Module 9: Substance-Related and Addictive Disorders
Case studies: substance-abuse disorders, learning objectives.
- Identify substance abuse disorders in case studies

Case Study: Benny
The following story comes from Benny, a 28-year-old living in the Metro Detroit area, USA. Read through the interview as he recounts his experiences dealing with addiction and recovery.
Q : How long have you been in recovery?
Benny : I have been in recovery for nine years. My sobriety date is April 21, 2010.
Q: What can you tell us about the last months/years of your drinking before you gave up?
Benny : To sum it up, it was a living hell. Every day I would wake up and promise myself I would not drink that day and by the evening I was intoxicated once again. I was a hardcore drug user and excessively taking ADHD medication such as Adderall, Vyvance, and Ritalin. I would abuse pills throughout the day and take sedatives at night, whether it was alcohol or a benzodiazepine. During the last month of my drinking, I was detached from reality, friends, and family, but also myself. I was isolated in my dark, cold, dorm room and suffered from extreme paranoia for weeks. I gave up going to school and the only person I was in contact with was my drug dealer.
Q : What was the final straw that led you to get sober?
Benny : I had been to drug rehab before and always relapsed afterwards. There were many situations that I can consider the final straw that led me to sobriety. However, the most notable was on an overcast, chilly October day. I was on an Adderall bender. I didn’t rest or sleep for five days. One morning I took a handful of Adderall in an effort to take the pain of addiction away. I knew it wouldn’t, but I was seeking any sort of relief. The damage this dosage caused to my brain led to a drug-induced psychosis. I was having small hallucinations here and there from the chemicals and a lack of sleep, but this time was different. I was in my own reality and my heart was racing. I had an awful reaction. The hallucinations got so real and my heart rate was beyond thumping. That day I ended up in the psych ward with very little recollection of how I ended up there. I had never been so afraid in my life. I could have died and that was enough for me to want to change.
Q : How was it for you in the early days? What was most difficult?
Benny : I had a different experience than most do in early sobriety. I was stuck in a drug-induced psychosis for the first four months of sobriety. My life was consumed by Alcoholics Anonymous meetings every day and sometimes two a day. I found guidance, friendship, and strength through these meetings. To say early sobriety was fun and easy would be a lie. However, I did learn it was possible to live a life without the use of drugs and alcohol. I also learned how to have fun once again. The most difficult part about early sobriety was dealing with my emotions. Since I started using drugs and alcohol that is what I used to deal with my emotions. If I was happy I used, if I was sad I used, if I was anxious I used, and if I couldn’t handle a situation I used. Now that the drinking and drugs were out of my life, I had to find new ways to cope with my emotions. It was also very hard leaving my old friends in the past.
Q : What reaction did you get from family and friends when you started getting sober?
Benny : My family and close friends were very supportive of me while getting sober. Everyone close to me knew I had a problem and were more than grateful when I started recovery. At first they were very skeptical because of my history of relapsing after treatment. But once they realized I was serious this time around, I received nothing but loving support from everyone close to me. My mother was especially helpful as she stopped enabling my behavior and sought help through Alcoholics Anonymous. I have amazing relationships with everyone close to me in my life today.
Q : Have you ever experienced a relapse?
Benny : I experienced many relapses before actually surrendering. I was constantly in trouble as a teenager and tried quitting many times on my own. This always resulted in me going back to the drugs or alcohol. My first experience with trying to become sober, I was 15 years old. I failed and did not get sober until I was 19. Each time I relapsed my addiction got worse and worse. Each time I gave away my sobriety, the alcohol refunded my misery.
Q : How long did it take for things to start to calm down for you emotionally and physically?
Benny : Getting over the physical pain was less of a challenge. It only lasted a few weeks. The emotional pain took a long time to heal from. It wasn’t until at least six months into my sobriety that my emotions calmed down. I was so used to being numb all the time that when I was confronted by my emotions, I often freaked out and didn’t know how to handle it. However, after working through the 12 steps of AA, I quickly learned how to deal with my emotions without the aid of drugs or alcohol.
Q : How hard was it getting used to socializing sober?
Benny : It was very hard in the beginning. I had very low self-esteem and had an extremely hard time looking anyone in the eyes. But after practice, building up my self-esteem and going to AA meetings, I quickly learned how to socialize. I have always been a social person, so after building some confidence I had no issue at all. I went back to school right after I left drug rehab and got a degree in communications. Upon taking many communication classes, I became very comfortable socializing in any situation.
Q : Was there anything surprising that you learned about yourself when you stopped drinking?
Benny : There are surprises all the time. At first it was simple things, such as the ability to make people smile. Simple gifts in life such as cracking a joke to make someone laugh when they are having a bad day. I was surprised at the fact that people actually liked me when I wasn’t intoxicated. I used to think people only liked being around me because I was the life of the party or someone they could go to and score drugs from. But after gaining experience in sobriety, I learned that people actually enjoyed my company and I wasn’t the “prick” I thought I was. The most surprising thing I learned about myself is that I can do anything as long as I am sober and I have sufficient reason to do it.
Q : How did your life change?
Benny : I could write a book to fully answer this question. My life is 100 times different than it was nine years ago. I went from being a lonely drug addict with virtually no goals, no aspirations, no friends, and no family to a productive member of society. When I was using drugs, I honestly didn’t think I would make it past the age of 21. Now, I am 28, working a dream job sharing my experience to inspire others, and constantly growing. Nine years ago I was a hopeless, miserable human being. Now, I consider myself an inspiration to others who are struggling with addiction.
Q : What are the main benefits that emerged for you from getting sober?
Benny : There are so many benefits of being sober. The most important one is the fact that no matter what happens, I am experiencing everything with a clear mind. I live every day to the fullest and understand that every day I am sober is a miracle. The benefits of sobriety are endless. People respect me today and can count on me today. I grew up in sobriety and learned a level of maturity that I would have never experienced while using. I don’t have to rely on anyone or anything to make me happy. One of the greatest benefits from sobriety is that I no longer live in fear.
Case Study: Lorrie

Figure 1. Lorrie.
Lorrie Wiley grew up in a neighborhood on the west side of Baltimore, surrounded by family and friends struggling with drug issues. She started using marijuana and “popping pills” at the age of 13, and within the following decade, someone introduced her to cocaine and heroin. She lived with family and occasional boyfriends, and as she puts it, “I had no real home or belongings of my own.”
Before the age of 30, she was trying to survive as a heroin addict. She roamed from job to job, using whatever money she made to buy drugs. She occasionally tried support groups, but they did not work for her. By the time she was in her mid-forties, she was severely depressed and felt trapped and hopeless. “I was really tired.” About that time, she fell in love with a man who also struggled with drugs.
They both knew they needed help, but weren’t sure what to do. Her boyfriend was a military veteran so he courageously sought help with the VA. It was a stroke of luck that then connected Lorrie to friends who showed her an ad in the city paper, highlighting a research study at the National Institute of Drug Abuse (NIDA), part of the National Institutes of Health (NIH.) Lorrie made the call, visited the treatment intake center adjacent to the Johns Hopkins Bayview Medical Center, and qualified for the study.
“On the first day, they gave me some medication. I went home and did what addicts do—I tried to find a bag of heroin. I took it, but felt no effect.” The medication had stopped her from feeling it. “I thought—well that was a waste of money.” Lorrie says she has never taken another drug since. Drug treatment, of course is not quite that simple, but for Lorrie, the medication helped her resist drugs during a nine-month treatment cycle that included weekly counseling as well as small cash incentives for clean urine samples.
To help with heroin cravings, every day Lorrie was given the medication buprenorphine in addition to a new drug. The experimental part of the study was to test if a medication called clonidine, sometimes prescribed to help withdrawal symptoms, would also help prevent stress-induced relapse. Half of the patients received daily buprenorphine plus daily clonidine, and half received daily buprenorphine plus a daily placebo. To this day, Lorrie does not know which one she received, but she is deeply grateful that her involvement in the study worked for her.
The study results? Clonidine worked as the NIDA investigators had hoped.
“Before I was clean, I was so uncertain of myself and I was always depressed about things. Now I am confident in life, I speak my opinion, and I am productive. I cry tears of joy, not tears of sadness,” she says. Lorrie is now eight years drug free. And her boyfriend? His treatment at the VA was also effective, and they are now married. “I now feel joy at little things, like spending time with my husband or my niece, or I look around and see that I have my own apartment, my own car, even my own pots and pans. Sounds silly, but I never thought that would be possible. I feel so happy and so blessed, thanks to the wonderful research team at NIDA.”
- Liquor store. Authored by : Fletcher6. Located at : https://commons.wikimedia.org/wiki/File:The_Bunghole_Liquor_Store.jpg . License : CC BY-SA: Attribution-ShareAlike
- Benny Story. Provided by : Living Sober. Located at : https://livingsober.org.nz/sober-story-benny/ . License : CC BY: Attribution
- One patientu2019s story: NIDA clinical trials bring a new life to a woman struggling with opioid addiction. Provided by : NIH. Located at : https://www.drugabuse.gov/drug-topics/treatment/one-patients-story-nida-clinical-trials-bring-new-life-to-woman-struggling-opioid-addiction . License : Public Domain: No Known Copyright

Substance Use Disorders and Addiction: Mechanisms, Trends, and Treatment Implications
Information & authors, metrics & citations, view options, insights into mechanisms related to cocaine addiction using a novel imaging method for dopamine neurons, treatment implications of understanding brain function during early abstinence in patients with alcohol use disorder, relatively low amounts of alcohol intake during pregnancy are associated with subtle neurodevelopmental effects in preadolescent offspring, increased comorbidity between substance use and psychiatric disorders in sexual identity minorities, trends in nicotine use and dependence from 2001–2002 to 2012–2013, conclusions, information, published in.

- Substance-Related and Addictive Disorders
- Addiction Psychiatry
- Transgender (LGBT) Issues
Competing Interests
Export citations.
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download. For more information or tips please see 'Downloading to a citation manager' in the Help menu .
| Format | |
|---|---|
| Citation style | |
| Style | |
To download the citation to this article, select your reference manager software.
There are no citations for this item
View options
Login options.
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Not a subscriber?
Subscribe Now / Learn More
PsychiatryOnline subscription options offer access to the DSM-5-TR ® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).
Share article link
Copying failed.
NEXT ARTICLE
Request username.
Can't sign in? Forgot your username? Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username
Create a new account
Change password, password changed successfully.
Your password has been changed
Reset password
Can't sign in? Forgot your password?
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password.
Your Phone has been verified
As described within the American Psychiatric Association (APA)'s Privacy Policy and Terms of Use , this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences. Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
Drugs, Brains, and Behavior: The Science of Addiction Drug Misuse and Addiction
What is drug addiction.
Addiction is defined as a chronic, relapsing disorder characterized by compulsive drug seeking and use despite adverse consequences. † It is considered a brain disorder, because it involves functional changes to brain circuits involved in reward, stress, and self-control. Those changes may last a long time after a person has stopped taking drugs. 11
Addiction is a lot like other diseases, such as heart disease. Both disrupt the normal, healthy functioning of an organ in the body, both have serious harmful effects, and both are, in many cases, preventable and treatable. If left untreated, they can last a lifetime and may lead to death.
Why do people take drugs?
In general, people take drugs for a few reasons:
- To feel good. Drugs can produce intense feelings of pleasure. This initial euphoria is followed by other effects, which differ with the type of drug used. For example, with stimulants such as cocaine, the high is followed by feelings of power, self-confidence, and increased energy. In contrast, the euphoria caused by opioids such as heroin is followed by feelings of relaxation and satisfaction.
- To feel better. Some people who suffer from social anxiety, stress, and depression start using drugs to try to feel less anxious. Stress can play a major role in starting and continuing drug use as well as relapse (return to drug use) in patients recovering from addiction.
- To do better. Some people feel pressure to improve their focus in school or at work or their abilities in sports. This can play a role in trying or continuing to use drugs, such as prescription stimulants or cocaine.
- Curiosity and social pressure. In this respect, teens are particularly at risk because peer pressure can be very strong. Adolescence is a developmental period during which the presence of risk factors, such as peers who use drugs, may lead to substance use.
If taking drugs makes people feel good or better, what's the problem?

When they first use a drug, people may perceive what seem to be positive effects. They also may believe they can control their use. But drugs can quickly take over a person's life. Over time, if drug use continues, other pleasurable activities become less pleasurable, and the person has to take the drug just to feel “normal.” They have a hard time controlling their need to take drugs even though it causes many problems for themselves and their loved ones. Some people may start to feel the need to take more of a drug or take it more often, even in the early stages of their drug use. These are the signs of an addiction.
Even relatively moderate drug use poses dangers. Consider how a social drinker can become intoxicated, get behind the wheel of a car, and quickly turn a pleasurable activity into a tragedy that affects many lives. Occasional drug use, such as misusing an opioid to get high, can have similarly disastrous effects, including impaired driving and overdose.
Do people choose to keep using drugs?
The initial decision to take drugs is typically voluntary. But with continued use, a person's ability to exert self-control can become seriously impaired. This impairment in self-control is the hallmark of addiction.
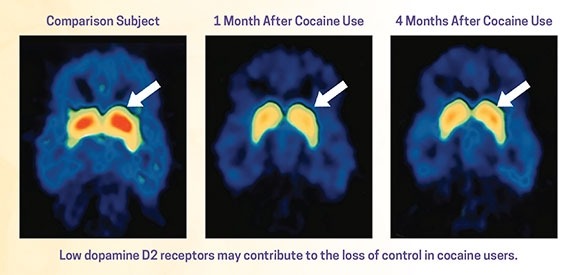
Brain imaging studies of people with addiction show physical changes in areas of the brain that are critical to judgment, decision-making, learning and memory, and behavior control. 12 These changes help explain the compulsive nature of addiction.
Why do some people become addicted to drugs, while others do not?
As with other diseases and disorders, the likelihood of developing an addiction differs from person to person, and no single factor determines whether a person will become addicted to drugs. In general, the more risk factors a person has, the greater the chance that taking drugs will lead to drug use and addiction. Protective factors, on the other hand, reduce a person's risk. Risk and protective factors may be either environmental or biological.
| Risk Factors | Protective Factors |
|---|---|
| Aggressive behavior in childhood | Self-efficacy (belief in self-control) |
| Lack of parental supervision | Parental monitoring and support |
| Low peer refusal skills | Positive relationships |
| Drug experimentation | Good grades |
| Availability of drugs at school | School anti-drug policies |
| Community poverty | Neighborhood resources |
What biological factors increase risk of addiction?
Biological factors that can affect a person's risk of addiction include their genes, stage of development, and even gender or ethnicity. Scientists estimate that genes, including the effects environmental factors have on a person's gene expression, called epigenetics, account for between 40 and 60 percent of a person's risk of addiction. 27 Also, teens and people with mental disorders are at greater risk of drug use and addiction than others. 28
What environmental factors increase the risk of addiction?
Environmental factors are those related to the family, school, and neighborhood. Factors that can increase a person's risk include the following:
- Home and Family. The home environment, especially during childhood, is a very important factor. Parents or older family members who use drugs or misuse alcohol, or who break the law, can increase children's risk of future drug problems. 29
- Peer and School. Friends and other peers can have an increasingly strong influence during the teen years. Teens who use drugs can sway even those without risk factors to try drugs for the first time. Struggling in school or having poor social skills can put a child at further risk for using or becoming addicted to drugs. 30
What other factors increase the risk of addiction?
- Early use. Although taking drugs at any age can lead to addiction, research shows that the earlier people begin to use drugs, the more likely they are to develop serious problems. 31 This may be due to the harmful effect that drugs can have on the developing brain. 32 It also may result from a mix of early social and biological risk factors, including lack of a stable home or family, exposure to physical or sexual abuse, genes, or mental illness. Still, the fact remains that early use is a strong indicator of problems ahead, including addiction.
- How the drug is taken. Smoking a drug or injecting it into a vein increases its addictive potential. 33,34 Both smoked and injected drugs enter the brain within seconds, producing a powerful rush of pleasure. However, this intense high can fade within a few minutes. Scientists believe this powerful contrast drives some people to repeatedly use drugs to recapture the fleeting pleasurable state.
Images of Brain Development in Healthy Children and Teens (Ages 5-20)
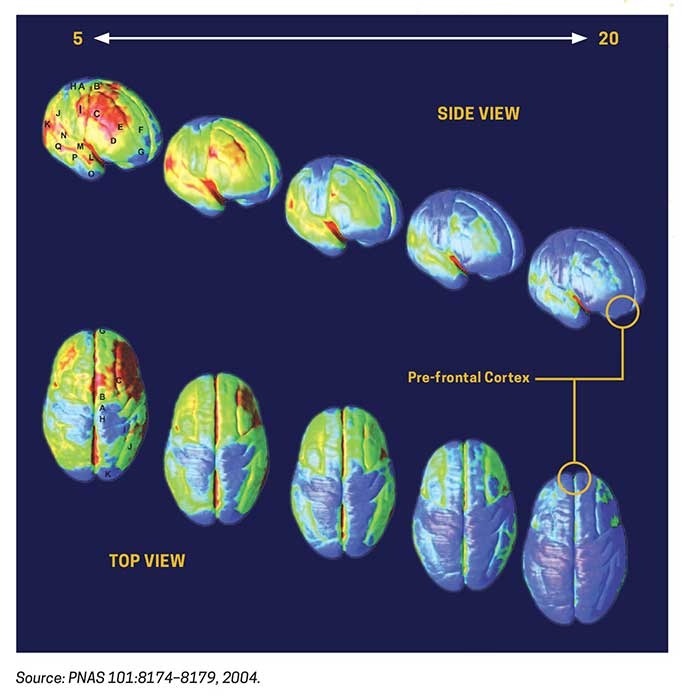
The brain continues to develop into adulthood and undergoes dramatic changes during adolescence.
One of the brain areas still maturing during adolescence is the prefrontal cortex—the part of the brain that allows people to assess situations, make sound decisions, and keep emotions and desires under control. The fact that this critical part of a teen’s brain is still a work in progress puts them at increased risk for trying drugs or continuing to take them. Introducing drugs during this period of development may cause brain changes that have profound and long-lasting consequences.
† The term addiction as used in this booklet is equivalent to a severe substance use disorder as defined by the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5, 2013).

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

The NIAAA is the lead agency for U.S. research on the causes, consequences, prevention and treatment of alcohol use disorder and alcohol-related problems.
National Institute on Alcohol Abuse and Alcoholism (NIAAA)
Major research initiatives.
Addressing alcohol-related issues—from basic science to clinical studies.
Extramural Research: Research at Grantee Institutions
Primary areas of research, funding opportunities, and staff listings for Extramural Research Divisions.
Intramural Research: Research in NIAAA Labs
Organization, primary areas of research, and staff listings for Intramural Research Labs.
Guidance and policies for scientists pursuing alcohol research.

