript was written by King R and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Laidsaar-Powell R. .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethics approval
This article does not contain any studies with human participants performed by any of the authors.
Consent to participate
As this was a meta-review and systematic review, no individual participants were involved, and consent was not necessary to obtain.
Consent for publication
Not applicable.
Conflict of interest
Additional information, publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (DOCX 17 KB)
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
R., K., L., S., P., B. et al. Psychosocial experiences of breast cancer survivors: a meta-review. J Cancer Surviv 18 , 84–123 (2024). https://doi.org/10.1007/s11764-023-01336-x
Download citation
Received : 12 October 2022
Accepted : 15 January 2023
Published : 01 March 2023
Issue Date : February 2024
DOI : https://doi.org/10.1007/s11764-023-01336-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Breast cancer
- Survivorship
- Qualitative
- Meta-review
- Systematic review
- Find a journal
- Publish with us
- Track your research
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Advances in the care...
Advances in the care of breast cancer survivors
Linked editorial.
Understanding inequalities in breast cancer screening uptake
Linked research
Effect of invitation letter in language of origin on screening attendance
- Related content
- Peer review
- Elizabeth J Cathcart-Rake , medical oncologist ,
- Amye J Tevaarwerk , medical oncologist ,
- Tufia C Haddad , medical oncologist ,
- Stacy D D’Andre , medical oncologist ,
- Kathryn J Ruddy , medical oncologist
- Mayo Clinic, Department of Oncology, Rochester, MN, USA
- Correspondence to: E J Cathcart-Rake Cathcart-rake.elizabeth{at}mayo.edu
Breast cancer survivors may experience significant after effects from diagnoses of breast cancer and cancer directed therapies. This review synthesizes the evidence about optimal management of the sequelae of a diagnosis of breast cancer. It describes the side effects of chemotherapy and endocrine therapy and evidence based strategies for management of such effects, with particular attention to effects of therapies with curative intent. It includes strategies to promote health and wellness among breast cancer survivors, along with data to support the use of integrative oncology strategies. In addition, this review examines models of survivorship care and ways in which digital tools may facilitate communication between clinicians and patients. The strategies outlined in this review are paramount to supporting breast cancer survivors’ quality of life.
Introduction
Breast cancer is the most common cancer in the world, with 2.26 million diagnoses in 2020. 1 People with breast cancer are living longer as a result of improvements in screening and treatment, such that in the US alone the number of survivors of breast cancer is expected to grow by more than 2 million in the next decade. 2 3 Unfortunately, survivors may experience significant after effects from breast cancer diagnoses and cancer directed therapies. Symptoms related to surgery, radiation, and systemic therapies may persist lifelong and limit quality of life.
This review synthesizes the evidence base on optimal management of treatment sequelae in survivors of breast cancer. We describe the side effects of chemotherapy and endocrine therapy and evidence based strategies for management of such effects, with particular attention to effects of therapies with curative intent. We include strategies to promote health and wellness among breast cancer survivors, along with data to support the use of integrative oncology strategies. In addition, we examine models of survivorship care and ways in which digital tools may facilitate communication between clinicians and patients.
Sources and selection criteria
We searched PubMed for the term “breast cancer survivorship” (without restricting the date range) on 17 August 2022 and limited our search to papers designated as randomized controlled trials (RCTs) or meta-analyses. This identified 245 peer reviewed publications, some of which we excluded because they were focused more on disease outcomes than on management of toxicity and models of survivorship care. We supplemented this search strategy by a hand search of the references of key articles. We achieved inclusion of identified articles by assessing a study’s impact and its methods, with preference given to RCTs. When RCT evidence was not available for certain topics, we included other study types, focusing on the highest level of evidence available and excluding lower level evidence. To ensure that we covered all critical data relevant to management of endocrine therapy toxicity, management of long term effects of chemotherapy, new models of care and digital tools to facilitate communication and symptom management, integrative oncology for breast cancer survivors, general health maintenance (including screening for second cancers), genetic testing, and surveillance for recurrence, we also added select additional studies for inclusion on the basis of consensus among our author group (medical oncologists with specific expertise in symptom control (ECR, KR), survivorship (KR, AT), integrative medicine (SD), and digital oncologic tools (TH, AT)).
Epidemiology
Breast cancer is the most commonly diagnosed cancer, accounting for nearly a quarter of all cancer cases globally. 4 More than 2.3 million people worldwide are given a diagnosis of breast cancer annually, and more than 7.8 million women are breast cancer survivors with diagnoses over the past five years, according to 2020 statistics. 4 Although the incidence of and mortality from breast cancer vary from region to region, these numbers are steadily growing, such that more than 3 million new cases of breast cancer are projected to be diagnosed by 2040. 4
Burden and management of long term effects of systemic therapies
Despite recent advances that help us to tailor and de-escalate treatment on the basis of estimates of clinical benefit to limit toxicity, 5 6 many curatively treated breast cancer patients still receive chemotherapy. This is particularly true among patients with triple negative breast cancer, who may receive up to four chemotherapies (anthracycline, cyclophosphamide, taxane, platinum) and an immunotherapy (pembrolizumab) (known as the KEYNOTE-522 regimen), with a fifth chemotherapy agent added if residual disease is present at the time of surgery. 7 The persistent (chronic) and future (late) side effects of these systemic therapies are mediated by a variety of host factors, including age, menopausal status, and existing comorbidities such as diabetes and hypertension. 8 9 10 11 12 13 Moreover, some toxicities, such as cancer related cognitive impairment (also known as “chemo brain”), are broadly linked to the use of cancer therapy but not tied to a particular agent. 14 The robustness of evidence based screening and prevention strategies varies between different treatment sequelae. 15
“Traditional” chemotherapeutic agents
Three chemotherapeutic classes (that is, anthracyclines, alkylating agents, and taxanes) have relatively well understood toxicity profiles in the curative setting based on decades of use in breast cancer ( table 1 ). For instance, anthracyclines increase the risk of cardiovascular events in the short term (for example, arrhythmias) and can cause long term irreversible left ventricular dysfunction. 23 24 Anthracyclines and cyclophosphamide carry a risk of secondary leukemia, although this may be less true for cyclophosphamide at the doses used in breast cancer. 25 26 27 Likewise, anthracyclines and cyclophosphamide are gonadotoxic, 28 29 affecting reproduction, menopausal symptom burden, and potentially bone and cardiac health. Taxanes contribute to chemotherapy induced peripheral neuropathy (CIPN), a primarily sensory peripheral neuropathy involving the feet and hands in a sock and glove-like distribution, which may persist lifelong in a small subset of patients. Although duloxetine can assuage CIPN related burning pain, more information is needed to inform strategies used to prevent CIPN and methods to treat numbness/tingling. 13 30
Chronic and late effects after treatment with common chemotherapeutics, immunotherapeutics, and associated targeted therapeutics used in (neo)adjuvant breast cancer setting
- View inline
Capecitabine and platinums —Despite longer track records in other disease settings, capecitabine and platinums (namely, carboplatin) are relatively new additions to the adjuvant breast cancer armamentarium. The persistent and future toxicity profiles, particularly when used in younger patients, are less well characterized. For instance, platinums can cause gonadal failure, 31 although the effect on ovarian function is poorly studied for carboplatin in the breast cancer setting. 16 32 33 34 This is despite routine use of carboplatin in combination with docetaxel and trastuzumab (with or witout pertuzumab) in the TCH(+/−P) regimens for human epidermal growth factor receptor 2 (HER2) positive disease for more than a decade. 35 The effect of platinum dosing (for example, weekly versus every three weeks) on ovarian reserve remains unassessed. 27 Platinums have been shown to increase the risk of secondary leukemia in ovarian cancer 33 ; the additive risk when used with anthracyclines and cyclophosphamide as in the Keynote-522 regimen remains understudied. 33
Targeted therapy and immunotherapy agents
HER2 targeted agents —Trastuzumab has been joined by pertuzumab, ado-trastuzumab emtansine, and neratinib in the adjuvant setting. Studies of these newer agents report lower incidences of cardiotoxicity compared with trastuzumab, but ado-trastuzumab emtansine is more hepatotoxic and carries a risk of persistent neuropathy. 22 36 The degree to which the cardiac effects of HER2 targeted agents are confined to the treatment period is not well studied for the newer agents but is presumably similar to that for trastuzumab. 37 38 Patients who do experience cardiotoxicity during HER2 directed therapy do not seem to develop this later, in the absence of other risk factors such as receipt of anthracycline.
Immunotherapy, PARP inhibitors, and abemaciclib —Routine use of pembrolizumab in higher risk triple negative breast cancer has followed the Keynote-522 results. Most of the available data on chronic and late toxicity profiles come from other disease settings, in which long term immune related side effects occurred in 43.2% of patients and ranged from mild disease, such as hypothyroidism (14.0%), to severely debilitating diagnoses, such as hypophysitis (2.1%), which may necessitate lifelong hydrocortisone treatment. 39 Similarly, the poly ADP ribose polymerase (PARP) inhibitor olaparib has recently emerged as a tool for BRCA carriers with high risk disease or residual disease after neoadjuvant chemotherapy. 40 Most of what is known about the chronic and late toxicity profile comes from patients with ovarian cancer and short term follow-up. 41 Finally, abemaciclib is a recent adjuvant therapy for estrogen sensitive breast cancers with a high risk of recurrence; knowledge of toxicities is largely based on that seen in patients with metastatic breast cancer.
Although many targeted agents have fewer listed side effects than do traditional chemotherapeutic agents, their acute toxicities become subacute and longer lasting problems owing to a longer duration of therapy (for example, two years for abemaciclib in the adjuvant setting). 40 42 Certain toxicities, such as interstitial lung disease from abemaciclib, may even be fatal (albeit rarely). 43 Furthermore, owing to short term follow-up of studies with relatively small numbers supporting the efficacy of these agents, long term toxicities in the adjuvant setting have not yet been fully described.
Endocrine therapy
Endocrine therapies improve survival for people with hormone receptor positive breast cancer. 44 45 46 Endocrine therapy encompasses a range of therapeutics, including oral drugs, such as tamoxifen and the aromatase inhibitors (letrozole, anastrozole, and exemestane), as well as gonadotropin releasing hormone (GNRH) agonists, such as goserelin and leuprolide. Endocrine therapies may be recommended for up to 10 years in people with early stage disease. 47
Whereas some patients report manageable or no side effects from endocrine therapy, other patients experience debilitating prolonged symptoms. 48 49 Because of the duration of endocrine therapy, both on-therapy and long term effects of endocrine therapy are within the scope of this survivorship review. Side effects of endocrine therapy are particularly predominant among premenopausal patients taking GNRH agonists for ovarian suppression. 50 These may worsen quality of life, and severe symptoms may also contribute to non-adherence to and/or early discontinuation of endocrine therapy, in turn worsening breast cancer survival. 51 52 53 54 55 Therefore, control of side effects related to endocrine therapy is essential in people with estrogen receptor positive breast cancer.
Vasomotor symptoms
Vasomotor symptoms have been seen in up to 80% of patients receiving endocrine therapy in population based studies. 56 Patients may experience relief from vasomotor symptoms through use of a variety of strategies, as delineated in table 2 .
Side effects of endocrine therapy
As the efficacies of therapeutic strategies have not been directly compared, individualized evaluations of potential benefits and side effects should be completed on a patient-by-patient basis. For instance, although paroxetine is an effective agent for hot flashes, it has the potential to interact with tamoxifen metabolism contributing to a potential decrease in the efficacy of tamoxifen. 86 Patients treated with gabapentinoids for alternative diagnoses, such as diabetic neuropathy, might see improvements in their hot flashes, but in one randomized, crossover trial of 66 patients assigned to gabapentin or venlafaxine, 68% reported an overall preference for venlafaxine (P=0.01) over gabapentin. In this study, patients randomized to venlafaxine and to gabapentin both had a 66% reduction in hot flash scores, but patients receiving venlfaxine reported greated reduction in severity and frequency of hot flashes and fewer adverse effects. 87 Furthermore, patients who do not experience benefit from one drug may glean benefit from another, so trialing a second drug is worthwhile if the first is ineffective. 88
Finally, although estrogen based hormone replacement therapy should be avoided in this setting, data on the benefit-to-risk ratio of progestin monotherapy are limited. 89 Megestrol acetate was compared with placebo in an RCT including 97 women with breast cancer; 74% of the megestrol acetate group, compared with 20% of the placebo group, had a decrease of 50% or more in the frequency of hot flashes (P<0.001). 90 Medroxyprogesterone seems to be particularly effective; an RCT of 218 women found that a depot injection of medroxyprogesterone versus venlafaxine significantly increased the number of women with >50% reduction in hot flashes (74% v 46%; P<0.001). 91
Genitourinary symptoms
Genitourinary symptoms are related to low estrogenic states and are pervasive among patients receiving aromatase inhibitors and ovarian suppression. 66 67 However, although many patients wish to discuss such problems with clinicians, such symptoms are infrequently discussed in oncology clinics, which exacerbates non-use of safe and evidence based treatments. 92 93 94 Vaginal dryness is commonly experienced, and efficacious treatment options are available; however, dyspareunia, poor libido, and other sexual health concerns are frequently distressing to breast cancer survivors and lack data driven management options ( table 2 ).
Vaginal estrogen is commonly recommended for vaginal dryness and its sequelae in patients with no history of breast cancer, but this approach may carry some risks in patients with a history of estrogen sensitive breast cancers. Systemic estrogen concentrations may be very mildly increased after vaginal estrogen in a dose dependent fashion, but this may or may not be clinically significant. 95 One recent cohort study of 8461 breast cancer survivors in Denmark reported a 39% higher risk of recurrence of breast cancer at a median follow-up of 9.8 years after diagnosis, but no difference in mortality, among patients who received concurrent vaginal estrogen therapy and aromatase inhibitors. 96 This study was non-randomized and therefore different doses of vaginal estrogen may have been used; however, the risk-to-benefit ratio of vaginal estrogen remains controversial. Of note, a topical vaginal androgen, dehydroepiandrosterone, does not seem to raise estrogen concentrations in patients taking aromatase inhibitors. 70
Musculoskeletal symptoms
Approximately half of breast cancer survivors taking aromatase inhibitors experience “aromatase inhibitor associated musculoskeletal symptoms” or AIMSS. 76 Various plausible pathogenic explanations have been proposed as to why AIMSS occurs: aromatase inhibitors have pro-inflammatory properties, estrogen helps to maintain synovial fluid health, and pain sensitivity may be altered by aromatase inhibitors. 97 98 99 Of note, tamoxifen may also contribute to musculoskeletal symptoms, more commonly muscle cramping, but insufficient evidence exists about effective treatments. 100
Both duloxetine and acupuncture have been shown to reduce AIMSS in placebo controlled clinical trials ( table 2 ), 101 but one common first approach to AIMSS is a brief hiatus in treatment to ensure symptom improvement or resolution, followed by a switch from one aromatase inhibitor to another (or to tamoxifen). 77 80 102 One prospective, multicenter, non-randomized study of 179 patients reported that 74% had less severe AIMSS after switching from anastrozole to letrozole. Another open label randomized trial of exemestane versus letrozole in 503 women reported that 39% of patients were able to stay on aromatase inhibitor after switching to a second aromatase inhibitor, whereas all patients who did not switch chose to discontinue therapy; however, complete resolution of AIMSS after such a switch is uncommon. 80 102 This approach is safe and low risk, and it typically does not require additional time or cost. 103
More than a third of breast cancer survivors taking endocrine therapy report hair thinning and loss, described as frontal and parietal hairline recession. 104 105 Prospective investigations into the clinical characteristics and incidence of endocrine therapy related alopecia are ongoing. Minoxidil, a vasodilative agent that causes hair follicles to transition into growth phase and increases the size of hair follicles, offers a promising potential therapy for endocrine therapy related alopecia; the use of topical and low dose oral minoxidil has been supported by early studies. Although this may be offered as an off-label treatment, RCT results are eagerly awaited. 106 107
Osteoporosis
Aromatase inhibitors increase risks for bone thinning, osteoporosis, and fractures, which are major drivers of cost, morbidity, and mortality, particularly in breast cancer survivors. 108 109 Bisphosphonates and receptor activator of nuclear factor-κB ligand (RANKL) inhibitors lessen the risks for bone loss and fractures among both postmenopausal patients and premenopausal patients taking ovarian function suppression or with chemotherapy related ovarian failure. 110 111 112 113 114 115 116 117 118 119 Additionally, these agents decrease risk for bone recurrence and improve breast cancer-free survival. 120 The most recently published double blinded RCT of 3425 postmenoapusal patients compared denosumab with placebo; denosumab improved disease-free survival with a hazard ratio of 0.83 (95% confidence interval 0.71 to 0.97; P=0.016) and reduced fractures with a hazard ratio of 0.76 (0.63 to 0.92; P=0.004) at a median follow-up of eight years. 121

Other important components of survivorship care
Screening for recurrence.
Screening for recurrence relies on regular (usually at least annual) visits with a cancer specialist or primary care provider for physical examination and assessment of symptoms that might indicate that cancer has returned. 122 123 124 Female survivors who have residual breast tissue (because they have not undergone bilateral mastectomy) and no evidence of distant metastases are generally recommended to undergo annual mammography at least until age 75 (unless medical comorbidities substantially limit the projected benefit of early detection of local recurrences and new primaries). 125 Supplemental screening imaging (for example, magnetic resonance imaging of the breast, ultrasonography, or molecular breast imaging) may also be considered for female survivors with dense breast tissue (for whom mammography is less sensitive) or for those with an elevated risk of new primary cancer. 126 127 Male survivors should also consider unilateral surveillance mammography if they had breast conserving therapy (to detect local recurrences). 128
Routine imaging or blood tests to assess for distant recurrence is not recommended by current guidelines. 122 124 If a survivor develops a sign or symptom of possible recurrence on physical examination or history, distant imaging (for example, positron emission tomography, computed tomography, or bone scan) may be warranted.
Genetic testing
For patients who do not meet criteria for genetic testing at the time of the initial cancer diagnosis (or who undergo only limited genetic testing at that time), periodically asking about new cancers diagnosed in family members that might affect the projected yield of genetic testing is important. Survivors who are found to carry pathogenic variants predisposing to cancer may warrant additional screening or risk reducing surgeries.
Financial toxicity
Advances in breast cancer management have enabled more cures; however, they have also contributed to the unsustainable rise in the cost of care, 129 with the overall financial burden disproportionately affecting patients. Financial toxicity has been described as a combination of objective financial burden and subjective financial distress, and this adverse event has a spectrum of severity with 79% of patients with cancer reporting moderate to catastrophic financial burden. 130 131 High costs of cancer care, particularly out-of-pocket costs, are associated with worse patient reported outcomes, lower quality of life, and poor adherence to treatment. 131 132 Several factors have been associated with risk of financial toxicity, including younger age, female sex, non-white race, employment changes, low average household income, increasing distance from treatment centers, and increasing out-of-pocket costs. 133 Furthermore, significant geographic disparities exist in financial burden across the world. Large out-of-pocket costs may be required in some parts of the world (for example, the US, Africa, and Central and South America), whereas other healthcare systems (for example, Canada, the EU, and the UK) protect patients against out-of-pocket costs. 134 Defined risk factors for financial toxicity now exist, along with a validated assessment tool. 135 Globally, cancer practices need to systematically screen patients for financial toxicity or proactively discuss finances associated with care during or after cancer care, notably when options with variable costs are available.
Fear of recurrence
Fear of recurrence is experienced by up to 80% of women with breast cancer. 136 This can lead to worsened quality of life, depression, anxiety, and lack of proper follow-up surveillance. 137 138 139 Assessing patient safety is important, as is consideration of referral to mental health professionals. 140 Cognitive behavioral therapy (CBT), discussed further below, has been shown in multiple trials (and a recent systematic review to decrease fear of recurrence, which assessed the quality of the 17 RCTs). 121 One included study ranodmized 56 patients to a form of CBT, termed cognitively based compassion training, over eight weeks and found reduced fear of cancer recurrence and psychologic stress (significant time × group interaction of 3.521; P<0.05). 141 Cognitive behavioral therapy can be delivered via individual therapy, group therapy, or digitally. 140 An RCT of mindfulness based stress reduction (MBSR; also discussed further, below) included 322 patients with breast cancer who were given a six week MBSR course versus usual care. Patients assigned to the MBSR group had significantly reduced fear of recurrence and anxiety scores (P<0.01), as assessed at baseline/six weeks and 12 weeks. 142
Survivorship care plans
Survivorship care plans were proposed in the 2005 Institute of Medicine report “From Cancer Patient to Cancer Survivor: Lost in Transition” as a potential way to support primary care providers in the provision of survivorship care (in part to control costs and in part to assure that survivors receive all of the non-cancer related care that they need). 143 However, subsequent clinical trials assessing the impact of survivorship care plans have shown mixed effects on a variety of survivorship outcomes. 144 145 A persistent need remains for novel approaches to facilitate dynamic transmission of knowledge between survivors and clinicians. As noted below, digital tools are showing potential in this arena and allow for a shared tool for primary care physicians and sub-specialists to communicate and improve care coordination. However, scaling and disseminating interventions into the “real world” is challenging. When asked about survivorship care plans, breast cancer survivors surveyed in one qualitative study recommended better education and personalization with regard to nutrition, exercise, managing side effects, comorbidities, and provision of resources, such as health coaches. 146 Breast cancer support groups can also help patients to cope with their diagnosis and treatment related side effects.
General health maintenance
Screening for and treating new non-breast cancers and managing other medical conditions are critical components of breast cancer survivorship care. Cardiovascular disease is common, especially in this population, in part as a result of the toxicities of breast cancer therapy. 147 148
Screening for second cancers
Breast cancer survivors face elevated risks of colorectal, ovarian, lung, endometrial, and thyroid carcinomas, as well as sarcoma and non-lymphocytic leukemia. 149 150 151 In addition, they face standard age related risks of many other cancers. For people who are not known carriers of genetic mutations predisposing them to cancer or otherwise at high risk of a second malignancy, guidelines recommend continuing with age appropriate cancer screening as recommended for the general population. 122 152 The primary differences between recommendations in the US and Europe pertain to the age range for screening for colorectal cancer and to the fact that screening for Helicobacter pylori is recommended in some EU countries. 153
Cholesterol, diabetes, and blood pressure monitoring and management
Hypertension, diabetes, coronary artery disease, and cerebrovascular disease share the following risk factors with breast cancer: obesity, metabolic syndrome, age, and lack of physical activity. In addition, certain breast cancer therapies, such as anthracycline based chemotherapies and anti-HER2 therapies, are associated with various cardiovascular toxicities, including heart failure. 154 155 Interestingly, a recent case-control Kaiser Permanente study, including 3642 women with breast cancer and 68 202 matched controls, found that breast cancer survivors were more likely to develop diabetes (subdistribution hazard ratio 1.16, 1.07 to 1.26) but less likely to develop dyslipidemia (0.90, 0.86 to 0.95) than matched women without cancer. 156 Although some early studies suggested that aromatase inhibitors might lead to more cardiovascular disease than tamoxifen, a recent cross sectional evaluation of 569 breast cancer survivors, 40% of whom had used aromatase inhibitors, found no difference in carotid intima media thickness (median 0.63 (interquartile range 0.56-0.71) mm with low exposure to aromatase inhibitors, 0.66 (0.59-0.75) mm with intermediate exposure, 0.64 (0.59-0.73) mm with high exposure), advanced glycation end products (median 2.13 (1.90-2.40) arbitrary units with low exposure to aromatase inhibitors, 2.20 (1.90-2.51) with intermediate exposure, 2.11 (1.90-2.43) with high exposure), or hyperlipidemia (data not provided) by exposure to aromatase inhibitors. 157
Thus, for most breast cancer survivors, a reasonable approach is to follow the United States Preventive Service Task Force (USPSTF) guidelines, which include office blood pressure and weight measurement for all patients aged ≥18; fasting plasma glucose, glycated hemaglobin, or oral glucose tolerance test to screen for diabetes in those aged 35-70; lipid panel to screen for dyslipidemia for those aged 40-70 (plus those aged 21-39 on the basis of clinical judgment); and counseling about smoking cessation for all adults who smoke. Optimal screening intervals for these assessments are unknown, but the USPSTF suggests annual screening for hypertension and weight, screening every three years for diabetes, and screening every five years for dyslipidemia. 158 Guidelines from the European Society of Cardiology are similar.
A meta-analysis that included data from 10 RCTs and 1095 breast cancer survivors found that diet and exercise interventions improved anthropomorphic measurements, systolic blood pressure, and C reactive protein but did not affect cholesterol, glucose, insulin, or leptin. 159 Drugs are often needed to optimize cardiovascular health in survivors with abnormal cholesterol, blood pressure, and/or glucose. Unfortunately, evidence that screening and aggressive management of cardiovascular risk factors improve long term cardiac outcomes in breast cancer survivors is limited.
Integrative oncology approaches to breast cancer survivorship
Exercise is one of the most important lifestyle interventions patients can engage in to prevent recurrence and decrease symptoms associated with breast cancer treatments. Research has shown that exercise reduces both recurrence of and death from breast cancer; one meta-analysis reported that meeting recommended physical activity guidelines (at least eight hours of moderate intesnity aerobic exercise a week) after diagnosis was associated with lower risk of breast cancer related death (hazard ratio 0.67, 95% confidence interval 0.50 to 0.90) during average follow-up periods ranging from 4.3 to 12.7 years. 160 161 162 163 164 Exercise has also been shown to improve fatigue, anxiety, depression, quality of life, physical function, strength, sleep, and bone health. 165 166 167 168 169 170 171 172 173 Resistance training is safe in patients with lymphedema and should be encouraged. 174 Unfortunately, most breast cancer survivors do not meet the recommended goals of 150 minutes of moderate aerobic exercise a week and twice weekly strength training. 175 The American Cancer Society also recognizes that people should move about during the day: “move more and sit less.” 176
The American Society of Clinical Oncology (ASCO) recommends aerobic and strength exercises during active treatment to reduce the side effects of therapy. 177 Exercise in patients undergoing chemotherapy has been shown to improve fatigue and cognition, 168 169 177 178 179 quality of life, depression/anxiety, and sleep quality. 165 180 In people taking aromatase inhibitors, exercise, including aerobic and strength training for a 12 month program, reduced pain scores by 30%. 181 This is important given that many people will stop aromatase inhibitors because of side effects.
Patients with no comorbidities do not need medical clearance before starting an exercise program. However, patients with neuropathy, bone/arthritis problems, or lymphedema should be referred for evaluation by a rehabilitation specialist and can consider medical clearance. Those with serious comorbidities, such as coronary artery disease, chronic obstructive pulmonary disease, recent surgeries, severe nutritional deficiencies, fatigue, or bone metastasis, should undergo medical clearance and rehabilitation evaluation before starting a program. 182
Yoga has additional benefits and is recommended by the Society for Integrative Oncology (SIO)/ASCO. 183 Yoga has been shown to improve quality of life (grade B) and may improve depression/anxiety (grade C) and fatigue (grade C). 183 Gentle yoga can be considered to help with sleep problems (grade C). SIO/ASCO also recommends consideration of yoga for aromatase inhibitor induced joint pain and pain after breast cancer therapy (both low level evidence). Yoga can be adapted for patients with functional limitations and is available in person or online. Patients with limited mobility or serious comorbidities should be evaluated and work with a certified instructor to avoid injury. 184
Dietary factors
No one specific diet is known to improve prognosis or quality of life during or after cancer treatment. However, some general recommendations can be made. The Women’s Health Initiative trial was a dietary prevention trial that randomized 41 835 women to low fat (20%) plus increased fruits/vegetables and whole grains versus a standard diet. Women in the intervention arm who developed breast cancer had improved overall survival compared with the usual diet group (10 year overall survival 82% v 78%; hazard ratio 0.78, 0.65 to 0.94; P=0.01). 185 Whether the observed benefits were due to decreased fat intake or the increase in other healthy foods is unclear. In another trial, 2437 women with early stage breast cancer were randomized to a low fat (20%) diet versus a standard diet. The primary endpoint, relapse-free survival, was improved in those in the low fat diet group (9.8% v 12.4% with events; hazard ratio 0.78, 0.60 to 0.98; P=0.03). This was more pronounced in women with hormone receptor negative tumors. However, the low fat group lost weight, and the benefits may have been just due to weight loss. 186 Other studies have shown increased all cause mortality in breast cancer survivors consuming the highest amounts of saturated/trans fats. 187 188 Therefore, a plant heavy diet (which includes the Mediterranean diet and some Asian diets), incorporating healthy fats and whole grains while avoiding processed meats and carbohydrates, sugar sweetened drinks, and artificial sweeteners, is recommended. 176 A Mediterranean diet containing nuts and extra virgin olive oil has cardiovascular benefits, 189 190 191 and incorporating high fiber foods may also be beneficial. 192
The effects of meal timing has also been studied. For example, data collected from 2413 women from the Women’s Healthy Eating and Living study showed that women who fasted <13 hours per night had increased recurrences of breast cancer compared with those who extended overnight fasting periods (hazard ratio 1.36, 1.05 to 1.76). 193 Longer fasting was also associated with improvement in glycated hemoglobin. Further evidence is needed to know the effect of extended overnight fasting on risk for recurrence.
Recommendations for limiting alcohol consumption for primary and secondary breast cancer prevention vary; however, most evidence suggests that alcohol increases the risk of recurrence, especially after the menopause. A recent review suggests limiting alcohol to less than three drinks a week, 194 whereas the National Comprehensive Cancer Network’s survivorship guidelines take a more stringent view on alcohol and state that women with breast cancer should abstain.
Dietary soy is safe for people with a history of breast cancer and may be beneficial. 195 However, soy supplements are not recommended. 196
Acupuncture
Acupuncture is an ancient Chinese medicine practice of placing fine needles into various points in the body. Heat (moxibustion) or electrostimulation can be added to standard needling. 197 The mechanism of action is not well understood. Traditional Chinese medicine explains acupuncture as a technique for balancing the flow of energy or life force that flows through meridians in the body. 198 Acupuncture may also stimulate nerves, fascia, or muscles to affect its action. 199 200 Sessions are generally weekly and often include other evaluations of the patient’s constitution, lifestyle advice, and herbal therapies. These components of traditional acupuncture are not often included in clinical trials in which only the acupuncture needle part of the treatment is assessed. 201 Studies of acupuncture are challenging to perform and evaluate owing to heterogeneity of providers, difficulty in choosing a control group (waitlist versus sham versus standard of care), not including other components of acupuncture treatment (pragmatic study), and difficulty in double blinding. The placebo effect is well established as playing a significant role in these studies. 202 However, evidence has been mounting, and SIO/ASCO recommends electro-acupuncture for consideration for chemotherapy induced nausea on the basis of RCTs and a consensus conference (in addition to standard drug therapies) (grade B, SIO). 197 203 204 SIO/ASCO guidelines for managing pain recommend acupuncture for aromatase inhibitor related joint pain and general pain/musculoskeletal pain from cancer (both with intermediate level evidence quality) and consideration of acupuncture for CIPN and procedural or surgical pain (both with low quality level evidence). 205 Acupuncture is generally safe but should be avoided in patients with severe cytopenias, and needles should not be inserted into areas of tumors or infections. 206 207 208
Acupressure is another technique in which manual pressure is applied to different body parts to achieve an effect, using pressure from fingers, bands, or beads. This has been most well studied for nausea/vomiting, using a pressure point called Neiguan located on the inner arm near the wrist. 209 210 211 212 This treatment is a grade B recommendation from SIO/ASCO. 183 It may also be useful for other cancer related symptoms, including pain and fatigue. 205 213 214
Cognitive behavioral therapy
CBT is a psychological treatment that treats anxiety/depression and insomnia and improves relaxation and quality of life. 215 216 It may also help people with the fear of recurrence. 121 The techniques included in this form of talking therapy involve trying to change thinking patterns to improve a particular condition; for instance, a therapist treating a patient with anxiety will often identify a patient’s anxious/nervous thought patterns and help to reframe these thoughts so that they are less detrimental. CBT has been shown to improve sleep and anxiety/depressive symptoms and increase quality of life in cancer patients. For instance, among 11 RCTs of patients with breast cancer, the overall effect size of CBT on quality of life of breast cancer survivors was 0.39 (95% confidence interval 0.12 to 0.66; P<0.001, I 2 =83%). 215 216 217 218 219 220 221 222 223 224 225
Insomnia is a common problem for patients with breast cancer, both during and after treatment, owing to direct treatment effects (including tamoxifen or steroids prescribed with chemotherapy), stress of diagnosis and treatment, or other causes. Insomnia often coexists with other symptoms such as pain, anxiety/depression, and fatigue, leading to reduced quality of life. 226 CBT-insomnia is a form of CBT that has been shown to improve insomnia in breast cancer patients for up to 12 months post-intervention 217 223 ; in one systematic review and meta-analysis of 22 studies, CBT-insomnia significantly reduced severity of insomnia (g=0.78). 217 CBT-insomnia involves stimulus control, sleep hygiene, cognitive therapy, and relaxation therapy. 219 227
Mindfulness
Mindfulness practice is a technique used to train attention and awareness to focus on the present moment in a non-judgmental way. 228 Mindfulness practice is recommended by SIO/ASCO for anxiety, depression, and quality of life (grade A). 183 Patients may practice mindfulness in different ways, including meditation, yoga, Tai Chi, breathing techniques, and body scans. Mindfulness practices improve anxiety, depression, sleep, and quality of life in cancer patients. 229 230 231 232 233 234 235 236 MBSR is a more formal program that teaches a variety of meditation practices either in person or online, weekly over six to eight weeks, 228 and may also improve mood, sleep, fatigue, and quality of life. 226 234 235 237 Studies have been mixed regarding the effects of MBSR on cognitive function. 238 The duration of beneficial effects of MBSR may not be long lasting, and more studies are needed to determine whether ongoing practice or repeat courses are needed to maintain benefits. 237 239
Supplements
Guidelines state that dietary supplements are not recommended for the treatment of cancer or prevention of recurrence and are not recommended for cancer survivors in the absence of a documented nutritional deficiency, poor diet, or other medical indication. 183 240 241 However, some dietary supplements may be useful in symptom management. For example, Wisconsin ginseng has been shown to reduce fatigue in breast cancer patients undergoing chemotherapy, 242 and ginger may help with nausea. 243 244 245 Treating vitamin D deficiency may be associated with improved breast cancer outcomes and bone health. 246 247 Dietary soy is safe, but supplements are not recommended or useful for hot flashes. 248 249 250 Some supplements, however, can be harmful and should be avoided. For example, acetyl-L carnitine was shown to worsen taxane induced neuropathy. 251 Vitamin B 12 before/during chemotherapy and iron during chemotherapy were associated with increased recurrence of and death from breast cancer. 252 Patients should also avoid supplemental antioxidants during chemotherapy, as some studies suggest worse cancer outcomes. 253 Supplements/herbal medicines can interfere with cancer treatments, generally, through cytochrome P450/P-glycoprotein interactions, which may increase the toxicity of therapy or decrease its effectiveness. 254 255 Many patients are taking dietary supplements and do not inform their care teams. 256 257 Asking whether patients are taking dietary supplements and assessing for potential interactions are important.
Other integrative modalities
Other therapies that have shown promise in helping patients with breast cancer with a variety of problems are listed in table 3 (adapted from SIO guidelines). 205 240
Level of evidence for integrative medicine strategies used for symptom management.
Digital tools to enhance survivorship care
With the burgeoning population of breast cancer survivors, transformation of delivery models for cancer care has become a necessity. Telehealth and virtual care have been adopted globally, and they may offer solutions to enable the transition of some aspects of survivorship care from the clinic into the home or community environment. Communication with care team members, symptom management, and disease surveillance can be facilitated by digital products and platforms, as summarized in this section.
Electronic/mobile health services
Digital technologies leveraged for electronic health (eHealth) interventions are most commonly mediated through the web or internet, whereas mobile health (mHealth) interventions are mediated through smartphone or tablet devices, most commonly via applications. Digital delivery of educational content for patients and online peer support groups accessible through a web browser or mobile device are a few examples of eHealth/mHealth tools that foster self-management.
A systematic review with meta-analyses (random effects model) of RCTs evaluated the effectiveness of eHealth delivered interventions in patients during and after breast cancer treatment. 258 Most interventions were web based and included videos, forums, and electronic reminder systems. The 32 unique studies (4790 participants) included were conducted within health systems globally, showing the broad reach of these interventions and diversity within the populations represented. A significant effect of eHealth interventions on quality of life (standardized mean difference 0.20, 95% confidence interval 0.03 to 0.36), self-efficacy (0.45, 0.24 to 0.65), distress (–0.41, –0.63 to –0.20), and fatigue (–0.37, –0.61 to –0.13) was seen. They had no effect on anxiety or depression. Studies (78.1%) measuring patient reported experience measures (n=25) found that acceptability (n=9) was high, with high ratings for satisfaction (range 71-100%), usefulness (71-95%), and ease of use (73-92%).
A systematic review of mHealth applications used across the breast cancer continuum was conducted by searching four databases with an objective of providing an overview of available, research tested interventions. Ten of the 29 identified studies targeted breast cancer survivorship (846 patients). 259 All aimed to assess lifestyle changes, and nearly all interventions were mobile applications, some of which included email or SMS text messaging features, as well as video enabled sessions with a healthcare professional. Several of the included studies showed a significant association for weight loss and increased physical activity with the mHealth intervention. 260 261 More high quality research is needed to better understand the effect of mHealth applications on these and other clinical outcomes.
Telehealth services
The electronic health record (EHR) has become the standard for storing and viewing patients’ health data and clinical documentation. A shift has taken place from passively viewing health information to an interactive EHR, and patients report that this facilitates better communication, enables a more effective partnership with providers, and helps to track their health information more proactively. 262
Asynchronous telehealth services are a form of eHealth/mHealth, often mediated respectively through the web or application based EHR patient portals. They can facilitate secure messaging between survivors and their care teams, as well as store-and-forward transmission of data. 263 The latter can be used for electronic patient reported outcomes, such as self-reported symptom assessments, or for patients to send images. The submitted data can be reviewed by a healthcare provider and care recommendations can be returned to patients at a convenient time outside of an in-person assessment,.
Synchronous telehealth services require an interactive audio and/or video telecommunication system to permit real time communication between providers at the distant site and the patient at the originating site. 263 Emerging literature suggests that patients’ acceptance of and satisfaction with video telemedicine visits in the breast surgical oncology practice have been high. 264 265 High patient satisfaction scores were also observed in a multisite, multiregional medical oncology practice. In that study, rates of use of telehealth visits were lower for patients ≥65 years of age and those residing in rural communities than for younger patients and those in urban areas. 266 Breast cancer clinicians have also expressed satisfaction with telemedicine and recognize it as a valuable option to enhance outpatient care and routine follow-up. 267 When appropriate, moving some follow-up care to the home via telehealth visits may improve access to facility based care while still serving the needs of breast cancer survivors.
Remotely delivered rehabilitation, weight loss, and physical activity programs
Beyond episodic visits, entire programs supporting cancer survivors have been transformed for virtual care delivery. As an example, telerehabilitation has been developed and implemented in several cancer practices to facilitate physical therapy for complications of breast cancer treatments, including lymphedema, limited shoulder range of motion, pain, fatigue, and loss of muscle strength. 268 Although remotely delivered physical therapy is a viable model of care delivery for survivors, research is needed to understand patients’ acceptance of and compliance with the telerehabilitation program, as well as its efficacy compared with traditional in-person physical therapy.
Additionally, the feasibility and effectiveness of a remotely delivered weight loss program has been compared with usual care in an RCT of patients who have completed treatment for early stage breast cancer. 269 Compared with usual care, the virtual weight loss program, including telephone calls and optional text messaging, was associated with significantly greater improvements in weight, metabolic syndrome risk score, physical quality of life, musculoskeletal pain, and other variables. Notably, the effects on weight, adiposity, and metabolic syndrome risk scores were sustained at 18 months. Bringing these weight loss programs into the home environment with a goal of improving overall health and wellness may improve patients’ access and adherence to them.
Remotely delivered physical activity programs for breast cancer survivors have also emerged separately or in concert with weight loss programs, and early results have shown their feasibility and acceptance in both older rural and young breast cancer survivors. 270 271 Interventions supporting these programs include the use of video enabled exercise sessions, web based education, wearable devices/accelerometers, and certified instruction or peer coaching. In an RCT of a remotely delivered exercise program versus a waitlist wellness control group of breast cancer survivors, those receiving the intervention had significantly greater reductions in sedentary behavior, and the increase in moderate to vigorous physical activity was inversely proportional to sedentary behavior. As shown in a separate study, remotely delivered programs for cancer survivors, when combined with telecoaching, can improve program retention and adherence enabling improved outcomes for patients. 272
This growing body of evidence supports continued investment in the development and study of remotely delivered programs for breast cancer survivors that foster rehabilitation, weight loss, and increased physical activity. They have the potential to improve health related quality of life and clinical outcomes, and they can furthermore break down barriers to access and adherence to these services that traditionally have been offered at limited institutions through traditional in-person care models.
Cancer treatment delivery at home
Home hospital programs can provide supportive care to patients with cancer in the home environment, and studies have shown the feasibility, safety, and effectiveness of oncology specific home hospital programs. 273 274 Initially developed and adopted several decades ago in single payer health systems globally, 275 276 the programs have expanded to include delivery of systemic cancer treatment in the home. Studies have shown that this is safe, improves patient and care giver experience, and reduces treatment costs. 277 Many breast cancer drugs administered to breast cancer survivors have a low risk for reactions and would be amenable to administration in the home, such as GNRH analogs, biologics, and bone supportive care. This could be transformative for care of breast cancer survivors and warrants investigation.
Emerging treatments
Many emerging treatments for long term toxicities of systemic therapies exist. Two upcoming clinical trials will focus on therapies that might prevent the development of long term peripheral neuropathy, one testing a compound called GM-1 and another a device that provides both cryotherapy and compression therapy (NCT number not yet assigned). For therapy related alopecia, a clinical trial is under way to study the benefits of minoxidil in a randomized controlled fashion ( NCT05417308 ).
Various national and international organizations have issued breast cancer survivorship guidelines, as well as guidelines for the management of specific symptoms facing breast cancer survivors, for integrative medicine approaches, and for surveillance strategies. General survivorship guidelines from the American Cancer Society, American Society of Clinical Oncology, European Society of Clinical Oncology, and National Comprehensive Cancer Network guidelines were reviewed in detail to inform this review.
Conclusions
In general, the complexity of after effects from breast cancer are likely to increase as new therapies are added to our armamentarium and treatment becomes increasingly tailored. As the sections above highlight, survivors and clinicians face challenges in monitoring persistent and late after effects from cancer and its treatment. Following up for multiple aftereffects in trials of cancer directed therapy over the long term can be costly, and many clinical trials may be too small to capture rare side effects. Digital tools may help to engage survivors in long term tracking, but reporting bias will be a potential confounder and care must be exercised to prevent under-representation of populations with lower digital literacy.
Questions for future research
How can we prevent and/or treat many of the challenging long term side effects of systemic therapy, including peripheral neuropathy, therapy related alopecia, and vaginal dryness?
What is the optimal way to help patients to differentiate between evidence based integrative oncology approaches and approaches that may not help and may actually harm patients?
How can digital tools enhance the benefit of survivorship care plans?
How patients were involved in the creation of this article
All of the authors of this manuscript are clinicians who interact with breast cancer survivors regularly. All also engage with patient advocates as part of their research efforts. A team of breast cancer survivors and patient advocates provided feedback on the long term side effects and integrative oncology strategies that are covered in this manuscript; we would personally like to acknowledge the following breast cancer survivors and advocates: Lisa Halverson, Anne Mehnke, Tracee Cole, and Jody Koubsky .
Series explanation: State of the Art Reviews are commissioned on the basis of their relevance to academics and specialists in the US and internationally. For this reason they are written predominantly by US authors
Contributors: KJ was responsible for the original conception and design of the article, with input from all co-authors; all authors were responsible for the acquisition and interpretation of data for the work, drafting the work, revising it critically, and final approval of the version to be published. All authors agreed to be accountable for all aspects of the work and will assure that questions related to the accuracy or integrity of any part of the work will be appropriately investigated and resolved.
Competing interests: We have read and understood the BMJ policy on declaration of interests and declare the following interests: none.
Provenance and peer review: Commissioned; externally peer reviewed.
- ↵ World Health Organization, International Agency for Research on Cancer Statistics. Breast cancer. https://www.iarc.who.int/cancer-type/breast-cancer/ .
- Siegel RL ,
- Miller KD ,
- ↵ American Cancer Society. Cancer Treatment and Survivorship Facts and Figures 2019-2021. 2019. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/cancer-treatment-and-survivorship-facts-and-figures/cancer-treatment-and-survivorship-facts-and-figures-2019-2021.pdf .
- Sparano JA ,
- Makower DF ,
- Kalinsky K ,
- Barlow WE ,
- Gralow JR ,
- Salgado R ,
- Seretny M ,
- Currie GL ,
- Upshaw JN ,
- Ruthazer R ,
- Nieboer P ,
- Rodenhuis S ,
- Valcovici M ,
- Andrica F ,
- Loprinzi CL ,
- Lacchetti C ,
- Bleeker J ,
- Tevaarwerk A ,
- Denlinger CS ,
- Arteaga CL ,
- de la Torre-Montero JC ,
- López-Tarruella S ,
- Lambertini M ,
- Anderson RA ,
- Phillips KA ,
- POEMS/S0230 Investigators
- Tolaney SM ,
- Armenian SH ,
- Mertens L ,
- Slorach C ,
- Curigliano G ,
- Lenihan D ,
- Fradley M ,
- ESMO Guidelines Committee. Electronic address: [email protected]
- Curtis RE ,
- Boice JD Jr . ,
- Stovall M ,
- Overbeek A ,
- van den Berg MH ,
- van Leeuwen FE ,
- Kaspers GJ ,
- Lambalk CB ,
- van Dulmen-den Broeder E
- Peccatori FA ,
- Demeestere I ,
- Margulies A ,
- Cardoso F ,
- ESMO Guidelines Committee. Electronic address: [email protected] ,
- EONS Education Working Group. Electronic address: [email protected] ,
- EANO Guideline Committee. Electronic address: [email protected]
- Loncharich MF ,
- Anderson CW
- Travis LB ,
- Holowaty EJ ,
- Bergfeldt K ,
- Jensen KC ,
- Vinayak S ,
- Eiermann W ,
- Breast Cancer International Research Group
- von Minckwitz G ,
- KATHERINE Investigators
- Fosbøl EL ,
- Goldhar HA ,
- Patrinely JR Jr . ,
- Johnson R ,
- Lawless AR ,
- Garber JE ,
- Kaufman B ,
- OlympiA Clinical Trial Steering Committee and Investigators
- Morice PM ,
- Dolladille C ,
- Johnston SRD ,
- O’Shaughnessy J ,
- monarchE Committee Members
- Taguchi Y ,
- ↵ Surveillance, Epidemiology, and End Results (SEER) Program. Cancer Stat Facts: Female Breast Cancer. https://seer.cancer.gov/statfacts/html/breast.html .
- Budzar AU ,
- ATAC Trialists’ Group
- Adjuvant Tamoxifen: Longer Against Shorter (ATLAS) Collaborative Group
- Harris PF ,
- Remington PL ,
- Trentham-Dietz A ,
- ↵ Ribi K, Luo W, Bernhard J, et al. Patient-reported endocrine symptoms, sexual functioning and quality of life (QoL) in the IBCSG SOFT trial: adjuvant treatment with tamoxifen (T) alone versus T plus ovarian function suppression (OFS) in premenopausal women with hormone receptor-positive (HR+) early breast cancer (BC). San Antonio Breast Cancer Symposium. 2014.
- Bernhard J ,
- Kidwell KM ,
- Chirgwin JH ,
- Giobbie-Hurder A ,
- Coates AS ,
- Hershman DL ,
- Ferreira AR ,
- Di Meglio A ,
- Pistilli B ,
- Jotwani AC ,
- Chlebowski RT ,
- Mortimer JE ,
- Crandall CJ ,
- Barton DL ,
- LaVasseur BI ,
- Freeman EW ,
- Guthrie KA ,
- Kugler JW ,
- Leon-Ferre RA ,
- Novotny PJ ,
- Stearns V ,
- Program to Reduce Incontinence by Diet and Exercise Investigators
- Tanasijevic A ,
- Schover LR ,
- Brewster A ,
- Melhem-Bertrandt A
- Chlebowski RT
- van der Kaaij M ,
- van Dorst E ,
- Creutzberg C ,
- Faubion SS ,
- Larkin LC ,
- Stuenkel CA ,
- Shuster LT ,
- Dockter T ,
- Goetsch MF ,
- Juraskova I ,
- Goldfrank DJ ,
- Mathias C ,
- Cardeal Mendes CM ,
- Pondé de Sena E ,
- Greenlee H ,
- Capodice J ,
- Loprinzi CL
- Baglia ML ,
- Cartmel B ,
- Galantino ML ,
- Demichele A ,
- Stricker CT ,
- Juurlink DN ,
- Bordeleau L ,
- Pritchard KI ,
- Carpenter LA ,
- Holmberg L ,
- Anderson H ,
- HABITS steering and data monitoring committees
- Michalak JC ,
- Quella SK ,
- Cathcart-Rake E ,
- O’Connor J ,
- Ridgeway JL ,
- Iglehart EI ,
- Schover LL ,
- Kingsberg S ,
- Santen RJ ,
- Bernick B ,
- Constantine GD
- Jensen MB ,
- Cronin-Fenton D ,
- Christiansen P ,
- Ejlertsen B
- Dietrich W ,
- Tschugguel W
- Karatas F ,
- Babacan T ,
- Saunders C ,
- Partridge A ,
- Santoro N ,
- Tubiana-Hulin M ,
- Colleoni M ,
- Karlsson P ,
- SOLE Investigators
- Gallicchio L ,
- Calhoun C ,
- Helzlsouer KJ
- Moscetti L ,
- Agnese Fabbri M ,
- Sperduti I ,
- Freites-Martinez A ,
- Shapiro J ,
- ↵ Kuo AM, Reingold RE, Ketosugbo K, et al. Oral minoxidil fo rthe treatment of late alopecia in cancer survivors, Abstract #12022. American Society of Clinical Oncology Annual Meeting 2022.
- Wolinsky FD ,
- Fitzgerald JF ,
- Chlebowski R ,
- Vehmanen L ,
- Välimäki M ,
- Blomqvist C
- Delmas PD ,
- Confravreux E ,
- Hardouin C ,
- Brufsky A ,
- Harker WG ,
- Mlineritsch B ,
- Schippinger W ,
- ABCSG-12 Trial Investigators
- Luschin-Ebengreuth G ,
- Austrian Breast and Colorectal Cancer Study Group
- Shapiro CL ,
- Majithia N ,
- Atherton PJ ,
- Frantal S ,
- Pfeiler G ,
- all ABCSG-18 investigators
- Runowicz CD ,
- Grunfeld E ,
- Levine MN ,
- Julian JA ,
- Kyriakides S ,
- Freedman RA ,
- Minami CA ,
- Monticciolo DL ,
- Newell MS ,
- Monsees B ,
- Hassett MJ ,
- Somerfield MR ,
- Mariotto AB ,
- Yabroff KR ,
- Carrera PM ,
- Kantarjian HM ,
- Peppercorn JM ,
- Dusetzina SB ,
- Huskamp HA ,
- Parikh DA ,
- Ragavan M ,
- Papanicolas I ,
- Woskie LR ,
- de Souza JA ,
- Wroblewski K ,
- ↵ Syrjala KL, Yi J. Overview of psychosocial issues in the adult cancer survivor. 2023. https://www.uptodate.com/contents/overview-of-psychosocial-issues-in-the-adult-cancer-survivor .
- Bertram H ,
- Ploos van Amstel FK ,
- van den Berg SW ,
- van Laarhoven HW ,
- Gielissen MF ,
- Ottevanger PB
- FCR Study Advisory Committee
- ↵ National Comprehensive Cancer Network. NCCN survivorship guidelines. www.nccn.org/professionals/physician_gls/pdf/survivorship.pdf .
- Gonzalez-Hernandez E ,
- Lengacher CA ,
- Paterson CL ,
- Institute of Medicine ,
- National Research Council ,
- Greenfield S ,
- Wakefield CE ,
- Krok-Schoen JL ,
- Naughton MJ ,
- Noonan AM ,
- Pisegna J ,
- DeSalvo J ,
- Lustberg MB
- Hooning MJ ,
- Aleman BM ,
- Patnaik JL ,
- DiGuiseppi C ,
- Dabelea D ,
- Molina-Montes E ,
- Dávila-Arias C ,
- ↵ US Preventive Services Task Force. Recommendations. https://www.uspreventiveservicestaskforce.org/uspstf/search_results?searchterm=cancer%20screening%20 .
- ↵ European Commission Initiative on Colorectal Cancer. Colorectal cancer guidelines and quality assurance. 2022. https://healthcare-quality.jrc.ec.europa.eu/ecicc .
- Watson KE ,
- American Heart Association Cardiovascular Disease in Women and Special Populations Committee of the Council on Clinical Cardiology; Council on Cardiovascular and Stroke Nursing; and Council on Quality of Care and Outcomes Research
- Zamorano JL ,
- Lancellotti P ,
- Rodriguez Muñoz D ,
- Authors/Task Force Members ,
- ESC Committee for Practice Guidelines (CPG) ,
- Document Reviewers
- Iribarren C ,
- van Ommen-Nijhof A ,
- Jacobse JN ,
- Steggink LC ,
- Whelton PK ,
- Lahart IM ,
- Metsios GS ,
- Nevill AM ,
- Carmichael AR
- McNeely ML ,
- Campbell KL ,
- Klassen TP ,
- Mackey JR ,
- Courneya KS
- Rees-Punia E ,
- Schmidt MD ,
- La Vecchia C ,
- Spence RR ,
- Steele ML ,
- Sandler CX ,
- Elvsaas IKO ,
- Campbell R ,
- Vansteenkiste M ,
- Delesie L ,
- Hilfiker R ,
- Meichtry A ,
- Robinson PD ,
- Cataudella D ,
- Mustian KM ,
- Alfano CM ,
- Heckler C ,
- Rogers LQ ,
- Courneya KS ,
- Vitale JA ,
- Schmitz KH ,
- Troeschel AN ,
- Thomson CA ,
- Sullivan KR ,
- Ligibel JA ,
- Furmaniak AC ,
- Ehlers DK ,
- Schmidt ME ,
- Steindorf K
- Gradishar WJ ,
- Abraham J ,
- Krucoff C ,
- Aragaki AK ,
- Anderson GL ,
- Blackburn GL
- Beasley JM ,
- Newcomb PA ,
- Kroenke CH ,
- Sweeney C ,
- Castillo A ,
- Estruch R ,
- Salas-Salvadó J ,
- PREDIMED Study Investigators
- Gensini GF ,
- Willett WC ,
- Trichopoulou A ,
- Farvid MS ,
- Spence ND ,
- Holmes MD ,
- Marinac CR ,
- Nelson SH ,
- Haslam DE ,
- Touillaud M ,
- Mesrine S ,
- ↵ NIH Consensus Conference. Acupuncture . JAMA 1998 ; 280 : 1518 - 24 . pmid: 9809733 OpenUrl CrossRef PubMed Web of Science
- Kaptchuk TJ
- Langevin HM
- Garcia MK ,
- McQuade J ,
- Georgiade G
- Ismaila N ,
- Höxtermann MD ,
- Aboudamaah S ,
- World Health Organization
- Dibble SL ,
- Cooper BA ,
- Molassiotis A ,
- Dabbour R ,
- Hummerston S
- Russell W ,
- Murphy SL ,
- Arnedt JT ,
- Mboineki JF ,
- Squires LR ,
- Fawcett J ,
- Savard MH ,
- Garland SN ,
- Johnson JA ,
- Casault L ,
- Matthews EE ,
- Berger AM ,
- Schmiege SJ ,
- Fiorentino L ,
- Rissling M ,
- Ancoli-Israel S
- Kabat-Zinn J
- Potters L ,
- Wernicke AG ,
- Christodoulou G ,
- Witek Janusek L ,
- Witek-Janusek L ,
- Albuquerque K ,
- Chroniak KR ,
- Chroniak C ,
- Durazo-Arvizu R ,
- Schell LK ,
- Shomstein S ,
- Winkler MM ,
- DuPont-Reyes MJ ,
- Balneaves LG ,
- Frenkel M ,
- Society for Integrative Oncology
- Dakhil SR ,
- Sahebkar A ,
- Hashemian F ,
- Taghikhani M ,
- Abolhasani E
- Heckler CE ,
- Roscoe JA ,
- Hankinson SE ,
- Bertone-Johnson ER ,
- Madden JM ,
- MacGregor CA ,
- Canney PA ,
- Patterson G ,
- McDonald R ,
- Van Patten CL ,
- Olivotto IA ,
- Chambers GK ,
- Ambrosone CB ,
- Zirpoli GR ,
- Hutson AD ,
- Mooiman KD ,
- Beijnen JH ,
- Schellens JH ,
- Meijerman I
- Blumberg JB ,
- Mullan BA ,
- Singleton AC ,
- Raeside R ,
- Jongerius C ,
- Mazzocco K ,
- Pravettoni G
- Zickmund SL ,
- ↵ Matters MLN. CY2022 Telehealth Update Medicare Physician Fee Schedule. 2022. https://www.cms.gov/files/document/mm12549-cy2022-telehealth-update-medicare-physician-fee-schedule.pdf .
- DeGirolamo K ,
- Johnson BA ,
- Lindgren BR ,
- Pritchett J ,
- Dholakia R ,
- Hardy-Abeloos C ,
- de Rezende LF ,
- Francisco VE ,
- Reeves MM ,
- Terranova CO ,
- Winkler EAH ,
- Weiner LS ,
- Irene Su H ,
- Wagner LI ,
- Titchener K ,
- Haaland B ,
- Gaufberg E ,
- Titchener K
- Divorne N ,
- Trémolières P ,
- Close the Gap
- SurvivorNetTV
- Clinical Trials
You Are Not Alone — 6 Inspiring Cancer Memoirs to Help Survivors and Caregivers Cope with Their Journeys SHARE
- Acute Myeloid Leukemia (AML)
- Bladder Cancer
- Breast Cancer
- Chronic Lymphocytic Leukemia (CLL)
- Chronic Myeloid Leukemia (CML)
- Colon Cancer
- Endometrial Cancer
- Esophageal Cancer
- Heart Failure
- Hypertrophic Cardiomyopathy (HCM)
- Liver Cancer
- Lung Cancer
Multiple Myeloma
Discover local multiple myeloma resources:.
- Multiple Sclerosis (MS)
- Myelodysplastic Syndrome (MDS)
- Myeloproliferative Neoplasms
- Non-Hodgkin Lymphoma
Ovarian Cancer
Discover local ovarian cancer resources:.
- Prostate Cancer
- Rare Diseases Cold Agglutinin Disease (CAD) Transthyretin Amyloid Cardiomyopathy (ATTR-CM) Von Hippel-Lindau Disease
- SN Guides: Critical information from SurvivorNet's experts
- Mental Health: Helping patients find the balance critical to treatment and recovery
- Clinical Trial Finder: Search for clinical trials that fit your profile
Multiple Myeloma: Main Page
Discover local multiple myeloma resources:, ovarian cancer: main page, discover local ovarian cancer resources:.
- Cold Agglutinin Disease (CAD)
- Mental Health
- Transthyretin Amyloid Cardiomyopathy (ATTR-CM)
- Von Hippel-Lindau Disease
- Newsletters and Guides
You Are Not Alone — 6 Inspiring Cancer Memoirs to Help Survivors and Caregivers Cope with Their Journeys
These remarkable books share the challenges of a disease that changes lives in an instant.
For anyone facing cancer themselves or the diagnosis of someone close to them, finding a community to lean on can be life changing. Friends, family and support groups can all help fill this need, but there’s another way, as well. Cancer memoirs, written by those who have been on the journey, can illuminate your own in unexpected, and often moving, ways. Whether you’re looking for someone to tell you the cold hard facts, or read a story to lift your spirits, it’s out there.
Here 6 remarkable cancer memoirs, each different in tone and story, and each uniquely able to teach, comfort and guide.
‘Not One of These Poems Is About You’: Teva Harrison
Read More View this post on Instagram ☆REVIEW☆ (#freebook | @houseofanansi ) • Not One Of These Poems is About You By Teva Harrison Available January 7th! • Thoughts~ My heart is heavy after reading this. And yet I am so appreciative and enamored by her grace and honesty in these poems. Diagnosed with metastatic breast cancer at age 37 she goes deep, opening up her heart for all to see. Sharing her innermost thoughts and fears. Her journey through her diagnosis and treatments and the way cancer has changed who she is. A devastatingly beautiful, heartbreaking read. I feel like no words I write will do this book justice. Her bravery and honesty is profound and complex. Thank You Teva for gifting this book to the world. A comfort for thoes who walk in your shoes and an insightful look inside this terrifying diagnosis for the rest of us. Sadly Teva Harrison passed away in April of this year. Her words and work will live on and continue to inspire. This collection is out in January. Highly reccomend checking it out. • Thank You to @houseofanansi for sending me this. ♡ . . [#bookalongreview] . . #notoneofthesepoemsisaboutyou #tevaharrison #poetry #canlit #canadareads #readthenorth #canadianauthor #poetrysunday #bookreview #bookreviewer #bookblogger #bookblog #bookdragon #bookphoto #allthebooks #bookstagram #bookstagrammer #bibliophile #bookcommunity #booksbooksbooks #booksandplants #booksandbeans #mustread #amreading #vscobooks #vscoreads #bookasthetic #2019reads A post shared by Kate | ???????? (@bookalong) on Dec 8, 2019 at 11:39am PST
In this posthumous book of essays, Teva Harrison shares her metastatic breast cancer journey. A follow up to Harrison’s “In-Between Days: A Memoir About Living with Cancer,” it dives deep into what it means to have cancer, the impact it has on her life, and how the disease has progressed. A look at her femininity, health and the great love of her life, it’s an honest and raw read.
‘TOUGH: Women Who Survived Cancer’
View this post on Instagram Thank you to everyone who came out to the ????Book Launch Party???? for ‘TOUGH: Women Who Survived Cancer’: https://amzn.to/31H1SCh Because of you, we are a #1 New Release on Amazon with over ????reviews! YES Love you all! ???? – Marquina Special Thanks: ????by @denniscahlo ????by #michna and @automaticstudios for the space #sharetriumph #cancer #survivor #survivorstories #metavivorstories #tough #hope #livenow #lovenow #book #booklaunch #party #photos #cancer #strongwomen #booklover #sisterhood #tellyourstory #cancersupport A post shared by Marquina Iliev-Piselli (@sharetriumph) on Sep 22, 2019 at 8:44am PDT
This cumulative work from 37 women who survived a variety of cancers shines a light on so many remarkable stories. Edited by cancer survivor Marquina Iliev-Piselli, “TOUGH: Women Who Survived Cancer” brings the reader along as these women follow creative pursuits from stand-up comedy to air guitar.
‘Memoir of a Debulked Woman: Enduring Ovarian Cancer’: Susan Gubar
View this post on Instagram #50booksmamareads2018 #memoirofadebulkedwoman #susangubar #cancer #ovariancancer #chemotherapy #fixthisplease #fundresearch #remission #memoir #nonfiction A post shared by A S W (@butyouhaveto) on Apr 12, 2018 at 8:28am PDT
In 2008, Susan Gubar’s life was turned upside down when she was diagnosed with ovarian cancer. Her memoir dives into the aftereffects and coping with what she describes as her body’s betrayal. She leans on her husband, children and friends while seeking a community through books and testimonies of those who had also faced cancer. In writing this book, she helps others find the community and support that is so critically needed while facing a cancer diagnosis.
“The Middle Place”: Kelly Corrigan
View this post on Instagram I had read Kelly Corrigan’s ‘Glitter and Glue’ a while ago and I know she has a new one out but I figured I’d had start with ‘The Middle Place’ given it’s one I hear friends rave about. And I can see why. She’s not only a great writer but an astute student, and observer, of this season of life that many of us find ourselves in: raising little ones while also still enjoying one’s role as a daughter of parents. But as in all seasons of life, these seasons are in constant flux, and when she receives a breast cancer diagnosis around the same time as her father receives one for bladder cancer, she goes back and forth between the role of daughter and mother daily, sometimes hourly. It’s a tender read, I loved how she has alternates chapters for her childhood and present tense. Reminding us of how life isn’t either/or but continues in the both/and, particularly when we are in that ‘middle place’. ????????✨ #livingbythepage A post shared by Natalie d’Aubermont Thompson (@livingbythepagewithnatalie) on Jan 26, 2018 at 9:33am PST
When Kelly Corrigan was 36, she had a happy marriage, two great kids and a weekly newspaper column. But when she discovered a lump in her breast just as her father discovers he has late-stage cancer, she finds herself in what she calls the Middle Place, “that sliver of time when parenthood and childhood overlap.”
“Don’t Stop Believin'”: Olivia Newton-John
View this post on Instagram For everyone living in the UK, #DontStopBelievin will be published on 13 June. Can’t wait for you all to read it! Available on Amazon now amzn.to/2VMiNQq A post shared by Olivia Newton-john (@therealonj) on Jun 3, 2019 at 11:33am PDT
Olivia Newton-John, who has stage 4 breast cancer — her third bout with the disease – and who says she recently received encouraging results from her last MRI, has been incredibly open and uplifting throughout her journey. "I've adjusted to living with cancer, which I'm very lucky to say I'm able to do," Newton-John told SurvivorNet in a previous conversation. Her memoir gives fans and supporters the story of her life, details of her cancer journey, and so much more.
‘The Bright Hour: A Memoir of Living and Dying’: Nina Riggs
John Duberstein lost his wife, writer Nina Riggs, to metastatic triple negative breast cancer. “She wanted to embrace the existence that she had, even before she knew she was going to die imminently. I did not want to talk about what was going to happen with me after Nina died. Nina is the one that really brought it up, she brought it up a number of times. She wanted to make sure that I knew that it was OK,” he told SurvivorNet in a previous conversation. Her book, The Bright Hour,” tells the story of their relationship and her outlook while staring down the end.
Learn more about SurvivorNet's rigorous medical review process.
Sarah Fielding is a reporter for SurvivorNet. You can follow her on Twitter at @sarahfielding_. Read More
SurvivorNetTV. Hope. Science. Inspiration.
Patient Pathfinder:
Clinical Trial Finder
Are you looking for other treatment options? Right now there are ... lung cancer trials in the U.S. within 100 miles of
Enter your zip code and travel distance to explore trials in your area...
Related Articles
For Young Detroit Photographer Extreme Back and Stomach Pains That Left Him Unable ‘To Do Anything’ Turned Out To Be Acute Lymphoblastic Leukemia (ALL)
After Losing Eddie Van Halen To Cancer, ‘Food Network’ Star Valerie Bertinelli Is Enjoying Life With New Man, Who Calls Their Relationship A ‘Gift’
Inspired By Kate Middleton— ‘Leverage Redemption’ Star Gina Bellman, 57, Now ‘Has The Courage’ To Share Her Breast Cancer Diagnosis
‘Dallas’ Actor Patrick Duffy Praised As ‘Happy Days’ Star Linda Purl’s ‘Remarkable Love’ On His Milestone 75th Birthday
Get SurvivorNet in Your Inbox
Our newsletter – vital information, hope, and healing, delivered weekly.
Introducing, the Journey Bar
Use this bar to access information about the steps in your cancer journey.
Sign Up for SN+
Sign up now for access to powerful tools, top experts, and customized information to help you fight cancer.
- Personalized content tailored to your profile and disease type
- Access exclusive patient guides
- Breaking treatment information and expert perspectives
- and more...
Already have an account? Sign In
- Sign-In with Google
Don't have an account? Sign In
Sign In to SN+
Username or email address *
Remember me
Lost your password?
Not a member yet? Register now.
Don't have an account? Sign Up

