Diagnosis and Management of Asthma in Adults: A Review
Affiliations.
- 1 Division of Allergy and Clinical Immunology, University of Texas Medical Branch, Galveston.
- 2 Department of Preventive Medicine and Community Health, University of Texas Medical Branch, Galveston.
- 3 Division of Pulmonary Critical Care and Sleep, Department of Internal Medicine, University of Texas Medical Branch, Galveston.
- PMID: 28719697
- DOI: 10.1001/jama.2017.8372
Importance: Asthma affects about 7.5% of the adult population. Evidence-based diagnosis, monitoring, and treatment can improve functioning and quality of life in adult patients with asthma.
Observations: Asthma is a heterogeneous clinical syndrome primarily affecting the lower respiratory tract, characterized by episodic or persistent symptoms of wheezing, dyspnea, and cough. The diagnosis of asthma requires these symptoms and demonstration of reversible airway obstruction using spirometry. Identifying clinically important allergen sensitivities is useful. Inhaled short-acting β2-agonists provide rapid relief of acute symptoms, but maintenance with daily inhaled corticosteroids is the standard of care for persistent asthma. Combination therapy, including inhaled corticosteroids and long-acting β2-agonists, is effective in patients for whom inhaled corticosteroids alone are insufficient. The use of inhaled long-acting β2-agonists alone is not appropriate. Other controller approaches include long-acting muscarinic antagonists (eg, tiotropium), and biological agents directed against proteins involved in the pathogenesis of asthma (eg, omalizumab, mepolizumab, reslizumab).
Conclusions and relevance: Asthma is characterized by variable airway obstruction, airway hyperresponsiveness, and airway inflammation. Management of persistent asthma requires avoidance of aggravating environmental factors, use of short-acting β2-agonists for rapid relief of symptoms, and daily use of inhaled corticosteroids. Other controller medications, such as long-acting bronchodilators and biologics, may be required in moderate and severe asthma. Patients with severe asthma generally benefit from consultation with an asthma specialist for consideration of additional treatment, including injectable biologic agents.

Publication types
- Administration, Inhalation
- Adrenal Cortex Hormones / adverse effects
- Adrenal Cortex Hormones / therapeutic use
- Adrenergic beta-Agonists / adverse effects
- Adrenergic beta-Agonists / therapeutic use
- Airway Obstruction / physiopathology
- Anti-Asthmatic Agents / adverse effects
- Anti-Asthmatic Agents / therapeutic use*
- Asthma / diagnosis*
- Asthma / drug therapy*
- Asthma / physiopathology
- Biological Products / therapeutic use
- Bronchial Hyperreactivity / physiopathology
- Drug Therapy, Combination
- Inflammation
- Muscarinic Antagonists / therapeutic use
- Adrenal Cortex Hormones
- Adrenergic beta-Agonists
- Anti-Asthmatic Agents
- Biological Products
- Muscarinic Antagonists
Grants and funding
- UL1 TR000071/TR/NCATS NIH HHS/United States

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Heart-Healthy Living
- High Blood Pressure
- Sickle Cell Disease
- Sleep Apnea
- Information & Resources on COVID-19
- The Heart Truth®
- Learn More Breathe Better®
- Blood Diseases and Disorders Education Program
- Publications and Resources
- Blood Disorders and Blood Safety
- Sleep Science and Sleep Disorders
- Lung Diseases
- Health Disparities and Inequities
- Heart and Vascular Diseases
- Precision Medicine Activities
- Obesity, Nutrition, and Physical Activity
- Population and Epidemiology Studies
- Women’s Health
- Research Topics
- Clinical Trials
- All Science A-Z
- Grants and Training Home
- Policies and Guidelines
- Funding Opportunities and Contacts
- Training and Career Development
- Email Alerts
- NHLBI in the Press
- Research Features
- Past Events
- Upcoming Events
- Mission and Strategic Vision
- Divisions, Offices and Centers
- Advisory Committees
- Budget and Legislative Information
- Jobs and Working at the NHLBI
- Contact and FAQs
- NIH Sleep Research Plan
- < Back To Research Topics
Asthma Research
Language switcher.
Over the years, and as part of our broader commitment to research on lung diseases, the NHLBI has led and supported asthma research to discover better prevention and treatment options. Research supported by the NHLBI has also helped us understand what leads to and affects asthma, and it has provided doctors with information about what treatments work best for people who have asthma.
NHLBI research that really made a difference
For nearly 20 years, the NHLBI Severe Asthma Research Program (SARP) has transformed our knowledge of severe asthma. Research supported through the program has identified secondhand smoke, pneumonia, and obesity as key risk factors for asthma . Studies have also found genetic variations linked with severe asthma and biomarkers for asthma severity. Researchers can request access to the data on dbGaP .
Research funded by the NHLBI
Our Division of Lung Diseases and its Airway Biology and Disease Branch oversee much of the research on asthma we fund. The Asthma Program supports research related to asthma, including the role of inflammation in the development of asthma, genetics and asthma, and clinical management of asthma in adults and children.
Find funding opportunities and program contacts for asthma research.
Current research on asthma treatment
- How ventilators may lead to asthma: The NHLBI-funded Post-Vent study will use data collected from the Prematurity-Related Ventilatory Control (Pre-Vent): Role in Respiratory Outcomes NHLBI Collaborative Program to study long-term health outcomes of premature birth and intermittent low oxygen levels shortly after babies are born prematurely. These babies often develop asthma. This study will try to predict which premature babies are most likely to develop asthma.
- Why medicines work: An NHLBI-funded study is assessing how an antibiotic called azithromycin (AZ) reduces severe wheezing in preschool children seen in the emergency room. While prior studies have shown that AZ benefits these children, it is unclear if the beneficial effects are because of the antibacterial activity of AZ or because of the anti-inflammatory activity of AZ. To help answer this question, this study will compare whether children with bacteria growing in their throats get more benefit from AZ treatment than children who do not have bacteria growing in their throats at the time they go to the emergency room with severe wheezing.
- Personalized medicine: The Precision Interventions for Severe and/or Exacerbation Prone Asthma Network (PrecISE) is conducting clinical trials to identify personalized medicine approaches that treat severe asthma more effectively. It has established 30 locations nationwide that will test new and approved treatments based on each patient’s specific biology and biomarkers.
Find more NHLBI-funded studies on asthma treatment at NIH RePORTER.

Learn about one PrecISE study that is looking at treatments that may help support people with severe asthma or asthma that hasn’t responded to traditional treatments: Personalizing treatment for severe asthma .
Current research on asthma biology
The different bacteria in a person’s body can affect the immune system. We support studies to figure out whether different bacteria play a role in developing certain types of asthma.
- Airway cells and asthma: NHLBI-funded research will look at how genes are regulated in airway epithelial cells to better understand how they affect the development of asthma. Epithelial cells line the lung’s airways. As researchers learn more about how changes in the cells lead to asthma, they hope to develop treatments to reprogram the epithelium and prevent or cure asthma and other lung diseases.
- Bacteria in the airways: An AsthmaNet study found different bacteria in the airways of people with asthma compared to those without asthma. Some of the observed differences could help predict the response to inhaled steroids. Researchers can request the data through our Biologic Specimen and Data Repository Information Coordinating Center.
- Targeted treatments for severe asthma: NHLBI-supported researchers are developing new and personalized approaches to treating severe asthma . The study builds on earlier research which led the researchers’ discovery of three mechanisms that are relevant to severe asthma.
Find more NHLBI-funded studies on asthma biology at NIH RePORTER.
Researchers have identified a key role for the circadian system — the biological clock that controls your sleep/wake cycle: Study of biological clock may explain why asthma worsens at night .
Current research on asthma disparities
African Americans are more likely to develop asthma and three times more likely to die from asthma-related causes than white Americans. Research on this topic is part our broader commitment to addressing health disparities and inequities .
- Genetic factors: The Consortium on Asthma among African-Ancestry Populations in the Americas (CAAPA) aims to discover genes that confer asthma risk among individuals of African ancestry and to study genetic diversity in populations of African descent. Read some of the results here or request access to the data on dbGaP .
- Comprehensive care for at-risk children: We also fund the Asthma Empowerment Collaborations to Reduce Childhood Asthma Disparities . We support clinical trials to evaluate programs that provide comprehensive care for children at high risk of poor asthma outcomes, such as low-income minority children.
- Race, sex, and socioeconomic factors: The NHLBI recently launched the DECIPHeR program to study differences in heart and lung diseases among groups defined by race and ethnicity, sex and/or gender, and socioeconomic status. The first projects began in September 2020, with one project focused on asthma in children in Colorado. Working with communities across the state, from rural to urban areas in Colorado, researchers will work with school-based asthma navigators and nurses to test a team approach to asthma control in school children in low-income areas.
Find more NHLBI-funded studies on asthma and health disparities .

