
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Variations in Fetal Position and Presentation |
During pregnancy, the fetus can be positioned in many different ways inside the mother's uterus. The fetus may be head up or down or facing the mother's back or front. At first, the fetus can move around easily or shift position as the mother moves. Toward the end of the pregnancy the fetus is larger, has less room to move, and stays in one position. How the fetus is positioned has an important effect on delivery and, for certain positions, a cesarean delivery is necessary. There are medical terms that describe precisely how the fetus is positioned, and identifying the fetal position helps doctors to anticipate potential difficulties during labor and delivery.
Presentation refers to the part of the fetus’s body that leads the way out through the birth canal (called the presenting part). Usually, the head leads the way, but sometimes the buttocks (breech presentation), shoulder, or face leads the way.
Position refers to whether the fetus is facing backward (occiput anterior) or forward (occiput posterior). The occiput is a bone at the back of the baby's head. Therefore, facing backward is called occiput anterior (facing the mother’s back and facing down when the mother lies on her back). Facing forward is called occiput posterior (facing toward the mother's pubic bone and facing up when the mother lies on her back).
Lie refers to the angle of the fetus in relation to the mother and the uterus. Up-and-down (with the baby's spine parallel to mother's spine, called longitudinal) is normal, but sometimes the lie is sideways (transverse) or at an angle (oblique).
For these aspects of fetal positioning, the combination that is the most common, safest, and easiest for the mother to deliver is the following:
Head first (called vertex or cephalic presentation)
Facing backward (occiput anterior position)
Spine parallel to mother's spine (longitudinal lie)
Neck bent forward with chin tucked
Arms folded across the chest
If the fetus is in a different position, lie, or presentation, labor may be more difficult, and a normal vaginal delivery may not be possible.
Variations in fetal presentation, position, or lie may occur when
The fetus is too large for the mother's pelvis (fetopelvic disproportion).
The uterus is abnormally shaped or contains growths such as fibroids .
The fetus has a birth defect .
There is more than one fetus (multiple gestation).

Position and Presentation of the Fetus
Variations in fetal position and presentation.
Some variations in position and presentation that make delivery difficult occur frequently.
Occiput posterior position
In occiput posterior position (sometimes called sunny-side up), the fetus is head first (vertex presentation) but is facing forward (toward the mother's pubic bone—that is, facing up when the mother lies on her back). This is a very common position that is not abnormal, but it makes delivery more difficult than when the fetus is in the occiput anterior position (facing toward the mother's spine—that is facing down when the mother lies on her back).
When a fetus faces up, the neck is often straightened rather than bent,which requires more room for the head to pass through the birth canal. Delivery assisted by a vacuum device or forceps or cesarean delivery may be necessary.
Breech presentation
In breech presentation, the baby's buttocks or sometimes the feet are positioned to deliver first (before the head).
When delivered vaginally, babies that present buttocks first are more at risk of injury or even death than those that present head first.
The reason for the risks to babies in breech presentation is that the baby's hips and buttocks are not as wide as the head. Therefore, when the hips and buttocks pass through the cervix first, the passageway may not be wide enough for the head to pass through. In addition, when the head follows the buttocks, the neck may be bent slightly backwards. The neck being bent backward increases the width required for delivery as compared to when the head is angled forward with the chin tucked, which is the position that is easiest for delivery. Thus, the baby’s body may be delivered and then the head may get caught and not be able to pass through the birth canal. When the baby’s head is caught, this puts pressure on the umbilical cord in the birth canal, so that very little oxygen can reach the baby. Brain damage due to lack of oxygen is more common among breech babies than among those presenting head first.
In a first delivery, these problems may occur more frequently because a woman’s tissues have not been stretched by previous deliveries. Because of risk of injury or even death to the baby, cesarean delivery is preferred when the fetus is in breech presentation, unless the doctor is very experienced with and skilled at delivering breech babies or there is not an adequate facility or equipment to safely perform a cesarean delivery.
Breech presentation is more likely to occur in the following circumstances:
Labor starts too soon (preterm labor).
The uterus is abnormally shaped or contains abnormal growths such as fibroids .
Other presentations
In face presentation, the baby's neck arches back so that the face presents first rather than the top of the head.
In brow presentation, the neck is moderately arched so that the brow presents first.
Usually, fetuses do not stay in a face or brow presentation. These presentations often change to a vertex (top of the head) presentation before or during labor. If they do not, a cesarean delivery is usually recommended.
In transverse lie, the fetus lies horizontally across the birth canal and presents shoulder first. A cesarean delivery is done, unless the fetus is the second in a set of twins. In such a case, the fetus may be turned to be delivered through the vagina.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic
RELATED TOPICS
INTRODUCTION
For patients who present in labor with a breech fetus, cesarean birth is the preferred approach in many hospitals in the United States and elsewhere. Cesarean is performed for over 90 percent of breech presentations, and this rate has increased worldwide [ 1,2 ]. However, even in institutions with a policy of routine cesarean birth for breech presentation, vaginal breech births occur because of situations such as patient preference, precipitous birth, out-of-hospital birth, and lethal fetal anomaly or fetal death. Therefore, it is essential for clinicians to maintain familiarity with the techniques required to assist in a vaginal breech birth.
In addition, some clinicians and patients consider vaginal breech birth preferable to cesarean birth. Recent trends, particularly in central Europe, support vaginal breech birth [ 3-5 ]. In selected cases, as described below and depicted in the algorithm ( algorithm 1 ), it is associated with a low risk of complications. The American College of Obstetricians and Gynecologists has opined that "Planned vaginal delivery of a term singleton breech fetus may be reasonable under hospital-specific protocol guidelines for eligibility and labor management" [ 6 ].
This topic will focus on vaginal birth of breech singletons, with a brief discussion of breech delivery at cesarean. Choosing the best route of birth for the fetus in breech presentation and delivery of the breech first or second twin are reviewed separately.
● (See "Overview of breech presentation", section on 'Approach to management at or near term' .)

- Pregnancy Classes

Breech Births
In the last weeks of pregnancy, a baby usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation. A breech presentation occurs when the baby’s buttocks, feet, or both are positioned to come out first during birth. This happens in 3–4% of full-term births.
What are the different types of breech birth presentations?
- Complete breech: Here, the buttocks are pointing downward with the legs folded at the knees and feet near the buttocks.
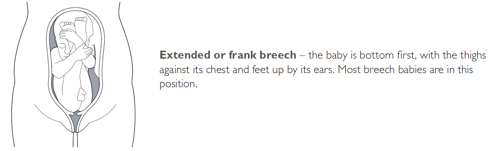
- Frank breech: In this position, the baby’s buttocks are aimed at the birth canal with its legs sticking straight up in front of his or her body and the feet near the head.
- Footling breech: In this position, one or both of the baby’s feet point downward and will deliver before the rest of the body.
What causes a breech presentation?
The causes of breech presentations are not fully understood. However, the data show that breech birth is more common when:
- You have been pregnant before
- In pregnancies of multiples
- When there is a history of premature delivery
- When the uterus has too much or too little amniotic fluid
- When there is an abnormally shaped uterus or a uterus with abnormal growths, such as fibroids
- The placenta covers all or part of the opening of the uterus placenta previa
How is a breech presentation diagnosed?
A few weeks prior to the due date, the health care provider will place her hands on the mother’s lower abdomen to locate the baby’s head, back, and buttocks. If it appears that the baby might be in a breech position, they can use ultrasound or pelvic exam to confirm the position. Special x-rays can also be used to determine the baby’s position and the size of the pelvis to determine if a vaginal delivery of a breech baby can be safely attempted.
Can a breech presentation mean something is wrong?
Even though most breech babies are born healthy, there is a slightly elevated risk for certain problems. Birth defects are slightly more common in breech babies and the defect might be the reason that the baby failed to move into the right position prior to delivery.
Can a breech presentation be changed?
It is preferable to try to turn a breech baby between the 32nd and 37th weeks of pregnancy . The methods of turning a baby will vary and the success rate for each method can also vary. It is best to discuss the options with the health care provider to see which method she recommends.
Medical Techniques
External Cephalic Version (EVC) is a non-surgical technique to move the baby in the uterus. In this procedure, a medication is given to help relax the uterus. There might also be the use of an ultrasound to determine the position of the baby, the location of the placenta and the amount of amniotic fluid in the uterus.
Gentle pushing on the lower abdomen can turn the baby into the head-down position. Throughout the external version the baby’s heartbeat will be closely monitored so that if a problem develops, the health care provider will immediately stop the procedure. ECV usually is done near a delivery room so if a problem occurs, a cesarean delivery can be performed quickly. The external version has a high success rate and can be considered if you have had a previous cesarean delivery.
ECV will not be tried if:
- You are carrying more than one fetus
- There are concerns about the health of the fetus
- You have certain abnormalities of the reproductive system
- The placenta is in the wrong place
- The placenta has come away from the wall of the uterus ( placental abruption )
Complications of EVC include:
- Prelabor rupture of membranes
- Changes in the fetus’s heart rate
- Placental abruption
- Preterm labor
Vaginal delivery versus cesarean for breech birth?
Most health care providers do not believe in attempting a vaginal delivery for a breech position. However, some will delay making a final decision until the woman is in labor. The following conditions are considered necessary in order to attempt a vaginal birth:
- The baby is full-term and in the frank breech presentation
- The baby does not show signs of distress while its heart rate is closely monitored.
- The process of labor is smooth and steady with the cervix widening as the baby descends.
- The health care provider estimates that the baby is not too big or the mother’s pelvis too narrow for the baby to pass safely through the birth canal.
- Anesthesia is available and a cesarean delivery possible on short notice
What are the risks and complications of a vaginal delivery?
In a breech birth, the baby’s head is the last part of its body to emerge making it more difficult to ease it through the birth canal. Sometimes forceps are used to guide the baby’s head out of the birth canal. Another potential problem is cord prolapse . In this situation the umbilical cord is squeezed as the baby moves toward the birth canal, thus slowing the baby’s supply of oxygen and blood. In a vaginal breech delivery, electronic fetal monitoring will be used to monitor the baby’s heartbeat throughout the course of labor. Cesarean delivery may be an option if signs develop that the baby may be in distress.
When is a cesarean delivery used with a breech presentation?
Most health care providers recommend a cesarean delivery for all babies in a breech position, especially babies that are premature. Since premature babies are small and more fragile, and because the head of a premature baby is relatively larger in proportion to its body, the baby is unlikely to stretch the cervix as much as a full-term baby. This means that there might be less room for the head to emerge.
Want to Know More?
- Creating Your Birth Plan
- Labor & Birth Terms to Know
- Cesarean Birth After Care
Compiled using information from the following sources:
- ACOG: If Your Baby is Breech
- William’s Obstetrics Twenty-Second Ed. Cunningham, F. Gary, et al, Ch. 24.
- Danforth’s Obstetrics and Gynecology Ninth Ed. Scott, James R., et al, Ch. 21.
BLOG CATEGORIES
- Can I get pregnant if… ? 3
- Child Adoption 19
- Fertility 54
- Pregnancy Loss 11
- Breastfeeding 29
- Changes In Your Body 5
- Cord Blood 4
- Genetic Disorders & Birth Defects 17
- Health & Nutrition 2
- Is it Safe While Pregnant 54
- Labor and Birth 65
- Multiple Births 10
- Planning and Preparing 24
- Pregnancy Complications 68
- Pregnancy Concerns 62
- Pregnancy Health and Wellness 149
- Pregnancy Products & Tests 8
- Pregnancy Supplements & Medications 14
- The First Year 41
- Week by Week Newsletter 40
- Your Developing Baby 16
- Options for Unplanned Pregnancy 18
- Paternity Tests 2
- Pregnancy Symptoms 5
- Prenatal Testing 16
- The Bumpy Truth Blog 7
- Uncategorized 4
- Abstinence 3
- Birth Control Pills, Patches & Devices 21
- Women's Health 34
- Thank You for Your Donation
- Unplanned Pregnancy
- Getting Pregnant
- Healthy Pregnancy
- Privacy Policy
Share this post:
Similar post.