Emma Campbell has been diagnosed with cancer three times since 2010.
They survived breast cancer. Now they’re baring their scars — and their souls
Photographs by Lynsey Addario Story by Kyle Almond, CNN
Emma Campbell lost one of her breasts nearly 10 years ago, when she was diagnosed with breast cancer just after giving birth to triplets.
She had to have a second mastectomy last year when the cancer invaded her other breast.
But she refuses to let cancer rob her of her spirit.
“Cancer has shown me how incredibly strong I am,” said Campbell, who was also diagnosed with skin cancer in 2014. “Cancer has taught me resilience. Cancer has brought my life into sharp, vivid, technicolored focus. I see life clearly now. I know what matters.”
Campbell is one of 12 breast cancer survivors — women of different ages and backgrounds — who are sharing their courageous stories as part of Stella McCartney’s annual campaign for Breast Cancer Awareness Month. This year, the fashion designer partnered with acclaimed photojournalist Lynsey Addario, who collaborated with each of the women to take powerful, inspiring portraits that bare their scars both physical and emotional.
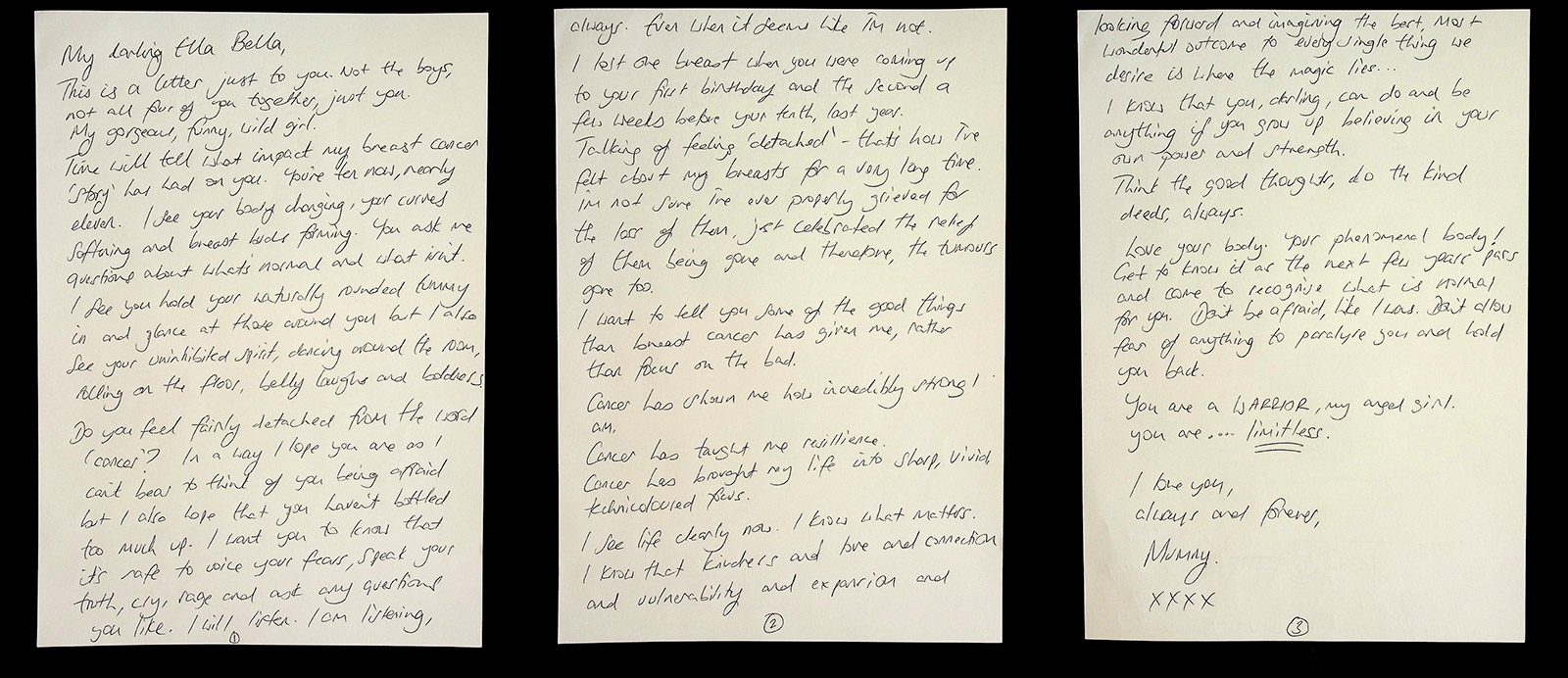
As part of the campaign, the women wrote letters to loved ones. Emma Campbell wrote to her 10-year-old daughter, Ella Bella.
“We don't often see these kinds of images, and I wanted to photograph them in a beautiful, empowering way,” said Addario, who shot the portraits in each woman’s home in the United Kingdom.
The portraits are paired with a letter from each woman where they tell their story in their own words.
“It was really important to let them tell their stories, and I think the letters and seeing their handwriting makes it even more personal,” Addario said.
The idea behind the “A Letter to My Loved Ones” campaign is to empower the women and highlight their resiliency.
“Many of the women expressed the fact that when they first had their mastectomy or when they first realized they were going to lose their breasts, that was a huge part of their femininity being taken away and they were really ashamed, self-conscious, embarrassed. A lot of those words came up over and over,” Addario said. “And each one of these women expressed that, over time, they learned to be proud of their scars.”

