- Patient Care & Health Information
- Diseases & Conditions
- Soft tissue sarcoma

Kaposi sarcoma
Kaposi sarcoma is a type of cancer that forms in the lining of blood vessels and lymph vessels. The cancer forms growths of cells, called lesions, on the skin. The lesions often form on the face, arms and legs. The lesions may look pink, red, purple or brown.
Lesions also can appear on the genitals or in the mouth. In severe Kaposi sarcoma, lesions can be in the digestive tract and lungs.
The cause of Kaposi sarcoma is infection with the virus human herpes virus 8, also called HHV-8. In healthy people, this infection usually causes no symptoms because the immune system keeps it under control. In someone with a weakened immune system, however, HHV-8 can lead to Kaposi sarcoma.
There are four types of Kaposi sarcoma:
- AIDS -related or epidemic Kaposi sarcoma. This type happens in people infected with human immunodeficiency virus, also called HIV. HIV is the virus that causes AIDS .
- Transplant-associated or iatrogenic Kaposi sarcoma. This type happens in people who take medicine to control the immune system after an organ transplant.
- Classic Kaposi sarcoma. This type occurs in older men of Eastern European, Mediterranean and Middle Eastern descent. It usually grows slowly and can cause swelling in areas such as the legs.
- Endemic Kaposi sarcoma. This type affects young people in Africa. It can grow slowly on the skin or quickly inside the body.
Taking a piece of skin for testing
A health care professional may recommend removing a small piece of a skin lesion for testing. This procedure is called a skin biopsy. The sample is sent to a lab for testing. Lab tests can look for signs of cancer.
A skin biopsy can confirm Kaposi sarcoma.
Testing for Kaposi sarcoma inside the body
Other tests might be needed to look for Kaposi sarcoma in the lungs or the digestive tract.
Test to find Kaposi sarcoma in the digestive tract might include:
- Fecal occult blood test. This test detects hidden blood in stool. If it shows hidden blood, other tests might be needed to find the source. Other tests include an endoscopy or colonoscopy. These tests are used to see if Kaposi sarcoma is causing the bleeding.
- Endoscopy. In this test, a thin tube, called an endoscope, is passed through the mouth. It allows a health care professional to look at the esophagus, stomach and first part of the small intestine.
- Colonoscopy. In this test, a thin tube called a colonoscope goes through the rectum and into the colon. It allows a health professional to look at the walls of these organs.
Tests to find Kaposi sarcoma in the lungs might include:
- Chest X-ray. A chest X-ray might show something unusual in the lungs. If so, a CT scan of the chest or a bronchoscopy might be used to see to see if the unusual finding is Kaposi sarcoma.
- CT scan. This imaging test uses X-rays to make detailed images of the lungs.
- Bronchoscopy. In this test, a thin tube called a bronchoscope passes through the nose or mouth into the lungs. This allows for viewing the lining of the lungs and taking samples of lung tissue.
There's no cure for Kaposi sarcoma. But there are many treatment options that can help control it. Some people may not need treatment right away. Instead, the condition might be monitored to make sure it's not getting worse. Treatment depends on:
- The type of Kaposi sarcoma.
- Number of lesions and where they are.
- Effects of the lesions, such as causing pain or getting in the way of eating or breathing.
- Your overall health.
Treatment for AIDS-related Kaposi sarcoma
Thanks to better antiviral medicines to treat AIDS and ways to prevent it, Kaposi sarcoma has become less common and less severe in people with AIDS . Taking antiviral medicines can lower the amount of the virus that causes HIV / AIDS and make the immune system stronger. This might be the only treatment needed for Kaposi sarcoma.
Treatment for transplant-related Kaposi sarcoma
Some people with transplant-related Kaposi sarcoma may be able to stop taking the medicines that are controlling the immune system or switch to another medicine.
Treatment for small skin lesions
These might include:
- Minor surgery, also called excision.
- Burning, called electrodessication, or freezing, called cryotherapy.
- Low-dose radiation, which is also helpful for lesions in the mouth.
- Laser therapy.
- An injection of the chemotherapy drug vinblastine into lesions.
- Applying a vitamin A-like medicine called a retinoid to the skin.
Lesions treated in any of these ways are likely to return within a couple of years. When this happens, treatment often can be repeated.
Treatment if there are many skin lesions
If the Kaposi sarcoma causes many skin lesions, other treatments might be needed, such as:
- Radiation therapy. Radiation therapy uses powerful energy beams to kill cancer cells. This is a treatment option if there are many skin lesions, but not enough to need chemotherapy.
- Chemotherapy. Chemotherapy uses strong medicines to kill cancer cells. Chemotherapy might an option when Kaposi sarcoma affects multiple parts of the body. For Kaposi sarcoma that's getting worse quickly, chemotherapy might help.
- Ferri FF. Kaposi sarcoma. In: Ferri's Clinical Advisor 2023. Elsevier; 2023. https://www.clinicalkey.com. Accessed April 25, 2023.
- Kaposi sarcoma treatment (PDQ) – Health professional version. National Cancer Institute. https://www.cancer.gov/types/soft-tissue-sarcoma/hp/kaposi-treatment-pdq. Accessed April 25, 2023.
- Groopman JE. AIDS-related Kaposi sarcoma: Clinical manifestations and diagnosis. https://www.uptodate.com/contents/search. Accessed April 25, 2023.
- Bennett JE, et al. Kaposi sarcoma-associated herpesvirus (human herpesvirus 8). In: Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed April 25, 2023.
- Groopman JE. AIDS-related Kaposi sarcoma: Staging and treatment. https://www.uptodate.com/contents/search. Accessed April 25, 2023.
- Zeinaty PE, et al. Endemic Kaposi sarcoma. Cancers. 2023; doi:10.3390/cancers15030872.
- Kaposi sarcoma. National Comprehensive Cancer Network. https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1485. Accessed April 28, 2023.
Associated Procedures
- Chemotherapy
- Needle biopsy
- Positron emission tomography scan
- Radiation therapy
News from Mayo Clinic
- Fluorescent green dye helps surgeons reduce complications after surgery for people with soft tissue sarcoma Dec. 24, 2023, 12:00 p.m. CDT
Products & Services
- A Book: Mayo Clinic Family Health Book
- Newsletter: Mayo Clinic Health Letter — Digital Edition
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
5X Challenge
Thanks to generous benefactors, your gift today can have 5X the impact to advance AI innovation at Mayo Clinic.
Masks Strongly Recommended but Not Required in Maryland
Respiratory viruses continue to circulate in Maryland, so masking remains strongly recommended when you visit Johns Hopkins Medicine clinical locations in Maryland. To protect your loved one, please do not visit if you are sick or have a COVID-19 positive test result. Get more resources on masking and COVID-19 precautions .
- Vaccines
- Masking Guidelines
- Visitor Guidelines
Kaposi Sarcoma
Kaposi sarcoma is a disease in which cancer cells are found in the skin or mucous membranes that line the gastrointestinal (GI) tract, from mouth to anus, including the stomach and intestines.
These tumors appear as purple patches or nodules on the skin and/or mucous membranes and can spread to lymph nodes and lungs. Kaposi sarcoma is more common in men and in patients with suppressed immune systems.
What causes Kaposi sarcoma?
Kaposi sarcoma is always caused by an infection with a virus called human herpesvirus 8, which is also known as Kaposi sarcoma-associated herpesvirus (KSHV). The virus, which is in the same family as Epstein-Barr virus, is rare in the United States. In fact, less than 1 percent of the general U.S. population is a carrier. The virus and the tumor are much more common in some other parts of the world.
How the virus is initially acquired and spread is poorly understood, but scientists have identified four distinct populations that represent nearly all cases of the disease. There is some evidence within those populations as to how KSHV is acquired and what causes some carriers to develop Kaposi sarcoma.
What are the risk factors for Kaposi sarcoma?
You must already be infected with Kaposi sarcoma-associated herpesvirus (KSHV) to develop Kaposi sarcoma. However, most people who have the virus will never get Kaposi sarcoma. The cancer is usually triggered by a weakened immune system in people who are HIV-positive, who have received an organ transplant or whose immune systems are weakened for other reasons, including age.
What are the types of Kaposi sarcoma?
Kaposi sarcoma occurs in four different settings. The approach to treatment depends in part on the setting in which the tumor occurs..
Epidemic (AIDS-Related) Kaposi Sarcoma
In the United States, most cases of Kaposi sarcoma are related to HIV . HIV only leads to the development of Kaposi sarcoma in patients who are also KSHV infected.
Among HIV-positive individuals, it appears that men who have sex with other men are more likely to get Kaposi sarcoma, probably because KSHV is more common in this population. While experts presume that there is some sexual transmission of the virus, it is generally detected in saliva rather than semen.
During the AIDS epidemic, cases of Kaposi sarcoma grew drastically in the U.S., reaching more than 20 times the pre-epidemic numbers, according to the American Cancer Society. At the worst point, the incidence of disease was 47 per cases per year for every 1 million people. Individuals with HIV had a 50 percent chance of developing the disease.
Since then, Kaposi sarcoma has become less common, yielding about 6 cases per 1 million people each year. Antiretroviral treatment in HIV-positive patients has helped control and prevent the disease.
Classic (Mediterranean) Kaposi Sarcoma
Classic Kaposi sarcoma mainly occurs in older men of Mediterranean, Middle Eastern and Eastern European descent. These areas of the world have a much greater incidence of KSHV. While the reasons aren’t clearly understood, some evidence indicates that populations with high rates of KSHV likely acquired the virus in childhood, possibly through saliva transmission from mother to child.
As in other types of Kaposi sarcoma, experts believe that classic Kaposi tumors emerge as a result of a compromised immune system. Although these men may have carried the virus their entire lives, the cancer develops in the setting of a natural, age-related decline in immune function.
Endemic (African) Kaposi Sarcoma
In some areas of Equatorial Africa, a high percentage of the population may be infected with KSHV and therefore have a greater risk of developing Kaposi sarcoma. Once again, medical experts think that the virus is being spread mostly through saliva transmission from mother to child. Women and children are also being affected. Why the tumor develops in young boys whereas classic KS occurs mainly in old men isn’t known.
Transplant-Related Kaposi Sarcoma
Most patients receiving an organ or bone marrow transplant must take immunosuppressant drugs to keep their immune system from attacking the transplanted organ. But if an immunosuppressed transplant patient is already infected with KSHV, they have the potential to develop Kaposi sarcoma. Getting a transplant in a country where KSHV is more common (e.g., Italy or Saudi Arabia) further increases risk as the virus may be transmitted with the organ transplant.
What are the symptoms of Kaposi sarcoma?
Kaposi sarcoma symptoms include the following:
- Lesions on the skin. The first signs of Kaposi are usually cancerous lesions (spots) on the skin that are purple, red or brown and can appear flat or raised. These may appear in just one area, or they can show up in many areas. Often they are disfiguring. Common locations for lesions are the feet, legs and face.
- Lesions on mucous membranes. Lesions can also occur in the mouth, anus or elsewhere in the gastroinstestinal tract.
- Lesions inside the body. When lesions form inside the lungs, breathing can be restricted or the patient may cough up blood. Inside the GI tract, lesions can cause pain and bleeding, which may eventually lead to anemia .
- Lymph nodes. Involvement of lymph nodes, particularly in the groin can be associated with painful swelling in the legs.
How is Kaposi sarcoma diagnosed?
The disease has become so rare in the United States that not every doctor has seen it. Its rarity can lead to patients being seen by multiple doctors before getting a diagnosis. As with all cancers, early diagnosis can improve outcomes and lessen the risk of the disease spreading to other organs.
If you have signs of Kaposi sarcoma, a doctor will do a physical examination of your skin, mouth and rectum. The doctor will also check your lymph nodes.
- Skin biopsy . During this procedure, small pieces of tissue will be removed from the lesion(s). A pathologist will examine the samples in a lab to confirm the presence of Kaposi sarcoma.
- Chest X-ray . Since Kaposi sarcoma commonly spreads to the lungs, most patients will receive a chest X-ray. This noninvasive test may be used even if there appears to be no lung involvement.
- Bronchoscopy . If the chest X-ray shows an abnormality, or if you’re coughing up blood or having breathing problems, your doctor may order a bronchoscopy to look at your trachea and airways in greater detail.
- Endoscopy . An upper endoscopy and/or colonoscopy may be required if you have blood in the stool , abdominal pain or anemia.
In the past, it was much more common for patients with Kaposi sarcoma to have more advanced stages of disease. Today, only about 20 percent of patients have tumors beyond their skin or lymph nodes. This decrease in advanced disease has largely resulted from the success of antiretroviral therapies.
Newly Diagnosed
A new Kaposi sarcoma diagnosis can be scary and cause you to ask many questions. Learning everything you can about your cancer and its treatment options can help you feel less afraid. It will also make it easier for you to work with your health care team to make the best treatment decisions.
Working with Your Health Care Team
Your health care team may include the following:
- Dermatologist . This is a doctor who specializes in treating skin diseases.
- Infectious disease specialist . This is a doctor who treats infectious diseases such as AIDS.
- Medical oncologist . This is a doctor who specializes in treating cancer with medicines such as chemotherapy.
- Radiation oncologist . This is a doctor who specializes in treating cancer with radiation.
Many other health care professionals will be part of your team as well. They will help you by:
- Answering your questions
- Guiding you through tests and explaining your test results
- Helping you make treatment decisions
- Providing support during treatment
- Explaining your follow-up care plan
Because Kaposi sarcoma is rare, it’s helpful to receive care from a cancer center with experts who have experience treating this disease.
Getting Support
Coping with cancer can be very stressful. Talk with your health care team about referring you to a counselor for emotional support. You may also want to ask your health care team about joining a local or online support group. These groups are designed to help patients with Kaposi sarcoma share coping strategies.
What is the treatment for Kaposi sarcoma?
KSHV, the virus that causes Kaposi, cannot be treated. Once you contract KSHV, you will always have it. Treatment for Kaposi sarcoma is focused on managing symptoms and treating the cancer. The best approach will depend on your specific diagnosis and the extent of the disease.
Experts advise against regarding the disease as localized, even if it physically appears to be so. It should be treated with the assumption that it has spread beyond any visible signs.
The following treatment strategies may be used for patients with Kaposi sarcoma:
- Improving immune system function .The most effective and important therapy for patients with Kaposi sarcoma is addressing the immune deficiency that may allow the cancer to grow. For AIDS patients, the same antiretroviral therapy used for AIDS may be all that’s needed to treat Kaposi sarcoma. For transplant recipients, changing or decreasing the dosage of immunosuppressant drugs may be recommended. The top priority in treating Kaposi sarcoma patients is strengthening the immune system. Additional treatments such as chemotherapy are not tolerated for long periods in people with existing immunity concerns.
- Local therapies . Some doctors may suggest topical treatments including injection of chemotherapy directly into lesions, cryosurgery , excisions, phototherapy or local radiation when there are only a few small lesions.
- Chemotherapy . Patients who do not see improvement in Kaposi sarcoma after addressing immune deficiencies may require chemotherapy as a follow-up treatment. Chemotherapy is usually administered intravenously, although some oral therapies are now being used.
- Immunotherapy . This type of treatment works by activating the immune system’s natural ability to fight cancer. Since it has already proven to be effective in treating many types of cancer, researchers are studying its application in Kaposi sarcoma treatment. Ask your doctor about clinical trials for immunotherapy and other emerging treatment approaches.
Surgery is not usually recommended because it is ineffective at curing the disease and lesions can recur.
What is the prognosis for Kaposi sarcoma?
Unlike early in the AIDS epidemic, Kaposi is very treatable. Very few people die from the disease because it usually responds to one treatment or another.
Data from the National Cancer Institute indicates that the five-year relative survival is about 72 percent. This means that five years after diagnosis, a person with Kaposi sarcoma is 72 percent as likely as the average person without Kaposi to still be living. With improvements in treatment, these numbers are likely to continue rising.
It’s also important to note that the cause of death for patients with Kaposi sarcoma is often something other than Kaposi sarcoma (e.g., HIV or AIDS-related diseases). And remember that survival rates are an average of a large group of people. Your own prognosis, which should be discussed with your doctor, depends on many factors, including your age, health and immune status as well as the extent of your disease.
[[sarcoma_pages]]
The Johns Hopkins Proton Therapy Center
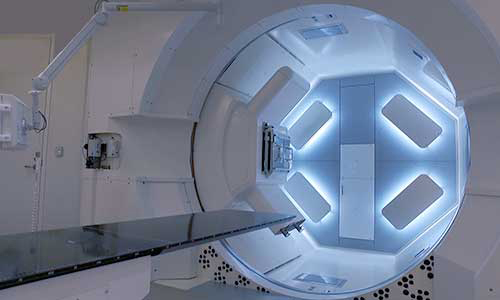
Proton therapy is used to treat certain tumors in children and adults. Our treatment center, located at Sibley Memorial Hospital in Washington, D.C., combines advanced proton therapy technology, the latest research and caring specialists.
Find a Doctor
Specializing In:
- Chondrosarcoma
- Bone Sarcoma
- Bone Cancer
- HIV/HCV Psychiatry
- HIV Treatment and Prevention
- HIV-Associated Lipodystrophy
- HIV Pathogenesis
- HIV Related Kidney Disease
- HIV/AIDS Associated Neuropathies
- HIV-Associated Metabolic Abnormalities
- HIV/STD Interaction
- HBV/HIV coinfection
- HCV/HIV coinfection
- Infectious Diseases and International Health
- Infectious Diseases
- AIDS Psychiatry
- AIDS-Related Cancers
Find a Treatment Center
- Neuroimmunology and Neurological Infections
- Orthopaedic Oncology
- Pediatric Oncology
Find Additional Treatment Centers at:
- Howard County Medical Center
- Sibley Memorial Hospital
- Suburban Hospital
Request an Appointment

Neurological Complications of HIV

Dealing with Discrimination When You Have HIV

Traveling With HIV
Related Topics
- HIV and AIDS
Kaposi Sarcoma
(kaposi's sarcoma; multiple idiopathic hemorrhagic sarcoma).
- Classification |
- Symptoms and Signs |
- Diagnosis |
- Treatment |
- Key Points |
Kaposi sarcoma is a multicentric vascular tumor caused by herpesvirus type 8. It is categorized into 5 types: classic (sporadic), AIDS-associated (epidemic), non-epidemic, endemic (in Africa), and iatrogenic (eg, after organ transplantation). Diagnosis is by biopsy. Treatment for indolent superficial lesions involves cryotherapy, electrocoagulation, excision, or electron beam radiation therapy. Radiation therapy is used for more extensive disease. In the AIDS-associated form, treatment includes antiretrovirals.
(See also Overview of Skin Cancer .)
Kaposi sarcoma originates from endothelial cells in response to infection by human herpesvirus type 8 (HHV-8). Immunosuppression (particularly due to organ transplantation or AIDS) markedly increases the likelihood of Kaposi sarcoma in patients infected with HHV-8.
The tumor cells have a spindle shape, resembling smooth muscle cells, fibroblasts, and myofibroblasts.

Photo courtesy of Karen McKoy, MD.
Classification of Kaposi Sarcoma
Classic kaposi sarcoma.
This type occurs most often in older ( > 60 years) men of Mediterranean, Eastern European, or Ashkenazi Jewish ancestry.
The course is indolent, and the disease is usually confined to a small number of lesions on the skin of the lower extremities; visceral involvement occurs in < 10%.
This type is usually not fatal.

AIDS-associated Kaposi sarcoma (epidemic Kaposi sarcoma)
This type is the most common AIDS-associated cancer and is more aggressive than classic Kaposi sarcoma.
Multiple cutaneous lesions are typically present, often involving the face and trunk. Mucosal, lymph node, and gastrointestinal (GI) involvement is common. Sometimes Kaposi sarcoma is the first manifestation of AIDS.