An NHLBI-funded study found that African-American boys, but not girls, with higher levels of BPA (Bisphenol A) tended to have more asthma symptoms: Study links exposure to higher levels of BPA plasticizer to more asthma symptoms in black boys .
Asthma research labs at the NHLBI
The Laboratory of Asthma and Lung Inflammation , located within the Pulmonary Branch , is focused on developing new treatment approaches for people with severe asthma. Headed by Stewart J. Levine, M.D., the lab’s researchers found a new biological pathway that leads to asthma. They continue to study this pathway, as well as an important molecule in it called apolipoprotein E (ApoE).
“By studying the pathways of the disease, we identified a new biological mechanism that leads to asthma,” explained Stewart J. Levine, M.D. Read the research feature: Disease pathways lead to possible new treatment for severe asthma .
Learn about research opportunities in the lab:
- Post-doctoral Fellowship on Apolipoprotein Pathways in Asthma
- Graduate Medical Education (GME): NHLBI/UMD Pulmonary-Critical Care Fellowship
Related asthma programs and guidelines
- The NAEPP’s Expert Panel Report 4 (EPR-4) Working Group was established in 2018 to update the 2007 Guidelines for the Diagnosis and Management of Asthma (EPR-3) in focused topic areas. The working group members reviewed the latest research to update the guidelines on treatments and management of asthma, including the role of immunotherapy, the effectiveness of indoor allergen reduction, and the use of fractional exhaled nitric oxide (FeNO). Read Asthma Management Guidelines: Focused Updates 2020 .
- Learn More Breathe Better® is a national health education program for asthma, COPD, and other lung and respiratory diseases. The program raises awareness about asthma and other lung conditions and supports the promotion, implementation, and adoption of evidence-based care. Learn More Breathe Better® Asthma offers a series of asthma handouts to patients and caregivers, including tips for talking to your doctor.
- Since 1989, the National Asthma Education and Prevention Program (NAEPP) has worked with medical associations, voluntary health organizations, and community programs to educate patients, healthcare professionals, and the public about asthma.
- The Lung Tissue Research Consortium (LTRC) provides human lung tissues to qualified investigators for use in their research. The program enrolls patients who are planning to have lung surgery, collects blood and other clinical data from these donors, and stores donated tissue that otherwise would be discarded after the lung surgery. The LTRC provides tissue samples and data at no cost to approved investigators.
Explore more NHLBI research on asthma
The sections above provide you with the highlights of NHLBI-supported research on asthma. You can explore the full list of NHLBI-funded studies on the NIH RePORTER .
To find more studies:
- Type your search words into the Quick Search box and press enter.
- Check Active Projects if you want current research.
- Select the Agencies arrow, then the NIH arrow, then check NHLBI .
If you want to sort the projects by budget size — from the biggest to the smallest — click on the FY Total Cost by IC column heading.
- Search by keyword
- Search by citation
Page 1 of 2
Psychological distress and associated factors among asthmatic patients in Southern, Ethiopia, 2021
There is an increased prevalence of psychological distress in adults with asthma. Psychological distress describes unpleasant feelings or emotions that impact the level of functioning. It is a significant exac...
- View Full Text
Retrospective assessment of a collaborative digital asthma program for Medicaid-enrolled children in southwest Detroit: reductions in short-acting beta-agonist (SABA) medication use
Real-world evidence for digitally-supported asthma programs among Medicaid-enrolled children remains limited. Using data from a collaborative quality improvement program, we evaluated the impact of a digital i...
Nonadherence to antiasthmatic medications and its predictors among asthmatic patients in public hospitals of Bahir Dar City, North West Ethiopia: using ASK-12 tool
Globally, adequate asthma control is not yet achieved. The main cause of uncontrollability is nonadherence to prescribed medications.
The hen and the egg question in atopic dermatitis: allergy or eczema comes first
Atopic dermatitis (AD) as a chronic inflammatory systemic condition is far more than skin deep. Co-morbidities such as asthma and allergic rhinitis as well as the psychological impact influence seriously the q...
Medication regimen complexity and its impact on medication adherence and asthma control among patients with asthma in Ethiopian referral hospitals
Various studies have found that medication adherence is generally low among patients with asthma, and that the complexity of the regimen may be a potential factor. However, there is no information on the compl...
Monoclonal antibodies targeting small airways: a new perspective for biological therapies in severe asthma
Small airway dysfunction (SAD) in asthma is characterized by the inflammation and narrowing of airways with less of 2 mm in diameter between generations 8 and 23 of the bronchial tree. It is now widely accepte...
Level of asthma control and its determinants among adults living with asthma attending selected public hospitals in northwestern, Ethiopia: using an ordinal logistic regression model
Asthma is a major public health challenge and is characterized by recurrent attacks of breathlessness and wheezing that vary in severity and frequency from person to person. Asthma control is an important meas...
Static lung volumes and diffusion capacity in adults 30 years after being diagnosed with asthma
Long-term follow-up studies of adults with well-characterized asthma are sparse. We aimed to explore static lung volumes and diffusion capacity after 30 + years with asthma.
Over-prescription of short-acting β 2 -agonists and asthma management in the Gulf region: a multicountry observational study
The overuse of short-acting β 2 -agonists (SABA) is associated with poor asthma control. However, data on SABA use in the Gulf region are limited. Herein, we describe SABA prescription practices and clinical outcom...
A serological biomarker of type I collagen degradation is related to a more severe, high neutrophilic, obese asthma subtype
Asthma is a heterogeneous disease; therefore, biomarkers that can assist in the identification of subtypes and direct therapy are highly desirable. Asthma is a chronic inflammatory disease that leads to change...
Adherence to inhalers and associated factors among adult asthma patients: an outpatient-based study in a tertiary hospital of Rajshahi, Bangladesh
Adherence to inhaler medication is an important contributor to optimum asthma control along with adequate pharmacotherapy. The objective of the present study was to assess self-reported adherence levels and to...
The link between atopic dermatitis and asthma- immunological imbalance and beyond
Atopic diseases are multifactorial chronic disturbances which may evolve one into another and have overlapping pathogenetic mechanisms. Atopic dermatitis is in most cases the first step towards the development...
The effects of nebulized ketamine and intravenous magnesium sulfate on corticosteroid resistant asthma exacerbation; a randomized clinical trial
Asthma exacerbation is defined as an acute attack of shortness of breath with more than 25% decrease in morning peak flow compared to the baseline on 2 consecutive days, which requires immediate standard thera...
Determinants of asthma in Ethiopia: age and sex matched case control study with special reference to household fuel exposure and housing characteristics
Asthma is a chronic inflammatory disorder characterized by airway obstruction and hyper-responsiveness. Studies suggest that household fuel exposure and housing characteristics are associated with air way rela...
Feasibility and acceptability of monitoring personal air pollution exposure with sensors for asthma self-management
Exposure to fine particulate matter (PM 2.5 ) increases the risk of asthma exacerbations, and thus, monitoring personal exposure to PM 2.5 may aid in disease self-management. Low-cost, portable air pollution sensors...
Biological therapy for severe asthma
Around 5–10% of the total asthmatic population suffer from severe or uncontrolled asthma, which is associated with increased mortality and hospitalization, increased health care burden and worse quality of lif...
Treatment outcome clustering patterns correspond to discrete asthma phenotypes in children
Despite widely and regularly used therapy asthma in children is not fully controlled. Recognizing the complexity of asthma phenotypes and endotypes imposed the concept of precision medicine in asthma treatment...
Positive change in asthma control using therapeutic patient education in severe uncontrolled asthma: a one-year prospective study
Severe asthma is difficult to control. Therapeutic patient education enables patients to better understand their disease and cope with treatment, but the effect of therapeutic patient education in severe uncon...
Asthma and COVID-19: a dangerous liaison?
The coronavirus disease 2019 (COVID-19) pandemic, caused by the new severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), provoked the most striking international public health crisis of our time. COVI...
Knowledge, attitude, and practice towards COVID-19 among chronic disease patients at Aksum Hospital, Northern Ethiopia, 2020: a cross-sectional study
The Coronavirus disease 2019 outbreak is the first reported case in Wuhan, China in December 2019 and suddenly became a major global health concern. Currently, there is no vaccine and treatment have been repor...
Self-reported vs. objectively assessed adherence to inhaled corticosteroids in asthma
Adherence to inhaled corticosteroids (ICS) in asthma is vital for disease control. However, obtaining reliable and clinically useful measures of adherence remains a major challenge. We investigated the associa...
Association between prevalence of obstructive lung disease and obesity: results from The Vermont Diabetes Information System
The association of obesity with the development of obstructive lung disease, namely asthma and/or chronic obstructive pulmonary disease, has been found to be significant in general population studies, and weig...
Changes in quantifiable breathing pattern components predict asthma control: an observational cross-sectional study
Breathing pattern disorders are frequently reported in uncontrolled asthma. At present, this is primarily assessed by questionnaires, which are subjective. Objective measures of breathing pattern components ma...
The role of leukotriene modifying agent treatment in neuropsychiatric events of elderly asthma patients: a nested case control study
In March 2020, the US Food and Drug Administration decided that the dangers related to neuropsychiatric events (NPEs) of montelukast, one of the leukotriene modifying agents (LTMAs), should be communicated thr...
Asthma and stroke: a narrative review
Asthma is a heterogeneous disease, usually characterized by chronic airway inflammation, bronchial reversible obstruction and hyperresponsiveness to direct or indirect stimuli. It is a severe disease causing a...
Comparison of dental caries (DMFT and DMFS indices) between asthmatic patients and control group in Iran: a meta-analysis
The association between caries index, which is diagnosed by Decayed, Missing, and Filled Teeth (DMFT), and asthma has been assessed in several studies, which yielded contradictory results. Meta-analysis is the...
ICS/formoterol in the management of asthma in the clinical practice of pulmonologists: an international survey on GINA strategy
The treatment with short-acting beta-2 agonists (SABA) alone is no longer recommended due to safety issues. Instead, the current Global Initiative for Asthma (GINA) Report recommends the use of the combination...
Sustainability of residential environmental interventions and health outcomes in the elderly
Research has documented that housing conditions can negatively impact the health of residents. Asthma has many known indoor environmental triggers including dust, pests, smoke and mold, as evidenced by the 25 ...
Non-adherence to inhaled medications among adult asthmatic patients in Ethiopia: a systematic review and meta-analysis
Medication non-adherence is one of a common problem in asthma management and it is the main factor for uncontrolled asthma. It can result in poor asthma control, which leads to decreased quality of life, incre...
The outcome of COVID-19 among the geriatric age group in African countries: protocol for a systematic review and meta-analysis
According to the World Health Organization (WHO), the outbreak of coronavirus disease in 2019 (COVID-19) has been declared as a pandemic and public health emergency that infected more than 5 million people wor...
Correction to: A comparison of biologicals in the treatment of adults with severe asthma – real-life experiences
An amendment to this paper has been published and can be accessed via the original article.
The original article was published in Asthma Research and Practice 2020 6 :2
Disease control in patients with asthma and respiratory symptoms (wheezing, cough) during sleep
The Global Initiative for Asthma ( GINA)-defined criteria for asthma control include questions about daytime symptoms, limitation of activity, nocturnal symptoms, need for reliever treatment and patients’ satisfac...
The burden, admission, and outcomes of COVID-19 among asthmatic patients in Africa: protocol for a systematic review and meta-analysis
Coronavirus disease 2019 outbreak is the first reported case in Wuhan, China in December 2019 and suddenly became a major global health concern. According to the European Centre for Disease Prevention and Cont...
The healthcare seeking behaviour of adult patients with asthma at Chitungwiza Central Hospital, Zimbabwe
Although asthma is a serious public health concern in Zimbabwe, there is lack of information regarding the decision to seek for healthcare services among patients. This study aimed to determine the health care...
Continuous versus intermittent short-acting β2-agonists nebulization as first-line therapy in hospitalized children with severe asthma exacerbation: a propensity score matching analysis
Short-acting β2-agonist (SABA) nebulization is commonly prescribed for children hospitalized with severe asthma exacerbation. Either intermittent or continuous delivery has been considered safe and efficient. ...
Patient perceived barriers to exercise and their clinical associations in difficult asthma
Exercise is recommended in guidelines for asthma management and has beneficial effects on symptom control, inflammation and lung function in patients with sub-optimally controlled asthma. Despite this, physica...
Asthma management with breath-triggered inhalers: innovation through design
Asthma affects the lives of hundred million people around the World. Despite notable progresses in disease management, asthma control remains largely insufficient worldwide, influencing patients’ wellbeing and...
A nationwide study of asthma correlates among adolescents in Saudi Arabia
Asthma is a chronic airway inflammation disease that is frequently found in children and adolescents with an increasing prevalence. Several studies are linking its presence to many lifestyle and health correla...
A comparison of biologicals in the treatment of adults with severe asthma – real-life experiences
Anti-IgE (omalizumab) and anti-IL5/IL5R (reslizumab, mepolizumab and benralizumab) treatments are available for severe allergic and eosinophilic asthma. In these patients, studies have shown beneficial effects...
The Correction to this article has been published in Asthma Research and Practice 2020 6 :10
Determinants of Acute Asthma Attack among adult asthmatic patients visiting hospitals of Tigray, Ethiopia, 2019: case control study
Acute asthma attack is one of the most common causes of visits to hospital emergency departments in all age groups of the population and accounts for the greater part of healthcare burden from the disease. Des...
Determinants of non-adherence to inhaled steroids in adult asthmatic patients on follow up in referral hospital, Ethiopia: cross-sectional study
Asthma is one of the major non-communicable diseases worldwide. The prevalence of asthma has continuously increased over the last five decades, resulting in 235 million people suffering from it. One of the mai...
Development of a framework for increasing asthma awareness in Chitungwiza, Zimbabwe
Asthma accounts for significant global morbidity and health-care costs. It is still poorly understood among health professionals and the general population. Consequently, there are significant morbidity and mo...
Epidemiology and utilization of primary health care services in Qatar by asthmatic children 5–12 years old: secondary data analysis 2016–2017
Childhood asthma is a growing clinical problem and a burden on the health care system due to repetitive visits to children’s emergency departments and frequent hospital admissions where it is poorly controlled...
Is asthma in the elderly different? Functional and clinical characteristics of asthma in individuals aged 65 years and older
The prevalence of chronic diseases in the elderly (> 65 years), including asthma, is growing, yet information available on asthma in this population is scarce.
Factors associated with exacerbations among adults with asthma according to electronic health record data
Asthma is a chronic inflammatory lung disease that affects 18.7 million U.S. adults. Electronic health records (EHRs) are a unique source of information that can be leveraged to understand factors associated w...
What is safe enough - asthma in pregnancy - a review of current literature and recommendations
Although asthma is one of the most serious diseases causing complications during pregnancy, half of the women discontinue therapy thus diminishing the control of the disease, mostly due to the inadequate educa...
Biomarkers in asthma: state of the art
Asthma is a heterogenous disease characterized by multiple phenotypes driven by different mechanisms. The implementation of precision medicine in the management of asthma requires the identification of phenoty...
Exhaled biomarkers in childhood asthma: old and new approaches
Asthma is a chronic condition usually characterized by underlying inflammation. The study of asthmatic inflammation is of the utmost importance for both diagnostic and monitoring purposes. The gold standard fo...
Assessment of predictors for acute asthma attack in asthmatic patients visiting an Ethiopian hospital: are the potential factors still a threat?
Recurrent exacerbations in patients with moderate or severe asthma are the major causes of morbidity, mortality and medical expenditure. Identifying predictors of frequent asthma attack might offer the fertile...
Effect of adjusting the combination of budesonide/formoterol on the alleviation of asthma symptoms
The combination of budesonide + formoterol (BFC) offers the advantages of dose adjustment in a single inhaler according to asthma symptoms. We analyzed the relationship between asthma symptoms in terms of peak...
Asthma Research and Practice
ISSN: 2054-7064
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Bronchial Asthma: Symptoms, Triggers, and More
Causes and types of asthma.
- Signs and Symptoms
Frequently Asked Questions
Asthma is a chronic disease that affects your breathing. All types of asthma impact the tubes that move air in and out of your lungs, called bronchial tubes or bronchi. These tubes become swollen and inflamed in people with asthma, earning this condition its name.
This article will explore the different asthma types, what sets them apart, and how to manage them.
LAW Ho Ming / Getty Images
An asthma diagnosis means you have chronic swelling and inflammation in the bronchioles. Also referred to as wheezing or bronchial asthma, this condition can run in families or be triggered by allergies and irritants .
There are different types of asthma, which are classified by the cause of the condition or what triggers symptoms.
Allergies and Bronchial Asthma
Allergies are a major trigger of bronchial asthma. Inhaling certain substances called allergens can trigger an allergic reaction, causing your airways to become irritated, inflamed, and swollen.
Swelling and inflammation narrow the opening that air passes through, making it more difficult to breathe. Wheezing sounds and coughing are common symptoms that can develop with an allergic asthma attack.
Many allergens can lead to an asthma attack. Food allergies and allergic skin reactions are linked to a higher risk of asthma.
Types of Asthma
Allergies aren't the only triggers for an asthma attack. Bronchial asthma develops in the bronchioles and includes nearly every type of asthma.
A more effective way to categorize asthma types is by cause or trigger. Common types of asthma besides allergic asthma include:
- Allergic asthma : Triggered by an allergen or allergens
- Nonallergic asthma : Triggered by inhaled irritants, chemicals, a respiratory infection, cold weather, or tobacco smoke
- Occupational asthma : Caused by inhaled chemicals or industrial dust in the workplace
- Exercise-induced asthma : Triggered by exercise and physical exertion, especially when the air is dry
Bronchial Asthma Triggers
Anyone can develop asthma, but it is most common in people who:
- Have a family history of asthma
- Had severe respiratory infections in childhood
- Are affected by obesity
- Use tobacco
- Are exposed to irritants in the workplace
- Live in areas with high levels of pollution
- Have other allergic conditions like eczema or hay fever
When allergies trigger a bronchial asthma attack, specific culprits can vary from person to person. Some common allergens that trigger asthma attacks include:
- Tobacco smoke
- Dander and waste from rodents or insects
- Chemicals or cleaning products
Signs and Symptoms of Bronchial Asthma
If you have asthma, you may notice regular changes in your breathing that range from mild to severe. But when an asthma attack occurs, your symptoms can become severe quickly and may even require immediate medical treatment.
Some common signs and symptoms of bronchial asthma are:
- Tightness or pain in your chest
- Coughing, especially in the morning and at night
- Shortness of breath
Diagnosing Bronchial Asthma
Diagnosing asthma is a multistep process that begins with your healthcare provider reviewing your personal and family medical histories, going over your types of allergies (or doing an allergy test to identify any allergies), and performing a physical exam.
Allergy and immune system testing using blood or skin tests are standard, and in most cases, you will also undergo testing that evaluates your lung function and respiratory system.
Spirometry is a type of lung function test that measures the overall health of your lungs. This test requires you to breathe into a device with different strengths and at different rates. It measures how much air you can move in and out of your lungs with each breath and how easily air moves through your respiratory system.
Peak Expiratory Flow (PEF)
Peak expiratory flow (PEF) is another type of lung function test. This test measures how quickly you can force air out of your lungs after a full inhalation.
Peak flow testing is measured with a handheld device that can help your healthcare provider understand how much the space in your airways is limited by inflammation and can help you manage your asthma daily.
Fractional Exhaled Nitric Oxide (FeNO)
This test measures the level of nitric oxide in your breath when you exhale. High levels of nitric oxide can signal inflammation in your lungs. This test is done by breathing into a machine that will measure your nitric oxide levels.
Chest X-Ray
A chest X-ray can give your healthcare provider a look inside your lungs. While this test isn't beneficial for diagnosing asthma, chest X-rays can identify other problems affecting your breathing, like pneumonia or lung cancer .
Treating Bronchial Asthma
Bronchial asthma treatment includes avoiding triggers, maintenance medications, and treating flare-ups (occasions when symptoms worsen).
Knowing your triggers and working to avoid or manage them is vital, as this can help prevent severe asthma attacks . Daily maintenance medications are essential for prevention, as these medications help keep inflammation and swelling from developing in the bronchioles.
When these strategies are ineffective, a quick-acting medication (also called a rescue medication) can be used before or after an activity known to increase asthma symptoms. Short-acting inhaled bronchodilators (medications to relax your airways) and oral corticosteroids (medications to reduce lung inflammation) are examples of rescue medications.
If your asthma attack is severe , you may also require hospitalization for additional treatments like intravenous medications or supplemental oxygen.
Bronchial asthma is a term that is used interchangeably with asthma. All types of asthma affect the tubes that bring air in and out of your lungs (bronchioles). In all types of asthma, an allergen, irritant, or other condition causes these bronchioles to swell and limits air movement. Your healthcare provider can help you manage your asthma with daily control medications and treatments for flare-ups or asthma attacks.
A Word From Verywell
Asthma is a lifelong condition that impacts your breathing. All types of asthma affect the bronchi, earning this condition the nickname "bronchial asthma." If asthma runs in your family or if you experience wheezing and other breathing problems in certain environments or after activities, talk to your healthcare provider about your asthma risk and how to best manage your condition.
"Bronchial asthma" is just another name for asthma. All types of asthma affect your bronchial tubes.
Bronchial asthma is best treated by avoiding triggers and using maintenance medications to control inflammation. Asthma attacks are treated with rescue medications or direct medical care.
Bronchial asthma is a chronic condition. Once diagnosed, it is a health condition you will need to control for the rest of your life.
Bronchial asthma never goes away, and symptoms can range from mild to severe. If you experience difficulty breathing and your bronchioles are too swollen to pass air through, you may experience a medical emergency.
There are many types of asthma, but allergic asthma, nonallergic asthma, and exercise-induced asthma are among the most common.
MedlinePlus. Asthma .
American College of Allergy Asthma and Immunology. Allergic asthma .
Zimmerman P, et al. Association between the intestinal microbiota and allergic sensitization, eczema, and asthma: A systematic review . J Allergy Clin Immunol. February 2018; 143(2):467-485. doi:10.1016/j.jaci.2018.09.025.
Emons JAM, Gerth van Wijk R. Food allergy and asthma: Is there a link ? Curr Treat Options Allergy. October 2018; 5:436-444. doi: 10.1007/s40521-018-0185-1.
American Lung Association. Asthma risk factors .
Centers for Disease Control and Prevention. Common asthma triggers .
American Lung Association. Spirometry.
Johns Hopkins Medicine. Peak flow measurement.
American Lung Association. Exhaled nitric oxide test.
NIH National Heart, Lung, and Blood Institute. Tests for lung disease .
By Rachael Zimlich, BSN, RN Zimlich is a critical care nurse who has been writing about health care and clinical developments for over 10 years.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 26 April 2024
How to make Asthma Right Care ‘easy’ in primary care: learnings from the 2023 Asthma Right Care Summit
- Siân Williams 1 ,
- Jaime Correia de Sousa ORCID: orcid.org/0000-0001-6459-7908 1 , 2 ,
- Ee Ming Khoo ORCID: orcid.org/0000-0003-3191-1264 1 , 3 ,
- Habib Ghedira 4 , 5 ,
- Vincent Mak 1 , 6 ,
- Mar Martínez Vázquez 7 , 8 ,
- Cláudia Vicente 9 , 10 &
- Darush Attar-Zadeh 1 , 11
npj Primary Care Respiratory Medicine volume 34 , Article number: 4 ( 2024 ) Cite this article
102 Accesses
2 Altmetric
Metrics details
- Health policy
- Health services
- Patient education
- Respiratory signs and symptoms
Introduction
Asthma affects approximately 262 million people worldwide with an estimated 1000 people dying from asthma attacks each day 1 , 2 . The majority of asthma attacks are preventable and the substantial mortality, morbidity, healthcare utilisation, environmental and economic burden asthma causes are all largely avoidable. Owing to its impact on the individual and society, asthma warrants a biopsychosocial, holistic approach best provided by primary care. However, the lack of universal health coverage and investment in primary care creates preventable harm, inequalities and inequity within and between countries 3 , 4 .
Despite knowledge about how to manage it effectively, asthma is often overlooked as a clinical, health and research priority. Currently, a key problem in asthma management is the over-reliance on episodic care defined as a system-wide over-reliance on symptom relief and rescue. This includes inhaled short-acting β 2 -receptor agonists (SABAs), systemic steroids and the overuse of emergency services and hospitalisation, which may partly be caused by lack of adherence to the appropriate medication and disregard of symptoms by patients.
Since 2019, the Global Initiative for Asthma (GINA) no longer recommends treatment of asthma with SABA monotherapy in adults, adolescents and children over 6 years. For the best outcomes, inhaled corticosteroids (ICS)-containing treatment should be initiated when (or as soon as possible after) asthma is diagnosed. All patients should also be provided with a reliever inhaler for quick symptom relief, preferably an anti-inflammatory reliever (AIR), including ICS-formoterol and ICS-SABA 5 .
In 2017, the International Primary Care Respiratory Group (IPCRG) initiated a social movement, Asthma Right Care, to mobilise stakeholders firstly to acknowledge that problems exist, particularly over-reliance on SABA, and secondly to take responsibility for remedying them 3 . This movement aims to disrupt the current system by demonstrating the scale of the problem, and then build on adult-learning principles, offering problem-based education about right care 6 , 7 , guided by national guidelines and/or GINA.
Making Asthma Right Care ‘easy’ in primary care
To obtain a greater understanding of current asthma management worldwide, a survey (see Supplementary Information) based on the IPCRG’s situational analyses for its Teach the Teacher ® programmes and structured according to IPCRG’s eight person-centred statements ( https://www.ipcrg.org/asthmarightcare/what-does-good-quality-asthma-care-look-like , see Supplementary Information) was sent out as an online form to representatives from 47 countries where IPCRG had active contacts with practising clinicians. There was representation from low-, middle- and high-income countries and, in some cases, there was more than one response from a country where different disciplines were represented, including family medicine, community pharmacy and pulmonology (seeing primary care patients). We received 57 responses from 33 countries: 40/57 from respiratory-interested clinicians working in primary care and 17/57 from respiratory specialists. Following the analysis of responses, on the 9 September 2023, an international summit facilitated by a multinational IPCRG faculty took place in Milan, Italy, called ‘Making Asthma Right Care “easy” in primary care’. IPCRG primary care colleagues familiar with Asthma Right Care were joined by 19 delegates from 13 countries from Asia, Latin America and Africa who had expressed interest in engaging in the movement. Figure 1 highlights the objectives of the summit.
Objectives from the ‘Making Asthma Right Care “easy” in primary care’ summit.
Current asthma management worldwide
The survey responses reported a variation in asthma care, diagnosis and management worldwide—the responses to all questions and representativity from countries are available in the Supplementary Information.
Overall, 47/57 (82%) respondents reported the existence of local or national guidelines for asthma management (Fig. 2 ) and about one third of them considered that these were frequently implemented in practice. Approximately three quarters of the respondents felt that there were no national policies to support the implementation of local/national guidelines.
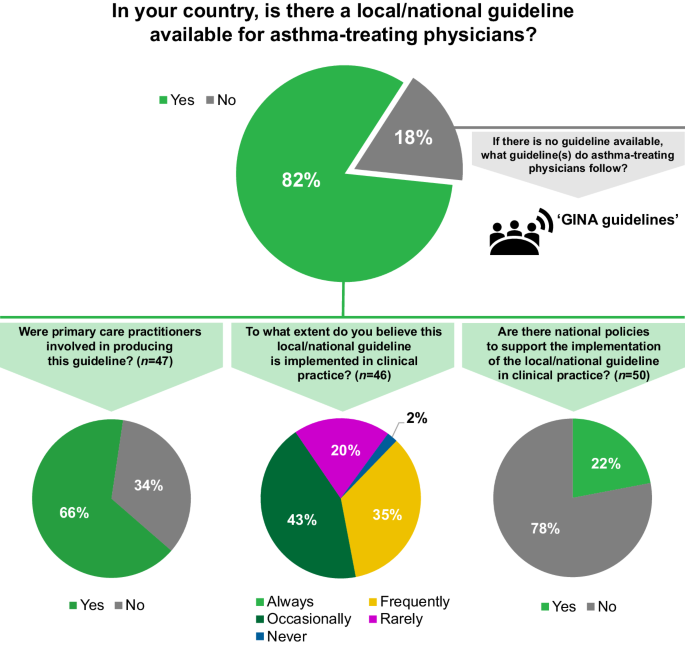
N =57 respondents from 33 countries, unless otherwise stated. The responses include representation from low- (1/33), lower-middle- (7/33), upper-middle- (12/33) and high- (13/33) income countries, according to the World Bank classification 17 . GINA Global Initiative for Asthma.
Key elements of right care were reported missing in many of the countries (Fig. 3 ). Only approximately a third of respondents noted that asthma inhaler technique training is given always or frequently in their country when a device is prescribed.
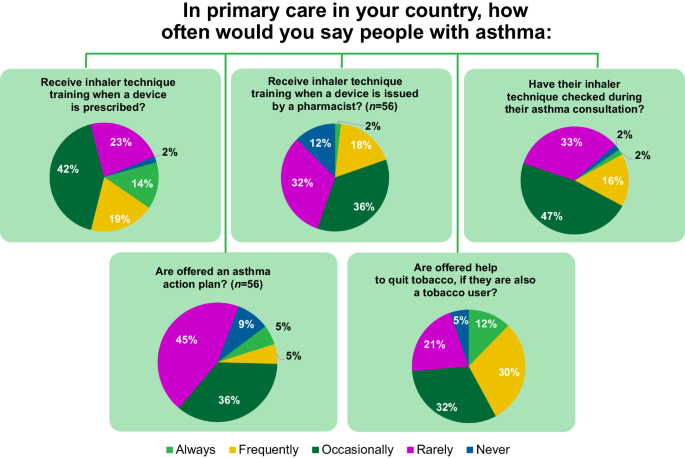
N =57 respondents from 33 countries, unless otherwise stated. The responses include representation from low- (1/33), lower-middle- (7/33), upper-middle- (12/33) and high- (13/33) income countries, according to the World Bank classification 17 .
Identifying the key barriers to the delivery of right care
Given time constraints, the meeting mainly focused on asthma management, but diagnostic challenges were also acknowledged as significant. During small-group discussions, delegates considered the drivers and barriers for implementation of right care in their countries. These can be characterised as lack of: (1) education and awareness; (2) capacity and investment in publicly funded healthcare; (3) access to and affordability of medicines; and (4) optimised systems.
There was a strong consensus that improved context-specific asthma education is essential. Some primary care physicians do not consider asthma an important condition that warrants their time to learn about or manage. There is a lack of incentive and of confidence to diagnose asthma in some regions and, in general, confidence and capability in asthma management is too variable to ensure right care for all patients. Family physicians, nurses, pharmacists and patients need to receive better education to recognise when asthma is poorly controlled, to understand the need to treat the underlying inflammation and the risks of over-reliance on SABA monotherapy. Overcoming a lack of disease awareness through education is particularly important in countries where the term ‘asthma’ is not used owing to cultural stigma; alternative incorrect terms such as ‘allergic bronchitis’ contribute to misunderstanding and incorrect treatment. Moreover, appropriate education could facilitate the involvement of people with asthma in their treatment decisions. There is an additional wider need to educate the public and those with the power to influence the public (e.g. journalists, who frequently use wrong inhaler images—for a selection of appropriate images visit: https://www.ipcrg.org/gallery ). Educational interventions should be tailored to different levels of asthma awareness and literacy, and the messages should be framed appropriately; for example, emphasis on patient safety is a key element in clinician education, discussions with health administrators and managers, or when speaking with patient organisations. Teachers with the capability to teach primary care and with the knowledge about right care are needed to lead the improvement.
The lack of capacity, resources and time remain universal issues in primary care. Family physicians and nurses often manage many different health conditions, so chronic respiratory diseases are not always a priority. An insufficient number of skilled professionals (i.e. physicians, nurses, pharmacists) able to diagnose asthma is a major barrier in most countries. This can also lead to pulmonologists feeling overburdened.
Ideally, investment in publicly funded healthcare should be a focus to ensure equal access to diagnostic skills, tools and treatments across sectors. Economic constraints and affordability of asthma treatments are major barriers; many countries lack reimbursement schemes and/or apply prescription charges for treatments. The goal should be for universal health coverage to include evidence-based treatment options for asthma.
Continuity of care is key for successful management of asthma. Where primary care is empowered to deliver asthma care, electronic patient records and systems to invite patients at highest risk for follow-up appointments are essential but are not always available. Effective referral systems and compatible electronic patient records are also vital to achieving optimal patient-centred communication between primary, secondary and tertiary care. Depending on the region, access to secondary care may be restricted or permission from respiratory specialists to initiate or change treatment in primary care may be required, which can delay care and compromise safety. Since SABA is available over the counter or can easily be bought online without a prescription in many countries, patients may bypass medical care and self-manage. Optimising systems could facilitate the implementation of guidelines in clinical practice and ensure the delivery of right care.
Tools to improve asthma care
Social movements mobilise followers by prompting conversations that raise awareness of the problem and seek solutions 8 . In small groups divided by region and language and facilitated by IPCRG, the delegates reviewed three Asthma Right Care tools that the IPCRG has developed to facilitate these conversations (Fig. 4 ). All three tools can be used in clinical practice and also clinical education settings to start conversations that begin to shift perceptions about either a problem or the potential solutions 9 .
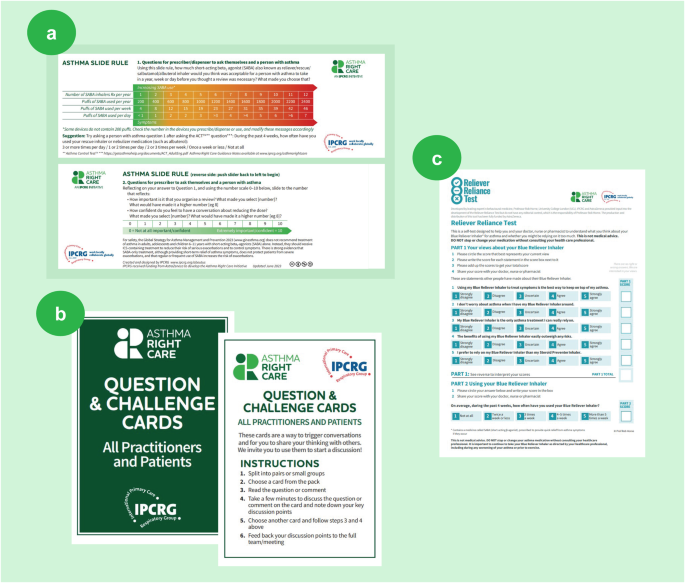
a Asthma SABA slide rule; b ‘Question and challenge’ cards; c Reliever Reliance Test. IPCRG. Asthma Right Care Key Resources. Available at: https://www.ipcrg.org/asthmarightcare/asthma-right-care-key-resources (Accessed February 2024). IPCRG International Primary Care Respiratory Group, SABA short-acting β 2 -receptor agonist.
(a) Asthma SABA slide rule : invites the user to explore how many puffs (as opposed to doses) of SABA inhaler are being used compared with the international guideline advice. Inspired by the Readiness Ruler, on the reverse are a visual analogue scale and Motivational Interviewing questions exploring the importance of requesting a review and confidence to have conversations with healthcare professionals 3 .
(b) ‘Question and challenge’ cards : useful cards for icebreakers, discussion fora and social media, inspired by the ‘Whose Shoes’ game 3 ( http://nutshellcomms.co.uk/ ).
(c) Reliever Reliance Test : a self-administered test based on the Beliefs About Medicines Questionnaire 10 and SABA Reliance Questionnaire, co-developed with behavioural scientists, which aims to identify patients at risk of over-reliance on SABA medication and elicit their beliefs 11 .
Since 2017, IPCRG Asthma Right Care country programmes have tested these tools in multiple settings, adapting them in context. More recently, additional tools have also been co-developed and can be shared to help drive change 12 .
Initiatives to improve asthma care
In addition to reviewing the tools, summit delegates considered the feasibility of adapting several success stories in their countries.
Three-step AIR Treatment Guideline in New Zealand 13
In 2020, New Zealand national asthma guidelines, which had strong primary care involvement, recommended AIR therapy as the preferred management approach (Fig. 5 ). The guidelines were launched with a structured communication plan for wide distribution and encouragement for implementation in practice. A recently published evaluation of the impact of these guidelines identified a significant increase in the dispensing of ICS–formoterol and a reduction in the dispensing of SABA inhalers since the release of the recommendations 14 . This evidence suggests that widespread transition to AIR therapy regimens as recommended by GINA could be achieved if recommended in national asthma guidelines, jointly developed and endorsed as the preferred therapeutic approach by primary and secondary care, and supported by optimised systems for access to medicines and appropriate clinician reimbursement. It is also important to consider the patients’ preference as it will likely impact their adherence to the medication.
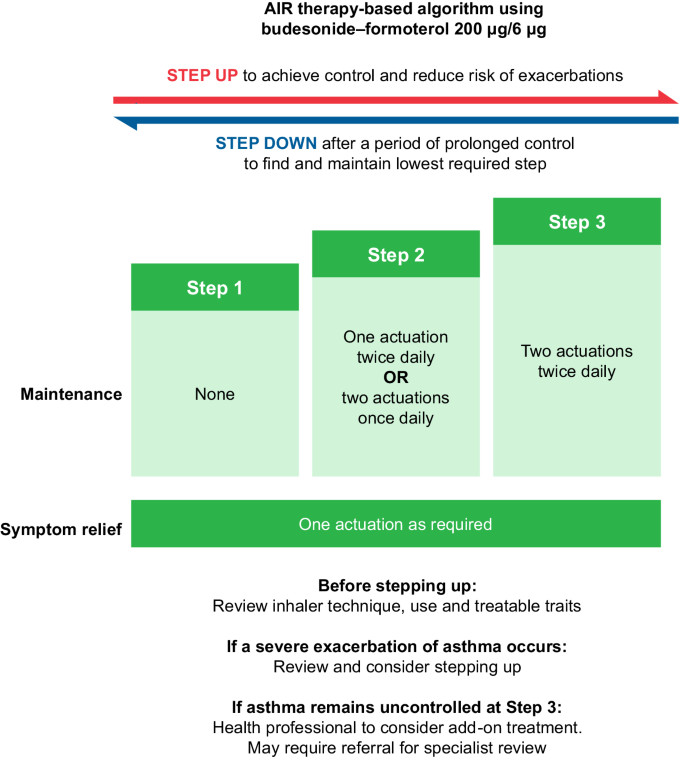
Reproduced with permission from: Asthma and Respiratory Foundation NZ, New Zealand Adolescent and Adult Asthma Guidelines 2020 13 . AIR anti-inflammatory reliever.
Taking advantage of teachable moments in Spain
In Spain, community pharmacist capability and confidence have been improved through a Teach the Teacher ® 15 programme led by IPCRG-taught pharmacists and family physician teachers. This recognises the opportunity for community pharmacists when a SABA inhaler is requested over the counter to take advantage of the teachable moment that it might offer. Strong relationships among patients, family physicians and community pharmacists have been developed to change the asthma pathway, moving away from providing SABA canisters on demand over the counter in pharmacies to using Asthma Right Care tools with individuals, offering advice about right care and prompting those with poorly controlled asthma to visit their family physician for review 16 . This approach resulted in 500,000 fewer SABA canisters sold in 2020 compared with 2018.
Patient and public engagement in Portugal
In Portugal, creative bottom-up approaches to patient and public engagement have been used. To date, more than 50 organised walks and talks (‘Caminhasma’, meaning ‘walk with asthma’) planned by primary care physicians, nurses and community pharmacists involving almost 4000 people within their communities, have taken place to improve asthma literacy and awareness. Subsequently, the initiative has been replicated in Brazil. Also, the Asthma Right Care (known as ‘CAPA’) team has co-created a teaching film and delivered a series of television interviews for a health channel, as well as clinical webinars. A new campaign aimed at adolescents with a video promoting a game between the viewers to teach about asthma is being developed in partnership with the Ministry of Education of Portugal.
Draft national asthma law in Argentina
In Argentina, respiratory-interested clinicians have advocated to the national senate for an asthma law to allow equal access to care for every person with asthma. They have separately worked with colleagues in other specialities to raise awareness about specific at-risk groups such as pregnant women who, according to an unpublished national survey, often stop taking their asthma prescription during pregnancy.
Asthma lexicon in Tunisia
In Tunisia, a multidisciplinary Asthma Right Care steering group prioritised a SABA overuse awareness programme in community pharmacies supported by the Pharmacists Union and the Private Physicians Union. The programme was presented to the Minister of Health who encouraged the initiative. IPCRG’s tools, such as the Reliever Reliance Test and Asthma Slide Rule, were translated to Tunisian dialect to support the nationwide programme. The group also developed a lexicon of Tunisian dialect’s usual asthma and allergy words with their translation in French and English. This lexicon ensures that the terminology used in communication becomes more consistent across the healthcare system.
Many other success stories are emerging, demonstrating the value of bottom-up approaches that engage primary care and patients in highlighting the problem of episodic care and then taking responsibility to address it through education and advocacy for system change.
Nine statements to improve respiratory care
The delegates were shown and supported nine key actions to improve respiratory care that IPCRG and the World Organization of Family Doctors (WONCA) Europe agreed at the 2023 WONCA Council meeting (see Fig. 6 ).
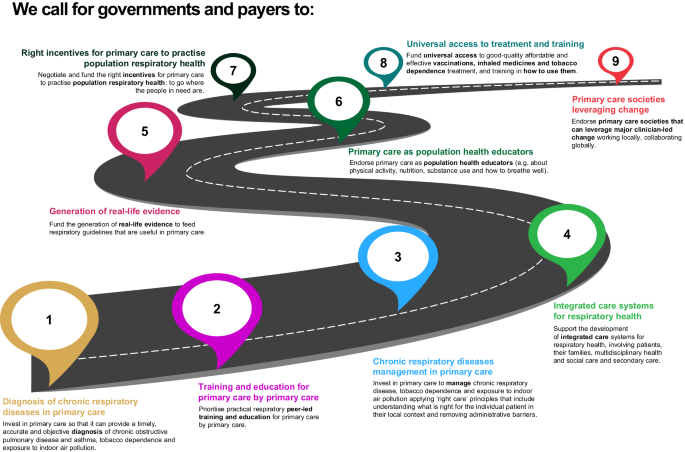
IPCRG International Primary Care Respiratory Group, WONCA World Organization of Family Doctors.
Conclusions
Currently, no universal approach exists to tackle the obstacles to right care in asthma, but the Asthma Right Care movement has demonstrated that change is possible with leadership, teamwork, community involvement and commitment. There are a number of tools available that can be used and adapted considering local contexts. To achieve large-scale improvements, context-specific strategies that engage as many parts of the healthcare system in as many geographic areas as possible, are needed; the aim is for improved awareness and behaviour change. At the end of the summit, it was agreed that to generate and sustain change every country needs ‘Asthma Right Care champions’ passionate about engaging all stakeholders using Asthma Right Care tools. The IPCRG commits to building these champions’ capacity to advocate for and lead change, and to teach their peers through IPCRG Teach the Teacher © cascade models 15 .
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
All data supporting the findings presented in this manuscript are available within the paper and its Supplementary Information.
World Health Organization. Asthma. WHO newsroom. Fact sheets. https://www.who.int/news-room/fact-sheets/detail/asthma (2023).
Global Asthma Network. Global Asthma Report 2022. http://globalasthmanetwork.org/Global_Asthma_Report_2022.pdf (2022).
Williams, S. Asthma Right Care: what will you commit to? J. Gen. Pract. Nurs. 7 , 12 (2021).
Google Scholar
Williams, S. et al. Respiratory research funding is inadequate, inequitable, and a missed opportunity. Lancet Respir. Med. 8 , e67 (2020).
Article CAS PubMed PubMed Central Google Scholar
GINA. Global strategy for asthma management and prevention; updated 2023. https://www.ginasthma.org (2023).
Saini, V. Right Care Series: The Lancet. https://www.thelancet.com/series/right-care (2017).
Tsiligianni, I., Christodoulakis, A. & Williams, S. Improving primary healthcare education through lessons from a flock of birds. NPJ Prim. Care Respir. Med. 33 , 22 (2023).
Article Google Scholar
Nesta. We change the world report. https://media.nesta.org.uk/documents/we_change_the_world_report.pdf (2023).
Boghossian, P. & Lindsay, J. How to have impossible conversations: a very practical guide. First. Life long; 2019. Conversational leadership. https://conversational-leadership.net/ (2019).
Horne, R., Weinman, J. & Hankins, M. The Beliefs about Medicines Questionnaire: the development and evaluation of a new method for assessing the cognitive representation of medication. Psychol. Health 14 , 1 (1999).
Chan, A. H. Y. et al. SABA Reliance Questionnaire (SRQ): identifying patient beliefs underpinning reliever overreliance in asthma. J. Allergy Clin. Immunol. Pract. 8 , 3482.e1–3489.e1 (2020).
The International Primary Care Respiratory Group. Asthma Right Care key resources. https://www.ipcrg.org/asthmarightcare/asthma-right-care-key-resources (2023).
Beasley, R. et al. Asthma and Respiratory Foundation NZ Adolescent and Adult Asthma Guidelines 2020: a quick reference guide. NZ Med. J. 133 , 73 (2020).
Hatter, L. et al. Patterns of asthma medication use in New Zealand after publication of National Asthma Guidelines. J. Allergy Clin. Immunol. Pract. 11 , 2757.e5–2764.e5 (2023).
The International Primary Care Respiratory Group. Teach the teacher. https://www.ipcrg.org/projects/education/teach-the-teacher (2023).
Grupo de Respiratorio en Atención primaria (GRAP), Sociedad Española de Farmacia Clinica, Familiar y Comunitaria (SEFAC), International Primary Care Respiratory Group (IPCRG) & Local Spanish Colleges of Pharmacists. How Spanish pharmacists have improved their role in asthma management from supplying SABA without restriction to prescription-only dispensing. https://www.ipcrg.org/resources/search-resources/how-spanish-pharmacists-have-improved-their-role-in-asthma-management (2021).
World Bank. World Bank country and lending groups. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (2024).
Download references
Acknowledgements
The authors acknowledge 3 Stories High, UK, for medical writing support, which was funded by AstraZeneca. IPCRG received funding from AstraZeneca to develop the Asthma Right Care initiative. IPCRG would like to thank all the IPCRG member countries who participated in the survey. For further information on the survey and participants, please see Supplementary Information.
Author information
Authors and affiliations.
International Primary Care Respiratory Group, London, UK
Siân Williams, Jaime Correia de Sousa, Ee Ming Khoo, Vincent Mak & Darush Attar-Zadeh
Life and Health Sciences Research Institute (ICVS), School of Medicine, University of Minho, Braga, Portugal
Jaime Correia de Sousa
Department of Primary Care Medicine, Faculty of Medicine, Universiti Malaya, Kuala Lumpur, Malaysia
Ee Ming Khoo
Pulmonologist, Lac II, Tunis, Tunisia
Habib Ghedira
International Primary Care Respiratory Group, Tunis, Tunisia
Imperial College Healthcare National Health Service Trust, London, UK
Vincent Mak
Zorroza Primary Care Unit, Bilbao, Spain
Mar Martínez Vázquez
International Primary Care Respiratory Group, Bilbao, Spain
Araceti Family Health Unit, Coimbra, Portugal
Cláudia Vicente
International Primary Care Respiratory Group, Coimbra, Portugal
National Health Service North West London Integrated Care Board, London, UK
Darush Attar-Zadeh
You can also search for this author in PubMed Google Scholar
Contributions
S.W. was responsible for conceptualisation, methodology, supervision, validation and writing of the original draft. S.W. and E.M.K. drafted the questionnaire. S.W., J.C.S., E.M.K., H.G., V.M., M.M.V., C.V. and D.A.-Z. contributed equally to the design of the workshop, writing and reviewing of the final manuscript.
Corresponding author
Correspondence to Siân Williams .
Ethics declarations
Competing interests.
S.W. is the CEO of IPCRG. IPCRG reports educational grants from GSK, AstraZeneca, Boehringer Ingelheim and membership subscription from Vitalograph, as well as current research grants from RESPIRE and UK Research and Innovation (FRESHAIR4Life). J.C.d.S. reports grant funding to his institution from AstraZeneca and GSK, and advisory board and consulting fees paid to him from Boehringer Ingelheim, GSK, AstraZeneca, Bial and Medinfar. He also received payment for lectures from GSK, AstraZeneca and Sanofi Pasteur; support for attending meetings from Mundipharma and Mylan; and has a leadership role at IPCRG. E.M.K. reports grants from the National Institute for Health and Care Research Global Health Research Unit on Respiratory Health (RESPIRE); personal fees from AstraZeneca; and is the President of the IPCRG and the Primary Care Respiratory Group Malaysia. H.G. reports advisory board and lecture honoraria from AstraZeneca, Sanofi, Boehringer Ingelheim and travel bursary from Recordati. V.M. reports lecture/advisory board honoraria and travel bursaries from Chiesi and AstraZeneca. M.M.V. reports advisory board honoraria, lecture honoraria and travel bursary from AstraZeneca, Gebro and Menarini. C.V. is the GRESP coordinator in Portugal, the secretary in group 01.03 of ERS and has a leadership role at IPCRG. C.V. reports advisory board honoraria and lecture honoraria from AstraZeneca, GSK, Pfizer, Viatris and Medinfar. D.A.-Z. reports advisory board honoraria/lecture honoraria/travel bursary from AstraZeneca, Boehringer Ingelheim, Chiesi, Clement Clarke International, GSK, Janssen-Cilag, Orion, Pfizer and Trudell Medical.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information, reporting summary, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Williams, S., Correia de Sousa, J., Khoo, E.M. et al. How to make Asthma Right Care ‘easy’ in primary care: learnings from the 2023 Asthma Right Care Summit. npj Prim. Care Respir. Med. 34 , 4 (2024). https://doi.org/10.1038/s41533-024-00366-x
Download citation
Received : 18 December 2023
Accepted : 10 April 2024
Published : 26 April 2024
DOI : https://doi.org/10.1038/s41533-024-00366-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Open access
- Published: 15 August 2020
Treatment strategies for asthma: reshaping the concept of asthma management
- Alberto Papi 1 , 7 ,
- Francesco Blasi 2 , 3 ,
- Giorgio Walter Canonica 4 ,
- Luca Morandi 1 , 7 ,
- Luca Richeldi 5 &
- Andrea Rossi 6
Allergy, Asthma & Clinical Immunology volume 16 , Article number: 75 ( 2020 ) Cite this article
46k Accesses
54 Citations
4 Altmetric
Metrics details
Asthma is a common chronic disease characterized by episodic or persistent respiratory symptoms and airflow limitation. Asthma treatment is based on a stepwise and control-based approach that involves an iterative cycle of assessment, adjustment of the treatment and review of the response aimed to minimize symptom burden and risk of exacerbations. Anti-inflammatory treatment is the mainstay of asthma management. In this review we will discuss the rationale and barriers to the treatment of asthma that may result in poor outcomes. The benefits of currently available treatments and the possible strategies to overcome the barriers that limit the achievement of asthma control in real-life conditions and how these led to the GINA 2019 guidelines for asthma treatment and prevention will also be discussed.
Asthma, a major global health problem affecting as many as 235 million people worldwide [ 1 ], is a common, non-communicable, and variable chronic disease that can result in episodic or persistent respiratory symptoms (e.g. shortness of breath, wheezing, chest tightness, cough) and airflow limitation, the latter being due to bronchoconstriction, airway wall thickening, and increased mucus.
The pathophysiology of the disease is complex and heterogeneous, involving various host-environment interactions occurring at various scales, from genes to organ [ 2 ].
Asthma is a chronic disease requiring ongoing and comprehensive treatment aimed to reduce the symptom burden (i.e. good symptom control while maintaining normal activity levels), and minimize the risk of adverse events such as exacerbations, fixed airflow limitation and treatment side effects [ 3 , 4 ].
Asthma treatment is based on a stepwise approach. The management of the patient is control-based; that is, it involves an iterative cycle of assessment (e.g. symptoms, risk factors, etc.), adjustment of treatment (i.e. pharmacological, non-pharmacological and treatment of modifiable risk factors) and review of the response (e.g. symptoms, side effects, exacerbations, etc.). Patients’ preferences should be taken into account and effective asthma management should be the result of a partnership between the health care provider and the person with asthma, particularly when considering that patients and clinicians might aim for different goals [ 4 ].
This review will discuss the rationale and barriers to the treatment of asthma, that may result in poor patient outcomes. The benefits of currently available treatments and the possible strategies to overcome the barriers that limit the achievement of asthma control in real-life situations will also be discussed.
The treatment of asthma: where are we? Evolution of a concept
Asthma control medications reduce airway inflammation and help to prevent asthma symptoms; among these, inhaled corticosteroids (ICS) are the mainstay in the treatment of asthma, whereas quick-relief (reliever) or rescue medicines quickly ease symptoms that may arise acutely. Among these, short-acting beta-agonists (SABAs) rapidly reduce airway bronchoconstriction (causing relaxation of airway smooth muscles).
National and international guidelines have recommended SABAs as first-line treatment for patients with mild asthma, since the Global Initiative for Asthma guidelines (GINA) were first published in 1995, adopting an approach aimed to control the symptoms rather than the underlying condition; a SABA has been the recommended rescue medication for rapid symptom relief. This approach stems from the dated idea that asthma symptoms are related to bronchial smooth muscle contraction (bronchoconstriction) rather than a condition concomitantly caused by airway inflammation. In 2019, the GINA guidelines review (GINA 2019) [ 4 ] introduced substantial changes overcoming some of the limitations and “weaknesses” of the previously proposed stepwise approach to adjusting asthma treatment for individual patients. The concept of an anti-inflammatory reliever has been adopted at all degrees of severity as a crucial component in the management of the disease, increasing the efficacy of the treatment while lowering SABA risks associated with patients’ tendency to rely or over-rely on the as-needed medication.
Until 2017, the GINA strategy proposed a pharmacological approach based on a controller treatment (an anti-inflammatory, the pillar of asthma treatment), with a SABA as an additional rescue intervention. The reliever, a short-acting bronc hodilator, was merely an addendum , a medication to be used in case the real treatment (the controller) failed to maintain disease control: SABAs effectively induce rapid symptom relief but are ineffective on the underlying inflammatory process. Based on the requirement to achieve control, the intensity of the controller treatment was related to the severity of the disease, varying from low-dose ICS to combination low-dose ICS/long-acting beta-agonist (LABA), medium-dose ICS/LABA, up to high-dose ICS/LABA, as preferred controller choice, with a SABA as the rescue medication. As a result, milder patients were left without any anti-inflammatory treatment and could only rely on SABA rescue treatment.
Poor adherence to therapy is a major limitation of a treatment strategy based on the early introduction of the regular use of controller therapy [ 5 ]. Indeed, a number of surveys have highlighted a common pattern in the use of inhaled medication [ 6 ], in which treatment is administered only when asthma symptoms occur; in the absence of symptoms, treatment is avoided as patients perceive it as unnecessary. When symptoms worsen, patients prefer to use reliever therapies, which may result in the overuse of SABAs [ 7 ]. Indirect evidence suggests that the overuse of beta-agonists alone is associated with increased risk of death from asthma [ 8 ].
In patients with mild persistent disease, low-dose ICS decreases the risk of severe exacerbations leading to hospitalization and improves asthma control [ 9 ]. When low-dose ICS are ineffective in controlling the disease (Step 3 of the stepwise approach), a combination of low-dose ICS with LABA maintenance was the recommended first-choice treatment, plus as-needed SABA [ 3 , 10 ]. Alternatively, the combination low-dose ICS/LABA (formoterol) was to be used as single maintenance and reliever treatment (SMART). The SMART strategy containing the rapid-acting formoterol was recommended throughout GINA Steps 3 to 5 based on solid clinical-data evidence [ 3 ].
The addition of a LABA to ICS treatment reduces both severe and mild asthma exacerbation rates, as shown in the one-year, randomized, double-blind, parallel-group FACET study [ 11 ]. This study focused on patients with persistent asthma symptoms despite receiving ICS and investigated the efficacy of the addition of formoterol to two dose levels of budesonide (100 and 400 µg bid ) in decreasing the incidence of both severe and mild asthma exacerbations. Adding formoterol decreased the incidence of both severe and mild asthma exacerbations, independent of ICS dose. Severe and mild exacerbation rates were reduced by 26% and 40%, respectively, with the addition of formoterol to the lower dose of budesonide; the corresponding reductions were 63% and 62%, respectively, when formoterol was added to budesonide at the higher dose.
The efficacy of the ICS/LABA combination was confirmed in the post hoc analysis of the FACET study, in which patients were exposed to a combination of formoterol and low-dose budesonide [ 12 ]. However, such high levels of asthma control are not achieved in real life [ 5 ]. An explanation for this is that asthma is a variable condition and this variability might include the exposure of patients to factors which may cause a transient steroid insensitivity in the inflammatory process. This, in turn, may lead to an uncontrolled inflammatory response and to exacerbations, despite optimal controller treatment. A typical example of this mechanism is given by viral infections, the most frequent triggers of asthma exacerbations. Rhinoviruses, the most common viruses found in patients with asthma exacerbations, interfere with the mechanism of action of corticosteroids making the anti-inflammatory treatment transiently ineffective. A transient increase in the anti-inflammatory dose would overcome the trigger-induced anti-inflammatory resistance, avoiding uncontrolled inflammation leading to an exacerbation episode [ 13 , 14 , 15 ].
Indeed, symptoms are associated with worsening inflammation and not only with bronchoconstriction. Romagnoli et al. showed that inflammation, as evidenced by sputum eosinophilia and eosinophilic markers, is associated with symptomatic asthma [ 16 ]. A transient escalation of the ICS dose would prevent loss of control over inflammation and decrease the risk of progression toward an acute episode. In real life, when experiencing a deterioration of asthma control, patients self-treat by substantially increasing their SABA medication (Fig. 1 ); it is only subsequently that they (modestly) increase the maintenance treatment [ 17 ].
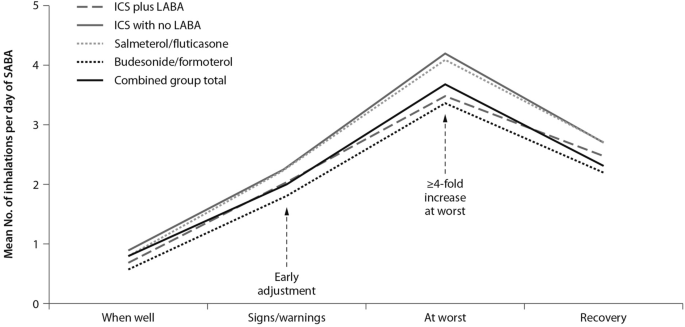
Mean use of SABA at different stages of asthma worsening. Patients have been grouped according to maintenance therapy shown in the legend. From [ 17 ], modified
As bronchodilators, SABAs do not control the underlying inflammation associated with increased symptoms. The “as required” use of SABAs is not the most effective therapeutic option in controlling a worsening of inflammation, as signaled by the occurrence of symptoms; instead, an anti-inflammatory therapy included in the rescue medication along with a rapid-acting bronchodilator could provide both rapid symptom relief and control over the underlying inflammation. Thus, there is a need for a paradigm shift, a new therapeutic approach based on the rescue use of an inhaled rapid-acting beta-agonist combined with an ICS: an anti-inflammatory reliever strategy [ 18 ].
The symptoms of an exacerbation episode, as reported by Tattersfield and colleagues in their extension of the FACET study, increase gradually before the peak of the exacerbation (Fig. 2 ); and the best marker of worsening asthma is the increased use of rescue beta-agonist treatment that follows exactly the pattern of worsening symptomatology [ 19 ]. When an ICS is administered with the rescue bronchodilator, the patient would receive anti-inflammatory therapy when it is required; that is, when the inflammation is uncontrolled, thus increasing the efficiency of the anti-inflammatory treatment.
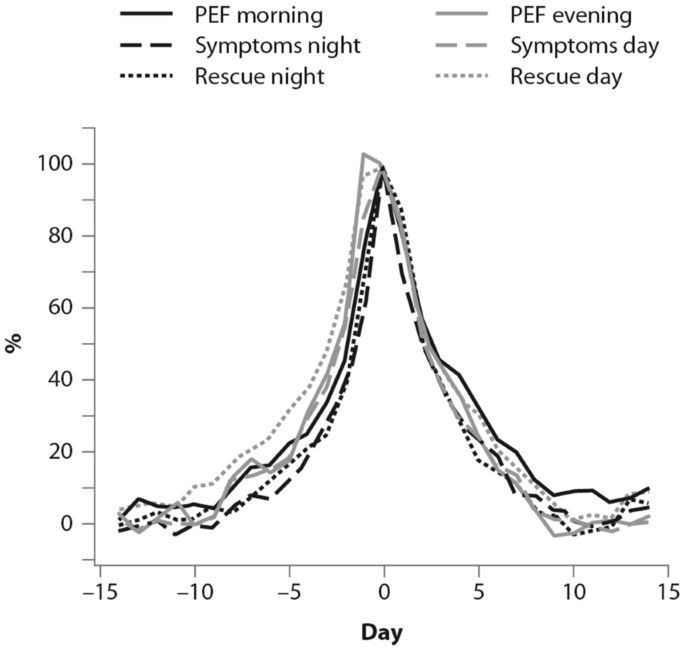
(From [ 19 ])
Percent variation in symptoms, rescue beta-agonist use and peak expiratory flow (PEF) during an exacerbation. In order to allow comparison over time, data have been standardized (Day-14 = 0%; maximum change = 100%)
Barriers and paradoxes of asthma management
A number of barriers and controversies in the pharmacological treatment of asthma have prevented the achievement of effective disease management [ 20 ]. O’Byrne and colleagues described several such controversies in a commentary published in 2017, including: (1) the recommendation in Step 1 of earlier guidelines for SABA bronchodilator use alone, despite asthma being a chronic inflammatory condition; and (2) the autonomy given to patients over perception of need and disease control at Step 1, as opposed to the recommendation of a fixed-dose approach with treatment-step increase, regardless of the level of symptoms [ 20 ]. Other controversies outlined were: (3) a difficulty for patients in understanding the recommendation to minimize SABA use at Step 2 and switch to a fixed-dose ICS regimen, when they perceive SABA use as more effective; (4) apparent conflicting safety messages within the guidelines that patient-administered SABA monotherapy is safe, but patient-administered LABA monotherapy is not; and (5) a discrepancy as to patients’ understanding of “controlled asthma” and their symptom frequency, impact and severity [ 20 ].
Controversies (1) and (2) can both establish an early over-dependence on SABAs. Indeed, asthma patients freely use (and possibly overuse) SABAs as rescue medication. UK registry data have recently suggested SABA overuse or overreliance may be linked to asthma-related deaths: among 165 patients on short-acting relievers at the time of death, 56%, 39%, and 4% had been prescribed > 6, > 12, and > 50 SABA inhalers respectively in the previous year [ 21 ]. Registry studies have shown the number of SABA canisters used per year to be directly related to the risk of death in patients with asthma. Conversely, the number of ICS canisters used per year is inversely related to the rate of death from asthma, when compared with non-users of ICS [ 8 , 22 ]. Furthermore, low-dose ICS used regularly are associated with a decreased risk of asthma death, with discontinuation of these agents possibly detrimental [ 22 ].
Other barriers to asthma pharmacotherapy have included the suggestion that prolonged treatment with LABAs may mask airway inflammation or promote tolerance to their effects. Investigating this, Pauwels and colleagues found that in patients with asthma symptoms that were persistent despite taking inhaled glucocorticoids, the addition of regular treatment with formoterol to budesonide for a 12-month period did not decrease asthma control, and improved asthma symptoms and lung function [ 11 ].
Treatment strategies across all levels of asthma severity
Focusing on risk reduction, the 2014 update of the GINA guidelines recommended as-needed SABA for Step 1 of the stepwise treatment approach, with low-dose ICS maintenance therapy as an alternative approach for long-term anti-inflammatory treatment [ 23 ]. Such a strategy was only supported by the evidence from a post hoc efficacy analysis of the START study in patients with recently diagnosed mild asthma [ 24 ]. The authors showed that low-dose budesonide reduced the decline of lung-function over 3 years and consistently reduced severe exacerbations, regardless of symptom frequency at baseline, even in subjects with symptoms below the then-threshold of eligibility for ICS [ 24 ]. However, as for all post hoc analyses, the study by Reddel and colleagues does not provide conclusive evidence and, even so, their results could have questionable clinical significance for the management of patients with early mild asthma. To be effective, this approach would require patients to be compliant to regular twice-daily ICS for 10 years to have the number of exacerbations reduce by one. In real life, it is highly unlikely that patients with mild asthma would adhere to such a regular regimen [ 25 ].
The 2016 update to the GINA guidelines lowered the threshold for the use of low-dose ICS (GINA Step 2) to two episodes of asthma symptoms per month (in the absence of any supportive evidence for the previous cut-off). The objective was to effectively increase the asthma population eligible to receive regular ICS treatment and reduce the population treated with a SABA only, given the lack of robust evidence of the latter’s efficacy and safety and the fact that asthma is a variable condition characterized by acute exacerbations [ 26 ]. Similarly, UK authorities recommended low-dose ICS treatment in mild asthma, even for patients with suspected asthma, rather than treatment with a SABA alone [ 10 ]. However, these patients are unlikely to have good adherence to the regular use of an ICS. It is well known that poor adherence to treatment is a major problem in asthma management, even for patients with severe asthma. In their prospective study of 2004, Krishnan and colleagues evaluated the adherence to ICS and oral corticosteroids (OCS) in a cohort of patients hospitalized for asthma exacerbations [ 27 ]. The trend in the data showed that adherence to ICS and OCS treatment in patients dropped rapidly to reach nearly 50% within 7 days of hospital discharge, with the rate of OCS discontinuation per day nearly double the rate of ICS discontinuation per day (− 5.2% vs. − 2.7%; p < 0.0001 respectively, Fig. 3 ), thus showing that even after a severe event, patients’ adherence to treatment is suboptimal [ 27 ].

