- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board

Preparation and Procedures Involved in Gender Affirmation Surgeries
If you or a loved one are considering gender affirmation surgery , you are probably wondering what steps you must go through before the surgery can be done. Let's look at what is required to be a candidate for these surgeries, the potential positive effects and side effects of hormonal therapy, and the types of surgeries that are available.
Gender affirmation surgery, also known as gender confirmation surgery, is performed to align or transition individuals with gender dysphoria to their true gender.
A transgender woman, man, or non-binary person may choose to undergo gender affirmation surgery.
The term "transexual" was previously used by the medical community to describe people who undergo gender affirmation surgery. The term is no longer accepted by many members of the trans community as it is often weaponized as a slur. While some trans people do identify as "transexual", it is best to use the term "transgender" to describe members of this community.
Transitioning
Transitioning may involve:
- Social transitioning : going by different pronouns, changing one’s style, adopting a new name, etc., to affirm one’s gender
- Medical transitioning : taking hormones and/or surgically removing or modifying genitals and reproductive organs
Transgender individuals do not need to undergo medical intervention to have valid identities.
Reasons for Undergoing Surgery
Many transgender people experience a marked incongruence between their gender and their assigned sex at birth. The American Psychiatric Association (APA) has identified this as gender dysphoria.
Gender dysphoria is the distress some trans people feel when their appearance does not reflect their gender. Dysphoria can be the cause of poor mental health or trigger mental illness in transgender people.
For these individuals, social transitioning, hormone therapy, and gender confirmation surgery permit their outside appearance to match their true gender.
Steps Required Before Surgery
In addition to a comprehensive understanding of the procedures, hormones, and other risks involved in gender-affirming surgery, there are other steps that must be accomplished before surgery is performed. These steps are one way the medical community and insurance companies limit access to gender affirmative procedures.
Steps may include:
- Mental health evaluation : A mental health evaluation is required to look for any mental health concerns that could influence an individual’s mental state, and to assess a person’s readiness to undergo the physical and emotional stresses of the transition.
- Clear and consistent documentation of gender dysphoria
- A "real life" test : The individual must take on the role of their gender in everyday activities, both socially and professionally (known as “real-life experience” or “real-life test”).
Firstly, not all transgender experience physical body dysphoria. The “real life” test is also very dangerous to execute, as trans people have to make themselves vulnerable in public to be considered for affirmative procedures. When a trans person does not pass (easily identified as their gender), they can be clocked (found out to be transgender), putting them at risk for violence and discrimination.
Requiring trans people to conduct a “real-life” test despite the ongoing violence out transgender people face is extremely dangerous, especially because some transgender people only want surgery to lower their risk of experiencing transphobic violence.
Hormone Therapy & Transitioning
Hormone therapy involves taking progesterone, estrogen, or testosterone. An individual has to have undergone hormone therapy for a year before having gender affirmation surgery.
The purpose of hormone therapy is to change the physical appearance to reflect gender identity.
Effects of Testosterone
When a trans person begins taking testosterone , changes include both a reduction in assigned female sexual characteristics and an increase in assigned male sexual characteristics.
Bodily changes can include:
- Beard and mustache growth
- Deepening of the voice
- Enlargement of the clitoris
- Increased growth of body hair
- Increased muscle mass and strength
- Increase in the number of red blood cells
- Redistribution of fat from the breasts, hips, and thighs to the abdominal area
- Development of acne, similar to male puberty
- Baldness or localized hair loss, especially at the temples and crown of the head
- Atrophy of the uterus and ovaries, resulting in an inability to have children
Behavioral changes include:
- Aggression
- Increased sex drive
Effects of Estrogen
When a trans person begins taking estrogen , changes include both a reduction in assigned male sexual characteristics and an increase in assigned female characteristics.
Changes to the body can include:
- Breast development
- Loss of erection
- Shrinkage of testicles
- Decreased acne
- Decreased facial and body hair
- Decreased muscle mass and strength
- Softer and smoother skin
- Slowing of balding
- Redistribution of fat from abdomen to the hips, thighs, and buttocks
- Decreased sex drive
- Mood swings
When Are the Hormonal Therapy Effects Noticed?
The feminizing effects of estrogen and the masculinizing effects of testosterone may appear after the first couple of doses, although it may be several years before a person is satisfied with their transition. This is especially true for breast development.
Timeline of Surgical Process
Surgery is delayed until at least one year after the start of hormone therapy and at least two years after a mental health evaluation. Once the surgical procedures begin, the amount of time until completion is variable depending on the number of procedures desired, recovery time, and more.
Transfeminine Surgeries
Transfeminine is an umbrella term inclusive of trans women and non-binary trans people who were assigned male at birth.
Most often, surgeries involved in gender affirmation surgery are broken down into those that occur above the belt (top surgery) and those below the belt (bottom surgery). Not everyone undergoes all of these surgeries, but procedures that may be considered for transfeminine individuals are listed below.
Top surgery includes:
- Breast augmentation
- Facial feminization
- Nose surgery: Rhinoplasty may be done to narrow the nose and refine the tip.
- Eyebrows: A brow lift may be done to feminize the curvature and position of the eyebrows.
- Jaw surgery: The jaw bone may be shaved down.
- Chin reduction: Chin reduction may be performed to soften the chin's angles.
- Cheekbones: Cheekbones may be enhanced, often via collagen injections as well as other plastic surgery techniques.
- Lips: A lip lift may be done.
- Alteration to hairline
- Male pattern hair removal
- Reduction of Adam’s apple
- Voice change surgery
Bottom surgery includes:
- Removal of the penis (penectomy) and scrotum (orchiectomy)
- Creation of a vagina and labia
Transmasculine Surgeries
Transmasculine is an umbrella term inclusive of trans men and non-binary trans people who were assigned female at birth.
Surgery for this group involves top surgery and bottom surgery as well.
Top surgery includes :
- Subcutaneous mastectomy/breast reduction surgery.
- Removal of the uterus and ovaries
- Creation of a penis and scrotum either through metoidioplasty and/or phalloplasty
Complications and Side Effects
Surgery is not without potential risks and complications. Estrogen therapy has been associated with an elevated risk of blood clots ( deep vein thrombosis and pulmonary emboli ) for transfeminine people. There is also the potential of increased risk of breast cancer (even without hormones, breast cancer may develop).
Testosterone use in transmasculine people has been associated with an increase in blood pressure, insulin resistance, and lipid abnormalities, though it's not certain exactly what role these changes play in the development of heart disease.
With surgery, there are surgical risks such as bleeding and infection, as well as side effects of anesthesia . Those who are considering these treatments should have a careful discussion with their doctor about potential risks related to hormone therapy as well as the surgeries.
Cost of Gender Confirmation Surgery
Surgery can be prohibitively expensive for many transgender individuals. Costs including counseling, hormones, electrolysis, and operations can amount to well over $100,000. Transfeminine procedures tend to be more expensive than transmasculine ones. Health insurance sometimes covers a portion of the expenses.
Quality of Life After Surgery
Quality of life appears to improve after gender-affirming surgery for all trans people who medically transition. One 2017 study found that surgical satisfaction ranged from 94% to 100%.
Since there are many steps and sometimes uncomfortable surgeries involved, this number supports the benefits of surgery for those who feel it is their best choice.
A Word From Verywell
Gender affirmation surgery is a lengthy process that begins with counseling and a mental health evaluation to determine if a person can be diagnosed with gender dysphoria.
After this is complete, hormonal treatment is begun with testosterone for transmasculine individuals and estrogen for transfeminine people. Some of the physical and behavioral changes associated with hormonal treatment are listed above.
After hormone therapy has been continued for at least one year, a number of surgical procedures may be considered. These are broken down into "top" procedures and "bottom" procedures.
Surgery is costly, but precise estimates are difficult due to many variables. Finding a surgeon who focuses solely on gender confirmation surgery and has performed many of these procedures is a plus. Speaking to a surgeon's past patients can be a helpful way to gain insight on the physician's practices as well.
For those who follow through with these preparation steps, hormone treatment, and surgeries, studies show quality of life appears to improve. Many people who undergo these procedures express satisfaction with their results.
Bizic MR, Jeftovic M, Pusica S, et al. Gender dysphoria: Bioethical aspects of medical treatment . Biomed Res Int . 2018;2018:9652305. doi:10.1155/2018/9652305
American Psychiatric Association. What is gender dysphoria? . 2016.
The World Professional Association for Transgender Health. Standards of care for the health of transsexual, transgender, and gender-nonconforming people . 2012.
Tomlins L. Prescribing for transgender patients . Aust Prescr . 2019;42(1): 10–13. doi:10.18773/austprescr.2019.003
T'sjoen G, Arcelus J, Gooren L, Klink DT, Tangpricha V. Endocrinology of transgender medicine . Endocr Rev . 2019;40(1):97-117. doi:10.1210/er.2018-00011
Unger CA. Hormone therapy for transgender patients . Transl Androl Urol . 2016;5(6):877-884. doi:10.21037/tau.2016.09.04
Seal LJ. A review of the physical and metabolic effects of cross-sex hormonal therapy in the treatment of gender dysphoria . Ann Clin Biochem . 2016;53(Pt 1):10-20. doi:10.1177/0004563215587763
Schechter LS. Gender confirmation surgery: An update for the primary care provider . Transgend Health . 2016;1(1):32-40. doi:10.1089/trgh.2015.0006
Altman K. Facial feminization surgery: current state of the art . Int J Oral Maxillofac Surg . 2012;41(8):885-94. doi:10.1016/j.ijom.2012.04.024
Therattil PJ, Hazim NY, Cohen WA, Keith JD. Esthetic reduction of the thyroid cartilage: A systematic review of chondrolaryngoplasty . JPRAS Open. 2019;22:27-32. doi:10.1016/j.jpra.2019.07.002
Top H, Balta S. Transsexual mastectomy: Selection of appropriate technique according to breast characteristics . Balkan Med J . 2017;34(2):147-155. doi:10.4274/balkanmedj.2016.0093
Chan W, Drummond A, Kelly M. Deep vein thrombosis in a transgender woman . CMAJ . 2017;189(13):E502-E504. doi:10.1503/cmaj.160408
Streed CG, Harfouch O, Marvel F, Blumenthal RS, Martin SS, Mukherjee M. Cardiovascular disease among transgender adults receiving hormone therapy: A narrative review . Ann Intern Med . 2017;167(4):256-267. doi:10.7326/M17-0577
Hashemi L, Weinreb J, Weimer AK, Weiss RL. Transgender care in the primary care setting: A review of guidelines and literature . Fed Pract . 2018;35(7):30-37.
Van de grift TC, Elaut E, Cerwenka SC, Cohen-kettenis PT, Kreukels BPC. Surgical satisfaction, quality of life, and their association after gender-affirming aurgery: A follow-up atudy . J Sex Marital Ther . 2018;44(2):138-148. doi:10.1080/0092623X.2017.1326190
American Society of Plastic Surgeons. Gender confirmation surgeries .
American Psychological Association. Transgender people, gender identity, and gender expression .
Colebunders B, Brondeel S, D'Arpa S, Hoebeke P, Monstrey S. An update on the surgical treatment for transgender patients . Sex Med Rev . 2017 Jan;5(1):103-109. doi:10.1016/j.sxmr.2016.08.001
- Patient Care & Health Information
- Tests & Procedures
- Feminizing surgery
Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation. Bottom surgery can involve removal of the testicles, or removal of the testicles and penis and the creation of a vagina, labia and clitoris. Facial procedures or body-contouring procedures can be used as well.
Not everybody chooses to have feminizing surgery. These surgeries can be expensive, carry risks and complications, and involve follow-up medical care and procedures. Certain surgeries change fertility and sexual sensations. They also may change how you feel about your body.
Your health care team can talk with you about your options and help you weigh the risks and benefits.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Available Sexual Health Solutions at Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
Many people seek feminizing surgery as a step in the process of treating discomfort or distress because their gender identity differs from their sex assigned at birth. The medical term for this is gender dysphoria.
For some people, having feminizing surgery feels like a natural step. It's important to their sense of self. Others choose not to have surgery. All people relate to their bodies differently and should make individual choices that best suit their needs.
Feminizing surgery may include:
- Removal of the testicles alone. This is called orchiectomy.
- Removal of the penis, called penectomy.
- Removal of the testicles.
- Creation of a vagina, called vaginoplasty.
- Creation of a clitoris, called clitoroplasty.
- Creation of labia, called labioplasty.
- Breast surgery. Surgery to increase breast size is called top surgery or breast augmentation. It can be done through implants, the placement of tissue expanders under breast tissue, or the transplantation of fat from other parts of the body into the breast.
- Plastic surgery on the face. This is called facial feminization surgery. It involves plastic surgery techniques in which the jaw, chin, cheeks, forehead, nose, and areas surrounding the eyes, ears or lips are changed to create a more feminine appearance.
- Tummy tuck, called abdominoplasty.
- Buttock lift, called gluteal augmentation.
- Liposuction, a surgical procedure that uses a suction technique to remove fat from specific areas of the body.
- Voice feminizing therapy and surgery. These are techniques used to raise voice pitch.
- Tracheal shave. This surgery reduces the thyroid cartilage, also called the Adam's apple.
- Scalp hair transplant. This procedure removes hair follicles from the back and side of the head and transplants them to balding areas.
- Hair removal. A laser can be used to remove unwanted hair. Another option is electrolysis, a procedure that involves inserting a tiny needle into each hair follicle. The needle emits a pulse of electric current that damages and eventually destroys the follicle.
Your health care provider might advise against these surgeries if you have:
- Significant medical conditions that haven't been addressed.
- Behavioral health conditions that haven't been addressed.
- Any condition that limits your ability to give your informed consent.
Like any other type of major surgery, many types of feminizing surgery pose a risk of bleeding, infection and a reaction to anesthesia. Other complications might include:
- Delayed wound healing
- Fluid buildup beneath the skin, called seroma
- Bruising, also called hematoma
- Changes in skin sensation such as pain that doesn't go away, tingling, reduced sensation or numbness
- Damaged or dead body tissue — a condition known as tissue necrosis — such as in the vagina or labia
- A blood clot in a deep vein, called deep vein thrombosis, or a blood clot in the lung, called pulmonary embolism
- Development of an irregular connection between two body parts, called a fistula, such as between the bladder or bowel into the vagina
- Urinary problems, such as incontinence
- Pelvic floor problems
- Permanent scarring
- Loss of sexual pleasure or function
- Worsening of a behavioral health problem
Certain types of feminizing surgery may limit or end fertility. If you want to have biological children and you're having surgery that involves your reproductive organs, talk to your health care provider before surgery. You may be able to freeze sperm with a technique called sperm cryopreservation.
How you prepare
Before surgery, you meet with your surgeon. Work with a surgeon who is board certified and experienced in the procedures you want. Your surgeon talks with you about your options and the potential results. The surgeon also may provide information on details such as the type of anesthesia that will be used during surgery and the kind of follow-up care that you may need.
Follow your health care team's directions on preparing for your procedures. This may include guidelines on eating and drinking. You may need to make changes in the medicine you take and stop using nicotine, including vaping, smoking and chewing tobacco.
