

Supplementary Material for: Employment in Myasthenia Gravis: A Systematic Literature Review and Meta-Analysis
Usage metrics.

Introduction
Discussion/conclusion, acknowledgment, statement of ethics, disclosure statement, funding sources, author contributions, employment in myasthenia gravis: a systematic literature review and meta-analysis.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
Erika Guastafierro , Irene Tramacere , Claudia Toppo , Matilde Leonardi , Renato Mantegazza , Silvia Bonanno , Rita Frangiamore , Alberto Raggi; Employment in Myasthenia Gravis: A Systematic Literature Review and Meta-Analysis. Neuroepidemiology 17 July 2020; 54 (4): 304–312. https://doi.org/10.1159/000506310
Download citation file:
- Ris (Zotero)
- Reference Manager
Introduction: Myasthenia gravis (MG) is an autoimmune disease whose period of typical onset is around 20–40 years (i.e., early onset), thus in the peak of working age, or around 60–80 years (i.e., late onset). However, the information on work-related issues and employment status are sparse and not systematically reported. Therefore, we performed a systematic literature review with meta-analysis to address the employment status of MG patients. Methods: We searched for papers reporting employment status on participants with MG published between January 2000 and May 2019. Information on employment was extracted. Random-effects models were used to produce meta-analytic estimates for the proportion of employed patients. Results: In total, 1,045 records were retrieved, of which 19 fitted the inclusion criteria. In total, 3,600 participants (average age 47.5, range 35–60) were included in the studies and 1,579 of them were employed. The proportion of employed patients varied from 28 to 82%, with an extreme heterogeneity between studies. Overall, the pooled proportion of workers was 50% (95% CI 41–60%). Subgroup analyses suggested a possible, although not significant, higher proportion of workers among women, younger participants, those with a higher level of education, shorter MG duration, and less frequently thymectomized, whereas a lower proportion was observed among those with generalized, bulbar, and respiratory symptoms. Conclusions: The results of our meta-analysis show that the percentage of employment is considerably low if we take into account that the mean age of MG patients involved in the included studies was around 48 years, thus in peak of working life. Therefore, it is important to understand what kind of influence MG exerts on work dynamics.
Myasthenia gravis (MG) is an autoimmune disease caused by autoantibodies to the postsynaptic site of the neuromuscular junction that induces weakness and fatigability of skeletal muscles [ 1, 2 ]. MG has different forms, and its impact on patients’ daily life depends on symptoms’ severity and on muscle involvement, which is usually categorized as ocular, generalized, bulbar, or respiratory [ 3, 4 ]. In recent studies, the prevalence rate of MG varies between 10.66 and 32.89 per 100,000 [ 5-7 ]. It is more common among women (about 70%), and the period of onset is around 20–40 years old (i.e., early onset), but late onset, which may span also up to 60–80 years old, is frequent as well [ 3, 8, 9 ].
Thus, MG affects persons of working age and causes significant limitations in daily life activities [ 10, 11 ], including patients’ involvement in work duties and therefore employment status [ 12 ]. The severity of interference in physical activities induces MG patients to modify the amount of physical work and, for example, to reduce working hours or to limit the kind of work activities to those not involving physical exertion [ 12 ]. However, many studies analyzed only the physical symptoms and limitations [ 13-15 ], and some psychosocial aspects, such as quality of life (QoL) [ 10, 16, 17 ], largely ignoring work-related issues. In addition, only few studies focused on the burden of MG in terms of costs, participation, work-related difficulties, sick leave, and job loss. For example, the study by Twork et al. [ 18 ] highlighted that 30.8% of respondents were employed but only 25.8% of patients worked >15 h/week. Conversely, in a study by Frost et al. [ 19 ], 82.1% of the sample was employed but after the diagnosis of MG 41.2% of patients experienced 9 or more weeks per years of sick leave. Thus, these studies report very different data on the proportion of employed patients and focused on different aspects of working life, and the information on work-related issues are sparse and not systematically reported. Therefore, we performed a systematic literature review with meta-analysis to address the employment status of MG patients.
Data Sources and Data Extraction
We searched SCOPUS looking for records containing the term “Myasthenia” in title, abstract, or keywords published in the period comprised between January 2000 and May 2019, so to get recent data on employment, and written in English. We looked for primary research articles, so excluded editorials, reviews, letter to the editors, conference proceedings, notes and erratum, books, and retracted articles.
We applied SCOPUS filters to exclude papers indexed in those subject areas clearly not dealing with the topic (e.g., arts and humanities, energy, material sciences, veterinary) and that would retrieve papers in which sample of human tissues, rather than patients, are included (e.g., biochemistry, genetics and molecular biology, Pharmacology, Toxicology, and Pharmaceutics). We also applied filters to exclude keywords referred to nonhumans, children, adolescents, or people aged 65 or over, or patients with conditions different from MG. Please see online supplementary Materials (see www.karger.com/doi/10.1159/000506310 ) for the complete search strategy.
At abstract check, we excluded studies that were based on animals and on biological samples (e.g., thymus tissues or blood samples); were not written in English; were reviews, letters to editors, books, editorials, case studies, and studies based on <10 participants; included only patients of non-working age (i.e., children and people aged 65 or over). At full-text screening, we selected those manuscript that enabled the identification of the number of employed subjects in each study (i.e., “employed,” “unemployed,” “type of occupation”).
Extracted information included employment status, that is, the fact that a given number of patients were identified as “employed” at the time of enrolment in the study with any kind of contract: this include employees, employers, and freelancers. In addition to these information, we extracted the following variables: gender, age, and symptoms duration in years, education (primary, secondary, high, university), previous thymectomy, prescribed medications at the time of inclusion in the study (pyridostigmine bromide, steroids, and immunomodulators, e.g., azathioprine, cyclosporin, mycophenolate mofetil, and cyclophosphamide), and MG type at the time of inclusion in the study. MG type was defined relying on the MG Foundation of America or on the Besta Neurological Institute rating scale for MG classification systems [ 20, 21 ], based on data availability.
Data Analysis
The measure of interest was the proportion of workers among subjects with MG. The confidence intervals were based on the score (Wilson) procedure [ 22 ]. All the meta-analytic estimates were derived using random-effects models [ 23 ]. The pooled estimates were calculated after Freeman-Tukey Double Arcsine Transformation [ 24 ] to stabilize the variances. We assessed the heterogeneity among studies using the χ 2 test [ 25 ], defining a significant heterogeneity as a p value of <0.10, and quantified the inconsistency using the I 2 statistic [ 26 ]. The following subgroup analyses were performed: by sex; age; educational level that was divided into primary and secondary school, high school and university; symptom duration; thymectomy; type of medication that was divided into pyridostigmine, steroids, and immunomodulatory treatments; type of MG-related muscle involvement divided into asymptomatic, ocular, and a single group for generalized, bulbar, and respiratory. We adopted such a division for MG-related muscle involvement because it is not infrequent that studies address one kind of patients (e.g., only with bulbar symptoms) or discern between ocular and the other ones. In each subgroup analysis, the included studies were divided into 2 groups based on the corresponding median value (e.g., in the subgroup analysis by sex, we compared studies with a proportion of women ≥ median value calculated on all studies, that is, 59% versus those with a proportion of women <59%).
The search yielded 1,045 results. Of these, 19 articles fitted the inclusion criteria related to the employment status and thus were considered for the analysis (Fig. 1 ) [ 17-19, 27-42 ]. Table 1 reports the information extracted for each single study. In total, 3,600 participants were included in the different studies, of whom 2,140 were females and with an average age of 47.5 (range 35–60): of all included participants, 1,579 were employed.
Characteristics of the included studies

Flow chart of papers’ selection.
Figure 2 shows the forest plot of the proportion of workers in each study: such a proportion varied from 28 [ 31 ] to 82% [ 19 ], with an extreme heterogeneity between studies. Overall, the pooled proportion of workers was 50% (95% CI 41–60%).

Forest plot for the overall employment rate. Estimated proportion (ES) of workers.
Table 2 reports the summary statistics of the subgroup analyses. Results showed no significant differences between groups, although higher proportions were observed in studies with a percentage of women higher than 59% (+7% compared to studies with a percentage of women lower than 59%); with participants on average younger than 48 years (+15% compared to studies with participants on average older than 48 years); with >22% of participants achieved university degree (+14% compared to studies with a percentage of participants achieved university degree lower than 22%); with participants with mean symptom duration lower than 8.85 years (+17% compared to studies with participants with mean symptom duration higher than 8.85 years); with a percentage of participants thymectomized lower than 48% (+11% compared to studies with a percentage of participants thymectomized higher than 48%); and with a percentage of participants with generalized, bulbar, or respiratory symptoms lower than 61% of patients (+10% compared to studies with a percentage of participants with generalized, bulbar, or respiratory symptoms higher than 61%).
Percentage of workers in subgroups analysis

The results of our meta-analysis show that the proportion of employed people with MG was 50% (95% CI 41–60%). This percentage is considerably low if we take into account that the average age of MG participants involved in the included studies was around 48 years, thus in peak of working life. Our results also show that there were no significant differences in the proportion of employed patients by age, gender, education, symptoms duration, thymectomy, treatment, and muscle involvement. However, higher proportions were observed in studies with a higher percentage of women, younger participants, with a higher level of education, shorter MG duration, and less frequently thymectomized, whereas a lower proportion was observed among those with generalized, bulbar, and respiratory symptoms.
Considering the mean age of participants involved in the included studies, the impact of MG on employment is relevant. The employment rate of people with chronic disease is less than half compared with that of economically active population [ 43 ]. In 2018, the employment rate of general European population aged 20–64 was 73.2% [ 44 ]. In a Dutch study [ 45 ] that evaluated the impact of several chronic diseases on work, patients with musculoskeletal diseases had higher probabilities to have work disability and a living allowance, but they had a lower probability to be unemployed. In another study conducted on the factors related to unemployment in Europe [ 46 ], the employment rate of people with no chronic conditions was 75.5%, while the employment rate of people with one or more chronic conditions was around 59%. The proportion of employed patients found in our study (i.e., 50%, 95% CI 41–60%) therefore show that the impact of MG on employment status is slightly stronger than the average of chronic conditions in general. If we contrast proportion of employed MG patients to the employment rates of the general population described above, that is, around 75% [ 44-46 ], we can reasonably presume that MG is responsible for a 15–35% decrease. Such an information is however to be read with caution. In fact the mean age of participants to the different studies ranged between 35 and 60 years: so it is reasonable that a portion of participants may be retired due to age.
Therefore, it is important to understand what kind of influence MG exerts on work dynamics. Although we found no significant differences in the proportion of employed MG patients by age, gender, education, symptoms duration, thymectomy, treatment, and muscle involvement, some trends can be reported. Our data in fact suggested a possible higher proportion of workers among women, younger participants, those with a higher level of education, shorter MG duration, and non-thymectomized ones, whereas a lower proportion was observed among those with generalized, bulbar, and respiratory symptoms. It has however to be carefully considered that we could rely on a limited number of studies, namely, 19 drawn out of a set of 1,045 records, that is, <2%: these variables need therefore to be exploited in future retrospective and prospective analyses, to ascertain whether they are or not predictors of job loss. It is moreover desirable that information on employment status in MG patients is routinely reported, so that future analyses may collect relevant data also on investments on health on containment of indirect costs. Heterogeneity of results emerged here as a problem with interpretation of data, as the percentage of employed patients ranged between 28 and 82%. Other reviews facing the same problem, for example, Wo et al. [ 47 ] did not perform meta-analysis and decided to report trends between variables, such as the inverse trend between clinical severity and employment rates, or differences by countries or year in which the study was carried out. In our case, choosing to highlight the heterogeneity of results by a meta-analysis was a way to focus the attention of researchers on employment in MG patients.
The connection between MG and job loss deserves more attention given the obvious implication of unemployment in terms of societal costs of the disease, as well as in terms of its effect on patients’ QoL. Research has shown that QoL and employment status are strictly connected variables [ 48-50 ], and QoL in MG is an outcome of importance, as treatment for MG is a lifelong one [ 50 ], and QoL in MG patients is lower than normative values [ 27, 51-54 ]. However, the majority of papers addressing QoL of MG patients did not account for employment status and even less for the way MG can affect work performance. Only Twork et al. [ 18 ] took into consideration the employment status and found that work-related capabilities of MG patients are limited by physical impairments, which is consistent with the features of MG. However, many people carry out work-related tasks that involve cognitive rather than physical skills, and in which fatigue may likewise exert some effect, but the understanding of the existence and the degree of such an association is in its infancy.
Job loss of course is a driver of increased financial burden of MG. Most of the studies, such as those by Guptill et al. [ 55, 56 ], addressed only direct healthcare cost related to MG. Indirect costs were addressed by a German study [ 57 ], where the total annual costs of MG were around Euro 14,950 per patient, of whom 2,790 (i.e., 19%) was due to indirect cost, and premature retirement held the second rank among MG cost categories. In the analysis of Twork et al. [ 18 ], MG had an influence on patient’s workforce participation, as 8.5% of MG patients changed their job due to MG, 21% experienced difficulties in their job and 28.3% early retired. Issues connected to employment have however to be defined also on the actual reasons for not being employed, which include, for example, age-related retirement, sick leave, maternity leave, or personal decision (e.g., being an housekeeper). Future prospective studies should address such differences.
Limitations of this study are referred, first of all, to the use of SCOPUS only for the search. Such a choice was based on its wide coverage, which would have enable to reach a wide set of document, including those of nonmedical journals. Second, we used only “myasthenia” as a search term and excluded those areas that were likely not relevant (e.g., nonhuman, child/adolescents, human tissue): we cannot be completely sure that some of these documents contained information on employment status.
In conclusion, our meta-analytic review on employment status of patients with MG, covering the period from January 2000 to May 2019, shows that the proportion of employed MG patients was 50% (95% CI 41–60%). It has to be noted that the information herein produced was based on a limited number of studies, the main reason being the overall lack of data on employment status in the vast majority of the studies retrieved by our search. If contrasted to data on the general populations, for whom employment rates were reported around 75%, we can presume that MG is responsible for a 15–35% decrease in the proportion of employed subjects.
As a chronic disease, MG has a severe impact on patients’ lives and their socioeconomic status. The loss of productivity, premature retirement, or job loss can cause relevant problems both on outcomes of the diseases and on QoL. Future studies should explore the effect of MG on employment status, either retrospectively and prospectively, and the information on employment status of MG patients should routinely be reported: in this way, future meta-analytic reviews might collect more data and give more consistent results on the effect of investments on health over indirect cost reduction.
A.R. is supported by a grant from the Italian Ministry of Health (Ricerca Corrente, Fondazione Istituto Neurologico C. Besta, Linea 4 – Outcome Research: dagli Indicatori alle Raccomandazioni Cliniche).
Not applicable.
The authors have no conflicts of interest to declare.
No funding was available for this manuscript.
E.G. conception, literature review phase, writing of the first draft, review, and critique. I.T. analysis, review, and critique. C.T. literature review phase, review, and critique. M.L. and R.M. conception, review, and critique. S.B. and R.F. review and critique. A.R. conception, literature review phase, review, and critique.
Email alerts
Citing articles via, suggested reading.
- Online ISSN 1423-0208
- Print ISSN 0251-5350
INFORMATION
- Contact & Support
- Information & Downloads
- Rights & Permissions
- Terms & Conditions
- Catalogue & Pricing
- Policies & Information
- People & Organization
- Stay Up-to-Date
- Regional Offices
- Community Voice
SERVICES FOR
- Researchers
- Healthcare Professionals
- Patients & Supporters
- Health Sciences Industry
- Medical Societies
- Agents & Booksellers
Karger International
- S. Karger AG
- P.O Box, CH-4009 Basel (Switzerland)
- Allschwilerstrasse 10, CH-4055 Basel
- Tel: +41 61 306 11 11
- Fax: +41 61 306 12 34
- Contact: Front Office
- Experience Blog
- Privacy Policy
- Terms of Use
This Feature Is Available To Subscribers Only
Sign In or Create an Account
- Open access
- Published: 20 December 2021
Global prevalence of myasthenia gravis and the effectiveness of common drugs in its treatment: a systematic review and meta-analysis
- Nader Salari 1 ,
- Behnaz Fatahi 2 ,
- Yalda Bartina 3 ,
- Mohsen Kazeminia 2 ,
- Reza Fatahian 4 ,
- Payam Mohammadi 5 ,
- Shamarina Shohaimi 6 &
- Masoud Mohammadi ORCID: orcid.org/0000-0002-5722-8300 7
Journal of Translational Medicine volume 19 , Article number: 516 ( 2021 ) Cite this article
14k Accesses
23 Citations
319 Altmetric
Metrics details
Myasthenia gravis is a neuromuscular autoimmune disorder characterized by weakness and disability in the voluntary muscles. There have been several preliminary studies on the epidemiology of myasthenia gravis in different parts of the world and the effectiveness of common drugs in its treatment, but there has been no comprehensive study of the efficacy of common drugs in the treatment of myasthenia gravis. Therefore, this study aimed to determine the epidemiology of myasthenia gravis globally and the effectiveness of common drugs in its treatment using systematic review and meta-analysis.
Research studies were extracted from IranDoc, MagIran, IranMedex, SID, ScienceDirect, Web of Sciences (WoS), ProQuest, Medline (PubMed), Scopus and Google Scholar based on Cochran's seven-step guidelines using existing keywords extracted in MeSH browser. The I 2 test was used to calculate the heterogeneity of studies, and Begg and Mazumdar rank correlation tests were used to assess publication bias. Data were analyzed using Comprehensive Meta-Analysis software (Version 2).
In the search for descriptive studies based on the research question, 7374 articles were found. After deleting articles unrelated to the research question, finally, 63 articles with a sample size of 1,206,961,907 people were included in the meta-analysis. The prevalence of MG worldwide was estimated to be 12.4 people (95% CI 10.6–14.5) per 100,000 population. For analytical studies on the effectiveness of common myasthenia gravis drugs, 4672 articles were found initially, and after removing articles unrelated to the research question, finally, 20 articles with a sample size of 643 people in the drug group and 619 people in the placebo group were included in the study. As a result of the combination of studies, the difference between the mean QMGS score index after taking Mycophenolate and Immunoglobulin or plasma exchange drugs in the group of patients showed a significant decrease of 1.4 ± 0.77 and 0.62 ± 0.28, respectively (P < 0.01).
The results of systematic review of drug evaluation in patients with myasthenia gravis showed that Mycophenolate and Immunoglobulin or plasma exchange drugs have positive effects in the treatment of MG. It also represents the positive effect of immunoglobulin or plasma exchange on reducing SFEMG index and QMGS index and the positive effect of Mycophenolate in reducing MG-ADL index, SFEMG and Anti-AChR antibodies index. In addition, based on a meta-analysis of the random-effect model, the overall prevalence of MG in the world is 12.4 people per 100,000 population, which indicates the urgent need for attention to this disease for prevention and treatment.
Myasthenia gravis (MG) is a neuromuscular disease characterized by weakness in the voluntary muscles [ 1 , 2 ]. This disease has different symptoms that vary in different patients depending on the degree of involvement of the striated muscles. The most common type of symptom in patients with myasthenia gravis is ocular symptoms, which appear as ptosis and diplopia. These symptoms usually occur at the end of the day and follow activities such as watching TV or driving is more common, and excessive fatigue has been reported due to frequent activity in patients with this disease [ 3 ].
Myasthenia gravis is an autoimmune disease that connects the nerve to the muscle (NMJ) [ 4 ], which is produced by different antibodies against synaptic membrane proteins [ 5 ]. This is usually more than 85% of cases and is caused by a type of antibody against the skeletal muscle acetylcholine receptor (AChR-Ab) [ 6 , 7 ]. However, components other than AChR, such as muscle-specific tyrosine kinase receptor (MuSK) or lipoprotein-associated protein 4 (LRP4), may also be targeted for the autoimmune attack [ 6 , 8 , 9 ].
Based on the mechanism of autoimmune disease and antibodies, invasive skeletal muscle molecules, thymus status, genetic characteristics, disease phenotype and response to treatment, myasthenia gravis is divided into early and late ocular subtypes (OMG), seronegative, thymoma, LRP4, MuSk. Diagnosis of MG subtype influences treatment decisions and disease prognosis [ 10 , 11 ]. Approximately 50% of patients with OMG develop general myasthenia gravis (GMG) over a 2-year period, which affects other muscles and manifests as weakness and ocular symptoms [ 12 ].
According to a systematic population-based study, CAR et al. [ 13 ] estimated the incidence and prevalence of MG at 54 per million and 77.7 per million, respectively. However, significant changes have been reported in various studies. The incidence of this disease has shown a range between 1.77 and 21.3 per million people and the prevalence of 15 to 179 million people [ 13 ]. A large number of epidemiological studies, mainly in Western Europe and Asia, reported significant differences in the incidence and prevalence of MG. The incidence of myasthenia gravis ranged from 1.7 to 30 per million per year [ 14 , 15 , 16 , 17 ].
The disease has two age peaks: age 40–40 years, which mainly affects women, and another 80–60 years, which occurs equally in men and women [ 4 ].
Current treatment options mainly include acetylcholinesterase inhibitors, glucocorticoids (GC), intravenous immunoglobulin (IVIg), plasma replacement (PLEX), thymectomy, and immunosuppressive agents including azathioprine prednisone, cyclosporine, cyclosporine, and cyclosporine [ 18 , 19 , 20 , 21 , 22 , 23 , 24 ]. However, the use of corticosteroids and immunosuppressants such as azathioprine manages MG. However, many patients do not tolerate or respond adequately to these drugs, and long-term treatment with GC is associated with a significant risk of side effects such as diabetes, obesity, and high blood pressure. This has led to the introduction of newer immunosuppressants such as mycophenolate mofetil (MMF) [ 12 , 25 , 26 , 27 ].
About 15% of patients with general myasthenia gravis do not respond to immunosuppressants and require intravenous immunoglobulin (IVIg) or plasma replacement (PLEX) to improve their symptoms [ 28 , 29 ]. Intensified cases and myasthenia gravis crisis also require immediate treatment due to poor swallowing or respiratory failure that threatens the lives of these patients and muscle defects that may be a major disability for their daily activities [ 30 ].
Therefore, additional immunosuppression is often treated with Plasma Freesia (PLEX) and intravenous immunoglobulin (IVIg) to relieve symptoms. Plasma freeze uses filtration to kill pathological antibodies used in patients with myasthenia gravis and severe MG [ 31 , 32 , 33 ].
Myasthenia gravis has high direct health care costs (including long-term treatment and periodic hospitalization costs) and indirect costs such as loss of income and reduced care productivity [ 34 ]. Therefore, accurate identification of patients with MG is vital for organizing health care services and implementing preventive health measures. Many early articles have been done on the prevalence of myasthenia gravis and the effect of different drugs on the treatment process, but appropriate policy to control, diagnose and treat this disease requires coherent, accurate and uniform information. Therefore, the present study was performed to estimate the prevalence of myasthenia gravis globally and determine the effectiveness of the most common drugs in the treatment of patients by systematic review and meta-analysis.
The present systematic review and meta-analysis were conducted according to the Cochrane seven-step approach, including selecting research questions, determining inclusion and exclusion criteria, identifying descriptive articles, selecting studies, qualitative evaluation of studies, data extraction, analysis and interpretation of findings [ 35 ].
Research question and determining the keywords of the descriptive section
According to the research question in the descriptive section, "How has the prevalence of MG in the world changed?" The population included: MG patients, Outcome included MG prevalence, Time or duration Included: Date of publication of the first related article until 15 November 2020 and type of study (study design) Included: cross-sectional (descriptive) studies. Keywords were extracted from the MeSH browser. Keywords related to the studied population (P): Myasthenia Gravis, MG and outcome keywords (O); Prevalence and Epidemiology.
Research question and determining the keywords of the analytical section
According to the research question of the analytical section, "What is the effectiveness of Corticosteroids, Mycophenolate and Immunoglobulin or plasma exchange drugs in the treatment of MG?" According to the PICO guidelines, the study population (Population) includes patients with MG, intervention (intervention) including Corticosteroids, Mycophenolate and Immunoglobulin or plasma exchange, analogous (Comparison) including QMGS index score, Anti-AChR antibodies, SFEMG And MG-ADL before and after the intervention, the outcome (Outcome) included: changes in QMGS, Anti-AChR antibodies, SFEMG and MG-ADL after the intervention. Keywords were extracted from the MeSH browser according to PICO instructions. Keywords related to the study population (P): Myasthenia Gravis, MG Keywords related to the intervention (I); Corticosteroids, Corticotropin, Alternate-day prednisone, Methylprednisone, Prednisolone, Mycophenolate, Immunoglobulin or plasma exchange, Intravenous immunoglobulin, IVIG and keywords related to analogy (C) and outcome (O); QMGS, QMG, Anti-AChRantibodies, Anti-AChR ab, SFEMG and MG-ADL.
Criteria for inclusion and exclusion according to the descriptive research question
Cross-sectional (descriptive) studies in chronic patients reporting the prevalence of MG in different parts of the world published in English, and the full text was available. Observational studies, cohort, case–control, analytical and interventional studies, case reports, short reports, letters to the editor and studies unrelated to the research question were excluded from the study.
Criteria for inclusion and exclusion according to the research question of the analytical section
Clinical trial studies that reported the mean and standard deviation of the effect of Corticosteroids, Mycophenolate and Immunoglobulin or plasma exchange on at least one of the indicators of QMGS, Anti-AChR antibodies, SFEMG and MG-ADL in patients with MG, in Persian and were printed in English and their full text was available and included in the study. Descriptive studies, cross-sectional studies, reviews, case reports, short reports, letters to the editor, and other studies unrelated to the research question were excluded from the study.
Articles identification
To find studies related to research questions, four Persian databases, including IranDoc, MagIran, IranMedex and SID and five international databases: ScienceDirect, Web of Science (WoS), ProQuest, Medline (PubMed), Scopus were searched. The Google Scholar scientific search engine was reviewed for final review. No time limit was set for the search to retrieve the relevant research, so all articles published by November 15, 2020, were reviewed. The search was limited to studies published in Persian and English. The search strategy in each database was determined using Advanced Search (Advanced Search) with the help of all possible keyword combinations with the help of (AND) and (OR) operators. For example, the search strategy in the PubMed database for the descriptive part of the research was determined as follows:
(((Prevalence [Title/Abstract]) OR (Epidemiology [Title/Abstract])) AND (Myasthenia Gravis [Title/Abstract])) OR (chronic patients [Title/Abstract]) OR (MG [Title/Abstract]).
Also, the search strategy in the PubMed database for the analytical part of the research was determined as follows:
((((((((((((((((Corticosteroids[Title/Abstract]) OR (Corticotropin[Title/Abstract])) OR (Alternate-day prednisone[Title/Abstract])) OR (Methylprednisone [Title/Abstract])) OR (chronic patients [Title/Abstract]) OR (Prednisolone[Title/Abstract])) OR (Mycophenolate[Title/Abstract])) OR (Immunoglobulin[Title/Abstract] OR plasma exchange[Title/Abstract])) OR (Intravenous immunoglobulin[Title/Abstract])) OR (IVIG[Title/Abstract])) AND (QMGS[Title/Abstract])) OR (QMG[Title/Abstract])) OR (Anti-AChR antibodies[Title/Abstract])) OR (Anti-AChR ab[Title/Abstract])) OR (SFEMG[Title/Abstract])) OR (MG-ADL[Title/Abstract])) AND (Myasthenia Gravis[Title/Abstract])) OR (MG[Title/Abstract]).
In order to access the latest published studies, an alert was created on several databases, including PubMed and Scopus, to check if new articles were published during the study. Also, in order to access all related studies, the sources of articles that met the inclusion criteria were manually reviewed. To avoid errors, all steps of article search, study selection, qualitative evaluation and data extraction were performed independently by two researchers (M.K. and B.F.). If there was a difference of opinion between the researchers regarding the inclusion of the article in the study, in order to avoid the risk of bias for specific studies, first a final agreement was reached through discussion and in some cases with the participation and opinion of a third party (MM).
Selection of studies based on entry and exit criteria
Based on the 4-step PRISMA process, including article identification, screening, eligibility, and inclusion in the study, three researchers reviewed this process as follows, and studies were selected based on inclusion and exclusion criteria. All articles found in each database were transferred to EndNote X8 software. After completing the search in all the databases, the articles repeated in different databases were deleted. Then, in order to avoid the risk of bias in selecting studies, the names of the authors and the titles of the journals were removed, and a checklist was prepared based on the titles and abstracts of the studies. In the next step, two authors (M.K. and B.F.) independently examined the title and abstract of the studies and eliminated studies that were not related to the research based on the inclusion and exclusion criteria of the study and in case of discrepancy, it was examined by the third researcher (M.M). Studies whose full text was not found were also excluded from the systematic review and meta-analysis process. The full text of all remaining articles was then evaluated. Studies that did not meet the inclusion criteria based on the research question were excluded.
Qualitative evaluation of descriptive studies
Qualitative evaluation of studies was performed using the STROBE checklist, a suitable tool for the qualitative assessment of descriptive studies. This checklist has 22 general items, each of which has sub-items (32 sub-items in total) and to evaluate different parts of a study, including title and abstract, study objectives, problem statement, study type, sampling method, study statistical population, the sample size is the definition of variables, tools for collecting study data, statistical analysis, findings and discussion. In order to rate the articles, if each article referred to the items considered in the checklist, it was given a score of 1, and if it was not mentioned, a score of zero was given. The minimum and maximum scores in this checklist are 0 and 32, respectively. Articles with scores of 16 and above were considered high and medium quality studies and were included in the systematic review and meta-analysis process, and articles with scores below 16 were considered low-quality studies [ 36 ].
Qualitative evaluation of analytical studies
Qualitative evaluation of studies was performed using the CONSORT checklist, a suitable tool for the qualitative assessment of interventional studies. This checklist has 25 general items, each with minor items (a total of 37 minor items). Different sections include Title and Abstract, Introduction and Background, Methods, Participants, Interventions, Objectives, Consequences, Sample Size, Randomization, How to Assign Participants, Blind Allocation, Execution, Blindness of Study, Statistical Methods, Results, Flow Participants' presence, sampling method, initial data of the number of people analyzed, consequences and estimates, auxiliary analysis, adverse reactions, explanations, interpretation, generalizability and general evidence. In this study, all general checklist items were reviewed by two authors (M.K. and B.F.). In order to rate the articles, if each article referred to the items in the checklist, it was given a score of 1, and if it was not mentioned, a score of zero was given. The minimum and maximum scores in this checklist are 0 and 37, respectively. Studies with 75% or more of the maximum achievable score (score greater than or equal to 27) with “high quality”, studies with a score between 75 and 50% (score 18–26) as “average quality” and studies with a score below 50% (less than or equal to 17) were considered “low quality” studies [ 37 ]. Based on this checklist, medium and high-quality articles were included in the study, and low-quality articles were excluded.
Data extraction
After selecting the studies to enter the systematic review and meta-analysis process, the data were extracted, and the studies were summarized. For this purpose, two electronic checklists (one for the descriptive section and one for the analytical section) were prepared. The various items in the descriptive checklist included: name of the first author, year of publication and year of the report, place of study, age, sample size and prevalence, and various items in the analytical checklist, including the name of the first author, year of publication, place of research, the sample size of the drug group and the placebo group was the type of drug, mean and standard deviation before and after the intervention.
Statistical analysis of the descriptive part
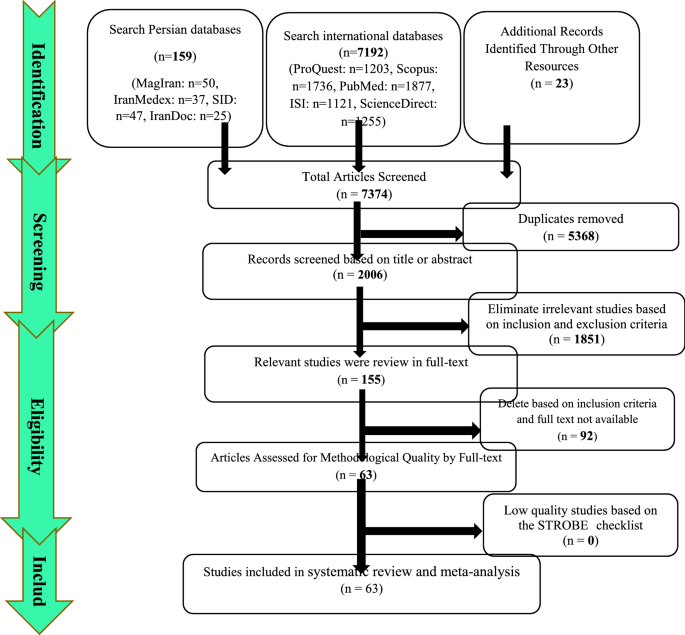
To analyze and combine the results of different studies, in each study, the prevalence of MG was considered as the probability of binomial distribution and its variance was calculated through binomial distribution. Heterogeneity of studies was assessed using the I 2 test, and the random-effects model was used in the case of the I 2 index above 50%. In this model, parametric changes between studies are also considered in the calculations, so it can be said that the results of this model in heterogeneous conditions can be more generalized than the model with a fixed effect. Publication bias assessment was performed using Funnel Plot and Begg and Mazumdar rank correlation test. Data were analyzed using Comprehensive Meta-Analysis (Version 2) software, and the significance level of the test was P < 0.05.
Statistical analysis of the analytical section
In this study, the standardized mean difference was calculated. The main outcome of this study was the mean score of the studied indicators before and after the intervention in patients with MG. As a result, the mean and standard deviation of the studied indices before and after the intervention were extracted. I 2 index was used to evaluate heterogeneity. Funnel Plot and Begg and Mazumdar rank correlation tests were used to assess the publication bias. The significance level of the test was considered 0.1. Data were analyzed using Comprehensive Meta-Analysis software (Version 2).
Descriptive part of the study
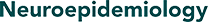
Summary of how articles enter meta-analysis: In the first stage, 7374 articles (7192 articles in international databases, 159 articles in Persian databases and 23 studies in reviewing article sources) were found, of which 5368 studies were repeated in different databases were removed. A total of 2006 studies were entered the in the screening stage and 1851 articles were deleted based on the inclusion and exclusion criteria by reviewing the title and abstract of the study. In the next stage (competency assessment), out of the remaining 155 studies from the screening stage, 92 articles were removed by reviewing the full text of the article because it was not relevant to the research. The quality evaluation of 63 articles included in this study was performed using the STROBE checklist, all of which were of medium and high quality according to the criteria of this tool. Thus, 63 articles related to the descriptive part of the study entered the process of systematic review and meta-analysis (Fig. 1 ).
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA 2009) flow diagram Descriptive section
General characteristics of the studies
The total sample size of the studies was 1,206,961,907 people. The studies were published between 1969 and November 15, 2020. There were 8 studies in Asia, 42 in Europe, 7 in the United States, 5 in Africa, and 1 in Australia. Summary of study characteristics, including the name of the first author, year of publication and year of the report, place of study, mean age of patients, sample size and prevalence of MG, are reported in Table 1 .
Systematic meta-analysis and descriptive review
The result of the I 2 test for the prevalence of MG in the world indicates a significant heterogeneity between studies (I 2 = 99.9), so the data were analyzed by meta-analysis using a random-effects model. Due to the high heterogeneity of the studies, sensitivity analysis was performed, and each study's effect on the final result and the degree of heterogeneity was evaluated. None (P = 0.103) (Fig. 2 ). As a result of the combination of studies, the overall estimate of the global prevalence of MG 1 2 . 4 people (95% confidence interval: 10-14-5.5) per 100,000 population was based on a random-effects model. The black square is the prevalence and the length of the line segment on which the 95% confidence interval per It is a study, the rhombus symbol shows the worldwide prevalence for all studies (Fig. 3 ). The highest prevalence was reported in Salvado et al. [ 61 ]; 3463 per 100,000 population and the lowest prevalence Bettini et al. [ 58 ]; 0.006 people reported per 100,000 population.
Funnel plot Results for estimating the prevalence of Myasthenia Gravis worldwide

