Advertisement

Socio-ecological determinants of distress in Filipino adults during COVID-19 crisis
- Published: 03 January 2021
- Volume 41 , pages 7482–7492, ( 2022 )
Cite this article

- John Jamir Benzon R. Aruta 1
9376 Accesses
23 Citations
Explore all metrics
The present study examined the socio-ecological factors that influenced psychological distress (combined index of depression and anxiety symptoms) among Filipino adults during the COVID-19 crisis. The study involved 401 adult participants currently residing in the Philippines. Data were collected using a self-reported online questionnaire administered to the participants. Findings revealed that one individual level factor, such as individual resilience, and two family level factors, such as safety at home and being a parent, negatively influenced psychological distress. On the other hand, a family level factor, family’s financial difficulties, positively predicted psychological distress. Societal level factor such as national resilience, but not the community level factor, community resilience, positively predicted psychological distress in Filipino adults. Findings identified individual resilience, national resilience, and financial difficulties as the strongest predictors of psychological distress among Filipino adults during the COVID-19 crisis. Implications, limitations, and future directions are discussed.
Similar content being viewed by others

Prediction of individual, community and societal resilience in the Czech Republic compared to Slovakia during the war in Ukraine

Social Support and Religiosity as Contributing Factors to Resilience and Mental Wellbeing in Latino Immigrants: A Community-Based Participatory Research Study
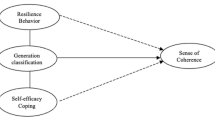
Intergenerational differences on resilience, sense of coherence, and self-efficacy coping of family during covid19 crisis: a salutogenic perspective
Avoid common mistakes on your manuscript.
Introduction
Covid-19 worldwide.
In December 31, 2019, China announced the discovery of the novel coronavirus (COVID-19) in Wuhan. From that point, COVID-19 has quickly spread across the world. By March 11, 2020, the World Health Organization declared COVID-19 as a pandemic (World Health Organization [WHO], 2020 ). Consequently, its highly contagious nature has affected millions of lives worldwide (WHO, 2020 ) leading to world leaders putting their respective countries on lockdown with varying degrees of tightness (WHO, 2020 ). As of the second week of October in 2020, there are >36 million confirmed cases and >1 million deaths worldwide (WHO, 2020 ). Corollary to the massive loss of life, the COVID-19 crisis was estimated to precipitate a global economic recession (International Monetary Fund, 2020 ). Furthermore, the COVID-19 crisis has also led to a spike in the number of individuals experiencing mental health concerns (United Nations [UN], 2020 ). The present study aims to advance the literature on mental health by examining the socio-ecological predictors of psychological distress during the COVID-19 crisis in the Philippines.
The Philippine Context
Historically, the Philippines has been constantly facing natural disasters, including typhoons and volcanic eruptions, among others. For example, the country faces more than 20 cyclones every year. In 2018, 21 strong tropical cyclones hit the country which affected thousands of families, killed hundreds of people, damaged thousands of properties, and ruined livelihoods (PAGASA, 2018 ). Moreover, the eruption of Taal Volcano in January 2020 which is located in the southern part of the Luzon island, has affected the livelihood of thousands of Filipino families (Liu et al., 2020 ). United Nations University Institute for Environment and Human Security’s (UNU-EHS) World Risk Report has consistently listed the Philippines as highly prone in terms of high disaster risk (UNU-EHS, 2011 ). However, the disasters and adversities that the country has faced in the past only required regional governmental response. It is undeniable that the COVID-19 crisis is the widest adversity that the country has ever faced, which required an unprecedented national level public response.
In the third week of March 2020, the Philippine government implemented varying types of community quarantine (lockdown) in which regulation strictness was based on the extent of infection spread in an area (“ECQ and GCQ”, 2020 ). Community quarantine required stopping the operations of non-essential services such as businesses, public transportations, and other operations. Work-from-home and skeletal workforce policies were implemented in public and private sectors, including schools and businesses, to minimize physical contact across the country (“ECQ and GCQ”, 2020 ). The community quarantine in the country, especially in its capital Manila, was implemented for several months and was considered the longest lockdown in the world to date (Yee, 2020 ). As of the second week of October, the Philippines has >329,000 COVID-19 cases, with approximately 6000 deaths, ranking as one of the countries most affected by the COVID-19 crisis worldwide (WHO, 2020 ). Economically, COVID-19 crisis in the Philippines has resulted in an nationwide unemployment rate of about 18% (7.3 million job losses) in April 2020 (Philippine Statistics Authority [PSA], 2020 ). In July 2020, a mobile phone-based survey showed that unemployment has skyrocketed to 46% (Social Weather Stations [SWS], 2020 ). Given the scale of adversities that the Philippines is facing, the present study aims to examine Filipino adults’ psychological distress and its socio-ecological determinants during the COVID-19 crisis.
COVID-19 Crisis and Mental Health
Although the vast majority of the population is not expected to suffer directly from the physical symptoms caused by the COVID-19 disease, nobody has immunity from the psychological consequences brought about by the COVID-19 crisis. It was projected that the COVID-19 crisis could lead to a surge in mental health concerns worldwide (UN, 2020 ). Recent studies showed that the COVID-19 pandemic had caused alarming mental health consequences, including stress, anxiety, and depression, among others, across the world (Lieberoth, Lin, Stockli, Han, et al., 2020 ; Salari, Hosseinian-Far, Jalali, Vaisi-Raygani, et al., 2020 ). In the Philippines, the increasing number of COVID-19 infections required long months of community quarantine (Yee, 2020 ), resulting in prolonged isolation and increase in mental health problems including depression, anxiety, and trauma, among others among Filipinos (Talidong & Toquero, 2020 ; Tee, Tee, Anlacan, et al., 2020 ). Furthermore, living in a developing country can make Filipinos especially vulnerable to the consequences brought about by the COVID-19 crisis. Therefore, it is imperative to investigate the factors within a person’s socio-ecological environment which serve as protective factors against and vulnerability for psychological distress among Filipinos within the context of the COVID-19 pandemic.
Socio-Ecological Determinants of Distress
While previous research focused on individual level factors that influence mental health, there is a dearth of research that takes into account the indirect role of socio-ecological factors on psychological distress. In the present study, individual level factors including age, religiosity, and individual resilience were identified as predictors of psychological distress during the COVID-19 crisis. There is mixed evidence on the relationship between age and psychological distress in times of adversities. For instance, previous findings demonstrated that age has no association with distress among Israeli adults during the aftermath of the second Lebanon war (Kimhi, Eshel, Zysberg, & Hantman, 2010 ). On the other hand, recent evidence showed that during times of war and other adversities, older adults in Israel experience less psychological distress, compared to younger adults, due to more refined emotion regulation skills that developed over time (Eshel, Kimhi, Lahad, & Leykin, 2016 ). Age differences in psychological distress may vary based on the nature of the disaster. In terms of the COVID-19 pandemic, older individuals are highly at risk to the health threat of coronavirus (Garnier-Crussard, Forestier, Gilbert, and Krolak-Salmon 2020 ). Religiosity was found to buffer the impact of stressful life events on psychological distress among African American adults (Lesniak, Rudman, Rector, & Elkin, 2006 ). Individual resilience , or a person’s capacity to recover from life’s adversities (Connor & Davidson, 2003 ) was found to protect individuals with experience of trauma and abuse against depression (Wingo et al., 2010 ) and adult Israeli Arabs and Jews from psychological distress during the COVID-19 pandemic (Kimhi, Eshel, Marciano, & Adini, 2020a ).
In terms of family level factors, safety at home, parenthood, and financial difficulties in the family were selected as predictors of psychological distress during the COVID-19 pandemic. Evidence suggests that sense of safety at home in times of stressful life events reduced COVID-19 distress among adult Israeli Jews (Kimhi, Marciano, Eshel, & Adini, 2020b ). Moreover, parenthood or having children was found to boost adults’ well-being, meaning in life, life satisfaction, positive emotions (Nelson, Kushlev, & Lyubomirsky, 2014 ), and decrease distress during challenging life events (Kimhi, Marciano, et al., 2020b ). On the other hand, financial difficulties in the family were found to be a strong predisposing factor for mental health problems, including depression and anxiety (DeForge, Belcher, Orourke, & Lindsey, 2008 ; Robbins, Dollard, Armstrong, Kutash, & Vergon, 2008 ). Historically, financial difficulties in the Philippines caused Filipinos to live through substandard living conditions causing mental health concerns (Tuason, 2010 ). In the time of COVID-19 crisis, millions of Filipino families have lost sources of income (PSA, 2020 ; SWS, 2020 ).
In terms of community level factor, accumulating evidence points out that community resilience , or people’s perception of the community’s capacity to withstand disasters (Leykin, Lahad, Cohen, Goldberg, & Aharonson-Daniel, 2013 ), can be a protective resource against mental health concerns (Kimhi, Eshel, Leykin, & Lahad, 2017 ; Kimhi & Shamai, 2004 ). For instance, community resilience was found to reduce psychological distress among Israeli adults living in the Israel-Lebanon border who have greater exposure to threats of war (Kimhi & Shamai, 2004 ) and among Israeli adults who experienced terror attacks (Kimhi et al., 2017 ). In addition, national resilience , or a person’s perception of the capacity of one’s nation to recover from adversities while keeping its social fabric intact (Kimhi, Eshel, Lahad, & Leykin, 2019 ), was found to be an important protective factor against distress symptoms in times of great adversities such as wars and terror attacks (Kimhi et al., 2017 ).
In summary, the above-mentioned socio-ecological factors were selected as predictors of psychological distress due to their important role in determining psychological distress in times of adversities as proven by empirical evidence. The present study aims to advance this line of research by examining how these factors influence psychological distress within a socio-ecological framework among Filipino adults during the COVID-19 crisis.
Theoretical Perspective
Ecological Systems Theory (Bronfenbrenner, 1979 ) proposed that there are several environmental systems that influence people’s mental health: microsystem, mesosystem, exosystem, macrosystem, and chronosystem. Microsystem (individual and family level factors) includes factors within a person’s immediate environment, such as personal and family characteristics. Similar to microsystem, mesosystem (community level factors) includes factors within one’s proximal environment, including school, neighborhood, and peers. Exosystem (societal level factors) includes economic, political, and government factors that indirectly influence a person’s way of living. Macrosystem involves distant collections of society’s overarching cultural beliefs and values that indirectly influence one’s development. Lastly, chronosystem (dimension of time) consists of environmental events including transitions throughout a person’s life.
Guided by Ecological Systems Theory, the present study investigated the factors within a person’s socio-ecological environment that directly and indirectly influenced psychological distress (combined index of depression and anxiety) in the context of COVID-19 crisis in the Philippines. The current research examined the individual, family (microsystem), community (mesosystem), and societal (exosystem) determinants of psychological distress in Filipino adults. Given that the fight against the COVID-19 crisis requires a multilevel response, it is imperative to determine the factors at the different levels of a person’s socio-ecological environment that contribute to mental health problems. This is necessary in order to inform more holistic mental health policies and interventions in times of adversities.
Research Objectives and Hypotheses
To date, no research has been conducted on the socio-ecological determinants of psychological distress during the COVID-19 pandemic in the Philippines. In light of the foregoing literature, the present study proposed the following hypotheses:
In terms of individual level factors, Filipinos who are older, less religious, and have lower individual resilience will report greater levels of psychological distress.
In terms of family level factors, Filipinos who have greater financial difficulties in the family, and a lower sense of safety at home will report psychological greater distress. In addition, Filipino adults with no children will report higher levels of psychological distress compared to those who have children.
In terms of community level factor, individuals with perception of higher community resilience will experience lower psychological distress.
In terms of societal level factor, individuals with perception of greater national resilience will experience lower psychological distress.
Participants
The present study collected responses from 401 adults currently residing in the Philippines. There were 254 (63.34%) females, 146 (36.41%) males, and 1 did not report gender. The participants’ ages ranged from 18 to 68 years old ( M age = 30.09, SD age = 11.15) with more than half of them in the age bracket 22–29 years (55.36%). In terms of civil status, most participants were single (72.57%). The majority of the participants earned bachelor’s degrees (66.83%) and more than a third of them reported receiving higher than average income (39.40%).
Instruments
Individual resilience.
The present study used the 10-item Connor-Davidson Resilience Scale (CD-RISC 10) to measure an individual’s capacity to bounce back from the COVID-19 crisis (Campbell-Sills & Stein, 2007 ; Connor & Davidson, 2003 ). Respondents rated each item (e.g., “ Tend to bounce back after an illness or hardship” ) on a 5-point scale (0 = Not true at all times to 4 = True nearly all of the time ), with a higher score indicating a greater level of individual resilience. CD-RISC 10 has demonstrated a stable single-factor structural validity based on adult samples in Spain (Blanco, Guisande, Sánchez, Otero, & Vázquez, 2019 ) and China (Wang, Shi, Zhang, & Zhang, 2010 ). Moreover, previous studies showed an excellent reliability α = .86 for CD-RISC 10 (Blanco et al., 2019 ). In the present study, the reliability index of CD-RISC 10 was α = .90.
Community Resilience
The 10-item Conjoint Community Resilience Assessment Measure (CCRAM-10) was utilized to assess participants’ perceptions on the ability of a community to deal with Coronavirus crisis (Leykin et al., 2013 ). Participants responded to each item (e.g., “ The municipal authority functions well in the current Coronavirus crisis. ”) on a 5-point scale (1 = Strongly disagree to 5 = Strongly agree ), with a higher score indicating a greater level of community resilience. Previous studies based on data from adult samples in Israel (Leykin et al., 2013 ) and China (Cui & Han, 2019 ) showed a stable five-factor model (i.e., leadership, collective efficacy, preparedness, place attachment, & social trust ) of the CCRAM-10. The reliability of CCRAM-10 was adequate for all factors and overall scores, ranging from α = .66 to α = .86 (Cui & Han, 2019 ). In the present study, the overall reliability of CCRAM-10 was α = .90.
National Resilience
National resilience, or one’s perception of a nation’s capacity to recover from adversities, specifically during the COVID-19 crisis, was measured using a 16-item scale, with 14 items (e.g., “I am optimistic about the future of my country” ) adapted from the original 25-item NRAS (Kimhi et al., 2019 ) and the remaining two items ( “I have full faith in the ability of my country’s health system to care for the population in the current Coronavirus crisis.” and “I have complete confidence in the ability of my government to take care of all aspects relevant to overcoming the current Coronavirus crisis.” ) were developed by Shaul Kimhi and colleagues to increase the content relevance of the scale during the COVID-19 crisis. Participants responded using a 5-point scale (1 = Strongly disagree to 5 = Strongly agree ) , with a higher score indicating a greater level of national resilience. Recent research using Filipino samples showed stable four factors of national resilience (Callueng, Aruta, Antazo, & Diato, 2020 ). Previous studies using Israeli adults demonstrated reliability coefficients of α = .88 (Kimhi, Eshel, et al., 2020a ) and α = .91 (Kimhi, Marciano, et al., 2020b ) for national resilience during the COVID-19 pandemic. In the current study, the overall reliability of national resilience was α = .95.
Psychological Distress
The present study measured the severity of participants’ distress during the COVID-19 crisis by using the 8-item instrument which was based on the anxiety (e.g., “ Lack of calm so that it is impossible to sit in one place ”) and depression (e.g., “ Hopelessness about the future ”) subscales of the Brief Symptoms Inventory (BSI; Derogatis & Savitz, 2000 ; Derogatis & Spencer, 1982 ). Respondents responded using a 5-point scale (1 = Not at all to 5 = To a very great extent ) with a higher score indicating more severe distress symptoms. Previous research utilized BSI as a valid and reliable tool in assessing distress symptoms in Filipino (Callueng et al., 2020 ) and Jewish Israeli (Kimhi et al., 2019 ) adults. In the current study, CFA solution of the BSI yielded an adequate data fit for a modified single-factor model: χ2 = 69.21, df = 18, p = .00, CFI = .96, TLI = .94, SRMR = .04, RMSEA = .08. All items showed strong factor loadings (λ), ranging from .51 to .81. The current research used the combined scores of depression and anxiety items as an index of distress with overall reliability of α = .90.
Safety at Home
Participants reported the extent to which they feel secured at home during the Coronavirus crisis by answering one item ( “How safe are you at your home during this period of the Coronavirus crisis?” ) using a 5-point scale (1 = Not at all to 5 = To a very great extent ). Recent studies have used this item in assessing people’s sense of safety at home in times of adversities including, during the COVID-19 crisis (Kimhi, Marciano, et al., 2020b ).
Financial Difficulties in the Family
To measure the extent of financial difficulties in one’s family brought about by the Coronavirus crisis, participants rated one item (“Do you or your family currently experience financial difficulties due to the Coronavirus crisis [such as unemployment, reduced business activity and so on]?” ) using a 5-point scale (1 = Not at all to 5 = To a very great extent ).
Demographic Variables
Parenthood was assessed by asking the participants the question, “Do you have children?” , where 68.8% reported having no children, 32% reported having at least one child, and 0.2% did not report. Religiosity was measured by asking the participants to describe their religious identity ( 1 = Secular, 2 = Traditional, 3 = Religious, 4 = Very religious). Participants then reported their age and gender.
The survey materials were translated from English to Filipino, which is the national language of the participants. After securing the informed consent from the participants, they were instructed to complete the online version of the survey. The respondents were invited to participate in the study using convenience and snowball sampling. That is, an online survey link was sent to the participants through social media, private messages, among others. Participants were then asked to forward the link to other adults that may qualify to participate in the study. The participants were recruited during the early phase (between the last week of April and the second week of May in 2020) of community quarantine (lockdown) in the Philippines.
Table 1 shows the descriptive statistics (mean and standard deviation) of the variables, including the estimate of normality (skewness and kurtosis <|2|), which indicates approximately normal distribution in all the variables. As shown in Table 2 , bivariate correlations indicated that all the predictor variables, except gender, were significantly correlated with psychological distress, and that the directionality of the correlations was in the expected directions. Sizes of the relationships of the predictor variables with psychological distress ranged from low (−.15 for religiosity) to moderate (−.40 for individual resilience). Gender was not included in the main analysis as it did not show a significant correlation with psychological distress in the preliminary examination.
Sequential regression analysis was conducted to determine the influence of socio-ecological factors at the individual, family, community, and societal levels on distress. In Step 1 of the regression equation, individual level factors such as age, religiosity, and individual resilience were entered. In Step 2, family level factors such as family’s financial difficulties due to Coronavirus crisis, parenthood (having a child/ren or not), and sense of safety at home were added. Step 3 added community resilience as a community level factor; and finally, national resilience was factored in as a societal level factor in Step 4. To determine potential multicollinearity, indices of variance inflation factor (VIF) and tolerance (TOL) from the regression analysis were utilized. As general guidelines, VIF above 10 or TOL below .10 may indicate the presence of multicollinearity of the variables (Oakland, Callueng, & Harris, 2012 ). There was no multicollinearity noted in the analysis, with VIFs ranging from 1.01 to 1.86 and TOLs ranging from .53 to .98.
As summarized in Table 3 , results of the regression analysis indicated that in Step 1, the three individual level factors collectively explained approximately 19.9% ( ΔR 2 = .199, ΔF (3, 390) = 32.23, p ≤ .001) of the variance in psychological distress. Participants who are younger (β = −.18, t = −3.86, p ≤ .001) and those with lower individual resilience (β = −.37, t = −7.94, p ≤ .001) tend to experience greater psychological distress. On the other hand, level of religiosity was not a significant predictor of psychological distress (β = −.08, t = −1.78, p =.059). In Step 2, the addition of family level factors accounted for approximately 5.9% increase in the variance of psychological distress ( ΔR 2 = .059, ΔF (6, 387) = 22.36, p ≤ .001). People with greater financial difficulties in the family (β = .18, t = 4.00, p ≤ .001), individuals without a child or children (β = −.13, t = −2.38, p ≤ .05), and those with lower levels of sense of safety at home (β = −.12, t = −2.63, p ≤ .01) tend to experience greater levels of psychological distress. In Step 3, the addition of a community level factor accounted for approximately .05% increase in the variance of psychological distress ( ΔR 2 = .005, ΔF (7, 386) = 19.59, p ≤ .001). However, community resilience was not a significant predictor of distress (β = −.08, t = −1.56, p = .12). In Step 4, the addition of a societal level factor accounted for approximately 1.5% increase in the variance of distress ( ΔR 2 = .015, ΔF (8, 385) = 18.48, p ≤ .001). Individuals with perceptions of higher national resilience tend to experience lower distress (β = −.17, t = −2.86, p ≤ .01). However, age did not significantly predict distress (β = −.07, t = −1.35, p = .18) when family, community, and societal level factors are added in the regression equation.
In total, the variance of distress explained by the combined levels of socio-ecological factors was approximately 27.7%, with individual resilience, family’s financial difficulties, and national resilience as the strongest predictors of psychological distress relative to other variables in the study.
Across the globe, the COVID-19 pandemic has posed serious threats not only to people’s health but also to their mental health. The United Nations estimated that the consequences brought about by the COVID-19 pandemic have overwhelmed the different levels of society in many countries, and that the deleterious impact of COVID-19 crisis may be more pronounced in developing nations like the Philippines (Bruckner & Mollerus, 2020 ). Due to nationwide community quarantine, the Philippine economy has shut down and millions of Filipinos have lost their jobs (PSA, 2020 ; SWS, 2020 ), causing serious problems (e.g., lack of resources for rent, bills, and food) down to family and individual levels. Using Ecological Systems Theory (Bronfenbrenner, 1979 ), the overarching goal of the current study was to examine the individual, family, community, and societal level determinants of psychological distress in Filipino adults during the COVID-19 crisis. Overall, findings revealed that factors within the individual, family, and societal layers of the socio-ecological environment predicted psychological distress in Filipino adults during the COVID-19 pandemic. Specifically, findings showed that individual resilience, national resilience, and financial difficulties were the strongest determinants of psychological distress.
Key Findings
Socio-ecological determinants of psychological distress, individual level.
The present study examined the individual level factors that influenced psychological distress during the COVID-19 crisis. Findings showed that individuals with higher levels of individual resilience reported lower psychological distress. This finding suggests that people who have a greater capacity to withstand life’s adversities tend to experience lower levels of depression and anxiety symptoms caused by the COVID-19 crisis. This finding echoes previous findings showing the protective role of individual resilience in preventing distress in times of adversities (Ben-Zur & Gilbar, 2011 ; Cenat, Charles, & Kebedom, 2020 ), including the challenges caused by the COVID-19 pandemic (Kimhi, Marciano, et al., 2020b ). Contrary to the posited hypothesis, it appears that regardless of age and religiosity, people may experience psychological distress during the COVID-19 crisis. An explanation is that the positive and negative aspects of being old may have counterbalanced its influence on distress. That is, older adults were expected to experience greater distress since they are considered highly vulnerable to COVID-19 illness due to lower immunity and a higher possibility of comorbid illnesses (Chen, Wu, Chen, Yan, et al., 2020 ). However, the influence of age on psychological distress may have been suppressed because older adults may have developed effective strategies in regulating negative emotions (Zimmermann & Iwanski, 2014 ) as a result of years of experience in facing life’s adversities (Eshel et al., 2016 ). In addition, religiosity did not predict distress during the COVID-19 crisis. One possible explanation is that the COVID-19 pandemic may have made people realize that everyone could be a potential victim of the contagious disease regardless of economic, racial, and religious background. Overall, partial support for hypothesis 1 was found by showing that an individual level factor, individual resilience, but not age and religiosity, was a significant determinant of lower psychological distress during the COVID-19 pandemic.
Family Level
Hypothesis 2 proposed that family level factors, including parenthood and sense of safety at home will negatively influence psychological distress. On the other hand, one’s family’s financial difficulties due to the COVID-19 crisis will positively predict psychological distress. Current findings found support for hypothesis 2 by demonstrating that participants with children tend to report lower levels of depression and anxiety symptoms compared to participants without children. Given that the relationships between childlessness, mental health, and well-being are complex and contextual (Umberson, Pudrovska, & Reczek, 2010 ), the present study contributes to the literature by demonstrating that in the context of COVID-19 crisis in the Philippines, Filipino adults who have children experienced lower levels of psychological distress despite the challenges during the pandemic. Past evidence posited that parents experience greater meaning in life, satisfaction, and greater positive emotions explaining why parents tend to report less psychological distress (Nelson et al., 2014 ) compared to non-parent participants. Culturally, Filipinos place a high premium on family-centered values (Morillo, Capuno, & Mendoza, 2013 ). Despite the weight and pressure of responsibilities that Filipino parents shoulder (Aassve, Goisis, & Sironi, 2012 ), it appears that their children serve as a protective factor from severe mental health problems by serving as parents’ main sources of joy, inspiration, and meaning (Aassve et al., 2012 ; Nelson, Kushlev, English, Dunn, & Lyubomirsky, 2013 ) in the midst of the pandemic.
Moreover, findings revealed that individuals who have a greater sense of safety at home reported lower levels of psychological distress during the COVID-19 crisis. This finding strengthens the recent evidence that demonstrated that safety at home suppresses distress symptoms in times of great adversities (Eshel & Kimhi, 2016 ) including the COVID-19 crisis (Kimhi, Marciano, et al., 2020b ). Given that one’s safety from COVID-19 depends on adherence to physical distancing measures, and that staying at home is considered as one of the protective measures against the coronavirus, it is understandable that one’s sense of safety at home significantly decreases psychological distress during the COVID-19 pandemic. Furthermore, staying at home during the lockdown may have provided opportunities to spend more quality time with one’s family as family support could protect people from experiencing severe depression and anxiety (Kimhi et al., 2010 ).
The present findings demonstrated that people who faced worse financial difficulties in the family brought about by the COVID-19 crisis experienced greater symptoms of sadness and excessive worrying. This finding is consistent with earlier studies which showed that economic difficulties have detrimental effects on mental health (DeForge et al., 2008 ; Robbins et al., 2008 ; Utsey & Constantine, 2008 ). Due to community quarantine imposed in the Philippines during the pandemic, millions of Filipinos lost their sources of income (PSA, 2020 ; SWS, 2020 ). The detrimental influence of financial difficulties on mental health appeared pronounced because the participants in the present study were adults who are likely shouldering family responsibilities. Moreover, the uncertainty of the length of the community may explain greater uncertainties about the family’s income leading to excessive worrying and emotional distress.
Overall, the findings confirmed hypothesis 2 that family level factors such as parenthood and safety at home could serve as a protective factor from severe psychological distress. In contrast, financial difficulties in the family can cause greater psychological distress in Filipino adults during the COVID-19 crisis.
Community Level
As a community level factor, community resilience was hypothesized to negatively influence psychological distress. The present study did not find support for hypothesis 3 as community resilience did not significantly predict psychological distress. A possible explanation is that although local communities play a crucial role in fighting the pandemic, much of the decision-making in facing the COVID-19 crisis in the Philippines comes from the national government. For example, the guidelines and regulations in the observance of social distancing, curfew implementation, and relief support, among others, are primarily decided by the national government (“ECQ and GCQ”, 2020 ). The whole nation constantly awaits nationwide announcements from the national government as every decision from that level would largely dictate how Filipinos would live their lives in the succeeding months. Additionally, it is possible that the participants view COVID-19 not only as a threat at the community level, but more so at the national and global levels.
Societal Level
Hypothesis 4 proposed that the societal level factor, national resilience, will negatively predict psychological distress. Confirming this prediction, the findings revealed that Filipinos who perceive greater levels of national resilience tend to experience lower depression and anxiety symptoms. That is, when individuals believe that the nation as a whole is capable of recovering from the COVID-19 crisis, they are less likely to experience severe sadness, hopelessness, and excessive worries. Viewed differently, people who believe that the nation is not capable of effectively responding to the adversities caused by the COVID-19 crisis are more likely to experience extreme levels of distress, sadness, and worries. This finding provided support for previous research showing that national resilience is associated with lower levels of distress symptoms in the time of large-scale adversities (Kimhi et al., 2017 ; Kimhi et al., 2019 ; Kimhi & Eshel, 2019 ), as the impact of crises as wide as the COVID-19 crisis in a country depends heavily on the actions taken at the national level.
Interestingly, the present findings revealed that individual resilience, national resilience, and financial difficulties were the strongest determinants of psychological distress among Filipino adults in the days of COVID-19 crisis. These findings suggest that as people face the challenges caused by the COVID-19 pandemic, the personal capacity to cope with life’s adversities, society’s ability to effectively respond to crises, and the trustworthiness of public institutions could decrease people’s vulnerability to depression and anxiety symptoms, confirming previous research (Ben-Zur & Gilbar, 2011 ; Cenat et al., 2020 ; Kimhi et al., 2019 ; Kimhi, Marciano, et al., 2020b ). It appears that resilience, not only at the individual level but also at the societal level, operates as safeguard against psychological distress in times of great adversities. On the other hand, individuals facing greater financial consequences of the COVID-19 crisis have a higher risk of developing depression and anxiety, confirming past evidence on the detrimental impact of financial instability on people’s mental health (DeForge et al., 2008 ; Robbins et al., 2008 ; Utsey & Constantine, 2008 ). As discussed in the earlier part of this section, the fact the participants in the current study were adults shouldering family responsibilities, and the exceptionally high unemployment caused by the COVID-19 crisis (PSA, 2020 ; SWS, 2020 ) explain why family’s financial losses have a strong detrimental impact on the mental health among Filipino adults during the COVID-19 pandemic.
Putting together, findings of the present study indicate that different factors within the socio-ecological environment influenced psychological distress in Filipino adults in the days of COVID-19 crisis. The current findings provided support for the proposition of Ecological Systems Theory (Bronfenbrenner, 1979 ) that factors within a person’s immediate environment (microsystem) are not the only elements that contribute to one’s mental health status. The theory argued that there are other layers within a person’s broader ecological environment including family, peers, school, community (mesosystem), economic, political, government system (exosystem), overarching beliefs and values (macrosystem), and dimension of time (chronosystem) that indirectly influence an individual’s mental health status during times of adversities. The findings of the present research indicate that while an individual level factor such as individual resilience, but not age and religiosity, contributes to lower psychological distress among Filipino adults during the COVID-19 crisis, family level factors such as family’s financial difficulties, parenthood, and safety at home also predicted depression and anxiety symptoms. Moreover, the societal level factor , national resilience, but not the community level factor, community resilience, predicted psychological distress. Ecological Systems Theory (Bronfenbrenner, 1979 ) provided a holistic lens in understanding the dynamic nature of people’s mental health by taking into account how individual, family, community, and societal factors simultaneously influence the development of better mental health in times of great adversities. The findings of the present study contributed to the literature by demonstrating that Ecological Systems Theory (Bronfenbrenner, 1979 ) can be applied in determining the different protective and suppressing factors of psychological distress within Filipino adults’ socio-ecological environment in the midst of the COVID-19 pandemic.
Implications
The present study provides an empirical and practical contribution to the sparse literature on mental health during the COVID-19 crisis in several ways. First, the present study found that lack of safety at home and financial difficulties due to income losses of at least one family member could lead to greater levels of depression and anxiety symptoms in Filipino adults. Hence, it is recommended that effective mechanisms that provide community safety and sustainable financial security to Filipino families during great crises such as the COVID-19 pandemic be considered. Findings of the current research indicate that safety at home and financial security may not only help solve basic material needs, but may also safeguard Filipinos from the inimical psychological consequences of financial problems. Second, despite the challenges that Filipinos faced during the COVID-19 pandemic, two different levels of resiliencies, such as individual and national resilience, emerged as important factors that play as a protective mechanism against severe mental health concerns. Therefore, programs geared toward improving individual resilience may be beneficial by equipping people coping skills in times of challenging life events. In addition, it is imperative that people visibly witness that the nation and its public institutions (i.e., police, health, education, media, and congress sectors) could effectively respond to the challenges caused by the COVID-19 crisis. The current findings indicate that when the nation, government, and public institutions are perceived as trustworthy and competent, it could partly contribute in reducing people’s vulnerability for severe mental health problems. Lastly, the current research indicates that being a parent can serve as a protective factor from psychological distress during difficult times as children may serve as sources of meaning and inspiration to overcome life’s adversities (Aassve et al., 2012 ; Nelson et al., 2013 ). In the context of counseling and psychotherapy, this may be an important finding as providing greater focus on the joy and meaning that children bring into one’s life could be beneficial when dealing with parent-clients who present severe depression and anxiety.
Limitations and Future Directions
The limitations of the present study provides opportunities for future research. First, limited factors at the different levels were utilized in the study. Future research may examine the impact of other important factors (e.g., emotion regulation, economic status, and trust in public institutions) across the various levels of the socio-ecological environment. This can give further insights on the factors that contribute to mental health in times of adversities. Second, the present study focused on Filipino adults and did not claim that the participants are representative samples. Future studies may focus on more representative samples across different developmental levels and Philippine regions. Third, the criterion variable used in the study was psychological distress representing the combined scores of depression and anxiety. It does not represent other possible negative emotional reactions from the COVID-19 crisis. Future studies may focus on other psychological reactions such as fear and trauma. Fourth, the present findings showed that community resilience did not predict distress, which was contrary to the posited hypothesis. The study recommends future research to identify the moderators between community resilience and psychological distress. The capacity of one’s local community to address crises may play an important role in protecting people from developing distress symptoms in times of adversities. Lastly, current findings indicate that individuals with children experienced lower distress in the days of COVID-19 crisis. However, the present study used a dichotomous measure (i.e., no child versus with child/ren) of parenthood and did not identify when the connection between number of children and distress plateaus. It is possible that having children may not always lead to lower distress because parents who have more children relative to their financial capacity may experience higher pressure in providing for the children’s needs, and hence, may experience greater levels of distress. The present study recommends that future researchers consider looking at the interaction between parents’ number of children and socioeconomic status on people’s psychological distress in times of adversities. Nonetheless, the present study provided novel insights on the importance of taking into account socio-ecological factors in preserving Filipino adults’ mental health in times of great adversities such as the COVID-19 pandemic.
Aassve, A., Goisis, A., & Sironi, M. (2012). Happiness and childbearing across Europe. Social Indicators Research, 108 , 65–86. https://doi.org/10.1007/s11205-011-9866-x .
Article Google Scholar
Ben-Zur, H., & Gilbar, O. (2011). Resilience and distress: Israelis respond to the disengagement from Gaza and the second Lebanese war. Community Mental Health Journal, 47 , 551–559. https://doi.org/10.1007/s10597-011-9371-3 .
Article PubMed Google Scholar
Blanco, V., Guisande, M. A., Sánchez, M. T., Otero, P., & Vázquez, F. L. (2019). Spanish validation of the 10-item Connor–Davidson resilience scale (CD-RISC 10) with non-professional caregivers. Aging & Mental Health, 23 (2), 183–188. https://doi.org/10.1080/13607863.2017.1399340 .
Bronfenbrenner, U. (1979). The ecology of human development: Experiments by nature and design . Cambridge: Harvard University Press.
Google Scholar
Bruckner, M. & Mollerus, R. (2020). UN/DESA Policy Brief #66: COVID-19 and the least developed countries . Retrieved from: https://www.un.org/development/desa/dpad/publication/un-desa-policy-brief-66-covid-1 -and-the-least-developed-countries/
Callueng, C., Aruta, J. J. B., Antazo, B., & Diato, A. (2020). Measurement and antecedents of national resilience in Filipino adults during coronavirus crisis. Journal of Community Psychology, 48 , 2608–2624. https://doi.org/10.1002/jcop.22438 .
Article PubMed PubMed Central Google Scholar
Campbell-Sills, L., & Stein, M. B. (2007). Psychometric analysis and refinement of the Connor–Davidson resilience scale (CD-RISC): Validation of a 10-item measure of resilience. Journal of Traumatic Stress, 20 (6), 1019–1028.
Cenat, J. M., Charles, C. H., & Kebedom, P. (2020). Multiple traumas, health problems and resilience among Haitian asylum seekers in Canada’s 2017 migration crisis: Psychopathology of crossing. Journal of Loss and Trauma, 25 (5), 416–437. https://doi.org/10.1080/15325024.2019.1703610 .
Chen, T., Wu, D., Chen, H., Yan, W., … & Ning, Q. (2020). Clinical characteristics of 113 deceased patients with coronavirus disease 2019: Retrospective study. BMJ 2020; 368:m1091.
Connor, K. M., & Davidson, J. R. T. (2003). Development of a new resilience scale: The Connor-Davidson resilience scale (CD-RISC). Depression and Anxiety, 18 , 71–82.
Cui, K., & Han, Z. (2019). Cross-cultural adaptation adaptation and validation of the 10-item conjoint community resiliency assessment measurement in a community-based sample in Southwest China. International Journal of Disaster Risk Science, 10 , 439–448. https://doi.org/10.1007/s13753-019-00240-2 .
DeForge, B. R., Belcher, J. R., Orourke, M., & Lindsey, M. A. (2008). Personal resources and homelessness in early life: Predictors of depression in consumers of homeless MultiService Centers. Journal of Loss and Trauma, 13 (2–3), 222–242. https://doi.org/10.1080/15325020701769105 .
Derogatis, L. R., & Savitz, K. L. (2000). The SCL–90–R and brief symptom inventory (BSI) in primary care. In M. E. Maruish (Ed.), Handbook of psychological assessment in primary care settings (p. 297–334). Lawrence Erlbaum Associates Publishers.
Derogatis, L. R., & Spencer, P. M. (1982). The brief symptom inventory (BSI): Administration, and procedures manual-I . Baltimore: Clinical Psychometric Research.
ECQ and GCQ Guidelines. (2020). Retrieved from https://www.covid19.gov.ph/ecq-gcq-guidelines/
Eshel, Y., & Kimhi, S. (2016). Postwar recovery to stress symptoms ratio as a measure of resilience, individual characteristics, sense of danger, and age. Journal of Loss and Trauma, 21 (2), 160–177. https://doi.org/10.1080/15325024.2014.965970 .
Eshel, Y., Kimhi, S., Lahad, M., & Leykin, D. (2016). Individual, community, and national resiliencies and age: Are older people less resilient than younger individuals? American Journal of Geriatric Psychiatry, 24 (8), 644–647. https://doi.org/10.1016/j.jagp.2016.03.002 .
Garnier-Crussard, A., Forestier, E., Gilbert, T., & Krolak-Salmon, P. (2020). Novel coronavirus (COVID-19) epidemic: What are the risks for older patients? Journal of the American Geriatric Society, 68 (5), 939–940. https://doi.org/10.1111/jgs.16407 .
International Monetary Fund. (2020). The great lockdown: Worst economic downturn since the great depression [Press release]. Retrieved from https://www.imf.org/en/News/Articles/2020/03/23/pr2098-imf-managing-director-stateetfollowing-a-g20-ministerial-call-on-the-coronavirus-emergency
Kimhi, S., & Eshel, Y. (2019). Measuring national resilience: A new short version of the scale (NR-13). Journal of Community Psychology, 47 , 517–528. https://doi.org/10.1002/jcop.22135 .
Kimhi, S., Eshel, Y., Lahad, M., & Leykin, D. (2019). National resilience: A new self-report assessment scale. Community Mental Health Journal, 55 , 721–731. https://doi.org/10.1007/s10597-018-0362-5 .
Kimhi, S., Eshel, Y., Leykin, D., & Lahad, M. (2017). Individual, community, and national resilience in peace time and in the face of terror: A longitudinal study. Journal of Loss and Trauma, 22 (8), 698–713. https://doi.org/10.1080/15325024.2017.1391943 .
Kimhi, S., Eshel, Y., Marciano, H., & Adini, B. (2020a). Distress and resilience in the days of COVID-19: Comparing two ethnicities. International Journal of Environmental Research and Public Health, 17 , 3956. https://doi.org/10.3390/ijerph17113956 .
Article PubMed Central Google Scholar
Kimhi, S., Eshel, Y., Zysberg, L., & Hantman, S. (2010). Postwar winners and losers in the long run: Determinants of war related stress symptoms and posttraumatic growth. Community Mental Health Journal, 46 , 10–19. https://doi.org/10.1007/s10597-009-9183-x .
Kimhi, S., Marciano, H., Eshel, Y., & Adini, B. (2020b). Recovery from the COVID-19 pandemic: Distress and resilience. International Journal of Disaster Risk Reduction, 50 , 101843. https://doi.org/10.1016/j.ijdrr.2020.101843 .
Kimhi, S., & Shamai, M. (2004). Community resilience and the impact of stress: Adult response to Israel’s withdrawal from Lebanon. Journal of Community Psychology, 32 , 439–451.
Lesniak, W., Rudman, W., Rector, M., & Elkin, D. (2006). Psychological distress, stressful life events, and religiosity in younger African American adults. Mental Health, Religion, & Culture, 9 (1), 15–28.
Leykin, D., Lahad, M., Cohen, O., Goldberg, A., & Aharonson-Daniel, L. (2013). Conjoint community resiliency assessment Measure-28/10 items (CCRAM28 and CCRAM10): A self-report tool for assessing community resilience. American Journal of Community Psychology, 52 , 313–323.
Lieberoth, A. Lin, S., Stockli, S., Han, H … et al. (2020). Stress and worry in the 2020 coronavirus pandemic: Relationships to trust and compliance with preventive measures across 45* countries. Royal Society Open Science. https://www.forskningsdatabasen.dk/en/catalog/2547433597
Liu, F., Xing, C., Li, J., Wang, B., Chai, J., et al. (2020). Could the recent Taal volcano eruption trigger an El Niño and lead to Eurasian warming? Advances in Atmospheric Sciences, 37 , 663–670. https://doi.org/10.1007/s00376-020-2041-z .
Morillo, H. M., Capuno, J. J., & Mendoza, A. M. (2013). Views and values on family among Filipinos: An empirical exploration. Asian Journal of Social Science, 41 (1), 5–28. https://doi.org/10.1163/15685314-12341278 .
Nelson, S. K., Kushlev, K., English, T., Dunn, E. W., & Lyubomirsky, S. (2013). In defense of parenthood: Children are associated with more joy than misery. Psychological Science, 12 (1), 3–10. https://doi.org/10.1177/0956797612447798 .
Nelson, S. K., Kushlev, K., & Lyubomirsky, S. (2014). The pains and pleasures of parenting: When, why, and how is parenthood associated with more or less well-being? Psychological Bulletin, 140 (3), 846–895. https://doi.org/10.1037/a0035444 .
Oakland, T., Callueng, C., & Harris, J. G. (2012). The impact of test-taking behaviors on WISC-IV Spanish domain scores in its standardization sample. Journal of Psychoeducational Assessment, 30 (2), 139–147. https://doi.org/10.1177/0734282911423358 .
Philippine Atmospheric, Geophysical and Astronomical Services Administration (PAGASA) (2018). Tropical cyclone summary. Retrieved from: http://bagong.pagasa.dost.gov.ph/tropical-cyclone/tropical-cyclone-summary
Philippine Statistics Authority (2020). Employment situation in April 2020 . Retrieved from: https://psa.gov.ph/content/employment-situation-april-2020
Robbins, V., Dollard, N., Armstrong, B. J., Kutash, K., & Vergon, K. S. (2008). Mental health needs of poor suburban and rural children and their families. Journal of Loss and Trauma, 13 (2–3), 94–122. https://doi.org/10.1080/15325020701769170 .
Salari, N., Hosseinian-Far, A., Jalali, R., Vaisi-Raygani, A., et al. (2020). Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Globalization and Health, 16 (57), 57. https://doi.org/10.1186/s12992-020-00589-w .
Social Weather Stations (2020). SWS July 3–6, 2020 National Mobile Phone Survey – Report No. 16: Adult joblessness rises to record-high 45.5%. Retrieved from: http://www.sws.org.ph/swsmain/generalArtclSrchPage/?page=1&srchprm=&arttyp=3&stdtrng=&endtrng=&swityp=8
Talidong, K. B., & Toquero, C. D. (2020). Philippine teachers’ practices to deal with anxiety amid COVID-19. Journal of Loss and Trauma, 25 , 573–579. https://doi.org/10.1080/15325024.2020.1759225 .
Tee, M., Tee, C., Anlacan, J., et al. (2020). Psychological impact of COVID-19 in the Philippines. Journal of Affective Disorders, 277 , 379–391. https://doi.org/10.1016/j.jad.2020.08.043 .
Tuason, M. T. (2010). The poor in the Philippines: Some insights from psychological research. Psychology and Developing Societies, 22 (2), 299–330. https://doi.org/10.1177/097133361002200204 .
Umberson, D., Pudrovska, T., & Reczek, C. (2010). Parenthood, childlessness, and well-being: A life course perspective. Journal of Marriage and Family, 72 (3), 612–629. https://doi.org/10.1111/j.1741-3737.2010.00721.x .
United Nations. (2020). Launch of the policy brief on COVID-19 and mental health. Retrieved from https://www.un.org/en/coronavirus/mental-health-services-are-essential-part-all-government-responses-covid-19
UNU-EHS (United Nations University – Institute for Environment and Human Security). World Risk Report. (2011). Germany: Bündnis Entwicklung Hilft. URL: http://www.ehs.unu.edu/file/get/9018 [consulted 19 July 2012].
Utsey, S. O., & Constantine, M. G. (2008). Mediating and moderating effects of racism-related stress on the relation between poverty-related risk factors and subjective well-being in a community sample of African Americans. Journal of Loss and Trauma, 13 (2–3), 186–204. https://doi.org/10.1080/15325020701769204 .
Wang, L., Shi, Z., Zhang, Y., & Zhang, Z. (2010). Psychometric properties of the 10-item Connor–Davidson resilience scale in Chinese earthquake victims. Psychiatry and Clinical Neurosciences, 64 , 499–504. https://doi.org/10.1111/j.1440-1819.2010.02130.x .
Wingo, A. P., Wrenn, G., Pelletier, T., Gutman, A. R., Bradley, B., & Ressler, K. J. (2010). Moderating effects of resilience on depression in individuals with a history of childhood abuse or trauma exposure. Journal of Affective Disorders, 126 (3), 411–414.
World Health Organization (WHO). (2020). Coronavirus disease 2019 (COVID-19): Situation report, 122. Retrieved from https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports
World Health Organization. (2020). Mental health and psychosocial considerations during the COVID-19 outbreak . https://www.who.int/docs/default-source/coronaviruse/mental-health-considerations.pdf
Yee, J. (2020). Longest lockdown, lost opportunities: PH COVID-19 cases go past 300,000. Inquirer . Net . Retrieved from https://newsinfo.inquirer.net/1340659/longest-lockdown-lost-opportunities-300k-cases
Zimmermann, P., & Iwanski, A. (2014). Emotion regulation from early adolescence to emerging adulthood and middle adulthood: Age differences, gender differences, and emotion-specific developmental variations. International Journal of Behavioral Development, 38 (2), 182–194. https://doi.org/10.1177/0165025413515405 .
Download references
Acknowledgments
The author would like to thank Judith Paceño for proofreading the manuscript.
Author information
Authors and affiliations.
De La Salle University, 2401 Taft Avenue, Malate, 1004, Manila, Philippines
John Jamir Benzon R. Aruta
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to John Jamir Benzon R. Aruta .
Ethics declarations
Conflict of interest.
The author/s claimed no conflict of interest in the present study.
Ethics Approval
The study was part of a cross-national study approved by the Institutional Review Board of Tel Aviv University, Israel.
Code Availability
Data, materials, and codes for analysis can be made available by the author/s upon written request by any party.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Aruta, J.J.B.R. Socio-ecological determinants of distress in Filipino adults during COVID-19 crisis. Curr Psychol 41 , 7482–7492 (2022). https://doi.org/10.1007/s12144-020-01322-x
Download citation
Accepted : 22 December 2020
Published : 03 January 2021
Issue Date : November 2022
DOI : https://doi.org/10.1007/s12144-020-01322-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Socio-ecological factors
- Psychological distress
- Find a journal
- Publish with us
- Track your research
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

DEPRESYON: ISA SA DAHILAN NG KAWALAN NG GANA SA PAG-AARAL

Related Papers
Ariel A. Diccion
Sa mga pag-aaral ukol sa Simbahang Aglipay o Iglesia Filipina Independiente, karaniwang tinatalakay ang rebolusyonaryo nitong pinagmulan at separatista nitong simulain. Salat ang mga pag-aaral ukol sa mga tiyak na Aglipayanong kongregasyon sa kapuluan, partikular sa patuloy nilang pag-iral sa kontemporanyong panahon sa kanilang mga tiyak na konteksto. Sa talakayang ito, sinuri ang pagdaraos ng prusisyon ng Salubong ng Aglipayanong kongregasyon sa Paliparan, Santo Nino, Lungsod ng Marikina bilang isang pagtatanghal ng dalawang naratibo. Ang una bilang paggunita ng muling pagkabuhay ni Hesukristo na siyang rurok ng pananampalatayang Kristiyano; at ikalawa bilang muling pag-uulit at pag-aangkin ng mga Aglipayanong mananampalataya ng kanilang mga gawi matapos lisanin ang dating lunan ng pagsamba. Sa pagsipat sa mga aspekto ng Bigkis ng Bisa at Aliw mula kay Richard Schechner, hinimay sa pag-aaral na ito ang mga ritwalistiko at teatrikal na katangian ng nasabing pagtatanghal bilang isang...
ANGELICA MALIGALIG
Ang Asignaturang Filipino ay kabilang sa K to 12 Curriculum na idinisenyo ng mga eskperto sa Kagawaran ng Edukasyon upang mapalawak ang kaalaman ng bawat Filipino patungkol sa sariling wika at ang mga kagamitan nito. Sa kasalukuyan, maraming mag-aaral ang nahihirapan sa Asignaturang Filipino at maging pagpapahayag ng kanilang mga ideya at saloobin sa paraang pasulat ay apektado. Kapansin-pansin na nawawalan sila ng kawilihan, kadalasang hindi pinakikinggan ang mga aralin at kinatatamaran ang pagsulat kung nakasusulat man ay kulang sa kasanayan. Kaya't ninais ng mananaliksik na gumamit ng ibang estratehiya na maaaring makatulong sa pagpapaunlad ng kasanayan sa pagsulat ng sanaysay ng mga magaaral, ang Cloze Passage bilang estratehiya sa pagtuturo ng Filipino. Ginamit sa pananaliksik ang eksperimentalna disenyo, Pauna at Panghuling Pagsulat ng Sanaysay (Pre-test& Post-test) upang matamo ang mga layunin ng pag-aaral: (1) Ano ang kasanayan sa pagsulat ng sanaysay ng mga mag-aaral ba...
The Normal Lights
Rodrigo Abenes
Layunin ng pananaliksik ang makabuo ng mga lunsarang aralin at gawaing angkla sa MELCs o Most Essential Learning Competencies sa primaryang antas. Pangunahing metodo ang disenyong palarawan at pagbuo ng mga lokalisado at kontekstuwalisadong may temang katutubo, kabuhayan, kalinangan, kapaligiran, at diskursong kasarian na angkop sa pagtuturo sa anyong modyular, harapan, o blended. Ginamit ang sarbey at panayam sa mga piling kalahok. Lumabas sa pag-aaral na epektibo ang mga aralin kapag nakadikit sa karanasan, kaligiran, at interes ng mga mag-aaral. Ang mga kontekstuwalisadong aralin na pinagtibay sa konteksto ng pandemya at bagong kadawyan o new normal ay mainam na gamiting sandigang kaalaman sa kasanayan at kahusayang komunikatibo sa Filipino at iba pang kaugnay na disiplina.
Kritike: An Online Journal of Philosophy
Danica Lorraine Garena
Ang pag-aaral na ito ay isinagawa upang mabatid ang pananaw ng mag-aaral sa paggamit ng mga sariling komposisyon ng panitikang pambata at antas ng pang-unawa. Sa pag-aaral na ito binibigyang katugunan ang mga sumusunod na katanungan: Ano ang pananaw ng mga tagasagot sa paggamit ng mga Sariling Komposisyon ngPanitikang Pambata bataysa nilalaman,layunin,disensyo/istilo, kasanayan/gawain; Ano ang antas ng pang-unawa ng mga tagasagot sa paggamit ng mga Sariling Komposisyon ng Panitikang Pambata batay sa Pang-unawang Literal at Pang-unawangKritikal; May makabuluhang kaugnayan ba ang pananaw ng mag-aaral sa paggamit ng mga Sariling Komposisyon ng Panitikang Pambata at Antas ng Pang- unawa sa Pagbasa; Ang pamamaraang palarawan-correlation ang ginamit ng mananaliksik upang makalap ang mahalaga at makatotohanang impormasyon na kinakailangan sa pag-aaral. Ang istatistikal na pamamaraan na ginamit sa pagsasaliksik ay weighted mean at standard deviation para sa pananawng mga tagasagot sa Mga Sa...
Jurnal Bisnis Strategi
Harry Susanto
International Journal of Research Studies in Education
JOHN EMIL ESTERA
Springer eBooks
Peta Colbert
African Arts
susan vogel
Likhaan: The Journal of Contemporary Philippine Literature
Napoleon Arcilla
Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
RELATED PAPERS
Veturliði Óskarsson
Media Akuakultur
Arief Taslihan
Dewan Bahasa dan Pustaka eBooks
Wan Ahmad Fauzi Wan Husain
Robert Paull
American Journal of Bioethics
Mansa Gurjar
Peeters Publishers
György Heidl
Tulane Studies in Philosophy
David Auerbach
The Australian journal of agricultural economics
Jock Anderson
Journal of Forensic Sciences
Dr. Ronald Wright
Cabdi axmed Cali
Verification
Steve Fetter
Nambiyath Balakrishnan
Aditya Pratama
Kennedy Institute of Ethics Journal
Nancy Sherman
Journal of Anatolia Nursing and Health Sciences
Fusun Terzioglu
Silvia Vautretto
Folia Linguist
Yves Duhoux
Oxford Art Journal
Abigail Solomon-Godeau
Debajit Sarma
Language Resources and Evaluation
Akinori Abe
Georgios T . Halkias
Modeling of Adhesively Bonded Joints
Marcelo Fsf De Moura
Teaching Mathematics and Computer Science
Bujdosó Gyöngyi
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Factors Associated with Depressive Symptoms among Filipino University Students
* E-mail: [email protected]
Affiliation Department of Behavioral Sciences, de la Salle University, Manila, The Philippines
- Madelene Sta. Maria,
Affiliation Office of Counselling and Career Services, de la Salle University, Manila, The Philippines
- Romeo B. Lee,
- Madelene Sta. Maria,
- Susana Estanislao,
- Cristina Rodriguez