Episiotomy: Advantages & Complications

Retained Placenta

What is Dilation in Pregnancy?
Track your baby’s development, subscribe to our week-by-week pregnancy newsletter.
- The Bumpy Truth Blog
- Fertility Products Resource Guide
Pregnancy Tools
- Ovulation Calendar
- Baby Names Directory
- Pregnancy Due Date Calculator
- Pregnancy Quiz
Pregnancy Journeys
- Partner With Us
- Corporate Sponsors
Clinical exam
Palpation of the abdomen to determine the position of the baby's head
Palpation of the abdomen to confirm the position of the fetal spine on one side and fetal extremities on the other
Palpation of the area above the symphysis pubis to locate the fetal presenting part
Palpation of the presenting part to confirm presentation, to determine how far the fetus has descended and whether the fetus is engaged.
Ultrasound examination
Premature fetus.
Prematurity is consistently associated with breech presentation. [ 6 ] [ 9 ] This may be due to the smaller size of preterm infants, who are more likely to change their in utero position.
Increasing duration of pregnancy may allow breech-presenting fetuses time to grow, turn spontaneously or by external cephalic version, and remain cephalic-presenting.
Larger fetuses may be forced into a cephalic presentation in late pregnancy due to space or alignment constraints within the uterus.
small for gestational age fetus
Low birth-weight is a risk factor for breech presentation. [ 9 ] [ 11 ] [ 12 ] [ 13 ] [ 14 ] Term breech births are associated with a smaller fetal size for gestational age, highlighting the association with low birth-weight rather than prematurity. [ 6 ]
nulliparity
Women having a first birth have increased rates of breech presentation, probably due to the increased likelihood of smaller fetal size. [ 6 ] [ 9 ]
Relaxation of the uterine wall in multiparous women may reduce the odds of breech birth and contribute to a higher spontaneous or external cephalic version rate. [ 10 ]
fetal congenital anomalies
Congenital anomalies in the fetus may result in a small fetal size or inappropriate fetal growth. [ 9 ] [ 12 ] [ 14 ] [ 15 ]
Anencephaly, hydrocephaly, Down syndrome, and fetal neuromuscular dysfunction are associated with breech presentation, the latter due to its effect on the quality of fetal movements. [ 9 ] [ 14 ]
previous breech delivery
The risk of recurrent breech delivery is 8%, the risk increasing from 4% after one breech delivery to 28% after three. [ 16 ]
The effects of recurrence may be due to recurring specific causal factors, either genetic or environmental in origin.
uterine abnormalities
Women with uterine abnormalities have a high incidence of breech presentation. [ 14 ] [ 17 ] [ 18 ] [ 19 ]
female fetus
Fifty-four percent of breech-presenting fetuses are female. [ 14 ]
abnormal amniotic fluid volume
Both oligohydramnios and polyhydramnios are associated with breech presentation. [ 1 ] [ 12 ] [ 14 ]
Low amniotic fluid volume decreases the likelihood of a fetus turning to a cephalic position; an increased amniotic fluid volume may facilitate frequent change in position.
placental abnormalities
An association between placental implantation in the cornual-fundal region and breech presentation has been reported, although some studies have not found it a risk factor. [ 8 ] [ 20 ] [ 21 ] [ 22 ] [ 10 ] [ 14 ]
The association with placenta previa is also inconsistent. [ 8 ] [ 9 ] [ 22 ] Placenta previa is associated with preterm birth and may be an indirect risk factor.
Pelvic or vaginal examination reveals the buttocks and/or feet, felt as a yielding, irregular mass, as the presenting part. [ 26 ] In cephalic presentation, a hard, round, regular fetal head can be palpated. [ 26 ]
The Leopold maneuver on examination suggests breech position by palpation of the fetal head under the costal margin. [ 26 ]
The baby's heartbeat should be auscultated using a Pinard stethoscope or a hand-held Doppler to indicate the position of the fetus. The fetal heartbeat lies above the maternal umbilicus in breech presentation. [ 1 ]
Tenderness under one or other costal margin as a result of pressure by the harder fetal head.
Pain due to fetal kicks in the maternal pelvis or bladder.
breech position
Visualizes the fetus and reveals its position.
Used to confirm a clinically suspected breech presentation. [ 28 ]
Should be performed by practitioners with appropriate skills in obstetric ultrasound.
Establishes the type of breech presentation by imaging the fetal femurs and their relationship to the distal bones.
Transverse lie
Differentiating Signs/Symptoms
Fetus lies horizontally across the uterus with the shoulder as the presenting part.
Similar predisposing factors such as placenta previa, abnormal amniotic fluid volume, and uterine anomalies, although more common in multiparity. [ 1 ] [ 2 ] [ 29 ]
Differentiating Tests
Clinical examination and fetal auscultation may be indicative.
Ultrasound confirms presentation.
Treatment Approach
Breech presentation <37 weeks' gestation.
The UK Royal College of Obstetricians and Gynaecologists (RCOG) recommends that corticosteroids should be offered to women between 24 and 34+6 weeks' gestation, in whom imminent preterm birth is anticipated. Corticosteroids should only be considered after discussion of risks/benefits at 35 to 36+6 weeks. Given within 7 days of preterm birth, corticosteroids may reduce perinatal and neonatal death and respiratory distress syndrome. [ 32 ] The American College of Obstetricians and Gynecologists (ACOG) recommends a single course of corticosteroids for pregnant women between 24 and 33+6 weeks' gestation who are at risk of preterm delivery within 7 days, including those with ruptured membranes and multiple gestations. It may also be considered for pregnant women starting at 23 weeks' gestation who are at risk of preterm delivery within 7 days. A single course of betamethasone is recommended for pregnant women between 34 and 36+6 weeks' gestation at risk of preterm birth within 7 days, and who have not received a previous course of prenatal corticosteroids. Regularly scheduled repeat courses or serial courses (more than two) are not currently recommended. A single repeat course of prenatal corticosteroids should be considered in women who are less than 34 weeks' gestation, who are at risk of preterm delivery within 7 days, and whose prior course of prenatal corticosteroids was administered more than 14 days previously. Rescue course corticosteroids could be provided as early as 7 days from the prior dose, if indicated by the clinical scenario. [ 33 ]
Magnesium sulfate given before anticipated early preterm birth reduces the risk of cerebral palsy in surviving infants. Physicians electing to use magnesium sulfate for fetal neuroprotection should develop specific guidelines regarding inclusion criteria, treatment regimens, and concurrent tocolysis. [ 34 ]
Breech presentation from 37 weeks' gestation, before labor
ECV is the initial treatment for a breech presentation at term when the patient is not in labor. It involves turning a fetus presenting by the breech to a cephalic (head-down) presentation to increase the likelihood of vaginal birth. [ 35 ] [ 36 ] Where available, it should be offered to all women in late pregnancy, by an experienced clinician, in hospitals with facilities for emergency delivery, and no contraindications to the procedure. [ 35 ] There is no upper time limit on the appropriate gestation for ECV, with success reported at 42 weeks.
There is no general consensus on contraindications to ECV. Contraindications include multiple pregnancy (except after delivery of a first twin), ruptured membranes, current or recent (<1 week) vaginal bleeding, rhesus isoimmunization, other indications for cesarean section (e.g., placenta previa or uterine malformation), or abnormal electronic fetal monitoring. [ 35 ] One systematic review of relative contraindications for ECV highlighted that most contraindications do not have clear empirical evidence. Exceptions include placental abruption, severe preeclampsia/HELLP syndrome, or signs of fetal distress (abnormal cardiotocography and/or Doppler flow). [ 36 ]
The procedure involves applying external pressure and firmly pushing or palpating the mother's abdomen to coerce the fetus to somersault (either forward or backward) into a cephalic position. [ 37 ]
The overall ECV success rate varies but, in a large series, 47% of women following an ECV attempt had a cephalic presentation at birth. [ 35 ] [ 38 ] Various factors influence the success rate. One systematic review found ECV success rates to be 68% overall, with the rate significantly higher for women from African countries (89%) compared with women from non-African countries (62%), and higher among multiparous (78%) than nulliparous women (48%). [ 39 ] Overall, the ECV success rates for nulliparous and multiparous non-African women were 43% and 73%, respectively, while for nulliparous and multiparous African women rates were 79% and 91%, respectively. Another study reported no difference in success rate or rate of cesarean section among women with previous cesarean section undergoing ECV compared with women with previous vaginal birth. However, numbers were small and further studies in this regard are required. [ 40 ]
Women's preference for vaginal delivery is a major contributing factor in their decision for ECV. However, studies suggest women with a breech presentation at term may not receive complete and/or evidence-based information about the benefits and risks of ECV. [ 41 ] [ 42 ] Although up to 60% of women reported ECV to be painful, the majority highlighted the benefits outweigh the risks (71%) and would recommend ECV to their friends or be willing to repeat for themselves (84%). [ 41 ] [ 42 ]
Cardiotocography and ultrasound should be performed before and after the procedure. Tocolysis should be used to facilitate the maneuver, and Rho(D) immune globulin should be administered to women who are Rhesus negative. [ 35 ] Tocolytic agents include adrenergic beta-2 receptor stimulants such as albuterol, terbutaline, or ritodrine (widely used with ECV in some countries, but not yet available in the US). One Cochrane review of tocolytic beta stimulants demonstrates that these are less likely to be associated with failed ECV, and are effective in increasing cephalic presentation and reducing cesarean section. [ 43 ] There is no current evidence to recommend one beta-2 adrenergic receptor agonist over another. Until these data are available, adherence to a local protocol for tocolysis is recommended. The Food and Drug Administration has issued a warning against using injectable terbutaline beyond 48 to 72 hours, or acute or prolonged treatment with oral terbutaline, in pregnant women for the prevention or prolonged treatment of preterm labor, due to potential serious maternal cardiac adverse effects and death. [ 44 ] Whether this warning applies to the subcutaneous administration of terbutaline in ECV is still unclear; however, studies currently support this use. The European Medicines Agency (EMA) recommends that injectable beta agonists should be used for up to 48 hours between the 22nd and 37th week of pregnancy only. They should be used under specialist supervision with continuous monitoring of the mother and unborn baby owing to the risk of adverse cardiovascular effects in both the mother and baby. The EMA no longer recommends oral or rectal formulations for obstetric indications. [ 45 ]
If ECV is successful, pregnancy care should continue as usual for any cephalic presentation. One systematic review assessing the mode of delivery after a successful ECV found that these women were at increased risk for cesarean section and instrumental vaginal delivery compared with women with spontaneous cephalic pregnancies. However, they still had a lower rate of cesarean section following ECV (i.e., 47%) compared with the cesarean section rate for those with a persisting breech (i.e., 85%). With a number needed to treat of three, ECV is still considered to be an effective means of preventing the need for cesarean section. [ 46 ]
Planned cesarean section should be offered as the safest mode of delivery for the baby, even though it carries a small increase in serious immediate maternal complications compared with vaginal birth. [ 24 ] [ 25 ] [ 31 ] In the US, most unsuccessful ECV with persistent breech will be delivered via cesarean section.
A vaginal mode of delivery may be considered by some clinicians as an option, particularly when maternal request is provided, senior and experienced staff are available, there is no absolute contraindication to vaginal birth (e.g., placenta previa, compromised fetal condition), and with optimal fetal growth (estimated weight above the tenth centile and up to 3800 g). Other factors that make planned vaginal birth higher risk include hyperextended neck on ultrasound and footling presentation. [ 24 ]
Breech presentation from 37 weeks' gestation, during labor
The first option should be a planned cesarean section.
There is a small increase in the risk of serious immediate maternal complications compared with vaginal birth (RR 1.29, 95% CI 1.03 to 1.61), including pulmonary embolism, infection, bleeding, damage to the bladder and bowel, slower recovery from the delivery, longer hospitalization, and delayed bonding and breast-feeding. [ 23 ] [ 31 ] [ 47 ] [ 48 ] [ 49 ] [ 50 ] [ 51 ] [ 52 ] [ 53 ] [ 54 ] [ 55 ] [ 56 ] [ 57 ] [ 58 ] Consider using antimicrobial triclosan-coated sutures for wound closure to reduce the risk of surgical site infection. [ 59 ]
The long-term risks include potential compromise of future obstetric performance, increased risk of repeat cesarean section, infertility, uterine rupture, placenta accreta, placental abruption, and emergency hysterectomy. [ 60 ] [ 61 ] [ 62 ] [ 63 ]
Planned cesarean section is safer for babies, but is associated with increased neonatal respiratory distress. The risk is reduced when the section is performed at 39 weeks' gestation. [ 64 ] [ 65 ] [ 66 ] For women undergoing a planned cesarean section, RCOG recommends an informed discussion about the potential risks and benefits of a course of prenatal corticosteroids between 37 and 38+6 weeks' gestation. Although prenatal corticosteroids may reduce admission to the neonatal unit for respiratory morbidity, it is uncertain if there is any reduction in respiratory distress syndrome, transient tachypnea of the newborn, or neonatal unit admission overall. In addition, prenatal corticosteroids may result in harm to the neonate, including hypoglycemia and potential developmental delay. [ 32 ] ACOG does not recommend corticosteroids in women >37 weeks' gestation. [ 33 ]
Undiagnosed breech in labor generally results in cesarean section after the onset of labor, higher rates of emergency cesarean section associated with the least favorable maternal outcomes, a greater likelihood of cord prolapse, and other poor infant outcomes. [ 23 ] [ 67 ] [ 49 ] [ 68 ] [ 69 ] [ 70 ] [ 71 ]
This mode of delivery may be considered by some clinicians as an option for women who are in labor, particularly when delivery is imminent. Vaginal breech delivery may also be considered, where suitable, when delivery is not imminent, maternal request is provided, senior and experienced staff are available, there is no absolute contraindication to vaginal birth (e.g., placenta previa, compromised fetal condition), and with optimal fetal growth (estimated weight above the tenth centile and up to 3800 g). Other factors that make planned vaginal birth higher risk include hyperextended neck on ultrasound and footling presentation. [ 24 ]
Findings from one systematic review of 27 observational studies revealed that the absolute risks of perinatal mortality, fetal neurologic morbidity, birth trauma, 5-minute Apgar score <7, and neonatal asphyxia in the planned vaginal delivery group were low at 0.3%, 0.7%, 0.7%, 2.4%, and 3.3%, respectively. However, the relative risks of perinatal mortality and morbidity were 2- to 5-fold higher in the planned vaginal than in the planned cesarean delivery group. Authors recommend ongoing judicious decision-making for vaginal breech delivery for selected singleton, term breech babies. [ 72 ]
ECV may also be considered an option for women with breech presentation in early labor, when delivery is not imminent, provided that the membranes are intact.
A woman presenting with a breech presentation <37 weeks is an area of clinical controversy. Optimal mode of delivery for preterm breech has not been fully evaluated in clinical trials, and the relative risks for the preterm infant and mother remain unclear. In the absence of good evidence, if diagnosis of breech presentation prior to 37 weeks' gestation is made, prematurity and clinical circumstances should determine management and mode of delivery.
Primary Options
12 mg intramuscularly every 24 hours for 2 doses
6 mg intramuscularly every 12 hours for 4 doses
The UK Royal College of Obstetricians and Gynaecologists recommends that corticosteroids should be offered to women between 24 and 34+6 weeks' gestation, in whom imminent preterm birth is anticipated. Corticosteroids should only be considered after discussion of risks/benefits at 35 to 36+6 weeks. Given within 7 days of preterm birth, corticosteroids may reduce perinatal and neonatal death and respiratory distress syndrome. [ 32 ]
The American College of Obstetricians and Gynecologists recommends a single course of corticosteroids for pregnant women between 24 and 33+6 weeks' gestation who are at risk of preterm delivery within 7 days, including those with ruptured membranes and multiple gestations. It may also be considered for pregnant women starting at 23 weeks' gestation who are at risk of preterm delivery within 7 days. A single course of betamethasone is recommended for pregnant women between 34 and 36+6 weeks' gestation at risk of preterm birth within 7 days, and who have not received a previous course of prenatal corticosteroids. Regularly scheduled repeat courses or serial courses (more than two) are not currently recommended. A single repeat course of prenatal corticosteroids should be considered in women who are less than 34 weeks' gestation, who are at risk of preterm delivery within 7 days, and whose prior course of prenatal corticosteroids was administered more than 14 days previously. Rescue course corticosteroids could be provided as early as 7 days from the prior dose, if indicated by the clinical scenario. [ 33 ]
consult specialist for guidance on dose
external cephalic version (ECV)
There is no upper time limit on the appropriate gestation for ECV; it should be offered to all women in late pregnancy by an experienced clinician in hospitals with facilities for emergency delivery and no contraindications to the procedure. [ 35 ] [ 36 ]
ECV involves applying external pressure and firmly pushing or palpating the mother's abdomen to coerce the fetus to somersault (either forward or backward) into a cephalic position. [ 37 ]
There is no general consensus on contraindications to ECV. Contraindications include multiple pregnancy (except after delivery of a first twin), ruptured membranes, current or recent (<1 week) vaginal bleeding, rhesus isoimmunization, other indications for cesarean section (e.g., placenta previa or uterine malformation), or abnormal electronic fetal monitoring. [ 35 ] One systematic review of relative contraindications for ECV highlighted that most contraindications do not have clear empirical evidence. Exceptions include placental abruption, severe preeclampsia/HELLP syndrome, or signs of fetal distress (abnormal cardiotocography and/or Doppler flow). [ 36 ]
Cardiotocography and ultrasound should be performed before and after the procedure.
If ECV is successful, pregnancy care should continue as usual for any cephalic presentation. A systematic review assessing the mode of delivery after a successful ECV found that these women were at increased risk for cesarean section and instrumental vaginal delivery compared with women with spontaneous cephalic pregnancies. However, they still had a lower rate of cesarean section following ECV (i.e., 47%) compared with the cesarean section rate for those with a persisting breech (i.e., 85%). With a number needed to treat of 3, ECV is still considered to be an effective means of preventing the need for cesarean section. [ 46 ]
tocolytic agents
see local specialist protocol for dosing guidelines
Tocolytic agents include adrenergic beta-2 receptor stimulants such as albuterol, terbutaline, or ritodrine (widely used with external cephalic version [ECV] in some countries, but not yet available in the US). They are used to delay or inhibit labor and increase the success rate of ECV. There is no current evidence to recommend one beta-2 adrenergic receptor agonist over another. Until these data are available, adherence to a local protocol for tocolysis is recommended.
The Food and Drug Administration has issued a warning against using injectable terbutaline beyond 48-72 hours, or acute or prolonged treatment with oral terbutaline, in pregnant women for the prevention or prolonged treatment of preterm labor, due to potential serious maternal cardiac adverse effects and death. [ 44 ] Whether this warning applies to the subcutaneous administration of terbutaline in ECV is still unclear; however, studies currently support this use. The European Medicines Agency (EMA) recommends that injectable beta agonists should be used for up to 48 hours between the 22nd and 37th week of pregnancy only. They should be used under specialist supervision with continuous monitoring of the mother and unborn baby owing to the risk of adverse cardiovascular effects in both the mother and baby. The EMA no longer recommends oral or rectal formulations for obstetric indications. [ 45 ]
A systematic review found there was no evidence to support the use of nifedipine for tocolysis. [ 73 ]
There is insufficient evidence to evaluate other interventions to help ECV, such as fetal acoustic stimulation in midline fetal spine positions, or epidural or spinal analgesia. [ 43 ]
Rho(D) immune globulin
300 micrograms intramuscularly as a single dose
Nonsensitized Rh-negative women should receive Rho(D) immune globulin. [ 35 ]
The indication for its administration is to prevent rhesus isoimmunization, which may affect subsequent pregnancy outcomes.
Rho(D) immune globulin needs to be given at the time of external cephalic version and should be given again postpartum to those women who give birth to an Rh-positive baby. [ 74 ]
It is best administered as soon as possible after the procedure, usually within 72 hours.
Dose depends on brand used. Dose given below pertains to most commonly used brands. Consult specialist for further guidance on dose.
elective cesarean section/vaginal breech delivery
Mode of delivery (cesarean section or vaginal breech delivery) should be based on the experience of the attending clinician, hospital policies, maternal request, and the presence or absence of complicating factors. In the US, most unsuccessful external cephalic version (ECV) with persistent breech will be delivered via cesarean section.
Cesarean section, at 39 weeks or greater, has been shown to significantly reduce perinatal mortality and neonatal morbidity compared with vaginal breech delivery (RR 0.33, 95% CI 0.19 to 0.56). [ 31 ] Although safer for these babies, there is a small increase in serious immediate maternal complications compared with vaginal birth (RR 1.29, 95% CI 1.03 to 1.61), as well as long-term risks for future pregnancies, including pulmonary embolism, bleeding, infection, damage to the bladder and bowel, slower recovery from the delivery, longer hospitalization, and delayed bonding and breast-feeding. [ 23 ] [ 31 ] [ 47 ] [ 48 ] [ 49 ] [ 50 ] [ 51 ] [ 52 ] [ 53 ] [ 54 ] [ 55 ] [ 56 ] [ 57 ] [ 58 ] Consider using antimicrobial triclosan-coated sutures for wound closure to reduce the risk of surgical site infection. [ 59 ]
Vaginal delivery may be considered by some clinicians as an option, particularly when maternal request is provided, when senior and experienced staff are available, when there is no absolute contraindication to vaginal birth (e.g., placenta previa, compromised fetal condition), and with optimal fetal growth (estimated weight above the tenth centile and up to 3800 g). Other factors that make planned vaginal birth higher risk include hyperextended neck on ultrasound and footling presentation. [ 24 ]
For women undergoing a planned cesarean section, the UK Royal College of Obstetricians and Gynaecologists recommends an informed discussion about the potential risks and benefits of a course of prenatal corticosteroids between 37 and 38+6 weeks' gestation. Although prenatal corticosteroids may reduce admission to the neonatal unit for respiratory morbidity, it is uncertain if there is any reduction in respiratory distress syndrome, transient tachypnea of the newborn, or neonatal unit admission overall. In addition, prenatal corticosteroids may result in harm to the neonate, including hypoglycemia and potential developmental delay. [ 32 ] The American College of Obstetricians and Gynecologists does not recommend corticosteroids in women >37 weeks' gestation. [ 33 ]
It is best administered as soon as possible after delivery, usually within 72 hours.
Administration of postpartum Rho (D) immune globulin should not be affected by previous routine prenatal prophylaxis or previous administration for a potentially sensitizing event. [ 74 ]
≥37 weeks' gestation in labor: no imminent delivery
planned cesarean section
For women with breech presentation in labor, planned cesarean section at 39 weeks or greater has been shown to significantly reduce perinatal mortality and neonatal morbidity compared with vaginal breech delivery (RR 0.33, 95% CI 0.19 to 0.56). [ 31 ]
Although safer for these babies, there is a small increase in serious immediate maternal complications compared with vaginal birth (RR 1.29, 95% CI 1.03 to 1.61), as well as long-term risks for future pregnancies, including pulmonary embolism, infection, bleeding, damage to the bladder and bowel, slower recovery from the delivery, longer hospitalization, and delayed bonding and breast-feeding. [ 23 ] [ 31 ] [ 47 ] [ 48 ] [ 49 ] [ 50 ] [ 51 ] [ 52 ] [ 53 ] [ 54 ] [ 55 ] [ 56 ] [ 57 ] [ 58 ] Consider using antimicrobial triclosan-coated sutures for wound closure to reduce the risk of surgical site infection. [ 59 ]
Continuous cardiotocography monitoring should continue until delivery. [ 24 ] [ 25 ]
vaginal breech delivery
Mode of delivery (cesarean section or vaginal breech delivery) should be based on the experience of the attending clinician, hospital policies, maternal request, and the presence or absence of complicating factors.
This mode of delivery may be considered by some clinicians as an option, particularly when maternal request is provided, when senior and experienced staff are available, when there is no absolute contraindication to vaginal birth (e.g., placenta previa, compromised fetal condition), and with optimal fetal growth (estimated weight above the tenth centile and up to 3800 g). Other factors that make planned vaginal birth higher risk include hyperextended neck on ultrasound and footling presentation. [ 24 ]
For women with persisting breech presentation, planned cesarean section has, however, been shown to significantly reduce perinatal mortality and neonatal morbidity compared with vaginal breech delivery (RR 0.33, 95% CI 0.19 to 0.56). [ 31 ]
ECV may also be considered an option for women with breech presentation in early labor, provided that the membranes are intact.
There is no upper time limit on the appropriate gestation for ECV. [ 35 ]
Involves applying external pressure and firmly pushing or palpating the mother's abdomen to coerce the fetus to somersault (either forward or backward) into a cephalic position. [ 37 ]
Relative contraindications include placental abruption, severe preeclampsia/HELLP syndrome, and signs of fetal distress (abnormal cardiotocography and/or abnormal Doppler flow). [ 35 ] [ 36 ]
Rho(D) immune globulin needs to be given at the time of ECV and should be given again postpartum to those women who give birth to an Rh-positive baby. [ 74 ]
≥37 weeks' gestation in labor: imminent delivery
cesarean section
For women with persistent breech presentation, planned cesarean section has been shown to significantly reduce perinatal mortality and neonatal morbidity compared with vaginal breech delivery (RR 0.33, 95% CI 0.19 to 0.56). [ 31 ] Although safer for these babies, there is a small increase in serious immediate maternal complications compared with vaginal birth (RR 1.29, 95% CI 1.03 to 1.61), as well as long-term risks for future pregnancies, including pulmonary embolism, infection, bleeding, damage to the bladder and bowel, slower recovery from the delivery, longer hospitalization, and delayed bonding and breast-feeding. [ 23 ] [ 31 ] [ 47 ] [ 48 ] [ 49 ] [ 50 ] [ 51 ] [ 52 ] [ 53 ] [ 54 ] [ 55 ] [ 56 ] [ 57 ] [ 58 ] Consider using antimicrobial triclosan-coated sutures for wound closure to reduce the risk of surgical site infection. [ 59 ]
This mode of delivery may be considered by some clinicians as an option, particularly when delivery is imminent, maternal request is provided, when senior and experienced staff are available, when there is no absolute contraindication to vaginal birth (e.g., placenta previa, compromised fetal condition), and with optimal fetal growth (estimated weight above the tenth centile and up to 3800 g). Other factors that make planned vaginal birth higher risk include hyperextended neck on ultrasound and footling presentation. [ 24 ]
It is best administered as soon as possible after the delivery, usually within 72 hours.
External cephalic version before term
Moxibustion, postural management, follow-up overview, perinatal complications.
Compared with cephalic presentation, persistent breech presentation has increased frequency of cord prolapse, abruptio placentae, prelabor rupture of membranes, perinatal mortality, fetal distress (heart rate <100 bpm), preterm delivery, lower fetal weight. [ 10 ] [ 11 ] [ 67 ]
complications of cesarean section
There is a small increase in the risk of serious immediate maternal complications compared with vaginal birth (RR 1.29, 95% CI 1.03 to 1.61), including pulmonary embolism, infection, bleeding, damage to the bladder and bowel, slower recovery from the delivery, longer hospitalization, and delayed bonding and breast-feeding. [ 23 ] [ 31 ] [ 47 ] [ 48 ] [ 49 ] [ 50 ] [ 51 ] [ 52 ] [ 53 ] [ 54 ] [ 55 ] [ 56 ] [ 57 ] [ 58 ]
The long-term risks include potential compromise of future obstetric performance, increased risk of repeat cesarean section, infertility, uterine rupture, placenta accreta, placental abruption, and emergency hysterectomy. [ 60 ] [ 61 ] [ 62 ] [ 63 ] The evidence suggests that using sutures, rather than staples, for wound closure after cesarean section reduces the incidence of wound dehiscence. [ 59 ]
Emergency cesarean section, compared with planned cesarean section, has demonstrated a higher risk of severe obstetric morbidity, intra-operative complications, postoperative complications, infection, blood loss >1500 mL, fever, pain, tiredness, and breast-feeding problems. [ 23 ] [ 48 ] [ 50 ] [ 70 ] [ 81 ]
Key Articles
Impey LWM, Murphy DJ, Griffiths M, et al; Royal College of Obstetricians and Gynaecologists. Management of breech presentation: green-top guideline no. 20b. BJOG. 2017 Jun;124(7):e151-77. [Full Text]
Hofmeyr GJ, Hannah M, Lawrie TA. Planned caesarean section for term breech delivery. Cochrane Database Syst Rev. 2015 Jul 21;(7):CD000166. [Abstract] [Full Text]
Royal College of Obstetricians and Gynaecologists. External cephalic version and reducing the incidence of term breech presentation. March 2017 [internet publication]. [Full Text]
Cluver C, Gyte GM, Sinclair M, et al. Interventions for helping to turn term breech babies to head first presentation when using external cephalic version. Cochrane Database Syst Rev. 2015 Feb 9;(2):CD000184. [Abstract] [Full Text]
de Hundt M, Velzel J, de Groot CJ, et al. Mode of delivery after successful external cephalic version: a systematic review and meta-analysis. Obstet Gynecol. 2014 Jun;123(6):1327-34. [Abstract]
Referenced Articles
1. Cunningham F, Gant N, Leveno K, et al. Williams obstetrics. 21st ed. New York: McGraw-Hill; 1997.
2. Kish K, Collea JV. Malpresentation and cord prolapse. In: DeCherney AH, Nathan L, eds. Current obstetric and gynecologic diagnosis and treatment. New York: McGraw-Hill Professional; 2002.
3. Scheer K, Nubar J. Variation of fetal presentation with gestational age. Am J Obstet Gynecol. 1976 May 15;125(2):269-70. [Abstract]
4. Nassar N, Roberts CL, Cameron CA, et al. Diagnostic accuracy of clinical examination for detection of non-cephalic presentation in late pregnancy: cross sectional analytic study. BMJ. 2006 Sep 16;333(7568):578-80. [Abstract] [Full Text]
5. Roberts CL, Peat B, Algert CS, et al. Term breech birth in New South Wales, 1990-1997. Aust N Z J Obstet Gynaecol. 2000 Feb;40(1):23-9. [Abstract]
6. Roberts CL, Algert CS, Peat B, et al. Small fetal size: a risk factor for breech birth at term. Int J Gynaecol Obstet. 1999 Oct;67(1):1-8. [Abstract]
7. Brar HS, Platt LD, DeVore GR, et al. Fetal umbilical velocimetry for the surveillance of pregnancies complicated by placenta previa. J Reprod Med. 1988 Sep;33(9):741-4. [Abstract]
8. Kian L. The role of the placental site in the aetiology of breech presentation. J Obstet Gynaecol Br Commonw. 1963 Oct;70:795-7. [Abstract]
9. Rayl J, Gibson PJ, Hickok DE. A population-based case-control study of risk factors for breech presentation. Am J Obstet Gynecol. 1996 Jan;174(1 Pt 1):28-32. [Abstract]
10. Westgren M, Edvall H, Nordstrom L, et al. Spontaneous cephalic version of breech presentation in the last trimester. Br J Obstet Gynaecol. 1985 Jan;92(1):19-22. [Abstract]
11. Brenner WE, Bruce RD, Hendricks CH. The characteristics and perils of breech presentation. Am J Obstet Gynecol. 1974 Mar 1;118(5):700-12. [Abstract]
12. Hall JE, Kohl S. Breech presentation. Am J Obstet Gynecol. 1956 Nov;72(5):977-90. [Abstract]
13. Morgan HS, Kane SH. An analysis of 16,327 breech births. JAMA. 1964 Jan 25;187:262-4. [Abstract]
14. Luterkort M, Persson P, Weldner B. Maternal and fetal factors in breech presentation. Obstet Gynecol. 1984 Jul;64(1):55-9. [Abstract]
15. Braun FH, Jones KL, Smith DW. Breech presentation as an indicator of fetal abnormality. J Pediatr. 1975 Mar;86(3):419-21. [Abstract]
16. Albrechtsen S, Rasmussen S, Dalaker K, et al. Reproductive career after breech presentation: subsequent pregnancy rates, interpregnancy interval, and recurrence. Obstet Gynecol. 1998 Sep;92(3):345-50. [Abstract]
17. Zlopasa G, Skrablin S, Kalafatić D, et al. Uterine anomalies and pregnancy outcome following resectoscope metroplasty. Int J Gynaecol Obstet. 2007 Aug;98(2):129-33. [Abstract]
18. Acién P. Breech presentation in Spain, 1992: a collaborative study. Eur J Obstet Gynecol Reprod Biol. 1995 Sep;62(1):19-24. [Abstract]
19. Michalas SP. Outcome of pregnancy in women with uterine malformation: evaluation of 62 cases. Int J Gynaecol Obstet. 1991 Jul;35(3):215-9. [Abstract]
20. Fianu S, Vaclavinkova V. The site of placental attachment as a factor in the aetiology of breech presentation. Acta Obstet Gynecol Scand. 1978;57(4):371-2. [Abstract]
21. Haruyama Y. Placental implantation as the cause of breech presentation [in Japanese]. Nihon Sanka Fujinka Gakkai Zasshi. 1987 Jan;39(1):92-8. [Abstract]
22. Filipov E, Borisov I, Kolarov G. Placental location and its influence on the position of the fetus in the uterus [in Bulgarian]. Akush Ginekol (Sofiia). 2000;40(4):11-2. [Abstract]
23. Waterstone M, Bewley S, Wolfe C. Incidence and predictors of severe obstetric morbidity: case-control study. BMJ. 2001 May 5;322(7294):1089-93. [Abstract] [Full Text]
24. Impey LWM, Murphy DJ, Griffiths M, et al; Royal College of Obstetricians and Gynaecologists. Management of breech presentation: green-top guideline no. 20b. BJOG. 2017 Jun;124(7):e151-77. [Full Text]
25. American College of Obstetricians and Gynecologists Committee on Obstetric Practice. ACOG committee opinion no. 745: mode of term singleton breech delivery. Obstet Gynecol. 2018 Aug;132(2):e60-3. [Abstract] [Full Text]
26. Beischer NA, Mackay EV, Colditz P, eds. Obstetrics and the newborn: an illustrated textbook. 3rd ed. London: W.B. Saunders; 1997.
27. Royal College of Obstetricians and Gynaecologists. Antepartum haemorrhage: green-top guideline no. 63. November 2011 [internet publication]. [Full Text]
28. American College of Obstetricians and Gynecologists. Practice bulletin no. 175: ultrasound in pregnancy. Obstet Gynecol. 2016 Dec;128(6):e241-56. [Abstract]
29. Enkin M, Keirse MJNC, Neilson J, et al. Guide to effective care in pregnancy and childbirth. 3rd ed. Oxford: Oxford University Press; 2000.
30. Hofmeyr GJ, Kulier R, West HM. External cephalic version for breech presentation at term. Cochrane Database Syst Rev. 2012 Oct 17;(10):CD000083. [Abstract] [Full Text]
31. Hofmeyr GJ, Hannah M, Lawrie TA. Planned caesarean section for term breech delivery. Cochrane Database Syst Rev. 2015 Jul 21;(7):CD000166. [Abstract] [Full Text]
32. Stock SJ, Thomson AJ, Papworth S, et al. Antenatal corticosteroids to reduce neonatal morbidity and mortality: Green-top Guideline No. 74. BJOG. 2022 Jul;129(8):e35-60. [Abstract] [Full Text]
33. American College of Obstetricians and Gynaecologists Committee on Obstetric Practice. Committee opinion no. 713: antenatal corticosteroid therapy for fetal maturation. August 2017 (reaffirmed 2020) [internet publication]. [Full Text]
34. American College of Obstetricians and Gynecologists Committee on Obstetric Practice. Committee opinion no. 455: magnesium sulfate before anticipated preterm birth for neuroprotection. March 2010 (reaffirmed 2020) [internet publication]. [Full Text]
35. Royal College of Obstetricians and Gynaecologists. External cephalic version and reducing the incidence of term breech presentation. March 2017 [internet publication]. [Full Text]
36. Rosman AN, Guijt A, Vlemmix F, et al. Contraindications for external cephalic version in breech position at term: a systematic review. Acta Obstet Gynecol Scand. 2013 Feb;92(2):137-42. [Abstract]
37. Hofmeyr GJ. Effect of external cephalic version in late pregnancy on breech presentation and caesarean section rate: a controlled trial. Br J Obstet Gynaecol. 1983 May;90(5):392-9. [Abstract]
38. Beuckens A, Rijnders M, Verburgt-Doeleman GH, et al. An observational study of the success and complications of 2546 external cephalic versions in low-risk pregnant women performed by trained midwives. BJOG. 2016 Feb;123(3):415-23. [Abstract]
39. Nassar N, Roberts CL, Barratt A, et al. Systematic review of adverse outcomes of external cephalic version and persisting breech presentation at term. Paediatr Perinat Epidemiol. 2006 Mar;20(2):163-71. [Abstract]
40. Sela HY, Fiegenberg T, Ben-Meir A, et al. Safety and efficacy of external cephalic version for women with a previous cesarean delivery. Eur J Obstet Gynecol Reprod Biol. 2009 Feb;142(2):111-4. [Abstract]
41. Pichon M, Guittier MJ, Irion O, et al. External cephalic version in case of persisting breech presentation at term: motivations and women's experience of the intervention [in French]. Gynecol Obstet Fertil. 2013 Jul-Aug;41(7-8):427-32. [Abstract]
42. Nassar N, Roberts CL, Raynes-Greenow CH, et al. Evaluation of a decision aid for women with breech presentation at term: a randomised controlled trial [ISRCTN14570598]. BJOG. 2007 Mar;114(3):325-33. [Abstract] [Full Text]
43. Cluver C, Gyte GM, Sinclair M, et al. Interventions for helping to turn term breech babies to head first presentation when using external cephalic version. Cochrane Database Syst Rev. 2015 Feb 9;(2):CD000184. [Abstract] [Full Text]
44. US Food & Drug Administration. FDA Drug Safety Communication: new warnings against use of terbutaline to treat preterm labor. Feb 2011 [internet publication]. [Full Text]
45. European Medicines Agency. Restrictions on use of short-acting beta-agonists in obstetric indications - CMDh endorses PRAC recommendations. October 2013 [internet publication]. [Full Text]
46. de Hundt M, Velzel J, de Groot CJ, et al. Mode of delivery after successful external cephalic version: a systematic review and meta-analysis. Obstet Gynecol. 2014 Jun;123(6):1327-34. [Abstract]
47. Lydon-Rochelle M, Holt VL, Martin DP, et al. Association between method of delivery and maternal rehospitalisation. JAMA. 2000 May 10;283(18):2411-6. [Abstract]
48. Yokoe DS, Christiansen CL, Johnson R, et al. Epidemiology of and surveillance for postpartum infections. Emerg Infect Dis. 2001 Sep-Oct;7(5):837-41. [Abstract]
49. van Ham MA, van Dongen PW, Mulder J. Maternal consequences of caesarean section. A retrospective study of intra-operative and postoperative maternal complications of caesarean section during a 10-year period. Eur J Obstet Gynecol Reprod Biol. 1997 Jul;74(1):1-6. [Abstract]
50. Murphy DJ, Liebling RE, Verity L, et al. Early maternal and neonatal morbidity associated with operative delivery in second stage of labour: a cohort study. Lancet. 2001 Oct 13;358(9289):1203-7. [Abstract]
51. Lydon-Rochelle MT, Holt VL, Martin DP. Delivery method and self-reported postpartum general health status among primiparous women. Paediatr Perinat Epidemiol. 2001 Jul;15(3):232-40. [Abstract]
52. Wilson PD, Herbison RM, Herbison GP. Obstetric practice and the prevalence of urinary incontinence three months after delivery. Br J Obstet Gynaecol. 1996 Feb;103(2):154-61. [Abstract]
53. Persson J, Wolner-Hanssen P, Rydhstroem H. Obstetric risk factors for stress urinary incontinence: a population-based study. Obstet Gynecol. 2000 Sep;96(3):440-5. [Abstract]
54. MacLennan AH, Taylor AW, Wilson DH, et al. The prevalence of pelvic disorders and their relationship to gender, age, parity and mode of delivery. BJOG. 2000 Dec;107(12):1460-70. [Abstract]
55. Thompson JF, Roberts CL, Currie M, et al. Prevalence and persistence of health problems after childbirth: associations with parity and method of birth. Birth. 2002 Jun;29(2):83-94. [Abstract]
56. Australian Institute of Health and Welfare. Australia's mothers and babies 2015 - in brief. October 2017 [internet publication]. [Full Text]
57. Mutryn CS. Psychosocial impact of cesarean section on the family: a literature review. Soc Sci Med. 1993 Nov;37(10):1271-81. [Abstract]
58. DiMatteo MR, Morton SC, Lepper HS, et al. Cesarean childbirth and psychosocial outcomes: a meta-analysis. Health Psychol. 1996 Jul;15(4):303-14. [Abstract]
59. National Institute for Health and Care Excellence. Caesarean birth. Mar 2021 [internet publication]. [Full Text]
60. Greene R, Gardeit F, Turner MJ. Long-term implications of cesarean section. Am J Obstet Gynecol. 1997 Jan;176(1 Pt 1):254-5. [Abstract]
61. Coughlan C, Kearney R, Turner MJ. What are the implications for the next delivery in primigravidae who have an elective caesarean section for breech presentation? BJOG. 2002 Jun;109(6):624-6. [Abstract]