Estimation of the prevalence of Myasthenia Gravis in the world based on a random-effects model
According to different reports of MG prevalence in different parts of the world, subgroup analysis by different continents (Asia, Europe, Africa and America) is reported in Table 2 , which has the highest prevalence in the Americas with 19 people (95% CI 15–23.8) (Table 2 ).
The analytical part of the study
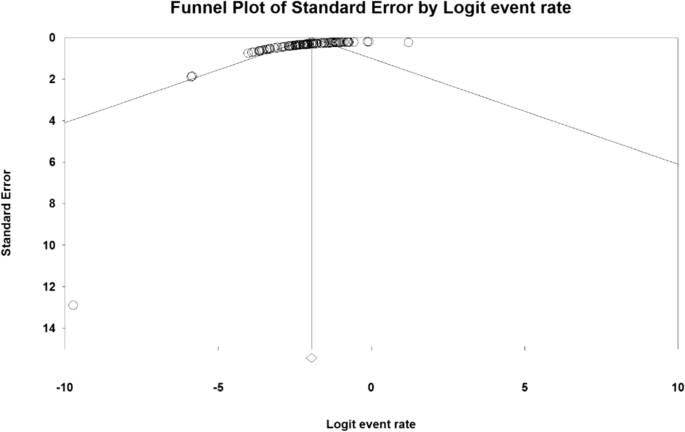
Summary of how to enter articles: In the first stage, 4672 articles (4596 articles in international databases, 45 articles in Persian databases and 31 studies in reviewing the sources of articles) were found, and 3126 studies that were repeated in different databases were deleted. 1546 studies were entered in the screening stage, and based on the inclusion and exclusion criteria, the article was removed by reviewing the title and abstract of the 1992 studies. In the next stage (competency assessment), out of the remaining 175 studies from the screening stage, 183 articles were removed by reviewing the full text of the article because it was not relevant to the research. The remaining 22 articles were evaluated qualitatively by the CONSORT checklist, of which 2 studies were of low quality according to the criteria of this tool and were excluded from the study. Therefore, 20 articles related to the analytical part of the study were included in the systematic review and meta-analysis process (Fig. 4 ).
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA 2009) flow diagram Analytical section
General characteristics of analytical studies
The total sample size was 643 in the drug group and 619 in the placebo group. The studies were published between 1976 and November 15, 2020. The smallest sample size was related to the study of Benatar et al. [ 109 ] with 6 patients in the drug group and 5 patients in the placebo group, and the largest sample size was related to the study of Sanders et al. [ 112 ] with 88 patients in the drug group and 88 patients in the placebo group. Summary of study characteristics including the name of the first author, year of publication, place of study, sample size, type of drug, and mean and standard deviation before and after the intervention of QMGS, Anti-AchR antibodies, SFEMG and MG-ADL indices are reported in Table 3 .
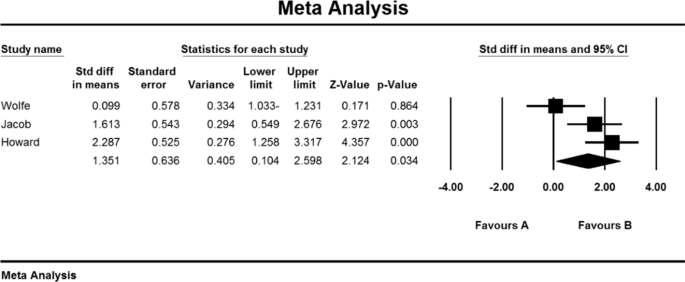
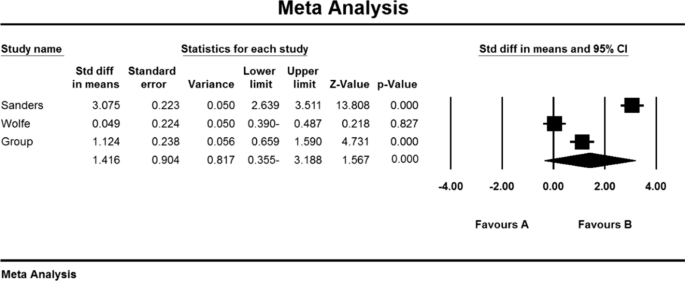
Immunoglobulin or plasma exchange drugs
A total of 13 studies examined the effect of immunoglobulin or plasma exchange drugs on MG patients. Studies were reported from 1997 to 2020. 11 studies examined the QMGS index, 4 studies the Anti-AChR antibodies, 4 studies the SFEMG index, and 3 the MG-ADL index.
MG-ADL index
The Daily Living Activity Scale (MG-ADL) is an 8-item scale to assess secondary ocular disability (two items), bulbar (three items), respiratory (one item), limb (two items) related to myasthenia gravis effects. This scale has a linear rating from zero to 3, and its overall scoring range is from zero to 24 [ 115 ]. The patient's MG-ADL questionnaire is completely reported without training and specialized equipment and usually lasts less than five minutes [ 116 ].
Based on the present meta-analysis results between studies, there is a lot of heterogeneity (I 2 = 78.5), so the stochastic effects model was used to combine the studies and the final result. Begg and Mazumdar rank correlation to test the publication bias in the studies for the MG-ADL index (P = 1.000) (Table 4 ).
As a result of the combination of studies, the mean score of MG-ADL indices before the intervention in the drug group was 8.2 ± 1.3. After the intervention was 4.0 ± 4.84 (Table 4 ), as well as the difference between the mean of the MG-ADL index before and after the intervention, 1.3 ± 0.63 was obtained (P < 0.01) (Fig. 5 ), which indicates the positive effect of Immunoglobulin or plasma exchange on the reduction of MG-ADL index.
Accumulation chart of studies included in the meta-analysis based on the difference between the mean MG-ADL index before and after the intervention for Immunoglobulin or plasma exchange
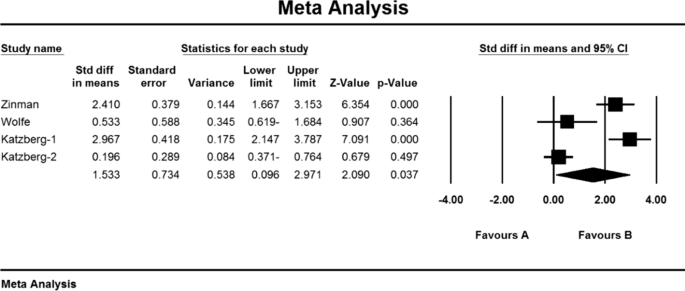
SFEMG index
Single-fiber electromyography (SFEMG) is an efficient tool to investigate neurotransmitter disorders. In this method, with the help of bipolar needle electrodes, the action potential of two adjacent muscle fibres belonging to a motor unit that have been activated voluntarily or electrically stimulated can be recorded [ 117 ]. This technique is more time consuming than conventional EMG, and patient cooperation in this method is effective because even small movements by the patient can lead to loss or change of action potential [ 118 ].
Based on the present meta-analysis results between studies, there is a lot of heterogeneity (I 2 = 43.5), so the stochastic effects model was used to combine the studies and the final result. Begg and Mazumdar rank correlation tests were not available in studies for the SFEMG index (P = 1.000) (Table 4 ). As a result of the combination of studies, the mean score of SFEMG indices before the intervention in the drug group was 82.2 ± 1.43, and after the intervention was 54/5 ± 27/5 (Table 4 ), also, the difference between the mean of SFEMG index before and after the intervention was 1.5 ± 0.73 (P < 0.01) (Fig. 6 ), which indicates the positive effect of immunoglobulin or plasma exchange on the reduction of SFEMG index.
Accumulation chart of studies included in the meta-analysis based on the difference between the mean SFEMG index before and after the intervention for Immunoglobulin or plasma exchange
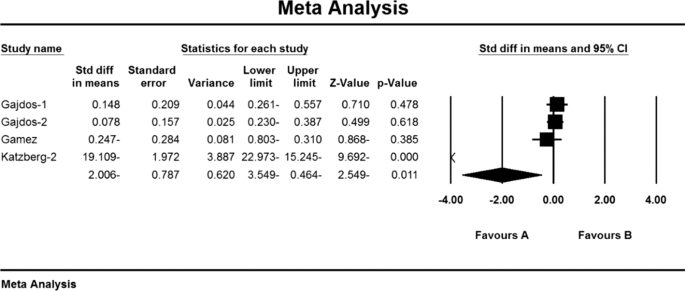
Anti-AChR antibodies index
Weakness and fatigue in myasthenia gravis are caused by a decrease in acetylcholine receptors due to an autoimmune attack of antibodies at the neuromuscular junction. Specific antibodies induce this autoimmune response against the acetylcholine receptor by blocking or binding to the receptor or postsynaptic membrane damage [ 119 ].
Based on the present meta-analysis results, there is a lot of heterogeneity between studies (I 2 = 99.8), so the stochastic effects model was used to combine the studies and the final result. Begg and Mazumdar rank correlation test Emission bias was not presented in studies for Anti-AChR antibodies index (P = 1.000) (Table 4 ). As a result of the combination of studies, the mean score of Anti-AChR antibodies before the intervention in the drug group was 10.8 ± 4.6 and after the intervention was 52.7 ± 34.1 (Table 4 ). AChR antibodies were obtained before and after the intervention at − 2.006 ± 78.7 (P < 0.01) (Fig. 7 ), indicating that Immunoglobulin or plasma exchange did not affect the Anti-AChR antibodies index. QMGS index.
Accumulation chart of studies included in the meta-analysis based on the mean difference of the anti-AChR antibodies index before and after the intervention for Immunoglobulin or plasma exchange
Myasthenia Gravis Quantitative Score (QMGS) is a 13-item scale developed by Tindall et al. [ 120 ] and modified by Barohn et al. [ 121 ] to be used to determine the severity of myasthenia gravis. This scale measures ocular, bulbar, respiratory, and limb function and scores each finding from zero (no myasthenic findings) to 39 (maximum myasthenic defects) [ 122 , 123 ].
Based on the present meta-analysis results, there is a lot of heterogeneity between studies (I 2 = 98.6), so the random-effects model was used to combine the studies and the final result. Begg and Mazumdar rank correlation test was not possible in the studies for the QMGS index (P = 0.391) (Table 4 ).
As a result of the combination of studies, the mean score of QMGS indices before the intervention in the drug group was 11.2 ± 1.6 and after the intervention was 9/1 ± 4/8 (Table 4 ), as well as the difference between the mean of the QMGS index before and after the intervention. 0.62 ± 0.28 was obtained (P < 0.01) (Fig. 8 ), which indicates the positive effect of Immunoglobulin or plasma exchange on QMGS index reduction.
Accumulation diagram of meta-analysis studies based on mean differences in mean QMGS before and after intervention for Immunoglobulin or plasma exchange
Mycophenolate
In total, 4 studies examined the effect of Mycophenolate on MG patients. 4 studies reviewed the QMGS index, 2 studies the Anti-AChR antibodies index, 1 study the SFEMG index and 3 studies the MG-ADL index.
Based on the results of the present meta-analysis studies, there is a lot of heterogeneity (I 2 = 85.3), so the stochastic effects model was used to combine the studies and the outcome. Begg and Mazumdar rank correlation test of publication bias was not possible in the studies for MG-ADL index (P = 1.000) (Table 4 ).
As a result of the combination of studies, the mean score of MG-ADL indices before the intervention in the drug group was 5.9 ± 0.87 and after the intervention was 7.4 ± 5.09 (Table 4 ), as well as the difference between the mean of the MGADL index before and after The intervention showed 1.4 ± 0.9 (P < 0.01) (Fig. 9 ) which indicates the positive effect of Mycophenolate on the reduction of MG-ADL index.
Accumulation chart of studies entered for meta-analysis based on the difference between the mean MG-ADL index before and after intervention for Mycophenolate
Based on the present meta-analysis results between studies, according to a study, there was no heterogeneity (I 2 = 0), so the fixed effects model was used to combine the study and the final result. It was not possible to perform Begg and Mazumdar rank correlation test in the studies for the SFEMG index according to the study of only one research (Table 4 ).
As a result of the combination of studies, the mean score of SFEMG indices before the intervention in the drug group was 71.5 ± 11.3 and after the intervention was 60.5 ± 13.1 (Table 4 ), as well as the difference between the mean of the SFEMG index before and after the intervention. 0.9 ± 0.56 was obtained (P < 0.01), indicating Mycophenolate's positive effect on SFEMG index reduction.
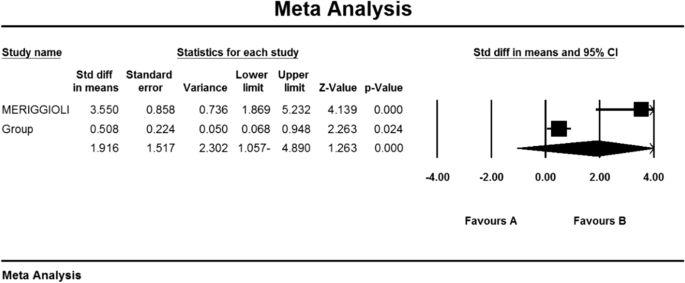
Index of anti-AChR antibodies
Based on the present meta-analysis results between studies, there is a lot of heterogeneity (I 2 = 79.1), so the stochastic effects model was used to combine the studies and the final result. It was not possible to perform Begg and Mazumdar rank correlation test, publication bias in studies for Anti AChR antibodies index due to review of only 2 studies (Table 4 ).
As a result of the combination of studies, the mean score of Anti-AChR antibodies before the intervention in the drug group was 11.1 ± 2.1 and after the intervention was 5.5 ± 2.4 (Table 4 ) and the difference between the mean of the anti-AChR index. Antibodies were obtained before and after the intervention (1.9 ± 1.5 (P < 0.01) (Fig. 10 )), which indicates the positive effect of Mycophenolate on the Anti-AChR antibodies index.
Accumulation chart of studies included in the meta-analysis based on the mean difference of the anti-AChR antibodies index before and after the intervention for Mycophenolate
Based on the present meta-analysis results between studies, there is a lot of heterogeneity (I 2 = 67.9), so the stochastic effects model was used to combine the studies and the final results.
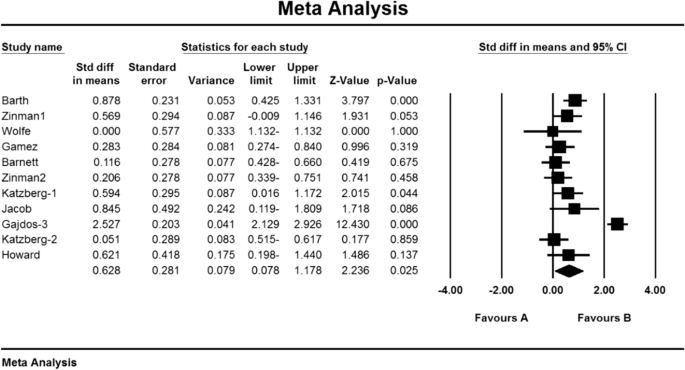
As a result of the combination of studies, the mean score of QMGS indices before the intervention in the drug group was 12.3 ± 0.71 and after the intervention was 8.0 ± 0.59 (Table 4 ). It was obtained 1.4 ± 0.77 (P < 0.01) (Fig. 11 ), indicating Mycophenolate's positive effect on QMGS index reduction.
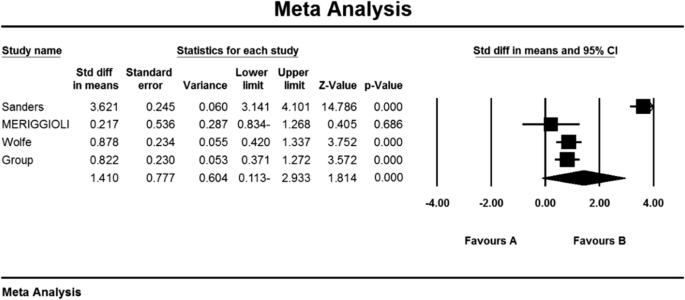
Accumulation chart of studies entered for meta-analysis based on the mean difference of QMGS index before and after intervention for Mycophenolate
Corticosteroids
In the study of studies in the field of corticosteroids, only the QMGS index could be examined. Based on this, 3 studies examined the effect of corticosteroids on MG patients. In the study of Benatar et al. [ 109 ], the QMGS index before the intervention in the placebo group was 6.5 ± 1.8 units and in the drug group was 6.0 ± 0.2 units, and after the intervention in the placebo group decreased by 0.05 units (P > 0.05). There was a significant decrease of 2.25 units (P < 0.05) [ 109 ]. Also, in the study of Howard et al. [ 110 ] QMGS index before the intervention in the placebo group was 7.97 ± 0.91 units and in the drug group was 8.18 ± 0.63 units and after the intervention in the placebo group increased by 0.07 units (P > 0.05) and in the drug group had a decrease of 0.03 units (P > 0.05) [ 110 ]. In the study of Lindberg et al. [ 111 ], The anti-AChR antibodies index was reported before intervention in the placebo group of 264 ± 401 (μmol/L) and in the drug group of 354 m 290 (μmol/L) [ 111 ].
Based on the present meta-analysis results between studies, there is a lot of heterogeneity (I 2 = 99.4), so the stochastic effects model was used to combine the studies and the final result of the outcomes. According to the review of only two studies, it was not possible to use the Begg and Mazumdar rank correlation test for the QMGS index studies according to the review of only 2 studies (Table 4 ).
As a result of the combination of studies, the mean score of QMGS indices before the intervention in the drug group was 7.08 09 1.09 and after the intervention was 5.9 2 2.2 (Table 4 ), as well as the difference between the mean scores of the QMGS index before and after the intervention. 1.64 1 1.6 was obtained (P.010.01) (Fig. 12 ), which indicates the positive effect of corticosteroids on reducing the QMGS index.

