Fastest Nurse Insight Engine
- MEDICAL ASSISSTANT
- Abdominal Key
- Anesthesia Key
- Basicmedical Key
- Otolaryngology & Ophthalmology
- Musculoskeletal Key
- Obstetric, Gynecology and Pediatric
- Oncology & Hematology
- Plastic Surgery & Dermatology
- Clinical Dentistry
- Radiology Key
- Thoracic Key
- Veterinary Medicine
- Gold Membership

Making Decisions and Solving Problems
CHAPTER 6 Making Decisions and Solving Problems Rose Aguilar Welch This chapter describes the key concepts related to problem solving and decision making. The primary steps of the problem-solving and decision-making processes, as well as analytical tools used for these processes, are explored. Moreover, strategies for individual or group problem solving and decision making are presented. Objectives • Apply a decision-making format to list options to solve a problem, identify the pros and cons of each option, rank the options, and select the best option. • Evaluate the effect of faulty information gathering on a decision-making experience. • Analyze the decision-making style of a nurse leader/manager. • Critique resources on the Internet that focus on critical thinking, problem solving, and decision making. Terms to Know autocratic creativity critical thinking decision making democratic optimizing decision participative problem solving satisficing decision The Challenge Vickie Lemmon RN, MSN Director of Clinical Strategies and Operations, WellPoint, Inc., Ventura, California Healthcare managers today are faced with numerous and complex issues that pertain to providing quality services for patients within a resource-scarce environment. Stress levels among staff can escalate when problems are not resolved, leading to a decrease in morale, productivity, and quality service. This was the situation I encountered in my previous job as administrator for California Children Services (CCS). When I began my tenure as the new CCS administrator, staff expressed frustration and dissatisfaction with staffing, workload, and team communications. This was evidenced by high staff turnover, lack of teamwork, customer complaints, unmet deadlines for referral and enrollment cycle times, and poor documentation. The team was in crisis, characterized by in-fighting, blaming, lack of respectful communication, and lack of commitment to program goals and objectives. I had not worked as a case manager in this program. It was hard for me to determine how to address the problems the staff presented to me. I wanted to be fair but thought that I did not have enough information to make immediate changes. My challenge was to lead this team to greater compliance with state-mandated performance measures. What do you think you would do if you were this nurse? Introduction Problem solving and decision making are essential skills for effective nursing practice. Carol Huston (2008) identified “expert decision-making skills” as one of the eight vital leadership competencies for 2020. These processes not only are involved in managing and delivering care but also are essential for engaging in planned change. Myriad technologic, social, political, and economic changes have dramatically affected health care and nursing. Increased patient acuity, shorter hospital stays, shortage of healthcare providers, increased technology, greater emphasis on quality and patient safety, and the continuing shift from inpatient to ambulatory and home health care are some of the changes that require nurses to make rational and valid decisions. Moreover, increased diversity in patient populations, employment settings, and types of healthcare providers demands efficient and effective decision making and problem solving. More emphasis is now placed on involving patients in decision making and problem solving and using multidisciplinary teams to achieve results. Nurses must possess the basic knowledge and skills required for effective problem solving and decision making. These competencies are especially important for nurses with leadership and management responsibilities. Definitions Problem solving and decision making are not synonymous terms. However, the processes for engaging in both processes are similar. Both skills require critical thinking, which is a high-level cognitive process, and both can be improved with practice. Decision making is a purposeful and goal-directed effort that uses a systematic process to choose among options. Not all decision making begins with a problem situation. Instead, the hallmark of decision making is the identification and selection of options or alternatives. Problem solving, which includes a decision-making step, is focused on trying to solve an immediate problem, which can be viewed as a gap between “what is” and “what should be.” Effective problem solving and decision making are predicated on an individual’s ability to think critically. Although critical thinking has been defined in numerous ways, Scriven and Paul (2007) refer to it as “ the intellectually disciplined process of actively and skillfully conceptualizing, applying, analyzing, synthesizing, and/or evaluating information gathered from, or generated by, observation, experience, reflection, reasoning, or communication, as a guide to belief and action.” Effective critical thinkers are self-aware individuals who strive to improve their reasoning abilities by asking “why,” “what,” or “how.” A nurse who questions why a patient is restless is thinking critically. Compare the analytical abilities of a nurse who assumes a patient is restless because of anxiety related to an upcoming procedure with those of a nurse who asks if there could be another explanation and proceeds to investigate possible causes. It is important for nurse leaders and managers to assess staff members’ ability to think critically and enhance their knowledge and skills through staff-development programs, coaching, and role modeling. Establishing a positive and motivating work environment can enhance attitudes and dispositions to think critically. Creativity is essential for the generation of options or solutions. Creative individuals can conceptualize new and innovative approaches to a problem or issue by being more flexible and independent in their thinking. It takes just one person to plant a seed for new ideas to generate . The model depicted in Figure 6-1 demonstrates the relationship among related concepts such as professional judgment, decision making, problem solving, creativity, and critical thinking. Sound clinical judgment requires critical or reflective thinking. Critical thinking is the concept that interweaves and links the others. An individual, through the application of critical-thinking skills, engages in problem solving and decision making in an environment that can promote or inhibit these skills. It is the nurse leader’s and manager’s task to model these skills and promote them in others. FiGURE 6-1 Problem-solving and decision-making model. Decision Making This section presents an overview of concepts related to decision models, decision-making styles, factors affecting decision making, group decision making (advantages and challenges), and strategies and tools. The phases of the decision-making process include defining objectives, generating options, identifying advantages and disadvantages of each option, ranking the options, selecting the option most likely to achieve the predefined objectives, implementing the option, and evaluating the result. Box 6-1 contains a form that can be used to complete these steps. BOX 6-1 Decision-Making Format Objective: _____________________________________ Options Advantages Disadvantages Ranking Add more rows as necessary. Rank priority of options, with “1” being most preferred. Select the best option. Implementation plan: ______________________________________________________________________________ Evaluation plan: __________________________________________________________________________________ A poor-quality decision is likely if the objectives are not clearly identified or if they are inconsistent with the values of the individual or organization. Lewis Carroll illustrates the essential step of defining the goal, purpose, or objectives in the following excerpt from Alice’s Adventures in Wonderland: One day Alice came to a fork in the road and saw a Cheshire Cat in a tree. “Which road do I take?” she asked. His response was a question: “Where do you want to go?” “I don’t know,” Alice answered. “Then,” said the cat, “it doesn’t matter.” Decision Models The decision model that a nurse uses depends on the circumstances. Is the situation routine and predictable or complex and uncertain? Is the goal of the decision to make a decision conservatively that is just good enough or one that is optimal? If the situation is fairly routine, nurse leaders and managers can use a normative or prescriptive approach. Agency policy, standard procedures, and analytical tools can be applied to situations that are structured and in which options are known. If the situation is subjective, non-routine, and unstructured or if outcomes are unknown or unpredictable, the nurse leader and manager may need to take a different approach. In this case, a descriptive or behavioral approach is required. More information will need to be gathered to address the situation effectively. Creativity, experience, and group process are useful in dealing with the unknown. In the business world, Camillus described complex problems that are difficult to describe or resolve as “wicked” (as cited in Huston, 2008 ). This term is apt in describing the issues that nurse leaders face. In these situations, it is especially important for nurse leaders to seek expert opinion and involve key stakeholders. Another strategy is satisficing. In this approach, the decision maker selects the solution that minimally meets the objective or standard for a decision. It allows for quick decisions and may be the most appropriate when time is an issue. Optimizing is a decision style in which the decision maker selects the option that is best, based on an analysis of the pros and cons associated with each option. A better decision is more likely using this approach, although it does take longer to arrive at a decision. For example, a nursing student approaching graduation is contemplating seeking employment in one of three acute care hospitals located within a 40-mile radius of home. The choices are a medium-size, not-for-profit community hospital; a large, corporate-owned hospital; and a county facility. A satisficing decision might result if the student nurse picked the hospital that offered a decent salary and benefit packet or the one closest to home. However, an optimizing decision is more likely to occur if the student nurse lists the pros and cons of each acute care hospital being considered such as salary, benefits, opportunities for advancement, staff development, and mentorship programs. Decision-Making Styles The decision-making style of a nurse manager is similar to the leadership style that the manager is likely to use. A manager who leans toward an autocratic style may choose to make decisions independent of the input or participation of others. This has been referred to as the “decide and announce” approach, an authoritative style. On the other hand, a manager who uses a democratic or participative approach to management involves the appropriate personnel in the decision-making process. It is imperative for managers to involve nursing personnel in making decisions that affect patient care. One mechanism for doing so is by seeking nursing representation on various committees or task forces. Participative management has been shown to increase work performance and productivity, decrease employee turnover, and enhance employee satisfaction. Any decision style can be used appropriately or inappropriately. Like the tenets of situational leadership theory, the situation and circumstances should dictate which decision-making style is most appropriate. A Code Blue is not the time for managers to democratically solicit volunteers for chest compressions! The autocratic method results in more rapid decision making and is appropriate in crisis situations or when groups are likely to accept this type of decision style. However, followers are generally more supportive of consultative and group approaches. Although these approaches take more time, they are more appropriate when conflict is likely to occur, when the problem is unstructured, or when the manager does not have the knowledge or skills to solve the problem. Exercise 6-1 Interview colleagues about their most preferred decision-making model and style. What barriers or obstacles to effective decision making have your colleagues encountered? What strategies are used to increase the effectiveness of the decisions made? Based on your interview, is the style effective? Why or why not? Factors Affecting Decision Making Numerous factors affect individuals and groups in the decision-making process. Tanner (2006) conducted an extensive review of the literature to develop a Clinical Judgment Model. Out of the research, she concluded that five principle factors influence decision making. (See the Literature Perspective below.) Literature Perspective Resource: Tanner, C. A. (2006). Thinking like a nurse: A research-based model of clinical judgment in nursing. Journal of Nursing Education, 45 (6), 204-211. Tanner engaged in an extensive review of 200 studies focusing on clinical judgment and clinical decision making to derive a model of clinical judgment that can be used as a framework for instruction. The first review summarized 120 articles and was published in 1998. The 2006 article reviewed an additional 71 studies published since 1998. Based on an analysis of the entire set of articles, Tanner proposed five conclusions which are listed below. The reader is referred to the article for detailed explanation of each of the five conclusions. The author considers clinical judgment as a “problem-solving activity.” She notes that the terms “clinical judgment,” “problem solving,” “decision making,” and “critical thinking” are often used interchangeably. For the purpose of aiding in the development of the model, Tanner defined clinical judgment as actions taken based on the assessment of the patient’s needs. Clinical reasoning is the process by which nurses make their judgments (e.g., the decision-making process of selecting the most appropriate option) ( Tanner, 2006 , p. 204): 1. Clinical judgments are more influenced by what nurses bring to the situation than the objective data about the situation at hand. 2. Sound clinical judgment rests to some degree on knowing the patient and his or her typical pattern of responses, as well as an engagement with the patient and his or her concerns. 3. Clinical judgments are influenced by the context in which the situation occurs and the culture of the nursing care unit. 4. Nurses use a variety of reasoning patterns alone or in combination. 5. Reflection on practice is often triggered by a breakdown in clinical judgment and is critical for the development of clinical knowledge and improvement in clinical reasoning. The Clinical Judgment Model developed through the review of the literature involves four steps that are similar to problem-solving and decision-making steps described in this chapter. The model starts with a phase called “Noticing.” In this phase, the nurse comes to expect certain responses resulting from knowledge gleaned from similar patient situations, experiences, and knowledge. External factors influence nurses in this phase such as the complexity of the environment and values and typical practices within the unit culture. The second phase of the model is “Interpreting,” during which the nurse understands the situation that requires a response. The nurse employs various reasoning patterns to make sense of the issue and to derive an appropriate action plan. The third phase is “Responding,” during which the nurse decides on the best option for handling the situation. This is followed by the fourth phase, “Reflecting,” during which the nurse assesses the patient’s responses to the actions taken. Tanner emphasized that “reflection-in-action” and “reflection-on-action” are major processes required in the model. Reflection-in-action is real-time reflection on the patient’s responses to nursing action with modifications to the plan based on the ongoing assessment. On the other hand, reflection-on-action is a review of the experience, which promotes learning for future similar experiences. Nurse educators and managers can employ this model with new and experienced nurses to aid in understanding thought processes involved in decision making. As Tanner (2006) so eloquently concludes, “If we, as nurse educators, help our students understand and develop as moral agents, advance their clinical knowledge through expert guidance and coaching, and become habitual in reflection-on-practice, they will have learned to think like a nurse” ( p. 210 ). Implications for Practice Nurse educators and managers can employ this model with new and experienced nurses to aid in understanding thought processes involved in decision making. For example, students and practicing nurses can be encouraged to maintain reflective journals to record observations and impressions from clinical experiences. In clinical post-conferences or staff development meetings, the nurse educator and manager can engage them in applying to their lived experiences the five conclusions Tanner proposed. The ultimate goal of analyzing their decisions and decision-making processes is to improve clinical judgment, problem-solving, decision-making, and critical-thinking skills. Internal and external factors can influence how the situation is perceived. Internal factors include variables such as the decision maker’s physical and emotional state, personal philosophy, biases, values, interests, experience, knowledge, attitudes, and risk-seeking or risk-avoiding behaviors. External factors include environmental conditions, time, and resources. Decision-making options are externally limited when time is short or when the environment is characterized by a “we’ve always done it this way” attitude. Values affect all aspects of decision making, from the statement of the problem/issue through the evaluation. Values, determined by one’s cultural, social, and philosophical background, provide the foundation for one’s ethical stance. The steps for engaging in ethical decision making are similar to the steps described earlier; however, alternatives or options identified in the decision-making process are evaluated with the use of ethical resources. Resources that can facilitate ethical decision making include institutional policy; principles such as autonomy, nonmaleficence, beneficence, veracity, paternalism, respect, justice, and fidelity; personal judgment; trusted co-workers; institutional ethics committees; and legal precedent. Certain personality factors, such as self-esteem and self-confidence, affect whether one is willing to take risks in solving problems or making decisions. Keynes (2008) asserts that individuals may be influenced based on social pressures. For example, are you inclined to make decisions to satisfy people to whom you are accountable or from whom you feel social pressure? Characteristics of an effective decision maker include courage, a willingness to take risks, self-awareness, energy, creativity, sensitivity, and flexibility. Ask yourself, “Do I prefer to let others make the decisions? Am I more comfortable in the role of ‘follower’ than leader? If so, why?” Exercise 6-2 Identify a current or past situation that involved resource allocation, end-of-life issues, conflict among healthcare providers or patient/family/significant others, or some other ethical dilemma. Describe how the internal and external factors previously described influenced the decision options, the option selected, and the outcome. Group Decision Making There are two primary criteria for effective decision making. First, the decision must be of a high quality; that is, it achieves the predefined goals, objectives, and outcomes. Second, those who are responsible for its implementation must accept the decision. Higher-quality decisions are more likely to result if groups are involved in the problem-solving and decision-making process. In reality, with the increased focus on quality and safety, decisions cannot be made alone. When individuals are allowed input into the process, they tend to function more productively and the quality of the decision is generally superior. Taking ownership of the process and outcome provides a smoother transition. Multidisciplinary teams should be used in the decision-making process, especially if the issue, options, or outcome involves other disciplines. Research findings suggest that groups are more likely to be effective if members are actively involved, the group is cohesive, communication is encouraged, and members demonstrate some understanding of the group process. In deciding to use the group process for decision making, it is important to consider group size and composition. If the group is too small, a limited number of options will be generated and fewer points of view expressed. Conversely, if the group is too large, it may lack structure, and consensus becomes more difficult. Homogeneous groups may be more compatible; however, heterogeneous groups may be more successful in problem solving. Research has demonstrated that the most productive groups are those that are moderately cohesive. In other words, divergent thinking is useful to create the best decision. For groups to be able to work effectively, the group facilitator or leader should carefully select members on the basis of their knowledge and skills in decision making and problem solving. Individuals who are aggressive, are authoritarian, or manifest self-oriented behaviors tend to decrease the effectiveness of groups. The nurse leader or manager should provide a nonthreatening and positive environment in which group members are encouraged to participate actively. Using tact and diplomacy, the facilitator can control aggressive individuals who tend to monopolize the discussion and can encourage more passive individuals to contribute by asking direct, open-ended questions. Providing positive feedback such as “You raised a good point,” protecting members and their suggestions from attack, and keeping the group focused on the task are strategies that create an environment conducive to problem solving. Advantages of Group Decision Making The advantages of group decision making are numerous. The adage “two heads are better than one” illustrates that when individuals with different knowledge, skills, and resources collaborate to solve a problem or make a decision, the likelihood of a quality outcome is increased. More ideas can be generated by groups than by individuals functioning alone. In addition, when followers are directly involved in this process, they are more apt to accept the decision, because they have an increased sense of ownership or commitment to the decision. Implementing solutions becomes easier when individuals have been actively involved in the decision-making process. Involvement can be enhanced by making information readily available to the appropriate personnel, requesting input, establishing committees and task forces with broad representation, and using group decision-making techniques. The group leader must establish with the participants what decision rule will be followed. Will the group strive to achieve consensus, or will the majority rule? In determining which decision rule to use, the group leader should consider the necessity for quality and acceptance of the decision. Achieving both a high-quality and an acceptable decision is possible, but it requires more involvement and approval from individuals affected by the decision. Groups will be more committed to an idea if it is derived by consensus rather than as an outcome of individual decision making or majority rule. Consensus requires that all participants agree to go along with the decision. Although achieving consensus requires considerable time, it results in both high-quality and high-acceptance decisions and reduces the risk of sabotage. Majority rule can be used to compromise when 100% agreement cannot be achieved. This method saves time, but the solution may only partially achieve the goals of quality and acceptance. In addition, majority rule carries certain risks. First, if the informal group leaders happen to fall in the minority opinion, they may not support the decision of the majority. Certain members may go so far as to build coalitions to gain support for their position and block the majority choice. After all, the majority may represent only 51% of the group. In addition, group members may support the position of the formal leader, although they do not agree with the decision, because they fear reprisal or they wish to obtain the leader’s approval. In general, as the importance of the decision increases, so does the percentage of group members required to approve it. To secure the support of the group, the leader should maintain open communication with those affected by the decision and be honest about the advantages and disadvantages of the decision. The leader should also demonstrate how the advantages outweigh the disadvantages, suggest ways the unwanted outcomes can be minimized, and be available to assist when necessary.
Share this:
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
Related posts:
- Patient Safety
- Developing the Role of Manager
- Care Delivery Strategies
Stay updated, free articles. Join our Telegram channel
Comments are closed for this page.