Non-epidemic Kaposi sarcoma
An additional type of Kaposi sarcoma that has been increasingly recognized occurs in men who are HIV-negative and who have sex with men ( 1 ). The reasons for increased prevalence in this group is uncertain and remains an area of ongoing investigation.
Endemic Kaposi sarcoma
This type occurs in Africa independent of HIV infection. There are 2 main forms:
Prepubertal lymphadenopathic form: It predominantly affects children; primary tumors involve lymph nodes, with or without skin lesions. The course is usually fulminant and fatal.
Adult form: This form resembles classic Kaposi sarcoma.
Iatrogenic Kaposi sarcoma (immunosuppressive Kaposi sarcoma)
This type typically develops several years after organ transplantation. The course is more or less fulminant, depending on the degree of immunosuppression.
Classification reference
1. Vangipuram R, Tyring SK : Epidemiology of Kaposi sarcoma: review and description of the nonepidemic variant. Int J Dermatol 58(5):538-542, 2019. doi: 10.1111/ijd.14080
Symptoms and Signs of Kaposi Sarcoma
Cutaneous lesions are asymptomatic purple, pink, brown, or red macules that may coalesce into blue-violet to black plaques and nodules. Some edema may be present. Occasionally, nodules fungate or penetrate soft tissue and invade bone.
Although less common, visceral involvement most often involves the oral cavity, gastrointestinal (GI) tract, and the lungs. Symptoms depend on specific organ involvement. Mucosal lesions appear as bluish to violaceous macules, plaques, and tumors. GI lesions can bleed, sometimes extensively, but usually are asymptomatic.
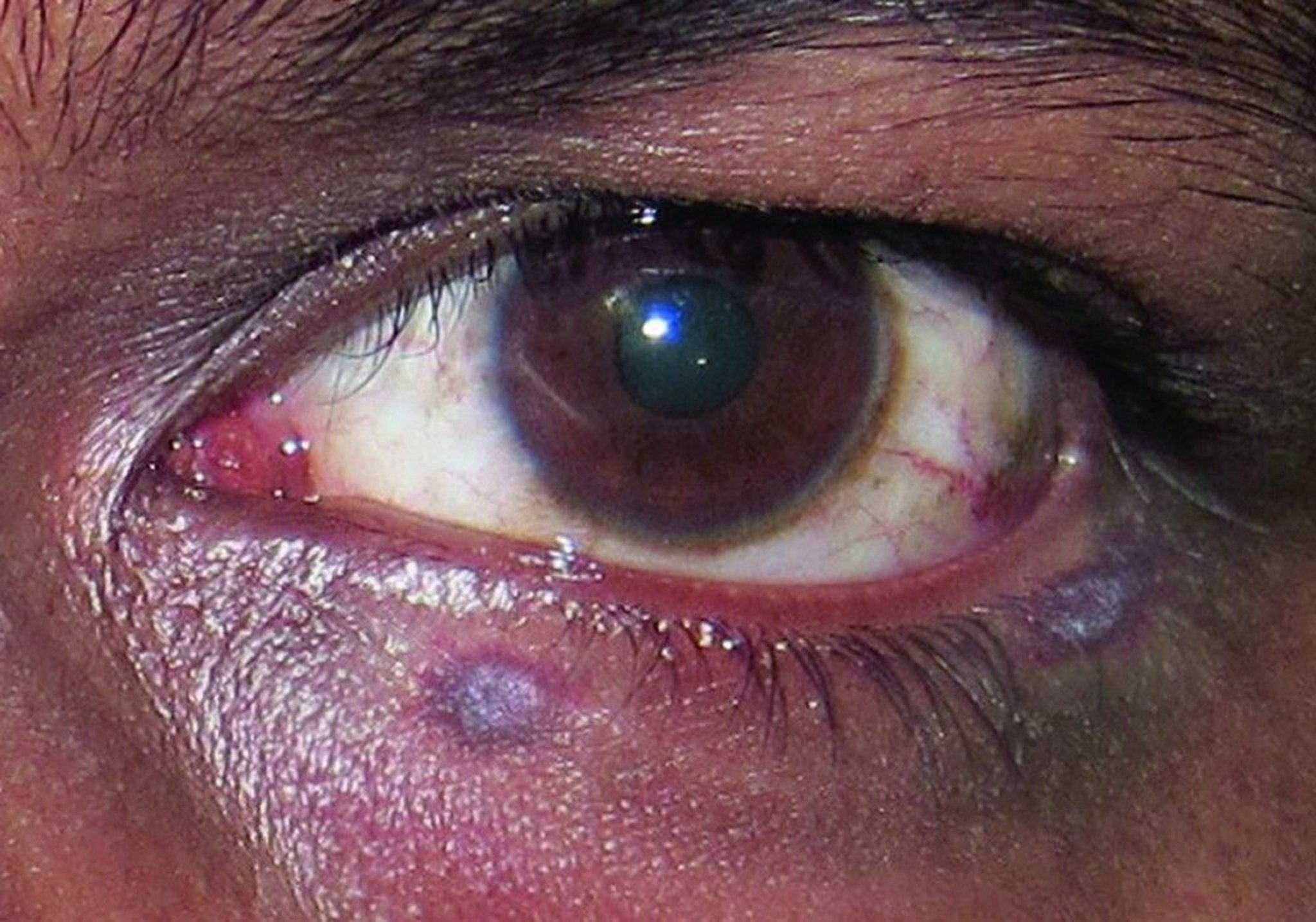
© Springer Science+Business Media

Diagnosis of Kaposi Sarcoma
Diagnosis of Kaposi sarcoma is confirmed by punch biopsy.
Patients with AIDS or immunosuppression require evaluation for visceral spread by CT of the chest and abdomen.
If CT is negative but pulmonary or GI symptoms are present, bronchoscopy or endoscopy should be considered.
Treatment of Kaposi Sarcoma
Surgical excision, cryotherapy, electrocoagulation, intralesional chemotherapy, or possibly topical imiquimod or alitretinoin for superficial lesions
Local radiation therapy and chemotherapy for multiple lesions, diffuse involvement, or lymph node disease
Antiretroviral therapy with similar local treatments or chemotherapy depending on extent of disease for AIDS-associated Kaposi sarcoma
Reduction of immunosuppressants for iatrogenic Kaposi sarcoma
Treatments for classic Kaposi sarcoma and AIDS-associated Kaposi sarcoma overlap considerably.
AIDS-associated Kaposi sarcoma responds markedly to antiretroviral therapy (ART), probably because the CD4+ count increases and the HIV viral load decreases; however, there is some evidence that protease inhibitors in this regimen may block angiogenesis (although this has not been shown to have beneficial clinical effects in humans).
In patients with AIDS who have indolent local disease, CD4+ counts > 150/mcL, and HIV RNA <
2 doxorubicin fails.
Other agents being investigated as adjuncts include interleukin (IL)-12, desferrioxamine, and oral retinoids. Treatment of Kaposi sarcoma does not prolong life in most patients with AIDS because infections dominate the clinical course.
Non-epidemic classic Kaposi sarcoma requires treatment of indolent lesions as described above .
Iatrogenic Kaposi sarcoma
Endemic Kaposi sarcoma treatment is challenging and typically palliative.
Consider Kaposi sarcoma in older men, Africans, and patients with organ transplants or AIDS.
Test patients with immunosuppression (including AIDS) for metastases.
Treat superficial lesions with locally ablative methods.
Treat multiple lesions, diffuse involvement, or lymph node disease with local radiation therapy and chemotherapy.

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
- Cookie Preferences

0 Changes From Previous Versions
2.1 definition and background information, 2.2 epidemiology, 2.2.1 classic kaposi's sarcoma, 2.2.2 endemic kaposi's sarcoma, 2.2.3 iatrogenic immunosuppression-associated kaposi's sarcoma - epidemiology, 2.2.4 epidemic or aids-associated kaposi's sarcoma - epidemiology, 2.2.5 kaposi's sarcoma in msm without hiv infection, 2.3 pathogenesis, 4 clinical characteristics, 4.1 symptoms, 5 diagnosis, 5.2 diagnostics, 5.2.1 primary work-up, 5.3 classification, 5.3.1 subtypes of kaposi’s sarcoma, 5.3.1.1 histology, 5.3.1.1.1 spot (patch) stage, 5.3.1.2 plaque stage, 5.3.1.3 node or tumor stage, 5.3.1.4 immunohistology, 5.4 prognostic factors, 5.5 differential diagnosis, 6.1 treatment structure, 6.1.1 classic kaposi's sarcoma, 6.1.2 endemic kaposi's sarcoma, 6.1.3 iatrogenic immunosuppression-associated kaposi's sarcoma, 6.1.4 epidemic or aids-associated kaposi's sarcoma, 6.2 therapy modalities, 6.2.1 systemic tumor treatment, 6.2.2 local treatment options, 8 follow-up / surveillance, 8.2 follow-up, 9 references, 15 authors' affiliations, 16 disclosure of potential conflicts of interest, kaposi's sarcoma, compliance rules.
- Conflict of interests
- Print version
Authors and societies
No history available so far!
Kaposi's sarcoma (KS) most likely originates from lymphatic endothelial cells, and human herpesvirus 8 infection contributes to their malignant transformation. Immunosuppression fosters the occurrence, persistence, and progression of KS, which belongs to the most common AIDS-defining neoplasms in HIV-infected individuals. KS is rare among the general population. Advanced, extensive KS can usually be improved clinically and controlled long-term with systemic chemotherapy. Smaller localized manifestations can be treated intralesionally, surgically, or with radiotherapy. In HIV-infected patients, starting antiretroviral therapy, resulting in immune reconstitution, and in immunosuppressed patients, the reduction of immunosuppressive drugs may lead to healing of KS.
Other soft tissue sarcoma entities are addressed in separate Onkopedia guidelines, see Onkopedia Soft Tissue Sarcomas, Onkopedia Gastrointestinal Stromal Tumors (GIST) , and Onkopedia Ewing Sarcoma . For further recommendations, we also refer to the S1 guideline Kaposi's sarcoma of the AWMF [ 1 ] and the European guideline from EDF/EADO/EORTC [ 18 ] .
In 1872, Moriz Kaposi, a Hungarian dermatologist, described five patients with aggressive idiopathic pigmented sarcoma of the skin ('sarcoma idiopathicum multiplex hemorrhagicum') [ 15 ] . One of these patients died of gastrointestinal hemorrhage 15 months after the emergence of the skin lesions. Biopsies showed visceral spread to the lungs and the gastrointestinal tract.
Five different epidemiological/clinical variants have been described, which occur in specific populations or have different manifestations or rates of progression [ 1 , 18 ] . These variants are thought to represent different clinical courses based on the same pathomechanism.
Classic KS primarily affects older men (m:w approx. 15:1) of Eastern European-Mediterranean or Jewish origin with an age peak in the 7th decade of life. Multiple, reddish-bluish-brown plaques and nodules are often found, especially in the lower extremities. The overall course is not markedly progressive over years or decades and rarely involves other organs. Sometimes lymphedema or hyperkeratosis are found.
Histologically, there are infiltrates of spindle-cell endothelia, slit-like new thin-walled, partly incomplete blood vessels with erythrocyte extravasations and hemosiderin deposits, furthermore a lymphocytic inflammatory infiltrate.
Since the middle of the last century, an increasing incidence of KS in sub-Saharan Africa has been reported. In 1971, KS accounted for 3% to 9% of all cancers in Uganda. In 1983, a dramatic increase in the incidence of KS was reported in Zambia. Once the acquired immunodeficiency syndrome (AIDS) could be reliably diagnosed, it was possible to distinguish HIV-negative endemic Kaposi's sarcoma from HIV-positive epidemic KS. Four clinical courses are described for African endemic KS:
relatively benign: nodular skin lesions similar to those seen in classic KS. This mainly affects young men around the age of 35;
aggressively localized: cutaneous form of progression with infiltration into soft tissue and bone with fatal outcome within 5 to 7 years;
diffuse: mucocutaneous involvement and visceral involvement;
fulminant course: lymphadenopathy and involvement of visceral organs usually without skin involvement, occurring preferably in young children.
KS has been described as a consequence of iatrogenic immunosuppression, usually associated with organ transplantation, but also in other types of immunosuppression. In this regard, there appears to be an increased risk in certain ethnic groups, which are also at increased risk for classic KS. Although the course can be both chronic and rapidly progressive, remission usually occurs after cessation of immunosuppressive therapy.
In 1981, Friedmann-Kien et al. described fifty previously healthy young homosexual men with KS, affecting lymph nodes, visceral organs, mucosa and skin. At the same time, life-threatening opportunistic infections were present in association with a massive defect in T-cell-mediated immunity. Shortly after that, this disease was described as Acquired Immunodeficiency Syndrome (AIDS) and HIV infection was proven to be the cause. Although the incidence of Kaposi's sarcoma has now decreased significantly as a result of effective antiretroviral therapy for HIV infection, this tumor remains the most common AIDS-associated malignancy in the United States. The same is true for Germany [ 13 ] . Overall, the risk for HIV patients to develop KS is increased by 20,000-fold compared to the normal population and by 300-fold compared to other immunosuppressed patients [ 2 ] . Among the different HIV transmission groups, the risk of developing KS is 20-fold higher in homosexual men than in patients with hemophilia. KS rarely occurs in women.
In recent years, an increasing number of HIV-associated KS have also been reported in patients with higher T helper cell counts and low HIV viral load, including patients on successful cART (combined Anti-Retroviral Therapy) [ 26 ] .
At first diagnosis - usually in HIV-infected persons who have not yet received antiretroviral treatment - a multilocular manifestation is typically present. The characteristic skin lesions may develop within a few days. They begin as macules in the skin cleavage lines and progress to papules or papular tumors. Before the cART era, oral lesions were found as the primary manifestation in many patients, but lesions on the penis were also typically found.
While the skin lesions can be highly stigmatizing for the affected patient, organ involvement is clinically most relevant. Since almost all organs, including the entire gastrointestinal tract, but also the heart, liver and lungs can be affected, life-threatening complications may rapidly emerge. Involvement of the CNS and the eyes is rare.
In recent years, KS has been increasingly reported in younger HIV-negative men who have sex with men (MSM) from geographic regions with low HHV-8 seroprevalence (e.g., France, England, or Germany) [ 10 , 17 , 21 ] .
Similar to classic KS, the course is rather indolent, lesions occur on the entire integument, whereas visceral or organ involvement is very rare. CD4 cell count and CD4/CD8 ratio seem to correlate with disease severity. Because of these features and differences from the previously 4 recognized subtypes of KS, this form is newly classified as an additional (5th) epidemiologic subtype [ 5 , 6 ] .
The pathogenesis of KS is increasingly well understood. Using molecular biology methods and PCR-assisted in situ hybridization, the detection of DNA sequences of a human herpesvirus designated as KS-associated (KSHV) or HHV-8 was achieved in endothelial cells and spindle cells in both AIDS-associated KS and KS from HIV-negative patients in >95% of cases [ 19 , 24 ] . Therefore, HHV-8, which can be transmitted sexually but also via saliva and blood, is considered to play a crucial role in the development of KS. HHV-8 is not only regularly found in KS, but also in certain B-cell lymphomas ('body cavity-based large B-cell lymphoma') and in multicentric Castleman's disease, but not in other vascular tumors. In addition, leukocytes infected with HHV-8 as well as KS cells were found in the peripheral blood of HIV-positive KS patients. In some regions, e.g., in Italy or Central Africa, HHV-8 is also detectable in up to 50% of the normal population. Probably like other herpesviruses, HHV-8 is transmitted predominantly by saliva, but also sexually, vertically, and via blood.
For the development of KS, HHV-8 is a necessary, but not sufficient condition on its own. Cofactors include the HIV-TAT (trans-activator of transcription) gene and cytokines such as interferon-γ and vascular endothelial cell growth factor (VEGF). Genes with oncogenic properties (c-myc, bcl-2) (transforming, chemoattractant, growth-promoting, anti-apoptotic) and others affecting adherence, cell growth, inflammation, and angiogenesis have been identified in the genome of HHV-8. Expression of these gene products in KS spindle cells in vivo contributes critically to KS development.
3 [Chapter not relevant]
KS mainly affects the skin and mucous membranes. Mostly symmetrical on the distal extremities, initially indurated reddish-brown to purplish-red macules often appear in the course of the skin cleavage lines, transforming into extensively infiltrated plaques and hardened painful nodules. Spread is in proximal direction, increasingly disseminated with frequent mucosal involvement. Spontaneous regressions result in hemorrhagic hyperpigmentation, and hemorrhages result in perilesional discoloration (ochre yellow purpura). KS may immure regional lymphatic structures, causing edema up to elephantiasis-like swelling in the affected drainage area. Mechanical stress and trauma may cause ulcerative rupture, especially affecting the feet.
Internal organs such as lymph nodes, gastrointestinal tract, liver, lungs, kidney and spleen may also be affected. Lymphatic or visceral involvement sometimes occurs without skin involvement.
The course of KS is highly variable, ranging from single lesions that remain stationary for years to markedly aggressive courses that lead to death within a few weeks, especially in HIV-infected individuals.
5.1 [Chapter not relevant]
A stepwise diagnostic approach is recommended. It starts with confirming the diagnosis, see Table 1 , followed by staging procedures, see Table 2 .
Procedure | Note |
|---|---|
Procedure | Note |
|---|---|
Sporadic, classic KS
KS associated with iatrogenic immunosuppression
Endemic, African KS
Epidemic, HIV-associated KS
KS in men who have sex with men (MSM) without HIV infection.
KS is a mesenchymal tumor of blood vessels and lymphatic vessels. The histologic image of KS is multifaceted and changes with clinical progression. KS consist of three components [ 8 ] :
Angiomatous phase
Spindle cell phase
Inflammatory phase
Closely adjacent to larger plexus vessels in the mid and upper stratum reticulare of the dermis, multicentric discrete perivascular spindle cell proliferations with slit-like clefts accompanied by lymphoplasmacytic infiltrates, extravascular erythrocytes, hemosiderin deposits, and siderophages ('pseudogranulomatous pattern') are found in early KS, initially omitting the papillary body and its vessels. In addition, endothelium-lined vascular clefts with empty lumina may dominate. Adnexa and preexisting vascular structures are partially encompassed by the newly formed vascular clefts and lacunae in a semi-island-like fashion ('promontory sign'). In early KS, mitoses and endothelial apoptosis are rare, and cellular and nuclear atypia are absent.
Spindle cells encroaching on the papillary body intersperse the entire corium bundled into short, cell-rich fascicles or strands. Sieve-like, the spindle cell aggregates are broken up by slit-like erythrocyte-rich clefts.
The tumor periphery is dominated by congested, dilated, serum-free vessels engorged with erythrocytes that appear stuffed ('stuffing'). Spindle cell apoptosis but no significant nuclear atypia is observed. Intracellularly and extracellularly, erythrocytic degradation is present in the form of hyaline PAS-positive globi ('hyaline globules').
Mitotic-rich, densely packed, factor XIIIa positive, CD31 positive, and CD34 positive, fascicular-structured spindle cell tumors with enclosed erythrocyte-rich clefts, moderate nuclear atypia (exceptionally marked atypia in anaplastic equatorial African variants) often surrounded by an epithelial collerette in exophytic growth, and by a connective tissue pseudocapsule in expansive nodular variants. PAS-positive hyaline erythrocytic globi and apoptotic spindle cells occur in clusters. Older lesions show necrosis in addition to hemorrhages and iron storage.
At regression, a plasma cell-rich, inflammatory round cell infiltrate develops.
Molecular detection of KS herpesvirus HHV-8 is helpful for differential diagnosis.
Prognostic factors are summarized in the TIS (Tumor, Immune system, Systemic Illness) classification of the ACTG (AIDS Clinical Trials Group) [ 15 ] , see Table 3 .
Criteria | |||
|---|---|---|---|
Prognosis | Tumor characteristics | Immune system | Systemic involvement |
Differential diagnosis of KS should include acroangiodermatitis in chronic venous insufficiency, other angiosarcomas, hemangiomas, bacillary angiomatosis, Gougerot-Blum disease, melanoma metastases, and erythema elevatum et diutinum. In case of doubt, an excisional biopsy should be performed to confirm the histological diagnosis.
The treatment approach is based on the four epidemiologic clinical variants [ 1 , 17 ] . An overview of the primary therapeutic procedures is summarized in Figure 1 .
In classical KS, individualized treatment concepts and often only local therapy are preferred due to the typically higher age of the patients [ 22 ] . Since KS is radiosensitive, fractionated soft X-ray therapy, irradiation with fast electrons or cobalt irradiation are suitable [ 11 ] . Cryotherapies may also be used locally, as well as intralesionally applied vinca alkaloids, bleomycin, or interferons [ 4 , 20 ] . Excision should be considered only in cases of functionally compromising changes and rapid need for action. Systemic chemotherapy, usually with pegylated liposomal doxorubicin, is indicated for extensive primaries, systemic involvement, and progressive courses [ 12 , 23 ] .
The endemic African KS usually responds well to systemic therapy, with the exception of the lymphadenopathic variant.
In iatrogenic immunosuppression-associated KS, tumor lesions usually regress completely after cessation of immunosuppression.
In epidemic AIDS-associated KS, initiation of combined antiretroviral therapy (cART) in previously non-antiretrovirally treated patients often leads to an arrest of progression or even complete disappearance of the sarcoma lesions [ 7 ] . Therefore, antiretroviral therapy should be initiated at the latest with the occurrence of KS in HIV patients. The type of cART does not play a crucial role in KS response, but rather its virologic efficacy and cART-related immune reconstitution. In some cases, a transient, often substantial worsening of the condition may occur as part of the immune reconstitution syndrome. These patients should be treated additionally with systemic chemotherapy. Also, in cases of concurrent new diagnosis of advanced KS with organ involvement and HIV infection, concurrent initiation of antiretroviral and systemic KS therapy as described below is also recommended. If KS is diagnosed in patients already receiving antiretroviral therapy, its effectiveness should be reviewed and eventually be optimized using resistance testing.
Regardless of the clinical course, progressive KS should be treated systemically. In the past, a variety of substances were used for this purpose. These include interferon, vinca alkaloids, bleomycin and anthracyclines [ 9 ] .
Standard therapy for AIDS-associated or advanced KS consists of administration of pegylated liposomal doxorubicin at a dose of 20 mg per m² of body surface area at two to three weeks intervals until complete clinical remission. Generally, clinical follow-up is scheduled at 2-3 months. In case of good regression of tumor lesions without complete remission, further course is awaited after 4-6 months.
As with any initiation of anthracycline therapy, cardiac evaluation with echocardiography should be performed to determine left ventricular ejection fraction, as there is a risk of cardiotoxicity in addition to myelotoxicity. Painful macular erythema (palmoplantar erythrodysesthesia) may occur on the hands and feet associated with the administration of liposomal doxorubicin. However, this side effect is rarely observed at the doses recommended for KS, and more often at higher single doses.
The taxane paclitaxel is available for second-line therapy. In the original report by Gill et al., a dose of 100 mg/m² every two weeks was used [ 25 ] . However, since weekly administration at reduced doses has now been shown to be better tolerated and at least as effective in other diseases such as breast carcinoma, weekly administration may also be discussed in KS, see Onkopedia Female Breast Cancer . Myelotoxicity, alopecia, and onychodystrophy should also be noted. Interactions with cART should be considered in HIV-infected patients with KS.
In HIV-associated KS, systemic interferons can be used alternatively if CD4 cell counts are good (>350 cells/µl) or immune status is good. Pegylated interferons (weekly administration possible, better tolerated than classical interferons) are not approved for KS, but may be more effective and easier to administer, as shown by case reports in AIDS-associated, but also in classical Kaposi's sarcoma [ 16 ] .
For local compromising (feet, face) KS lesions, local surgery or local drug application are often sufficient. These are inexpensive and well tolerated. Recurrence in the scars is common after surgical excision. KS are radiosensitive, so radiotherapy may also be used, preferably fractionated single doses of soft X-rays [ 8 ] . Other local therapies range from camouflage to intralesional injection of vincristine and to experimental topical use of retinoids [ 3 ] .
After successful treatment of KS, esthetically disturbing postinflammatory hyperpigmentation often remains visible for a long time, which should not be confused with active KS.
7 [Chapter not relevant]
8.1 [chapter not relevant].
Since KS is prone to recurrence, regular surveillance must be performed.
AWMF Guideline S1 Kaposi's sarcoma, 2021. https://register.awmf.org/de/leitlinien/detail/032-025 .
Brockmeyer NH, Mertins L. Therapy of HIV-associated Kaposi's sarcoma. IN: Brockmeyer NH, Mertins L (eds.): HIV infection, pathogenesis, diagnosis, therapy. Springer Verlag Berlin Heidelberg New York 1997. p. 93-122. ISBN 3-540-62544-5.
Bodsworth NJ, Bloch M, Bower M et al. Phase III vehicle-controlled, multi-centered study of topical alitretinoin gel 0.1% in cutaneous AIDS-related Kaposi`s sarcoma. Am J Clin Dermatol 2:77-87, 2001. PMID:11705307
Boudreaux AA, Smith LL, Cosby CD et al. Intralesional vinblastine for cutaneous Kaposi`s sarcoma associated with acquired immunodeficiency syndrome. J Am Acad Dermatol 28:61-65. 1993. PMID:8381146
Cesarman E, Damania B, Krown SE et al. Kaposi sarcoma. Nat Rev Dis Primers 5:9, 2019. DOI:10.1038/s41572-019-0060-9
Denis D, Seta V, Regnier-Rosencher E et al. A fifth subtype of Kaposi's sarcoma, classic Kaposi's sarcoma in men who have sex with men: a cohort study in Paris. J Eur Acad Dermatol Venereol 32:1377-1384, 2018. DOI:10.1111/jdv.14831
Dupont C, Vasseur E, Beauchet A et al. Long-term efficacy on Kaposi's sarcoma of highly active antiretroviral therapy in a cohort of HIV-positive patients. CISIH 92. centre d'information et de soins de l'immunodéficience humaine. AIDS 14:987-993, 2000. PMID:10853980
Fritsch P, Zelger B, Sepp N. Kaposi's sarcoma. Histology. IN: Fritsch P (ed.) Dermatology and venereology. Springer Verlag. Berlin, Heidelberg, New York. p. 617. ISBN 3-540-61169-X.
Gill PS, Wenz J, Scadden DT et al. Randomized phase III trial of daunorubicin versus doxorubicin, bleomycin, and vincristine in AIDS-related Kaposi’s sarcoma. J Clin Oncol 8:2353-2364, 1996. DOI:10.1200/JCO.1996.14.8.2353
Guo LN, Nambudiri VE. Kaposi sarcoma in HIV-negative men who have sex with men: a case series of nonepidemic Kaposi sarcoma. Clin Exp Dermatol 585-587, 2020. DOI:10.1111/ced.14146
Hamilton CR, Cummings BJ, Harwood AR. Radiotherapy of Kaposi's sarcoma. Int J Radiat Oncol Biol Phys 12:1931-1935, 1986. PMID:3771313
Hengge UR, Esser S, Rudel HP, Goos M. Long-term chemotherapy of HIV-associated Kaposi's sarcoma with liposomal doxorubicin. Eur J Cancer 37:878-883, 2001. PMID:11313176
Hensel M, Goetzenich A, Lutz T et al. HIV and cancer in Germany. Dtsch Arztebl Int 108:117-122, 2011. DOI:10.3238/arztebl.2010.0117
Kaposi M. Idiopathic multiple pigmentary sarcoma of the skin. Arch Derm Syph 4:265-273, 1872.
Krown SE, Metroka C, Wernz JC. Kaposi's sarcoma in the acquired immune deficiency syndrome: a proposal for uniform evaluation, response, and staging criteria. AIDS Clinical Trials Group Oncology Committee. J Clin Oncol 7:1201-1207, 1989. DOI:10.1200/JCO.1989.7.9.1201
Krown SE, Li P, Von Roenn JH et al. Efficacy of low-dose interferon with antiretroviral therapy in Kaposi`s sarcoma: a randomized phase II AIDS clinical trials group study. J Interferon Cytokine Res 22:295-303, 2002. DOI:10.1089/107999002753675712
Lanternier F, Lebbe C, Schartz N et al. Kaposi's sarcoma in HIV-negative men having sex with men. AIDS 22:1163-1168, 2008. DOI:10.1097/QAD.0b013e3283031a8a
Lebbe C, Garbe C, Stratigos AJ et al. Diagnosis and treatment of Kaposi's sarcoma: European consensus-based interdisciplinary guideline (EDF/EADO/EORTC). Eur J Cancer 114:117-127, 2019. DOI:10.1016/j.ejca.2018.12.036
Moore PS, Chang Y. Detection of herpesvirus-like DNA sequences in Kaposi's sarcoma in patients with and without HIV infection. N Engl J Med 332:1181-1185, 1995. DOI:10.1056/NEJM1995043321801
Myskowski PL. Intralesional interferon a-2b produces responses in Kaposi’s sarcoma. Dermatology 3:11, 1992.
Rashidghamat E, Bunker CB, Bower M, Banerjee P. Kaposi sarcoma in HIV-negative men who have sex with men. Br J Dermatol 171:1267-1268, 2014. DOI:10.1111/bjd.13102
Régnier-Rosencher E, Guillot B, Dupin N. Treatments for classic Kaposi sarcoma: a systematic review of the literature. J Am Acad Dermatol 68: 313-331, 2013. DOI:10.1016/j.jaad.2012.04.018
Stewart S, Jablonowski H, Goebel FD et al. Randomized comparative trial of pegylated liposomal doxorubicin versus bleomycin and vincristine in the treatment of AIDS-related Kaposi's sarcoma. International Pegylated Liposomal Doxorubicin Study Group. J Clin Oncol 16: 683-691, 1998. DOI:10.1200/JCO.1998.16.2.683
Stürzl M, Blasig C, Schreier A et al. Expression of HHV-8 latency-associated T0.7 RNA in spindle cells and endothelial cells of AIDS-associated, classical and African Kaposi's sarcoma. Int J Cancer 72:68-71, 1997 PMID:9212225
Tulpule A, Groopman J, Saville MW et al. Multicenter trial of low-dose paclitaxel in patients with advanced AIDS-related Kaposi sarcoma. Cancer 95:147-154, 2002. DOI:10.1002/cncr.10634
Yanik EL, Achenbach CJ, Gopal S et al. Changes in clinical context for Kaposi's Sarcoma and Non-Hodgkin Lymphoma among people with HIV infection in the United States J Clin Oncol 34: 3276-3283, 2016. DOI:10.1200/JCO.2016.67.6999
10 Active studies
11 systemic therapy - protocols, 12 study results, 13 certification status.
| Author | Employer | Consulting / Expert opinion | Shares / Funds | Patent / Copyright / License | Fees | Funding of scientific research | Other financial relations | Personal relationship with authorized representatives |
|---|---|---|---|---|---|---|---|---|
| Mosthaf, Franz A. | ||||||||
| Esser, Stefan |
- (DE) Kaposi-Sarkom
Quellenangabe:
Onkopedia-Leitlinien werden kontinuierlich an den Stand des Wissens angepasst. Die jeweils gültige Version, AGB und Nutzungsbedingungen finden Sie unter www.onkopedia.com.
Für die kommerzielle Nutzung wenden Sie sich bitte an [email protected] .
Onkopedia guidelines are continuously adapted to the state of knowledge. The currently valid version, terms of use and general terms and conditions can be found at onkopedia-guidelines.info .
For commercial use, please contact [email protected] .