Accumulation diagram of studies included in the meta-analysis based on the difference between the mean QMGS index before and after the intervention for Corticosteroids
Myasthenia gravis (MG) is the largest group of neuromuscular disorders caused by autoimmune antibodies against postsynaptic components of the voluntary muscle endplate [ 124 , 125 , 126 ]. Acetylcholine receptor antibodies (AChR), muscle-specific kinase (MuSK), and lipoprotein-associated protein (LRP4) have been well established as sensitive diagnostic markers and pathogens, in addition to antibodies in the classification of patients with Myasthenia gravis also play a key role [ 127 ].
Although the clinical features of MG can vary, increasing muscle weakness with continued skeletal muscle activity is one way to diagnose the disease [ 128 ]. Unlike ocular involvement, which is often asymmetric and involves several muscles, the pattern of muscle involvement in myasthenia gravis is usually symmetrical. Muscle weakness usually increases with exercise and frequent muscle use, and its intensity varies from day to day and fluctuates throughout the day [ 129 ].
In the current systematic review and meta-analysis study, the overall prevalence of MG in the world; 12.4 people per 100,000 population were obtained. Most prevalent in Salvado et al. [ 61 ]; 3463 per 100,000 population and the lowest prevalence Bettini et al. [ 58 ]; 0.006 people per 100,000 population reported.
Due to the different reports of MG prevalence in different parts of the world, a detailed study of the prevalence of this disease in different continents in order to pay more attention to planners and its consequences seemed necessary. Therefore, according to the subgroup analysis by different continents (Asia, Europe, Africa, and America), the highest prevalence of myasthenigraphy was reported in the Americas with 19 per 100,000 people and the lowest in continental Europe with 10 per 100,000 people.
Symptomatic, safe, and supportive approaches are very effective in treating myasthenia gravis, and treatment should be aimed at complete or almost complete drug recovery [ 130 ]. Most patients with myasthenia gravis to achieve therapeutic goals of full physical function or relatively high quality of life need immunosuppressive drugs. Immunosuppressive drugs are prescribed to all patients who respond only to symptomatic and supportive treatment [ 131 ].
Only the QMGS index could be assessed in studies of corticosteroids, which measures the severity of myasthenia gravis in 13 items [ 120 ]. The mean score of the QMGS index before and after the intervention in the drug group was 7.08 09 1.09 and 5.9 2 2.2, which indicates the positive effect of corticosteroid use on reducing the QMGS index improving myasthenia gravis.
Oral corticosteroid therapy has been used since the 1950s with a dramatic improvement in approximately 70 to 80% of patients with myasthenia gravis [ 132 , 133 ]. The usefulness of oral steroids is determined by the occurrence of a wide range of dose and time-dependent side effects [ 134 , 135 ]. Intermittent intravenous methylprednisolone (IVMP) is used to treat several autoimmune disorders, including MG, on the assumption that it is more effective and has fewer side effects than oral steroids [ 136 ]. IVMP is also effective in severe cases of MG [ 137 ].
Mycophenolate mofetil (MMF) is an immunosuppressive agent that is primarily used to prevent acute rejection of organ transplants [ 138 ] which have reported preliminary use of this drug in the treatment of myasthenia gravis [ 139 ].
Regarding the effectiveness of mycophenolate mofetil, the mean score of MG-ADL index before and after the intervention in the drug group was 5.9 87 0.87 and 7.4 09 5.09, respectively. This scale assesses daily life activity in people with myasthenia gravis through 8 items [ 115 ]. The mean score of the SFEMG (single-strand electromyography) index, which is used to evaluate neuromuscular site abnormalities [ 117 ], was reported to be 71.5 ± 11.3 and 60.13 5 5.1, respectively, before and after the intervention in the drug group. Also, the mean score of Anti-AChR antibodies before and after the intervention in the drug group was 5/5 ± 2/4 and 11/2 ± 1/1. The mean score of QMGS indices before and after the intervention in the drug group was 12.3 ± 0.71 and 8.0 ± 1.59, which the results show the positive effect of using Mycophenolate on reducing the above 4 indicators and thus improving the treatment status of patients with MG.
Certain cure requires suppression or modulation of the immune system by intravenous immunoglobulin (IVIg) or plasma replacement (PLEX) [ 140 ]. Immune system modification is used when rapid recovery is required, such as exacerbated myasthenia gravis, power optimization before thymectomy, and patients who do not tolerate and respond adequately to immunosuppressive drugs [ 100 , 141 , 142 ]. In recent years, the administration of 2 g/kg intravenous IVIg immunoglobulin has been proven to treat moderate to severe myasthenia gravis and is continuously used to manage intensified MG [ 143 ].
Therapeutic plasmapheresis or plasma replacement (PLEX) is the first line of treatment in patients with myasthenia gravis with respiratory failure, inability to swallow, myasthenic crisis, or inadequate response to drug therapy [ 144 , 145 ]. In therapeutic plasmapheresis, plasma containing pathogenic antibodies is separated from the patient's blood and returned to other cells. Plasma replacement is prescribed five times in 10 to 14 days, through which and by repeating it, plasma levels of acetylcholine receptor antibody are reduced, and clinical improvement is achieved [ 119 ].
Due to the high prevalence of myasthenia gravis globally and its many negative consequences for individuals and society. Therefore, it seems useful to take measures to achieve better therapies or to use supportive therapies to reduce the symptoms of the disease. Common drug treatments in MG were evaluated to show the effectiveness of immunosuppressive drugs, including steroids and their modulators, including intravenous immunoglobulin (IVIg and plasma replacement) (PLEX). These studies can provide useful information to health care providers, enrich health care interventions, improve the quality of services, and ultimately improve the quality of life of these people. Therefore, it is suggested that physicians and the health care system give these drug classes more attention.
The application of nanotechnology is promising, given frustrating problems in therapeutic neurology [ 146 ]. Nanotechnology involves the manipulation of technological machinery at the atomic scale. For perspective, a nucleus is about 6 μm across, a ribosome 20 nm in diameter, and a single strand of DNA 2 nm wide [ 146 ]. A typical human being is composed of 100 trillion cells. Nanotechnology has created novel devices for the treatment of various neurological diseases. Shrinkage of machinery, chip-based technologies, and the creation of unprecedented nanomaterials are contributing immensely to the reduction of morbidity [ 146 , 147 ]
Considerable efforts are being focused on using nanoneuromedicine for disease treatment in the research laboratory. In the case of neurodegenerative diseases such as myasthenia gravis (MG), Alzheimer's disease (AD), Parkinson's disease (PD), amyotrophic lateral sclerosis (ALS), and multiple sclerosis (MS), nanomedicines have emerged as promising treatment options. Pathophysiological processes involving neuron inflammation and protein misfolding initiate a degeneration cycle within the cell. This can be thwarted using better drug targeting. Diagnosing and monitoring the end-effects of therapeutics is possible using nanoneurotechnology [ 146 , 147 , 148 ].
In addition to what has been said, the interest in graphene-based nanomaterials (GBNs) application in nanomedicine, particularly neurology, steadily increased in the last decades. GBNs peculiar physical–chemical properties allow the design of innovative therapeutic tools to manipulate biological structures with subcellular resolution [ 148 , 149 ]. Based on the study, it can also be said that to develop effective antioxidant therapies the best strategy may be to create new nanoscale drug delivery systems [ 150 ].
Limitations
Among the limitations of this study, it can be asserted that some samples were not based on random selection. Also, non-uniform reporting of articles, inconsistent implementation method, non-copying and unavailability of the full text of articles presented at the conference can be mentioned as other limitations.
Suggestion for future works
The meta-analysis results enable the overall prevalence to be presented to the policy-maker and thus manage the cost, time and future diagnostic and treatment decisions commensurate with the overall prevalence. A systematic review also reveals drugs effective in treating myasthenia gravis, which can guide physicians and encourage the researcher to conduct future clinical trial studies and a network meta-analysis to determine therapeutic supplements for the disease.
The results of systematic review of drug evaluation in patients with myasthenia gravis showed that Mycophenolate and Immunoglobulin or plasma exchange drugs have positive effects in the treatment of MG. It also represents the positive effect of immunoglobulin or plasma exchange on reducing SFEMG index and QMGS index and the positive effect of Mycophenolate on reducing MG-ADL index, SFEMG and Anti-AChR antibodies index. In addition to what was mentioned, based on a meta-analysis of the random-effect model, the overall prevalence of MG in the world is 12.4 people per 100,000 populations, which indicates the urgent need for the attention of officials and specialists to this disease for prevention and treatment.
Availability of data and materials
Datasets are available through the corresponding author upon reasonable request.
Abbreviations
Scientific Information Database
Medical Subject Headings
Web of science
Preferred Reporting Items for Systematic Reviews and Meta-Analysis
Consolidated Standards of Reporting Trials
Strengthening the reporting of observational studies in epidemiology for a cross-sectional study
Myasthenia Gravis
Anti-acetylcholine receptor antibodies
Intravenous immunoglobulin
Quantitative Myasthenia Gravis Score
Myasthenia Gravis Activities of Daily Living
Single-fibre electromyography
Sanders DB, Wolfe GI, Benatar M, Evoli A, Gilhus NE, Illa I, et al. International consensus guidance for management of myasthenia gravis: executive summary. Neurology. 2016;87(4):419–25.
PubMed PubMed Central Google Scholar
Gilhus NE, Verschuuren JJ. Myasthenia gravis: subgroup classification and therapeutic strategies. Lancet Neurol. 2015;14(10):1023–36.
CAS PubMed Google Scholar
Shield TW, editor. General thoracic surgery, 7th ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2010. pp. 2323–64.
Conti-Fine BM, Milani M, Kaminski HJ. Myasthenia gravis: past, present, and future. J Clin Invest. 2006;116(11):2843–54.
CAS PubMed PubMed Central Google Scholar
Benatar M. A systematic review of diagnostic studies in myasthenia gravis. Neuromuscul Disord. 2006;16(7):459–67.
PubMed Google Scholar
Berrih-Aknin S, Frenkian-Cuvelier M, Eymard B. Diagnostic and clinical classification of autoimmune myasthenia gravis. J Autoimmun. 2014;48–49:143–8.
Meriggioli MN, Sanders DB. Autoimmune myasthenia gravis: emerging clinical and biological heterogeneity. Lancet Neurol. 2009;8(5):475–90.
Hoch W, McConville J, Helms S, Newsom-Davis J, Melms A, Vincent A. Auto-antibodies to the receptor tyrosine kinase MuSK in patients with myasthenia gravis without acetylcholine receptor antibodies. Nat Med. 2001;7(3):365–8.
Higuchi O, Hamuro J, Motomura M, Yamanashi Y. Autoantibodies to low-density lipoprotein receptor-related protein 4 in myasthenia gravis. Ann Neurol. 2011;69(2):418–22.
Kerty E, Elsais A, Argov Z, Evoli A, Gilhus NE. EFNS/ENS guidelines for the treatment of ocular myasthenia. Eur J Neurol. 2014;21:687–93.
Heldal AT, Owe JF, Gilhus NE, Romi F. Seropositive myasthenia gravis: a nationwide epidemiologic study. Neurology. 2009;73:150–1.
Wang L, Zhang S, Xi J, Li W, Zhou L, Lu J, et al. Efficacy and safety of tacrolimus for myasthenia gravis: a systematic review and meta-analysis. J Neurol. 2017;264(11):2191–200.
Carr AS, Cardwell CR, McCarron PO, McConville J. A systematic review of population-based epidemiological studies in myasthenia Gra-vis. BMC Neurol. 2010;10:46.
MacDonald BK, Cockerell OC, Sander JW, Shorvon SD. The incidence and lifetime prevalence of neurological disorders in a prospective community-based study in the UK. Brain J Neurol. 2000;123(Pt 4):665–76.
Google Scholar
Breiner A, Widdifield J, Katzberg HD, Barnett C, Bril V, Tu K. Epidemiology of myasthenia gravis in Ontario, Canada. Neuromuscular Disord. 2016;26(1):41–6.
Kurtzke JF. Epidemiology of myasthenia gravis. Adv Neurol. 1978;19:545–66.
Eaton WW, Rose NR, Kalaydjian A, Pedersen MG, Mortensen PB. Epidemiology of autoimmune diseases in Denmark. J Autoimmun. 2007;29(1):1–9.
Mh H, Ms F. The clinical outcome of thymectomy in myasthenia gravis. Tehran Univ Med J TUMS Publications. 2009;66(11):821–5.
Chen S, Xu M-B, Zhou X-L, Rong P-Q, Jin T-Y, Zheng G-Q. Chinese herbal medicine for myasthenia gravis: a systematic review and meta-analysis. Front Pharmacol. 2018;9:969.
Li H-F, Xie Y, Yue Y-X. Myasthenia gravis: subgroup classifications. Lancet Neurol. 2016;15(4):355–6.
Meriggioli MN, Rowin J, Richman JG, Leurgans S. Mycophenolate mofetil for myasthenia gravis: a double-blind, placebo-controlled study. Ann NY Acad Sci. 2003;998:494–9.
Sieb J. Myasthenia gravis: an update for the clinician. Clin Exp Immunol. 2014;175(3):408–18.
De Feo LG, Schottlender J, Martelli NA, Molfino NA. Use of intravenous pulsed cyclophosphamide in severe, generalized myasthenia gravies. Muscle Nerve. 2002;26(1):31–6.
García-Carrasco M, Escárcega RO, Fuentes-Alexandro S, Riebeling C, Cervera R. Therapeutic options in autoimmune myasthenia gravis. Autoimmun Rev. 2007;6(6):373–8.
Ciafaloni E. Mycophenolate mofetil and myasthenia gravis. Lupus. 2005;14(3-suppl):46–9.
Skeie GO, Apostolski S, Evoli A, et al. Guidelines for the treatment of autoimmune neuromuscular transmission disorders. Eur J Neurol. 2006;13(7):691–9.
Rozsa C, Lovas G, Fornadi L, Szabo G, Komoly S. Safety of long-term combined immunosuppressive treatment in myasthenia gravis: analysis of adverse effects of 163 patients. Eur J Neurol. 2006;13(9):947–52.
Drachman DB, Adams RN, Hu R, et al. Rebooting the immune system with high-dose cyclophosphamide for the treatment of refractory myasthenia gravis. Ann N Y Acad Sci. 2008;1132:305–14.
Suh J, Goldstein JM, Nowak RJ. Clinical characteristics of refractory myasthenia gravis patients. Yale J Biol Med. 2013;86(2):255–60.
Gajdos P, Tranchant C, Clair B, Bolgert F, Eymard B, Stojkovic T, et al. Treatment of myasthenia gravis exacerbation with intravenous immunoglobulin: a randomized double-blind clinical trial. Arch Neurol. 2005;62(11):1689–93.
Barth D, Nabavi Nouri M, Ng E, Nwe P, Bril V. Comparison of IVIgand PLEX in patients with myasthenia gravis. Neurology. 2011;76(23):2017–23.
Katzberg HD, Barnett C, Bril V. Predictors of response to immunomodulation in patients with myasthenia gravis. Muscle Nerve. 2012;45(5):648–52.
Nagayasu T, Yamayoshi T, Matsumoto K, Ide N, Hasazumi S, Nomura M, et al. Beneficial effects of plasmapheresis before thymectomy on the outcome in myasthenia gravis. Jpn J Thorac Cardiovasc Surg. 2005;53(1):2–7.
Guptill JT, Sharma BK, Marano A, Soucy A, Krueger A, Sanders DB. The estimated cost of treating myasthenia gravis in an insured US population. Muscle Nerve. 2012;45(3):363–6.
Henderson LK, Craig JC, Willis NS, Tovey D, Webster AC. How to write a cochrane systematic review. Nephrology. 2010;15(6):617–24.
Ramke J, Palagyi A, Jordan V, Petkovic J, Gilbert CE. Using the STROBE statement to assess reporting in blindness prevalence surveys in low and middle-income countries. PloS One. 2017;12(5):e0176178.
Schulz KF, Altman DG, Moher D, Group C. CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Trials. 2010;11(1):32.
Murai H, Yamashita N, Watanabe M, Nomura Y, Motomura M, Yoshikawa H, et al. Characteristics of myasthenia gravis according to onset-age: Japanese nationwide survey. J Neurol Sci. 2011;305(1–2):97–102.
Nemet AY, Kaiserman I, Mimouni M, Segal O, Vinker S. High prevalence of myasthenia gravis among rural adult populations. J Clin Neuromuscul Dis. 2014;16(2):47–50.
Park S-Y, Lee JY, Lim NG, Hong Y-H. Incidence and prevalence of myasthenia gravis in Korea: a population-based study using the National Health Insurance claims database. J Clin Neurol. 2016;12(3):340–4.
Lee HS, Lee HS, Shin HY, Choi Y-C, Kim SM. The epidemiology of myasthenia gravis in Korea. Yonsei Med J. 2016;57(2):419–25.
Okinaka S, Reese HH, Katsuki S, et al. The prevalence of multiple sclerosis and other neurological diseases in Japan. Acta Neurologica Scandinavica. 1966;47(Suppl 19):68–76.
Araki S, Uchino M, Yoshida O. Epidemiologic study of multiple sclerosis, myasthenia gravis and polymyositis in the city of Kumamoto, Japan. Clin Neurol. 1983;23:838–41.
CAS Google Scholar
Kondo K, Takasu T, Ahmed A. Neurological diseases in Karachi, Pakistan—elevated occurrence of subacute sclerosing panencephalitis. Neuroepidemiology. 1988;7:66–80.
Yu YL, Hawkins BR, Ip MS, Wong V, Woo E. Myasthenia gravis in Hong Kong Chinese: epidemiology and adult disease. Acta Neurol Scand. 1992;86(2):113–9.
Zieda A, Ravina K, Glazere I, Pelcere L, Naudina M, Liepina L, et al. A nationwide epidemiological study of myasthenia gravis in Latvia. Eur J Neurol. 2018;25(3):519–26.
Lavrnic D, Basta I, Rakocevic-Stojanovic V, Stevic Z, Peric S, Nikolic A, et al. Epidemiological study of adult-onset myasthenia gravis in the area of Belgrade (Serbia) in the period 1979–2008. Neuroepidemiology. 2013;40(3):190–4.
Tola M, Granieri E, Paolino E, Caniatti L, Quatrale R, Mazzanti B, et al. Epidemiological study of myasthenia gravis in the province of Ferrara, Italy. J Neurol. 1989;236(7):388–90.
Montomoli C, Citterio A, Piccolo G, Cioccale R, Ferretti VV, Fratti C, et al. Epidemiology and geographical variation of myasthenia gravis in the province of Pavia, Italy. Neuroepidemiology. 2012;38(2):100–5.
Cetin H, Fülöp G, Zach H, Auff E, Zimprich F. Epidemiology of myasthenia gravis in Austria: rising prevalence in an ageing society. Wien Klin Wochenschr. 2012;124(21–22):763–8.
Storm-Mathisen A. Epidemiology of myasthenia gravis in Norway. Acta Neurol Scand. 1984;70(4):274–84.
Westerberg E, Punga AR. Epidemiology of Myasthenia gravis in Sweden 2006–2016. Brain Behav. 2020;10:e01819.
Kalb B, Matell G, Pirskanen R, Lambe M. Epidemiology of myasthenia gravis: a population-based study in Stockholm, Sweden. Neuroepidemiology. 2002;21(5):221–5.
Aiello I, Pastorino M, Sotgiu S, Pirastru M, Sau G, Sanna G, et al. Epidemiology of myasthenia gravis in northwestern Sardinia. Neuroepidemiology. 1997;16(4):199–206.
Guidetti D, Sabadini R, Cavalletti S, Lodesani M, Mantegazza R, Solime FCV. Epidemiological study of myasthenia gravis in the province of Reggio Emilia, Italy. Eur J Epidemiol. 1998;14(4):381–7.
Foldvari A, Kovacs N, Sipos V, Merth G, Vincze F, Szucs M, et al. Estimation of incidence, prevalence, and age-at-diagnosis of myasthenia gravis among adults by hospital discharge records. Wien Klin Wochenschr. 2015;127(11–12):459–64.
Zivadinov R, Jurjevic A, Willheim K, Cazzato G, Zorzon M. Incidence and prevalence of myasthenia gravis in the County of the Coast and Gorski kotar, Croatia, 1976 through 19961. Neuroepidemiology. 1998;17(5):265–72.
Bettini M, Chaves M, Cristiano E, Pagotto V, Perez L, Giunta D, et al. Incidence of autoimmune myasthenia gravis in a health maintenance organization in Buenos Aires, Argentina. Neuroepidemiology. 2017;48(3–4):119–23.
Andersen J, Heldal A, Engeland A, Gilhus N. Myasthenia gravis epidemiology in a national cohort; combining multiple disease registries. Acta Neurol Scand. 2014;129:26–31.
Aragones J, Altimiras J, Roura P, Alonso F, Bufill E, Munmany A, et al. Prevalence of myasthenia gravis in the Catalan county of Osona. Neurología (English Edition). 2017;32(1):1–5.
Salvado M, Canela M, Ponseti JM, Lorenzo L, Garcia C, Cazorla S, et al. Study of the prevalence of familial autoimmune myasthenia gravis in a Spanish cohort. J Neurol Sci. 2016;360:110–4.
Christensen P, Jensen T, Tsiropoulos I, Søsrensen T, Kjser M, Højer-Pedersen E, et al. Incidence and prevalence of myasthenia gravis in western Denmark: 1975 to 1989. Neurology. 1993;43(9):1779.
Robertson N, Deans J, Compston D. Myasthenia gravis: a population-based epidemiological study in Cambridgeshire, England. J Neurol Neurosurg Psychiatry. 1998;65(4):492–6.
Garland H, Clark ANG. Myasthenia gravis, a personal study of 60 cases. BMJ. 1956;1:1259–62.
Pennington GW, Wilson A. Incidence of myasthenia gravis in the Merseyside conurbation. In: Veits HR, editor. Myasthenia Gravis. Proceedings of the second international symposium. Springfield IL: Charles C Thomas; 1961; pp. 337–45.
Gudmundsson KR. The prevalence of some neurological diseases in Iceland. Acta Neurol Scand. 1968;44:55–69.
Oosterhuis: Epidemiologie dei myasthenie in Amsterdam. Neurologie Deutsche Jesells. 1977; 103–108.
Hokkanen E. Epidemiology of myasthenia gravis in Finland. J Neurol Sci. 1969;9:463–78.
Giagheddu M, Puggioni G, Sanna G, et al. Epidemiological study of myasthenia gravis in Sardinia Italy (1958–1986). Acta Neurol Scand. 1989;79:326–33.
D’Alessamdro R, Granieri E, Benassi G, et al. Comparative study on the prevalence of myasthenia gravis in the provinces of Bologna and Ferrera Italy. Acta Neurol Scand. 1991;83(2):83–8.
Sorensen TT, Holm EB. Myasthenia gravis in the county of Viborg, Denmark. Eur Neurol. 1989;29:177–9.
Somnier FE, Keiding N, Paulson OB. Epidemiology of myasthenia gravis in Denmark: a longitudinal and comprehensive population survey. Arch Neurol. 1991;48(7):733–9.
Christensen PB, Jensen TS, Tsiropoulos I, et al. Mortality and survival in myasthenia gravis: a Danish population-based study. JNNP. 1998;64(1):78–83.
Ferrari G, Lovaste MG. Epidemiology of myasthenia gravis in the province of Trento (northern Italy). Neuroepidemiology. 1992;11(3):135–42.
Krivopusk ME. Clinico-epidemiological aspects of hereditary neuromuscular diseases in the Krasnodar territory. Zhurnal Nevropatologii I Psikhiatrii Imeni SS Korsakova. 1991;91(9):3–5.
Lavrnic D, Jarebinski M, Rakocevic-Stojanovic V, et al. Epidemiological and clinical characteristics of myasthenia gravis in Belgrade, Yugoslavia (1983–1992). Acta Neurologica Scandanavica. 1999;100(3):168–74.
Kyriallis K, Hristova A, Middleton I. What is the real epidemiology of myasthenia gravis? Neurology. 1995; A351.
Holtsema H, Mourik J, Rico RE, et al. Myasthenia gravis on the Dutch Antilles: an epidemiological study. Clin Neurol Neurosurg. 2000;102(4):195–8.
Villagra-Cocco A, Villagra-Cocco P. Prevalence of myasthenia gravis on the island of La Palma. Revista Neurol. 1997;25(148):2068–9.
Oopik M, Kaasik AE, Jakobson J. A population-based epidemiological study of myasthenia gravis in Estonia. JNNP. 2003;74(12):1638–43.
Wirtz PW, Nijnuis MG, Sotodeh M, et al. The epidemiology of myasthenia gravis, Lambert Eaton myasthenic syndrome and their associated tumours in the northern part of Southern Holland. J Neurol. 2003;250(6):698–701.
Kotov SV, Neretin VI, Agafonov BV, Sidorova OP. Population-based study of Myasthenia in Moscow region. Zhurnal Nevrologii I Psikhiatrii Imeni SS Korsakova. 2006;106(5):52–5.
Somnier FE. Increasing incidence of late-onset anti-AChR antibody-seropositive myasthenia gravis. Neurology. 2005;65:928–30.
Poulas K, Tsibri E, Kokla A, et al. Epidemiology of seropositive myasthenia gravis in Greece. JNNP. 2001;71(3):352–6.
Niks EH, Kuks JB, Verschuuren JJ, et al. Epidemiology of myasthenia gravis with anti-muscle specific kinase antibodies in The Netherlands. JNNP. 2007;78(4):417–8.
Tsiamalos P, Kordas G, Kokla A, et al. Epidemiological and immunological profile of muscle-specific kinase myasthenia gravis in Greece. Eu J Neurol. 2009;16(8):925–30.
Maharaj J, Bahadursingh S, Ramcharan K. Myasthenia gravis in South Trinidad. West Indian Med J. 2013;62(6):510–4.
Gordon B, Noone J, Van Doren B, Zacherle E, Blanchette C. Prevalence and cost of myasthenia gravis in the medicare beneficiary sample. Value Health. 2015;18(7):A661.
Phillips LH, Torner JC, Anderson MS, Cox GM. The epidemiology of myasthenia gravis in central and western Virginia. Neurology. 1992;42(10):1888.
Kurland LT. Descriptive epidemiology if selected neurologic and myopathic disorders with particular reference to a survey in Rochester, Minnesota. J Chronic Disorders. 1958;8(4):378.
Alter M, Rhett-Talbert O, Kurland LT. Myasthenia gravis in a southern community. Arch Neurol. 1960;3:65–9.
Kvirkveliia NB. Clinico-epidemiologic aspects of Myasthenia in the Georgian SSR. Zh Nevropatol Psikhiatr Im S S Korsakova. 1986;86(3):327–30.
Cisernos AD, Luis RS, Leon R, Carrera PL. Some epidemiological aspects of myasthenia gravis in Cuba. Revista de Neurol. 1996;24(128):435–9.
Sanchez JL, Uribe CS, Franco AF, Jimeniz ME, Arcos-Burgos OM, Palacio LG. Prevalence of myasthenia gravis in Antioquia, Colombia. Revista de Neurologia. 2002;34(11):1010–2.
Deffeminis Rospide HA, Petra de Mirabel M, Piazza de Silva N, et al. Estudio epidemiologico de la miastenia en el Uruguay. Acta Neurol Latinoamer 1975; 53–65.
Khedr EM, Fawi G, Abbas MA-A, El-Fetoh AN, Zaki AF, Gamea A, et al. Prevalence of neuromuscular disorders in Qena governorate/Egypt: a population-based survey. Neurol Res. 2016; 38(12):1056–63
El-Tallawy HN, Khedr EM, Qayed MH, Helliwell TR, Kamel NF. Epidemiological study of neuromuscular disorders in Assuit, Egypt. Neuroepidemiology. 2005;25(4):205–11.
Gattellari M, Goumas C, Worthington J. A national epidemiological study of myasthenia gravis in Australia. Eur J Neurol. 2012;19(11):1413–20.
Gajdos P, Chevret S, Clair B, Tranchant C, Chastang C, Group MGCS. Clinical trial of plasma exchange and high-dose intravenous immunoglobulin in myasthenia gravis. Ann Neurol. 1997;41(6):789–96.
Zinman L, Ng E, Bril V. IV immunoglobulin in patients with myasthenia gravis: a randomized controlled trial. Neurology. 2007;68(11):837–41.
Wolfe GI, Barohn RJ, Foster BM, Jackson CE, Kissel JT, Day JW, Thornton CA, Nations SP, Bryan WW, Amato AA. Randomized, controlled trial of intravenous immunoglobulin in myasthenia gravis. Muscle Nerve. 2002;26(4):549–52.
Gamez J, Salvadó M, Carmona F, de Nadal M, Romero L, Ruiz D, Jáuregui A, Martínez O, Pérez J, Suñé P. Intravenous immunoglobulin to prevent myasthenic crisis after thymectomy and other procedures can be omitted in patients with well-controlled myasthenia gravis. Ther Adv Neurol Disord. 2019;12:1756286419864497.
Barnett TC, Bril V, Davis AM. Performance of individual items of the quantitative myasthenia gravis score. Neuromuscul Disord. 2013;23(5):413–7.
Zinman L, Bril V. IVIG treatment for myasthenia gravis: effectiveness, limitations, and novel therapeutic strategies. Ann N Y Acad Sci. 2008;1132(1):264–70.
Katzberg HD, Barnett C, Merkies IS, Bril V. Minimal clinically important difference in myasthenia gravis: outcomes from a randomized trial. Muscle Nerve. 2014;49(5):661–5.
Jacob S, Murai H, Utsugisawa K, Nowak RJ, Wiendl H, Fujita KP, O’Brien F, Howard JF Jr. Response to eculizumab in patients with myasthenia gravis recently treated with chronic IVIg: a subgroup analysis of REGAIN and its open-label extension study. Ther Adv Neurol Disord. 2020;13:1756286420911784.
Gajdos P, Chevret S. Treatment of myasthenia gravis acute exacerbations with intravenous immunoglobulin. Ann N Y Acad Sci. 2008;1132(1):271–5.
Howard JF, Bril V, Burns TM, Mantegazza R, Bilinska M, Szczudlik A, Beydoun S. Garrido FJRDR, Piehl F, Rottoli M: Randomized phase 2 study of FcRn antagonist efgartigimod in generalized myasthenia gravis. Neurology. 2019;92(23):e2661–73.
Benatar M, Mcdermott MP, Sanders DB, Wolfe GI, Barohn RJ, Nowak RJ, Hehir M, Juel V, Katzberg H, Tawil R. Efficacy of prednisone for the treatment of ocular Myasthenia (EPITOME): a randomized, controlled trial. Muscle Nerve. 2016;53(3):363–9.
Howard FM Jr, Duane DD, Lambert EH, Daube JR. Alternate-day prednisone: preliminary report of a double-blind controlled study. Ann N Y Acad Sci. 1976;274:596–607.
Lindberg C, Andersen O, Lefvert A. Treatment of myasthenia gravis with methylprednisolone pulse: a double-blind study. Acta Neurol Scand. 1998;97(6):370–3.
Sanders D, Hart I, Mantegazza R, Shukla S, Siddiqi Z, De Baets M, Melms A, Nicolle M, Solomons N, Richman DP. An international, phase III, randomized trial of mycophenolate mofetil in myasthenia gravis. Neurology. 2008;71(6):400–6.
Wolfe GI, Barohn RJ, Sanders DB, McDermott MP. Comparison of outcome measures from a trial of mycophenolate mofetil in myasthenia gravis. Muscle Nerve. 2008;38(5):1429–33.
Group MS. A trial of mycophenolate mofetil with prednisone as initial immunotherapy in myasthenia gravis. Neurology. 2008;71(6):394–9.
Muppidi S. The myasthenia gravis-specific activities of daily living profile. Ann N Y Acad Sci. 2012;1274(1):114–9.
Muppidi S, Wolfe GI, Conaway M, Burns TM, Composite M, Group MQS. MG-ADL: still a relevant outcome measure. Muscle Nerve. 2011;44(5):727–31.
Dumitru D, Amato A, Zwarts M, editors. Electrodiagnostic medicine, 2nd ed. Philadelphia: Hanley & belfus, INC, 2002; pp. 1148–1177.
Jabre JF, Chirico-Post J, Weiner M. Stimulation SFEMG in myasthenia gravis. Muscle Nerve. 1989;12(1):38–42.
Kasper D, Fauci A, Hauser S, Longo D, Jameson J, Loscalzo J. Harrison's principles of internal medicine, 19th ed. New York: McGraw-Hill Education; 2015; pp. 2704–6.
Tindall RS, Rollins JT, Phillips JT, et al. Preliminary results of a double-blind, randomized, placebo-controlled trial of cyclosporine in myasthenia gravis. N Engl J Med. 1987;316:719–24.
Barohn RJ, McIntire D, Herbelin L, et al. Reliability testing of the quantitative myasthenia gravis score. Ann N Y Acad Sci. 1998;841:769–72.
Sharshar T, Chevret S, Mazighi M, et al. Validity and reliability of two muscle strength scores commonly used as endpoints in assessing treatment of myasthenia gravis. J Neurol. 2000;247:286–90.
Bedlack RS, Simmel D, Bosworth H, et al. Quantitative myasthenia gravis score: assessment of responsiveness and longitudinal validity. Neurology. 2005;64:1968–70.
Gilhus NE. Myasthenia and neuromuscular junction. Curr Opin Neurol. 2012;25:523–9.
Querol L, Illa I. Myasthenia and the neuromuscular junction. Curr Opin Neurol. 2013;26:459–65.
Verschuuren JJ, Huijbers MG, Plomp JJ, et al. Pathophysiology of myasthenia gravis with antibodies to the acetylcholine receptor, muscle-specific kinase and low-density lipoprotein receptor-related protein 4. Autoimmun Rev. 2013;12:918–23.
Huijbers M, Lipka A, Plomp J, Niks E, van der Maarel S, Verschuuren J. Pathogenic immune mechanisms at the neuromuscular synapse: specific antibody-binding epitopes’ role in myasthenia gravis. J Intern Med. 2014;275(1):12–26.
Zisimopoulou P, Brenner T, Trakas N, Tzartos SJ. Serological diagnostics in myasthenia gravis based on novel assays and recently identified antigens. Autoimmun Rev. 2013;12:924–30.
Verschuuren J, Strijbos E, Vincent A. Neuromuscular junction disorders. Handb Clin Neurol. 2016;133:447–66.
Skeie GO, Apostolski S, Evoli A, et al. Guidelines for treatment of autoimmune neuromuscular transmission disorders. Eur J Neurol. 2010;17:893–902.
Hart IK, Sathasivam S, Sharshar T. Immunosuppressive agents for myasthenia gravis. Cochrane Database Syst Rev. 2007;4:CD005224.
Brunner NG, Namba T, Grob D. Corticosteroids in management of severe, generalized myasthenia gravis. Effectiveness and comparison with corticotropin therapy. Neurology. 1972;22:603–10.
Mann JD, Johns TR, Campa JF, Muller WH. Long-term prednisone followed by thymectomy in myasthenia gravis. Ann NY Acad Sci. 1976;274:608–22.
Pascuzzi RM, Coslett HB, Johns TR. Long-term cortico- steroid treatment of myasthenia gravis: report of 116 patients. Ann Neurol. 1984;15:291–8.
Evoli A, Batocchi AP, Palmisani MT, Monaco ML, Tonali P. Long-term results of corticosteroid therapy in patients with myasthenia gravis. Eur Neurol. 1992;32:37–43.
Matell G, Baerendtz S, Hulting J, Malmlund HO. Effects on Myasthenia of twin shock doses of methylprednisolone (TSDMP). 1982. 5th Int Congr Neuromusc Diseases.
Arsura E, Brunner NG, Namba T, Grob D. High-dose intravenous methylprednisolone in myasthenia gravis. Arch Neurol. 1985;42:1149–53.
Chaudhry V, Cornblath D, Griffin J, O’Brien R, Drachman DB. Mycophenolate mofetil: a safe and promising immunosuppressant in neuromuscular diseases. Neurology. 2001;56(1):94–6.
Ciafaloni E, Massey J, Tucker-Lipscomb B, Sanders D. Mycophenolate mofetil for myasthenia gravis: an open-label pilot study. Neurology. 2001;56(1):97–9.
Keesey JC. Clinical evaluation and management of myasthenia gravis. Muscle Nerve. 2004;29:484–505.
Gajdos P, Chevret S, Toyka K. Plasma exchange for myas-thenia gravis. Cochrane Database Syst Rev. 2002. https://doi.org/10.1002/14651858.cd002275 .
Article PubMed PubMed Central Google Scholar
Jnsen P, Bril V. A comparison of the effectiveness of intravenous immunoglobulin and plasma exchange as preoperative therapy of myasthenia gravis. J Clin NeuromusculDis. 2008;9:352–5.
Ronager J, Ravnborg M, Hermansen I, Vorstrup S. Immunoglobulintreatment versus plasma exchange in patients with chronic moderate to severe myasthenia gravis. Artif Organs. 2001;25:967–73.
Chegini A. Therapeutic plasmapheresis in myasthenic crisis after botox injection (case report). 2016 (In Persian).
McLeod BC, Weinstein R, Winters JL. Textbook of apheresis principles and practice, 3rd ed. USA: AABB; 2010. pp. 295–317.
Cellot G, Franceschi Biagioni A, Ballerini L. Nanomedicine and graphene-based materials: advanced technologies for potential treatments of diseases in the developing nervous system. Pediatr Res. 2021. https://doi.org/10.1038/s41390-021-01681-6 .
Article PubMed Google Scholar
Ambesh P, Gregory AD. Nanotechnology in neurology: genesis, current status, and prospects. Ann Indian Acad Neurol. 2015;18(4):382–6.
Sriramoju B, Kanwar RK, Kanwar JR. Nanomedicine based nanoparticles for neurological disorders. Curr Med Chem. 2014;21(36):4154–68.
Kumar Nath U, Bhattacharyya D, Chattopadhya D, Dhingra G, Azad SH, Mohanty A. Visceral leishmaniasis masquerading as drug-induced pancytopenia in myasthenia gravis. Drug Discov Therapeutics. 2021;15(1):48–50.
Eftekhari A, Maleki Dizaj S, Chodari L, Sunar S, Hasanzadeh A, Ahmadian E, Hasanzadeh M. The promising future of nano-antioxidant therapy against environmental pollutants induced-toxicities. Biomed Pharmacother. 2018;103:1018–27.
Download references
Acknowledgements
This study results from research project No. 4000257 approved by the Student Research Committee of Kermanshah University of Medical Sciences. We would like to thank the esteemed officials of the centre for the financial affords of this study.
By Deputy for Research and Technology, Kermanshah University of Medical Sciences (IR) (4000257). This deputy has no role in the study process.
Author information
Authors and affiliations.
Department of Biostatistics, School of Health, Kermanshah University of Medical Sciences, Kermanshah, Iran
Nader Salari
Student Research Committee, Kermanshah University of Medical Sciences, Kermanshah, Iran
Behnaz Fatahi & Mohsen Kazeminia
Department of Translation Studies, Faculty of Literature, Istanbul University, Istanbul, Turkey
Yalda Bartina
Department of Neurosurgery, School of Medicine, Kermanshah University of Medical Sciences, Kermanshah, Iran
Reza Fatahian
Department of Neurology, School of Medicine, Kermanshah University of Medical Sciences, Kermanshah, Iran
Payam Mohammadi
Department of Biology, Faculty of Science, University Putra Malaysia, Serdang, Selangor, Malaysia
Shamarina Shohaimi
Cellular and Molecular Research Center, Gerash University of Medical Sciences, Gerash, Iran
Masoud Mohammadi
You can also search for this author in PubMed Google Scholar
Contributions
NS, BF, and MK contributed to the design and MM statistical analysis and participated in most study steps. MM and BF, and MK prepared the manuscript. YB and RF and MM and BF and PM and SS helped design and interpret the study. All authors read and approved the content of the manuscript.
Corresponding author
Correspondence to Masoud Mohammadi .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval was received from the deputy of the research and technology ethics committee, Kermanshah University of Medical Sciences (IR.KUMS.REC.1400.116).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Salari, N., Fatahi, B., Bartina, Y. et al. Global prevalence of myasthenia gravis and the effectiveness of common drugs in its treatment: a systematic review and meta-analysis. J Transl Med 19 , 516 (2021). https://doi.org/10.1186/s12967-021-03185-7
Download citation
Received : 27 October 2021
Accepted : 06 December 2021
Published : 20 December 2021
DOI : https://doi.org/10.1186/s12967-021-03185-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Myasthenia gravis
- Systematic review
- Meta-analysis
Journal of Translational Medicine
ISSN: 1479-5876
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
SYSTEMATIC REVIEW article
Therapeutic plasma exchange in myasthenia gravis: a systematic literature review and meta-analysis of comparative evidence.

