Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
Methodology

Semi-Structured Interview | Definition, Guide & Examples
Published on January 27, 2022 by Tegan George . Revised on June 22, 2023.
A semi-structured interview is a data collection method that relies on asking questions within a predetermined thematic framework. However, the questions are not set in order or in phrasing.
In research, semi-structured interviews are often qualitative in nature. They are generally used as an exploratory tool in marketing, social science, survey methodology, and other research fields.
They are also common in field research with many interviewers, giving everyone the same theoretical framework, but allowing them to investigate different facets of the research question .
- Structured interviews : The questions are predetermined in both topic and order.
- Unstructured interviews : None of the questions are predetermined.
- Focus group interviews : The questions are presented to a group instead of one individual.
Table of contents
What is a semi-structured interview, when to use a semi-structured interview, advantages of semi-structured interviews, disadvantages of semi-structured interviews, semi-structured interview questions, how to conduct a semi-structured interview, how to analyze a semi-structured interview, presenting your results (with example), other interesting articles, frequently asked questions about semi-structured interviews.
Semi-structured interviews are a blend of structured and unstructured types of interviews.
- Unlike in an unstructured interview, the interviewer has an idea of what questions they will ask.
- Unlike in a structured interview, the phrasing and order of the questions is not set.
Semi-structured interviews are often open-ended, allowing for flexibility. Asking set questions in a set order allows for easy comparison between respondents, but it can be limiting. Having less structure can help you see patterns, while still allowing for comparisons between respondents.
Semi-structured interviews are best used when:
- You have prior interview experience. Spontaneous questions are deceptively challenging, and it’s easy to accidentally ask a leading question or make a participant uneasy.
- Your research question is exploratory in nature. Participant answers can guide future research questions and help you develop a more robust knowledge base for future research.
Just like in structured interviews, it is critical that you remain organized and develop a system for keeping track of participant responses. However, since the questions are less set than in a structured interview, the data collection and analysis become a bit more complex.
Differences between different types of interviews
Make sure to choose the type of interview that suits your research best. This table shows the most important differences between the four types.
Semi-structured interviews come with many advantages.
Best of both worlds
No distractions, detail and richness.
However, semi-structured interviews also have their downsides.
Low validity
High risk of research bias, difficult to develop good semi-structured interview questions.
Since they are often open-ended in style, it can be challenging to write semi-structured interview questions that get you the information you’re looking for without biasing your responses. Here are a few tips:
- Define what areas or topics you will be focusing on prior to the interview. This will help you write a framework of questions that zero in on the information you seek.
- Write yourself a guide to refer to during the interview, so you stay focused. It can help to start with the simpler questions first, moving into the more complex ones after you have established a comfortable rapport.
- Be as clear and concise as possible, avoiding jargon and compound sentences.
- How often per week do you go to the gym? a) 1 time; b) 2 times; c) 3 times; d) 4 or more times
- If yes: What feelings does going to the gym bring out in you?
- If no: What do you prefer to do instead?
- If yes: How did this membership affect your job performance? Did you stay longer in the role than you would have if there were no membership?
Once you’ve determined that a semi-structured interview is the right fit for your research topic , you can proceed with the following steps.
Step 1: Set your goals and objectives
You can use guiding questions as you conceptualize your research question, such as:
- What are you trying to learn or achieve from a semi-structured interview?
- Why are you choosing a semi-structured interview as opposed to a different type of interview, or another research method?
If you want to proceed with a semi-structured interview, you can start designing your questions.
Step 2: Design your questions
Try to stay simple and concise, and phrase your questions clearly. If your topic is sensitive or could cause an emotional response, be mindful of your word choices.
One of the most challenging parts of a semi-structured interview is knowing when to ask follow-up or spontaneous related questions. For this reason, having a guide to refer back to is critical. Hypothesizing what other questions could arise from your participants’ answers may also be helpful.
Step 3: Assemble your participants
There are a few sampling methods you can use to recruit your interview participants, such as:
- Voluntary response sampling : For example, sending an email to a campus mailing list and sourcing participants from responses.
- Stratified sampling of a particular characteristic trait of interest to your research, such as age, race, ethnicity, or gender identity.
Step 4: Decide on your medium
It’s important to determine ahead of time how you will be conducting your interview. You should decide whether you’ll be conducting it live or with a pen-and-paper format. If conducted in real time, you also need to decide if in person, over the phone, or via videoconferencing is the best option for you.
Note that each of these methods has its own advantages and disadvantages:
- Pen-and-paper may be easier for you to organize and analyze, but you will receive more prepared answers, which may affect the reliability of your data.
- In-person interviews can lead to nervousness or interviewer effects, where the respondent feels pressured to respond in a manner they believe will please you or incentivize you to like them.
Step 5: Conduct your interviews
As you conduct your interviews, keep environmental conditions as constant as you can to avoid bias. Pay attention to your body language (e.g., nodding, raising eyebrows), and moderate your tone of voice.
Relatedly, one of the biggest challenges with semi-structured interviews is ensuring that your questions remain unbiased. This can be especially challenging with any spontaneous questions or unscripted follow-ups that you ask your participants.
After you’re finished conducting your interviews, it’s time to analyze your results. First, assign each of your participants a number or pseudonym for organizational purposes.
The next step in your analysis is to transcribe the audio or video recordings. You can then conduct a content or thematic analysis to determine your categories, looking for patterns of responses that stand out to you and test your hypotheses .
Transcribing interviews
Before you get started with transcription, decide whether to conduct verbatim transcription or intelligent verbatim transcription.
- If pauses, laughter, or filler words like “umm” or “like” affect your analysis and research conclusions, conduct verbatim transcription and include them.
- If not, you can conduct intelligent verbatim transcription, which excludes fillers, fixes any grammatical issues, and is usually easier to analyze.
Transcribing presents a great opportunity for you to cleanse your data . Here, you can identify and address any inconsistencies or questions that come up as you listen.
Your supervisor might ask you to add the transcriptions to the appendix of your paper.
Coding semi-structured interviews
Next, it’s time to conduct your thematic or content analysis . This often involves “coding” words, patterns, or recurring responses, separating them into labels or categories for more robust analysis.
Due to the open-ended nature of many semi-structured interviews, you will most likely be conducting thematic analysis, rather than content analysis.
- You closely examine your data to identify common topics, ideas, or patterns. This can help you draw preliminary conclusions about your participants’ views, knowledge or experiences.
- After you have been through your responses a few times, you can collect the data into groups identified by their “code.” These codes give you a condensed overview of the main points and patterns identified by your data.
- Next, it’s time to organize these codes into themes. Themes are generally broader than codes, and you’ll often combine a few codes under one theme. After identifying your themes, make sure that these themes appropriately represent patterns in responses.
Analyzing semi-structured interviews
Once you’re confident in your themes, you can take either an inductive or a deductive approach.
- An inductive approach is more open-ended, allowing your data to determine your themes.
- A deductive approach is the opposite. It involves investigating whether your data confirm preconceived themes or ideas.
After your data analysis, the next step is to report your findings in a research paper .
- Your methodology section describes how you collected the data (in this case, describing your semi-structured interview process) and explains how you justify or conceptualize your analysis.
- Your discussion and results sections usually address each of your coded categories.
- You can then conclude with the main takeaways and avenues for further research.
Example of interview methodology for a research paper
Let’s say you are interested in vegan students on your campus. You have noticed that the number of vegan students seems to have increased since your first year, and you are curious what caused this shift.
You identify a few potential options based on literature:
- Perceptions about personal health or the perceived “healthiness” of a vegan diet
- Concerns about animal welfare and the meat industry
- Increased climate awareness, especially in regards to animal products
- Availability of more vegan options, making the lifestyle change easier
Anecdotally, you hypothesize that students are more aware of the impact of animal products on the ongoing climate crisis, and this has influenced many to go vegan. However, you cannot rule out the possibility of the other options, such as the new vegan bar in the dining hall.
Since your topic is exploratory in nature and you have a lot of experience conducting interviews in your work-study role as a research assistant, you decide to conduct semi-structured interviews.
You have a friend who is a member of a campus club for vegans and vegetarians, so you send a message to the club to ask for volunteers. You also spend some time at the campus dining hall, approaching students at the vegan bar asking if they’d like to participate.
Here are some questions you could ask:
- Do you find vegan options on campus to be: excellent; good; fair; average; poor?
- How long have you been a vegan?
- Follow-up questions can probe the strength of this decision (i.e., was it overwhelmingly one reason, or more of a mix?)
Depending on your participants’ answers to these questions, ask follow-ups as needed for clarification, further information, or elaboration.
- Do you think consuming animal products contributes to climate change? → The phrasing implies that you, the interviewer, do think so. This could bias your respondents, incentivizing them to answer affirmatively as well.
- What do you think is the biggest effect of animal product consumption? → This phrasing ensures the participant is giving their own opinion, and may even yield some surprising responses that enrich your analysis.
After conducting your interviews and transcribing your data, you can then conduct thematic analysis, coding responses into different categories. Since you began your research with several theories about campus veganism that you found equally compelling, you would use the inductive approach.
Once you’ve identified themes and patterns from your data, you can draw inferences and conclusions. Your results section usually addresses each theme or pattern you found, describing each in turn, as well as how often you came across them in your analysis. Feel free to include lots of (properly anonymized) examples from the data as evidence, too.
If you want to know more about statistics , methodology , or research bias , make sure to check out some of our other articles with explanations and examples.
- Student’s t -distribution
- Normal distribution
- Null and Alternative Hypotheses
- Chi square tests
- Confidence interval
- Quartiles & Quantiles
- Cluster sampling
- Stratified sampling
- Data cleansing
- Reproducibility vs Replicability
- Peer review
- Prospective cohort study
Research bias
- Implicit bias
- Cognitive bias
- Placebo effect
- Hawthorne effect
- Hindsight bias
- Affect heuristic
- Social desirability bias
A semi-structured interview is a blend of structured and unstructured types of interviews. Semi-structured interviews are best used when:
- You have prior interview experience. Spontaneous questions are deceptively challenging, and it’s easy to accidentally ask a leading question or make a participant uncomfortable.
The four most common types of interviews are:
- Structured interviews : The questions are predetermined in both topic and order.
- Semi-structured interviews : A few questions are predetermined, but other questions aren’t planned.
Social desirability bias is the tendency for interview participants to give responses that will be viewed favorably by the interviewer or other participants. It occurs in all types of interviews and surveys , but is most common in semi-structured interviews , unstructured interviews , and focus groups .
Social desirability bias can be mitigated by ensuring participants feel at ease and comfortable sharing their views. Make sure to pay attention to your own body language and any physical or verbal cues, such as nodding or widening your eyes.
This type of bias can also occur in observations if the participants know they’re being observed. They might alter their behavior accordingly.
The interviewer effect is a type of bias that emerges when a characteristic of an interviewer (race, age, gender identity, etc.) influences the responses given by the interviewee.
There is a risk of an interviewer effect in all types of interviews , but it can be mitigated by writing really high-quality interview questions.
Inductive reasoning is a bottom-up approach, while deductive reasoning is top-down.
Inductive reasoning takes you from the specific to the general, while in deductive reasoning, you make inferences by going from general premises to specific conclusions.
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
George, T. (2023, June 22). Semi-Structured Interview | Definition, Guide & Examples. Scribbr. Retrieved April 15, 2024, from https://www.scribbr.com/methodology/semi-structured-interview/
Is this article helpful?
Tegan George
Other students also liked, structured interview | definition, guide & examples, unstructured interview | definition, guide & examples, what is a focus group | step-by-step guide & examples, "i thought ai proofreading was useless but..".
I've been using Scribbr for years now and I know it's a service that won't disappoint. It does a good job spotting mistakes”
- What is a semi-structured interview?
Last updated
5 February 2023
Reviewed by
Cathy Heath
When designed correctly, user interviews go much deeper than surface-level survey responses. They can provide new information about how people interact with your products and services, and shed light on the underlying reasons behind these habits.
Semi-structured user interviews are widely considered one of the most effective tools for doing this kind of qualitative research , depending on your specific goals. As the name suggests, the semi-structured format allows for a more natural, conversational flow, while still being organized enough to collect plenty of actionable data .
Analyze semi-structured interviews
Bring all your semi-structured interviews into one place to analyze and understand
A semi-structured interview is a qualitative research method used to gain an in-depth understanding of the respondent's feelings and beliefs on specific topics. As the interviewer prepares the questions ahead of time, they can adjust the order, skip any that are redundant, or create new ones. Additionally, the interviewer should be prepared to ask follow-up questions and probe for more detail.
Semi-structured interviews typically last between 30 and 60 minutes and are usually conducted either in person or via a video call. Ideally, the interviewer can observe the participant's verbal and non-verbal cues in real-time, allowing them to adjust their approach accordingly. The interviewer aims for a conversational flow that helps the participant talk openly while still focusing on the primary topics being researched.
Once the interview is over, the researcher analyzes the data in detail to draw meaningful results. This involves sorting the data into categories and looking for patterns and trends. This semi-structured interview approach provides an ideal framework for obtaining open-ended data and insights.
- When to use a semi-structured interview?
Semi-structured interviews are considered the "best of both worlds" as they tap into the strengths of structured and unstructured methods. Researchers can gather reliable data while also getting unexpected insights from in-depth user feedback.
Semi-structured interviews can be useful during any stage of the UX product-development process, including exploratory research to better understand a new market or service. Further down the line, this approach is ideal for refining existing designs and discovering areas for improvement. Semi-structured interviews can even be the first step when planning future research projects using another method of data collection.
- Advantages of semi-structured interviews
Flexibility
This style of interview is meant to be adapted according to the answers and reactions of the respondent, which gives a lot of flexibility. Semi-structured interviews encourage two-way communication, allowing themes and ideas to emerge organically.
Respondent comfort
The semi-structured format feels more natural and casual for participants than a formal interview. This can help to build rapport and more meaningful dialogue.
Semi-structured interviews are excellent for user experience research because they provide rich, qualitative data about how people really experience your products and services.
Open-ended questions allow the respondent to provide nuanced answers, with the potential for more valuable insights than other forms of data collection, like structured interviews , surveys , or questionnaires.
- Disadvantages of semi-structured interviews
Can be unpredictable
Less structure brings less control, especially if the respondent goes off tangent or doesn't provide useful information. If the conversation derails, it can take a lot of effort to bring the focus back to the relevant topics.
Lack of standardization
Every semi-structured interview is unique, including potentially different questions, so the responses collected are very subjective. This can make it difficult to draw meaningful conclusions from the data unless your team invests the time in a comprehensive analysis.
Compared to other research methods, unstructured interviews are not as consistent or "ready to use."
- Best practices when preparing for a semi-structured interview
While semi-structured interviews provide a lot of flexibility, they still require thoughtful planning. Maximizing the potential of this research method will depend on having clear goals that help you narrow the focus of the interviews and keep each session on track.
After taking the time to specify these parameters, create an interview guide to serve as a framework for each conversation. This involves crafting a range of questions that can explore the necessary themes and steer the conversation in the right direction. Everything in your interview guide is optional (that's the beauty of being "semi" structured), but it's still an essential tool to help the conversation flow and collect useful data.
Best practices to consider while designing your interview questions include:
Prioritize open-ended questions
Promote a more interactive, meaningful dialogue by avoiding questions that can be answered with a simple yes or no, otherwise known as close-ended questions.
Stick with "what," "when," "who," "where," "why," and "how" questions, which allow the participant to go beyond the superficial to express their ideas and opinions. This approach also helps avoid jargon and needless complexity in your questions.
Open-ended questions help the interviewer uncover richer, qualitative details, which they can build on to get even more valuable insights.
Plan some follow-up questions
When preparing questions for the interview guide, consider the responses you're likely to get and pair them up with some effective, relevant follow-up questions. Factual questions should be followed by ones that ask an opinion.
Planning potential follow-up questions will help you to get the most out of a semi-structured interview. They allow you to delve deeper into the participant's responses or hone in on the most important themes of your research focus.
Follow-up questions are also invaluable when the interviewer feels stuck and needs a meaningful prompt to continue the conversation.
Avoid leading questions
Leading questions are framed toward a predetermined answer. This makes them likely to result in data that is biased, inaccurate, or otherwise unreliable.
For example, asking "Why do you think our services are a good solution?" or "How satisfied have you been with our services?" will leave the interviewee feeling pressured to agree with some baseline assumptions.
Interviewers must take the time to evaluate their questions and make a conscious effort to remove any potential bias that could get in the way of authentic feedback.
Asking neutral questions is key to encouraging honest responses in a semi-structured interview. For example, "What do you consider to be the advantages of using our services?" or simply "What has been your experience with using our services?"
Neutral questions are effective in capturing a broader range of opinions than closed questions, which is ultimately one of the biggest benefits of using semi-structured interviews for research.
Use the critical incident method
The critical incident method is an approach to interviewing that focuses on the past behavior of respondents, as opposed to hypothetical scenarios. One of the challenges of all interview research methods is that people are not great at accurately recalling past experiences, or answering future-facing, abstract questions.
The critical incident method helps avoid these limitations by asking participants to recall extreme situations or 'critical incidents' which stand out in their memory as either particularly positive or negative. Extreme situations are more vivid so they can be recalled more accurately, potentially providing more meaningful insights into the interviewee’s experience with your products or services.
- Best practices while conducting semi-structured interviews
Encouraging interaction is the key to collecting more specific data than is typically possible during a formal interview. Facilitating an effective semi-structured interview is a balancing act between asking prepared questions and creating the space for organic conversation. Here are some guidelines for striking the right tone.
Beginning the interview
Make participants feel comfortable by introducing yourself and your role at the organization and displaying appropriate body language.
Outline the purpose of the interview to give them an idea of what to expect. For example, explain that you want to learn more about how people use your product or service.
It's also important to thank them for their time in advance and emphasize there are no right or wrong answers.
Practice active listening
Build trust and rapport throughout the interview with active listening techniques, focusing on being present and demonstrating that you're paying attention by responding thoughtfully. Engage with the participant by making eye contact, nodding, and giving verbal cues like "Okay, I see," "I understand," and "M-hm."
Avoid the temptation to rush to fill any silences while they're in the middle of responding, even if it feels awkward. Give them time to finish their train of thought before interrupting with feedback or another prompt. Embracing these silences is essential for active listening because it's a sign of a productive interview with meaningful, candid responses.
Practicing these techniques will ensure the respondent feels heard and respected, which is critical for gathering high-quality information.
Ask clarifying questions in real time
In a semi-structured interview, the researcher should always be on the lookout for opportunities to probe into the participant's thoughts and opinions.
Along with preparing follow-up questions, get in the habit of asking clarifying questions whenever possible. Clarifying questions are especially important for user interviews because people often provide vague responses when discussing how they interact with products and services.
Being asked to go deeper will encourage them to give more detail and show them you’re taking their opinions seriously and are genuinely interested in understanding their experiences.
Some clarifying questions that can be asked in real-time include:
"That's interesting. Could you give me some examples of X?"
"What do you mean when you say "X"?"
"Why is that?"
"It sounds like you're saying [rephrase their response], is that correct?"
Minimize note-taking
In a wide-ranging conversation, it's easy to miss out on potentially valuable insights by not staying focused on the user. This is why semi-structured interviews are generally recorded (audio or video), and it's common to have a second researcher present to take notes.
The person conducting the interview should avoid taking notes because it's a distraction from:
Keeping track of the conversation
Engaging with the user
Asking thought-provoking questions
Watching you take notes can also have the unintended effect of making the participant feel pressured to give shallower, shorter responses—the opposite of what you want.
Concluding the interview
Semi-structured interviews don't come with a set number of questions, so it can be tricky to bring them to an end. Give the participant a sense of closure by asking whether they have anything to add before wrapping up, or if they want to ask you any questions, and then give sincere thanks for providing honest feedback.
Don't stop abruptly once all the relevant topics have been discussed or you're nearing the end of the time that was set aside. Make them feel appreciated!
- Analyzing the data from semi-structured interviews
In some ways, the real work of semi-structured interviews begins after all the conversations are over, and it's time to analyze the data you've collected. This process will focus on sorting and coding each interview to identify patterns, often using a mix of qualitative and quantitative methods.
Some of the strategies for making sense of semi-structured interviews include:
Thematic analysis : focuses on the content of the interviews and identifying common themes
Discourse analysis : looks at how people express feelings about themes such as those involving politics, culture, and power
Qualitative data mapping: a visual way to map out the correlations between different elements of the data
Narrative analysis : uses stories and language to unlock perspectives on an issue
Grounded theory : can be applied when there is no existing theory that could explain a new phenomenon
Get started today
Go from raw data to valuable insights with a flexible research platform
Editor’s picks
Last updated: 21 December 2023
Last updated: 16 December 2023
Last updated: 6 October 2023
Last updated: 5 March 2024
Last updated: 25 November 2023
Last updated: 15 February 2024
Last updated: 11 March 2024
Last updated: 12 December 2023
Last updated: 6 March 2024
Last updated: 10 April 2023
Last updated: 20 December 2023
Latest articles
Related topics, log in or sign up.
Get started for free
Semi-structured Interviews
- Reference work entry
- First Online: 01 January 2020
- pp 4825–4830
- Cite this reference work entry
- Danielle Magaldi 3 &
- Matthew Berler 4
19k Accesses
52 Citations
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Baumbusch, J. (2010). Semi-structured interviewing in practice-close research. Journal for Specialists in Pediatric Nursing; Hoboken, 15 (3), 255–258.
Article Google Scholar
Clarkin, A. J., Ammaniti, M., & Fontana, A. (2015). The use of a psychodynamic semi-structured personality assessment interview in school settings. Adolescent Psychiatry, 5 (4), 237–244. https://doi.org/10.2174/2210676606666160502125435 .
Cooper, Z., & Fairburn, C. (1987). The Eating Disorder Examination: A semi-structured interview for the assessment of the specific psychopathology of eating disorders. International Journal of Eating Disorders, 6 (1), 1–8. https://doi.org/10.1002/1098-108X(198701)6:1<1::AID-EAT2260060102>3.0.CO;2-9 .
Creswell, J. W. (2007). Qualitative inquiry and research design: Choosing among five approaches (3rd ed.). Thousand Oaks: Sage.
Google Scholar
Dearnley, C. (2005). A reflection on the use of semi-structured interviews. Nurse Researcher, 13 (1), 19–28. https://doi.org/10.7748/nr2005.07.13.1.19.c5997 .
Article PubMed Google Scholar
DiCicco-Bloom, B., & Crabtree, B. F. (2006). The qualitative research interview. Medical Education, 40 (4), 314–321. https://doi.org/10.1111/j.1365-2929.2006.02418.x .
Elliott, R., Fischer, C. T., & Rennie, D. L. (1999). Evolving guidelines for publication of qualitative research studies in psychology and related fields. British Journal of Clinical Psychology, 38 (3), 215–229.
Fylan, F. (2005). Semi-structured interviewing. In A handbook of research methods for clinical and health psychology (pp. 65–77). New York: Oxford University Press.
Galanter, C. A., & Patel, V. L. (2005). Medical decision making: A selective review for child psychiatrists and psychologists. Journal of Child Psychology and Psychiatry, 46 (7), 675–689. https://doi.org/10.1111/j.1469-7610.2005.01452.x .
Galletta, A. (2013). Mastering the semi-structured interview and beyond: From research design to analysis and publication . New York: New York University Press.
Book Google Scholar
Gibbs, L., Kealy, M., Willis, K., Green, J., Welch, N., & Daly, J. (2007). What have sampling and data collection got to do with good qualitative research? Australian and New Zealand Journal of Public Health, 31 (6), 291–295. https://doi.org/10.1028/bdj.2008.192 .
Glenn, C. R., Weinberg, A., & Klonsky, E. D. (2009). Relationship of the Borderline Symptom List to DSM-IV borderline personality disorder criteria assessed by semi-structured interview. Psychopathology; Basel, 42 (6), 394–398.
Haverkamp, B. E. (2005). Ethical perspectives on qualitative research in applied psychology. Journal of Counseling Psychology, 52 (2), 146.
Hill, C., Knox, S., Thompson, B., Williams, E., Hess, S., & Ladany, N. (2005). Consensual qualitative research: An update. Journal of Counseling Psychology . Retrieved from http://epublications.marquette.edu/edu_fac/18
Hutsebaut, J., Kamphuis, J. H., Feenstra, D. J., Weekers, L. C., & De Saeger, H. (2017). Assessing DSM–5-oriented level of personality functioning: Development and psychometric evaluation of the Semi-Structured Interview for Personality Functioning DSM–5 (STiP-5.1). Personality Disorders: Theory, Research, and Treatment, 8 (1), 94–101. https://doi.org/10.1037/per0000197 .
Kallio, H., Pietilä, A., Johnson, M., & Kangasniemi, M. (2016). Systematic methodological review: Developing a framework for a qualitative semi-structured interview guide. Journal of Advanced Nursing, 72 (12), 2954–2965. https://doi.org/10.1111/jan.13031 .
Kaufman, J., Birmaher, B., Brent, D., Rao, U., Flynn, C., Moreci, P., … Ryan, N. (1997). Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child & Adolescent Psychiatry, 36 (7), 980–988. https://doi.org/10.1097/00004583-199707000-00021 .
Knox, S., & Burkard, A. W. (2014). Qualitative research interviews: An update. In W. Lutz, S. Knox, W. Lutz, & S. Knox (Eds.), Quantitative and qualitative methods in psychotherapy research (pp. 342–354). New York: Routledge/Taylor & Francis Group.
Chapter Google Scholar
Kraus, S. E., Hamzah, A., Omar, Z., Suandi, T., Ismail, I. A., & Zahari, M. Z. (2009). Preliminary investigation and interview guide development for studying how Malaysian farmers form their mental models of farming. The Qualitative Report, 14 (2), 245–260.
McTate, E. A., & Leffler, J. M. (2017). Diagnosing disruptive mood dysregulation disorder: Integrating semi-structured and unstructured interviews. Clinical Child Psychology and Psychiatry, 22 (2), 187–203. https://doi.org/10.1177/1359104516658190 .
Pierucci-Lagha, A., Gelernter, J., Chan, G., Arias, A., Cubells, J. F., Farrer, L., & Kranzler, H. R. (2007). Reliability of DSM-IV diagnostic criteria using the semi-structured assessment for drug dependence and alcoholism (SSADDA). Drug and Alcohol Dependence, 91 (1), 85–90. https://doi.org/10.1016/j.drugalcdep.2007.04.014 .
Article PubMed PubMed Central Google Scholar
Polit, D. F., & Beck, C. T. (2010a). Essentials of nursing research: Appraising evidence for nursing practice . Philadelphia: Lippincott Williams & Wilkins.
Polit, D. S., & Beck, C. T. (2010b). Essentials of nursing research. Appraising evidence for nursing practice (7th ed.). Philadelphia: Lippincott-Raven Publishers.
Ramos-Quiroga, J. A., Nasillo, V., Richarte, V., Corrales, M., Palma, F., Ibáñez, P., … Kooij, J. J. S. (2016). Criteria and concurrent validity of DIVA 2.0: A semi-structured diagnostic interview for adult ADHD. Journal of Attention Disorders . https://doi.org/10.1177/1087054716646451 .
Rennie, D. L. (2004). Reflexivity and person-centered counseling. Journal of Humanistic Psychology, 44 , 182–203.
Rubin, H. J., & Rubin, I. S. (2005). Qualitative interviewing: The art of hearing data (2nd ed.). Thousand Oaks: Sage.
Ryan, A. B. (2006). Post-positivist approaches to research. In Researching and writing your thesis: A guide for postgraduate students (pp. 12–26). Ireland: MACE: Maynooth Adult and Community Education.
Turner, D. W. (2010). Qualitative interview design: A practical guide for novice researcher. The Qualitative Report, 15 (3), 754–760.
Whiting, L. S. (2008). Semi-structured interviews: Guidance for novice researchers. Nursing Standard, 22 (23), 35–40.
Williams, E. N., & Morrow, S. L. (2009). Achieving trustworthiness in qualitative research: A pan-paradigmatic perspective. Psychotherapy Research, 19 (4–5), 576–582.
Download references
Author information
Authors and affiliations.
City University of New York, Lehman College, New York City, NY, USA
Danielle Magaldi
Pace University, New York City, NY, USA
Matthew Berler
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Danielle Magaldi .
Editor information
Editors and affiliations.
Oakland University, Rochester, MI, USA
Virgil Zeigler-Hill
Todd K. Shackelford
Section Editor information
Department of Educational Sciences, University of Genoa, Genoa, Italy
Patrizia Velotti
Sapienza University of Rome, Rome, Italy
Rights and permissions
Reprints and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this entry
Cite this entry.
Magaldi, D., Berler, M. (2020). Semi-structured Interviews. In: Zeigler-Hill, V., Shackelford, T.K. (eds) Encyclopedia of Personality and Individual Differences. Springer, Cham. https://doi.org/10.1007/978-3-319-24612-3_857
Download citation
DOI : https://doi.org/10.1007/978-3-319-24612-3_857
Published : 22 April 2020
Publisher Name : Springer, Cham
Print ISBN : 978-3-319-24610-9
Online ISBN : 978-3-319-24612-3
eBook Packages : Behavioral Science and Psychology Reference Module Humanities and Social Sciences Reference Module Business, Economics and Social Sciences
Share this entry
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Semi-Structured Interviews in Qualitative Research
Unveiling insights of semi-structured interviews in qualitative research, the methods for nuanced understanding and robust data analysis.
Qualitative research explores the rich complexities of human experiences, perceptions, and meanings. In the research area, semi-structured interviews emerge as a versatile method to gather in-depth insights from participants. Unlike rigidly structured interviews, semi-structured interviews provide a flexible framework that combines predetermined questions with the freedom to explore emergent topics and probe deeper into participants’ thoughts and experiences. This article aims to show the purpose, benefits, and best practices of utilizing semi-structured interviews in qualitative research. By understanding how this approach facilitates a nuanced exploration of research questions, researchers can harness its potential to capture the multifaceted nature of human phenomena and gain rich and meaningful data that enhances the understanding of diverse social, psychological, and cultural phenomena.
What Are Semi-structured Interviews In Qualitative Research?
A semi-structured interview is a qualitative research method that combines aspects of both structured and unstructured interviews. In a semi-structured interview, the researcher prepares a set of predetermined questions or topics to guide the conversation with the participant, but there is also room for flexibility and follow-up questions based on the participant’s responses. This allows for a more conversational and exploratory approach, enabling the researcher to delve deeper into specific areas of interest and capture detailed and nuanced information.
Also read: What’s the Difference: Qualitative vs Quantitative Research?
Semi-structured interviews enable researchers to explore participants’ perspectives, experiences, and perceptions in-depth. They can uncover rich narratives, personal insights, and contextual details that may not emerge in more standardized interview formats. The open-ended nature of semi-structured interviews allows for a holistic understanding of the research topic and captures the complexity of human experiences.
The Purpose Of Semi-Structured Interviews
Semi-structured interviews serve as a dynamic means of collecting qualitative data, allowing researchers to engage in a conversation with participants while maintaining a certain level of flexibility. These interviews enable researchers to explore research questions, delve into participants’ perspectives, and gain a comprehensive understanding of the studied phenomena. The purpose of semi-structured interviews extends beyond factual information; it aims to uncover participants’ perceptions, beliefs, values, and emotions, providing valuable insights into their subjective experiences.
When To Use A Semi-Structured Interview?
When conducting qualitative research, the decision to use a semi-structured interview approach is influenced by various factors. Semi-structured interviews are particularly suitable when exploring complex and multifaceted topics that require full understanding. They are valuable when researchers aim to capture participants’ perspectives, experiences, and narratives in a flexible and open-ended manner. Semi-structured interviews are effective when the research objectives involve exploring diverse viewpoints, identifying patterns and themes, and gaining insights into individuals’ thoughts and emotions. Additionally, this approach is advantageous when researchers seek to establish rapport and build a collaborative relationship with participants, as it allows for meaningful and interactive conversations. The use of semi-structured interviews empowers researchers to investigate the richness of participants’ experiences while maintaining a level of versatility and adaptability in data collection.
Benefits Of Semi-Structured Interviews
Flexibility and Adaptability: Semi-structured interviews offer a balance between structure and flexibility, allowing researchers to adapt their questioning based on participant responses. This approach enables researchers to examine specific areas of interest, explore unexpected avenues, and capture nuanced information that may not emerge in rigidly structured interviews.
Participant-Centered Approach: Semi-structured interviews place participants at the center of the research process, valuing their perspectives and experiences. By creating a conversational and comfortable atmosphere, researchers can foster trust and rapport, encouraging participants to share their thoughts openly. This approach facilitates a collaborative and co-constructed knowledge-building process, capturing the complexity of participants’ lived experiences.
In-Depth Exploration: Through semi-structured interviews, researchers can delve deeply into participants’ narratives, unraveling intricate details and uncovering hidden meanings. The open-ended nature of these interviews allows for rich descriptions, personal anecdotes, and contextual insights, enabling researchers to gain a comprehensive understanding of the research topic.
Disadvantages Of Semi-Structured Interviews
While semi-structured interviews offer several benefits, it is important to consider their potential disadvantages in qualitative research. One disadvantage is the possibility of interviewer bias or influence. As the interviewer plays an active role in guiding the interview, their personal biases, assumptions, or interpretations may inadvertently shape the participants’ responses. This can compromise the objectivity of the data collected. Another challenge is the time-consuming nature of semi-structured interviews. Conducting interviews, transcribing, and analyzing the data can be a lengthy process, requiring substantial time and resources.
Also read: A Problem Called Sampling Bias
Additionally, the quality of the data obtained may depend on the interviewer’s skills and experience in conducting interviews and eliciting rich responses from participants. If the interviewer lacks proper training or expertise, the quality and depth of the data collected may be compromised. Lastly, the open-ended nature of semi-structured interviews may lead to a vast amount of qualitative data that can be challenging to analyze and interpret, requiring careful attention and rigorous analysis techniques.
Key Considerations For Conducting Semi-Structured Interviews
After confirming that a semi-structured interview aligns with the research topic, the following sequential steps are used to prepare and conduct a semi-structured interview:
Step 1: Define The Objective And Research Scope
Begin by clarifying the purpose of the semi-structured interview and why it is the most suitable research method for the study. Consider the specific knowledge or insights that are intended to be gained through the interview process.
Step 2: Develop Well-Designed Interview Questions
Craft the interview questions to be open-ended, simple, and concise. Take care with the choice of words, particularly when discussing sensitive topics. Ensure that the questions allow for participants to provide detailed and nuanced responses.
Step 3: Identify The Target Group(s) For The Interview
Determine the specific population or groups to engage with during the semi-structured interview. Depending on the size of the target group, utilize random or stratified sampling techniques to select a representative sample. Alternatively, if the group is small, the interview may be with all potential participants.
Step 4: Plan The Logistics Of The Interview
Decide on the details of how, when, and where the interview will take place. Obtain consent from participants and provide them with advance notice of the interview date, time, and location. Choose an environment conducive to open and comfortable communication.
Step 5: Conduct The Interviews
Initiate the interviews by engaging in a casual conversation to establish rapport and build trust with the participants. During face-to-face interviews, actively listen to respondents, paying attention to their non-verbal cues such as body language, gestures, and vocal changes. Maintain a non-judgmental, empathetic, and friendly demeanor throughout the interview process.
Step 6: Transcribe The Interview Recordings
Transcribe the audio or video recordings of the semi-structured interviews. Transcription converts spoken content into written form, aiding in data analysis. Seek appropriate resources or tools to assist you in effectively transcribing the interviews.
Step 7: Code And Categorize The Data
Next, analyze the data collected from the semi-structured interviews. Coding involves carefully examining the transcribed data to identify recurring patterns, themes, and categories. This process helps in organizing and making sense of the information obtained. Consider using specialized coding interview software to streamline this task.
Also read: Mastering Analysis: The Role of Codebook Qualitative Research
Step 8: Analyze The Coded Data
Once the coding process is complete, analyze the coded data to gain meaningful insights. Utilize qualitative data analysis tools, such as Delve, to explore the data more deeply and uncover valuable findings. Draw connections between themes and patterns to develop a comprehensive understanding of the interview outcomes.
Step 9: Present Findings In A Research Paper Or Report
Transform the analysis into a coherent narrative by presenting the results in a research paper or report. Communicate the story behind the data, emphasizing key insights and supporting evidence. Structure the paper to effectively convey the significance and implications of findings in relation to research objectives.
Add Visual Impact To Your Posters With Scientific Illustrations And Graphics
Mind The Graph platform revolutionizes scientific communication by empowering scientists to add visual impact to their posters through scientific illustrations and graphics. With a user-friendly interface and a vast library of pre-designed elements, researchers can effortlessly create visually captivating posters that effectively convey complex scientific concepts. The platform offers a wide range of customizable templates, allowing scientists to tailor their posters to their specific research needs. Whether presenting at conferences, sharing research with colleagues, or publishing scientific papers, Mind the Graph empowers scientists to create visually stunning posters that leave a lasting impression and elevate the impact of their scientific work.
Subscribe to our newsletter
Exclusive high quality content about effective visual communication in science.
Unlock Your Creativity
Create infographics, presentations and other scientifically-accurate designs without hassle — absolutely free for 7 days!
Content tags
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Basic Clin Pharm
- v.5(4); September 2014-November 2014
Qualitative research method-interviewing and observation
Shazia jamshed.
Department of Pharmacy Practice, Kulliyyah of Pharmacy, International Islamic University Malaysia, Kuantan Campus, Pahang, Malaysia
Buckley and Chiang define research methodology as “a strategy or architectural design by which the researcher maps out an approach to problem-finding or problem-solving.”[ 1 ] According to Crotty, research methodology is a comprehensive strategy ‘that silhouettes our choice and use of specific methods relating them to the anticipated outcomes,[ 2 ] but the choice of research methodology is based upon the type and features of the research problem.[ 3 ] According to Johnson et al . mixed method research is “a class of research where the researcher mixes or combines quantitative and qualitative research techniques, methods, approaches, theories and or language into a single study.[ 4 ] In order to have diverse opinions and views, qualitative findings need to be supplemented with quantitative results.[ 5 ] Therefore, these research methodologies are considered to be complementary to each other rather than incompatible to each other.[ 6 ]
Qualitative research methodology is considered to be suitable when the researcher or the investigator either investigates new field of study or intends to ascertain and theorize prominent issues.[ 6 , 7 ] There are many qualitative methods which are developed to have an in depth and extensive understanding of the issues by means of their textual interpretation and the most common types are interviewing and observation.[ 7 ]
Interviewing
This is the most common format of data collection in qualitative research. According to Oakley, qualitative interview is a type of framework in which the practices and standards be not only recorded, but also achieved, challenged and as well as reinforced.[ 8 ] As no research interview lacks structure[ 9 ] most of the qualitative research interviews are either semi-structured, lightly structured or in-depth.[ 9 ] Unstructured interviews are generally suggested in conducting long-term field work and allow respondents to let them express in their own ways and pace, with minimal hold on respondents’ responses.[ 10 ]
Pioneers of ethnography developed the use of unstructured interviews with local key informants that is., by collecting the data through observation and record field notes as well as to involve themselves with study participants. To be precise, unstructured interview resembles a conversation more than an interview and is always thought to be a “controlled conversation,” which is skewed towards the interests of the interviewer.[ 11 ] Non-directive interviews, form of unstructured interviews are aimed to gather in-depth information and usually do not have pre-planned set of questions.[ 11 ] Another type of the unstructured interview is the focused interview in which the interviewer is well aware of the respondent and in times of deviating away from the main issue the interviewer generally refocuses the respondent towards key subject.[ 11 ] Another type of the unstructured interview is an informal, conversational interview, based on unplanned set of questions that are generated instantaneously during the interview.[ 11 ]
In contrast, semi-structured interviews are those in-depth interviews where the respondents have to answer preset open-ended questions and thus are widely employed by different healthcare professionals in their research. Semi-structured, in-depth interviews are utilized extensively as interviewing format possibly with an individual or sometimes even with a group.[ 6 ] These types of interviews are conducted once only, with an individual or with a group and generally cover the duration of 30 min to more than an hour.[ 12 ] Semi-structured interviews are based on semi-structured interview guide, which is a schematic presentation of questions or topics and need to be explored by the interviewer.[ 12 ] To achieve optimum use of interview time, interview guides serve the useful purpose of exploring many respondents more systematically and comprehensively as well as to keep the interview focused on the desired line of action.[ 12 ] The questions in the interview guide comprise of the core question and many associated questions related to the central question, which in turn, improve further through pilot testing of the interview guide.[ 7 ] In order to have the interview data captured more effectively, recording of the interviews is considered an appropriate choice but sometimes a matter of controversy among the researcher and the respondent. Hand written notes during the interview are relatively unreliable, and the researcher might miss some key points. The recording of the interview makes it easier for the researcher to focus on the interview content and the verbal prompts and thus enables the transcriptionist to generate “verbatim transcript” of the interview.
Similarly, in focus groups, invited groups of people are interviewed in a discussion setting in the presence of the session moderator and generally these discussions last for 90 min.[ 7 ] Like every research technique having its own merits and demerits, group discussions have some intrinsic worth of expressing the opinions openly by the participants. On the contrary in these types of discussion settings, limited issues can be focused, and this may lead to the generation of fewer initiatives and suggestions about research topic.
Observation
Observation is a type of qualitative research method which not only included participant's observation, but also covered ethnography and research work in the field. In the observational research design, multiple study sites are involved. Observational data can be integrated as auxiliary or confirmatory research.[ 11 ]
Research can be visualized and perceived as painstaking methodical efforts to examine, investigate as well as restructure the realities, theories and applications. Research methods reflect the approach to tackling the research problem. Depending upon the need, research method could be either an amalgam of both qualitative and quantitative or qualitative or quantitative independently. By adopting qualitative methodology, a prospective researcher is going to fine-tune the pre-conceived notions as well as extrapolate the thought process, analyzing and estimating the issues from an in-depth perspective. This could be carried out by one-to-one interviews or as issue-directed discussions. Observational methods are, sometimes, supplemental means for corroborating research findings.
Strengths and Weaknesses of Semi-Structured Interviews in Qualitative Research: A Critical Essay
A semi-structured interview (SSI) is one of the essential tools in conduction qualitative research. This essay draws upon the pros and cons of applying semi-structured interviews (SSI) in the qualitative research method. Moreover, the challenges of SSI during the coronavirus pandemic are critically discussed to provide plausible recommendations.
- Related Documents
Exploring the consequences of teachers’ self-efficacy: a case of teachers of English as a foreign language
AbstractTeacher self-efficacy has been abundantly studied. However, it seems that the consequences of teachers’ self-efficacy have not been appropriately explored yet. The research objective was to investigate the consequences of teachers’ teaching self-efficacy. The researchers used a qualitative research method. They collected the data through semi-structured interviews with 20 EFL teachers who were selected through purposive sampling. The interviews were content analyzed thematically. Findings showed that self-efficacy has different consequences: pedagogical, learner-related, and psychological. Each consequence has several sub-categories. It is concluded that high self-efficacy affects teachers’ teaching practices, learners’ motivation, and achievement. It also affects teachers’ burn-out status, psychological being, as well as their job satisfaction. The findings can be theoretically and pedagogically important to EFL teachers, teacher-trainers, and administrators of educational settings.
Experiences of partners of professional nurses venting traumatic information
Background: Professional nurses employed in trauma units encounter numerous stressors in their practice environment. They use different strategies to cope with this stress, including venting traumatic information to their partners and other family members. Aims: To describe how partners of professional nurses cope with traumatic information being vented to them. Methods: A qualitative research method with an interpretive descriptive inquiry design was used to explore, interpret and describe the coping experiences of the nurses’ partners. Purposive sampling was used to select a total of 14 partners, but only ten participated in semi-structured interviews. Tesch’s eight steps of open coding were used for data analysis. Results: Four main themes were identified indicating adaptive and maladaptive coping skills, namely partners’ experiences of traumatic information vented to them; partners’ coping activities; reciprocal communication and relationship support between partners and nurses; and resilience of partners to deal with the nursing profession. Conclusion: Partners employed different ways to cope with traumatic information. It was essential for partners and nurses to be supported by nurses’ practice environments and to develop resilience to fulfil reciprocal supportive roles in their relationships.
Dispersion, Diaspora Identity and Belonging
Turks are one of those migrants living in Europe with constituting majority of the migrants in the country of residence and Denmark is among those countries that opened its doors to Turks since 1960's. In this research, I specifically focus on the diaspora consciousness, relations and belonging of the Turkish migrants in Denmark. In doing that, Copenhagen is chosen as the city for the case study. Focusing on the Turkish diaspora and reflection of the sociological realities in the issue of integration to Denmark is the basis of this research. I use qualitative research method and interviewed with 7 migrants from Turkey in living in Copenhagen while conducting my research applying structured interview method. In this study, I have found out that diaspora identity has a significant role in getting integrated to Denmark. As a result of these, migrant Turkish identity becomes bolder which has a direct affect in the level of integration to Denmark.
Leader–member exchange in public organizations: a qualitative study
Purpose The purpose of this paper is to propose the new typologies of leader–member exchange (LMX) theory. Design/methodology/approach This research conducted a thorough, targeted literature review along with a qualitative research method involving in-depth, open-ended and semi-structured interviews. The interviews were conducted with 21 managers and 70 employees of different public organizations during the two years. After interviews, data were transcribed and the qualitative research method of theory elaboration was used to extract the themes from the transcripts. Findings The results showed that the LMX has a dynamic nature with four different versions. Also, the results discovered the multi-level of LMX with three different types of leaders’ styles. In addition, four factors that cause damage to high-quality relationships have been identified (i.e. perceived dissimilarity, feeling of being betrayed, failure to meet the expectations and impression management). Finally, the results discovered five dark sides of LMX. Originality/value This research proposes the new typologies of LMX and the approach and findings of this research contribute to the literature of leadership theories.
PENUTUPAN LOKALISASI DOROKANDANG: ANTARA PERTIMBANGAN MORAL, SOSIAL DAN KEBUTUHAN EKONOMI
This study aims to determine the background of the closure of localization in the area of Dorokandang Village, Lasem District, Rembang Regency. The dominant factors towards the closure of localization in Dorokandang Village are important to note given that so far the existence of localization in the middle of the community always reaped various pros and cons. The decision to close the localization was carried out by the Dorokandang Village government in order to deal with social problems in the form of prostitution or prostitution in the region. The research method used is a qualitative research method. The results of the study show that the background of the closure of localization in Dorokandang Village is based on several factors including moral, social and economic considerations. The hope of the Dorokandang village government with the closure of the localization was the cooperation of both the local village community, the Rembang Regency government and the Satpol PP in the supervision of the ex-localization area so that the practice of prostitution in the area would not occur in secret.
Exploring the Consequences of Teachers’ Self-efficacy: A Case of Teachers of English as a Foreign Language
Abstract Teacher self-efficacy, as a socio-affective concept, has been abundantly studied in relation to different factors. However, it seems that the consequences of teachers' self-efficacy have not been appropriately explored to the present date. The present study aimed at investigating the consequences of EFL teachers' teaching self-efficacy. In so doing, a qualitative research method was used. The data were collected through semi-structured interviews with 20 EFL teachers who were selected through purposive sampling. The interviews were content analyzed thematically. Findings showed that self-efficacy has three main consequences: pedagogical, learner-related, and psychological. Each of these consequences has several sub-categories. It can be concluded that high self-efficacy affects teachers’ teaching practices, learners’ motivation, and achievement. It also affects teachers’ burn-out status, psychological being, as well as their job satisfaction. The findings can be theoretically and pedagogically important to EFL teachers, teacher-trainers, and administrators of educational settings.
Opinions of Graduate Students of Social Studies Education About Qualitative Research Method
The purpose of the study is to determine the opinions of graduate students from social studies education regarding the qualitative research method. The study was conducted in accordance with the phenomenological design, one of the qualitative research designs. The sample group of the study was composed of 25 postgraduate students including 11 females and 14 males studying in the Department of Social Studies Education in Division of Turkish Language and Social Sciences Education of Educational Sciences Institute, in Firat University in the spring semester of the 2019-2020 academic year. The sample group was determined with criterion sampling, one of the purposeful sampling methods. The data of the study were obtained through interview method by using semi-structured interview form. Content analysis method was used in the analysis of the data obtained in the study and the qualitative data analysis program was employed to assess the data. It was determined as a result of the study that the graduate students expressed the qualitative research method as sensitivity to the natural environment, in-depth examination of a social phenomenon, and revealing perception and experiences. Since the qualitative research experience positively affect the knowledge and skills of the graduate students towards the study, they should be included more in the research environment and process. In addition, during the qualitative research process, graduate students should be encouraged and directed to academic activities.
Role of Tuition Centers in the Performance and Achievement of Students: A Case of Hyderabad District, Sindh, Pakistan
This research is designed to explore the importance of tuition centers in the perception of students. It tries to find out the role, supporting methods, environment and good characteristics of tuition centers, their owners and management to support the student to learn effectively and bring good grades in their board examinations. A qualitative research method employed to collect data from the 30 participating students who receive tuition at different centers of Hyderabad district. Semi-structured interview protocol was design; discussed with five experts of field; improved as per suggestions of field experts; piloted on three students; and then implemented and conducted on the recruited sample of students of class Higher Secondary Certificate -II (XII) in order to collect data. The results revealed that the students who receive tuition at different centers bring good grades in their examination and have suitable knowledge about their subjects taught at centers. Their previous grades were found good and attractive such as A-1 and A with more than 80% and 70% marks respectively, due to coaching received at tuition centers that time, reveled from experiences shared by students.
A Folia de Reis “Fulô da Mantiqueira” do Município de Itajubá – MG na Perspectiva da Geografia Cultutal / The Folia de Reis “Fulô da Mantiqueira” of Itajubá - MG in Geographic Cultural Perspective
<p>A Folia de Reis Fulô da Mantiqueira localizada no município de Itajubá – MG é analisada levando em conta as questões de identidade, pertencimento, território e o processo de globalização da sociedade contemporânea. Este trabalho tem como objetivo relacionar a Folia de Reis com a Geografia Cultural e identificar a importância desta para a sociedade e o seu espaço, na busca de um maior reconhecimento desta manifestação folclórico-cultural. A metodologia utilizada foi a pesquisa qualitativa; no estudo de caso foi utilizada a história oral com entrevistas semiestruturadas para o melhor entrosamento com os entrevistados e assim ser possível obter informações mais ricas. Esta pesquisa foi feita sob o olhar de quem de alguma forma participa dessa manifestação, levando em conta a identidade cultural, religiosidade e simbolismo dos entrevistados.</p><p><strong>Palavras-chave: </strong>Cultura; Folclore; Folia de Reis; Itajubá.</p><p><strong>Abstract</strong></p><p>The Fulô da Mantiqueira Folia de Reis is located in Itajubá, in state of Minas Gerais, it is analyzed considering certain issues such as identity, belonging, territory and the globalization process of contemporary society. This article aims to relate Folia de Reis with Cultural Geography and to identify its importance for society and its space, focusing on the recognition of this folkloric and cultural manifestation. In this paper was used a qualitative research method, in the study case was utilized oral stories with semi structured interviews in order to have a rapport with other participants, in this way it is possible to obtain richer information. This project was done by someone who participates of this event and it approaches cultural identity, religiosity and symbolisms of the interviewed.</p><p><strong>Keywords</strong>: Culture; folklore; Folia de Reis; Itajubá.</p>
”I Am Satisfied with My Marriage”: An Experience from Madurese Women who Married Early
The research aimed at examining ways by which Madurese women could achieve satisfaction in early marriage. Its used a qualitative research method with an interpretative phenomenological analysis (IPA). To understand the meaning of one’s experience by looking for themes from available data, IPA rested on three pillars, namely phenomenology, hermeneutics, and idiography. The researchers used semi-structured interviews to collect data and purposive homogeneous sampling. The participants involved were three married women under 18 years old who were living in Madura. The results of the research show that the three women are satisfied with their marriage. The satisfaction of their marriage can be seen from taking care of each other when sick, giving her enough money, and always happy with her husband, not far apart. Furthermore, Madurese women dissatisfaction in her marriage can be seen from anger if she is not given money and is not helped in doing household.
Export Citation Format
Share document.
Designing a semi-structured interview guide for qualitative interviews
But what exactly do semi structured interviews mean? What exactly counts as in-depth? How structured are semi-structured interviews?

Daniel Turner
Interviews are a frequently used research method in qualitative studies. You will see dozens of papers that state something like “We conducted n in-depth semi-structured interviews with key informants”. But what exactly does this mean? What exactly counts as in-depth? How structured are semi-structured interviews?
This post is hosted by Quirkos, simple and affordable software for qualitative analysis. Download a 14 day free trial !
The term “in-depth” is defined fairly vaguely in the literature: it generally means a one-to-one interview on one general topic, which is covered in detail. Usually these qualitative interviews last about an hour, although sometimes much longer. It sounds like two people having a discussion, but there are differences in the power dynamics, and end goal: for the classic sociologist Burgess (2002) these are “conversations with a purpose”.
Qualitative interviews generally differ from quantitative survey based questions in that they are looking for a more detailed and nuanced response. They also acknowledge there is no ‘one-size fits all’, especially when asking someone to recall a personal narrative about their experiences. Instead of a fixed “research protocol” that asks the same question to each respondent, most interviewees adopt a more flexible approach. However there is still a need “...to ensure that the same general areas of information are collected from each interviewee; this provides more focus than the conversational approach, but still allows a degree of freedom and adaptability in getting information from the interviewee” – MacNamara (2009) .
Turner (2010) (who coincidentally shares the same name as me) describes three different types of qualitative interview; Informal Conversation, General Interview Guide, and Standardised Open-Ended. These can be seen as a scale from least to most structured, and we are going to focus on the ‘interview guide’ approach, which takes a middle ground.
An interview guide is like a cheat-sheet for the interviewer – it contains a list of questions and topic areas that should be covered in the interview. However, these are not to be read verbatim and in order, in fact they are more like an aide-mémoire. “Usually the interviewer will have a prepared set of questions but these are only used as a guide, and departures from the guidelines are not seen as a problem but are often encouraged” – Silverman (2013) . That way, the interviewer can add extra questions about an unexpected but relevant area that emerges, and sections that don’t apply to the participant can be negated.
So what do these look like, and how does one go about writing a suitable semi-structured interview guide? Unfortunately, it is rare in journal articles for researchers to share the interview guide, and it’s difficult to find good examples on the internet. Basically they look like a list of short questions and follow-on prompts, grouped by topic. There will generally be about a dozen. I’ve written my fair share of interview guides for qualitative research projects over the years, either on my own or with the collaboration of colleagues, so I’m happy to share some tips.
Questions should answer your research questions Your research project should have one or several main research questions, and these should be used to guide the topics covered in the interviews, and hopefully answer the research questions. However, you can’t just ask your respondents “Can the experience of male My Little Pony fans be described through the lens of Derridean deconstruction?”. You will need to break down your research into questions that have meaning for the participant and that they can engage with. The questions should be fairly informal and jargon free (unless that person is an expert in that field of jargon), open ended - so they can’t be easily answered with a yes or no, and non-leading so that respondents aren’t pushed down a certain interpretation.
Link to your proposed analytical approach The questions on your guide should also be constructed in such a way that they will work well for your proposed method of analysis – which again you should already have decided. If you are doing narrative analysis, questions should be encouraging respondents to tell their story and history. In Interpretative Phenomenological Analysis you may want to ask more detail about people’s interpretations of their experiences. Think how you will want to analyse, compare and write up your research, and make sure that the questioning style fits your own approach.
Specific ‘Why’ and prompt questions It is very rare in semi-structured interviews that you will ask one question, get a response, and then move on to the next topic. Firstly you will need to provide some structure for the participant, so they are not expected (or encouraged) to recite their whole life story. But on the other level, you will usually want to probe more about specific issues or conditions. That is where the flexible approach comes in. Someone might reveal something that you are interested in, and is relevant to the research project. So ask more! It’s often useful in the guide to list a series of prompt words that remind you of more areas of detail that might be covered. For example, the question “When did you first visit the doctor?” might be annotated with optional prompts such as “Why did you go then?”, “Were you afraid?” or “Did anyone go with you?”. Prompt words might reduce this to ‘Why THEN / afraid / with someone’.
Be flexible with order Generally, an interview guide will be grouped into several topics, each with a few questions. One of the most difficult skills is how to segue from one topic or question to the next, while still seeming like a normal conversation. The best way to manage this is to make sure that you are always listening to the interviewee, and thinking at the same time about how what they are saying links to other discussion topics. If someone starts talking about how they felt isolated visiting the doctor, and one of your topics is about their experience with their doctor, you can ask ‘Did you doctor make you feel less isolated?’. You might then be asking about topic 4, when you are only on topic 1, but you now have a logical link to ask the more general written question ‘Did you feel the doctor supported you?’. The ability to flow from topic to topic as the conversation evolves (while still covering everything on the interview guide) is tricky, and requires you to:
Know your guide backwards - literally I almost never went into an interview without a printed copy of the interview guide in front of me, but it was kind of like Dumbo’s magic feather : it made me feel safe, but I didn’t really need it. You should know everything on your interview guide off by heart, and in any sequence. Since things will crop up in unpredictable ways, you should be comfortable asking questions in different orders to help the conversational flow. Still, it’s always good to have the interview guide in front of you; it lets you tick off questions as they are asked (so you can see what hasn’t been covered), is space to write notes, and also can be less intimidating for the interviewee, as you can look at your notes occasionally rather than staring them in the eye all the time.
Try for natural conversation Legard, Keegan and Ward (2003) note that “Although a good in-depth interview will appear naturalistic, it will bear little resemblance to an everyday conversation”. You will usually find that the most honest and rich responses come from relaxed, non-combative discussions. Make the first question easy, to ease the participant into the interview, and get them used to the question-answer format. But don’t let it feel like a tennis match, where you are always asking the questions. If they ask something of you, reply! Don’t sit in silence: nod, say ‘Yes’, or ‘Of course’ every now and then, to show you are listening and empathising like a normal human being. Yet do be careful about sharing your own potentially leading opinions, and making the discussion about yourself.
Discuss with your research team / supervisors You should take the time to get feedback and suggestions from peers, be they other people on your research project, or your PhD supervisors. This means preparing the interview guide well in advance of your first interview, leaving time for discussion and revisions. Seasoned interviewers will have tips about wording and structuring questions, and even the most experienced researcher can benefit from a second opinion. Getting it right at this stage is very important, it’s no good discovering after you’ve done all your interviews that you didn’t ask about something important.
Adapting the guide While these are semi-structured interviews, in general you will usually want to cover the same general areas every time you do an interview, no least so that there is some point of comparison. It’s also common to do a first few interviews and realise that you are not asking about a critical area, or that some new potential insight is emerging (especially if you are taking a grounded theory approach). In qualitative research, this need not be a disaster (if this flexibility is methodologically appropriate), and it is possible to revise your interview guide. However, if you do end up making significant revisions, make sure you keep both versions, and a note of which respondents were interviewed with each version of the guide.
Test the timing Inevitably, you will not have exactly the same amount of time for each interview, and respondents will differ in how fast they talk and how often they go off-topic! Make sure you have enough questions to get the detail you need, but also have ‘lower priority’ questions you can drop if things are taking too long. Test the timing of your interview guide with a few participants, or even friends before you settle on it, and revise as necessary. Try and get your interview guide down to one side of paper at the most: it is a prompt, not an encyclopaedia!
Hopefully these points will help demystify qualitative interview guides, and help you craft a useful tool to shape your semi-structured interviews. I’d also caution that semi-structured interviewing is a very difficult process, and benefits majorly from practice. I have been with many new researchers who tend to fall back on the interview guide too much, and read it verbatim. This generally leads to closed-off responses, and missed opportunities to further explore interesting revelations. Treat your interview guide as a guide, not a gospel, and be flexible. It’s extra hard, because you have to juggle asking questions, listening, choosing the next question, keeping the research topic in your head and making sure everything is covered – but when you do it right, you’ll get rich research data that you will actually be excited to go home and analyse.

Don’t forget to check out some of the references above, as well as the myriad of excellent articles and textbooks on qualitative interviews. There’s also Quirkos itself , software to help you make the research process engaging and visual, with a free trial to download of this innovative tool. We also have a rapidly growing series of blog post articles on qualitative interviews. These now include 10 tips for qualitative interviewing , transcribing qualitative interviews and focus groups , and how to make sure you get good recordings . Our blog is updated with articles like this every week, and you can hear about it first by following our Twitter feed @quirkossoftware .
Sign up for more like this.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Call for Papers
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 7, Issue 2
- Semistructured interviewing in primary care research: a balance of relationship and rigour
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-2660-3358 Melissa DeJonckheere 1 and
- Lisa M Vaughn 2 , 3
- 1 Department of Family Medicine , University of Michigan , Ann Arbor , Michigan , USA
- 2 Department of Pediatrics , University of Cincinnati College of Medicine , Cincinnati , Ohio , USA
- 3 Division of Emergency Medicine , Cincinnati Children's Hospital Medical Center , Cincinnati , Ohio , USA
- Correspondence to Dr Melissa DeJonckheere; mdejonck{at}med.umich.edu
Semistructured in-depth interviews are commonly used in qualitative research and are the most frequent qualitative data source in health services research. This method typically consists of a dialogue between researcher and participant, guided by a flexible interview protocol and supplemented by follow-up questions, probes and comments. The method allows the researcher to collect open-ended data, to explore participant thoughts, feelings and beliefs about a particular topic and to delve deeply into personal and sometimes sensitive issues. The purpose of this article was to identify and describe the essential skills to designing and conducting semistructured interviews in family medicine and primary care research settings. We reviewed the literature on semistructured interviewing to identify key skills and components for using this method in family medicine and primary care research settings. Overall, semistructured interviewing requires both a relational focus and practice in the skills of facilitation. Skills include: (1) determining the purpose and scope of the study; (2) identifying participants; (3) considering ethical issues; (4) planning logistical aspects; (5) developing the interview guide; (6) establishing trust and rapport; (7) conducting the interview; (8) memoing and reflection; (9) analysing the data; (10) demonstrating the trustworthiness of the research; and (11) presenting findings in a paper or report. Semistructured interviews provide an effective and feasible research method for family physicians to conduct in primary care research settings. Researchers using semistructured interviews for data collection should take on a relational focus and consider the skills of interviewing to ensure quality. Semistructured interviewing can be a powerful tool for family physicians, primary care providers and other health services researchers to use to understand the thoughts, beliefs and experiences of individuals. Despite the utility, semistructured interviews can be intimidating and challenging for researchers not familiar with qualitative approaches. In order to elucidate this method, we provide practical guidance for researchers, including novice researchers and those with few resources, to use semistructured interviewing as a data collection strategy. We provide recommendations for the essential steps to follow in order to best implement semistructured interviews in family medicine and primary care research settings.
- qualitative research
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0
https://doi.org/10.1136/fmch-2018-000057
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Introduction
Semistructured interviews can be used by family medicine researchers in clinical settings or academic settings even with few resources. In contrast to large-scale epidemiological studies, or even surveys, a family medicine researcher can conduct a highly meaningful project with interviews with as few as 8–12 participants. For example, Chang and her colleagues, all family physicians, conducted semistructured interviews with 10 providers to understand their perspectives on weight gain in pregnant patients. 1 The interviewers asked questions about providers’ overall perceptions on weight gain, their clinical approach to weight gain during pregnancy and challenges when managing weight gain among pregnant patients. Additional examples conducted by or with family physicians or in primary care settings are summarised in table 1 . 1–6
- View inline
Examples of research articles using semistructured interviews in primary care research
From our perspective as seasoned qualitative researchers, conducting effective semistructured interviews requires: (1) a relational focus, including active engagement and curiosity, and (2) practice in the skills of interviewing. First, a relational focus emphasises the unique relationship between interviewer and interviewee. To obtain quality data, interviews should not be conducted with a transactional question-answer approach but rather should be unfolding, iterative interactions between the interviewer and interviewee. Second, interview skills can be learnt. Some of us will naturally be more comfortable and skilful at conducting interviews but all aspects of interviews are learnable and through practice and feedback will improve. Throughout this article, we highlight strategies to balance relationship and rigour when conducting semistructured interviews in primary care and the healthcare setting.
Qualitative research interviews are ‘attempts to understand the world from the subjects’ point of view, to unfold the meaning of peoples’ experiences, to uncover their lived world prior to scientific explanations’ (p 1). 7 Qualitative research interviews unfold as an interviewer asks questions of the interviewee in order to gather subjective information about a particular topic or experience. Though the definitions and purposes of qualitative research interviews vary slightly in the literature, there is common emphasis on the experiences of interviewees and the ways in which the interviewee perceives the world (see table 2 for summary of definitions from seminal texts).
Definitions of qualitative interviews
The most common type of interview used in qualitative research and the healthcare context is semistructured interview. 8 Figure 1 highlights the key features of this data collection method, which is guided by a list of topics or questions with follow-up questions, probes and comments. Typically, the sequencing and wording of the questions are modified by the interviewer to best fit the interviewee and interview context. Semistructured interviews can be conducted in multiple ways (ie, face to face, telephone, text/email, individual, group, brief, in-depth), each of which have advantages and disadvantages. We will focus on the most common form of semistructured interviews within qualitative research—individual, face-to-face, in-depth interviews.
- Download figure
- Open in new tab
- Download powerpoint
Key characteristics of semistructured interviews.
Purpose of semistructured interviews
The overall purpose of using semistructured interviews for data collection is to gather information from key informants who have personal experiences, attitudes, perceptions and beliefs related to the topic of interest. Researchers can use semistructured interviews to collect new, exploratory data related to a research topic, triangulate other data sources or validate findings through member checking (respondent feedback about research results). 9 If using a mixed methods approach, semistructured interviews can also be used in a qualitative phase to explore new concepts to generate hypotheses or explain results from a quantitative phase that tests hypotheses. Semistructured interviews are an effective method for data collection when the researcher wants: (1) to collect qualitative, open-ended data; (2) to explore participant thoughts, feelings and beliefs about a particular topic; and (3) to delve deeply into personal and sometimes sensitive issues.
Designing and conducting semistructured interviews
In the following section, we provide recommendations for the steps required to carefully design and conduct semistructured interviews with emphasis on applications in family medicine and primary care research (see table 3 ).
Steps to designing and conducting semistructured interviews
Steps for designing and conducting semistructured interviews
Step 1: determining the purpose and scope of the study.
The purpose of the study is the primary objective of your project and may be based on an anecdotal experience, a review of the literature or previous research finding. The purpose is developed in response to an identified gap or problem that needs to be addressed.
Research questions are the driving force of a study because they are associated with every other aspect of the design. They should be succinct and clearly indicate that you are using a qualitative approach. Qualitative research questions typically start with ‘What’, ‘How’ or ‘Why’ and focus on the exploration of a single concept based on participant perspectives. 10
Step 2: identifying participants
After deciding on the purpose of the study and research question(s), the next step is to determine who will provide the best information to answer the research question. Good interviewees are those who are available, willing to be interviewed and have lived experiences and knowledge about the topic of interest. 11 12 Working with gatekeepers or informants to get access to potential participants can be extremely helpful as they are trusted sources that control access to the target sample.
Sampling strategies are influenced by the research question and the purpose of the study. Unlike quantitative studies, statistical representativeness is not the goal of qualitative research. There is no calculation of statistical power and the goal is not a large sample size. Instead, qualitative approaches seek an in-depth and detailed understanding and typically use purposeful sampling. See the study of Hatch for a summary of various types of purposeful sampling that can be used for interview studies. 12
‘How many participants are needed?’ The most common answer is, ‘it depends’—it depends on the purpose of the study, what kind of study is planned and what questions the study is trying to answer. 12–14 One common standard in qualitative sample sizes is reaching thematic saturation, which refers to the point at which no new thematic information is gathered from participants. Malterud and colleagues discuss the concept of information power , or a qualitative equivalent to statistical power, to determine how many interviews should be collected in a study. They suggest that the size of a sample should depend on the aim, homogeneity of the sample, theory, interview quality and analytic strategy. 14
Step 3: considering ethical issues
An ethical attitude should be present from the very beginning of the research project even before you decide who to interview. 15 This ethical attitude should incorporate respect, sensitivity and tact towards participants throughout the research process. Because semistructured interviewing often requires the participant to reveal sensitive and personal information directly to the interviewer, it is important to consider the power imbalance between the researcher and the participant. In healthcare settings, the interviewer or researcher may be a part of the patient’s healthcare team or have contact with the healthcare team. The researchers should ensure the interviewee that their participation and answers will not influence the care they receive or their relationship with their providers. Other issues to consider include: reducing the risk of harm; protecting the interviewee’s information; adequately informing interviewees about the study purpose and format; and reducing the risk of exploitation. 10
Step 4: planning logistical aspects
Careful planning particularly around the technical aspects of interviews can be the difference between a great interview and a not so great interview. During the preparation phase, the researcher will need to plan and make decisions about the best ways to contact potential interviewees, obtain informed consent, arrange interview times and locations convenient for both participant and researcher, and test recording equipment. Although many experienced researchers have found themselves conducting interviews in less than ideal locations, the interview location should avoid (or at least minimise) interruptions and be appropriate for the interview (quiet, private and able to get a clear recording). 16 For some research projects, the participants’ homes may make sense as the best interview location. 16
Initial contacts can be made through telephone or email and followed up with more details so the individual can make an informed decision about whether they wish to be interviewed. Potential participants should know what to expect in terms of length of time, purpose of the study, why they have been selected and who will be there. In addition, participants should be informed that they can refuse to answer questions or can withdraw from the study at any time, including during the interview itself.
Audio recording the interview is recommended so that the interviewer can concentrate on the interview and build rapport rather than being distracted with extensive note taking 16 (see table 4 for audio-recording tips). Participants should be informed that audio recording is used for data collection and that they can refuse to be audio recorded should they prefer.
Suggestions for successful audio recording of interviews
Most researchers will want to have interviews transcribed verbatim from the audio recording. This allows you to refer to the exact words of participants during the analysis. Although it is possible to conduct analyses from the audio recordings themselves or from notes, it is not ideal. However, transcription can be extremely time consuming and, if not done yourself, can be costly.
In the planning phase of research, you will want to consider whether qualitative research software (eg, NVivo, ATLAS.ti, MAXQDA, Dedoose, and so on) will be used to assist with organising, managing and analysis. While these tools are helpful in the management of qualitative data, it is important to consider your research budget, the cost of the software and the learning curve associated with using a new system.
Step 5: developing the interview guide
Semistructured interviews include a short list of ‘guiding’ questions that are supplemented by follow-up and probing questions that are dependent on the interviewee’s responses. 8 17 All questions should be open ended, neutral, clear and avoid leading language. In addition, questions should use familiar language and avoid jargon.
Most interviews will start with an easy, context-setting question before moving to more difficult or in-depth questions. 17 Table 5 gives details of the types of guiding questions including ‘grand tour’ questions, 18 core questions and planned and unplanned follow-up questions.
Questions and prompts in semistructured interviewing
To illustrate, online supplementary appendix A presents a sample interview guide from our study of weight gain during pregnancy among young women. We start with the prompt, ‘Tell me about how your pregnancy has been so far’ to initiate conversation about their thoughts and feelings during pregnancy. The subsequent questions will elicit responses to help answer our research question about young women’s perspectives related to weight gain during pregnancy.
Supplemental material
After developing the guiding questions, it is important to pilot test the interview. Having a good sense of the guide helps you to pace the interview (and not run out of time), use a conversational tone and make necessary adjustments to the questions.
Like all qualitative research, interviewing is iterative in nature—data collection and analysis occur simultaneously, which may result in changes to the guiding questions as the study progresses. Questions that are not effective may be replaced with other questions and additional probes can be added to explore new topics that are introduced by participants in previous interviews. 10
Step 6: establishing trust and rapport
Interviews are a special form of relationship, where the interviewer and interviewee converse about important and often personal topics. The interviewer must build rapport quickly by listening attentively and respectfully to the information shared by the interviewee. 19 As the interview progresses, the interviewer must continue to demonstrate respect, encourage the interviewee to share their perspectives and acknowledge the sensitive nature of the conversation. 20
To establish rapport, it is important to be authentic and open to the interviewee’s point of view. It is possible that the participants you recruit for your study will have preconceived notions about research, which may include mistrust. As a result, it is important to describe why you are conducting the research and how their participation is meaningful. In an interview relationship, the interviewee is the expert and should be treated as such—you are relying on the interviewee to enhance your understanding and add to your research. Small behaviours that can enhance rapport include: dressing professionally but not overly formal; avoiding jargon or slang; and using a normal conversational tone. Because interviewees will be discussing their experience, having some awareness of contextual or cultural factors that may influence their perspectives may be helpful as background knowledge.
Step 7: conducting the interview
Location and set-up.
The interview should have already been scheduled at a convenient time and location for the interviewee. The location should be private, ideally with a closed door, rather than a public place. It is helpful if there is a room where you can speak privately without interruption, and where it is quiet enough to hear and audio record the interview. Within the interview space, Josselson 15 suggests an arrangement with a comfortable distance between the interviewer and interviewee with a low table in between for the recorder and any materials (consent forms, questionnaires, water, and so on).
Beginning the interview
Many interviewers start with chatting to break the ice and attempt to establish commonalities, rapport and trust. Most interviews will need to begin with a brief explanation of the research study, consent/assent procedures, rationale for talking to that particular interviewee and description of the interview format and agenda. 11 It can also be helpful if the interviewer shares a little about who they are and why they are interested in the topic. The recording equipment should have already been tested thoroughly but interviewers may want to double-check that the audio equipment is working and remind participants about the reason for recording.

Interviewer stance
During the interview, the interviewer should adopt a friendly and non-judgemental attitude. You will want to maintain a warm and conversational tone, rather than a rote, question-answer approach. It is important to recognise the potential power differential as a researcher. Conveying a sense of being in the interview together and that you as the interviewer are a person just like the interviewee can help ease any discomfort. 15
Active listening
During a face-to-face interview, there is an opportunity to observe social and non-verbal cues of the interviewee. These cues may come in the form of voice, body language, gestures and intonation, and can supplement the interviewee’s verbal response and can give clues to the interviewer about the process of the interview. 21 Listening is the key to successful interviewing. 22 Listening should be ‘attentive, empathic, nonjudgmental, listening in order to invite, and engender talk’ 15 15 (p 66). Silence, nods, smiles and utterances can also encourage further elaboration from the interviewee.
Continuing the interview
As the interview progresses, the interviewer can repeat the words used by the interviewee, use planned and unplanned follow-up questions that invite further clarification, exploration or elaboration. As DiCicco-Bloom and Crabtree 10 explain: ‘Throughout the interview, the goal of the interviewer is to encourage the interviewee to share as much information as possible, unselfconsciously and in his or her own words’ (p 317). Some interviewees are more forthcoming and will offer many details of their experiences without much probing required. Others will require prompting and follow-up to elicit sufficient detail.
As a result, follow-up questions are equally important to the core questions in a semistructured interview. Prompts encourage people to continue talking and they can elicit more details needed to understand the topic. Examples of verbal probes are repeating the participant’s words, summarising the main idea or expressing interest with verbal agreement. 8 11 See table 6 for probing techniques and example probes we have used in our own interviewing.
Probing techniques for semistructured interviews (modified from Bernard 30 )
Step 8: memoing and reflection
After an interview, it is essential for the interviewer to begin to reflect on both the process and the content of the interview. During the actual interview, it can be difficult to take notes or begin reflecting. Even if you think you will remember a particular moment, you likely will not be able to recall each moment with sufficient detail. Therefore, interviewers should always record memos —notes about what you are learning from the data. 23 24 There are different approaches to recording memos: you can reflect on several specific ideas, or create a running list of thoughts. Memos are also useful for improving the quality of subsequent interviews.
Step 9: analysing the data
The data analysis strategy should also be developed during planning stages because analysis occurs concurrently with data collection. 25 The researcher will take notes, modify the data collection procedures and write reflective memos throughout the data collection process. This begins the process of data analysis.
The data analysis strategy used in your study will depend on your research question and qualitative design—see the study of Creswell for an overview of major qualitative approaches. 26 The general process for analysing and interpreting most interviews involves reviewing the data (in the form of transcripts, audio recordings or detailed notes), applying descriptive codes to the data and condensing and categorising codes to look for patterns. 24 27 These patterns can exist within a single interview or across multiple interviews depending on the research question and design. Qualitative computer software programs can be used to help organise and manage interview data.
Step 10: demonstrating the trustworthiness of the research
Similar to validity and reliability, qualitative research can be assessed on trustworthiness. 9 28 There are several criteria used to establish trustworthiness: credibility (whether the findings accurately and fairly represent the data), transferability (whether the findings can be applied to other settings and contexts), confirmability (whether the findings are biased by the researcher) and dependability (whether the findings are consistent and sustainable over time).
Step 11: presenting findings in a paper or report
When presenting the results of interview analysis, researchers will often report themes or narratives that describe the broad range of experiences evidenced in the data. This involves providing an in-depth description of participant perspectives and being sure to include multiple perspectives. 12 In interview research, the participant words are your data. Presenting findings in a report requires the integration of quotes into a more traditional written format.
Conclusions
Though semistructured interviews are often an effective way to collect open-ended data, there are some disadvantages as well. One common problem with interviewing is that not all interviewees make great participants. 12 29 Some individuals are hard to engage in conversation or may be reluctant to share about sensitive or personal topics. Difficulty interviewing some participants can affect experienced and novice interviewers. Some common problems include not doing a good job of probing or asking for follow-up questions, failure to actively listen, not having a well-developed interview guide with open-ended questions and asking questions in an insensitive way. Outside of pitfalls during the actual interview, other problems with semistructured interviewing may be underestimating the resources required to recruit participants, interview, transcribe and analyse the data.
Despite their limitations, semistructured interviews can be a productive way to collect open-ended data from participants. In our research, we have interviewed children and adolescents about their stress experiences and coping behaviours, young women about their thoughts and behaviours during pregnancy, practitioners about the care they provide to patients and countless other key informants about health-related topics. Because the intent is to understand participant experiences, the possible research topics are endless.
Due to the close relationships family physicians have with their patients, the unique settings in which they work, and in their advocacy, semistructured interviews are an attractive approach for family medicine researchers, even if working in a setting with limited research resources. When seeking to balance both the relational focus of interviewing and the necessary rigour of research, we recommend: prioritising listening over talking; using clear language and avoiding jargon; and deeply engaging in the interview process by actively listening, expressing empathy, demonstrating openness to the participant’s worldview and thanking the participant for helping you to understand their experience.
Further Reading
Edwards R, & Holland J. (2013). What is qualitative interviewing?: A&C Black.
Josselson R. Interviewing for qualitative inquiry: A relational approach. Guilford Press, 2013.
Kvale S. InterViews: An Introduction to Qualitative Research Interviewing. SAGE, London, 1996.
Pope C, & Mays N. (Eds). (2006). Qualitative research in health care.
- Gold KJ , et al
- Croxson CH ,
- Ashdown HF ,
- DeJonckheere M ,
- Robinson CH ,
- Evans L , et al
- Griffiths F ,
- Boardman F , et al
- Takemura Y ,
- Nishiue T , et al
- Schoenborn NL ,
- Pollack CE , et al
- Pietilä A-M ,
- Johnson M , et al
- Lincoln YS ,
- DiCicco-Bloom B ,
- Crabtree BF
- Malterud K ,
- Siersma VD ,
- Guassora AD
- Josselson R
- Edwards R ,
- Spradley JP
- Opdenakker R
- Anderson K ,
- Huberman AM
- Huberman AM ,
- Creswell JW
- Damschroder L
Contributors Both authors contributed equally to this work.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Patient consent for publication Not required.
Provenance and peer review Not commissioned; internally peer reviewed.
Read the full text or download the PDF:
- Open access
- Published: 11 April 2024
Perceptions of medical students on narrow learning objectives and structured debriefing in medical escape rooms: a qualitative study
- Tami Jørgensen 1 , 2 ,
- Oscar Rosenkrantz 1 , 3 ,
- Kristine Elisabeth Eberhard 1 , 4 ,
- Theo Walther Jensen 1 , 5 &
- Peter Dieckmann 1 , 7 , 6
BMC Medical Education volume 24 , Article number: 403 ( 2024 ) Cite this article
171 Accesses
8 Altmetric
Metrics details
Escape rooms are increasingly used in medical education as a complementary learning technique or even alternative to traditional educational approaches. Few studies focus on debriefing following medical escape rooms and how escape rooms can be used to achieve pre-defined learning objectives. Evaluating the use of narrow learning objectives may increase the depth of reflections and transform an engaging team event into an effective learning opportunity. This study aimed to explore participants’ experiences and perceived learning outcomes of narrow learning objectives in a medical escape room with debriefing.
In this explorative, qualitative study, participants saw a video lecture, participated in an escape room experience, and in a following debriefing. Throughout this learning session, the learning objectives concerned “exchange of information” and are therefore relatively narrow. Participants then participated in a semi-structured focus group interview and completed a demographic questionnaire. Participants were volunteer final-year medical students. Focus group interview recordings were transcribed and analysed using systematic text condensation.
Thirty-two students in eight groups completed the study. Five themes were described in the analysis of the focus group interviews: Experience with the narrow learning objectives, topics discussed in the debriefing, learning mechanisms, learning outcomes concerning exchange of information and influences of the learning approach.
Conclusions
Narrow learning objectives and structured debriefing seem to increase perceived learning depth of medical escape room sessions. Using semi-structured debriefing still allows for discussions of other elements relevant to the students.
Clinical trials
Clinical.trials ID NCT04783259.
Peer Review reports
There is increasing evidence that medical students prefer interactive education styles with elements of gamification [ 1 , 2 , 3 ]. Gamification is applying game mechanics to a non-gaming environment [ 4 ], which improves achievement of learning goals compared to traditional teaching methods [ 5 , 6 , 7 ].
One interactive gamification technique is escape rooms, a themed exercise that involves solving puzzles and riddles to get out of a room within a specific time limit [ 8 ]. An example of an educational escape room is the Medical Escape Room Game Experience (MERGE) [ 9 ]. It is designed to raise awareness about non-technical skills (NTS) [ 10 , 11 ] among healthcare students by presenting medically themed logic- and skill-based puzzles to be solved as a team. NTS are defined as the social, cognitive and personal management skills necessary for safe and effective performance. These skills are important across various high risk industries including nuclear power, aviation and healthcare [ 12 ].
Like simulations, escape rooms are experiential learning settings. Compared to a simulation, however, participants engage less in role-play and more in a game. Where a simulation at least sometimes asks participants to assume a professional role other than their own, participants in an escape room typically enter as “themselves.”
In such a learning situation, participants share the experience but perceive it from different angles. Debriefing can enlighten differences and strengthen the learning outcome from experiential learning situations by allowing reflection on the educational experience [ 13 , 14 , 15 ]. Therefore, debriefing will supplement an escape room’s inherent entertainment value to increase learning [ 16 ]. Further, the debriefer can be a peer to the learners as peer-to-peer feedback is suggested to affect the learning outcome positively [ 17 ].
The considerable number of debriefing structures published indicate that there is value in organising the debriefing in one way or another. The research group also experienced that structure in the debriefing is appreciated by participants and facilitators. On a theoretical basis, structured debriefings might positively affect the collaboration between facilitators and participants, as both know what to expect, once the structure is established [ 18 , 19 ].
In a debriefing, learning objectives can be predetermined [ 14 , 20 ] with narrow or broad wording. The research group differentiates between narrow and broad learning objectives. Narrow learning objectives concern focused and well-defined questions as opposed to broad learning objectives that are more open and likely to spur many different discussions depending on the learner. The “breadth” metaphor is always relative: “Knowing how errors occur” or “Discussing communication” are examples of broader learning goals with many possible subtopics whereas “Understanding the role of eye contact in non-verbal communication” in contrast is relatively narrow. When using narrow rather than broad learning objectives, the discussion can reach deeper reflection levels, as fewer topics are covered [ 21 , 22 ]. The discussion might not cover topics of interest to participants if they are outside the narrow learning objectives, resulting in discussions being terminated during a debriefing.
Only four studies evaluated escape room debriefing [ 23 , 24 , 25 , 26 ] and concluded that participants would have preferred more structured debriefing relating to specific outcomes for the escape room sessions.
Published studies applied broad learning objectives or had no pre-set learning objective. Thus, no knowledge exists about how narrow learning objectives in a medical escape room are perceived by participants and how they affect the learning experience. The research group believes this knowledge might optimise the overall learning outcome of medical escape rooms by helping educators choose suitable learning objectives. Focusing on learning objectives during debriefing can optimise learning and emphasise the educational character of these entertaining activities. When having learning objectives tailored to the needs of the participants, it is, in the research group’s experience, easier for the educator to provide a high-quality learning session. This can be done by emphasising certain aspects of the learning objectives (e.g., spending more time on discussing them) to satisfy the learning needs and wishes of the participants.
For other experiential learning settings, like simulation, debriefing was declared the “heart and soul” of learning [ 27 ]. Therefore, the research group assumes that debriefing is valuable for escape rooms as well. Given the richness and openness of the learning situation in an escape room it is unclear whether the debriefing should focus on “everything” or specific potentials in the situation. Both approaches likely have advantages and disadvantages.
This study aimed to explore participants’ experiences and perceived learning outcomes of narrow learning objectives in a medical escape room with debriefing.
This was a qualitative study using semi-structured focus group interviews and text condensing. The research group was interested in exploring participants’ perceptions and needed a method that allowed participants to express those experiences. Given the character of the learning objectives, the cognitive aspects of participants’ learning were of interest. Therefore, verbal descriptions in an interview would be a valuable method to collect data and answer the research question [ 28 ]. The research group operated within the constructivist paradigm as it tried to understand a phenomenon from the perspective of those experiencing it.
This section describes the approach, but the supplementary material should be read to understand the experimental work clearly.
The escape room followed the MERGE manual [ 9 ] and was conducted at Copenhagen Academy of Medical Education and Simulation (CAMES) at Herlev Hospital, Denmark. The theme was a zombie apocalypse. It consisted of seven medically themed, logic- and skill-based puzzles that had to be solved sequentially, and the award at the end was the cure for the fictive zombie virus. The MERGE ‘Triage’ puzzle was exchanged with a puzzle box with laparoscopic forceps, focussing on teamwork (see Appendix 2 ). Behind a see-through mirror, a facilitator monitored the escape room events. Participants had 45 min to solve the puzzles. If they struggled in progress, the facilitator provided planned scenario lifesavers to help keep the time frame [ 29 ]. All the faculty had experience facilitating experiential learning settings, including simulation and escape room experiences.
Data collection
Following the escape room, participants were interviewed semi-structured in focus groups and the individuals involved answered a questionnaire about their experience, perceived learning outcome, and demographic information (see Appendix 1 ).
The puzzles in the escape room were in English, while participants communicated in Danish. The video lecture, debriefing, focus group interview, and questionnaire were in Danish. Illustrative citations from the condensation process were translated from Danish into English.
Participants
Participants were medical students who had completed four out of six years of their studies at the University of Copenhagen (UCPH), Denmark. Participants had completed at least four months of internship, experienced clinical practice close to that experienced by young physicians, and had some experience with simulation. Participants were recruited via social media, signed up in groups of four to five, and chosen based on the order of application. Participants did not receive any compensation.
Intervention
The intervention was a structured learning session comprising four parts: a video lecture, focused instructions before the escape room, the escape room scenario, and a post-session debriefing. It was conducted in March 2021.
The learning session focused on two narrow learning objectives: “ Recognising the different ways of exchanging information ” and “ Discussing the impact of exchanging information on problem solving ”. These were chosen based on previous focus points and learning wishes by former participants [ 9 ]. The first learning objective concerned knowledge and comprehension of Bloom’s taxonomy, and the second concerned application and analysis [ 30 ].
The video lecture concerned theory of exchange of information in general terms, thus preparing participants to work with the concrete learning objectives and was developed within the research team (see Appendix 3 ). The focused instructions included practical information on the escape room’s course and emphasised the need to focus on exchange of information, as it was the learning objective. Debriefing was a semi-structured conversation steered by TJ, who has practical experience in the peer-to-peer debriefing of medical students and facilitated the discussion following a manual (Appendix 4 ) based on an established debriefing model [ 13 ].
Semi-structured focus group interviews
Immediately after debriefing, participants were focus group interviewed with a semi-structured interview guide by KE or PD (see interview guide, Appendix 5 ). Focus group interviews concerned participants’ experiences and perceived learning outcomes of narrow learning objectives in a medical escape room with debriefing. Some of the main questions explored how they felt about the format, if and why participants would have preferred a less structured format and whether or not they felt limited by the narrow focus of the debriefing. Furthermore, participants were asked when they experienced learning outcomes and what these were.
Focus group interviews were estimated to last 30 to 45 min and were video and audio recorded. Interviewers emphasised that all points of view were relevant and essential, including perceived challenges.
Focus group interviews were transcribed ad verbatim by TJ and OR and analysed using systematic text condensation [ 31 ]. Condensation focussed on participants’ statements. Unclear and explicitly irrelevant citations (e.g. chit-chat) were excluded. The coding was done in Microsoft Excel. The citations were loaded into one column, where each row represented a different speaker. After initially reading the focus group interview transcripts several times, the coding proceeded with paraphrasing each cell in the next column on a similar level of abstraction by TJ. Themes were assigned to each paraphrase, condensing content of the focus group interviews. Themes were used by TJ and OR to identify all citations relevant to the study aim. These steps were repeated until researchers concluded that saturation had been reached by watching the remaining focus group interviews, and no more codes or themes were identified. TJ condensed the statements, selecting and translating representative citations from Danish to English before grouping them into main themes. Three research group members not involved in the coding and condensation (KE, TWJ, PD) cross-checked the coding and condensation process.
Because of the qualitative character of this study, the purpose was to describe participants’ perceptions as detailed as possible but not to describe how widespread each perception was. Further quantifications were avoided, as the semi-structured nature of the focus group interviews possibly would strongly influence how often a point was made (e.g. when a follow-up question was posed). Points made by a single participant were therefore reported and treated equally important as those made by “some” or “all”.
The questionnaire provided some quantifiable information used in the discussion and conclusion to describe the general tendencies.
Several themes of interest not directly associated with the narrow learning objectives were included in a separate analysis, as they provided valuable insights into escape rooms and debriefings in general; the protocol did not cover this. The study protocol was uploaded to clinicaltrials.gov on 05/03/2021 (ClinicalTrials ID: NCT04783259).
Focus group interviews and participants
Eight groups, with a total of 32 participants completed the study. Participants were in their late twenties and evenly distributed amongst gender (see Table 1 ). In the post-interview questionnaire, they reported prior experience, educational preferences and familiarity (see Table 2 ). Focus group interview duration had a median of 36 min and ranged from 23 to 43 min. After coding and analysing six focus group interviews, saturation was reached, as no new themes could be identified from the last two focus group interviews. This was confirmed by TJ and OR watching the remaining focus group interviews on video. The remaining two focus group interviews were neither transcribed nor analysed.
Themes related to narrow learning objectives
Five main themes were identified from the focus group interviews (Table 2 ).
Within the first theme, experience with narrow learning objectives , participants expressed that they did not feel restricted by the narrow learning objectives but experienced the possibility of discussing other topics important to them.
Topics discussed in the debriefing were mainly about exchange of information . Participants understood the term communication as broader than exchange of information . Participants also discussed leadership and situational awareness .
Learning mechanisms : The single and narrow focus was seen to increase the depth and perceived outcome of the debriefing. Participants explained that the debriefer helped maintain focus on the learning objectives and increased the perceived learning outcome by guiding participants in their reflection.
Perceived learning outcomes in relation to exchange of information that were identified included: Knowledge of different ways of communicating and the importance of optimising communication when working together; skills in ignoring redundant information; and change of attitude by becoming aware that others perceive a situation differently. A few participants reported no learning outcome due to being familiar with the learning objectives prior to the intervention.
Influence of the learning approach covered the parts of the whole learning experience besides the debriefing, focussing on how each of the different phases affected perceived learning of participants. Participants expressed that the video lecture contained little educational value but supported the rest of the approach by setting the scene. Regarding the scenario briefing, some participants wished for more emphasis on the learning objectives just before entering the room. Some participants explained that they got caught up in the game and did not focus on the learning objectives during the escape room. Finally, participants indicated that they liked the coherence of the experience in that each part supported the next and enabled deeper reflection.
Other findings
The focus group interviews provided points beyond discussing the narrow learning objectives (Appendix 6 ). Two main themes were identified. Meta-learning regarding the debriefing itself, where participants realised the usefulness of debriefings in an educational context. And the general experience of the escape room , where participants stated that the experience was relevant to clinical practice. Some participants also described how learning within an escape room differed from conventional communication training because the lack of formal pressure promoted more genuine communication that reflected real-life behaviour. Furthermore, the format was engaging and fun, and the low requirements on medical expertise were appreciated as they did not steal focus.
Post-interview questionnaire
The questionnaire results concerning the learning objectives and their perceived learning outcome are presented in Table 3 . It shows that all participants experienced learning about exchange of information and many about other topics as well. The vast majority liked the narrow focus of the learning objectives and would not have preferred a broader learning objective.
This qualitative study identified narrow learning objectives and structured debriefing to increase perceived learning depth and general outcome of medical escape room sessions. Using semi-structured debriefing allowed for discussions of other elements relevant to the students.
Narrow learning objectives were not restricting
Unstructured game-like learning exercises allows for many different learning objectives catering to participants’ interests but can result in superficial and erratic discussions with frequent changes in topics. To increase the learning outcome, there is a need for some structure. According to the questionnaire, most participants preferred a narrow learning objective though they did not have a comparable experience with a broad learning objective. During the focus group interviews, participants did not feel restricted by the narrow learning objectives and felt free to discuss other topics of their interest. This is a benefit of the semi-structured rather than fully-structured debriefing format and illustrates an educational duality: participants feel a need for autonomy but also for being paced by the educator to focus on the learning objectives and return to the topic when getting off-topic. The results suggest that many educators’ fear– that guiding the debriefing is seen as negative by participants [ 32 ]– might not have an empirical basis. However, the current setting took several steps to focus on the narrow learning objectives (video lecture, scenario briefing, and debriefing). Therefore, this focus was more stringent than is typical in simulation practice.
Structuring debriefings affect perceived learning outcomes
By making participants verbalise perceptions and experiences during the escape room and their perception of aspects of the experience related to the narrow learning objective, the educator increased the perceived learning outcome by increasing the depth of the debriefing. Though the research group defines this as facilitation techniques, the participants refer to it as structure . This complies with others’ findings that participants prefer structured debriefing sessions [ 23 , 24 , 25 ]. This study emphasises that such structure indeed can improve– at least the perceived– learning outcome.
Medical expertise in the escape room
Participants expressed it as an advantage that the level of ambition for medical expertise in the escape room puzzles was low. If there had been difficult medical challenges, these could have reduced learning related to exchange of information . This could be related to matching the amount of new information to avoid an overload, as described in cognitive load theory [ 33 ]. It can also be challenging, especially for novice facilitators, not to overwhelm learners, as they might do so to avoid risking the participants perceiving the learning session as boring [ 34 ]. This study can make it easier for educators to accept that less can be more: participants see the value of discussing fewer topics in more depth.
Exchange of information as a learning objective
The learning objectives were “Recognising the different ways of exchanging information” and “Discussing the impact of exchanging information on problem solving”. Participants were thoroughly introduced to the definition of exchanging information and reminded of the learning objectives throughout the learning experience, yet participants widely used the term communication during the focus group interview. When asked, participants explained that they perceived exchange of information as a more narrow and instrumental term than communication . Participants considered the reflections in the debriefing to concern both the instrumental factors, such as structuring a message and taking notes, and elements, such as non-verbal communication and the distribution of roles within the group.
This exemplifies a challenge in concept learning [ 35 ]: Educators need to balance conceptual sharpness and keep learners motivated about a new concept. The literature on learning (second) languages shows that it may lead to steeper learning and acceptance curves if skills are presented practically with a focus on implementation instead of insisting on conceptual sharpness in using terms [ 36 , 37 , 38 ]. However, this may increase the risk of misunderstanding concepts and terms. Focusing on definitions can be frustrating for many and may slow down learning.
Limitations
In participant recruitment, the research group may have created a selection bias by having voluntary admissions for the study, thus risking a sample of the general population with a specific interest in innovative and interactive education. This potential bias is of little concern since the aim concerned the learning objectives, not the innovative and interactive education style.
The study design increases the risk of a social-desirability bias. The researchers attempted to pre-empt this by explicitly informing the participants of the importance of enlightening both positive and negative aspects.
As a medical student at UPCH, TJ had met some of the participants before, but none of the interviewers had met the participants. Although it cannot be ruled out that familiarity between participants and TJ affected the debriefing, the data collected during the focus group interview session is without this bias.
Narrow learning objectives and structured debriefing can increase perceived learning depth of medical escape room sessions. Using semi-structured debriefing still allows for discussions of other elements relevant to the students.
The findings of this study encourage the use of narrow learning objectives and semi-structured debriefings in future conductions of medical escape room sessions. This will hopefully aid educators in choosing suitable learning objectives to optimise the overall learning outcome of medical escape rooms.
Data availability
Not applicable.
Abbreviations
Copenhagen Academy of Medical Education and Simulation
Medical Escape Room Gaming Experience
Non-technical skills
University of Copenhagen
Moore K, Frazier RS. Engineering education for generation Z. Am J Eng Educ (AJEE). 2017;8(2):111–26.
Article Google Scholar
Shatto B, Erwin K. Teaching millennials and Generation Z: bridging the generational divide. Creat Nurs. 2017;23(1):24–8.
Schenarts PJ. Now arriving: Surgical trainees from Generation Z. J Surg Educ. 2020;77(2):246–53.
Sardi L, Idri A, Fernández-Alemán JL. A systematic review of gamification in e-Health. J Biomed Inform. 2017;71:31–48.
van Gaalen AEJ, Brouwer J, Schönrock-Adema J, Bouwkamp-Timmer T, Jaarsma ADC, Georgiadis JR. Gamification of health professions education: a systematic review. Advances in health sciences education: theory and practice. 2020.
Gentry SV, Gauthier A, L’Estrade Ehrstrom B, Wortley D, Lilienthal A, Tudor Car L, et al. Serious gaming and Gamification Education in Health professions: systematic review. J Med Internet Res. 2019;21(3):e12994.
McClarty KL, Orr A, Frey PM, Dolan RP, Vassileva V, McVay A. A literature review of gaming in education. Gaming Educ. 2012:1–35.
Nicholson S. Peeking behind the locked door: A survey of escape room facilities. Pozyskano z http://scottnicholsoncom/pubs/erfacwhite.pdf. 2015.
Rosenkrantz O, Jensen TW, Sarmasoglu S, Madsen S, Eberhard K, Ersbøll AK, et al. Priming healthcare students on the importance of non-technical skills in healthcare: how to set up a medical escape room game experience. Med Teach. 2019;41(11):1285–92.
Flin R, Patey R, Glavin R, Maran N. Anaesthetists’ non-technical skills. BJA: Br J Anaesth. 2010;105(1):38–44.
Flin R, Patey R. Improving patient safety through training in non-technical skills. BMJ. 2009;339:b3595.
Applied Psychology and Human Factors group TUoA. Non-technical skills n.d. [Available from: https://research.abdn.ac.uk/applied-psych-hf/non-technical-skills/ .
Steinwachs B. How to facilitate a debriefing. Simul Gaming. 1992;23(2):186–95.
Fanning RM, Gaba DM. The role of debriefing in simulation-based learning. Simul Healthcare: J Soc Simul Healthc. 2007;2(2):115–25.
Felix HM, Beecham GB, Simon LV. Debriefing theories and philosophies in Medical Simulation. StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2020. StatPearls Publishing LLC.; 2020.
Kolb A, Kolb D. Eight important things to know about the experiential learning cycle. Australian Council for Educational Leaders; 2018. pp. 8–14.
Lerchenfeldt S, Mi M, Eng M. The utilization of peer feedback during collaborative learning in undergraduate medical education: a systematic review. BMC Med Educ. 2019;19(1):321.
Kolbe M, Grande B, Spahn DR. Briefing and debriefing during simulation-based training and beyond: Content, structure, attitude and setting. Best Pract Res Clin Anaesthesiol. 2015;29(1):87–96.
Palaganas JC, Fey M, Simon R. Structured debriefing in Simulation-Based Education. AACN Adv Crit Care. 2016;27(1):78–85.
Dieckmann P, Molin Friis S, Lippert A, Ostergaard D. The art and science of debriefing in simulation: Ideal and practice. Med Teach. 2009;31(7):e287–94.
Husebø SE, Dieckmann P, Rystedt H, Søreide E, Friberg F. The Relationship between facilitators’ questions and the level of reflection in Postsimulation Debriefing. Simul Healthcare: J Soc Med Simul. 2013;8(3):135–42.
Kihlgren P, Spanager L, Dieckmann P. Investigating novice doctors’ reflections in debriefings after simulation scenarios. Med Teach. 2015;37(5):437–43.
Friedrich C, Teaford H, Taubenheim A, Boland P, Sick B. Escaping the professional silo: an escape room implemented in an interprofessional education curriculum. J Interprof Care. 2019;33(5):573–5.
Zhang XC, Diemer G, Lee H, Jaffe R, Papanagnou D. Finding the ‘QR’ to Patient Safety: applying gamification to Incorporate Patient Safety priorities through a simulated ‘Escape room’ experience. Cureus. 2019;11(2):e4014–e.
Google Scholar
Zhang XC, Lee H, Rodriguez C, Rudner J, Chan TM, Papanagnou D. Trapped as a Group, escape as a team: applying gamification to Incorporate Team-building skills through an ‘Escape room’ experience. Cureus. 2018;10(3):e2256.
Khanna A, Ravindran A, Ewing B, Zinnerstrom K, Grabowski C, Mishra A, et al. Escape MD: using an escape room as a Gamified Educational and Skill-Building Teaching Tool for Internal Medicine residents. Cureus. 2021;13(9):e18314–e.
Rall M, Manser T, Howard SK. Key elements of debriefing for simulator training. Eur J Anaesthesiol. 2000;17(8):516–7.
Hobson A, Townsend A. Interviewing as Educational Research Method(s). 2010. p. 223– 38.
Dieckmann P, Lippert A, Glavin R, Rall M. When things do not go as expected: scenario life savers. Simul Healthcare: J Soc Med Simul. 2010;5(4):219–25.
Adams NE. Bloom’s taxonomy of cognitive learning objectives. J Med Libr Association: JMLA. 2015;103(3):152–3.
Malterud K. Systematic text condensation: a strategy for qualitative analysis. Scand J Public Health. 2012;40(8):795–805.
Dieckmann P, Friis SM, Lippert A, Østergaard D, Goals. Success factors, and barriers for Simulation-based learning:a qualitative interview study in Health Care. Simul Gaming. 2012;43(5):627–47.
van Merriënboer JJ, Sweller J. Cognitive load theory in health professional education: design principles and strategies. Med Educ. 2010;44(1):85–93.
Dieckmann P, Rall M, Sadler C. What competence do simulation instructors need. Minerva Anestesiol. 2008;74:277–81.
Dieckmann P, Glavin R, Hartvigsen Grønholm Jepsen RM, Krage R. Non-technical skills Bingo—a game to facilitate the learning of complex concepts. Adv Simul. 2016;1(1):23.
Muñoz A, Ramirez M. Teachers’ conceptions of motivation and motivating practices in second-language learning: a self-determination theory perspective. Theory Res Educ. 2015;13(2):198–220.
Jugo RR. Language anxiety in Focus: the case of Filipino Undergraduate Teacher Education Learners. Educ Res Int. 2020;2020:7049837.
Mekhriban A, Error and error correction in, teaching speaking. JournalNX - Multidisciplinary Peer Reviewed Journa. 2021;7(2):188–90.
Download references
Acknowledgements
We thank CAMES for funding the expenses required to set up and run the escape room and the participants for their time and insights.
No external funding was received for the conduct of the study.
Author information
Authors and affiliations.
Copenhagen Academy for Medical Education and Simulation (CAMES), Capital Region of Denmark, Borgmester Ib Juuls Vej 1, 2730, Copenhagen, Denmark
Tami Jørgensen, Oscar Rosenkrantz, Kristine Elisabeth Eberhard, Theo Walther Jensen & Peter Dieckmann
Department of Cardiology, Bispebjerg Hospital, Copenhagen, Denmark
Tami Jørgensen
Department of Anaesthesia, Center of Head and Orthopaedics, Copenhagen University Hospital - Rigshospitalet, Copenhagen, Denmark
Oscar Rosenkrantz
Copenhagen University Hospital - Rigshospitalet, Copenhagen, Denmark
Kristine Elisabeth Eberhard
Prehospital Center, Region Zealand, Denmark
Theo Walther Jensen
Department of Public Health, University of Copenhagen, Copenhagen , Denmark
Peter Dieckmann
Department of Quality and Health Technology, University of Stavanger, Stavanger, Norway
You can also search for this author in PubMed Google Scholar
Contributions
T.J. wrote the main manuscript and prepared Tables 1, 2, 3 and 4. All authors participated in conducting the intervention, analysing the data and reviewing the manuscript.
Corresponding author
Correspondence to Tami Jørgensen .
Ethics declarations
Ethics approval and consent to participate.
A formal review was waived by the National Committee on Health Research Ethics (nr.: 21014792). Participants were informed about study procedures and publication plans and were informed that they could withdraw consent at any moment without consequences. They also gave written consent before participation. Thus, informed consent was obtained from all the participants in the study. All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Competing interests.
Dieckmann holds a professorship with the University of Stavanger, Norway, which was established by an unconditional grant to the university by the Laerdal Foundation and is today financed by the university itself. Dieckmann is part of the leadership of the EuSim group, a network of simulation educators and centres providing faculty development courses. We believe that these activities do not substantially impact the study presented here. The other authors report no conflicts of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Jørgensen, T., Rosenkrantz, O., Eberhard, K.E. et al. Perceptions of medical students on narrow learning objectives and structured debriefing in medical escape rooms: a qualitative study. BMC Med Educ 24 , 403 (2024). https://doi.org/10.1186/s12909-024-05295-4
Download citation
Received : 02 December 2022
Accepted : 11 March 2024
Published : 11 April 2024
DOI : https://doi.org/10.1186/s12909-024-05295-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Gamification
- Innovative teaching
- Escape room
- Learning objectives
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Open access
- Published: 17 April 2024
Navigating outpatient care of patients with type 2 diabetes after hospital discharge - a qualitative longitudinal study
- Léa Solh Dost 1 , 2 ,
- Giacomo Gastaldi 3 ,
- Marcelo Dos Santos Mamed 4 , 5 &
- Marie P. Schneider 1 , 2
BMC Health Services Research volume 24 , Article number: 476 ( 2024 ) Cite this article
Metrics details
The transition from hospital to outpatient care is a particularly vulnerable period for patients as they move from regular health monitoring to self-management. This study aimed to map and investigate the journey of patients with polymorbidities, including type 2 diabetes (T2D), in the 2 months following hospital discharge and examine patients’ encounters with healthcare professionals (HCPs).
Patients discharged with T2D and at least two other comorbidities were recruited during hospitalization. This qualitative longitudinal study consisted of four semi-structured interviews per participant conducted from discharge up to 2 months after discharge. The interviews were based on a guide, transcribed verbatim, and thematically analyzed. Patient journeys through the healthcare system were represented using the patient journey mapping methodology.
Seventy-five interviews with 21 participants were conducted from October 2020 to July 2021. The participants had a median of 11 encounters (min–max: 6–28) with HCPs. The patient journey was categorized into six key steps: hospitalization, discharge, dispensing prescribed medications by the community pharmacist, follow-up calls, the first medical appointment, and outpatient care.
Conclusions
The outpatient journey in the 2 months following discharge is a complex and adaptive process. Despite the active role of numerous HCPs, navigation in outpatient care after discharge relies heavily on the involvement and responsibilities of patients. Preparation for discharge, post-hospitalization follow-up, and the first visit to the pharmacy and general practitioner are key moments for carefully considering patient care. Our findings underline the need for clarified roles and a standardized approach to discharge planning and post-discharge care in partnership with patients, family caregivers, and all stakeholders involved.
Peer Review reports
Care transition is defined as “the movement patients make between healthcare practitioners and settings as their condition and care needs change in the course of a chronic or acute illness” [ 1 ]. The transition from hospital to outpatient care is a particularly vulnerable period for patients as they move from a medical environment with regular health monitoring to self-management, where they must implement a large amount of information received during their hospital stay [ 2 , 3 , 4 , 5 , 6 ]. This transition period can be defined as “the post-hospital syndrome,” which corresponds to a transient period of vulnerability (e.g., 30 days) for various health problems, such as stress, immobility, confusion, and even cognitive decline in older adults, leading to complications [ 7 ]. Furthermore, discharged patients may experience a lack of care coordination, receive incomplete information, and inadequate follow-ups, leading to potential adverse events and hospital readmissions [ 8 , 9 , 10 ].
People with type 2 diabetes mellitus (T2D) represent a high proportion of hospitalized patients, and their condition and medications are associated with a higher rate of hospital readmission [ 11 , 12 , 13 ]. Moreover, T2D is generally associated with multiple comorbidities. This complex disease requires time-consuming self-management tasks such as polypharmacy, adaptations of medication dosages, diet, exercise, and medical follow-up, especially during care transition [ 14 , 15 , 16 ].
Various interventions and practices, such as enhanced patient education, discharge counseling, and timely follow-up, have been studied to improve care transition for patients with chronic diseases; however, they have shown mixed results in reducing costs and rehospitalization [ 17 , 18 , 19 , 20 ]. In addition, patient perspectives and patient-reported outcomes are rarely considered; however, their involvement and monitoring are essential for seamless and integrated care [ 21 , 22 ]. Care integration, an approach to strengthening healthcare systems in partnership with people, focuses on patient health needs, the quality of professional services, and interprofessional collaboration. This approach prevents care fragmentation for patients with complex needs [ 23 , 24 ]. Therefore, knowledge of healthcare system practices is essential to ensure integrated, coordinated, and high-quality care. Patient perspectives are critical, considering the lack of literature on how patients perceive their transition from hospital to autonomous care management [ 25 , 26 ].
Patients’ journeys during hospitalization have been described in the literature using various methods such as shadowing, personal diaries, and interviews; however, patients’ experiences after hospital discharge are rarely described [ 26 , 27 ]. Jackson et al. described the complexity of patient journeys in outpatient care after discharge using a multiple case study method to follow three patients with chronic obstructive pulmonary disease from hospitalization to 3 months post-discharge [ 26 ]. The literature does not provide an in-depth understanding of the experiences of patients with comorbidities during care transition upon hospital discharge. The assumption about the patient journey after discharge is that multiple and multi-professional encounters will ensure the transition of care from hospitalization to self-management, but often without care coordination.
This study aimed to investigate the healthcare trajectories of patients with comorbidities, including T2D, during the 2 months following hospital discharge and to examine patients’ encounters with healthcare professionals (HCPs).
While this article focuses on patients’ journeys to outpatient care, another article describes and analyzes patients’ medication management, knowledge, and adherence [ 28 ]. This study followed the Consolidated Criteria for Reporting Qualitative Research (COREQ).
Study design and population
A qualitative longitudinal research approach was adopted, with four individual semi-structured interviews over 2 months after discharge (approximately 3, 10, 30, and 60 days after discharge) that took place at home, by telephone, secured video call, or at the university at the participant’s convenience. Participants were recruited during hospitalization. The inclusion criteria were patients with T2D, with at least two other comorbidities, at least one medication change during hospitalization, hospitalization duration of at least 3 days, and those who returned home after discharge and self-managed their medications. A family caregiver could also participate in the interviews alongside to participants.
Researcher characteristics
All the researchers were trained in qualitative studies. The ward diabetologist and researcher (GG) who enrolled the patients in the study participated in most participants’ care during hospitalization. LS (Ph.D. student and community pharmacist) was unknown to participants and presented herself during hospitalization as a “researcher” rather than a pharmacist to avoid any risk of influencing participants’ answers. MS is a professor in pharmacy, whose research focuses on medication adherence in chronic diseases and aims at better understanding this behavior and its consequences for patients and the healthcare system. MDS is a researcher, linguist, and clinical psychologist, with a particular interest in patients living with chronic conditions such as diabetes and a strong experience in qualitative methodology and verbal data analysis.
Data collection
The interviews were based on four semi-structured interview guides based on existing frameworks and theories: the World Health Organization’s five dimensions for adherence, the Information-Motivation-Behavioral Skills model, and the Social Cognitive Theory [ 29 , 30 , 31 ]. For in-depth documentation of participants’ itinerary in the healthcare system, the interview guides included questions on the type, reason, and moment of the HCP’s encounters and patient relationships with HCPs. Interview guides are available in Supplementary File 1 . During the development phase of the study, the interview guides were reviewed for clarity and validity and adapted by two patient partners from the Geneva University Hospitals’ Patient Partner Platform for Research and Patient and Public Involvement. Thematic saturation was considered reached when no new code or theme emerged and new data repeated previously coded information [ 32 ]. Sociodemographic and clinical data were collected from hospital databases and patient questionnaires. The interviews were audio-recorded, anonymized, and transcribed verbatim.
Data analysis
The sociodemographic and clinical characteristics were descriptively analyzed. Transcriptions were double-coded until similar codes were obtained, and thematic analysis, as described by Braun and Clarke [ 33 , 34 ], was used in a systematic, iterative, and comparative manner. A patient journey mapping methodology was used to illustrate the trajectories of each participant and provide a comprehensive understanding of their experiences. Patient journey mapping is a visual method adapted from the marketing industry that is increasingly used in various health settings and contexts to illustrate and evaluate healthcare services and patient experiences [ 35 ]. In this analysis, we used the term “healthcare professionals” when more than one profession could be involved in participants’ healthcare. Otherwise, when a specific HCP was involved, we used the designated profession (e.g. physicians, pharmacists).
A. Participants description
Twenty-one participants were interviewed between October 2020 and September 2021, generating 75 interviews. All participants took part in Interview 1, 19 participants in Interview 2, 16 participants in Interview 3 and 19 participants in Interview 4, with a median duration of 41 minutes (IQR: 34-49) per interview. Interviews 1,2,3 and 4 took place respectively 5 days (IQR: 4-7), 14 days (13-20), 35 days (33-38), and 63 days (61-68) after discharge. Nine patients were newly diagnosed with T2D, and 12 had a previous diagnosis of T2D, two of whom were untreated. Further information on participants is described in Table 1 . The median number of comorbidities was six (range: 3–11), and participants newly diagnosed with diabetes tended to have fewer comorbidities (median: 4; range: 3–8). More detailed information regarding sociodemographic characteristics and medications has been published previously [ 28 ].
B. Journey mappings
Generic patient journey mapping, presented in Fig. 1 , summarizes the main and usual encounters participants had with their HCPs during the study period. Generic mapping results from all individual patient journey mappings from discharge to 2 months after discharge are available in Supplementary File 2 .
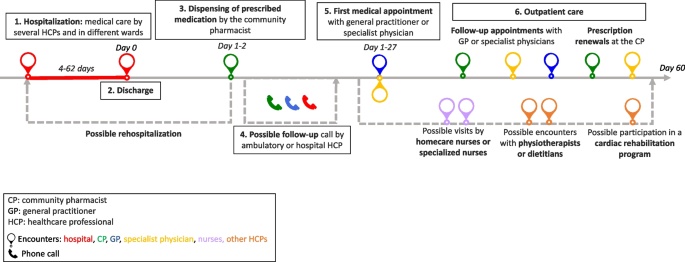
Generic patient journey mapping from hospitalization to two months after discharge
During the 2 months following discharge, the participants had a median number of 10 (range: 6–28) encounters with HCPs. The HCPs met by participants are represented in Fig. 2 . All participants visited their pharmacists at least once, and 16 of the 21 participants met their general practitioners (GPs) at least once. Five participants received home care assistance, four went to an outpatient cardiac rehabilitation program, and five were readmitted during the study period.
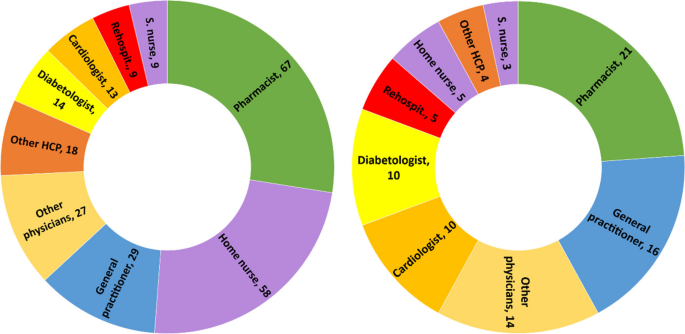
Healthcare professionals seen by participants during the study period. left: n=cumulative encounters; right: n=encountered at least once. Abbreviation: S.nurse: specialized nurse; Other physicians: ophthalmologists, neurologists, hematologists, immunologists, addictologists; other HCP: physiotherapists, dietitians, massage therapist
The first HCP encountered was at the community pharmacy on the same day or day after discharge, except for one participant who did not pick up her medication. The first medical appointment with a physician occurred between days 1 and 27 after discharge (median: 8; IQR: 6-14).
Participants newly diagnosed with diabetes had a closer follow-up after discharge than participants with a former diagnosis of T2D (median: 7; IQR: 6–10 vs median: 9; IQR: 5–19), fewer encounters with HCPs (median: 8; IQR: 7–10 vs. 11; IQR: 8–17), and fewer comorbidities (median: 4; IQR: 4–7 vs. 7; IQR: 5–9). Most participants newly diagnosed with T2D or receiving insulin treatment benefited from either a follow-up call, home visit by a nurse, or diabetes care appointment.
C. Qualitative analysis
Transcripts were analyzed longitudinally and categorized into six key steps based on the verbal data. These key steps, shown in Fig. 1 , represent the identified thematic categories and refer to the following elements: 1. Hospitalization, 2. Discharge, 3. Dispensing of prescribed medications at the pharmacy, 4. Possible follow-up call, 5. First medical appointment, and 6. Outpatient care.
Hospitalization: hospital constraints and care organization
Most participants thought they had benefited from adequate medical care by committed and attentive HCPs but highlighted different constraints and gaps. Some participants noted constraints related to the hospital environment, such as loss of autonomy during their stay, lack of privacy, and the large number of hospital staff encountered. This resulted in participants repeating the same information several times, causing frustration, misunderstanding and a lack of coordination for some participants:
“Twenty or thirty staff members come in during the day! So, it's hard to keep track of [what] is bein g said or done. The best thing for me [...] would be to have clear information from just one person.” Participant 8; interview 1 (P18.1)
Participants had different opinions on the hospital’s care organization. Some participants found that care coordination between the wards was well-organized. In contrast, others highlighted poor coordination and communication between the hospital wards, resulting in long waiting times, care fragmentation, and contradictory or unclear information. Some participants felt that they did not benefit from comprehensive and integrated care and that the hospital staff focused on the cause of their hospitalization, neglecting other comorbidities:
“They were not interested [in my diabetes and my sight]. I was there for the heart and that was where [my care] stopped.” P17.1
Patients’ involvement in decision-making regarding medical care varied. Some participants were involved in their care and took part in medical decisions. Written information, adequate communication, and health professionals’ interest in patients were highlighted by some participants:
“They took the information sheet and they explained everything to me. They didn't just come once; they came several times to explain everything to me.” P5.1
Other participants found the information difficult to understand, particularly because of their fatigue and because the information was provided orally.
Discharge: an unclear process
The discharge process was unclear for patients who could not identify a specific related outpatient medical visit or a key step that summarized their hospital stay and prepared them for discharge:
“Well, there's no real preparation [for discharge]. I was waiting for them to give me the go-ahead so I could go home, that’s all...” P7.4
For some participants, outpatient care follow-up was organized before discharge by the hospital team (generally by making an appointment with the patient’s GP before discharge), whereas others had no post-discharge follow-up scheduled during their hospitalization. Approximately half of the participants refused follow-ups during their hospitalization, such as home care services provided by a nurse, or a rehabilitation hospital stay. The main reason for this refusal was that patients did not perceive the need for follow-up:
“It's true that I was offered a lot of services, which I turned down because I didn't realize how I would manage back at home.” P22.2
Dispensing prescribed medications by the community pharmacist: the first HCP seen after discharge
On behalf of half the participants, a family caregiver went to the usual community or hospital outpatient pharmacy to pick up the medications. The main reasons for delegation were tiredness or difficulty moving. In some cases, this missed encounter would have allowed participants to discuss newly prescribed medications with the pharmacist:
“[My husband] went to get the medication. And I thought afterward, […] that I could have asked [the pharmacist]: “But listen, what is this medication for?” I would have asked questions” P2.3
Participants who met their pharmacist after hospital discharge reported a range of pharmaceutical practices, such as checking the prescribed medication against medication history, providing information and explanations, and offering services such as the preparation of pillboxes. For some, the pharmacists’ work at discharge did not differ from regular prescriptions, whereas others found that they received further support and explanations:
“She took the prescription […] checked thoroughly everything and then she wrote how, when, and how much to take on each medication box. She managed it very well and I had good explanations.” P20.3
Some participants experienced problems with generic substitution, the unavailability of medications, or dispensing errors, complicating their journey through the healthcare system.
Possible follow-up call by HCP: an unsystematic practice
Some participants received a call from their GP or hospital physician a few days after discharge to check their health or answer questions. These calls reassured participants and their caregivers, who knew they had a point of contact in case of difficulty. Occasionally, participants received calls from their community pharmacists to ensure proper understanding and validate medication changes issued during hospitalization. Some participants did not receive any calls and were disappointed by the lack of follow-up:
“There is no follow-up! Nobody called me from the hospital to see how I was doing […]” P8.2
First medical appointment: a key step in the transition of care
The first medical appointment was made in advance by the hospital staff or the patient after discharge. For some participants, this first appointment did not differ from usual care. For most, it was a crucial appointment that allowed them to discuss their hospitalization and new medications and organize their follow-up care. Being cared for by a trusted HCP enabled some patients to feel safe, relieved, and well-cared for, as illustrated by the exchange between a patient and her daughter:
Daughter: When [my mom] came back from the GP, she felt much better [...] It was as if a cork had popped. Was it psychological? Patient: Maybe… I just felt better. D: Do you think it was the fact that she paid attention to you as a doctor? P: She took care of me. She did it in a delicate way. [silence] - P23.2
Some participants complained that their physicians did not receive the hospital discharge letter, making it difficult to discuss hospitalization and sometimes resulting in delayed care.
Outpatient care: a multifaceted experience
During the 2 months after hospital discharge, participants visited several physicians (Fig. 2 ), such as their GP and specialist physicians, for follow-ups, routine check-ups, medical examinations, and new prescriptions. Most participants went to their regular pharmacies to renew their prescriptions, for additional medication information, or for health advice.
Some participants had home care nurses providing various services, such as toileting, care, checks on vital functions, or preparing weekly pill boxes. While some participants were satisfied with this service, others complained that home nurses were unreliable about appointment times or that this service was unnecessary. Some participants were reluctant to use these services:
“The [homecare nurse] makes you feel like you're sick... It's a bit humiliating.” P22.2
Specialized nurses, mostly in diabetology, were appreciated by patients who had dedicated time to talk about different issues concerning diabetes and medication and adapted explanations to the patient’s knowledge. Participants who participated in cardiac rehabilitation said that being in a group and talking to people with the same health problems motivated them to undertake lifestyle and dietary changes:
“In the rehabilitation program, I’m part of a team [of healthcare professionals and patients], I have companions who have gone through the same thing as me, so I’m not by myself. That's better for motivation.” P16.2
Navigating the outpatient healthcare system: the central role of patients
Managing medical appointments is time-consuming and complex for many participants. Some had difficulty knowing with whom to discuss and monitor their health problems. Others had difficulty scheduling medical appointments, especially with specialist physicians or during holidays. A few participants did not attend some of their appointments because of physical or mental vulnerabilities. Restrictions linked to the type of health insurance coverage made navigating the healthcare system difficult for some participants:
“Some medications weren't prescribed by my GP [...] but by the cardiologist. So, I must ask my GP for a delegation to see the cardiologist. And I have to do this for three or four specialists... Well, it’s a bit of a hassle […] it's not always easy or straightforward”. P11.2
Some participants had financial difficulties or constraints, such as expenses from their hospitalization, ambulance transportation, and medications not covered by their health insurance plans. This led to misunderstandings, stress, and anxiety, especially because some participants could not return to work or, to a lesser extent, because of their medical condition.
To ensure continuity of care, some participants were proactive in their case management, for example, by calling to confirm or obtain further information on an appointment or to ensure information transfer. Written convocations for upcoming medical appointments and tailored explanations helped the participants organize their care. Family caregivers were also key in taking participants to various consultations, reminding them, and managing their medical appointments.
Information transfer: incomplete and missing information
Information transfer between and within settings was occasionally lacking. Even weeks after hospitalization, some documents were not transmitted to outpatient physicians, sometimes delaying medical care. Some participants reported receiving incomplete, unclear, or contradictory information from different HCPs, sometimes leading to doubts, seeking a second medical opinion, or personal searches for information. A few proactive participants ensured good information transmission by making a copy of the prescription or sending copies of their documents to physicians:
“My GP hasn't received anything from the hospital yet. I’ve sent him the PDF with the medication I take before our appointment […] Yes, It’s the patient that does all the job.” P10.3
Interprofessional work: a practice highlighted by some participants
Several participants highlighted the interprofessional work they observed in the outpatient setting, especially because they had several comorbidities; therefore, several physicians followed their care:
“My case is very complex! For example, between the cardiologist and the diabetologist, they need to communicate closely because there could be consequences or interactions with the medications I take [for my heart and my diabetes].” P4.2
Health professionals referred their patients to the most appropriate provider for better follow-up (e.g., a nurse specializing in addictology referred a patient to a nurse specializing in diabetology for questions and follow-up on blood sugar levels). Interprofessional collaboration between physicians and pharmacists was noted by some participants, especially for prescription refills or ordering medications.
Patient-HCPs relationships: the importance of trust
Trust in the care relationship was discussed by the participants regarding different HCPs, especially GPs and community pharmacists. Most participants highlighted the communication skills and active listening of healthcare providers. Knowing an HCP for several years helped build trust and ensure an updated medical history:
“I've trusted this pharmacist for 20 years. I can phone her or go to the pharmacy to ask any question[...] I feel supported.” P3.2
Some participants experienced poor encounters owing to a lack of attentive listening or adapted communication, especially when delivering bad news (new diagnoses or deterioration of health status). Professional competencies were an important aspect of the patient-HCP relationship, and some participants lost confidence in their physician or pharmacist because of inadequate medical or pharmaceutical care management or errors, such as the physician prescribing the wrong medication dosage, the pharmacist delivering the wrong pillbox or the general practitioner refusing to see a patient:
“I think I'll find another doctor… In fact, the day I was hospitalized, I called before to make an appointment with her and she refused to see me […] because I had a fever, and I hadn’t done a [COVID] test.” P6.2
Most participants underlined the importance of their GP because they were available, attentive to their health issues, and had a comprehensive view of their medications and health, especially after hospitalization:
“Fortunately, there are general practitioners, who know everything. With some specialists, the body is fragmented, but my GP knows the whole body.” P14.1
After hospitalization, the GP’s role changed for some participants who saw their GP infrequently but now played a central role.
Community pharmacist: an indistinct role
Pharmacists and their teams were appreciated by most participants for their interpersonal competencies, such as kindness, availability, professional flexibility, and adaptability to patients’ needs to ensure medication continuity (e.g., extension of the prescription, home delivery, or extending time to pay for medications). The role of community pharmacists varied according to the participants. Some viewed pharmacists as simple salespeople:
“It's like a grocery store. [...] I go there, it's ordered, I take my medication, I pay and I leave.” P23.3
For others, the pharmacist provided medication and advice and was a timely source of information but did not play a central role in their care. For others, the pharmacist’s role is essential for medication monitoring and safety:
“I always go to the same pharmacy […] because I know I have protection: when [the pharmacist] enters the medications in his computer, if two medications are incompatible, he can verify. [...] There is this follow-up that I will not have if I go each time somewhere else.” P10.4
The patient journey mapping methodology, coupled with qualitative thematic analysis, enabled us to understand and shed light on the intricacies of the journey of polypharmacy patients with T2Din the healthcare system after discharge. This provided valuable insights into their experiences, challenges, and opportunities for improvement.
This study highlights the complex pathways of patients with comorbidities by considering the population of patients with T2D as an example. Our population included a wide variety of patients, both newly diagnosed and with known diabetes, hospitalized for T2D or other reasons. Navigating the healthcare system was influenced by the reason for hospitalization and diagnosis. For example, newly diagnosed participants with T2D had a closer follow-up after discharge, participants were more likely to undergo cardiac rehabilitation after infarction, and participants with a former T2D diagnosis were more complex, with more comorbidities and more HCP encounters. Our aim was not to compare these populations but to highlight particularities and differences in their health care and these qualitative data reveal the need for further studies to improve diabetes management during inpatient to outpatient care transition.
The variability in discharge practices and coordination with outpatient care highlights the lack of standardization during and after hospital discharge. Some participants had a planned appointment with their GP before discharge, others had a telephone call with a hospital or ambulatory physician, and some had no planned follow-up, causing confusion and stress. Although various local or national guidelines exist for managing patients discharged from the hospital [ 36 , 37 , 38 , 39 ], there are no standard practices regarding care coordination implemented in the setting of this study. The lack of local coordination has also been mentioned in other studies [ 5 , 40 , 41 ].
Our results also raise questions about the responsibility gap in the transition of care. Once discharged from the hospital, who is responsible for the patient until their first medical appointment? This responsibility is not clearly defined among hospital and outpatient care providers, with more than 25% of internal medicine residents indicating their responsibility for patients ending at discharge [ 42 , 43 ]. Importance should be given to clarifying when and who will take over the responsibility of guaranteeing patient safety and continuity of care and avoiding rehospitalization [ 44 ].
The first visit with the community pharmacist after discharge and the referring physician were the key encounters. While the role of the GP at hospital discharge is well-defined, the community pharmacist’s role lacks clarity, even though they are the first HCP encountered upon hospital discharge. A meta-analysis showed the added value of community pharmacists and how their active participation during care transition can reduce readmission [ 18 ]. A better definition of the pharmacist’s role and integration into care coordination could benefit patient safety during the transition and should be assessed in future studies.
Our findings showed that the time elapsed between discharge and the first medical appointment varied widely (from 1 to 27 days), correlating with findings in the literature showing that more than 80% of patients see their GP within 30 days [ 45 ]. Despite the first medical appointment being within the first month after discharge, some patients in our study reported a lack of support and follow-up during the first few days after discharge. Care coordination at discharge is critical, as close outpatient follow-up within the first 7–10 days can reduce hospital readmission rates [ 46 , 47 ]. Furthermore, trust and communication skills are fundamental components of the patient-HCP relationship, underlined in our results, particularly during the first medical appointment. Relational continuity, especially with a particular HCP who has comprehensive patient knowledge, is crucial when patients interact with multiple clinicians and navigate various settings [ 48 , 49 ].
Navigating the outpatient healthcare system after discharge was complex for most participants and relied heavily on patient involvement and responsibility. While some participants who received clear information felt more empowered and engaged in their care, others highlighted the difficulty in organizing their care during this vulnerable period. Such difficulties in case management have been described previously [ 50 , 51 ]. Moreover, services proposed by HCPs (e.g., home assistance) do not always correspond to patient needs and are sometimes refused. This highlights the tension between HCPs’ medical recommendations, priorities, and patient expectations. This tension between medical priorities and patient needs was felt during hospitalization and shaped the 2 months following discharge. HCPs need to assess patient needs and preferences during hospitalization and transition for follow-up services. They must also ensure that the offered services meet at least the most relevant of patients’ perceived needs to improve seamless care and patient safety [ 52 , 53 ].
Examples of a lack of communication and information transfer were described in our results at different levels among HCPs, between participants or family caregivers, and HCPs, and these findings correlate with the literature [ 3 , 54 , 55 , 56 ]. Although family caregivers play an important role in supporting patients in the healthcare system, they are also additional interlocutors, leading to missed opportunities for patient-pharmacist interactions when dispensing discharged medication. Therefore, it is paramount to integrate and involve family caregivers in shared decision-making and communicate with patients remotely when they are not present [ 57 ].
Opportunities to improve the discharge of patients returning home after discharge without home care are highlighted in this article. Our insights can serve as a valuable foundation for healthcare providers and policymakers seeking to optimize patient experience and quality of care in the post-discharge phase. Different professionals should be integrated into standard practice through guidelines to ensure improved collaboration from hospital discharge to outpatient care. During hospitalization:
an appointment should be scheduled with the referring physician shortly after discharge to guarantee continuity of care
a hospital discharge interview should be conducted in a systematic way to summarize and securely close the hospitalization
the community pharmacist should be informed before the patient’s discharge to prepare and reconcile medications before and after hospitalization
In outpatient care:
an in-person or phone encounter with the pharmacy team should be scheduled for the patient and/or caregivers at discharge
a contact point (phone number, email, or virtual chat assistant) or scheduled follow-up should be implemented to answer questions and redirect patients before they can meet with the referring physician
a long-term and active communication channel between HCPs should be established.
In other countries, several outpatient services are already available for patients discharged home to enhance continuity of care and patient safety after discharge. The telehealth-based Transitional Care Management Programme, a local initiative in a New York hospital, involves contacting discharged patients 24 to 48 hours after discharge to support understanding of discharge instructions, medication access, follow-up appointments, and social needs [ 58 ]. The Australian Government has introduced the Transition Care Program that provides short-term care for older people, including social work, nursing support, personal care, and allied health care [ 59 ]. In England, the NHS has introduced the Discharge Medicines Service (DMS) in community pharmacies, which aims to improve communication between hospitals and community pharmacies and to ensure that patients understand changes to their medications [ 60 ].
Limitations
This study has several limitations. First, the accuracy of the encounter dates with HCPs, as described by the participants, could not be verified using a second data source (e.g., medical or pharmacy records). Additionally, recall biases cannot be excluded, especially during interviews 3 and 4, which took place at longer intervals (20 days between interviews 2 and 3 and 30 days between interviews 3 and 4). Nevertheless, our findings express a patient's representation of their healthcare system navigation experience. Secondly, these results may not be generalizable to populations with other long-term diseases, even though we recruited patients with different reasons for hospitalization, including age, sex, and comorbidities. In addition, the study region is predominantly an urban area with a high density of HCPs, which may influence patient journeys in the healthcare system. Finally, we excluded patients whose medications were managed by HCPs because these patients might have had different experiences, difficulties, and needs. This exclusion criterion was chosen because our objective was to investigate patients’ medication self-management, as described in another article [ 28 ].
A patient’s journey in the 2 months following discharge is unique for each individual and constitutes a complex and adaptive process. Despite the active role of numerous HCPs, navigation in outpatient care after discharge relies heavily on the involvement and responsibilities of polypharmacy. The findings of this study highlight the need to standardize the approach for discharge planning and post-discharge care in partnership with patients and caregivers. Preparation for discharge, the first visit to the pharmacy, and the first appointment with the GP are key moments for all patients, along with the involvement of other medical and nurse specialists, as needed. Standardizing practices, clarifying responsibilities, integrating community pharmacists during the transition, empowering patients, and enhancing interprofessional communication and collaboration should be explored and implemented to achieve better patient outcomes and a more seamless healthcare journey for individuals transitioning from the hospital to the community.
Availability of data and materials
The qualitative codes in French and anonymized patient datasets are available from the corresponding author on reasonable request. Individual patient journeys are provided in the Supplementary Files.
Abbreviations
General practitioner
Healthcare professional
type 2 diabetes mellitus
Coleman EA, Boult C. Improving the quality of transitional care for persons with complex care needs. J Am Geriatr Soc. 2003;51(4):556–7.
Article PubMed Google Scholar
Allen J, Hutchinson AM, Brown R, Livingston PM. User experience and care for older people transitioning from hospital to home: Patients’ and carers’ perspectives. Health Expect. 2018;21(2):518–27.
Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. Jama. 2007;297(8):831–41.
Article CAS PubMed Google Scholar
Allen J, Hutchinson AM, Brown R, Livingston PM. Quality care outcomes following transitional care interventions for older people from hospital to home: a systematic review. BMC Health Serv Res. 2014;14:346.
Article PubMed PubMed Central Google Scholar
Hesselink G, Flink M, Olsson M, Barach P, Dudzik-Urbaniak E, Orrego C, et al. Are patients discharged with care? A qualitative study of perceptions and experiences of patients, family members and care providers. BMJ Qual Saf. 2012;21(Suppl 1):i39-49.
World Health Organization (WHO). Transitions of Care. 2016.
Google Scholar
Krumholz HM. Post-hospital syndrome–an acquired, transient condition of generalized risk. N Engl J Med. 2013;368(2):100–2.
Article CAS PubMed PubMed Central Google Scholar
Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–28.
Banholzer S, Dunkelmann L, Haschke M, Derungs A, Exadaktylos A, Krähenbühl S, et al. Retrospective analysis of adverse drug reactions leading to short-term emergency hospital readmission. Swiss Med Wkly. 2021;151:w20400.
World Health Organization (WHO). Medication Safety in Transitions of Care. 2019.
Müller-Wieland D, Merkel M, Hamann A, Siegel E, Ottillinger B, Woker R, et al. Survey to estimate the prevalence of type 2 diabetes mellitus in hospital patients in Germany by systematic HbA1c measurement upon admission. Int J Clin Pract. 2018;72(12):e13273.
Blanc AL, Fumeaux T, Stirnemann J, Dupuis Lozeron E, Ourhamoune A, Desmeules J, et al. Development of a predictive score for potentially avoidable hospital readmissions for general internal medicine patients. PLoS One. 2019;14(7):e0219348.
Hansen LO, Greenwald JL, Budnitz T, Howell E, Halasyamani L, Maynard G, et al. Project BOOST: effectiveness of a multihospital effort to reduce rehospitalization. J Hosp Med. 2013;8(8):421–7.
Khan MAB, Hashim MJ, King JK, Govender RD, Mustafa H, Al Kaabi J. Epidemiology of Type 2 Diabetes - Global Burden of Disease and Forecasted Trends. J Epidemiol Glob Health. 2020;10(1):107–11.
Iglay K, Hannachi H, Joseph Howie P, Xu J, Li X, Engel SS, et al. Prevalence and co-prevalence of comorbidities among patients with type 2 diabetes mellitus. Curr Med Res Opin. 2016;32(7):1243–52.
Russell LB, Suh DC, Safford MA. Time requirements for diabetes self-management: too much for many? J Fam Pract. 2005;54(1):52–6.
PubMed Google Scholar
Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155(8):520–8.
Lussier ME, Evans HJ, Wright EA, Gionfriddo MR. The impact of community pharmacist involvement on transitions of care: a systematic review and meta-analysis. J Am Pharm Assoc. 2020;60(1):153.
Article Google Scholar
Donzé J, John G, Genné D, Mancinetti M, Gouveia A, Méan M, et al. Effects of a Multimodal Transitional Care Intervention in Patients at High Risk of Readmission: The TARGET-READ Randomized Clinical Trial. JAMA Intern Med. 2023.
Leppin AL, Gionfriddo MR, Kessler M, Brito JP, Mair FS, Gallacher K, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med. 2014;174(7):1095–107.
Noonan VK, Lyddiatt A, Ware P, Jaglal SB, Riopelle RJ, Bingham CO 3rd, et al. Montreal Accord on Patient-Reported Outcomes (PROs) use series - Paper 3: patient-reported outcomes can facilitate shared decision-making and guide self-management. J Clin Epidemiol. 2017;89:125–35.
Hesselink G, Schoonhoven L, Barach P, Spijker A, Gademan P, Kalkman C, et al. Improving patient handovers from hospital to primary care: a systematic review. Ann Intern Med. 2012;157(6):417–28.
(WHO) WHO. Systems in the who European region: framework for action on integrated health services delivery. Copenhagen: WHO; 2016.
Damery S, Flanagan S, Combes G. The effectiveness of interventions to achieve co-ordinated multidisciplinary care and reduce hospital use for people with chronic diseases: study protocol for a systematic review of reviews. Syst Revi. 2015;4(1):64.
Noor F, Gulis G, Karlsson LE. Exploration of understanding of integrated care from a public health perspective: a scoping review. J Public Health Res. 2023;12(3):22799036231181210.
Jackson K, Oelke ND, Besner J, Harrison A. Patient journey: implications for improving and integrating care for older adults with chronic obstructive pulmonary disease. Can J Aging. 2012;31(2):223–33.
Gualandi R, Masella C, Viglione D, Tartaglini D. Exploring the hospital patient journey: what does the patient experience? PLoS One. 2019;14(12):e0224899.
Solh Dost L, Gastaldi G, Schneider M. Patient medication management, understanding and adherence during the transition from hospital to ambulatory care – a qualitative longitudinal study in polymorbid type 2 diabetes patients. BMC Health Services Research, in press
World Health Organization (WHO). Adherence to long-term therapies: Evidence for action. 2003.
Fisher JD, Fisher WA, Amico KR, Harman JJ. An information-motivation-behavioral skills model of adherence to antiretroviral therapy. Health Psychol. 2006;25(4):462–73.
Bandura A. Health promotion from the perspective of social cognitive theory. Psychol Health. 1998;13(4):623–49.
Hennink MM, Kaiser BN, Marconi VC. Code saturation versus meaning saturation: how many interviews are enough? Qual Health Res. 2016;27(4):591–608.
Braun V, Clarke V. Reflecting on reflexive thematic analysis. Qual Res Sport Exercise Health. 2019;11(4):589–97.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Davies EL, Bulto LN, Walsh A, Pollock D, Langton VM, Laing RE, et al. Reporting and conducting patient journey mapping research in healthcare: a scoping review. J Adv Nurs. 2023;79(1):83–100.
California pharmacists association. Transitions of Care Resource Guide https://cdn.ymaws.com/www.cshp.org/resource/resmgr/Files/Practice-Policy/For_Pharmacists/transitions_of_care_final_10.pdf . Accessed 20 Nov 2023.
National Health Service (NHS). Guidance: Hospital discharge and community support guidance. 2022. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1087354/Hospital-Discharge-and-Community-Support-Guidance-2022-v2.pdf . Accessed 01 Apr 2024.
Winnipeg Regional Health Authority. Safe Patient Discahrge Guideline. 2017. https://wrha.mb.ca/files/guideline-safe-discharge.pdf . Accessed 01 Apr 2024.
Haute Autorité de Santé, France. Check-List de Sortie d'hospitalisation supérieure à 24 heures https://www.has-sante.fr/jcms/c_2035081/fr/check-list-de-sortie-d-hospitalisation-superieure-a-24h . Accessed 04 Apr 2024.
Wong ELY, Yam CHK, Cheung AWL, Leung MCM, Chan FWK, Wong FYY, et al. Barriers to effective discharge planning: a qualitative study investigating the perspectives of frontline healthcare professionals. BMC Health Serv Res. 2011;11(1):242.
Urban R, Paloumpi E, Rana N, Morgan J. Communicating medication changes to community pharmacy post-discharge: the good, the bad, and the improvements. Int J Clin Pharm. 2013;35(5):813–20.
Young E, Stickrath C, McNulty MC, Calderon AJ, Chapman E, Gonzalo JD, et al. Internal medicine residents’ perceived responsibility for patients at hospital discharge: a national survey. J Gen Intern Med. 2016;31(12):1490–5.
Jones CD, Vu MB, O’Donnell CM, Anderson ME, Patel S, Wald HL, et al. A failure to communicate: a qualitative exploration of care coordination between hospitalists and primary care providers around patient hospitalizations. J Gen Intern Med. 2015;30(4):417–24.
Watts R, Pierson J, Gardner H. Co-ordination of the discharge planning process in critical care. J Clin Nurs. 2007;16(1):194–202.
Roughead EE, Kalisch LM, Ramsay EN, Ryan P, Gilbert AL. Continuity of care: when do patients visit community healthcare providers after leaving hospital? Intern Med J. 2011;41(9):662–7.
Riverin BD, Strumpf EC, Naimi AI, Li P. Optimal timing of physician visits after hospital discharge to reduce readmission. Health Serv Res. 2018;53(6):4682–703.
Coppa K, Kim EJ, Oppenheim MI, Bock KR, Conigliaro J, Hirsch JS. Examination of post-discharge follow-up appointment status and 30-day readmission. J Gen Intern Med. 2021;36(5):1214–21.
Haggerty JL, Roberge D, Freeman GK, Beaulieu C. Experienced continuity of care when patients see multiple clinicians: a qualitative metasummary. Ann Fam Med. 2013;11(3):262–71.
Baker R, Freeman G, Boulton M, Windridge K, Tarrant C, Low J, et al. Continuity of care: patients’ and carers’ views and choices in their use of primary care services. Report for the national co-ordinating center for NHS Service Delivery and Organisation R & D (NCCSDO). 2006.
Arora VM, Prochaska ML, Farnan JM, D’Arcy MJt, Schwanz KJ, Vinci LM, et al. Problems after discharge and understanding of communication with their primary care physicians among hospitalized seniors: a mixed methods study. J Hosp Med. 2010;5(7):385–91.
Allen J, Hutchinson AM, Brown R, Livingston PM. User experience and care integration in transitional care for older people from hospital to home: a meta-synthesis. Qual Health Res. 2016;27(1):24–36.
Krook M, Iwarzon M, Siouta E. The discharge process-from a patient’s perspective. SAGE Open Nurs. 2020;6:2377960819900707.
PubMed PubMed Central Google Scholar
Huber DL, McClelland E. Patient preferences and discharge planning transitions. J Prof Nurs. 2003;19(4):204–10.
Ravenscroft E. Navigating the health care system: insights from consumers with multimorbidity. J Nurs Healthcare Chronic Illness. 2010;2:215–24.
Ancker JS, Witteman HO, Hafeez B, Provencher T, Van de Graaf M, Wei E. The invisible work of personal health information management among people with multiple chronic conditions: qualitative interview study among patients and providers. J Med Internet Res. 2015;17(6):e137.
Manias E, Gerdtz M, Williams A, McGuiness J, Dooley M. Communicating about the management of medications as patients move across transition points of care: an observation and interview study. J Eval Clin Pract. 2016;22(5):635–43.
Mackie BR, Mitchell M, Marshall AP. Patient and family members’ perceptions of family participation in care on acute care wards. Scandinavian J Caring Sci. 2019;33(2):359–70.
Michelle E, Rachel CSF, Jonathan S, Priscilla H, Farrukh NJ. Telehealth-based transitional care management programme to improve access to care. BMJ Open Qual. 2023;12(4):e002495.
Department of Health and Aged Care, Australia. Transition Care Programme. https://www.health.gov.au/our-work/transition-care-programme . Accessed 03 Apr 2024
National Health Service (NHS) Discharge Medicines Service. 2021. https://www.england.nhs.uk/primary-care/pharmacy/pharmacy-services/nhs-discharge-medicines-service/ . Accessed 03 Apr 2024
Download references
Acknowledgments
The authors would like to thank all the patients who took part in this study. We would also like to thank the Geneva University Hospitals Patients Partners +3P platform as well as Mrs Tourane Corbière and Mr Joël Mermoud, patient partners, who reviewed interview guides for clarity and significance.
Open access funding provided by University of Geneva This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
School of Pharmaceutical Sciences, University of Geneva, Geneva, Switzerland
Léa Solh Dost & Marie P. Schneider
Institute of Pharmaceutical Sciences of Western Switzerland, University of Geneva, Geneva, Switzerland
Division of Endocrinology, Diabetes, Hypertension and Nutrition, Department of Medicine, Geneva University Hospitals, Geneva, Switzerland
Giacomo Gastaldi
Institute of Psychology and Education, University of Neuchatel, Neuchâtel, Switzerland
Marcelo Dos Santos Mamed
Institute of Psychology, University of Lausanne, Lausanne, Switzerland
You can also search for this author in PubMed Google Scholar
Contributions
LS, GG, and MS conceptualized and designed the study. LS and GG screened and recruited participants. LS conducted the interviews. LS, GG, and MS performed data analysis and interpretation. LS drafted the manuscript and LS and MS worked on the different versions. MDS contributed its expertise and external opinion as a clinical psychologist and linguist. All authors read and approved the final manuscript.
Corresponding authors
Correspondence to Léa Solh Dost or Marie P. Schneider .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval was sought and granted by the Cantonal Research Ethics Commission, Geneva (CCER) (2020-01779). Informed consent to participate was obtained for all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Interview guides.
Additional file 2.
Individual patient journey mappings from discharge to 2 months after discharge.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Solh Dost, L., Gastaldi, G., Dos Santos Mamed, M. et al. Navigating outpatient care of patients with type 2 diabetes after hospital discharge - a qualitative longitudinal study. BMC Health Serv Res 24 , 476 (2024). https://doi.org/10.1186/s12913-024-10959-4
Download citation
Received : 17 January 2024
Accepted : 07 April 2024
Published : 17 April 2024
DOI : https://doi.org/10.1186/s12913-024-10959-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Type 2 diabetes mellitus
- Outpatient care
- Hospital discharge
- Qualitative research
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- Open access
- Published: 12 April 2024
Qualitative analysis of mothers’ perception related to the delivery of information regarding preterm births
- Doriane Randriamboarison 1 na1 ,
- Elisa Fustec 2 na1 ,
- Isabelle Enderlé 2 , 3 ,
- Mathilde Yverneau 1 , 3 ,
- Karine Le Breton 1 , 2 ,
- Linda Lassel 2 ,
- Nadia Mazille-Orfanos 1 &
- Patrick Pladys 1 , 3
BMC Pregnancy and Childbirth volume 24 , Article number: 272 ( 2024 ) Cite this article
75 Accesses
1 Altmetric
Metrics details
Preterm birth is a major health issue due to its potential outcomes and socioeconomic impact. Prenatal counseling is of major importance for parents because it is believed that the risk of preterm birth is associated with a higher parental mental burden. Nowadays in France, the content and delivery of antenatal counseling is based on personal experience since there is a lack of official guidelines. The goal of the study was to evaluate maternal perception of antenatal information delivered in the setting of preterm births.
A qualitative study was performed using semi-structured individual interviews of 15 mothers with a child born > 26–34 GW. Data analysis was based on a constant comparative method.
Concerning prenatal counseling content, parents wanted to be informed of their role in the care of their preterm child more so than statistics that were not always considered relevant. Parents’ reactions to the announcement of the risk of a preterm birth was dominated by stupefaction, uncertainty and anxiety. When it comes to the setting of prenatal counseling, patients’ room was deemed an appropriate setting by parents and ideally the presence of a coparent was appreciated as it increased patients’ understanding. The physicians’ attitude during the counseling was considered appropriate and described as empathic and optimistic. The importance of support throughout the hospitalization in the form of other parents’ experiences, healthcare professionals and the possibility to preemptively visit the NICU was emphasized by participants. Delivery experience was dominated by a sense of uncertainty, and urgency. Some leads for improvement included additional support of information such as virtual NICU visit; participants also insisted on continuity of care and the multidisciplinary aspect of counseling (obstetrician, neonatologist, midwife, nurse, lactation consultant and psychologist).
Highlighting parents’ expectations about prenatal counseling could lead to the establishment of overall general guidelines. However, some topics like the use of statistics and mentioning the risk of death underline the importance of a personalized information.
Peer Review reports
Introduction
According to the latest French National Prenatal Survey (NPS), the rate of preterm birth was 7% in 2021, which represents about 46,000 newborns [ 1 ].This rate has remained stable since 2016. Most of preterm deliveries happen between 32 and 36 GW (5.3%), and1.7% occurbetween 22 and 31 GW [ 1 ].
Preterm birth has long term effects and even though survival without neuromotor or sensory disabilities has improved in the last decades from 45.5% in 1997 to 62% in 2011 [ 2 ], ex-preterm infants present more neurodevelopmental complications and motor disorders such as cerebral palsy, cognitive disabilities, school learning disabilities [ 3 , 4 ]. Considering all these outcomes and their socioeconomic impact,preterm birth represents a major health issue. Therefore, preventingpreterm labor and neonatal complications associated with a preterm birth is of utmost importance [ 2 ]. An integral part of high-risk pregnancy management is announcing to the parents that their pregnancy is no longer as they had envisioned it. It is the healthcare professional’s responsibility to make sure the patient understands all the information necessary to apprehend the medical course and to make informed decisions [ 5 ]. In this setting, communication in addition to bringing emotional support and conveying empathy also plays a legal role. This information is delivered during an antenatal consultation.
During the antenatal consultation, neonatologists focus on neonatal complications and how to manage them. This has been shown to be helpful for parents [ 6 ]. It contributes to psycho-social support, lowers risk of postpartum depression and mother-infant bonding disorder [ 7 ]. However, this new knowledge may also contribute to parents’ anxiety [ 8 ]. Parents’ needs and expectations regarding antenatal counseling are not always correctly understood by clinicians [ 9 , 10 ]. Furthermore, this information is often delivered in a stressful environment, where there is a concomitant concern for the mother’s health. Information concerning obstetrical outcomes must also be provided including causes of preterm birth, treatments, and prognosis. In this setting, delivery becomes an abrupt and unanticipated event which can generate an important amount of stress. High-risk pregnancies and emergency deliveries are more at risk to generate posttraumatic stress disorder than regular pregnancies (18.5% versus 4%) [ 11 ].Neonatal outcomes are deeply connected to the obstetrical path and perinatal collaboration between neonatal and maternal caregivers improves families’ experience in all aspects of preterm birth [ 12 ]. Therefore, the way in which information is delivered in the antenatal period has a major impact on the parents’ experience throughout their subsequent path.
Nowadays in France, the content and delivery of antenatal counseling is based on personal experience since there is a lack of official guidelines. Most studies evaluating antenatal counseling are focusing on extreme preterm birth [ 13 , 14 , 15 , 16 ]. However, even though preterm infants born after 26 GW are at lower risk of adverse outcomes, they represent an important population in terms of prognosis. Moreover, these studies essentially focus on parents’ role in deciding between active support and palliative care [ 17 ], overlooking all other aspects of prenatal information. Most research has also been conducted from a neonatological point of view without the obstetricians’ input.
The aim of this qualitative study is to evaluate maternal perception of antenatal information delivery in the setting of preterm birth between 26 and 34 GW. Our goal is to improve our practice by bringing some insights on how to best counsel patients at risk of preterm birth and help them understand complex information [ 18 ].
Study context
The neonatal and obstetric departments of the university hospital of Rennes offer prenatal counseling and maternal care to all patients at risk of preterm delivery. Information delivered is based on healthcare professionals’ experience. Concerning neonatal antenatal counseling, interviews are conducted by a senior neonatologist as soon as possible after patient’s hospital admission. If the situation evolves or if patient asks for an update, follow-up consultations may be conducted by the neonatal physician. The obstetric team (senior obstetricians and neonatologists, residents and midwives) informs patients on obstetrical care and prognostication. All information given is adjusted on clinical context and patient’s history.
A qualitative study was performed. We followed Consolidated Criteria for Reporting Qualitative Studies (COREQ) guidelines [ 19 ]. Then we analyzed quantitative population’s characteristics.
Participants
Mothers with a child born between 26 and 34 gestation weeks admitted to the NICU at the tertiary care university hospital of Rennes from January 2019 to April 2020 and discharged from the hospital at the time of inclusion were selected. The time lag between birth and interview ranged from 6 months post-discharge to a maximum of 18 months, in order to minimize memory bias We included in our study mothers who had been hospitalized in the level 3 high risk pregnancy unit of the University hospital of Rennes and received prenatal counseling from a neonatal attending physician. Some patients had their first medical care at another hospital and then were transferred to the hospital of Rennes before birth. Transferred patients were also included. Our exclusion criteria were children born before 26 GW, deceased children, deceased mother, patients under 18 years old, patients who did not speak fluently French, patients with cognitive disabilities, patients without contact information, patients who gave birth in another hospital and patients whose child (or one of the children in case of multiple pregnancy) was still hospitalized at the time of the study.
Setting and sample
A physician was responsible for explaining the research project to potential participants and for sending an email newsletter describing the purpose and outline of the research. Mothers were invited to participate in a semi-structured interview. Participants responded to this invitation via email. Investigators who conducted the interviews informed participants, in the letter and then orally, about the aim of the study and their right to withdraw their participation at any time without giving any reason. Reminders were then sent via emails to the participants who did not respond to the letter. Patients who did not have an email address were recruited by phone calls made by one of the investigators. All mothers gave their informed consent before participating. We planned on stopping inclusion of patients when saturation was achieved (i.e. no new themes or ideas were generated by subsequent interviews).
Considering the difficulty for patients to come to the hospital for the interview, we initially let participants choose between a face-to-face interview or over the phone according to their convenience. In the face of the Sars-CoV-2 pandemic and its associated restrictions, all interviews were then conducted over the phone.
Data collection
Semi-structured interviews were conducted in French by one or both interviewers who were a neonatal resident (DR) and an obstetrician-gynecologist (OB/GYN) resident (EF). Data collection spanned from June 2020 to March 2021. Interviews were semi-structured, with a predefined list of open-ended questions focusing first on the information received concerning the hospitalization, treatments, and prenatal counseling, and then on desired improvements, and open suggestions. The interview guide was developed by authors (DR, EF, NM, IE and KL) after a review of the literature before starting the study. If applicable, face-to-face interviews were conducted at a private office space located in the NICU.
To ensure consistency, we used the same interview guide in every interview (Table 1 ). The interviewers received preliminary training on reformulation to carry out the in-depth interviews with qualitative method referents. They reported their involvement after each interview. Sessions were recorded with the consent of each participant and then transcribed verbatim and de-identified. The aims and rational for the research were disclosed to the participants in the newsletter. We confirmed patient’s understanding during the interview.
Throughout the session, the moderator summarized and reformulated the results and presented them back to the participants to ensure information was accurate and that their comments had been correctly understood. At the end of the session, participants completed a short quantitative questionnaire to obtain their socio-demographic characteristics. We obtained remaining socio-demographic data from the patient electronic medical record.
Data analysis
The analysis procedure was conducted byfour researchers (EF, DR, NM and IE) using an inductive approach to identify themes that emerged from the data. Each transcript was independently read several times to facilitate immersion in the data.The thematic analysis of the data promoted a logic of emergence. The interviews were first analyzed using a manual method of coding the themes and sub-themes. The researchers used open coding process to summarize participants’ views by assigning words to quotes or paragraphs. The coding of the researchers were then compared and in the event of any discrepancies or a disagreement, other physicians (MY, KL, LL and PP) adjudicated. This method enhances the validity of the assigned themes. We kept including participants in the study until saturation was achieved (i.e. no new themes or ideas were generated by subsequent interviews).
The list of themes and sub-themes was then generated and extracted in tabular form. Constant comparative analysis was used to assess overall saturation [ 20 ]. Authors selected verbatim quotes to illustrate the thematic findings. We coded data from transcripts using the Saldaña method [ 21 ] To ensure the reliability of the coding and analysis of the data, findings were discussed among the authors. At the same time we used the NVivo® 12 Plus software interface (QSR International) to support the coding tree. The software was also used to check the frequency of occurrence of themes and to ensure that our main themes were consistent. NVivo’s contribution was also to facilitate the link between the highlighted themes and the verbatim references.
Ethical considerations
The study was approved by the local Ethics Committee (reference number 20.61). Participation was on a voluntary basis. The university hospital of Rennes recorded the material in accordance with all French ethical regulations (ref: MR-003).
We conducted a total of 15 interviews, which took place between June 2020 and March 2021.We obtained data saturation after 12 interviews. Amongst the three first participants who were given the choice of the interview setting, two of them decided on a face-to-face interview, and the last one over the phone. For all remaining participants, we only conducted phone interviews.Average length of interviews is 44 min ± 11 min (minimum 25 min, maximum 66 min). Face to face interviews lasted 32 and 42 min each.
Participant’s characteristics are presented in Table 2 . On average, participating mothers were 31.4 years old (± 4.9 years). Newborns were on average 30.2 ± 2.5 weeks of gestation at birth.
Characteristics of prenatal counseling
Circumstances of prenatal counseling are reported in Table 3 . Interviews mostly took place in the patient’s hospital room, and within the first days after admission.
Thematic analysis
Seven themes were extracted from our data analysis. We subdivided each theme into sub-themes and illustrated some of them with participants’ quotes from the interview (presented in Table 4 ).
Prenatal counseling content.
Neonatal complications and care .
Information delivered during prenatal counseling was the most mentioned during the interviews. Participants recalled being told about neonatal complications. They talked about respiratory outcomes first, short and long term. Then neurological complications were evoked including specific follow-up and neurosensorial risks. Mothers also reported receiving information concerning the NICU: the rooms, the equipment, the incubator. They remembered being told about the usual medical course and the steps during hospitalization.
Parents’ role .
How participants should act with their preterm newborn is commonly addressed during antenatal consultation. Mentioning the baby’s future life makes parenthood more real. For instance, practical aspects such as transferring parents’ smell through comfort blankets and cuddly toys were greatly appreciated. Being able to spend unlimited time with their child was also reassuring. Breastfeeding is another important topic, especially knowing that it is feasible even in case of preterm delivery. This notion was carried by the obstetric team. Midwives adapted their support to patients’ need, no matter what they first wished. A participant explained that she changed her mind based on the information she received about the role of breast milk for preterm babies: ‘Midwives who listened, who taught me how to pump my milk even though I was totally reluctant to breastfeed’ (patient no 2).
Finally, participants mentioned skin to skin as a beneficial act to their child’s well-being. Mothers report highly on it, as shown by patient no 8’s quote: “they told me that I could stay close to her, that I was going to be able to touch her […] to hold her against me. When I was told that, I felt a lot better because I didn’t know I would have the opportunity to hold her.”
Use of statistics .
To participants, statistics and numbers were either not mentioned or considered irrelevant. Indeed, seven patients reported not receiving any and seven had no recall of any statistics. Only one patient was looking for statistical data in the prenatal counseling and insisted on receiving some. When asked if they wished they were given some, four participants were against, four would have appreciated it and seven had no opinion. The ones in favor explained they wanted to hear positive numbers such as survival rates. Some participants described themselves as wanting to know everything and be as informed as possible. Participants who did not wish to receive any statistics argued that it would have scared them, and made them worry about worst case scenario.
Risk of death .
Mortality of preterm children was not mentioned to every participant as four participants reported death not being talked about during antenatal counseling. Avoiding this subject was appreciated by some participants. One mentioned they felt like practitioners could sense which information was relevant to them. To other participants, not talking about death could lead parents to imagine the worst-case scenario.
Mothers’ feelings and reactions.
Announcement of a risk of preterm birth .
Participants often reported feeling paradoxically in good health while being diagnosed with a risk of preterm birth. Therefore, such a diagnosis was reported as being a shock. Another feeling commonly mentioned is fear for the child’s health. On the contrary, some participants felt optimistic.
Prenatal hospitalization experience .
When asked how their hospital stay went, participants reported as many positive aspects as negative ones. They generally appreciated the close medical attention and support which were reassuring. However, some of them also mentioned the difficulty to accept the fact that they needed to stay in the hospital. Feelings mentioned by order of frequency were stupefaction, uncertainty, hope and anxiety. The sudden change during their pregnancy brought disorientation to some participants. Another feeling described was not knowing exactly what would happen to them and when delivery would occur. Participants also mentioned developing some hope during their hospital stay, especially for participants who were hospitalized for the longest period of time. As time went by and nothing serious was happening, they found themselves hoping they would slowly escape preterm birth’s adverse outcomes. The whole experience of a risk of preterm birth generated anxiety for several participants. They continuously feared for their child’s life. Moreover, being hospitalized, away from their homes and relatives, could enhance this anxiety.
Circumstances of prenatal counseling.
Co-parent present .
Both parents being present during antenatal counseling was the most frequent situation. Having the other parent present allowed to reflect further on what had just been said. It kept the information alive and encouraged questions.
Organization of prenatal counseling .
All participants could describe how prenatal counseling went. Consultations happened in their hospital room, which participants found appropriate.
Counselor’s attitude .
Participants commented on the physician’s skills. Fourteen of them defined the neonatologist as optimistic, and showing empathy. They reported the physician using understandable language to them. According to participants, the counselor also personalized information according to the patient and the situation, as Patient no 1 mentioned: ‘I think they really understood [me] and told me what I needed to know without telling me too much.’
Support during prenatal hospitalization.
Close relatives seemed to be the most important emotional support throughout hospitalization. The other parent was the most mentioned, followed by first-degree family members, especially mothers and sisters, and for some participants, friends. Healthcare professionals were also referred as supportive. Midwives and assistant nurses were in the first line of patient’s care and mothers relied on them. The psychologist was also cited, bringing moral, psychological, and emotional support. Shared experience with other parents who went through a similar path were appreciated by participants. They mentioned feedback from relatives who had a preterm delivery, letters, and pictures from former parents of NICU’s babies, who are now doing well. One patient said she had the need to search the internet, even though it did not necessarily bring her comfort. The tour of the NICU was also appreciated by mothers and considered as a real source of support.
Delivery experience.
Participants described information on delivery as clear but mentioned the difficulty dealing with delivery’s unpredictability. They had questions on how far in their pregnancy they could possibly go, whether they were going to deliver vaginally or by cesarean, if they were going to be induced. Mothers also talked a lot about the urgency of delivery and reported a feeling of being rushed. The need for support in this difficult situation was important. The presence of the co-parent was requested by participants, although it may not always have been possible if delivery was impending. They counted on the midwives and the obstetric team to support them as well.
Additional sources of information.
The most mentioned source of information was the tour of the NICU, when the patient’s health allowed it, and delivery was not impending. Written documents were also presented to patients and appreciated. Most participants mentioned receiving paper documents, including one on breastfeeding and one explaining planned cesarean section. Some participants reported searching information on the internet.
Suggestions for improvement.
Additional support of information .
Participants suggested pictures and videos. A virtual tour of the NICU to show the rooms with their equipment was also mentioned. The expectation of what the photographs should describe was controversial. Pamphlets with pictures of staff members to help identify each professional’s face and tasks were suggested. Written documents about local neonatal units, from highly intensive care to current care, and how they connect to each other, would be appreciated as well. Explanations on milk collection centers (lactarium) were also requested as several participants did not have a complete understanding of their functioning.
Antenatal information .
Participants wanted the same practitioners to perform the consultation, as they sought continuity of care and commitment from healthcare professionals. Several participants also mentioned that the presence of a neonatal nurse during the neonatologist’s counseling would be beneficial. One participant suggested having the psychologist present to adjust psychological follow-up after the meeting. Sharing other parents’ experiences was also brought up. Participants wished they could have joined talk groups in the high pregnancy risks unit. Participant no 9 suggested to tell future parents confronted with a risk of preterm birth about the care of a preterm child: “And to tell them it’s a fight for the baby and it’s a fight for the parents.”
Postpartum care .
Several participants addressed postpartum mothers’ care. They expressed the need to be hospitalized in a unit without any newborn instead of the usual post-delivery maternity units, as it made the absence of their child harder to endure. Some of them even wished to be in the same room as their infant, included in the intensive care unit, such as Kangaroo Mother Care (KMC) units. Another commonly mentioned topic was breastfeeding: they wished for more help and support during the first steps of setting breastfeeding.
This study on the information related to preterm birth and its consequences, delivered during prenatal care, gives a thorough insight into the perception of mothers faced with the care of a preterm infant. The announcement of a risk ofpreterm birth came as a shock for patients, as there often was no forerunner. However, the information delivered byneonatologists was overall described as clear, adapted, and carried out with optimism and empathy. Concerning hospitalization in the high-risk pregnancy unit, participants emphasized the importance of having different sources of support to help them cope with anxiety and unpredictability. The feedback provided by participants to improve the delivery of information included the development of visual sources of information.
Providing information on a situation that cannot be predicted is a difficult task. Parents need to be aware that the ability to give an accurate prognosis before delivery remains limited [ 22 ]. Our study shows that some parents wish to have as much information as possible to be fully prepared, whereas others would like to only hear what is very necessary. Many studies on prenatal counseling have shown the importance of personalized information. Most of them focus on the field of extreme prematurity. However, Gaucher et al. demonstrated, in a preliminary qualitative study of 5 interviews [ 23 ], results comparable to our own on the content of patients’ expectations during this antenatal interview. This initial study was followed by a quantitative study [ 24 ] designed to verify their results on a larger scale using a quantitative method. This is one of the few studies which has focused on the maternal experience beyond extreme prematurity, but with a quantitative approach. Healthcare professionals must try to identify parents’ expectations and adapt their speech accordingly [ 18 ]. Culture and social background should also be taken into consideration, as well as level of understanding [ 25 ]. Personalization is probably the most important aspect and should be applied to all parts of antenatal care [ 26 , 27 ](. We also found these results in our study, but our qualitative approach, which is relevant for assessing mothers’ experiences, provided additional data on the way in which parents wish to receive this information. Learning how to identify parents’ wishes should be a part of residents’ training as it is not an easy task. Moreover, delivering unwanted information can create the wrong environment and hinder the parents and healthcare providers relationship [ 13 , 14 ]. Misunderstanding can generate miscommunication and dissatisfaction which can lead to suboptimal care [ 18 ]. What practicians think parents understood may not reflect what parents actually report being told [ 22 ].
In our findings, the wish for statistics and figures varies from one participant to another. Physicians may be confronted with the question of whether or not to share them. A study showed that some mothers, especially those with a high education level appreciated exact statistics more than general facts [ 6 ]. It brings us back to the idea of personalizing our counsel. Geurtzen et al. showed that parents’ choice on statistics was divided, and if given, these should be well explained [ 26 ]. However, a systematic review on parent communication needs during antenatal consultations found that parents wished for more than only quantitative data concerning mortality and morbidity. For instance, they expect information on their role [ 14 ]. So before giving statistical data, physicians should seek if parents want them and provide them in a way that is understandable and relevant to this individual situation.
In our study, physician’s skills and attitude are well remembered by mothers, suggesting the idea that if parents feel in a safe and trusting environment, they will be more willing to listen, understand and ask questions. Other studies found that in order to improve pedagogy, the speaker should be compassionate, empathic, honest, and caring [ 10 ]. Nevertheless, parents also expect truth and real outcomes and importantly, in words they can understand [ 14 ]. Our study shows that participants had a positive experience with well conducted antenatal counseling, even though the risk of neonatal death was brought up by the physician. As pointed in previous research work, truthful information, even when difficult, can be expected from physicians regarding prenatal information. Some hope should also be provided, however some physicians may fear giving false hope [ 16 ]. The timing of the information delivery is another aspect of prenatal counseling that also needs to be personalized. Too soon can be stressful if the patient is still accommodating to their new situation [ 18 ]. On the contrary, too late may increase mother’s stress. Uncertainty of the prognosis and the possible threat of sudden emergency delivery add difficulty to the timing of antenatal counseling.
Several participants from our study brought up the positive impact of a nurse being present during counseling, which illustrates the importance of multidisciplinarity. Indeed, it has been shown that nurses can rephrase and check parents’ understanding [ 14 ]. Moreover, in the Netherlands, guidelines mention antenatal counseling should be performed with both an obstetrician and aneonatologist [ 15 ]. An American study supports the idea that optimal communication between the obstetric and neonatal teams improves outcomes and safety during the peripartum period [ 28 ]. When combined with an obstetric expertise, neonatal information can be more accurate and adapted to the degree of emergency. .
The use of multiple means of information delivery was supported by our participants including written, oral and visual. A study on the use of a decision aid in antenatal counseling showed that written information was often too complicated and understanding relied on parents’ educational level. Consequently, written information should be completed by oral explanations from a professional [ 18 ]. This has proven its efficacy in the obstetric field [ 25 ]. Such documents should be preferably personalized and adjusted to parents’ needs [ 26 ]. A visual support can decrease mothers’ anxiety [ 7 ]. Indeed, the time between antenatal counseling and the actual day of delivery can be long and mothers’ memory of the information delivered may fade. Visual aid can help parents remember information, even more so in a stressful environment [ 29 ]. A. D. Muthusamy et al. [ 30 ] found that submission of the medium before or while the information is being delivered improved recall of the information and decreased anxiety. However, providing this support after the information has been delivered is not very effective. Written information may not improve factual recall after verbal counseling of mothers in preterm labor [ 31 ]. Concerning the support of written information, Nicole M Rau and al provided that a paper handout and multimedia tablet were equally effective in the labor unit to supplement verbal preterm birth counseling and decrease parental anxiety [ 32 ]. This approach could be used in the setting of antenatal counseling. Alongside official documents provided by the hospital, the use of the Internet as a means of information has become increasingly important for pregnant women over the years [ 28 ]. In our study, the internet was depicted as negative because mothers mostly reported on their “worst case scenario” findings. However, other research show that even though internet findings may generate anxiety, they can also reassure mothers-to-be and be a rich and accessible source of support [ 33 ].
Strengths and limitations
Our study is novel as it explores the obstetric side, and the research team was multidisciplinary, including neonatologists, obstetricians, and a psychologist. Moreover, the fact that we did not focus on periviable terms enabled us to study several aspects of prenatal counseling other than decision-making. Even though our interviews were conducted over the phone for the most part due to the sanitary conditions, the interview durations were satisfactory which shows participants’ trust towards researchers. Furthermore, we included patients who gave birth at least 6 months before the interview, and whose child was discharged which gave participants time to process what happened, allowing them to tell their experience. Another asset of this study is that it reflects real world experience and not a simulation like many previous studies [ 34 ].
One of the limitations of our study is that our results are impacted by some mothers’ characteristics: our participants mostly had preeclampsia. In consequence, we cannot generalize our results to all high-risk pregnancy hospitalizations, in particular spontaneous preterm labor. However, preeclampsia causes longer hospital stays and thus allows deeper insights on the hospital experience. Patients who present with spontaneous preterm labor sometimes don’t have time to receive antenatal counseling before delivery. Other biases to consider are gestational age at admission and delivery, and pathology of the newborns, as they may have influenced participants’ experiences. We also did not include mothers who had lost their child. They probably have a very different insight that is important to consider. This stems from the fact that we decided to not include very extreme preterm children, therefore mortality was less important in our population. In order to explore mothers’ point of view after the loss of their child, the research team would have to be well prepared to deal with grief and bring emotional support during the study. Another population that was not included was mothers who had gotten prenatal counseling but ended up delivering at full term. We did not explore the impact of such information on preterm birth and the stress generated on those patients. Fish et al. showed that prenatal counseling improved parental knowledge and satisfaction without increasing anxiety [ 35 ]. Finally, in this study we focused on mothers’ experiences. It would be interesting to compare them with the coparents’ point of views, as there could be differences in psychosocial perceptions between them.
To improve the delivery of information related to preterm births, several leads could be explored. Using simulation to personalize the information in prenatal counseling remains interesting and has been widely described in the literature, but an evaluation of the clinical implementation after this simulation training is essential. Furthermore, multidisciplinarity could be developed by training different specialists to perform prenatal counseling. Written documents and videos may be elaborated to improve patients’ understanding.
The risk of preterm birth is a complex situation and all involved healthcare professionals should reflect on the best way to inform and support patients. Providing some general guidelines on how to respond to mothers’ expectations could be relevant, however personalization is the most fundamental aspect to keep in mind when delivering information on preterm birth. Hence the skills associated with information delivery in preterm births could benefit from the development and improvement of tools like: healthcare professionals’ training, interview guide for physicians that integrates parents’ expectations, and multidisciplinary counseling including all actors involved in the care of the mother and the child.
Data availability
All authors had full access to the data and materials. Data is available from Nadia Mazille-Orfanos ([email protected]) upon reasonable request.
Le Ray C, Lelong N, Cinelli H, Blondel B, Le Ray C, Lelong N, et al. Results of the 2021 French National Perinatal Survey and trends in perinatal health in metropolitan France since 1995. J Gynecol Obstet Hum Reprod. 2022;51(10):102509.
Article PubMed Google Scholar
Glover AV, Manuck TA. Screening for spontaneous preterm birth and resultant therapies to reduce neonatal morbidity and mortality: a review. Semin Fetal Neonatal Med. 2018;23(2):126–32.
Pierrat V, Marchand-Martin L, Arnaud C, Kaminski M, Resche-Rigon M, Lebeaux C et al. Neurodevelopmental outcome at 2 years for preterm children born at 22 to 34 weeks’ gestation in France in 2011: EPIPAGE-2 cohort study. BMJ. 2017;j3448.
Larroque B, Delobel M, Arnaud C, Marchand L, Groupe Epipage. [Outcome at 5 and 8 years of children born very preterm]. Arch Pediatr. 2008;15(5):589–91.
Article CAS PubMed Google Scholar
Haute Autorité de Santé [Internet]. [cited 2022 May 6]. Délivrance de l’information à la personne sur son état de santé. Available from: https://www.has-sante.fr/jcms/c_1261551/fr/delivrance-de-l-information-a-la-personne-sur-son-etat-de-sante .
Paul DA, Epps S, Leef KH, Stefano JL. Prenatal consultation with a neonatologist prior to preterm delivery. J Perinatol. 2001;21(7):431–7.
Dekens C, Fontaine C, Carpentier E, Barcat L, Gondry J, Tourneux P. [Maternal anxiety related to how the pediatrician provided prenatal information about preterm birth]. Arch Pediatr. 2017;24(11):1076–82.
Yee WH, Sauve R. What information do parents want from the antenatal consultation? Paediatr Child Health. 2007;12(3):191–6.
Article PubMed PubMed Central Google Scholar
Zupancic Ja, Kirpalani F, Barrett H, Stewart J, Gafni S, Streiner A. Characterising doctor-parent communication in counselling for impending preterm delivery. Arch Dis Child Fetal Neonatal Ed. 2002;87(2):F113–117.
Article CAS PubMed PubMed Central Google Scholar
Janvier A, Lantos J, Investigators POST. Ethics and etiquette in neonatal intensive care. JAMA Pediatr. 2014;168(9):857–8.
Yildiz PD, Ayers S, Phillips L. The prevalence of posttraumatic stress disorder in pregnancy and after birth: a systematic review and meta-analysis. J Affect Disord. 2017;208:634–45.
Ohlinger J, Kantak A, Lavin JP, Fofah O, Hagen E, Suresh G, et al. Evaluation and development of potentially better practices for perinatal and neonatal communication and collaboration. Pediatrics. 2006;118(Suppl 2):S147–152.
Young E, Tsai E, O’Riordan A. A qualitative study of predelivery counselling for extreme prematurity. Paediatr Child Health. 2012;17(8):432–6.
Kharrat A, Moore GP, Beckett S, Nicholls SG, Sampson M, Daboval T. Antenatal consultations at Extreme Prematurity: a systematic review of parent communication needs. J Pediatr. 2018;196:109–e1157.
Geurtzen R, van Heijst AFJ, Draaisma JMT, Kuijpers LJMK, Woiski M, Scheepers HCJ, et al. Development of Nationwide recommendations to support prenatal counseling in Extreme Prematurity. Pediatrics. 2019;143(6):e20183253.
Grobman WA, Kavanaugh K, Moro T, DeRegnier RA, Savage T. Providing advice to parents for women at acutely high risk of periviable delivery. Obstet Gynecol. 2010;115(5):904–9.
Article R4127-36. - Code de la santé publique - Légifrance [Internet]. [cited 2022 May 6]. Available from: https://www.legifrance.gouv.fr/codes/article_lc/LEGIARTI000032973595/ .
Guillén Ú, Mackley A, Laventhal N, Kukora S, Christ L, Derrick M, et al. Evaluating the Use of a decision aid for parents facing extremely premature delivery: a Randomized Trial. J Pediatr. 2019;209:52–e601.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57.
Côté L, Turgeon J. Appraising qualitative research articles in medicine and medical education. Med Teach. 2005;27(1):71–5.
The Coding Manual for Qualitative Researchers. | Online Resources [Internet]. [cited 2022 May 6]. Available from: https://study.sagepub.com/saldanacoding3e .
Batton DG, Committee on Fetus and Newborn. Clinical report–antenatal counseling regarding resuscitation at an extremely low gestational age. Pediatrics. 2009;124(1):422–7.
Gaucher N, Payot A. From powerlessness to empowerment: mothers expect more than information from the prenatal consultation for preterm labour. Paediatr Child Health. 2011;16(10):638–42.
Gaucher N, Nadeau S, Barbier A, Janvier A, Payot A. Personalized Antenatal consultations for Preterm Labor: responding to mothers’ expectations. J Pediatr. 2016;178:130–e1347.
Pierre F. [Woman’s information and consent in obstetrics: CNGOF Perineal Prevention and Protection in Obstetrics Guidelines]. Gynecol Obstet Fertil Senol. 2018;46(12):986–93.
CAS PubMed Google Scholar
Geurtzen R, van Heijst A, Draaisma J, Ouwerkerk L, Scheepers H, Hogeveen M, et al. Prenatal counseling in extreme prematurity - insight into preferences from experienced parents. Patient Educ Couns. 2019;102(8):1541–9.
De Proost L, Geurtzen R, Ismaili M’hamdi, Reiss H, Irwin IKM, Steegers EAP, Eric. (Joanne) Verweij EJ. Prenatal counseling for extreme prematurity at the limit of viability: a scoping review. Patient Educ Couns. 2022;105(7):1743–60.
Yuill C, McCourt C, Cheyne H, Leister N. Women’s experiences of decision-making and informed choice about pregnancy and birth care: a systematic review and meta-synthesis of qualitative research. BMC Pregnancy Childbirth. 2020;20(1):343.
Kakkilaya V, Groome LJ, Platt D, Kurepa D, Pramanik A, Caldito G, et al. Use of a visual aid to improve counseling at the threshold of viability. Pediatrics. 2011;128(6):e1511–1519.
Muthusamy AD, Leuthner S, Gaebler-Uhing C, Li SH, Basir MA. Supplemental Writ Inform Improves Prenatal Counseling: Randomized Trial. 2012;129(5).
Kett JC, Mohamed MA, Bathgate S, Larsen JW, Aly H. Written Information May not improve factual recall after verbal counseling of mothers in premature labor – a Randomized Controlled Trial. J Clin Neonatology. 2016;5(1):39.
Article Google Scholar
Rau NM, Mcintosh JJ, Flynn KE, Szabo A, Ahamed SI, Asan O, et al. Multimedia tablet or paper handout to supplement counseling during preterm birth hospitalization: a randomized controlled trial. Am J Obstet Gynecol MFM. 2023;5(4):100875.
Lagan BM, Sinclair M, Kernohan WG. What is the impact of the internet on decision-making in pregnancy? A global study. Birth. 2011;38(4):336–45.
Pedrini L, Prefumo F, Frusca T, Ghilardi A. Counselling about the risk of Preterm Delivery: a systematic review. Biomed Res Int. 2017;2017:7320583.
Fish R, Weber A, Crowley M, March M, Thompson C, Voos K. Early antenatal counseling in the outpatient setting for high-risk pregnancies: a randomized control trial. J Perinatol. 2021;41(7):1595–604.
Download references
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Doriane Randriamboarison, Elisa Fustec Contributed equally.
Authors and Affiliations
Department of Neonatology, University Hospital of Rennes, Rennes, 35000, France
Doriane Randriamboarison, Mathilde Yverneau, Karine Le Breton, Nadia Mazille-Orfanos & Patrick Pladys
Department of Obstetrics and Gynecology, University Hospital of Rennes, Rennes, 35000, France
Elisa Fustec, Isabelle Enderlé, Karine Le Breton & Linda Lassel
Faculty of Medicine Rennes 1 University, Rennes, France
Isabelle Enderlé, Mathilde Yverneau & Patrick Pladys
You can also search for this author in PubMed Google Scholar
Contributions
DR, EF, IE, KL, NM participated in the study design, collection and analysis of the data and the writing of the report. NM, IE and MY participated in the study design, trained the interviewers, guaranteed the expertise of the qualitative method and participated in the analysis of the data through N Vivo software. LL and PP participated in study design, data collection, writing and the interpretation of the data. DR and EF participated in organisation of the interviews and collection of the data. All authors revised this article critically, approved the final manuscript and agreed to its being submitted for publication. DR, EF, IE, KL, MY, LL, NM, and PP had complete access to the study data that support the publication.
Corresponding author
Correspondence to Nadia Mazille-Orfanos .
Ethics declarations
Ethics approval and consent to participate.
The study was reviewed and approved by the Rennes University Hospital Ethics Committee (reference number 20.61). The University Hospital of Rennes recorded the material in accordance with all French ethical regulations (ref: MR-003). All methods were carried out in accordance with relevant guidelines and regulations. Participation was on a voluntary basis. All participants provided written informed consent to participate in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Randriamboarison, D., Fustec, E., Enderlé, I. et al. Qualitative analysis of mothers’ perception related to the delivery of information regarding preterm births. BMC Pregnancy Childbirth 24 , 272 (2024). https://doi.org/10.1186/s12884-024-06404-3
Download citation
Received : 05 March 2023
Accepted : 11 March 2024
Published : 12 April 2024
DOI : https://doi.org/10.1186/s12884-024-06404-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Preterm birth
- Qualitative
BMC Pregnancy and Childbirth
ISSN: 1471-2393
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Search Menu
- Advance Articles
- Supplements
- Virtual Collections
- Author Guidelines
- Submission Site
- Open Access
- Self-Archiving Policy
- Benefits of Publishing with JBCR
- About Journal of Burn Care and Research
- About the American Burn Association
- Editorial Board
- Advertising & Corporate Services
- Journals Career Network
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
- < Previous
30 A Qualitative Descriptive Exploration of the Experiences of Burn Therapists
- Article contents
- Figures & tables
- Supplementary Data
Miranda L Yelvington, Rachel E Wood, Tyler Corson, Jiale Hu, Stacey Reynolds, 30 A Qualitative Descriptive Exploration of the Experiences of Burn Therapists, Journal of Burn Care & Research , Volume 45, Issue Supplement_1, May/June 2024, Page 24, https://doi.org/10.1093/jbcr/irae036.030
- Permissions Icon Permissions
Exposure to patients who have experienced major traumatic events places burn therapists at risk for developing high levels of anxiety and stress, directly impacting their quality of life. Poor professional quality of life has been associated with negative physical and emotional characteristics in healthcare professionals and can subsequently influence patient safety and satisfaction, job retention, and productivity. The purpose of this study was to understand and describe the experiences of occupational and physical therapists who provide acute therapy to people who have sustained burn injuries.
The study utilized a qualitative descriptive approach. Participants were selected using a maximum variation sampling strategy. Years of burn experience ranged from 2 to 37 years, and participants practiced in adult (40%), pediatric (20%), or mixed burn care (40%). Participating therapists represented all five American Burn Association Regions. Semi-structured interviews were completed with 10 participants (8 female, 7 physical therapists) to explore their experiences in their own words. Conventional content analysis was used to analyze the data collected from semi-structured interviews.
Six themes emerged after content analysis. These themes were: 1) the importance of therapeutic relationships to patient successes and therapists’ retention; 2) the autonomy and flexibility of burn therapists; 3) the impact of career longevity on compassion; 4) the uniqueness of burn team relationships and camaraderie; 5) the challenges of operating within the business of a healthcare system; and 6) the physical, mental and emotional challenges to the burn therapists’ resiliency.
The overarching themes reflected the importance of therapeutic relationships to patient successes and therapists’ retention. The autonomy and flexibility of burn therapists were found to be a driver of professional quality of life as therapists were empowered by their ability to lead patient change. Therapists endorsed developing boundaries and methods to decrease the emotional impact of patient losses as their career progresses. Participants spoke about the positive and negative impact of being part of a multidisciplinary team, often feeling limited by the challenges inherent in operating within the business of a healthcare system.
This research brings to light the physical, mental, and emotional challenges that impact burn therapists’ resiliency and which should be considered when creating programs to increase retention and professional quality of life in this population.
Email alerts
Citing articles via, looking for your next opportunity.
- Recommend to Your Librarian
- Advertising and Corporate Services
Affiliations
- Online ISSN 1559-0488
- Print ISSN 1559-047X
- Copyright © 2024 American Burn Association
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.

IMAGES
VIDEO
COMMENTS
A semi-structured interview is a data collection method that relies on asking questions within a predetermined thematic framework. However, the questions are not set in order or in phrasing. In research, semi-structured interviews are often qualitative in nature. They are generally used as an exploratory tool in marketing, social science ...
From our perspective as seasoned qualitative researchers, conducting effective semistructured interviews requires: (1) a relational focus, including active engagement and curiosity, and (2) practice in the skills of interviewing. First, a relational focus emphasises the unique relationship between interviewer and interviewee.
First, the semi-structured interview is more powerful than other types of interviews for qualitative research because it allows for researchers to acquire in-depth information and evidence from ...
A semi-structured interview is a qualitative research method used to gain an in-depth understanding of the respondent's feelings and beliefs on specific topics. As the interviewer prepares the questions ahead of time, they can adjust the order, skip any that are redundant, or create new ones. Additionally, the interviewer should be prepared to ...
The semi-structured interview is an exploratory interview used most often in the social sciences for qualitative research purposes or to gather clinical data. While it generally follows a guide or protocol that is devised prior to the interview and is focused on a core topic to provide a general structure, the semi-structured interview also ...
Semi-structured interviews are characterized by open-ended questions and the use of an interview guide (or topic guide/list) in which the broad areas of interest, sometimes including sub-questions, are defined . The pre-defined topics in the interview guide can be derived from the literature, previous research or a preliminary method of data ...
In qualitative research, researchers often conduct semi-structured interviews with people familiar to them, but there are limited guidelines for researchers who conduct interviews to obtain curriculum-related information with academic colleagues who work in the same area of practice but at different higher education institutions.
A semi-structured interview is a qualitative research method that combines aspects of both structured and unstructured interviews. In a semi-structured interview, the researcher prepares a set of predetermined questions or topics to guide the conversation with the participant, but there is also room for flexibility and follow-up questions based ...
This book offers an in-depth and captivating step-by-step guide to the use of semi-structured interviews in qualitative research. By tracing the life of an actual research project as a consistent example threaded across the volume, Anne Galletta shows in concrete terms how readers can approach the planning and execution of their own new research endeavor and illuminates unexpected, real-life ...
Qualitative research using semi-structured interviews typically employs an iterative process in which data collection and analysis occur concurrently to refine questions and add new prompts to explore relevant topics inspired by participants in previous interviews to gain an in-depth understanding of the research question (DeJonckheere & Vaughn, 2019).
The popularity and value of qualitative research has increasingly been recognized in health and pharmacy services research. Although there is certainly an appropriate place in qualitative research for other data collection methods, a primary benefit of the semi-structured interview is that it permits interviews to be focused while still giving the investigator the autonomy to explore pertinent ...
Interviewing. This is the most common format of data collection in qualitative research. According to Oakley, qualitative interview is a type of framework in which the practices and standards be not only recorded, but also achieved, challenged and as well as reinforced.[] As no research interview lacks structure[] most of the qualitative research interviews are either semi-structured, lightly ...
Semi-Structured Interviews and Focus Groups Margaret C. Harrell Melissa A. Bradley Th is course provides an overview of two types of qualitative data collection methodologies: semi-structured interviews and focus groups. Th ese techniques are commonly used in policy research and are applicable to many research questions.
A semi-structured interview is a method of research used most often in the social sciences. ... to the qualitative research. And they could more easily give the reasons for their answers during the interviews. Plus, the structured part of semi-structured interviews gives the interviewers reliable, comparable qualitative data as well. ...
Abstract. This chapter gives an introduction to qualitative interviewing in its unstructured and semistructured forms. Initially, the human world is depicted as a conversational reality in which interviewing takes a central position as a research method.
Although semi-structured interviews (SSIs) are used extensively in research, scant attention is given to their diversity, underlying assumptions, construction, and broad applications to qualitative and mixed-method research.
The semi-structured interview is considered and referred to as a conversation with a purpose ( Burgress, 1984) it is a widely used technique and method in qualitative research, it focuses on ...
Abstract. Conducted conversationally with one respondent at a time, the semi-structured interview (SSI) employs a blend of closed- and open-ended questions, often accompanied by follow-up why or ...
A semi-structured interview (SSI) is one of the essential tools in conduction qualitative research. This essay draws upon the pros and cons of applying semi-structured interviews (SSI) in the qualitative research method. Moreover, the challenges of SSI during the coronavirus pandemic are critically discussed to provide plausible recommendations.
Think how you will want to analyse, compare and write up your research, and make sure that the questioning style fits your own approach. Specific 'Why' and prompt questions. It is very rare in semi-structured interviews that you will ask one question, get a response, and then move on to the next topic.
Semistructured in-depth interviews are commonly used in qualitative research and are the most frequent qualitative data source in health services research. This method typically consists of a dialogue between researcher and participant, guided by a flexible interview protocol and supplemented by follow-up questions, probes and comments. The method allows the researcher to collect open-ended ...
The semi-structured interview guide provides a clear set of instructions for interviewers and can provide reliable, comparable qualitative data. Semi-structured interviews are often preceded by observation, informal and unstructured interviewing in order to allow the researchers to develop a keen understanding of the topic of interest necessary ...
Semi-structured interviews in qualitative research are used to collect qualitative, open-ended data. The researcher and participants engage in a formal interview. The researcher develops and utilizes an interview guide, a list of open-ended questions, and topics that the researcher will cover in the interview.
This was a qualitative study using semi-structured focus group interviews and text condensing. The research group was interested in exploring participants' perceptions and needed a method that allowed participants to express those experiences.
A qualitative longitudinal research approach was adopted, with four individual semi-structured interviews over 2 months after discharge (approximately 3, 10, 30, and 60 days after discharge) that took place at home, by telephone, secured video call, or at the university at the participant's convenience.
There are currently no methodological frameworks available to conduct semi-structured interviews in the education and social sciences fields with children of primary school age, ... and qualitative research textbooks offer little guidance. For example, the book The Qualitative Research Interview (Boutin, 2018, free translation from French) ...
The goal of the study was to evaluate maternal perception of antenatal information delivered in the setting of preterm births. A qualitative study was performed using semi-structured individual interviews of 15 mothers with a child born > 26-34 GW. Data analysis was based on a constant comparative method.
Journal of Burn Care & Research, Volume 45, Issue Supplement_1, May/June 2024, ... The study utilized a qualitative descriptive approach. Participants were selected using a maximum variation sampling strategy. ... Conventional content analysis was used to analyze the data collected from semi-structured interviews. Results.
We found that using traditional semi-structured interviews with children brings inherent challenges and that adaptation of current methods is not sufficient. A preliminary set of interviewing guidelines emphasizing a flexible and laissez-faire approach as well as a list of alternatives to the semi-structured interview for elementary-aged ...
by individuals engaged in qualitative research within the Saudi context. To do so, I conducted semi-structured interviews with eight doctoral students and employed a qualitative case study design for this paper. Utilizing the MAXQDA software, I also applied thematic analysis to the data gathered from the interviews.