Ihr Browser wird nicht unterstützt. Damit die Browsersicherheit gewährt ist, muss die aktuellste Browserversion installiert sein. Überprüfen Sie, ob Sie die neueste Browserversion nützen und laden Sie diese ggf. herunter
Kaposi Sarcoma Treatment (PDQ®)–Patient Version
General information about kaposi sarcoma, kaposi sarcoma is a disease in which malignant lesions (cancer) can form in the skin, mucous membranes, lymph nodes, and other organs., tests that examine the skin, lungs, and gastrointestinal tract are used to diagnose kaposi sarcoma., after kaposi sarcoma has been diagnosed, tests are done to find out if cancer cells have spread to other parts of the body., certain factors affect prognosis (chance of recovery) and treatment options..
Kaposi sarcoma is a cancer that causes lesions ( abnormal tissue ) to grow in the skin; the mucous membranes lining the mouth, nose, and throat ; lymph nodes ; or other organs . The lesions are usually purple and are made of cancer cells , new blood vessels , red blood cells , and white blood cells . Kaposi sarcoma is different from other cancers in that lesions may begin in more than one place in the body at the same time.
Human herpesvirus-8 (HHV-8) is found in the lesions of all patients with Kaposi sarcoma. This virus is also called Kaposi sarcoma herpesvirus (KSHV). Most people with HHV-8 do not get Kaposi sarcoma. People with HHV-8 are more likely to develop Kaposi sarcoma if their immune system is weakened by disease, such as human immunodeficiency virus (HIV), or by drugs given after an organ transplant .
There are several types of Kaposi sarcoma. The two types discussed in this summary include:
- Classic Kaposi sarcoma .
- Epidemic Kaposi sarcoma (HIV-associated Kaposi sarcoma) .
In addition to asking about your personal and family health history and doing a physical exam , your doctor may perform the following tests and procedures:
- Chest x-ray : An x-ray of the organs and bones inside the chest. An x-ray is a type of energy beam that can go through the body and onto film, making a picture of areas inside the body. This is used to find Kaposi sarcoma in the lungs .
One of the following types of biopsies may be done to check for Kaposi sarcoma lesions in the skin:
- Excisional biopsy : A scalpel is used to remove the entire skin growth.
- Incisional biopsy : A scalpel is used to remove part of a skin growth.
- Core biopsy : A wide needle is used to remove part of a skin growth.
- Fine-needle aspiration (FNA) biopsy : A thin needle is used to remove part of a skin growth.
An endoscopy or bronchoscopy may be done to check for Kaposi sarcoma lesions in the gastrointestinal tract or lungs.
- Endoscopy for biopsy : A procedure to look at organs and tissues inside the body to check for abnormal areas. An endoscope is inserted through an incision (cut) in the skin or opening in the body, such as the mouth. An endoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue or lymph node samples, which are checked under a microscope for signs of disease. This is used to find Kaposi sarcoma lesions in the gastrointestinal tract.
- Bronchoscopy for biopsy : A procedure to look inside the trachea and large airways in the lung for abnormal areas. A bronchoscope is inserted through the nose or mouth into the trachea and lungs. A bronchoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue samples, which are checked under a microscope for signs of disease. This is used to find Kaposi sarcoma lesions in the lungs.
The following tests and procedures may be used to find out if cancer has spread to other parts of the body:
- Blood chemistry studies : A procedure in which a blood sample is checked to measure the amounts of certain substances released into the blood by organs and tissues in the body. An unusual (higher or lower than normal) amount of a substance can be a sign of disease.
- CT scan (CAT scan) : A procedure that makes a series of detailed pictures of areas inside the body, such as the lung, liver , and spleen , taken from different angles. The pictures are made by a computer linked to an x-ray machine. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography.
- PET scan (positron emission tomography scan) : A procedure to find malignant lesions in the body. A small amount of radioactive glucose (sugar) is injected into a vein. The PET scanner rotates around the body and makes a picture of where glucose is being used in the body. Malignant lesions show up brighter in the picture because they are more active and take up more glucose than normal cells do. This imaging test checks for signs of cancer in the lung, liver, and spleen.
- CD34 lymphocyte count : A procedure in which a blood sample is checked to measure the amount of CD34 cells (a type of white blood cell). A lower than normal amount of CD34 cells can be a sign the immune system is not working well.
The prognosis and treatment options depend on the following:
- The type of Kaposi sarcoma.
- The general health of the patient, especially the patient's immune system.
- Whether the cancer has just been diagnosed or has recurred (come back).

Classic Kaposi Sarcoma
Classic kaposi sarcoma is found most often in older men of italian or eastern european jewish origin., signs of classic kaposi sarcoma may include slow-growing lesions on the legs and feet., another cancer may develop..
Classic Kaposi sarcoma is a rare disease that gets worse slowly over many years.
Patients may have one or more red, purple, or brown skin lesions on the legs and feet, most often on the ankles or soles of the feet. Over time, lesions may form in other parts of the body, such as the stomach , intestines , or lymph nodes . The lesions usually don't cause any symptoms but may grow in size and number over a period of 10 years or more. Pressure from the lesions may block the flow of lymph and blood in the legs and cause painful swelling. Lesions in the digestive tract may cause gastrointestinal bleeding.
Some patients with classic Kaposi sarcoma may develop another type of cancer before the Kaposi sarcoma lesions appear or later in life. Most often, this second cancer is non-Hodgkin lymphoma . Frequent follow-up is needed to watch for these second cancers.
Epidemic Kaposi Sarcoma (HIV-Associated Kaposi Sarcoma)
Patients with hiv are at risk of developing epidemic kaposi sarcoma (hiv-associated kaposi sarcoma)., the use of drug therapy called highly active antiretroviral therapy (haart) reduces the risk of epidemic kaposi sarcoma in patients with hiv., signs of epidemic kaposi sarcoma can include lesions that form in many parts of the body..
AIDS is caused by HIV , which attacks and weakens the body's immune system . A weakened immune system is unable to fight infection and disease. People with HIV have an increased risk of infection and cancer .
A person with HIV and certain types of infection or cancer, such as Kaposi sarcoma , is diagnosed as having AIDS. Sometimes, a person is diagnosed with AIDS and epidemic Kaposi sarcoma at the same time.
HAART is a combination of several drugs used to lessen the damage to the immune system caused by HIV infection. Treatment with HAART reduces the risk of epidemic Kaposi sarcoma, although it is possible for a person to develop epidemic Kaposi sarcoma while taking HAART.
For information about AIDS and its treatment, see the HIVinfo website .
The signs of epidemic Kaposi sarcoma can include lesions in different parts of the body, including any of the following:
- Lining of the mouth.
- Lymph nodes .
- Stomach and intestines .
- Lungs and lining of the chest.
Kaposi sarcoma is sometimes found in the lining of the mouth during a regular dental check-up.
In most patients with epidemic Kaposi sarcoma, the disease will spread to other parts of the body over time.
Treatment Option Overview
There are different types of treatment for patients with kaposi sarcoma., radiation therapy, cryosurgery, chemotherapy, immunotherapy, targeted therapy, treatment for kaposi sarcoma may cause side effects., patients may want to think about taking part in a clinical trial., patients can enter clinical trials before, during, or after starting their cancer treatment., follow-up tests may be needed..
Different types of treatments are available for patients with Kaposi sarcoma . Some treatments are standard (the currently used treatment), and some are being tested in clinical trials . A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer . When clinical trials show that a new treatment is better than the standard treatment, the new treatment may become the standard treatment. Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
The following types of treatment are used to treat Kaposi sarcoma:
Treatment of epidemic Kaposi sarcoma combines treatment for Kaposi sarcoma with treatment for acquired immunodeficiency syndrome (AIDS). The types of treatment used to treat Kaposi sarcoma include:
Highly active antiretroviral therapy (HAART) is a combination of several drugs used to lessen the damage to the immune system caused by human immunodeficiency virus (HIV) infection. For many patients, HAART alone may be enough to treat epidemic Kaposi sarcoma. For other patients, HAART may be combined with other standard treatments to treat epidemic Kaposi sarcoma.
Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. There are two types of radiation therapy:
- External radiation therapy uses a machine outside the body to send radiation toward the area of the body with cancer.
- Internal radiation therapy uses a radioactive substance sealed in needles, seeds , wires, or catheters that are placed directly into or near the cancer.
The way the radiation therapy is given depends on the type of the cancer being treated. Certain types of external radiation therapy are used to treat Kaposi sarcoma lesions . Photon radiation therapy treats lesions with high-energy light. Electron beam radiation therapy uses tiny negatively charged particles called electrons .
The following surgical procedures may be used for Kaposi sarcoma to treat small, surface lesions:
- Local excision : The cancer is cut from the skin along with a small amount of normal tissue around it.
- Electrodesiccation and curettage : The tumor is cut from the skin with a curette (a sharp, spoon-shaped tool). A needle-shaped electrode is then used to treat the area with an electric current that stops the bleeding and destroys cancer cells that remain around the edge of the wound . The process may be repeated one to three times during the surgery to remove all of the cancer.
Cryosurgery is a treatment that uses an instrument to freeze and destroy abnormal tissue. This type of treatment is also called cryotherapy.
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body ( systemic chemotherapy ). When chemotherapy is placed directly into the cerebrospinal fluid , an organ , tissue, or a body cavity such as the abdomen , the drugs mainly affect cancer cells in those areas ( regional chemotherapy ).
In electrochemotherapy, intravenous chemotherapy is given and a probe is used to send electric pulses to the tumor. The pulses make an opening in the membrane around the tumor cell and allow the chemotherapy to get inside.
The way the chemotherapy is given depends on where the Kaposi sarcoma lesions occur in the body. In Kaposi sarcoma, chemotherapy may be given in the following ways:
- For local Kaposi sarcoma lesions, such as in the mouth, anticancer drugs may be injected directly into the lesion ( intralesional chemotherapy).
- For local lesions on the skin, a topical agent may be applied to the skin as a gel. Electrochemotherapy may also be used.
- For widespread lesions on the skin, intravenous chemotherapy may be given.
Liposomal chemotherapy uses liposomes (very tiny fat particles) to carry anticancer drugs. Liposomal doxorubicin is used to treat Kaposi sarcoma. The liposomes build up in Kaposi sarcoma tissue more than in healthy tissue, and the doxorubicin is released slowly. This increases the effect of the doxorubicin and causes less damage to healthy tissue.
See Drugs Approved for Kaposi Sarcoma for more information.
Immunotherapy is a treatment that uses the patient's immune system to fight cancer. Substances made by the body or made in a laboratory are used to boost, direct, or restore the body's natural defenses against cancer. Immunotherapy with interferon alfa and interleukin-12 may be used to treat Kaposi sarcoma.
New types of treatment are being tested in clinical trials.
This summary section describes treatments that are being studied in clinical trials. It may not mention every new treatment being studied. Information about clinical trials is available from the NCI website .
Targeted therapy is a type of treatment that uses drugs or other substances to identify and attack specific cancer cells. Monoclonal antibody therapy and tyrosine kinase inhibitors (TKIs) are types of targeted therapy being studied in the treatment of Kaposi sarcoma.
Monoclonal antibodies are immune system proteins made in the laboratory to treat many diseases, including cancer. As a cancer treatment, these antibodies can attach to a specific target on cancer cells or other cells that may help cancer cells grow. The antibodies are able to then kill the cancer cells, block their growth, or keep them from spreading. Monoclonal antibodies are given by infusion . They may be used alone or to carry drugs, toxins , or radioactive material directly to cancer cells. Bevacizumab is a monoclonal antibody that may be used to treat Kaposi sarcoma.
TKIs block signals needed for tumors to grow. Imatinib mesylate is a TKI that may be used to treat Kaposi sarcoma.
For information about side effects caused by treatment for cancer, visit our Side Effects page.
For some patients, taking part in a clinical trial may be the best treatment choice. Clinical trials are part of the cancer research process. Clinical trials are done to find out if new cancer treatments are safe and effective or better than the standard treatment .
Many of today's standard treatments for cancer are based on earlier clinical trials. Patients who take part in a clinical trial may receive the standard treatment or be among the first to receive a new treatment.
Patients who take part in clinical trials also help improve the way cancer will be treated in the future. Even when clinical trials do not lead to effective new treatments, they often answer important questions and help move research forward.
Some clinical trials only include patients who have not yet received treatment. Other trials test treatments for patients whose cancer has not gotten better. There are also clinical trials that test new ways to stop cancer from recurring (coming back) or reduce the side effects of cancer treatment.
Clinical trials are taking place in many parts of the country. Information about clinical trials supported by NCI can be found on NCI’s clinical trials search webpage. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
As you go through treatment, you will have follow-up tests or check-ups. Some tests that were done to diagnose or stage the cancer may be repeated to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your condition has changed or if the cancer has recurred (come back).
Treatment of Classic Kaposi Sarcoma
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment for single skin lesions may include the following:
- Radiation therapy .
Treatment for skin lesions all over the body may include the following:
- Radiation therapy.
- Chemotherapy .
- Electrochemotherapy.
Treatment for Kaposi sarcoma that affects lymph nodes or the gastrointestinal tract usually includes chemotherapy with or without radiation therapy.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Epidemic Kaposi Sarcoma
Treatment for epidemic Kaposi sarcoma may include the following:
- Surgery , including local excision or electrodesiccation and curettage .
- Cryosurgery .
- Chemotherapy using one or more anticancer drugs .
- Immunotherapy using interferon alfa or interleukin-12 .
- Targeted therapy using imatinib or bevacizumab .
To Learn More About Kaposi Sarcoma
For more information from the National Cancer Institute about Kaposi sarcoma, see the following:
- Cryosurgery to Treat Cancer
- Drugs Approved for Kaposi Sarcoma
- Immunotherapy to Treat Cancer
- Targeted Therapy to Treat Cancer
For general cancer information and other resources from the National Cancer Institute, visit:
- About Cancer
- Chemotherapy and You: Support for People With Cancer
- Radiation Therapy and You: Support for People With Cancer
- Coping with Cancer
- Questions to Ask Your Doctor about Cancer
- For Survivors and Caregivers
About This PDQ Summary
Physician Data Query (PDQ) is the National Cancer Institute's (NCI's) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish .
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government’s center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about the treatment of Kaposi sarcoma. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Updated") is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Adult Treatment Editorial Board .
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials can be found online at NCI's website . For more information, call the Cancer Information Service (CIS), NCI's contact center, at 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as “NCI’s PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary].”
The best way to cite this PDQ summary is:
PDQ® Adult Treatment Editorial Board. PDQ Kaposi Sarcoma Treatment. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/soft-tissue-sarcoma/patient/kaposi-treatment-pdq . Accessed <MM/DD/YYYY>. [PMID: 26389178]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online . Visuals Online is a collection of more than 3,000 scientific images.
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website’s E-mail Us .
- News and Features
- Conferences
- Clinical Tools
- Special Collections
Kaposi's Sarcoma (KS)

Are You Confident of the Diagnosis?
What you should be alert for in the history.
Kaposi’s sarcoma is characterized by the appearance of purplish, reddish-blue, or dark brown/black macules, plaques, or nodules on the skin. With classic Kaposi’s sarcoma, the lesions most commonly appear on the lower extremities (Figure 1).
Classical KS on the lower extremity. (Courtesy of Bryan Anderson, MD)