Full access? Get Clinical Tree

- Research article
- Open access
- Published: 07 October 2020
Impact of social problem-solving training on critical thinking and decision making of nursing students
- Soleiman Ahmady 1 &
- Sara Shahbazi ORCID: orcid.org/0000-0001-8397-6233 2 , 3
BMC Nursing volume 19 , Article number: 94 ( 2020 ) Cite this article
28k Accesses
21 Citations
1 Altmetric
Metrics details
The complex health system and challenging patient care environment require experienced nurses, especially those with high cognitive skills such as problem-solving, decision- making and critical thinking. Therefore, this study investigated the impact of social problem-solving training on nursing students’ critical thinking and decision-making.
This study was quasi-experimental research and pre-test and post-test design and performed on 40 undergraduate/four-year students of nursing in Borujen Nursing School/Iran that was randomly divided into 2 groups; experimental ( n = 20) and control (n = 20). Then, a social problem-solving course was held for the experimental group. A demographic questionnaire, social problem-solving inventory-revised, California critical thinking test, and decision-making questionnaire was used to collect the information. The reliability and validity of all of them were confirmed. Data analysis was performed using SPSS software and independent sampled T-test, paired T-test, square chi, and Pearson correlation coefficient.
The finding indicated that the social problem-solving course positively affected the student’ social problem-solving and decision-making and critical thinking skills after the instructional course in the experimental group ( P < 0.05), but this result was not observed in the control group ( P > 0.05).
Conclusions
The results showed that structured social problem-solving training could improve cognitive problem-solving, critical thinking, and decision-making skills. Considering this result, nursing education should be presented using new strategies and creative and different ways from traditional education methods. Cognitive skills training should be integrated in the nursing curriculum. Therefore, training cognitive skills such as problem- solving to nursing students is recommended.
Peer Review reports
Continuous monitoring and providing high-quality care to patients is one of the main tasks of nurses. Nurses’ roles are diverse and include care, educational, supportive, and interventional roles when dealing with patients’ clinical problems [ 1 , 2 ].
Providing professional nursing services requires the cognitive skills such as problem-solving, decision-making and critical thinking, and information synthesis [ 3 ].
Problem-solving is an essential skill in nursing. Improving this skill is very important for nurses because it is an intellectual process which requires the reflection and creative thinking [ 4 ].
Problem-solving skill means acquiring knowledge to reach a solution, and a person’s ability to use this knowledge to find a solution requires critical thinking. The promotion of these skills is considered a necessary condition for nurses’ performance in the nursing profession [ 5 , 6 ].
Managing the complexities and challenges of health systems requires competent nurses with high levels of critical thinking skills. A nurse’s critical thinking skills can affect patient safety because it enables nurses to correctly diagnose the patient’s initial problem and take the right action for the right reason [ 4 , 7 , 8 ].
Problem-solving and decision-making are complex and difficult processes for nurses, because they have to care for multiple patients with different problems in complex and unpredictable treatment environments [ 9 , 10 ].
Clinical decision making is an important element of professional nursing care; nurses’ ability to form effective clinical decisions is the most significant issue affecting the care standard. Nurses build 2 kinds of choices associated with the practice: patient care decisions that affect direct patient care and occupational decisions that affect the work context or teams [ 11 , 12 , 13 , 14 , 15 , 16 ].
The utilization of nursing process guarantees the provision of professional and effective care. The nursing process provides nurses with the chance to learn problem-solving skills through teamwork, health management, and patient care. Problem-solving is at the heart of nursing process which is why this skill underlies all nursing practices. Therefore, proper training of this skill in an undergraduate nursing program is essential [ 17 ].
Nursing students face unique problems which are specific to the clinical and therapeutic environment, causing a lot of stresses during clinical education. This stress can affect their problem- solving skills [ 18 , 19 , 20 , 21 ]. They need to promote their problem-solving and critical thinking skills to meet the complex needs of current healthcare settings and should be able to respond to changing circumstances and apply knowledge and skills in different clinical situations [ 22 ]. Institutions should provide this important opportunity for them.
Despite, the results of studies in nursing students show the weakness of their problem-solving skills, while in complex health environments and exposure to emerging diseases, nurses need to diagnose problems and solve them rapidly accurately. The teaching of these skills should begin in college and continue in health care environments [ 5 , 23 , 24 ].
It should not be forgotten that in addition to the problems caused by the patients’ disease, a large proportion of the problems facing nurses are related to the procedures of the natural life of their patients and their families, the majority of nurses with the rest of health team and the various roles defined for nurses [ 25 ].
Therefore, in addition to above- mentioned issues, other ability is required to deal with common problems in the working environment for nurses, the skill is “social problem solving”, because the term social problem-solving includes a method of problem-solving in the “natural context” or the “real world” [ 26 , 27 ]. In reviewing the existing research literature on the competencies and skills required by nursing students, what attracts a lot of attention is the weakness of basic skills and the lack of formal and systematic training of these skills in the nursing curriculum, it indicates a gap in this area [ 5 , 24 , 25 ]. In this regard, the researchers tried to reduce this significant gap by holding a formal problem-solving skills training course, emphasizing the common social issues in the real world of work. Therefore, this study was conducted to investigate the impact of social problem-solving skills training on nursing students’ critical thinking and decision-making.
Setting and sample
This quasi-experimental study with pretest and post-test design was performed on 40 undergraduate/four-year nursing students in Borujen nursing school in Shahrekord University of Medical Sciences. The periods of data collection were 4 months.
According to the fact that senior students of nursing have passed clinical training and internship programs, they have more familiarity with wards and treatment areas, patients and issues in treatment areas and also they have faced the problems which the nurses have with other health team personnel and patients and their families, they have been chosen for this study. Therefore, this study’s sampling method was based on the purpose, and the sample size was equal to the total population. The whole of four-year nursing students participated in this study and the sample size was 40 members. Participants was randomly divided in 2 groups; experimental ( n = 20) and control (n = 20).
The inclusion criteria to take part in the present research were students’ willingness to take part, studying in the four-year nursing, not having the record of psychological sickness or using the related drugs (all based on their self-utterance).
Intervention
At the beginning of study, all students completed the demographic information’ questionnaire. The study’s intervening variables were controlled between the two groups [such as age, marital status, work experience, training courses, psychological illness, psychiatric medication use and improving cognitive skills courses (critical thinking, problem- solving, and decision making in the last 6 months)]. Both groups were homogeneous in terms of demographic variables ( P > 0.05). Decision making and critical thinking skills and social problem solving of participants in 2 groups was evaluated before and 1 month after the intervention.
All questionnaires were anonymous and had an identification code which carefully distributed by the researcher.
To control the transfer of information among the students of two groups, the classification list of students for internships, provided by the head of nursing department at the beginning of semester, was used.
Furthermore, the groups with the odd number of experimental group and the groups with the even number formed the control group and thus were less in contact with each other.
The importance of not transferring information among groups was fully described to the experimental group. They were asked not to provide any information about the course to the students of the control group.
Then, training a course of social problem-solving skills for the experimental group, given in a separate course and the period from the nursing curriculum and was held in 8 sessions during 2 months, using small group discussion, brainstorming, case-based discussion, and reaching the solution in small 4 member groups, taking results of the social problem-solving model as mentioned by D-zurilla and gold fried [ 26 ]. The instructor was an assistant professor of university and had a history of teaching problem-solving courses. This model’ stages are explained in Table 1 .
All training sessions were performed due to the model, and one step of the model was implemented in each session. In each session, the teacher stated the educational objectives and asked the students to share their experiences in dealing to various workplace problems, home and community due to the topic of session. Besides, in each session, a case-based scenario was presented and thoroughly analyzed, and students discussed it.
Instruments
In this study, the data were collected using demographic variables questionnaire and social problem- solving inventory – revised (SPSI-R) developed by D’zurilla and Nezu (2002) [ 26 ], California critical thinking skills test- form B (CCTST; 1994) [ 27 , 28 ] and decision-making questionnaire.
SPSI-R is a self - reporting tool with 52 questions ranging from a Likert scale (1: Absolutely not – 5: very much).
The minimum score maybe 25 and at a maximum of 125, therefore:
The score 25 and 50: weak social problem-solving skills.
The score 50–75: moderate social problem-solving skills.
The score higher of 75: strong social problem-solving skills.
The reliability assessed by repeated tests is between 0.68 and 0.91, and its alpha coefficient between 0.69 and 0.95 was reported [ 26 ]. The structural validity of questionnaire has also been confirmed. All validity analyses have confirmed SPSI as a social problem - solving scale.
In Iran, the alpha coefficient of 0.85 is measured for five factors, and the retest reliability coefficient was obtained 0.88. All of the narratives analyzes confirmed SPSI as a social problem- solving scale [ 29 ].
California critical thinking skills test- form B(CCTST; 1994): This test is a standard tool for assessing the basic skills of critical thinking at the high school and higher education levels (Facione & Facione, 1992, 1998) [ 27 ].
This tool has 34 multiple-choice questions which assessed analysis, inference, and argument evaluation. Facione and Facione (1993) reported that a KR-20 range of 0.65 to 0.75 for this tool is acceptable [ 27 ].
In Iran, the KR-20 for the total scale was 0.62. This coefficient is acceptable for questionnaires that measure the level of thinking ability of individuals.
After changing the English names of this questionnaire to Persian, its content validity was approved by the Board of Experts.
The subscale analysis of Persian version of CCTST showed a positive high level of correlation between total test score and the components (analysis, r = 0.61; evaluation, r = 0.71; inference, r = 0.88; inductive reasoning, r = 0.73; and deductive reasoning, r = 0.74) [ 28 ].
A decision-making questionnaire with 20 questions was used to measure decision-making skills. This questionnaire was made by a researcher and was prepared under the supervision of a professor with psychometric expertise. Five professors confirmed the face and content validity of this questionnaire. The reliability was obtained at 0.87 which confirmed for 30 students using the test-retest method at a time interval of 2 weeks. Each question had four levels and a score from 0.25 to 1. The minimum score of this questionnaire was 5, and the maximum score was 20 [ 30 ].
Statistical analysis
For analyzing the applied data, the SPSS Version 16, and descriptive statistics tests, independent sample T-test, paired T-test, Pearson correlation coefficient, and square chi were used. The significant level was taken P < 0.05.
The average age of students was 21.7 ± 1.34, and the academic average total score was 16.32 ± 2.83. Other demographic characteristics are presented in Table 2 .
None of the students had a history of psychiatric illness or psychiatric drug use. Findings obtained from the chi-square test showed that there is not any significant difference between the two groups statistically in terms of demographic variables.
The mean scores in social decision making, critical thinking, and decision-making in whole samples before intervention showed no significant difference between the two groups statistically ( P > 0.05), but showed a significant difference after the intervention ( P < 0.05) (Table 3 ).
Scores in Table 4 showed a significant positive difference before and after intervention in the “experimental” group ( P < 0.05), but this difference was not seen in the control group ( P > 0.05).
Among the demographic variables, only a positive relationship was seen between marital status and decision-making skills (r = 0.72, P < 0.05).
Also, the scores of critical thinking skill’ subgroups and social problem solving’ subgroups are presented in Tables 5 and 6 which showed a significant positive difference before and after intervention in the “experimental” group (P < 0.05), but this difference was not seen in the control group ( P > 0.05).
In the present study conducted by some studies, problem-solving and critical thinking and decision-making scores of nursing students are moderate [ 5 , 24 , 31 ].
The results showed that problem-solving skills, critical thinking, and decision-making in nursing students were promoted through a social problem-solving training course. Unfortunately, no study has examined the effect of teaching social problem-solving skills on nursing students’ critical thinking and decision-making skills.
Altun (2018) believes that if the values of truth and human dignity are promoted in students, it will help them acquire problem-solving skills. Free discussion between students and faculty on value topics can lead to the development of students’ information processing in values. Developing self-awareness increases students’ impartiality and problem-solving ability [ 5 ]. The results of this study are consistent to the results of present study.
Erozkan (2017), in his study, reported there is a significant relationship between social problem solving and social self-efficacy and the sub-dimensions of social problem solving [ 32 ]. In the present study, social problem -solving skills training has improved problem -solving skills and its subdivisions.
The results of study by Moshirabadi (2015) showed that the mean score of total problem-solving skills was 89.52 ± 21.58 and this average was lower in fourth-year students than other students. He explained that education should improve students’ problem-solving skills. Because nursing students with advanced problem-solving skills are vital to today’s evolving society [ 22 ]. In the present study, the results showed students’ weakness in the skills in question, and holding a social problem-solving skills training course could increase the level of these skills.
Çinar (2010) reported midwives and nurses are expected to use problem-solving strategies and effective decision-making in their work, using rich basic knowledge.
These skills should be developed throughout one’s profession. The results of this study showed that academic education could increase problem-solving skills of nursing and midwifery students, and final year students have higher skill levels [ 23 ].
Bayani (2012) reported that the ability to solve social problems has a determining role in mental health. Problem-solving training can lead to a level upgrade of mental health and quality of life [ 33 ]; These results agree with the results obtained in our study.
Conducted by this study, Kocoglu (2016) reported nurses’ understanding of their problem-solving skills is moderate. Receiving advice and support from qualified nursing managers and educators can enhance this skill and positively impact their behavior [ 31 ].
Kashaninia (2015), in her study, reported teaching critical thinking skills can promote critical thinking and the application of rational decision-making styles by nurses.
One of the main components of sound performance in nursing is nurses’ ability to process information and make good decisions; these abilities themselves require critical thinking. Therefore, universities should envisage educational and supportive programs emphasizing critical thinking to cultivate their students’ professional competencies, decision-making, problem-solving, and self-efficacy [ 34 ].
The study results of Kirmizi (2015) also showed a moderate positive relationship between critical thinking and problem-solving skills [ 35 ].
Hong (2015) reported that using continuing PBL training promotes reflection and critical thinking in clinical nurses. Applying brainstorming in PBL increases the motivation to participate collaboratively and encourages teamwork. Learners become familiar with different perspectives on patients’ problems and gain a more comprehensive understanding. Achieving these competencies is the basis of clinical decision-making in nursing. The dynamic and ongoing involvement of clinical staff can bridge the gap between theory and practice [ 36 ].
Ancel (2016) emphasizes that structured and managed problem-solving training can increase students’ confidence in applying problem-solving skills and help them achieve self-confidence. He reported that nursing students want to be taught in more innovative ways than traditional teaching methods which cognitive skills training should be included in their curriculum. To this end, university faculties and lecturers should believe in the importance of strategies used in teaching and the richness of educational content offered to students [ 17 ].
The results of these recent studies are adjusted with the finding of recent research and emphasize the importance of structured teaching cognitive skills to nurses and nursing students.
Based on the results of this study on improving critical thinking and decision-making skills in the intervention group, researchers guess the reasons to achieve the results of study in the following cases:
In nursing internationally, problem-solving skills (PS) have been introduced as a key strategy for better patient care [ 17 ]. Problem-solving can be defined as a self-oriented cognitive-behavioral process used to identify or discover effective solutions to a special problem in everyday life. In particular, the application of this cognitive-behavioral methodology identifies a wide range of possible effective solutions to a particular problem and enhancement the likelihood of selecting the most effective solution from among the various options [ 27 ].
In social problem-solving theory, there is a difference among the concepts of problem-solving and solution implementation, because the concepts of these two processes are different, and in practice, they require different skills.
In the problem-solving process, we seek to find solutions to specific problems, while in the implementation of solution, the process of implementing those solutions in the real problematic situation is considered [ 25 , 26 ].
The use of D’zurilla and Goldfride’s social problem-solving model was effective in achieving the study results because of its theoretical foundations and the usage of the principles of cognitive reinforcement skills. Social problem solving is considered an intellectual, logical, effort-based, and deliberate activity [ 26 , 32 ]; therefore, using this model can also affect other skills that need recognition.
In this study, problem-solving training from case studies and group discussion methods, brainstorming, and activity in small groups, was used.
There are significant educational achievements in using small- group learning strategies. The limited number of learners in each group increases the interaction between learners, instructors, and content. In this way, the teacher will be able to predict activities and apply techniques that will lead students to achieve high cognitive taxonomy levels. That is, confront students with assignments and activities that force them to use cognitive processes such as analysis, reasoning, evaluation, and criticism.
In small groups, students are given the opportunity to the enquiry, discuss differences of opinion, and come up with solutions. This method creates a comprehensive understanding of the subject for the student [ 36 ].
According to the results, social problem solving increases the nurses’ decision-making ability and critical thinking regarding identifying the patient’s needs and choosing the best nursing procedures. According to what was discussed, the implementation of this intervention in larger groups and in different levels of education by teaching other cognitive skills and examining their impact on other cognitive skills of nursing students, in the future, is recommended.
Social problem- solving training by affecting critical thinking skills and decision-making of nursing students increases patient safety. It improves the quality of care because patients’ needs are better identified and analyzed, and the best solutions are adopted to solve the problem.
In the end, the implementation of this intervention in larger groups in different levels of education by teaching other cognitive skills and examining their impact on other cognitive skills of nursing students in the future is recommended.
Study limitations
This study was performed on fourth-year nursing students, but the students of other levels should be studied during a cohort from the beginning to the end of course to monitor the cognitive skills improvement.
The promotion of high-level cognitive skills is one of the main goals of higher education. It is very necessary to adopt appropriate approaches to improve the level of thinking. According to this study results, the teachers and planners are expected to use effective approaches and models such as D’zurilla and Goldfride social problem solving to improve problem-solving, critical thinking, and decision-making skills. What has been confirmed in this study is that the routine training in the control group should, as it should, has not been able to improve the students’ critical thinking skills, and the traditional educational system needs to be transformed and reviewed to achieve this goal.
Availability of data and materials
The datasets used and analyzed during the present study are available from the corresponding author on reasonable request.
Abbreviations
California critical thinking skills test
Social problem-solving inventory – revised
Pesudovs L. Medical/surgical nursing in the home. Aust Nurs Midwifery J. 2014;22(3):24.
PubMed Google Scholar
Szeri C, et al. Problem solving skills of the nursing and midwifery students and influential factors. Revista Eletrônica de Enfermagem. 2010;12(4).
Friese CR, et al. Pod nursing on a medical/surgical unit: implementation and outcomes evaluation. J Nurs Adm. 2014;44(4):207–11.
Article Google Scholar
Lyneham J. A conceptual model for medical-surgical nursing: moving toward an international clinical specialty. Medsurg Nurs. 2013;22(4):215–20 263.
Altun I. The perceived problem solving ability and values of student nurses and midwives. Nurse Educ Today. 2003;23(8):575–84.
Deniz Kocoglu R, et al. Problem solving training for first line nurse managers. Int J Caring Sci. 2016;9(3):955.
Google Scholar
Mahoney C, et al. Implementing an 'arts in nursing' program on a medical-surgical unit. Medsurg Nurs. 2011;20(5):273–4.
Pardue SF. Decision-making skills and critical thinking ability among associate degree, diploma, baccalaureate, and master's-prepared nurses. J Nurs Educ. 1987;26(9):354–61.
Article CAS Google Scholar
Kozlowski D, et al. The role of emotion in clinical decision making: an integrative literature review. BMC Med Educ. 2017;17(1):255.
Kuiper RA, Pesut DJ. Promoting cognitive and metacognitive reflective reasoning skills in nursing practice: self-regulated learning theory. J Adv Nurs. 2004;45(4):381–91.
Huitzi-Egilegor JX, et al. Implementation of the nursing process in a health area: models and assessment structures used. Rev Lat Am Enfermagem. 2014;22(5):772–7.
Lauri S. Development of the nursing process through action research. J Adv Nurs. 1982;7(4):301–7.
Muller-Staub M, de Graaf-Waar H, Paans W. An internationally consented standard for nursing process-clinical decision support Systems in Electronic Health Records. Comput Inform Nurs. 2016;34(11):493–502.
Neville K, Roan N. Challenges in nursing practice: nurses' perceptions in caring for hospitalized medical-surgical patients with substance abuse/dependence. J Nurs Adm. 2014;44(6):339–46.
Rabelo-Silva ER, et al. Advanced nursing process quality: comparing the international classification for nursing practice (ICNP) with the NANDA-international (NANDA-I) and nursing interventions classification (NIC). J Clin Nurs. 2017;26(3–4):379–87.
Varcoe C. Disparagement of the nursing process: the new dogma? J Adv Nurs. 1996;23(1):120–5.
Ancel G. Problem-solving training: effects on the problem-solving skills and self-efficacy of nursing students. Eurasian J Educ Res. 2016;64:231–46.
Fang J, et al. Social problem-solving in Chinese baccalaureate nursing students. J Evid Based Med. 2016;9(4):181–7.
Kanbay Y, Okanli A. The effect of critical thinking education on nursing students' problem-solving skills. Contemp Nurse. 2017;53(3):313–21.
Lau Y. Factors affecting the social problem-solving ability of baccalaureate nursing students. Nurse Educ Today. 2014;34(1):121–6.
Terzioglu F. The perceived problem-solving ability of nurse managers. J Nurs Manag. 2006;14(5):340–7.
Moshirabadi, Z., et al., The perceived problem solving skill of Iranian nursing students . 2015.
Cinar N. Problem solving skills of the nursing and midwifery students and influential factors. Revista Eletrônica de Enfermagem. 2010;12(4):601–6.
Moattari M, et al. Clinical concept mapping: does it improve discipline-based critical thinking of nursing students? Iran J Nurs Midwifery Res. 2014;19(1):70–6.
PubMed PubMed Central Google Scholar
Elliott TR, Grant JS, Miller DM. Social Problem-Solving Abilities and Behavioral Health. In Chang EC, D'Zurilla TJ, Sanna LJ, editors. Social problem solving: Theory, research, and training. American Psychological Association; 2004. p. 117–33.
D'Zurilla TJ, Maydeu-Olivares A. Conceptual and methodological issues in social problem-solving assessment. Behav Ther. 1995;26(3):409–32.
Facione PA. The California Critical Thinking Skills Test--College Level. Technical Report# 1. Experimental Validation and Content Validity; 1990.
Khalili H, Zadeh MH. Investigation of reliability, validity and normality Persian version of the California Critical Thinking Skills Test; Form B (CCTST). J Med Educ. 2003;3(1).
Mokhberi A. Questionnaire, psychometrics, and standardization of indicators of social problem solving ability. Educ Measurement. 2011;1(4):1–21.
Heidari M, Shahbazi S. Effect of training problem-solving skill on decision-making and critical thinking of personnel at medical emergencies. Int J Crit Illn Inj Sci. 2016;6(4):182–7.
Kocoglu D, Duygulu S, Abaan S, Akin B. Problem Solving Training for First Line Nurse Managers. Int J Caring Sci. 2016;9(13):955–65.
Erozkan A. Analysis of social problem solving and social self-efficacy in prospective teachers. Educational Sciences: Theory and Practice. 2014;14(2):447–55.
Bayani AA, Ranjbar M, Bayani A. The study of relationship between social problem-solving and depression and social phobia among students. J Mazandaran Univ Med Sci. 2012;22(94):91–8.
Kashaninia Z, et al. The effect of teaching critical thinking skills on the decision making style of nursing managers. J Client-Centered Nurs Care. 2015;1(4):197–204.
Kirmizi FS, Saygi C, Yurdakal IH. Determine the relationship between the disposition of critical thinking and the perception about problem solving skills. Procedia Soc Behav Sci. 2015;191:657–61.
Hung CH, Lin CY. Using concept mapping to evaluate knowledge structure in problem-based learning. BMC Med Educ. 2015;15:212.
Download references
Acknowledgments
This article results from research project No. 980 approved by the Research and Technology Department of Shahrekord University of Medical Sciences. We would like to appreciate to all personnel and students of the Borujen Nursing School. The efforts of all those who assisted us throughout this research.
‘Not applicable.
Author information
Authors and affiliations.
Department of Medical Education, Virtual School of Medical Education and Management, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Soleiman Ahmady
Virtual School of Medical Education and management, Shahid Beheshty University of Medical Sciences, Tehran, Iran
Sara Shahbazi
Community-Oriented Nursing Midwifery Research Center, Shahrekord University of Medical Sciences, Shahrekord, Iran
You can also search for this author in PubMed Google Scholar
Contributions
SA and SSH conceptualized the study, developed the proposal, coordinated the project, completed initial data entry and analysis, and wrote the report. SSH conducted the statistical analyses. SA and SSH assisted in writing and editing the final report. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Sara Shahbazi .
Ethics declarations
Ethics approval and consent to participate.
This study was reviewed and given exempt status by the Institutional Review Board of the research and technology department of Shahrekord University of Medical Sciences (IRB No. 08–2017-109). Before the survey, students completed a research consent form and were assured that their information would remain confidential. After the end of the study, a training course for the control group students was held.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ahmady, S., Shahbazi, S. Impact of social problem-solving training on critical thinking and decision making of nursing students. BMC Nurs 19 , 94 (2020). https://doi.org/10.1186/s12912-020-00487-x
Download citation
Received : 11 March 2020
Accepted : 29 September 2020
Published : 07 October 2020
DOI : https://doi.org/10.1186/s12912-020-00487-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Social problem solving
- Decision making
- Critical thinking
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Nursing professional development evidence-based practice.
Barbara A. Brunt ; Melanie M. Morris .
Affiliations
Last Update: March 4, 2023 .
- Introduction
Evidence-based practice is “integrating the best available evidence with the healthcare educator’s expertise and the client’s needs while considering the practice environment. [1] One of the roles of the NPD practitioner in the 2022 edition of the Nursing Scope and Standards of Practice is a champion for scientific inquiry. In this role, the NPD practitioner promotes a spirit of inquiry, the generation and dissemination of new knowledge, and the use of evidence to advance NPD practice, guide clinical practice, and improve the quality of care for the healthcare consumer/partner. Scholarly inquiry is a standard of practice within that role. It is defined as “The nursing professional development (NPD) practitioner integrates scholarship, evidence, and research findings into practice” (p. 104).
There is often confusion between quality improvement, evidence-based practice, and research. A seminal article by Shirey and colleagues. [2] differentiated these three topics. Evidence-based practice is a systematic problem-solving approach that is evidence-driven and translates new knowledge into clinical, administrative, and educational practice. Institutional Review Board (IRB) approval is usually not required unless outcomes are intended for publication, or the project could potentially expose individuals to harm.
The EBP process, as defined by Melnyk and Fineout-Overholt, includes seven steps:
- Encouraging and supporting a spirit of inquiry
- Asking questions
- Searching for evidence
- Appraising the evidence
- Integrating evidence into practice
- Evaluating outcomes
- Sharing results
Implementing EBP in practice has been shown to lead to a higher quality of care and better patient outcomes, but nurses encounter many barriers when implementing EBP. NPD practitioners can facilitate the implementation of EBP by ensuring a supportive environment for EBP, providing educational sessions to nurses about the EBP process, being role models, and mentoring nurses.
- Issues of Concern
PICOT Question
The foundation of EBP is developing a PICOT question, which identifies the terms to be used to search for the best evidence to answer a burning clinical question. [3] This framework breaks down the question into keywords. P stands for patient/population; I refers to Intervention; C stands for comparison/control; O stands for the outcome; and T refers to the time frame. When looking at the population, it is important to consider the relevant patients, including age, sex, geographic location, or specific characteristics that would be important to the question.
The intervention examines the management strategy, diagnostic test, or exposure of interest. There may not always be a comparison in the PICOT analysis. If there is, this would be a control or alternative management strategy compared to the intervention. Outcomes should be measurable, as the best evidence comes from rigorous studies with statistically significant findings. The time factor looks at what period should be considered. There are a variety of clinical domains that PICOT questions can evaluate, such as intervention, diagnosis, etiology, prevention, prognosis/prediction, quality of life, or therapy. Writing a good PICOT question for an effective search and making robust, evidence-based recommendations to improve care and outcomes is critical.
The Evidence
While there are multiple ways to evaluate and rank evidence in the literature, one of the most widely used in nursing in the United States uses seven levels. These seven accepted levels of evidence are assigned to studies based on the methodological quality of the design, validity, and application to patient care. In addition, these levels provide the “grade” or strength of the recommendation.
- Level I – Evidence from a systematic review or meta-analysis of all relevant randomized controlled trials (RCTs) or evidence-based clinical practice guidelines based on a systematic review of RCTs or three or more RCTs of decent quality with comparable results.
- Level II - Evidence obtained from at least one well-designed RCT
- Level III – Evidence obtained from well-designed controlled trials without randomization
- Level IV - Evidence from well-designed case-control or cohort studies
- Level V - Evidence from a systematic review of descriptive and qualitative studies (meta-syntheses)
- Level VI – Evidence from a single or descriptive or qualitative study
- Level VII - Evidence from the opinion of authorities and/or reports of expert committees.
Roe-Prior discussed the strength of evidence by comparing it to a murder trial. A suspect’s conviction should require more than the testimony of one witness. If a crowd of people all agree that the suspect was the perpetrator or there was DNA evidence, that evidence is much stronger. Studies without a comparative group, methodologically weak studies, or poorly controlled studies could be likened to one witness. Roe Prior encouraged individuals to also look at non-nursing research findings since research centered on other disciplines, like psychology or education, could be appropriate.
Other frameworks for identifying levels of evidence include The Oxford Centre for Evidence-Based Medicine Levels of Evidence and Burns framework. [4] The Oxford Centre describes five levels with various subparts as listed here:
- 1a Systematic review of RCTs
- 1b Individual RCT
- 2a Systematic review of cohort studies
- 2b Individual cohort study
- 2c Outcomes research
- 3a Systematic review of case-control studies
- 3b Individual case-control study
- 4 Case series
- 5 Expert opinion
Burns uses three levels to differentiate the strength of the evidence presented:
- I At least 1 RCT with proper randomization
- II.1 Well-designed cohort or case-control study
- II.2 Time series comparisons or dramatic results from uncontrolled studies
- III Expert opinions
Roe Prior outlined guidelines for the literature review. [5] Use keywords from the PICOT question to perform simple, then more complex searches in reliable databases, preferably limited to the past five years, although landmark studies can be included. Limit the review to peer-reviewed and research articles and use caution when including only full-text articles, as some key papers may be missed. Check the validity of any online sources and use original research where possible. Remember that textbooks are often obsolete by their publication date, and books are considered secondary sources.
The Cochran Library is comprised of multiple databases where systematic reviews on healthcare topics can be found. Using the Preferred Reporting Items for Systemic Review and Meta-Analysis (PRISMA) Guidelines to evaluate a systemic review or meta-analysis can help the individual ensure the findings are valid and reliable. Findings from the literature review are put into an evidence-based table. There are various formats for these tables, but they all include information about the source, design, sample, summary of findings, and level of evidence for each of the articles included.
The most frequently used EBP models are the Iowa Model, the Advancing Research and Clinical Practice through Close Collaboration (ARCC) Model, the Star Model of Knowledge Transformation, and the John Hopkins Nursing Evidence-based Practice (JHNEBP) Model. The IOWA Model focuses on implementing evidence-based practice changes, and the ARCC model on advancing EBP in systems by using EBP mentors and control and cognitive behavioral therapies. The Star Model provides a framework for approaching EBP, and the John Hopkins Model is a problem-based approach to clinical decision-making accompanied by tools to guide its use.
The Iowa model was revised and updated in 2017 by the Iowa Model Collaborative. [6] Changes in the healthcare environment, such as a focus on implementation science and emphasis on patient engagement, prompted a reevaluation, revision, and validation of the model. This model differs from other frameworks by linking practice changes within the system. Model changes included an expansion of piloting, implementation, patient engagement, and sustaining change.
Support for the ARCC Model was outlined in an article by Melnyk and colleagues in a study exploring how an evidence-based culture and mentorship predicted EBP implementation, nurse job satisfaction, and intent to stay. [7] This model involves assessing organizational culture and readiness for EBP using EBP mentors who work with clinicians to facilitate the implementation of evidence-based practice.
A concept analysis of feelings of entrapment during the COVID-19 pandemic, using the ACE Star Model, was completed by Lee and Park. The ACE Star model is used to understand the cycle, nature, and characteristics of knowledge used in various aspects of EBP. The model consists of five steps: discovery research, evidence summary, translation to guidelines, practice integration, and process and outcome evaluation.
The JHNEBP Model is a problem-solving approach to clinical decision-making with user-friendly tools to guide individual or group use. It is explicitly designed to meet the needs of the practicing nurse and uses a three-step process called PET: practice question, evidence, and translation. In a study conducted by Speroni and colleagues on using EBP models across the United States, this was the second most frequently used model by the 127 nurse leaders who responded to the questionnaire. [8]
EBP Competence and Implementation
NPD practitioners are instrumental in implementing EBP. Harper and colleagues conducted a national study to examine NPD practitioners’ beliefs and competencies, frequency of implementing EBP, and perceptions of organizational culture and readiness for EBP. [9] The Association for Nursing Professional Development (ANPD) collaborated with the Center for Transdisciplinary Evidence-Based Practice at The Ohio State University to explore the NPD practitioners’ beliefs and experiences with EBP, as well as to explore relationships among NPD practitioner characteristics and healthcare organizational outcomes such as nursing sensitive quality indicator scores and core measures. A total of 253 NPD practitioners from 43 states and the District of Columbia participated in this study. Findings indicated that NPD practitioners need to develop personal competence in EBP, become involved in shared governance, collaborate with others to facilitate the implementation of EBP, and become comfortable with using quality metrics to demonstrate the effectiveness of NPD activities.
The Helene Fuld Health Trust National Institute for Evidence-based Practice in Nursing and Healthcare of the Ohio State University developed an Evidence-Based Practice Certificate, which was approved by the Accreditation Board for Specialty Nursing Certification in 2018. There are 24 EBP competencies; 13 for practicing registered nurses and an additional 11 competencies for practicing advanced practice nurses and EBP experts. These competencies are outlined in an article by Melnyk et al. [10]
Although these competencies were initially written for nurses, they apply to other interprofessional team members who have received advanced EBP education. In addition to demonstrating completion of the EBP coursework, applicants must demonstrate current EBP knowledge through content review and successful testing and submit a portfolio to review that shows an EBP practice change project before receiving a certificate.
In 2020, ANPD worked with the Helene Fuld Health Trust National Institute for Evidence-Based Practice in Nursing and Healthcare to develop a curriculum for the Nursing Professional Development EBP Academy. [11] The program consists of live webinars, 26 asynchronous modules, and the completion of an EBP change initiative/project. This Academy curriculum aligns with the EBP Certificate educational requirements.
There are numerous resources available for NPD practitioners on evidence-based practice. There is a peer-reviewed journal published by Sigma Theta Tau International, Worldviews on Evidence-based Nursing, which includes original research with recommendations applicable to use as best practices to improve patient care. ANPD has a year-long evidence-based fellowship consisting of theory and completion of an evidence-based project. The Nursing Professional Development Evidence-Based Practice (EBP) Academy is a 12-month mentored program designed to guide the NPD practitioner through creating PICOT questions, gathering and critically appraising literature, and EBP implementation, evaluation, dissemination, and sustainment. Participation in the EBP Academy enhances the evidence-based competencies of nursing professional development practitioners to enable them to fulfill their role as champions of scientific inquiry and mentor other healthcare professionals in implementing EBP practices.
EBP in Action
One organization evaluated the use of evidence-based practice in clinical practice after nurses attended a formal evidence-based practice course. [12] Nurses who attended the organization’s EBP course were invited to participate in focus groups to provide additional qualitative data. Data from two focus groups highlighted the impact of the EBP course, areas for further development, and potential barriers to the use of EBP. The nurses indicated that the course changed their way of thinking and enhanced their patient care. They stated there was a need for mentoring and that time was a significant barrier to EBP. That information was used by organizational leadership to help identify areas needing consideration for educational offerings and support mechanisms.
Another large academic medical center evaluated the implementation of an EBP program. [13] They noted that although their approach to educating professional staff on EBP provided initial benefits, holding the gains over a one-year period was difficult. The “train-the-trainer” model envisioned by the team was not realistic, as the participants did not feel well-versed enough to teach others. They concluded future efforts require attention to participant feedback and the implementation of measures to decrease the barriers to implementing EBP.
There are numerous examples in the literature of individuals/organizations using evidence-based principles to develop programs in a variety of settings. McGarity and colleagues examined frontline nurse leaders oriented with only on-the-job training questioning whether their level of competence is improved with a professional development program. [14] This project used a pre-and post-survey design to evaluate a leadership development curriculum. The intervention was an evidence-based leadership curriculum that consisted of twelve four-hour classes. The fact that all 38 frontline nurse leaders who participated in this project improved their competencies reinforced the need for formal professional development. The outcome of this training program showed that all 38 frontline nurse leaders who attended it were more confident in their skills and improved their competence in leading effective teams, reinforcing the need for education.
Ydrogo and colleagues discussed a multifaceted approach to strengthening nurses’ EBP capabilities in a comprehensive cancer center. [15] They created a program designed to promote a spirit of inquiry, strengthen EBP facilitators, overcome barriers to EBP, and expand nurses’ knowledge of EBP. The program consisted of a blended interactive seminar with leader-directed discussion on promoting a spirit of inquiry, a seven-week course on retrieving, reading, analyzing, and evaluating research papers, and a monthly challenge emailed to staff, posted to the hospital intranet, and included in a weekly nursing newsletter. Both leadership and staff gained increased confidence and a foundation to initiate two research projects and one EBP project shortly after completing the course.
Integrating EBP into an emergency department nurse residency program was the subject of an article by Asselta. [16] In addition to extensive training in the core competencies of emergency nursing, this 6-month program included exemplars in EBP and its positive impact on patient care and/or ED workflow. One of the requirements for this program was for the nurses to participate in developing an EBP project specific to emergency nursing practice. An example of a project comparing intravenous (IV) push medications versus IV piggyback medications was shared. This project demonstrated the advantages of the IV push route of administration, which yielded significant cost savings for the organization.
Pediatric nurses were the focus of a project described by Cline et al. [17] They evaluated nurses’ perceptions of barriers, facilitators, confidence, and attitudes toward research and evidence-based practice. There were 369 nurses who completed the survey during the baseline data collection period, 288 nurses completed the 6-month survey, and 284 nurses completed the 12-month survey. The results indicated that implementation of a curriculum focused on research and EBP may be most successful when implemented with the availability of mentors, in a research-supported environment, with grant funding support for novice researchers, and with an ample amount of time allotted to complete a research study.
Many nurses work in long-term care. Higuchi and colleagues described a study that examined the impact of EBP practice change in ten long-term care (LTC) settings in Canada. [18] Introducing and sustaining practice changes that enhance the quality of care is a significant challenge in LTC facilities. A full-day workshop that included identifying success stories, describing current practice challenges, building a case for change, seizing the moment, and identifying an action plan was presented at each site. Participants completed a questionnaire at the end of the workshop, and all participants were invited to participate in semi-structured interviews five months after the program. The benefits identified in the follow-up interviews were initiating the change process and enhancing team collaboration. This study demonstrated that an interactive workshop had important positive effects on LTC staff.
Clinical nurse educators were the focus of a study conducted by Dagg and colleagues. [19] Centralization of a new clinical nurse educator (CNE) role created role confusion and poor role outcomes. An evidence-based quality improvement project was completed to integrate the ANPD practice model and transition to the practice fellowship program. An ANPD competency assessment survey tool was selected because it included information specific to the CNE role expectations. The nurse-sensitive indicators selected were fall rates and indwelling urinary catheter rates. Self-assessed competencies and nurse-sensitive quality outcomes of the CNEs were measured before and after the ANPD practice model was integrated into their daily practice. There were only 5 CNEs who completed both the pre-and post-assessment, but results supported that CNEs influenced patient quality outcomes and improved their self-assessed competency.
Phan and Hampton described an evidence-based project focused on promoting civility in the workplace by addressing bullying in new graduate nurses using simulation and cognitive rehearsal. [20] Nurse bullying (NB) has been a problem for many years, and this can threaten the safety of patients, nurses, and organizations. This study used a mixed-methods, quasi-experimental design.
The NPD Scope and Standards were used to assess, plan, implement, and evaluate the project. In addition to the demographic data collected at baseline, participants completed the Clark Workplace Civility Index (CWCI) at baseline and three times after the intervention (immediately, 2.5 months, and five months). The sample included 36 new graduate nurses (NGNs). The intervention consisted of 2.75 hours of didactic, polling, reflection, simulation role-play, and debriefing. The training was developed virtually on the Zoom platform, and breakout rooms facilitated small group discussions and role-playing. Although there was no statistically significant increase in civility scores, the qualitative data indicated the participants could apply knowledge and skills from the intervention to improve communication, peer relationships, teamwork, patient safety, and care.
- Clinical Significance
Evidence-based practice falls under the champion for scientific inquiry role of the NPD practitioner. According to the NPD scope and standards of practice, the NPD practitioner promotes a spirit of inquiry and assists with generating and disseminating new knowledge. The NPD practitioner also uses evidence to advance the specialty of NPD and guide practice.
The ultimate goal is to promote the quality of care for the healthcare consumer. Competencies for scholarly inquiry include acting as a champion for inquiry, generating new knowledge, and integrating the best available evidence into practice. In addition, the standards include disseminating inquiry findings, including evidence-based practice and quality improvement activities, through educational and professional development activities.
- Enhancing Healthcare Team Outcomes
The healthcare consumer is the ultimate recipient of NPD practice. Therefore, NPD practitioners collaborate with the interprofessional team to ensure quality care, leading to optimal care outcomes and population health. Interprofessional partnerships are critical factors in achieving safe, effective, high-quality care.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Barbara Brunt declares no relevant financial relationships with ineligible companies.
Disclosure: Melanie Morris declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Brunt BA, Morris MM. Nursing Professional Development Evidence-Based Practice. [Updated 2023 Mar 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Beliefs and implementation of evidence-based practice among nurses in the nursing homes of a Swiss canton: An observational cross-sectional study. [J Clin Nurs. 2021] Beliefs and implementation of evidence-based practice among nurses in the nursing homes of a Swiss canton: An observational cross-sectional study. Perruchoud E, Fernandes S, Verloo H, Pereira F. J Clin Nurs. 2021 Nov; 30(21-22):3218-3229. Epub 2021 May 7.
- The Experience and Effectiveness of Nurse Practitioners in Orthopaedic Settings: A Comprehensive Systematic Review. [JBI Libr Syst Rev. 2012] The Experience and Effectiveness of Nurse Practitioners in Orthopaedic Settings: A Comprehensive Systematic Review. Taylor A, Staruchowicz L. JBI Libr Syst Rev. 2012; 10(42 Suppl):1-22.
- Strategies for advancing evidence-based practice in clinical settings. [J N Y State Nurses Assoc. 2004] Strategies for advancing evidence-based practice in clinical settings. Fineout-Overholt E, Levin RF, Melnyk BM. J N Y State Nurses Assoc. 2004 Fall-2005 Winter; 35(2):28-32.
- Review Evidence Brief: The Quality of Care Provided by Advanced Practice Nurses [ 2014] Review Evidence Brief: The Quality of Care Provided by Advanced Practice Nurses McCleery E, Christensen V, Peterson K, Humphrey L, Helfand M. 2014 Sep
- Review Critical Appraisal Tools and Reporting Guidelines for Evidence-Based Practice. [Worldviews Evid Based Nurs. 2017] Review Critical Appraisal Tools and Reporting Guidelines for Evidence-Based Practice. Buccheri RK, Sharifi C. Worldviews Evid Based Nurs. 2017 Dec; 14(6):463-472. Epub 2017 Sep 12.
Recent Activity
- Nursing Professional Development Evidence-Based Practice - StatPearls Nursing Professional Development Evidence-Based Practice - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Faye Abdellah: 21 Nursing Problems Theory