- Published: November 6, 2013
- https://doi.org/10.1371/journal.pone.0079825
- Reader Comments
Depression can be prevented if its symptoms are addressed early and effectively. Prevention against depression among university students is rare in the Philippines, but is urgent because of the rising rates of suicide among the group. Evidence is needed to systematically identify and assist students with higher levels of depressive symptoms. We carried out a survey to determine the social and demographic factors associated with higher levels of depressive symptoms among 2,436 Filipino university students. The University Students Depression Inventory with measures on lethargy, cognition-emotion, and academic motivation, was used. Six of the 11 factors analyzed were found to be statistically significantly associated with more intense levels of depressive symptoms. These factors were: frequency of smoking, frequency of drinking, not living with biological parents, dissatisfaction with one’s financial condition, level of closeness with parents, and level of closeness with peers. Sex, age category, course category, year level and religion were not significantly related. In identifying students with greater risk for depression, characteristics related to lifestyle, financial condition, parents and peers are crucial. There is a need to carry out more surveys to develop the pool of local knowledge on student depression.
Citation: Lee RB, Maria MS, Estanislao S, Rodriguez C (2013) Factors Associated with Depressive Symptoms among Filipino University Students. PLoS ONE 8(11): e79825. https://doi.org/10.1371/journal.pone.0079825
Editor: Hamid Reza Baradaran, Iran University of Medical Sciences, Islamic Republic of Iran
Received: June 9, 2013; Accepted: October 4, 2013; Published: November 6, 2013
Copyright: © 2013 Lee et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Funding: The authors have no support or funding to report. The study was carried out as part of the community engagement activities of the authors.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Depression is a major source of the burden of disease throughout the world [ 1 ]. In much of the developing world, however, depression is largely unexplored as a research topic. A social mapping revealed that, even though the mental disorder has been recognized as a research priority, only a sparse number of relevant studies have been carried out in low- and middle-income countries [ 2 ]. Roughly 60% of these countries have contributed fewer than five articles to the international mental health indexed literature [ 2 ]. Strategic evidence is needed in order to prevent the occurrence of depression, including its pernicious effects and prohibitive treatment cost.
Prevention of depression, particularly among university students in developing countries, is urgent. With their large student populations and the developmental propensity of students for depression [ 3 ], the burden of the mental disorder is heavy on this demographic sector [ 4 – 6 ]. Preventive efforts in the developing world, however, are rare. Consistent with observations elsewhere [ 7 , 8 ], depression is widely perceived in this part of the world as innocuous and as part and parcel of normal adolescent development. Students with the mental disorder are not only suffering in silence, but are also placing their academic and future life goals in peril. Depression can be averted if students with depressive symptoms, comprising not only physical but also non-physical conditions (e.g., cognition-emotion and motivation) [ 9 ], are promptly and properly identified and helped.
Extant studies suggest that students with higher levels of symptoms tend to be women [ 10 , 11 ], older and in their senior year [ 5 ], and Catholics and/or Jews [ 12 , 13 ]. Moreover, research indicates that highly symptomatic students do not reside with their parents in one household [ 14 ], and are smoking [ 15 ] and drinking alcohol [ 16 ], and belong to the low-income bracket [ 6 ]. Furthermore, students with more severe levels of depressive symptoms have lower levels of closeness with their parents or with friends [ 7 ].
The context of the present study
The Philippines has a total population of 92.3 million that is very young (median age: 23) and growing at 1.9% annually. In 2009-2010, 2.8 million university students were enrolled in the country’s 2,247 higher education institutions. Of every 10 Filipino students, 6 and 4 are enrolled in private and public universities, respectively. Of these students, 26% are enrolled in business, 16% in medicine and allied programs, and 13% each are in engineering, information science and education [ 17 ]. In contrast to their counterparts throughout most of the world, Filipino students commence their university education at the age of 15 or 16 years.
Filipinos place a high premium on formal education; a university degree is strongly regarded as a primary requirement for social and economic mobility. In the context of the collective aspirations of Filipinos to go abroad for lucrative employments, the need for university education is even more compelling. Individual students are thus pressured to excel or complete a degree, lest they bring dishonor to their family and friends, and endanger their employment and life prospects. In this respect, academic-related matters are salient issues for individual students and in their relationships and conflicts with parents; these, too, can induce higher levels of depressive symptoms in students.
We carried out this research as part of our community engagement activities to help in the prevention of mental disorders, and subsequently, of suicide among Filipino university students. The connection between depression and suicide is well-established [ 18 ]. The spate of suicide events among local students had served as the impetus to conceive and implement this study. There is paucity of data on university student depressive symptomatology in the Philippines, and in the absence of published relevant articles in indexed journals, little is understood about depressive symptoms among Filipino university students at the international level. This survey examined the social and demographic factors associated with higher levels of depressive symptoms among Filipino university students. The University Student Depression Inventory (USDI), a newly-developed and psychometrically sound scale with measures on academic motivation in addition to lethargy and cognition-emotion, was used.
Participants
Data were derived from a complete enumeration survey undertaken in 2012 covering all 67 undergraduate classes in general social sciences (e.g., introductory sociology) at a large private university (total student population: >16,000) in Manila, the Philippines. Roughly half of the 67 classes were surveyed in the middle of Term 1 and the other half in the middle of Term 2. A total of 2,591 Filipino students anonymously completed the 10-page self-accomplished questionnaire. Only the questionnaires of 2,436 students were considered for the purpose of this report (126 questionnaires of international students were excluded and 29 questionnaires with at least 10 unanswered items were invalidated). Our sample represents about 15% of the university’s total undergraduate student population.
We utilized the USDI to measure depressive symptoms as a continuous variable. The USDI, developed by Khawaja & Kelly [ 9 ], measures the academic motivational aspect of depressive symptoms in addition to physical and cognitive-emotive dimensions. The USDI has 3 sub-scales having a total of 30 statements: lethargy (9 statements on lethargy, concentration difficulties and task performance); cognitive-emotional (14 statements on suicide ideation, worthlessness, emotional emptiness and sadness); and academic motivation (7 statements on class attendance and motivation to study) ( Table 1 ). Statements have score-bearing response options ranging from “none at all” (1) to “all the time” (5). The USDI has a high level of internal consistency (Cronbach α=0.95) [ 9 ].
| Parents |
|---|
| 1. I like spending time with my parents. |
| 2. My parent/s show/s how much she/she/they love me. |
| 3. I feel good being with my parents. |
| 4. My parent/s does/do not really care about me.* |
| 5. I disclose my private concerns to my parent/s. |
| 6. I am not happy when I spend time with my parent/s.* |
| 7. I think my parent/s is/are the best in the world. |
| 8. I wish my parent/s paid more attention to me.* |
| Peers |
| 1. I feel happy when I am with my friends. |
| 2. I would rather be alone than spend time with my friends.* |
| 3. My friends show me their support. |
| 4. My friends do not treat me well.* |
| 5. I wish I had more supportive friends.* |
| 6. I am satisfied with the friendships I develop in school. |
| 7. I like spending time with my friends. |
| 8. I do not enjoy spending time with my friends.* |
| 9. I am happiest when I am with my friends. |
| Depressive symptoms |
| A. Lethargy |
| 1. I am more tired than I used to be. |
| 2. I do not have the energy to study at my usual level. |
| 3. My energy is low. |
| 4. I find it hard to concentrate. |
| 5. I don't feel rested even after sleeping. |
| 6. I am overwhelmed by the challenges I encounter in my studies. |
| 7. My mood affects my ability to carry out assigned tasks. |
| 8. Daily tasks take me longer than they used to. |
| 9. My study is disrupted by distracting thoughts. |
| B. Cognitive/emotional |
| 10. I wonder whether life is worth living. |
| 11. I feel worthless. |
| 12. I have thought about killing myself. |
| 13. No one cares about me. |
| 14. I feel emotionally empty. |
| 15. I feel sad. |
| 16. I worry I will not amount to anything. |
| 17. The activities I used to enjoy no longer interest me. |
| 18. I feel like I cannot control my emotions. |
| 19. I spend more time alone than I used to. |
| 20. I feel disappointed in myself. |
| 21. I feel withdrawn when I'm around with others. |
| 22. I do not cope well. |
| 23. I think most people are better than me. |
| Academic motivation |
| 24. I do not have any desire to go to my classes. |
| 25. I do not attend classes as much as I used to. |
| 26. I don't feel motivated to study. |
| 27. Going to university is pointless. |
| 28. I have trouble starting assignments. |
| 29. I do not find study as interesting as I used to. |
| 30. I have trouble completing study tasks. |
| *Reverse coded |
Table 1. Statements used for measuring levels of closeness with parents and with peers, and depressive symptoms.
The socio-demographic characteristics include sex, age category, course category, year level, religion, frequency of smoking, frequency of drinking, living/not living with both biological parents, level of satisfaction with one’s financial condition, level of closeness with parents, and level of closeness with peers. The last 2 variables were measured using a series of 8 statements on parents and 9 statements on peers. The statements were drawn from published studies on parental and peer relationships among adolescents [ 7 , 19 ]. Each series had 4 score-bearing response options: definitely not true (1), mostly not true (2), mostly true (3), and definitely true (4) ( Table 1 ).
Ethical standards
The study was approved by the ethics review committee of the university. After evaluating the contents of the survey instrument, the Committee assessed that the study would have no known risk to research participants. Verbal consent was thus obtained; however, students were informed that they could decline participation and that they could stop completing the questionnaire if they wished to. The benefits of the study (i.e., findings would be used to draw attention towards mental health in Filipino students) were especially stressed in order to trigger a sense of social responsibility and citizenship, and therefore, research participation among students. These instructions were written on the cover page of the survey instrument that was administered. On the same cover page, we also included our full names and contact numbers in which we enjoined students to ask us questions about the study and related matters.
We did not seek the consent of the students’ parents anymore. The survey focused on real-life conditions (e.g., feeling bored and having low energy) which are normally shared between and among Filipino students. During our pre-test of the questionnaire, student-respondents perceived the topic of the study as personally acceptable, one they felt they would not be asking their parents for permission should they decide to discuss it. The foregoing ethical standards, especially with respect to studies with no known harmful risks and the waiving of a signed certification of consent, are in line with the practices of most Institutional Review Boards elsewhere.
We conducted the survey in classrooms during the first quarter of the 90-minute classes. Each class was informed about the importance and rationale, and the anonymity and confidentiality of the study. Afterwards, students were invited to participate and were each given a questionnaire to accomplish. Students were reminded not to write any mark in the instrument that would identify them. Whether completely accomplished or not, all questionnaires were collected. Students were thanked for their participation. No incentive of any form was given.
Using the Statistical Package for the Social Sciences Version 20, differences in the mean depressive symptoms scores were examined based on social and demographic characteristics. The characteristics that were statistically significantly related with higher levels of depressive symptoms were further examined at the sub-scale levels. The analysis of variance was used.
The independent variables, except for sex (male, female), were recoded into variables with 2-3 categories each ( Table 2 ). The levels of closeness with parents and with peers were constructed by adding the scores corresponding to responses given to the series of statements. For level of closeness with parents, the score range is 8 to 32 (low-moderate, 8-23; high, 24-32); and for level of closeness with peers, the range is 9 to 36 (low-moderate, 9-26; high, 27-36). Our analyses revealed a high level of internal consistency for both series (parents: α=0.77; peers α=0.79).
| Variables | Categories | N | % | Means | Standard deviation |
|---|---|---|---|---|---|
| Sex | Male | 1063 | 43.6 | 71.39 | 19.21 |
| Female | 1373 | 56.4 | 71.47 | 18.18 | |
| Age category | <17 | 1034 | 42.5 | 71.43 | 18.9 |
| 17 | 724 | 29.8 | 71.17 | 18.23 | |
| >17 | 674 | 27.7 | 71.75 | 18.71 | |
| Course category | Social sciences and humanities | 941 | 39.0 | 72.14 | 18.78 |
| Business, economics and management | 714 | 29.6 | 70.02 | 18.15 | |
| Double major and interdisciplinary | 198 | 8.2 | 70.54 | 19.73 | |
| Engineering, natural sciences and computer science | 561 | 23.2 | 72.47 | 18.57 | |
| Year level | 1 | 1731 | 71.1 | 71.16 | 18.69 |
| 2 -4 | 704 | 28.9 | 72.13 | 18.47 | |
| Religion | Catholic | 1968 | 80.9 | 71.55 | 18.38 |
| Non-Catholic/others | 466 | 19.1 | 71.04 | 19.69 | |
| Frequency of smoking (in days)** | 0 | 2108 | 86.5 | 70.84 | 18.50 |
| ≤10 | 182 | 7.5 | 76.82 | 18.64 | |
| >10 | 146 | 6.0 | 73.30 | 19.47 | |
| Frequency of drinking (in days)** | ≤10 | 885 | 36.5 | 73.29 | 19.03 |
| >10 | 1541 | 63.5 | 70.33 | 18.28 | |
| Living with both biological parents* | Yes | 1895 | 77.9 | 70.99 | 18.51 |
| No | 539 | 22.1 | 72.99 | 19.03 | |
| Level of satisfaction with one's financial condition** | Not satisfied | 140 | 5.8 | 81.97 | 20.84 |
| Somewhat satisfied | 583 | 24.0 | 77.19 | 18.84 | |
| Satisfied | 1252 | 51.6 | 69.19 | 17.43 | |
| Very satisfied | 452 | 18.6 | 66.78 | 17.86 | |
| Level of closeness with parents** | Low/moderate | 427 | 17.5 | 81.65 | 19.77 |
| High | 2006 | 82.5 | 69.2 | 17.65 | |
| Level of closeness with peers** | Low/moderate | 289 | 11.9 | 84.58 | 20.69 |
| High | 2138 | 88.1 | 69.66 | 17.61 |
Table 2. Means and standard deviations for depressive symptoms scale scores by social and demographic characteristics.
| Variables | Lethargy | Cognition/emotion | Academic motivation | |||
|---|---|---|---|---|---|---|
| Means | p-values | Means | p-values | Mean | p-values | |
| Frequency of smoking (in days) | =0.001** | =0.007** | =0.000** | |||
| 0 | 28.42 | 28.41 | 14.05 | |||
| ≤10 | 30.03 | 30.76 | 16.03 | |||
| >10 | 29.51 | 27.62 | 16.24 | |||
| F =6.56, SS=556.88, MS=278.44 | F =5.03, SS=1066.29, MS=533.14 | F =22.82, SS=1222.83, MS=611.41 | ||||
| Frequency of drinking (in days) | =0.001** | =0.033* | =0.000** | |||
| ≤10 | 29.17 | 29.11 | 15.11 | |||
| >10 | 28.29 | 28.18 | 13.87 | |||
| F =10.28, SS=435.77 | F =4.53, SS=479.96 | F =32.03, SS=861.29 | ||||
| Living with both biological parents | =0.098 NS | =0.042* | =0.104 NS | |||
| Yes | 28.49 | 28.30 | 14.24 | |||
| No | 29.02 | 29.32 | 14.65 | |||
| F =2.74, SS=116.89 | F =4.15, SS=441.32 | F =2.65, SS=72.24, MS=72.24 | ||||
| Level of satisfaction with one’s financial condition | =0.000** | =0.000** | =0.000** | |||
| Not satisfied | 31.37 | 33.69 | 16.91 | |||
| Somewhat satisfied | 29.91 | 31.83 | 15.46 | |||
| Satisfied | 28.09 | 27.40 | 13.76 | |||
| Very satisfied | 27.51 | 25.68 | 13.59 | |||
| F =23.56, SS=2934, MS=978.00 | F =51.08, SS=15351.53, MS=5117.18 | F =29.36, SS=2319.56, MS=773.18 | ||||
| Level of closeness with parents | =0.000** | =0.000** | =0.000** | |||
| Low/moderate | 30.74 | 34.35 | 16.56 | |||
| High | 28.16 | 27.29 | 13.86 | |||
| F =56.15, SS=2342.5 | F =176.73, SS=17563.84 | F =98.06, SS=2571.45 | ||||
| Level of closeness with peers | =0.000** | =0.000** | =0.000** | |||
| Low/moderate | 30.86 | 37.10 | 16.91 | |||
| High | 28.30 | 27.37 | 13.98 | |||
| F =39.59, SS=1658.98 | F =248.31, SS=24038.13 | F =82.43, SS=2178.29 | ||||
Table 3. Means, F-values and p-values for depressive symptoms sub-scale scores by selected social and demographic characteristics.
The dependent variable (levels of depressive symptoms) was constructed by adding the scores corresponding to the responses given to the series of statements. The scale score ranges from 30 to 150 while the sub-scale scores range from 9 to 45 for lethargy, 14 to 70 for cognition-emotion, and 7 to 35 for academic motivation; higher scores suggest higher levels of depressive symptoms Our analyses revealed a high level of internal consistency for the USDI (α=0.93).
Profile of respondents
The majority were female while 43.6% were male. 42.5% were 16 years of age or younger, 29.8% were 17 years old and a similar number were older. 39.0% were in social sciences/humanities; 29.6% were in business/economics/management and 23.2% were in engineering/natural/computer sciences. Seven of every 10 were first year students. Most were Catholic (80.9%) and reported not having smoked in the past 30 days prior to the survey. In the past 30 days, about 6 of every 10 students had taken alcohol for more than 10 days, while 4 for ≤10 days. Most respondents (77.9%) currently lived with both biological parents. About 70% were satisfied and very satisfied with their financial condition; the rest were not or were only somewhat satisfied. Most had high levels of closeness with parents (82.5%) and peers (88.1%).
Differences in mean scale scores based on social and demographic characteristics
The means and standard deviations for depressive symptoms scale scores are shown in Table 2 . Higher means suggest higher or more severe levels of depressive symptoms. Results indicate that male and female students did not differ in their symptoms levels. No significant differences were observed across age groups. The level of depressive symptoms statistically significantly varied according to course category but only marginally (F (3,2410) =2.54, p<.06). Means were not significantly dissimilar across year level and religion.
Means comparison related to frequency of smoking suggests significant differences among the categories (F (2,2411) =9.65, p<.01). Results of post-hoc Tukey test indicate that those who smoked for ≤10 days had a higher level of depressive symptoms than those who did not smoke in the past 30 days (p<.01). Significant means differences were observed based on frequency of drinking (F (1,2424) =14.31, p<.01). Students not living with both parents had a significantly higher level of symptoms compared to those living with parents (F (1,2432) =4.87, p<.05). Moreover, depressive symptoms level significantly varied according to satisfaction with one’s financial condition (F (3,2423) =52.03, p<.01). Based on post-hoc Tukey test findings, students who were not satisfied with their financial status had a more elevated level of depressive symptoms than those who were somewhat satisfied (p<.05), satisfied (p<.01) and very satisfied (p<.01).
Students with a low to a moderate level of closeness with parents had a significantly higher level of depressive symptoms than students with a high level of closeness with parents (F (1,2431) =165.76, p<.01). Students with a low-moderate level of closeness with peers had a significantly higher level of symptoms than those with a high level of closeness with peers (F (1,2425) =176.91, p<.01).
The 6 independent variables with statistically significant relationships with higher levels of depressive symptoms were further examined for their interactions. The two-way analysis of variance results indicate an absence of any interaction.
Differences in mean sub-scale scores based on statistically significant social and demographic factors
Additional analyses using the one-way analysis of variance were performed to determine if the statistically significant associations of the 6 independent variables (i.e., frequency of smoking, frequency of drinking, living/not living with both biological parents, level of satisfaction with financial condition, level of closeness with parents, and level of closeness with peers) would hold at the sub-scale level. The means, F-values and p-values are given in Table 3 .
Results indicate that the associations of the 5 variables (i.e., frequency of drinking, level of satisfaction with financial condition, and levels of closeness with parents and with peers) persisted at all sub-scales of depressive symptoms (p-values at <0.01 or <0.05). The significant sub-scale association of the remaining variable (i.e., living/not living with both biological parents) was confined only to the cognitive-emotional sub-scale.
This survey identified a set of social and demographic factors that are statistically significantly associated with higher levels of depressive symptoms among Filipino university students. The aim is to help prevent depression among the domestic university student population. If students with elevated risks are known and assisted early, their depression would be promptly averted. Data suggest that the factors with significant associations with depressive symptoms, mostly at both the scale and sub-scale levels, were frequency of smoking, frequency of drinking, living/not living with both biological parents, level of satisfaction with one’s financial condition, and levels of closeness with parents and with peers.
The significant associations of frequencies of smoking and of drinking with depressive symptoms are aligned with extant empirical findings [ 20 , 21 ]. The present study revealed that Filipino students who smoked for some days (against those who did not smoke) and who took alcohol for some days (against those who consumed alcohol for longer durations) had higher depressive symptoms levels. In explaining the associations of smoking and drinking, some studies tend to highlight the psychopharmacological [ 20 ] and symbiotic [ 22 ] dimensions of these bivariate relationships. This implies that students could have smoked or taken alcohol as an escape route from the burdens of psychosocial difficulties. In the case of drinking, in particular, the use of alcohol usually precedes the symptoms of lethargy and social difficulties associated with depression [ 23 , 24 ]. Caution should be taken in appreciating these interpretations, however. The variables were measured in this study based on the number of days of smoking and drinking rather than the quantities of cigarettes and alcohol consumed (these two are not necessarily equivalent indicators). Considering that the rates of smoking and drinking among the Filipino youth are relatively high (21.0% and 41.4%, respectively) [ 25 ], these twin behaviors, specifically their frequencies, need closer examination vis-à-vis depressive symptoms.
The association between not living in the household with both biological parents and having more serious levels of depressive symptoms has ample empirical support [ 14 , 26 ]. Across the country, many Filipino students do not reside with both parents while pursuing their university education, because they live away from home in dormitories and/or their biological parents are single, separated, or are working abroad. Either as a permanent or a temporary condition, not living with both biological parents may induce depressive symptoms, primarily in cognitive-emotive terms as this study revealed, probably as a result of having restricted access to parental presence and support.
Satisfaction or dissatisfaction with one’s financial condition is well-confirmed in several other investigations for its significant role in mental health [ 27 ]. It is usually expensive to study in a private Philippine university compared to studying in the country’s state colleges and universities. Students in private universities would generally belong to higher levels of socioeconomic status and may influence a peer culture that promotes greater awareness of a person’s socioeconomic standing in society. Such an educational environment is, in turn, likely to enhance sensitivities about one’s own social status in comparison to one’s peers. Those who perceive themselves as higher in status also have higher levels of optimism and perceived control, and therefore, are also likely to exhibit lower levels of depressive symptoms [ 28 , 29 ].
The current study findings on the significant associations between the levels of closeness with parents and peers and depressive symptoms are to be expected; these are within the realm of the evidence widely reported in other investigations [ 7 , 30 ]. That most of the Filipino university students who participated in this study had high closeness levels with their parents and peers is hardly unexpected. Parents and friends are basic yet very significant primary groups for Filipino adolescents. Their provisions, including the immediate care, security and support that they bestow and the secure attachments that they consequently foster, are effective protectors and buffers of university students against depressive symptoms [ 31 , 32 ].
In the absence of high level of closeness of Filipino students with parents, in which the parent-child relationship would be characterized by communication problems, excessive parental control, low levels of cohesion, and high levels of conflict in the families, adolescents are bound to experience depressive symptoms [ 33 , 34 ]. Without high level of closeness with peers, local students are also predisposed to be at risk. Students are in a stage when they mostly need their peers for emotional support. Peer acceptance is important to the growing individual and is therefore associated with depressive symptoms [ 35 ]. Compared to the association of the lack of parental warmth and acceptance with adolescents’ depressive symptoms, which is largely unidirectional, the association between depressive symptoms and peer-relational problems tends to be bidirectional [ 36 ]. Filipino students exhibiting depressive symptoms are likely to be spending less time interacting with their peers and are prone to relate with them aggressively. This interaction pattern, in turn, is likely to cultivate further peer rejection and neglect.
Sex, age category, course category, year level and religion were not statistically significant factors as our analyses revealed. As a general rule, females show higher rates of depression than males [ 37 , 38 ] due to their tendency to be more expressive and more sensitive to the support provided by their social networks [ 39 ]. However, this normative rule on gender differences does not seem to hold true for university students [ 37 ]. The exception may be accounted for by the homogeneous university life experiences, similarities in parental education, or common socio-demographic conditions among the youth in general [ 37 , 39 ]. The lack of significant associations of age category, course category and year level among Filipino students could be due to this homogeneity factor as well, particularly that most of them were young, freshmen and completing general education rather than major subjects at the time of their interview. Religion was not significantly associated with depressive symptoms and this is to be expected: the Filipino youth, including university students, are largely nominal Catholics who seldom practice their faith [ 40 ]. Elsewhere, one’s religiousness rather than religious affiliation per se has been observed to be significantly related with lower levels of depressive symptoms in students [ 41 ].
The survey has some limitations. Since the study’s respondents were from general education classes with mostly first year students from middle- and high-income backgrounds, the findings cannot be generalized to the entire student population of the university surveyed or student populations from other universities in the Philippines. Another limitation of the survey is that it did not include other factors that may have potential relationships with higher levels of depressive symptoms. For instance, since completing a university degree is culturally valued among Filipinos, the academic performance of students could be a critical factor for assessing depressive symptoms. Also, the study is cross-sectional, and as such, its conclusions only refer to associations rather than causal relationships between the independent and dependent variables. Moreover, the level of depressive symptoms measured through the USDI pertains not to the sequence of the occurrence of high levels of depressive symptoms, but to the amount of depressive symptoms weighted by frequency of occurrence students experienced in the past fortnight.
More surveys using the USDI are needed in the Philippines. Future studies have to involve representative samples of Filipino university students from other socio-economic backgrounds. If feasible, longitudinal studies, which will provide repeated observations of the levels and associated factors of depressive symptoms, are a better alternative. Variables related to students’ academic performance should be included as well. Some variable measures (e.g., frequency of smoking) need to capture more nuanced dimensions of the social and demographic conditions of students at greater risk, For example, variables related to smoking and drinking should ask follow-up questions regarding the specific quantities of cigarettes and alcohol consumed by students in a given period. In addition, the association of religion with depressive symptoms will be better understood by a follow-up question on religiousness.
The present survey is a pioneering large-scale research on the social and demographic factors of higher levels of depressive symptoms among Filipino university students. These initial findings can help guide the development of a campus-based prevention program at the university surveyed. Towards addressing depressive symptoms and depression in students, lifestyle and factors related to financial condition and parental and peer relationships are important considerations for identifying those at greater risk. More research is needed towards building additional local knowledge on the topic.
Author Contributions
Conceived and designed the experiments: RBL MS SE CR. Analyzed the data: RBL MS SE CR. Wrote the manuscript: RBL MS SE CR.
- View Article
- Google Scholar
- 2. World Health Organization (2007) Research capacity for mental health in low- and middle income countries. Geneva: WHO.
- 3. Rudolph KD, Hammen C, Daley SE (2006) Mood disorders. In: DA WolfeEJ Mash. Behavioral and emotional disorders in adolescents: Nature, assessment and treatment. New York: Guilford Publishing House.
- 7. Bushnik T (2005) Youth depressive symptoms and changes in relationships with parents and peers. Children and Youth Research Paper Series. Ottawa: Ministry of Industry.
- 10. World Federationof Mental Health (2012) Depression: A global crisis. Occoquan, VA: World Federation for Mental Health, European Regional Council.
- 16. Zawawi JA, Hamaideh SH (2009) Depressive symptoms and their correlates with locus of control and satisfaction with life among Jordanian college students. Eur J Psychol 4: 71-103.
- 17. Commission on Higher Education (2010) Higher education enrolment and graduates by sector, discipline group, sex and academic year: AY 2004/5-AY 2009/10. Quezon City, Philippines: CHED. Available: http://www.ched.gov.ph/chedwww/index.php/eng/Information/Statistics . Accessed 25 February 2013.
- 25. University of the Philippines Population Institute (2002) The Filipino youth: 2002 YAFS data sheet. Quezon City, Philippines: UPPI.
- 35. Hutcherson MS (2011) An examination of the interrelation of risk and protective factors associated with interpersonal relationships and internalizing problems in undergraduate college students (doctoral dissertation). Texas: Texas Tech University.
- 40. Catholic Bishops Conference of the Philippines (2002) National Filipino Catholic youth survey. Manila: CBCP.
Mental Health Care of Filipino Americans
Information & authors, metrics & citations, view options, history and demography, effects of regionalism, mental illness among filipino americans.
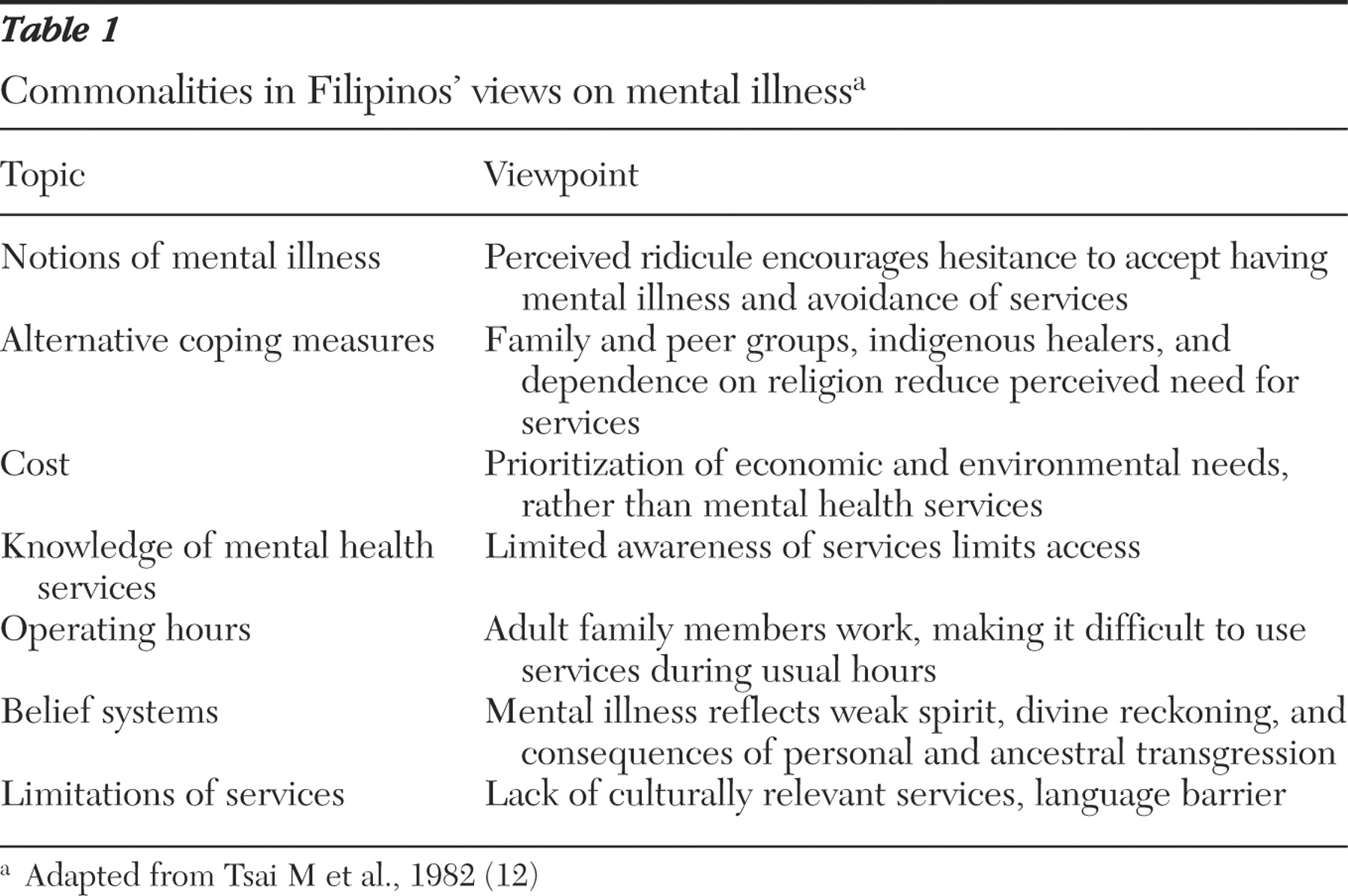
Contributors to perceptions of mental health
Family and support systems, indigenous traits and coping styles, clinical implications in treating filipino americans, therapeutic interventions, conclusions, acknowledgments and disclosures, information, published in.

Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download. For more information or tips please see 'Downloading to a citation manager' in the Help menu .
| Format | |
|---|---|
| Citation style | |
| Style | |
To download the citation to this article, select your reference manager software.
There are no citations for this item
View options
Login options.
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Purchase Options
Purchase this article to access the full text.
PPV Articles - Psychiatric Services
Not a subscriber?
Subscribe Now / Learn More
PsychiatryOnline subscription options offer access to the DSM-5-TR ® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).
Share article link
Copying failed.
PREVIOUS ARTICLE
Next article, request username.
Can't sign in? Forgot your username? Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username
Create a new account
Change password, password changed successfully.
Your password has been changed
Reset password
Can't sign in? Forgot your password?
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password.
Your Phone has been verified
As described within the American Psychiatric Association (APA)'s Privacy Policy and Terms of Use , this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences. Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
- Research article
- Open access
- Published: 05 October 2018
A qualitative study on the stigma experienced by people with mental health problems and epilepsy in the Philippines
- Chika Tanaka ORCID: orcid.org/0000-0002-6288-5532 1 ,
- Maria Teresa Reyes Tuliao 2 ,
- Eizaburo Tanaka 3 ,
- Tadashi Yamashita 4 &
- Hiroya Matsuo 1
BMC Psychiatry volume 18 , Article number: 325 ( 2018 ) Cite this article
144k Accesses
35 Citations
8 Altmetric
Metrics details
Stigma towards people with mental health problems (PMHP) is known to have substantial negative impacts on their lives. More in-depth exploration of the stigma and discrimination experienced by PMHP in low- and middle-income countries is needed. Previous research suggests that negative attitudes towards PMHP are widespread among the Filipino general public. However, no study has investigated PMHP’s own experiences of being stigmatised in the Philippines.
A qualitative study was conducted on the stigma experienced by PMHP (including people with epilepsy) and its related factors in the Philippines, employing the constructivist grounded theory approach. We analysed data on 39 PMHP collected through interviews with PMHP, their carers, and community health volunteers who know them well.
The findings highlight the culturally and socio-economically specific contexts, consequences, and impact modifiers of experiences of stigma. Participants emphasised that PMHP face stigma because of the cultural traits such as the perception of mental health problem as a disease of the family and the tendency to be overly optimistic about the severity of the mental health problem and its impact on their life. Further, stigma was experienced under conditions where mental health care was not readily available and people in the local community could not resolve the PMHP’s mental health crisis. Stigma experiences reduced social networks and opportunities for PMHP, threatened the economic survival of their entire family, and exacerbated their mental health problems. An individual’s reaction to negative experiences can be fatalistic in nature (e.g. believing in it is God’s will). This fatalism can help PMHP to remain hopeful. In addition, traditional communal unity alleviated some of the social exclusion associated with stigma.

Conclusions
The study indicates that existing stigma-reduction strategies might have limitations in their effectiveness across cultural settings. Therefore, we propose context-specific practical implications (e.g. emphasis on environmental factors as a cause of mental health problems, messages to increase understanding not only of the possibility of recovery but also of challenges PMHP face) for the Philippines.
Peer Review reports
Stigma and discrimination against people with mental health problems (PMHP) are a global public health issue [ 1 , 2 , 3 ] and can have substantial negative impacts on all aspects of a person’s life, from employment and housing to social and family life [ 4 , 5 , 6 , 7 ]. Public stigma, the general public’s reaction towards a stigmatised group, can be conceptualised as having three distinct elements [ 8 ]. First, a negative belief about a stigmatised group is seen as stereotype. Second, an emotional reaction to the stereotype is seen as prejudice. Third, a behavioural manifestation of the prejudice is discrimination. Historically, research on stigma related to mental health has been conducted mainly on stereotypes, prejudices, and intentions to discriminate that are held by the general public with regard to PMHP. Such research revealed that the general public frequently label PMHP as dangerous, blameworthy, incompetent and weak, which is often accompanied with emotions of fear and anger and can lead to behavioural intention of avoidance, punishment, and coercion [ 9 , 10 , 11 , 12 ]. Further, the literature shows that internalisation of public stigma or self-stigma is also frequent among PMHP, which reduces self-esteem, causes social isolation, and inhibits help-seeking behaviour [ 6 , 13 , 14 , 15 ].
Recent research has more often investigated levels of discrimination using direct reports from PMHP. The results of such research suggest that discrimination against PMHP is a universal phenomenon around the world [ 2 , 3 , 16 ]; however, PMHP’s experiences of discrimination and its related factors might differ in high-income countries (HICs) versus low- and middle- income countries (LMICs). Some studies suggest that PMHP experience a lower level of stigma in LMICs [ 17 ], such as India [ 18 ], China [ 19 ], and Nigeria [ 20 ], compared with HICs. The reasons for the more positive acceptance of PMHP in those settings have been considered to be a more supportive environment with social cohesion as well as more social role options that PMHP are able to fulfil [ 21 , 22 ]. At the same time, there is also accumulating evidence revealing that in LMICs, experiences of stigma, discrimination and human rights abuses related to mental health problems are common and severe [ 23 , 24 , 25 , 26 , 27 ]. The stigmatisation in LMICs has been attributed to the combined effects of socioeconomic and ethno-cultural characteristics of the setting [ 28 ]. For example, the economic situation of widespread poverty may contribute to further marginalisation of PMHP who are not able to financially contribute to society [ 29 ]. Moreover, the cultural value of collectivism may results in discrimination towards PMHP especially with regarding to marriage and childrearing, since a person’s mental health problem is often seen as the family’s mental health problem [ 30 ]. Overall, practices and outcomes of stigma differ across cultures and socioeconomic backgrounds [ 29 , 31 , 32 ], and meaningful comparison across cultural settings may not be achievable with cross-cultural measures [ 33 ]. In consideration of this, researchers have called for an in-depth qualitative exploration of the experiences of stigma among PMHP in LMICs settings, where about 85% of the world’s population live [ 21 ].
PMHP in the Philippines, a lower-middle income country in Asia, might experience a significant level of stigma and discrimination. Filipino immigrants believed that personal characteristics (i.e. self-centeredness and “soul weakness”) resulted in mental health problems [ 34 , 35 ], which have been shown to be related to blaming PMHP and discriminatory behaviour in other settings [ 36 ]. Also, a multi-country survey revealed that, among 16 countries surveyed, the Philippines had the second highest proportion of citizens who agreed that PMHP should not be hired for a job even if they are qualified [ 37 ]. Further, some studies that involved interviews with Filipino immigrants living in Australia and the United States and that sampled from the general population revealed that a fear of being labelled as ‘crazy’ and spoiling their family’s reputation made Filipinos hesitate to seek help from mental health professionals [ 35 , 38 , 39 ]. Although these previous studies provide some knowledge regarding public stigma in the Filipino context, all of them looked at stereotypes, prejudices and intentions to discriminate held by the general public towards PMHP. To our knowledge, there is no study investigating PMHP’s own experiences of being stigmatised and discriminated against and the related factors in the Philippines.
To fill the gaps in the literature, we conducted a qualitative study on the factors related to experiences of stigma as well as the experiences itself of PMHP in the Philippines, using interviews with PMHP and people who know them well. Revealing the existence, types, and sources of stigma experienced by PMHP in the Philippines can contribute to the stigma research in Asian LMIC settings. Further, exploring the experiences of stigma and its related factors can provide fundamental knowledge for the design of an effective stigma reduction program in the Filipino setting.
The current research utilised the principles of constructivist grounded theory, which is deemed suitable for revealing the social phenomenon of PMHP’s experiences of stigma [ 40 ] in the Filipino context. The constructivist grounded theory assumes a relativist ontology (accepting that multiple realities exist) and a subjectivist epistemology (involving a co-construction of meaning through interaction between the researcher and participant) [ 41 ]. It provides a means of studying power, inequality, and marginality [ 42 ].
Our study was conducted in Muntinlupa, the southernmost city in the Philippines’ National Capital Region. The city has a population of 481,461 as of 2016. The majority comprises Tagalog ethnic groups and professes Christian, primarily Roman Catholic, faith. Households below the food threshold, the minimum income required to meet basic food needs, account for 21.5% of the total in the city [ 43 ]. The majority of citizens cannot afford private medical services, which cost five times more than the public medical services [ 44 ]. With respect to public psychiatric service, the city has one outpatient and no in-patient facility. The nearest public in-patient psychiatric facility is located about 23 km away.
Main data collection
Participants.
We collected data on PMHP from three different sources of information: PMHP themselves, their carers, and community health volunteers who knew them well. The eligibility criteria for PMHP were 1) having a mental health problem, listed in the Diagnostic and Statistical Manual of Mental Disorders 5 (DSM-5), or epilepsy, and 2) currently not using residential care. Epilepsy was included for several reasons. First, people with epilepsy are known to suffer stigma and discrimination [ 45 , 46 ]. Second, the condition has a long history of being classified as a psychiatric problem [ 47 ]. Third, even with the present-day efforts promoting mental health in LMICs, epilepsy is often treated together with mental health issues [ 48 ]. Last, pilot interviews revealed that local lay people do not clearly differentiate epilepsy from mental health problems.
For the recruitment, we approached 42 PMHP in person; one of them declined to participate owing to time constraints. Thus, we obtained informed consent from 41 PMHP. Among them, two PMHP were excluded because they were confirmed to have only physical health problems and no mental health problems as listed in DSM-5. Consequently, we used data of 39 PMHP for our analysis. The profiles of the final sample are shown in Table 1 . In 20 of the PMHP, we interviewed the PMHP and their main carer, usually a parent or sibling. In the remaining 19 PMHP, only a main carer was interviewed, as the 19 PMHP had communication difficulties that hindered them from answering interview questions. Additionally, in 11 PMHP, we conducted interviews with a community health volunteer who was in charge of the district in which the PMHP lived.
Recruitment
We aimed to include a wide variation in the characteristics of the PMHP, namely, gender, age, marital status, educational attainment, employment status, religion, type of mental health problem, and history of using health and welfare services. To achieve this, the participants were recruited by purposive sampling in cooperation with two different collaborating stakeholders. First, as stigma was considered to inhibit Filipino people from seeking professional help for their mental condition [ 35 , 49 ], we recruited the majority of PMHP ( n = 36) in cooperation with community health volunteers, which enabled us to recruit PMHP regardless of their history of receiving health care. The community health volunteers had good knowledge of the profiles of the residents of the district under their charge and covered all the areas of the city. Second, we recruited a small number of PMHP ( n = 3) with common mental health problems (e.g. anxiety and depressive problems) from the outpatient clinical practice of a psychiatrist, as the community health volunteers did not identify any people with these types of problems.
To check the eligibility of those who had never been diagnosed by a specialist as having a mental health problem, a research member, ET, carefully reviewed the data of the individual participants, including interview recordings, transcriptions, and field notes, and then provided informed presumption if the participants had a mental health problem or not. ET also assessed which chapter, the broadest classification in DSM-5, the participant most fitted. ET has clinical experience as a psychiatrist in Japan for over 15 years.
Interview procedures
Data on the PMHP were collected through semi-structured in-depth interviews. Prior to the beginning of data collection, an interview guide was developed, referring to previous research [ 18 , 50 ], and then modified based on six pilot interviews in the setting. The interview guide had a series of open questions on three major topics: onset of mental health problems and coping behaviours, experiences of being treated negatively owing to the problem and its consequences, and activities PMHP gave up because of how others might respond to their health problem. The interview guides for interviews with PMHP and for interviews with carers and community health volunteers can be accessed in Additional files 1 and 2 , respectively. Consistent with the grounded theory methods, we used the interview guide as a flexible tool that could be revised as the analysis progressed. The carers and community health volunteers were not asked about their own experiences of stigma as a carer or person working in mental health. Instead, we asked them about the PMHP’s experiences regarding the same topics, based on their observations. Demographic data of the PMHP were also obtained at the beginning of the interview.
The first author, CT (female, a Japanese public health nurse), conducted all of the data collection between January and March 2017. During the interview, Tagalog or English was used as preferred by the participants. When Tagalog was chosen, the interviews were interpreted by one of two health workers who had lived in the city for more than 30 years and were fluent in both Tagalog and English. After explaining the study and gaining informed consent, the interviews were conducted in their home, a health centre, or the city hospital, depending on the participants’ preference. Wherever possible, we conducted interviews in a space where there was no one but the interviewee, interviewer, and interpreter around. However, five PMHP were not willing to be interviewed alone. In which case, a family member was in the same place and assisted the interview. All the interviews were digitally recorded with interviewees’ permission and lasted between 19 and 53 min; the median length was 29 min. The participants received 100 Philippine pesos (1.9 US dollars) as acknowledgement for their participation.
Supplementary data collection
We included data of interviews with seven health workers into our analysis to gain a wider perspective on the stigma experienced by PMHP. CT conducted the interviews during her one-month participant observation at health services provided by the city government. During the observation, CT discussed the role of stigma and its impact on PMHP with more than 85 health and welfare workers. We analysed seven interviews with those who shared episodes on PMHP with whom they were in direct contact as a part of their duty at work. The interviewees were three community health volunteers, two nurses, one doctor, and one rehabilitation program officer. Notes were taken during the interviews and six out of seven interviews were audiotaped with their permission.
All of the recordings were transcribed verbatim by two trained transcribers. Tagalog recordings were simultaneously translated into English by the transcribers fluent in English and Tagalog. An independent research assistant randomly selected 10% of the English transcripts and checked their accuracy by matching them with the Tagalog and English recordings. During this checking process, no significant errors were found thus the transcripts were quality assured.
Data analysis started as soon as the initial data were collected. We set aside theoretical ideas from the existing literature; instead, we remained open to exploring the theoretical possibilities we could discern from the data. After reading each of the transcripts at least twice, CT and ET independently conducted the initial coding. Simple codes were created to describe the phenomenon in each segment of data, using the qualitative data analysis software, Nvivo Version 11.4.1 (QSR International, 2016). The initial codes with identical meanings were merged through discussion, whereas those with different meanings were left unchanged to increase the variety in the interpretation of the data. We used data from interviews with cares, health volunteers, health and welfare workers to increase variety of data on stigma experienced by PMHP and gain comprehensive understanding of its context. Thus, when accounts showed some discrepancy between a person with mental health problem and his/her carer or a person who knew him/her well, we used the data from both accounts for our analysis.
The authors gradually moved on to the focus coding, in which the initial codes were concentrated on or collapsed into categories that make analytical sense, and then tested these against extensive data. The interpersonal interaction between people with and without mental health problems was treated as the central phenomenon of our interest. To explore comprehensively PMHP’s experiences of stigma, we decided to treat any “uncomfortable treatments from others” reported as stigma experience, regardless of the actors’ motivation. We constantly compared data on similarities and differences within a participant as well as across participants to examine the categories and develop links among them. CT led the preliminary focus coding. Subsequently, discussions were held between CT, ET, and HM, in which we reviewed the developed categories and links to determine if they were grounded in data and sufficiently explained the phenomenon.
After analysing the data of the 35 PMHP, a tentative model that explains the relations between categories was developed. We then collected and analysed data on four additional PMHP. Through discussion, the full research team determined that the categories and themes were sufficiently relevant and that the model held true for these additional PMHP. We then concluded that the model was theoretically saturated.
Analyses revealed four interrelated themes surrounding stigma experienced by PMHP: (1) the context affecting stigma experience, (2) stigma experience, (3) impact modifier of the stigma experience, and (4) consequence of the stigma experience. Figure 1 shows the relationship among the themes.
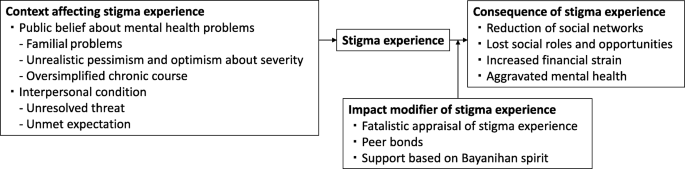
Stigma experienced by people with mental health problems and its related factors in the Philippines
Context affecting stigma experience
We identified two contextual categories that changed how others treated PMHP in a negative way.
Public belief about mental health problems
Public beliefs surrounding mental health issues are a contextual category of stigma experienced by PMHP in the Philippines. It consists of three themes: familial problems, unrealistic pessimism and optimism about severity, and oversimplified chronic course.
Familial problems
Community health volunteers and health workers observed that families of PMHP and people in the local community do not provide appropriate support for PMHP because they perceive mental affliction as a family problem and indicative of so-called “bad blood”. The belief that mental health problems can be transmitted among relatives pushed families of PMHP to deny the existence of mental health issues and people in the community to distance themselves from PMHP. A nurse shared an episode of a male patient with depression:
His family could not accept the idea that one of their relatives is actually depressed. (…) It’s because in our culture, when it comes to mental illness, it tends to be a family affair. People think if one of you has a history of mental illness, there is a chance that almost all of you already have that as well. We care about how others think about our family more than anything else. And other people feel that it is not their place to intervene in some family matters. (Interview 48, Nurse, Female)
In particular, marrying age PMHP faced stigma because of the belief in heredity. People in the community often believe that PMHP have mental health problems in their family’s blood and are afraid of developing those problems in their kinship via marriage.
I had one neighbour that I reported to the barangay [district government] because she mocked me. She was saying that I had mental illness in our blood and no one dare marry me and get in trouble. (Interview 51, PMHP, Male)
Unrealistic pessimism and optimism about severity
PMHP experienced stigma when others were overly pessimistic about the severity of a mental health problem. Participants often criticised those who believe that mental health problems generally cause severe functional impairments. This belief has resulted in unfair treatment towards PMHP in the Philippines.
[Researcher: What is the biggest challenge for the [social inclusion] program?] Finding a job. It’s very difficult. The community people don’t believe they [PMHP] are functional and don’t hire them. (…) So now some barangays [district governments] have started to hire them. We hope people see them working hard and start to trust them. (Interview 27, Rehabilitation program officer, Male)
Meanwhile, unrealistic optimism about its severity also caused stigma. The commonly held belief is that individuals are able to overcome any psychological suffering by themselves, and as a result, it will not become a serious problem. It was common for PMHP to be doubted or withheld empathy in such a culture that emphasises resilience and humour under stressful situations.
Filipinos are proud of being resilient. We find something funny in any difficult situation. But when you have this illness, that kind of thinking gives you a huge pressure. (…) One day, I opened up about my mental illness to my friends, but they all had the same reaction. They laughed at me and didn’t take it seriously. (Interview 71, PMHP, Female)
Oversimplified chronic course
The oversimplified chronic course of mental health problems emerged as one of the causes of stigma. People without any experience of a mental health problem often misunderstand the repetitive relapse and remission in the course of a mental health problem. They tend to apply an acute illness model and expect a complete cure in the short term. However, as the symptoms are prolonged, they begin to mistrust the PMHP’s account.
After one month of no work, I was able to work and sleep. But in February, it came back. I couldn’t sleep for several days. (...) My supervisors were thinking that I should be working a night shift duty, but I told them that I would have to take sick leave. But because it was the same reason for my previous absent, they are already thinking that I am making up stories. (Interview 30, PMHP, Male)
Interpersonal condition
Interpersonal condition was identified as a direct trigger of stigma experience. It consists of two themes: unresolved threat and unmet expectation.
Unresolved threat
Unresolved threat is a condition where PMHP are at risk of hurting themselves or others owing to their mental health problems, with the people in contact with the PMHP failing to manage such risks. Under such conditions, PMHP often experience physical violence, being avoided, and being restricted by others. Although the PMHP, their families, and community health volunteers attributed the threats to PMHP’s personal factors, such as personality and outwardly noticeable symptoms, they also emphasised the culpability of people in the local community for their lack of understanding and skills in interacting with PMHP. When others became familiar with PMHP, they successfully managed those threats and prevented PMHP from experiencing stigma. The mother of a boy with a neurodevelopmental problem told us:
My son easily becomes violent. For example, when someone takes and plays with his toy. The neighbours don’t understand why he is angry and they bully him. But there are also some playmates who fully understand him. When they know that my son is about to be angry, they immediately keep distance from him. And after a while, my son calms down and they start playing around together. (Interview 4, Mother of a boy with a mental health problem)
Unmet expectation
Unmet expectation was another context of stigma. In this context, there is a gap between PMHP’s abilities and other people’s expectations of them. Some PMHP reported suffering from stigma when others’ expectations were too high for their situation. People in this cultural setting tend to value strong bonds and reciprocity among families and neighbours. PMHP sometimes were unable to perform in accordance with this value owing to their mental health conditions. Violation of this value was judged as morally wrong.
They [the neighbours] say I should help my mum by doing washing, cleaning, and taking care of my brother, even when I say I feel weak or don’t know how to. (Interview 5, PMHP, Female) She is big but still doesn’t help her mother. That’s why the neighbours don’t like her. They say she is not a good daughter. (Interview 18, Community health volunteer, Female)
Meanwhile, some other PMHP experienced stigma when others underestimated PMHP’s abilities. Families often criticised other people that looked only at PMHP’s disabilities but not at their abilities.
When someone in our neighbourhood was trying to talk to my sister and she did not respond back, they started bullying her and calling her crazy. [Researcher: How do you think we can change such situation?] I think proper communication towards her would be the best since she’s really a good listener. The problem is that other people don’t know she actually understands things really well. (Interview 8, Sister of a woman with a mental health problem)
Stigma experience
Although we frequently found that PMHP were positively treated by others because of their mental health problems, we also discovered that almost all the PMHP participants were faced with negative treatment from others. PMHP experienced psychological abuse (e.g. being verbally insulted, laughed at, stared at, gossiped about, doubted), physical violence (e.g. being hit, stones being thrown at them), being restricted (e.g. being told not to go outside alone, tied with a rope to a pillar), not being supported (e.g. lack of understanding and sympathy), being taken advantage of (e.g. being cheated out of money and belongings), being neglected (e.g. privacy not being protected, medical care not being provided), and being rejected (e.g. not being associated with, not being hired). Families were an important source of stigma in terms of prominence as stigma from families was often repetitive (e.g. frequently being slapped) and prolonged (e.g. being locked up in a room for several months). PMHP also experienced stigma frequently from their neighbours, and sometimes from school friends, co-workers and employers. People who were involved with PMHP as a part of their duty at work (i.e. health workers and public safety officers) were a source of stigma as well. For complete information on the stigma experience by source, please see Table 2 .
Impact modifier of stigma experience
Even if the nature of stigma experiences were similar, the extent and degree of its influence on PMHP’s life varied depending on impact modifier of stigma experience . PMHP had three impact modifiers consisting of internal (i.e. fatalistic appraisal) and external (i.e. peer bonds, community unity) factors.
Fatalistic appraisal of stigma experience
Fatalistic appraisal of stigma experience offered PMHP and their families a strategy to cope with the emotional pain caused by stigma experience. People in the setting generally believed that God predetermined life events in the past, present and future. Some PMHP and their family accepted unfair treatments from others as “fate.” They were able to remain hopeful because they believed that God would help them if they had faith in God.
Sometimes people say he is crazy. [Researcher: What do you do in response to that?] Nothing. People say what they want to say. We just say “God is good.” As long as we believe in Him, it will be alright. (Interview 23, Sister of a man with a mental health problem)
Peer bonds , the emotional bonds with other people with similar mental health problems, empowered PMHP to change their stigmatised situation in a positive way. Stigma experience could marginalise them in the community, but when they were together with peers who understood not only their health condition but also their lowered social status, they were empowered and motivated to change the situation for themselves and their peers.
[Researcher: What are the barriers to your recovery?] The different perceptions of people towards us [she and other people with mental health problems]. It is so discouraging for us. And we are the only ones who can understand each other very well. We are like brothers and sisters already. Nevertheless, we make sure that the reason we join the [rehabilitation] program is not only for ourselves but to show them that we can change ourselves for the better. If we will be given a chance to work again, we will make 100 percent effort to get things done accordingly. (Interview 34, PMHP, Female)
Support based on Bayanihan spirit
Support based on Bayanihan spirit , a traditional concept of community unity, relieved the negative impacts of stigma on PMHP. It was not rare that community people gave food or rented a house free to PMHP and their family who had little income. Helping one another in a time of need was inherent in their lives, called Bayanihan in Tagalog. For example, a homeless woman with schizophrenia told us that she had felt hopeless because she had been bullied at school and was in a materially deprived circumstance. However, she was now enjoying her life and managing to make a living because some of her neighbours treated her as a valued community member (e.g. regularly invited her to a local dancing event) and occasionally gave her food. A community health volunteer explained why she had good relationships with the community as follows:
That is natural here. When your family member is sick, neighbours and friends are there to pay for medicines, bring food, help with housework, and take care of small kids. We call it Bayanihan. (Interview 3, Community health volunteer, Female)
Consequence of stigma experience
Stigma experience was found to bring about a substantial negative impact on PMHP’s social networks, roles, opportunities, and mental health.
Reduction of social networks
Stigma experience reduced PMHP’s social networks, which led to them spending their days isolated at home without any interaction with people outside of their immediate family. This was due not only to the direct influence of experiences of stigma (i.e. being physically restrained , being avoided by others ) but also the indirect influence of changes in three aspects: PMHP’s behaviour, restriction by families, and relationships with others. First, after being negatively treated, PMHP tended to “close off to everybody” and distanced themselves from others.
Going out is sometimes like an obstacle. (…) After that [hearing my friends gossiping about me], I have been afraid of people’s judgments. (Interview 62, PMHP, Female)
Second, families started to restrict PMHP’s behaviour to protect them from further stigma experiences.
We do not allow him to go out. We are afraid that something like that [neighbours calling him crazy] might happen to him again or someone might abduct him. (Interview 9, Sister of a man with a mental health problem)
Third, stigma experiences provoked conflicts, from a quarrel to a physical fight, and worsened the relationship between PMHP and others. The conflicting relationships produced a further stigmatising attitude towards PMHP.
He got into a fight with his playmates because they said bad words to him. (…) Many of our neighbours told me that he should be in a cell. They told me that they knew a policeman who could put him in jail. (Interview 1, Mother of a man with metal health problem)
Lost social roles and opportunities
As a result of stigma experience, PMHP lost social roles and opportunities , such as being employed, going to school, having a romantic partner, getting married, parenting, helping with household chores and the family business, taking care of younger siblings and joining religious activities.
She was a member of the choir in church. She likes singing and has a good voice. And plenty of friends visited her in the past and they went to church together. But no more. Nobody visits her, and she quit attending it. (Interview 10, Mother of a woman with a mental health problem)
Increased financial strain
Lost social roles and opportunities increased financial strain, which negatively affected the families as well as PMHP themselves. In this setting, PMHP and their families lived in communities where many people find it difficult to make a living. The cost of transportation to medical facilities and treatment fees put them in a further difficult situation economically. In such conditions, entire families often suffered from the financial strain that was due to stigma to the degree that they could not afford basic items including food and clothing.
If only I could find a good job like when I was well. Even though we do not have enough money to buy things, my family really makes an effort to find ways that we can buy those medicines. (Interview 20, PMHP, Male)
Aggravated mental health
The participants reported that the stigma experiences aggravated mental health in PMHP. The memory of negative treatment from others often stuck in their mind and its influence lasted for a long time. A 32-year-old woman with anxiety problem explained how the experience of being bullied when she was a teenager influenced her current condition:
It triggers my anxiety. When I remember their facial expressions, even now, I feel overwhelmed and breathless (Interview 39, PMHP, Female).
The experience of stigma also affected the mental health condition of PMHP by preventing them from seeking help. Some PMHP and their families choose to keep their mental health status a secret. However, families have limited capacities to take care of a person with a mental health problem, especially in the case of someone with severe symptoms. In the worst case in terms of the influence of stigma on PMHP’s mental health, a community health volunteer reported that the parents of a daughter with a mental health problem locked her up in her room and took care of her without seeking professional help. However, her condition kept deteriorating and eventually she committed suicide inside her room.
To our knowledge, this is the first study to document the stigma experienced by PMHP in the Philippines. This study adds to the understanding of discrimination in LMIC settings and its related contextual factors in the Philippines.
First, our results showed that PMHP in the Philippines experienced stigma, which brought about negative impacts on PMHP’s social networks, roles and opportunities, financial burden, and mental health. Although stigma types, sources, and areas of impact were generally consistent with the existing literature in this field [ 4 , 6 , 51 ], we found that experiences of stigma threatened the economic survival of the entire family of PMHP and increased the mental health crisis in the LMIC context, given the minimal welfare and mental health care provisions. Several studies with participants recruited from clinical settings have shown that PMHP in LMICs suffered less from stigma [ 2 , 18 , 19 , 20 ]. In this study, we involved PMHP without psychiatric service use, which prevented us from overlooking the stigma experienced by the poorest and most marginalised PMHP. Our findings might better reflect the reality in LMIC settings, where it is estimated that more than 70% of PMHP receive no treatment for their mental health conditions [ 52 ].
Second, we found that pessimistic and over-optimistic reactions to a mental health problem are among the important contexts of experiences of stigma in the Philippines. Historically, stigma research has mainly focused on the pessimistic view on the prognosis and its negative effects [ 10 , 53 , 54 , 55 , 56 ]. Meanwhile, when the over-optimistic view on the outcome of mental health problems has been documented among Filipino immigrants, it was only recognised as a barrier to help-seeking [ 35 , 39 ]. Our qualitative exploration’s original finding is that the over-optimistic belief among the community regarding the severity of mental health problems results in PMHP’s receiving inappropriate or negative treatment. This is an important finding for the Philippines, because resilience and optimism under difficult situations are among the well-known cultural traits of Filipinos [ 57 , 58 ]. Stigma resulting from optimism might be prevalent in the Philippines; a prior study showed that among the 16 countries, the Philippines posted the highest proportion of respondents who agreed that mental illness would improve on its own [ 59 ].
Third, the results indicated that mental health problems were perceived as problems of the family and discouraged people from accepting mental health problems. The finding is consistent with psychiatrists’ clinical experiences with Filipino patients [ 60 , 61 ]. We also found that a belief in transmissibility among relatives led to PMHP experiencing reduced marriage opportunities. Previous studies conducted on Chinese descent groups [ 62 , 63 , 64 ] showed that the threat of genetic contamination was related to endorsement of reproductive restriction. We propose that it might hold true in the Filipino context, meaning that the threat to family lineage through genetic contamination via marriage accounts for some of the discrimination experienced by PMHP.
Fourth, we revealed a context-specific impact modifier of stigma experiences, namely, fatalistic appraisal of stigma experience . Existing studies have discussed that Filipinos typically attribute illness to “the will of God” [ 39 , 49 , 65 ]. A new finding of this study is that negative treatments from others were also attributed to fate. Globally, it is known that fatalistic appraisal of negative events inhibits active coping and worsens health [ 66 , 67 ]. However, we found that fatalism offered a spiritual coping strategy and shielded PMHP from the adverse effects of stigma in the Catholic dominant setting of the Philippines. These findings are consistent with the literature that have showed that fatalism facilitates adjustment to negative life events [ 49 , 68 , 69 ]. Moreover, support based on Bayanihan spirit was another culturally relevant impact modifier. The origin of the Bayanihan spirit is traced back to the country’s tradition wherein towns’ people cooperate to carry a family’s entire house on their shoulders to a new location. It is considered a core essence of the Filipino culture. Our finding supports the arguments by Lasalvia [ 21 ] and Mascayano et al. [ 29 ] that communal network, which tends to be better maintained in LMICs, is among the existing strengths to reduce the negative effects of stigma.
Lastly, the research method of obtaining perspectives from multiple participants who witnessed and experienced stigma allowed us to reveal that the interpersonal conditions (i.e. unresolved threat and unmet expectations ) preceded stigma experiences. Consistent with previous research from India [ 24 ] and Indonesia [ 70 ], in the setting where mental health care is not readily available at a local level, people in the community needed to cope with the possible danger of PMHP to self or others and can violate PMHP’s human rights. Similar to the results of prior qualitative analyses of interviews with PMHP and their families [ 18 , 71 ], the expectations of others in contrast to PMHP’s actual capabilities caused negative reactions from others. Those interpersonal conditions might be a more important determinant of stigma experiences than PMHP’s personal factors, considering the previous studies showing individual variables (e.g. employment status, symptom, and treatment experiences) accounted for only less than 30% of total variance of experienced stigma [ 2 , 3 ].
Practical implications
Our results suggest that mental health care must have the objective of the reduction of stigma towards PMHP. The Department of Health and Local Government Units are required by the Mental Health Act [ 72 ], established in 2018 as the first law of its kind in the Philippines, to initiate and sustain nationwide campaigns to raise the level of awareness on the protection and promotion of mental health and rights. In conducting stigma reduction campaigns, they should: 1) target families of PMHP, community people, health workers, and public safety officers; 2) avoid genetic explanations for mental health problems and emphasise the role of environmental and social factors as its cause; 3) increase public understanding of not only the possibility of recovery but also the challenges that PMHP face; and 4) improve families’ and community members’ skills in assessing and coping with possible danger posed by PMHP to self or others [ 73 , 74 , 75 , 76 ]. These interventions might be more effective when they utilise the existing communal network and increase social contact between PMHP and others [ 77 , 78 ] We also propose that mental health and welfare services for PMHP should: 1) be community-based and support PMHP in meeting expectations that are meaningful for themselves and others; 2) provide opportunities for PMHP to share their experiences with peers to empower them [ 79 , 80 , 81 ]; and 3) prevent PMHP from internalising experiences of stigma with acknowledgement of fatalistic appraisal of them as a coping strategy. Lastly, to mitigate the adverse influences of stigma, it is necessary to change the structure of health care and welfare service provision for PMHP (e.g. inclusive education, welfare benefits, and job schemes). It is also essential to provide effective and accessible mental health care.
Study limitations
We were unable to recruit people with common mental health problems who were not using psychiatric services. In fact, community health volunteers do not recognise any people having common mental health problems. This may reflect stigma-related situations where local people do not recognise the manifestation of symptoms of those problems as a health issue, or where people with those problems hide their conditions. Additionally, cultural and language barriers may have played a part in data collection and interpretation. However, we also encountered a number of situations where the interviewee provided the data collector, who was from another cultural background, with further explanations, especially on their culture. Further, some interviews were too short to be considered an in-depth interview. Also, we needed to rely in part on data from narratives of people who know PMHP well, instead of from PMHP themselves. These were because the interviewer had difficulty encouraging some participants, especially PMHP, to talk about sensitive topics. Thus, there might be experiences and related themes that we could not explore. Lastly, we conducted the study in one city; thus, the results may not be generalisable to another part of the Philippines (e.g. rural and Muslim-dominant areas).
Our findings highlight that PMHP in the Philippines experience substantial discrimination and its adverse effects are severe to the degree that it threatens the financial survival of the entire family. Culture-bound beliefs and social structure (e.g. perceiving mental health problems as a familial problems, traditional communal unity) played important roles in shaping and modifying stigma experiences. More research is needed to develop stigma reduction interventions utilising these findings and to evaluate their effectiveness.
Abbreviations
The Diagnostic and Statistical Manual of Mental Disorders
High-income countries
Low- and middle-income countries
People with mental health problems
Seeman N, Tang S, Brown AD, Ing A. World survey of mental illness stigma. J Affect Disord. 2016;190:115–121. Available from: https://doi.org/10.1016/j.jad.2015.10.011 Elsevier.
Article Google Scholar
Lasalvia A, Zoppei S, Van Bortel T, Bonetto C, Cristofalo D, Wahlbeck K, et al. Global pattern of experienced and anticipated discrimination reported by people with major depressive disorder: a cross-sectional survey. Lancet. 2013;381:55–62. Available from: https://doi.org/10.1016/S0140-6736(12)61379-8 Elsevier Ltd
Thornicroft G, Brohan E, Rose D, Sartorius N, Leese M. Global pattern of experienced and anticipated discrimination against people with schizophrenia: a cross-sectional survey. Lancet; 2009;373:408–415. Available from: https://doi.org/10.1016/S0140-6736(08)61817-6 . Elsevier Ltd
Sharac J, McCrone P, Clement S, Thornicroft G. The economic impact of mental health stigma and discrimination: a systematic review. Epidemiol Psichiatr Soc. 2010;19:223. Available from: https://www.ncbi.nlm.nih.gov/pubmed/21261218 .
Clement S, Schauman O, Graham T, Maggioni F, Evans-Lacko S, Bezborodovs N, et al. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol Med. 2015;45:11–27 Available from: http://www.ncbi.nlm.nih.gov/pubmed/24569086 .
Article CAS Google Scholar
Livingston JD, Boyd JE. Correlates and consequences of internalized stigma for people living with mental illness: a systematic review and meta-analysis. Soc Sci Med. 2010;71:2150–2161. Available from: https://doi.org/10.1016/j.socscimed.2010.09.030 Elsevier Ltd
Link BG, Phelan JC. Conceptualising stigma. Annu Rev Sociol. 2001 [cited 2018 Jul 3];27:363–385. Available from: https://www.annualreviews.org/doi/pdf/10.1146/annurev.soc.27.1.363
Corrigan PW. Mental health stigma as social attribution: implications for research methods and attitude change. Clin Psychol Sci Pract. 2006;7:48–67 Available from: http://doi.wiley.com/10.1093/clipsy.7.1.48 .
Mannarini S, Boffo M. Anxiety, bulimia, drug and alcohol addiction, depression, and schizophrenia: what do you think about their aetiology, dangerousness, social distance, and treatment? A latent class analysis approach. Soc Psychiatry Psychiatr Epidemiol. 2015;50:27–37.
McGinty EE, Goldman HH, Pescosolido B, Barry CL. Portraying mental illness and drug addiction as treatable health conditions: effects of a randomized experiment on stigma and discrimination. Soc Sci Med; 2015;126:73–85. Available from: https://doi.org/10.1016/j.socscimed.2014.12.010 . Elsevier Ltd
Angermeyer MC, Dietrich S. Public beliefs about and attitudes towards people with mental illness: a review of population studies. Acta Psychiatr Scand. 2006;113:163–79.
Corrigan PW, Markowitz FE, Watson A, Rowan D, Kubiak MA. An attribution model of public discrimination towards persons with mental illness. J Health Soc Behav. 2003;44:162–79.
Corrigan P, Watson A. The paradox of self-stigma and mental illness. Clin Psychol Sci Pract. 2002;9:35–53 Available from: https://onlinelibrary.wiley.com/doi/10.1093/clipsy.9.1.35 .
Google Scholar
Evans-Lacko S, Brohan E, Mojtabai R, Thornicroft G. Association between public views of mental illness and self-stigma among individuals with mental illness in 14 European countries. Psychol Med. 2012;42:1741–52.
Mccann TV, Renzaho A, Mugavin J, Lubman DI. Stigma of mental illness and substance misuse in sub-Saharan African migrants: a qualitative study. Int J Ment Health Nurs. 2017;27:956–65.
Camden Schizoph E, Corker EA, Beldie A, Brain C, Jakovljevic M, Jarema M, et al. Experience of stigma and discrimination reported by people experiencing the first episode of schizophrenia and those with a first episode of depression: The FEDORA project Anamaria Vasilache 2 , Margda Waern 3,4 , Norman Sartorius 10 , Graham Thornicroft 1 and the FEDORA study group. Int J Soc Psychiatry. 2015 [cited 2018 Jul 3];61:438–445. Available from: http://journals.sagepub.com/doi/pdf/10.1177/0020764014551941
Lasalvia A, Van Bortel T, Bonetto C, Jayaram G, Van Weeghel J, Zoppei S, et al. Cross-national variations in reported discrimination among people treated for major depression worldwide : the ASPEN / INDIGO international study. Br J Psychiatry. 2015;207:507–14.
Koschorke M, Padmavati R, Kumar S, Cohen A, Weiss HA, Chatterjee S, et al. Experiences of stigma and discrimination of people with schizophrenia in India. Soc Sci Med; 2014;123:149–159. Available from: https://doi.org/10.1016/j.socscimed.2014.10.035 . Elsevier Ltd
Lv Y, Wolf A, Wang X. Experienced stigma and self-stigma in Chinese patients with schizophrenia. Gen Hosp Psychiatry. 2013;35:83–8. Available from: https://doi.org/10.1016/j.genhosppsych.2012.07.007 Elsevier Inc.
Oshodi YO, Abdulmalik J, Ola B, James BO, Bonetto C, Cristofalo D, et al. Pattern of experienced and anticipated discrimination among people with depression in Nigeria: a cross-sectional study. Soc Psychiatry Psychiatr Epidemiol. 2014;49:259–66.
Lasalvia A. Tackling the mental illness stigma in low- and middle-income countries: lessons learned from high-income countries and mistakes to avoid. Epidemiol Psychiatr Sci. 2015;24:395–8 Available from: https://www.cambridge.org/core/journals/epidemiology-and-psychiatric-sciences/article/tackling-the-mental-illness-stigma-in-low-and-middleincome-countries-lessonslearned-from-highincome-countries-and-mistakes-to-avoid/83D63EA7FD15A3A3F2F9085E7E1700A2 .
Rosen A. Destigmatizing day-to-day practices: what developed countries can learn from developing countries. World Psychiatry. 2006;5:21–24. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1472257/ .
Alonso J, Buron A, Bruffaerts R, He Y, Posada-Villa J, Lepine JP, et al. Association of perceived stigma and mood and anxiety disorders: results from the world mental health surveys. Acta Psychiatr Scand. 2008;118:305–14.
Mathias K, Kermode M, San Sebastian M, Koschorke M, Goicolea I. Under the banyan tree--exclusion and inclusion of people with mental disorders in rural North India. BMC Public Health. 2015;15:–446 Available from: https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-015-1778-2 .
Maramis A, Van Tuan N, Minas H. Mental health in Southeast Asia. Lancet. 2011;377:700–2.
Minas H, Diatri H. Pasung: Physical restraint and confinement of the mentally ill in the community. Int J Ment Health Syst. 2008;2 Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2442049/ .
Tawiah PE, Adongo PB, Aikins M. Mental Health-Related Stigma and Discrimination in Ghana: Experience of Patients and Their Caregivers. Ghana Med J. 2015 [cited 2018 Jul 3];49:30–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26339082 .
Lauber C, Rössler W. Stigma towards people with mental illness in developing countries in Asia. Int Rev Psychiatry [Internet]. 2007;19:157–78 Available from: https://www.ncbi.nlm.nih.gov/pubmed/17464793 .
Mascayano F, Armijo JE, Yang LH. Addressing stigma relating to mental illness in low- and middle-income countries. Front Psychiatry. 2015;6:1–4.
Abdullah T, Brown TL. Mental illness stigma and ethnocultural beliefs, values, and norms. Clin Psychol Rev. 2011;31:934–48.
Semrau M, Evans-Lacko S, Koschorke M, Ashenafi L, Thornicroft G. stugma and discrimination related to mental illness in low- and middle-income countries. Epidemiol. Psychiatr. Sci. [Internet]. 2015;24:382–94. Available from: https://www.ncbi.nlm.nih.gov/pubmed/25937022 .
Yang LH, Kleinman A, Link BG, Phelan JC, Lee S, Good B. Culture and stigma: adding moral experience to stigma theory. Soc Sci Med. 2007;64:1524–35.
Yang LH, Thornicroft G, Alvarado R, Vega E, Link BG. Recent advances in cross-cultural measurement in psychiatric epidemiology: utilizing “what matters most” to identify culture-specific aspects of stigma. Int. J. Epidemiol. [internet]. 2014;43:494–510. Available from. https://www.ncbi.nlm.nih.gov/pubmed/24639447 .
Edman JL, Johnson RC. Filipino American and Caucasian American beliefs about the causes and treatment of mental problems. Cultur Divers Ethnic Minor Psychol. 1999;5:380–6.
Thompson S, Hartel G, Manderson L, Woelz-Stirling N, Kelaher M. The mental health status of Filipinas in Queensland. Aust N Z J Psychiatry. 2002;36:674–80.
Corrigan PW, Rowan D, Green A, Lundin R, River P, Uphoff-Wasowski K, et al. Challenging two mental illness Stigmas : personal responsibility and dangerousness. Schizophr Bull. 2002;28:293–310.
Pescosolido BA, Medina TR, Martin JK, Long JS. The “Backbone” of Stigma: Identifying the Global Core of Public Prejudice Associated With Mental Illness. Am. J. Public Health [Internet]. 2013;103:853–60. Available from: https://www.ncbi.nlm.nih.gov/pubmed/23488508 .
Gong F, Gage SJL, Tacata LA. Helpseeking behavior among Filipino Americans: a cultural analysis of face and language. J Community Psychol. 2003;31:469–88.
Javier JR, Supan J, Lansang A, Beyer W, Kubicek K, Palinkas LA. Preventing Filipino mental health disparities: perspectives from adolescents, caregivers, providers, and advocates. Asian Am J Psychol [Internet]. 2014;5:316–24 Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4319658/ .
Charmaz K. Constructing Grounded Theory. 2nd ed. SAGE Publications Ltd; 2014.
Charmaz K. Grounded theory methods in social justice research. In: Denzin NK, Lincoln YS, editors. SAGE Handb. Qual. Res. SAGE; 2011. p. 359–380.
Charmaz K. The Power of Constructivist Grounded Theory for Critical Inquiry. Qual. Inq. [Internet]. 2017;23:34–45. Available from: http://journals.sagepub.com/doi/10.1177/1077800416657105
City Government of Muntinlupa. POVERTY AND EMPLOYMENT STATISTICS [Internet]. 2017 [cited 2017 Jun 30].
Philippine Statistics Authority. Philippines National Demographic and Health Survey 2013. 2013 [cited 2017 Jun 30]. Available from: https://dhsprogram.com/pubs/pdf/FR294/FR294.pdf .
Boling W, Means M, Fletcher A. Quality of Life and Stigma in Epilepsy, Perspectives from Selected Regions of Asia and Sub-Saharan Africa. Brain Sci. [Internet]. Multidisciplinary Digital Publishing Institute (MDPI); 2018 [cited 2018 Jun 27];8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29614761 .
Herrmann LK, Welter E, Berg AT, Perzynski AT, Van Doren JR, Sajatovic M. Epilepsy misconceptions and stigma reduction: Current status in Western countries. Epilepsy Behav. [Internet]. 2016 [cited 2018 Jun 27];60:165–73. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27208826 .
Koch-Stoecker S. Neuropsychiatric issues in epilepsy. In: Matsuura M, Inoue Y, editors. Neuropsychiatr. issues epilepsy [Internet]. John Libbey Eurotext; 2010 [cited 2018 Jun 27]. p. 233. Available from: https://books.google.co.jp/books?id=FQXhAAAAQBAJ&pg=PA174&lpg=PA174&dq=epilepsy+Emil+Kraepelin&source=bl&ots=r35Oh0rwjA&sig=IZa-67-5hrTVkzSl4HEIoGkaobQ&hl=en&sa=X&ved=0ahUKEwjd26SwkvPbAhWEnZQKHUvrDZsQ6AEIsAEwEw#v=onepage&q=epilepsyAQ28EmilKraepelin&f=false .
World Health Organization. mhGAP Training Manuals - for the mhGAP Intervention Guide for mental, neurological and substance use disorders in non-specialized health settings, version 2.0 [Internet]. WHO. World Health Organization; 2017 [cited 2018 Jun 27]. Available from: http://www.who.int/mental_health/mhgap/training_manuals/en/
Tuliao AP. Mental health help seeking among Filipinos: a review of the literature. Asia Pacific J Couns Psychother [Internet]. 2014;5:124–36 Available from: http://www.tandfonline.com/doi/abs/10.1080/21507686.2014.913641 .
Yang LH, Valencia E, Alvarado R, Link B, Huynh N, Nguyen K, et al. A theoretical and empirical framework for constructing culture-specific stigma instruments for Chile. Cad. saude coletiva [Internet]. 2013;21:71–9. Available from: /pmc/articles/PMC3753780/?report=abstract.
Hamilton S, Pinfold V, Cotney J, Couperthwaite L, Matthews J, Barret K, et al. Qualitative analysis of mental health service users’ reported experiences of discrimination. Acta Psychiatr Scand. 2016;134:14–22.
Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I, Kovess V, Lepine JP, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization world mental health surveys. JAMA [internet]. 2004;291:2581–90. Available from. http://www.ncbi.nlm.nih.gov/pubmed/15173149 .
Wig NN, Suleiman MA, Routledge R, Murthy RS, Ladrido-Ignacio L, Ibrahim HH, et al. Community reactions to mental disorders. A key informant study in three developing countries. Acta Psychiatr. Scand. [Internet]. 1980;61:111–26. Available from: https://www.ncbi.nlm.nih.gov/pubmed/7361584 .
Ando S, Yamaguchi S, Aoki Y, Thornicroft G. Review of mental-health-related stigma in Japan. Psychiatry Clin Neurosci. 2013;67:471–82.
van Boekel LC, Brouwers EP, van Weeghel J, Garretsen HF. Comparing stigmatising attitudes towards people with substance use disorders between the general public, GPs, mental health and addiction specialists and clients. Int J Soc Psychiatry [Internet]. 2014;61:539–49 Available from: http://isp.sagepub.com/cgi/doi/10.1177/0020764014562051 .
Clement S, Jarrett M, Henderson C, Thornicroft G. Messages to use in population-level campaigns to reduce mental health-related stigma: consensus development study. Epidemiol Psichiatr Soc. 2010;19:72–9.
Dy MB. Values in Philippine culture and education. Washington, DC: CRVP; 1994.
Social Weather Stations. Social Weather Station Survey. [Internet]. 2017 [cited 2017 Nov 9]. Available from: https://www.sws.org.ph/swsmain/artcldisppage/?artcsyscode=ART-20170816103037
Pescosolido BA, Martin JK, Olafsdottir S, Long JS, Medina TR, Martin JK. The theory of industrial society and cultural schemata: does the “cultural myth of stigma” underlie the WHO schizophrenia paradox? Am J Sociol. 2015;121:783–825.
Araneta EG. Psychiatric Care of Pilipino Americans. In: Gaw AC, editor. Cult. Ethn. Ment. Illn. Washington, DC: American Psychiatric Press; 1993. p. 377–412.
Sanchez F, Gaw A. Mental health Care of Filipino Americans. Psychiatr Serv [Internet] 2007;58:810–815. Available from: https://www.ncbi.nlm.nih.gov/pubmed/17535941
Wonpat-Borja AJ, Yang LH, Link BG, Phelan JC. Eugenics, genetics, and mental illness stigma in Chinese Americans. Soc Psychiatry Psychiatr Epidemiol. 2012;47:145–56.
Yang LH, Purdie-Vaughns V, Kotabe H, Link BG, Saw A, Wong G, et al. Culture, threat, and mental illness stigma: identifying culture-specific threat among Chinese-American groups. Soc. Sci. Med. [internet]. Elsevier Ltd. 2013;88:56–67 Available from: https://doi.org/10.1016/j.socscimed.2013.03.036 .
Yang LH, Kleinman A. “Face” and the embodiment of stigma in China: the cases of schizophrenia and AIDS. Soc Sci Med. 2008;67:398–408.
Abad PJB, Tan ML, Baluyot MMP, Villa AQ, Talapian GL, Reyes ME, et al. Cultural beliefs on disease causation in the Philippines: challenge and implications in genetic counseling. J Community Genet. 2014;5:399–407.
De Los Monteros KE, Gallo LC. The relevance of fatalism in the study of Latinas’ cancer screening behavior: a systematic review of the literature. Int J Behav Med. 2011;18:310–8.
Roberts RE, Roberts CR, Chen IG. Fatalism and risk of adolescent depression. Psychiatry [internet]. 2000;63:239–52. Available from. http://www.ncbi.nlm.nih.gov/pubmed/11125670 .
Cheng H, Sit JWH, Twinn SF, Cheng KKF, Thorne S. Coping with breast Cancer survivorship in Chinese women the role of fatalism or fatalistic voluntarism. Cancer Nurs. 2013;36:236–44.
Gonzalez P, Nuñez A, Wang-Letzkus M, Lim J-W, Flores KF, Nápoles AM. Coping with breast cancer: reflections from Chinese American, Korean American, and Mexican American women. Heal Psychol [Internet] 2016;35:19–28. Available from: https://www.ncbi.nlm.nih.gov/pubmed/26389720 .
Nurjannah I ,Mills J PT& UK. Human rights of the mentally ill in Indonesia. Int Nurs Rev. 2015;62:153–61.
Habtamu K, Alem A, Hanlon C. Conceptualizing and contextualizing functioning in people with severe mental disorders in rural Ethiopia: a qualitative study. BMC psychiatry [internet]. 2015;15:34. Available from: https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-015-0418-9 .
An act establishing a national mental health policy for the purpose of enhancing the delivery of integrated mental health services, promoting and protecting the rights of persons utilizing psychiatric, neurologic and psychosocial health services, APPROPRI [Internet]. Republic of the Philippines; 2018. Available from: http://www.officialgazette.gov.ph/2018/06/20/republic-act-no-11036/
Kitchener B, Jorm A. Mental health first aid training for the public: evaluation of effects on knowledge, attitudes and helping behavior. BMC Psychiatry [Internet]. 2002;2:10. Available from: http://www.biomedcentral.com/1471-244X/2/10
Morgan AJ, Ross A, Reavley NJ. Systematic review and meta-analysis of Mental Health First Aid training: Effects on knowledge, stigma, and helping behaviour. Doran CM, editor. PLoS One [Internet]. 2018 [cited 2018 Jun 28];13:e0197102. Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0197102 .
Bond KS, Jorm AF, Kitchener BA, Reavley NJ. Mental health first aid training for Australian medical and nursing students: an evaluation study. BMC Psychol. [Internet]. 2015 [cited 2018 Jun 28];3:11. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25914827 .
Jorm AF, Kitchener BA, Fischer J-A, Cvetkovski S. Mental Health First Aid Training by e-Learning: A Randomized Controlled Trial. Aust. New Zeal. J. Psychiatry [Internet]. 2010 [cited 2018 Jun 28];44:1072–81. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21070103 .
Corrigan PW, Morris SB, Michaels PJ, Rafacz JDRN. Challenging the public stigma of mental illness: a meta-analysis of outcome studies. Psychiatr. Serv. [Internet]. 2012;63:963–73 Available from: https://www.ncbi.nlm.nih.gov/pubmed/23032675 .
Corrigan PW, Michaels PJ, Vega E, Gause M, Larson J, Krzyzanowski R, et al. Key ingredients to contact-based stigma change: A cross-validation. Psychiatr. Rehabil. J. [Internet]. 2014 [cited 2018 Jun 28];37:62–4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24417232 .
Corrigan PW, Larson JE, Michaels PJ, Buchholz BA, Del Rossi R, Fontecchio MJ, et al. Diminishing the self-stigma of mental illness by coming out proud. Psychiatry Res. 2015;229:148–54.
Rüsch N, Abbruzzese E, Hagedorn E, Hartenhauer D, Kaufmann I, Curschellas J, et al. Efficacy of Coming Out Proud to reduce stigma’s impact among people with mental illness: pilot randomised controlled trial. Br. J. Psychiatry [Internet]. 2014 [cited 2018 Jun 28];204:391–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24434073 .
Corrigan PW, Rüsch N, Scior K. Adapting disclosure programs to reduce the stigma of mental illness. Psychiatr. Serv. [internet]. 2018 [cited 2018 Jun 28];appi.Ps.2017004. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29606076 .
Download references
Acknowledgments
We are grateful to the interviewees for their participation. We would like to thank Dr. Magdalena C. Meana, Dr. Ma. Luisa Babaran-Echavez, and barangay health workers for their assistance with data collection.
Availability of data and materials
The transcripts from the interviews are confidential and will not be shared.
Author information
Authors and affiliations.
Graduate School of Health Sciences, Kobe University, 701, 2-6-2, Yamamoto-dori, Chuo-ku, Kobe, Hyogo, 650-0003, Japan
Chika Tanaka & Hiroya Matsuo
City Health Office, City Government of Muntinlupa, Muntinlupa, Philippines
Maria Teresa Reyes Tuliao
Hyogo Institute for Traumatic Stress, Kobe, Japan
Eizaburo Tanaka
Kobe City College of Nursing, Kobe, Japan
Tadashi Yamashita
You can also search for this author in PubMed Google Scholar
Contributions
CT had a major role in the conception of the study, undertook the data collection, carried out the data analysis, and had a major role in writing the manuscript. MT contributed to the design of the study, assisted the data collection and interpretation, and supervised writing the manuscript. ET assisted data collection, conducted data analysis, and revised the manuscript. YT assisted data collection and revised the manuscript. HM supervised the design of the study, had a role in data analysis, and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Chika Tanaka .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was obtained from the ethical committee of the Graduate School of Health Sciences, Kobe University, Japan (reference number 561). The study was conducted in accordance with the ethical guidelines set forth by the Declaration of Helsinki and the Ethical Guidelines for Medical and Health Research Involving Human Subjects provided by the Ministry of Health, Labour, and Welfare of Japan. The City Health Office of the local government approved a head of time our study protocol, especially ethical aspects for potentially participating citizens. Potential participants received written and oral information about the study. It was emphasized that participation was voluntary. During the data collection, we obtained written consent from all the interviewees and verbal assent from PMHP whose carers participated in the interviews. In the case where the interviewee was under 18 years old, we gained verbal assent from them and written consent from their parents.
Consent for publication
Participants were informed that the information they shared in the interviews would be published in anonymised form. Written informed consent for publication was obtained.
Competing interests
The authors declare that they have no competing interest.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:.
Interview guide for interviews with people with mental health problems. A set of questions we referred while interviewing PMHP. (DOCX 88 kb)
Additional file 2:
Interview guide for interviews with carers and community health volunteers. A set of questions we referred while interviewing carers and community health volunteers. (DOCX 90 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Tanaka, C., Tuliao, M.T.R., Tanaka, E. et al. A qualitative study on the stigma experienced by people with mental health problems and epilepsy in the Philippines. BMC Psychiatry 18 , 325 (2018). https://doi.org/10.1186/s12888-018-1902-9
Download citation
Received : 20 December 2017
Accepted : 20 September 2018
Published : 05 October 2018
DOI : https://doi.org/10.1186/s12888-018-1902-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Discrimination
- Mental illness
- The Philippines
- Qualitative
BMC Psychiatry
ISSN: 1471-244X
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Health Promot Perspect
- v.11(3); 2021
Mental health and well-being of children in the Philippine setting during the COVID-19 pandemic
Grace zurielle c. malolos.
1 College of Medicine, University of the Philippines Manila, Manila, Philippines
Maria Beatriz C. Baron
Faith ann j. apat.
2 Matias H. Aznar Memorial College of Medicine, Cebu City, Philippines
Hannah Andrea A. Sagsagat
3 West Visayas State University-College of Medicine, La Paz, Iloilo City, Philippines
Pamela Bianca M. Pasco
Emma teresa carmela l. aportadera.
4 Faculty of Medicine and Surgery, University of Santo Tomas, Manila, Philippines
Roland Joseph D. Tan
5 Baguio General Hospital and Medical Center, Baguio City, Philippines
Angelica Joyce Gacutno-Evardone
6 Department of Pediatrics, Eastern Visayas Regional Medical Center, Tacloban City, Philippines
Don Eliseo Lucero-Prisno III
7 Faculty of Management and Development Studies, University of the Philippines Open University, Los Banos, Laguna, Philippines
8 Department of Global Health and Development, London School of Hygiene and Tropical Medicine, London, United Kingdom
The coronavirus disease 2019 (COVID-19) pandemic has subjected the mental health and well-being of Filipino children under drastic conditions. While children are more vulnerable to these detriments, there remains the absence of unified and comprehensive strategies in mitigating the deterioration of the mental health of Filipino children. Existing interventions focus on more general solutions that fail to acknowledge the circumstances that a Filipino child is subjected under. Moreover, these strategies also fail to address the multilayered issues faced by a lower-middle-income country, such as the Philippines. As the mental well-being of Filipino children continues to be neglected, a subsequent and enduring mental health epidemic can only be expected for years to come.
Introduction
The Philippine Development Plan for 2017-2023 highlights that children are among the most vulnerable population groups in society, including them in strategies for risk reduction and adaptive capacity strengthening. 1 Approximately 40% of the total Philippine population is comprised of Filipinos below 18 years of age. 2 Despite having a large portion of the Philippine population declared as vulnerable, concerning issues involving them still persist and remain unaddressed.
Among Filipino children aged 5 to 15, 10% to 15% are affected by mental health problems. 3 According to the World Health Organization (WHO), 16.8% of Filipino students aged 13 to 17 have attempted suicide at least once within a year before the 2015 Global School-based Student Health survey. 4 This is just one of the many indicators showing the state of mental health of these children. These statistics involving children’s mental health are concerning as childhood is a crucial period where most mental health disorders begin. Efforts should be made to identify these issues early for proper treatment in prevention of negative health and social outcomes. 4 Childhood mental and developmental disorders also frequently persist into adulthood, making it more likely for them to have compromised growth with greater need for medical and disability services and higher risk of getting involved with law enforcement agencies. 5 In this context, the COVID-19 pandemic threatens to worsen these numbers, affecting the delivery of the Philippines’ health care services, including those for children’s mental health.
Since the beginning of the pandemic, children have been subjected to multiple threats to their mental health. Adding insult to injury, several concurrent factors in the Philippine society exacerbate this. While these are experiences shared by all people regardless of age, impediments to emotional and social development are greater in children than in adults. 6 They may also be more vulnerable to developing mental health issues such as depression and anxiety. 7 Together with these circumstances and the weakened health care system, children’s vulnerability towards mental health problems may be worsened by the pandemic, leading to more new cases and exacerbating existing ones. 2
Status of mental health system for children in the Philippines
According to the National Statistics Office (NSO), mental health illnesses rank as the third most common form of morbidity among Filipinos. 8 In the assessment conducted on the Philippine mental health system, a prevalence of 16% of mental disorders among children was reported. 9 With this alarming number of cases, it is surprising to see how the Philippines is currently responding to this problem. To date, there are only five government hospitals with psychiatric facilities for children, 84 general hospitals with psychiatric units, and 46 outpatient facilities from which there are only 11 that are designated for children and adolescents. Additionally, there are only 60 child psychiatrists practicing in the Philippines, with the majority of them practicing in urban areas such as the National Capital Region. Hence, children with mental health problems who are in rural areas have less access to such services. 10
As the pandemic continues, combined with the menace of the typhoon season, thousands of children are placed in a situation where the future is uncertain. A local study showed that youth age and students are among those with significant association to a greater psychological impact due to the pandemic. 11 In addition, UNICEF also reports that children nowadays face a trifecta of threats which include direct consequences of the disease itself, interruption in essential services, and increasing poverty and inequality. All of these can lead to higher incidences of stress, anxiety, and depression. 12
General mental health implications of COVID-19 on Filipino children
The fear and anxiety of contracting the virus, the suspension of physical classes, the disruption of regular daily routine, and the decrease of social support from school peers collectively add burden to the mental well-being of children. 7 , 13 The shift to online classes increases the burden on the mental well-being of children. Excessive use of these technologies has been associated with developmental delays and has resulted in sleep schedule disruptions. 14 This situation is aggravated by the strict implementation of the confinement of children at home. Children living with preexisting mental health concerns, 13 and living in cramped households and communities face worse circumstances.
Militarization of the Philippine COVID-19 response
Aside from being regarded as one of the countries with the longest lockdown, the Philippines has also been called out by the United Nations for employing a highly militaristic approach in response to the COVID-19 pandemic. 15 Militarization may come across as threatening, because it implies a potential for violence. 16 Furthermore, few studies abroad have reported that children and adolescents may tend to view police forces as punitive figures whom they fear. 17 , 18 While these qualitative studies were conducted long before the current health crisis began, it may be possible for increased military presence in communities to exacerbate the fears already emanating from the pandemic itself; this can negatively impact a child’s psychological development. 4 Still, local evidence to confirm these associations, especially in the context of the pandemic, is lacking. Many studies have already documented the impact of lockdown on children, but none of them have looked into how the strategies for implementation may also be contributory to their mental health or well-being.
Typhoons and the mental health of Filipino children
The Philippines has been hit by 22 tropical typhoons during the COVID-19 pandemic, leaving thousands of families homeless. 19 Children who are already frightened of COVID-19 and previous tropical storms have had to relive their experience with each new typhoon that came. In addition, children in crowded evacuation centers are at increased risk of contracting diseases and experiencing gender-based violence. 20 Given how past typhoons of similar strength and destruction have caused lasting adverse mental health effects on children, 21 the same or even worse, may be expected as a result of the more recent calamities. Super typhoons Goni and Vamco have caused further disruptions in schooling and livelihood, therefore leaving more children vulnerable to the effects of the pandemic. Those who have been forced to seek refuge in evacuation centers are at an increased risk of acquiring COVID-19, among other diseases. 20
Child Labor and Abuse in the Time of COVID-19
The COVID-19 crisis caused an unprecedented reduction in economic activity and working time, thus increasing poverty. Fewer employment opportunities and lower wages drive exploitative work. Further suppression of wages induces child labor. There may be deliberate recruitment of children to cut costs and boost earnings. 22
In addition to the threats of child labor, a study entitled The Hidden Impact of COVID-19 on Children reported that violence occurred in nearly one-third (32%) of households. Lesser household incomes were associated with more reports of violence towards children. 23 According to UNICEF, the Philippine government saw a 260% increase in online child abuse reports from March-May. Many victims are first abused by their parents, who livestream sexual violence for predators in wealthy Western nations. This occurrence resulted from job and income loss and more time spent at home due to strict quarantine measures. The abuse in children occurs at an average of 2 years before being rescued. 24
Strategies Addressing the mental health implications of COVID-19 on Filipino children
Numerous strategies have been utilized to address the mental health impacts of COVID-19 on Filipinos. With the mental health implications predicted at the beginning of the pandemic, the Psychological Association of the Philippines has compiled a list of free telemedicine consultations. As of August 24, the Philippine Red Cross has also established a COVID-19 hotline with 9790 helpline volunteers to address mental health and other similar concerns. The Department of Health has also conducted nationwide campaigns in observance of the National Mental Health Week. 25
Albeit present, these interventions are limited to the general population, and strategies specific to addressing the mental health situation of children remain scarce and staggered. Compounding factors of classifying among the lower- to middle-income countries of militarization, natural disasters, and child labor and abuse have yet to be considered. In addition, it is also important to consider that happiness, with its multifactorial nature, is a vital component of an individual’s overall wellbeing. 26
The already-challenged state of mental well-being of Filipino children has been worsened by the pandemic and the lack of good mental health policies by the government. While there is increasing awareness for mental health, children-centered interventions remain deficient. Approaches must integrate commonly-known mental health effects on children with existing and anticipated Philippine societal issues. Without doing so, it may be expected that as the COVID-19 pandemic is mitigated, a mental health epidemic will replace it.
Competing interests
The authors have no conflicts of interest.
Ethical approval
Not applicable.
Authors’ contributions
GZCM and DELP were involved in the conception of the paper. GZCM led the writing of the manuscript and acted as corresponding author. GZCM, MBCB, FAJA, HAAS, PBMB, ETCA and RJDT wrote sections of the manuscript. AJGE and DELP reviewed and edited the initial draft of the manuscript prior to submission. All authors have reviewed and agreed to the final version of the paper.
Online Game Addiction and the Level of Depression Among Adolescents in Manila, Philippines
- December 2020
- Central Asian Journal of Global Health 9(1)

- Polytechnic University of the Philippines

- This person is not on ResearchGate, or hasn't claimed this research yet.
Abstract and Figures

Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations
- Ronald D. Derla
- Greg Adrian D Cañamo
- Trishia Nicole G Lantaco
- Hazel D Omblero
- Claire Lynn Culajara
- Janu V. Peralta

- Suciani Latif
- Maria Criszel Joy L. Alpe
- Recylyn I. Bayna-Mariano

- Kenneth Marius R Raval
- ADDICT BEHAV

- Julie Balzer

- mohammad herangza

- Mohammad Narimani

- Widya Rahma Syari
- Edo Gusdiansyah
- BMC PUBLIC HEALTH

- Jennifer Hafekost

- Lota A. Teh

- Natasha F. Veltri

- Neena Kalayamthanam

- Maliheh Chashmi
- Nasim Hedayati
- Charles Lumbay
- Christian Caben M. Larisma
- Catalino L. Centillas Jr
- Committee on the Science of Changing Behavioral Health Social Norms
- Board on Behavioral, Cognitive, and Sensory Sciences
- Division of Behavioral and Social Sciences and Education
- National Academies of Sciences, Engineering, and Medicine
- Robert L. Spitzer

- Curr Psychiatr Rev

- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up

COMMENTS
Introduction. Mental illness is the third most common disability in the Philippines. Around 6 million Filipinos are estimated to live with depression and/or anxiety, making the Philippines the country with the third highest rate of mental health problems in the Western Pacific Region [].Suicide rates are pegged at 3.2 per 100,000 population with numbers possibly higher due to underreporting or ...
Research Paper. Depressive symptoms among young adults in the Philippines: Results from a nationwide cross-sectional survey ... The prevalence of moderate to severe depression in Filipino young adults is higher among females than males. ... The CES-D scale: a self-report depression scale for research in the general population. Appl. Psychol ...
A literature review was conducted and records describing patient journey touchpoints in terms of disease awareness, screening, diagnosis, treatment, adherence, and remission of depression in the Philippines were screened over a period of 10 years (01 January 2010 to 31 December 2019). The methods of conducting the review have been detailed ...
Purpose This systematic review aims to synthesise the evidence on behavioural and attitudinal patterns as well as barriers and enablers in Filipino formal help-seeking. Methods Using PRISMA framework, 15 studies conducted in 7 countries on Filipino help-seeking were appraised through narrative synthesis. Results Filipinos across the world have general reluctance and unfavourable attitude ...
We carried out a survey to determine the social and demographic factors associated with higher levels of depressive symptoms among 2,436 Filipino university students. The University Students Depression Inventory with measures on lethargy, cognition-emotion, and academic motivation, was used. Six of the 11 factors analyzed were found to be ...
Depression is a mental illness that negatively affects how a person feels, thinks and acts. In this work, we used an online survey to ask 501 Filipino university-age students on symptoms commonly associated with depression: sadness or isolation, headaches or migraine, anxiety over everyday activities, moodiness or irritability or agitation, chronic fatigue, and low self-esteem or motivation.
Filipino college students attributed depression to what professionals would commonly describe as triggers such as day-to-day problems, childhood problems, and guilt over wrongful acts, trauma, etc. People they suggested as helpful to a person suffering from depression are counselors, family, friends, psychologist, and psychiatrist. Social
Limitations The version of CES-D included in the survey has not been validated for use among young Filipino adults. Conclusions Close to 1 in 10 young adults (8.9%) in the Philippines experience ...
The present study examined the socio-ecological factors that influenced psychological distress (combined index of depression and anxiety symptoms) among Filipino adults during the COVID-19 crisis. The study involved 401 adult participants currently residing in the Philippines. Data were collected using a self-reported online questionnaire administered to the participants. Findings revealed ...
The high depression rates that we observed in our study are consistent with findings from a research study among Filipino Americans in the U.S. (Kim et al., 2010). Researchers also reported a similar prevalence rate for depression (22%) among Filipino patients with cancer in a tertiary hospital ( Que et al., 2013 ).
The findings suggest comorbidities of an alcohol use disorder, depression, and anxiety among Filipino sexual minorities that can be addressed through cost-effective online treatment modalities ...
Academia.edu is a platform for academics to share research papers. ... Ang Asignaturang Filipino ay kabilang sa K to 12 Curriculum na idinisenyo ng mga eskperto sa Kagawaran ng Edukasyon upang mapalawak ang kaalaman ng bawat Filipino patungkol sa sariling wika at ang mga kagamitan nito. ... Sayson, Elynor. 2005. Depression case among college ...
Hindi parehas ang tanda ng depression ng bata at adult, kaya kailangang mag-ingat. Karaniwan, ang mga batang may depresyon ay nagpupumilit magsabi ng kanilang damdamin at kalooban. Maaaring tanda ng depression ang mga sintomas na pisikal kagaya ng sakit sa ulo, sakit sa tiyan, pagbaba ng score o pagsasabi ng ayaw pumasok sa paaralan.
Facebook usage, depression, adolescents, college students 1. Introduction There is an estimated 350 million people suffering from depression worldwide (World Health Organization [WHO], 2016). Depression is the current leading cause of disability and likely to be the second leading cause of death across the globe by 2020 (WHO, 2018).
Thus, this paper aims to discover, in-depth, some basic realities regarding the effects of the pandemic on the various aspects of mental health of Filipino college students. With the explored contextualized themes, appropriate interventions can be formulated for future research which can be beneficial in addressing related issues.
Abstract. This paper aimed to provide a review of mental health stigma in the Philippines, its implications on policy and. programs, and in terventions on addressing the issue. Stigma t owards ...
Depression can be prevented if its symptoms are addressed early and effectively. Prevention against depression among university students is rare in the Philippines, but is urgent because of the rising rates of suicide among the group. Evidence is needed to systematically identify and assist students with higher levels of depressive symptoms. We carried out a survey to determine the social and ...
Filipino Americans considered interpersonal factors (time with family, friendship, and support groups) as important treatments for depression ( 18). Filipino Americans cited significant barriers to treatment, including dealing with family hierarchy and reputation, fatalistic attitude and religious fanaticism, lack of belief in one's capacity to ...
The current research utilised the principles of constructivist grounded theory, which is deemed suitable for revealing the social phenomenon of PMHP's experiences of stigma [] in the Filipino context.The constructivist grounded theory assumes a relativist ontology (accepting that multiple realities exist) and a subjectivist epistemology (involving a co-construction of meaning through ...
Experiences of Stress and Coping Responses in Filipinos. The enduring presence of colonial mentality (David & Nadal, 2013; Tuazon et al., 2019) and cultural influences on wellness (Samaco-Zamora & Fernandez, 2016) affect experiences of stress and coping within Filipino communities. Colonial mentality is the "automatic and uncritical rejection of anything Filipino and an automatic and ...
Amidst this worldwide pandemic, depression is a significant and pervasive public health issue. Furthermore, there is the possibility of using social media postings as a new lens for studying ...
Among Filipino children aged 5 to 15, 10% to 15% are affected by mental health problems. 3 According to the World Health Organization (WHO), 16.8% of Filipino students aged 13 to 17 have attempted suicide at least once within a year before the 2015 Global School-based Student Health survey. 4 This is just one of the many indicators showing the ...
depression in Filipino adolescents. Methods: A paper - and - pencil self - administered questionnaire assessing depression and o nline game addiction was distributed from August to November , 2018.