There are four types of Kaposi’s sarcoma:classic (sporadic), endemic (African), immunosuppression related and acquired immunodeficiency syndrome (AIDS) associated. In the cutaneous presentation is most often on the distal lower extremities the classic Kaposi’s and the immunosuppression related variety. In the endemic and AIDS-associated varieties, the disease is more often disseminated and aggressive, but invariably has cutaneous manifestations.
Visceral involvement, including the gastrointestinal tract and regional lymph nodes, is less common in the classic variety but more likely in the other subtypes. There are at least ten different morphologic variants of the cutaneous lesions of Kaposi’s sarcoma.
Characteristic findings on physical examination
The skin lesions may appear as a plaque, patch, nodule, exophytic infiltrative, or lymphadenopathy. The lesions may appear cavernous and lymphangioma-like, and produce chronic lymphedema in the lower extremities. These lesions may consist of compressible nodules that appear as fluid-filled cysts, or they can coalesce and anastomose in networks, producing areas of extensive raised plaques.
Regional lymphadenopathy in the inguinal nodes may be present but does not influence prognosis or treatment options in patients with classic Kaposi’s.
Expected results of diagnostic studies
Immunohistochemical staining of the biopsies can also be useful to detect the presence of LANA-1 (latency-associated nuclear antigen) within the spindle cells (Figure 2, Figure 3).
Histology of KS (H&E). Low power view. (Courtesy of Bryan Anderson, MD)

Histology of KS (H&E). High power view. (Courtesy of Bryan Anderson, MD)

Radiological studies are rarely necessary to evaluate potential metastatic disease sites in patients with classic Kaposi’s. Gastrointestinal involvement rarely complicates cases of classic Kaposi’s, except those with extensive skin involvement of the lower extremities. Patients with Kaposi’s related to endemic, immunosuppression, and AIDS are much more likely to have extensive disease involvement that is extracutaneous.
Involvement of the oral cavity occurs in approximately a third of patients with AIDS-related Kaposi’s, and in 15% of cases, it is the initial presentation of this disease. The palate is the most commonly affected area, followed by the gingiva. Intraoral lesions can be easily traumatized, causing pain, bleeding, ulceration, and secondary infection. Oral lesions may interfere with nutrition and speech, and are often a major reason for treating patients urgently.
Evaluation of gastrointestinal involvement should be performed by endoscopic examination, as these lesions are rarely seen radiologically. Gastrointestinal lesions may be asymptomatic, or can cause weight loss, abdominal pain, nausea, vomiting, upper or lower gastrointestinal bleeding, malabsorption, intestinal obstruction, or diarrhea.
Pulmonary involvement is common in AIDS-related Kaposi’s, usually presenting as shortness of breath, fever, cough, hemoptysis, or chest pain (or patients may be asymptomatic).
Radiological findings are variable, and include infiltrates and densities, effusions, and adenopathy. Diagnosis of pulmonary involvement with Kaposi’s sarcoma is usually made by bronchoscopy, by observing cherry-red raised lesions on the endobronchial surface.
Since a number of other organs can be involved by Kaposi’s computed tomography (CT) and magnetic resonance imaging (MRI) scans are usually needed to evaluate organ involvement including involvement of the lymph nodes, liver, pancreas, cardiovascular system, , testes, bone marrow, bone, or skeletal muscle.
Staging and prognosis are established by determining CD4 count, human immunodeficiency virus (HIV) viral load, and the presence of human herpes virus 8 (HHV-8) DNA. The most commonly used staging system developed by the AIDS clinical trial group separates patients into good and poor risk categories according to extent of tumor, immune status, and severity of illness. These factors were much more important in the period before highly active retroviral therapy. Since the introduction of highly active retroviral therapy, the incidence of and prognosis for Kaposi’s have improved substantially in all risk categories.
Diagnosis confirmation
The diagnosis of classic Kaposi’s sarcoma is suspected based on the appearance and location of the lesions. Lesions located on the lower extremities can be mistaken for changes due to peripheral vascular disease or venous stasis.
Bacillary angiomatosis is a rare infection caused by the Bartonella species, which are gram-negative bacilli that are readily treated with antibiotics. Lesions due to this infection usually present as numerous small red-purple papules that may expand into larger exophytic lesions and become friable. The rash may be associated with fevers, chills, malaise, headache, and anorexia. Bacillary angiomatosis can infect both immunocompromised and immunocompetent patients.
Bacillary angiomatosis was described in the 1980s and found to be associated with AIDS at presentation. This condition may simulate Kaposi’s in patients with AIDS by its dermatological presentation and systemic spread; however, this disorder responds to antibiotics, including oral erythromycin as well as other antibiotics. Anti-tuberculosis medications are also effective. Bacillary angiomatosis is treatable and curable, but it may also be life-threatening, if undiagnosed.
Other rare infections that may produce similar and confusing nodular violaceous skin lesions include S. schenckii (sporotrichosis) and M. marium. Biopsy of these skin lesions allows a definitive diagnosis to be made. Biopsies demonstrate typical histological features under standard microscopy. Additional studies, including polymerase chain reaction, can be performed on obvious skin lesions to detect amplified HHV-8 DNA sequences.
Who is at Risk for Developing this Disease?
There are four subgroups of Kaposi’s sarcoma:
1. Classic Kaposi’s is characteristically seen in older men of Mediterranean and Jewish origin.
2. Endemic or African Kaposi’s is found in all parts of equatorial Africa, particularly in sub-Saharan Africa, and is not associated with immunodeficiency.
HHV-8, also known as Kaposi’s-sarcoma-associated herpes virus (KSHV), is necessary but not sufficient for the development of Kaposi’s sarcoma. A secondary factor results in a reactivation of this virus, which is important in the pathogenesis of Kaposi’s and the distinctive and largely unexplained geographic distributions of classic Kaposi’s.
3. Immunosuppression due to transplantation, particularly solid organ transplant, is a risk factor for Kaposi’s sarcoma. Patients receiving immunosuppressive agents are not at risk for developing Kaposi’s; thus it appears that the immunological derangements that occur in patients with solid organ transplants and in those on immunosuppressive agents is a distinctive risk factor for Kaposi’s.
4. AIDS-related Kaposi’s (epidemic KS) is associated with HIV and severe immunosuppression with low CD4 counts. Kaposi’s sarcoma in patients with HIV defines AIDS. Treatment with highly active retroviral therapy not only helps control Kaposi’s disease, but also has been associated with a marked reduction in the incidence of Kaposi’s in patients on highly active retroviral therapy.
What is the Cause of the Disease?
Kaposi’s sarcoma is a low-grade vascular tumor associated with infection with HHV-8 also known as KSHV. These vascular tumors primarily develop in the skin and lower extremities in classic Kaposi’s sarcoma and remain confined to the lower extremities, causing lymphedema and disfigurement.
Classic Kaposi’s patients are not immunosuppressed, and their disease involves chronic lower extremity edema due to this invasive tumor. This tumor rarely metastasizes distantly, other than to local regional nodes.
Endemic Kaposi’s follows a similar pattern, with lower extremity involvement, but generally is more aggressive and can disseminate to distant organs, unlike classic Kaposi’s.
Immunosuppression-related Kaposi’s occurs during immunosuppression for solid tumor organs. Lesions usually present in the skin and lower extremity, but are much more likely to disseminate. The control and progression of the lesions, both locally and with dissemination, are related to the ability to restore the immune system by eliminating or changing immunosuppressive agents.
AIDS-related Kaposi’s is a much more aggressive and widely disseminated disease, causing significant morbidity and mortality. The degree of immunosuppression is directly correlated with the risk of developing Kaposi’s sarcoma and treatment with highly active retroviral therapy; the resultant restoration of the immune system has reduced the incidence of Kaposi’s and provided an improved outcome.
- Systemic Implications and Complications
Patients with AIDS-associated Kaposi’s or immunosuppression-mediated Kaposi’s who are treated with corticosteroids are more likely to have exacerbation of existing Kaposi’s lesions and progression of their lesions. Patients with Kaposi’s who are on corticosteroids also have a higher incidence of opportunistic infections.
Patients with AIDS-associated Kaposi’s that arises during immunosuppression are also at risk for other malignancies. Non-Hodgkin’s lymphoma is a common second malignancy in patients on immunosuppression. Non-Hodgkin’s lymphoma is a complication for patients with HIV-AIDS and for solid organ transplant patients that are being treated with immunosuppressive agents.
The subtype of Kaposi’s sarcoma will dictate the extent of clinical workup. For example, patients with classic Kaposi’s do not require any extensive radiological surveillance. On the other hand, patients with AIDS-related Kaposi’s will need very careful attention to various organs, and will require radiological studies, especially an endoscopic evaluation including careful oral and dental evaluations.
Chest x-rays are useful for screening for pulmonary lesions; bronchoscopy should be reserved for patients with abnormal radiographs or respiratory symptoms. Visceral disease is much more likely in patients with low CD4 counts (CD4 counts of 200 or less are usually associated with a higher risk of developing Kaposi’s and also with more aggressive and extensive disease at the time of presentation).
Testing stool for occult blood is a good screen for gastrointestinal involvement and endoscopy should be reserved for patients who have positive occult blood or have gastrointestinal symptoms.
Treatment Options
Treatment options will vary according to the subtype of Kaposi’s.
CLASSIC KAPOSI’S SARCOMA
-observation of asymptomatic lesions
-compression therapy
-topical allotretinoin cream
-topical imiquimod
-intralesional interferon
-surgical excision
-cryosurgery
-laser (pulsed-dye laser)
-systemic chemotherapy (peglyated doxorubicin)
AFRICAN KAPOSI’S SARCOMA
African Kaposi’s sarcoma can be treated with the same approach used for patients with classic Kaposi’s.
IMMUNOSUPPRESSION-MEDIATED KAPOSI’S
-withdrawal of immunosuppressive agents
AIDS-ASSOCIATED KAPOSI’S SARCOMA
-highly active antiretroviral treatment
-intralesional chemotherapy (vincristine or bleomycin)
-laser ablation—pulsed dye laser
-systemic chemotherapy (liposomal anthracycline)
AIDS-associated Kaposi’s sarcoma patients who receive highly active retroviral therapy and develop immune reconstitution inflammatory syndrome and progressive Kaposi’s within weeks after initiation of highly active retroviral therapy should be treated with chemotherapy (vincristine, bleomycin, adriamycin, or paclitaxel based) during this phase.
Optimal Therapeutic Approach for this Disease
Classic Kaposi’s sarcoma can be treated with surgical excision of small isolated lesions. If there is extensive skin involvement, then radiation therapy is the treatment of choice.
The goal of therapy is to alleviate symptoms, including reducing lymphedema, improving the function of lower extremities, decreasing the size of cutaneous lesions, and preventing progression. Patients with limited disease involvement may be observed without active therapy. Asymptomatic patients and those who do not have impairment of ambulation (if lower extremity edema can be managed with compressive stockings) may be observed without active therapy.
Patients with a limited volume of disease causing bleeding or cosmetic disfigurement can be treated with local therapy; radiation therapy, excision, cryotherapy, and laser ablation are useful, depending on the number of sites and the extent of involvement, as well as clinician and patient preference.
Patients with bulky disease that cannot be managed with local modalities should be considered for systemic therapy and first-line preference given to pegylated liposomal doxorubicin. African Kaposi’s can be treated with the same approach used for patients with classic Kaposi’s.
The recommendation is to initially diagnose the suspicious skin lesion and classify the subtype of Kaposi’s sarcoma. As indicated above, the various subtypes of Kaposi’s sarcoma will have different natural histories of disease. Once a diagnosis has been established, the patient can be referred to a medical oncologist and infectious disease specialist. For patients with a solid organ transplant who are on immunosuppression, the treatment decisions are usually difficult and require a balance of maintaining immunosuppression for the transplanted organ and controlling and eradicating the Kaposi’s sarcoma.
Immunosuppression-mediated Kaposi’s can often respond to withdrawal of the immunosuppressive agents used to control graft-versus-host disease. These maneuvers can often result in complete responses and remissions. Case reports have described regression of Kaposi’s sarcoma in patients treated with the mTOR inhibitor rapamycin (sirolimus), suggesting that this approach (rather than using an alternative immunosuppressive agent in transplant-associated Kaposi’s) may be much more rational and applicable to transplant patients.
Systemic chemotherapy with pegylated liposomal doxorubicin as a first-line therapy, followed by other second-line agents, can be used to control the disease in patients where immunosuppression cannot be altered.
Patients with AIDS-associated Kaposi’s who develop either limited or advanced Kaposi’s sarcoma should initially be treated with highly active retroviral therapy. For patients who have limited disease-causing symptoms or cosmetic disfigurement, local therapy rather than systemic therapy, in addition to highly active retroviral therapy, is the recommended approach. The treatment approach for local regional disease, including intralesional chemotherapy, surgery, cryotherapy, and laser ablation should be reserved for patients with small lesions.
Patients with larger lesions or bulky local regional disease should receive radiation therapy.
Patients with extensive cutaneous disease and symptomatic visceral involvement or local cutaneous disease unresponsive to local measures should receive systemic chemotherapy with the recommended liposomal anthracycline.
AIDS-associated Kaposi’s sarcoma patients who receive highly active retroviral therapy and develop immune reconstitution inflammatory syndrome and progressive Kaposi’s within weeks after initiation of highly active retroviral therapy should be treated with chemotherapy during this phase.
Patient Management
Classic Kaposi’s sarcoma requires the identification of the appropriate patient subgroup, namely older males of Mediterranean or Jewish ancestry. The lesions are typically extensive, involving the lower extremities, and treated with local regional control efforts. Laboratory studies need to be ordered to rule out HIV infection, and CD4 counts should be monitored. Radiological studies such as CT scans should be ordered only if there are symptoms and concern about organ involvement. There is no role for routine radiological surveillance.
African Kaposi’s sarcoma presents in a fashion similar to classic Kaposi’s, with lower extremity involvement; however, this disease tends to be more aggressive and infiltrative. Laboratory studies need to be ordered to rule out HIV infection, and CD4 counts should be monitored. Radiological studies, including CT scans and pulmonary and GI endoscopy, should be considered, especially in patients with symptoms and in those with extensive disease involvement.
AIDS-associated Kaposi’s sarcoma is a much more aggressive and widespread disease. Routine radiological surveillance and pulmonary and GI endoscopic studies should be performed. Physical examination should include a careful oral and dental evaluation. Laboratory studies include monitoring of viral load and CD4 counts.
Kaposi’s sarcoma that develops in patients with solid organ transplants is established once a positive skin biopsy is obtained. Radiological surveillance should include CT scans and endoscopic surveillance of the pulmonary system and GI tract. Laboratory studies will include monitoring of the immune system and viral serology, including HIV testing. Treatment decisions will be made by collaboration between the medical oncologist and transplant physician.
- Unusual Clinical Scenarios to Consider in Patient Management
One must be vigilant for the possibility of secondary malignancies, most notably non-Hodgkin’s lymphoma.
Patients may be at risk for the immune reconstitution syndrome after the commencement of highly active antiretroviral therapy.
What is the Evidence?
Gill, PS, Wernz, J, Scadden, DT. “Randomized phase 3 trial of liposomal doxorubicin in AIDS related Kaposi's sarcoma”. JClini Oncol. vol. 14. 1996. pp. 2353 (Nice study on the use of systemic chemotherapy for AIDS-related Kaposi's sarcoma)
Leidner, RS, Aboulafia, DM. “Recrudescent Kaposi's sarcoma after initiation of HAART: manifestation of immune reconstitution syndrome”. AIDS Patient Care STDS. vol. 19. 2005. pp. 635 (Kaposi's sarcoma manifests after the start of HAAART. Mechanisms and theories are discussed.)
Gallafent, JH, Buskin, SE, De Turk, PB, Aboulafia, DM. “Profile of patients with Kaposi's sarcoma in the era of highly active retroviral therapy”. JClini Oncol. vol. 23. 2005. pp. 1253 (Characterization of patients with Kaposi's, with special focus on those undergoing antiretroviral therapy)
Gill, PS, Loureiro, C, Bernstein-Singer, M. “Clinical effects of glucocorticoids on Kaposi's sarcoma related to acquired immunodeficiency syndrome”. Ann Intern Med. vol. 110. 1989. pp. 937 (Short paper on corticosteroids for the treatment of Kaposi's in patients with AIDS .)
Fenig, E, Brenner, B, Rakowsky, E. “Classic Kaposi's sarcoma: experience at Rabin Medical Center in Israel”. Am J Clin Oncol. vol. 21. 1998. pp. 498 (Wonderful review of the classical form of Kaposi's sarcoma. Discussion deals with etiology, pathogenesis, epidemiology, and therapy.)
Copyright © 2017, 2013 Decision Support in Medicine, LLC. All rights reserved.
No sponsor or advertiser has participated in, approved or paid for the content provided by Decision Support in Medicine LLC. The Licensed Content is the property of and copyrighted by DSM.
Picked For You
Latest News
Want to read more?
Please login or register first to view this content.
Login Register
Enjoying our content? Thanks for visiting Dermatology Advisor . We hope you’re enjoying the latest clinical news, full-length features, case studies, and more.
You’ve viewed {{metering-count}} of {{metering-total}} articles this month. If you wish to read unlimited content, please log in or register below. Registration is free.
{{login-button}} {{register-button}}
Log in to continue reading this article.
Don’t miss out on today’s top content on Dermatology Advisor . Register for free and gain unlimited access to:
- Clinical Updates, with personalized daily picks for you - Evidence-Based Guidance - Conference Coverage - Full-Length Features - Drug Monographs - And More
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Dermatol Ther (Heidelb)
- v.6(4); 2016 Dec