Faye Abdellah is a celebrated nurse theorist, military nurse, and leader in nursing research. Get to know the major concepts of her “ 21 Nursing Problems ” nursing theory , its application, and its impact on nursing.
Table of Contents
Early life of faye abdellah, as an educator, as a researcher, established nursing standards, military nursing service, abdellah’s typology of 21 nursing problems, awards and honors, assumptions, nursing problems, problem solving, basic needs, sustenal care needs, remedial care needs, restorative care needs, patient-centered approaches to nursing, 21 nursing problems and the nursing process, recommended resources, external links, biography of faye glenn abdellah.
Faye Glenn Abdellah (March 13, 1919 – present) is a nursing research pioneer who developed the “Twenty-One Nursing Problems.” Her nursing model was progressive for the time in that it refers to a nursing diagnosis during a time in which nurses were taught that diagnoses were not part of their role in health care.
She was the first nurse officer to rank a two-star rear admiral, the first nurse, and the first woman to serve as a Deputy Surgeon General.
On March 13, 1919, Faye Abdellah was born in New York to a father of Algerian heritage and a Scottish mother. Her family subsequently moved to New Jersey, where she attended high school.
Years later, on May 6, 1937, the German hydrogen-fueled airship Hindenburg exploded over Lakehurst.

Abdellah and her brother witnessed the explosion, destruction, and fire after the ignited hydrogen killed many people. That incident became the turning point in Abdellah’s life. It was that time when she realized that she would never again be powerless to assist when people were in such a dire need of assistance. It was at that moment she vowed that she would learn to nurse and become a professional nurse.
Faye Abdellah earned a nursing diploma from Fitkin Memorial Hospital’s School of Nursing, now known as Ann May School of Nursing.
It was sufficient to practice nursing during her time in the 1940s, but she believed that nursing care should be based on research, not hours of care.
Abdellah went on to earn three degrees from Columbia University: a bachelor of science degree in nursing in 1945, a master of arts degree in physiology in 1947, and a doctor of education degree in 1955.

With her advanced education, Abdellah could have chosen to become a doctor. However, as she explained in one of her interviews that she wanted to be an M.D. because she could do all she wanted to do in nursing, which is a caring profession.
Career and Appointments
In her early twenties, Faye Abdellah worked as a health nurse at a private school, and her first administrative position was on the faculty of Yale University from 1945-1949. At that time, she was required to teach a class called “120 Principles of Nursing Practice,” using a standard nursing textbook published by the National League for Nursing. The book included guidelines that had no scientific basis, which challenged Abdellah to explain everything she called the “brilliant” students.

After a year, Abdellah became so frustrated that she gathered her colleagues in the Yale courtyard and burned the textbooks. The next morning the school’s dean told her she would have to pay for the destroyed texts. It took a year for Abdellah to settle the debt, but she never regretted her actions because it started her on the long road to pursue the scientific basis of the nursing practice.
In 1949, she met Lucile Petry Leone, the first Nurse Officer, and decided to join the Public Health Service. Her first assignment was with the division of nursing that focused on research and studies. They performed studies with numerous hospitals to improve nursing practice.
Abdellah was an advocate of degree programs for nursing. Diploma programs, she believes, were never meant to prepare nurses at the professional level. Nursing education, she argued, should be based on research; she herself became among the first in her role as an educator to focus on theory and research. Her first studies were qualitative; they simply described situations. As her career progressed, her research evolved to include physiology, chemistry, and behavioral sciences.
In 1957, Abdellah spearheaded a research team in Manchester, Connecticut, that established the groundwork for what became known as progressive patient care. In this framework, critical care patients were treated in an intensive care unit, followed by a transition to immediate care and then home care. The first two segments of the care program proved very popular within the caregiver profession. Abdellah is also credited with developing the first nationally tested coronary care unit as an outgrowth of her work in Manchester.

Home care, which is the third phase of the progressive patient care equation, was not widely accepted in the mid-twentieth century. Abdellah explained that people at the time kept saying home care would mean having a maid or a nurse in everyone’s home. They could not figure out that home care with nurses teaching self-care would help patients regain independent function. Forty years later, home care had become an essential part of long-term health care.
In another innovation within her field, Abdellah developed the Patient Assessment of Care Evaluation (PACE), a system of standards used to measure the relative quality of individual health-care facilities that were still used in the healthcare industry into the 21st century. She was also one of the first people in the healthcare industry to develop a classification system for patient care and patient-oriented records.

Classification systems have evolved in different ways within the health-care industry, and Abdellah’s work was foundational in developing the most widely used form: Diagnostic related groups, or DRGs. DRGs, which became the standard coding system used by Medicare, categorize patients according to particular primary and secondary diagnoses. This system keeps health-care costs down because each DRG code includes the maximum amount Medicare will payout for a specific diagnosis or procedure while also taking into account patient age and length of stay in a healthcare facility. Providers are given an incentive to keep costs down because they only realize a profit if costs are less than the amount specified by the relevant DRG category.

During her 40-year career as a Commissioned Officer in the U.S. Public Health Service from 1949 to 1989, Abdellah was assigned to work with the Korean people during the Korean War. As a senior officer, she was alternatively assigned to Japan, China , Russia, Australia, and the Scandinavian countries to identify the Public Health Service’s role in dealing with various health problems. She was able to assist and initiate, in an advisory role, numerous studies in those countries.
She served as Chief Nurse Officer from 1970 to 1987 and was the first nurse to achieve the rank of a two-star Flag Officer named by U.S. Surgeon General C. Everett Koop as the first woman and nurse Deputy Surgeon General from 1982 to 1989. After retirement, Abdellah founded and served as the first dean in the Graduate School of Nursing, GSN, Uniformed Services University of the Health Sciences (USUHS).
Faye Abdellah is well known for developing the “Twenty-One Nursing Problems Theory” that has interrelated the concepts of health, nursing problems, and problem-solving.
She views nursing as an art and a science that molds the attitude, intellectual competencies, and technical skills of the individual nurse into the desire and ability to help individuals cope with their health needs, whether they are ill or well.
She used Henderson’s 14 basic human needs and nursing research to establish the classification of nursing problems.
Faye Abdellah’s theory is further discussed below.
As a consultant and educator, Faye Abdellah shared her nursing theories with caregivers around the world. She led seminars in France, Portugal, Israel, Japan, China, New Zealand, Australia, and the former Soviet Union. She also served as a research consultant to the World Health Organization. From her global perspective, Abdellah learned to appreciate nontraditional and complementary medical treatments and developed the belief such non-Western treatments deserved scientific research.

Also, she has been active in professional nursing associations and is a prolific author, with more than 150 publications. Her publications include Better Nursing Care Through Nursing Research and Patient-Centered Approaches to Nursing . She also developed educational materials in many areas of public health, including AIDS , hospice care , and drug addiction.
Abdellah considers her greatest accomplishment being able to “play a role in establishing a foundation for nursing research as a science.” Her book, Patient-Centered Approaches to Nursing , emphasizes nursing science and has elicited changes throughout nursing curricula. Her work, which is based on the problem-solving method, serves as a vehicle for delineating nursing (patient) problems as the patient moves toward a healthy outcome.

Faye Abdellah is recognized as a leader in nursing research and nursing as a profession within the Public Health Service (PHS) and as an international expert on health problems. She was named a “living legend” by the American Academy of Nursing in 1994 and was inducted into the National Women’s Hall of Fame in 2000 for a lifetime spent establishing and leading essential health care programs for the United States. In 2012, Abdellah was inducted into the American Nurses Association Hall of Fame for a lifetime of contributions to nursing.
Her contributions to nursing and public health have been recognized with almost 90 professional and academic honors, such as the Allied Signal Achievement Award for pioneering research in aging and Sigma Theta Tau’s Lifetime Achievement Award.
Abdellah’s leadership, her publications, and her lifelong contributions have set a new standard for nursing and health care. Her legacy of more than 60 years of extraordinary accomplishments lives nationally and globally.
Aside from being the first nurse and the first woman to serve as a Deputy Surgeon General, Faye Glenn Abdellah also made a name in the nursing profession to formulate her “21 Nursing Problems Theory.” Her theory changed the focus of nursing from disease-centered to patient-centered and began to include the care of families and the elderly in nursing care. The Patient Assessment of Care Evaluation developed by Abdellah is now the standard used in the United States.
Abdellah’s 21 Nursing Problems Theory
According to Faye Glenn Abdellah’s theory, “Nursing is based on an art and science that molds the attitudes, intellectual competencies, and technical skills of the individual nurse into the desire and ability to help people, sick or well, cope with their health needs.”
The patient-centered approach to nursing was developed from Abdellah’s practice, and the theory is considered a human needs theory. It was formulated to be an instrument for nursing education, so it most suitable and useful in that field. The nursing model is intended to guide care in hospital institutions but can also be applied to community health nursing, as well.
The assumptions Abdellah’s “21 Nursing Problems Theory” relate to change and anticipated changes that affect nursing; the need to appreciate the interconnectedness of social enterprises and social problems; the impact of problems such as poverty, racism, pollution, education, and so forth on health and health care delivery; changing nursing education; continuing education for professional nurses; and development of nursing leaders from underserved groups.
- Learn to know the patient.
- Sort out relevant and significant data.
- Make generalizations about available data concerning similar nursing problems presented by other patients.
- Identify the therapeutic plan.
- Test generalizations with the patient and make additional generalizations.
- Validate the patient’s conclusions about his nursing problems.
- Continue to observe and evaluate the patient over a period of time to identify any attitudes and clues affecting this behavior.
- Explore the patient’s and family’s reaction to the therapeutic plan and involve them in the plan.
- Identify how the nurse feels about the patient’s nursing problems.
- Discuss and develop a comprehensive nursing care plan .
Major Concepts of 21 Nursing Problems Theory
The model has interrelated concepts of health and nursing problems and problem-solving, which is inherently logical in nature.
She describes nursing recipients as individuals (and families), although she does not delineate her beliefs or assumptions about the nature of human beings.
Health, or the achieving of it, is the purpose of nursing services. Although Abdellah does not define health, she speaks to “total health needs” and “a healthy state of mind and body.”
Health may be defined as the dynamic pattern of functioning whereby there is a continued interaction with internal and external forces that results in the optimal use of necessary resources to minimize vulnerabilities.
Society is included in “planning for optimum health on local, state, and international levels.” However, as Abdellah further delineates her ideas, the focus of nursing service is clearly the individual.
The client’s health needs can be viewed as problems, overt as an apparent condition, or covert as a hidden or concealed one.
Because covert problems can be emotional, sociological, and interpersonal in nature, they are often missed or misunderstood. Yet, in many instances, solving the covert problems may solve the overt problems as well.
Quality professional nursing care requires that nurses be able to identify and solve overt and covert nursing problems. The problem-solving process can meet these requirements by identifying the problem, selecting pertinent data, formulating hypotheses, testing hypotheses through collecting data, and revising hypotheses when necessary based on conclusions obtained from the data.
Subconcepts
The following are the subconcepts of Faye Abdellah’s “21 Nursing Problems” theory and their definitions.
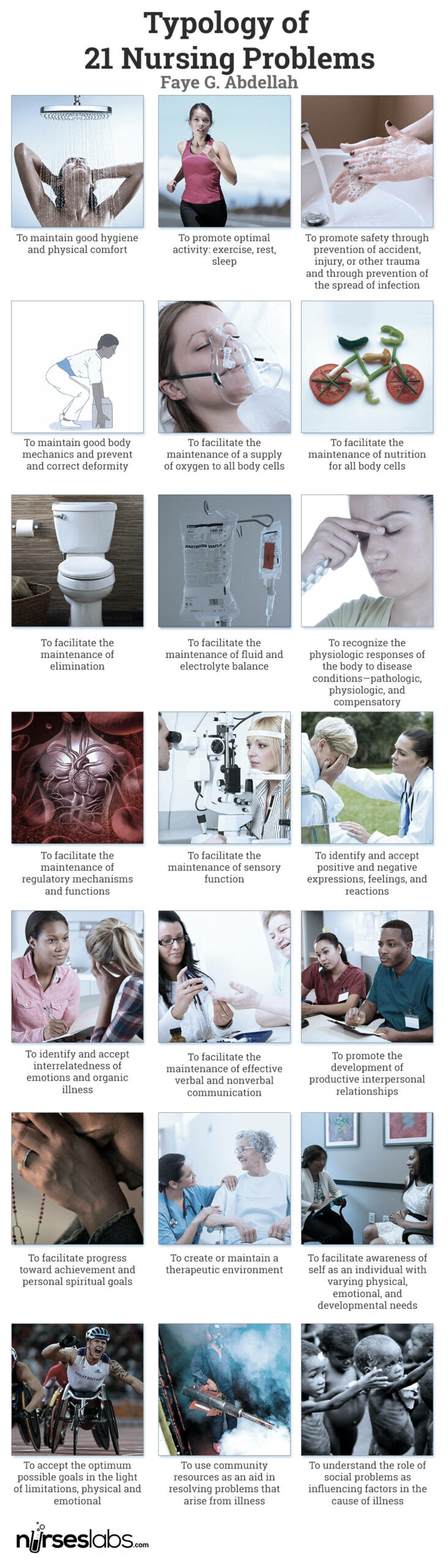
The 21 nursing problems fall into three categories: physical, sociological, and emotional needs of patients; types of interpersonal relationships between the patient and nurse; and common elements of patient care. She used Henderson’s 14 basic human needs and nursing research to establish the classification of nursing problems. Abdellah’s 21 Nursing Problems are the following:
- To maintain good hygiene and physical comfort.
- To promote optimal activity: exercise, rest, sleep
- To promote safety by preventing accidents, injuries, or other trauma and preventing the spread of infection .
- To maintain good body mechanics and prevent and correct the deformity.
- To facilitate the maintenance of a supply of oxygen to all body cells.
- To facilitate the maintenance of nutrition for all body cells.
- To facilitate the maintenance of elimination.
- To facilitate the maintenance of fluid and electrolyte balance.
- To recognize the physiologic responses of the body to disease conditions—pathologic, physiologic, and compensatory.
- To facilitate the maintenance of regulatory mechanisms and functions.
- To facilitate the maintenance of sensory function.
- To identify and accept positive and negative expressions, feelings, and reactions.
- To identify and accept interrelatedness of emotions and organic illness.
- To facilitate the maintenance of effective verbal and nonverbal communication.
- To promote the development of productive interpersonal relationships.
- To facilitate progress toward achievement and personal spiritual goals.
- To create or maintain a therapeutic environment.
- To facilitate awareness of self as an individual with varying physical, emotional, and developmental needs.
- To accept the optimum possible goals in the light of limitations, physical and emotional.
- To use community resources as an aid in resolving problems that arise from an illness.
- To understand the role of social problems as influencing factors in the cause of illness.
Moreover, patients’ needs are further divided into four categories: basic to all patients , sustenance care needs , remedial care needs , and restorative care needs .
The basic needs of an individual patient are to maintain good hygiene and physical comfort; promote optimal health through healthy activities, such as exercise, rest, and sleep ; promote safety through the prevention of health hazards like accidents, injury , or other trauma and the prevention of the spread of infection; and maintain good body mechanics and prevent or correct deformity.
Sustenal care needs to facilitate the maintenance of a supply of oxygen to all body cells; facilitate the maintenance of nutrition of all body cells; facilitate the maintenance of elimination; facilitate the maintenance of fluid and electrolyte balance; recognize the physiological responses of the body to disease conditions; facilitate the maintenance of regulatory mechanisms and functions, and facilitate the maintenance of sensory function.
Remedial care needs to identify and accept positive and negative expressions, feelings, and reactions; identify and accept the interrelatedness of emotions and organic illness; facilitate the maintenance of effective verbal and non- verbal communication ; promote the development of productive interpersonal relationships; facilitate progress toward achievement of personal spiritual goals; create and maintain a therapeutic environment; and facilitate awareness of the self as an individual with varying physical, emotional, and developmental needs.
Restorative care needs include the acceptance of the optimum possible goals in light of limitations, both physical and emotional; the use of community resources as an aid to resolving problems that arise from an illness; and the understanding of the role of social problems as influential factors in the case of illness.
Abdellah’s work, based on the problem-solving method, serves as a vehicle for delineating nursing (patient) problems as the patient moves toward a healthy outcome. The theory identifies ten steps to identify the patient’s problem and 11 nursing skills to develop a treatment typology.

The ten steps are:
- Validate the patient’s conclusions about his nursing problems.
- Continue to observe and evaluate the patient over a period of time to identify any attitudes and clues affecting his or her behavior.
- Explore the patient and their family’s reactions to the therapeutic plan and involve them in the plan.
- Identify how the nurses feel about the patient’s nursing problems.
- Discuss and develop a comprehensive nursing care plan.
The 11 nursing skills are:
- observation of health status
- skills of communication
- application of knowledge
- the teaching of patients and families
- planning and organization of work
- use of resource materials
- use of personnel resources
- problem-solving
- the direction of work of others
- therapeutic uses of the self
- nursing procedure
Abdellah also explained nursing as a comprehensive service, which includes:
- Recognizing the nursing problems of the patient
- Deciding the appropriate course of action to take in terms of relevant nursing principles
- Providing continuous care of the individual’s total needs
- Providing continuous care to relieve pain and discomfort and provide immediate security for the individual
- Adjusting the total nursing care plan to meet the patient’s individual needs
- Helping the individual to become more self-directing in attaining or maintaining a healthy state of body and mind
- Instructing nursing personnel and family to help the individual do for himself that which he can within his limitations
- Helping the individual to adjust to his limitations and emotional problems
- Working with allied health professions in planning for optimum health on local, state, national, and international levels
- Carrying out continuous evaluation and research to improve nursing techniques and to develop new techniques to meet people’s health needs
Faye Abdellah’s work is a set of problems formulated in terms of nursing-centered services used to determine the patient’s needs. The nursing-centered orientation to client care appears to be contradicting the client-centered approach that Abdellah professes to support. This can be observed by her desire to move away from a disease-centered orientation.
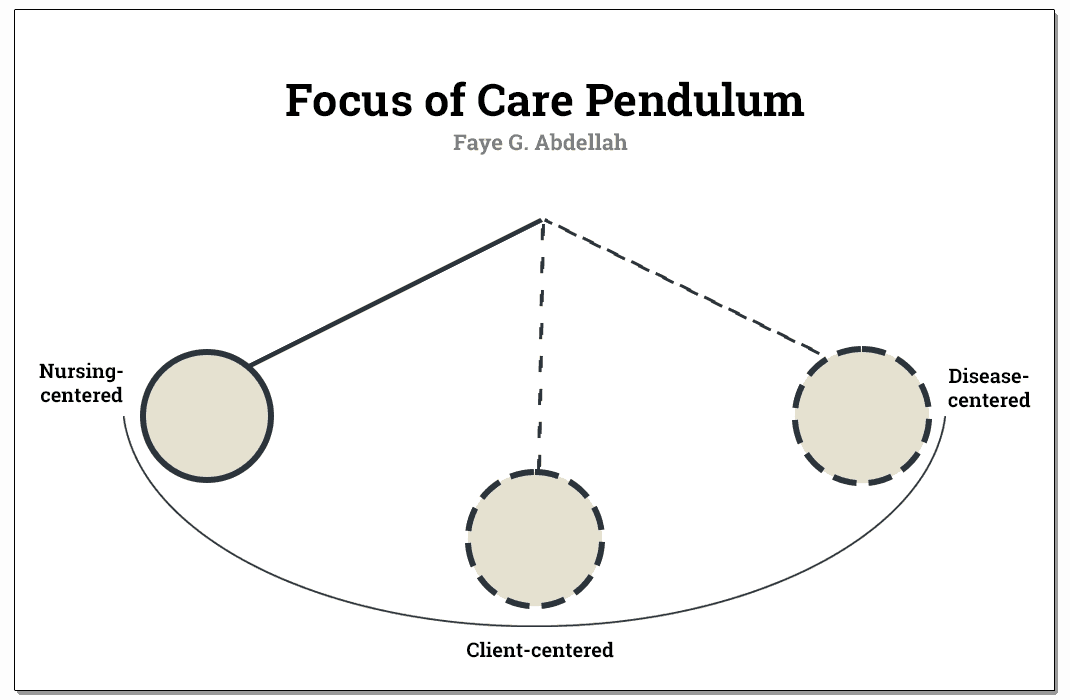
In her attempt to bring the nursing practice to its proper relationship with restorative and preventive measures for meeting total client needs, she seems to swing the pendulum to the opposite pole, from the disease orientation to nursing orientation, while leaving the client somewhere in the middle.
The nursing process in Abdellah’s theory includes assessment , nursing diagnosis, planning, implementation, and evaluation.
In the assessment phase , the nursing problems implement a standard procedure for data collection. A principle underlying the problem-solving approach is that for each identified problem, pertinent data is collected. The overt or covert nature of problems necessitates a direct or indirect approach, respectively.
The outcome of the collection of data in the first phase concludes the patient’s possible problems, which can be grouped under one or more of the broader nursing problems. This will further lead to the nursing diagnosis .
After formulating the diagnosis, a nursing care plan is developed, and appropriate nursing interventions are determined. The nurse now sets those interventions in action, which complete the implementation phase of the nursing process .
The evaluation takes place after the interventions have been carried out. The most convenient evaluation would be the nurse’s progress or lack of progress toward achieving the goals established in the planning phase.
With Faye Abdellah’s aim in formulating a clear categorization of patient’s problems as health needs, she rather conceptualized nurses’ actions in nursing care, which is contrary to her aim. Nurses’ roles were defined to alleviate the problems assessed through the proposed problem-solving approach.
The problem-solving approach introduced by Abdellah has the advantage of increasing the nurse’s critical and analytical thinking skills since the care to be provided would be based on sound assessment and validation of findings.
One can identify that the framework is strongly applied to individuals as the focus of nursing care. The inclusion of an aggregate of people such as the community or society would make the theory of Abdellah more generalizable since nurses do not only provide one-person service, especially now that the community healthcare level is sought to have higher importance than curative efforts in the hospital.
The following are the strengths of Faye Abdellah’s “21 Nursing Problems” theory.
- The problem-solving approach is readily generalizable to the client with specific health needs and specific nursing problems.
- With the model’s nature, healthcare providers and practitioners can use Abdellah’s problem-solving approach to guide various activities within the clinical setting. This is true when considering a nursing practice that deals with clients with specific needs and specific nursing problems.
- The language of Faye Abdellah’s framework is simple and easy to comprehend.
- The theoretical statement greatly focuses on problem-solving, an activity that is inherently logical in nature.
The following are the limitations of Faye Abdellah’s “21 Nursing Problems” theory.
- The major limitation to Abdellah’s theory and the 21 nursing problems is their robust nurse-centered orientation. She rather conceptualized nurses’ actions in nursing care which is contrary to her aim.
- Another point is the lack of emphasis on what the client is to achieve was given in client care.
- The framework seems to focus quite heavily on nursing practice and individuals. This somewhat limits the generalizing ability, although the problem-solving approach is readily generalizable to clients with specific health needs and specific nursing.
- Also, Abdellah’s framework is inconsistent with the concept of holism. The nature of the 21 nursing problems attests to this. As a result, the client may be diagnosed with numerous problems leading to fractionalized care efforts. Potential problems might be overlooked because the client is not deemed to be in a particular illness stage.
Abdellah’s typology of 21 nursing problems is a conceptual model mainly concerned with patient’s needs and nurses’ role in problem identification using a problem analysis approach.
According to the model, patients are described as having physical, emotional, and sociological needs. People are also the only justification for the existence of nursing. Without people, nursing would not be a profession since they are the recipients of nursing.
Patient-centered approaches to nursing health are described as a state mutually exclusive of illness. Abdellah does not define health but speaks to “total health needs” and “a healthy state of mind and body” in her nursing description.
However, Abdellah rather conceptualized nurses’ actions in nursing care, contrary to her aim of formulating a clear categorization of patients’ problems as health needs. Nurses’ roles were defined to alleviate the problems assessed through the proposed problem-solving approach.
As a whole, the theory is intended to guide care not just in the hospital setting but can also be applied to community nursing, as well. The model has interrelated concepts of health and nursing problems and problem-solving, which is inherently logical in nature.
Furthermore, the 21 nursing problems progressed to a second-generation development referred to as patient problems and patient outcomes. Abdellah educated the public on AIDS , drug addiction, violence, smoking, and alcoholism. Her work is a problem-centered approach or philosophy of nursing.
Recommended books and resources to learn more about nursing theory:
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. For more information, check out our privacy policy .
- Nursing Theorists and Their Work (10th Edition) by Alligood Nursing Theorists and Their Work, 10th Edition provides a clear, in-depth look at nursing theories of historical and international significance. Each chapter presents a key nursing theory or philosophy, showing how systematic theoretical evidence can enhance decision making, professionalism, and quality of care.
- Knowledge Development in Nursing: Theory and Process (11th Edition) Use the five patterns of knowing to help you develop sound clinical judgment. This edition reflects the latest thinking in nursing knowledge development and adds emphasis to real-world application. The content in this edition aligns with the new 2021 AACN Essentials for Nursing Education.
- Nursing Knowledge and Theory Innovation, Second Edition: Advancing the Science of Practice (2nd Edition) This text for graduate-level nursing students focuses on the science and philosophy of nursing knowledge development. It is distinguished by its focus on practical applications of theory for scholarly, evidence-based approaches. The second edition features important updates and a reorganization of information to better highlight the roles of theory and major philosophical perspectives.
- Nursing Theories and Nursing Practice (5th Edition) The only nursing research and theory book with primary works by the original theorists. Explore the historical and contemporary theories that are the foundation of nursing practice today. The 5th Edition, continues to meet the needs of today’s students with an expanded focus on the middle range theories and practice models.
- Strategies for Theory Construction in Nursing (6th Edition) The clearest, most useful introduction to theory development methods. Reflecting vast changes in nursing practice, it covers advances both in theory development and in strategies for concept, statement, and theory development. It also builds further connections between nursing theory and evidence-based practice.
- Middle Range Theory for Nursing (4th Edition) This nursing book’s ability to break down complex ideas is part of what made this book a three-time recipient of the AJN Book of the Year award. This edition includes five completely new chapters of content essential for nursing books. New exemplars linking middle range theory to advanced nursing practice make it even more useful and expand the content to make it better.
- Nursing Research: Methods and Critical Appraisal for Evidence-Based Practice This book offers balanced coverage of both qualitative and quantitative research methodologies. This edition features new content on trending topics, including the Next-Generation NCLEX® Exam (NGN).
- Nursing Research (11th Edition) AJN award-winning authors Denise Polit and Cheryl Beck detail the latest methodologic innovations in nursing, medicine, and the social sciences. The updated 11th Edition adds two new chapters designed to help students ensure the accuracy and effectiveness of research methods. Extensively revised content throughout strengthens students’ ability to locate and rank clinical evidence.
Recommended site resources related to nursing theory:
- Nursing Theories and Theorists: The Definitive Guide for Nurses MUST READ! In this guide for nursing theories, we aim to help you understand what comprises a nursing theory and its importance, purpose, history, types or classifications, and give you an overview through summaries of selected nursing theories.
Other resources related to nursing theory:
- Betty Neuman: Neuman Systems Model
- Dorothea Orem: Self-Care Deficit Theory
- Dorothy Johnson: Behavioral System Model
- Florence Nightingale: Environmental Theory
- Hildegard Peplau: Interpersonal Relations Theory
- Ida Jean Orlando: Deliberative Nursing Process Theory
- Imogene King: Theory of Goal Attainment
- Jean Watson: Theory of Human Caring
- Lydia Hall: Care, Cure, Core Nursing Theory
- Madeleine Leininger: Transcultural Nursing Theory
- Martha Rogers: Science of Unitary Human Beings
- Myra Estrin Levine: The Conservation Model of Nursing
- Nola Pender: Health Promotion Model
- Sister Callista Roy: Adaptation Model of Nursing
- Virginia Henderson: Nursing Need Theory
- Abdellah, F.G. The federal role in nursing education. Nursing outlook. 1987, 35(5),224-225.
- Abdellah, F.G. Public policy impacting on nursing care of older adults. In E.M. Baines (Ed.), perspectives on gerontological nursing. Newbury, CA: Sage publications. 1991.
- Abdellah, F.G., & Levine, E. Preparing nursing research for the 21st century. New York: Springer. 1994.
- Abdellah, F.G., Beland, I.L., Martin, A., & Matheney, R.V. Patient-centered approaches to nursing (2nd ed.). New York: Mac Millan. 1968.
- Abdellah, F.G. Evolution of nursing as a profession: perspective on manpower development. International Nursing Review, 1972); 19, 3..
- Abdellah, F.G.). The nature of nursing science. In L.H. Nicholl (Ed.), perspectives on nursing theory. Boston: Little, Brown, 1986.
- Craddock, J. (2013). Encyclopedia of world biography supplement. Detroit, Mich.: Gale. https://www.encyclopedia.com/doc/1G2-3435000010.html
- Better Patient Care Through Nursing Research
- Preparing Nursing Research for the 21st Century: Evolution, Methodologies, Challenges
With contributions by Wayne, G. (for Biography), Vera, M.

6 thoughts on “Faye Abdellah: 21 Nursing Problems Theory”
Thank you for sharing Angelo
I mean no disrespect to RADM Abdellah’s service to our nation, but the USPHS is not part of the military. It is part of the Uniformed Services, but not in the Dept of Defense.
Oh! Good to know! Thanks for clarifying :)
An insightful information 👌
I was a brand new lieutenant US Army and just graduated from college to become a nurse. I had used Faye Abdellah’s Theories as the rationale for nursing care plans in school papers, so I was very familiar. A big professional regret was I had the opportunity to meet Faye at a nursing conference in Germany. I was a timid young nurse and somewhat shy and saw her in one of the conference sessions sitting by herself. I wish I introduced myself and talked to her. I really respected her as a pioneer in nursing theory.
thanks for sharing.
Leave a Comment Cancel reply

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
6.3 Ethical Dilemmas
Nurses frequently find themselves involved in conflicts during patient care related to opposing values and ethical principles. These conflicts are referred to as ethical dilemmas. An ethical dilemma results from conflict of competing values and requires a decision to be made from equally desirable or undesirable options. See Figure 6.11 [1] for an illustration of conflict resulting from an ethical dilemma.
An ethical dilemma can involve conflicting patient’s values, nurse values, health care provider’s values, organizational values, and societal values associated with unique facts of a specific situation. For this reason, it can be challenging to arrive at a clearly superior solution for all stakeholders involved in an ethical dilemma. Nurses may also encounter moral dilemmas where the right course of action is known but the nurse is limited by forces outside their control. See Table 6.3a for an example of ethical dilemmas a nurse may experience in their nursing practice.
Table 6.3a Examples of Ethical Issues Involving Nurses
Read more about Ethics Topics and Articles on the ANA website.
According to the American Nurses Association (ANA), a nurse’s ethical competence depends on several factors: [2]
- Continuous appraisal of personal and professional values and how they may impact interpretation of an issue and decision-making
- An awareness of ethical obligations as mandated in the Code of Ethics for Nurses with Interpretive Statements [3]
- Knowledge of ethical principles and their application to ethical decision-making
- Motivation and skills to implement an ethical decision
Nurses and nursing students must have moral courage to address the conflicts involved in ethical dilemmas with “the willingness to speak out and do what is right in the face of forces that would lead us to act in some other way.” [4] See Figure 6.12 [5] for an illustration of nurses’ moral courage.