Because feminizing surgery might cause physical changes that cannot be reversed, you must give informed consent after thoroughly discussing:
- Risks and benefits
- Alternatives to surgery
- Expectations and goals
- Social and legal implications
- Potential complications
- Impact on sexual function and fertility
Evaluation for surgery
Before surgery, a health care provider evaluates your health to address any medical conditions that might prevent you from having surgery or that could affect the procedure. This evaluation may be done by a provider with expertise in transgender medicine. The evaluation might include:
- A review of your personal and family medical history
- A physical exam
- A review of your vaccinations
- Screening tests for some conditions and diseases
- Identification and management, if needed, of tobacco use, drug use, alcohol use disorder, HIV or other sexually transmitted infections
- Discussion about birth control, fertility and sexual function
You also may have a behavioral health evaluation by a health care provider with expertise in transgender health. That evaluation might assess:
- Gender identity
- Gender dysphoria
- Mental health concerns
- Sexual health concerns
- The impact of gender identity at work, at school, at home and in social settings
- The role of social transitioning and hormone therapy before surgery
- Risky behaviors, such as substance use or use of unapproved hormone therapy or supplements
- Support from family, friends and caregivers
- Your goals and expectations of treatment
- Care planning and follow-up after surgery
Other considerations
Health insurance coverage for feminizing surgery varies widely. Before you have surgery, check with your insurance provider to see what will be covered.
Before surgery, you might consider talking to others who have had feminizing surgery. If you don't know someone, ask your health care provider about support groups in your area or online resources you can trust. People who have gone through the process may be able to help you set your expectations and offer a point of comparison for your own goals of the surgery.
What you can expect
Facial feminization surgery.
Facial feminization surgery may involve a range of procedures to change facial features, including:
- Moving the hairline to create a smaller forehead
- Enlarging the lips and cheekbones with implants
- Reshaping the jaw and chin
- Undergoing skin-tightening surgery after bone reduction
These surgeries are typically done on an outpatient basis, requiring no hospital stay. Recovery time for most of them is several weeks. Recovering from jaw procedures takes longer.
Tracheal shave
A tracheal shave minimizes the thyroid cartilage, also called the Adam's apple. During this procedure, a small cut is made under the chin, in the shadow of the neck or in a skin fold to conceal the scar. The surgeon then reduces and reshapes the cartilage. This is typically an outpatient procedure, requiring no hospital stay.
Top surgery
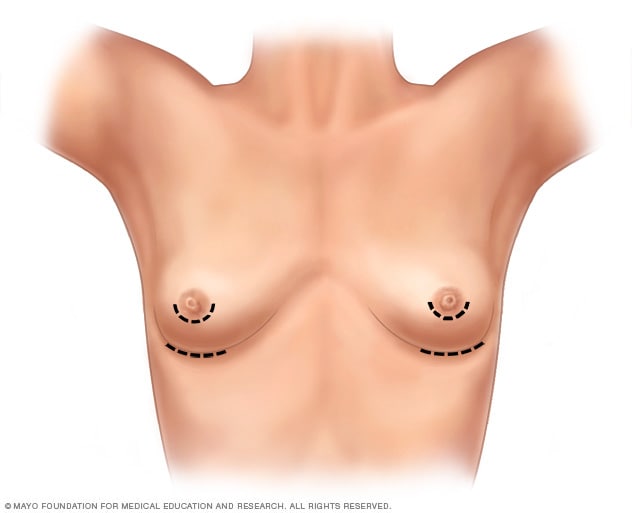
- Breast augmentation incisions
As part of top surgery, the surgeon makes cuts around the areola, near the armpit or in the crease under the breast.
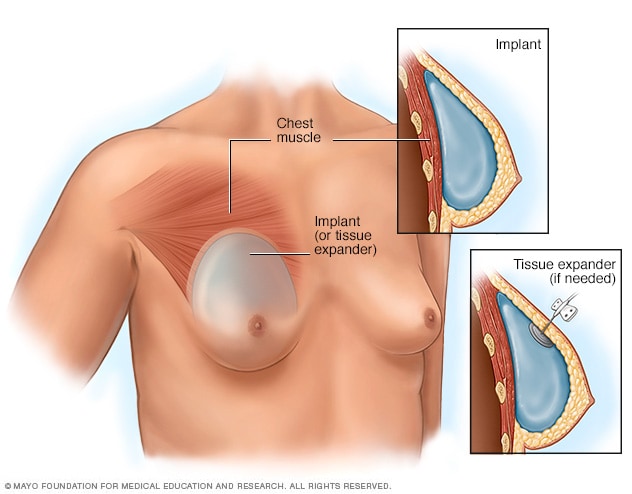
- Placement of breast implants or tissue expanders
During top surgery, the surgeon places the implants under the breast tissue. If feminizing hormones haven't made the breasts large enough, an initial surgery might be needed to have devices called tissue expanders placed in front of the chest muscles.
Hormone therapy with estrogen stimulates breast growth, but many people aren't satisfied with that growth alone. Top surgery is a surgical procedure to increase breast size that may involve implants, fat grafting or both.
During this surgery, a surgeon makes cuts around the areola, near the armpit or in the crease under the breast. Next, silicone or saline implants are placed under the breast tissue. Another option is to transplant fat, muscles or tissue from other parts of the body into the breasts.
If feminizing hormones haven't made the breasts large enough for top surgery, an initial surgery may be needed to place devices called tissue expanders in front of the chest muscles. After that surgery, visits to a health care provider are needed every few weeks to have a small amount of saline injected into the tissue expanders. This slowly stretches the chest skin and other tissues to make room for the implants. When the skin has been stretched enough, another surgery is done to remove the expanders and place the implants.
Genital surgery
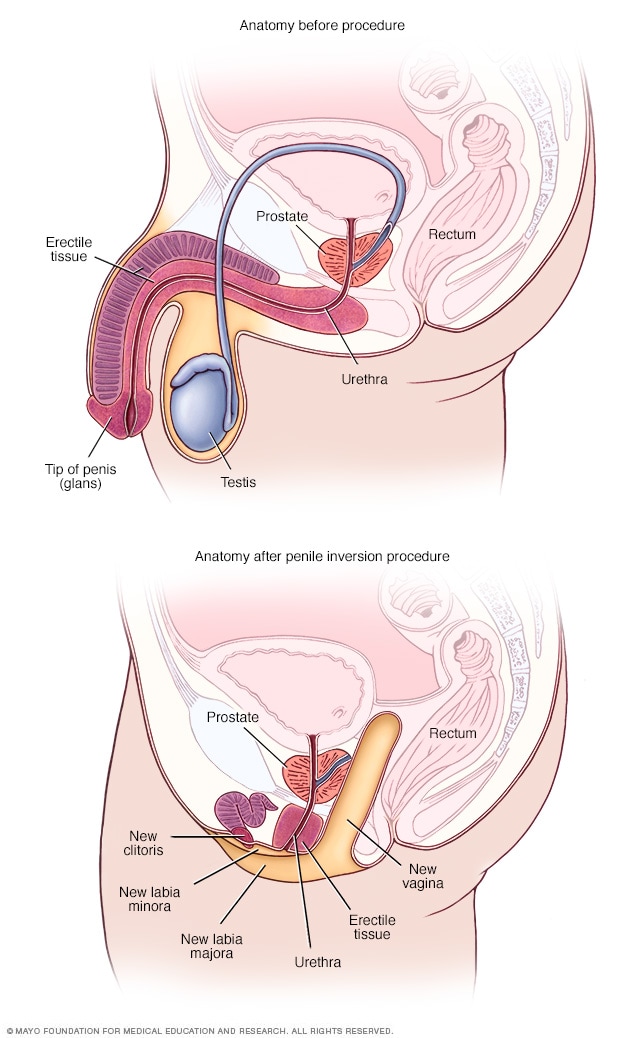
- Anatomy before and after penile inversion
During penile inversion, the surgeon makes a cut in the area between the rectum and the urethra and prostate. This forms a tunnel that becomes the new vagina. The surgeon lines the inside of the tunnel with skin from the scrotum, the penis or both. If there's not enough penile or scrotal skin, the surgeon might take skin from another area of the body and use it for the new vagina as well.
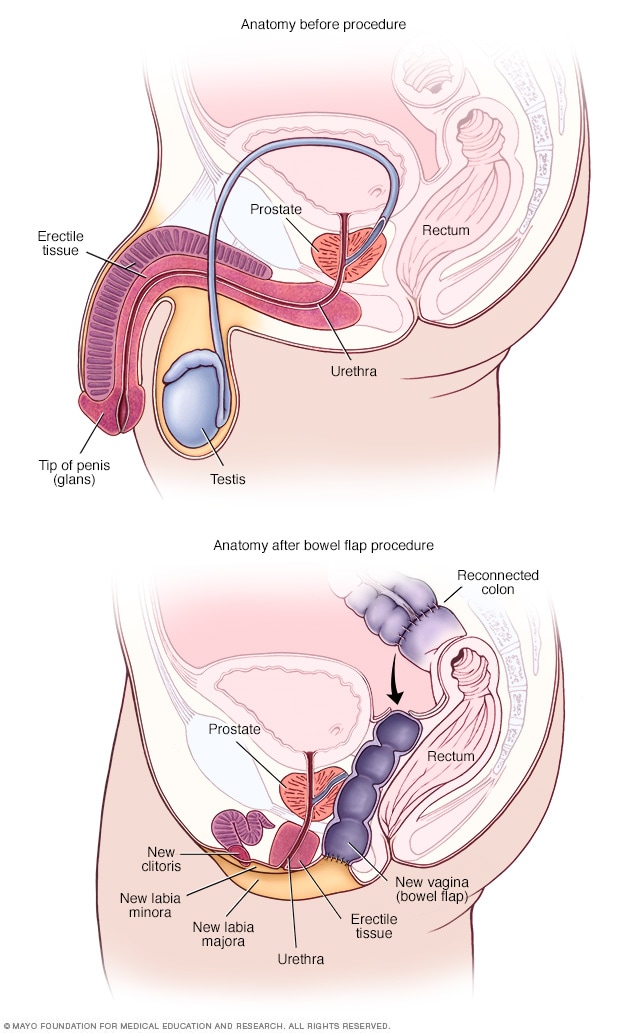
- Anatomy before and after bowel flap procedure
A bowel flap procedure might be done if there's not enough tissue or skin in the penis or scrotum. The surgeon moves a segment of the colon or small bowel to form a new vagina. That segment is called a bowel flap or conduit. The surgeon reconnects the remaining parts of the colon.
Orchiectomy
Orchiectomy is a surgery to remove the testicles. Because testicles produce sperm and the hormone testosterone, an orchiectomy might eliminate the need to use testosterone blockers. It also may lower the amount of estrogen needed to achieve and maintain the appearance you want.
This type of surgery is typically done on an outpatient basis. A local anesthetic may be used, so only the testicular area is numbed. Or the surgery may be done using general anesthesia. This means you are in a sleep-like state during the procedure.
To remove the testicles, a surgeon makes a cut in the scrotum and removes the testicles through the opening. Orchiectomy is typically done as part of the surgery for vaginoplasty. But some people prefer to have it done alone without other genital surgery.
Vaginoplasty
Vaginoplasty is the surgical creation of a vagina. During vaginoplasty, skin from the shaft of the penis and the scrotum is used to create a vaginal canal. This surgical approach is called penile inversion. In some techniques, the skin also is used to create the labia. That procedure is called labiaplasty. To surgically create a clitoris, the tip of the penis and the nerves that supply it are used. This procedure is called a clitoroplasty. In some cases, skin can be taken from another area of the body or tissue from the colon may be used to create the vagina. This approach is called a bowel flap procedure. During vaginoplasty, the testicles are removed if that has not been done previously.
Some surgeons use a technique that requires laser hair removal in the area of the penis and scrotum to provide hair-free tissue for the procedure. That process can take several months. Other techniques don't require hair removal prior to surgery because the hair follicles are destroyed during the procedure.
After vaginoplasty, a tube called a catheter is placed in the urethra to collect urine for several days. You need to be closely watched for about a week after surgery. Recovery can take up to two months. Your health care provider gives you instructions about when you may begin sexual activity with your new vagina.
After surgery, you're given a set of vaginal dilators of increasing sizes. You insert the dilators in your vagina to maintain, lengthen and stretch it. Follow your health care provider's directions on how often to use the dilators. To keep the vagina open, dilation needs to continue long term.
Because the prostate gland isn't removed during surgery, you need to follow age-appropriate recommendations for prostate cancer screening. Following surgery, it is possible to develop urinary symptoms from enlargement of the prostate.
Dilation after gender-affirming surgery
This material is for your education and information only. This content does not replace medical advice, diagnosis and treatment. If you have questions about a medical condition, always talk with your health care provider.
Narrator: Vaginal dilation is important to your recovery and ongoing care. You have to dilate to maintain the size and shape of your vaginal canal and to keep it open.
Jessi: I think for many trans women, including myself, but especially myself, I looked forward to one day having surgery for a long time. So that meant looking up on the internet what the routines would be, what the surgery entailed. So I knew going into it that dilation was going to be a very big part of my routine post-op, but just going forward, permanently.
Narrator: Vaginal dilation is part of your self-care. You will need to do vaginal dilation for the rest of your life.
Alissa (nurse): If you do not do dilation, your vagina may shrink or close. If that happens, these changes might not be able to be reversed.
Narrator: For the first year after surgery, you will dilate many times a day. After the first year, you may only need to dilate once a week. Most people dilate for the rest of their life.
Jessi: The dilation became easier mostly because I healed the scars, the stitches held up a little bit better, and I knew how to do it better. Each transgender woman's vagina is going to be a little bit different based on anatomy, and I grew to learn mine. I understand, you know, what position I needed to put the dilator in, how much force I needed to use, and once I learned how far I needed to put it in and I didn't force it and I didn't worry so much on oh, did I put it in too far, am I not putting it in far enough, and I have all these worries and then I stress out and then my body tenses up. Once I stopped having those thoughts, I relaxed more and it was a lot easier.
Narrator: You will have dilators of different sizes. Your health care provider will determine which sizes are best for you. Dilation will most likely be painful at first. It's important to dilate even if you have pain.
Alissa (nurse): Learning how to relax the muscles and breathe as you dilate will help. If you wish, you can take the pain medication recommended by your health care team before you dilate.
Narrator: Dilation requires time and privacy. Plan ahead so you have a private area at home or at work. Be sure to have your dilators, a mirror, water-based lubricant and towels available. Wash your hands and the dilators with warm soapy water, rinse well and dry on a clean towel. Use a water-based lubricant to moisten the rounded end of the dilators. Water-based lubricants are available over-the-counter. Do not use oil-based lubricants, such as petroleum jelly or baby oil. These can irritate the vagina. Find a comfortable position in bed or elsewhere. Use pillows to support your back and thighs as you lean back to a 45-degree angle. Start your dilation session with the smallest dilator. Hold a mirror in one hand. Use the other hand to find the opening of your vagina. Separate the skin. Relax through your hips, abdomen and pelvic floor. Take slow, deep breaths. Position the rounded end of the dilator with the lubricant at the opening to your vaginal canal. The rounded end should point toward your back. Insert the dilator. Go slowly and gently. Think of its path as a gentle curving swoop. The dilator doesn't go straight in. It follows the natural curve of the vaginal canal. Keep gentle down and inward pressure on the dilator as you insert it. Stop when the dilator's rounded end reaches the end of your vaginal canal. The dilators have dots or markers that measure depth. Hold the dilator in place in your vaginal canal. Use gentle but constant inward pressure for the correct amount of time at the right depth for you. If you're feeling pain, breathe and relax the muscles. When time is up, slowly remove the dilator, then repeat with the other dilators you need to use. Wash the dilators and your hands. If you have increased discharge following dilation, you may want to wear a pad to protect your clothing.
Jessi: I mean, it's such a strange, unfamiliar feeling to dilate and to have a dilator, you know to insert a dilator into your own vagina. Because it's not a pleasurable experience, and it's quite painful at first when you start to dilate. It feels much like a foreign body entering and it doesn't feel familiar and your body kind of wants to get it out of there. It's really tough at the beginning, but if you can get through the first month, couple months, it's going to be a lot easier and it's not going to be so much of an emotional and uncomfortable experience.
Narrator: You need to stay on schedule even when traveling. Bring your dilators with you. If your schedule at work creates challenges, ask your health care team if some of your dilation sessions can be done overnight.
Alissa (nurse): You can't skip days now and do more dilation later. You must do dilation on schedule to keep vaginal depth and width. It is important to dilate even if you have pain. Dilation should cause less pain over time.
Jessi: I hear that from a lot of other women that it's an overwhelming experience. There's lots of emotions that are coming through all at once. But at the end of the day for me, it was a very happy experience. I was glad to have the opportunity because that meant that while I have a vagina now, at the end of the day I had a vagina. Yes, it hurts, and it's not pleasant to dilate, but I have the vagina and it's worth it. It's a long process and it's not going to be easy. But you can do it.
Narrator: If you feel dilation may not be working or you have any questions about dilation, please talk with a member of your health care team.
Research has found that gender-affirming surgery can have a positive impact on well-being and sexual function. It's important to follow your health care provider's advice for long-term care and follow-up after surgery. Continued care after surgery is associated with good outcomes for long-term health.
Before you have surgery, talk to members of your health care team about what to expect after surgery and the ongoing care you may need.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Feminizing surgery care at Mayo Clinic
- Tangpricha V, et al. Transgender women: Evaluation and management. https://www.uptodate.com/ contents/search. Accessed Aug. 16, 2022.
- Erickson-Schroth L, ed. Surgical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Coleman E, et al. Standards of care for the health of transgender and gender diverse people, version 8. International Journal of Transgender Health. 2022; doi:10.1080/26895269.2022.2100644.
- AskMayoExpert. Gender-affirming procedures (adult). Mayo Clinic; 2022.
- Nahabedian, M. Implant-based breast reconstruction and augmentation. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Erickson-Schroth L, ed. Medical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Ferrando C, et al. Gender-affirming surgery: Male to female. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Doctors & Departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
- Search the site GO Please fill out this field.
- Newsletters
- Mental Health
- Social and Public Health
What Is Gender Affirmation Surgery?
:max_bytes(150000):strip_icc():format(webp)/KP-Headshot-IMG_1661-0d48c6ea46f14ab19a91e7b121b49f59.jpg)
A gender affirmation surgery allows individuals, such as those who identify as transgender or nonbinary, to change one or more of their sex characteristics. This type of procedure offers a person the opportunity to have features that align with their gender identity.
For example, this type of surgery may be a transgender surgery like a male-to-female or female-to-male surgery. Read on to learn more about what masculinizing, feminizing, and gender-nullification surgeries may involve, including potential risks and complications.
Why Is Gender Affirmation Surgery Performed?
A person may have gender affirmation surgery for different reasons. They may choose to have the surgery so their physical features and functional ability align more closely with their gender identity.
For example, one study found that 48,019 people underwent gender affirmation surgeries between 2016 and 2020. Most procedures were breast- and chest-related, while the remaining procedures concerned genital reconstruction or facial and cosmetic procedures.
In some cases, surgery may be medically necessary to treat dysphoria. Dysphoria refers to the distress that transgender people may experience when their gender identity doesn't match their sex assigned at birth. One study found that people with gender dysphoria who had gender affirmation surgeries experienced:
- Decreased antidepressant use
- Decreased anxiety, depression, and suicidal ideation
- Decreased alcohol and drug abuse
However, these surgeries are only performed if appropriate for a person's case. The appropriateness comes about as a result of consultations with mental health professionals and healthcare providers.
Transgender vs Nonbinary
Transgender and nonbinary people can get gender affirmation surgeries. However, there are some key ways that these gender identities differ.
Transgender is a term that refers to people who have gender identities that aren't the same as their assigned sex at birth. Identifying as nonbinary means that a person doesn't identify only as a man or a woman. A nonbinary individual may consider themselves to be:
- Both a man and a woman
- Neither a man nor a woman
- An identity between or beyond a man or a woman
Hormone Therapy
