
An SLP writes about swallowing, communication, and cognition
- Browse by topic
- Eat (swallowing)
Speak (communication)
- Think (cognition)
- Being an SLP
- Continuing Education


Articulation therapy for dysarthria: Part 1
Articulation therapy for dysarthria focuses on improving the speech mechanism itself. We can administer articulation therapy alongside teaching compensatory speaking strategies, AAC, partner strategies, and modifying the environment. Wonder why a gift is the featured image? Read on!
Free DIRECT downloads: Articulation therapy: Part 1 and 20+ speech tasks (cheat sheets). ( Email subscribers get free access to all the resources in the Free Subscription Library .)
- Go beyond compensatory strategies .
- Talking “a lot” is not sufficient for recovery .
- Therapy tip .
- Drill, drill, drill !
- Practice more than once a day .
- Begin by explicitly teaching the strategies .
- Informally assess carryover frequently .
- Repetition to start, then variable practice .
- Example therapy sequence for a mod-severe dysarthria .
- Why we should make the task unpredictable .
- How we can make the next trial unpredictable .
- 20+ speech tasks, from simple to hard .
- Be sensitive to your patient’s frustration level .
- Related Eat, Speak, & Think posts .
- More coming up in Part 2 .
- References .
Go beyond compensatory strategies
We should include articulation therapy in our care plan unless our patient is unable to participate. Joseph Duffy, PhD, BC-ANCDS, F-ASHA , wrote that most clinicians focus on compensatory strategies, which may be a disservice to our patients. He went on to say:
Focus on compensation may actually limit activity-dependent neural reorganization that is necessary to the reduction of specific impairment. Duffy, J. R. (2005). Motor speech disorders: Substrates, differential diagnosis, and management . St. Louis, Mo: Elsevier Mosby, page 442.
Not only can we directly reduce the specific impairment, we can also begin teaching our patient to be independent with their speech work from day one. This is especially important when insurance or other factors don’t allow a patient to stay on caseload very long.
return to top
Practice what you want to improve
Specificity is a key principle of motor learning. If someone wants to improve talking, then they have to talk (a lot).
…recovery of speech in people with MSDs, at least when they have a nonprogressive disease, requires speaking, and probably lots of it. Duffy, J. R. (2005). Motor speech disorders: Substrates, differential diagnosis, and management . St. Louis, Mo: Elsevier Mosby, page 446.
One exception is if our patient doesn’t have any ability to produce speech, in which case we can work on non-speech movements or eliciting sounds that can be shaped into speech sounds.
Another exception is if we have to focus on the foundations of speech, such as posture, breath support, and laryngeal strength, before our patient is able to produce speech.
So skip the non-speech exercises, unless you have a good rationale for doing them with that particular patient.
Talking “a lot” is not sufficient for recovery
Most people do not improve simply by talking. Duffy, J. R. (2005). Motor speech disorders: Substrates, differential diagnosis, and management . St. Louis, Mo: Elsevier Mosby, page 450.
Just talking a lot is not sufficient for most people to recover speech function. That’s where skilled intervention comes in, determining the what, when, and how of speech work, following the principles of motor learning.
Choose the level of speech that matches the goal
Most of our patients likely want speech therapy to improve their ability to communicate natural-sounding, comprehensible messages to others.
Joseph Duffy says that we shouldn’t practice skills that are less advanced than what our patients demonstrate in assessment. And we shouldn’t work on improving skills beyond what is necessary to achieve the goals of treatment. (Duffy, 451)
And Maas et al (2008) points out that motor learning is better when we practice the whole movement sequence rather than repeatedly practicing individual movement elements.
Therapy tip
Since we generally communicate in multi-word units, we should progress to phrases and sentences as quickly as possible. If we want to maximize motor learning, it would be a mistake to target speech sounds in the traditional hierarchy, mastering one level before progressing to the next.
In most cases, spending time on word lists is not functional. At least put each word in a phrase, even if it’s a carrier phrase!
Drill, drill, drill!
Maximize outcomes by getting in as many trials as you can in each session. Although you may repeat each target many times in a row in the beginning of a session (constant practice), move into variable practice as soon as you can during the same session.
Example of constant practice for /k/: Repeating the word “car” over and over.
Example of variable practice for /k/: Repeating words with /k/ in different places. “Car, take, parking, skirt”.
Practice more than once a day
Distributed practice is better than massed practice for overall outcomes. It’s the same concept we know from our own learning experiences. If we practice a skill for 15 minutes every day, we’re much more likely to master it than if we only practice for 90 minutes on Saturdays.
Ideally, we’d distribute articulation practice in smaller sessions over the course of the day. So on days with speech therapy, our patient may practice for a short period of time later in the day. And on days without speech therapy, they may do two practice sessions on their own.
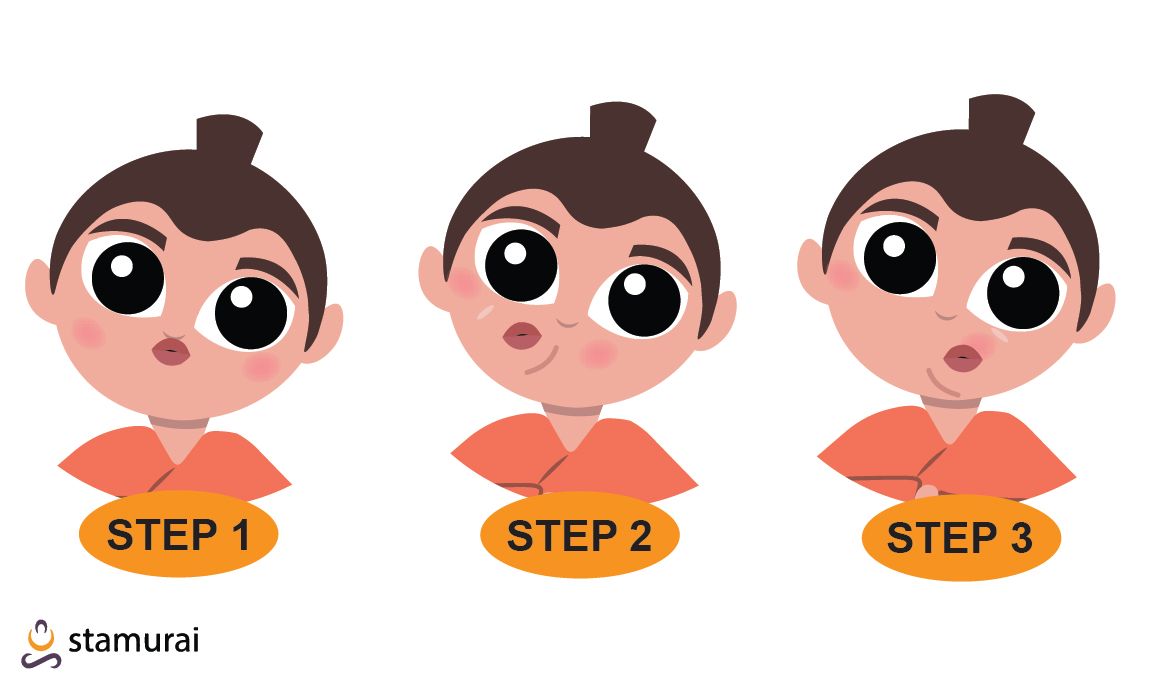
Begin by explicitly teaching the strategies
In the beginning, we should deliberately teach and demonstrate what we want our patients to do. People generally have better outcomes when they understand their problem and why we want them to follow our instructions.
We shouldn’t assume that our patient will connect the dots on their own.
Actively engaging our patient, we can ask them to tell us in their own words what strategy they’re using and why. Or we can ask them to tell a family member who wasn’t present during the session. This allows us to gauge how well they understand.
Informally assess carryover frequently
Although our patients are likely to improve their speech during structured speech therapy, it doesn’t mean they’ll be able to carryover those new skills.
We can probe spontaneous performance at the beginning and end of each session to get a sense of how well our patient is retaining what we’re teaching.
Be a little patient though. Following the principles of motor learning means that immediate performance will be less accurate in the early stages, but if therapy is successful, our patient will have better recovery.
Repetition to start, then variable practice
Repeating the same movement over and over is constant practice. You may find this useful at the start of the session, to help your patient achieve success. Constant practice can be done at any level of speech. You can repeat any sound, word, phrase, or sentence over and over.
While a person will be more likely to have higher accuracy with constant practice, this is a short-term effect. So once your patient achieves a reasonable level of success, it’s time to switch to variable practice.