62. Hemminki E, Merilainen J. Long-term effects of cesarean sections: ectopic pregnancies and placental problems. Am J Obstet Gynecol. 1996 May;174(5):1569-74. [Abstract]
63. Gilliam M, Rosenberg D, Davis F. The likelihood of placenta previa with greater number of cesarean deliveries and higher parity. Obstet Gynecol. 2002 Jun;99(6):976-80. [Abstract]
64. Morrison JJ, Rennie JM, Milton PJ. Neonatal respiratory morbidity and mode of delivery at term: influence of timing of elective caesarean section. Br J Obstet Gynaecol. 1995 Feb;102(2):101-6. [Abstract]
65. Annibale DJ, Hulsey TC, Wagner CL, et al. Comparative neonatal morbidity of abdominal and vaginal deliveries after uncomplicated pregnancies. Arch Pediatr Adolesc Med. 1995 Aug;149(8):862-7. [Abstract]
66. Hook B, Kiwi R, Amini SB, et al. Neonatal morbidity after elective repeat cesarean section and trial of labor. Pediatrics. 1997 Sep;100(3 Pt 1):348-53. [Abstract]
67. Nassar N, Roberts CL, Cameron CA, et al. Outcomes of external cephalic version and breech presentation at term: an audit of deliveries at a Sydney tertiary obstetric hospital, 1997-2004. Acta Obstet Gynecol Scand. 2006;85(10):1231-8. [Abstract]
68. Nwosu EC, Walkinshaw S, Chia P, et al. Undiagnosed breech. Br J Obstet Gynaecol. 1993 Jun;100(6):531-5. [Abstract]
69. Flamm BL, Ruffini RM. Undetected breech presentation: impact on external version and cesarean rates. Am J Perinatol. 1998 May;15(5):287-9. [Abstract]
70. Cockburn J, Foong C, Cockburn P. Undiagnosed breech. Br J Obstet Gynaecol. 1994 Jul;101(7):648-9. [Abstract]
71. Leung WC, Pun TC, Wong WM. Undiagnosed breech revisited. Br J Obstet Gynaecol. 1999 Jul;106(7):638-41. [Abstract]
72. Berhan Y, Haileamlak A. The risks of planned vaginal breech delivery versus planned caesarean section for term breech birth: a meta-analysis including observational studies. BJOG. 2016 Jan;123(1):49-57. [Abstract] [Full Text]
73. Wilcox C, Nassar N, Roberts C. Effectiveness of nifedipine tocolysis to facilitate external cephalic version: a systematic review. BJOG. 2011 Mar;118(4):423-8. [Abstract]
74. Qureshi H, Massey E, Kirwan D, et al. BCSH guideline for the use of anti-D immunoglobulin for the prevention of haemolytic disease of the fetus and newborn. Transfus Med. 2014 Feb;24(1):8-20. [Abstract] [Full Text]
75. Hutton EK, Hofmeyr GJ, Dowswell T. External cephalic version for breech presentation before term. Cochrane Database Syst Rev. 2015 Jul 29;(7):CD000084. [Abstract] [Full Text]
76. Coyle ME, Smith CA, Peat B. Cephalic version by moxibustion for breech presentation. Cochrane Database Syst Rev. 2012 May 16;(5):CD003928. [Abstract] [Full Text]
77. Hofmeyr GJ, Kulier R. Cephalic version by postural management for breech presentation. Cochrane Database Syst Rev. 2012 Oct 17;(10):CD000051. [Abstract] [Full Text]
78. Hannah ME, Whyte H, Hannah WJ, et al. Maternal outcomes at 2 years after planned cesarean section versus planned vaginal birth for breech presentation at term: the International Randomized Term Breech Trial. Am J Obstet Gynecol. 2004 Sep;191(3):917-27. [Abstract]
79. Eide MG, Oyen N, Skjaerven R, et al. Breech delivery and Intelligence: a population-based study of 8,738 breech infants. Obstet Gynecol. 2005 Jan;105(1):4-11. [Abstract]
80. Whyte H, Hannah ME, Saigal S, et al. Outcomes of children at 2 years after planned cesarean birth versus planned vaginal birth for breech presentation at term: the International Randomized Term Breech Trial. Am J Obstet Gynecol. 2004 Sep;191(3):864-71. [Abstract]
81. Brown S, Lumley J. Maternal health after childbirth: results of an Australian population based survey. Br J Obstet Gynaecol. 1998 Feb;105(2):156-61. [Abstract]
Published by
American College of Obstetricians and Gynecologists
2016 (reaffirmed 2022)
Royal College of Obstetricians and Gynaecologists (UK)
National Institute for Health and Care Excellence (UK)
Topic last updated: 2024-03-05
Natasha Nassar , PhD
Associate Professor
Menzies Centre for Health Policy
Sydney School of Public Health
University of Sydney
Christine L. Roberts , MBBS, FAFPHM, DrPH
Research Director
Clinical and Population Health Division
Perinatal Medicine Group
Kolling Institute of Medical Research
Jonathan Morris , MBChB, FRANZCOG, PhD
Professor of Obstetrics and Gynaecology and Head of Department
Peer Reviewers
John W. Bachman , MD
Consultant in Family Medicine
Department of Family Medicine
Mayo Clinic
Rhona Hughes , MBChB
Lead Obstetrician
Lothian Simpson Centre for Reproductive Health
The Royal Infirmary
Brian Peat , MD
Director of Obstetrics
Women's and Children's Hospital
North Adelaide
South Australia
Lelia Duley , MBChB
Professor of Obstetric Epidemiology
University of Leeds
Bradford Institute of Health Research
Temple Bank House
Bradford Royal Infirmary
Justus Hofmeyr , MD
Head of the Department of Obstetrics and Gynaecology
East London Private Hospital
East London
South Africa
Breech baby at the end of pregnancy
Published: July 2017
Please note that this information will be reviewed every 3 years after publication.
This patient information page provides advice if your baby is breech towards the end of pregnancy and the options available to you.
It may also be helpful if you are a partner, relative or friend of someone who is in this situation.
The information here aims to help you better understand your health and your options for treatment and care. Your healthcare team is there to support you in making decisions that are right for you. They can help by discussing your situation with you and answering your questions.
This information is for you if your baby remains in the breech position after 36 weeks of pregnancy. Babies lying bottom first or feet first in the uterus (womb) instead of in the usual head-first position are called breech babies.
This information includes:
- What breech is and why your baby may be breech
- The different types of breech
- The options if your baby is breech towards the end of your pregnancy
- What turning a breech baby in the uterus involves (external cephalic version or ECV)
- How safe ECV is for you and your baby
- Options for birth if your baby remains breech
- Other information and support available
Within this information, we may use the terms ‘woman’ and ‘women’. However, it is not only people who identify as women who may want to access this information. Your care should be personalised, inclusive and sensitive to your needs, whatever your gender identity.
A glossary of medical terms is available at A-Z of medical terms .
- Breech is very common in early pregnancy, and by 36–37 weeks of pregnancy most babies will turn into the head-first position. If your baby remains breech, it does not usually mean that you or your baby have any problems.
- Turning your baby into the head-first position so that you can have a vaginal delivery is a safe option.
- The alternative to turning your baby into the head-first position is to have a planned caesarean section or a planned vaginal breech birth.
Babies lying bottom first or feet first in the uterus (womb) instead of in the usual head-first position are called breech babies. Breech is very common in early pregnancy, and by 36-37 weeks of pregnancy, most babies turn naturally into the head-first position.
Towards the end of pregnancy, only 3-4 in every 100 (3-4%) babies are in the breech position.
A breech baby may be lying in one of the following positions:
It may just be a matter of chance that your baby has not turned into the head-first position. However, there are certain factors that make it more difficult for your baby to turn during pregnancy and therefore more likely to stay in the breech position. These include:
- if this is your first pregnancy
- if your placenta is in a low-lying position (also known as placenta praevia); see the RCOG patient information Placenta praevia, placenta accreta and vasa praevia
- if you have too much or too little fluid ( amniotic fluid ) around your baby
- if you are having more than one baby.
Very rarely, breech may be a sign of a problem with the baby. If this is the case, such problems may be picked up during the scan you are offered at around 20 weeks of pregnancy.
If your baby is breech at 36 weeks of pregnancy, your healthcare professional will discuss the following options with you:
- trying to turn your baby in the uterus into the head-first position by external cephalic version (ECV)
- planned caesarean section
- planned vaginal breech birth.
What does ECV involve?
ECV involves applying gentle but firm pressure on your abdomen to help your baby turn in the uterus to lie head-first.
Relaxing the muscle of your uterus with medication has been shown to improve the chances of turning your baby. This medication is given by injection before the ECV and is safe for both you and your baby. It may make you feel flushed and you may become aware of your heart beating faster than usual but this will only be for a short time.
Before the ECV you will have an ultrasound scan to confirm your baby is breech, and your pulse and blood pressure will be checked. After the ECV, the ultrasound scan will be repeated to see whether your baby has turned. Your baby’s heart rate will also be monitored before and after the procedure. You will be advised to contact the hospital if you have any bleeding, abdominal pain, contractions or reduced fetal movements after ECV.
ECV is usually performed after 36 or 37 weeks of pregnancy. However, it can be performed right up until the early stages of labour. You do not need to make any preparations for your ECV.
ECV can be uncomfortable and occasionally painful but your healthcare professional will stop if you are experiencing pain and the procedure will only last for a few minutes. If your healthcare professional is unsuccessful at their first attempt in turning your baby then, with your consent, they may try again on another day.
If your blood type is rhesus D negative, you will be advised to have an anti-D injection after the ECV and to have a blood test. See the NICE patient information Routine antenatal anti-D prophylaxis for women who are rhesus D negative , which is available at: www.nice.org.uk/guidance/ta156/informationforpublic .
Why turn my baby head-first?
If your ECV is successful and your baby is turned into the head-first position you are more likely to have a vaginal birth. Successful ECV lowers your chances of requiring a caesarean section and its associated risks.
Is ECV safe for me and my baby?
ECV is generally safe with a very low complication rate. Overall, there does not appear to be an increased risk to your baby from having ECV. After ECV has been performed, you will normally be able to go home on the same day.
When you do go into labour, your chances of needing an emergency caesarean section, forceps or vacuum (suction cup) birth is slightly higher than if your baby had always been in a head-down position.
Immediately after ECV, there is a 1 in 200 chance of you needing an emergency caesarean section because of bleeding from the placenta and/or changes in your baby’s heartbeat.
ECV should be carried out by a doctor or a midwife trained in ECV. It should be carried out in a hospital where you can have an emergency caesarean section if needed.
ECV can be carried out on most women, even if they have had one caesarean section before.
ECV should not be carried out if:
- you need a caesarean section for other reasons, such as placenta praevia; see the RCOG patient information Placenta praevia, placenta accreta and vasa praevia
- you have had recent vaginal bleeding
- your baby’s heart rate tracing (also known as CTG) is abnormal
- your waters have broken
- you are pregnant with more than one baby; see the RCOG patient information Multiple pregnancy: having more than one baby .
Is ECV always successful?
ECV is successful for about 50% of women. It is more likely to work if you have had a vaginal birth before. Your healthcare team should give you information about the chances of your baby turning based on their assessment of your pregnancy.
If your baby does not turn then your healthcare professional will discuss your options for birth (see below). It is possible to have another attempt at ECV on a different day.
If ECV is successful, there is still a small chance that your baby will turn back to the breech position. However, this happens to less than 5 in 100 (5%) women who have had a successful ECV.
There is no scientific evidence that lying down or sitting in a particular position can help your baby to turn. There is some evidence that the use of moxibustion (burning a Chinese herb called mugwort) at 33–35 weeks of pregnancy may help your baby to turn into the head-first position, possibly by encouraging your baby’s movements. This should be performed under the direction of a registered healthcare practitioner.
Depending on your situation, your choices are:
There are benefits and risks associated with both caesarean section and vaginal breech birth, and these should be discussed with you so that you can choose what is best for you and your baby.
Caesarean section
If your baby remains breech towards the end of pregnancy, you should be given the option of a caesarean section. Research has shown that planned caesarean section is safer for your baby than a vaginal breech birth. Caesarean section carries slightly more risk for you than a vaginal birth.
Caesarean section can increase your chances of problems in future pregnancies. These may include placental problems, difficulty with repeat caesarean section surgery and a small increase in stillbirth in subsequent pregnancies. See the RCOG patient information Choosing to have a caesarean section .
If you choose to have a caesarean section but then go into labour before your planned operation, your healthcare professional will examine you to assess whether it is safe to go ahead. If the baby is close to being born, it may be safer for you to have a vaginal breech birth.
Vaginal breech birth
After discussion with your healthcare professional about you and your baby’s suitability for a breech delivery, you may choose to have a vaginal breech birth. If you choose this option, you will need to be cared for by a team trained in helping women to have breech babies vaginally. You should plan a hospital birth where you can have an emergency caesarean section if needed, as 4 in 10 (40%) women planning a vaginal breech birth do need a caesarean section. Induction of labour is not usually recommended.
While a successful vaginal birth carries the least risks for you, it carries a small increased risk of your baby dying around the time of delivery. A vaginal breech birth may also cause serious short-term complications for your baby. However, these complications do not seem to have any long-term effects on your baby. Your individual risks should be discussed with you by your healthcare team.
Before choosing a vaginal breech birth, it is advised that you and your baby are assessed by your healthcare professional. They may advise against a vaginal birth if:
- your baby is a footling breech (one or both of the baby’s feet are below its bottom)
- your baby is larger or smaller than average (your healthcare team will discuss this with you)
- your baby is in a certain position, for example, if its neck is very tilted back (hyper extended)
- you have a low-lying placenta (placenta praevia); see the RCOG patient information Placenta Praevia, placenta accreta and vasa praevia
- you have pre-eclampsia or any other pregnancy problems; see the RCOG patient information Pre-eclampsia .
With a breech baby you have the same choices for pain relief as with a baby who is in the head-first position. If you choose to have an epidural, there is an increased chance of a caesarean section. However, whatever you choose, a calm atmosphere with continuous support should be provided.
If you have a vaginal breech birth, your baby’s heart rate will usually be monitored continuously as this has been shown to improve your baby’s chance of a good outcome.
In some circumstances, for example, if there are concerns about your baby’s heart rate or if your labour is not progressing, you may need an emergency caesarean section during labour. A paediatrician (a doctor who specialises in the care of babies, children and teenagers) will attend the birth to check your baby is doing well.
If you go into labour before 37 weeks of pregnancy, the balance of the benefits and risks of having a caesarean section or vaginal birth changes and will be discussed with you.
If you are having twins and the first baby is breech, your healthcare professional will usually recommend a planned caesarean section.
If, however, the first baby is head-first, the position of the second baby is less important. This is because, after the birth of the first baby, the second baby has lots more room to move. It may turn naturally into a head-first position or a doctor may be able to help the baby to turn. See the RCOG patient information Multiple pregnancy: having more than one baby .
If you would like further information on breech babies and breech birth, you should speak with your healthcare professional.
Further information
- NHS information on breech babies
- NCT information on breech babies
If you are asked to make a choice, you may have lots of questions that you want to ask. You may also want to talk over your options with your family or friends. It can help to write a list of the questions you want answered and take it to your appointment.
Ask 3 Questions
To begin with, try to make sure you get the answers to 3 key questions , if you are asked to make a choice about your healthcare:
- What are my options?
- What are the pros and cons of each option for me?
- How do I get support to help me make a decision that is right for me?
*Ask 3 Questions is based on Shepherd et al. Three questions that patients can ask to improve the quality of information physicians give about treatment options: A cross-over trial. Patient Education and Counselling, 2011;84:379-85
- https://aqua.nhs.uk/resources/shared-decision-making-case-studies/
Sources and acknowledgements
This information has been developed by the RCOG Patient Information Committee. It is based on the RCOG Green-top Clinical Guidelines No. 20a External Cephalic Version and Reducing Incidence of Term Breech Presentation and No. 20b Management of Breech Presentation . The guidelines contain a full list of the sources of evidence we have used.
This information was reviewed before publication by women attending clinics in Nottingham, Essex, Inverness, Manchester, London, Sussex, Bristol, Basildon and Oxford, by the RCOG Women’s Network and by the RCOG Women’s Voices Involvement Panel.
Please give us feedback by completing our feedback survey:
- Members of the public – patient information feedback
- Healthcare professionals – patient information feedback
External Cephalic Version and Reducing the Incidence of Term Breech Presentation Green-top Guideline
Management of Breech Presentation Green-top Guideline
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Cochrane Database Syst Rev
External cephalic version for breech presentation at term
Management of breech presentation is controversial, particularly in regard to manipulation of the position of the fetus by external cephalic version (ECV). ECV may reduce the number of breech presentations and caesarean sections, but there also have been reports of complications with the procedure.
The objective of this review was to assess the effects of ECV at or near term on measures of pregnancy outcome. Methods of facilitating ECV, and ECV before term are reviewed separately.
Search methods
We searched the Cochrane Pregnancy and Childbirth Trials Register (28 February 2015) and reference lists of retrieved studies.
Selection criteria
Randomised trials of ECV at or near term (with or without tocolysis) compared with no attempt at ECV in women with breech presentation.
Data collection and analysis
Two review authors assessed eligibility and trial quality, and extracted the data.
Main results
We included eight studies, with a total of 1308 women randomised. The pooled data from these studies show a statistically significant and clinically meaningful reduction in non‐cephalic presentation at birth (average risk ratio (RR) 0.42, 95% confidence interval (CI) 0.29 to 0.61, eight trials, 1305 women); vaginal cephalic birth not achieved (average RR 0.46, 95% CI 0.33 to 0.62, seven trials, 1253 women, evidence graded very low); and caesarean section (average RR 0.57, 95% CI 0.40 to 0.82, eight trials, 1305 women, evidence graded very low) when ECV was attempted in comparison to no ECV attempted. There were no significant differences in the incidence of Apgar score ratings below seven at one minute (average RR 0.67, 95% CI 0.32 to 1.37, three trials, 168 infants) or five minutes (RR 0.63, 95% CI 0.29 to 1.36, five trials, 428 infants, evidence graded very low), low umbilical vein pH levels (RR 0.65, 95% CI 0.17 to 2.44, one trial, 52 infants, evidence graded very low), neonatal admission (RR 0.80, 95% CI 0.48 to 1.34, four trials, 368 infants, evidence graded very low), perinatal death (RR 0.39, 95% CI 0.09 to 1.64, eight trials, 1305 infants, evidence graded low), nor time from enrolment to delivery (mean difference ‐0.25 days, 95% CI ‐2.81 to 2.31, two trials, 256 women).
All of the trials included in this review had design limitations, and the level of evidence was graded low or very low. No studies attempted to blind the intervention, and the process of random allocation was suboptimal in several studies. Three of the eight trials had serious design limitations, however excluding these studies in a sensitivity analysis for outcomes with substantial heterogeneity did not alter the results.
Authors' conclusions
Attempting cephalic version at term reduces the chance of non‐cephalic presentation at birth, vaginal cephalic birth not achieved and caesarean section. There is not enough evidence from randomised trials to assess complications of ECV at term. Large observational studies suggest that complications are rare.
A visual summary of some of the results from this review can be found here.
Plain language summary
Effects of turning unborn babies from bottom first to head first at the end of pregnancy (around 36 weeks or more) for reducing problems during childbirth
What is the issue?
The best outcomes in childbirth for both mothers and babies are when the baby is born head‐first. If the baby is in another position, there is a higher risk of complications including the need for caesarean section. In a ‘breech presentation’ the baby is bottom‐down instead of head‐down. External cephalic version (ECV) is a technique for turning the unborn baby so it lies head‐down. This review looked at the effects of using ECV on babies that were in the breech position at the end of pregnancy (around 36 weeks or more).
Why is this important?
Everyone wants to avoid complications in childbirth and many women want to avoid having a caesarean section. Avoiding the need for surgery is very important in countries with limited resources for healthcare. ECV is sometimes used before the end of pregnancy (around 34 weeks) but the results might be different when it is used just before childbirth. Also, it might not be possible to turn the unborn baby at this late stage. We wanted to know if using ECV at the end of pregnancy resulted in safer childbirth or was harmful.
What evidence did we find?
We found 8 studies involving 1308 women. (We included studies up to 28 February 2015.) All the studies were randomised and involved women with low‐risk pregnancies. Using ECV around 36 weeks or more increased the chance that babies were born head‐first and reduced the risk of having a caesarean section. There were no clear differences in other outcomes such as the risk of babies dying. The quality of the studies and therefore the strength of the evidence was varied.
What does this mean?
If an unborn baby is lying bottom‐down, turning it by ECV just before birth can reduce some of the problems this position can cause. These studies are too small to show if ECV is safe to use in women with low‐risk pregnancies, however other types of studies suggest that it is safe. We also do not know if it should be used in high‐risk cases, such as mothers who have already had a caesarean section, or who are expecting twins.
Summary of findings
Summary of findings for the main comparison.
1 Most studies contributing data had design limitations, with more than 40% of weight from a study with serious design limitations. 2 Statistical heterogeneity (I 2 > 30%). Variation in size of effect. 3 Statistical heterogeneity (I 2 > 30%). Variation in size and direction of effect. 4 Most studies contributing data had design limitations. 5 Wide confidence interval crossing the line of no effect and few events. 6 One study with design limitations. 7 Wide confidence interval crossing the line of no effect, few events and small sample size. 8 Wide confidence interval crossing the line of no effect.
Description of the condition
Approximately 3% to 4% of all pregnant women who reach full term will have a fetus in breech presentation. This may be caused by an underlying fetal or maternal abnormality, or could be an apparently chance occurrence, or related to an otherwise benign variant such as cornual placental position. In the latter instance, breech presentation places a healthy fetus and mother at increased risk of a complicated vaginal delivery or caesarean section.
Breech delivery, whether vaginally or by caesarean section, has a higher incidence of poor perinatal outcomes than cephalic birth. For example, the incidence of minor childhood handicap following breech presentation has been found to be high (19.4%) and similar for those delivered following trial of labour and those following an elective caesarean section ( Danielian 1996 ).
The majority of women with a breech presenting baby would prefer a vaginal birth although most would choose caesarean section if there is a medical indication ( Gamble 2000 ; Geary 1997 ; Hildingsson 2002 ; Turnbull 1999 ). For the singleton fetus in breech presentation, caesarean section has been shown to be safer for the fetus than vaginal birth in many settings ( Hofmeyr 2005 ), although a large prospective study suggested that vaginal breech delivery may be safe under certain conditions with experienced practitioners ( Goffinet 2006 ).
The risks associated with caesarean section are low, however caesarean section is not without maternal risk and in developed countries remains the largest contributing factor to the incidence of maternal mortality and morbidity following childbirth ( Minkoff 2003 ). A Cochrane review of planned caesarean section versus planned vaginal delivery for breech pregnancy at term, reported that even though 45% of women in the planned vaginal delivery group were delivered by caesarean section, planned caesarean section was associated with an increase in maternal morbidity (risk ratio (RR) 1.29, 95% confidence interval (CI) 1.03 to 1.61) ( Hofmeyr 2003 ). Furthermore, although the overall risk is very small, recent estimates of the incidence of mortality associated with elective caesarean section were nearly tripled compared to vaginal birth ( Cooper 2002 ; Hall 1999 ). In addition to the increase in immediate morbidity following caesarean section, intra‐abdominal adhesions may occur after caesarean section resulting in subsequent infertility ( LaSala 1987 ). The presence of the uterine scar puts future pregnancies at increased risk of complications such as ectopic pregnancy, placenta previa, accreta and abruption, and uterine rupture ( Dashe 2002 ; Gilliam 2002 ; Lydon‐Rochelle 2001 ; Minkoff 2003 ). A further deterrent to caesarean section is that the procedure requires the expertise of an obstetrician or other health worker with surgical training, and limits the role for low‐risk obstetrical care providers such as midwives and family practitioners. A review of strategies to reduce caesarean section rates identified external cephalic version (ECV) as the only clinical intervention with demonstrated Level 1 evidence for reducing primary caesarean section rates overall ( Walker 2002 ).
Description of the intervention
Considering the complications that can arise from breech delivery, it is not surprising that, over the years, the possibility of manipulating the baby from the breech to the cephalic presentation has intrigued obstetric caregivers. ECV is a procedure in which the baby is manipulated by pressure through the mother's abdominal wall into a cephalic (head‐down) position.
ECV before term (usually before 34 weeks' gestation) came into routine obstetric practice on the basis of the self‐evident immediate effectiveness of the procedure as well as reassuring results from several non‐randomised trials, and in spite of the negative results of the only randomised trial reported prior to 1980 ( Brosset 1956 ). The popularity of ECV before term waned after the mid‐1970s, partly because of reports of a substantial perinatal mortality associated with the procedure ( Bradley‐Watson 1975 ), and the increasing perception of caesarean section as a safer option than ECV or breech delivery.
Prior to the mid‐1970s, ECV was usually attempted before term because of the belief that the procedure would seldom be successful at term. Subsequent studies showed that with the use of tocolysis (medication to relax the uterus), ECV could be achieved in a substantial proportion of women with breech presentation at term. ECV at term differs in many fundamental ways from that performed before term. These include the fact that the fetus is mature and may be delivered more readily in the event of complications, and that spontaneous versions without ECV attempt, or reversion after successful ECV, are less common at term. ECV before term is therefore evaluated as a separate procedure ( see ' External cephalic version for breech presentation before term ' ( Hutton 2006 )). The current review includes studies in which the intention was to include pregnant women at or near term (i.e. from 36 weeks' gestation).
External cephalic version at term has been shown to be feasible in two small uncontrolled trials in women with previous caesarean section ( Flamm 1991 ; Schachter 1994 ), and in two in women in labour ( Ferguson 1985 ; Fortunato 1988 ). El‐Muzaini 2008a and El‐Muzaini 2008b are abstract reports of prospective controlled studies of ECV in labour and with previous caesarean section respectively, with results in favour of ECV, but it is not clear whether these studies were randomised. To our knowledge, no randomised trials of these interventions have been reported.
Several authors have investigated which factors are associated with an increased chance of successful external cephalic version ( Boucher 2003 ; Fortunato 1988 ; Guyer 2001 ; Lau 1997 ; Le Bret 2004 ). Factors which have been found to predict failure of ECV attempt include engagement of the presenting part, difficulty in palpating the fetal head and a tense uterus on palpation ( Lau 1997 ), and increased amniotic fluid volume ( Boucher 2003 ). However, a prediction model based on clinical parameters was found to be insufficiently accurate to be useful in predicting the outcome of ECV attempts ( Chan 2004 ).
The majority of women prefer vaginal birth over caesarean birth ( Hildingsson 2002 ). As ECV is the primary intervention to achieve a vaginal delivery when the baby is in breech presentation, it would seem logical that women would be highly motivated to try it. The preferences of women with breech presentation regarding their care appear to have changed over the past couple of decades, and vary by location. In an Israeli study in 1995, 54% were willing to consider ECV and 65% preferred planned caesarean section if the breech presentation persisted, compared with 24% and 97% respectively in 2001 ( Yogev 2002 ). In an Australian study in 2001, 39% of women attending antenatal clinic would choose ECV if needed, and 22% were undecided ( Raynes‐Greenow 2004 ). In another Australian study, Nassar 2007 evaluated a decision aid for women with breech presentation at term. The decision aid was not intended to increase or decrease intervention rates, but rather aim to support informed decision‐making that is consistent with personal values. Seventy‐four per cent of women who were randomised to receive the decision aid expressed an intention to have ECV if needed, while 66% of women who received normal care would choose ECV. A higher proportion of women who received the additional information reported that they had enough information to make a decision (95.7%, compared with 73.6%, at first follow‐up). The women who received the decision aid experienced lower decisional conflict, increased knowledge, and greater satisfaction with their decision. Murray‐Davis 2012 reported that women participating in a trial comparing the timing of ECV preferred the procedure to be carried out at 34 to 36 weeks' gestation rather than after 37 weeks, as it was perceived to have physiological and practical advantages. However, their sample is likely to have over‐estimated preferences for early ECV as that option was only available to trial participants.
Complications reported following ECV at term include fracture of the baby's femur ( Papp 2004 ), prolonged tachycardia (rapid heartbeat) of the baby ( Nzewi 1999 ), sinusoidal baby's heart rate pattern (a fluctuating pattern sometimes indicating compromise) ( Ferber 1999 ), and fetal‐maternal haemorrhage (bleeding from the baby's to the mother's circulation in the placenta) ( Shankar 2004 ). The rate of caesarean section during labour has been found to be greater following successful ECV than in spontaneous cephalic presentation: 20% versus 6.3%, RR 3.2 ( Ben‐Haroush 2002 ); 27.6% versus 12.5%, RR 2.04; 95% CI 1.43 to 2.91 ( Chan 2004b ); odds ratio 2.04 for nulliparous women, 4.30 for multiparous ( Vezina 2004 ). This is not surprising, given that women with persistent breech presentation in the first instance are a high‐risk group. Cord blood gases at delivery were no different ( Chan 2004c ).
However, series of cases have reported very low complication rates with ECV ( Boucher 2003 ; Impey 1999 ; Impey 2005 ; Tong 2012 ). A review of 44 studies of ECV (7377 participants) from 1990 to 2002 found the most frequently reported complication to be transient abnormal baby's heart rate patterns (5.7%). Less frequent complications were persisting pathological baby's heart rate patterns (0.37%); vaginal bleeding (0.47%); placental abruption (0.12%); emergency caesarean section (0.43%); and perinatal mortality (0.16%) ( Collaris 2004 ). Because of the risk of allo‐immunisation, anti‐D prophylaxis is recommended for non‐sensitised D‐negative women following ECV attempts ( Fung Kee Fung 2003 ).
Contra‐indications to ECV include: multiple pregnancy, severe abnormality, unsatisfactory condition or death of the baby, caesarean section necessary irrespective of the presentation (e.g. major placenta praevia), and ruptured membranes. Relative contraindications include previous caesarean section, poor growth of the baby, and bleeding from the uterus.
The question of whether ECV might increase the risk of mother‐to‐child transmission of viral infections such as HIV is important and, in the absence of direct evidence, we have reviewed the relevant biological evidence and concluded that, unlike fetal‐maternal transfusion (bleeding from the baby's to the mother's circulation in the placenta), maternal‐fetal transfusion is extremely rare, and unlikely to be precipitated by ECV ( Holmes 2004 ). It is also reassuring that in a randomised trial of fundal pressure to expel the baby during caesarean section, no evidence of maternal‐fetal transfusion was found ( Owens 2003 ).
Several authors have reported success rates for ECV at term in routine clinical practice in the region of 40% to 50%: 53% ( Hughes 1997 ); 39% ( Williams 1999 ); 55% ( Guyer 2001 ); 45% ( Devendra 2002 ); 43% ( Lojacono 2003 ); 51% ( Skupski 2003 ); 42% to 65% (depending on amniotic fluid volume ( Boucher 2003 )); and 51% ( Le Bret 2004 ).
Readers are referred to previous reviews of the topic ( Hofmeyr 1989 ; Hofmeyr 1991 ; Hofmeyr 1992 ; Hofmeyr 1993 ; Zhang 1993 ). See also related Cochrane systematic reviews: ' External cephalic version for breech presentation before term ', ' Cephalic version by postural management for breech presentation ' and ' Interventions for helping to turn term breech babies to head first presentation when using external cephalic version .' ( Hutton 2006 ; Hofmeyr 2000 ; Cluver 2012 ).
Why it is important to do this review
There is a higher risk of complications when delivering a baby presenting in the breech rather than in the cephalic position. Caesarean section appears to be safer for the baby, but presents a higher level of maternal morbidity. Achieving a cephalic vaginal delivery by successfully rotating the baby in utero therefore, potentially offers a way to reduce the caesarean section rate, and improve perinatal and maternal outcomes. It may be of particular importance in resource‐poor situations in which women may be unable to reach health services during labour, and caesarean sections are unavailable or unsafe ( Hofmeyr 2004 ).
To assess, using the best available evidence, the effects of external cephalic version (ECV) at or near term for breech presentation on: presentation at and method of delivery; and perinatal and maternal morbidity and mortality.
Criteria for considering studies for this review
Types of studies.
Clinical trials comparing the effects of external cephalic version (ECV) at or near term, with or without tocolysis, with a control group (no ECV attempt). Cluster‐randomised studies and cross‐over studies were eligible for inclusion, as mentioned in Unit of analysis issues . Quasi‐randomised controlled trials were not eligible for inclusion.
Types of participants
Pregnant women with babies in the breech presentation at or near term and no contraindications to ECV.
Types of interventions
ECV attempt at term, with or without the use of tocolysis, compared with no ECV attempt.
Types of outcome measures
Outcomes were included if:
- they were determined to be clinically meaningful;
- reasonable measures were taken to minimise observer bias;
- missing data were insufficient to materially influence conclusions;
- data were available for analysis according to original allocation, irrespective of protocol violations;
- and data were available in a format suitable for analysis.
Primary outcomes
- Vaginal cephalic birth not achieved (not prespecified)
- Caesarean section
Secondary outcomes
- Non cephalic presentation at delivery
- Vaginal breech birth (not prespecified)
- Apgar score less than seven at one minute (not prespecified)
- Apgar score less than seven at five minutes
- Umbilical vessel pH below 7.2
- Perinatal death
- Neonatal admission
- Enrolment‐delivery interval (not prespecified)
Search methods for identification of studies
The following methods section of this review is based on a standard template used by the Cochrane Pregnancy and Childbirth Group.
Electronic searches
We searched the Cochrane Pregnancy and Childbirth Group’s Trials Register by contacting the Trials Search Co‐ordinator (28 February 2015).
The Cochrane Pregnancy and Childbirth Group’s Trials Register is maintained by the Trials Search Co‐ordinator and contains trials identified from:
- monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
- weekly searches of MEDLINE (Ovid);
- weekly searches of Embase (Ovid);
- monthly searches of CINAHL (EBSCO);
- handsearches of 30 journals and the proceedings of major conferences;
- weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Details of the search strategies for CENTRAL, MEDLINE, Embase and CINAHL, the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service can be found in the ‘Specialized Register’ section within the editorial information about the Cochrane Pregnancy and Childbirth Group.
Trials identified through the searching activities described above are each assigned to a review topic (or topics). The Trials Search Co‐ordinator searches the register for each review using the topic list rather than keywords.
[For details of additional searches we carried out for the previous version of this review ( Hofmeyr 2012 ), see Appendix 1 .]
Searching other resources
We searched the reference lists of retrieved studies.
We did not apply any language or date restrictions.
For methods used when assessing the trials identified in the previous version of this review ( see Hofmeyr 2012 ). For this update, the following methods were used for assessing the trial identified by the updated search ( Rita 2012 ).
Selection of studies
Two review authors independently assessed for inclusion all the potential studies identified as a result of the search strategy. We resolved any disagreement through discussion and, if required, would have consulted a third assessor.
Data extraction and management
We designed a form to extract data. For eligible studies, two review authors extracted the data using the agreed form. We entered data into Review Manager software ( RevMan 2014 ) and checked for accuracy.
When information was unclear, we attempted to contact authors of the original reports to provide further details.
Assessment of risk of bias in included studies
Two review authors independently assessed the risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions ( Higgins 2011 ). We resolved any disagreement through discussion and, if required, would have consulted R Kulier.
(1) Random sequence generation (checking for possible selection bias)
We described for each included study the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
We assessed the method as:
- low risk of bias (any truly random process, e.g. random number table; computer random number generator);
- high risk of bias (any non‐random process, e.g. odd or even date of birth; hospital or clinic record number);
- unclear risk of bias.
(2) Allocation concealment (checking for possible selection bias)
We described for each included study the method used to conceal allocation to interventions prior to assignment and assessed whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We assessed the methods as:
- low risk of bias (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
- high risk of bias (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth);
(3.1) Blinding of participants and personnel (checking for possible performance bias)
We described for each included study the methods used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. We considered that studies were at low risk of bias if they were blinded, or if we judged that the lack of blinding unlikely to affect results. We assessed blinding separately for different outcomes or classes of outcomes.
- low, high or unclear risk of bias for participants;
- low, high or unclear risk of bias for personnel.