Gender-affirming hormone therapy uses sex hormones and hormone blockers to help align the person's physical appearance with their gender identity. For example, some people may take masculinizing hormones.
"They start growing hair, their voice deepens, they get more muscle mass," Heidi Wittenberg, MD , medical director of the Gender Institute at Saint Francis Memorial Hospital in San Francisco and director of MoZaic Care Inc., which specializes in gender-related genital, urinary, and pelvic surgeries, told Health .
Types of hormone therapy include:
- Masculinizing hormone therapy uses testosterone. This helps to suppress the menstrual cycle, grow facial and body hair, increase muscle mass, and promote other male secondary sex characteristics.
- Feminizing hormone therapy includes estrogens and testosterone blockers. These medications promote breast growth, slow the growth of body and facial hair, increase body fat, shrink the testicles, and decrease erectile function.
- Non-binary hormone therapy is typically tailored to the individual and may include female or male sex hormones and/or hormone blockers.
It can include oral or topical medications, injections, a patch you wear on your skin, or a drug implant. The therapy is also typically recommended before gender affirmation surgery unless hormone therapy is medically contraindicated or not desired by the individual.
Masculinizing Surgeries
Masculinizing surgeries can include top surgery, bottom surgery, or both. Common trans male surgeries include:
- Chest masculinization (breast tissue removal and areola and nipple repositioning/reshaping)
- Hysterectomy (uterus removal)
- Metoidioplasty (lengthening the clitoris and possibly extending the urethra)
- Oophorectomy (ovary removal)
- Phalloplasty (surgery to create a penis)
- Scrotoplasty (surgery to create a scrotum)
Top Surgery
Chest masculinization surgery, or top surgery, often involves removing breast tissue and reshaping the areola and nipple. There are two main types of chest masculinization surgeries:
- Double-incision approach : Used to remove moderate to large amounts of breast tissue, this surgery involves two horizontal incisions below the breast to remove breast tissue and accentuate the contours of pectoral muscles. The nipples and areolas are removed and, in many cases, resized, reshaped, and replaced.
- Short scar top surgery : For people with smaller breasts and firm skin, the procedure involves a small incision along the lower half of the areola to remove breast tissue. The nipple and areola may be resized before closing the incision.
Metoidioplasty
Some trans men elect to do metoidioplasty, also called a meta, which involves lengthening the clitoris to create a small penis. Both a penis and a clitoris are made of the same type of tissue and experience similar sensations.
Before metoidioplasty, testosterone therapy may be used to enlarge the clitoris. The procedure can be completed in one surgery, which may also include:
- Constructing a glans (head) to look more like a penis
- Extending the urethra (the tube urine passes through), which allows the person to urinate while standing
- Creating a scrotum (scrotoplasty) from labia majora tissue
Phalloplasty
Other trans men opt for phalloplasty to give them a phallic structure (penis) with sensation. Phalloplasty typically requires several procedures but results in a larger penis than metoidioplasty.
The first and most challenging step is to harvest tissue from another part of the body, often the forearm or back, along with an artery and vein or two, to create the phallus, Nicholas Kim, MD, assistant professor in the division of plastic and reconstructive surgery in the department of surgery at the University of Minnesota Medical School in Minneapolis, told Health .
Those structures are reconnected under an operative microscope using very fine sutures—"thinner than our hair," said Dr. Kim. That surgery alone can take six to eight hours, he added.
In a separate operation, called urethral reconstruction, the surgeons connect the urinary system to the new structure so that urine can pass through it, said Dr. Kim. Urethral reconstruction, however, has a high rate of complications, which include fistulas or strictures.
According to Dr. Kim, some trans men prefer to skip that step, especially if standing to urinate is not a priority. People who want to have penetrative sex will also need prosthesis implant surgery.
Hysterectomy and Oophorectomy
Masculinizing surgery often includes the removal of the uterus (hysterectomy) and ovaries (oophorectomy). People may want a hysterectomy to address their dysphoria, said Dr. Wittenberg, and it may be necessary if their gender-affirming surgery involves removing the vagina.
Many also opt for an oophorectomy to remove the ovaries, almond-shaped organs on either side of the uterus that contain eggs and produce female sex hormones. In this case, oocytes (eggs) can be extracted and stored for a future surrogate pregnancy, if desired. However, this is a highly personal decision, and some trans men choose to keep their uterus to preserve fertility.
Feminizing Surgeries
Surgeries are often used to feminize facial features, enhance breast size and shape, reduce the size of an Adam’s apple , and reconstruct genitals. Feminizing surgeries can include:
- Breast augmentation
- Facial feminization surgery
- Penis removal (penectomy)
- Scrotum removal (scrotectomy)
- Testicle removal (orchiectomy)
- Tracheal shave (chondrolaryngoplasty) to reduce an Adam's apple
- Vaginoplasty
- Voice feminization
Breast Augmentation
Top surgery, also known as breast augmentation or breast mammoplasty, is often used to increase breast size for a more feminine appearance. The procedure can involve placing breast implants, tissue expanders, or fat from other parts of the body under the chest tissue.
Breast augmentation can significantly improve gender dysphoria. Studies show most people who undergo top surgery are happier, more satisfied with their chest, and would undergo the surgery again.
Most surgeons recommend 12 months of feminizing hormone therapy before breast augmentation. Since hormone therapy itself can lead to breast tissue development, transgender women may or may not decide to have surgical breast augmentation.
Facial Feminization and Adam's Apple Removal
Facial feminization surgery (FFS) is a series of plastic surgery procedures that reshape the forehead, hairline, eyebrows, nose, cheeks, and jawline. Nonsurgical treatments like cosmetic fillers, botox, fat grafting, and liposuction may also be used to create a more feminine appearance.
Some trans women opt for chondrolaryngoplasty, also known as a tracheal shave. The procedure reduces the size of the Adam's apple, an area of cartilage around the larynx (voice box) that tends to be larger in people assigned male at birth.
Vulvoplasty and Vaginoplasty
As for bottom surgery, there are various feminizing procedures from which to choose. Vulvoplasty (to create external genitalia without a vagina) or vaginoplasty (to create a vulva and vaginal canal) are two of the most common procedures.
Dr. Wittenberg noted that people might undergo six to 12 months of electrolysis or laser hair removal before surgery to remove pubic hair from the skin that will be used for the vaginal lining.
Surgeons have different techniques for creating a vaginal canal. A common one is a penile inversion, where the masculine structures are emptied and inverted into a created cavity, explained Dr. Kim. Vaginoplasty may be done in one or two stages, said Dr. Wittenberg, and the initial recovery is three months—but it will be a full year until people see results.
Surgical removal of the penis or penectomy is sometimes used in feminization treatment. This can be performed along with an orchiectomy and scrotectomy.
However, a total penectomy is not commonly used in feminizing surgeries . Instead, many people opt for penile-inversion surgery, a technique that hollows out the penis and repurposes the tissue to create a vagina during vaginoplasty.
Orchiectomy and Scrotectomy
An orchiectomy is a surgery to remove the testicles —male reproductive organs that produce sperm. Scrotectomy is surgery to remove the scrotum, that sac just below the penis that holds the testicles.
However, some people opt to retain the scrotum. Scrotum skin can be used in vulvoplasty or vaginoplasty, surgeries to construct a vulva or vagina.
Other Surgical Options
Some gender non-conforming people opt for other types of surgeries. This can include:
- Gender nullification procedures
- Penile preservation vaginoplasty
- Vaginal preservation phalloplasty
Gender Nullification
People who are agender or asexual may opt for gender nullification, sometimes called nullo. This involves the removal of all sex organs. The external genitalia is removed, leaving an opening for urine to pass and creating a smooth transition from the abdomen to the groin.
Depending on the person's sex assigned at birth, nullification surgeries can include:
- Breast tissue removal
- Nipple and areola augmentation or removal
Penile Preservation Vaginoplasty
Some gender non-conforming people assigned male at birth want a vagina but also want to preserve their penis, said Dr. Wittenberg. Often, that involves taking skin from the lining of the abdomen to create a vagina with full depth.
Vaginal Preservation Phalloplasty
Alternatively, a patient assigned female at birth can undergo phalloplasty (surgery to create a penis) and retain the vaginal opening. Known as vaginal preservation phalloplasty, it is often used as a way to resolve gender dysphoria while retaining fertility.
The recovery time for a gender affirmation surgery will depend on the type of surgery performed. For example, healing for facial surgeries may last for weeks, while transmasculine bottom surgery healing may take months.
Your recovery process may also include additional treatments or therapies. Mental health support and pelvic floor physiotherapy are a few options that may be needed or desired during recovery.
Risks and Complications
The risk and complications of gender affirmation surgeries will vary depending on which surgeries you have. Common risks across procedures could include:
- Anesthesia risks
- Hematoma, which is bad bruising
- Poor incision healing
Complications from these procedures may be:
- Acute kidney injury
- Blood transfusion
- Deep vein thrombosis, which is blood clot formation
- Pulmonary embolism, blood vessel blockage for vessels going to the lung
- Rectovaginal fistula, which is a connection between two body parts—in this case, the rectum and vagina
- Surgical site infection
- Urethral stricture or stenosis, which is when the urethra narrows
- Urinary tract infection (UTI)
- Wound disruption
What To Consider
It's important to note that an individual does not need surgery to transition. If the person has surgery, it is usually only one part of the transition process.
There's also psychotherapy . People may find it helpful to work through the negative mental health effects of dysphoria. Typically, people seeking gender affirmation surgery must be evaluated by a qualified mental health professional to obtain a referral.
Some people may find that living in their preferred gender is all that's needed to ease their dysphoria. Doing so for one full year prior is a prerequisite for many surgeries.
All in all, the entire transition process—living as your identified gender, obtaining mental health referrals, getting insurance approvals, taking hormones, going through hair removal, and having various surgeries—can take years, healthcare providers explained.
A Quick Review
Whether you're in the process of transitioning or supporting someone who is, it's important to be informed about gender affirmation surgeries. Gender affirmation procedures often involve multiple surgeries, which can be masculinizing, feminizing, or gender-nullifying in nature.
It is a highly personalized process that looks different for each person and can often take several months or years. The procedures also vary regarding risks and complications, so consultations with healthcare providers and mental health professionals are essential before having these procedures.
American Society of Plastic Surgeons. Gender affirmation surgeries .
Wright JD, Chen L, Suzuki Y, Matsuo K, Hershman DL. National estimates of gender-affirming surgery in the US . JAMA Netw Open . 2023;6(8):e2330348-e2330348. doi:10.1001/jamanetworkopen.2023.30348
Coleman E, Radix AE, Bouman WP, et al. Standards of care for the health of transgender and gender diverse people, version 8 . Int J Transgend Health . 2022;23(S1):S1-S260. doi:10.1080/26895269.2022.2100644
Chou J, Kilmer LH, Campbell CA, DeGeorge BR, Stranix JY. Gender-affirming surgery improves mental health outcomes and decreases anti-depressant use in patients with gender dysphoria . Plast Reconstr Surg Glob Open . 2023;11(6 Suppl):1. doi:10.1097/01.GOX.0000944280.62632.8c
Human Rights Campaign. Get the facts on gender-affirming care .
Human Rights Campaign. Transgender and non-binary people FAQ .
Unger CA. Hormone therapy for transgender patients . Transl Androl Urol . 2016;5(6):877–84. doi:10.21037/tau.2016.09.04
Richards JE, Hawley RS. Chapter 8: Sex Determination: How Genes Determine a Developmental Choice . In: Richards JE, Hawley RS, eds. The Human Genome . 3rd ed. Academic Press; 2011: 273-298.
Randolph JF Jr. Gender-affirming hormone therapy for transgender females . Clin Obstet Gynecol . 2018;61(4):705-721. doi:10.1097/GRF.0000000000000396
Cocchetti C, Ristori J, Romani A, Maggi M, Fisher AD. Hormonal treatment strategies tailored to non-binary transgender individuals . J Clin Med . 2020;9(6):1609. doi:10.3390/jcm9061609
Van Boerum MS, Salibian AA, Bluebond-Langner R, Agarwal C. Chest and facial surgery for the transgender patient . Transl Androl Urol . 2019;8(3):219-227. doi:10.21037/tau.2019.06.18
Djordjevic ML, Stojanovic B, Bizic M. Metoidioplasty: techniques and outcomes . Transl Androl Urol . 2019;8(3):248–53. doi:10.21037/tau.2019.06.12
Bordas N, Stojanovic B, Bizic M, Szanto A, Djordjevic ML. Metoidioplasty: surgical options and outcomes in 813 cases . Front Endocrinol . 2021;12:760284. doi:10.3389/fendo.2021.760284
Al-Tamimi M, Pigot GL, van der Sluis WB, et al. The surgical techniques and outcomes of secondary phalloplasty after metoidioplasty in transgender men: an international, multi-center case series . The Journal of Sexual Medicine . 2019;16(11):1849-1859. doi:10.1016/j.jsxm.2019.07.027
Waterschoot M, Hoebeke P, Verla W, et al. Urethral complications after metoidioplasty for genital gender affirming surgery . J Sex Med . 2021;18(7):1271–9. doi:10.1016/j.jsxm.2020.06.023
Nikolavsky D, Hughes M, Zhao LC. Urologic complications after phalloplasty or metoidioplasty . Clin Plast Surg . 2018;45(3):425–35. doi:10.1016/j.cps.2018.03.013
Nota NM, den Heijer M, Gooren LJ. Evaluation and treatment of gender-dysphoric/gender incongruent adults . In: Feingold KR, Anawalt B, Boyce A, et al., eds. Endotext . MDText.com, Inc.; 2000.
Carbonnel M, Karpel L, Cordier B, Pirtea P, Ayoubi JM. The uterus in transgender men . Fertil Steril . 2021;116(4):931–5. doi:10.1016/j.fertnstert.2021.07.005
Miller TJ, Wilson SC, Massie JP, Morrison SD, Satterwhite T. Breast augmentation in male-to-female transgender patients: Technical considerations and outcomes . JPRAS Open . 2019;21:63-74. doi:10.1016/j.jpra.2019.03.003
Claes KEY, D'Arpa S, Monstrey SJ. Chest surgery for transgender and gender nonconforming individuals . Clin Plast Surg . 2018;45(3):369–80. doi:10.1016/j.cps.2018.03.010
De Boulle K, Furuyama N, Heydenrych I, et al. Considerations for the use of minimally invasive aesthetic procedures for facial remodeling in transgender individuals . Clin Cosmet Investig Dermatol . 2021;14:513-525. doi:10.2147/CCID.S304032
Asokan A, Sudheendran MK. Gender affirming body contouring and physical transformation in transgender individuals . Indian J Plast Surg . 2022;55(2):179-187. doi:10.1055/s-0042-1749099
Sturm A, Chaiet SR. Chondrolaryngoplasty-thyroid cartilage reduction . Facial Plast Surg Clin North Am . 2019;27(2):267–72. doi:10.1016/j.fsc.2019.01.005
Chen ML, Reyblat P, Poh MM, Chi AC. Overview of surgical techniques in gender-affirming genital surgery . Transl Androl Urol . 2019;8(3):191-208. doi:10.21037/tau.2019.06.19
Wangjiraniran B, Selvaggi G, Chokrungvaranont P, Jindarak S, Khobunsongserm S, Tiewtranon P. Male-to-female vaginoplasty: Preecha's surgical technique . J Plast Surg Hand Surg . 2015;49(3):153-9. doi:10.3109/2000656X.2014.967253
Okoye E, Saikali SW. Orchiectomy . In: StatPearls [Internet] . Treasure Island (FL): StatPearls Publishing; 2022.
Salgado CJ, Yu K, Lalama MJ. Vaginal and reproductive organ preservation in trans men undergoing gender-affirming phalloplasty: technical considerations . J Surg Case Rep . 2021;2021(12):rjab553. doi:10.1093/jscr/rjab553
American Society of Plastic Surgeons. What should I expect during my recovery after facial feminization surgery?
American Society of Plastic Surgeons. What should I expect during my recovery after transmasculine bottom surgery?
de Brouwer IJ, Elaut E, Becker-Hebly I, et al. Aftercare needs following gender-affirming surgeries: findings from the ENIGI multicenter European follow-up study . The Journal of Sexual Medicine . 2021;18(11):1921-1932. doi:10.1016/j.jsxm.2021.08.005
American Society of Plastic Surgeons. What are the risks of transfeminine bottom surgery?
American Society of Plastic Surgeons. What are the risks of transmasculine top surgery?
Khusid E, Sturgis MR, Dorafshar AH, et al. Association between mental health conditions and postoperative complications after gender-affirming surgery . JAMA Surg . 2022;157(12):1159-1162. doi:10.1001/jamasurg.2022.3917
Related Articles
Masks Strongly Recommended but Not Required in Maryland, Starting Immediately
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines

Gender Affirmation Surgeries
Featured Expert:

Fan Liang, M.D.
Surgeries are not required for gender affirmation, but many patients choose to undergo one or more surgical procedures. Talk with your doctor to discuss what surgical options may be right for you. The following is an overview of gender affirmation surgeries.
- Penile construction (phalloplasty/metoidioplasty) : This surgical procedure can include removal of the vagina (vaginectomy), reconstruction of the urethra and penile reconstruction. Surgeons may use either vaginal tissue or tissue from another part of the body to construct the penis.
- Vaginal construction (vaginoplasty) : This surgical procedure is a multistage process during which surgeons may remove the penis (penectomy) and the testes (orchiectomy), if still present, and use tissues from the penis to construct the vagina, the clitoris (clitoroplasty) and the labia (labiaplasty).
- Top surgery is surgery that removes or augments breast tissue and reshapes the chest to create a more masculine or feminine appearance for transgender and nonbinary people.
- Facial gender surgery can include a variety of procedures to create more feminine features , like reshaping the nose; brow lift (or forehead lift); chin, cheek and jaw reshaping; Adam’s apple reduction; lip augmentation; hairline restoration; and earlobe reduction.
- Facial gender surgery can also include a series of procedures to create more masculine features , such as forehead lengthening and augmentation; cheek augmentation; reshaping the nose and chin; jaw augmentation ; and thyroid cartilage enhancement to construct an Adam’s apple.
- Hysterectomy : This surgical procedure includes the removal of the uterus and ovaries (oophorectomy). There are options for oocyte storage and fertility preservation that you may want to discuss with your doctor.
- Some people may combine this procedure with a scrotectomy , which is surgery to remove all or part of the scrotum. For others, the skin of the scrotum can be used in vulvoplasty or vaginoplasty ― the surgical construction of a vulva or vagina.
- The procedure reduces testosterone production and may eliminate the need for continuing therapy with estrogen and androgen-suppressing medications. Your health care practitioner will discuss options such as sperm freezing before orchiectomy that can preserve your ability to become a biological parent.
Recovery After Gender Affirmation Surgeries
Recovery time from a gender affirmation surgery or procedure varies, depending on the procedure. Talk to your doctor about what you can expect.

Treatment Caring for Transgender Patients
Fearing discrimination and hostility, transgender people are often reluctant to seek care. Discover how Paula Neira, Program Director of LGBTQ+ Equity and Education, Johns Hopkins Medicine Office of Diversity, Inclusion and Health Equity, is working to ensure that all patients — regardless of gender identity — are treated with dignity and respect.
Find a Treatment Center
- Center for Transgender and Gender Expansive Health
Find Additional Treatment Centers at:
- Howard County Medical Center
- Sibley Memorial Hospital
- Suburban Hospital

Request an Appointment

Gender Affirmation: Do I Need Surgery?

Gender Affirmation Nonsurgical Services

Facial Masculinization Surgery
Related Topics
Jump to content
Updated visitor policies
Other michigan medicine sites.
- About Michigan Medicine
- UofMHealth.org
- Medical School
- Find a Clinical Trial

Michigan Medicine
Federated search page form block, quick links.
- Patient Portal Login
- For Health Providers
- Maps & Directions
Gender Confirmation Surgery
The University of Michigan Health System offers procedures for surgical gender transition. Working together, the surgical team of the Comprehensive Gender Services Program, which includes specialists in plastic surgery, urology and gynecology, bring expertise, experience and safety to procedures for our transgender patients.
Access to gender-related surgical procedures for patients is made through the University of Michigan Health System Comprehensive Gender Services Program .
The Comprehensive Gender Services Program adheres to the WPATH Standards of Care , including the requirement for a second-opinion prior to genital sex reassignment.
Available surgeries:
Male-to-Female: Tracheal Shave Breast Augmentation Facial Feminization Male-to-Female genital sex reassignment
Female-to-Male: Hysterectomy, oophorectomy, vaginectomy Chest Reconstruction Female-to-male genital sex reassignment
Sex Reassignment Surgeries (SRS)
At the University of Michigan Health System, we are dedicated to offering the safest proven surgical options for sex reassignment (SRS.) Because sex reassignment surgery is just one step for transitioning people, the Comprehensive Gender Services Program has access to providers for mental health services, hormone therapy, pelvic floor physiotherapy, and speech therapy. Surgical procedures are done by a team that includes, as appropriate, gynecologists, urologists, pelvic pain specialists and a reconstructive plastic surgeon. A multi-disciplinary team helps to best protect the health of the patient.
For patients receiving mental health and medical services within the University of Michigan Health System, the UMHS-CGSP will coordinate all care including surgical referrals. For patients who have prepared for surgery elsewhere, the UMHS-CGSP will help organize the needed records, meet WPATH standards, and coordinate surgical referrals. Surgical referrals are made through Sara Wiener the Comprehensive Gender Services Program Director.
Male-to-female sex reassignment surgery
At the University of Michigan, participants of the Comprehensive Gender Services Program who are ready for a male-to-female sex reassignment surgery will be offered a penile inversion vaginoplasty with a neurovascular neoclitoris.
During this procedure, a surgeon makes “like become like,” using parts of the original penis to create a sensate neo-vagina. The testicles are removed, a procedure called orchiectomy. The skin from the scrotum is used to make the labia. The erectile tissue of the penis is used to make the neoclitoris. The urethra is preserved and functional.
This procedure provides for aesthetic and functional female genitalia in one 4-5 hour operation. The details of the procedure, the course of recovery, the expected outcomes, and the possible complications will be covered in detail during your surgical consultation. What to Expect: Vaginoplasty at Michigan Medicine .
Female-to-male sex reassignment
At the University of Michigan, participants of the Comprehensive Gender Services Program who are ready for a female-to-male sex reassignment surgery will be offered a phalloplasty, generally using the radial forearm flap method.
This procedure, which can be done at the same time as a hysterectomy/vaginectomy, creates an aesthetically appropriate phallus and creates a urethera for standing urination. Construction of a scrotum with testicular implants is done as a second stage. The details of the procedure, the course of recovery, the expected outcomes, and the possible complications will be covered in detail during your surgical consultation.
Individuals who desire surgical procedures who have not been part of the Comprehensive Gender Services Program should contact the program office at (734) 998-2150 or email [email protected] . W e will assist you in obtaining what you need to qualify for surgery.
The Go-To Guide to Gender Surgeons
Find a qualified surgeon for gender-affirming care.
Start Your Search
Find a Surgeon
Search by U.S. State, Procedure and Insurance Search by Country and Procedure Browse the Global Surgeon Maps
The Go-To Guide To Gender Surgeons

- Introduction
- Conclusions
- Article Information
Error bars represent 95% CIs. GAS indicates gender-affirming surgery.
Percentages are based on the number of procedures divided by number of patients; thus, as some patients underwent multiple procedures the total may be greater than 100%. Error bars represent 95% CIs.
eTable. ICD-10 and CPT Codes of Gender-Affirming Surgery
eFigure. Percentage of Patients With Codes for Gender Identity Disorder Who Underwent GAS
Data Sharing Statement
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Wright JD , Chen L , Suzuki Y , Matsuo K , Hershman DL. National Estimates of Gender-Affirming Surgery in the US. JAMA Netw Open. 2023;6(8):e2330348. doi:10.1001/jamanetworkopen.2023.30348
Manage citations:
© 2024
- Permissions
National Estimates of Gender-Affirming Surgery in the US
- 1 Department of Obstetrics and Gynecology, Columbia University College of Physicians and Surgeons, New York, New York
- 2 Department of Obstetrics and Gynecology, University of Southern California, Los Angeles
Question What are the temporal trends in gender-affirming surgery (GAS) in the US?
Findings In this cohort study of 48 019 patients, GAS increased significantly, nearly tripling from 2016 to 2019. Breast and chest surgery was the most common class of procedures performed overall; genital reconstructive procedures were more common among older individuals.
Meaning These findings suggest that there will be a greater need for clinicians knowledgeable in the care of transgender individuals with the requisite expertise to perform gender-affirming procedures.
Importance While changes in federal and state laws mandating coverage of gender-affirming surgery (GAS) may have led to an increase in the number of annual cases, comprehensive data describing trends in both inpatient and outpatient procedures are limited.
Objective To examine trends in inpatient and outpatient GAS procedures in the US and to explore the temporal trends in the types of GAS performed across age groups.
Design, Setting, and Participants This cohort study includes data from 2016 to 2020 in the Nationwide Ambulatory Surgery Sample and the National Inpatient Sample. Patients with diagnosis codes for gender identity disorder, transsexualism, or a personal history of sex reassignment were identified, and the performance of GAS, including breast and chest procedures, genital reconstructive procedures, and other facial and cosmetic surgical procedures, were identified.
Main Outcome Measures Weighted estimates of the annual number of inpatient and outpatient procedures performed and the distribution of each class of procedure overall and by age were analyzed.
Results A total of 48 019 patients who underwent GAS were identified, including 25 099 (52.3%) who were aged 19 to 30 years. The most common procedures were breast and chest procedures, which occurred in 27 187 patients (56.6%), followed by genital reconstruction (16 872 [35.1%]) and other facial and cosmetic procedures (6669 [13.9%]). The absolute number of GAS procedures rose from 4552 in 2016 to a peak of 13 011 in 2019 and then declined slightly to 12 818 in 2020. Overall, 25 099 patients (52.3%) were aged 19 to 30 years, 10 476 (21.8%) were aged 31 to 40, and 3678 (7.7%) were aged12 to 18 years. When stratified by the type of procedure performed, breast and chest procedures made up a greater percentage of the surgical interventions in younger patients, while genital surgical procedures were greater in older patients.
Conclusions and Relevance Performance of GAS has increased substantially in the US. Breast and chest surgery was the most common group of procedures performed. The number of genital surgical procedures performed increased with increasing age.
Gender dysphoria is characterized as an incongruence between an individual’s experienced or expressed gender and the gender that was assigned at birth. 1 Transgender individuals may pursue multiple treatments, including behavioral therapy, hormonal therapy, and gender-affirming surgery (GAS). 2 GAS encompasses a variety of procedures that align an individual patient’s gender identity with their physical appearance. 2 - 4
While numerous surgical interventions can be considered GAS, the procedures have been broadly classified as breast and chest surgical procedures, facial and cosmetic interventions, and genital reconstructive surgery. 2 , 4 Prior studies 2 - 7 have shown that GAS is associated with improved quality of life, high rates of satisfaction, and a reduction in gender dysphoria. Furthermore, some studies have reported that GAS is associated with decreased depression and anxiety. 8 Lastly, the procedures appear to be associated with acceptable morbidity and reasonable rates of perioperative complications. 2 , 4
Given the benefits of GAS, the performance of GAS in the US has increased over time. 9 The increase in GAS is likely due in part to federal and state laws requiring coverage of transition-related care, although actual insurance coverage of specific procedures is variable. 10 , 11 While prior work has shown that the use of inpatient GAS has increased, national estimates of inpatient and outpatient GAS are lacking. 9 This is important as many GAS procedures occur in ambulatory settings. We performed a population-based analysis to examine trends in GAS in the US and explored the temporal trends in the types of GAS performed across age groups.
To capture both inpatient and outpatient surgical procedures, we used data from the Nationwide Ambulatory Surgery Sample (NASS) and the National Inpatient Sample (NIS). NASS is an ambulatory surgery database and captures major ambulatory surgical procedures at nearly 2800 hospital-owned facilities from up to 35 states, approximating a 63% to 67% stratified sample of hospital-owned facilities. NIS comprehensively captures approximately 20% of inpatient hospital encounters from all community hospitals across 48 states participating in the Healthcare Cost and Utilization Project (HCUP), covering more than 97% of the US population. Both NIS and NASS contain weights that can be used to produce US population estimates. 12 , 13 Informed consent was waived because data sources contain deidentified data, and the study was deemed exempt by the Columbia University institutional review board. This cohort study followed the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline.
We selected patients of all ages with an International Statistical Classification of Diseases and Related Health Problems, Tenth Revision ( ICD-10 ) diagnosis codes for gender identity disorder or transsexualism ( ICD-10 F64) or a personal history of sex reassignment ( ICD-10 Z87.890) from 2016 to 2020 (eTable in Supplement 1 ). We first examined all hospital (NIS) and ambulatory surgical (NASS) encounters for patients with these codes and then analyzed encounters for GAS within this cohort. GAS was identified using ICD-10 procedure codes and Common Procedural Terminology codes and classified as breast and chest procedures, genital reconstructive procedures, and other facial and cosmetic surgical procedures. 2 , 4 Breast and chest surgical procedures encompassed breast reconstruction, mammoplasty and mastopexy, or nipple reconstruction. Genital reconstructive procedures included any surgical intervention of the male or female genital tract. Other facial and cosmetic procedures included cosmetic facial procedures and other cosmetic procedures including hair removal or transplantation, liposuction, and collagen injections (eTable in Supplement 1 ). Patients might have undergone procedures from multiple different surgical groups. We measured the total number of procedures and the distribution of procedures within each procedural group.
Within the data sets, sex was based on patient self-report. The sex of patients in NIS who underwent inpatient surgery was classified as either male, female, missing, or inconsistent. The inconsistent classification denoted patients who underwent a procedure that was not consistent with the sex recorded on their medical record. Similar to prior analyses, patients in NIS with a sex variable not compatible with the procedure performed were classified as having undergone genital reconstructive surgery (GAS not otherwise specified). 9
Clinical variables in the analysis included patient clinical and demographic factors and hospital characteristics. Demographic characteristics included age at the time of surgery (12 to 18 years, 19 to 30 years, 31 to 40 years, 41 to 50 years, 51 to 60 years, 61 to 70 years, and older than 70 years), year of the procedure (2016-2020), and primary insurance coverage (private, Medicare, Medicaid, self-pay, and other). Race and ethnicity were only reported in NIS and were classified as White, Black, Hispanic and other. Race and ethnicity were considered in this study because prior studies have shown an association between race and GAS. The income status captured national quartiles of median household income based of a patient’s zip code and was recorded as less than 25% (low), 26% to 50% (medium-low), 51% to 75% (medium-high), and 76% or more (high). The Elixhauser Comorbidity Index was estimated for each patient based on the codes for common medical comorbidities and weighted for a final score. 14 Patients were classified as 0, 1, 2, or 3 or more. We separately reported coding for HIV and AIDS; substance abuse, including alcohol and drug abuse; and recorded mental health diagnoses, including depression and psychoses. Hospital characteristics included a composite of teaching status and location (rural, urban teaching, and urban nonteaching) and hospital region (Northeast, Midwest, South, and West). Hospital bed sizes were classified as small, medium, and large. The cutoffs were less than 100 (small), 100 to 299 (medium), and 300 or more (large) short-term acute care beds of the facilities from NASS and were varied based on region, urban-rural designation, and teaching status of the hospital from NIS. 8 Patients with missing data were classified as the unknown group and were included in the analysis.
National estimates of the number of GAS procedures among all hospital encounters for patients with gender identity disorder were derived using discharge or encounter weight provided by the databases. 15 The clinical and demographic characteristics of the patients undergoing GAS were reported descriptively. The number of encounters for gender identity disorder, the percentage of GAS procedures among those encounters, and the absolute number of each procedure performed over time were estimated. The difference by age group was examined and tested using Rao-Scott χ 2 test. All hypothesis tests were 2-sided, and P < .05 was considered statistically significant. All analyses were conducted using SAS version 9.4 (SAS Institute Inc).
A total of 48 019 patients who underwent GAS were identified ( Table 1 ). Overall, 25 099 patients (52.3%) were aged 19 to 30 years, 10 476 (21.8%) were aged 31 to 40, and 3678 (7.7%) were aged 12 to 18 years. Private insurance coverage was most common in 29 064 patients (60.5%), while 12 127 (25.3%) were Medicaid recipients. Depression was reported in 7192 patients (15.0%). Most patients (42 467 [88.4%]) were treated at urban, teaching hospitals, and there was a disproportionate number of patients in the West (22 037 [45.9%]) and Northeast (12 396 [25.8%]). Within the cohort, 31 668 patients (65.9%) underwent 1 procedure while 13 415 (27.9%) underwent 2 procedures, and the remainder underwent multiple procedures concurrently ( Table 1 ).
The overall number of health system encounters for gender identity disorder rose from 13 855 in 2016 to 38 470 in 2020. Among encounters with a billing code for gender identity disorder, there was a consistent rise in the percentage that were for GAS from 4552 (32.9%) in 2016 to 13 011 (37.1%) in 2019, followed by a decline to 12 818 (33.3%) in 2020 ( Figure 1 and eFigure in Supplement 1 ). Among patients undergoing ambulatory surgical procedures, 37 394 (80.3%) of the surgical procedures included gender-affirming surgical procedures. For those with hospital admissions with gender identity disorder, 10 625 (11.8%) of admissions were for GAS.
Breast and chest procedures were most common and were performed for 27 187 patients (56.6%). Genital reconstruction was performed for 16 872 patients (35.1%), and other facial and cosmetic procedures for 6669 patients (13.9%) ( Table 2 ). The most common individual procedure was breast reconstruction in 21 244 (44.2%), while the most common genital reconstructive procedure was hysterectomy (4489 [9.3%]), followed by orchiectomy (3425 [7.1%]), and vaginoplasty (3381 [7.0%]). Among patients who underwent other facial and cosmetic procedures, liposuction (2945 [6.1%]) was most common, followed by rhinoplasty (2446 [5.1%]) and facial feminizing surgery and chin augmentation (1874 [3.9%]).
The absolute number of GAS procedures rose from 4552 in 2016 to a peak of 13 011 in 2019 and then declined slightly to 12 818 in 2020 ( Figure 1 ). Similar trends were noted for breast and chest surgical procedures as well as genital surgery, while the rate of other facial and cosmetic procedures increased consistently from 2016 to 2020. The distribution of the individual procedures performed in each class were largely similar across the years of analysis ( Table 3 ).
When stratified by age, patients 19 to 30 years had the greatest number of procedures, 25 099 ( Figure 2 ). There were 10 476 procedures performed in those aged 31 to 40 years and 4359 in those aged 41 to 50 years. Among patients younger than 19 years, 3678 GAS procedures were performed. GAS was less common in those cohorts older than 50 years. Overall, the greatest number of breast and chest surgical procedures, genital surgical procedures, and facial and other cosmetic surgical procedures were performed in patients aged 19 to 30 years.
When stratified by the type of procedure performed, breast and chest procedures made up the greatest percentage of the surgical interventions in younger patients while genital surgical procedures were greater in older patients ( Figure 2 ). Additionally, 3215 patients (87.4%) aged 12 to 18 years underwent GAS and had breast or chest procedures. This decreased to 16 067 patients (64.0%) in those aged 19 to 30 years, 4918 (46.9%) in those aged 31 to 40 years, and 1650 (37.9%) in patients aged 41 to 50 years ( P < .001). In contrast, 405 patients (11.0%) aged 12 to 18 years underwent genital surgery. The percentage of patients who underwent genital surgery rose sequentially to 4423 (42.2%) in those aged 31 to 40 years, 1546 (52.3%) in those aged 51 to 60 years, and 742 (58.4%) in those aged 61 to 70 years ( P < .001). The percentage of patients who underwent facial and other cosmetic surgical procedures rose with age from 9.5% in those aged 12 to 18 years to 20.6% in those aged 51 to 60 years, then gradually declined ( P < .001). Figure 2 displays the absolute number of procedure classes performed by year stratified by age. The greatest magnitude of the decline in 2020 was in younger patients and for breast and chest procedures.
These findings suggest that the number of GAS procedures performed in the US has increased dramatically, nearly tripling from 2016 to 2019. Breast and chest surgery is the most common class of procedure performed while patients are most likely to undergo surgery between the ages of 19 and 30 years. The number of genital surgical procedures performed increased with increasing age.
Consistent with prior studies, we identified a remarkable increase in the number of GAS procedures performed over time. 9 , 16 A prior study examining national estimates of inpatient GAS procedures noted that the absolute number of procedures performed nearly doubled between 2000 to 2005 and from 2006 to 2011. In our analysis, the number of GAS procedures nearly tripled from 2016 to 2020. 9 , 17 Not unexpectedly, a large number of the procedures we captured were performed in the ambulatory setting, highlighting the need to capture both inpatient and outpatient procedures when analyzing data on trends. Like many prior studies, we noted a decrease in the number of procedures performed in 2020, likely reflective of the COVID-19 pandemic. 18 However, the decline in the number of procedures performed between 2019 and 2020 was relatively modest, particularly as these procedures are largely elective.
Analysis of procedure-specific trends by age revealed a number of important findings. First, GAS procedures were most common in patients aged 19 to 30 years. This is in line with prior work that demonstrated that most patients first experience gender dysphoria at a young age, with approximately three-quarters of patients reporting gender dysphoria by age 7 years. These patients subsequently lived for a mean of 23 years for transgender men and 27 years for transgender women before beginning gender transition treatments. 19 Our findings were also notable that GAS procedures were relatively uncommon in patients aged 18 years or younger. In our cohort, fewer than 1200 patients in this age group underwent GAS, even in the highest volume years. GAS in adolescents has been the focus of intense debate and led to legislative initiatives to limit access to these procedures in adolescents in several states. 20 , 21
Second, there was a marked difference in the distribution of procedures in the different age groups. Breast and chest procedures were more common in younger patients, while genital surgery was more frequent in older individuals. In our cohort of individuals aged 19 to 30 years, breast and chest procedures were twice as common as genital procedures. Genital surgery gradually increased with advancing age, and these procedures became the most common in patients older than 40 years. A prior study of patients with commercial insurance who underwent GAS noted that the mean age for mastectomy was 28 years, significantly lower than for hysterectomy at age 31 years, vaginoplasty at age 40 years, and orchiectomy at age 37 years. 16 These trends likely reflect the increased complexity of genital surgery compared with breast and chest surgery as well as the definitive nature of removal of the reproductive organs.
This study has limitations. First, there may be under-capture of both transgender individuals and GAS procedures. In both data sets analyzed, gender is based on self-report. NIS specifically makes notation of procedures that are considered inconsistent with a patient’s reported gender (eg, a male patient who underwent oophorectomy). Similar to prior work, we assumed that patients with a code for gender identity disorder or transsexualism along with a surgical procedure classified as inconsistent underwent GAS. 9 Second, we captured procedures commonly reported as GAS procedures; however, it is possible that some of these procedures were performed for other underlying indications or diseases rather than solely for gender affirmation. Third, our trends showed a significant increase in procedures through 2019, with a decline in 2020. The decline in services in 2020 is likely related to COVID-19 service alterations. Additionally, while we comprehensively captured inpatient and ambulatory surgical procedures in large, nationwide data sets, undoubtedly, a small number of procedures were performed in other settings; thus, our estimates may underrepresent the actual number of procedures performed each year in the US.
These data have important implications in providing an understanding of the use of services that can help inform care for transgender populations. The rapid rise in the performance of GAS suggests that there will be a greater need for clinicians knowledgeable in the care of transgender individuals and with the requisite expertise to perform GAS procedures. However, numerous reports have described the political considerations and challenges in the delivery of transgender care. 22 Despite many medical societies recognizing the necessity of gender-affirming care, several states have enacted legislation or policies that restrict gender-affirming care and services, particularly in adolescence. 20 , 21 These regulations are barriers for patients who seek gender-affirming care and provide legal and ethical challenges for clinicians. As the use of GAS increases, delivering equitable gender-affirming care in this complex landscape will remain a public health challenge.
Accepted for Publication: July 15, 2023.
Published: August 23, 2023. doi:10.1001/jamanetworkopen.2023.30348
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2023 Wright JD et al. JAMA Network Open .
Corresponding Author: Jason D. Wright, MD, Division of Gynecologic Oncology, Department of Obstetrics and Gynecology, Columbia University College of Physicians and Surgeons, 161 Fort Washington Ave, 4th Floor, New York, NY 10032 ( [email protected] ).
Author Contributions: Dr Wright had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Wright, Chen.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Wright.
Critical review of the manuscript for important intellectual content: All authors.
Statistical analysis: Wright, Chen.
Administrative, technical, or material support: Wright, Suzuki.
Conflict of Interest Disclosures: Dr Wright reported receiving grants from Merck and personal fees from UpToDate outside the submitted work. No other disclosures were reported.
Data Sharing Statement: See Supplement 2 .
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- For Journalists
- News Releases
- Latest Releases
- News Release
Age restriction lifted for gender-affirming surgery in new international guidelines
'Will result in the need for parental consent before doctors would likely perform surgeries'
Media Information
- Release Date: September 16, 2022
Media Contacts
Kristin Samuelson
- (847) 491-4888
- Email Kristin
- Expert can speak to transgender peoples’ right to bodily autonomy, how guidelines affect insurance coverage, how the U.S. gender regulations compare to other countries, more
CHICAGO --- The World Professional Association for Transgender Health (WPATH) today today announced its updated Standards of Care and Ethical Guidelines for health professionals. Among the updates is a new suggestion to lift the age restriction for youth seeking gender-affirming surgical treatment, in comparison to previous suggestion of surgery at 17 or older.
Alithia Zamantakis (she/her), a member of the Institute of Sexual & Gender Minority Health at Northwestern University Feinberg School of Medicine, is available to speak to media about the new guidelines. Contact Kristin Samuelson at [email protected] to schedule an interview.
“Lifting the age restriction will greatly increase access to care for transgender adolescents, but will also result in the need for parental consent for surgeries before doctors would likely perform them,” said Zamantakis, a postdoctoral fellow at Northwestern, who has researched trans youth and resilience. “Additionally, changes in age restriction are not likely to change much in practice in states like Alabama, Arkansas, Texas and Arizona, where gender-affirming care for youth is currently banned.”
Zamantakis also can speak about transgender peoples’ right to bodily autonomy, how guidelines affect insurance coverage and how U.S. gender regulations compare to other countries.
Guidelines are thorough but WPATH ‘still has work to do’
“The systematic reviews conducted as part of the development of the standards of care are fantastic syntheses of the literature on gender-affirming care that should inform doctors' work,” Zamantakis said. “They are used by numerous providers and insurance companies to determine who gets access to care and who does not.
“However, WPATH still has work to do to ensure its standards of care are representative of the needs and experiences of all non-cisgender people and that the standards of care are used to ensure that individuals receive adequate care rather than to gatekeep who gets access to care. WPATH largely has been run by white and/or cisgender individuals. It has only had three transgender presidents thus far, with Marci Bower soon to be the second trans woman president.
“Future iterations of the standards of care must include more stakeholders per committee, greater representation of transgender experts and stakeholders of color, and greater representation of experts and stakeholders outside the U.S.”
Transgender individuals’ right to bodily autonomy
“WPATH does not recommend prior hormone replacement therapy or ‘presenting’ as one's gender for a certain period of time for surgery for nonbinary people, yet it still does for transgender women and men,” Zamantakis said. “The reality is that neither should be requirements for accessing care for people of any gender.
“The recommendation of requiring documentation of persistent gender incongruence is meant to prevent regret. However, it's important to ask who ultimately has the authority to determine whether individuals have the right to make decisions about their bodily autonomy that they may or may not regret? Cisgender women undergo breast augmentation regularly, which is not an entirely reversible procedure, yet they are not required to have proof of documented incongruence. It is assumed that if they regret the surgery, they will learn to cope with the regret or will have an additional surgery. Transgender individuals also deserve the right to bodily autonomy and ultimately to regret the decisions they make if they later do not align with how they experience themselves.”
Long-term Outcomes After Gender-Affirming Surgery: 40-Year Follow-up Study
Affiliations.
- 1 From the Department of Plastic and Reconstructive Surgery.
- 2 School of Medicine.
- 3 Department of Obstetrics and Gynecology.
- 4 Department of Urology.
- 5 Department of Psychiatry and Neurobehavioral Sciences, University of Virginia, Charlottesville, VA.
- PMID: 36149983
- DOI: 10.1097/SAP.0000000000003233
Background: Gender dysphoria is a condition that often leads to significant patient morbidity and mortality. Although gender-affirming surgery (GAS) has been offered for more than half a century with clear significant short-term improvement in patient well-being, few studies have evaluated the long-term durability of these outcomes.
Methods: Chart review identified 97 patients who were seen for gender dysphoria at a tertiary care center from 1970 to 1990 with comprehensive preoperative evaluations. These evaluations were used to generate a matched follow-up survey regarding their GAS, appearance, and mental/social health for standardized outcome measures. Of 97 patients, 15 agreed to participate in the phone interview and survey. Preoperative and postoperative body congruency score, mental health status, surgical outcomes, and patient satisfaction were compared.
Results: Both transmasculine and transfeminine groups were more satisfied with their body postoperatively with significantly less dysphoria. Body congruency score for chest, body hair, and voice improved significantly in 40 years' postoperative settings, with average scores ranging from 84.2 to 96.2. Body congruency scores for genitals ranged from 67.5 to 79 with free flap phalloplasty showing highest scores. Long-term overall body congruency score was 89.6. Improved mental health outcomes persisted following surgery with significantly reduced suicidal ideation and reported resolution of any mental health comorbidity secondary to gender dysphoria.
Conclusion: Gender-affirming surgery is a durable treatment that improves overall patient well-being. High patient satisfaction, improved dysphoria, and reduced mental health comorbidities persist decades after GAS without any reported patient regret.
Copyright © 2022 Wolters Kluwer Health, Inc. All rights reserved.
- Follow-Up Studies
- Gender Dysphoria* / surgery
- Sex Reassignment Surgery*
- Transgender Persons* / psychology
- Transsexualism* / psychology
How Gender Reassignment Surgery Works (Infographic)
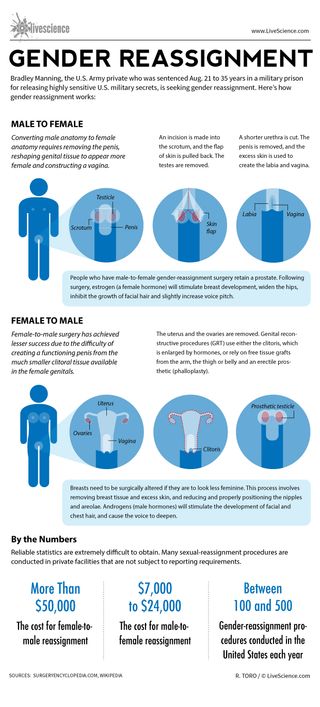
Bradley Manning, the U.S. Army private who was sentenced Aug. 21 to 35 years in a military prison for releasing highly sensitive U.S. military secrets, is seeking gender reassignment. Here’s how gender reassignment works:
Converting male anatomy to female anatomy requires removing the penis, reshaping genital tissue to appear more female and constructing a vagina.
An incision is made into the scrotum, and the flap of skin is pulled back. The testes are removed.
A shorter urethra is cut. The penis is removed, and the excess skin is used to create the labia and vagina.
People who have male-to-female gender-reassignment surgery retain a prostate. Following surgery, estrogen (a female hormone) will stimulate breast development, widen the hips, inhibit the growth of facial hair and slightly increase voice pitch.
Female-to-male surgery has achieved lesser success due to the difficulty of creating a functioning penis from the much smaller clitoral tissue available in the female genitals.
The uterus and the ovaries are removed. Genital reconstructive procedures (GRT) use either the clitoris, which is enlarged by hormones, or rely on free tissue grafts from the arm, the thigh or belly and an erectile prosthetic (phalloplasty).
Breasts need to be surgically altered if they are to look less feminine. This process involves removing breast tissue and excess skin, and reducing and properly positioning the nipples and areolae. Androgens (male hormones) will stimulate the development of facial and chest hair, and cause the voice to deepen.
Reliable statistics are extremely difficult to obtain. Many sexual-reassignment procedures are conducted in private facilities that are not subject to reporting requirements.
The cost for female-to-male reassignment can be more than $50,000. The cost for male-to-female reassignment can be $7,000 to $24,000.
Between 100 to 500 gender-reassignment procedures are conducted in the United States each year.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Man's years of premature ejaculation had a rare cause
Viagra alternatives? Study of mouse erections hints at new ways to treat erectile dysfunction
China launches Chang'e 6 sample-return mission to moon's far side
Most Popular
- 2 Cave of Crystals: The deadly cavern in Mexico dubbed 'the Sistine Chapel of crystals'
- 3 1,700-year-old Roman shipwreck was stuffed to the gills with fish sauce when it sank
- 4 Asteroid that exploded over Berlin was fastest-spinning space rock ever recorded
- 5 'You certainly don't see this every day': Ultra-rare backward-spinning tornado formed over Oklahoma
- 2 Optical illusion reveals key brain rule that governs consciousness
- 3 Cave of Crystals: The deadly cavern in Mexico dubbed 'the Sistine Chapel of crystals'
- 4 1st Americans came over in 4 different waves from Siberia, linguist argues
- 5 Stunning image shows atoms transforming into quantum waves — just as Schrödinger predicted

The Gender Reassignment Controversy
When people opt for surgery, are they satisfied with the outcome.
Posted March 16, 2018 | Reviewed by Ekua Hagan
In an age of increasing gender fluidity, it is surprising that so many find it difficult to accept the gender of their birth and take the drastic step of changing it through surgery. What are their motives? Are they satisfied with the outcome?
Gender may be the most important dimension of human variation, whether that is either desirable, or inevitable. In every society, male and female children are raised differently and acquire different expectations, and aspirations, for their work lives, emotional experiences, and leisure pursuits.
These differences may be shaped by how children are raised but gender reassignment, even early in life, is difficult, and problematic. Reassignment in adulthood is even more difficult.
Such efforts are of interest not just for medical reasons but also for the light they shed on gender differences.
The first effort at reassignment, by John Money, involved David Reimer whose penis was accidentally damaged at eight months due to a botched circumcision.
The Money Perspective
Money believed that while children are mostly born with unambiguous genitalia, their gender identity is neutral. He felt that which gender a child identifies with is determined primarily by how parents treat it and that parental views are shaped by the appearance of the genitals.
Accordingly, Money advised the parents to have the child surgically altered to resemble a female and raise it as “Brenda.” For many years, Money claimed that the reassignment had been a complete success. Such was his influence as a well-known Johns Hopkins gender researcher that his views came to be widely accepted by scholars and the general public.
Unfortunately for Brenda, the outcome was far from happy. When he was 14, Reimer began the process of reassignment to being a male. As an adult, he married a woman but depression and drug abuse ensued, culminating in suicide at the age of 38 (1).
Money's ideas about gender identity were forcefully challenged by Paul McHugh (2), a leading psychiatrist at the same institution as Money. The brunt of this challenge came from an analysis of gender reassignment cases in terms of both motivation and outcomes.
Adult Reassignment Surgery Motivation
Why do people (predominantly men) seek surgical reassignment (as a woman)? In a controversial take, McHugh argued that there are two main motives.
In one category fall homosexual men who are morally uncomfortable about their orientation and see reassignment as a way of solving the problem. If they are actually women, sexual interactions with men get redefined as heterosexual.
McHugh argued that many of the others seeking reassignment are cross-dressers. These are heterosexual men who derive sexual pleasure from wearing women's clothing. According to McHugh, surgery is the logical extreme of identifying with a female identity through cross-dressing.
If his thesis is correct, McHugh denies that reassignment surgery is ever either medically necessary or ethically defensible. He feels that the surgeon is merely cooperating with delusional thinking. It is analogous to providing liposuction treatment for an anorexic who is extremely slender but believes themselves to be overweight.
To bolster his case, McHugh looked at the clinical outcomes for gender reassignment surgeries.
Adult Reassignment Results
Anecdotally, the first hurdle for reassignment is how the result is perceived by others. This problem is familiar to anyone who looked at Dustin Hoffman's depiction of a woman ( Tootsie ). Diligent as the actor was in his preparation, his character looked masculine.
For male-to-female transsexuals, the toughest audience to convince is women. As McHugh reported, one of his female colleagues said: “Gals know gals, and that's a guy.”
According to McHugh, although transsexuals did not regret their surgery, there were little or no psychological benefits:
“They had much the same problems with relationships, work, and emotions, as before. The hope that they would emerge now from their emotional difficulties to flourish psychologically had not been fulfilled (2)”.

Thanks to McHugh's influence, gender reassignment surgeries were halted at Johns Hopkins. The surgeries were resumed, however, and are now carried out in many hospitals here and around the world.
What changed? One likely influence was the rise of the gay rights movement that now includes transgender people under its umbrella and has made many political strides in work and family.
McHugh's views are associated with the religious right-wing that has lost ground in this area.
Transgender surgery is now covered by medical insurance reflecting more positive views of the psychological benefits.
Aspirational Surgery
Why do people who are born as males want to be women? Why do females want to be men? There seems to be no easy biological explanation for the transgender phenomenon (2).
Transgender people commonly report a lifelong sense that they feel different from their biological category and express satisfaction after surgery (now called gender affirmation) that permits them to be who they really are.
The motivation for surgical change is thus aspirational rather than medical, as is true of most cosmetic surgery also. Following surgery, patients report lower gender dysphoria and improved sexual relationships (3).
All surgeries have potential costs, however. According to a Swedish study of 324 patients (3, 41 percent of whom were born female) surgery was associated with “considerably higher risks for mortality, suicidal behavior, and psychiatric morbidity than the general population.”
1 Blumberg, M. S. (2005). Basic instinct: The genesis of behavior. New York: Thunder's Mouth Press.
2 McHugh, P. R. (1995). Witches, multiple personalities, and other psychiatric artifacts. Nature Medicine, 1, 110-114.
3 Dhejne, S., Lichtenstein, P., Boman, M., et al. (2011). Long-term follow-up of transsexual persons undergoing sex reassignment surgery: Cohort study of Sweden . Plos One.

Nigel Barber, Ph.D., is an evolutionary psychologist as well as the author of Why Parents Matter and The Science of Romance , among other books.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
State health plans must cover gender-affirming surgery, US appeals court rules
- Medium Text

Sign up here.
Reporting By Brendan Pierson in New York, Editing by Alexia Garamfalvi and Bill Berkrot
Our Standards: The Thomson Reuters Trust Principles. New Tab , opens new tab

Thomson Reuters
Brendan Pierson reports on product liability litigation and on all areas of health care law. He can be reached at [email protected].
Read Next / Editor's Picks

Industry Insight Chevron
Mike Scarcella, David Thomas

Karen Sloan

Henry Engler

Diana Novak Jones
Court says state health-care plans can’t exclude gender-affirming surgery

A federal appellate court in Richmond became the first in the country to rule that state health-care plans must pay for gender-affirming surgeries, a major win for transgender rights amid a nationwide wave of anti-trans activism and legislation.
The decision came from a set of cases out of North Carolina and West Virginia, where state officials argued that their policies were based on cost concerns rather than bias. The U.S. Court of Appeals for the 4th Circuit rejected that argument, saying the plans were discriminating against trans people in need of treatment.
Judge Roger L. Gregory, an appointee of President Bill Clinton, wrote for the majority that the restrictions were “obviously discriminatory” based on both sex and gender.
“In this case, discriminating on the basis of diagnosis is discriminating on the basis of gender identity and sex,” Gregory wrote, because “gender dysphoria is so intimately related to transgender status as to be virtually indistinguishable from it.”
The majority ruled that West Virginia’s policy also violated the Affordable Care Act’s anti-discrimination provision, a finding that has broad implications for other states’ Medicaid programs.
It’s the second ruling in favor of trans rights this month from the 4th Circuit, a once-conservative court that has become a trailblazer in the realm of transgender rights. The court was the first to say trans students had a right to use the bathrooms that align with their gender identity and the first to recognize gender dysphoria as a protected disability. Earlier this month, the court said a federally funded middle school could not ban a trans 13-year-old from playing on the girls’ track and field team.
The decision will be appealed to the Supreme Court, which recently allowed Idaho to enforce a ban on gender-affirming care for minors. West Virginia Attorney General Patrick Morrisey, who is running for governor, said in a statement Monday that he would “take this up to the Supreme Court and win.”
But the conservative-led Supreme Court has been reluctant to engage on these issues, letting multiple 4th Circuit rulings in favor of transgender rights stand. The court also generally waits until there is disagreement between circuit courts before getting involved.
All of these rulings split the 4th Circuit court down ideological lines, with judges appointed by Democrats joining the majority opinion and those appointed by Republicans dissenting. In the lead dissent from the ruling Monday, Judge Jay Richardson, a Trump appointee, wrote that there was no role for the federal court in policing what treatments health-care plans decide to cover.
The majority opinion, Richardson wrote, “treats these cases as new fronts upon which this conflict must be waged. But not every battle is part of a larger war. In the majority’s haste to champion plaintiffs’ cause, today’s result oversteps the bounds of the law.”
Richardson said what mattered is that trans patients have the same coverage of the same conditions as others. For example, he said, a trans patient with uterine cancer could get a hysterectomy under these plans.
“The different coverage accorded to treatments for different diagnoses is … based on medical judgment of biological reality,” he wrote. “States can reasonably decide that certain gender-dysphoria services are not cost-justified, in part because they question the services’ medical efficacy and necessity.”
Other states have banned hormonal treatment and surgery for trans minors; some have restricted care for transgender adults as well. Multiple other states have similar laws against insurance coverage for transition-related treatment. The Biden administration has moved to protect trans Americans through federal regulations, including guidelines released Monday that treat misuse of pronouns or refusal to let transgender employees use their preferred bathroom as workplace harassment.
In West Virginia, transgender Medicaid users challenged the state’s program, which since 2004 has by law banned “transsexual surgeries.” In North Carolina, state employees challenged their coverage, which in 2018 excluded surgical treatment of gender dysphoria — the clinical diagnosis of a disconnect between a person’s gender and birth sex.
Both states insisted that there was no bias in their coverage limitations, only cost concerns. Trans patients, they argued, were entitled to the same health treatments as everyone else but not specialized care.
“There is no service that is covered for a cisgendered person that is not covered for a transgender person meeting the same criteria,” Caleb David, an attorney for West Virginia, told judges on the appellate court during the oral argument. David added that the state had decided to provide psychiatric and hormonal treatment for gender dysphoria — just not surgery.
Advocates for trans patients said there was no medical justification for drawing the line there, when the state would cover such procedures for other conditions. They also said the financial explanation was suspect because so few people get gender-affirming surgery. It’s “a drop in the bucket,” Lambda Legal attorney Tara Borelli said during oral arguments. But even if the cost was significant, she argued, the cost of public health insurance “has to be a shared burden. It can’t be shunted onto the backs of a vulnerable minority group.”
The court agreed, saying cost-cutting could not justify covering the same treatments for health concerns other than gender dysphoria. For example, Gregory noted that under these plans, “cisgender people do receive coverage for certain gender-affirming surgeries,” including breast reconstruction for cancer patients after a mastectomy.
North Carolina began covering gender-affirming care in 2017 and stopped the following year, when Republican Dale Folwell became state treasurer. Julia McKeown, a professor at North Carolina State University, accepted her job in 2016, a few years into fully transitioning after a lifetime of “being adamant about what my gender was” but being limited in expressing it. She spent months preparing for surgery, only to be forced to cover the full cost along with all other treatment.
“It’s like having the rug pulled out from under you,” she said. “In some ways it’s worse than going in and knowing it was going to be denied.” She cut into her retirement savings rather than delay the surgery, calling herself “fortunate” to be able to do so.
McKeown grew up in a rural town in Florida and spent years pretending to be a man for fear of social and professional exclusion. Joining the lawsuit meant exposing herself to hate mail from strangers.
“In an ideal world, I would have loved to just move on with my life” after the surgery, she said. “At the same time, I feel a moral obligation to help those who can’t speak up for themselves, and for those who risk being fired or who have dependents on the state health-care plan who need access to treatment.”
Twenty-one Republican-led states asked the court to rule against the plaintiffs, focusing on disagreement over what physical interventions should be available to trans youth. But most major medical plans and the federal government cover gender transition treatment, which has been endorsed by mainstream medical associations. Studies indicate very few people who transition regret doing so or seek to reverse the changes, including those who start treatment in their teens.
Seventeen Democratic-led states and the District of Columbia urged the court to rule for the coverage, saying their “experience demonstrates that protecting access to gender-affirming care improves health outcomes for our transgender residents at little cost.”
An earlier version of this story reported that the contested insurance plans covered mastectomies for cancer patients but not for trans women. The plans covered mastectomies for all cancer patients, but did not cover the procedure for trans men who wanted their breasts removed to treat gender dysphoria.

Advertisement
Free Newsletters
Sign up now

Help us raise $225,000 for NCR!
We have raised $42,616 from 298 supporters. We are 18.9% of the way to our goal!
Is the Vatican's condemnation of trans surgery new? Theologians discuss.

Demonstrators in Lisbon, Portugal, take part in a march to celebrate International Transgender Day of Visibility March 31. (AP/Armando Franca)

by Katie Collins Scott
Staff Reporter
View Author Profile
Join the Conversation
Pope Francis warmly and repeatedly interacts with transgender individuals, sanctioned a document that affirms trans people can serve as Catholic godparents, and has praised the work of LGBTQ advocacy groups previously denounced by the Vatican.
But he also recently approved a new treatise on human dignity that lists "gender theory" and gender-affirming surgeries — which many, though not all, trans people undergo — among the "grave violations of human dignity in our time," placing them alongside sexual abuse, human trafficking, poverty and abortion.
NCR asked three Catholic theologians how they view Dignitas Infinita ("Infinite Dignity"), issued by the Dicastery for the Doctrine of the Faith on April 8, in light of the pope's notable actions of welcome toward the trans community.
Their answers have points of agreement but also mirror the broader discourse in the U.S. church, where portions of the document have been met with praise , gratitude , disappointment and fear .
Does Dignitas Infinita say anything new?
The theologians agreed that the Vatican document is a rearticulation of previous church teachings on gender, but they disagreed as to whether it addresses the concrete realities of trans people, and whether further doctrinal developments are possible.
Ish Ruiz is a theologian, ethicist and postdoctoral teaching fellow at Emory University in Atlanta. He told NCR that while Dignitas Infinita contains a synthesis of past teachings, it is the first time the highest doctrinal office at the Vatican has affirmed a doctrine on "gender theory" and "sex change" surgeries.
"It elevates these ideas to a definitively magisterial doctrine on gender-affirming surgery, offering a forceful condemnation by calling it a threat to human dignity," he said.

Ish Ruiz is a queer Latino Catholic theologian, ethicist and postdoctoral teaching fellow at Emory University in Atlanta. (Courtesy of Ish Ruiz)
Ruiz, who identifies as queer, said he sees that as a problem.
"Doctrine develops over time, and I'm afraid a doctrine like this is a setback for those of us who seek to expand LGBTQ+ inclusion in the church," he said.
Quoting Amoris Laetitia , Francis' 2016 apostolic exhortation on family life, Dignitas Infinita states that gender theory "envisages a society without sexual differences, thereby eliminating the anthropological basis of the family."
This argument is "a boogeyman, a monster that is somehow threatening to destroy us, but it doesn't really exist," Ruiz said.
"Transgender persons are not trying to eliminate gender differences; they are not trying to erase the so-called foundation for the human family — not at all," he said. "They are trying to live faithfully to their God-given identity, even at the risk of oppression, and undergoing gender-affirming surgeries so they can experience the very same human dignity that is being extended to everyone else."
Ruiz contends that, because Dignitas Infinita did not consult and ultimately misrepresented the experiences of trans people, it does not represent magisterial doctrine on transgender people "as we understand them today or as they see themselves."
Dawn Eden Goldstein, a theologian, canonist and author in Washington, D.C., said the church always will teach that there are just two sexes and that "nothing is going to change with regard to the doctrine."
( Trans advocates say being transgender does not necessarily mean people have a "third gender," since most trans people identify with being either male or female after being assigned the opposite gender at birth.)
What can change, said Goldstein, is the church speaking more forcefully with regard to "how we as Catholics are to show charity to people."
Dawn Eden Goldstein is a theologian, canonist and author in Washington, D.C. (Courtesy of Dawn Eden Goldstein)
For guidance on how to respond to trans people, she said, Catholics can look to Francis, who, while affirming that there are only two sexes, "will still refer to people by their preferred pronouns — out of charity."
The recent Vatican document does not address pastoral questions around pronouns, but Goldstein said she can imagine the church saying it is not sinful to use someone's preferred name and pronoun, although with room for people to follow their conscience on the matter in a sensitive way.
In the United States, many diocesan gender policies currently prohibit the use of preferred pronouns.
Although Dignitas Infinita is a reaffirmation of traditional positions on gender, a new addition is that the Vatican does not only condemn unjust discrimination but also denounces the practice in some parts of the world to imprison and torture people because of their "sexual orientation," said Elizabeth Sweeny Block, a Catholic moral theologian and associate professor of Christian ethics at St. Louis University.
The Catechism of the Catholic Church , in a section on people who are homosexual, says "every sign of unjust discrimination in their regard should be avoided.'"
Dignitas Infinita goes further, said Block.

Elizabeth Sweeny Block, an associate professor of Christian ethics at St. Louis University, said the Eucharist should not be weaponized. (Courtesy of Elizabeth Sweeny Block)
Goldstein told NCR this stronger wording is significant given that, for instance, the Center for Family and Human Rights (C-Fam), a nongovernmental organization that claims to represent Catholic understanding on human rights at the United Nations, "supports efforts to criminalize homosexuality in places like Africa."
C-FAM is listed as an anti-LGBT hate group by the Southern Poverty Law Center, and its president, Austin Ruse , reportedly supports the criminalization of homosexuality. Ruse told NCR that neither he nor his organization have ever argued for criminalizing homosexuality.*
A group cannot say it advocates for the Catholic understanding of the human person while it backs that view, said Goldstein.
The Vatican document's firm repudiation of unjust discrimination toward every person "regardless of sexual orientation" precedes the section on "gender theory," a placement that seems to put sexual orientation and gender identity under the same umbrella. The document never uses the terms "transgender" or "gender dysphoria."
Ruiz said the conflation of sexual orientation (related to people's sexual attraction) and gender identity (one's concept of self as male, female or nonbinary) "further demonstrates a lack of familiarity with contemporary conversations about sexuality and shows a misunderstanding of different realities."
More generally, added Block, when it comes to understanding human bodies, sexuality and gender, the church has always relied on a traditional and narrow interpretation of Scripture to support the claims it wishes to uphold, instead of learning from other disciplines, including science.
She contrasted that approach with how Francis went to great lengths in his latest apostolic exhortation on the climate crisis, Laudate Deum , to provide scientific evidence of climate change.
"A continued openness to varied sources of wisdom is critical," Block said.
Pastoral vs. doctrinal?
Last fall, Cardinal Víctor Manuel Fernández, head of the Vatican's doctrine office, said in a written response to questions from a Brazilian bishop that transgender people may be baptized, serve as godparents and be witnesses at Catholic weddings, if it would not cause confusion or "public scandal" among fellow Catholics.
Fernández said this would apply even to "transsexuals" (the term used in the 2023 document, written in Italian, and considered outdated by some trans advocates) who have undergone gender reassignment surgery and hormone treatment.
Goldstein — who is concerned people are focused far more on gender identity issues in Dignitas Infinita than on its striking, important statements on the death penalty, war and other issues — said the new 2024 document is doctrinal and Fernández's answers are pastoral.
"Doctrine informs our pastoral understanding, but pastoral ministry also takes up questions that aren't taken up by doctrine," she said. "Sometimes charity will require us to do things that require a kind of broadness that we couldn't exercise if we were teaching the doctrine."
Because a person with gender dysphoria may experience "psychological issues that cause them to feel pain in their biological sex," Goldstein said, that may "mitigate their culpability" in choosing to undergo surgery.
However, Dignitas Infinita buttresses arguments for conscience protections for doctors, said Goldstein. "It is certainly saying that Catholic doctors can't participate in operations to change the way that their sex appears," she said.
For Ruiz, the pastoral and the doctrinal documents together "show an inconsistency."
"The idea that transgender persons should be treated with respect and welcome, but at the same time we are going to consider their queerness, their trans identities and the way they live those out as a threat to human dignity — there's a disconnect there," he said.
"At the end of the day, it's a question of integrity," said Ruiz. "These matters of human sexuality are incredibly mysterious, and we're still trying to understand them. We have to be honest about that instead of feigning certainty when we are still learning."
* Editor's Note : This article was updated after initial publication to include a comment from Austin Ruse, president of C-Fam.
Most Read Stories

#1 Catholic students, theologians, ministers write an open letter to Pope Francis

#2 Pope responds with 'open heart' to Vatican document criticism from parents of LGBTQ children

#3 Pope asks lay Catholics to prepare for synod's 'prophetic' stage
#4 'It's a different time': Relations between US sisters, Vatican have changed radically
Latest news.
What Doubting Thomas can teach us about not knowing

The problems with criticisms of 'Dignitas Infinita'
Inspired by 'Laudato Si' ', Catholics in Bangladesh work to protect environment

Despair in the Holy Land
Subscribe to ncr's free newsletters.
Select any of the newsletters below, then enter your email address and click "subscribe"
- Election 2024
- Entertainment
- Newsletters
- Photography
- Personal Finance
- AP Investigations
- AP Buyline Personal Finance
- AP Buyline Shopping
- Press Releases
- Israel-Hamas War
- Russia-Ukraine War
- Global elections
- Asia Pacific
- Latin America
- Middle East
- Election Results
- Delegate Tracker
- AP & Elections
- Auto Racing
- 2024 Paris Olympic Games
- Movie reviews
- Book reviews
- Personal finance
- Financial Markets
- Business Highlights
- Financial wellness
- Artificial Intelligence
- Social Media
Tennessee lawmakers OK bill penalizing adults who help minors receive gender-affirming care
FILE - The Tennessee Capitol is seen, Jan. 22, 2024, in Nashville, Tenn. On Thursday, April 25, 2024, Tennessee’s GOP-controlled Statehouse gave their final approval to legislation criminalizing adults who help minors receive gender-affirming care without parental consent, clearing the way for the first-in-the-nation proposal to be sent to Gov. Bill Lee’s desk for his signature. (AP Photo/George Walker IV, File)
- Copy Link copied
NASHVILLE, Tenn. (AP) — Tennessee’s GOP-controlled Statehouse on Thursday gave their final approval to legislation penalizing adults who help minors receive gender-affirming care without parental consent, clearing the way for the first-in-the-nation proposal to be sent to Gov. Bill Lee’s desk for his signature.
The bill mirrors almost the same language from a so-called anti-abortion trafficking proposal Tennessee Republican lawmakers approved just a day prior. In that version, supporters are hoping to stop adults from helping young people obtain abortions without permission from their parents or guardians.
Lee, a Republican, hasn’t publicly commented on either bill, but supporters are confident he will sign them into law. Lee eagerly approved a sweeping abortion ban and a ban on gender-affirming care for children . He has also never issued a veto during his time as governor.
While the Republican supermajority touted the proposed statutes as necessary to protect parental rights, critics warned about the possible broad application. Violations could range from talking to an adolescent about a website on where to find care to helping that young person travel to another state with looser restrictions on gender-affirming care services.
The original bill included criminal penalties, but supporters agreed to civil penalties for violators.
“This is a parent’s rights bill, nothing more, nothing less,” Republican Rep. Bryan Richey, the bill’s sponsor, said during House debate earlier this week. “At the end of the day, parents should have final say what medical procedures their children are receiving, and nobody else.”
The Human Rights Campaign says Tennessee has enacted more anti-LGBTQ+ laws more than any other state since 2015, identifying more than 20 bills that advanced out of the Legislature over the past few months.
That included sending Gov. Lee a bill banning the spending of state money on hormone therapy or sex reassignment procedures for prisoners — though it would not apply to state inmates currently receiving hormone therapy — and requiring public school employees to out transgender students to their parents .
Republicans in the state also passed a measure that would let LGBTQ+ foster children be placed with families that hold anti-LGBTQ+ beliefs. Lee signed it into law this month.
“Tennessee lawmakers are on the verge of enacting more than twice as many anti-LGBTQ+ laws as any other state, a staggering assault on their own constituents,” Cathryn Oakley, senior director of legal policy at the Human Rights Campaign, said in a statement.
To date, no state has placed restrictions on helping young people receive gender-affirming care, despite the recent push among more than 20 Republican-led states — including Tennessee — to ban such care for most minors.
Instead some Democratic-led states have been pushing to shield health care providers if they provide services that are banned in a patient’s home state. Most recently Maine’s Democratic governor signed a bill Wednesday protecting providers of abortion and gender-affirming care from legal action brought by other states.
The proposal has created a disagreement between Maine Attorney General Aaron Frey and attorneys general in several other states, including Tennessee. The other states have warned of legal action over the law; Frey dismissed such threats as “meritless.”

- Election 2024
- Environment
- Politics + Government
Kansas House fails to override veto on bill that would ban gender-affirming care for kids
By: sherman smith - april 29, 2024 7:50 pm.