Nurse leaders and organizations can support moral courage by creating environments where nurses feel safe and supported to speak up. [6] Nurses may experience moral conflict when they are uncertain about what values or principles should be applied to an ethical issue that arises during patient care. Moral conflict can progress to moral distress when the nurse identifies the correct ethical action but feels constrained by competing values of an organization or other individuals. Nurses may also feel moral outrage when witnessing immoral acts or practices they feel powerless to change. For this reason, it is essential for nurses and nursing students to be aware of frameworks for solving ethical dilemmas that consider ethical theories, ethical principles, personal values, societal values, and professionally sanctioned guidelines such as the ANA Nursing Code of Ethics.
Frameworks for Solving Ethical Dilemmas
Systematically working through an ethical dilemma is key to identifying a solution. Many frameworks exist for solving an ethical dilemma, including the nursing process, four quadrant approach, the MORAL model, and the organization-focused PLUS Ethical Decision-Making Model. [7] When nurses use a structured, systematic approach to resolving ethical dilemmas with appropriate data collection, identification and analysis of options, and inclusion of stakeholders, they have met their legal, ethical, and moral responsibilities, even if the outcome is less than ideal.
Nursing Process Model
The nursing process is a structured problem-solving approach that nurses may apply in ethical decision-making to guide data collection and analysis. See Table 6.3b for suggestions on how to use the nursing process model during an ethical dilemma. [8]
Table 6.3b Using the Nursing Process in Ethical Situations [9]
Four Quadrant Approach
The four quadrant approach integrates ethical principles (i.e., beneficence, nonmaleficence, autonomy, and justice) in conjunction with health care indications, individual and family preferences, quality of life, and contextual features. [10] See Table 6.3c for sample questions used during the four quadrant approach.
Table 6.3c Four Quadrant Approach [11]
MORAL Model
The MORAL model is a nurse-generated, decision-making model originating from research on nursing-specific moral dilemmas involving client autonomy, quality of life, distributing resources, and maintaining professional standards. The model provides guidance for nurses to systematically analyze and address real-life ethical dilemmas. The steps in the process may be remembered by using the mnemonic MORAL. See Table 6.3d for a description of each step of the MORAL Model [12] , [13]
Table 6.3d MORAL Model
PLUS Ethical Decision-Making Model
The PLUS Ethical Decision-Making Model was created by the Ethics and Compliance Initiative to help organizations empower employees to make ethical decisions in the workplace. This model uses four filters throughout the ethical decision-making process, referred to by the mnemonic PLUS:
- P: Policies, procedures, and guidelines of an organization
- L: Laws and regulations
- U: Universal values and principles of an organization
- S: Self-identification of what is good, right, fair and equitable [14]
The seven steps of the PLUS Ethical Decision-Making Model are as follows: [15]
- Define the problem using PLUS filters
- Seek relevant assistance, guidance, and support
- Identify available alternatives
- Evaluate the alternatives using PLUS to identify their impact
- Make the decision
- Implement the decision
- Evaluate the decision using PLUS filters
- “Ethical dilema.png” by Meredith Pomietlo for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2015). Code of ethics for nurses with interpretive statements. American Nurses Association. https://www.nursingworld.org/practice-policy/nursing-excellence/ethics/code-of-ethics-for-nurses/coe-view-only / ↵
- American Nurses Association (ANA). Ethics topics and articles. https://www.nursingworld.org/practice-policy/nursing-excellence/ethics/ethics-topics-and-articles/ ↵
- “Moral courage.png” by Meredith Pomietlo for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- Crisham, P. (1985). Moral: How can I do what is right? Nursing Management, 16 (3), 44. https://journals.lww.com/nursingmanagement/citation/1985/03000/moral__how_can_i_do_what_s_right_.6.aspx ↵
- Ethics & Compliance Initiative. (2021). The PLUS Ethical Decision Making Model . https://www.ethics.org/resources/free-toolkit/decision-making-model/ ↵
Conflict resulting from competing values that requires a decision to be made from equally desirable or undesirable options.
The willingness of an individual to speak out and do what is right in the face of forces that would lead us to act in some other way.
Feelings occurring when an individual is uncertain about what values or principles should be applied to an ethical issue.
Feelings occurring when correct ethical action is identified but the individual feels constrained by competing values of an organization or other individuals.
Feelings occurring when an individual witnesses immoral acts or practices they feel powerless to change.
Leadership and Management of Nursing Care Copyright © 2022 by Kim Belcik and Open Resources for Nursing is licensed under a Creative Commons Attribution 4.0 International License , except where otherwise noted.
Share This Book
An integrated ethical decision-making model for nurses
Affiliation.
- 1 Department of Nursing, Kyungwon University, San 65 Bokjeong-Dong, Gyeonggi-Do, Korea. [email protected]
- PMID: 22156941
- DOI: 10.1177/0969733011413491
The study reviewed 20 currently-available structured ethical decision-making models and developed an integrated model consisting of six steps with useful questions and tools that help better performance each step: (1) the identification of an ethical problem; (2) the collection of additional information to identify the problem and develop solutions; (3) the development of alternatives for analysis and comparison; (4) the selection of the best alternatives and justification; (5) the development of diverse, practical ways to implement ethical decisions and actions; and (6) the evaluation of effects and development of strategies to prevent a similar occurrence. From a pilot-test of the model, nursing students reported positive experiences, including being satisfied with having access to a comprehensive review process of the ethical aspects of decision making and becoming more confident in their decisions. There is a need for the model to be further tested and refined in both the educational and practical environments.
Publication types
- Research Support, Non-U.S. Gov't
- Attitude of Health Personnel
- Decision Support Techniques*
- Ethics, Nursing*
- Models, Nursing*
- Nursing Evaluation Research
- Pilot Projects
- Students, Nursing / psychology
- Open access
- Published: 19 April 2024
Impact of virtual problem-based learning of cardiopulmonary resuscitation on fourth-year nursing students’ satisfaction and performance: a quasi-experimental study
- Seyedeh Nayereh Falahan 1 ,
- Edris Habibi 2 ,
- Naser Kamyari 3 &
- Vahid Yousofvand ORCID: orcid.org/0000-0002-2958-0681 4
BMC Medical Education volume 24 , Article number: 425 ( 2024 ) Cite this article
Metrics details
Regarding competency of nursing students in cardiopulmonary resuscitation (CPR), nursing students frequently exhibit inadequate performance and low satisfaction levels regarding CPR training methods. The problem-based learning (PBL) method, characterized by a constructivist approach, has been underutilized for CPR training, particularly in a virtual format. Hence, this study aims to assess the influence of virtual problem-based learning in cardiopulmonary resuscitation on the satisfaction and performance of fourth-year nursing students.
This quasi-experimental study, conducted in 2022, involved 80 final-year nursing students from Hamadan University of Medical Sciences, Iran. The participants were randomly assigned to either the experimental group ( N = 40) or the control group ( N = 40). The experimental group was further divided into six smaller groups on WhatsApp. Both groups initially received routine training sessions, after which the experimental group engaged in four problem-based learning sessions across three different scenarios. Data collection included demographic information, a teaching satisfaction questionnaire, and cardiopulmonary resuscitation checklists administered immediately and one month after the intervention.
The study was initiated and concluded with 80 participants. The study commenced with no significant disparity in the mean scores of cardiopulmonary resuscitation performance, encompassing chest compressions ( P = 0.451) and airway management ( P = 0.378), as well as teaching satisfaction ( p = 0.115) among the nursing students between the experimental and control groups. However, subsequent to the intervention, both immediately and one month later, the experimental group displayed notable enhancements in mean scores for cardiopulmonary resuscitation performance, comprising chest compressions ( p < 0.001) and airway management ( p < 0.001), as well as teaching satisfaction ( p < 0.001) compared to the control group.
Based on the study’s findings, it is recommended that nursing educators implement this approach in their teaching practices.
Peer Review reports
Cardiopulmonary arrest, being a life-threatening condition, demands prompt interventions from healthcare professionals, particularly nurses, to safeguard lives and avert irreversible harm to vital organs [ 1 ]. Consequently, nurses and nursing students must possess the competence to initiate and execute effective cardiopulmonary resuscitation (CPR) at the onset of their nursing careers [ 2 ]. Despite this imperative, various studies have documented suboptimal CPR performance [ 3 , 4 , 5 ]. Liou et al. additionally noted that nursing students frequently encounter challenges and difficulties in comprehending the educational content and mastering the clinical skills associated with cardiopulmonary resuscitation [ 6 ].
Spinelli et al.‘s investigation revealed inadequacies not only among nursing students but also among nursing staff and medical personnel concerning CPR training and knowledge, indicating a notable gap in this domain [ 7 ]. Furthermore, Nasr-Esfahani et al.‘s study underscored suboptimal performance levels among nursing students in correctly executing cardiopulmonary resuscitation [ 8 ]. Another study evaluating the knowledge and proficiency of nursing students in adhering to standard cardiopulmonary resuscitation protocols reported exceptionally low levels of competence [ 9 ]. Some research attributes nursing students’ deficient competence and subpar performance in accurately conducting cardiopulmonary resuscitation to insufficient training and the dissatisfaction of nursing students with the teaching methodology [ 10 , 11 ].
A study conducted in Iran indicated that students’ express dissatisfaction with the traditional, teacher-centered approach to CPR education [ 12 ]. Similarly, another study found that graduate nurses exhibited lower satisfaction levels with conventional cardiopulmonary resuscitation instruction compared to an electronic delivery method [ 13 ]. It was suggested in a study that the dissatisfaction among medical or nursing students in CPR training groups might be attributed to the high number of participants, highlighting the potential benefits of smaller group sizes [ 14 ]. In a qualitative study, nursing students emphasized the importance of smaller groups, particularly during the COVID-19 pandemic, to allow teachers to allocate more time for individualized instruction with each student [ 15 ]. Thus, for the effective achievement of CPR objectives aimed at saving lives, it is advisable to educate nursing students in smaller groups, enabling instructors to correct mistakes and provide personalized feedback on performance [ 16 ].
In the study conducted by Nabecker et al., it was suggested that reducing the size of training groups, particularly during the initial sessions of basic life support, may enhance trainers’ proficiency in detecting performance errors [ 17 ]. Furthermore, a qualitative inquiry by Dziurka et al. revealed that a significant proportion of nursing students expressed discontent with the pedagogical approach of solely imparting theoretical knowledge, particularly its teacher-centered nature. They tend to have opportunities to utilize various instructional methods to enhance nursing skills and performance throughout their academic trajectory [ 15 ].
Numerous studies indicate that over time, the knowledge and performance of nursing students, as well as nursing graduates, tend to decline [ 18 ]. To uphold patient safety and enhance students’ self-confidence in executing clinical procedures such as CPR, it is imperative for university professors to deliver accurate training in clinical skills through innovative teaching methods [ 19 ]. Despite the critical importance of CPR training, insufficient attention has been directed toward employing engaging and suitable instructional techniques. Consequently, the current imperative extends beyond merely expanding cardiopulmonary resuscitation training; rather, it underscores the paramount need to enhance the quality of this training [ 20 ].
It is crucial to acknowledge that while all forms of training contribute to learning, the depth and sustainability of learning may vary across different training methods [ 21 ]. Various studies have scrutinized educational approaches aimed at enhancing the quality of CPR training. These approaches encompass both direct and indirect methods, including workshops, lectures, videos, brochures, pamphlets, e-learning, and multimedia software [ 9 ].
Presently, lectures represent a prevalent method for CPR training in Iran; however, achieving comprehensive and effective training to enhance the quality of instruction necessitates the incorporation of additional complementary methods [ 22 ]. Even brief training sessions conducted in clinical skill centers fall short of providing a comprehensive grasp of all pertinent skills. There remains a dearth of knowledge remains regarding the optimal teaching methods for imparting this critical and essential skill [ 23 ].
On the other hand, certain studies argue that acquiring and applying CPR-related training for nursing students necessitates engaging in a problem-solving process through critical thinking [ 6 ]. Despite nursing curricula placing emphasis on fostering critical thinking skills in nursing students and graduates, findings from previous studies in Iran indicate varying levels of competence in these skills, ranging from weak to moderate, among nursing students and nurses [ 24 ]. Nevertheless, a study conducted in Malaysia reported a high level of critical thinking among nursing students [ 25 ]. Ahmady and colleagues attributed the consequences of poor critical thinking skills and the inability of nursing students to solve problems to a widening gap between theory and practice, a deficiency in timely decision-making, and suboptimal clinical reasoning [ 26 ].
Thus, nursing students are encouraged to employ problem-solving and critical thinking strategies to unravel intricate solutions to complex issues such as CPR [ 27 ]. In this context, considerable attention has been directed towards problem-based learning (PBL), anticipating its role in enhancing students’ critical thinking skills for competent CPR performance and increased satisfaction in learning it [ 28 ]. Problem-based learning is an educational approach that shifts the teacher’s role to a more student-centered dynamic, grounded in self-directed learning principles [ 29 ].
According to Ghani et al., PBL emphasizes learning behaviors conducive to critical thinking, problem-solving, communication, and collaborative skills in student preparation. The study by Ghani et al. identified internal empowerment, delegation, and performance skills as three pivotal elements effective in attaining learning outcomes through PBL [ 30 ]. A comprehensive review indicated that PBL is an effective and gratifying method in medical education, suggesting that medical students, through PBL, acquire not only knowledge but also essential competencies requisite for the medical profession [ 29 ]. Prior research has demonstrated that students instructed through PBL exhibit superior problem-solving abilities compared to those receiving traditional lectures [ 31 ].
Perdana et al.‘s study found the problem-solving method to be more effective in enhancing students’ digital literacy than the online laboratory simulation method with concept maps [ 32 ]. Another study concluded that PBL more effectively promotes nursing students’ progress and academic motivation compared to the lecture method [ 33 ]. However, a singular study posited that the PBL approach in first-year medical students did not significantly enhance critical thinking/knowledge, problem-solving, and self-direction compared to conventional teaching methods [ 34 ].
Simultaneously, the surge in communication facilities and equipment has propelled the popularity of online learning and virtual technologies in education [ 35 ]. Leveraging modern technologies, including virtual space, is imperative in the practical training of nursing students. This utilization aims to equip students with the skills to navigate challenging and novel situations, foster decision-making proficiency, and enhance problem-solving capabilities [ 15 ]. A study conducted in Indonesia demonstrated that the implementation of the problem-based learning model through electronic learning media resulted in improved learning outcomes, coupled with high satisfaction levels among students [ 36 ]. In a study by Aslan et al., participants engaged in live online classes using the PBL approach exhibited elevated levels of learning achievement, problem-solving skills, and direct interaction during online sessions. Nevertheless, no significant difference was observed in the communication skills of the groups [ 37 ].
In Iran, several studies have revealed that a majority of nursing educators predominantly employ content-based educational methods and exhibit a preference for a formal educational setting characterized by limited student participation [ 38 , 39 ]. Given that Iranian nursing students have demonstrated subpar and moderate performance levels in prior investigations, coupled with their low satisfaction with CPR training methods, and considering that PBL, a constructivist approach, has been underutilized for CPR training, the current study seeks to assess the impact of a virtual problem-based learning (PBL) approach of cardiopulmonary resuscitation on the satisfaction and performance of fourth-year nursing students.
Design and setting
This pre-post-test quasi-experimental study was undertaken at the School of Nursing and Midwifery, Hamadan University of Medical Sciences, between February 2021 and June 2022. The study sample comprised 80 fourth-year nursing students enrolled in semesters seven and eight.
Participants and sampling
The sample size for the current study was determined in accordance with a precedent study [ 40 ], considering a confidence level of 95%, a test power of 80%, an effect size of 0.69, and factoring in a potential attrition rate of 18%. As a result, a total of 80 participants, with 40 individuals allocated to each group, were deemed sufficient for the study.
Following the inclusion criteria, 80 fourth-year students were selected for the study and then randomly assigned to either the experimental group ( N = 40) or the control group ( N = 40). Both groups were evenly distributed with a mix of 7th and 8th semester nursing students (fourth year) (Fig. 1 ). The experimental group was further divided into six subgroups using a random number table in WhatsApp. Similarly, the control group was also organized into a WhatsApp group. It is important to note that all study participants had received routine CPR training during their sixth academic semester.
The inclusion criteria for this study required participants to have successfully completed the cardiopulmonary resuscitation course as outlined in the academic curriculum, and not to have taken additional CPR courses from external organizations outside of the nursing and midwifery faculty. The exclusion criteria encompassed being absent for more than one training session and failing to complete the questionnaire. Prior to participation in the study, written informed consent was obtained from the students, with a total of 80 nursing students ultimately taking part in the research (comprising fifty 8th-semester students and sixty 7th-semester students).
CONSORT diagram
Tools and measurements
Demographic information form.
The demographic information form included age, gender, marital status, student employment history, time spent in the student workplace, student workplace department, and cardiopulmonary resuscitation experience. In terms of face validity, ten Hamadan Nursing and Midwifery Faculty members reviewed and approved this form.
Teaching satisfaction for nursing student’s questionnaire
The questionnaire utilized in this study was developed by Borim Nejad et al. (2015) through an extensive literature review, examination of other satisfaction questionnaires, and consultations with academic experts. Comprising 16 items on a 3-point Likert scale (completely = 3, somewhat = 2, not at all = 1), the questionnaire assesses aspects such as increased interest in the subject and the application of gained knowledge and skills in communication. Scores on this questionnaire range from 16 to 48, with a higher score indicating greater satisfaction. Student satisfaction levels with teaching are categorized into three tiers: low (scores between 0 and 16), medium (16–32), and high (scores above 32). The validity of the questionnaire was established through input from 15 specialists, resulting in necessary adjustments for form and content. The content validity index (CVI), calculated based on Waltz and Basel standards, was determined to be 0.85. Reliability was assessed using the test-retest method, with a reported correlation of 0.90 [ 41 ]. In the current study, the internal consistency of the questionnaire was found to be 0.93, indicating a high level of reliability.
In this study, the final-year nursing students had previously received cardiopulmonary resuscitation (CPR) training in the emergency department during the preceding semester as part of their curriculum, utilizing a teacher-centered approach. Their satisfaction with this teaching method was assessed before the intervention. Following the implementation of the intervention, their satisfaction with teaching, particularly in comparison to the Problem-Based Learning (PBL) method, was evaluated. Some of the questions pertaining to teaching satisfaction in the questionnaire are provided below:
I found this teaching method enjoyable.
This method adequately addressed my information needs.
The knowledge and skills acquired through this method are applicable to my profession.
I believe my performance improved with this method.
Learning occurred more efficiently with this method.
I perceive learning to be more effective with this approach.
This method enhanced my motivation to learn.
I found the subject matter more engaging with this approach.
This method contributed to the enhancement of my clinical judgment.
Overall, I am satisfied with this teaching method.
I would recommend implementing this method in other educational settings.
Cardiopulmonary resuscitation procedure checklist
The Ministry of Health of Iran has presented a standardized 20-item scale for evaluating the competency of nursing students in cardiopulmonary resuscitation. This scale comprises ten inquiries pertaining to cardiac massage techniques and ten inquiries concerning airway management during adult resuscitation. Each item is evaluated using a three-point Likert scale, with options for weak = 1, moderate = 2, and good = 3. The cumulative score for each section is determined by adding together the individual item scores. The performance of nursing students in each section is classified into three tiers: inadequate (scores between 0 and 10), moderate (11–20), and proficient (21–30).
Before and after the intervention, the performance of students in cardiopulmonary resuscitation (CPR), covering chest compressions and airway management, was evaluated by two assessors. The assessment panel comprised an instructor with a medical-surgical nursing degree, 17 years of experience in the emergency department, and a PhD student in medical-surgical nursing with five years of experience in emergency and intensive care units. Evaluations were conducted both concurrently and separately. In cases where both assessors reached a consensus on the assigned grades for the students, the same grade was recorded. If a discrepancy arose between the two assessors, the opinion of a third assessor, a PhD holder in emergency nursing with 25 years of experience, was solicited. Subsequently, all three assessors reached a consensus, and grades were allocated to the students accordingly. The evaluation took place in the Faculty of Nursing and Midwifery simulation lab, utilizing pre-prepared mannequins.
Intervention
Prior to the intervention, both the experimental and control groups completed a demographic information form and the Satisfaction teaching for nursing students’ questionnaire. Additionally, an observational cardiopulmonary resuscitation practical test was conducted as a pre-test to complete the cardiopulmonary resuscitation checklist.
Subsequently, as an initial session, both the control and experimental groups received identical educational content via WhatsApp, including voice slides, educational videos, and questions. Twenty participants from each group were selected based on random numbers and were questioned to ensure their comprehension of the training content. Those who required further understanding of the educational content were provided with additional instruction after one or two days and were subsequently questioned about it.
The intervention consisted of four sessions, each lasting one hour per week. The first intervention session was uniform for both groups. However, from the second session onwards, the control group did not receive any further training. In contrast, the remaining three sessions for the experimental group focused on problem-based learning. During these sessions, students utilized PDF files to implement the ESI triage manual, 4th edition, to three scenarios [ 42 ]. At each session, researchers presented a scenario along with necessary explanations. Subsequently, students asked questions to clarify any ambiguities and received appropriate answers. Following receipt of the scenario, students were required to study it carefully during the week and solve it based on the steps described in Table 1 .
In the initial session, a hypothetical scenario was presented involving a 65-year-old male patient diagnosed with asystole, with a medical history including myocardial infarction and diabetes. The students were tasked with mentally placing themselves in the clinical setting and initiating the initial steps of cardiopulmonary resuscitation (CPR) while providing the rationale for their actions. Subsequently, they were required to continue CPR and provide ongoing care during and after resuscitation efforts. Initially, one of the researchers provided a comprehensive case overview.
Following this, students were instructed to review the latest Cardiopulmonary Resuscitation Guidelines (2020) provided by the researchers in group settings, and then apply the steps outlined in the problem-based learning (PBL) approach. The researchers monitored each group’s progress, offering guidance when necessary, and facilitated group discussions to analyze the scenario comprehensively. Prior training had been provided to the students on how to effectively analyze CPR-related problems, considering various dimensions such as their responsibilities in the situation, necessary actions, potential risks to the patient, composition of the resuscitation team, required resources, and possible further interventions.
Students were encouraged to identify and discuss any uncertainties or ambiguities within the scenario, providing justification and rationale for their perspectives. In subsequent stages, students were prompted to share both correct and incorrect responses within their groups without judgment. All steps outlined in Table 1 were sequentially implemented. At the conclusion of each session, students and researchers collectively reviewed the PBL process, and each group presented their final conclusions. The resources available to students included CPR guidelines for different scenarios, PDF files containing the Emergency Severity Index (ESI) triage manual (4th edition), and guidance from the researchers. Subsequent sessions aimed to increase the level of challenge by presenting more complex scenarios to the students.
Data collection methods
At the outset (pre-test), immediately following the intervention (post-test 1), and one month thereafter (post-test 2), the nursing students were tasked with completing a demographic information form and a teaching satisfaction questionnaire. Furthermore, the researchers administered a cardiopulmonary resuscitation performance checklist in a practical setting. Both the experimental and control groups were requested to complete the teaching satisfaction questionnaire immediately and one month after the intervention at the designated location within the nursing school. Following the practical examination of cardiopulmonary resuscitation, the researchers conducted an assessment of the students’ performance in this course. Adhering to research ethics, the material presented to the experimental group was also made available to the control group upon conclusion of the study.
Data analysis
Upon completion of data collection, statistical analysis was conducted using SPSS version 22. Descriptive statistics, including mean, standard deviation, frequency, and percentage, were used to describe the data. The normality of the data was assessed using the Kolmogorov-Smirnov and Shapiro-Wilk tests. Subsequently, independent t-tests, chi-square tests, Fisher’s exact tests, repeated measures ANOVA, and Bonferroni’s post hoc tests were employed for data analysis. The significance level for this study was set at 0.05.
Ethical considerations
The current study received approval from the Ethics Committee of Hamadan University of Medical Sciences (ethical code: IR.UMSHA.REC.1400.884). Prior to commencing the research, the researchers provided a detailed explanation of the study objectives to the participants. Subsequently, written informed consent was obtained from the students in order for them to participate in the study and for the results to be published. Furthermore, the researchers assured the participants that all information provided would be kept confidential and emphasized their right to withdraw from the study at any point.
The baseline analysis of socio-demographic characteristics revealed that there were no significant differences between the experimental and control groups, indicating homogeneity (Table 2 ).
Prior to the intervention, the performance of fourth-year nursing students in chest compression and airway management was found to be moderate to weak, as indicated by mean scores of 11.93 (SD = 1.11) and 10.95 (SD = 1.10) in the experimental group, and 11.73 (SD = 1.24) and 10.75 (SD = 0.89) in the control group, respectively. There were no significant differences between the groups at baseline ( P = 0.451 for chest compression and P = 0.378 for airway management). However, immediately and one month after the intervention, significant differences were observed between the groups ( P < 0.001). Additionally, the experimental group showed a significant improvement in performance scores from baseline to one month after the intervention ( p < 0.001), while the control group did not show significant improvement ( P > 0.05) (Table 3 ).