(3.2) Blinding of outcome assessment (checking for possible detection bias)
We described for each included study the methods used, if any, to blind outcome assessors from knowledge of which intervention a participant received. We assessed blinding separately for different outcomes or classes of outcomes.
We have assessed methods used to blind outcome assessment as:
- low, high or unclear risk of bias.
(4) Incomplete outcome data (checking for possible attrition bias due to the amount, nature and handling of incomplete outcome data)
We described for each included study, and for each outcome or class of outcomes, the completeness of data including attrition and exclusions from the analysis. We stated whether attrition and exclusions were reported and the numbers included in the analysis at each stage (compared with the total randomised participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported, or could be supplied by the trial authors, we planned to re‐include missing data in the analyses which we undertook.
We assessed methods as:
- low risk of bias (e.g. no missing outcome data; missing outcome data balanced across groups);
- high risk of bias (e.g. numbers or reasons for missing data imbalanced across groups; ‘as treated’ analysis done with substantial departure of intervention received from that assigned at randomisation);
(5) Selective reporting (checking for reporting bias)
We described for each included study how we investigated the possibility of selective outcome reporting bias and what we found.
- low risk of bias (where it is clear that all of the study’s prespecified outcomes and all expected outcomes of interest to the review have been reported);
- high risk of bias (where not all the study’s prespecified outcomes have been reported; one or more reported primary outcomes were not prespecified; outcomes of interest are reported incompletely and so cannot be used; study fails to include results of a key outcome that would have been expected to have been reported);
(6) Other bias (checking for bias due to problems not covered by (1) to (5) above)
We described for each included study any important concerns we had about other possible sources of bias.
(7) Overall risk of bias
We made explicit judgements about whether studies were at high risk of bias, according to the criteria given in the Handbook (Higgins 2011). With reference to (1) to (6) above, we planned to assess the likely magnitude and direction of the bias and whether we considered it is likely to impact on the findings. In future updates, we will explore the impact of the level of bias through undertaking sensitivity analyses ‐ see Sensitivity analysis .
For this update the quality of the evidence was assessed using the GRADE approach ( Schunemann 2009 ) in order to assess the quality of the body of evidence relating to the following outcomes for the main comparisons.
- Vaginal cephalic birth not achieved
- Umbilical pH below 7.2
The GRADE profiler ( Grade 2008 ) was used to import data from Review Manager 5.3 ( RevMan 2014 ) in order to create a ’Summary of findings’ table. A summary of the intervention effect and a measure of quality for each of the above outcomes was produced using the GRADE approach. The GRADE approach uses five considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the quality of the body of evidence for each outcome. The evidence can be downgraded from 'high quality' by one level for serious (or by two levels for very serious) limitations, depending on assessments for risk of bias, indirectness of evidence, serious inconsistency, imprecision of effect estimates or potential publication bias.
Measures of treatment effect
Dichotomous data.
For dichotomous data, we present results as summary risk ratio with 95% confidence intervals.
Continuous data
For continuous data, we used the mean difference if outcomes were measured in the same way between trials. We planned to use the standardised mean difference to combine trials that measured the same outcome, but used different methods, if required.
Unit of analysis issues
Cluster‐randomised trials.
We would have included cluster‐randomised trials in the analyses along with individually‐randomised trials had there been any. We would have adjusted their sample sizes or standard errors using the methods described in the Handbook in Section 16.3.4 and 16.3.6 ( Higgins 2011 ) using an estimate of the intracluster correlation co‐efficient (ICC) derived from the trial (if possible), from a similar trial or from a study of a similar population. In future updates of the review, if we use ICCs from other sources, we will report this and conduct sensitivity analyses to investigate the effect of variation in the ICC. Had we identified both cluster‐randomised trials and individually‐randomised trials, we planned to synthesise the relevant information. We would consider it reasonable to combine the results from both if there was little heterogeneity between the study designs and the interaction between the effect of intervention and the choice of randomisation unit was considered to be unlikely.
We would also acknowledge heterogeneity in the randomisation unit and perform a sensitivity or subgroup analysis to investigate the effects of the randomisation unit.
Cross‐over trials
We identified no cross‐over trials on this topic for the update, but if such trials were identified and deemed eligible for inclusion, we would include them in the analyses with parallel group trials, using methods described by Elbourne 2002 .
Dealing with missing data
For included studies, we noted levels of attrition. We explored the impact of including studies with high levels of missing data in the overall assessment of treatment effect by using sensitivity analysis.
For all outcomes we have carried out analyses, as far as possible, on an intention‐to‐treat basis, i.e. we attempted to include all participants randomised to each group in the analyses. The denominator for each outcome in each trial was the number randomised minus any participants whose outcomes were known to be missing.
Assessment of heterogeneity
We assessed statistical heterogeneity in each meta‐analysis using the Tau², I² and Chi² statistics. We regarded heterogeneity as substantial if an I² was greater than 30% and either a Tau² was greater than zero, or there was a low P value (less than 0.10) in the Chi² test for heterogeneity. Had we identified substantial heterogeneity (above 30%), we planned to explore it by prespecified subgroup analysis.
Assessment of reporting biases
Where we suspected reporting bias ( see ‘Selective reporting bias’ above), we attempted to contact study authors, asking them to provide missing outcome data. Where this was not possible, and the missing data were thought to introduce serious bias, we explored the impact of including such studies in the overall assessment of results by a sensitivity analysis.
In future updates, if there are 10 or more studies in the meta‐analysis we will investigate reporting biases (such as publication bias) using funnel plots. We will assess funnel plot asymmetry visually. If asymmetry is suggested by a visual assessment, we will perform exploratory analyses to investigate it.
Data synthesis
We carried out statistical analysis using the Review Manager software ( RevMan 2014 ). We used fixed‐effect meta‐analysis for combining data where trials were examining the same intervention, and the trials’ populations and methods were judged sufficiently similar.
If there was clinical heterogeneity sufficient to expect that the underlying treatment effects differed between trials, or if substantial statistical heterogeneity was detected, we used random‐effects meta‐analysis to produce an overall summary, if an average treatment effect across trials was considered clinically meaningful. The random‐effects summary was treated as the average of the range of possible treatment effects and we discussed the clinical implications of treatment effects differing between trials. If the average treatment effect was not clinically meaningful, we would not have combined trials. Where we used random‐effects analyses, the results were presented as the average treatment effect with 95% confidence intervals, and the estimates of Tau² and I².
Subgroup analysis and investigation of heterogeneity
We did not perform any subgroup analyses in the original review or this update (2015). If we identified substantial heterogeneity in a fixed‐effect meta‐analysis, we noted this and repeated the analysis using a random‐effects method. In future updates, if sufficient data become available, we will conduct the following subgroup analyses on primary outcomes.
- Nulliparous women versus multiparous women versus parity mixed or not stated.
- Frank breech presentation versus non‐frank breech presentation versus presentation mixed or not stated
- Studies recruiting mainly black African women versus studies recruiting mainly Caucasian women versus other studies.
We will assess subgroup differences by interaction tests available within RevMan ( RevMan 2014 ) and report the results of subgroup analyses quoting the Chi² statistic and P value, and the interaction test I² value.
Sensitivity analysis
Due to the potentially high risk of bias in three of the studies ( Brocks 1984 ; Dafallah 2004 ; Hindawi 2005 ) and our lack of success in contacting the latter two trial authors, we undertook the meta‐analyses of included studies twice: first, including all the studies and second, excluding the studies at high risk of bias. When sensitivity analyses showed that the overall results and conclusions from primary outcomes were not affected by their inclusion, we regarded the results of the review with a higher degree of certainty. If both or either of these studies had greatly influenced the findings of the review, we would have recommended an appropriate degree of caution.
It has been suggested that ECV may be more successful (and spontaneous version more common) in black African than Caucasian women, possibly because of the tendency for the presenting part to remain high until the onset of labour ( Hofmeyr 1986 ). Ethnicity was not a pre‐defined subgroup analysis for the original review. However for this update (2015), post‐hoc sensitivity analysis excluding the three studies in black African women ( Dafallah 2004 ; Hofmeyr 1983 ; Mahomed 1991 ) was conducted.
Description of studies
Results of the search.
Eight studies were included in the review (one from an updated search: Rita 2012 ).
Included studies
See Characteristics of included studies .
All eight studies were two‐arm randomised controlled trials, in which women were randomised to either receive attempted ECV or no attempt at ECV.
Sample sizes
The total number of women included in the eight included studies was 1308. Five of the studies included 65 or fewer women ( Brocks 1984 ; Hofmeyr 1983 ; Rita 2012 ; Van de Pavert 1990 ; Van Dorsten 1981 ), two recruited around 200 women ( Hindawi 2005 ; Mahomed 1991 ), and one included over 600 women ( Dafallah 2004 ).
Studies were carried out in Denmark, India, Jordan, the Netherlands, South Africa, Sudan, the USA and Zimbabwe. The recruitment and any intervention happened in an outpatient clinic in Brocks 1984 ; Dafallah 2004 ; Hindawi 2005 ; Van Dorsten 1981 , women in Hofmeyr 1983 were recruited when admitted to hospital from antenatal clinics and subsequently referred back to the antenatal clinic, and the setting was not described in the other studies ( Mahomed 1991 ; Rita 2012 ; Van de Pavert 1990 ).
Participants
Pregnant women with a breech presentation baby were included in all studies. Women were recruited during the 37th week of pregnancy ( Brocks 1984 ), 36 to 38 weeks' gestation ( Dafallah 2004 ), from 37 weeks' gestation ( Hindawi 2005 ; Mahomed 1991 ; Rita 2012 ) after 36 weeks' gestation ( Hofmeyr 1983 ; Van de Pavert 1990 ), and 37 to 39 weeks' gestation ( Van Dorsten 1981 ). Several reports explicitly stated that only women with singleton pregnancies were eligible ( Brocks 1984 ; Hindawi 2005 ; Mahomed 1991 ; Rita 2012 ). The women included in these studies had low‐risk pregnancies and medical histories, with no contra‐indications to vaginal delivery or external version. Women with a previous caesarean section or uterine scar were excluded from all studies except Rita 2012 , which excluded those with two or more previous caesarean sections.
Interventions
A variety of different techniques and maternal positions were used to perform ECV (classic forward roll technique ( Dafallah 2004 , Van de Pavert 1990 ), forward roll or back flip ( Hofmeyr 1983 ; Mahomed 1991 ; Van Dorsten 1981 ), woman lying in left lateral tilt ( Brocks 1984 ; Rita 2012 ), in the Trendelberg position ( Dafallah 2004 ). lying with left or right lateral tilt ( Hofmeyr 1983 ). An ultrasound scan confirming breech presentation was carried out prior to ECV in all studies ( Brocks 1984 ; Dafallah 2004 ; Hindawi 2005 ; Hofmeyr 1983 ; Mahomed 1991 ; Rita 2012 ; Van de Pavert 1990 ; Van Dorsten 1981 ), and a reactive non‐stress test/unstressed cardiotocogram was often recorded ( Brocks 1984 ; Mahomed 1991 ; Van de Pavert 1990 ; Van Dorsten 1981 ).
A single attempt at ECV was carried out in Brocks 1984 ; Hindawi 2005 ; Mahomed 1991 ; and Rita 2012 . Repeat attempts were allowed in Dafallah 2004 (up to three attempts), Hofmeyr 1983 and Van Dorsten 1981 (in the opposite direction to the initial attempt if it failed), and in Van de Pavert 1990 if the first attempt without tocolysis was unsuccessful, ritodrine was administered and ECV was attempted again.
No analgesia was used in these studies. This review included trials with and without tocolysis. Four trials used tocolysis routinely for ECV (ritodrine: Brocks 1984 and Hindawi 2005 ; hexaprenaline: Mahomed 1991 ; terbutaline sulphate: Van Dorsten 1981 ). In two trials, tocolysis was used if the initial ECV attempt was unsuccessful (hexaprenaline: Hofmeyr 1983 ; ritodrine: Van de Pavert 1990 ). No tocolysis was used in Dafallah 2004 and Rita 2012 .
All studies reported caesarean section and perinatal death. Outcomes regarding presentation at delivery were not reported in a consistent way, however in most reports the information was available to impute the outcomes of interest (e.g. vaginal cephalic birth not achieved by adding caesarean section and breech vaginal delivery).
Excluded studies
Six studies identified by the search strategy were excluded from this review (see Characteristics of excluded studies ). They were excluded because group allocation was not randomised ( Besio 1994 ; El‐Muzaini 2008a ; El‐Muzaini 2008b ; Stine 1985 ), compared early with late ECV ( Rust 2005 ), and ECV attempts started at 33 weeks' gestation ( Van Veelen 1989 ).
Risk of bias in included studies
See Characteristics of included studies , Figure 1 and Figure 2 .