(From [ 27 ])
Use of inhaled (ICS) and oral (OCS) corticosteroids in patients after hospital discharge among high-risk adult patients with asthma. The corticosteroid use was monitored electronically. Error bars represent the standard errors of the measured ICS and OCS use
Guidelines set criteria with the aim of achieving optimal control of asthma; however, the attitude of patients towards asthma management is suboptimal. Partridge and colleagues were the first in 2006 to evaluate the level of asthma control and the attitude of patients towards asthma management. Patients self-managed their condition using their medication as and when they felt the need, and adjusted their treatment by increasing their intake of SABA, aiming for an immediate relief from symptoms [ 17 ]. The authors concluded that the adoption of a patient-centered approach in asthma management could be advantageous to improve asthma control.
The concomitant administration of an as-needed bronchodilator and ICS would provide rapid relief while administering anti-inflammatory therapy. This concept is not new: in the maintenance and reliever approach, patients are treated with ICS/formoterol (fast-acting, long-acting bronchodilator) combinations for both maintenance and reliever therapy. An effective example of this therapeutic approach is provided in the SMILE study in which symptomatic patients with moderate to severe asthma and treated with budesonide/formoterol as maintenance therapy were exposed to three different as-needed options: SABA (terbutaline), rapid-onset LABA (formoterol) and a combination of LABA and ICS (budesonide/formoterol) [ 28 ]. When compared with formoterol, budesonide/formoterol as reliever therapy significantly reduced the risk of severe exacerbations, indicating the efficacy of ICS as rescue medication and the importance of the as-needed use of the anti-inflammatory reliever.
The combination of an ICS and a LABA (budesonide/formoterol) in one inhaler for both maintenance and reliever therapy is even more effective than higher doses of maintenance ICS and LABA, as evidenced by Kuna and colleagues and Bousquet and colleagues (Fig. 4 ) [ 29 , 30 ].
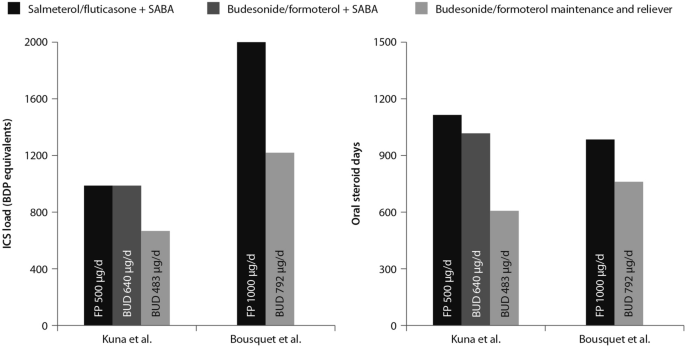
(Data from [ 29 , 30 ])
Comparison between the improvements in daily asthma control resulting from the use of budesonide/formoterol maintenance and reliever therapy vs. higher dose of ICS/LABA + SABAZ and steroid load for the two regimens
The effects of single maintenance and reliever therapy versus ICS with or without LABA (controller therapy) and SABA (reliever therapy) have been recently addressed in the meta-analysis by Sobieraj and colleagues, who analysed 16 randomized clinical trials involving patients with persistent asthma [ 31 ]. The systematic review supported the use of single maintenance and reliever therapy, which reduces the risk of exacerbations requiring systemic corticosteroids and/or hospitalization when compared with various strategies using SABA as rescue medication [ 31 ].
This concept was applied to mild asthma by the BEST study group, who were the first to challenge the regular use of ICS. A pilot study by Papi and colleagues evaluated the efficacy of the symptom-driven use of beclomethasone dipropionate plus albuterol in a single inhaler versus maintenance with inhaled beclomethasone and as-needed albuterol. In this six-month, double-blind, double-dummy, randomized, parallel-group trial, 455 patients with mild asthma were randomized to one of four treatment groups: an as-needed combination therapy of placebo bid plus 250 μg of beclomethasone and 100 μg of albuterol in a single inhaler; an as-needed albuterol combination therapy consisting of placebo bid plus 100 μg of albuterol; regular beclomethasone therapy, comprising beclomethasone 250 μg bid and 100 μg albuterol as needed); and regular combination therapy with beclomethasone 250 μg and albuterol 100 μg in a single inhaler bid plus albuterol 100 μg as needed.
The rescue use of beclomethasone/albuterol in a single inhaler was as efficacious as the regular use of inhaled beclomethasone (250 μg bid ) and it was associated with a lower 6-month cumulative dose of the ICS [ 32 ].
The time to first exacerbation differed significantly among groups ( p = 0.003), with the shortest in the as-needed albuterol and placebo group (Fig. 5 ). Figure 5 also shows equivalence between the as-needed combination therapy and the regular beclomethasone therapy. However, these results were not conclusive since the study was not powered to evaluate the effect of the treatment on exacerbations. In conclusion, as suggested by the study findings, mild asthma patients may require the use of an as-needed ICS and an inhaled bronchodilator rather than a regular treatment with ICS [ 32 ].
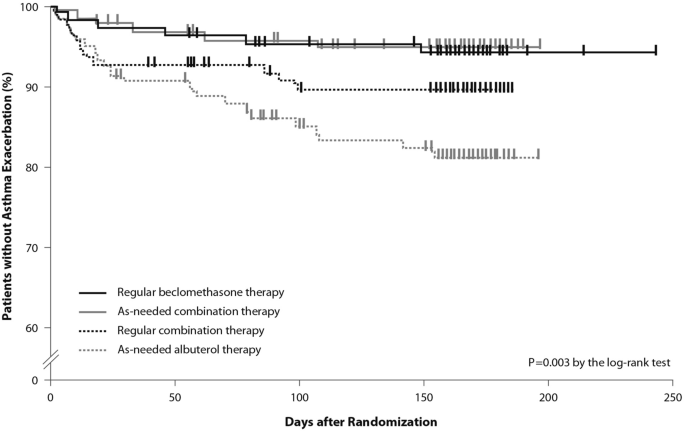
(From [ 32 ])
Kaplan Meier analysis of the time to first exacerbation (modified intention-to-treat population). First asthma exacerbations are shown as thick marks. As-needed albuterol therapy = placebo bid plus 100 μg of albuterol as needed; regular combination therapy = 250 μg of beclomethasone and 100 μg of albuterol in a single inhaler bid plus 100 μg of albuterol as needed; regular beclomethasone therapy = 250 μg of beclomethasone bid and 100 μg of albuterol as needed; as-needed combination therapy = placebo bid plus 250 μg of beclomethasone and 100 μg of albuterol in a single inhaler as needed
Moving forward: a new approach to the management of asthma patients
Nearly a decade after the publication of the BEST study in 2007, the use of this alternative therapeutic strategy was addressed in the SYGMA 1 and SYGMA 2 trials. These double-blind, randomized, parallel-group, 52-week phase III trials evaluated the efficacy of as-needed use of combination formoterol (LABA) and the ICS budesonide as an anti-inflammatory reliever in patients requiring GINA Step 2 treatment, with the current reliever therapy (e.g. as-needed SABA) or with low-dose maintenance ICS (inhaled budesonide bid ) plus as-needed SABA, administered as regular controller therapy [ 33 , 34 ].
The SYGMA 1 trial, which enrolled 3849 patients, aimed to demonstrate the superiority of the as-needed use of the combination budesonide/formoterol over as-needed terbutaline, as measured by the electronically-recorded proportion of weeks with well-controlled asthma [ 34 ]. The more pragmatic SYGMA 2 trial enrolled 4215 patients with the aim to demonstrate that the budesonide/formoterol combination is non-inferior to budesonide plus as-needed terbutaline in reducing the relative rate of annual severe asthma exacerbations [ 33 ]. Both trials met their primary efficacy outcomes. In particular, as-needed budesonide/formoterol was superior to as-needed SABA in controlling asthma symptoms (34.4% versus 31.1%) and preventing exacerbations, achieving a 64% reduction in exacerbations. In both trials, budesonide/formoterol as-needed was similar to budesonide maintenance bid at preventing severe exacerbations, with a substantial reduction of the inhaled steroid load over the study period (83% in the SYGMA 1 trial and 75% in the SYGMA 2 trial). The time to first exacerbation did not differ significantly between the two regimens; however, budesonide/formoterol was superior to SABA in prolonging the time to first severe exacerbation [ 33 , 34 ].
The double-blind, placebo-controlled design of the SYGMA trials does not fully address the advantages of anti-inflammatory reliever strategy in patients who often rely on SABAs for symptom relief, so to what extent the study findings could apply to real-life practice settings was unclear.
These limitations were overcome by the results of the Novel START study, an open-label, randomized, parallel-group, controlled trial designed to reflect real-world practice, which demonstrated the effectiveness in mild asthma of budesonide/formoterol as an anti-inflammatory reliever therapy [ 35 ].
In real-world practice, mild asthma patients are treated with an as-needed SABA reliever or with daily low-dose ICS maintenance therapy plus a SABA reliever. In the Novel START study, 668 patients with mild asthma were randomized to receive either as-needed albuterol 100 µg, two inhalations (SABA reliever as a continuation of the Step 1 treatment according to the 2017 GINA guidelines), budesonide 200 µg (ICS maintenance treatment) plus as-needed albuterol (Step 2 therapy of the GINA 2017 guidelines), or 200 µg/6 µg budesonide/formoterol as anti-inflammatory reliever therapy taken as-needed for a 52-week study period.
In this study, the rate of asthma exacerbations for budesonide/formoterol was lower compared with albuterol (51%) and similar to the twice-daily maintenance budesonide plus albuterol, despite a 52% reduction in the mean steroid dose with the single combination inhaler treatment [ 35 ]. In addition, severe exacerbation rate was lower with budesonide/formoterol as compared with as-needed albuterol and regular twice-daily budesonide. These data support the findings of the SYGMA 1 and 2 trials, highlighting the need for a critical re-examination of current clinical practice. Along with the results of the SYGMA trials, they provide convincing evidence of the advantages of the anti-inflammatory reliever strategy, particularly in real-life settings.
The SYGMA 1, SYGMA 2 and the novel START studies complete the picture of the treatment strategies for asthma at any degree of severity, including mild asthma. A growing body of evidence shows that an anti-inflammatory reliever strategy, when compared with all other strategies with SABA reliever, consistently reduces the rate of exacerbations across all levels of asthma severity (Fig. 6 ) [ 28 , 29 , 34 , 36 , 37 , 38 , 39 ].
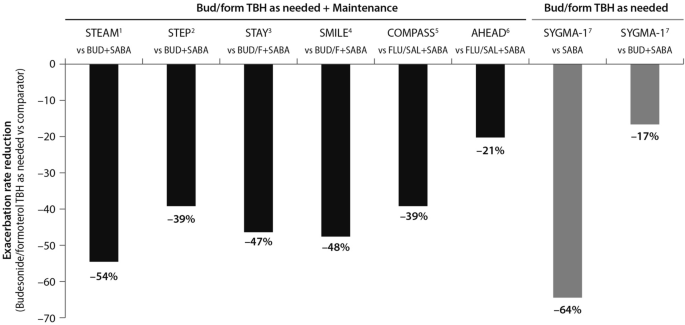
(Data source: [ 39 ])
Risk reduction of severe asthma attack of anti-inflammatory reliever versus SABA across all levels of asthma severity. Bud = budesonide; form = formoterol; TBH = turbohaler. Data from: 1: [ 36 ]; 2: [ 37 ]; 3: [ 38 ]; 4: [ 28 ]; 5: [ 29 ]; 6: [ 30 ]; 7: [ 34 ]
This evidence set the ground (Fig. 7 ) for the release of the 2019 GINA strategy updates. The document provides a consistent approach towards the management of the disease and aims to avoid the overreliance and overuse of SABAs, even in the early course of the disease. The 2019 GINA has introduced key changes in the treatment of mild asthma: for safety reasons, asthmatic adults and adolescents should receive ICS-containing controller treatment instead of the SABA-only treatment, which is no longer recommended.
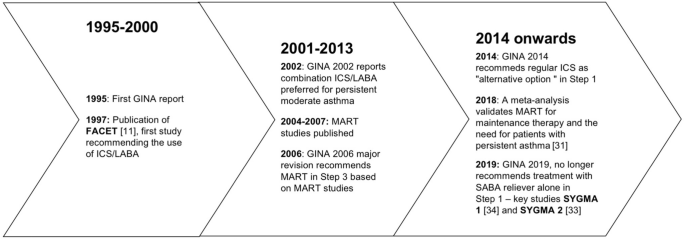
Timeline of key randomized controlled trials and meta-analyses providing the supporting evidence base leading to the Global Initiative for Asthma (GINA) 2019 guidelines. GINA global initiative for asthma, MART maintenance and reliever therapy, SMART single inhaler maintenance and reliever therapy
In Step 1 of the stepwise approach to adjusting asthma treatment, the preferred controller option for patients with fewer than two symptoms/month and no exacerbation risk factors is low-dose ICS/formoterol as needed. This strategy is indirectly supported by the results of the SYGMA 1 study which evaluated the efficacy and safety of budesonide/formoterol as needed, compared with as-needed terbutaline and budesonide bid plus as-needed terbutaline (see above). In patients with mild asthma, the use of an ICS/LABA (budesonide/formoterol) combination as needed provided superior symptom control to as-needed SABA, resulting in a 64% lower rate of exacerbations (p = 0.07) with a lower steroid dose (17% of the budesonide maintenance dose) [ 34 ]. The changes extend to the other controller options as well. In the 2017 GINA guidelines, the preferred treatment was as-needed SABA with the option to consider adding a regular low-dose ICS to the reliever. In order to overcome the poor adherence with the ICS regimen, and with the aim to reduce the risk of severe exacerbations, the 2019 GINA document recommends taking low-dose ICS whenever SABA is taken, with the daily ICS option no longer listed.
Previous studies including the TREXA study in children and adolescents [ 40 ], the BASALT study [ 41 ] and research conducted by the BEST study group [ 32 ] have already added to the evidence that a low-dose ICS with a bronchodilator is an effective strategy for symptom control in patients with mild asthma. A recently published study in African-American children with mild asthma found that the use of as-needed ICS with SABA provides similar asthma control, exacerbation rates and lung function measures at 1 year, compared with daily ICS controller therapy [ 42 ], adding support to TREXA findings that in children with well controlled, mild asthma, ICS used as rescue medication with SABA may be an efficacious step-down strategy [ 40 ].
In Step 2 of the stepwise approach, there are now two preferred controller options: (a) a daily low-dose ICS plus an as-needed SABA; and (b) as-needed low-dose ICS/formoterol. Recommendation (a) is supported by a large body of evidence from randomized controlled trials and observations showing a substantial reduction of exacerbation, hospitalization, and death with regular low-dose ICS [ 7 , 8 , 9 , 24 , 43 ], whereas recommendation (b) stems from evidence on the reduction or non-inferiority for severe exacerbations when as-needed low-dose ICS/formoterol is compared with regular ICS [ 33 , 34 ].
The new GINA document also suggests low-dose ICS is taken whenever SABA is taken, either as separate inhalers or in combination. This recommendation is supported by studies showing reduced exacerbation rates compared with taking a SABA only [ 32 , 40 ], or similar rates compared with regular ICS [ 32 , 40 , 41 ]. Low-dose theophylline, suggested as an alternative controller in the 2017 GINA guidelines, is no longer recommended.
Airway inflammation is present in the majority of patients with asthma, and although patients with mild asthma may have only infrequent symptoms, they face ongoing chronic inflammation of the lower airways and risk acute exacerbations. The GINA 2019 strategy recognizes the importance of reducing the risk of asthma exacerbations, even in patients with mild asthma (Steps 1 and 2) [ 4 ]. In this regard, the new recommendations note that SABA alone for symptomatic treatment is non-protective against severe exacerbation and may actually increase exacerbation risk if used regularly or frequently [ 4 ].
The reluctance by patients to regularly use an ICS controller means they may instead try and manage their asthma symptoms by increasing their SABA reliever use. This can result in SABA overuse and increased prescribing, and increased risk of exacerbations.
As part of the global SABINA (SABA use IN Asthma) observational study programme, a UK study examined primary care records to describe the pattern of SABA and ICS use over a 10-year period in 373,256 patients with mild asthma [ 44 ]. Results showed that year-to-year SABA prescribing was more variable than that of ICS indicating that, in response to fluctuations in asthma symptom control, SABA use was increased in preference to ICS use. Furthermore, more than 33% of patients were prescribed SABA inhalers at a level equivalent to around ≥ 3 puffs per week which, according to GINA, suggests inadequate asthma control.
The problem of SABA overuse is further highlighted by two studies [ 45 , 46 ], also as part of the SABINA programme. These analysed data from 365,324 patients in a Swedish cohort prescribed two medications for obstructive lung disease in any 12-month period (HERA).
The first study identified SABA overuse (defined as ≥ 3 SABA canisters a year) in 30% of patients, irrespective of their ICS use; 21% of patients were collecting 3–5 canisters annually, 7% were collecting 6–10, and 2% more than 11 [ 45 ]. Those patients who were overusing SABA had significantly more asthma exacerbations relative to those using < 3 canisters (20.0 versus 12.5 per 100 patient years; relative risk 1.60, 95% CI 1.57–1.63, p < 0.001). Moreover, patients overusing SABA and whose asthma was more severe (GINA Steps 3 and 4) had greater exacerbation risk compared with overusing patients whose asthma was milder (GINA Steps 1 and 2).
The second study found those patients using three or more SABA reliever canisters a year had an increased all-cause mortality risk relative to patients using fewer SABA canisters: hazard ratios after adjustment were 1.26 (95% CI 1.14–1.39) for 3–5 canisters annually, 1.67 (1.49–1.87) for 6–10 canisters, and 2.35 (2.02–2.72) for > 11 canisters, relative to patients collecting < 3 canisters annually [ 46 ].
The recently published PRACTICAL study lends further support to as-needed low-dose ICS/formoterol as an alternative option to daily low-dose ICS plus as-needed SABA, outlined in Step 2 of the guidelines [ 47 ]. In their one-year, open-label, multicentre, randomized, superiority trial in 890 patients with mild to moderate asthma, Hardy and colleagues found that the rate of severe exacerbations per patient per year (the primary outcome) was lower in patients who received as-needed budesonide/formoterol than in patients who received controller budesonide plus as-needed terbutaline (relative rate 0.69, 95% CI 0.48–1.00; p < 0.05). Indeed, they suggest that of these two treatment options, as-needed low-dose ICS/formoterol may be preferred over controller low-dose ICS plus as-needed SABA for the prevention of severe exacerbations in this patient population.
Step 3 recommendations have been left unchanged from 2017, whereas Step 4 treatment has changed from recommending medium/high-dose ICS/LABA [ 3 ] to medium-dose ICS/LABA; the high-dose recommendation has been escalated to Step 5. Patients who have asthma that remains uncontrolled after Step 4 treatment should be referred for phenotypic assessment with or without add-on therapy.
To summarise, the use of ICS medications is of paramount importance for optimal asthma control. The onset and increase of symptoms are indicative of a worsening inflammation leading to severe exacerbations, the risk of which is reduced by a maintenance plus as-needed ICS/LABA combination therapy. The inhaled ICS/bronchodilator combination is as effective as the regular use of inhaled steroids.
The efficacy of anti-inflammatory reliever therapy (budesonide/formoterol) versus current standard-of-care therapies in mild asthma (e.g. reliever therapy with a SABA as needed and regular maintenance controller therapy plus a SABA as-needed) has been evaluated in two randomized, phase III trials which confirmed that, with respect to as-needed SABA, the anti-inflammatory reliever as needed is superior in controlling asthma and reduces exacerbation rates, exposing the patients to a substantially lower glucocorticoid dose.
Conclusions
A growing body of evidence shows that anti-inflammatory reliever strategy is more effective than other strategies with SABA reliever in controlling asthma and reducing exacerbations across all levels of asthma severity. A budesonide/formoterol therapy exposes asthma patients to a substantially lower glucocorticoid dose while cutting the need for adherence to scheduled therapy.
Availability of data and materials
Not applicable.