An Update on Kaposi’s Sarcoma: Epidemiology, Pathogenesis and Treatment
Paul curtiss.
The Ronald O. Perelman Department of Dermatology, New York University School of Medicine, New York, NY USA
Lauren C. Strazzulla
Alvin e. friedman-kien.
Kaposi’s sarcoma is an angioproliferative neoplasm which has undergone considerable epidemiologic change since the original description by Moritz Kaposi in the late 1800s. This opportunistic neoplasm gained widespread notoriety within the US during the height of the AIDS epidemic, where it was frequently found co-occurring with opportunistic infections. With the advent of modern antiretroviral therapies, as well as an increasing number of individuals on immunosuppression for autoimmune disease or organ transplantation, the landscape of the immunocompromised individual has changed. It is now important for clinicians to be mindful of Kaposi’s sarcoma manifesting in a growing variety of clinical contexts.
The Four Epidemiological Forms of Kaposi’s Sarcoma
Aids-associated kaposi’s sarcoma.
Kaposi’s sarcoma (KS) is a multi-focal, angioproliferative neoplasm that usually appears on the skin, but can also involve the visceral organs. In 1981, 26 cases of KS were reported as occurring in young homosexual men in New York and California. Many of these patients also had concomitant pneumocystis carinii pneumonia (PCP) and a variety of other “opportunistic infections” [ 1 ]. At that time, the underlying cause of AIDS was unknown, but, remarkably, one-third of these patients developed a disseminated form of KS. In 1983, it was postulated that KS was driven by the host’s profoundly immunocompromised state. Interestingly, 95% of these cases had occurred in homosexual men. Furthermore, it appeared that the clinical presentation of AIDS-associated KS (AIDS-KS) differed significantly from previously described clinical variants of this unusual neoplasm [ 2 ]. In these immunocompromised patients, KS behaved more aggressively, often involving mucosal tissues, and progressed to visceral involvement leading to organ dysfunction and death [ 3 ].
In the early 1980s, a significant proportion of homosexual men with AIDS were affected by KS; for example, in San Francisco, this opportunistic neoplasm occurred in 40% of homosexual men with AIDS. This suggested that a major risk factor for KS might be homosexual intercourse [ 4 ]. In fact, several early studies showed a connection between the number of sexual partners and the prevalence of KS. For example, in Vancouver, 56% of homosexual men with AIDS and more than 20 partners developed KS [ 5 ]. As the widespread use of highly active antiretroviral therapy (HAART) gained popularity in the early and mid-1990s, an 8.8% annual decline from 1990 to 1998 in KS incidence in the United States was observed, along with a 50% reduction in KS incidence among those on triple antiretroviral therapy [ 6 ]. A cancer surveillance program in San Francisco revealed similar patterns, with the incidence of KS in 1973 (prior to the AIDS epidemic) at 0.5 cases per 100,000 people, while during the peak of the AIDS epidemic in 1991, this number was 33.3 cases per 100,000 people and then declined in 1998 (post-HAART) to 2.8 cases per 100,000 people [ 7 ].
The Classic Form
In 1872, Moritz Kaposi first described the “classic” variant of KS that is typically observed in elderly men of Mediterranean or eastern European origin [ 8 ]. This form of KS generally presents with lesions confined to the lower extremity, affects men more commonly than women in a 15:1 ratio, and is usually indolent with patients living 10 years or more [ 9 ]. The incidence of KS in the Mediterranean is significantly higher than in the rest of Europe and the United States. For example, prior to the AIDS epidemic, there was a two- to threefold higher prevalence of KS among the Italian population compared to that of the USA, and a ten times greater prevalence compared to England [ 10 ].
The Endemic Form
In the 1950s, an endemic form of KS was reported to be one of the most common neoplasms observed in central Africa, affecting men, women and children [ 11 ]. Notably, following the AIDS epidemic, the incidence of KS in Africa increased markedly, and from 1968 to 1970, KS accounted for 6.6% of all cancers occurring in men; however, from 1989 to 1991, KS became the most commonly reported cancer occurring in men (48.6% of male cancer patients), while the prevalence in female cancer patients rose to 17.9% [ 12 ].
The Iatrogenic Form
In the 1970s, an “iatrogenic” form of KS was also observed among organ transplant recipients, as well as other patients on long-term immunosuppression for other diseases [ 2 ]. Recently, there have been a growing number of cases of this iatrogenic variant of KS. For example, there are an increasing number of reports in the literature describing individuals who develop KS arising in the context of long-term corticosteroid therapy and other biologic therapies, including rituximab, infliximab, and abatacept administered for chronic inflammatory and autoimmune conditions, including autoimmune thrombocytopenia, polyangiitis and pemphigus vulgaris [ 13 – 15 ]. The occurrence of KS in such patients frequently resolves spontaneously when the immunosuppressive therapies are discontinued [ 16 ]. As the increasing use of these immunomodulatory medications becomes more widespread, it is important to be aware of the possibility of KS occurring among these individuals who previously had not been considered “high-risk”.
New attention has been focused on the increased occurrence of KS among patients who are significantly immunosuppressed following organ transplantation. In fact, the incidence of KS is 400–500 times higher among such patients than the general population [ 17 ]. This may be due to reactivation of latent HHV-8 virus or perhaps through acquisition of the virus from the donor organ [ 18 ]. However, certain immunosuppressants may be less likely to put patients at risk for iatrogenic KS. For example, sirolimus or everolimus (mTOR inhibitors) appear to inhibit the occurrence and/or progression of KS in transplant recipients while preventing organ rejection [ 19 , 20 ]. These drugs may reduce the effect of vascular endothelial growth factor (VEGF) which is believed to play a pivotal role in the pathogenesis of KS [ 20 ]. Therefore, clinicians need to be aware of the oncogenic potential of immunosuppressive therapy in these organ transplant recipients.
Pathogenesis
For many years, the cause of KS was initially perplexing, with the occurrence of KS in patients such as those on long-term immunosuppressant therapy strongly suggesting the possibility that this neoplasm might be related to a transmissible agent. Interestingly, in the 1990s, there were also case reports of KS occurring in gay or bisexual HIV-negative immunocompetent individuals, supporting the hypothesis that KS was a neoplasm that could be due to a sexually transmitted infection occurring within that community [ 21 ]. It still remains unclear exactly why KS is almost exclusively observed in homosexual AIDS patients, and is very rarely if ever observed in IV drug users, or in individuals receiving blood products through transfusions, such as hemophiliacs. Perhaps the pathogenesis of KS may be hormone-dependent, which would account for the predominance in males and for the observation that KS is transferred between men through homosexual intercourse more commonly than from a male to a female partner through heterosexual intercourse [ 22 ].
In 1996, a newly discovered virus was found to be associated with every specimen of KS examined. Kaposi’s sarcoma-associated herpesvirus (KSHV), now known as human herpesvirus-8 (HHV8), was sequenced and identified as the infectious agent previously associated with KS among different populations, including individuals in Eastern Europe, Africa and the United States [ 23 ]. Since this discovery, new research has shed light on the molecular mechanisms of KS. The lesions found in KS are known to contain several cell types, such as infiltrating inflammatory cells, endothelium and spindle cells, which have been postulated to derive from either vascular or lymphatic precursors. One paper has shown a monoclonal antibody that stains specifically for lymphatic endothelium and also stains spindle cells from KS lesions, suggesting that the tumor cell of KS may be of lymphatic origin [ 24 ]. Moreover, spindle cell viability is likely dependent on the tumor milieu, which in KS consists of elevated levels of growth factors and cytokines, such as interleukin (IL)-1, IL-6, platelet-derived growth factor, tumor necrosis factor, IFN-gamma, and VEGF [ 25 ].
In HIV-infected individuals, Th1-type cytokines have been suggested to potentiate KSHV activation, which can lead to an increased viral load and a greater likelihood of the development of KS [ 26 ]. Also, HIV-1-associated trans-activating regulatory (Tat) protein is needed for replication of the HIV virus and is also released from acutely infected T cells. This protein may induce KS by stimulating proangiogenic chemokines, and by enhancing KS cell growth by synergizing with basic fibroblast growth factor (bFGF), which is an essential factor for lesion formation [ 3 ]. This may account for the more aggressive behavior of KS lesions in HIV-infected individuals compared to the classic variant [ 27 ]. However, the Tat protein is only able to interact with endothelial cells through a RGD motif, which is absent in HIV-2. This may explain why KS is less commonly found in individuals with HIV-2 compared to HIV-1 infection [ 28 ].
A variety of treatment options are available for the classic variant of KS. Since these lesions often recur, but are less often life-threatening, one viable treatment strategy is recurrent use of local cryotherapy which typically resolves the isolated lesions [ 29 ]. Another well-described approach is the use of intralesional chemotherapeutics such as vincristine which are also efficacious [ 30 ].
For patients with extensive disease and/or widespread rapidly progressive disease, it may be necessary to resort to more generalized therapies. Pegylated liposomal doxorubicin has been used as a first-line treatment, with a favorable 71% response rate, and is significantly better tolerated than traditional chemotherapeutics [ 31 , 32 ]. Another option is the use of localized radiation to the lower extremity which has shown a high rate of resolution to the affected fields [ 33 ].
Kaposi’s sarcoma occurring in patients on significant immunosuppression will resolve in the majority of patients when the immunosuppressive therapy is altered, reduced or discontinued. Commonly, when KS arises in renal transplant recipients, a decrease in the level of immunosuppression is a first reasonable strategy [ 34 ]. When this does not promote resolution of the disease, or begins to compromise graft viability, some patients may benefit from transition of typical calcineurin inhibitors such as cyclosporine to proliferation signal inhibitors such as sirolimus, which often results in complete resolution of active KS without rejection of the graft [ 20 ].
The mainstay of treatment for AIDS-related KS involves the initiation of HAART, which typically results in a subsequent decrease in tumor burden as the CD4 count rises and is able to adequately suppress the HHV8 virus. Interestingly, a subset of these patients may experience a progression of their disease following initiation of HAART in an immune reconstitution inflammatory syndrome (IRIS) [ 35 , 36 ]. Typically, these patients are able to continue therapy, but in some cases adjuvant chemotherapy may be required to control the tumor burden.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors.
Acknowledgements
No funding or sponsorship was received for this study or publication of this article. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published.
Disclosures
Paul Curtiss, Lauren C. Strazzulla and Alvin E. Friedman-Kien have nothing to disclose.
Online Help
Our 24/7 cancer helpline provides information and answers for people dealing with cancer. We can connect you with trained cancer information specialists who will answer questions about a cancer diagnosis and provide guidance and a compassionate ear.
Chat live online
Select the Live Chat button at the bottom of the page
Call us at 1-800-227-2345
Available any time of day or night
Our highly trained specialists are available 24/7 via phone and on weekdays can assist through online chat. We connect patients, caregivers, and family members with essential services and resources at every step of their cancer journey. Ask us how you can get involved and support the fight against cancer. Some of the topics we can assist with include:
- Referrals to patient-related programs or resources
- Donations, website, or event-related assistance
- Tobacco-related topics
- Volunteer opportunities
- Cancer Information
For medical questions, we encourage you to review our information with your doctor.
- About Kaposi Sarcoma
Get an overview of Kaposi sarcoma and the latest key statistics in the US.
Overview and Types
If you have been diagnosed with Kaposi sarcoma or are worried about it, you likely have a lot of questions. Learning some basics is a good place to start.
- What Is Kaposi Sarcoma?
Research and Statistics
See the estimates for cases of Kaposi sarcoma in the US and what research is currently being done.
- Key Statistics About Kaposi Sarcoma
- What’s New in Kaposi Sarcoma Research?
More in Kaposi Sarcoma
- Causes, Risk Factors, and Prevention
- Early Detection, Diagnosis, and Staging
- After Treatment
Help us end cancer as we know it, for everyone.

If this was helpful, donate to help fund patient support services, research, and cancer content updates.

Ophthalmologic Manifestations of Kaposi Sarcoma Clinical Presentation
- Author: Jacqueline Freudenthal, MD; Chief Editor: Edsel B Ing, MD, PhD, MBA, MEd, MPH, MA, FRCSC more...
- Sections Ophthalmologic Manifestations of Kaposi Sarcoma
- Pathophysiology
- Epidemiology
- Laboratory Studies
- Imaging Studies
- Histologic Findings
- Medical Care
- Surgical Care
- Consultations
- Medication Summary
- Antineoplastics
- Interferons
- Further Outpatient Care
- Inpatient & Outpatient Medications
- Complications
- Patient Education
- Questions & Answers
- Media Gallery
Identify risk factors for Kaposi sarcoma. The clinician should ask about the following:
Demographics
Immune status
Previous skin lesions
Previous treatment for Kaposi sarcoma
History of opportunistic infections
Current medication use
Symptoms of Kaposi sarcoma include the following:
Photophobia
Recurrent red or bloody eyes
Irritation and foreign body sensation
Mucopurulent discharge
Heavy or swollen eyelids
Cosmetic disfigurement of the eyelids
Eyelashes rubbing against the eyes
Inability to close the eyes
Visual obstruction
Blurred vision
Full ocular examination should include the following:
Inspect and evert the eyelids and lashes
Perform slit lamp biomicroscopy
Examine palpebral and bulbar conjunctivae and fornices in detail
Palpate the lacrimal gland, and examine for masses
Examine both eyes for proptosis in the rare likelihood of orbital involvement; fortunately, intraocular Kaposi sarcoma has never been reported
The lesions are purplish-red to bright-red and highly vascular with surrounding telangiectatic vessels. They may be macular, plaquelike, or nodular. Ophthalmic Kaposi sarcoma lesions are found on the eyelids, conjunctiva, caruncle, and lacrimal sac. They rarely are found inside the orbit (1 case of choroidal involvement). [ 16 ]
See the image below.

Dugel et al described 3 clinical stages that may help direct therapy. Stage I and II tumors are patchy and flat. These lesions have a thickness of less than 3 mm in vertical height and are younger than 4 months. Stage III tumors are nodular and elevated with a vertical height of greater than 3 mm. They tend to be older than 4 months. [ 17 ]
Of ophthalmic Kaposi sarcoma cases, 6-16% are eyelid lesions, and the superior and inferior eyelids tend to be involved equally. Of ophthalmic Kaposi sarcoma cases, 7-18% are conjunctival lesions. Many conjunctival lesions tend to involve the inferior conjunctiva (as is shown in the image below) and fornix.

Lesions tend to be indolent, but, as the tumor grows, it can alter ocular adnexal structures [ 14 ] and the ocular surface. The mass effect of the tumor on the eyelids can cause mechanical ectropion or entropion with trichiasis and lagophthalmos and irregular astigmatism. Ectropion or entropion can result in poor lid apposition, trichiasis, and lagophthalmos. Consequently, the patient may experience epiphora, poor tear clearance and drainage, recurrent corneal abrasions, pain and discomfort, foreign body sensation, dry eyes, and photophobia. Long-standing trichiasis and exposure can result in corneal infection, scarring, and opacification.
Rarely, tumor bulk may block the visual axis by ptosis or direct obstruction. Tumor bulk may even prevent the complete closure of the eyelid.
Conjunctival involvement may present with subconjunctival hemorrhage, injection, and chemosis.
Human herpesvirus-8 (HHV-8) DNA or Kaposi sarcoma–associated herpesvirus (KSHV) has been implicated with patients who are HIV-negative or HIV-positive. [ 18 ]
Homosexual males with HIV infection are at an increased risk. This risk is markedly increased with the number of partners.
Patients who have had organ transplants and use immunosuppressive agents and steroids are at an increased risk.
Elderly males of Mediterranean or Ashkenazi ancestry are at an increased risk.
Kaposi M. Idiopathisches multiple Pigment-sarkom der Haut. Arch Dermatol . Syphilol. 1872:4. [QxMD MEDLINE Link] .
Jones JL, Hanson DL, Dworkin MS, et al. Surveillance for AIDS-defining opportunistic illnesses, 1992-1997. MMWR CDC Surveill Summ . 1999 Apr 16. 48(2):1-22. [QxMD MEDLINE Link] .
Holland GN, Gottlieb MS, Yee RD, et al. Ocular disorders associated with a new severe acquired cellular immunodeficiency syndrome. Am J Ophthalmol . 1982 Apr. 93(4):393-402. [QxMD MEDLINE Link] .
Mowatt L. Ophthalmic manifestations of HIV in the highly active anti-retroviral therapy era. West Indian Med J . 2013. 62(4):305-12. [QxMD MEDLINE Link] .
Becker KN, Becker NM. Ocular manifestations seen in HIV. Dis Mon . 2014 Jun. 60(6):268-75. [QxMD MEDLINE Link] .
Verma V, Shen D, Sieving PC, Chan CC. The role of infectious agents in the etiology of ocular adnexal neoplasia. Surv Ophthalmol . 2008 Jul-Aug. 53(4):312-31. [QxMD MEDLINE Link] . [Full Text] .
Chang Y, Cesarman E, Pessin MS, et al. Identification of herpesvirus-like DNA sequences in AIDS-associated Kaposi's sarcoma. Science . 1994 Dec 16. 266(5192):1865-9. [QxMD MEDLINE Link] .
Pantry SN, Medveczky PG. Epigenetic regulation of Kaposi's sarcoma-associated herpesvirus replication. Semin Cancer Biol . 2009 Jun. 19(3):153-7. [QxMD MEDLINE Link] . [Full Text] .
Ye F, Zhou F, Bedolla RG, Jones T, Lei X, Kang T, et al. Reactive oxygen species hydrogen peroxide mediates Kaposi's sarcoma-associated herpesvirus reactivation from latency. PLoS Pathog . 2011 May. 7(5):e1002054. [QxMD MEDLINE Link] . [Full Text] .
Sakakibara S, Tosato G. Viral interleukin-6: role in Kaposi's sarcoma-associated herpesvirus: associated malignancies. J Interferon Cytokine Res . 2011 Nov. 31(11):791-801. [QxMD MEDLINE Link] . [Full Text] .
Ye F, Lei X, Gao SJ. Mechanisms of Kaposi's Sarcoma-Associated Herpesvirus Latency and Reactivation. Adv Virol . 2011. 2011: [QxMD MEDLINE Link] . [Full Text] .
Traylen CM, Patel HR, Fondaw W, et al. Virus reactivation: a panoramic view in human infections. Future Virol . 2011 Apr. 6(4):451-463. [QxMD MEDLINE Link] . [Full Text] .
Centers for Disease Control and Prevention. Update: AIDS--United States, 2000. JAMA . 2002 Aug 14. 288(6):691-2. [QxMD MEDLINE Link] .
Mansour AM. Adnexal findings in AIDS. Ophthal Plast Reconstr Surg . 1993 Dec. 9(4):273-9. [QxMD MEDLINE Link] .
Gigase PL, de Muynck A, de Feyter M. Kaposi's sarcoma in Zaire. IARC Sci Publ . 1984. 549-57. [QxMD MEDLINE Link] .
Pantanowitz L, Dezube BJ. Kaposi sarcoma in unusual locations. BMC Cancer . 2008. 8:190. [QxMD MEDLINE Link] . [Full Text] .
Dugel PU, Gill PS, Frangieh GT, Rao NA. Ocular adnexal Kaposi's sarcoma in acquired immunodeficiency syndrome. Am J Ophthalmol . 1990 Nov 15. 110(5):500-3. [QxMD MEDLINE Link] .
Meyers D. Eye signs that alert the clinician to a diagnosis of AIDS. SADJ . 2005. 60:386-387. [QxMD MEDLINE Link] .
Emina MO, Odjimogho SE. Ocular problems in HIV and AIDS patients in Nigeria. Optom Vis Sci . 2010 Dec. 87(12):979-84. [QxMD MEDLINE Link] .
[Guideline] Mofenson LM, Brady MT, Danner SP, et al. Guidelines for the Prevention and Treatment of Opportunistic Infections among HIV-exposed and HIV-infected children: recommendations from CDC, the National Institutes of Health, the HIV Medicine Association of the Infectious Diseases Society of America, the Pediatric Infectious Diseases Society, and the American Academy of Pediatrics. MMWR Recomm Rep . 2009 Sep 4. 58:1-166. [QxMD MEDLINE Link] . [Full Text] .
Macken M, Dale H, Moyo D, Chakmata E, Depani S, Israels T, et al. Triple therapy of vincristine, bleomycin and etoposide for children with Kaposi sarcoma: Results of a study in Malawian children. Pediatr Blood Cancer . 2018 Feb. 65 (2): [QxMD MEDLINE Link] .
Hoffmann C, Sabranski M, Esser S. HIV-Associated Kaposi's Sarcoma. Oncol Res Treat . 2017. 40 (3):94-98. [QxMD MEDLINE Link] . [Full Text] .
Brasnu E, Wechsler B, Bron A, et al. Efficacy of interferon-alpha for the treatment of Kaposi's sarcoma herpesvirus-associated uveitis. Am J Ophthalmol . 2005 Oct. 140(4):746-8. [QxMD MEDLINE Link] .
Hummer J, Gass JD, Huang AJ. Conjunctival Kaposi's sarcoma treated with interferon alpha-2a. Am J Ophthalmol . 1993 Oct 15. 116(4):502-3. [QxMD MEDLINE Link] .
Qureshi YA, Karp CL, Dubovy SR. Intralesional interferon alpha-2b therapy for adnexal Kaposi sarcoma. Cornea . 2009 Sep. 28(8):941-3. [QxMD MEDLINE Link] .
Hermans P. Epidemiology, etiology and pathogenesis, clinical presentations and therapeutic approaches in Kaposi's sarcoma: 15-year lessons from AIDS. Biomed Pharmacother . 1998. 52(10):440-6. [QxMD MEDLINE Link] .
Samaniego F, Bryant JL, Liu N, et al. Induction of programmed cell death in Kaposi's sarcoma cells by preparations of human chorionic gonadotropin. J Natl Cancer Inst . 1999 Jan 20. 91(2):135-43. [QxMD MEDLINE Link] .
Simonart T, Noel JC, Andrei G, et al. Iron as a potential co-factor in the pathogenesis of Kaposi's sarcoma?. Int J Cancer . 1998 Dec 9. 78(6):720-6. [QxMD MEDLINE Link] .
Hermans P, Clumeck N, Picard O, et al. AIDS-related Kaposi's sarcoma patients with visceral manifestations. Response to human chorionic gonadotropin preparations. J Hum Virol . 1998 Jan-Feb. 1(2):82-9. [QxMD MEDLINE Link] .
Bailey J, Pluda JM, Foli A, et al. Phase I/II study of intermittent all-trans-retinoic acid, alone and in combination with interferon alfa-2a, in patients with epidemic Kaposi's sarcoma. J Clin Oncol . 1995 Aug. 13(8):1966-74. [QxMD MEDLINE Link] .
Dugel PU, Gill PS, Frangieh GT, Rao NA. Treatment of ocular adnexal Kaposi's sarcoma in acquired immune deficiency syndrome. Ophthalmology . 1992 Jul. 99(7):1127-32. [QxMD MEDLINE Link] .
Korn BS, Park DJ, Kikkawa DO. Intralesional mitomycin-C for the treatment of conjunctival Kaposi sarcoma. Ophthal Plast Reconstr Surg . 2011 Jul-Aug. 27(4):e88-90. [QxMD MEDLINE Link] .
Shuler JD, Holland GN, Miles SA, et al. Kaposi sarcoma of the conjunctiva and eyelids associated with the acquired immunodeficiency syndrome. Arch Ophthalmol . 1989 Jun. 107(6):858-62. [QxMD MEDLINE Link] .
Jackson CC, Dickson MA, Sadjadi M, Gessain A, Abel L, Jouanguy E, et al. Kaposi Sarcoma of Childhood: Inborn or Acquired Immunodeficiency to Oncogenic HHV-8. Pediatr Blood Cancer . 2016 Mar. 63 (3):392-7. [QxMD MEDLINE Link] . [Full Text] .
Gill PS, Wernz J, Scadden DT, et al. Randomized phase III trial of liposomal daunorubicin versus doxorubicin, bleomycin, and vincristine in AIDS-related Kaposi's sarcoma. J Clin Oncol . 1996 Aug. 14(8):2353-64. [QxMD MEDLINE Link] .
Northfelt DW, Dezube BJ, Thommes JA, et al. Efficacy of pegylated-liposomal doxorubicin in the treatment of AIDS-related Kaposi's sarcoma after failure of standard chemotherapy. J Clin Oncol . 1997 Feb. 15(2):653-9. [QxMD MEDLINE Link] .
Welles L, Saville MW, Lietzau J, et al. Phase II trial with dose titration of paclitaxel for the therapy of human immunodeficiency virus-associated Kaposi's sarcoma. J Clin Oncol . 1998 Mar. 16(3):1112-21. [QxMD MEDLINE Link] .
- Section of eyelid with Kaposi sarcoma lesion under high magnification. This tissue section demonstrates increased angiogenesis and spindle-shaped cells. Courtesy of Ben Glasgow, MD, University of California, Los Angeles, Department of Ophthalmology, Jules Stein Eye Institute.
- Section of eyelid with Kaposi sarcoma lesion under high magnification. This tissue section demonstrates endothelium-lined vascular channels and proliferation of spindle-shaped cells. Increased angiogenesis with erythrocyte extravasation is observed. Courtesy of Ben Glasgow, MD, University of California, Los Angeles, Department of Ophthalmology, Jules Stein Eye Institute.
- The inferior conjunctiva is involved more commonly than the superior conjunctiva in Kaposi sarcoma. Courtesy of Gary N Holland, MD, University of California, Los Angeles, Department of Ophthalmology, Jules Stein Eye Institute.
- Kaposi sarcoma involvement of the eyelid. Courtesy of Gary N Holland, MD, University of California, Los Angeles, Department of Ophthalmology, Jules Stein Eye Institute.

Contributor Information and Disclosures
Jacqueline Freudenthal, MD Co-Investigator, Ophthalmic Consultants Centre, Toronto Jacqueline Freudenthal, MD is a member of the following medical societies: American Academy of Ophthalmology , Association for Research in Vision and Ophthalmology , Canadian Ophthalmological Society Disclosure: Nothing to disclose.
Kevin Ryan Yuhan, MD Attending Physician, Cornea, Cataract, Refractive and External Diseases, Southern California Permanente Medical Group Kevin Ryan Yuhan, MD is a member of the following medical societies: Alpha Omega Alpha , American Medical Association , Association for Research in Vision and Ophthalmology , Phi Beta Kappa , American Academy of Ophthalmology , American Society of Cataract and Refractive Surgery Disclosure: Nothing to disclose.
Timothy T You, MD Consulting Surgeon in Ophthalmology, Private Practice Timothy T You, MD is a member of the following medical societies: American Academy of Ophthalmology , American Society of Retina Specialists Disclosure: Nothing to disclose.
Simon K Law, MD, PharmD Clinical Professor of Health Sciences, Department of Ophthalmology, Jules Stein Eye Institute, University of California, Los Angeles, David Geffen School of Medicine Simon K Law, MD, PharmD is a member of the following medical societies: American Academy of Ophthalmology , Association for Research in Vision and Ophthalmology , American Glaucoma Society Disclosure: Nothing to disclose.
Christopher J Rapuano, MD Professor, Department of Ophthalmology, Sidney Kimmel Medical College of Thomas Jefferson University; Director of the Cornea Service, Wills Eye Hospital Christopher J Rapuano, MD is a member of the following medical societies: American Academy of Ophthalmology , American Ophthalmological Society , American Society of Cataract and Refractive Surgery , Contact Lens Association of Ophthalmologists , Cornea Society , Eye Bank Association of America , International Society of Refractive Surgery Disclosure: Serve(d) as a director, officer, partner, employee, advisor, consultant or trustee for: AAO; OMIC; American Society of Ophthalmic Trauma (ASOT); Avellino, Baxis; Bio-Tissue; Celularity; Dompe; Emmecell; Glaukos; Kala; Oyster Point; Tarsus; TearLab<br/>Serve(d) as a speaker or a member of a speakers bureau for: Dompe<br/>Received research grant from: Glaukos<br/>Received income in an amount equal to or greater than $250 from: AAO; OMIC; Baxis; Bio-Tissue; Cellularity; Dompe; Glaukos; Kala; TearLab<br/>stock options for: RPS, Fount Bio.
Edsel B Ing, MD, PhD, MBA, MEd, MPH, MA, FRCSC Professor, Department of Ophthalmology and Vision Sciences, Sunnybrook Hospital, University of Toronto Faculty of Medicine; Incoming Chair of Ophthalmology, University of Alberta Faculty of Medicine and Dentistry, Canada Edsel B Ing, MD, PhD, MBA, MEd, MPH, MA, FRCSC is a member of the following medical societies: American Academy of Ophthalmology , American Association for Pediatric Ophthalmology and Strabismus , American Society of Ophthalmic Plastic and Reconstructive Surgery , Canadian Medical Association , Canadian Ophthalmological Society , Canadian Society of Oculoplastic Surgery , Chinese Canadian Medical Society, European Society of Ophthalmic Plastic and Reconstructive Surgery, North American Neuro-Ophthalmology Society , Ontario Medical Association , Royal College of Physicians and Surgeons of Canada , Statistical Society of Canada Disclosure: Nothing to disclose.
Anastasios J Kanellopoulos, MD Assistant Program Director, Clinical Associate Professor, Department of Ophthalmology, Manhattan Eye, Ear, and Throat Hospital, New York University
Anastasios J Kanellopoulos, MD is a member of the following medical societies: American Academy of Ophthalmology , Association for Research in Vision and Ophthalmology , Eye Bank Association of America , and International Society of Refractive Surgery
Disclosure: Nothing to disclose.
What would you like to print?
- Print this section
- Print the entire contents of
- Print the entire contents of article

- Kaposi Sarcoma Staging
- Pathology - Sarcomas of the Head and Neck
- Osteogenic Sarcoma Staging
- Soft Tissue Sarcoma Staging
- Soft Tissue Sarcoma Guidelines
- Synovial Sarcoma Imaging
- Cardiac Sarcoma
- Rare Cutaneous Sarcoma Incidence Twice as High in Black Individuals vs White Individuals
- Medscape Rare Diseases

- Drug Interaction Checker
- Pill Identifier
- Calculators

- 20022007306-overviewDiseases & Conditions Diseases & Conditions Osteogenic Sarcoma Staging
- 20022007127-overviewDiseases & Conditions Diseases & Conditions Kaposi Sarcoma Staging
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
The state-of-the-art of mycobacterium chimaera infections and the causal link with health settings: a systematic review.

1. Introduction
2. materials and methods, 4. discussion, 4.1. mycobacterium chimaera’s characteristics and ecosystem, 4.2. heater-cooler units, medical devices, water, and air-conditioned implants, 4.3. incubation period and symptoms presentation, 4.4. presence in the lung system, 4.5. modality of transmission, 4.6. detection, 4.7. disinfection, 4.8. causal link assessment, 5. limitations, 6. conclusions, supplementary materials, author contributions, institutional review board statement, informed consent statement, data availability statement, conflicts of interest, abbreviations.
| MAC | mycobacterium avium complex |
| NTM | non-tuberculosis mycobacterium |
| M. chimaera | Mycobacterium chimaera |
| HCU | heater-cooler units |
| OPPP | opportunistic premise plumbing pathogens |
| ECMO | extra-corporal mechanical oxygenation |
| HAI | healthcare-associated infection |
- Vendramin, I.; Peghin, M.; Tascini, C.; Livi, U. Longest Incubation Period of Mycobacterium chimaera Infection after Cardiac Surgery. Eur. J. Cardio-Thoracic Surg. 2021 , 59 , 506–508. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Biswas, M.; Rahaman, S.; Biswas, T.K.; Haque, Z.; Ibrahim, B. Association of Sex, Age, and Comorbidities with Mortality in COVID-19 Patients: A Systematic Review and Meta-Analysis. Intervirology 2020 , 64 , 36–47. [ Google Scholar ] [ CrossRef ]
- Treglia, M.; Pallocci, M.; Passalacqua, P.; Sabatelli, G.; De Luca, L.; Zanovello, C.; Messineo, A.; Quintavalle, G.; Cisterna, A.M.; Marsella, L.T. Medico-Legal Aspects of Hospital-Acquired Infections: 5-Years of Judgements of the Civil Court of Rome. Healthcare 2022 , 10 , 1336. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bolcato, V.; Tronconi, L.P.; Odone, A.; Blandi, L. Healthcare-Acquired Sars-Cov-2 Infection: A Viable Legal Category? Int. J. Risk Saf. Med. 2023 , 34 , 129–134. [ Google Scholar ] [ CrossRef ]
- Tattoli, L.; Dell’erba, A.; Ferorelli, D.; Gasbarro, A.; Solarino, B. Sepsis and Nosocomial Infections: The Role of Medico-Legal Experts in Italy. Antibiotics 2019 , 8 , 199. [ Google Scholar ] [ CrossRef ]
- Barranco, R.; Caristo, I.; Spigno, F.; Ponzano, M.; Trevisan, A.; Signori, A.; Di Biagio, A.; Ventura, F. Management of the Medico-Legal Dispute of Healthcare-Related SARS-CoV-2 Infections: Evaluation Criteria and Case Study in a Large University Hospital in Northwest Italy from 2020 to 2021. Int. J. Environ. Res. Public Health 2022 , 19 , 16764. [ Google Scholar ] [ CrossRef ]
- Goldenberg, S.D.; Volpé, H.; French, G.L. Clinical Negligence, Litigation and Healthcare-Associated Infections. J. Hosp. Infect. 2012 , 81 , 156–162. [ Google Scholar ] [ CrossRef ]
- Rizzo, N. La Causalità Civile ; Jus Civile; Giappichelli Editore: Torino, Italy, 2022. [ Google Scholar ]
- Riccardi, N.; Monticelli, J.; Antonello, R.M.; Luzzati, R.; Gabrielli, M.; Ferrarese, M.; Codecasa, L.; Di Bella, S.; Giacobbe, D.R. Mycobacterium chimaera Infections: An Update. J. Infect. Chemother. 2020 , 26 , 199–205. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Natanti, A.; Palpacelli, M.; Valsecchi, M.; Tagliabracci, A.; Pesaresi, M. Mycobacterium chimaera : A Report of 2 New Cases and Literature Review. Int. J. Leg. Med. 2021 , 135 , 2667–2679. [ Google Scholar ] [ CrossRef ]
- Wetzstein, N.; Kohl, T.A.; Diricks, M.; Mas-Peiro, S.; Holubec, T.; Kessel, J.; Graf, C.; Koch, B.; Herrmann, E.; Vehreschild, M.J.G.T.; et al. Clinical Characteristics and Outcome of Mycobacterium chimaera Infections after Cardiac Surgery: Systematic Review and Meta-Analysis of 180 Heater-Cooler Unit-Associated Cases. Clin. Microbiol. Infect. 2023 , 29 , 1008–1014. [ Google Scholar ] [ CrossRef ]
- Desai, A.N.; Hurtado, R.M. Infections and Outbreaks of Nontuberculous Mycobacteria in Hospital Settings. Curr. Treat. Options Infect. Dis. 2018 , 10 , 169–181. [ Google Scholar ] [ CrossRef ]
- van Ingen, J.; Kohl, T.A.; Kranzer, K.; Hasse, B.; Keller, P.M.; Katarzyna Szafrańska, A.; Hillemann, D.; Chand, M.; Schreiber, P.W.; Sommerstein, R.; et al. Global Outbreak of Severe Mycobacterium chimaera Disease after Cardiac Surgery: A Molecular Epidemiological Study. Lancet Infect. Dis. 2017 , 17 , 1033–1041. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bisognin, F.; Messina, F.; Butera, O.; Nisii, C.; Mazzarelli, A.; Cristino, S.; Pascale, M.R.; Lombardi, G.; Cannas, A.; Dal Monte, P. Investigating the Origin of Mycobacterium chimaera Contamination in Heater-Cooler Units: Integrated Analysis with Fourier Transform Infrared Spectroscopy and Whole-Genome Sequencing. Microbiol. Spectr. 2022 , 10 , e0289322. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Pinzauti, D.; De Giorgi, S.; Fox, V.; Lazzeri, E.; Messina, G.; Santoro, F.; Iannelli, F.; Ricci, S.; Pozzi, G. Complete Genome Sequences of Mycobacterium chimaera Strains 850 and 852, Isolated from Heater-Cooler Unit Water. Microbiol. Resour. Announc. 2022 , 11 , e0102121. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hasan, N.A.; Warren, R.L.; Elaine Epperson, L.; Malecha, A.; Alexander, D.C.; Turenne, C.Y.; MacMillan, D.; Birol, I.; Pleasance, S.; Coope, R.; et al. Complete Genome Sequence of Mycobacterium chimaera SJ42, a Nonoutbreak Strain from an Immunocompromised Patient with Pulmonary Disease. Genome Announc. 2017 , 5 , e00963-17. [ Google Scholar ] [ CrossRef ]
- Wallace, R.J.; Iakhiaeva, E.; Williams, M.D.; Brown-Elliott, B.A.; Vasireddy, S.; Vasireddy, R.; Lande, L.; Peterson, D.D.; Sawicki, J.; Kwait, R.; et al. Absence of Mycobacterium Intracellulare and Presence of Mycobacterium chimaera in Household Water and Biofilm Samples of Patients in the United States with Mycobacterium avium Complex Respiratory Disease. J. Clin. Microbiol. 2013 , 51 , 1747–1752. [ Google Scholar ] [ CrossRef ]
- Falkinham, J.O.; Hilborn, E.D.; Arduino, M.J.; Pruden, A.; Edwards, M.A. Epidemiology and Ecology of Opportunistic Premise Plumbing Pathogens: Legionella pneumophila , Mycobacterium avium , and Pseudomonas aeruginosa . Environ. Health Perspect. 2015 , 123 , 749–758. [ Google Scholar ] [ CrossRef ]
- European Centre for Disease Prevention and Control. EU Protocol for Testing of M. chimaera Infections Potentially Associated with Heater-Cooler Units Environmental Microbiology Investigations ; Technical Document; European Centre for Disease Prevention and Control: Solna, Sweden, 2015. [ Google Scholar ]
- Ministero della Salute. Raccomandazioni per Il Controllo Dell’infezione da Mycobacterium chimaera in Italia ; Ministero della Salute: Roma, Italy, 2019.
- Bolcato, M.; Rodriguez, D.; Aprile, A. Risk Management in the New Frontier of Professional Liability for Nosocomial Infection: Review of the Literature on Mycobacterium chimaera . Int. J. Environ. Res. Public Health 2020 , 17 , 7328. [ Google Scholar ] [ CrossRef ]
- Achermann, Y.; Rössle, M.; Hoffmann, M.; Deggim, V.; Kuster, S.; Zimmermann, D.R.; Bloemberg, G.; Hombach, M.; Hasse, B. Prosthetic Valve Endocarditis and Bloodstream Infection Due to Mycobacterium chimaera . J. Clin. Microbiol. 2013 , 51 , 1769–1773. [ Google Scholar ] [ CrossRef ]
- Zabost, A.T.; Szturmowicz, M.; Brzezińska, S.A.; Klatt, M.D.; Augustynowicz-Kopeć, E.M. Mycobacterium chimaera as an Underestimated Cause of NTM Lung Diseases in Patients Hospitalized in Pulmonary Wards. Pol. J. Microbiol. 2021 , 70 , 315–320. [ Google Scholar ] [ CrossRef ]
- Truden, S.; Žolnir-Dovč, M.; Sodja, E.; Starčič Erjavec, M. Nationwide Analysis of Mycobacterium chimaera and Mycobacterium intracellulare Isolates: Frequency, Clinical Importance, and Molecular and Phenotypic Resistance Profiles. Infect. Genet. Evol. 2020 , 82 , 104311. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021 , 372 , 71. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bills, N.D.; Hinrichs, S.H.; Aden, T.A.; Wickert, R.S.; Iwen, P.C. Molecular Identification of Mycobacterium chimaera as a Cause of Infection in a Patient with Chronic Obstructive Pulmonary Disease. Diagn. Microbiol. Infect. Dis. 2009 , 63 , 292–295. [ Google Scholar ] [ CrossRef ]
- Cohen-Bacrie, S.; David, M.; Stremler, N.; Dubus, J.-C.; Rolain, J.-M.; Drancourt, M. Mycobacterium chimaera Pulmonary Infection Complicating Cystic Fibrosis: A Case Report. J. Med. Case Rep. 2011 , 5 , 473. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Alhanna, J.; Purucker, M.; Steppert, C.; Grigull-Daborn, A.; Schiffel, G.; Gruber, H.; Borgmann, S. Mycobacterium chimaera Causes Tuberculosis-like Infection in a Male Patient with Anorexia Nervosa. Int. J. Eat. Disord. 2012 , 45 , 450–452. [ Google Scholar ] [ CrossRef ]
- Gunaydin, M.; Yanik, K.; Eroglu, C.; Sanic, A.; Ceyhan, I.; Erturan, Z.; Durmaz, R. Distribution of Nontuberculous Mycobacteria Strains. Ann. Clin. Microbiol. Antimicrob. 2013 , 12 , 33. [ Google Scholar ] [ CrossRef ]
- Boyle, D.P.; Zembower, T.R.; Reddy, S.; Qi, C. Comparison of Clinical Features, Virulence, and Relapse among Mycobacterium avium Complex Species. Am. J. Respir. Crit. Care Med. 2015 , 191 , 1310–1317. [ Google Scholar ] [ CrossRef ]
- Mwikuma, G.; Kwenda, G.; Hang’ombe, B.M.; Simulundu, E.; Kaile, T.; Nzala, S.; Siziya, S.; Suzuki, Y. Molecular Identification of Non-Tuberculous Mycobacteria Isolated from Clinical Specimens in Zambia. Ann. Clin. Microbiol. Antimicrob. 2015 , 14 , 1. [ Google Scholar ] [ CrossRef ]
- Moon, S.M.; Kim, S.Y.; Jhun, B.W.; Lee, H.; Park, H.Y.; Jeon, K.; Huh, H.J.; Ki, C.S.; Lee, N.Y.; Shin, S.J.; et al. Clinical Characteristics and Treatment Outcomes of Pulmonary Disease Caused by Mycobacterium chimaera . Diagn. Microbiol. Infect. Dis. 2016 , 86 , 382–384. [ Google Scholar ] [ CrossRef ]
- Moutsoglou, D.M.; Merritt, F.; Cumbler, E. Disseminated Mycobacterium chimaera Presenting as Vertebral Osteomyelitis. Case Rep. Infect. Dis. 2017 , 2017 , 9893743. [ Google Scholar ] [ CrossRef ]
- Bursle, E.; Playford, E.G.; Coulter, C.; Griffin, P. First Australian Case of Disseminated Mycobacterium chimaera Infection Post-Cardiothoracic Surgery. Infect. Dis. Health 2017 , 22 , 1–5. [ Google Scholar ] [ CrossRef ]
- Kim, S.-Y.; Shin, S.H.; Moon, S.M.; Yang, B.; Kim, H.; Kwon, O.J.; Huh, H.J.; Ki, C.-S.; Lee, N.Y.; Shin, S.J.; et al. Distribution and Clinical Significance of Mycobacterium avium Complex Species Isolated from Respiratory Specimens. Diagn. Microbiol. Infect. Dis. 2017 , 88 , 125–137. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Chand, M.; Lamagni, T.; Kranzer, K.; Hedge, J.; Moore, G.; Parks, S.; Collins, S.; Del Ojo Elias, C.; Ahmed, N.; Brown, T.; et al. Insidious Risk of Severe Mycobacterium chimaera Infection in Cardiac Surgery Patients. Clin. Infect. Dis. 2017 , 64 , 335–342. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Truden, S.; Žolnir-Dovč, M.; Sodja, E.; Starčič Erjavec, M. Retrospective Analysis of Slovenian Mycobacterium avium Complex and Mycobacterium abscessus Complex Isolates and Molecular Resistance Profile. Russ. J. Infect. Immun. 2018 , 8 , 447–451. [ Google Scholar ] [ CrossRef ]
- Larcher, R.; Lounnas, M.; Dumont, Y.; Michon, A.L.; Bonzon, L.; Chiron, R.; Carriere, C.; Klouche, K.; Godreuil, S. Mycobacterium chimaera Pulmonary Disease in Cystic Fibrosis Patients, France, 2010–2017. Emerg. Infect. Dis. 2019 , 25 , 611–613. [ Google Scholar ] [ CrossRef ]
- Shafizadeh, N.; Hale, G.; Bhatnagar, J.; Alshak, N.S.; Nomura, J. Mycobacterium chimaera Hepatitis: A New Disease Entity. Am. J. Surg. Pathol. 2019 , 43 , 244–250. [ Google Scholar ] [ CrossRef ]
- Rosero, C.I.; Shams, W.E. Mycobacterium chimaera Infection Masquerading as a Lung Mass in a Healthcare Worker. IDCases 2019 , 15 , e00526. [ Google Scholar ] [ CrossRef ]
- Watanabe, R.; Seino, H.; Taniuchi, S.; Igusa, R. Mycobacterium chimaera -Induced Tenosynovitis in a Patient with Rheumatoid Arthritis. BMJ Case Rep. 2020 , 13 , e233868. [ Google Scholar ] [ CrossRef ]
- Chen, L.C.; Huang, H.N.; Yu, C.J.; Chien, J.Y.; Hsueh, P.R. Clinical Features and Treatment Outcomes of Mycobacterium chimaera Lung Disease and Antimicrobial Susceptibility of the Mycobacterial Isolates. J. Infect. 2020 , 80 , 437–443. [ Google Scholar ] [ CrossRef ]
- Maalouly, C.; Devresse, A.; Martin, A.; Rodriguez-Villalobos, H.; Kanaan, N.; Belkhir, L. Coinfection of Mycobacterium malmoense and Mycobacterium chimaera in a Kidney Transplant Recipient: A Case Report and Review of the Literature. Transpl. Infect. Dis. 2020 , 22 , e13241. [ Google Scholar ] [ CrossRef ]
- de Melo Carvalho, R.; Nunes, A.L.; Sa, R.; Ramos, I.; Valente, C.; Saraiva da Cunha, J. Mycobacterium chimaera Disseminated Infection. J. Med. Cases 2020 , 11 , 35–36. [ Google Scholar ] [ CrossRef ]
- Sharma, K.; Sharma, M.; Modi, M.; Joshi, H.; Goyal, M.; Sharma, A.; Ray, P.; Rowlinson, M.C. Mycobacterium chimaera and Chronic Meningitis. QJM Int. J. Med. 2020 , 113 , 563–564. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kim, M.J.; Kim, K.M.; Shin, J.I.; Ha, J.H.; Lee, D.H.; Choi, J.G.; Park, J.S.; Byun, J.H.; Yoo, J.W.; Eum, S.; et al. Identification of Nontuberculous Mycobacteria in Patients with Pulmonary Diseases in Gyeongnam, Korea, Using Multiplex PCR and Multigene Sequence-Based Analysis. Can. J. Infect. Dis. Med. Microbiol. 2021 , 2021 , 8844306. [ Google Scholar ] [ CrossRef ]
- Kavvalou, A.; Stehling, F.; Tschiedel, E.; Kehrmann, J.; Walkenfort, B.; Hasenberg, M.; Olivier, M.; Steindor, M. Biofilm Infection of a Central Venous Port-Catheter Caused by Mycobacterium avium Complex in an Immunocompetent Child with Cystic Fibrosis. BMC Infect. Dis. 2022 , 22 , 321. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Robinson, B.; Chaudhri, M.; Miskoff, J.A. A Case of Cavitary Mycobacterium chimaera . Cureus 2022 , 14 , e26984. [ Google Scholar ] [ CrossRef ]
- Ahmad, M.; Yousaf, A.; Khan, H.M.W.; Munir, A.; Chandran, A. Mycobacterium chimaera Lung Infection and Empyema in a Patient without Cardiopulmonary Bypass. Bayl. Univ. Med. Cent. Proc. 2022 , 35 , 817–819. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- George, M.; Afra, T.P.; Santhosh, P.; Nandakumar, G.; Balagopalan, D.; Sreedharan, S. Ulcerating Nodules on the Face Due to Mycobacterium chimaera in a Patient with Diabetes. Clin. Exp. Dermatol. 2022 , 47 , 587–589. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Lin, Y.F.; Lee, T.F.; Wu, U.I.; Huang, C.F.; Cheng, A.; Lin, K.Y.; Hung, C.C. Disseminated Mycobacterium chimaera Infection in a Patient with Adult-Onset Immunodeficiency Syndrome: Case Report. BMC Infect. Dis. 2022 , 22 , 665. [ Google Scholar ] [ CrossRef ]
- Łyżwa, E.; Siemion-Szcześniak, I.; Sobiecka, M.; Lewandowska, K.; Zimna, K.; Bartosiewicz, M.; Jakubowska, L.; Augustynowicz-Kopeć, E.; Tomkowski, W. An Unfavorable Outcome of M. Chimaera Infection in Patient with Silicosis. Diagnostics 2022 , 12 , 1826. [ Google Scholar ] [ CrossRef ]
- McLaughlin, C.M.; Schade, M.; Cochran, E.; Taylor, K.F. A Case Report of a Novel Atypical Mycobacterial Infection: Mycobacterium chimaera Hand Tenosynovitis. JBJS Case Connect. 2022 , 12 , e22. [ Google Scholar ] [ CrossRef ]
- Gross, J.E.; Teneback, C.C.; Sweet, J.G.; Caceres, S.M.; Poch, K.R.; Hasan, N.A.; Jia, F.; Epperson, L.E.; Lipner, E.M.; Vang, C.K.; et al. Molecular Epidemiologic Investigation of Mycobacterium intracellulare Subspecies Chimaera Lung Infections at an Adult Cystic Fibrosis Program. Ann. Am. Thorac. Soc. 2023 , 20 , 677–686. [ Google Scholar ] [ CrossRef ]
- Azzarà, C.; Lombardi, A.; Gramegna, A.; Ori, M.; Gori, A.; Blasi, F.; Bandera, A. Non-Tuberculous Mycobacteria Lung Disease Due to Mycobacterium chimaera in a 67-Year-Old Man Treated with Immune Checkpoint Inhibitors for Lung Adenocarcinoma: Infection Due to Dysregulated Immunity? BMC Infect. Dis. 2023 , 23 , 573. [ Google Scholar ] [ CrossRef ]
- Pradhan, A.; Martinez, E.; Sintchenko, V.; Post, J.; Overton, K. Case of Mycobacterium chimaera Vertebral Osteomyelitis Diagnosed 7 Years after Cardiac Surgery. Intern. Med. J. 2023 , 53 , 150–151. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Garcia-Prieto, F.; Rodríguez Perojo, A.; Río Ramírez, M.T. Endobronchial Fibroanthracosis Associated with Mycobacterium chimaera Infection: An Exceptional Case. Open Respir. Arch. 2024 , 6 , 100309. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Paul, S.; MacNair, A.; Lostarakos, V.; Capstick, R. Non-Tuberculous Mycobacterial Pulmonary Infection Presenting in a Patient with Unilateral Pulmonary Artery Agenesis. BMJ Case Rep. 2024 , 17 , e259125. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bittner, M.J.; Preheim, L.C. Other Slow-Growing Nontuberculous Mycobacteria. Microbiol. Spectr. 2016 , 4 , 767–776. [ Google Scholar ] [ CrossRef ]
- Tortoli, E.; Rindi, L.; Garcia, M.J.; Chiaradonna, P.; Dei, R.; Garzelli, C.; Kroppenstedt, R.M.; Lari, N.; Mattei, R.; Mariottini, A.; et al. Proposal to Elevate the Genetic Variant MAC-A Included in the Mycobacterium avium Complex, to Species Rank as Mycobacterium chimaera sp. nov. Int. J. Syst. Evol. Microbiol. 2004 , 54 , 1277–1285. [ Google Scholar ] [ CrossRef ]
- Turankar, R.P.; Singh, V.; Gupta, H.; Pathak, V.K.; Ahuja, M.; Singh, I.; Lavania, M.; Dinda, A.K.; Sengupta, U. Association of Non-Tuberculous Mycobacteria with Mycobacterium leprae in Environment of Leprosy Endemic Regions in India. Infect. Genet. Evol. 2019 , 72 , 191–198. [ Google Scholar ] [ CrossRef ]
- Makovcova, J.; Slany, M.; Babak, V.; Slana, I.; Kralik, P. The Water Environment as a Source of Potentially Pathogenic Mycobacteria. J. Water Health 2014 , 12 , 254–263. [ Google Scholar ] [ CrossRef ]
- Falkinham, J.O. Ecology of Nontuberculous Mycobacteria-Where Do Human Infections Come From? Semin. Respir. Crit. Care Med. 2013 , 34 , 95–102. [ Google Scholar ] [ CrossRef ]
- Norton, G.J.; Williams, M.; Falkinham, J.O., III; Honda, J.R. Physical Measures to Reduce Exposure to Tap Water-Associated Nontuberculous Mycobacteria. Front. Public Health 2020 , 8 , 190. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Durnez, L.; Eddyani, M.; Mgode, G.F.; Katakweba, A.; Katholi, C.R.; Machang’u, R.R.; Kazwala, R.R.; Portaels, F.; Leirs, H. First Detection of Mycobacteria in African Rodents and Insectivores, Using Stratified Pool Screening. Appl. Environ. Microbiol. 2008 , 74 , 768. [ Google Scholar ] [ CrossRef ]
- Sax, H.; Bloemberg, G.; Hasse, B.; Sommerstein, R.; Kohler, P.; Achermann, Y.; Rössle, M.; Falk, V.; Kuster, S.P.; Böttger, E.C.; et al. Prolonged Outbreak of Mycobacterium chimaera Infection after Open-Chest Heart Surgery. Clin. Infect. Dis. 2015 , 61 , 67–75. [ Google Scholar ] [ CrossRef ]
- Falkinham, J.O.; Williams, M.D. Desiccation-Tolerance of Mycobacterium avium , Mycobacterium intracellulare , Mycobacterium chimaera , Mycobacterium abscessus and Mycobacterium chelonae . Pathogens 2022 , 11 , 463. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Gebert, M.J.; Delgado-Baquerizo, M.; Oliverio, A.M.; Webster, T.M.; Nichols, L.M.; Honda, J.R.; Chan, E.D.; Adjemian, J.; Dunn, R.R.; Fierer, N. Ecological Analyses of Mycobacteria in Showerhead Biofilms and Their Relevance to Human Health. mBio 2018 , 9 , e01614–e01618. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Cao, Y.; Yuan, S.; Pang, L.; Xie, J.; Gao, Y.; Zhang, J.; Zhao, Z.; Yao, S. Study on Microbial Diversity of Washing Machines. Biodegradation 2024 , 1–13. [ Google Scholar ] [ CrossRef ]
- Liu, H.; Jiao, P.; Guan, L.; Wang, C.; Zhang, X.X.; Ma, L. Functional Traits and Health Implications of the Global Household Drinking-Water Microbiome Retrieved Using an Integrative Genome-Centric Approach. Water Res. 2024 , 250 , 121094. [ Google Scholar ] [ CrossRef ]
- Choi, J.Y.; Sim, B.R.; Park, Y.; Yong, S.H.; Shin, S.J.; Kang, Y.A. Identification of Nontuberculous Mycobacteria Isolated from Household Showerheads of Patients with Nontuberculous Mycobacteria. Sci. Rep. 2022 , 12 , 8648. [ Google Scholar ] [ CrossRef ]
- Shen, Y.; Haig, S.J.; Prussin, A.J.; Lipuma, J.J.; Marr, L.C.; Raskin, L. Shower Water Contributes Viable Nontuberculous Mycobacteria to Indoor Air. PNAS Nexus 2022 , 1 , pgac145. [ Google Scholar ] [ CrossRef ]
- Struelens, M.J.; Plachouras, D. Mycobacterium chimaera Infections Associated with Heater-Cooler Units (HCU): Closing Another Loophole in Patient Safety. Eurosurveillance 2016 , 21 , 30397. [ Google Scholar ] [ CrossRef ]
- Trudzinski, F.C.; Schlotthauer, U.; Kamp, A.; Hennemann, K.; Muellenbach, R.M.; Reischl, U.; Gärtner, B.; Wilkens, H.; Bals, R.; Herrmann, M.; et al. Clinical Implications of Mycobacterium chimaera Detection in Thermoregulatory Devices Used for Extracorporeal Membrane Oxygenation (ECMO), Germany, 2015 to 2016. Eurosurveillance 2016 , 21 , 30398. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Schnetzinger, M.; Heger, F.; Indra, A.; Kimberger, O. Bacterial Contamination of Water Used as Thermal Transfer Fluid in Fluid-Warming Devices. J. Hosp. Infect. 2023 , 141 , 49–54. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Barker, T.A.; Dandekar, U.; Fraser, N.; Dawkin, L.; Sweeney, P.; Heron, F.; Simmons, J.; Parmar, J. Minimising the Risk of Mycobacterium chimaera Infection during Cardiopulmonary Bypass by the Removal of Heater-Cooler Units from the Operating Room. Perfusion 2018 , 33 , 264–269. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Barnes, S.; Twomey, C.; Carrico, R.; Murphy, C.; Warye, K. OR Air Quality: Is It Time to Consider Adjunctive Air Cleaning Technology? AORN J. 2018 , 108 , 503–515. [ Google Scholar ] [ CrossRef ]
- Walker, J.T.; Lamagni, T.; Chand, M. Evidence That Mycobacterium chimaera Aerosols Penetrate Laminar Airflow and Result in Infections at the Surgical Field. Lancet Infect. Dis. 2017 , 17 , 1019. [ Google Scholar ] [ CrossRef ]
- Schlotthauer, U.; Hennemann, K.; Gärtner, B.C.; Schäfers, H.-J.; Becker, S.L. Microbiological Surveillance of Heater-Cooler Units Used in Cardiothoracic Surgery for Detection of Mycobacterium chimaera . Thorac. Cardiovasc. Surg. 2022 , 72 , 59–62. [ Google Scholar ] [ CrossRef ]
- Gross, J.E.; Caceres, S.; Poch, K.; Epperson, L.E.; Hasan, N.A.; Jia, F.; de Moura, V.C.N.; Strand, M.; Lipner, E.M.; Honda, J.R.; et al. Prospective Healthcare-Associated Links in Transmission of Nontuberculous Mycobacteria among People with Cystic Fibrosis (PHALT NTM) Study: Rationale and Study Design. PLoS ONE 2023 , 18 , e0291910. [ Google Scholar ] [ CrossRef ]
- Nakamura, S.; Azuma, M.; Sato, M.; Fujiwara, N.; Nishino, S.; Wada, T.; Yoshida, S. Pseudo-Outbreak of Mycobacterium chimaera through Aerators of Hand-Washing Machines at a Hematopoietic Stem Cell Transplantation Center. Infect. Control Hosp. Epidemiol. 2019 , 40 , 1433–1435. [ Google Scholar ] [ CrossRef ]
- Kanamori, H.; Weber, D.J.; Rutala, W.A. Healthcare-Associated Mycobacterium chimaera Transmission and Infection Prevention Challenges: Role of Heater-Cooler Units as a Water Source in Cardiac Surgery. Clin. Infect. Dis. 2017 , 64 , 343–346. [ Google Scholar ] [ CrossRef ]
- Rao, M.; Silveira, F.P. Non-Tuberculous Mycobacterial Infections in Thoracic Transplant Candidates and Recipients. Curr. Infect. Dis. Rep. 2018 , 20 , 14. [ Google Scholar ] [ CrossRef ]
- Walker, J.; Moore, G.; Collins, S.; Parks, S.; Garvey, M.I.; Lamagni, T.; Smith, G.; Dawkin, L.; Goldenberg, S.; Chand, M. Microbiological Problems and Biofilms Associated with Mycobacterium chimaera in Heater–Cooler Units Used for Cardiopulmonary Bypass. J. Hosp. Infect. 2017 , 96 , 209–220. [ Google Scholar ] [ CrossRef ]
- Born, F.; Wieser, A.; Oberbach, A.; Oberbach, A.; Ellgass, R.; Peterss, S.; Kur, F.; Grabein, B.; Hagl, C. Five Years without Mycobacterium chimaera . Thorac. Cardiovasc. Surg. 2020 , 68 , S1–S72. [ Google Scholar ] [ CrossRef ]
- Scriven, J.E.; Scobie, A.; Verlander, N.Q.; Houston, A.; Collyns, T.; Cajic, V.; Kon, O.M.; Mitchell, T.; Rahama, O.; Robinson, A.; et al. Mycobacterium chimaera Infection Following Cardiac Surgery in the United Kingdom: Clinical Features and Outcome of the First 30 Cases. Clin. Microbiol. Infect. 2018 , 24 , 1164–1170. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Olatidoye, O.A.; Samat, S.H.; Yin, K.; Bates, M.J. Pulmonary Valve Infective Endocarditis Caused by Mycobacterium abscessus . J. Cardiothorac. Surg. 2023 , 18 , 221. [ Google Scholar ] [ CrossRef ]
- Ganatra, S.; Sharma, A.; D’Agostino, R.; Gage, T.; Kinnunen, P. Mycobacterium chimaera Mimicking Sarcoidosis. Methodist Debakey Cardiovasc. J. 2018 , 14 , 301–302. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Buchanan, R.; Agarwal, A.; Mathai, E.; Cherian, B. Mycobacterium chimaera : A Novel Pathogen with Potential Risk to Cardiac Surgical Patients. Natl. Med. J. India 2020 , 33 , 284–287. [ Google Scholar ] [ CrossRef ]
- McHugh, J.; Saleh, O.A. Updates in Culture-Negative Endocarditis. Pathogens 2023 , 12 , 1027. [ Google Scholar ] [ CrossRef ]
- Delgado, V.; Ajmone Marsan, N.; De Waha, S.; Bonaros, N.; Brida, M.; Burri, H.; Caselli, S.; Doenst, T.; Ederhy, S.; Erba, P.A.; et al. 2023 ESC Guidelines for the Management of Endocarditis. Eur. Heart J. 2023 , 44 , 3948–4042. [ Google Scholar ] [ CrossRef ]
- Kohler, P.; Kuster, S.P.; Bloemberg, G.; Schulthess, B.; Frank, M.; Tanner, F.C.; Rössle, M.; Böni, C.; Falk, V.; Wilhelm, M.J.; et al. Healthcare-Associated Prosthetic Heart Valve, Aortic Vascular Graft, and Disseminated Mycobacterium chimaera Infections Subsequent to Open Heart Surgery. Eur. Heart J. 2015 , 36 , 2745–2753. [ Google Scholar ] [ CrossRef ]
- Wyrostkiewicz, D.; Opoka, L.; Filipczak, D.; Jankowska, E.; Skorupa, W.; Augustynowicz-Kopeć, E.; Szturmowicz, M. Nontuberculous Mycobacterial Lung Disease in the Patients with Cystic Fibrosis—A Challenging Diagnostic Problem. Diagnostics 2022 , 12 , 1514. [ Google Scholar ] [ CrossRef ]
- Virdi, R.; Lowe, M.E.; Norton, G.J.; Dawrs, S.N.; Hasan, N.A.; Epperson, L.E.; Glickman, C.M.; Chan, E.D.; Strong, M.; Crooks, J.L.; et al. Lower Recovery of Nontuberculous Mycobacteria from Outdoor Hawai’i Environmental Water Biofilms Compared to Indoor Samples. Microorganisms 2021 , 9 , 224. [ Google Scholar ] [ CrossRef ]
- Schweickert, B.; Goldenberg, O.; Richter, E.; Göbel, U.B.; Petrich, A.; Buchholz, P.; Moter, A. Occurrence and Clinical Relevance of Mycobacterium chimaera sp. nov., Germany. Emerg. Infect. Dis. 2008 , 14 , 1443–1446. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Boyle, D.P.; Zembower, T.R.; Qi, C. Evaluation of Vitek MS for Rapid Classification of Clinical Isolates Belonging to Mycobacterium avium Complex. Diagn. Microbiol. Infect. Dis. 2015 , 81 , 41–43. [ Google Scholar ] [ CrossRef ]
- Sommerstein, R.; Rüegg, C.; Kohler, P.; Bloemberg, G.; Kuster, S.P.; Sax, H. Transmission of Mycobacterium chimaera from Heater-Cooler Units during Cardiac Surgery despite an Ultraclean Air Ventilation System. Emerg. Infect. Dis. 2016 , 22 , 1008–1013. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Balsam, L.B.; Louie, E.; Hill, F.; Levine, J.; Phillips, M.S. Mycobacterium chimaera Left Ventricular Assist Device Infections. J. Card. Surg. 2017 , 32 , 402–404. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sanchez-Nadales, A.; Diaz-Sierra, A.; Mocadie, M.; Asher, C.; Gordon, S.; Xu, B. Advanced Cardiovascular Imaging for the Diagnosis of Mycobacterium chimaera Prosthetic Valve Infective Endocarditis After Open-Heart Surgery: A Contemporary Systematic Review. Curr. Probl. Cardiol. 2022 , 47 , 101392. [ Google Scholar ] [ CrossRef ]
- Cannas, A.; Campanale, A.; Minella, D.; Messina, F.; Butera, O.; Nisii, C.; Mazzarelli, A.; Fontana, C.; Lispi, L.; Maraglino, F.; et al. Epidemiological and Molecular Investigation of the Heater–Cooler Unit (HCU)-Related Outbreak of Invasive Mycobacterium chimaera Infection Occurred in Italy. Microorganisms 2023 , 11 , 2251. [ Google Scholar ] [ CrossRef ]
- Schreiber, P.W.; Kohl, T.A.; Kuster, S.P.; Niemann, S.; Sax, H. The Global Outbreak of Mycobacterium chimaera Infections in Cardiac Surgery—A Systematic Review of Whole-Genome Sequencing Studies and Joint Analysis. Clin. Microbiol. Infect. 2021 , 27 , 1613–1620. [ Google Scholar ] [ CrossRef ]
- Rubinstein, M.; Grossman, R.; Nissan, I.; Schwaber, M.J.; Carmeli, Y.; Kaidar-Shwartz, H.; Dveyrin, Z.; Rorman, E. Mycobacterium intracellulare Subsp. Chimaera from Cardio Surgery Heating-Cooling Units and from Clinical Samples in Israel Are Genetically Unrelated. Pathogens 2021 , 10 , 1392. [ Google Scholar ] [ CrossRef ]
- Mercaldo, R.A.; Marshall, J.E.; Prevots, D.R.; Lipner, E.M.; French, J.P. Detecting Clusters of High Nontuberculous Mycobacteria Infection Risk for Persons with Cystic Fibrosis—An Analysis of U.S. Counties. Tuberculosis 2023 , 138 , 102296. [ Google Scholar ] [ CrossRef ]
- Asadi, T.; Mullin, K.; Roselli, E.; Johnston, D.; Tan, C.D.; Rodriguez, E.R.; Gordon, S. Disseminated Mycobacterium chimaera Infection Associated with Heater-Cooler Units after Aortic Valve Surgery without Endocarditis. J. Thorac. Cardiovasc. Surg. 2018 , 155 , 2369–2374. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Clemente, T.; Spagnuolo, V.; Bottanelli, M.; Ripa, M.; Del Forno, B.; Busnardo, E.; Di Lucca, G.; Castagna, A.; Danise, A. Disseminated Mycobacterium chimaera Infection Favoring the Development of Kaposi’s Sarcoma: A Case Report. Ann. Clin. Microbiol. Antimicrob. 2022 , 21 , 57. [ Google Scholar ] [ CrossRef ]
- Schaeffer, T.; Kuster, S.; Koechlin, L.; Khanna, N.; Eckstein, F.S.; Reuthebuch, O. Long-Term Follow-Up after Mycobacterium chimaera Infection Following Cardiac Surgery: Single-Center Experience. J. Clin. Med. 2023 , 12 , 948. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Trauth, J.; Matt, U.; Kohl, T.A.; Niemann, S.; Herold, S. Blind Spot in Endocarditis Guidelines: Mycobacterium chimaera Prosthetic Valve Endocarditis after Cardiac Surgery—A Case Series. Eur. Heart J. Case Rep. 2023 , 7 , ytad400. [ Google Scholar ] [ CrossRef ]
- Sanavio, M.; Anna, A.; Bolcato, M. Mycobacterium chimaera : Clinical and Medico-Legal Considerations Starting from a Case of Sudden Acoustic Damage. Leg. Med. 2020 , 47 , 101747. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- van Ingen, J. Microbiological Diagnosis of Nontuberculous Mycobacterial Pulmonary Disease. Clin. Chest Med. 2015 , 36 , 43–54. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Wang, H.; Bédard, E.; Prévost, M.; Camper, A.K.; Hill, V.R.; Pruden, A. Methodological Approaches for Monitoring Opportunistic Pathogens in Premise Plumbing: A Review. Water Res. 2017 , 117 , 68–86. [ Google Scholar ] [ CrossRef ]
- Hasse, B.; Hannan, M.M.; Keller, P.M.; Maurer, F.P.; Sommerstein, R.; Mertz, D.; Wagner, D.; Fernández-Hidalgo, N.; Nomura, J.; Manfrin, V.; et al. International Society of Cardiovascular Infectious Diseases Guidelines for the Diagnosis, Treatment and Prevention of Disseminated Mycobacterium chimaera Infection Following Cardiac Surgery with Cardiopulmonary Bypass. J. Hosp. Infect. 2020 , 104 , 214–235. [ Google Scholar ] [ CrossRef ]
- Schreiber, P.W.; Köhler, N.; Cervera, R.; Hasse, B.; Sax, H.; Keller, P.M. Detection Limit of Mycobacterium chimaera in Water Samples for Monitoring Medical Device Safety: Insights from a Pilot Experimental Series. J. Hosp. Infect. 2018 , 99 , 284–289. [ Google Scholar ] [ CrossRef ]
- Daley, C.L.; Iaccarino, J.M.; Lange, C.; Cambau, E.; Wallace, R.J.; Andrejak, C.; Böttger, E.C.; Brozek, J.; Griffith, D.E.; Guglielmetti, L.; et al. Treatment of Nontuberculous Mycobacterial Pulmonary Disease: An Official ATS/ERS/ESCMID/IDSA Clinical Practice Guideline. Clin. Infect. Dis. 2020 , 71 , e1–e36. [ Google Scholar ] [ CrossRef ]
- Lecorche, E.; Haenn, S.; Mougari, F.; Kumanski, S.; Veziris, N.; Benmansour, H.; Raskine, L.; Moulin, L.; Cambau, E.; Aubry, A.; et al. Comparison of Methods Available for Identification of Mycobacterium chimaera . Clin. Microbiol. Infect. 2018 , 24 , 409–413. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Lyamin, A.V.; Ereshchenko, A.A.; Gusyakova, O.A.; Yanchenko, A.V.; Kozlov, A.V.; Khaliulin, A.V. Comparison of Laboratory Methods for Identifying Members of the Family Mycobacteriaceae. Int. J. Mycobacteriol 2023 , 12 , 129–134. [ Google Scholar ] [ CrossRef ]
- Togawa, A.; Chikamatsu, K.; Takaki, A.; Matsumoto, Y.; Yoshimura, M.; Tsuchiya, S.; Nakamura, S.; Mitarai, S. Multiple Mutations of Mycobacterium ntracellulare Subsp. Chimaera Causing False-Negative Reaction to the Transcription-Reverse Transcription Concerted Method for Pathogen Detection. Int. J. Infect. Dis. 2023 , 133 , 14–17. [ Google Scholar ] [ CrossRef ]
- Kuehl, R.; Banderet, F.; Egli, A.; Keller, P.M.; Frei, R.; Döbele, T.; Eckstein, F.; Widmer, A.F. Different Types of Heater-Cooler Units and Their Risk of Transmission of Mycobacterium chimaera during Open-Heart Surgery: Clues from Device Design. Infect. Control Hosp. Epidemiol. 2018 , 39 , 834–840. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Quintás Viqueira, A.; Pérez Romero, C.; Toro Rueda, C.; Sánchez Calles, A.M.; Blázquez González, J.A.; Alejandre Leyva, M. Mycobacterium chimaera in Heater-Cooler Devices: An Experience in a Tertiary Hospital in Spain. New Microbes New Infect. 2021 , 39 , 100757. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Falkinham, J.O., III. Disinfection and Cleaning of Heater-Cooler Units: Suspension- and Biofilm-Killing. J. Hosp. Infect. 2020 , 105 , 552–557. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hammer-Dedet, F.; Dupont, C.; Evrevin, M.; Jumas-Bilak, E.; Romano-Bertrand, S. Improved Detection of Non-Tuberculous Mycobacteria in Hospital Water Samples. Infect. Dis. Now 2021 , 51 , 488–491. [ Google Scholar ] [ CrossRef ]
- Romano-Bertrand, S.; Evrevin, M.; Dupont, C.; Frapier, J.M.; Sinquet, J.C.; Bousquet, E.; Albat, B.; Jumas-Bilak, E. Persistent Contamination of Heater-Cooler Units for Extracorporeal Circulation Cured by Chlorhexidine-Alcohol in Water Tanks. J. Hosp. Infect. 2018 , 99 , 290–294. [ Google Scholar ] [ CrossRef ]
- Colangelo, N.; Giambuzzi, I.; Moro, M.; Pasqualini, N.; Aina, A.; De Simone, F.; Blasio, A.; Alfieri, O.; Castiglioni, A.; De Bonis, M. Mycobacterium chimaera in Heater–Cooler Units: New Technical Approach for Treatment, Cleaning and Disinfection Protocol. Perfusion 2019 , 34 , 272–276. [ Google Scholar ] [ CrossRef ]
- Ditommaso, S.; Giacomuzzi, M.; Memoli, G.; Garlasco, J.; Curtoni, A.; Iannaccone, M.; Zotti, C.M. Chemical Susceptibility Testing of Non-Tuberculous Mycobacterium strains and Other Aquatic Bacteria: Results of a Study for the Development of a More Sensitive and Simple Method for the Detection of NTM in Environmental Samples. J. Microbiol. Methods 2022 , 193 , 106405. [ Google Scholar ] [ CrossRef ]
- Shrimpton, N.Y.R. Evaluation of Disinfection Processes for Water Heater Devices Used for Extracorporeal Life Support. Perfusion 2019 , 34 , 428–432. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sarink, M.J.; van Cappellen, W.A.; Tielens, A.G.M.; van Dijk, A.; Bogers, A.J.J.C.; de Steenwinkel, J.E.M.; Vos, M.C.; Severin, J.A.; van Hellemond, J.J. Vermamoeba Vermiformis Resides in Water-Based Heater–Cooler Units and Can Enhance Mycobacterium chimaera Survival after Chlorine Exposure. J. Hosp. Infect. 2023 , 132 , 73–77. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bengtsson, D.; Westerberg, M.; Nielsen, S.; Ridell, M.; Jönsson, B. Mycobacterium chimaera in Heater-Cooler Units Used during Cardiac Surgery–Growth and Decontamination. Infect. Dis. 2018 , 50 , 736–742. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Weitkemper, H.H.; Spilker, A.; Knobl, H.J.; Körfer, R. The Heater-Cooler Unit-A Conceivable Source of Infection. J. Extra Corpor. Technol. 2016 , 48 , 62–66. [ Google Scholar ] [ CrossRef ]
- Foltan, M.; Nikisch, A.; Dembianny, J.; Miano, A.L.; Heinze, J.; Klar, D.; Göbölös, L.; Lehle, K.; Schmid, C. A Solution for Global Hygienic Challenges Regarding the Application of Heater-Cooler Systems in Cardiac Surgery. Perfusion 2023 , 38 , 28–36. [ Google Scholar ] [ CrossRef ]
- Pradal, I.; Esteban, J.; Mediero, A.; García-Coca, M.; Aguilera-Correa, J.J. Contact Effect of a Methylobacterium sp. Extract on Biofilm of a Mycobacterium chimaera Strain Isolated from a 3T Heater-Cooler System. Antibiotics 2020 , 9 , 474. [ Google Scholar ] [ CrossRef ]
- Masaka, E.; Reed, S.; Davidson, M.; Oosthuizen, J. Opportunistic Premise Plumbing Pathogens. A Potential Health Risk in Water Mist Systems Used as a Cooling Intervention. Pathogens 2021 , 10 , 462. [ Google Scholar ] [ CrossRef ]
- Treglia, M.; Pallocci, M.; Ricciardi Tenore, G.; Castellani, P.; Pizzuti, F.; Bianco, G.; Passalacqua, P.; De Luca, L.; Zanovello, C.; Mazzuca, D.; et al. Legionella and Air Transport: A Study of Environmental Contamination. Int. J. Environ. Res. Public Health 2022 , 19 , 8069. [ Google Scholar ] [ CrossRef ]
- Glassmeyer, S.T.; Burns, E.E.; Focazio, M.J.; Furlong, E.T.; Gribble, M.O.; Jahne, M.A.; Keely, S.P.; Kennicutt, A.R.; Kolpin, D.W.; Medlock Kakaley, E.K.; et al. Water, Water Everywhere, but Every Drop Unique: Challenges in the Science to Understand the Role of Contaminants of Emerging Concern in the Management of Drinking Water Supplies. Geohealth 2023 , 7 , e2022GH000716. [ Google Scholar ] [ CrossRef ]
- Ortiz-Martínez, Y. Mycobacterium chimaera : An under-Diagnosed Pathogen in Developing Countries? J. Hosp. Infect. 2017 , 97 , 125–126. [ Google Scholar ] [ CrossRef ]
- Becker, J.B.; Moisés, V.A.; Guerra-Martín, M.D.; Barbosa, D.A. Epidemiological Differences, Clinical Aspects, and Short-Term Prognosis of Patients with Healthcare-Associated and Community-Acquired Infective Endocarditis. Infect. Prev. Pract. 2024 , 6 , 100343. [ Google Scholar ] [ CrossRef ]
- Ferrara, S.D.; Baccino, E.; Bajanowski, T.; Boscolo-Berto, R.; Castellano, M.; De Angel, R.; Pauliukevičius, A.; Ricci, P.; Vanezis, P.; Vieira, D.N.; et al. Malpractice and Medical Liability. European Guidelines on Methods of Ascertainment and Criteria of Evaluation. Int. J. Leg. Med. 2013 , 127 , 545–557. [ Google Scholar ] [ CrossRef ]
Click here to enlarge figure
| References | Author, Year | N. of Patients | Surgery | Mean Time of Presentation If Previous Surgery | Setting (Country) | Organ and/or Tissue Involved |
|---|---|---|---|---|---|---|
| [ ] | (Bills et al., 2009) | 1 | None | Na | Not healthcare (USA) | Lung, nodules in chronic obstructive pulmonary disease |
| [ ] | (Cohen-Bacrie et al., 2011) | 1 | None | Na | Possible frequent healthcare contact (Réunion Island, FR) | Lung infections in cystic fibrosis |
| [ ] | (Alhanna et al., 2012) | 1 | None | Na | Not healthcare (Germany) | Lung infection |
| [ ] | (Gunaydin et al., 2013) | 5 (of 90) | None | Na | Possible healthcare contact (Turkey) | Lung (reassessment of sputum specimens) |
| [ ] | (Boyle et al., 2015) | 125 (of 448) | None | Na | Possible healthcare contact (USA) | Lung (reassessment of sputum specimens) |
| [ ] | (Mwikuma et al., 2015) | 1 (of 54) | None | Na | Not healthcare (Zambia) | Lung (reassessment of sputum specimens) |
| [ ] | (Moon et al., 2016) | 11 | None | Na | Not healthcare (South Korea) | Lung infection (reassessment of sputum specimens) |
| [ ] | (Moutsoglou et al., 2017) | 1 | None | Na | Not healthcare (USA) | Disseminated with spinal osteomyelitis and discitis |
| [ ] | (Bursle et al., 2017) | 1 | Tricuspid valve repair and mitral annuloplasty | 13 months | Underwent surgery (Australia) | Disseminated |
| [ ] | Kim et al., 2017 | 8 (of 91) | None | Na | Possible healthcare contact (Korea) | Lung (reassessment of sputum specimens) |
| [ ] | (Chand et al., 2017) * | 4 | Valvular cardiac surgery | 1.15 (0.25–5.1) years | Underwent surgery (UK) | 1 osteomyelitis and 3 disseminated |
| [ ] | (Truden et al., 2018) | 49 (of 102) | None | Na | Possible healthcare contact (Slovenia) | Lung (reassessment of sputum specimens) |
| [ ] | (Larcher et al., 2019) | 4 | None | Na | Possible frequent healthcare contact (France) | Lung (reassessment of sputum specimens in cystic fibrosis) |
| [ ] | (Shafizadeh et al., 2019) * | 5 | Valvular cardiac surgery | 20.6 (14–29) months | Underwent surgery (USA) | Disseminated with liver infection |
| [ ] | (Rosero and Shams, 2019) | 1 | None but operating room nurse 10 years ago | >10 years | Possible frequent healthcare contact (USA) | Lung infection |
| [ ] | (Watanabe et al., 2020) | 1 | None | Na | Not healthcare (Japan) | Tendons, hand tenosynovitis |
| [ ] | (Chen et al., 2020) | 28 | None | Na | Not healthcare (Taiwan) | Lung infection (reassessment of sputum specimens) |
| [ ] | (Maalouly et al., 2020) | 1 | Kidney transplantation | One week | Underwent surgery (Belgium) | Kidney, urinary tract infection in a kidney transplant recipient with concomitant Mycobacterium malmoense lung infection and fibro anthracosis |
| [ ] | (de Melo Carvalho et al., 2020) | 1 | None | Na | Possible healthcare contact (Portugal) | Disseminated in B-cell lymphoma |
| [ ] | (Sharma et al., 2020) | 2 | None | Na | Not healthcare (India) | Meninges, meningitis |
| [ ] | (Zabost et al., 2021) | 88 (of 200) | None | Na | Possible healthcare contact (Poland) | Lung infection (reassessment of sputum specimens) |
| [ ] | (Kim et al., 2021) | 4 (of 320) | None | Na | Possible healthcare contact (Korea) | Lung infection (reassessment of sputum specimens) |
| [ ] | (Kavvalou et al., 2022) | 1 | None | Na | Possible healthcare contact (Germany) | Central venous catheter infection in cystic fibrosis |
| [ ] | (Robinson et al., 2022) | 1 | None | Na | Not healthcare (USA) | Lung infection in drug abuser |
| [ ] | (Ahmad et al., 2022) | 1 | None | Na | Not healthcare (USA) | Lung infection in sarcoidosis |
| [ ] | (George et al., 2022) | 1 | None | Na | Not healthcare (India) | Skin, periapical abscess with chin ulcer |
| [ ] | (Lin et al., 2022) | 1 | None | Na | Possible frequent healthcare contact (Taiwan) | Disseminated in adult-onset immunodeficiency syndrome |
| [ ] | (Łyżwa et al., 2022) | 1 | None | Na | Not healthcare (Poland) | Lung infection in silicosis |
| [ ] | (McLaughlin et al., 2022) | 1 | Coronary artery bypass grafting | 1 year | Underwent surgery (USA) | Tendons, hand tenosynovitis in ipsilateral elbow wound in fisherman |
| [ ] | (Gross et al., 2023) | 23 | None | Na | Healthcare (USA) | Lung infections in cystic fibrosis (genomic analysis for cluster correlation to hospital outbreaks) |
| [ ] | (Azzarà et al., 2023) | 1 | None | Na | Possible healthcare contact (Italy) | Lung infection in lung adenocarcinoma treated with immune checkpoint inhibitors |
| [ ] | (Pradhan et al., 2023) | 1 | Bioprosthetic mitral valve replacement | 7 years | Underwent surgery (Australia) | Spinal osteomyelitis and discitis |
| [ ] | (Garcia-Prieto et al., 2024) | 1 | None | Na | Not healthcare (Spain) | Lung infection in fibro anthracosis |
| [ ] | (Paul et al., 2024) | 1 | None | Na | Possible healthcare contact (UK) | Lung infection in unilateral pulmonary artery agenesis on the right side |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Bolcato, V.; Bassetti, M.; Basile, G.; Bianco Prevot, L.; Speziale, G.; Tremoli, E.; Maffessanti, F.; Tronconi, L.P. The State-of-the-Art of Mycobacterium chimaera Infections and the Causal Link with Health Settings: A Systematic Review. Healthcare 2024 , 12 , 1788. https://doi.org/10.3390/healthcare12171788
Bolcato V, Bassetti M, Basile G, Bianco Prevot L, Speziale G, Tremoli E, Maffessanti F, Tronconi LP. The State-of-the-Art of Mycobacterium chimaera Infections and the Causal Link with Health Settings: A Systematic Review. Healthcare . 2024; 12(17):1788. https://doi.org/10.3390/healthcare12171788
Bolcato, Vittorio, Matteo Bassetti, Giuseppe Basile, Luca Bianco Prevot, Giuseppe Speziale, Elena Tremoli, Francesco Maffessanti, and Livio Pietro Tronconi. 2024. "The State-of-the-Art of Mycobacterium chimaera Infections and the Causal Link with Health Settings: A Systematic Review" Healthcare 12, no. 17: 1788. https://doi.org/10.3390/healthcare12171788
Article Metrics
Article access statistics, supplementary material.
ZIP-Document (ZIP, 83 KiB)
Further Information
Mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals

COMMENTS
Kaposi sarcoma (KS) is an angioproliferative disorder that requires infection with human herpes virus 8 (HHV-8), also known as Kaposi sarcoma-associated herpes virus ... This review will focus on the clinical presentation, staging, diagnosis, and treatment of classic KS. The epidemiology, risk factors, pathology, and molecular pathogenesis of ...
Kaposi sarcoma is an interesting soft tissue tumor occurring in several distinct populations with a variety of presentations and courses. In its most well-known form, Kaposi sarcoma occurs in patients with immunosuppression, such as those with acquired immunodeficiency syndrome (AIDs) or those undergoing immunosuppression due to an organ transplant. Initially described in 1872 by Moritz Kaposi ...
Kaposi sarcoma is a type of cancer that forms in the lining of blood vessels and lymph vessels. The cancer forms growths of cells, called lesions, on the skin. The lesions often form on the face, arms and legs. The lesions may look pink, red, purple or brown. Lesions also can appear on the genitals or in the mouth.
Kaposi Sarcoma. Kaposi sarcoma is a disease in which cancer cells are found in the skin or mucous membranes that line the gastrointestinal (GI) tract, from mouth to anus, including the stomach and intestines. These tumors appear as purple patches or nodules on the skin and/or mucous membranes and can spread to lymph nodes and lungs.
Kaposi sarcoma is a multicentric vascular tumor caused by herpesvirus type 8. It is categorized into 5 types: classic (sporadic), AIDS-associated (epidemic), non-epidemic, endemic (in Africa), and iatrogenic (eg, after organ transplantation). Diagnosis is by biopsy. Treatment for indolent superficial lesions involves cryotherapy ...
This entity occurs in patients with advanced HIV infection and is the most common presentation of Kaposi sarcoma. It is an AIDS-defining cancer, and is approximately 500 times more common in HIV-infected patients than the general US population. Kaposi sarcoma accounts for 12% of cancers in people living with HIV, with 765 to 910 new cases per ...
Kaposi sarcoma (KS) is an angioproliferative disorder that requires infection with human herpesvirus 8 (HHV-8), also known as Kaposi sarcoma-associated herpesvirus ... pathology, and molecular pathogenesis of classic KS. The clinical presentation, diagnosis, staging, and treatment of classic KS is discussed elsewhere, as is AIDS-related KS and ...
1 Summary. Kaposi's sarcoma (KS) most likely originates from lymphatic endothelial cells, and human herpesvirus 8 infection contributes to their malignant transformation. Immunosuppression fosters the occurrence, persistence, and progression of KS, which belongs to the most common AIDS-defining neoplasms in HIV-infected individuals.
Kaposi's sarcoma is the most common tumor associated with human immunodeficiency virus infection and is found in homosexual and bisexual men, injection drug users, and hemophiliacs. ... Clinical Presentation. Natural History of Disease. The natural course of Kaposi's sarcoma can take 1 of 2 forms: (1) a very slowly progressing disease over ...
Kaposi's sarcoma (KS) is a rare angioproliferative tumor classified in four different clinical-epidemiological forms. ... (77.9%) while 5.8% had an exclusively extracutaneous presentation of the disease. Patients presenting with both cutaneous and extracutaneous involvement were 12.2%. Epidemic KS, thus related to HIV-1 and 2, constituted a ...
Kaposi sarcoma (KS) usually appears first as spots (called lesions) on the skin.The lesions can be purple, red, or brown. KS lesions can be flat and not raised above the surrounding skin (called patches), flat but slightly raised (called plaques), or bumps (called nodules).The skin lesions of KS most often develop on the legs or face, but they can also appear in other areas.
Kaposi sarcoma (KS) is a cancer that develops from the cells that line lymph or blood vessels. It usually appears as tumors on the skin or on mucosal surfaces such as inside the mouth, but these tumors can also develop in other parts of the body, such as in the lymph nodes (bean-sized collections of immune cells throughout the body), the lungs ...
Kaposi sarcoma is a disease in which malignant lesions (cancer) can form in the skin, mucous membranes, lymph nodes, and other organs. Kaposi sarcoma is a cancer that causes lesions (abnormal tissue) to grow in the skin; the mucous membranes lining the mouth, nose, and throat; lymph nodes; or other organs.The lesions are usually purple and are made of cancer cells, new blood vessels, red blood ...
Kaposi sarcoma typically starts as small, flat patches on the skin or inside the mouth. These patches may be red, purple, pink, brown, black, or blue and look like bruises. They don't usually cause pain at first but can turn into bumps as they grow and may form open wounds. More widespread Kaposi sarcoma can cause: Bleeding or blockage in the ...
Abstract. Kaposi Sarcoma (KS) is the most common neoplasm of people living with HIV today. In Sub-Saharan Africa KS is among the most common cancers in men, overall. Not only HIV+ individuals present with KS; any immune compromised person infected with Kaposi Sarcoma-associated herpesvirus (KSHV) or human herpesvirus 8 is at risk: the elderly ...
Kaposi's sarcoma (KS) is a type of cancer that can form masses on the skin, in lymph nodes, in the mouth, or in other organs. [4] [6] The skin lesions are usually painless, purple and may be flat or raised.[6] [8] Lesions can occur singly, multiply in a limited area, or may be widespread. [6]Depending on the sub-type of disease and level of immune suppression, KS may worsen either gradually or ...
History. AIDS-related Kaposi sarcoma (KS) has a variable clinical course ranging from minimal mucocutaneous disease to widespread organ involvement. The lesions may involve the skin, oral mucosa, lymph nodes, and visceral organs. Most patients present with cutaneous disease. Visceral disease may occasionally precede cutaneous manifestations.
Soft tissue Kaposi sarcoma is a vascular neoplasm caused by human herpesvirus 8 (HHV8); it tends to be indolent but may be locally aggressive. Menu. Chapters By Subspecialty . ... 23 year old HIV+ man with Kaposi sarcoma as a presentation for HIV (Cureus 2021;13:e18936)
Kaposi's sarcoma is characterized by the appearance of purplish, reddish-blue, or dark brown/black macules, plaques, or nodules on the skin. ... (African), immunosuppression related and acquired immunodeficiency syndrome (AIDS) associated. In the cutaneous presentation is most often on the distal lower extremities the classic Kaposi's and ...
Kaposi's sarcoma (KS) is a multi-focal, angioproliferative neoplasm that usually appears on the skin, but can also involve the visceral organs. In 1981, 26 cases of KS were reported as occurring in young homosexual men in New York and California. Many of these patients also had concomitant pneumocystis carinii pneumonia (PCP) and a variety of ...
Research and Statistics. See the estimates for cases of Kaposi sarcoma in the US and what research is currently being done. Key Statistics About Kaposi Sarcoma. What's New in Kaposi Sarcoma Research? About Kaposi Sarcoma. Causes, Risk Factors, and Prevention. Early Detection, Diagnosis, and Staging. Treatment.
Of ophthalmic Kaposi sarcoma cases, 6-16% are eyelid lesions, and the superior and inferior eyelids tend to be involved equally. Of ophthalmic Kaposi sarcoma cases, 7-18% are conjunctival lesions. Many conjunctival lesions tend to involve the inferior conjunctiva (as is shown in the image below) and fornix. The inferior conjunctiva is involved ...
(1) Background. A definition of healthcare-associated infections is essential also for the attribution of the restorative burden to healthcare facilities in case of harm and for clinical risk management strategies. Regarding M. chimaera infections, there remains several issues on the ecosystem and pathogenesis. We aim to review the scientific evidence on M. chimaera beyond cardiac surgery, and ...