SYSTEMATIC REVIEW article
Lung cancer mortality and associated predictors: systematic review using 32 scientific research findings.

- 1 Departement of Statistics, Bahir Dar University, Bahir Dar, Ethiopia
- 2 Epidemiology and Biostatistics Division, School of Public Health, Queensland University, Brisbane, QLD, Australia
- 3 School of Mathematics, Statistics and Computer Science, University of KwaZulu-Natal, Durban, South Africa
Background: Cancer is a chronic disease brought on by mutations to the genes that control our cells’ functions and become the most common cause of mortality and comorbidities. Thus, this study aimed to assess the comprehensive and common mortality-related risk factors of lung cancer using more than thirty scientific research papers.
Methods: Possible risk factors contributing to lung cancer mortality were assessed across 201 studies sourced from electronic databases, including Google Scholar, Cochrane Library, Web of Science (WOS), EMBASE, Medline/PubMed, the Lung Cancer Open Research Dataset Challenge, and Scopus. Out of these, 32 studies meeting the eligibility criteria for meta-analysis were included. Due to the heterogeneous nature of the studies, a random-effects model was applied to estimate the pooled effects of covariates.
Results: The overall prevalence of mortality rate was 10% with a 95% confidence interval of 6 and 16%. Twenty studies (62.50%) studies included in this study considered the ages of lung cancer patients as the risk factors for mortality. Whereas, eighteen (56.25%) and thirteen (40.63%) studies incorporated the gender and smoking status of patients respectively. The comorbidities of lung cancer mortality such as cardiovascular disease, hypertension, diabetes, and pneumonia were also involved in 7 (21.90%), 6 (18.75%), 5 (15.63%), and 2 (6.25%) studies, respectively. Patients of older age are more likely to die as compared to patients of younger age. Similarly, lung patients who had smoking practice were more likely to die as compared to patients who hadn’t practiced smoking
Conclusion: The mortality rate of lung cancer patients is considerably high. Older age, gender, stage, and comorbidities such as cardiovascular, hypertension, and diabetes have a significant positive effect on lung cancer mortality. The study results will contribute to future research, management, and prevention strategies for lung cancer.