Abbreviations
Global Initiative for Asthma
Inhaled corticosteroids
Long-acting beta-agonists
Oral corticosteroids
Short-acting beta-agonists
Single inhaler maintenance and reliever treatment
World Health Organization. Asthma. 2017. https://www.who.int/news-room/fact-sheets/detail/asthma . Accessed 9 April 2019.
Papi A, Brightling C, Pedersen SE, Reddel HK. Asthma. Lancet. 2018;391(10122):783–800.
Article PubMed Google Scholar
Global Initiative for Asthma. Global strategy for asthma management and prevention, 2017. http://www.ginasthma.org . Accessed 1 June 2019.
Global Initiative for Asthma. Pocket guide for asthma management and prevention. 2019, pp. 1–32. www.ginasthma.org . Accessed 1 June 2019.
Rabe KF, Vermeire PA, Soriano JB, Maier WC. Clinical management of asthma in 1999: the Asthma Insights and Reality in Europe (AIRE) study. Eur Respir J. 2000;16(5):802–7.
Article CAS PubMed Google Scholar
Price D, Fletcher M, Molen V. Asthma control and management in 8,000 European patients: the REcognise Asthma and LInk to Symptoms and Experience (REALISE) survey. NPJ Prim Care Respir Med. 2014;24:14009.
Article PubMed Central PubMed Google Scholar
Suissa S, Ernst P, Kezouh A. Regular use of inhaled corticosteroids and the long term prevention of hospitalisation for asthma. Thorax. 2002;57(10):880–4.
Article CAS PubMed Central PubMed Google Scholar
Suissa S, Ernst P, Benayoun S, Baltzan M, Cai B. Low-dose inhaled corticosteroids and the prevention of death from asthma. New Engl J Med. 2000;343(5):332–6.
Pauwels RA, Pedersen S, Busse WW, Tan WC, Chen YZ, Ohlsson SV, et al. Early intervention with budesonide in mild persistent asthma: a randomised, double-blind trial. Lancet. 2003;361(9363):1071–6.
Healthcare Improvement Scotland and British Thoracic Society. SIGN 153: British guideline on the management of asthma. 2016. https://www.sign.ac.uk/sign-153-british-guideline-on-the-management-of-asthma.html .
Pauwels RA, Löfdahl CG, Postma DS, Tattersfield AE, O’Byrne P, Barnes PJ, Ullman A. Effect of inhaled formoterol and budesonide on exacerbations of asthma. N Engl J Med. 1997;337(20):1405–11.
O’Byrne PM, Naya IP, Kallen A, Postma DS, Barnes PJ. Increasing doses of inhaled corticosteroids compared to adding long-acting inhaled β2-agonists in achieving asthma control. Chest. 2008;134(6):1192–9.
Johnston SL, Pattemore PK, Sanderson G, Smith S, Lampe F, Josephs L, et al. Community study of role of viral infections in exacerbations of asthma in 9–11 year old children. BMJ. 1995;310(6989):1225–9.
Corne JM, Marshall C, Smith S, Schreiber J, Sanderson G, Holgate ST, Johnston SL. Frequency, severity, and duration of rhinovirus infections in asthmatic and non-asthmatic individuals: a longitudinal cohort study. Lancet. 2002;359(9309):831–4.
Papi A, Contoli M, Adcock IM, Bellettato C, Padovani A, Casolari P, et al. Rhinovirus infection causes steroid resistance in airway epithelium through nuclear factor κb and c-Jun N-terminal kinase activation. J Allergy Clin Immunol. 2013;132(5):1075–85.
Romagnoli M, Vachier I, Tarodo de la Fuente P, Meziane H, Chavis C, Bousquet J, et al. Eosinophilic inflammation in sputum of poorly controlled asthmatics. Eur Respir J. 2002;20(6):1370–7.
Partridge MR, van der Molen T, Myrseth SE, Busse WW. Attitudes and actions of asthma patients on regular maintenance therapy: the INSPIRE study. BMC Pulm Med. 2006;6:13.
Papi A, Caramori G, Adcock IM, Barnes PJ. Rescue treatment in asthma. More than as-needed bronchodilation. Chest. 2009;135(6):1628–33.
PubMed Google Scholar
Tattersfield AE, Postma DS, Barnes PJ, Svensson K, Bauer CA, Byrne PM, et al. Exacerbations of asthma: a descriptive study of 425 severe exacerbations The FACET International Study Group. Am J Respir Crit Care Med. 1999;160(2):594–9.
O’Byrne PM, Jenkins C, Bateman ED. The paradoxes of asthma management: time for a new approach? Eur Respir J. 2017. https://doi.org/10.1183/13993003.01103-2017 .
Royal College of Physicians. Why asthma still kills: the National Review of Asthma Deaths (NRAD). Confidential Enquiry report. London: RCP; 2014.
Google Scholar
Suissa S, Ernst P, Boivin JF, Horwitz RI, Habbick B, Cockroft D, et al. A cohort analysis of excess mortality in asthma and the use of inhaled β-agonists. Am J Respir Crit Care Med. 1994;149(3 Pt 1):604–10.
Global Initiative for Asthma. Global strategy for asthma management and prevention, 2014. https://ginasthma.org/wp-content/uploads/2019/01/2014-GINA.pdf .
Reddel HK, Busse WW, Pedersen S, Tan WC, Chen YZ, Jorup C, et al. Should recommendations about starting inhaled corticosteroid treatment for mild asthma be based on symptom frequency: a post hoc efficacy analysis of the START study. Lancet. 2017;389(10065):157–66.
Papi A, Fabbri LM. Management of patients with early mild asthma and infrequent symptoms. Lancet. 2017;389(10065):129–30.
Global Initiative for Asthma. Global strategy for asthma management and prevention, 2016. https://ginasthma.org/wp-content/uploads/2016/04/GINA-Appendix-2016-final.pdf .
Krishnan JA, Riekert KA, McCoy JV, Stewart DY, Schmidt S, Chanmugam A, et al. Corticosteroid use after hospital discharge among high-risk adults with asthma. Am J Respir Crit Care Med. 2004;170(12):1281–5.
Rabe KF, Atienza T, Magyar P, Larsson P, Jorup C, Lalloo UG. Effect of budesonide in combination with formoterol for reliever therapy in asthma exacerbations: a randomised controlled, double-blind study. Lancet. 2006;368(9537):744–53.
Kuna P, Peters MJ, Manjra AI, Jorup C, Naya IP, Martínez-Jimenez NE, Buhl R. Effect of budesonide/formoterol maintenance and reliever therapy on asthma exacerbations. Int J Clin Pract. 2007;61(5):725–36.
Bousquet J, Boulet LP, Peters MJ, Magnussen H, Quiralte J, Martinez-Aguilar NE, Carlsheimer A. Budesonide/formoterol for maintenance and relief in uncontrolled asthma vs. high-dose salmeterol/fluticasone. Respir Med. 2007;101(12):2437–46.
Sobieraj DM, Weeda ER, Nguyen E, Coleman CI, White CM, Lazarus SC, et al. Association of inhaled corticosteroids and long-acting β-agonists as controller and quick relief therapy with exacerbations and symptom control in persistent asthma a systematic review and meta-analysis. JAMA. 2018;319(14):1485–96.
Papi A, Canonica GW, Maestrelli P, Paggiaro P, Olivieri D, Pozzi E, BEST Study Group, et al. Rescue use of beclomethasone and albuterol in a single inhaler for mild asthma. New Engl J Med. 2007;356(20):2040–52.
Bateman ED, Reddel HK, O’Byrne PM, Barnes PJ, Zhong N, Keen C, et al. As-needed budesonide–formoterol versus maintenance budesonide in mild asthma. New Engl J Med. 2018;378(20):1877–87.
O’Byrne PM, FitzGerald JM, Bateman ED, Barnes PJ, Zhong N, Keen C, et al. Inhaled combined budesonide-formoterol as needed in mild asthma. New Engl J Med. 2018;378(20):1865–76.
Beasley R, Holliday M, Reddel HK, Braithwaite I, Ebmeier S, Hancox RJ, Novel START Study Team, et al. Controlled trial of budesonide-formoterol as needed for mild asthma. New Engl J Med. 2019;380(21):2020–30.
Rabe K, Pizzichini E, Ställberg B, Romero S, Balanzat AM, Atienza T, et al. Budesonide/formoterol in a single inhaler for maintenance and relief in mild-to-moderate asthma: a randomized, double-blind trial. Chest. 2006;129(2):246–56.
Scicchitano R, Aalbers R, Ukena D, Manjra A, Fouquert L, Centanni S, et al. Efficacy and safety of budesonide/formoterol single inhaler therapy versus a higher dose of budesonide in moderate to severe asthma. Curr Med Res Opin. 2004;20(9):1403–18.
O’Byrne PM, Bisgaard H, Godard PP, Pistolesi M, Palmqvist M, Zhu Y, et al. Budesonide/formoterol combination therapy as both maintenance and reliever medication in asthma. Am J Respir Crit Care Med. 2005;171(2):129–36.
Pavord ID, Beasley R, Agusti A, Anderson GP, Bel E, Brusselle G, et al. After asthma: redefining airways diseases. Lancet. 2017;391(10118):350–400.
Martinez FD, Chinchilli VM, Morgan WJ, Boehmer SJ, Lemanske RF Jr, Mauger DT, et al. Use of beclomethasone dipropionate as rescue treatment for children with mild persistent asthma (TREXA): a randomised, double-blind, placebo-controlled trial. Lancet. 2011;377(9766):650–7.
Calhoun WJ, Ameredes BT, King TS, Icitovic N, Bleecker ER, Castro M, et al. Comparison of physician-, biomarker-, and symptom-based strategies for adjustment of inhaled corticosteroid therapy in adults with asthma: the BASALT randomized controlled trial. JAMA. 2012;308(10):987–97.
Sumino K, Bacharier LB, Taylor J, et al. A pragmatic trial of symptom-based inhaled corticosteroid use in African-American children with mild asthma. J Allergy Clin Immunol Pract. 2020;8(176–85):e2.
Byrne PM, Barnes PJ, Rodriguez-Roisin R, Runnerstrom E, Sandstrom T, Svensson K, Tattersfield A. Low dose inhaled budesonide and formoterol in mild persistent asthma: the OPTIMA randomized trial. Am J Respir Crit Care Med. 2001;164(8):1392–7.
Article Google Scholar
Bloom C, Quint J, Cabrera C. SABA and ICS prescriptions among mild asthma patients in UK primary care. Poster presented at the European Respiratory Society International Congress; 2019 Sep 28–Oct 2; Madrid, Spain.
Janson C, Nwaru B, Hasvold P, Wicklund F, Telg G, Ekstrom M. Use of short-acting beta-2 agonists (SABA) and exacerbations in a nationwide Swedish asthma cohort (HERA). Poster presented at the European Respiratory Society International Congress; 2019 Sep 28–Oct 2; Madrid, Spain.
Janson C, Nwaru B, Hasvold P, Wicklund F, Telg G, Ekstrom M. SABA overuse and risk of mortality in a nationwide Swedish asthma cohort (HERA). Late Breaker abstract at the European Respiratory Society International Congress; 2019 Sep 28–Oct 2; Madrid, Spain.
Hardy J, Baggott C, Fingleton J, Reddel HK, Hancox RJ, Harwood M, et al. Budesonide-formoterol reliever therapy versus maintenance budesonide plus terbutaline reliever therapy in adults with mild to moderate asthma (PRACTICAL): a 52-week, open-label, multicentre, superiority, randomised controlled trial. Lancet. 2019;394(10202):919–28.
Download references
Acknowledgements
The Authors thank Maurizio Tarzia and Gayle Robins, independent medical writers who provided editorial assistance on behalf of Springer Healthcare Communications. The editorial assistance was funded by AstraZeneca.
No funding was received for this study. The editorial assistance was funded by AstraZeneca.
Author information
Authors and affiliations.
Section of Cardiorespiratory and Internal Medicine, Department of Morphology, Surgery and Experimental Medicine, University of Ferrara, Ferrara, Italy
Alberto Papi & Luca Morandi
Internal Medicine Department, Respiratory Unit and Adult Cystic Fibrosis Center, Fondazione IRCCS Cà Granda Ospedale Maggiore Policlinico, Milan, Italy
Francesco Blasi
Department of Pathophysiology and Transplantation, Università degli Studi di Milano, Milan, Italy
Personalized Medicine Asthma & Allergy Clinic, Humanitas University & Istituto Clinico Humanitas, Milan, Italy
Giorgio Walter Canonica
Università Cattolica del Sacro Cuore, Fondazione Policlinico A. Gemelli IRCCS, Rome, Italy
Luca Richeldi
Respiratory Section, Department of Medicine, University of Verona, Verona, Italy
Andrea Rossi
Respiratory Unit, Emergency Department, University Hospital S. Anna, Via Aldo Moro 8, 44124, Ferrara, Italy
You can also search for this author in PubMed Google Scholar
Contributions
AP, FB, GWC, LM, LR and AR contributed to writing. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Alberto Papi .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
AP reports grants, personal fees, non-financial support and payment for advisory board membership, consultancy, payment for lectures, grants for research, and travel expenses reimbursement from Chiesi, AstraZeneca, GlaxoSmithKline, Boehringer Ingelheim, Mundipharma and Teva, and personal fees and non-financial support from Menarini, Novartis, Zambon and Sanofi.
FB reports having received in the last three years research grants as well as lecture or advisory board fees from: Alk-Abelló, AstraZeneca, Boehringer Ingelheim, Chiesi, Guidotti, Glaxo Smith Kline, Grifols, Menarini, Novartis, Sanofi, Valeas, Zambon.
GWC reports having received in the last 3 years research grants as well as lecture or advisory board fees from: A. Menarini, Alk-Abelló, AstraZeneca-Medimmune, Boehringer Ingelheim, Chiesi Farmaceutici, Genentech, Guidotti-Malesci, Glaxo Smith Kline, Hal Allergy, Merck Sharp & Dohme, Mundipharma, Novartis, Orion, Sanofi-Aventis, Sanofi Genzyme/Regeneron, Stallergenes-Greers, UCB Pharma, Uriach Pharma, Valeas.
LR Receipt of grants/research supports: Roche, Boehringer Ingelheim.
Receipt of honoraria or consultation fees: Boehringer Ingelheim, Roche, Biogen, FibroGen,
Sanofi-Aventis, Anthera, Promedior, ImmuneWorks, Asahi-Kasei, Bayer, Celgene, RespiVant,
Nitto, Bristol Myers Squibb, Prometic, Pliant Therapeutics, Toray, Global Blood Therapeutics,
Zambon, Veracyte, Acceleron, CSL Behring.
LM and AR reports no conflicts of interest in the last 3 years.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Papi, A., Blasi, F., Canonica, G.W. et al. Treatment strategies for asthma: reshaping the concept of asthma management. Allergy Asthma Clin Immunol 16 , 75 (2020). https://doi.org/10.1186/s13223-020-00472-8
Download citation
Received : 18 March 2020
Accepted : 05 August 2020
Published : 15 August 2020
DOI : https://doi.org/10.1186/s13223-020-00472-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Anti-inflammatory treatment
- Disease control
- Patient outcomes
Allergy, Asthma & Clinical Immunology
ISSN: 1710-1492
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Patient Care & Health Information
- Diseases & Conditions
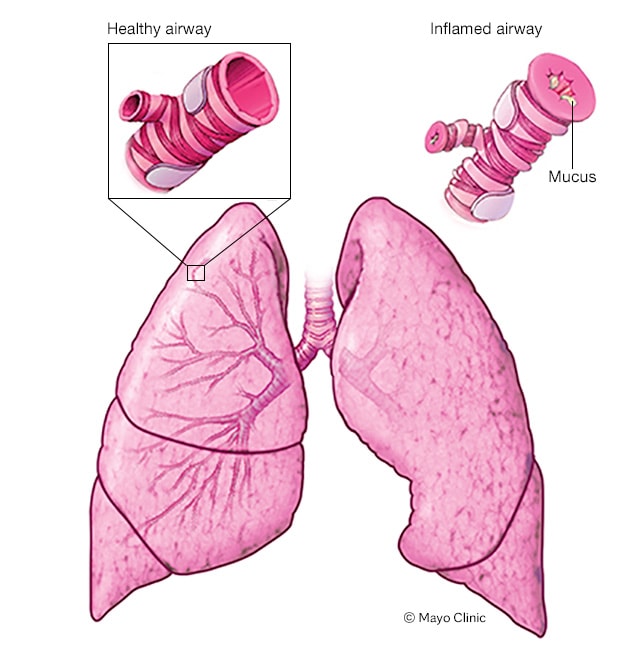
Asthma attack
When a person has asthma, the inside walls of the airways in the lungs can narrow and swell. Also, the airway linings may make too much mucus. The result is an asthma attack. During an asthma attack, narrowed airways make breathing difficult and may cause coughing and wheezing.
Asthma is a condition in which your airways narrow and swell and may produce extra mucus. This can make breathing difficult and trigger coughing, a whistling sound (wheezing) when you breathe out and shortness of breath.
For some people, asthma is a minor nuisance. For others, it can be a major problem that interferes with daily activities and may lead to a life-threatening asthma attack.
Asthma can't be cured, but its symptoms can be controlled. Because asthma often changes over time, it's important that you work with your doctor to track your signs and symptoms and adjust your treatment as needed.
Products & Services
- A Book: Mayo Clinic Book of Home Remedies
Asthma symptoms vary from person to person. You may have infrequent asthma attacks, have symptoms only at certain times — such as when exercising — or have symptoms all the time.
Asthma signs and symptoms include:
- Shortness of breath
- Chest tightness or pain
- Wheezing when exhaling, which is a common sign of asthma in children
- Trouble sleeping caused by shortness of breath, coughing or wheezing
- Coughing or wheezing attacks that are worsened by a respiratory virus, such as a cold or the flu
Signs that your asthma is probably worsening include:
- Asthma signs and symptoms that are more frequent and bothersome
- Increasing difficulty breathing, as measured with a device used to check how well your lungs are working (peak flow meter)
- The need to use a quick-relief inhaler more often
For some people, asthma signs and symptoms flare up in certain situations:
- Exercise-induced asthma, which may be worse when the air is cold and dry
- Occupational asthma, triggered by workplace irritants such as chemical fumes, gases or dust
- Allergy-induced asthma, triggered by airborne substances, such as pollen, mold spores, cockroach waste, or particles of skin and dried saliva shed by pets (pet dander)
When to see a doctor
Seek emergency treatment.
Severe asthma attacks can be life-threatening. Work with your doctor to determine what to do when your signs and symptoms worsen — and when you need emergency treatment. Signs of an asthma emergency include:
- Rapid worsening of shortness of breath or wheezing
- No improvement even after using a quick-relief inhaler
- Shortness of breath when you are doing minimal physical activity
Contact your doctor
See your doctor:
- If you think you have asthma. If you have frequent coughing or wheezing that lasts more than a few days or any other signs or symptoms of asthma, see your doctor. Treating asthma early may prevent long-term lung damage and help keep the condition from getting worse over time.
- To monitor your asthma after diagnosis. If you know you have asthma, work with your doctor to keep it under control. Good long-term control helps you feel better from day to day and can prevent a life-threatening asthma attack.
If your asthma symptoms get worse. Contact your doctor right away if your medication doesn't seem to ease your symptoms or if you need to use your quick-relief inhaler more often.
Don't take more medication than prescribed without consulting your doctor first. Overusing asthma medication can cause side effects and may make your asthma worse.
- To review your treatment. Asthma often changes over time. Meet with your doctor regularly to discuss your symptoms and make any needed treatment adjustments.
More Information
Asthma care at Mayo Clinic
- Vocal cord dysfunction
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
It isn't clear why some people get asthma and others don't, but it's probably due to a combination of environmental and inherited (genetic) factors.
Asthma triggers
Exposure to various irritants and substances that trigger allergies (allergens) can trigger signs and symptoms of asthma. Asthma triggers are different from person to person and can include:
- Airborne allergens, such as pollen, dust mites, mold spores, pet dander or particles of cockroach waste
- Respiratory infections, such as the common cold
- Physical activity
- Air pollutants and irritants, such as smoke
- Certain medications, including beta blockers, aspirin, and nonsteroidal anti-inflammatory drugs, such as ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve)
- Strong emotions and stress
- Sulfites and preservatives added to some types of foods and beverages, including shrimp, dried fruit, processed potatoes, beer and wine
- Gastroesophageal reflux disease (GERD), a condition in which stomach acids back up into your throat
- Asthma and acid reflux
Risk factors
A number of factors are thought to increase your chances of developing asthma. They include:
- Having a blood relative with asthma, such as a parent or sibling
- Having another allergic condition, such as atopic dermatitis — which causes red, itchy skin — or hay fever — which causes a runny nose, congestion and itchy eyes
- Being overweight
- Being a smoker
- Exposure to secondhand smoke
- Exposure to exhaust fumes or other types of pollution
- Exposure to occupational triggers, such as chemicals used in farming, hairdressing and manufacturing
Complications
Asthma complications include:
- Signs and symptoms that interfere with sleep, work and other activities
- Sick days from work or school during asthma flare-ups
- A permanent narrowing of the tubes that carry air to and from your lungs (bronchial tubes), which affects how well you can breathe
- Emergency room visits and hospitalizations for severe asthma attacks
- Side effects from long-term use of some medications used to stabilize severe asthma
Proper treatment makes a big difference in preventing both short-term and long-term complications caused by asthma.
While there's no way to prevent asthma, you and your doctor can design a step-by-step plan for living with your condition and preventing asthma attacks.
Follow your asthma action plan. With your doctor and health care team, write a detailed plan for taking medications and managing an asthma attack. Then be sure to follow your plan.
Asthma is an ongoing condition that needs regular monitoring and treatment. Taking control of your treatment can make you feel more in control of your life.
- Get vaccinated for influenza and pneumonia. Staying current with vaccinations can prevent flu and pneumonia from triggering asthma flare-ups.
- Identify and avoid asthma triggers. A number of outdoor allergens and irritants — ranging from pollen and mold to cold air and air pollution — can trigger asthma attacks. Find out what causes or worsens your asthma, and take steps to avoid those triggers.
Monitor your breathing. You may learn to recognize warning signs of an impending attack, such as slight coughing, wheezing or shortness of breath.
But because your lung function may decrease before you notice any signs or symptoms, regularly measure and record your peak airflow with a home peak flow meter. A peak flow meter measures how hard you can breathe out. Your doctor can show you how to monitor your peak flow at home.
Identify and treat attacks early. If you act quickly, you're less likely to have a severe attack. You also won't need as much medication to control your symptoms.
When your peak flow measurements decrease and alert you to an oncoming attack, take your medication as instructed. Also, immediately stop any activity that may have triggered the attack. If your symptoms don't improve, get medical help as directed in your action plan.
- Take your medication as prescribed. Don't change your medications without first talking to your doctor, even if your asthma seems to be improving. It's a good idea to bring your medications with you to each doctor visit. Your doctor can make sure you're using your medications correctly and taking the right dose.
- Pay attention to increasing quick-relief inhaler use. If you find yourself relying on your quick-relief inhaler, such as albuterol, your asthma isn't under control. See your doctor about adjusting your treatment.
- Weinberger SE, et al. Asthma. In: Principles of Pulmonary Medicine. 7th ed. Elsevier; 2019. https://www.clinicalkey.com. Accessed March 30, 2020.
- Asthma. National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health-topics/asthma. Accessed March 25, 2020.
- AskMayoExpert. Asthma (adult). Mayo Clinic; 2020.
- Global strategy for asthma management and prevention (2019 update). Global Initiative for Asthma. https://ginasthma.org/gina-reports/. Accessed March 27, 2020.
- Khurana S, et al. Systematic approach to asthma of varying severity. Clinics in Chest Medicine. 2019; doi:10.1016/j.ccm.2018.10.004.
- Ferri FF. Asthma. In: Ferri's Clinical Advisor 2020. Elsevier; 2020. https://www.clinicalkey.com. Accessed March 30, 2020.
- Wu TD, et al. Asthma in the primary care setting. Medical Clinics of North America. 2019; doi:10.1016/j.mcna.2018.12.004.
- Fanta CH. An overview of asthma management. https://www.uptodate.com/contents/search. Accessed March 30, 2020.
- Santino TA, et al. Breathing exercises for adults with asthma. Cochrane Database of Systematic Reviews. 2020; doi:10.1002/14651858.CD001277.pub4.
- Amaral-Machado L, et al. Use of natural products in asthma treatment. Evidence-based Complementary and Alternative Medicine. 2020; doi:10.1155/2020/1021258.
- Montelukast. IBM Micromedex. https://www.micromedexsoluitions.com. Accessed April 6, 2020.
- Whyand T, et al. Pollution and respiratory disease: Can diet or supplements help? A review. Respiratory Research. 2018; doi:10.1186/s12931-018-0785-0.
- O'Keefe JH, et al. Coffee for cardioprotection and longevity. Progress in Cardiovascular Diseases. 2018; doi:10.1016/j.pcad.2018.02.002.
- Allergies and asthma
- Asthma diet
- Asthma inhalers: Which one's right for you?
- Asthma medications
- Asthma treatment: 3 steps
- Asthma: Testing and diagnosis
- Dry powder disk inhaler
- Dry powder tube inhaler
- Ozone air purifiers
- Single-dose dry powder inhaler
- Using a metered dose asthma inhaler and spacer
- Video: How to use a peak flow meter
- What is aspirin-exacerbated respiratory disease (AERD)?
Associated Procedures
- Allergy shots
News from Mayo Clinic
- Mayo Clinic Minute: Can aspirin make your breathing worse? March 26, 2024, 04:00 p.m. CDT
- Mayo Clinic Minute: How to use an asthma inhaler Sept. 22, 2023, 04:00 p.m. CDT
- Mayo Clinic Minute: Signs and symptoms of asthma April 24, 2023, 04:30 p.m. CDT
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Make twice the impact
Your gift can go twice as far to advance cancer research and care!

- Center on Health Equity and Access
- Health Care Cost
- Health Care Delivery
- Value-Based Care
Bronchial Thermoplasty Improves Ventilation Heterogeneity in Severe Asthma
Significant improvements were seen in ventilation heterogeneity in patients with severe asthma after 12 months of bronchial thermoplasty.
Patients with severe asthma experienced clinical benefits of bronchial thermoplasty (BT) measured by improvements in ventilation heterogeneity assessed by functional respiratory imaging (FRI), according to a prospective study is published in the Journal of Asthma and Allergy .

Close up of doctor hand holding blue asthma inhaler and writing medical prescription on rx form for treatment asthma | Orawan - stock.adobe.com

Most patients with severe asthma already undergo chest computed tomography (CT) to exclude other differentials, which means performing BT to study lung ventilation is a minor inconvenience for these patients, the authors explained.
“Moreover, successful detection of changes in ventilation heterogeneity using FRI [functional respiratory imaging] may provide a means of assessing response to therapy and identifying suitable patients, not only in the application of BT but also other relevant interventions," they wrote.
To the researchers’ knowledge, this study is the first of its kind to measure changes in ventilation heterogeneity using FRI in patients undergoing BT.
Patients were prospectively recruited from a tertiary hospital severe asthma clinic, who were aged 18 years and older, had diagnosis of severe asthma, and were scheduled for a clinically indicated BT by their treating physician.
Patients with altnerative respiratory conditions, including chronic obstructive pulmonary disease or bronchiectasis, as well as females who were pregnant or lactating were excluded from the study.
A total of 18 patients were recruited for the study and were assessed at baseline, 4 weeks after treatment of the left lung, and 12 months after treatment of the right lung.
Additionally, the researchers assessed short-acting β-agonist (SABA) and oral prednisolone (OCS) use, asthma control questionnaire (ACQ-5) score, and exacerbation history. Furthermore, patients underwent lung function tests and CT, with ventilation parameters including interquartile distance (IQD) using FRI.
Significant improvements were observed 12 months after BT in SABA and OCS use, ACQ-5, and the number of OCS-requiring exacerbations, with median (IQR) ACQ score reduced from 3.3 (2.7-4.2) to 1.9 (1.1-2.7); P < .001.
SABA rescue therapy was reduced from a median of 11 (8-20) puffs per day to 2.5 (1.3-6.8) puffs per day ( P < .001). Additionally, all 15 patients who required maintenance OCS at baseline reduced their daily OCS dose from 7.5 (5-25) mg per day to 4.5 (0-10) mg per day ( P = .01).
Ventilation heterogeneity was significantly improved after treatment of the left lung (0.18 ± 0.04 vs 0.20 ± 0.04; P = .045), with treatment effect persisting up to 12 months later (0.18 ± 0.05 vs 0.20 ± 0.04; P = .028). Ventilation heterogeneity also improved after treatment of the right lung but did not reach statistical significance (0.18 ± 0.05 vs 0.19 ± 0.04; P = .06).
However, the researchers acknowledged some limitations to the study, including a small sample size, being conducted in a single center, and not having a comparative control group.
Despite these limitations, the researchers believe there are clinical benefits of BT, observed in improvements in ventilation heterogeneity as measured by FRI.
“In this study, we demonstrated an improvement in ventilation heterogeneity, as reflected by a reduction in IQD, along with clinical improvements after BT,” wrote the researchers. “These findings are consistent with mathematical modeling of the physiological behavior of the asthmatic lung when subjected to BT, namely that improvements in ventilation heterogeneity are expected, particularly at higher levels of ASM [airway smooth muscle] activation.”
Foo CT, Donovan GM, Thien F, et al. Bronchial thermoplasty improves ventilation heterogeneity measured by functional respiratory imaging in severe asthma. J Asthma Allergy . 2024;17:399-409 doi:10.2147/JAA.S454951

Vitamin D Supplementation Linked to Reduced In-Hospital, ICU Mortality in Patients With COPD
Vitamin D supplementation may decrease in-hospital and intensive care unit (ICU) mortality in patients with chronic obstructive pulmonary disease (COPD), a study found.

Updates on Adagrasib in CRC and the Importance of Genomic Testing With Dr Jun Gong
Jun Gong, MD, of Cedars-Sinai Medical Center, discusses the latest data on adagrasib in colorectal cancer, the importance of conducting genomic testing, and more.

Research Unveils UGT2B17 as Key Prognostic Marker in CLL
UGT2B17, a metabolic enzyme known for regulating various endogenous molecules, has been identified to have heightened expression in the B cells of patients who have chronic lymphocytic leukemia (CLL).
Managed Care Cast Presents: Insights Into Precision Medicine in NSCLC
In this podcast, a trio of experts discuss precision medicine in non–small cell lung cancer (NSCLC), current immunotherapies, and more.

Patients With DMD Receiving Eteplirsen Show Prolonged Survival, Study Finds
The study provides evidence of survival benefits among patients with Duchenne muscular dystrophy (DMD) receiving eteplirsen compared with the natural history of the condition.

When Uncontrolled Diabetes and a Fungus Meet: Emergency Treatment of Rhino-Orbital-Cerebral Mucormycosis
JAMA used a case report of rhino-orbital-cerebral mucormycosis in a patient with uncontrolled diabetes to demonstrate correct and incorrect treatment choices.
2 Commerce Drive Cranbury, NJ 08512
609-716-7777
Institutes, Divisions & Centers Asthma Research
Innovative leader in asthma research.
The Division of Asthma Research aims to accelerate the bidirectional flow of knowledge between the clinical beside and research settings. We translate clinical challenges in asthma into well-designed research studies that integrate the collective expertise of individuals in the division and across Cincinnati Children's and take advantage of transdisciplinary approaches that span the use of human cohorts, animal models, in vitro and ex vivo models, and innovative methodologies. We have brought together physician scientists, basic scientists, clinical researchers, epidemiologists, exposure experts, geneticists and epigeneticists who work together on many aspects of asthma research.
Our Mission
To improve the health of children with asthma through a combination of clinically relevant research designed to delineate the mechanisms underlying asthma and the biologic basis for individual variations in asthma presentation, treatment response, and outcome.
Top-notch clinical care requires a top-notch research base is the basic principal that guides the Division of Asthma at Cincinnati Children’s. The central goal is to contribute to new standards for clinical care through novel scientific discoveries and cutting edge research. We also strive to develop new treatment strategies and management paradigms based on research findings, which can be systematically evaluated in investigator initiated clinical trials and through our involvement in national networks.
Interested in Joining Our Division?
The Division of Asthma Research is devoted to providing each individual within our division an outstanding educational and work experience. We are interested in recruiting self-driven individuals who want to join us and make a difference for children with Asthma. Click here to see our available positions .

Statistics at a Glance
Research and training.
- Joint Appointment Faculty: 4
- Research Graduate Students: 2
- Research Fellows and Post Docs: 6
@AsthmaResCincy

Connect With Us
3333 Burnet Avenue, Cincinnati, Ohio 45229-3026
© 1999-2024 Cincinnati Children's Hospital Medical Center. All rights reserved.