The Strategic Plan describes research goals, themes, and programs.

NIAAA’s peer-reviewed scientific journal.

About NIAAA's Small Business Research Funding Programs

NIAAA surveillance reports on alcohol-related problems.
Research on factors that compel youth to begin and continue drinking.
Research on medications in development for treatment of alcohol use disorder.
The NIAAA data archive is a data repository that houses and shares human subjects data generated by NIAAA-funded research.
Resources include biological specimens, animals, data, materials, tools, or services made available to any qualified investigato r to accelerate alcohol-related research in a cost-effective manner.
Current and potential alcohol research investigators and trainees are encouraged to subscribe to our new email list to receive NIAAA information and updates relevant to the research community. To sign up, enter your contact information below.
Sign Up for Email Updates
niaaa.nih.gov
An official website of the National Institutes of Health and the National Institute on Alcohol Abuse and Alcoholism
Alcohol Abuse in Society: Case Studies
Cite this chapter.

- Adrian Bonner 3 &
- James Waterhouse 4
34 Accesses
The last three chapters have demonstrated how routine data may be collected from the health service and forensic medicine. These data present a view of the occurrence of alcohol and drug abuse in society which is generated from a ‘medical model’. As useful as this approach is, it does not take into account the nature and needs of specific groups. To do this a more ‘socially appropriate perspective’ can be used. The following case studies illustrate some of the problems resulting from methodological issues in this area of investigation and, in particular, from studies undertaken in short-term projects undertaken by graduate students. Important discussions relating to: ‘what level of consumption constitutes abuse ’ ‘alcohol usage by the elderly’, and ‘the effectiveness of health education’ will be introduced.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Unable to display preview. Download preview PDF.
Similar content being viewed by others

Alcohol Use

Sociological Testimony in Alcohol- and Other Drug-Associated Litigation

Alcohol Use in Sub-Saharan Africa
Anderson, P. (1984) ‘Alcohol Consumption of Undergraduates at Oxford University’, Alcohol and Alcoholism , 19:pp. 77–84.
Google Scholar
Black, D. and Weare, K. (1989) ‘Knowledge and Attitudes about Alcohol in 17- and 18-Year-Olds’, Health Education Journal , 48 (2):pp. 69–73.
Article Google Scholar
Cyster, R. and McEwen, J. (1987) ‘Alcohol Education in the Workplace’, Health Education Journal , 46 (4):pp. 156–61.
Davies, J. (1991) ‘Learning to Drink’, paper presented at a national conference on ‘Alcohol and Young People’, 8 October 1991, Queen Mother Conference Centre, Royal College of Physicians, Edinburgh.
Gillies, P. (1991) ‘What Can Education Achieve?’, paper presented at a national conference on ‘Alcohol and Young People’, 8 October 1991, Queen Mother Conference Centre, Royal College of Physicians, Edinburgh.
Grant, M. (1981) ‘Aims, Form and Content: First Steps in Developing a Taxonomy of Preventative Education in Drug and Alcohol Abuse’, in L. R. H. Drew et al . (eds), Man, Drugs, and Society: Current Perspectives (Canberra: Australian Foundation on Alcoholism and Drug Dependence).
Haack, M. (1988) ‘Stress and Impairment among Nursing Students’, Research in Nursing and Health , 11:pp. 125–34.
Haack, M. and Harford, T. (1984) ‘Drinking Patterns among Student Nurses’, The International Journal of the Addictions , 19 (5):pp. 577–83.
Hopkins, R., Maussa, A., Kearney, K. and Weisheit, R. (1988) ‘Comprehensive Evaluation of a Model Alcohol Education Curriculum’, Journal of Studies on Alcohol , 49 (1):pp. 38–50.
Hutchison, S. (1986) ‘Chemically Dependent Nurses: The Trajectory towards Self Annihilation’, Nursing Research , 35 (July/August):pp. 196–201.
Maussa, A., Hopkins, R., Weisheit, R., and Kearney, K. (1988) The Problematic Prospects for Prevention in the Classroom: Should Alcohol Education Programmes be Expected to Reduce Drinking by Youth?’, Journal of Studies in Alcohol , 49 (1):pp. 51–61.
Plant, M. (1991) ‘Heavy Drinkers: Are They Distinctive?’, paper presented at a national conference on ‘Alcohol and Young People’, 8 October 1991, Queen Mother Conference Centre, Royal College of Physicians, Edinburgh.
Plant, M. L., Plant, M. A. and Foster, J. (1991) ‘Alcohol, Tobacco and Illicit Drug Use Amongst Nurses: A Scottish Study’, Drug and Alcohol Dependence , 28:pp. 195–202.
Roberts, R. (1988) ‘Hiccups in Alcohol Education’, Health Education Journal , 47 (213):pp. 73–5.
Royal College of General Practitioners (1986) Alcohol: A Balanced View (London: Tavistock).
Saltz, R., and Elandt, D. (1986) ‘College Students Drinking Studies 1976–1985’, Contemporary Drug Problems (Spring):pp. 117–59.
Wallace, P., Brennan, P., and Haines, A. (1987) ‘Drinking Patterns in General Practice Patients’, Journal of the Royal College of General Practitioners , 37:pp. 354–7.
Weichsler, H. and McFadden, M. (1979) ‘Drinking among College Students in New England; Extent, Social Correlates and Consequences of Alcohol’, Journal of Studies on Alcohol , 40:pp. 969–99.
West, R., Drummond, C., and Eames, K. (1990) ‘Alcohol Consumption, Problem Drinking and Anti-Social Behaviour in a Sample of College Students’, British Journal of Addiction , 85:pp. 479–86.
Download references
Author information
Authors and affiliations.
Addictive Behaviour Centre Roehampton Institute, London, UK
Adrian Bonner ( Director )
School of Biological Sciences, School of Human Biology, University of Manchester, UK
James Waterhouse ( Senior Research Fellow, Lecturer in Physiology )
You can also search for this author in PubMed Google Scholar
Editor information
Editors and affiliations.
Adrian Bonner ( Director ) ( Director )
James Waterhouse ( Senior Research Fellow, Lecturer in Physiology ) ( Senior Research Fellow, Lecturer in Physiology )
Copyright information
© 1996 Adrian Bonner and James Waterhouse
About this chapter
Bonner, A., Waterhouse, J. (1996). Alcohol Abuse in Society: Case Studies. In: Bonner, A., Waterhouse, J. (eds) Addictive Behaviour: Molecules to Mankind. Palgrave Macmillan, London. https://doi.org/10.1007/978-1-349-24657-1_17
Download citation
DOI : https://doi.org/10.1007/978-1-349-24657-1_17
Publisher Name : Palgrave Macmillan, London
Print ISBN : 978-0-333-64556-7
Online ISBN : 978-1-349-24657-1
eBook Packages : Palgrave Social & Cultural Studies Collection Social Sciences (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

In Crisis? Call or Text 988
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Alcohol, Tobacco, and Other Drugs
The use and misuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans.
The National Survey on Drug Use and Health (NSDUH) estimates allow researchers, clinicians, policymakers, and the general public to better understand and improve the nation’s behavioral health.
We know that drinking too much can harm your health . The Dietary Guidelines for Americans recommends that if adults (age 21 and older) choose to drink alcohol, drinking less is better for health than drinking more.
Tobacco, E-Cigarettes, and Vaping
Smoking harms nearly every organ in the body ― heart and blood vessel disease; lung disease; cancer (almost anywhere in your body); and impacts to your bones, eyes, teeth, gums, fertility and pregnancy.
Marijuana and CBD
Marijuana use comes with risks to health. Today’s marijuana is stronger than ever before.
States that have legalized marijuana regulate the drug in widely different ways ― and often it’s not being checked for its ingredients, purity, strength, or safety.
Prescriptions, Opioids, and Fake Pills
Opioid overdose is life-threatening. Overdose can happen, even with a prescription opioid. Naloxone can reverse an opioid overdose.
Other Drugs, Prevention, and Addiction
There’s a science to what works in prevention.
Drug addiction is a complex disease. Drugs change the brain, in ways that make it hard to quit.
Resources, Events, and Campaigns
Find resources to help individuals, families, schools, and communities.
- Open access
- Published: 30 August 2024
Research landscape analysis on dual diagnosis of substance use and mental health disorders: key contributors, research hotspots, and emerging research topics
- Waleed M. Sweileh 1
Annals of General Psychiatry volume 23 , Article number: 32 ( 2024 ) Cite this article
Metrics details
Substance use disorders (SUDs) and mental health disorders (MHDs) are significant public health challenges with far-reaching consequences on individuals and society. Dual diagnosis, the coexistence of SUDs and MHDs, poses unique complexities and impacts treatment outcomes. A research landscape analysis was conducted to explore the growth, active countries, and active journals in this field, identify research hotspots, and emerging research topics.
A systematic research landscape analysis was conducted using Scopus to retrieve articles on dual diagnosis of SUDs and MHDs. Inclusion and exclusion criteria were applied to focus on research articles published in English up to December 2022. Data were processed and mapped using VOSviewer to visualize research trends.
A total of 935 research articles were found. The number of research articles on has been increasing steadily since the mid-1990s, with a peak of publications between 2003 and 2012, followed by a fluctuating steady state from 2013 to 2022. The United States contributed the most articles (62.5%), followed by Canada (9.4%). The Journal of Dual Diagnosis , Journal of Substance Abuse Treatment , and Mental Health and Substance Use Dual Diagnosis were the top active journals in the field. Key research hotspots include the comorbidity of SUDs and MHDs, treatment interventions, quality of life and functioning, epidemiology, and the implications of comorbidity. Emerging research topics include neurobiological and psychosocial aspects, environmental and sociocultural factors, innovative interventions, special populations, and public health implications.
Conclusions
The research landscape analysis provides valuable insights into dual diagnosis research trends, active countries, journals, and emerging topics. Integrated approaches, evidence-based interventions, and targeted policies are crucial for addressing the complex interplay between substance use and mental health disorders and improving patient outcomes.

Introduction
Substance use disorders (SUDs) refer to a range of conditions characterized by problematic use of psychoactive substances, leading to significant impairment in physical, psychological, and social functioning [ 1 ]. These substances may include alcohol, tobacco, illicit drugs (e.g., cocaine, opioids, cannabis), and prescription medications. The global burden of SUDs is substantial, with far-reaching consequences on public health, socio-economic development, and overall well-being. For instance, alcohol abuse accounts for 3 million deaths worldwide annually, while the opioid crisis has escalated to unprecedented levels in certain regions, such as North America, resulting in tens of thousands of overdose deaths per year [ 2 , 3 , 4 ]. Mental health disorders (MHDs) encompass a wide range of conditions that affect mood, thinking, behavior, and emotional well-being [ 5 ]. Examples of MHDs include depression, anxiety disorders, post-traumatic stress disorder (PTSD), bipolar disorder, schizophrenia, and eating disorders. These conditions can significantly impair an individual's ability to function, negatively impacting their quality of life, relationships, and overall productivity [ 6 , 7 , 8 ]. Furthermore, certain MHD such as major depressive disorder and anxiety are often associated with specific affective temperaments, hopelessness, and suicidal behavior and grasping such connections can help in crafting customized interventions to reduce suicide risk [ 9 ]. In addition, a systematic review of 18 studies found that demoralization with somatic or psychiatric disorders is a significant independent risk factor for suicide and negative clinical outcomes across various populations [ 10 ]. The coexistence of SUDs and MHDs, often referred to as dual diagnosis or comorbidity, represents a complex and prevalent phenomenon that significantly impacts affected individuals and healthcare systems [ 11 , 12 , 13 , 14 , 15 ]. For instance, individuals with depression may be more likely to self-medicate with alcohol or drugs to cope with emotional distress [ 16 ]. Similarly, PTSD has been linked to increased rates of substance abuse, as individuals attempt to alleviate the symptoms of trauma [ 17 , 18 ]. Moreover, chronic substance use can lead to changes in brain chemistry, increasing the risk of developing MHDs or exacerbating existing conditions [ 17 , 19 , 20 , 21 ]. The coexistence of SUDs and MHDs presents unique challenges from a medical and clinical standpoint. Dual diagnosis often leads to more severe symptoms, poorer treatment outcomes, increased risk of relapse, and higher rates of hospitalization compared to either disorder alone [ 22 ]. Additionally, diagnosing and treating dual diagnosis cases can be complex due to overlapping symptoms and interactions between substances and psychiatric medications. Integrated treatment approaches that address both conditions simultaneously are essential for successful recovery and improved patient outcomes [ 20 ]. Patients grappling with dual diagnosis encounter a multifaceted web of barriers when attempting to access essential mental health services. These barriers significantly compound the complexity of their clinical presentation. The first barrier pertains to stigma, where societal prejudices surrounding mental health and substance use disorders deter individuals from seeking help, fearing discrimination or social repercussions [ 23 ]. A lack of integrated care, stemming from fragmented healthcare systems, poses another significant hurdle as patients often struggle to navigate separate mental health and addiction treatment systems [ 24 ]. Insurance disparities contribute by limiting coverage for mental health services and imposing strict criteria for reimbursement [ 25 ]. Moreover, there is a shortage of adequately trained professionals equipped to address both substance use and mental health issues, creating a workforce barrier [ 26 ]. Geographical disparities in access further hinder care, particularly in rural areas with limited resources [ 27 ]. These barriers collectively serve to exacerbate the clinical complexity of patients with dual diagnosis, and ultimately contributing to poorer outcomes.
A research landscape analysis involves a systematic review and synthesis of existing literature on a specific topic to identify key trends, knowledge gaps, and research priorities [ 28 , 29 ]. Scientific research landscape analysis, is motivated by various factors. First, the rapid growth of scientific literature poses a challenge for researchers to stay up-to-date with the latest developments in their respective fields. Research landscape analysis provides a structured approach to comprehend the vast body of literature, identifying crucial insights and emerging trends. Additionally, it plays a vital role in identifying knowledge gaps, areas with limited research, or inadequate understanding. This pinpointing allows researchers to focus on critical areas that demand further investigation, fostering more targeted and impactful research efforts [ 30 ]. Furthermore, in the realm of policymaking and resource allocation, evidence-based decision-making is crucial. Policymakers and funding agencies seek reliable information to make informed decisions about research priorities. Research landscape analysis offers a comprehensive view of existing evidence, facilitating evidence-based decision-making processes [ 28 ]. When it comes to the research landscape analysis of dual diagnosis of SUDs and MHDs, there are several compelling justifications to explore this complex comorbidity and gain a comprehensive understanding of its interplay and impact on patient outcomes. Firstly, the complexity of the interplay between SUDs and MHDs demands a comprehensive examination of current research to unravel the intricacies of this comorbidity [ 31 ]. Secondly, dual diagnosis presents unique challenges for treatment and intervention strategies due to the overlapping symptoms and interactions between substances and psychiatric medications. A research landscape analysis can shed light on effective integrated treatment approaches and identify areas for improvement [ 18 ]. Moreover, the public health impact of co-occurring SUDs and MHDs is substantial, resulting in more severe symptoms, poorer treatment outcomes, increased risk of relapse, and higher rates of hospitalization. Understanding the research landscape can inform public health policies and interventions to address this issue more effectively [ 32 ]. Lastly, the holistic approach of research landscape analysis enables a comprehensive understanding of current knowledge, encompassing epidemiological data, risk factors, treatment modalities, and emerging interventions. This integrative approach can lead to more coordinated and effective care for individuals with dual diagnosis [ 22 ]. Based on the above argument, the current study aims to conduct a research landscape analysis of dual diagnosis of SUDs and MHDs. The research landscape analysis bears a lot of significance for individuals and society. First and foremost, it’s a beacon of hope for individuals seeking help. Research isn’t just about dry statistics; it's about finding better ways to treat and support those facing dual diagnosis. By being informed about the latest breakthroughs, healthcare professionals can offer more effective, evidence-backed care, opening the door to improved treatment outcomes and a brighter future for those they serve. Beyond the individual level, this understanding has profound societal implications. It has the power to chip away at the walls of stigma that often surround mental health and substance use issues. Greater awareness and knowledge about the complexities of dual diagnosis can challenge stereotypes and biases, fostering a more compassionate and inclusive society. Additionally, society allocates resources based on research findings. When we understand the prevalence and evolving nature of dual diagnosis, policymakers and healthcare leaders can make informed decisions about where to channel resources most effectively. This ensures that the needs of individuals struggling with co-occurring disorders are not overlooked or under-prioritized. Moreover, research helps identify risk factors and early warning signs related to dual diagnosis. Armed with this information, we can develop prevention strategies and early intervention programs, potentially reducing the incidence of co-occurring disorders and mitigating their impact. Legal and criminal justice systems also stand to benefit. Understanding dual diagnosis trends can inform policies related to diversion programs, treatment alternatives to incarceration, and the rehabilitation of individuals with co-occurring disorders, potentially reducing rates of reoffending. Moreover, dual diagnosis research contributes to public health planning by highlighting the need for integrated mental health and addiction services. This knowledge can guide the development of comprehensive healthcare systems that offer holistic care to individuals with co-occurring disorders. Families and communities, too, are vital players in this narrative. With a grasp of research findings, they can provide informed, empathetic, and effective support to their loved ones, contributing to better outcomes.
The present research landscape analysis of dual diagnosis of SUDs and MHDs was conducted using a systematic approach to retrieve, process, and analyze relevant articles. The following methodology outlines the key steps taken to address the research questions:
Research Design The present study constitutes a thorough and robust analysis of the research landscape concerning the dual diagnosis of SUD and MHD. It's important to note that the research landscape analysis differs from traditional systematic or scoping reviews. In conducting research landscape analysis, we made deliberate methodological choices aimed at achieving both timely completion and unwavering research quality. These choices included a strategic decision to focus our search exclusively on a single comprehensive database, a departure from the customary practice of utilizing multiple databases. Furthermore, we streamlined the quality control process by assigning specific quality checks to a single author, rather than following the conventional dual-reviewer approach. This approach prioritized efficiency and expediency without compromising the rigor of our analysis. To expedite the research process further, we opted for a narrative synthesis instead of a quantitative one, ensuring that we provide a succinct yet highly informative summary of the available evidence. We place a premium on research transparency and, as such, are committed to sharing the detailed search string employed for data retrieval. This commitment underscores our dedication to fostering reproducibility and transparency in research practices.
Ethical considerations Since the research landscape analysis involved the use of existing and publicly available literature, and no human subjects were directly involved, no formal ethical approval was required.
Article retrieval Scopus, a comprehensive bibliographic database, was utilized to retrieve articles related to the dual diagnosis of SUDs and MHDs. Scopus is a multidisciplinary abstract and citation database that covers a wide range of scientific disciplines, including life sciences, physical sciences, social sciences, and health sciences. It includes content from thousands of scholarly journals.
Keywords used To optimize the search process and ensure the inclusion of pertinent articles, a set of relevant keywords and equivalent terms were employed. Keywords for “dual diagnosis” included dual diagnosis, co-occurring disorders, comorbid substance use, comorbid addiction, coexisting substance use, combined substance use, simultaneous substance use, substance use and psychiatric, co-occurring substance use and psychiatric, concurrent substance use and mental, coexisting addiction and mental, combined addiction and mental, simultaneous addiction and mental, substance-related and psychiatric, comorbid mental health and substance use, co-occurring substance use and psychiatric, concurrent mental health and substance use, coexisting mental health and substance use, combined mental health and substance use, simultaneous mental health and substance use, substance-related and coexisting psychiatric, comorbid psychiatric and substance abuse, co-occurring mental health and substance-related, concurrent psychiatric and substance use, coexisting psychiatric and substance abuse, combined psychiatric and substance use, simultaneous psychiatric and substance use, substance-related and concurrent mental, substance abuse comorbidity. Keywords for “Substance use disorders” included substance abuse, substance dependence, drug use disorders, addiction, substance-related disorders, drug abuse, opioid use disorder, cocaine use disorder, alcohol use disorder, substance misuse, substance use disorder, substance-related, substance addiction. Keywords for “Mental health disorders” included psychiatric disorders, mental illnesses, mental disorders, emotional disorders, psychological disorders, schizophrenia, depression, PTSD, ADHD, anxiety, bipolar disorder, eating disorders, personality disorders, mood disorders, psychotic disorders, mood and anxiety disorders, mental health conditions. To narrow down the search to focus specifically on dual diagnosis, we adopted a strategy that involved the simultaneous presence of SUDs and MHDs in the presence of specific keywords in the titles and abstracts such as “dual,” “co-occurring,” “concurrent,” “co-occurring disorders,” “dual disorders,” “dual diagnosis,” “comorbid psychiatric,” “cooccurring psychiatric,” “comorbid*,” and “coexisting”.
Inclusion and exclusion criteria To maintain the study’s focus and relevance, specific inclusion and exclusion criteria were applied. Included articles were required to be research article, written in English, and published in peer-reviewed journals up to December 31, 2022, Articles focusing on animal studies, internet addiction, obesity, pain, and validity of instruments and tools were excluded.
Flow chart of the search strategy Supplement 1 shows the overall search strategy and the number of articles retrieved in each step. The total number of research articles that met the inclusion and exclusion criteria were 935.
Validation of search strategy The effectiveness of our search strategy was rigorously assessed through three distinct methods, collectively demonstrating its ability to retrieve pertinent articles while minimizing false positives. First, to gauge precision, we meticulously examined a sample of 30 retrieved articles, scrutinizing their alignment with our research question and their contributions to the topic of dual diagnosis. This manual review revealed that the majority of the assessed articles were highly relevant to our research focus. Second, for a comprehensive evaluation, we compared the articles obtained through our search strategy with a set of randomly selected articles from another source. This set comprised 10 references sourced from Google Scholar [ 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 ], and the aim was to determine if our strategy successfully identified articles selected at random from an alternative database. Impressively, our analysis showed that the search strategy had a notably high success rate in capturing these randomly selected articles. Lastly, to further corroborate the relevance of our retrieved articles, we investigated the research interests of the top 10 active authors and the subject scope of the top 10 active journals. This exploration confirmed that their areas of expertise and the journal scopes were in alignment with the field of mental health and/or substance use disorders. These three validation methods collectively reinforce the reliability of our search strategy, affirming that the vast majority of the retrieved articles are indeed pertinent to our research inquiry.
Data processing and mapping Data extracted from the selected articles were processed and organized using Microsoft Excel. Information on the titles/abstracts/author keywords, year of publication, journal name, authors, institution and country affiliation, and number of citations received by the article were extracted. To visualize and analyze the research landscape, VOSviewer, a bibliometric analysis tool, was employed [ 43 ]. This software enables mapping and clustering of co-occurring terms, authors, and countries, providing a comprehensive overview of the dual diagnosis research domain.
Interpreting VOSviewer maps and generating research topics
We conducted a rigorous analysis and generated a comprehensive research landscape using VOSviewer, a widely acclaimed software tool renowned for its expertise in mapping research domains. We seamlessly integrated pertinent data extracted from the Scopus database, including publication metadata, into VOSviewer to delve into the frequency of author keywords and terminologies. The resulting visualizations provided us with profound insights into the intricate web of interconnected research topics and their relationships within the field. Interpreting VOSviewer maps is akin to navigating a vibrant and interconnected tapestry of knowledge. Each term or keyword in the dataset is depicted as a point on the map, represented by a circle or node. These nodes come in varying sizes and colors and are interconnected by lines of differing thicknesses. The size of a node serves as an indicator of the term’s significance or prevalence within the dataset. Larger nodes denote that a specific term is frequently discussed or plays a pivotal role in the body of research, while smaller nodes signify less commonly mentioned concepts. The colors assigned to these nodes serve a dual purpose. Firstly, they facilitate the categorization of terms into thematic groups, with terms of the same color typically belonging to the same cluster or sharing a common thematic thread. Secondly, they aid in the identification of distinct research clusters or thematic groups within the dataset. For instance, a cluster of blue nodes might indicate that these terms are all associated with a particular area of research. The spatial proximity of nodes on the map reflects their closeness in meaning or concept. Nodes positioned closely together share a robust semantic or contextual connection and are likely to be co-mentioned in research articles or share a similar thematic focus. Conversely, nodes situated farther apart indicate less commonality in terms of their usage in the literature. The lines that link these nodes represent the relationships between terms. The thickness of these lines provides insights into the strength and frequency of these connections. Thick lines indicate that the linked terms are frequently discussed together or exhibit a robust thematic association, while thinner lines imply weaker or less frequent connections. In essence, VOSviewer maps offer a visual narrative of the underlying structure and relationships within your dataset. By examining node size and color, you can pinpoint pivotal terms and thematic clusters. Simultaneously, analyzing the distance between nodes and line thickness unveils the semantic closeness and strength of associations between terms. These visual insights are invaluable for researchers seeking to unearth key concepts, identify research clusters, and track emerging trends within their field of study.
Growth pattern, active countries, and active journals
The growth pattern of the 935 research articles on dual diagnosis of substance use disorders and mental health disorders shows an increasing trend in the number of published articles over the years. Starting from the late 1980s and early 1990s with only a few publications, the research interest gradually picked up momentum, and the number of articles has been consistently rising since the mid-1990s. Table 1 shows the number of articles published in three different periods. The majority of publications (52.2%) were produced between 2003 and 2012, indicating a significant surge in research during that decade. The subsequent period from 2013 to 2022 saw a continued interest in the subject, accounting for 35.5% of the total publications. The number of articles published per year during the period from 2013 to 2022 showed a fluctuating steady state with an average of approximately 33 articles per year. The earliest period from 1983 to 2002 comprised 12.3% of the total publications, reflecting the initial stages of research and the gradual development of interest in the field.
Out of the total 935 publications, the United States contributed the most with 585 publications, accounting for approximately 62.5% of the total research output. Canada follows with 88 publications, making up around 9.4% of the total. The United Kingdom and Australia also made substantial contributions with 70 and 53 publications, accounting for 7.5 and 5.7%, respectively. Table 2 shows the top 10 active countries.
Based on the list of top active journals in the field of dual diagnosis of substance use and mental health disorders, it is evident that there are several reputable and specialized journals that focus on this important area of research (Table 3 ). These journals cover a wide range of topics related to dual diagnosis, including comorbidity, treatment approaches, intervention strategies, and epidemiological studies. The Journal of Dual Diagnosis appears to be a leading and comprehensive platform for research on dual diagnosis. It covers a broad spectrum of studies related to substance use disorders and mental health conditions. The Journal of Substance Abuse Treatment ranked second while the Mental Health and Substance Use Dual Diagnosis journal ranked third and seems to be dedicated specifically to the intersection of substance use disorder and mental health disorders, providing valuable insights and research findings related to comorbidities and integrated treatment approaches.
Most frequent author keywords
Mapping author keywords with a minimum occurrence of five (n = 96) provides insights in research related to dual diagnosis. Figure 1 shows the 96 author keywords and their links with other keywords. The number of occurrences represent the number of times each author keyword appears in the dataset, while the total link strength (TLS) indicates the combined strength of connections between keywords based on their co-occurrence patterns. The most frequent author keywords with high occurrences and TLS represent the key areas of focus in research on the dual diagnosis of substance use and mental health disorders.
“Comorbidity” is the most frequent keyword, with 144 occurrences and a high TLS of 356. This reflects the central theme of exploring the co-occurrence of substance use disorders and mental health conditions and their complex relationship. “Substance use disorder” and “dual diagnosis” are also highly prevalent keywords with 122 and 101 occurrences, respectively. These terms highlight the primary focus on studying individuals with both substance use disorders and mental health disorders, underscoring the significance of dual diagnosis in research. “Co-occurring disorders” and “substance use disorders” are frequently used, indicating a focus on understanding the relationship between different types of disorders and the impact of substance use on mental health. Several specific mental health disorders such as “schizophrenia,” “depression,” “bipolar disorder,” and “PTSD” are prominent keywords, indicating a strong emphasis on exploring the comorbidity of these disorders with substance use. “Mental health” and “mental illness” are relevant keywords, reflecting the broader context of research on mental health conditions and their interaction with substance use. “Treatment” is a significant keyword with 34 occurrences, indicating a focus on investigating effective interventions and treatment approaches for individuals with dual diagnosis. “Addiction” and “recovery” are important keywords, highlighting the interest in understanding the addictive nature of substance use and the potential for recovery in this population. The mention of “veterans” as a keyword suggests a specific focus on the dual diagnosis of substance use and mental health disorders in the veteran population. “Integrated treatment” is an important keyword, indicating an interest in studying treatment approaches that address both substance use and mental health disorders together in an integrated manner.
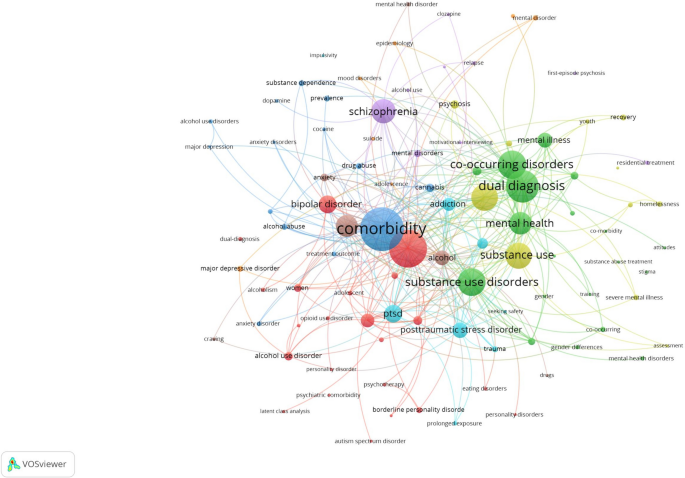
Network visualization map of author keywords with a minimum occurrence of five in the retrieved articles on dual diagnosis of substance use and mental health disorders
Most impactful research topics
To have an insight into the most impactful research topics on dual diagnosis, the top 100 research articles were visualized and the terms with the largest node size and TLS were used to. To come up with the five most common investigated research topics:
Dual diagnosis and comorbidity of SUDs and MHDs: This topic focuses on the co-occurrence of substance use disorders and various mental health conditions, such as schizophrenia, bipolar disorder, PTSD, anxiety disorders, and major depressive disorder. This research topic explored the prevalence, characteristics, and consequences of comorbidity in different populations, including veterans, adolescents, and individuals experiencing homelessness [ 13 , 19 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 ].
Treatment and interventions for co-occurring disorders: This topic involves studies on different treatment approaches and interventions for individuals with dual diagnosis. These interventions may include motivational interviewing, cognitive-behavioral therapy, family intervention, integrated treatment models, assertive community treatment, and prolonged exposure therapy. The goal is to improve treatment outcomes and recovery for individuals with co-occurring substance use and mental health disorders [ 48 , 53 , 54 , 55 , 56 , 57 , 58 , 59 ].
Quality of life and functioning in individuals with dual diagnosis: This research topic explores the impact of dual diagnosis on the quality of life and functioning of affected individuals. It assesses the relationship between dual diagnosis and various aspects of well-being, including social functioning, physical health, and overall quality of life [ 60 , 61 , 62 , 63 , 64 ].
Epidemiology and prevalence of co-occurring disorders: This topic involves population-based studies that investigate the prevalence of comorbid substance use and mental health disorders. It examines the demographic and clinical correlates of dual diagnosis, as well as risk factors associated with the development of co-occurring conditions [ 50 , 52 , 60 , 65 , 66 , 67 ].
Implications and consequences of comorbidity: This research topic explores the consequences of comorbidity between substance use and mental health disorders, such as treatment utilization, service access barriers, criminal recidivism, and the impact on suicidality. It also investigates the implications of comorbidity for treatment outcomes and the potential risks associated with specific comorbidities [ 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 ].
Emerging research topics
Upon scrutinizing the titles, abstracts, author keywords, and a visualization map of the 100 recently published articles, the research themes listed below came to the forefront. It’s worth noting that some of the research themes in the 100 recently published articles were not groundbreaking; rather, they represented a natural progression of ongoing research endeavors, and that is why they were not listed as emerging research themes. For instance, there was a continuation of research into the prevalence and epidemiology of co-occurring mental illnesses and substance use disorders and characteristics of various cases of co-morbid cases of SUDs and MHDs. The list below included such emergent themes. It might seem that certain aspects within these research themes duplicate the initial research topics, but it’s crucial to emphasize that this is not the case. For example, both themes delve into investigations concerning treatment, yet the differentiation lies in the treatment approach adopted.
Neurobiological and psychosocial aspects of dual diagnosis: This research topic focuses on exploring the neurobiological etiology and underlying mechanisms of comorbid substance use and mental health disorders. It investigates brain regions, neurotransmitter systems, hormonal pathways, and other neurobiological factors contributing to the development and maintenance of dual diagnosis. Additionally, this topic may examine psychosocial aspects, such as trauma exposure, adverse childhood experiences, and social support, that interact with neurobiological factors in the context of comorbidity [ 76 ].
Impact of environmental and sociocultural factors on dual diagnosis: This research topic delves into the influence of environmental and sociocultural factors on the occurrence and course of comorbid substance use and mental health disorders. It may explore how cultural norms, socioeconomic status, access to healthcare, and societal attitudes toward mental health and substance use affect the prevalence, treatment outcomes, and quality of life of individuals with dual diagnosis [ 77 , 78 ].
New interventions and treatment approaches for dual diagnosis: This topic involves studies that propose and evaluate innovative interventions and treatment approaches for individuals with dual diagnosis. These interventions may include novel psychotherapeutic techniques, pharmacological treatments, digital health interventions, and integrated care models. The research aims to improve treatment effectiveness, adherence, and long-term recovery outcomes in individuals with comorbid substance use and mental health disorders [ 79 , 80 , 81 , 82 , 83 , 84 ].
Mental health and substance use in special populations with dual diagnosis: This research topic focuses on exploring the prevalence and unique characteristics of comorbid substance use and mental health disorders in specific populations, such as individuals with eating disorders, incarcerated individuals, and people with autism spectrum disorder. It aims to identify the specific needs and challenges faced by these populations and develop tailored interventions to address their dual diagnosis [ 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 ].
Public health implications and policy interventions for dual diagnosis: This topic involves research that addresses the public health implications of dual diagnosis and the need for policy interventions to address this complex issue. It may include studies on the economic burden of comorbidity, the impact on healthcare systems, and the evaluation of policy initiatives aimed at improving prevention, early intervention, and access to integrated care for individuals with dual diagnosis [ 81 , 96 , 97 , 98 , 99 , 100 , 101 ].
Comparison in research topics
The comparison between the most impactful research topics and emerging research topics in the field of dual diagnosis reveals intriguing insights into the evolving landscape of this critical area of study (Table 4 ). In the most impactful research topics, there is a strong emphasis on the epidemiology of dual diagnosis, indicating a well-established foundation in understanding the prevalence, characteristics, and consequences of comorbid SUDs and MHDs. Treatment and interventions also receive considerable attention, highlighting the ongoing efforts to improve outcomes and recovery for individuals with dual diagnosis. Quality of life and medical consequences are additional focal points, reflecting the concern for the holistic well-being of affected individuals and the health-related implications of comorbidity.
On the other hand, emerging research topics signify a shift towards newer methods and interventions. The exploration of neurobiology in the context of dual diagnosis reflects a growing interest in unraveling the underlying neurobiological mechanisms contributing to comorbidity. This shift suggests a deeper understanding of the neural pathways and potential targets for intervention. The consideration of dual diagnosis in special groups underscores a recognition of the unique needs and challenges faced by specific populations, such as individuals with autism spectrum disorder. This tailored approach acknowledges that one size does not fit all in addressing dual diagnosis. Finally, the exploration of environmental and psychosocial contexts highlights the importance of socio-cultural factors, policy interventions, and societal attitudes in shaping the experience of individuals with dual diagnosis, signaling a broader perspective that extends beyond clinical interventions. In summary, while the most impactful research topics have laid a strong foundation in epidemiology, treatment, quality of life, and medical consequences, the emerging research topics point to a promising future with a deeper dive into the neurobiology of dual diagnosis, a focus on special populations, and a broader consideration of the environmental and psychosocial context. This evolution reflects the dynamic nature of dual diagnosis research as it strives to advance our understanding and improve the lives of those affected by comorbid substance use and mental health disorders.
The main hypothesis underlying the study was that dual diagnosis, or the comorbidity of SUDs and MHDs, was historically underrecognized and under-researched. Over time, however, there has been a significant increase in understanding, appreciation, and research into this complex interplay in clinical settings. This was expected to manifest through a growing number of publications, increased attention to integrated treatment approaches, and a heightened recognition of the complexities and public health implications associated with dual diagnosis. The study aims to analyze this progression and its implications through a research landscape analysis, identifying key trends, knowledge gaps, and research priorities. The research landscape analysis of the dual diagnosis of SUDs and MHDs has unveiled a substantial and evolving body of knowledge, with a notable rise in publications since the mid-1990s and a significant surge between 2003 and 2012. This growing research interest underscores the increasing recognition of the importance and complexity of dual diagnosis in clinical and public health contexts. The United States has emerged as the most active contributor, followed by Canada, the United Kingdom, and Australia, with specialized journals such as the Journal of Dual Diagnosis playing a pivotal role in disseminating research findings. Common keywords such as “comorbidity,” “substance use disorder,” “dual diagnosis,” and specific mental health disorders highlight the primary focus areas, with impactful research topics identified as the comorbidity of SUDs and MHDs, treatment and interventions, quality of life, epidemiology, and the implications of comorbidity. Emerging research themes emphasize neurobiological and psychosocial aspects, the impact of environmental and sociocultural factors, innovative treatment approaches, and the needs of special populations with dual diagnosis, reflecting a shift towards a more holistic and nuanced understanding. The study highlights a shift from traditional epidemiological studies towards understanding the underlying mechanisms and broader social determinants of dual diagnosis, with a need for continued research into integrated treatment models, specific needs of diverse populations, and the development of tailored interventions.
The findings of this research landscape analysis have significant implications for clinical practice, public health initiatives, policy development, and future research endeavors. Clinicians and healthcare providers working with individuals with dual diagnosis can benefit from the identified research hotspots, as they highlight crucial aspects that require attention in diagnosis, treatment, and support. The prominence of treatment and intervention topics indicates the need for evidence-based integrated approaches that address both substance use and mental health disorders concurrently [ 102 , 103 , 104 ]. The research on the impact of dual diagnosis on quality of life and functioning underscores the importance of holistic care that addresses psychosocial and functional well-being [ 63 ]. For public health initiatives, understanding the prevalence and epidemiological aspects of dual diagnosis is vital for resource allocation and the development of effective prevention and early intervention programs. Policymakers can use the research landscape analysis to inform policies that promote integrated care, reduce barriers to treatment, and improve access to mental health and substance abuse services [ 15 , 105 ]. Furthermore, the identification of emerging topics offers opportunities for investment in research areas that are gaining momentum and importance.
The present study lays a robust groundwork, serving as a catalyst for the advancement of research initiatives and the formulation of comprehensive policies and programs aimed at elevating the quality of life for individuals grappling with the intricate confluence of SUDs and MHDs. Within the realm of significance, it underscores a critical imperative—the urgent necessity to revolutionize the landscape of tailored mental health services offered to patients harboring this challenging comorbidity. The paper distinctly illuminates the exigency for a heightened quantity of research endeavors that delve deeper into unraveling the temporal intricacies underpinning the relationship between SUDs and MHDs. In so doing, it not only unveils potential risk factors but also delves into the far-reaching consequences of treatment modalities over the extended course of time. This illumination, therefore, not only beckons but virtually ushers in a promising trajectory for prospective research endeavors, a path designed to uncover the intricate and evolving journey of dual diagnosis. A profound implication of this study is the direct applicability of its findings in the corridors of policymaking. By leveraging the insights encapsulated within the paper, policymakers stand uniquely equipped to sculpt policies that unequivocally champion the cause of integrated care. The remarkable emphasis on themes of treatment and intervention, permeating the research's core, emphatically underscores the urgent demand for dismantling barriers obstructing access to mental health and substance abuse services. It is incumbent upon policymakers to heed this call, for policies fostering the integration of care can inexorably elevate the outcomes experienced by patients grappling with dual diagnosis. Furthermore, this study artfully directs policymakers to allocate their resources judiciously by identifying burgeoning areas of research that are surging in prominence and pertinence. These emergent topics, discerned within the study, are not just topics; they are emblematic of windows of opportunity. By investing in these areas, policymakers can tangibly bolster research initiatives that are primed to tackle the multifaceted challenges inherent in the realm of dual diagnosis, addressing both current exigencies and future prospects. Additionally, the paper furnishes the foundational blueprint essential for the development of screening guidelines and clinical practice protocols that truly grasp the complexity of dual diagnosis. Clinical practitioners and healthcare establishments would be remiss not to harness this invaluable information to augment their own practices, thereby delivering more effective and empathetic care to individuals contending with dual diagnosis. In essence, this study serves as the compass guiding the way toward a more compassionate, comprehensive, and efficacious approach to mental health and substance abuse care for those in need.
The current landscape analysis of reveals significant implications and highlights the growing research interest in this field since the late 1980s. This increasing trend underscores the complexities and prevalence of comorbid conditions, which necessitate focused research and intervention strategies. The results can be generalized to guide future research priorities, inform clinical guidelines, shape healthcare policies, and provide a framework for other countries to adapt and build upon in their context.
The key take-home message emphasizes the importance of recognizing the high prevalence and intricate relationship between SUDs and MHDs, necessitating integrated and tailored treatment approaches. Additionally, the study advocates for employing efficient research methodologies to synthesize vast amounts of literature and identify emerging trends, focusing on quality of life, treatment outcomes, and the broader socio-cultural and policy contexts to improve care and support for individuals with dual diagnosis. Finally, the research underscores the critical need for continued focus on dual diagnosis, advocating for comprehensive, integrated, and innovative approaches to research, clinical practice, and policymaking to improve outcomes for affected individuals.
Despite the comprehensive approach adopted in this research landscape analysis, several limitations must be acknowledged. The exclusive reliance on Scopus, while extensive, inherently limits the scope of the analysis, potentially omitting relevant articles indexed in other databases such as the Chinese scientific database, thus not fully representing the entire research landscape on dual diagnosis of SUDs and MHDs. Assigning quality control responsibilities to a single author, rather than employing a dual-reviewer system, may introduce bias and affect the reliability of the quality assessment. Although this approach was chosen to expedite the process, it might have compromised the thoroughness of quality checks. The use of narrative synthesis instead of a quantitative synthesis limits the ability to perform meta-analytical calculations that could provide more robust statistical insights. This choice was made for efficiency, but it may affect the depth of the analysis and the generalizability of the conclusions. The reliance on specific keywords to retrieve articles means that any relevant studies not containing these exact terms in their titles or abstracts may have been overlooked, potentially leading to an incomplete representation of the research domain. The restriction to English-language articles and peer-reviewed journals may exclude significant research published in other languages or in non-peer-reviewed formats, introducing linguistic and publication type bias that could skew the results towards predominantly English-speaking regions and established academic journals. The inclusion of articles up to December 31, 2022, means that any significant research published after this date is not considered, potentially missing the latest developments in the field. The validation of the search strategy using a small sample of 30 articles and a comparison with 10 randomly selected articles from Google Scholar may not be sufficient to comprehensively assess the effectiveness of the search strategy; a larger sample size might provide a more accurate validation. Some of the research topics and findings may be specific to particular populations (e.g., veterans) and might not be generalizable to other groups, highlighting the need for caution when extrapolating the results to broader contexts. Although no formal ethical approval was required due to the use of existing literature, ethical considerations related to the interpretation and application of findings must still be acknowledged, particularly in terms of representing vulnerable populations accurately and sensitively. Acknowledging these limitations is crucial for interpreting the findings of this research landscape analysis and for guiding future research efforts to address these gaps and enhance the robustness and comprehensiveness of studies on the dual diagnosis of SUDs and MHDs.
In conclusion, the research landscape analysis of dual diagnosis of substance abuse and mental health disorders provides valuable insights into the growth, active countries, and active journals in this field. The identification of research hotspots and emerging topics informs the scientific community about prevailing interests and potential areas for future investigation. Addressing research gaps can lead to a more comprehensive understanding of dual diagnosis, while the implications of the findings extend to clinical practice, public health initiatives, policy development, and future research priorities. This comprehensive understanding is crucial in advancing knowledge, improving care, and addressing the multifaceted challenges posed by dual diagnosis to individuals and society.
Availability of data and materials
All data presented in this manuscript are available on the Scopus database using the search query listed in the methodology section.
Hasin DS, O’Brien CP, Auriacombe M, Borges G, Bucholz K, Budney A, et al. DSM-5 criteria for substance use disorders: recommendations and rationale. Am J Psychiatry. 2013;170(8):834–51. https://doi.org/10.1176/appi.ajp.2013.12060782 .
Article PubMed PubMed Central Google Scholar
Collaborators GA. Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet. 2018;392(10152):1015–35. https://doi.org/10.1016/s0140-6736(18)31310-2 .
Article Google Scholar
Ayalew M, Tafere M, Asmare Y. Prevalence, trends, and consequences of substance use among university students: implication for intervention. Int Q Community Health Educ. 2018;38(3):169–73. https://doi.org/10.1177/0272684x17749570 .
Article PubMed Google Scholar
Raftery D, Kelly PJ, Deane FP, Baker AL, Ingram I, Goh MCW, et al. Insight in substance use disorder: a systematic review of the literature. Addict Behav. 2020;111:106549. https://doi.org/10.1016/j.addbeh.2020.106549 .
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62(6):593–602. https://doi.org/10.1001/archpsyc.62.6.593 .
Hossain MM, Nesa F, Das J, Aggad R, Tasnim S, Bairwa M, et al. Global burden of mental health problems among children and adolescents during COVID-19 pandemic: an umbrella review. Psychiatry Res. 2022;317:114814. https://doi.org/10.1016/j.psychres.2022.114814 .
Article CAS PubMed PubMed Central Google Scholar
Kurdyak P, Patten S. The burden of mental illness and evidence-informed mental health policy development. Can J Psychiatry. 2022;67(2):104–6. https://doi.org/10.1177/07067437211021299 .
Stumbrys D, Jasilionis D, Pūras D. The burden of mental health-related mortality in the Baltic States in 2007–2018. BMC Public Health. 2022;22(1):1776. https://doi.org/10.1186/s12889-022-14175-9 .
Pompili M, Innamorati M, Gonda X, Serafini G, Sarno S, Erbuto D, et al. Affective temperaments and hopelessness as predictors of health and social functioning in mood disorder patients: a prospective follow-up study. J Affect Disord. 2013;150(2):216–22. https://doi.org/10.1016/j.jad.2013.03.026 .
Costanza A, Vasileios C, Ambrosetti J, Shah S, Amerio A, Aguglia A, et al. Demoralization in suicide: a systematic review. J Psychosom Res. 2022;157:110788. https://doi.org/10.1016/j.jpsychores.2022.110788 .
Arias F, Szerman N, Vega P, Mesías B, Basurte I, Rentero D. Bipolar disorder and substance use disorders. Madrid study on the prevalence of dual disorders/pathology. Adicciones. 2017;29(3):186–94. https://doi.org/10.2088/adicciones.782 .
Brewer S, Godley MD, Hulvershorn LA. Treating mental health and substance use disorders in adolescents: what is on the menu? Curr Psychiatry Rep. 2017;19(1):5. https://doi.org/10.1007/s11920-017-0755-0 .
Jones CM, McCance-Katz EF. Co-occurring substance use and mental disorders among adults with opioid use disorder. Drug Alcohol Depend. 2019;197:78–82. https://doi.org/10.1016/j.drugalcdep.2018.12.030 .
Murthy P, Mahadevan J, Chand PK. Treatment of substance use disorders with co-occurring severe mental health disorders. Curr Opin Psychiatry. 2019;32(4):293–9. https://doi.org/10.1097/yco.0000000000000510 .
Saddichha S, Schütz CG, Sinha BN, Manjunatha N. Substance use and dual diagnosis disorders: future epidemiology, determinants, and policies. Biomed Res Int. 2015;2015:145905. https://doi.org/10.1155/2015/145905 .
Hammen C. Adolescent depression: stressful interpersonal contexts and risk for recurrence. Curr Dir Psychol Sci. 2009;18(4):200–4. https://doi.org/10.1111/j.1467-8721.2009.01636.x .
Wolitzky-Taylor K, Bobova L, Zinbarg RE, Mineka S, Craske MG. Longitudinal investigation of the impact of anxiety and mood disorders in adolescence on subsequent substance use disorder onset and vice versa. Addict Behav. 2012;37(8):982–5. https://doi.org/10.1016/j.addbeh.2012.03.026 .
Mueser KT, Drake RE, Wallach MA. Dual diagnosis: a review of etiological theories. Addict Behav. 1998;23(6):717–34.
Article CAS PubMed Google Scholar
Hartz SM, Pato CN, Medeiros H, Cavazos-Rehg P, Sobell JL, Knowles JA, et al. Comorbidity of severe psychotic disorders with measures of substance use. JAMA Psychiat. 2014;71(3):248–54. https://doi.org/10.1001/jamapsychiatry.2013.3726 .
Carroll KM, Kiluk BD, Nich C, Babuscio TA, Brewer JA, Potenza MN, et al. Cognitive function and treatment response in a randomized clinical trial of computer-based training in cognitive-behavioral therapy. Subst Use Misuse. 2011;46(1):23–34. https://doi.org/10.3109/10826084.2011.521069 .
Drake RE, Mueser KT. Psychosocial approaches to dual diagnosis. Schizophr Bull. 2000;26(1):105–18. https://doi.org/10.1093/oxfordjournals.schbul.a033429 .
Ruggeri M, Leese M, Thornicroft G, Bisoffi G, Tansella M. Definition and prevalence of severe and persistent mental illness. Br J Psychiatry. 2000;177:149–55. https://doi.org/10.1192/bjp.177.2.149 .
Reavley NJ, Jorm AF. Stigmatizing attitudes towards people with mental disorders: findings from an Australian national survey of mental health literacy and stigma. Aust N Z J Psychiatry. 2011;45(12):1086–93. https://doi.org/10.3109/00048674.2011.621061 .
Torrey WC, Tepper M, Greenwold J. Implementing integrated services for adults with co-occurring substance use disorders and psychiatric illnesses: a research review. J Dual Diagn. 2011;7(3):150–61. https://doi.org/10.1080/15504263.2011.592769 .
Bouchery EE, Harwood HJ, Dilonardo J, Vandivort-Warren R. Type of health insurance and the substance abuse treatment gap. J Subst Abuse Treat. 2012;42(3):289–300. https://doi.org/10.1016/j.jsat.2011.09.002 .
Abuse S, Administration MHS. National Mental Health Services Survey (N-MHSS): 2014. Data on mental health treatment facilities. Department of Health and Human Services, Substance Abuse and Mental Health …; 2014.
Shiner B, Gottlieb D, Rice K, Forehand JA, Snitkin M, Watts BV. Evaluating policies to improve access to mental health services in rural areas. J Rural Health. 2022;38(4):805–16. https://doi.org/10.1111/jrh.12674 .
Ioannidis JP, Greenland S, Hlatky MA, Khoury MJ, Macleod MR, Moher D, et al. Increasing value and reducing waste in research design, conduct, and analysis. Lancet. 2014;383(9912):166–75. https://doi.org/10.1016/s0140-6736(13)62227-8 .
Bornmann L, Bowman BF, Bauer J, Marx W, Schier H, Palzenberger MJBbHmiosi. (2014): 11 Bibliometric standards for evaluating research institutes in the natural sciences.201.
Hicks D, Wouters P, Waltman L, de Rijcke S, Rafols I. Bibliometrics: the Leiden manifesto for research metrics. Nature. 2015;520(7548):429–31. https://doi.org/10.1038/520429a .
Ziedonis D, Brady K. Dual diagnosis in primary care. Detecting and treating both the addiction and mental illness. Med Clin North Am. 1997;81(4):1017–36. https://doi.org/10.1016/s0025-7125(05)70561-7 .
Kim JI, Kim B, Kim BN, Hong SB, Lee DW, Chung JY, et al. Prevalence of psychiatric disorders, comorbidity patterns, and repeat offending among male juvenile detainees in South Korea: a cross-sectional study. Child Adolesc Psychiatry Ment Health. 2017;11:6. https://doi.org/10.1186/s13034-017-0143-x .
Astals M, Domingo-Salvany A, Buenaventura CC, Tato J, Vazquez JM, Martín-Santos R, et al. Impact of substance dependence and dual diagnosis on the quality of life of heroin users seeking treatment. Subst Use Misuse. 2008;43(5):612–32. https://doi.org/10.1080/10826080701204813 .
Buckley PF. Prevalence and consequences of the dual diagnosis of substance abuse and severe mental illness. J Clin Psychiatry. 2006;67(Suppl 7):5–9.
PubMed Google Scholar
Buckley PF, Brown ES. Prevalence and consequences of dual diagnosis. J Clin Psychiatry. 2006;67(7):e01. https://doi.org/10.4088/jcp.0706e01 .
Canaway R, Merkes M. Barriers to comorbidity service delivery: the complexities of dual diagnosis and the need to agree on terminology and conceptual frameworks. Aust Health Rev. 2010;34(3):262–8. https://doi.org/10.1071/ah08723 .
Edward KL, Munro I. Nursing considerations for dual diagnosis in mental health. Int J Nurs Pract. 2009;15(2):74–9. https://doi.org/10.1111/j.1440-172X.2009.01731.x .
Healey C, Peters S, Kinderman P, McCracken C, Morriss R. Reasons for substance use in dual diagnosis bipolar disorder and substance use disorders: a qualitative study. J Affect Disord. 2009;113(1–2):118–26. https://doi.org/10.1016/j.jad.2008.05.010 .
Horsfall J, Cleary M, Hunt GE, Walter G. Psychosocial treatments for people with co-occurring severe mental illnesses and substance use disorders (dual diagnosis): a review of empirical evidence. Harv Rev Psychiatry. 2009;17(1):24–34. https://doi.org/10.1080/10673220902724599 .
Kerfoot KE, Petrakis IL, Rosenheck RA. Dual diagnosis in an aging population: prevalence of psychiatric disorders, comorbid substance abuse, and mental health service utilization in the department of veterans affairs. J Dual Diagn. 2011;7(1–2):4–13. https://doi.org/10.1080/15504263.2011.568306 .
Morojele NK, Saban A, Seedat S. Clinical presentations and diagnostic issues in dual diagnosis disorders. Curr Opin Psychiatry. 2012;25(3):181–6. https://doi.org/10.1097/YCO.0b013e328351a429 .
Thylstrup B, Johansen KS. Dual diagnosis and psychosocial interventions–introduction and commentary. Nord J Psychiatry. 2009;63(3):202–8. https://doi.org/10.1080/08039480802571069 .
van Eck NJ, Waltman L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics. 2010;84(2):523–38. https://doi.org/10.1007/s11192-009-0146-3 .
Arndt S, Tyrrell G, Flaum M, Andreasen NC. Comorbidity of substance abuse and schizophrenia: the role of pre-morbid adjustment. Psychol Med. 1992;22(2):379–88. https://doi.org/10.1017/S0033291700030324 .
Barnes TRE, Mutsatsa SH, Hutton SB, Watt HC, Joyce EM. Comorbid substance use and age at onset of schizophrenia. Br J Psychiatry. 2006;188:237–42. https://doi.org/10.1192/bjp.bp.104.007237 .
Brady KT, Killeen T, Saladin ME, Dansky B, Becker S. Comorbid substance abuse and posttraumatic stress disorder: characteristics of women in treatment. Am J Addict. 1994;3(2):160–4. https://doi.org/10.1111/j.1521-0391.1994.tb00383.x .
Brière FN, Rohde P, Seeley JR, Klein D, Lewinsohn PM. Comorbidity between major depression and alcohol use disorder from adolescence to adulthood. Compr Psychiatry. 2014;55(3):526–33. https://doi.org/10.1016/j.comppsych.2013.10.007 .
Brown PJ, Stout RL, Mueller T. Substance use disorder and posttraumatic stress disorder comorbidity: addiction and psychiatric treatment rates. Psychol Addict Behav. 1999;13(2):115–22. https://doi.org/10.1037/0893-164X.13.2.115 .
Bulik CM, Klump KL, Thornton L, Kaplan AS, Devlin B, Fichter MM, et al. Alcohol use disorder comorbidity in eating disorders: a multicenter study. J Clin Psychiatry. 2004;65(7):1000–6. https://doi.org/10.4088/JCP.v65n0718 .
Compton WM, Conway KP, Stinson FS, Grant BF. Changes in the prevalence of major depression and comorbid substance use disorders in the United States between 1991–1992 and 2001–2002. Am J Psychiatry. 2006;163(12):2141–7. https://doi.org/10.1176/ajp.2006.163.12.2141 .
Green AI, Drake RE, Brunette MF, Noordsy DL. Schizophrenia and co-occurring substance use disorder. Am J Psychiatry. 2007;164(3):402–8. https://doi.org/10.1176/ajp.2007.164.3.402 .
Morgenstern J, Langenbucher J, Labouvie E, Miller KJ. The comorbidity of alcoholism and personality disorders in a clinical population: prevalence rates and relation to alcohol typology variables. J Abnorm Psychol. 1997;106(1):74–84. https://doi.org/10.1037/0021-843X.106.1.74 .
Back SE, Waldrop AE, Brady KT. Treatment challenges associated with comorbid substance use and posttraumatic stress disorder: clinicians’ perspectives. Am J Addict. 2009;18(1):15–20. https://doi.org/10.1080/10550490802545141 .
Brown PJ, Recupero PR, Stout R. PTSD substance abuse comorbidity and treatment utilization. Addict Behav. 1995;20(2):251–4. https://doi.org/10.1016/0306-4603(94)00060-3 .
Harris KM, Edlund MJ. Use of mental health care and substance abuse treatment among adults with co-occurring disorders. Psychiatr Serv. 2005;56(8):954–9. https://doi.org/10.1176/appi.ps.56.8.954 .
Hien DA, Cohen LR, Miele GM, Litt LC, Capstick C. Promising treatments for women with comorbid PTSD and substance use disorders. Am J Psychiatry. 2004;161(8):1426–32. https://doi.org/10.1176/appi.ajp.161.8.1426 .
Manwani SG, Szilagyi KA, Zablotsky B, Hennen J, Griffin ML, Weiss RD. Adherence to pharmacotherapy in bipolar disorder patients with and without co-occurring substance use disorders. J Clin Psychiatry. 2007;68(8):1172–6. https://doi.org/10.4088/JCP.v68n0802 .
Minkoff K. An integrated treatment model for dual diagnosis of psychosis and addiction. Hosp Community Psychiatry. 1989;40(10):1031–6. https://doi.org/10.1176/ps.40.10.1031 .
Smith JP, Book SW. Comorbidity of generalized anxiety disorder and alcohol use disorders among individuals seeking outpatient substance abuse treatment. Addict Behav. 2010;35(1):42–5. https://doi.org/10.1016/j.addbeh.2009.07.002 .
Kamali M, Kelly L, Gervin M, Browne S, Larkin C, O’Callaghan E. The prevalence of comorbid substance misuse and its influence on suicidal ideation among in-patients with schizophrenia. Acta Psychiatr Scand. 2000;101(6):452–6. https://doi.org/10.1034/j.1600-0447.2000.101006452.x .
Padgett DK, Gulcur L, Tsemberis S. Housing first services for people who are homeless with co-occurring serious mental illness and substance abuse. Res Soc Work Pract. 2006;16(1):74–83. https://doi.org/10.1177/1049731505282593 .
Schmidt LM, Hesse M, Lykke J. The impact of substance use disorders on the course of schizophrenia-A 15-year follow-up study. Dual diagnosis over 15 years. Schizophr Res. 2011;130(1–3):228–33. https://doi.org/10.1016/j.schres.2011.04.011 .
Singh J, Mattoo SK, Sharan P, Basu D. Quality of life and its correlates in patients with dual diagnosis of bipolar affective disorder and substance dependence. Bipolar Disord. 2005;7(2):187–91. https://doi.org/10.1111/j.1399-5618.2004.00173.x .
Urboanoski KA, Cairney J, Bassani DG, Rush BR. Perceived unmet need for mental health care for Canadians with co-occurring mental and substance use disorders. Psychiatr Serv. 2008;59(3):283–9. https://doi.org/10.1176/appi.ps.59.3.283 .
Kingston REF, Marel C, Mills KL. A systematic review of the prevalence of comorbid mental health disorders in people presenting for substance use treatment in Australia. Drug Alcohol Rev. 2017;36(4):527–39. https://doi.org/10.1111/dar.12448 .
Klinkenberg WD, Caslyn RJ, Morse GA, Yonker RD, McCudden S, Ketema F, et al. Prevalence of human immunodeficiency virus, hepatitis B, and hepatitis C among homeless persons with co-occurring severe mental illness and substance use disorders. Compr Psychiatry. 2003;44(4):293–302. https://doi.org/10.1016/S0010-440X(03)00094-4 .
Wallace C, Mullen PE, Burgess P. Criminal offending in schizophrenia over a 25-year period marked by deinstitutionalization and increasing prevalence of comorbid substance use disorders. Am J Psychiatry. 2004;161(4):716–27. https://doi.org/10.1176/appi.ajp.161.4.716 .
Bronisch T, Wittchen HU. Suicidal ideation and suicide attempts: comorbidity with depression, anxiety disorders, and substance abuse disorder. Eur Arch Psychiatry Clin Neurosci. 1994;244(2):93–8. https://doi.org/10.1007/BF02193525 .
Hatzenbuehler ML, Keyes KM, Narrow WE, Grant BF, Hasin DS. Racial/ethnic disparities in service utilization for individuals with co-occurring mental health and substance use disorders in the general population: Results from the national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry. 2008;69(7):1112–21. https://doi.org/10.4088/JCP.v69n0711 .
Hodgins S, Tiihonen J, Ross D. The consequences of conduct disorder for males who develop schizophrenia: associations with criminality, aggressive behavior, substance use, and psychiatric services. Schizophr Res. 2005;78(2–3):323–35. https://doi.org/10.1016/j.schres.2005.05.021 .
Hunt GE, Bergen J, Bashir M. Medication compliance and comorbid substance abuse in schizophrenia: impact on community survival 4 years after a relapse. Schizophr Res. 2002;54(3):253–64. https://doi.org/10.1016/S0920-9964(01)00261-4 .
Link BG, Struening EL, Rahav M, Phelan JC, Nuttbrock L. On stigma and its consequences: evidence from a longitudinal study of men with dual diagnoses of mental illness and substance abuse. J Health Soc Behav. 1997;38(2):177–90. https://doi.org/10.2307/2955424 .
Priester MA, Browne T, Iachini A, Clone S, DeHart D, Seay KD. Treatment access barriers and disparities among individuals with co-occurring mental health and substance use disorders: an integrative literature review. J Subst Abuse Treat. 2016;61:47–59. https://doi.org/10.1016/j.jsat.2015.09.006 .
Talamo A, Centorrino F, Tondo L, Dimitri A, Hennen J, Baldessarini RJ. Comorbid substance-use in schizophrenia: relation to positive and negative symptoms. Schizophr Res. 2006;86(1–3):251–5. https://doi.org/10.1016/j.schres.2006.04.004 .
Teplin LA, Elkington KS, McClelland GM, Abram KM, Mericle AA, Washburn JJ. Major mental disorders, substance use disorders, comorbidity, and HIV-AIDS risk behaviors in juvenile detainees. Psychiatr Serv. 2005;56(7):823–8. https://doi.org/10.1176/appi.ps.56.7.823 .
Hinckley JD, Danielson CK. Elucidating the neurobiologic etiology of comorbid PTSD and substance use disorders. Brain Sci. 2022. https://doi.org/10.3390/brainsci12091166 .
Jarnecke AM, Saraiya TC, Brown DG, Richardson J, Killeen T, Back SE. Examining the role of social support in treatment for co-occurring substance use disorder and posttraumatic stress disorder. Addict Behav Rep. 2022. https://doi.org/10.1016/j.abrep.2022.100427 .
Kyster NB, Tranberg K, Osler M, Hjorthøj C, Mårtensson S. The influence of childhood aspirations on the risk of developing psychotic disorders, substance use disorders, and dual diagnosis in adulthood based on the Metropolit 1953 Danish male birth cohort. Eur Child Adolesc Psychiatry. 2022. https://doi.org/10.1007/s00787-022-02091-7 .
Cunill R, Castells X, González-Pinto A, Arrojo M, Bernardo M, Sáiz PA, et al. Clinical practice guideline on pharmacological and psychological management of adult patients with attention deficit and hyperactivity disorder and comorbid substance use. Adicciones. 2022;34(2):168–78. https://doi.org/10.2088/adicciones.1569 .
Margolese HC, Boucher M, Therrien F, Clerzius G. Treatment with aripiprazole once-monthly injectable formulation is effective in improving symptoms and global functioning in schizophrenia with and without comorbid substance use—a post hoc analysis of the ReLiAM study. BMC Psychiatry. 2022. https://doi.org/10.1186/s12888-022-04397-x .
Minkoff K, Covell NH. Recommendations for integrated systems and services for people with co-occurring mental health and substance use conditions. Psychiatric Serv. 2022;73(6):686–9. https://doi.org/10.1176/appi.ps.202000839 .
Oliva V, De Prisco M, Pons-Cabrera MT, Guzmán P, Anmella G, Hidalgo-Mazzei D, et al. Machine learning prediction of comorbid substance use disorders among people with bipolar disorder. J Clin Med. 2022. https://doi.org/10.3390/jcm11143935 .
Somohano VC, Kaplan J, Newman AG, O’Neil M, Lovejoy T. Formal mindfulness practice predicts reductions in PTSD symptom severity following a mindfulness-based intervention for women with co-occurring PTSD and substance use disorder. Addict Sci Clin Pract. 2022. https://doi.org/10.1186/s13722-022-00333-2 .
Watkins LE, Patton SC, Drexler K, Rauch SAM, Rothbaum BO. Clinical effectiveness of an intensive outpatient program for integrated treatment of comorbid substance abuse and mental health disorders. Cogn Behav Pract. 2022. https://doi.org/10.1016/j.cbpra.2022.05.005 .
Bertulies-Esposito B, Ouellet-Plamondon C, Jutras-Aswad D, Gagnon J, Abdel-Baki A. The impact of treatment orders for residential treatment of comorbid severe substance use disorders for youth suffering from early psychosis: a case series. Int J Ment Heal Addict. 2021;19(6):2233–44. https://doi.org/10.1007/s11469-020-00317-w .
Butler A, Nicholls T, Samji H, Fabian S, Lavergne MR. Prevalence of mental health needs, substance use, and co-occurring disorders among people admitted to prison. Psychiatric Serv. 2022;73(7):737–44. https://doi.org/10.1176/appi.ps.202000927 .
Henderson JL, Wilkins LK, Hawke LD, Wang W, Sanches M, Brownlie EB, et al. Longitudinal emergence of concurrent mental health and substance use concerns in an ontario school-based sample: the research and action for teens study. J Can Acad Child Adolesc Psychiatry. 2021;30(4):249–63.
PubMed PubMed Central Google Scholar
Huang JS, Yang FC, Chien WC, Yeh TC, Chung CH, Tsai CK, et al. Risk of substance use disorder and its associations with comorbidities and psychotropic agents in patients with autism. JAMA Pediatr. 2021. https://doi.org/10.1001/jamapediatrics.2020.5371 .
Lu W, Muñoz-Laboy M, Sohler N, Goodwin RD. Trends and disparities in treatment for co-occurring major depression and substance use disorders among US adolescents from 2011 to 2019. JAMA Netw Open. 2021. https://doi.org/10.1001/jamanetworkopen.2021.30280 .
Melkonian AJ, Flanagan JC, Calhoun CD, Hogan JN, Back SE. Craving moderates the effects of intranasal oxytocin on anger in response to social stress among veterans with co-occurring posttraumatic stress disorder and alcohol use disorder. J Clin Psychopharmacol. 2021;41(4):465–9. https://doi.org/10.1097/JCP.0000000000001434 .
Otasowie J. Co-occurring mental disorder and substance use disorder in young people: aetiology, assessment and treatment. BJPsych Adv. 2021;27(4):272–81. https://doi.org/10.1192/bja.2020.64 .
Saraiya TC, Badour CL, Jones AC, Jarnecke AM, Brown DG, Flanagan JC, et al. The role of posttraumatic guilt and anger in integrated treatment for PTSD and co-occurring substance use disorders among primarily male veterans. Psychol Trauma: Theory Res Pract Policy. 2022. https://doi.org/10.1037/tra0001204 .
Walhout SJN, Zanten JV, DeFuentes-Merillas L, Sonneborn CKME, Bosma M. Patients with autism spectrum disorder and co-occurring substance use disorder: a clinical intervention study. Subst Abuse: Res Treat. 2022. https://doi.org/10.1177/11782218221085599 .
Walker D, Infante AA, Knight D. Examining the impact of mental health, substance use, and co-occurring disorders on juvenile court outcomes. J Res Crime Delinq. 2022;59(6):820–53. https://doi.org/10.1177/00224278221084981 .
Warfield SC, Pack RP, Degenhardt L, Larney S, Bharat C, Ashrafioun L, et al. The next wave? Mental health comorbidities and patients with substance use disorders in under-resourced and rural areas. J Subst Abuse Treat. 2021. https://doi.org/10.1016/j.jsat.2020.108189 .
Hien DA, Fitzpatrick S, Saavedra LM, Ebrahimi CT, Norman SB, Tripp J, et al. What’s in a name? A data-driven method to identify optimal psychotherapy classifications to advance treatment research on co-occurring PTSD and substance use disorders. Eur J Psychotraumatol. 2022. https://doi.org/10.1080/20008198.2021.2001191 .
Leonhardt M, Brodahl M, Cogan N, Lien L. How did the first COVID-19 lockdown affect persons with concurrent mental health and substance use disorders in Norway? A qualitative study. BMC Psychiatry. 2022. https://doi.org/10.1186/s12888-022-03812-7 .
Leonhardt M, Kyrdalen E, Holstad A, Hurlen-Solbakken H, Chiu MYL, Lien L. Norwegian cross-cultural adaptation of the social and communities opportunities profile-mini for persons with concurrent mental health and substance use disorders. J Psychosoc Rehabil Mental Health. 2022. https://doi.org/10.1007/s40737-022-00309-0 .
Sell L, Lund HL, Johansen KS. Past, present, and future labor market participation among patients admitted to hospital with concurrent substance use and mental health disorder, and what we can learn from it. J Occup Environ Med. 2022;64(12):1041–5. https://doi.org/10.1097/JOM.0000000000002633 .
Sverdlichenko I, Hawke LD, Henderson J. Understanding the service needs of youth with opioid use: a descriptive study of demographics and co-occurring substance use and mental health concerns. J Subst Abuse Treat. 2022. https://doi.org/10.1016/j.jsat.2021.108592 .
Yerriah J, Tomita A, Paruk S. Surviving but not thriving: Burden of care and quality of life for caregivers of patients with schizophrenia spectrum disorders and comorbid substance use in South Africa. Early Interv Psychiatry. 2022;16(2):153–61. https://doi.org/10.1111/eip.13141 .
Murthy P, Chand P. Treatment of dual diagnosis disorders. Curr Opin Psychiatry. 2012;25(3):194–200. https://doi.org/10.1097/YCO.0b013e328351a3e0 .
Schneier M. Better treatment for dual diagnosis patients. Psychiatr Serv. 2000;51(9):1079. https://doi.org/10.1176/appi.ps.51.9.1079 .
Tirado Muñoz J, Farré A, Mestre-Pintó J, Szerman N, Torrens M. Dual diagnosis in depression: treatment recommendations. Adicciones. 2018;30(1):66–76. https://doi.org/10.2088/adicciones.868 .
Carrà G, Clerici M. Dual diagnosis–policy and practice in Italy. Am J Addict. 2006;15(2):125–30. https://doi.org/10.1080/10550490500528340 .
Download references
Acknowledgements
Author information, authors and affiliations.
Department of Physiology and Pharmacology/Toxicology, Division of Biomedical Sciences, College of Medicine and Health Sciences, An-Najah National University, Nablus, Palestine
Waleed M. Sweileh
You can also search for this author in PubMed Google Scholar
Contributions
W.S started the idea, designed the methodology; did the data analysis, graphics, and data interpretation; wrote and submitted the manuscript. This was a single-authored manuscript. W.S wrote and submitted the manuscript.
Corresponding author
Correspondence to Waleed M. Sweileh .
Ethics declarations
Ethics approval and consent to participate.
IRB at An-Najah National University (Palestine) requires no approval for bibliometric studies.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Sweileh, W.M. Research landscape analysis on dual diagnosis of substance use and mental health disorders: key contributors, research hotspots, and emerging research topics. Ann Gen Psychiatry 23 , 32 (2024). https://doi.org/10.1186/s12991-024-00517-x
Download citation
Received : 28 July 2023
Accepted : 21 August 2024
Published : 30 August 2024
DOI : https://doi.org/10.1186/s12991-024-00517-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Substance use disorders
- Mental health disorders
- Dual diagnosis
- Research landscape analysis
- Treatment interventions
- Comorbidity
Annals of General Psychiatry
ISSN: 1744-859X
- Submission enquiries: [email protected]
Pardon Our Interruption
As you were browsing something about your browser made us think you were a bot. There are a few reasons this might happen:
- You've disabled JavaScript in your web browser.
- You're a power user moving through this website with super-human speed.
- You've disabled cookies in your web browser.
- A third-party browser plugin, such as Ghostery or NoScript, is preventing JavaScript from running. Additional information is available in this support article .
To regain access, please make sure that cookies and JavaScript are enabled before reloading the page.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.10(9); 2020