Sharon Marshall-Green with her son Pharrell
Marshall-Green was diagnosed with stage 3 breast cancer in May 2016, 18 days before her 45th birthday. Her treatment included two lumpectomies and eight rounds of chemotherapy. She has four children, three of whom are now adults.
“Pharrell was 4 years old when I was diagnosed,” she said, “and I just felt I needed to fight that bit more so I could be there for him, so I could teach and instill those certain same beliefs and strengths that I had with all the other children.”
She wrote a letter to her four kids as part of the Stella McCartney campaign.
“I have been through so much since my diagnosis in terms of physical and mental pain, anguish, insomnia, depression and fear,” she wrote. “However, in saying all of this I feel I have come out triumphant! The reason I say this is because whilst having treatment I had time to think, evaluate life.”
She said she had always been very critical of herself, and her ordeal has taught her to love herself — a lesson she wants to pass down to her kids.
“No one is perfect, but it’s important to accept ourselves for who we are and work on the bits of us we don’t like. It’s OK to have flaws,” she wrote.

Carolina Boore
Boore was 34 years old when she was diagnosed with stage 2 inflammatory breast cancer, an extremely rare form of breast cancer with no lump to be detected by hand or by mammogram. Instead, there may be swelling, redness and a dimpling of the breast skin that may look and feel like an orange peel.
Boore underwent chemotherapy and had a mastectomy. Two years later, the cancer had spread to her spine.
“I don't live like I did before,” she said. “I live every minute to the fullest. I've got a conscious thing of, you've got to make every second, minute, hour, day, count. You have to have and live your best life. I've looked at my life, what I was doing, how I was living. And I was like, am I happy? Do I want more? And I made a lot of changes to how I do things. I accept my secondary diagnosis. I respect it. I know I could be here for five years or I could be here for 25 years.”
She wrote her letter to her mother, who was also diagnosed with cancer twice.
“I am so proud of the strong, confident, positive woman I have become,” Boore wrote. “Seeing you fight cancer so gracefully head on, like you do with everything in your life, gives me strength and courage. You are a warrior! You are my warrior!”

Nisha Tanna with her children Asara, left, and Jaiden
Tanna was diagnosed with stage 3 breast cancer nearly five years ago, just after her 35th birthday. At the time, her daughter was 2 years old and her son was 1.
“I think most of us mothers, new mothers, young mothers, put pressure on ourselves to be the best that we can, look the best that we can, give our children the best that we can,” she said. “Going through my treatment, especially initially, there still was this real need to want to do that, to still be this model mother.
“Slowly, as my treatment progressed, there was this huge sense of acceptance of it was OK not to be OK. It was OK to let my hair down and literally take my wig off and just be, and that was enough for the children. It was enough for myself. It was enough for my husband. And I think that's when I felt a real sense of resilience.”
She dedicated her letter to her children and described how her diagnosis made her stronger.
“I learnt that sometimes when we fall, when we get back up again, we stand a little taller,” she wrote. “We find alternative ways of thinking, of looking, of being. I learnt that trauma, stress and adversity can become your allies, helping you to grow when otherwise you may not. It’s like weight training for the mind.”

Keely Joseph
Joseph, 37, is fighting stage 4 breast cancer. She had a single mastectomy and reconstruction, and she has been undergoing chemotherapy three times a week to fight the tumors that have spread across her chest.
She has a 17-year-old son and a 10-year-old daughter.
“They know that I love them, but I don't think they realize just how much they mean to me in that they are literally my reason for being,” she said. “If it wasn't for them, I would have given up quite easily. I think when you're going through chemo, it's easy to kind of wallow and to get yourself in a really negative state. I was never allowed to do that.“
She penned a letter to her daughter, Alyssa.
“I hope that one day you will sit down and tell my grandchildren (absolutely zero pressure there) all about me,” she wrote. “Tell them that I constantly talked about boobs and that I had topless portraits taken to help me love my body even with its scars. I hope that you can tell them that seeing me like that helped you in some way not to get hung up on what might be imperfections to some because I taught you that it was OK to love yourself just as you are.”

Leanne Hughes
Hughes was diagnosed with stage 4 breast cancer when she was 31. She is fighting it with hormone therapy and oral chemotherapy.
“It's been two and a half years of some real ups and downs,” she said. “There's been some really scary moments, and then moments of just like, ‘Oh my God, this could be going in the right direction.’ It's a never-ending roller coaster. Literally every single month is different.”
For the Stella McCartney campaign, she wrote a love letter to her body.
“I was too busy following advice from others as to how I should treat you, focusing on the outside and forgetting to listen to you,” she wrote. “I am with you now, whatever you need. To be your biggest advocate and support, nourish and love you unconditionally.”

“My mastectomy scar felt weird,” she recalled. “And I can't tell you anything else other than it just felt weird. So I kept saying, ‘It feels weird and I can't explain why.’ ”
An MRI confirmed the reoccurrence in the same breast. Shah then had a lumpectomy and hormone treatment to fight it.
In her letter, she thanks her friend Jonelle for being there when “it all became too much.”
“Thank you for being the best friend a girl can have,” she wrote. “You are a true friend and sister and give me the space to be my full authentic self.”

Mel Bastien
Bastien was 46 years old when she was diagnosed with breast cancer in October 2018. She had a total mastectomy with reconstruction in June 2019, followed by radiation therapy.
“I didn’t know anyone who had had a mastectomy,” she said. “I didn’t know where to turn, to be honest. I really felt lost. I didn’t tell my family I was having a mastectomy until after I had it.”
She went online to try to see what a mastectomy breast looked like. She rarely saw anyone who looked like her. “Nine times out of 10, it just came up with White ladies,” she said.
In her letter to her loved ones, Bastien says she’s always been a positive person. “I’ve learnt that being happy and surrounding myself with people that make me happy and are uplifting is the only way to be. I’ve learnt about toxic people and how toxic behavior can impact my mental state, and I will no longer tolerate this. Going through cancer messes with your mental state, and it’s so important to block out and stay away from negativity.”

