- Open access
- Published: 09 August 2023

The effectiveness of theory-based smoking cessation interventions in patients with chronic obstructive pulmonary disease: a meta-analysis
- Mengjing Han 1 na1 ,
- Yingping Fu 1 na1 ,
- Quanyue Ji 1 ,
- Xiaoli Deng 2 &
- Xuewen Fang 2
BMC Public Health volume 23 , Article number: 1510 ( 2023 ) Cite this article
3198 Accesses
1 Citations
15 Altmetric
Metrics details
Smoking cessation can effectively reduce the risk of death, alleviate respiratory symptoms, and decrease the frequency of acute exacerbations in patients with chronic obstructive pulmonary disease (COPD). Effective smoking cessation strategies are crucial for the prevention and treatment of COPD. Currently, clinical interventions based on theoretical frameworks are being increasingly used to help patients quit smoking and have shown promising results. However, theory-guided smoking cessation interventions have not been systematically evaluated or meta-analyzed for their effectiveness in COPD patients. To improve smoking cessation rates, this study sought to examine the effects of theory-based smoking cessation interventions on COPD patients.
We adhered to the PRISMA guidelines for our systematic review and meta-analysis. The Cochrane Library, Web of Science, PubMed, Embase, Wanfang, CNKI, VIP Information Services Platform, and China Biomedical Literature Service System were searched from the establishment of the database to April 20, 2023. The study quality was assessed using the Cochrane Collaboration's risk assessment tool for bias. The revman5.4 software was used for meta-analysis. The I 2 test was used for the heterogeneity test, the random effect model and fixed effect model were used for meta-analysis, and sensitivity analysis was performed by excluding individual studies.
A total of 11 RCTs involving 3,830 patients were included in the meta-analysis. Results showed that theory-based smoking cessation interventions improved smoking cessation rates, quality of life, and lung function in COPD patients compared to conventional nursing. However, these interventions did not significantly affect the level of nicotine dependence in patients.
Theory-based smoking cessation intervention as a non-pharmacologically assisted smoking cessation strategy has a positive impact on motivating COPD patients to quit smoking and improving their lung function and quality of life.
Trial registration
PROSPERO registration Number: CRD42023434357.
Peer Review reports
Introduction
Chronic Obstructive Pulmonary Disease (COPD) is a heterogeneous lung disease characterized by persistent respiratory symptoms and airflow limitation caused by airway and/or alveolar abnormalities, as defined by the 2023 Global Initiative for Chronic Obstructive Lung Disease (GOLD) [ 1 ]. In China, the overall prevalence of COPD is 8.6%, with a rate of 13.7% in the population over 40 years old [ 2 ]. Smoking is a major risk factor for COPD, with smokers having 10.92 times the risk of developing COPD compared to non-smokers [ 3 ]. Additionally, smoking COPD patients have more respiratory symptoms than non-smokers and higher mortality rates [ 4 ]. Smoking cessation is considered the most effective and cost-effective strategy for preventing and treating COPD [ 5 ]. For COPD smokers, it is important to adopt effective methods to control their smoking behavior [ 6 ]. However, smoking cessation is challenging, and conventional approaches may not be effective for all patients. Although conventional smoking cessation methods such as telephone hotlines [ 7 ], medication [ 8 ], and comprehensive interventions [ 9 ] have been shown to improve patients' smoking cessation rates and lung function to some extent, patients' smoking cessation behavior is highly influenced by their health knowledge and behavior change.
Therefore, some scholars have attempted to use theory-guided interventions to improve COPD patients' smoking cessation rates, achieving good results. Currently, the theories related to the management of smoking cessation in COPD include "timing theory" [ 10 ], "theory of planned behavior" [ 11 ], "the 5A nursing model" [ 12 ], and "cognitive-behavioral theory" [ 13 ]. The timing theory was proposed by Canadian scholars Cameron et al [ 10 ]. According to this theory, targeted intervention should be implemented according to the disease stage of patients, emphasizing the importance of understanding the different stages of the disease, focusing on the patients themselves, increasing their confidence in treating the disease, improving their current negative behaviors and emotions, and ultimately achieving a positive health outcome [ 14 , 15 ]. The planned behavior theory was proposed by Ajzen [ 11 ], who believed that individual behavior is mainly influenced by individual behavioral intentions, including attitudes, subjective norms, and perceived behavioral control. Attitude refers to the positive or negative evaluation and experience of behavior; subjective norms refer to the social pressure felt when adopting behavior; and perceived behavioral control refers to self-efficacy and control over behavior [ 16 , 17 ]. The 5A nursing model [ 12 ] includes five components: assess, advise, agree, assist, and arrange. The aim is to improve patients' self-efficacy and self-management skills [ 18 , 19 ]. Cognitive-behavioral theory is an integration of cognitive theory and behavioral theory that utilizes methods to change negative cognitions, beliefs, and behaviors [ 13 ]. Cognitive-behavioral interventions involve selecting theories related to cognition and/or behavior, considering individual, behavioral, and environmental factors, and designing intervention plans based on the individual's understanding of behavior change and available resources. This approach promotes the formation of healthy behaviors and corrects negative ones [ 20 ]. Theory-based smoking cessation interventions are designed to provide patients with the knowledge, skills, and support necessary to quit smoking successfully [ 21 ]. By understanding these theories, healthcare providers can design interventions that are tailored to the individual patient's needs and increase the likelihood of successful smoking cessation [ 22 ].
Currently, there has yet to be a systematic evaluation or meta-analysis of the effectiveness of theory-based smoking cessation interventions in COPD patients. Therefore, this study aims to synthesize randomized controlled trials of theory-based smoking cessation interventions in COPD patients and evaluate their effectiveness and impact on patients through meta-analysis, providing evidence-based medicine for their clinical application.
Our aim was to evaluate the effectiveness of theory-based smoking cessation interventions in patients with COPD.
We followed the Cochrane Collaboration's Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [ 23 ]. The review protocol is registered on the PROSPERO database (Registration No: CRD42023434357).
Literature search
Two researchers searched for RCT studies published in the Cochrane Library, Web of Science, PubMed, Embase, Wanfang Knowledge Service Platform, CNKI, VIP Resource Integration Service Platform, and China Biomedical Literature Database. The search terms included chronic obstructive pulmonary disease*/chronic obstructive lung disease*/COPD, smoking/smoking cessation/smoking intervention, theory/model/theoretical. We conducted the search by combining subject terms and free words, and expanded our search by tracing the references included in the study in a snowball manner. The retrieval deadline for this search is from the establishment of the database up until April 20, 2023.
Study selection
The inclusion and exclusion criteria were formulated according to the Population, Intervention, Comparison, Outcome, Study design (PICOS) framework. Inclusion criteria: (i) the study participants met the diagnostic criteria for COPD of the Chinese Medical Association Respiratory Disease Society (2021 revised edition) [ 24 ] and also met the relevant criteria for tobacco dependence in the Chinese Clinical Smoking Cessation Guidelines (2015 edition) [ 25 ]; (ii) the intervention was based on theoretical smoking cessation methods; (iii) the outcome indicators: at least one of smoking cessation rate, nicotine dependence level, lung function, quality of life, clinical composite symptom score, and number of clinical symptom exacerbations; (iv) the study type was a randomized controlled trial. Exclusion criteria: Exclusion criteria: (i) duplicate publications; (ii) there were no relevant outcome indicators; (iii) literature with incomplete data and outcome index data that cannot be transformed and used; (iv) literature of low quality (based on a Cochrane Collaboration risk of bias assessment quality grade of C).
Quality assessment
The Cochrane Collaboration's risk of bias assessment tool (RoB 2.0) [ 26 ] was used to evaluate the methodological quality of the included studies. Involving seven items: (i) random sequence generation, (ii) allocation concealment, (iii) blinding of participants and personnel, (iv) blinding of outcome assessment, (v) incomplete outcome data (loss to follow-up or withdrawal), (vi) selective reporting, (vii) other biases. High-risk, low-risk, and unclear were used to evaluate the risk of bias for each item. If all of the above criteria are fully met, the study quality level is A, indicating a low possibility of various biases occurring. If some of the above criteria are met, the study quality level is B, indicating a moderate possibility of bias occurring. If none of the above criteria are met, the study quality level is C, indicating a high possibility of bias occurring. In the event of disagreement between the two researchers, a third-party researcher should be consulted to reach a consensus.
Data extraction
Two researchers independently screened articles, extracted data, and cross-checked them. The data were extracted according to the designed extraction strategy, which included: (i) basic information of the included studies, including title, first author, publication year, abstract, and source of the literature; (ii) study characteristics, including sample size, age of the experimental and control groups, and intervention measures; (iii) outcome indicators, including observation indicators, measurement tools or assessment criteria, measurement values, and research conclusions.
Data synthesis and analysis
RevMan5.4 software was used for meta-analysis. The heterogeneity test was performed using the I 2 test. If P>0.1 and I 2 <50%, heterogeneity was considered acceptable, and the fixed effect model was selected; if P ≤0.1 and I 2 ≥50%, indicated that there was heterogeneity among studies, and the random effect model was selected. A sensitivity analysis was conducted to identify sources of heterogeneity. The effect size of count data was expressed as odds ratio (OR) with a 95% confidence interval (CI), while continuous data were expressed as mean difference (MD) or standardized mean difference (SMD) with a 95% confidence interval (CI).
Literature search outcomes
We searched 431 relevant articles in the database and obtained one article by reading the references to related studies. The EndNote software was applied to remove 207 duplicate literatures. 156 articles were excluded based on reading the titles and abstracts, as they included non-randomized controlled trials, inconsistent research subjects, and poor correlation. Further reading of the full text was re-screened to exclude 58 papers with the same data, outcome indicators that did not match, data that could not be translated into application, and lower quality. Ultimately, we included 11 articles [ 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 ] in our analysis, consisting of 9 Chinese-language articles [ 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 ] and 2 English-language articles [ 36 , 37 ]. A total of 3830 patients were included, including 1989 in the experimental group and 1841 in the control group. The literature screening process and results are shown in Fig. 1 .
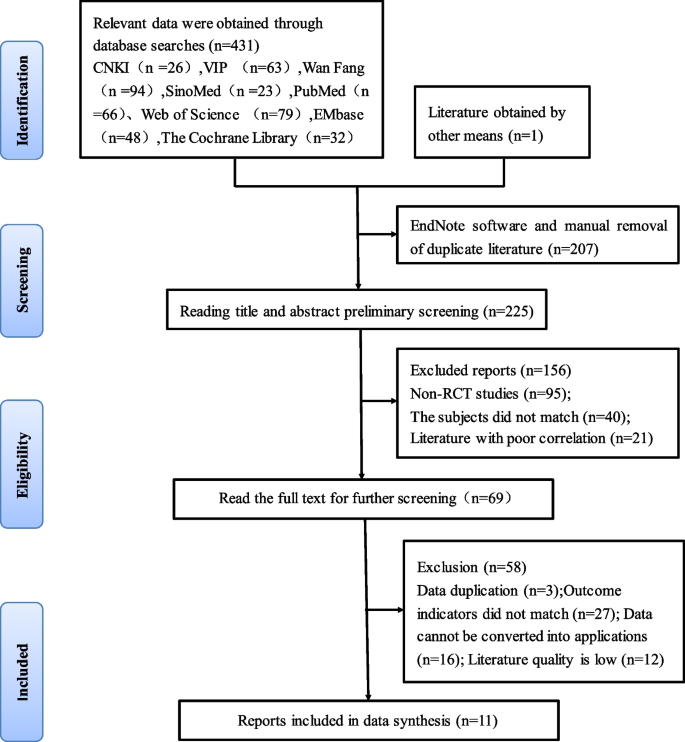
Flow chart of literature screening
The basic characteristics of studies
11 RCTs published between 2013 and 2023 were included in the meta-analysis. The studies were based on three different theories, including seven on the timing theory [ 27 , 28 , 29 , 30 , 31 , 32 , 33 ], two on the 5A nursing model [ 34 , 35 ], and two on the cognitive-behavioral theory [ 36 , 37 ]. One study on the theory of planned behavior [ 38 ] was not included in the meta-analysis because it was not an RCT. The basic characteristics of the literature are shown in Table 1 .
Two researchers evaluated and graded the 11 included studies according to the RTC bias risk assessment tool [ 26 ] provided by the Cochrane Collaboration. The results are shown in Table 2 and Fig. 2 . All studies were graded B in quality. Ten studies [ 27 , 28 , 29 , 30 , 31 , 32 , 34 , 35 , 36 , 37 ] described the generation of randomized sequences, with seven studies [ 27 , 28 , 29 , 30 , 32 , 35 , 37 ] using random number tables for grouping, one study [ 31 ] using odd-even numbering for grouping, one study [ 34 ] grouping according to patient preference, and one study [ 36 ] mentioning randomization but not specifying the method used. None of the 11 studies had any dropouts or missing data reports, and the experimental and control groups were comparable in terms of baseline levels before the intervention ( P > 0.05). This suggests that the methodological quality of the included literature is fair, the risk of bias is low, and the credibility of the evidence is high.
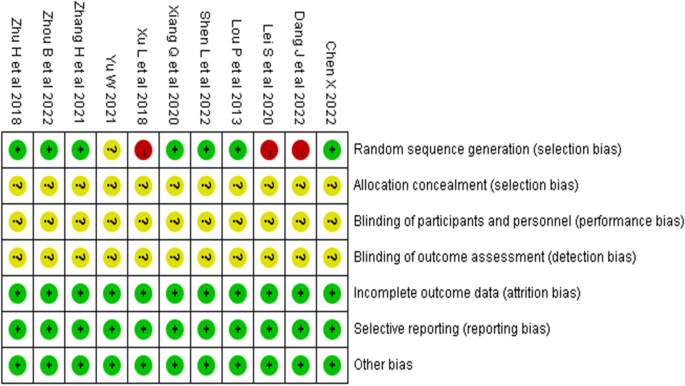
Risk of bias summary
Meta-analysis results and sensitivity analysis
Smoking cessation rates.
Ten studies [ 27 , 28 , 29 , 33 , 35 , 36 , 37 ] were evaluated for smoking cessation rates. Four studies [ 27 , 28 , 30 , 32 ] reported smoking cessation rates at one month after the intervention, and nine studies [ 27 , 29 , 30 , 31 , 32 , 33 , 35 , 36 , 37 ] reported smoking cessation rates at six months after the intervention. Fewer studies reported smoking cessation rates at three and twelve months after the intervention, so they were not included in the meta-analysis. The heterogeneity test was conducted, I 2 =48% and P =0.03, and the heterogeneity was acceptable. A fix-effects model was used for analysis, which showed that smoking cessation interventions at different intervention times were more effective in increasing smoking cessation rates than the control group [ OR =4.04, 95%CI (3.23, 5.06), P <0.001, Fig. 3 ].
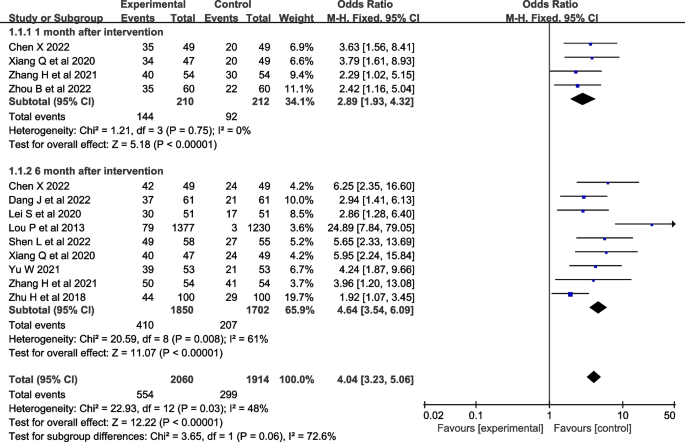
Forest plot of smoking cessation rate
Nicotine dependence
Seven studies [ 27 , 28 , 29 , 30 , 31 , 32 , 37 ] evaluated nicotine dependence. However, one study [ 27 ] used percentile and interquartile range to describe nicotine dependence, two studies [ 29 , 32 ] used percentile and interquartile range to describe nicotine dependence, and four studies [ 28 , 30 , 31 , 37 ] described nicotine dependence as mild, moderate, and severe, so four studies [ 28 , 30 , 31 , 37 ] were included in the meta-analysis. A heterogeneity test was conducted, resulting in an I 2 =71% and P <0.001. A random-effects model was used for analysis, which showed that the effect of theory-based smoking cessation interventions on nicotine dependence could not be determined [ OR =1.00, 95%CI (0.78, 1.29), P <0.001, Fig. 4 ]. Sensitivity analysis was performed by excluding individual studies, and the results still showed significant heterogeneity, indicating that the heterogeneity was stable.
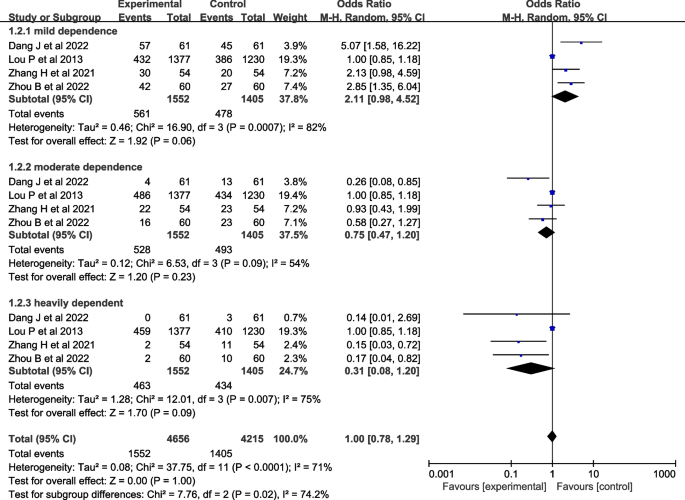
Forest plot of nicotine dependence level
Pulmonary function
Seven studies [ 28 , 29 , 30 , 32 , 33 , 35 , 36 ] evaluated lung function, including FEV1 (forced expiratory volume in the first second) [ 28 , 29 , 32 , 33 , 34 , 35 ], FEV1/Pre (ratio of forced expiratory volume in the first second to estimated vital capacity) [ 30 , 32 , 33 , 34 , 35 , 36 ], and FEV1/FVC (ratio of forced expiratory volume in the first second to forced vital capacity) [ 28 , 30 , 32 , 33 , 35 , 36 ]. The heterogeneity test showed that there was significant heterogeneity in FEV1 and FEV1/FVC among the studies ( I 2 >50%, P <0.001), and there was no heterogeneity in FEV1/Pre ( I 2 =0%, P =0.86). A random-effects model was used for analysis, which showed that the effect of theory-based smoking cessation interventions on lung function was better in the experimental group than in the control group [ MD =0.51, 95% CI (0.28, 0.74), P <0.001, Fig. 5 ]. Sensitivity analysis was performed by excluding individual studies, and the results still showed significant heterogeneity, indicating that the heterogeneity was stable.
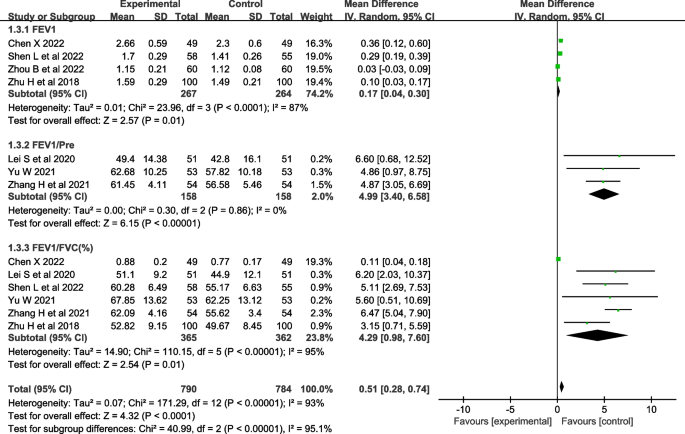
Forest plot of lung function
Quality of life
Four studies [ 29 , 30 , 31 , 35 ] evaluated quality of life. One study [ 29 ] used the Seattle COPD questionnaire [ 39 ] for evaluation, and three studies [ 30 , 31 , 35 ] used the St. George's Respiratory Questionnaire (SGRQ) [ 40 ] for evaluation, so three studies [ 30 , 31 , 35 ] were included in the meta-analysis. The heterogeneity test showed that there was significant heterogeneity ( I 2 =78%, P <0.001). A random-effects model was used for analysis, which showed that the effect of theory-based smoking cessation interventions on quality of life was better in the experimental group than in the control group [ MD =-4.87, 95% CI (-6.34, -3.40), P < 0.001, Fig. 6 ]. Sensitivity analysis was performed by excluding individual studies, and the results still showed significant heterogeneity, indicating that the heterogeneity was stable.
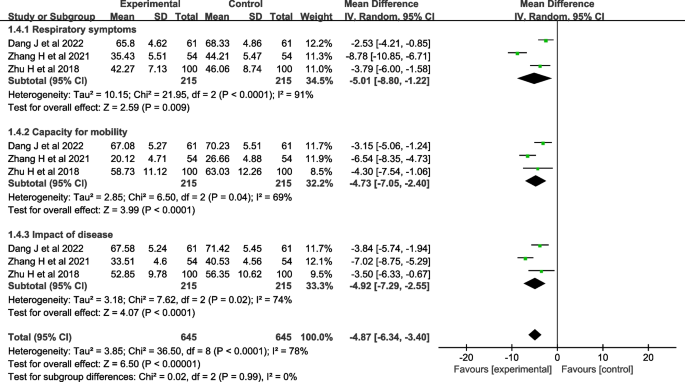
Forest plot of quality of life
Clinical symptom score
Two studies [ 28 , 34 ] reported clinical symptom scores, which are not suitable for meta-analysis because of the paucity of literature. Both studies [ 28 , 34 ] showed that the clinical composite symptom scores were significantly lower in the experimental group than in the control group ( P <0.05).
Frequency of clinical symptom exacerbation
Two studies [ 33 , 34 ] reported the frequency of clinical symptom exacerbation, which was not suitable for meta-analysis due to the small number of studies. The two studies [ 33 , 34 ] both showed that the frequency of clinical symptom aggravation in the experimental group was significantly lower than that in the control group ( P <0.05).
This study conducted a meta-analysis of data from 11 randomized controlled trials to assess the effectiveness of smoking cessation interventions in patients with COPD. This meta-analysis demonstrated that based on timing theory [ 10 ], 5A nursing model [ 12 ], and cognitive behavioral theory [ 13 ] smoking cessation interventions significantly improved smoking cessation rates, lung function, and quality of life in COPD patients. However, these interventions did not significantly affect nicotine dependence levels.
The timing theory proposes that smoking cessation strategies should be targeted based on the disease stage of COPD patients. This approach emphasizes understanding the different stages of the disease, improving negative behaviors, and increasing patients' confidence to quit smoking [ 27 , 28 , 29 , 30 , 31 , 32 , 33 ]. The 5A nursing model involves individualized assessment, setting goals, and providing help and regular follow-up to change COPD patients' cognition of the disease and the harm of smoking so that they can establish correct health beliefs [ 34 , 35 ]. Cognitive behavioral theory emphasizes the importance of addressing patients' smoking-related thoughts and behaviors for successful smoking cessation [ 36 , 37 ]. Healthcare providers can develop interventions by targeting the specific needs of patients at each stage of the disease, identifying the underlying causes of their smoking behavior, and selecting an appropriate rationale. The goal is to help COPD patients develop effective strategies to quit smoking and manage their disease symptoms. This study provides valuable insights into the effectiveness of theory-based smoking cessation interventions for COPD patients.
Theory-based smoking cessation interventions can improve the smoking cessation rate of COPD patients
The findings of this study suggest that theory-based smoking cessation interventions can improve smoking cessation rates in patients with COPD. Given the strong association between COPD and smoking, it is crucial to address smoking cessation as a key component of COPD management [ 41 ]. Previous studies mainly used smoking cessation drugs to relieve withdrawal symptoms or used auxiliary methods to improve the success rate of smokers who wanted to quit, but not all patients were willing to accept or needed to use smoking cessation drugs to quit successfully [ 42 , 41 , 42 , 43 , 44 ]. The positive impact of theory-based smoking cessation interventions on smoking cessation rates can be attributed to their emphasis on understanding patients' individual needs, motivations, and barriers to quitting smoking, as well as providing tailored support and strategies to overcome these challenges. By addressing the psychological aspects of smoking behavior and incorporating behavioral change theories, these interventions can help patients develop the necessary skills and confidence to successfully quit smoking. The use of theory-based interventions is particularly promising because it allows for a more systematic and evidence-based approach to smoking cessation. It is more conducive for patients to form a strong desire to quit smoking and take action to bring about more effective and sustainable smoking cessation effects for patients. The sensitivity analysis showed that the heterogeneity among the studies included in the meta-analysis was acceptable, indicating that the evidence results were relatively reliable.
The effect of theory-based smoking cessation interventions on nicotine dependence levels is uncertain
Nicotine dependence, also known as tobacco dependence, is a chronic disease [ 45 ]. A considerable number of COPD patients, know the harm of smoking and have the intention to quit, but because they are addicted to smoking, it is difficult to quit, which means that their degree of tobacco dependence has not improved and they still have a high risk of relapse after discharge [ 46 ]. The lack of significant effect on nicotine dependence levels may be due to several factors, including the relatively short duration of the interventions and follow-up periods in the included studies, as well as potential differences in the measurement and reporting of nicotine dependence levels across studies. For patients, in addition to providing professional and scientific help throughout the smoking cessation process, better results can be achieved by combining drug control and encouraging family members to provide adequate emotional support throughout the process. It is recommended that future studies be guided by theory and combined with pharmacological control to investigate the improvement effect.
Theory-based smoking cessation interventions improve lung function and quality of life in COPD patients
Lung function is the gold standard for diagnosing and evaluating the severity of COPD, which can objectively reflect the degree of airflow restriction or obstruction in patients [ 47 ]. Due to the intake of a large amount of nicotine, tar, and some radioactive substances, COPD smokers have a serious impact on their lung health, which not only causes inflammatory changes but also threatens the lung function of the body's respiratory system [ 48 ]. As the duration of smoking increases, the lung function of patients also decreases, which further triggers a series of lung diseases and reduces their quality of life [ 49 , 50 ], so it is urgent to control their smoking behavior.
The improvement in lung function observed in this meta-analysis is consistent with previous research showing that smoking cessation can lead to significant improvements in lung function and reduce the risk of COPD exacerbations. By helping patients quit smoking, theory-based interventions may contribute to slowing down the progression of COPD and improving patients' overall respiratory health. The observed improvement in quality of life is also an important finding, as COPD is known to have a significant impact on patients' physical, emotional, and social well-being. By addressing both the physical and psychological aspects of smoking behavior, theory-based interventions may help improve patient’s overall well-being and quality of life.
Limitations
Several limitations of this study remain: (i) Due to language limitations, only publicly available Chinese and English literature was searched, which may result in incomplete literature collection; (ii) The included studies did not mention allocation concealment and blinding methods, resulting in medium-quality research quality, which may affect the reliability of the results to some extent. It is hoped that subsequent relevant research will further improve the rigor of allocation concealment and blinding methods to achieve higher quality levels. (iii) Currently, most studies only report short-term effects of theory-based smoking cessation interventions on COPD patients.
The findings of this study demonstrated that implementing theory-based smoking cessation interventions in conventional healthcare can have a positive effect on the smoking cessation rate, lung function, and quality of life of COPD patients. It is recommended that these interventions be widely implemented in clinical practice. Further investigation is required to confirm these findings due to the limitations in the standardization and homogeneity of the included studies.
Availability of data and materials
The study is conducted using open-source data from published articles. Additional data can be made available upon request to Mengjing Han([email protected]).
Liang Z, Wang F, Chen Z, et al. Updated key points interpretation of global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (2023 Report). Chinese General Practice. 2023;26(11):1287–98.
Google Scholar
Wang C, Xu J, Yang L, et al. Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China Pulmonary Health [CPH] study): a national cross-sectional study. Lancet. 2018;391(10131):1706–17.
PubMed Google Scholar
Salvi SS, Brashier BB, Londhe J, et al. Phenotypic comparison between smoking and non-smoking chronic obstructive pulmonary disease. Respir Res. 2020;21(1):50.
CAS PubMed PubMed Central Google Scholar
Li X, Wu Z, Xue M, et al. Smoking status affects clinical characteristics and disease course of acute exacerbation of chronic obstructive pulmonary disease: a prospectively observational study. Chron Respir Dis. 2020;17:1479973120916184.
PubMed PubMed Central Google Scholar
Hirai K, Tanaka A, Homma T, et al. Characteristics of and reasons for patients with chronic obstructive pulmonary disease to continue smoking, quit smoking, and switch to heated tobacco products. Tob Induc Dis. 2021;19(1):85.
Thomson NC. The role of smoking in asthma and chronic obstructive pulmonary disease overlap. Immunol Allergy Clin North Am. 2022;42(3):615–30.
McCabe C, McCann M, Brady AM. Computer and mobile technology interventions for self-management in chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2017;5(5):CD011425.
Antoniu SA, Buculei I, Mihaltan F, et al. Pharmacological strategies for smoking cessation in patients with chronic obstructive pulmonary disease: a pragmatic review. Expert Opin Pharmacother. 2021;22(7):835–47.
CAS PubMed Google Scholar
Saeed MI, Sivapalan P, Eklöf J, et al. TOB-STOP-COP (TOBacco STOP in COPd trial): study protocol-a randomized open-label, superiority, multicenter, two-arm intervention study of the effect of “high-intensity” vs. “low-intensity” smoking cessation intervention in active smokers with chronic obstructive pulmonary disease. Trials. 2020;21(1):730.
Cameron JI, Gignac MA. “Timing It Right”: a conceptual framework for addressing the support needs of family caregivers to stroke survivors from the hospital to the home. Patient Educ Couns. 2008;70(3):305–14.
Ajzen I. Perceived behavioral control, self-efficacy, locus of control, and the theory of planned behavior. Journal of Applied Social Psychology. 2002;32(4):665–83.
Martínez C, Castellano Y, Andrés A, et al. Factors associated with implementation of the 5A’s smoking cessation model. Tob Induc Dis. 2017;1(1):15:41.
Zeng G, Wang W, Qin X. Research progress on the theory and mechanism of health behavior intervention. Chinese Nursing Research. 2021;35(8):1428–34.
Jiang X, Gu Q, Jiang Z, et al. Effect of family-centered nursing based on timing it right framework in patients with acute cerebral infarction. Am J Transl Res. 2021;13(4):3147–55.
Xu Y, Song W, Wang Q, et al. The effect of a psychological nursing intervention program based on the “Timing it Right” (TIR) framework on elderly patients’ anxiety, psychology, and self-efficacy. Am J Transl Res. 2021;13(8):9600–6.
Bosnjak M, Ajzen I, Schmidt P. The Theory of Planned Behavior: Selected Recent Advances and Applications. Eur J Psychol. 2020;16(3):352–6.
Şanlıtürk D, Ayaz-Alkaya S. The Effect of a Theory of Planned Behavior Education Program on Asthma Control and Medication Adherence: A Randomized Controlled Trial. J Allergy Clin Immunol Pract. 2021;9(9):3371–9.
Zhang X, Lai M, Wu D, et al. The Effect of 5A nursing intervention on living quality and self-care efficacy of patients undergoing chemotherapy after hepatocellular carcinoma surgery. Am J Transl Res. 2021;13(6):6638–45.
Rokni S, Rezaei Z, Noghabi AD, et al. Evaluation of the effects of diabetes self-management education based on 5A model on the quality of life and blood glucose of women with gestational diabetes mellitus: an experimental study in eastern Iran. J Prev Med Hyg. 2022;63(3):E442–7.
Williams MT, Johnston KN, Paquet C. Cognitive behavioral therapy for people with chronic obstructive pulmonary disease: rapid review. Int J Chron Obstruct Pulmon Dis. 2020;15(1):903–19.
Bhatt G, Goel S, Soundappan K, et al. Theoretical constructs of smoking cessation among current tobacco smokers in India: a secondary analysis of Global Adult Tobacco Survey-2 (2016–2017). BMJ Open. 2022;12(1): e050916.
Campbell KA, Fergie L, Coleman-Haynes T, et al. Improving behavioral support for smoking cessation in pregnancy: What are the barriers to stopping and which behavior change techniques can influence these? Application of theoretical domains framework. Int J Environ Res Public Health. 2018;15(2):359.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71.
Chronic obstructive pulmonary Disease Group, Respiratory Branch, Medical Association, et al. Guidelines for the management and Treatment of chronic obstructive pulmonary Disease (2021 revised). Chinese J Tubercul Resp Dis. 2021;44(3):170–205.
National health and family planning commission of the people’s republic of China. Chinese clinical smoking cessation guidelines (2015 edition). Chinese J Health Management. 2016;10(2):88–95.
Cumpston M, Li T, Page MJ, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019;10:ED000142.
Xiang Q, Zhang C, Xu S, et al. Effects of a smoking cessation intervention based on Timing It Right in patients with chronic obstructive pulmonary disease. Chinese Journal of Nursing. 2020;55(5):684–9.
Zhou B, Chui Y, Wang X. Application of smoking cessation intervention based on timing theory in elderly patients with COPD complicated with tobacco dependence. Chinese Journal of Modern Nursing. 2022;28(36):5084–9.
Shen L, Zhang Q, Wang J, et al. Application effect of timing theory based smoking cessation intervention in patients with chronic obstructive pulmonary disease. Modern Nurse. 2022;29(10):24–7.
Zhang H, Yan X. Clinical effect of smoking cessation intervention based on timing theory on patients with chronic obstructive pulmonary disease. Journal of Clinical and Pathological Research. 2021;41(9):2052–8.
Dang J. Effect of wooden ball training combined with timing theory of smoking cessation intervention on cardiopulmonary endurance and quality of life of patients with chronic obstructive pulmonary disease in stable stage. Medical Journal of Liaoning. 2022;36(2):49–52.
Chen X. Application of smoking cessation intervention based on timing theory in patients with chronic obstructive pulmonary disease. The Journal of Medical Theory and Practice. 2022;35(2):343–5.
Yu W. Effect of a staged smoking cessation intervention program based on timing theory on the prognosis of elderly COPD patients. Zhejiang Clinical Medicine Journal. 2021;23(11):1642–4.
Xu L, Hu X, Sun H, et al. Application of smoking cessation intervention based on 5A model in patients with chronic obstructive pulmonary disease. Nursing Practice and Research. 2018;15(10):33–5.
Zhu H, Zhang Y, Zeng Y. Effects of smoking cessation intervention on smoking cessation efficacy in patients with chronic obstructive pulmonary disease. Academic Journal of Guangzhou Medical University. 2018;46(02):86–9.
Lei S, Li M, Duan W, et al. The long-term outcomes of tobacco control strategies based on the cognitive intervention for smoking cessation in COPD patients. RESP MED. 2020;172:106155.
Lou P, Zhu Y, Chen P, et al. Supporting smoking cessation in chronic obstructive pulmonary disease with behavioral intervention: a randomized controlled trial. BMC Fam Pract. 2013;14:91.
Xiang Q, Zeng H, Yu F, et al. Application of smoking cessation intervention based on planned behavior theory in community patients with chronic obstructive pulmonary disease. Journal of Nursing Administration. 2022;22(12):853–7+867.
Tu SP, McDonell MB, Spertus JA, et al. A new self-administered questionnaire to monitor health-related quality of life in patients with COPD. Ambulatory Care Quality Improvement Project (ACQUIP) Investigators. Chest. 1997;112(2):614–22.
Hardin M, Rennard SI. What’s New with the St George’s Respiratory Questionnaire and Why Do We Care? Chronic Obstr Pulm Dis. 2017;4(2):83–6.
Liu Z, Xiao D, Wang C. Smoking cessation is the most effective measure for the prevention and treatment of chronic obstructive pulmonary disease. Chinese Journal of Tuberculosis and Respiratory Diseases. 2017;40(12):894–7.
Wei X, Guo K, Shang X, et al. Effects of different interventions on smoking cessation in chronic obstructive pulmonary disease patients: a systematic review and network meta-analysis. Int J Nurs Stud. 2022;136(1): 104362.
van Eerd EA, van der Meer RM, van Schayck OC, et al. Smoking cessation for people with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2016;1(8):CD010744.
Feng L, Lv X, Wang Y, et al. Developments in smoking cessation interventions for patients with chronic obstructive pulmonary disease in the past 5 years: a scoping review. Expert Rev Respir Med. 2022;16(7):749–64.
Wills L, Kenny PJ. Addiction-related neuroadaptations following chronic nicotine exposure. J Neurochem. 2021;157(5):1652–73.
Hashimoto R, Tomioka H, Wada T, et al. Outcomes and predictive factors for successful smoking cessation therapy in COPD patients with nicotine dependence. Respir Investig. 2020;58(5):387–94.
Neder JA, Torres JP, Milne KM, et al. Lung Function Testing in Chronic Obstructive Pulmonary Disease. Clin Chest Med. 2020;41(3):347–66.
Keogan S, Alonso T, Sunday S, et al. Lung function changes in patients with chronic obstructive pulmonary disease (COPD) and asthma exposed to secondhand smoke in outdoor areas. J Asthma. 2021;58(9):1169–75.
Ding Q, Li J, Xu S, et al. Different smoking statuses on survival and emphysema in patients with acute exacerbation of chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2022;17(1):505–15.
Boulet LP, Boulay ME, Milot J, et al. Longitudinal comparison of outcomes in patients with smoking-related asthma-COPD overlap and in non-smoking asthmatics with incomplete reversibility of airway obstruction. Int J Chron Obstruct Pulmon Dis. 2019;14(1):493–8.
Download references
Acknowledgements
Not applicable.
This study was supported by the Open Program of the Clinical Medical Center of the First People's Hospital of Yunnan Province, PRC (Grant NO. 2021LCZXXF-HX05).
Author information
MengjingHan and YingpingFu contributed equally to this work.
Authors and Affiliations
Yunnan University of Chinese Medicine, Kunming, Yunnan, People’s Republic of China
Mengjing Han, Yingping Fu & Quanyue Ji
The First People’s Hospital of Yunnan Province, Kunming, Yunnan, People’s Republic of China
Xiaoli Deng & Xuewen Fang
You can also search for this author in PubMed Google Scholar
Contributions
Research plan and framework: Mengjing Han. Data acquisition and analysis: Mengjing Han, Yingping Fu. Methodological approach: Xiaoli Deng, Xuewen Fang. Validation: Quanyue Ji. Drafting of the manuscript: Mengjing Han, Yingping Fu. Critical revision: Mengjing Han, Xiaoli Deng, Xuewen Fang. The work was equally contributed by Mengjing Han and Yingping Fu.
Corresponding author
Correspondence to Xiaoli Deng .
Ethics declarations
Ethics approval and consent to participate, consent for publication.
Not applicable
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Search terms and strategies.
Additional file 2.
PRISMA Checklist.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Han, M., Fu, Y., Ji, Q. et al. The effectiveness of theory-based smoking cessation interventions in patients with chronic obstructive pulmonary disease: a meta-analysis. BMC Public Health 23 , 1510 (2023). https://doi.org/10.1186/s12889-023-16441-w
Download citation
Received : 28 June 2023
Accepted : 02 August 2023
Published : 09 August 2023
DOI : https://doi.org/10.1186/s12889-023-16441-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Chronic obstructive pulmonary disease
- Smoking cessation
- Clinical trial
- Meta-analysis
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Smoking cessation: strategies and effects in primary and secondary cardiovascular prevention
Affiliations.
- 1 Department of Respiratory Medicine, Wythenshawe Hospital, Manchester University NHS Foundation Trust, Wythenshawe, UK.
- 2 Department of Respiratory Medicine, Wythenshawe Hospital, Manchester University NHS Foundation Trust, Wythenshawe, UK - [email protected].
- PMID: 33325671
- DOI: 10.23736/S0031-0808.20.04241-X
Although smoking is seen as a major health problem by most clinicians, few are able to provide evidence based smoking cessation interventions to their patients. Most individuals who smoke actually want to quit. Unfortunately, smoking is still seen as a vice or lifestyle choice, when it is actually a chronic disease which often starts in adolescence. Nicotine dependence is complex and must be quantified and treated differently for each patient in order to achieve high quit rates. Smoking has a significant impact on the development and progression of cardiovascular disease. Smoking cessation is a cost effective and often overlooked prevention tool which improves both short- and long-term outcomes. There are both pharmacological and non-pharmacological strategies for smoking cessation that can be applied in clinical practice. Brief advice, specialized counseling including therapeutic education and behavioral support, and first- and second-line pharmacological interventions have been proven to be effective to help smokers quit. Although classically tobacco dependence was seen in relation to smoking, since the early 2000s, new nicotine delivery systems have appeared on the market, which despite being marketed as "healthy" alternatives, can often complicate smoking cessation efforts and act as gateway devices for new generations of smokers. In this article we review the results of several large systematic reviews and meta-analyses, which have shown that many cessation strategies are effective. We also offer practical tips on providing brief cessation advice and how pharmacotherapy can be prescribed and incorporated into clinical practice in both primary and secondary cardiovascular prevention.
Publication types
- Cardiovascular Diseases / prevention & control*
- Primary Prevention*
- Secondary Prevention*
- Smoking / adverse effects
- Smoking Cessation*
- Tobacco Use Disorder / complications*
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
An overview of systematic reviews on predictors of smoking cessation among young people
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliations Institute of Medical Science, University of Toronto, Toronto, Canada, Centre for Addiction and Mental Health, Toronto, Canada
Roles Investigation, Writing – original draft
Affiliation Dalla Lana School of Public Health, University of Toronto, Toronto, Canada
Roles Methodology, Writing – review & editing
Affiliations Institute of Medical Science, University of Toronto, Toronto, Canada, Centre for Addiction and Mental Health, Toronto, Canada, Dalla Lana School of Public Health, University of Toronto, Toronto, Canada
Affiliations Institute of Medical Science, University of Toronto, Toronto, Canada, The Hospital for Sick Children (SickKids), Toronto, Canada, Department of Paediatrics, University of Toronto, Toronto, Canada
Roles Methodology, Supervision, Writing – review & editing
Affiliations Institute of Medical Science, University of Toronto, Toronto, Canada, Centre for Addiction and Mental Health, Toronto, Canada, Department of Family and Community Medicine, University of Toronto, Toronto, Canada
Roles Conceptualization, Methodology, Supervision, Writing – review & editing
- Anasua Kundu,
- Nahid Sultana,
- Daniel Felsky,
- Theo J. Moraes,
- Peter Selby,
- Michael Chaiton