- 1 Department of Pathology and Laboratory Medicine, University of Arkansas for Medical Sciences, Little Rock, AR, United States
- 2 Terumo Blood and Cell Technologies, Lakewood, CO, United States
- 3 Department of Pathology, University of New Mexico, Albuquerque, NM, United States
Background: Patients with Myasthenia Gravis (MG) can be treated acutely with therapeutic plasma exchange (TPE) or intravenous immune globulin (IVIG). To date, there is no definitive understanding of which of the two treatments is more effective and safer. The purpose of this study was to systematically review the literature on the comparative efficacy and safety of TPE to other available treatments for MG.
Methods: A systematic literature search for studies published between 1997 and 2017 was performed per Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines using two database sources, MEDLINE (through the PubMed database) and Cochrane Library.
Results: The search strategy resulted in 535 articles whose abstracts were reviewed. Among these, 165 full texts articles were reviewed for eligibility and 101 articles were excluded. Of the 165 articles, 64 articles were included for a systematic literature and 11 articles for a meta-analysis.
Conclusions: This systematic literature review and meta-analysis of treatment options showed that there was a higher response rate with TPE than IVIG in acute MG patients and patients undergoing thymectomy. There was no difference in mortality between the two treatment options. Our findings highlight the need for additional randomized clinical trials in these patients with MG.
Introduction
Myasthenia gravis (MG) is an autoimmune, neuromuscular transmission disease characterized by a fluctuating weakness of skeletal muscle. It is estimated to affect about 60,000–80,000 people in the United States and about 700,000 people worldwide ( 1 , 2 ). The disease is clinically classified into two main categories: restrictive ocular MG commonly affecting ocular muscles and generalized MG affecting multiple muscle sets including, but not limited to, ocular muscles. Generalized MG, a focus of this review, accounts for about 80% of all MG ( 3 ). MG is commonly caused by antibodies that target the receptors at the neuromuscular junction and is often defined based on those targeted receptors, such as acetylcholine receptor positive (AChR+) MG (~85% of MG), muscle-specific tyrosine-kinase receptor positive (MuSK+) MG (~5% of MG) and low-density lipoprotein receptor-related protein 4 positive (LRP4+) MG (~3% of MG) ( 4 – 7 ). In MG with no detectable levels of any antibodies (~7% of MG), referred to as seronegative MG, the source of immune attack is unclear but the clinical manifestation, treatment options, and treatment response are similar to those of seropositive MG patients.
The hallmark of the disorder is a fluctuating degree and variable combination of weakness in ocular, bulbar, limb, and respiratory muscles. Weakness is the result of an antibody-mediated, T-cell dependent immunological attack directed at proteins in the postsynaptic membrane of the neuromuscular junction (acetylcholine receptors and/or receptor-associated proteins). Thus, MG patients typically exhibit symptoms such as drooping eyelids (ptosis), blurred or double vision (diplopia), change in facial expression, difficulty swallowing, impaired speech, shortness of breath, and progressive muscle weakness of the limbs ( 7 ). Because disease progression is gradual and symptoms fluctuate, diagnosis is often delayed in many patients by months or even years. Disease severity rises with the number of muscles affected from moderate affecting only a few muscles to severe affecting multiple muscle groups. MG is typically a chronic condition, yet about 15–20% of patients experience severe acute symptoms within 2 years of diagnosis ( 3 ). Disease burden in acute patients is significant as these patients can experience impaired breathing; in some cases, these patients require emergency ventilation due to weakening of breathing muscles leading to a condition called myasthenic crisis or MG crisis.
The diagnosis of MG is based on results of one or more physical and neurological examinations as well as tests such as edrophonium test, blood test, electrodiagnostics, diagnostic imaging, and pulmonary function testing ( 7 ). Treatment options vary depending on the patient's state at the time of presentation. Treatment in chronic MG patients is directed at symptom management and typically includes anticholinesterase inhibitors as well as immunosuppressive agents, such as corticosteroids, azathioprine and cyclosporine ( 4 , 7 ). For the ~15% of MG patients that have a tumor in their thymus they often undergo thymectomy to reduce the risk of myasthenic crisis and improve disease prognosis ( 8 ). Acute or severe patients generally receive short term disease stabilizing therapies such as therapeutic plasma exchange (TPE) and intravenous immunoglobulin (IVIG) ( 9 , 10 ). Management of acute patients is critically important because failure to intervene with a proper treatment option can lead to respiratory failure, paralysis, and potentially death. TPE stabilizes acute patients by removing the destructive antibodies; it does this by replacing plasma containing harmful antibodies with a disease-free replacement fluid (either albumin or plasma) ( 11 , 12 ). The mechanism of action of IVIG has yet to be fully elucidated. However, it has been shown that IVIG, when injected, directly binds to the disease-causing antibodies and neutralizes them for relief from immune attack ( 13 ).
TPE, the focus of this review, is a type of apheresis therapy in which plasma that contains disease-causing antibodies is separated and removed from the patient's bloodstream. The TPE procedure can take place through central or peripheral venous access points. There are several TPE systems available from different manufacturers. In the treatment of acute MG patients, including but not limited to myasthenic crisis, TPE, and IVIG are often used interchangeably. Despite several literature reviews ( 14 – 25 ) on TPE, IVIG, or both, there is not a clear agreement as to which of the two acute therapy options is more effective or safer; results can vary across studies and patient types. The decision to use TPE vs. IVIG may also depend on factors such as access and convenience.
The purpose of this literature review and meta-analysis is to assess the comparative efficacy and safety of TPE against available treatment modalities and/or untreated patients.
Materials and Methods
Literature search and review.
The systematic literature review was conducted per Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines with two independent database sources, MEDLINE (through the PubMed database) and Cochrane Library ( 26 ). A systematic search of both database sources was conducted for studies published between 1997 and 2017 using predefined search terminology focusing on TPE and MG. Table 1 presents search terms and combinations used to search both databases. In the report, therapeutic plasma exchange was used unless a reference did not specify the specific type of plasmapheresis. “Plasmapheresis” is a slightly broader term, which includes TPE, and was used within the report only when a particular type of plasmapheresis was not specified in a cited reference. Only studies published in English addressing the efficacy and/or safety of TPE in MG were included. Efficacy endpoints to be included were pre-defined prior to the full text review ( Table 2 ). Safety endpoints, on the other hand, were not pre-defined; all available data were captured except for those reported as “any adverse event (AE)” or “any complication” rates due to the variable or omitted definitions for these terms in many publications. Original clinical research articles and consensus guidelines were included for use in the report. Systematic reviews & meta-analyses were included for context and as potential sources of additional references. All other publication types were excluded: non-systematic reviews, unofficial guidelines, preclinical research, and journal article comments. Abstracts of all studies identified through the search were scored by two independent reviewers to assess eligibility for inclusion.
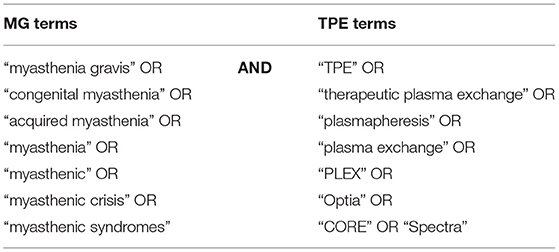
Table 1 . Search terminology.
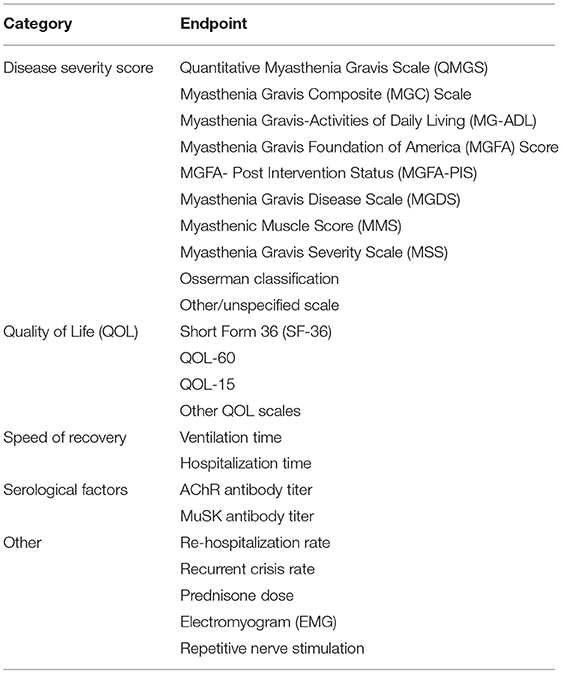
Table 2 . Efficacy endpoints of interest.
Study Selection Process
A total of 526 studies from MEDLINE and 38 studies from the Cochrane Library were identified based on search terminology. Following the removal of duplicates, 535 papers were selected for abstract screening. Abstract screening led to a total of 165 1 articles as eligible candidates for full text review. Bibliographies were checked for additional references, including pre-1997 publications. In cases where an article was not available for download, inquiries were sent to the publisher and corresponding author. Despite these efforts, 3 articles could not be obtained for full text review ( 27 – 29 ). All eligible papers were reviewed and a total of 64 papers met the final criteria and were included in the literature review. Of these 64 papers, 13 cited one or more specific TPE systems, including 6 that cited the COBE Spectra Apheresis System and 1 that cited the Spectra Optia Apheresis System (Terumo BCT, Inc., Lakewood, CO, USA; formerly Caridian BCT). There were numerous non-comparative studies of TPE in MG that are not included in this review. Figure 1 presents the study selection process applied during abstract screening and full text review.
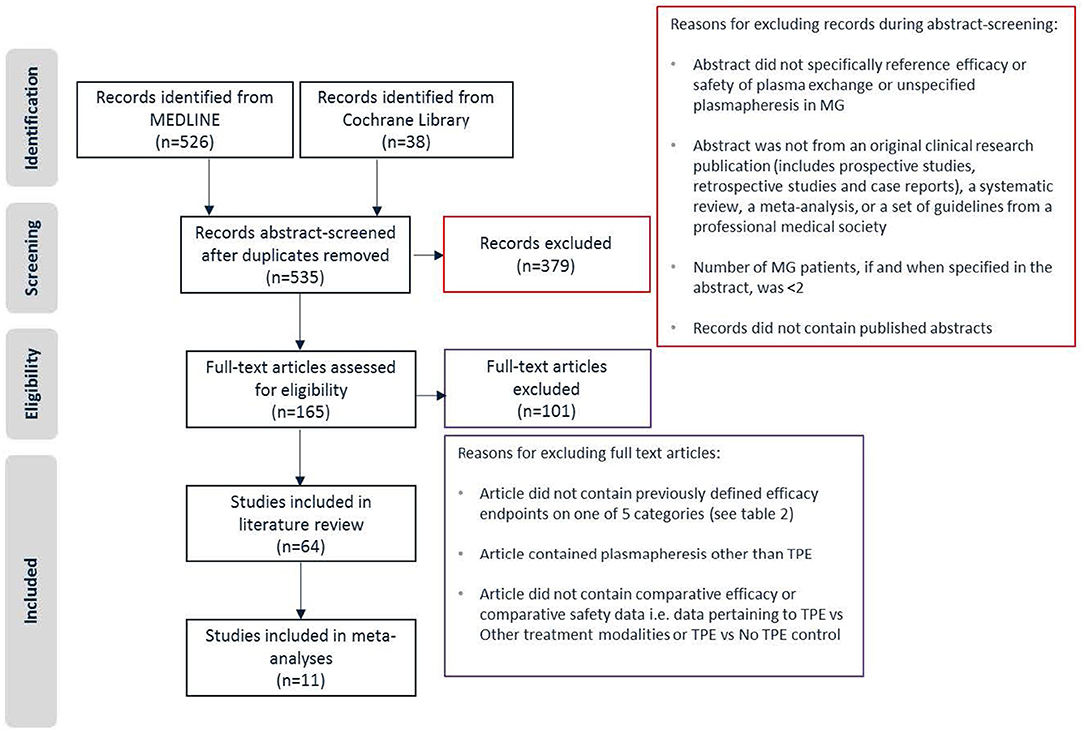
Figure 1 . Study selection.
Data Extraction
During data extraction, reviewers noted and discussed potential sources of biases including imbalances in baseline characteristics, non-randomized nature of studies, and unmasked outcomes. In some cases where data was presented graphically, but not in explicit numerical form, WebPlotDigitizer was used to extract data points from figure images. Where available, statistical summaries including p -values from studies are reported. Where original publications did not provide a test of statistical significance, p -values were calculated using Fisher's exact test for categorical data and student's t -test for continuous data, if appropriate. Continuous variables are described as mean ± standard deviation unless otherwise noted.
Meta-Analysis
All efficacy and safety endpoints captured by 36 comparative safety and comparative efficacy papers were qualified as candidates for meta-analysis. The decision to run a meta-analysis on a specific endpoint was based on two criteria: a) there must be at least 3 papers containing data on that endpoint and b) available data on that endpoint across studies must contain a matching comparator treatment and a comparable study background including treatment context, age group, and outcome measures. Based on these criteria, two endpoints qualified for the meta-analysis. Both compare TPE and IVIG in acute MG patients, with one analysis focused on response rate and the other mortality rate.
Meta-analysis was performed using a random-effects model to account for the fact that the treatment effect may vary due to a variation in patient populations across studies. The outcome of the meta-analysis was reported as risk differences between TPE and IVIG along with 95% confidence intervals (95% CI). The model was fit using the DerSimonian and Laird method with a continuity correction of 0.5 in studies with 0 cell frequencies ( 30 ). Bias in meta-analyses was assessed using Egger's method ( 31 ).
Professional Guidelines and Guidance Statements on the Use of TPE in MG
Three sets of prominent US and EU professional guidelines & guidance statements recommend the use of TPE in one or more MG clinical situations ( 2 , 4 , 32 – 36 ). The most recent guidance from the MG Foundation of America (MGFA) Task Force and guidelines from the European Federation of Neurological Societies (EFNS) and American Society for Apheresis (ASFA) all recommend the use of TPE in cases of severe acute MG, including myasthenic crisis, and in preparation for thymectomy. The ASFA guidelines go further to include patients with moderate disease severity. The MGFA Task Force recommendations expand the set of appropriate clinical situations to include maintenance treatment in juvenile, refractory, or immunosuppressant-contraindicated patients, short term treatment during pregnancy, or any other time that a rapid response is required.
In contrast to the references above that recommend the use of TPE in MG, 2011 guidelines from the American Academy of Neurology (AAN) conclude that there is not enough evidence to support or refute the use of TPE in MG citing a lack of randomized, controlled clinical trials with masked outcomes ( 37 ) 2 . However, the AAN guidelines acknowledge that TPE is being used at many medical centers for the treatment of myasthenic crisis and MG pre-thymectomy.
The MGFA Task Force, ASFA, and EFNS provide further commentary on the tradeoffs between TPE and IVIG. All three guidelines describe TPE and IVIG as equally effective, but tentatively suggest potential advantages for each. The MGFA Task Force guidance and EFNS guidelines state that TPE may work faster in general and may be more effective in MuSK+ patients than IVIG ( 2 , 33 ). The MGFA Task Force guidance and ASFA guidelines describe a more favorable safety profile for IVIG compared to TPE ( 2 , 4 ). No strong recommendation for one over the other is given, though EFNS guidelines state that IVIG may be preferred due to fewer and less severe side effects, while the MGFA Task Force says that expert consensus suggests that TPE is more effective.
Recommendations from on optimizing TPE outcomes include the use of peripheral rather than central venous access ( 2 ), early rather than delayed initiation of TPE during crisis ( 33 ), and delay of corticosteroid treatment during crisis until initial improvement is achieved via TPE ( 2 ). The guidelines are careful to note that although the clinical effect of TPE is rapid (1–7 days), durability is limited & variable (2–12 weeks).
Older ( 38 ) or regional ( 39 ) guidelines on the use and limitations of TPE in MG have also been published. Consensus statements recommending TPE as a valuable treatment for both acute MG crisis and pre-thymectomy date back at least as far as 1986 ( 38 ). A summary of German Society for Neurology guidelines notes that TPE, IVIG, and immunoadsorption (IA) are equivalently recommended for the treatment of myasthenic crisis ( 40 ).
TPE Efficacy
Efficacy of tpe in the treatment of acute mg.
Acute MG patients require immediate medical attention to prevent worsening of symptoms and possibly death. There is a large body of evidence associating TPE with improved disease severity and recovery from crisis in acute MG patients ( 5 , 41 – 46 ). In comparison to IVIG, meta-analysis results indicate a higher overall response rate in patients treated with TPE. Shorter ventilation times have been observed with TPE, while shorter overall hospitalization times have been reported with IVIG. However, for most endpoints, including QOL scores, response time, electrophysiological metrics, and antibody titers, no significant evidence exists for a difference between the two treatments. It is important to note that studies comparing TPE to “no treatment” are not found in the literature likely due to the seriousness of acute MG and the timeframe in which the treatment was developed.
TPE vs. IVIG
Numerous studies have compared the effectiveness of TPE and IVIG in the treatment of acute MG. The majority of these, comprising 2 prospective, randomized trials ( 5 , 41 ) and 4 retrospective analyses ( 42 – 44 , 47 ) included a measure of the impact of TPE and IVIG on overall disease burden. All response rates to TPE treatment were ≥50% of patients and all changes from baseline on established MG disease severity scales were statistically significant. In each of the 6 studies, reported response rates and/or mean response magnitude was greater among patients treated with TPE than among those treated with IVIG 3 . However, the difference reached statistical significance in only one of the studies ( 44 ).
To further explore the difference in efficacy across studies, a meta-analysis of response rates for TPE vs. IVIG in acute MG was performed ( Table 3 ). Data from 4 studies were determined to be sufficiently comparable for inclusion in the analysis (see Table 4 for study design summaries). Studies with response rates that were not based on a specific disease severity or outcome scale were excluded ( 42 , 47 ). The summary statistic, response risk difference (TPE % responders minus IVIG % responders), ranged from +7% to +32% for the 4 eligible studies; a positive risk difference indicates that more patients responded to TPE vs. IVIG. The pooled estimate based on a random effects model was a +19% response risk difference in favor of TPE vs. IVIG in acute MG. This result was statistically significant ( p = 0.002). Egger's test did not indicate bias ( p = 0.6729), but the small number of studies used limits the power of this assessment ( 31 ).
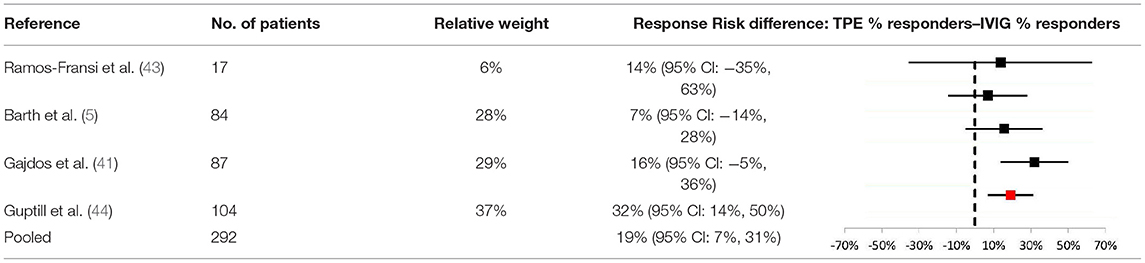
Table 3 . Meta-analysis results comparing response risk differences between TPE and IVIG in acute MG patients.
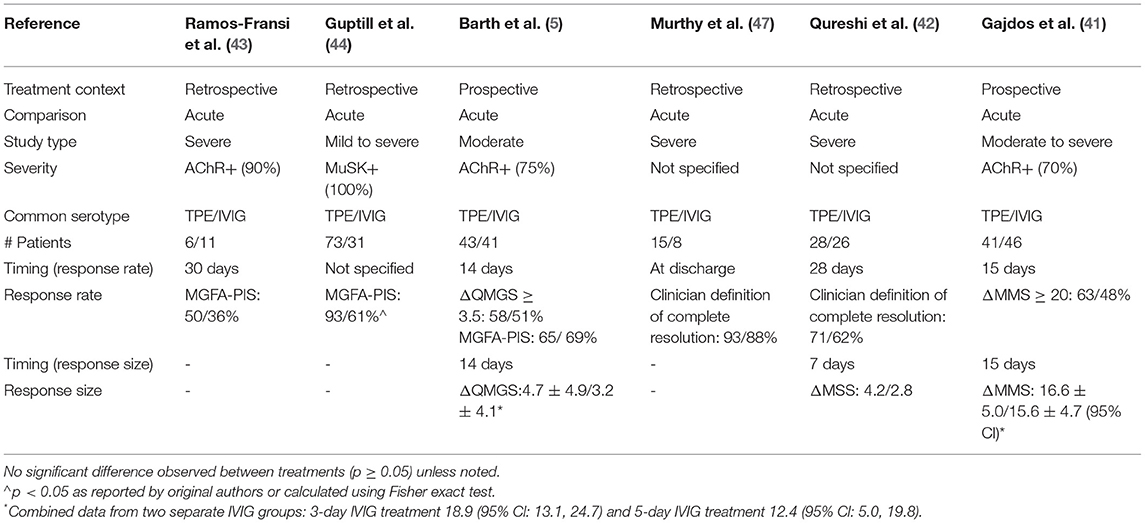
Table 4 . TPE vs. IVIG response rates and sizes in acute MG data.
When comparing TPE to IVIG for other key endpoints, published evidence shows limited differences between the two treatment modalities. However, evidence suggests that compared to IVIG, patients treated with TPE experience shorter ventilation times but longer hospitalizations.
In general, studies comparing TPE and IVIG have not found significant differences for most endpoints. For example, improvements in quality of life scores ( 48 ), response times ( 41 , 42 ), electrophysiological improvement ( 5 ), and decrease in AChR antibody titers ( 41 ) are all key endpoints for which no significant differences between TPE and IVIG have been reported in acute MG. However, there is indirect evidence that responses to TPE may be faster ( 42 ) 4 , but less durable ( 5 ), than responses to IVIG based on response time and electrophysiological data, respectively. Direct comparison of response times also showed a noticeably shorter median response time for TPE vs. IVIG, though the difference did not reach statistical significance ( 42 ).
In contrast, speed of recovery, as measured by ventilation and hospitalization times, is an area in which significant differences between TPE and IVIG have been observed. Specifically, a higher rate of early extubation and superior ventilation status at 2 weeks was observed for TPE vs. IVIG in one study ( 42 ). Conversely, significantly longer hospitalization times were observed among MG crisis patients treated with TPE vs. IVIG ( 1 ). For both of these endpoints, there are studies providing indirect ( 49 ) or directional ( 42 , 50 ) support for these conclusion.
TPE vs. Other Treatment Modalities
In addition to IVIG, the efficacy of TPE has been compared to other treatment modalities in acute MG including immunoadsorption and as an addition to other treatment backgrounds. In 2 studies comparing TPE to IA in acute MG, no significant differences between the two treatments were observed ( 51 , 52 ). However, the combination of TPE + immunoadsorption was associated with significantly shorter hospitalization times than TPE alone ( 51 ).
Studies of other treatment backgrounds with or without TPE have either found better outcomes with TPE ( 49 ) or did not observe significant differences ( 53 , 54 ) among patients receiving treatment for acute MG.
Efficacy of Pre-thymectomy TPE in MG
Studies have found pre-operative TPE to be associated with better thymectomy outcomes. However, there is not strong evidence to support TPE as a superior treatment to IVIG in the pre-thymectomy setting.