- Open access
- Published: 25 April 2024
TFEB regulates dendritic cell antigen presentation to modulate immune balance in asthma
- JinYing Xiang 1 ,
- Yinying Ren 1 ,
- Yuehan Li 1 ,
- Mi Zhou 1 ,
- Jinyue Yu 3 , 4 ,
- Zhengxiu Luo 1 ,
- Enmei Liu 1 ,
- Zhou Fu 1 &
- Fengxia Ding 1
Respiratory Research volume 25 , Article number: 182 ( 2024 ) Cite this article
11 Accesses
Metrics details
Asthma stands as one of the most prevalent chronic respiratory conditions in children, with its pathogenesis tied to the actived antigen presentation by dendritic cells (DCs) and the imbalance within T cell subgroups. This study seeks to investigate the role of the transcription factor EB (TFEB) in modulating the antigen presentation process of DCs and its impact on the differentiation of T cell subgroups.
Bone marrow dendritic cells (BMDCs) were activated using house dust mites (HDM) and underwent RNA sequencing (RNA-seq) to pinpoint differentially expressed genes. TFEB mRNA expression levels were assessed in the peripheral blood mononuclear cells (PBMCs) of both healthy children and those diagnosed with asthma. In an asthma mouse model induced by HDM, the TFEB expression in lung tissue DCs was evaluated. Further experiments involved LV-shTFEB BMDCs co-cultured with T cells to explore the influence of TFEB on DCs’ antigen presentation, T cell subset differentiation, and cytokine production.
Transcriptomic sequencing identified TFEB as a significantly differentially expressed gene associated with immune system pathways and antigen presentation. Notably, TFEB expression showed a significant increase in the PBMCs of children diagnosed with asthma compared to healthy counterparts. Moreover, TFEB exhibited heightened expression in lung tissue DCs of HDM-induced asthmatic mice and HDM-stimulated BMDCs. Silencing TFEB resulted in the downregulation of MHC II, CD80, CD86, and CD40 on DCs. This action reinstated the equilibrium among Th1/Th2 and Th17/Treg cell subgroups, suppressed the expression of pro-inflammatory cytokines like IL-4, IL-5, IL-13, and IL-17, while augmenting the expression of the anti-inflammatory cytokine IL-10.
TFEB might have a vital role in asthma’s development by impacting the antigen presentation of DCs, regulating T cell subgroup differentiation, and influencing cytokine secretion. Its involvement could be pivotal in rebalancing the immune system in asthma. These research findings could potentially unveil novel therapeutic avenues for treating asthma.
Introduction
Asthma is among the prevalent chronic respiratory conditions in children, characterized by chronic airway inflammation, hyperresponsiveness, and irreversible airway wall remodeling [ 1 ]. Allergic asthma, the most prevalent type of the disease, results from exposure to innocuous environmental allergens such as house dust mites (HDM), pollen, and fungi [ 2 ]. The development of asthma is directly linked to the disruption of the body’s immune homeostasis, in which the activation of antigen-presenting cells and the imbalance between effector T cells and regulatory T cells (Treg) play a crucial role in this process [ 3 ]. DCs are the most effective antigen-presenting cells in stimulating adaptive immune responses. Upon stimulation by external triggers, these cells’ antigen presentation functions are activated, thereby promoting the immune responses mediated by effector T cells [ 4 ]. DCs are also the most common antigen-presenting cells in the lungs, playing a critical role in maintaining pulmonary immune homeostasis [ 5 , 6 ]. When the respiratory tract is exposed to an allergen, DCs process it into small peptides and migrate to the mediastinal lymph nodes, binding to the MHC II receptor and co-stimulatory molecules on the surface of naïve CD4 + T helper cells, consequently achieving antigen presentation of the allergen. Subsequently, naïve CD4 + T helper cells differentiate into various T cell subtypes, producing corresponding cytokines [ 7 , 8 ].
TFEB is a member of the MiTF/TFE family of basic helix-loop-helix leucine zipper transcription factors, linked to a range of conditions including neurodegenerative diseases, metabolic disorders, obesity, tumors, and lysosomal storage diseases [ 9 , 10 ]. Previous research has shown that TFEB is involved in both the non-specific and adaptive immune responses [ 11 ]. When macrophages are exposed to pathogens, TFEB facilitates the transcription of various chemokines and pro-inflammatory cytokines that are essential for the immune response [ 12 ]. Additionally, TFEB’s transcriptional activity is upregulated during CD4 + T cell activation and significantly contributes to humoral immunity by enhancing the production of IgG and IgA [ 13 ]. Recent studies indicate that TFEB aids DCs in capturing and transporting antigens to lysosomes. TFEB elevates intracellular Ca2 + concentration by activating the lysosomal calcium channel TRPML1, which drives the fusion of lysosomes with the plasma membrane. This process facilitates the transportation of antigen-bound MHC II molecules for expression on the outer surface of the cell membrane, resulting in a shift towards MHC II for cross-antigen presentation, and enhancing the activation of CD4 + T cells [ 14 , 15 ]. Additionally, the migration of DCs from the periphery to the lymph nodes is regulated by a TFEB-TRPML1 axis feedback loop, which originates from lysosomes [ 16 ]. These findings suggest that TFEB could play a pivotal role as a transcription factor in initiating antigen presentation by DCs and mediating the immune response of CD4 + T cells. However, it is currently unclear how TFEB changes in asthma and what impact it has on the antigen-presenting function of DCs and T-cell differentiation. Therefore, in this study, we employed RNA-seq to identify differentially expressed genes, while concurrently evaluating the expression of TFEB mRNA in peripheral blood mononuclear cells (PBMCs) from both healthy children and children diagnosed with asthma. Moreover, by constructing a mouse model of HDM-induced asthma and a co-culture system of bone marrow dendritic cells (BMDCs) and T cells, we comprehensively analyze the role of TFEB in the process of antigen presentation by DCs and in mediating the immune response of CD4 + T cells.
Materials and methods
Cell culture.
BMDCs were obtained from mouse femurs and tibiae according to previously described methods [ 17 ]. T cells were obtained from the spleens of C57BL/6 mice using the Mouse Spleen Lymphocyte Isolation Kit (Hao Yang Bio, Tianjin, China) according to the manufacturer’s instructions. T cells were inoculated with BMDCs in a 5:1 ratio into 12-well plates and co-cultured for 36 h with or without HDM (20ug/ml) stimulation.The co-cultured cell culture supernatant and co-cultured cells were collected for subsequent experiments. All cells were cultured in an incubator at 37 °C containing 5% CO2.
RNA-Seq and data analysis
BMDCs with stable culture condition were inoculated into 6 cm petri dishes, and 5 petri dishes were randomly selected as experimental group to be stimulated with HDM (20ug/ml), and 5 other petri dishes were randomly selected as control group to be not stimulated with HDM. After incubating at 37 °C with 5% CO2 for 36 h, collected control and experimental groups for RNA-seq (Boho Biotech Co., Ltd, Shanghai, China). Differential genes (DEGs) between the two groups were screened according to the criteria of |log2FC|>1 and P <0.05, and the volcano map was plotted using the “ggplot2” R package, and the enrichment analysis was performed by the “clusterProfiler” R package.
Human subjects
Thirty-eight subjects were recruited from the outpatient department of the Children’s Hospital of Chongqing Medical University, comprising a ratio of approximately 1:1.5 between healthy children ( n = 15) and children diagnosed with asthma ( n = 23). Inclusion criteria for the asthma group included children aged 4 years or older who met the diagnostic criteria for asthma outlined in the Global Initiative for Asthma (GINA) Management and Prevention guidelines published in 2023 [ 18 ]. Patients with other respiratory diseases, a history of respiratory infections within the last 2 weeks, and a history of immunosuppressant or glucocorticoid use within 4 weeks before the start of the study were excluded. Healthy children over 4 years of age without respiratory disease and no recent history of infection were used as controls. A total of 3 ml of peripheral blood was collected from each subject, from which peripheral blood mononuclear cells (PBMCs) were isolated using the Human Peripheral Mononuclear Cells Isolation Kit (Hao Yang Bio, Tianjin, China). Total RNA was then extracted from the PBMCs using the SimplyP Total RNA Extraction Kit (BioFlux, USA), following the manufacturer’s instructions.
HDM-induced allergic asthma mouse model
C57BL/6 mice (female, 6–8 weeks old) were purchased from Chongqing Enswell Biotechnology Co Ltd (Chongqing, China). Mice were housed in an environment with a humidity level of 40–70%, at a temperature of 24 °C, and subjected to a 12-hour light/dark cycle. Adequate food and water were provided and all were sterilised. Twenty female C57BL/6 mice were randomly assigned to the control group ( n = 10) and the asthma group ( n = 10). On days 0 and 14, mice were intranasally administered 40 µl of HDM (20 µg) solution (Greer, Los Angeles, CA, USA) for sensitization, followed by intranasal administration of 40 µl HDM (20 µg) solution on days 21, 23, 25, 27, and 29 for challenge. The control group received saline instead of the HDM solution. On day 31, all mice were sacrificed for relevant experimental tests and analyses [ 17 ].
Lung histopathological staining and immunohistochemistry
The left lung tissue of mice was fixed with 4% paraformaldehyde, embedded in paraffin, and then sliced into 4 μm thick lung tissue paraffin sections. The inflammation around the bronchi, blood vessels, and pulmonary interstitium was assessed using hematoxylin and eosin (H&E) staining, and graded from 0 to 3. A score of 0 indicated no inflammatory response; 1 indicated inflammatory infiltration around the bronchi, blood vessels, and pulmonary interstitium without thickening; 2 indicated obvious inflammatory infiltration and mild thickening around the bronchi, blood vessels, and pulmonary interstitium; and 3 indicated significant inflammatory infiltration and marked thickening around the bronchi, blood vessels, and pulmonary interstitium. For immunohistochemistry, sections were incubated with primary anti-TFEB antibody (1:150, Proteintech, Wuhan, China) overnight, followed by 30 min of incubation with the secondary antibody. DAB (Zhongshang JinQiao Biotechnology Co., Ltd., Beijing, China) was used for visualization. The mean optical density (MOD) was analyzed using Image J software.
Immunofluorescence of lung sections and cells
4% paraformaldehyde was utilized to fix 4-µm lung tissue paraffin sections and BMDCs, followed by permeabilization with 0.2% Triton X100 (Solarbio, Beijing, China), and blocking with 5% BSA (Solarbio, Beijing, China). The samples were incubated overnight at 4 °C with rabbit anti-mouse TFEB primary antibody (diluted 1:300, Proteintech, Wuhan, China) and CoraLite Plus 488-conjugated CD11c (diluted 1:200, Proteintech, Wuhan, China). Afterward, the samples were incubated at room temperature in the dark for 1 h with FITC- or cy3-conjugated goat anti-rabbit secondary antibody (diluted 1:200, Proteintech, Wuhan, China). DAPI (Beyotime, Shanghai, China) was used as a nuclear stain and incubated in the dark at room temperature for 15 min. Actin-Tracker Red-555 (diluted 1:100, Beyotime, Shanghai, China) was employed as a cytoskeletal dye and incubated for 1 h at room temperature. After mounting with anti-fluorescence quencher (Beyotime, Shanghai, China), the images were captured under a confocal microscope (Nikon, Tokyo, Japan), and analyzed using ImageJ software.
Bronchoalveolar lavage and differential cell counting
The left bronchus of mice was ligated, and bronchoalveolar lavage fluid (BALF) was collected using pre-cooled PBS. After centrifugation at 2500 rpm for 20 min at 4 °C, the cells were lysed with erythrocyte lysate, and the total BALF cell count was determined using a cell counter. The centrifuged BALF cell sediment was placed on slides, and the cells were stained with rapid Rhee’s staining solution (Built Technology Co., Ltd., Nanjing, China). Subsequently, at least 200 cells were enumerated under the microscope, and the number and proportion of macrophages, neutrophils, eosinophils, and lymphocytes were recorded separately.
Enzymelinked immunosorbent assay (ELISA)
Mouse ocular blood was collected and centrifuged at 2500 rpm for 15 min at room temperature, and serum was obtained for the determination of IgE levels. According to the protocol, the mouse IgE ELISA kit (Ruixin Bio, Guangzhou, China) was used to measure the total IgE level in the serum. The supernatant of mouse bronchoalveolar lavage fluid (BALF) was obtained after centrifugation at 4 °C for 20 min, and the expression levels of IL-4, IL-10, IL-17, and IFN-γ were measured using the Mouse IL-4, IL-10, IL-17, and IFN-γ ELISA kit (Ruixin Bio, Guangzhou, China). The medium was collected after co-culturing T cells and BMDCs, then centrifuged at 2500 rpm for 15 min at room temperature, and the levels of IL-4, IFN-γ, and IL-17 in the culture medium supernatant were determined using the Mouse IL-4, IFN-γ, and IL-17 ELISA Kit (Ruixin Bio, Guangzhou, China).
Measurement of airway hyperresponsiveness (AHR)
After the last HDM stimulation for 24 h, the resistance of the lung to different doses of acetylcholine was measured using a non-invasive lung function meter (EMKA Technologies, Paris, France). Mice were placed in a body plethysmograph, and non-invasive whole-body plethysmography (WBP) was utilized to evaluate bronchial constriction in awake, freely active mice by assessing their respiratory physiological parameters. Baseline measurements were recorded prior to stimulating the mice with the bronchoconstrictor acetyl-β-methylcholine (Sigma, Missouri, USA) at doses of 0, 3.125, 6.25, 12.5, 25, and 50 mg/ml using a nebulization system. The lung resistance at each concentration was calculated.
RNA interference
The shRNA sequences for mouse TFEB (shTFEB-1-5ʹ--3ʹ, shTFEB-2-5ʹ--3ʹ, shTFEB-3-5ʹ--3ʹ) were synthesized by GeneChem company (Shanghai, China). shGFP was used as a control group. BMDCs were seeded into a 24-well plate, and transduced with shGFP or shTFEB at a virus titer of MOI 75. Additionally, HitransG P infection enhancement solution (GeneChem, Shanghai, China) was added to improve the infection efficiency of the lentivirus. The culture medium was replaced with fresh, virus-free medium after 24 h. GFP expression in BMDCs was observed under a fluorescence microscope 72 h after lentiviral infection. Lentivirus infection efficiency was assessed using flow cytometry. The efficiency of TFEB gene knockdown was determined through RT-qPCR, western blotting, and immunofluorescence detection.
Wound healing assay
To assess the migration ability of the BMDCs, we performed a scratch wound healing assay. The BMDCs transfected with LV-GFP or LV-shTFEB were cultured in a 6-well plate until reaching 100% confluence. Subsequently, the cells were subjected to scratching with a 200µL pipette tip, followed by two washes with PBS and then incubation in medium containing 1% serum. Microscopic images were taken at 6 and 12 h. ImageJ was employed for image analysis and quantitative measurements.
Flow cytometry
After collecting cultured cells and blocking with rat serum for 30 min, the following flow cytometry antibodies were used for phenotypic analysis: anti-CD11c-APC (Biolegend, California, USA), anti-MHCII-BV421 (Biolegend, California, USA), anti-CD80-Percp/cy5.5 (Biolegend, California, USA), anti-CD86-PE (Biolegend, California, USA), anti-CD40-PE/Cy7 (Elabscience, Wuhan, China). Data was acquired using FACS Canto II (BD Biosciences, USA) and analyzed using FlowJo software.
RNA extraction and RT-qPCR
We used the SimplyP Total RNA Extraction Kit (BioFlux, USA) to extract total RNA from PBMCs, mouse lung tissue and BMDCs. The RNA was then reverse-transcribed into cDNA using the Evo M-MLV Reverse Transcription Kit (Aike Rui Biotechnology, Hunan, China). RT-qPCR was performed using the SYBR Green Pro Taq pre-mix kit (Aike Rui Biotechnology, Hunan, China) to detect gene expression. Mouse β-actin and human GAPDH were used as internal controls for mouse samples and human PBMCs samples, respectively. The primer sequences we used were as follows:
Mouse TFEB (forward 5’-GCATCAGAAGGTTCGGGAGTATC-3’, reverse 5’-AGGCGCATAATGTTGTCAATGAC-3), mouse IL-4 (forward 5’-GGAGATGGATGTGCCAAACG-3’, reverse 5’-TGGAAGCCCTACAGACGAG-3’), mouse IL-5 (forward 5’-AGCAATGAGACGATGAGGCTT-3’, reverse 5’-TACCCCCACGGACAGTTTGA-3’), mouse IL-6 (forward 5’-GCCTTCTTGGGACTGATGCT-3’, reverse 5’-GGTCTGTTGGGAGTGGTATCC-3’), mouse IL-10 (forward 5’-CAACATACTGCTAACCGACTCCT-3’, reverse 5’-GCCTGGGGCATCACTTCTAC-3’), mouse IL-12 (forward 5’-GCCAGGGTCATTCCAGTCTC-3’, reverse 5’-TGGTTTGGTCCCGTGTGATG-3’), mouse IL-13 (forward 5’-GTATGGAGTGTGGACCTGGC-3’, reverse 5’-TTTTGGTATCGGGGAGGCTG-3’), mouse IFN-γ (forward 5’-GAGGTCAACAACCCACAGGTC-3’, reverse 5’-TCTTC CCCACCCCGAATCA-3’), mouse TRPML1 (forward 5’-CGGTGTCATTCGCTACCTGA-3’, reverse 5’-CAGCGAGCGGAACTTCACAT-3’), mouse Foxp3 (forward 5’-AGAGCGAGAAGGGAGCAGT-3’, reverse 5’-GCAGGGATTGGAGCACTTGT-3’), mouse GATA3 (forward 5’-CCATTACCACCTATCCGCCC-3’, reverse 5’-TTCACACACTCCCTGCCTTC-3’), mouse RORγt (forward 5’-GCAAAGAAGACCCACACCTCA-3’, reverse 5’-ACATTACACTGCTGGCTGCG-3’), mouse T-bet (forward 5’-GCCTACCAGAACGCAGAGAT-3’, reverse 5’-CCCCCAAGCAGTTGACAGTT-3’), mouse β-actin (forward 5’-GTGCTATGTTGCTCTAGACTTCG-3’, reverse 5’-AGCCACAGGATTCCATACC-3’), human TFEB (forward 5’-ACCTGACCCAGAAGCGAGA-3’, reverse 5’-TGAGGATGGTGCCCTTGTTC-3’), human GAPDH (forward 5’-AATGGGCAGCCGTTAGGAAA-3’, reverse 5’-GCGCCCAATACGACCAAATC-3’).
Western blotting
The mouse lung tissue and BMDCs were lysed using RIPA buffer (Kaige Biotechnology, Jiangsu, China) containing 1x protease inhibitor, 1x phosphatase inhibitor, and 1x PMSF. After centrifugation at 12,000 rpm for 20 min at 4 °C, the supernatant containing the proteins was collected. The protein concentration was measured using a spectrophotometer (Thermo Fisher Scientific, USA). The proteins were separated by SDS-PAGE gel electrophoresis, then transferred to a PVDF membrane, blocked with 5% BSA at room temperature for 1 h. The primary antibodies rabbit anti-mouse TFEB (diluted 1:2000, Proteintech, Wuhan, China) and β-actin (diluted 1:10000, Zen Bioscience, Chengdu, China) were incubated overnight at 4 °C. The membranes were then incubated with HRP-conjugated goat anti-rabbit IgG (diluted 1:1000, Proteintech, Wuhan, China) at room temperature for 1 h. The chemiluminescence was detected using ECL reagent (Zen Bioscience, Chengdu, China) and visualized with a Bio-Rad imaging system (California, USA). Protein expression was quantified using Image J software.
Statistical analysis
Graph Pad Prism Version 9.5 (Graph Pad Software Inc.) was used for all statistical analyses. Data are presented as mean ± s.e.m. of at least 3 independent experiments. Statistical comparisons were performed with analyzes of variance (ANOVA) or two-tailed Student’s t-test with paired or unpaired wherever appropriate. A P value < 0.05 was considered statistically significant.
TFEB appears as an up-regulated gene within the RNA-seq findings of BMDCs
In the analysis of the RNA-seq results of BMDCs, we observed that TFEB is a gene that is differentially expressed, with its expression being up-regulated in BMDCs following HDM treatment (Fig. 1 A). Additionally, the KEGG Classification results exhibit associations with the immune system (Fig. 1 B). Notably, the top 30 enriched pathways identified in the KEGG analysis encompass the antigen processing and presentation pathway (Fig. 1 C).
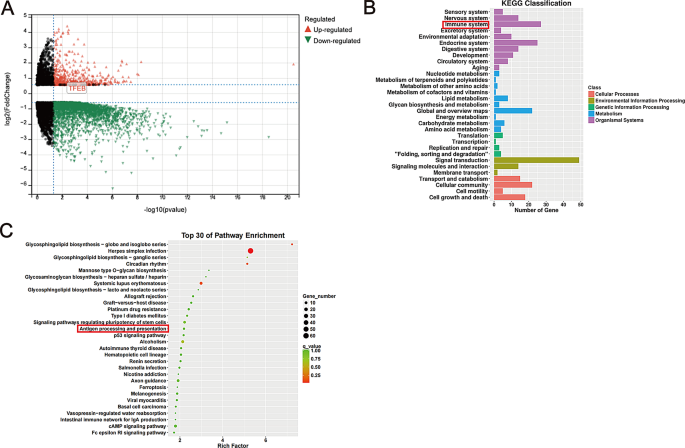
The results of RNA-seq. ( A ) Volcano map of DEGs: Each colored dot represents a DEG based on the criteria of ( P < 0.01) and |log2FC| > 1; red denotes up-regulation, green denotes down-regulation, and black indicates normally expressed mRNA. ( B ) KEGG classification of DEGs in our sequencing results. ( C ) The 30 most significantly enriched KEGG pathways of DEGs in our sequencing results
Characteristics of the subjects
We recruited a total of 38 subjects, comprising 15 healthy children and 23 children diagnosed with asthma (refer to Table 1 ). The mean serum total IgE levels and allergen-specific IgE levels were notably higher in children with asthma compared to their healthy counterparts ( P < 0.05). Among children with asthma, 52.17% were allergic to dust mites. Furthermore, a significantly higher percentage of asthmatic children reported a history of secondhand smoke exposure, as well as a family history of allergy or asthma, in contrast to healthy children ( P < 0.05). Importantly, lung function assessments revealed significantly lower FEV1%pred and FEV1/FVC ratios in children with asthma compared to healthy children, suggesting impaired lung function in the asthmatic group.
Elevated expression of TFEB in PBMCs of children with asthma
Total RNA was extracted from PBMCs of 38 children, followed by reverse transcription into cDNA, and subsequent analysis using RT-qPCR. The results revealed a significantly elevated expression of TFEB mRNA in the PBMCs of children with asthma compared to healthy controls, demonstrating statistical significance (Fig. 2 , P < 0.0001).
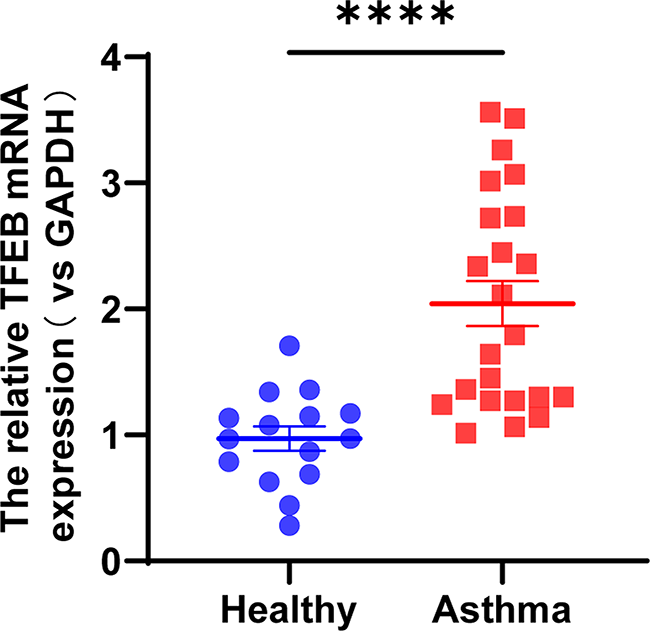
TFEB expression is increased in PBMCs of asthmatic patients. TFEB mRNA expression in PBMCs of healthy subjects ( n = 15) and asthmatic patients ( n = 23). **** P < 0.0001
Exacerbation of pulmonary inflammation in HDM-induced asthmatic mice
To establish a mouse model of asthma, we sensitized and challenged C57BL/6 mice aged 6–8 weeks with HDM (Fig. 3 A). Subsequently, on the 31st day of modeling, the mice were euthanized, and relevant experimental tests and analyses were conducted to validate the successful establishment of the mouse asthma model. The histological analysis of mouse lung tissues using HE staining revealed a marked increase in inflammatory cell infiltration around the trachea, bronchioles, and blood vessels in the asthma group as compared to the control group. Additionally, the lung interstitium exhibited significant thickening (Fig. 3 B). According to the pathological findings, we conducted a scoring of lung inflammation (Fig. 3 C). The results demonstrated a notably higher inflammation score in the lungs of the mice in the asthmatic group compared to those in the control group (Fig. 3 D, P < 0.0001). Compared to the control group, mice in the asthma group showed a significant increase in total cell count, eosinophil count, and neutrophil count in the BALF (Fig. 3 E-F, P < 0.001). Furthermore, non-invasive pulmonary function testing indicated that the lung resistance of both groups of mice increased gradually with the rise of acetyl-β-methylcholine concentration. Once the concentration of acetyl-β-methylcholine reached 12.5 mg/ml, 25 mg/ml, and 50 mg/ml, the lung resistance of the mice in asthma group significantly surpassed that of the mice in control group (Fig. 3 G, P < 0.001).
In addition, the total IgE levels in the serum were determined, revealing significantly higher levels in the asthma group than in the control group (Fig. 3 H, P < 0.0001). ELISA was utilized to measure the levels of IL-4, IL-10, IL-17, and IFN-γ in the BALF of the mice. The findings revealed that the levels of IL-4 and IL-17, as pro-inflammatory cytokines in the BALF of the asthmatic group mice, were significantly higher than those in the control group (Fig. 3 I, P < 0.01). Additionally, no significant variance was observed in the expression levels of IL-10 and IFN-γ between the asthma group and the control group (Fig. 3 I). These findings indicate the successful establishment of a mouse asthma model induced by HDM.
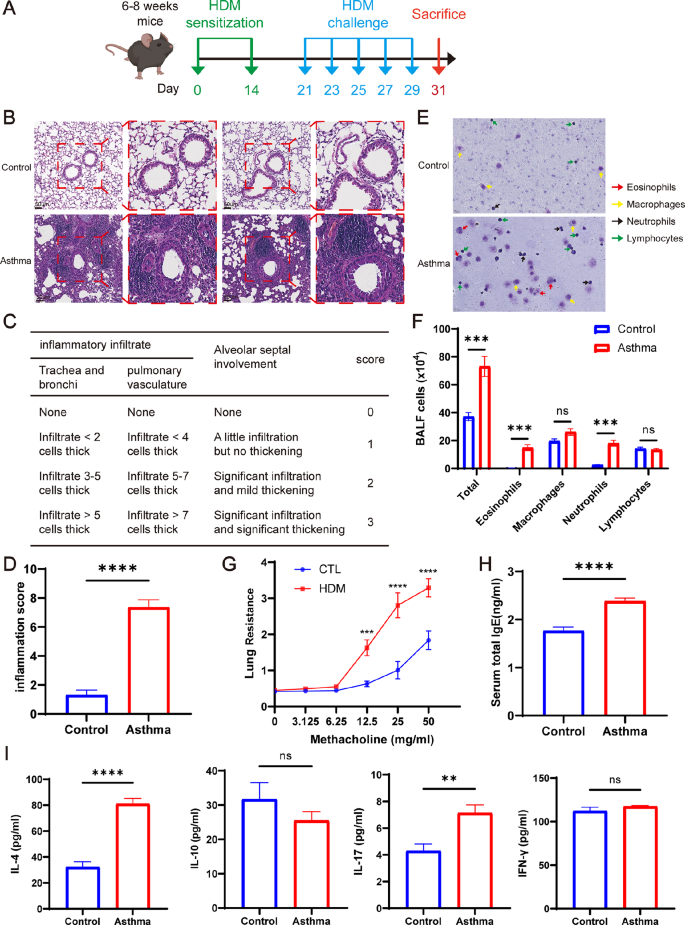
HDM-induced exacerbation of lung inflammation in asthmatic mice. ( A ) Establishment of mice-asthma model induced by HDM. ( B ) Representative lung tissue sections stained with hematoxylin and eosin (H&E). Scale bar = 4 μm. ( C ) Lung tissue inflammation scale in mice. ( D ) The scores of lung inflammation in mice. ( E ) Rachel’s staining of BALF cells. ( F ) Total cell count and leukocyte differential count in BALF. ( G ) Detection of lung resistance in mice after inhalation of methacholine. ( H ) Total serum IgE content of mice. ( I ) Expression of IL-4, IL-10, IL-17 and IFN-γ in BALF supernatant of mice. * P < 0.05; ** P < 0.01; *** P < 0.001 **** P < 0.0001
TFEB expression is increased in the lungs of mice with HDM-induced asthma
To detect TFEB mRNA expression in mouse lungs, RT-qPCR was employed. The results revealed a significantly elevated TFEB mRNA level in the lung tissue of mice within the asthma group compared to the control group (Fig. 4 A, P < 0.01). The Western blot analysis revealed a significant increase in TFEB protein expression in the lung tissue of mice in the asthma group compared to the control group (Fig. 4 B-C, P < 0.01). Immunohistochemistry results showed that the lungs of mice in the asthma group had a large number of inflammatory cells infiltrated and TFEB was highly expressed (Fig. 4 D-E, P < 0.0001). Additionally, immunofluorescence of sections showed significantly higher TFEB expression on DCs in the asthma group compared to the control group (Fig. 4 F-G, P < 0.001). The above results collectively demonstrated an increase in TFEB expression in DCs within the lung tissues of HDM-induced asthmatic mice, corroborating our previous sequencing findings.
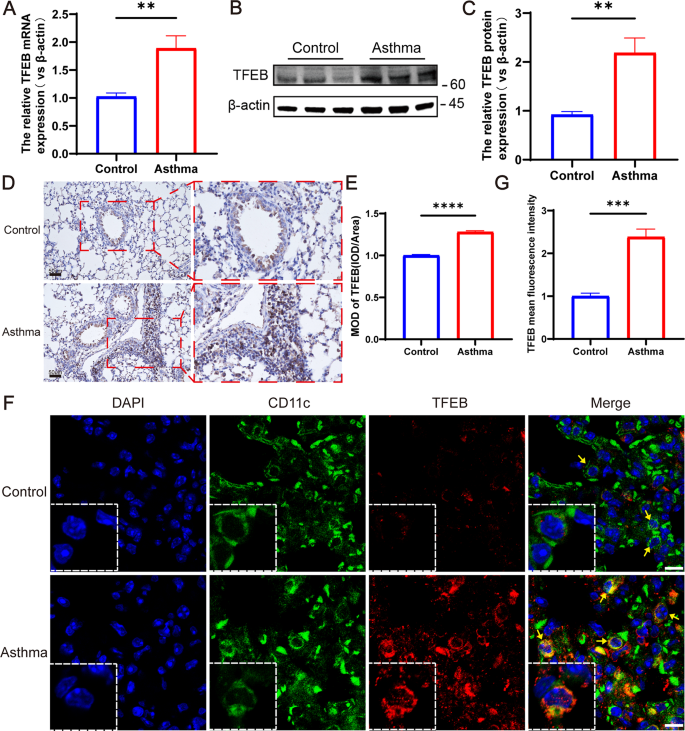
TFEB expression is increased in lung tissues of HDM-induced asthma mice. ( A ) TFEB mRNA expression in lung tissues of HDM-induced asthma mice and control mice. ( B ) Expression and quantification of TFEB protein in lung tissues via western blotting. ( C ) Quantification of western blotting results. ( D ) Immunohistochemical staining of TFEB in lung tissue of mice. ( E ) Quantification of immunohistochemical staining. ( F ) Immunofluorescent staining was performed on lung dendritic cells from mouse lung sections. In the images, blue fluorescence indicates nuclear staining, green fluorescence represents CD11c + dendritic cells, and red fluorescence represents TFEB. ( G ) Mean fluorescence intensity of TFEB in lung tissue immunofluorescence. ** P < 0.01; *** P < 0.001 **** P < 0.0001
TFEB expression increased in mouse BMDCs after HDM stimulation
BMDCs were stimulated with HDM concentrations ranging from 0 to 25 µg/ml for 36 h. The results revealed a concentration-dependent increase in TFEB expression corresponding to the HDM concentration, with the most significant and statistically significant increase observed at 20 µg/ml (Fig. 5 A, P < 0.001). Subsequently, BMDCs were stimulated with a concentration of 20 µg/ml HDM for 36 h, leading to elevated TFEB expression levels compared to the control group, with a statistically significant difference observed at 36 h of stimulation (Fig. 5 B, P < 0.0001). Consequently, we selected to stimulate mouse BMDCs with 20 µg/ml of HDM for 36 h for subsequent experiments. RT-qPCR (Fig. 5 C), western blot (Fig. 5 D-E), and immunofluorescence (Fig. 5 F-G) results demonstrated an elevation in TFEB expression following HDM stimulation of BMDCs ( P < 0.01), with enhanced nuclear expression.
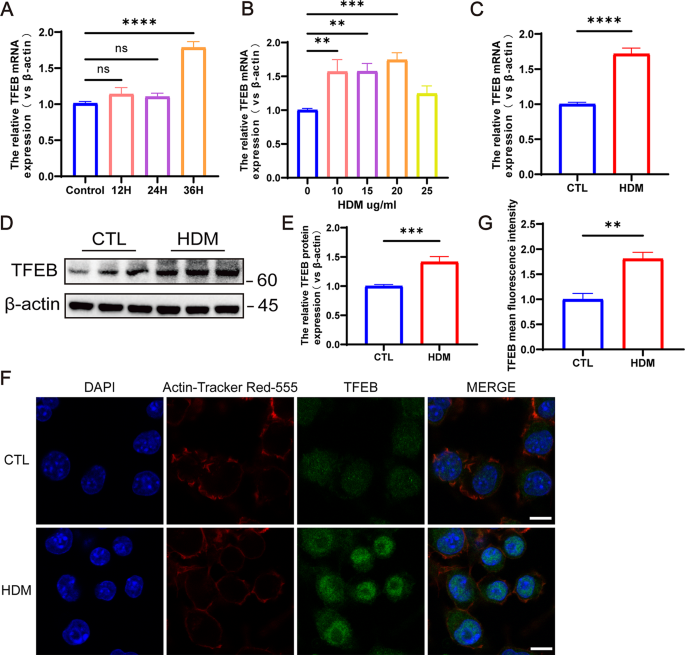
TFEB expression is increased after HDM stimulation of mouse BMDCs. ( A ) TFEB expression in BMDCs stimulated by different concentrations of HDM. ( B ) TFEB expression in BMDCs after HDM stimulation at different times. ( C ) TFEB mRNA expression in BMDCs after 36 h stimulation with HDM at 20 ug/ml. ( D ) TFEB protein expression in BMDCs after 36 h of HDM stimulation at 20 ug/ml. ( E ) Quantification of western blotting results. ( F ) Immunofluorescence staining of TFEB in BMDCs following 36-hour stimulation with 20 µg/ml HDM. Blue fluorescence represents DAPI, red fluorescence represents Actin-Tracker Red-555, and green fluorescence represents TFEB. ( G ) Quantification of the mean fluorescence intensity of TFEB. ** P < 0.01; *** P < 0.001; **** P < 0.0001
TFEB expression is inhibited after transfection of BMDCs with lentivirus
To investigate the role of TFEB in DCs, BMDCs were transfected with LV-shTFEB, and lentiviral transfection was visualized using confocal microscopy (Fig. 6 A). Flow cytometry analysis revealed that approximately 90% of cells were GFP-positive post-transfection (Fig. 6 B). Subsequent RT-qPCR analysis showed that LV-shTFEB-3 achieved the most effective knockdown, resulting in a significant reduction of approximately 50% in TFEB expression (Fig. 6 C, P < 0.001). Consequently, LV-shTFEB-3 was selected for further experiments. Western blot results confirmed the successful knockdown of TFEB (Fig. 6 D-E, P < 0.0001). Immunofluorescence analysis further demonstrated a reduction in TFEB expression following lentiviral transfection of BMDCs (Fig. 6 F-G, P < 0.0001). These findings collectively indicate that LV-shTFEB effectively reduces TFEB expression after BMDCs transfection.
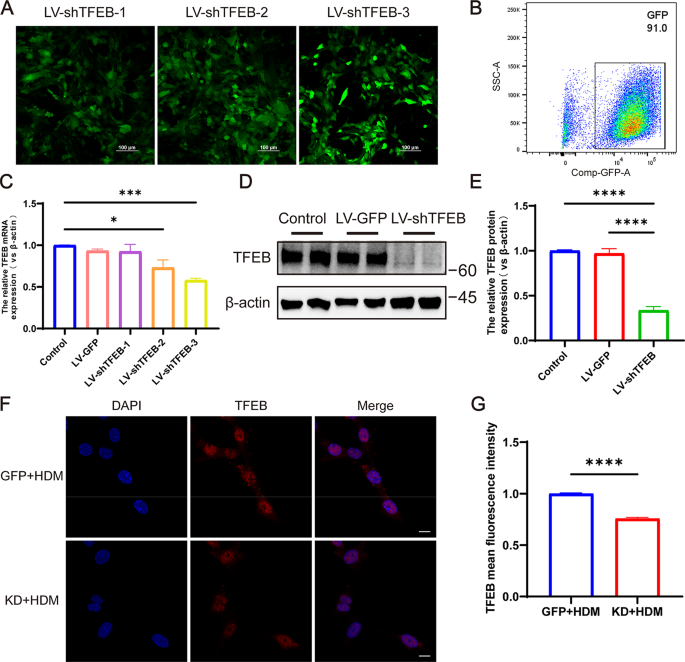
TFEB expression decreased after transfection of BMDCs with lentivirus. ( A ) Confocal microscopy of three lentivirally transfected BMDCs. ( B ) The transfection efficiency of cells by flow cytometry. ( C ) The expression of TFEB mRNA in BMDCs after transfection with 3 different lentiviruses. ( D ) Western blots analysis of TFEB from these three groups. ( E ) Quantification of western blotting results. ( F ) Immunofluorescent staining for TFEB in HDM-treated LV-GFP and LV-shTFEB BMDCs. ( G ) Quantification of the mean fluorescence intensity of TFEB. * P < 0.05; *** P < 0.001 **** P < 0.0001
Knockdown of TFEB inhibits the migratory capacity of BMDCs
The migration ability can reflect the antigen presentation and activation status of BMDCs. Therefore, we first investigated whether knocking down TFEB affects the migration ability of BMDCs. The cell wound healing assay results demonstrated a significant inhibition of BMDCs migration following TFEB knockdown (Fig. 7 A-B, P < 0.01). Next we co-cultured BMDCs knocked down TFEB with spleen T cells (Fig. 7 C). As previously mentioned, the migration of DCs to lymph nodes may be positively regulated by the TFEB-TRPML1 axis, so we examined the expression levels of TRPML1 molecules in the co-cultured cells by RT-qPCR. We found that the expression of TRPML1 molecules was elevated after HDM stimulation of the co-cultured cells (Fig. 7 D, P < 0.05), and the expression of TRPML1 molecules was significantly decreased after knockdown of TFEB (Fig. 7 D, P < 0.0001).
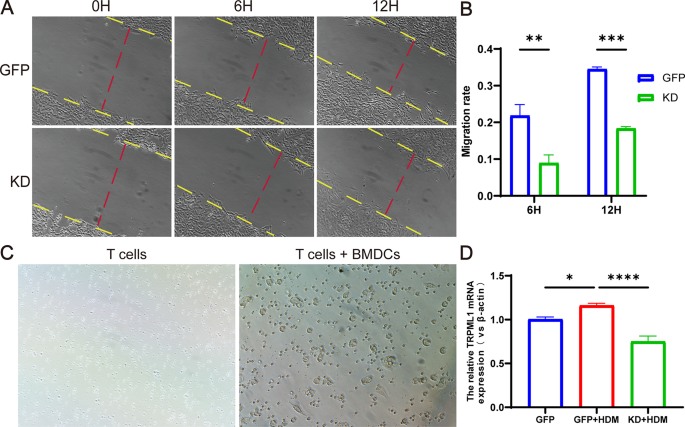
Knockdown of TFEB inhibits the migratory capacity of BMDCs. ( A ) The migratory capacity of BMDCs determined by wound healing assays. ( B ) Quantification of Wound-Healing Assay results. ( C ) BMDCs were co-cultured with spleen T cells. ( D ) The expression of TRPML1 mRNA in co-cultured cells detected by RT-qPCR. * P < 0.05; ** P < 0.01; *** P < 0.001; **** P < 0.0001
Knockdown of TFEB inhibits BMDCs’ antigen presentation capability
In order to investigate whether knocking down TFEB affects the antigen presentation process of BMDCs, we first used flow cytometry to detect the expression of antigen recognition molecule MHCII and co-stimulatory molecules CD40, CD80, and CD86 on the surface of BMDCs in co-cultured cells to assess the antigen presentation ability of BMDCs. The results revealed that following HDM stimulation, the Mean Fluorescence Intensity (MFI) of surface molecules MHCII, CD40, CD80, and CD86 on BMDCs increased. However, upon knockdown of TFEB, these MFIs decreased significantly (Fig. 8 A-B, P < 0.05).
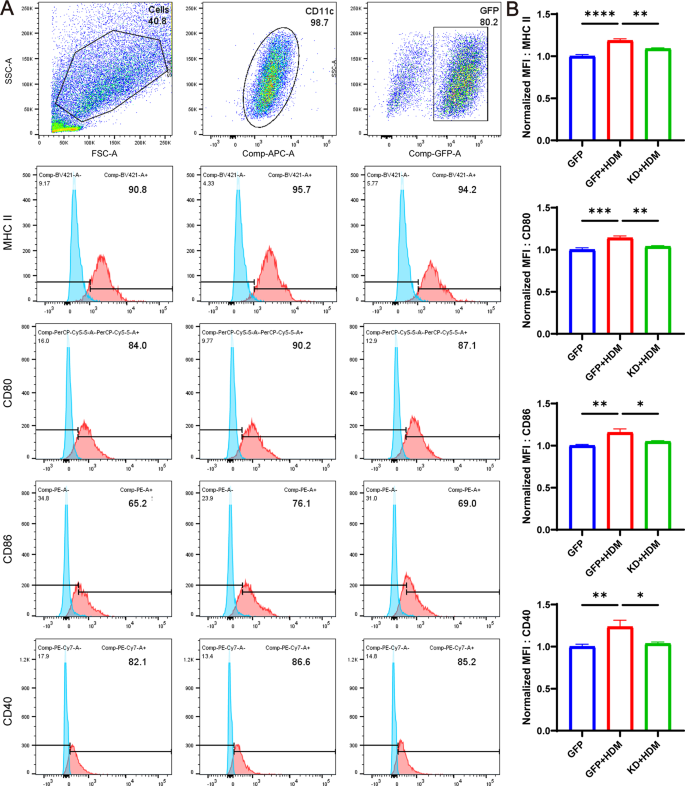
Knockdown of TFEB inhibits the antigen presentation ability of BMDCs. ( A ) The expression of MHC II, CD80, CD86 and CD40 molecules on the surface of BMDCs was analyzed by flow cytometry. ( B ) Statistical analysis of flow cytometry. * P < 0.05; ** P < 0.01; *** P < 0.001; **** P < 0.0001
Knockdown of TFEB in BMDCs co-cultured with T cells can reshape the balance of Th1/Th2 and Treg/Th17 cells
In order to further investigate the impact of BMDCs on T cell subpopulation differentiation after knockdown of TFEB, we examined the expression levels of factors such as FOXP3, RORγ-T, GATA3 and T-bet in co-cultured cells by RT-qPCR. Compared with the control group, the expression of FOXP3 and T-bet in co-cultured cells after HDM stimulation was significantly decreased, while the expression of RORγ-T and GATA3 was significantly increased. However, knockdown of TFEB resulted in increased expression of FOXP3 and T-bet and decreased expression of RORγ-T and GATA3 in co-cultured cells (Fig. 9 A, P < 0.05). To examine the impact of TFEB knockdown on cytokine secretion by BMDCs and T cells, we used RT-qPCR to detect the expression levels of cytokine mRNA such as IL-6, IL-10, IL-12, IFN-γ, IL-4, IL-5, and IL-13 in co-cultured cells. Additionally, we measured the expression of IL-4, IFN-γ and IL-17 in the supernatants of co-cultured cell medium through ELISA. After HDM stimulation, we observed a decrease in IFN-γ secretion by T cells, an increase in the expression of IL-4, IL-5, IL-13, and an elevation in IL-17 secretion. These alterations were mitigated following TFEB knockdown (Fig. 9 B-C, P < 0.05). It indicates that knocking down TFEB alters the expression or secretion of pro-inflammatory/anti-inflammatory cytokines, which may be related to its reshaping of the balance of Th1/Th2 and Treg/Th17 cells.
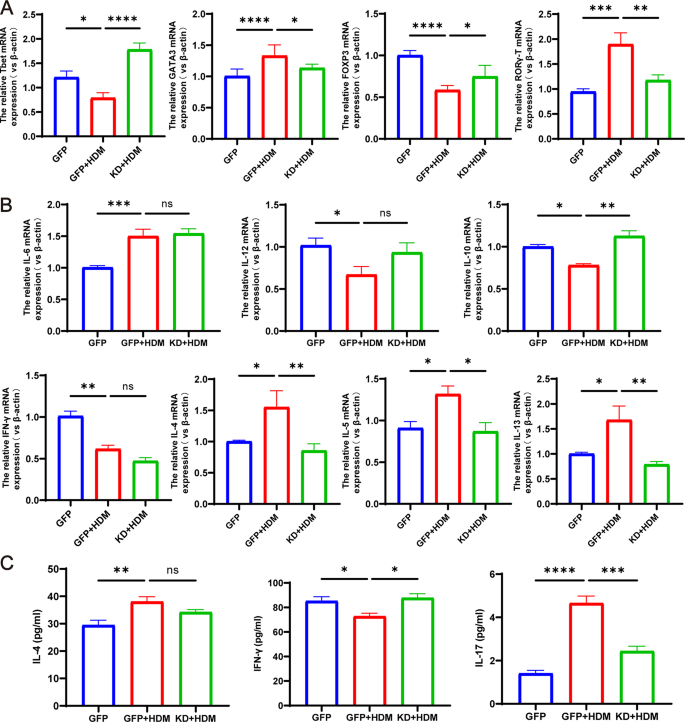
Co-culture of TFEB-knockdown BMDCs with T cells remodels the balance of Th1/Th2 and Treg/Th17 cells. ( A ) T- bet, GATA3, Foxp3 and RORγt mRNA expression in each group. ( B ) The expression of IL-6, IL-12, IL-10, IFN-γ, IL-4, IL-5 and IL-13 in co-cultured cells detected by RT-qPCR. ( C ) Expression of IL-4, IFN-γ and IL-17 in the supernatant of co-cultured cells detected by ELISA. * P < 0.05; ** P < 0.01; *** P < 0.001; **** P < 0.0001
In this study, our initial RNA-seq analysis validated the differential expression of the TFEB gene in HDM-induced BMDCs, suggesting its potential involvement in immune system modulation and antigen presentation pathways. Next, we confirmed the increased expression of TFEB in PBMCs from asthmatic children as well as in the lung tissues of asthmatic mice. By constructing a co-culture system of BMDCs and T cells, we observed that knocking down TFEB inhibited the migration and surface expression of antigen presentation and co-stimulatory molecules of BMDCs. The above results indicate that the knockdown of TFEB inhibited the antigen presentation process of DCs. Furthermore, we observed that the knockdown of TFEB affected the differentiation of naïve T cells, resulting in a decrease in the expression or secretion of pro-inflammatory cytokines and an increase in the expression or secretion of anti-inflammatory cytokines. This led to a re-regulation of the balance between Th1/Th2 and Treg/Th17 cells (Fig. 10 ).
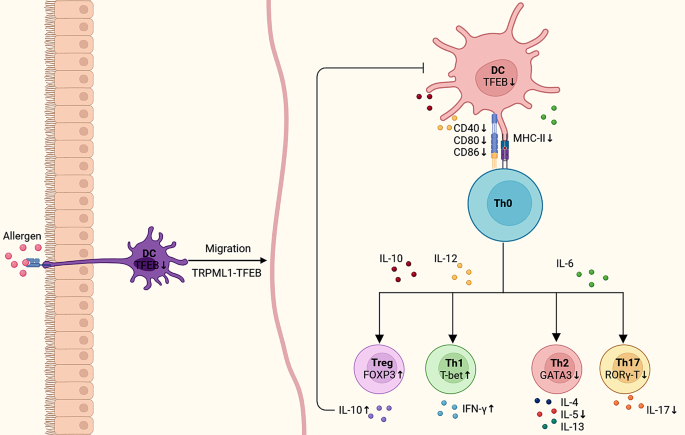
Schematic representation of knockdown of TFEB regulating Th0 cell subpopulation differentiation through inhibition of dendritic cell antigen presentation. The suppression of TFEB hindered the migratory ability of dendritic cells and reduced the surface expression of CD40, CD80, CD86, and MHC-II on DC cells, thereby impacting the differentiation of Th0 cell subtypes. This inhibition led to decreased expression of pro-inflammatory factors and increased expression of anti-inflammatory factors, ultimately rebalancing the Th1/Th2 and Treg/Th17 cell equilibrium
The pathogenesis of asthma is very complex, and it is currently believed to be mainly related to the antigen presentation of dendritic cells and T cell activation [ 19 , 20 ]. Dendritic cells are considered to be the most important antigen-presenting cells, mediating immune responses and tolerance of T cells by continuously presenting co-stimulatory molecules and/or cytokines to T cells [ 21 ]. The activation of T cells requires the completion of a dual-signal pathway involving DCs, which includes the antigen recognition signal and the co-stimulatory signal. The antigen recognition signal acts as the first signal, during which dendritic cells present exogenously derived peptide antigens to CD8 + T cells and CD4 + T cells by expressing MHC class I and MHC class II molecules. The co-stimulatory molecules on the surface of dendritic cells then bind to and interact with the corresponding receptors on the surface of T cells to initiate a second signal, the coordinated stimulatory signal [ 22 , 23 , 24 ]. In asthma, dendritic cells present antigens to CD4 + T cells by expressing MHC class II molecules and rely on co-stimulatory molecules such as CD40, CD80, CD86 to induce T cell activation [ 20 , 25 ]. In addition, the cytokines secreted by DCs after antigen stimulation can also regulate the subset differentiation of naïve T helper cells [ 26 , 27 ]. Among them, IL-12 and IFN-γ are important cytokines in inducing the differentiation of Th0 cells into Th1 cells [ 28 ]. IL-6 induces Th0 to Th2 and/or Th17 differentiation [ 29 ]. Whereas IL-10 induces the differentiation of Th0 cells into Treg cells. At the same time, IL-10 can also act on DCs to inhibit their maturation and suppress the expression of MHC-II, co-stimulatory molecules, and chemokines [ 27 , 30 , 31 ]. Therefore, after clarifying the antigen presentation of DCs and the immune response process of T cells in asthma, we want to identify important regulatory targets for this process from the source, in order to provide more effective prevention and treatment for asthma.
TFEB is one of the MiTF/TFE family members of the leucine zip (bHLH-LZ) class of transcription factors, which have been found to potentially play an important role in a variety of diseases such as lysosomal storage disorders, neurodegenerative diseases, hepatic metabolic disorders, obesity, and others [ 9 , 10 , 32 ]. Liu et al. found that promotion of nuclear translocation in tumour cell TFEB was able to induce PD-L1 degradation and mediate anti-tumour immune responses [ 33 ]. In another study, TFEB was also shown to synergistically regulate the involvement of B cells in the humoral immune response by regulating CD40L expression in T cells [ 11 ]. Furthermore, in a mouse model of autoimmune disease, deletion of TFEB in Treg cells resulted in reduced Treg accumulation and impaired Treg function [ 34 ]. The above studies suggest that TFEB may play an important role in regulating immune cell-mediated immune responses. Based on the above research background, we want to understand whether TFEB is involved in the immune response of asthma DCs. Our study results first suggested that TFEB has differential expression in asthma DCs, and may be involved in antigen presentation and the immune response process. The above results lay the groundwork for further exploration of the role of TFEB in antigen presentation by DCs. Recent studies have identified TFEB as a key transcription factor regulating lysosomes, and the migration of DCs from the periphery to the lymph nodes is controlled by a positive feedback loop mediated by the TFEB-TRPML1 axis in lysosomes [ 16 , 35 ]. In this study, we also observed that after knocking down TFEB, the migration of BMDCs was significantly inhibited, and the expression of TRPML1 in BMDCs decreased. At the same time, our research results also suggest that knocking down TFEB will inhibit the expression of MHC II molecules, as well as co-stimulatory molecules CD80, CD86, and CD40 on the surface of BMDCs, indicating that TFEB may be involved simultaneously in antigen recognition and co-stimulation of DCs, affecting the antigen presentation process of DCs.
It is currently believed that the imbalance of Th1/Th2 and/or Th17/Treg cell subgroups and the excessive secretion of cytokines are critical factors in the pathogenesis of allergic asthma [ 36 , 37 , 38 , 39 ]. Therefore, we further investigated whether regulating the expression of TFEB affects the differentiation of Th0 cell subgroups and the expression of cytokines. Initially, we investigated the mRNA expression of T-bet, GATA3, RORγ-T, and Foxp3 in co-culture systems of BMDCs and T cells induced by HDM. These transcription factors play a crucial role in regulating the differentiation of Th0 cells into Th1, Th2, Th17, and Treg cells, respectively, and thus were utilized to signify the differentiation of subpopulations within the Th0 cells [ 40 , 41 , 42 ]. Our results indicate that the expression of GATA3 and RORγ-T decreased after knocking down TFEB, while the expression of T-bet and FOXP3 increased. This suggests that the differentiation of Th0 towards Th2 and Th17 is inhibited after knocking down TFEB, while the differentiation towards Th1 and Treg is increased. Therefore, knocking down TFEB can rebalance the Th1/Th2 and Treg/Th17 cells. In addition, the differentiation of Th0 cells may also be regulated by the cytokines secreted by DCs [ 27 ]. However, our research results show that the knockdown of TFEB did not significantly alter the cytokines (IL-6 and IL-12) secreted by DCs, indicating that TFEB does not completely depend ons this pathway but is more likely to affect the differentiation of T cells by inhibiting the antigen presentation process of DCs.
It is well known that IFN-γ, IL-4/IL-5/IL-13 and IL-17 are pro-inflammatory cytokines expressed or secreted by activated Th1, Th2 and TH17 cells, respectively, and play key roles in various immune diseases [ 42 ]. In contrast, Treg cells can express or secrete the anti-inflammatory cytokine IL-10, which is thought to have immunosuppressive functions and play an important role in immune tolerance [ 43 , 44 ]. In this study, we found that knockdown of TFEB inhibited the expression of IL-4, IL-5, and IL-13, while inhibiting the secretion of IL-17, and increasing the secretion of IFN-γ and the expression of IL-10. The aforementioned findings suggest that upon TFEB knockdown in DCs, there is a decrease in pro-inflammatory factors and an increase in anti-inflammatory factors, providing additional evidence that modulating TFEB can recalibrate the Th1/Th2 and Treg/Th17 cell balance.
In summary, our study demonstrated up-regulation of TFEB expression in asthmatic dendritic cells. Manipulating TFEB expression enabled regulation of dendritic cell migration and antigen presentation processes, modulation of the immune response of CD4 + T cells, and remodeling of the subpopulation balance of Th1/Th2 and Th17/Treg cells. These findings are anticipated to identify new therapeutic targets for preventing and treating asthma, with potential clinical applications.
Data availability
All data generated or analysed during this study are included in this published article. The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request. Data obtained from RNA-seq, which provide the evidence for the conclusions made in this study, are supervised by FengXia Ding. Access to these data is restricted, as they were generated under a license specific to the current study and are not publicly available. Nonetheless, the author can make the data available upon reasonable request and with FengXia Ding’s permission. FengXia Ding’spermission.
Abbreviations
Dendritic cells
Transcription Factor EB
House dust mite
Bone marrow dendritic cells
Peripheral blood mononuclear cells
Regulatory T cell
Differential genes
RNA sequencing
Hematoxylin and eosin
Airway hyperresponsiveness
Enzyme-linked immunosorbent assay
Immunohisto-chemical
Mean optical density
Bronchoalveolar lavage fluid
Lentiviral vectors
Green fluorescent protein
Fuchs O, Bahmer T, Rabe KF, von Mutius E. Asthma transition from childhood into adulthood. Lancet Respiratory Med. 2017;5(3):224–34.
Article Google Scholar
Holgate ST, Wenzel S, Postma DS, Weiss ST, Renz H, Sly PD. Asthma Nat Reviews Disease Primers. 2015;1(1).
Brusselle GG, Taichman DB, Koppelman GH. Biologic therapies for severe asthma. N Engl J Med. 2022;386(2):157–71.
Article CAS PubMed Google Scholar
Kashem SW, Igyarto BZ, Gerami-Nejad M, Kumamoto Y, Mohammed JA, Jarrett E, et al. Candida albicans morphology and dendritic cell subsets determine T helper cell differentiation. Immunity. 2015;42(2):356–66.
Article CAS PubMed PubMed Central Google Scholar
Morianos I, Semitekolou M. Dendritic cells: critical regulators of allergic asthma. Int J Mol Sci. 2020;21(21).
Hasegawa H, Matsumoto T. Mechanisms of Tolerance induction by dendritic cells in vivo. Front Immunol. 2018;9:350.
Article PubMed PubMed Central Google Scholar
Hammad H, Lambrecht BN. Barrier epithelial cells and the control of type 2 immunity. Immunity. 2015;43(1):29–40.
Semitekolou M, Morianos I, Banos A, Konstantopoulos D, Adamou-Tzani M, Sparwasser T, et al. Dendritic cells conditioned by activin A-induced regulatory T cells exhibit enhanced tolerogenic properties and protect against experimental asthma. J Allergy Clin Immunol. 2018;141(2):671-84.e7.
Tan A, Prasad R, Lee C, Jho EH. Past, present, and future perspectives of transcription factor EB (TFEB): mechanisms of regulation and association with disease. Cell Death Differ. 2022;29(8):1433–49.
Napolitano G, Ballabio A. TFEB at a glance. J Cell Sci. 2016.
Brady OA, Martina JA, Puertollano R. Emerging roles for TFEB in the immune response and inflammation. Autophagy. 2017;14(2):181–9.
El-Houjeiri L, Possik E, Vijayaraghavan T, Paquette M, Martina JA, Kazan JM, et al. The transcription factors TFEB and TFE3 link the FLCN-AMPK Signaling Axis to Innate Immune Response and Pathogen Resistance. Cell Rep. 2019;26(13):3613–e286.
Huan C, Kelly ML, Steele R, Shapira I, Gottesman SR, Roman CA. Transcription factors TFE3 and TFEB are critical for CD40 ligand expression and thymus-dependent humoral immunity. Nat Immunol. 2006;7(10):1082–91.
Samie M, Cresswell P. The transcription factor TFEB acts as a molecular switch that regulates exogenous antigen-presentation pathways. Nat Immunol. 2015;16(7):729–36.
Joffre OP, Segura E, Savina A, Amigorena S. Cross-presentation by dendritic cells. Nat Rev Immunol. 2012;12(8):557–69.
Bretou M, Sáez PJ, Sanséau D, Maurin M, Lankar D, Chabaud M, et al. Lysosome signaling controls the migration of dendritic cells. Sci Immunol. 2017;2:16.
Wang Y, Liao K, Liu B, Niu C, Zou W, Yang L et al. GITRL on dendritic cells aggravates house dust mite-induced airway inflammation and airway hyperresponsiveness by modulating CD4 + T cell differentiation. Respir Res. 2021;22(1).
Global Initiative for Asthma. Global strategy for Asthma Management and Prevention,2023.Updated July 2023. Available from: www.ginasthma.org.
Hammad H, Kool M, Soullié T, Narumiya S, Trottein F, Hoogsteden HC, et al. Activation of the D prostanoid 1 receptor suppresses asthma by modulation of lung dendritic cell function and induction of regulatory T cells. J Exp Med. 2007;204(2):357–67.
Vroman H, Hendriks RW, Kool M. Dendritic cell subsets in Asthma: impaired tolerance or exaggerated inflammation? Front Immunol. 2017;8:941.
Eisenbarth SC. Dendritic cell subsets in T cell programming: location dictates function. Nat Rev Immunol. 2019;19(2):89–103.
Waisman A, Lukas D, Clausen BE, Yogev N. Dendritic cells as gatekeepers of tolerance. Semin Immunopathol. 2016;39(2):153–63.
Article PubMed Google Scholar
Bar-On L, Birnberg T, Kim KW, Jung S. Dendritic cell-restricted CD80/86 deficiency results in peripheral regulatory T-cell reduction but is not associated with lymphocyte hyperactivation. Eur J Immunol. 2011;41(2):291–8.
Waisman A, Lukas D, Clausen BE, Yogev N. Dendritic cells as gatekeepers of tolerance. Semin Immunopathol. 2017;39(2):153–63.
Schuijs MJ, Hammad H, Lambrecht BN. Professional and ‘Amateur’ Antigen-presenting cells in type 2 immunity. Trends Immunol. 2019;40(1):22–34.
Ohno Y, Kitamura H, Takahashi N, Ohtake J, Kaneumi S, Sumida K, et al. IL-6 down-regulates HLA class II expression and IL-12 production of human dendritic cells to impair activation of antigen-specific CD4(+) T cells. Cancer Immunol Immunother. 2016;65(2):193–204.
Yin X, Chen S, Eisenbarth SC. Dendritic cell regulation of T Helper cells. Annu Rev Immunol. 2021;39(1):759–90.
Conejero L, Khouili SC, Martínez-Cano S, Izquierdo HM, Brandi P, Sancho D. Lung CD103 + dendritic cells restrain allergic airway inflammation through IL-12 production. JCI Insight. 2017;2(10).
Heink S, Yogev N, Garbers C, Herwerth M, Aly L, Gasperi C, et al. Trans-presentation of IL-6 by dendritic cells is required for the priming of pathogenic T(H)17 cells. Nat Immunol. 2017;18(1):74–85.
Clement M, Ladell K, Miners KL, Marsden M, Chapman L, Cardus Figueras A et al. Inhibitory IL-10-producing CD4(+) T cells are T-bet-dependent and facilitate cytomegalovirus persistence via coexpression of arginase-1. Elife. 2023;12.
Qiao J, Liu Z, Dong C, Luan Y, Zhang A, Moore C, et al. Targeting tumors with IL-10 prevents dendritic cell-mediated CD8(+) T cell apoptosis. Cancer Cell. 2019;35(6):901–e154.
Goding CR, Arnheiter H. MITF-the first 25 years. Genes Dev. 2019;33(15–16):983–1007.
Liu X, Yin M, Dong J, Mao G, Min W, Kuang Z, et al. Tubeimoside-1 induces TFEB-dependent lysosomal degradation of PD-L1 and promotes antitumor immunity by targeting mTOR. Acta Pharm Sin B. 2021;11(10):3134–49.
Xia M, Zhang C, Chen Y, Zhao X, Zhang S, Liu Y, et al. Transcription factor EB coordinates environmental cues to regulate T regulatory cells’ mitochondrial fitness and function. Proc Natl Acad Sci U S A. 2022;119(31):e2205469119.
Idoyaga J, Fiorese C, Zbytnuik L, Lubkin A, Miller J, Malissen B, et al. Specialized role of migratory dendritic cells in peripheral tolerance induction. J Clin Invest. 2013;123(2):844–54.
CAS PubMed PubMed Central Google Scholar
Hirahara K, Nakayama T. CD4 + T-cell subsets in inflammatory diseases: beyond the Th1/Th2 paradigm. Int Immunol. 2016;28(4):163–71.
Norimoto A, Hirose K, Iwata A, Tamachi T, Yokota M, Takahashi K, et al. Dectin-2 promotes house dust mite-induced T helper type 2 and type 17 cell differentiation and allergic airway inflammation in mice. Am J Respir Cell Mol Biol. 2014;51(2):201–9.
Lambrecht BN, Hammad H. The immunology of asthma. Nat Immunol. 2015;16(1):45–56.
Ding F, Fu Z, Liu B. Lipopolysaccharide exposure alleviates asthma in mice by regulating Th1/Th2 and Treg/Th17 Balance. Med Sci Monit. 2018;24:3220–9.
Chalmin F, Humblin E, Ghiringhelli F, Végran F. Transcriptional programs underlying Cd4 T cell differentiation and functions. Int Rev Cell Mol Biol. 2018;341:1–61.
Chen W, Cao Y, Zhong Y, Sun J, Dong J. The mechanisms of Effector Th cell responses contribute to Treg cell function: New insights into Pathogenesis and Therapy of Asthma. Front Immunol. 2022;13:862866.
Zhu JT, Helper Cell. Differentiation, heterogeneity, and plasticity. Cold Spring Harb Perspect Biol. 2018;10(10).
Boonpiyathad T, Satitsuksanoa P, Akdis M, Akdis CA. Il-10 producing T and B cells in allergy. Semin Immunol. 2019;44:101326.
van Oosterhout AJ, Bloksma N. Regulatory T-lymphocytes in asthma. Eur Respir J. 2005;26(5):918–32.
Download references
Acknowledgements
We wish to thank Dr. RuiZong Wang from Chongqing Medical University Children’s Hospital for assistance in the successful implementation of this study.
Author information
Authors and affiliations.
Department of Respiratory Medicine, Ministry of Education Key Laboratory of Child Development and Disorders, Chongqing Engineering Research Center of Stem Cell Therapy, National Clinical Research Center for Child Health and Disorders, China International Science and Technology Cooperation base of Child development and Critical Disorders, Children’s Hospital of Chongqing Medical University, No. 136, Zhongshan 2nd Road, Yuzhong Dis, 400014, Chongqing, PR China
JinYing Xiang, Yan Li, Yinying Ren, Yuehan Li, Mi Zhou, Zhengxiu Luo, Enmei Liu, Zhou Fu & Fengxia Ding
Department of Cardiothoracic Surgery, Ministry of Education Key Laboratory of Child Development and Disorders, Chongqing Engineering Research Center of Stem Cell Therapy, National Clinical Research Center for Child Health and Disorders, China International Science and Technology Cooperation base of Child development and Critical Disorders, Children’s Hospital of Chongqing Medical University, No. 136, Zhongshan 2nd Road, Yuzhong Dis, 400014, Chongqing, PR China
Bristol Medical School, University of Bristol, Bristol, UK
Great Ormond Street Institute of Child Health, University College London, London, UK
You can also search for this author in PubMed Google Scholar
Contributions
J.X., E.L., Z.L., Z.F., B.L. and F.D. were responsible for the overall conception and design of the study. J.X. performed most of the experiments and the data analysis, collected the data, and wrote the manuscript. J.Y., B.L. and F.D. revising the manuscript. Y.L., Y.R., Y.H.L. and M.Z. contributed to the sample collection. All authors reviewed, edited and approved the manuscript.
Corresponding authors
Correspondence to Bo Liu or Fengxia Ding .
Ethics declarations
Ethics approval and consent to participate.
The animal and human experiments were approved by the Ethics Committee of the Children’s Hospital of Chongqing Medical University (No. 2022-006/2023 − 225). The animal experiments adhered to the guidelines for the care and use of laboratory animals approved by the Institutional Animal Care and Use Committee (IACUC). The human experiments were conducted in compliance with the principles of the Helsinki Declaration, and informed consent was obtained from the children’s guardians.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Xiang, J., Liu, B., Li, Y. et al. TFEB regulates dendritic cell antigen presentation to modulate immune balance in asthma. Respir Res 25 , 182 (2024). https://doi.org/10.1186/s12931-024-02806-1
Download citation
Received : 28 November 2023
Accepted : 04 April 2024
Published : 25 April 2024
DOI : https://doi.org/10.1186/s12931-024-02806-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Dendritic cell
- Antigen presentation
Respiratory Research
ISSN: 1465-993X
- General enquiries: [email protected]
- Original research article
- Open access
- Published: 08 July 2014
Bronchial asthma and chronic obstructive pulmonary disease: research activity in Arab countries
- Waleed M Sweileh 1 ,
- Samah W Al-Jabi 2 ,
- Sa’ed H Zyoud 2 &
- Ansam F Sawalha 1
Multidisciplinary Respiratory Medicine volume 9 , Article number: 38 ( 2014 ) Cite this article
8105 Accesses
15 Citations
1 Altmetric
Metrics details
Chronic respiratory diseases, like bronchial asthma and chronic obstructive pulmonary disease (COPD), are a worldwide health problem. Quantitative and qualitative assessment of asthma and COPD-related research from Arab countries has not been explored and there are few internationally published reports on such field. The main objectives of this study were to analyze research output originating from Arab countries in the field of bronchial asthma and COPD.
Original scientific articles or reviews published from the 22 Arab countries were screened using specific words pertaining to asthma and COPD using Scopus database and search engine. Research productivity was evaluated based on: (a) total and trends of contribution of each Arab country to asthma and COPD research and (b) journals in which researchers from Arab countries published their research.
The total number of original research and review articles published globally about bronchial asthma and COPD was 163,964. The leading country in bronchial asthma and COPD research was United States of America (38,632; 23.56%). Worldwide, Turkey ranked 19th while Israel and Iran ranked 25th and 29th respectively. Among Arab countries, Egypt and Kingdom of Saudi Arabia came on positions 39th and 43rd, respectively. A total of 1,304 documents about bronchial asthma and COPD were published from Arab countries which represents 0.8% of the global research output. Research in bronchial asthma was almost double that in COPD. Research from Arab countries was low and showed a significant increase after 2000. Approximately 12% of research activity in asthma and COPD from Arab countries was published in Saudi Medical Journal, Annals of Saudi Medicine, Eastern Mediterranean Health Journal and Tunisie Medicale . Kingdom of Saudi Arabia, with a total publication of 353 (27.07%) ranked first among the Arab countries while University of Kuwait was the most productive institution with a total of 123 (9.43%) documents.
Conclusions
The present data showed relatively low research productivity about bronchial asthma and COPD in Arab countries. Research output can be improved by investing more in international and national collaborative research projects in the field of asthma and COPD.
Chronic respiratory diseases are chronic diseases of the airways and other parts of the lung. Bronchial asthma and chronic obstructive pulmonary disease (COPD) are the most common types of chronic respiratory diseases [ 1 ]. The global burden of asthma and COPD is increasing and it is estimated that more than 500 million people suffer from bronchial asthma and COPD ( http://www.who.int/respiratory/en/ ) [ 2 ]. The world health organization (WHO) is leading a global effort to expand understanding of chronic obstructive pulmonary disease (COPD) and advocate for better patients care. One such aspect of fighting COPD is carried out through the “Global Alliance against Chronic Respiratory Diseases” (GARD) which is a global alliance dedicated to reduce the global burden of COPD ( http://www.who.int/respiratory/gard/en/ ). The WHO also plays a major role in coordinating international efforts against bronchial asthma to reduce the disability and premature death related to asthma particularly in low and middle income member countries. Another global alliance for asthma is GINA which was launched in 1993 in collaboration with the National Heart, Lung, and Blood Institute, National Institutes of Health, USA, and the World Health Organization ( http://www.ginasthma.org/ ).
Research about bronchial asthma and COPD is one important aspect that each country needs to provide in the struggle against such emotionally difficult type of chronic diseases. Research in chronic respiratory diseases will shed light on the environmental and genetic risk factors as well as cultural and regional differences in the epidemiology of such diseases. An important goal of medical research is to help in initiating communication, exchange of findings and building a network of scientists sharing similar research interest. One thoughtful approach to achieve and implement such goal is through assessing and evaluating research productivity in a particular field or particular disease. It is believed that the quality, quantity and type of research publications shape up the prestige of the researcher and the research institution. Furthermore, the annual number and type of research from a particular institute or country reflects the health concern and health agenda of that country. Research about bronchial asthma and COPD can positively reflect on clinical practice in any particular region.
One method to assess research contribution from any country is bibliometric analysis which refers to the implementation of statistical methods for evaluating the research productivity, for individuals, institutes and countries [ 3 ]. Bibliometric analysis is a useful tool to obtain information about the current state of research in particular areas [ 4 – 6 ]. Bibliometrics has been applied to various diseases and is now widely accepted as a method of measuring research and literacy output in any particular area [ 7 – 14 ]. Therefore, the objective of this study was to analyze research output from 22 Arab countries about bronchial asthma and COPD. The Arab countries cover a large geographic area including North Africa and the Arabic Peninsula with around 380 million inhabitants. Up to the authors’ knowledge, no bibliometric studies have been published from the Arab world about bronchial asthma and/or COPD. Such study will lead to a better understanding of the past, current and future status of research in chronic respiratory diseases in the Arab world which, hopefully, can lead to better preventive disease strategies and better patient-oriented health services [ 15 – 19 ]. The results of the study will help health policy makers and people in academia and clinical practice to shape up bronchial asthma and COPD research in the future. In addition, research activity needs to be encouraged and maintained through analysis of publications from researchers so as to provide feedback to health policy makers and education planners.