Original research
Prevalence of psychoactive substance use among acutely hospitalised patients in oslo and moscow: a cross-sectional, observational study, danil gamboa.
1 Department of Forensic Sciences, Oslo University Hospital, Oslo, Norway
2 Department of Internal Medicine, Lovisenberg Diaconal Hospital, Oslo, Norway
Benedicte Jørgenrud
Evgeny a bryun.
3 Moscow Research and Practical Centre on Addictions, Moscow Department of Health, Moscow, Russia
4 Russian Medical Academy of Continuous Professional Education, Moscow, Russia
Vigdis Vindenes
5 Norwegian Centre for Addiction Research, University of Oslo, Oslo, Norway
Evgenya A Koshkina
Aleksei v nadezhdin, saranda kabashi.
6 Institute of Health and Society, Faculty of Medicine, University of Oslo, Oslo, Norway
Elena J Tetenova
Thomas berg, anna armika tussilago nyman, alexey j kolgashkin, aleksei e petukhov.
7 Sechenov First Moscow State Medical University, Moscow, Russia
Sergey N Perekhodov
8 Demikhov Moscow Clinical Hospital, Moscow, Russia
Elena N Davydova
Anners lerdal.
9 Department of Interdisciplinary Health Sciences, Institute of Health and Society, Faculty of Medicine, University of Oslo, Oslo, Norway
10 Department of Research, Lovisenberg Diaconal Hospital, Oslo, Norway
Gudmund Nordby
Stig tore bogstrand, associated data.
bmjopen-2019-032572supp001.pdf
The use of psychoactive prescription medication is increasing in the general population. This is a cause for concern, particularly among the elderly, where physiological changes related to senescence increase the risk for adverse effects. While previous studies regarding psychoactive substance use have generally been population based, we sought to determine the frequency of such use among acutely hospitalised patients.
Two emergency departments (EDs), one in Oslo and one in Moscow, admitting patients to Departments of Internal Medicine.
Participants
5583 patients aged ≥18 years participated, distributed evenly between genders and study locations. Patients unable to give informed consent were excluded. The study sites did not admit patients with surgical conditions and/or injuries.
Primary and secondary outcomes
The presence of psychoactive substances was determined through blood analysis using liquid chromatography-mass spectrometry. Secondary outcomes comprised demographic data (including age, gender, employment and marital status), degree of psychological distress, concurrent alcohol use, and self-reported alcohol, psychoactive drug and illicit substance use.
32.3% in Oslo and 12% in Moscow were positive for one or more psychoactive medicinal drugs (benzodiazepines, z-hypnotics, opioids or barbiturates). In Oslo, medicinal drug use was associated with being aged 61 to 70 years (OR 2.40, 95% CI 1.61 to 3.58) compared with 18 to 40 years, and psychological distress (OR 2.61, 95% CI 2.06 to 3.30). In Moscow, psychoactive medicinal drug use was also associated with psychological distress (OR 1.68, 95% CI 1.18 to 2.39), and was less common among patients aged 41 to 60 years (OR 0.62, 95% CI 0.43 to 0.88) than among patients aged 18 to 40 years.
A significant proportion of admitted patients used one or more psychoactive medicinal drugs, in particular benzodiazepines (Oslo and Moscow) and opiates (Oslo). We suggest formalised screening for inappropriate prescription drug use and increased adherence to clinical prescription guidelines.
Strengths and limitations of this study
- Blood sample analysis was used in addition to self-reporting to accurately assess the prevalence of psychoactive substance use.
- Large sample size divided across two sites, with an inclusion period lasting 1 year.
- Differences in laboratory methods, legislation and prescription practices for psychoactive substances between the selected sites limit comparability.
Introduction
While the deleterious effects of harmful alcohol use and tobacco smoking are well known, several studies have also called attention to increasing rates of psychoactive prescription drug use in Western countries, especially among the elderly. 1–3 These drugs include opioids, benzodiazepines and z-hypnotics. In addition to increased usage rates, there seems to be an apparent increase in the non-medical use and abuse of psychoactive medication, 4 as well as inappropriate prescription practices and diversion from clinical guidelines. 2
Several studies have prospectively assessed the impact and usage rates of alcohol, psychoactive medication and illicit substances in the ED. 5–8 Alcohol-related presentations to the ED have been quantified both through the use of questionnaires, and classification through the International Classification of Diseases, Tenth Revision (ICD-10). However, patients may under-report alcohol consumption when presented with a questionnaire, and self-reporting may be limited by recall bias. 9 Potentially harmful, but not clinically apparent, alcohol-related presentations may also remain undetected by health professionals and thus misclassified. These limitations may attenuate the accuracy of prevalence data in such studies. A study published in 2011 10 used blood sample analysis using highly selective methods to assess the prevalence of psychoactive substances among patients acutely admitted due to injury—this provided accurate and reliable prevalence data. However, blood sample analysis has not been used to assess the prevalence of psychoactive substances among patients acutely admitted to Departments of Internal Medicine.
Patients admitted to Departments of Internal Medicine are likely to be older than the general population. 11 The elderly are more vulnerable to any potential adverse effects from psychoactive medication use due to age-related changes in the pharmacodynamic and pharmacokinetic properties of various drugs. 12 13 Changes in physiology and body composition related to ageing increases the susceptibility to adverse effects from alcohol consumption, 14 and the concurrent use of psychoactive drugs and alcohol also exacerbates the respective adverse effects of each substance. Drowsiness and reduced postural stability are common effects of psychoactive drugs, and these are enhanced by alcohol consumption. Consequently, both drug-drug and drug-alcohol interactions may cause clinically significant adverse reactions in the elderly, such as falls, injury and infections. 1 These events may be precipitated even by low-to-moderate doses of the substances mentioned. Polypharmacy—the concurrent use of multiple medications—increases in frequency with age, with rates ranging from 12 % to 35 % among the elderly in Western countries. 15 This may contribute to the additive risk for adverse drug-drug interactions. Considering the high frequency of use among older adults, knowledge regarding the prevalence of these substances among acutely hospitalised patients may be of clinical significance. Psychoactive medication, specifically benzodiazepines and z-hypnotics, is also often used to treat psychological distress and sleep disorders, which are common among the elderly. 16 Contrary to alcohol, which is usually independently procured, and where ingestion is user-initiated, the distribution of psychoactive medication is generally mediated by health professionals. In light of increased rates of non-medical use and abuse of these drugs, 4 the presence of reliable and accurate prevalence data may mediate prudence regarding prescription practices, and lead to more critical appraisals of when these drugs are necessary or should be discontinued.
In this study, we sought to assess the prevalence of psychoactive substances among patients acutely hospitalised to Departments of Internal Medicine.
Specifically, we wished to:
- Measure the rate of psychoactive substance use through the use of blood sampling and highly selective analytical methods.
- Investigate patient characteristics when a psychoactive substance is detected; namely age, gender, employment status, marital status, degree of psychological distress and self-reported alcohol consumption.
- Investigate the concurrent rate of alcohol and illicit drug use when psychoactive substances are detected.
This study is part of a larger collaborative project between Oslo University Hospital and the Moscow Research Center on Addiction.
Study design, setting and participants
Design and site selection.
We have employed an observational, cross-sectional approach. We chose two study sites—
Lovisenberg Diaconal Hospital (LDS) in Oslo, Norway (site 1) and Hospital No. 68 in Moscow, Russia (site 2). Both sites are medium-sized urban hospitals. The mean life expectancy in Norway is 84.2 years for women and 80.6 years for men, 17 which is significantly higher than in Russia, where the mean life expectancy is 72.1 years. 18 However, due to socioeconomic disparities within the various districts in Oslo, the life expectancy in several populations belonging to the catchment area for LDS approaches that in Russia, ranging from 72 to 76 years for men and 79 to 81 years for women,. 19 Due to differences in laboratory techniques, prescription practices as well as guidelines and legislation for psychoactive drug use in each nation, results for each site will be presented separately.
Inclusion and exclusion criteria
In Oslo, patients were generally either recruited by emergency department (ED) nurses while awaiting ward transfer or examinations such as radiographic imaging, or shortly after arrival to their respective ward, while in Moscow, patients were recruited on arrival to the ward by physicians serving as dedicated study and recruitment coordinators. The EDs in Oslo and Moscow were both located at the Department of Internal Medicine, and therefore did not admit patients with injuries or surgical conditions. Patients were transferred to an appropriate ward after an initial evaluation, which in Oslo was General Internal Medicine, Infectious Diseases, Cardiology, Pulmonary Medicine, Cerebrovascular and Geriatric conditions, Haematology or Gastroenterology, and in Moscow patients were transferred to General Internal Medicine, Cardiology, Pulmonary Medicine or Neurology. Only patients aged 18 years and above and able to give informed consent were included. Patients unable to consent on admission due to reversible or transient causes (such as intoxication or severe illness) were approached at a later time by dedicated research assistants, and were offered to participate when they were able to consent. The inclusion period lasted from November 2016 to December 2017, and patients were included at all hours of the day, to account for any seasonal or diurnal variations. We employed the following exclusion criteria: (1) permanently unable to give an informed consent; (2) elective transfer from other hospitals; and (3) limited or no ability to read or write the national language, either Russian or Norwegian, as translated copies of both the consent form and accompanying questionnaire were unavailable. Figures 1 and 2 detail the flow of patient recruitment.

Flow diagram for patient recruitment in Oslo. All admitted patients were screened for eligibility. Patients permanently unable to give an informed consent, as well as patients electively transferred from other hospitals, were excluded.

Flow diagram for patient recruitment in Moscow. All admitted patients were screened for eligibility. Patients permanently unable to give an informed consent, as well as patients electively transferred from other hospitals, were excluded.
Patient and public involvement
There was no patient or public involvement in the design and implementation of this study. In addition to disseminating results to clinicians and policy makers, we intend to inform and involve patient interest organisations in the field of substance use disorders.
Study design, variables and analytical methods were jointly developed by the research teams at both study sites to maintain consistency in data collection and collation. The study sites were also visited by the respective study researchers to ensure methodological continuity.
Blood analysis
Whole blood was drawn from every study participant and secured in 5 mL BD Vacutainer blood collection glass tubes (BD Vacutainer Systems, Franklin Lakes, New Jersey, USA). The blood samples were stored at 4°C for a maximum of 7 days before analysis. In Oslo, the samples were analysed at the Division of Laboratory Medicine, Section of Drug Abuse Research, Oslo University Hospital. We prepared the samples by 96-well supported liquid extraction, which were then analysed by liquid chromatography-tandem mass spectrometry (LC-MS/MS). This is the same sample preparation and LC-MS/MS method used by Kristoffersen et al . 20 Stable isotope-labelled internal standards were used for all compounds. Two multiple reaction monitor (MRM) transitions were used for each compound and each internal standard. The chosen detection limits (cut-off limit) were based on validation data and signal/noise (S/N) ratio of the quantifier MRM transition (S/N≥10). For tetrahydrocannabinol (THC), S/N≥3 was used. The Russian samples were analysed at the Moscow Research Center for Addiction. Blood samples were prepared by protein precipitation and analysed by ultra-high performance LC-MS/MS. Two MRM transitions were used for each compound. The cut-off level for each analyte was defined as a signal corresponding to S/N=1000 for the quantifier MRM transition. We have provided additional methodological details and validation data for the Oslo site in online supplemental table 1 .
Supplementary data
Any sample in which the patient was administered a psychoactive medicinal drug by healthcare personnel prior to blood sampling was omitted from the results—specifically, morphine and diazepam at the Oslo site, and diazepam, phenazepam and tramadol at the Moscow site. In order to distinguish medicinal morphine use from heroin use, a morphine/codeine ratio cut-off value of >1 was used. 21 Similarly, concentration ratios of methamphetamine to amphetamine were used to distinguish methamphetamine use from various mixtures of the two stimulants. 22
Questionnaire
Upon enrolment, every patient filled out a questionnaire containing demographic data: age ranges (18 to 40, 41 to 60, 61 to 70 and ≥71 years), gender (male/female), marital status (single, married or widowed) and employment status (employed, retired, unemployed or student). Psychological distress was measured using the Symptom Checklist 5 (SCL-5), a short-form screening tool which performs almost as well as the full version. 23 A value above two points indicates psychological distress. Self-reported alcohol use was measured through the Alcohol Use Disorder Identification Test-4 (AUDIT-4), which has been validated as a simple yet effective screening tool for identifying alcohol use disorders. 24 25 A value of 7 points or more for men and 5 points or more for women indicates at-risk alcohol consumption patterns. Both questionnaires have been validated for use in their respective nations. 26–28 The questionnaires were filled out by the patients themselves, with occasional aid from emergency room (ER) nurses at the Oslo site if questions arose. The ER nurses were also instructed beforehand by the study coordinator, and a data collection pilot preceded the inclusion period. We also included self-reported use of benzodiazepines and/or barbiturates (termed ‘sedatives’), z-hypnotics (termed ‘sleeping medication’), opioids (termed ‘painkillers’) and illicit drugs (termed ‘narcotic substances’). All drug groups had example trade or colloquial names to improve question comprehension.
Questionnaires were manually entered, controlled and later transferred to the electronic project database.
Psychoactive substances
Our primary outcome was the presence of a psychoactive substance, determined through analytical cut-off values ( tables 1 and 2 ). Psychoactive medicinal drugs were defined as opioids, benzodiazepines, z-hypnotics or barbiturates. The specific drugs were selected based on prescription practices among primary care and hospital physicians, as well as hospital usage rates. Due to differences in prescription practices, certain substances were omitted at the Moscow site, and vice versa for the Oslo site. Specifically, the use of z-hypnotics in Russia is very uncommon, and phenazepam, a commonly prescribed benzodiazepine in Russia, is not marketed in Norway. 29 Barbiturates are also commonly used as a sedative in Russia, but this use is uncommon in Norway.
Prevalence of illicit substances and psychoactive medication among all admitted patients in Oslo
| Cut-off (nmol/L) | Mean concentration (nmol/L) | Number of positive samples | Per cent | |
| Illicit | 167 | 6.4 | ||
| Amphetamines | 55 | 2.1 | ||
| Amphetamine | 200 | 1696 | 21 | 0.8 |
| Methamphetamine | 200 | 1859 | 45 | 1.7 |
| Cocaine* | 30 | 1.2 | ||
| Benzoylecgonine | 10 | 1587 | 22 | 0.8 |
| Cocaine | 0.6 | 242 | 26 | 1.0 |
| Heroin | M/C>1 | 24 | 0.9 | |
| MDMA ecstasy | 200 | 1063 | 4 | 0.2 |
| THC | 2 | 15 | 97 | 3.7 |
| Medicinal | 843 | 32.3 | ||
| Alprazolam | 1 | 40 | 19 | 0.7 |
| Buprenorphine | 4 | 10 | 7 | 0.3 |
| Clonazepam | 0.4 | 127 | 98 | 3.8 |
| Codeine | 3 | 167 | 181 | 6.9 |
| Diazepam | 20 | 402 | 251 | 9.6 |
| Flunitrazepam | 0.5 | 5 | 6 | 0.2 |
| Methadone | 20 | 1142 | 46 | 1.8 |
| Morphine | 3 | 90 | 107 | 4.1 |
| Nitrazepam | 5 | 139 | 93 | 3.6 |
| Oxycodone | 5 | 193 | 91 | 3.5 |
| Oxazepam | 50 | 822 | 215 | 8.2 |
| Tramadol | 20 | 743 | 121 | 4.6 |
| Zolpidem | 70 | 406 | 32 | 1.2 |
| Zopiclone | 20 | 57 | 139 | 5.3 |
| Z-hypnotics | 171 | 6.6 | ||
| Benzodiazepines | 482 | 18.5 | ||
| Opioids | 507 | 19.5 | ||
| Alcohol | 94 | 3.6 | ||
| Medicinal and/or illicit | 900 | 34.5 |
*Cocaine-positive is defined as a sample positive for either cocaine or benzoylecgonine. Because the recovery of benzoylecgonine is very low using SLE extraction, a patient may be positive for cocaine, but negative for benzoylecgonine.
†Alcohol-positive is defined as blood alcohol content >0.1 g/kg.
M/C, morphine/codeine ratio; MDMA, 3,4-Methylenedioxymethamphetamine; SLE, supported liquid extraction; THC, tetrahydrocannabinol.
Prevalence of illicit substances and psychoactive medication among all admitted patients in Moscow
| S/N ratio* | Number of positive samples | Percent† | |
| Illicit | 43 | 1.4 | |
| Amphetamines | 1000 | 5 | 0.2 |
| Amphetamine | 4 | 0.14 | |
| Methamphetamine | 1 | 0.03 | |
| Cocaine‡ | 1 | 0.03 | |
| Benzoylecgonine | 1 | 0.03 | |
| Heroin | 2 | 0.07 | |
| MDMA ecstasy | 2 | 0.07 | |
| THC | 32 | 1.1 | |
| Alpha PVP | 3 | 0.10 | |
| Methadone | 6 | 0.20 | |
| Medicinal | 361 | 12.0 | |
| Clonazepam | 1 | 0.03 | |
| Codeine | 1 | 0.03 | |
| Dextromethorphan | 1 | 0.03 | |
| Diazepam | 61 | 2.0 | |
| Phenazepam | 240 | 8.0 | |
| Phenobarbital | 68 | 2.3 | |
| Pregabalin | 9 | 0.3 | |
| Tramadol | 13 | 0.4 | |
| Barbiturates | 68 | 2.3 | |
| Benzodiazepines | 291 | 9.7 | |
| Opioids | 28 | 0.9 | |
| Alcohol | 30 | 1.0 | |
| Medicinal and/or illicit | 393 | 13.1 |
*In Moscow, the detection limit was based on a S/N ratio above 1000, which applies for all substances listed. In Oslo, absolute lower detection limits were used.
†In instances of substances being detected in a very small number of samples, percentages are presented with 2 decimal points.
‡Cocaine-positive is defined as a sample positive for either cocaine or benzoylecgonine. Because the recovery of benzoylecgonine is very low using SLE extraction, a patient may be positive for cocaine, but negative for benzoylecgonine
§In Moscow, several other substances were analysed in addition to those listed in table 2—these were omitted due to lack of positive samples.
¶Alcohol-positive is defined as blood alcohol content >0.1 g/kg.
alpha PVP, alpha-pyrrolidinovalerophenone; MDMA, 3,4-Methylenedioxymethamphetamine; SLE, supported liquid extraction; S/N, signal/noise; THC, tetrahydrocannabinol.
The presence of alcohol was determined through direct analysis of blood alcohol content. Based on population studies, the most common illicit drugs and their metabolites were analysed—these comprise amphetamines, methamphetamines, cocaine, MDMA (3,4-Methylenedioxymethamphetamine)/ecstasy, heroin and THC. So-called ‘new psychoactive substances’ were not analysed—the rapid introduction of new compounds poses significant analytical challenges, and selecting which substance to analyse is complicated by limited knowledge regarding their availability in the general population. 30 Polyuse was defined as the presence of two or more psychoactive substances (prescription medication and/or illicit drugs) in any given blood sample.
Statistical analysis
We analysed the data using IBM SPSS 25.0 (Armonk, New York, USA). The prevalence of various psychoactive substances is shown through descriptive tables. We employed bivariate cross tables to analyse associations between the presence of a psychoactive substance and sample characteristics. χ 2 statistics with ORs were used to assess statistical significance. Our primary dependent variable was the presence of any psychoactive medicinal substance. Our covariates were age ranges, marital status, employment status, positive blood alcohol content, presence of illicit drugs, polyuse, presence of psychological distress and self-reported alcohol use. We performed logistic regression analyses to test the association between our dependent values, which were medicinal drug use, illicit drug use and polyuse, and independent covariates, which were age, gender, SCL-5 values, marital status, employment status and AUDIT-4 zones. Our reference categories for each variable were age 18 to 40 years, male gender, SCL-5 score ≤2, married, active in the workforce and an AUDIT score of 0 to 3. The level of significance was set at p<0.05. Continuous data are presented as means, with 95% CIs.
A total of 2874 patients in the Oslo site and 3009 patients in the Moscow site were included, with a participation rate of 81% and 90%, respectively—47.6% were women in Oslo and 52.9% were women in Moscow. Distribution across age ranges was similar at both sites ( tables 3 and 4 ).
Medicinal drug use* and demographic data, SCL-5, concurrent illicit drug use and AUDIT-4 in Oslo
| Medicinal no N (%) | Medicinal yes N (%) | Total N (%) | P value (χ ) | |
| Gender | p=0.66 | |||
| Female | 832 (48) | 388 (47) | 1220 (48) | |
| Male | 907 (52) | 439 (53) | 1346 (52) | |
| Total | 1739 | 827 | 2566 | |
| Age (years) | p<0.001 | |||
| 18 to 40 | 593 (34) | 113 (14) | 706 (28) | |
| 41 to 60 | 424 (25) | 214 (26) | 638 (25) | |
| 61 to 70 | 317 (18) | 222 (27) | 539 (21) | |
| ≥71 | 398 (23) | 276 (34) | 674 (26) | |
| Total | 1732 | 825 | 2557 | |
| Marital status | p<0.001 | |||
| Married/co-habitant | 814 (48) | 266 (34) | 1080 (43) | |
| Divorced | 242 (14) | 176 (22) | 418 (17) | |
| Widowed | 124 (7) | 99 (13) | 223 (9) | |
| Single | 525 (31) | 245 (31) | 770 (31) | |
| Total | 1705 | 786 | 2491 | |
| Employment | p<0.001 | |||
| Active | 985 (58) | 188 (24) | 1173 (47) | |
| Retired | 548 (33) | 393 (50) | 941 (38) | |
| Non-active | 154 (9) | 211 (27) | 365 (15) | |
| Total | 1687 | 792 | 2479 | |
| SCL-5 | p<0.001 | |||
| ≤2 | 1383 (84) | 460 (62) | 1843 (77) | |
| >2 | 263 (16) | 279 (38) | 542 (23) | |
| Total | 1646 | 739 | 2367 | |
| Illicit drugs in blood | p<0.001 | |||
| No | 1707 (97) | 733 (87) | 2440 (94) | |
| Yes | 57 (3) | 110 (13) | 167 (6) | |
| Total | 1764 | 843 | 2607 | |
| AUDIT-4 | p<0.001 | |||
| 0 to 3 | 901 (54) | 506 (64) | 1407 (57) | |
| 4 to 6 | 537 (32) | 147 (19) | 684 (28) | |
| 7 to 8 | 126 (8) | 52 (7) | 178 (7) | |
| 9 to 16 | 107 (6) | 85 (11) | 192 (8) | |
| Total | 1671 | 790 | 2461 | |
| Blood alcohol content | p=0.03 | |||
| <0.1% | 1710 (97) | 803 (95) | 2513 (96) | |
| ≥0.1% | 54 (3) | 40 (5) | 94 (4) | |
| Total | 1764 | 843 | 2607 | |
| Polyuse | p<0.001 | |||
| <2 | 1760 (100) | 462 (55) | 2222 (85) | |
| ≥2 | 4 (0.2) | 381 (45) | 385 (15) | |
| Total | 1764 | 843 | 2607 |
*Medicinal drugs are defined as the presence of benzodiazepines, z-hypnotics or opioids.
AUDIT-4, Alcohol Use Disorder Identification Test-4; SCL-5, Symptom Checklist 5.
Medicinal drug use* and demographic data, SCL-5, concurrent illicit drug use and AUDIT-4 in Moscow
| Medicinal no N (%) | Medicinal yes N (%) | Total N (%) | P value (χ ) | |
| Gender | p=0.18 | |||
| Female | 1412 (53) | 179 (50) | 1591 (53) | |
| Male | 1236 (47) | 182 (50) | 1418 (47) | |
| Total | 2648 | 361 | 3009 | |
| Age (years) | p=0.14 | |||
| 18 to 40 | 451 (17) | 77 (21) | 528 (17) | |
| 41 to 60 | 821 (31) | 103 (29) | 924 (31) | |
| 61 to 70 | 663 (25) | 79 (22) | 742 (25) | |
| ≥71 | 719 (27) | 102 (28) | 815 (27) | |
| Total | 2654 | 361 | 3009 | |
| Marital status | p=0.03 | |||
| Married/co-habitant | 1305 (49) | 152 (42) | 1457 (49) | |
| Divorced | 336 (13) | 62 (17) | 398 (13) | |
| Widowed | 704 (27) | 106 (29) | 810 (27) | |
| Single | 303 (11) | 41 (11) | 344 (11) | |
| Total | 2648 | 361 | 3009 | |
| Employment | p<0.001 | |||
| Active | 816 (31) | 81 (22) | 897 (30) | |
| Retired | 401 (15) | 90 (25) | 491 (16) | |
| Non-active | 1430 (54) | 190 (53) | 1620 (54) | |
| Total | 2647 | 361 | 3008 | |
| SCL-5 | p<0.001 | |||
| ≤2 | 2454 (93) | 310 (86) | 2414 (92) | |
| >2 | 189 (7) | 49 (14) | 238 (8) | |
| Total | 2643 | 359 | 3002 | |
| Illicit drugs in blood | p=0.02 | |||
| No | 2615 (99) | 351 (97) | 2966 (99) | |
| Yes | 33 (1) | 10 (3) | 43 (1) | |
| Total | 2648 | 361 | 3009 | |
| AUDIT-4 | p<0.001 | |||
| 0 to 3 | 1986 (75) | 228 (63) | 2214 (74) | |
| 4 to 6 | 222 (8) | 16 (4) | 238 (8) | |
| 7 to 8 | 110 (4) | 13 (4) | 123 (4) | |
| 9 to 16 | 326 (12) | 103 (29) | 429 (14) | |
| 2644 | 360 | 3004 | ||
| Blood alcohol content | p=0.51 | |||
| <0.1% | 2626 (99) | 353 (98) | 2979 (99) | |
| ≥0.1% | 22 (1) | 8 (2) | 30 (1) | |
| Total | 2648 | 361 | 3009 | |
| Polyuse | p<0.001 | |||
| <2 | 2642 (100) | 319 (88) | 2961 (98) | |
| ≥2 | 6 (0) | 42 (12) | 48 (2) | |
| Total | 2648 | 361 | 3009 |
*Medicinal drugs are defined as the presence of benzodiazepines, barbiturates or opioids.
Prevalence data and sample characteristics
Prevalence data.
Tables 1 and 2 depict the main findings in our study, showing prevalence data for all psychoactive substances analysed and their analytical cut-off values. In Oslo, psychoactive medicinal drugs were detected in 32.3% of analysed samples. The most common drug class detected was opioids (19.5 %), followed by benzodiazepines (18.5 %). Z-hypnotics were found in 6.6% of samples. In the Moscow site, psychoactive medicinal drugs were detected in 12% of samples—benzodiazepines were the most frequently detected drug class (9.7 %). The rates for other drug classes were low, with opioids found in 0.9%.
In Oslo, illicit drugs were detected in 6.4% of all samples, with THC (3.7 %) being the most common. In the Moscow site, the total rate for illicit drug use was lower compared with the Oslo site, at 1.4 %, with THC being the most common (1.1 %). The rates for the remaining substances in both sites were low.
Cut-off values at each of the two sites were not identical due to differences in analytical methods, with a lower S/N ratio at the Oslo site. We have therefore provided mean concentrations for the substances detected at the Oslo site, which in the majority of substances are well above the analytical cut-off.
Sample characteristics
Tables 3 and 4 show the unadjusted distribution for psychoactive medicinal drug users and non-users across all covariates measured in Oslo and Moscow, respectively. Medicinal drug use was evenly distributed among genders at both sites. In Oslo, the highest proportion of medicinal drug use was found among patients aged older than 40 years, as well as among those being retired, and/or in the lowest AUDIT-4 ranges. In Moscow, medicinal drug use was more evenly distributed across all age groups, with the highest proportion of use among patients that were non-active in the workforce.
Table 5 depicts logistic regression analysis for various covariates in the Oslo site. Compared with patients aged 18 to 40 years, the likelihood for medicinal drug use was higher among patients aged 41 years and older. There was no significant gender difference among medicinal drug users. The likelihood for polyuse was higher among non-employed patients compared with patients being active in the workforce—this was also observed in regards to illicit substances as well as medicinal drug use. In the Oslo site, female patients were also significantly less likely to use illicit drugs than male patients. Patients aged 18 to 40 years were more likely to use illicit drugs than other age groups. The use of medicinal drugs, illicit drugs, and polyuse was significantly more likely in patients scoring above the cut-off value for SCL-5 (>2).
Logistic regression analysis of demographic characteristics, AUDIT-4 and SCL-5 for medicinal drugs*, illicit drugs and polyuse in Oslo
| Illicit drugs | Medicinal drugs | Polyuse | |||||||
| OR | 95% CI | P value | OR | 95% CI | P value | OR | 95% CI | P value | |
| Age (years) | |||||||||
| 18 to 40 | Reference | ||||||||
| 41 to 60 | 0.40 | 0.23 to 0.67 | <0.001 | 1.71 | 1.24 to 2.38 | <0.05 | 1.34 | 0.83 to 2.15 | 0.23 |
| 61 to 70 | 0.12 | 0.05 to 0.27 | <0.001 | 2.40 | 1.61 to 3.58 | <0.001 | 1.51 | 0.87 to 2.64 | 0.15 |
| 71+ | 0.02 | 0.00 to 0.12 | <0.001 | 2.22 | 1.36 to 3.65 | <0.05 | 1.00 | 0.51 to 1.95 | 1.00 |
| Gender | |||||||||
| Male | Reference | ||||||||
| Female | 0.37 | 0.24 to 0.58 | <0.001 | 0.86 | 0.70 to 1.06 | 0.15 | 0.79 | 0.60 to 1.05 | 0.10 |
| SCL-5 | |||||||||
| ≤2 | Reference | ||||||||
| >2 | 2.07 | 1.35 to 3.17 | <0.001 | 2.61 | 2.06 to 3.30 | <0.001 | 3.47 | 2.61 to 4.61 | <0.001 |
| Marital status | |||||||||
| Married/co-habitant | Reference | ||||||||
| Divorced | 3.30 | 1.79 to 6.10 | <0.001 | 1.30 | 0.98 to 1.74 | 0.07 | 1.75 | 1.21 to 2.53 | <0.05 |
| Widowed | 0.74 | 0.09 to 5.92 | 0.77 | 1.47 | 1.01 to 2.12 | 0.04 | 1.49 | 0.90 to 2.45 | 0.12 |
| Single | 1.78 | 1.12 to 2.85 | <0.05 | 1.28 | 1.01 to 1.64 | 0.05 | 1.28 | 0.91 to 1.79 | 0.16 |
| Employment | |||||||||
| Active | Reference | ||||||||
| Retired | 2.20 | 0.83 to 5.83 | 0.11 | 2.07 | 1.40 to 3.07 | <0.001 | 3.82 | 2.22 to 6.59 | <0.001 |
| Non-active | 6.29 | 3.74 to 10.58 | <0.001 | 3.82 | 2.80 to 5.21 | <0.001 | 7.36 | 4.87 to 11.14 | <0.001 |
| AUDIT-4 | |||||||||
| 0 to 3 | Reference | ||||||||
| 4 to 6 | 1.03 | 0.62 to 1.72 | 0.91 | 0.77 | 0.60 to 0.98 | <0.05 | 0.72 | 0.51 to 1.04 | 0.08 |
| 7 to 8 | 1.63 | 0.85 to 3.10 | 0.14 | 1.02 | 0.68 to 1.54 | 0.93 | 1.34 | 0.79 to 2.28 | 0.28 |
| 9 to 16 | 0.85 | 0.46 to 1.58 | 0.61 | 1.12 | 0.77 to 1.62 | 0.55 | 0.89 | 0.56 to 1.41 | 0.61 |
*Medicinal drugs defined as benzodiazepines, z-hypnotics or opioids.
In the Moscow site ( table 6 ), similar trends for SCL-5 were observed, where patients scoring above the cut-off value were more likely to use medicinal drugs. However, there was no significant difference in the likelihood for polyuse and illicit drug use. Contrary to the Oslo site, the presence of medicinal drugs and polyuse was significantly less likely in patients aged 41 to 60 years. Being retired increased the likelihood for medicinal drug use compared with patients being actively employed—the same association was not statistically significant for patients being non-active in the workforce.
Logistic regression analysis of demographic characteristics, AUDIT-4 and SCL-5 for medicinal drugs,* illicit drugs and polyuse in Moscow
| Illicit drugs | Medicinal drugs | Polyuse | |||||||
| OR | 95% CI | P value | OR | 95% CI | P value | OR | 95% CI | P value | |
| Age (years) | |||||||||
| 18 to 40 | Reference | ||||||||
| 41 to 60 | 0.19 | 0.09 to 0.42 | <0.001 | 0.62 | 0.43 to 0.88 | 0.01 | 0.29 | 0.12 to 0.70 | <0.05 |
| 61 to 70 | 0.07 | 0.05 to 0.83 | <0.05 | 0.67 | 0.40 to 1.12 | 0.13 | 0.10 | 0.02 to 0.39 | <0.05 |
| 71+ | 0.00 | 0.00 | 0.99 | 0.81 | 0.47 to 1.40 | 0.44 | 0.12 | 0.03 to 0.50 | <0.05 |
| Gender | |||||||||
| Male | Reference | ||||||||
| Female | 0.22 | 0.09 to 0.53 | <0.001 | 1.02 | 0.77 to 1.34 | 0.91 | 0.50 | 0.25 to 1.02 | 0.06 |
| SCL-5 | |||||||||
| ≤2 | Reference | ||||||||
| >2 | 1.44 | 0.53 to 3.91 | 0.47 | 1.68 | 1.18 to 2.39 | <0.05 | 2.09 | 0.94 to 4.63 | 0.07 |
| Marital status | |||||||||
| Married/co-habitant | Reference | ||||||||
| Divorced | 2.14 | 0.90 to 5.08 | 0.09 | 1.39 | 1.00 to 1.95 | 0.05 | 1.49 | 0.66 to 3.34 | 0.34 |
| Widowed | 3.27 | 0.66 to 16.10 | 0.15 | 1.34 | 0.96 to 1.85 | 0.08 | 1.22 | 0.47 to 3.17 | 0.68 |
| Single | 1.65 | 0.78 to 3.46 | 0.19 | 0.95 | 0.63 to 1.44 | 0.81 | 1.19 | 0.50 to 2.84 | 0.70 |
| Employment | |||||||||
| Active | Reference | ||||||||
| Retired | 1.13 | 0.57 to 2.23 | 1.13 | 1.90 | 1.35 to 2.66 | <0.001 | 2.21 | 0.96 to 4.90 | 0.05 |
| Non-active | 0.23 | 0.02 to 2.84 | 0.23 | 1.46 | 0.94 to 2.27 | 0.09 | 4.89 | 1.52 to 15.71 | <0.05 |
| AUDIT-4 | |||||||||
| 0 to 3 | Reference | ||||||||
| 4 to 6 | 0.86 | 0.31 to 2.40 | 0.87 | 0.73 | 0.42 to 1.26 | 0.26 | 1.04 | 0.35 to 3.13 | 0.94 |
| 7 to 8 | 1.14 | 0.36 to 3.61 | 1.14 | 1.22 | 0.66 to 2.28 | 0.53 | 0.48 | 0.06 to 3.72 | 0.48 |
| 9 to 16 | 0.87 | 0.39 to 1.91 | 0.87 | 2.81 | 2.04 to 3.87 | <0.001 | 1.59 | 0.75 to 3.37 | 0.23 |
*Medicinal drugs defined as benzodiazepines, barbiturates or opioids.
Tables 7 and 8 show the distribution of self-reported use if a sample is positive for either benzodiazepines, opioids, z-hypnotics and illicit drugs, with both benzodiazepines and barbiturates categorised as ‘sedatives’ in Moscow. If a sample is negative, this is generally mirrored in questionnaires regarding self-reported use. The highest concordance between positive samples and confirmatory self-reported use in Oslo was for z-hypnotics (75.8 %), followed by opioids (62.5 %), illicit drugs (49.4 %) and benzodiazepines (48.9 %). In Moscow, there was a high concordance between negative samples for opioids and illicit drugs, and self-reported non-use. This percentage was lower for sedatives (83.2% for barbiturates and 83.8% for benzodiazepines). The percentage of sample-positive self-reported use ranged from 7.1% for opioids to 55.9% for barbiturates.
Comparison between self-reported intake and laboratory detection of z-hypnotics, opioids, benzodiazepines and illicit drugs at the Oslo site
| Laboratory analysis | No | Yes | Not sure | |
| Z-hypnotics | p<0.0001 | |||
| Negative | 2066 (87.2 %) | 291 (12.3 %) | 12 (0.5 %) | |
| Positive | 40 (24.2 %) | 125 (75.8 %) | 0 (0 %) | |
| Opioids | p<0.0001 | |||
| Negative | 1875 (92.4 %) | 135 (6.6 %) | 19 (0.9 %) | |
| Positive | 178 (36.7 %) | 304 (62.5 %) | 4 (0.8 %) | |
| Benzodiazepines | p<0.0001 | |||
| Negative | 1984 (96.2 %) | 63 (3.1 %) | 15 (0.7 %) | |
| Positive | 226 (49.6 %) | 223 (48.9 %) | 7 (1.5 %) | |
| Illicit drugs | p<0.0001 | |||
| Negative | 2344 (98.7 %) | 28 (1.2 %) | 3 (0.1 %) | |
| Positive | 82 (50.0 %) | 81 (49.4 %) | 1 (0.6 %) | |
Comparison between self-reported intake and laboratory detection of barbiturates, benzodiazepines, opioids and illicit drugs at the Moscow site
| Laboratory analysis | No | Yes | Not sure | |
| Barbiturates | p<0.0001 | |||
| Negative | 2447 (83.2 %) | 493 (16.8 %) | 1 (0.0 %) | |
| Positive | 29 (42.6 %) | 38 (55.9 %) | 1 (1.5 %) | |
| Benzodiazepines | p<0.0001 | |||
| Negative | 2279 (83.8 %) | 438 (16.1 %) | 1 (0.1 %) | |
| Positive | 197 (67.7 %) | 93 (32.0 %) | 1 (0.3 %) | |
| Opioids | p<0.05 | |||
| Negative | 2952 (99 %) | 27 (0.9 %) | 2 (0.1 %) | |
| Positive | 26 (92.9 %) | 2 (7.1 %) | 0 (0.0 %) | |
| Illicit drugs | p<0.0001 | |||
| Negative | 2959 (99.8 %) | 7 (0.2 %) | 0 (0.0 %) | |
| Positive | 38 (88.4 %) | 5 (11.6 %) | 0 (0.0 %) | |
*Z-hypnotics are almost completely unavailable in Russia due to various regulatory practices, and there are no drug classes typically marketed as ‘sleeping medication’. Barbiturates and benzodiazepines are generally used to treat both anxiety as well as sleep disorders.
Figure 3 shows the distribution of psychoactive substances within different AUDIT-4 ranges in Oslo. The highest prevalence of benzodiazepine use was found in the highest AUDIT-4 range (9 to 16 points), with a rate of 31 %, compared with 18.5% for the whole study population. The use of opioids is more prevalent at the lowest and highest AUDIT-4 ranges. The use of THC, stimulants and z-hypnotics is evenly distributed along all AUDIT-4 ranges. In Moscow ( figure 4 ), the highest rate of benzodiazepine use is also found among the highest AUDIT-4 range, while the usage rate for other psychoactive substances is uniformly low in all other AUDIT-4 ranges.