Teaching satisfaction among fourth-year nursing students was moderate before the intervention, with mean scores of 19.83 (SD = 4.29) in the experimental group and 18.63 (SD = 2.07) in the control group. There was no significant difference between the groups before the intervention ( p = 0.115). However, significant differences were observed between the groups immediately and one month after the intervention ( p < 0.001). The mean teaching satisfaction scores of nursing students in the experimental group significantly improved from baseline to one month after the intervention ( p < 0.001), while no significant differences were observed for the control group ( p = 0.175) (Table 4 ).
The present study assessed the impact of problem-based learning virtual training on cardiopulmonary resuscitation on the teaching satisfaction and performance of fourth-year nursing students. Prior to the intervention, there were no significant differences in the mean scores of chest compression and airway management in cardiopulmonary resuscitation between the experimental and control groups, indicating that students had a moderate to weak skill level in this area. This may be attributed to the limited education provided before graduation, as well as the need for access to recognized instructional resources from international organizations and institutes that evaluate these principles.
However, this study’s results demonstrated a significant difference between groups immediately after the intervention and one month afterward. Additionally, the experimental group’s mean performance scores in chest compression and airway management increased from baseline to one month after the intervention. Therefore, problem-based learning virtual education courses on cardiopulmonary resuscitation effectively improve nursing students’ performance.
Aligned with our study, Habibli et al. demonstrated that nursing students exhibited significantly higher performance scores immediately after the intervention and at a three-month follow-up compared to the control group, indicating that simulation-based training enhanced the proficiency of nursing students in Basic Life Support-Cardiopulmonary Resuscitation (BLS-CPR) [ 43 ]. Similarly, Ren et al.‘s investigation corroborated our findings by illustrating that Problem-Based Learning (PBL) modules yielded more effective medical education outcomes across various medical science specialties, fostering both theoretical knowledge and practical skills compared to traditional lecture-based approaches. Participants receiving PBL reported more positive feedback and satisfaction than those exposed to conventional methods [ 44 ].
Echoing our research, Hazrati et al.‘s comprehensive review highlighted the efficacy of PBL in Iranian medical education, showcasing its role in enhancing student performance, fostering critical thinking, and garnering student satisfaction [ 45 ]. Additionally, Towfik et al. demonstrated the significant impact of problem-based learning on strengthening critical thinking skills, clinical satisfaction, academic progress, and course learning achievements (skills and values) among nursing students [ 46 ]. GU Deng-yu et al.‘s study further supported the benefits of problem-based learning, particularly in conjunction with case-based learning, for improving performance and clinical practice skills among nurse anesthesia trainees compared to lecture-based learning [ 47 ].
Park et al.‘s investigation aimed to assess the educational effects of a blended e-learning program for nursing graduate students on self-efficacy, problem-solving, and psychomotor skills for core nursing skills. Their results indicated that participants who underwent combined e-learning experienced enhancements in problem-solving abilities and self-efficacy related to nursing performance, particularly in cardiopulmonary resuscitation and defibrillation. Although most psychomotor skills demonstrated excellent post-intervention performance rates ranging from 80 to 90%, certain aspects such as chest compression location, compression rate per minute, artificial respiration, and patient outcome verification still exhibited lower performance levels [ 48 ].
Baccin et al. found that PBL education through mobile phones has been shown to enhance nursing students’ knowledge of diagnosing and taking timely action at the patient’s bedside. The authors also emphasized that using PBL through mobile phones could serve as a valuable learning strategy for nurses, and suggested that nursing students should be actively involved in this process [ 49 ]. Several other studies have highlighted that nursing students can access clinical opportunities and educational topics via mobile phones, with many nurses and nursing students reporting a positive and progressive impact on their knowledge acquisition process [ 33 , 36 , 37 , 50 ].
Additionally, Lee et al. demonstrated that simulation problem-based learning can enhance nursing students’ communication attitudes, suggesting its potential for application in clinical practice to improve communication attitudes and facilitate the application of learned knowledge to simulated nursing situations through experiential learning [ 51 ]. The utilization of mobile phone capabilities and communication applications has the potential to enhance nursing education beyond traditional settings such as the university and the patient’s bedside [ 52 , 53 ]. Furthermore, problem-based learning (PBL) methods have been shown to improve students’ abilities in analyzing information, critical thinking, and problem-solving skills [ 30 ].
The findings of the current study contrast with those of Kang et al.‘s study, “The Effect of Virtual Education on Nursing Students’ Learning in Caring for Children with Asthma,” which found that virtual education did not significantly improve students’ knowledge. It appears that simply preparing and sending educational materials may not be sufficient to enhance the knowledge of the research sample. The current study suggests that incorporating online simulated or face-to-face courses, as well as the opportunity for live participation and discussion, leads to greater participant satisfaction due to the convenience and unrestricted access to content [ 54 ]. Additionally, Manuaba et al.‘s study demonstrated that problem-based learning (PBL) is not effective at enhancing critical thinking, problem-solving, and self-direction among first-year medical students [ 34 ]. Meanwhile, Mendel et al.‘s research at the Washburn School of Nursing in the USA concluded that virtual education has a minimal impact on reducing moral distress in neonatal intensive care unit nurses, whereas face-to-face meetings related to palliative care for infants reduced moral distress among nurses in neonatal intensive care units. The author suggests that palliative care meetings in the final stages of life may alleviate some of these distresses [ 55 ]. These studies collectively indicate that a primary obstacle to raising awareness of virtual training courses is inadequate follow-up and participants’ need for more focus on the content of the training sessions.
Prior to the intervention, fourth-year nursing students expressed a moderate level of satisfaction with the teaching of cardiopulmonary resuscitation. Following the intervention, the mean scores of teaching satisfaction among fourth-year students in the experimental group showed a significant increase from baseline to one-month post-intervention in comparison to the control group. Thus, the findings of the study suggest that virtual education utilizing problem-based learning (PBL) for cardiopulmonary resuscitation courses had a positive impact on students’ satisfaction with the teaching.
In alignment with our research, Jannah et al.‘s findings revealed that approximately two-thirds of nursing students expressed satisfaction with the Problem-Based Learning (PBL) approach and its instructional methodology [ 56 ]. Similarly, Forouzan Jahromi et al. demonstrated that nursing students reported significantly higher levels of learning satisfaction when engaged in problem-based learning than outcome-based learning, particularly within the intensive care unit setting [ 57 ]. Tadesse et al.‘s study further supported these results by indicating higher academic satisfaction among students in problem-based learning programs than lecture-based learning environments [ 58 ]. Additionally, González Hernando et al. observed a positive reception to PBL, with 78% of students expressing a preference for this method post-implementation. Following active engagement in PBL, students demonstrated heightened motivation and satisfaction across educational content, instructional methods, the learning process, instructor involvement, and student roles [ 59 ].
Moreover, Son’s study underscored the efficacy of integrating simulator programs with PBL as a strategy to enhance clinical reasoning abilities and foster learning satisfaction among nursing students [ 60 ]. Consistent with our investigation, a comprehensive review by Hazrati et al. highlighted the advantageous impact of PBL on increasing teaching satisfaction in medical education within Iran [ 45 ]. Furthermore, GU Deng-yu et al.‘s research indicated that students in the intervention group, exposed to a combination of problem-based learning and case-based learning, exhibited higher overall satisfaction, greater acceptance of the teaching model, and superior knowledge mastery compared to those in the control group receiving lecture-based instruction [ 47 ].
In their study, Berger et al. found that nursing students exhibited higher levels of satisfaction with teaching when utilizing mobile phones and PBL methods compared to traditional teaching approaches. They recommended the use of mobile phones and PBL to enhance student satisfaction [ 61 ]. Similarly, Trullàs et al. reported that the PBL method resulted in high levels of teaching satisfaction among nursing and medical students [ 29 ]. Furthermore, Xing et al. demonstrated that CPBL and SBAR improved nursing students’ problem-solving and critical thinking abilities, with both students and teachers expressing satisfaction with the new teaching method [ 62 ]. Sangestani et al. also observed increased satisfaction among midwifery students when utilizing the PBL method [ 63 ]. Lastly, Sharma’s research indicated that PBL increased nursing students’ self-efficacy and improved learning outcomes [ 64 ].
However, Jannah et al.‘s study highlights that despite nursing students’ satisfaction with the teaching method, several challenges persist within the learning process. For instance, students express concerns regarding inadequate time to fully comprehend the subject matter. Additionally, when learning topics involve practical field-related facts, students may exhibit reluctance to engage in discussions. Moreover, there are limitations in learning resources, indicating a need for effective management of e-learning tools and regulation of students’ access to ensure the availability of pertinent learning materials for sharing among peers [ 56 ].
The findings of this study underscore the potential of modern, learner-centered teaching methods, exemplified by Problem-Based Learning (PBL), to supplant traditional teacher-centered approaches in nursing education. PBL emerges as a transformative pedagogical strategy that not only enhances nurses’ preparedness for skills and behavioral challenges but also empowers students to attain diverse educational objectives through the integration of mobile technology and social media. Consequently, it is recommended that future research endeavors capitalize on the implications of employing PBL within the educational landscape, contributing to the advancement of educational methodologies. Furthermore, it is advisable to conduct additional research to comprehensively elucidate the impact of the PBL teaching method on nursing students’ teaching satisfaction and performance.
Limitations
In the present study, there is a potential limitation regarding the participants’ comprehensive understanding of the training content. To address this limitation, a random selection of 20 students from both the experimental and control groups was made, and they were assessed through a series of questions related to the educational content. Subsequently, the training content was reviewed with those who did not fully comprehend it, and after a few days, they were re-evaluated through a question-answer session. Another limitation of this study pertains to the need for follow-up on nursing students’ performance and satisfaction post-intervention. Therefore, it is recommended that future research includes observations of nursing students at the patient’s bedside during cardiopulmonary resuscitation to strengthen this innovative learning method further. Furthermore, additional research is necessary to fully understand the impact of the PBL education method on nursing student performance.
The present study’s findings suggest that PBL virtual training can effectively maintain CPR skills and enhance teaching satisfaction among nursing students. As such, it is recommended that nursing educators consider incorporating this educational approach to enhance knowledge and satisfaction levels among their students.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to keeping participants’ information confidential but are available from the corresponding author at reasonable request.
Lott C, Truhlář A, Alfonzo A, Barelli A, González-Salvado V, Hinkelbein J, Nolan JP, Paal P, Perkins GD, Thies K-C. European Resuscitation Council guidelines 2021: cardiac arrest in special circumstances. Resuscitation. 2021;161:152–219. https://doi.org/10.1016/j.resuscitation.2021.02.011 .
Article Google Scholar
Janatolmakan M, Nouri R, Soroush A, Andayeshgar B, Khatony A. Barriers to the success of cardiopulmonary resuscitation from the perspective of Iranian nurses: a qualitative content analysis. Int Emerg Nurs. 2021;54:100954. https://doi.org/10.1016/j.ienj.2020.100954 .
Greif R, Bhanji F, Bigham BL, Bray J, Breckwoldt J, Cheng A, Duff JP, Gilfoyle E, Hsieh M-J, Iwami T. Education, implementation, and teams: 2020 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2020;142(16suppl1):S222–83. https://doi.org/10.1161/CIR.0000000000000896 .
Berg KM, Soar J, Andersen LW, Böttiger BW, Cacciola S, Callaway CW, Couper K, Cronberg T, D’Arrigo S, Deakin CD. Adult advanced life support: 2020 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2020;142(16suppl1):S92–139. https://doi.org/10.1016/j.resuscitation.2020.09.012 .
Olasveengen TM, Mancini ME, Perkins GD, Avis S, Brooks S, Castrén M, Chung SP, Considine J, Couper K, Escalante R. Adult basic life support: international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation. 2020;156:A35–79. https://doi.org/10.1016/j.resuscitation.2020.09.010 .
Liou SR, Liu HC, Tsai SL, Chu TP, Cheng CY. Performance competence of pregraduate nursing students and hospital nurses: a comparison study. J Clin Nurs. 2020;29(13–14):2652–62. https://doi.org/10.1111/jocn.15287 .
Spinelli G, Brogi E, Sidoti A, Pagnucci N, Forfori F. Assessment of the knowledge level and experience of healthcare personnel concerning CPR and early defibrillation: an internal survey. BMC Cardiovasc Disord. 2021;21(1):195. https://doi.org/10.1186/s12872-021-02009-2 .
Nasr-Esfahani M, Yazdannik A, Mohamadiriz S. Development of nursing students’ performance in advanced cardiopulmonary resuscitation through role-playing learning model. J Educ Health Promotion. 2019;8:151. https://doi.org/10.4103/jehp.jehp_125_18 .
Habibli T, Ghezeljeh TN, Haghani S. The effect of simulation-based education on nursing students’ knowledge and performance of adult basic cardiopulmonary resuscitation: a randomized clinical trial. Nurs Pract Today. 2020. https://doi.org/10.18502/npt.v7i2.2730 .
Roel S, Bjørk IT. Comparing nursing student competence in CPR before and after a pedagogical intervention. Nurs Res Pract. 2020;2020:7459084. https://doi.org/10.1155/2020/7459084 .
Dehnoalian A, Zare Z, Tatari F. Evaluating nursing students, performance with on Objective Structured Clinical Examination. Res Med Educ. 2020;12(4):29–39. https://doi.org/10.52547/rme.12.4.29 .
heidarzadeh a. Kazemi m, Forouzi m, jahani y: comparing the effect of two methods of cardiopulmonary resuscitation education including computer-based stimulation and mannequin stimulation on nursing students knowledge and satisfaction. J Med Educ Dev. 2015;8(17):12–20.
Google Scholar
Khoshnoodifar M, Rafie S, Nasrabadi M, Alavi N. The effects of CPR training using two traditional and electronic training methods on the knowledge, skill, and satisfaction of nurses from in Service Education of Cardiopulmonary Resuscitation. Qom Univ Med Sci J. 2019;13:34–43. https://doi.org/10.29252/qums.13.9.34 .
Kwon Y, Lee H, Kim W. Design of an IoT-Based remote Learning System for Medical Skill Training in the age of COVID-19: focusing on CPR skill training. Appl Sci. 2022;12(17):8840. https://doi.org/10.3390/app12178840 .
Dziurka M, Machul M, Ozdoba P, Obuchowska A, Kotowski M, Grzegorczyk A, Pydyś A, Dobrowolska B. Clinical training during the COVID-19 pandemic: experiences of nursing students and implications for education. Int J Environ Res Public Health. 2022;19(10):6352. https://doi.org/10.3390/ijerph19106352 .
Nuuyoma V. Feedback in clinical settings: nursing students’ perceptions at the district hospital in the southern part of Namibia. Curationis. 2021;44(1):e1–12. https://doi.org/10.4102/curationis.v44i1.2147 .
Nabecker S, Huwendiek S, Theiler L, Huber M, Petrowski K, Greif R. The effective group size for teaching cardiopulmonary resuscitation skills– A randomized controlled simulation trial. Resuscitation. 2021;165:77–82. https://doi.org/10.1016/j.resuscitation.2021.05.034 .
Lanahan M, Montalvo B, Cohn T. The perception of preparedness in undergraduate nursing students during COVID-19. J Prof Nurs. 2022;42:111–21. https://doi.org/10.1016/j.profnurs.2022.06.002 .
Chen P-J, Liou W-K. The effects of an augmented reality application developed for paediatric first aid training on the knowledge and skill levels of nursing students: an experimental controlled study. Nurse Educ Today. 2023;120:105629. https://doi.org/10.1016/j.nedt.2022.105629 .
Rodríguez-Matesanz M, Guzmán-García C, Oropesa I, Rubio-Bolivar J, Quintana-Díaz M, Sánchez-González P. A New Immersive virtual reality station for cardiopulmonary resuscitation objective structured clinical exam evaluation. Sensors. 2022;22(13):4913. https://doi.org/10.3390/s22134913 .
Farsi Z, Sajadi SA, Afaghi E, Fournier A, Aliyari S, Ahmadi Y, Hazrati E. Explaining the experiences of nursing administrators, educators, and students about education process in the COVID-19 pandemic: a qualitative study. BMC Nurs. 2021;20:1–13. https://doi.org/10.1186/s12912-021-00666-4 .
Tajiki I, Vizeshfar F, Keshtkaran Z. The effect of training program based on health belief model on burn prevention knowledge in mothers of children aged to 1–3 years: a randomized controlled. Burns. 2022;48(4):808–15. https://doi.org/10.1016/j.burns.2021.11.001 .
Burgess A, van Diggele C, Roberts C, Mellis C. Tips for teaching procedural skills. BMC Med Educ. 2020;20(2):458. https://doi.org/10.1186/s12909-020-02284-1 .
Tajvidi M, Moghimi Hanjani S. The relationship between critical thinking and clinical competence in nurses. Strides Dev Med Educ. 2019;16(1). https://doi.org/10.5812/sdme.80152 .
Yee L, Lim sg, Ho A, Lian. Level of critical thinking ability among nursing students. Malaysian J Nurs. 2019;11:31. https://doi.org/10.31674/mjn.2019.v11i02.004 .
Ahmady S, Shahbazi S. Impact of social problem-solving training on critical thinking and decision making of nursing students. BMC Nurs. 2020;19(1):94. https://doi.org/10.1186/s12912-020-00487-x .
Thrift JR. Nursing student perceptions of Presence in a virtual learning environment: a qualitative description study. Mercer University; 2022.
Gooney M, Jennings H, Kennedy S, Maher R, Moylan M, Purcell G. Clinical skills in undergraduate nurse education: transforming and Harnessing Student Engagement through Problem Based Learning utilising a blended Teaching Approach. All Irel J High Educ 2022, 14(2).
Trullàs JC, Blay C, Sarri E, Pujol R. Effectiveness of problem-based learning methodology in undergraduate medical education: a scoping review. BMC Med Educ. 2022;22(1):104. https://doi.org/10.1186/s12909-022-03154-8 .
Ghani ASA, Rahim AFA, Yusoff MSB, Hadie SNH. Effective learning behavior in Problem-based learning: a scoping review. Med Sci Educ. 2021;31(3):1199–211. https://doi.org/10.1007/s40670-021-01292-0 .
Nantha C. A quasi-experimental evaluation of classes using traditional methods, problem-based learning, and flipped learning to Enhance Thai Student-Teacher Problem-solving skills and academic achievement. Int J Emerg Technol Learn (Online). 2022;17(14):20. https://doi.org/10.3991/ijet.v17i14.30903 .
Perdana R, Jumadi J, Rosana D, Riwayani R. The online laboratory simulation with concept mapping and problem-based learning (ols-cmpbl): is it effective in improving students’ digital literacy skills? Jurnal Cakrawala Pendidikan. 2020;39:382–94. https://doi.org/10.21831/cp.v39i2.31491 .
Arian M, Kamali A, Oghazian MB. Comparing the efficacy of problem-based learning vs. lectures on the academic achievement and educational motivation of nursing students: a 3-year quasi-experimental study. Res Dev Med Educ. 2022;11(1):3–3. https://doi.org/10.34172/rdme.2022.003 .
Manuaba IBAP, -No Y, Wu C-C. The effectiveness of problem based learning in improving critical thinking, problem-solving and self-directed learning in first-year medical students: a meta-analysis. PLoS ONE. 2022;17(11):e0277339. https://doi.org/10.1371/journal.pone.0277339 .
Yao S, Li D, Yohannes A, Song H. Exploration for network distance teaching and resource sharing system for higher education in epidemic situation of COVID-19. Procedia Comput Sci. 2021;183:807–13. https://doi.org/10.1016/j.procs.2021.03.002 .
Nurrohma RI, Adistana GAYP. Penerapan Model Pembelajaran Problem Based Learning dengan media E-Learning Melalui Aplikasi Edmodo pada Mekanika Teknik. Edukatif: Jurnal Ilmu Pendidikan. 2021;3(4):1199–209. https://doi.org/10.31004/edukatif.v3i4.544 .
Aslan A. Problem-based learning in live online classes: learning achievement, problem-solving skill, communication skill, and interaction. Comput Educ. 2021;171:104237. https://doi.org/10.1016/j.compedu.2021.104237 .
Delam H, Kavi E, Eidi A, Sookhak F. Assessing students’ satisfaction regarding the use of virtual learning at Larestan University of Medical Sciences. Interdisciplinary J Virtual Learn Med Sci. 2022;13(2):118–26. https://doi.org/10.30476/IJVLMS.2022.94627.1140 .
Salmani N, Bagheri I, Dadgari A. Iranian nursing students experiences regarding the status of e-learning during COVID-19 pandemic. PLoS ONE. 2022;17(2):e0263388. https://doi.org/10.1371/journal.pone.0263388 .
Habibli T, Ghezeljeh TN, Haghani S. The effect of simulation-based education on nursing students’ knowledge and performance of adult basic cardiopulmonary resuscitation: a randomized clinical trial. Nurs Pract Today. 2020;7(2):87–96. https://doi.org/10.18502/npt.v7i2.2730 .
Borim Nejad L, Sajadi Hezaveh M, Khosravi S. The Effect of Learning Contract on Self-directed learning and satisfaction of nursing students in Clinical Education. Iran J Med Educ. 2015;14(12):1084–92.
Gilboy N, Tanabe P, Travers D, Rosenau A. Emergency Severity Index Implementation Handbook 2020 edition. A Triage Tool for Emergency Department Care, version 4; 2020.
Habibli T, Tahereh Najafi G, Shima H. The effect of simulation-based education on nursing students’ knowledge and performance of adult basic cardiopulmonary resuscitation: a randomized clinical trial. Nurs Pract Today. 2020;7(2). https://doi.org/10.18502/npt.v7i2.2730 .
Ren S, Li Y, Pu L, Feng Y. Effects of problem-based learning on delivering medical and nursing education: a systematic review and meta‐analysis of randomized controlled trials. Worldviews Evidence‐Based Nurs. 2023;20(5):500–12. https://doi.org/10.1111/wvn.12663 .
Hazrati H, Zaregavgani V, Ghojazadeh M, Vahedi L. A systematic review of the Effect of ProblemBased Learning on learning satisfaction and efficacy of the Iranian Medical Education. Strides Dev Med Educ. 2016;13(3):246–54.
Towfik AF, Hafez SH, Abualruz H, Mohamed HA, Mohamed NA. Mahgoub SAE-f: bridging the gap between theory and practice: applying Problem based Learning Strategy to improve nursing students’ achievement. Tanta Sci Nurs J. 2023;30(3):127–37. https://doi.org/10.21608/tsnj.2023.307830 .
Deng-yu GU, Fu-qi WCXU, Hui-fen LI, Yan ZHU, Qiu-rui HUANG. Effect of PBL combined with CBL on interns in anesthesia nursing resident teaching class. J Nurs. 2023;30(6):12–4. https://doi.org/10.16460/j.issn1008-9969.2023.06.012 .
Park JY, Woo CH, Yoo JY. Effects of blended cardiopulmonary resuscitation and defibrillation E-learning on nursing students’ Self-efficacy, problem solving, and psychomotor skills. Comput Inf Nurs. 2016;34(6):272–80. https://doi.org/10.1097/cin.0000000000000227 .
Baccin CRA, Dal Sasso GTM, Paixão CA, de Sousa PAF. Mobile Application as a learning aid for nurses and nursing students to identify and care for Stroke patients: Pretest and Posttest results. Computers Inf Nursing: CIN. 2020;38(7):358–66. https://doi.org/10.1097/cin.0000000000000623 .
Kim JH, Park H. Effects of Smartphone-based mobile learning in nursing education: a systematic review and Meta-analysis. Asian Nurs Res. 2019;13(1):20–9. https://doi.org/10.1016/j.anr.2019.01.005 .
Lee J, Son HK. Effects of simulation problem-based learning based on Peplau’s interpersonal relationship model for cesarean section maternity nursing on communication skills, communication attitudes and team efficacy. Nurse Educ Today. 2022;113:105373. https://doi.org/10.1016/j.nedt.2022.105373 .
Raghunathan K, McKenna L, Peddle M. Factors in integrating academic electronic medical records in nursing curricula: a qualitative multiple case studies approach. Nurse Educ Today. 2023;120:105626. https://doi.org/10.1016/j.nedt.2022.105626 .
Haleem A, Javaid M, Pratap Singh R, Suman R. Medical 4.0 technologies for healthcare: features, capabilities, and applications. Internet Things Cyber-Physical Syst. 2022;2:12–30. https://doi.org/10.1016/j.iotcps.2022.04.001 .
Kang KA, Kim SJ, Lee MN, Kim M, Kim S. Comparison of Learning effects of virtual reality Simulation on nursing students caring for children with asthma. Int J Environ Res Public Health. 2020;17(22):8417. https://doi.org/10.3390/ijerph17228417 .
Mendel TR. The use of neonatal palliative care: reducing moral distress in NICU nurses. J Neonatal Nurs. 2014;20(6):290–3. https://doi.org/10.1016/j.jnn.2014.03.004 .
Jannah N, Fitrisia D, Fitriani SS, Safira RY. Nursing students’ attitude towards problem-based learning in the classroom. Enfermería Clínica. 2022;32:S24–9. https://doi.org/10.1016/j.enfcli.2022.03.012 .
Forouzan jahromi F, Mahdood B. Evaluation of nursing students’ satisfaction with two methods of problem-solving-based learning and outcome-based learning in the Cardiac Care Unit. Paramedical Sci Military Health. 2022;17(3):51–7.
Tadesse SG, Tadesse DG, Dagnaw EH. Problem based learning approach increases the academic satisfaction of health science students in Ethiopian universities: a comparative cross sectional study. BMC Med Educ. 2022;22(1):334. https://doi.org/10.1186/s12909-022-03397-5 .
González Hernando C, Carbonero Martín MÁ, Lara Ortega F, Martín Villamor P. Nursing students’ satisfaction in problem-based learning. Enfermería Global. 2014;13(3):97–103.
Son HK. Effects of simulation with problem-based learning (S-PBL) on nursing students’ clinical reasoning ability: based on Tanner’s clinical judgment model. BMC Med Educ. 2023;23(1):601. https://doi.org/10.1186/s12909-023-04567-9 .
Berger C, Brinkrolf P, Ertmer C, Becker J, Friederichs H, Wenk M, Van Aken H, Hahnenkamp K. Combination of problem-based learning with high-fidelity simulation in CPR training improves short and long-term CPR skills: a randomised single blinded trial. BMC Med Educ. 2019;19(1):180. https://doi.org/10.1186/s12909-019-1626-7 .
Xing C, Zhou Y, Li M, Wu Q, Zhou Q, Wang Q, Liu X. The effects of CPBL + SBAR teaching mode among the nursing students. Nurse Educ Today. 2021;100:104828. https://doi.org/10.1016/j.nedt.2021.104828 .
Sangestani G, Khatiban M. Comparison of problem-based learning and lecture-based learning in midwifery. Nurse Educ Today. 2013;33(8):791–5. https://doi.org/10.1016/j.nedt.2012.03.010 .
Sharma S, Saragih ID, Tarihoran DETAU, Chou F-H. Outcomes of problem-based learning in nurse education: a systematic review and meta-analysis. Nurse Educ Today. 2023;120:105631. https://doi.org/10.1016/j.nedt.2022.105631 .
Download references
Acknowledgements
This article is the result of a research project approved by Hamadan University of Medical Sciences (project number: 14010123244, ethics code: IR.UMSHA.REC.1400.884) as a financial provider. This study was conducted with the participation of nursing students, and the researchers wish to express their sincere gratitude to them.
This work was supported by Hamadan University of Medical Sciences (grant number: 14010123244).
Author information
Authors and affiliations.
School of Nursing and Midwifery, Hamadan University of Medical Sciences, Hamadan, Iran
Seyedeh Nayereh Falahan
Student Research Committee, Hamadan University of Medical Sciences, Hamadan, Iran
Edris Habibi
Department of Biostatistics and Epidemiology, School of Health, Abadan University of Medical Sciences, Abadan, Iran
Naser Kamyari
Student Research Committee, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Vahid Yousofvand
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the study’s conception and design. Study conception and design: S N. F, V. Y, N. K Data collection: S N. F, V. Y, E.H Data analysis and interpretation: N.K Drafting of the article: S N. F, V. Y, E.H Critical revision of the article: S N. F, V. Y, N. K.
Corresponding author
Correspondence to Vahid Yousofvand .
Ethics declarations
Ethics approval and consent to participate.
The present study was approved by the Ethics Committee of Hamadan University of Medical Sciences (ethical code: IR.UMSHA.REC.1400.884). Before conducting the research, the researchers explained the study objectives to the participants. Then, in order to participate in the study and publish the results, the researchers obtained written informed consent from the students. Additionally, the researchers explained to the participants that all information was confidential and they could withdraw from the study anytime.
Consent for publication
Not applicable.
Conflict of interest
All the authors of this paper agree on the absence of any conflict of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Falahan, S.N., Habibi, E., Kamyari, N. et al. Impact of virtual problem-based learning of cardiopulmonary resuscitation on fourth-year nursing students’ satisfaction and performance: a quasi-experimental study. BMC Med Educ 24 , 425 (2024). https://doi.org/10.1186/s12909-024-05375-5
Download citation
Received : 11 November 2023
Accepted : 30 March 2024
Published : 19 April 2024
DOI : https://doi.org/10.1186/s12909-024-05375-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Problem-based learning
- Cardiopulmonary resuscitation
- Nursing students
- Performance
- Satisfaction
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
AI Prompt Engineering Isn’t the Future
- Oguz A. Acar