Louisa Rasmussen
Rasmussen was 34 when she was diagnosed with stage 4 breast cancer that had spread to her liver. For treatment, she has been undergoing hormone therapy and taking chemotherapy drugs.
She wrote her letter to her mother and her brother, Christian, referencing her late father who also had cancer.
“It was hard and painful at times when Daddy had his cancer journey, but he lived it!” she wrote. “He lived all the 8 years in such great spirits. That has taught me well.
“I do wish that I knew then what I know now. … When it came to my turn, I’ve tried everything I can. I’m trying the best that I can to heal, to be healthy and happy and lead an easy life.”

Lizzi England and her daughter Violet
England was diagnosed with breast cancer while pregnant with Violet, her third child. England was 29 at the time.
“One day I noticed a lump and I called the (general practitioner). They got me in quite quickly, but I was met with: ‘No, you're too young. The changes are likely to be hormonal. This is not going to be breast cancer. So we want you to come back if you're still worried, and we'll go from there,’ ” England recalled. “I went back (two weeks later), I was still worried, and they reluctantly sent me for a referral. And yeah, when I was referred, I was diagnosed with stage 2, grade 3, breast cancer.”
England had a mastectomy and underwent chemotherapy while she was pregnant. She wrote her letter to Violet, who she called a “little miracle who proved herself to be a warrior from day one.”
“You did everything you needed to and more,” England wrote. “You were incredible, just like your brother, sister and Daddy.”

Jane Hutchison
Hutchison was 35 years old when she was diagnosed with breast cancer in 2012.
A year later, she founded the Hello Beautiful Foundation, a UK-based charity.
“We provide cancer patients with free access to counseling, holistic practice, nutritional workshops and functional medicine,” she said. “The aim being to help people cultivate a nontoxic lifestyle that is sustainable on a day-to-day basis.”
In her letter, Hutchison provides advice that might be helpful to anyone going through what she has.
“Your journey will feel tough at times, but embrace the daily practices that allow your mind, body and spiritual consciousness to flourish,” she wrote. “Be still, be calm and breathe.”

Gemma Longland
Longland had a mastectomy, reconstructive surgery, eight rounds of chemotherapy and 15 rounds of radiotherapy after being diagnosed with stage 3 breast cancer at the age of 35.
She wrote her letter to her two young children, Olly and Sienna.
“You kept me sane on the days I thought I was going crazy and brought me joy when I was in so much pain,” she wrote. “I hope that in harder times in both your lives that you will look back at what we went through when you were young and that you will be stronger people for it.
“Maybe one day I can inspire you the way you did me.”
Lynsey Addario is an award-winning photojournalist and author of the best-selling memoir “It’s What I Do.” You can follow her on Instagram, Facebook and Twitter.
More on Stella McCartney’s “A Letter to My Loved Ones” campaign can be found on the fashion designer’s website.
Editors: Brett Roegiers, Rebecca Wright, Sandee LaMotte
Psychosocial experiences of breast cancer survivors: a meta-review
Affiliations.
- 1 Melbourne School of Psychological Sciences, The University of Melbourne, Melbourne, Australia.
- 2 Centre for Medical Psychology and Evidence-Based Decision-Making, School of Psychology, The University of Sydney, Sydney, Australia.
- 3 Centre for Medical Psychology and Evidence-Based Decision-Making, School of Psychology, The University of Sydney, Sydney, Australia. [email protected].
- PMID: 36854799
- PMCID: PMC10866753
- DOI: 10.1007/s11764-023-01336-x
Purpose: Advances in breast cancer care have led to a high rate of survivorship. This meta-review (systematic review of reviews) assesses and synthesises the voluminous qualitative survivorship evidence-base, providing a comprehensive overview of the main themes regarding breast cancer survivorship experiences, and areas requiring further investigation.
Methods: Sixteen breast cancer reviews identified by a previous mixed cancer survivorship meta-review were included, with additional reviews published between 1998 and 2020, and primary papers published after the last comprehensive systematic review between 2018 and 2020, identified via database searches (MEDLINE, Embase, CINAHL, PsycINFO). Quality was assessed using the Joanna Briggs Institute Critical Appraisal Checklist for Systematic Reviews and the CASP (Critical Appraisal Skills Programme Qualitative) checklist for primary studies. A meta-ethnographic approach was used to synthesise data.
Results: Of 1673 review titles retrieved, 9 additional reviews were eligible (25 reviews included in total). Additionally, 76 individual papers were eligible from 2273 unique papers. Reviews and studies commonly focused on specific survivorship groups (including those from ethnic minorities, younger/older, or with metastatic/advanced disease), and topics (including return to work). Eight themes emerged: (1) Ongoing impact and search for normalcy, (2) Uncertainty, (3) Identity: Loss and change, (4) Isolation and being misunderstood, (5) Posttraumatic growth, (6) Return to work, (7) Quality of care, and (8) Support needs and coping strategies.
Conclusions: Breast cancer survivors continue to face challenges and require interventions to address these.
Implications for cancer survivors: Breast cancer survivors may need to prepare for ongoing psychosocial challenges in survivorship and proactively seek support to overcome these.
Keywords: Breast cancer; Meta-review; Qualitative; Survivorship; Systematic review.
© 2023. The Author(s).
Publication types
- Research Support, Non-U.S. Gov't
- Breast Neoplasms* / therapy
- Cancer Survivors* / psychology
- Qualitative Research
- Systematic Reviews as Topic
- History, Facts & Figures
- YSM Dean & Deputy Deans
- YSM Administration
- Department Chairs
- YSM Executive Group
- YSM Board of Permanent Officers
- FAC Documents
- Current FAC Members
- Appointments & Promotions Committees
- Ad Hoc Committees and Working Groups
- Chair Searches
- Leadership Searches
- Organization Charts
- Faculty Demographic Data
- Professionalism Reporting Data
- 2022 Diversity Engagement Survey
- State of the School Archive
- Faculty Climate Survey: YSM Results
- Strategic Planning
- Mission Statement & Process
- Beyond Sterling Hall
- COVID-19 Series Workshops
- Previous Workshops
- Departments & Centers
- Find People
- Biomedical Data Science
- Health Equity
- Inflammation
- Neuroscience
- Global Health
- Diabetes and Metabolism
- Policies & Procedures
- Media Relations
- A to Z YSM Lab Websites
- A-Z Faculty List
- A-Z Staff List
- A to Z Abbreviations
- Dept. Diversity Vice Chairs & Champions
- Dean’s Advisory Council on Lesbian, Gay, Bisexual, Transgender, Queer and Intersex Affairs Website
- Minority Organization for Retention and Expansion Website
- Office for Women in Medicine and Science
- Committee on the Status of Women in Medicine Website
- Director of Scientist Diversity and Inclusion
- Diversity Supplements
- Frequently Asked Questions
- Recruitment
- By Department & Program
- News & Events
- Executive Committee
- Aperture: Women in Medicine
- Self-Reflection
- Portraits of Strength
- Mindful: Mental Health Through Art
- Event Photo Galleries
- Additional Support
- MD-PhD Program
- PA Online Program
- Joint MD Programs
- How to Apply
- Advanced Health Sciences Research
- Clinical Informatics & Data Science
- Clinical Investigation
- Medical Education
- Visiting Student Programs
- Special Programs & Student Opportunities
- Residency & Fellowship Programs
- Center for Med Ed
- Organizational Chart
- Leadership & Staff
- Committee Procedural Info (Login Required)
- Faculty Affairs Department Teams
- Recent Appointments & Promotions
- Academic Clinician Track
- Clinician Educator-Scholar Track
- Clinican-Scientist Track
- Investigator Track
- Traditional Track
- Research Ranks
- Instructor/Lecturer
- Social Work Ranks
- Voluntary Ranks
- Adjunct Ranks
- Other Appt Types
- Appointments
- Reappointments
- Transfer of Track
- Term Extensions
- Timeline for A&P Processes
- Interfolio Faculty Search
- Interfolio A&P Processes
- Yale CV Part 1 (CV1)
- Yale CV Part 2 (CV2)
- Samples of Scholarship
- Teaching Evaluations
- Letters of Evaluation
- Dept A&P Narrative
- A&P Voting
- Faculty Affairs Staff Pages
- OAPD Faculty Workshops
- Leadership & Development Seminars
- List of Faculty Mentors
- Incoming Faculty Orientation
- Faculty Onboarding
- Past YSM Award Recipients
- Past PA Award Recipients
- Past YM Award Recipients
- International Award Recipients
- Nominations Calendar
- OAPD Newsletter
- Fostering a Shared Vision of Professionalism
- Academic Integrity
- Addressing Professionalism Concerns
- Consultation Support for Chairs & Section Chiefs
- Policies & Codes of Conduct
- First Fridays
- Fund for Physician-Scientist Mentorship
- Grant Library
- Grant Writing Course
- Mock Study Section
- Research Paper Writing
- Establishing a Thriving Research Program
- Funding Opportunities
- Join Our Voluntary Faculty
- Child Mental Health: Fostering Wellness in Children
- Faculty Resources
- Research by Keyword
- Research by Department
- Research by Global Location
- Translational Research
- Research Cores & Services
- Program for the Promotion of Interdisciplinary Team Science (POINTS)
- CEnR Steering Committee
- Experiential Learning Subcommittee
- Goals & Objectives
- Issues List
- Print Magazine PDFs
- Print Newsletter PDFs
- YSM Events Newsletter
- Social Media
- Patient Care
INFORMATION FOR
- Residents & Fellows
- Researchers
“In Our Own Words”: Cancer patients tell their stories
- Features When art and medicine meet Closing the circle—medicine re-engages with the humanities Thirty years of the humanities at the School of Medicine Students share their “sharp and poignant moments” in literary journal Selections from Murmurs On the other side: listening to patients Writing toward better care How art sharpens students’ clinical skills “In Our Own Words”: Cancer patients tell their stories Art therapy: helping families cope with cancer In the midst of an epidemic ¡ANDA! Walk and Run raises more than $25,000
- News Crossing disciplines, Yale scientists unravel Zika’s secrets Robert Rock, art, justice, and medicine Immune system also controls weight In Syria, the world’s shame Deputy dean deeply mourned at the School of Medicine A thesis in three minutes An opioid crisis in the city and a bad night in the emergency room “Blue state” parents more likely to vaccinate their teens Wildfire surge traced to climate change Ancestral role for female orgasm Town hall features new dean for diversity
- People Through writing, a psychologist extends her reach From English lit to gene expression in neurons How grassroots activism Vivek Murthy dismissed as U.S. Surgeon
- Dialogue What the humanities mean to medicine An alternative to the Affordable Care Act Medical student wellness Second Opinion Is there a standard for evaluation?
By turns ironic, inspiring, sobering, and funny, essays in a booklet called “In Our Own Words” relate key moments in diagnosis and treatment, as well as observations and realizations made along the way.
The cedar strings quartet, composed of medical students aishwarya vijay, michelle ferreira, william chen, and charles hsu.
For Christine Shadle, Ph.D., the writers group for patients at Smilow Cancer Hospital at Yale New Haven Health was a godsend.
She seized the opportunity to write frankly about her breast cancer and share her writing with fellow patients, without softening the “gory and disgusting” realities of her disease. “It’s really lonely to have a severe illness,” said Shadle, who is now in remission. “This is a way of telling my story, and it ends up being a way to find ourselves.”
Shadle and nine other patients shared their work in a booklet called “In Our Own Words,” published thanks in part to a grant from the annual Closer to Free fundraising campaign. On a Thursday evening in October, four patients and three guest readers read essays from the booklet before an audience of physicians, caregivers, and family members in the Park Building. The authors and guest readers, including Yale New Haven Health CEO Marna P. Borgstrom, M.P.H. ’79, read from the works. By turns ironic, inspiring, sobering, and funny, the essays relate key moments in diagnosis and treatment, as well as observations and realizations made along the way. “I feel honored to have been part of this program and have a chance to look into some of your personal moments,” said Dana Shaffer, Smilow’s art expression coordinator.
In her essay, Shadle, a research scientist at the Haskins Laboratories in New Haven, noted that oncotype scores that determine whether she’ll need chemotherapy and National Institutes of Health scores for grant applications share one characteristic—a low score is better. And in both cases a score over 31 is bad. “I saw my oncologist this morning, and she told me my score,” Shadle wrote. “It’s 34. A new era is starting.”
Judith Drew Mauzaka wrote of her yearning to take a vacation and “swim with sea turtles in the warm blue waters of the Caribbean” despite the risks involved. Mauzaka, who has since died, indeed made the trip.
Kathleen Miles Schumacher, a breast cancer survivor, described an elevator ride with a hospital employee who pretended he was an elevator operator. “Sixth floor! Menswear!” he called out. “Fifth floor! Cocktail lounge! Fourth floor! Baked goods!” That ride, Schumacher wrote, turned a car full of strangers into a temporary community, and the ride into “an interactive comedy club for a few brief minutes.” As she read her essay, Donald Macmillan, the hospital’s flight services coordinator who provides helicopter transportation for patients and the employee in her story, stood at her side barking out the floor announcements.
The writers’ program was founded in 2013 thanks to retired New York Times editor and reporter Charlotte Evans, Shaffer said. During her journalism career, Evans said, she felt her work was important to readers, but at a distance from them. In retirement, however, she sought a closer connection. “I thought it would be rewarding to try to help people one on one and get to know them as people,” she said.
The group meets every other week and typically includes four to six patients, Shaffer said. About 30 patients have taken part since its inception, she said.
The program is one of many run by Integrative Medicine at Smilow Cancer Hospital, including art, yoga, and meditation, to address cancer patients’ psychological and emotional needs. “These are all things that help you step back and put you more in tune with yourself,” she said.
The booklet is just the beginning, Shaffer said. She is already choosing essays for a second collection.
- Graduate School of Arts & Sciences
- Diseases & Conditions
Featured in this article
- Marna Borgstrom, MPH Lecturer in Public Health (Health Policy); President and CEO, Yale New Haven Health System