Search strategy
The data used in this study were based on the Scopus online database. A comprehensive online search was performed using SciVerse Scopus, which is one of the world’s largest databases of peer-reviewed literature. Scopus covers nearly 18,000 titles from 5,000 publishers worldwide, contains 41 million records and provides 100% coverage of MEDLINE [ 20 ]. Elsevier, combining the characteristics of both the Web of Science and PubMed, developed the Scopus database. These characteristics allow for an enhanced service for educational and academic needs, as well as for medical literature research and bibliometric analysis. Scopus offers basic search and advanced search features. In the basic search, the results for the chosen keywords can be limited by the date of publication, subject area or document type [ 12 , 21 ]. The search output from Scopus can be presented as a list of 20–200 items per page and extracted documents can be exported to Microsoft Excel®. The results can be refined by document type, author name, source title and publications per year and/or subject area. In addition, a new search can be initiated within the results [ 21 , 22 ].
The keywords entered into the Scopus search engine to achieve the objectives of this study were entered as part of the “Article Title” or “Abstract”. All subject areas were selected for this search: health sciences, social sciences, life sciences and physical sciences, including all previous years up to the date of December 31st, 2012. The resulting search was as follows: AFFILCOUNTRY(qatar) OR AFFILCOUNTRY(jordan) OR AFFILCOUNTRY(egypt) OR AFFILCOUNTRY(emirates) OR AFFILCOUNTRY(saudi) OR AFFILCOUNTRY(palestine) OR AFFILCOUNTRY(bahrain) OR AFFILCOUNTRY(yemen) OR AFFILCOUNTRY(syrian) OR AFFILCOUNTRY(iraq) OR AFFILCOUNTRY(kuwait) OR AFFILCOUNTRY(oman) OR AFFILCOUNTRY(lebanon) OR AFFILCOUNTRY(morocco) OR AFFILCOUNTRY(tunisia) OR AFFILCOUNTRY(sudan) OR AFFILCOUNTRY(algeria) OR AFFILCOUNTRY(comoros) OR AFFILCOUNTRY(djibouti) OR AFFILCOUNTRY(libya) OR AFFILCOUNTRY(mauritania) OR AFFILCOUNTRY(somalia) AND (TITLE(asthma) OR ABS(asthma) OR TITLE(asthmatic) OR ABS(asthmatic) OR TITLE(chronic obstructive pulmonary disease) OR ABS(chronic obstructive pulmonary disease) OR TITLE(chronic obstructive lung disease) OR ABS(chronic obstructive lung disease) OR TITLE(copd) OR ABS(copd) OR TITLE(emphysema) OR ABS(emphysema) OR TITLE(chronic bronchitis) OR ABS(chronic bronchitis)).
We excluded documents that were published as an erratum. Scientific research productivity in the years 2013 and 2014 was excluded because these years were still open for new journal issues and therefore inclusion of the year 2013 would create error and bias. All searches were completed on March 28, 2014 to avoid bias due to the daily updating of the database.
Scientific output was evaluated based on a methodology developed and used in other bibliometric studies [ 12 , 23 – 26 ]. The collected data were used to generate the following information: (a) total and trends of contributions in asthma and COPD research during all previous years up to December 31st, 2012; (b) research productivity by country; (c) journals in which Arab researchers published; (d) the productivity and impact of the most prolific institutions; and (e) the citations received by the publications.
Indices of research productivity
The measurements of bibliometric analysis (e.g. countries, cited articles, institutions) were converted to the rank order using the standard competition ranking (SCR). We took in our consideration only the ten top-ranked. If the measurements of bibliometric analysis have the same ranking number, then a gap is left in the following ranking numbers. The h -index for data collected from Scopus is presented. The h -index is a country’s number of articles (h) that have received at least h citations. It quantifies both country scientific productivity and scientific impact and it is also applicable to scientists, journals, etc. [ 27 ]. That is to say, a country with an h-index of 10 has published 10 documents, each have attracted at least 10 citations. Documents with fewer than 10 citations are not calculated by the index. The h -index was originally developed as a way of qualifying research performance [ 28 ]. Journal impact factor (IF) was evaluated using the Journal Citation Report (JCR; Web of Knowledge) 2012 science edition by Thomson Reuters (New York, NY, USA).
Ethical approval
The Institutional Review Board (IRB) at An-Najah National University does not require submission of an IRB application for a bibliometric study. The IRB confirmed that there is no risk to human subjects in this type of research since the data are based on published literature and, as secondary data, did not involve any interactions with human subjects.
Statistical analysis
Data from Scopus were exported to Microsoft Excel® and then transferred to the Statistical Package for Social Sciences, Version 15 (SPSS; SPSS Inc., Chicago, IL, USA) program for analysis.
The total number of original and review documents retrieved from Scopus without specifying the name of any country and using the keywords listed in the methodology was 163,964. This number represents the global research productivity (original research articles and reviews) in bronchial asthma and COPD using the key words listed in methodology. The leading countries in bronchial asthma and COPD research were United States of America (USA) (38,632; 23.56%) followed by United Kingdom (UK) (15,535; 9.47%) and Japan (8,092; 4.93%). Worldwide, Turkey ranked 19th while Israel and Iran ranked 25th and 29th respectively. Among Arab countries, Egypt and Kingdom of Saudi Arabia (KSA) ranked 39th and 43rd respectively. The 163,964 documents were written in 41 different languages, mainly English (126,408; 77.09%) followed by German, French and Japanese languages with a total of 6,428 (3.92%); 5,025 (3.06%); and 4,763 (2.90%) respectively. The annual global research productivity about bronchial asthma and COPD showed steady growth over the past 50 years. The number of documents published in 2005 was approximately 7 folds more than that published in 1975 (Figure 1 ). The majority of globally published documents were in the subject area of Medicine (137,825; 84.05%) followed by Immunology and Microbiology (17,671; 10.78%); Biochemistry, Genetics and Molecular Biology (13,312; 8.12%) and Pharmacology, Toxicology and Pharmaceutics (11,747; 7.16%). The most common journals in which asthma and COPD documents appeared were Journal of Allergy and Clinical Immunology ; Chest ; and Thorax with total number of documents of 5,537 (3.37%), 4,167 (2.54%), and 3,144 (1.92%) respectively. The most productive institutions of asthma and COPD research were VA Medical Center (USA), National Heart and Lung Institute (USA), and Brigham and Women’s Hospital with a total of 1,904 (1.16%), 1,481 (0.90%), and 1,299 (0.79%) documents respectively.When the same methodology was applied using the list of the 22 Arab countries, 1,304 asthma and COPD documents were retrieved. Therefore, research about asthma and COPD published from Arab countries represents approximately 0.80% of the global research productivity in the field. Out of the 1,304 documents, 1,152 (88.34%) were written in English language. The annual number of documents published from Arab countries indicated that research activity in this field was low and steady until early 2000 and showed a sharp increase in the last decade (Figure 2 ).
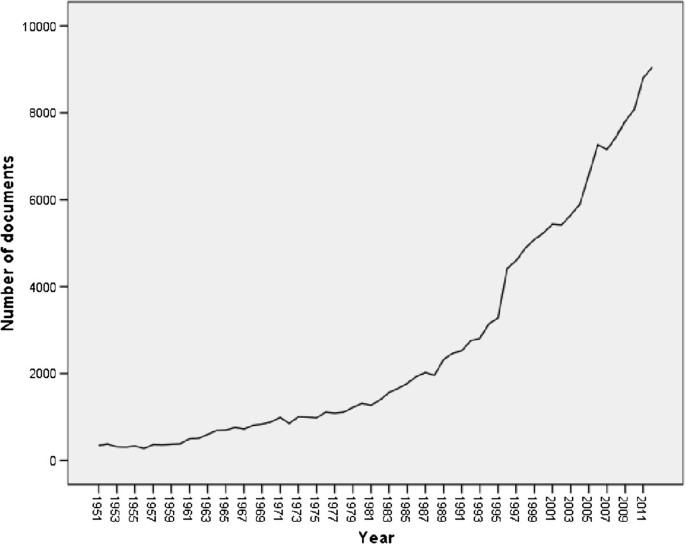
Worldwide research productivity in bronchial asthma and COPD as extracted from Scopus database.
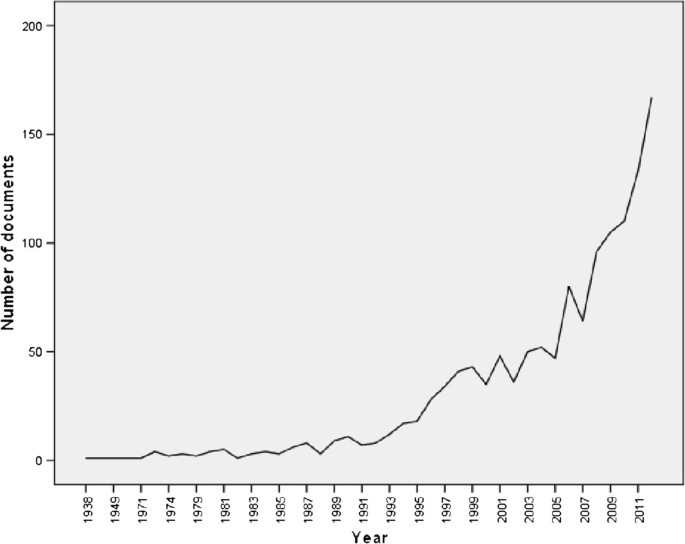
Research productivity about asthma and COPD from Arab countries as extracted from ISI Web of Science.
When retrieved data were analyzed by country, Kingdom of Saudi Arabia (KSA) (353; 27.07%) had the highest research output followed by Egypt (242; 18.56%) and Tunisia (169; 12.96%). More than half (58.58%) of asthma and COPD research from Arab world came from the three Arab countries; KSA, Egypt and Tunisia. No data related to asthma and COPD were found from Somalia, Djibouti, Mauritania and Comoros (Table 1 ). The first article about asthma and/or COPD published from an Arab country appeared in 1938 (Bilharzial asthma. Bronchial asthma in Schistosoma infection) [ 29 ]. Collaboration between Arab countries and non-Arab countries in asthma and COPD research and publication was evident. Countries whose researchers collaborated most with investigators in the Arab world include France (89; 6.8%), United States of America (USA) (87; 6.67%), and England (81; 6.21%).
The majority of published documents from Arab countries were in the subject area of Medicine (1,095; 83.97%). Top 10 subject areas of research interest of asthma and COPD publications from Arab countries are shown in Table 2 . The key word “asthma” was used in 806 documents while COPD key word was used in 355 documents. The 1,304 documents were published in 160 different journals. Table 3 lists the top 10 journals in which documents about asthma and COPD from Arab countries were published. One hundred and fifty eight (12.11%) documents appeared in 4 medical journals that are based in Arab countries, particularly Saudi Medical Journal, Annals of Saudi Medicine, Eastern Mediterranean Health Journal and Tunisie Medicale. The 4 journals have a wide medical scope. Out of the top 10 journals, 3 ( Annals of Thoracic Medicine; Respiratory Medicine; Revue Des Maladies Respiratoires ) were in the specific field of Respiratory/ Thoracic medicine whereas 2 were in allergy/ immunology and 1 in the field of asthma ( Journal of Asthma ). Interest of Arab gulf researchers in asthma and COPD research is evident in top 10 Arabic institutions involved in asthma and COPD research (Table 4 ). The most productive institution was University of Kuwait (123; 9.43%) followed by King Saud University in KSA and King Faisal Specialist Hospital and Research Centre KSA with a total of 114 (8.74%) and 65 (4.98%) publications respectively. Except for the King Faisal Specialist Hospital Research Centre, all institutions in the top 10 list were academic institutions. Five of the top 10 institutions were based in the Arab Gulf and 3 were based in Egypt while the remaining 2 were based in Jordan and Lebanon. The total number of citations for bronchial asthma and COPD documents from the Arab world, at the time of data analysis (April 12th, 2014), was 13,354. Out of the 1304 documents considered for the h -index, 44 had been cited at least 44 times at the time of data analysis.
Chronic respiratory diseases are considered a worldwide health problem. The prevalence of chronic respiratory diseases in Arab countries is believed to be increasing in the light of urbanization and industrialization especially in certain rich Arab countries. With more funds and governmental financial support to medical research, more accurate publications about epidemiology and triggering factors are expected to appear with regard to chronic respiratory diseases in Arab countries. Recent literature indicated that non-communicable diseases, including COPD, are becoming the real future health challenge and burden for Arab countries [ 30 ]. Several epidemiological studies indicated that bronchial asthma is common in Arab world and is mostly associated with allergic disorders [ 31 – 59 ]. Furthermore, bronchial asthma is affecting both children and adults and is imposing an economic burden on individuals and on health systems [ 60 ]. In contrast to asthma, epidemiological studies about COPD in Arab countries are fewer and most information regarding COPD in Arab countries is obtained from BREATHE study which indicated that the prevalence of COPD was lower than that reported in developed countries mostly due to under-reporting or the presence of other non-smoking factors [ 61 – 66 ]. Screening the net showed that there is one poster published in a scientific conference (Dhubai, UAE in 2010) regarding research activity about asthma in Arab world. The authors of the poster used PubMed to screen for asthma publications and found that the number of asthma related publications originating from Arab countries over the last 10 years totaled 275 articles ( https://wao.confex.com/wao/2010isc/webprogram/Paper1414.html ). However, up to the author’s best knowledge, there are no published full articles about bibliometric analysis of research activity regarding respiratory system, respiratory medicine, asthma and/ or COPD in Arab countries. However, several articles were published from other parts of the world [ 67 – 72 ]. These international publications are important for readers in the field of respiratory medicine, public health and health system research.
Reducing chronic respiratory diseases-related morbidity and mortality in Arab countries requires periodic assessment of how these various countries progress in scientific research pertaining to epidemiology, awareness, control and risk factors associated with asthma and COPD. Furthermore, identifying research output and research activity in asthma and COPD is of great importance to public health and pharmaceutical industry. Better delivery systems might help increase compliance and therapeutic outcomes among patients with asthma/ COPD. The main goal of such a study is to direct attention of professionals, academics, researchers and pharmaceutical industry to the current status of asthma and COPD research activity. Academic institutions in the Arab world are advised to initiate more research about bronchial asthma and COPD and to strengthen research collaboration with international researchers and institutions. For future studies in this direction, it is recommended that similar quantitative and qualitative research analyses for other disciplines, particularly allergy and immunology is needed.
Our study was based on 1,304 documents extracted from Scopus, and therefore, cannot be generalized to bronchial asthma and COPD literature published from other Arab countries covered by other databases such as Google Scholar. However, the study does give a clear and a close picture about the characteristics of published asthma and COPD documents from Arab countries. Our results indicated that asthma research is almost double that of the COPD and more efforts are needed to promote research about COPD. Our results also showed that the majority of top 10 institutions in asthma and COPD research were universities with medical schools. Research productivity reveals intellectual output by the institution and is useful to university administrators when evaluating performance of university faculties in the light of university ranking among various universities [ 73 ].
Our study is not without limitations, most of which are the same as those of studies performed in other biomedical fields [ 11 , 26 , 74 , 75 ]. First of all, articles published in journals not indexed in Scopus were not included in the analysis, although they might contribute to scientific productivity. Another limitation is the keywords used to screen for asthma and COPD publications. The authors did their best to include all possible and commonly used terms in this field. However, some articles might have been missed because they might have used some keywords that are different than the ones used in our research methodology. Finally, it should be noted that research output for certain institutions could have been under-estimated because of writing their English names differently in different articles. Therefore, such authors might have 2 or more institute profiles in Scopus database because their names were written differently in different articles.
The present data showed that Arab countries have relatively low research productivity in the field of asthma and COPD. Research output can be improved by investing in more international and national collaborative research projects. Pharmaceutical industry should benefit from the data presented and invest in research leading to the transfer of recent technology pertaining to asthma and COPD therapy.
Abbreviations
Statistical Package for Social Sciences
Institute for Scientific Information
Kingdom of Saudi Arabia
United Arab Emirates
Syrian Arab Republic
United States of America
World Health Organization
Journal Citation Report
Institutional Review Board
Standard Competition Ranking
Impact factors.
Wu W, Kaminski N: Chronic lung diseases. Wiley Interdiscip Rev Syst Biol Med. 2009, 1: 298-308.
Article CAS PubMed Google Scholar
Halbert R, Natoli J, Gano A, Badamgarav E, Buist A, Mannino DM: Global burden of COPD: systematic review and meta-analysis. Eur Respir J. 2006, 28: 523-532.
Wallin JA: Bibliometric methods: pitfalls and possibilities. Basic Clin Pharmacol Toxicol. 2005, 97: 261-275.
De Battisti F, Salini S: Robust analysis of bibliometric data. Stat Methods Appl. 2013, 22: 269-283.
Article Google Scholar
Smith D: Impact factors, scientometrics and the history of citation-based research. Scientometrics. 2012, 92: 419-427.
Smith DR: Citation analysis and impact factor trends of 5 core journals in occupational medicine, 1985–2006. Arch Environ Occup Health. 2008, 63: 114-122.
Article PubMed Google Scholar
Bramness JG, Henriksen B, Person O, Mann K: A bibliometric analysis of European versus USA research in the field of addiction. Research on alcohol, narcotics, prescription drug abuse, tobacco and steroids 2001–2011. Eur Addict Res. 2014, 20: 16-22.
Hofman K, Ryce A, Prudhomme W, Kotzin S: Reporting of non-communicable disease research in low- and middle-income countries: a pilot bibliometric analysis. J Med Libr Assoc. 2006, 94: 415-420.
PubMed Central PubMed Google Scholar
Huber JT, Gullion JS: Complementary and alternative medicine as represented in the HIV/AIDS body of knowledge: a bibliometric analysis. Med Ref Ser v Q. 2003, 22: 23-32.
Rashidi A, Rahimi B, Delirrad M: Bibliometric analysis of parasitological research in iran and Turkey: a comparative study. Iran J Parasitol. 2013, 8: 313-322.
PubMed Central CAS PubMed Google Scholar
Zyoud SH, Al-Jabi SW, Sweileh WM, Awang R: Assessing the scientific research productivity of a leading toxicology journal: a case study of human & experimental toxicology from 2003 to 2012. SAGE Open Med. 2014, 2: 2050312114523424.
Zyoud SH, Al-Jabi SW, Sweileh WM, Awang R: A bibliometric analysis of toxicology research productivity in Middle Eastern Arab countries during a 10-year period (2003–2012). Health Res Policy Syst. 2014, 12: 4.
Article PubMed Central PubMed Google Scholar
Smith DR: Identifying a set of ‘core’journals in occupational health, part 2: lists derived by bibliometric techniques. Arch Environ Occup Health. 2010, 65: 173-175.
Smith DR: Identifying a set of ‘core’ journals in occupational health, Part 1: lists proposed by others. Arch Environ Occup Health. 2010, 65: 106-110.
Allison MM: Mapping the literature of nephrology nursing. J Med Libr Assoc. 2006, 94: E74-E79.
Fedder J, Nielsen GL, Petersen LJ, Rasmussen C, Lauszus FF, Frost L, Hornung N, Lederballe O, Andersen JP: A substantial number of scientific publications originate from non-university hospitals. Dan Med Bull. 2011, 58: A4332.
PubMed Google Scholar
Garg AX, Iansavichus AV, Kastner M, Walters LA, Wilczynski N, McKibbon KA, Yang RC, Rehman F, Haynes RB: Lost in publication: half of all renal practice evidence is published in non-renal journals. Kidney Int. 2006, 70: 1995-2005.
CAS PubMed Google Scholar
Hari Kumar KV, Aravinda K: Publication trends of a biomedical journal from India. Indian J Med Sci. 2010, 64: 253-258.
Thomas GR, Eng L, de Wolff JF, Grover SC: An evaluation of Wikipedia as a resource for patient education in nephrology. Semin Dial. 2013, 26: 159-163.
Scopus: SciVerse Scopus fact sheet. SciVerse® Scopus. 2013, [cited 2013 14, September]; Available from: http://www.elsevier.com/online-tools/scopus
Google Scholar
Falagas ME, Pitsouni EI, Malietzis GA, Pappas G: Comparison of PubMed, Scopus, web of science, and Google scholar: strengths and weaknesses. FASEB J. 2008, 22: 338-342.
Burnham JF: Scopus database: a review. Biomed Digit Libr. 2006, 3: 1.
Zyoud S, Al-Jabi S, Sweileh W: Bibliometric analysis of scientific publications on waterpipe (narghile, shisha, hookah) tobacco smoking during the period 2003–2012. Tob Induc Dis. 2014, 12: 7.
Zyoud SH, Al-Jabi SW, Sweileh WM: A Scopus-based examination of tobacco use publications in Middle Eastern Arab countries during the period 2003–2012. Harm Reduct J. 2014, 11: 14.
Zyoud SH, Al-Jabi SW, Sweileh WM: Worldwide research productivity of paracetamol (acetaminophen) poisoning: a bibliometric analysis (2003–2012). Hum Exp Toxicol. 2014, Article in Press
Zyoud SH, Al-Jabi SW, Sweileh WM, Awang R: A bibliometric analysis of research productivity of Malaysian publications in leading toxicology journals during a 10-year period (2003–2012). Hum Exp Toxicol. 2014, Article in Press
Hirsch JE: An index to quantify an individual’s scientific research output. Proc Natl Acad Sci U S A. 2005, 102: 16569-16572.
Article PubMed Central CAS PubMed Google Scholar
Meho LI, Rogers Y: Citation counting, citation ranking, and h‒index of human‒computer interaction researchers: a comparison of Scopus and Web of Science. J Am Soc Inf Sci Technol. 2008, 59: 1711-1726.
Mainzer F: Bilharzial asthma: bronchial asthma in Schistosoma infection. Trans R Soc Trop Med Hyg. 1938, 32: 253-264.
Alwan A: Responding to priority health challenges in the Arab world. Lancet. 2014, 383: 284-286.
Mahboub BH, Al-Hammadi S, Rafique M, Sulaiman N, Pawankar R, Al Redha AI, Mehta AC: Population prevalence of asthma and its determinants based on European Community Respiratory Health Survey in the United Arab Emirates. BMC Pulm Med. 2012, 12: 4.
Hassan Mahboub BH, Santhakumar S, Soriano JB, Pawankar R: Asthma insights and reality in the United Arab Emirates. Ann Thorac Med. 2010, 5: 217-221.
Mohammad Y, Tabbah K, Mohammad S, Yassine F, Clayton T, Hassan M: International study of asthma and allergies in childhood: phase 3 in the Syrian Arab Republic. East Mediterr Health J. 2010, 16: 710-716.
Alsowaidi S, Abdulle A, Bernsen R, Zuberbier T: Allergic rhinitis and asthma: a large cross-sectional study in the United Arab Emirates. Int Arch Allergy Immunol. 2010, 153: 274-279.
Alsowaidi S, Abdulle A, Bernsen R: Prevalence and risk factors of asthma among adolescents and their parents in Al-Ain (United Arab Emirates). Respiration. 2010, 79: 105-111.
Joseph M, Zoubeidi T, Al-Dhaheri SM, Al-Dhaheri AA, Al-Kaabi FM, Al-Muhairi SJ, Joseph J: Paternal asthma is a predictor for childhood asthma in the consanguineous families from the United Arab Emirates. J Asthma. 2009, 46: 175-178.
Johnson M, Nriagu J, Hammad A, Savoie K, Jamil H: Asthma, environmental risk factors, and hypertension among Arab Americans in metro Detroit. J Immigr Minor Health. 2010, 12: 640-651.
Johnson M, Nriagu J, Hammad A, Savoie K, Jamil H: Asthma prevalence and severity in Arab American communities in the Detroit area, Michigan. J Immigr Health. 2005, 7: 165-178.
Swadi H: Psychiatric morbidity in a community sample of Arab children with asthma. J Trop Pediatr. 2001, 47: 106-107.
al-Maskari F, Bener A, al-Kaabi A, al-Suwaidi N, Norman N, Brebner J: Asthma and respiratory symptoms among school children in United Arab Emirates. Allerg Immunol (Paris). 2000, 32: 159-163.
CAS Google Scholar
Amir J, Horev Z, Jaber L, Varsano I: Prevalence of asthma in Israeli schoolchildren. A comparative study of Jewish and Arab populations. Isr J Med Sci. 1992, 28: 789-792.
el-Hefny AM: The allergens of asthma in children in the United Arab Republic. J Egypt Med Assoc. 1966, 49: 257-266.
Binsaeed AA, Torchyan AA, Alsadhan AA, Almidani GM, Alsubaie AA, Aldakhail AA, Alrashed AA, Alfawaz MA, Alsaadi MM: Determinants of asthma control among children in Saudi Arabia. J Asthma. 2014, 51: 435-439.
Abd El-Kader MS, Al-Jiffri O, Ashmawy EM: Impact of weight loss on markers of systemic inflammation in obese Saudi children with asthma. Afr Health Sci. 2013, 13: 682-688.
Al-Moamary MS, Alhaider SA, Al-Hajjaj MS, Al-Ghobain MO, Idrees MM, Zeitouni MO, Al-Harbi AS, Al Dabbagh MM, Al-Matar H, Alorainy HS: The Saudi initiative for asthma - 2012 update: Guidelines for the diagnosis and management of asthma in adults and children. Ann Thorac Med. 2012, 7: 175-204.
Wahabi HA, Alziedan RA: Reasons behind non-adherence of healthcare practitioners to pediatric asthma guidelines in an emergency department in Saudi Arabia. BMC Health Serv Res. 2012, 12: 226.
Al-Binali AM, Mahfouz AA, Al-Fifi S, Naser SM, Al-Gelban KS: Asthma knowledge and behaviours among mothers of asthmatic children in Aseer, south-west Saudi Arabia. East Mediterr Health J. 2010, 16: 1153-1158.
Sabry EY: Relation of perimenstrual asthma with disease severity and other allergic co-morbidities–the first report of perimenstrual asthma prevalence in Saudi Arabia. Allergol Immunopathol (Madr). 2011, 39: 23-26.
Article CAS Google Scholar
Abudahish A, Bella H: Primary care physicians perceptions and practices on asthma care in Aseer region, Saudi Arabia. Saudi Med J. 2006, 27: 333-337.
Al-Dawood KM: Schoolboys with bronchial asthma in Al-Khobar City, Saudi Arabia: are they at increased risk of school absenteeism?. J Asthma. 2002, 39: 413-420.
Al-Dawood KM: School boys with bronchial asthma in Al-khobar city, Saudi Arabia: are they at increased risk of school absenteeism?. J Fam Commun Med. 2001, 8: 25-33.
Al-Dawood KM: Epidemiology of bronchial asthma among school boys in Al-Khobar city, Saudi Arabia. Saudi Med J. 2001, 22: 61-66.
Al-Mazam A, Mohamed AG: Risk factors of bronchial asthma in Bahrah, Saudi Arabia. J Fam Commun Med. 2001, 8: 33-39.
Al-Dawood K: Epidemiology of bronchial asthma among schoolboys in Al-Khobar city, Saudi Arabia: cross-sectional study. Croat Med J. 2000, 41: 437-441.
Hijazi N, Abalkhail B, Seaton A: Asthma and respiratory symptoms in urban and rural Saudi Arabia. Eur Respir J. 1998, 12: 41-44.
Ballal SG, Ali BA, Albar AA, Ahmed HO, al-Hasan AY: Bronchial asthma in two chemical fertilizer producing factories in eastern Saudi Arabia. Int J Tuberc Lung Dis. 1998, 2: 330-335.
Bener A, al-Jawadi TQ, Ozkaragoz F, Anderson JA: Prevalence of asthma and wheeze in two different climatic areas of Saudi Arabia. Indian J Chest Dis Allied Sci. 1993, 35: 9-15.
Bener A, al-Jawadi TQ, Simsek M, al-Nassar KE: Heredity of asthma in Saudi population. Eur J Epidemiol. 1992, 8: 733-736.
Al Frayh AR: Asthma patterns in Saudi Arabian children. J R Soc Health. 1990, 110: 98-100.
Mahboub BH, Safarini B, AbdulAziz M, Mustafa G: Cost of Asthma in Dubai, United Arab Emirates (UAE). J Pulmon Resp Med. 2013, 3: 2.
Al Ghobain M: The prevalence of chronic obstructive pulmonary disease in Saudi Arabia: Where do we stand?. Ann Thorac Med. 2011, 6: 185-186.
Al-Kassimi FA, Alhamad EH: Re: prevalence of chronic obstructive pulmonary disease among smokers attending primary healthcare clinics in Saudi Arabia. Ann Saudi Med. 2011, 31: 433-434. author reply 434
Al Ghobain M, Al-Hajjaj MS, Wali SO: Prevalence of chronic obstructive pulmonary disease among smokers attending primary healthcare clinics in Saudi Arabia. Ann Saudi Med. 2011, 31: 129-133.
El Hasnaoui A, Rashid N, Lahlou A, Salhi H, Doble A, Nejjari C: Chronic obstructive pulmonary disease in the adult population within the Middle East and North Africa region: rationale and design of the BREATHE study. Respir Med. 2012, 106: S3-S15.
Tageldin MA, Nafti S, Khan JA, Nejjari C, Beji M, Mahboub B, Obeidat NM, Uzaslan E, Sayiner A, Wali S: Distribution of COPD-related symptoms in the Middle East and North Africa: Results of the BREATHE study. Respir Med. 2012, 106: S25-S32.
Døssing M, Khan J, Al-Rabiah F: Risk factors for chronic obstructive lung disease in Saudi Arabia. Respir Med. 1994, 88: 519-522.
Klaewsongkram J, Reantragoon R: Asthma research performance in Asia-Pacific: a bibliometric analysis by searching PubMed database. J Asthma. 2009, 46: 1013-1020.
Gupta B, Bala A: Mapping of asthma research in India: a scientometric analysis of publications output during 1999–2008. Lung India. 2011, 28: 239-246.
Michalopoulos A, Falagas ME: A bibliometric analysis of global research production in respiratory medicine. CHEST. 2005, 128: 3993-3998.
Chen S-R, Chiu W-T, Ho Y: Asthma in children: mapping the literature by bibliometric analysis. Rev Fr Allergol Immunol Clin. 2005, 45: 442-446.
Xie S, Zhang J, Ho Y-S: Assessment of world aerosol research trends by bibliometric analysis. Scientometrics. 2008, 77: 113-130.
Groneberg-Kloft B, Scutaru C, Dinh QT, Welte T, Chung KF, Fischer A, Quarcoo D: Inter-disease comparison of research quantity and quality: bronchial asthma and chronic obstructive pulmonary disease. J Asthma. 2009, 46: 147-152.
Zainal H, Zainab AN: Biomedical and health sciences publication productivity from Malaysia. Health Inform Libr J. 2011, 28: 216-225.
Li XQ, Tao KM, Zhou QH, Ling CQ: Scientific publications from mainland China, Taiwan, and Hong Kong in integrative and complementary medicine journals: a ten-year literature survey. Am J Chin Med. 2011, 39: 639-649.
Sweileh WM, Zyoud SH, Sawalha AF, Abu-Taha A, Hussein A, Al-Jabi SW: Medical and biomedical research productivity from Palestine, 2002–2011. BMC Res Notes. 2013, 6: 41.
Download references
Acknowledgements
The authors would like to thank An-Najah National University for providing the opportunities to access most recent information sources, such as the Scopus database.
Author information
Authors and affiliations.
Department of Pharmacology/Toxicology, College of Medicine and Health Sciences, An-Najah National University, Nablus, Palestine
Waleed M Sweileh & Ansam F Sawalha
Department of Clinical and Community Pharmacy, College of Medicine and Health Sciences, An-Najah National University, Nablus, Palestine
Samah W Al-Jabi & Sa’ed H Zyoud
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Waleed M Sweileh .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors’ contributions
All authors were involved in drafting the article, and all authors approved the final version to be submitted for publication. WS and SZ contributed to idea and design while S.A and A.S contributed to data analysis, critical thinking and manuscript writing and submission.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Authors’ original file for figure 2, rights and permissions.
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/4.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly credited. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Sweileh, W.M., Al-Jabi, S.W., Zyoud, S.H. et al. Bronchial asthma and chronic obstructive pulmonary disease: research activity in Arab countries. Multidiscip Respir Med 9 , 38 (2014). https://doi.org/10.1186/2049-6958-9-38
Download citation
Received : 25 May 2014
Accepted : 23 June 2014
Published : 08 July 2014
DOI : https://doi.org/10.1186/2049-6958-9-38
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Arab countries
- Bronchial asthma
Multidisciplinary Respiratory Medicine
ISSN: 2049-6958
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Clin Diagn Res
- v.8(8); 2014 Aug
Evaluation of Efficacy of Curcumin as an Add-on therapy in Patients of Bronchial Asthma
Afroz abidi.
1 Associate Professor, Department of Pharmacology,Era‘s Lucknow Medical College, Lucknow, U.P., India.
Surabhi Gupta
2 Professor, Department of Pharmacology,Subharti Medical College, Meerut, U.P., India.
Manu Agarwal
3 Junior Resident, Department of Pharmacology,Subharti Medical College, Meerut, U.P., India.
H.L. Bhalla
4 Associate Professor, Department of Pharmacology,Subharti Medical College, Meerut, U.P., India.
Mahip Saluja
5 Professor, Department of TB & Chest,Subharti Medical College, Meerut, U.P., India.
Background: Bronchial asthma being a chronic inflammatory disease of airways has numerous treatment options none of which have disease modifying properties. Curcumin, a yellow dietary pigment has varied pharmacological activities, prominent among which is an anti-inflammatory activity which may be crucial in bronchial asthma as has been proved by various in vitro and in vivo animal studies.
Aims: To determine the efficacy and safety of curcumin as an ‘add-on’ therapy in patients of bronchial asthma.
Settings and Design: This study was conducted on 77 patients of mild to moderate Bronchial asthma who had a documented positive bronchodilator reversibility test with ≥15% improvement in forced expiratory volume one second (FEV1).
Materials and Methods: Seventy seven patients were recruited for the study and randomized into either of the two groups, but 17 patients were lost to follow up. Thus Group A – Receiving standard therapy for bronchial asthma for 30d (n=30) and Group B – Receiving standard therapy for bronchial asthma + Cap Curcumin 500mg BD daily for 30d (n=30). The predefined primary endpoints were clinical assessments of dyspnoea, wheezing, cough, chest tightness and nocturnal symptoms, change in the pre-bronchodilator FEV1 during the treatment and hematological improvement. The secondary end points were assessed by the change in the post-bronchodilator FEV1, C-reactive protein (CRP) concentration and incidence of adverse events.
Statistical Analysis used: The data was analysed by SPSS 17.0 software using one-way ANOVA or Paired t-test.
Results and Conclusion: The results showed that curcumin capsules help in improving the airway obstruction which was evident by significant improvement in the mean FEV1 values. There was also significant improvement in the hematological parameters and absence of any clinically significant adverse events indicates dependable safety profile of curcumin capsules, though there was no apparent clinical efficacy. Therefore, it is concluded that curcumin is effective and safe as an add-on therapy for the treatment of bronchial asthma.
Introduction
Bronchial asthma affects 100-150 million people worldwide and approximately 180,000 deaths annually are attributed to asthma [ 1 ]. According to WHO, India is home to 15-20 million asthmatics. Asthma is a chronic inflammatory disorder of the airways characterized by recurrent episodes of wheezing, breathlessness, chest tightness and coughing due to reversible airway obstruction, cellular inflammation, mucus hypersecretion, airway remodeling, blood vessel proliferation and mucous gland hyperplasia and hypersecretion. The broncho-constrictor and inflammatory mediators of asthma include cytokines, chemokines, cysteinyl leukotrines, histamine, nitric oxide, PGD2 adhesion molecules, enzymes and kinases which are mostly regulated by NF-kB pathway. This pathway has now been recognized to be involved in asthma and mediates the complex inflammatory response in the airways therefore the agents that downregulates NF-kB pathway could have a potential efficacy against the disease [ 2 ].
The diagnosis of asthma is established by demonstrating reversible airway obstruction. Pulmonary Function Test (PFT) is the gold standard for evaluating airway obstruction and/or restriction. The FEVl/FVC ratio, also called Tiffeneau index, whose normal values are approximately 80%. This ratio is reduced in obstructive while normal in restrictive lung diseases. Reversibility is traditionally defined as a 15% or greater increase in FEV1 after two puffs of a b2 adrenergic agonist.
Medications to treat asthma can be classified as controllers or relievers. Controller drugs like corticosteroids keep asthma under clinical control by inhibiting airway inflammation by modulating cytokine and chemokine production, inhibiting eicosanoid synthesis, markedly inhibiting cellular infiltration in lung tissues and decreasing the vascular permeability [ 3 ], but its use is limited by the risk of local and systemic adverse effects. Relievers are medications used on an as-needed basis that act quickly to reverse bronchoconstriction and relieve its symptoms. They include rapid-acting inhaled and oral β2-agonists, inhaled anticholinergics, leukotriene modifiers, cromones and short-acting theophylline [ 3 ]. Immunotherapy by IgE antibody Omalizumab reduces exacerbations in patient with severe asthma and may improve bronchial hyper-reactivity helping in asthma control.
Bronchial thermoplasty is a treatment for severe asthma approved by the FDA in 2010 that involves the delivery of controlled therapeutic radiofrequency energy to the airway wall, thus heating the tissue leading to acute epithelial destruction and reducing the amount of oedema in the airway wall [ 4 ]. Non-pharmacologic alternative treatments including hypnosis, acupuncture, chiropraxy, breathing control, yoga and speleotherapy may be popular with some patients. However, placebo-controlled studies have shown that each of these treatments lacks efficacy and cannot be recommended. However, they are not detrimental and may be used as long as conventional pharmacologic therapy is continued.
In spite of voluminous literature on the subject, the treatment of bronchial asthma continues to be far from satisfactory. The available treatment options for bronchial asthma have major limitations due to low efficacy, associated adverse events, lack of disease modifying property and compliance issues. Therefore, there is a need to explore for new anti-asthmatic agents with extended pulmonary efficacy and minimal systemic side effects.
WHO has recognized herbal medicines as an essential building block for primary health care in developing countries like India. It has been reported in the past that 11-40% asthma patients use herbal medicines [ 5 ].
In recent years, turmeric, a spice used in Asian countries, has attracted the attention of researchers due to its reported effectiveness in inflammatory and other disorders. Curcumin, a natural product from the rhizomes of Curcuma longa (Turmeric), has a wide range of beneficial properties including anti-inflammatory, anti-oxidant, anti-rheumatic, anti-carcinogenic, anti-coagulant, anti-fertility, anti-diabetic, anti-bacterial, anti-protozoal, anti-viral, anti-fibrotic, hypolipidemic and hypoglycemic activities [ 6 ]. Curcumin modulates the inflammatory response by down-regulating intercellular signaling proteins, such as protein kinase C [ 7 ], modulating the activity of transcription factors like activating protein-1 (AP-1) and inhibiting NF-KB pathway which is involved in regulation of inflammation, cellular proliferation, transformation and tumourogenesis. Curcumin is thought to suppress NF-kB activation and proinflammatory gene expression by blocking phosphorylation of inhibitory factor l-kappa B kinase (I-rcB) [ 8 ], thereby subsequently suppressing cyclooxygenases, lipoxygenase pathways and iNOS expression. All these activities inhibit the production of the inflammatory cytokines, tumor necrosis factor-alpha (TNF-a), interleukins (IL-1,2,6,8,12) monocyte chemoattractant protein (MCP) and migration inhibitory protein. It also inhibits transcription factor products such as signal transducer and activator of transcription (STAT), PPAR-g and down-regulates Janus kinases [ 9 ].
Our study focuses on one of its best explored actions, the anti-inflammatory effects. There were only a few studies to explore the action of curcumin in asthma but all were with different methodologies and end points. Based on the anti-inflammatory properties, we hypothesized that curcumin could have an effective role in the treatment of asthma. Hence, the present comparative study has been designed to investigate the efficacy and safety of curcumin as an add-on therapy in mild-to-moderate bronchial asthma patients.
Materials and Methods
The present study was an open labelled, randomized, single centre study assessing the efficacy of orally administered curcumin capsules in addition to the normally prescribed medication for the treatment of asthma. Approval of Institutional Ethical Committee was obtained. Written informed consent was taken from all patients.
Human studies have showed that curcumin at doses ranging from 0.9 to 3.6 g/day for 1-4 months has been classified as ‘generally recognized as safe’ (GRAS) by the National cancer Institute and Food and Drug Administration but exhibited some adverse effects [ 10 ] . Thus, we selected a safe dose of 1gm i.e. 1000mg given in two divided doses [ 7 , 11 ].
Selection of the Patients
Inclusion Criteria
Bronchial asthma patients in the age group of 18 to 55 y of either sex who had a documented positive bronchodilator reversibility test with ≥15% improvement in FEV1 from 15 to 30 minutes after inhalation of at least 200 μg of salbutamol, patients who had never smoked/had left smoking since past three months; with prebronchodilator FEV1 values in range of 60-80%; with normal serum glutamic pyruvic transaminase (SGPT) and normal serum creatinine levels were included in the study.
Exclusion Criteria
Children, bronchial asthma patients who were currently smoking were excluded from the study. Patients with severe asthma, chest infections, bile duct obstruction (or history of gallstones), abnormal SGPT levels & serum creatinine values, those on warfarin or anti-platelet drugs were not included in the study. Pregnant females, patients having chronic bronchitis and/or emphysema, or patients suffering from concurent systemic diseases like cardiopulmonary, tuberculosis, pulmonary eosinophilia, bronchiectasis, cancer, congestive heart failure, hepatic dysfunction, neurological disorders and diarrheal disorders or having a hemoglobin level less than 10 g/dl were also excluded from the study.
Methodology
At initial visit, a comprehensive assessment comprising detailed medical history, a thorough clinical examination with special emphasis on respiratory system examination, hematological test (haemoglobin, TLC, DLC, ESR, C-reactive protein), biochemical test (SGPT, serum creatinine), urine analysis, chest x-ray and pulmonary function test (FEV1) were performed.
After a medical examination 77 subjects satisfying the inclusion criteria were recruited in the study and written informed consent was obtained from each of the patient. All the selected patients were randomized by a computer generated random number in either of the two groups:
Group A – Receiving standard therapy for bronchial asthma- Formonide Resicaps BD German Remedies (Zydus Cadila HealthcareLtd) [Budesonide 100 mcg, formoterol 6 mcg], Cap ABflo BD Lupin Laboratories Ltd [Acebrophylline 100 mg], Tab Montek LC hs Sun Pharmaceutical Industries Ltd (Montelukast 10 mg, levocetirizine 5mg) for 30d;
Group B – Receiving standard therapy for bronchial asthma as above + Cap Curcumin 500 mg BD daily for 30d.
The curcumin capsules were dispensed to patients by the prescribing doctor while other medications were purchased from the chemist. The curcumin capsules CUR- 500 (Curcumin 500 mg) were purchased by us from authorized manufacturer (M/s Indsaff & Charak International Private Limited, O/s Pahari Gate, Batala, Punjab -143505, India) and were provided free of cost to the study participants.
All the patients were followed up every tenth day for a period of one month. At each visit clinical symptoms like dyspnoea, wheezing, cough, chest tightness and nocturnal symptoms were assessed. Pulmonary function test (Spirometry): FEV1, blood Pressure, temperature, hematological test like Hb, TLC, DLC, ESR, C-Reactive Protein (CRP), biochemical tests like Serum Glutamic Pyruvic Transaminase (SGPT), serum creatinine and anthropometric measurements like height and weight were recorded from which Basal Metabolic Index (BMI) was calculated.
Spirometry - FEV1 was measured by a computerized spirometer RMS Medspiror (Platfurm Win 98, Version 1.0). It was performed by the same technician on all patients and with the same instrument to avoid bias. Spirometry is best performed with the patient seated. Patients who were anxious about the tests were reassured and counseled before starting the procedure. The pre bronchodilator FEV1 value was taken after careful explanation of the test accompanied by a demonstration. The best of three reproducible measurements was taken for analysis. The post-bronchodilator FEV1 value was assessed at 20 min after the inhalation of 200 μg salbutamol using a metered dose inhaler with a spacer device. The percentage of predicted values and the percent of difference between the pre-bronchodilator and post-bronchodilator values were calculated.
Hematological tests- Hb, TLC, DLC was analysed using autoanalyser MS-9, ESR was analysed using Westergren method and CRP was analysed using either latex agglutination or turbidimetry method.
The predefined primary endpoints were rapid symptomatic control clinically assessed by dyspnoea, wheezing, cough, chest tightness and nocturnal symptoms, change in the pre-bronchodilator FEV1 during the treatment and hematological improvement. The secondary end points were change in the post-bronchodilator FEV1 (change from baseline during the treatment) and C - reactive protein (CRP) concentration.
All adverse events either reported or observed by patients were recorded in CDSCO forms. Patients were allowed to voluntarily withdraw from the study but efforts were made to ascertain the reason for dropout. Subjects were asked to maintain a daily diary regarding use of all medications and were asked to bring back the curcumin bottles to monitor medication compliance.
Statistical Analysis
The data was analysed using SPSS 17.0 software. The two groups were compared with each other for changes in various parameters either by one-way ANOVA (comparing reduction in severity of asthma symptoms) or paired t-test (comparing improvement in FEV1 values and improvement in hematological parameters). The level of significance was fixed at p<0.05.
Seventy-seven patients, meeting the inclusion criteria were recruited in the study. Out of 77 enrolled patients, 17 patients were lost to follow-up (10 patients in Group A and 07 patients in Group B) and the remaining 60 patient’s data was analysed.
Group A: Receiving standard therapy for asthma (n=30)
Group B: Receiving standard therapy for asthma + Curcumin (n=30)
Demographic data: The mean age of the study population in years, the distribution of female and male patients, the mean height in cms and mean weight in kgs was comparable in both group A and group B patients [ Table/Fig-1 ].
[Table/Fig-1]:
Shows the demographic data i.e Mean age in years, the Male and Female population, Mean height in cms and Mean weight in kgs in each group which are comparable in both the groups
Clinical symptoms: The severities of clinical symptoms were analysed individually for both Group A and Group B, and the mean baseline (0 visit), 10th day (1st visit), 20th day (2nd visit) and 30th day (3rd visit) values were calculated. The reductions in symptoms of dyspnea, wheezing, cough, chest tightness, nocturnal symptoms and the total symptom score were compared in both the groups by one way ANOVA. All the values were found to be insignificant [ Table/Fig-2 ].
[Table/Fig-2]:
Compares the reduction in severity of asthma symptoms like dyspnea, wheezing, cough, chest tightness, nocturnal symptoms and total score in both the groups by one way ANOVA
Pulmonary Function Tests: FEV1 values were analysed individually for both Group A and Group B, on day 0, 10th, 20th and 30th day. Also, the improvements in FEV1 values in both the groups were compared to evaluate the efficacy of curcumin as an ‘add-on’ therapy. Analyzing improvement in FEV1 values of both the groups by using paired‘t’ test it was revealed that Group B patients showed significant improvement in FEV1 values as compared to Group A patients [ Table/Fig-3 ].
[Table/Fig-3]:
Compares the Pre-bronchodilator FEV1, Post-bronchodilator FEV1 and % reduction in Reversibility in both the groups by Paired ‘t’ test. All values are expressed as Mean±SD
* p< 0.05 indicates significant values
Hematological values: Hematological parameters were analysed individually for both Group A and Group B, and the mean baseline (0 visit) and 30th day (3rd visit) values were calculated. On comparing the improvement of hematological values in both the groups by paired t-test it was noted that decrease in total leukocyte count was more in Group B patients as compared to Group A patients, p < 0.05 (significant); increase in neutrophils was more in Group A patients as compared to Group B patients; decrease in lymphocytes was more in Group A patients as compared to Group B patients;decrease in eosinophils and decrease in ESR was more in Group B as compared to Group A, p< 0.05 (significant) [ Table/Fig-4 ].
[Table/Fig-4]:
Comparing improvement of Hematological Parameters in both the groups (0 visit to 3rd visit)
Adverse events: Although the Group B patients recorded less number of adverse events in comparison with the Group A patients, the comparison is statistically insignificant. While headache and insomnia was recorded in both the study groups; weight gain was observed only in Group B and decrease in appetite was reported with Group A only. There were no clinically significant reported or observed adverse events [ Table/Fig-5 ].
[Table/Fig-5]:
Shows the incidence of adverse effects in both the groups in number and %
Bronchial asthma, a chronic bronchial inflammatory disorder, is characterized by bronchoconstriction, increased mucus production and airway hyper-responsiveness. The increased inflammatory infiltrate, tenacious plugs of exudates and mucus and enlargement of bronchial smooth muscle particularly in medium sized bronchi leads to the resultant symptomatology of wheezing, coughing and dyspnea. Bronchodilators and inhaled/systemic corticosteroids are commonly used as the first-line treatment for symptomatic management but their use is limited due to long-term adverse effects. Prophylactic therapy is essential in asthma but they do not prevent recurrent episodes.
Despite major advances in treating asthma, until now disease-modifying efficacy has not been demonstrated for any of the existing drugs, therefore there is an essential need to develop new drugs that might be of additional benefit in clinical settings. Since herbal medicines offer a positive beneficial effect in most chronic diseases, we aimed to investigate this aspect in our study. Over the years, there has been increasing evidence that curcumin, a phytochemical present in Curcuma longa (Turmeric or haldi), has a wide spectrum of therapeutic properties including modulation of inflammation and oxidative stress. Various studies have clearly established it’s anti-inflammatory effect both in vitro and in vivo by inhibiting iNOS production and scavenging the free radicals, inhibiting the activation of NF-kappaB and activating protein 1 (AP 1) and suppressing the production of proinflammatory cytokines [ 2 ]. Studies have also demonstrated that curcumin decreases the level of iNOS-induced by IFN-γ in lung tissue and expression of cytokines such as IL-2,IL-5 and GM-GSF by acting as a histone deacetylases (HDAC) activator and inhibits histamine release from mast cells. It has been proved that curcumin can also restore HDAC activity, thereby restoring corticosteroid function [ 12 ]. Previous data from various studies have demonstrated the efficacy of curcumin in animal models of asthma, but there are very few human trials which explored the efficacy of oral curcumin in asthma. Hence, we decided to undertake this study.
Kobayashi T et al., showed that curcumin when added to Dermatophagoides farineae (Der-f)-stimulated lymphocyte cell cultures from allergic asthmatics inhibited Der-f-induced lymphocyte proliferation and production of IL-2, IL-4, IL-5 and GM-CSF thereby proving that curcumin blocks the allergen- triggered release of inflammatory chemicals in white blood cells taken from asthma patients. It also demonstrated that curcumin may have potential effects on controlling allergic diseases through inhibiting the production of cytokines, eosinophil function and IgE synthesis [ 13 ].
South et al., investigated the effects of dietary curcumin (1, 20 or 40 mg/kg) for five wks on antibody (IgG) production, delayed-type hypersensitivity and natural killer cell activity in rats. The highest doses of curcumin, significantly enhanced IgG levels. Neither delayed-type hypersensitivity nor natural killer cell activity was different from control values at any dietary concentration of curcumin [ 14 ].
Another significant study by Ram A et al., studied the effect of curcumin on airway hyperresponsiveness in sensitized guinea pigs and demonstrated by a constant volume body plethysmograph that curcumin significantly inhibited ovalbumin-induced airway constriction and airway hyperreactivity in guinea pigs [ 15 ].
It was shown by Kohli K et al., that curcumin in a dose of 200 mg/kg body weight helps to prevent allergic airway inflammation by inhibiting the actions of an inflammatory protein called NF-κB [ 16 ].
Kurup et al., used a murine model of latex allergy to investigate the role of curcumin as an immunomodulator. BALB/c mice were exposed to latex allergens and developed latex allergy with a T helper 2 lymphocycets (Th2) type immune response. These animals were treated with curcumin and the immunologic and inflammatory responses were evaluated. Animals exposed to latex showed enhanced serum IgE, latex-specific IgGl, IL-4, IL-5, IL-13, and eosinophils and inflammation in the lungs. Intragastric treatment of latex-sensitized mice with curcumin demonstrated a diminished Th2 response with a concurrent reduction in lung inflammation. Eosinophilia in curcumin-treated mice was markedly reduced, co-stimulatory molecule expression (CD80 and CD86) on antigen-presenting cells was decreased and expression of MMP-9 and OAT genes was also attenuated. These results suggest that curcumin has potential therapeutic value for arresting and reversing tissue, specifically lung inflammation in mice due to a controlled allergic reaction with exposure to latex [ 17 ] .
Moon et al., investigated the anti-inflammatory effect of curcumin in a different model of ovalbumin induced murine asthma and found that pre-treatment with curcumin caused low levels of ovalbumin induced nitric oxide, IL-4, IL-5, IFN-γ and IgE antibodies [ 18 ].
In another study by Aggarwal BB et al., curcumin significantly inhibited the activity of NF-κB, thus inhibiting the airway inflammation and cell infiltration in asthma. It also proved that curcumin decreases the expression and release of eotaxin, MCP-1 and MCP-3 from IL-1-stimulated human airway smooth muscle cells [ 19 ].
Oh SW et al., proved that curcumin attenuates the allergic airway inflammation and hyper-responsiveness of asthma in mice by inhibiting NF-κB activation [ 20 ].
Karaman M et al., demonstrated that curcumin was as effective as the prescription steroid dexamethasone and had equal ability to reverse ovalbumin induced histopathological airway changes due to inflammation [ 21 ].
Xin Zeng et al., demonstrated that the proliferation of airway smooth muscle cells is inhibited by curcumin in vitro and in vivo by upregulating the expression of caveolin-1 and blocking the activation of extracellular signal-regulated kinase (ERK) pathway [ 22 ].
Antiinflammatory activity of curcumin was demonstrated by various authors. Kang BY et al., demonstrated that curcumin significantly inhibits production of IL-12, reduces the induction of IFN-γ, IL-4 in CD4+ T-cells by macrophages, leading to the inhibition of Th1 cytokine profile [ 23 ]. Chainani Wu N showed that curcumin inhibits several agents involved in inflammation including phospholipase, lipoxygenase, cyclooxygenase-2, leukotrienes, thromboxane, prostaglandins, nitric oxide, collagenase, elastase, hyaluronidase, monocyte chemoattractant protein-1, interferon-inducible protein, tumour necrosis factor alpha and interleukin-12 [ 24 ]. Hong et al., confirmed that curcumin is a dual inhibitor of arachidonic acid metabolism, inhibiting both the enzymes 5-lipoxygenase and cyclooxygenase [ 24 ]. Similarly a study by Jagetia GC et al., proved that curcumin is a potent immunomodulatory agent that can modulate the activation of T cells, B cells, macrophages, neutrophils, natural killer cells and dendritic cells and can also downregulate the expression of various proinflammatory cytokines including TNF-α, IL-1, IL-2, IL-6, IL-8, IL-12, and chemokines [ 25 ]. Another important study by Biswas S et al., illustrates that curcumin can down-regulate expression of pro-inflammatory mediators, matrix metalloproteinases, adhesion molecules and growth factor receptor genes and they up-regulate HDAC2 in the lungs. It also showed that curcumin can directly scavenge free radicals such as superoxide anion and nitric oxide and modulate important signaling pathways mediated via NF-B and mitogen-activated protein kinase pathways [ 26 ].
There are numerous clinical studies of curcumin in patients of rheumatoid arthritis, chronic anterior uveitis, inflammatory orbital pseudotumor, cancers of oral cavity, breast, skin etc and various other diseases [ 16 ]. But there are few published studies which have evaluated the clinical effect of oral curcumin on asthmatics patients. In reference to all the above studies we hypothesized that curcumin being a strong anti-inflammatory agent could prove efficacious as add-on therapy in mild to moderate asthma patients. Therefore, the present study was conducted to compare the effects of 4 weeks of treatment with curcumin capsules as add-on therapy (Group B) on lung function, severity of symptoms, hematological parameters and on treatment related adverse outcomes with that of 4 weeks of standard treatment for patients having mild-to-moderate asthma (Group A).
In our study, the mean age of the population was approximately thirty two years with almost similar gender distribution in both the groups [ Table/Fig-1 ] . Thus the two groups were demographically comparable to each other. This it is in accordance with previous studies stating that occurrence of bronchial asthma is more before the age of forty with equal sex ratio in the adults [ 27 ].
When both the groups were analysed individually for reductions in severity of asthma symptoms, it was observed that there was significant reduction (p< 0.05) in the mean scores for cough, dyspnoea, wheezing, chest tightness, nocturnal symptoms and total asthma symptom score in both the groups between baseline and 30th day i.e. 3rd visit. However, when reductions in severity of asthma symptoms in both the groups were compared, the results were found to be insignificant (p>0.05); thus it is unlikely that curcumin has an effect on reduction in severity of asthma symptoms [ Table/Fig-2 ]. Our results differ with the uncontrolled trial conducted in India, where 60% of asthma patients administered plain or ghee-fried turmeric powder showed a relief in their symptoms [ 28 ]; but since they have used turmeric, it cannot be ascertained whether reduction in severity of asthma symptoms was due to curcumin or due to some other component of turmeric. In our study curcumin does not have any effect on asthma symptoms may be because patients were recruited from the community with mild to moderate asthma and the symptomatic impairment may have been severe enough not to get cured with either the studied dose or duration of curcumin administered.
When both the groups were analysed individually for improvement in FEV1 values, it was observed that there was a significant reduction (p < 0.05) in the mean improvement of FEV1 values, between baseline (0 visits) and 30th day (3rd visit) in both the groups. Further, when improvements in FEV1 values in both the groups were compared, the results revealed that Group B patients showed significant (p < 0.05) improvement in Pre-FEV1, Post FEV1 and % reversibility values as compared to Group A patients groups [ Table/Fig-3 , Table/Fig-6 ]. Thus, it is suggested that curcumin causes improvement in FEV1 values. Our results are in consistence with the study of Ng TP et al., indicating an improvement in FEV1 values and FEV1/FVC values indicating a significant decrease in airway constriction and inflammation [ 29 ].