Introduction
Cancer is a chronic disease brought on by mutations to the genes that control our cells’ functions, particularly their growth and division, which results in uncontrolled cell growth and division that forms malignant tumors and spreads to nearby organs ( 1 ). In 2015, the Global Burden of Disease Cancer study found that, with 8 million deaths, cancer was the second greatest cause of death worldwide, with cardiovascular illnesses taking the top spot ( 2 ).
According to 2018 World Cancer statistics, there were an estimated 18 million cancer cases around the world, of which 9.5 million cases were males and 8.5 million in females ( 3 ). Recently National Cancer Institute showed that there are more than 100 types of cancer which are usually named for the organs or tissues where the cancers form ( 2 , 4 ). With 2,093,876 cases or 12.3% of the total, lung cancer is the first and most often diagnosed cancer worldwide. Among the top five most frequently diagnosed cancers, breast (2,088,849 cases, 12.2% of the total), colorectal (1,800,977 cases, 10% of the total), prostate (1,276,106 cases, 9.8% of the total), and stomach (1,033,701 cases, 5% of the total) are ranked second, third, fourth, and fifth, respectively ( 2 ). As a result, this study was focused on a meta-analysis of mortality-related risk factors of lung cancer.
Lung cancer is a malignancy that typically develops in the cells lining the airways of the lung. It remained the leading cause of cancer death, with an estimated 1.8 million deaths (18%), followed by colorectal (9.4%), liver (8.3%), stomach (7.7%), and female breast (6.9%) cancers ( 4 , 5 ). Lung cancer has already become a threat to public health around the world with nearly 2 million cases and deaths in 2020. The cases of lung cancer annually are anticipated to reach 3.8 million in 2050, even with current risk levels and age-specific rates ( 6 ). Several studies reported that socioeconomic, demographic, biological, and behavioral factors are important determinants of lung cancer mortality ( 5 ). Among these age ( 7 – 10 ), sex ( 11 – 14 ), cigarette smoking ( 8 , 9 , 12 , 13 ), stage ( 10 , 14 – 16 ), infectious lung disease (ILD) ( 7 , 17 , 18 ), body mass index (BMI) ( 12 , 13 , 19 , 20 ), diabetes ( 13 , 15 , 19 , 21 ), and hypertension ( 12 , 17 , 19 ) are the most common factors associated with lung cancer mortality.
In regards to gender, following prostate and colorectal cancer, lung cancer is the most common cancer and the main cause of cancer death in men. The lung cancer death rates among women whose husbands had ever smoked during the current marriage were 20% higher than those among those who were married to never-smokers. Cigarette smoking is the most important preventable risk factor for lung cancer, which is the leading cause of cancer mortality ( 6 ). Lung cancer risk is higher in people with low BMI. When the analysis was limited to lifetime nonsmokers, an increased risk of lung cancer associated with a family history of the disease was found, though this did not reach statistical significance ( 11 , 22 ).
Despite, the lung cancer mortality rates are increasing and numerous studies conducted ( 8 , 17 , 18 , 21 , 23 , 24 ) to identify the potential risk factors, still a lack of studies that show common causes of mortality due to lung cancer. Several studies were done on lung cancer to identify associated factors of it. However, they are limited to some specific locations, cases, and attributes. Thus, this study aimed to assess the comprehensive and common mortality-related risk factors of lung cancer using more than thirty scientific research papers. In this study, we provide a comprehensive and comparable investigation of mortality-related risk factors of lung cancer global level.
Materials and methods
Study protocol.
To evaluate the association between lung cancer mortality and comorbidities, as well as other socioeconomic, demographic, and biological factors. The study implemented and followed PRISMA procedures to execute the meta-analysis of the articles identified through our systematic reviews.
Search strategy
We systematically searched electronic databases up until 10 December 2022, including Google Scholar, Cochrane Library, Web of Sciences (WOS), EMBASE, Medline/PubMed, lung cancer Open Research Dataset Challenge, and Scopus. The search strategy was as follows: (lung cancer mortality OR lung neoplasms mortality OR cancer death rate) AND (risk factors OR predictors OR determinants) AND (adult patients OR lung cancer patients OR lung cancer survivors). The search was also narrowed down to articles that examined laboratory data, pre-existing comorbidities, clinical status, and demographic traits as potential indicators of lung cancer’s fatal outcome. The time and language of publications were not subject to any limitations. We downloaded the literature results into EndNote X9 to speed up the screening procedure.
Eligibility criteria
After duplicates were eliminated, the initial search results were checked for relevance by both authors using titles and abstracts. The eligibility requirements were examined in the complete texts ( Figure 1 ). Excluded from the analysis were studies without an abstract or full text, correspondence, studies on infants only, editorials, reviews, qualitative studies, books, theses, expert opinion papers, and review articles. We also used studies that only provided odds ratios (ORs), hazard ratios (HRs), or relative risks (RR) along with 95% confidence intervals (CI) for the association between demographic, epidemiological, or clinical characteristics and fatal outcomes of lung cancer among the eligible studies. The overall studies included in this study was presented in Table 1 .
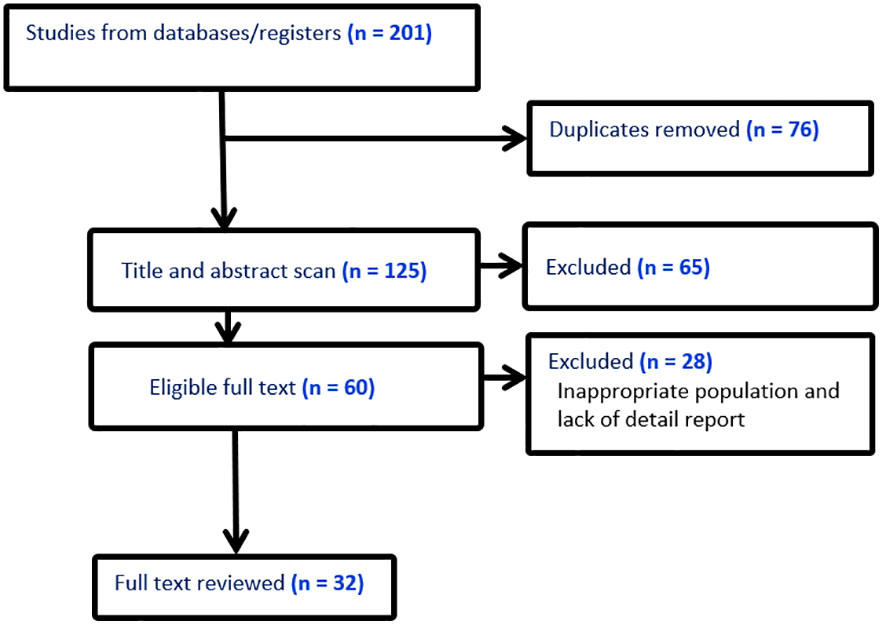
Figure 1 Literature screening flow chart.
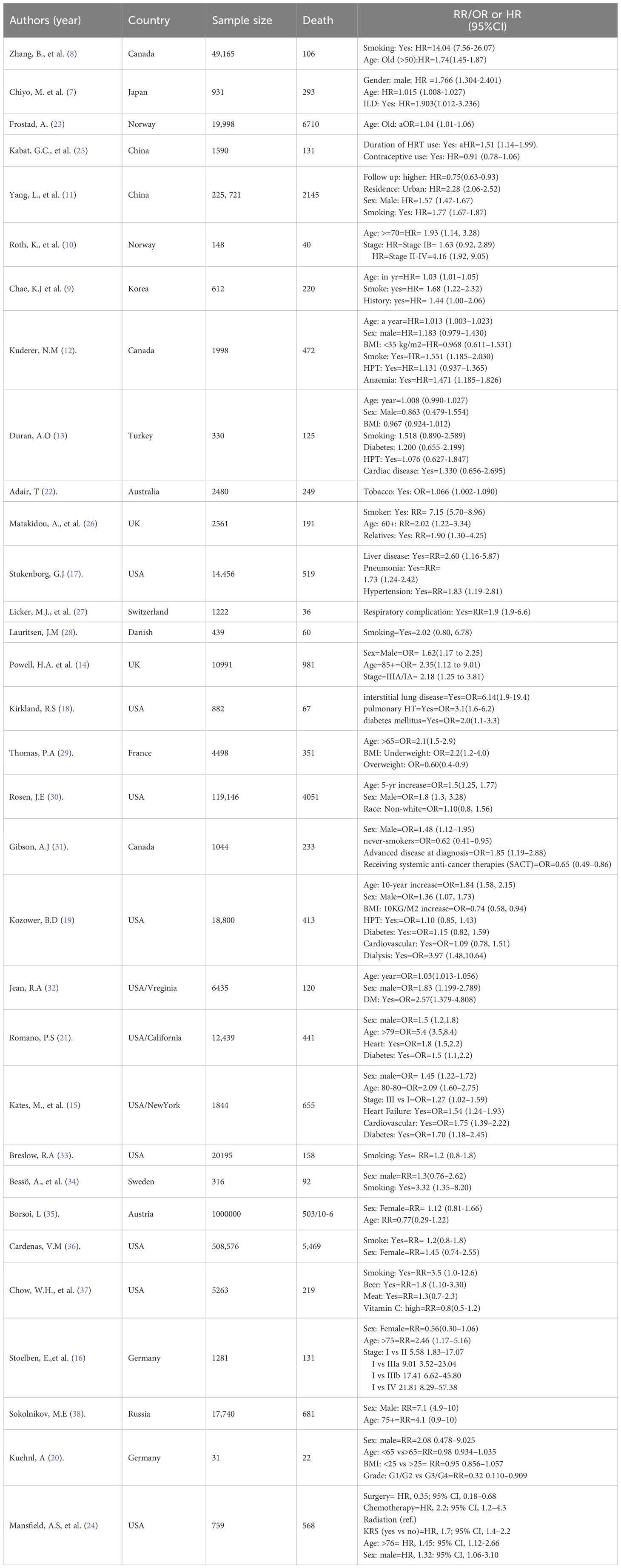
Table 1 Characteristics of studies included in the systematic review and meta-analysis on lung cancer mortality.
Data extraction and assessment for study quality
The downloaded EndNote X9 search outputs were independently reviewed for inclusion by each author. Discussion and consensus among the authors were used to settle any differences. The first author’s name, country, assessment techniques, sample size, study design, publication year, demographic and clinical variables (such as gender, age, and comorbidities), outcome (mortality), exposure (risk factors), and adjusted odds ratios or hazard ratios or relative risks were all extracted by all authors.
Using the Newcastle-Ottawa method, the authors independently assessed the articles’ quality methodological approach. This method relied on three main elements to evaluate the quality of the papers: evaluation of the results, comparability of the study groups, and patient selection methods. The seven domains in the Newcastle-Ottawa technique were scored from 3 to 0 (i.e., from low to high bias), and their average score was taken.
Statistical analysis
To determine the relationship between risk factors and the likelihood that lung cancer will be fatal, we used ORs, RRs, or HRs (and their 95%CI) that were peer-reviewed and published. The expected between-study heterogeneity has been taken into consideration when computing a mixed-effect model. Cochran’s Q test was used to determine whether there was heterogeneity in effect sizes; a significant Q value suggests that there is heterogeneity rather than homogeneity. The I 2 statistic was used to calculate the percentage of the total variance that could be attributed to study heterogeneity ( 39 ). The I 2 values between 60% and 90%, 40% and 59%, and 0% and 39% were regarded as severe, moderate, and mild, respectively. For evaluating publication bias, funnel plots with an Egger-weighted regression test were used ( 40 ). The pooled odds ratio, relative risk, and hazard ratio were calculated and publication bias was examined using STATA version 17 and R-4.0.2 statistical software, respectively.
In this study, a total of 201 publications on the mortality of lung cancer were identified using so many sites such as Google Scholar, Cochrane Library, Web of Sciences (WOS), EMBASE, Medline/PubMed, cancer research database (WHO), lung cancer open research dataset challenge, and Scopus database, of which, 15 studies that did not have numbers of hospital death, 35 reviews, 15 non-English, and 76 duplicates were excluded. Among the remaining 60 studies, 28 did not report cross-tabulation with ORs or HRs, or RRs. Consequently, we got only 32 studies that satisfied all the eligibility criteria (see Figure 1 ). The studies considered in this meta-analysis consists of numerous mortality-related risk factor of lung cancer diseases ( 6 , 8 , 10 , 11 , 16 , 18 , 25 , 26 , 29 , 30 , 32 ) (see Table 1 ). The effect of each risk factor on mortality of lung cancer was measured and estimated using adjusted odds ratio (OR), relative risk (RR), or hazard ratio (HR).
The estimate of each risk factor was the pooled of OR, RR, and HR. This was done using a forest plot in Figures 1 – 4 for risk factors age, BMI; sex, smoking; cardiovascular, stage; hypertension, diabetes; and Interstitial Lung Disease (ILD), Pneumonia, respectively. Out of the 32 studies, ten, fourteen, and eight studies provided the effect of risk factors were estimated using HR, OR, and RR respectively. The Meta-analysis included studies with retrospective and prospective study designs. The mortality rate noticed in retrospective studies was lower as compared to prospective studies. For instance, in the retrospective study conducted by Zhang et al. the mortality rate was 106 to 49165 which is almost null, whereas, in the prospective study conducted by Mansfield et al, the mortality rate was 568 to 759 which is almost 75 percent of the total. The overall prevalence of mortality rate was 10% with a 95% confidence interval of 6 and 16% (see Figure 2 ).
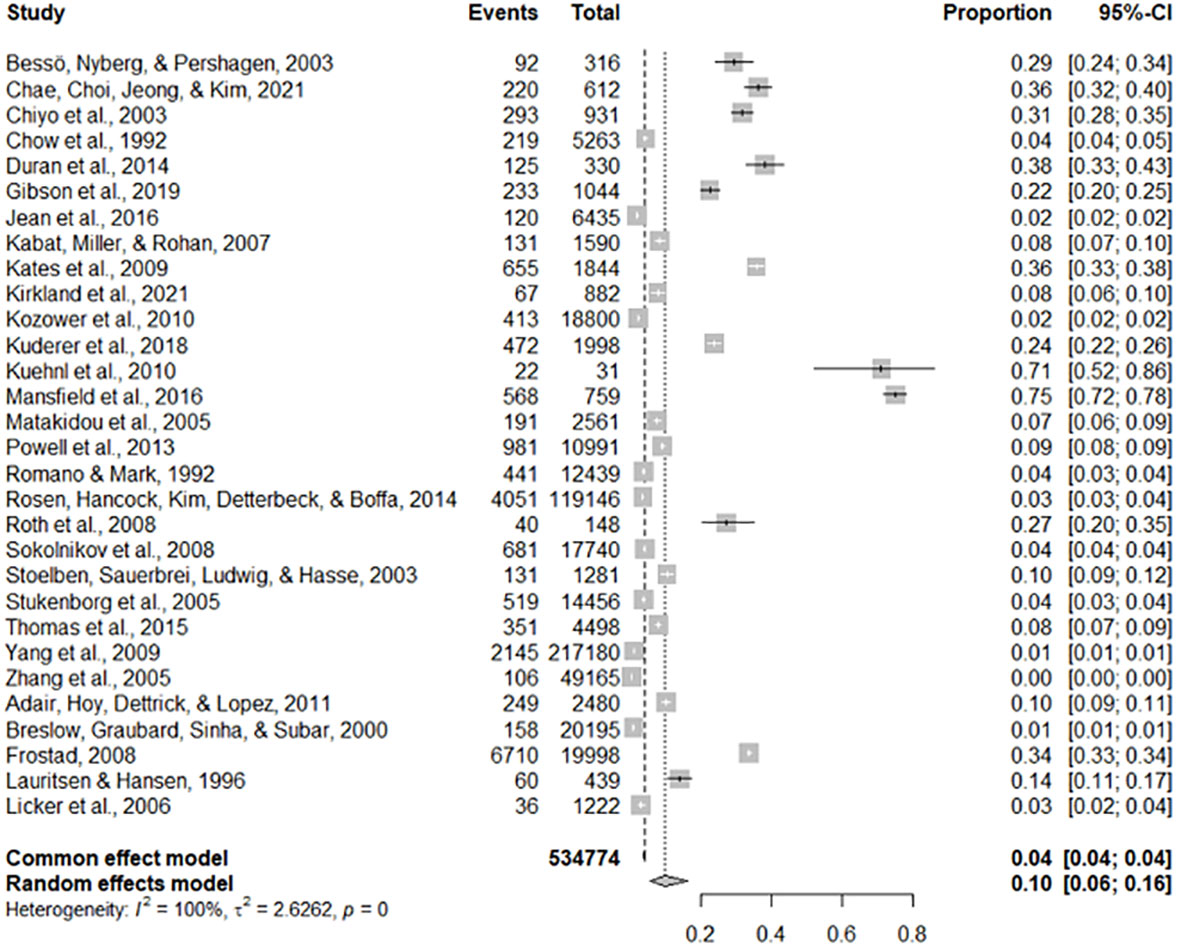
Figure 2 The overall mortality rate of lung cancer.
Figure 3 The forest plot of the effect size age (A) and BMI (B) .
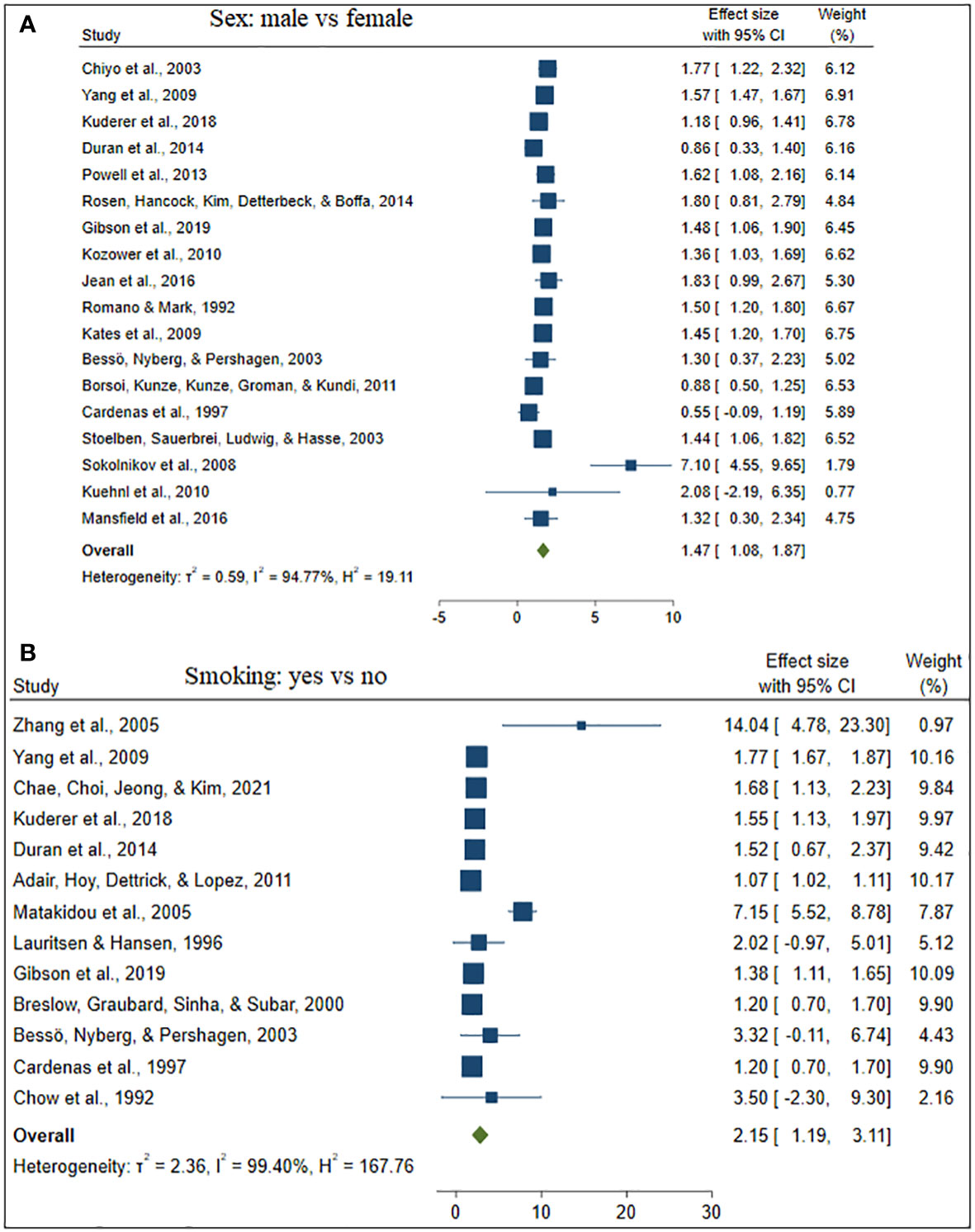
Figure 4 The forest plot of the effect size sex (A) and smoking (B) .
Twenty studies (62.50%) studies included in this study considered the ages of lung cancer patients as the risk factors for mortality. Whereas, eighteen (56.25%) and thirteen (40.63%) studies were incorporate the gender and smoking status of patients respectively. The comorbidities of lung cancer mortality such as cardiovascular disease, hypertension, diabetes, and pneumonia were also involved in 7 (21.90%), 6 (18.75%), 5 (15.63%), and 2 (6.25%) studies, respectively (see Table 2 ).
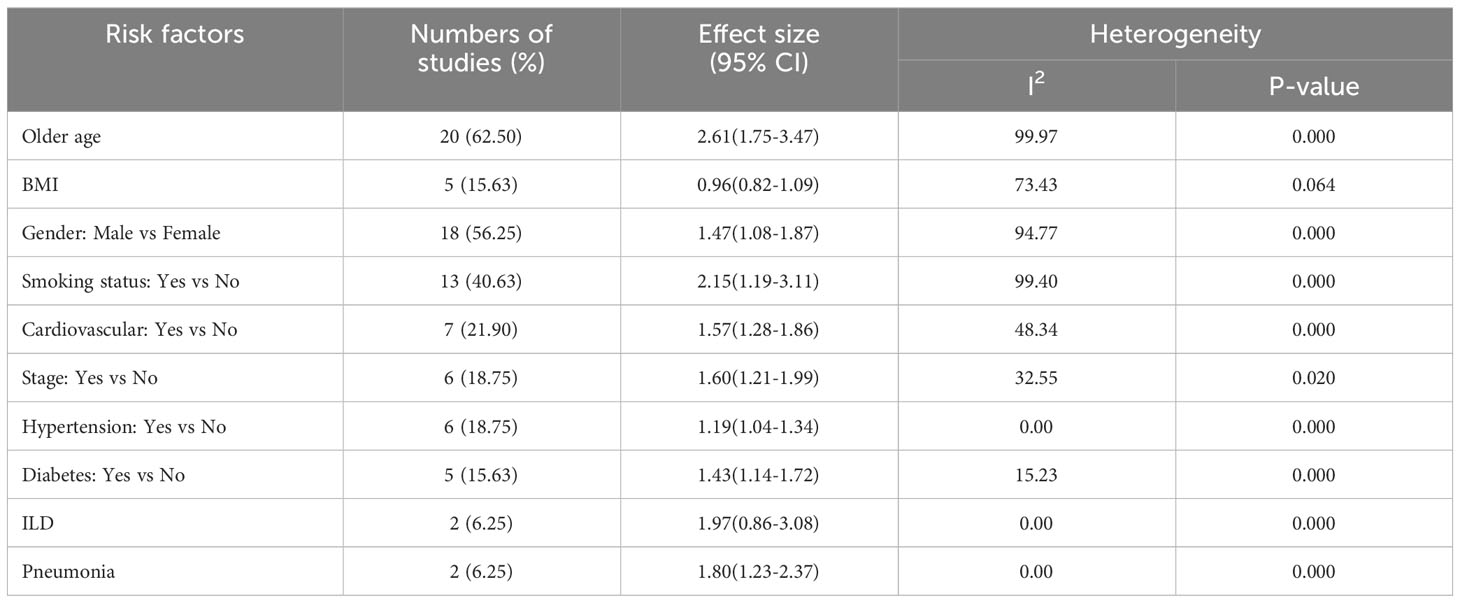
Table 2 Results of meta-analysis based on demographic and clinical variables associated with lung cancer mortality.
Besides, Table 2 depicted the overall effect size demographic and clinical variables associated with lung cancer mortality. Except for the BMI of the patient determinants such as patient age, gender, smoking, cardiovascular, stage of cancer metastasis, diabetes and pneumonia has a significant positive effect on lung cancer mortality. For instance, patients of older age are more likely to die as compared to patients of younger age. Similarly, lung patients who had smoking practice were more likely to die as compared to patients who hadn’t practiced smoking. The estimated effects of covariates for each study separately and aggregate/overall estimated effect were also presented using a forest plot in Figures 3 – 6 .
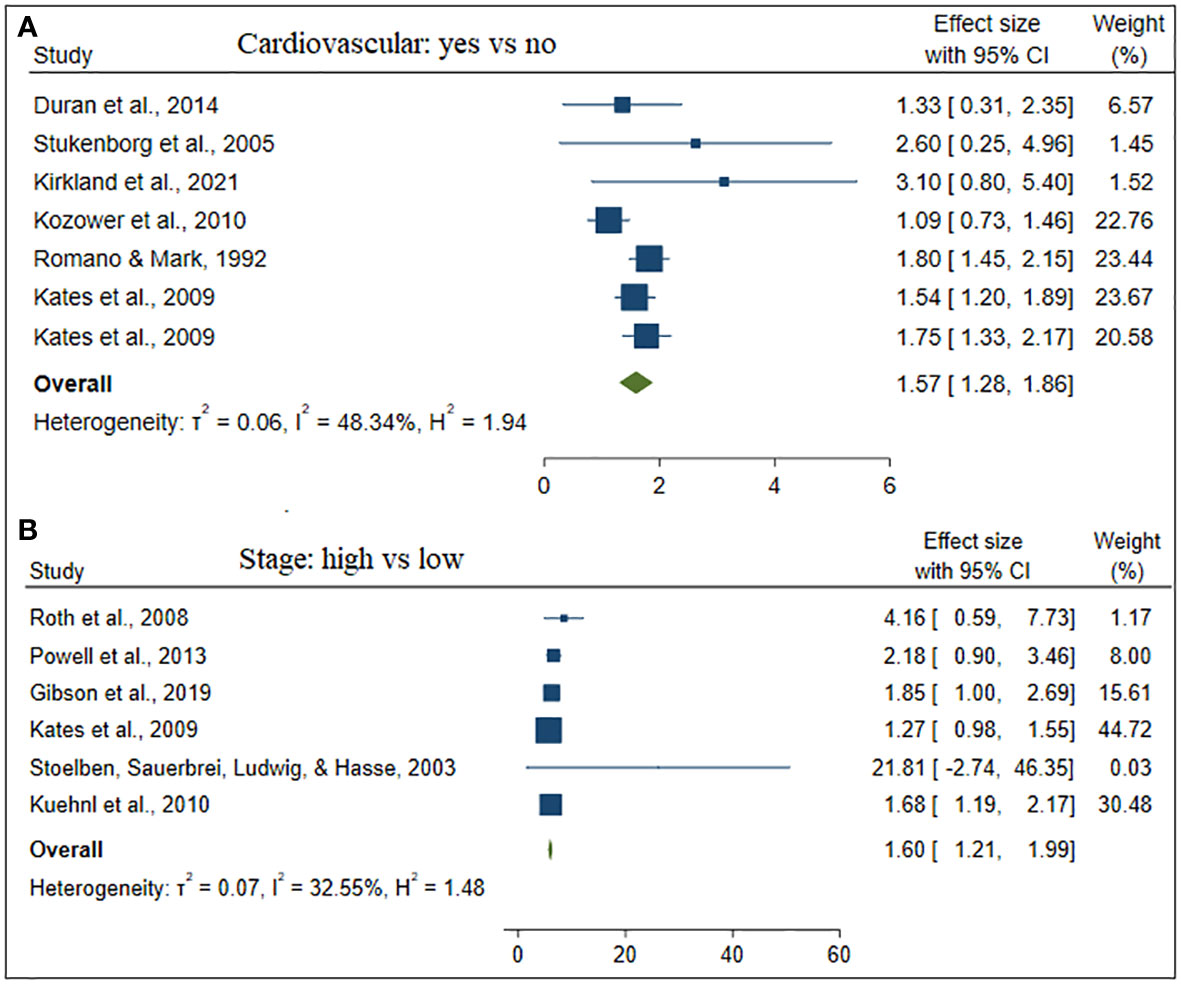
Figure 5 The forest plot of the effect size cardiovascular (A) and stage (B) .
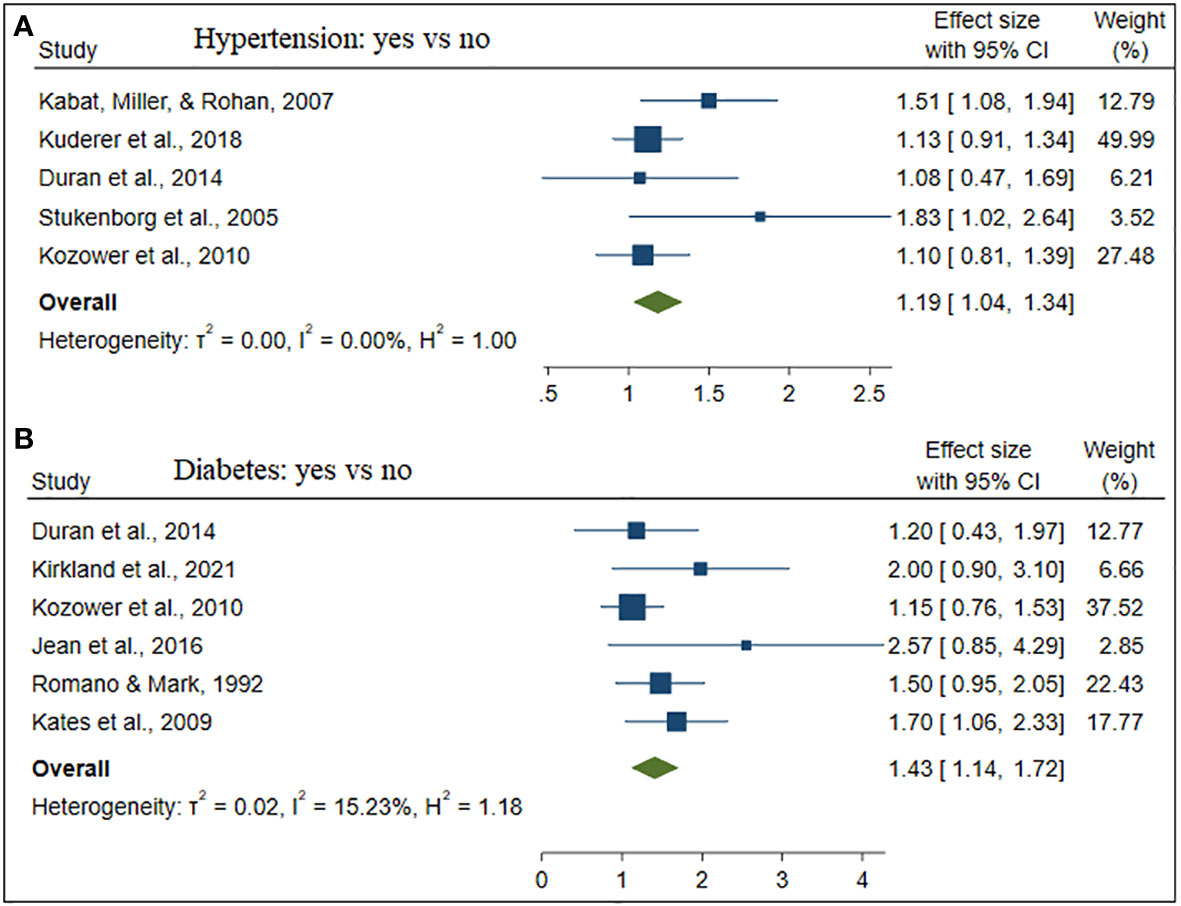
Figure 6 The forest plot of the effect size hypertension (A) and diabetes (B) .
Despite this, only one single study on the effect of anemia, residence, and receiving systematic anti-cancer treatment (SACT) on lung cancer mortality was included in this study (see Figure 7 ). Patients who had and lived in rural areas were more likely to die. In contrast, patients who took SACT were less likely to die.
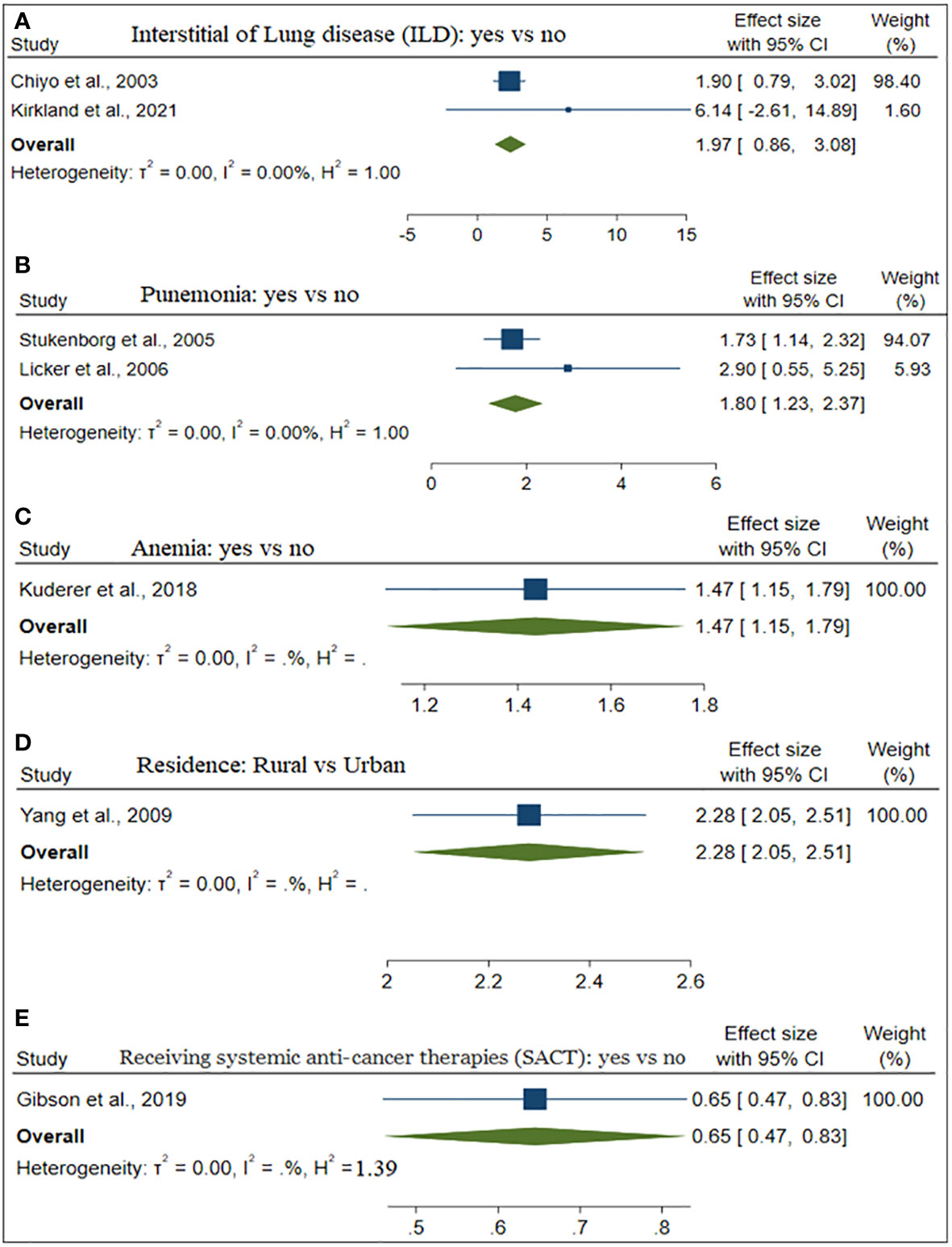
Figure 7 The forest plot of the effect size ILD (A) , Pneumonia (B) , Anemia (C) , and Residence (D) .
The goodness of the meta-analysis for each factor was considered using a funnel plot in Figure 8 . The points within the funnel line indicate the systematic review analysis for the corresponding variable is a good fit.
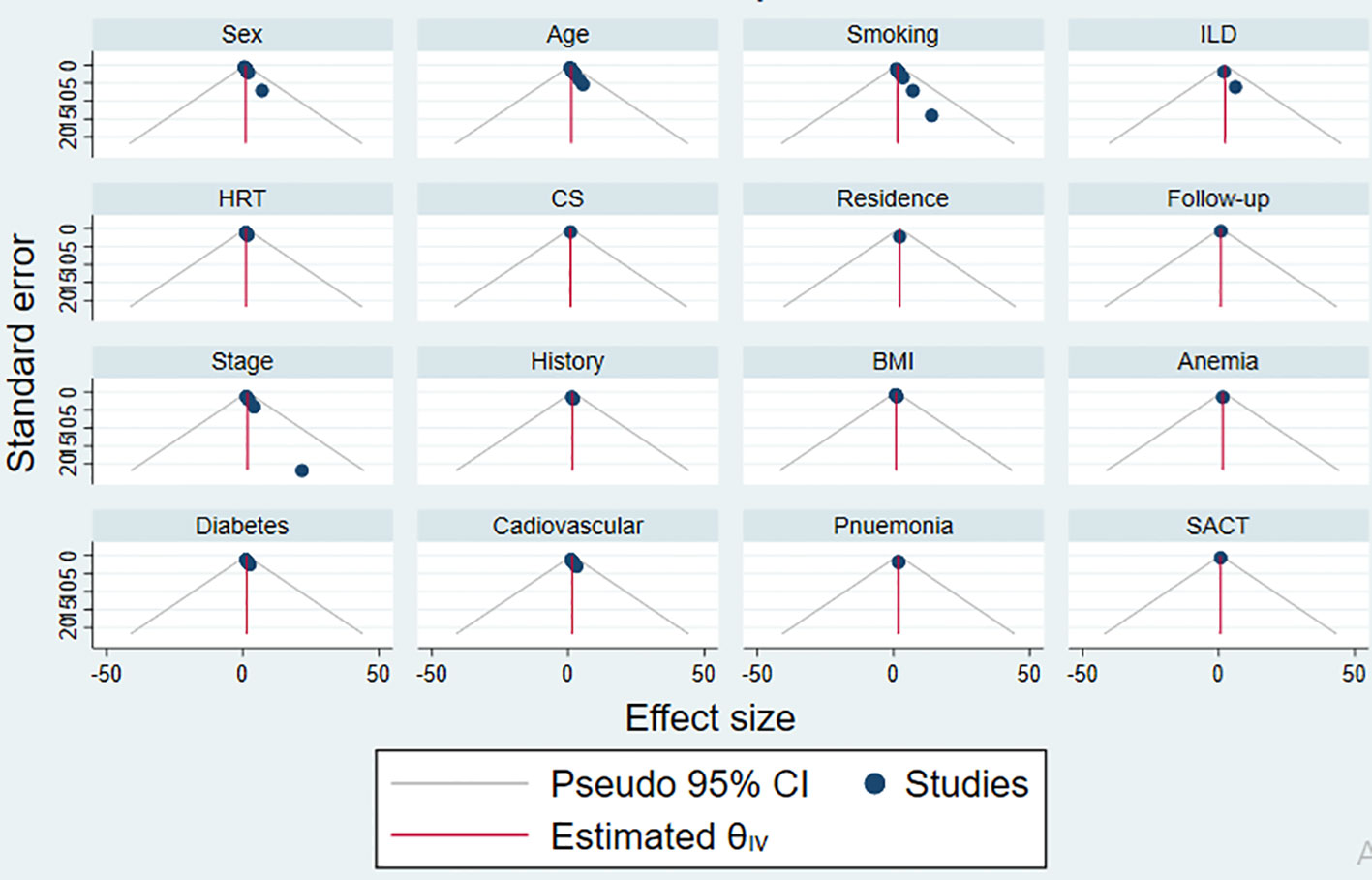
Figure 8 The funnel plot of each risk factors publication bias.
This study presents a comprehensive systematic review examining the risk factors associated with lung cancer mortality. The objective was to comprehensively explore potential risk factors, including demographic, biological, behavioral, and socioeconomic determinants associated with lung cancer mortality, and to estimate the overall prevalence of lung cancer mortality. We delved into a total of 201 lung cancer studies sourced from diverse electronic databases, including Google Scholar, Cochrane Library, Web of Sciences (WOS), EMBASE, Medline/PubMed, the Lung Cancer Open Research Dataset Challenge, and Scopus. In the meantime, 32 studies that satisfy the eligibility criteria of the Meta-analysis were involved in this study. The majority of the studies consist of patients’ age, gender, and smoking status ( 7 – 15 , 21 , 24 , 26 , 29 , 31 ).
Despite reports indicating a decline in the mortality rate of patients with lung cancer, it remains substantial. The overall mortality rate stands at 10%, signifying that, on average, ten out of every hundred lung cancer patients succumb to the disease. Put differently, there is a one in ten likelihood that a lung cancer patient will die. In 2012, an estimated 1.8 million new cases, accounting for 12.9% of the total, were recorded ( 41 ). In 2012, the regions with the highest lung cancer mortality rates per 100,000 were Central and Eastern Europe and Eastern Asia for males, and Northern America and Northern Europe for females. Conversely, the lowest rates were observed in sub-Saharan Africa for both males and females ( 42 ).
This study depicted that older age, gender, stage, and comorbidities such as cardiovascular, hypertension, and diabetes have a significant positive effect on lung cancer mortality. A study conducted on global trends of lung mortality revealed that the overall trend of lung cancer mortality among females is higher than among males ( 42 ), which contradicts the findings of this study states that males have a higher likelihood to be died as compared to females. The probability that an individual is affected by lung cancer increases as age does. This was in line with studies in ( 43 , 44 ), which reported that lung cancer incidence and mortality rates steadily rise after the age of 30, reaching a peak between the ages of 75 and 79 for men and 70 to 74 for women. Due to less concomitant illness, younger individuals may be able to tolerate more rigorous multimodal therapy. Various factors, including higher prevalence of occupational hazards like asbestos exposure and common settings such as kitchens, where staff are exposed to smoke, may contribute to increased lung cancer risk among females in the population.
The majority of patients visit the hospital during the advanced stage (III/IV) of cancer, which leads to having an effective prescription or treatment. Thus, the stage of the cancer diseases affected the survival time of the patient ( 43 ). Communities who are living in rural areas had more vulnerability to death. This is common because of poor health facilities and leads unable to take treatment in time in rural areas as compared to the urban. If lung cancer is detected early and the right treatment is available, it may be curable. The place of residence of patients interrelates with lifestyle, which is a considerable risk factor for cancer ( 45 ). A potential obstacle to the effective management of future changes in incidence and mortality rate is the lack of or limited access to health care services in rural areas, particularly in developing nations.
The most frequent factor in both lung cancer incidence and mortality is smoking which is in line with studies ( 8 , 46 ) state that lung cancer is directly caused by tobacco use, particularly cigarette smoking. Thus, an essential behavioral strategy for preventing lung cancer is quitting smoking. However, since this risk never goes back to normal, former smokers continue to have heightened risk compared to never smokers. Former smokers account for over 50% of instances of diagnosed lung cancer. About 58 percent of these occurrences happened in less developed areas, which is probably a reflection of the rising cigarette usage in these nations. Lung cancer is the most frequent kind of cancer death globally, accounting for 1.59 million projected deaths in 2012, even though exposure to tobacco smoke is avoidable ( 47 , 48 ). In the last, this review synthesizes evidence from multiple studies, offering a more robust and reliable overview than individual studies. This helps in drawing more accurate conclusions. It provides a comprehensive understanding of the current state of knowledge regarding factors influencing lung cancer mortality. This is valuable for researchers, healthcare professionals, and policymakers.
Despite providing pooled estimates from 32 studies across 13 geographical locations, which may be seen as broadly representative of the pandemic, our systematic review has several limitations. Firstly, there is high heterogeneity, potentially due to substantial variations in sample sizes among studies and differences in study designs. Secondly, even with careful statistical adjustments, confounding variables can affect the validity of the results, as not all factors influencing lung cancer mortality are incorporated. Thirdly, it’s important to note that this study did not consider covariates related to treatment outcomes, survival rates, and disease progression in cancer patients. Lastly, some included studies had very small sample sizes, possibly limiting the identification of factors influencing lung cancer mortality.
The mortality rate among lung cancer patients is notably elevated. Several factors contribute significantly to lung cancer mortality, including older age, gender, disease stage, and the presence of comorbidities such as cardiovascular conditions, hypertension, and diabetes. These findings hold substantial implications for the field of lung cancer research, management, and future prevention strategies. By shedding light on the influential factors behind lung cancer mortality, this study offers valuable insights that can inform more effective approaches to Comprehensive tobacco control policies, public awareness campaigns highlighting the dangers of smoking, and measures to improve air quality and regulate occupational exposures are essential. Access to healthcare services needs enhancement, focusing on early detection and treatment. Supporting smoking cessation efforts, promoting a healthy lifestyle, and integrating preventive measures into primary healthcare systems are vital components. International collaboration for knowledge sharing and resource allocation further strengthens the global fight against lung cancer combatting this deadly disease, ultimately leading to improved patient outcomes and reduced mortality rates.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Author contributions
LT: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. ZD: Data curation, Investigation, Methodology, Software, Supervision, Validation, Writing – review & editing. HF: Data curation, Formal Analysis, Investigation, Methodology, Software, Validation, Visualization, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to thank the School of Mathematics, Statistics and Computer Science, University of KwaZulu-Natal, South Africa for providing their guidance and support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Meyerson M, Gabriel S, Getz G. Advances in understanding cancer genomes through second-generation sequencing. Nat Rev Genet (2010) 11(10):685–96. doi: 10.1038/nrg2841
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Tesfaw LM, Muluneh EK. Modeling the spatial distribution of cancer and determining the associated risk factors. Cancer Inf (2020) 19:1176935120939898. doi: 10.1177/1176935120939898
CrossRef Full Text | Google Scholar
3. Torre L, Siegel R, Jemal A. Global cancer facts & figures. Atlanta: Am Cancer Soc (2015) 2.
Google Scholar
4. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: Cancer J Clin (2018) 68(6):394–424. doi: 10.3322/caac.21492
5. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: Cancer J Clin (2021) 71(3):209–49. doi: 10.3322/caac.21660
6. Sharma R. Mapping of global, regional and national incidence, mortality and mortality-to-incidence ratio of lung cancer in 2020 and 2050. Int J Clin Oncol (2022) 27(4):665–75. doi: 10.1007/s10147-021-02108-2
7. Chiyo M, Sekine Y, Iwata T, Tatsumi K, Yasufuku K, Iyoda A, et al. Impact of interstitial lung disease on surgical morbidity and mortality for lung cancer: analyses of short-term and long-term outcomes. J Thorac Cardiovasc Surg (2003) 126(4):1141–6. doi: 10.1016/S0022-5223(03)00791-8
8. Zhang B, Ferrence R, Cohen J, Bondy S, Ashley MJ, Rehm J, et al. Smoking cessation and lung cancer mortality in a cohort of middle-aged Canadian women. Ann Epidemiol (2005) 15(4):302–9. doi: 10.1016/j.annepidem.2004.08.013
9. Chae KJ, Choi H, Jeong WG, Kim J. The value of the illness-death model for predicting outcomes in patients with non–small cell lung cancer. Cancer Res Treat (2021). doi: 10.4143/crt.2021.902
10. Roth K, Nilsen TIL, Hatlen E, Sørensen KS, Hole T, Haaverstad R. Predictors of long time survival after lung cancer surgery: a retrospective cohort study. BMC pulmonary Med (2008) 8(1):1–8. doi: 10.1186/1471-2466-8-22
11. Yang L, Yang G, Zhou M, Smith M, Ge H, Boreham J, et al. Body mass index and mortality from lung cancer in smokers and nonsmokers: a nationally representative prospective study of 220,000 men in China. Int J Cancer (2009) 125(9):2136–43. doi: 10.1002/ijc.24527
12. Kuderer NM, Poniewierski MS, Culakova E, Lyman GH, Khorana AA, Pabinger I, et al. Predictors of venous thromboembolism and early mortality in lung cancer: results from a global prospective study (CANTARISK). Oncologist (2018) 23(2):247–55. doi: 10.1634/theoncologist.2017-0205
13. Duran AO, Inanc M, Karaca H, Dogan I, Berk V, Bozkurt, et al. Albumin-globulin ratio for prediction of long-term mortality in lung adenocarcinoma patients. Asian Pacific J Cancer Prev (2014) 15(15):6449–53. doi: 10.7314/APJCP.2014.15.15.6449
14. Powell HA, Tata LJ, Baldwin DR, Stanley RA, Khakwani A, Hubbard RB. Early mortality after surgical resection for lung cancer: an analysis of the English National Lung cancer audit. Thorax (2013) 68(9):826–34. doi: 10.1136/thoraxjnl-2012-203123
15. Kates M, Perez X, Gribetz J, Swanson SJ, McGinn T, Wisnivesky JP. Validation of a model to predict perioperative mortality from lung cancer resection in the elderly. Am J Respir Crit Care Med (2009) 179(5):390–5. doi: 10.1164/rccm.200808-1342OC
16. Stoelben E, Sauerbrei W, Ludwig C, Hasse J. Tumor stage and early mortality for surgical resections in lung cancer. Langenbeck's Arch Surg (2003) 388(2):116–21. doi: 10.1007/s00423-003-0354-x
17. Stukenborg GJ, Kilbridge KL, Wagner DP, Harrell FE Jr, Oliver MN, Lyman JA, et al. Present-at-admission diagnoses improve mortality risk adjustment and allow more accurate assessment of the relationship between volume of lung cancer operations and mortality risk. Surgery (2005) 138(3):498–507. doi: 10.1016/j.surg.2005.04.004
18. Kirkland RS, Kole AJ, Batra H, Boggs DH, Spencer SA, Dobelbower MC, et al. Predictors of in-hospital death in patients with lung cancer admitted for acute radiation pneumonitis: A healthcare cost and utilization project (HCUP) analysis. Clin Lung Cancer (2021) 22(5):e716–22. doi: 10.1016/j.cllc.2021.01.016
19. Kozower BD, Sheng S, O'Brien SM, Liptay MJ, Lau CL, Jones , et al. STS database risk models: predictors of mortality and major morbidity for lung cancer resection. Ann Thorac Surg (2010) 90(3):875–83. doi: 10.1016/j.athoracsur.2010.03.115
20. Kuehnl A, Lindner M, Hornung HM, Winter H, Jauch KW, et al. Atrial resection for lung cancer: morbidity, mortality, and long-term follow-up. World J Surg (2010) 34(9):2233–9. doi: 10.1007/s00268-010-0596-z
21. Romano PS, Mark DH. Patient and hospital characteristics related to in-hospital mortality after lung cancer resection. Chest (1992) 101(5):1332–7. doi: 10.1378/chest.101.5.1332
22. Adair T, Hoy D, Dettrick Z, Lopez AD. Reconstruction of long-term tobacco consumption trends in Australia and their relationship to lung cancer mortality. Cancer Causes Control (2011) 22(7):1047–53. doi: 10.1007/s10552-011-9781-0
23. Frostad A. Association between respiratory symptom score and 30-year cause-specific mortality and lung cancer incidence. Clin Respir J (2008) 2:53–8. doi: 10.1111/j.1752-699X.2008.00084.x
24. Mansfield A, Tafur AJ, Wang CE, Kourelis TV, Wysokinska EM, Yang P. Predictors of active cancer thromboembolic outcomes: validation of the Khorana score among patients with lung cancer. J Thromb Haemostasis (2016) 14(9):1773–8. doi: 10.1111/jth.13378
25. Kabat GC, Miller AB, Rohan TE. Reproductive and hormonal factors and risk of lung cancer in women: a prospective cohort study. Int J Cancer (2007) 120(10):2214–20. doi: 10.1002/ijc.22543
26. Matakidou A, Eisen T, Bridle H, O'Brien M, Mutch R, Houlston RS, et al. Case-control study of familial lung cancer risks in UK women. Int J Cancer (2005) 116(3):445–50. doi: 10.1002/ijc.21012
27. Licker MJ, Widikker I, Robert J, Frey JG, Spiliopoulos A, Ellenberger C, et al. Operative mortality and respiratory complications after lung resection for cancer: impact of chronic obstructive pulmonary disease and time trends. Ann Thorac Surg (2006) 81(5):1830–7. doi: 10.1016/j.athoracsur.2005.11.048
28. Lauritsen JM, Hansen KS. Lung cancer mortality in stainless steel and mild steel welders: A nested case-referent study. Am J Ind Med (1996) 30(4):383–91. doi: 10.1002/(SICI)1097-0274(199610)30:4<383::AID-AJIM2>3.0.CO;2-X
29. Thomas PA, Berbis J, Baste JM, Le Pimpec-Barthes F, Tronc F, Falcoz PE, et al. Pneumonectomy for lung cancer: contemporary national early morbidity and mortality outcomes. J Thorac Cardiovasc Surg (2015) 149(1):73–83. doi: 10.1016/j.jtcvs.2014.09.063
30. Rosen JE, Hancock JG, Kim AW, Detterbeck FC, Boffa DJ. Predictors of mortality after surgical management of lung cancer in the National Cancer Database. Ann Thorac Surg (2014) 98(6):1953–60. doi: 10.1016/j.athoracsur.2014.07.007
31. Gibson AJ, Li H, D’Silva A, Elegbede AA, Tudor RA, Otsuka S, Bebb DG, et al. Factors associated with early mortality in non-small cell lung cancer patients following systemic anti-cancer therapy: a 10 year population-based study. Lung Cancer (2019) 134:141–6. doi: 10.1016/j.lungcan.2019.06.003
32. Jean RA, DeLuzio MR, Kraev AI, Wang G, Boffa DJ, Detterbeck FC, et al. Analyzing risk factors for morbidity and mortality after lung resection for lung cancer using the NSQIP database. J Am Coll Surgeons (2016) 222(6):992–1000.e1. doi: 10.1016/j.jamcollsurg.2016.02.020
33. Breslow RA, et al. Diet and lung cancer mortality: a 1987 National Health Interview Survey cohort study. Cancer Causes Control (2000) 11(5):419–31. doi: 10.1023/A:1008996208313
34. Bessö A, Nyberg F, Pershagen G. Air pollution and lung cancer mortality in the vicinity of a nonferrous metal smelter in Sweden. Int J Cancer (2003) 107(3):448–52. doi: 10.1002/ijc.11412
35. Borsoi L, Kunze U, Kunze M, Groman E, Kundi M. Trends in mortality and mean age at death from lung cancer in Austria (1975–2007). Cancer Epidemiol (2011) 35(2):120–5. doi: 10.1016/j.canep.2010.06.018
36. Cardenas VM, Thun MJ, Austin H, Lally CA, Clark WS, Greenberg RS, et al. Environmental tobacco smoke and lung cancer mortality in the American Cancer Society's Cancer Prevention Study II. Cancer Causes Control (1997) 8(1):57–64. doi: 10.1023/A:1018483121625
37. Chow W-H, Schuman LM, McLaughlin JK, Bjelke E, Gridley G, Wacholder S, et al. A cohort study of tobacco use, diet, occupation, and lung cancer mortality. Cancer Causes Control (1992) 3(3):247–54. doi: 10.1007/BF00124258
38. Sokolnikov ME, Gilbert ES, Preston DL, Ron E, Shilnikova NS, Khokhryakov VV, et al. Lung, liver and bone cancer mortality in Mayak workers. Int J Cancer (2008) 123(4):905–11. doi: 10.1002/ijc.23581
39. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ (2003) 327(7414):557–60. doi: 10.1136/bmj.327.7414.557
40. Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L. Comparison of two methods to detect publication bias in meta-analysis. JAMA (2006) 295(6):676–80. doi: 10.1001/jama.295.6.676
41. Grewal AS, Padera RF, Boukedes S, Divo M, Rosas IO, Camp PC, et al. Prevalence and outcome of lung cancer in lung transplant recipients. Respir Med (2015) 109(3):427–33. doi: 10.1016/j.rmed.2014.12.013
42. Islami F, Torre LA, Jemal A. Global trends of lung cancer mortality and smoking prevalence. Trans Lung Cancer Res (2015) 4(4):327.
43. Skarin AT, Herbst RS, Leong TL, Bailey A, Sugarbaker D. Lung cancer in patients under age 40. Lung Cancer (2001) 32(3):255–64. doi: 10.1016/S0169-5002(00)00233-6
44. O'Rourke MA, Feussner JR, Feigl P, Laszlo J. Age trends of lung cancer stage at diagnosis: implications for lung cancer screening in the elderly. Jama (1987) 258(7):921–6. doi: 10.1001/jama.1987.03400070059035
45. Khaltaev N, Axelrod S. Global lung cancer mortality trends and lifestyle modifications: preliminary analysis. Chin Med J (2020) 133(13):1526–32. doi: 10.1097/CM9.0000000000000918
46. Rahal Z, El Nemr S, Sinjab A, Chami H, Tfayli A, Kadara H. Smoking and lung cancer: a geo-regional perspective. Front Oncol (2017) 7:194. doi: 10.3389/fonc.2017.00194
47. Loeb LA, Emster VL, Warner KE, Abbotts J, Laszlo J. Smoking and lung cancer: an overview. Cancer Res (1984) 44(12_Part_1):5940–58.
PubMed Abstract | Google Scholar
48. Ozlü T, Bülbül Y. Smoking and lung cancer. Tuberkuloz ve toraks (2005) 53(2):200–9.
Keywords: lung cancer, mortality, predictors, systematic review, global
Citation: Tesfaw LM, Dessie ZG and Mekonnen Fenta H (2023) Lung cancer mortality and associated predictors: systematic review using 32 scientific research findings. Front. Oncol. 13:1308897. doi: 10.3389/fonc.2023.1308897
Received: 07 October 2023; Accepted: 28 November 2023; Published: 14 December 2023.
Reviewed by:
Copyright © 2023 Tesfaw, Dessie and Mekonnen Fenta. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lijalem Melie Tesfaw, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- Introduction
- Article Information
The forest plot presents 2022 lung cancer screening prevalence estimates and 95% CIs for individuals meeting 2013 and 2021 US Preventive Services Task Force eligibility criteria. Vertical lines indicate national 2022 lung cancer screening prevalence estimates using 2013 and 2021 eligibility criteria.
Data Sharing Statement
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Henderson LM , Su I , Rivera MP, et al. Prevalence of Lung Cancer Screening in the US, 2022. JAMA Netw Open. 2024;7(3):e243190. doi:10.1001/jamanetworkopen.2024.3190
Manage citations:
© 2024
- Permissions
Prevalence of Lung Cancer Screening in the US, 2022
- 1 Department of Radiology, University of North Carolina at Chapel Hill
- 2 Lineberger Comprehensive Cancer Center, University of North Carolina at Chapel Hill
- 3 Department of Epidemiology, University of North Carolina at Chapel Hill
- 4 Department of Medicine, University of Rochester Medical Center, Rochester, New York
- 5 Department of Medicine, University of North Carolina at Chapel Hill
The National Lung Screening Trial reported a reduction in lung cancer mortality with low-dose computed tomography lung cancer screening (LCS) among individuals with significant smoking exposure. In 2013, the US Preventive Services Task Force (USPSTF) recommended annual LCS with low-dose computed tomography (CT) for individuals ages 55 to 80 years who currently or formerly smoked (quit within 15 years) with a 30 pack-year (PY) smoking history. 1 In 2021, the USPSTF revised its recommendation to initiate LCS at age 50 years and lowered the smoking requirement to 20 PY, in part to address concerns over disparities in eligibility by race and ethnicity and sex. 2 Despite recommendations, LCS uptake has been low, with 2021 data from 4 states reporting 21% of eligible individuals screened. 3 National estimates of LCS prevalence are limited. Hence, we sought to compare LCS prevalence in 2022 by sociodemographic characteristics and by state among individuals eligible per 2013 vs 2021 USPSTF recommendations.
The University of North Carolina at Chapel Hill institutional review board exempted this cross-sectional study from review and informed consent because data used are publicly available. We followed the STROBE reporting guideline.
We analyzed Center for Disease Control and Prevention Behavioral Risk Factor Surveillance System (BRFSS) data for 2022, which included LCS as a core section for all states. 4 We included adults ages 50 to 79 years who self-reported currently smoking or quitting within the last 15 years with at least a 20-PY smoking history. Because USPSTF recommends yearly LCS, we classified responders who reported a chest CT scan to “check or screen for” lung cancer within the past year as having LCS per recommendations ( Table ).
We created 2 nested groups by USPSTF eligibility criteria: individuals ages 55 to 79 years with a smoking history of 30 or more PYs or ages 50 to 79 years with 20 or more PYs (2013 and 2021 criteria, respectively). We applied BRFSS survey weights to calculate the weighted number of LCS-eligible and screened individuals, then calculated LCS prevalence rates with 95% CIs in each group by characteristics and state. Data were analyzed using SAS statistical software version 9.4 (SAS Institute) and visualized using R statistical software version 4.3.2 (R Project for Statistical Computing).
In 2022, the weighted LCS-eligible population was 13 526 348 individuals vs 8 154 440 individuals per 2021 vs 2013 criteria (an increase of 5 371 908 individuals [65.9%]) ( Table ). The 2022 LCS prevalence was 16.4% and 19.6% using 2021 and 2013 criteria, respectively; the number screened increased by 619 054 individuals. Among individuals newly eligible for LCS under 2021 criteria, 2 063 840 individuals were aged 50 to 54 years, with 6.1% reporting LCS, and 4 020 879 individuals had a 20- to 29-PY smoking history, with 13.1% reporting LCS. Expanded criteria were associated with the greatest relative increase in the LCS-eligible population among Asian (88% increase), Black (109% increase), and Hispanic (86% increase) groups. The number of females eligible for LCS increased by 78% vs 57% for males.
Using 2021 criteria, 2022 LCS prevalence estimates ranged from 8.6% in Wyoming to 28.7% in Rhode Island ( Figure ). In general, Northeastern and Mid-Atlantic states had higher LCS prevalence rates. There were no significant differences in LCS prevalence rates for 2021 vs 2013 criteria by state or territory, including the District of Columbia (23.9% vs 19.3%), Illinois (17.5% vs 14.6%), Guam (19.1% vs 10.6%), and Virgin Islands (14.1% vs 3.5%).
In this cross-sectional study, expanded USPSTF eligibility criteria were associated with 5 371 908 additional individuals eligible for LCS, with relative increases highest for Asian, Black, Hispanic, and female individuals, aligning with the goal of reducing race and ethnic and sex disparities in eligibility. 2 , 5 While approximately 619 054 newly eligible individuals were screened under expanded recommendations, 2022 LCS prevalence remained low (16.4%). Prior BRFSS analyses using 2013 USPSTF criteria reported LCS prevalence rates of 12.8% in 2019 (20 states) 6 and 21.2% in 2021 (4 states), 3 indicating a similar LCS prevalence rate in 2021 and 2022 (19.6%). A limitation of our study was that BRFSS LCS data are self-reported. Our findings suggest that updated LCS eligibility criteria may be an important first step to reducing lung cancer disparities, although screening rates remained low. Increasing LCS uptake nationwide should be a major public health priority.
Accepted for Publication: January 28, 2024.
Published: March 21, 2024. doi:10.1001/jamanetworkopen.2024.3190
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2024 Henderson LM et al. JAMA Network Open .
Corresponding Author: Louise M. Henderson, PhD, Department of Radiology, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599-7515 ( [email protected] ).
Author Contributions: Dr Henderson and Ms Su had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Henderson, Su, Rivera, Lund.
Acquisition, analysis, or interpretation of data: Henderson, Su, Pak, Chen, Reuland, Lund.
Drafting of the manuscript: Henderson.
Critical review of the manuscript for important intellectual content: All authors.
Statistical analysis: Henderson, Su, Pak, Reuland, Lund.
Obtained funding: Henderson, Rivera, Lund.
Administrative, technical, or material support: Henderson, Chen, Lund.
Supervision: Henderson, Lund.
Conflict of Interest Disclosures: Dr. Henderson reported receiving grants from the National Institutes of Health during the conduct of the study. Dr Su reported receiving the Bristol-Myers Squibb (BMS)-University of North Carolina (UNC) Worldwide Health Economics and Outcomes Research Predoctoral Fellowship, with funds distributed through UNC and not directly from BMS, outside the submitted work. No other disclosures were reported.
Funding/Support: This work was supported through grants R01CA277756, R01CA292014, and R01CA251686 from the National Cancer Institute of the National Institutes of Health.
Role of the Funder/Sponsor: The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Data Sharing Statement: See the Supplement .
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Advances in Lung Cancer Research

Lung cancer cells driven by the KRAS oncogene, which is highlighted in purple.
NCI-funded researchers are working to advance our understanding of how to prevent, detect, and treat lung cancer. In particular, scientists have made progress in identifying many different genetic alterations that can drive lung cancer growth.
This page highlights some of the latest research in non-small cell lung cancer (NSCLC), the most common form of lung cancer, including clinical advances that may soon translate into improved care, NCI-supported programs that are fueling progress, and research findings from recent studies.
Early Detection of Lung Cancer
A great deal of research has been conducted in ways to find lung cancer early. Several methods are currently being studied to see if they decrease the risk of dying from lung cancer.
The NCI-sponsored National Lung Screening Trial (NLST) showed that low-dose CT scans can be used to screen for lung cancer in people with a history of heavy smoking. Using this screening can decrease their risk of dying from lung cancer. Now researchers are looking for ways to refine CT screening to better predict whether cancer is present.
Markers in Blood and Sputum
Scientists are trying to develop or refine tests of sputum and blood that could be used to detect lung cancer early. Two active areas of research are:
- Analyzing blood samples to learn whether finding tumor cells or molecular markers in the blood will help diagnose lung cancer early.
- Examining sputum samples for the presence of abnormal cells or molecular markers that identify individuals who may need more follow-up.
Machine Learning
Machine learning is a method that allows computers to learn how to predict certain outcomes. In lung cancer, researchers are using computer algorithms to create computer-aided programs that are better able to identify cancer in CT scans than radiologists or pathologists. For example, in one artificial intelligence study , researchers trained a computer program to diagnose two types of lung cancer with 97% accuracy, as well as detect cancer-related genetic mutations.
Lung Cancer Treatment
Treatment options for lung cancer are surgery , radiation , chemotherapy , targeted therapy , immunotherapy , and combinations of these approaches. Researchers continue to look for new treatment options for all stages of lung cancer.
Treatments for early-stage lung cancer
Early-stage lung cancer can often be treated with surgery. Researchers are developing approaches to make surgery safer and more effective.
- When lung cancer is found early, people usually have surgery to remove an entire section ( lobe ) of the lung that contains the tumor. However, a recent clinical trial showed that, for certain people with early-stage NSCLC, removing a piece of the affected lobe is as effective as surgery to remove the whole lobe .
- The targeted therapy Osimertinib (Tagrisso ) was approved by the FDA in 2021 to be given after surgery—that is, as adjuvant therapy —to people with early-stage NSCLC that has certain mutations in the EGFR gene.
- Two immunotherapy drugs, atezolizumab (Tecentriq) and pembrolizumab (Keytruda) have been approved by the FDA to be used as adjuvant treatments after surgery and chemotherapy, for some patients with early-stage NSCLC.
- The immunotherapy drug nivolumab (Opdivo) is approved to be used, together with chemotherapy, to treat patients with early-stage lung cancer before surgery (called neoadjuvant ). This approval, which came in 2022, was based on the results of the CheckMate 816 trial, which showed that patients who received neoadjuvant nivolumab plus chemotherapy lived longer than those who received chemotherapy alone .
- In another trial (Keynote-671), patients with early-stage NSCLC who received pembrolizumab plus chemotherapy before surgery and pembrolizumab after surgery had better outcomes than those who received just neoadjuvant or just adjuvant treatment.
Treatments for advanced lung cancer
Newer therapies are available for people with advanced lung cancer. These primarily include immunotherapies and targeted therapies, which continue to show benefits as research evolves.
Immunotherapy
Immunotherapies work with the body's immune system to help fight cancer. They are a major focus in lung cancer treatment research today. Clinical trials are ongoing to look at new combinations of immunotherapies with or without chemotherapy to treat lung cancer.
Immune checkpoint inhibitor s are drugs that block an interaction between proteins on immune cells and cancer cells which, in turn, lowers the immune response to the cancer. Several immune checkpoint inhibitors have been approved for advanced lung cancer, including p embrolizumab (Keytruda) . a tezolizumab (Tecentriq) , c emiplimab (Libtayo) , d urvalumab (Imfinzi) , and n ivolumab (Opdivo) .
A key issue with immunotherapies is deciding which patients are most likely to benefit. There is some evidence that patients whose tumor cells have high levels of an immune checkpoint protein called PD-L1 may be more responsive to immune checkpoint inhibitors. Another marker for immunotherapy response is tumor mutational burden , or TMB, which refers to the amount of mutations in the DNA of the cancer cells. In some lung cancer trials, positive responses to immune checkpoint inhibitors have been linked with a high TMB. However, these markers cannot always predict a response and there is ongoing work to find better markers.
To learn more, see Immunotherapy to Treat Cancer .
Targeted Therapies
Targeted treatments identify and attack certain types of cancer cells with less harm to normal cells. In recent years, many targeted therapies have become available for advanced lung cancer and more are in development. Targeted treatments for lung cancer include the below.
Anaplastic lymphoma kinase (ALK) Inhibitors
ALK inhibitors target cancer-causing rearrangements in a protein called ALK. These drugs continue to be refined for the 5% of NSCLC patients who have an ALK gene alteration. Approved treatments include ceritinib (Zykadia) , alectinib (Alecensa) , brigatinib (Alunbrig) , and lorlatinib (Lorbrena) .
These ALK inhibitors are improvements from previous ones in their enhanced ability to cross the blood–brain barrier. This progress is critical because, in non-small cell lung cancer patients with ALK alterations, disease progression tends to occur in the brain.
EGFR Inhibitors
- Lung Cancer Trial of Osimertinib Draws Praise—and Some Criticism
The drug improved survival in a large clinical trial, but some question the trial’s design.
EGFR inhibitors block the activity of a protein called epidermal growth factor receptor (EGFR). Altered forms of EGFR are found at high levels in some lung cancers, causing them to grow rapidly. Osimertinib (Tagrisso) is the most effective and most widely used EGFR inhibitor. It is also used for adjuvant therapy after surgery for resectable NSCLC. Other drugs that target EGFR that are approved for treating NSCLC include afatinib (Gilotrif) , dacomitinib (Vizimpro) , erlotinib (Tarceva) , gefitinib (Iressa) . For people with Exon 20 mutations, amivantamab (Rybrevant) is an approved targeted therapy.
ROS1 Inhibitors
The ROS1 protein is involved in cell signaling and cell growth. A small percentage of people with NSCLC have rearranged forms of the ROS1 gene. Crizotinib (Xalkori) and entrectinib (Rozlytrek) are approved as treatments for patients with these alterations. In late 2023, the FDA approved repotrectinib (Augtyro) for advanced or metastatic NSCLC with ROS1 fusions as an initial treatment and as a second-line treatment in those who previously received a ROS1-targeted drug.
BRAF Inhibitors
The B-Raf protein is involved in sending signals in cells and cell growth. Certain changes in the B-Raf gene can increase the growth and spread of NSCLC cells.
The combination of the B-Raf-targeted drug dabrafenib (Tafinlar) and trametinib (Mekinist ), which targets a protein called MEK, has been approved as treatment for patients with NSCLC that has a specific mutation in the BRAF gene.
Encorafenib (Braftovi) combined with binimetinib (Mektovi) is approved for patients with metastatic NSCLC with a BRAF V600E mutation .
Other Inhibitors
Some NSCLCs have mutations in the genes NRTK-1 and NRTK-2 that can be treated with the targeted therapy larotrectinib (Vitrakvi). Those with certain mutations in the MET gene can be treated with tepotinib (Tepmetko) or capmatinib (Tabrecta) . And those with alterations in the RET gene are treated with selpercatinib (Retevmo) and pralsetinib (Gavreto) . A 2023 clinical trial showed that treatment with selpercatinib led to longer progression-free survival compared with people who received chemotherapy with or without pembrolizumab. Inhibitors of other targets that drive some lung cancers are being tested in clinical trials.
See a complete list of targeted therapies for lung cancer .
NCI-Supported Research Programs
Many NCI-funded researchers at the NIH campus, and across the United States and the world, are seeking ways to address lung cancer more effectively. Some research is basic, exploring questions as diverse as the biological underpinnings of cancer and the social factors that affect cancer risk. And some is more clinical, seeking to translate basic information into improved patient outcomes. The programs listed below are a small sampling of NCI’s research efforts in lung cancer.

Pragmatica-Lung Study Enrolling Patients
The simplified trial may serve as a model for future cancer clinical trials.
- The Pragmatica-Lung Study is a randomized trial that will compare the combination of the targeted therapy ramucirumab (Cyramza) and the immunotherapy pembrolizumab (Keytruda) with standard chemotherapy in people with advanced NSCLC whose disease has progressed after previous treatment with immunotherapy and chemotherapy. In addition to looking at an important clinical question, the trial will serve as a model for future trials because it is designed to remove many of the barriers that prevent people from joining clinical trials.
- Begun in 2014, ALCHEMIST is a multicenter NCI trial for patients with early stage non-small cell lung cancer. It tests to see whether adding a targeted therapy after surgery, based on the genetics of a patient’s tumor, will improve survival.
- The Lung MAP trial is an ongoing multicenter trial for patients with advanced non-small cell lung cancer who have not responded to earlier treatment. Patients are assigned to specific targeted therapies based on their tumor’s genetic makeup.
- The Small Cell Lung Cancer Consortium was created to coordinate efforts and provide a network for investigators who focus on preclinical studies of small-cell lung cancer. The goal of the consortium is to accelerate progress on this disease through information exchange, data sharing and analysis, and face-to-face meetings.
- NCI funds eight lung cancer Specialized Programs of Research Excellence (Lung SPOREs) . These programs are designed to quickly move basic scientific findings into clinical settings. Each SPORE has multiple lung cancer projects underway.
Clinical Trials
NCI funds and oversees both early- and late-phase clinical trials to develop new treatments and improve patient care. Trials are available for both non-small cell lung cancer treatment and small cell lung cancer treatment .
Lung Cancer Research Results
The following are some of our latest news articles on lung cancer research:
- Repotrectinib Expands Treatment Options for Lung Cancers with ROS1 Fusions
- Tarlatamab Shows Promise for Some People with Small Cell Lung Cancer
- Selpercatinib Slows Progression of RET-Positive Lung, Medullary Thyroid Cancers
- Lung-Sparing Surgery Is Effective for Some with Early-Stage Lung Cancer
- Enhertu Marks First Targeted Therapy for HER2-Mutant Lung Cancer
View the full list of Lung Cancer Research Results and Study Updates .
- Search Menu
- Browse content in Acquired Cardiac
- Arrhythmias
- Congestive Heart Failure
- Coronary Disease (Acquired Cardiac)
- Education (Acquired Cardiac)
- Experimental (Acquired Cardiac)
- Great Vessels
- Heart Failure Surgery (Acquired Cardiac)
- Mechanical Circulatory Support
- Minimally Invasive Procedures (Acquired Cardiac)
- Myocardial Infarction
- Organ Protection (Acquired Cardiac)
- Pericardium
- Transcatheter Procedures
- Translational Research (Acquired Cardiac)
- Tumours (Acquired Cardiac)
- Valve Disorders (Acquired Cardiac)
- Browse content in Congenital
- Anomalies of LVOT and RVOT
- Double Inlet or Double Outlet Ventricle
- Education (Congenital)
- Experimental (Congenital)
- Fontan Operation
- Grown-up Congenital Heart Disease
- Heart Failure Surgery (Congenital)
- Interventional Procedures (Congenital)
- Neurodevelopment (Congenital)
- Organ Protection (Congenital)
- Perioperative Care (Congenital)
- Septal Defects (Congenital)
- Tetralogy of Fallot
- Translational Research (Congenital)
- Transposition Surgery
- Tumours (Congenital)
- Univentricular Palliation
- Valvular Anomalies (Congenital)
- Vessel Anomalies (Congenital)
- Browse content in General Interest
- Basic Science
- Clinical Epidemiology
- Education (General Interest)
- Essential Surgical Skills
- Experimental (General Interest)
- Perioperative Care (General Interest)
- Research Methods
- Browse content in Thoracic
- Education (Thoracic)
- Experimental (Thoracic)
- Mediastinum
- Minimally Invasive Procedures (Thoracic)
- Organ Protection (Thoracic)
- Trachea and Bronchi
- Translational Research (Thoracic)
- Trauma (Thoracic)
- Browse content in Vascular
- Aortic Disorders
- Aorto-iliac Disease
- Cerebrovascular Disease
- Education (Vascular)
- Endovascular Procedures
- Experimental (Vascular)
- Organ Protection (Vascular)
- Peripheral Arteries and Veins
- Renal and Visceral Arteries
- Translational Research (Vascular)
- Vascular Malformations
- Venous Disease
- Advance articles
- Editor's Choice
- Supplements
- Residents' Corner
- Author Guidelines
- Statistical Primers
- Publishing Tips
- Why Publish with EJCTS
- About European Journal of Cardio-Thoracic Surgery
- About the European Association for Cardio-Thoracic Surgery
- About the European Society of Thoracic Surgeons
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Contact EACTS
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Perioperative immune checkpoint blockades improve prognosis of resectable non-small cell lung cancer.
Yu Tian, Zhichao Liu, Hanbo Pan authors contributed equally to this paper.
- Article contents
- Figures & tables
- Supplementary Data
Yu Tian, Zhichao Liu, Hanbo Pan, Hongda Zhu, Ningyuan Zou, Long Jiang, Ziming Li, Jia Huang, Yingjie Hu, Qingquan Luo, Perioperative immune checkpoint blockades improve prognosis of resectable non-small cell lung cancer, European Journal of Cardio-Thoracic Surgery , 2024;, ezae110, https://doi.org/10.1093/ejcts/ezae110
- Permissions Icon Permissions
Immune checkpoint blockades (ICB) have been proven to improve prognosis of non-small cell lung (NSCLC) in the neoadjuvant setting, while whether its perioperative use could bring extra benefit remained unidentified. We aimed to demonstrate the prognostic benefit of perioperative ICB over preoperative-only use and investigate who could benefit from this “sandwich ICB therapy”.
Patients undergoing neoadjuvant therapy followed by surgery from 2018 to 2022 was retrospectively reviewed, and were divided into four groups based on the perioperative regimens: pre-ICB + post-CT, pre-ICB-only, pre-CT + post-ICB, and pre-CT-only. Treatment-related adverse events, surgical outcomes, therapeutic response, recurrence-free survival (RFS) and overall survival (OS) were compared.
Of 214 enrolled patients with preoperative therapy, 108 underwent immunochemotherapy and 106 underwent platinum-based chemotherapy. Compared with preoperative chemotherapy, preoperative immunochemotherapy was demonstrated with significantly higher major pathologic response (MPR, 57/108 vs 12/106) and pathologic complete response (pCR, 35/108 vs 4/106) rates with comparable adverse events. Regarding survival, perioperative ICB significantly improved the RFS (vs pre-CT-only HR, 0.15; 95% CI, 0.09–0.27; vs pre-ICB-only HR, 0.36; 95% CI, 0.15–0.88) and OS (vs pre-CT-only HR, 0.24; 95% CI, 0.08–0.68). In patients without MPR, perioperative ICB was observed to decrease the risk of recurrence (HR, 0.31; 95% CI 0.11–0.83) compared with preoperative ICB, and was an independent prognostic factor (p < 0.05) for RFS.
Perioperative ICB showed promising efficacy in improving pathological response and survival outcomes of resectable NSCLC. For patients without MPR after resection followed by preoperative ICB, sequential ICB treatment could be considered.

Author notes
- non-small-cell lung carcinoma
- perioperative care
- preoperative care
- cell cycle checkpoint
Supplementary data
Email alerts, citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1873-734X
- Copyright © 2024 European Association for Cardio-Thoracic Surgery
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 26 March 2024
Background and clinical significance of biomarker-based patient enrichment in non-small-cell lung cancer drug development
- Kenji Harada 1 , 2 &
- Shunsuke Ono 1
Scientific Reports volume 14 , Article number: 7194 ( 2024 ) Cite this article
151 Accesses
7 Altmetric
Metrics details
- Business strategy in drug development
- Clinical trials
- Drug development
- Drug discovery
- Non-small-cell lung cancer
Pharmaceutical companies have adopted biomarker-based enrichment (personalized) strategies to improve research and development productivity. We explored the background in which personalized strategies are adopted and examined whether their adoption is linked to improved efficacy of new drugs approved for non-small cell lung cancer (NSCLC) by US Food and Drug Administration (FDA). We extracted data from the first labels of drugs approved for NSCLC between May 2003 and February 2021, and performed a qualitative comparative analysis and meta-analysis. Personalized strategies were adopted in more than half of the trials (16/27) and were often used in trials aimed at obtaining first-line indications and in drugs that were not first-in-class. The meta-analysis showed that personalized trials had significantly improved progression-free survival (PFS) hazard ratio (HR) than trials without personalization but not for relative response rate ratio (RRR) or overall survival (OS) HR. Trials in which PFS HR was the primary endpoint tended to have improved PFS HR, and trials in which OS HR was the primary endpoint had worse PFS HR. The efficacy endpoints that are substantially affected by personalized strategies appear to differ, especially for new drugs with novel mechanism of action (MOA), because trial designs are employed to validate drug-specific advantages.
Similar content being viewed by others

The National Lung Matrix Trial of personalized therapy in lung cancer
Gary Middleton, Peter Fletcher, … Lucinda Billingham

Defining subpopulations of differential drug response to reveal novel target populations
Nirmal Keshava, Tzen S. Toh, … Dennis Wang

Evaluating eligibility criteria of oncology trials using real-world data and AI
Ruishan Liu, Shemra Rizzo, … James Zou
Introduction
The recent rise in pharmaceutical Research & Development (R&D) costs and the decline in the number of approved drugs have long called for the need to improve drug development efficiency 1 , 2 . Approaches based on pharmacogenomics (PGx), a field of research that clarifies the causal relationship between drug response and genetic polymorphisms in organisms, are expected to optimize the efficacy and safety profile of drugs based on individual genome information 3 . The practical application of PGx is a personalized approach that uses biomarkers in clinical trials. There are several drugs for which the patient enrichment biomarkers specified by PGx are listed on the drug label 4 . Examples include crizotinib and dabrafenib. Crizotinib is a kinase inhibitor indicated for the treatment of adult patients with metastatic NSCLC whose tumors are anaplastic lymphoma kinase (ALK) or ROS1-positive as detected by an FDA-approved test. Dabrafenib is a kinase inhibitor indicated for the treatment of patients with unresectable or metastatic melanoma with BRAF V600E mutation as detected by an FDA-approved test.
The recent emergence of anticancer drugs with innovative mechanisms of action has significantly changed the methods and strategies for new drug development. For example, immune checkpoint inhibitors, such as PD-1/PD-L1 inhibitors, have dramatically improved the prognosis of patients with cancer 5 . The mode of cancer treatment is also changing, as evidenced by extensive advances in gene therapy. In this increasingly competitive anticancer drug market, it is natural for companies to conduct clinical development to demonstrate the most obvious advantages of their products based on their characteristics. The application of personalized strategies to new drug development serves as the objective of companies.
A previous study analyzing FDA-approved anticancer drugs found that the adoption of personalized strategies is associated with improved efficacy 6 . In addition, studies on the impact of personalized strategies on drug development showed that the phase transition rates were higher for products using patient enrichment biomarkers than for those not using them 7 and that personalized strategies were associated with higher median response rates (RR) and longer median PFS in phase I and II trials 8 , 9 .
However, from the perspective of optimizing the pharmaceutical business, companies do not unconditionally apply personalization strategies to all drugs. Personalized strategies necessarily involve some type of market segmentation that may reduce potential future revenue. Strategies that seek competitive advantages of a drug other than its high efficacy (e.g., improved safety) may also be reasonable in certain therapeutic areas. Pharmaceutical companies are expected to use personalized strategies not only to improve the efficacy observed in clinical trials, but also to optimize the positioning of their products in individual markets.
In this study, we investigated the adoption of personalized strategies in recent pivotal and/or phase III trials of anticancer drugs approved in the US for the treatment of NSCLC, one of the cancers to which personalized strategies are most applied. Since NSCLC has high genetic heterogeneity and the prognosis and safety of treatment with existing drugs are still insufficient, the application of personalized medicine (i.e., patient selection by biomarker) has been pursued. Furthermore, it has become clear that drugs with PD-1/L1 inhibition as described above are effective for NSCLC. We applied logical analysis and identified the conditions in which companies adopted personalized strategies. We then examined the relationship between personalized strategies and the effect size in these trials. As several efficacy endpoints have been examined in oncological trials, we explored whether the observed relationship was the same across different endpoints. Based on the results of these analyses, we discuss what should be considered when interpreting and generalizing the results of pivotal trials conducted to obtain regulatory approval.
All anti-cancer drugs approved for NSCLC between May 2003 and February 2021 were identified by the FDA 10 . In 2003, gefitinib was approved as the first molecularly targeted drug for the treatment of NSCLC. Among these drugs, those listed in the FDA’s Table of Pharmacogenomic Biomarkers in Drug Labeling as of February 2021, and those with a patient enrichment biomarker listed in the “Indication and usage” section of the label were classified as anticancer drugs, for which a personalized strategy was adopted. We reviewed the first label approved for the treatment of NSCLC and extracted data on efficacy endpoints, including RR, PFS, and OS. There were six drugs for which results with and without a personalized strategy were indicated. For drugs that received accelerated approval, we used data at the time of final approval. Drugs with only single-arm trials listed on the label were excluded from the analysis because it is difficult to reliably estimate the effect size (e.g., risk ratio, HR) (Fig. 1 ). Biosimilars were also excluded from the analysis because they basically follow the personalized/non-personalized strategy of their predecessors and could not choose the personalized/non-personalized strategy itself as a strategic option in drug development (Fig. 1 ). Informed consent was not sought for this study because it is not a research involving human participants.
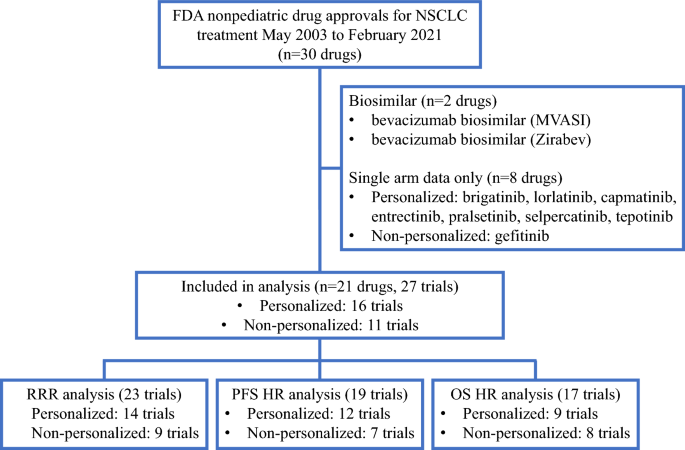
Flow diagram of search strategy and study selection.
To classify the background of a company’s choice to adopt a personalized/non-personalized drug strategy, we performed qualitative comparative analysis (QCA). QCA uses set theory and Boolean algebra to infer the causal relationship between the characteristics of individual cases and their results, enabling a logical examination of similarities and differences among cases. The QCA results are expressed in the form of multiple conditional expressions that provide clues for deciphering causal relationships. After reviewing the “Indication and usage” section of the labels, we obtained the following six background conditions for each drug that may have contributed to the decision to adopt a personalized strategy:(1) whether the personalized strategy has been taken in other cancers before development in NSCLC, (2) whether the drug has indication for squamous NSCLC only (this cancer type is known to have few genetic mutations), (3) whether the drug has received orphan designation, (4) whether the drug is an immune checkpoint inhibitor (i.e., a new MOA), (5) whether the drug is the first anticancer drug targeting the molecule in NSCLC, (6) whether the drug has a first-line indication. The logical remainder (i.e., the parsimonious solution) was applied to the QCA. Tosmana ver. 1.6.1.0) was used for statistical analysis.
We performed a meta-analysis (random-effects model) to determine the association between personalized strategies and effect size. The effect size of the HR for PFS and OS and the relative response rate ratio (RRR) for RR were calculated. The mediators or confounders included personalization, randomization, drug type (cytotoxic vs. targeted), concomitant medications, control drug (active treatment vs. placebo), crossover, tumor immunity-related target, FDA approval date (before the median vs. after), effect size pertaining to the primary endpoint of the trial, first-line treatment, first-in-class target, priority review, and orphan drug designation. Independent samples were assessed using the Wilcoxon rank-sum test.
We further investigated the effect sizes of PFS and OS using meta-regression analysis (random-effects model) with independent variables (for PFS: personalization, OS HR pertains to the primary endpoint; for OS: drug type, tumor immunity-related target, and priority review), all of which were significantly associated with PFS HR and OS HR in each meta-analysis.
Differences were considered statistically significant at p < 0.05. Statistical analyses were performed using Stata 14 software (StataCorp, College Station, TX, USA).
We identified 21 drugs approved for the treatment of NSCLC between May 2003 and February 2021 that met the criteria described in the Methods section (Fig. 1 ). For the 21 drugs, 27 trials were phase III and/or pivotal trials, 16 were personalized trials, and 11 were non-personalized trials (Supplemental Tables 1 and 2 ). All drugs, except for paclitaxel protein-bound particles and pemetrexed disodium, were molecularly targeted drugs, the targets of which were epidermal growth factor receptor (EGFR)-related targets (EGFR, human epidermal growth factor (HER)2, and HER4), anaplastic lymphoma kinase (ALK), immuno-onco-targets (Programmed death receptor-1/Programmed cell Death ligand 1 and Cytotoxic T-lymphocyte associated antigen-4), and others (vascular endothelial growth factor-2, v-raf murine sarcoma viral oncogene homolog B1, and mitogen-activated extracellular signal-regulated kinase 1/2).
Descriptive characteristics of personalized and non-personalized trials that met the selection criteria
The characteristics of personalized and non-personalized trials that met the selection criteria are summarized and compared in Table 1 . Recently, the number of personalized trials has increased. Personalized trials were performed only for molecularly targeted drugs (100% [16/16]) and mostly for drugs that were not first-in-class (75% [12/16] vs. 36% [4/11]). They were administered more often as first-line drugs (88% [14/16] vs. 36% [4/11]) and orphan drugs (56% [9/16] vs. 18% [2/11]). Placebo controls were not used in personalized trials. Personalized trials more often adopted the PFS HR as the primary endpoint (75% [12/16] vs. 18% [2/11]), whereas non-personalized trials tended to use the OS HR as the primary endpoint (31% [5/16] vs. 64% [7/11]).
These findings were consistent when viewed separately for each endpoint employed in the study (Table 1 ). PFS was the primary endpoint in all personalized trials in which it was evaluated.
The results of the logical analysis (QCA) of the background of the personalized and non-personalized trials are shown in Table 2 . The truth table is presented in Supplementary Table 3 . Two trials (personalized pembrolizumab and non-personalized durvalumab) were acknowledged as exceptional cases.
The backgrounds of the trials with and without personalized strategies were classified into five and six categories, respectively ((1)–(5) and (6)–(11) in Table 2 ). No personalized trials have been conducted for squamous NSCLC. Personalized strategies have been employed in trials for first-line applications and follow-on trials (i.e., not first-in-class) drugs. Orphan designation is generally linked to the conduct of personalized trials. Orphan drug background was associated with the conduct of personalized trials, not alone, but in conjunction with other backgrounds.
Effect sizes and personalized strategies for each endpoint (meta-analysis)
The results of meta-analysis are presented in Fig. 2 and Table 3 .
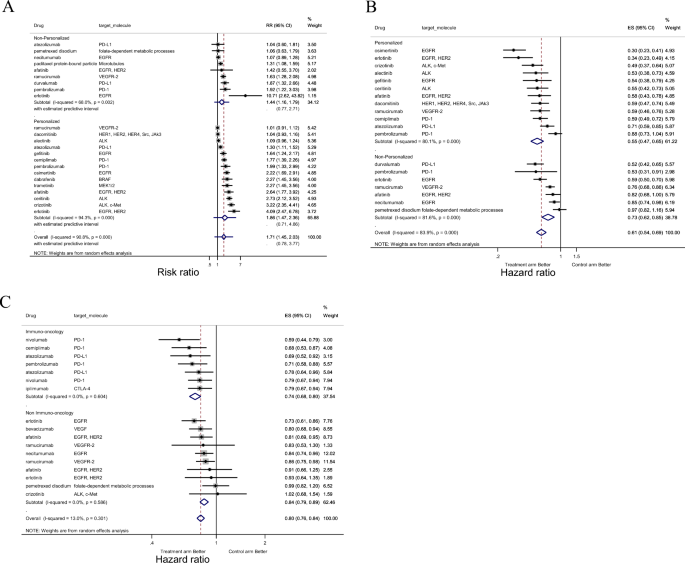
Forest-plot representing the relative response rate ratio (RRR) ( A ), hazard ratios (HRs) for progression-free survival (PFS) ( B ), and HRs for overall survival (OS) (C) between the experimental and control arms by personalized therapy status (( A ), ( B )), or by imuno-onco target status ( C ) in trials. In ( A ), RRR is shown and lines to the right of the vertical line indicate improvement in the experimental arm. In ( B and C ), the plots show HRs and, therefore, lines to the left of the vertical line indicate improvement (i.e., lower HR for PFS or OS) for the experimental arm.
Adoption of a personalized strategy was associated with improved PFS HR (HR, 0.76; p = 0.048) but not with RRR or OS HR (Table 3 ). For PFS HR, being a molecular-targeted drug (HR, 0.61; p = 0.086) and having a primary endpoint of PFS HR (HR, 0.75; p = 0.062) also tended to be associated with an improved PFS HR. In contrast, having a primary endpoint of OS HR was associated with worse PFS HR (HR, 1.43; p = 0.004). Being a molecular-targeted drug (HR, 0.80; p = 0.042), being an immune checkpoint inhibitor (HR, 0.88; p = 0.023), and priority review (HR, 0.87; p = 0.013) were associated with improved OS HR. Heterogeneity between the trials for RRR and PFS HR was classified as high (I 2 > 75%) or low (I 2 < 50%) for OS HR.
Meta-regression analysis with two independent variables showing a significant association in the meta-analysis of PFS HR indicated that trials with OS HR as the primary endpoint were associated with worse PFS HR (HR, 1.36; p = 0.016).
We analyzed clinical trials that have been submitted as the basis for regulatory approval for NSCLC since 2003 to evaluate the context in which personalized strategies have been adopted and whether these strategies improve the efficacy observed in such trials.
Personalized strategies were adopted in more than half of the trials (16/27 [59%]). Personalized trials were more likely to include the HR for PFS as the primary endpoint, whereas non-personalized trials included the HR for OS as the primary endpoint. The analysis also revealed that personalized strategies are often used in trials aimed at obtaining first-line indications and in trials of drugs that are not first-in-class. QCA also revealed that overall, the orphan drug designation status is associated with the adoption of personalized strategies and may also be a contributing factor to the relationship between other background factors and the adoption of personalized strategies.
Our meta-analysis showed a significant positive correlation between personalized strategies and improvement in PFS HR, but not in RRR or OS HR. Our results also revealed that the relationship between personalized strategies and outcomes varies depending on what is employed as the primary endpoint of the trial: in trials where PFS was the primary endpoint, PFS HR improved with the adoption of personalized strategies, whereas in trials where OS was the primary endpoint, the improvement did not occur. New drugs with tumor immune-related targets that have not been investigated in previous studies have shown a clear improvement in OS, indicating that the emergence of such drugs may weaken the correlation between personalized strategies and effect sizes, particularly for OS HR.
The QCA results, which enable logical linking of the background conditions of trials to the adoption of personalized designs, provide interesting clues for inferring why a company would (or would not) conduct personalized trials. These results could also help explain the consistent distribution patterns shown in Table 1 .
Several combinations of conditions were found to correspond to the use or non-use of personalized strategies, and these combinations led to the following interpretation: First, a personalized strategy was adopted when the target indication was NSCLC with targeted driver oncogene mutations 11 , 12 , 13 , 14 ((1) and (6) in Table 2 ). Second, personalized strategies tend to be adopted in trials aimed at obtaining approval for first-line treatments ((2), (8), (10), and (11) in Table 2 ). This finding may reflect the fact that patients eligible for first-line treatment are more heterogeneous than those eligible for second-line or subsequent treatment and that the magnitude of the efficacy signal expected for approval is greater for first-line treatment than for second-line treatment. Third, personalized strategies are often used in trials for drugs that are not first-in-class (i.e., follow-on drugs (3), (4), (9), and (11) in Table 2 ). In the development of first-in-class drugs, companies tend to approach broader patient populations, but there may be a lack of validated and appropriate biomarkers. In contrast, companies developing follow-on new drugs with the same mechanism of action can take advantage of richer, accumulated information on patient selection. The existence of treatment-resistant patients is gradually becoming more evident, leading to a growing need for personalization through the appropriate use of biomarkers. In some cases, if the preceding drug has adopted a personalized strategy, follow-on products may have no choice but to adopt the same strategy 15 , 16 . Fourth, personalized strategies are more likely to be adopted when the target indication is given orphan status ((1), (5), (8), and (9) in Table 2 ). This relationship naturally arises because orphan designation is usually provided when attempts are made to subdivide patients with NSCLC using biomarkers.
Our observation that the background of personalization through the use of biomarkers can be classified into several patterns reflects the reality of the recent development strategies of industries, regulatory approval policies, and trends relevant to anticancer drugs. The results can also be seen as an example of the successful exploitation of the potential of recent drugs with distinctive characteristics and a delicate balance of risk–benefit profiles.
Regardless of the background and purpose of personalization, we expect it to improve efficacy and/or safety in clinical trials. A previous study 6 reported that the adoption of a personalized strategy was significantly correlated with improvements in RRR and HR for PFS and that a positive correlation with improvements in HR for OS was also observed, but weakly ( p = 0.07). Our results showed that the personalized strategy was associated only with the HR for PFS, and not with the RRR or HR for OS. The observed differences can be explained by the different types of drugs and clinical trials analyzed.
Our results may reflect the inclusion of newly introduced drugs with distinctive features in terms of their mechanisms of action. Compared to previous studies, the targeted drugs in this study included a larger number of drugs that, due to resistance to treatment, may be evaluated more favorably by PFS than by OS. Several studies have suggested that drugs that exert effects on specific molecules in the body may be highly effective in the early stages of treatment and improve PFS HR; however, with continued treatment, drug resistance may develop due to the acquisition of resistance mutations, and OS HR may not improve 17 , 18 , 19 , 20 , 21 . The samples in the previous study 6 were anticancer drugs approved between September 1998 and June 2013 and did not include second-generation EGFR tyrosine kinase inhibitors (TKIs) (afatinib), third-generation EGFR TKIs (osimertinib), or each generation of ALK inhibitors (crizotinib, ceritinib, and alectinib), which are known to acquire resistance in clinical settings 22 , 23 .
Immune checkpoint inhibitors have not been fully analyzed in previous studies 6 . These inhibitors cause the acquisition of tumor immunity by immune cells in patients and the long-term retention of antitumor activity 24 , 25 , 26 . They showed improved OS HR in this study, and this advantage may have masked potential efficacy gains from personalized strategies. In fact, 44.4% (4/9) of trials of immune checkpoint inhibitors in our sample achieved efficacy levels sufficient for approval without a personalized strategy.
The finding that the relationship between personalized strategy and effect size varied by endpoint may also be explained by the fact that we examined only trials that provided evidence to justify successful marketing approval. Our analysis showed that the PFS HR was improved in trials in which PFS was the primary endpoint and worse in trials in which OS was the primary endpoint (Table 3 ). This indicates that the observed efficacy for each endpoint was used flexibly as a basis for approval, depending on the type of drug and its indication.
The endpoints emphasized in regulatory approval have also changed over time. Approval for NSCLC used to be granted based on trials with OS as the primary endpoint. However, the discussion at the Oncologic Drugs Advisory Committee (ODAC) on December 3, 2003, concluded that PFS may be used as an endpoint to evaluate drug effects in metastatic disease for consideration of regular approval. The FDA issued guidance 27 based on the discussion at the ODAC to encourage the use of PFS as the primary endpoint and as the basis for approval. In contrast, recent evaluations of immune checkpoint inhibitors have focused more on OS than on PFS as an endpoint owing to their unique mechanism of action. They may cause pseudo progression 5 , 28 , which results in transient disease progression and worsening of PFS HR even when the OS HR eventually improves.
As seen from the background analysis of the trials mentioned above, a personalized strategy appears to be adopted as an option for a company’s development and life cycle management. Six drugs in our sample had both personalized and non-personalized indications. First, afatinib and pembrolizumab obtained approval for personalized indications and then for non-personalized indications. In contrast, atezolizumab, erlotinib, nivolumab, and ramucirumab were approved for non-personalized indications first and then obtained approval for personalized indications. The effect sizes of the latter indications for each drug were not necessarily large (Supplementary Table 2 ).
Although it is unclear how much of the relationship found in the study can be attributed to the pharmacological response of drugs related to indications and to the background of trials (i.e., successful trials used to obtain marketing approval), it has been revealed that background factors in the choice of study design may confound the results of efficacy. When comparing drug effect sizes or extrapolating trial results, one must be cautious about the purpose and context of the trial.
The results of this study seem to support the appropriate adoption of a personalized strategy to obtain a favorable effect size and present compelling evidence for regulators. This study does not necessarily provide an answer to the question of whether selecting a personalized approach is appropriate as an industrial development strategy. Nevertheless, since 2003, more than half of the molecular-targeted drugs approved for NSCLC have used personalized strategies for different purposes, suggesting that companies can benefit from strategic options in their drug development. In a competitive environment, biomarker-based personalization will not merely create a downside to market fragmentation, but will also ensure the proper positioning of drugs in the anticancer treatment and pharmaceutical business.
Therefore, it is critical to discover and develop superior biomarkers that enable more efficient and effective enrichment and utilization in cancer treatment. Especially in immuno-oncology, not only the expression of target antigens, but also the tumor mutation burden and the degree of infiltration of immune cells (CD8 + T cells) into the tumor environment may be useful biomarkers 29 , 30 .

Conclusions
The current analysis of clinical trials that formed the basis for the approval of NSCLC indications revealed that whether a personalized strategy (biomarker-based enrichment) is adopted in trials is associated with background factors, such as the drug’s MOA and competition from similar drugs in the market. The impact of adopting personalized strategies on endpoint outcomes depends on the characteristics of the drug and its indication, especially for recently developed drugs with novel MOA profiles, as trial designs are often employed to clearly validate such drug-specific advantages. When assessing the relationship between personalized strategies and efficacy, careful consideration should be given to the context in which the clinical trials were conducted.
Data availability
Data available from the corresponding author ([email protected]) upon request.
Scannell, J. W., Blanckley, A., Boldon, H. & Warrington, B. Diagnosing the decline in pharmaceutical R&D efficiency. Nat. Rev. Drug Discov. 11 (3), 191–200 (2012).
Article CAS PubMed Google Scholar
Schuhmacher, A. et al. R&D efficiency of leading pharmaceutical companies—A 20-year analysis. Drug. Discov. Today. 26 (8), 1784–1789 (2021).
Article PubMed Google Scholar
U.S. Department of Health and Human Services. Guidance for Industry: Enrichment strategies for clinical trials to support determination of effectiveness of human drugs and biological products. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/enrichment-strategies-clinical-trials-support-approval-human-drugs-and-biological-products . Accessed February 22, (2021)
FDA Table of Pharmacogenomic Biomarkers in Drug Labeling. https://www.fda.gov/drugs/science-and-research-drugs/table-pharmacogenomic-biomarkers-drug-labeling . Accessed February 22, (2021).
Brahmer, J. et al. Nivolumab versus docetaxel in advanced squamous-cell non-small-cell lung cancer. N. Engl. J. Med. 373 (2), 123–135 (2015).
Article CAS PubMed PubMed Central Google Scholar
Jardim, D. L. et al. Impact of a biomarker-based strategy on oncology drug development: A meta-analysis of clinical trials leading to FDA approval. J. Natl. Cancer Inst. 107 (11), 253 (2015).
Article Google Scholar
Hayashi, K., Masuda, S. & Kimura, H. Impact of biomarker usage on oncology drug development. J. Clin. Pharm. Ther. 38 (1), 62–67 (2013).
Schwaederle, M. et al. Association of biomarker-based treatment strategies with response rates and progression-free survival in refractory malignant neoplasms: A meta-analysis. JAMA Oncol. 2 (11), 1452–1459 (2016).
Schwaederle, M. et al. Impact of precision medicine in diverse cancers: A meta-analysis of phase II clinical trials. J. Clin. Oncol. 33 (32), 3817–3825 (2015).
Drugs@FDA: FDA-Approved Drugs https://www.accessdata.fda.gov/scripts/cder/daf/ . Accessed February 22, (2021)
Marchetti, A. et al. EGFR mutations in non-small-cell lung cancer: analysis of a large series of cases and development of a rapid and sensitive method for diagnostic screening with potential implications on pharmacologic treatment. J. Clin. Oncol. 23 (4), 857–865 (2005).
Miyamae, Y. et al. Significance of epidermal growth factor receptor gene mutations in squamous cell lung carcinoma. Oncol. Rep. 25 (4), 921–928 (2011).
CAS PubMed Google Scholar
Boland, J. M. et al. Anaplastic lymphoma kinase immunoreactivity correlates with ALK gene rearrangement and transcriptional up-regulation in non-small cell lung carcinomas. Hum. Pathol. 40 (8), 1152–1158 (2009).
Inamura, K. et al. EML4-ALK fusion is linked to histological characteristics in a subset of lung cancers. J. Thorac. Oncol. 3 (1), 13–17 (2008).
Mok, T. S. et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N. Engl. J. Med. 361 (10), 947–957 (2009).
Casaluce, F. et al. ALK inhibitors: A new targeted therapy in the treatment of advanced NSCLC. Target. Oncol. 8 (1), 55–67 (2013).
Kobayashi, S. et al. EGFR mutation and resistance of non-small-cell lung cancer to gefitinib. N. Engl. J. Med. 352 (8), 786–792 (2005).
Pao, W. et al. EGF receptor gene mutations are common in lung cancers from “never smokers” and are associated with sensitivity of tumors to gefitinib and erlotinib. Proc. Natl. Acad. Sci. U. S A. 101 (36), 13306–13311 (2004).
Article ADS CAS PubMed PubMed Central Google Scholar
Suda, K., Mizuuchi, H., Maehara, Y. & Mitsudomi, T. Acquired resistance mechanisms to tyrosine kinase inhibitors in lung cancer with activating epidermal growth factor receptor mutation–diversity, ductility, and destiny. Cancer Metastasis. Rev. 31 (3–4), 807–814 (2012).
Katayama, R. et al. Mechanisms of acquired crizotinib resistance in ALK-rearranged lung Cancers. Sci Transl Med. 4 (120), 120ra17 (2012).
Article PubMed PubMed Central Google Scholar
Shi, H. et al. Melanoma whole-exome sequencing identifies (V600E)B-RAF amplification-mediated acquired B-RAF inhibitor resistance. Nat. Commun. 3 , 724 (2012).
Article ADS PubMed Google Scholar
Thress, K. S. et al. Acquired EGFR C797S mutation mediates resistance to AZD9291 in non-small cell lung cancer harboring EGFR T790M. Nat. Med. 21 (6), 560–562 (2015).
Gainor, J. F. et al. Molecular mechanisms of resistance to first- and second-generation ALK inhibitors in ALK-rearranged lung cancer. Cancer Discov. 6 (10), 1118–1133 (2016).
Im, S. J. et al. Defining CD8+ T cells that provide the proliferative burst after PD-1 therapy. Nature. 537 (7620), 417–421 (2016).
Jameson, S. C. & Masopust, D. Diversity in T cell memory: An embarrassment of riches. Immunity. 31 (6), 859–871 (2009).
Jansen, C. S. et al. An intra-tumoral niche maintains and differentiates stem-like CD8 T cells. Nature. 576 (7787), 465–470 (2019).
Clinical Trial Endpoints for the Approval of Non-Small Cell Lung Cancer Drugs and Biologics Guidance for Industry April 2015 https://www.fda.gov/media/116860/download Accessed June 5, (2023)
Hodi, F. S. et al. Evaluation of immune-related response criteria and RECIST v1.1 in patients with advanced melanoma treated with pembrolizumab. J. Clin. Oncol. 34 (13), 1510–1517 (2016).
Yu, Y. et al. Association of survival and immune-related biomarkers with immunotherapy in patients with non-small cell lung cancer: A meta-analysis and individual patient-level analysis. JAMA Netw. Open. 2 (7), e196879 (2019).
Chan, T. A. et al. Development of tumor mutation burden as an immunotherapy biomarker: utility for the oncology clinic. Ann. Oncol. 30 (1), 44–56 (2019).
Download references
Acknowledgements
This study was funded by a Japanese government-based grant-in-aid from the Ministry of Education, Culture, Sports, Science and Technology, Tokyo, Japan (KAKEN-HI:19K07215). We would like to thank Editage ( www.editage.com ) for English language editing.
Author information
Authors and affiliations.
Laboratory of Pharmaceutical Regulatory Science, Graduate School of Pharmaceutical Sciences, The University of Tokyo, 7-3-1 Hongo, Bunkyo-ku, Tokyo, 113-0033, Japan
Kenji Harada & Shunsuke Ono
Kyowa Kirin Co., Ltd., Tokyo, Japan
Kenji Harada
You can also search for this author in PubMed Google Scholar
Contributions
K.H. and S.O. contributed to the design of the study. K.H. collected and analyzed the data. K.H. and S.O. drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Shunsuke Ono .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary tables., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Harada, K., Ono, S. Background and clinical significance of biomarker-based patient enrichment in non-small-cell lung cancer drug development. Sci Rep 14 , 7194 (2024). https://doi.org/10.1038/s41598-024-57556-3
Download citation
Received : 22 December 2023
Accepted : 19 March 2024
Published : 26 March 2024
DOI : https://doi.org/10.1038/s41598-024-57556-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Translational Research newsletter — top stories in biotechnology, drug discovery and pharma.
Together we are beating cancer
- Cancer types
- Breast cancer
- Bowel cancer
- Lung cancer
- Prostate cancer
- Cancers in general
- Clinical trials
- Causes of cancer
- Coping with cancer
- Managing symptoms and side effects
- Mental health and cancer
- Money and travel
- Death and dying
- Cancer Chat forum
- Health Professionals
- Cancer Statistics
- Cancer Screening
- Learning and Support
- NICE suspected cancer referral guidelines
- Make a donation
- By cancer type
- Leave a legacy gift
- Donate in Memory
- Find an event
- Race for Life
- Charity runs
- Charity walks
- Search events
- Relay for Life
- Volunteer in our shops
- Help at an event
- Help us raise money
- Campaign for us
- Do your own fundraising
- Fundraising ideas
- Get a fundraising pack
- Return fundraising money
- Fundraise by cancer type
- Set up a Cancer Research UK Giving Page
- Find a shop or superstore
- Become a partner
- Cancer Research UK for Children & Young People
- Our Play Your Part campaign
- Brain tumours
- Skin cancer
- All cancer types
- By cancer topic
- New treatments
- Cancer biology
- Cancer drugs
- All cancer subjects
- All locations
- By Researcher
- Professor Duncan Baird
- Professor Fran Balkwill
- Professor Andrew Biankin
- See all researchers
- Our achievements timeline
- Our research strategy
- Involving animals in research
- Research opportunities
- For discovery researchers
- For clinical researchers
- For population researchers
- In drug discovery & development
- In early detection & diagnosis
- For students & postdocs
- Our funding schemes
- Career Development Fellowship
- Discovery Programme Awards
- Clinical Trial Award
- Biology to Prevention Award
- View all schemes and deadlines
- Applying for funding
- Start your application online
- How to make a successful applicant
- Funding committees
- Successful applicant case studies
- How we deliver research
- Our research infrastructure
- Events and conferences
- Our research partnerships
- Facts & figures about our funding
- Develop your research career
- Recently funded awards
- Manage your research grant
- Notify us of new publications
- Find a shop
- Volunteer in a shop
- Donate goods to a shop
- Our superstores
- Shop online
- Wedding favours
- Cancer Care
- Flower Shop
- Our eBay store
- Shoes and boots
- Bags and purses
- We beat cancer
- We fundraise
- We develop policy
- Our global role
- Our organisation
- Our strategy
- Our Trustees
- CEO and Executive Board
- How we spend your money
- Early careers
- Your development
Cancer News
- For Researchers
- For Supporters
- Press office
- Publications
- Update your contact preferences
- About cancer
- Get involved
- Our research
- Funding for researchers
The latest news, analysis and opinion from Cancer Research UK
- Science & Technology
- Health & Medicine
- Personal Stories
- Charity News
- Science & Technology
£1.7 million for the world’s first vaccine to prevent lung cancer

22 March 2024

Researchers at the University of Oxford, the Francis Crick Institute and University College London have been granted £1.7 million of funding from Cancer Research UK and the CRIS Cancer Foundation to develop a lung cancer vaccine .
The team are seeking to create ‘LungVax’, the world’s first vaccine to prevent lung cancer in people with a high risk of the disease.
From COVID-19 breakthrough to lung cancer vaccine
The LungVax vaccine will use technology similar to the highly successful Oxford/AstraZeneca COVID-19 vaccine.
In the same way traditional vaccines use part of a virus to train our bodies to fight disease, cancer vaccines use harmless proteins from the surface of cancer cells known as neoantigens.
Neoantigens appear on the surface of the cell because of cancer-causing mutations within the cell’s DNA. When they are introduced into the body they act as a ‘red flag’, which trains the immune system to recognise them on abnormal lung cells.
This lung cancer vaccine will help activate the immune system to kill these cells and stop lung cancer.
“Cancer is a disease of our own bodies and it’s hard for the immune system to distinguish between what’s normal and what’s cancer,” said Professor Tim Elliott, research lead for the LungVax project.
“Getting the immune system to recognise and attack cancer is one of the biggest challenges in cancer research today. If we can replicate the kind of success seen in trials during the pandemic, we could save the lives of tens of thousands of people every year in the UK alone.”
The scientists developing this lung cancer vaccine will first use lab tests to see if it successfully triggers an immune response. And if the results are positive, the vaccine will move straight into a clinical trial .
Projects like LungVax are a really important step forward into an exciting future, where cancer is much more preventable. We’re in a golden age of research and this is one of many projects which we hope will transform lung cancer survival.
Expanding out
Over the next 2 years the team will receive funding to support lab research and initial manufacturing of 3,000 doses of the vaccine at the Oxford Clinical BioManufacturing Facility.
The vaccine could then be scaled up to bigger trials for people at high risk of lung cancer, which could include people aged 55-74 who are current smokers, or have previously smoked. This is the same group that currently qualifies for targeted lung health checks in some parts of the UK.
“Fewer than 10% of people with lung cancer survive their disease for 10 years or more. That must change,” said Professor Mariam Jamal-Hanjani of University College London and the Francis Crick Institute, who will be leading the LungVax clinical trial.
“LungVax will not replace stopping smoking as the best way to reduce your risk of lung cancer. But it could offer a viable route to preventing some of the earliest stage cancers from emerging in the first place.”
Researchers think the vaccine could cover around 90% of all lung cancers, and this funding will be the first step towards getting it to patients.

The Cancer News newsletter brings the latest on cancer research direct to your inbox
I am Copd patient, smoked in past, this is brilliant news. X
Good news, Your article doesn’t mention patients who have previously had lung cancer and are in remission, or whether this vaccine is suitable for them. Also what type of lung cancer, NSCLC or SCLC.
Tell us what you think
Leave a reply cancel reply.
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Read our comment policy .
Highlighted content

Can vaping cause changes in our cells?

A message to MPs: Don’t miss the opportunity to make smoking history
From lemonade stand to grand challenge: changing how we treat cancer in children and young people

Cancer Grand Challenges gives a record £100m to five cancer research teams
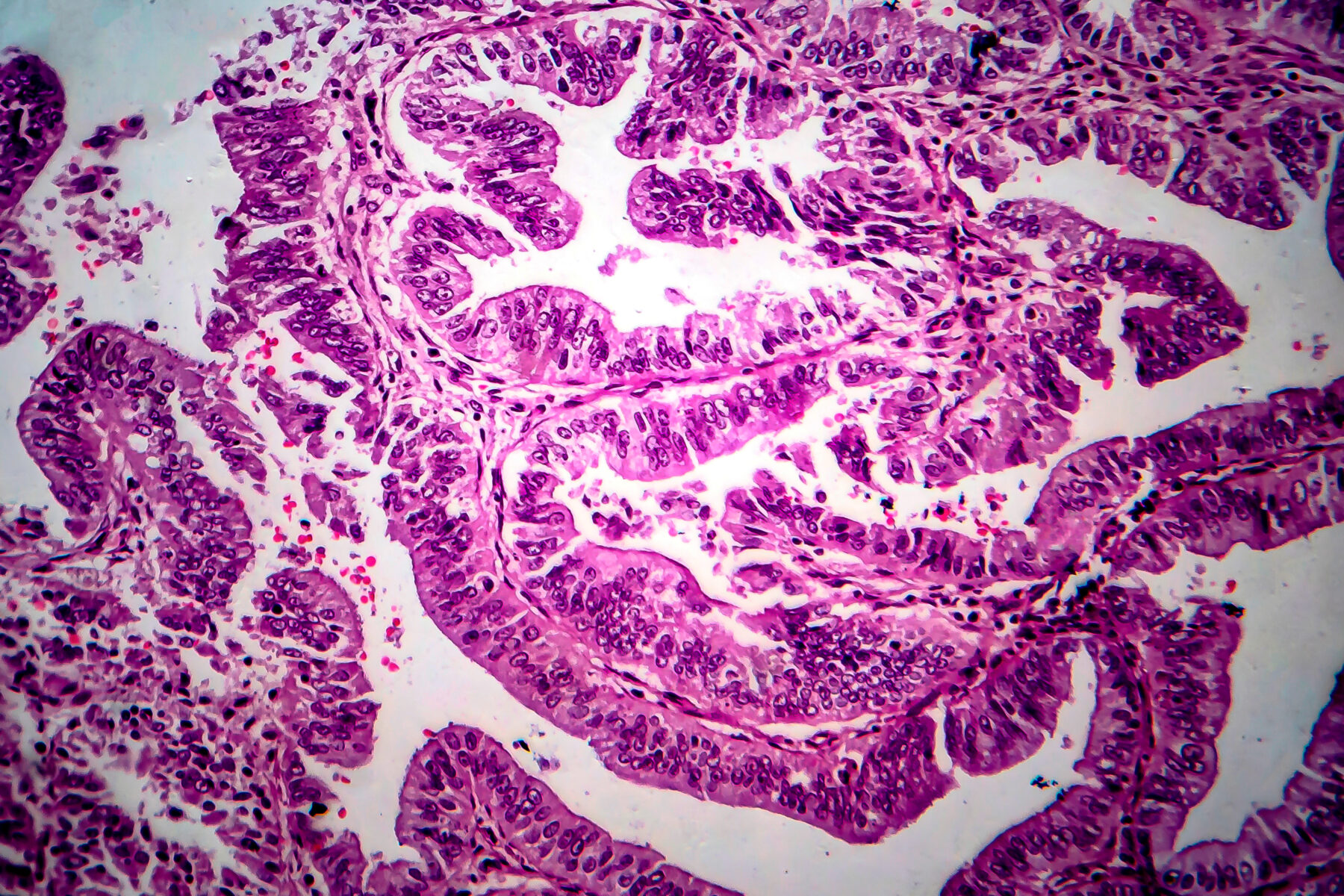
New treatment option made available for advanced womb cancers

Cancer deaths plummet in middle-aged people
Related topics.
- Vaccination
- Cancer in the news
Lung cancer: a review
Affiliation.
- 1 Northeastern University, 360 Huntington Avenue, Boston, MA 02115, USA.
- PMID: 11944603
- DOI: 10.1093/ajhp/59.7.611
The frequency, risk factors, pathophysiology, diagnosis, and management of lung cancer are reviewed. An estimated 157,400 Americans died of lung cancer in 2001. Lung cancer is the second most frequent cancer in both men and women. The major risk factor for lung cancer is smoking, which accounts for 75-80% of lung cancer-related deaths. Lung cancers can be broadly classified into two forms, small-cell carcinomas and non-small-cell carcinomas. Non-small-cell lung cancer is more common, accounting for up to 75% of lung cancers. Lung cancer is diagnosed by chest radiography, sputum cytology, bronchoscopy, needle biopsy, and other techniques. Surgery plays a major role in managing stage I and stage II non-small-cell lung cancer and may be used for stage III disease. Patients with stage IIIa disease may be surgical candidates, but involvement of mediastinal lymph nodes reduces the probability of survival. Adjuvant irradiation may reduce the rate of local recurrence but does not increase survival time. Adjuvant chemotherapy may confer a small survival-time advantage if the regimen includes cisplatin. Chemotherapy combined with radiation therapy may produce a survival advantage over irradiation alone. Patients with advanced non-small-cell lung cancer should receive combination chemotherapy. Several regimens have shown a survival advantage over best supportive care. Paclitaxel, docetaxel, gemcitabine, vinorelbine, irinotecan, and topotecan have activity both as single agents and in combination. Surgery has only a limited role in the management of small-cell lung cancer. Patients with limited disease should receive a platinum-based chemotherapy regimen plus radiation therapy. Combination chemotherapy should be offered to patients with extensive disease. The most active regimens contain cisplatin or carboplatin. Paclitaxel, docetaxel, gemcitabine, vinorelbine, irinotecan, and topotecan combinations have shown some promise. Lung cancer, although highly preventable, is usually diagnosed at an incurable stage. Chemotherapy is playing an increasingly important role alongside surgery and radiation therapy in the management of this disease.
Publication types
- Antineoplastic Combined Chemotherapy Protocols / therapeutic use*
- Carcinoma, Non-Small-Cell Lung* / diagnosis
- Carcinoma, Non-Small-Cell Lung* / drug therapy
- Carcinoma, Non-Small-Cell Lung* / physiopathology
- Combined Modality Therapy
- Lung / anatomy & histology*
- Lung / physiology
- Lung Neoplasms* / diagnosis
- Lung Neoplasms* / drug therapy
- Lung Neoplasms* / physiopathology
- Randomized Controlled Trials as Topic
- Risk Factors
- Survival Rate
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.8(10); 2018

Smoking as a risk factor for lung cancer in women and men: a systematic review and meta-analysis
Linda m o’keeffe.
1 MRC Integrative Epidemiology Unit at the University of Bristol, Bristol Medical School, University of Bristol, Bristol, UK
2 Population Health Sciences, Bristol Medical School, University of Bristol, Bristol, UK
Gemma Taylor
3 UK Centre for Tobacco and Alcohol Studies, School of Experimental Psychology, University of Bristol, Bristol, UK
4 Department of Psychology, University of Bath, Bath, UK
Rachel R Huxley
5 College of Science, Health and Engineering, La Trobe University, Melbourne, Australia
6 The George Institute for Global Health, University of New South Wales, Sydney, New South Wales, Australia
Paul Mitchell
7 Olivia Newton-John Cancer and Wellness Centre, Austin Health and Olivia Newton-John Cancer Research Institute, Heidelberg, Victoria, Australia
Mark Woodward
8 The George Institute for Global Health, University of Oxford, Oxford, UK
9 Department of Epidemiology, John Hopkins University, Baltimore, Maryland, USA
Sanne A E Peters
Associated data.
bmjopen-2018-021611supp001.pdf
To investigate the sex-specific association between smoking and lung cancer.
Systematic review and meta-analysis.
Data sources
We searched PubMed and EMBASE from 1 January 1999 to 15 April 2016 for cohort studies. Cohort studies before 1 January 1999 were retrieved from a previous meta-analysis. Individual participant data from three sources were also available to supplement analyses of published literature.
Eligibility criteria for selecting studies
Cohort studies reporting the sex-specific relative risk (RR) of lung cancer associated with smoking.
Data from 29 studies representing 99 cohort studies, 7 million individuals and >50 000 incident lung cancer cases were included. The sex-specific RRs and their ratio comparing women with men were pooled using random-effects meta-analysis with inverse-variance weighting. The pooled multiple-adjusted lung cancer RR was 6.99 (95% Confidence Interval (CI) 5.09 to 9.59) in women and 7.33 (95% CI 4.90 to 10.96) in men. The pooled ratio of the RRs was 0.92 (95% CI 0.72 to 1.16; I 2 =89%; p<0.001), with no evidence of publication bias or differences across major pre-defined participant and study subtypes. The women-to-men ratio of RRs was 0.99 (95% CI 0.65 to 1.52), 1.11 (95% CI 0.75 to 1.64) and 0.94 (95% CI 0.69 to 1.30), for light, moderate and heavy smoking, respectively.
Conclusions
Smoking yields similar risks of lung cancer in women compared with men. However, these data may underestimate the true risks of lung cancer among women, as the smoking epidemic has not yet reached full maturity in women. Continued efforts to measure the sex-specific association of smoking and lung cancer are required.
Strengths and limitations of this study
- Evidence on the sex-specific association of smoking and lung cancer was meta-analysed in over 7 million participants across 99 cohort studies.
- Several subgroup analyses were performed to examine the robustness of findings across different population subgroups.
- However, the smoking epidemic is not yet fully mature in women and risks of lung cancer in women may still be underestimated.
- Detailed data on smoking behaviour and data on specific subtypes of lung cancer were not available.
Introduction
Lung cancer is the leading cause of cancer death worldwide with 1.7 million global deaths attributed to cigarette smoking in 2015. 1 Tobacco use is the leading cause of lung cancer; 55% of lung cancer deaths in women and over 70% of lung cancer deaths in men are due to smoking. 1 These global estimates, however, mask major differences in smoking prevalence in men and women across populations, with rates below 5% for women in most Asian and African countries to 40% and above for men in many parts of Asia and Eastern Europe. 2 In addition, smoking behaviour varies significantly by sex. For example, compared with women, men smoke more cigars and pipes, 3 take puffs of longer duration and leave shorter butts, 4 which each could potentially predispose them to greater risks of smoking-related lung cancer. Substantial physiological differences between the sexes may also result in sex differences in the effects of smoking, particularly for women. For example, compared with men, women have a smaller lung size and different airway behaviour, 5 which may increase their susceptibility to lung cancer at lower levels of smoking. A recent meta-analysis showed that cigarette smoking confers a greater coronary hazard in women compared with men, which suggests the possibility that this may also be true for the risk of smoking-related lung cancer. 6
A study of 50-year trends in smoking-related mortality in the USA found that the relative risks of smoking-related lung cancer mortality were higher in men than women. 7 However, this sex difference was only apparent in the oldest cohorts with the longest follow-up, possibly reflecting greater cumulative tobacco exposure in men than in women. In contrast, a recent study in Korea, a population where smoking patterns continue to differ between the sexes, suggested that sex differences in the impact of smoking on lung cancer risk exist and differ by histological subtype. 8 Analyses of a large UK primary care database showed that moderate and heavy smoking more strongly increase the risks of lung cancer in women than in men. 9
Two recent meta-analyses examined the sex-specific association between smoking and lung cancer. In the most recent of these, men were found to have a greater risk of lung cancer associated with smoking compared with women. 10 However, virtually all data were from historical case–control studies, which have several limitations, and the three included prospective studies provided contradictory results. While a previous meta-analysis by Lee et al 11 included 287 cohort and case–control studies and provided sex-specific estimates, single-sex cohorts were also included, sex differences in the smoking-related risk of lung cancer were not formally compared within studies, and only studies published up to 1999 were included.
To resolve this uncertainty, we performed a systematic review and meta-analysis of prospective cohort studies published to date on the sex-specific association of smoking with the risk of fatal and non-fatal lung cancer. Our systematic review builds on these previous meta-analyses by adding literature from 1999 onwards and restricting the analyses to cohort studies, which are less prone to bias than case–control studies. In addition, we perform several predefined subgroup analyses which have not been performed in meta-analyses of cohort studies included in previous reviews and supplement our findings with results from three sources of individual participant data (IPD), not published previously. An important a priori consideration is the substantial sex difference in the maturity of the smoking epidemic with men being at a more advanced stage than women in most parts of the world. 2 This would be expected to translate into lower relative risk (RR) estimates for lung cancer in women than in men. Hence, the null hypothesis that smoking confers the same lung cancer hazard in both women and men, would be met if the ratio of the RRs (RRRs) for lung cancer (women:men) was less than unity (reflecting a greater hazard in men than women). However, if the RRRs were found to be unity (or higher) then this would suggest a greater hazard associated with tobacco exposure in women than in men.
Search strategy
This review was conducted using a predefined protocol and in accordance to the Meta-analysis Of Observational Studies in Epidemiology guidelines (online supplementary eappendix 1 ). We systematically searched PubMed and EMBASE for studies published between 1 January 1999 and 15 April 2016 that reported on the relationship between smoking and lung cancer in men and women from a general population. The computer-based searches combined medical subject headings and free-text terms related to ‘tobacco/smoking’, ‘cancer’, ‘sex’ and ‘cohort studies’. The full search criteria are available in online supplementary eappendix 2 . Articles published before 1 January 1999 were retrieved from a previous systematic review. 11 The reference lists of all relevant original research and review articles were scanned to capture missed studies. Two authors (LMOK and GT) independently conducted the screening of studies and any disagreement was mediated by a third author (SAEP).
Supplementary file 1
Data extraction.
Data were extracted, in duplicate, from studies deemed to meet the eligibility criteria. These included details on general study characteristics (study name, duration of follow-up, year of publication), information about the studied population (prevalence of smoking, mean age, number of men and women, incidence of lung cancer, whether lung cancer was fatal or non-fatal and level of adjustment for covariates). We extracted sex-specific adjusted measures of RR and 95% confidence intervals (CIs).
Study selection
Observational cohort studies were included if they reported sex-specific RRs or equivalent, on the relationship between smoking and lung cancer. Studies were excluded if the variability around the point estimate was not reported, if they had not been adjusted for at least age, or if the study was performed in a population selected on the basis of prior lung cancer or another major underlying chronic disease. In the case of duplicate reports from the same study, the report with the longest follow-up or the highest number of cases was included. IPD from studies available to the authors were also used; the Asia Pacific Cohort Studies Collaboration (APCSC), the National Health and Nutrition Examination Survey III (NHANES III) and the Scottish Heart Health Extended Cohort Study (SHHEC). The Newcastle-Ottawa Scale assessment (NOS) was used to assess the methodological quality of all included studies, on a 9-point scale (online supplementary eappendix 3 and etable 1 ). 12
Meta-analysis
The primary analysis was a comparison of the sex-specific RR of lung cancer (fatal or non-fatal) in current smokers versus non-smokers (defined either as former or never smokers). For each study, we obtained the natural log of the sex-specific RRs and calculated the differences. The differences were pooled across studies using random-effects meta-analysis which allows the RR of lung cancer to vary from study to study, weighted by the inverse of the variances of the log RRs and then back-transformed to obtain the pooled women-to-men RRRs. The SE of the log RRR was calculated as the square root of the sum of the variance of the two sex-specific log RRs for each study. Pooled RRRs were computed separately for studies with only age-adjusted estimates and then for those studies with multiple-adjusted estimates. The set of multiple adjustments made was allowed to vary by study, but had to include at least one other risk factor in addition to age. The I² statistic was used to estimate the percentage of variability across studies due to between-study heterogeneity. The presence of publication bias was graphically examined using contour funnel plots, plotting the natural log of the RRR against its SE and tested using Begg’s test. Predefined subgroup analyses were conducted to obtain the adjusted RRRs by study region (Asia or non-Asia and Asia, Europe, USA, and Australia and New Zealand (ANZ)), year of study baseline (pre-1985 or post-1985), study endpoint (fatal only or fatal and non-fatal combined), number of cigarettes smoked per day (>0 to 10, 10–20, >20), study quality ≤6 vs >6 points) and follow-up time (≤10 vs >10 years). Random-effects meta-analyses were used for all subgroup analyses and differences between subgroups were examined using meta-regression. To include the largest number of studies available, we combined the age-adjusted and multiple-adjusted estimates, taking the maximum adjustment set available. In secondary analyses, we obtained the sex-specific RRs and RRRs comparing former smokers to never smokers and performed the same set of subgroup analyses. All analyses were performed using Stata V.12.0.
Patient and public involvement
There were no patients or applicable public involved in this review.
Of the 9519 unique records that were identified through the systematic search, 227 qualified for full-text evaluation ( figure 1 ). Of these, 25 separate studies provided information about sex differences in the association between smoking and lung cancer. This database was extended with IPD from APCSC (separately for Asia and ANZ), NHANES III and SHHEC leading to a total of 29 individual estimates, representing a total of 99 cohort studies available for meta-analysis.

Flow chart of study selection. IPD, individual participant data.
The characteristics of the included studies are described in table 1 . Overall, data were available from 99 cohorts, including 7 113 303 individuals (46% women)—not accounting for two cohorts that used Census data—and at least 51 161 incident cases of lung cancer (31% women). Forty-six cohorts were from Asia (61% of the individuals), 6 were from the USA (28%), 37 were from Europe (10%) and 10 were from ANZ (1%). Of 29 studies, 4 studies had a quality score of 5 out of 9, 9 studies had a score of 6, 12 studies had a score of 7 and 4 studies with a score of 8 (online supplementary etable 1 ).
Characteristics of included studies
*Note that where several studies are cited for a single cohort, data may be extracted from multiple studies if all data required is not available in the most up-to-date and relevant study.
ANZ, Australia and New Zealand; ARIC, Atherosclerosis Risk in Communities study; APCSC, Asia Pacific Cohort Studies Collaboration; BMI, body mass index; CHD, coronary heart disease; CPS, Cancer Prevention Study; DM, diabetes mellitus; EHS, Elderly Health Services; EPIC, European Prospective Investigation into Cancer; F, fatal; FEV, forced expiratory volume; JACC, Japan Collaborative Cohort Study; JPHC, Japan Public Health CentreStudy; NF, non-fatal; NHANES III, National Health And Nutrition Examination Survey III; NHIS, National Health Interview Survey; NIH-AARP, National Institutes of Health American Association of Retired Persons Diet and Health Study; NOS, Newcastle-Ottawa Scale; NR, not reported; PA, physical activity; SBP, systolic blood pressure; SES, socioeconomic status; SHHEC, Scottish Heart Health Extended Cohort Study; TC, total cholesterol; TG, triglycerides; TPCS, Three-Prefecture Cohort Study.
Eighteen studies reported on the prevalence of smoking, which varied widely by study, region and sex. The prevalence of smoking ranged from 1% to 47% in women and from 1% to 70% in men. In all but two studies, the prevalence of smoking was higher in men than women, especially in Asia where typically less than 10% of women were smokers compared with over 50% of men. Smoking cessation rates were also higher among men (7%–61%) than women (<1%–39%).
Risk of lung cancer in current smokers versus non-smokers
Compared with non-smoking, current smoking was associated with an age-adjusted RR of lung cancer of 7.48 (95% CI 5.29 to 10.60) in women and 8.78 (95% CI 6.13 to 12.57) in men ( table 2 and online supplementary efigure 1 ). The pooled age-adjusted women-to-men RRR was 0.81 (95% CI 0.62 to 1.04), with substantial between-study heterogeneity (I 2 =86%; p<0.001) ( table 2 and online supplementary efigure 2 ). The multiple-adjusted RR of lung cancer associated with current smoking was 6.99 (95% CI 5.09 to 9.59) in women and 7.33 (95% CI 4.90 to 10.96) in men ( table 2 and figure 2 ). The corresponding RRR was 0.92 (95% CI 0.72 to 1.16) and between-study heterogeneity was substantial (I 2 =89%; p<0.001) ( table 2 and figure 3 ). There was no evidence of publication bias based on the Begg’s test (p=0.75) (online supplementary efigure 3 ).

Multiple-adjusted relative risk (RR) for incident lung cancer in women and men, comparing current smokers to non-smokers. Multiple-adjusted includes anything that adjusted for more than just age. These covariates are listed in table 1 . Figures may contain less than 29 studies because we report age-adjusted and multiple-adjusted results separately. Some studies only contributed age-adjusted results whereas others only provided multiple-adjusted results. However, the count of unique studies that contributed to at least one of these analyses is 29. APCSC, Asia Pacific Cohort Studies Collaboration; ARIC, Atherosclerosis Risk in Communities study; CPS, Cancer Prevention Study; EHS, Elderly Health Services; EPIC, European Prospective Investigation into Cancer; JACC, Japan Collaborative Cohort Study; JPHC, Japan Public Health Centre Study; NHANES III, National Health And Nutrition Examination Survey III; NHIS, National Health Interview Survey; NIH-AARP, National Institutes of Health American Association of Retrired Persons Diet and Health Study; SHHEC, Scottish Heart Health Extended Cohort Study; TPCS, Three-Prefecture Cohort Study.