TPE vs. No Immunomodulatory Treatment
The majority of published evidence has demonstrated that outcomes in patients undergoing thymectomy are superior for those who receive TPE prior to surgery compared to those who do not receive immunomodulatory therapy ( Table 5 ). Retrospective studies comparing TPE to no pre-thymectomy treatment have found that TPE significantly increases speed of post-operative recovery ( 55 , 57 ), improves long-term response rate and magnitude ( 10 , 55 ) and decreases incidence of crisis during follow up ( 10 , 55 ). The single exception to this trend was a retrospective study in which a lower immediate extubation rate and longer hospitalization time were reported for TPE, though in neither case were the differences statistically significant ( 56 ).
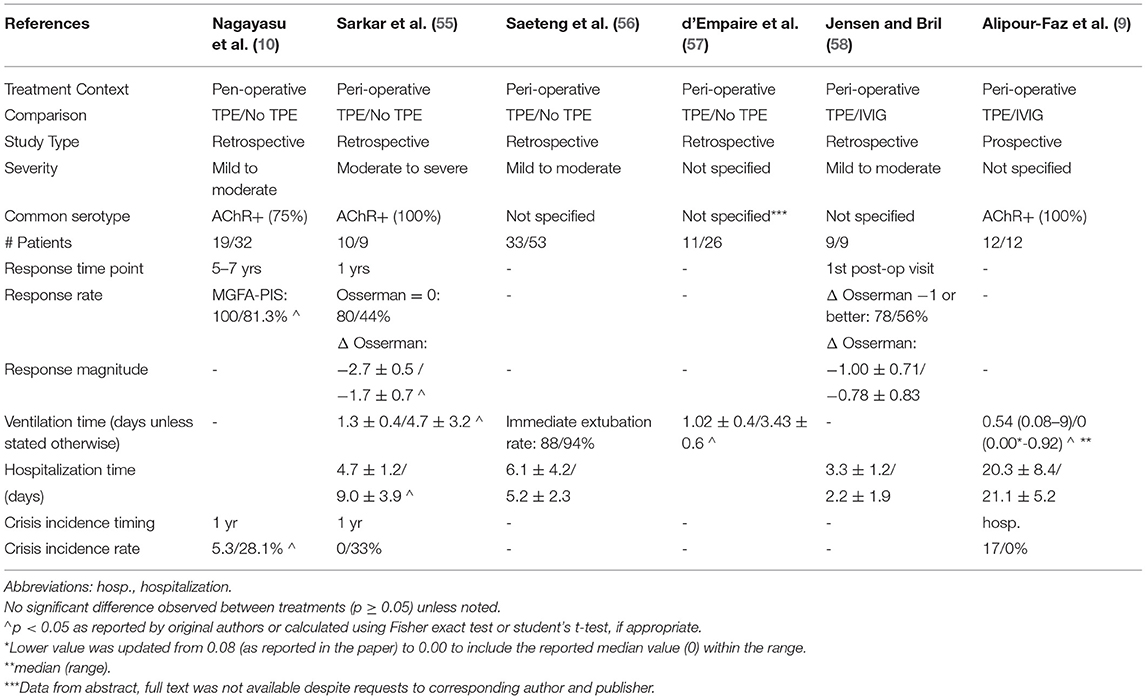
Table 5 . Pre-thymectomy TPE comparative efficacy data.
When compared to IVIG in the pre-thymectomy context, there is no available evidence to suggest that TPE leads to superior outcomes. Across one prospective and one retrospective comparison, no significant differences in response rate or magnitude, hospitalization time, or incidence of crisis were observed between TPE and IVIG ( 9 , 58 ). However, in the prospective study, patients receiving TPE were intubated for a significantly longer time than those receiving IVIG ( 9 ).
Efficacy of TPE in Chronic MG
While TPE is routinely used in the treatment of acute MG patients and those undergoing thymectomy, comparative data is sparse in the maintenance treatment of chronic, stable patients. However, in the limited literature for chronic MG that is available, there is data showing higher response rates to TPE vs. IVIG among juvenile patients ( 25 ) and no evidence of a significant difference between the two treatments in adults ( 45 ).
A controlled crossover trial of TPE and IVIG in chronic, stable adult MG patients tracked QMGS and AChR titers for 16 weeks after an initial course of treatment ( 45 ). During the TPE phase, a statistically significant improvement from baseline QMGS was observed at 1 week, maintained at 4 weeks, but was no longer significant by 8 weeks ( p < 0.05). In contrast, a statistically significant improvement from baseline was not reached until 4 weeks for IVIG and, similarly, was no longer significant by 8 weeks. No statistically significant differences between TPE and IVIG were observed at any timepoint as measured by QMGS. TPE, but not IVIG, led to a statistically significant reduction in AChR titers at 1 week (average decline of 79%, p < 0.001) 5 . In the longer timeframe, neither group showed any statistically significant reduction in AChR titers (4–16 weeks).
Additionally, retrospective analysis of maintenance therapies in juvenile MG patients found that the response rate to TPE was significantly higher than IVIG (100 vs. 50%; p = 0.04) ( 25 ).
In addition to IVIG, the efficacy of TPE has been compared to other treatment modalities in acute MG including pyridostigmine and as an addition to other treatment modalities, such as glucocorticosteroids. In a prospective study of chronic stable moderate patients treated with pyridostigmine or TPE, significantly larger improvements in several pulmonary function metrics was observed with TPE ( 59 ). Studies of steroid treatment backgrounds (i.e., prednisolone, prednisone) with or without TPE have not observed significant differences in maintenance therapy ( 60 , 61 ). One prospective study of long term TPE and prednisone treatment found a faster response when TPE was added to a background of prednisone, although the trend did not continue over a longer period of 24 months ( 61 ); a higher rate of exacerbations was noted in the TPE group, but the difference was not significant.
Considerations to Maximize TPE Efficacy
Some studies have looked at ways to optimize TPE efficacy ( 62 – 66 ). For example, published evidence shows that treatment schedule and venous access route can impact TPE efficacy in MG.
Treatment Schedule
Timing and frequency of TPE in MG may impact speed of recovery. A randomized trial of acute MG patients reported that patients receiving daily TPE spent a median of 17.5 days in the hospital whereas those receiving TPE on alternate days spent a median of 26 days, though this difference was not statistically significant ( p = 0.054) ( 65 ). Similarly, timing of TPE can affect recovery speed as evidenced by a study which showed that MG crisis patients receiving TPE within 2 days of admission had a significantly shorter hospital stay compared to those receiving TPE >2 days after admission (6 days vs. 14 days; p < 0.001) ( 63 ).
Venous Access Route
Peripheral venous access is associated with faster recovery compared to central venous access. A retrospective analysis of MG patients treated with TPE found that patients who received TPE via peripheral venous access spent significantly less time in the hospital compared to those who received TPE via a central venous line (median: 9 days [range 6–10] versus 12 days [range: 8–18], p = 0.002; 84 and 94% acute patients, respectively) ( 62 ).
Specific Population: MuSK+ Patients
There is a small body of evidence demonstrating the efficacy of TPE specifically in MuSK+ MG patients including evidence of higher response rates with TPE vs. IVIG. A retrospective analysis of 110 MuSK+ acute MG patients reported that 93% of patients who received TPE and 61% of patients on IVIG saw clinical improvements based on MGFA-PIS ( p = 0.0002) ( 44 ). A prospective trial in MuSK+ patients compared the efficacy of TPE ( N = 3) against that of early prednisone ( N = 6) and thymectomy ( N = 3) by grading patients on MGFA classification at the onset of myasthenic symptoms, in the maximally deteriorated state, and at the last clinic visit after or during treatment ( 60 ). It found that while all patients on TPE and early prednisone improved ( p = 1.0), no patient improved post-thymectomy. It is important to note, however, that patients in the prednisone and TPE groups had more severe baselines (IIb to V) than the thymectomy group (all IIb) and differences in response rate for TPE vs. thymectomy in MuSK+ patients did not reach statistical significance ( p = 0.1). Although other studies exist that highlight the benefits of TPE over IVIG in MuSK+ patients, they do not provide clear comparative evidence [i.e., one study reports response rates for TPE and IVIG, but the number of patients who received only TPE, only IVIG, or both TPE and IVIG is not specified ( 67 ); another publication studied TPE in patients that had failed IVIG rather than a side by side comparison ( 68 )].
COBE Spectra and Spectra Optia Apheresis Systems
As noted, several types of TPE systems are available to perform TPE procedures in MG patients. Although preclinical publications exist, data comparing the clinical efficacy of different TPE systems was not found in published literature. Most comparative papers either use more than one in a single study or do not specify which was used.
Among publications included in this review that specified one or more specific TPE systems, the Spectra line of systems, COBE Spectra and Spectra Optia Apheresis Systems were the most commonly cited ( 5 , 51 , 62 , 64 ). Comparative studies that exclusively used both COBE Spectra and Spectra Optia Apheresis Systems include a prospective, randomized trial of TPE vs. IVIG in acute MG ( 5 ). In the TPE group, mean QMGS scores were significantly improved at day 14 and this improvement was maintained through day 28 ( p < 0.0001). The majority of TPE patients responded to treatment according to two separate scales 6 , but no significant difference was observed in response rate to TPE vs. IVIG on either scale ( p = 0.5 to 0.74). Although mean values of QMGS improvement were greater at all time points for TPE compared to IVIG, none of the differences were statistically significant ( p = 0.07 to 0.13).
A retrospective analysis from an institution solely using the COBE Spectra Apheresis System for TPE found that patients receiving pre-operative TPE using the COBE Spectra Apheresis System saw improvements following thymectomy compared to those who did not receive a pre-operative TPE ( 64 ). Another retrospective analysis, which exclusively used the COBE Spectra Apheresis System, found that peripheral venous access is associated with shorter hospitalizations compared to central venous access among acute MG patients treated via TPE ( 62 ). Lastly, a retrospective analysis comparing TPE vs. immunoadsorption in acute MG was published by an institution that utilized COBE Spectra Apheresis System as one of its two TPE systems (AS104 from Fresenius Kabi, Bad Homburg, Germany also used). Findings in the TPE group included a statistically significant improvement in QMGS from baseline to time of discharge ( p < 0.0001) ( 51 ). However, there was no statistically significant difference in efficacy between the TPE and immunoadsorption groups.
No significant increase in mortality risk has been reported for TPE compared to other MG treatment modalities, including IVIG. In the pre-thymectomy context, the use of TPE has not been shown to significantly affect mortality compared to untreated patients. In myasthenic crisis, TPE with corticosteroid treatment is associated with significantly lower mortality than treatment with corticosteroids alone. This report provides a complete summary of TPE in MG studies with comparative all-cause mortality data.
TPE vs. No TPE
Most published studies that compare TPE to an untreated group are within the peri-operative context. In a retrospective analysis of patients receiving ( N = 10) or not receiving ( N = 9) pre-thymectomy TPE, no deaths were reported among either patient group through 1 year of follow-up ( 55 ). Another retrospective analysis compared two pre-thymectomy protocols: a universal protocol in which all patients underwent TPE ( N = 74) and a selective protocol in which only “high risk” patients underwent TPE ( N = 90). No deaths were reported under either protocol during hospitalization ( 64 ). A third retrospective study, comparing patients receiving ( N = 33) or not receiving ( N = 53) pre-thymectomy TPE, reported 1 death during hospitalization in each group and no statistically significant difference between the two options ( p = 1.00) ( 56 ).
One very small prospective study reported outcomes for myasthenic crisis patients treated with intravenous methylprednisone (MP) with or without TPE ( 54 ). During hospitalization, mortality was significantly higher in patients treated only with MP compared to those who received both MP and TPE (100% mortality, N = 3 vs. 0% mortality, N = 4; p = 0.03). The authors note that although all patients were mechanically ventilated, some patients were not treated in the ICU due to limited resources. Another, older (1970–1995) retrospective analysis reported high mortality rates among myasthenic crisis patients treated with or without TPE in a background of pyridostigmine ± prednisolone, but there was no significant difference between the +TPE and -TPE groups (19 vs. 10%, p = 0.42) ( 53 ).
As with efficacy, studies of TPE vs. IVIG represent the greatest volume of comparative TPE mortality data. No statistically significant differences between the two have been reported across treatment contexts. For example, the largest published cohort is a retrospective analysis of the Healthcare Cost and Utilization Project-Nationwide Inpatient Sample (HCUPNIS) administrative database, which reported in-patient mortality rates across all MG diagnoses & treatment contexts ( 1 ). Although the unadjusted mortality rate was higher in TPE than in IVIG (2.6 and 0.6%), the adjusted odds ratio of 2.6 was not found to be statistically significant ( p = 0.21).
To provide greater strength of evidence within a single treatment context, a meta-analysis of TPE vs. IVIG all-cause mortality in acute MG was performed ( Table 6 ). Data from 7 studies were determined to be sufficiently comparable for inclusion in the analysis (See Table 7 for study design and demographic summary). Chronic, maintenance studies ( 25 , 45 ) and mixed cohorts ( 1 ) 7 were excluded. Mortality risk difference (TPE mortality % minus IVIG mortality %), ranged from−5.8% to +5.1%. The pooled estimate based on a random effects model was a +1.5% mortality risk difference (higher risk in TPE) but was not statistically significant ( p = 0.264). Egger's test did not indicate bias ( p = 0.065), but the small number of studies used limits the power of this assessment ( 31 ). Thus, even when aggregating data from all published comparisons, there is insufficient evidence to conclude that TPE and IVIG have different all-cause mortality rates in acute MG.
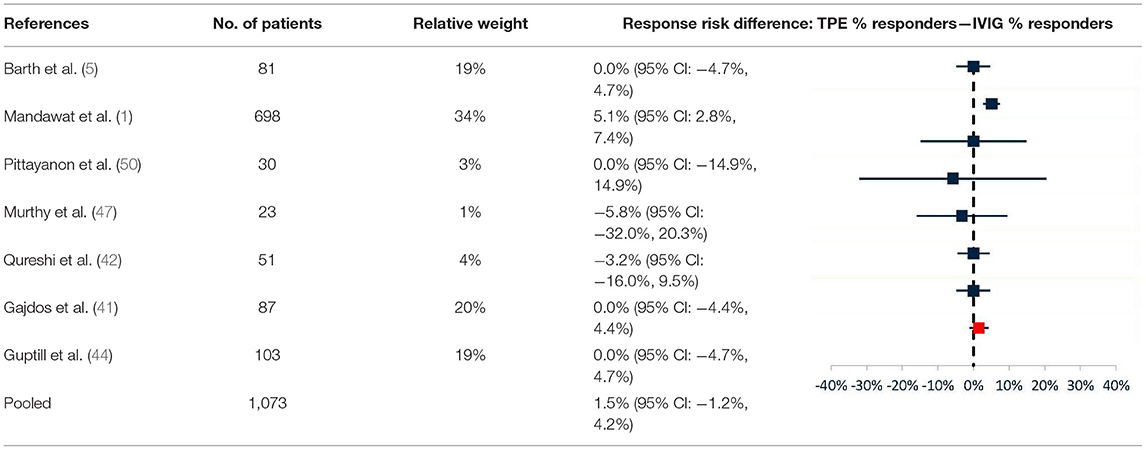
Table 6 . Results of meta-analysis (TPE vs. IVIG) of mortality risk difference in acute MG.
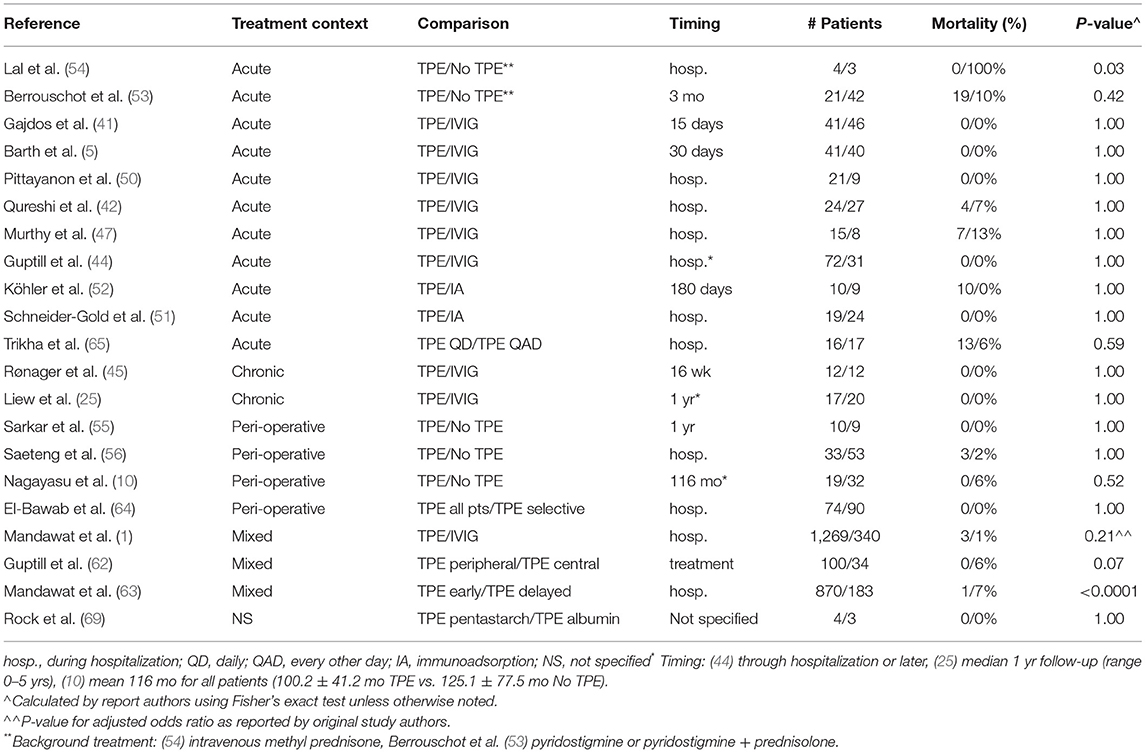
Table 7 . Comparative all-cause mortality data for TPE in MG.
Mortality data has also been published in the chronic/maintenance setting, though the number of published comparisons of TPE vs. IVIG is far fewer than in acute MG. In one retrospective analysis, 27 juvenile MG patients were treated with TPE or IVIG every other week, with tapering if possible ( 25 ). Over a median 1-year follow-up, no deaths were reported in either group. Lastly, in a prospective controlled crossover trial, 12 stable, chronic MG patients were treated with a course of TPE or IVIG ( 45 ). Through 16 weeks of follow-up, no deaths were reported in either group.
Optimizing TPE
A few studies have also looked at the effects of procedural factors on mortality in MG patients treated with TPE. In a retrospective analysis of the HCUPNIS administrative database, inpatient mortality was reported for patients receiving early TPE (0–2 days from admission) or delayed TPE (>2 days from admission) under any MG treatment context ( 63 ). All-cause mortality was significantly higher in patients who received delayed vs. early TPE (6.6% N = 183 vs. 1.2% N = 870, p < 0.0001: adjusted odds ratio 1.86, p < 0.0001).
A retrospective study of the impact of access route on TPE complications in MG compared mortality for peripheral vs. central venous access ( 62 ). Across a mix of treatment contexts, no deaths were reported in patients receiving TPE via peripheral venous access ( N = 100). Two deaths occurred among patients receiving TPE via central access ( N = 34), but this difference did not reach statistical significance ( p = 0.07).
As noted above for efficacy, data comparing the mortality associated with different TPE systems was not found in published literature. However, Table 7 includes all-cause mortality data from several studies captured in this report that used the Spectra systems, COBE Spectra and Spectra Optia Apheresis Systems, exclusively ( 5 , 62 , 64 ) or as one of two cited systems ( 51 , 69 ). Across all treatment contexts in the studies using COBE Spectra and Spectra Optia Apheresis Systems exclusively, 2 deaths were reported among 284 treated patients. Both deaths occurred in patients described as having MG-related immobility and were suspected to have been caused by central venous catheter complications: urosepsis and pulmonary embolism ( 62 ).
Other Adverse Events
Studies which resulted in statistically significant differences between TPE, and any comparator treatment were limited to a handful of publications comparing TPE vs. IVIG. While incidence of certain AEs is greater in TPE, there are other AEs more frequently seen in IVIG. Existing evidence points to peripheral venous access and early treatment as the TPE procedural factors most strongly associated with lower AE rates. A compilation of all vascular, cardiac, infection, and other 8 AE rates from comparative studies, including those for which significant differences were not observed, are shown in Tables 8 – 11 , respectively. As seen in Tables 8 – 11 , AEs other than those listed here may have had higher rates reported in either TPE or IVIG, but the differences were not significant, and sufficiently comparable studies could not be identified for a meta-analysis of >2 studies.
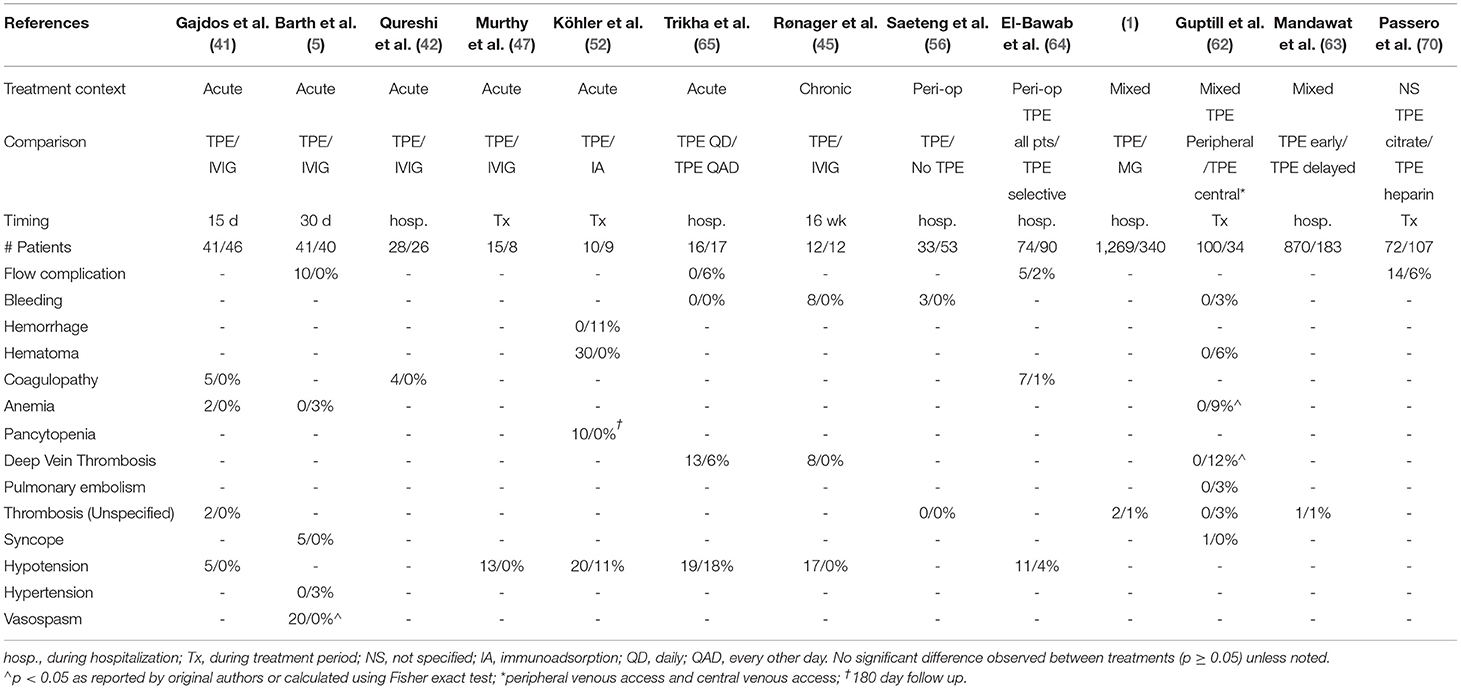
Table 8 . Comparative vascular adverse event data for TPE in MG.
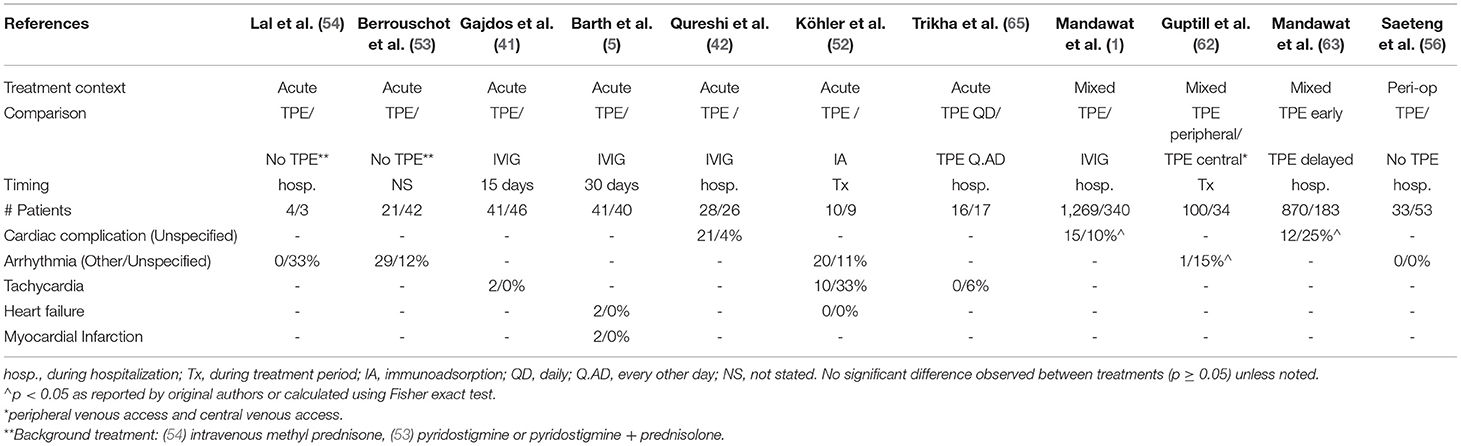
Table 9 . Comparative cardiac adverse event data for TPE in MG.
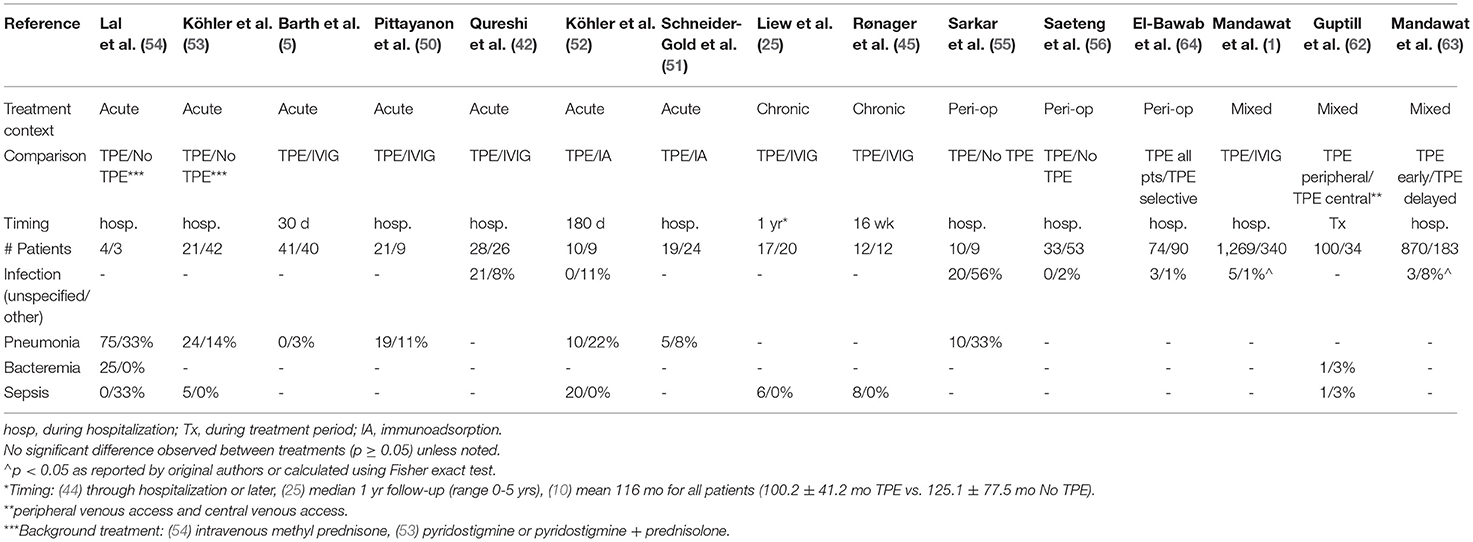
Table 10 . Comparative infection adverse event data for TPE in MG.
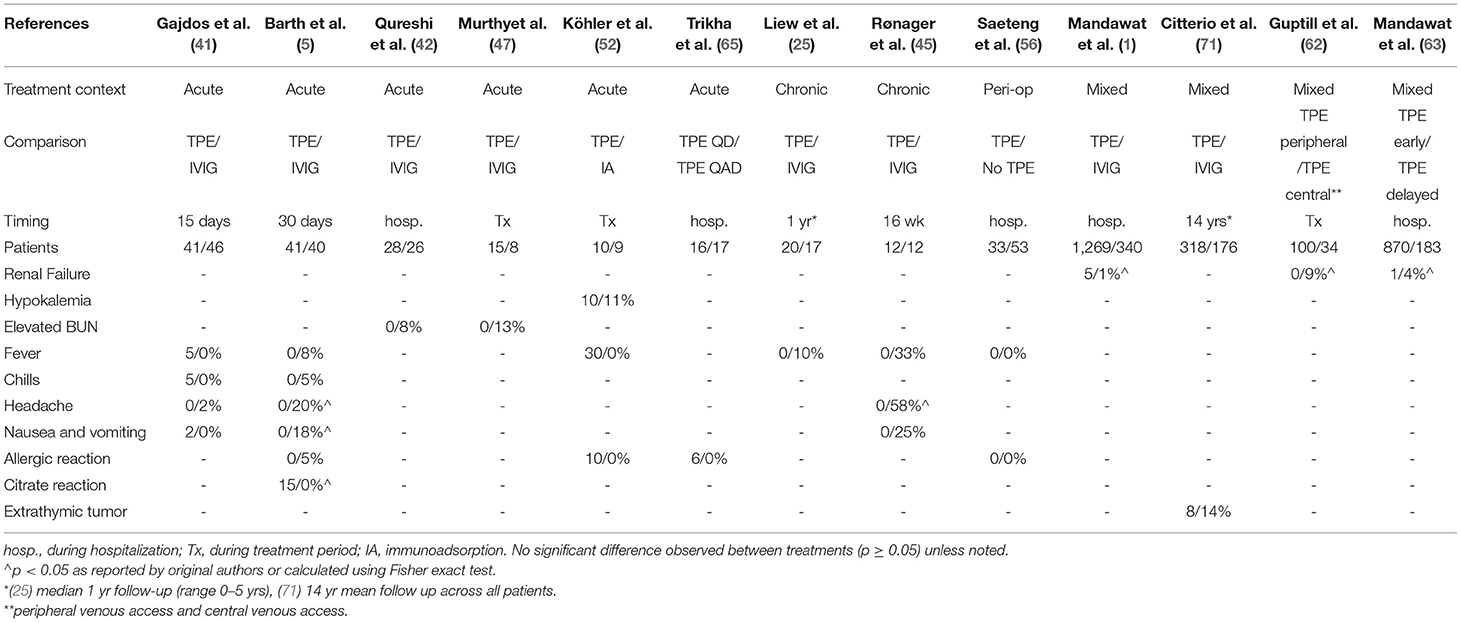
Table 11 . Additional comparative adverse event data for TPE in MG.
PE vs. IVIG
AEs with significantly higher rates in TPE included cardiovascular AEs, infections, renal failure, and citrate reactions, while IVIG showed higher rates of extra-thymic tumor formation, headache, and nausea and vomiting.
In a combined analysis of all MG patients (crisis and non-crisis) in a retrospective HCUPNIS analysis ( 1 ), the adjusted odds ratio for any severe complication favored IVIG, but did not reach statistical significance (odds ratio IVIG/TPE: 0.71, p = 0.07). However, among myasthenic crisis patients treated with TPE or IVIG, the rates of cardiac complications, systemic infections, and acute renal failure were all significantly higher among TPE-treated patients. Cardiac complications, comprising hypotension, fluid overloading, arrhythmias, myocardial infarction, and cardiac arrest, was the most frequently observed category in both TPE and IVIG (22.68 vs. 11.83%, p = 0.001). The most significant difference between TPE and IVIG was observed in systemic infections, which included bacteremia, sepsis, systemic inflammatory response syndrome, and anaphylaxis (9.45 vs. 1.18%, p < 0.0001). Acute renal failure was significantly higher in the TPE cohort (4.73 vs. 1.18%, p = 0.038). In contrast, rates for non-crisis MG patients were lower for each category and no statistically significant differences were observed between TPE and IVIG (cardiac: 9.50 vs. 7.60%, p = 0.55; infection: 1.63 vs. 1.17%, p = 1.00; renal failure: 0.27 vs. 1.17%, p = 0.16; N = 737 and 171, respectively). A fourth AE category, thrombotic complications, exhibited a higher rate in TPE among crisis patients and a lower rate in TPE among non-crisis patients, though neither was statistically significant (crisis: 3.40 vs. 0.59%, p = 0.05; non-crisis: 0.27 vs. 0.58%, p = 0.46).
A prospective, randomized study comparing TPE ( N = 41) and IVIG ( N = 40) in acute MG found significant differences in the rate of several AEs ( 5 , 72 ). Citrate reaction (14.6 vs. 0%, p = 0.03) and vasospasm (19.5 vs. 0%, p = 0.0054) were observed specifically in TPE. In contrast, headache (0 vs. 20.0%, p = 0.0024) and nausea & vomiting (0 vs. 17.5%, p = 0.0054) occurred solely in the IVIG group. A prospective controlled crossover comparison of TPE vs. IVIG as maintenance therapies similarly reported headache as an IVIG-specific adverse event (0 vs. 58%, p = 0.0046) ( 45 ).
A large, retrospective survey examined the risk factors associated with extrathymic tumor formation in 2,479 MG patients over long term follow-up (mean 14 years) ( 71 ). Increased risk of extrathymic tumor formation as a function of MG treatment history was summarized by odds ratios for several common MG treatments, including TPE (OR: 1.1, 95% CI 0.6–1.7) and IVIG (OR: 1.8, 95% CI 1.1–3.0). Among all treatments considered, only history of IVIG treatment was confirmed by multivariate logistic regression analysis to have a statistically significant association with extrathymic tumor formation (adjusted OR: 1.8, 95% CI 1.1–2.9).
A few studies have also looked at the effects of procedural factors on specific adverse events, beyond mortality, in MG patients treated with TPE. Significantly better safety outcomes were achieved when TPE was performed soon after hospital admission and via peripheral venous access.
A retrospective study compared adverse event rates in TPE for MG performed via peripheral ( N = 100) vs. central venous access ( N = 34) ( 62 ). Cohorts included TPE use under any MG treatment context. Rates of several specific AEs were significantly lower for peripheral access: anemia or coagulopathy requiring transfusion (0 vs. 9%, p = 0.015), deep vein thrombosis (0 vs. 12%, p = 0.0033), arrhythmia (atrial fibrillation with rapid ventricular response: 1 vs. 15%, p = 0.0041), and acute renal failure (0 vs. 9%, p = 0.015).
The retrospective analysis of TPE timing within HCUPNIS found that the rates of several major AE categories were lower in early TPE (0–2 days from admission, N = 870) vs. delayed TPE (>2 days from admission, N = 183) ( 63 ). Specifically, the rates of cardiac complications (11.8 vs. 24.6%, p < 0.0001), systemic infections (2.9 vs. 7.7%, p < 0.001), and acute renal failure (1.0 vs. 3.8%, p = 0.009) were all statistically lower when TPE was performed early. The adjusted odds ratio for any complication from the above categories showed a significant increase in risk when TPE treatment was delayed (odds ratio delayed/early: 1.49, p < 0.0001).
As noted for efficacy and mortality, data comparing other adverse events associated with different TPE systems was not found in published literature. Tables 8 – 11 include adverse event data from several studies captured in this report that used the Spectra systems, COBE Spectra and Spectra Optia Apheresis Systems, exclusively ( 5 , 62 , 64 , 70 ) or as one of two cited systems ( 51 , 69 ). Safety findings from studies exclusively using COBE Spectra and Spectra Optia Apheresis Systems in comparison to IVIG ( 5 , 72 ) and that used COBE Spectra Apheresis System exclusively in comparing between peripheral and central venous access ( 62 ) have been described in previous sections. Safety data in other TPE optimization studies using COBE Spectra Apheresis System reported higher rates of several AEs under certain conditions, but differences did not reach statistical significance in any case ( 64 , 69 , 70 ). Lastly, in a retrospective analysis comparing TPE vs. immunoadsorption in acute MG from an institution that utilized COBE Spectra Apheresis System as one of its two TPE systems, a higher overall adverse event rate was reported with TPE (36.9 vs. 4.2%, p < 0.05) ( 51 ). Other than pneumonia, for which there was no significant difference between the two treatments, rates of specific AEs were not reported.
Limitations
There are several limitations of this report and the body of literature on which it is based. As has been noted by many authors in the past, establishing a baseline benefit of TPE is not possible from the available literature given the lack of placebo-controlled studies, likely due to the life-threatening nature of the condition in the acute context. Others have noted that decades of observational experience likely preclude and render unethical the performance of a randomized trial with a placebo arm ( 73 , 74 ). As such, this report was designed to capture comparative data between TPE and other key treatments in use within MG. The included studies are mostly retrospective or prospective, but not blinded, not adjusted for potential geographic differences, and the majority do not specify the TPE system or separation method. Although we highlighted one system, comparison of other devices in the future would be beneficial. Other systematic reviews and some guidelines utilized more narrow inclusion criteria, which can be complemented by the more inclusive approach of this report. Another meta-analysis comparing plasmapheresis with IVIG looked strictly at prospective studies but also included other forms of plasmapheresis ( 75 ). Lastly, predominately retrospective or prospective studies were used in the analysis; randomized controlled studies would be preferred but unfortunately this is a limitation of available data.
Despite a comprehensive, inclusive approach, it is possible that our search may not have captured all relevant studies. Potential gaps include non-English articles, articles published prior to 1997, but not cited in later literature, articles not indexed in either of the databases utilized, or articles for which full text copies could not be obtained. Furthermore, the strategy was not designed to specifically look at data for MG patients seronegative for MuSK antibodies or positive for LRP 4, but this area remains of interest. Given the dearth of available data to determine if seropositive or seronegative patients should be treated differently with the available treatment, the currently available studies indicate that these patients should be treated similarly.
Regarding professional treatment guidelines, the most recent versions were given precedence. Several of these are more than 5 years old and more recent data might have altered the perspectives of their developers ( 4 , 37 ).
In the meta-analyses, because of design limitations in the available studies, including variable disease scale, serotype, and timepoint, additional variables cannot be ruled out as potentially affecting TPE vs. IVIG outcomes. Baseline disease severity could also impact both efficacy and safety results, as was specifically noted in the largest retrospective analysis included in this report ( 1 ). It is also notable that in several instances an AE commonly mentioned in the literature to be associated with TPE was higher than a comparator, but the difference was not significant, which could be an unavoidable limitation of the small size of many of the included studies ( Tables 8 – 11 ).
Conclusions
TPE is an effective and appropriate MG treatment as evidenced by original research studies and professional guideline recommendations.
Although placebo controlled studies are not available, studies report high response rates among acute MG patients treated with TPE, as has been summarized previously ( 76 ). There is a large body of evidence associating TPE with improved disease severity and recovery from crisis in acute MG patients. In acute MG, a risk/benefit tradeoff appears to exist between TPE and IVIG. The meta-analysis results from this report indicate a higher response rate with TPE vs. IVIG in acute MG patients. The meta-analysis did not find differences in mortality; however, IVIG was associated with a lower risk of potentially serious adverse events. If peripheral rather than central venous access can be utilized in TPE treatment of myasthenic crisis, evidence shows a significant drop in most serious AE rates. Some evidence suggests that fast responses and shorter ventilation times are more likely with TPE, which might increase the favorability of TPE when a rapid response is particularly important. TPE might be preferred over IVIG in patients with a higher baseline risk of extrathymic tumor formation than the broader MG population, or in patients particularly sensitive to headache or nausea & vomiting. Conversely, IVIG might be preferred in patients with a higher baseline risk of cardiovascular AEs, infections, and renal failure than the broader MG population. It is important to note that these factors potentially impacting risk/benefit tradeoffs have not been evaluated prospectively but warrant further investigation. Irrespective of IVIG, peripheral venous access and early intervention are associated with significantly more favorable outcomes of TPE treatment in acute MG. There is direct of evidence that TPE is superior to IVIG in MuSK+ patients from a single comparative study, which is reflected in professional guidelines. Other studies in which TPE and IVIG are used in MuSK+ patients, but they do not provide clear comparative evidence and further investigation would be valuable.
Most published evidence has demonstrated that outcomes in patients undergoing thymectomy are superior for those who receive TPE prior to surgery compared to those who do not receive acute immunomodulatory therapy. However, there is no available evidence to suggest that TPE has superior efficacy over IVIG when used pre-thymectomy, and TPE vs. IVIG adverse event rates have not been reported in this context.
In maintenance therapy for chronic MG, the overall body of evidence comparing TPE to other treatments is quite limited and the limitation of the transient response is burdensome. In juvenile patients, there is evidence supporting the use of TPE over IVIG for maintenance therapy, but further investigation is needed beyond the single published comparative study. However, the relatively high response rates and lack of a statistically significant safety downsides to IVIG in available maintenance studies suggest that this treatment area warrants further investigation to further establish both comparative efficacy and safety.
In summary, available literature and professional recommendations strongly indicate that TPE has clear clinical utility in the treatment of acute MG and in improving thymectomy outcomes. There are notable side effects that should be considered, but neither a significantly increased risk of mortality nor a consistent pattern of serious adverse events exists across studies. TPE outcomes can be improved further with early intervention and peripheral venous access.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author Contributions
TSI and JSR: study concept, design, and drafting of the manuscript. All authors contributed to critically revising the manuscript.
The authors declare that this study received funding from Terumo Blood and Cell Technologies. The funder was not involved in the study design, collection, interpretation of data, the writing of this article, or the decision to submit it for publication.
Conflict of Interest
TSI and JSR are consultants for Terumo Blood and Cell Technologies. ARD was an employee of Terumo Blood and Cell Technologies.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. ^ 9 of the 165 articles were added from citations during full-text review.
2. ^ AAN scale “Level U” recommendation – very low confidence in evidence.
3. ^ One study reported a higher rate for TPE vs. IVIG when response was defined as clinically meaningful improvement in the primary outcome metric (ΔQMGS≥3.5) (58 vs. 51%), but an opposing trend when response was defined as an MGFA-PIS of improved or better (65 vs. 69%).
4. ^ Direct statistical comparison between TPE and IVIG not reported and not possible from published data because no variance metric was reported.
5. ^ The study did not report on the statistical differences between the efficacies of two treatments as measured by AChR titers.
6. ^ ΔQMGS ≥ 3.5: 57% response rate, MGFA-PIS “improved” or better: 65% response rate.
7. ^ HCUPNIS analysis comprised a mixed cohort (“Myasthenia gravis”), which was excluded from the meta-analysis, and an acute cohort (“myasthenia gravis crisis”), which was included in the meta-analysis.
8. ^ Includes any other specific AEs meeting at least one of the following criteria (1) appearing in >1 publication, (2) associated with TPE according to other existing literature, (3) subjectively evaluated by report authors as potentially serious (e.g., vasospasm, extrathymic tumors).
1. Mandawat A, Kaminski HJ, Cutter G, Katirji B, Alshekhlee A. Comparative analysis of therapeutic options used for myasthenia gravis. Ann. Neurol. (2010) 68:797–805. doi: 10.1002/ana.22139
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Sanders DB, Wolfe GI, Benatar M, Evoli A, Gilhus NE, Illa I, et al. International consensus guidance for management of myasthenia gravis: Executive summary. Neurology. (2016) 87:419–25. doi: 10.1212/WNL.0000000000002790
3. Abbas Jowkar C, Lorenzo N. Myasthenia gravis: practice essentials, background, anatomy. Medscape . (2017). Available online at: https://emedicine.medscape.com/article/1171206-overview (accessed September, 2019).
4. Skeie GO, Apostolski S, Evoli A, Gilhus NE, Illa I, Harms L, et al. Guidelines for treatment of autoimmune neuromuscular transmission disorders. Eur J Neurol. (2010) 17:893–902. doi: 10.1111/j.1468-1331.2010.03019.x
5. Barth D, Nabavi Nouri M, Ng E, Nwe P, Bril V. Comparison of IVIg and PLEX in patients with myasthenia gravis. Neurology. (2011) 76:2017–23. doi: 10.1212/WNL.0b013e31821e5505
6. Zisimopoulou P, Evangelakou P, Tzartos J, Lazaridis K, Zouvelou V, Mantegazza R, et al. A comprehensive analysis of the epidemiology and clinical characteristics of anti-LRP4 in myasthenia gravis. J Autoimmun. (2014) 52:139–45. doi: 10.1016/j.jaut.2013.12.004
7. NIH. Myasthenia Gravis Fact Sheet. (2017). Available online at: https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Myasthenia-Gravis-Fact-Sheet (accessed September, 2019).
Google Scholar
8. Linda M, Wendell C, Joshua Levine M. Myasthenic crisis neuroanesthesia neurocritical care. Case Stud . (2011) 1:321–3. doi: 10.1177/1941875210382918
9. Alipour-Faz A, Shojaei M, Peyvandi H, Ramzi D, Oroei M, Ghadiri F, et al. A comparison between IVIG and plasma exchange as preparations before thymectomy in myasthenia gravis patients. Acta Neurol Belg. (2017) 117:245–9. doi: 10.1007/s13760-016-0689-z
10. Nagayasu T, Yamayoshi T, Matsumoto K, Ide N, Hashizume S, Nomura M, et al. Beneficial effects of plasmapheresis before thymectomy on the outcome in myasthenia gravis. Jpn J Thorac Cardiovasc Surg. (2005) 53:2–7. doi: 10.1007/s11748-005-1001-y
11. Guptill JT, Juel VC, Massey JM, Anderson AC, Chopra M, Yi JS, et al. Effect of therapeutic plasma exchange on immunoglobulins in myasthenia gravis. Autoimmunity. (2016) 49:472–9. doi: 10.1080/08916934.2016.1214823
12. Reeves HM, Winters JL. The mechanisms of action of plasma exchange. Br J Haematol . (2014) 164:342–51. doi: 10.1111/bjh.12629
13. Lehmann HC, Hartung HP. Plasma exchange and intravenous immunoglobulins: Mechanism of action in immune-mediated neuropathies. J Neuroimmunol. (2011) 231:61–9. doi: 10.1016/j.jneuroim.2010.09.015
14. Dhawan PS, Goodman BP, Harper CM, Bosch PE, Hoffman-Snyder CR, Wellik KE, et al. IVIG versus PLEX in the treatment of worsening myasthenia gravis: What is the evidence? A critically appraised topic. Neurologist. (2015) 19:145–8. doi: 10.1097/NRL.0000000000000026
15. Gajdos P, Chevret S, Toyka K. Intravenous immunoglobulin for myasthenia gravis. Cochrane Database Syst Rev. (2003) 12:CD002277. doi: 10.1002/14651858.CD002277
16. McDaneld LM, Fields JD, Bourdette DN, Bhardwaj A. Immunomodulatory therapies in neurologic critical care. Neurocrit Care. (2010) 12:132–43. doi: 10.1007/s12028-009-9274-0
17. Gajdos P, Chevret S, Toyka K. Intravenous immunoglobulin for myasthenia gravis. Cochrane Database Syst Rev. (2006) 12:CD002277. doi: 10.1002/14651858.CD002277.pub2
18. Dalakas MC. Intravenous Immunoglobulin in autoimmune neuromuscular diseases. JAMA . (2004) 291:2367–75. doi: 10.1001/jama.291.19.2367
19. Winters JL, Pineda AA. New directions in plasma exchange. Curr Opin Hematol. (2003) 10:424–8. doi: 10.1097/00062752-200311000-00005
20. Gajdos P, Chevret S, Toyka K. Plasma exchange for generalised myasthenia gravis. Cochrane Database Syst Rev. (2002) 4:2002. doi: 10.1002/14651858.CD002275
21. Gajdos P, Chevret S, Toyka KV. Intravenous immunoglobulin for myasthenia gravis. Cochrane Database Syst Rev. (2012) 12:CD002277. doi: 10.1002/14651858.CD002277.pub4
22. Gajdos P, Chevret S. Treatment of myasthenia gravis acute exacerbations with intravenous immunoglobulin. Ann N Y Acad Sci. (2008) 1132:271–5. doi: 10.1196/annals.1405.001
23. Gajdos P, Chevret S, Toyka KV. Intravenous immunoglobulin for myasthenia gravis. Cochrane Database Syst Rev . (2008) 1:CD002277. doi: 10.1002/14651858.CD002277.pub3
24. Ng JK, Ng CS, Underwood MJ, Lau KK. Does repeat thymectomy improve symptoms in patients with refractory myasthenia gravis?. Interact Cardiovasc Thorac Surg. (2014) 8:376–80. doi: 10.1093/icvts/ivt493
25. Liew WK, Powell CA, Sloan SR, Shamberger RC, Weldon CB, Darras BT, et al. Comparison of plasmapheresis and intravenous immunoglobulin as maintenance therapies for juvenile myasthenia gravis. JAMA Neurol. (2014) 71:575–80. doi: 10.1001/jamaneurol.2014.17
26. Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. PRISMA-P (preferred reporting items for systematic review and meta-analysis protocols) 2015 checklist : recommended items to address in a systematic review protocol. BMJ. (2015) 349:2015. doi: 10.1136/bmj.g7647
27. Iani C, Caramia M, Morosetti M, Loberti M, Palmieri MG, Meloni C, et al. The treatment of severe forms of myasthenia gravis. Funct Neurol. (1998) 13:231–7.
PubMed Abstract | Google Scholar
28. Tireli H, Karlikaya G, Tutkavul K, Akpinar A, Okay T. Myasthenia gravis: how to treat?. Myopathies cardiomyopathies Off. J Mediterr Soc Myol. (2004) 23:140–5.
29. Pérez Nellar J, Domínguez AM, Llorens-Figueroa JA, Ferrá-Betancourt A, Pardo A, Quiala M, et al. [A comparative study of intravenous immunoglobulin and plasmapheresis preoperatively in myasthenia]. Rev Neurol. (2001) 33:413–6. doi: 10.33588/rn.3305.2001132
30. DerSimonian R, Laird N. Meta-analysis in clinical trials revisited. Contemp Clin Trials. (2015) 45:139–45. doi: 10.1016/j.cct.2015.09.002
31. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
32. Skeie GO, Apostolski S, Evoli A, Gilhus NE, Illa I, Harms L, et al. Guidelines for the treatment of autoimmune neuromuscular transmission disorders. Eur J Neurol. (2006) 13:691–9. doi: 10.1111/j.1468-1331.2006.01476.x
33. Padmanabhan A, Connelly-Smith L, Aqui N, Balogun RA, Klingel R, Meyer E, et al. Guidelines on the use of therapeutic apheresis in clinical practice-evidence-based approach from the writing committee of the American society for apheresis: the seventh special issue. J Clin Apheresis. (2016) 31:149–62. doi: 10.1002/jca.21470
34. Schwartz J, Winters JL, Padmanabhan A, Balogun RA, Delaney M, Linenberger ML, et al. Guidelines on the use of therapeutic apheresis in clinical practice-evidence-based approach from the writing committee of the American society for apheresis: the sixth special issue. J Clin Apher. (2013) 28:145–284. doi: 10.1002/jca.21276
35. Szczepiorkowski ZM, Winters JL, Bandarenko N, Kim HC, Linenberger ML, Marques MB, et al. Guidelines on the use of therapeutic apheresis in clinical practice - Evidence-based approach from the apheresis applications committee of the American Society for Apheresis. J Clin Apheresis. (2010) 22:106–75.
36. Szczepiorkowski ZM, Bandarenko N, Kim HC, Linenberger ML, Marques MB, Sarode R, et al. Guidelines on the use of therapeutic apheresis in clinical practice: evidence-based approach from the Apheresis Applications Committee of the American Society for Apheresis. J Clin Apher. (2007) 22:106–75. doi: 10.1002/jca.20129
37. Cortese I, Chaudhry V, So YT, Cantor F, Cornblath DR, Rae-Grant A. Evidence-based guideline update : plasmapheresis in neurologic disorders report of the therapeutics and technology assessment. Neurology. (2011) 76:294–300. doi: 10.1212/WNL.0b013e318207b1f6
38. The utility of therapeutic plasmapheresis for neurological disorders. NIH Consensus Development. JAMA . (1986) 256:1333–7. doi: 10.1001/jama.256.10.1333
CrossRef Full Text | Google Scholar
39. Diener HC, Weimar C, Berlit P, Deuschl G, Elger C, Gold R, et al. Leitlinien für Diagnostik und Therapie in der Neurologie . Stuttgart: Georg Thieme Verlag (2008).
40. Klingel R, Heibges A, Fassbender C. Plasma exchange and immunoadsorption for autoimmune neurologic diseases - current guidelines and future perspectives. Atheroscler. (2009) 10:129–32. doi: 10.1016/S1567-5688(09)71827-6
41. Gajdos P, Chevret S, Clair B, Tranchant C, Chastang C. Clinical trial of plasma exchange and high-dose intravenous immunoglobulin in myasthenia gravis. Myasthenia Gravis Clinical Study Group. Ann Neurol. (1997) 41:789–96. doi: 10.1002/ana.410410615
42. Qureshi AI, Choudhry MA, Akbar MS, Mohammad Y, Chua HC, Yahia AM, et al. Plasma exchange versus intravenous immunoglobulin treatment in myasthenic crisis. Neurology. (1999) 52:629. doi: 10.1212/WNL.52.3.629
43. Ramos-Fransi A, Rojas-García R, Segovia S, Márquez-Infante C, Pardo J, Coll-Cantí J, et al. Myasthenia gravis: Descriptive analysis of life-threatening events in a recent nationwide registry. Eur J Neurol. (2015) 22:1056–61. doi: 10.1111/ene.12703
44. Guptill JTT, Sanders DBB, Evoli A. Anti-MuSK antibody myasthenia gravis: clinical findings and response to treatment in two large cohorts. Muscle Nerve. (2011) 44:36–40. doi: 10.1002/mus.22006
45. Rønager J, Ravnborg M, Hermansen I, Vorstrup S. Immunoglobulin treatment versus plasma exchange in patients with chronic moderate to severe myasthenia gravis. Artif Organs. (2001) 25:967–731. doi: 10.1046/j.1525-1594.2001.06717.x
46. Katzberg HDD, Barnett C, Bril V. Predictors of response to immunomodulation in patients with myasthenia gravis. Muscle Nerve. (2012) 45:648–52. doi: 10.1002/mus.23236
47. Murthy J, Meena A, Chowdary G, Naryanan J. Myasthenic crisis: clinical features, complications and mortality. Neurol India. (2005) 53:37. doi: 10.4103/0028-3886.15050
48. Barnett C, Wilson G, Barth D, Katzberg HD, Bril V. Changes in quality of life scores with intravenous immunoglobulin or plasmapheresis in patients with myasthenia gravis. J Neurol Neurosurg Psychiatry. (2013) 84:94–7. doi: 10.1136/jnnp-2011-301449
49. Liu Z, Yao S, Zhou Q, Deng Z, Zou J, Feng H, et al. Predictors of extubation outcomes following myasthenic crisis. J Int Med Res . (2016) 44:1524–33. doi: 10.1177/0300060516669893
50. Pittayanon R, Treeprasertsuk S, Phanthumchinda K. Plasmapheresis or intravenous immunoglobulin for myasthenia gravis crisis in King Chulalongkorn Memorial Hospital. J Med Assoc Thail. (2009) 92:478–82.
51. Schneider-Gold C, Krenzer M, Klinker E, Mansouri-Thalegani B, Müllges W, Toyka KV, et al. Immunoadsorption versus plasma exchange versus combination for treatment of myasthenic deterioration. Ther Adv Neurol Disord. (2016) 9:297–303. doi: 10.1177/1756285616637046
52. Köhler W, Bucka C, Klingel R. A randomized and controlled study comparing immunoadsorption and plasma exchange in myasthenic crisis. J Clin Apher. (2011) 26:347–55. doi: 10.1002/jca.20317
53. Berrouschot J, Baumann I, Kalischewski P, Sterker M, Schneider D. Therapy of myasthenic crisis. Crit Care Med. (1997) 25:1228–35. doi: 10.1097/00003246-199707000-00027
54. Lal V, Prabhakar S, Agarwal R, Sharma S. Clinical profile and outcome of myasthenic crisis in a tertiary care hospital: A prospective study. Ann Indian Acad Neurol. (2013) 16:203. doi: 10.4103/0972-2327.112466
55. Sarkar BKK, Sengupta P, Sarkar UNN. Surgical outcome in thymic tumors with myasthenia gravis after plasmapheresis - a comparative study. Interact Cardiovasc Thorac Surg. (2008) 7:1007–10. doi: 10.1510/icvts.2007.170894
56. Saeteng S, Tantraworasin A, Siwachat S, Lertprasertsuke N, Euathrongchit J, Wannasopha Y. Preoperative plasmapheresis for elective thymectomy in myasthenia patient: is it necessary?. ISRN Neurol. (2013) 2013:238783. doi: 10.1155/2013/238783
57. d'Empaire G, Hoaglin DC, Perlo VP, Pontoppidan H. Effect of prethymectomy plasma exchange on postoperative respiratory function in myasthenia gravis. J Thorac Cardiovasc Surg. (1985) 89:592–6. doi: 10.1016/S0022-5223(19)38763-X
58. Jensen P, Bril V. Short report a comparison of the effectiveness of intravenous immunoglobulin and plasma exchange as preoperative therapy of myasthenia gravis. J Clin Neuromuscul Dis. (2008) 9:352–5. doi: 10.1097/CND.0b013e3181660807
59. Goti P, Spinelli A, Marconi G, Duranti R, Gigliotti F, Pizzi A, et al. Comparative effects of plasma exchange and pyridostigmine on respiratory muscle strength and breathing pattern in patients with myasthenia gravis. Thorax. (1995) 50:1080–6. doi: 10.1136/thx.50.10.1080
60. Ohta K, Shigemoto K, Fujinami A, Maruyama N, Konishi T, Ohta M. Clinical and experimental features of MuSK antibody positive MG in Japan. Eur J Neurol. (2007) 14:1029–34. doi: 10.1111/j.1468-1331.2007.01870.x
61. Gajdos P, Simon N, de Rohan-Chabot P, Raphael JC, Goulon M. Long-term effects of plasma exchange in myasthenia. Results of a randomized study. Presse Med. (1983) 12:939–42.
62. Guptill JT, Oakley D, Kuchibhatla M, Guidon AC, Hobson-Webb LD, Massey JM, et al. A Retrospective study of complications of therapeutic plasma exchange in myasthenia. Muscle Nerve. (2013) 47:170–6. doi: 10.1002/mus.23508
63. Mandawat AAA, Mandawat AAA, Kaminski HJJ, Shaker ZAA, Alawi AAA, Alshekhlee A. Outcome of plasmapheresis in myasthenia gravis: Delayed therapy is not favorable. Muscle Nerve. (2011) 43:578–84. doi: 10.1002/mus.21924
64. El-Bawab H, Hajjar W, Rafay M, Bamousa A, Khalil A, Al-Kattan K. Plasmapheresis before thymectomy in myasthenia gravis: routine versus selective protocols. Eur J Cardio-Thoracic Surg . (2009) 35:392–7. doi: 10.1016/j.ejcts.2008.11.006
65. Trikha I, Singh S, Goyal V, Shukla G, Bhasin R, Behari M. Comparative efficacy of low dose, daily versus alternate day plasma exchange in severe myasthenia gravis: A randomised trial. J Neurol. (2007) 254:989–95. doi: 10.1007/s00415-006-0235-7
66. Hawkey CJ, Newsom-davis J, Vincent A. Plasma exchange and immunosuppressive drug treatment in myasthenia gravis : no evidence for synergy. J Neurol Neurosurg Psychiatry. (1981) 1981:469–75. doi: 10.1136/jnnp.44.6.469
67. Pasnoor M, Wolfe GI, Nations S, Trivedi J, Barohn RJ, Herbelin L, et al. Clinical findings in MuSK-antibody positive myasthenia gravis: a U.S. experience. Muscle Nerve. (2010) 41:370–4. doi: 10.1002/mus.21533
68. Yamada C, Pham HP, Wu Y, Cooling L, Kim HC, Morgan S, et al. Report of the ASFA apheresis registry on muscle specific kinase antibody positive myasthenia gravis. J Clin Apher. (2017) 32:5–11. doi: 10.1002/jca.21454
69. Rock G, Sutton DM, Freedman J, Nair RC. Pentastarch instead of albumin as replacement fluid for therapeutic plasma exchange. J Clin Apher. (1997) 12:165–9. doi: 10.1002/(SICI)1098-1101(1997)12:4<165::AID-JCA2>3.0.CO;2-8
70. Passero BA, Zappone P, Lee HE, Novak C, Maceira EL, Naber M. Citrate versus heparin for apheresis catheter locks: An efficacy analysis. J Clin Apher. (2015) 30:22–7. doi: 10.1002/jca.21346
71. Citterio A, Beghi E, Millul A, Evoli A, Mantegazza R, Antozzi C, et al. Risk factors for tumor occurrence in patients with myasthenia gravis. J Neurol. (2009) 256:1221–7. doi: 10.1007/s00415-009-5091-9
72. Ebadi H, Barth D, Bril V. Safety of plasma exchange therapy in patients with myasthenia gravis. Muscle Nerve. (2013) 47:510–4. doi: 10.1002/mus.23626
73. Chhibber V, Weinstein R. Evidence-based review of therapeutic plasma exchange in neurological disorders. Semin Dial. (2012) 25:132–9. doi: 10.1111/j.1525-139X.2011.01023.x
74. Kaminski HJ, Cutter G, Ruff R. Practice parameters and focusing research: plasma exchange for myasthenia gravis. Muscle Nerve. (2011) 43:625–6. doi: 10.1002/mus.22080
75. Ortiz Salas PA, Gaviria Carrillo M, Cortés Bernal GA, Moreno Medina K, Roa LF, Rodríguez Quintana JH. Human immunoglobulin versus plasmapheresis in guillain-barre syndrome and myasthenia gravis. J Clin Neuromuscul Dis. (2016) 18:1–11. doi: 10.1097/CND.0000000000000119
76. Kuks JBM, Skallebaek D. Plasmapheresis in myasthenia gravis. A survey. Transfus Sci. (1998) 19:129–36. doi: 10.1016/S0955-3886(98)00022-8
Keywords: plasmapheresis, myasthenia (myasthenia gravis-MG), autoimmune disorders, neurological diseases, therapies and management
Citation: Ipe TS, Davis AR and Raval JS (2021) Therapeutic Plasma Exchange in Myasthenia Gravis: A Systematic Literature Review and Meta-Analysis of Comparative Evidence. Front. Neurol. 12:662856. doi: 10.3389/fneur.2021.662856
Received: 01 February 2021; Accepted: 12 July 2021; Published: 31 August 2021.
Reviewed by:
Copyright © 2021 Ipe, Davis and Raval. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tina S. Ipe, tipe@uams.edu
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Efficacy of innovative therapies in myasthenia gravis: A systematic review, meta-analysis and network meta-analysis
Affiliations.
- 1 Department of Neurosciences and Reproductive and Odontostomatological Sciences, University "Federico II", Naples, Italy.
- 2 Department of Health Sciences, University of Genoa, Genoa, Italy.
- PMID: 37204031
- DOI: 10.1111/ene.15872
Background and purpose: Therapy for myasthenia gravis (MG) is undergoing a profound change, with new treatments being tested. These include complement inhibitors and neonatal Fc receptor (FcRn) blockers. The aim of this study was to perform a meta-analysis and network meta-analysis of randomized and placebo-controlled trials of innovative therapies in MG with available efficacy data.
Methods: We assessed statistical heterogeneity across trials based on the Cochrane Q test and I 2 values, and mean differences were pooled using the random-effects model. Treatment efficacy was assessed after 26 weeks of eculizumab and ravulizumab, 28 days of efgartigimod, 43 days of rozanolixizumab, 12 weeks of zilucoplan, and 16, 24 or 52 weeks of rituximab treatment.
Results: We observed an overall mean Myasthenia Gravis-Activities of Daily Living scale (MG-ADL) score change of -2.17 points (95% confidence interval [CI] -2.67, -1.67; p < 0.001) as compared to placebo. No significant difference emerged between complement inhibitors and anti-FcRn treatment (p = 0.16). The change in Quantitative Myasthenia Gravis scale (QMG) score was -3.46 (95% CI -4.53, -2.39; p < 0.001), with a higher reduction with FcRns (-4.78 vs. -2.60; p < 0.001). Rituximab did not significantly improve the MG-ADL (-0.92 [95% CI -2.24, 0.39]; p = 0.17) or QMG scores (-1.9 [95% CI -3.97, 0.18]; p = 0.07). In the network meta-analysis, efgartigimod had the highest probability of being the best treatment, followed by rozanolixizumab.
Conclusion: Anti-complement and FcRn treatments both proved to be effective in MG patients, whereas rituximab did not show a significant benefit for patients. Within the limitations of this meta-analysis, including efficacy time points, FcRn treatments showed a greater effect on QMG score in the short term. Real-life studies with long-term measurements are needed to confirm our results.
Keywords: FcRn inhibitor; comparative; complement inhibitor; innovative treatment; trial.
© 2023 The Authors. European Journal of Neurology published by John Wiley & Sons Ltd on behalf of European Academy of Neurology.
Publication types
- Systematic Review
- Meta-Analysis
- Activities of Daily Living*
- Complement Inactivating Agents / therapeutic use
- Infant, Newborn
- Myasthenia Gravis* / drug therapy
- Network Meta-Analysis
- Rituximab / therapeutic use
- Therapies, Investigational
- Complement Inactivating Agents
Europe PMC requires Javascript to function effectively.
Either your web browser doesn't support Javascript or it is currently turned off. In the latter case, please turn on Javascript support in your web browser and reload this page.
Search life-sciences literature (43,991,122 articles, preprints and more)
- Full text links
- Citations & impact
- Similar Articles
Employment in Myasthenia Gravis: A Systematic Literature Review and Meta-Analysis.
Author information, affiliations.
- Guastafierro E 1
- Tramacere I 2
- Leonardi M 3
- Mantegazza R 4
- Bonanno S 4
- Frangiamore R 4
ORCIDs linked to this article
- Tramacere I | 0000-0001-5550-3412
- | 0000-0002-0383-3791
- Toppo C | 0000-0002-1312-6679
- Guastafierro E | 0000-0002-5051-0207
- Bonanno S | 0000-0002-8823-6821
Neuroepidemiology , 25 Feb 2020 , 54(4): 304-312 https://doi.org/10.1159/000506310 PMID: 32097937
Abstract
Introduction, conclusions, full text links .
Read article at publisher's site: https://doi.org/10.1159/000506310
Citations & impact
Impact metrics, citations of article over time, alternative metrics.