Prevalence of psychoactive substances within AUDIT-4 in Oslo. Percentage of samples positive for stimulants (amphetamines or cocaine), THC, opiates, benzodiazepines and z-hypnotics across AUDIT-4 ranges in Oslo. Results are combined for both men and women. AUDIT-4, Alcohol Use Disorder Identification Test-4; THC, tetrahydrocannabinol.

Prevalence of psychoactive substances within AUDIT-4 in Moscow. Percentage of samples positive for stimulants (amphetamines or cocaine), THC, opiates, benzodiazepines and barbiturates across AUDIT-4 ranges in Moscow. Results are combined for both men and women. AUDIT-4, Alcohol Use Disorder Identification Test-4; THC, tetrahydrocannabinol.
Our study demonstrates that the use of psychoactive substances among patients admitted to Departments of Internal Medicine is highly prevalent, while simultaneously highlighting differences in sample characteristics between Oslo and Moscow. Based on previous studies, the volume of participants and rate of inclusion provide representative and accurate data. The number of positive sample for psychoactive substances was far higher in Oslo than in Moscow. The use of psychoactive substances in Oslo was significantly associated with older age, psychological distress and being unemployed. The latter two characteristics are known to be associated with substance use. 31 There was no significant gender disparity among positive samples—this may be explained by a higher percentage of positive samples among younger males compared with females, and vice versa for older females compared with older males. Previous population-based studies 3 32 33 also show an apparent increase in the use of psychoactive prescription medication in the general population, particularly among the elderly. However, the drug use statistics were extracted from national prescription databases, and whether or not the patient took the prescribed drug as well as the duration of drug use was not measured. Additionally, substance abuse disorders are more prevalent among non-participants in health surveys. 34 35 These factors may underestimate the prevalence of psychoactive substance use—as far as we are aware, this is the first study to demonstrate the frequency of substance use among internal medicine patients.
The high rate of psychoactive substance use among the elderly is a cause for concern. The changes in pharmacodynamics and pharmacokinetics associated with senescence increase complexity when prescribing medications to the elderly. 36 Inter-individual variability to drugs increases with age, partly explained by reduced physiological reserves during stressors such as inter-current illness or disease. Half-life of elimination is prolonged by changes in body composition, affecting the volume of distribution of lipid-soluble drugs, and reduced renal and hepatic clearance. 12 These factors alter and increase the sensitivity to psychoactive substances. Elderly patients are particularly sensitive to the effects of benzodiazepines on the central nervous system. Sedation may occur at lower doses than in younger patients. Drowsiness and decreased motor skills, combined with the age-related reduction in functional reserves, increase the risk for immobility and falls. 37
Physiological reserves in many elderly people may be adequate at normal homeostasis. However, the introduction of a stressor, such as an illness requiring acute hospitalisation, may deplete these reserves, even after the precipitating cause has been corrected. 38 Concurrent use of psychoactive substances and the increased vulnerability to their adverse effects may exacerbate this course. Additionally, conditions which increase in frequency and severity with old age, such as chronic obstructive pulmonary disease, have increased rates of adverse events among users of benzodiazepines and opioids. 39 Increasing age also increases morbidity and multimorbidity, which in turn is associated with polypharmacy, 40 with a concurrent increased risk for drug-drug interactions and other adverse effects. 41 While physicians may be aware of these factors, there is evidence that diversion from clinical guidelines for the prescription of psychoactive medication, in particular benzodiazepines, is widespread. 2
Regarding self-reported use of benzodiazepines, opioids, z-hypnotics and illicit drugs, there appears to be a high negative predictive value if a patient reports non-use. However, if a sample is positive, under-reporting seems to be prevalent. This differs based on substance category. Patient uncertainty regarding their medication list may contribute 42 and lead to under-reporting, as well as any potential stigma associated with illicit substance or psychoactive medication use.
The co-occurrence of harmful alcohol use and non-medical prescription drug use is also well established. 43 Our study demonstrates primarily increased rates of benzodiazepine use in the upper AUDIT-4 ranges ( figures 3 and 4 ). Whether this reflects co-occurring non-medical prescription drug use or as a reflection of treatment of symptoms related to harmful alcohol use is uncertain.
Clinical implications
The above considerations, combined with the findings from our study, should prompt an increased awareness regarding the use of psychoactive substances among acutely hospitalised patients. A reduction in inappropriate use or misuse of psychoactive substances may have a positive impact on hospitalisation rates, risk of re-admittance and healthcare costs. Specifically, strengthening and implementing the following practices may contribute to improved patient outcomes:
- Screening for inappropriate or harmful psychoactive substance use
- Critically assessing the indications for psychoactive medicinal drug use and considering discontinuation or tapering if inappropriate prescribing is present
- Assess the degree of increased risk for adverse events in specific conditions when using psychoactive substances, such as chronic obstructive pulmonary disease
- Assess concomitant alcohol use if psychoactive substance use is present
Hospital admissions may serve as opportunities to screen for unapparent harmful use or misuse of psychoactive substances, but this practice is less likely to be performed among elderly patients than among younger individuals. 32 Health professionals may experience hesitation in screening for unhealthy psychoactive substances use due to the perceived sensitive nature of the subject, 44 but guidelines for proper communicative techniques exist, which may ameliorate any associated stigma. 45 46 Due to the commonality of substance use disorders among acutely admitted patients, 47 clinicians may benefit from assessing psychoactive medication use in addition to alcohol and illicit drugs, particularly among the elderly. Similar to screening for alcohol, 48 validated single-question screening tools exist for illicit drug use and non-medical use of psychoactive medication. 49 However, these tools were validated in a primary care setting. Older adults may also perceive symptoms of harmful psychoactive substance use as symptoms of ageing, and adverse effects stemming from psychoactive drug use may be similar to manifestations of other conditions. 32 Single-question screening tools may therefore better serve as an adjunct to the general clinical assessment of every admitted patient.
The use of psychoactive medication is usually mediated by healthcare professionals, which mandates adherence to prescription guidelines. However, based on prescription databases, inappropriate use of benzodiazepines and z-hypnotics is widespread. 2 Hospital clinicians have the opportunity to prudently assess medication use among admitted patients, and are in a position to inform and co-operate with primary care physicians or other health professionals. Any identified instances of harmful or inappropriate use may then be managed by targeted interventions, or discontinuation or drug-tapering. In the event of specific illnesses, it is important to consider whether harmful, inappropriate or even therapeutic use may have precipitated an adverse event. As several illnesses that are more commonly occurring in old age progress, physiological reserves may be depleted. For instance, respiratory depression associated with benzodiazepine use 50 may cause adverse respiratory events in patients with chronic pulmonary obstructive disease if pulmonary function continues to decrease.
Brief interventions for substance use disorders have shown varying degrees of efficacy in the reduction of harmful alcohol use 51–53 and illicit drug use, 54 55 with some studies showing a reduction in at-risk drinking, while brief interventions have shown no increased efficacy in reducing illicit drug misuse compared with control groups. These studies also did not include elderly patients (above 64 years of age) or the critically ill. Additionally, study participation and the screening process itself may cause a reduction in harmful substance use in both the control group and the groups receiving brief interventions. 56
While the above recommendations may be valid for Norway and other similar countries in the West, the number of samples positive for psychoactive substances was markedly lower across all age groups in Moscow, at 12%. Plausible causes may be differences in prescription guidelines and legislative practices. Additionally, there were significant differences in the cut-off values used at both sites—in Moscow, the S/N ratio cut-off was set at 1000 versus an S/N ratio set at 10 in Oslo—this may have underestimated the number of positive samples. However, the usage frequency of psychoactive medications in a Russian ED population may still warrant prudence regarding adherence to prescription guidelines and adverse effects. Their use may also reflect a different selection of illnesses in that particular population—further discussion regarding these elements is beyond the scope of this article.
Limitations
Previous studies have used both self-reporting and registry-based data to assess substance use among acutely hospitalised patients—a major strength in our study is the addition of blood sample analysis. The analytical methods used have allowed us to identify individual substances, thus increasing the descriptive accuracy in our data. Our inclusion criteria were broad, increasing the likelihood for a representative sample size—this is also strengthened by a high participation rate. The use of two to different hospital sites in two different nations increased our sample size; however, external generalisability to other ED populations is limited to due to differences in medical practice and cultural norms. Differences in analytical cut-off values between Oslo and Moscow also limit the comparability between the two data sets. In order to satisfy necessary ethical considerations, patients unable to give informed consent were excluded. Their cognitive limitations may have been caused by or exacerbated by psychoactive substances or alcohol use—consequently, prevalence data for this patient group remains unavailable. The prevalence of substance use among patients who declined to participate is also a potential bias, as they may have been unwilling to participate due to concerns regarding the disclosure of substance or alcohol use, or may have been incapacitated due to illicit drug use. Finally, substances with a long half-life (such as certain benzodiazepines and z-hypnotics) may have a detection window longer than 24 hours—this may result in a substance-positive sample, but a negative reply regarding self-reported ingestion the past 24 hours.
The use of psychoactive substances among patients acutely admitted to Departments of Internal Medicine is common, and may cause both readily identifiable as well as oblique adverse effects. Health professionals should be aware that the use of benzodiazepines and opiates is highly prevalent, particularly among elderly patients, and should exact prudence when prescribing these drug classes. Implementing screening practices may improve the identification of inappropriate psychoactive substance use.
Supplementary Material
Contributors: DG drafted the manuscript. BJ, SK and AAN did the initial data analysis. TB performed supplementary data analysis. BJ, SK, VV, DG, AL, GN and STB organised or contributed to the Oslo data collection. EB, EK, AN, ET, AK, AP, SP and ED organised or contributed to the Moscow data collection. All authors were responsible for study design, interpretation of the results, as well as final revision and approval of the manuscript.
Funding: The study was supported by the Norwegian Ministry of Health’s Funding for Norwegian-Russian Collaboration in Health and Social issues grant B-1408.
Disclaimer: The Norwegian Ministry of Health had no role in the design of the study, in the collection, analysis or interpretation of the data, nor in writing the manuscript or in the decision to submit the article for publication.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Patient consent for publication: Not required.
Ethics approval: This study was approved by the Regional Ethics Committee for South Eastern Norway (2015/2404), and by the Moscow Local Ethical Committee of Moscow Research and Practical Center on Addiction.
Provenance and peer review: Not commissioned; externally peer-reviewed.
Data availability statement: No data are available due to institutional policies.

COMMENTS
A 16-Year-old Boy with Combined Volatile and Alcohol ...
Case Study: Lorrie. Figure 1. Lorrie. Lorrie Wiley grew up in a neighborhood on the west side of Baltimore, surrounded by family and friends struggling with drug issues. She started using marijuana and "popping pills" at the age of 13, and within the following decade, someone introduced her to cocaine and heroin.
Introduction and background. Drug misuse is a widespread issue; in 2016, 5.6% of people aged 15 to 26 reported using drugs at least once [].Because alcohol and illegal drugs represent significant issues for public health and urgent care, children and adolescents frequently visit emergency rooms [].It is well known that younger people take drugs more often than older adults for most drugs.
KEVIN CASE CONCEPTUALIZATION & TREATMENT PLAN
A Case of Alcohol Abuse. The patient is a 65-year-old white woman, married for 35 years to an accountant. They have 5 grown children and 12 grandchildren. She taught elementary school for 28 years and has not worked since retiring 15 years ago.
ubstance Abuse Treatment Client With Borderline Personality DisorderMing L., an Asian female, was 32 years old when. she was taken by ambulance to the local hospital's emergency room. Ming L. had taken 80 T. lenol capsules and an unknown amount of Ativan in a suicide attempt. Once medically stable, Ming L. was evaluat.
Substance Use Disorders and Addiction: Mechanisms, Trends ...
National Institute on Alcohol Abuse and Alcoholism (NIAAA) NIAAA supports and conducts research on the impact of alcohol use on human health and well-being. Learn About Alcohol's Effects on Health. NIAAA is now on LinkedIn The Healthcare Professional's Core Resource on Alcohol from NIAAA
Drug Misuse and Addiction
In this article, a case-based format is used to address complex clinical issues in addiction medicine. The cases were developed from the authors' practice experience, and were presented at the American College of Medical Toxicology Addiction Academy in 2015. Section I: Drug and Alcohol Dependence and Pain explores cases of patients with co-occurring pain and substance use disorders. Section ...
How would you diagnose and treat a 54-year-old man with alcohol withdrawal and altered mental status? Read this case challenge and test your knowledge.
the effects of substance abuse on parents and siblings
Alcohol Research Resource (R24 and R28) Awards. Resources include biological specimens, animals, data, materials, tools, or services made available to any qualified investigato r to accelerate alcohol-related research in a cost-effective manner. Current and potential alcohol research investigators and trainees are encouraged to subscribe to our ...
Abstract. In this article, a case-based format is used to address complex clinical issues in addiction medicine. The cases were developed from the authors' practice experience, and were presented at the American College of Medical Toxicology Addiction Academy in 2015. Section I: Drug and Alcohol Dependence and Pain explores cases of patients ...
Poverty, homelessness, and social stigma make addiction ...
These data present a view of the occurrence of alcohol and drug abuse in society which is generated from a 'medical model'. As useful as this approach is, it does not take into account the nature and needs of specific groups. To do this a more 'socially appropriate perspective' can be used. The following case studies illustrate some of ...
Study design. We conducted a scoping review to appraise the evidence that exists on drug and substance abuse in Africa. Scoping review is defined as "a form of knowledge synthesis that addresses an exploratory research question aimed at mapping key concepts, types of evidence, and gaps in research related to a defined area or field by systematically searching, selecting, and synthesizing ...
The use and misuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. The National Survey on Drug Use and Health (NSDUH) estimates allow researchers, clinicians, policymakers, and the general public to better understand and improve the nation's behavioral health.
Background Substance use disorders (SUDs) and mental health disorders (MHDs) are significant public health challenges with far-reaching consequences on individuals and society. Dual diagnosis, the coexistence of SUDs and MHDs, poses unique complexities and impacts treatment outcomes. A research landscape analysis was conducted to explore the growth, active countries, and active journals in ...
Alcohol, Aggression, and Violence: From Public Health to ...
Challenges in addiction-affected families: a systematic ...
The new Alcohol and Drug Studies program offers both a local degree and a certificate, designed to meet the growing demand for certified counselors in the field of chemical dependency and substance abuse. This comprehensive vocational, academic, and clinical program focuses on the prevention, treatment, and recovery of individuals affected by ...
During this study, "Post-treatment, 2 participants had ended their drug and alcohol abuse completely, 1 had reduced his abuse, and 1 still had a heavy abuse of alcohol." Helverschou, S. B., Brunvold, A. R., & Arnevik, E. A. claim, "This study addresses ways of improving services for individuals with ASD and SUD by enhancing the competence of ...
Russia's National Concept to Reduce Alcohol Abuse and ...
1. Introduction. The illicit drug overdose crisis is an ongoing epidemic that continues to take lives at unprecedented rates. British Columbia, Canada has been identified as the epicenter in Canada, where approximately seven deaths per day are linked to unregulated substances most often including fentanyl [].Increasingly drug checking is being pursued as a potential response to the rapid ...
Background. While the deleterious effects of harmful alcohol use and tobacco smoking are well known, several studies have also called attention to increasing rates of psychoactive prescription drug use in Western countries, especially among the elderly. 1-3 These drugs include opioids, benzodiazepines and z-hypnotics. In addition to increased usage rates, there seems to be an apparent ...