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
In four trials, randomly ordered sealed envelopes or cards were used for allocation ( Hofmeyr 1983 ; Mahomed 1991 ; Rita 2012 ; Van de Pavert 1990 ), but only two ( Mahomed 1991 ; Rita 2012 ) specified that the cards were sequentially numbered. Van Dorsten 1981 used a random number table and Brocks 1984 used 'random' allocation without specifying the mechanism. Concealment of allocation was thus not optimal.
Dafallah 2004 and Hindawi 2005 did not describe the methods of randomisation and allocation concealment at all. Attempts to contact the respective authors for more information failed. See Sensitivity analysis .
Due to the nature of the intervention, no studies attempted to blind participants or clinicians to group allocation. Women would have been aware of the intervention and this may have affected decisions regarding care in later pregnancy and at the birth. Staff would be aware of the intervention and this may have affected other aspects of care and decision‐making at the birth. This may have had an impact on outcomes such as caesarean section. In one study ( Van de Pavert 1990 ), it was much more likely that women would have a caesarean section if external cephalic version (ECV) had been attempted and failed than in women where ECV had never been attempted, so it is possible than attempt and failure of ECV affects decision‐making about caesarean section.
One study ( Mahomed 1991 ) described blinding assessors to some outcomes (Apgar scores, admission to neonatal unit, stillbirth, neonatal death). In one study ( Hofmeyr 1983 ), outcome assessment was from records (it was not clear whether attempted ECV or randomisation group was stated in the records). It states that "there was no subsequent intervention in their management by the investigator". In all other studies, it was not clear whether outcome assessment was carried out by staff who were involved in women's care. It is unlikely that lack of blinding of outcome assessors could have influenced most of the outcomes measured, but assessment of the infant may have been affected by knowledge of randomisation group.
Incomplete outcome data
Brocks 1984 studied 65 women who agreed to randomisation and a further 65 who either specifically requested or refused an ECV attempt. Since factors that may have a bearing on the outcome of pregnancy may influence the decision to accept ECV, we have limited this review to an analysis of the 65 randomised cases. Hindawi 2005 gives no explanation for the large difference in group size (90 versus 102).
The exclusion of three women after enrolment in Van Dorsten 1981 is unlikely to have affected the results materially. Van de Pavert 1990 attempted ECV without tocolysis in 21/25 of the study group, and with tocolysis in 16/20 initial failures. Thus 8/25 (32%) received no ECV attempt (4) or incomplete ECV protocol (4). ECV was attempted on request in 5/27 of the control group, tocolysis being used in the three which were successful. While the analysis was appropriate according to intention‐to‐treat, the rate of non‐compliance with the allocated treatment reduces the power of the study to detect differences resulting from ECV attempt.
Selective reporting
Neonatal outcomes were given according to presentation not allocation in Brocks 1984 , so were not included in this review. Dafallah 2004 did not report on all prespecified outcomes, e.g. Apgar scores, or other key outcomes of interest, e.g. morbidity. In Hindawi 2005 , outcomes are not clearly prespecified. Studies were generally assessed from published reports, without access to the protocols, so it was unclear whether all prespecified outcomes had been reported ( Brocks 1984 ; Mahomed 1991 ; Rita 2012 ; Van de Pavert 1990 ; Van Dorsten 1981 ).
Other potential sources of bias
In two trials, higher numbers of women in the ECV group had fundal placentas ( Mahomed 1991 ; Rita 2012 ), however the clinical implications are unclear.
Group sizes differ by 13% and outcomes are not clearly prespecified in Hindawi 2005 .
Overall, all studies had some design limitations. It was judged that three studies had serious design limitations and were at high risk of bias ( Brocks 1984 ; Dafallah 2004 ; Hindawi 2005 ). A sensitivity analysis was carried out to assess the effect of these limitations on the results.
Effects of interventions
See: Table 1
External cephalic version at term versus no ECV attempt
There was significant heterogeneity in the results for the outcomes vaginal cephalic birth not achieved, caesarean section, non‐cephalic presentation at birth, vaginal breech birth, and Apgar score less than seven at one minute, therefore these were pooled using the random‐effects model. For all other data we used the fixed‐effect model.
Primary outcomes: Vaginal cephalic birth not achieved and caesarean section
Overall, the pooled data from included studies show a statistically significant and clinically meaningful reduction in vaginal cephalic birth not being achieved (average risk ratio (RR) 0.46, 95% confidence interval (CI) 0.33 to 0.62, seven trials, 1253 women, evidence graded very low, Analysis 1.1 ), and caesarean section (average RR 0.57, 95% CI 0.40 to 0.82, eight trials, 1305 women, evidence graded very low, Analysis 1.2 ) when ECV was attempted.