Shows the improvement in FEV1 values at 3rd visit i.e. on 30th day- Pre-bronchodilator FEV1, Post-bronchodilator FEV1 and % reduction in reversibility
When both the groups were analysed individually for reduction in hematological parameters (TLC, DLC, ESR), it was observed that there was significant reduction (p < 0.05) in the mean scores for hematological parameters between baseline (0 visit) and 30th day (3rd visit) in both the groups. Further, when improvement of hematological parameters in both the groups were compared, the results revealed that Group B patients showed significant improvement (p<0.05) in the hematological parameters as compared to Group A patients [ Table/Fig-4 ]. These results are in agreement with the studies of Kurup et al., [ 17 ] Jagetia GC et al., [ 25 ] and Vachharajini V et al.,[ 30 ] all of which showed improvement in haematological profile with curcumin. This modulation of hematological parameters probably emphasizes on the anti-inflammatory properties of curcumin.
No safety concerns emerged over the use of curcumin during the study; neither of the group showed any significant drug-related adverse events [ Table/Fig-5 ]. Hepatic and renal functioning was assessed both at the beginning and end of the study. All the known adverse effects of curcumin were monitored vigorously on regular basis, making sure that no ADR went unnoticed. This is supported by the review of the previous literature stating that curcumin does not cause significant short-term toxicity at doses up to 8 g/day [ 7 ].
Overall, our study demonstrated efficacious FEV1 control and significant improvement in the hematological parameters at the end of the treatment compared to their baseline values in group B patients. The significance can be attributed to the use of curcumin capsules as an add-on therapy in bronchial asthma patients. Thus, our study proved the beneficial role of curcumin as an add-on therapy in asthma.
There is no effect of curcumin add-on therapy on improvement of asthma symptoms. This may be because the number of the study subjects were only 60, who completed the study, which may be insufficient numbers to provide a statistically significant result in the patient centered outcome measures (like asthma symptoms). Besides the dose and duration of curcumin administered may not be sufficient enough to produce clinically beneficial effect. Moreover the severity of clinical symptoms were assessed by an individual (as absent, mild, moderate and severe with scores of 0, 1, 2 and 3) thus were not much reliable. A further study with large subjects and modified dose is now required to investigate the effects of curcumin on symptomatic control. In addition, the study only explored the use of curcumin as an add-on therapy, and no information can be inferred on the use of this agent as monotherapy or as a steroidsparing agent. These areas need further exploration.
This study evaluated the clinical efficacy and safety of curcumin capsules as an add on therapy in patients of mild to moderate asthma and proved therapeutic improvement in FEV1 values along with improvement in concerned hematological parameters. This corroborates the fact that there is a definite improvement in lung function due to the anti-inflammatory effect of curcumin though there is no visible clinical efficacy. Therefore a further clinical evaluation is needed with more number of subjects, a higher tolerated dose and for a longer duration. Absence of any clinically significant adverse events indicates dependable safety profile of curcumin. Therefore, it is concluded that curcumin is effective and safe as an add-on therapy for the treatment of bronchial asthma.
Financial or Other Competing Interests