Reasonably successful can be defined as >50% accurate or close approximation on 3-5 trials.
With variable practice, we change up the movement patterns. This can be done in many ways, and we can change things in more than one way at the same time. For instance, we can:
- Use different words with the same target sound in different positions.
- Increase the length of utterance.
- Change the speech task difficulty , for instance from repetition to sentence completion.
- Increase the cognitive load, for instance by randomly inserting a working memory task.
The literature from motor learning indicates that we see better outcomes from varying the tasks we practice during a session. We’re likely to see less accurate performance during the session, but long-term motor learning is better.
Move up and down the articulation hierarchy
Start at the highest level you think the person will be successful. Move from one level to the next as soon as the patient can produce the target reasonably well. Drop down a level if a person has too much difficulty.
- Single sound: “k”.
- Initial: Car, coat, cup.
- Final: Back, neck, take.
- Medial: Bacon, hockey, making.
- Increasing syllable length, no consonant blends.
- Initial: Clean, crumb, quit.
- Final: Milk, dark, box.
- Medial: Likely, secret, parking.
- Increasing syllable length, with consonant blends.
- Phrases: Come here. Can you? Find coat.
- Short sentences: Come here now. Can I eat? I like cake.
- Longer sentences: Can you come here now? Can you find my coat? I like to eat birthday cake.
Work at the level the person is reasonably successful, and occasionally probe the next higher level in the hierarchy. We can move up and down the hierarchy many times over the course of a single session.
It’s ok to skip a level. Our focus is on helping our patient to produce the longest utterances they can, not to make sure we hit every level in the hierarchy.
Example therapy sequence for a mod-severe dysarthria
Here’s an example order of stimuli used when working with someone who has a moderate to severe dysarthria. We practiced each level a couple of times before moving to the next, until we reached a level that was too hard.
- Establish /k/ sound: “k”.
- Put it at start of one-syllable word: Come.
- Add a word: Come here.
- Add another word: Come here now.
- Make a longer sentence: Can you come here now?
- Oops, too hard. Drop back down: Come here now.
- Now do the other part: Can you?
- Now add a word back in: Can you come?
- Finally, repeat the longer sentence: Can you come here now?
This is an example of a patient who needed a lot of cueing to even make the /k/ sound, but after several minutes was able to say “Can you come here now?” reasonably well.
Not only is this following the principles of motor learning, but imagine how the patient felt at successfully saying a complete sentence with the difficult sound!
Make the task unpredictable
Why we should make the task unpredictable.
If the next trial is predictable, then our patient may already have the motor plan activated. It’s a mental short-cut. They’re more likely to be accurate during the session, but it doesn’t reflect normal conversation which requires activating each motor plan as we use it.
Instead, we should make our patient start from scratch for each trial. This will probably decrease accuracy during the session, because they’ll be more likely to make an error. However, over the long run, they’ll likely have better recovery.
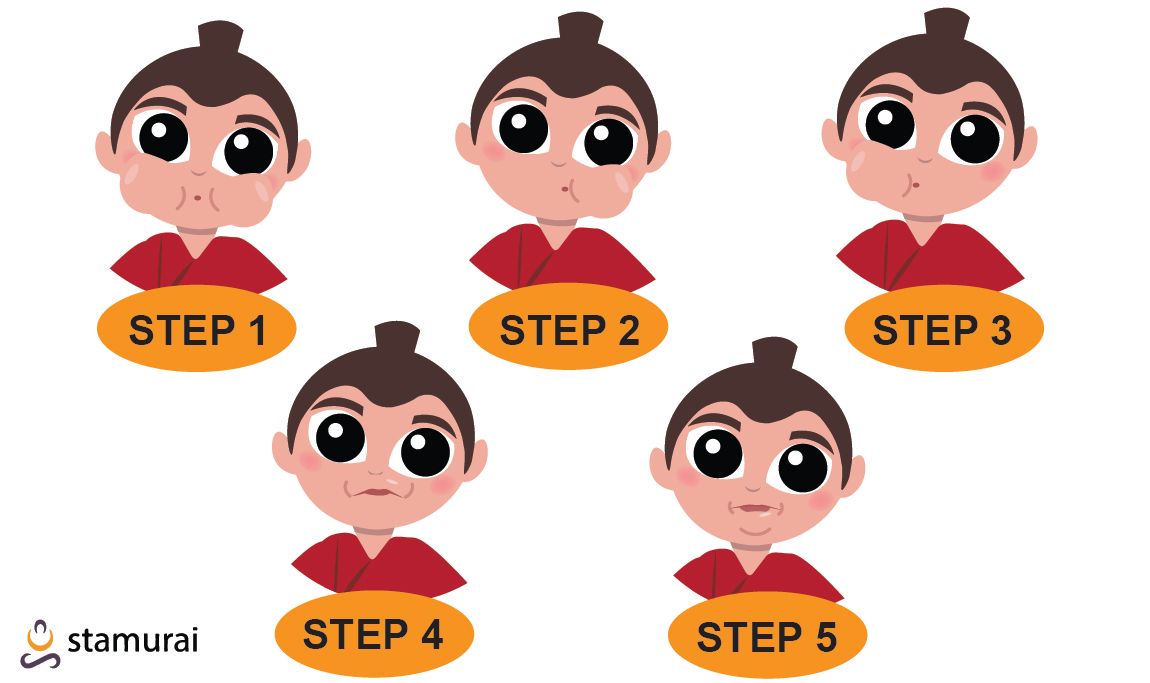
This is such an important principle, and one that we may not remember to follow, that I highlighted the concept of surprise with my featured image.
How we can make the next trial unpredictable
To maximize outcomes, we can mix two or more therapy targets together. We have a lot of flexibility for what counts as a therapy target. For instance:
- Targeting the impaired sound in different word positions.
- Treating multiple impaired sounds.
- Moving between different levels on the articulation hierarcy.
- Switching between speech strategies (for example, speaking slowly vs loudly).
- Changing the emotion we convey (pretend to be happy, angry, surprised, etc…).
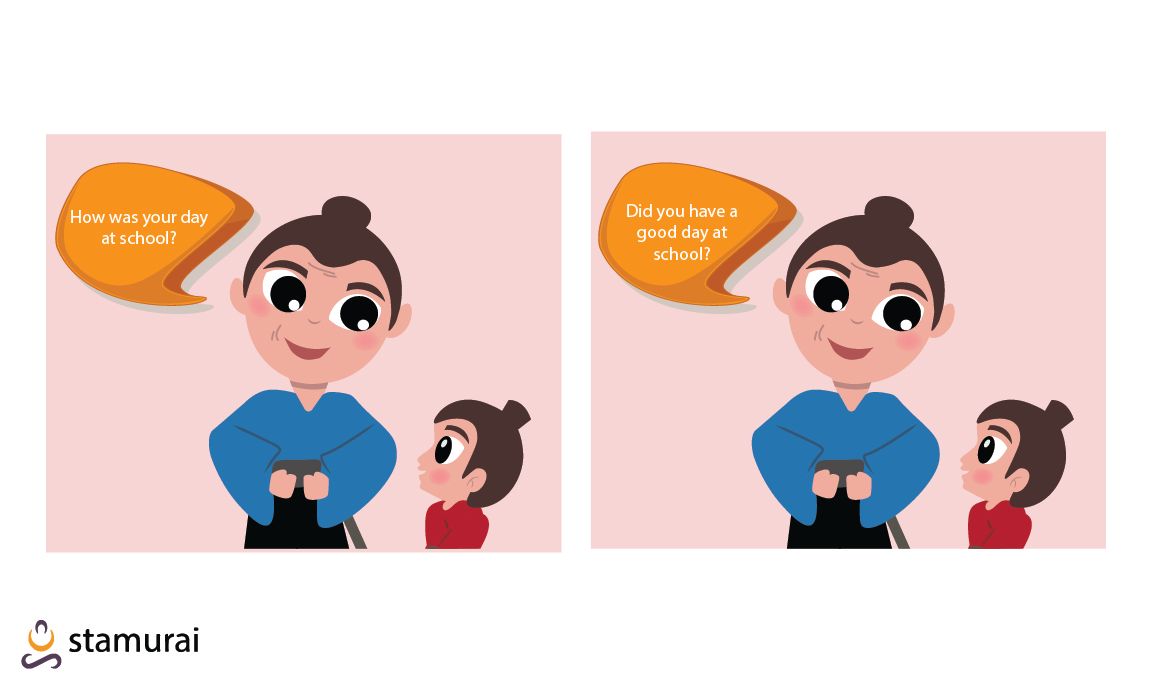
- Varying the speaking context (talk to a different person, move to a different area, imagine different scenario).
- Changing the difficulty of the speech task.
- Non-articulation therapy goal (for example, memory or word-finding).
20+ speech tasks, from simple to hard
This hierarchy of task difficulty is not fixed. It changes according to the abilities of your patient and other factors of the speech work you’re doing. But this list may give you some ideas for how to adjust the difficulty of the speech task to be appropriate for your patient at that moment.
- Choral speech (speaking in unison).
- Automatic speech (example, counting to 10).
- Imitate (repeat).
- Recite familiar material (example, a poem).
- Cloze sentence completion. (example, “Roses are red, violets are ____.”)
- Open-ended sentence completion.
- Convergent naming.
- Confrontation naming.
- Divergent naming.
- Name by function or attribute.
- Generate synonyms, antonyms, or homonyms.
- Create a sentence around a given word.
- Picture description.
- Answer wh-questions.
- Ask wh-questions about picture or using a given word.
- Describe steps to complete a task.
- Personal narrative.
- Answer problem-solving questions.
- Working memory tasks.
- Provide opinions.
- Read passage aloud, then restate in own words.
- Watch short video and recall key points.
- Listen to passage and recall key points.
- Do something while talking (walk, move objects from one bin to another, sort cards by suit, etc).
Be sensitive to your patient’s frustration level
Always bear in mind the frustration level of your patient. If we make it clear to them WHY we’re practicing the way we are, they are more likely to persist with the difficult exercise. But we all have our limits for tackling difficult work.
If you sense frustration, try one of these:
- Drop down the articulation hierarchy.
- Make the speech task easier.
- Pick a different therapy target.
- Honestly praise the good aspects you noticed.
- Make a recording and compare to one from evaluation day.
- Take a break.
Try to begin and end each session with success.
Related Eat, Speak, & Think posts
- Motor learning for articulation: Focus and feedback .
- Tips for dynamic speech assessment .
- Free multimedia resources for the SLP .
More coming up in Part 2
I’m continuing this post in Part 2 , which will include two very important topics: focus of attention and the role of feedback. It will include the cueing hierarchy, and how to use dynamic cueing during articulation therapy with specific examples.
- Duffy, J. R. (2005). Motor speech disorders: Substrates, differential diagnosis, and management . St. Louis, Mo: Elsevier Mosby.
- Maas, E., Robin, D.A., Austermann Hula, S.N., Freedman, S.E., Wulf, G., Ballard, K.J., & Schmidt, R.A. (2008). Principles of Motor Learning in Treatment of Motor Speech Disorders. American Journal of Speech-Language Pathology, 17, 277-298. [ PubMed ]

Lisa A Young M.A. CCC-SLP
Lisa earned her M.A. in Speech-Language Pathology from the University of Maryland, College Park and her M.A. in Linguistics from the University of California, San Diego.
She participated in research studies with the National Institute on Deafness and other Communication Disorders (NIDCD) and the University of Maryland in the areas of aphasia, Parkinson’s Disease, epilepsy, and fluency disorders.
Lisa has been working as a medical speech-language pathologist since 2008. She has a strong passion for evidence-based assessment and therapy, having earned five ASHA Awards for Professional Participation in Continuing Education.
She launched EatSpeakThink.com in June 2018 to help other clinicians be more successful working in home health, as well as to provide strategies and resources to people living with problems eating, speaking, or thinking.
- Lisa A Young M.A. CCC-SLP https://eatspeakthink.com/author/admin/ Home health SLP survey results may surprise you
- Lisa A Young M.A. CCC-SLP https://eatspeakthink.com/author/admin/ An easy way to write participation-level speech therapy goals
- Lisa A Young M.A. CCC-SLP https://eatspeakthink.com/author/admin/ Learn how Goal Attainment Scaling makes SMART goals better
- Lisa A Young M.A. CCC-SLP https://eatspeakthink.com/author/admin/ Quick guide to self-management training in Parkinson's
I had a stroke Dec. 2018 I have dysarthia and dysphagia.. I attended inhouse Rehab for 4 months and out patient speech therapy for over a year. My speech is still not normal. I have found more information on this site that will help me regain my normal speech than over 18 months of therapy
Thank you for letting me know! I’m happy I’ve given some helpful information.
Here’s another site you might want to check out, written by another speech-language therapist: Tactus Therapy ( https://tactustherapy.com/ ).
[…] Articulation therapy for dysarthria: Part 1. […]
I was diagnosed with ataxia and dysarthria three years ago. I’ve been fortunate to have regular speech therapy sessions. This article has helped me understand more clearly the strategies my therapist uses. Additionally this article has given me a new ways to look at my personal practice. I will first split my time up, and instead of practicing for 30 minutes a day, commit to 15 minutes twice a day. Next rather than just drilling stumble words, I like the idea of using them in novel ways, or even combining them with other stumble words. My therapy today was reading this article aloud, thinking about volume and support and mastering stumble words in context.
Ascot, thank you for your feedback on the article. I’m happy it helped you understand the therapy approach better, and that it’s given you ideas on how to maximize your practice! Good luck with your practice!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Your Comment
Your Website URL
This site uses Akismet to reduce spam. Learn how your comment data is processed .
9 Most Effective Dysarthria Treatment Exercises
Dysarthria is a speech disorder that makes it hard to speak clearly, control pitch and volume, and keep a steady pace . It can really impact communication and social interactions, affecting someone’s overall quality of life.
But there are exercises to help manage and improve speech clarity when dealing with communication disorders such as Dysarthria.
“Mewing” is a technique that has lately acquired popularity as a therapeutic exercise for dysarthria. Placing the tongue on the roof of the mouth can assist in strengthening the muscles involved in speech production and enhance overall speech clarity . If you wish to understand mewing better, and learn more about its benefits, take a quiz below .
In this article, we’ll also explore:
- 📝 What is dysarthria and how it affects speech production
- 👄 The importance of dysarthria treatment exercises
- ✔️ The benefits of mewing and other non-speech exercises

What Causes Dysarthria?
Motor speech disorders result from a damaged nervous system preventing the full control of particular body parts, in this case, the jaw, the tongue, and the larynx.
Dysarthria can be caused by a range of neurological conditions, injuries, and disorders that affect the parts of the brain responsible for controlling the muscles used in speech production such as the unilateral upper motor neuron.
Here are some of the most common causes of dysarthria:
- Stroke: A stroke is a serious condition that can cause damage to the brain and affect speech production, resulting in dysarthria.
- Traumatic Brain Injury: A severe head injury, such as a concussion or skull fracture, can also damage the brain and cause dysarthria.
- Neurodegenerative Diseases: Conditions such as Parkinson’s, multiple sclerosis, and ALS can cause degeneration of the nerves and muscles involved in speech production. Patients suffering from these medical conditions can have dysarthria.
- Brain Tumors: A tumor in the brain can cause dysarthria by interfering with the normal function of the speech muscles.
- Cerebral Palsy: This condition affects the brain’s development and can cause difficulties with motor function, including speech.
- Alcohol or Drug Abuse: Chronic use of alcohol or drugs resulting in dysarthria. They can cause damage to the brain and nerves involved in speech production.
- Infections: Certain infections, such as meningitis or encephalitis, can cause inflammation and damage to the brain that may lead to dysarthria.
- Medications: Some medications can affect the nerves and muscles used in speech production, causing dysarthria as a side effect.
Dysarthria: Types, Symptoms, and Treatment Approaches
Dysarthria is a speech disorder caused by damage or injury to the parts of the brain responsible for controlling the muscles used in speech production. There are different types of dysarthria, each with its own set of characteristics and treatment approaches.
Spastic Dysarthria Treatment
Spastic dysarthria is a motor speech disorder that results in slow, effortful speech with a harsh-sounding voice. Treatment focuses on strengthening weak muscles and improving articulation through exercises. Augmentative and alternative communication (AAC) devices can also be used as dysarthria treatment techniques.
Ataxic Dysarthria Treatment
Ataxic dysarthria is a motor speech disorder that causes slurred speech with irregular pauses and a lack of coordination in the speech muscles. Dysarthria exercises may help to improve speech by focusing on practicing rhythm and timing, breathing correctly , and using a monotone voice.
You may also use other approaches, like speaking at a slower pace and emphasizing sounds or words. Working with a speech-language pathologist can help individuals with ataxic dysarthria develop personalized dysarthria exercises for adults, such as word lists, to practice communication abilities.
Flaccid Dysarthria Treatment
Flaccid dysarthria is a motor speech disorder that results in weak, breathy speech with reduced volume and poor articulation. This type of dysarthria is caused by damage to the lower motor neurons or nerves that control the speech muscles.
Treatment exercises may aim to strengthen the speech muscles, improve breath control, and increase vocal resonance to improve speech quality.
Hyperkinetic Dysarthria Treatment
Hypokinetic dysarthria is a speech disorder often associated with Parkinson’s disease. It is characterized by speaking slowly, lacking inflection, and a reduced volume. The speech muscles become rigid and slow. This results in difficulty with exercising your facial expression and speech production.
Treatment exercises for hypokinetic dysarthria may include practicing loud and clear speech and improving breath support and vocal control.
Mixed Dysarthria Treatment
Mixed dysarthria is a complex condition that combines features of different types of dysarthria. It can present a unique challenge for speech-language pathologists as the symptoms vary depending on the specific combination of dysarthria types.
Treatment approaches for mixed dysarthria may involve a combination of exercises that target various speech subsystems, such as respiratory, phonatory, and articulatory systems. The treatment plan may also involve augmentative and alternative communication strategies to supplement speech.
9 Effective Dysarthria Treatment Exercises for Children and Adults
1. orthotropics.
Orthotropics or mewing refers to a set of lip and tongue exercises that aim to improve facial structure and overall oral posture. They involve techniques, such as tongue twisters and blowing bubbles, to strengthen the muscles by exercising your jaw .
Mobile apps are also available that promote mewing exercises and provide guidance on proper technique. One of them is our own product: Mewing.coach. The app is designed to provide users with a comprehensive guide to practicing mewing exercises to enhance their jawline and facial appearance.
The app offers a range of features, including instructional videos, progress tracking, and customized workout plans to help users achieve their desired results.
Take a quick quiz to receive a workout program to improve your jaw, facial muscles and overall appearance.

2. Exercises for Breathing Support
Breathing support exercises are methods that help improve the way air exits the lungs. These workouts sometimes entail activities such as blowing up balloons or blowing bubbles to develop the respiratory muscles.
These exercises can be especially beneficial for those who use their voice professionally, such as singers or public speakers, and those with respiratory problems, such as asthma.
3. Speaking Exercises
Different tongue exercises frequently include a variety of activities, such as singing, imitating animal sounds, or performing tongue twisters to help develop the muscles required for speaking.
Children and adults with dysarthria can enhance their speech sounds, breath support, and general facial expressions by completing these exercises on a daily basis. This may be achieved and aided by seeing an expert in speech-language pathology.
4. Expression or Enunciation Exercises
These exercises frequently involve repeating certain sounds, syllables, or phrases that can aid in improving articulation and speech clarity. Children and adults with dysarthria can enhance their capacity to speak and be understood by completing these activities on a daily basis. These exercises may be adjusted to each person’s specific requirements and speech therapy.
5. Steady and Overemphasized Speaking Drills
These exercises include practicing speaking slowly and deliberately, stressing each word and syllable to improve clarity and effectiveness. Individuals may enhance their enunciation, rhythm, and tempo by frequently doing these dysarthria exercises, making their speech more interesting and easier to comprehend.
6. Exercises for Improving Oral-Motor Skills
Oral-motor exercises are techniques for improving the function of the mouth and throat muscles, which can aid in speech, eating, and drinking. Strengthening the tongue, lips, and cheeks requires exercises that include chewing gum for jawline , sucking on straws, or blowing bubbles.
Individuals who practice these exercises on a regular basis can improve their oral-motor skills, allowing them to eat, speak, and communicate more effectively.
7. Improving Communication Skills Through Conversing with Family and Peers
In addition to dysarthria therapy activities, practicing communication skills with family members or peers can help enhance speaking ability. Conversation with others can assist people with fluency disorders in improving their articulation, vocal intensity, and conversation skills in a natural and comfortable situation.
Individuals may boost their confidence and ability to express themselves successfully in a range of contexts by practicing communication on a regular basis.
8. Implementing Communication Techniques
Exercises for dysarthria therapy are crucial for enhancing speech output in people with this speech problem. Incorporating communication techniques that can improve all aspects of communication, particularly for kids and adults with dysarthria, is equally crucial.
These tactics may include approaches like speaking more slowly, employing gestures or visual aids, and getting comfortable taking turns in conversations.
People with dysarthria can communicate more effectively in their daily lives, enhancing their quality of life and social connections by combining these tactics with dysarthria therapy activities. Overall, effective dysarthria treatment requires a thorough strategy that includes both speech production and communication techniques.
9. Use Visual or Technological Tools
These techniques can help people communicate in settings where speech is difficult or inefficient, such as in loud environments or with strangers. Speech-generating devices, for example, are electronic gadgets that may generate speech from text sentences or symbols that the user selects.
Communication boards, on the other hand, are actual boards containing symbols or pictures that people may point to in order to convey their message.
Other visual aids, in addition to these tools, can be beneficial to people who have disorders. Picture books, visual timetables, and other sorts of visual dysarthria treatment activities for adults.
Collaborating with a Speech Therapists
Collaboration with a speech-language therapist may be tremendously useful for people seeking dysarthria therapy. Speech therapists are skilled practitioners who specialize in diagnosing and treating voice disorders such as speech deficits.
Patients with dysarthria who work with a speech-language therapist can get compensatory strategies and focus on enhancing their speech intelligibility.
Some of the benefits of working with a speech-language therapist for differential diagnosis include:
- Assessment and Diagnosis: A speech-language therapist can conduct a comprehensive assessment to determine the specific type and severity of dysarthria, essential for developing an effective treatment plan.
- Tailored Treatment Plan: Based on the neurogenic speech disorders, a speech-language therapist can create a personalized treatment plan that is tailored to the individual’s specific needs and goals. Some may even recommend nonspeech exercises.
- Therapy and Exercises: Speech-language therapy for dysarthria may involve various exercises and techniques to improve articulation, voice production, and overall communication skills.
- Communication Strategies: A speech-language therapist can provide communication strategies and techniques to individuals with dysarthria to enhance their ability to communicate effectively in different situations.
- Support and Counseling: Working with a speech-language therapist can provide emotional support and counseling to help individuals cope with the challenges of living with dysarthria.
Working with a speech-language therapist may be a great resource for people with dysarthria who want to enhance their communication skills, quality of life, and general well-being. A therapist will also give you more information on other dysarthria-causing factors and general guidance on uneven lip exercises .
How Long Does it Take to Recover from Dysarthria?
The time it takes to recover from dysarthria varies substantially depending on the underlying cause and severity of the ailment. Dysarthria may be a transient ailment that cures on its own after a few days or weeks. However, in some cases, it may be a chronic condition that necessitates ongoing treatment and management.
Age, overall health, and the individual’s dedication to treatment can all impact the recovery duration for dysarthria. Individuals who receive early and consistent treatment for dysarthria tend to have better outcomes and recover faster.
Final Thoughts
Dysarthria treatment exercises are essential for improving communication skills and enhancing the quality of life for individuals with this speech disorder. Engaging in therapy with a speech-language therapist, using visual aids, and regular exercising can help to strengthen the muscles used in speech production and improve overall speech clarity.
Individuals with dysarthria need to seek professional help and exercise daily to achieve their communication goals and enhance their quality of life. By doing so, individuals with dysarthria can significantly improve their communication skills, confidence, and well-being.
How useful was this post?
Vote count: 6
Thank you for rating this post!

Emma Erickson
Orthodontist, lecturer, face yoga expert.
Share this article
Sculpt your face into desired look with mewing. Answer a quick quiz to receive your workout program.
- Patient Care & Health Information
- Diseases & Conditions
A speech-language pathologist might evaluate your speech to help determine the type of dysarthria you have. This can be helpful to the neurologist, who will look for the underlying cause.
Besides conducting a physical exam, your doctor might order tests to identify underlying conditions, including:
- Imaging tests. Imaging tests, such as an MRI or CT scan, create detailed images of your brain, head and neck that may help identify the cause of your speech problem.
- Brain and nerve studies. These can help pinpoint the source of your symptoms. An electroencephalogram (EEG) measures electrical activity in your brain. An electromyogram (EMG) evaluates electrical activity in your nerves as they transmit messages to your muscles. Nerve conduction studies measure the strength and speed of the electrical signals as they travel through your nerves to your muscles.
- Blood and urine tests. These can help determine if an infectious or inflammatory disease is causing your symptoms.
- Lumbar puncture (spinal tap). In this procedure, a doctor or nurse inserts a needle in your lower back to remove a small sample of cerebrospinal fluid for laboratory testing. A lumbar puncture can help diagnose serious infections, disorders of the central nervous system, and cancers of the brain or spinal cord.
- Brain biopsy. If a brain tumor is suspected, your doctor may remove a small sample of your brain tissue to test.
- Neuropsychological tests. These measure your thinking (cognitive) skills, your ability to understand speech, your ability to understand reading and writing, and other skills. Dysarthria doesn't affect your cognitive skills and understanding of speech and writing, but an underlying condition can.
More Information
- EEG (electroencephalogram)
- Electromyography (EMG)
- Lumbar puncture (spinal tap)

Speech therapy is often a part of stroke rehabilitation.
Your treatment will depend on the cause and severity of your symptoms and the type of dysarthria you have.
Your doctor will treat the cause of your dysarthria when possible, which may improve your speech. If your dysarthria is caused by prescription medications, talk to your doctor about changing or stopping such medications.
Speech and language therapy
You may have speech and language therapy to help you regain normal speech and improve communication. Your speech therapy goals might include adjusting speech rate, strengthening muscles, increasing breath support, improving articulation and helping family members communicate with you.
Your speech-language pathologist may recommend trying other communication methods if speech and language therapy isn't effective. These communication methods could include visual cues, gestures, an alphabet board or computer-based technology.
Coping and support
If you have significant dysarthria that makes your speech difficult to understand, these suggestions may help you communicate more effectively:
- Speak slowly. Listeners may understand you better with additional time to think about what they're hearing.
- Start small. Introduce your topic with one word or a short phrase before speaking in longer sentences.
- Gauge understanding. Ask listeners to confirm that they know what you're saying.
- If you're tired, keep it short. Fatigue can make your speech more difficult to understand.
- Have a backup. Writing messages can be helpful. Type messages on a cellphone or hand-held device, or carry a pencil and small pad of paper with you.
- Use shortcuts. Create drawings and diagrams or use photos during conversations, so you don't have to say everything. Gesturing or pointing to an object also can help convey your message.
Family and friends
If you have a family member or friend with dysarthria, the following suggestions may help you better communicate with that person:
- Allow the person time to talk.
- Don't finish sentences or correct errors.
- Look at the person when he or she is speaking.
- Reduce distracting noises in the environment.
- Ask yes or no questions.
- Tell the person if you're having trouble understanding.
- Keep paper and pencils or pens readily available.
- Help the person with dysarthria create a book of words, pictures and photos to assist with conversations.
- Involve the person with dysarthria in conversations as much as possible.
- Talk normally. Many people with dysarthria understand others without difficulty, so there's no need to slow down or speak loudly when you talk.
Preparing for your appointment
Dysarthria requires prompt medical attention. See a doctor right away if you have sudden or unexplained changes in your ability to speak.
If the changes are more subtle, you'll likely start by seeing your primary care doctor. If your doctor suspects a medical condition is causing your symptoms, he or she will likely refer you to a nervous system specialist (neurologist) for further evaluation.
Here's what you can do to get ready for your appointment.
- Be aware of pre-appointment restrictions. Ask if there's anything you need to do in advance, such as restrict your diet for blood tests.
- Write down your symptoms, including any that may seem unrelated to the reason for which you scheduled the appointment.
- Write down key personal information, including major stresses or recent life changes.
- List all medications, vitamins and supplements you take.
- Take a family member or friend along, if possible. Someone who accompanies you can help you remember information.
- Write down questions to ask your doctor.
For dysarthria, some basic questions to ask your doctor include:
- What's the most likely cause of my symptoms?
- What tests do I need?
- Will I need to see a specialist?
- What treatments are available?
- Are there brochures or other printed material that I can have? What websites do you recommend?
Don't hesitate to ask other questions, as well.
What to expect from your doctor
Your doctor is likely to ask you a number of questions, including:
- When did your symptoms begin?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- Does anything seem to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
- Daroff RB, et al., eds. Bradley's Neurology in Clinical Practice. 7th ed. Elsevier; 2016. https://www.clinicalkey.com. Accessed April 10, 2020.
- Dysarthria. American Speech-Language-Hearing Association. https://www.asha.org/public/speech/disorders/dysarthria/. Accessed April 6, 2020.
- Maitin IB, et al., eds. Current Diagnosis & Treatment: Physical Medicine & Rehabilitation. McGraw-Hill Education; 2020. https://accessmedicine.mhmedical.com. Accessed April 10, 2020.
- Dysarthria in adults. American Speech-Language-Hearing Association. https://www.asha.org/PRPPrintTemplate.aspx?folderid=8589943481. Accessed April 6, 2020.
- Drugs that cause dysarthria. IBM Micromedex. https://www.micromedexsolutions.com. Accessed April 10, 2020.
- Lirani-Silva C, et al. Dysarthria and quality of life in neurologically healthy elderly and patients with Parkinson's disease. CoDAS. 2015; doi:10.1590/2317-1782/20152014083.
- Signs and symptoms of untreated Lyme disease. Centers for Disease Control and Prevention. https://www.cdc.gov/lyme/signs_symptoms/index.html. Accessed April 6, 2020.
- Neurological diagnostic tests and procedures fact sheet. National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Neurological-Diagnostic-Tests-and-Procedures-Fact. Accessed April 6, 2020.

Associated Procedures
Products & services.
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.

Dysarthria Speech Therapy
Convenient & Effective Speech Therapy

What is dysarthria?
Dysarthria is a motor speech disorder typically caused by some sort of accident or illness that has attacked or injured the brain (i.e., stroke, traumatic brain injury, brain tumor, etc.) The accident or illness damages the portions/nerves of the brain that control the tongue, lips, vocal cords, and diaphragm (many of which are typically just referred to as the ‘articulators’). Dysarthria is typically characterized by muscles weakness and imprecise movements of said articulators.
Because it follows some sort of trauma or illness to the brain, a speech-language pathologist will typically conduct an assessment while the patient is still in the early stages of recovery. The sooner treatment begins, typically, the better the outcome. The outcome of treatment is also influenced by how extensive the damage to the brain is (i.e., the severity of the stroke or the traumatic brain injury). Unfortunately, dysarthria does not always present itself physically, but can also cause emotional distress for the individual with dysarthria. This can be due to frustration, sadness, or even anxiety and depression surrounding their inability to communicate effectively with loved ones and strangers.

TYPES OF DYSARTHRIA
What are the types of dysarthria?
There are several types of dysarthria that can be caused by different localized damage to the brain. The type a patient may have is dependent on where in the brain the damage has occurred and the severity of the damage to the brain. This is because more severe damage can cause more than one dysarthria to be present if several portions of the brain are damaged. Some of these different types of dysarthria include:
Flaccid: Breathy/nasally voice. Attributed to lower motor neuron damage.
Spastic: Strained voice with a slow rate of speech. Attributed to bilateral motor neuron damage or unilateral upper motor neuron damage.
Ataxic: Excessive stress. Attributed to cerebellum damage.
Hypokinetic: Rapid rate of speech. Attributed to extrapyramidal damage.
Hyperkinetic: Voice stoppages/inappropriate pauses. Similar to hyperkinetic, in that it is also typically attributed to extrapyramidal damage.
Spastic and Flaccid: Hypernasality and harsh vocal quality. Attributed to both upper and lower motor neuron damage.
DYSARTHRIA CAUSES
What causes dysarthria?
Several contributing factors can cause dysarthria or just one overarching issue can cause it as well. Some of the most common causes of dysarthria include:
Traumatic Brain Injury (TBI) : A TBI can be caused by a variety of accidents or illnesses. Car accidents, falls, anoxic brain injury, etc. can all be attributed to dysarthria caused by a TBI.
Cerebrovascular Accident (Stroke) : A CVA or otherwise known as a stroke, is when blood flow to the brain is disrupted in some manner.
Illness : Certain illnesses that attack the brain can cause dysarthria in some individuals. This could include certain types of cancers or degenerative diseases (i.e. brain tumor, Parkinson’s disease, multiple sclerosis, etc.)
The severity and specific symptoms of dysarthria can vary depending on the underlying cause and the extent of the damage. In some cases, dysarthria may be temporary and improve over time with appropriate treatment. In other cases, it may be a permanent condition that requires ongoing management and support.
DYSARTHRIA DIAGNOSIS
How is dysarthria diagnosed?
Dysarthria is usually diagnosed while an individual is still recovering from the accident or illness that has caused the dysarthria. An individual may be referred for a speech-language evaluation, either through inpatient or outpatient services depending on where they are in their recovery.The diagnosis usually involves a comprehensive evaluation by a speech-language pathologist (SLP):
Case History & Background: The SLP will review the patient’s medical history, as well as gather their own background from the individual/the individual’s family. Once this background is collected, and the speech-language pathologist has a grasp on where the patient was, speech-wise, prior to the event, they may follow up with an in-depth assessment.
Physical Examination: The SLP will examine the patient's mouth, tongue, and throat to look for any physical abnormalities or signs of weakness.
Speech Assessment: The SLP will listen to the patient speak and assess their speech intelligibility, voice quality, and articulation.
Depending on the results of this assessment and the background collection, the speech-language pathologist will suggest an individualized treatment plan that addresses the patient's specific needs and goals.

DYSARTHRIA TREATMENT AND THERAPY
How speech language pathologists treat patients with dysarthria?
Dysarthria treatment looks different for every individual, and is also dependent on the type of dysarthria/the location and severity of damage to the brain. A speech-language pathologist will try to individualize the speech therapy in order to most benefit the patient, while including the patient’s wants/needs as well as the goals of their caregivers. Some focuses of dysarthria treatment include:
Motor exercises: Muscular weakness is often associated with dysarthria, so motor exercises are often utilized to restrengthen said muscles as well as relearn coordination for speech.
Alternative forms of communication: An individual may need to learn alternative forms of communication , whether it be temporarily or long term. Some of these alternative forms of communication can include an AAC device (i.e., an iPad) or they can include a communication board or even just a notebook.
Speech drills: Another form of treatment for dysarthria can include speech drills. Similarly, to motor exercises, speech drills assist in the relearning and restrengthening of the articulators/muscles.
A speech-language pathologist can also offer emotional support as well as refer patients to professionals to assist in counseling, if that is something the patient is interested in and in need of.
How to Improve Your Speech?

Join Better Speech

We'll Match You With the Ideal Therapist
No Waitlists - Start This Week

Improve Speech
Live Weekly Zoom Sessions

150+ Licensed and Experienced Therapists

Our speech therapists are all licensed and certified, with ~10 years of experience. We cover every state in the USA. We offer speech therapy services for children and adults.

WHY PEOPLE LOVE US
Our Shining Testimonials

It's really convenient, easy and affordable. My son speech really got better.

We have seen our son just explode in terms of speech, language and confidence. It gets our highest recommendation!

I love the flexibility of the online schedule. Also with insurance, it was a fraction of the cost of a clinic, I wish I have tried Better Speech sooner.

Get Free Guide to Improve Speech
Improve your communication skills

Improve your child’s speech


What is Dysarthria?
4 min read
Dysarthria is a motor-speech disorder that results in unclear speech. This inability to speak clearly is because of weakness, slowness, or lack of coordination in the muscles of the mouth, voice, and lungs.
Dysarthria results from damage to the nervous system. There are several different types of dysarthria. The type of dysarthria a person has is determined by the area of the nervous system that’s damaged.
In unilateral dysarthria, just one side of the face and tongue is weak. In spastic dysarthria, the muscles on both sides are stiff and uncoordinated. With flaccid dysarthria, the muscles are loose and floppy. In ataxic dysarthria, muscle movements are uncoordinated. Hyperkinetic dysarthria involves involuntary muscle movements, while hypokinetic dysarthria features muscle movements that are slow to start. There are also many mixed dysarthrias that include features of more than one type.
Dysarthria can be a mild annoyance, or it can have a devastating effect on a person’s ability to make him or herself understood.
Download a Free Patient Education Handout about Dysarthria
Get your free PDF summarizing what dysarthria is, what you might notice, & how you can help . A perfect handout for families.

In addition to receiving your free download, you will also be added to our mailing list. You can unsubscribe at any time. Please make sure you read our Privacy Policy and Terms & Conditions .
What Causes Dysarthria
Dysarthria can be caused by a stroke, head injury, or brain tumor. It can also be caused by a congenital disorder such as cerebral palsy (CP), or a degenerative disease such as motor neurone disease (MND / ALS) or Parkinson’s disease (PD). Dysarthria can also be a symptom of autoimmune disorders like myasthenia gravis (MG), multiple sclerosis (MS), or Guillain–Barré syndrome (GBS).
Dysarthria is NOT a problem with speech caused by a structural problem, such as a cleft palate or tongue resection. These speech problems are classified as dysglossias . Dysarthria must involve the brain (central nervous system) or nerves (peripheral nervous system).
What You Might Notice
Dysarthria affects different people in different ways.
Some people sound like they’re mumbling or slurring their words. Some sound like they’re talking through their noses, while others sound stuffed up.
Some speak in a monotone, while others make extreme pitch changes. Some speak slowly, some speak very quickly, and some fluctuate. Some speak loudly, some speak softly, and some are irregular in volume. Their voices may sound unusually hoarse, breathy, or strained.
Dysarthria can affect more than just speech. Someone with dysarthria may look like his or her face is drooping. They may have difficulty swallowing, or get food caught in the cheeks. Due to limited movement of the tongue, lips, or jaw, the person may drool or have trouble keeping dentures in place. Even breathing may be irregular, if the lungs are affected.
If You Have Dysarthria
If you have dysarthria, you may find talking to be difficult and frustrating. Take your time and follow these tips:
- Sit up and face your listener if possible. It’s important to make eye contact so your listeners can understand you better by watching your lips. You might want to avoid wearing a moustache that hides your upper lip.
- Speak slowly and loudly, exaggerating how each word is supposed to sound. Pause to take a breath when you need one.
- Use facial expressions, gestures, drawing, and pointing to help get your message across.
- If your listener has trouble understanding you, try using different words if repeating the exact words hasn’t worked.
- If you need to, write down what you want to say or key words. You can also point to the first letter of words on a letter board .
- Swallow before speaking to clear your mouth of saliva. Clear your throat if you need to so your voice will be clear.
- Try to relax and stay calm. If you have trouble, it’s okay to give up and come back to the subject later. Avoid important conversations when you’re tired or feeling emotional.
5 Ways to Help a Person with Dysarthria
A person with dysarthria can improve a great deal through speech therapy. Meanwhile, you can help the person communicate by taking a few simple actions:
- Make sure your surroundings are quiet and well lit. Turn off the TV and radio, and shut the door, so you won’t be interrupted. Be sure the lights are on or the curtains are open.
- Sit across from the person, so you can make eye contact. His or her body language and lip movements can tell you a lot.
- Establish the topic, so you both know what you’re discussing.
- Be patient. Give the person plenty of time to speak.
- If you don’t understand what the person is trying to say, don’t pretend you do. Instead, say what you do understand, using his or her exact words. Then ask specifically for the words that are unclear.
Want to learn more about dysarthria or other communication disorders in adults? Visit our Learn section to discover helpful resources. We also have a wide variety of apps for dysarthria therapy you can download to get started on improving communication today.
If you liked this article, Share It !

Megan S. Sutton , MS, CCC-SLP is a speech-language pathologist and co-founder of Tactus Therapy. She is an international speaker, writer, and educator on the use of technology in adult medical speech therapy. Megan believes that technology plays a critical role in improving aphasia outcomes and humanizing clinical services.
More in ‘ What Is ’
What is the Communication Problem?
Learn about the 4 types of acquired communication disorders that may affect the way a stroke survivor speaks. Find out what you can do once you understand what's happening.
What is Brain Injury?
Damage to the brain can result in problems in every area of life. Learn more about the types, causes, and effects of brain injury, as well as how SLPs can help to recover function.
6 min read
What is Dysphagia?
Dysphagia means difficulty swallowing. Learn more about the causes, symptoms, diagnosis, and treatment of dysphagia for people with swallowing disorders.
5 min read
What is a Stroke?
Find out the types, causes, how to prevent a stroke, how to spot one happening, and what happens afterwards as survivors try to recover through rehabilitation.
What is Apraxia?
Apraxia of speech is common after a stroke, leaving the patient with impaired communication. Find out what this acquired disorder is all about & what to do.
What is a Cognitive-Communication Disorder?
After a stroke, brain injury, or in dementia, communication can suffer along with cognition. Learn why and what to do for cognitive-communication disorders.
7 min read
What is Primary Progressive Aphasia?
PPA is a type of dementia that gradually impairs the ability to use language over time. Learn what it is, how it is diagnosed & treated, and what you can do to help.

What is Global Aphasia?
Global aphasia is the most severe and devastating type of aphasia. Learn what it is and how you can better communicate with a person who has global aphasia.
What is Fluent Aphasia?
Fluent aphasia is a disorder with effortless but largely meaningless speech. Learn what it is, see a video, and find out how to help Wernicke's-type aphasia.
What is Broca’s Aphasia?
Learn what Broca's aphasia is, see a video of what it sounds like, and find out how to help a person with the frustrating condition of expressive or non-fluent aphasia.
What is Aphasia?
Aphasia is a language disorder after a stroke. Learn what causes it, what you can do when you meet a person with aphasia, and how it can vary.
What is Left Neglect?
A step-by-step guide to visual scanning treatment, an evidence-based cognitive therapy technique to improve visual attention for right or left neglect.
8 min read
Best Exercises for Children with Dysarthria
Dysarthria is a collective term used to describe motor-speech disorders. It can affect anyone irrespective of age, gender, and family history.
Childhood dysarthria of speech is typically a result of neurological damage that causes weakness in the muscles necessary for producing speech. The nerve damage resulting in this motor-speech disorder may be due to traumatic brain injury (TMI), stroke(s), aneurysm(s), or neurodegenerative disease.
If you or your loved one has been diagnosed with dysarthria, it is wise to consult a neurologist to determine the actual cause.
What Causes Dysarthria?
The neurological damage that may contribute to or cause dysarthria include –
- Brain tumors
- Congenital conditions (cerebral palsy, congenital suprabulbar palsy, Chiari malformation)
- Degenerative disorders conditions (ALS, Huntington’s disease, and Parkinson's disease)
- Demyelinating diseases (multiple sclerosis, Guillain-Barre, and other autoimmune disorders)
- Inflammatory conditions (encephalitis and meningitis)
- Vascular conditions (strokes, aneurysms, or Moyamoya disease)
- Exposure to heavy metals or toxins
These are some of the more common causes of dysarthria. There can be lesser-known conditions and disorders that lead to dysarthria as well.
What Are Some Of The Best Exercises For Dysarthria Treatment?
Although dysarthria can be of various types, it is characterized by weakness in the face, lips, tongue, and throat muscles. Therefore, the treatment for childhood dysarthria primarily focuses on strengthening these muscles through daily exercises.
These are a few exercises trained speech therapists use to stimulate muscle movement in children with dysarthria –
Here's the thing – children don't like boring exercises, especially when they have to do it every day. So, we need to find more than one way to make speech therapy for slurred speech fun, interactive, and rewarding for them.
Dysarthria: Exercises For Their Lips
1. Let's begin with something fun – tell your child to mimic you . Say "ooooo" with an exaggerated lip movement. Follow it up with "eeee." Now, combine them to say "ooooeeee."

You can tell your child that you are making the sound a police car makes and repeat “oooo-eeee” a couple of times with them.
Every time you do this exercise, you can tell your child, “Hey, what sound does a police car make?”
2. Blow bubbles. Get a bubble maker or make your own at home. Children typically love to blow bubbles and play with them. You can also switch your game up with kazoos, whistles, and horns!

It might get a little loud in the house for about 2 minutes, but your child is going to love this exercise!
3. Try to say “puh” with an emphasis on the pop.
You can tell them that this is the sound a bubble makes when it pops. And when it's time for their exercise, you can ask them, "So what sound does a popping bubble make?"
You can combine exercises 2 and 3 for some fun and effectiveness!
4. Pose for selfies with your child . While striking out cool poses, ask them to say “cheese” and smile as widely as they can.

You can use the photos for future reference of improvement as well! Repeat this at least 5 times during the exercise each day.
5. Get a couple of metal straws. Encourage your child to drink through the straws most of the time. It is a great activity for the lips, cheeks, and tongue.

Note: Try this only if your child has enough oral-motor control to not choke on the fluid. Drinking through a straw will require your child to tighten the cheeks and tongue, retract the tongue, and purse the lips.
Ask your speech therapist if your child is ready to begin drinking through a straw. A speech therapist can teach your child to drink through a straw if they don’t know how to already!
6. Tell your child to puff up both cheeks and hold the air . Shift all the air to one cheek, hold for 2 seconds, and then transfer it to the other cheek. Tell them to puff out their upper lip, and next, the lower lip!
You can tell them this is how we hold our breath while taking a dip in the pool. This activity for children with dysarthria will be enjoyable for your child.
7. Teach your child how to blow a kiss. Ask them to purse their lips to make a kiss. Next, tell them to move the kiss to the right and next to the left.
You could encourage them by blowing a kiss back. And move from left to right as they move their kiss!
Dysarthria: Exercises For The Tongue
1. What do we sing when we forget the lyrics? Say “lalalalalala” by only moving the tip of the tongue. Tell your child to follow, but they should not move their jaws at all.
You can do this now and then with your child since it is a simple exercise for kids with Dysarthria that is entertaining!
2. You need to help your child practice tongue-tip sounds. It may not be as fun as the other exercises, but it's helpful.
Ask your child to follow as you say, “t-t-t-t-t-t-t,” “n-n-n-n-n” and “d-d-d-d-d-d”. For keeping things interesting, you can move to a combination of these sounds once they master the singular sounds.
3. Teach your child to do a tongue-pop. Young children typically enjoy making new sounds, especially if they sound like animals, toys, or vehicles.
You may tell them that a tongue pop sounds like a lizard or gecko! They should have fun mimicking one since this exercise has to be done 25-times in a row.
4. The aim of this exercise is to get your child to say "go" with exaggeration. You can make it a part of a word-play, where you say "come," and your child replies with "go." Or you can find nursery rhyme verses that have "go" in them and ask your child to fill the word in for you as you recite the rhyme.

5. Is there a candy your child loves, or maybe a lollipop flavor? Rub the candy on the lips and get them to lick it off.

You can use frosting, chocolate, or peanut butter to add variation to this exercise. Just ensure that your child licks the entire food off each time to extend their tongue as much as possible.
6. This exercise is a little tricky, and you may need the help of a speech therapist. Your child should place the tongue on the roof of their mouth. Next, they should hold it with suction for around 10 seconds.
Once they have mastered this, they should move their jaw down and up while the tongue is still in suction.
Dysarthria: Exercises For The Cheeks
1. Ask them to put their lips together and suck their cheeks in. Isn’t that the face fish make?
Well, when it’s time to repeat the exercise, you can ask your child to make the fish-face for you. And you can make the same face with them for them to model and for some pure fun.
2. You can use drinking through a straw technique to strengthen cheek muscles, as well as lip muscles.
Dysarthria: Exercises For The Jaws
1. Request your child to follow your jaw movements. Open your jaw wide so that it's fully stretched, but doesn't hurt. Hold it for 5 seconds before relaxing.
Repeat this 5 times each day.