Interview With Cancer Survivor Jenn!
- February 4, 2016

Today we are continuing with one of our features, personal interviews! You can read our past interviews here . Today Cactus Cancer Society talks with cancer survivor, Jenn . She is a two-time breast cancer survivor, talks to us about her book , parenting during a cancer diagnosis, and so much more!
Cactus Cancer Society: When were you diagnosed and what is your diagnosis?
Jennifer: I found a lump in my breast in 2007 when I was 38. I assumed it was a cyst, it felt rubbery – not rock hard. I figured it would go away after I got my period – but it didn’t. I had gone for a mammogram 18 months prior (as a baseline and it was normal) so I called the imaging center at my husband’s urging (he didn’t like the way it felt at all) and they took me right away. After the mammo they sent me down for an ultrasound…and I began freaking out. No one would tell me anything – but they kept patting my shoulder. I knew it wasn’t going to be good news. A core needle biopsy came back inconclusive but two weeks later the surgical biopsy revealed invasive ductal breast cancer, stage IIA.
CCS: How did you feel when you were first diagnosed?
J: I was so deeply in denial. I really couldn’t wrap my head around it. I felt like I was telling a lie each time I told someone about my diagnosis. I thought breast cancer only ran in families or only happened to women over 40. I was clearly mistaken and I had a lot to learn. My surgeon told me that because the mass was contained and relatively small I would be a candidate for a lumpectomy. Fine by me – get it out, get it over with was my mindset. Once I saw an oncologist though he kept using the words aggressive and fast growing. Which made me nervous. I just wanted to get through treatment and get on with my life. I had no idea that my life would never be the same.
CCS: Who/what/where did you turn to?
J: I had terrific support from my family and friends but none of them had any experience with breast cancer. I went online and the pages I was directed to were terrifying and filled with statistics I was not ready to know yet. I struggled to find books or support groups geared toward young women. Everything I found was aimed at older women and the advice was to look at this as a gift, slow down, retire, and enjoy the grandkids. What the WHAT??? I had little boys at the time (age 9 and 11). This wasn’t a gift, gifts make people happy, cancer makes people cry. And retire? I was just getting my career back on track after taking a few years off while my boys were babies. Nothing made sense to me. I wanted to know what treatment would really be like, because in my head getting chemo meant that once the drip started I would immediately begin throwing up and all my hair would fall out at once in the doctors office, (clearly I’ve watched too much Lifetime television).
CCS: What (if any) additional outlets could you have used/turned to that you do not feel you had at the time?
J: I eventually found support at my local Cancer Support Community but typically I was the youngest of the bunch. There were only about three of us under 40 and in active treatment. There are so many wonderful resources that exist now that didn’t in 2007. Facebook groups and online support groups like Cure Diva and the LBBC both of whom also have a strong Facebook following.
CCS: How did you choose to share your diagnosis with your children?
J: Once we knew the stage and planned treatment we told them in very simple, honest terms that were age appropriate. I was diagnosed two days before my youngest son’s birthday so we waited until after his birthday to tell them both. They knew something was going on because I’d been home from work for over a week and we wanted to make sure they heard it directly from us rather than over hearing a conversation or voicemail message that would frighten them. We sat them down after dinner and explained that a few weeks prior mommy found something hard in her chest and when you feel something in your body that doesn’t feel right you go to the doctor to get it checked out. I told them that I went to the doctor and he ran tests and did a small operation and found out that I have breast cancer. I explained I was going to take medicine that might make me sick and tired and my hair might fall out but it would grow back in again. Very, very hard conversation to have, I felt like I stole their childhood away from them. They were amazing though, lots of hugs and kisses and support – even still to this day as young men!
CCS: What was your biggest parenting challenge during cancer treatment and into survivorship?
J: I lost my job during treatment so I used the opportunity to volunteer at their schools and participate as team mom for the sports they played. Yea, I was the bald mom at football practice and in art class but I used it as a teaching moment for all the kids. Some asked to see my head without my hat or scarf and I happily obliged. I wanted my kids to know that no matter what I’d still be their mom and I’d always be there for them. The toughest part though was when another child told one of mine that I was probably going to die. I had to do a lot of damage control, I certainly couldn’t predict the future but I couldn’t have my kids living in fear either. I always tell them (still to this day) I’m fine right now.
CCS: Any words of wisdom to other young adult cancer survivor moms (and dads) out there?
J: Break everything down into two categories; what you can control and what you cannot control. A cancer diagnosis makes you feel very out of control. You cannot control the treatment or the surgeries or how you will feel but there will still be things in your life that you can control so focus on that. It helps to feel empowered. Also, take it one day at a time. Rest when you need to, listen to your body, and take care of yourself first and foremost. You’re allowed to be selfish, you’ve earned it.
CCS: What kinds of things did you do to distract yourself when you were going through treatments (either at home or at the hospital… Or both)?
J: I began writing the book I needed to read . As I said earlier I couldn’t find a book that I could relate to and I had also lost my job while I was in treatment. I began keeping notes and eventually thought if I recorded, honestly, what it was like for me to go through treatments as a young mom then maybe I could make a pamphlet to help others. Once I hit over 100 pages I realized that my pamphlet was going to be a book. Does This Outfit Make Me Look Bald? was published in 2012, at the same time as my 5th cancerversary. I also listened to music, watched movies and napped – a lot!
CCS: How did you decide to start blogging about your experiences?
J: Interestingly enough, when I was promoting my book I had decided to have a prophylactic bilateral mastectomy. Since my initial diagnosis I had several false alarms (benign growths) and I also had a complication of severe radiation deformity, which was physically and emotionally painful, it had become too much to bear. During the MRI prior to the surgery they found a small cancerous lesion at my lumpectomy sight. It was not a recurrence but a brand new cancer with different properties than the first one, this can happen 20% of the time – I had no idea. I knew the drill at this point though. I booked a haircut and a bilateral mastectomy on the same day. Once I was home and on disability leave I began blogging to help me process what I had been through and to keep my friends updated, it was incredibly cathartic. Since I had become such an outspoken advocate for empowering young women with breast cancer I had made multiple media contacts that had promoted my book I ended up with several sites running my blogs too.
CCS: Could you describe how sharing your story has affected your journey with Cancer?
J: I’ve helped women that I’ve never met and that means the world to me. I have no idea why or how I got cancer once – never mind twice. I always felt that if I could make the road a bit smoother for someone else then all the stuff I went though makes sense. I needed to give back to others and help them through my own experience. I have a Facebook fan page for the book where I post current articles about research, blogs (my own and others that I like), and also a lot of humor – because I know that during my darkest days I still wanted to laugh. I needed to find some humor. Being sick is so damn scary and so serious that on the days I laughed I felt like I was taking a vacation from cancer. I’m also a National Cancer Survivor’s Day (NCSD) recommended speaker; which is pretty cool. I’m asked to give about 4 or 5 speeches a year – and I love knowing that those talks reach even more people than my book and blogs do.
CCS: Where are you now in your journey with Cancer?
J: I’m fine until a doctor tells me otherwise. My blood work gets checked every six months and I see my surgeons once a year. I still deal with mild PTSD but I have my coping tools so I know how to manage that. I’m both a 9 year and 3 year survivor.
CCS: What do you like to do in your spare time?
J: I live near the beach so if the weather is nice – my toes are in the sand! I like to run a few times a week while listening to very loud music. I continue to write my blogs and I’m also working on a fictional novel. I also love going out to dinner with my husband and kids.
CCS: What “words of wisdom” and/or advice would you give any young adult facing Cancer or another life-threatening illness?
J: You’ll be amazed by your strength and you’ll have far more good days than bad so relish those. Breathe deep, relax, laugh and love in equal measure and cherish yourself first and foremost. Listen to your doctors and partner with them, be your own best advocate. And if you feel as if they are dismissive…fire them! You get to be the boss of cancer.
Thank you for sharing your story with us, Jenn! Look forward to a few more pieces from Jenn soon!
Are you a young adult cancer survivor, caregiver, or do you have a long term illness? Interested in being interviewed by Lacuna Loft? Let us know! We’d love to hear from you!
Latest Articles

Christina’s Corner: May 2024

May 2024 Programs

10 Questions with Scarlett

10 Questions with Robynne

Dating Through Cancer?!

Financial Aid & College Scholarships for Cancer Survivors
College is an exciting time of life filled with new experiences, knowledge, and relationships. Although it is expensive, childhood cancer patients and survivors have several college scholarship and financial aid options.
Many organizations provide scholarships for cancer patients and survivors. In addition, there are financial aid opportunities available for people with certain disabilities.
Some scholarships are available for family members of cancer patients. Be sure to check the application criteria for all scholarships.

Tips for successful scholarship applications
- Every scholarship is different. Read the application and the organization’s website carefully. Note the application deadline as well as contact information, application requirements, and ability to renew the scholarship each year. Don’t miss an opportunity because of a simple mistake.
- In general, applicants must provide a letter from a doctor stating the original diagnosis and the age the patient began treatment. Allow the doctor plenty of time to write the letter.
- Some applications may also request letters of reference from teachers, coaches, or employers. Ask these people in advance. Don’t wait until the last minute.

Every scholarship is different. Read the application and the organization’s website carefully.
Scholarship essay tips
Many scholarship applications require an essay. Some will ask the same types of essay questions. You may be able to tweak an essay written for one scholarship to meet requirements for other applications.
Make sure to have someone knowledgeable about writing and grammar proofread your application and essay.
List of scholarships for cancer patients and survivors
The organizations that offer these scholarships are often funded by donations and endowments given in honor or in memory of other pediatric and young adult cancer patients.
Beyond the Cure
These scholarships are for childhood cancer survivors who have demonstrated the ability to overcome the difficult challenges of cancer with determination and motivation. Fifty-eight (58) $3,500 scholarships are awarded each academic year. The scholarship application period is from January – March of each calendar year.
Applicants must be:
- A childhood cancer survivor under the age of 25
- Diagnosed before the age of 18 with cancer or a high-grade or anaplastic brain tumor
- A citizen of the United States living within the country and attending school in the U.S.
- Accepted into a post-secondary school in the fall of the upcoming school year.
Visit the website for an application:
Beyond the Cure Ambassador Scholarship Program
Cancer for College
The website provides a number of different scholarship offers to different regions of the United States. Scholarship application period is November 1-January 31 each year. Applicants must be planning to attend a degree-earning program in the United States. Certain scholarships listed are relevant only for particular states.
Applicants need:
- Their parents’ tax return(s)
- Their own personal tax return or proof of any income if they do not file a tax return
- A letter of good standing from the university attending
- 2 years of academic transcripts, confirmation of diagnosis letter
- Confirmation of Diagnosis letter
- A letter of recommendation from 1 person outside your family
- Total annual cost of attendance
Cancer for College Scholarship Application
National Collegiate Cancer Foundation
This organization provides services and support to young adults whose lives have been impacted by cancer and who have continued with their education throughout treatment or after their treatment. Each award is $1,000. Applications available in March. Deadline is May 15.
- A young adult cancer survivor or current patient between the ages of 18-35. Exceptions are made for age 17 if entering college in the fall following application.
- A U.S. citizen or permanent resident
- Attending or planning to attend an accredited college, university or vocational institution in pursuit of an associate’s, bachelor’s, master’s, doctorate or certificate as of the fall following application
National Collegiate Cancer Foundation Scholarships
The Ortlieb Foundation
The foundation was created to honor cancer survivor Evan Ortleib, who was diagnosed with non-Hodgkin lymphoma at age 16. Scholarships are awarded twice each year (spring and fall) and are valued at $1,000 each. The submission deadline for the spring semester is December 15, and the deadline for the fall semester is June 15.
Eligibility requirements include:
- Letter of cancer diagnosis and treatment of chemotherapy , radiation , or proton therapy from oncologist
- Proof of enrollment in full-time study at a four-year college or university
- Transcripts from high school or college
- Standardized test scores (ACT or SAT)
- 1040 tax documents from parents and self
- 2 letters of recommendation from teachers, mentors, or employers
- 250-word essay on academic and career goals
Ortlieb Foundation Scholarship Application
Ronald McDonald House Charities
The network of U.S. chapters, along with the global office of RMHC, offers scholarships to students in financial need who have demonstrated academic achievement, leadership, and community involvement. Since 1985, more than $56 million in scholarships have been awarded.
Scholarships are awarded by local RMHC chapters.
Find Your Local RMHC Chapter
The Ulman Fund for Young Adults
Scholarships available to young adults affected by cancer through their own diagnosis or through the diagnosis of a parent or sibling. Applicants must be between the ages of 15 and 39 during the time of diagnosis/treatment. Recipients will be awarded a total of $2,500 over two academic semesters, paid directly to the recipient’s school. Deadline is March 1.
Ulman Cancer Fund Scholarships
Scholarship databases
Finaid: the smartstudent guide to financial aid.
This page contains information about scholarships for cancer patients, cancer survivors, children of a cancer patient or survivor, students who lost a parent to cancer, and students pursuing careers in cancer treatment.
FinAid Scholarships
The Samfund
Grants and scholarships provided by the Samfund cover a wide range of post-treatment financial needs, such as (but not limited to): rent and mortgage assistance; health insurance premiums; car payments, insurance, and repairs; continuing education and loans; gym memberships; and mental health expenses. This group is no longer accepting applications for undergraduate tuition, as they have in the past, but rather is focusing on other school-related expenses. Applications open in the spring.
Applicants need to:
- Be between the ages of 21 and 39
- Either (1) finished active treatment with no evidence of disease, (2) completed one year of planned treatment and be in a stable condition, or (3) be receiving long-term hormonal or targeted therapy.
Samfund Cancer Survivor Grants
Scholarship resources for students with physical disabilities
San francisco state university disability resource center.
The Disability Programs and Resource Center at San Francisco State University has compiled a list of scholarships for students of various disabilities. A chart lists the organization offering the scholarship as well as general information and a link to each scholarship page.
SFSU Disability Resource Center Scholarships
University of Washington Disability Resource Page
The University of Washington has put together a page with tips on searching for funding for students with disabilities. In addition to links to sites offering scholarships, it also discusses other ways students might find information on funding, such as vocational rehab and other state programs. Scholarships are listed by type of disability.
Scholarships for vision-impaired students
American council of the blind (acb).
This organization offers scholarships to legally blind student going to technical, undergraduate, or graduate school. Scholarships range from $1,500-$7,500. Application deadline is February 15.
American Council of the Blind Scholarships
American Foundation for the Blind (AFB)
The AFB offers multiple scholarships to legally blind students. Application deadline is April 1.
Descriptions of the scholarships, as well as the online application can be found at the above website.
American Foundation for the Blind Scholarship
Council of Citizens with Low Vision International – Fred Scheigert Scholarship
This program awards 3 students an individual prize of $3,000 to full-time college students with low vision. Applicants must meet visual acuity and academic guidelines. Scholarship guidelines, application, and vision certification are offered on the website from January 1 to March 15 of each year. The scholarship application must be completed online. Selected finalists will be required to complete a phone interview with committee members. Chosen winners are expected to attend an annual meeting in conjunction with the American Council of the Blind National Convention (usually in July).
CCLVI Scheigert Scholarship
National Federation of the Blind (NFB)
The NFB offers 30 scholarships to legally blind students each year, worth from $3,000 to $12,000. The winner must participate in the NFB national convention in July and all its scheduled scholarship program activities. Assistance is available for convention needs. Application due in March 31.
- Legally blind in both eyes
- A resident of the United States or Puerto Rico
- Planning to attend postsecondary study in the United States
National Federation of the Blind Scholarship Program
Christian Record Services for the Blind
The Anne Lowe Scholarship is awarded to blind students based on academic achievement and citizenship. Applications must be submitted or postmarked by April 15.
Application information/requirements:
- Currently registered as a full-time student in undergraduate studies at accredited college or university in the U.S.
- Minimum 3.0 GPA
- Written essay
- 3 letters of recommendation from non-family members
Scholarship is distributed in two parts during the school year
Anne Lowe Scholarship — Christian Record Services for the Blind
Scholarships for hearing-impaired students
Sertoma – service to mankind.
This group offers scholarships to individuals with hearing impairments and communicative disorders. Scholarships are available in $1,000 amounts. Application deadline is May 1.
Qualifications:
- Must have a minimum 40dB bilateral hearing loss, as evidenced on audiogram by an SRT & PTA of 40dB or greater in both ears
- Must be a citizen of the U.S.
- Must be pursuing a bachelor’s degree on a full-time basis at a college or university in the United States
- Must have a minimum cumulative 3.2 GPA on a 4.0 unweighted scale
- 2 letters of recommendation
- High school and/or college transcript
- Recent audiogram from a hearing health professional (must not be any older than two years)
- Hearing loss on application must be verifiable from audiogram
Sertoma Scholarships
AG Bell College Scholarship Program
AG Bell Scholarships are for high-achieving students who have bilateral hearing loss that was diagnosed before age 4.
- Must be using listening and spoken language as your primary communication mode
- Must attend a mainstream university and working toward a four-year undergraduate degree or a graduate degree
Hydrocephalus
Hydrocephalus association.
Scholarships applicants must be 17 or older with hydrocephalus. The scholarship funds must be used for an educational purpose, including, but not limited to, a 2-year or 4-year college, a high school post-graduate year to prepare for college, technical or trade school, an accredited employment-training program, or a post–graduate program. Scholarships are $1,000 each.
Application opens in January and is due April 15.
Hydrocephalus Association’s Scholarship Program
Learning-disabled
National center for learning disabilities.
Scholarships are available for 2 graduating high school seniors with documented learning disabilities and/or attention deficit hyperactivity disorder who are pursuing postsecondary educatoin.
National Center for Learning Disabilities Scholarships
- Epsilon Sigma Alpha (ESA)
- Sallie Mae Student Loans
- Federal Student Aid
- Financial Aid Scholarships
— Together does not endorse any branded product mentioned in this article.
— Reviewed: February 2020
College Classroom Accommodations
College and trade schools likely have services to help you when you need academic or physical accommodations for cancer-related problems. Sometimes cancer and treatment side effects can affect thinking and learning skills or your ability to get around from place to place.
Keep Up with School
Cancer treatment and side effects will likely disrupt your regular school schedule. Find resources to help you make the most of your education.
ACT or SAT Accommodations
Cancer patients may qualify for accommodations on ACT and SAT tests. Accommodations are changes made to the regular testing environment to allow people with disabilities to demonstrate their true ability on tests.

