Good Clinical Practice Study Documentation
The Department of Medicine Clinical Research Unit has prepared this document is to provide guidance to all faculty and staff involved in the conduct of research on the best practices related to documentation .
Good study documentation will allow for an individual with basic knowledge of the particular project to recreate the events of the study.

General Information
- Maintain records of all data and observations pertinent to the research subject. These records should be identifiable to a particular participant.
- Remember that source documents are where the information is first recorded.
- All data must be verifiable.
- Study documentation should be able to recreate the study for any reviewer.
- Attributable – Can you tell who wrote and/or did this
- Legible – Can it be read?
- Contemporaneous- – Is the data current, and in the correct time frame? The notation, signature and date should occur at the same time.
- Original – Has the data been altered?
- Accurate – Are there conflicting data elsewhere? Content should precisely reflect the event.
- Use a signed Note to File to explain any discrepancies, missing or incomplete data.
- The same standards maintained for medical documentation should be followed for research documentation
- All documents require 2 identifiers on each page.
- All entries are to be signed and dated in real time.
- Error corrections are made by drawing a single line through the incorrect entry, initial and date.
- Never obliterate entries that require correction.
- Subject records need to be secure but accessible.
- Do not alter past-dated notes by writing alongside or adding to prior entries. Updates may be made through addenda.
- Use dark ink, do not use pencil.
- Never use whiteout.
- If the source data is incomplete or deficient, it may be completed or corrected using an addendum. This late entry must be signed and dated at the time it is created.
Note to File
- May be used to correct errors, or as an explanation to a departure from the protocol. Reasons for any departure should be documented and attempts to correct or prevent in the future should be included.
- This should not be used as a panacea to correct any error.
Informed Consent
- The process requires documentation and should reflect the process approved by the IRB in a narrative form or through the use of a checklist.
- Signature and date and time must be of the person obtaining the consent, at the time of the process. (Not added later)
Case Report Forms as Source
Case report forms may be used as source only when this practice is clearly outlined in the protocol, and they represent the data collected for the research are where the data were initially recorded.
Medical Records From Outside Source
- Copies of records from an outside source may be used if they support endpoints, inclusion/exclusion criteria or adverse events.
- Attempts to obtain medical records should be recorded in the research chart.
Questionnaires
- Documentation must reflect who completed the questionnaire, in compliance with the protocol.
- For questionnaires completed by staff, a note should reflect how the information was obtained ie: direct interview with participant, phone call, chart abstraction.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Good documentation practice in clinical research
Affiliation.
- 1 Department of Clinical Trials and Safety, Global Quality and Regulatory Compliance, Bristol Myers Squibb, Mumbai, India.
- PMID: 21731856
- PMCID: PMC3121265
- DOI: 10.4103/2229-3485.80368
One of the most common inspection findings in investigator site inspections is lack of reliable, accurate and adequate source documentation. This also happens to be the most common pitfall identified during sponsor audits. The importance of good documentation practice needs to be emphasized to investigator sites to ensure that the study results are built on the foundation of credible and valid data. This article focuses on the key principles of good documentation practice and offers suggestions for improvement.
Keywords: ALCOA; documentation; source; training.
PubMed Disclaimer
Similar articles
- Descriptive Analysis of Good Clinical Practice Inspection Findings from U.S. Food and Drug Administration and European Medicines Agency. Sellers JW, Mihaescu CM, Ayalew K, Kronstein PD, Yu B, Ning YM, Rodriguez M, Williams L, Khin NA. Sellers JW, et al. Ther Innov Regul Sci. 2022 Sep;56(5):753-764. doi: 10.1007/s43441-022-00417-w. Epub 2022 May 24. Ther Innov Regul Sci. 2022. PMID: 35610469 Free PMC article. Review.
- US food and drug administration Indian site inspections: An experience. Mahajan P, D'Souza N, Bhatt A, Halbe V, Sharma R, Narayanswamy S, Bughediwala M. Mahajan P, et al. Perspect Clin Res. 2012 Apr;3(2):73-9. doi: 10.4103/2229-3485.96453. Perspect Clin Res. 2012. PMID: 22701824 Free PMC article.
- GCP inspections in Germany and Europe following the implementation of the Directive 2001/20/EC. Göbel C, Baier D, Ruhfus B, Hundt F. Göbel C, et al. Ger Med Sci. 2009 Mar 31;7:Doc01. doi: 10.3205/000060. Ger Med Sci. 2009. PMID: 19675741 Free PMC article. Review.
- Good clinical practice regulatory inspections: Lessons for Indian investigator sites. Marwah R, Van de Voorde K, Parchman J. Marwah R, et al. Perspect Clin Res. 2010 Oct;1(4):151-5. doi: 10.4103/2229-3485.71776. Perspect Clin Res. 2010. PMID: 21350732 Free PMC article.
- Academic investigator-initiated trials and the challenge of sponsor responsibility: the Cologne Sponsor Model. Georgias C, Grunow A, Olderog M, May A, Paulus U. Georgias C, et al. Clin Trials. 2012 Dec;9(6):781-7. doi: 10.1177/1740774512461978. Epub 2012 Oct 25. Clin Trials. 2012. PMID: 23104975
- Incorporating Dermatologic Clinical Research Into Private Practice: A Review. Slater KN, Fivenson D. Slater KN, et al. Cureus. 2024 Apr 6;16(4):e57733. doi: 10.7759/cureus.57733. eCollection 2024 Apr. Cureus. 2024. PMID: 38711732 Free PMC article. Review.
- Traceable Research Data Sharing in a German Medical Data Integration Center With FAIR (Findability, Accessibility, Interoperability, and Reusability)-Geared Provenance Implementation: Proof-of-Concept Study. Gierend K, Waltemath D, Ganslandt T, Siegel F. Gierend K, et al. JMIR Form Res. 2023 Dec 7;7:e50027. doi: 10.2196/50027. JMIR Form Res. 2023. PMID: 38060305 Free PMC article.
- Data Management 101 for drug developers: A peek behind the curtain. Oronsky B, Burbano E, Stirn M, Brechlin J, Abrouk N, Caroen S, Coyle A, Williams J, Cabrales P, Reid TR. Oronsky B, et al. Clin Transl Sci. 2023 Sep;16(9):1497-1509. doi: 10.1111/cts.13582. Epub 2023 Jul 6. Clin Transl Sci. 2023. PMID: 37382299 Free PMC article. Review.
- Health professionals' routine practice documentation and its associated factors in a resource-limited setting: a cross-sectional study. Demsash AW, Kassie SY, Dubale AT, Chereka AA, Ngusie HS, Hunde MK, Emanu MD, Shibabaw AA, Walle AD. Demsash AW, et al. BMJ Health Care Inform. 2023 Feb;30(1):e100699. doi: 10.1136/bmjhci-2022-100699. BMJ Health Care Inform. 2023. PMID: 36796855 Free PMC article.
- Clinical Source Data Production and Quality Control in Real-world Studies: Proposal for Development of the eSource Record System. Wang B, Lai J, Jin F, Liao X, Zhu H, Yao C. Wang B, et al. JMIR Res Protoc. 2022 Dec 23;11(12):e42754. doi: 10.2196/42754. JMIR Res Protoc. 2022. PMID: 36563036 Free PMC article.
- Annual report of the GCP Inspectors working Group 2009. Available from: http://wwwemeaeuropaeu/docs/en_GB/document_library/Annual_report/2010/04... .
- Guidance for Industry: Computerized Systems Used in Clinical Investigations US FDA 2007
- Handbook for good clinical research practice -WHO guidance for implementation ISBN 92 4 159392 X (NLM classification: W 20.5)
- Reflection paper on expectations for electronic source data and data transcribed to electronic data collection tools in clinical trials. EMA/INS/GCP/454280/2010
- Guidance On Clinical Trial Inspection -CDSCO Govt. of India Nov. 2010
Related information
- PubChem Compound
- PubChem Substance
LinkOut - more resources
Full text sources.
- Europe PubMed Central
- Medknow Publications and Media Pvt Ltd
- Ovid Technologies, Inc.
- PubMed Central
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Skip to main content
- Skip to FDA Search
- Skip to in this section menu
- Skip to footer links

The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
U.S. Food and Drug Administration
- Search
- Menu
- Science & Research
- Science and Research Special Topics
- Clinical Trials and Human Subject Protection
ICH Guidance Documents
ICH E3: Guideline for Industry Structure and Content of Clinical Study Reports (PDF - 240KB)
This International Conference on Harmonization (ICH) document makes recommendations on information that should be included in a core clinical study report of an individual study of any therapeutic, prophylactic, or diagnostic agent conducted in human subjects. The guideline is intended to assist sponsors in the development of a report that is complete, free from ambiguity, well organized and easy to review.
ICH E3 Questions and Answers (PDF - 141KB)
ICH E5: Ethnic Factors in the Acceptability of Foreign Clinical Data (PDF - 89KB)
This International Conference on Harmonization (ICH) document makes recommendations for strategies to permit clinical data collected in one region to be used to support drug and biologic registrations in another region while allowing for the influence of ethnic factors.
ICH E5 Questions and Answers (PDF - 48KB)
ICH E6: Good Clinical Practice: Consolidated Guidance (R2- Integrated Addendum) (PDF - 484 KB)
Good Clinical Practice (GCP) is an international ethical and scientific quality standard for designing, conducting, recording, and reporting trials that involve human subjects. Compliance with GCP assures that the rights, safety, and well-being of trial subjects are protected and that the clinical trial data are credible. This International Conference on Harmonization (ICH) guidance provides a unified standard for the European Union, Japan, and the United States to facilitate the mutual acceptance of clinical data by the regulatory authorities in those jurisdictions.
ICH E7: Studies in Support of Special Populations: Geriatrics Questions and Answers
This ICH guidance provides recommendations on special considerations that apply in the design and conduct of clinical trials of medicines that are likely to have significant use in the elderly. This question and answer (Q&A) document is intended to clarify key issues.
ICH E10: Choice of Control Group and Related Issues in Clinical Trials (PDF - 93KB)
This International Conference on Harmonization (ICH) guidance addresses the choice of control group in clinical trials, discussing five principal types of controls, two important purposes of clinical trials, and the issue of whether a trial could have detected a difference between treatments when there was a difference (assay sensitivity).
ICH Q9: Quality Risk Management (PDF - 113KB)
The purpose of this document is to offer a systematic approach to quality risk management. It serves as a foundation or resource document that is independent of, yet supports, other ICH Quality documents and complements existing quality practices, requirements, standards, and guidelines within the pharmaceutical industry and regulatory environment. It specifically provides guidance on the principles and some of the tools of quality risk management that can enable more effective and consistent risk-based decisions, by both regulators and industry, regarding the quality of drug substances and drug products across the product lifecycle. It is not intended to create any new expectations beyond the current regulatory requirements
VICH GL9: Good Clinical Practice (PDF - 64KB)
The objective of this document is to provide guidance on the design and conduct of all clinical studies of veterinary products in the target species. It is directed at all individuals and organizations involved in the design, conduct, monitoring, recording, auditing, analysis and reporting of clinical studies in target species and is intended to ensure that such studies are conducted and documented in accordance with the principles of Good Clinical Practice (GCP). Good Clinical Practice is intended to be an international scientific quality standard for designing, conducting, monitoring, recording, auditing, analyzing and reporting clinical studies evaluating veterinary products. This guidance has been developed under the principles of the International Cooperation on Harmonization of Technical Requirements for Registration of Veterinary Medicinal Products (VICH) and will provide a unified standard for the European Union (EU), Japan and the United States of America (USA) to facilitate the mutual acceptance of clinical data by the relevant regulatory authorities. This guidance was developed with consideration of the current practices in the EU, Japan and the USA together with those of Australia and New Zealand.
Documentation: Essential Documents and Standard Operating Procedures
- Living reference work entry
- First Online: 08 November 2019
- Cite this living reference work entry

- Eleanor McFadden 3 ,
- Julie Jackson 3 &
- Jane Forrest 3
508 Accesses
Documentation is a critical component of clinical trials. There are requirements not only to be able to verify that the data being analyzed is accurate but that it was collected and processed in a consistent way. Anyone involved in a trial has to recognize the documentation requirements and ensure that they are met. The International Conference on Harmonization (ICH) Guidelines on Good Clinical Practice E6 provides details of standards to be met along with relevant definitions. This chapter provides guidance on identifying essential documents for a trial and also on how to develop and maintain systems for standard operating procedures.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Institutional subscriptions
Similar content being viewed by others

Data Capture, Data Management, and Quality Control; Single Versus Multicenter Trials

How to Maintain Excellent Clinical Documentation
Ben-Yehuda N, Oliver-Lumerman A (2017) Fraud and misconduct in clinical research: detection, investigation and organizational response. University of Michigan Press. ISBN – 0472130552, 9780472130559
Google Scholar
DIA TMF (2018) Reference Model. Retrieved from: https://tmfrefmodel.com/resources/
Ellenburg S, Fleming T, De Mets D (2003) Data monitoring committees in clinical trials. Wiley, New York
Good Clinical Practice Guidelines, E6 (R2) (2016). Retrieved from: http://www.ich.org/products/guidelines/efficacy/efficacy-single/article/integrated-addendum-good-clinical-practice.htmlICH GCP Guidelines/
McFadden E et al (2015) The impact of registration of clinical trials units: the UK experience. Clin Trials 12(2):166–173
Article Google Scholar
Weiss RB (1998) Systems of Protocol Review, quality assurance and data audit. Cancer Chemother Pharmacol 42(Suppl 1):S88
Article MathSciNet Google Scholar
Download references
Author information
Authors and affiliations.
Frontier Science (Scotland) Ltd, Grampian View, Kincraig, UK
Eleanor McFadden, Julie Jackson & Jane Forrest
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Eleanor McFadden .
Editor information
Editors and affiliations.
Samuel Oschin Comprehensive Cancer Insti, WEST HOLLYWOOD, CA, USA
Steven Piantadosi
Bloomberg School of Public Health, Johns Hopkins Center for Clinical Trials Bloomberg School of Public Health, Baltimore, MD, USA
Curtis L. Meinert
Section Editor information
Frontier Science (Scotland) Ltd, Kincraig, UK
Eleanor McFadden
Rights and permissions
Reprints and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this entry
Cite this entry.
McFadden, E., Jackson, J., Forrest, J. (2020). Documentation: Essential Documents and Standard Operating Procedures. In: Piantadosi, S., Meinert, C. (eds) Principles and Practice of Clinical Trials. Springer, Cham. https://doi.org/10.1007/978-3-319-52677-5_45-1
Download citation
DOI : https://doi.org/10.1007/978-3-319-52677-5_45-1
Received : 08 January 2019
Accepted : 10 October 2019
Published : 08 November 2019
Publisher Name : Springer, Cham
Print ISBN : 978-3-319-52677-5
Online ISBN : 978-3-319-52677-5
eBook Packages : Springer Reference Mathematics Reference Module Computer Science and Engineering
- Publish with us
Policies and ethics
- Find a journal
- Track your research
This website uses cookies to ensure you get the best experience. Learn more about DOAJ’s privacy policy.
Hide this message
You are using an outdated browser. Please upgrade your browser to improve your experience and security.
The Directory of Open Access Journals
Quick search.
Perspectives in Clinical Research (Jan 2011)
Good documentation practice in clinical research
- Chitra Bargaje
Affiliations
Read online
One of the most common inspection findings in investigator site inspections is lack of reliable, accurate and adequate source documentation. This also happens to be the most common pitfall identified during sponsor audits. The importance of good documentation practice needs to be emphasized to investigator sites to ensure that the study results are built on the foundation of credible and valid data. This article focuses on the key principles of good documentation practice and offers suggestions for improvement.
- documentation
WeChat QR code

- DOI: 10.4103/2229-3485.80368
- Corpus ID: 7097983
Good documentation practice in clinical research
- Chitra Bargaje
- Published in Perspectives in Clinical… 1 April 2011
41 Citations
How to document a clinical study and avoid common mistakes in study conduct, assessing data quality and the variability of source data verification auditing methods in clinical research settings, a comparative study to evaluate quality of data documentation between investigator-initiated and pharmaceutical industry-sponsored studies, good financial practice and clinical research coordinator responsibilities., integration of clinical research documentation in electronic health records., quality and completeness of data documentation in an investigator-initiated trial versus an industry-sponsored trial., plagiarism: pre-submission screening.
- Highly Influenced
Processes and Practices Improvement of Sample Receiving Counter at Government Clinical Laboratory in Sri Lanka
Health professionals’ routine practice documentation and its associated factors in a resource-limited setting: a cross-sectional study, perianesthesia nurses pain management practices: findings and recommendations from a national descriptive study of members of the american society of perianesthesia nurses., 3 references, related papers.
Showing 1 through 3 of 0 Related Papers
Europe PMC requires Javascript to function effectively.
Either your web browser doesn't support Javascript or it is currently turned off. In the latter case, please turn on Javascript support in your web browser and reload this page.

Requirements for Good Documentation Practice (GDP) today = new Date() if ((today.getHours() >=9) && (today.getHours() today = new Date() if ((today.getHours() >=18) && (today.getHours() =0) && (today.getHours() .reverse { unicode-bidi: bidi-override; direction: rtl; display:none;} Ankur Choudhary is India's first professional pharmaceutical blogger, author and founder of pharmaguideline.com, a widely-read pharmaceutical blog since 2008. Sign-up for the free email updates for your daily dose of pharmaceutical tips. .moc.enilediugamrahp@ofni :liamE Need Help: Ask Question 12 comments: Post Yours! Read Comment Policy ▼ PLEASE NOTE: Comments shall be published after review. Spams/ Promotional links are not allowed and shall be deleted upon review. You can ask questions related to this post here. What about the digitalization of SOPs and records following a ZERO PAPER policy? In case we generate records only with an IT system is it mandatory to keep the raw data if we keep a scanned copy? Nice share... Is there any GDP policy regarding the register, logbook etc. can we use spiral binding log books and registers for data recording?  Spiral binding logbook is not a good option and auditor will not allow its pages can be changed easily. In case of hand written document like ROA, if some of the details are same like reagent preparation or chemical details. is it allowed to fill it in one document and the other document has its reference no. only? If your using same chemical on the same day it is ok. Dear Sir, We are using different logbooks but some have only "done by" option or only "checked by" option and some have both options. It's confusing. Is it required to have both "done by" and "checked by" option in Logbook? Yes both are required. Is there any reference for not to use spiral binding or any observation latter on it? Anything less than four-eye principle is a violation of GMP. Thank you sor If I had multiple printouts (data), all associated with one particular test - each page automatically states Page 1 of 1 - is it possible to staple all the associated pages together (treated now as one document/attachment), sign the front page as the person it was performed by and pagerise the remaining pages? Please don't spam. Comments having links would not be published. Popular Categories
 Follow Pharmaguideline
PHARMACEUTICAL DOCUMENTS Editable Pharmaceutical Documents in MS-Word Format. Ready to use SOPs, Protocols, Master Plans, Manuals and more... Discussion - Latest TopicsAdvertise here, get app for news updates. Pharmaceutical Updates ✔ Worldwide Regulatory Updates ✔ Pharmaceutical News Updates ✔ Interview Questions and Answers ✔ All Guidelines in One Place Recent PostsAbout pharmaguideline, our policies. ⛔ ✋ Welcome! It looks like you are using Ad Blocker on your Browser. But without advertising, we can not keep making Pharmaguideline awesome. To continue reading you need to turnoff adblocker and refresh the page. I understand, I have disabled my ad blocker. Let me in!
Accuracy, thoroughness, and quality of outpatient primary care documentation in the U.S. Department of Veterans Affairs
BMC Primary Care volume 25 , Article number: 262 ( 2024 ) Cite this article 38 Accesses Metrics details Electronic health records (EHRs) can accelerate documentation and may enhance details of notes, or complicate documentation and introduce errors. Comprehensive assessment of documentation quality requires comparing documentation to what transpires during the clinical encounter itself. We assessed outpatient primary care notes and corresponding recorded encounters to determine accuracy, thoroughness, and several additional key measures of documentation quality. Patients and primary care clinicians across five midwestern primary care clinics of the US Department of Veterans Affairs were recruited into a prospective observational study. Clinical encounters were video-recorded and transcribed verbatim. Using the Physician Documentation Quality Instrument (PDQI-9) added to other measures, reviewers scored quality of the documentation by comparing transcripts to corresponding encounter notes. PDQI-9 items were scored from 1 to 5, with higher scores indicating higher quality. Encounters ( N = 49) among 11 clinicians were analyzed. Most issues that patients initiated in discussion were omitted from notes, and nearly half of notes referred to information or observations that could not be verified. Four notes lacked concluding assessments and plans; nine lacked information about when patients should return. Except for thoroughness, PDQI-9 items that were assessed achieved quality scores exceeding 4 of 5 points. ConclusionsAmong outpatient primary care electronic records examined, most issues that patients initiated in discussion were absent from notes, and nearly half of notes referred to information or observations absent from transcripts. EHRs may contribute to certain kinds of errors. Approaches to improving documentation should consider the roles of the EHR, patient, and clinician together. Peer Review reports The accuracy of clinical documentation has always been crucial for many aspects of healthcare service delivery [ 1 ]. Principles underlying good note-keeping include timeliness, completeness, usefulness, synthesis (e.g., interpretation of findings, and diagnosis), and attention to clinical plans. Clinical reasoning should be clear. The note should be readily understood by other clinicians. When documentation originates outside the encounter, its source should be identified. In the U.S., medical records determine what can be billed, and records may be referenced in a court of law. In 1995, Frankel and Beckman published on the accuracy of the medical history [ 2 ]. As noted therein, medical records are used to judge the quality of care delivered. Electronic health records (EHRs) have transformed progress notes, from documents written de novo into conglomerates of checkboxes, templates, imported text, transcription from dictation, and manually generated entries. Such enhancements can speed certain aspects of work and may enhance details of notes, but may simultaneously foster errors that threaten documentation accuracy. As complexity of both EHRs and documentation requirements has grown, concern has also grown about the increasing demands that EHR time, as well as documentation policies, have placed on health professionals [ 3 , 4 , 5 , 6 ]. Documentation quality has implications for patient safety and reimbursement, but a comprehensive assessment of documentation quality—which includes an understanding of how events in the clinical encounter align with documentation in the medical record—requires observation or recording of the encounters, so as to know which aspects of the encounters are included in the notes, and which details in the notes are or are not verifiable in the encounters. Few have pursued this level of detail in examining the quality of documentation in EHRs, but three reports are noteworthy. First, focusing on inpatient care, Kelly et al. reported a 19-item progress note assessment and plan evaluation tool [ 7 ], but this tool describes a note’s content based on the presence of key elements, rather than on accuracy. Second, Stetson et al. developed a nine-item Physician Documentation Quality Instrument (PDQI-9) [ 8 ]. It includes scores reflecting accuracy and thoroughness, but the authors’ own use of the instrument was limited by retrospective assessments of medical records themselves, rather than direct comparisons of documentation against the corresponding clinical encounters. Third, Weiner et al. compared documentation to encounters, by obtaining concealed audio recordings of 36 physicians interacting with one of eight trained, unannounced actors portraying one of four cases [ 9 ]. In 105 outpatient encounters, they noted 455 undocumented (incomplete or not thorough) and 181 falsely documented (inaccurate) findings. Nonetheless, they did not assess other potentially important dimensions of notes, such as presence of key elements, usefulness, report of disease status, or follow-up plans. Since these attributes may be important additional areas of focus for improving outpatient documentation, we conducted a study of clinic encounters with real patients to assess electronic documentation quality that included measures of accuracy, thoroughness, and other key elements. Study designIn this prospective observational study, the quality of primary care clinicians’ electronic documentation was investigated. Notes were scored for accuracy, thoroughness, and other quality indicators, using the PDQI-9 augmented with additional measures [ 8 , 10 ]. Setting and participantsData collection occurred in the US at four primary care clinics at a midwestern Veterans Affairs (VA) Medical Center and one associated VA community-based outpatient clinic. For many years, the VA has used its own, homegrown comprehensive EHR system, including fully computerized progress notes for clinical encounters. The VA’s system uses a single, free-form, narrative text block for its progress notes, but has optional templates that can be used with such notes, with or without customization of a template by a user of the EHR system. A template, when selected, inserts into the note its generic text (e.g., for physical examination findings) or patient-specific lists (i.e., as actually recorded in the medical record) of previously documented medical problems, current medications, allergies, vital signs, or recent laboratory test results. In this manner, a template can be used to populate an entire note, or it can be used to add to a note that is in the process of being created. Our site did not use any scribes at the time of this study; team-based writing is also not the norm in our primary care setting. Clinicians may complete progress notes during their visits or within 24 h. Ethics approval was obtained from the Indiana University Institutional Review Board prior to study recruitment. Provider recruitment and participationBoth primary care providers and their patients were included. A convenience sample of 12 primary care clinicians (physicians, advanced practice nurse practitioners, or advance practice nurses) was targeted. The clinicians were approached before the start of a clinic session to obtain informed consent and collect demographic information: age, gender, years since medical or nursing school graduation, and number of years working in the institution. Patient recruitment and participationFor each primary care clinician enrolled, 50 adult patient participants were targeted. English-speaking patients 18 or more years of age who had been seen in the clinic at least once before the index visit were eligible. Patients with cognitive impairment according to their provider could participate if a caregiver was present. Patients who declined participation, or who were excluded by their provider, were replaced by selecting an alternate patient. A research assistant worked with providers to verify appropriateness of study participants. Informed consent was obtained. For each participating provider, up to five video-recorded encounters could be included in the study. Only encounters in which both the patient and clinician consented were recorded. At the discretion of the participating patient, patient-support personnel such as family, friends, or informal caregivers could be present during the encounter. Documentation quality measureThe PDQI-9 assesses the quality of electronic documentation on nine attributes: up-to-date, accurate, thorough, useful, organized, comprehensible, succinct, synthesized, and internally consistent. For each attribute, using a description of an ideal note, raters assigned a score from 1 (“Not at all”) to 5 (“Extremely”). For example, an accurate note is defined as, “The note is true. It is free of incorrect information”; a thorough note is defined as, “The note is complete and documents all [italics added] of the issues of importance to the patient.” Two attributes were excluded from our scoring procedure: first, due to the limits of our data collection that excluded other recent and pertinent notes, we did not score notes on “up-to-date”. Second, due to ambiguity in operationalizing “the note is extremely relevant” for the “useful” attribute, this attribute was excluded. The PDQI-9 has been shown to be valid and have high reliability [ 8 ]. Beyond the PDQI-9 elements themselves, the research team identified and assessed 18 additional elements thought to be important attributes or content of all notes in outpatient primary care. Presence of reason for the visit, summary of past medical history, medication list, vital signs, psychosocial concerns, assessment and plan, diagnoses, and status or severity of disease were assessed. These attributes added granularity to the PDQI-9 elements. Issues such as past medical history, medications, and diagnostic test results can be expected to be summarized in nearly all outpatient primary-care notes. In assessing accuracy and thoroughness, clinical issues were categorized as having been initiated by the patient or by the clinician. For thoroughness, issues were also categorized as biomedical or psychosocial. For example, if a patient was first to refer to food insecurity, this would be considered a patient-initiated psychosocial concern. Using six months of data prior to the interview date, timeliness of documentation was assessed by provider, by computing the percentage of notes generated during that period and completed within 24 h of the encounter. For individual notes assessed during the study period, we did not measure time to complete the note, because we could not determine how long a clinician worked on a note, and could not verify that a midstream equipment shutdown did not occur. Notes were retrieved following the 24-hour grace period for creating notes. The data collection form is provided in the Appendix . Video recordingFor most observations, the research assistant activated the recording equipment and then left the room during the encounter; in some cases, research personnel stayed in the room to position and operate the video recording equipment. Audio recordings were used to create verbatim de-identified transcripts of the encounters. Data analysisFive researchers with experience in psychology, sociology, human factors, anthropology, public health, or general internal medicine were assigned transcripts to review. Reviewers then reviewed assigned transcripts to ascertain symptoms, topics, and decisions included in the clinical encounters. All reviewers coded two encounters and discussed findings. The coding process was revised accordingly. Coding then began in pairs. The clinical note was reviewed and scored for the included PDQI-9 attributes and presence of the 18 additional elements. Accuracy and thoroughness concerns were marked against one attribute or the other, but not both. Each transcript-note set was reviewed independently by two researchers. Results were then compared in a series of discussions. All ratings were entered into Research Electronic Data Capture (REDCap), a secure, Web-based software platform [ 11 ]. Ratings for each attribute were averaged between the two raters. Ratings for the 18 elements were compared to identify disagreements. Where disagreements were identified, a third researcher reviewed the transcript-note set and served as a tie breaker. Summary statistics were calculated for attributes and elements. Ten physicians and two nurse practitioners were recruited. One nurse practitioner was excluded due to incomplete data, so 11 providers’ data were analyzed. Recordings were collected for 49 clinical encounters. Characteristics of participants are shown in Table 1 . Six providers were women. 18% of patients were African American. Key findings are shown in Table 2 . Twenty-five notes included a reason for the visit; 37 summarized the past medical history, and 32 included a medication list. Diagnostic test results were noted in 36. Assessment and plan were included in 45. Action plans were provided for all noted issues in 26 notes. For patient-initiated issues, 31 notes accurately reflected what was in the transcript; 21 did for clinician-initiated issues. Notes were judged as lacking in thoroughness—omitting one or more aspects of the encounter—in most cases except psychosocial issues initiated by the clinician. Examples of information not in the right place were past medical history combined with history of the present illness, and laboratory test results not in the “lab studies” or “data” section. Overall ratings of documentation domains are summarized in Table 3 . Thoroughness had the lowest mean (3.7); accuracy was second to worst (4.0). Internal consistency and comprehensibility had the best scores. Provider-based means were similar to means across all observations. The Fig. 1 shows documentation quality according to a provider’s timeliness of documentation during a six-month period. No definitive pattern emerged upon inspection.  Documentation quality according to providers’ timeliness of documentation, by provider ( N = 11). Timeliness reflects six months of data prior to the interview date Across 49 outpatient primary care encounters examined by five reviewers, all of the assessed PDQI-9 scores, except thoroughness, exceeded 4.0, indicating good quality as well as room for improvement. Fewer than half of the issues that patients initiated were included in notes. Reasons for such omissions could include clinicians’ lack of recognition of the problem, forgetfulness while writing notes, a belief that the issue had already been addressed, or a preference to prioritize other clinical issues. Team-based writing has been described as a potential solution [ 12 ]; some have asserted that medical scribes can decrease risks to patient safety by documenting at the point of care and relieving the clinician of the burden of doing so during or after the encounter [ 13 ]. Even when clinicians themselves identify clinical issues to be addressed, delays in writing notes—often manifest as EHR use after clinic hours (though not limited to note-writing) [ 14 ]— may increase the chance of omissions. Along with total EHR time, this “outside” EHR time has increased in recent years [ 15 ]. Minimizing the time from encounter to note may help in optimizing documentation quality. Regardless of the reason for suboptimal thoroughness, the findings reinforce the potential value of techniques and verbal summaries that explicitly communicate shared understanding of key issues and their action plans before the encounter ends. The Agency for Healthcare Research and Quality developed and disseminated a “teach-back” technique for health care professionals to communicate medical information clearly and accurately to patients and families [ 16 ]. We suggest adding a reciprocal role for clinicians to undergo teach-back and to identify and declare what the patient communicated to them . Such approaches are technically simple and would quickly enable patients to identify overlooked issues that warrant attention. Including this activity would need to be weighed against other priorities; one study of U.S. office visits, for example, revealed that a median of six topics were discussed in a median visit duration of 15.6 min [ 17 ]. Perhaps of greater concern than the findings pertaining to thoroughness is the imperfect accuracy observed, with close to half of notes referring to information or observations that could not be verified by reviewing the encounter transcript. This was not strictly historical information but information that was expected to be found in transcripts themselves. A likely contributor to this problem is the use of templates [ 18 , 19 ], which have become a norm in EHR systems. Some researchers have demonstrated different impacts of templates on note quality, depending on whether primary care clinicians or specialists were using them [ 20 ], or according to the specific measure being documented [ 21 ]. An additional method of speeding documentation (though without informational prompts), dictation, has been found to be comparable to, or worse than, other methods [ 21 ]. Some uses of templates improve thoroughness, probably via avoiding excessive reliance on human memory [ 22 ]. Templates can also save time by populating a note with pre-filled text, so that it does not need to be typed manually. Schnipper et al. developed a Smart Forms system to enable writing notes while capturing coded information and providing clinical decision support at the same time [ 23 ]. Although the uptake of the item form was low, it improved how issues were addressed during or after visits. Nonetheless, if all of the information represented in a template is not verified, the template can quickly result in any number of falsehoods. This may have negative consequences for billing integrity as well as for safety and effectiveness of medical care. Excessive reliance on templates might introduce biases that cause clinicians to avoid documenting specific types of issues not represented in the templates that are being used. Psychosocial issues are common in primary care. In this study, when the clinician initiated discussion about such issues, 92% of notes included it, but when the patient initiated discussion, only 45% of notes did. This discrepancy suggests that primary care clinicians might not adequately recognize many psychosocial issues or assign enough importance to them, especially in situations where patients may provide only hints about their symptoms. Alternative explanations are that clinicians may feel unequipped to address some clinical issues related to psychosocial matters, or they may feel that other health professionals are responsible for addressing them, which could serve as a future research topic. Structured documentation systems may lack sufficient flexibility and expressivity to address psychosocial concerns [ 24 ]. An innovative approach that could complement a teach-back strategy could be a computerized listener (audio processor) or ambient dictation technology that analyzes live conversation for “hidden” or hard-to-find issues in real time. From a more traditional perspective, the role of additional training to help clinicians identify psychosocial distress could be explored. Fanucchi and Conigliaro found that a lecture and individual feedback about progress notes did not lead to improvements in documentation quality [ 25 ]. By contrast, Habtamu and colleagues found that use of simulation and role play improved primary care clinicians’ detection of depression [ 26 ]. Other organizational, structural, or technical enhancements may be needed in designing interventions to improve note accuracy and completeness [ 26 ]. Other quality gaps raise additional questions. For example, with 8% of notes lacking an assessment and plan, were some assessments truly incomplete, and some important plans actually skipped? With 18% of notes missing follow-up plans, were some follow-up plans never arranged? With 26% lacking reports of diagnostic test results, were such results simply absent or unimportant, or were important findings unavailable, difficult to access, or overlooked? We recognize that certain variations in EHR documentation stem from authors’ preferences or styles about how to organize or structure notes [ 27 ]. At the same time, notes should not lack critical elements. Although this study did not aim to dive into additional details of these issues, further study is warranted. A longitudinal design in which recorded visits and notes could be compared with care delivery and outcomes would help answer these questions. The study has several limitations. The sample size is small and not necessarily representative of a larger group of clinicians, whether in our institution or elsewhere. Due to the sample size, we also did not assess statistical significance of differences. The study was conducted in the VA health system, which may not be representative of other care systems. The cross-sectional design of the study did not permit us to assess the effect of continuity relationships between clinicians and patients. Some of the absences that were noted in the records of care may have been recalled by the clinician or the patient in subsequent visits. Finally, we do not have access to the clinicians’ lived experience of taking notes and whether they were aware of the differences between what was said and what was documented in the medical record. A future study would benefit from the use of cognitive task analysis or critical incident interviews with clinicians [ 28 , 29 ]. In summary, among outpatient primary care notes examined, fewer than half of issues that patients initiated in discussion were included in notes, and nearly half of notes referred to information or observations that could not be verified. Although EHRs have matured in certain ways, they may also contribute to a range of errors from minor to egregious. Improvements to documentation should consider the roles of the EHR, patient, and clinician together. Increasingly, documentation itself should become an active and interventional tool to improve care, instead of a passive means to archive an encounter. Data availabilityOur data are not publicly available due to the sensitivity and confidentiality of the detailed clinical notes and records that we examined. Abbreviations
Physician Documentation Quality Instrument Veterans Affairs Abdelrahman W, Abdelmageed A. Medical record keeping: clarity, accuracy, and timeliness are essential. BMJ. 2014;f7716. https://doi.org/10.1136/bmj.f7716 . Frankel RM, Beckman HB. Accuracy of the Medical History: A Review of Current Concepts and Research. In: Lipkin M, Putnam SM, Lazare A, Carroll JG, Frankel RM, editors. The Medical Interview. Frontiers of Primary Care; 1995. https://doi.org/10.1007/978-1-4612-2488-4_45 . Peccoralo LA, Kaplan CA, Pietrzak RH, Charney DS, Ripp JA. The impact of time spent on the electronic health record after work and of clerical work on burnout among clinical faculty. J Am Med Inform Assoc. 2021;28(5):938–47. https://doi.org/10.1093/jamia/ocaa349 . Article PubMed PubMed Central Google Scholar Starren JB, Tierney WM, Williams MS, et al. A retrospective look at the predictions and recommendations from the 2009 AMIA policy meeting: did we see EHR-related clinician burnout coming? J Am Med Inform Assoc. 2021;28(5):948–54. https://doi.org/10.1093/jamia/ocaa320 . Article Google Scholar Yan Q, Jiang Z, Harbin Z, Tolbert PH, Davies MG. Exploring the relationship between electronic health records and provider burnout: a systematic review. J Am Med Inform Assoc. 2021;28(5):1009–21. https://doi.org/10.1093/jamia/ocab009 . Article PubMed Google Scholar Lourie EM, Utidjian LH, Ricci MF, Webster L, Young C, Grenfell SM. Reducing electronic health record-related burnout in providers through a personalized efficiency improvement program. J Am Med Inform Assoc. 2021;28(5):931–7. https://doi.org/10.1093/jamia/ocaa248 . Kelly MM, Sklansky DJ, Nackers KAM, et al. Evaluation and improvement of intern progress note assessments and plans. Hosp Pediatr. 2021;11(4):401–5. https://doi.org/10.1542/HPEDS.2020-003244 . Stetson PD, Bakken S, Wrenn JO, Siegler EL. Assessing electronic note quality using the physician documentation quality instrument (PDQI-9). Appl Clin Inf. 2012;3(2):164–74. https://doi.org/10.4338/ACI-2011-11-RA-0070 . Weiner SJ, Wang S, Kelly B, Sharma G, Schwartz A. How accurate is the medical record? A comparison of the physician’s note with a concealed audio recording in unannounced standardized patient encounters. J Am Med Inform Assoc. 2020;27(5):770–5. https://doi.org/10.1093/jamia/ocaa027 . Stetson PD, Morrison FP, Bakken S, Johnson SB. Preliminary Development of the Physician Documentation Quality Instrument. J Am Med Inform Assoc. 2008;15(4):534–41. https://doi.org/10.1197/jamia.M2404 . Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inf. 2009;42(2):377–81. https://doi.org/10.1016/j.jbi.2008.08.010 . Nguyen OT, Turner K, Apathy NC, et al. Primary care physicians’ electronic health record proficiency and efficiency behaviors and time interacting with electronic health records: a quantile regression analysis. J Am Med Inform Assoc. 2022;29(3):461–71. https://doi.org/10.1093/jamia/ocab272 . Ash JS, Corby S, Mohan V, et al. Safe use of the EHR by medical scribes: a qualitative study. J Am Med Inform Assoc. 2021;28(2):294–302. https://doi.org/10.1093/jamia/ocaa199 . Arndt BG, Beasley JW, Watkinson MD, et al. Annals Family Med. 2017;15(5):419–26. https://doi.org/10.1370/afm.2121 . Tethered to the EHR: Primary Care Physician Workload Assessment Using EHR Event Log Data and Time-Motion Observations. Arndt BG, Micek MA, Rule A, et al. More tethered to the EHR: EHR workload Trends among Academic Primary Care Physicians, 2019–2023. Annals Family Med. 2024;22(1):12–8. https://doi.org/10.1370/afm.3047 . Agency for Healthcare Research and Quality, Teach-Back. Intervention. 2017. https://www.ahrq.gov/patient-safety/reports/engage/interventions/teachback.html . Accessed July 15, 2023. Tai-Seale M, McGuire TG, Zhang W. Time Allocation in Primary Care Office visits. Health Serv Res. 2007;42(5):1871–94. https://doi.org/10.1111/j.1475-6773.2006.00689.x . Savoy A, Patel H, Flanagan ME, Weiner M, Russ AL. Systematic heuristic evaluation of Computerized Consultation Order templates: clinicians’ and human factors engineers’ perspectives. J Med Syst. 2017;41(8):129. https://doi.org/10.1007/s10916-017-0775-7 . Savoy A, Frankel R, Weiner M. Clinical thinking via electronic note templates: who benefits? J Gen Intern Med. 2021;36(3):577–9. https://doi.org/10.1007/s11606-020-06376-y . Neri PM, Volk LA, Samaha S, et al. Relationship between documentation method and quality of chronic disease visit notes. Appl Clin Inf. 2014;05(02):480–90. https://doi.org/10.4338/ACI-2014-01-RA-0007 . Article CAS Google Scholar Linder JA, Schnipper JL, Middleton B. Method of electronic health record documentation and quality of primary care. J Am Med Inform Assoc. 2012;19(6):1019–24. https://doi.org/10.1136/amiajnl-2011-000788 . Lobo SEM, Rucker J, Kerr M, et al. A comparison of mental state examination documentation by junior clinicians in electronic health records before and after the introduction of a semi-structured assessment template (OPCRIT+). Int J Med Inf. 2015;84(9):675–82. https://doi.org/10.1016/j.ijmedinf.2015.05.001 . Schnipper JL, Linder JA, Palchuk MB, et al. Effects of documentation-based decision support on chronic disease management. Am J Manag Care. 2010;16(12 Suppl HIT):SP72–81. PubMed Google Scholar Rosenbloom ST, Denny JC, Xu H, Lorenzi N, Stead WW, Johnson KB. Data from clinical notes: a perspective on the tension between structure and flexible documentation. J Am Med Inform Assoc. 2011;18(2):181–6. https://doi.org/10.1136/jamia.2010.007237 . Article PubMed Central Google Scholar Fanucchi L, Yan D, Conigliaro R. Duly noted: lessons from a two-site intervention to assess and improve the quality of clinical documentation in the electronic health record. Appl Clin Inf. 2016;07(03):653–9. https://doi.org/10.4338/ACI-2016-02-CR-0025 . Habtamu K, Birhane R, Demissie M, Fekadu A. Interventions to improve the detection of depression in primary healthcare: systematic review. Syst Rev. 2023;12(1):25. https://doi.org/10.1186/s13643-023-02177-6 . Cohen GR, Friedman CP, Ryan AM, et al. Variation in Physicians’ Electronic Health Record Documentation and potential patient harm from that variation. J Gen Intern Med. 2019;34(11):2355–67. https://doi.org/10.1007/s11606-019-05025-3 . Hoffman RR, Militello LG. Perspectives on Cognitive Task Analysis: historical origins and Modern communities of Practice. Psychology; 2008. Crandall B, Klein G, Hoffman RR. Working minds. A Practitioners Guide to Cognitive Task Analysis. MIT Press; 2006. Download references AcknowledgementsWe would like to acknowledge Melissa R. Thomas and Steve Becraft for their careful review of the manuscript. The views expressed in this article are those of the authors and do not necessarily represent the views of the U.S. Department of Veterans Affairs or the United States government. Source of funding: U.S. Department of Veterans Affairs (HX002519). Author informationAuthors and affiliations. Center for Health Information and Communication, Department of Veterans Affairs, Health Services Research and Development Service, Veterans Health Administration, Richard L. Roudebush VA Medical Center, CIN 13 416, Indianapolis, IN, USA Michael Weiner, Mindy E. Flanagan, Nicholas A. Rattray, Zamal Franks, April W. Savoy & Richard M. Frankel Department of Medicine, Indiana University School of Medicine, Indianapolis, IN, USA Michael Weiner, Nicholas A. Rattray & Richard M. Frankel Indiana University Center for Health Services and Outcomes Research, Regenstrief Institute, Inc, 1101 West 10th Street, 46202-4800, Indianapolis, IN, USA Michael Weiner, Ann H. Cottingham, Nicholas A. Rattray, April W. Savoy & Richard M. Frankel Applied Decision Science LLC, Cincinnati, OH, USA Katie Ernst Purdue School of Engineering and Technology, Indiana University-Purdue University Indianapolis, Indianapolis, IN, USA April W. Savoy Department of Population and Quantitative Health Sciences, University of Massachusetts Chan Medical School, Worcester, MA, USA You can also search for this author in PubMed Google Scholar ContributionsRF and NR recruited providers in the study. MW, AC, MF, KE, and RF each reviewed and coded the transcripts. All authors read and approved the final manuscript. Corresponding authorCorrespondence to Michael Weiner . Ethics declarationsEthics approval and consent to participate. Informed consent was obtained from all participants. Ethics approval was obtained from the Indiana University Institutional Review Board. The study was conducted in accordance with the Declaration of Helsinki. Consent for publicationNot applicable (IRB documents available upon request). Competing interestsMichael Weiner reports stock holdings in Allscripts Healthcare Solutions, Apple, Centene, DXC Technology, General Electric, Hewlett Packard, International Business Machines, Kyndryl Holdings, Micro Focus International, Microsoft, Oracle Cerner, Perkinelmer, Qualcomm, Walgreens, Zimmer Biomet, Intel, Cellcom Israel, Exact Sciences, IRhythm Technologies, Senseonics, Teladoc Health, and Varex Imaging. Remaining authors have no competing interest to declare. Additional informationPublisher’s note. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Electronic supplementary materialBelow is the link to the electronic supplementary material. Supplementary Material 1Rights and permissions. Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data. Reprints and permissions About this articleCite this article. Weiner, M., Flanagan, M.E., Ernst, K. et al. Accuracy, thoroughness, and quality of outpatient primary care documentation in the U.S. Department of Veterans Affairs. BMC Prim. Care 25 , 262 (2024). https://doi.org/10.1186/s12875-024-02501-6 Download citation Received : 07 January 2024 Accepted : 27 June 2024 Published : 18 July 2024 DOI : https://doi.org/10.1186/s12875-024-02501-6 Share this articleAnyone you share the following link with will be able to read this content: Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative
BMC Primary CareISSN: 2731-4553
An official website of the United States government The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site. The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
 Health professionals’ routine practice documentation and its associated factors in a resource-limited setting: a cross-sectional studyAddisalem workie demsash. 1 College of Health Science, Health Informatics Department, Mettu University, Mettu, Ethiopia Sisay Yitayih KassieAbiy tasew dubale, alex ayenew chereka, habtamu setegn ngusie. 2 College of Health Science, Health Informatics Department, Woldia University, Woldia, Ethiopia Mekonnen Kenate Hunde3 College of Education and Behavioral Science, Lifelong Learning and Community Development Department, Mettu University, Mettu, Ethiopia Milkias Dugassa Emanu4 College of Health Science, Nursing Department, Mettu University, Mettu, Ethiopia Adamu Ambachew ShibabawAgmasie damtew walle, associated data. All the data generated and analysed during this study are included, in the table and text form, in this article. If required, the data will be available on request from the corresponding author. Not applicable. Documenting routine practice is significant for better diagnosis, treatment, continuity of care and medicolegal issues. However, health professionals’ routine practice documentation is poorly practised. Therefore, this study aimed to assess health professionals’ routine practice documentation and associated factors in a resource-limited setting. An institution-based cross-sectional study design was used from 24 March up to 19 April 2022. Stratified random sampling and a pretested self-administered questionnaire were used among 423 samples. Epi Info V.7.1 and STATA V.15 software were used for data entry and analysis, respectively. Descriptive statistics and a logistic regression model were employed to describe the study subjects and to measure the strength of association between dependent and independent variables, respectively. A variable with a p value of <0.2 in bivariate logistic regression was considered for multivariable logistic regression. In multivariable logistic regression, ORs with 95% CIs and a p value of <0.05 were considered to determine the strength of association between dependent and independent variables. Health professionals’ documentation practice was 51.1% (95% CI: 48.64 to 53.1). Lack of motivation (adjusted OR (AOR): 0.41, 95% CI: 0.22 to 0.76), good knowledge (AOR: 1.35, 95% CI: 0.72 to 2.97), taking training (AOR: 4.18, 95% CI: 2.99 to 8.28), using electronic systems (AOR: 2.19, 95% CI: 1.36 to 3.28), availability of standard documentation tools (AOR: 2.45, 95% CI: 1.35 to 4.43) were statistically associated factors.  ConclusionsHealth professionals’ documentation practice is good. Lack of motivation, good knowledge, taking training, using electronic systems and the availability of documentation tools were significant factors. Stakeholders should provide additional training, and encourage professionals to use an electronic system for documentation practices. WHAT IS ALREADY KNOWN ON THIS TOPIC
WHAT THIS STUDY ADDS
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
IntroductionIn routine healthcare practice, evidence about the care and treatment of patients, progress notes, assessments and care plans, 1 laboratory tests and results, medication and drug prescription information, patient education and counselling 2 are some of the routine practices of health professionals. Therefore, documenting the health professionals’ routine practices are important for various purposes. Documentation is a standard way of keeping ongoing patient care information. It is the relevant facts of routine health information and patient care plans, 3 such as professionals’ evaluation and judgement about the patients, evaluation charts, tests, reports, subjective notes or professionals’ reflections. 4 Documenting routine practices is essential for the continuity of patient care, legal defence, reimbursement, communication among healthcare professionals and better patient diagnoses and treatments. 5 Maintaining routine practice is part of the health professional obligation. Healthcare facilities’ by-laws or policies should require health professionals to complete patient records. 6 Whether the documentation is a paper-based or electronic system, it should be patient-focused, accurate, relevant, clear, permanent, confidential and timely. Electronic patient record systems are better for reducing the time spent on documenting patient information and enhancing the quality of documentation. 7 Poor documentation practice affects patient management, continuity of patient care and medicolegal issues, which arise from incomplete and inadequate documentation, lack of accuracy and poor quality. 8 It leads to adverse patient outcomes, medication errors and patient deaths. 9 Distorted health information may influence health professionals’ decision-making capabilities due to inappropriate and misleading documentation practices. 10 Globally, poor communication between health professionals is a reason for medical error and patient mortality. 9 Many health professionals’ documentation practice is incomplete, inaccurate and of poor quality. According to evidence from the USA, documentation errors are a cause of at least one death and 1.3 million injuries annually. 11 Moreover, health professionals’ documentation practice is inadequate such as 33.3% in Indonesia, 12 47% in England 13 and 50% in Iran. 14 In the low-income and middle-income regions, a qualitative study undertaken in Uganda stated that documentation practice is limited by constraints and poor support from the administration. 15 In Ghana, 46% of care is provided, and progress notes are not documented after the first day of patient admission. 16 In Nigeria, only 44% of health professionals had good documentation knowledge and practice. 17 In Ethiopia, documentation is poorly practised and has been reported as being left undone. 3 Health professionals’ documentation practice is 47.8% in the Tigray 18 and 37.4% 3 in Amhara regions. Surprisingly, 88% of the medication provided has been wrongly documented. 19 A study report in the Amhara region states that 87% of the medications had documentation errors. 19 Age, sex, experience, income, levels of education, health professionals’ knowledge and attitude, 3 12 18 motivation, workload and training about documentation 20 are factors associated with routine practice documentation. Documenting health professionals’ routine activities is valuable for sharing knowledge and learning from history. This has a significant impact on better decision-making and accuracy in patient diagnosis and treatment. As per our literature review, studies have not been undertaken in the current study setting. Few studies in similar settings have been carried out with only nursing as a study participants, education and counselling given to the patient were not assessed. So, assessment documentation practice in both medical and non-medical practices, including all health professionals is crucial. Therefore, this study aimed to determine health professionals’ routine practice documentation and associated factors. Study design and periodAn institutional-based cross-sectional study design was employed among health professionals working in public health facilities in the Ilu Aba bora Zone, from 24 March up to 19 April 2022. Study settingIlu Aba Bora Zone is found in Southwest Ethiopia. The zone is located 600 km away from Addis Ababa, the capital city of Ethiopia. In the zone, there are 44 total health facilities and 2 hospitals (1 general hospital and 1 referral hospital). The public health facilities provide different health services for more than a million of the population in southwest parts of the country coming from Gambela, Southern Nation Nationality and People’s region. Study population and eligibility criteriaAll healthcare professionals working in the public health facilities of Ilu Aba Bora Zone and those who were found during the data collection period were the sources and study population, respectively. Healthcare professionals who were not permanently employed, those who were not present during the study period and who worked as data clerks were excluded. Sampling size determinationA sample size (n) was determined by using a single population proportion formula, N=(Z a/2 ) 2 ×P(1−P)/d 2 , where n=the required sample size, (Za /2 ) 2 =the value of standard normal distribution or 1.96, p=the prevalence of documentation practice among health professionals and so the default maximum value of 50% was used for P, d=degree of precision or 0.05. Taking this, the required sample size was calculated to be 384. After adding a 10% non-response rate, a total of 423 healthcare professionals participated in this study. Sampling producerA stratified simple random sampling method was used. Due to the limited resources, we have to cover all types of health facilities, we have included two hospitals directly and three randomly selected health centres. Once the sample was stratified based on the types of randomly selected health facilities, the sample was allocated to each stratum proportionally. Then, a simple random sampling technique was used to select the study subjects in each public health facility. The list of health professionals was taken from human resource departments. Accordingly, there are 1043 health professionals from 5 randomly selected health facilities. The sampling procedure has been presented in figure 1 .  Sampling procedures of study participant selection. HC, health centres. Operationalisations and measurementsIn the healthcare system, patient status, medical diagnoses, planned care, medical interventions or treatments, laboratory tests, result confirmations, medications, patient education and counselling, communication and delivering service are activities of health professionals. All the mentioned activities of health professionals are either medical or non-medical activities (patient education and counselling), but all are routine activities for health professionals. As a result, health professionals use standard documentation tools such as manual records and/or electronic systems to document their routine activities correctly and on time while respecting the rules of ethics. 21 Accordingly, health professionals’ routine practice documentation was assessed by using 12 ‘yes’ and ‘no’ questions. 3 22 The level of health professionals’ routine practice documentation was determined using the mean value as a cut-off point. Hence, the level of health professionals’ routine practice documentation is good if the score is above or equal to the mean value, and otherwise poor documentation practice. The study participants’ level of knowledge was measured by using 10 ‘yes’ and ‘no’ options. Health professionals who scored above or equal to the mean score were considered to have good knowledge, and those who scored below the mean value had poor knowledge. 3 The study participants’ level of attitude was measured by using nine Likert scale questions with responses ranging from 1 ‘strongly agree’ to 5 ‘strongly disagree’. 3 18 Health professionals who scored above or equal to the mean score were considered to have a good attitude, otherwise, poor attitude. Data collection tool and quality assuranceThe tool used was developed based on reviewing similar studies. 3 18 22 A pretested, self-administered questionnaire was used. Two supervisors and three data collectors received 2 days of intensive training on the study objectives and how to approach study participants. A pretest was done outside the study area with 10% of the study subjects to check the readability and consistency of the questionnaire. The data obtained from the pretest were used to check the validity and reliability of the tool. The Cronbach’s alpha was used to check the reliability of the tool with a value of 83. Data processing and analysisThe data entry was performed using Epi Info V.7.1 software packages and analysed using STATA V.15 software. Descriptive statistics were computed to describe the sociodemographic characteristics of the healthcare professionals, their knowledge and their attitudes towards routine practice documentation. Bivariable and multivariable binary logistic regression analyses were conducted to measure the association between the dependent and independent variables. In the bivariable regression analysis, variables with a p value of <0.2 were considered for further multivariable logistic regression analysis. The OR with a 95% CI level was assumed to assess the strength of the association between dependent and predictor variables. For all significantly associated variables, a p value <0.05 was used as a cut-off point. A variance inflation factor was performed. Consequently, its value for all predictors was between one and three. This revealed that there was no correlation between the variables. The Hosmer-Lemeshow test was performed to assess the model fitness, and so model was fitted (p=0.271). Description of study subjectsFrom 423 participants, 415 responded to a questionnaire with a 98.11% response rate. The mean age of the study subjects was 29.28 (SD±2.21) years with a minimum age of 21 years and a maximum age of 59 years. Half (51.1%) of the study subjects were male. The majority (66.7%) of study subjects were BSc degree holders or below. Of the total respondents, around 6–10 (62.4%) of the study participants had up to 5 years of working experience. Less than half (32.3%) of the study subjects were trained in routine practice documentation. Of 415 study participants, 235 (56.6%) health professionals earned 4500–7500 Ethiopian Birr per month, and 8–10 (80.2%) health professionals responded that standard documentation tools were available in the working area. One hundred twenty-five (54.22%) health professionals used manual forms for documentation purposes ( table 1 ). Sociodemographic characteristics of health professionals
Health professionals’ routine practice documentationOverall, 51.1% (95% CI: 46.29% to 53.55%) of health professionals had good routine practice documentation; 6.99% of different laboratory test request forms were not completed and documented; 6.025% of the physicians’ prediagnosis was completed and documented; 5.54% of drug prescription and laboratory result forms were not completed and documented. Documentation incompleteness accounted for 32.52% of health professionals’ poor routine practice documentation ( table 2 ). Checklists examine health professionals’ routine practice documentation adopted from the Ethiopian health institution reform implementation guidelines
Factors associated with routine practice documentationBivariate and multivariate logistic regressions were used to measure the association between dependent and independent predictors. In the bivariate logistic regression, p<0.2 was used and sex, age, training, knowledge, attitude, types of documentation tools, availability of standard documentation tools, workload and motivation of study subjects were the candidate variables for the multivariable regression analysis. In the multivariable regression model, knowledge, training, motivation, types and availability of the standard documentation tools were significant factors for routine practice documentation ( table 3 ). Bivariate and multivariate analysis of factors associated with health professionals’ routine practice documentation (n=415)
Reference category=1. *Significant in COR. †Significant in AOR. AOR, adjusted OR; COR, crude OR. Health professionals who lack motivation were 59% (adjusted OR (AOR): 0.41, 95% CI: 0.22 to 0.76) less likely to document routine practices. Health professionals who had good knowledge of routine practice documentation were 1.4 (AOR: 1.35, 95% CI: 0.72 to 2.97) times more likely to document routine practice than those who had poor knowledge. Health professionals who were trained in routine practice documentation were 4.2 (AOR: 4.18, 95% CI: 2.99 to 8.28) times more likely to document routine practices than those who were not trained. Health professionals who used electronic systems for routine practice documentation were 2.2 (AOR: 2.19, 95% CI: 1.36 to 3.28) times more likely to document their routine practices than those who used manual forms for documentation. The availability of standard documentation tools were 2.5 (AOR: 2.45, 95% CI: 1.35 to 4.43) times more odds for health professionals to document their routine practices ( table 3 ). This study assesses health professionals’ routine practice documentation and associated factors. Health professionals who had good knowledge about routine practice documentation, training on documentation, using electronic systems for documentation, the availability of standard documentation tools and a lack of motivation towards routine practice documentation were statistically significant factors associated with health professionals’ routine practice documentation. The study revealed that health professionals’ routine practice documentation was good (51.1%). This finding is higher than previous similar studies, which found 44.2% in Nigeria, 17 33.3% in Indonesia 12 and 37.4%–48.8% in different parts of Ethiopia. 3 18 23 However, the finding is lower than the study done in Jamaica, which reports that health professionals’ documentation practice is 98%. 24 This might be due to the utilisation of technologies such as the electronic medical record and district health information system V.2 (DHIS2), the accessibility of required tools for documentation and health professionals’ good commitment to using DHIS2 data. 19 Additionally, this variation might be due to the information difference, the time gap between studies, the high patient flow, the shortage of time and the workload of health professionals. Health professionals who lack motivation were 59% less likely to have documentation practices when compared with those who had gained motivation. This finding is inconsistence with studies done in Ethiopia. 23 25 This might be poor professional encouragement, poor financial support, less opportunities for further educational development, poor infrastructures and low hospital management support. 25 Health professionals for whom standard documentation tools were available were 2.5 times more likely to document routine practices than those for whom standard documentation tools were not available. This finding is consistence with a study done in Australia, 26 Tigray 18 and Amhara regions. 23 This might be due to familiarisation with standard documentation sheets, and the accessibility of integrated routine health information forms for recording and reporting. 27 Health professionals who had good knowledge of routine practice documentation were more likely to document their routine practice. This result is supported by studies done in Ethiopia, 3 the USA 28 and Australia. 29 This might be due to health professionals’ familiarity with documentation guidelines and manual forms that improve health professionals’ knowledge of routine practice documentation. 3 Additionally, the reason might be that health professionals understand the importance of documenting routine practice, the viability of reading materials, know that record-keeping is required for medicolegal issues and have good competency in the area of documentation. 29 Moreover, spending on documentation courses may promote health professionals’ knowledge. 30 Health professionals who were trained in routine practice documentation were 4.2 times more likely to document routine practices than those who were not trained. This evidence is supported by studies done in Ethiopia 3 and Iran. 30 This might be due to training, which might enhance health professionals’ knowledge and motivation for documentation and provide team-based learning, intrapersonal skills sharing and consultation gained from colleagues. Plus, training may force health professionals to develop a positive attitude towards routine practice documentation. 3 Health professionals who used electronic systems for routine practice documentation were 2.2 times more likely to document their routine practices than those who used manual forms. This study is supported by a study done in Ethiopia 20 and a study done about maintaining practices and record-keeping. 1 This might be due to the capability of electronic systems to reduce the time spent documenting patient care. 7 Additionally, record-keeping in the light of recent public inquiries, national interests in shifting from paper to digital storage of data, the capability of electronic health records to generate a complete record of an episode of care and the longitudinal nature of the electronic system might be possible reasons. 1 Moreover, a need for real-time access to health information when and where it is needed might be reason why an electronic system could be more likely to be good for documentation. 23 Strength and limitationSince the data were collected at a specific time, social desirability bias may occur. Significant variables may have a temporal relationship. This study assesses the use of electronic systems for documentation as an independent variable. All health professionals were included, and documentation regarding education and counselling was assessed. Hence, the finding is unique as compared with previous studies. Moreover, the mean value was used as a cut-off point to determine level of health professionals’ routine practice documentation to consider the weighted average values. In this study, health professionals have good routine practice documentation. Knowledge, training, using an electronic system, availability of standard documentation tools and lack of motivation are statistically significant factors for routine practice documentation. Health policy formulators and stakeholders give additional training to health professionals, and encourage them to use an electronic system for documentation. Stakeholders should improve health professionals’ knowledge and motivation of routine practice documentation. Additional high-quality studies are required on a similar topic. Contributors: AWD had made a substantial contribution in writing the conception, designing the study, analyzing the data, and discussing the findings. SYK and ATD were involved in drafting the manuscript and interpreting the results. AAC and HSN had revised the manuscript. MKH, AAS, ADW, and MDE all made significant contributions to revising the manuscript, and managing the data. All authors read and approved the final manuscript submission for publication. Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors. Competing interests: None declared. Provenance and peer review: Not commissioned; externally peer reviewed. Data availability statementEthics statements, patient consent for publication. Not applicable. Ethics approvalEthics approval was obtained from the Institutional Review Committee of the health science college of Mettu University with reference number ARcsu/271/24. Informed verbal and written consent from the study participant was obtained. Clinical Researcher Guidance for Preparing Standard Operating Procedures (SOPs)Clinical Researcher October 17, 2023  Clinical Researcher—October 2023 (Volume 37, Issue 5) CULTIVATING QUALITY Olena Chervonenko, MS Standard operating procedures (SOPs) play a vital role in ensuring quality, compliance, and safety across a pharmaceutical company’s operations. SOPs are key to ensuring users follow current requirements and best practices and perform tasks consistently and uniformly. An SOP is a documented set of step-by-step instructions that outline the approved methods and practices for carrying out specific tasks or processes within an organization. When writing SOPs, it’s important to strike the right balance between providing enough detail and avoiding excessive complexity. Insufficient detail increases the likelihood of users improvising on the spot or following widely used, but perhaps inadequate, methods. On the other hand, excessive information can lead to confusion, errors, and mistakes. In the pharmaceutical industry, improvising or deviating from established methods can have serious consequences and may result in the company becoming noncompliant with one or more of the internationally agreed-upon “Good x Practices,” where “x” may stand for Clinical,{1} Manufacturing,{2} Laboratory,{3} etc. SOPs must ensure the robustness, traceability, and integrity of a Pharmaceutical Quality System (PQS) of an organization and contribute to maintaining quality, safety, and compliance standards within the organization. Robustness of the PQSSOPs provide a systematic and documented approach to performing critical tasks and processes within an organization. By outlining specific procedures, controls, and requirements, SOPs help ensure the robustness of the PQS. They establish a framework that promotes consistency, traceability, and accountability in all operations. SOPs incorporate safety considerations and guidelines to mitigate risks and protect personnel, patients, and the environment. They outline business workflows, safety protocols, personal protective equipment requirements, handling procedures for hazardous substances, and emergency response measures. By adhering to SOPs, organizations promote a culture of safety and minimize the potential for accidents or incidents. In short, SOPs are essential tools in assuring the robustness of the PQS. TraceabilityEnsuring the traceability of the PQS is a critical aspect of SOPs within the pharmaceutical industry. Traceability provides a clear and documented path that demonstrates the implementation and effectiveness of the PQS. Here are some key considerations to incorporate traceability into your SOPs: Documented References: SOPs should reference the relevant sections of the PQS documentation, such as quality manuals, policies, and guidelines. This ensures that SOPs are aligned with the overall quality system and current edition of guides. Version Control: SOPs should have a version control system in place, indicating the specific version number, date of revision, and any relevant updates. This allows for easy identification of the most current version and facilitates traceability. Cross-Referencing: SOPs should cross-reference other related SOPs or documents within the PQS. This ensures that interdependencies between procedures are clearly identified and maintained. Change Control Process: The revision history of an SOP should clearly outline the specific changes that were made, accompanied by a linked change control document. This document should include thorough documentation of any modifications to the SOPs, along with justification and, if applicable, a risk assessment. This facilitates traceability and identification of the chronology of changes. By incorporating these traceability elements into your SOPs, you establish a clear link between the procedures outlined in the SOPs and the overall PQS, ensuring transparency, compliance, and effective quality management. Data IntegrityData integrity is a critical aspect of SOPs within the pharmaceutical industry. It ensures that data generated, recorded, and reported during operations are accurate, complete, and reliable. SOPs must declare data integrity principles to prevent data manipulation, fraud, and errors. Key considerations for maintaining data integrity via SOPs include: Data Recording: SOPs should outline the proper methods for recording data accurately, including clear instructions on data entry, identification, and verification. Audit Trails: SOPs should define procedures for creating and maintaining audit trails, which provide a chronological record of data changes, ensuring data integrity and traceability. Data Security: SOPs should incorporate measures to protect data integrity, such as access controls, data encryption, and regular data backups. Bringing in the Right PeopleIt is important to involve quality assurance (QA) and senior management in all stages of SOP creation — from ideation to assessing the effectiveness of implemented SOPs. The QA department plays a crucial role in ensuring the effectiveness of SOPs within the pharmaceutical industry. QA staff are responsible for overseeing the development, implementation, and maintenance of SOPs to guarantee compliance with industry regulations and standards. Chiefly, they are responsible for SOP review, collaborating with subject matter experts to ensure SOPs are accurate, comprehensive, and aligned with regulatory requirements. Senior management plays a key role in supporting and driving the effective implementation of SOPs. Their responsibilities include: Policy and Strategy: Establishing clear policies and strategies that emphasize the importance of SOPs in ensuring quality, safety, and compliance throughout the organization. Leadership and Communication: Promoting a culture of quality and compliance, fostering a shared understanding of the significance of SOPs at all levels of the organization. Senior management also communicates expectations, provides guidance, and encourages employee engagement. Continuous Improvement: Supporting a continuous improvement mindset by encouraging feedback, monitoring of performance metrics, and implementing initiatives to enhance SOP effectiveness. Focus of InspectionDuring inspections, regulatory authorities and auditors focus on evaluating the implementation and effectiveness of SOPs. They assess whether the organization has well-documented and controlled SOPs, that these SOPs are followed, and that they are in compliance with regulatory requirements. Key areas of inspections related to SOPs include: Process Description: Inspectors assess whether the organization has cohesively documented all GxP relevant activities. SOP Availability: Inspectors verify that SOPs are readily available to personnel and accessible in relevant areas where tasks are performed. Adherence to SOPs: Inspectors assess whether employees follow SOPs consistently, ensuring that documented procedures are being executed as specified. Further ConsiderationsWhen creating or updating SOPs, it is important to keep in mind the following points to avoid unnecessary complexity: Author and Reviewer: The author of the procedure should be someone who performs the task or possesses a deep understanding of it. They should strike a balance between providing adequate detail and avoiding excessive elaboration. The reviewer’s role is to ensure that the SOP achieves the appropriate level of detail. Ask Why: Simplify and improve the workflow by questioning the necessity of each step in the SOP. This technique involves creating a comprehensive list of all the steps in a work process and critically evaluating their purpose. Field Testing: Red line the procedure in the field to assess its relevance and coherence. This practice involves documenting and accurately recording the process while onsite, often accompanied by clear photos that can be included in the SOP. Embrace Simplicity: Lengthy and intricate SOPs are challenging to follow. Strive to keep SOPs simple and user-friendly while ensuring that all important steps are included. Complex tasks can be broken down into smaller sub-steps. Sentences should generally be kept short to ensure clarity. Visual Aids: Humans process visual information more easily than text. Improve the understandability of SOPs by incorporating photos, drawings, and flowcharts. Visual aids can significantly assist in conveying complex information. Minimize Involvement: Involving fewer individuals in a task reduces the likelihood of human error. Streamlining the number of people involved in a task enhances efficiency and accuracy. Audience Consideration: SOPs should be tailored to the education, experience, knowledge, and abilities of the personnel who will use them. Language: SOPs should be written using vocabulary relevant to the area of use, experience, knowledge, and abilities of the personnel who will use them. Testing and Verification: Before finalizing an SOP, conduct tests with individuals who will use it regularly. Their feedback can help identify unclear information, missing steps, or incorrect sequencing. It can also be beneficial to have someone with limited knowledge of the process test the SOP to ensure its accessibility to a broader audience. Preserve Simplification Efforts: During the review process, carefully evaluate any additional or removed steps. Justification should be provided before incorporating any changes, being cautious to maintain the simplified nature of the SOP. This approach ensures that deviations are properly identified through root cause analysis. Regular Review and Revision: Seek feedback from those who have direct experience using the SOP after several weeks of implementation. Evaluate clarity, effectiveness, readability, and ease of use. Revise the SOP based on the feedback received. Keep SOPs Updated: Regularly review and update SOPs to align with current practices and requirements. Failure to periodically review and update SOPs can quickly render them obsolete. A recommended review frequency is every two to three years. The review frequency should be justified. By following these guidelines and incorporating the necessary elements, SOPs can effectively guide pharmaceutical industry professionals, promote efficiency, support compliance and data integrity, and contribute to the overall success of an organization.
A list of SOPs required by the U.S. Food and Drug Administration, the European Union Guideline to Good Manufacturing Practice (GMP), and the World Health Organization for GMP activities can be found at http://www.gmp-compliance.org/gmp-news/which-sops-are-required-by-gmp . For Good Documentation Practice (GDP), the Health Products Regulatory Authority in Ireland has published a guidance document that includes the SOPs that are needed for compliance with GDP and details the general framework for each SOP at https://www.hpra.ie/docs/default-source/publications-forms/guidance-documents/ia-g0038-guide-to-quality-system-for-general-sale-wholesale-distributors-v2.pdf?sfvrsn=14 . European Medicines Agency Procedures, EMA: https://www.ema.europa.eu/en/procedures Manual of Policies and Procedures, FDA: https://www.fda.gov/media/90280/download The contents of this article are solely the opinion of the author and do not represent the opinions of PharmaLex GmbH or its parent Cencora Inc. PharmaLex and Cencora strongly encourage readers to review the references provided with this article and all available information related to the topics mentioned herein and to rely on their own experience and expertise in making decisions related thereto.  Sorry, we couldn't find any jobs that match your criteria.  Improving Cardiovascular Research for Transgender and Gender Diverse Populations Disruptive Technologies Redefining the Path of Clinical Trials How an Innovative Statistical Methodology Enables More Patient-Centric Design and Analysis of Clinical TrialsJobs in the acrp career center.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
Reporting guidelines for precision medicine research of clinical relevance: the BePRECISE checklist
Nature Medicine volume 30 , pages 1874–1881 ( 2024 ) Cite this article 673 Accesses 5 Altmetric Metrics details
Precision medicine should aspire to reduce error and improve accuracy in medical and health recommendations by comparison with contemporary practice, while maintaining safety and cost-effectiveness. The etiology, clinical manifestation and prognosis of diseases such as obesity, diabetes, cardiovascular disease, kidney disease and fatty liver disease are heterogeneous. Without standardized reporting, this heterogeneity, combined with the diversity of research tools used in precision medicine studies, makes comparisons across studies and implementation of the findings challenging. Specific recommendations for reporting precision medicine research do not currently exist. The BePRECISE (Better Precision-data Reporting of Evidence from Clinical Intervention Studies & Epidemiology) consortium, comprising 23 experts in precision medicine, cardiometabolic diseases, statistics, editorial and lived experience, conducted a scoping review and participated in a modified Delphi and nominal group technique process to develop guidelines for reporting precision medicine research. The BePRECISE checklist comprises 23 items organized into 5 sections that align with typical sections of a scientific publication. A specific section about health equity serves to encourage precision medicine research to be inclusive of individuals and communities that are traditionally under-represented in clinical research and/or underserved by health systems. Adoption of BePRECISE by investigators, reviewers and editors will facilitate and accelerate equitable clinical implementation of precision medicine. Similar content being viewed by others Translating evidence into practice: eligibility criteria fail to eliminate clinically significant differences between real-world and study populations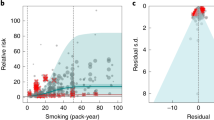 The Burden of Proof studies: assessing the evidence of risk Constructing a finer-grained representation of clinical trial results from ClinicalTrials.govPrecision medicine represents an evolution in the long history of evidence-based medicine and healthcare. Spanning disease classifications and risk factor boundaries, precision medicine is underpinned by four key ‘pillars’ (prevention, diagnosis, treatment and prognosis) 1 , 2 . The overarching objective of precision medicine is to reduce error and improve accuracy in medical and health recommendations compared with contemporary approaches 3 . Precision medicine solutions should meet or improve on existing standards for safety. They should also be compatible with the individual’s preferences, capabilities and needs and tailored to the cultural and societal conditions of the population. Furthermore, precision medicine should be cost-effective and enhance health equity by increasing access to better medical and healthcare practices for the people most in need. Cardiometabolic diseases are the leading causes of mortality globally 4 . With this burden projected to worsen over the coming decades 5 , innovative approaches to disease prevention, diagnosis and treatment are urgently needed. A plethora of precision medicine approaches are being explored in translational and clinical research. However, translating, scaling and implementing these findings for clinical practice have proved difficult. The heterogeneous nature of disease presentation and the etiology of cardiometabolic diseases contribute to these challenges, as does the range and diversity of clinical information, molecular data types and computational analyses used in precision medicine research. The ability to synthesize data and reproduce research findings are tenets of the modern scientific process, which help maximize progress in evidence-based healthcare and medicine. The ‘Second international consensus report on gaps and opportunities for the clinical translation of precision diabetes medicine’ 3 was supported by a series of systematic evidence reviews 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 . The report focused on key dimensions of precision diabetes medicine, including evidence for prevention, diagnosis, treatment and prognosis in monogenic forms of diabetes, gestational diabetes, and type 1 and type 2 diabetes. A key finding from the report and the systematic evidence reviews underpinning it is that the published literature on precision diabetes medicine lacks evidence standardization or benchmarking against contemporary standards and often overlooks under-represented populations, who tend to bear the greatest burden of diabetes and its complications. In the present report, we present reporting guidelines for clinically relevant precision medicine research, using common cardiometabolic diseases as the example. We first evaluated a representative sample of the literature on precision medicine in cardiometabolic diseases, determining that the quality of evidence reporting is low, akin to the level previously observed for precision diabetes medicine 3 . We then generated consensus guidelines and a corresponding checklist for reporting of research germane to precision medicine. The purpose of these guidelines is to improve reporting standards so that: (1) evidence can be combined and synthesized in a way that yields meaningful insights from collective efforts; (2) claims of clinical utility can be benchmarked against contemporary standards; and (3) end-user engagement and health equity will be strengthened. Scoping reviewThe literature search focused on identifying precision medicine publications using the term ‘precision medicine’ and associated proxy nomenclature, among other keywords and phrases ( Supplementary Methods ). The search identified 2,679 publications, of which 13 were excluded owing to duplication. The remaining 2,666 papers were screened, of which 47 were randomly selected (through computer-generated, random-number sequence) for full text review and quality assessment. The summary (count and percentage) of each quality assessment item across all papers and the quality assessment results for each paper are shown in Supplementary Tables 2 and 3 . This quality assessment yielded a median score of 6 (interquartile range = 4–7) with none of the papers achieving a positive quality evaluation across all 11 items (Fig. 1 ).  Median scores of 47 published precision medicine manuscripts randomly selected for full text review and quality assessment through computer-generated, random-number sequence. IQR, Interquartile range. A summary of the itemized evidence reporting quality is shown in Supplementary Table 2 . Most abstracts (81%) reported findings relevant to the four pillars of precision medicine (prevention, diagnosis, treatment and/or prognosis) and provided sufficient detail in the methods sections to determine whether the study was designed to test hypotheses on precision medicine (77%), details about participant eligibility (75%) and descriptions of standard reporting definitions (70%). The items that were less frequently reported were the description of patient and public involvement and engagement (PPIE) in determining the impact and utility of precision medicine (15%), the inclusion of the term ‘precision medicine’ in the title or abstract (17%), the reporting of measures of discriminative or predictive accuracy (23%), the description of the approach used to control risk of false-positive reporting (28%), the reporting of effect estimates with 95% confidence intervals and units underlying effect estimates (57%) and the reporting of a statistical test for comparisons of subgroups (for example, interaction test) (60%). Stakeholder surveyDelphi panel demographics. Of the 23 Delphi panelists, 22 (96%) completed Delphi survey 1, 18 (78%) and attended the full-panel consensus meeting and 22 (96%) completed Delphi survey 2. All panelists engaged in further extensive dialog around key topics through online communication. Delphi resultsThe initial checklist in Delphi survey 1 contained 68 items. After Delphi survey 1 and the full-panel consensus meeting, 2 items were added, resulting in 70 items in Delphi survey 2. At the Consensus meeting, it was determined that the checklist should be used together with existing relevant checklists. These include the CONSORT (Consolidated Standards of Reporting Trials) 17 and STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) 18 checklists for interventional trials and observational studies, respectively. This led to a recommendation to remove items covered in established checklists (Supplementary Fig. 1 ). The scoring from Delphi survey 1, Delphi survey 2 and notes from the Consensus meetings are as shown in Supplementary Table 4 . After Delphi survey 2, the consensus was to retain 25 items across 6 core categories. Guidelines finalizationThe executive oversight committee reviewed the panel scores and free-text comments from all the rounds of Delphi surveys to determine the final checklist items and wording. The group discussed five items with inconsistent consensus (between 70% and 80% consensus), resulting in the removal of one item because it overlapped conceptually with another item (17b and 17g in Supplementary Table 4 ). It was also determined that ‘health equity’ should be included as an overarching theme, thereby encouraging users of the checklist to consider this topic more broadly when describing precision medicine research. This resulted in removal of two items. The final checklist comprised 23 items that the executive oversight committee concluded are unique and essential for reporting standards in precision medicine. The final BePRECISE checklist is presented in Table 1 , with a downloadable version of the checklist available online ( https://www.be-precise.org , and https://www.equator-network.org/reporting-guidelines/ ). Explanation of checklist ItemsThe checklist and the explanation of each item are presented in Table 1 . The BePRECISE checklist is intended to complement existing guidelines such as CONSORT 17 , STROBE 18 and PRISMA (Preferred Reporting System for Systematic Reviews and Meta-Analyses) 19 . These reporting guidelines use the terms ‘precision medicine’ and ‘personalized medicine’ as defined in the ‘Second international consensus report on gaps and opportunities for the clinical translation of precision diabetes medicine’ 3 , as follows: ‘Precision medicine focuses on minimizing errors and improving accuracy in medical decisions and health recommendations. It seeks to maximize efficacy, cost-effectiveness, safety, access for those in need and compliance compared with contemporary evidence-based medicine. Precision medicine emphasizes tailoring diagnostics or therapeutics (prevention or treatment) to subgroups of populations sharing similar characteristics.’ Personalized medicine refers to ‘the use of a person’s own data to objectively gauge the efficacy, safety, and tolerability of therapeutics, and, subjectively, to tailor health recommendations and/or medical decisions to the individual’s preferences, circumstances, and capabilities’. Accordingly, personalized medicine can be viewed as being nested within the broader concept of precision medicine. Equity and PPIE (E1–E4)Equity, diversity and inclusivity considerations and the involvement of patients and public is a crosscutting theme in this checklist. Where relevant, papers should include a description of how equity has been considered, including diversity and inclusivity of study participants, and whether there was PPIE. Cohort selection biases and probable risks when extrapolating the study’s results to other populations should be clearly described. The selection of participants should consider racial, ethnic, ancestral, geographic and sociodemographic characteristics 20 , and include an explanation for the inclusion or exclusion of groups that are typically under-represented in clinical research (E1 and E2). Race and ethnicity are social constructs but, as they are categories recognized by some government and health authorities in contexts that are relevant to precision medicine, we have elected to retain inclusion of these somewhat controversial terms here. PPIE in any part of the study should be described, including but not limited to design, conduct and reporting (E3). Where possible, and ideally with guidance from those with lived experience, the potential impact of the research findings on the target population(s) should be discussed (E4). Consider co-writing these aspects with PPIE representatives. Title and abstract (1.1–1.4)In the title and/or abstract, the term ‘precision medicine’ should be included to highlight that the research is relevant to precision medicine (1.1). Given that precision medicine is an approach that can be used in several research contexts, the study design (for example, randomized clinical trial (RCT), retrospective observational) and the research question should be stated clearly (1.2). Use of the terms ‘prevention’, ‘diagnostics’, ‘treatment’ or ‘prognostics’ is needed to highlight which pillar of precision medicine the study concerns 3 (1.3). To ensure transparency about generalizability and/or applicability of the findings to a specific population or subgroup, the study population must be described (1.4). Background and objectives (2.1–2.2)The background should clearly describe the rationale for the chosen precision medicine approach, including the context and prior work that led to it and the specific hypothesis being tested (2.1). To provide the reader with greater context, papers should also state the nature and objective of the precision medicine study as ‘etiological’, ‘discovery’, ‘predictive’ and/or ‘confirmatory’ (2.2). Methods (general)Although this reporting guide focuses on clarifying elements of papers that are germane to precision medicine, authors are strongly encouraged to ensure that methods also adhere to other appropriate reporting guidelines (for example, CONSORT and STROBE), with the overarching goal of ensuring that the study protocol described therein could, in principle, be accurately reproduced by third-party investigators. Methods (3.1–3.7)Methods should describe the aspects of a study design relating to precision medicine in such detail that the design can be understood and replicated (3.1). The rationale for the choice of primary outcome should be clearly stated (3.2). To enable readers to assess bias and interpret the study findings, this section should state how the participants were identified and enrolled in the study (4.1) and (if applicable) how a subset of a broader group of participants was selected from an existing study (3.3). Any markers used for stratification or prediction should be explicitly stated with an explanation of how the marker(s) was(were) chosen (3.4). The sample size and how it was derived should be described, for example, following a priori power calculations, or if the sample size was limited primarily by availability or cost, and any implications that this might have for type 2 error (3.5). Authors should also describe attempts to minimize false-positive discovery, especially when multiple testing has occurred (3.5). If any replication and/or validation analyses were undertaken, a clear description should be given of the approach, including whether these analyses were planned and relevant datasets identified before or after conclusion of primary analyses (3.6), in addition to justification for the sample size and choice of replication cohort (3.7). Results (4.1–4.4)The number of participants in the study should be provided, along with a table of baseline characteristics (4.1). If the analysis involves comparison (rather than discovery) of subgroups, the baseline characteristics and numbers of participants should be provided by the subgroup. Results from any statistical tests done should be reported. Any comparisons of subgroups should include appropriate test statistics, which may include tests of interaction and heterogeneity, and in cluster analyses tests of probability for cluster assignment (for example, relative entropy statistic) (4.2). Key findings should be benchmarked against current reference standards or practice, if they exist, so that the reader can determine the likely benefit of translating the study’s findings into clinical practice. This may include, for example, the comparison of the new and existing approaches using tests of discriminative (cross-sectional) or predictive (prospective) accuracy, or estimation of net reclassification or changes in numbers needed to treat. If benchmarking has not been done, a clear explanation should be given (4.3). If validation and/or replication analyses were undertaken, the results of all such attempts at analyses should be clearly described (4.4). Discussion (5.1–5.2)The paper should include a balanced and nuanced discussion of any limitations to the interpretation and/or implementation of the reported findings. The limitations section should consider biases that might prevent fair and equitable generalization of the study’s findings to other populations, particularly to groups that are under-represented within the published literature. Authors are also encouraged to consider other potential biases that might arise with stratified and subgroup analyses (5.1). If there is a direct clinical implication of the study’s findings, authors should describe how their findings might be applied in clinical practice. This might, for example, include an explanation of how any algorithms, technologies or risk markers that stem directly from the research might benefit clinical practice. The BePRECISE guidelines are intended to enhance publication of research on precision medicine by improving quality and standardization of reporting. In turn, it is anticipated that this will help improve and accelerate the impact of precision medicine research on the health and well-being of target populations and individuals. BePRECISE was initiated to follow up on recommendations from the ‘Second international consensus report on gaps and opportunities for the clinical translation of precision diabetes medicine’ 3 . The report, founded on 16 systematic evidence reviews summarizing research described in >100,000 published papers, found a low degree of standardization across the published literature, with a broad absence of key information needed for benchmarking against contemporary standards, validation analyses and meaningful interpretation of research findings. Implementation of the checklistThese reporting guidelines were derived through structured evaluation and consensus processes undertaken by subject-matter experts in precision medicine for complex traits. The report is premised on cardiometabolic disease translational research but is relevant to translation of research in other complex diseases. These guidelines are directed toward authors describing translational research in precision medicine, as well as for journal editors handling submissions in this field. These guidelines may also be of value to funding agencies, policy advisers and health educators. The BePRECISE guidelines are designed to be used together with existing study-specific checklists such as CONSORT 17 , STROBE 18 and STORMS (Strengthening the Organization and Reporting of Microbiome Studies) 21 . Publications relevant to precision medicine cover diverse topics and study designs; thus, to accommodate this diversity, we recommend that authors elaborate on relevant details related to checklist items to facilitate manuscript evaluations by journal editors and peer reviewers who will determine whether a given paper has addressed the BePRECISE checklist criteria. Health equityPrecision medicine has the potential to improve health equity by making health advice and medical therapies more accessible to those in most need and by being more effective and acceptable to the recipient than contemporary clinical approaches. Nevertheless, as the ‘inverse care law’ 22 highlights, the best healthcare often reaches those who need it least. We believe that precision medicine research should place emphasis on the development of solutions for people in greatest need, regardless of who or where they are. Ensuring representation of underserved populations, where the disease burden can be high, is important because determining the effectiveness of precision medicine solutions requires data from the target populations. Research in population genetics provides clear evidence of this, where the predictive accuracy of polygenic burden scores can be low when applied outside the data-source population, even when these populations are geographically proximal 23 , 24 . Raising awareness of these challenges by discussing them in the health literature and, ultimately, by addressing them through improved study design could facilitate enhancement of health equity using precision medicine approaches. Promoting equity through precision medicine requires awareness of the many biases. For this reason, the BePRECISE guidelines place emphasis on equity, diversity and inclusion as an overarching concept throughout the checklist. As with health equity, the BePRECISE guidelines position PPIE as a crosscutting theme to motivate its consideration in all elements of precision medicine translational research. We encourage those using the BePRECISE checklist to follow existing guidance on PPIE 25 . Ensuring that the eventual recipients of precision medicine solutions are adequately represented in the planning, execution and reporting of precision medicine research will help maximize the translational value of the research. Ideally, research teams should include members of the communities that will eventually benefit from this work, including in leadership roles, although to achieve this will often require long-term capacity strengthening. This engagement will help ensure that the relevance and utility of the research output are maximized. It will also strengthen the potential for target populations to determine their own health trajectories. Where this is not immediately achievable, establishing authentic partnerships with representatives from these target populations should be prioritized. This may involve community consultations, training opportunities and co-creation of research proposals with assigned community members, through dissemination and translation of research findings. Moreover, the selection of study participants should be done equitably and result in study cohorts that are representative of the populations who are the focus of the research 26 . The use of patient-reported outcome measures and patient-reported experience measures should be considered during the research design and execution phases, and reported in research papers wherever possible following established guidelines 27 , 28 . Doing so will amplify the patient voice and maximize the relevance of the research to the target populations and individuals. Cost-effectivenessThe translation of precision medicine research into practice will invariably depend on it being cost-effective, affordable and accessible. This initial version of the BePRECISE checklist does not include checklist items pertaining directly to these important factors. The consensus view was that such analyses are sufficiently complex to stand alone and are likely to be outside the scope of most current precision medicine research. This topic may be revisited in subsequent versions of the checklist. Strengths and limitationsWe believe that implementation of the BePRECISE checklist in the context of academic publishing will strengthen standardization of reporting across precision medicine research, ultimately enabling improved and equitable translation of research findings into the clinical and public health settings. The checklist will also encourage investigators to improve study design, particularly with respect to health equity. Other strengths include rigor of our consensus methods and the diverse range of societal backgrounds and expertise of our group. We acknowledge that precision medicine in many complex diseases is relatively nascent (with the exception of precision oncology), with the needs of the field and stakeholders evolving. We plan to evaluate uptake of the checklist among journals and authors to assess whether items should be added or removed from the checklist as the field matures. An additional limitation is that the BePRECISE consensus group is small by comparison with similar efforts in other fields of research. We will involve a larger group of experts with broader global and technical representation in future efforts, including increased representation from low- and middle-income countries and individuals with more diverse lived experiences. Additional technical expertise may also be needed from other disciplines, including health economics and health systems administration, for example. We acknowledge that journal formatting requirements and procedures may not always entirely align with the checklist specifications. We removed a checklist item for provision of a plain language summary, for example, because many journal formats are presently unable to accommodate this type of additional material. However, we hope that in the future editors and publishers of medical and scientific journals will include space for this incredibly important component that facilitates scientific communication with the public. We defer to editorial and reviewer discretion in implementation of the BePRECISE checklist. Although the BePRECISE checklist items are included to support best scientific practices, at least in the short term, some ongoing precision medicine studies will not have addressed the health equity or PPIE considerations in their design. We do not expect that insufficient attention to these items would be a sole reason for not considering a manuscript for review, unless blatant disregard for participant and/or community safety, privacy or respect has occurred in the study design and/or conduct. Over time, however, we hope that health equity and PPIE will be considered as standard practice in precision medicine research and implementation. ConclusionsThe BePRECISE reporting guidelines have been generated through a structured consensus process to address the need for better reporting of clinical translational research in precision medicine in common complex diseases. The burgeoning literature on this topic is reported inconsistently, impeding the assimilation, syntheses and interpretation of evidence. There is a general lack of benchmarking against contemporary standards, a situation that makes it impossible to determine whether new precision medicine approaches might be beneficial, feasible and sustainable. Moreover, very little existing precision medicine research has incorporated PPIE or focused on the groups within societies most in need of innovative precision medicine solutions. These barriers limit the positive impact that precision medicine could have on the health and well-being of those most in need. The BePRECISE reporting guidelines are intended to help address these and other important challenges. Consortium structureThe BePRECISE Consortium comprised an executive oversight committee (S.S.L., Z.S.-A., M.L.M., A.H.N., S.S.R., J.L.S. and P.W.F.), which oversaw the full process, with representation across key domain areas, and an evidence evaluation group (Z.S.-A., M.L.M., A.A., H.F., M.-F.H., M.F.G., J.M., D.K.T., M.I.T., S.S.R., J.L.S. and P.W.F.), which undertook the scoping review to determine current reporting standards. All consortium members participated in a Delphi consensus process 29 . The Consortium chair and co-chair were P.W.F. and S.S.L., respectively (Supplementary Table 1 ). Protocols and registrationsA scoping review protocol was developed before initiating the literature review or consensus activities and was registered in the Open Science Framework (http://osf-registrations-nh4g2-v1). The consensus process followed the EQUATOR (Enhancing the QUAlity and TRansparency of health Research) Network recommendations for reporting guidelines development ( https://www.equator-network.org/library/equator-network-reporting-guideline-manual ) and was registered with EQUATOR as ‘Reporting guidelines under development’ ( https://www.equator-network.org/library/reporting-guidelines-under-development/reporting-guidelines-under-development-for-other-study-designs ). The final BePRECISE guidelines are available on the Equator website ( https://www.equator-network.org/reporting-guidelines/ ). The purpose of the scoping review was to determine whether the published literature on precision medicine in cardiometabolic diseases met a minimum threshold for reporting quality. We set the minimum expectation as a condition where most (that is, ≥50%) published papers in this domain are adequately reported. To define a study as adequately or inadequately reported (as a binary variable), members of the scoping review committee identified, through consultation, 11 key items (Supplementary Tables 2 and 3 ). Papers that met all 11 reporting criteria were deemed, a priori, to be adequately reported. The checklist items used to assess the reporting quality of studies captured in the scoping review were determined before the Delphi surveys were undertaken. These scoping review checklist items correspond with some of those used in the Delphi surveys that formed the basis of the final BePRECISE checklist, because both the scoping review and Delphi surveys are, to varying degrees, derived from the findings of the ‘Second international consensus report on gaps and opportunities for the clinical translation of precision diabetes medicine’ 3 . The scoping review was intended to provide a snapshot of the quality of reporting in a subset of literature relating to precision medicine. It was not undertaken to inform the items in the BePRECISE checklist; this purpose was served by the systematic evidence reviews 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 and the Consensus report 3 described above. Based on the findings of the precision diabetes medicine Consensus report 3 , we hypothesized that no more than 30% of currently published studies are adequately reported. This assumption was tested by full text reviewing a statistically powered, random subsample of published papers on precision medicine across cardiometabolic diseases (ʻSearch strategyʼ and ʻSample size estimationʼ). This scoping review was conducted in accordance with the PRISMA Extension for Scoping Review guidelines 30 to identify and assess the current literature on precision medicine in cardiometabolic diseases and was completed before the ‘guidelines consensus process’ described below. Sample size estimationThe literature search was not intended to be a comprehensive evaluation of the published evidence, but instead to provide an unbiased representation of this literature. To determine how many papers should be reviewed as a representative sample of the published literature, an a priori sample size calculation was performed using SAS software v.9.4 (SAS Institute). Given the scenario described, we used a two-sided test with a type 1 error threshold (critical α) of 0.05, assuming a null hypothesis proportion of 0.50, which corresponds to our minimum expectation, an expected number of adequately reported papers of <30% and nominal power of 80%. This calculation determined that 47 randomly selected papers should be full text reviewed to ascertain whether the assumed proportion of adequately reported studies is significantly lower than the prespecified null proportion (that is, to infer that the quality of papers reported in this field is lower than the minimum expectation). Search strategyWe searched the PubMed database ( https://pubmed.ncbi.nlm.nih.gov ) to identify relevant articles published in the past 5 years (January 2019 to January 2024). The search strategy incorporated keywords and terms ( https://www.ncbi.nlm.nih.gov/mesh ) in human epidemiological cohorts and clinical trials representing: (1) precision medicine, (2) cardiometabolic diseases and (3) clinical translation (see Supplementary Methods for the detailed search strategy). The search was constrained to publications written in English. Conference abstracts, case reports, study protocols, reviews and animal studies were excluded. Study selection and quality assessmentCovidence software ( https://www.covidence.org ; Veritas Health Innovation) was used to manage the scoping review selection process. Studies were filtered in three stages: (1) removal of duplicate publications; (2) ascertainment of study eligibility based on title and abstract by at least two independent reviewers; and (3) full text review of 47 randomly selected studies, where at least 2 independent reviewers assessed the eligibility of each publication according to the inclusion and exclusion criteria. Each paper was further evaluated to determine whether it met the 11 predetermined quality criteria. Any conflicts were subsequently resolved by an independent reviewer. Consensus processThe five-step consensus process was based on a modified Delphi and nominal group technique 29 . The consensus process involved: (1) completion of an initial Delphi survey (6–13 February 2024); (2) a consensus meeting (15–16 February 2024); and (3) a second Delphi survey (19–26 February 2024). Finalization of the checklist was conducted at a second consensus meeting by the executive oversight committee (5–6 March 2024), who reviewed the voting of all rounds of the Delphi survey, made final decisions about item inclusion and refined wording of the BePRECISE checklist. The executive oversight committee also evaluated the checklist against two publications on precision medicine determined through the scoping review to be of high and low quality, respectively. The final version of the checklist was circulated to all panel members for consultation and approval (13–19 March 2024). The items in the first iteration of Delphi survey 1 were derived from existing checklists: CONSORT 17 , STROBE 18 , CONSORT-Equity 2017 extension 31 and STrengthening the REporting of Genetic Association Studies (STREGA)—an extension of the STROBE guidelines 32 . Additional items specific to precision medicine were generated based on the reporting gaps identified from the series of systematic reviews (11 published) that underpinned the ‘Second international consensus report on gaps and opportunities for the clinical translation of precision diabetes medicine’ 3 . The draft of Delphi survey 1 was presented to the full panel at a roundtable discussion followed by co-development with the full panel through an online document-sharing platform. The final items for Delphi survey 1, including the input sources for its development, are shown in Supplementary Table 3 . The Delphi survey response scale had five options: ‘Completely inappropriate’, ‘Somewhat inappropriate’, ‘Neither appropriate nor inappropriate’, ‘Somewhat appropriate’ and ‘Completely appropriate’. The consensus threshold was defined a priori as at least 80% of the panel voting for ‘Completely appropriate’ or ‘Somewhat appropriate’. Items with voting scores under this consensus threshold were discussed at the Consensus meetings. The Delphi surveys were administered online and were anonymous. Panelists were invited to provide free-text comments to suggest new items (survey 1 only), suggest a change of wording for a given item or justify their voting decision. The voting scores and anonymous comments for each item from the previous consensus round were provided to panelists at the subsequent rounds, such that consensus was reached iteratively. Delphi panel and executive oversight committeeThe BePRECISE checklist panelists cover the core areas of expertise outlined in the EQUATOR Network recommendations for reporting guidelines development ( https://www.equator-network.org/library/equator-network-reporting-guideline-manual ). The panel includes subject-matter experts across relevant disease areas and with expertise in the topics highlighted as gaps in the ‘Second international consensus report on gaps and opportunities for the clinical translation of precision diabetes medicine’. Moreover, the BePRECISE panelist selection focused on ensuring diversity: (1) global representation (Europe, North America, sub-Saharan Africa and Australia); (2) career stages (23% early career researchers within 10 years of research experience, 27% of mid-career researchers of 11–15 years of experience and 50% of senior researchers of >20 years of experience); and (3) gender (55% of authors being female). Accordingly, the Delphi panel comprised subject-matter experts in key cardiometabolic disorders (diabetes, obesity, cardiovascular disease, fatty liver disease, renal disease), statistics, study design (epidemiologists and clinical trialists), journal editorial, lived experience, benchmarking and technology, education and translation, health equity, community engagement and clinical practice. Several of these experts are based in or have worked extensively with investigators in low- and middle-income countries (M.R., N.S., J.L.S. and P.W.F.). The executive oversight committee for this report consisted of multidisciplinary experts in cardiometabolic disorders, equity research, medical journal editorial and lived experience (P.W.F., S.S.L., S.S.R., J.L.S., A.H.N., Z.S.A. and M.L.M.). Chung, W. K. et al. Precision medicine in diabetes: a consensus report from the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 43 , 1617–1635 (2020). Article CAS PubMed PubMed Central Google Scholar Chung, W. K. et al. Precision medicine in diabetes: a consensus report from the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 63 , 1671–1693 (2020). Article PubMed PubMed Central Google Scholar Tobias, D. K. et al. Second international consensus report on gaps and opportunities for the clinical translation of precision diabetes medicine. Nat. Med. 29 , 2438–2457 (2023). GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396 , 1204–1222 (2020). Article Google Scholar Sun, H. et al. IDF diabetes atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res. Clin. Pract. 183 , 109119 (2022). Article PubMed Google Scholar Ahmad, A. et al. Precision prognostics for cardiovascular disease in type 2 diabetes: a systematic review and meta-analysis. Commun. Med. 4 , 11 (2024). Semnani-Azad, Z. et al. Precision stratification of prognostic risk factors associated with outcomes in gestational diabetes mellitus: a systematic review. Commun. Med. 4 , 9 (2024). Francis, E. C. et al. Refining the diagnosis of gestational diabetes mellitus: a systematic review and meta-analysis. Commun. Med. 3 , 185 (2023). Misra, S. et al. Precision subclassification of type 2 diabetes: a systematic review. Commun. Med. 3 , 138 (2023). Benham, J. L. et al. Precision gestational diabetes treatment: a systematic review and meta-analyses. Commun. Med. 3 , 135 (2023). Felton, J. L. et al. Disease-modifying therapies and features linked to treatment response in type 1 diabetes prevention: a systematic review. Commun. Med. 3 , 130 (2023). Murphy, R. et al. The use of precision diagnostics for monogenic diabetes: a systematic review and expert opinion. Commun. Med. 3 , 136 (2023). Lim, S. et al. Participant characteristics in the prevention of gestational diabetes as evidence for precision medicine: a systematic review and meta-analysis. Commun. Med. 3 , 137 (2023). Jacobsen, L. M. et al. Utility and precision evidence of technology in the treatment of type 1 diabetes: a systematic review. Commun. Med. 3 , 132 (2023). Semple, R. K., Patel, K. A., Auh, S., Ada/Easd, P. & Brown, R. J. Genotype-stratified treatment for monogenic insulin resistance: a systematic review. Commun. Med. 3 , 134 (2023). Naylor, R. N. et al. Systematic review of treatment of beta-cell monogenic diabetes. Preprint at medRxiv https://doi.org/10.1101/2023.05.12.23289807 (2023). Schulz, K. F., Altman, D. G., Moher, D.& the CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. PLoS Med. 7 , e1000251 (2010). Cuschieri, S. The STROBE guidelines. Saudi J. Anaesth. 13 , S31–S34 (2019). Page, M. J. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br. Med. J. 372 , n71 (2021). O’Neill, J. et al. Applying an equity lens to interventions: using PROGRESS ensures consideration of socially stratifying factors to illuminate inequities in health. J. Clin. Epidemiol. 67 , 56–64 (2014). Mirzayi, C. et al. Reporting guidelines for human microbiome research: the STORMS checklist. Nat. Med. 27 , 1885–1892 (2021). Hart, J. T. The inverse care law. Lancet i , 405–412 (1971). Kamiza, A. B. et al. Transferability of genetic risk scores in African populations. Nat. Med. 28 , 1163–1166 (2022). Choudhury, A. et al. Meta-analysis of sub-Saharan African studies provides insights into genetic architecture of lipid traits. Nat. Commun. 13 , 2578 (2022). Aiyegbusi, O. L. et al. Considerations for patient and public involvement and engagement in health research. Nat. Med. 29 , 1922–1929 (2023). Article CAS PubMed Google Scholar Retzer, A. et al. A toolkit for capturing a representative and equitable sample in health research. Nat. Med. 29 , 3259–3267 (2023). Calvert, M. et al. Reporting of patient-reported outcomes in randomized trials: the CONSORT PRO extension. J. Am. Med. Assoc. 309 , 814–822 (2013). Article CAS Google Scholar Calvert, M. et al. Guidelines for inclusion of patient-reported outcomes in clinical trial protocols: the SPIRIT-PRO extension. J. Am. Med. Assoc. 319 , 483–494 (2018). Rankin, N. M. et al. Adapting the nominal group technique for priority setting of evidence-practice gaps in implementation science. BMC Med. Res. Methodol. 16 , 110 (2016). Tricco, A. C. et al. PRISMA extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann. Intern. Med. 169 , 467–473 (2018). Welch, V. A. et al. CONSORT-Equity 2017 extension and elaboration for better reporting of health equity in randomised trials. Br. Med. J. 359 , j5085 (2017). Little, J. et al. STrengthening the REporting of Genetic Association studies (STREGA)—an extension of the STROBE statement. Eur. J. Clin. Invest. 39 , 247–266 (2009). Download references AcknowledgementsAs a PPIE representative from Australia, A.H.N. was remunerated by the Cardiometabolic Health Implementation Research in Postpartum women (CHIRP) consumer group, Eastern Health Clinical School, Monash University according to the Monash Partners Remuneration and Reimbursement Guidelines for Consumer and Community Involvement Activity. The Covidence license was paid for in part by Lund University’s Medical Library (Faculty of Medicine, Lund University, Lund, Sweden). Z.S.-A. was supported by the Canadian Institutes of Health Research Fellowship; M.L.M. by the Italian Ministry of Health Grant ‘Ricerca Finalizzata 2019’ (no. GR-2019-12369702); A.A. by Swedish Heart–Lung Foundation (grant no. 20190470), Swedish Research Council (2018-02837), EU H2020-JTI-lMl2-2015-05 (grant no. 115974—BEAt-DKD) and HORIZON-RIA project (grant no. 101095146—PRIME-CKD); H.F. by EU H2020-JTI-lMl2-2015-05 (grant no. 115974—BEAt-DKD) and HORIZON-RIA project (grant no. 101095146—PRIME-CKD). J.M.D. is a Wellcome Trust Early Career Fellow (no. 227070/Z/23/Z) and is supported by the Medical Research Council (UK) (grant no. MR/N00633X/1) and the National Institute for Health and Care Research (NIHR), Exeter Biomedical Research Centre. The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care. R.J.F.L. is employed at the Novo Nordisk Foundation Center for Basic Metabolic Research, which is supported by grants from the Novo Nordisk Foundation (nos. NNF23SA0084103 and NNF18CC0034900), and in addition by personal grants from the Novo Nordisk Foundation (Laureate award no. NNF20OC0059313) and the Danish National Research Fund (Chair DNRF161). M.R. is a South African Research Chair on the Genomics and Bioinformatics of African Populations, funded by the Department of Science and Innovation. N.S. is Chair of the Obesity Mission for the Office of Life Science, UK Government. M.F.G. is supported by the Swedish Research Council (EXODIAB, no. 2009-1039), Swedish Foundation for Strategic Research (LUDC-IRC, no. 15-0067) and EU H2020-JTI-lMl2-2015-05 (grant no. 115974—BEAt-DKD). A.H.N’.s salary is supported by funding from the Medical Research Future Fund and Monash Centre for Health Research and Implementation. S.S.R. is supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases (no. R01 DK122586), the Juvenile Diabetes Research Foundation (no. 2-SRA-202201260-S-B) and the Leona M. and Harry B. Helmsley Charitable Trust (no. 2204–05134). P.W.F. is supported by grants from the Swedish Research Council (no. 2019-01348), the European Commission (ERC-2015-CoG-681742-NASCENT), and Swedish Foundation for Strategic Research (no. LUDC-IRC, 15-0067). Author informationAuthors and affiliations. Health Systems and Equity, Eastern Health Clinical School, Monash University, Box Hill, Victoria, Australia Siew S. Lim & Jacqueline Boyle Department of Nutrition, Harvard T.H. Chan School of Public Health, Boston, MA, USA Zhila Semnani-Azad, Deirdre K. Tobias & Paul W. Franks Unit of Metabolic Disease, University-Hospital of Padua, Padua, Italy Mario L. Morieri Department of Medicine, University of Padua, Padua, Italy Monash Centre for Health Research Implementation, Monash University and Monash Health, Melbourne, Victoria, Australia Ashley H. Ng Monash Partners Academic Health Science Centre, Melbourne, Victoria, Australia Precision Healthcare University Research Institute, Queen Mary University of London, London, UK Ashley H. Ng & Claudia Langenberg Diabetic Complications Unit, Department of Clinical Sciences, Lund University Diabetes Centre, Malmo, Sweden Abrar Ahmad, Hugo Fitipaldi & Maria F. Gomez Board of Directors, Steno Diabetes Center, Copenhagen, Denmark Christian Collin Department of Clinical and Biomedical Sciences, University of Exeter Medical School, Exeter, UK John M. Dennis Computational Medicine, Berlin Institute of Health at Charité—Universitätsmedizin Berlin, Berlin, Germany Claudia Langenberg Novo Nordisk Foundation Center for Basic Metabolic Research, Faculty of Health and Medical Sciences, University of Copenhagen, Copenhagen, Denmark Ruth J. F. Loos & Jordi Merino Charles Bronfman Institute for Personalized Medicine, Icahn School of Medicine at Mount Sinai, New York, NY, USA Ruth J. F. Loos Diabetes Australia, Canberra, Australian Capital Territory, Australia Melinda Morrison Sydney Brenner Institute for Molecular Bioscience, University of the Witwatersrand, Faculty of Health Sciences, Johannesburg, South Africa Michele Ramsay Division of Gastroenterology, Hepatology and Nutrition, Virginia Commonwealth University School of Medicine, Richmond, VA, USA Arun J. Sanyal School of Cardiovascular and Metabolic Health, University of Glasgow, Glasgow, UK Naveed Sattar Division of Chronic Disease Research Across the Lifecourse, Department of Population Medicine, Harvard Medical School, Harvard Pilgrim Health Care Institute; Diabetes Unit, Massachusetts General Hospital, Boston, MA, USA Marie-France Hivert Diabetes Unit, Endocrine Division, Massachusetts General Hospital, Boston, MA, USA Jordi Merino Center for Genomic Medicine, Massachusetts General Hospital, Boston, MA, USA Novo Nordisk Foundation Center for Genomic Mechanisms of Disease, Broad Institute of MIT and Harvard, Cambridge, MA, USA Division of Preventive Medicine, Department of Medicine, Brigham and Women’s Hospital and Harvard Medical School, Boston, MA, USA Deirdre K. Tobias Population Health Sciences Institute, Newcastle University, Newcastle upon Tyne, UK Michael I. Trenell Center for Public Health Genomics, Department of Public Health Sciences, University of Virginia, Charlottesville, VA, USA Stephen S. Rich School of Public Health, Imperial College London, London, UK Jennifer L. Sargent Department of Clinical Sciences, Lund University, Helsingborg, Sweden Paul W. Franks You can also search for this author in PubMed Google Scholar ContributionsS.S.L. (co-chair), Z.S.-A., M.L.M., A.H.N., S.S.R., J.L.S. and P.W.F. (chair) formed the executive oversight committee. Z.S.-A. (lead), M.L.M., A.A., H.F., M.-F.H., M.F.G., J.M., D.K.T., M.I.T., S.S.R., J.L.S. and P.W.F. formed the evidence evaluation group. S.S.L. (lead), Z.S.-A., M.L.M., A.A., H.F., J.B., C.C., J.M.D., C.L., R.J.F.L., M.M., M.R., A.J.S., N.S., M.-F.H., M.F.G., J.M., D.K.T., M.I.T., A.H.N., S.S.R., J.L.S. and P.W.F. formed the consensus review panel. A.H.N. and C.C. were the PPIE representatives. S.S.L., Z.S.-A., M.L.M., A.H.N., S.S.R., J.L.S. and P.W.F. wrote the first draft of the manuscript. All the authors edited and approved the final version of the manuscript before submission for journal review. Corresponding authorCorrespondence to Paul W. Franks . Ethics declarationsCompeting interests. M.L.M. has consulted for and/or received speaker honoraria from Amarin, Amgen, AstraZeneca, Boehringer Ingelheim, Daichi, Eli Lilly, Merck Sharp & Dohme, Novo Nordisk, Novartis and Servier. In the past 5 years, A.H.N. has received an investigator-initiated grant from Abbott Diabetes Care and consulting honoraria from Roche Diabetes Care, Australia and the Australian Diabetes Educators Association. There are no perceived conflicts from previous involvements on this work. C.C. is a member of the Board of Directors for the Steno Diabetes Center in Copenhagen, Denmark. The views expressed in this paper do not necessarily reflect those of the Steno Center. M.R. is a consultant on the Genentech. ‘One Roche: Race, Ethnicity and Ancestry (“REA”) Initiative’. A.J.S. received research grants (paid to the institution) from: Intercept, Lilly, Novo Nordisk, Echosense, Boehringer Ingelhiem, Pfizer, Merck, Bristol Myers Squibb, Hanmi, Madrigal, Galmed, Gilead, Salix and Malinckrodt; was a consultant for Intercept, Gilead, Merck, NGM Bio, Terns, Regeneron, Alnylam, Amgen, Genentech, Pfizer, Novo Nordisk, AstraZeneca, Salix, Malinckrodt, Lilly, Histoindex, Path AI, Rivus, Hemoshear, Northsea, 89Bio, Altimmune, Surrozen and Poxel; and had ownership interests in Tiziana, Durect, Exhalenz, GENFIT, Galmed, Northsea and Hemoshear. N.S. has consulted for and/or received speaker honoraria from Abbott Laboratories, AbbVie, Amgen, AstraZeneca, Boehringer Ingelheim, Eli Lilly, Hanmi Pharmaceuticals, Janssen, Menarini-Ricerche, Novartis, Novo Nordisk, Pfizer, Roche Diagnostics and Sanofi; and received grant support (paid to the institution) from AstraZeneca, Boehringer Ingelheim, Novartis and Roche Diagnostics outside the submitted work. M.F.G. received financial and nonfinancial (in-kind) support (paid to the institution) from Boehringer Ingelheim Pharma, JDRF International, Eli Lilly, AbbVie, Sanofi-Aventis, Astellas, Novo Nordisk, Bayer, within EU grant H2020-JTI-lMl2-2015-05 (grant no. 115974—BEAt-DKD); also received financial and in-kind support from Novo Nordisk, Pfizer, Follicum, Coegin Pharma, Abcentra, Probi and Johnson & Johnson, within a project funded by the Swedish Foundation for Strategic Research on precision medicine in diabetes (LUDC-IRC no. 15-0067); and received personal consultancy fees from Lilly and Tribune Therapeutics AB. M.I.T. has, within the past 5 years, received consulting/honoraria from the Novo Nordisk Foundation, Abbott Nutrition, Changing Health and DAISER. This work is independent and does not represent the opinions of these organizations. S.S.R. has received consulting honoraria from Westat and investigator-initiated grants from the US National Institutes of Health, the Juvenile Diabetes Research Foundation and the Leona M. and Harry B. Helmsley Charitable Trust. J.L.S. receives consulting fees from the World Health Organization and the University of Bergen. This work was done outside these roles and the opinions expressed in these guidelines do not necessarily reflect those of the World Health Organization or the University of Bergen. J.L.S. was deputy editor of Nature Medicine until December 2023. She left employment at Springer Nature before any of her work on this Consensus Statement was initiated. P.W.F. was an employee of the Novo Nordisk Foundation at the time that these guidelines were written, although this work was done entirely within his academic capacity. The opinions expressed in these guidelines do not necessarily reflect those of the Novo Nordisk Foundation. Within the past 5 years, he has received consulting honoraria from Eli Lilly, Novo Nordisk Foundation, Novo Nordisk, UBS and Zoe, and previously had other financial interests in Zoe. He has also received investigator-initiated grants (paid to the institution) from numerous pharmaceutical companies as part of the Innovative Medicines Initiative of the European Union. The remaining authors declare no competing interests. J.A.B. received royalties from Elsevier as an editor on a medical textbook that does not impact this work. A.J.S. has stock options in Rivus, is a consultant to Boehringer Ingelhiem and Akero, and has grants from Takeda. Peer reviewPeer review information. Nature Medicine thanks Jose Florez and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editor: Joao Monteiro, in collaboration with the Nature Medicine team. Additional informationPublisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Supplementary informationSupplementary information, rights and permissions. Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law. Reprints and permissions About this articleCite this article. Lim, S.S., Semnani-Azad, Z., Morieri, M.L. et al. Reporting guidelines for precision medicine research of clinical relevance: the BePRECISE checklist. Nat Med 30 , 1874–1881 (2024). https://doi.org/10.1038/s41591-024-03033-3 Download citation Received : 21 March 2024 Accepted : 29 April 2024 Published : 19 July 2024 Issue Date : July 2024 DOI : https://doi.org/10.1038/s41591-024-03033-3 Share this articleAnyone you share the following link with will be able to read this content: Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative Quick links
Sign up for the Nature Briefing: Translational Research newsletter — top stories in biotechnology, drug discovery and pharma.  | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
IMAGES
VIDEO
COMMENTS
The importance of good documentation practice needs to be emphasized to investigator sites to ensure that the study results are built on the foundation of credible and valid data. This article focuses on the key principles of good documentation practice and offers suggestions for improvement. ... Clinical research documentation involves a ...
Additionally, good documentation practices in source documentation are an essential part of a well-run clinical trial. Source documents are medical records providing documentation prior to, during ...
A ccurateAccurate, consistent and real representation. C ompleteThe information should be complete (i.e., to answer who, what, when, where, why, and how).- All of the elements of the acronym ALCOA must be applied to both paper and electronic source data, and the records that hold. hat data. Serving as evidence of the events that took place ...
The Department of Medicine Clinical Research Unit has prepared this document is to provide guidance to all faculty and staff involved in the conduct of research on the best practices related to documentation. Good study documentation will allow for an individual with basic knowledge of the particular project to recreate the events of the study.
The importance of good documentation practice needs to be emphasized to investigator sites to ensure that the study results are built on the foundation of credible and valid data. This article focuses on the key principles of good documentation practice and offers suggestions for improvement. Keywords: ALCOA; documentation; source; training ...
Good Clinical Research Practice (GCP) is a process that incorporates established ethical and scientifi c quality standards for the design, ... ating valid observations and sound documentation of the fi ndings, GCP not only serves the interests of the parties actively involved in the research process, but also protects the rights, safety and ...
Good Clinical Practice is intended to be an international scientific quality standard for designing, conducting, monitoring, recording, auditing, analyzing and reporting clinical studies ...
The version of ICH E6 Guidelines on Good Clinical Practice (GCP) published in November 2016 defines Documentation as "All records in any form (including, but not limited to, written, electronic, magnetic, and optical records, and scans, x-rays, and electrocardiograms) that describe or record the methods, conduct, and/or results of a trial, the factors affecting a trial, and the actions taken."
Documentation in clinical trials adheres to the principles of Good Clinical Practice (GCP), and healthcare professionals involved in the conduct of clinical trials—including students—are obliged to perform documentation in accordance with GCP principles. Unprecedented challenges have arisen with regard to the appropriate training of ...
Similarly, source documentation issues ranked 5th among the top 10 findings from European Medicines Agency (EMA) inspections of investigator sites in 2009 [ 1] and in some instances the findings were classified 'critical'. Not surprisingly, clinical trial monitors and auditors also report documentation issues as a frequent area of GCP concern.
Introduction. Clinical documentation is the process of creating a text record that summarizes the interaction between patients and healthcare providers during clinical encounters [].The quality of clinical documentation is important as it impacts quality of patient care, patient safety, and the number of medical errors [2-4].Furthermore, clinical documentation is increasingly used for other ...
The importance of good documentation practice needs to be emphasized to investigator sites to ensure that the study results are built on the foundation of credible and valid data. This article focuses on the key principles of good documentation practice and offers suggestions for improvement. One of the most common inspection findings in ...
The importance of good documentation practice needs to be emphasized to investigator sites to ensure that the study results are built on the foundation of credible and valid data. This article focuses on the key principles of good documentation practice and offers suggestions for improvement [1]. Inadequate/misguided case histories shape the ...
The importance of good documentation practice needs to be emphasized to investigator sites to ensure that the study results are built on the foundation of credible and valid data. One of the most common inspection findings in investigator site inspections is lack of reliable, accurate and adequate source documentation. This also happens to be the most common pitfall identified during sponsor ...
Complete -. There should be no empty blanks without notation. • Complete all entries or document why data not obtained. Original. • Investigator should have access to the original source document. Accurate. • The information should be accurate, consistent and real representation of the facts. • All blanks filled in.
Good documentation practice (recommended to abbreviate as GDocP to distinguish from "good distribution practice" also abbreviated GDP) is a term in the pharmaceutical and medical device industries to describe standards by which documents are created and maintained. While some GDocP standards are codified by various competent authorities, others are not but are considered cGMP (with emphasis on ...
This ensures good practices AND allows for source documentation to be available at the time of a data abstraction, monitoring visit or audit. • If at anytime there is conflicting documentation/ discrepancies in source documents a clarification note is required. Examples: • fellow note, dictated note, and/or nursing note have differing
Moreover clinical research happens over a long period of time which adds to the challenge of maintaining continuity in the documentation practice. Inadequacies in documentation could be the result of lack of training and experience in good understanding of clinical research and documentation requirements.
An overview of good documentation practices applicable to those working in the pharmaceutical and healthcare sectors is presented. Discover the world's research 25+ million members
Good documentation practice GDP is a systematic procedure of preparation, reviewing, approving, issuing, recording, storing and archival of documents. The importance of documentation: As per GMP documentation control "If it is not written down, then it did not happen". The document provides information on when, where, who, why and how to ...
The accuracy of clinical documentation has always been crucial for many aspects of healthcare service delivery [].Principles underlying good note-keeping include timeliness, completeness, usefulness, synthesis (e.g., interpretation of findings, and diagnosis), and attention to clinical plans.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY. ... of health professionals had good routine practice documentation; 6.99% of different laboratory test request forms were not completed and documented; 6.025% of the physicians' prediagnosis was completed and documented; 5.54% of drug prescription and laboratory result forms were not ...
For Good Documentation Practice (GDP), ... With more than 16,500 members, the Association of Clinical Research Professionals (ACRP) is the only non-profit organization solely dedicated to representing, supporting, and advocating for clinical research professionals. ACRP supports individuals and life science organizations globally by providing ...
Here we explore the exciting Good documentation practices (DGP) in clinical research and Pharma industry and explain the standards, guidelines and what are c...
The BePRECISE (Better Precision-data Reporting of Evidence from Clinical Intervention Studies & Epidemiology) consortium, comprising 23 experts in precision medicine, cardiometabolic diseases ...