Article citations
Impact of ravulizumab on patient outcomes and quality of life in generalized myasthenia gravis..
Antozzi C , Mantegazza R
Patient Relat Outcome Meas , 14:305-312, 18 Oct 2023
Cited by: 0 articles | PMID: 37876920 | PMCID: PMC10590807
The economic burden of individuals living with generalized myasthenia gravis and facing social determinants of health challenges.
Hughes T , Howard JF , Silvestri NJ , Anderson AEL , Sato M , Suchotliff S , Guptill JT , Phillips G
Front Public Health , 11:1247931, 12 Sep 2023
Cited by: 0 articles | PMID: 37766748 | PMCID: PMC10520715
Understanding the Symptom Burden and Impact of Myasthenia Gravis from the Patient's Perspective: A Qualitative Study.
Jackson K , Parthan A , Lauher-Charest M , Broderick L , Law N , Barnett C
Neurol Ther , 12(1):107-128, 02 Nov 2022
Cited by: 8 articles | PMID: 36322146 | PMCID: PMC9837342
Academic and Employment Status in Patients With Generalized Myasthenia Gravis Treated With Eculizumab: A Case Series.
Kang SA , Sweeney M , Govindarajan R
J Clin Neuromuscul Dis , 23(4):210-218, 01 Jun 2022
Cited by: 1 article | PMID: 35608645 | PMCID: PMC9126260
Physician-Reported Perspectives on Myasthenia Gravis in the United States: A Real-World Survey.
Mahic M , Bozorg AM , DeCourcy JJ , Golden KJ , Gibson GA , Taylor CF , Ting A , Story TJ , Scowcroft A
Neurol Ther , 11(4):1535-1551, 20 Jul 2022
Cited by: 4 articles | PMID: 35859033 | PMCID: PMC9298707
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Employment in refractory myasthenia gravis: A Myasthenia Gravis Foundation of America Registry analysis.
Harris L , Aban IB , Xin H , Cutter G
Muscle Nerve , 60(6):700-706, 22 Oct 2019
Cited by: 10 articles | PMID: 31478207 | PMCID: PMC6900169
Prevalence and risk factors of myasthenia gravis recurrence post-thymectomy.
Alqarni F , Almalki D , Aljohani Z , Ali A , AlSaleem A , Alotaibi N , Odeh S , Dalbhi SA
Neurosciences (Riyadh) , 26(1):4-14, 01 Jan 2021
Cited by: 4 articles | PMID: 33530037 | PMCID: PMC8015504
Clinical features and impact of myasthenia gravis disease in Australian patients.
Blum S , Lee D , Gillis D , McEniery DF , Reddel S , McCombe P
J Clin Neurosci , 22(7):1164-1169, 26 May 2015
Cited by: 37 articles | PMID: 26021730
Prevalence of depression and anxiety among myasthenia gravis (MG) patients: A systematic review and meta-analysis.
Nadali J , Ghavampour N , Beiranvand F , Maleki Takhtegahi M , Heidari ME , Salarvand S , Arabzadeh T , Narimani Charan O
Brain Behav , 13(1):e2840, 10 Dec 2022
Cited by: 5 articles | PMID: 36495116 | PMCID: PMC9847616
Thymectomy is a beneficial therapy for patients with non-thymomatous ocular myasthenia gravis: a systematic review and meta-analysis.
Zhu K , Li J , Huang X , Xu W , Liu W , Chen J , Chen P , Feng H
Neurol Sci , 38(10):1753-1760, 13 Jul 2017
Cited by: 18 articles | PMID: 28707128
Europe PMC is part of the ELIXIR infrastructure
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Brain Behav
- v.13(1); 2023 Jan
Prevalence of depression and anxiety among myasthenia gravis (MG) patients: A systematic review and meta‐analysis
Javad nadali.
1 School of Nursing and Midwifery, Shahroud University of Medical Sciences, Shahroud Iran
Neda Ghavampour
2 School of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran Iran
Farzaneh Beiranvand
Mona maleki takhtegahi, mohammad eghbal heidari.
3 Student's Scientific Research Center, School of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran Iran
Shahin Salarvand
4 Hepatitis Research Center, Nursing and midwifery faculty, Lorestan University of Medical Sciences, Lorestan Iran
Tina Arabzadeh
Omid narimani charan, associated data.
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Myasthenia gravis (MG) people experience adverse psychiatric outcomes, which may impact on their life and disturb their daily activity. Depression and anxiety are identified as significant psychiatric problems that MG people face. However, there is no sufficient epidemiological information about depression and anxiety‐based publication. Due to this limitation, the aim of this study was to review the prevalence of depression and anxiety in MG patients.
Original and international databases were searched to find papers about the estimation of anxiety and depression. Random‐effects analysis was used for calculating the proportions of anxiety and depression. For estimating anxiety and depression based the severity, instruments, type of studies, and study regions, subgroup analysis was performed.
38 studies met inclusion criteria and entered study. The pooling of the prevalence of depression was found at 36%, (95% CI 28% to 45%). Also, prevalence of anxiety was found at 33%, (95% CI 25% to 42%). Prevalence of depression based on mild, moderate, and severe level was 27%, 14%, and 9%, respectively.
Conclusions
Anxiety and depression are a major concern among MG individuals. The estimation of both anxiety and depression are high even when compared to other autoimmune diseases. It seems depression and anxiety are important issues and more attention needs to be paid to these psychiatric disorders.