- Published: March 11, 2024
- https://doi.org/10.1371/journal.pone.0299728
- Reader Comments
Understanding the factors that influence smoking cessation among young people is crucial for planning targeted cessation approaches. The objective of this review was to comprehensively summarize evidence for predictors of different smoking cessation related behaviors among young people from currently available systematic reviews. We searched six databases and reference lists of the included articles for studies published up to October 20, 2023. All systematic reviews summarizing predictors of intention to quit smoking, quit attempts, or smoking abstinence among people aged 10–35 years were included. We excluded reviews on effectiveness of smoking cessation intervention; smoking prevention and other smoking behaviors; cessation of other tobacco products use, dual use, and polysubstance use. We categorized the identified predictors into 5 different categories for 3 overlapping age groups. JBI critical appraisal tool and GRADE-CERqual approach were used for quality and certainty assessment respectively. A total of 11 systematic reviews were included in this study; all summarized predictors of smoking abstinence/quit attempts and two also identified predictors of intention to quit smoking. Seven reviews had satisfactory critical appraisal score and there was minimal overlapping between the reviews. We found 4 ‘possible’ predictors of intention to quit smoking and 119 predictors of smoking abstinence/quit attempts. Most of these 119 predictors were applicable for ~10–29 years age group. We had moderate confidence on the ‘probable’, ‘possible’, ‘insufficient evidence’, and ‘inconsistent direction’ predictors and low confidence on the ‘probably unrelated’ factors. The ‘probable’ predictors include a wide variety of socio-demographic factors, nicotine dependence, mental health, attitudes, behavioral and psychological factors, peer and family related factors, and jurisdictional policies. These predictors can guide improvement of existing smoking cessation interventions or planning of new targeted intervention programs. Other predictors as well as predictors of intention to quit smoking need to be further investigated among adolescents and young adults separately.
Citation: Kundu A, Sultana N, Felsky D, Moraes TJ, Selby P, Chaiton M (2024) An overview of systematic reviews on predictors of smoking cessation among young people. PLoS ONE 19(3): e0299728. https://doi.org/10.1371/journal.pone.0299728
Editor: Mohammed Nasser Alhajj, Thamar University: Dhamar University, YEMEN
Received: August 10, 2023; Accepted: February 15, 2024; Published: March 11, 2024
Copyright: © 2024 Kundu et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the paper and its Supporting Information files.
Funding: The authors received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Worldwide approximately 8 million deaths and 200 million disability-adjusted life-years were attributed to smoking tobacco in the year 2019 [ 1 ]. Although smoking prevalence has decreased considerably over past years, still 1.1% of the Canadians aged 12 to 17 years and 11.4% aged 18 to 34 years reported currently smoking cigarettes in 2021 [ 2 ]. Almost 90% of the adult cigarette smokers start smoking cigarettes by the age of 18 years [ 3 ]. The risk of smoking-related disease development as well as the likelihood of dying from cancer increases as a function of duration of smoking [ 3 , 4 ]. However, quitting smoking at younger ages reduces this risk significantly and quitting by the age of 34 years avoids approximately 100% of the cancer mortality risk associated with continued smoking [ 4 ]. While many young people desire to quit smoking and the highest rate of quit attempts is seen among 18–24 years age group [ 5 ], most of them have a great deal of difficulty in successfully quitting smoking [ 5 – 7 ]. A previous longitudinal study reported that smokers may take on average 30 or more quit attempts before finally being successful in quitting [ 7 ]. Hence, it is important to explore the individual and environmental predictors that influence different smoking cessation related behaviors among populations before tobacco related morbidity and mortality are manifested.
Although the reasons and motivations to quit smoking are not much different between youths and adults (e.g., health concerns and costs) [ 8 , 9 ], they differ in other aspects. For example, youths are more likely to report concomitant nicotine and cannabis use, have higher nicotine and alcohol dependence, better physical functioning, and lower psychological functioning than older adults [ 10 ]. Moreover, smoking cessation is a behaviorally different process for youths in comparison to adults due to their high sensitivity to unique intrapersonal and interpersonal factors as well as different social determinants of health [ 3 , 11 ]. While previous systematic reviews have addressed different types of predictors of smoking cessation among youth, most of them are heterogenous with some focused on a single predictor, some included only a specific population group, and reviews conducted in different time periods over the years [ 12 – 14 ]. Moreover, it is not clear which predictors should be prioritized in terms of significance, and which predictors are needed to be studied further. Hence, we conducted a comprehensive overview where we included published systematic reviews on predictors of smoking cessation among the young population. It will improve our existing knowledge on this topic; guide us to identify higher-risk population; and eventually minimize smoking related mortality and morbidity by intervening in these individuals as young as possible [ 4 ]. The objective of this overview was to summarize individual and environmental factors that predict smoking cessation related behaviors among young people aged 10–35 years from currently available systematic reviews and categorize them according to their reported statistical significance.
Materials and methods
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines by adhering to the four-phase flow diagram and 27-item checklist for this study [ 15 ]. This protocol was registered on the Open Science Framework ( https://osf.io/48mja/ ) [ 16 ]. The review was conducted in five steps: (1) database search and exclusion of duplicate articles, (2) review of the titles and abstracts to exclude clearly irrelevant articles, (3) in-depth full-text review of articles to determine inclusion, (4) extraction of relevant data from the included articles, and 5) synthesis of the extracted data, critical appraisal of the included articles, and certainty assessment of the evidence.
Information sources and search strategy
We searched MEDLINE, PubMed, PsycINFO, CINAHL Plus and Scopus as sources of academic databases and Google Scholar as a source of grey literature. We conducted our initial literature search in September 26, 2022, but later updated our search in October 20, 2023 by using various combinations of medical subject headings (MeSH terms) and keywords (e.g., “smoking cessation”, “cigarette*”, “quit”, “abstinence”, “predict*”, “risk factors”, “correlate*”, “associate*”, “emerging adulthood”, “youth*”, “adolescent*”, and “young adult*”) (see S1 Appendix ). From the initial Google Scholar search, first 200 results were considered for title and abstract screening, because we did not get any relevant article following this threshold. Later, we additionally screened first 100 results of the most recently published articles from the updated Google Scholar search. All search results were further limited to review articles on humans and English language papers. We also searched the reference lists of the included articles. One reviewer (AK) conducted both academic and grey literature search and imported the articles to the Covidence workflow platform where duplicate articles were automatically removed. Another reviewer (NS) searched the reference lists of the finally included articles looking for any potential paper which matched the eligibility criteria.
Eligibility criteria
We included any systematic reviews which summarized factors possibly influencing smoking cessation related behaviors including intention to quit smoking, quit attempts and smoking abstinence among young people between age 10 and 35 years. Hence, other types of literature reviews including scoping and narrative reviews were excluded. Although World Health Organization (WHO) has defined people between age 10 and 24 years as adolescents and young adults [ 17 ], several studies identified people up to age 35 years as young adults [ 18 – 20 ]. Moreover, previous research has shown that quitting smoking by 34 years significantly lowers smoking mortality and morbidities [ 4 ]. Hence, we decided to expand our target population to people between the ages of 10 and 35 years, so that the findings of this study could be applicable for a broader group of young population. We also included reviews where the target population included people between 10 and 35 years as sub-population, or the review assessed predictors of smoking cessation as one of the various other outcomes. We excluded systematic reviews on 1) efficacy of smoking cessation interventions; 2) predictors of adverse health effects of smoking; 3) predictors of smoking prevention and other smoking behaviors such as smoking initiation, escalation, and smoking prevalence; 4) predictors of other tobacco products (OTPs) cessation; and 5) predictors of cessation of dual use of cigarettes and e-cigarettes or polysubstance use. We excluded reviews that assessed the efficacy of smoking cessation interventions because most of the studies included in these types of reviews were randomized controlled trials [ 21 , 22 ], which are most suitable for examining cause and effect relationship. However, rather than identifying which intervention will be more effective for causing smoking cessation, we intended to summarize the individual and environmental risk factors that influence young peoples’ smoking cessation related behaviors.
Selection process
Two reviewers (AK and NS) independently screened each title and abstract in accordance with the inclusion and exclusion criteria. Next, each full text of the remaining articles was reviewed by the two reviewers (AK and NS) and any disagreements were resolved by further discussions among them.
Data collection process, data items, and effect measures
We used a custom-made data extraction form to extract relevant data on general characteristics of the included reviews (author and year, number of databases searched, search period, number of included studies, study design of included studies, age group, primary outcome, number of predictors identified, key findings, special features and critical appraisal score). For any given review, we also extracted data on all predictors (both statistically significant and insignificant) of smoking cessation related behaviors reported in the review. The included reviews reported statistical significance of the predictors using either a narrative data synthesis approach, or by considering p-values < 0.05 or 95% confidence intervals reported in their included studies. We also extracted data on the direction of association of the predictors as reported in the reviews, which were either positive or negative or inconsistent. One particular review [ 12 ] did not report the direction of association of their identified predictors clearly. We contacted the corresponding author enquiring about details of the findings but did not receive any responses. Hence, we documented the direction of association for these predictors as unclear. For the reviews which assessed predictors of different cigarette or tobacco use related behaviors, we limited our data extraction to the studies included in their review that evaluated only smoking cessation behaviors. While one reviewer (AK) extracted the data from all final included reviews, another reviewer (NS) checked for accuracy of the extracted data. Disagreements were resolved by discussion between the reviewers.
Synthesis methods
We grouped outcomes in the included reviews into two categories: intention to quit smoking and smoking abstinence/quit attempts. While intention to quit smoking was indicated by future intention to quit among current smokers, smoking abstinence was usually defined by the reviews as successfully quitting smoking for a defined time-period such as 6 months. Some reviews used the term ‘smoking cessation’ as their outcomes which was non-specific and could be interpreted as either smoking abstinence or previous quit attempts. So, we combined these outcomes with smoking abstinence and made a category named smoking abstinence/quit attempts. Most of the included reviews used broader age groups as target population. Hence, we made three categories of overlapping age groups and summarized the predictors of smoking abstinence/quit attempts for individual age groups.
By following the categorization method used in a previous systematic review [ 14 ], each identified predictor was further categorized into the following groups based on the frequency of their reported significant association in the reviews: 1) probable predictor (the predictor was reported by at least 2 reviews and found statistically significant in at least 50% of the reviews); 2) possible predictor (statistical significance was observed in only one review or <50% of the total reviews); 3) insufficient evidence (when the predictor was reported by only one review and no statistically significant association was found); 4) probably unrelated (no statistically significant effect identified in at least 2 reviews). We determined the direction of effect for each individual predictor as positive or negative based on the reported direction of association observed in majority of the reviews. For any given predictor, if an unclear association was identified for one particular review [ 12 ], we ignored it and considered the direction of association found in other reviews while determining the final direction of effect. If a predictor with unclear direction of association was examined by a single review, we grouped it as ‘insufficient evidence’ factor. An additional category- ‘inconsistent direction’ was added to the previous 4 categories to represent the predictors for which 1) equal number of reviews reported positive and negative associations; or 2) equal number of reviews reported positive/negative and inconsistent associations. Data synthesis was conducted by one reviewer (AK) and checked for accuracy by another reviewer (NS).
Quality assessment
For quality assessment of the included reviews, we used the Joanna Briggs Institute (JBI) critical appraisal checklist for systematic reviews [ 23 ]. We choose the JBI critical appraisal checklist instead of other critical appraisal tools (e.g., A measurement tool to assess systematic reviews (AMSTAR) [ 24 ] or Risk of bias in systematic review (ROBIS) [ 25 ]), because the applicability of this tool is wide and more appropriate for systematic review of non-experimental studies [ 26 , 27 ]. It contains an 11-item checklist, where for each item appraised, we assigned a score of 1, if the criterion was met, and 0, if the criterion was not met or was unclear. We modified the 11-item checklist to a 10-item checklist for selective reviews of qualitative studies, because item no. 9 was not applicable for these type of reviews [ 23 ]. Finally, all critical appraisal scores were reported as a percentage of the assigned total numerical scores instead of individual points. We followed a recent overview [ 28 ] to present our results for the JBI critical appraisal checklist and determined an overall score of at least 70% indicating satisfactory methodological quality. Two reviewers (AK and NS) independently scored all reviews, and any disagreement was resolved by discussion.
Certainty assessment and overlapping between the reviews
As the included reviews did not conduct any meta-analysis and mostly presented their findings by narrative data synthesis, we used the Confidence in Evidence from Reviews of Qualitative Research (GRADE-CERQual) approach [ 29 ] for assessing certainty or confidence in the body of evidence. Although the GRADE-CERQual [ 29 ] is mainly built for conducting systematic review of primary studies, we followed similar approach applied in previous research [ 30 ] and recommendations on adapting existing tools for assessing certainty of the evidence in an overview [ 31 ]. The certainty assessment in GRADE-CERQual is based on four components- methodological limitations, coherence, adequacy of data, and relevance [ 29 ]. We evaluated the confidence in evidence on categories of the predictors for each individual outcome by assessing whether the involved reviews had any concerns regarding these four components. Based on the judgements made for each of the four components, an overall assessment of certainty or confidence was made as high, moderate, low, or very low confidence [ 29 ]. Two reviewers (AK and NS) independently provided their judgements, and any disagreement was resolved by discussion.
Here, N is the number of total studies across all reviews (including multiple counting of the same study), r is the number of primary studies and c is the number of reviews. The CCA value 0–5 indicates slight overlap, 6–10 moderate overlap, 11–15 high overlap and >15 means very high overlap between the reviews [ 32 ].
Although one of our included reviews [ 12 ] reported including total 51 studies in the final review, we could only retrieve 18 studies from their reference list. Our efforts to get the full reference list failed to get any responses from the authors of the review [ 12 ]. Hence, we counted only the retrieved 18 original studies for measuring the final CA and CCA measures.
Study selection
The search of academic electronic databases yielded 999 articles. Following removal of 307 duplicates, a total of 692 articles were reviewed by title and abstract screening. An additional 300 articles were screened through Google Scholar search and 1 article was added from searching reference lists of the final included articles. Finally, a total of 24 articles were selected for full-text screening. After removing 13 articles for various reasons ( Fig 1 ), we included total 11 articles [ 11 – 14 , 33 – 39 ] in the final review. The detailed selection process of the articles is presented in the PRISMA flow diagram ( Fig 1 ).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0299728.g001
Study characteristics and results of individual studies
The summary statistics of the included studies and general characteristics of individual reviews are presented in Tables 1 and 2 respectively. Out of 11 final systematic reviews [ 11 – 14 , 33 – 39 ], only 2 [ 12 , 33 ] were published before 2010, the remaining 9 were published between 2011 and 2022. Only 2 reviews [ 35 , 37 ] assessed predictors of intention to quit smoking, while all reviews [ 11 – 14 , 33 – 39 ] identified predictors of smoking abstinence/quit attempts. Four [ 13 , 34 , 36 , 37 ] out of 11 reviews included only 1–5 studies on smoking cessation in their review, 2 reviews [ 35 , 39 ] included 6–10 studies, 2 reviews [ 11 , 33 ] included 11–20 studies, and 3 reviews [ 12 , 14 , 38 ] included >20 studies. The highest number of studies included in one review [ 12 ] was 51 studies, however, only 18 of them were retrievable. The second highest number of studies included in one review [ 38 ] was 39. Five reviews [ 13 , 34 – 37 ] detected <20 predictors, while 4 reviews [ 11 , 12 , 33 , 38 ] detected 21–50 predictors and 2 reviews [ 14 , 39 ] detected >51 predictors. The highest number of predictors identified by a single review [ 14 ] was 67 ( Table 2 ).
https://doi.org/10.1371/journal.pone.0299728.t001
https://doi.org/10.1371/journal.pone.0299728.t002
Synthesis of results on predictors of smoking cessation
We identified a total of 123 predictors, of which 4 were predictors of intention to quit smoking and 119 were predictors of smoking abstinence/quit attempts. There was no ‘probable’ predictor for intention to quit smoking, because the low number of studies (n = 2) examining this outcome focused on completely different factors. Hence, it did not meet our criteria of ‘probable’ predictors and we categorized these 4 factors as ‘possible’ predictors. Among them, self-recognizing smoker identity, and interactions between smoker identity and other identity like being a mother increased the likelihood, while positive risk acceptance with smoker identity decreased the likelihood of having intention to quit smoking among 16–34 years age people [ 35 ]. Additionally, using flavored tobacco was found to lower the probability of future intention to quit smoking among 12–18 years age group [ 37 ].
Tables 3 – 5 and S2 Appendix presents the distribution of 119 predictors of smoking abstinence/quit attempts by 3 overlapping age groups- ~12–21 years, ~16–34 years, and ~10–29 years. While the predictors for the first two age groups were very small in number, the four reviews [ 14 , 33 , 38 , 39 ] conducted on the ~10–29 years age group identified on an average of 46.5 predictors. No ‘probable’ and ‘probably unrelated’ predictors were found for ~12–21 years age group, while 22 ‘possible’ predictors, 3 predictors of ‘insufficient evidence’, and 1 predictor of ‘inconsistent direction’ were identified. Among the predictors identified for the ~16–34 years age group, 2 were ‘probable’, 6 were ‘possible’, 17 had ‘insufficient evidence’, and 2 were ‘inconsistent direction’ predictors. The 2 ‘probable” predictors were self-efficacy/confidence in quitting and tobacco price increase, both were found to have positive direction of association with smoking abstinence/quit attempts ( Table 3 ). No ‘probably unrelated’ predictors were found for this age group.
https://doi.org/10.1371/journal.pone.0299728.t003
https://doi.org/10.1371/journal.pone.0299728.t004
https://doi.org/10.1371/journal.pone.0299728.t005
For the ~10–29 years age group, we detected 29 ‘probable’, 39 ‘possible’, 26 ‘insufficient evidence’, 2 ‘probably unrelated’, and 14 ‘inconsistent direction’ predictors of smoking abstinence/quit attempts. The ‘probable’ predictors included a wide variety of factors including socio-demographic factors, nicotine dependence, attitudes regarding smoking, mental health and psychological factors, behavioral factors, peer and family related factors, and policy related factors. ( Table 3 ). The socio-demographic factors- older age at smoking initiation, higher education, married/living with partners, and pregnancy/becoming parent had positive association with smoking abstinence/quit attempts, while factors related to dependence- level of nicotine dependence, cravings, frequency, and intensity of smoking had negative association. Higher self-efficacy/self-confidence in quitting increased the likelihood, but having pro-smoking attitudes, and susceptibility to smoking reduced the likelihood of smoking abstinence/quit attempts. Among the mental health and psychological factors, good self-management skills had a positive association, and stress level and depression had negative association. Additionally, having good self-perceived general health increased the probabilities of smoking abstinence/quit attempts, while previous history of cigarette use, alcohol or other substance use lowered the likelihood of smoking abstinence/quit attempts. Among the peer and family related factors, parental monitoring, parental or peer support, and parents/family members quitting, friends/peers quitting were positive predictors, and family/household smoking, peer smoking, and social acceptability of smoking were negative predictors. Additionally, increasing tobacco prices, restricting cigarette availability, and ban on cigarette coupons were found to have positive associations with smoking abstinence/quit attempts ( Table 3 ).
Quality assessment findings
The average critical appraisal score of the 11 reviews was 71.4% with a standard deviation of 156%, and 95% confidence interval of 60.6% to 82.1% ( Table 1 ). Seven reviews [ 11 , 13 , 34 – 38 ] had a total critical appraisal score of at least 70%, indicating satisfactory methodological quality, while two [ 13 , 38 ] reviews were considered to have a score of at least 90% ( Table 2 ). Three reviews [ 14 , 33 , 39 ] had a critical appraisal score between 50 and 69% and one review [ 12 ] had a score of less than 50%. None of the reviews assessed the likelihood of publication bias in their review. Thirty percent (n = 3) of the reviews used adequate sources for searching studies and 45% (n = 5) of the reviews had an appropriate search strategy. Seventy-three percent of the reviews had conducted appropriate critical appraisals by two or more reviewers. Approximately 80% to 90% of the reviews had clear and explicit research questions, appropriate inclusion criteria, adequate methods of data extraction and data synthesis. All reviews provided recommendations for policy and/or practice based on their findings and direction for future research (see S1 Table ).
Tables 6 and S2 of the Supporting Information summarizes the findings and evidence profile on individual components of the GRADE-CERQual certainty assessment. Overall, we had moderate confidence on the ‘probable’, ‘possible’, ‘insufficient evidence’, and ‘inconsistent direction’ predictors of smoking abstinence/quit attempts. However, our confidence on the ‘probably unrelated’ factors of smoking abstinence/quit attempts and 4 ‘possible’ predictors of intention to quit smoking were low.
https://doi.org/10.1371/journal.pone.0299728.t006
We identified a total of 138 primary or index publications out of the 11 reviews [ 11 – 14 , 33 – 39 ] (see S3 Table ). We found only 7 primary studies which were included in multiple reviews. The percentage of overlap was 0.05%, CA was 0.10 and CCA value was 0.01. Hence, the degree of overlap between the reviews was slight or minimal.
In this overview, we identified 119 predictors of smoking abstinence/quit attempts among young people of 3 overlapping age groups between 10 and 35 years and categorized them into 5 different groups. Among them, we have moderate confidence in support of all predictors except ‘probably unrelated’ factors (Tables 3 – 5 ). However, we found only 4 ‘possible’ predictors of low confidence for intention to quit smoking. Finding out these predictors is important to plan effective smoking prevention and intervention programs targeting young smokers who have a higher probability of showing future intention to quit. While several studies have already been published on this topic [ 40 , 41 ], we need well-designed comprehensive systematic reviews to summarize these predictors. Additionally, the ‘possible’, ‘insufficient evidence’, and ‘inconsistent direction’ predictors of smoking abstinence/quit attempts ( Table 5 ) should be further investigated by future longitudinal research to determine their direction of effects or statistically significant association with smoking cessation.
Our findings on the ‘probable’ predictors of smoking abstinence/quit attempts have great implications for smoking cessation programs and policies. We found that young people aged ~10–29 years and who had lower level of nicotine dependence and cravings, had a higher chance of quitting smoking ( Table 3 ). Similarly, we also found that high frequency and intensity of smoking act as barriers for smoking abstinence/quit attempts. Hence, ‘cutting down’ on smoking or gradual cessation approach targets lowering level of nicotine dependence and increasing probability of quitting. Although a recent meta-analysis showed that the ‘cold turkey’ or abrupt cessation approach is more effective for achieving long-term abstinence than ‘cutting down’ on smoking [ 42 ], people who find it hard to quit might better engage with the later one [ 43 ]. Our findings showed that stress and depression act as barriers of quitting ( Table 3 ). Previous research also found that smoking cessation lowers stress level and improves depression [ 44 , 45 ]. This feature suggests that integrating smoking cessation with the treatment of mental health conditions might be a beneficial intervention approach for young people [ 46 ]. Similarly, not using alcohol or other substances were seen to increase probability of smoking abstinence/quit attempts ( Table 3 ). These factors should be taken into consideration while modifying personal behaviors to increase the likelihood of quitting and planning smoking cessation interventions for young polysubstance users who face unique challenges while quitting [ 47 , 48 ].
Additionally, we found that higher self-confidence in quitting, good self-management skills, and being less susceptible to smoking increased probabilities of smoking abstinence/quit attempts among ~10–29 years age young people. Self-efficacy/confidence in quitting also came out as a ‘probable’ predictor of ~16–34 years age group. These factors have considerable public health policy implications. Experimental studies have found evidence that programs focusing on building self-confidence and self-control, changing attitude towards smoking, and informing about related health risk of smoking were effective in increasing intention to quit and smoking cessation rate among adolescents [ 49 , 50 ]. Undertaking smoking cessation campaigns and incorporating these measures to minimize pro-smoking attitudes in the society might benefit at the individual, community, and national level. While peer smoking or family or household smoking are established predictors of smoking initiation [ 51 ], our findings show that they also may act as barriers for smoking abstinence/quit attempts ( Table 3 ). Similarly, parental monitoring or support, seeing parents or families or friends quitting, as well as peer support, and low social acceptability of smoking is linked with smoking cessation among young people. This suggests that group therapy-based smoking cessation programs might work better than individual interventions for young smokers who want to quit smoking [ 52 ].
Among the other ‘probable’ predictors, starting smoking at an older age, tobacco price increase, restricting cigarette availability, and ban on cigarette coupons were seen to promote cessation in ~10–29 years age people ( Table 3 ). While the later three factors are already been proven effective and adapted by the policy makers in several countries [ 53 ], making the minimum age to sell tobacco products 21 years instead of 18 might be a possible approach to delay smoking initiation and promote cessation among young people [ 54 ]. Among the socio-demographic predictors, attaining higher education was found to promote smoking abstinence/quit attempts. This finding suggests that having a social determinant of health approach for tobacco control is crucial for removing tobacco-related disparities [ 55 ]. Moreover, people with higher education have higher harm perception of smoking than those with low education [ 56 ]. Health concerns is one of the top reasons for quitting smoking among young people [ 57 , 58 ]; hence, public awareness program is recommended as a broader tobacco control policy [ 59 ]. Although our findings showed that being married/living with partners, pregnancy/becoming parent were positive ‘probable’ predictors, and ‘living with children’ was negative ‘possible’ predictors of smoking abstinence/quit attempts among ~10–29 years age young people, these might be more relevant for people who are older in this age group. Hence, further investigations into this association particularly among young adult population are warranted.
We could only identify 2 ‘probable’ predictors of ~16–34 years age group and no ‘probable’ predictors for ~12–21 years age group ( Table 3 ). One of the reasons behind it was identifying the majority of the predictors by only four reviews which focused on a target population aged ~10 to 29. It also indicates that although our target population was people between age 10 and 35 years, the findings of this overview are more applicable for age 10–29 years. Hence, future reviews should look for predictors of smoking cessation related behaviors among adolescents (10–19 years) and young adults (20–35 years) separately.
Most of the reviews included in our study achieved a satisfactory (≥70%) total critical appraisal score. However, four [ 12 , 14 , 33 , 39 ] out of six reviews, which yielded the highest number of predictors, were found to have total critical appraisal scores less than 70%. Moreover, one [ 12 ] of these four reviews included 51 studies in their review, out of which only 18 were retrievable. They also did not provide any clear direction of association, which in turn considerably lowered our ability to determine the direction of effects for several smoking abstinence/cessation predictors. Hence, future systematic reviews should adhere to the established guidelines (e.g., PRISMA, Cochrane, JBI guideline for systematic reviews) [ 15 , 60 , 61 ] to improve their methodological qualities and increase confidence in their results. Finally, in the context of evidence-based impact of the patient engagement in public health research [ 62 , 63 ], future researchers should consider incorporating patient and public involvement to support quitting smoking among young people.
The findings of this overview should be considered with a few limitations. First of all, we did not have high confidence in our findings ( Table 5 ); hence, the interpretation of these findings should be done with caution. We acknowledge that we considered a wide age group (10–35 years) as the target population. Although we divided this population into three overlapping age groups, still these age groups (i.e., ~10–29 years) encroached on both the adolescent and young adulthood periods. Hence, the readers should keep this fact in mind while interpreting the findings. While we used the term smoking abstinence/quit attempts as one of our outcomes, it does not indicate which predictors increase probability of remaining abstinent and which factors increase probability of relapse. Therefore, future systematic reviews should investigate smoking abstinence and quit attempts separately and identify predictors for each. We excluded non-English literatures, which might lead to missing reviews published in other languages. However, the search periods in the included reviews ranged from 1970 to 2023, capturing studies conducted in different time-periods and locations. Still, conducting another overview looking for reviews published in non-English language might complement our findings. Due to including highly heterogenous reviews of mainly observational studies, we could not conduct a meta-analysis. Moreover, our intention was to summarize the predictors of smoking cessation, rather than evaluating effect sizes or effectiveness of smoking cessation interventions.
Conclusions
The findings of this overview have significant public health and policy implications. We identified a wide variety of ‘probable’ predictors of smoking abstinence/quit attempts among young people aged 10–35 years, which can be used for screening high risk population, improving existing smoking cessation interventions, or planning new targeted interventions programs. In addition, some of our identified predictors can be used for behavioral modification for increasing the likelihood of successful quitting. However, due to wide age range of 10–35 years and lack of high confidence in our findings, the interpretations should be done with caution. We also provided direction for future research by informing researchers about the predictors that need further testing (‘possible’, ‘insufficient evidence’ and ‘inconsistent direction’ predictors of smoking abstinence/quit attempts), the predictors that require further attention (predictors of intention to quit smoking) as well as the age groups that need to be focused.
Supporting information
S1 checklist. prisma 2020 checklist..
https://doi.org/10.1371/journal.pone.0299728.s001
S1 Appendix. Database search strategies.
https://doi.org/10.1371/journal.pone.0299728.s002
S2 Appendix. Summary of predictors of smoking abstinence/quit attempts by different age groups.
https://doi.org/10.1371/journal.pone.0299728.s003
S1 Table. Quality assessment of included reviews using JBI critical appraisal tools for systematic review.
https://doi.org/10.1371/journal.pone.0299728.s004
S2 Table. GRADE-CERQual evidence profile to assess certainty or confidence in the body of evidence.
https://doi.org/10.1371/journal.pone.0299728.s005
S3 Table. Overlapping between reviews (N = 11) and CCA calculation.
https://doi.org/10.1371/journal.pone.0299728.s006
- View Article
- PubMed/NCBI
- Google Scholar
- 5. United States Public Health Service Office of the Surgeon General, National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Smoking Cessation: A Report of the Surgeon General. Washington (DC): US Department of Health and Human Services; 2020. Available: https://www.ncbi.nlm.nih.gov/books/NBK555591/ .
- 54. Institute of Medicine. Public Health Implications of Raising the Minimum Age of Legal Access to Tobacco Products. Washington, DC: National Academies Press (US); 2015 Jul. https://doi.org/10.17226/18997
- Open access
- Published: 19 January 2019
Effectiveness of stop smoking interventions among adults: protocol for an overview of systematic reviews and an updated systematic review
- Mona Hersi ORCID: orcid.org/0000-0003-1784-1167 1 na1 ,
- Gregory Traversy 2 na1 ,
- Brett D. Thombs 3 , 4 ,
- Andrew Beck 1 ,
- Becky Skidmore 1 ,
- Stéphane Groulx 5 , 6 ,
- Eddy Lang 7 , 8 ,
- Donna L. Reynolds 9 , 10 ,
- Brenda Wilson 11 ,
- Steven L. Bernstein 12 ,
- Peter Selby 10 , 13 ,
- Stephanie Johnson-Obaseki 14 , 15 ,
- Douglas Manuel 15 , 16 , 17 , 18 , 19 ,
- Smita Pakhale 15 , 17 , 18 ,
- Justin Presseau 17 , 18 , 20 ,
- Susan Courage 2 ,
- Brian Hutton 1 , 18 ,
- Beverley J. Shea 1 , 18 ,
- Vivian Welch 17 , 18 , 19 ,
- Matt Morrow 21 ,
- Julian Little 18 &
- Adrienne Stevens 1
Systematic Reviews volume 8 , Article number: 28 ( 2019 ) Cite this article
26k Accesses
15 Citations
26 Altmetric
Metrics details
Tobacco smoking is the leading cause of cancer, preventable death, and disability. Smoking cessation can increase life expectancy by nearly a decade if achieved in the third or fourth decades of life. Various stop smoking interventions are available including pharmacotherapies, electronic cigarettes, behavioural support, and alternative therapies. This protocol outlines an evidence review which will evaluate the benefits and harms of stop smoking interventions in adults.
The evidence review will consist of two stages. First, an overview of systematic reviews evaluating the benefits and harms of various stop smoking interventions delivered in or referred from the primary care setting will be conducted. The second stage will involve updating a systematic review on electronic cigarettes identified in the overview; randomized controlled trials will be considered for outcomes relating to benefits while randomized controlled trials, non-randomized controlled trials, and comparative observational studies will be considered for evaluating harms. Search strategies will be developed and peer-reviewed by medical information specialists. The search strategy for the updated review on e-cigarettes will be developed using that of the candidate systematic review. The MEDLINE®, PsycINFO, Embase, and the Cochrane Library electronic databases will be searched as of 2008 for the overview of reviews and from the last search date of the selected review for the updated review. Organizational websites and trial registries will be searched for unpublished or ongoing reviews/studies. Two reviewers will independently screen the title and abstracts of citations using the liberal accelerated method. Full-text screening will be performed independently by two reviewers. Extracted data will be verified by a second reviewer. Disagreements regarding full-text screening and data extraction will be resolved by consensus or third-party adjudication. The methodological quality of systematic reviews, risk of bias of randomized and non-randomized trials, and methodological quality of cohort studies will be evaluated using AMSTAR 2, the Cochrane risk of bias tool, and a modified version of the Scottish Intercollegiate Guidelines Network critical appraisal tool, respectively. The GRADE framework will be used to assess the quality of the evidence for outcomes.
The evidence review will evaluate the benefits and harms of various stop smoking interventions for adults. Findings will be used to inform a national tobacco cessation guideline by the Canadian Task Force on Preventive Health Care.
Systematic review registration
PROSPERO (CRD42018099691, CRD42018099692)
Peer Review reports
Prevalence and burden of tobacco smoking
In 2012, approximately 45,500 deaths (18% of all deaths in Canada) were attributed to tobacco smoking [ 1 ]. Smoking continues to be a leading cause of preventable death and disability [ 2 , 3 ]. Among smoking-related deaths, most were attributable to cancers, cardiovascular disease, and respiratory diseases [ 1 , 4 ].
Worldwide, it is estimated that nearly one in seven adults smoke tobacco daily [ 5 ]. According to the Canadian Community Health Survey (CCHS), five million (16%) Canadians over the age of 12 years in 2017 smoked tobacco [ 6 ]. In Canada, daily or occasional smoking is higher in males (19% versus 13%), particularly among those 20 to 34 years of age (24%) [ 6 ]. Among females, smoking is most prevalent in those 50 to 64 years of age (17%) [ 6 ]. Higher rates of smoking have been shown in people with lower education (<secondary education: 20%; completion of university: 10%) and lower income (lowest household income: 23%; highest household income: 12%) [ 7 , 8 ]. The rate of smoking in Indigenous populations is two to three times the national average, ranging from 34 to 53% across First Nations, Métis, and Inuit populations [ 9 ]. Studies suggest that smoking rates are also higher in people with substance use disorders and mental health issues [ 10 , 11 , 12 ]. Although smoking prevalence has declined overall across Canada, smoking rates vary across the country, with Prince Edward Island reporting the lowest (12%) and Newfoundland and Labrador reporting the highest (20%) rates [ 13 ].
Smoking is the leading cause of cancer with evidence linking it to increased risk of several types of cancers including lung, mouth, upper aerodigestive tract, bladder, cervix, colon, and rectum [ 14 ]. Smoking also increases the risk of non-malignant respiratory diseases (e.g. chronic obstructive pulmonary disease, tuberculosis), cardiovascular disease (e.g. coronary heart disease, stroke, artherosclerosis, aortic aneurysm, peripheral vascular disease), reproductive issues (e.g. infertility, spontaneous abortion, premature birth, low birth weight), neonatal death, sudden infant death syndrome, early menopause, osteoporosis, and many other chronic health conditions [ 15 , 16 , 17 , 18 , 19 ]. Tobacco smoking using a water pipe or hookah is associated with lung and esophageal cancer as well as infectious diseases due to sharing of the pipe [ 20 , 21 , 22 ]. Exposure to second- and third-hand smoke also increases the risk of many diseases including stroke, lung cancer, cervical cancer, respiratory diseases, infections, perinatal and neonatal death, and sudden infant death syndrome [ 16 , 23 , 24 , 25 , 26 ].
Smoking is associated with lower health-related quality of life. Longitudinal data from the Canadian National Population Health Survey found that individuals who smoke tobacco had a lower health-related quality of life compared to those who had never smoked. Smoking cessation was associated with improvement in health-related quality of life. In women, health-related quality of life was similar to those who had never smoked tobacco after 10 years of cessation. In men, it took 20 years of cessation to achieve a health-related quality of life equivalent to those who had never smoked tobacco [ 27 ].
In 2012, the total cost of tobacco use in Canada was estimated at $16 billion CDN [ 1 ]. This estimate includes both direct (i.e. hospital expenditure, physician care, medications) and indirect (i.e. economic loss associated with premature death and disability) costs which were approximately $6.5 billion and $9.5 billion, respectively [ 1 ].
Smoking cessation, defined as quitting or the discontinuation of tobacco smoking, reduces the risk of smoking-related diseases and premature death [ 3 , 28 , 29 ]. Quitting at 30 years of age increases life expectancy by a decade while quitting at 40 and 50 years of age increases expectancy by 9 and 6 years, respectively [ 30 ]. For every two individuals who quit smoking tobacco, one will avoid a tobacco-related death [ 31 ]. According to the 2017 Canadian Tobacco, Alcohol and Drugs Survey, about 63% of Canadians who reported smoking at some point in their life have successfully quit smoking [ 13 ]. Among the 44% of respondents who made an attempt to quit in the past year, 16% made a single attempt while 12% attempted four or more times [ 13 ]. In 2017, reducing smoking consumption was the most common cessation method (approximately 63%) among survey respondents, followed by the use of pharmacotherapies (approximately 55%) [ 13 ]. Approximately 32% of those who attempted to quit tobacco smoking in 2017 used electronic cigarettes (e-cigarette) as a cessation method [ 13 ].
Stop smoking interventions
Approved pharmacotherapies.
Nicotine replacement therapy (NRT) and cytisine are available over-the-counter while varenicline and bupropion are available by prescription [ 32 ]. NRT is the most widely used pharmacotherapy for smoking cessation available over the counter. NRT products administer nicotine thereby reducing withdrawal symptoms and cigarette cravings [ 33 ]. It is available in various forms (e.g. patches, chewing gum, lozenges, tablets, buccal spray, and inhalers) and nicotine dosages [ 34 ]. Cytisine is a naturally occurring nicotine partial agonist found in the laburnum plant and is pharmacologically similar to varenicline [ 35 ]. It is approved as a natural remedy for smoking cessation in Canada [ 36 ].
Varenicline and bupropion do not contain nicotine. Varenicline is a nicotine receptor partial agonist that triggers the release of dopamine thereby reducing nicotine withdrawal symptoms and relieving cravings [ 37 ]. Varenicline also prevents the stimulating effects of nicotine [ 38 ]. Bupropion, the only antidepressant medication approved for smoking cessation [ 39 ], is a non-competitive antagonist of nicotinic acetylcholine receptors [ 40 ] and also inhibits uptake of dopamine, serotonin, and noradrenaline [ 41 ]. Although the mechanism of action is unclear, bupropion may promote cessation by reducing nicotine withdrawal symptoms via inhibition of dopamine and noradrenaline reuptake [ 42 ].
Electronic cigarettes
Electronic cigarettes, also known as e-cigarettes, electronic nicotine (or non-nicotine) delivery systems, or vaporizers, represent another potential intervention strategy by which individuals employ behaviour substitution in their efforts to quit smoking. Most e-cigarettes are battery-operated and are used to inhale a vapour that can contain nicotine and other chemicals such as flavourings, propylene glycol, and/or vegetable glycerin [ 43 , 44 ]. A heating element within the device releases liquid that is vaporized into a fog or smoke-like cloud [ 43 ]. These devices can provide similar behavioural and sensory cues of smoking with no or lower levels of nicotine [ 44 ]. There is some evidence to suggest that e-cigarettes significantly reduce exposure to other toxic compounds found in combusted cigarette smoke such as carbon monoxide, acrolein, acetaldehyde, and formaldehyde [ 45 , 46 ]. However, other studies have found that some e-cigarette brands contain high levels of toxic metals including nickel, cadmium, chromium, lead, and manganese [ 47 ]. The recently passed Canadian Tobacco and Vaping Products Act (Bill S-5) now allows adults to legally purchase e-cigarettes containing nicotine in Canada. However, it bans the sale of e-cigarettes to individuals under 18 years of age, specific flavours that are appealing to youth (e.g. confectionary, soft drink), ingredients that suggest health benefits (e.g. vitamin, caffeine), and certain types of advertising and promotion (e.g. health benefits, products using tobacco brands) [ 48 ].
Behavioural therapies
There are various behavioural interventions used for tobacco cessation. Broadly, behavioural interventions may promote smoking cessation directly, be directed to improve adherence to smoking cessation pharmacotherapies, or promote other health behaviour change along with the stopping smoking behaviour (e.g. healthy eating, alcohol reduction).
Behavioural interventions can be classified by intensity (very brief, brief, intensive), frequency of contact, modality of contact, type of provider, and content. These factors can influence the effectiveness of the intervention. Details on the specific behavioural change technique(s) (i.e. the content or “the smallest active ingredients of interventions capable of inducing change in behaviour” [ 49 ]) that are being targeted are essential in determining not only what components of behaviour support systems are effective, but how they can be replicated in practice [ 49 ]. A taxonomy of behavioural change techniques used in individual behavioural support for smoking cessation has been developed to support such evaluations [ 50 ]. Examples of behavioural change techniques include goal setting (e.g. setting a quit date), advice on altering routines to avoid exposure to smoking cues, and providing information regarding withdrawal symptoms [ 50 ].
Another aspect of behavioural change interventions is understanding the psychological theory underpinning the design of the intervention. For example, the Transtheoretical Model of Change, also known as the ‘Stages of Change’ model, is highly used in the smoking cessation literature, but not supported empirically in systematic review evaluations [ 51 , 52 ]. Although these theories may have face validity, evaluating them is important not only to understand effectiveness but also to avoid harms. Evidence suggests that stage-based approaches for smoking cessation are not more effective than non-stage interventions indicating that readiness or motivation to stop smoking may not be integral for quitting [ 51 , 52 ]. Further, stage-based interventions might prevent providers from offering effective treatment to those deemed unmotivated to stop smoking thereby prolonging their exposure to the toxic constituents of smoke.
Brief advice interventions consist of healthcare professionals providing verbal instructions with a “stop smoking message” [ 53 ]. These interventions may vary in intensity, frequency, and duration but generally only last a few minutes. Individual or group therapies are led by counsellors such as physicians, nurses, clinical psychologists, and counsellors. The objective of such interventions is to provide an opportunity for people who smoke to share cessation experiences; derive support; learn coping skills to manage cravings, lapses, and relapses; and promote self-control [ 54 ]. More intensive face-to-face interventions require greater effort and resources and may only reach a small segment of the smoking population [ 55 ]. Telephone counselling can supplement or replace these therapies as a way of providing services to a larger number of people [ 56 ]. These can take the form of proactive (i.e. counsellor-initiated) or reactive counselling (i.e. tobacco smoker-initiated) [ 57 ].
Self-help interventions are information aids, such as manuals or programmes, used by individuals without the direct support of healthcare professionals [ 55 ]. The goal is to provide some of the benefits of brief advice and counselling but without the necessary attendance. Traditional self-help materials, such as print, audio, and video recordings, can be more widely accessible and are increasing their reach via newer technology (e.g. web-based, mobile applications and games, streaming content) [ 58 ]. However, increased reach may not necessarily be more effective if the content of the instruction is not effective.
Some therapies, such as exercise-based interventions, have been used alone or as adjuncts to other interventions. Exercise alleviates withdrawal symptoms and relieves cravings [ 59 ]. Although the mechanism of action is unclear, several hypotheses have been proposed [ 59 , 60 ]. The biological hypothesis suggests that exercise and nicotine have similar impacts on beta-endorphins, cortisol, noradrenaline, and adrenaline [ 59 , 60 ]. For example, like nicotine, exercise stimulates the release of adrenaline and noradrenaline thereby relieving cravings [ 59 ]. Although the evidence is inconsistent, the beneficial effect of exercise on cessation may also be attributed to increases in positive affect or distraction from withdrawal symptoms and cravings [ 59 , 60 ].
Alternative therapies
Alternative therapies for smoking cessation include hypnosis, acupuncture (including acupressure and electrostimulation), and laser therapy [ 59 , 61 ]. It is hypothesized that acupuncture, acupressure, and laser therapy alleviate withdrawal symptoms by stimulating peripheral nerves which triggers release of opioid peptides, dopamine, enkephalin, and serotonin [ 62 ]. The mechanism of action underpinning the effect of hypnotherapy on smoking cessation is related to strengthening impulse control [ 63 ]. St. John’s Wort is a herbal product commonly used by patients as an alternative to standard antidepressant medications [ 64 ]. St. John’s Wort may promote smoking cessation by alleviating tobacco withdrawal symptoms and decreasing negative affect through various mechanisms including inhibition of monoamine oxidase A and B and dopamine and noradrenaline reuptake [ 39 , 65 ]. S-Adenosylmethionine (SAMe), a natural health product, promotes the production of dopamine and norepinephrine and may therefore alleviate tobacco withdrawal symptoms [ 66 ].
Current clinical practice and recommendations
Canadian guidelines.
In 2011, the Canadian Action Network for the Advancement, Dissemination and Adoption of Practice-informed Tobacco Treatment (CAN-ADAPTT) published recommendations for adults and specific populations (e.g. Indigenous, hospital-based, mental health, substance use disorders, pregnant and breastfeeding women, and youth) that were informed by six guidelines [ 67 ]. CAN-ADAPTT recommends that healthcare providers routinely ask patients about their tobacco use and advise those who smoke tobacco to quit. Those willing to begin treatment should be offered assistance such as brief advice, individual and group counselling (focused on problem-solving skills or skills training and providing support), self-help materials, motivational interviewing, or pharmacotherapies. Where possible, CAN-ADAPTT recommends combining counselling and pharmacotherapies as the preferred approach. Providers are encouraged to follow-up regularly and modify treatment as needed.
The Registered Nurses’ Association of Ontario (2017) released recommendations based on previous guidelines and a systematic review [ 68 ]. They recommend using brief interventions to screen individuals for tobacco use, developing person-centered tobacco intervention plans, referring tobacco users to intensive interventions and counselling on the use of pharmacotherapies (i.e. NRT, varenicline, bupropion), and evaluating the effectiveness of these interventions and adjusting as needed. They conclude that there is insufficient evidence regarding e-cigarettes, hypnotherapy, laser therapy, electrostimulation, acupressure, and acupuncture as cessation tools. For pregnant or postpartum women, they recommended intensive behavioural counselling, in conjunction with NRT.
Guidelines from international organizations
Guidelines from international organizations are consistent in recommending behavioural interventions and/or pharmacotherapies (i.e. NRT, bupropion, and varenicline) for smoking cessation. The UK National Institute for Health and Care Excellence (NICE, 2018) recommends individual or group behavioural support, very brief advice, bupropion, combination of short- and long-acting NRT, or varenicline in conjunction with behavioural support [ 69 ]. New Zealand’s Ministry of Health (2014) recommends brief advice (approximately 30 s), behavioural support, NRT, buproprion, varenicline, and nortriptyline. They consider a combination of behavioural and pharmacotherapy to be the most effective [ 70 ]. As part of their “Risk estimation and the prevention of cardiovascular disease” guideline, the Scottish Intercollegiate Guidelines Network (2017) recommends (1) varenicline or combination NRT (i.e. “interventions involving more than one type of nicotine replacement delivery”) alone or as part of a smoking cessation programme, and (2) bupropion and single NRT [ 71 ]. The US Preventive Services Task Force is currently updating their 2015 guideline [ 17 ]. The 2015 guideline, based on an overview of reviews [ 72 ], recommends behavioural interventions and approved pharmacotherapies (i.e. bupropion, varenicline, NRT). Only behavioural interventions are recommended for pregnant women as the evidence regarding pharmacotherapies was insufficient for this subgroup.
We did not identify any guideline that recommends the use of e-cigarettes for smoking cessation. However, NICE recommends that, when advising those interested in using e-cigarettes containing nicotine, primary health care providers should communicate that “many people have found them helpful to quit smoking cigarettes” and that e-cigarettes, while not without risk, are less harmful than tobacco smoking [ 69 ]. Similarly, Public Health England’s recently developed guidance for clinicians includes e-cigarettes as a smoking cessation option to discuss with patients. The guidance indicates that e-cigarettes present less risk than smoking and that they may be as or more effective than nicotine replacement therapy [ 73 ]. Other organizations state that there is currently insufficient evidence regarding the beneficial effects of e-cigarettes to make recommendations [ 17 , 71 ].
A majority of the available guidelines are out of date (i.e. last database search range: 2008 to 2015). Although recent, the NICE guideline excludes several smoking cessation interventions including varenicline, exercise, and alternative therapies (e.g. acupuncture, hypnotherapy) [ 69 ]. Limitations in existing clinical practice guidelines necessitate the development of a Canadian guideline on tobacco cessation strategies for adults.
Objective and key questions
The goal of this evidence review is to determine the effectiveness of stop smoking strategies for adults. Pharmacotherapy, behaviour change interventions, electronic cigarettes, exercise interventions, and complementary and alternative medicine interventions will be considered. Adult populations will include subgroups of interest such as those with co-morbid conditions, pregnant women, various demographic factors, and the distinction of opportunistic and treatment-seeking individuals. This synthesis will be used by the Canadian Task Force on Preventive Health Care (Task Force) to inform their development of a clinical practice guideline on stop smoking interventions.
The evidence review will consist of two stages. First, the overview of stop smoking interventions will be conducted. An overview of systematic reviews approach was selected to compile the evidence base in light of the large volume of primary and synthesized evidence that exists. The second stage will involve updating the most recent, comprehensive, and high-quality systematic review on e-cigarettes identified in the overview of reviews. Only the e-cigarettes strategy will be updated because of the increasing use of this strategy and its quickly evolving evidence base. This protocol document serves to outline the methodology for both review types.
For the purpose of the evidence review, tobacco smoking will refer to any form of smoked tobacco (e.g. cigarettes, pipes, cigars, cigarillos, via water pipe or hookah). This will not include tobacco use for traditional or ceremonial purposes such as that used by Indigenous people in sacred rituals and prayers for healing and purification [ 74 , 75 ].
Stage 1: Overview of systematic reviews of stop smoking interventions
The overview will evaluate the benefits and harms of stop smoking interventions among adults. If feasible, the overview will also evaluate the benefits and harms of behavioural change techniques (i.e. “the smallest active ingredients of interventions capable of inducing change in behaviour” [ 49 ]). Figure 1 illustrates the framework of the overview of systematic reviews. The overview will address the following key questions:
Key question 1a ( KQ1a ). What are the benefits and harms of interventions to promote cessation of tobacco smoking among adults?
Key question 1b ( KQ1b ). What is the comparative effectiveness (benefits and harms) of interventions to promote cessation of tobacco smoking among adults?
Key question 1c ( KQ1c ). What are the benefits and harms of behavioural change techniques or clusters of techniques to promote cessation of tobacco smoking among adults?
Stage 2: Updated systematic review on e-cigarette use for smoking cessation
This update will evaluate the benefit and harms of e-cigarettes to promote cessation of tobacco smoking among adults. This protocol outlines key questions and eligibility criteria for the updated review. However, should the candidate review from which to update have slightly different parameters, we will transparently declare any necessary changes from the protocol in the final report.
Key question 2a ( KQ2a ). What are the benefits and harms of electronic cigarettes for tobacco smoking cessation in adults?
Key question 2b ( KQ2b ). What is the comparative effectiveness (benefits and harms) of electronic cigarettes for tobacco smoking cessation in adults?
Analytic framework for the overview of reviews. *Practitioner advice (of varying length/intensity, and by various provider types); Intensive individual counselling (of varying length, of varying number of sessions, and by various provider types); Intensive group counselling (of varying length, of varying number of sessions, and by various provider types); Self-help interventions (print-based or web-/computer-based); Internet or computer-based interventions with counselling/support; Telephone-based interventions (e.g., mobile phone-based, quit lines/help lines) with counselling/support; Nicotine receptor partial agonists (varenicline and cytisine); Bupropion; Nicotine replacement therapy (e.g., patch, gum, lozenge, mist, inhaler); Ecigarettes; Exercise interventions; ‘Alternative’ therapies (e.g., acupuncture, acupressure, electrostimulation, hypnosis, St. John’s Wort, S-adenosylmethionine); Combinations of interventions. **Practitioner advice (of varying length/intensity, and by various provider types); Intensive individual counselling (of varying length, of varying number of sessions, and by various provider types); Intensive group counselling (of varying length, of varying number of sessions, and by various provider types); Self-help interventions (print-based or web-/computer-based); Internet or computer-based interventions with counselling/support; Telephone-based interventions (e.g., mobile phone-based, quit lines/help lines) with counselling/support; Other behaviour change interventions evaluated on a case-by-case basis with the Working Group
The evidence review will be completed by the Evidence Review and Synthesis Centre (ERSC) at the Ottawa Hospital Research Institute. A working group (WG) of Task Force members and external content experts was formed for development of the topic, refinement of the key questions and scope, and rating of outcomes. Outcomes were rated on a scale of 1 to 9 according to the Grading of Recommendations Assessment, Development and Evaluation (GRADE) methodology; those rated as critical (mean score 7 to 9) and important (mean score 4 to 6) for decision-making were selected. Patients identified through patient engagement activities conducted by the St. Michael’s Hospital Knowledge Translation Program have also rated the outcomes. The process of incorporating patient priorities is described in the CTFPHC’s Patient Engagement Protocol ( https://canadiantaskforce.ca/methods/patient-preferences-protocol/ ).
Reporting of this protocol was guided by the PRISMA Statement for Protocols (PRISMA-P) to the extent possible and where appropriate [ 76 ] (Additional file 1 ). The protocol is registered in PROSPERO ( https://www.crd.york.ac.uk/PROSPERO/ ) (CRD42018099691, CRD42018099692). The final overview will be reported using the Preferred Reporting Items for Overviews of systematic reviews including harms pilot checklist (PRIO-harms) [ 77 ], and the updated systematic review will be reported using PRISMA [ 78 ].
A team of clinical and content experts will be consulted at key points during the conduct of the evidence review. Amendments to this protocol will be noted in the final report.
Guidelines for the conduct of overviews of reviews are currently lacking [ 79 ]. Given this current gap, the methodology for this overview will be guided by the Cochrane Handbook of Systematic Reviews of Interventions ( Chapter 22 ) [ 80 ] as well as other available reports on overview methodology [ 79 , 81 , 82 , 83 , 84 , 85 ].
Literature search
The search strategy will be developed and tested through an iterative process by an experienced medical information specialist in consultation with the review team. We will search Ovid MEDLINE®, Ovid MEDLINE® Epub Ahead of Print, In-Process & Other Non-Indexed Citations, PsycINFO, Embase Classic + Embase, and the Cochrane Library on Wiley. Databases will be searched from 2008 to the current date. The draft search strategy can be found in Additional file 2 . The search strategy will be peer-reviewed using the PRESS 2015 guideline [ 86 ]. Results of the PRESS reviews will be provided in an appendix in the final report.
We will search for unpublished literature and reports of ongoing and completed reports using the Canadian Agency for Drugs and Technologies in Health (CADTH) Grey Matters checklist [ 87 ] and through searches of the following websites: CADTH, Ontario Tobacco Research Unit, The Canadian Partnership Against Cancer (cancerview.ca), SurgeonGeneral.gov , Philip Morris, Foundation for a Smoke-free World, Public Health England, Tobacco.org , Truth Initiative, Physicians for a Smoke-Free Canada, Centers for Disease Control and Prevention Smoking and Health Resource Library, Canadian Cancer Society, American Cancer Society, American Thoracic Society, US National Cancer Institute, US National Comprehensive Cancer Network, National Institute for Health and Care Excellence, World Health Organization Framework Convention on Tobacco Control, World Health Organization’s International Clinical Trials Registry Platform, OpenTrials.net , International Prevention Research Institute, North American Quitline Consortium website, and the Ottawa Heart Institute’s Ottawa Model for Smoking Cessation. We will also scan the bibliographies of relevant reviews and other identified overviews for grey literature and references not identified in our database search. Grey literature searching will be restricted to English and French language documents and will be limited to what can be completed within 1 week by one reviewer.
Eligibility criteria
KQ1a and KQ1b will examine interventions that can be delivered or referred to in the primary care setting. This includes certain behavioural change interventions, pharmacotherapies, e-cigarettes, exercise interventions, and alternative therapies (Table 1 ). Interventions that cannot be delivered or referred to by a wide variety of primary care practitioners (e.g. quit-to-win contests, biomedical risk assessment, aversive smoking, incentivized cessation) as well as specific behavioural counselling techniques (e.g. motivational interviewing, stage of change-based counselling) which require specialized training that has been shown to vary [ 88 ] and may not be readily available to all primary care practitioners will be excluded. We will also exclude reviews on broader public health interventions (e.g. mass media, taxation, packaging restrictions) as well as those on broad lifestyle interventions not specific to tobacco smoking behaviour and that do not attempt to isolate for the effect of our included interventions (i.e. when delivered as part of a multifaceted lifestyle intervention). Generally, pharmacotherapies that are not approved by Health Canada as smoking cessation aids (e.g. clonidine, lobeline, anxiolytics, nortriptyline, opioid antagonists, silver acetate, rimonabant) or not available in Canada (e.g. Nicobrevin, Nicobloc, nicotine vaccines, mecamylamine) will be excluded. However, due to their ease of access, an exception will be made for St. John’s Wort (sold in various forms in pharmacies and health stores across Canada), cytisine, and S-adenosylmethionine (SAMe) (licensed natural health products).
Systematic reviews for KQ1a and KQ1b will be selected for inclusion according to the eligibility criteria outlined in Table 1 [ 89 , 90 ].
In addition to the other interventions listed in Table 1 , the intent of KQ1a/b is to capture reviews which examine behavioural change interventions (e.g. practitioner advice, counselling, self-help interventions). These reviews may provide information on the active components of these interventions, referred to as behavioural change techniques . Examples of such techniques include providing information on consequences of smoking, explaining the importance of abrupt cessation, strengthening ex-smoker identity, and receiving prompt commitment from the patient [ 50 ]. If there is sufficient data, subgroup analysis by behavioural change technique or clusters of techniques will be performed for KQ1a/b (see the “ Subgroup analysis ” section).
While the intent of KQ1a/b is to synthesize reviews of behavioural change intervention s (these reviews may or may not report the behavioural change techniques used as part of these interventions), the intent of KQ1c is to capture reviews which specifically examine the effectiveness of behavioural change techniques or cluster of techniques. A taxonomy of behavioural change techniques used in smoking cessation interventions will guide the coding of techniques encountered in the literature [ 50 ].
Eligibility of reviews for KQ1c will be evaluated in consultation with the WG on a case-by-case basis with selection for inclusion dependent on applicability to the primary care setting. For example, the WG may decide to include behavioural change interventions outside of those listed in Table 2 or may decide to include reviews in specialty settings if the review examines behavioural change techniques that can reasonably be applied in primary care. Selection of reviews for KQ1c will be guided by the eligibility criteria outlined in Table 2 . All decisions regarding the selection of reviews will be reported in the completed review.
Study selection
Duplicates will be identified and removed using Reference Manager [ 91 ]. Title and abstract and full-text screening will be conducted using an online systematic review managing software, Distiller Systematic Review (DistillerSR) Software© [ 92 ]. Two reviewers will independently screen the title and abstracts of citations using the liberal accelerated method (i.e. a second reviewer verifies records excluded by a first reviewer). References will be randomized, and screening will be done concurrently to ensure that each reviewer cannot determine whether a given reference was excluded by another reviewer. The full text of potentially relevant citations will be retrieved, and two reviewers will independently assess the article for relevancy. If unclear whether a review is eligible after duplicate review, a third person will be consulted before excluding the review. Conflicts will be resolved by consensus or by consulting with a third team member. The reasons for exclusion at full-text screening will be documented.
Both screening forms will be piloted by reviewers prior to commencement of screening, with adjustments made, as needed, to maximize efficiency. If necessary, articles will be ordered via interlibrary loan. Only those received within 30 days will be included. Exclusions due to unavailability of articles will be noted.
A list of potentially relevant reviews available only in abstract form will be made available, but these studies will not be included in the overview.
Data mapping and overlap detection
Given the proliferation of systematic reviews [ 81 ], we anticipate that we will encounter multiple systematic reviews covering the same research question (i.e. population, intervention, comparison, outcomes, time points, and settings). Such reviews are expected to rely on the same evidence base (i.e. same studies and data); therefore, inclusion of these overlapping systematic reviews may potentially bias the overview findings as the same primary studies are counted more than once [ 93 ].
While there is currently no optimal approach for addressing the issue of overlapping reviews [ 79 ], existing options include the following: (1) limiting inclusion to a single systematic review using a priori established criteria or (2) including all available reviews and computing the degree of overlap [ 79 , 81 , 93 ]. Limiting inclusion to a single systematic review for a given research question may result in missing data, and while inclusion of all available reviews may improve comprehensiveness, it also increases workload and complexity [ 81 ].
To detect and address overlapping systematic reviews, we will first map the research questions (i.e. population, intervention, comparator, outcomes, time points, setting) and characteristics (i.e. date of last search, comprehensiveness, and quality) of all eligible systematic reviews. Where there are multiple reviews addressing the same research question, we will compare the review characteristics and exclude those which are “superseded by a later review, or (contain) no additional (studies) compared with a review of similar, or higher, methodological quality” [ 79 , 94 ]. For example, an up-to-date, high-quality systematic review may report on a single intervention (e.g. acupuncture) while another review, of lower methodological quality and with an older search date, may report on a number of alternative therapies including acupuncture. Although superseded by the former in terms of quality and recency, the latter review captures evidence on additional interventions. Inclusion of both reviews would be necessary to capture all available information on alternative therapies for smoking cessation. In this particular example, we would rely on the former review for data on acupuncture and on the latter for all other interventions (i.e. excluding acupuncture). As described by Pollock et al., the decision to exclude reviews based on these criteria can be a complex process often due to slight differences in research questions [ 94 ]. The criteria above will be used as a guide; with the pool of candidate reviews in hand, information will be mapped to facilitate decisions about potential exclusion. Decisions to exclude reviews due to redundancy will be tracked and documented in a table of characteristics of excluded reviews.
In cases where overlapping data cannot be avoided (i.e. overlapping reviews with similar search dates, quality, and comprehensiveness), we will include overlapping reviews and calculate the degree of overlap using the corrected covered area (CCA) [ 83 , 93 ]. Although reporting the degree of overlap is recommended, it does not minimize or omit potential bias caused by inclusion of overlapping reviews [ 83 , 93 ]. The CCA is calculated using the formula below, where N is the total number of studies across reviews (including multiple occurrences of the same study), r is the number of unique (first occurrence) studies, and c is the number of reviews.
The benefit of the correction for primary studies is that it diminishes the impact of large reviews that may add area but not necessarily overlap. Hence, the CCA corrects for the first time that studies are counted. The higher the CCA value, the greater the overlap among reviews: CCA value 0–5 would represent slight overlap, 6–10 of moderate overlap, 11–15 of high overlap, and > 15 of very high overlap.
Mapping of review characteristics will be conducted by a single reviewer. The decision to exclude a review, using the criteria described above, will be made by two reviewers via discussion, with review by the guideline WG. Where overlapping reviews are included, concordance of results/conclusions will be explored (see the “ Discordance ” section of the manuscript).
Quality assessment of systematic reviews
The methodological quality of reviews will be evaluated according to the AMSTAR 2 instrument (Additional file 3 ). This updated version of the original AMSTAR tool allows for the appraisal of systematic reviews of randomized and non-randomized studies of interventions [ 95 ]. We will evaluate each review against the 16-item instrument. An overall rating of quality will be assigned according to the algorithm suggested by Shea et al. [ 95 ]. Reviews failing to meet any of the seven critical AMSTAR 2 items will be deemed to have a “critical flaw” while non-fulfillment of the remaining items will be deemed a “non-critical weakness” of the review (Additional file 4 ). Reviews with one or more critical flaws will receive a low or critically low rating, respectively. Reviews with no critical flaws will be considered either high or moderate quality depending on the number of non-critical weaknesses (i.e. high-quality reviews have a maximum of one non-critical weaknesses and moderate-quality reviews have more than one weakness). Aside from decisions on inclusion related to assessing duplicate or overlapping reviews, reviews will not need to meet a particular threshold for methodological quality to be included.
The quality of systematic reviews will be evaluated by one reviewer and verified by another. Disagreements regarding by-item and overall rating of quality will be resolved by consensus or third-party adjudication if consensus cannot be reached.
Data extraction and management
Data extraction forms will be developed a priori in DistillerSR and pilot tested on a sample of studies to adjust forms, where needed, to maximize efficiency. Full data abstraction will be completed by one reviewer and verified by a second reviewer. Disagreements will be resolved by consensus or third party adjudication if consensus cannot be reached.
Additional file 5 lists draft items to be collected from reviews during data extraction. We will extract data as synthesized and/or reported in the reviews. We will not consult primary studies for the purpose of data extraction, risk of bias assessment, or for verifying the accuracy of the data reported in the systematic reviews.
We will collect data regarding outcomes of interest as reported by review authors. For reviews reporting a meta-analysis, we will collect the pooled effect estimates, corresponding confidence intervals, and results of statistical tests for heterogeneity (e.g. number of studies, number of participants, chi-square, Cochrane Q, corresponding p values, I 2 ).
For network meta-analyses, ideally sufficient evidence from direct comparisons will be available, and treatment effect estimates along with measures of uncertainty from those analyses will be extracted. However, where little to no evidence from direct comparisons is available and indirect comparison data exist, we will extract both analyses and determine extent of consistency of results and make appropriate interpretations. For indirect comparison analyses, effect estimates and corresponding credible intervals will be collected from indirect comparisons. We will extract and transparently describe if and how authors’ ranking of treatments was used, ensuring appropriateness; ranking may take the form of rank probabilities, mean/median rank, surface under the cumulative ranking (SUCRA) curve, or a P-score [ 96 , 97 , 98 ].
For outcomes where a pooled analysis was not performed, how data are extracted will be informed by authors’ reporting. For example, if effect estimates from primary studies are reported, then a range of those effects could be extracted. In the absence of optimal quantitative data, a narrative summary of findings will be extracted from the reviews. Data will be collected for all reported and relevant (see Table 1 ) time points of follow-up.
Where reviews partially overlap with the scope of interest, such that a subset of studies may be conducted in a different population (e.g. adolescents), setting (not relevant to primary care), or other relevant parameter, we will attempt to determine whether the analyses undertaken are sufficiently direct to the overview question by considering the relative contribution of those studies to the analysis, subject to adequate reporting of this information. How these analyses are handled (inclusion versus exclusion) will be reviewed with the WG for their input; those decisions and any accompanying uncertainty in the applicability of the included results will be detailed in the report.
Subgroup analysis
The overview will seek information on various factors that would typically be considered variables for effect modification. In the case of an overview, we expect to encounter reviews that have undertaken subgroup or meta-regression analyses. There may also be reviews through the process of defining scope that would have focused their interest according to a particular factor, such as evaluating the effects of an intervention in a particular setting. Reviews addressing both of these approaches will be included. Variables of interest listed below are those that we have considered as being potentially important effect modifiers that would influence the development of guideline recommendations or implementation considerations. According to guidance, we have restricted subgroup analysis to characteristics that are measured at baseline rather than after randomization [ 99 ].
Populations
Fewer versus more quit attempts (specific groupings will depend on what is found in the literature)
Opportunistic versus individuals seeking treatment
Baseline level of nicotine dependence (e.g. using a validated scale or cigarettes per day as a proxy)
By demographic factors (age, SES, sex, ethnicity, LGBTQ+)
By comorbid conditions (e.g. mental illness, HIV infection, cardiovascular disease, COPD, obesity, substance use disorder)
By pregnancy status
Intervention-related variables
Dose, type, duration, number of sessions
Specific forms of an intervention (e.g. yoga as a form of exercise)
KQ1a/b: behavioural change technique (e.g. providing information on consequences of smoking, explaining the importance of abrupt cessation, receiving prompt commitment from the patient)
Family medicine clinics
Walk-in clinics
Smoking cessation clinics
Urgent care facilities
Emergency departments
Public health units
Dental offices
Behavioural health/substance use treatment facilities (ambulatory or outpatient)
Academic research settings
Other variables
By industry funding status (subgroup and/or sensitivity analyses performed in eligible reviews will be sought)
Evidence synthesis
While there are both simple (e.g. comparing 95% confidence intervals, statistical test of summary estimates) and complex (e.g. Bucher method, network meta-analysis) methods available for indirect comparisons of treatments across reviews, all approaches are based on the assumption that the primary studies are similar [ 85 , 100 ]. This would require overview authors to be familiar with the primary study literature and not to rely solely on review authors’ reporting of the primary studies [ 85 ]. Given that we will not have opportunity to read and become familiar with the primary study reports themselves, conducting network meta-analyses or informal indirect comparisons of interventions will not be performed. As noted above, any existing network meta-analyses located in the literature will be included and commented on.
Similarly, subgroup analyses within reviews will provide evidence for effect modification. For factors that comprise the focused scope of a given review, as described in the previous section, we will provide the appropriate statements relating to interpretation but be unable to perform comparisons across reviews in the absence of the direct familiarity with the primary studies. Where possible, we will evaluate the credibility of subgroup analyses [ 99 , 101 , 102 ].
Although a narrative synthesis of available evidence to ensure appropriate interpretation will be provided for readers, the use of GRADE tables will facilitate appropriate presentation of this information in tabular form to avoid juxtaposition that may lend to inappropriate comparisons on the part of the reader [ 83 , 85 , 103 ]. Comparisons across reviews with similar scope will be limited to an assessment of the extent of concordance or discordance of the review results and, for discordance, an exploration of a potential explanation.
Discordance
Reviews that overlap in terms of scope may present discordant results and/or conclusions due to variation in eligibility criteria, data extraction, risk of bias assessment, data synthesis approach, or interpretation of the results [ 104 ]. In those instances, we will investigate the source(s) of discordance using the algorithm developed by Jadad et al. as a guide [ 104 , 105 ].
Where overlapping reviews of similar quality rely on the exact same studies, we will investigate whether discordance was due to differences in data extraction (e.g. reviews may have extracted data at different time points of follow-up or reviews may vary regarding definitions of outcomes or outcome measurement methods), heterogeneity testing (e.g. reviews differ in their investigation of clinical and methodological heterogeneity and the decision in which to conduct a meta-analysis), or the synthesis approach (e.g. quantitative versus qualitative synthesis or in the statistical methods used).
If overlapping reviews do not rely on the exact same studies, we will investigate differences in the eligibility criteria. If similar, we will evaluate whether discordance is attributable to differences in the search strategies (e.g. number and type of databases searched, whether grey literature was searched) or in the application of the eligibility criteria. If reviews use different eligibility criteria, Jadad et al. [ 105 ] recommend comparing the publication status of primary studies (e.g. whether there are differences in the inclusion of unpublished reports), evaluation of the methodological quality of primary studies (e.g. differences across reviews regarding the assessment of quality of primary studies and how quality was used in interpreting the results of the review), language restrictions, and quantitative synthesis [ 105 ].
In addition to exploring sources of discordance, we will categorize discordance as follows: (1) direction of effect (i.e. reviews report results in opposite directions), (2) magnitude of effect (i.e. reviews report results in the same direction but differ in the size of the effect estimate), and (3) statistical significance (i.e. statistical significance reached in one review but not others) [ 105 ].
Quality of the body of evidence
The Task Force endorses the use of GRADE methodology for assessing the quality of the body of evidence for critical and important outcomes [ 106 ]. Currently, there are no methods to evaluate the strength of evidence across systematic reviews [ 83 ]. For each outcome of interest reported in each individual review, we will provide GRADE assessments by intervention/comparison [ 107 ]. We will not evaluate the strength of the evidence across reviews.
For reviews that have used GRADE methods, we will provide results for the overall quality of evidence, including reasons for downgrading. If available, we will also report the ratings for each of the five domains of GRADE (i.e. risk of bias, imprecision, indirectness, inconsistency, publication bias). We will not consult primary studies as a quality control measure.
If GRADE methods were not used in a given review, we will attempt to conduct GRADE assessments using information available in the review (e.g. risk of bias assessments). This will likely be challenging due to reporting issues; therefore, we will provide our best interpretation based on the available information and note any limitations. For systematic reviews that include a network meta-analysis, using information reported in the review, we will evaluate the quality of evidence using the GRADE extension for network meta-analysis [ 108 ]. As above, we will not consult primary studies for the purpose of conducting GRADE assessments. We will make note if it is not possible to conduct GRADE for a given review or outcome.
Stage 2: Updated systematic review on electronic cigarettes for smoking cessation
The search strategy for this update will be developed using the search strategy of the candidate systematic review, once identified. The search strategy of the candidate review will be evaluated and modified as necessary. Databases will be searched from the last search date of the review. Using the OVID platform, we will search Ovid MEDLINE®, Ovid MEDLINE® Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Embase Classic + Embase, and PsycINFO. We will also search the Cochrane Library on Wiley. The final search will be peer-reviewed using the PRESS 2015 guideline [ 86 ]. Results of the PRESS reviews will be provided in an appendix in the final report. The grey literature will be searched using the same approach outlined for the overview of reviews.
Studies will be selected for inclusion using the criteria outlined in Table 3 .
Study selection and data extraction
Study selection and data extraction will follow the same process described for the overview of reviews. Where study eligibility is unclear, authors will be contacted by email twice over 2 weeks for additional information.
We will collect both self-report and biochemically validated tobacco abstinence and relapse. Data will be collected for all reported and relevant (see Table 3 ) time points of follow-up. Where needed, we will convert data (e.g. standard error to standard deviation) to facilitate consistent presentation of results across studies. Authors will be contacted by email twice over 2 weeks if any information is missing or unclear. Refer to Additional file 6 for a list of draft items to be collected during data extraction
We will consult studies included in the original review to ensure that all outcomes of interest (Table 3 ) have been captured.
Risk of bias assessment
For consistency, risk of bias assessments/quality appraisal will be performed for all available studies (i.e. studies included in the original review and newly identified studies). The risk of bias of randomized and non-randomized controlled trials will be assessed by one reviewer using the Cochrane risk of bias (ROB) tool [ 109 ] (Additional file 7 ). We will consider industry funding under the “other sources of bias” domain of the tool. A modified version of the Scottish Intercollegiate Guidelines Network critical appraisal tool [ 110 ] (Additional file 8 ), which accounts for potential sources of bias including that arising from industry funding, will be used to evaluate the quality of prospective cohort studies. Verification will be done by a second reviewer. Disagreements will be resolved by consensus or third-party adjudication.
Some domains are outcome-specific and will be assessed at the outcome level. Overall risk of bias for the body of evidence will be evaluated according to the importance of domains, the likely direction of bias, and the likely magnitude of bias [ 109 ]. The Agency for Healthcare Research and Quality guidance will be followed for evaluating risk of bias for outcome and analysis reporting bias [ 111 ].
Study characteristics will be summarized narratively and presented in summary tables. Where possible, relative and absolute effects with 95% confidence intervals will be calculated for the GRADE summary of findings and evidence profile tables. Risk ratios and risk differences will be used to report effects for dichotomous data. For calculating the risk difference from meta-analyzed data, we will use the median baseline risk for the control group in the included studies, although we may perform sensitivity analysis using differing baseline risks if thought to be suitable. For continuous outcomes, mean difference (i.e. difference in means) effect measures will be used for outcomes using the same measure and standardized mean differences for outcomes using different measures, consistent with GRADE guidance [ 112 ].
Meta-analysis
We will examine the extent of clinical and methodological heterogeneity to determine appropriateness of performing meta-analysis. The Cochrane’s Q (considered statistically significant at p < 0.10) and I 2 statistic will be used to assess the statistical heterogeneity across included studies [ 113 , 114 ]. If appropriate, data from the original systematic review will be meta-analyzed with data from newly identified studies, using random effects models. For time-to-event data, the hazard ratio will be pooled using the generic inverse variance method. Analyses will be stratified by study design. For observational studies, we will use adjusted risk estimates in the meta-analysis.
Should meta-analysis not be appropriate due to considerable heterogeneity, the range of effects will be presented and results will be discussed narratively. Studies will also be presented in a forest plot without a pooled risk estimate. Clinical and methodological sources of heterogeneity will also be explored using subgroup, sensitivity, and/or meta-regression analyses, depending on how data are reported in studies. We will follow previously published guidance for meta-regression [ 115 ].
Sparse binary data and studies with zero events
Results will be synthesized narratively if studies report rare events. The risk difference will be used for outcomes (e.g. serious adverse events) where at least one intervention group contains zero events.
If there are sufficient data, the following subgroup analyses will be conducted:
By use of other substances (alcohol, cannabis, opioids)
By setting (e.g. family medicine clinics, walk-in clinics, urgent care facilities)
Nicotine content (groupings will depend on what is found in the literature)
Intensity of behavioural therapy (groupings will depend on what is found in the literature)
Duration of e-cigarette usage as part of the intervention (groupings will depend on what is found in the literature)
By type or generation of e-cigarette device
By industry funding
Sensitivity analysis
Sensitivity analyses restricted to low risk of bias studies may be performed. Sensitivity analyses may also be performed to explore statistical heterogeneity or to evaluate the impact of various decisions made during the conduct of the review.
Small study effects
To evaluate small study effects, a combination of graphical aids and/or statistical tests will be performed if there are at least 10 studies in the analysis.
The Cochrane Review Manager software version 5.3 [ 116 ] will be used to conduct analyses. Where needed, Comprehensive Meta-Analysis (CMA) or Stata may be used.
Grading the quality of evidence and interpretation
For critical and important outcomes, the GRADE framework [ 106 , 117 ] will be used to assess the quality of the evidence.
Smoking is a leading cause of preventable death and disability, accounting for nearly 20% of all deaths in Canada. It is estimated that the cost of tobacco use in Canada is around $16 billion CDN, when considering factors such as hospital expenditure, physician care, and economic losses associated with premature death and disability. In response to this important public health care issue, the Canadian Task Force on Preventive Health Care will be developing a national tobacco smoking cessation guideline informed by an overview of systematic reviews of the benefits and harms of various stop smoking interventions for adults and relevant subpopulations, where available. This document has outlined the methods for undertaking the overview and an update of e-cigarette evidence for that overview.
Abbreviations
Canadian Action Network for the Advancement, Dissemination and Adoption of Practice-informed Tobacco Treatment
Chronic obstructive pulmonary disorder
Electronic cigarette
Human immunodeficiency virus
Key question
National Institute for Health and Care Excellence
Nicotine replacement therapy
Randomized controlled trial
Socioeconomic status
Working group
Dobrescu A, Bhandari A, Sutherland G, Dinh T (2017) The costs of tobacco use in Canada, 2012. The Conference Board of Canada. https://www.conferenceboard.ca/e-Library/abstract.aspx?did=9185 . Accessed 20 June 2018.
Public Health Agency of Canada (2017) How healthy are Canadians? https://www.canada.ca/en/public-health/services/publications/healthy-living/how-healthy-canadians.html . Accessed 20 June 2018.
Reid RD, Pritchard G, Walker K, Aitken D, Mullen K-A, Pipe AL. Managing smoking cessation. Can Med Assoc J. 2016;188:E484–92.
Article Google Scholar
Baliunas D, Patra J, Rehm J, Popova S, Kaiserman M, Taylor B. Smoking-attributable mortality and expected years of life lost in Canada 2002: conclusions for prevention and policy. Chronic Dis Inj Can. 2007;27:154.
Google Scholar
Peacock A, Leung J, Larney S, Colledge S, Hickman M, Rehm J, Giovino GA, West R, Hall W, Griffiths P. Global statistics on alcohol, tobacco and illicit drug use: 2017 status report. Addiction. 2018. https://doi.org/10.1111/add.14234 .
Statistics Canada (2018) Smoking, 2017. https://www150.statcan.gc.ca/n1/pub/82-625-x/2018001/article/54974-eng.htm. Accessed 16 July 2018.
Health Canada (2013) Canadian Tobacco Use Monitoring Survey (CTUMS) 2012: supplementary tables. In: Can. Tob. Use Monit. Surv. CTUMS 2012 Suppl. Tables - Canadaca. https://www.canada.ca/en/health-canada/services/publications/healthy-living/canadian-tobacco-use-monitoring-survey-2012-supplementary-tables.html . Accessed 20 June 2018.
Statistics Canada (2017) Smoking, 2016. https://www150.statcan.gc.ca/n1/en/pub/82-625-x/2017001/article/54864-eng.pdf?st=gEUMVM40 . Accessed 20 June 2018.
Statistics Canada Table 13-10-0457-01 Health indicators, by Aboriginal identity, four-year period estimates. https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310045701 . Accessed 20 June 2018.
CAN-ADAPTT (2011) Canadian smoking cessation guideline - specific populations: mental health and/or other addiction(s).
Kirst M, Mecredy G, Chaiton M (2013) The prevalence of tobacco use co-morbidities in Canada. Can J public health rev can Sante Publique 104:e210–e215.
Guydish J, Passalacqua E, Tajima B, Chan M, Chun J, Bostrom A. Smoking prevalence in addiction treatment: a review. Nicotine Tob Res. 2011;13:401–11.
Article PubMed PubMed Central Google Scholar
Health Canada (2018) Canadian Tobacco Alcohol and Drugs (CTADS) Survey: 2017 summary. https://www.canada.ca/en/health-canada/services/canadian-tobacco-alcohol-drugs-survey/2017-summary.html . Accessed 7 Nov 2018.
Cancer Research UK (2015) How smoking causes cancer. https://www.cancerresearchuk.org/about-cancer/causes-of-cancer/smoking-and-cancer/how-smoking-causes-cancer . Accessed 24 Aug 2018.
Alberg AJ, Shopland DR, Cummings KM. The 2014 Surgeon General’s Report: commemorating the 50th Anniversary of the 1964 Report of the Advisory Committee to the US Surgeon General and updating the evidence on the health consequences of cigarette smoking. Am J Epidemiol. 2014;179:403–12.
US Department of Health and Human Services (2014) The health consequences of smoking—50 years of progress: a report of the surgeon general. Centers for Disease Control and Prevention (US), Atlanta (GA). http://www.ncbi.nlm.nih.gov/books/NBK179276/
Siu AL. Behavioral and pharmacotherapy interventions for tobacco smoking cessation in adults, including pregnant women: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2015;163:622–34.
Article PubMed Google Scholar
International Agency for Research on Cancer (ed) (2012) A review of human carcinogens. Part E: personal habits and indoor combustions. IARC, Lyon. http://monographs.iarc.fr/ENG/Monographs/vol100E/mono100E.pdf
Global Initiative for Asthma (2018) Global strategy for asthma management and prevention.
Montazeri Z, Nyiraneza C, El-Katerji H, Little J. Waterpipe smoking and cancer: systematic review and meta-analysis. Tob Control. 2017;26:92–97.
Urkin J, Ochaion R, Peleg A. Hubble bubble equals trouble: the hazards of water pipe smoking. ScientificWorldJournal. 2006;6:1990–7.
Knishkowy B, Amitai Y. Water-pipe (narghile) smoking: an emerging health risk behavior. Pediatrics. 2005;116:e113–9.
Cao S, Yang C, Gan Y, Lu Z. The health effects of passive smoking: an overview of systematic reviews based on observational epidemiological evidence. PLoS One. 2015;10:e0139907.
World Health Organization (WHO) (2017) WHO report on the global tobacco epidemic, 2017: monitoring tobacco use and prevention policies. http://www.who.int/tobacco/global_report/2017/en/.
Hori M, Tanaka H, Wakai K, Sasazuki S, Katanoda K. Secondhand smoke exposure and risk of lung cancer in Japan: a systematic review and meta-analysis of epidemiologic studies. Jpn J Clin Oncol. 2016;46:942–51.
Fischer F, Kraemer A. Meta-analysis of the association between second-hand smoke exposure and ischaemic heart diseases, COPD and stroke. BMC Public Health. 2015;15:1202.
Shields M, Garner RE, Wilkins K. Dynamics of smoking cessation and health-related quality of life among Canadians. Health Rep. 2013;24:3.
PubMed Google Scholar
Pirie K, Peto R, Reeves GK, Green J, Beral V, Million Women Study Collaborators (2013) The 21st century hazards of smoking and benefits of stopping: a prospective study of one million women in the UK. Lancet Lond Engl 381:133–141.
Mons U, Müezzinler A, Gellert C, Schöttker B, Abnet CC, Bobak M, de Groot L, Freedman ND, Jansen E, Kee F. Impact of smoking and smoking cessation on cardiovascular events and mortality among older adults: meta-analysis of individual participant data from prospective cohort studies of the CHANCES consortium. BMJ. 2015;350:h1551.
Jha P, Peto R. Global effects of smoking, of quitting, and of taxing tobacco. N Engl J Med. 2014;370:60–8.
Article CAS PubMed Google Scholar
Lam TH. Absolute risk of tobacco deaths: one in two smokers will be killed by smoking: comment on “smoking and all-cause mortality in older people”. Arch Intern Med. 2012;172:845–6.
McIvor A. Tobacco control and nicotine addiction in Canada: current trends, management and challenges. Can Respir J J Can Thorac Soc. 2009;16:21–6.
Wadgave U, Nagesh L. Nicotine replacement therapy: an overview. Int J Health Sci. 2016;10:425.
Cahill K, Stevens S, Perera R, Lancaster T. Pharmacological interventions for smoking cessation: an overview and network meta-analysis. Cochrane Libr. 2013. https://doi.org/10.1002/14651858.CD009329.pub2 .
Prochaska JJ, Das S, Benowitz NL. Cytisine, the world’s oldest smoking cessation aid. BMJ. 2013;347:f5198.
Government of Canada HC (2014) Licensed Natural Health Products Database (LNHPD). https://health-products.canada.ca/lnhpd-bdpsnh/info.do?licence=80072525 . Accessed 16 July 2018.
Brandon TH, Drobes DJ, Unrod M, Heckman BW, Oliver JA, Roetzheim RC, Karver SB, Small BJ. Varenicline effects on craving, cue reactivity, and smoking reward. Psychopharmacology. 2011;218:391–403.
Article CAS PubMed PubMed Central Google Scholar
Westergaard CG, Porsbjerg C, Backer V. The effect of Varenicline on smoking cessation in a group of young asthma patients. Respir Med. 2015;109:1416–22.
Hughes JR, Stead LF, Hartmann-Boyce J, Cahill K, Lancaster T. Antidepressants for smoking cessation. Cochrane Database Syst Rev. 2014. https://doi.org/10.1002/14651858.CD000031.pub4 .
Slemmer JE, Martin BR, Damaj MI. Bupropion is a nicotinic antagonist. J Pharmacol Exp Ther. 2000;295:321–7.
CAS PubMed Google Scholar
McCarthy DE, Jorenby DE, Minami H, Yeh V. Treatment options in smoking cessation: what place for bupropion sustained-release? Clin Med Ther. 2009;1:CMT.S2044.
Roddy E. Bupropion and other non-nicotine pharmacotherapies. BMJ. 2004;328:509–11.
World Health Organization (WHO) (2015) Electronic cigarettes (e-cigarettes) or electronic nicotine delivery systems. http://www.who.int/tobacco/communications/statements/eletronic_cigarettes/en/ . Accessed 20 June 2018.
Hartmann-Boyce J, McRobbie H, Bullen C, Begh R, Stead LF, Hajek P. Electronic cigarettes for smoking cessation. Cochrane Libr. 2016. https://doi.org/10.1002/14651858.CD010216.pub3 .
Farsalinos KE, Gillman G. Carbonyl emissions in e-cigarette aerosol: a systematic review and methodological considerations. Front Physiol. 2018. https://doi.org/10.3389/fphys.2017.01119 .
Institute for Quality and Efficiency in Health Care (IQWiG) (2017) Smoking: E-cigarettes: an alternative to tobacco, or a quitting aid?, Cologne, Germany. https://www.ncbi.nlm.nih.gov/books/NBK453108/
Hess CA, Olmedo P, Navas-Acien A, Goessler W, Cohen JE, Rule AM. E-cigarettes as a source of toxic and potentially carcinogenic metals. Environ Res. 2017;152:221–5.
Health Canada (2017) Bill S-5, an act to amend the tobacco act and the non-smokers’ health act and to make consequential amendments to other acts: an overview. In: Bill -5 Act Amend Tob. Act non-smokers health act make consequential amend. Acts Overv. - Canadaca. https://www.canada.ca/en/health-canada/programs/consultation-regulation-vaping-products/s5-overview-regulate-vaping-products.html . Accessed 20 June 2018.
de Bruin M, Viechtbauer W, Eisma MC, Hartmann-Boyce J, West R, Bull E, Michie S, Johnston M. Identifying effective behavioural components of Intervention and Comparison group support provided in SMOKing cEssation (IC-SMOKE) interventions: a systematic review protocol. Syst Rev. 2016. https://doi.org/10.1186/s13643-016-0253-1 .
Michie S, Hyder N, Walia A, West R. Development of a taxonomy of behaviour change techniques used in individual behavioural support for smoking cessation. Addict Behav. 2011;36:315–9.
Riemsma RP, Pattenden J, Bridle C, Sowden AJ, Mather L, Watt IS, Walker A. Systematic review of the effectiveness of stage based interventions to promote smoking cessation. BMJ. 2003;326:1175.
Cahill K, Lancaster T, Green N. Stage‐based interventions for smoking cessation. Cochrane Database of Systematic Reviews. 2010, Issue 11. Art. No.: CD004492. https://doi.org/10.1002/14651858.CD004492.pub4 .
Stead LF, Buitrago D, Preciado N, Sanchez G, Hartmann‐Boyce J, Lancaster T. Physician advice for smoking cessation. Cochrane Database of Systematic Reviews 2013, Issue 5. Art. No.: CD000165. https://doi.org/10.1002/14651858.CD000165.pub4 .
Stead LF, Carroll AJ, Lancaster T. Group behaviour therapy programmes for smoking cessation. Cochrane Libr. 2017. https://doi.org/10.1002/14651858.CD001007.pub3 .
Hartmann-Boyce J, Lancaster T, Stead LF. Print-based self-help interventions for smoking cessation. Cochrane Libr. 2014. https://doi.org/10.1002/14651858.CD001118.pub3 .
Zhu S-H, Anderson CM, Tedeschi GJ, Rosbrook B, Johnson CE, Byrd M, Gutiérrez-Terrell E. Evidence of real-world effectiveness of a telephone quitline for smokers. N Engl J Med. 2002;347:1087–93.
Gilbert H, Sutton S. Evaluating the effectiveness of proactive telephone counselling for smoking cessation in a randomized controlled trial. Addiction. 2006;101:590–8.
Taylor GMJ, Dalili MN, Semwal M, Civljak M, Sheikh A, Car J. Internet-based interventions for smoking cessation. Cochrane Libr. 2017. https://doi.org/10.1002/14651858.CD007078.pub5 .
Ussher MH, Taylor AH, Faulkner GE. Exercise interventions for smoking cessation. Cochrane Libr. 2014. https://doi.org/10.1002/14651858.CD002295.pub5 .
Hassandra M, Goudas M, Theodorakis Y. Exercise and smoking: a literature overview. Health (N Y). 2015;07:1477–91.
White AR, Rampes H, Liu JP, Stead LF, Campbell J. Acupuncture and related interventions for smoking cessation. Cochrane Libr. 2014. https://doi.org/10.1002/14651858.CD000009.pub4 .
White AR, Rampes H, Liu JP, Stead LF, Campbell J (2011) Acupuncture and related interventions for smoking cessation Cochrane Database Syst Rev CD000009.
Barnes J, Dong CY, McRobbie H, Walker N, Mehta M, Stead LF. Hypnotherapy for smoking cessation. Cochrane Database Syst Rev, CD001008. 2010.
Jurcic J, Pereira JA, Kavanaugh D. St John’s wort versus paroxetine for depression. Can Fam Physician. 2007;53:1511–3.
PubMed PubMed Central Google Scholar
Sood A, Ebbert JO, Prasad K, Croghan IT, Bauer B, Schroeder DR. A randomized clinical trial of St. John’s wort for smoking cessation. J Altern Complement Med. 2010;16:761–7.
Sood A, Prasad K, Croghan IT, Schroeder DR, Ehlers SL, Ebbert JO. S-Adenosyl-l-methionine (SAMe) for smoking abstinence: a randomized clinical trial. J Altern Complement Med. 2012;18:854–9.
CAN-ADAPTT (2012) Canadian smoking cessation clinical practice guideline. http://www.strokebestpractices.ca/wp-content/uploads/2012/04/CAN-ADAPTT2.pdf.
Registered Nurses’ Association of Ontario (2017) Integrating tobacco interventions into daily practice. http://rnao.ca/bpg/guidelines/integrating-tobacco-interventions-daily-practice . Accessed 20 June 2018.
National Institute for Health and Care Excellence (NICE). Stop smoking interventions and services. In: NICE guideline; 2018. https://www.nice.org.uk/guidance/ng92/resources/stop-smoking-interventions-and-services-pdf-1837751801029 .
New Zealand Ministry of Health (2014) The New Zealand guidelines for helping people to stop smoking. https://www.health.govt.nz/publication/new-zealand-guidelines-helping-people-stop-smoking .
Scottish Intercollegiate Guidelines Network (SIGN) Risk estimation and the prevention of cardiovascular disease. SIGN publication no. 149. https://www.sign.ac.uk/assets/sign149.pdf .
Patnode CD, O’connor E, Whitlock EP, Perdue LA, Soh C, Hollis J. Primary care–relevant interventions for tobacco use prevention and cessation in children and adolescents: a systematic evidence review for the US Preventive Services Task Force. Ann Intern Med. 2013;158:253–60.
Public Health England (2018) Stop smoking options: guidance for conversations with patients. In: GOV.UK. https://www.gov.uk/government/publications/stop-smoking-options-guidance-for-conversations-with-patients/stop-smoking-options-guidance-for-conversations-with-patients . Accessed 30 Oct 2018.
Aboriginal Tobacco Program First Nations. In: First Nations - Tobaccowise. http://www.tobaccowise.com/first_nations . Accessed 30 Oct 2018.
National Collaborating Centre for Aboriginal Health (2013) Tobacco fact sheet.
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;349:g7647.
Bougioukas KI, Liakos A, Tsapas A, Ntzani E, Haidich A-B. Preferred reporting items for overviews of systematic reviews including harms checklist: a pilot tool to be used for balanced reporting of benefits and harms. J Clin Epidemiol. 2018;93:9–24.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100.
Pollock A, Campbell P, Brunton G, Hunt H, Estcourt L. Selecting and implementing overview methods: implications from five exemplar overviews. Syst Rev. 2017;6:145.
Becker L, Oxman AD. Chapter 22: overviews of reviews. Cochrane Handb. Syst Rev Interv. 2011 Version 5.1.0.
McKenzie JE, Brennan SE (2017) Overviews of systematic reviews: great promise, greater challenge. Syst Rev. doi: https://doi.org/10.1186/s13643-017-0582-8 .
Pollock M, Fernandes RM, Becker LA, Featherstone R, Hartling L. What guidance is available for researchers conducting overviews of reviews of healthcare interventions? A scoping review and qualitative metasummary. Syst Rev. 2016;5:190.
Ballard M, Montgomery P. Risk of bias in overviews of reviews: a scoping review of methodological guidance and four-item checklist. Res Synth Methods. 2017;8:92–108.
Hartling L, Vandermeer B, Fernandes RM. Systematic reviews, overviews of reviews and comparative effectiveness reviews: a discussion of approaches to knowledge synthesis. Evidence-Based Child Health Cochrane Rev J. 2014;9:486–94.
Becker L, Caldwell D, Higgins JPT, Li T, Salanti G, Schmid CH Comparing multiple interventions in Cochrane reviews http://methods.cochrane.org/cmi/sites/methods.cochrane.org.cmi/files/public/uploads/Comparing%20Multiple%20Interventions%20in%20Cochrane%20Reviews%20-%202003%2003%2023.pdf .
McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol. 2016;75:40–6.
Canadian Agency for Drugs and Technologies in Health (CADTH) (2015) Grey matters: a practical search tool for evidenced-based medicine. https://www.cadth.ca/resources/finding-evidence/grey-matters .
Lindson-Hawley N, Thompson TP, Begh R. Motivational interviewing for smoking cessation. Cochrane Database Syst Rev. 2015. https://doi.org/10.1002/14651858.CD006936.pub3 .
Shiplo S, Czoli CD, Hammond D. E-cigarette use in Canada: prevalence and patterns of use in a regulated market. BMJ Open. 2015;5:e007971.
Caraballo RS, Shafer PR, Patel D, Davis KC, McAfee TA. Peer reviewed: quit methods used by US adult cigarette smokers, 2014–2016. Prev Chronic Dis. 2017;14.
Thomson Reuters Reference Manager 12. Thomson Reuters, New York.
Evidence Partners (2011) DistillerSR. Ottawa, Canada. https://www.evidencepartners.com/
Pieper D, Antoine S-L, Mathes T, Neugebauer EA, Eikermann M. Systematic review finds overlapping reviews were not mentioned in every other overview. J Clin Epidemiol. 2014;67:368–75.
Pollock A, Farmer SE, Brady MC, Langhorne P, Mead GE, Mehrholz J, van Wijck F (2013) Interventions for improving upper limb function after stroke. Cochrane Database Syst Rev doi: https://doi.org/10.1002/14651858.CD010820.pub2 .
Shea BJ, Reeves BC, Wells G, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
Mills EJ, Kanters S, Thorlund K, Chaimani A, Veroniki A-A, Ioannidis JP. The effects of excluding treatments from network meta-analyses: survey. BMJ. 2013;347:f5195.
Brignardello-Petersen R, Johnston BC, Jadad AR, Tomlinson G. Using decision thresholds for ranking treatments in network meta-analysis results in more informative rankings. J Clin Epidemiol. 2018;98:62–9.
Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. 2011;64:163–71.
Sun X, Briel M, Walter SD, Guyatt GH. Is a subgroup effect believable? Updating criteria to evaluate the credibility of subgroup analyses. BMJ. 2010;340:c117.
Edwards SJ, Clarke MJ, Wordsworth S, Borrill J. Indirect comparisons of treatments based on systematic reviews of randomised controlled trials. Int J Clin Pract. 2009;63:841–54.
Sun X, Ioannidis JPA, Agoritsas T, Alba AC, Guyatt G. How to use a subgroup analysis: users’ guide to the medical literature. JAMA. 2014;311:405–11.
Guyatt GH, Oxman AD, Kunz R, et al. GRADE guidelines: 7. Rating the quality of evidence--inconsistency. J Clin Epidemiol. 2011;64:1294–302.
Ioannidis JP. Integration of evidence from multiple meta-analyses: a primer on umbrella reviews, treatment networks and multiple treatments meta-analyses. Can Med Assoc J. 2009;181:488–93.
Moja L, Del Rio MPF, Banzi R, Cusi C, D’Amico R, Liberati A, Lodi G, Lucenteforte E, Minozzi S, Pecoraro V. Multiple systematic reviews: methods for assessing discordances of results. Intern Emerg Med. 2012;7:563–8.
Jadad AR, Cook DJ, Browman GP. A guide to interpreting discordant systematic reviews. Can Med Assoc J. 1997;156:1411–6.
CAS Google Scholar
Canadian Task Force on Preventive Health Care (2014) Canadian Task Force on preventive health care procedure manual. https://canadiantaskforce.ca/methods /.
Atkins D, Best D, Briss PA, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328:1490.
Puhan MA, Schünemann HJ, Murad MH, Li T, Brignardello-Petersen R, Singh JA, Kessels AG, Guyatt GH. A GRADE Working Group approach for rating the quality of treatment effect estimates from network meta-analysis. Bmj. 2014;349:g5630.
Higgins JPT, Altman DG, Sterne JAC. Chapter 8: assessing risk of bias in included studies. Cochrane Handb. Syst Rev Interv; 2011.
Scottish Intercollegiate Guidelines Network (SIGN) (2012) Methodology checklist 3: cohort studies. http://www.sign.ac.uk/checklists-and-notes.html . Accessed 20 June 2018.
Balshem H, Stevens A, Ansari M, Norris S, Kansagara D, Shamliyan T, Chou R, Chung M, Moher D, Dickersin K. Finding Grey Literature Evidence and Assessing for Outcome and Analysis Reporting Biases When Comparing Medical Interventions: AHRQ and the Effective Health Care Program. Methods Guide for Comparative Effectiveness Reviews. (Prepared by the Oregon Health and Science University and the University of Ottawa Evidencebased Practice Centers under Contract Nos. 290-2007-10057-I and 290-2007-10059-I.) AHRQ Publication No. 13(14)-EHC096-EF. Rockville, MD: Agency for Healthcare Research and Quality. November 2013. www.effectivehealthcare.ahrq.gov/reports/final.cfm .
Guyatt GH, Thorlund K, Oxman AD, et al. GRADE guidelines: 13. Preparing summary of findings tables and evidence profiles-continuous outcomes. J Clin Epidemiol. 2013;66:173–83.
Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
Sterne JAC, Sutton AJ, Ioannidis JPA, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343:d4002.
Morton SC, Murad MH, O’Connor E, et al (2018) Quantitative Synthesis—An Update. Methods Guide for Comparative Effectiveness Reviews. AHRQ Publication No. 18-EHC007-EF. Rockville, MD: Agency for Healthcare Research and Quality. https://effectivehealthcare.ahrq.gov/topics/methods-quantitative-synthesis-update/methods . Accessed 30 Oct 2018.
The Cochrane Collaboration Review Manager (RevMan). The Nordic Cochrane Centre. Copenhagen; 2015.
GRADE Working Group. Grading quality of evidence and strength of recommendations. BMJ. 2004;328:1490.
Article PubMed Central Google Scholar
Download references
Acknowledgements
Other members of the Canadian Task Force on Preventive Health Care who provided additional comments: John Leblanc, Guylène Thériault, John Riva. Detailed descriptions of each member are available at https://canadiantaskforce.ca . The authors also acknowledge Marion Doull and Rachel Rodin from the Public Health Agency of Canada for their input and direction during project scoping and refinement.
Funding for this protocol and subsequent evidence review is provided by the Public Health Agency of Canada. This funding will support all phases of conduct of the evidence review, including the search and selection of the evidence, collection of the data, data management, analyses, and writing. The funder was involved in the development of the protocol and will give approval to the final version. For the conduct of the review, the funder will also be given opportunity to comment, but final decisions will be made by the review team. In addition, the funder will not be involved in study selection, data extraction, or analysis.
Availability of data and materials
Not applicable.
Author information
Mona Hersi and Gregory Traversy contributed equally to this work.
Authors and Affiliations
Knowledge Synthesis Group, Clinical Epidemiology Program, Ottawa Hospital Research Institute, Centre for Practice-Changing Research, 501 Smyth Road, Box 201, Ottawa, Ontario, K1H 8L6, Canada
Mona Hersi, Andrew Beck, Becky Skidmore, Brian Hutton, Beverley J. Shea & Adrienne Stevens
Public Health Agency of Canada, Ottawa, Ontario, Canada
Gregory Traversy & Susan Courage
Lady Davis Institute of the Jewish General Hospital, Montreal, Quebec, Canada
Brett D. Thombs
Department of Psychiatry, McGill University, Montreal, Quebec, Canada
Department of Community Health Sciences, University of Sherbrooke, Sherbrooke, Quebec, Canada
Stéphane Groulx
Centre de recherche Charles-Le Moyne – Saguenay–Lac-Saint-Jean sur les innovations en santé (CR-CSIS), Université de Sherbrooke, Quebec, Quebec, Canada
University of Calgary Cumming School of Medicine, Calgary, Alberta, Canada
Alberta Health Services, Calgary, Alberta, Canada
Department of Family and Community Medicine, University of Toronto, Toronto, Ontario, Canada
Donna L. Reynolds
Dalla Lana School of Public Health, University of Toronto, Toronto, Ontario, Canada
Donna L. Reynolds & Peter Selby
Division of Community Health and Humanities, Memorial University of Newfoundland, St. John’s, Newfoundland, Canada
Brenda Wilson
Department of Emergency Medicine, Yale School of Medicine, New Haven, CT, USA
Steven L. Bernstein
Addictions Division, Centre for Addiction and Mental Health, Toronto, Ontario, Canada
Peter Selby
Department of Otolaryngology, University of Ottawa, Ottawa, Ontario, Canada
Stephanie Johnson-Obaseki
The Ottawa Hospital, Ottawa, Ontario, Canada
Stephanie Johnson-Obaseki, Douglas Manuel & Smita Pakhale
Department of Family Medicine, University of Ottawa, Ottawa, Ontario, Canada
Douglas Manuel
Ottawa Hospital Research Institute, Ottawa, Ontario, Canada
Douglas Manuel, Smita Pakhale, Justin Presseau & Vivian Welch
School of Epidemiology and Public Health, Faculty of Medicine, University of Ottawa, Ottawa, Ontario, Canada
Douglas Manuel, Smita Pakhale, Justin Presseau, Brian Hutton, Beverley J. Shea, Vivian Welch & Julian Little
Bruyere Research Institute, Ottawa, Ontario, Canada
Douglas Manuel & Vivian Welch
School of Psychology, University of Ottawa, Ottawa, Ontario, Canada
Justin Presseau
Patient representative, Vancouver, British Columbia, Canada
Matt Morrow
You can also search for this author in PubMed Google Scholar
Contributions
MH, GT, AB, and AS drafted the protocol. BS developed the search strategy and provided text for the protocol. JL, BJS, BH, and VW critically reviewed the protocol and provided methodological expertise. SLB, PS, SJO, DM, SP, and JP reviewed the protocol and provided clinical expertise for the review. MM provided a patient perspective for the protocol. Members of the Tobacco Working Group for the Canadian Task Force on Preventive Health Care (BT, SG, EL, DLR, BW) critically reviewed and provided feedback on the protocol. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Mona Hersi .
Ethics declarations
Ethics approval and consent to participate, consent for publication.
Written informed consent to publish was obtained from the stakeholders who provided feedback on the protocol. A copy of the written consent is available for review by the Editors-in-Chief of this journal. The stakeholder feedback has been anonymized and included as Additional file 9 .
Competing interests
BH has received consultancy fees from Cornerstone Research Group for methodologic advice related to systematic reviews and meta-analysis and is a member of the Editorial team for Systematic Reviews . PS reports grants and research support from Pfizer Inc., Bhasin Consulting Fund, and Patient Centered Outcomes Research Institute; consulting fees from Pfizer Canada Inc., Evidera Inc., Johnson & Johnson Group of Companies, Medcan Clinic, NVision Insight Group, and Myelin & Associates; receival of drugs free of charge or at a discounted rate for study through open tender process from Johnson & Johnson, Novartis, and Pfizer Inc.; assisted in organizing the Pfizer Canada Inc. Advisory Board events; and speaking engagements (content not subject to sponsor approval)/honoraria from Pfizer Inc. The remaining authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:.
PRISMA Statement for Protocols (PRISMA-P) checklist. (DOCX 18 kb)
Additional file 2:
Search strategy for the overview of reviews. (DOCX 16 kb)
Additional file 3:
AMSTAR 2 Critical Appraisal Tool. (DOCX 77 kb)
Additional file 4:
AMSTAR 2 critical domains for assessing overall rating of quality. (DOCX 14 kb)
Additional file 5:
Draft data extraction items for the overview of reviews. (DOCX 13 kb)
Additional file 6:
Draft data extraction items for the updated review of e-cigarettes for smoking cessation. (DOCX 12 kb)
Additional file 7:
Cochrane risk of bias tool. (DOCX 29 kb)
Additional file 8:
Modified SIGN methodology checklist for cohort studies. (DOCX 26 kb)
Additional file 9:
Stakeholder feedback. (DOCX 34 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Hersi, M., Traversy, G., Thombs, B.D. et al. Effectiveness of stop smoking interventions among adults: protocol for an overview of systematic reviews and an updated systematic review. Syst Rev 8 , 28 (2019). https://doi.org/10.1186/s13643-018-0928-x
Download citation
Received : 29 August 2018
Accepted : 20 December 2018
Published : 19 January 2019
DOI : https://doi.org/10.1186/s13643-018-0928-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Stop smoking
- Systematic review
Systematic Reviews
ISSN: 2046-4053
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Featured Clinical Reviews
- Screening for Atrial Fibrillation: US Preventive Services Task Force Recommendation Statement JAMA Recommendation Statement January 25, 2022
- Evaluating the Patient With a Pulmonary Nodule: A Review JAMA Review January 18, 2022
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Smoking Cessation—Progress, Barriers, and New Opportunities : The Surgeon General’s Report on Smoking Cessation
- 1 Office of the Surgeon General, Public Health Service, Department of Health and Human Services, Washington, DC
- US Preventive Services Task Force USPSTF Recommendation: Tobacco Use Prevention and Cessation in Children and Adolescents US Preventive Services Task Force; Douglas K. Owens, MD, MS; Karina W. Davidson, PhD, MASc; Alex H. Krist, MD, MPH; Michael J. Barry, MD; Michael Cabana, MD, MA, MPH; Aaron B. Caughey, MD, PhD; Susan J. Curry, PhD; Katrina Donahue, MD, MPH; Chyke A. Doubeni, MD, MPH; John W. Epling Jr, MD, MSEd; Martha Kubik, PhD, RN; Gbenga Ogedegbe, MD, MPH; Lori Pbert, PhD; Michael Silverstein, MD, MPH; Melissa A. Simon, MD, MPH; Chien-Wen Tseng, MD, MPH, MSEE; John B. Wong, MD JAMA
- Medical News & Perspectives COVID-19 and the “Lost Year” for Smokers Trying to Quit Mary Chris Jaklevic, MSJ JAMA
- Viewpoint The Need for a Smoking Cessation “Care Package” Robert M. Califf, MD; Brian A. King, PhD, MPH JAMA
- In the News WHO Report–Tobacco Use Decreasing Globally, but Not on Track to Meet 2025 Target Joan Stephenson, PhD JAMA Health Forum
The reduction in cigarette smoking is one of the most significant public health successes in modern US history. As noted in the landmark 50th anniversary report of the surgeon general, more than an estimated 8 million deaths were averted over the past half century through evidence-based tobacco control efforts, 1 and recent data show that cigarette smoking among US adults is now at an all-time low of 14%. 2 However, 34 million US adults continue to smoke cigarettes, with marked disparities across the population. 2 Moreover, 16 million adults in the United States currently live with a smoking-related disease. 1 In addition to these human costs, smoking places a significant burden on the US economy, with estimated societal costs of smoking projected at more than $300 billion annually, including an estimated $170 billion in health care spending. 1
Read More About
Adams JM. Smoking Cessation—Progress, Barriers, and New Opportunities : The Surgeon General’s Report on Smoking Cessation . JAMA. 2020;323(24):2470–2471. doi:10.1001/jama.2020.6647
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- Open access
- Published: 14 September 2023
Health professional’s perception of a smoking cessation intervention among disadvantaged patients participating in a pragmatic randomized trial
- Aurélia Manns 1 ,
- Sarah Mahdjoub 1 ,
- Gladys Ibanez 1 , 2 ,
- Emilie Jarrier 1 ,
- Ava Daeipour 1 ,
- Maria Melchior 1 &
- Fabienne El-Khoury 1
BMC Health Services Research volume 23 , Article number: 993 ( 2023 ) Cite this article
785 Accesses
Metrics details
Introduction
Individuals who have a low socio-economic position (SEP) are more likely to smoke and face greater barriers to quitting tobacco. However, the effectiveness of tailored interventions has been limited probably due to specific challenges relative to this population. We conducted a mixed-method study to better understand health professionals’ perceptions and barriers when implementing a preference-based smoking cessation (SC) intervention among disadvantaged smokers.
A self-administered online questionnaire was sent to health professionals (doctors’ and other health professionals specialized in SC) participating in “STOP” a pragmatic multicentre randomized controlled trial. Perceptions regarding patient eligibility, the doctor-patient relationship, general study organization, and satisfaction were measured.
Twenty-eight STOP study investigators responded. Health professionals prioritize smoking cessation for disadvantaged patients, but face challenges in approaching and following them. A research intervention providing cessation tools based on preference was deemed useful but generally undermined by time constraints. Health professionals’ preconceptions regarding patients in low SEP having other “pressing problems” which might be exacerbated by quitting smoking were also identified. Further, participation in a research intervention was perceived as not satisfactory due to workload and lack of time.
Our results highlight general barriers inherent to implementing pragmatic trials. They also present specific challenges in smoking cessation trials among disadvantaged population, essential to advance equity in tobacco control.
Peer Review reports
Smoking is a major public health concern and one of the leading causes of preventable death and disease worldwide [ 1 ]. Despite multiple tobacco-control efforts, smoking prevalence remains high in most Western countries, particularly among individuals in low socio-economic positions (SEP) [ 2 ]. In France, almost one adult in 4 (25.3%) smokes cigarettes daily, with a higher prevalence in people in low SEP (32% of French adults with no high school diploma smoke) [ 3 ]. Individuals with socioeconomic disadvantages are not only more likely to smoke, they also have higher rates of nicotine dependence, and face greater barriers to quitting smoking than those who belong to higher socio-economic backgrounds [ 4 ].
Hence, tailored interventions were developed to support smoking cessation among disadvantaged populations [ 5 ]. However, these interventions face specific challenges when working with individuals with low SEP, who often have several concomitant medical and psychosocial needs that can make it difficult for health professionals to support them in quitting smoking [ 6 , 7 ].
Smokers with socioeconomic disadvantages report lower quitting rates compared to more affluent smokers, regardless of the smoking cessation intervention method [ 8 , 9 ]. Combining pharmacotherapy and structured behavioral support has shown some success in helping smokers with socioeconomic disadvantages quit, but their quit rates are still lower than those of more affluent smokers. Lack of support for quit attempts, stronger nicotine dependence, lower motivation to quit, and less compliance with treatment are other possible reasons explaining why quitting is more difficult for low SEP smokers. Disadvantaged smokers may also have less support from their family or community because they are more likely to have smokers in their social network. Motivation, use of pharmacotherapy and smoking cessation services, and the nature of smoking cessation programs can also affect quitting success, but inconsistent findings have been reported [ 8 ]. A systematic review by Kock et al. (2019) [ 10 ] indicates that individual-level interventions can be effective in helping disadvantaged smokers quit. However, tailoring these interventions specifically for disadvantaged smokers did not show significant benefits [ 10 ]. The authors concluded that to achieve positive smoking cessation outcomes for this group, it may be necessary to improve the development of more equitable interventions that are better tailored to their needs.
There is evidence that smoking cessation interventions in primary care settings can be effective in reducing tobacco-related health inequalities [ 11 ], however, these types of interventions are under-utilised [ 12 ]. Moreover, delivering smoking cessation interventions in low SEP populations presents specific challenges, particularly in the context of a research trial. These challenges include issues such as low literacy, lack of trust in the medical system, and difficulties in communication [ 13 ]. Identifying such barriers can inform the development of more effective smoking cessation interventions for disadvantaged populations, as well as provide guidance for researchers and tobacco-control health professionals.
To address these challenges, our team launched a pragmatic randomized controlled trial (RCT) assessing the effectiveness of a preference-based smoking cessation intervention centred on the patient’s preference : the STOP (Sevrage Tabagique à l’aide d’Outils dédiés selon la Préférence: Smoking cessation using preference-based tools) RCT. Participants randomized to the intervention group of this RCT receive smoking cessation tools delivered free of charge by a health professional, according to their choice. Doctors and other health professionals specialized in smoking cessation are responsible for enrolling and randomizing eligible patients, as well delivering the intervention in both arms [ 14 ]. As a pragmatic trial, the intervention was designed to be integrated into routine care and approximate a real-life setting.
The objective of this pragmatic trial is to determine treatments’ effects in ‘real-life’ conditions, by getting as close as possible to the actual conditions under which the treatment could be implemented. Health professionals who usually participate in pragmatic trials are chosen not because they are specialists in their field but because they conform to usual care. Thus, understanding the perceptions and barriers to implementation of this intervention among health professionals is essential to optimize both research and routine practices [ 15 ]. The present analysis aims to better understand the challenges and barriers faced by health professionals when implementing smoking cessation interventions among low SEP individuals in a research context.
This article therefore presents findings based on a questionnaire administered to these health professionnals, and provides a critical reflection on the challenges of implementing smoking cessation interventions among low SEP individuals in ‘real-life settings’.
STOP : study design and outcomes
The design of the STOP pragmatic multicenter randomized controlled trial (RCT) is described in more details elsewhere [ 16 ]. Trial registration number NCT04654585.
The primary outcome is smoking abstinence at 6 months after inclusion, defined as self-reported continuous abstinence for at least 7 days. Secondary outcomes include the total number of days of abstinence at 6 months after inclusion, continuous abstinence for at least 7 days at one and three months after inclusion and number of relapses.
Participants in the STOP RCT
The main inclusion criteria is regular smoking of at least five cigarettes per day, a willingness to quit or reduce tobacco consumption, and a low socio-economic position (low SEP). To assess SEP, individuals had to be either unemployed or eligible for a social benefit reserved to low-income individuals living in France. Participants also have to be at least 18 years of age, available for four follow-up appointments over the course of six months, and covered by the French national health insurance system. Patients who are already attempting to quit smoking, or those under guardianship or legal curatorship were not eligible to be included, as were persons who did not speak French.
Study centers and recruitment – STOP RCT
The study is being implemented in eighteen medical centers in France, including eight in the greater Paris area, four in Lyon and six in other cities as presented in supplementary Figure S1 . Participating medical centers include public hospitals, municipal health centers, or addiction treatment and prevention facilities, which concentrate a high proportion of patients with low SEP. The recruitments are carried out by physicians (general practitioners, addiction specialists, or smoking cessation specialists), or other health professionals specialized in smoking cessation (i.e. nurses or pharmacists). After receiving oral information about the study protocol, individuals who agree to participate are asked to answer a pre-inclusion questionnaire, and, if eligible, to sign a written informed consent. They are then randomized into two groups (control group vs. intervention group). The study is conducted in a single-blind fashion.
Ethical approval
The study protocol was approved by a French Ethical Committee (CPP) - n°: 20.01.31.65528 RIPH2 HPS.
STOP intervention
Participants in both groups are treated for smoking cessation according to the latest recommendations and usual medical practice [ 17 ]. In addition, patients in the intervention group directly receive free Nicotine Replacement Treatment (NRT: patches, inhalers, gum, sublingual tablets, and lozenges) and/or an electronic cigarette (supplied with e-liquid), according to their preference. A brief and clear description of each smoking cessation tool is given by the health professional and, depending on the participant’s subsequent choice, a sufficient quantity of the tool or tools of choice is provided to last until the next appointment.
Health professionals’ questionnaire
An email containing a link to an online questionnaire on the Lime Survey platform was sent to each healthcare professional participating in the STOP RCT, months after recruitment started in their center. The questionnaire examined perceptions regarding four possible barriers or facilitating factors in the trial’s implementation:
Patient eligibility: Health professionals were asked how often they met ‘eligible’ patients (i.e. persons who smoke, are willing to stop smoking, and have a low SEP). Practitioners’ routine practices were also examined, by asking if they generally brought up smoking and if they thought that smoking cessation for low SEP patients was a priority.
Doctor-patient relationship: Health professionals were asked whether, compared to other patients, low SEP patients were generally different in terms of patient-physician trust, adherence to care, regular follow-up, difficulty in undertaking long consultations, adherence to treatment, follow-up, addressing the issue of smoking cessation, and participating in a research study.
Study organization: participants’ views on difficulties (ranging from very simple to very complex) regarding the evaluation of eligibility criteria and the RCT’s integration into clinical practice were assessed. Difficulties related to time constraints were also assessed, by asking how much time the study added per week in terms of: 1/ paperwork, 2/ study presentation to patients, and 3/additional appointment time (ranging from less than ten minutes to more than two hours).
Satisfaction: we also examined health practitioner’s perceptions of the research’s merits and whether participating in the study had benefits for them in terms of: 1/ more frequent discussions relative to smoking cessation, 2/ new knowledge about NRT and e-cigarettes, and 3/ changes in perceptions of smoking cessation among patients with socioeconomic disadvantages. They were also asked if giving out free smoking cessation tools made them feel like they were providing a better treatment than a prescription, or resulted in better patient compliance. Finally, a question was asked about possible treatment contamination among patients part of the intervention and control groups (the study being single blind).
Most of the questions followed the Likert scale [ 18 ].
We also collected data regarding health professionals’ sex, age, occupation (nurse specialized in smoking cessation, general practitioner, doctor specialized in smoking cessation, addictologist doctor, other) and smoking status. Occupations were classified into two categories: doctors and other health professionals (according to their profession). We also identified smoking cessation specialists (‘tobbacologist’ Yes/No).
Open-ended questions
Four questions in the online questionnaire were open-ended with no character limits. They are presented in Fig. 1 .
Open ended questions addressed to health professionals participating in the STOP RCT
All statistical analyses performed were descriptive. The frequencies of each response were calculated and compared across different categories of health professionals (occupation, specialty, health professional’s smoking status) when relevant. All analyses were conducted using SAS 9.2.
Twenty-eight health professionals participating in the STOP study completed the questionnaire. The mean age was 47 years old (sd = 10). Their characteristics are presented in Table 1 .
Health professional’s perceptions
Patient’s eligibility.
As shown in supplementary Table s1 , health professionals declared that they are often treating patients with a low SEP. They also reported that the majority of their patients are smokers who are not spontaneously requesting to quit smoking and who are not yet treated for smoking cessation.
Participating health professionals indicated that many of their patients met eligibility criteria for the STOP RCT. However, several comments on barriers for recrutment were reported in Fig. 2 -A.

Perceptions reported health professionals participating in the STOP RCT concerning barriers for recruitmenet, and constraints relative to study organization
For tobacco-cessation specialists other types of barriers to recruitment were identified:
“We are already doing too much smoking cessation (we are even proactive; we teach medical students on rotation to prescribe patches to smokers who come for bronchitis, even if they don’t ask for it, in the belief that this proactive approach described in some studies will lead patients to at least try and discuss the experience with a doctor). Therefore, recruitment [for the STOP RCT] is not easy. In the health center where we already do a lot of smoking cessation (the doctors and the specialized nurse); thus the majority of eligible patients encountered already have patches or had already been offered them in the past year.”
“Very often my patients are already on NRT so it is rather difficult to recruit new ones.”
Doctor-patient relationship
Health professionals mostly agreed with the statement “As a professional, I think that smoking cessation is a priority for my patients with low SEP”. Some differences can be observed depending on the health professional’s occupation, and depending on their smoking status, as described in Fig. 3 .
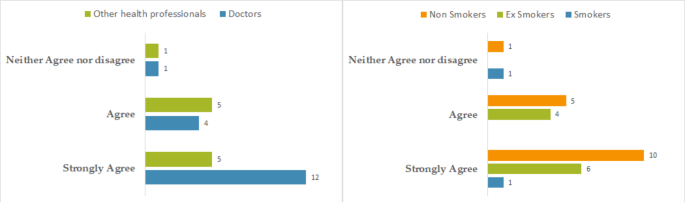
Health professionals participating in the STOP pragmatic RCT perceptions concerning “Priority given to smoking cessation in low SEP patients” according to the health professionals’ profession and smoking status (France, 2023)
Compared to other patients, initiating a smoking cessation for a disadvantaged patient was perceived as more difficult. Participating in a research study was also perceived as less convenient when participants are in low SEP. Interviewed health professionals also reported that it was more difficult to schedule multiple appointments (i.e. asking the patient to come back only due to the study), follow-up was less consistent, and treatment adherence was perceived as lower than among patients with high SEP (Table 2 ).
Satisfaction
Participating health professionals were mostly convinced of the merits of the STOP RCT. However, they did not report being more interested in e-cigarette or NRT because of the study, and not having discussed smoking cessation more frequently with their patients. Their perception of the low SEP patients’ desire to stop smoking has not changed compared to their views prior to study participation (supplementary table s2 ).
Figure 4 illustrates perceptions regarding the delivery of free smoking cessation tools according to the occupation or specialty of the health professional. Compared to other health professionals specialized in smoking cessation and non-smoking cessation specialists, doctors and smoking cessation specialists adhere more to the fact that giving free products allows better treatment adherence. Similarly, they report feeling that they are better able to help patients by giving free nicotine replacement products than by simply prescribing them.
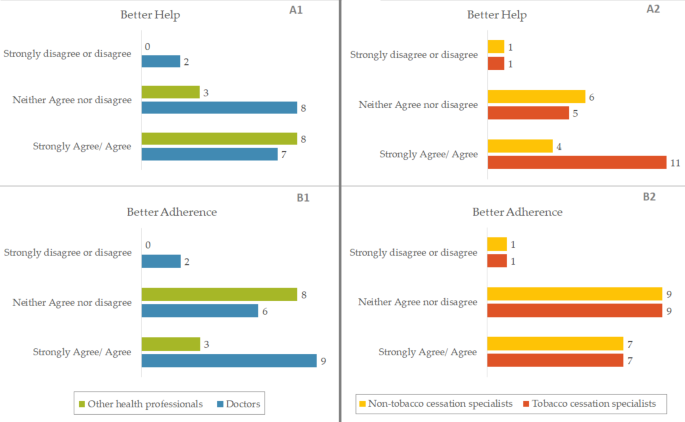
Answers to the questions « Giving products free of charge allowed me to provide a better help than with a simple prescription ( A ) » and « Giving products free of charge allowed patients to have a better adherence to treatment ( B ) », according to profession or specialty of health professionals participating in the STOP RCT.(France, 2023)
Study organization and time constraint
Overall, the study took approximately 10 min to present the aims 30 min to explain the procedures in addition to a standard appointment time, 30 min of time dedicated to administrative procedures and data colelction (Table 3 ). Time is the most frequent constraint to study participation reported by participating health professionals. This was in fact mentioned in almost half of the open-ended comments (31 out of 81).
In addition, the other reported constraints relative to study organization are presented in Fig. 2 -B.
But it also has been reported that participation in the study can have positive impacts on routine care and practices:
“[The intervention] helps address aspects of perception of nicotine substitutes and e-cigarettes that are not necessarily spontaneously addressed. It also makes it easier to discuss questions of preference related to the taste of NRTs, the concentration of e-liquids.“,
“An improvement in my patient-centered approach”.
Regarding participation in an academic research study, the following remarks were noted by participating health professionals:
“The times of care and research should be seperated”.
“Multiplicity of studies with the fear of making mistakes and distorting the study”.
“The overall workload at the public hospital, any study requires additional explanations and lengthens consultations”.
“Several patients did not wish to participate in the study on principle, as they did not want to be included in a research protocol, even after I explained that it would not change anything in their treatment. Moreover, it is sometimes difficult to explain to patients the benefits of the study (their interest as patients) without mentioning the two randomized groups (without telling them that they may potentially receive free treatments).“
“The act of participating in an interventional study modifies practices (in any arm, for that matter).“
“The training for field research in primary care is not widely disseminated, and still not sufficiently integrated into practice. However, the daily operational question remains: on-site support from clinical research assistants would help ensure the proper conduct of research and a form of acculturation for primary care physicians.“
The contribution of a clinical research assistant was noted three times as being valuable.
Health professionals in our study sample routinely meet low SEP patients who smoke, and consider it a priority to offer them smoking cessation treatment. However, they are confronted with challenges specific to these patients, with whom the uptake of smoking cessation, regular follow-up, and adherence to care are perceived as complex.
We also highlighted perceived obstacles to study implementation that are inherent in the study organization and design, mainly due to time constraints. However, health professionals were mostly convinced of the usefulness of this research and felt they were providing better help through the intervention, by delivering smoking cessation tools free of charge according to the patient’s choice, than with a standard prescription. In clinical practice outside of a research trial, this intervention does not present the same type of administrative time constraints, but it does require consultation time dedicated to explaining the smoking cessation tools that the patient has at his disposal so that he or she can make an informed choice.
Interpretation
Barriers to patients recruitment.
Patients received in consultation by health professionals mostly correspond to the target population of our study, however several difficulties relative to recruitment were reported, which can be grouped into four categories:
Exclusion criteria (lack of French language skills, a high income, a center policy that results in patients being mostly already treated, under legal guardianship),
Difficulties to evaluate eligibility criteria (detecting social benefits/ low SEP),
Problems inherent to the patient (hospitalized, geographical distance),
And finally, some health professionals’ preconceived idea that the desire to stop smoking is not a priority for smokers with low SEP, and quitting is perceived as more challenging among this population.
This last point calls for vigilance regarding the prejudices that some health professionals might have relative to what the patient thinks is a priority for him/her.
Although health professionals agreed that smoking cessation is a priority for their low-SEP patients, some comments indicated otherwise.
A study based on the National Health Interview Survey (NHIS) of 2001 in the US [ 19 ], revealed that assistance with smoking cessation was less frequently reported by patients with high or mid-levels of disadvantage compared to those with low levels. Levels of disadvantage were scored depending on education, income, and health insurance. The authors explain this by the fact that patients in these situations are those among whom prevalences of smoking and associated comorbidities are the highest. Thus, health care professionals may feel that they are less likely to be successful in quitting. In addition, the facilities that provide care for this patient population are often in busy, under-staffed environments, which limit the smoking cessation treatments.
A systematic review on perceived barriers to smoking cessation among vulnerable groups reports cases where health professionals discourage smoking cessation because they were concerned about their mental health, or because they thought smoking was their only source of pleasure [ 20 ]. Several studies cited in this review highlight lack of support to quit from health professionals [ 20 ]. These results based on a systematic review of the literature suggest that some health professionals might have the preconception that disadvantaged patients have other “higher priority” problems and that quitting smoking could add to or exacerbate them.
Finally, health professionals report that smokers with low SEP have inherent difficulties in smoking cessation. Withdrawal is perceived as more complicated, as is smoking cessation initiation or participation in a study. Follow-up and adherence to care are also perceived as more difficult for these patients.
A literature review on barriers faced by low SEP patients to smoking cessation reports a lower ability to reach smoking cessation support because of low mobility, low social support, and a tendency to perceive it as inappropriate or inaccessible [ 21 ].
Participation of health professionals in a research intervention
Health professionals did not report high satisfaction with their participation in the study. They mostly did not report gaining more information about NRT and e-cigarettes, discussing smoking cessation more often, or changing their perception concerning the desire to quit among low SEP populations. However, one of the goals of the study is to prove that giving free cessation tools to these patients according to their own choice would lead to greater success in quitting smoking. The professionals most convinced that this intervention would allow them to better help their patients, or would allow a better adherence to the care of their patients, were the smoking cessation specialists and the medical doctors.
The most frequently cited barriers and constraints related to participating in the study were the lack of time combined with the already present heavy workload. Indeed, since the investigating centers are public hospitals or health centers, the lack of staff and the influx of patients beyond capacity can make research take second place to care. Consultations must be quick and efficient in order to see as many patients as possible, and the addition of time that is not strictly necessary is perceived as burdening and therefore denied. The SESMAT qualitative survey [ 22 ] asked physicians about work difficulty. The results highlight physicians’ frustration over chronic extensive workload (quantity, time, lack of recognition), administrative burden and lack of time. Since these issues are already present in everyday life, the addition of a research intervention can represent a constraint rather than a motivation.
Health professionals may also have been uncomfortable by the content of some questions in the questionnaire, such as questions on socio-economic background by fear of stigma. They reported that it could be complicated to submit it into the middle of a specific appointment, and that it may strain the already fragile therapeutic alliance with low SEP patients. Moreover, due to lack of time, sometimes these questionnaires replaced routine questioning that the professional would have liked to carry out. Thus, it may be considered more relevant to separate the time of care and the time of research by avoiding integrating the data collection in the consultation. In addition, they may be apprehensive about patients’ reluctance to participate in research. Patients may experience it as a “test”, and this may weaken the physician-patient trust relationship. Finally, health care professionals are sometimes not well trained in research and may be afraid of making errors and distorting the study.
Our results are consistent with a qualitative study on perceptions of recruiters in six Randomized Control Trials (RCTs) [ 23 ]. Doctors struggled to balance their roles as recruiters and clinicians, leading to conflicts with clinical practice, uncertainty about the best treatment, and willingness to recruit patients. Nurses also faced conflicts between their roles as caring clinical nurses, patient advocates, and recruiters/scientists, causing considerable discomfort and difficulty. Organizational difficulties, lack of eligible patients, and patients’ strong treatment preferences were identified as recruitment barriers, but they were not straightforward and were often reinforced by recruiters’ views. Recruiters’ discomfort and difficulty were significant, leading to low morale and poor recruitment levels, as they had conflicts between carrying out research and ensuring individual patients’ best interests, and strong treatment preferences or clinical instincts that made them uncomfortable recruiting patients outside their comfort zone.
Our results highlight the desire of some health professionals to separate research time from clinical practice time. However, the aim of this pragmatic research, and therefore of the pragmatic trial, was to integrate research into routine, so that the intervention would be as close as possible to real-life conditions. This is so the intervention could be more easily generalized outside the research context.
Some professionals did have positive feedback on the integration of the intervention into their medical practice: it allowed them to refocus on patient preferences and thus improve their patient-centered approach to care. The co-construction of interventions with the target audience is indeed a criterion of effectiveness according to a synthesis of the literature conducted by Guignard et al. on smoking cessation interventions in low SEP patients [ 24 ]. The value of relying on patient preference has already been explained in the STOP study protocol justification [ 16 ].
A qualitative study asked key stakeholders about the challenges raised by pragmatic trials [ 25 ]. It was noted that the difference between research, quality improvement, and practice is sometimes unclear. The boundary is also not well defined for the patient during the consultation time (the point at which one moves from care to research). This may explain why the health professionals in our study would prefer to separate the two components. Moreover, it is requested to compare the intervention to usual care. which can differ between each patient, and between each caregiver. Therefore the difference between the intervention and usual care may vary within the same study. The workload generated by the administrative aspect of the research would then seem disproportionate, for a lesser addition to the usual care given.
Finally, in real life, health professionals are confronted with specific problems while treating low SEP patients. This is why a pragmatic trial specifically tailored to this population has been set up. However, these same issues recur as barriers to the implementation of the research, which illustrates all the complexity of pragmatic trials not just those targeting individuals with lown SEP.
Limitations
Despite the valuable insights provided by this study, there are some limitations that should be acknowledged. Firstly, the sample size was relatively small, with only 28 doctors and other health professionals specialized in smoking cessation participating in the study. This limited sample size may affect the generalizability of the findings and the representativeness of the sample.
Secondly, the study was conducted in France, which has a unique healthcare system and cultural context. This may limit the applicability of the findings to other countries with no universal health care system.
Thirdly, the questionnaire used in this study was auto-filled, which may have led to some bias in the responses. While the use of an auto-filled questionnaire ensured consistency in the responses, it may have limited the depth and richness of the data collected.
Finally, the recruiters who participated in the study were not working in the same conditions. This may have influenced their perceptions and experiences with delivering the intervention and may have affected the results.
Addressing these limitations in future studies will enhance our understanding of the issues facing disadvantaged populations and inform the development of more effective smoking cessation interventions.
Conclusions
This study highlights the challenges and barriers faced by health professionals when implementing smoking cessation interventions among low SEP individuals in a pragmatic trial context. A patient-preference intervention where smoking cessation tools were freely delivered was seen as useful and effective, but several challenges limited recruitment and implementation.
The findings suggest that while health professionals recognize the importance of offering smoking cessation interventions to this population, they face specific constraints in their routine that must be addressed. There is a need to address preconceptions and a better understanding of the health problems of low SEP patients. An improvement of research training among health professionals would help integrate the time of research in their daily practice in order to ensure successful implementation of such interventions, without having to separate time of research and time of medical consultation.
The insights gained from this study can inform the development of more effective smoking cessation interventions for disadvantaged populations, as well as provide guidance for researchers and health professionals working in this field, notably those looking to set up pragmatic trials which are increasingly encouraged.
Data Availability
Available upon request from corresponding author, at fabienne.khoury(at)inserm(.)fr.
Abbreviations
Comité de Protection de Personnes
Institut National de Cancer
National Health Interview Survey
Nicotine Replacement Treatment
Randomized controlled trial
Low socio-economic position
Sevrage Tabagique à l’aide d’Outils dédiés selon la Préférence:Smoking cessation using preference-based tools
Standard deviation
Reference category
Tobacco. https://www.who.int/news-room/fact-sheets/detail/tobacco . Accessed 12 Apr 2023.
Hiscock R, Bauld L, Amos A, Fidler JA, Munafò M. Socioeconomic status and smoking: a review. Ann N Y Acad Sci. 2012;1248:107–23.
Article PubMed Google Scholar
Pasquereau A, Andler R, Guignard R, Gautier A, Soullier N, Richard JB, et al. Prévalence nationale et régionale du tabagisme en France en 2021 parmi les 18–75 ans, d’après le Baromètre de Santé publique France. Bull Épidemiol Hebd. 2022;26:470–80.
Google Scholar
Hobkirk AL, Krebs NM, Muscat JE. Income as a moderator of psychological stress and nicotine dependence among adult smokers. Addict Behav. 2018;84:215–23.
Article PubMed PubMed Central Google Scholar
Bryant J, Bonevski B, Paul C, McElduff P, Attia J. A systematic review and meta-analysis of the effectiveness of behavioural smoking cessation interventions in selected disadvantaged groups. Addiction. 2011;106:1568–85.
Kotz D, West R. Explaining the social gradient in smoking cessation: it’s not in the trying, but in the succeeding. Tob Control. 2009;18:43–6.
Article CAS PubMed Google Scholar
Gollust SE, Schroeder SA, Warner KE. Helping smokers quit: understanding the barriers to utilization of smoking cessation services. Milbank Q. 2008;86:601–27.
Hiscock R, Judge K, Bauld L. Social inequalities in quitting smoking: what factors mediate the relationship between socioeconomic position and smoking cessation? J Public Health. 2011;33:39–47.
Article Google Scholar
Leventhal AM, Dai H, Higgins ST. Smoking Cessation Prevalence and Inequalities in the United States: 2014–2019. JNCI J Natl Cancer Inst. 2022;114:381–90.
Kock L, Brown J, Hiscock R, Tattan-Birch H, Smith C, Shahab L. Individual-level behavioural smoking cessation interventions tailored for disadvantaged socioeconomic position: a systematic review and meta-regression. Lancet Public Health. 2019;4:e628–44.
Smith CE, Hill SE, Amos A. Impact of specialist and primary care stop smoking support on socio-economic inequalities in cessation in the United Kingdom: a systematic review and national equity analysis. Addiction. 2020;115:34–46.
Geletko KW, Graves K, Lateef H, Harman J. Tobacco Cessation Counseling and Medications provided by Physicians to Tobacco users during primary care visits. J Prim Care Community Health. 2022;13:215013192210931.
Price KN, Lyons AB, Hamzavi IH, Hsiao JL, Shi VY. Facilitating clinical trials participation of low socioeconomic status patients. Dermatology. 2021;237:843–6.
Héron M, Le Faou A-L, Ibanez G, Métadieu B, Melchior M, El-Khoury Lesueur F. Smoking cessation using preference-based tools: a mixed method pilot study of a novel intervention among smokers with low socioeconomic position. Addict Sci Clin Pract. 2021;16:43.
Patsopoulos NA. A pragmatic view on pragmatic trials. Dialogues Clin Neurosci. 2011;13:217–24.
El-Khoury F, El Aarbaoui T, Héron M, Hejblum G, Métadieu B, Le Faou A-L, et al. Smoking cessation using preference-based tools among socially disadvantaged smokers: study protocol for a pragmatic, multicentre randomised controlled trial. BMJ Open. 2021;11:e048859.
HAS. Arrêt de la consommation de tabac : du dépistage individuel au maintien de l’abstinence en premier recours. 2014.
Joshi A, Kale S, Chandel S, Pal D. Likert Scale: explored and explained. Br J Appl Sci Technol. 2015;7:396–403.
Browning KK, Ferketich AK, Salsberry PJ, Wewers ME. Socioeconomic disparity in provider-delivered assistance to quit smoking. Nicotine Tob Res. 2008;10:55–61.
Twyman L, Bonevski B, Paul C, Bryant J. Perceived barriers to smoking cessation in selected vulnerable groups: a systematic review of the qualitative and quantitative literature. BMJ Open. 2014;4:e006414.
van Wijk EC, Landais LL, Harting J. Understanding the multitude of barriers that prevent smokers in lower socioeconomic groups from accessing smoking cessation support: a literature review. Prev Med. 2019;123:143–51.
Estryn-Béhar M, Leimdorfer F, Picot G. Comment des médecins hospitaliers apprécient leurs conditions de travail. Réponses aux questions ouvertes d’une enquête nationale. Rev Fr Aff Soc. 2010;:27–52.
Donovan JL, Paramasivan S, de Salis I, Toerien M. Clear obstacles and hidden challenges: understanding recruiter perspectives in six pragmatic randomised controlled trials. Trials. 2014;15:5.
Guignard R, Nguyen-Thanh V, Delmer O, Lenormand M-C, Blanchoz J-M, Arwidson P. Interventions pour l’arrêt du tabac chez les fumeurs de faible niveau socio-économique: synthèse de la littérature. Santé Publique. 2018;30:45–60.
Nicholls SG, Carroll K, Zwarenstein M, Brehaut JC, Weijer C, Hey SP, et al. The ethical challenges raised in the design and conduct of pragmatic trials: an interview study with key stakeholders. Trials. 2019;20:765.
Download references
Acknowledgements
We thank members of the STOP pilot committee, and all study investigators and participants.
This work was supported by a grant from the French National Cancer Institute (INCA). Award/Grant number: IRESP- AAP TABAC 2018. The funders of the study had no role in study design, data collection, data analysis, data interpretation, writing of the report, or in the decision to submit the article for publication.
Author information
Authors and affiliations.
Department of social epidemiology, Sorbonne Université, Institut Pierre Louis d’Epidémiologie et de Santé Publique, INSERM, IPLESP, 27 rue Chaligny, Paris, 75012, France
Aurélia Manns, Sarah Mahdjoub, Gladys Ibanez, Emilie Jarrier, Ava Daeipour, Maria Melchior & Fabienne El-Khoury
Faculty of Medicine Pierre et Marie Curie, Department of Education and Research in General Medicine, Sorbonne Université, Paris, F75012, France
Gladys Ibanez
You can also search for this author in PubMed Google Scholar
Contributions
FEK is the Principal investigator of the STOP RCT. MM and GI were implicated in the study design, funding application, and study implementation. AM, SM and FEK designed the health professional survey. EJ and AD implemented the survey. AM carried out the data analysis and wrote the first draft of the manuscript. All authors contributed valuable remarks, helped draft and have approved the final manuscript.
Corresponding author
Correspondence to Fabienne El-Khoury .
Ethics declarations
Ethics approval guidelines and consent to participate.
All study procedures were performed in accordance with relevant guidelines and regulations. The study protocol was approved by a French Ethical Committee (CPP) - n°: 20.01.31.65528 RIPH2 HPS. Written informed consent was obtained from study participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Manns, A., Mahdjoub, S., Ibanez, G. et al. Health professional’s perception of a smoking cessation intervention among disadvantaged patients participating in a pragmatic randomized trial. BMC Health Serv Res 23 , 993 (2023). https://doi.org/10.1186/s12913-023-09950-2
Download citation
Received : 17 May 2023
Accepted : 22 August 2023
Published : 14 September 2023
DOI : https://doi.org/10.1186/s12913-023-09950-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Smoking cessation
- Low socioeconomic position
- Perceived barriers
- Research intervention implementation
- Health professionals
- Pragmatic trials
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- Search Menu
- Supplements
- Advance articles
- Editor's Choice
- Special Issues
- Author Guidelines
- Submission Site
- Why Publish With Us?
- Open Access
- About Nicotine & Tobacco Research
- About Society for Nicotine & Tobacco Research
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, declaration of interests, author contributions, data availability.
- < Previous
The Natural Trajectory of Smoking Cessation Among Cancer Patients Who Want to Quit “On Their Own”: A Mixed-Methods, Longitudinal Study
- Article contents
- Figures & tables
- Supplementary Data
Tia Borger, Abigayle R Feather, Kathleen E Wakeman, William Bowling, Jessica L Burris, The Natural Trajectory of Smoking Cessation Among Cancer Patients Who Want to Quit “On Their Own”: A Mixed-Methods, Longitudinal Study, Nicotine & Tobacco Research , Volume 26, Issue 5, May 2024, Pages 629–633, https://doi.org/10.1093/ntr/ntad207
- Permissions Icon Permissions
Many cancer patients who smoke cigarettes want to quit. Unfortunately, many of these cancer patients prefer to quit without the aid of pharmacotherapy or behavioral counseling. The teachable moment of cancer diagnosis might still position these cancer patients to make meaningful changes in their smoking behavior, but no study has documented the trajectory of smoking cessation outcomes among cancer patients who want to quit “on their own.” This study aimed to fill this gap in the literature.
In this mixed-methods, longitudinal study, 35 cancer patients who declined tobacco treatment because of the desire to quit “on their own” provided data via three surveys and 1–2 semi-structured interviews. The observation period spanned 60 days. Participants were recently diagnosed at and recruited from outpatient cancer clinics.
Participants were mostly female (68.57%), White, non-Hispanic (85.71%), unemployed due to disability (57.14%), and rural residents (54.29%). Across time, 43.76% of participants achieved 50% smoking reduction, 21.88% achieved 3-day floating abstinence, 18.75% achieved 7-day floating abstinence, and 12.50% achieved 30-day point-prevalence abstinence. Key themes that emerged from the interviews centered on intention and confidence to quit and types of tobacco treatment used/received.
This study with cancer patients who desired to quit smoking without assistance found some evidence of quit success, but success waned as criteria grew more stringent. Results showed participants’ initial intention to quit unassisted was quite strong, as few reported tobacco treatment use. Interventions to increase the uptake of evidence-based tobacco treatment among cancer patients are sorely needed.
The preference to quit smoking without assistance is common among cancer patients, even given lack of evidence supporting its effectiveness. This study is the first to explore the trajectory of smoking cessation outcomes among cancer patients who desire to quit without assistance. These data can be used to develop interventions to increase the uptake of tobacco treatment and increase quit success among cancer patients.
Smoking after a cancer diagnosis can have negative health outcomes (eg, early mortality, recurrence) 1 while smoking cessation has many positive outcomes (eg, improved survival, better function). 2 Despite this, 20%–30% of cancer survivors currently smoke and/or use other tobacco products. 3 , 4 Cancer care organizations recommend provision of evidence-based tobacco treatment for cancer patients. 5 However, research shows many cancer patients desire to quit tobacco “on their own” (ie, without Federal Drug Administration (FDA)-approved pharmacotherapy, behavioral counseling, or other professional help). 6 This approach is problematic as little to no treatment use is a well-recognized reason for quit failure. 7 Indeed, less than 10% of people in the general population who smoke successfully quit without using tobacco treatment. 7 While the outcomes of unassisted quit attempts have been tracked in the general population of adults who smoke, 8 , 9 little is known about this preference in cancer patients. Due to the health implications of smoking versus quitting after a cancer diagnosis, it is imperative to better understand the smoking behavior of cancer patients who desire to quit “on their own.” Therefore, this mixed-methods, longitudinal study examines the natural trajectory of smoking cessation attempts and outcomes among cancer patients who desire to quit “on their own.”
Participants
Participants were 35 adult cancer patients who smoked in the past month. To be eligible, and in the context of cancer care delivery, patients must have declined an offer of quit assistance/tobacco treatment specifically because they wanted to quit “on their own.” Other inclusion criteria included (1) reliable phone access, (2) ability to communicate in English, and (3) ability to answer questions about daily life.
Participants were recruited through an National Cancer Institute (NCI)-designated cancer center’s outpatient clinics. Tobacco-related eligibility was determined via a chart review of patients’ responses to standardized questions asked of all adult outpatients. Patients were contacted by investigators and screened for eligibility by phone. Eligible patients completed written informed consent and HIPAA authorization either via mail or e-consent. Data were collected between August 2022 and January 2023, and 71.19% of eligible patients chose to participate. Assessment involved surveys and brief semi-structured interviews over 60 days. Surveys were completed via phone or mail form at days 0, 30, and 60 ( n s = 35, 34, and 32, respectively), and interviews were completed by phone at days 0 and 60 ( n s = 35 and 15, respectively). Participants were purposively selected for the second interview based on the desire to get follow-up information from participants who did and did not report 50% smoking reduction and/or tobacco treatment use at day 30. Participants received $10 checks for each survey and $15 checks for each interview completed. Procedures were approved by the University of Kentucky’s Institutional Review Board (IRB# 78001).
Participants responded to demographic questions from a Behavioral Risk Factors Surveillance System survey. 10 Clinical information was obtained from medical records.
At baseline, motivation to abstain from smoking for the next 30 days was measured via commonly used, validated 11-point Contemplation Ladders, 11 with these verbal anchors for intention and confidence, respectively: 0 = very definitely no and not at all confident to 10 = very definitely yes and extremely confident. At follow-up, the observation period was the past 30 days and participants’ number of smoking days, number of quit attempts, occurrence of 3- and 7-day floating abstinence (ie, 3 or 7 consecutive days of not smoking, respectively), occurrence of 30-day point-prevalence abstinence, and type of tobacco treatment were assessed. 12 Finally, at every assessment, cigarettes per day in the past week were assessed via timeline follow-back.
A standardized interview guide that included a core set of prompts and open-ended questions was used (see Supplementary Appendix ).
Data Analysis
Descriptive statistics were calculated using SPSS. Analysis of interview responses involved thematic analysis. 13 This included (1) reading four randomly selected interviews, (2) identifying key concepts, (3) organizing key concepts into a codebook, (4) double-coding the initial four interviews, (5) finalizing the codebook (see Table 1 ), (6) revising the four previously coded interviews, (7) double-coding all remaining interviews, and (8) analyzing all coded interviews in NVivo.
Semi-Structured Interview Codebook
a The participant’s identification number is in parentheses.
Sample Characteristics
Participants were 54.43 ± 10.86 years old. Most participants identified as female (68.57%, n = 24) and White, non-Hispanic (85.71%, n = 30). Most participants were unemployed due to disability (57.14%, n = 20) and separated, divorced, or widowed (54.29%, n = 19). Most resided in a rural county (54.29%, n = 19). Medicaid was the most common insurance type (54.29%, n = 19). Participants were diagnosed with cancer 7.46 ± 4.94 months pre-enrollment. Common cancer sites were gynecological (28.57%, n = 10), lung (21.26%, n = 8), and head/neck (14.29%, n = 5). Just under half the sample had stage III or IV disease (42.86%, n = 15). Most participants received >1 cancer treatment modality (60.00%, n = 21). Finally, at baseline, participants smoked 12.20 ± 7.78 cigarettes per day. Intention and confidence to abstain from smoking were 4.76 ± 3.68 and 3.32 ± 3.90, respectively.
Survey Results
Participants reported smoking on 25.37 ± 10.21 of the last 30 days (range = 1–30). They reported 13.60 ± 10.72 cigarettes per day (range = 1–40) on smoking days. Seven participants (20.00%) reported using another tobacco product in the past month, most commonly vape products (14.29%, n = 5).
Across time, 31.25% ( n = 10) of participants reported making a quit attempt, with 18.75% reporting a 24-hour quit attempt. Participants reported 5.65 ± 15.23 total quit attempts (range = 0-60) and 2.94 ± 9.79 24-hour quit attempts (range = 0–40). Abstinence and tobacco treatment use outcomes for the 60-day observation period appear in Figure 1 . On day 30, participants reported 25.37 ± 9.37 smoking days (range = 1–30) and 12.77 ± 8.42 cigarettes on smoking days (range = 1–40). On day 60, participants reported 23.41 ± 11.42 smoking days (range = 1–30) and 11.53 ± 8.49 cigarettes on smoking days (range = 1–40). On day 30, 23.53% ( n = 8) of participants achieved 50% smoking reduction from baseline, and at day 60, 31.25% ( n = 10) of participants achieved 50% smoking reduction from day 30. On day 30, four participants achieved 3-day floating abstinence (11.76%) and three achieved 7-day floating abstinence (8.82%), both of which increased by day 60 (21.88% ( n = 7) and 18.75% ( n = 6), respectively). Figure 1 shows 30-day point-prevalence abstinence outcomes. On both days 30 and 60, just over 20% of participants reported using tobacco treatment in the past month. On day 30, 17.65% ( n = 6) used pharmacotherapy and 2.94% ( n = 1) used behavioral treatment. On day 60, participants only reported using pharmacotherapy (21.88%, n = 7). Finally, some participants reported receiving brief advice to quit (see Figure 1 ).

Participants’ smoking cessation outcomes across the 60 days a . Participants’ tobacco treatment use across the 60 days b .
Interview Findings
No meaningful differences were observed between day 0 and 60 interview findings, so the results are integrated later.
While most participants said they would like to quit for good, some admitted not having given quitting a serious try and many had low self-efficacy about quitting. For example, “I haven’t had any [success] with that because I’ve literally not tried. When I think about it, I always think ‘I would love to lay these down.” (126, Day 0). Confidence to quit “on one’s own” was low, even though this was participants’ preferred strategy: “I’d like to do it that way, but I don’t know if I can do it that way.” (102, day 60, emphasis added).
Tobacco Treatment
Some participants discussed receiving brief advice to quit from a health care provider. However, participants were generally unhappy with these interactions: “They all tell me the same thing: ‘You need to quit, you need to quit, you need to quit’” (126, day 0). Very few participants discussed having tried behavioral treatment: “I haven’t even thought about havin’ experience at all with any counseling” (130, day 0). Finally, some participants had never tried pharmacotherapy (eg, “The patches and stuff, I’ve never used anything like that, and I didn’t know if it would make me sick, which I’m sure, just not knowin’ I guess and just wantin’ to quit my own” [124, day 0]) while others discussed trying it in the past, and talked about the perceived ineffectiveness of this approach: “The nicotine patches really didn’t have any effect at all. I tried Wellbutrin once and it just had no effect either” (112, day 60).
Many cancer patients who smoke either decline tobacco treatment or use treatment at a dose or duration that is ineffective for quit success. 14 , 15 Little is known about the natural trajectory of smoking cessation among cancer patients who prefer to quit without assistance. This study aimed to track the quit attempts, abstinence, and tobacco treatment outcomes of cancer patients who initially stated a desire to quit without assistance. Better understanding this preference and its likelihood of success could inform patient–provider communication around optimal approaches to smoking cessation in the context of cancer care delivery.
At baseline, participants smoked over a half of a pack of cigarettes per day on average. Two months later, roughly 4 in 10 were able to reduce the number of cigarettes smoked per day by half. Research in the general population suggests gradual smoking reduction is an inferior quit strategy than abrupt, assisted quitting. 16 , 17 Plus, the health risks of persistent smoking after cancer diagnosis are high, and smoking reduction does not eliminate these dangers. While cancer patients’ efforts to reduce smoking should be viewed positively, it should not be adopted as the “end-goal.” Regarding abstinence, few participants achieved 3-day floating abstinence, with even fewer achieving 7-day floating abstinence, and fewer still achieving 30-day point prevalence abstinence. In the interview, participants reported intention to quit on their own but little confidence in their ability to do so successfully, even though this was their preferred cessation strategy. It is possible participants’ remarks of low confidence directly resulted from their difficulties with smoking cessation. To summarize, for the cancer patients in this brief longitudinal study—all of whom indicated the desire to quit without assistance—there was little evidence of quitting for good .
Unsurprisingly, few participants in this study used tobacco treatment. Only one-quarter of participants opted for pharmacotherapy use and only one participant engaged in behavioral treatment. Interview results corroborate these findings, as many participants discussed either ineffectiveness of past pharmacotherapy use or never having tried pharmacotherapy or behavioral treatment in the past. Additionally, any brief advice to quit patients received from health care professionals was reported in interviews to be unhelpful. While suboptimal, these findings are expected given this study’s focus on cancer patients who were intentional about quitting “on their own.” The importance of educating cancer patients who use tobacco about the benefits of tobacco treatment and employing motivational interviewing or other techniques to encourage its use cannot be understated.
There are study limitations. First, the sample size was insufficient to power inferential statistics regarding change over time. However, retention was very high for an observational study that for many coincided with cancer treatment. Second, even though this study focused on cancer patients who wanted to quit on their own, it would have been advantageous to collect greater detail about tobacco treatment use (eg, number of use days). Finally, one cannot rule out the possibility that some participants stated the desire to quit “on their own” because they deemed it more socially acceptable than admitting they were not ready to quit. However, it is believed that participants’ stated intention was reflective of a true preference to quit unassisted, as this approach is observed and viewed favorably in the general population of people who smoke. 18 , 19
This sample of cancer patients achieved fleeting success with smoking cessation. This is likely due to low rates of tobacco treatment use in combination with other well-established barriers to quit success in cancer patients (eg, distress, other smokers in the home; (eg, see Puelo et al. 20 ). Given low tobacco treatment use and reports of ineffectiveness of pharmacotherapy among participants in this sample, interventions with cancer patients are needed to evoke more positive attitudes toward, provide education about, and increase uptake of tobacco treatment.
This work was supported by the Patient-Oriented and Population Sciences Shared Resource Facility of the University of Kentucky Markey Cancer Center (P30 CA177558), an administrative supplement to the Markey Cancer Center Support grant (P30 CA177558-05S5), and a Center for Advancing Translational Sciences grant (UL1 TR001998).
None declared.
Tia Borger (Conceptualization [equal], Data curation [equal], Formal analysis [equal], Investigation [equal], Methodology [equal], Project administration [equal], Writing—original draft [equal], Writing—review & editing [equal]), Abigayle Feather (Conceptualization [supporting], Investigation [supporting], Methodology [supporting], Project administration [supporting], Writing—review & editing [supporting]), Kathleen Wakeman (Project administration [supporting]), William Bowling (Conceptualization [supporting], Project administration [supporting]), and Jessica Burris (Conceptualization [equal], Funding acquisition [equal], Investigation [equal], Methodology [equal], Resources [equal], Software [equal], Supervision [equal], Writing—review & editing [equal])
The data generated during and/or analyzed for the current study are not publicly available. Ethics approval, participant permissions, and all other relevant approvals were granted for this data sharing.
US Department of Health and Human Services . Atlanta GA : US Department of Health and Human Services, Center for Disease Control and Prevention, Office on Smoking and Health ; 2014 .
Sheikh M , Mukeriya A , Shangina O , Brennan P , Zaridze D. Postdiagnosis smoking cessation and reduced risk for lung cancer progression and mortality: a prospective cohort study . Ann Intern Med. 2021 ; 174 ( 9 ): 1232 – 1239 .
Google Scholar
Swoboda CM , Walker DM , Huerta TR. Likelihood of smoking among cancer survivors: an updated Health Information National Trends Survey analysis . Nicotine Tob Res . 2019 ; 21 ( 12 ): 1636 – 1643 . https://doi.org/10.1093/ntr/ntz007
Gallaway MS , Glover-Kudon R , Momin B , et al. . Smoking cessation attitudes and practices among cancer survivors—United States, 2015 . J Cancer Surviv. 2019 ; 13 ( 1 ): 66 – 74 . https://doi.org/10.1007/s11764-018-0728-2
Lowy DR , Fiore MC , Willis G , et al. . Treating smoking in cancer patients: an essential component of cancer care—the new National Cancer Institute tobacco control monograph . JCO Oncol Pract . 2022 ; 18 ( 12 ): e1971 – e1976 .
Burris JL , Borger TN , Shelton B , et al. . Cancer patients’ tobacco use and treatment referral response: implementation outcomes at a National Cancer Institute-Designated Cancer Center . J Oncol Pract . 2022 ; 18 ( 2 ): e261 – e270 .
Babb S , Malarcher A , Schauer G , Asman K , Jamal A. Quitting Smoking Among Adults—United States, 2000–2015 . MMWR Morb Mortal Wkly Rep. 2017 Jan 6 ; 65 ( 52 ): 1457 – 1464 .
Google Preview
Bachmann MS , Znoj H , Brodbeck J. Identifying distinct quitting trajectories after an unassisted smoking cessation smoking cessation attempt: an ecological momentary assessment study . Open J Med Psychol . 2012 ; 1 ( 3 ): 44 – 50 .
Soulakova JN , Crockett LJ. Unassisted quitting and smoking cessation methods used in the United States: analyses of 2010-2011 tobacco use supplement to the current population survey data . Nicotine Tob Res. 2018 ; 20 ( 1 ): ntw273 – ntw239 .
Centers for Disease Control and Prevention . Behavioral risk factor surveillance system questionnaire, 2021 . Atlanta, GA : U.S. Department of Health and Human Services, Centers for Disease Control and Prevention ; 2021 .
Biener L , Abrams DB. The contemplation ladder: validation of a measure of readiness to consider smoking cessation . J. Health Psychol. 1991 ; 10 ( 5 ): 360 – 365 .
Land SR , Toll BA , Moinpour CM , et al. . Research priorities, measures, and recommendations for assessment of tobacco use in clinical cancer research . Clin Cancer Res. 2016 ; 22 ( 8 ): 1907 – 1913 .
Hsieh HF , Shannon SE. Three approaches to qualitative content analysis . Qual Health Res. 2005 ; 15 ( 9 ): 1277 – 1288 .
Gravely S , Cummings KM , Hammond D , et al. . Self-reported quit aids and assistance used by smokers at their most recent quit attempt: findings from the 2020 International Tobacco Control Four Country Smoking and Vaping Survey . Nicotine Tob Res . 2021 ; 23 ( 10 ): 1699 – 1707 .
Borger T , Shelton BJ , Valentino J , et al. . A daily assessment study of smoking cessation after a head and neck cancer diagnosis . Nicotine Tob Res . 2022 ; 24 ( 11 ): 1781 – 1788 .
Lindson-Hawley N , Aveyard P , Hughes JR. Gradual reduction vs abrupt cessation as a smoking cessation strategy in smokers who want to quit . JAMA. 2013 ; 310 ( 1 ): 91 – 92 .
Lindson-Hawley N , Banting M , West R , et al. . Gradual versus abrupt smoking cessation: a randomized, controlled noninferiority trial . Ann Intern Med. 2016 ; 164 ( 9 ): 585 – 592 .
Smith AL , Carter SM , Dunlop SM , Freeman B. The views and experiences of smokers who quit smoking unassisted: a systematic review of the qualitative evidence . PLoS One . 2015 ; 10 ( 5 ): e0127144 . https://doi.org/10.1371/journal.pone.0127144
Morphett K , Partridge B , Gartner C , Carter A , Hall W. Why don’t smokers want help to quit? A qualitative study of smokers’ attitudes towards assisted vs unassisted quitting . International Journal of Environmental Research and Public Health . 2015 ; 12 ( 6 ): 6591 – 6607 . https://doi.org/10.3390/ijerph120606591
Puelo GE , Borger T , Bowling WR , Burris JL. The state of the science on cancer diagnosis as a “teachable moment” for smoking cessation: a scoping review . Nicotine Tob Res. 2022 ; 160 ( 168 ): 160 – 168 .
Supplementary data
Email alerts, citing articles via.
- About Nicotine & Tobacco Research
- Recommend to your Library
Affiliations
- Online ISSN 1469-994X
- Copyright © 2024 Society for Research on Nicotine and Tobacco
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 41, Issue 5
- Cessation of Smoking Trial in the Emergency Department (COSTED): a multicentre randomised controlled trial
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-5623-4178 Ian Pope 1 ,
- http://orcid.org/0000-0001-7162-0512 Lucy V Clark 1 ,
- http://orcid.org/0000-0003-2965-8941 Allan Clark 1 ,
- http://orcid.org/0000-0002-7579-3215 Emma Ward 1 ,
- http://orcid.org/0000-0003-2065-6878 Pippa Belderson 1 ,
- Susan Stirling 1 ,
- http://orcid.org/0000-0002-0165-1150 Steve Parrott 2 ,
- http://orcid.org/0000-0003-1496-7450 Jinshuo Li 2 ,
- http://orcid.org/0000-0003-2736-2784 Tim Coats 3 ,
- http://orcid.org/0000-0001-7411-4260 Linda Bauld 4 ,
- http://orcid.org/0000-0002-4663-6923 Richard Holland 5 ,
- http://orcid.org/0000-0002-0805-0200 Sarah Gentry 1 ,
- http://orcid.org/0000-0001-7873-0300 Sanjay Agrawal 6 ,
- http://orcid.org/0000-0002-3016-4925 Benjamin Michael Bloom 7 ,
- http://orcid.org/0000-0002-9009-5423 Adrian A Boyle 8 ,
- Alasdair J Gray 9 ,
- M Geraint Morris 10 ,
- http://orcid.org/0000-0002-3757-5591 Jonathan Livingstone-Banks 11 ,
- http://orcid.org/0000-0003-0876-3304 Caitlin Notley 1
- 1 Norwich Medical School , University of East Anglia Norwich Medical School , Norwich , UK
- 2 Department of Health Sciences , University of York , York , UK
- 3 Department of Cardiovascular Sciences , University of Leicester , Leicester , UK
- 4 Usher Institute , The University of Edinburgh , Edinburgh , UK
- 5 University of Exeter , Exeter , UK
- 6 Leicester Royal Infirmary , Leicester , UK
- 7 Emergency Department , Barts Health NHS Trust , London , UK
- 8 Emergency Department , Addenbrooke's Hospital , Cambridge , UK
- 9 Emergency Department , Royal Infirmary of Edinburgh , Edinburgh , Edinburgh , UK
- 10 Emergency Department , Homerton University Hospital NHS Foundation Trust , London , UK
- 11 Nuffield Department of Primary Care Health Sciences , University of Oxford , Oxford , UK
- Correspondence to Dr Ian Pope, Norwich Medical School, University of East Anglia, Norwich, UK; i.pope{at}uea.ac.uk
Background Supporting people to quit smoking is one of the most powerful interventions to improve health. The Emergency Department (ED) represents a potentially valuable opportunity to deliver a smoking cessation intervention if it is sufficiently resourced. The objective of this trial was to determine whether an opportunistic ED-based smoking cessation intervention can help people to quit smoking.
Methods In this multicentre, parallel-group, randomised controlled superiority trial conducted between January and August 2022, adults who smoked daily and attended one of six UK EDs were randomised to intervention (brief advice, e-cigarette starter kit and referral to stop smoking services) or control (written information on stop smoking services). The primary outcome was biochemically validated abstinence at 6 months.
Results An intention-to-treat analysis included 972 of 1443 people screened for inclusion (484 in the intervention group, 488 in the control group). Of 975 participants randomised, 3 were subsequently excluded, 17 withdrew and 287 were lost to follow-up. The 6-month biochemically-verified abstinence rate was 7.2% in the intervention group and 4.1% in the control group (relative risk 1.76; 95% CI 1.03 to 3.01; p=0.038). Self-reported 7-day abstinence at 6 months was 23.3% in the intervention group and 12.9% in the control group (relative risk 1.80; 95% CI 1.36 to 2.38; p<0.001). No serious adverse events related to taking part in the trial were reported.
Conclusions An opportunistic smoking cessation intervention comprising brief advice, an e-cigarette starter kit and referral to stop smoking services is effective for sustained smoking abstinence with few reported adverse events.
Trial registration number NCT04854616 .
- emergency departments
- substance-related disorders
- Clinical Trial
Data availability statement
Data are available upon reasonable request. The protocol, consent form, statistical analysis plan, medical ethics committee approvals, training materials and other relevant study materials are available online at https://osf.io/8hbne/ . Deidentified participant data will be made publicly available within 3 months at the above address.
This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/ .
https://doi.org/10.1136/emermed-2023-213824
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
WHAT IS ALREADY KNOWN ON THIS TOPIC
Emergency Department (ED)-based smoking cessation interventions have shown promise but there is uncertainty about the best intervention components and longer term outcomes.
E-cigarettes have been shown to be one of the most effective smoking cessation tools but have never been tested in the ED environment.
WHAT THIS STUDY ADDS
In this trial significantly more people receiving a smoking cessation intervention in the ED achieved long-term smoking abstinence compared with those receiving usual care. Findings were limited by relatively low biochemical validation rates and slightly differential rates of follow-up.
This trial contributes to the existing evidence that ED-based interventions are effective and is the first trial to test e-cigarettes in the ED setting.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Policy makers should consider the ED as a location to deliver smoking cessation interventions as long as appropriate funding is available for dedicated staff.
This study shows that it is possible to recruit efficiently and to deliver a brief opportunistic intervention to support sustained tobacco smoking abstinence in the ED setting.
Introduction
Tobacco kills more than 8 million people each year worldwide. 1 In the UK 6.4 million people continue to smoke, with those in ‘routine and manual’ occupations having a smoking rate of 22.8% compared with 8.3% for those in ‘managerial and professional’ occupations. 2 Treating tobacco addiction is a powerful tool to combat premature death, address health inequalities and to reduce healthcare utilisation. 3 4 Emergency Departments (EDs) see large numbers of people, and those who attend the ED are more likely to smoke 5 and suffer complex health inequalities. 6
Smoking cessation interventions embedded in EDs have shown promise; however, there is uncertainty about the long-term impact and optimal intervention components. 7 Previous studies in ED settings have evaluated behavioural support alone, or behavioural support combined with an offer of nicotine replacement therapy (NRT). 7 Evidence shows that e-cigarettes are more effective than NRT in supporting people to quit smoking, but the majority of trial evidence comes from people who are motivated to stop smoking rather than people who potentially have no prior intention to quit. 8 An intervention to treat tobacco dependency in an ED setting using e-cigarettes has not previously been tested.
In this trial we aimed to test the real-world effectiveness of an ED-based brief tailored smoking cessation intervention in comparison with usual care, by comparing continuous smoking abstinence at 6-month follow-up between trial groups.
Trial design
The Cessation of Smoking Trial in the Emergency Department (COSTED) is a two-arm pragmatic, multicentre, parallel-group, individually randomised controlled trial carried out at six UK NHS EDs. 9 The study protocol has been published 9 and is available in online supplemental file 1 and the statistical analysis plan is available online. 10 A full economic evaluation and process evaluation were embedded and will be published separately.
Supplemental material
Participants.
We recruited adults (aged 18 years or older) who reported smoking tobacco daily, attending the ED for medical treatment or accompanying someone attending for medical treatment. Participants were screened while they were in the ED. People were excluded if they had an expired carbon monoxide (CO) of <8 parts per million (ppm), required immediate medical treatment, were in police custody, had a known allergy to nicotine, were current dual users (defined as daily e-cigarette use), were considered not to have capacity to consent or had already taken part in the trial.
Where the person accompanying an included patient met the inclusion criteria and wished to participate, they were enrolled in a similar way to the patients and assigned to the same treatment group as the patient they accompanied. They were followed up but are not included in the analysis reported in this paper as they were not randomised individually (as per the protocol).
Randomisation
People who met the inclusion criteria and gave consent were individually randomised (1:1) to the intervention or control groups through a web-based service provided by the Norwich Clinical Trials Unit. This computer-generated randomisation employed varying block sizes and was stratified by the recruitment sites which allowed for concealment of allocation. Due to the participatory nature of the intervention, it was not feasible to blind participants or those delivering the intervention to group allocation.
Interventions
Participants allocated to the intervention group received an opportunistic smoking cessation intervention undertaken face-to-face in the ED, comprising three elements: (1) brief smoking cessation advice (up to 15 min), (2) the provision of an e-cigarette starter kit plus advice on its use (up to 15 min) and (3) referral to local stop smoking services.
The advice was delivered individually (or with an accompanying person) by a dedicated smoking cessation advisor based in the ED. Protocol-driven 10 theory-based 11 smoking cessation advice addressed key aspects of the importance of switching away from tobacco smoking, tailored to the participants’ presenting condition (eg, discussing improved wound healing for patients attending with a laceration). This part of the intervention was a single session undertaken within the ED while patients were waiting to be seen or after discharge.
The e-cigarette starter kit (DotPro, manufactured by Liberty Flights, an independent e-cigarette manufacturer not funded by the tobacco industry) is a ‘pod’ device. The kit included 11 pods (3 tobacco flavoured, 4 berry flavoured and 4 menthol flavoured) of 20 mg/mL nicotine strength. This device was chosen based on in-depth patient and public consultation, considering ease of use, nicotine delivery, satisfaction, price and availability.
Participants were electronically referred to the local stop smoking service which provided routinely available follow-up support. This typically consisted of a telephone call offering support and, if taken up, advice on how to quit and free provision of NRT.
The intervention was delivered by smoking cessation advisors trained specifically for the role. The advisors were either research nurses, research practitioners, ED nurses or healthcare assistants seconded to the trial and received 2.5 days of training. A TIDieR checklist, 12 logic model and intervention manual are available on the Open Science Framework. 10
Participants allocated to the control group were given details of local NHS stop smoking services via written material but were not referred directly.
Research assessments were undertaken at baseline and then 1, 3 and 6 months after randomisation. Local site research teams undertook the baseline assessments face-to-face in the ED. Follow-up questionnaires were sent as a link in a text message or email, or by mail with freepost envelopes for return. We attempted to contact all participants who did not respond to the initial request at least twice. Those who reported smoking abstinence at 6 months were invited to undertake a CO reading either at the ED, at a convenient location or remotely by being sent a CO monitor and having a video call with a researcher. Participants were not given details about CO test cut-offs or that it was being used to verify abstinence. All measures except for the CO verification at baseline and 6 months were self-reported. It was not possible to blind outcome assessors to study group.
On completion of the 6-month follow-up questionnaires, participants received a £30 shopping voucher for taking part. A further £30 voucher was offered to participants who reported being smoke-free for providing a CO reading. Participants were, however, unaware they would be offered the additional £30 when completing follow-up questionnaires to avoid it acting as an incentive.
The primary effectiveness outcome was self-reported continuous smoking abstinence, biochemically validated by CO monitoring at 6 months with a cut-off of <8 ppm (according to the Russell standard). 13 If smoking status or CO readings could not be obtained, the participant was assumed to be smoking as is agreed practice in smoking cessation trials. 13 14 Bedfont Micro Smokerlyzers (Bedfont Scientific, Maidstone, UK) were used at baseline and follow-up to measure CO levels. Participants were classified as having been biochemically-verified continuously abstinent if they reported having fewer than six lapses in the last 6 months and gave a CO reading of <8 ppm. Self-reported 7-day abstinence rates were defined as answering ‘no’ to the question “‘Have you smoked a tobacco cigarette in the past 7 days?”
Secondary outcomes were self-reported 7-day point prevalence smoking status at 1 and 3 months, biochemically-validated 7-day point prevalence abstinence at 6 months, number of quit attempts, time to relapse (if applicable), number of cigarettes per day, nicotine dependence, 15 number of times using an e-cigarette per day, incidence of self-reported dry cough or mouth or throat irritation, motivation to stop smoking, 16 self-reported use of healthcare services in the last 6 months, self-reported use of smoking cessation services in the last 6 months and quality of life (using the EQ-5D-5L). 17
Adverse events were self-reported by participants in the follow-up questionnaire in response to the experience of symptoms of a dry cough and throat/mouth irritation. Attendance at hospital was asked about at 1, 3 and 6 months.
Further details of secondary outcomes and adverse events are available in the published protocol. 9
Sample size
A sample size of 972 (486 per group) conferred 90% power to detect a difference between a biochemically-confirmed control quit rate of 6.2% and biochemically-confirmed intervention quit rate of 12.2% at the 5% level of significance. This was based on a US trial of an ED smoking cessation intervention using a brief intervention, referral to smoking cessation services and nicotine replacement. 18 A quit rate of 6.2% was used in the control group based on an average of three studies of unmotivated quitters who received either contact details for stop smoking services or no intervention. 19–21
Statistical analysis
The primary outcome measure was compared between the two groups using a binary regression model with a log link to estimate the relative risk and with an identity link to estimate the difference in risk; both models included fixed effects for randomisation group and site. In cases when the convergence failed for the identity link model, a Gaussian model with robust variance was used. Full details of the statistical analysis can be found in the statistical analysis plan online. 10 Those conducting the analysis were not blinded.
Patient and public involvement
This trial was initially informed by patient and public involvement (PPI) consultations in three EDs, assessing the acceptability and feasibility of approaching people about smoking cessation. We actively recruited further PPI volunteers who were then involved in trial set-up through advising on study materials, checking Case Report Form burden and advising on language use. A separate PPI panel was recruited to inform intervention components (choice of e-cigarette). We recruited two independent PPI members to be involved in our trial steering group, providing a lay perspective in oversight of the trial. We have shared the results with all our PPI representatives.
Between January and August 2022 we screened patients in the ED of whom 2888 reported current smoking; 1443 agreed to take part in the trial and were assessed for eligibility and 484 were subsequently randomised to the intervention group and 488 to the control group ( figure 1 ).
- Download figure
- Open in new tab
- Download powerpoint
Trial profile. *Where the person accompanying an included patient met the inclusion criteria and wished to participate, they were enrolled in a similar way to the patients and assigned to the same treatment group as the patient they accompanied. They were followed up but are not included in this analysis.
The most common reasons for declining to take part were: no reason given (n=409, 29.1%), feeling too unwell (n=296, 21.0%) and not wanting to quit (n=161, 11.4%). The most common reasons for being excluded were providing a CO reading of <8 ppm (n=308, 65.8%), currently using an e-cigarette daily (n=52, 11.1%) and not smoking daily (n=31, 6.6%).
Three participants were found later to be ineligible and were considered post-randomisation exclusions, two due to being randomised twice and one who subsequently reported daily use of an e-cigarette.
There were 5 (1.0%) withdrawals in the intervention group and 12 (2.5%) in the control group. Reasons for withdrawals were no reason given (n=7), wanting the intervention (n=3), did not want to answer the questions (n=6) and reporting a new allergy to nicotine (n=1).
The baseline characteristics of the participants are shown in table 1 and were broadly equivalent across the two groups. The mean deprivation decile was 4.31 in the intervention group and 4.53 in the control group (1=most deprived, 10=least), indicating that participants were generally from more deprived neighbourhoods than average.
- View inline
Baseline characteristics of the intention-to-treat population
Primary outcome
Biochemically-verified self-reported continuous abstinence at 6 months was 7.2% (35/484) in the intervention group and 4.1% (20/488) in the control group (relative risk (RR) 1.76 (95% CI 1.03 to 3.01), risk difference 3.3% (95% CI 0.3% to 6.3%)).
In total, 351 (72.5%) participants in the intervention group and 317 (65.0%) in the control group reported their smoking status at 6 months ( figure 1 ). Of those who reported continuous abstinence, 35/122 (28.7%) in the intervention group and 20/64 (31.3%) in the control group went on to have their abstinence biochemically verified. Sixty-eight participants in the intervention group and 32 in the control group declined to provide a CO reading, and 19 in the intervention group and 12 in the control group had a CO reading ≥8 ppm.
The online supplemental material shows a sensitivity analysis for the assumption that those who did not respond or did not provide a CO reading were still smoking. Provided the dropouts have <0.2 times the odds of being abstinent than those who remain, the intervention is statistically significant. Even under the assumption that the dropouts are equally likely to smoke as those who remain, the estimated adjusted OR is still larger than 1.5 (1.56, 95% CI 0.88 to 2.76), but no longer statistically significant.
Secondary outcomes
Self-reported 7-day abstinence at 6 months was 23.3% (113/484) in the intervention group and 12.9% (63/488) in the control group (RR 1.80 (95% CI 1.36 to 2.38); p<0.0001). Table 2 shows the abstinence rates at all time points.
Abstinence rates at different time points
The number needed to treat to achieve biochemically-validated smoking continuous abstinence at 6 months was 30 (95% CI 16 to 343) and for self-reported abstinence at 6 months it was 9 (95% CI 6 to 11).
At 6 months the median (IQR) number of quit attempts was 2 (1–4) in the intervention group and 1 (0–3) in the control group (p<0.0001). Of those who responded, the number of participants using an e-cigarette daily at 6 months was 39.4% (125/317) in the intervention group and 17.5% (53/303) in the control group ( table 3 ). The number reporting not having used an e-cigarette in the past 6 months was 14.8% (47/317) in the intervention group and 54.5% (165/303) in the control group.
Secondary outcome measures
The number of participants reporting serious adverse events was 5.2% (25/484) in the intervention group and 5.1% (25/488) in the control group ( table 4 ). None were related to the intervention.
Adverse event by type
Principal findings
In this trial adults attending the ED who smoked and received the intervention of brief advice, an e-cigarette starter kit and referral to stop smoking services were statistically significantly more likely to achieve sustained smoking abstinence than those who received signposting to stop smoking services alone. The biochemically-verified quit rate was not as high as the assumptions underpinning the power calculation; however, the difference found achieved statistical significance, with the potential to impact on population smoking prevalence. There was a much larger difference in self-reported abstinence compared with the power calculation, which may indicate that the biochemically-verified quit rate is an underestimate of the true effect of the intervention.
Comparison with previous studies
These results strengthen previous findings that ED-based smoking cessation interventions are effective. 7 To our knowledge, the 6-month self-reported quit rate is the highest reported by any ED-based smoking cessation intervention trial to date. As the first ED-based trial to include an e-cigarette starter kit as part of the intervention, this suggests that the e-cigarette itself, in addition to brief advice, may have contributed to the size of the effect. The findings are in keeping with existing evidence that e-cigarettes are effective in aiding smoking cessation, 8 22 but are novel as this is the first trial to use them opportunistically to support abstinence in those who smoke and are accessing healthcare services, but who are not actively seeking help to quit.
Of people who smoke attending the ED, half were willing to take part in the trial, indicating that the ED represents an acceptable location for smoking cessation intervention and therefore offers a valuable opportunity to engage those who smoke who are not currently seeking to quit.
Strengths and limitations
The strengths of this study include: its large sample size; it was inclusive, being delivered across multiple UK centres recruiting a diverse population; it used an objective primary outcome measure; inclusion criteria were broad to ensure generalisability; it had a robust study design with appropriate randomisation and allocation concealment and the trial had a pragmatic design with an intervention that should be easy to replicate in day-to-day practice assuming it is appropriately resourced.
A limitation of the study was that control participants did not simply receive a leaflet signposting them to stop smoking services, as in order to collect the data needed from the control group there was a discussion with researchers that may have affected smoking behaviour. They underwent CO breath testing, were asked extensive questions about their smoking, received written information on stop smoking services and were asked their smoking status three times over the follow-up period. This may have caused a higher quit rate in the control group compared with true usual care (which is likely to have no mention of quitting smoking) and therefore potentially underestimates the impact of the intervention.
Successfully encouraging our trial participants to submit a CO reading at 6 months proved to be very challenging. This may in part be due to the transient and sometimes chaotic nature of the lives of many ED attendees, the large geographical catchment area of participating EDs and transportation complexities. Thus, the biochemically confirmed cessation rates (while statistically significant) may underestimate the true effect size. Equally, it is possible that being part of the intervention group encouraged more of those to provide biochemical confirmation, although our biochemical confirmation findings mirrored our self-report findings and the percentage of CO verifications at 6 months was similar across the intervention and control groups. While the biochemically confirmed quit rates in the intervention and control groups were not as large as the power calculation had been based on, the self-reported continuous abstinence rate was much larger. The difference is likely a result of the difficulty with collecting CO readings. There was a difference in response rate between the intervention and control groups. As is convention in smoking cessation trials, we assumed that those who did not respond were still smoking; 23 however, this assumption may be conservative and has been examined in a sensitivity analysis in the online supplemental material . The challenges achieving biochemical verification and the differences in response rates between the groups are limitations which arise from this being a pragmatic trial which attempted to replicate real life. This is in keeping with other ED-based smoking cessation trials which attempted to biochemically verify smoking status with loss to follow-up rates of around 30% and biochemical verification of those reporting abstinence of around 50%.
Policy implications
This trial has demonstrated the effectiveness of a simple, opportunistic and acceptable intervention in a real-world setting with no serious adverse effects. We consider that this could be rolled out to reach a large proportion of current smokers, although dedicated staff are clearly needed to deliver the intervention so as not to burden clinical staff. Those attending EDs are generally from more deprived communities and more likely to smoke than the general population. 5 6 Therefore, this intervention has the potential to address health inequalities that arise from disparities in smoking rates between different socioeconomic groups. 3
Given high accessibility to an at-risk population, future research might explore the use of EDs as a location to support people to change other behaviours such as excess alcohol use or low physical activity.
In this study of adults who smoke and who were attending the ED, an intervention comprising brief advice, provision of an e-cigarette starter kit and referral to stop smoking services resulted in significantly increased sustained smoking abstinence 6 months later compared with those signposted to stop smoking services. Providing smoking cessation support in the ED should be considered to reach groups of the population that may not routinely engage with stop smoking services but have the most to gain from stopping smoking.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
The study was approved by the UK National Research Ethics Committee – Oxford B (reference 21/SC/0288). Participants gave informed consent to participate in the study before taking part.
Acknowledgments
We thank the study sponsor, Norfolk and Norwich University Hospital NHS Foundation Trust. The study was led by researchers at the University of East Anglia and managed by the Norwich Clinical Trials Unit (specifically Mei-See Man, Matthew Hammond, Tom Conway, Ollie Ellacott, Antony Colles, Erica Berardi and Zuzanna Halicka). Our thanks go to the research teams at the organisations involved in recruitment and in supporting delivery of the trial and the sites’ local stop smoking services. We would also like to thank PPI contributors who were critical in defining the choice of e-cigarette starter kit and shaping the intervention. We acknowledge the contribution of the smoking cessation advisors who underwent training to deliver the intervention. We thank SmokeFree Norfolk for supporting the study by training the advisors. Thanks also to our independent Trial Steering Committee and Data Monitoring Committee members (Professor Steve Goodacre, Dr Gary Abel, Dr Sarah Jackson, Carmen Glover, Dr Francesca Pesola, Deb Smith, Dr Kirsty Challen, Professor Jamie Brown, Professor Paul McCrone). We thank all the participants for taking part. The e-cigarette and pods were DotPro produced by Liberty Flight and were purchased at wholesale price. Liberty Flight had no role in the study design, data collection, data analysis, data interpretation or writing of this report.
- World Health Organization
- Office for National Statistics
- Action on Smoking and Health (ASH)
- Mullen KA ,
- Manuel DG ,
- Hawken SJ , et al
- Lowenstein SR ,
- Tomlinson D ,
- Koziol-McLain J , et al
- NHS Digital
- Lemhoefer C ,
- Wellmann J , et al
- Hartmann-Boyce J ,
- Lindson N ,
- Butler AR , et al
- Belderson P , et al
- Pope I , et al
- van Stralen MM ,
- Hoffmann TC ,
- Glasziou PP ,
- Boutron I , et al
- Stead L , et al
- Ferguson J ,
- Chesterman J , et al
- Heatherton TF ,
- Kozlowski LT ,
- Frecker RC , et al
- Crittenden KS ,
- Manfredi C ,
- Lacey L , et al
- ↵ Eq-5D-5L . 2020 . Available : https://euroqol.org/eq-5d-instruments/eq-5d-5l-about/
- Bernstein SL ,
- D’Onofrio G ,
- Rosner J , et al
- Hennrikus D ,
- Joseph AM ,
- Lando HA , et al
- Pieterse ME ,
- Seydel ER ,
- DeVries H , et al
- Malte CA , et al
- Theodoulou A ,
- Ordóñez-Mena JM , et al
- Barnes SA ,
- Larsen MD ,
- Schroeder D , et al
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
- Data supplement 2
Handling editor Jason E Smith
X @drianpope, @dradrianboyle, @AddictionUEA
Contributors IP and CN conceived the original idea for the trial and obtained funding. IP is the guarantor for the study. EW, PB, CN and IP designed the intervention. EW and PB undertook PPI work to determine the optimal device to use. IP, SA, BMB, AAB, AJG and MGM were principal investigators for each of the participating centres. TC, LB, RH and SG provided advice on methodology and implementation. LVC acted as trial manager. AC and SS designed the statistical method, wrote the statistical analysis plan and independently undertook the statistical analysis. SP and JL wrote the health economic evaluation plan and undertook the economic analysis. JLB undertook the literature search. All authors made a substantial contribution to drafting or revising the article and gave final approval of the version to be published.
Funding This study is funded by the NIHR (Health Technology Assessment (NIHR129438)). The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care. The funder had no role in considering the study design or in the collection, analysis, interpretation of data, writing of the report, or decision to submit the article for publication.
Competing interests None declared.
Patient and public involvement Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Linked Articles
- Commentary Electronic cigarettes: beneficial for smoking cessation but harmful to public health? Gina Kruse Jon Samet Joaquin Barnoya Emergency Medicine Journal 2024; 41 283-284 Published Online First: 26 Mar 2024. doi: 10.1136/emermed-2024-213940
- Commentary Opportunistic screening in the emergency department James France Emergency Medicine Journal 2024; 41 285-286 Published Online First: 10 Apr 2024. doi: 10.1136/emermed-2024-214073
Read the full text or download the PDF:
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- 17 April 2024
- Correction 18 April 2024
Smoking bans are coming: what does the evidence say?
- Carissa Wong
You can also search for this author in PubMed Google Scholar
Smoking rates have declined globally over the past few decades. Credit: Debbie Bragg/Everynight Images via Alamy
You have full access to this article via your institution.
Nations worldwide are aiming to introduce some of the tightest restrictions ever on smoking and vaping, especially among young people.
On 16 April, UK lawmakers backed one of the world’s most ambitious plans — to create by 2040 a ‘smoke-free’ generation of people who will never be able to legally buy tobacco. The proposal is now a step closer to becoming law. The UK, Australian and French governments are also clamping down on vaping with e-cigarettes. These countries’ bold policies are currently in the minority, say researchers, but such measures would almost certainly prevent diseases, as well as save lives and billions of dollars in health-care costs.

Smoking scars the immune system for years after quitting
The UK plan would probably “be the most impactful public-health policy ever introduced”, says health-policy researcher Duncan Gillespie at the University of Sheffield, UK. The Conservative government’s Prime Minister Rishi Sunak initiated the proposal. The government hopes that the smoking restrictions, alongside offering health benefits for individuals, will reduce toxic chemicals leaching from used vapes into the environment.
Smoke-free generations
The health harms of smoking tobacco have been established for decades — it substantially raises the risk of diseases including cancer, heart disease and diabetes. Increased awareness of these health risks has led to a global decline in the deadly habit in the past few decades (see ‘Smoke clearing’).
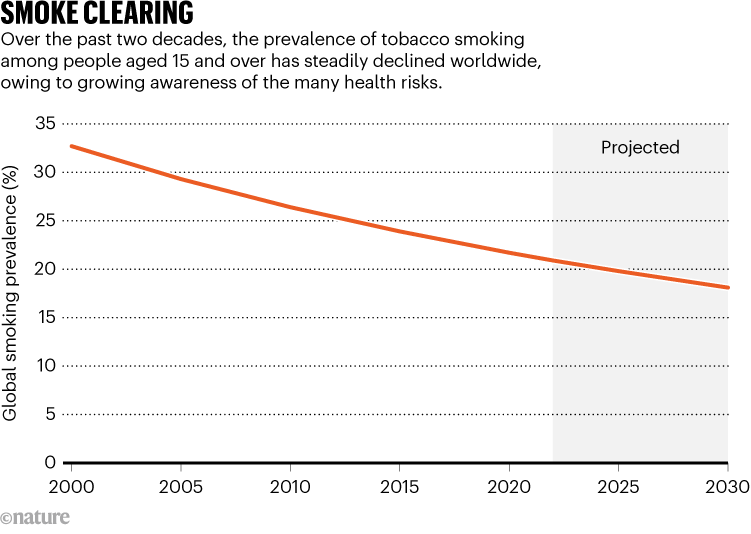
Source: WHO
Any drop in smoking rates saves money and reduces the burden on health-care systems, says Alison Commar, who studies tobacco policy at the World Health Organization (WHO) in Geneva, Switzerland. The WHO estimates that tobacco use costs the world US$1.4 trillion every year in health expenditures and lost productivity. “Every tobacco-related illness is adding to the burden on the health system unnecessarily,” says Commar.
The UK proposal, announced last October, would ban the sale of tobacco to any person born in or after 2009. That would prevent anyone who turns 15 or younger this year from ever buying cigarettes legally in the country. From 2027, the minimum legal age to purchase tobacco products would increase from 18 years old by one year each year — meaning that the threshold in 2028, for instance, would be 20. This strategy, the government hopes, will by 2040 create a smoke-free generation. The UK move follows similar legislation announced in 2021 by New Zealand. The nation reversed its intended ban because tobacco sales were needed to help pay for tax cuts, but the government said last month that it will seek to ban disposable vapes.
Modelling smokers
The UK government’s policies are backed by a modelling study published in December that predicts how the proposal would affect smoking rates and people over time. Its ‘pessimistic’ model predicts that the policy could reduce the smoking rate among people aged 14–30 from 13% in 2023 to around 8% in 2030. By 2040, just 5% of this age group would smoke. In the baseline scenario, 8% of 14- to 30-year-olds would smoke. In the ‘optimistic’ scenario, only 0.4% of that age group would start smoking by 2040 (see ‘Ban plan’). That model suggests that, by 2075, the policy would save tens of thousands of lives and £11 billion ($13.7 billion) in health-care costs by preventing smoking-related diseases.
These projections are based on solid evidence and are of high quality, says tobacco researcher Allen Gallagher at the University of Bath, UK.
Still, no country has ever introduced a policy that raises the minimum tobacco-purchasing age in this way — only time will tell what the effects will be, says Commar.
Vaping bans
Nations are also targeting vaping, a trend that began around 2010 and has surged among younger people. Many people have perceived it as a potentially healthier alternative to smoking — for which there is substantial evidence. But whether vaping itself harms health has long been controversial, and the evidence is uncertain.
“The results are not super clear, but certainly hint towards vaping causing damage to the lungs and other organs,” says Carolyn Baglole, who studies lung disease at the McGill University Health Centre in Montreal, Canada.
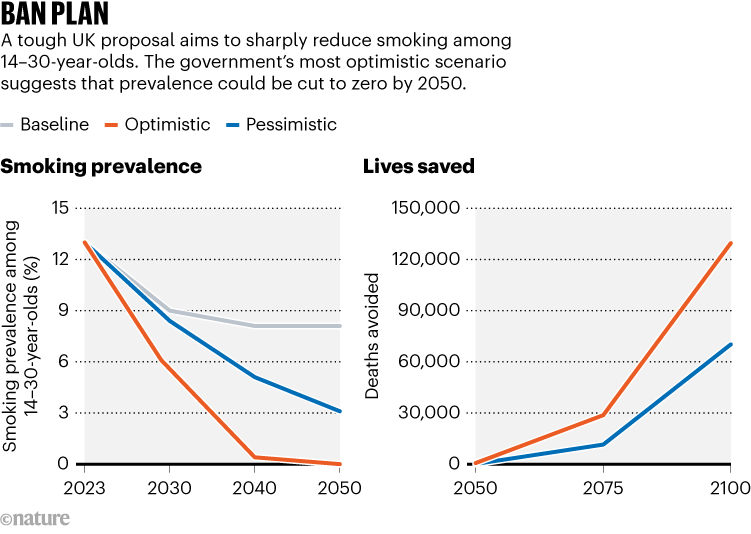
Source: UK government
Vapes are made of a box filled with liquid that usually contains nicotine, a heating element that turns the liquid into aerosols and a mouthpiece to inhale the aerosol ‘vape’ clouds, which are often fruity or dessert-flavoured. Although vapes lack tobacco and most of the toxic chemicals in cigarettes, the nicotine is still harmful. Nicotine can raise blood pressure, increase the risk of heart and lung disease and disrupt brain development in children and adolescents. In turn, this can lead to impairments in attention, memory and learning.
The UK plan includes banning disposable vapes, restricting vape flavours that appeal to young users and limiting how vapes are advertised. Most young people in Great Britain use disposable vapes rather than rechargeable ones than can be refilled with liquid, according to a survey by the public-health charity Action on Smoking and Health, based in London. Rechargeable vapes would remain legal.
Global policies
The French government also wants to ban disposable vapes this year, and in December its parliament unanimously backed the proposal. And in 2021, Australia restricted e-cigarette sales to smokers who have a prescription for using vapes to quit smoking. “There is a good consensus that vaping is likely to pose only a small fraction of risks of smoking over the long term,” says psychologist Peter Hajek at Queen Mary University of London, who led a study 1 that suggested vaping safely helped pregnant women to stop smoking.
But illegal vaping is still surging among people under the legal age of 18 in Australia, according to research by the Australian Institute of Health and Welfare. That’s led the government to tighten rules on vape products. “This policy push should see the upswing in youth vaping contained and reversed,” says epidemiologist Tony Blakely at the University of Melbourne in Australia.
The flavoured liquid in vapes also contains solvents such as propylene glycol and glycerin. Agencies including the US and European Union drug regulators have approved these chemicals for oral consumption. But animal studies suggest that inhaling them could cause damage and inflammation, raising the risk of lung and heart disease 2 . “The issue is we don’t know much about what happens when you heat these products and aerosolize them for inhalation,” says Baglole.
One thing researchers know is that the heating element in e-cigarettes can release heavy metals into the inhaled aerosols. These particles have been linked to a raised risk of heart and respiratory disease, she says.
Ultimately, scientists seem to be overwhelmingly in favour of tough restrictions on smoking and vaping. Research is needed to establish the long-term health impacts of such policies, says Baglole. “Hopefully, different types of studies, different models, in addition to human participants, will start to paint a more complete picture,” she says.
Nature 628 , 695-696 (2024)
doi: https://doi.org/10.1038/d41586-024-00472-3
Updates & Corrections
Correction 18 April 2024 : The graphic ‘Smoking prevalence’ wrongly coloured the chart lines for the optimistic and pessimistic scenarios. This has been corrected.
Pesola, F. et al. Addiction 119 , 875–884 (2024).
Article PubMed Google Scholar
Traboulsi, H. et al. Int. J. Mol. Sci. 21 , 3495 (2020).
Download references
Reprints and permissions
Related Articles

- Public health

Want to make a difference? Try working at an environmental non-profit organization
Career Feature 26 APR 24

NIH pay rise for postdocs and PhD students could have US ripple effect
News 25 APR 24
India’s 50-year-old Chipko movement is a model for environmental activism
Correspondence 23 APR 24

Bird flu virus has been spreading in US cows for months, RNA reveals
News 27 APR 24

WHO redefines airborne transmission: what does that mean for future pandemics?
News 24 APR 24
More work is needed to take on the rural wastewater challenge
Berlin (DE)
Springer Nature Group
ECUST Seeking Global Talents
Join Us and Create a Bright Future Together!
Shanghai, China
East China University of Science and Technology (ECUST)
Position Recruitment of Guangzhou Medical University
Seeking talents around the world.
Guangzhou, Guangdong, China
Guangzhou Medical University
Junior Group Leader
The Imagine Institute is a leading European research centre dedicated to genetic diseases, with the primary objective to better understand and trea...
Paris, Ile-de-France (FR)
Imagine Institute
Director of the Czech Advanced Technology and Research Institute of Palacký University Olomouc
The Rector of Palacký University Olomouc announces a Call for the Position of Director of the Czech Advanced Technology and Research Institute of P...
Czech Republic (CZ)
Palacký University Olomouc
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- MUSC Health MyChart
- Schedule an Appointment
- Adult Patient Care
- Children's Health
- Education at MUSC
- Research at MUSC
- Latest News
- E-cigarettes
Tobacco researchers suggest health care providers talk with adult patients who smoke about relative risks of tobacco products, including e-cigarettes

Health care providers who are working with adult patients struggling to stop smoking should consider discussing e-cigarettes as a potential tool if they’ve already tried FDA-approved medications, say tobacco researchers with MUSC Hollings Cancer Center .
Benjamin Toll, Ph.D. , director of the MUSC Health Tobacco Treatment Program , and Tracy Smith, Ph.D. , associate professor in the Addiction Sciences Division of the Department of Psychiatry and Behavioral Sciences, partnered with Brian King, Ph.D. , director of the Center for Tobacco Products at the U.S. Food and Drug Administration, to write a commentary in Nature Medicine that lays out the relative risk of e-cigarettes compared with traditional combustible cigarettes. Existing scientific evidence indicates that both products have health risks, but that e-cigarettes generally have lower risks than cigarettes.
To be clear – neither option is good for your health, Toll and Smith said. And they certainly don’t want any youth, or adults who don’t smoke, to take up e-cigarette use. But among adults who have already tried FDA-approved cessation medicines, if the choice is between continuing to smoke traditional cigarettes or switching completely to e-cigarettes, then a complete switch should be encouraged, they said. They were motivated to work with King to write this commentary because they saw confusion among the general public and doctors about the relative harms of each product.
“It really bothered me that there are well-intentioned, smart health care providers who think that e-cigarettes are worse than smoking cigarettes,” Toll said. “It’s simply not true.”
Toll, who is currently serving as president of the Society for Research on Nicotine and Tobacco, wanted to expand the conversation that health care providers can have with patients about ways to stop smoking.
There are seven FDA-approved smoking cessation aids, including medication and nicotine replacement options like the patch. These smoking cessation products, especially when combined with behavioral counseling, improve a person’s chances of quitting smoking. But because nicotine is so addictive, many people still struggle. That’s where Smith and Toll see a place for e-cigarettes.
“Doctors and other health care professionals don't know what to say or how to talk about it,” Smith said. “I always say, ‘If you have somebody who smokes cigarettes, they are standing in a convenience store every single day, buying the most harmful tobacco product they could possibly be buying.’ And it’s a real injustice not to say to them, ‘Hey, there are nicotine products you could buy every day that would be a whole lot less likely to kill you.’”
However, Toll and Smith are very specific about which types of e-cigarettes they’re referring to. When they say that e-cigarettes have fewer toxicants and cause less harm than cigarettes, they’re referring specifically to the 23 products that have received FDA authorization for marketing. It’s worth noting that all 23 of these products are tobacco-flavored, not fruity, chocolatey or candy-flavored.
Smith explained that the FDA created two paths for e-cigarette manufacturers to gain authorization. The first path would allow manufacturers to market their e-cigarettes as smoking cessation devices.
“Thus far, no company has done that – as far as we know, they have not even applied,” Smith said.
The second path allows companies to market their products as tobacco products, but makes no claims about smoking cessation. Companies have to show that their products are appropriate for the protection of public health – specifically, that the benefits of the product for helping adults who smoke to transition completely outweighs the known risk of these products to youth and nonusers.
Besides the likelihood that the product will entice young people, the FDA looks at everything from environmental impact to whether users completely switch to the e-cigarette product from cigarettes. Complete switching, rather than going back and forth between e-cigarettes and cigarettes, is an important factor. If people use both products – something that researchers call “dual use” – then they’re still exposing themselves to the carcinogens and toxicants in cigarettes.
“So far, the FDA has issued more than a million denials and 23 authorizations,” Smith said.
Due to the rigorous nature of the reviews, Smith and Toll believe that doctors can reasonably share that list of 23 authorized e-cigarettes with people who are struggling to stop smoking.
In addition, there’s increasing evidence suggesting that e-cigarettes can help adults who smoke to completely transition away from cigarettes, they said. Recent large-scale studies published in JAMA Internal Medicine and the New England Journal of Medicine showed that e-cigarettes helped people to stop smoking. Further, Smith said, a Cochrane Review conducted earlier this year concluded that there is evidence from enough high-quality studies to say that e-cigarettes are more likely to help people to quit than nicotine replacement therapy, which includes nicotine gum, nicotine lozenges and the patch.
E-cigarettes remain controversial though.
“Some believe that we shouldn’t be allowing new tobacco products on the market that could potentially be appealing to youth, no matter what the benefit is to adults who smoke. And I’m just not in that camp because cigarettes are the primary way that tobacco kills people,” Smith said. “For me, because cigarettes are responsible for the vast majority of the deaths and illnesses from tobacco, I think that having less harmful alternatives out there for adults, especially if we can reduce the appeal to youth, is really important.”

Vaping on the Rise
New research shows that, for the first time, there are more young people who begin to use nicotine through vaping rather than through cigarettes.
A tobacco researcher at MUSC Hollings Cancer Center was honored by the American Society of Preventive Oncology for his work.

Doll-Wynder Award
Dr. Michael Cummings was honored for the groundbreaking advances he's made over a 40-year career in tobacco control research.
Related Links
More MUSC Hollings Cancer Center news
Subscribe to our newsletter
Hollings Horizons magazine
About the Author
Leslie Cantu MUSC Hollings Cancer Center
Categories: Cancer , Influence , Research
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
April 23, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
Smoking cessation before laryngeal cancer treatment improves survival, retention of voice box, study shows
by University of Oklahoma

In a study of patients who smoked when they were diagnosed with laryngeal cancer, those who quit smoking before starting chemotherapy or radiation responded better to treatment, were less likely to need their voice boxes surgically removed, and lived significantly longer than those who continued to smoke. The research , from the University of Oklahoma, is published in the journal Otolaryngology-Head and Neck Surgery .
The study's senior author, Lurdes Queimado, M.D., Ph.D., said the findings underscore the importance of integrating tobacco cessation programs into treatment plans for cancer of the larynx, an area of the throat involved in breathing, swallowing, and talking.
An abundance of research exists showing that smokers fare worse with laryngeal cancer than those who never smoked or who quit before receiving a diagnosis. But Queimado narrowed her analysis to understand what happened to people who quit smoking between the time of their diagnosis and the start of treatment, typically a period of just a few weeks.
"To the best of our knowledge, this is the first study to suggest that in newly diagnosed laryngeal cancer patients who are smokers at the time of diagnosis, those who quit before treatment begins will have a much better prognosis than those who continue smoking," said Queimado, a professor of otolaryngology-head and neck surgery in the OU College of Medicine.
"We are excited about these findings because it gives our patients some hope. If chemotherapy and radiation don't work, they may need to have their voice box removed, and that often brings stigma and depression. Their quality of life significantly decreases because they have a lot of difficulty swallowing and have to talk through a tube."
Queimado's research team analyzed data from patients with laryngeal cancer who were treated at OU Health Stephenson Cancer Center, Oklahoma's only National Cancer Institute-designated cancer center. Those who quit smoking before starting treatment were nearly four times as likely as smokers to have a complete response to chemotherapy and radiation, meaning doctors could find no evidence of cancer.
The research team then studied patient data for seven years following treatment. Those who quit smoking before treatment were half as likely as smokers to require surgery to remove their voice box in order to eradicate the cancer.
In addition, those who quit smoking before treatment lived longer than those who continued to smoke. At the three-year point following treatment, 83% of those who quit smoking were still living, vs. 66% of those who continued to smoke. At five years, the statistics were 79% vs. 60%, and at seven years, 75% vs. 56%.
"To have such an improved quality of life for seven years is significant. In most patients, we treat with chemotherapy and radiation first to try to spare the voice box because it is so vital for speaking and swallowing. Because of those quality of life issues, the impact of this study is beyond what we measured," said Queimado, who also directs the Tobacco Regulatory Science Lab in the TSET Health Promotion Research Center, a program of OU Health Stephenson Cancer Center.
Queimado has now launched a prospective study following the outcomes of current patients who quit smoking at diagnosis and those who continue to smoke. She is also working with her clinical colleagues to place her findings on informational cards in patient care areas. However, her longer-term goal is to make tobacco cessation help much more accessible for patients.
"We are applying for a grant that would allow us to take tobacco cessation products and assistance directly to the patient rather than simply pointing them toward resources," she said.
"A diagnosis of cancer is overwhelming, and people's lives are turned upside down, so unless services are taken to them, they are less likely to pursue them on their own. It is very difficult to quit smoking, but I think it will make a difference if we can surround the patient with the support and tools they need to quit. And if they quit during their treatment, maybe they will never go back to it."
Explore further
Feedback to editors

Research shows 'profound' link between dietary choices and brain health
Apr 27, 2024

Component of keto diet plus immunotherapy may reduce prostate cancer

Study finds big jump in addiction treatment at community health clinics

Positive childhood experiences can boost mental health and reduce depression and anxiety in teens

Gene linked to epilepsy and autism decoded in new study
Apr 26, 2024

Blood test finds knee osteoarthritis up to eight years before it appears on X-rays

Researchers find pregnancy cytokine levels impact fetal brain development and offspring behavior

Study finds biomarkers for psychiatric symptoms in patients with rare genetic condition 22q

Clinical trial evaluates azithromycin for preventing chronic lung disease in premature babies

Scientists report that new gene therapy slows down amyotrophic lateral sclerosis disease progression
Related stories.

Exposure to secondhand smoke during chemotherapy makes treatment less effective, study finds
Feb 27, 2024

Only 1 in 4 rural US smokers attempted to quit during a one year period, study finds
Mar 5, 2024

What's the relationship between cancer survivors' tobacco use, symptom burden, and motivation to quit smoking?
May 22, 2023

Smoking cessation after cancer diagnosis associated with improved survival
Jan 4, 2022

Quitting smoking is hard—increase your chance of success
Nov 15, 2022

Cancer survivors who quit smoking sooner can live longer
Sep 12, 2017
Recommended for you

Study identifies driver of liver cancer that could be target for treatment

Analysis identifies 50 new genomic regions associated with kidney cancer risk

Biomarkers identified for successful treatment of bone marrow tumors

Study finds vitamin D alters mouse gut bacteria to give better cancer immunity
Apr 25, 2024
Let us know if there is a problem with our content
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.

E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
This paper is in the following e-collection/theme issue:
Published on 24.4.2024 in Vol 13 (2024)
An Integrated mHealth App for Smoking Cessation in Black Smokers With HIV: Protocol for a Randomized Controlled Trial
Authors of this article:

- Andre Bizier 1 , BS ;
- Arielle Jones 1 , BS ;
- Michael Businelle 2, 3 , PhD ;
- Krista Kezbers 2 , PhD ;
- Bettina B Hoeppner 4, 5 , PhD ;
- Thomas P Giordano 6 , MD, MPH ;
- Jessica M Thai 1 , BSc ;
- Jacqueline Charles 1 , MA ;
- Audrey Montgomery 2 , MEd ;
- Matthew W Gallagher 1, 7, 8 , PhD ;
- Marshall K Cheney 9 , PhD ;
- Michael Zvolensky 1, 7, 10 , PhD ;
- Lorra Garey 1, 7 , PhD
1 University of Houston, Houston, TX, United States
2 TSET Health Promotion Research Center, Stephenson Cancer Center, Oklahoma City, OK, United States
3 Department of Family and Preventive Medicine, University of Oklahoma Health Sciences Center, Oklahoma City, OK, United States
4 Massachusetts General Hospital, Boston, MA, United States
5 Harvard Medical School, Boston, MA, United States
6 Baylor College of Medicine, Houston, TX, United States
7 HEALTH Institute, Houston, TX, United States
8 Texas Institute for Measurement, Evaluation, and Statistics, Houston, TX, United States
9 Department of Health and Exercise Science, University of Oklahoma, Norman, OK, United States
10 The University of Texas MD Anderson Cancer Center, Houston, TX, United States
Corresponding Author:
Lorra Garey, PhD
University of Houston
3695 Cullen Blvd, Fred J. Heyne Building, Suite 126
Houston, TX
United States
Phone: 1 7137438056
Email: [email protected]
Background: Black adults who smoke and have HIV experience immense stressors (eg, racial discrimination and HIV stigma) that impede smoking cessation success and perpetuate smoking-related health disparities. These stressors also place Black adults who smoke and have HIV at an increased risk of elevated interoceptive stress (eg, anxiety and uncomfortable bodily sensations) and smoking to manage symptoms. In turn, this population is more likely to smoke to manage interoceptive stress, which contributes to worse HIV-related outcomes in this group. However, no specialized treatment exists to address smoking cessation, interoceptive stress, and HIV management for Black smokers with HIV.
Objective: This study aims to test a culturally adapted and novel mobile intervention that targets combustible cigarette smoking, HIV treatment engagement and adherence, and anxiety sensitivity (a proxy for difficulty and responsivity to interoceptive stress) among Black smokers with HIV (ie, Mobile Anxiety Sensitivity Program for Smoking and HIV [MASP+]). Various culturally tailored components of the app are being evaluated for their ability to help users quit smoking, manage physiological stress, and improve health care management.
Methods: This study is a pilot randomized controlled trial in which Black combustible cigarette smokers with HIV (N=72) are being recruited and randomly assigned to use either (1) the National Cancer Institute’s QuitGuide app or (2) MASP+. Study procedures include a web-based prescreener; active intervention period for 6 weeks; smartphone-based assessments, including daily app-based ecological momentary assessments for 6 weeks (4 ecological momentary assessments each day); a video-based qualitative interview using Zoom Video Communications software at week 6 for participants in all study conditions; and smartphone-based follow-up assessments at 0, 1, 2 (quit date), 3, 4, 5, 6, and 28 weeks postbaseline (26 weeks postquitting date).
Results: Primary outcomes include biochemically verified 7-day point prevalence of abstinence, HIV-related quality of life, use of antiretroviral therapy, and HIV care appointment adherence at 26 weeks postquitting date. Qualitative data are also being collected and assessed to obtain feedback that will guide further tailoring of app content and evaluation of efficacy.
Conclusions: The results of this study will determine whether the MASP+ app serves as a successful aid for combustible cigarette smoking cessation, HIV treatment engagement, and physiological stress outcomes among Black people with HIV infection. If successful, this study will provide evidence for the efficacy of a new means of addressing major mental and physical health difficulties for this high-risk population. If the results are promising, the data from this study will be used to update and tailor the MASP+ app for testing in a fully powered randomized controlled trial that will evaluate its efficacy in real-world behavioral health and social service settings.
Trial Registration: ClinicalTrials.gov NCT05709002; https://clinicaltrials.gov/study/NCT05709002
International Registered Report Identifier (IRRID): PRR1-10.2196/52090
Introduction
People with HIV/AIDS smoke at a rate 3 times higher (33.6% vs 12.5%) than that of the general population [ 1 , 2 ]. This group is also less likely to quit smoking and is more susceptible to the harmful effects of smoking (eg, increased risk for cancer and lung disease) [ 1 , 3 , 4 ], likely due to the combined impact of several social determinants of health, including behavioral risk factors, limited resources, and diminished access to health care, as well as immune system dysfunction and chronic inflammation caused by HIV [ 5 - 10 ]. Indeed, cigarette smoking is a leading risk factor for HIV-related and non–HIV-related morbidity and mortality among people with HIV/AIDS [ 11 , 12 ], even among those taking antiretroviral medications [ 13 ], and contributes to more life-years lost than HIV-related complications among those effectively treated with antiretroviral therapy (ART) [ 13 - 15 ]. Furthermore, people with HIV/AIDS who smoke are less adherent to ART than nonsmokers and experience poorer viral and immunologic responses to ART [ 16 , 17 ], a greater risk of virologic rebound, and more frequent immunologic failure [ 18 ].
Among people with HIV/AIDS who smoke, those who identify as members of a racial minority group are at an elevated risk for negative health consequences of smoking and poorer HIV-related outcomes. Evidence suggests that Black adults with HIV, in particular, experience high rates of discrimination and stigma that lead to the onset and maintenance of maladaptive coping, including smoking [ 19 , 20 ]. Consistent with these data, Black adults with HIV are more likely to smoke [ 4 ], less likely to quit [ 4 , 21 - 24 ], and experience greater quit difficulty when attempting to quit than White smokers or smokers without HIV [ 21 ]. Black adults with HIV also have lower rates of compliance with routine HIV care (ie, ART adherence), retention in long-term care, and are less likely to be virally suppressed relative to other groups [ 25 - 28 ]. This is a public health problem because Black adults account for the highest proportion (42%) of new HIV diagnoses and experience higher mortality than White adults with HIV [ 25 , 27 , 28 ]. From an intersectional stigma and discrimination perspective and socioecological models of social determinants of health [ 29 , 30 ], Black adults who smoke and have HIV may be at elevated risk for worse HIV disease management and smoking outcomes and ultimately experience increased health disparities [ 6 ].
Emotional models of coping suggest that Black adults with HIV may smoke and continue to smoke despite health problems to manage interoceptive stress and uncomfortable physiological arousal associated with minority status stressors such as racial discrimination and HIV-related stigma. Anxiety sensitivity (AS) is one of the most noteworthy constructs related to physiological distress and manifestations of elevated internal distress, including psychopathologies. AS refers to the fear of anxiety or anxiety-related symptoms [ 31 ]. AS amplifies negative mood states via enhanced threat perception (eg anxiety) [ 32 , 33 ], contributing to the development of anxiety and depressive problems [ 34 ]. Notably, anxiety and depression contribute to an increased likelihood of poor ART adherence [ 35 ]. Among people with HIV/AIDS, AS is related to more severe social anxiety symptoms, anxious arousal symptoms, HIV-related stigma, and HIV symptom distress [ 36 , 37 ]. AS has also been implicated as a contributing factor in smoking initiation, maintenance, and relapse [ 38 , 39 ]. Emerging data indicate that AS is elevated in both Black adults who smoke and people with HIV/AIDS who smoke [ 40 ], placing this group at greater odds of early lapse and relapse [ 41 , 42 ]. Without appropriate interventions to address susceptibility to the negative impact of interoceptive stress, Black adults with HIV who smoke and have elevated AS may be inclined to return to smoking to alleviate abstinence-induced increases in anxiety and to manage uncomfortable HIV-related bodily symptoms that may increase with smoking cessation.
Although smoking cessation treatments that target AS exist, they are limited in their reach, adaptability, and potential for adoption and do not consider critical barriers to smoking cessation or HIV treatment engagement and adherence. For example, current combined AS and smoking treatments focus primarily on multisession, intensive treatments, particularly those that rely on in-person, clinician-administered psychosocial protocols [ 43 - 46 ]. Participation in these treatments often requires notable time commitments, practical limitations, and expense [ 47 ]. Such burdens are barriers to treatment and may contribute to the low treatment participation rates [ 47 ]. An additional limitation of current treatments is that no readily available smoking cessation treatments that target AS integrate information to improve HIV treatment engagement and adherence. Given the robust evidence that targeting AS and promoting smoking cessation may lead to improved HIV outcomes, this is a major limitation. Finally, the required human resources, specialized training, and financial support that are needed to administer currently available combined AS and smoking treatments discourage the adoption of these treatments in communities most in need, such as those that serve Black adults with HIV who smoke. Therefore, it is essential to develop a digital AS intervention that can be culturally adapted for this population.
On the basis of our prior work [ 48 ], we modified our previously developed and tested novel, integrated, smartphone-delivered intervention for AS reduction and smoking (ie, Mobile Anxiety Sensitivity Program [MASP]) [ 49 ] for Black people with HIV/AIDS who smoke, integrating HIV information and care support that is culturally tailored to create the new smartphone-based app: Mobile Anxiety Sensitivity Program for Smoking and HIV (MASP+). MASP+ contains features and content designed to aid Black adults with combustible smoking cessation, HIV care adherence, and AS reduction. The initial efficacy of MASP+ relative to an established control intervention, the National Cancer Institute’s (NCI) QuitGuide app, on combustible cigarette smoking cessation, HIV-related outcomes, and AS reduction is currently being tested in a pilot randomized controlled trial (RCT). We expect that MASP+ participants will report greater biochemically confirmed smoking abstinence at 26 weeks postquitting date relative to the QuitGuide group. In addition, we hypothesize that MASP+ participants will report greater HIV-specific quality of life, ART adherence, and HIV treatment engagement at 26 weeks postquitting date relative to the QuitGuide group. Finally, we expect that improvement in AS will mediate the relationship between treatment and (1) smoking abstinence and (2) HIV-related outcomes and that daily experiences of discrimination (race and HIV) will moderate these relationships. We will also examine qualitative and quantitative data to guide the refinement and further adaptation of MASP+ and support the development of a high-quality, culturally relevant, and scalable intervention.
Ethical Consideration
The Institutional Review Board at the University of Houston (UH) approved the protocol presented in this study under STUDY00003811, whereas the University of Oklahoma Health Sciences Center and Baylor College of Medicine relied on the UH Institutional Review Board. This trial has been registered at ClinicalTrials.gov (NCT05709002; protocol ID: QKWEF8XLMTT3).
Study Eligibility
The study eligibility criteria included being aged ≥18 years, having HIV, self-identification as Black or African American, providing a current picture of their cigarette package to verify smoking status [ 48 ], possessing at least a grade 6 reading level (≥4 on the Rapid Estimate of Adult Literacy in Medicine [REALM]) [ 50 ], experiencing elevated AS (ie, Short Scale Anxiety Sensitivity Index [SSASI] score of ≥5) [ 51 ], reporting daily smoking with a minimum of 10 cigarettes per day for at least 2 years, being motivated to quit smoking (>5 on a 10-point scale) [ 52 ], willingness to complete all study surveys or assessments, agreeing to use nicotine replacement medications (nicotine replacement therapy [NRT]; nicotine patch and lozenges), and agreeing to attempt to quit smoking 2 weeks after the date of randomization. Exclusion criteria included not being fluent in English; high blood pressure that is not under control (eg, medicated); experiencing a heart attack (myocardial infarction) within the past 2 weeks; use of any pharmacotherapy targeting smoking cessation beyond what is provided by this study; legal status that would interfere with participation (eg, incarceration with restricted access to mobile devices); cognitive impairment (assessed via the 6-item Cognitive Impairment Test) [ 53 ]; and being non-Black, pregnant, or younger than 18 years.
Recruitment and Procedures
Participants are recruited via web-based advertisement materials, as well as physical materials placed throughout the city of Houston. Study materials provide contact information for UH if a potential participant has questions about the study. Study advertisements also include a QR code linked to a REDCap (Research Electronic Data Capture; Vanderbilt University) prescreener survey. Those who complete the prescreening are deemed either ineligible or pre-eligible. For those recruited from Thomas Street at Quentin Mease Health Center, a clinic in Houston that provides routine medical care to ≥5000 people with HIV/AIDS study team members at Thomas Street perform a chart review to confirm HIV status. Pre-eligible participants are then contacted to complete an enrollment call wherein they provide informed consent and complete the final eligibility screening for the study (refer to Figure 1 for the participant enrollment flowchart).

Persons deemed eligible at the enrollment call download the Insight app onto their personal smartphone or study phone. The Insight app houses the MASP+ content and is used to administer smartphone-based surveys and ecological momentary assessments (EMAs) to all participants. The study smartphones are provided to those without a smartphone and those with a smartphone that is incompatible with the Insight platform. Insight is supported on most Android smartphones (Android versions 6.0-14.0). Participants with a personal phone that is incompatible with Insight are sent a study phone. For those using their personal smartphone, the study staff instruct participants on how to download the app onto their personal phone. Insight adjusts according to the font size selected by participants on their phones. Participants who experience issues reading text in the app due to font size are instructed to increase font size in the phone settings. Once Insight is downloaded, participants are given a unique single-use code that enables them to use the app to complete the baseline assessment, which must be completed within 6 days after inputting the code. If participants do not complete the baseline survey within 6 days, they are no longer eligible to participate in the study. All participants are mailed a baseline package that includes a Bedfont iCO (iCarbon Monoxide) quit smokerlyzer, a Greenphire Mastercard, and NRT. The Bedfont iCO is used to biochemically verify self-reported abstinence at follow-ups.
Upon completion of the baseline survey and receipt of the baseline package, the participants complete a randomization call with the study staff. During the randomization call, the participants are randomized to receive the MASP+ or QuitGuide interventions based on the randomization chart developed by the study statistician (MWG). Block randomization was used and stratified according to binary sex (assigned at birth). Variable-sized permuted block randomization (block sizes vary from 4 to 12) is used. Before data analyses, the balance of randomization will be checked and controlled for imbalanced factors by including any factors that differ between groups as covariates. The participants are provided with a unique code to access the app to which they are randomized. MASP+ participants have access to all MASP+ features (ie, Treatment Videos, Coping Toolkit, Quit Tips, and Stress Management Trainings) through the Insight platform. Participants randomized to the control intervention (ie, QuitGuide) have access to limited features (ie, App Instructions, Payment Tracking, Call Staff, and Record Stress) through the Insight platform and receive intervention content (ie, Track My Craving, Manage My Mood, and Learn To Quit) through the QuitGuide app. Participants assigned to the control intervention receive assistance with downloading the QuitGuide app through the Google Play Store. Both intervention groups use the Insight app to complete the study assessments, which include the baseline survey, weekly follow-ups, the 28-week follow-up, and EMAs. Once the code is entered, the research staff orients the participant to the app features and the iCO carbon monoxide (CO) breath testing device. Participants have access to MASP+ or QuitGuide content through the final follow-up (ie, the 28-week follow-up). At the end of the randomization call, participants are directed to take a brief postrandomization survey, which must be completed within 6 days after the randomization call. Failure to complete the postrandomization survey within 6 days does not affect participants’ status in the study.
Following randomization, the participants complete 4 daily EMAs for 6 weeks. Participants also complete app-based follow-up surveys each week of the treatment period (ie, weeks 1-6) and at 26 weeks postquitting date (28 weeks postbaseline). Between weeks 6 and 28, all participants are prompted to complete a brief check-in survey each month, which reminds them about available app features and assesses their current smoking status. The participants complete a final series of EMAs (4 per day) for 7 days before the 28-week follow-up assessment. The Insight app prompts daily EMAs and follow-up assessments for both treatment groups. In addition, participants complete a Zoom-based qualitative interview to assess their experience with the app and capture recommendations for improving app features and content at 6 weeks postrandomization. Participants who received loaned study smartphones are required to return them after their final follow-up assessment at week 28.
Compensation
Each participant who enrolls receives a Greenphire Mastercard gift card that is loaded with compensation for survey completion. Participants receive all compensation in USD. Participants receive US $30 for completing the baseline assessment and US $10 for completing the postrandomization survey. Participants receive US $10 for completing each weekly follow-up assessment at weeks 1, 2 (quit date), 3, 4, and 5 as well as 6 weeks postbaseline (including the app-based survey, iCO breath test, and Zoom-based qualitative interview at week 6 only). Participants receive US $50 for completing the 28-week follow-up assessment (via Insight) and iCO breath test. Participants are compensated at the end of week 6 for EMA completion during weeks 1 to 6 and at the end of week 28 for EMAs completed during week 28. Specifically, participants receive a total of US $60 for completing 50% to 74% of the brief EMAs (4 per day×7 days=28 weekly EMAs) prompted during weeks 1 to 6, US $90 for completing 75% to 89% of EMAs, or US $120 for completing ≥90% of EMAs. For week 28, participants will receive US $10 for completing 50% to 74% of the brief EMAs, US $15 for completing 75% to 89% of EMAs, or US $20 for completing ≥90% of EMAs. Participants can use the “Payment” and “Weekly Survey Payment” buttons on the app’s home screen whenever desired to view an up-to-the-moment summary of EMAs presented and their current completion rate. Payments for completed EMAs are loaded onto participants’ Greenphire cards following week 6 and week 28.
Study Conditions
Both conditions.
Given that clinical guidelines recommend that all smokers attempting to quit should receive and use pharmacotherapy [ 54 ], both MASP+ and QuitGuide participants are sent NRT with their baseline package. Transdermal nicotine patches and nicotine lozenges are provided for use during the first 4 weeks postquitting date, and each participant is given the option order up to 4 weeks of additional NRT. For those in the MASP+ condition, an additional NRT can be ordered by clicking a button on the app home screen, which sends an encrypted email to the study team informing them of NRT requests. For those in the QuitGuide condition, NRT orders are placed by calling the number provided to participants and speaking with a member of the study team ( Figure 2 ). In a prior study, 66% of enrolled participants used a similar app button or feature to place NRT orders [ 55 ]. Patches and lozenges were chosen for use in this study because of their safety and effectiveness (especially in combination with NRT), ease of use, and relatively benign side effects compared to other forms of NRT [ 56 , 57 ].

NCI QuitGuide Condition
The NCI’s QuitGuide app (available for free by request from the NCI Smokefree [ 58 ] server, on Google Play, or from the Google Play Store) is a free smartphone app that complies with many of the clinical practice guidelines for quitting smoking [ 54 ]. QuitGuide aims to orient smokers to their own smoking patterns and support users in developing the skills needed to quit smoking. Participants with a compatible smartphone who are randomly assigned to use QuitGuide are directed to download the app to their personal devices. Those who do not own a compatible device receive a study smartphone and are directed to download the QuitGuide app during the randomization call. Information explaining how to use the QuitGuide app is shared and reviewed during the randomization phone call. QuitGuide participants also download and use a modified version of the Insight EMA app with all MASP+ intervention features removed, which allows participants to receive EMAs and baseline or follow-up assessments. Refer to Table 1 for a list of QuitGuide features.
a Some treatment components will be available to all participants regardless of group or app assignment during randomization (eg, smoking cessation psychoeducation and inspirational messages). Other components will be exclusive to either the MASP + condition (eg, content specific to Black smokers with HIV and guidance for challenging automatic thoughts) or the QuitGuide condition (eg, scheduled tips and individualized quit plan).
b MASP+: Mobile Anxiety Sensitivity Program for Smoking and HIV.
c EMA: ecological momentary assessment.
d NRT: nicotine replacement therapy.
e AS: anxiety sensitivity.
MASP+ Condition
The MASP+ app was adapted from MASP materials and focuses on smoking cessation, HIV treatment engagement or adherence, and AS reduction among Black smokers with HIV [ 59 , 60 ]. Specifically, treatment video scripts were updated from MASP to reflect language and life experiences particular to those with HIV (eg, “Smoking can cause infections, slow down healing, and make it harder for HIV medications to keep your immune system strong.”). EMA messages underwent similar tailoring (eg, “Thinking about the stress of HIV treatment can sometimes feel overwhelming. Relieve your stress by doing one of the relaxation exercises in the app’s Coping Toolkit.”), and 2 new features were added to the app: “How to Improve my Treatment Outcomes” and “Tips on Living with a Chronic Disease.”
Within a culturally adapted framework, MASP+ integrates both standard cognitive behavioral therapy practices for smoking cessation (in accordance with clinical practice guidelines) and transdiagnostic treatment for AS reduction [ 54 ]. MASP+ provides participants with (1) scheduled treatment content, (2) participant-initiated and scheduled stress exposure sessions, (3) personalized messages following each completed EMA (both pre- and postquit), and (4) numerous “on-demand” features (eg, Quit Tips and Coping Toolkit; both pre- and postquit). Culturally tailored components (eg, educational content related to menthol tobacco products in the Black community, the history of tobacco marketing directly to Black people, HIV treatment management and HIV disparities, and the impact of discrimination and racism on smoking and stress) are featured throughout MASP+. To support cultural tailoring, subject matter experts, including coinvestigators specializing in health disparities and HIV research and members of a Community Research Advisory Board, provided feedback on the cultural tailoring of the study materials for Black participants with HIV.
MASP+ App Features
Treatment on a schedule.
MASP+ includes 17 videos that are 4 to 6 minutes long. These videos provide psychoeducation on topics such as nicotine withdrawal, unhelpful thinking, coping with others smoking nearby, managing uncomfortable sensations, chronic stress and HIV, myths about smoking, strategies for cessation and relapse prevention, smoking as a temporary coping mechanism to avoid experiencing negative emotions, thinking flexibly, stress management, stress and smoking, interoceptive exposure techniques, and the importance of using NRT. All videos were based on those deployed in the MASP study; however, scripts and content were updated to reflect the life experiences of Black adults with HIV (eg, smoking can cause infections, slow down healing, and make it harder for HIV medications to keep your immune system strong). In addition, 1 video was split into 2 videos to reduce the length of individual videos and thereby reduce participant burden. Two new videos become available each day for the first 8 days of the intervention. Participants are able to watch videos as they become available or later by clicking on the on-demand “Treatment Videos” button ( Figure 2 ). There is no limit on how frequently each video can be viewed. The app records date-, time-, and location-stamped information each time a video is watched. This process occurs at both initiation and completion.
Exposure Sessions
Empirical studies demonstrate that internet-based stress exposure is well tolerated, acceptable, and effective [ 61 , 62 ]. The MASP+ treatment videos introduce graduated exposure to anxiety- and distress-provoking situations and response prevention to target AS. Originally, these exposure exercises were created for the MASP pilot study (that is, straw breathing, running in place, head rush, overbreathing, and chair spinning) [ 49 ]. Participants are instructed to press the “Stress Management Trainings” button to initiate a stress exposure session ( Figure 2 ). The MASP+ app randomly selects 1 of the 5 exercises each time a participant presses the Stress Management Trainings button. The participants are then guided through stress exposures: the app explains to the participant the purpose of the assigned activity and how to perform it, normalizes the physiological symptoms experienced during the exercise, and relates this experience to their quit attempt. As in the MASP pilot [ 49 ], when the participant is ready to begin, the app assesses their level of distress (0-100 scale), displays a countdown timer while the exercise is being completed, and then assesses their level of distress again (0-100 scale) following the expiration of the countdown. The app suggests repeating the exercise up to 3 additional times if the participant’s current reported distress is >50 on a 1 to 100 scale. The aim of this strategy is to increase habituation to feared physiological sensations. Participants in the MASP pilot study accessed the Stress Management Training exercises on 6 out of 13 days before their quit date [ 63 ]. A recent review of phone-delivered interventions for anxiety and depression showed that treatments involving interoceptive exposure were safe and effective for participants [ 61 , 62 , 64 ].
EMAs With Tailored Real-Time Treatment Messages
During the prequit date period (ie, a participant’s first 2 weeks in the study), the MASP+ app delivers a message at the end of each EMA (4 per day) intended to increase motivation and provide information about quitting (eg, “Everyone experiences negative emotions, such as stress. These emotions do not last forever, but they can lead to relapse. Make a specific plan to cope with such feelings.”). During the postquitting date period (weeks 3-6 postbaseline), participants receive tailored messages following each EMA. These messages are based upon their responses to the EMA items they answered, which assess constructs such as ART adherence (eg, “Did you miss a dose of your HIV medication yesterday?”) and reported the likelihood of smoking today (ie, 0%-100%). HIV-related EMA messages were specifically developed for the MASP+ study. When participants report that they missed a dose of medication, they are prompted to select the reason that they missed their medication (eg, “Simply forgot” or “Away from home”). On the basis of the response or responses they provide, a tailored message is shared with the participant. For example, selecting that a dose was missed due to forgetting leads the app to display 1 of several possible messages to encourage participants to take their medication as prescribed (eg, “Taking your medications every day is a step toward improving your health!”). The type of message (eg, motivational, coping with urges or stress, and tips for HIV care management) that is delivered following each EMA is recorded and uploaded to our server for future analyses that examine the effects of messages on targeted smoking lapse triggers, HIV outcomes, and anxiety or depression in future EMAs. In addition, participants are instructed to review and practice stress management exercises (ie, interoceptive exposure exercises) to normalize and learn to manage symptoms of anxiety and withdrawal. These exposure exercises have been deployed without incident in the MASP study [ 49 ].
On-Demand Features
On-demand features including Quit Tips ( Figure 3 ) and Coping Toolkit ( Figure 4 ) are available to participants via buttons found on the MASP+ home screen. Each of the available icons provides a specific message related to the content area or an activity to support participants in that moment. The research team has developed hundreds of unique messages that address various triggers for smoking relapse [ 55 , 65 ]; the large message bank is intended to reduce repetition. Two new on-demand features were developed for this study: How to Improve My Treatment Outcomes and Tips on Living with a Chronic Disease. When selected, these features provide on-demand tips and messages of support regarding managing HIV care (eg, “Set reminders on your phone to help you remember appointments and when to take your medication.”) and coping with health stress (eg, “Going on a daily walk, even if just for a few minutes, can help you relax and sort through your thoughts!”), respectively. LG and MB led the development of these messages and activities.

To reduce the potential for data entry errors and the need to retain paper copies of raw data, baseline and follow-up data are collected via smartphone using the Insight mHealth platform app software [ 66 ]. Questions appear on the phone screen, and answers are provided via touch screen. Tables 2 - 4 provides the schedule for when each measure is administered. The baseline survey takes approximately 30 minutes to complete; the postrandomization survey takes approximately 10 minutes to complete, the EMAs take approximately 2 to 4 minutes to complete, and the follow-up assessments take up to 15 minutes to complete.
a Various measures will be deployed during the eligibility screener, baseline and randomization surveys, weekly surveys, and daily EMAs. Daily EMAs will include items assessing sleep quality, HIV medication adherence, and discrimination, whereas random and event EMAs will include items assessing social interactions and smoking availability.
b Not available.
c MASP+: Mobile Anxiety Sensitivity Program for Smoking and HIV.
d QG: QuitGuide.
e ART: antiretroviral therapy.
f WHO: World Health Organization.
g iCO: iCarbon Monoxide.
h SSASI: Short Scale Anxiety Sensitivity Index.
a Not available.
b NRT: nicotine replacement therapy.
The prescreener includes a demographic questionnaire that assesses demographics (eg, sex, age, race, and ethnicity), smoking history, motivation to quit, and smartphone and data plan details. The REALM-Short Form was used to assess literacy (>grade 6 English literacy level is required to complete EMAs) [ 50 ]. Participants read the REALM words from their phone screen back to the research assistant during the enrollment call. If a participant has trouble reading the words due to vision issues, they have the option to use their phone settings to enlarge the font. The 6-item Cognitive Impairment Test is used to assess impairment in cognitive function (participants with scores <8 will be excluded) [ 53 ]. After participants recruited from Thomas Street Clinic complete the prescreener, a team member at Thomas Street Clinic performs a chart review to verify HIV status and record relevant details of health history, including history of respiratory illnesses related to smoking (eg, chronic obstructive pulmonary disease; COPD), height or weight, and number of missed appointments in preceding months. All other participants progress without a chart review.
Smoking Outcomes
During each weekly follow-up survey, smoking status is biochemically confirmed using the Insight platform and the Bedfont Scientific iCO smokerlyzer device. Biochemically confirmed 7-day point prevalence abstinence (PPA) at 26 weeks postquitting date is the primary study outcome. This is consistent with best practices as well as most published smoking cessation RCTs (refer to the clinical practice guidelines) [ 54 , 67 ]. In their baseline package, participants receive the Bedfont iCO smokerlyzer, which they use to verify smoking status at each weekly follow-up assessment (weeks 1-6 and week 26 postquitting date). At the end of each assessment, the participants are directed by the Insight app to connect the iCO device to the smartphone (simply by pressing the power button on the device) and complete the iCO test. The date and time of completion are collected and saved to our server along with the test results. Our CO criteria are informed by numerous studies that have used CO cutoffs of <7 ppm [ 68 - 74 ]. The CO level is a validated indicator of smoking status and outcomes and is strongly correlated with cotinine and other biochemical measures that have longer detection windows [ 75 - 77 ].
HIV Outcomes
HIV outcomes are assessed using several measures. HIV-specific quality of life is assessed using the World Health Organization Quality of Life-HIV [ 78 ], a questionnaire comprising 36 items related to the quality of life in individuals with HIV. The items assess psychological well-being, functional limitations resulting from HIV status, pain, and the impact of HIV status on interpersonal relationships. ART adherence is assessed using 2 measures: the ART Adherence Scale [ 79 ], which consists of 7 items that assess adherence to ART medication regimens and attendance of HIV-specific medical appointments, and the AIDS Clinical Trial Group Adherence Baseline Questionnaire [ 80 ], which assesses ART adherence and reasons for missed medication, and nonadherence across 20 items. HIV treatment engagement is assessed using the Index of Engagement in HIV Care [ 81 ], a 10-item scale that asks participants about their experience of HIV care.
Discrimination
Race-based and HIV status–based discrimination is assessed using the Everyday Discrimination Scale [ 82 ]. This 5-item measure allows participants to report how often they face various forms of discrimination. Consistent with past work [ 83 ], the 5 items were adapted to assess both race-based and HIV status–based discrimination for a total of 10 items.
Anxiety Sensitivity
We assess AS using the SSASI [ 51 ]. The SSASI is derived from the ASI-3 and consists of 5 items that measure AS using a 5-point Likert-type scale (0=very little to 4=very much) [ 31 ].
MASP+ Feedback
We assess the perceived utility of MASP+ using the standardized System Usability Scale (a participant-completed, reliable, and valid metric for measuring usability and acceptability of technologies), which is administered during a 6-week follow-up survey [ 84 - 86 ]. Using a 5-point Likert-type scale (1=strongly agree to 5=strongly disagree), participants indicate their level of agreement with statements about the app’s usefulness (eg, “I thought the smoking cessation app was easy to use”).
MASP+ Feedback: Qualitative Interviews
Participant experience is assessed via a Zoom-based qualitative interview conducted at the end of treatment (week 6). The semistructured qualitative interview is conducted by trained members of the research team and audio recorded. These interviews focus on the ease of interacting with the app, the usefulness of app features, how the app can be improved, how sociocultural factors that affect Black smokers with HIV could be further woven into the intervention, and their willingness to refer the app to a friend. As participants in both study arms use the Insight app to complete EMAs and receive intervention content via the Insight app or QuitGuide app, the qualitative interview questions primarily concern participants’ experiences with Insight (MASP+ and EMA, or EMA only) and QuitGuide (intervention content). During the qualitative interviews, participants provide details about the features of the different apps that they did and did not like (eg, “What did you like about the app?”), how app features impacted relevant study outcomes (eg, “Which, if any, app features helped you manage your HIV better?”), and how the app or apps they used could be improved (eg, “How can we make the app fit better with your life experiences?”). Combined with the primary outcomes and other quantitative data, qualitative interview data will be used to refine MASP+, which will then be tested in a large-scale RCT.
Ecological Momentary Assessments
At present, EMAs are the most accurate way to measure phenomena in real-time, natural settings [ 87 , 88 ]. EMA items are less biased than traditional in-person assessments and identify fluctuations in key variables related to the study outcomes. EMA data are used to tailor the MASP+ treatment content and identify both treatment mechanisms and moments of high risk for smoking lapse.
The EMA methodology used in this study mimics that used in our previous studies and by other researchers [ 49 , 55 , 65 , 87 , 89 - 95 ]. The EMA items assess multiple constructs hypothesized to be related to HIV care and smoking lapse. Three types of EMAs are used in this study: daily diary, random sampling, and event sampling. Random and daily diary EMAs are prompted and initiated by the app. The phone audibly and visually notifies the participants of these EMAs for 30 seconds. If participants do not respond after 5 prompts, the assessment is recorded as “missed. All assessments are date and time stamped for future analyses.
Daily Diary
Each morning during weeks 1 to 6 and week 28, participants complete a daily diary EMA, for which they receive a notification 30 minutes after waking. Likewise, participants receive a notification to complete their evening daily diary 75 minutes before their reported bedtime. Questions from the morning daily diary ask about thoughts, experiences, feelings, and behaviors from both the previous day and the present (eg, “Did you miss a dose of your HIV medication yesterday?” and “Today, how long ago did you last smoke a cigarette?”). The participants are also asked about smoking cessation medication use, ART adherence, and sleep quality from the previous day. During evening daily diaries, participants are asked about thoughts, experiences, feelings, and behaviors from the same day (eg, “How is your health in general today?” and “How would you rate your quality of life today?”).
Random Sampling
Twice each day during weeks 1 to 6 and week 28, participants are prompted to complete EMAs that are scheduled to occur randomly during each participant’s normal waking hours. Participants rate their affect by indicating their level of agreement with several statements on a 5-point scale from “strongly disagree” to “strongly agree” (eg, “I feel stressed”). In addition, participants are asked about smoking triggers (eg, “I have an urge to smoke”), current depression level (“Rate your current level of depression [feeling sad]”), and anxiety level (“Rate your current level of anxiety [feeling nervous]”). Participants are also asked to describe their current environment (eg, home and work) and social setting.
Event Sampling
Throughout the treatment period, participants are asked to initiate Smoking Assessments (prequit date), Lapse Assessments (postquitting date), and Stress Assessments (pre- and postquitting date).
Before their quit date, participants are instructed to click a Record Cigarette button every time they feel they are about to smoke or have already smoked a cigarette. In addition, 10% of the time, this triggers a brief survey asking participants about their affect, stress, and experiences while smoking (eg, “Smoking improved my mood” and “Smoking was pleasurable”). These smoking assessments are date, time, and location stamped for future analyses.
Participants are instructed to press the Record Cigarette I Am About to Slip or the I Already Slipped button and complete a lapse assessment each time they smoke after their quitting date. Items on these assessments are similar to those presented in the random and smoking assessments and worded to separately assess the participants’ responses immediately before and after the lapse.
Participants are instructed to press the Report Stress button and complete the resulting assessment each time they “experience a significant increase in stress.”
Importantly, each MASP+ pre- and postquitting date EMA is followed by a treatment message that is tailored to the participant’s responses and current situation. Those assigned to the QuitGuide group complete EMAs identical to the MASP+ group, although they do not receive tailored intervention messages after completion.
EMA Alert Settings
During the enrollment call, the participants’ sleep-wake times for each day of the week are recorded and stored (Note: these sleep-wake times can be changed by calling the study team). This practice is intended to prevent or reduce the chance of the phone ringing while participants are asleep. When an EMA is prompted, participants can delay (“snooze”) EMAs by up to 30 minutes by clicking the Snooze Assessment option on the smartphone screen.
Data Loss Prevention
To avoid potential data loss as a result of participants losing their phones, each device is programmed to synchronize and upload encrypted data with our secure server multiple times each day (Note: in most studies, <1% of phones have been lost) [ 48 ]. These procedures prevent the collected EMA data from being lost, allow the researchers to remotely monitor participants’ EMA completion rates, and identify when participants need to be contacted for low survey completion. Notably, EMA data are encrypted and password protected on each study phone. Therefore, the study data are only accessible to the research team. The lost phones are wiped remotely. Participants who lose their phones are provided up to 1 replacement.
The Insight Platform
The Insight mHealth platform was developed by the mHealth Shared Resource at the University of Oklahoma Health Sciences Center and the Stephenson Cancer Center. This platform offers resources to help researchers build, test, and launch technology-based assessment and intervention tools [ 66 ]. The mHealth resource uses a sizeable team that includes 1 program manager, 4 project coordinators, and 4.5 computer scientists or engineers. Together, they develop and maintain web and mobile apps and relational databases. These apps are developed using cutting-edge, cross-platform design tools.
Smartphone Training
Our team has developed and implemented a brief user-friendly training protocol to aid those with limited smartphone experience. During the randomization call, all participants, depending on condition assignment, receive training on how to use either the MASP+ app or the EMA-only Insight app and the QuitGuide app. Both versions of the Insight app (MASP+ and EMA only) contain an “App Instructions” button to remind participants of how each app feature functions ( Figure 2 ). In previous studies, similar protocols have resulted in high EMA compliance rates (eg, 82%-87% of all EMAs completed) in samples of socioeconomically disadvantaged and nondisadvantaged adults [ 55 , 65 , 95 , 96 ]. All smartphones used in this study automatically collect data on intervention delivery (eg, number of times features are used and number of minutes treatment videos are watched).
Data Analyses
To test the hypothesis that MASP+ produces higher rates of smoking abstinence compared to the NCI QuitGuide app, a biochemically verified measure of 7-day PPA that is collected during weekly assessments via Bedfont iCO will be used. PPA is defined as no smoking, not even a puff, in the 7 days before follow-up assessments and biochemical verification of smoking abstinence (ie, CO levels <7 ppm according to an iCO test). We will calculate odds ratio effect sizes (with 95% CI) to estimate between-group differences for PPA at each follow-up assessment. The effect size for the comparison between conditions at the 26-week postquitting date assessment will serve as the primary analysis of the impact of treatment condition on smoking cessation.
We will then conduct a series of conditional latent growth curve models (LGM) to examine the impact of treatment condition on abstinence trajectories. First, an LGM will be specified using CO breath tests at 2 (quit date), 3, 4, 5, 6, and 28 weeks. The intercept of these models will be centered on the baseline assessment and will be specified to model linear change across the major assessments. A dummy code representing the treatment condition will be specified as a predictor of the intercept and slope factors to quantify the effect of MASP+ on the longitudinal course of abstinence.
The impact of treatment conditions on HIV quality of life, ART adherence, and HIV treatment engagement (hypothesis 2) will be examined using the same sequence of analyses: between-condition effect sizes followed by conditional LGM. We will then conduct univariate LGM to explore changes in AS a function of treatment (hypothesis 3), followed by a series of parallel process LGM to examine how changes in AS relate to changes in smoking and HIV outcomes. The indirect effects of treatment via AS will be evaluated by calculating bootstrapped CIs of the indirect effect using the MODEL INDIRECT command in MPlus.
Mixed Methodology
Triangulation mixed methods quantitative and qualitative data analysis will be used to evaluate quantitative and qualitative data [ 97 ]. Using an explanatory sequential mixed methods design, qualitative data collection and analysis will increase the investigators’ understanding of participant experiences of the tailored material for both cultural relevance and relevance to living with HIV.
Quantitative Data
Quantitative data analysis will focus on (1) behavioral markers of engagement with the app (ie, completion of >75% of all assigned videos and completion of >75% of all assigned exercises); (2) self-report evaluations of the app including ease of interacting with the app (ie, >75% of all participants agreeing that MASP+ is easy to use based on a rating of ≥3 on the scale), that the MASP+ features (eg, automated treatment messages that follow EMA and treatment videos) are useful and helpful on a similar scale, and that at least 75% of participants would be likely to recommend the app to a friend; and (3) data from the System Usability Scale [ 98 - 100 ]. Low engagement and evaluation of MASP+ will be discussed with each participant during the qualitative interview.
Qualitative Data
Qualitative data analysis will focus on participants’ experiences with the app and incorporating their feedback to improve the app interface and features. Individual interviews will be transcribed following completion of participant treatment and then reviewed by the research team to monitor data quality. The transcribed interviews will be coded using NVivo (version 12; Lumivero). Following a first reading of the transcripts, the interviews will be coded using 2 coding passes [ 101 ]. The first coding pass will be use focused [ 102 ], with initial codes developed from the question path questions and additional codes based on responses to the System Usability Scale. The qualitative researcher (MKC) will code the interviews, and the coding will be reviewed by a second member of the research team trained in qualitative methods. The coding disagreements will then be discussed and resolved. Memos and notes will be reviewed and discussed. A second coding pass will then be conducted based on additional codes identified during the discussion, which may be process based or theoretically based, depending on what emerges from the first round of coding. Following the review of both coding passes, the research team will conduct a thematic analysis in several steps, beginning with the MASP+ participants, where themes will be identified both within and between codes. The team will then create data displays and review the patterns of responses between related sets of codes [ 103 ]. Points of integration between the MASP+ qualitative and quantitative data will be identified, a joint analysis will be conducted, and joint displays will be created [ 104 ]. Following the joint analysis, the transcripts will be read again for additional confirming and disconfirming evidence of themes [ 103 ], and representative quotes will then be selected. The QuitGuide responses will then be analyzed and compared to the MASP+ responses.
Sample Size Determination
As this is the first empirical evaluation of the MASP+ intervention in this population, our focus is on determining the feasibility of the new intervention and obtaining preliminary estimates of effect sizes on smoking and HIV outcomes and the hypothesized mechanism of change, rather than conducting a full-scale and statistically powered examination of comparative efficacy. We expect that MASP+ will be superior to the NCI QuitGuide on all outcomes examined, but that the effects of MASP+ may vary and be larger for smoking outcomes than for HIV outcomes. On the basis of power calculations conducted using Repeated Measures and Sample Size and simulation studies identifying the sample sizes necessary to detect indirect effects [ 105 , 106 ], a target sample size of 72 would provide sufficient statistical power to detect a medium to large effect (Cohen d ≥0.6) and an indirect effect for H3 if the treatment effect on AS is large (Cohen d =0.8) and the effect of AS on outcomes is medium to large (Cohen d =0.5). Our conclusions will primarily be based on effect sizes and associated CIs, and the effect size estimates (and associated CIs) from this trial will be used to guide future larger trials of comparative efficacy.
Qualitative interviews are conducted with all MASP+ and QuitGuide participants. The recommended minimum size for any subgroup is 20 interviews [ 107 ]. However, based on our prior work [ 48 ], interviews vary substantially in the content provided, so interviews will be conducted with all enrolled study participants in MASP+ and QuitGuide to meet the saturation of key study questions. Interviewing all MASP+ participants should be sufficient for the saturation of key study questions. The QuitGuide interviews will be used as a comparative group following the analysis of the MASP+ content, based on our prior work.
This study received IRB approval on November 29, 2022, under STUDY00003811 and began data collection on October 16, 2023. As of manuscript submission, a total of 9 participants have been fully enrolled in this trial. Data enrollment is scheduled to be completed by June 2024, and data collection is scheduled to be completed by December 2024. Data analysis will begin February 2025 and results will be published March 2024.
Expected Findings
Data collection is currently underway. Results are expected to indicate that MASP+, relative to QuitGuide, will lead to improved biochemically verified 7-day PPA, increased adherence to ART, and improved attendance at HIV-related health appointments at 26 weeks postquitting date. Qualitative interviews will be integrated with quantitative data to further refine and adapt MASP+ and support the development of an iterative intervention that is high quality, culturally relevant, scalable, and ready for rigorous testing as part of an R01-level grant.
Study Implications
This study is the first to culturally tailor a smoking cessation smartphone-delivered intervention that is integrated with AS reduction skills for Black people with HIV/AIDS who smoke and elevated AS. Smartphone interventions such as MASP+ have the potential to provide low-cost, scalable treatments to diverse populations who may not be as likely to have access to in-person treatment or may not have health insurance to cover costs. A 2021 survey found that 85% of US adults reported owning a smartphone [ 108 ], and other studies have found that smartphone ownership is high among minoritized populations (83% among Black adults) as well as individuals with low socioeconomic status (76% among those earning <US $30,000/y) [ 108 ]. Given the widespread ownership of smartphones, MASP+ has the potential to overcome traditional barriers to care and enhance the accessibility and reach of culturally appropriate, clinical-grade care for hard-to-reach populations.
Clinically, the cultural tailoring and integration of AS reduction skills within MASP+ represents a groundbreaking approach. Experiences of AS and related mental health factors (eg, anxiety, depression, and drug withdrawal or craving) can vary over time and among individuals [ 109 ]. By assessing these factors throughout the day and providing support as these symptoms arise, MASP+ constitutes a just-in-time tailored intervention for smoking cessation, AS, and HIV management. Such an approach may serve as a potential solution to address the documented health disparities experienced by Black people with HIV/AIDS who smoke [ 6 , 110 ]. MASP+ is also distinguished by the specificity with which it can respond to the unique stressors, needs, and challenges experienced by Black smokers with HIV and AS. This underscores the potential for MASP+ to serve as a stand-alone or adjunctive treatment for smoking cessation. Indeed, MASP+ offers personalized care to address factors that impede successful behavioral change in a culturally appropriate and person-centered manner, which may have strong implications for mitigating health disparities for Black smokers with HIV.
Understanding the role of AS in the process of quitting cigarettes and better managing HIV among Black adults with HIV has several theoretical implications. First, this work bridges together disparate yet complementary work on AS, smoking, and HIV [ 111 , 112 ]. Thus, findings from this trial may provide a holistic understanding of how these constructs relate to and influence one another. This greatly advances the current models for the role of interoceptive distress as a risk factor for worse smoking cessation and HIV-related outcomes [ 113 - 116 ]. Second, several models related to minority stress indicate the need for culturally tailored interventions, particularly those targeting smoking cessation [ 117 - 119 ]. Expanding these efforts to produce tailored interventions for Black smokers with HIV that focus on a mechanism implicated in worse health outcomes among this group (ie, AS) allows providers and researchers to address documented health disparities among this population in a culturally specific manner [ 120 ]. Further studies of the mechanisms underlying quit success among Black smokers with HIV and AS will guide future efforts to tailor smoking cessation interventions for this population. This study will provide insights about which risk factors to target during smoking cessation treatment among this group, the ideal timing of intervention efforts, and the preferred content of intervention messages.
Anticipated Limitations
This study has several limitations. Daily EMAs can be disruptive as they are prompted throughout the day rather than clustered in a single study appointment. This could potentially discourage participation in the daily EMA component of this study. In addition, some study measures rely on self-reporting, and participants may not respond in real time. In addition, recruiting a population as specific as Black people with HIV/AIDS who smoke only combustible cigarettes may prove challenging for the study team. Finally, although participants will be responding to items while navigating daily life, thereby increasing ecological validity, this comes at the expense of depriving experimenters of a high degree of control over participants’ environmental conditions.
Conclusions
This study may provide insights into precision medicine treatment that is not otherwise available by providing a smoking cessation and HIV management intervention with tailored treatment content based on the psychological and environmental context in real time. Pending tests of its efficacy, an intervention that is automated, scalable, and culturally informed could be easily incorporated into other real-world settings and aid in the reduction of health disparities. This novel mobile intervention has the potential to address the mental and physical barriers to smoking cessation and treatment engagement that are unique to Black people with HIV/AIDS. Despite any potential difficulties in recruiting such a specific group or capturing EMA data, the benefits of this study far outweigh any drawbacks.
Additional work is essential for the successful translation and cultural adaption of effective in-person smoking cessation interventions into mobile, remotely delivered treatments such as MASP+. Compared to current treatment options, mobile interventions have the potential to produce even greater cessation outcomes and provide wider access for historically oppressed and underserved populations such as Black smokers with HIV and high AS. In light of prior studies that demonstrate the feasibility of mobile smoking cessation technology [ 49 , 55 , 121 ], mobile treatments that integrate AS constitute a vital “next step” for addressing tobacco-related health disparities among Black smokers with HIV. This study will extend our work in this area as well as in the wider field of smoking–emotional disorder comorbidity by adapting and testing a fully automated, culturally tailored, mobile AS smoking cessation intervention for Black smokers with HIV. Future work will focus on testing the MASP+ app in a larger, fully powered efficacy trial; national dissemination of intervention materials; and implementation across diverse health care settings.
Acknowledgments
This study was supported by funding from the National Institute on Minority Health and Health Disparities to the University of Houston (U54MD015946; principal investigator: Ezemenari Obasi). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. LG and MB are the Multiple Principal Investigators in the Supplement Project titled MASP+ described in this paper. This work was also partially supported by the Oklahoma Tobacco Settlement Endowment Trust (R21-02 to MSB) and the National Cancer Institute (P30CA225520) awarded to the Stephenson Cancer Center, and the work used the Stephenson Cancer Center’s mHealth Shared Resource. TPG is supported by the MD Anderson Foundation Chair at Baylor College of Medicine and the Texas Developmental Center for AIDS Research (P01AI161943; principal investigator: TPG). The manuscript and its revisions were supported by the National Institute on Drug Abuse of the National Institutes of Health (R25DA054015; Multiple Principal Investigators: Obasi and Reitzel).
Data Availability
The data sets generated or analyzed during this study are available from the corresponding author upon reasonable request.
Conflicts of Interest
MB is an inventor of the Insight mobile health platform and receives royalties related to the use of this platform by investigators external to the University of Oklahoma Health Sciences Center. As MB is one of multiple principal investigators in this study, he did not receive royalties for the use of the platform to create the Mobile Anxiety Sensitivity Program for Smoking and HIV (MASP+) app.
- Frazier EL, Sutton MY, Brooks JT, Shouse RL, Weiser J. Trends in cigarette smoking among adults with HIV compared with the general adult population, United States - 2009-2014. Prev Med. Jun 2018;111:231-234. [ CrossRef ] [ Medline ]
- Cornelius ME, Loretan CG, Wang TW, Jamal A, Homa DM. Tobacco product use among adults - United States, 2020. MMWR Morb Mortal Wkly Rep. Mar 18, 2022;71(11):397-405. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Rahmanian S, Wewers ME, Koletar S, Reynolds N, Ferketich A, Diaz P. Cigarette smoking in the HIV-infected population. Proc Am Thorac Soc. Jun 2011;8(3):313-319. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Mdodo R, Frazier EL, Dube SR, Mattson CL, Sutton MY, Brooks JT, et al. Cigarette smoking prevalence among adults with HIV compared with the general adult population in the United States: cross-sectional surveys. Ann Intern Med. Mar 03, 2015;162(5):335-344. [ CrossRef ] [ Medline ]
- Burkhalter JE, Springer CM, Chhabra R, Ostroff JS, Rapkin BD. Tobacco use and readiness to quit smoking in low-income HIV-infected persons. Nicotine Tob Res. Aug 1, 2005;7(4):511-522. [ CrossRef ] [ Medline ]
- Gritz ER, Vidrine DJ, Lazev AB, Amick BC, Arduino RC. Smoking behavior in a low-income multiethnic HIV/AIDS population. Nicotine Tob Res. Feb 1, 2004;6(1):71-77. [ CrossRef ] [ Medline ]
- Sigel K, Makinson A, Thaler J. Lung cancer in persons with HIV. Curr Opin HIV AIDS. Jan 2017;12(1):31-38. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Presti RM, Flores SC, Palmer BE, Atkinson JJ, Lesko CR, Lau B, et al. Mechanisms underlying HIV-associated noninfectious lung disease. Chest. Nov 2017;152(5):1053-1060. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ntsekhe M, Baker JV. Cardiovascular disease among persons living with HIV: new insights into pathogenesis and clinical manifestations in a global context. Circulation. Jan 03, 2023;147(1):83-100. [ CrossRef ]
- Feinstein MJ, Hsue PY, Benjamin LA, Bloomfield GS, Currier JS, Freiberg MS, et al. Characteristics, prevention, and management of cardiovascular disease in people living with HIV: a scientific statement from the American Heart Association. Circulation. Jul 09, 2019;140(2):e98-124. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hemkens LG, Bucher HC. HIV infection and cardiovascular disease. Eur Heart J. Jun 01, 2014;35(21):1373-1381. [ CrossRef ] [ Medline ]
- Islam F, Wu J, Jansson J, Wilson D. Relative risk of cardiovascular disease among people living with HIV: a systematic review and meta-analysis. HIV Med. Sep 14, 2012;13(8):453-468. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Helleberg M, May MT, Ingle SM, Dabis F, Reiss P, Fätkenheuer G, et al. Smoking and life expectancy among HIV-infected individuals on antiretroviral therapy in Europe and North America. AIDS. Jan 14, 2015;29(2):221-229. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Helleberg M, Gerstoft J, Afzal S, Kronborg G, Larsen CS, Pedersen C, et al. Risk of cancer among HIV-infected individuals compared to the background population: impact of smoking and HIV. AIDS. Jun 19, 2014;28(10):1499-1508. [ CrossRef ] [ Medline ]
- Reddy KP, Parker RA, Losina E, Baggett TP, Paltiel AD, Rigotti NA, et al. Impact of cigarette smoking and smoking cessation on life expectancy among people with HIV: a US-based modeling study. J Infect Dis. Dec 01, 2016;214(11):1672-1681. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ditre JW, Brandon TH, Zale EL, Meagher MM. Pain, nicotine, and smoking: research findings and mechanistic considerations. Psychol Bull. Nov 2011;137(6):1065-1093. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Pomerleau OF, Turk DC, Fertig JB. The effects of cigarette smoking on pain and anxiety. Addict Behav. Jan 1984;9(3):265-271. [ CrossRef ] [ Medline ]
- Labbe AK, Wilner JG, Kosiba JD, Gonzalez A, Smits JA, Zvolensky MJ, et al. Demonstration of an integrated treatment for smoking cessation and anxiety symptoms in people with HIV: a clinical case study. Cogn Behav Pract. May 2017;24(2):200-214. [ CrossRef ]
- Crockett KB, Rice WS, Turan B. Associations between multiple forms of discrimination and tobacco use among people living with HIV: the mediating role of avoidance coping. J Acquir Immune Defic Syndr. May 01, 2018;78(1):9-15. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Martinez DA, Goggin K, Catley D, Gerkovich MM, Williams K, Wright J, et al. MOTIV8. Do coping styles mediate the relationship between substance use and educational attainment and antiretroviral adherence? AIDS Behav. Nov 7, 2012;16(8):2319-2329. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lloyd-Richardson EE, Stanton CA, Papandonatos GD, Shadel WG, Stein M, Tashima K, et al. Motivation and patch treatment for HIV+ smokers: a randomized controlled trial. Addiction. Nov 09, 2009;104(11):1891-1900. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Simoni JM, Huh D, Wilson IB, Shen J, Goggin K, Reynolds NR, et al. Racial/Ethnic disparities in ART adherence in the United States: findings from the MACH14 study. J Acquir Immune Defic Syndr. Aug 15, 2012;60(5):466-472. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Silverberg MJ, Leyden W, Quesenberry CP, Horberg MA. Race/ethnicity and risk of AIDS and death among HIV-infected patients with access to care. J Gen Intern Med. Sep 16, 2009;24(9):1065-1072. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Mugavero MJ, Lin HY, Allison JJ, Giordano TP, Willig JH, Raper JL, et al. Racial disparities in HIV virologic failure: do missed visits matter? J Acquir Immune Defic Syndr. Jan 01, 2009;50(1):100-108. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Beer L, McCree DH, Jeffries WL, Lemons A, Sionean C. Recent US Centers for Disease Control and Prevention activities to reduce HIV stigma. J Int Assoc Provid AIDS Care. Jan 24, 2019;18:2325958218823541. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lyons SJ, Johnson AS, Hu X, Yu C, Jin C, Yu C, et al. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data: United States and 6 dependent areas. Centers for Disease Control and Prevention. 2018. URL: https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-supplemental-report-vol-25-2.pdf [accessed 2024-03-05]
- HIV surveillance reports. Centers for Disease Control and Prevention. 2019. URL: https://www.cdc.gov/hiv/library/reports/hiv-surveillance.html [accessed 2024-03-05]
- Randolph SD, Golin C, Welgus H, Lightfoot AF, Harding CJ, Riggins LF. How perceived structural racism and discrimination and medical mistrust in the health system influences participation in HIV health services for black women living in the United States South: a qualitative, descriptive study. J Assoc Nurses AIDS Care. 2020;31(5):598-605. [ CrossRef ] [ Medline ]
- Kilanowski JF. Breadth of the socio-ecological model. J Agromedicine. 2017;22(4):295-297. [ CrossRef ] [ Medline ]
- Crenshaw K. Demarginalizing the intersection of race and sex: a black feminist critique of antidiscrimination doctrine, feminist theory, and antiracist politics. In: Bartlett K, editor. Feminist Legal Theory. New York, NY. Routledge; 2013;23-51.
- Taylor S, Zvolensky MJ, Cox BJ, Deacon B, Heimberg RG, Ledley DR, et al. Robust dimensions of anxiety sensitivity: development and initial validation of the Anxiety Sensitivity Index-3. Psychol Assess. Jun 2007;19(2):176-188. [ CrossRef ] [ Medline ]
- Reiss S. Expectancy model of fear, anxiety, and panic. Clin Psychol Rev. Jan 1991;11(2):141-153. [ FREE Full text ] [ CrossRef ]
- Zinbarg RE, Barlow DH, Brown TA. Hierarchical structure and general factor saturation of the Anxiety Sensitivity Index: evidence and implications. Psychol Assess. 1997;9(3):277-284. [ CrossRef ]
- Taylor S. Anxiety Sensitivity: Theory, Research, and Treatment of the Fear of Anxiety. Oxfordshire, UK. Routledge; 1999.
- Wykowski J, Kemp CG, Velloza J, Rao D, Drain PK. Associations between anxiety and adherence to antiretroviral medications in low- and middle-income countries: a systematic review and meta-analysis. AIDS Behav. Aug 18, 2019;23(8):2059-2071. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Leyro TM, Vujanovic AA, Bonn-Miller MO. Examining associations between cognitive-affective vulnerability and HIV symptom severity, perceived barriers to treatment adherence, and viral load among HIV-positive adults. Int J Behav Med. Feb 19, 2015;22(1):139-148. [ CrossRef ] [ Medline ]
- Brandt CP, Paulus DJ, Jardin C, Heggeness L, Lemaire C, Zvolensky MJ. Examining anxiety sensitivity as an explanatory construct underlying HIV-related stigma: relations to anxious arousal, social anxiety, and HIV symptoms among persons living with HIV. J Anxiety Disord. May 2017;48:95-101. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Leventhal AM, Zvolensky MJ. Anxiety, depression, and cigarette smoking: a transdiagnostic vulnerability framework to understanding emotion-smoking comorbidity. Psychol Bull. Jan 2015;141(1):176-212. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Gregor KL, Zvolensky MJ, McLeish AC, Bernstein A, Morissette S. Anxiety sensitivity and perceived control over anxiety-related events: associations with smoking outcome expectancies and perceived cessation barriers among daily smokers. Nicotine Tob Res. Apr 2008;10(4):627-635. [ CrossRef ] [ Medline ]
- Alcántara C, Giorgio Cosenzo LA, Fan W, Doyle DM, Shaffer JA. Anxiety sensitivity and racial differences in sleep duration: results from a national survey of adults with cardiovascular disease. J Anxiety Disord. May 2017;48:102-108. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Assayag Y, Bernstein A, Zvolensky MJ, Steeves D, Stewart SS. Nature and role of change in anxiety sensitivity during NRT-aided cognitive-behavioral smoking cessation treatment. Cogn Behav Ther. Mar 2012;41(1):51-62. [ CrossRef ] [ Medline ]
- Brown RA, Kahler CW, Zvolensky MJ, Lejuez C, Ramsey SE. Anxiety sensitivity: relationship to negative affect smoking and smoking cessation in smokers with past major depressive disorder. Addict Behav. Nov 2001;26(6):887-899. [ CrossRef ] [ Medline ]
- Smits JA, Zvolensky MJ, Davis ML, Rosenfield D, Marcus BH, Church TS, et al. The efficacy of vigorous-intensity exercise as an aid to smoking cessation in adults with high anxiety sensitivity: a randomized controlled trial. Psychosom Med. Apr 2016;78(3):354-364. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Zvolensky MJ, Bogiaizian D, Salazar PL, Farris SG, Bakhshaie J. An anxiety sensitivity reduction smoking-cessation program for Spanish-speaking smokers (Argentina). Cognitive and Behavioral Practice. Aug 2014;21(3):350-363. [ CrossRef ]
- Zvolensky MJ, Lejuez C, Kahler CW, Brown RA. Integrating an interoceptive exposure-based smoking cessation program into the cognitive-behavioral treatment of panic disorder: theoretical relevance and case demonstration. Cogn Behav Pract. Sep 2003;10(4):347-357. [ CrossRef ]
- Schmidt NB, Raines AM, Allan NP, Zvolensky MJ. Anxiety sensitivity risk reduction in smokers: a randomized control trial examining effects on panic. Behav Res Ther. Feb 2016;77:138-146. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Shiffman S, Brockwell SE, Pillitteri JL, Gitchell JG. Use of smoking-cessation treatments in the United States. Am J Prev Med. Feb 2008;34(2):102-111. [ CrossRef ] [ Medline ]
- Businelle MS, Garey L, Gallagher MW, Hébert ET, Vujanovic A, Alexander A, et al. An integrated mHealth app for smoking cessation in black smokers with anxiety: protocol for a randomized controlled trial. JMIR Res Protoc. May 30, 2022;11(5):e38905. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Garey L, Hébert ET, Mayorga NA, Chavez J, Shepherd JM, Businelle MS, et al. Evaluating the feasibility and acceptability of a mobile-based health technology for smoking cessation: mobile anxiety sensitivity program. Br J Clin Psychol. Jan 03, 2022;61 Suppl 1(Suppl 1):111-129. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Arozullah AM, Yarnold PR, Bennett CL, Soltysik RC, Wolf MS, Ferreira RM, et al. Development and validation of a short-form, rapid estimate of adult literacy in medicine. Med Care. Nov 2007;45(11):1026-1033. [ CrossRef ] [ Medline ]
- Zvolensky MJ, Garey L, Fergus TA, Gallagher MW, Viana AG, Shepherd JM, et al. Refinement of anxiety sensitivity measurement: the Short Scale Anxiety Sensitivity Index (SSASI). Psychiatry Res. Nov 2018;269:549-557. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Boardman T, Catley D, Mayo MS, Ahluwalia JS. Self-efficacy and motivation to quit during participation in a smoking cessation program. Int J Behav Med. Dec 2005;12(4):266-272. [ CrossRef ] [ Medline ]
- Brooke P, Bullock R. Validation of a 6 item cognitive impairment test with a view to primary care usage. Int J Geriatr Psychiatry. Nov 1999;14(11):936-940. [ Medline ]
- 2008 PHS Guideline Update Panel‚ Liaisons‚Staff. Treating tobacco use and dependence: 2008 update U.S. public health service clinical practice guideline executive summary. Respir Care. Sep 2008;53(9):1217-1222. [ FREE Full text ] [ Medline ]
- Hébert ET, Ra CK, Alexander AC, Helt A, Moisiuc R, Kendzor DE, et al. A mobile just-in-time adaptive intervention for smoking cessation: pilot randomized controlled trial. J Med Internet Res. Mar 09, 2020;22(3):e16907. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Treating tobacco use and dependence: 2008 update. US Department of Health and Human Services. 2008. URL: https://www.ncbi.nlm.nih.gov/books/NBK63952/ [accessed 2024-03-05]
- Sweeney CT, Fant RV, Fagerstrom KO, McGovern JF, Henningfield JE. Combination nicotine replacement therapy for smoking cessation: rationale, efficacy and tolerability. CNS Drugs. 2001;15(6):453-467. [ CrossRef ] [ Medline ]
- Home page. U.S. Department of Health and Human Services. URL: https://smokefree.gov/ [accessed 2024-04-03]
- Forney DJ, Sheehan DM, Dale SK, Li T, De La Rosa M, Spencer EC, et al. The impact of HIV-related stigma on racial/ethnic disparities in retention in HIV care among adults living with HIV in Florida. J Racial Ethn Health Disparities (Forthcoming). Jul 26, 2023. [ CrossRef ] [ Medline ]
- Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. Feb 22, 2009;32(1):20-47. [ FREE Full text ] [ CrossRef ] [ Medline ]
- van Ballegooijen W, Klein B, Lindefors N. ICBT for panic disorder and agoraphobia: from the computer at home to real-life ‘In Vivo’ exposure. In: Lindefors N, Andersson G, editors. Guided Internet-Based Treatments in Psychiatry. Cham, Switzerland. Springer; 2016;33-52.
- Ebenfeld L, Kleine Stegemann S, Lehr D, Ebert DD, Jazaieri H, van Ballegooijen W, et al. Efficacy of a hybrid online training for panic symptoms and agoraphobia: study protocol for a randomized controlled trial. Trials. Nov 04, 2014;15(1):427. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Neal AM, Turner SM. Anxiety disorders research with African Americans: current status. Psychol Bull. 1991;109(3):400-410. [ CrossRef ]
- Coughtrey AE, Pistrang N. The effectiveness of telephone-delivered psychological therapies for depression and anxiety: a systematic review. J Telemed Telecare. Feb 2018;24(2):65-74. [ CrossRef ] [ Medline ]
- Businelle MS, Ma P, Kendzor DE, Frank SG, Vidrine DJ, Wetter DW. An ecological momentary intervention for smoking cessation: evaluation of feasibility and effectiveness. J Med Internet Res. Dec 12, 2016;18(12):e321. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Insight mHealth platform on the app store. Apple Store. URL: https://apps.apple.com/us/app/insight-mhealth-platform/id1582652446 [accessed 2024-03-05]
- Benowitz NL, Bernert JT, Foulds J, Hecht SS, Jacob III P, Jarvis MJ, et al. Biochemical verification of tobacco use and abstinence: 2019 update. Nicotine Tob Res. Jun 12, 2020;22(7):1086-1097. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Perkins KA, Karelitz JL, Jao NC. Optimal carbon monoxide criteria to confirm 24-hr smoking abstinence. Nicotine Tob Res. May 18, 2013;15(5):978-982. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Tevyaw TO, Colby SM, Tidey JW, Kahler CW, Rohsenow DJ, Barnett NP, et al. Contingency management and motivational enhancement: a randomized clinical trial for college student smokers. Nicotine Tob Res. Jun 2009;11(6):739-749. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Heil SH, Higgins ST, Bernstein IM, Solomon LJ, Rogers RE, Thomas CS, et al. Effects of voucher-based incentives on abstinence from cigarette smoking and fetal growth among pregnant women. Addiction. Jun 28, 2008;103(6):1009-1018. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Higgins ST, Bernstein IM, Washio Y, Heil SH, Badger GJ, Skelly JM, et al. Effects of smoking cessation with voucher-based contingency management on birth outcomes. Addiction. Nov 15, 2010;105(11):2023-2030. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Stoops WW, Dallery J, Fields NM, Nuzzo PA, Schoenberg NE, Martin CA, et al. An internet-based abstinence reinforcement smoking cessation intervention in rural smokers. Drug Alcohol Depend. Nov 01, 2009;105(1-2):56-62. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Dunn KE, Sigmon SC, Thomas CS, Heil SH, Higgins ST. Voucher-based contingent reinforcement of smoking abstinence among methadone-maintained patients: a pilot study. J Appl Behav Anal. Feb 27, 2008;41(4):527-538. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Etter JF. Financial incentives for smoking cessation in low-income smokers: study protocol for a randomized controlled trial. Trials. Jun 21, 2012;13(1):88. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Berlin I, Radzius A, Henningfield JE, Moolchan ET. Correlates of expired air carbon monoxide: effect of ethnicity and relationship with saliva cotinine and nicotine. Nicotine Tob Res. Nov 1, 2001;3(4):325-331. [ CrossRef ] [ Medline ]
- Jarvis MJ, Tunstall-Pedoe H, Feyerabend C, Vesey C, Saloojee Y. Comparison of tests used to distinguish smokers from nonsmokers. Am J Public Health. Nov 1987;77(11):1435-1438. [ CrossRef ] [ Medline ]
- Fritz M, Wallner R, Grohs U, Kemmler G, Saria A, Zernig G. Comparable sensitivities of urine cotinine and breath carbon monoxide at follow-up time points of three months or more in a smoking cessation trial. Pharmacology. Mar 17, 2010;85(4):234-240. [ CrossRef ] [ Medline ]
- WHOQOL-HIV BREF, 2012 revision. World Health Organization. URL: https://www.who.int/publications/i/item/WHO-MSD-MER-Rev-2012-02 [accessed 2024-03-05]
- Lu M, Safren SA, Skolnik PR, Rogers WH, Coady W, Hardy H, et al. Optimal recall period and response task for self-reported HIV medication adherence. AIDS Behav. Jan 19, 2008;12(1):86-94. [ CrossRef ] [ Medline ]
- Chesney MA, Ickovics JR, Chambers DB, Gifford AL, Neidig J, Zwickl B, et al. AIDS Care. Jun 27, 2000;12(3):255-266. [ CrossRef ] [ Medline ]
- Johnson MO, Neilands TB, Koester KA, Wood T, Sauceda JA, Dilworth SE, et al. Detecting disengagement from HIV care before it is too late: development and preliminary validation of a novel index of engagement in HIV care. J Acquir Immune Defic Syndr. Jun 01, 2019;81(2):145-152. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Sternthal MJ, Slopen N, Williams DR. Racial disparities in health: how much does stress really matter? Du Bois Rev. 2011;8(1):95-113. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Peek ME, Nunez-Smith M, Drum M, Lewis TT. Adapting the everyday discrimination scale to medical settings: reliability and validity testing in a sample of African American patients. Ethn Dis. 2011;21(4):502-509. [ FREE Full text ] [ Medline ]
- Bevan N, Kirakowski J, Maissel J. What is usability? In: Bullinger HJ, editor. Human Aspects in Computing: Design and Use of Interactive Systems and Work With Terminals. Cambridge, MA. Elsevier Academic Press; 1991.
- Kirakowski J, Corbett M. Measuring user satisfaction. In: Proceedings of the 4th Conference of the British Computer Society on People and computers IV. 1988. Presented at: BSC HCI '88; August 5-9, 1988;329-338; Manchester, UK. URL: https://dl.acm.org/doi/proceedings/10.5555/54675
- Lewis JR. The system usability scale: past, present, and future. Int J Hum Comput Interact. Mar 30, 2018;34(7):577-590. [ CrossRef ]
- Shiffman S, Hufford M, Hickcox M, Paty JA, Gnys M, Kassel JD. Remember that? A comparison of real-time versus retrospective recall of smoking lapses. J Consult Clin Psychol. Apr 1997;65(2):292-300. [ CrossRef ] [ Medline ]
- Stone AA, Shiffman S, Schwartz JE, Broderick JE, Hufford MR. Patient non-compliance with paper diaries. BMJ. May 18, 2002;324(7347):1193-1194. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Wetter DW, McClure JB, Cofta-Woerpel L, Costello TJ, Reitzel LR, Businelle MS, et al. A randomized clinical trial of a palmtop computer-delivered treatment for smoking relapse prevention among women. Psychol Addict Behav. Jun 2011;25(2):365-371. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Stone AA, Schwartz JE, Neale JM, Shiffman S, Marco CA, Hickcox M, et al. A comparison of coping assessed by ecological momentary assessment and retrospective recall. J Pers Soc Psychol. Jun 1998;74(6):1670-1680. [ CrossRef ] [ Medline ]
- Shiffman S, Paty JA, Gnys M, Kassel JA, Hickcox M. First lapses to smoking: within-subjects analysis of real-time reports. J Consult Clin Psychol. Apr 1996;64(2):366-379. [ CrossRef ] [ Medline ]
- Piasecki TM, Cooper ML, Wood PK, Sher KJ, Shiffman S, Heath AC. Dispositional drinking motives: associations with appraised alcohol effects and alcohol consumption in an ecological momentary assessment investigation. Psychol Assess. Jun 2014;26(2):363-369. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Simons JS, Dvorak RD, Batien BD, Wray TB. Event-level associations between affect, alcohol intoxication, and acute dependence symptoms: effects of urgency, self-control, and drinking experience. Addict Behav. Dec 2010;35(12):1045-1053. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Swendsen JD, Tennen H, Carney MA, Affleck G, Willard A, Hromi A. Mood and alcohol consumption: an experience sampling test of the self-medication hypothesis. J Abnorm Psychol. 2000;109(2):198-204. [ CrossRef ]
- Kendzor DE, Shuval K, Gabriel KP, Businelle MS, Ma P, High RR, et al. Impact of a mobile phone intervention to reduce sedentary behavior in a community sample of adults: a quasi-experimental evaluation. J Med Internet Res. Jan 25, 2016;18(1):e19. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Businelle MS, Kendzor DE, Kesh A, Cuate EL, Poonawalla IB, Reitzel LR, et al. Small financial incentives increase smoking cessation in homeless smokers: a pilot study. Addict Behav. Mar 2014;39(3):717-720. [ CrossRef ] [ Medline ]
- Wilson V. Research methods: triangulation. Evid Based Libr Inf Pract. Mar 05, 2014;9(1):74-75. [ FREE Full text ] [ CrossRef ]
- Rooke SE, Gates PJ, Norberg MM, Copeland J. Applying technology to the treatment of cannabis use disorder: comparing telephone versus Internet delivery using data from two completed trials. J Subst Abuse Treat. Jan 2014;46(1):78-84. [ CrossRef ] [ Medline ]
- Hindson J, Hanstock T, Dunlop A, Kay-Lambkin F. Internet-delivered tobacco treatment for people using cannabis: a randomized trial in two Australian cannabis clinics. JMIR Form Res. Dec 07, 2020;4(12):e14344. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Macatee RJ, Albanese BJ, Okey SA, Afshar K, Carr M, Rosenthal MZ, et al. Impact of a computerized intervention for high distress intolerance on cannabis use outcomes: a randomized controlled trial. J Subst Abuse Treat. Feb 2021;121:108194. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Saldaña J. The Coding Manual for Qualitative Researchers. Thousand Oaks, CA. Sage Publications; Oct 18, 2016.
- Patton MQ, Campbell-Patton CE. Utilization-Focused Evaluation. Thousand Oaks, CA. Sage Publications; 2008.
- Miles MB, Huberman AM, Saldaña J. Qualitative Data Analysis: A Methods Sourcebook. Thousand Oaks, CA. Sage Publications; 2019.
- Creswell JW, Clark VL. Designing and Conducting Mixed Methods Research. Thousand Oaks, CA. Sage Publications; 2017.
- Hedeker D, Gibbons RD, Waternaux C. Sample size estimation for longitudinal designs with attrition: comparing time-related contrasts between two groups. J Educ Behav Stat. 1999;24(1):70. [ CrossRef ]
- Fritz MS, Mackinnon DP. Required sample size to detect the mediated effect. Psychol Sci. Mar 04, 2007;18(3):233-239. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Morse JM. Strategies for sampling. In: Morse JM, editor. Qualitative Nursing Research: A Contemporary Dialogue. Thousand Oaks, CA. Sage Publications; 1991;127-145.
- Mobile fact sheet. Pew Research Center. 2021. URL: https://www.pewresearch.org/internet/fact-sheet/mobile/ [accessed 2024-03-05]
- Hovenkamp-Hermelink JH, van der Veen DC, Oude Voshaar RC, Batelaan NM, Penninx BW, Jeronimus BF, et al. Anxiety sensitivity, its stability and longitudinal association with severity of anxiety symptoms. Sci Rep. Mar 13, 2019;9(1):4314. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Aral SO, Adimora AA, Fenton KA. Understanding and responding to disparities in HIV and other sexually transmitted infections in African Americans. Lancet. Jul 2008;372(9635):337-340. [ CrossRef ]
- Brandt CP, Bakhshaie J, Jardin C, Lemaire C, Kauffman BY, Sharp C, et al. The moderating effect of smoking status on the relation between anxiety sensitivity, sexual compulsivity, and suicidality among people with HIV/AIDS. Int J Behav Med. Feb 11, 2017;24(1):92-100. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Paulus DJ, Jardin C, Bakhshaie J, Sharp C, Woods SP, Lemaire C, et al. Anxiety sensitivity and hazardous drinking among persons living with HIV/AIDS: an examination of the role of emotion dysregulation. Addict Behav. Dec 2016;63:141-148. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Millon EM, Shors TJ. How mental health relates to everyday stress, rumination, trauma and interoception in women living with HIV: a factor analytic study. Learn Motiv. Feb 2021;73:101680. [ CrossRef ]
- Farris SG, Langdon KJ, DiBello AM, Zvolensky MJ. Why do anxiety sensitive smokers perceive quitting as difficult? The role of expecting “interoceptive threat” during acute abstinence. Cogn Ther Res. Sep 26, 2014;39(2):236-244. [ CrossRef ]
- Hina F, Aspell JE. Altered interoceptive processing in smokers: evidence from the heartbeat tracking task. Int J Psychophysiol. Aug 2019;142:10-16. [ CrossRef ] [ Medline ]
- Kim M, Park YJ, Kim K, Lee JH. Effect of heightened interoceptive awareness among smokers on misinterpretation of emotional arousal. Soc Behav Pers. Feb 05, 2020;48(2):1-8. [ CrossRef ]
- Matthews AK, McConnell EA, Li CC, Vargas MC, King A. Design of a comparative effectiveness evaluation of a culturally tailored versus standard community-based smoking cessation treatment program for LGBT smokers. BMC Psychol. May 30, 2014;2(1):12. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kong G, Singh N, Krishnan-Sarin S. A review of culturally targeted/tailored tobacco prevention and cessation interventions for minority adolescents. Nicotine Tob Res. Dec 21, 2012;14(12):1394-1406. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Tan AS, Chen JT, Keen R, Scout N, Gordon B, Applegate J, et al. Culturally tailored anti-smoking messages: a randomized trial with U.S. sexual minority young women. Am J Prev Med (Forthcoming). Dec 07, 2023. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hai AH, Batey DS, Lee CS, Li S, Schnall R. Examining the intersection of ethnoracial disparities and HIV status in substance use risks among U.S. adults. AIDS Behav (Forthcoming). Jan 31, 2024. [ CrossRef ] [ Medline ]
- Bricker JB, Watson NL, Mull KE, Sullivan BM, Heffner JL. Efficacy of smartphone applications for smoking cessation: a randomized clinical trial. JAMA Intern Med. Nov 01, 2020;180(11):1472-1480. [ FREE Full text ] [ CrossRef ] [ Medline ]
Abbreviations
Edited by A Mavragani; submitted 22.08.23; peer-reviewed by R Rosen, C Baxter; comments to author 17.12.23; revised version received 09.02.24; accepted 14.02.24; published 24.04.24.
©Andre Bizier, Arielle Jones, Michael Businelle, Krista Kezbers, Bettina B Hoeppner, Thomas P Giordano, Jessica M Thai, Jacqueline Charles, Audrey Montgomery, Matthew W Gallagher, Marshall K Cheney, Michael Zvolensky, Lorra Garey. Originally published in JMIR Research Protocols (https://www.researchprotocols.org), 24.04.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in JMIR Research Protocols, is properly cited. The complete bibliographic information, a link to the original publication on https://www.researchprotocols.org, as well as this copyright and license information must be included.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Cochrane Database Syst Rev
Nursing interventions for smoking cessation
Healthcare professionals, including nurses, frequently advise people to improve their health by stopping smoking. Such advice may be brief, or part of more intensive interventions.
To determine the effectiveness of nursing‐delivered smoking cessation interventions in adults. To establish whether nursing‐delivered smoking cessation interventions are more effective than no intervention; are more effective if the intervention is more intensive; differ in effectiveness with health state and setting of the participants; are more effective if they include follow‐ups; are more effective if they include aids that demonstrate the pathophysiological effect of smoking.
Search methods
We searched the Cochrane Tobacco Addiction Group Specialized Register and CINAHL in January 2017.
Selection criteria
Randomized trials of smoking cessation interventions delivered by nurses or health visitors with follow‐up of at least six months.
Data collection and analysis
Two review authors extracted data independently. The main outcome measure was abstinence from smoking after at least six months of follow‐up. We used the most rigorous definition of abstinence for each trial, and biochemically‐validated rates if available. Where statistically and clinically appropriate, we pooled studies using a Mantel‐Haenszel fixed‐effect model and reported the outcome as a risk ratio (RR) with a 95% confidence interval (CI).
Main results
Fifty‐eight studies met the inclusion criteria, nine of which are new for this update. Pooling 44 studies (over 20,000 participants) comparing a nursing intervention to a control or to usual care, we found the intervention increased the likelihood of quitting (RR 1.29, 95% CI 1.21 to 1.38); however, statistical heterogeneity was moderate (I 2 = 50%) and not explained by subgroup analysis. Because of this, we judged the quality of evidence to be moderate. Despite most studies being at unclear risk of bias in at least one domain, we did not downgrade the quality of evidence further, as restricting the main analysis to only those studies at low risk of bias did not significantly alter the effect estimate. Subgroup analyses found no evidence that high‐intensity interventions, interventions with additional follow‐up or interventions including aids that demonstrate the pathophysiological effect of smoking are more effective than lower intensity interventions, or interventions without additional follow‐up or aids. There was no evidence that the effect of support differed by patient group or across healthcare settings.
Authors' conclusions
There is moderate quality evidence that behavioural support to motivate and sustain smoking cessation delivered by nurses can lead to a modest increase in the number of people who achieve prolonged abstinence. There is insufficient evidence to assess whether more intensive interventions, those incorporating additional follow‐up, or those incorporating pathophysiological feedback are more effective than one‐off support. There was no evidence that the effect of support differed by patient group or across healthcare settings.
Plain language summary
Does support and intervention from nurses help people to stop smoking?
Most smokers want to quit, and may be helped by advice and support from healthcare professionals. Nurses are the largest healthcare workforce, and are involved in virtually all levels of health care. The main aim of this review was to determine if nursing‐delivered interventions can help adult smokers to stop smoking.
Study characteristics
This review of clinical trials covered 58 studies in which nurses delivered a stop‐smoking intervention to smokers. More than 20,000 participants were included in the main analysis, including hospitalized adults and adults in the general community. The most recent search was conducted in January 2017. All studies reported whether or not participants had quit smoking at six months or longer.
Key Results
This review found moderate‐quality evidence that advice and support from nurses could increase people's success in quitting smoking, whether in hospitals or in community settings. Eleven studies compared different nurse‐delivered interventions and did not find that adding more components changed the effect.
Quality of evidence
The quality of evidence was moderate, meaning that further research may change our confidence in the result. This is because results were not consistent across all of the studies, and in some cases there were not very many studies contributing to comparisons.
Summary of findings
Summary of findings for the main comparison.
1 Control group quit rate based on average across all included studies. 2 Not downgraded for risk of bias: Sensitivity analyses excluding studies at high or unclear risk of bias did not significantly alter the effect size. 3 Downgraded one level for inconsistency: Unexplained statistical heterogeneity present. 4 Downgraded one level for imprecision: Total number of events < 300, confidence intervals include a significant effect and no effect.
Tobacco‐related deaths and disabilities are on the increase worldwide because of continued use of tobacco (mainly cigarettes). Tobacco use has reached epidemic proportions in many low‐ and middle‐income countries, while steady use continues in high‐income nations like the USA ( The Tobacco Atlas 2015 ; CDC 2016 ). According to the Centers for Disease Control, 68% of adult smokers in the USA want to quit and millions have tried ( CDC 2017 ), with 70% of smokers visiting a healthcare professional each year ( AHRQ 2008 ). Nurses, representing the largest number of healthcare providers worldwide, are involved in most of these visits, and therefore have the potential for a profound effect on the reduction of tobacco use ( Youdan 2005 ).
Systematic reviews (e.g. Stead 2013 ) have confirmed the effectiveness of advice from physicians to stop smoking. The Agency for Health Care Research and Quality Clinical Practice Guideline ( AHRQ 2008 ) lists nurses as one of the many providers from whom advice to stop smoking could increase quit rates, but identifies the effectiveness of advice to quit smoking given by clinicians other than physicians (including nurses) as an area requiring further research. The American Nurses Association ( ANA 2012 ) state that nurses have tremendous potential to implement smoking cessation interventions effectively and advance tobacco use reduction goals proposed by Healthy People 2020, and note that nurses must be equipped to assist with smoking cessation, to prevent tobacco use, and to promote strategies to decrease exposure to second‐hand smoke. The American Nurses Association/American Nurses Foundation promotes the mission of Tobacco‐Free Nurses to the nation’s registered nurses through its constituent associations, members, and organizational affiliates ( ANA 2012 ).
A review of nursing's specific role in smoking cessation is essential if the profession is to endorse the International Council of Nurses' (ICN) call to encourage nurses to "...integrate tobacco use prevention and cessation ... as part of their regular nursing practice" ( ICN 2012 ).
The aim of this review is to examine and summarize randomized controlled trials where nurses provided smoking cessation interventions. The review therefore focuses on the nurse as the intervention provider, rather than on a particular type of intervention. We do not include smoking cessation interventions targeting pregnant women, because of the particular circumstances and motivations among this population. Interventions for pregnant smokers have been reviewed elsewhere ( Chamberlain 2017 ; Coleman 2015 ).
To determine the effectiveness of nursing‐delivered interventions on smoking behavior in adults. To establish whether nursing‐delivered smoking cessation interventions: (i) are more effective than no intervention; (ii) are more effective if the intervention is more intensive; (iii) differ in effectiveness with health state and setting of the participants; (iv) are more effective if they include follow‐ups; (v) are more effective if they include aids that demonstrate the pathophysiological effect of smoking.
Criteria for considering studies for this review
Types of studies.
Inclusion criteria for studies were: (i) they had to have at least two treatment groups; (ii) allocation to treatment groups must have been stated to be 'random'. We excluded studies that used historical controls.
Types of participants
Participants were adult smokers, 18 years and older, of either gender and recruited in any type of healthcare or other setting. The only exceptions were studies that had exclusively recruited pregnant women. We included trials in which 'recent quitters' were classified as smokers, but conducted sensitivity analyses to determine whether they differed from trials that excluded such individuals.
Types of interventions
We define 'nursing intervention' as the provision of advice, counseling, and/or strategies to help people quit smoking. The review includes cessation studies that compared usual care with an intervention, brief advice with a more intensive smoking cessation intervention or different types of interventions. We included studies of smoking cessation interventions as a part of multifactorial lifestyle counseling or rehabilitation only if it was possible to discern the specific nature and timing of the intervention, and to extract data on the outcomes for those who were smokers at baseline. We define 'advice' as verbal instructions from the nurse to stop smoking, whether or not they provided information about the harmful effects of smoking. We grouped interventions into low and high intensity for comparison. We categorize as 'low intensity' those trials where advice was provided (with or without a leaflet) during a single consultation lasting 10 minutes or less, with up to one follow‐up visit. We categorize as 'high intensity' those trials where the initial contact lasted more than 10 minutes, there were additional materials (e.g. manuals) or strategies or both, other than simple leaflets, and usually participants had more than one follow‐up contact. We excluded studies where participants were randomized to receive advice versus advice plus some form of pharmacotherapy, since these were primarily comparisons of the effectiveness of pharmacotherapies rather than nursing interventions. These are covered in separate reviews ( Cahill 2016 ; Hughes 2014 ; Stead 2012 ).
Types of outcome measures
The primary outcome was smoking cessation rather than a reduction in withdrawal symptoms or a reduction in the number of cigarettes smoked. Trials had to report follow‐up of at least six months for inclusion in the review. We excluded trials which did not include data on smoking cessation rates. We used the strictest available criteria to define abstinence in each study, e.g. sustained cessation rather than point prevalence. Where biochemical validation was used, we regarded only participants meeting the biochemical criteria for cessation as abstainers. We counted participants lost to follow‐up as continuing smokers (in intention‐to‐treat analyses).
Search methods for identification of studies
We searched the Tobacco Addiction Review Group Specialized Register for trials (most recent search 10 January 2017). This Register includes trials located from systematic searches of electronic databases and handsearching of specialist journals, conference proceedings, and reference lists of previous trials and overviews. At the time of the search the Register included the results of searches of:
- Cochrane Central Register of Controlled trials (CENTRAL), in the Cochrane Library 2016, Issue 11;
- MEDLINE (via OVID) to update 20161202;
- Embase (via OVID) to week 201650;
- PsycINFO (via OVID) to update 20160926.
See the Tobaco Addiction Group module in the Cochrane Library for full search strategies and a list of other resources searched. We checked all trials with 'nurse*' or 'nursing' or 'health visitor' in the title, abstract, or keywords for relevance. See Appendix 1 for the search strategy. We also searched the Cumulative Index to Nursing and Allied Health Literature (CINAHL) on OVID for 'nursing' and 'smoking cessation' from 1983 to January 2017.
Selection of studies
For this update, two review authors independently screened titles and abstracts. Where there was uncertainty, we requested the full text. Two review authors checked the full text of articles flagged for inclusion, with discrepancies resolved by discussion or by referral to a third review author.
Data extraction and management
Two review authors independently extracted data from the published reports, contacting study authors where necessary, and resolving disagreements by referral to a third person. For each trial, we extracted the following data:
(i) Author(s) and year; (ii) Country of origin, study setting, and design; (iii) Number and characteristics of participants and definition of 'smoker'; (iv) Description of the intervention and designation of its intensity (high or low); (v) Outcomes and biochemical validation.
Assessment of risk of bias in included studies
We used the Cochrane 'Risk of bias' tool to assess bias in four domains:
- random sequence generation (a potential source of selection bias);
- allocation concealment (also a potential source of selection bias);
- incomplete outcome data (attrition bias);
- other biases.
We did not judge the trials on the basis of blinding, as we tested behavioral interventions where blinding of participants and providers is not possible.
We judged each included study to be at high, unclear, or low risk of bias in each of the above domains, according to the guidelines in the Cochrane Handbook .
Measures of treatment effect
We use the risk ratio (RR) for summarizing individual trial outcomes and for the estimate of the pooled effect. Where we judged a group of studies to be sufficiently clinically and statistically homogeneous, we used the Mantel‐Haenszel fixed‐effect method ( Greenland 1985 ) to calculate a weighted average of the risk ratios of the individual trials, with a 95% confidence interval.
Dealing with missing data
In trials where the details of the methodology were unclear or where the results were expressed in a form that did not allow for extraction of key data, we approached the original investigators for additional information. We treated participants lost to follow‐up as continuing smokers. We excluded from totals only those participants who died before follow‐up or were known to have moved to an untraceable address.
Assessment of heterogeneity
To assess statistical heterogeneity between trials we used the I 2 statistic ( Higgins 2003 ). This measures the percentage of total variation across studies due to heterogeneity rather than to chance. Values of I 2 over 75% indicate a considerable level of heterogeneity (Chapter 8, Cochrane Handbook ).
'Summary of findings' table
Following standard Cochrane methodology, we created a 'Summary of findings' table for our primary outcome, smoking cessation at longest follow‐up. This includes a GRADE evaluation of the quality of evidence, based on the five standard considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias).
Description of studies
Included studies.
Fifty‐eight trials met the inclusion criteria, of which nine are new for this update ( Kim 2003 ; Jorstad 2013 ; Berndt 2014 ; Hornnes 2014 ; Gilbody 2015 ; Kadda 2015 ; Pardavila‐Belio 2015 ; Zwar 2015 ; Smit 2016 ). Trials were of nursing interventions for smoking cessation in adults who used tobacco (primarily cigarettes), published between 1987 and 2017. One trial ( Sanders 1989a ; Sanders 1989b ) had two parts with randomization at each stage, so is treated here as two separate studies, making a total of 59 studies in the Characteristics of included studies table. Forty‐four studies contributed to the primary meta‐analysis that compared a nursing intervention to a usual‐care or minimal‐intervention control. Eleven studies included a comparison between two nursing interventions, involving different components or different numbers of contacts, and contribute to a secondary meta‐analysis. Six further studies did not contribute to a meta‐analysis and their results are described separately. Sample sizes of studies contributing to a meta‐analysis ranged from 25 to 2700, but were typically between 150 and 500. Figure 1 documents the flow of studies screened and included in this update.

Study flow diagram for 2017 update
Seventeen trials took place in the USA, 11 in the UK, five in The Netherlands, four in Canada, three in Australia, Denmark, and Spain, and two each in China, Japan, Norway, and South Korea. One trial took place in Belgium, one in Greece, and one in Sweden. One multicenter study was conducted in multiple European countries.
Twenty‐two trials intervened with hospitalized participants ( Taylor 1990 ; DeBusk 1994 ; Rigotti 1994 ; Lewis 1998 ; Allen 1996 ; Carlsson 1997 ; Miller 1997 ; Feeney 2001 ; Bolman 2002 ; Hajek 2002 ; Quist‐Paulsen 2003 ; Froelicher 2004 ; Hasuo 2004 ; Chouinard 2005 ; Hennrikus 2005 ; Nagle 2005 ; Hanssen 2007 ; Wood 2008 ; Meysman 2010 ; Cossette 2011 ; Berndt 2014 ; Hornnes 2014 ). Two trials ( Rice 1994 ; Jorstad 2013 ) recruited hospitalized participants, but with follow‐up after discharge. Kadda 2015 recruited participants following discharge after open‐heart surgery. Twenty‐eight studies recruited from primary care or outpatient clinics ( Sanders 1989b ; Janz 1987 ; Vetter 1990 ; Sanders 1989a ; Risser 1990 ; Hollis 1993 ; Nebot 1992 ; Family Heart 1994 ; OXCHECK 1994 ; Tønnesen 1996 ; Campbell 1998 ; Lancaster 1999 ; Steptoe 1999 ; Canga 2000 ; Aveyard 2003 ; Kim 2003 ; Ratner 2004 ; Hilberink 2005 ; Kim 2005 ; Duffy 2006 ; Sanz‐Pozo 2006 ; Tønnesen 2006 ; Aveyard 2007 ; Jiang 2007 ; Wood 2008 ; Chan 2012 ; Gilbody 2015 ; Zwar 2015 ; Smit 2016 ). In some trials, the recruitment took place during a clinic visit, whilst in others the invitation to enroll was made by letter. One study ( Terazawa 2001 ) recruited employees during a workplace health check, two studies enrolled community‐based adults motivated to make a quit attempt ( Davies 1992 ; Alterman 2001 ), one study recruited mothers taking their child to a pediatric clinic ( Curry 2003 ), one study recruited people being visited by a home healthcare nurse ( Borrelli 2005 ), and one study recruited university students on campus ( Pardavila‐Belio 2015 ).
Eighteen studies focused on adults with diagnosed cardiovascular health problems ( Taylor 1990 ; DeBusk 1994 ; Family Heart 1994 ; Rice 1994 ; Rigotti 1994 ; Allen 1996 ; Carlsson 1997 ; Miller 1997 ; Campbell 1998 ; Feeney 2001 ; Bolman 2002 ; Hajek 2002 ; Jiang 2007 ; Chan 2012 (subgroup with cardiovascular disease); Cossette 2011 ; Jorstad 2013 ; Berndt 2014 ; Hornnes 2014 ; Kadda 2015 ), two studies were in participants with respiratory diseases ( Tønnesen 1996 ; Tønnesen 2006 ), one was in people with diabetes ( Canga 2000 ), and one was in people with severe mental illness ( Gilbody 2015 ). One study recruited participants either with diagnosed cardiovascular health problems or judged to be at high risk of developing heart disease ( Wood 2008 ). Two studies recruited surgical patients: Ratner 2004 recruited people attending a surgical pre‐admission clinic and Meysman 2010 recruited people admitted to surgical wards. One study recruited head‐and‐neck‐cancer patients at four medical centres ( Duffy 2006 ).
All studies included adults 18 years and older who used some form of tobacco. Allen 1996 , Curry 2003 and Froelicher 2004 studied women only, and Terazawa 2001 and Kim 2003 studied men only. The definition of tobacco use varied and in some cases included recent quitters.
Nine studies examined a smoking cessation intervention as a component of multiple risk factor reduction interventions in adults with cardiovascular disease ( DeBusk 1994 ; Allen 1996 ; Carlsson 1997 ; Campbell 1998 ; Hanssen 2007 ; Jiang 2007 ; Wood 2008 ; Jorstad 2013 ; Kadda 2015 ). In four studies, the smoking cessation component was clearly defined, of high intensity, and independently measurable ( DeBusk 1994 ; Allen 1996 ; Carlsson 1997 ; Jiang 2007 ), whereas in the remaining five the smoking component was less clearly specified ( Campbell 1998 ; Hanssen 2007 ; Wood 2008 ; Jorstad 2013 ; Kadda 2015 ).
Fourty‐four studies with a total of over 20,000 participants contributed to the main comparison of nursing intervention versus control. We classified 36 as high‐intensity on the basis of the planned intervention, although in some cases implementation may have been incomplete. In seven, we classified the intervention as low‐intensity ( Janz 1987 ; Vetter 1990 ; Davies 1992 ; Nebot 1992 ; Tønnesen 1996 ; Aveyard 2003 ; Nagle 2005 ). All of these were conducted in outpatient, primary care or community settings. One further study ( Hajek 2002 ) may be considered as a comparison between a low‐intensity intervention and usual care. Participants in the usual‐care control group received systematic brief advice and self‐help materials from the same nurses who provided the intervention. Unlike the other trials in the low‐intensity subgroup, this trial was conducted amongst inpatients with cardiovascular disease. Since the control group received a form of nursing intervention, we primarily classified the trial as a comparison of two intensities of nursing intervention. But since other studies had usual‐care groups that may have received advice from other healthcare professionals, we also report the sensitivity of the main analysis results to including it as a low‐intensity nursing intervention compared to usual‐care control.
Hajek 2002 and 10 other studies contributed to a second group comparing two interventions involving a nursing intervention. Three of these tested additional components as part of a session: demonstration of carbon monoxide (CO) levels to increase motivation to quit ( Sanders 1989b ); CO and spirometry feedback ( Risser 1990 ); and CO feedback plus additional materials and an offer to find a support buddy ( Hajek 2002 ). Five involved additional counseling sessions from a nurse ( Alterman 2001 ; Feeney 2001 ; Tønnesen 2006 ; Aveyard 2007 ; Jiang 2007 ). One other study compared two interventions with a usual‐care control ( Miller 1997 ). The minimal intervention condition included a counseling session and one telephone call after discharge from hospital. In the intensive condition, participants received three additional telephone calls, and those who relapsed were offered further face‐to‐face meetings, and nicotine replacement therapy if needed. We classified both interventions as intensive in the main meta‐analysis, but compared the intensive and minimal conditions in a separate analysis of the effect of additional follow‐up. Chouinard 2005 also assessed the effect of additional telephone support as an adjunct to an inpatient counseling session, so is pooled in a subgroup with Miller 1997 . We included in the same subgroup a study that tested additional telephone follow‐up as a relapse prevention intervention for people who had inpatient counseling ( Hasuo 2004 ).
Five studies ( Family Heart 1994 ; OXCHECK 1994 ; Campbell 1998 ; Steptoe 1999 ; Wood 2008 ) were not included in any meta‐analysis and do not have results displayed graphically because their designs did not allow us to extract appropriate outcome data. The first part of a two‐stage intervention study is also included in this group ( Sanders 1989a ); the second part ( Sanders 1989b ) is included in one of the meta‐analyses. These studies are discussed separately in the Effects of interventions section below.
We determined whether the nurses delivering the intervention were providing it alongside clinical duties that were not smoking‐related, were working in health promotion roles, or were employed specifically as project nurses. Of the high‐intensity intervention studies, 21 used nurses for whom the intervention was a core component of their role ( Hollis 1993 ; DeBusk 1994 ; Allen 1996 ; Carlsson 1997 ; Terazawa 2001 ; Kim 2003 ; Quist‐Paulsen 2003 ; Froelicher 2004 ; Duffy 2006 ; Aveyard 2007 ; Chan 2012 ; Meysman 2010 ; Cossette 2011 ; Jorstad 2013 ; Berndt 2014 ; Hornnes 2014 ; Gilbody 2015 ; Kadda 2015 ; Pardavila‐Belio 2015 ; Zwar 2015 ; Smit 2016 ). One study ( Kim 2005 ) employed retired nurses who were trained to provide a brief intervention using the '5 As' framework. In only four studies were intensive interventions intended to be delivered by nurses for whom it was not a core task ( Lancaster 1999 ; Bolman 2002 ; Curry 2003 ; Sanz‐Pozo 2006 ). Most of the low‐intensity interventions were delivered by primary care or outpatient clinic nurses. One low‐intensity inpatient intervention was delivered by a clinical nurse specialist ( Nagle 2005 ).
Follow‐up periods for reinforcement and outcome measurements varied across studies, with a tendency for limited reinforcement and shorter follow‐up periods in the older studies. All trials had some contact with participants in the first three months of follow‐up for restatement of the intervention or point prevalence data collection or both. Eight of the studies had less than one year final outcome data collection ( Janz 1987 ; Vetter 1990 ; Davies 1992 ; Lewis 1998 ; Canga 2000 ; Kim 2003 ; Berndt 2014 ; Pardavila‐Belio 2015 ). The rest had follow‐up at one year or beyond. The outcome used for the meta‐analysis was the longest follow‐up (six months and beyond), with the exception of Hanssen 2007 , in which we preferred 12‐month over 18‐month data. The outcome in this study was point prevalence abstinence and we judged the 18‐month data to be too conservative, due to a rise in abstinent participants in the control group.
A brief description of the main components of each intervention is provided in the ' Characteristics of included studies ' table.
Excluded studies
Sixty studies that we had identified as potentially relevant but subsequently excluded are listed in the Characteristics of excluded studies table, along with the reason for exclusion for each. The most common reasons for exclusion were: study design (not a randomized clinical trial); less than six months follow‐up; multicomponent studies with insufficient detail on smoking intervention/outcome; and studies in which the impact of the nursing intervention was confounded by additional pharmacological or behavioral treatment that was not provided to the control arm.
Risk of bias in included studies
As seen in Figure 2 , we rated most studies at low or unclear risk of selection bias (random sequence generation and allocation concealment) and attrition bias (loss to follow‐up). As seen in Figure 3 , we judged 16 studies to be at low risk of bias across all domains, and 16 at high risk of bias in at least one domain. The rest were at unclear risk of bias.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Thirty studies provided details of a method of random sequence generation judged to be at low risk of bias, and a further 23 studies did not report how the sequence was generated and were hence rated as unclear for this domain. We judged five studies to be at high risk based on their reported methods of random sequence generation: Bolman 2002 was a cluster‐randomized study in which some hospitals picked their allocation; in Curry 2003 participants drew a colored ball from a bag; Davies 1992 allocated based on order of attendance; Hollis 1993 randomized participants based on health record number; and Sanders 1989a / Sanders 1989b randomized participants based on day of attendance. In addition to these five studies, we rated three further studies in which providers rather than participants were randomized at high risk of selection bias: Hilberink 2005 reported that self‐selection at practice level may have affected the results; in Janz 1987 allocation was determined by clinic session; and in Nebot 1992 the providers were also responsible for allocating participants, rendering allocation concealment impossible. Overall, we judged 26 studies to be at low risk of bias for allocation concealment, 24 studies had unclear risk of bias because concealments was unspecified, and we rated eight studies at high risk of bias for concealment. A sensitivity analysis including only the results of studies judged to be at low risk of selection bias did not alter the main conclusions.
Incomplete outcome data
We judged 33 studies that reported minimal to moderate loss to follow‐up and accounted for all participants in their reporting to be at low risk of attrition bias. A further 20 studies did not provide sufficient detail with which to judge the likelihood of attrition bias and hence we rated them as 'unclear' for this domain. We judged five studies to be at high risk of attrition bias: in Feeney 2001 , 79% of usual‐care participants were not followed up; OXCHECK 1994 stated that their methods of accounting for missing participants may have overestimated the effect; in Sanders 1989a / Sanders 1989b only a subsample of participants from the control group was followed up; and in Steptoe 1999 and in Hornnes 2014 overall dropout rates were high and varied between intervention and control groups.
Other potential sources of bias
Definitions of abstinence ranged from single point prevalence to sustained abstinence (multiple point prevalence with self‐report of no slips or relapses). In one study ( Miller 1997 ) we used validated abstinence at one year rather than continuous self‐reported abstinence, because only the former outcome was reported for disease diagnosis subgroups.
Of the 44 studies included in the primary meta‐analysis, 22 biochemically validated self‐reports of abstinence using either urinary/saliva cotinine or exhaled CO. One study tested CO levels only amongst people followed up in person ( Curry 2003 ), and five studies used some validation but did not report rates based on biochemical validation of every self‐reported quitter ( Nebot 1992 ; Rice 1994 ; Miller 1997 ; Froelicher 2004 ; Borrelli 2005 ). Fifteen studies did not use any biochemical validation and relied on self‐reported smoking cessation at a single follow‐up, although two warned participants that samples might be requested for testing (i.e. 'bogus pipeline'), and Jiang 2007 sought confirmation of smoking status from a family member.
We judged three studies ( Rice 1994 ; Hennrikus 2005 ; Kim 2005 ) to be at high risk of other bias because of differences between intervention and control groups in validation rates for reported cessation. We judged two studies to be at unclear risk of bias. In Canga 2000 , the same nurse conducted all interviews and follow‐up examinations, allowing the potential for observer bias, and in Chan 2012 there was potential for the study intervention to overlap with the standard care received by participants in the control group.
Effects of interventions
See: Table 1
Effects of intervention versus control/usual care
Smokers offered advice by a nursing professional had an increased likelihood of quitting compared to smokers without intervention, with evidence of moderate statistical heterogeneity between the results of the 44 studies contributing to this comparison (I 2 = 50%). Heterogeneity was marginally more apparent in the subgroup of 37 high‐intensity trials (I 2 = 53%). There was one trial with a significant negative effect for treatment ( Rice 1994 ). This result may be explained by the fact that participants in both arms were advised to quit and more people in the control group had had coronary artery bypass graft surgery. Further, a multivariate analysis of one‐year follow‐up data revealed quitters were significantly more likely to be less than 48 years old, male, to have had individualized versus group or no cessation instruction, and to have had a high degree of perceived threat relative to their health state. In addition to this, three studies reported particularly large positive effects ( Canga 2000 ; Terazawa 2001 ; Pardavila‐Belio 2015 ). Pooling all 44 studies using a fixed‐effect model gave a risk ratio (RR) of 1.29 with a 95% confidence interval (CI) 1.21 to 1.38 at the longest follow‐up ( Figure 4 ; Analysis 1.1 ). Because of the heterogeneity we tested the sensitivity to pooling the studies using a random‐effects model. This did not materially alter the estimated effect size or greatly widen the confidence interval (RR 1.31, 95% CI 1.18 to 1.45, analysis not shown ). A sensitivity analysis excluding the four outlying trials widened the CI but did not alter the point estimate whilst greatly reducing statistical heterogeneity in the high‐intensity subgroup (I 2 = 15%). A further sensitivity analysis restricted to only those studies at low risk of bias across all domains also did not significantly alter the point estimate (RR 1.25, 95% CI 1.10 to 1.51, analysis not shown ).

Trials of nursing intervention versus control grouped by intensity of intervention. Outcome: Smoking cessation at longest follow‐up.

Comparison 1 All nursing intervention vs control trials, grouped by intensity of intervention, Outcome 1 Smoking cessation at longest follow‐up.
We also tested the sensitivity of these results to excluding studies that did not validate all reports of abstinence, and limiting the analysis to studies judged to be at low risk of selection bias. None of these altered the estimates to any great extent, although confidence intervals became wider due to the smaller number of studies. Excluding one study ( Bolman 2002 ) for which we were not able to enter the numbers of quitters directly did not alter the results.
Some participants in Taylor 1990 had been encouraged to use nicotine replacement therapy (NRT). Exclusion of these people did not alter the significant effect of the intervention in this study. In Miller 1997 more people in the intervention conditions than the controls used NRT (44% of intensive and 39% of minimal intervention versus 29% of control). People who were prescribed NRT had lower quit rates than those who were not, but the relative differences in quit rates between the usual‐care and intervention groups were similar for the subgroups that did and did not use NRT. However, because of the different rates of use of NRT, it is probable that the increased use of NRT contributed to the effects of the nursing intervention. Use of NRT was also encouraged as part of the Canga 2000 intervention, with 17% of the intervention group accepting a prescription, and as part of the Duffy 2006 intervention, although at six months similar percentages in the intervention and control groups had used NRT over the course of the study.
Six further studies which compared a nursing intervention to control/usual care were not included in the meta‐analysis ( Sanders 1989a ; Family Heart 1994 ; OXCHECK 1994 ; Campbell 1998 ; Steptoe 1999 ; Wood 2008 ). Although they met the main inclusion criteria, in five trials the design did not allow data extraction for meta‐analysis in a comparable format to other studies, and in Sanders 1989a only a random sample of the control group was followed up.
Sanders 1989a , in which smokers visiting their family doctor were asked to make an appointment for cardiovascular health screening, reported that only 25.9% of the patients made and kept such an appointment. The percentage that had quit at one month and at one year and reported last smoking before the one‐month follow‐up was higher both in the attenders (4.7%) and the non‐attenders (3.3%) than in the usual‐care controls (0.9%). This suggests that the invitation to make an appointment for health screening could have been an anti‐smoking intervention in itself, and that the additional effect of the structured nursing intervention was small.
We do not have comparable data for OXCHECK 1994 , which used similar health checks, because the households had been randomized to be offered the health check in different years. The authors compared the proportions of smokers in the intervention group who reported stopping smoking in the previous year to patients attending for their one‐year follow‐up, and to controls attending for their first health check. They found no difference in the proportions that reported stopping smoking in the previous year.
The Family Heart 1994 study offered nurse‐led cardiovascular screening for men aged 40 to 59 and for their partners, with smoking cessation as one of the recommended lifestyle changes. Cigarette smokers were invited to attend up to three further visits. Smoking prevalence was lower amongst those who returned for the one‐year follow up than amongst the control group screened at one year. This difference was reduced if non‐returners were assumed to have continued to smoke, and if CO‐validated quitting was used. In that case there was a reduction of only about one percentage point, with weak evidence of a true reduction.
Campbell 1998 invited people with a diagnosis of coronary heart disease to nurse‐run clinics promoting medical and lifestyle aspects of secondary prevention. There was no significant effect on smoking cessation. At one year the decline in smoking prevalence was greater in the control group than in the intervention group. Four‐year follow‐up did not alter the effect of a lack of benefit.
Steptoe 1999 recruited people at increased risk of coronary heart disease for a multicomponent intervention. The quit rate amongst smokers followed up after one year was not significantly higher in the intervention group (9.4%, 95% CI ‐9.6 to 28.3), and there was greater loss to follow‐up of smokers in the intervention group.
Wood 2008 recruited people with established or increased risk of coronary heart disease for a multicomponent lifestyle intervention, coordinated by nurses. The authors reported results separately for those participants recruited in hospital and those recruited in general practice. For coronary patients recruited in hospital who had smoked within one month at baseline, abstinence at one year favored the intervention group (58% versus 47%), but the difference was not significant (P = 0.06). For participants at high risk of coronary heart disease recruited in general practice, the prevalence of smoking fell from baseline but did not differ between conditions.
Effect of intervention intensity
We detected no evidence from our indirect comparison between subgroups that the trials we classified as using higher‐intensity interventions had larger treatment effects. In this update of the review the point estimate for the pooled effect of the seven lower‐intensity trials is effectively the same as for the 37 of higher intensity. For the low‐intensity group the confidence interval does not exclude 1, but there were fewer studies (high‐intensity subgroup RR 1.29, 95% CI 1.21 to 1.38, I 2 = 53%, 16,865 participants, Analysis 1.1 .1; low‐intensity subgroup RR 1.27, 95% CI 0.99 to 1.62, I 2 = 36%, 4016 participants, Analysis 1.1 .2). In a sensitivity analysis we included Hajek 2002 , a study for which we were uncertain about the classification of the control group (as noted above in the Description of studies section), in the low‐intensity subgroup. Including this study in the low‐intensity subgroup reduced the point estimate and there was no evidence of a treatment effect (RR 1.09, 95% CI 0.92 to 1.29). Compared to the other trials in the low‐intensity subgroup, the Hajek 2002 trial was conducted amongst hospitalized participants with cardiovascular disease and the overall quit rates were high. The large number of events gave this trial a high weight in the meta‐analysis.
The distinction between low‐ and high‐intensity subgroups was based on our categorization of the intended intervention. We particularly noted low levels of implementation in the trial reports for Lancaster 1999 , Bolman 2002 and Curry 2003 , so we tested the effect of moving them from the high‐ to the low‐intensity subgroup. This reduced the point estimate of effect in the low‐intensity subgroup and increased it in the high‐intensity one. If these three studies and Hajek 2002 are included in the low‐intensity subgroup, the pooled estimate of effect is small and non‐significant (RR 1.09, 95% CI 0.96 to 1.25, 6056 participants, Analysis 4.1 ). We also assessed the sensitivity of the results to using additional participants in the control group for Aveyard 2003 (see Characteristics of included studies for details). This reduced the size of the effect in the low‐intensity subgroup but did not alter our conclusions.

Comparison 4 Sensitivity analysis by intensity, including Hajek 2002, with Lancaster, Bolman, Curry as low intensity, Outcome 1 Smoking cessation at longest follow‐up.
Effects of differing health states and client settings
Trials in hospitals recruited participants with health problems, but some trials specifically recruited those with cardiovascular disease, and amongst these some interventions addressed multiple risks whilst most only addressed smoking. Trials in primary care generally did not select participants with a particular health problem. We combined setting and disease diagnosis in one set of subgroups ( Analysis 2.1 ).

Comparison 2 All nursing intervention vs control trials, grouped by setting and population, Outcome 1 Smoking cessation at longest follow‐up.
Seven trials that included a smoking cessation intervention from a nurse as part of cardiac rehabilitation showed a significant pooled effect on smoking (RR 1.25, 95% CI 1.11 to 1.41, I 2 = 0%, 1007 participants, Analysis 2.1 .1). Six of these ( Allen 1996 ; Carlsson 1997 ; Hanssen 2007 ; Jiang 2007 ; Jorstad 2013 ; Kadda 2015 ) did not use biochemical validation of quitting, and in the seventh ( DeBusk 1994 ) we were unable to confirm the proportion of dropouts with the study authors.
There was some heterogeneity (I 2 = 42%) among eight trials of smoking‐specific interventions in hospitalized smokers with cardiovascular disease, due to the strong intervention effect in one of the eight trials ( Taylor 1990 ). The RR was 1.29 (95% CI 1.16 to 1.43, 2668 participants, Analysis 2.1 .2) and the effect remained significant if we excluded Taylor 1990 (reducing the I 2 to 0%) or if we applied a random‐effects model. A sensitivity analysis of the effect of including Hajek 2002 in this category increased the heterogeneity (I 2 = 56%), and the pooled effect was significant whether we used a fixed‐effect or a random‐effects model ( Analysis 5.1 ). Excluding Taylor 1990 again removed heterogeneity but the point estimate decreased (RR 1.14, 95% CI 1.02 to 1.27, analysis not shown).

Comparison 5 Sensitivity analysis by setting and population, including Hajek 2002, Outcome 1 Smoking cessation at longest follow‐up.
Among the seven trials in non‐cardiac hospitalized smokers the risk ratio was small and the confidence interval did not exclude no effect (RR 1.12, 95% CI 0.96 to 1.30, 4872 participants, Analysis 2.1 .3). We included in this subgroup one trial that began the intervention in a pre‐admission clinic for elective surgery patients ( Ratner 2004 ).
Heterogeneity was high (I 2 = 94%) between two trials of interventions delivered to non‐hospitalized adults with cardiovascular disease ( Rice 1994 ; Chan 2012 ; Analysis 2.1 .4). Subgroup analysis in Rice 1994 , however, suggested that smokers who had experienced cardiovascular bypass surgery were more likely to quit, and these participants were over‐represented in the control group who received advice to quit but no structured intervention.
Pooling 20 trials of cessation interventions for other non‐hospitalized adults showed an increase in the success rates (RR 1.70, 95% CI 1.45 to 2.00, 10,368 participants, Analysis 2.1 .5). A sensitivity analysis testing the effect of excluding those trials ( Janz 1987 ; Vetter 1990 ; Curry 2003 ; Hilberink 2005 ) where a combination of a nursing intervention and advice from a physician was used did not substantially alter this.
Higher‐ versus lower‐intensity interventions
Effects of physiological feedback.
Two trials ( Sanders 1989b ; Risser 1990 ) evaluated the effect of physiological feedback as an adjunct to a nursing intervention compared to nursing without physiological feedback. Neither found any evidence of an effect at maximum follow‐up ( Analysis 3.1 .1 (RR 1.06, 95% CI 0.55 to 2.02, 751 participants) and Analysis 3.1 .2 (RR 0.33, 95% CI 0.10 to 1.15, 90 participants)).

Comparison 3 Effect of additional strategies: Higher versus lower intensity, Outcome 1 Additional components at single contact. Smoking cessation at longest follow‐up.
Effects of other components at a single contact
One trial in hospitalized smokers with cardiovascular disease ( Hajek 2002 ) found no evidence of a significant benefit of additional support from a nurse giving additional written materials, a written quiz, an offer of a support buddy, and CO measurement compared to controls receiving brief advice and a self‐help booklet (RR 0.91, 95% CI 0.73 to 1.13, 505 participants, Analysis 3.1 .3).
Effects of additional telephone support
There was weak evidence from pooling three trials ( Miller 1997 ; Hasuo 2004 ; Chouinard 2005 ) that additional telephone support increased cessation compared to less or no telephone support, as the lower limit of the confidence interval was at the boundary of no effect (RR 1.25, 95% CI 1.00 to 1.56, I 2 = 0%; 1220 participants, Analysis 3.2 .1).