Multiple-adjusted women-to-men ratio of relative risks (RRR) for incident lung cancer, comparing current smokers to non-smokers. Multiple-adjusted includes anything that adjusted for more than just age. These covariates are listed in table 1 . Figures may contain less than 29 studies because we report age-adjusted and multiple-adjusted results separately. Some studies only contributed age-adjusted results whereas others only provided multiple-adjusted results. However, the count of unique studies that contributed to at least one of these analyses is 29. APCSC, Asia Pacific Cohort Studies Collaboration; ARIC, Atherosclerosis Risk in Communities study; CPS, Cancer Prevention Study; EHS, Elderly Health Services; EPIC, European Prospective Investigation into Cancer; JACC, Japan Collaborative Cohort Study; JPHC, Japan Public Health Centre Study; NHANES III, National Health And Nutrition Examination Survey III; NHIS, National Health Interview Survey; NIH-AARP, National Institutes of Health American Association of Retired Persons Diet and Health Study; SHHEC, Scottish Heart Health Extended Cohort Study; TPCS, Three-Prefecture Cohort Study.
Sex-specific pooled relative risks (RR) and ratio of relative risks (RRR) for lung cancer associated with smoking
Multiple adjusted includes anything that adjusted for more than just age. Maximum available adjustment refers to the most adjustments provided in the study. For some studies, this would have been age adjusted whereas other studies adjusted for more factors than age only (ie, multiple adjusted). These covariates are listed in table 1 .
The sex difference in the risk of smoking-related lung cancer in our main analysis did not differ in subgroup analyses stratified by the women-to-men ratio of current smokers (p=0.90), women-to-men ratio of lung cancer incidence in the studies (p=0.64), year of study baseline (p=0.66), study endpoint (p=0.21) or study region (p=0.73) ( table 3 ). The sex difference in the risk of smoking-related lung cancer in our main analysis also did not differ by follow-up time (p=0.83) or study quality (p=0.69). The RRR was 0.93 (95% CI 0.72 to 1.20) for studies from Asia and 0.87 (95% CI 0.66 to 1.14) for studies from USA, Europe or ANZ.
Maximally adjusted pooled women to men ratio of relative risks (RRR) for lung cancer associated with smoking, in subgroup analyses
Random-effects meta-analyses were used for all subgroup analyses and differences between subgroups were examined using meta-regression.
*P for interaction assessed using meta-regression.
ANZ, Australia and New Zealand.
The risk of smoking-related lung cancer increased according to the number of cigarettes smoked per day in both sexes ( table 2 ). In women, the RRs were 5.30 (95% CI 3.52 to 7.97), 10.67 (95% CI 7.43 to 15.33) and 17.09 (95% CI 12.11 to 24.11) across subgroups of <10, 10 to 20 and >20 cigarettes per day versus non-smoking, respectively. Corresponding RRs in men were 4.97 (95% CI 2.74 to 9.03), 8.93 (95% CI 4.90 to 16.28) and 14.61 (95% CI 8.33 to 25.59), respectively. The RRRs in these subgroups were 0.99 (95% CI 0.65 to 1.52), 1.11 (95% CI 0.75 to 1.64) and 0.94 (95% CI 0.69 to 1.30), respectively.
Risk of lung cancer in former smokers versus never smokers
Data from 89 cohorts, including 6 006 725 individuals and 38 244 cases of lung cancer, reported on the risk of lung cancer in former smokers compared with never smokers. The age-adjusted RR of lung cancer associated with former smoking was 2.82 (95% CI 2.25 to 3.54) in women and 3.01 (95% CI 2.23 to 4.08) in men ( table 2 and online supplementary efigure 4 ); the age-adjusted RRR was 0.88 (95% CI 0.69 to 1.14) (I 2 =64%; p<0.001) ( table 2 and online supplementary efigure 5 ). The corresponding multiple-adjusted RRs were 3.14 (95% CI 2.45 to 4.03) in women and 3.13 (95% CI 2.06 to 4.76) in men ( table 2 and online supplementary efigure 6 ). There was no statistical evidence that the effects of smoking cessation on risk of lung cancer differed between the sexes; the multiple-adjusted RRR was 0.89 (95% CI 0.69 to 1.13) (I 2 =69%; p<0.001) ( table 2 and online supplementary efigure 7 ). There was no evidence that the RRR differed across various subgroup analyses ( table 3 ).
In this systematic review and meta-analysis, comprising data from more than 7 million participants, 99 cohort studies and over 50 000 incident cases of lung cancer, there was no evidence for a difference in the risk of smoking-related lung cancer in women compared with men. This was true across a range of subgroup and sensitivity analyses. However, as smoking prevalence and intensity were higher in men compared with women in most studies included in this analysis, there may yet be an unrealised sex difference in the risk of smoking-related lung cancer that will only become fully manifest as the smoking epidemic reaches full maturity in women. 2
The sevenfold higher RRs of lung cancer associated with smoking found in the present meta-analysis are considerably smaller than the 20-fold increased risks reported in the Million Women’s Study 13 and the British Doctors Study. 14 Both of these studies had the advantage of capturing smoking-related risks in populations that had smoked for long enough for the effects to become fully manifest, highlighting the importance of taking into consideration the stage of the tobacco epidemic in each sex. The lack of any appreciable sex difference in the RRs of lung cancer is surprising given men’s greater cumulative exposure to smoking, in most populations, compared with women. In addition, men have a greater exposure to other risk factors for lung cancer including occupational carcinogens. 15 Men also smoke more cigars and pipes, 3 take longer puffs of longer duration and leave shorter butts compared with women. 4 Hence, it may be reasonable to surmise that the RR estimates of smoking-related lung cancer in women may eventually exceed those of men, once cumulative exposure to smoking in women is comparable to that in men. In a previous meta-analysis, using similar methodology, we found that smoking conferred a 25% greater RR of coronary heart disease (CHD) in women than in men. Two possible explanations for why a similar pattern is not observed for lung cancer are that, first, the lag-time between smoking and CHD is considerably shorter than for lung cancer, 16 and second the pathways by which smoking increases risk are different between CHD and lung cancer.
Although not assessed in this analysis, evidence suggests that there are sex differences in the pattern of lung cancer among never smokers, with a higher prevalence of lung cancer among never-smoking women than never-smoking men. 17 18 A US study among 500000 people found a 30% higher incidence of lung cancer in women never smokers compared with men never smokers. 19 An Australian study found the proportion of patients with lung cancer who had never smoked was approximately 18% in women and 3% of men. 20 The reasons for this sex difference are not clear, but women may have increased exposure to environmental tobacco smoke 21 or other environmental carcinogens such as indoor air pollution 22 or sex-related differences in the metabolism of environmental carcinogens. The possibility of greater exposure to environmental tobacco smoke and other environmental carcinogens in women compared with men could have resulted in a greater underestimation of the association between smoking and lung cancer in women than men. This, in turn, could have impacted the sex difference in risk of smoking-related lung cancer reported in this study.
Our study has several strengths including restriction to cohort studies which provide more robust evidence of the associations compared with case–control studies. Differences between case–control and cohort studies may also explain why a previous meta-analysis of case–control studies (which included only three cohort studies) showed a higher RR of lung cancer in men compared with women. 10 Other strengths to our study include an update of findings to include studies published after 1999, 11 with supplementation of published literature with IPD from three established population databases. We have also performed a range of prespecified sensitivity analyses and several subgroup analyses which were not performed in previous meta-analyses. Our results were consistent across regions and irrespective of the women-to-men smoking ratio, suggesting that underestimation of the association of smoking and lung cancer in women due to sex differences in smoking prevalence and under-reporting of smoking is unlikely. This is especially relevant for parts of Asia where the prevalence of smoking in women is typically <10% and where smoking among women remains relatively socially unacceptable. As the up-take of smoking continues among women in countries where significant sex differences in smoking prevalence exist, the sex-specific risks of lung cancer due to smoking may become further apparent. This is also true for Western countries where differences in prevalence between women and men have reduced substantially over time, with prevalence of smoking in younger cohorts of women and men approaching unity. 23 The limitations of this study include heterogeneity across studies in study design, study population, verification of smoking status and outcome ascertainment. Assessment of smoking status differed across studies and was generally self-reported, which may have introduced measurement error. 24 Notably, compared with men, women are more likely to under-report smoking status, and under-reporting is especially prevalent in countries where smoking among women is not culturally acceptable. 25 The lack of standardisation across studies in how smoking status was obtained, including how smoking dose and duration were measured is also a major limitation. In addition, there was insufficient data available to examine whether there were sex differences in the impact of age at smoking initiation and smoking duration on the risk of lung cancer. The reference group of non-smokers in our analysis of current smoking was composed of former and never smokers which may inflate the risks of smoking-related lung cancer risk among non-smokers. However, we have also examined former smoking compared with never smoking and demonstrated no appreciable sex differences in the risks of smoking-related lung cancer in this group, which provides some evidence that the inclusion of former smokers in the reference category is unlikely to have biased the sex difference in our main analysis. We quantified sex differences in the risk of lung cancer associated with smoking based on RRs rather than absolute risks. This might introduce a statistical artefact, in which the generally higher absolute risk for lung cancer in men, and the same risk difference subsequent to smoking in each sex, would translate to a greater RR in women than men. However, our previous meta-analyses on risk factors for cardiovascular diseases demonstrated that sex differences in RRs are not inevitable, 26 despite differences in absolute risks. Compared with absolute risks, RRs are more stable across populations with different background risks, which makes them suitable for meta-analyses. In addition, RRs are reported much more commonly than absolute risks. In our review, no studies reported adjusted absolute risks, with standard errors, that allow for meta-analyses. We, therefore, believe that use of RRs in the present analysis is appropriate. In addition, while we have aimed to assess study quality using the widely accepted and used NOS, the value and contribution of quality assessment scales such as this to systematic reviews and meta-analyses continues to be debated. 27–29 Finally, there are differences between men and women in histological subtypes of lung cancer. Adenocarcinoma is more common in women and squamous cell carcinoma is more common in men. 30 Smoking is more strongly associated with squamous cell carcinoma than adenocarcinoma. 30 Few studies reported the sex-specific association of smoking with histological subtypes of cancer, which precluded the examination of sex differences in the association of smoking-related lung cancer subtypes and this remains an important limitation of our review. 30 Further studies of the smoking-related risks of lung cancer in women and men are required as the smoking epidemic reaches its full maturity in women. Given the later up-take of smoking in women, studies which allow sufficient lag time for lung cancer to develop are essential. In addition, reducing under-reporting of smoking in women, using standardised and robust methods for the ascertainment of smoking status and smoking behaviours and more extensive measurement and adjustment for confounders which differ by sex (such as exposure to environmental tobacco smoke) is also important for future work, as well as examination of histological subtypes of lung cancer which was not possible in this review.
In conclusion, this meta-analysis, summarising all available literature to date, shows that the effect of smoking on risk of lung cancer is similar in women and men. However, these data may yet underestimate the true RR of smoking-related lung cancer in women, given later uptake and lower intensity of smoking in women. Although strides have been made in reducing smoking rates particularly in high-income countries, continuing efforts to measure the effects of smoking on disease outcomes are required, as the smoking epidemic has not yet reached its global peak, particularly among women. In addition, tobacco control programmes that dissuade both sexes from smoking but which also encourage individuals to quit remain a priority.
Supplementary Material
LMO’K and GT contributed equally.
Contributors: LMOK, GT, SAEP, RRH and MW designed the study. LMOK and GT performed systematic searches, retrieved literature and performed data extraction. SAEP performed the analysis of the data. LMOK and GT wrote the first draft of the article. RRH, MW and PM contributed important intellectual content and critical expertise and revisions to the manuscript.
Funding: The MRC Integrative Epidemiology Unit at the University of Bristol is supported by the University of Bristol and the Medical Research Council [MC_UU_12013/2, MC_UU_12013/3, MC_UU_12013/4, MC_UU_12013/6, MC_UU_12013/9]. LMOK is supported by a UK Medical Research Council Population Health Scientist fellowship (MR/M014509/1). GT is funded by a Cancer Research UK Postdoctoral Fellowship ( {"type":"entrez-nucleotide","attrs":{"text":"C56067","term_id":"2400668","term_text":"C56067"}} C56067 /A21330). SAEP is supported by a UK Medical Research Council Skills Development Fellowship (MR/P014550/1).
Competing interests: None declared.
Patient consent: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Technical appendix, statistical code and dataset (of published data only) available from authors on request.

IMAGES
COMMENTS
Abstract. Lung cancer is one of the most frequently diagnosed cancers and the leading cause of cancer-related deaths worldwide with an estimated 2 million new cases and 1·76 million deaths per year. Substantial improvements in our understanding of disease biology, application of predictive biomarkers, and refinements in treatment have led to ...
Lung cancer remains the leading cause of cancer mortality in men and women in the U.S. and worldwide. About 90% of lung cancer cases are caused by smoking and the use of tobacco products. However, other factors such as radon gas, asbestos, air pollution exposures, and chronic infections can contribute to lung carcinogenesis.
Tobacco smoking remains the predominant risk factor for lung cancer development. Nontobacco risk factors include environmental and occupational exposures, chronic lung disease, lung infections, and lifestyle factors. Because tobacco remains the leading risk factor for lung cancer, disease prevention is focused on smoking avoidance and cessation ...
According to the National Cancer Institute's Surveillance, Epidemiology, and End Results (SEER) program, there were an estimated 229,000 new cases of lung cancer in the US in 2020, accounting for 12.7% of all cancer diagnoses. The current incidence of 45.6/100,000 is down from a peak of 69.5/100,000 in 1992, largely due to smoking cessation.
Globally, lung cancer is the largest contributor to new cancer diagnoses (1,350,000 new cases and 12.4% of total new cancer cases) and to death from cancer (1,180,000 deaths and 17.6% of total cancer deaths). The 5-year survival rate in the United States for lung cancer is 15.6%, and although there has been some improvement in survival during ...
Lung cancer is the leading cause of global cancer incidence and mortality, accounting for an estimated 2 million diagnoses and 1.8 million deaths. Neoplasms of the lungs are the second most common cancer diagnosis in men and women (after prostate and breast cancer, respectively). With increasing access to tobacco and industrialization in ...
Lung cancer incidence largely reflects trends in smoking patterns, which generally vary by sex and economic development. ... a GRADE concept paper. ... Lung Cancer 10, 107-124 (2019). PubMed ...
Lung cancer is one of the most frequently diagnosed cancers and the leading cause of cancer-related deaths worldwide with an estimated 2 million new cases and 1·76 million deaths per year. Substantial improvements in our understanding of disease biology, application of predictive biomarkers, and refinements in treatment have led to remarkable progress in the past two decades and transformed ...
In 2022, approximately 236,000 lung cancer diagnoses and 130,000 lung cancer deaths were expected to occur in the United States (US) 1.Every day, roughly 350 patients are expected to die from lung ...
Lung cancer persists as the main cause of cancer death in people globally, driven by the ongoing tobacco epidemic and the emergence of risk factors such as ionising radiation exposure and ambient pollution. Nearly 2 million people die of lung cancer each year, a far higher death rate than other common cancer types. However, developments over the past 10 years have dramatically improved the ...
In this study, a total of 201 publications on the mortality of lung cancer were identified using so many sites such as Google Scholar, Cochrane Library, Web of Sciences (WOS), EMBASE, Medline/PubMed, cancer research database (WHO), lung cancer open research dataset challenge, and Scopus database, of which, 15 studies that did not have numbers ...
In 2018, a total of 47,838 people had lung cancer diagnoses with 35,137 deaths recorded. Incidence across the United Kingdom is illustrated in Figure 1. In the past decade, lung cancer age-standardized incidence rates increased by 1% overall with a 15% increase in females and 11% decrease in males ( Fig. 2 ), and lung cancer age-standardized ...
Introduction. For several decades lung cancer has been the most common cancer in the world. 1 In 2014 there were 46,403 new cases of lung cancer diagnosed in the UK. 2 It is the third most common cancer after breast and prostate, but has the largest proportion of all cancer-related deaths (22%). 2 The overall age standardised incidence has declined slightly over the past 40 years, which is a ...
There has been a lot of research done on lung cancer classification. However, there are still some accuracy difficulties. ... Article CAS PubMed Google Scholar ... Basis Dis. 1866, Paper ID ...
The types of research cited by the CPGs were primarily clinical trials, as well as three treatment modalities (chemotherapy, radiotherapy and surgery). Genetics, palliative care and quality of life were largely neglected. The median time gap between papers cited on a lung CPG and its publication was 3.5 years longer than for WoS citations.
In 2022, the weighted LCS-eligible population was 13 526 348 individuals vs 8 154 440 individuals per 2021 vs 2013 criteria (an increase of 5 371 908 individuals [65.9%]) ( Table ). The 2022 LCS prevalence was 16.4% and 19.6% using 2021 and 2013 criteria, respectively; the number screened increased by 619 054 individuals.
The Lung Cancer Master Protocol, or Lung-MAP, is a precision medicine research study for people with advanced non-small cell lung cancer that has continued to grow after treatment. Patients are assigned to different study drug combinations based on the results of genomic profiling of their tumors.
The NCI-sponsored National Lung Screening Trial (NLST) showed that low-dose CT scans can be used to screen for lung cancer in people with a history of heavy smoking. Using this screening can decrease their risk of dying from lung cancer. Now researchers are looking for ways to refine CT screening to better predict whether cancer is present.
Perioperative immune checkpoint blockades improve prognosis of resectable non-small cell lung cancer Yu Tian, MD ... Zhichao Liu, Hanbo Pan authors contributed equally to this paper. Author Notes. European Journal of Cardio-Thoracic Surgery ... It furthers the University's objective of excellence in research, scholarship, and education by ...
Abstract. Lung cancer is the leading cause of mortality and person-years of life lost from cancer among US men and women. Early detection has been shown to be associated with reduced lung cancer mortality. Our objective was to update the American Cancer Society (ACS) 2013 lung cancer screening (LCS) guideline for adults at high risk for lung ...
Introduction. Lung cancer (LC) is the number one cause of cancer-related deaths in the United States and the world in both men and women [1, 2].Worldwide, there are approximately 1.8 million new cases and 1.6 million deaths every year [], and in the US alone, LC accounts for approximately 23% of cancer related mortality [].The overall 5-year survival rate for LC remains poor at approximately ...
Lung cancer is the leading global cause of cancer-related deaths. Although smoking cessation is the best prevention, 50% of lung cancer diagnoses occur in people who have quit smoking. Research into treatment options for high-risk patients is constrained to rodent models, which are time-consuming, expensive, and require large cohorts.
Introduction. SCLC accounts for about 15% −20% of lung cancer cases. Citation 1 SCLC belongs to one of neuroendocrine tumors, which is characterized by rapid tumor proliferation, tendency for early and extensive metastases, and poor prognosis. Citation 1 About 60% of the SCLC patients are in an extensive stage at the time of diagnosis. Citation 2 The first-line standard treatment for ...
Marchetti, A. et al. EGFR mutations in non-small-cell lung cancer: analysis of a large series of cases and development of a rapid and sensitive method for diagnostic screening with potential ...
The initial introduction of cancer screening programs was decided based on experts' opinions. Since 2003, the research groups funded by the National Cancer Center have published screening guidelines for gastric, colorectal, lung, prostate, cervical, and breast cancers.
Lung cancer or bronchogenic carcinoma refers to tumors originating in the lung parenchyma or within the bronchi. It is one of the leading causes of cancer-related deaths in the United States. Since 1987, lung cancer has been responsible for more deaths in women than breast cancer. It is estimated that there are 225,000 new cases of lung cancer in the United States annually, and approximately ...
Researchers at the University of Oxford, the Francis Crick Institute and University College London have been granted £1.7 million of funding from Cancer Research UK and the CRIS Cancer Foundation to develop a lung cancer vaccine.. The team are seeking to create 'LungVax', the world's first vaccine to prevent lung cancer in people with a high risk of the disease.
An estimated 157,400 Americans died of lung cancer in 2001. Lung cancer is the second most frequent cancer in both men and women. The major risk factor for lung cancer is smoking, which accounts for 75-80% of lung cancer-related deaths. Lung cancers can be broadly classified into two forms, small-cell carcinomas and non-small-cell carcinomas.
A total of 89.6% of the participants without any advanced colorectal neoplasia (colorectal cancer or advanced precancerous lesions) identified on colonoscopy had a negative cfDNA blood-based test ...
Introduction. Lung cancer is the leading cause of cancer death worldwide with 1.7 million global deaths attributed to cigarette smoking in 2015. 1 Tobacco use is the leading cause of lung cancer; 55% of lung cancer deaths in women and over 70% of lung cancer deaths in men are due to smoking. 1 These global estimates, however, mask major differences in smoking prevalence in men and women across ...