Comparison 1 External cephalic version at term versus no ECV attempt, Outcome 1 Vaginal cephalic birth not achieved (CS + breech vaginal birth) (not prespecified).

Comparison 1 External cephalic version at term versus no ECV attempt, Outcome 2 Caesarean section.
Secondary outcomes: Perinatal and maternal morbidity and mortality
The pooled data from included studies show a statistically significant and clinically meaningful reduction in non‐cephalic presentation at birth (average RR 0.42, 95% CI 0.29 to 0.61, eight trials, 1305 women, Analysis 1.3 ), and vaginal breech delivery (not prespecified, average RR 0.35, 95% CI 0.24 to 0.50, seven trials, 685 women, Analysis 1.4 ).

Comparison 1 External cephalic version at term versus no ECV attempt, Outcome 3 Non‐cephalic presentation at birth.

Comparison 1 External cephalic version at term versus no ECV attempt, Outcome 4 Vaginal breech birth (not prespecified).
Data were not available from all the trials for the remaining outcomes. There were no significant differences in the incidence of Apgar score ratings below seven at one minute (not prespecified, random‐effects model: average RR 0.67, 95% CI 0.32 to 1.37; three trials, 168 infants, Analysis 1.5 ) or five minutes (RR 0.63, 95% CI 0.29 to 1.36, five trials, 428 infants, evidence graded very low, Analysis 1.6 ), low umbilical vein pH levels (RR 0.65, 95% CI 0.17 to 2.44, one trial, 52 infants, evidence graded very low, Analysis 1.7 ), neonatal admission (RR 0.80, 95% CI 0.48 to 1.34, four trials, 368 infants, evidence graded very low, Analysis 1.9 ), perinatal death (RR 0.39, 95% CI 0.09 to 1.64, eight trials, 1305 infants, evidence graded low, Analysis 1.8 ), nor time from enrolment to delivery (not prespecified, mean difference ‐0.25 days, 95% CI ‐2.81 to 2.31, two trials, 256 women, Analysis 1.10 ).

Comparison 1 External cephalic version at term versus no ECV attempt, Outcome 5 Apgar score < 7 at 1 minute (not prespecified).

Comparison 1 External cephalic version at term versus no ECV attempt, Outcome 6 Apgar score < 7 at 5 minutes.

Comparison 1 External cephalic version at term versus no ECV attempt, Outcome 7 Umbilical vein pH < 7.20.

Comparison 1 External cephalic version at term versus no ECV attempt, Outcome 8 Perinatal death.

Comparison 1 External cephalic version at term versus no ECV attempt, Outcome 9 Neonatal admission.

Comparison 1 External cephalic version at term versus no ECV attempt, Outcome 10 Enrolment‐delivery interval (not prespecified).
Sensitivity analyses
Three studies were judged to have serious design limitations and were at high risk of bias ( Brocks 1984 ; Dafallah 2004 ; Hindawi 2005 ). However, a sensitivity analysis excluding these studies from the analyses showed that the overall results were not greatly influenced by their inclusion (random‐effect model) (vaginal cephalic birth not being achieved: average RR 0.32, 95% CI 0.25 to 0.41, four trials, 376 women, Analysis 2.1 ; caesarean section: average RR 0.46, 95% CI 0.27 to 0.79, five trials, 428 women, Analysis 2.2 ; non‐cephalic presentation at birth: average RR 0.29, 95% CI 0.12 to 0.68, five trials, 428 women, Analysis 2.3 ; and vaginal breech delivery: average RR 0.38, 95% CI 0.21 to 0.69, five trials, 428 women, Analysis 2.4 ).

Comparison 2 Sensitivity analysis (excluding studies with high risk of bias), Outcome 1 Vaginal cephalic birth not achieved (CS + breech vaginal birth).

Comparison 2 Sensitivity analysis (excluding studies with high risk of bias), Outcome 2 Caesarean section.

Comparison 2 Sensitivity analysis (excluding studies with high risk of bias), Outcome 3 Non cephalic presentation at birth.

Comparison 2 Sensitivity analysis (excluding studies with high risk of bias), Outcome 4 Vaginal breech birth.
It has been suggested that ECV may be more successful (and spontaneous version more common) in black African than Caucasian women, possibly because of the tendency for the presenting part to remain high until the onset of labour ( Hofmeyr 1986 ). Ethnicity was not a pre‐defined subgroup analysis for the original review. However, post‐hoc sensitivity analysis excluding the three studies in black African women ( Dafallah 2004 ; Hofmeyr 1983 ; Mahomed 1991 ) produced the following results (fixed‐effect model): vaginal cephalic birth not achieved: RR 0.49, 95% CI 0.41 to 0.58, 4 trials, 365 women, Analysis 3.1 ; caesarean section: RR 0.57, 95% CI 0.45 to 0.73, five trials, 417 women, Analysis 3.2 , non‐cephalic presentation at birth: RR 0.46, 95% CI 0.39 to 0.55, five trials, 417 women Analysis 3.3 ; vaginal breech birth: RR 0.38, 95% CI 0.27 to 0.54, five trials, 417 women, Analysis 3.4 .