Asking the perfect question is less important than really understanding the problem you’re trying to solve.
Despite the buzz surrounding it, the prominence of prompt engineering may be fleeting. A more enduring and adaptable skill will keep enabling us to harness the potential of generative AI? It is called problem formulation — the ability to identify, analyze, and delineate problems.
Prompt engineering has taken the generative AI world by storm. The job, which entails optimizing textual input to effectively communicate with large language models, has been hailed by World Economic Forum as the number one “job of the future” while Open AI CEO Sam Altman characterized it as an “amazingly high-leveraged skill.” Social media brims with a new wave of influencers showcasing “magic prompts” and pledging amazing outcomes.
- Oguz A. Acar is a Chair in Marketing at King’s Business School, King’s College London.
Partner Center

IMAGES
VIDEO
COMMENTS
Typical decision theory approaches to the identification of problem solving in nursing have viewed the process as a series of decision formulations that include: ... Status quo of postgraduate education model of master of nursing specialist. Chinese Nursing Research, 32 (21), 3370-3372. 10.12102/j.1009-6493.2018.21.016 ...
The structural model for relationships among clinical nurses' communication skills, problem-solving ability, understanding of patients' condition, and nurse's perception of professionalism that would be suitable for predicting the influencing relationships was verified. ... Kim M. Influence of nursing informatics competencies and problem ...
Here are some essentials for building a culture of innovation that encourages problem solving: Present problems as opportunities instead of obstacles. Strive to be a positive role model. Support creative thinking and staff collaboration. Encourage feedback and embrace new ideas. Respect staff knowledge and abilities.
In this model, clinical judgment is viewed as a problem-solving activity, beginning with assessment and nursing diagnosis, pro-ceeding with planning and implementing nursing inter-ventions directed toward the resolution of the diagnosed problems, and culminating in the evaluation of the effec-tiveness of the interventions. While this model may be
The nursing process, which is heavily used and frequently described as a problem-solving approach to nursing care, requires a deductive reasoning process which is not the problem-solving process in use during care-giving activities. ... None of the research approaches used to date has resulted in the identification of a general model of problem ...
Nurse leaders perceive their role as a problem-solver, which is a necessary step in advocacy. 27 Problem-solving is a process that contains the elements of decision-making and critical thinking. 28. The theory that emerged from the core categories explicitly focused on the central phenomenon of LHV in the nursing work environment.
The primary steps of the problem-solving and decision-making processes, as well as analytical tools used for these processes, are explored. ... FiGURE 6-1 Problem-solving and decision-making model. ... Thinking like a nurse: A research-based model of clinical judgment in nursing. Journal of Nursing Education, 45(6), 204-211.
The study reviewed 20 currently-available structured ethical decision-making models and developed an integrated model consisting of six steps with useful questions and tools that help better performance each step: (1) the identification of an ethical problem; (2) the collection of additional information to identify the problem and develop solutions; (3) the development of alternatives for ...
Critical thinking is applied by nurses in the process of solving problems of patients and decision-making process with creativity to enhance the effect. It is an essential process for a safe, efficient and skillful nursing intervention. Critical thinking according to Scriven and Paul is the mental active process and subtle perception, analysis ...
This paper analyses the role of problem solving in nursing practice including the process, acquisition and measurement of problem-solving skills It is argued that while problem-solving ability is acknowledged as critical if today's nurse practitioner is to maintain effective clinical practice, to date it retains a marginal place in nurse education curricula Further, it has attracted limited ...
This chapter explores the problem-solving approach to care, and shows how it relates to nursing students everyday work as a nurse. It also explores the ideas of the problem-solving process (APIE) as described by Yura and Walsh, and expands them to include two extra stages. ASPIRE also offers an explanation of what experienced practitioners do ...
• Discuss 7 steps to problem-solving. Introduction As medicine becomes more and more complex and nursing responsibilities increase, critical thinking—the ability to question and make rational decisions—becomes even more important. Too often, healthcare providers simply follow routines and accept the word of
Three studies were pooled to generate data for problem-solving of nursing students; one study used the Problem-Solving Scale for College Students (Choi et al., ... Use of a problem-based learning teaching model for undergraduate medical and nursing education: a systematic review and meta-analysis. Adv. Med. Educ. Pract., 8 (2017), p. 691.
Step 2: Analyze the Problem. Break down the problem to get an understanding of the problem. Determine how the problem developed. Determine the impact of the problem. Step 3: Develop Solutions. Brainstorm and list all possible solutions that focus on resolving the identified problem. Do not eliminate any possible solutions at this stage.
Background The complex health system and challenging patient care environment require experienced nurses, especially those with high cognitive skills such as problem-solving, decision- making and critical thinking. Therefore, this study investigated the impact of social problem-solving training on nursing students' critical thinking and decision-making. Methods This study was quasi ...
The knowledge-driven model emphasizes the organization and availability of relevant content knowledge stored in memory as the prime determinant of clinical problem solving. This contention is discussed in relation to the development of a clinical problem-solving task for nursing students and its implications for nursing curricula.
It is defined as "The nursing professional development (NPD) practitioner integrates scholarship, evidence, and research findings into practice" (p. 104). ... The JHNEBP Model is a problem-solving approach to clinical decision-making with user-friendly tools to guide individual or group use. It is explicitly designed to meet the needs of ...
The model has interrelated concepts of health and nursing problems and problem-solving, which is inherently logical in nature. Furthermore, the 21 nursing problems progressed to a second-generation development referred to as patient problems and patient outcomes.
Abstract. This paper analyses the role of problem solving in nursing practice including the process, acquisition and measurement of problem-solving skills. It is argued that while problem-solving ability is acknowledged as critical if today's nurse practitioner is to maintain effective clinical practice, to date it retains a marginal place in ...
The subjects' mean problem-solving ability score was 3.63 out of 5. Factors affecting problem-solving ability were age, communication competence, and metacognition, among which metacognition had the greatest influence. These variables explained 51.2% of the problem-solving ability of nursing students. Thus, it is necessary to provide guidance ...
Nursing is a profession that requires critical thinking, problem-solving, and decision making skills to provide quality care to patients. In this article, we will discuss the different decision making models in nursing, their advantages, disadvantages, and when to use them. By the end of this article, you will have a better understanding of ...
Nursing Process Model. The nursing process is a structured problem-solving approach that nurses may apply in ethical decision-making to guide data collection and analysis. See Table 6.3b for suggestions on how to use the nursing process model during an ethical dilemma. [8] Table 6.3b Using the Nursing Process in Ethical Situations [9]
The study reviewed 20 currently-available structured ethical decision-making models and developed an integrated model consisting of six steps with useful questions and tools that help better performance each step: (1) the identification of an ethical problem; (2) the collection of additional information to identify the problem and develop solutions; (3) the development of alternatives for ...
Background Regarding competency of nursing students in cardiopulmonary resuscitation (CPR), nursing students frequently exhibit inadequate performance and low satisfaction levels regarding CPR training methods. The problem-based learning (PBL) method, characterized by a constructivist approach, has been underutilized for CPR training, particularly in a virtual format. Hence, this study aims to ...
It is called problem formulation — the ability to identify, analyze, and delineate problems. Prompt engineering has taken the generative AI world by storm. The job, which entails optimizing ...
To address the issue of centrifugal force affecting the vertical load during the stability and trajectory planning of autonomous vehicles during high-speed cornering and obstacle avoidance, a model predictive control of trajectory planning and tracking is proposed that considers the roll factor using only a two-degrees-of-freedom vehicle dynamics model. Firstly, a trajectory planning ...