- Biochemistry and Molecular Biology
- Biostatistics
- Environmental Health and Engineering
- Epidemiology
- Health Policy and Management
- Health, Behavior and Society
- International Health
- Mental Health
- Molecular Microbiology and Immunology
- Population, Family and Reproductive Health
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?

Bringing Informed Decision-Making to Cancer Screening
“Get screened” shouldn’t be the full message, says one cancer prevention expert.
Aliza Rosen
Screening for various cancers before a person experiences symptoms can help detect cancer in the early stages when treatment is often more effective. But there’s more to the message of “get screened” than most people realize, says Otis Brawley , MD, a Bloomberg Distinguished Professor with joint appointments in Epidemiology and the Sidney Kimmel Comprehensive Cancer Center, who emphasizes the importance of routine, high-quality screening with adequate follow-up.
For Cancer Prevention Awareness Month, Brawley talked with Public Health On Call host Stephanie Desmon about why it’s important for everyone to understand both the benefits and the risks of cancer screening in order to make informed decisions. This article is adapted from their conversation.
Cancer screening is more complex than just getting a test.
Many people think you just get the test, and if the test finds cancer, there is benefit. In fact, it’s far more complicated than that.
While family practice doctors and internal medicine doctors tend to be educated on it, it’s not something all doctors learn about in medical school.
There are cancers—for example, in the prostate and breast—that a person will never be bothered by, because they will ultimately die from something totally unrelated.
Cervical cancer screening saves lives.
In the case of cervical cancer —detected early with a Pap smear or advanced HPV testing— screening clearly saves lives . Women should be screened starting in their 20s. Certain tests should only be done once women are in their 30s through their 60s.
Don’t just get a mammogram. Get routine, high-quality mammography.
Screening for breast cancer saves lives, and it’s recommended that most women start at age 45. However, the message so frequently is to get a mammogram, when the message should be to get into a program of routine, high-quality mammography.
For example, most mammogram vans do not offer the opportunity for previous mammograms to be looked at. High-quality mammography, in my opinion, means that a person’s mammograms from last year and the year before are compared to this year’s.
Colonoscopies aren’t the only way to screen for colorectal cancer.
With colorectal cancer screening , everybody thinks “colonoscopy, colonoscopy.” Colonoscopies save lives and they can be done every 10 years. There’s also stool blood testing, which can be done every year, and stool DNA tests, which can be done every three years. Starting at age 45, those things should be done with adequate follow-up .
Lung cancer screening saves lives, but it’s not without risks.
There are about 140,000 to 150,000 lung cancer deaths a year in the United States. If we had full-scale lung cancer screening , we know that we would prevent perhaps 10,000 of them, but we would actually cause 1,500 to 1,800 deaths because of the diagnostics .
In lung cancer screening, it’s common that a radiologist will see something on an image that could be lung cancer, but could also be an old fungal infection or a scar from a bacterial infection 60 years prior. The only way to figure out whether or not it’s lung cancer is a transthoracic needle biopsy, which involves a controlled stab of a needle through a person’s chest and into the lesion while the person is in a CT scanner. If you stab enough people, you’re going to potentially cause a collapsed lung, and it’s possible the person will have a heart attack.
It’s recommended that people with an extensive smoking history understand the potential risks and benefits, and then find a high-quality screening program. That means a hospital or clinic that has thoracic surgery, good radiology, and good pulmonary medicine.
Prostate cancer screening is controversial. Here’s why.
The approach to prostate cancer screening has changed dramatically over the last 20 years. Now, about half of all men with screen-detected prostate cancer are told that the next step should be observation. The majority of those men are never going to be treated because they don’t need to be cured.
Most professional organizations, including the U.S. Preventive Services Task Force and Medicare, recommend “fair balance,” meaning informed decision-making. There have been studies that show that prostate cancer screening doesn’t save lives, and at least one study that shows that it does save lives, but very few.
One study suggests that prostate cancer screening with a blood test and digital rectal exam will reduce risk of death by 20%. Here’s what that actually means:
If you screen 1,000 men in their 50s on a regular basis over 15 to 20 years, you will diagnose 100 of those 1,000 men with prostate cancer, and ultimately four will die. If you take 1,000 men of the same age, and you don’t screen them over that same period of time, you will diagnose about 60 with prostate cancer because of symptoms, and five will die. That five per 1,000 unscreened going to four per 1,000 screened is where the 20% reduction in risk of death comes from. But it’s at a cost of almost doubling the man’s risk of being diagnosed with prostate cancer.
After an abnormal screen, follow-up is essential.
One of the problems we find is people have an abnormal screen and then don't get the diagnostics or treatment. Women will get a mammogram, be told there’s an abnormality, and a repeat mammogram and additional testing may be needed. A larger portion of poorer women don’t return for that follow-up evaluation.
One study suggests that of the 45,000 or so women who die from breast cancer every year, approximately 10% die because they never got a mammogram. And somewhere around 20-25% die because they did not get adequate follow-up or treatment following an abnormal mammogram.
Not everyone has access to the same quality screening.
In the case of mammography in the U.S., the proportion of Black women and white women in their 50s and 60s who get screened is the same, about 60%. The problem is that Black women more often get screened in centers that don't have previous mammograms for comparison.
With lung cancer screening, we see middle- and upper-middle-class individuals going to high-quality centers and poorer people going to community hospitals that don't offer all the various specialties that ensure high-quality screening.
One famous study of colon cancer screening and treatment showed that poor people in California were going to overcrowded hospitals, and the quality of the screening and diagnosis was impacted. In the hospitals poor people went to, a pathologist had to deal with six patients a day, but in the hospitals where middle-class people with good insurance went, the pathologist only had to deal with two patients a day. So there was a difference in quality because the doctor spent more time analyzing the patients with better insurance.
Each person should make their own informed decisions around screening.
Cancer screening saves lives. But that doesn't mean the recommendation is for everyone to get it. It means that we should have a conversation and respect people’s concerns. Those who are concerned or hesitant to get screened, perhaps ought not to. Those who want to get screened ought to be able to get screened, and we should remove financial barriers for them to do so.
Aliza Rosen is a digital content strategist at the Johns Hopkins Bloomberg School of Public Health.
RELATED:
- Otis Brawley on Cancer's Critical Socioeconomic—Not Just Racial—Disparities
- Cervical Cancer is Preventable
- The Promise and Perils of the Lung Cancer Screening Tool (Podcast)
Related Content

Study Estimates Home Blood Pressure Devices Don’t Fit Properly for More than 17 Million U.S. Adults

New Research Sheds Light on Treatment and Harm Reduction Gaps Among Drug Users

Understanding the Impact of Economic and Social Conditions on Health

Study Reveals Significant Barriers for TGNC Adults Accessing Healthcare in the U.S.
Medical Misinformation Harms People from Communities that are Marginalized
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
Science, health, and public trust.
April 27, 2022
Putting Cancer Screening in Perspective

By Paul Pinsky, Ph.D., Chief, Early Detection Research Group, NCI Division of Cancer Prevention; Philip Castle, Ph.D., M.P.H., Director, NCI Division of Cancer Prevention; Maureen Johnson, Ph.D., Executive Secretary, President’s Cancer Panel; and Samantha Finstad, Ph.D., Senior Health Science Policy Advisor, President’s Cancer Panel
It’s common wisdom that “catching the cancer early” is always a good thing. It can be a key factor in being able to survive cancer. You often hear, “luckily, they caught it early,” or the converse, “unfortunately, they didn’t detect it until it had spread” when people talk about friends or relatives with a cancer diagnosis. But the reality of cancer screening is not that simple.
The overall goal of cancer screening is to reduce cancer morbidity (illness) and mortality (death). There is no question that appropriate screening reduces illnesses and deaths due to cancer. Cervical and colorectal cancer incidence has declined in the last few decades by about 55% and 45%, respectively. Death rates have declined even more. These have been due primarily to routine screening.
Some types of screenings can detect cancer early (e.g., mammography for breast cancer and low-dose CT for lung cancer). Others can detect cancer early as well as detect cancer precursors, which can prompt action to prevent the development of cancer (e.g., colonoscopy screening for colorectal cancer and Pap smears and/or HPV testing for cervical cancer). Preventing cancer, even a curable cancer, is a large benefit in itself because it can reduce the many burdens to patients associated with a cancer diagnosis.
But when communicating information about cancer screenings to the public, it’s important to discuss the benefits and the risks. Cancer screening will not necessarily benefit every patient who gets it. A patient could still succumb to cancer despite it being detected early. Others may survive even if their cancer was missed early on and caught at a later stage. And for some patients, screening can actually cause harms.
Screening may lead to the overdiagnosis of indolent (symptomless) cancers. These are cancers detected through screening that would never have become symptomatic in the patient’s lifetime. There is evidence of overdiagnosis associated with various types of screening, most notably PSA screening for prostate cancer. Overdiagnosis of cancer can lead to treatment, or overtreatment, and have serious side effects. For example, impotence and urinary incontinence are associated with prostate cancer surgery.
Screening can also lead to false positives—when people get a positive screening test but no cancer is found. Since screening tests are usually given to healthy people with a low risk of harboring cancer, the tests need to have a high specificity, or the ability to avoid too many false-positive results. A false-positive result can cause anxiety, require additional clinical visits and diagnostic procedures like imaging and biopsies, and lead to high costs for both the medical system and patient. For example, for mammography screening, around 8−12% of women will receive a false positive result at any given screening visit, and up to 45% will receive at least one false positive result over a ten year period of regular screening.
Since cancer screening is intended for those who have no signs or symptoms of cancer, it is important that the benefits strongly outweigh the risks. Cancer screening guidelines can change as new research shows which populations would benefit most from screening with the least harm. For example, more people became eligible for lung cancer screening in 2021, when the U.S. Preventive Services Task Force updated their eligibility recommendations, lowering the minimum age and the amount a person has smoked over their lifetime (or smoking pack-years).
For new screening approaches, establishing the high sensitivity of a test—the ability to find someone who does have cancer—is an important first step in determining its clinical utility. But it is only a first step. Researchers must also demonstrate that the benefits outweigh the harms. Such evidence generally requires a randomized clinical trial in which subjects are randomized to a screening and control arm. The primary outcome is typically mortality from the cancer in question.
There is much discussion lately about the new “multi-cancer early detection” (MCED) tests. Also called liquid biopsies, these are blood tests that can detect multiple different cancer types simultaneously. To date, there has been limited research on the clinical utility of such tests—in other words, if they actually reduce illness and death. As these tests develop, it’s crucial to keep in mind that a sensitive test does not necessarily indicate clinical utility, or that the benefits of MCED screening would outweigh the harms.
While the benefits of appropriate screening are undeniable, it is important to acknowledge that harms can also be associated with screening; more is not always better. When describing cancer screening, make sure to refer to the current guidelines and clarify that screening isn’t for everyone. It should be done only for the right people at the right time.
Connect with Us
- More Social Media from NIH
- Search Menu
- Sign in through your institution
- Advance articles
- Editor's Choice
- Supplements
- Author Guidelines
- Submission Site
- Open Access
- About Journal of Public Health
- About the Faculty of Public Health of the Royal Colleges of Physicians of the United Kingdom
- Editorial Board
- Self-Archiving Policy
- Dispatch Dates
- Advertising and Corporate Services
- Journals Career Network
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, supplementary data, conflict of interest.
- < Previous
Factors influencing the decision to attend screening for cancer in the UK: a meta-ethnography of qualitative research
- Article contents
- Figures & tables
- Supplementary Data
B Young, L Bedford, D Kendrick, K Vedhara, J F R Robertson, R das Nair, Factors influencing the decision to attend screening for cancer in the UK: a meta-ethnography of qualitative research, Journal of Public Health , Volume 40, Issue 2, June 2018, Pages 315–339, https://doi.org/10.1093/pubmed/fdx026
- Permissions Icon Permissions
This review aimed to better understand experiences of being invited to cancer screening and associated decision-making.
Qualitative evidence explaining UK cancer screening attendance decisions was systematically identified. Data were extracted and meta-ethnography used to identify shared themes, synthesize findings and generate higher level interpretations.
Thirty-four studies met inclusion criteria. They related to uptake of breast, cervical, colorectal, prostate, ovarian and lung cancer screening. Three primary themes emerged from the synthesis. ‘Relationships with the health service’ shaped decisions, influenced by trust, compliance with power, resistance to control or surveillance and perceived failures to meet cultural, religious and language needs. ‘Fear of cancer screening’ was both a motivator and barrier in different ways and to varying degrees. Strategies to negotiate moderate fear levels were evident. ‘Experiences of risk’ included the creation of alternative personal risk discourses and the use of screening as a coping strategy, influenced by disease beliefs and feelings of health and wellness.
The findings highlight the importance of the provider–patient relationship in screening uptake and enrich our understanding of how fear and risk are experienced and negotiated. This knowledge can help promote uptake and improve the effectiveness of cancer screening.
More than 50% of people in the UK born after 1960 will be diagnosed with cancer in their lifetime. 1 In order for screening to be effective in reducing cancer mortality, it is important that uptake is high. National Health Service (NHS) population screening tests for breast, cervical and colorectal cancer have uptake rates of 71%, 2 73% 3 and 52%, 4 respectively in England. Those who do not attend are more likely to be at higher risk; improving uptake is therefore a key public health strategy to reduce health inequalities in outcomes at every stage of the cancer patient pathway. 5 Ethnicity, social deprivation and gender are important determinants of cancer screening uptake. 6 Factors influencing screening uptake identified in quantitative research include practical barriers, such as difficulty making an appointment, forgetting to do so and dependency on others to carry out the activities of daily living. 7 , 8 Psychosocial motivators and barriers, including embarrassment, worry, anxiety and self-efficacy have also been identified. 9 , 10 Interventions to improve uptake targeting structural and system factors, such as invitation and reminder methods, and education have been demonstrated to be effective. 11 – 13
Public debate about communication of the benefits and harms of screening has led to a shift from the objective of maximizing uptake to the promotion of informed uptake. 14 A systematic review of interventions to promote informed choice about health screening found some evidence that greater informed choice does not reduce uptake but this was based on a limited number of studies. 15 A randomized controlled trial of information about overdetection in breast cancer screening found that greater knowledge about the potential harms of screening may reduce intentions to be screened. 16 Higher awareness of the risks of screening could contribute to a decline in the positive social attitudes to cancer screening which have generally been observed. 17 , 18 This highlights the importance of using an exploratory approach to investigate thoughts and experiences of recipients of cancer screening invitations to better understand why a proportion of individuals do not attend when invited.
The aim of this meta-ethnography was to systematically identify and synthesize qualitative evidence which explains cancer screening attendance decisions in the UK.
Eligibility criteria
Studies were eligible for inclusion if they utilized qualitative methodology and included evidence of factors influencing decisions to attend screening for cancer. We limited our search to UK studies because there are international differences in the organization and delivery of screening and a need for uptake strategies to consider health service context and cultural and societal norms. 6 At least one factor must have been described, either by a participant or the author, as having influenced the participant's prior real-life screening attendance decision.
Screening programmes eligible for inclusion were organised population screening and research trials of screening methods. Opportunistic screening, self-examination, second stage screening (e.g. a diagnostic test following an abnormal screen), genetic testing and family history counselling were all ineligible. Reports solely of the views of people other than the screening invitation recipient (e.g. healthcare practitioners) were ineligible. Research which reported screening attendance decisions exclusively in individuals with symptoms of the disease, a previous cancer diagnosis, physical or learning disabilities, or who had experienced sexual abuse were ineligible.
Several data sources were searched (see Supplementary data, Table S1 ), reference lists of included studies were searched for further relevant references and Web of Science was used to search for papers citing the included studies. Search results from each source were combined and duplicates removed. Titles and abstracts were screened for eligibility independently by B.Y. and L.B. A third researcher (R.d.N.) was available to resolve any disagreements. Full text papers were retrieved and the eligibility of each paper for inclusion was assessed by B.Y. and L.B. Papers assessed as eligible were then classified independently by both B.Y. and L.B. according to a typology of findings in qualitative research. 19 This addressed the problem that methodologies stated by qualitative study authors often do not accurately reflect those which are used. The typology outlines five categories which classify study findings as qualitative or not qualitative depending on the degree of data transformation (see Supplementary data, Table S2 ). Studies classified as ‘qualitative findings’ were included and others were excluded.
Study characteristics were extracted from included papers. Quotes and text from papers which met the criteria were extracted into a spreadsheet by B.Y., coded as first- or second-order constructs 20 and as primary or secondary data ( Supplementary data, Fig. S1 ).
Appraisal of included papers was conducted independently by both B.Y. and L.B. using the Critical Appraisal Skills Programme (CASP) tool for qualitative research. 21 The tool has 10 questions which assist in forming a judgement of the validity and value of reports. It was not used to numerically score papers on their quality. By taking into account the CASP tool, typology of findings, conceptual richness and relevance and contribution to the review question, papers were categorized as a key paper, satisfactory paper or fatally flawed. Such an approach allows the value and importance of qualitative studies in answering a research question to be tempered by the validity of the findings. 22 This categorization was used to guide the synthesis, allowing more emphasis to be placed on key papers.
The synthesis of findings involved interpretative analysis using meta-ethnography ( Supplementary data, Fig. S2 ). 23 Included papers were carefully read and the relationships between the concepts arising in the papers considered using a matrix of shared themes. Thematic coding was undertaken, firstly with data extracted from key papers and continued through all included studies. When a new theme was identified, the other papers were reviewed to check for the presence of the theme, forming a cyclical process. Studies were compared and contrasted via an interpretative reading of meaning of conceptual data. Third-order constructs 24 were developed by taking the first- and second-order constructs and analysing them thematically to form a new interpretation.
Summary of included studies
Thirty-six papers reporting 34 different studies were included in a ‘reciprocal synthesis’ 23 (Fig. 1 ). The characteristics and relevant findings of included studies are shown in Table 1 . Twenty-one papers had cancer screening uptake as the main focus of the reports. 25 – 45 The primary focus of other reports included wider knowledge and attitudes to cancer and prevention, 46 – 52 responses to information about screening, 53 – 56 experiences of screening test results 57 , 58 and risk management options which included screening. 59 , 60 Cervical, breast and colorectal cancer accounted for 29 of the 34 studies. Two related to prostate cancer, two to ovarian and one to lung cancer. Five papers were categorized as key papers 32 , 35 , 36 , 42 , 53 and the rest as satisfactory.

PRISMA flowchart.
Characteristics and relevant findings of included studies
| . | (disease, method and context) (collection and analysis method as described by authors) . | . | (explicitly linked to screening attendance) . |
|---|---|---|---|
| . | = 42 (focus groups), = 8 (interviews) | ||
| = 7 | |||
| = 35 | |||
| As above | |||
| a | As above | ||
| . | = 53 | | |
| . | = 21 | ||
| . | = 21 | ||
| = 17 eligible for meta-ethnography. Study also included ineligible interviews with facilitators of cancer awareness sessions and focus groups with health advocates | Themes may be derived partly from ineligible data from facilitators and health advocates or due to age of interviewee | ||
| . | = 28 | ||
| . | = 10 | ||
| = 35 | |||
| . | = 44 | a civic duty | |
| . | = 12 from 1 of 21 centres in the UK | ||
| . | = 45 eligible for meta-ethnography. Study also included ineligible interviews with NHS professionals | ||
| . | = 50 | ||
| . | = 33 | ||
| . | = 27 | ||
| . | = 32 = 20 Poland = 18, Romania = 9, Slovakia = 5, Poland = 11, Romania = 2, Slovakia = 7; London | ||
| . | = 68 19–55 years, 50–65 years, 50–60 years; 11 men, 57 women; ethnic group not reported; Tayside and Lothian | ||
| . | = 24 | ||
| . | = 48 | ||
| = 48 | |||
| . | = 54 | ||
| . | = 60 participants sampled from group aged 55–64; 30 men, 30 women; ethnic group not reported; Leicester | ||
| . | = 20 | ||
| . | = 128 | Themes common across non-professional and professional occupational groups: | |
| . | = 60 ‘limited numbers of ethnic minority patients’; location not reported | ||
| = 70 (of eligible screening age) | |||
| . | = 10 | ||
| . | = 22 | ||
| . | = 28 = 9, not reported = 4; Leyton, north-east London | ||
| . | = 135 | (believing in the importance of screening but not translating positive screening intentions into action) | |
| . | = 27 (focus groups) = 19 (interviews) | (making an active decision not to attend) | |
| . | = 40 | ||
| . | = 86 |
| . | (disease, method and context) (collection and analysis method as described by authors) . | . | (explicitly linked to screening attendance) . |
|---|---|---|---|
| . | = 42 (focus groups), = 8 (interviews) | ||
| = 7 | |||
| = 35 | |||
| As above | |||
| a | As above | ||
| . | = 53 | | |
| . | = 21 | ||
| . | = 21 | ||
| = 17 eligible for meta-ethnography. Study also included ineligible interviews with facilitators of cancer awareness sessions and focus groups with health advocates | Themes may be derived partly from ineligible data from facilitators and health advocates or due to age of interviewee | ||
| . | = 28 | ||
| . | = 10 | ||
| = 35 | |||
| . | = 44 | a civic duty | |
| . | = 12 from 1 of 21 centres in the UK | ||
| . | = 45 eligible for meta-ethnography. Study also included ineligible interviews with NHS professionals | ||
| . | = 50 | ||
| . | = 33 | ||
| . | = 27 | ||
| . | = 32 = 20 Poland = 18, Romania = 9, Slovakia = 5, Poland = 11, Romania = 2, Slovakia = 7; London | ||
| . | = 68 19–55 years, 50–65 years, 50–60 years; 11 men, 57 women; ethnic group not reported; Tayside and Lothian | ||
| . | = 24 | ||
| . | = 48 | ||
| = 48 | |||
| . | = 54 | ||
| . | = 60 participants sampled from group aged 55–64; 30 men, 30 women; ethnic group not reported; Leicester | ||
| . | = 20 | ||
| . | = 128 | Themes common across non-professional and professional occupational groups: | |
| . | = 60 ‘limited numbers of ethnic minority patients’; location not reported | ||
| = 70 (of eligible screening age) | |||
| . | = 10 | ||
| . | = 22 | ||
| . | = 28 = 9, not reported = 4; Leyton, north-east London | ||
| . | = 135 | (believing in the importance of screening but not translating positive screening intentions into action) | |
| . | = 27 (focus groups) = 19 (interviews) | (making an active decision not to attend) | |
| . | = 40 | ||
| . | = 86 |
a Same study as Armstrong 2005
Evidence synthesis
Three primary themes emerged from the analysis: first, screening attendance decisions were shaped by individuals’ relationships with the health service. Second, fear was a dominant influence on both decisions to attend and to not attend. Third, experiences of risk were expressed throughout the data. Additionally, a range of other factors interacted with these primary themes as described below. The distribution of themes across the 36 papers is shown in the Supplementary data, Table S3 . Illustrative quotes from study participants (P) and authors (A) are provided below and further supporting data excerpts are shown in the Supplementary data, Table S4 . A diagram of third-order constructs and their relationships is shown in Fig. 2 .