Comparison 3 Sensitivity analysis (excluding studies in Africa), Outcome 1 Vaginal cephalic birth not achieved (CS + breech vaginal birth).

Comparison 3 Sensitivity analysis (excluding studies in Africa), Outcome 2 Caesarean section.

Comparison 3 Sensitivity analysis (excluding studies in Africa), Outcome 3 Non cephalic presentation at birth.

Comparison 3 Sensitivity analysis (excluding studies in Africa), Outcome 4 Vaginal breech birth.
Summary of main results
The evidence from randomised trials shows that attempting external cephalic version at term increases the chance of vaginal cephalic birth, and reduces the chance of caesarean section and vaginal breech delivery. There is not enough evidence from randomised trials to assess complications of external cephalic version at term, however large observational studies suggest that complications are rare ( Boucher 2003 ; Impey 1999 ; Impey 2005 ).
Overall completeness and applicability of evidence
The absolute numbers of non‐cephalic births and caesarean sections vary considerably between trials. This probably reflects differences in study populations and caesarean section policies. The direction of effects is, however, consistent, with the exception of the rates of caesarean section in the study of Van de Pavert 1990 . Considerable cross‐over between groups in the latter study may have reduced the power of the study to show differences related to external cephalic version (ECV). The study authors suggest that against a background of low caesarean section rates for breech presentation, the negative experience of failed ECV may render the woman or doctors more likely to opt for caesarean section.
The women included in these studies had low‐risk pregnancies and medical histories. Women with previous caesarean sections were excluded, for example. This limits the applicability of the evidence to other populations of women.
The recent trend to routine caesarean section for persistent breech presentation may result in a greater impact of ECV on caesarean section rates than was apparent in the studies reviewed.
The trials reviewed do not give information on women's views.
No analgesia was used in these studies. This review included trials with and without tocolysis. Four trials used tocolysis routinely for ECV (ritodrine: Brocks 1984 and Hindawi 2005 , hexaprenaline: Mahomed 1991 , terbutaline sulphate: Van Dorsten 1981 ). In two trials tocolysis was used if the initial ECV attempt was unsuccessful (hexaprenaline: Hofmeyr 1983 , ritodrine: Van de Pavert 1990 ). No tocolysis was used in Dafallah 2004 and Rita 2012 . The use of tocolytic drugs and other interventions to help ECV is covered by a separate Cochrane review ( Cluver 2012 ).
Quality of the evidence
All of the trials included in this review had design limitations. Due to the nature of the intervention, no studies attempted to blind participants or clinicians to group allocation. Women would have been aware of the intervention and this may have affected decisions regarding care in later pregnancy and at the birth. Staff would be aware of intervention and this may have affected other aspects of care and decision‐making at the birth. This may have had an impact on outcomes such as caesarean section. In one study ( Van de Pavert 1990 ), it was much more likely that women would have a caesarean section if ECV had been attempted and failed than in women where ECV had never been attempted, so it is possible than attempt and failure of ECV affects decision‐making about caesarean section.
The descriptions of randomisation and allocation procedures were not optimal in several studies ( Brocks 1984 ; Dafallah 2004 ; Hindawi 2005 ; Rita 2012 ; Van de Pavert 1990 ; Van Dorsten 1981 ). It is unclear whether this is due to omissions in the reporting of the studies, or limitations of study design.
The level of evidence was graded low (perinatal death) or very low (vaginal cephalic birth not achieved, caesarean section, Apgar score < 7 at five minutes, umbilical vein pH < 7.20, neonatal admission) ( Table 1 ). The two graded outcomes addressing mode of delivery (vaginal cephalic birth not achieved, caesarean section) were downgraded for quality of evidence due to design limitations in the studies, and inconsistency due to statistical heterogeneity. The four graded outcomes addressing perinatal outcomes (Apgar score < 7 at five minutes, umbilical vein pH < 7.20, neonatal admission, perinatal death) were downgraded for quality evidence due to design limitations in the studies, and imprecision due to wide confidence intervals and few events.
Potential biases in the review process
The assessment of risk of bias involves subjective judgements. This potential limitation is minimised by following the procedures in the Cochrane Handbook for Systematic Reviews of Interventions ( Higgins 2011 ), with review authors independently assessing studies and resolving any disagreement through discussion, and if required involving a third assessor in the decision.
Agreements and disagreements with other studies or reviews
No recent systematic reviews of randomised trials were found. A systematic review of cohort studies (three) and case‐control studies (eight), found an increased caesarean delivery rate for women with a successful external cephalic version (21%; odds ratio 2.2, 95% confidence interval 1.6 to 3.0) ( De Hundt 2014 ).
Implications for practice
The studies in this review provide convincing evidence that the chance of breech birth and caesarean section may be substantially reduced by attempting external cephalic version (ECV) at or near term. The numbers studied are too small to give an accurate assessment of the risks of ECV, though data from observation studies are reassuring. There is sound reason for the clinical use of ECV at term, with the appropriate precautions, in any woman in whom the value of an improved chance of a cephalic birth outweighs the risk of the procedure.
Implications for research
Future research should be directed towards refining the selection of women suitable for ECV attempt at term. For example, previous caesarean section has been regarded as a contraindication to ECV. In an uncontrolled series, ECV was found to be successful in 82% of 56 women with one or two previous caesarean sections ( Flamm 1991 ).
The place of ECV during labour requires further study. This procedure was reported to be successful in 11 (73%) out of 15 women in labour considered unsuitable for vaginal breech delivery. Caesarean section was avoided in 10 (67%) of the women ( Ferguson 1985 ).
Further research is needed to define more accurately the effect of ECV on perinatal outcome, and the place of ECV in non‐longitudinal lies.
Future studies should include an assessment of women's views.
Protocol first published: Issue 2, 1996 Review first published: Issue 2, 1996
Acknowledgements
In this update: Therese Dowswell for assessing the blinding of outcome assessors in included studies, Leanne Jones and Denise Atherton for editorial and administrative support, Lynn Hampson for the literature search.
In previous versions: Tess Lawrie for assistance with study selection, data extraction and help preparing this update; Sonja Henderson and Denise Atherton for administrative support; Lynn Hampson and Jill Hampson for the literature search.
Helen West's work is supported by the NIHR Cochrane Programme Grant Project: 13/89/05 – Pregnancy and childbirth systematic reviews to support clinical guidelines.
This project was supported by the National Institute for Health Research, via Cochrane Infrastructure and Cochrane Programme Grant funding to Cochrane Pregnancy and Childbirth. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Appendix 1. Previous searches conducted by authors
CENTRAL ( The Cochrane Library, 2010, Issue 3) and PubMed (1966 to September 2010) using the terms external cephalic version OR ECV.
Edited (no change to conclusions)
Data and analyses
Comparison 1, comparison 2, comparison 3, characteristics of studies, characteristics of included studies [ordered by study id].
APH: antepartum haemorrhage CS: caesarean section CTG: cardiotocograph ECV: external cephalic version GA: gestational age IUGR: intrauterine growth restriction IVI: intravenous
Characteristics of excluded studies [ordered by study ID]
ECV: external cephalic version
Differences between protocol and review
The outcomes vaginal cephalic delivery not achieved and vaginal breech delivery were added for this 2015 update. Outcomes that were not prespecified in the original protocol include: vaginal cephalic delivery not achieved, vaginal breech delivery, Apgar score less than seven at one minute, and enrolment‐delivery interval.
Methods for subgroup analysis for future updates were added. It has been suggested that ECV may be more successful (and spontaneous version more common) in black African than Caucasian women, possibly because of the tendency for the presenting part to remain high until the onset of labour ( Hofmeyr 1986 ). Post‐hoc sensitivity analysis excluding the three studies in black African women ( Dafallah 2004 ; Hofmeyr 1983 ; Mahomed 1991 ) was conducted.
Contributions of authors
GJ Hofmeyr prepared the original version, maintains the review and reviewed the updated version. H West revised the text, assessed studies, extracted and analysed data for the updated version of the review. R Kulier assessed studies and extracted data for the updated version of the review, and revised and quality‐checked the previous version of the review.
Sources of support
Internal sources.
- (GJH) Effective Care Research Unit, University of the Witwatersrand/Fort Hare, Eastern Cape Department of Health, South Africa.
- Department of Obstetrics and Gynaecology, Geneva University Hospital, Switzerland.
- (HW) Cochrane Pregnancy and Childbirth Group, Department of Women's and Children's Health, The University of Liverpool, Liverpool, UK.
External sources
- (GJH) South African Medical Research Council, South Africa.
- (GJH) HRP‐UNDP/UNFPA/WHO/World Bank Special Programme in Human Reproduction, Geneva, Switzerland.
- Rockefeller Foundation, USA.
- (HW) National Institute for Health Research (NIHR), UKNIHR Cochrane Programme Grant Project: 13/89/05 – Pregnancy and childbirth systematic reviews to support clinical guidelines, UK.
Declarations of interest
GJ Hofmeyr (GJH) is an author of one of the papers included in this review ( Hofmeyr 1983 ) but he was not involved in assessing this study for inclusion, assessing trial quality, or data extraction. GJH receives royalties from UpToDate for chapters related to breech pregnancy, delivery of a baby in breech presentation and external cephalic version. UpToDate is an electronic publication by Wolters Kluwer to disseminate evidence‐based medicine (such as Cochrane reviews).
References to studies included in this review
Brocks 1984 {published data only}.
- Brocks V, Philipsen T, Secher NJ. A randomized trial of external cephalic version with tocolysis in late pregnancy . British Journal of Obstetrics and Gynaecology 1984; 91 :653‐6. [ PubMed ] [ Google Scholar ]
Dafallah 2004 {published data only}
- Dafallah SE, Elhag SM. The role of external cephalic version on the presentation at delivery . Saudi Medical Journal 2004; 25 ( 3 ):386‐8. [ PubMed ] [ Google Scholar ]
Hindawi 2005 {published data only}
- Hindawi I. Value and pregnancy outcome of external cephalic version . Eastern Mediterranean Health Journal 2005; 11 ( 4 ):633‐9. [ PubMed ] [ Google Scholar ]
Hofmeyr 1983 {published data only}
- Hofmeyr GJ. Effect of external cephalic version in late pregnancy on breech presentation and caesarean section rate: a controlled trial . British Journal of Obstetrics and Gynaecology 1983; 90 :392‐9. [ PubMed ] [ Google Scholar ]
Mahomed 1991 {published data only}
- Mahomed K, Seeras R, Coulson R. External cephalic version at term. A randomised controlled trial using tocolysis . British Journal of Obstetrics and Gynaecology 1991; 98 :8‐13. [ PubMed ] [ Google Scholar ]
Rita 2012 {published data only}
- Rita, Mehbooba, Sultana S, Khurshid R. A randomized trial of external cephalic version in late pregnancy . JK Science 2012; 14 ( 1 ):25‐9. [ Google Scholar ]
Van de Pavert 1990 {published data only}
- Pavert R, Gravenhorst JB, Keirse MJNC. Value of external version in breech presentation at term . Nederlands Tijdschrift voor Geneeskunde 1990; 134 :2245‐8. [ PubMed ] [ Google Scholar ]
Van Dorsten 1981 {published data only}
- Dorsten JP, Schifrin BS, Wallace RL. Randomized control trial of external cephalic version with tocolysis in late pregnancy . American Journal of Obstetrics and Gynecology 1981; 141 :417‐24. [ PubMed ] [ Google Scholar ]
References to studies excluded from this review
Besio 1994 {published data only}.
- Besio M, Coto M. Evaluation of the external cephalic version in the management of dystocia (published erratum appears in Revista Chilena de Obstetricia y Ginecologia 1995;60(2):145) . Revista Chilena de Obstetricia y Ginecologia 1994; 59 :422‐7. [ PubMed ] [ Google Scholar ]
El‐Muzaini 2008a {published data only}
- El‐Muzaini MF, Felimban HM, Al‐Hazmi NM, Shabaan LA, Namankani FY, Fathudein MA. Breech in labor, to turn or not to turn? . BJOG: an international journal of obstetrics and gynaecology 2008; 115 ( s1 ):77. [ Google Scholar ]
El‐Muzaini 2008b {published data only}
- El‐Muzaini MF, Felimban HM, Al‐Hazmi NM, Shabaan LA, Namankani FY, Fathudein MA. Breech with previous scar, is ECV a good option? . BJOG: an international journal of obstetrics and gynaecology 2008; 115 ( s1 ):77‐8. [ Google Scholar ]
Rust 2005 {published data only}
- Rust O, Atlas R, Gersbach E, Roberts W, Larkin R, Hess LW. A randomized trial of late versus early external cephalic version for the treatment of abnormal presentation at term [abstract] . American Journal of Obstetrics and Gynecology 2005; 193 ( 6 Suppl ):S129. [ Google Scholar ]
Stine 1985 {published data only}
- Stine LE, Phelan JP, Wallace R, Eglinton GS, Dorsten JP, Schifrin BS. Update on external cephalic version performed at term . Obstetrics & Gynecology 1985; 65 :642‐6. [ PubMed ] [ Google Scholar ]
Van Veelen 1989 {published data only}
- Veelen AJ, Cappellen AW, Flu PK, Straub MJPF, Wallenburg HCS. Effect of external cephalic version in late pregnancy on presentation at delivery: a randomized controlled trial . British Journal of Obstetrics and Gynaecology 1989; 96 :916‐21. [ PubMed ] [ Google Scholar ]
Additional references
Ben‐haroush 2002.
- Ben‐Haroush A, Perri T, Bar J, Yogev Y, Bar‐Hava I, Hod M, et al. Mode of delivery following successful external cephalic version . American Journal of Perinatology 2002; 19 :355‐60. [ PubMed ] [ Google Scholar ]
Boucher 2003
- Boucher M, Bujold E, Marquette GP, Vezina Y. The relationship between amniotic fluid index and successful external cephalic version: a 14‐year experience . American Journal of Obstetrics and Gynecology 2003; 189 :751‐4. [ PubMed ] [ Google Scholar ]
Bradley‐Watson 1975
- Bradley‐Watson PJ. The decreasing value of external cephalic version in modern obstetric practice . American Journal of Obstetrics and Gynecology 1975; 123 :237‐40. [ PubMed ] [ Google Scholar ]
Brosset 1956
- Brosset A. The value of prophylactic external version in cases of breech presentation . Acta Obstetricia et Gynecologica Scandinavica 1956; 35 :555‐62. [ PubMed ] [ Google Scholar ]
- Chan LY, Leung TY, Fok WY, Chan LW, Lau TK. Prediction of successful vaginal delivery in women undergoing external cephalic version at term for breech presentation . European Journal of Obstetrics & Gynecology and Reproductive Biology 2004; 116 :39‐42. [ PubMed ] [ Google Scholar ]
- Chan LY, Tang JL, Tsoi KF, Fok WY, Chan LW, Lau TK. Intrapartum cesarean delivery after successful external cephalic version: a meta‐analysis . Obstetrics & Gynecology 2004; 104 :155‐60. [ PubMed ] [ Google Scholar ]
- Chan LY, Leung TY, Fok WY, Chan LW, Lau TK. Cord blood acid‐base status at delivery after successful external cephalic version . Acta Obstetricia et Gynecologica Scandinavica 2004; 83 :436‐9. [ PubMed ] [ Google Scholar ]
Cluver 2012
- Cluver C, Hofmeyr GJ, Gyte GML, Sinclair M. Interventions for helping to turn term breech babies to head first presentation when using external cephalic version . Cochrane Database of Systematic Reviews 2012, Issue 1 . [DOI: 10.1002/14651858.CD000184.pub3] [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Collaris 2004
- Collaris RJ, Oei SG. External cephalic version: a safe procedure? A systematic review of version‐related risks . Acta Obstetricia et Gynecologica Scandinavica 2004; 83 :511‐8. [ PubMed ] [ Google Scholar ]
Cooper 2002
- Cooper GM, Lewis G, Neilson J. Editorial: confidential enquiries into maternal deaths . British Journal of Anaesthesia 2002; 89 ( 3 ):369‐72. [ PubMed ] [ Google Scholar ]
Danielian 1996
- Danielian PJ, Wang J, Hall MH. Long term outcome by method of delivery of fetuses in breech presentation at term: population based follow up . BMJ 1996; 312 :1451‐3. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dashe JS, McIntire DD, Ramus RM, Santos‐Ramos R, Twickler DM. Persistence of placenta previa according to gestational age at ultrasound . Obstetrics & Gynecology 2002; 99 ( 5 Pt 1 ):692‐7. [ PubMed ] [ Google Scholar ]
De Hundt 2014
- Hundt M, Velzel J, Groot CJ, Mol BW, Kok M. Mode of delivery after successful external cephalic version: a systematic review and meta‐analysis . Obstetrics & Gynecology 2014; 123 ( 6 ):1327‐34. [ PubMed ] [ Google Scholar ]
Devendra 2002
- Devendra K. Introducing routine external cephalic version for the management of the malpresenting fetus near term . Medical Journal of Malaysia 2002; 57 :454‐9. [ PubMed ] [ Google Scholar ]
Elbourne 2002
- Elbourne DR, Altman DG, Higgins JPT, Curtin F, Vaillancourt JM. Meta‐analyses involving cross‐over trials: methodological issues . International Journal of Epidemiology 2002; 31 :140‐9. [ PubMed ] [ Google Scholar ]
Ferber 1999
- Ferber A, Peleg D, Bar‐Hava I, Orvieto R, Ben‐Rafael Z. Optimal fetal outcome despite persistent sinusoidal pattern after external cephalic version . Journal of Obstetrics and Gynaecology 1999; 19 :314‐5. [ PubMed ] [ Google Scholar ]
Ferguson 1985
- Ferguson JE, Dyson DC. Intrapartum external cephalic version . American Journal of Obstetrics and Gynecology 1985; 152 :297‐8. [ PubMed ] [ Google Scholar ]
- Flamm BL, Fried MW, Lonky NM, Giles WS. External cephalic version after previous cesarean section . American Journal of Obstetrics and Gynecology 1991; 165 :370‐2. [ PubMed ] [ Google Scholar ]
Fortunato 1988
- Fortunato SJ, Mercer LJ, Guzick DS. External cephalic version with tocolysis: factors associated with success . Obstetrics & Gynecology 1988; 72 :59‐62. [ PubMed ] [ Google Scholar ]
Fung Kee Fung 2003
- Fung Kee Fung K, Eason E, Crane J, Armson A, Ronde S, Farine D, et al. Prevention of Rh alloimmunization . Journal of Obstetrics and Gynaecology Canada: JOGC 2003; 25 :765‐73. [ PubMed ] [ Google Scholar ]
Gamble 2000
- Gamble JA, Creedy DK. Women's request for a cesarean section: a critique of the literature . Birth 2000; 27 ( 4 ):256‐63. [ PubMed ] [ Google Scholar ]
- Geary M, Fanagan M, Boylan P. Maternal satisfaction with management of labour and preference for mode of delivery . Journal of Perinatal Medicine 1997; 25 ( 5 ):433‐9. [ PubMed ] [ Google Scholar ]
Gilliam 2002
- Gilliam M, Rosenberg D, Davis F. The likelihood of placenta previa with greater number of cesarean deliveries and higher parity . Obstetrics & Gynecology 2002; 99 ( 6 ):976‐80. [ PubMed ] [ Google Scholar ]
Goffinet 2006
- Goffinet F, Carayol M, Foidart JM, Alexander S, Uzan S, Subtil D, Bréart G, PREMODA Study Group. Is planned vaginal delivery for breech presentation at term still an option? Results of an observational prospective survey in France and Belgium . American Journal of Obstetrics and Gynecology 2006; 194 ( 4 ):1002‐11. [ PubMed ] [ Google Scholar ]
Grade 2008 [Computer program]
- Version 3.6 for Windows. GRADEpro [Computer program]. Jan Brozek, Andrew Oxman, Holger Schünemann . Version 3.6 for Windows, 2008.
- Guyer CH, Heard MJ. A prospective audit of external cephalic version at term: are ultrasound parameters predictive of outcome? . Journal of Obstetrics and Gynaecology 2001; 21 :580‐2. [ PubMed ] [ Google Scholar ]
- Hall MH, Bewley S. Maternal mortality and mode of delivery . Lancet 1999; 354 ( 1180 ):776. [ PubMed ] [ Google Scholar ]
Higgins 2011
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011 . Available from www.cochrane‐handbook.org .
Hildingsson 2002
- Hildingsson I, Radestad I, Rubertsson C. Waldenstrom U. Few women wish to be delivered by caesarean section . BJOG: an international journal of obstetrics and gynaecology 2002; 109 ( 6 ):618‐23. [ PubMed ] [ Google Scholar ]
Hofmeyr 1986
- Hofmeyr GJ, Sadan O, Myer IG, Gallal KC, Simko G. External cephalic version and spontaneous version rates: ethnic and other determinants . British Journal of Obstetrics and Gynaecology 1986; 93 :13‐6. [ PubMed ] [ Google Scholar ]
Hofmeyr 1989
- Hofmeyr GJ. Breech presentation and abnormal lie in late pregnancy . In: Chalmers I, Enkin MW, Keirse MJNC editor(s). Effective Care in Pregnancy and Childbirth . Oxford: Oxford University Press, 1989:653‐65. [ Google Scholar ]
Hofmeyr 1991
- Hofmeyr GJ. External cephalic version at term: how high are the stakes? . British Journal of Obstetrics and Gynaecology 1991; 98 :1‐3. [ PubMed ] [ Google Scholar ]
Hofmeyr 1992
- Hofmeyr GJ. Breech presentation and shoulder dystocia in childbirth . Current Opinion in Obstetrics and Gynecology 1992; 4 :807‐12. [ PubMed ] [ Google Scholar ]
Hofmeyr 1993
- Hofmeyr GJ. External cephalic version at term . Fetal Maternal Medicine Review 1993; 5 :213‐22. [ Google Scholar ]
Hofmeyr 2000
- Hofmeyr GJ, Kulier R. Cephalic version by postural management for breech presentation . Cochrane Database of Systematic Reviews 2000, Issue 3 . [DOI: 10.1002/14651858.CD000051] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Hofmeyr 2003
- Hofmeyr GJ, Hannah M, Lawrie TA. Planned caesarean section for term breech delivery . Cochrane Database of Systematic Reviews 2003, Issue 2 . [DOI: 10.1002/14651858.CD000166] [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Hofmeyr 2004
- Hofmeyr GJ. Obstructed labor: using better technologies to reduce mortality . International Journal of Gynaecology & Obstetrics 2004; 85 Suppl 1 :S62‐72. [ PubMed ] [ Google Scholar ]
Hofmeyr 2005
Holmes 2004.
- Holmes W, Hofmeyr GJ. Management of breech presentation in areas with high prevalence of HIV infection . International Journal of Gynaecology & Obstetrics 2004; 87 :272‐6. [ PubMed ] [ Google Scholar ]
Hughes 1997
- Hughes GW. Establishing an external cephalic version clinic: outcome of the first year . Journal of Obstetrics and Gynaecology 1997; 17 :127‐31. [ PubMed ] [ Google Scholar ]
Hutton 2006
- Hutton EK, Hofmeyr GJ. External cephalic version for breech presentation before term . Cochrane Database of Systematic Reviews 2006, Issue 1 . [DOI: 10.1002/14651858.CD000084.pub2] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Impey L, Lissoni D. Outcome of external cephalic version after 36 weeks' gestation without tocolysis . Journal of Maternal‐Fetal Medicine 1999; 8(5) :203‐7. [ PubMed ] [ Google Scholar ]
- Impey L, Pandit M. Tocolysis for repeat external cephalic version in breech presentation at term: a randomised, double‐blinded, placebo‐controlled trial . BJOG: an international journal of obstetrics and gynaecology 2005; 112(5) :627‐31. [ PubMed ] [ Google Scholar ]
LaSala 1987
- LaSala AP, Berkeley AS. Primary cesarean section and subsequent fertility . American Journal of Obstetrics and Gynecology 1987; 157 ( 2 ):379‐83. [ PubMed ] [ Google Scholar ]
- Lau TK, Lo KWK, Wan D, Rogers MS. Predictors of successful external cephalic version at term: a prospective study . British Journal of Obstetrics and Gynaecology 1997; 104 :798‐802. [ PubMed ] [ Google Scholar ]
Le Bret 2004
- Bret T, Grange G, Goffinet F, Cabrol D. External cephalic version: experience about 237 versions at Port‐Royal maternity . Journal de Gynecologie, Obstetrique et Biologie de la Reproduction (Paris) 2004; 33 :297‐303. [ PubMed ] [ Google Scholar ]
Lojacono 2003
- Lojacono A, Donarini G, Valcamonico A, Soregaroli M, Frusca T. External cephalic version for breech presentation at term: an effective procedure to reduce the caesarean section rate . Minerva Ginecologica 2003; 55 :519‐24. [ PubMed ] [ Google Scholar ]
Lydon‐Rochelle 2001
- Lydon‐Rochelle M, Holt VL, Easterling TR, Martin DP. First‐birth cesarean and placental abruption or previa at second birth . Obstetrics & Gynecology 2001; 97 ( 5 Pt 1 ):765‐9. [ PubMed ] [ Google Scholar ]
Minkoff 2003
- Minkoff H, Chervenak FA. Elective primary cesarean delivery . New England Journal of Medicine 2003; 384 ( 10 ):946‐50. [ PubMed ] [ Google Scholar ]
Murray‐Davis 2012
- Murray‐Davis B, Marion A, Malott A, Reitsma A, Hutton RM and the Early ECV2 Trial Collaborative Group. Women's experiences of participating in the early external cephalic version 2 trial . Birth 2012; 39 ( 1 ):30‐8. [ PubMed ] [ Google Scholar ]
Nassar 2007
- Nassar N, Roberts CL, Raynes‐Greenow CH, Barratt A, Peat B, on behalf of the Decision Aid for Breech Presentation Trial Collaborators. Evaluation of a decision aid for women with breech presentation at term: a randomised controlled trial . British Journal of Obstetrics and Gynaecology 2007; 114 :325‐33. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Nzewi N, Clerk P, Bowen‐Simpkins C. Prolonged fetal tachycardia‐an unusual complication of external cephalic version . Journal of Obstetrics and Gynaecology 1999; 19 :427‐8. [ PubMed ] [ Google Scholar ]
- Owens M, Bhullar A, Carlan SJ, O'Brien WF, Hirano K. Effect of fundal pressure on maternal to fetal microtransfusion at the time of cesarean delivery . Journal of Obstetrics and Gynaecology Research 2003; 29 :152‐6. [ PubMed ] [ Google Scholar ]
- Papp S, Dhaliwal G, Davies G, Borschneck D. Fetal femur fracture and external cephalic version . Obstetrics & Gynecology 2004; 104 :1154‐6. [ PubMed ] [ Google Scholar ]
Raynes‐Greenow 2004
- Raynes‐Greenow CH, Roberts CL, Barratt A, Brodrick B, Peat B. Pregnant women's preferences and knowledge of term breech management, in an Australian setting . Midwifery 2004; 20 :181‐7. [ PubMed ] [ Google Scholar ]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan) . Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Schachter 1994
- Schachter M, Kogan S, Blickstein I. External cephalic version after previous cesarean section ‐ a clinical dilemma . International Journal of Gynecology & Obstetrics 1994; 45 :17‐20. [ PubMed ] [ Google Scholar ]
Schunemann 2009
- Schunemann HJ. GRADE: from grading the evidence to developing recommendations. A description of the system and a proposal regarding the transferability of the results of clinical research to clinical practice [GRADE: Von der Evidenz zur Empfehlung. Beschreibung des Systems und Losungsbeitrag zur Ubertragbarkeit von Studienergebnissen]. Zeitschrift fur Evidenz, Fortbildung und Qualitat im Gesundheitswesen 2009; 103 ( 6 ):391‐400. [PUBMED: 19839216] [ PubMed ] [ Google Scholar ]
Shankar 2004
- Shankar M, Gough GW, Chakravarti S, Vellacott ID. Massive feto‐maternal haemorrhage with good perinatal outcome following failed external cephalic version . Fetal Diagnosis and Therapy 2004; 19 :68‐71. [ PubMed ] [ Google Scholar ]
Skupski 2003
- Skupski DW, Harrison‐Restelli C, Dupont RB. External cephalic version: an approach with few complications . Gynecologic and Obstetric Investigation 2003; 56 :83‐8. [ PubMed ] [ Google Scholar ]
- Tong Leung VK, Suen SS, Singh Sahota D, Lau TK, Yeung Leung T. External cephalic version does not increase the risk of intra‐uterine death: a 17‐year experience and literature review . Journal of Maternal‐Fetal & Neonatal Medicine 2012; 25 ( 9 ):1774‐8. [ PubMed ] [ Google Scholar ]
Turnbull 1999
- Turnbull DA, Wilkinson C, Yaser A, Carty V, Svigos JM, Robinson JS. Women's role and satisfaction in the decision to have a caesarean section . Medical Journal of Australia 1999; 170 ( 12 ):580‐3. [ PubMed ] [ Google Scholar ]
Vezina 2004
- Vezina Y, Bujold E, Varin J, Marquette GP, Boucher M. Cesarean delivery after successful external cephalic version of breech presentation at term: a comparative study . American Journal of Obstetrics and Gynecology 2004; 190 :763‐8. [ PubMed ] [ Google Scholar ]
Walker 2002
- Walker R, Turnbull D, Wilkinson C. Strategies to address global cesarean section rates: a review of the evidence . Birth 2002; 29 ( 1 ):28‐39. [ PubMed ] [ Google Scholar ]
Williams 1999
- Williams J, Bjornsson S, Cameron AD, Mathers A, Yahya SZS, Pell JP. Prospective study of external cephalic version in Glasgow: patient selection, outcome and factors associated with outcome . Journal of Obstetrics and Gynaecology 1999; 19 :598‐601. [ PubMed ] [ Google Scholar ]
- Yogev Y, Horowitz E, Ben‐Haroush A, Chen R, Kaplan B. Changing attitudes toward mode of delivery and external cephalic version in breech presentations . International Journal of Gynecology & Obstetrics 2002; 79 :221‐4. [ PubMed ] [ Google Scholar ]
- Zhang J, Bowes WA, Fortney JA. Efficacy of external cephalic version: a review . Obstetrics & Gynecology 1993; 82 :306‐12. [ PubMed ] [ Google Scholar ]
References to other published versions of this review
Hofmeyr 1995.
- Hofmeyr GJ. External cephalic version at term. [revised 04 October 1993] . In: Enkin MW, Keirse MJNC, Renfrew MJ, Neilson JP, Crowther C (eds.) Pregnancy and Childbirth Module. In: The Cochrane Pregnancy and Childbirth Database [database on disk and CDROM]. The Cochrane Collaboration; Issue 2, Oxford: Update Software; 1995 .
Hofmeyr 1996
- Hofmeyr GJ, Kulier R. External cephalic version for breech presentation at term . Cochrane Database of Systematic Reviews 1996, Issue 1 . [DOI: 10.1002/14651858.CD000083] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Hofmeyr 2012
- Hofmeyr GJ, Kulier R. External cephalic version for breech presentation at term . Cochrane Database of Systematic Reviews 2012, Issue 10 . [DOI: 10.1002/14651858.CD000083.pub2] [ PubMed ] [ CrossRef ] [ Google Scholar ]

IMAGES
VIDEO
COMMENTS
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The three types of breech presentation include frank breech, complete breech, and incomplete breech. ... a planned cesarean section for delivery sometime after 39 weeks. Regarding the premature breech, gestational age ...
The main types of breech presentation are: Frank breech - Both hips are flexed and both knees are extended so that the feet are adjacent to the head ( figure 1 ); accounts for 50 to 70 percent of breech fetuses at term. Complete breech - Both hips and both knees are flexed ( figure 2 ); accounts for 5 to 10 percent of breech fetuses at term.
This head-first position is called vertex presentation and is the safest position for birth. Advertisement. ... (C-section). How does a breech baby affect delivery? If your baby presents in a breech position after 36 weeks of pregnancy, your birthing plan will likely change. It's usually unsafe for a breech baby to be born vaginally due to ...
In a breech presentation, the body comes out first, leaving the baby's head to be delivered last. The baby's body may not stretch the cervix enough to allow room for the baby's head to come out easily. There is a risk that the baby's head or shoulders may become wedged against the bones of the mother's pelvis.
Labour with a preterm breech should be managed as with a term breech. C. Where there is head entrapment, incisions in the cervix (vaginal birth) or vertical uterine D incision extension (caesarean section) may be used, with or without tocolysis. Evidence concerning the management of preterm labour with a breech presentation is lacking.
Because of risk of injury or even death to the baby, cesarean delivery is preferred when the fetus is in breech presentation, unless the doctor is very experienced with and skilled at delivering breech babies or there is not an adequate facility or equipment to safely perform a cesarean delivery.
(See "Overview of breech presentation" and "External cephalic version".) For patients who present in labor with a breech fetus, cesarean birth is the preferred approach in many hospitals in the United States and elsewhere. Cesarean is performed for over 90 percent of breech presentations, and this rate has increased worldwide . However, even in ...
Breech Births. In the last weeks of pregnancy, a baby usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation. A breech presentation occurs when the baby's buttocks, feet, or both are positioned to come out first during birth. This happens in 3-4% of full-term births.
A caesarian section booked as an elective procedure at term is the most common management for breech presentation. Caesarean section is preferred for preterm babies (due to an increased head to abdominal circumference ratio in preterm babies) and is used if the external cephalic version is unsuccessful or as a maternal preference. This option ...
Observational, usually retrospective, series have consistently favoured elective caesarean birth over vaginal breech delivery. A meta-analysis of 27 studies examining term breech birth, 5 which included 258 953 births between 1993 and 2014, suggested that elective caesarean section was associated with a two- to five-fold reduction in perinatal mortality when compared with vaginal breech ...
At full term, around 3%-4% of births are breech. The different types of breech presentations include: Complete: The fetus's knees are bent, and the buttocks are presenting first. Frank: The fetus's legs are stretched upward toward the head, and the buttocks are presenting first. Footling: The fetus's foot is showing first.
Breech presentation is defined as a fetus in a longitudinal lie with the buttocks or feet closest to the cervix. This occurs in 3-4% of all deliveries. The percentage of breech deliveries decreases with advancing gestational age from 22-25% of births prior to 28 weeks' gestation to 7-15% of births at 32 weeks' gestation to 3-4% of births at term.
Cesarean section in breech or transverse presentation involves more complicated procedures than cesarean section in cephalic presentation because the former requires additional manipulations for guiding the presenting part of the fetus, liberation of the arms, and the after-coming head delivery; therefore, those cesarean sections are likely to be more invasive.
Learn more about the types, causes, and risks of breech presentation, along with how breech babies are typically delivered. ... Takeda S. Clinical Tips of Cesarean Section in Case of Breech ...
For women with breech presentation in labor, planned cesarean section at 39 weeks or greater has been shown to significantly reduce perinatal mortality and neonatal morbidity compared with vaginal breech delivery (RR 0.33, 95% CI 0.19 to 0.56).
Babies lying bottom first or feet first in the uterus (womb) instead of in the usual head-first position are called breech babies. Breech is very common in early pregnancy, and by 36-37 weeks of pregnancy, most babies turn naturally into the head-first position. Towards the end of pregnancy, only 3-4 in every 100 (3-4%) babies are in the breech ...
1. For a woman with breech presentation near term, pre- or early-labour ultrasound should be performed to assess type of breech presentation, flexion of the fetal head, and fetal growth. If a woman presents in labour and ultrasound is unavailable and has not recently been performed, Caesarean section is recommended (strong; moderate). 2.
With a policy of routine caesarean section for breech presentation at term, in time, the clinical skills of vaginal breech delivery will be eroded, placing women who deliver vaginally at increased risk. Implications for research. Childbirth is a profound and unique human experience. Little is known about the evolutionary importance of the birth ...
Between 1998 and 2002, 35,453 term infants were delivered. The cesarean delivery rate for breech presentation increased from 50% to 80% within 2 months of the trial's publication and remained elevated. The combined neonatal mortality rate decreased from 0.35% to 0.18%, and the incidence of reported birth trauma decreased from 0.29% to 0.08%.
Meta-analysis of 5-minute Apgar <7 score in term singleton breech presentation (planned vaginal delivery vs planned caesarean section) (n = 92 135). Admittance to neonatal ICU assessment included 9 studies, 32 438 single foetus, full-term, breech presentation deliveries (9053 planned vaginal deliveries and 23 385 elective caesareans) were included.
Breech presentation is common in about 15% of pregnancies at 29 to 32 weeks. ... Planned c-section for breech birth has been found to lower both perinatal and neonatal death rates, lower short ...
Incidence of breech presentation was 2.1 %, prematurity was the most common cause. 113 (42.6 %) women delivered vaginally. 54 (20.4 %) were planned for cesarean section. ... When assisted vaginal breech delivery is accomplished after proper selection and counseling for women with breech presentation, cesarean section in preterm as well as term ...
If the baby is in another position, there is a higher risk of complications including the need for caesarean section. In a 'breech presentation' the baby is bottom‐down instead of head‐down. External cephalic version (ECV) is a technique for turning the unborn baby so it lies head‐down. This review looked at the effects of using ECV ...