2. Move your jaw to the right until it's stretched but not painful. Tell your child to do the same. Hold it for 5 seconds and then relax.
Repeat by stretching it to the left. Hold it for 5 seconds and relax.
Repeat this set 5 times.
3. Make a circular movement with your jaw slowly. Stretch it in each direction fully. When you complete a circle, you can relax your jaw.
Repeat this movement 5 times per day.
Dysarthria: Additional Tools for Help
Sometimes, it is not enough to tell a child to "put your tongue against the roof of your mouth." They need tactile cues. For that, several speech therapists use a probe or Z-vibe. These are safe and simple tools to guide your child during these dysarthria speech therapy exercises. Using tactile cues can tell your child exactly where they need to put their tongue, where they need to exert pressure, and how they need to move their cheeks.
You can also do these exercises for dysarthria at home with your child in front of a mirror. It will help them see the difference and similarities between your performances.
Treatment Goals for Dysarthria
Speech therapists leverage a range of exercises to treat dysarthria. Tongue, lips, cheek, and jaw exercises are commonly utilized in dysarthria treatment to boost the strength of the weakened muscles.
These are mostly non-speech oral motor exercises (NSOME), which are different from the speech therapy exercises used for the treatment of stuttering and other fluency disorders.
The main goal of therapy for dysarthria is to make one’s speech more understandable. These exercises may help to –
- Improve the person’s pronunciation
- Slow their rate of speech to reduce pressure
- Control their breathing so they don’t run out of breath while talking
- Modulate the loudness of their voice while speaking
- Increase the strength and range of movement of the muscles involved in producing speech
What Can You Do?
A person with dysarthria may find it difficult to express themselves with spoken words. While practicing these exercises with them, you can also introduce alternative augmentative communication (AAC) methods. You can also use sign language or gestures to communicate with each other.
When they are speaking, make sure to hold eye contact, speak slowly and ask yes-or-no questions only. Do let them know when you have trouble understanding them, but do so politely. Try not to speak for them unless it is absolutely necessary!
Research shows that progress after starting regular NSOME exercises may be slow. Therefore, it is important to not give up once you have begun these exercises.
Related Posts
- Therapy Protocol
- Group Video Calls
- Privacy Policy
- Terms of Service
- Cancellation & Refund

IMAGES
VIDEO
COMMENTS
During articulation treatment, give: Phonetic placement cues (how to position the mouth, tongue, lips, or jaw during speech) Biofeedback about positioning (use a mirror, take pictures or video, etc.) Models of correct positioning. Encouragement! For more articulation exercises and materials, visit our shop. 3.
Therapy tip. Drill, drill, drill! Practice more than once a day. Begin by explicitly teaching the strategies. Informally assess carryover frequently. Repetition to start, then variable practice. Move up and down the articulation hierarchy . Example therapy sequence for a mod-severe dysarthria. Make the task unpredictable .
Therapy and Exercises: Speech-language therapy for dysarthria may involve various exercises and techniques to improve articulation, voice production, and overall communication skills. Communication Strategies: A speech-language therapist can provide communication strategies and techniques to individuals with dysarthria to enhance their ability ...
Dysarthria refers to a group of neurogenic speech disorders characterized by "abnormalities in the strength, speed, range, steadiness, tone, or accuracy of movements required for breathing, phonatory, resonatory, articulatory, or prosodic aspects of speech production" (Duffy, 2020, p. 3). These changes are due to one or more sensorimotor ...
Dysarthria is a motor speech disorder. This happens when brain or nerve damage changes the way your muscles work. It can be mild to severe. Children and adults can have dysarthria. There are many reasons people have trouble talking. Dysarthria can happen with other speech and language problems.
Dysarthria is a motor speech disorder involving weakness, paralysis, spasticity, or incoordination of speech-producing muscles. It results from damage to the nervous system and may affect approximately 1 in 1,000 children. Speech in these children can be slow, strained, monotone, breathy, and quiet, with imprecise articulation.
People with dysarthria often benefit from speech therapy to improve communication. A speech-language pathologist can also work with your family and loved ones to teach them how to communicate with you better. During speech therapy sessions, you may learn: Exercises to strengthen your tongue, lips and jaw muscles.
improving speech articulation for patients with dysarthria. Slowing down the words themselves, and/or performing a half-second pause between words is another way to perform a speech articulation rate change. It is recommended to first practice this strategy in reading tasks, as this will be a strategy that requires some
Treatment. Speech therapy is often a part of stroke rehabilitation. Your treatment will depend on the cause and severity of your symptoms and the type of dysarthria you have. Your doctor will treat the cause of your dysarthria when possible, which may improve your speech. If your dysarthria is caused by prescription medications, talk to your ...
Dysarthria is caused by damage to areas of the brain that control motor aspects of speech. Dysarthria can vary from being mild to severe; causing the individual great difficulty when trying to communicate verbally. Signs of dysarthria may include: • Slurred speech • Speaking slowly • Speaking too fast • Effortful speech • Face, lips ...
Dysarthria is a motor speech disorder that results from stroke, brain injury, brain tumor or other neurologic conditions. Dysarthria is characterized by weakness, incoordination or paralysis of the muscles used for speech production. It generally effects one side of the face and/or neck. In some cases, the muscle deficits are easy to see, such ...
Speech drills: Another form of treatment for dysarthria can include speech drills. Similarly, to motor exercises, speech drills assist in the relearning and restrengthening of the articulators/muscles. A speech-language pathologist can also offer emotional support as well as refer patients to professionals to assist in counseling, if that is ...
dysarthria (and sometimes apraxia): CP, the most common neuromotor disability in children-3.1-3.6 per 1000 children (Christensen et al., 2014)-So dysarthria in children with CP is a good place to start • Paucity of treatment research on children with dysarthria, regardless of etiology (CP or other) or type (spastic or other)
Dysarthria is a motor-speech disorder that results in unclear speech. This inability to speak clearly is because of weakness, slowness, or lack of coordination in the muscles of the mouth, voice, and lungs. Dysarthria results from damage to the nervous system. There are several different types of dysarthria.
Speech disorders can result (1) from sensorimotor impairments of articulatory movements = dysarthria, or (2) from structural changes of the speech organs, in adults particularly after surgical and radiochemical treatment of tumors = dysglossia. The decrease of intelligibility, a reduced vocal stamina, the stigmatization of a conspicuous voice ...
Dysarthria represents a group of motor speech disorders (MSDs) characterized by weakness, slowness, and/or lack of coordination of the speech musculature as a result of damage to the nervous system. This article reviews the history of our attempt to provide an evidence base for dysarthria intervention, to describe some recent efforts, and to ...
Severe spas-tic-ataxic dysarthria in a child with traumatic brain injury: Questions for management.. K.M. Yorkston & D.R. Beukelman (Eds.), Recent ... Speech and language therapy for dysarthria due to nonprogressive brain damage: A systematic Cochrane review. Clinical Rehabilitation, 16(1), 61-68. ...
Tongue, lips, cheek, and jaw exercises are commonly utilized in dysarthria treatment to boost the strength of the weakened muscles. These are mostly non-speech oral motor exercises (NSOME), which are different from the speech therapy exercises used for the treatment of stuttering and other fluency disorders.
IntroductionSpastic dysarthria is a motor speech disorder produced by bilateral damage to the activation pathways of the central nervous system. ... New therapy for treating hypernasal speech using continuous positive airway pressure (CPAP). ... A randomized study comparing the shaker exercise with traditional therapy: A preliminary study ...
treatment of speech rate and intonation with the Prosodietrainer can have a positive effect on the intelligibility of individuals with hypokinetic dysarthria due to Parkinson's disease. The perspective of potential progress in a relatively short time can be beneficial for motivation and therapeutic compliance.
Call UMMC Speech-Language Pathology 601-815-6064 or email [email protected]. Back to ENT Patient Information. Your tongue is responsible for touching very specific places in your mouth at a high rate of speed to create clear speech. This can be difficult following a surgery where tissue in the mouth is removed. Your tongue will be less mobile and ...