Diagram of primary third-order constructs and their relationships.
Relationship with health service
Responses to screening invitations were largely explained in terms of individuals’ relationship with the health service. There was a wide range of levels of trust evident in the data, ranging from those who interpreted the invitation as a command to be obeyed, to those who perceived it as an attempt at control to be resisted. Between these two extremes, individuals cited other aspects of the relationship which influenced their decision.
There was evidence that the NHS is seen as a higher power in the relationship: ‘Many interviewees referred to having a smear test as a “correct” form of behaviour: as the right/correct/proper thing for women to do. Notions of deviance were associated with non-attendance.’(A) 48 Some felt obliged to comply with the ‘system’ in order that they are taken seriously when presenting with other health problems in the future. 41 In this sense, they viewed trust as something to be demonstrated and maintained in both directions in the relationship. In contrast, others felt privileged to be invited to screening 56 and viewed it as the offer of a valuable service at no financial cost to them. 36
Immigrant populations with limited experience of the NHS lacked trust in its services and employees, sometimes opting to be screened in their home country where a stronger relationship existed with the healthcare provider. 40 Language problems inhibited them from asking questions and forming a trusting relationship. 38 There was distrust of interpreters provided by the NHS who were described as unqualified to translate using medical terminology. 44 There were perceptions from ethnic minority groups that screening services did not (or would not) meet their cultural and religious needs. ‘They just make you feel uncomfortable [for requesting a female nurse]. So that is why I don't go, if I got the test I would say no I don't want to go because of this thing.’(P) 25 Associations of cervical screening with promiscuity raised concerns about confidentiality in women who did not trust clinicians and receptionists to meet these needs. 45
Another aspect of the relationship which influenced decisions was the communication flowing from the health service to the individual containing information about screening and the potential harms and benefits. Different levels of knowledge about screening resulted from this information, but in those who did not attend there was often a deficit in knowledge and understanding about screening, which they were not motivated to overcome: ‘Throughout the focus groups the women expressed a lack of awareness about the need for cervical screening, resulting in the women ignoring an invite for cervical screening.’(A) 33 ‘Expressions such as ‘never knew anything about cancer before’; ‘I never knew’; ‘I didn't know what is cancer’ were common.’(A) 50 There were expectations that screening should take place in a clinical setting and that patients are the passive receiver of care from the screening provider. 35 The receipt of home testing kits for colorectal cancer, for example, was interpreted as unusual and impersonal. The detachment of screening from clinical settings was linked to non-uptake: ‘Self-testing at home … undermined the value and relevance of screening.’(A) 35 Invitations endorsed by general practitioners (GPs) carried additional weight and were revered, especially in those holding a biomedical view of the health service relationship in which the medical profession was seen as the sole decision-makers. 25
For women, the relationship with the health service was sometimes not perceived to be strong enough to entertain the prospect of attending screening, during which they would be required to reveal private parts of their body to a stranger. 45 There was a theme of control and surveillance experienced by women, within a discourse from the provider of the female body being a site of risk in need of medical observation, 48 or feelings their bodies were being used to fulfil quotas 45 or achieve other objectives. 55
Fears about cancer screening manifested as both a motivator and barrier to screening attendance. Four key sources of fear were screening invitations, the threat of cancer in the absence of screening, the threat of abnormal test results and screening methods.
The receipt of a cancer screening invitation was experienced as provoking varying levels of fear, often explaining avoidance or delay in participation. Non-attenders described being ‘terrified’ and ‘frightened to death’ by the invitation, 42 leading to a quick decision to not respond. Less extreme experiences of fear were carefully negotiated by talking to others and seeking more information about screening. An incentive to take up screening was anticipation that in doing so fear may be reduced. Fear of developing cancer in the absence of screening was a powerful motivator to attend which facilitated the overcoming of other perceived barriers to screening: ‘Fear appeared to be the main driving force behind the decision to have smear tests.’(A) 48
Implications of an abnormal screening test result were a principal source of fear in the data. This was interpreted as ‘fear of the unknown’ and fear of an inability to cope with a diagnosis and ‘the word cancer’ itself. 42 Fears about screening methods were commonly cited, either from previous experience or from anecdotes heard from others. These were anticipated as leading to other negative emotions including pain, discomfort and embarrassment.
Other sources of fear were the potential social inadequacy in the performance of an unfamiliar event under professional scrutiny, 36 anticipation of having to wait for screening results, a general fear of hospitals and medical procedures 42 and stigma associated with cancer or cancer risk. 50
Experiences of risk
Closely related to the first two themes was that of risk. Individuals were subject to external discourses of risk and also created their own ‘game of chance’. 36 The official discourse on screening from the health service was one which labels individuals as ‘at risk’, non-attenders as at even higher risk and attenders as at lower risk. There was, however, some resistance to this discourse, influenced by themes of beliefs about the disease and current health and wellness. For example, individuals who believed that an absence of symptoms and a feeling of wellness placed them at low risk cited this as a reason for either attending or not attending screening: ‘I'd almost be surprised if I did get it, I don't feel anything.’(P) 43 They felt they had either nothing to gain or nothing to lose by screening. Beliefs were expressed that risk of cancer was reduced by participation in screening. This may be a coping strategy to gain protection from the risk and uncertainty of the threat of cancer. Beliefs about cancer also influenced risk in minority ethnic groups, for example beliefs that talking about cancer or being in close proximity to someone with cancer can put one at risk. 50 This likely represents a culture in which cancer is a taboo subject and is avoided.
Main findings of this study
This meta-ethnography provides an insight into the thoughts and experiences which explained participants’ screening attendance decisions. Three primary themes emerged from the synthesis.
Individuals’ relationship with the health service was the most important factor, influenced by underlying dynamics of trust, power, control and authority. Some were compliant with screening requests, particularly when received from a known source. For example, invitations received from GPs were more trusted than those received from screening hubs. This is consistent with experimental research demonstrating that GP endorsement promotes higher uptake. 61 However, in a society where ever more areas of our lives are under routine surveillance, this synthesis found individuals can be sceptical of the requirement to adhere to a screening regime. Their resistance is interpreted as an attempt to maintain control over their own bodies and their right to decide when they are unwell and need medical attention. 48 A general distrust of those in power is a social dynamic that can include the NHS, which is viewed by some as an extension of the Government. 36
A further demonstration of the level of trust necessary in the relationship was the cultural and language needs which were seen as being unmet. Immigrant groups experience additional barriers due to a lack of familiarity with the NHS and limited knowledge of services. A fundamental aspect to the relationship with the screening provider is the information received and resulting knowledge and understanding. In screening, this communication typically occurs in writing and many of the nuances of communication that could contribute to a trusting relationship are lost. Home visits combined with an educational video have been shown to be particularly effective in promoting screening uptake in hard to reach groups, while written translated materials were ineffective. 62
According to our analysis, ultimately it was the sender's characteristics, rather than the content of the message itself, which were important. Interventions to modify invitation materials to address other barriers may therefore have limited potential to promote uptake beyond that which has already been achieved. 11 , 12 , 63 Improvements in uptake may be achieved by patient-oriented interventions targeting perceptions of the wider health service, rather than screening invitation materials or methods alone. For certain groups, there may be a benefit in including key community figures (e.g. local religious leaders) in communicating the health agenda. An extension of GP involvement in cancer screening could utilize an existing trusted relationship to promote uptake. For example, a banner on the invitation letter indicating endorsement from the patient's GP practice has been shown to increase uptake of colorectal screening. 64 Such interventions could lead to other desirable outcomes as a result of increased levels of trust in the relationship.
There are consistencies with other qualitative syntheses, which report cervical screening as an emotional experience 65 and fear as a barrier in colorectal screening. 66 Our finding of experiences of fear from a number of sources in cancer screening is consistent with patients’ reported experiences of seeking help for cancer symptoms. 67 , 68 The role of fear and its link with cancer worry and perceived susceptibility in cancer screening uptake has received much attention. Fear of a number of aspects of screening, including the hospital setting, pain from screening procedures, test results and their consequences, was strongly associated with non-attendance in a survey. 69 In a colorectal screening trial, desire for screening was higher in people who reported worrying about cancer, but individuals were less likely to attend if they had reported feeling uncomfortable at the thought of cancer. 70 It has been suggested that fear combined with high-efficacy messages promotes health behaviour change and fear with low-efficacy messages creates defensive responses. 71 The importance of response efficacy (the perception that a behaviour will alleviate a threat) in behaviour change has been demonstrated. 72 This relationship between fear and cancer screening attendance is complex and our findings provide an insight into the different ways fear is experienced and interpreted in this context. Specifically, the synthesis supports the theory that very high levels of fear about cancer screening, from sources including screening invitations, the perceived threat of cancer, abnormal test results or the screening methods, can promote avoidance. Some overcame their fear having been persuaded by another person to attend. Increasing familiarity and trust in relation to the health service might have a similar effect in enabling individuals to negotiate moderate levels of fear in deciding to attend screening.
The analysis showed how the experience of being identified as ‘at risk’ by the health service led to some resistance and the creation of alternative explanations based on a range of beliefs about the disease. Evidence shows a moderate level of perceived risk optimizes screening uptake, with high levels leading to avoidance and low levels a lack of motivation. 73 A meta-analysis of a range of behaviours suggests that this relationship between a threat and behaviour holds only when accompanied by high self- and response-efficacy. 74 Our study found individuals create their own perceptions of risk irrespective of the ‘official discourse’ and use screening as a coping strategy.
A better understanding of the complex determinants of uptake could lead to the identification of modifiable psychological variables as targets for intervention. Current screening invitation materials emphasize the recipient's choice in deciding whether or not to take part. To complement this, the perceived control an individual has over other aspects of the process could be promoted. Rather than screening being experienced as a mass surveillance programme in which people are systematically called and recalled by a computer, personalized aspects of screening could be enhanced and the element of individual control emphasized. The aims of ensuring that individuals have the knowledge to decide what they want to do and that they feel the communication is personalized could potentially be achieved in synergy. For example, interactive methods could be used in decision aids which address gaps in knowledge, tailored to individual levels of fear and perceived risk.
Our findings could also help in understanding why certain sociodemographic groups engage less with other health processes, as there may be common barriers generalizable beyond cancer screening. The findings could further contribute to understanding of delays in help-seeking when experiencing cancer symptoms.
What is already known on this topic
There is evidence that ethnic minorities, younger aged and economically deprived groups are less likely to attend cancer screening. Quantitative research has identified some practical and psychosocial factors influencing screening uptake but has not fully explained why a proportion of individuals do not attend. Qualitative studies have reported experiences of cancer screening uptake, focusing on specific groups and types of screening tests. Their findings have not been synthesized in a way that can be integrated with the existing hierarchy of evidence to inform future research, policy and practice.
What this study adds
A synthesis of evidence from a systematic review of qualitative studies has identified important themes which influence cancer screening uptake in the UK. A higher level interpretation of data demonstrated how an individual's relationship with the health service, their fear of cancer screening and their experiences of risk influence their response to a screening invitation. This review makes this important body of evidence more accessible to clinicians, policy-makers and researchers.
Limitations of this study
Reasons for taking part or not taking part in a cancer screening research trial may differ to those for routine NHS screening. As an example, altruistic reasons for participation were particularly evident in trials of ovarian and lung screening methods. 43 , 59 However, the majority of included studies related to NHS cervical, breast and colorectal screening. The studies were published over a wide time frame (1994–2016) and therefore the experiences of participants may not all necessarily reflect the current state of screening in the UK. Recall bias could have influenced the data because participants reported past experiences. Those who are least likely to engage in screening were probably underrepresented in the data since they might be less likely to take part in a research study on the topic.
This synthesis highlights important factors which underpin the uptake of cancer screening. It emphasizes the importance of the provider–patient relationship in promoting informed uptake and enriches our understanding of how fear and risk are experienced and negotiated in the screening attendance decision. Further research should use quantitative methods to explore in which groups the barriers identified are prevalent and the extent to which they are experienced. The qualitative literature could be examined further to draw out differences between screening programmes and population subgroups. Interventions could be piloted to promote a perception of personalized care, improved trust in the health service and prevent extreme levels of fear and perceived risk. As cancer screening invitations change in the future, due to the use of new screening methods and the growth in importance of concepts such as informed choice and risk stratification, there will be a continuing need to explore experiences of being invited to cancer screening.
Supplementary data are available at Journal of Public Health online.
This work received no specific grant from any funding agency.
The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Ahmad AS , Ormiston-Smith N , Sasieni PD . Trends in the lifetime risk of developing cancer in Great Britain: comparison of risk for those born from 1930 to 1960 . Br J Cancer 2015 ; 112 : 943 – 7 .
Google Scholar
Health and Social Care Information Centre. Breast Screening Programme, England – 2014–15. 2016; http://www.hscic.gov.uk/catalogue/PUB20018/bres-scre-prog-eng-2014-15-rep.pdf (24 January 2017, date last accessed).
Health and Social Care Information Centre. Cervical Screening Programme, England – 2015-2016. 2016; http://www.content.digital.nhs.uk/catalogue/PUB22414/nhs-cerv-scre-prog-eng-2015-16-rep.pdf (24 January 2017, date last accessed).
Logan RFA , Patnick J , Nickerson C et al. . Outcomes of the Bowel Cancer Screening Programme (BCSP) in England after the first 1 million tests . Gut 2012 ; 61 : 1439 – 46 .
Department of Health . Improving Outcomes: a Strategy for Cancer 2011 . http://www.gov.uk/government/uploads/system/uploads/attachment_data/file/213785/dh_123394.pdf (24 January 2017, date last accessed).
Google Preview
Weller DP , Campbell C . Uptake in cancer screening programmes: a priority in cancer control . Br J Cancer 2009 ; 101 : S55 – S9 .
Jepson R , Clegg A , Forbes C et al. . The determinants of screening uptake and interventions for increasing uptake: a systematic review . Health Technol Assess 2000 ; 4 ( i-vii ): 1 – 133 .
Waller J , Bartoszek M , Marlow L et al. . Barriers to cervical cancer screening attendance in England: a population-based survey . J Med Screen 2009 ; 16 : 199 – 204 .
Bish A , Sutton S , Golombok S . Predicting uptake of a routine cervical smear test: a comparison of the health belief model and the theory of planned behaviour . Psychol Health 2000 ; 15 : 35 – 50 .
Bukowska-Durawa A , Luszczynska A . Cervical cancer screening and psychosocial barriers perceived by patients: a systematic review . Contemp Oncol 2014 ; 18 : 153 – 9 .
Everett T , Bryant A , Griffin MF et al. . Interventions targeted at women to encourage the uptake of cervical screening . Cochrane Database Syst Rev 2011 ; 11 : CD002834 .
Bonfill X , Marzo M , Pladevall M et al. . Strategies for increasing women participation in community breast cancer screening . Cochrane Database Syst Rev 2001 : CD002943 .
Sabatino SA , Lawrence B , Elder R et al. . Effectiveness of interventions to increase screening for breast, cervical, and colorectal cancers: nine updated systematic reviews for the Guide to Community Preventive Services . Am J Prev Med 2012 ; 43 : 97 – 118 .
Raffle AE . Information about screening: is it to achieve high uptake or to ensure informed choice? Health Expect 2001 ; 4 : 92 – 8 .
Biesecker BB , Schwartz MD , Marteau TM . Enhancing informed choice to undergo health screening: a systematic review . Am J Health Behav 2013 ; 37 : 351 – 9 .
Hersch J , Barratt A , Jansen J et al. . Use of a decision aid including information on overdetection to support informed choice about breast cancer screening: a randomised controlled trial . Lancet 2015 ; 385 : 1642 – 52 .
Domenighetti G , D'Avanzo B , Egger M et al. . Women's perception of the benefits of mammography screening: population-based survey in four countries . Int J Epidemiol 2003 ; 32 : 816 – 21 .
Waller J , Osborne K , Wardle J . Enthusiasm for cancer screening in Great Britain: a general population survey . Br J Cancer 2015 ; 112 : 562 – 6 .
Sandelowski M , Barroso J . Classifying the findings in qualitative studies . Qual Health Res 2003 ; 13 : 905 – 23 .
Schutz A . Collected Papers , Vol. 1. The Hague : Martinus Nijhoff , 1962 .
Public Health Resource Unit. Critical Appraisal Skills Programme (CASP). Making sense of evidence about clinical effectiveness: 10 questions to help you make sense of qualitative research. 2013 ; http://www.casp-uk.net/checklists (24 January 2017, date last accessed).
Edwards A , Elwyn G , Hood K et al. . Judging the ‘weight of evidence’ in systematic reviews: introducing rigour into the qualitative overview stage by assessing signal and noise . J Eval Clin Pract 2000 ; 6 : 177 – 84 .
Noblit GW , Hare RD . Meta-ethnography: Synthesizing Qualitative Studies . Newbury Park, CA : SAGE Publications , 1988 .
Britten N , Campbell R , Pope C et al. . Using meta ethnography to synthesise qualitative research: a worked example . J Health Serv Res Policy 2002 ; 7 : 209 – 15 .
Austin KL , Power E , Solarin I et al. . Perceived barriers to flexible sigmoidoscopy screening for colorectal cancer among UK ethnic minority groups: a qualitative study . J Med Screen 2009 ; 16 : 174 – 9 .
Avery KN , Blazeby JM , Lane JA et al. . Decision-making about PSA testing and prostate biopsies: a qualitative study embedded in a primary care randomised trial . Eur Urol 2008 ; 53 : 1186 – 93 .
Bradley DT , Treanor C , McMullan C et al. . Reasons for non-participation in the Northern Ireland Bowel Cancer Screening Programme: a qualitative study . BMJ Open 2015 ; 5 : e008266 .
Chapple A , Ziebland S , Hewitson P et al. . What affects the uptake of screening for bowel cancer using a faecal occult blood test (FOBt): a qualitative study . Soc Sci Med 2008 ; 66 : 2425 – 35 .
Clifton A , Burgess C , Clement S et al. . Influences on uptake of cancer screening in mental health service users: a qualitative study . BMC Health Serv Res 2016 ; 16 : 257 .
Dharni N , Armstrong D , Chung-Faye G et al. . Factors influencing participation in colorectal cancer screening-a qualitative study in an ethnic and socio-economically diverse inner city population . Health Expect 2016 . Epub ahead of print.
Ekberg M , Callender M , Hamer H et al. . Exploring the decision to participate in the National Health Service Bowel Cancer Screening Programme . Eur J Cancer Prev 2014 ; 23 : 391 – 7 .
Hall NJ , Rubin GP , Dobson C et al. . Attitudes and beliefs of non-participants in a population-based screening programme for colorectal cancer . Health Expect 2015 ; 18 : 1645 – 57 .
Logan L , McIlfatrick S . Exploring women's knowledge, experiences and perceptions of cervical cancer screening in an area of social deprivation . Eur J Cancer Care (Engl) 2011 ; 20 : 720 – 7 .
Marlow LAV , Waller J , Wardle J Barriers to cervical cancer screening among ethnic minority women: a qualitative study . Fam Plan Reprod Health Care 2015 .
Palmer CK , Thomas MC , von Wagner C et al. . Reasons for non-uptake and subsequent participation in the NHS Bowel Cancer Screening Programme: a qualitative study . Br J Cancer 2014 ; 110 : 1705 – 11 .
Pfeffer N . Screening for breast cancer: candidacy and compliance . Soc Sci Med 2004 ; 58 : 151 – 60 .
Szarewski A , Cadman L , Ashdown-Barr L et al. . Exploring the acceptability of two self-sampling devices for human papillomavirus testing in the cervical screening context: a qualitative study of Muslim women in London . J Med Screen 2009 ; 16 : 193 – 8 .
Thomas VN , Saleem T , Abraham R . Barriers to effective uptake of cancer screening among Black and minority ethnic groups . Int J Palliat Nurs 2005 ; 11 ( 562 ): 4 – 71 .
Waller J , Jackowska M , Marlow L et al. . Exploring age differences in reasons for nonattendance for cervical screening: a qualitative study . BJOG 2012 ; 119 : 26 – 32 .
Jackowska M , von Wagner C , Wardle J et al. . Cervical screening among migrant women: a qualitative study of Polish, Slovak and Romanian women in London, UK . J Fam Plann Reprod Health Care 2012 ; 38 : 229 – 38 .
Jepson RG , Hewison J , Thompson A et al. . Patient perspectives on information and choice in cancer screening: a qualitative study in the UK . Soc Sci Med 2007 ; 65 : 890 – 9 .
McCaffery K , Borril J , Williamson S et al. . Declining the offer of flexible sigmoidoscopy screening for bowel cancer: a qualitative investigation of the decision-making process . Soc Sci Med 2001 ; 53 : 679 – 91 .
Patel D , Akporobaro A , Chinyanganya N et al. . Attitudes to participation in a lung cancer screening trial: a qualitative study . Thorax 2012 ; 67 : 418 – 25 .
Abdullahi A , Copping J , Kessel A et al. . Cervical screening: perceptions and barriers to uptake among Somali women in Camden . Public Health 2009 ; 123 : 680 – 5 .
Box V . Cervical screening: the knowledge and opinions of black and minority ethnic women and of health advocates in East London . Health Educ J 1998 ; 57 : 3 – 15 .
Armstrong N . Resistance through risk: women and cervical cancer screening . Health Risk Soc 2005 ; 7 : 161 – 76 .
Armstrong N , Murphy E . Weaving meaning? An exploration of the interplay between lay and professional understandings of cervical cancer risk . Soc Sci Med 2008 ; 67 : 1074 – 82 .
Bush J . ‘It's just part of being a woman’: cervical screening, the body and femininity . Soc Sci Med 2000 ; 50 : 429 – 44 .
Clements A , Henderson BJ , Tyndel S et al. . Diagnosed with breast cancer while on a family history screening programme: an exploratory qualitative study . Eur J Cancer Care (Engl) 2008 ; 17 : 245 – 52 .
Karbani G , Lim JN , Hewison J et al. . Culture, attitude and knowledge about breast cancer and preventive measures: a qualitative study of South Asian breast cancer patients in the UK . Asian Pac J Cancer Prev 2011 ; 12 : 1619 – 26 .
Michie S , McDonald V , Marteau T . Understanding responses to predictive genetic testing: a grounded theory approach . Psychol Health 1996 ; 11 : 455 – 70 .
Shang CY , Beaver K , Campbell M . Social cultural influences on breast cancer views and breast health practices among Chinese women in the United Kingdom . Cancer Nurs 2015 ; 38 : 343 – 9 .
Armstrong N . Discourse and the individual in cervical cancer screening . Health 2007 ; 11 : 69 – 85 .