Sen. Mary Ware, seen during an April 6, 2023, hearing, says Senate Bill 233 tramples on the rights of transgender Kansans. (Sherman Smith/Kansas Reflector)
TOPEKA — As the Kansas Legislature renewed its yearslong assault on transgender children, Sen. Mary Ware told her Senate colleagues Monday she had a “simple” question for them.
“What is the acceptable number of youth suicides?” Ware asked.
The Suicide and Crisis Lifeline is a hotline for individuals in crisis or for those looking to help someone else. To speak with a certified listener, call 988.
Crisis Text Line is a texting service for emotional crisis support. To speak with a trained listener, text HELLO to 741741. It is free, available 24/7, and confidential.
Ware’s question set the tone for debate in the Senate, which voted 27-13 to override Gov. Laura Kelly’s veto of Senate Bill 233, legislation that would ban gender-affirming care for anyone younger than 18. But the override attempt fell short in the House on an 82-43 vote , two short of the two-thirds majority required.
The bill would have blocked teenagers from receiving hormone therapy and other treatments recognized as necessary by medical professionals. And it would have banned state employees from supporting “social transitioning,” which is defined to include an individual changing their preferred pronouns or manner of dress.
Rep. Susan Concannon, R-Beloit, and Rep. Jesse Borjon, R-Topeka, flipped their votes from earlier in the month to sustain the governor’s veto. Two other Republicans — Rep. Mark Schreiber of Emporia and Rep. David Younger of Ulysses — also joined Democrats in blocking the legislation from becoming law.
“We hear about mental health, about suicide, and ask why,” Concannon said. “We’re not listening to the impact of youth. Government involvement is not the answer.”
On the Senate side, Sen. John Doll, R-Garden City, and Sen. Carolyn McGinn, R-Sedgwick, joined the chamber’s 11 Democrats in supporting the veto.
Opponents of the bill pointed to extensive medical research that shows transgender children, who are already at an elevated risk for suicide, are more likely to die from suicide if they don’t receive gender-affirming care.
“This bill ignores, or should I say tramples, on the rights of some Kansas citizens to live peaceably, lawfully and free to make their own decisions about their own bodies,” Ware said.
Republicans argued the bill would protect children from life-altering decisions they could end up regretting.
Sen. Beverly Gossage, R-Eudora, said she receives “beautiful cards” and emails from parents who thank her for pursuing the legislation.
“We all sympathize to those who are suffering from gender dysphoria,” Gossage said.
Sen. Mark Steffen, R-Hutchinson, said the predators in today’s society are “woke” health care providers who are preying on “confused” children and parents.
“No more than we would ever tell somebody with anorexia that they’re fat would we tell a boy that they’re a girl or girl that they’re a boy,” Steffen said.
In a teary speech, Senate Minority Leader Dinah Sykes, D-Lenexa, said she has heard from hundreds of Kansans who see hormone treatment as a life raft — and are concerned the Legislature is about to rip that away.
Research consistently shows that supportive environments, including access to gender-affirming care, reduces the mental health risk for kids, Sykes said, while denying that care amplifies feelings of isolation, shame and hopelessness.
“So for our transgender community, I will say there are some, who, we are in your camp,” Sykes said. “We may not understand all the complexities that you go through, but you have a place in this state. And we accept you and we cherish you. And regardless of where this vote goes, there is someone who is here, who cares.”
The House delayed taking action as Republican leadership tried to secure enough votes to override the governor’s veto. Before closing the roll call, Republicans locked the chamber doors and issued a procedural declaration that requires every member to cast a vote, rather than abstain.
Borjon said he would support a ban on gender reassignment surgery and limits on the use of hormone blockers for minors. But for him, the bill went too far in restricting speech and behavioral health care for transgender youths.
Rep. Tobias Schlingensiepen, a Topeka Democrat and pastor, said it was clear the “politically motivated bill” would make the lives of trans kids and their families more difficult.
“It is clear to me that this Legislature would be choosing to interfere in the most sacred of relationships — between parents and children, between families and health care providers, and yes, between all of these people and their God,” Schlingensiepen said. “I am confident that zero Kansas residents who would be affected by this bill have asked for it to pass. On the contrary, they have instead been pleading for this legislature to reject this policy.”
Our stories may be republished online or in print under Creative Commons license CC BY-NC-ND 4.0. We ask that you edit only for style or to shorten, provide proper attribution and link to our website. AP and Getty images may not be republished. Please see our republishing guidelines for use of any other photos and graphics.

Sherman Smith
Sherman Smith is the editor in chief of Kansas Reflector. He writes about things that powerful people don't want you to know. A two-time Kansas Press Association journalist of the year, his award-winning reporting includes stories about education, technology, foster care, voting, COVID-19, sex abuse, and access to reproductive health care. Before founding Kansas Reflector in 2020, he spent 16 years at the Topeka Capital-Journal. He graduated from Emporia State University in 2004, back when the school still valued English and journalism. He was raised in the country at the end of a dead end road in Lyon County.
Kansas Reflector is part of States Newsroom , the nation’s largest state-focused nonprofit news organization.
Related News

LGBTQ+ rights in Iraq: how morality laws ramped up
Same-sex relationships and gender reassignment surgery are now criminalised in latest attack on targeted community
- Newsletter sign up Newsletter

Human rights groups have condemned a bill passed by Iraq's parliament that criminalises s ame-sex relationships, with jail terms of between 10 and 15 years.
According to a copy of the legislation seen by Reuters , the law aims to "protect Iraqi society from moral depravity and the calls for homosexuality that have overtaken the world".
Amnesty International's Iraq researcher Razaw Salihy said that Iraq had "effectively codified in law the discrimination and violence" that members of the LGBTQ+ community have "been subjected to with absolute impunity for years".
Subscribe to The Week
Escape your echo chamber. Get the facts behind the news, plus analysis from multiple perspectives.
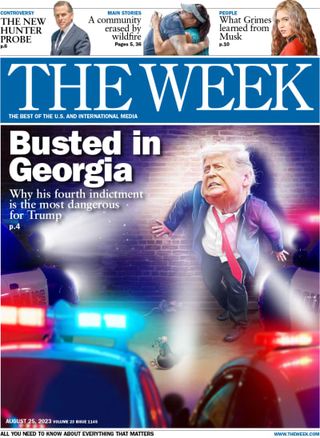
Sign up for The Week's Free Newsletters
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
What is in the new law?
As well as a penalty of between 10 and 15 years in prison for same-sex relations, the Law on Combating Prostitution and Homosexuality mandates at least seven years in jail for anybody who promotes homosexuality or prostitution, and between one and three years for anyone who changes their "biological gender" or wilfully dresses in an effeminate manner.
Doctors who perform gender reassignment surgery, men who "intentionally" act like women and those who engage in "wife swapping" will also face prison terms under the new legislation, said the BBC .
Why has it been introduced now?
Iraq had been among the few Islamic nations that did not explicitly criminalise same-sex relations , but "loosely defined" morality clauses in its penal code have been used to "target" LGBTQ+ people, said The Independent .
The new legislation was backed by conservative Shia Muslim parties that form the largest coalition in Iraq's mainly Muslim parliament. It is "a significant step in combating sexual deviancy given the infiltration of unique cases contradicting Islamic and societal values", Amir al-Maamouri, an independent MP, told Shafaq News.
It is indeed "sweeping", said Pink News , although "less extreme than originally planned", after a clause in an earlier version of the bill that called for the death penalty for same-sex acts was removed due to opposition from the US and Europe.
What has the reaction been?
The amended legislation has sparked condemnation from human rights groups and the international community.
It is "dangerous and worrying", said UK Foreign Secretary David Cameron. A statement from the US State Department said the law "threatens those most at risk in Iraqi society" and "can be used to hamper free speech and expression and inhibit the operations of NGOs across Iraq". The law would also weaken Iraq's ability to diversify its economy and attract foreign investment, the department said.
Data collected in 2022, reported by Pink News , suggested that just 2% of Iraq's population support homosexuality, while 55% oppose it. Ordinary Iraqis interviewed on Sunday expressed "mixed views" on the new law, said The Associated Press .
What was the law before?
"Public perception and morality clauses in its penal code" mean that LGBTQ+ people have been "routinely targeted domestically and institutionally", said Pink News.
A 2022 report by Human Rights Watch said armed groups in Iraq were abducting, raping, torturing and killing lesbian, gay, bisexual and transgender people, and accused the Iraqi government of failing to hold perpetrators accountable.
The words "homosexual" and "gender" were banned in the media and on social media platforms in 2023. Officials claimed the move would safeguard societal values and maintain public order.
Over the past year, major Iraqi parties have "stepped up" criticism of LGBTQ+ rights, said Al Jazeera , "with rainbow flags frequently being burned in protests by both governing and opposition conservative Shia Muslim factions".
Renewed outbreaks of violence against Iraq's LGBTQ+ community have seen several people killed, including 28-year-old trans blogger Simsim, who was stabbed to death by unknown assailants in the city of Diwaniyah in February.
The new law "rubber-stamps" the country's "appalling record of rights violations", said Rasha Younes, deputy director of the LGBTQ+ rights programme at Human Rights Watch, marking "a serious blow to fundamental human rights".
Sign up for Today's Best Articles in your inbox
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com

Cartoons Artists take on apolitical camping, the National Guard, and more
By The Week US Published 5 May 24

Talking Point Gabriel Attal announces 'bold' intervention to tackle rise in violent incidents
By The Week UK Published 5 May 24

The Week Recommends The sanctuary is a 'roaring' conservation success

Speed Read Greece becomes the first Orthodox Christian country to enshrine marriage equality in law
By Peter Weber, The Week US Published 16 February 24

The Explainer Relatives of victims bring case against controversial legislation to High Court
By Julia O'Driscoll, The Week UK Published 21 November 23

Speed Read Why do so many Middle Eastern countries have anti-LGBTQ laws, and what can be done to make a change?
By Justin Klawans Published 24 November 22

Speed Read Calls for foreign intervention have mounted as the island nation's situation has deteriorated
By Justin Klawans Published 25 October 22

In Depth Nationwide protests intensify as activists call for overhaul of government following controversial appointment
By Gabriel Power Last updated 3 February 20

In Depth UN official urges Scotland to delay plans to make it easier for transgender people to be granted legal recognition
By Arion McNicoll Last updated 29 November 22

In Depth Taiwan becomes the latest place to legalise same-sex marriage, prompting dispute with the government of China
By The Week Staff Last updated 21 May 19

In Depth Qatar World Cup ambassador describes homosexuality as ‘a damage in the mind’
By The Week Staff Last updated 14 November 22
- Contact Future's experts
- Terms and Conditions
- Privacy Policy
- Cookie Policy
- Advertise With Us
The Week is part of Future plc, an international media group and leading digital publisher. Visit our corporate site . © Future US, Inc. Full 7th Floor, 130 West 42nd Street, New York, NY 10036.

IMAGES
VIDEO
COMMENTS
Research consistently shows that people who choose gender affirmation surgery experience reduced gender incongruence and improved quality of life. Depending on the procedure, 94% to 100% of people report satisfaction with their surgery results. Gender-affirming surgery provides long-term mental health benefits, too.
The cost of transitioning can often exceed $100,000 in the United States, depending upon the procedures needed. A typical genitoplasty alone averages about $18,000. Rhinoplasty, or a nose job, averaged $5,409 in 2019. Insurance Coverage for Sex Reassignment Surgery.
Gender-affirming surgery is a surgical procedure, or series of procedures, that alters a person's physical appearance and sexual characteristics to resemble those associated with their identified gender.The phrase is most often associated with transgender health care and intersex medical interventions, although many such treatments are also pursued by cisgender and non-intersex individuals.
Gender affirmation surgery, also known as gender confirmation surgery, is performed to align or transition individuals with gender dysphoria to their true gender. A transgender woman, man, or non-binary person may choose to undergo gender affirmation surgery. The term "transexual" was previously used by the medical community to describe people ...
Overview. Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation.
Gender-affirming surgery for male-to-female transgender women or transfeminine non-binary people describes a variety of surgical procedures that alter the body to provide physical traits more comfortable and affirming to an individual's gender identity and overall functioning.. Often used to refer to vaginoplasty, sex reassignment surgery can also more broadly refer to other gender-affirming ...
Facial feminization surgery (FFS) is a series of plastic surgery procedures that reshape the forehead, hairline, eyebrows, nose, cheeks, and jawline. Nonsurgical treatments like cosmetic fillers ...
Request an Appointment. 844-546-5645 United States. +1-410-502-7683 International. To help provide guidance for those considering gender affirmation surgery, two experts from the Johns Hopkins Center for Transgender Health answer questions about what to expect before and after your surgery.
Top surgery is surgery that removes or augments breast tissue and reshapes the chest to create a more masculine or feminine appearance for transgender and nonbinary people. Facial gender surgery: While hormone replacement therapy can help achieve gender affirming changes to the face, surgery may help. Facial gender surgery can include a variety ...
A trans person can choose from multiple procedures to make their appearance match their self-identified gender identity. Doctors refer to this as gender "affirmation" surgery. Trans people might ...
Female-to-male surgery is a type of gender-affirmation or gender-affirming surgery. There are multiple forms of gender-affirming surgery, including altering the genital region, known as "bottom ...
Individuals who desire surgical procedures who have not been part of the Comprehensive Gender Services Program should contact the program office at (734) 998-2150 or email [email protected]. We will assist you in obtaining what you need to qualify for surgery. University of Michigan Comprehensive Gender Services Program brings ...
Facial Feminizations. Facial feminization surgery (FFS) involves several surgeries that can be done to feminize the facial features. These procedures include but are not limited to: rhinoplasty, forehead contouring, jaw angle reduction, chin width reduction, lowering the hairline, hair transplantation, cheek augmentation, lip augmentation and upper lip shortening.
1 Gender affirming surgery has historically been referred to as sexual reassignment surgery (SRS). 2 Gender affirming care is an umbrella term referring to any medical care a TGD individual might pursue that affirms their gender identity, including primary care, mental health care, GAH or GAS.
The Crane Center for Transgender Surgery has announced the launch of a gender-affirming hormone clinic at their transgender wellness center in Austin, Texas. The new clinic offers hormone replacement therapy for transgender and non-binary adults through an informed consent model. Both in-office and telemedicine appointments are available.
The most common procedures were breast and chest procedures, which occurred in 27 187 patients (56.6%), followed by genital reconstruction (16 872 [35.1%]) and other facial and cosmetic procedures (6669 [13.9%]). The absolute number of GAS procedures rose from 4552 in 2016 to a peak of 13 011 in 2019 and then declined slightly to 12 818 in 2020.
The World Professional Association for Transgender Health (WPATH) today announced its updated Standards of Care and Ethical Guidelines for health professionals. Among the updates is a new suggestion to lift the age restriction for youth seeking gender-affirming surgical treatment, in comparison to previous suggestion of surgery at 17 or older.
Masculinizing Procedures. "Mansculpture". Some trans men feel a sense of dysphoria about their hips, thighs, stomach, or other areas and wish to get liposuction to create a more masculine body contour. Complications are similar to any other liposuction treatment, and include bruising, pain, bleeding, and infection. Hysterectomy.
Background: Gender dysphoria is a condition that often leads to significant patient morbidity and mortality. Although gender-affirming surgery (GAS) has been offered for more than half a century with clear significant short-term improvement in patient well-being, few studies have evaluated the long-term durability of these outcomes.
Here's how gender reassignment works: Converting male anatomy to female anatomy requires removing the penis, reshaping genital tissue to appear more female and constructing a vagina. An incision ...
When he was 14, Reimer began the process of reassignment to being a male. As an adult, he married a woman but depression and drug abuse ensued, culminating in suicide at the age of 38 (1). Money's ...
April 29 (Reuters) - Health insurance plans run by U.S. states must cover gender-affirming surgeries for transgender people, a U.S. appeals court ruled on Monday. The 8-6 opinion , opens new tab ...
5 min. A federal appellate court in Richmond became the first in the country to rule that state health-care plans must pay for gender-affirming surgeries, a major win for transgender rights amid a ...
"I strongly support prohibiting gender reassignment surgery and limiting the use of hormone blockers … (some parts of the bill) go too far in restricting mental and behavioral health care for ...
Fernández said this would apply even to "transsexuals" (the term used in the 2023 document, written in Italian, and considered outdated by some trans advocates) who have undergone gender ...
FILE - The Tennessee Capitol is seen, Jan. 22, 2024, in Nashville, Tenn. On Thursday, April 25, 2024, Tennessee's GOP-controlled Statehouse gave their final approval to legislation criminalizing adults who help minors receive gender-affirming care without parental consent, clearing the way for the first-in-the-nation proposal to be sent to Gov. Bill Lee's desk for his signature.
Ware's question set the tone for debate in the Senate, which voted 27-13 to override Gov. Laura Kelly's veto of Senate Bill 233, legislation that would ban gender-affirming care for anyone younger than 18. But the override attempt fell short in the House on an 82-43 vote, two short of the two-thirds majority required.. The bill would have blocked teenagers from receiving hormone therapy ...
LGBTQ+ rights in Iraq: how morality laws ramped up. Same-sex relationships and gender reassignment surgery are now criminalised in latest attack on targeted community. Just 2% of Iraqis support ...
CNN —. Iraq has passed a new law that penalizes same-sex relations with up to 15 years in prison, a move condemned by rights advocates as the latest attack on the country's LGBTQ community ...
8 likes, 0 comments - gender_reassignment_clinic on January 7, 2024: "Affordable breast enlargement (silicone implant)Surgery..... contact.....+91-7698938615 # ...