1. INTRODUCTION
Myasthenia gravis (MG) is identified as a prevalent autoimmune disease and the most common form of neuromuscular junction disease. The estimated prevalence of MG is about 20 individuals per 100,000 persons. Among gender, women are more susceptible rather than men (Cherukupally et al., 2020 ). It is predicted that MG affects 36,000 to 60,000 patients in the United States and more than 700,000 people worldwide annually. Age and sex are important factors in the incidence and prevalence of MG (Yamamoto et al., 2019 ). In MG, the transmission of nerve impulses to the muscles is disrupted. When there is no nerve–muscle connection, muscles are disrupted and cause neuromuscular disorders in these patients (Leopardi et al., 2021 ).
MG often occurs in adults and its common clinical manifestations include ocular, bulbar, or generalized weakness. Ocular complaints are the most common and are seen in 50% of cases. Due to the severity of symptoms such as weakness or fatigue, 30% of patients have respiratory problems and weakness and need mechanical ventilation (Hendricks et al., 2019 ).
Evidence showed that MG people experience psychological outcomes because of complication and recurrent symptoms. Mood disorders are the most common psychological outcomes among MG people (Kulaksizoglu, 2007 ; Paul et al., 2000 ; Qiu et al., 2010 ; Vitturi et al., 2021 ) Furthermore, about 20% of MG patients suffer from a psychiatric orpsychological disorder. Studies showed that prevalence of mental disorders and anxiety in people with MG are more than in the general population (Alanazy, 2019 ).
Furthermore, MG people experience different and complex treatments and invasive interventions which might impact their life and mental health. As the disease progresses, patients experience more disabilities and problems in their treatment that may reduce their quality of life and increase the incidence of mental disorders such as depression and anxiety (Yang et al., 2016 ). Numerous studies have reported that MG patients suffer from disability due to their symptoms, treatment, or complication (Alanazy, 2019 ; Qiu et al., 2010 ). Fatigue, drowsiness, anxiety, and depression are the most important complaints of patients (Alekseeva et al., 2019 ).
Psychological outcomes affect family, social, occupational, and personal aspects of patients (Parada et al., 2014 ). In addition, psychiatric and emotional disorders may lead to increased risk of mortality (Gavrilov et al., 2020 ; Kulaksizoglu, 2007 ).
According to studies about the prevalence of anxiety and depression in MG, the epidemiology of depression in MG varies from 6% to 76% (Kalbus et al., 2020 ; Sivadasan et al., 2019 ) and anxiety varies from 3% to 71% (Sivadasan et al., 2019 ; Ybarra et al., 2011 ). So, evidence showed that MG individuals are inclined to show high rate of depression and anxiety, and studies confirmed that anxiety and depression affect the mental health of MG people.
To sum up, many researchers have been evaluating the prevalence of depression and anxiety in MG patients and have had diverse results. For prevention and promotion of quality of life and treatment in MG patients, knowing the prevalence of depression and anxiety is necessary. Such information is essential for understanding the epidemiology of MG and is also helpful for developing strategies that help us to overcome the burdens caused by psychological manifestations of MG. Therefore, for achieving epidemiologic purposes, additional studies in different regions are necessary. According to the above statements and the absence of a systematic review or meta‐analysis of these issues, we conducted this study to determine the prevalence of depression and anxiety among MG patients all around the world.
2. MATERIALS AND METHODS
Preferred Reporting Items for Systematic Reviews and Meta‐analyses (PRISMA) were considered as guidelines for designing, performing, and writing study (Moher et al., 2009 ).
2.1. Search strategy
We fulfilled extensive search by searching the original databases of Web of Science, PUBMED, EMBASE, Ovid, and Scopus to find relevant and appropriate papers about estimate of anxiety and depression in MG patients. Search strategy was applied from 1960 to July 28, 2022 without any limitation on language and date. Manual searching in key journals for finding relevant articles was conducted after an initial search of databases and checking the reference list of included articles. Mesh terms, free text method, expert opinions as well as related articles and abstracts were checked to find the equivalent of search strategy terms. The terms used to search the databases were: (MG OR Myasthenia gravis) AND (depression OR Depressive disorder OR Cognitive disorder OR Anxiety OR mental disorder).
2.2. Study eligibility
Two authors (O.N. and M.E.H.) independently reviewed and retrieved articles to find out relevant study for including in the study according to titles and abstracts. Then, the full texts of papers were reviewed and studies were selected according to the inclusion criteria.
The inclusion criteria were: (1) observational studies (cohort, cross‐sectional), (2) papers which calculated or mentioned the proportions of depressive disorder or depression symptoms and anxiety, (3) an MG patient diagnosed by a physician, and 4) valid self‐reporting tools or structured diagnostic interviews for evaluating depression and anxiety. Case reports, interventional studies, magazine articles, case series, newspaper articles, or commentaries were considered as exclusion criteria. Articles that did not have complete information, had incomplete abstract or text, or did not provide sufficient and relevant data to estimate depression and anxiety were also excluded. Disagreements regarding the eligibility of studies were resolved by the third author (J,N).
2.3. Data extraction
The list of data extraction included publication year, study year, first author's name, design of study, study country, prevalence of depression and anxiety, mean age of participants, sample size, and score of Newcastle–Ottawa risk of bias. Articles that did not have the necessary information to calculate the prevalence of anxiety and depression were corresponded with the authors of the articles, and if they did not respond to the email more than three times, the studies were removed from the list of included studies.
2.4. Risk of bias (quality) assessment
Two authors investigated the quality assessment of articles. For evaluating the quality of studies, Newcastle–Ottawa risk of bias was used (Peterson et al., 2011 ).
2.5. Statistical analysis
STATA, version 12.0 (STATA Corporation, College Station, TX, USA) was used for data analysis. For each study, point estimates and 95% confidence intervals were calculated for the prevalence of depression and anxiety. The forest plot was also used to comprehensively represent selected studies based on consolidated estimated prevalence and 95% confidence interval. Meta regression was used to estimate the extent to which the measured covariates (year of release, sample size, and duration of disease) could explain the heterogeneity observed in prevalence estimates across studies. Publication bias was first assessed by visual inspection of the distribution of studies observed in a funnel design. Egger regression tracking (Vitturi et al., 2021 ) and Begg rank correlation test (Vitturi et al., 2021 ) were used to quantify the degree of bias shown in the funnel diagram.
3.1. Characteristics of included studies
2432 citations were reviewed based on title and abstracts; 280 retrieved by assessing full text articles. So, 38 studies remained for final analysis (Figure 1 ). Table 1 outlines the characteristics of studies (2, 7–9, 12, 14–17, 20–48).

Four‐phase PRISMA flow diagram showing the number of studies identified, screened, eligible, and included in the systematic review and meta‐analysis
Characteristics of the studies included in this meta‐analysis
Abbrevations: BDI, Beck Depression Inventory; CES‐D, Center for Epidemiological Studies Depression; HDRS, Hamilton Depression Rating Scale; HADS, Hospital Anxiety and Depression Scale; PHQ, Patient Health Questionnaire; SCID‐1V, Structured Clinical Interview for DSM Disorders; DSM‐IV, Diagnostic and Statistical Manual of Mental Disorders; MINI, mini international neuropsychiatric interview; HAM‐D, Hamilton Depression Rating Scale; CMDI, Chicago Multiscale Depression Inventory.
In total, 38 studies involving 4108 individuals from 20 countries were included (Figure 1 ). Mean duration of disease was between 8.87 and 1.95 years. The mean age of participants was 47.04 (7.96) years. Dates of publication ranged from 2000 to 2021. Eleven studies were conducted in America, 15 were conducted in Asia, 10 were conducted in Europe, and 2 were conducted in African countries. Twenty‐four studies were cross‐sectional studies and 14 were cohort studies (Table 1 ). According to Myasthenia Gravis Foundation of America (MGFA), 835 individuals were in stages I and II, 365 patients in stage III, and 158 people with MG were in classification of IV.
The included studies applied different types of screening tools to assess anxiety. These tools included Beck Anxiety Inventory (BAI, four studies), Hospital Anxiety and Depression Scale (HADS, three studies), ADIS‐R, Diagnostic and Statistical Manual of Mental Disorders (DSM‐IV), GAD, HARS, STAI, and Structured Clinical Interview for DSM Disorders (SCID). For screening depression, used Beck Depression Inventory (BDI, 11 studies), HADS (3 studies), Hamilton Depression Rating Scale (HDRS, 3 studies), BDI‐II (2 studies), DSM‐IV (2 studies), CES‐D, PHQ‐9, SCID, HAMD, and Chicago Multiscale Depression Inventory (CMDI).
3.2. Results of the meta‐analysis
The pooled prevalence of depression reported was found at 36% (95% CI 28% to 45%) (Figure 2 ). Also, prevalence of anxiety was found at 33% (95% CI 25% to 42%) (Figure 3 ). Significant heterogeneity was found between studies in anxiety and depression. The test I 2 were 96.18% and 91.93% in depression and anxiety estimates, respectively. The prevalence of depression by the individual studies ranged from 1% to 76% and in anxiety ranged from 3% to 71%. Sensitivity analysis indicated that no individual study affected the overall prevalence estimate by more than 0.1%.

Forest plot of the prevalence of depression in MG patients. The 95% confidence interval for each study is shown in the form of horizontal lines around the central mean and midpoint of the dotted line represents the mean of the overall score and the lozenge shape shows the confidence interval of the prevalence of this disorder.

Forest plot of the prevalence of anxiety in MG patients. The 95% confidence interval for each study is shown in the form of horizontal lines around the central mean and midpoint of the dotted line represents the mean of the overall score and the lozenge shape shows the confidence interval of the prevalence of this disorder.
3.3. Subgroup analysis
For finding the source of heterogeneity and to characterize the range of depression and anxiety, subgroup analysis was performed based on the instrument, severity, continents, duration of disease, and type of studies. Prevalence of mild, moderate, and severe depression in MG people were 27%, 14%, and 9%, respectively. Also, further analysis based on severity of depression was conducted and the estimates of minor and major depression in MG were found at 31% and 26%, respectively. Based on the continent, the highest and lowest prevalence of depression was recorded in Europe (56%) and Asia (28%), respectively. Also, the prevalence of depression was 52% and 21% based on BDI and HADS, respectively (Table 2 ). In the cross‐sectional and cohort studies, the pooled prevalence of depression was 40% (95% CI: 30% to 50%) and 31% (95% CI: 16% to 48%), respectively (Table 2 ). Also, subgroup analysis showed the highest and lowest prevalence of anxiety was recorded in America (53%) and Asia (25%), respectively. In the cross‐sectional and cohort studies, the pooled prevalence of anxiety was 40% (95% CI: 31% to 51%) and 20% (95% CI: 8% to 36%), respectively.
Results of subgroup analysis
3.4. Meta‐regression test
The prevalence of depression and anxiety in MG patients was not significantly related to mean age ( p = .393), year of publication ( p = .64), and duration of disease ( p = .123).
3.5. Publication bias
This study showed that the publication bias was significant among the studies ( p < .001). Sensitivity test also showed that none of the studies alone had an impressive effect on the overall prevalence of depression and anxiety (Figure 4 ).

Funnel plot to detect publication bias‐based depression. Circles show selected studies, and the area of each circle is equivalent to the weight of each study. The horizontal axis represents accuracy, and the vertical axis represents the standardized effect.
4. DISCUSSION
To the extent of our knowledge, this study is the first systematic review and meta‐analysis that investigated the prevalence of overall anxiety and depression in MG people. Thirty‐eight studies were included in this study and the total population was 4108 individuals. We estimated the proportions of depression among MG patients at 36%, (95% CI 28% to 45%), which is higher compared to other autoimmune diseases like multiple sclerosis (30.5%) (Boeschoten et al., 2017 ) and systemic lupus erythematosus (35.0%) (Moustafa et al., 2020 ). We also estimated the pooled prevalence of anxiety at 33%, (95% CI 25% to 42%) which is also higher compared to multiple sclerosis (22.1%) (Boeschoten et al., 2017 ) and systemic lupus erythematosus (25.8%) (Moustafa et al., 2020 ). According to the finding, the rate of depression is higher than other neurological diseases such as dementia (30.3%) (Orgeta et al., 2015 ), ALS (34%) (Heidari et al., 2021 ), multiple sclerosis (30.5%) (Moustafa et al., 2020 ), and mild cognitive impairment (32%) (Ismail et al., 2017 ), and elderly patients with hip fracture (23%) (Irvani et al., 2020 ). Also, rate of depression was lower than in Alzheimer's patients (42%) (Zhao et al., 2016 ).
MG mainly affects acetylcholine receptors and disturbs their mechanism ( O'Connell et al., 2020 ). In most MG cases, the first symptoms are the weakness of extraocular muscles and ocular misalignment, which is considered as ocular MG. Within 3 years, in around 90% of cases, ocular MG develops to generalized MG (Yang et al., 2016 ), which is defined by symptoms of weakness and fatigue in skeletal muscles and its effects on swallowing, chewing, breathing, and talking of MG patients (Chu et al., 2019 ). Disabilities resulting from MG often affect patients’ quality of life and interfere with their daily routine and activity (Vitturi et al., 2021 ). Additionally, Instability of MG symptoms, prolonged illness, and treatment with steroids can cause psychiatric symptoms in MG patients (Yamamoto et al., 2019 ). Mood disorders are very common among patients with neurological conditions and MG patients are no exception. It was reported that 41% of MG patients experience mood disorders (Law et al., 2020 ). According to studies, depressive and anxiety symptoms are very prevalent in MG patients (Cherukupally et al., 2020 ; Law et al., 2020 ). In a cross‐sectional study by Alanazy, it was reported that about a quarter of MG patients (26.0%) experienced moderate–severe depression (Alanazy, 2019 ). In another study by Gavrilov et al., the prevalence of moderate–severe depression among MG patients was estimated at 20.5%. The results of a study by Braz et al. showed that around half (43.75%) of the MG patients had anxiety and 27.5% had depressive symptoms (Braz et al., 2018 ).
In a literature review by Law et al., it was reported that factors such as older age and disease duration can affect depression and anxiety in MG patients (Law et al., 2020 ), but our meta‐regression test showed no significant relation between prevalence of anxiety and depression with age and disease duration. Further research is recommended on this matter.
In our study, range of depression varied from 1% to 76% and in anxiety ranged from 3% to 71%. This might be due to the difference in methodological approach and the use of different screening tools. The most used screening tools for anxiety were BAI and HADS and for depression were BDI and HADS. The BAI is one of the most common screening tools for measuring anxiety (Bardhoshi et al., 2016 ). It was first developed to measure anxiety independently from depression (Toledano‐Toledano et al., 2020 ). BAI is a self‐report tool focusing on the physical symptoms of anxiety. It contains 21 items to measure the severity of anxiety symptoms and asks patients to rate each symptom on a four‐point scale (0 to 3). Final score can be varied from 0 to 63. Higher scores indicate more severe anxiety symptoms (Julian, 2011 ; Lee et al., 2018 ). Studies reported that the BAI is a valid and reliable instrument for assessing anxiety symptoms (Bardhoshi et al., 2016 ; Toledano‐Toledano et al., 2020 ). The HADS is a self‐report questionnaire, which was originally developed to assess depression and anxiety in non‐psychiatric patients. The HADS consisted of two sub‐scales: anxiety (HADS‐A) and depression (HADS‐D). This questionnaire has 14 items, 7 items for assessing anxiety and 7 items for assessing depression. The HADS asks individuals to rate each question on a four‐point scale (0 to 3) and the total score can range from 0 to 42, or 0 to 21 for each HADS‐A and HADS‐D (Annunziata et al., 2020 ; Djukanovic et al., 2017 ; Julian, 2011 ; Smarr & Keefer, 2011 ). Many studies with different populations reported HADS as a reliable and valid instrument to measure anxiety and depression (Bjelland et al., 2002 ; Bocéréan & Dupret, 2014 ; Cassiani‐Miranda et al., 2022 ; Djukanovic et al., 2017 ). The BDI is a 21 item self‐report questionnaire used to measure depression symptoms and severity. It is probably the most used screening tool for assessing depression in both psychiatric and non‐psychiatric populations (Moher et al., 2009 ; Крейс et al., 2020 ). The BDI has several versions including BDI‐I, BDI‐IA, BDI‐II, and BDI‐FS, which unlike others has seven items (Moher et al., 2009 ). The BDI consisted of 21 items to measure depression symptoms and severity, it asks patients to rate each symptom on a four‐point scale (from 0 to 3), and the final score can range between 0 and 63; higher scores indicate more severe depression symptoms. BDI‐II is a newer version designed to meet the DSM‐IV criteria for depressive disorders and includes items that measure cognitive, emotional, and physical symptoms (García‐Batista et al., 2018 ; Smarr & Keefer, 2011 ). Many studies with different types of population considered the BDI as a reliable and valid screening tool (García‐Batista et al., 2018 ; Lee et al., 2017 ; Sacco et al., 2016 ; Smarr & Keefer, 2011 ). Most of the screening tools for depression and anxiety consider somatic symptoms as an item; it can cause false results for the diagnosis of depression and anxiety in disease or conditions like MG that have somatic symptoms similar to somatic symptoms of depression and anxiety (e.g., fatigue, tiredness, etc.).
Prevalence of depression based on BDI and HADS in our results was 52% and 21%, respectively. We think that the reason for this gap is due to the difference and heterogeneity of cut points. Europe (56%) and Asia (28%) had highest and lowest prevalence of depression among continents. For anxiety, American (53%) and Asian (25%) individuals had highest and lowest prevalence in the present study.
This study is the first study that systematically reviewed the prevalence of anxiety and depression in MG patients. The search strategy, paper screening, and data extraction for this study were comprehensive. Also, PRISMA guidelines were considered for conducting study. Of course, there were some limitations in this study. First, included studies were different in design, screening tools, population origin, publication year, and setting which resulted in heterogeneity among studies. Second, some of the included studies used self‐report questionnaires to assess anxiety and depression in MG patients, which can decrease the reliability of the results. Finally, the possibility of publication bias could not be fully ignored.
5. CONCLUSION
According to our results, anxiety and depression are major problems among MG patients and the prevalence of both anxiety and depression is high even when compared to other autoimmune diseases. Symptoms such as depression and anxiety in MG patients are often overlooked or delayed in diagnosis, leading to an increase in severity of symptoms and delayed onset of treatment. Therefore, identifying the related factors and developing effective intervention strategies for MG patients are needed.
AUTHOR CONTRIBUTIONS
Javad Nadali, Mohammad Eghbal Heidari, and Neda Ghavampour: design of study, literature search, identification and selection, data extraction, quality assessment, conducting analysis, writing paper, and critical revision of paper. Mona Maleki Takhtegahi, Farzaneh Beiranvand, and Omid Narimani Charan: literature search, identification and selection, quality assessment, and critical revision of paper. Tina Arabzadeh and Shahin Salarvand: literature search, identification and selection, and critical revision of paper.
CONFLICT OF INTEREST
The authors declare no conflict of interests.
Funding information
Peer review.
The peer review history for this article is available at https://publons.com/publon/10.1002/brb3.2840
TRANSPARENT PEER REVIEW
Acknowledgments.
We would like to express our thanks and acknowledge the help of Hooman Shahsavari and Sahar Dalvand in the development of our search strategy.
Nadali, J. , Ghavampour, N. , Beiranvand, F. , Maleki Takhtegahi, M. , Heidari, M. E. , Salarvand, S. , Arabzadeh, T. , & Narimani Charan, O. (2023). Prevalence of depression and anxiety among myasthenia gravis (MG) patients: A systematic review and meta‐analysis . Brain and Behavior , 13 , e2840. 10.1002/brb3.2840 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Contributor Information
Javad Nadali, Email: ri.ca.smut.sunmula@iladanj .
Neda Ghavampour, Email: moc.liamg@adenruopmavahG .
Farzaneh Beiranvand, Email: moc.liamg@5631iebenazraf .
Mona Maleki Takhtegahi, Email: [email protected] .
Mohammad Eghbal Heidari, Email: [email protected] .
Shahin Salarvand, Email: ri.ca.smul@dnavralashs .
Tina Arabzadeh, Email: [email protected] .
Omid Narimani Charan, Email: [email protected] .
DATA AVAILABILITY STATEMENT
- Cherukupally, K. R. , Kodjo, K. , Ogunsakin, O. , Olayinka, O. , & Fouron, P. (2020). Comorbid depressive and anxiety symptoms in a patient with myasthenia gravis . Case Reports in Psychiatry , 2020 , 8967818. 10.1155/2020/8967818 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yamamoto, A. , Kimura, T. , Watanabe, S. , & Yoshikawa, H. (2019). Clinical characteristics of patients with myasthenia gravis accompanied by psychiatric disorders . Neurology and Clinical Neuroscience , 7 ( 2 ), 65–70. 10.1111/ncn3.12267 [ CrossRef ] [ Google Scholar ]
- Leopardi, V. , Chang, Y.‐M. , Pham, A. , Luo, J. , & Garden, O. A. (2021). A systematic review of the potential implication of infectious agents in myasthenia gravis . Frontiers in Neurology , 12 , 857. 10.3389/fneur.2021.618021 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hendricks, T. M. , Bhatti, M. T , Hodge, D. O. , & Chen, J J. (2019). Incidence, epidemiology, and transformation of ocular myasthenia gravis: A population‐based study . American Journal of Ophthalmology , 205 , 99–105. 10.1016/j.ajo.2019.04.017 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Vitturi, B. K. , Kim, A. I. H. , Mitre, L. P. , Pellegrinelli, A. , & Valerio, B. C. O. (2021). Social, professional and neuropsychiatric outcomes in patients with myasthenia gravis . Neurological Sciences , 42 ( 1 ), 167–173. 10.1007/s10072-020-04528-w [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kulaksizoglu, I. B. (2007). Mood and anxiety disorders in patients with myasthenia gravis . CNS Drugs , 21 ( 6 ), 473–481. 10.2165/00023210-200721060-00004 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Paul, R. H. , Cohen, R. A. , Goldstein, J. M. , & Gilchrist, J. M. (2000). Severity of mood, self‐evaluative, and vegetative symptoms of depression in myasthenia gravis . The Journal of Neuropsychiatry and Clinical Neurosciences , 12 ( 4 ), 499–501. 10.1176/jnp.12.4.499 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Qiu, L. , Feng, H. Y. , Huang, X. , Mo, R. , Ou, C. Y. , Luo, C. M. , Li, Y. , & Liu, W. B. (2010). Study of incidence and correlation factors of depression, anxiety and insomnia in patients with myasthenia gravis . Zhonghua Yi Xue Za Zhi , 90 ( 45 ), 3176–9. [ PubMed ] [ Google Scholar ]
- Alanazy, M. H. (2019). Prevalence and associated factors of depressive symptoms in patients with myasthenia gravis: A cross‐sectional study of two tertiary hospitals in Riyadh, Saudi Arabia . Behavioural Neurology , 2019 , 9367453. 10.1155/2019/9367453 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yang, Y. , Zhang, M. , Guo, J. , Ma, S. , Fan, L. , Wang, X. , Li, C. , Guo, P. , Wang, J. , Li, H. , & Li, Z. (2016). Quality of life in 188 patients with myasthenia gravis in China . The International journal of Neuroscience , 126 ( 5 ), 455–462. 10.3109/00207454.2015.1038712 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Alanazy, M. H. (2019). Prevalence and associated factors of depressive symptoms in patients with myasthenia gravis: A cross‐sectional study of two tertiary hospitals in Riyadh, Saudi Arabia . Behavioural Neurology , 2019 , 10.1155/2019/9367453 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Alekseeva, T. M. , Kreis, O. A. , Gavrilov, Y. V. , Valko, P. O. , Weber, K. P. , & Valko, Y. (2019). Impact of autoimmune comorbidity on fatigue, sleepiness and mood in myasthenia gravis . Journal of Neurology , 266 ( 8 ), 2027–2034. 10.1007/s00415-019-09374-1 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Parada, P. , Oliva, M. , Lázaro, E. , Amayra, I. , Paz, J. F. L. , & Martínez, O. (2014). Anxiety, depression and self‐efficacy in patients with myasthenia gravis . International Journal of Psychology and Psychological Therapy , 14 ( 1 ), 105–113. [ Google Scholar ]
- Gavrilov, Y. V. , Alekseeva, T. M. , Kreis, O. A. , Valko, P. O. , Weber, K. P. , & Valko, Y. (2020). Depression in myasthenia gravis: A heterogeneous and intriguing entity . Journal of Neurology , 267 ( 6 ), 1802–1811. 10.1007/s00415-020-09767-7 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sivadasan, A. , Alexander, M. , Aaron, S. , Mathew, V. , Nair, S. , Muthusamy, K. , Prabhakar, A. T. , Benjamin, R. N. , Shaikh, A. , & Rynjah, G. (2019). Comorbidities and long‐term outcomes in a cohort with myasthenic crisis: Experiences from a tertiary care center . Annals of Indian Academy of Neurology , 22 ( 4 ), 464. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kalbus, O. , Makarov, S. , Shastun, N. , & Somilo, O. (2020). Features of depression development in myasthenia gravis . Медичні перспективи , 25 ( 1 ), 96–104. [ Google Scholar ]
- Ybarra, M. I. , Kummer, A. , Frota, E. R. C. , Oliveira, J. T. , Gomez, R. S. , & Teixeira, A. L. (2011). Psychiatric disorders in myasthenia gravis . Arquivos de Neuro‐Psiquiatria , 69 ( 2A ), 176–179. 10.1590/S0004-282X2011000200006 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Moher, D. , Liberati, A. , Tetzlaff, J. , & Altman, D G. (2009). Preferred reporting items for systematic reviews and meta‐analyses: The PRISMA statement . PLoS Medicine , 6 ( 7 ), e1000097. 10.1371/journal.pmed.1000097 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Peterson, J. , Welch, V. , Losos, M. , & Tugwell, P. (2011). The Newcastle‐Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta‐analyses (pp. 1–12). Ottawa Hospital Research Institute. [ Google Scholar ]
- Vitturi, B. K. , Kim, A. I. H , Mitre, L. P. , Pellegrinelli, A. , & Valerio, B. C. O. (2021). Social, professional and neuropsychiatric outcomes in patients with myasthenia gravis . Neurological Sciences : Official Journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology , 42 ( 1 ), 167–173. 10.1007/s10072-020-04528-w [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Liu, C. , Li, T. , Wang, Q. , Xu, A. , & Wu, B. (2021). Post‐traumatic stress disorder symptoms after respiratory insufficiency in patients with myasthenia gravis . Psychology, Health & Medicine , 26 ( 2 ), 221–7. [ PubMed ] [ Google Scholar ]
- Крейс, О. , Алексеева, Т. , Гаврилов, Ю. , Валко, Ф. , & Валко, Ю. (2020). Диагностика сонливости, усталости и депрессии у пациентов с миастенией гравис . Нервно‐мышечные болезни , 10 ( 4 ), 27–37. [ Google Scholar ]
- Bogdan, A. , Barnett, C. , Ali, A. , Alqwaifly, M. , Abraham, A. , Mannan, S. , Ng, E. , & Bril, V. (2020). Chronic stress, depression and personality type in patients with myasthenia gravis . European Journal of Neurology , 27 ( 1 ), 204–209. 10.1111/ene.14057 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ayres, A. , Winckler, P. B. , Jacinto‐Scudeiro, L. A. , Rech, R. S. , Jotz, G. P. , & Olchik, M. R. (2020). Cognitive performance in patients with myasthenia gravis: An association with glucocorticosteroid use and depression . Dementia & Neuropsychologia , 14 , 315–23. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Amani, K. , Sarraf, P. , Abkhoo, A. , Tafakhori, A. , Fatehi, F. , & Bitarafan, S. (2020). Prevalence of depression among Iranian patients with myasthenia gravis during 2017–2018 . Current Journal of Neurology , 19 ( 4 ), 162–166. [ Google Scholar ]
- Siddig, A. , Hussein, A. , Aladil, O. , Abbashare, H. , Abbashar, M. , Alamin, M. , & Abbasher, K. M A (2019). Prevalence of depression among sudanese patients with myasthenia gravis . Journal of the Neurological Sciences , 405 , 5–6. 10.1016/j.jns.2019.10.1555 [ CrossRef ] [ Google Scholar ]
- Chu, H.‐T. , Tseng, C.‐C. , Liang, C.‐S. , Yeh, T.‐C. , Hu, L.‐Y. , Yang, A. C. , Tsai, S.‐J. , & Shen, C.‐C. (2019). Risk of depressive disorders following myasthenia gravis: A Nationwide population‐based retrospective cohort study . Frontiers in Psychiatry , 10 , 481. 10.3389/fpsyt.2019.00481 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bacci, E. D. , Coyne, K. S. , Poon, J.‐L. , Harris, L. , & Boscoe, A. N. (2019). Understanding side effects of therapy for myasthenia gravis and their impact on daily life . BMC Neurology , 19 ( 1 ), 1–13. 10.1186/s12883-019-1573-2 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tascilar, N. F. , Saracli, O. , Kurcer, M. A. , Ankarali, H. , & Emre, U. (2018). Is there any relationship between quality of life and polysomnographically detected sleep parameters/disorders in stable myasthenia gravis? Acta Neurologica Belgica , 118 ( 1 ), 29–37. 10.1007/s13760-017-0787-6 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Braz, N. F. T. , Rocha, N. P. , Vieira, É. L. M. , Barbosa, I. G. , Gomez, R. S. , Kakehasi, A. M. , & Teixeira, A. L. (2018). Muscle strength and psychiatric symptoms influence health‐related quality of life in patients with myasthenia gravis . Journal of Clinical Neuroscience : Official Journal of the Neurosurgical Society of Australasia , 50 , 41–44. 10.1016/j.jocn.2018.01.011 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Deneva, V. , Milanova, M. , Stamenova, P. , & Isakov, S. (2017). Depression and other risk factors for myasthenic crisis–A clinical study in bulgarian patients . Comptes rendus de l'Académie bulgare des Sciences , 70 ( 4 ), 571–9. [ Google Scholar ]
- Zou, J. , Su, C. , Lun, X. , Liu, W. , Yang, W. , Zhong, B. , Zhu, H. , Lei, Y. , Luo, H. , & Chen, Z. (2016). Preoperative anxiety in patients with myasthenia gravis and risk for myasthenic crisis after extended transsternal thymectomy: A CONSORT study . Medicine , 95 ( 10 ), e2828. 10.1097/MD.0000000000002828 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Uyaroğlu, F. G. , Bilgin, Ş. , Keleş, E. H. , & Zorlu, Y. (2016). Anxiety and depression symptoms in patients with generalized myasthenia gravis . The Journal of Tepecik Education and Research Hospital , 26 ( 2 ), 97–103. [ Google Scholar ]
- Hoffmann, S. , Ramm, J. , Grittner, U. , Kohler, S. , Siedler, J. , & Meisel, A. (2016). Fatigue in myasthenia gravis: Risk factors and impact on quality of life . Brain and Behavior , 6 ( 10 ), e00538. 10.1002/brb3.538 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- El‐Ghonemy, S. H. , Salem, H. H. , El‐Missiry, M. A. , El‐Ghamry, R. H. , & Mukhtar, Y. S. (2016). Myasthenia gravis and psychiatric comorbidities . Middle East Current Psychiatry , 23 ( 2 ), 99–105. 10.1097/01.XME.0000481469.56478.b0 [ CrossRef ] [ Google Scholar ]
- Blum, S. , Lee, D. , Gillis, D. , Mceniery, D. F. , Reddel, S. , & Mccombe, P. (2015). Clinical features and impact of myasthenia gravis disease in Australian patients . Journal of Clinical Neuroscience , 22 ( 7 ), 1164–1169. 10.1016/j.jocn.2015.01.022 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Freeman, C. , Lewis, I. , & Heckmann, J. M. (2014). Neuropsychiatric symptoms in patients with thymomaassociated and non‐thymoma myasthenia gravis . South African Journal of Psychiatry , 20 ( 2 ), 50–3. 10.4102/sajpsychiatry.v20i2.519 [ CrossRef ] [ Google Scholar ]
- Tetsuka, S. , Fujimoto, K.‐I. , & Ikeguchi, K. (2013). Preoperative high‐dose steroid has long‐term beneficial effects for myasthenia gravis . Neurology Research International , 2013 , 709480. 10.1155/2013/709480 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Suzuki, Y. , Utsugisawa, K. , Suzuki, S. , Nagane, Y. , Masuda, M. , Kabasawa, C. , Shimizu, Y. , Utsumi, H. , Uchiyama, S. , Fujihara, K. , & Suzuki, N. (2011). Factors associated with depressive state in patients with myasthenia gravis: A multicentre cross‐sectional study . BMJ Open , 1 ( 2 ), e000313. 10.1136/bmjopen-2011-000313 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Aysal, F. , Karamustafalioğlu, O. , Özçelik, B. , Yilmaz, M. , Karamustafalioğlu, N. , Yumrukçal, H. , & Tankaya, O. (2013). The relationship of symptoms of anxiety and depression with disease severity and treatment modality in myasthenia gravis: A cross‐sectional study . Nöro Psikiyatri Arşivi. , 50 ( 4 ), 295. 10.4274/npa.y5611 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Winter, Y. , Schepelmann, K. , Spottke, A E. , Claus, D. , Grothe, C. , Schröder, R. , Heuss, D. , Vielhaber, S. , Tackenberg, B. , Mylius, V. , Reese, J.‐P. , Kiefer, R. , Schrank, B. , Oertel, W. H. , & Dodel, R. (2010). Health‐related quality of life in ALS, myasthenia gravis and facioscapulohumeral muscular dystrophy . Journal of Neurology , 257 ( 9 ), 1473–1481. 10.1007/s00415-010-5549-9 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Di Blasi, C. , Quartuccio, M. , Pontecorvo, S. , Francia, A. , & Prencipe, M. (2009). Neuropsychological disorders and myasthenia gravis: A pilot study . Journal of the Peripheral Nervous System , 14 . [ Google Scholar ]
- Stewart, S. B. , Robertson, K. R. , Johnson, K. M. , & Howard, J. F. (2007). The prevalence of depression in myasthenia gravis . Journal of Clinical Neuromuscular Disease , 8 ( 3 ), 111–115. 10.1097/CND.0b013e3180316324 [ CrossRef ] [ Google Scholar ]
- Lundeen, J. , Fisher, J. , & Kothari, M. J. (2004). Frequency of anxiety in myasthenia gravis . Journal of Clinical Neuromuscular Disease , 6 ( 1 ), 9–12. 10.1097/01.cnd.0000138445.13978.e4 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fisher, J. , Parkinson, K. , & Kothari, M. J. (2003). Self‐reported depressive symptoms in myasthenia gravis . Journal of Clinical Neuromuscular Disease , 4 ( 3 ), 105–108. 10.1097/00131402-200303000-00001 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Alekseeva, T. M. , Gavrilov, Y. V. , Kreis, O. A. , Valko, P. O. , Weber, K. P. , & Valko, Y. (2018). Fatigue in patients with myasthenia gravis . Journal of Neurology , 265 ( 10 ), 2312–2321. 10.1007/s00415-018-8995-4 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Paradis, C. M. , Friedman, S. , Lazar, R. M. , & Kula, R. (1993). Anxiety disorders in a neuromuscular clinic . The American Journal of Psychiatry , 150 ( 7 ), 1102–4. [ PubMed ] [ Google Scholar ]
- Hong, S. (2010). Surveys on depressive disorders in patients with myasthenia gravis . Journal of Shandong Medical College , 4 , 019. [ Google Scholar ]
- Boeschoten, R. E. , Braamse, A. M. J. , Beekman, A. T. F. , Cuijpers, P. , Van Oppen, P. , Dekker, J. , & Uitdehaag, B. M. J. (2017). Prevalence of depression and anxiety in multiple sclerosis: A systematic review and meta‐analysis . Journal of the Neurological Sciences , 372 , 331–341. 10.1016/j.jns.2016.11.067 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Moustafa, A. T. , Moazzami, M. , Engel, L. , Bangert, E. , Hassanein, M. , Marzouk, S. , Kravtsenyuk, M. , Fung, W. , Eder, L. , Su, J. , Wither, J. E. , & Touma, Z. , editors. (2020). Prevalence and metric of depression and anxiety in systemic lupus erythematosus: A systematic review and meta‐analysis. Seminars in arthritis and rheumatism . Elsevier. [ PubMed ] [ Google Scholar ]
- Orgeta, V. , Qazi, A. , Spector, A. , & Orrell, M. (2015). Psychological treatments for depression and anxiety in dementia and mild cognitive impairment: Systematic review and meta‐analysis . The British Journal of Psychiatry , 207 ( 4 ), 293–298. 10.1192/bjp.bp.114.148130 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Heidari, M. E. , Nadali, J. , Parouhan, A. , Azarafraz, M. , Tabatabai, S. M. , Irvani, S. S. N. , Eskandari, F. , & Gharebaghi, A. (2021). Prevalence of depressive disorder among amyotrophic lateral sclerosis (ALS) patients: Systematic review and meta‐analysis . Journal of Affective Disorders , 287 , 182–190. 10.1016/j.jad.2021.03.015 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ismail, Z. , Elbayoumi, H. , Fischer, C. E. , Hogan, D. B. , Millikin, C. P. , Schweizer, T. , Mortby, M. E. , Smith, E. E. , Patten, S. B. , & Fiest, K. M. (2017). Prevalence of depression in patients with mild cognitive impairment: A systematic review and meta‐analysis . JAMA Psychiatry , 74 ( 1 ), 58–67. 10.1001/jamapsychiatry.2016.3162 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Irvani, S. S. N. , Khadem, M. , Torabi, F. , & Shahsavari, H. (2020). Prevalence of depression in elderly hip fracture: A systematic review and meta‐analysis . International Journal of Orthopaedic and Trauma Nursing , 40 , 100813. [ PubMed ] [ Google Scholar ]
- Zhao, Q.‐F. , Tan, L. , Wang, H.‐F. , Jiang, T. , Tan, M.‐S. , Tan, L. , Xu, W. , Li, J.‐Q. , Wang, J. , Lai, T.‐J. , & Yu, J.‐T. (2016). The prevalence of neuropsychiatric symptoms in Alzheimer's disease: Systematic review and meta‐analysis . Journal of Affective Disorders , 190 , 264–271. 10.1016/j.jad.2015.09.069 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- O'connell, K. , Ramdas, S. , & Palace, J. (2020). Management of juvenile myasthenia gravis . Frontiers in Neurology , 11 , 743. 10.3389/fneur.2020.00743 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yang, Y. , Zhang, M. , Guo, J. , Ma, S. , Fan, L. , Wang, X. , Li, C. , Guo, P. , Wang, J. , Li, H. , & Li, Z. (2016). Quality of life in 188 patients with myasthenia gravis in China . International Journal of Neuroscience , 126 ( 5 ), 455–462. 10.3109/00207454.2015.1038712 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Law, C. , Flaherty, C. V. , & Bandyopadhyay, S. (2020). A review of psychiatric comorbidity in myasthenia gravis . Cureus , 12 ( 7 ), e9184. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cherukupally, K. R. , Kodjo, K. , Ogunsakin, O. , Olayinka, O. , & Fouron, P. (2020). Comorbid depressive and anxiety symptoms in a patient with myasthenia gravis . Case Reports in Psychiatry , 2020 , 8967818. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Braz, N. F. T. , Rocha, N. P. , Vieira, É. L. M. , Barbosa, I. G. , Gomez, R. S. , Kakehasi, A. M. , & Teixeira, A. L. (2018). Muscle strength and psychiatric symptoms influence health‐related quality of life in patients with myasthenia gravis . Journal of Clinical Neuroscience , 50 , 41–44. 10.1016/j.jocn.2018.01.011 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bardhoshi, G. , Duncan, K. , & Erford, B. T. (2016). Psychometric meta‐analysis of the English version of the Beck Anxiety Inventory . Journal of Counseling & Development , 94 ( 3 ), 356–73. [ Google Scholar ]
- Toledano‐Toledano, F. , Moral De La Rubia, J. , Domínguez‐Guedea, M. T. , Nabors, L. A. , Barcelata‐Eguiarte, B. E. , Rocha‐Pérez, E. , Luna, D. , Leyva‐López, A. , & Rivera‐Rivera, L. (2020). Validity and reliability of the Beck Anxiety Inventory (BAI) for family caregivers of children with cancer . International Journal of Environmental Research and Public Health , 17 ( 21 ), 7765. 10.3390/ijerph17217765 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Julian, L. J. (2011). Measures of anxiety . Arthritis Care & Research , 63 ( 0 11 ). [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lee, K. , Kim, D. , & Cho, Y. (2018). Exploratory factor analysis of the Beck anxiety inventory and the Beck depression inventory‐II in a psychiatric outpatient population . Journal of Korean Medical Science , 33 ( 16 ). 10.3346/jkms.2018.33.e128 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Julian, L. J. (2011). Measures of anxiety: State‐Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale‐Anxiety (HADS‐A) . Arthritis Care & Research , 63 , Suppl 11(0 11), S467–72. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Annunziata, M. A. , Muzzatti, B. , Bidoli, E. , Flaiban, C. , Bomben, F. , Piccinin, M. , Gipponi, K. M. , Mariutti, G. , Busato, S. , & Mella, S. (2020). Hospital anxiety and depression scale (HADS) accuracy in cancer patients . Supportive Care in Cancer , 28 ( 8 ), 3921–3926. [ PubMed ] [ Google Scholar ]
- Djukanovic, I. , Carlsson, J. , & Årestedt, K. (2017). Is the Hospital Anxiety and Depression Scale (HADS) a valid measure in a general population 65–80 years old? A psychometric evaluation study . Health and Quality of life Outcomes , 15 ( 1 ), 1–10. 10.1186/s12955-017-0759-9 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Smarr, K. L. , & Keefer, A. L. (2011). Measures of depression and depressive symptoms: Beck depression Inventory‐II (BDI‐II), center for epidemiologic studies depression scale (CES‐D), geriatric depression scale (GDS), hospital anxiety and depression scale (HADS), and patient health Questionnaire‐9 (PHQ‐9) . Arthritis Care & Research , 63 ( S11 ), S454–S66. [ PubMed ] [ Google Scholar ]
- Bocéréan, C. , & Dupret, E. (2014). A validation study of the Hospital Anxiety and Depression Scale (HADS) in a large sample of French employees . BMC Psychiatry [Electronic Resource] , 14 ( 1 ), 1–11. 10.1186/s12888-014-0354-0 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cassiani‐Miranda, C. A. , & Scoppetta, O. , & Cabanzo‐Arenas, D. F. (2022). Validity of the hospital anxiety and depression scale (HADS) in primary care patients in Colombia . General Hospital Psychiatry , 74 , 102–109. [ PubMed ] [ Google Scholar ]
- Bjelland, I. , Dahl, A. A. , Haug, T. T. , & Neckelmann, D. (2002). The validity of the Hospital Anxiety and Depression Scale: An updated literature review . Journal of Psychosomatic Research , 52 ( 2 ), 69–77. 10.1016/S0022-3999(01)00296-3 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- García‐Batista, Z. E. , Guerra‐Peña, K. , Cano‐Vindel, A. , Herrera‐Martínez, S. X. , & Medrano, L. A. (2018). Validity and reliability of the Beck Depression Inventory (BDI‐II) in general and hospital population of Dominican Republic . PLoS ONE , 13 ( 6 ), e0199750. 10.1371/journal.pone.0199750 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sacco, R. , Santangelo, G. , Stamenova, S. , Bisecco, A. , Bonavita, S. , Lavorgna, L. , Trojano, L. , D'ambrosio, A. , Tedeschi, G. , & Gallo, A. (2016). Psychometric properties and validity of Beck Depression Inventory II in multiple sclerosis . European Journal of Neurology , 23 ( 4 ), 744–750. 10.1111/ene.12932 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lee, E.‐H. , Lee, S.‐J. , Hwang, S.‐T. , Hong, S.‐H. , & Kim, J.‐H. (2017). Reliability and validity of the Beck Depression Inventory‐II among Korean adolescents . Psychiatry Investigation , 14 ( 1 ), 30. 10.4306/pi.2017.14.1.30 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]

IMAGES
VIDEO
COMMENTS
Introduction: Myasthenia gravis (MG) is an autoimmune disease whose period of typical onset is around 20-40 years (i.e., early onset), thus in the peak of working age, or around 60-80 years (i.e., late onset). However, the information on work-related issues and employment status are sparse and not systematically reported. Therefore, we performed a systematic literature review with meta ...
Myasthenia gravis · Work · Employment · Systematic review · Meta-analysis Abstract Introduction: Myasthenia gravis (MG) is an autoimmune dis-ease whose period of typical onset is around 20-40 years (i.e., early onset), thus in the peak of working age, or around 60-80 years (i.e., late onset). However, the information on
Request PDF | Employment in Myasthenia Gravis: A Systematic Literature Review and Meta-Analysis | Introduction: Myasthenia gravis (MG) is an autoimmune disease whose period of typical onset is ...
The results of the meta-analysis show that the percentage of employment is considerably low if the authors take into account that the mean age of MG patients involved in the included studies was around 48 years, thus in peak of working life, which is important to understand what kind of influence MG exerts on work dynamics. Introduction: Myasthenia gravis (MG) is an autoimmune disease whose ...
Employment in myasthenia gravis: a systematic literature review and meta-analysis. Neuroepidemiology. 2020; 54:304-312. [Google Scholar] 18. Harris L, Aban IB, Xin H, et al.. Employment in refractory myasthenia gravis: a Myasthenia Gravis Foundation of America registry analysis. Muscle ...
Abstract. Myasthenia gravis (MG), a rare disease, is the most common neuromuscular junction problem. It's the quintessential autoimmune disease with ocular, bulbar, respiratory, axial, and limb muscles exhibiting a typical fatigable weakening due to the development of antibodies against the acetylcholine receptor (AChR).
Introduction: Myasthenia gravis (MG) is an autoimmune disease whose period of typical onset is around 20-40 years (i.e., early onset), thus in the peak of working age, or around 60-80 years (i.e., late onset). However, the information on work-related issues and employment status are sparse and not systematically reported. Therefore, we performed a systematic literature review with meta ...
People with myasthenia gravis (MG) experience impaired quality of life. However, the impact of MG symptoms on work productivity has not been well-studied. We aimed to evaluate this impact and to examine associations between disease severity and the degree of impairment. Methods
A systematic literature search was carried out mainly in PubMed, the Cochrane Library, and the American Academy of Neurology, European Academy of Neurology, and Myasthenia Gravis Foundation of America (MGFA) International Conference on Myasthenia and Related Disorders abstracts (all 1995-2022) to identify double-blind, randomized, placebo ...
2.1. Study Eligibility Criteria and Report Eligibility Criteria. The following study eligibility criteria were applied for this systematic review: (a) patients of any age affected by MG; (b) rehabilitation applied to at least a proportion of the patients; (c) enough data provided for the purpose of the review; (d) no limits applied as to the minimum length of the follow-up.
Introduction: Myasthenia gravis (MG) is an autoimmune disease whose period of typical onset is around 20-40 years (i.e., early onset), thus in the peak of working age, or around 60-80 years (i.e., late onset). However, the information on work-related issues and employment status are sparse and not systematically reported. Therefore, we performed a systematic literature review with meta ...
Background Myasthenia gravis is a neuromuscular autoimmune disorder characterized by weakness and disability in the voluntary muscles. There have been several preliminary studies on the epidemiology of myasthenia gravis in different parts of the world and the effectiveness of common drugs in its treatment, but there has been no comprehensive study of the efficacy of common drugs in the ...
excluded. Of the 165 articles, 64 articles were included for a systematic literature and 11 articles for a meta-analysis. Conclusions: This systematic literature review and meta-analysis of treatment options showed that there was a higher response rate with TPE than IVIG in acute MG patients and patients undergoing thymectomy.
Of the 165 articles, 64 articles were included for a systematic literature and 11 articles for a meta-analysis. Conclusions: This systematic literature review and meta-analysis of treatment options showed that there was a higher response rate with TPE than IVIG in acute MG patients and patients undergoing thymectomy. There was no difference in ...
This systematic review was performed in accordance with the PRISMA reporting guidelines for conducting a systematic review or a meta-analysis of intervention trials [32]. 2.1. Study Eligibility Criteria and Report Eligibility Criteria The following study eligibility criteria were applied for this systematic review: (a) patients of any
This systematic review, meta-analysis and network meta-analysis compares the efficacy of different innovative therapies for myasthenia gravis, a rare autoimmune disorder affecting neuromuscular transmission. Find out how anti-complement and FcRn treatments perform against rituximab and other conventional therapies in improving patients' symptoms and quality of life.
Background and purpose: Therapy for myasthenia gravis (MG) is undergoing a profound change, with new treatments being tested. These include complement inhibitors and ne-onatal Fc receptor (FcRn) blockers. The aim of this study was to perform a meta-analysis and network meta-analysis of randomized and placebo-controlled trials of innovative
Myasthenia gravis (MG) is an autoimmune disease whose period of typical onset is around 20-40 years (i.e., early onset), thus in the peak of working age, or around 60-80 years (i.e., late onset). However, the information on work-related issues and employment status are sparse and not systematically reported. Therefore, we performed a systematic ...
However, many patients with myasthenia gravis have a poor socioeconomic status. 24 The unemployment rate of patients with myasthenia gravis in Brazil, Japan, Germany, and Australia varies from 28.3% to 39.4%. 23,25-27 Moreover, myasthenic crises and infections lead to more frequent and longer hospitalizations, impacting the overall ...
Semantic Scholar extracted view of "Treatment of Depression in Adolescents With Myasthenia Gravis" by Mariana I Arce et al. ... patients: A systematic review and meta‐analysis. Javad Nadali Neda Ghavampour +5 authors Omid Narimani Charan. Medicine, Psychology. ... AI-powered research tool for scientific literature, based at the Allen ...
Introduction/Aims. Myasthenia gravis (MG) is a rare neuromuscular disorder with geographically variable prevalence and incidence rates. A global trend of increasing prevalence of MG has been observed in the last few decades, and this study aimed to assess the current prevalence and incidence rates of MG in the United States.
Myasthenia gravis (MG) is an autoimmune disease whose period of typical onset is around 20-40 years (i.e., early onset), thus in the peak of working age, or around 60-80 years (i.e., late onset). However, the information on work-related issues and employment status are sparse and not systematically reported. Therefore, we performed a systematic literature review with meta-analysis to address ...
DOI: 10.7759/cureus.58812 Corpus ID: 269339286; A Breath of Relief: Oxymetazoline and Flunisolide Nasal Spray in the Management of Myasthenia Gravis Ptosis @article{Aloyan2024ABO, title={A Breath of Relief: Oxymetazoline and Flunisolide Nasal Spray in the Management of Myasthenia Gravis Ptosis}, author={Toni Aloyan and Najla Shilleh and Arjun Sharma and Barsam Barsamian and Lisa Herring Sovory ...
Of the 165 articles, 64 articles were included for a systematic literature and 11 articles for a meta-analysis. Conclusions: This systematic literature review and meta-analysis of treatment options showed that there was a higher response rate with TPE than IVIG in acute MG patients and patients undergoing thymectomy. There was no difference in ...
Anti-signal recognition particle myopathy (anti-SRP myopathy) is a rare subtype of immune-mediated inflammatory myopathy characterized by muscle weakness and anti-SRP autoantibodies. Although plasma exchange (PE) is used in severe cases, its role remains unclear. A systematic review was conducted following PRISMA guidelines, identifying 23 patients with anti-SRP myopathy treated with PE.
Systematic meta-analysis and descriptive review. The result of the I 2 test for the prevalence of MG in the world indicates a significant heterogeneity between studies (I 2 = 99.9), so the data were analyzed by meta-analysis using a random-effects model. Due to the high heterogeneity of the studies, sensitivity analysis was performed, and each ...
Therefore, for achieving epidemiologic purposes, additional studies in different regions are necessary. According to the above statements and the absence of a systematic review or meta‐analysis of these issues, we conducted this study to determine the prevalence of depression and anxiety among MG patients all around the world.