Prinjha S , Evans J , McPherson A . Women's information needs about ductal carcinoma in situ before mammographic screening and after diagnosis: a qualitative study . J Med Screen 2006 ; 13 : 110 – 4 .
Waller J , Douglas E , Whitaker KL et al. . Women's responses to information about overdiagnosis in the UK breast cancer screening programme: a qualitative study . BMJ Open 2013 ; 3 : e002703 .
Woodrow C , Watson E , Rozmovits L et al. . Public perceptions of communicating information about bowel cancer screening . Health Expect 2008 ; 11 : 16 – 25 .
Archer J , Hayter M . Screening men for prostate cancer in general practice: experiences of men receiving an equivocal PSA (prostate specific antigen) test result . Prim Health Care Res Dev 2006 ; 7 : 124 – 34 .
Bond M , Garside R , Hyde C . A crisis of visibility: the psychological consequences of false-positive screening mammograms, an interview study . Br J Health Psychol 2015 ; 20 : 792 – 806 .
Lifford KJ , Clements A , Fraser L et al. . A qualitative study of women's experiences of familial ovarian cancer screening . Psychooncology 2013 ; 22 : 2576 – 84 .
Brain K , Gravell C , France E et al. . An exploratory qualitative study of women's perceptions of risk management options for familial ovarian cancer: implications for informed decision making . Gynecol Oncol 2004 ; 92 : 905 – 13 .
Hewitson P , Ward AM , Heneghan C et al. . Primary care endorsement letter and a patient leaflet to improve participation in colorectal cancer screening: results of a factorial randomised trial . Br J Cancer 2011 ; 105 : 475 – 80 .
McAvoy BR , Raza R . Can health education increase uptake of cervical smear testing among Asian women? BMJ 1991 ; 302 : 833 – 6 .
Baron RC , Rimer BK , Breslow RA et al. . Client-directed interventions to increase community demand for breast, cervical, and colorectal cancer screening a systematic review . Am J Prev Med 2008 ; 35 : S34 – 55 .
Wardle J , von Wagner C , Kralj-Hans I et al. . Effects of evidence-based strategies to reduce the socioeconomic gradient of uptake in the English NHS Bowel Cancer Screening Programme (ASCEND): four cluster-randomised controlled trials . Lancet 2016 ; 387 : 751 – 9 .
Chorley AJ , Marlow LA , Forster AS et al. . Experiences of cervical screening and barriers to participation in the context of an organised programme: a systematic review and thematic synthesis . Psychooncology 2016 ; 26 : 161 – 72 .
Honein-AbouHaidar GN , Kastner M , Vuong V et al. . Systematic review and meta-study synthesis of qualitative studies evaluating facilitators and barriers to participation in colorectal cancer screening . Cancer Epidemiol Biomarkers Prev 2016 ; 25 : 907 .
Smith LK , Pope C , Botha JL . Patients’ help-seeking experiences and delay in cancer presentation: a qualitative synthesis . Lancet 2005 ; 366 : 825 – 31 .
Licqurish S , Phillipson L , Chiang P et al. . Cancer beliefs in ethnic minority populations: a review and meta-synthesis of qualitative studies . Eur J Cancer Care (Engl) 2017 ; 26 : e12556 .
Murray M , McMillan C . Health beliefs, locus of control, emotional control and women's cancer screening behaviour . Br J Clin Psychol 1993 ; 32 : 87 – 100 .
Vrinten C , Waller J , von Wagner C et al. . Cancer fear: facilitator and deterrent to participation in colorectal cancer screening . Cancer Epidemiol Biomarkers Prev 2015 ; 24 : 400 .
Witte K , Allen M . A meta-analysis of fear appeals: implications for effective public health campaigns . Health Educ Behav 2000 ; 27 : 591 – 615 .
Sheeran P , Harris PR , Epton T . Does heightening risk appraisals change people's intentions and behavior? A meta-analysis of experimental studies . Psychol Bull 2014 ; 140 : 511 – 43 .
Hay JL , Buckley TR , Ostroff JS . The role of cancer worry in cancer screening: a theoretical and empirical review of the literature . Psychooncology 2005 ; 14 : 517 – 34 .
Peters G-JY , Ruiter RAC , Kok G . Threatening communication: a critical re-analysis and a revised meta-analytic test of fear appeal theory . Health Psychol Rev 2013 ; 7 : S8 – 31 .
- health services
- cancer screening
| Month: | Total Views: |
|---|---|
| May 2017 | 68 |
| June 2017 | 33 |
| July 2017 | 95 |
| August 2017 | 37 |
| September 2017 | 29 |
| October 2017 | 44 |
| November 2017 | 44 |
| December 2017 | 20 |
| January 2018 | 45 |
| February 2018 | 21 |
| March 2018 | 32 |
| April 2018 | 19 |
| May 2018 | 48 |
| June 2018 | 41 |
| July 2018 | 50 |
| August 2018 | 25 |
| September 2018 | 34 |
| October 2018 | 48 |
| November 2018 | 61 |
| December 2018 | 56 |
| January 2019 | 53 |
| February 2019 | 44 |
| March 2019 | 69 |
| April 2019 | 73 |
| May 2019 | 58 |
| June 2019 | 78 |
| July 2019 | 99 |
| August 2019 | 68 |
| September 2019 | 92 |
| October 2019 | 133 |
| November 2019 | 173 |
| December 2019 | 147 |
| January 2020 | 254 |
| February 2020 | 220 |
| March 2020 | 231 |
| April 2020 | 253 |
| May 2020 | 195 |
| June 2020 | 162 |
| July 2020 | 352 |
| August 2020 | 219 |
| September 2020 | 185 |
| October 2020 | 250 |
| November 2020 | 261 |
| December 2020 | 232 |
| January 2021 | 303 |
| February 2021 | 358 |
| March 2021 | 426 |
| April 2021 | 392 |
| May 2021 | 415 |
| June 2021 | 359 |
| July 2021 | 313 |
| August 2021 | 251 |
| September 2021 | 271 |
| October 2021 | 312 |
| November 2021 | 351 |
| December 2021 | 263 |
| January 2022 | 297 |
| February 2022 | 290 |
| March 2022 | 438 |
| April 2022 | 342 |
| May 2022 | 349 |
| June 2022 | 183 |
| July 2022 | 193 |
| August 2022 | 121 |
| September 2022 | 139 |
| October 2022 | 256 |
| November 2022 | 254 |
| December 2022 | 226 |
| January 2023 | 383 |
| February 2023 | 271 |
| March 2023 | 430 |
| April 2023 | 277 |
| May 2023 | 285 |
| June 2023 | 304 |
| July 2023 | 217 |
| August 2023 | 251 |
| September 2023 | 256 |
| October 2023 | 313 |
| November 2023 | 378 |
| December 2023 | 357 |
| January 2024 | 438 |
| February 2024 | 301 |
| March 2024 | 438 |
| April 2024 | 370 |
| May 2024 | 379 |
| June 2024 | 229 |
| July 2024 | 212 |
| August 2024 | 269 |
| September 2024 | 39 |
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1741-3850
- Print ISSN 1741-3842
- Copyright © 2024 Faculty of Public Health
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Cancer Screening Overview (PDQ®)–Patient Version
What is cancer screening, cancer screening is looking for cancer before a person has any symptoms., there are different kinds of screening tests., some screening tests can cause serious problems., false-positive test results are possible., false-negative test results are possible., finding the cancer may not improve the person's health or help the person live longer..
Screening tests can help find cancer at an early stage , before symptoms appear. When abnormal tissue or cancer is found early, it may be easier to treat or cure . By the time symptoms appear, the cancer may have grown and spread. This can make the cancer harder to treat or cure.
It is important to remember that when your doctor suggests a screening test, it does not always mean he or she thinks you have cancer. Screening tests are done when you have no cancer symptoms.
Screening tests include the following:
- Physical exam and history : An exam of the body to check general signs of health, including checking for signs of disease, such as lumps or anything else that seems unusual. A history of the patient's health habits and past illnesses and treatments will also be taken.
- Laboratory tests : Medical procedures that test samples of tissue, blood , urine , or other substances in the body.
- Imaging procedures : Procedures that make pictures of areas inside the body.
- Genetic tests : A laboratory test in which cells or tissue are analyzed to look for changes in genes or chromosomes . These changes may be a sign that a person has or is at risk of having a specific disease or condition .
Screening tests have risks.
Not all screening tests are helpful and most have risks. It is important to know the risks of the test and whether it has been proven to decrease the chance of dying from cancer.
Some screening procedures can cause bleeding or other problems. For example, colon cancer screening with sigmoidoscopy or colonoscopy can cause tears in the lining of the colon .
Screening test results may appear to be abnormal even though there is no cancer. A false-positive test result (one that shows there is cancer when there really isn't) can cause anxiety and is usually followed by more tests and procedures, which also have risks.
Screening test results may appear to be normal even though there is cancer. A person who receives a false-negative test result (one that shows there is no cancer when there really is) may delay seeking medical care even if there are symptoms.
Some cancers never cause symptoms or become life-threatening, but if found by a screening test, the cancer may be treated. There is no way to know if treating the cancer would help the person live longer than if no treatment were given. In both teenagers and adults, there is a rare risk of attempted or actual suicide in the first year after being diagnosed with cancer. Also, treatments for cancer have side effects .
For some cancers, finding and treating the cancer early does not improve the chance of a cure or help the person live longer.
What Is Informed and Shared Decision-Making?
Understanding the benefits and harms of screening tests is important for making an informed choice about which screening tests are right for you..
Before having any screening test, discuss the test with your doctor or other health care provider . Every screening test has both benefits and harms. Your health care provider should talk to you about the benefits and harms of a screening test and include you in the decision about whether the screening test is right for you. This is called informed and shared decision-making.
- Your health care provider will talk to you about the possible benefits, harms, and unknowns of a screening test. This may include information about the benefits of finding a cancer early or the harms related to false test results, overdiagnosis , and overtreatment . Your health care provider may also give you information in a leaflet, booklet, video, website, or other material.
- After you understand the benefits and harms of a screening test, you can decide whether or not you want to have the screening test based on what is best for you. Sometimes the harms and benefits are closely matched and the decision about whether to have a screening test is hard to make.
- Your health care provider will write your decision down in your medical record and order the screening test, if that was your decision.
What Are the Goals of Screening Tests?
Screening tests have many goals., screening tests are not meant to diagnose cancer..
A screening test that works the way it should and is helpful does the following:
- Finds cancer before symptoms appear.
- Screens for a cancer that is easier to treat and cure when found early.
- Has few false-negative test results and false-positive test results .
- Decreases the chance of dying from cancer.
Screening tests usually do not diagnose cancer. If a screening test result is abnormal , more tests may be done to check for cancer. For example, a screening mammogram may find a lump in the breast . A lump may be cancer or something else. More tests need to be done to find out if the lump is cancer. These are called diagnostic tests . Diagnostic tests may include a biopsy , in which cells or tissues are removed so a pathologist can check them under a microscope for signs of cancer.
Who Needs to Be Screened?
Certain screening tests may be suggested only for people who have a high risk for certain cancers., cancer screening research includes finding out who has an increased risk of cancer..
Anything that increases the chance of cancer is called a cancer risk factor . Not every person with one or more risk factors will develop cancer, and it will develop in some people who don't have any known risk factors.
Some screening tests are used only for people who have known risk factors for certain types of cancer. People known to have a higher risk of cancer than others include those who have any of the following:
- A personal history of cancer.
- A family history of cancer.
- Certain gene mutations (changes) that have been linked to cancer.
- Exposure to cancer-causing agents such as tobacco smoke or workplace chemicals .
- A blood clot that develops for no known reason.
People who have a high risk of cancer may need to be screened more often or at an earlier age than other people.
Scientists are trying to better understand who is likely to get certain types of cancer. They study the things we do and the things around us to see if they cause cancer. This information helps doctors figure out who should be screened for cancer, which screening tests should be used, and how often the tests should be done.
Since 1973, the Surveillance, Epidemiology, and End Results (SEER) Program of the National Cancer Institute has been collecting information on people with cancer from different parts of the United States. Information from SEER, research studies, and other sources is used to study who is at risk.
How Is Cancer Risk Measured?
Cancer risk is measured in different ways. The findings from surveys and studies about cancer risk are studied and the results are explained in different ways. Some of the ways risk is explained include absolute risk , relative risk , and odds ratios .
This is the risk a person has of developing a disease, in a given population (for example, the entire US population) over a certain period of time. Researchers estimate the absolute risk by studying a large number of people that are part of a certain population (for example, women in a given age group). Researchers count the number of people in the group who get a certain disease over a certain period of time. For example, a group of 100,000 women between the ages of 20 and 29 are observed for one year, and 4 of them get breast cancer during that time. This means that the one-year absolute risk of breast cancer for a woman in this age group is 4 in 100,000, or 4 chances in 100,000.
This is often used in research studies to find out whether a trait or a factor can be linked to the risk of a disease. Researchers compare two groups of people who are a lot alike. However, the people in one of the groups must have the trait or factor being studied (they have been "exposed"). The people in the other group do not have it (they have not been exposed). To figure out relative risk, the percentage of people in the exposed group who have the disease is divided by the percentage of people in the unexposed group who have the disease.
Relative risks can be:
- Larger than 1: The trait or factor is linked to an increase in risk.
- Equal to 1: The trait or factor is not linked to risk.
- Less than 1: The trait or factor is linked to a decrease in risk.
Relative risks are also called risk ratios.
In some types of studies, researchers don't have enough information to figure out relative risks. They use something called an odds ratio instead. An odds ratio can be an estimate of relative risk.
One type of study that uses an odds ratio instead of relative risk is called a case-control study . In a case-control study, two groups of people are compared. However, the individuals in each group are chosen based on whether or not they have a certain disease. Researchers look at the odds that the people in each group were exposed to something (a trait or factor) that might have caused the disease. Odds describes the number of times the trait or factor was present or happened, divided by the number of times it wasn't present or didn't happen. To get an odds ratio, the odds for one group are divided by the odds for the other group.
Odds ratios can be:
Looking at traits and exposures in people with and without cancer can help find possible risk factors . Knowing who is at an increased risk for certain types of cancer can help doctors decide when and how often they should be screened.
Does Screening Help People Live Longer?
Finding some cancers at an early stage (before symptoms appear) may help decrease the chance of dying from those cancers., screening studies are done to see whether deaths from cancer decrease when people are screened., certain factors may cause survival times to look like they are getting better when they are not..
For many cancers , the chance of recovery depends on the stage (the amount or spread of cancer in the body) of the cancer when it was diagnosed . Cancers that are diagnosed at earlier stages are often easier to treat or cure .
Studies of cancer screening compare the death rate of people screened for a certain cancer with the death rate from that cancer in people who were not screened. Some screening tests have been shown to be helpful both in finding cancers early and in decreasing the chance of dying from those cancers. These include mammograms for breast cancer and sigmoidoscopy and fecal occult blood testing for colorectal cancer . Other tests are used because they have been shown to find a certain type of cancer in some people before symptoms appear, but they have not been proven to decrease the risk of dying from that cancer. If a cancer is fast-growing and spreads quickly, finding it early may not help the person survive the cancer.
When collecting information on how long people with cancer live, some studies define survival as living 5 years after the diagnosis. This is often used to measure how well cancer treatments work. However, to see if screening tests are useful, studies usually look at whether deaths from the cancer decrease in people who were screened. Over time, signs that a cancer screening test is working include:
- An increase in the number of early-stage cancers found.
- A decrease in the number of late-stage cancers found.
- A decrease in the number of deaths from the cancer.
The number of deaths from cancer is lower today than it was in the past. It is not always clear if this is because screening tests found the cancers earlier or because cancer treatments have gotten better, or both. The Surveillance, Epidemiology, and End Results (SEER) Program of the National Cancer Institute collects and reports information on survival times of people with cancer in the United States. This information is studied to see if finding cancer early affects how long these people live.
These factors include lead-time bias , overdiagnosis , and healthy screenee bias.
Survival time for people with cancer is usually measured from the day the cancer is diagnosed until the day they die. People are often diagnosed after they have signs and symptoms of cancer. If a screening test leads to a diagnosis before a person has any symptoms, the person's survival time is increased because the date of diagnosis is earlier. This increase in survival time makes it seem as though screening helps people live longer when that may not be happening. This is called lead-time bias. Survival time may appear to be longer because the date of diagnosis is earlier for the people who are screened, but they may die at the same time they would have without the screening test.
Sometimes, screening tests find cancers that don't matter because they would have gone away on their own or never caused any symptoms. These cancers would never have been found if not for the screening test (for example, a computed tomography scan ). Finding these cancers is called overdiagnosis. Overdiagnosis can make it seem like more people are surviving cancer longer, but in reality, these are people who would not have died from cancer anyway.
People who choose to have screening tests are often more health conscious than the general public and tend to make other healthy choices in their lives. People with early-stage cancer found by screening may live longer than people who don't get screened. They may live longer because of the benefits of their healthy lifestyle rather than screening. This is sometimes called healthy screenee bias.
How do Screening Tests Become Standard Tests?
Results from research studies help doctors decide when a screening test works well enough to be used as a standard test., different types of research studies are done to study cancer screening., randomized controlled trials, nonrandomized controlled trials, cohort studies, case-control studies, ecologic studies, expert opinions, screening tests for cancer are being studied in clinical trials..
Evidence about how safe, accurate, and useful cancer screening tests are comes from clinical trials (research studies with people) and other kinds of research studies. When enough evidence has been collected to show that a screening test is safe, accurate, and useful, it becomes a standard test. Examples of cancer screening tests that were once under study but are now standard tests include:
- Colonoscopy for colorectal cancer .
- Mammograms for breast cancer .
- Pap tests (Pap smears) for cervical cancer .
Cancer screening trials study new ways of finding cancer in people before they have symptoms . Screening trials also study screening tests that may find cancer earlier or are more accurate than existing tests, or that may be easier, safer, or cheaper to use. Screening trials are designed to find the possible benefits and possible harms of cancer screening tests. Different clinical trial designs are used to study cancer screening tests.
The strongest evidence about screening comes from research done in clinical trials. However, clinical trials cannot always be used to study questions about screening. Findings from other types of studies can give useful information about how safe, useful, and accurate cancer screening tests are.
The following types of studies are used to get information about cancer screening tests:
Randomized controlled trials give the highest level of evidence about how safe, accurate, and useful cancer screening tests are. In these trials, volunteers are assigned randomly (by chance) to one of two or more groups. The people in one group (the control group ) may be given a standard screening test (if one exists) or no screening test. The people in the other group(s) are given the new screening test(s). Test results for the groups are then compared to see if the new screening test works better than the standard test, and to see if there are any harmful side effects .
Using chance to assign people to groups means that the groups will probably be very much alike and that the trial results won't be affected by human choices or something else.
In nonrandomized clinical trials , volunteers are not assigned randomly (by chance) to different groups. They choose which group they want to be in or the study leaders assign them. Evidence from this type of research is not as strong as evidence from randomized controlled trials.
A cohort study follows a large number of people over time. The people are divided into groups, called cohorts, based on whether or not they have had a certain treatment or been exposed to certain things. In cohort studies, the information is collected and studied after certain outcomes (such as cancer or death) have occurred. For example, a cohort study might follow a group of women who have regular Pap tests, and divide them into those who test positive for the human papillomavirus (HPV) and those who test negative for HPV. The cohort study would show how the cervical cancer rates are different for the two groups over time.
Case-control studies are like cohort studies but are done in a shorter time. They do not include many years of follow-up . Instead of looking forward in time, they look backward. In case-control studies, information is collected from cases (people who already have a certain disease) and compared with information collected from controls (people who do not have the disease). For example, a group of patients with melanoma and a group without melanoma might be asked about how they check their skin for abnormal growths and how often they check it. Based on the different answers from the two groups, the study may show that checking your skin is a useful screening test to decrease the number of melanoma cases and deaths from melanoma.
Evidence from case-control studies is not as strong as evidence from clinical trials or cohort studies.
Ecologic studies report information collected on entire groups of people, such as people in one city or county. Information is reported about the whole group, not about any single person in the group. These studies may give some evidence about whether a screening test is useful.
The evidence from ecologic studies is not as strong as evidence from clinical trials or other types of research studies.
Expert opinions can be based on the experiences of doctors or reports of expert committees or panels. Expert opinions do not give strong evidence about the usefulness of screening tests.
Information about clinical trials supported by NCI can be found on NCI’s clinical trials search webpage. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
About This PDQ Summary
Physician Data Query (PDQ) is the National Cancer Institute's (NCI's) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish .
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government’s center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about cancer screening. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Updated") is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Screening and Prevention Editorial Board .
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials can be found online at NCI's website . For more information, call the Cancer Information Service (CIS), NCI's contact center, at 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as “NCI’s PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary].”
The best way to cite this PDQ summary is:
PDQ® Screening and Prevention Editorial Board. PDQ Cancer Screening Overview. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/about-cancer/screening/patient-screening-overview-pdq . Accessed <MM/DD/YYYY>. [PMID: 26389447]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online . Visuals Online is a collection of more than 3,000 scientific images.
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website’s E-mail Us .
Official websites use .gov
A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
Cancer Screening Prevalence and Associated Factors Among US Adults
GUEST EDITORIAL — Volume 19 — April 21, 2022
Zhen-Qiang Ma, MD, MPH, MS 1 ; Lisa C. Richardson, MD, MPH 2 ( View author affiliations )
Suggested citation for this article: Ma Z, Richardson LC. Cancer Screening Prevalence and Associated Factors Among US Adults. Prev Chronic Dis 2022;19:220063. DOI: http://dx.doi.org/10.5888/pcd19.220063 .
PEER REVIEWED
Acknowledgments
Author information.
Cancer is the second leading cause of death in the US, exceeded only by heart disease. In 2018, 1,708,921 people were newly diagnosed and 599,265 people died of cancer (1). Although age-adjusted cancer incidence decreased 9.5% over the past 20 years, from 481.7 per 100,000 in 2009 to 435.8 per 100,000 in 2018, the number of people diagnosed with cancer increased, from 1,292,222 in 2009 to 1,708,921 in 2018 (1,2). The estimated national expenditure for cancer care in the US rose from $190.2 billion in 2015 to $208.9 billion in 2020, a 10% increase mainly due to the aging and growth of the US population (3,4). Costs will likely increase in future years as the population grows and ages and new and often more expensive treatments are adopted as standards of care.
Approximately 30% to 50% of cancers diagnosed today could be prevented by reducing exposure to tobacco smoke and other environmental carcinogens, maintaining healthy body weight, and receiving recommended cancer screenings and vaccinations (5,6). Cancer screening, which is different from diagnostic testing, can detect cancer at early stages before symptoms occur, when it can be more successfully treated. In addition to early detection, screening can prevent colorectal and cervical cancers by identifying precancerous lesions that can be removed before they become cancer (7–9). Thus, understanding screening patterns and factors associated with screening will help public health policy makers and practitioners improve cancer prevention programs further by implementing evidence-based policies and practices (10,11). This special collection of articles from Preventing Chronic Disease presents research on determinants of cancer screening, public health practices that increase cancer screening uptake in specific populations, and cancer screening trends.
Screening is considered the primary factor in the steady decline in colorectal cancer incidence over the past decade (12). Richardson and colleagues used data from the Behavioral Risk Factor Surveillance System to present a GIS (geographic information system) snapshot of US states and the District of Columbia that displays the percentage of US adults who reported no screening for colorectal cancer (13). The overall percentage screened decreased from 27.4% in 2012 to 21.6% in 2020, a 5.8 percentage=point decrease that represents almost 4 million people. The average statewide percentage of adults aged 50 to 75 years who were not up to date with colorectal cancer screening in 2020 was 69.4% and ranged from 58.4% in California to 79.6% in Maine. Twenty-two states did not meet the Healthy People 2020 objective of 70.5% of population screened for colorectal cancer. And most adults not up to date with screening had never been screened. Future research on colorectal cancer screening could focus on population subgroups and on new outreach methods directed at the unscreened in those subgroups. Successful interventions could then be disseminated among other population subgroups.
Although overall age-adjusted cancer incidence has been stabilizing over the past several decades, Weir and colleagues used the age-period-cohort generalized linear model to predict that total cancer incidence in the US will increase approximately 50% from 2015 to 2050, from 1.5 million to 2.3 million (2). The largest increase in cancer incidence will occur in people aged 75 years or older; prevention and early detection do work in older populations (14). With the US population aging and age as a nonmodifiable risk factor for cancer, prevention programs can implement evidence-based risk-reduction strategies to reduce behavioral risk factors such as smoking, drinking, and exposure to environmental carcinogens and chronic conditions such as obesity and type 2 diabetes. Cancer screening could also be treated as a prevention priority to detect precancerous lesions that can be removed, thereby preventing cancer, and to detect cancers at early, treatable stages. State and local health departments could also use the age-period-cohort model to estimate their local cancer incidence in their respective state and local areas and develop actionable plans with innovative strategies to help residents change their behaviors by making healthy lifestyle choices, including increasing screening rates. State and local health departments can also use the model to evaluate cancer prevention program outcomes by comparing the time trends and differentials of cancer incidences with or without interventions.
Screening can prevent thousands of cancer deaths. Modern mammography programs can reduce breast cancer mortality by more than 40% (15–17). The over-50% decrease in cervical cancer incidence and mortality over the past 3 decades is largely due to screening with the Papanicolaou (Pap) test, which can detect cervical cancer at an early stage as well as precancerous abnormalities (9). With appropriate evaluation, follow-up, and treatment, survival for women diagnosed with precancerous cervical lesions is almost 100% (18). Sharma and colleagues used a model-based approach in a cohort of 50-year-old participants and estimated that 10,179 deaths from breast cancer, 27,166 from cervical cancer, and 74,740 from colorectal cancer could be prevented if current screening levels were maintained. In addition, an extra 1,300 deaths from breast cancer, 3,400 from cervical cancer, and 11,000 from colorectal cancer could be averted with an increase of 10 percentage points above current screening rates (19). However, even with its proven benefits and US Preventive Services Task Force (USPSTF) recommendations, cancer screening is still suboptimal. The median prevalence of women aged 50 to 74 years who had a mammogram within the past 2 years was about 78% in 2020 and varied substantially, from 66% to 87% among states, differing by race and ethnicity, household income, access to health care, age, and education level (20). However, in 2020 approximately 20% of women aged 21 to 65 years had not been screened for cervical cancer in the past 3 years (20). Moreover, the national median prevalence of people aged 50 to 75 years who have been screened for colorectal cancer per USPSTF recommendations remains less than 70% (13). Again, screening rates differ substantially by state, age group, race and ethnicity, access to health care, health insurance, household income, and education level (20).
Many factors could affect cancer screening behavior, including sociodemographic characteristics, screening cost, health insurance, education, income, travel distance to and location of screening sites, knowledge of the disease, patient and clinician attitudes, and availability of adequate health care facilities (1,15–17,21,22). Therefore, investigating factors influencing screening participation is crucial to creating and implementing population-based cancer screening programs. One such program is the National Breast and Cervical Cancer Early Detection Program (NBCCEDP; www.cdc.gov/cancer/nbccedp/), which was authorized under the Breast and Cervical Cancer Mortality Prevention Act of 1990. The program provides breast and cervical cancer screening and diagnostic services to low-income, underinsured, and uninsured women. NBCCEDP focuses on factors at the interpersonal, organizational, community, and policy levels that influence screening and has served more than 5.9 million women with more than 15.4 million breast and cervical cancer screenings since its inception in 1991. NBCCEDP has expanded and now funds 70 award recipients — all 50 states, the District of Columbia, Puerto Rico, 5 US Pacific Island territories, and 13 American Indian and Alaska Native tribes or tribal organizations. Such programs directed at medically underserved populations should be expanded throughout the country.
Benavidez and colleagues used 2018 BRFSS data to study women who met breast, cervical, and colorectal cancer screening consistent with USPSTF recommendations and found that screening disparities persisted among socioeconomically disadvantaged groups, especially low-income women and women without health insurance (23). They also found that Hispanic women had higher breast and cervical cancer screening prevalence but lower colorectal cancer screening prevalence than non-Hispanic White women. In addition, some racial and ethnic groups and rural populations are disproportionately affected by most cancers. Kruse-Diehr and colleagues compared colorectal cancer deaths in Black populations with White populations in the historically segregated and economically distressed Mississippi Delta. They reported that segregation affected Black and White populations differently. Deaths from colorectal cancer among Black people were higher in mildly and severely segregated urban counties than in moderately segregated counties. Segregation had no effect on colorectal cancer death rates among Black populations in rural counties and was not associated with death rates among White populations (24). Bhimla and colleagues evaluated factors related to colorectal cancer screening among populations of Asian descent by neighborhood ethnic density and psychosocial factors, including knowledge about colorectal cancer, self-efficacy about screening, and perceived barriers to screening behaviors. Their study found that Vietnamese and Filipino Americans had significantly lower screening rates than Korean Americans (25). They also showed that Asian Americans who lived in neighborhoods with high Asian ethnic density were unlikely to complete the colorectal cancer screening process. These findings suggest that the people providing health education to populations with low colorectal cancer screening prevalence could benefit from a better understanding of the cultural norms and beliefs of those populations. Research on cultural characteristics is warranted to understand better why screening differences exist among different racial and ethnic populations. One successful study funded by the Centers for Disease Control and Prevention (CDC) showed that designing interventions for breast and cervical cancer for Muslim women could facilitate screening (26).
In an analysis of a large federally qualified health center in central Texas, Zhan and colleagues found that colorectal cancer screening prevalence was low among people who lived more than 20 miles from a primary care clinic. On the other hand, they found that screening prevalence was high among people who visited their primary care provider regularly. They also used geospatial cluster analysis to identify clusters of patients not up to date with colorectal cancer screening (27).
A randomized clinical trial showed that 20% fewer lung cancer deaths occurred in a group that received an invitation to annual low-dose computed tomography (LDCT) screening compared with a group invited to receive annual chest x-rays (22). Rohatgi and colleagues completed a quantitative evaluation of geographic access to LDCT lung cancer screening in Missouri and Illinois. They reported that rural residents had significantly lower access to LDCT than urban residents (28).
Where a person lives can profoundly affect short- and long-term health (29). Much research into this relationship incorporates locality and geospatial analysis with mixed-model approaches, which can be adopted by state and local health departments by using patient data. Although some geospatial research was done at the county level because of data constraints, geospatial analysis could be further developed for small neighborhoods where homogeneity can be found at the subcounty level. To answer this need, CDC developed PLACES (www.cdc.gov/places/) with the support of the Robert Wood Johnson Foundation and the CDC Foundation. PLACES uses small area estimation methods to provide community estimates on health conditions, prevention, health risks, and health status down to the zip code tabulation area (30). The PLACES tool can help us better understand why the uptake of cancer screening did not reach Healthy People 2020 targets. These data also allow public health professionals to identify populations for implementing proven interventions.
The Community Preventive Services Task Force ( Community Guide ) provides many evidence-based findings and recommendations about cancer screening in community settings (31). These recommendations can be adopted and modified for specific localities and populations. Haverkamp and colleagues mailed a fecal immunochemical test (FIT) to the eligible population served by 3 health care facilities in Arizona operated by American Indian tribes. They found that direct mail to eligible tribe members with instructions and a follow-up telephone call and/or home visit improved the screening compliance rate significantly (32). Simply mailing the FIT test kit with instructions and a telephone call reminder to eligible patients with regular office visits increased the test kit return rate almost threefold.
CDC supports many evidence-based public health interventions. Their National Comprehensive Cancer Control Program (NCCCP; www.cdc.gov/cancer/ncccp/) funds every US state, territory, and tribe or tribal organization to develop and implement evidence-based plans to control cancer. CDC recommends that state comprehensive cancer control plans include evidence-based recommendations and guidelines, such as those from the Community Guide and the USPSTF. These interventions include patient reminders, reducing structural barriers, provider reminders, provider assessment and feedback, small media programs, one-on-one education for cancer screening, multicomponent interventions, and interventions that engage community health workers (31). The inclusion of evidence-based interventions in cancer control plans is an area for improvement. Soori and colleagues evaluated current comprehensive cancer control plans for 50 states and the District of Columbia for inclusion of evidence-based breast cancer control recommendations and guidelines (33). They found that only 6% to 37% of plans included USPSTF recommendations for breast cancer interventions, and only about half included mammogram prevalence in the burden statement. A previous mixed-method study done by CDC found that developers of comprehensive cancer control programs were familiar with evidence-based interventions but needed assistance in implementing them and evaluating their success (34).
Increasing cancer screening will require the collective effort of policy makers, public health practitioners, researchers, and primary care providers. Using evidence-based, multicomponent interventions can increase screening among populations with low screening rates (35). Culturally tailored strategies could be developed to address the needs of socioeconomically disadvantaged and medically underserved groups (29,36). Research and evaluations of public health programs need to focus on the roots of barriers and develop innovative strategies to increase screening. Factors that affect cancer screening behaviors are intertwined. Resolving just one will not solve the whole screening issue. For example, cancer screening rates are generally low among people with low incomes or who lack health insurance (37,38). However, offering health insurance to the uninsured may not be sufficient to increase rates. Medicaid beneficiaries have health coverage for cancer screening, but they may not be able to afford the cost of transportation or loss of a day’s pay for a colonoscopy (31,39–41). The financial burden associated with transportation and loss of work should be considered and evaluated. Developing innovative cancer screening techniques that are portable, noninvasive, and low cost could also increase the uptake of cancer screening.
The ultimate goal of cancer screening is to reduce cancer incidence and mortality (36). Thus, cancer screening can be coupled with primary cancer prevention strategies to reduce cancer risks and to increase proper follow-up care and treatment, especially with the ongoing COVID pandemic in which preventive medical procedures and tests may be delayed or postponed. Public health needs to build the infrastructure to be better prepared so that cancer education, screening, and early treatment are minimally affected by the next pandemic, thereby saving lives.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. No copyrighted material, surveys, instruments, or tools were used in this article.
Correspondence: Zhen-Qiang (Marshal) Ma, MD, MPH, MS, Division of Community Epidemiology, Bureau of Epidemiology, Pennsylvania Department of Health, 625 Forster St, Rm 925, Harrisburg, PA 17120. Telephone: 717-547-3484. Email: [email protected] .
Author Affiliations: 1 Pennsylvania Department of Health, Harrisburg, Pennsylvania. 2 Centers for Disease Control and Prevention, Atlanta, Georgia.
- US Cancer Statistics Working Group. US cancer statistics data visualizations tool, based on 2020 submission data (1999–2018): US Department of Health and Human Services, Centers for Disease Control and Prevention, and National Cancer Institute. Released in June 2021. www.cdc.gov/cancer/dataviz. Accessed March 3, 2022.
- Weir HK, Thompson TD, Stewart SL, White MC. Cancer incidence projections in the United States between 2015 and 2050. Prev Chronic Dis 2021;18:E59. CrossRef PubMed
- Mariotto AB, Enewold L, Zhao J, Zeruto CA, Yabroff KR. Medical care costs associated with cancer survivorship in the United States. Cancer Epidemiol Biomarkers Prev 2020;29(7):1304–12. CrossRef PubMed
- Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML. Projections of the cost of cancer care in the United States: 2010–2020. J Natl Cancer Inst 2011;103(2):117–28. CrossRef PubMed
- National Cancer Institute. Public health research and cancer. https://www.cancer.gov/research/areas/public-health. Updated August 31, 2020. Accessed January 30, 2022.
- World Health Organization. Preventing cancer. https://www.who.int/activities/preventing-cancer. Accessed January 30, 2022.
- Smith RA, Andrews KS, Brooks D, Fedewa SA, Manassaram-Baptiste D, Saslow D, et al. Cancer screening in the United States, 2018: a review of current American Cancer Society guidelines and current issues in cancer screening. CA Cancer J Clin 2018;68(4):297–316. CrossRef PubMed
- National Cancer Institute. Cancer screening overview (PDQ)–patient version. Updated August 19, 2020. https://www.cancer.gov/about-cancer/screening/patient-screening-overview-pdq. Accessed March 3, 2022.
- World Health Organization, International Agency for Cancer Research, Working Group on the Evaluation of Cancer Preventive Strategies. Cervix cancer screening. IARC handbooks of cancer prevention, volume 10. Lyon (FR): International Agency for Research on Cancer; 2005.
- Deppen SA, Aldrich MC, Hartge P, Berg CD, Colditz GA, Petitti DB, et al. Cancer screening: the journey from epidemiology to policy. Ann Epidemiol 2012;22(6):439–45. CrossRef PubMed
- Hall IJ, Tangka FKL, Sabatino SA, Thompson TD, Graubard BI, Breen N. Patterns and trends in cancer screening in the United States. Prev Chronic Dis 2018;15:E97. CrossRef PubMed
- Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA Cancer J Clin 2021;71(1):7–33. Erratum in: CA Cancer J Clin 2021;71(4):359. CrossRef PubMed
- Richardson LC, King JB, Thomas CC, Richard TB, Dowling NF, Coleman King S. Adults who have never been screened for colorectal cancer, Behavioral Risk Factor Surveillance System, 2012 and 2020. Prev Chronic Dis 2022.
- White MC, Holman DM, Goodman RA, Richardson LC. Cancer risk among older adults: time for cancer prevention to go silver. Gerontologist 2019;59(Suppl 1):S1–6. CrossRef PubMed
- Marmot MG, Altman DG, Cameron DA, Dewar JA, Thompson SG, Wilcox M. The benefits and harms of breast cancer screening: an independent review. Br J Cancer 2013;108(11):2205–40. CrossRef PubMed
- Coldman A, Phillips N, Wilson C, Decker K, Chiarelli AM, Brisson J, et al. Pan-Canadian study of mammography screening and mortality from breast cancer. J Natl Cancer Inst 2014;106(11):dju261. Erratum in: J Natl Cancer Inst. 2015;107(1):dju404 CrossRef PubMed
- Paci E, Broeders M, Hofvind S, Puliti D, Duffy SW; EUROSCREEN Working Group. European breast cancer service screening outcomes: a first balance sheet of the benefits and harms. Cancer Epidemiol Biomarkers Prev 2014;23(7):1159–63. CrossRef PubMed
- Leyden WA, Manos MM, Geiger AM, Weinmann S, Mouchawar J, Bischoff K, et al. Cervical cancer in women with comprehensive health care access: attributable factors in the screening process. J Natl Cancer Inst 2005;97(9):675–83. CrossRef PubMed
- Sharma KP, Grosse SD, Maciosek MV, Joseph D, Roy K, Richardson LC, et al. Preventing breast, cervical, and colorectal cancer deaths: assessing the impact of increased screening. Prev Chronic Dis 2020;17:E123. CrossRef PubMed
- Centers for Disease Control and Prevention. BRFSS prevalence & trends data. 2015. https://www.cdc.gov/brfss/brfssprevalence. Accessed December 29, 2021.
- Tabár L, Dean PB, Chen TH, Yen AM, Chen SL, Fann JC, et al. The incidence of fatal breast cancer measures the increased effectiveness of therapy in women participating in mammography screening. Cancer 2019;125(4):515–23. CrossRef PubMed
- Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, Fagerstrom RM, et al. ; National Lung Screening Trial Research Team. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011;365(5):395–409. CrossRef PubMed
- Benavidez GA, Zgodic A, Zahnd WE, Eberth JM. Disparities in meeting USPSTF breast, cervical, and colorectal cancer screening guidelines among women in the United States. Prev Chronic Dis 2021;18:E37. CrossRef PubMed
- Kruse-Diehr AJ, McDaniel JT, Lewis-Thames MW, James AS, Yahaya M. Racial residential segregation and colorectal cancer mortality in the Mississippi Delta region. Prev Chronic Dis 2021;18:E14. CrossRef PubMed
- Bhimla A, Mann-Barnes T, Park H, Yeh M-C, Do P, Aczon F, et al. Effects of neighborhood ethnic density and psychosocial factors on colorectal cancer screening behavior among Asian American adults, Greater Philadelphia and New Jersey, United States, 2014-2019. Prev Chronic Dis 2021;18:E90. CrossRef PubMed
- Islam N, Patel S. Best practices for partnering with ethnic minority–serving religious organizations on health promotion and prevention. AMA J Ethics 2018;20(7):E643–54. CrossRef PubMed
- Zhan FB, Morshed N, Kluz N, Candelaria B, Baykal-Caglar E, Khurshid A, et al. Spatial insights for understanding colorectal cancer screening in disproportionately affected populations, central Texas, 2019. Prev Chronic Dis 2021;18:E20. CrossRef PubMed
- Rohatgi KW, Marx CM, Lewis-Thames MW, Liu J, Colditz GA, James AS. Urban-rural disparities in access to low-dose computed tomography lung cancer screening in Missouri and Illinois. Prev Chronic Dis 2020;17:E140. CrossRef PubMed
- Institute of Medicine. Challenges and successes in reducing health disparities: workshop summary. Washington (DC): The National Academies Press; 2008.
- Centers for Disease Control and Prevention. PLACES: local data for better health. https://www.cdc.gov/places/. Updated January 5, 2022. Accessed January 30, 2022.
- Community Preventive Services Task Force. The Community Guide: cancer. https://www.thecommunityguide.org/topic/cancer. Accessed March 3, 2022.
- Haverkamp D, English K, Jacobs-Wingo J, Tjemsland A, Espey D. Effectiveness of interventions to increase colorectal cancer screening among American Indians and Alaska Natives. Prev Chronic Dis 2020;17:E62. CrossRef PubMed
- Soori M, Platz EA, Kanarek N. Inclusion of evidence-based breast cancer control recommendations and guidelines in state comprehensive cancer control plans. Prev Chronic Dis 2020;17:E129. CrossRef PubMed
- Steele CB, Rose JM, Chovnick G, Townsend JS, Stockmyer CK, Fonseka J, et al. Use of evidence-based practices and resources among comprehensive cancer control programs. J Public Health Manag Pract 2015;21(5):441–8. CrossRef PubMed
- Sharma KP, Leadbetter S, DeGroff A. Characterizing clinics with differential changes in the screening rate in the Colorectal Cancer Control Program of the Centers for Disease Control and Prevention. Cancer 2021;127(7):1049–56. CrossRef PubMed
- American Cancer Society. Cancer prevention & early detection facts & figures 2019–2020. Atlanta (GA): American Cancer Society; 2019.
- O’Malley AS, Forrest CB, Mandelblatt J. Adherence of low-income women to cancer screening recommendations. J Gen Intern Med 2002;17(2):144–54. CrossRef PubMed
- Alharbi AG, Khan MM, Horner R, Brandt H, Chapman C. Impact of Medicaid coverage expansion under the Affordable Care Act on mammography and pap tests utilization among low-income women. PLoS One 2019;14(4):e0214886. CrossRef PubMed
- Wang C. The impact of car ownership and public transport usage on cancer screening coverage: empirical evidence using a spatial analysis in England. J Transp Geogr 2016;56:15–22. CrossRef PubMed
- Davis MM, Renfro S, Pham R, Hassmiller Lich K, Shannon J, Coronado GD, et al. Geographic and population-level disparities in colorectal cancer testing: a multilevel analysis of Medicaid and commercial claims data. Prev Med 2017;101:44–52. CrossRef PubMed
- Hunleth JM, Steinmetz EK, McQueen A, James AS. Beyond adherence: health care disparities and the struggle to get screened for colon cancer. Qual Health Res 2016;26(1):17–31. CrossRef PubMed
The opinions expressed by authors contributing to this journal do not necessarily reflect the opinions of the U.S. Department of Health and Human Services, the Public Health Service, the Centers for Disease Control and Prevention, or the authors’ affiliated institutions.
- All topics »
- Fact sheets
- Feature stories
- Publications
- Questions & answers
- Tools and toolkits
- Coronavirus disease (COVID-19) pandemic
- Ukraine emergency
- Environment and health
Mpox (monkeypox)
- Calls for experts
- Initiatives
- European Programme of Work
- Sustainable Development Goals
- The Pan-European Mental Health Coalition
- Empowerment through Digital Health
- The European Immunization Agenda 2030
- Healthier behaviours: incorporating behavioural and cultural insights
- Moving towards UHC
- Protecting against health emergencies
- Promoting health and well-being
- News stories
- Media releases
- Photo stories
- Questions and answers
- Media Contacts
Newsletters
- European Health Information Gateway
- European health report
- Core health indicators
- WHO Immunization Data portal
- Noncommunicable diseases (NCD) dashboard
- Events
- Teams »
- Data and digital health
- Policy & Governance f. Health through the Life Course
- Groups and networks »
- Health Evidence Network (HEN)
The European Health Report 2021 »

- Conflict in Israel and the occupied Palestinian territory
- Armenian refugee health response
- Climate crisis: extreme weather
- Türkiye and Syria earthquakes
- About health emergencies
- Health emergencies newsletter
- Health emergencies list

- Regional Director
- Executive Council
- Technical centres
- Faces of WHO
- Regional Committee for Europe
- Standing Committee
- Partnerships
- Groups and networks
- WHO collaborating centres
74th session of the WHO Regional Committee for Europe

- Fact Sheets /
Cancer - Screening and early detection
Early detection of cancer greatly increases the chances for successful treatment. The 2 components of early detection of cancer are early diagnosis (or downstaging) and screening. Early diagnosis focuses on detecting symptomatic patients as early as possible, while screening consists of testing healthy individuals to identify those having cancers before any symptoms appear.
Early diagnosis
Early diagnosis programmes aim at reducing the proportion of patients who are diagnosed at a late stage. They have 2 main components:
- increased awareness of first signs of cancer, among physicians, nurses and other health care providers as well as among the general public; and
- improved accessibility and affordability of diagnosis and treatment services, and improved referral from first to secondary and tertiary levels of care.
Early diagnosis is particularly relevant to cancers of the breast, cervix, mouth, larynx, colon and rectum, and skin.
Screening refers to the use of simple tests across a healthy population to identify those individuals who have a disease, but do not yet have symptoms. Examples include breast cancer screening using mammography or clinical breast exam, and cervical cancer screening using pap smears, human papillomavirus test or visual inspection with acetic acid.
Screening programmes should be undertaken only when their effectiveness has been demonstrated, when resources (personnel, equipment, etc.) are sufficient to cover nearly all of the target group, when facilities exist for confirming diagnoses and for treatment and follow-up of those with abnormal results, and when prevalence of the disease is high enough to justify the effort and costs of screening.
Even when implemented properly, screening programmes are associated with undesirable effects which include:
- falsely positive screening tests that result in additional testing, invasive diagnostic procedures and patient anxiety;
- falsely negative screening tests that provide false reassurance and can result in delayed presentation/diagnosis when symptoms appear; and
- over diagnosis/treatment of preclinical cancers that could have never cause symptoms nor pose a serious health threat and which involve unnecessary treatment that injures the patient.
The importance of these harms varies according to the screening tests, population groups targeted for screening and quality of screening programmes.
Weighing the harms against the benefits of screening has led WHO not to recommend mammography screening in women less than 50 years of age. Based on the existing evidence, mass population screening can be advocated only for cervical, breast and colorectal cancer.
Systematic prostate cancer screening of all men above a certain age using prostate-specific antigen (PSA) is not recommended by WHO. The high harm/benefit ratio has resulted in the abandonment of population-based PSA screening for prostate cancer in many countries of western Europe in the past years.

Distinguishing cancer screening from early diagnosis
Screening, on the other hand, is relevant to a subset of cancer types only – namely cervical, colorectal and breast cancers, which together represent 28% of cancer cases in the WHO European Region. In the case of cervical cancer, screening enables cure at a precancerous stage of the disease with minor surgical treatments. This is not the case for breast cancer, or for colorectal cancer screening by fecal occult blood test.

Barriers to early cancer diagnosis and treatment
Early diagnosis programmes focus on reducing delays between the detection of first symptoms and treatment by ensuring that:
- people are sensitized enough to consult health professionals as soon as symptoms appear, without being delayed by any financial, logistical or psychosocial barriers;
- the health staff consulted react appropriately and rapidly, thanks to adequate training and clear referral guidelines; and
- diagnostic and treatment services are accessible rapidly and deliver optimal quality at an affordable cost.
At all stages, barriers can reduce patients’ chances of being diagnosed and treated quickly. These include poor cancer awareness among the public; suboptimal knowledge at the primary health care level about cancer symptoms and/or adequate diagnosis follow-up; poor accessibility; low affordability and/or quality of diagnosis and treatment services (waiting lists, errors in diagnosis, administrative red tape, unclear referral pathways, etc.); and the many logistical, financial and psychosocial barriers preventing patients from accessing services rapidly.
A major objective of early diagnosis programmes is to reduce the prevalence of these barriers. This is also a prerequisite for implementing screening programmes, as to be successful they require rapid, adequate-quality diagnosis follow-up and treatment for people screened positive.
Early diagnosis programmes are comparatively easy and inexpensive to implement; since they cover symptomatic patients only, they are less extensive than screening programmes that target entire populations.


Alonzo Mourning, Prostate Cancer Survivor
Online Help
Our 24/7 cancer helpline provides information and answers for people dealing with cancer. We can connect you with trained cancer information specialists who will answer questions about a cancer diagnosis and provide guidance and a compassionate ear.
Chat live online
Select the Live Chat button at the bottom of the page
Call us at 1-800-227-2345
Available any time of day or night
Our highly trained specialists are available 24/7 via phone and on weekdays can assist through online chat. We connect patients, caregivers, and family members with essential services and resources at every step of their cancer journey. Ask us how you can get involved and support the fight against cancer. Some of the topics we can assist with include:
- Referrals to patient-related programs or resources
- Donations, website, or event-related assistance
- Tobacco-related topics
- Volunteer opportunities
- Cancer Information
For medical questions, we encourage you to review our information with your doctor.
- Cancer Basics
- Living Well
- Screening Guidelines
Why We Screen for Some Cancers and Not Others

Screening means having a test that looks for cancer or another disease in people who don’t have any symptoms. Some screening tests can find growths and remove them before they have a chance to turn into cancer. Other screening tests, when done regularly, can find cancer early when it's small, hasn't spread, and might be easier to treat.
The benefits of screening tests should be weighed against any risks of the tests themselves. Risks may include anxiety, pain, bleeding, or other side effects. And screening isn’t perfect. Sometimes screening misses cancer. And sometimes it finds something suspicious that turns out to be harmless (called a false-positive), but still needs to be checked out through additional tests that also carry risks and may cause more stress.
This is why the American Cancer Society uses a formal process to review scientific evidence to create guidelines for cancer screening . The guidelines give recommendations about what screening tests people should get, when they should get them, and how frequently the tests should be done.
American Cancer Society Screening Guidelines
The American Cancer Society has guidelines for average-risk adults with recommendations that include regular screening for breast cancer, cervical cancer, prostate cancer, lung cancer, and colorectal cancer, based on eligibility and scientific evidence that shows getting screened regularly may help save lives. For many other cancer types, researchers continue to conduct studies to learn the best ways to find cancer before symptoms appear.
Breast Cancer: Women should have the choice to start yearly screening with a mammogram at age 40 if they wish to do so. All women at average risk of breast cancer should begin yearly screening with a mammogram by age 45. At age 55, women can switch to a mammogram every 2 years, or can continue yearly screening. Women should talk to a health care provider about their own personal risk for breast cancer and about any breast changes they notice. Regular screening should continue for as long as a woman is in good health and expects to live at least 10 more years.
Cervical Cancer : Women and people with a cervix should start regular screening at age 25. Those who are between 25 and 65 should get a primary HPV (human papillomavirus) test every 5 years. If a primary HPV test is not available, a co-test (HPV test combined with a Pap test) should be done every 5 years or a Pap test can be done every 3 years. Those over age 65 who have had regular screening tests with normal results in the past 10 years should no longer be screened for cervical cancer. Some women – because of their history – may need to be screened more often. People vaccinated for HPV should still follow the guideline recommendations. Talk to a health care provider about your history and risk for cervical cancer.
Colorectal Cancer : Adults at average risk should begin regular colorectal screening at age 45, but those at high risk for colorectal cancer based on family and/or personal history or other factors may need to start screening before age 45, be screened more often, or get specific tests. Several different tests can be used to screen for colorectal cancer, including colonoscopy, flexible sigmoidoscopy, guaiac-based fecal occult blood test, and more. Talk with a health care provider about your risk for colorectal cancer and which tests might be good for you, and talk to your insurance provider about your coverage. All abnormal results on non-colonoscopy screening tests should be followed up with a colonoscopy.
Lung Cancer : Screening is recommended for certain people at higher risk for lung cancer. If you are between the ages of 50 and 80 and smoke now or used to smoke, you might benefit from screening for lung cancer with a yearly low-dose CT scan (LDCT). Talk to a health care provider about your risk for lung cancer, how you can quit smoking if you still smoke, and the possible benefits, limits, and harms of lung cancer screening.
Prostate Cancer: Screening recommendations involve making an informed decision when it comes to screening for prostate cancer. This means men should discuss the possible risks and benefits of prostate cancer screening with a health care provider when deciding whether to be screened. Starting at age 50, men should have a discussion about the pros and cons of testing so they can decide if testing is the right choice for them. Men who are African American or have a father or brother who had prostate cancer before age 65, should have this talk with a health care provider starting at age 45.
- Reviewed by
- Helpful resources

The American Cancer Society medical and editorial content team
Our team is made up of doctors and oncology certified nurses with deep knowledge of cancer care as well as editors and translators with extensive experience in medical writing.
- Cancer Screening Guidelines
- Screening Recommendations by Age
- Exams and Tests for Cancer
American Cancer Society news stories are copyrighted material and are not intended to be used as press releases . For reprint requests, please see our Content Usage Policy .
Related News and Stories
- Colorectal Cancer Screening: What Are My Options?
- If You’re Called Back After a Mammogram
- Colorectal Cancer Rates Higher in African Americans, Rising in Younger People
Help us end cancer as we know it, for everyone.

Cervical Cancer Screening: Review of Issues Essay
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment
Introduction
Describing quantitative research, appraisal tools, studies, and matrix, article discussion, applicability to practice and future research, appendix a: individual evidence summary tool.
Cervical cancer continues to be a significant health problem in the United States. According to the latest statistics by the Centers for Disease Control and Prevention (2022), the US has approximately 13,000 new cases of this cancer annually, and about 4,000 of the diagnosed women die from cervical cancer. Although new screening methods were introduced in the last decades, and women were provided with additional tests, screening rates remain low (Bedell et al., 2020). Therefore, the question of how Advance Practice Nurses can aid patients in undergoing screening arises. Nurses should introduce such initiatives as self-completed test kits that can be used at home for human papillomavirus screening and patient navigation to create a supportive environment for cervical cancer screening.
Quantitative research includes studies that approach scientific inquiries with quantifiable measures. In such studies, data is collected for calculations that help answer the research question. For example, one may find a correlation between an independent and dependent variable to see how two or more elements are interconnected (Sürücü & Maslakçi, 2020). Furthermore, quantitative research may help compare group behavior depending on the intervention to which they are exposed (Vu, 2021). Regression and change are also possible investigation goals in this branch of scientific research. Some types of quantitative studies include descriptive, correlational, quasi-experimental, experimental, and more.
To explore the issue of cervical cancer screening, one may look at different types of qualitative research. The problem reviewed is the need to increase cancer screening rates with the help of nurse intervention. Therefore, one needs to look at studies that compare the effectiveness of nursing interventions and usual care regarding screening programs. An experimental study that divides the participants into two or more groups is a type of quantitative research that can support the thesis and provide more information on effective intervention types. Moreover, meta-analyses and systematic reviews of nursing interventions can provide a solid base for further research.
Two studies were chosen for the appraisal and analysis to support the topic of cervical cancer screening. The first one is a meta-analysis performed by Nelson et al. (2020) – the researchers aim to investigate the impact of patient navigation on cancer screening rates among underserved populations. As seen in Appendices A and B, the study shows a high level of quality, producing consistent results. This review was selected as it contains studies on cervical cancer, and its focus on screening rate improvement aligns with the topic of interest.
The second article under examination is a randomized controlled study. In the clinical research by Winer et al. (2019), the authors test whether mailing a test kit to patients is more effective than simple reminders to get screened for cervical cancer. Similar to the previous study, Appendices A and B demonstrate the high quality of available evidence. The research was chosen for this review due to its interest in additional measures for improving screening rates and a choice of nursing intervention.
To understand the selection of sources and appraise their quality, one has to discuss them in more detail. First, in the meta-analysis, Nelson et al. (2020) aim to analyze the outcomes of patient navigation on the participants’ cancer screening rates. Breast, colorectal, and cervical cancer are considered in the study, and patient navigation is defined as “services that improve engagement in healthcare by providing personal guidance through the healthcare system” (Nelson et al., 2020, p. 3028). The research design is a meta-analysis that considers quantitative studies. The investigators introduce a new way of appraising the results by adapting them into one measurement. As a result, the article’s methodology synthesizes evidence and calculates the risk ratio.
The data collection process is described in the article in detail. It is noted that the authors gathered sources from such databases as Ovid® MEDLINE®, PsycINFO®, and SocINDEX (Nelson et al. (2020). The inclusion criteria included randomized controlled trials and observational studies with control and intervention groups. Furthermore, the reviewed sources had to consider vulnerable populations, be relevant to US health and practice, and present clear results of screening rates (Nelson et al. (2020). As a result, the data was collected from 37 articles, including 29 randomized controlled trials and eight observational studies. The validity of the data in the papers and their analysis was checked by comparing the selected studies’ results (Vu, 2021). Articles show consistently high significance, but additional research is necessary due to the variance in rates (Nelson et al. (2020). The instrument’s reliability is based on its transparency and consistency, which is supported by the author’s detailed discussion of its operation.
The results of the meta-analysis show that the screening rates for all types of cancer were positively influenced by patient navigation. While studies analyzing cervical cancer were limited in number, the consistency of the results for the available sources and the outcomes for other types of cancer demonstrate the overall effectiveness of this approach (Vu, 2021). These findings have significant implications for practice as they support the idea of additional measures for engaging patients in cancer screening. The study emphasizes the value of individual approaches to patients and communication’s role in improving patients’ preparedness for regular screening. Based on the factors above, the study’s evidence quality level and the findings’ ratings are high, and the meta-analysis can be marked as IA.
The second source presents similarly high-quality results while testing another method of screening rates’ improvement. In a randomized controlled trial, Winer et al. (2019) analyze whether patients are more likely to undergo hospital cervical cancer screening if they receive home test kits for human papillomavirus (HPV). To complete the study, the researchers identified eligible participants using electronic health records and separated them into control and intervention groups. The inclusion criteria are women between 30 and 64 years old who did not have a hysterectomy and had a clinician within the selected system. The control group receives usual care, including yearly reminders to undergo screening and frequent messages from the clinic. For the treatment group, these activities are supplemented by mailing patients a self-sampling kit that tests for HPV (Winer et al., 2019). Then, the screening rate is compared in the next six months after the initiative.
The data collection process in the second study relied on electronic health records. Two major outcomes were considered: diagnosed and treated precancerous conditions, and other measures included increased test uptake and abnormal results (Winer et al., 2019). As a result of investigating health records, it was determined that the difference between control and intervention groups was significant, with the self-testing kits raising the screening uptake by almost 10% (Winer et al., 2019). These results have high validity due to standardized statistical calculations and electronic records use (Vu, 2021). The implication of this study is the effectiveness of reaching out to patients with opportunities for self-testing instead of calling. The quality of data and the transparent explanations of each step allow one to grade this study as IA on the quality scale.
The discussed studies can significantly impact practice and positively influence its quality. Based on the six domains presented by the AHRQ (2022), the findings can enhance safety, effectiveness, and focus on patient-centered care. First, the articles demonstrate ways to improve screening rates and better diagnosing for patients to prevent and treat cancer – a severe condition that endangers the lives of many people. Thus, the conclusions and recommendations support the aim of patient safety. Second, the effectiveness of care is improved by engaging patients in screening and providing timely care. The higher rate of timely diagnoses is a result of both studies, showing the positive impact of the considered interventions. Finally, as the research finds ways to solve a problem in patient outreach, especially among underserved populations, it is consistent with the patient-centered approach to care. The recommendations to communicate with patients and provide them with easy methods of pretesting should be implemented in practice to deliver better care.
Cervical cancer is a significant problem that poses risks to population health. Timely screening remains an issue, especially among women with health disparities. The selected studies offer several options for reaching out to patients to provide them with testing recommendations or tests to engage them in cancer detection and treatment. The articles present reliable evidence of the approaches’ effectiveness and demonstrate that patient-centered and effective care is possible with nursing interventions.
Agency for Healthcare Research and Quality [AHRQ]. (2022). Six domains of healthcare quality . Web.
Bedell, S. L., Goldstein, L. S., Goldstein, A. R., & Goldstein, A. T. (2020). Cervical cancer screening: Past, present, and future . Sexual Medicine Reviews , 8 (1), 28-37. Web.
Centers for Disease Control and Prevention. (2022). Cervical cancer: Statistics . Web.
Nelson, H. D., Cantor, A., Wagner, J., Jungbauer, R., Fu, R., Kondo, K., Stillman, L., & Quiñones, A. (2020). Effectiveness of patient navigation to increase cancer screening in populations adversely affected by health disparities: A meta-analysis . Journal of General Internal Medicine , 35 , 3026-3035. Web.
Sürücü, L., & Maslakçi, A. (2020). Validity and reliability in quantitative research . Business & Management Studies: An International Journal , 8 (3), 2694-2726. Web.
Vu, T. T. N. (2021). Understanding validity and reliability from qualitative and quantitative research traditions . VNU Journal of Foreign Studies , 37 (3). Web.
Winer, R. L., Lin, J., Tiro, J. A., Miglioretti, D. L., Beatty, T., Gao, H., Kimbel, K., Thayer, C., & Buist, D. S. (2019). Effect of mailed human papillomavirus test kits vs usual care reminders on cervical cancer screening uptake, precancer detection, and treatment: A randomized clinical trial . JAMA Network Open , 2 (11), e1914729-e1914729. Web.
EBP Question: In women, will additional screening advice from the Advanced Practice Nurse increase the rate of screening for cervical cancer in comparison to usual care?
| 1 | Nelson, H. D., Cantor, A., Wagner, J., Jungbauer, R., Fu, R., Kondo, K., Stillman, L., & Quiñones, A. (2020). Effectiveness of patient navigation to increase cancer screening in populations adversely affected by health disparities: A meta-analysis. | Meta-analysis | Patients in need of screening for cancer, 37 studies, hospital setting | Patient navigation – support for patients and individual guidance | Patients with navigation have higher rates of undergoing screening. For cervical cancer, the rates of screening were higher significantly (RR 1.11; 95% CI 1.05 to 1.19) | Risk ratio was used to see whether the patient was screened or not. | A small number of studies on cervical cancer – additional data collection is necessary. | IA |
| 2 | Winer, R. L., Lin, J., Tiro, J. A., Miglioretti, D. L., Beatty, T., Gao, H., Kimbel, K., Thayer, C., & Buist, D. S. (2019). Effect of mailed human papillomavirus test kits vs usual care reminders on cervical cancer screening uptake, precancer detection, and treatment: A randomized clinical trial. | Randomised clinical trial | Women between 30 and 64 years, 19 851 participants, a US health care delivery system | Mailed human papillomavirus kits for self-sampling as a measure to increase follow-ups for cervical cancer screening | Increased detection of cervical cancer within months of screening, quicker access to treatment. The rate of screening was higher in the intervention group in comparison to the control group – 26.3 and 17.4%. | Kaplan-Meier methods and log-rank tests | A necessity to follow-up in the clinic after at-home screening could limit participants’ participation. Exclusion of non-English speakers. | IA |
Research Evidence Appraisal Tool – Source 1
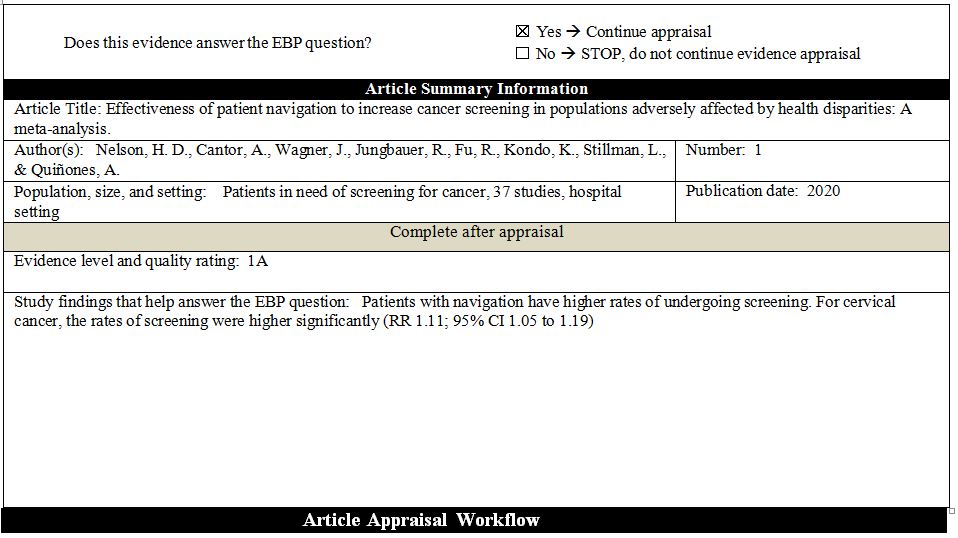
Research Evidence Appraisal Tool – Source 2
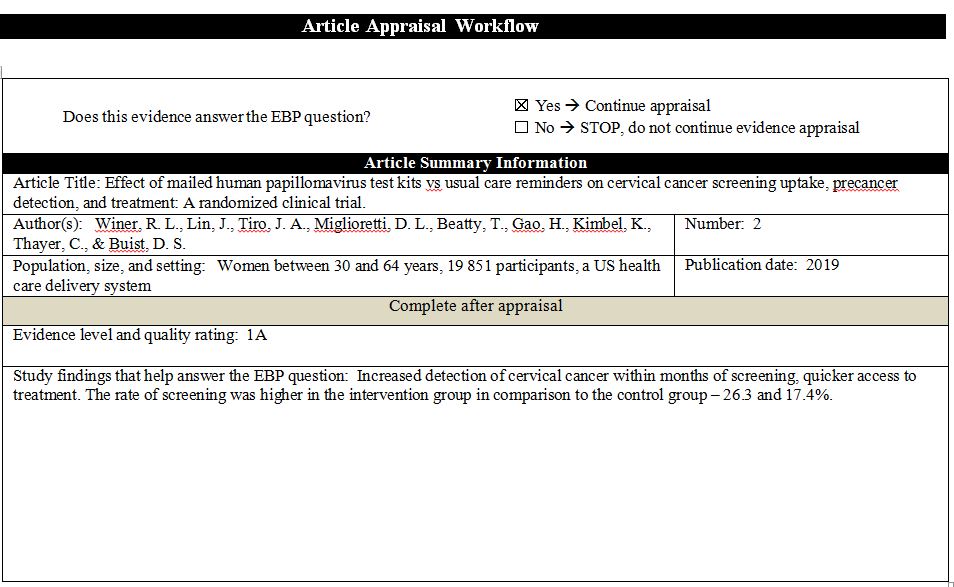
- Mammography Report: Radiology Cafe
- Hodgkin's Lymphoma: Symptoms, Stages and Therapies
- Cervical Cancer: Medical Imaging and Radiotherapy
- Cervical Cancer and Risk Factors
- Applying Roy's Adaptation Model to Cervical Cancer Patients
- Osteosarcoma: Innovative Treatment Strategies
- Breast Cancer and Its Population Burden
- Neurobiology of Disease: Article Summary
- Pap Smear and Cervical Cancer: Oncology Nursing
- Colorectal Cancer Screening Methodology
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, February 19). Cervical Cancer Screening: Review of Issues. https://ivypanda.com/essays/cervical-cancer-screening-review-of-issues/
"Cervical Cancer Screening: Review of Issues." IvyPanda , 19 Feb. 2024, ivypanda.com/essays/cervical-cancer-screening-review-of-issues/.
IvyPanda . (2024) 'Cervical Cancer Screening: Review of Issues'. 19 February.
IvyPanda . 2024. "Cervical Cancer Screening: Review of Issues." February 19, 2024. https://ivypanda.com/essays/cervical-cancer-screening-review-of-issues/.
1. IvyPanda . "Cervical Cancer Screening: Review of Issues." February 19, 2024. https://ivypanda.com/essays/cervical-cancer-screening-review-of-issues/.
Bibliography
IvyPanda . "Cervical Cancer Screening: Review of Issues." February 19, 2024. https://ivypanda.com/essays/cervical-cancer-screening-review-of-issues/.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.15(8); 2023 Aug
- PMC10498131

Addressing Cancer Disparities Through Community Engagement: Lessons and Best Practices
Swarali kale.
1 Medicine, Jawaharlal Nehru Medical College, Datta Meghe Institute of Higher Education and Research, Wardha, IND
Shoyeb Hirani
2 Medicine, Mahatma Gandhi Mission (MGM) Medical College and Hospital, Aurangabad, IND
Sauvik Vardhan
Aditi mishra, dewang b ghode.
3 General Surgery, Jawaharlal Nehru Medical College, Datta Meghe Institute of Higher Education and Research, Wardha, IND
Roshan Prasad
4 Medicine and Surgery, Jawaharlal Nehru Medical College, Datta Meghe Institute of Higher Education and Research, Wardha, IND
Mayur Wanjari
5 Research and Development, Jawaharlal Nehru Medical College, Datta Meghe Institute of Higher Education and Research, Wardha, IND
Cancer disparities continue to be a significant public health challenge, disproportionately affecting certain communities in terms of incidence, mortality, and access to quality care. Addressing these disparities requires a multifaceted approach that involves not only healthcare professionals and researchers but also the active participation and collaboration of the affected communities themselves. Community engagement has emerged as a promising strategy to reduce cancer disparities and promote health equity. This review article synthesizes the existing literature and examines the role of community engagement in addressing cancer disparities. It explores various approaches and best practices utilized in community engagement initiatives to empower and involve diverse populations in the fight against cancer. The review discusses key lessons learned from successful programs and identifies challenges faced in implementing such initiatives. The article highlights the importance of cultural competence, trust-building, and meaningful collaboration between stakeholders, including community leaders, healthcare providers, researchers, and policymakers. It emphasizes the significance of tailoring interventions to specific community needs, acknowledging cultural differences, and fostering a two-way exchange of knowledge and resources. Moreover, this review investigates the impact of community engagement on cancer prevention, early detection, treatment adherence, and survivorship outcomes. It sheds light on the role of community-based participatory research and other innovative strategies in generating evidence and facilitating the translation of research findings into real-world interventions. In conclusion, this review underlines the potential of community engagement in addressing cancer disparities and promoting health equity. By involving communities as active partners in cancer control efforts, healthcare systems can design more effective and sustainable interventions. This approach not only contributes to reducing cancer disparities but also fosters a sense of ownership and empowerment within the communities affected, paving the way for a more equitable and inclusive healthcare landscape.
Introduction and background
Cancer disparities refer to the unequal burden of cancer incidence, prevalence, mortality, and survivorship among different population groups. Various factors, including socioeconomic status, race/ethnicity, geographic location, and access to healthcare, influence these disparities. Studies have consistently shown that certain communities, such as racial and ethnic minorities, low-income individuals, and rural populations, experience higher cancer incidence rates, worse outcomes, and limited access to quality care [ 1 - 4 ].
Community engagement plays a crucial role in addressing cancer disparities by actively involving affected communities in designing, implementing, and evaluating initiatives and interventions. It recognizes that communities are experts in their own experiences, needs, and preferences and empowers them to actively participate in decision-making processes. Community engagement ensures that interventions are culturally appropriate, responsive, and sustainable by fostering collaborative partnerships between researchers, healthcare providers, policymakers, and community members [ 5 ].
This review article aims to explore the role of community engagement in addressing cancer disparities and highlight the lessons learned and best practices from existing initiatives. By examining successful community engagement models and strategies, this article provides insights and recommendations for researchers, healthcare providers, policymakers, and community leaders interested in developing effective approaches to reduce cancer disparities. The review will also identify challenges and limitations associated with community engagement and suggest potential future research and policy development directions in this field.
Methodology
The methodology employed for this review article involved conducting a comprehensive literature search to gather relevant information. Various electronic databases were utilized, including PubMed, Google Scholar, and academic libraries. The search strategy utilized a combination of keywords and controlled vocabulary related to cancer disparities, community engagement, and best practices. Publication dates did not limit the search to ensure a wide range of literature was considered. In selecting studies for inclusion, specific criteria were applied. Studies were included if they were relevant to the role of community engagement in addressing cancer disparities. This encompassed research articles, reviews, case studies, and reports that provided insights into community engagement initiatives, outcomes, and lessons learned. Only peer-reviewed studies published in English were considered to ensure the quality and accuracy of the information. Priority was given to studies that focused on lessons learned and best practices in community engagement, highlighting effective strategies, challenges, and recommendations. Studies were excluded if they did not meet the specified criteria or were primarily focused on theoretical frameworks or conceptual discussions without empirical evidence or practical examples. Additionally, studies that solely addressed individual-level interventions unrelated to community engagement in cancer disparities were excluded. The study selection process involved an initial screening of titles and abstracts, followed by a full-text review to assess eligibility. Disagreements were resolved through discussion and consensus among the reviewers.
Understanding cancer disparities
Definition and Scope of Cancer Disparities
Cancer disparities refer to the unequal distribution of cancer incidence, prevalence, mortality, and survivorship across different population groups. These disparities are characterized by variations in cancer outcomes based on race/ethnicity, socioeconomic status, age, gender, geographic location, and access to healthcare services. Disparities can manifest in different ways, including disparities in cancer screening and early detection, treatment utilization, access to clinical trials, and quality of care [ 1 ].
Factors Contributing to Cancer Disparities
Socioeconomic factors: Lower socioeconomic status is strongly associated with increased cancer disparities. Limited financial resources, a lack of health insurance, lower education levels, and inadequate access to healthcare facilities and services contribute to disparities in cancer prevention, detection, and treatment outcomes [ 6 ].
Racial and ethnic disparities: Racial and ethnic minorities often experience higher rates of certain cancers and poorer outcomes than non-Hispanic White populations. Factors such as systemic racism, discrimination, cultural beliefs, language barriers, and mistrust of the healthcare system contribute to these disparities [ 7 ].
Geographic disparities: Disparities in cancer incidence and outcomes are observed between urban and rural areas. Rural populations face unique challenges, including limited healthcare infrastructure, a shortage of healthcare providers, longer travel distances to access care, and reduced availability of specialized cancer services [ 8 ].
Access to healthcare: Limited access to quality healthcare services, including cancer screenings, diagnostic tests, and specialized treatments, contributes to disparities. Barriers to access may include a lack of health insurance, transportation issues, language barriers, and the inadequate availability of healthcare facilities in underserved areas [ 9 ].
Behavioral factors: Differences in health behaviors, such as tobacco use, physical inactivity, poor nutrition, and low adherence to recommended cancer screenings, contribute to disparities in cancer incidence and outcomes [ 10 ].
Impact of Cancer Disparities on Affected Communities
Cancer disparities have a significant impact on affected communities. They result in unequal disease burden, increased morbidity and mortality, decreased quality of life, and reduced survival rates for disadvantaged populations. Disparities also perpetuate social and economic inequalities, exacerbating existing health inequities. The emotional and financial toll on individuals and families affected by cancer disparities is substantial, further underscoring the urgency of addressing these disparities through targeted interventions and community engagement [ 11 ].
By understanding the factors contributing to cancer disparities and their impact on affected communities, we can develop targeted strategies and interventions that address the unique challenges different populations face. Community engagement is critical in ensuring that interventions are tailored to these communities' specific needs and contexts, ultimately leading to more equitable cancer care and outcomes [ 12 ].
Community engagement in cancer disparities
Definition and Significance of Community Engagement
Community engagement involves actively partnering with communities affected by cancer disparities in all stages of research, intervention development, implementation, and evaluation. It recognizes that community members possess valuable knowledge, experiences, and perspectives that can inform and guide efforts to address disparities. Community engagement moves beyond a passive recipient model to an active collaboration, empowering communities to be equal stakeholders in decision-making processes related to their health [ 13 , 14 ].
The significance of community engagement lies in its ability to ensure that interventions and strategies are culturally appropriate, relevant, and responsive to the unique needs of diverse populations. By actively involving community members, community engagement fosters trust, promotes health literacy, and enhances the acceptability and sustainability of interventions. It also facilitates the identification of community-specific barriers, strengths, and resources, leading to more effective and equitable approaches to reducing cancer disparities [ 15 ].
Benefits of Community Engagement in Addressing Cancer Disparities
Culturally appropriate interventions: Community engagement allows for developing and implementing interventions sensitive to cultural beliefs, values, and practices. By incorporating community perspectives, interventions can be tailored to overcome cultural barriers and increase acceptance and uptake among diverse populations [ 16 ].
Increased trust and engagement: Engaging communities builds trust between researchers, healthcare providers, and community members. Trust is crucial for improving health outcomes and encouraging individuals to participate in cancer prevention, screening, and treatment programs [ 17 ].
Enhanced relevance and acceptability: Community engagement ensures that interventions address the specific needs and priorities of the community. This increases the likelihood of community interventions being accepted, adopted, and sustained, leading to improved outcomes [ 5 ].
Effective dissemination of information: Community members often serve as trusted sources of information within their communities. By engaging community members, accurate and culturally relevant health information can be effectively disseminated, increasing awareness and understanding of cancer disparities and prevention measures [ 18 ].
Mobilization of community resources: Community engagement facilitates the identification and mobilization of community resources, including social support networks, community-based organizations, and local expertise. Leveraging these resources can enhance the reach and impact of interventions [ 19 ].
Role of Community Engagement in Reducing Health Inequities
Community engagement is a key strategy for reducing health inequities, including cancer disparities. By actively involving affected communities, community engagement helps to address the underlying social determinants of health, such as poverty, limited education, discrimination, and a lack of access to resources. It promotes equity by ensuring interventions are tailored to diverse populations' needs and contexts [ 20 ].
Community engagement also empowers communities, fostering a sense of ownership and agency in addressing health disparities. It encourages community members to become advocates, leaders, and partners in decision-making processes, enabling them to actively shape policies and practices that impact their health [ 21 ]. Furthermore, community engagement facilitates the implementation of comprehensive and integrated approaches that address multiple factors contributing to disparities. It promotes collaboration among various stakeholders, including community organizations, healthcare providers, policymakers, and researchers, to collectively work toward reducing health inequities.
Lessons learned from community engagement initiatives
Case Study: Community Health Workers in Cancer Prevention
This case study focuses on a community engagement initiative that utilized Community Health Workers (CHWs) to promote cancer prevention and education in underserved communities. CHWs are individuals from the community who serve as liaisons between healthcare systems and the community. They are crucial in bridging the gap by providing culturally tailored education, outreach, and support [ 22 ].
CHWs in breast cancer screening within the context of the initiative: The initiative aimed to address cancer prevention in target communities by involving the training and employment of CHWs to play crucial roles in delivering cancer prevention messages, conducting community outreach activities, and providing support to community members [ 23 ]. First, CHWs were actively engaged in education related to breast cancer screening. They played a vital role in disseminating crucial information about breast cancer, its risk factors, early detection methods, and the importance of screening. Their interactions with community members helped raise awareness and knowledge about breast cancer, empowering individuals to make informed decisions about their health. Second, CHWs provided direct assistance in breast cancer screening. As trained and trusted community members, they offered practical support in facilitating the screening process. This involved guiding individuals through getting screened, helping them schedule appointments, and addressing any concerns or fears related to the screening procedure. Their presence eased the process for many community members, increasing participation in breast cancer screening. Lastly, CHWs performed navigational services as a bridge between community members and healthcare facilities. They understood the cultural context and language of the community, enabling them to ensure that educational materials and messages about breast cancer were culturally appropriate and relevant. Additionally, they helped community members navigate the healthcare system, facilitating access to screening facilities, diagnostic tests, and further medical care when needed. Overall, the involvement of CHWs in the initiative played a pivotal role in enhancing breast cancer screening rates in the target communities. By focusing on education, direct assistance, and navigational services, they significantly contributed to promoting early detection and reducing barriers to breast cancer screening, ultimately improving the overall health outcomes in the communities they served [ 23 ].
The significance of this initiative's impact was rigorously assessed through a comprehensive evaluation process. To determine the effectiveness of the intervention, statistical analyses were conducted, employing both parametric and non-parametric tests, such as t-tests and chi-square tests, respectively. These tests were utilized to compare pre-and post-intervention data, assessing changes in cancer awareness levels, understanding of risk factors, and uptake of preventive measures among community members. Awareness levels were measured through pre- and post-intervention surveys, where participants were asked about their knowledge of cancer risk factors and preventive measures. A significant improvement in awareness was observed, with a considerable increase in correct responses in the post-intervention survey compared to the baseline. Quantitative data on the number of individuals undergoing cancer screening before and after the intervention was collected to evaluate the impact on screening rates. Additionally, qualitative assessments were conducted through focus group discussions and interviews with community members to understand their perceptions of the initiative and the factors influencing their decision to seek cancer screening services. The involvement of CHWs was particularly instrumental in creating a supportive and culturally sensitive environment, encouraging community members to feel more comfortable accessing screening services, which, in turn, contributed to the observed increase in screening rates. Moreover, preventive measures were assessed through community-level data on adopting healthier lifestyles and behaviors, such as tobacco cessation, dietary improvements, and increased physical activity. These measures were incorporated into the initiative with the support of CHWs, who played a pivotal role in promoting behavioral changes and providing continuous guidance to community members. As a result of this comprehensive initiative, notable reductions in cancer outcome disparities were observed within underserved communities. The combined effect of increased awareness, improved screening rates, and the adoption of preventive measures contributed to narrowing the gap in cancer outcomes between underserved communities and other populations [ 24 ].
Case Study: Culturally Tailored Cancer Education Programs
This case study examines a community engagement initiative that developed culturally tailored cancer education programs for specific ethnic or cultural communities. Recognizing the importance of cultural beliefs, values, and language preferences in effective communication, this initiative aimed to adapt educational materials and messages to align with the specific cultural context of the target communities [ 25 ].
The study highlighted a concerning lack of general awareness about cancer among the Indian population, particularly concerning its curability, preventability, and available screening methods. Our research indicated that education and place of residence (rural or urban) play pivotal roles in shaping cancer awareness. Notably, awareness of risk factors was predominantly limited to tobacco and alcohol consumption. On a positive note, we observed a favorable attitude toward screening modalities among the Indian population. However, despite this positive attitude, actual screening practices were found to be poor. The study identified the potential benefit of creating community-level awareness to enhance screening practices. The initiative focused on close collaboration with community members, cultural leaders, and healthcare providers to address this. Educational materials were thoughtfully designed to be culturally sensitive and linguistically accessible, incorporating familiar symbols, traditions, and real-life examples that resonated with the community's beliefs and experiences [ 26 ]. This culturally tailored approach aimed to bridge the knowledge gap and promote positive health-seeking behavior in cancer screening. By adopting such community-specific strategies and interventions, there is an opportunity to improve screening practices and subsequently reduce the burden of cancer in the Indian population. Understanding the cultural context and actively engaging with the community can prove instrumental in fostering greater awareness and encouraging timely screenings, leading to more effective cancer prevention and early detection efforts.
The positive outcomes of this initiative were notable. The culturally tailored cancer education programs increased awareness of cancer prevention, screening, and early detection within the target communities. Community members felt more empowered to take proactive steps toward cancer prevention and engage in regular screenings. This initiative also fostered a sense of community empowerment as individuals felt that their cultural values and perspectives were valued and included in the educational materials [ 27 ].
By highlighting these case studies, it becomes evident that community engagement initiatives, such as employing CHWs and developing culturally tailored programs, have effectively addressed cancer disparities. These examples underscore the importance of adapting interventions to specific community contexts, leveraging cultural strengths, and actively involving community members in the design and implementation of initiatives [ 28 ].
Evaluation of outcomes and impact of community engagement
Measurement of Intervention Outcomes
Evaluating community engagement initiatives involves employing various evaluation methodologies to assess the outcomes and impact of these interventions. Quantitative and qualitative measures are utilized to comprehensively understand community engagement's effects on addressing cancer disparities [ 29 ].
Quantitative measures may include assessing changes in cancer knowledge, behavior, screening rates, and access to care. For example, surveys or questionnaires can measure changes in cancer knowledge and screening behaviors before and after community engagement interventions. Data on screening rates and access to care can be collected from healthcare facilities or registries to evaluate the impact of community engagement on these outcomes [ 30 ].
Qualitative measures capture the experiences, perspectives, and stories of community members and stakeholders involved in community engagement initiatives. Interviews, focus groups, or qualitative surveys can be conducted to explore the qualitative impact of community engagement on individual and community-level outcomes. These measures provide insights into participants' lived experiences and allow for a deeper understanding of the effects of community engagement [ 31 ]. It is essential to incorporate community-defined indicators and outcome measures in the evaluation process. Community members should be actively involved in identifying meaningful indicators that reflect their priorities and values. This ensures that the evaluation captures the most relevant and important outcomes to the community, providing a comprehensive assessment of the impact of community engagement initiatives.
Impact on Disparities Reduction
Community engagement initiatives have demonstrated their potential to reduce cancer disparities significantly. These initiatives are instrumental in addressing the underlying factors contributing to disparities and are pivotal in promoting equitable access to cancer prevention, screening, and treatment services [ 32 ]. Participants in such initiatives have strongly preferred a community outreach approach to cancer screening, particularly favoring mobile community-based screening and community information sessions. Adopting an ethno-specific lens when tailoring these initiatives to the targeted communities is important. The feedback from participants highlighted the efficacy of models of primary care that extend support to the entire local community and offer some of their services directly within that community. Such an approach can potentially make a meaningful impact on cancer screening, especially for socially marginalized groups. By embedding screening services within the community, individuals facing barriers to healthcare access can benefit from more convenient and approachable avenues for early cancer detection. Mobile community-based screening units have emerged as a practical and efficient means of reaching underserved populations. These units can overcome geographical barriers, bringing cancer screening services directly to remote or isolated communities. Moreover, community information sessions have proven powerful tools for increasing awareness and knowledge about cancer prevention and screening. By actively engaging community members in these sessions, the initiatives can dispel misconceptions, enhance health literacy, and foster a sense of empowerment among participants [ 32 ].
One of the significant impacts of community engagement is the improvement in screening rates among marginalized populations. Community engagement interventions focusing on education, outreach, and navigation services have successfully increased awareness and utilization of cancer screenings. By tailoring interventions to the community's specific needs and cultural contexts, community engagement can effectively address barriers and increase screening rates among underserved populations [ 33 ].
Additionally, community engagement initiatives have played a crucial role in increasing access to care. By actively involving community members in decision-making processes and partnering with local healthcare providers, these initiatives have facilitated developing and implementing programs that address healthcare access barriers. By addressing these barriers, community engagement interventions have improved access to timely and appropriate cancer care, reducing disparities in treatment and healthcare outcomes [ 34 ].
Identification of key lessons learned from these initiatives
Building Trust and Partnerships
Establishing trusting relationships and partnerships with community members, organizations, and stakeholders is crucial to community engagement initiatives. Lessons learned emphasize the importance of fostering mutual respect, transparency, and effective communication to ensure meaningful engagement. Building trust involves actively listening to community concerns, addressing power dynamics, and demonstrating a commitment to collaboration. By prioritizing relationship-building and trust, community engagement initiatives can lay a strong foundation for successful interventions [ 35 ].
Culturally Appropriate Approaches
Tailoring interventions to the community's cultural, linguistic, and social contexts is essential to community engagement. Lessons learned highlight the significance of adapting educational materials, messages, and interventions to align with community values, practices, and beliefs. This involves understanding the community's cultural nuances, language preferences, and traditional practices. By incorporating cultural competency, interventions become more relatable, acceptable, and effective in addressing cancer disparities [ 36 ].
Capacity Building and Empowerment
A key lesson learned in community engagement initiatives is empowering community members through education, training, and leadership development. Supporting community-driven initiatives, mobilizing resources, and fostering sustainability beyond the duration of specific projects are important aspects. By providing opportunities for community members to build their skills, knowledge, and leadership capacity, they become active participants in decision-making processes and drivers of change within their communities. Empowerment fosters ownership, sustainability, and long-term impact in addressing cancer disparities [ 37 ].
Advocacy and Policy Change
Lessons learned highlight the value of leveraging community engagement to advocate for policy changes that address systemic barriers contributing to cancer disparities. Community engagement allows community members to share their experiences and perspectives, influencing policy decisions. Examples of successful advocacy efforts resulting in policy changes that have positively impacted cancer outcomes in marginalized communities serve as inspiration. By engaging in advocacy and policy change, community engagement initiatives can create systemic changes that address the root causes of cancer disparities [ 38 ].
Best practices for effective community engagement
Developing Strong Partnerships With Community Organizations
Developing strong partnerships with community organizations is a cornerstone of effective community engagement. This involves fostering collaborative partnerships with community-based organizations, community leaders, and stakeholders. It is essential to involve them in decision-making to ensure their active participation in identifying needs, setting goals, and implementing interventions [ 39 ].
Collaboration and co-creation are key principles in building partnerships. By working collaboratively with community organizations, researchers, healthcare providers, and policymakers can tap into these organizations' knowledge, expertise, and resources. This collaborative approach allows for a comprehensive understanding of the community's unique challenges and strengths, leading to the development of targeted interventions that address their specific needs [ 40 ].
Shared leadership is another vital element in developing strong partnerships. Recognizing and valuing community partners' expertise, knowledge, and experiences is important. Actively involving them in all aspects of the engagement process, from planning to implementation and evaluation, ensures that decision-making is inclusive and representative. By embracing shared leadership, power dynamics within partnerships become more equitable, allowing for a more balanced distribution of responsibilities and decision-making authority [ 41 ].
Cultivating long-term relationships with community organizations is crucial for building trust and continuity. It requires a commitment to sustained collaboration beyond the duration of specific projects or research studies. Long-term engagement allows for deeper connections, allowing time to establish rapport, understand community dynamics, and develop mutual trust. Building long-lasting relationships with community organizations creates a foundation for ongoing collaboration, enabling a more meaningful and sustained impact on addressing cancer disparities [ 42 ].
Cultural Competence and Sensitivity in Community Engagement
To effectively engage with communities, it is crucial to invest in developing cultural competence among researchers, healthcare providers, and professionals involved in community engagement. This involves understanding the community's cultural values, practices, and beliefs to ensure that interventions are respectful, relevant, and appropriate. Cultural understanding helps to avoid assumptions and stereotypes, allowing for a more meaningful and impactful engagement process [ 43 ].
In addition to cultural understanding, linguistic accessibility is vital for effective community engagement. It is essential to provide materials, resources, and communication in languages spoken by the community. Language barriers can hinder effective communication and understanding. Professional interpreters or bilingual staff can bridge these language barriers, ensuring community members accurately convey and understand information. Linguistic accessibility fosters inclusivity and promotes equal participation in community engagement [ 44 ].
Furthermore, tailoring interventions to align with the cultural context and preferences of the community is essential. By adapting interventions to the community's cultural context, interventions become more relatable and acceptable. This can involve incorporating culturally specific approaches and practices that resonate with community members. Tailoring interventions acknowledges and respects the diverse cultural backgrounds of the community, increasing the likelihood of community acceptance and engagement [ 45 ]. By investing in cultural understanding, linguistic accessibility, and tailoring interventions, community engagement efforts can effectively address cancer disparities. These practices foster a sense of respect, relevance, and cultural sensitivity, enhancing the overall effectiveness of interventions. They ensure community members feel heard, valued, and included in decision-making, leading to more meaningful and sustainable community engagement initiatives.
Strategies for Effective Communication and Collaboration
Clear and transparent communication is essential for effective community engagement. Using plain language and clear communication techniques helps ensure the community easily understands information. It is important to convey project goals, methodologies, and expected outcomes in a manner that is accessible to all community members. Transparency should be maintained throughout the engagement process, fostering trust and ensuring community members are well-informed about the initiatives' purpose, progress, and potential impact [ 46 ].
Active listening is a key component of successful community engagement. It involves genuinely understanding the community's needs, concerns, and aspirations. Community members' voices are valued and respected by creating spaces for community members to share their experiences, perspectives, and suggestions. Active listening enables a deeper understanding of the community's unique challenges, strengths, and preferences, which can inform the development of interventions that are more responsive and relevant [ 47 ].
Flexibility and adaptability are crucial when engaging with communities. Being open to adapting strategies and interventions based on community feedback and evolving needs is essential for success. Communities are dynamic, and their needs may change over time. By remaining flexible, engagement efforts can be adjusted to address emerging issues, incorporate community feedback, and ensure that interventions are tailored to specific contexts. This approach increases the effectiveness and acceptance of interventions by demonstrating a commitment to responding to unique circumstances and evolving community needs [ 48 ].
Building Trust and Meaningful Relationships With Community Members
Respect and empathy are essential when approaching community engagement initiatives. It is crucial to approach communities with genuine respect for their knowledge, experiences, and cultural diversity. Recognizing the community's strengths, resilience, and expertise fosters a collaborative and empowering environment. By valuing and amplifying the voices of community members, their contributions become integral to decision-making processes and the development of interventions [ 49 ].
Transparent and ethical practices are paramount in community engagement. Researchers and practitioners must maintain ethical standards throughout the research and engagement processes. This includes ensuring transparency in data collection, use, and dissemination. Obtaining informed consent from community members participating in research is essential to protecting their rights and privacy. Respecting ethical guidelines builds trust, credibility, and mutual understanding between researchers, practitioners, and the community [ 50 ].
Consistency and reliability are key factors in building trust and maintaining meaningful engagement. Demonstrating consistency in engagement efforts, including regular communication and updates, helps foster a sense of reliability and accountability. Upholding commitments and honoring agreements made with the community is essential to building trust and sustaining the partnership. By providing ongoing updates, community members feel valued, informed, and engaged, reinforcing trust and commitment between all parties involved [ 51 ].
Empowering Communities through Education and Resources
Empowering communities through education and resources is crucial to community engagement in addressing cancer disparities. This involves providing educational resources and training opportunities to enhance health literacy, empower community members to make informed decisions and build their capacity for active participation [ 52 ].
Education and skill building are vital to empowering community members to take control of their health. By providing educational resources tailored to the community's specific needs and cultural context, individuals can learn about cancer prevention, early detection, treatment options, and survivorship. This empowers them to make informed decisions and take proactive steps toward better health outcomes [ 5 ]. In addition to education, ensuring access to resources is essential for reducing cancer disparities. Identifying and addressing barriers to accessing resources and services is crucial. This includes advocating for equitable access to quality healthcare, cancer screenings, treatment options, and supportive care services. By addressing structural and systemic barriers, such as financial constraints, transportation issues, and language barriers, communities can overcome obstacles to receiving the necessary care.
Sustainable empowerment is another key aspect of community engagement. It involves facilitating community-led initiatives and supporting the development of community-driven solutions. Selflessness and sustainability can be fostered by empowering community leaders and organizations. This may involve providing resources, mentorship, and guidance to support the development and implementation of community-led interventions. By empowering communities to take ownership of their health, long-term impacts can be achieved beyond the duration of specific projects or interventions. Through education, access to resources, and sustainable empowerment, community engagement initiatives can empower communities to actively participate in addressing cancer disparities. By equipping individuals with knowledge, resources, and the skills needed to advocate for their health, long-lasting changes can be achieved, ultimately leading to improved cancer outcomes and reduced disparities.
Challenges and limitations of community engagement
Barriers to Community Engagement in Addressing Cancer Disparities
Limited resources: Insufficient funding, staffing, and infrastructure pose significant barriers to community engagement initiatives. A lack of resources can impede the capacity to sustain long-term partnerships and adequately support community-driven initiatives. Adequate funding and resources are essential to foster meaningful collaboration and ensure the sustainability of community engagement efforts [ 46 ].
Mistrust and historical trauma: Historical experiences of mistreatment, discrimination, and research abuses have contributed to a deep-rooted mistrust of researchers and healthcare systems among certain communities. Building trust and overcoming this historical trauma are crucial for successful community engagement. It requires transparency, cultural sensitivity, and a commitment to addressing past injustices [ 53 ].
Time and commitment: Effective community engagement requires significant time, effort, and sustained commitment. Engaging communities in decision-making processes, maintaining open lines of communication, and involving them throughout the entire engagement process can be challenging for researchers and healthcare professionals, who may face competing priorities and time constraints. However, prioritizing and allocating sufficient time and resources to community engagement efforts is critical for their success [ 54 ].
Language and cultural barriers: Language and cultural differences can challenge effective communication and understanding between researchers, healthcare providers, and community members. It is crucial to overcome these barriers through interpreters, culturally adapted materials, and culturally competent approaches. By addressing language and cultural differences, meaningful engagement can occur, ensuring community members' voices are heard and understood [ 55 ].
Diverse community needs: Communities affected by cancer disparities have unique needs, preferences, and priorities. Developing interventions that effectively address a community's diverse needs can be challenging. It requires a deep understanding of the community's cultural, social, and economic contexts and implementing tailored approaches responsive to these diverse needs. Engaging community members in designing and implementing interventions can help ensure their relevance and effectiveness [ 56 ].
Overcoming Challenges and Limitations
Community-driven approaches: Emphasizing community leadership and involvement in decision-making is crucial for effective community engagement. Engaging communities as equal partners allows them to have a voice and actively shape the direction and implementation of interventions. Community members are experts in their own experiences and have valuable insights into the challenges and solutions that are most relevant to their communities. Empowering communities to take ownership of interventions fosters a sense of ownership and commitment, leading to increased acceptance, sustainability, and, ultimately, better outcomes [ 57 ].
Culturally tailored strategies: Recognizing and respecting the cultural context, language preferences, and community-specific needs is essential to community engagement. Interventions should be tailored to align with the cultural nuances and values of the community. Employing cultural brokers or community health workers who deeply understand the community's cultural norms and customs can ensure that interventions are culturally sensitive and appropriate. By incorporating culturally tailored strategies, interventions become more accessible, relatable, and effective, leading to increased engagement and better outcomes [ 58 ].
Building trust and relationships: Building trust is foundational to successful community engagement. Transparency, honest communication, and consistent engagement are keys to establishing and maintaining trust with community members. Investing time and effort in building relationships allows for open dialogue, shared understanding, and mutual respect. Long-term partnerships demonstrate commitment and reliability, reinforcing trust over time. Trust is crucial for community members to feel comfortable sharing their perspectives, concerns, and ideas, leading to more meaningful collaborations and successful interventions [ 58 ].
Capacity building: Investing in the capacity building of community members is essential for sustainable community engagement. By providing training, education, and skill development opportunities, community members gain the knowledge and tools to actively participate in initiatives. Empowering community leaders to take ownership of interventions promotes sustainability beyond the duration of specific projects. Building community capacity ensures communities have the skills, resources, and confidence to continue addressing cancer disparities in the long run [ 5 ].
Flexibility and adaptability: Flexibility and adaptability are vital in community engagement, as needs and circumstances may change over time. Remaining flexible allows for adjustments in strategies and approaches based on community feedback and emerging challenges. Continuously assessing and responding to the community's evolving needs ensures that interventions remain relevant and effective. Being open to feedback, learning from mistakes, and adapting accordingly demonstrate a commitment to meeting the community's evolving needs and improving outcomes [ 59 ].
Addressing Ethical Considerations in Community-Engaged Research
Ethical considerations are of paramount importance in community-engaged research and engagement activities. Several key aspects should be emphasized to ensure ethical practices throughout the process. First, informed consent is essential. Community members participating in research and engagement activities should provide informed consent, understanding the purpose, risks, benefits, and privacy considerations involved. It is crucial to communicate this information in a culturally appropriate and accessible manner, enabling individuals to make informed decisions about their participation [ 60 ].
Confidentiality and privacy protection are vital to trust and respect within community engagement initiatives. Safeguarding the confidentiality of community members' information is crucial, and protocols should be established to handle data securely and ethically. This includes implementing appropriate data storage and management practices to ensure that personally identifiable information is kept confidential and that privacy is respected throughout the research process. Addressing power imbalances is essential for ethical community engagement. Researchers should recognize and actively work to mitigate power differentials between themselves and community members. A collaborative approach that values community expertise, decision-making autonomy, and shared leadership is important. This ensures the community's voice is heard, respected, and incorporated into the research and engagement process [ 61 ].
Community benefits should be a central consideration in community engagement initiatives. Beyond research participation, these initiatives should strive to provide tangible benefits to the community. This may include improving access to care, increasing health literacy, or offering capacity-building opportunities. By focusing on community benefits, ethical engagement practices promote the well-being and empowerment of the community beyond the immediate research objectives [ 5 ]. Lastly, continuous ethical reflection is crucial throughout the research and engagement processes. Engaging in ongoing dialogue with community members allows for regular assessment of ethical implications. Ethical reflection involves critically examining the potential impact of research and engagement activities on the community, continually evaluating the ethical considerations at play, and making necessary adjustments to protect community interests.
Future directions and recommendations
Areas for Further Research and Investigation
Long-term impact evaluation is essential to assess the sustained effects of community engagement interventions on cancer disparities. Conducting evaluations over an extended period allows for a comprehensive understanding of the long-term outcomes of cancer outcomes, healthcare utilization, and health equity. This evaluation can provide valuable insights into the effectiveness and durability of community engagement approaches to reducing disparities. Investigating the intersectionality of multiple social determinants of health and disparities is crucial. Understanding how factors such as race, socioeconomic status, gender, and geographic location intersect to influence cancer outcomes is essential for developing targeted interventions. By exploring these intersections, researchers can identify specific populations' unique challenges and needs and design interventions that address the complex interplay of multiple disparities.
The potential of innovative technologies, such as telehealth, mobile applications, and digital platforms, to enhance community engagement in cancer care, education, and support should be explored. Assessing their effectiveness and acceptability among diverse populations is important to ensure equitable access to technological advancements. Innovative technologies have the potential to enhance communication, education, and support for underserved communities, improving their engagement in cancer prevention, treatment, and survivorship. Fostering participatory and community-led research approaches empowers communities to actively participate in defining research questions, methodologies, and outcomes. Collaborating with community members throughout the research process enhances relevance, inclusivity, and cultural appropriateness. Community-driven research ensures that the priorities and perspectives of the community are incorporated, resulting in more meaningful and impactful research outcomes.
Policy Implications and Advocacy for Community Engagement
First, policy integration is essential. Advocating for integrating community engagement approaches into cancer-related policies, guidelines, and funding mechanisms helps ensure that community participation is prioritized in decision-making processes. By highlighting the importance of community involvement, policies can address cancer disparities more effectively and promote equitable outcomes. Securing funding support for community engagement initiatives is vital for their success and sustainability. Advocacy efforts should focus on increasing funding for these initiatives and ensuring sustained resources to support collaboration, capacity building, and community-led interventions. Promoting funding opportunities that prioritize projects with community engagement components can help establish and strengthen community-driven interventions.
A health equity focus is necessary for policy initiatives. Advocacy efforts should call for policies prioritizing health equity and addressing the root causes of cancer disparities. These policies should promote equal access to quality healthcare, cancer prevention, and screening programs. By addressing systemic barriers and promoting an equitable distribution of resources, policies can help reduce disparities and improve cancer outcomes for marginalized populations. Encouraging the establishment of collaborative networks is another important advocacy effort. These networks should include researchers, healthcare providers, policymakers, and community organizations. They facilitate knowledge exchange, resource sharing, and dissemination of best practices. Collaborative networks promote synergy and collective action, allowing stakeholders to learn from one another, share successful strategies, and work together toward reducing cancer disparities.
Recommendations for Integrating Community Engagement in Cancer Care and Research
First, institutional support is crucial. Institutions should prioritize community engagement by allocating resources and establishing dedicated positions or departments focused on it. This ensures that individuals and teams are responsible for coordinating and implementing community engagement initiatives. Furthermore, providing training and support for researchers and healthcare providers in community engagement principles and practices is essential to equip them with the necessary skills and knowledge. Education and training play a vital role in promoting effective community engagement. Incorporating community engagement principles and practices into educating and training healthcare professionals, researchers, and public health practitioners is important. This includes fostering an understanding of the significance of cultural competence, ethics, and community partnerships. By integrating these concepts into formal education programs, future healthcare professionals and researchers will be better prepared to engage with communities in a culturally sensitive and ethical manner.
Collaborative platforms are essential for facilitating effective community engagement. Developing platforms that enable collaboration, knowledge sharing, and best practice dissemination among researchers, healthcare providers, and community organizations is crucial. These platforms can be networks, forums, or online communities promoting ongoing dialogue, exchanging ideas, and sharing experiences and resources. By fostering collaboration and communication, these platforms enhance the collective understanding and implementation of community engagement initiatives. Continuous evaluation and learning are vital to the success of community engagement efforts. It is important to continuously evaluate community engagement initiatives' impact and outcomes, learning from successes and challenges. This evaluation process allows for the identification of effective strategies and areas for improvement. Findings and lessons learned should be shared widely within the research and healthcare communities to inform future efforts and contribute to the evidence base of effective community engagement approaches.
Conclusions
In conclusion, community engagement is a powerful strategy for addressing cancer disparities. By actively involving communities in all stages of research, intervention development, and evaluation, we can create meaningful and sustainable solutions. This review highlighted key points, including the importance of strong partnerships with community organizations, cultural competence, effective communication, trust-building, and community empowerment through education and resources. Ongoing community engagement efforts are crucial in the fight against cancer disparities. Through collaboration and shared decision-making, we can develop interventions tailored to diverse populations' unique needs and contexts. By fostering trust, we can bridge the gap between healthcare systems and communities, leading to improved acceptance and uptake of interventions. Empowering communities through education and resources ensures long-term sustainability and equips individuals with the tools to make informed decisions about their health. A call to action is needed to prioritize community engagement in cancer care and research. Researchers, healthcare providers, policymakers, and community leaders must recognize the transformative potential of community engagement and actively support its implementation. This includes advocating for policies promoting equitable access to care, funding initiatives prioritizing community engagement, and integrating community perspectives into decision-making processes. By working together, we can address cancer disparities, promote health equity, and create a future where every community has equal opportunities for optimal cancer prevention, treatment, and survivorship.
The authors have declared that no competing interests exist.

Preprints with The Lancet is part of SSRN´s First Look, a place where journals identify content of interest prior to publication. Authors have opted in at submission to The Lancet family of journals to post their preprints on Preprints with The Lancet. The usual SSRN checks and a Lancet-specific check for appropriateness and transparency have been applied. Preprints available here are not Lancet publications or necessarily under review with a Lancet journal. These preprints are early stage research papers that have not been peer-reviewed. The findings should not be used for clinical or public health decision making and should not be presented to a lay audience without highlighting that they are preliminary and have not been peer-reviewed. For more information on this collaboration, see the comments published in The Lancet about the trial period, and our decision to make this a permanent offering, or visit The Lancet´s FAQ page, and for any feedback please contact [email protected] .
Assessing the Efficacy of Faecal Immunochemical Testing for Early-Age Screening: A Propensity-Score-Matched Community Study in Taiwan
39 Pages Posted: 28 Aug 2024
Han-Mo Chiu
National Taiwan University - Department of Internal Medicine
Sam Li-Sheng Chen
Taipei Medical University
Chiu-Wen Su
Wen-feng hsu.
National Taiwan University - Graduate Institute of Epidemiology and Preventive Medicine
Ting-Yu Lin
National Taiwan University
Yi-Chia Lee
National Taiwan University - Department of Internal Medicine; National Taiwan University - Institute of Epidemiology and Preventive Medicine
Ming-Shiang Wu
Hsiu-hsi chen.
National Taiwan University - Graduate Institute of Epidemiology and Preventive Medicine; National Taiwan University - Innovation and Policy Center for Population Health and Sustainable Environment
Background: The rising incidence of young-onset colorectal cancer worldwide has prompted health policymakers to shift from regular screening to early-age screening in order to lower colorectal cancer incidence and mortality rates. However, there is currently no established evidence of its efficacy based on empirical population data. Method: Leveraging a community screening cohort of 263,125 residents aged 40-49 years between 2001 and 2009, a delayed screen design was naturally exploited to first identify the early screening group (the study arm) from 39,315 who began biennial FIT screening before 50 years of age and continued after 50 years of age into the nationwide FIT screening programme. The regular screening group (the control arm) was made up of the remaining residents (223,810) who were invited between ages of 40 and 49 but delayed screening till 50. This natural setting of real-world data between the two group was followed throughout time until the end of 2019 to identify incident colorectal cancer and death in both groups. To emulate a randomized controlled trial design, a propensity score-matched design and analysis to deal with self-selection biases was used to assess whether early screening can reduce colorectal cancer incidence and mortality. The double selection-bias method was developed to validate the consistency of the results from the propensity-score-matched method. Results: Before the propensity-score-matched design, the early screening group had lower incidence and mortality (per 105 person-years): 26·1 (178/682,112) and 3·2 (22/682,777) compared to the regular screening group [42·6 (1,620/3,803,860) and 7·4 (281/3,810,150). Early-screening significantly reduced colorectal cancer incidence and death (aRR=0·79 (95%CI:0·67-0·94) and aRR=0·61 (95%CI:0·38-0·98) using the propensity-score-matched analysis. Similar significant findings were observed when double self-selection biases were adjusted. Conclusion: When FIT screening began between the ages of 40 and 49, rather than at 50, it demonstrated a significant long-term incremental efficacy of 21% and 39% in reducing colorectal cancer incidence and mortality, respectively. Funding: This study was supported by the Health Promotion Administration, Ministry of Health and Welfare (A1011119, A1021227, A1031135, A1041122, A1051013 and A1061224) of the Taiwanese government. Declaration of Interest: Dr. Han-Mo Chiu received lecture fees from Boston Scientific, Olympus Medical, and Fujifilm Medical System. No other potential conflict of interest relevant to this article was reported. Ethical Approval: This study was approved by the Institutional Review Board of Taipei Medical University, under protocol number TMU-JIRBN No.: 202307023.
Keywords: Colorectal Cancer, Faecal Immunochemical Test, Screening, Young
Suggested Citation: Suggested Citation
National Taiwan University - Department of Internal Medicine ( email )
Taipei Taiwan
Taipei Medical University ( email )
250 Wu-Hsing Street Taipei Taiwan
National Taiwan University - Graduate Institute of Epidemiology and Preventive Medicine ( email )
National taiwan university ( email ), national taiwan university - institute of epidemiology and preventive medicine ( email ), hsiu-hsi chen (contact author).
1 Sec. 4, Roosevelt Road Taipei 106, 106 Taiwan
National Taiwan University - Innovation and Policy Center for Population Health and Sustainable Environment
Click here to go to thelancet.com, paper statistics, related ejournals, preprints with the lancet.
Subscribe to this free journal for more curated articles on this topic
Oncology eJournal
Subscribe to this fee journal for more curated articles on this topic
- Health Tech
- Health Insurance
- Medical Devices
- Gene Therapy
- Neuroscience
- H5N1 Bird Flu
- Health Disparities
- Infectious Disease
- Mental Health
- Cardiovascular Disease
- Chronic Disease
- Alzheimer's
- Coercive Care
- The Obesity Revolution
- The War on Recovery
- Adam Feuerstein
- Matthew Herper
- Jennifer Adaeze Okwerekwu
- Ed Silverman
- CRISPR Tracker
- Breakthrough Device Tracker
- Generative AI Tracker
- Obesity Drug Tracker
- 2024 STAT Summit
- All Summits
- STATUS List
- STAT Madness
- STAT Brand Studio
Don't miss out
Subscribe to STAT+ today, for the best life sciences journalism in the industry
First Opinion readers on cancer screening, mpox vaccines, and more
Keep those letters coming.
- Manage alerts for this article
- Email this article
- Share this article

By Torie Bosch
Sept. 7, 2024
Bosch is First Opinion editor.
First Opinion is STAT’s platform for interesting, illuminating, and provocative articles about the life sciences writ large, written by biotech insiders, health care workers, researchers, and others.
To encourage robust, good-faith discussion about issues raised in First Opinion essays, STAT publishes selected Letters to the Editor received in response to them. You can submit a Letter to the Editor here , or find the submission form at the end of any First Opinion essay.
advertisement
“ Doing more cancer screening won’t reduce Black-white health disparities ,” by Adewole Adamson, Vishal Patel, and H. Gilbert Welch
The response.
The op-ed unfairly and dangerously diminishes the value of cancer screening in reducing health disparities. As the writers acknowledge, numerous, complex factors contribute to poorer outcomes for Black patients than for white patients. Long-standing problems — like structural racism, poverty, lack of health insurance, and reduced care access — lead to poorer health and outcomes. Medtech innovators have forcefully advocated for Medicare, and other, policies to facilitate patient access to technologies, both established and emerging — including cancer screening — and are developing devices that are faster, more accurate, and more accessible than before. Cervical cancer screening kits for home use are in development. AI-enabled medtech devices are achieving more accurate diagnoses and helping clinicians find appropriate care pathways.
These devices have tremendous potential to reduce the number of tests needed for accurate diagnoses and to direct patients to the best care. Early detection can directly impact patient outcomes, treatment options, and financial burden. A patient whose cancer is detected early may have a better prognosis and may require less aggressive and/or less lengthy care. Longer care can be especially financially debilitating for under-resourced patients. Equal or higher rates of screening for Black patients relative to white patients is a positive development. It reflects years of dedicated advocacy toward getting patients what they need.
Of course, the work is far from over. For example, women with dense breast tissue need screening beyond mammograms, and access to supplemental screening is inadequate. Addressing health disparities in cancer diagnoses and care requires a comprehensive approach, and screening plays a vital role.
So rather than cast screening as the enemy, we should promote it alongside the necessary steps preceding and following it. Maybe screening gets an under-resourced patient in the door. If there’s a cancer diagnosis, the next step should be ensuring access to appropriate treatment, not devaluing the screening that led to the diagnosis.
The authors would have patients question the value of screening. Will that accomplish better health? Instead of dismissing cancer screening, which has been shown to work, those with a voice in health care debates should continue promoting equal access to all the resources that improve patient health.
— DeChane Dorsey and Deidre Washington, AdvaMed
“ Why you may not need a checkup every year ,” by Daniel Morgan
Dr. Morgan describes a health care philosophy embraced by many physicians. We are cogs in a medicoeconomic system that pays no heed to the interests of the patient. The chaos is united in only one central concept: financial gain. Any practicing physician must acknowledge this reality. Dr. Morgan gives more voice to those in the profession who have grown weary of the inherent conflicts of trying to practice good medicine, while at the same time being inundated with perverse incentives which feeds the bottom line.
— Walter Bortz
“ To stop mpox from becoming the next pandemic, we must address global vaccine inequities ,” by Wilfredo R. Matias
“Have we learned nothing from Covid-19?” That’s the right question, but Dr. Matias reaches the wrong conclusion. The real lesson is not to rely on the World Health Organization to look after the needs of developing nations. In the case of mpox, there isn’t a vaccine shortage. Both Bavarian Nordic (the manufacturer of the adult vaccine) and KM Biologics (manufacturer of the mpox vaccine for children) are ready and willing to ship their products to nations such as the Congo. What’s standing in their way is the unwillingness of the WHO to “precertify” that these products are safe and effective. Now the WHO says countries can begin to negotiate pricing before their process is complete. The WHO is in over its head. It is neither staffed nor financially resourced to undertake a thorough review of vaccine data — unlike either the European Medicines Agency or the Food and Drug Administration.
The WHO should step aside and let the expert judgment of gold standard global regulators expedite delivery to the Congo and other nations in Africa and elsewhere. Vaccine “prequalification” is a joke — a dangerous one — and a lesson we should have learned from the WHO’s debacle during the Covid-19 pandemic.
— Peter Pitts, Center for Medicine in the Public Interest
“ Health care price regulation is undemocratic ,” by Ge Bai
A for-profit health care system is immoral and amoral. It matters not that price regulation is undemocratic, it’s just necessary.
— Bruce Saunders
In general I agree with this opinion. However, in order to have competition, the consumer/prospective consumer needs to have adequate understandable information regarding the likely cost between providers, and there needs to be a bare minimum of providers competing with each other. In many nonurban areas, there is no real competition due to a shortage of providers for many services — and for some specialties there is no real competition even in major metros. These situations exist with or without any price regulation or incentives. And in order to have real competition, providers must be more transparent than they are — for most services there is little true transparency even after the recent transparency requirements were imposed. So if we are going to back off of pricing regulations, we will need a corresponding improvement in true transparency for competition to become a reality.
— Patrick Pine, Robert F. Kennedy Farmworkers Medical Plan
“ A harm-reduction approach to eating out ,” by Sophia Hua
Portion control is a key factor in achieving and maintaining a healthy weight, so the author’s exhortation to restaurants to offer two size options is sound. For those with just a bit of willpower, however, there’s another alternative: the doggie bag. When the plate of food arrives, just divide it all in half and take home the leftovers for tomorrow’s dinner. This limits calorie intake and proves a better bargain when the check arrives.
— Alison Sneider
About the reporting
STAT’s investigation is based on interviews with nearly 100 people around the country, including incarcerated patients and grieving families, prison officials, and legal and medical experts. Reporter Nicholas Florko also filed more than 225 public records requests and combed through thousands of pages of legal filings to tell these stories. His analysis of deaths in custody is based on a special data use agreement between STAT and the Department of Justice.
You can read more about the reporting for this project and the methodology behind our calculations.
The series is the culmination of a reporting fellowship sponsored by the Association of Health Care Journalists and supported by The Commonwealth Fund.
Torie Bosch
Editor, First Opinion
Torie Bosch is the First Opinion editor at STAT.
More on Long Covid

STAT Plus: As Humira biosimilars take over the market, CVS has created a new ploy: the drug ‘rebate credit’

The smartest thinkers in life sciences on what's happening — and what's to come
Your data will be processed in accordance with our Privacy Policy and Terms of Service . You may opt out of receiving STAT communications at any time.

A new era for drug development and research
Recommended

Presidential debate moderators should ask about mental health policy

Gaza polio vaccination drive must include measles shots

Eight former CDC directors: Hollowing out the CDC is a prescription for disaster

The truth behind that viral study on fluoride and IQ

The Snoo can’t help the people who need it most
Subscriber picks, stat plus: unitedhealth pledged a hands-off approach after buying a connecticut medical group. then it upended how doctors practice, stat plus: summit therapeutics vs. merck: prepping for a big lung cancer study reveal, stat plus: alnylam versus bridgebio: the attr-cm debate, stat plus: troubled for-profit chains are stealthily operating dozens of psychiatric hospitals under nonprofits’ names, doctors use problematic race-based algorithms to guide care every day. why are they so hard to change.

IMAGES
COMMENTS
In low-to-average risk populations, the recommended age to begin routine cancer screening is the age at which the risk of cancer begins to rise (e.g., 50 years for colorectal cancer screening) and when the tumor develops slowly. Slow tumor progression allows for the identification of a malignancy (or pre-malignancy) at an early stage which ...
Introduction. The American Cancer Society (ACS) provides an annual report for health care professionals and the public that summarizes the current ACS cancer screening guidelines, including current recommendations and updates, and guidance related to early cancer detection when a direct recommendation for screening cannot be made.
Balancing the Benefits and Risks of Cancer Screening
Cervical and colorectal cancer incidence has declined in the last few decades by about 55% and 45%, respectively. Death rates have declined even more. These have been due primarily to routine screening. Some types of screenings can detect cancer early (e.g., mammography for breast cancer and low-dose CT for lung cancer).
Twenty-one papers had cancer screening uptake as the main focus of the reports. 25- 45 The primary focus of other reports included wider knowledge and attitudes to cancer and prevention, 46- 52 responses to information about screening, 53- 56 experiences of screening test results 57, 58 and risk management options which included screening ...
Acomplementary strategy to preventing the occurrence of cancer (primary prevention) is early detection of cancer through screening (secondary prevention). The fundamental tenet of screening for cancer is that finding the disease before symptoms develop enables detection at a less advanced stage and that instituting treatment at that time leads ultimately to improved health outcomes. Although ...
What is cancer screening? The purpose of cancer screening tests is to detect pre-cancer or early-stage cancer in asymptomatic individuals so that timely diagnosis and early treatment can be offered, where this treatment can lead to better outcomes for some people. The aim of a cancer screening programme is either to reduce mortality and ...
Cancer Screening Overview (PDQ®)-Patient Version
The average statewide percentage of adults aged 50 to 75 years who were not up to date with colorectal cancer screening in 2020 was 69.4% and ranged from 58.4% in California to 79.6% in Maine. Twenty-two states did not meet the Healthy People 2020 objective of 70.5% of population screened for colorectal cancer.
The USPSTF updated their lung cancer screening recommendation in 2014, recommending lung cancer screening in adults aged 55 to 80 years who met the same smoking history and general health requirements listed above. 179 The Centers for Medicare and Medicaid (CMS) covers lung cancer screening for Medicare beneficiaries according to the NLST ...
Cancer - Screening and early detection
Colorectal cancer is one of the most common cancers worldwide. 1 In the United States, 147,000 individuals received a diagnosis of the disease in 2020, and 53,200 died from it. 2 Most patients with colorectal cancer are older than 50 years of age at diagnosis. 2 Men have a higher risk than do women and are on average 5 to 10 years younger than women when they receive the diagnosis. 3,4
INTRODUCTION. In 1980, the American Cancer Society (ACS) withdrew a prior recommendation for regular lung cancer screening (LCS) with chest radiography (CXR) in persons who currently or formerly smoked because a series of randomized controlled trials (RCTs) conducted in the 1970s had not demonstrated convincing evidence that LCS saved lives. 1 Thirty-three years later, after publication of the ...
UK Women's Views of the Concepts of Personalised Breast Cancer Risk Assessment and Risk-Stratified Breast Screening: A Qualitative Interview Study, Cancers, 13, 22, (5813), (2021). https://doi ...
Introduction and background. Cervical cancer remains a significant global health concern, particularly among underserved populations. Despite being largely preventable through early detection and screening, it continues to be a leading cause of cancer-related deaths among women worldwide [].The World Health Organization (WHO) has called for the elimination of cervical cancer as a public health ...
First, it is important to understand that cancer can occur in any age group, and maintaining routine health checkups with your primary care physician is essential. During such visits, use this opportunity to discuss whether cancer screening is appropriate for you. This is particularly important now given the ongoing COVID-19 pandemic, as ...
Cancer Screen Week is a public health initiative founded by Genentech, the American Cancer Society, Stand Up To Cancer and Optum to increase awareness of the benefits of screening for early detection of certain cancers. This nationwide collaborative effort to raise awareness about recommended cancer screening occurs the first full week of ...
This First Opinion essay by Dr. May accurately characterizes the potential pitfalls of a blood-based strategy; namely that it may shift the clinical performance of colorectal cancer screening ...
Colorectal Cancer: Adults at average risk should begin regular colorectal screening at age 45, but those at high risk for colorectal cancer based on family and/or personal history or other factors may need to start screening before age 45, be screened more often, or get specific tests. Several different tests can be used to screen for ...
The results of the meta-analysis show that the screening rates for all types of cancer were positively influenced by patient navigation. While studies analyzing cervical cancer were limited in number, the consistency of the results for the available sources and the outcomes for other types of cancer demonstrate the overall effectiveness of this approach (Vu, 2021).
You can submit a Letter to the Editor here, or find the submission form at the end of any First Opinion essay. " Doing more cancer screening won't reduce Black-white health disparities," by ...
Persuasive Essay On Cancer Screening. A cancer screening is a test or exam that checks for cancer. Your health care provider will recommend specific cancer screenings based on your age, personal history, and family history of cancer. Work with your health care provider to create a cancer screening schedule that protects your health.
Addressing Cancer Disparities Through Community ...
The regular screening group (the control arm) was made up of the remaining residents (223,810) who were invited between ages of 40 and 49 but delayed screening till 50. This natural setting of real-world data between the two group was followed throughout time until the end of 2019 to identify incident colorectal cancer and death in both groups.
380 Words. 2 Pages. Open Document. Cancer Screening Getting cancer is a really serious condition as a lot of people die from it. It is the uncontrolled division of cells. Cancer screening is used to check the body for cancer. Sometimes it could reduce the chances of dying.
Readers respond to recent First Opinion essays about mpox vaccination, cancer screening disparities, checkups, and more. ... Instead of dismissing cancer screening, which has been shown to work ...