Comparison 3 Effect of additional strategies: Higher versus lower intensity, Outcome 2 Additional contacts. Smoking cessation at longest follow‐up.
Effects of additional face‐to‐face sessions
One trial of additional support from an alcohol and drug assessment unit nurse for people admitted to a coronary care unit ( Feeney 2001 ) showed a very large benefit for the intervention (RR 32.68, 95% CI 4.55 to 234.56, 189 participants, Analysis 3.2 .2). The cessation rate among the controls, however, was very low (1/97), and there was a large number of dropouts, particularly from the control group. This could have underestimated the control group quit rate. Another trial ( Alterman 2001 ), offering four nurse sessions rather than one as an adjunct to nicotine patch, showed no benefit, with the control group having a significantly higher quit rate (RR 0.43, 95% CI 0.21 to 0.89, 157 participants, Analysis 3.2 .3). No explanation was offered for the lower than expected quit rates in the intervention group.
Effects of additional face‐to‐face sessions and telephone support
Pooled results from three trials ( Tønnesen 2006 ; Aveyard 2007 ; Cossette 2011 ) did not show an effect of providing additional clinic sessions and telephone support compared with fewer clinic sessions and less or no telephone support (RR 0.92, 95% CI 0.65 to 1.31, I 2 = 0%, 1335 participants, Analysis 3.2 .4).
Summary of main results
The results of this meta‐analysis support a modest but positive effect for smoking cessation interventions by nurses, but we rated the quality of evidence as moderate due to unexplained statistical heterogeneity (see Table 1 ). A structured smoking cessation intervention delivered by a nurse was more effective than usual care on smoking abstinence at six months or longer from the start of treatment. The direction of effect was consistent in different intensities of intervention, in different settings, and in smokers with and without tobacco‐related illnesses. In a subgroup of low‐intensity studies the confidence interval did not exclude no effect, but the point estimate was effectively the same as that in the larger group of high‐intensity studies. We found insufficient evidence to assess whether more intensive interventions, those incorporating additional follow‐up, or those incorporating pathophysiological feedback are more effective than one‐off support. There was no evidence that the effect of support differed by patient group or across healthcare settings.
Overall completeness and applicability of evidence
Overall, these meta‐analysis findings need to be interpreted carefully in light of the methodological limitations of both the review and the clinical trials. In terms of the review, it is possible that there was a publication selection bias due to using only tabulated data derived from published works ( Stewart 1993 ). Data from the unpublished or missed studies or both could have shown more or less favorable results, although a funnel plot for the main comparison did not suggest the presence of reporting bias. For recent updates, we have also searched clinical trials registries and 'grey' literature to identify relevant unpublished studies. Secondly, finding statistical heterogeneity between the incidences of cessation in different studies limits any assumption that interventions in any clinical setting and with any type of participant are equally effective.
The findings of this review, and in particular the estimated size of the treatment effect, have remained remarkably stable since its initial publication. In 1999, 15 studies contributed to the main analysis, with a pooled risk ratio of 1.30 (95% CI 1.16 to 1.44). Further studies have more than doubled the number of participants and thus narrowed the CIs, but have had very little impact on the point estimate, which in this most recent update is the same as it was in 1999.
Effectiveness by intervention characteristics and population
The effect estimates are similar for high‐ and low‐intensity smoking cessation interventions by nurses, as was found in a review of physicians' advice ( Stead 2013 ). Presumably, the more components added to the intervention the more intensive the intervention. However, assessing the contribution of factors such as total contact time, number of contacts, and content of the intervention was difficult. Our distinction between high and low intensity, based on the length of initial contact and number of planned follow‐ups, may not have accurately distinguished among the key elements that could have contributed to greater efficacy. We found that the nature of the smoking cessation interventions varied from advice alone, to more intensive interventions with multiple components, and that the description of what constituted 'advice only' varied. In most trials, advice was given with an emphasis on stopping smoking because of some existing health problem. To make most interventions more intensive, verbal advice was supplemented with a variety of counseling messages, including benefits of and barriers to cessation (e.g. Taylor 1990 ) and effective coping strategies (e.g. Allen 1996 ). Manuals and printed self‐help materials were also added to many interventions, along with repeated follow‐up ( Hollis 1993 ; Miller 1997 ). In some studies, the proposed intervention was not delivered consistently to all participants. In recent updates the evidence for the benefit of a low‐intensity intervention has become weaker than that for a more intensive intervention, and the estimated effect is sensitive to the inclusion of one additional study ( Hajek 2002 ) and to the classification of intensity of three studies. Almost all the intensive interventions were delivered either by dedicated project staff or by nurses with a health promotion role. Most studies in which the intensive intervention was intended to be delivered by a nurse with other roles consistently reported problems in delivering the intervention. None showed a statistically significant benefit for the intervention. We found no studies of brief opportunistic advice that were directly analogous to the low‐intensity interventions used in physician advice trials ( Stead 2013 ).
In two studies in the low‐intensity category ( Janz 1987 ; Vetter 1990 ), advice from a physician was also part of the intervention and this almost certainly contributed to the overall effect. The most highly‐weighted study in the high‐intensity subgroup ( Miller 1997 ) produced only relatively modest results. This was due in part to the effect of the minimal treatment condition that had just one follow‐up telephone call. However, using just the high‐intensity condition in the analysis did not materially alter the pooled estimate.
One study ( Miller 1997 ) provided data on the effect of the same intervention in smokers with different types of illness and suggested a greater effect in cardiovascular patients. In these individuals the intervention increased the 12‐month quit rate from 24% to 34%. In other types of patients, the rates were increased from 18.5% to 21%. However, this hypothesis was not formally tested. In this study participants were eligible if they had smoked any tobacco in the month prior to hospitalization, but were excluded if they had no intention of quitting (although they were also excluded if they wanted to quit on their own). These criteria may have contributed to the relatively high quit rates achieved. Also, a higher proportion of participants in the intensive treatment arm than in the minimal or usual‐care intervention arms were prescribed nicotine replacement therapy (NRT). However, the intervention was also effective in those not prescribed NRT. Those given NRT were heavier smokers (with higher levels of addiction) who achieved lower cessation rates than those who did not use NRT.
This suggests that nursing professionals may have an important 'window of opportunity' to intervene with patients in the hospital setting, or at least to introduce the notion of not resuming tobacco use upon hospital discharge. The size of the effect may be dependent on the reason for hospitalization. The additional telephone support, with the possibility of another counseling session for people who relapsed after discharge, seemed to contribute to more favorable outcomes in the intensive intervention used by Miller 1997 , although pooled results from three studies testing the addition of telephone counseling and further face‐to‐face contact did not detect an effect. A separate Cochrane Review of the efficacy of interventions for hospitalized patients ( Rigotti 2012 ) supports the efficacy of interventions for this patient group, but only when the interventions included post‐discharge support for at least one month.
Providing additional physiological feedback in the form of spirometry and demonstrated CO level as an adjunct to nursing intervention did not appear to have an effect. Three studies in primary care or outpatient settings used this approach ( Sanders 1989b ; Risser 1990 ; Hollis 1993 ). It was also used as part of the enhanced intervention in a study with hospitalized patients ( Hajek 2002 ). A separate Cochrane Review ( Bize 2012 ) found little evidence about the effects of most types of biomedical tests for risk assessment on smoking cessation.
The identification of an effect for a nurse‐mediated intervention in smokers who were not hospitalized is based on 20 studies. The largest study ( Hollis 1993 ) increased the quit rate from 2% in those who received only advice from a physician to 4% when a nurse delivered one of three additional interventions, including a video, written materials, and a follow‐up telephone call. Control group quit rates were less than 10% in almost all these studies, and more typically between 4% and 8%. The risk ratio in this group of studies (1.7) was a little higher than in some subgroups, but because of the low background quit rate the proportion of participants likely to become long‐term quitters as a result of a nursing intervention in these settings is likely to be small. However, because of the large number of people who could be reached by nurses, the effect would be important.
Combined efforts of many types of healthcare professionals are likely to be required. The US Public Health Service clinical practice guideline Treating Tobacco Use and Dependence ( AHRQ 2008 ) used logistic regression to estimate efficacy for interventions delivered by different types of providers. Their analysis did not distinguish among the non‐physician medical healthcare providers, so that dentists, health counselors, and pharmacists were included with nurses. The guideline concluded that these providers were effective (Table 15, odds ratio (OR) 1.7, 95% CI 1.3 to 2.1). They also concluded that interventions by multiple clinician types were more effective (Table 16, OR 2.5, 95% CI 1.9 to 23.4). Although it was recognized that there could be confounding between the number of providers and the overall intensity of the intervention, the findings confirmed that a nursing intervention that reinforces or complements advice from physicians or other healthcare providers or both is likely to be an important component in helping smokers to quit.
Implications for practice
Support for smoking cessation by a nurse leads to a modest improvement in tobacco abstinence. Most of these interventions were delivered by nurses with a specialist health promotion function and there was insufficient evidence to know whether general nurses can achieve the same benefits. Commissioners and providers of smoking cessation services need to consider the quality of delivery of smoking cessation services if these are to be provided by general nurses.
Implications for research
Further studies of nursing interventions are warranted, with more careful consideration of sample size, participant selection, refusals, dropouts, long‐term follow‐up, and biochemical verification. Additionally, controlled studies are needed that carefully examine the effects of 'brief advice by nursing', as this type of professional counseling may more accurately reflect the current standard of care. Work is now required to systematize interventions so that more rigorous comparisons can be made between studies. None of the trials reviewed was a replication study; this is a very important method to strengthen the science, and should be encouraged.
Protocol first published: Issue 3, 1998 Review first published: Issue 3, 1999
Acknowledgements
Lindsay Stead was an author for previous versions of this review. Nicky Cullum and Tim Coleman for their helpful peer review comments on the original version of this review. Hitomi Kobayasha, a doctoral student, for assistance with Japanese translation of a study. Jong‐Wook Ban and Hyunjik Kim for Korean language assistance. Thank you to Olga Kadda for providing additional study data for Kadda 2015 , and Harald Jorstad for providing additional study data for Jorstad 2013 .
Appendix 1. Register search strategy
Run using Cochrane Register of Studies (CRS) software
#1 (nurse* or nursing):TI,AB,XKY,MH,EMT,KY #2 (health visitor*):TI,AB,XKY,MH,EMT,KY #3 #1 OR #2
XKY, MH, EMT, KY are keyword fields. XKY field includes indexing terms added for the use of the tobacco addiction group.
Appendix 2. Glossary of terms
New search for studies and content updated (no change to conclusions)
Data and analyses
Comparison 1, comparison 2, comparison 3, comparison 4, comparison 5, characteristics of studies, characteristics of included studies [ordered by study id].
ACS = acute coronary syndrome AHCPR = Agency for Health Care Policy and Research CABG = Coronary Artery Bypass Graft CBT ‐ cognitive behavioural therapy CCU = Coronary Care Unit CHD = coronary heart disease CHF = congestive heart failure CO = carbon monoxide COPD = Chronic obstructive pulmonary disease cpd = cigarettes per day CVD = cardiovascular disease FTND: Fagerström Test for Nicotine Dependence ITT = intention‐to‐treat m = month(s) MA = meta‐analysis (A)MI = (Acute) Myocardial Infarction NRT = nicotine replacement therapy NS: not statistically significant PP = point prevalence PVD = peripheral vascular disease SMOCC = Smoking cessation for patients with COPD in general practice SoC = stage of change (precontemplation, contemplation, preparation, action) TQD = target quit date
Characteristics of excluded studies [ordered by study ID]
Characteristics of ongoing studies [ordered by study id], contributions of authors.
VHR wrote the original review. For the 2017 update, VHR & LH screened studies and extracted data, and JHB and JLB performed data extraction and updated the text and meta‐analysis.
Sources of support
Internal sources.
- Wayne State University College of Nursing, Adult Health & Administration, USA.
- Nuffield Department of Primary Care Health Sciences, University of Oxford, UK.
External sources
- American Heart Association, USA.
- National Institute of Health Research (NIHR), UK.
Declarations of interest
VHR was the principal investigator in one of the studies included in this review.
LH: None known
JLB: None known
JHB: None known
References to studies included in this review
Allen 1996 {published data only}.
- Allen JK. Coronary risk factor modification in women after coronary artery bypass surgery . Nursing Research 1996; 45 ( 5 ):260‐5. [ PubMed ] [ Google Scholar ]
Alterman 2001 {published data only}
- Alterman AI, Gariti P, Mulvaney F. Short‐ and long‐term smoking cessation for three levels of intensity of behavioral treatment . Psychology of Addictive Behaviors 2001; 15 ( 3 ):261‐4. [ PubMed ] [ Google Scholar ]
Aveyard 2003 {published data only}
- Aveyard P, Griffin C, Lawrence T, Cheng KK. A controlled trial of an expert system and self‐help manual intervention based on the stages of change versus standard self‐help materials in smoking cessation . Addiction 2003; 98 ( 3 ):345‐54. [ PubMed ] [ Google Scholar ]
Aveyard 2007 {published data only}
- Aveyard P, Brown K, Saunders C, Alexander A, Johnstone E, Munafo MR, et al. Weekly versus basic smoking cessation support in primary care: a randomised controlled trial . Thorax 2007; 62 ( 10 ):898‐903. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Berndt 2014 {published data only}
- Berndt N, Bolman C, Froelicher ES, Mudde A, Candel M, Vries H, et al. Effectiveness of a telephone delivered and a face‐to‐face delivered counseling intervention for smoking cessation in patients with coronary heart disease: a 6‐month follow‐up . Journal of Behavioral Medicine 2014; 37 ( 4 ):709‐24. [ PubMed ] [ Google Scholar ]
Bolman 2002 {published data only}
- Bolman C, Vries H, Breukelen G. A minimal‐contact intervention for cardiac inpatients: long‐term effects on smoking cessation . Preventive Medicine 2002; 35 ( 2 ):181‐92. [ PubMed ] [ Google Scholar ]
- Bolman C, Vries H, Breukelen G. Evaluation of a nurse‐managed minimal‐contact smoking cessation intervention for cardiac inpatients . Health Education Research 2002; 17 ( 1 ):99‐116. [ PubMed ] [ Google Scholar ]
- Segaar D, Willemsen MC, Bolman C, Vries H. Nurse adherence to a minimal‐contact smoking cessation intervention on cardiac wards . Research in Nursing & Health 2007; 30 ( 4 ):429‐44. [ PubMed ] [ Google Scholar ]
Borrelli 2005 {published data only}
- Borrelli B, Hayes RB, Dunsiger S, Fava JL. Risk perception and smoking behavior in medically ill smokers: a prospective study . Addiction 2010; 105 ( 6 ):1100‐8. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Borrelli B, Lee C, Novak S. Is provider training effective? Changes in attitudes towards smoking cessation counseling and counseling behaviors of home health care nurses . Preventive Medicine 2008; 46 ( 4 ):358‐63. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Borrelli B, Novak S, Hecht J, Emmons K, Papandonatos G, Abrams D. Home health care nurses as a new channel for smoking cessation treatment: outcomes from project CARES (Community‐nurse Assisted Research and Education on Smoking) . Preventive Medicine 2005; 41 ( 5‐6 ):815‐21. [ PubMed ] [ Google Scholar ]
- Hayes RB, Dunsiger S, Borrelli B. The influence of quality of life and depressed mood on smoking cessation among medically ill smokers . Journal of Behavioral Medicine 2010; 33 ( 3 ):209‐18. [ PubMed ] [ Google Scholar ]
Campbell 1998 {published data only}
- Campbell NC, Ritchie LD, Thain J, Deans HG, Rawles JM, Squair JL. Secondary prevention in coronary heart disease: a randomised trial of nurse led clinics in primary care . Heart 1998; 80 ( 5 ):447‐52. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Campbell NC, Thain J, Deans HG, Ritchie LD, Rawles JM, Squair JL. Secondary prevention clinics for coronary heart disease: randomised trial of effect on health . BMJ 1998; 316 ( 7142 ):1434‐7. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Murchie P, Campbell NC, Ritchie LD, Simpson JA, Thain J. Secondary prevention clinics for coronary heart disease: four year follow up of a randomised controlled trial in primary care . BMJ 2003; 326 ( 7380 ):84. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Canga 2000 {published data only}
- Canga N, Irala J, Vara E, Duaso MJ, Ferrer A, Martinez‐Gonzalez MA. Intervention study for smoking cessation in diabetic patients: a randomized controlled trial in both clinical and primary care settings . Diabetes Care 2000; 23 ( 10 ):1455‐60. [ PubMed ] [ Google Scholar ]
Carlsson 1997 {published data only}
- Carlsson R, Lindberg G, Westin L, Israelsson B. Influence of coronary nursing management follow up on lifestyle after acute myocardial infarction . Heart 1997; 77 ( 3 ):256‐9. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Chan 2012 {published data only}
- Chan SS, Leung DY, Lau C, Wong V, Lam T. Cost‐effectiveness analysis of a low intensity nurse‐led stage‐matched smoking cessation intervention to cardiac patients in Hong Kong . Circulation 2010; 122 ( 2 ):E87. [ Google Scholar ]
- Chan SS, Leung DY, Wong DC, Lau CP, Wong VT, Lam TH. A randomized controlled trial of stage‐matched intervention for smoking cessation in cardiac out‐patients . Addiction 2012; 107 ( 4 ):829‐37. [ PubMed ] [ Google Scholar ]
- Chan SSC, Lam TH, Lau C‐P. The effectiveness of a nurse‐delivered smoking cessation intervention for cardiac patients: a randomised controlled trial . Nicotine & Tobacco Research 2005; 7 :692. [ Google Scholar ]
Chouinard 2005 {published data only}
- Chouinard MC, Robichaud‐Ekstrand S. The effectiveness of a nursing inpatient smoking cessation program in individuals with cardiovascular disease . Nursing Research 2005; 54 ( 4 ):243‐54. [ PubMed ] [ Google Scholar ]
- Chouinard MC, .Robichaud‐Ekstrand S. Predictive value of the transtheoretical model to smoking cessation in hospitalized patients with cardiovascular disease . European Journal of Cardiovascular Prevention & Rehabilitation 2007; 14 ( 1 ):51‐8. [ PubMed ] [ Google Scholar ]
Cossette 2011 {published data only}
- Cossette S, Frasure‐Smith N, Robert M, Chouinard MC, Juneau M, Guertin MC, et al. A pilot randomized trial of a smoking cessation nursing intervention in cardiac patients after hospital discharge . Canadian Journal of Cardiovascular Nursing 2012; 22 ( 4 ):16‐26. [ PubMed ] [ Google Scholar ]
- Cossette S, Frasure‐Smith N, Robert M, Chouinard MC, Juneau M, Guertin MC, et al. A pre‐assessment for nursing intervention to support tobacco cessation in patients hospitalized for cardiac problems: a pilot study (So‐Live). [Évaluation préliminaire d'une intervention infirmière de soutien à la cessation tabagique chez des patients hospitalisés pour un problème cardiaque: étude pilote (So‐Live)]. Recherche en Soins Infirmiers 2011; 105 :60‐75. [ PubMed ] [ Google Scholar ]
Curry 2003 {published data only}
- Curry SJ, Ludman EJ, Graham E, Stout J, Grothaus L, Lozano P. Pediatric‐based smoking cessation intervention for low‐income women: a randomized trial . Archives of Pediatric and Adolescent Medicine 2003; 157 ( 3 ):295‐302. [ PubMed ] [ Google Scholar ]
Davies 1992 {published data only}
- Davies BL, Matte‐Lewis L, O'Connor AM, Dulberg CS, Drake ER. Evaluation of the "Time to Quit" self‐help smoking cessation program . Canadian Journal of Public Health 1992; 83 ( 1 ):19‐23. [ PubMed ] [ Google Scholar ]
DeBusk 1994 {published data only}
- DeBusk RF, Miller NH, Superko HR, Dennis CA, Thomas RJ, Lew HT, et al. A case‐management system for coronary risk factor modification after acute myocardial infarction . Annals of Internal Medicine 1994; 120 ( 9 ):721‐9. [ PubMed ] [ Google Scholar ]
Duffy 2006 {published data only}
- Duffy SA, Ronis DL, Valenstein M, Lambert MT, Fowler KE, Gregory L, et al. A tailored smoking, alcohol, and depression intervention for head and neck cancer patients . Cancer Epidemiology, Biomarkers & Prevention 2006; 15 ( 11 ):2203‐08. [ PubMed ] [ Google Scholar ]
- Duffy SA, Scheumann AL, Fowler KE, Darling‐Fisher C, Terrell JE. Perceived difficulty quitting predicts enrollment in a smoking‐cessation program for patients with head and neck cancer . Oncology Nursing Forum 2010; 37 ( 3 ):349‐56. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Family Heart 1994 {published data only}
- Family Heart Study Group. Randomised controlled trial evaluating cardiovascular screening and intervention in general practice: principal results of British family heart study . BMJ 1994; 308 ( 6924 ):313‐20. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wood DA, Kinmonth A‐L, Davies G, Thompson SG, Pyke SDM, Cramb R, et al. British family heart study: its design and method, and prevalence of cardiovascular risk factors . British Journal of General Practice 1994; 44 :62‐7. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Feeney 2001 {published data only}
- Feeney GF, McPherson A, Connor JP, McAlister A, Young MR, Garrahy P. Randomized controlled trial of two cigarette quit programmes in coronary care patients after acute myocardial infarction . Internal Medicine Journal 2001; 31 ( 8 ):470‐5. [ PubMed ] [ Google Scholar ]
Froelicher 2004 {published data only}
- Froelicher ES, Christopherson DJ. Women's Initiative for Nonsmoking (WINS) I: Design and methods . Heart & Lung 2000; 29 ( 6 ):429‐37. [ PubMed ] [ Google Scholar ]
- Froelicher ES, Christopherson DJ, Miller NH, Martin K. Women's initiative for nonsmoking (WINS) IV: description of 277 women smokers hospitalized with cardiovascular disease . Heart & Lung 2002; 31 ( 1 ):3‐14. [ PubMed ] [ Google Scholar ]
- Froelicher ES, Li WW, Mahrer‐Imhof R, Christopherson D, Stewart AL. Women's Initiative for Non‐Smoking (WINS) VI: Reliability and validity of health and psychosocial measures in women smokers with cardiovascular disease . Heart & Lung 2004; 33 ( 3 ):162‐75. [ PubMed ] [ Google Scholar ]
- Froelicher ES, Miller NH, Christopherson DJ, Martin K, Parker KM, Amonetti M, et al. High rates of sustained smoking cessation in women hospitalized with cardiovascular disease: the Women's Initiative for Nonsmoking (WINS) . Circulation 2004; 109 ( 5 ):587‐93. [ PubMed ] [ Google Scholar ]
- Mahrer‐Imhof R, Froelicher ES, Li WW, Parker KM, Benowitz N. Women's Initiative for Nonsmoking (WINS V): under‐use of nicotine replacement therapy . Heart & Lung 2002; 31 ( 5 ):368‐73. [ PubMed ] [ Google Scholar ]
- Martin K, Froelicher ES, Miller NH. Women's Initiative for Nonsmoking (WINS) II: The intervention . Heart & Lung 2000; 29 ( 6 ):438‐45. [ PubMed ] [ Google Scholar ]
Gilbody 2015 {published data only}
- Gilbody S, Peckham E, Man M‐S, Mitchell N, Li J, Becque T, et al. Bespoke smoking cessation for people with severe mental ill health (SCIMITAR): A pilot randomised controlled trial . Lancet Psychiatry 2015; 2 ( 5 ):395‐402. [ PubMed ] [ Google Scholar ]
Hajek 2002 {published data only}
- Hajek P, Taylor TZ, Mills P. Brief intervention during hospital admission to help patients to give up smoking after myocardial infarction and bypass surgery: randomised controlled trial . BMJ 2002; 324 ( 7329 ):87‐9. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Hanssen 2007 {published data only}
- Hanssen TA, Nordrehaug JE, Eide GE, Hanestad BR. Does a telephone follow‐up intervention for patients discharged with acute myocardial infarction have long‐term effects on health‐related quality of life? A randomised controlled trial . Journal of Clinical Nursing 2009; 18 ( 9 ):1334‐45. [ PubMed ] [ Google Scholar ]
- Hanssen TA, Nordrehaug JE, Eide GE, Hanestad BR. Improving outcomes after myocardial infarction: a randomized controlled trial evaluating effects of a telephone follow‐up intervention . European Journal of Cardiovascular Prevention and Rehabilitation 2007; 14 ( 3 ):429‐37. [ PubMed ] [ Google Scholar ]
Hasuo 2004 {published data only}
- Hasuo S, Tanaka H, Oshima A. Efficacy of a smoking relapse prevention program by postdischarge telephone contacts: a randomized trial . Nippon Koshu Eisei Zasshi (Japanese Journal of Public Health) 2004; 51 ( 6 ):403‐12. [ PubMed ] [ Google Scholar ]
Hennrikus 2005 {published data only}
- Hennrikus D, Lando HA, McCarty MC, Vessey JT. The effectiveness of a systems approach to smoking cessation in hospital inpatients . Society for Research on Nicotine and Tobacco 7th Annual Meeting March 23‐23 Seattle Washington . 2001:47.
- Hennrikus DJ, Lando HA, McCarty MC, Klevan D, Holtan N, Huebsch JA, et al. The TEAM project: the effectiveness of smoking cessation interventions with hospital patients . Preventive Medicine 2005; 40 ( 3 ):249‐58. [ PubMed ] [ Google Scholar ]
Hilberink 2005 {published data only}
- Hilberink SR, Jacobs JE, Bottema BJ, Vries H, Grol RP. Smoking cessation in patients with COPD in daily general practice (SMOCC): six months' results . Preventive Medicine 2005; 41 ( 5‐6 ):822‐7. [ PubMed ] [ Google Scholar ]
- Hilberink SR, Jacobs JE, Breteler MH, Vries H, Grol RP. General practice counseling for patients with chronic obstructive pulmonary disease to quit smoking: Impact after 1 year of two complex interventions . Patient Education and Counseling 2011; 83 ( 1 ):120‐4. [ PubMed ] [ Google Scholar ]
Hollis 1993 {published data only}
- Hollis JF, Lichtenstein E, Mount K, Vogt TM, Stevens VJ. Nurse‐assisted smoking counseling in medical settings: minimizing demands on physicians . Preventive Medicine 1991; 20 ( 4 ):497‐507. [ PubMed ] [ Google Scholar ]
- Hollis JF, Lichtenstein E, Vogt TM, Stevens VJ, Biglan A. Nurse‐assisted counseling for smokers in primary care . Annals of Internal Medicine 1993; 118 ( 7 ):521‐5. [ PubMed ] [ Google Scholar ]
Hornnes 2014 {published data only}
- Hornnes N, Larsen K, Brink‐Kjaer T, Boysen G. Specific antismoking advice after stroke . Danish Medical Journal 2014; 61 ( 4 ):A4816. [ PubMed ] [ Google Scholar ]
Janz 1987 {published data only}
- Janz NK, Becker MH, Kirscht JP, Eraker SA, Billi JE, Woolliscroft JO. Evaluation of a minimal‐contact smoking cessation intervention in an outpatient setting . American Journal of Public Health 1987; 77 :805‐9. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Jiang 2007 {published data only}
- Jiang X, Sit JW, Wong TK. A nurse‐led cardiac rehabilitation programme improves health behaviours and cardiac physiological risk parameters: evidence from Chengdu, China . Journal of Clinical Nursing 2007; 16 ( 10 ):1886‐97. [ PubMed ] [ Google Scholar ]
Jorstad 2013 {published data only}
- Jorstad HT, Birgelen C, Alings AM, Liem A, Dantzig JM, Jaarsma W, et al. Effect of a nurse‐coordinated prevention programme on cardiovascular risk after an acute coronary syndrome: main results of the RESPONSE randomised trial . Heart 2013; 99 ( 19 ):1421‐30. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Kadda 2015 {published data only}
- Kadda O, Kotanidou A, Manginas A, Stavridis G, Nanas S, Panagiotakos DB. Lifestyle intervention and one‐year prognosis of patients following open heart surgery: a randomised clinical trial . Journal of Clinical Nursing 2015; 24 ( 11‐12 ):1611‐21. [ PubMed ] [ Google Scholar ]
Kim 2003 {published data only}
- Kim YE, Song YM, Lee JK, Jung HS, Kang SC. A study evaluating the effect of telephone counselling on smoking performed by a nurse cessation: a preliminary, randomized, controlled trial . Journal of the Korean Academy of Family Medicine 2003; 24 ( 7 ):634‐41. [ Google Scholar ]
Kim 2005 {published data only}
- Kim JR, Lee MS, Hwang JY, Lee JD. Efficacy of a smoking cessation intervention using the AHCPR guideline tailored for Koreans: a randomized controlled trial . Health Promotion International 2005; 20 ( 1 ):51‐9. [ PubMed ] [ Google Scholar ]
Lancaster 1999 {published data only}
- Lancaster T, Dobbie W, Vos K, Yudkin P, Murphy M, Fowler G. Randomised trial of nurse‐assisted strategies for smoking cessation in primary care . British Journal of General Practice 1999; 49 ( 440 ):191‐4. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Lewis 1998 {published data only}
- Lewis SF, Piasecki TM, Fiore MC, Anderson JE, Baker TB. Transdermal nicotine replacement for hospitalized patients: A randomized clinical trial . Preventive Medicine 1998; 27 ( 2 ):296‐303. [ PubMed ] [ Google Scholar ]
Meysman 2010 {published data only}
- Meysman M, Boudrez H, Nackaerts K, Dieriks B, Indemans R, Vermeire P. Smoking cessation rates after a nurse‐led inpatient smoking cessation intervention . Journal of Smoking Cessation 2010; 5 ( 1 ):69‐76. [ Google Scholar ]
Miller 1997 {published data only}
- Miller NH, Smith PM, DeBusk RF, Sobel DS, Taylor CB. Smoking cessation in hospitalized patients. Results of a randomized trial . Archives of Internal Medicine 1997; 157 ( 4 ):409‐15. [ PubMed ] [ Google Scholar ]
- Miller NH, Smith PM, Taylor CB, Sobel D, DeBusk RF. Smoking cessation in hospitalized patients ‐ results of a randomized trial . Circulation 1995; 92 ( 8 ):SS179 (abstract 855). [ PubMed ] [ Google Scholar ]
- Taylor CB, Miller NH, Herman S, Smith PM, Sobel D, Fisher L, et al. A nurse‐managed smoking cessation program for hospitalized smokers . American Journal of Public Health 1996; 86 ( 11 ):1557‐60. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Nagle 2005 {published data only}
- Hensley MJ, Nagle AL, Schofield MJ, Koschel A. Efficacy of a brief nurse provided nicotine management intervention for hospitalised smokers . Respirology 2002; 7 :A12. [ Google Scholar ]
- Nagle AL, Hensley MJ, Schofield MJ, Koschel AJ. A randomised controlled trial to evaluate the efficacy of a nurse‐provided intervention for hospitalised smokers . Australian and New Zealand Journal of Public Health 2005; 29 ( 3 ):285‐91. [ PubMed ] [ Google Scholar ]
Nebot 1992 {published data only}
- Nebot M, Cabezas C. Does nurse counseling or offer of nicotine gum improve the effectiveness of physician smoking‐cessation advice? . Family Practice Research Journal 1992; 12 ( 3 ):263‐70. [ PubMed ] [ Google Scholar ]
OXCHECK 1994 {published data only}
- Imperial Cancer Research Fund OXCHECK Study Group. Effectiveness of health checks conducted by nurses in primary care: Results of the OXCHECK study after one year . BMJ 1994; 308 ( 6924 ):308‐12. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Imperial Cancer Research Fund OXCHECK Study Group. Effectiveness of health checks conducted by nurses in primary care: final results of the OXCHECK study . BMJ 1995; 310 ( 6987 ):1099‐104. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Pardavila‐Belio 2015 {published data only}
- Pardavila‐Belio MI, Garcia‐Vivar C, Pimenta AM, Canga‐Armayor A, Pueyo‐Garrigues S, Canga‐Armayor N. Intervention study for smoking cessation in Spanish college students: Pragmatic randomized controlled trial . Addiction 2015; 110 ( 10 ):1676‐83. [ PubMed ] [ Google Scholar ]
Quist‐Paulsen 2003 {published data only}
- Brown DW. Nurse‐led intervention increases smoking cessation among people with coronary heart disease . Evidence Based Healthcare 2004; 8 :128‐30. [ Google Scholar ]
- Quist‐Paulsen P, Bakke PS, Gallefoss F. Does smoking cessation improve quality of life in patients with coronary heart disease? . Scandinavian Cardiovascular Journal 2006; 40 ( 1 ):11‐16. [ PubMed ] [ Google Scholar ]
- Quist‐Paulsen P, Bakke PS, Gallefoss F. Predictors of smoking cessation in patients admitted for acute coronary heart disease . European Journal of Cardiovascular Prevention and Rehabilitation 2005; 12 ( 5 ):472‐7. [ PubMed ] [ Google Scholar ]
- Quist‐Paulsen P, Gallefoss F. Randomised controlled trial of smoking cessation intervention after admission for coronary heart disease . BMJ 2003; 327 ( 7426 ):1254‐7. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Quist‐Paulsen P, Lydersen S, Bakke PS, Gallefoss F. Cost effectiveness of a smoking cessation program in patients admitted for coronary heart disease . European Journal of Cardiovascular Prevention and Rehabilitation 2006; 13 ( 2 ):274‐80. [ PubMed ] [ Google Scholar ]
Ratner 2004 {published data only}
- Ratner PA, Johnson JL, Richardson CG, Bottorff JL, Moffat B, Mackay M, et al. Efficacy of a smoking‐cessation intervention for elective‐surgical patients . Research in Nursing and Health 2004; 27 ( 3 ):148‐61. [ PubMed ] [ Google Scholar ]
Rice 1994 {published data only}
- Rice VH, Fox DH, Lepczyk M, Sieggreen M, Mullin M, Jarosz P, et al. A comparison of nursing interventions for smoking cessation in adults with cardiovascular health problems . Heart and Lung 1994; 23 ( 6 ):473‐86. [ PubMed ] [ Google Scholar ]
Rigotti 1994 {published data only}
- Rigotti NA, McKool KM, Shiffman S. Predictors of smoking cessation after coronary artery bypass graft surgery. Results of a randomized trial with 5‐year follow‐up . Annals of Internal Medicine 1994; 120 ( 4 ):287‐93. [ PubMed ] [ Google Scholar ]
Risser 1990 {published data only}
- Risser NL, Belcher DW. Adding spirometry, carbon monoxide, and pulmonary symptom results to smoking cessation counseling: a randomized trial . Journal of General Internal Medicine 1990; 5 ( 1 ):16‐22. [ PubMed ] [ Google Scholar ]
Sanders 1989a {published data only}
- Sanders D, Fowler G, Mant D, Fuller A, Jones L, Marzillier J. Randomized controlled trial of anti‐smoking advice by nurses in general practice . Journal of the Royal College of General Practitioners 1989; 39 ( 324 ):273‐6. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Sanders 1989b {published data only}
Sanz‐pozo 2006 {published data only}.
- Sanz Pozo B, Miguel Díaz J, Aragón Blanco M, González González AI, Cortes Catalán M, Vázquez I. Effectiveness of non‐pharmacological primary care methods for giving up tobacco dependency [Efectividad de los métodos no farmacológicos para la deshabituación tabáquica en atención primaria]. Atencion Primaria 2003; 32 ( 6 ):366‐70. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sanz‐Pozo B, Miguel‐Díaz J, Aragón‐Blanco M, García‐Caballo M, Gomez‐Suarez E, Fernandez‐Dominguez JF. Effectiveness of a programme of intensive tobacco counselling by nursing professionals [Efectividad de un programa de consejo antitabaco intensivo realizado por profesionales de enfermería]. Atencion Primaria 2006; 37 :266‐72. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Smit 2016 {published data only}
- Smit ES, Vries H, Hoving C. Results of the PAS study: a randomized controlled trial evaluating the effectiveness of a web‐based multiple tailored smoking cessation program combined with tailored counseling by practice nurses . Health Communication 2016; 31 ( 9 ):1165‐73. [DOI: 10.1080/10410236.2015.1049727] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Smit ES, Vries H, Hoving C. The PAS study: a randomized controlled trial evaluating the effectiveness of a web‐based multiple tailored smoking cessation programme and tailored counselling by practice nurses . Contemporary Clinical Trials 2010; 31 ( 3 ):251‐8. [ PubMed ] [ Google Scholar ]
Steptoe 1999 {published data only}
- Steptoe A, Doherty S, Rink E, Kerry S, Kendrick T, Hilton S. Behavioural counselling in general practice for the promotion of healthy behaviour among adults at increased risk of coronary heart disease: randomised trial . BMJ 1999; 319 ( 7215 ):943‐7. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Taylor 1990 {published data only}
- Taylor CB, Houston‐Miller N, Killen JD, DeBusk RF. Smoking cessation after acute myocardial infarction: effects of a nurse‐managed intervention . Annals of Internal Medicine 1990; 113 ( 2 ):118‐23. [ PubMed ] [ Google Scholar ]
Terazawa 2001 {published data only}
- Terazawa T, Mamiya T, Masui S, Nakamura M. The effect of smoking cessation counseling at health checkup . Sangyo Eiseigaku Zasshi 2001; 43 ( 6 ):207‐13. [ PubMed ] [ Google Scholar ]
Tønnesen 1996 {published data only}
- Tønnesen P, Mikkelsen K, Markholst C, Ibsen A, Bendixen M, Pedersen L, et al. Nurse‐conducted smoking cessation with minimal intervention in a lung clinic: a randomized controlled study . European Respiratory Journal 1996; 9 ( 11 ):2351‐5. [ PubMed ] [ Google Scholar ]
Tønnesen 2006 {published data only}
- Tønnesen P, Mikkelsen K, Bremann L. Nurse‐conducted smoking cessation in patients with COPD using nicotine sublingual tablets and behavioral support . Chest 2006; 130 ( 2 ):334‐42. [ PubMed ] [ Google Scholar ]
Vetter 1990 {published data only}
- Vetter NJ, Ford D. Smoking prevention among people aged 60 and over: a randomized controlled trial . Age and Ageing 1990; 19 ( 3 ):164‐8. [ PubMed ] [ Google Scholar ]
Wood 2008 {published data only}
- Wood D, Kotseva K, Connolly S, Jennings C, Mead A, Jones J, et al. Nurse‐coordinated multidisciplinary, family‐based cardiovascular disease prevention programme (EUROACTION) for patients with coronary heart disease and asymptomatic individuals at high risk of cardiovascular disease: a paired, cluster‐randomised controlled trial . Lancet 2008; 371 ( 9629 ):1999‐2012. [ PubMed ] [ Google Scholar ]
Zwar 2015 {published data only}
- Zwar N, Richmond R, Halcomb E, Furler J, Smith J, Hermiz O, et al. Quit in general practice: a cluster randomised trial of enhanced in‐practice support for smoking cessation . BMC Family Practice 2010; 11 :59. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Zwar NA, Richmond RL, Halcomb EJ, Furler JS, Smith JP, Oshana Hermiz O, et al. Quit in general practice: a cluster randomized trial of enhanced in‐practice support for smoking cessation . Family Practice 2015; 32 ( 2 ):173‐180. [DOI: 10.1093/fampra/cmu089] [ PubMed ] [ CrossRef ] [ Google Scholar ]
References to studies excluded from this review
Aertsen‐van der kuip 2006 {published data only}.
- Aertsen‐Van der Kuip M, Besselink RM, Vlugt MJ, Peters E, Fouwels AJ, Wollersheim Hal. Successful motivational interviewing for smoking cessation in a secondary cardiovascular prevention clinic . European Heart Journal 2006; 27 ( Suppl 1 ):165. [ Google Scholar ]
Andrews 2007 {published data only}
- Andrews JO, Felton G, Wewers ME, Waller J, Tingen M. The effect of a multi‐component smoking cessation intervention in African American women residing in public housing . Research in Nursing & Health 2007; 30 ( 1 ):45‐60. [ PubMed ] [ Google Scholar ]
Avanzini 2011 {published data only}
- Avanzini F, Di GP, Amodeo R, Baldo S, Bergna ML, Busi G, et al. Effectiveness of a nurse‐led educational intervention for patients admitted for acute coronary syndrome [Efficacia di un intervento educativo infermieristico in pazienti ricoverati per una sindrome coronarica acuta]. Assistenza Infermieristica e Ricerca:Air 2011; 30 :16‐23. [ PubMed ] [ Google Scholar ]
Bredie 2011 {published data only}
- Bredie SJ, Fouwels AJ, Wollersheim H, Schippers GM. Effectiveness of nurse based motivational interviewing for smoking cessation in high risk cardiovascular outpatients: A randomized trial . European Journal of Cardiovascular Nursing 2011; 10 ( 3 ):174‐9. [ PubMed ] [ Google Scholar ]
Browning 2000 {published data only}
- Browning KK, Ahijevych KL, Ross P Jr, Wewers ME. Implementing the Agency for Health Care Policy and Research's Smoking Cessation Guideline in a lung cancer surgery clinic . Oncology Nursing Forum 2000; 27 ( 8 ):1248‐54. [ PubMed ] [ Google Scholar ]
Brunner‐Frandsen 2012 {published data only}
- Brunner Frandsen N, Sorensen M, Hyldahl TK, Henriksen RM, Bak S. Smoking cessation intervention after ischemic stroke or transient ischemic attack. A randomized controlled pilot trial . Nicotine & Tobacco Research 2012; 14 ( 4 ):443‐7. [ PubMed ] [ Google Scholar ]
- Brunner‐Frandsen NS, Bak S. Smoking cessation intervention after stroke or transient ischemic attack. A randomised controlled trial . Cerebrovascular Diseases 2010; 29 ( Suppl 2 ):323. [ Google Scholar ]
Cabezas 2011 {published data only}
- Cabezas C, Advani M, Puente D, Rodriguez T, Martin C, ISTAPS Study Group. Effectiveness of a stepped primary care smoking cessation intervention: cluster randomized clinical trial (ISTAPS study) . Addiction 2011; 106 ( 9 ):1696‐706. [ PubMed ] [ Google Scholar ]
- Cabezas C, Martin C, Granollers S, Morera C, Ballve JL, Zarza E, et al. Effectiveness of a stepped primary care smoking cessation intervention (ISTAPS study): design of a cluster randomised trial . BMC Public Health 2009; 9 :48. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Puente D, Cabezas C, Rodriguez‐Blanco T, Fernandez‐Alonso C, Cebrian T, Torrecilla M, et al. The role of gender in a smoking cessation intervention: a cluster randomized clinical trial . BMC Public Health 2011; 11 :369. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Carlsson 1998 {published data only}
- Carlsson R. Serum cholesterol, lifestyle, working capacity and quality of life in patients with coronary artery disease. Experiences from a hospital‐based secondary prevention programme . Scandinavian Cardiovascular Journal Supplement 1998; 50 :1‐20. [ PubMed ] [ Google Scholar ]
Caslin 2006 {published data only}
- Caslin EK, Newhouse R, Zissimos J, Murray P, Thompson KM, Ashen D, et al. Smoking Cessation Intervention and Nurse Initiation (SCINI) Trial . 13th World Conference on Tobacco & Health . 2006.
- Thompson KM, Caslin EK, Murray P, Zissimos J, Newhouse R, Yung R. Barriers to implementing nurse initiated inpatient smoking cessation [Abstract]. . Proceedings of the American Thoracic Society 2006: A294 . 2006.
Chan 2005 {published data only}
- Chan SS, Lam TH, Salili F, Leung GM, Wong DC, Botelho RJ, et al. A randomized controlled trial of an individualized motivational intervention on smoking cessation for parents of sick children: a pilot study . Applied Nursing Research 2005; 18 ( 3 ):178‐81. [ PubMed ] [ Google Scholar ]
Chan 2008 {published data only}
- Chan SS, Leung GM, Wong DC, Lam TH. Helping Chinese fathers quit smoking through educating their nonsmoking spouses: a randomized controlled trial . American Journal of Health Promotion 2008; 23 ( 1 ):31‐4. [ PubMed ] [ Google Scholar ]
- Chan SS, Wong DC, Lam T‐H. Will mothers of sick children help their husbands to stop smoking after receiving a brief intervention from nurses? Secondary analysis of a randomised controlled trial . BMC Pediatrics 2013; 13 :50. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Duffy 2014 {published data only}
- Duffy SA, Ronis DL, Karvonen‐Gutierrez CA, Ewing LA, Dalack GW, Smith PM, et al. Effectiveness of the tobacco tactics program in the Department of Veterans Affairs . Annals of Behavioral Medicine 2014; 48 ( 2 ):265‐74. [ PubMed ] [ Google Scholar ]
Efraimsson 2008 {published data only}
- Efraimsson EO, Hillervik C, Ehrenberg A. Effects of COPD self‐care management education at a nurse‐led primary health care clinic . Scandinavian Journal of Caring Sciences 2008; 22 ( 2 ):178‐85. [ PubMed ] [ Google Scholar ]
Fletcher 1987 {published data only}
- Fletcher V. An individualized teaching programme following primary uncomplicated myocardial infarction . Journal of Advanced Nursing 1987; 12 ( 2 ):195‐200. [ PubMed ] [ Google Scholar ]
French 2007 {published data only}
- French GM, Groner JA, Wewers ME, Ahijevych K. Staying smoke free: an intervention to prevent postpartum relapse . Nicotine & Tobacco Research 2007; 9 ( 6 ):663‐70. [ PubMed ] [ Google Scholar ]
Fritz 2008 {published data only}
- Fritz DJ, Hardin SB, Gore PA Jr, Bram D. A computerized smoking cessation intervention for high school smokers . Pediatric Nursing 2008; 34 ( 1 ):13‐7. [ PubMed ] [ Google Scholar ]
Galvin 2001 {published data only}
- Galvin K, Webb C, Hillier V. Assessing the impact of a nurse‐led health education intervention for people with peripheral vascular disease who smoke: the use of physiological markers, nicotine dependence and withdrawal . International Journal of Nursing Studies 2001; 38 ( 1 ):91‐105. [ PubMed ] [ Google Scholar ]
Gies 2008 {published data only}
- Gies CE, Buchman D, Robinson J, Smolen D. Effect of an inpatient nurse‐directed smoking cessation program . Western Journal of Nursing Research 2008; 30 ( 1 ):6‐19. [ PubMed ] [ Google Scholar ]
Griebel 1998 {published data only}
- Griebel B, Wewers ME, Baker CA. The effectiveness of a nurse‐managed minimal smoking‐cessation intervention among hospitalized patients with cancer . Oncology Nursing Forum 1998; 25 ( 5 ):897‐902. [ PubMed ] [ Google Scholar ]
Haddock 1997 {published data only}
- Haddock J, Burrows C. The role of the nurse in health promotion: an evaluation of a smoking cessation programme in surgical pre‐admission clinics . Journal of Advanced Nursing 1997; 26 ( 6 ):1098‐110. [ PubMed ] [ Google Scholar ]
Hall 2007 {published data only}
- Hall S, Reid E, Ukoumunne OC, Weinman J, Marteau TM. Brief smoking cessation advice from practice nurses during routine cervical smear tests appointments: a cluster randomised controlled trial assessing feasibility, acceptability and potential effectiveness . British Journal of Cancer 2007; 96 ( 7 ):1057‐61. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Happell 2014 {published data only}
- Happell B, Stanton R, Platania‐Phung C, McKenna B, Scott D. The cardiometabolic health nurse: physical health behaviour outcomes from a randomised controlled trial . Issues in Mental Health Nursing 2014; 35 ( 10 ):768‐75. [ PubMed ] [ Google Scholar ]
Heath 2012 {published data only}
- Heath J, Inglett S, Young S, Joshua TV, Sakievich N, Hawkins J, et al. The impact of the Georgia Health Sciences University nursing faculty practice on tobacco cessation rates . Nursing Clinics of North America 2012; 47 ( 1 ):1‐12. [ PubMed ] [ Google Scholar ]
Hjalmarson 2007 {published data only}
- Hjalmarson A, Boethius G. The effectiveness of brief advice and extended smoking cessation counseling programs when implemented routinely in hospitals . Preventive Medicine 2007; 45 ( 2‐3 ):202‐7. [ PubMed ] [ Google Scholar ]
Jansink 2013 {published data only}
- Jansink R, Braspenning J, Keizer E, Weijden T, Elwyn G, Grol R. No identifiable Hb1Ac or lifestyle change after a comprehensive diabetes programme including motivational interviewing: A cluster randomized trial . Scandinavian Journal of Primary Health Care 2013; 31 ( 2 ):119‐27. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Jansink R, Braspenning J, Weijden T, Niessen L, Elwyn G, Grol R. Nurse‐led motivational interviewing to change the lifestyle of patients with type 2 diabetes (MILD‐project): protocol for a cluster, randomized, controlled trial on implementing lifestyle recommendations . BMC Health Services Research 2009; 9 :19. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Jelley 1995 {published data only}
- Jelley MJ, Prochazka AV. A smoking cessation intervention in family planning clinics . Journal of Women's Health 1995; 4 :555‐67. [ Google Scholar ]
Johnson 1999 {published data only}
- Johnson JL, Budz B, Mackay M, Miller C. Evaluation of a nurse‐delivered smoking cessation intervention for hospitalized patients with cardiac disease . Heart and Lung 1999; 28 ( 1 ):55‐64. [ PubMed ] [ Google Scholar ]
Johnson 2000 {published data only}
- Johnson JL, Ratner PA, Bottorff JL, Hall W, Dahinten S. Preventing smoking relapse in postpartum women . Nursing Research 2000; 49 ( 1 ):44‐52. [ PubMed ] [ Google Scholar ]
- Ratner PA, Johnson JL, Bottorff JL, Dahinten S, Hall W. Twelve‐month follow‐up of a smoking relapse prevention intervention for postpartum women . Addictive Behaviors 2000; 25 ( 1 ):81‐92. [ PubMed ] [ Google Scholar ]
Jonsdottir 2015 {published data only}
- Jonsdottir H, Amundadottir OR, Gudmundsson G, Halldorsdottir BS, Hrafnkelsson B, Ingadottir TS, et al. Effectiveness of a partnership‐based self‐management programme for patients with mild and moderate chronic obstructive pulmonary disease: a pragmatic randomized controlled trial . Journal of Advanced Nursing 2015; 71 ( 11 ):2634‐49. [ PubMed ] [ Google Scholar ]
Katz 2012 {published data only}
- Katz DA, Vander Weg MW, Holman J, Nugent A, Baker L, Johnson S, et al. The Emergency Department Action in Smoking Cessation (EDASC) trial: impact on delivery of smoking cessation counseling . Academic Emergency Medicine 2012; 19 ( 4 ):409‐20. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Kendrick 1995 {published data only}
- Kendrick JS, Zahniser SC, Miller N, Salas N, Stine J, Gargiullo PM, et al. Integrating smoking cessation into routine public prenatal care: the Smoking Cessation in Pregnancy project . American Journal of Public Health 1995; 85 ( 2 ):217‐22. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Koelewijn‐van Loon 2009 {published data only}
- Koelewijn‐van Loon MS, Weijden T, Steenkiste B, Ronda G, Winkens B, Severens JL, et al. Involving patients in cardiovascular risk management with nurse‐led clinics: a cluster randomized controlled trial . Canadian Medical Association Journal 2009; 181 ( 12 ):E267‐74. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Kotz 2009 {published data only}
- Kotz D, Huibers MJH, West RJ, Wesseling G, Schayck OC. What mediates the effect of confrontational counselling on smoking cessation in smokers with COPD? . Patient Education and Counseling 2009; 76 ( 1 ):16‐24. [ PubMed ] [ Google Scholar ]
- Kotz D, Wesseling G, Huibers MJ, Schayck OC. Efficacy of confrontational counselling for smoking cessation in smokers with previously undiagnosed mild to moderate airflow limitation: study protocol of a randomized controlled trial . BMC Public Health 2007; 7 :332. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kotz D, Wesseling G, Huibers MJ, Schayck OC. Efficacy of confronting smokers with airflow limitation for smoking cessation.[see comment] . European Respiratory Journal 2009; 33 ( 4 ):754‐62. [ PubMed ] [ Google Scholar ]
Kruis 2014 {published data only}
- Kruis AL, Boland MR, Assendelft WJ, Gussekloo J, Tsiachristas A, Stijnen T, et al. Effectiveness of integrated disease management for primary care chronic obstructive pulmonary disease patients: Results of cluster randomised trial . Nederlands Tijdschrift voor Geneeskunde 2015; 159 ( 13 ). [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kruis AL, Boland MR, Assendelft WJ, Gussekloo J, Tsiachristas A, Stijnen T, et al. Effectiveness of integrated disease management for primary care chronic obstructive pulmonary disease patients: results of cluster randomised trial . BMJ 2014; 349 :1‐11. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Lakerveld 2010 {published data only}
- Lakerveld J, Bot SD, Chinapaw MJ, Kostense PJ, Nijpels G. An individual lifestyle intervention program is not more effective in changing diabetes risk and lifestyle behaviors than providing health brochures: The Hoorn Prevention Study . Diabetologia 2010; 53 :S82. [ Google Scholar ]
Lakerveld 2013 {published data only}
- Lakerveld J, Bot SD, Chinapaw MJ, Tulder MW, Kostense PJ, Dekker JM, et al. Motivational interviewing and problem solving treatment to reduce type 2 diabetes and cardiovascular disease risk in real life: A randomized controlled trial . International Journal of Behavioral Nutrition and Physical Activity 2013; 10 :47. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Lifrak 1997 {published data only}
- Lifrak P, Gariti P, Alterman AI, McKay J, Volpicelli J, Sparkman T, et al. Results of two levels of adjunctive treatment used with the nicotine patch . American Journal of Addiction 1997; 6 ( 2 ):93‐8. [ PubMed ] [ Google Scholar ]
Lou 2013 {published data only}
- Lou P, Zhu Y, Chen P, Zhang P, Yu J, Zhang N, et al. Supporting smoking cessation in chronic obstructive pulmonary disease with behavioral intervention: a randomized controlled trial . BMC Family Practice 2013; 14 :91. [ PMC free article ] [ PubMed ] [ Google Scholar ]
McHugh 2001 {published data only}
- McHugh F, Lindsay GM, Hanlon P, Hutton I, Brown MR, Morrison C, et al. Nurse led shared care for patients on the waiting list for coronary artery bypass surgery: a randomised controlled trial . Heart 2001; 86 ( 3 ):317‐23. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Meulepas 2007 {published data only}
- Meulepas MA, Jacobs JE, Smeenk FW, Smeele I, Lucas AE, Bottema BJ, et al. Effect of an integrated primary care model on the management of middle‐aged and old patients with obstructive lung diseases . Scandinavian Journal of Primary Health Care 2007; 25 ( 3 ):186‐92. [ PMC free article ] [ PubMed ] [ Google Scholar ]
O'Connor 1992 {published data only}
- O'Connor AM, Davies BL, Dulberg CS, Buhler PL, Nadon C, McBride BH, et al. Effectiveness of a pregnancy smoking cessation program . Journal of Obstetric, Gynecologic, and Neonatal Nursing 1992; 21 ( 5 ):385‐92. [ PubMed ] [ Google Scholar ]
Persson 2006 {published data only}
- Persson LG, Hjalmarson A. Smoking cessation in patients with diabetes mellitus: results from a controlled study of an intervention programme in primary healthcare in Sweden . Scandinavian Journal of Primary Health Care 2006; 24 ( 2 ):75‐80. [ PubMed ] [ Google Scholar ]
Planer 2011 {published data only}
- Planer D, Lev I, Elitzur Y, Sharon N, Ouzan E, Pugatsch T, et al. Bupropion for smoking cessation in patients with acute coronary syndrome . Archives of Internal Medicine 2011; 171 ( 12 ):1055‐60. [ PubMed ] [ Google Scholar ]
Pozen 1977 {published data only}
- Pozen MW, Stechmiller JA, Harris W, Smith S, Fried DD, Voigt GC. A nurse rehabilitator's impact on patients with myocardial infarction . Medical Care 1977; 15 ( 10 ):830‐7. [ PubMed ] [ Google Scholar ]
Reeve 2000 {published data only}
- Reeve K, Calabro K, Adams‐McNeill J. Tobacco cessation intervention in a nurse practitioner managed clinic . Journal of the American Academy of Nurse Practitioners 2000; 12 ( 5 ):163‐9. [ PubMed ] [ Google Scholar ]
Reid 2003 {published data only}
- Reid R, Pipe A, Higginson L, Johnson K, D'Angelo MS, Cooke D, et al. Stepped care approach to smoking cessation in patients hospitalized for coronary artery disease . Journal of Cardiopulmonary Rehabilitation 2003; 23 ( 3 ):176‐82. [ PubMed ] [ Google Scholar ]
Rigotti 1997 {published data only}
- Rigotti NA, Arnsten JH, McKool KM, Wood‐Reid KM, Pasternak RC, Singer DE. Efficacy of a smoking cessation program for hospital patients . Archives of Internal Medicine 1997; 157 ( 22 ):2653‐60. [ PubMed ] [ Google Scholar ]
Smith 2009 {published data only}
- Smith PM, Burgess E. Smoking cessation initiated during hospital stay for patients with coronary artery disease: a randomized controlled trial . Canadian Medical Association Journal 2009; 180 ( 13 ):1297‐303. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Stanislaw 1994 {published data only}
- Stanislaw AE, Wewers ME. A smoking cessation intervention with hospitalized surgical cancer patients: a pilot study . Cancer Nursing 1994; 17 ( 2 ):81‐6. [ PubMed ] [ Google Scholar ]
Sun 2000 {published data only}
- Sun C. Roles of psychological nursing played in the course of auricle point applying to help individuals giving up smoking . Shanxi Nursing Journal 2000; 14 ( 2 ):69‐70. [ Google Scholar ]
Targhetta 2011 {published data only}
- Targhetta R, Bernhard L, Sorokaty JM, Balmes JL, Nalpas B, Perney P. Intervention study to improve smoking cessation during hospitalization . Public Health 2011; 125 ( 7 ):457‐63. [ PubMed ] [ Google Scholar ]
Van Elderen 1994 {published data only}
- Elderen‐van Kemenade T, Maes S, Broek Y. Effects of a health education programme with telephone follow‐up during cardiac rehabilitation . British Journal of Clinical Psychology 1994; 33 ( 3 ):367‐78. [ PubMed ] [ Google Scholar ]
Van Zuilen 2011 {published data only}
- Zuilen AD, Blankestijn PJ, Buren M, Dam MA, Kaasjager KA, Ligtenberg G, et al. Nurse practitioners improve quality of care in chronic kidney disease: two‐year results of a randomised study . Netherlands Journal of Medicine 2011; 69 ( 11 ):517‐26. [ PubMed ] [ Google Scholar ]
- Zuilen AD, Bots ML, Dulger A, Tweel I, Buren M, Dam MA, et al. Multifactorial intervention with nurse practitioners does not change cardiovascular outcomes in patients with chronic kidney disease . Kidney International 2012; 82 ( 6 ):710‐7. [ PubMed ] [ Google Scholar ]
Wadland 1999 {published data only}
- Wadland WC, Stoffelmayr B, Berger E, Crombach A, Ives K. Enhancing smoking cessation rates in primary care . Journal of Family Practice 1999; 48 ( 9 ):711‐8. [ PubMed ] [ Google Scholar ]
Wadland 2001 {published data only}
- Wadland WC, Stoffelmayr B, Ives K. Enhancing smoking cessation of low‐income smokers in managed care . Journal of Family Practice 2001; 50 ( 2 ):138‐44. [ PubMed ] [ Google Scholar ]
Wewers 1994 {published data only}
- Wewers ME, Bowen JM, Stanislaw AE, Desimone VB. A nurse‐delivered smoking cessation intervention among hospitalized postoperative patients‐‐influence of a smoking‐related diagnosis: a pilot study . Heart and Lung 1994; 23 ( 2 ):151‐6. [ PubMed ] [ Google Scholar ]
Wewers 2009 {published data only}
- Wewers ME, Ferketich AK, Harness J, Paskett ED. Effectiveness of a nurse‐managed, lay‐led tobacco cessation intervention among Ohio Appalachian women . Cancer Epidemiology, Biomarkers and Prevention 2009; 18 ( 12 ):3451‐8. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Wilson 2008 {published data only}
- Wilson JS, Elborn JS, Fitzsimons D, McCrum‐Gardner E. Do smokers with chronic obstructive pulmonary disease report their smoking status reliably? A comparison of self‐report and bio‐chemical validation . International Journal of Nursing Studies 2011; 48 ( 7 ):856‐62. [ PubMed ] [ Google Scholar ]
- Wilson JS, Fitzsimons D, Bradbury I, Stuart EJ. Does additional support by nurses enhance the effect of a brief smoking cessation intervention in people with moderate to severe chronic obstructive pulmonary disease? A randomised controlled trial . International Journal of Nursing Studies 2008; 45 ( 4 ):508‐17. [ PubMed ] [ Google Scholar ]
Woollard 1995 {published data only}
- Woollard J, Beilin LJ, Lord T, Puddey I, MacAdam D, Rouse I. A controlled trial of nurse counselling of life‐style change for hypertensives treated in general practice ‐preliminary results . Clinical and Experimental Pharmacology and Physiology 1995; 22 ( 6‐7 ):466‐8. [ PubMed ] [ Google Scholar ]
Zakrisson 2011 {published data only}
- Zakrisson AB, Engfeldt P, Hägglund D, Odencrants S, Hasselgren M, Arne M, et al. Nurse‐led multidisciplinary programme for patients with COPD in primary health care: a controlled trial . Primary Care Respiratory Journal 2011; 20 ( 4 ):427‐33. [ PMC free article ] [ PubMed ] [ Google Scholar ]
References to ongoing studies
Lachman 2015 {published data only}.
- Lachman S, Minneboo M, Snaterse M, Jorstad HT, Ter Riet G, Scholte Op Reimer WJ, et al. Community‐based comprehensive lifestyle programs in patients with coronary artery disease: Objectives, design and expected results of Randomized Evaluation of Secondary Prevention by Outpatient Nurse SpEcialists 2 trial (RESPONSE 2) . American Heart Journal 2015; 170 ( 2 ):216‐22. [ PubMed ] [ Google Scholar ]
Mularski 2013 {published data only}
- Mularski RA, Leo MC, Waiwaiole LA, Carlson CA, Conn DE, Funkhouser KA, et al. Linking in‐hospital smoking cessation assistance with outpatient services and automated telephone follow‐up using dedicated nurse tobacco treatment specialists: A randomized controlled trial . American Journal of Respiratory and Critical Care Medicine 2013; 187 ( Meeting Abstracts ):A3905. [ Google Scholar ]
{"type":"clinical-trial","attrs":{"text":"NCT02106637","term_id":"NCT02106637"}} NCT02106637 {published data only}
- NCT02106637. Early in‐hospital Initiation of pharmacotherapy for smoking cessation, concomitant with nurse‐led support, in patients after an acute coronary syndrome (ACS) . clinicaltrials.gov/show/NCT02106637 (first received 8 April 2014).
Additional references
- Fiore MC, Jaen CR, Baker TB, Bailey WC, Benowitz NL, Curry SJ, et al. Treating Tobacco Use and Dependence: 2008 Update . Rockville, MD: US Dept of Health and Human Services, 2008. [ Google Scholar ]
- American Nurses Association. Tobacco Free Nurses . www.nursingworld.org/MainMenuCategories/WorkplaceSafety/Healthy‐Nurse/TobaccoFree.html (accessed 24 July 2013) .
- Bize R, Burnand B, Mueller Y, Rège‐Walther M, Camain JY, Cornuz J. Biomedical risk assessment as an aid for smoking cessation . Cochrane Database of Systematic Reviews 2012, Issue 12 . [DOI: 10.1002/14651858.CD004705.pub4] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Cahill 2016
- Cahill K, Lindson‐Hawley N, Thomas KH, Fanshawe TR, Lancaster T. Nicotine receptor partial agonists for smoking cessation . Cochrane Database of Systematic Reviews 2016, Issue 5 . [DOI: 10.1002/14651858.CD006103.pub7] [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Centers for Disease Control and Prevention. Current cigarette smoking among adults—United States, 2005‐2015 . Morbidity and Mortality Weekly Report 2016; 65 ( 44 ):1205‐11. [ PubMed ] [ Google Scholar ]
- Centers for Disease Control and Prevention. Quitting smoking among adults—United States, 2000–2015 . Morbidity and Mortality Weekly Report 2017; 65 ( 52 ):1457‐64. [ PubMed ] [ Google Scholar ]
Chamberlain 2017
- Chamberlain C, O'Mara‐Eves A, Porter J, Coleman T, Perlen SM, Thomas J, et al. Psychosocial interventions for supporting women to stop smoking in pregnancy . Cochrane Database of Systematic Reviews 2017, Issue 2 . [DOI: 10.1002/14651858.CD001055.pub5] [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Cochrane Handbook
- Higgins JPT, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011 . Available from handbook.cochrane.org .
Coleman 2015
- Coleman T, Chamberlain C, Davey MA, Cooper SE, Leonardi‐Bee J. Pharmacological interventions for promoting smoking cessation during pregnancy . Cochrane Database of Systematic Reviews 2015, Issue 12 . [DOI: 10.1002/14651858.CD010078.pub2] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Greenland 1985
- Greenland S, Robins J. Estimation of a common effect parameter from sparse follow‐up data . Biometrics 1985; 41 ( 1 ):55‐68. [ PubMed ] [ Google Scholar ]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses . BMJ 2003; 327 ( 7414 ):557‐60. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Hughes 2014
- Hughes JR, Stead LF, Hartmann‐Boyce J, Cahill K, Lancaster T. Antidepressants for smoking cessation . Cochrane Database of Systematic Reviews 2014, Issue 1 . [DOI: 10.1002/14651858.CD000031.pub4] [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- International Council of Nurses. Tobacco use and health: ICN position . www.icn.ch/publications/position‐statements/ (accessed 24 July 2013).
Rigotti 2012
- Rigotti NA, Clair C, Munafò MR, Stead LF. Interventions for smoking cessation in hospitalised patients . Cochrane Database of Systematic Reviews 2012, Issue 5 . [DOI: 10.1002/14651858.CD001837.pub3] [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Stead LF, Perera R, Bullen C, Mant D, Hartmann‐Boyce J, Cahill K, et al. Nicotine replacement therapy for smoking cessation . Cochrane Database of Systematic Reviews 2012, Issue 11 . [DOI: 10.1002/14651858.CD000146.pub4] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Stead LF, Buitrago D, Preciado N, Sanchez G, Hartmann‐Boyce J, Lancaster T. Physician advice for smoking cessation . Cochrane Database of Systematic Reviews 2013, Issue 5 . [DOI: 10.1002/14651858.CD000165.pub4] [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Stewart 1993
- Stewart LA, Parmar MK. Meta‐analysis of the literature or of individual patient data: is there a difference? . Lancet 1993; 341 ( 8842 ):418‐22. [ PubMed ] [ Google Scholar ]
The Tobacco Atlas 2015
- Eriksen M, Mackay J, Schluger N, Gomeshtapeh FI, Drope J. The Tobacco Atlas . www.tobaccoatlas.org . 5th. Atlanta, GA: American Cancer Society; New York, NY: World Lung Foundation, 2015; Vol. (accessed 22 November 2017).
Youdan 2005
- Youdan B, Queally B. Nurses' role in promoting and supporting smoking cessation . Nursing Times 2005; 101 ( 10 ):26. [ PubMed ] [ Google Scholar ]
References to other published versions of this review
- Rice VH, Stead LF. Nursing interventions for smoking cessation . Cochrane Database of Systematic Reviews 1999, Issue 3 . [DOI: 10.1002/14651858.CD001188] [ CrossRef ] [ Google Scholar ]
- Rice VH. Nursing intervention and smoking cessation: a meta‐analysis . Heart and Lung 1999; 28 ( 6 ):438‐54. [ PubMed ] [ Google Scholar ]
- Rice VH, Stead LF. Nursing interventions for smoking cessation . Cochrane Database of Systematic Reviews 2001, Issue 3 . [DOI: 10.1002/14651858.CD001188] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rice VH, Stead LF. Nursing interventions for smoking cessation . Cochrane Database of Systematic Reviews 2004, Issue 1 . [DOI: 10.1002/14651858.CD001188.pub2] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rice VH, Stead L. Nursing intervention and smoking cessation: meta‐analysis update . Heart and Lung 2006; 25 ( 3 ):147‐63. [ PubMed ] [ Google Scholar ]
- Rice VH, Stead LF. Nursing interventions for smoking cessation . Cochrane Database of Systematic Reviews 2008, Issue 1 . [DOI: 10.1002/14651858.CD001188.pub3] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rice VH, Hartmann‐Boyce J, Stead LF. Nursing interventions for smoking cessation . Cochrane Database of Systematic Reviews 2013. [DOI: 10.1002/14651858.CD001188.pub4] [ PubMed ] [ CrossRef ] [ Google Scholar ]

IMAGES
VIDEO
COMMENTS
The proven 4 steps to quit naturally without willpower, anxiety, weight gain, side effects. Follow a step-by-step process that rewires your brain and removes your desire to smoke.
Tobacco smoking is the leading cause of cancer, preventable death, and disability. Smoking cessation can increase life expectancy by nearly a decade if achieved in the third or fourth decades of life. Various stop smoking interventions are available including pharmacotherapies, electronic cigarettes, behavioural support, and alternative therapies.
Smoking cessation reduces the development and progression of markers of subclinical atherosclerosis, with larger reductions shown in cases where the cessation period has been substantial. In patients with existing stroke, smoking cessation reduces risk of stroke morbidity and mortality. ... (Oklahoma Tobacco Research Center, 2017), there was ...
Research indicates a dose-response connection between greater exposure to emotionally compelling mass media campaigns depicting the health risks of smoking and higher quit rates and quit line calls . According to the SimSmoke model, large-scale mass media campaigns can lead to a 6% short-term and 10% long-term reduction in smoking prevalence ...
Smoking cessation can effectively reduce the risk of death, alleviate respiratory symptoms, and decrease the frequency of acute exacerbations in patients with chronic obstructive pulmonary disease (COPD). Effective smoking cessation strategies are crucial for the prevention and treatment of COPD. Currently, clinical interventions based on theoretical frameworks are being increasingly used to ...
Importance Tobacco use is the leading preventable cause of disease, disability, and death in the US. In 2014, it was estimated that 480 000 deaths annually are attributed to cigarette smoking, including second hand smoke exposure. Smoking during pregnancy can increase the risk of numerous adverse pregnancy outcomes (eg, miscarriage and congenital anomalies) and complications in the offspring ...
How a 5-Day Stay in the Tobacco-Free Environment of the Stoptober House Supports Individuals to Quit Smoking: A Mixed Methods Pilot Study, European Addiction Research, 30, 2, (103-113), (2024 ...
Former smokers showed lower hazard ratios (1.3 in both women and men). Short-term cessation for fewer than 3 years was associated with a lower excess risk of 95% in women and 90% in men younger than 40 years of age, with notable beneficial associations also in women and men 40 to 49 years of age (81% and 61%, respectively) and 50 to 59 years of ...
Smoking cessation was measured after at least six months, using the most rigorous definition available, on an intention-to-treat basis. We calculated risk ratios (RRs) and 95% confidence intervals (CIs) for smoking cessation for each study, where possible. ... inconsistency and imprecision. Future research should aim to match any additional ...
Accordingly, the aims of the present scoping review were: (a) to map the existing literature published since 1990 to identify and assess the factors that may impact cessation for health professionals who smoke; (b) to identify knowledge gaps; and (c) to include recommendations on how to move research on this distinct population forward.
Tobacco Addiction. This Journal feature begins with a case vignette highlighting a common clinical problem. Evidence supporting various strategies is then presented, followed by a review of formal ...
3 Feinstein Institute for Medical Research at Northwell Health, Manhasset, New York. 4 University of California, Los Angeles. ... The USPSTF concludes that the evidence on the use of e-cigarettes for tobacco smoking cessation in adults, including pregnant persons, is insufficient, and the balance of benefits and harms cannot be determined. ...
This 2021 US Preventive Services Task Force Recommendation Statement recommends that clinicians ask all adults about tobacco use, advise them to stop using tobacco, and provide behavioral interventions and pharmacotherapy for cessation (A recommendation) and concludes that evidence is insufficient to assess the benefits and harms of tobacco cessation pharmacotherapy in pregnant persons and e ...
Smoking tobacco is causally related to many phenotypes of CVDs, it is linked to early onset atherosclerosis that starts in adolescents and young adults, increases the risk of acute myocardial infarction (AMI), stroke, peripheral artery disease, aortic aneurysm and sudden death (4-6,12,13).As far as secondhand smoke is concerned, several components of passive smoking (e.g., carbonyls and ...
Smoking cessation is a cost effective and often overlooked prevention tool which improves both short- and long-term outcomes. There are both pharmacological and non-pharmacological strategies for smoking cessation that can be applied in clinical practice. Brief advice, specialized counseling including therapeutic education and behavioral ...
Understanding the factors that influence smoking cessation among young people is crucial for planning targeted cessation approaches. The objective of this review was to comprehensively summarize evidence for predictors of different smoking cessation related behaviors among young people from currently available systematic reviews. We searched six databases and reference lists of the included ...
Background Tobacco smoking is the leading cause of cancer, preventable death, and disability. Smoking cessation can increase life expectancy by nearly a decade if achieved in the third or fourth decades of life. Various stop smoking interventions are available including pharmacotherapies, electronic cigarettes, behavioural support, and alternative therapies. This protocol outlines an evidence ...
Figure Box 1. Tobacco-related health risks have been known since 1964; however, it remains the leading cause of preventable disease and death. Smoking rates have declined from 20.9% in 2004 to 16.8% in 2014, largely due to population-based interventions such as tobacco price increases and smoke-free laws. 1,2 But significant work is required to reach the Healthy People 2020 objective of 12%. 3 ...
The reduction in cigarette smoking is one of the most significant public health successes in modern US history. As noted in the landmark 50th anniversary report of the surgeon general, more than an estimated 8 million deaths were averted over the past half century through evidence-based tobacco control efforts, 1 and recent data show that cigarette smoking among US adults is now at an all-time ...
Smoking is a major public health concern and one of the leading causes of preventable death and disease worldwide [].Despite multiple tobacco-control efforts, smoking prevalence remains high in most Western countries, particularly among individuals in low socio-economic positions (SEP) [].In France, almost one adult in 4 (25.3%) smokes cigarettes daily, with a higher prevalence in people in ...
Daily smoking amount, duration of smoking, duration of cessation, and background of individuals may play a critical role in the impact of smoking cessation on endothelial function. The method used ...
Tobacco use, primarily cigarette smoking, is the leading cause of preventable disease and death in the United States. It is well established that smoking increases the risk of different forms of cancer, including lung, liver, and colorectal. Eighty-five percent of lung cancers occur in smokers. Also, smoking increases the risk of respiratory diseases (such as chronic obstructive pulmonary ...
Research in the general population suggests gradual smoking reduction is an inferior quit strategy than abrupt, assisted quitting. 16, 17 Plus, the health risks of persistent smoking after cancer diagnosis are high, and smoking reduction does not eliminate these dangers. While cancer patients' efforts to reduce smoking should be viewed ...
Background Supporting people to quit smoking is one of the most powerful interventions to improve health. The Emergency Department (ED) represents a potentially valuable opportunity to deliver a smoking cessation intervention if it is sufficiently resourced. The objective of this trial was to determine whether an opportunistic ED-based smoking cessation intervention can help people to quit ...
Nations worldwide are aiming to introduce some of the tightest restrictions ever on smoking and vaping, especially among young people. On 16 April, UK lawmakers backed one of the world's most ...
In this study, we aimed to identify the most effective smoking cessation methods used in quit based upon a review of the literature. Methods: We did a search of PubMed, limited to English publications from 2000 to 2012. Two trained reviewers independently assessed titles, abstracts and full texts of articles after a pilot inter-rater ...
Toll, who is currently serving as president of the Society for Research on Nicotine and Tobacco, wanted to expand the conversation that health care providers can have with patients about ways to stop smoking. There are seven FDA-approved smoking cessation aids, including medication and nicotine replacement options like the patch.
The study's senior author, Lurdes Queimado, M.D., Ph.D., said the findings underscore the importance of integrating tobacco cessation programs into treatment plans for cancer of the larynx, an ...
Background: Black adults who smoke and have HIV experience immense stressors (eg, racial discrimination and HIV stigma) that impede smoking cessation success and perpetuate smoking-related health disparities. These stressors also place Black adults who smoke and have HIV at an increased risk of elevated interoceptive stress (eg, anxiety and uncomfortable bodily sensations) and smoking to ...
Smoking cessation at longest follow‐up ‐ High intensity intervention Follow‐up: 6+ months: 141 per 1000 1: 182 per 1000 (171 to 195) ... See: Shiffman et al 'Recommendations for the assessment of tobacco craving and withdrawal in smoking cessation trials' Nicotine & Tobacco Research 2004: 6(4): 599‐614: Open in a separate window. Notes.