Breast cancer survivors’ risk of secondary cancers studied by University of Cambridge researchers
S urvivors of breast cancer are at significantly higher risk of developing second cancers, including endometrial and ovarian cancer for women and prostate cancer for men, University of Cambridge research has found.
The study of data from almost 600,000 patients in England has also shown, for the first time, that this risk is higher among people living in areas of greater socioeconomic deprivation.
Breast cancer is the most commonly diagnosed cancer in the UK, with around 56,000 people in the UK diagnosed each year - more than 99 per cent of whom are women.
With improvements in earlier diagnosis and treatments, five-year survival rates reached 87 per cent by 2017 in England.
Those who survive breast cancer are known to be at risk of second primary cancer, but the nature of that risk has been unclear until now, with previously published research suggesting women and men who survive breast cancer are at a 24 per cent and 27 per cent greater risk of a non-breast second primary cancer than the wider population respectively.
It has also been suggested that second primary cancer risks differ by the age at breast cancer diagnosis.
The University of Cambridge team set out to provide a more accurate picture by analysing data from more than 580,000 female and more than 3,500 male breast cancer survivors diagnosed between 1995 and 2019 using the National Cancer Registration Dataset.
First author Isaac Allen, from Cambridge’s Department of Public Health and Primary Care, said: “It’s important for us to understand to what extent having one type of cancer puts you at risk of a second cancer at a different site. The female and male breast cancer survivors whose data we studied were at increased risk of a number of second cancers. Knowing this can help inform conversations with their care teams to look out for signs of potential new cancers.”
Females who survived breast cancer were at double the risk of contralateral breast cancer - that is, in the unaffected breast - compared to the general population and at 87 per cent greater risk of endometrial cancer, 58 per cent greater risk of myeloid leukaemia and 25 per cent greater risk of ovarian cancer.
Females diagnosed with breast cancer under the age of 50 were 86 per cent more likely to develop a second primary cancer compared to the general population of the same age, whereas women diagnosed after age 50 were at a 17 per cent increased risk.
This may be because a larger number of younger breast cancer survivors may have inherited genetic alterations that increase risk for multiple cancers. Women with inherited changes to the BRCA1 and BRCA2 genes , for example, are at increased risk of contralateral breast cancer, ovarian and pancreatic cancer.
Females from the most socio-economically deprived backgrounds were found to be at 35 per cent greater risk of a second primary cancer compared to females from the least deprived backgrounds
This difference was primarily driven by non-breast cancer risks, such as lung, kidney, head and neck, bladder, oesophageal and stomach cancers, and may be because smoking, obesity, and alcohol consumption are more common among more deprived groups and area established risk factors for these cancers.
Isaac, a PhD student at Clare Hall, added: “This is further evidence of the health inequalities that people from more deprived backgrounds experience. We need to fully understand why they are at greater risk of second cancers so that we can intervene and reduce this risk.”
Male breast cancer survivors, meanwhile, were 55 times more likely than the general male population to develop contralateral breast cancer, although the risk was still very low. For every 100 men diagnosed with breast cancer at age 50 or over, about three developed contralateral breast cancer during a 25-year period. Male breast cancer survivors were also 58 per cent more likely than the general male population to develop prostate cancer.
Prof Antonis Antoniou, from Cambridge’s Department of Public Health and Primary Care at the University of Cambridge, the study’s senior author, said: “This is the largest study to date to look at the risk in breast cancer survivors of developing a second cancer. We were able to carry this out and calculate more accurate estimates because of the outstanding data sets available to researchers through the NHS.”
Cancer Research UK’s senior cancer intelligence manager, Katrina Brown, said: “This study shows us that the risk of second primary cancers is higher in people who have had breast cancer, and this can differ depending on someone’s socioeconomic background. But more research is needed to understand what is driving this difference and how to tackle these health inequalities.”
The research, published in Lancet Regional Health – Europe, was funded by Cancer Research UK with support from the National Institute for Health and Care Research Cambridge Biomedical Research Centre.
People who are concerned about their cancer risk should contact their GP for advice. If you or someone close to you have been affected by cancer and you’ve got questions, you can call Cancer Research UK nurses on freephone 0808 800 4040, Monday to Friday.

- Share full article
Advertisement
Supported by
Kris Hallenga, Who Urged Early Breast Cancer Screenings, Dies at 38
After being diagnosed when she was 23, she became determined to educate other young people about early detection.

By Remy Tumin
When Kris Hallenga was diagnosed with stage four breast cancer at 23, questions swirled in her head: “Why didn’t anyone tell me to check my boobs? Why didn’t I know I could get breast cancer at 23?”
If she hadn’t known that she could get breast cancer so young, there was a very good chance that others were equally uninformed, she said in a 2021 interview with The Guardian. She spent the next 15 years educating young people about early detection through her nonprofit organization, CoppaFeel, and in a 2021 memoir, “Glittering a Turd.”
On Monday, a spokesman for CoppaFeel said Ms. Hallenga had died of breast cancer at her home in Cornwall, England. She was 38.
“Survival was never enough,” she said during a publicity tour in 2021. “I don’t just want to survive; I want to be able to really look at my life and go, ‘I’m glad to still be here, and I’m getting the most of what I want from life.’”
Kristen Hallenga was born on Nov. 11, 1985, in Norden, a small town in northern Germany, to a German father and an English mother, both of whom were teachers. When she was 9, she moved to Daventry in central England with her mother, Jane Hallenga; her twin sister, Maren; and their older sister Maike, all three of whom survive her. Her father, Reiner Hallenga, died of a heart attack when she was 20.
Ms. Hallenga first felt a lump in 2009, when she was in Beijing working for a travel company and teaching on the side. During a visit back home to the Midlands, Ms. Hallenga went to her internist, who attributed the lump to hormonal changes associated with her birth control pill, she told The Guardian.
But the lump grew more painful, and a bloody discharge developed. Another internist gave her a diagnosis similar to the first, tying her condition again to hormones and the pill. But because she didn’t know what would be considered normal, Ms. Hallenga didn’t have anything to judge by.
“I wasn’t touching my boobs at all,” she said. “I didn’t know anything about them.”
But her mother, whose own mother had breast cancer at an early age, insisted that Ms. Hallenga obtain a referral to a breast clinic. By the time she was diagnosed, eight months after finding the lump, the prognosis was terminal. The cancer had also spread to her spine.
After an aggressive round of chemotherapy, a mastectomy and hormone therapy, tests in 2011 revealed that the cancer had spread to her liver, she told The Huffington Post . A year later, doctors found that the cancer had spread to her brain. She underwent radiotherapy to remove a tumor.
But she continued to work through her illness. She wrote about her cancer diagnosis and her advocacy work in a column for her local newspaper, The Northampton Chronicle and Echo, and The Sun. But it was her work with CoppaFeel that reached her target audience: young people.
The organization has sent thousands of reminders about breast self-exams by text message; organized a group of women known as the Boobettes, who go into schools to talk about their experience with breast cancer at a young age; helped add cancer awareness to the education curriculum in Britain; and aired what was believed to be the first nipple in a daytime television commercial , which encouraged people to get to know their chests.
All of it was done in the hope that others could avoid a diagnosis like Ms. Hallenga’s.
“Cancer so often comes with a package of terms — survivor, thriver, warrior — and it’s great if someone wants to hang their existence on those words, if it helps them get through the day — if it helps them get perspective, great,” Ms. Hallenga said when her memoir was released . “But for me, I couldn’t really resonate with those words, ever. Because I say, unless I’m happy being alive, then what is the point in surviving?”
She stepped down as chief executive of CoppaFeel in 2017 and moved to Cornwall to spend more time with her sister Maren. Last June, she threw herself a living funeral at the Truro Cathedral in Cornwall. The dress code was YODO — you only die once. Dawn French, who played a village priest in the BBC sitcom “The Vicar of Dibley,” led the celebration of life .
“I’ve never felt love like it,” Ms. Hallenga wrote on Instagram after the event. “I’ve never felt joy like it. I’ve never felt such kinship with mortality. I’ve never felt so alive.”
Remy Tumin is a reporter for The Times covering breaking news and other topics. More about Remy Tumin

COMMENTS
February 1, 2024 Personal Stories. Because of a family history of breast cancer, Alecia Robinson underwent twice yearly breast MRIs. In April 2022, Alecia was diagnosed with stage 1A invasive ductal carcinoma ER, PR+, HER2+. This is her story in her own words. I felt no particular sense of anxiety when I left my breast MR I appointment in April ...
Here's Why I Said No To Reconstructive Surgery'. "You don't need implants to feel beautiful.". Christina Miner, 46, had both breasts removed during a double mastectomy in May 2020. She ...
Summary. Being a survivor of breast cancer means different things to different people. For many, it's part of their lifelong identity. Breast cancer has a high survivorship rate of 90% after five years; that rate varies depending on whether the cancer has spread and the person's race, age, and lifestyle factors.
It's imperative that you do speak up, though, because Black women are 40% more likely to die from breast cancer than white women. 7. Remember, this is your body. This is how you are feeling ...
Diana Abehssera is a mother, breast cancer survivor, and the Patient Experience Lead at Leal Health, an AI-powered platform dedicated to improving cancer treatment. View Diana's disclosures. When breast cancer comes knocking on the door, most people are never quite expecting it. I sure wasn't at the age of 32.
Cancer Survivors: In Their Words. June 20, 2020by Marci Landsmann. This year alone, an estimated 1.8 million people will hear their doctor say they have cancer. The individual impact of each person can be clouded in the vast statistics. In honor of National Cancer Survivor Month, Cancer Today would like to highlight several personal essays we ...
Help us end cancer as we know it, for everyone. Donate with Confidence. Learn more about living as a breast cancer survivor and get information about next steps, follow up care, and ways to look after your health.
Breast cancer survivorship is more than just surviving cancer. It includes your long-term physical, mental, emotional, and financial health.
Here, Barcenas shares three insights to help breast cancer patients with the transition into survivorship. 1. Survivorship means something different to everyone. "The definition of survivorship isn't exact," Barcenas says. "It depends on who you ask.". Mostly commonly, the survivorship phase is thought to start after completing active ...
Introduction. Breast cancer (BC) is the most frequent cancer in women worldwide, accounting for 11.7% of total cases, with 2.3 million cases newly diagnosed in 2020 [1•].Due to earlier diagnoses and more effective treatment, the 5-year survival rate has continued to improve over the last two decades and is now 86% in Italy and Turkey [].Male BC cases are less than 1% of all diagnosed breast ...
Breast cancer (BC), while highly prevalent globally (highest incidence cancer among women in 159/185 countries) [], has a high survival rateThe average five-year survival rate in Australia for BC from 2013 to 2017 was 91.5%, compared to 69.7% for all cancer types combined [].Cancer survivors are defined as individuals diagnosed with cancer who have completed their initial cancer treatment ...
Introduction. Breast cancer is the most common cancer in the world, with 2.26 million diagnoses in 2020.1 People with breast cancer are living longer as a result of improvements in screening and treatment, such that in the US alone the number of survivors of breast cancer is expected to grow by more than 2 million in the next decade.2 3 Unfortunately, survivors may experience significant after ...
In this posthumous book of essays, Teva Harrison shares her metastatic breast cancer journey. A follow up to Harrison's "In-Between Days: A Memoir About Living with Cancer," it dives deep into what it means to have cancer, the impact it has on her life, and how the disease has progressed. ... Edited by cancer survivor Marquina Iliev ...
754 Words. 4 Pages. Open Document. I am proud to say that I am a survivor of breast cancer. The years since I discovered I had cancer have, in many ways, been the best part of my life. My journey began when I signed up to play in a golf tournament for the benefit of the Breast Cancer Foundation when, ironically, I discovered a lump in one of my ...
As part of Stella McCartney's annual campaign for Breast Cancer Awareness Month, acclaimed photojournalist Lynsey Addario took powerful, inspiring portraits of 12 breast cancer survivors.
Breast cancer survivors may need to prepare for ongoing psychosocial challenges in survivorship and proactively seek support to overcome these. ... 76 individual papers were eligible from 2273 unique papers. Reviews and studies commonly focused on specific survivorship groups (including those from ethnic minorities, younger/older, or with ...
In her essay, Shadle, a research scientist at the Haskins Laboratories in New Haven, noted that oncotype scores that determine whether she'll need chemotherapy and National Institutes of Health scores for grant applications share one characteristic—a low score is better. ... Kathleen Miles Schumacher, a breast cancer survivor, described an ...
Today Cactus Cancer Society talks with cancer survivor, Jenn. She is a two-time breast cancer survivor, talks to us about her book, parenting during a cancer diagnosis, and so much more! — Cactus Cancer Society: When were you diagnosed and what is your diagnosis? Jennifer: I found a lump in my breast in 2007 when I was 38. I assumed it was a ...
Breast cancer is a disease in which abnormal breast cells grow out of control and form tumours. If left unchecked, the tumours can spread throughout the body and become fatal. Breast cancer cells begin inside the milk ducts and/or the milk-producing lobules of the breast. The earliest form (in situ) is not life-threatening and can be detected ...
Similarly, the high expression of miRNA-210 is related to tumor proliferation, invasion, and poor survival rates in breast cancer patients [238,239]. The miRNA-145 is an anti-cancer agent having the property of inhibiting migration and proliferation of breast cancer cells via regulating the TGF-β1 expression .
For primary breast cancer, Corradini et al. analysed the oncological outcomes of 7565 cases of breast cancer in a case-controlled cohort study comparing breast conserving surgery followed by radiotherapy with mastectomy, showing that the former was associated with better recurrence control and survival, and as such recommended physicians to ...
A childhood cancer survivor under the age of 25; Diagnosed before the age of 18 with cancer or a high-grade or anaplastic brain tumor; A citizen of the United States living within the country and attending school in the U.S. Accepted into a post-secondary school in the fall of the upcoming school year. Visit the website for an application:
With improvements in earlier diagnosis and treatments, five-year survival rates reached 87 per cent by 2017 in England. Those who survive breast cancer are known to be at risk of second primary ...
On Monday, a spokesman for CoppaFeel said Ms. Hallenga had died of breast cancer at her home in Cornwall, England. She was 38. "Survival was never enough," she said during a publicity tour in ...
Young woman in bed suffering from cancer. Breast cancer survivors are more likely to develop a second form of cancer if they live in the poorest parts of England. A study of nearly 600,000 people ...
Preclinical evidence suggests improved breast cancer survival associated with statin use, but findings from observational studies are conflicting and remain inconclusive. The objective of this study was to assess the association between statin use after cancer diagnosis and cancer outcomes among breast cancer patients. Methods
Semantic Scholar extracted view of "Assessing Lung Cancer Risk in Breast Cancer Survivors" by J.J. Lin et al. ... Semantic Scholar's Logo. Search 218,276,811 papers from all fields of science. Search. Sign In Create Free Account. DOI: 10.1164/ajrccm-conference.2024.209.1_meetingabstracts.a3054;
Background: Triple-negative breast cancer (TNBC) is a highly aggressive form of breast cancer subtype often treated with radiotherapy (RT). Due to its intrinsic heterogeneity and lack of effective targets, it is crucial to identify novel molecular targets that would increase RT efficacy. Here we demonstrate the role of BUB1 (cell cycle Ser/Thr kinase) in TNBC radioresistance and offer a novel ...
(1) Background: Abemaciclib combined with endocrine therapy is a standard first- or later--line of treatment for HR+/HER2− metastatic breast cancer (MBC). The aim of this retrospective cohort study was to describe the outcomes of patients treated in a real-world setting, with particular focus on elderly patients. (2) Patients and methods: Patients treated with abemaciclib between November ...