IMAGES
VIDEO
COMMENTS
Abstract. In this review, we discuss recent publications on asthma and review the studies that have reported on the different aspects of the prevalence, risk factors and prevention, mechanisms, diagnosis, and treatment of asthma. Many risk and protective factors and molecular mechanisms are involved in the development of asthma.
Asthma treatment is based on a stepwise approach. The management of the patient is control-based; that is, it involves an iterative cycle of assessment (e.g. symptoms, risk factors, etc.), adjustment of treatment (i.e. pharmacological, non-pharmacological and treatment of modifiable risk factors) and review of the response (e.g. symptoms, side ...
Results/Discussion. Bronchial asthma is a chronic inflammatory disease of the airways characterized by bronchial hyperreactivity and a variable degree of airway obstruction. It is diagnosed on the basis of the clinical history, physical examination, and pulmonary function tests, including reversibility testing and measurement of bronchial ...
The Severe Asthma Research Program (SARP) has identified five phenotypic clusters of severe asthma, including three clusters in adults and two clusters in children. ... Enterobacteriaceae in the sputum of patients with severe asthma and corticosteroid responsiveness with Actinobacteria in bronchial brushings. 52, 53, 54 Collectively, endotyping ...
Asthma is a chronic lung disease affecting people of all ages. It is caused by inflammation and muscle tightening around the airways, which makes it harder to breathe. Symptoms can include coughing, wheezing, shortness of breath and chest tightness. These symptoms can be mild or severe and can come and go over time.
Asthma articles from across Nature Portfolio. Asthma is a form of bronchial disorder caused by inflammation of the bronchi. It is characterized by spasmodic contraction of airway smooth muscle ...
Abstract. Asthma is the most common, long-lasting inflammatory airway disease that affects more than 10% of the world population. It is characterized by bronchial narrowing, airway hyperresponsiveness, vasodilatation, airway edema, and stimulation of sensory nerve endings that lead to recurring events of breathlessness, wheezing, chest tightness, and coughing.
Abstract. Importance: Asthma affects about 7.5% of the adult population. Evidence-based diagnosis, monitoring, and treatment can improve functioning and quality of life in adult patients with asthma. Observations: Asthma is a heterogeneous clinical syndrome primarily affecting the lower respiratory tract, characterized by episodic or persistent ...
To The Editor, The Global Initiative for Asthma (GINA) 2021 update was published on the 28th of April, 2021. [1]. There are significant changes, including treatment of mild asthma, the role of ...
Current research on asthma treatment. How ventilators may lead to asthma: The NHLBI-funded Post-Vent study will use data collected from the Prematurity-Related Ventilatory Control (Pre-Vent): Role in Respiratory Outcomes NHLBI Collaborative Program to study long-term health outcomes of premature birth and intermittent low oxygen levels shortly after babies are born prematurely.
Long-term follow-up studies of adults with well-characterized asthma are sparse. We aimed to explore static lung volumes and diffusion capacity after 30 + years with asthma. Conrad Uldall Becker Schultz, Oliver Djurhuus Tupper and Charlotte Suppli Ulrik. Asthma Research and Practice 2022 8 :4.
If you have asthma, you may notice regular changes in your breathing that range from mild to severe. But when an asthma attack occurs, your symptoms can become severe quickly and may even require immediate medical treatment. Some common signs and symptoms of bronchial asthma are: Tightness or pain in your chest.
Asthma affects approximately 262 million people worldwide with an estimated 1000 people dying from asthma attacks each day 1,2. The majority of asthma attacks are preventable and the substantial ...
Regular exercise can strengthen your heart and lungs, which helps relieve asthma symptoms. If you exercise in cold temperatures, wear a face mask to warm the air you breathe. Maintain a healthy weight. Being overweight can worsen asthma symptoms, and it puts you at higher risk of other health problems.
Asthma is a condition of acute, fully reversible airway inflammation, often following exposure to an environmental trigger. The pathological process begins with the inhalation of an irritant (e.g., cold air) or an allergen (e.g., pollen), which then, due to bronchial hypersensitivity, leads to airway inflammation and an increase in mucus ...
Asthma is a common chronic disease characterized by episodic or persistent respiratory symptoms and airflow limitation. Asthma treatment is based on a stepwise and control-based approach that involves an iterative cycle of assessment, adjustment of the treatment and review of the response aimed to minimize symptom burden and risk of exacerbations. Anti-inflammatory treatment is the mainstay of ...
Bronchial asthma is a heterogeneous disease, characterized by chronic inflammation of the airways and certain respiratory symptoms such as shortness of breath, chest tightness, cough, and sibilant ...
Asthma signs and symptoms include: Shortness of breath. Chest tightness or pain. Wheezing when exhaling, which is a common sign of asthma in children. Trouble sleeping caused by shortness of breath, coughing or wheezing. Coughing or wheezing attacks that are worsened by a respiratory virus, such as a cold or the flu.
In an interesting study, BAL and bronchial epithelial cells were obtained from patients with uncontrolled asthma before and after 12 weeks of TZP treatment. 80 The cells were cultured in vitro and exposed to the viral infection mimic poly(I:C) or rhinovirus mimic viral infection. Blocking TSLP with TZP in vivo in patients with asthma ...
Foo CT, Donovan GM, Thien F, et al. Bronchial thermoplasty improves ventilation heterogeneity measured by functional respiratory imaging in severe asthma. J Asthma Allergy. 2024;17:399-409 ...
The Division of Asthma Research aims to accelerate the bidirectional flow of knowledge between the clinical beside and research settings. We translate clinical challenges in asthma into well-designed research studies that integrate the collective expertise of individuals in the division and across Cincinnati Children's and take advantage of ...
Asthma stands as one of the most prevalent chronic respiratory conditions in children, with its pathogenesis tied to the actived antigen presentation by dendritic cells (DCs) and the imbalance within T cell subgroups. This study seeks to investigate the role of the transcription factor EB (TFEB) in modulating the antigen presentation process of DCs and its impact on the differentiation of T ...
With the increasing prevalence of bronchial asthma, the continuous lack of novel therapies and inefficient disease prevention, the demand for predictive biomarkers for allergic rhinitis and asthma is steadily increasing. ... Four inflammatory phenotypes have been identified in the Severe Asthma Research Program (SARP) cohort - eosinophilic ...
Background Chronic respiratory diseases, like bronchial asthma and chronic obstructive pulmonary disease (COPD), are a worldwide health problem. Quantitative and qualitative assessment of asthma and COPD-related research from Arab countries has not been explored and there are few internationally published reports on such field. The main objectives of this study were to analyze research output ...
Abstract. Aim: We compared the effectiveness of rush subcutaneous immunotherapy (SCIT) and sublingual immunotherapy (SLIT) using standardized house dust mite (HDM) extract for pediatric bronchial asthma (BA).Methods: We followed the pediatric BA treatment score during 3 years of treatment. We assessed the median time to no longer requiring long-term control pharmacotherapy (LTCP) for BA (LTCP ...
100. Prospective Study of Bronchial Asthma. Abstract. Bronchial asthma is an atopic disease characterized by chronic airway inflammation and hyper-responsiveness. Severe. acute asthma is a medical ...
Bronchial asthma is heterogeneous pulmonary disorder characterized by recurrent episodes of cough, breathlessness and wheezing, which may resolve spontaneously or after the use of bronchodilator medication 1.The global prevalence of asthma is anticipated to be approximately 4.5 per cent 2,3.There are about 334 million patients with asthma affecting all age groups, across the world 4.
Background: Bronchial asthma being a chronic inflammatory disease of airways has numerous treatment options none of which have disease modifying properties. Curcumin, a yellow dietary pigment has varied pharmacological activities, prominent among which is an anti-inflammatory activity which may be crucial in bronchial asthma as has been proved by various in vitro and in vivo animal studies.
Biden Repeats Dubious Oil Slicks Story, Claims He Ended Up with "Bronchial Asthma and Other Diseases" in Earth Day Speech (VIDEO) by Cristina Laila Apr. 22, 2024 4:40 pm. Truth; ... — RNC Research (@RNCResearch) April 22, 2024. Biden previously told this oil slicks story and blurted out he has cancer. WATCH: