Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Global health
- BMJ Journals

You are here
- Volume 2017, Issue
- Placental abruption leading to hysterectomy
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Hannah Catherine Sylvester ,
- Madeleine Stringer
- Department of Obstetrics and Gynaecology , King Edward Memorial Hospital , Subiaco, Western Australia , Australia
- Correspondence to Dr Hannah Catherine Sylvester, hannah.sylvester{at}trainee.ranzcog.edu.au
A 32-year-old multigravid patient at 21 weeks gestation presents with major concealed placental abruption and subsequent fetal demise. During an eventually failed misoprostol regime aiming for vaginal delivery she develops severe disseminated intravascular coagulopathy. Subsequent hysterotomy reveals Couvelaire uterus with major haemorrhage and requires subtotal hysterectomy for haemostasis. This case highlights the severity of the systemic response to abruption and fetal demise in utero and the multifactorial nature of its management.
https://doi.org/10.1136/bcr-2016-218349
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Contributors HCS is the primary author and initial preceptor of the idea of writing up this case. Carried out the literature review and is the writer of the discussion part of the case. Final editor of figures and text. Was the on call labour ward doctor during this patient's entire stay and assistant surgeon at the procedure in question. Have liaised with the patient and family and gained patient consent. MS is the coauthor, and was involved in the planning and development of the clinical part of the case write up. Designed the first draft of the case report and involved in subsequent editing.
Competing interests None declared.
Patient consent Obtained.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
Placental abruption: assessing trends in risk factors over time
- General Gynecology
- Published: 09 June 2022
- Volume 306 , pages 1547–1554, ( 2022 )
Cite this article

- Erga Schur ORCID: orcid.org/0000-0003-2170-3808 1 ,
- Yael Baumfeld 1 ,
- Reut Rotem 2 ,
- Adi Y. Weintraub 1 &
- Gali Pariente 1
524 Accesses
3 Citations
Explore all metrics
To evaluate changes in the independent contribution of different risk factors for placental abruption over time.
In this retrospective nested case–control study, trends of change in ORs for known risk factors for placental abruption occurring in three consecutive 8-year intervals were compared. A univariate assessment of factors associated with placental abruption and two multivariable logistic regression models were constructed to identify independent risk factors for placental abruption. Trends of change in the incidence and specific contribution of various risk factors were compared along the study time-period.
During the study period, 295,946 pregnancies met the inclusion criteria; of these, 2170 (0.73%) were complicated with placental abruption. Using logistic regression models, previous cesarean delivery, in vitro fertilization (IVF) pregnancy, hypertensive disorders, polyhydramnios, and inadequate prenatal care were recognized as independent risk factors for placental abruption. While the relative contribution of IVF pregnancy and polyhydramnios to the overall risk for abruption decreased over the course of the study, previous cesarean delivery became a stronger contributor for placental abruption.
In our study, a change over time in the specific contribution of different risk factors for placental abruption has been demonstrated.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Similar content being viewed by others

Abruption and Preterm Labor

Placenta previa: an outcome-based cohort study in a contemporary obstetric population

Placental pathology and neonatal morbidity: exploring the impact of gestational age at birth
Ananth CV, Lavery JA, Vintzileos AM, Skupski DW, Varner M, Saade G et al (2016) Severe placental abruption: clinical definition and associations with maternal complications. Am J Obstet Gynecol 214(2):272.e1-272.e9
Article Google Scholar
Oyelese Y, Ananth CV (2006) Placental abruption. Obstet Gynecol 108(4):1005–1016
Tikkanen M (2011) Placental abruption: epidemiology, risk factors and consequences. Acta Obstet Gynecol Scand 90(2):140–149
Pariente G, Wiznitzer A, Sergienko R, Mazor M, Holcberg G, Sheiner E (2011) Placental abruption: critical analysis of risk factors and perinatal outcomes. J Matern Fetal Neonatal Med 24(5):698–702
Downes KL, Shenassa ED, Grantz KL (2017) Neonatal outcomes associated with placental abruption. Am J Epidemiol 186(12):1319–1328
Shobeiri F, Masoumi SZ, Jenabi E (2017) The association between maternal smoking and placenta abruption: a meta-analysis. J Matern Fetal Neonatal Med 30(16):1963–1967
Article CAS Google Scholar
Ananth CV, Keyes KM, Hamilton A, Gissler M, Wu C, Liu S et al (2015) An international contrast of rates of placental abruption: an age-period-cohort analysis. PLoS One 10(5):0125246
Joseph KS, Young DC, Dodds L, O'Connell CM, Allen VM, Chandra S, et al. (2003) Changes in maternal characteristics and obstetric practice and recent increases in primary cesarean delivery. Obstet Gynecol 102(4):791–800.
Berkman L, Wainstock t, Sheiner E, Landau D, Pariente G (2019) Placental abruption and long-term cardiovascular morbidity of the offspring. Arch Gynecol Obstet 299(2): 393–401.
Li Y, Tian Y, Liu N et al (2019) Analysis of 62 placental abruption cases: risk factors and clinical outcomes. Taiwan J Obstet Gynecol 58(2):223–226
Kwan Yi C, Martin Ming HW, Sally S et al (2021) Dietary supplementation for gestational diabetes prevention and management: a meta-analysis of randomized controlled trials. Arch Gynecol Obstet 303:1381–1391
American College of Obstetricians and Gynecologists Gestational hypertension and preeclampsia (2020) ACOG practice bulletin summary, number 222. Obstet Gynecol 135(6):1492–1495
Twizer I, Sheiner E, Hallak M, Mazor M, Katz M, Shoham-Vardi I (2001) Lack of prenatal care in a traditional society. Is it an obstetric hazard? J Reprod Med 46(7):662
CAS PubMed Google Scholar
Kim A, Economidis MA, Stohl HE (2018) Placental abruption after amnioreduction for polyhydramnios caused by chorioangioma. BMJ Case Rep 2018:222399
Google Scholar
Nahavandi S, Price S, Sumithran P, Ekinci EI (2019) Exploration of the shared pathophysiological mechanisms of gestational diabetes and large for gestational age offspring. World J Diabet 10(6):333–340
Hung TH, Hsieh CC, Hsu JJ, Lo LM, Chiu TH, Hsieh TT (2007) Risk factors for placental abruption in an Asian population. Reprod Sci 14(1):59–65
Tikkanen M, Riihimäki O, Gissler M, Luukkaala T, Metsäranta M, Andersson S et al (2012) Decreasing incidence of placental abruption in Finland during 1980–2005. Acta Obstet Gynecol Scand 91(9):1046–1052
Klar M, Michels KB (2014) Cesarean section and placental disorders in subsequent pregnancies–a meta-analysis. J Perinat Med 42(5):571–583
Tikkanen M, Nuutila M, Hiilesmaa V, Paavonen J, Ylikorkala O (2006) Prepregnancy risk factors for placental abruption. Acta Obstet Gynecol Scand 85(1):40–44
Matsuda Y, Hayashi K, Shiozaki A, Kawamichi Y, Satoh S, Saito S (2011) Comparison of risk factors for placental abruption and placenta previa: case-cohort study. J Obstet Gynaecol Res 37(6):538–546
Sunderam S, Kissin DM, Zhang Y, Folger SG, Boulet SL, Warner L, et al (2019) Assisted reproductive technology surveillance—United States, 2016. In: Morbidity and mortality weekly report. Surveillance summaries (Washington, D.C) 68(4):1–23.
Zegers-Hochschild F, Mansour R, Ishihara O, Adamson GD, de Mouzon J, Nygren, KG. et al (2014) International committee for monitoring assisted reproductive technology: world report on assisted reproductive technology. Fert Steril 101(2):366–378.e14
De Geyter C, Calhaz-Jorge C, Kupka MS, Wyns C, Mocanu E, Motrenko T et al (2018) ART in Europe, 2014: results generated from European registries by ESHRE. Hum Reprod 33(9):1586–1601
Ananth CV, Peltier MR, Kinzler WL, Smulian JC, Vintzileos AM (2007) Chronic hypertension and risk of placental abruption: is the association modified by ischemic placental disease? Am J Obstet Gynecol 197(3):273–273
Auger N, Luo Z-Ch, Nuyt AM, Kaufman JS, Naimi AI, Platt RW, et al (2016) Secular Trends in preeclampsia incidence and outcomes in a large canada database: a longitudinal study over 24 years. Can J Cardiol 32(8):987.e15–987.e23
Basso O, Rasmussen S, Weinberg CR, Wilcox AJ, Irgens LM, Skjaerven R (2006) Trends in fetal and infant survival following preeclampsia. JAMA 296(11):1357–1362
Bibi S, Ghaffar S, Pir MA, Yousfani S (2009) Risk factors and clinical outcome of placental abruption: a retrospective analysis. J Pak Med Assoc 59(10):672–674
PubMed Google Scholar
Rosa CQ, Silveira DS, Costa JS (2014) Factors associated with lack of prenatal care in a large municipality. Rev Saude Publica 48(6):977–984
Ananth CV, Friedman AM (2014) Ischemic placental disease and risks of perinatal mortality and morbidity and neurodevelopmental outcomes. Semin Perinatol 38(3):151–158
Download references
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and affiliations.
Department of Obstetrics and Gynecology, Soroka University Medical Center, Faculty of Health Sciences, Ben-Gurion University of the Negev, POB 151, 84101, Beer-Sheva, Israel
Erga Schur, Yael Baumfeld, Adi Y. Weintraub & Gali Pariente
Department of Obstetrics and Gynecology, Shaare Zedek Medical Center, Jerusalem, affiliated with the Hebrew University Medical School of Jerusalem, Jerusalem, Israel
You can also search for this author in PubMed Google Scholar
Contributions
ES: Manuscript writing, data collection and management and manuscript editing. YB: data collection and management. RR: data collection and management. AYW: project development, data collection and management, and manuscript editing. GPG: project development, data collection and management, and manuscript editing.
Corresponding author
Correspondence to Erga Schur .
Ethics declarations
Conflict of interest.
The authors have no relevant financial or non-financial interests to disclose.
Additional information
In memory of Dr. David Yohay, a beloved physician and teacher who passed away while working on this study.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Schur, E., Baumfeld, Y., Rotem, R. et al. Placental abruption: assessing trends in risk factors over time. Arch Gynecol Obstet 306 , 1547–1554 (2022). https://doi.org/10.1007/s00404-022-06638-6
Download citation
Received : 10 February 2022
Accepted : 17 May 2022
Published : 09 June 2022
Issue Date : November 2022
DOI : https://doi.org/10.1007/s00404-022-06638-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Placental abruption
- Risk factors
- Time trend analysis
- Find a journal
- Publish with us
- Track your research
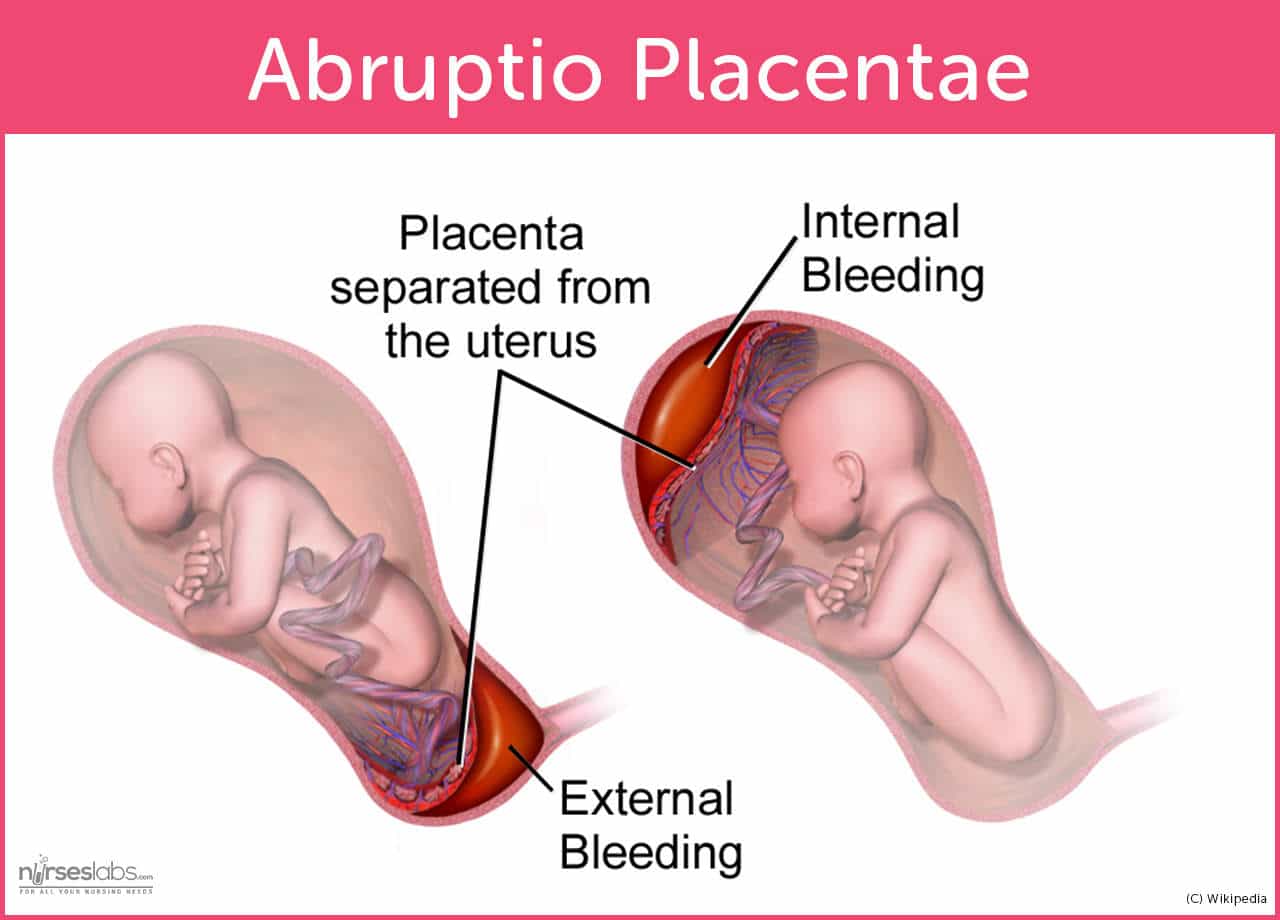
Abruptio Placentae

Abruptio placentae , also known as placental abruption, is a critical obstetric emergency characterized by the premature detachment of the placenta from the uterine wall before childbirth. This serious condition can result in significant maternal hemorrhage and jeopardize the well-being of the fetus. Early recognition, timely intervention, and skilled nursing care are essential in lessening the potential complications of abruptio placentae, ensuring the best possible outcomes for both the mother and the baby.
This nursing note provides a brief overview of this pregnancy complication, highlighting its significance in obstetrics and the crucial role of nursing in managing such cases effectively.
Table of Contents
What is abruptio placentae, pathophysiology, risk factors, signs and symptoms, diagnostic tests.
- Medical Management
- Surgical Management
Nursing Assessment
Nursing diagnosis, nursing care plans, nursing interventions.
- Abruptio placentae (also known as placental abruption) is the premature separation of the placenta that occurs late in the pregnancy.
- The placenta has been implanted in the correct location.
- For some unknown reason, it suddenly begins to separate, causing bleeding .
- This separation would occur late in pregnancy and accounts for 10% of perinatal deaths.
The following are the risk factors that surround abruptio placenta and these should be made known to all pregnant mothers to avoid the development of this fatal condition.
- High parity . A woman who has given birth multiple times predisposes herself to abruptio placentae.
- Short umbilical cord . A short umbilical cord could cause the separation of the placenta especially if trauma occurs.
- Advanced maternal age . Women over the age of 35 years old have a higher risk of acquiring abruptio placentae.
- Direct trauma . Any trauma to the abdomen could cause a separation of the placenta.
- Chorioamnionitis . This is an infection of the fetal membranes and fluid that could predispose the woman to premature placental separation.
The types of abruption placenta are measured according to the degree of placental separation that has occurred.
- Grade 0. No indication of placental separation and diagnosis of slight separation is made after birth.
- Grade 1 . There is minimal separation which causes vaginal bleeding , but no changes in fetal vital signs occur.
- Grade 2 . Moderate separation occurs and fetal distress is already evident. The uterus is also hard and painful upon palpation .
- Grade 3 . Extreme separation; maternal shock and fetal death is imminent if no interventions are done.
The signs and symptoms of abruption placenta must be monitored and detected early before it progresses to a critical stage.
- Sharp, stabbing pain . A woman may experience pain in the upper uterine fundus as initial separation occurs.
- Heavy bleeding . This usually happens after the separation of the placenta. External bleeding will only occur if the placenta separates first from the edges. Internal bleeding will occur if the placenta separates from the center because blood would pool under it.
- The uterus is tense and rigid . Most often called as Couvelaire uterus , it appears as a board-like, hard uterus without any bleeding.
These diagnostic procedures would be enforced by the physician to finally diagnose the presence of abruptio placenta.
- Hemoglobin level and fibrinogen level. These tests are performed to rule out disseminated intravascular coagulation .
Medical Management
To avoid a worsening condition, these medical procedures are implemented for both the mother and the fetus.
- Intravenous therapy . Once the woman starts to bleed, the physician would order a large gauge catheter to replace the fluid losses.
- Oxygen inhalation . Delivered via face mask, this would prevent fetal anoxia.
- Fibrinogen determination . This test would be taken several times before birth to detect DIC.
Surgical Management
Once the condition has reached a stage that mightily endangers the life of both patients, then surgical management is put into action.
- Cesarean delivery . If birth is imminent, it is safest to deliver the baby via cesarean delivery.
- Hysterectomy . The worst outcome would be for the woman to develop DIC, and to prevent exsanguinations, a hysterectomy must be performed.
Nursing Management
A vital role is also upheld by the nurses during this situation. Their accurate assessment would be one of the baseline data for all healthcare providers to plot the care plan for the patient.
- Assess for signs of shock, especially when heavy bleeding occurs.
- Assess if the bleeding is external or internal.
- Monitor contractions if separation occurs during labor .
- Obtain baseline vital signs.
- Assess the time the bleeding began, the amount and kind of bleeding, and interventions done when bleeding occurred if it started before admission.
- Assess for the quality of pain .
- Deficient fluid volume related to bleeding during premature placental separation.
- Check out our Nursing Care Plans page.
- Place the woman in a lateral , not supine position to avoid pressure in the vena cava .
- Monitor fetal heart sounds.
- Monitor maternal vital signs to establish baseline data.
- Avoid performing any vaginal or abdominal examinations to prevent further injury to the placenta.
- Maternal vital signs are all within the normal range, especially blood pressure .
- Urine output should be more than 30mL/hr.
- No bleeding or minimal amount of bleeding was observed.
- Uterus is not tense and rigid.
- Fetal heart sounds are within the normal range.
The team of health care providers could very well be the key towards the survival and safety of both the mother and the fetus. The role of the support system is also essential for this situation. Finally, the willpower of the mother to survive with both of their lives intact could be the turning point for those who care deeply for the patient and the child.
Leave a Comment Cancel reply
- Placental abruption
On this page
When to see a doctor, risk factors, complications.
Placental abruption (abruptio placentae) is an uncommon yet serious complication of pregnancy. The placenta develops in the uterus during pregnancy. It attaches to the wall of the uterus and supplies the baby with nutrients and oxygen.
Placental abruption occurs when the placenta partly or completely separates from the inner wall of the uterus before delivery. This can decrease or block the baby's supply of oxygen and nutrients and cause heavy bleeding in the mother.

The placenta is an organ that develops in the uterus during pregnancy. Placental abruption occurs when the placenta separates from the inner wall of the uterus before birth. Placental abruption can deprive the baby of oxygen and nutrients and cause heavy bleeding in the mother. In some cases, early delivery is needed.
Placental abruption often happens suddenly. Left untreated, it endangers both the mother and the baby.
Products & Services
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- Assortment Women's Health Products from Mayo Clinic Store
Placental abruption is most likely to occur in the last trimester of pregnancy, especially in the last few weeks before birth. Signs and symptoms of placental abruption include:
- Vaginal bleeding, although there might not be any
- Abdominal pain
- Uterine tenderness or rigidity
- Uterine contractions, often coming one right after another
Abdominal pain and back pain often begin suddenly. The amount of vaginal bleeding can vary greatly, and doesn't necessarily indicate how much of the placenta has separated from the uterus. It's possible for the blood to become trapped inside the uterus, so even with a severe placental abruption, there might be no visible bleeding.
In some cases, placental abruption develops slowly (chronic abruption), which can cause light, intermittent vaginal bleeding. Your baby might not grow as quickly as expected, and you might have low amniotic fluid or other complications.
Seek emergency care if you have signs or symptoms of placental abruption.
From Mayo Clinic to your inbox
The cause of placental abruption is often unknown. Possible causes include trauma or injury to the abdomen — from an auto accident or fall, for example — or rapid loss of the fluid that surrounds and cushions the baby in the uterus (amniotic fluid).
Factors that can increase the risk of placental abruption include:
- Placental abruption in a previous pregnancy that wasn't caused by abdominal trauma
- Chronic high blood pressure (hypertension)
- Hypertension-related problems during pregnancy, including preeclampsia, HELLP syndrome or eclampsia
- A fall or other type of blow to the abdomen
- Cocaine use during pregnancy
- Early rupture of membranes, which causes leaking amniotic fluid before the end of pregnancy
- Infection inside of the uterus during pregnancy (chorioamnionitis)
- Being older, especially older than 40
Placental abruption can cause life-threatening problems for both mother and baby.
For the mother, placental abruption can lead to:
- Shock due to blood loss
- Blood clotting problems
- The need for a blood transfusion
- Failure of the kidneys or other organs resulting from blood loss
- Rarely, the need for hysterectomy, if uterine bleeding can't be controlled
For the baby, placental abruption can lead to:
- Restricted growth from not getting enough nutrients
- Not getting enough oxygen
- Premature birth
You can't prevent placental abruption, but you can decrease certain risk factors. For example, don't smoke or use illegal drugs, such as cocaine. If you have high blood pressure, work with your health care provider to monitor the condition.
Always wear your seatbelt when in a motor vehicle. If you've had abdominal trauma — from an auto accident, fall or other injury — seek immediate medical help.
If you've had a placental abruption, and you're planning another pregnancy, talk to your health care provider before you conceive to see if there are ways to reduce the risk of another abruption.
Feb 25, 2022
- Ananth CV, et al. Placental abruption: Pathophysiology, clinical features, diagnosis and consequences. https://www.uptodate.com/contents/search. Accessed Nov. 16, 2019.
- Abruptio placentae. Merck Manual Professional Version. https://www.merckmanuals.com/professional/gynecology-and-obstetrics/abnormalities-of-pregnancy/abruptio-placentae. Accessed Nov. 16, 2019.
- Magowan BA, et al, eds. Obstetric haemorrhage. In: Clinical Obstetrics & Gynaecology. 4th ed. Elsevier; 2019. https://www.clinicalkey.com. Accessed Nov. 16, 2019.
- Oyelese Y, et al. Placental abruption: Management and long-term prognosis. https://www.uptodate.com/contents/search. Accessed Nov. 16, 2019.
- Downes KL. Maternal, labor, delivery and perinatal outcomes associated with placental abruption: A systematic review. American Journal of Perinatology. 2017; doi:10.1055/s-0037-1599149.
- Diseases & Conditions
- Placental abruption symptoms & causes
More Information
Associated procedures.
CON-XXXXXXXX
Double your impact on fighting cancer
Make a gift before July 31 and it can go twice as far to fight cancer.
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Changing risk factors for placental abruption: A case crossover study using routinely collected data from Finland, Malta and Aberdeen
Roles Formal analysis, Writing – original draft
Affiliation University of Aberdeen Medical School, Aberdeen, United Kingdom
Roles Formal analysis, Methodology, Supervision, Writing – review & editing
Affiliation Division of Applied Health Sciences, Medical Statistics Team, University of Aberdeen, Aberdeen, United Kingdom
Roles Conceptualization, Supervision, Writing – review & editing
Affiliation Aberdeen Maternity Hospital, Aberdeen, United Kingdom
Roles Data curation, Writing – review & editing
Affiliations Information Services Department, THL National Institute for Health and Welfare, Helsinki, Finland, Department of Neurobiology, Care Sciences and Society, Karolinska Institute, Stockholm, Sweden
Affiliation Strategy and Sustainability Division, Ministry for Health, Valletta, Malta
Affiliation School of Medicine, Medical Sciences and Nutrition, University of Aberdeen, Aberdeen, United Kingdom
Roles Conceptualization, Data curation, Supervision, Writing – review & editing
* E-mail: [email protected]
Affiliation Dugald Baird Centre for Research on Women’s Health, Aberdeen Maternity Hospital, Aberdeen, United Kingdom
- Emma Anderson,
- Edwin Amalraj Raja,
- Ashalatha Shetty,
- Mika Gissler,
- Miriam Gatt,
- Siladitya Bhattacharya,
- Sohinee Bhattacharya

- Published: June 11, 2020
- https://doi.org/10.1371/journal.pone.0233641
- Peer Review
- Reader Comments
To evaluate the effects of changes in risk factors between the first two pregnancies on the occurrence of placental abruption (PA) in the same woman.
Routinely collected obstetric data from Aberdeen Maternity and Neonatal Databank, the Maltese National Obstetric Information System and the Finnish Medical Birth Register were aggregated. Records of the first two singleton pregnancies from women who had PA in one pregnancy but not the other, were identified from this pooled dataset. A case-crossover study design was used; cases were pregnancies with abruption and matched controls were pregnancies without abruption in the same woman. Conditional logistic regression was used to investigate changes in risk factors for placental abruption in pregnancies with and without abruption.
A total of 2,991 women were included in the study. Of these 1,506 (50.4%) had PA in their first pregnancy and 1,485 (49.6%) in a second pregnancy. Pregnancies complicated by preeclampsia {194 (6.5%) versus 115 (3.8%) adj OR 1.69; (95% CI 1.23–2.33)}, antepartum haemorrhage of unknown origin {556 (18.6%) versus 69 (2.3%) adjOR 27.05; 95% CI 16.61–44.03)} and placenta praevia {80 (2.7%) versus 21 (0.7%) (adjOR 3.05; 95% CI 1.74–5.36)} were associated with PA. Compared to 20 to 25 years, maternal age of 35–39 years {365 (12.2) versus 323 (10.8) (adjOR 1.32; 95% CI 1.01–1.73) and single marital status (adjOR 1.36; 95% CI 1.04–1.76) were independently associated with PA. Maternal smoking, BMI and fetal gender were not associated with PA.
Advanced maternal age, pregnancies complicated with unexplained bleeding in pregnancy, placenta praevia and preeclampsia were independently associated with a higher risk of placental abruption.
Citation: Anderson E, Raja EA, Shetty A, Gissler M, Gatt M, Bhattacharya S, et al. (2020) Changing risk factors for placental abruption: A case crossover study using routinely collected data from Finland, Malta and Aberdeen. PLoS ONE 15(6): e0233641. https://doi.org/10.1371/journal.pone.0233641
Editor: Frank T. Spradley, University of Mississippi Medical Center, UNITED STATES
Received: February 5, 2020; Accepted: May 9, 2020; Published: June 11, 2020
Copyright: © 2020 Anderson et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: The dataset was created from three population based international datasets and permissions obtained from governing committees for the 3 databases. Therefore permission for public access to data will need to be given by all three committees. The Finnish register data have been given for this specific study, and the data cannot be shared without authorization from the register keepers. More information on the authorization application to researchers who meet the criteria for access to confidential data can be found at https://thl.fi/fi/web/thlfi-en/statistics/information-for-researchers/authorisation-application (THL). Similarly data from Aberdeen can be accessed by applying to the AMND steering committee found at https://www.abdn.ac.uk/iahs/research/obsgynae/amnd/access.php . The authors did not have special access privileges in accessing the data.
Funding: Funding was received from NHS Grampian Endowment Fund (Grant number RG14524-10) to cover data access and storage costs and for article processing charges for open access publication for this research project. The funders played no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: Prof Siladitya Bhattacharya receives honorarium and travel expenses from Oxford University Press as Editor in Chief of Human Reproduction Open journal. As invited speaker, has received funding for travel and accommodation at conferences supported by Industry and received research funding from National Institute for Health Research UK. The corresponding author Dr Sohinee Bhattacharya is the wife of Prof Siladitya Bhattacharya. She has received research grants from MRC that is not related to this project in the last 5 years. This does not alter our adherence to PLOS ONE policies on sharing data and materials. All other authors have declared that they have no competing interests.
Introduction
Placental abruption (PA) is an important cause of antepartum haemorrhage (APH) that affects 0.3–1% of pregnancies. [ 1 ] Defined as the premature separation of the placenta from the uterine wall, PA usually occurs without warning between 24 weeks gestation and delivery, [ 2 ] and is caused by rupture of the decidual vessels and haemorrhage within the placental bed. [ 3 ] Abruption can be revealed, indicated by vaginal bleeding, or concealed, where haemorrhage is contained behind the placenta. [ 4 ] The aetiology is unknown, and possibly part of a wider placental syndrome caused by underlying vascular pathology associated with defective deep placentation. [ 5 ] Oxygen supply to the fetus is compromised and maternal blood loss may be significant in affected women. Prompt fetal monitoring, maternal hemodynamic stabilization [ 2 ] and delivery, commonly by caesarean section (90%), is indicated within 24 hours of abruption. [ 4 , 6 ] PA may lead to antepartum fetal death and disseminated intravascular coagulopathy, though maternal mortality is rare with good healthcare access [ 6 ].
While PA can be triggered by abdominal trauma, most cases are not preceded by a clear pre-disposing event. Sociodemographic risk factors include maternal race/ethnic background, BMI, social class, marital status [ 7 ] and extremes of maternal age. [ 8 ] Behavioural risk factors include smoking, cocaine use, alcohol and short interpregnancy interval. [ 7 ] Smoking is one of the strongest established risk factors and exhibits a dose-response relationship. [ 9 ] Diabetes and hypertensive disease such as pre-eclampsia may aggravate the underpinning microvascular dysfunction, thus causing abruption. [ 10 ] Vaginal bleeding in pregnancy, placenta praevia and premature rupture of membranes (PROM) are also significant risk factors [ 7 ] as are stillbirth or abruption in a previous pregnancy. [ 2 , 11 ] PA shows aggregation within families [ 12 ] and has an association with heritable thrombophilias. [ 13 ] However, published literature is often inconsistent on the significance and importance of modifying these risk factors.
The objective of this study was to evaluate any changes in risk factors associated with PA across two consecutive pregnancies in the same woman by controlling for woman level variables such as inherited risk between pregnancies.
Materials and methods
Study design.
A case-crossover study design was used in women who experienced pregnancies with and without PA, such that they acted as their own controls.
Data sources
This study used anonymised data from three sources—the Aberdeen Maternity and Neonatal Databank (AMND) between 1986 and 2012, the Maltese National Obstetric Information System (NOIS) between 1999 and 2015 and Finnish Medical Birth Register (MBR) between 1987 and 2014. All three contain routinely collected clinical information on maternal, obstetric and neonatal characteristics of deliveries at or over 22 weeks’ gestation. Maltese NOIS and Finnish MBR are national databases collecting data from all maternity hospitals in the country, [ 14 , 15 ] while AMND collects data on all births within Aberdeen City District—a defined geographical region of Scotland. [ 16 ] The pooled dataset comprised women with their first two singleton pregnancies between 1986 and 2015. Women with missing information on placental abruption were excluded. The population selection process is shown in Fig 1 .
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0233641.g001
Ethical approval
Permissions to analyse anonymised data were obtained from the Caldicott guardians of all three databases: the steering committee of the Aberdeen Maternity and Neonatal Databank (AMND 3/2016); National Institute for Health and Welfare, Finland (THL 1719/5.05.00/2015); Directorate for Health Information Research Malta (28/04/2016). As routinely collected anonymised data were analysed formal ethical approval was not considered necessary by the North of Scotland Research Ethics Service. This analysis was part of a collaborative project looking at recurrence risk of stillbirth.
Case definition
Placental abruption was coded according to the International Classification of Diseases 9 th or 10 th Revision (ICD—9/10) in all three databases. ICD 10 defines placental abruption as ‘The separation of the placenta from the maternal uterine attachment when it occurs after the twentieth week of the pregnancy.’[ 17 ] Since 1 Oct 1990 Finland had a separate check-box for placental abruption. Pregnancies without placental abruption in the same women were the controls. Therefore the cases and control pregnancies were matched within each woman included in the study.
Risk factors
The potential risk factors under investigation included maternal age category (<20, 20–24, 25–29 [reference],30–34, 35–39 and ≥40 years), parity, BMI category (<18.5 as underweight, 18.5–24.9 as normal [reference], 25–29.9 as overweight and ≥30 as obese), smoking status (yes vs no), deprivation status (Deprived vs not deprived), marital status (single vs married), gestational diabetes, gestational hypertension, pre-eclampsia, threatened miscarriage, antepartum haemorrhage (APH) of unknown origin, placenta praevia, maternal anaemia, premature rupture of membranes (PROM) (yes versus no) and gender of the baby (male vs female). In each source database, variables were checked and re-coded, where necessary, to ensure homogenised coding amongst the three datasets. Continuous variables such as age and BMI were categorised prior to analysis; categorisation and reference bands were based on existing literature. Marital status ‘single’ denoted single, widowed, divorced, separated and ‘Married’ denoted marriage or co-habitation. Social class was measured differently between the three source data sets. These were re-coded into a new variable ‘Deprivation status’ for consistency and data merging. AMND recorded Registrar General’s paternal occupation based social class recoded as binary ‘not deprived’ and ‘deprived’. Finland used maternal occupational classification; ‘upper white-collar worker’ counted as ‘not deprived’, all others (lower white-collar, blue-collar and other including student and housewife) as deprived. Malta used maternal level of education attained as a proxy for social class. University level education was coded into ‘non-deprived’ and below this level as ‘deprived’.
Statistical analysis
Datasets were cleaned and merged using IBM SPSS version 24 (Statistical Package for the Social Sciences, SPSS Inc., Chicago, IL, USA). For univariable analysis, McNemar’s chi squared test of association was used to determine significant differences in the frequency of potential binary risk factors between pregnancies with and without abruption and conditional logistic regression for multinomial risk factors. Those maternal, obstetric and neonatal characteristics which were significant at p<0.2 in the univariable analysis were included in the multivariable model. However, as woman level factors such as country of origin were already matched for in the cases and controls, this was not included in the model. Multivariable conditional logistic regression with backward-selection method was used to find independent effect of risk factors on placental abruption. The strength of association was expressed as an Odds Ratio (OR) and 95% Confidence Intervals (CI). In cases where the p-value was less than 0.05 or the 95% confidence interval of the odds ratio did not include 1, the risk factor was considered to be statistically significant. Analyses were performed using Stata version 14 (StataCorp LP, College Station, TX, USA). Complete case analyses were performed after assigning a value to missing data.
Fig 1 presents cases of placental abruption by country and by pregnancy number. There were 0.8% and 0.6% cases of placental abruption in the first and second pregnancies respectively in the AMND. The incidence of placental abruption in both pregnancies was 0.3% in the Finnish and Maltese datasets. The study population comprised 2,991 women whose first two singleton pregnancies included one with PA and one without. Of these, 1,506 (50.4%) women had an abruption in pregnancy 1 and 1,485 (49.6%) experienced PA in pregnancy 2.
Tables 1 and 2 present the unadjusted (along with the counts and proportions) and adjusted models respectively investigating the association between various risk factors and placental abruption in the first and second pregnancies. Risk factors that were significantly associated with PA in the first pregnancy were maternal age 30–34 years {adj. OR1.35 (95% CI 1.16–1.57)} or 35–39 years {1.66 (1.31–2.12)}; smoking {1.91(1.64–2.21)}; pre-existing hypertension {1.89(1.38–2.61)}; preeclampsia {2.03(1.48–2.79)}; threatened miscarriage {2.64(1.70–4.09)}; unexplained antepartum haemorrhage {8.34(6.12–11.35)} and placenta praevia {7.26(4.71–11.19)}. After mutually adjusting for each other, risk factors that remained significantly associated with PA in the second pregnancy were: smoking {1.82 (1.40–2.36)}; pre-existing hypertension {2.25 (1.52–3.34)}; preeclampsia {2.61 (1.71–3.96)}; unexplained antepartum haemorrhage {9.28 (7.10–12.12)}; placenta praevia {2.70 (1.67–4.37)} and PA in the previous pregnancy {5.85 (2.84–12.04)}.
https://doi.org/10.1371/journal.pone.0233641.t001
https://doi.org/10.1371/journal.pone.0233641.t002
Maternal and obstetric characteristics in pregnancies with and without abruption are shown in Table 3 . Results of univariable and multivariable analyses are shown in Table 4 . On univariable analysis, pregnancies with abruption were significantly more likely to be associated with maternal age 35–39 years (OR 1.39; 95% CI 1.11–1.75), pre-eclampsia (OR 1.94; 95% CI 1.49–2.53), PROM (OR 1.58; 95% CI 1.11–2.25), anaemia (OR 1.66; 95% CI 1.04–2.62), threatened miscarriage (OR 1.59; 95% CI 1.20–2.11), placenta praevia (OR 4.11; 95% CI 2.49–6.78) and APH of unknown origin (OR 28.15; 95% CI 17.59–45.05) than pregnancies without abruption. Smoking status, BMI and fetal gender were not significantly associated with PA.
https://doi.org/10.1371/journal.pone.0233641.t003
https://doi.org/10.1371/journal.pone.0233641.t004
Results of multivariable analysis with backward elimination method for variable selection showed that maternal age 35–39 years (adjOR 1.32; 95% CI 1.01–1.73), single marital status (adjOR 1.36; 95% CI 1.04–1.76), preeclampsia (adjOR 1.69; 95% CI 1.23–2.33), APH of unknown origin (adjOR 27.05; 95% CI 16.61–44.03), placenta praevia (adjOR 3.05; 95% CI 1.74–5.36) were more likely to be independently, significantly associated with pregnancies with abruption. Maternal anemia, threatened miscarriage and PROM, which were significantly associated with abruption at univariable analysis were no longer statistically significant in the multivariable model.
Although this was not the primary focus of this study, the perinatal outcomes of pregnancies with and without placental abruption are presented as S1 , S2 and S3 Tables. In both pregnancies and in unadjusted as well as multi-adjusted models, placental abruption was significantly associated with Caesarean or instrumental delivery, stillbirth, preterm birth, low birth weight and IUGR.
Main findings
In a pooled dataset from three European populations comparing pregnancies occurring in the same woman we found that pregnancies with abruption were more likely to be associated with pre-eclampsia, placenta praevia and APH of unknown origin. Abruption was also more likely to occur in older women and those who were single. PPROM, threatened miscarriage and maternal anaemia were not confirmed as significant risk factors for PA in the multivariable model. Smoking status, BMI and fetal gender were not significantly associated with PA in univariable or multivariable models.
Comparison with existing literature
Our finding that pre-eclampsia increased the odds of abruption is supported by previous studies. Kramer found an odds ratio of 2.05 [ 18 ] and Lindqvist and Happach reported a 3.4-fold increased risk. [ 11 ]
Abruption was associated with maternal age 35–39 years—a finding which is consistent with the existing literature linking maternal age ≥35 years with PA with adjusted OR of 1.62 [ 19 ] We found no association with age ≥40 years but this is likely due to the small number of women in this group. The association between increased maternal age and abruption is suggested to be due to decreased vascularisation of the uterus which occurs with age and predisposes to placental insufficiency. [ 1 ] While other studies have also found a link between decreased maternal age (<20 years) and abruption, [ 20 ] this study found no evidence supporting this.
Kramer [ 18 ] also found that single marital status was associated with an increased risk of placental abruption and their odds ratio of 1.50 (95% CI 1.13–1.98) is comparable to our findings of 1.36 (95% CI 1.04–1.76).
It is notable that we did not find maternal smoking or BMI to be associated with abruption, this is probably explained by the fact that smoking status and BMI did not often change between successive pregnancies.
APH of unknown origin and placenta praevia were associated with pregnancies with placental abruption. Baumann [ 21 ] found the risk of abruption from bleeding >28 weeks’ gestation (adj OR 18.7 95% CI 14.2–24.6) and placenta praevia (adj OR 4.3; 95% CI 2.7–6.9) to be of a similar magnitude to the risk from APH of unknown origin and placenta praevia found in this study. Baumann admitted that they did not know in how many instances the APH coincided with the index abruption, thus having no predictive value. APH of unknown origin could be an early indicator or sign of placental abruption rather than a risk factor per se. An association with vaginal bleeding in early pregnancy (<27 weeks) was identified by Ananth, [ 5 ] who found it to increase risk of PA (adjusted relative risk 3.1; 95% CI 2.3, 4.1). They argued that this was a risk factor and not an early predictor due to the low positive predictive value of vaginal bleeding for placental abruption (3%), but high negative predictive value (98%), and that these results support the theory that PA is the result of chronic placental pathology beginning early in pregnancy—which manifests as abnormal bleeding.
Strengths and limitations
A major strength of this study is the novel use of a case-crossover design to compare risk factor exposure between pregnancies with and without PA. The existing literature consists of cohort and case-control analyses; this design adds a different and complementary perspective where women act as their own controls, thereby minimising within woman confounding. Similar results to previous studies verify the value of this design. The case cross-over study design is a relatively new epidemiological method that is a variation of a case control study and is self-matched. [ 22 ] It allows the study of transient exposures on an acute and rare outcome, in this case placental abruption. [ 23 ] This allowed us to examine the effect of risk factors such as age, pre-eclampsia and smoking status that may alter between pregnancies. Self-matching of cases reduces control-selection bias [ 23 ] and means that women act as their own control; the pregnancy with abruption is the case and the pregnancy without abruption is the control, with the PA/unaffected pregnancy in either order. Furthermore, self-matching removed the effect of genetic factors, which are known to play a role, [ 12 ] and other unmeasured confounding. This allowed reliable examination of the impact of transient clinical and socio-demographic risk factors such as age, fetal gender smoking and hypertension. The aim of the study was to look at the effect of changing some of the already known risk factors on the occurrence of placental abruption keeping the woman-based factors (eg. Genetic predisposition) constant. In fact our starting point was to identify the risk factors implicated in the literature for abruption and see what difference any change in these would make.
Further strengths of this study are related to the size and quality of the datasets. Pooling data from three sources provided a relatively large study population, thus allowing us to explore an uncommon condition. The databases used are reliable and well-established and contain information on complete populations of women for a long period of time and the data are recent, up to 2015. The detailed information allowed a comprehensive study of many potential risk factors in relation to PA.
While two data sources (Maltese NOIS and Finnish MBR) capture national data, AMND contains data gathered from Aberdeen Maternity Hospital (AMH) which is the only hospital to serve the entire population of the region (Aberdeen City District) which offers no other maternity facilities, either private or public. This represents two potential limitations. First, Aberdeen is a relatively affluent area which may not be representative of the total Scottish population. Second, as a tertiary referral centre, Aberdeen Maternity Hospital receives a disproportionate number of more complicated cases from outside the region. This is confirmed by the increased prevalence of PA seen in the Aberdeen data compared to Maltese and Finnish data. However, as only women who had a pregnancy with placental abruption were included in this study, this is unlikely to have a major effect on the findings.
Large amounts of missing or unrecorded data for some variables meant that substance misuse, alcohol use and in-vitro fertilisation (IVF) conception could not be included as co-variates. Tests of association would be weak with >60% missing data, and for drug and alcohol use self-reporting is likely to produce underestimations. [ 18 ] This can partially be attributed to some variables not being recorded in all three sources; drug and alcohol use was only recorded in the Maltese data. Excluding these variables meant that their effects could not be investigated and their unobserved effects could act as residual confounding.
COS are defined sets of outcomes relevant to a particular condition or topic, developed by the Core Research Outcomes in Women’s and Newborn Heath Initiative (CROWN). This initiative is in response to heterogeneity in the outcomes investigated by studies looking at the same problem. This variation limits their comparison and leads to outcome reporting bias and difficulty or inaccuracy in systematic reviews. [ 24 ] This lack of clarity is likely to hinder or delay the implementation of research findings into clinical practice. Additionally, the definition of covariates differed in the three datasets. For example, socioeconomic status was based on the mother’s occupation in the Finnish data, maternal education level in the Maltese data while post code based deprivation category was used in the AMND. Consequently, we had to arbitrarily categorise all data as ‘deprived’ and ‘non-deprived’ for consistency. The data although spanning three European countries, are derived from a mainly white Caucasian population and therefore may not be generalisable to other populations with different health care systems and access.
Interpretation
While a number of studies have previously established the presence and magnitude of risk of factors such as pre-eclampsia, few previous studies have investigated APH of unknown origin and placenta praevia as risk factors for placental abruption. This may be related to way data on APH is coded in registries—some have a hierarchical coding system whereby it is impossible for placental abruption and placenta praevia to be coded as comorbidities. In the Medical Birth Register in Finland there are two check boxes, and the birth hospitals report these diagnoses at the same time: Placenta previa; and Ablatio placentae (premature detachment of placenta) only if diagnosed during delivery. We looked at the overlap in these diagnoses and on average 5–6 cases were diagnosed as both over the years. Thus although the absolute numbers were small, the relative risk was high. While these results should be interpreted with caution, the size of the risk they confer in this study is substantial and warrants further investigation. These results suggest that clinicians should be aware that any unexplained bleeding or diagnosis of placenta praevia could mean that women are at a much higher risk of abruption later in pregnancy. In the U.K., a recent Royal College of Obstetricians and Gynaecologists guideline (2018) advises earlier planned delivery with confirmed placenta praevia at 36–37 weeks as the risk of increased bleeding and the need for emergency delivery increases with advancing gestation. [ 25 ] This risk increases rapidly after 36 weeks of gestation; below 5% by 35 weeks, 15% by 36 weeks, 30% by 37 weeks and 59% by 38 weeks of gestation. [ 25 ]. It could be argued that increased risk of bleeding could be in part due to a higher risk of PA in these women. In addition, the 2011 RCOG guidelines on antepartum haemorrhage state that following APH of unknown origin the pregnancy should be re-classified as high risk of PA; [ 2 ] this is in keeping with the results of this study.
Of all the risk factors that were found to be independently associated with PA in this study, advanced maternal age was the only one that was potentially modifiable. This increased risk was independent of parity, signifying that not only first pregnancies but also subsequent pregnancies were at higher risk of complications if occurring in women aged 35 and over. The UK Office for National Statistics (ONS) recently published data showing that in 2017 fertility rates decreased for every age group, except for women over 40 which increased by 1.6%. [ 26 ] Older women are making up an increased proportion of obstetric patients. Advanced maternal age comes with a spectrum of increased clinical risk; both maternal complications such as preeclampsia, gestational diabetes, placental abruption and adverse perinatal outcomes including preterm birth, miscarriage, stillbirth, growth restriction and genetic disorders. [ 27 ] This association is suggested to be due to placental dysfunction. Targeted public health messages should advise women of the higher risks associated with conceiving over the age of 35. Those planning to conceive a second time should also be advised not to wait too long as this study showed that advanced maternal age even in the second pregnancy conferred an increased risk of PA and other placental dysfunction.
Risk factors for PA include APH of unknown origin, placenta praevia, pre-eclampsia, maternal age ≥35 and single marital status. Women with APH of unknown origin and placenta praevia should be classified as at high risk for PA. Our data confirms preeclampsia as a well-established risk factor for PA. Knowledge that PA is more common in older women could help to inform clinical decision making in pregnancy.
Supporting information
S1 checklist. strobe statement—checklist of items that should be included in reports of observational studies..
https://doi.org/10.1371/journal.pone.0233641.s001
S1 Table. Comparison of perinatal outcomes of the first pregnancy with and without placental abruption.
https://doi.org/10.1371/journal.pone.0233641.s002
S2 Table. Comparison of perinatal outcomes of 2nd pregnancy with and without placental abruption.
https://doi.org/10.1371/journal.pone.0233641.s003
S3 Table. Unadjusted and adjusted odds ratios (95% Confidence Intervals) of perinatal outcomes in pregnancies 1 and 2.
https://doi.org/10.1371/journal.pone.0233641.s004
Acknowledgments
With thanks to the women from Malta, Finland and Aberdeen whose data is included and to all who contributed to the datasets used.
- View Article
- PubMed/NCBI
- Google Scholar
- 2. Royal College of Obstetricians and Gynaecology (2011, updated 2014), Antepartum Haemorrhage, Green-top Guideline no. 63
- 14. Department of Health Information and Research (2016) National Obstetric Information System (NOIS) Malta Third Quarterly Report [online] https://deputyprimeminister.gov.mt/en/dhir/Documents/Births/3rdquarter2016.pdf Accessed 20th January 2018.
- 15. THL (2016) Medical Birth Register Description. National Institute for Health and Welfare [online] https://www.thl.fi/fi/web/thlfi-en/statistics/information-on-statistics/register-descriptions/newborns . Accessed 20th January 2018.
- 17. International Classification of Diseases, 10th Revision. Version: 2016. https://icd.who.int/browse10/2016/en# . Accessed 6th March 2019.
- 22. Pennsylvania State University (2018) Case-Crossover Study Design. Epidemiological Research Methods, Department of Satistics Online Programme. [online] Avaliable from: https://onlinecourses.science.psu.edu/stat507/node/51 Accessed February 12th 2018
- 26. Office for National Statistics. (2017). Statistical bulletin: Births in England and Wales: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/livebirths/bulletins/birthsummarytablesenglandandwales/2017
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Placental abruption: a case study
- PMID: 8161949
Placental abruption is a clinical circumstance in which the anesthetist is confronted with a patient who is undergoing a variety of physiological insults. The principles of basic life support, appropriate fluid management, and cooperative gynecological surgeons will aid in the delivery of optimal care to both the mother and the fetus.
PubMed Disclaimer
Similar articles
- Anesthetic Management of a Patient With Type 1 von Willebrand Disease and Uterine Placental Abruption: A Case Report. Roberson MC, Wigley MD, Austin PN. Roberson MC, et al. AANA J. 2018 Jun;86(3):209-212. AANA J. 2018. PMID: 31580809
- [Abruptio placentae]. Atef Y, Nizar BA, Hasen M, Faouzi GM. Atef Y, et al. Tunis Med. 2005 Oct;83(10):603-6. Tunis Med. 2005. PMID: 16370210 French.
- Hemoperitoneum from a tubal pregnancy mimicking abruptio placentae: an obstetrical enigma. Mathelier AC, Jurado L, Karachorlu K. Mathelier AC, et al. Int J Fertil. 1992 Jan-Feb;37(1):29-32. Int J Fertil. 1992. PMID: 1348732
- Placental abruption. Oyelese Y, Ananth CV. Oyelese Y, et al. Obstet Gynecol. 2006 Oct;108(4):1005-16. doi: 10.1097/01.AOG.0000239439.04364.9a. Obstet Gynecol. 2006. PMID: 17012465 Review.
- [Abruptio placentae--a clinical diagnosis?]. Parslov M. Parslov M. Ugeskr Laeger. 1995 Jan 9;157(2):161-6. Ugeskr Laeger. 1995. PMID: 7831728 Review. Danish.
- The Association of Placental Abruption and Pediatric Neurological Outcome: A Systematic Review and Meta-Analysis. Oltean I, Rajaram A, Tang K, MacPherson J, Hondonga T, Rishi A, Toltesi R, Gowans R, Jahangirnia A, Nasr Y, Lawrence SL, El Demellawy D. Oltean I, et al. J Clin Med. 2022 Dec 27;12(1):205. doi: 10.3390/jcm12010205. J Clin Med. 2022. PMID: 36615006 Free PMC article. Review.
Publication types
- Search in MeSH
Related information
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Placental Abruption: a Case Study
International Journal of Scientific & Engineering Research Volume 9, Issue 2, February-2018 318 ISSN 2229-5518
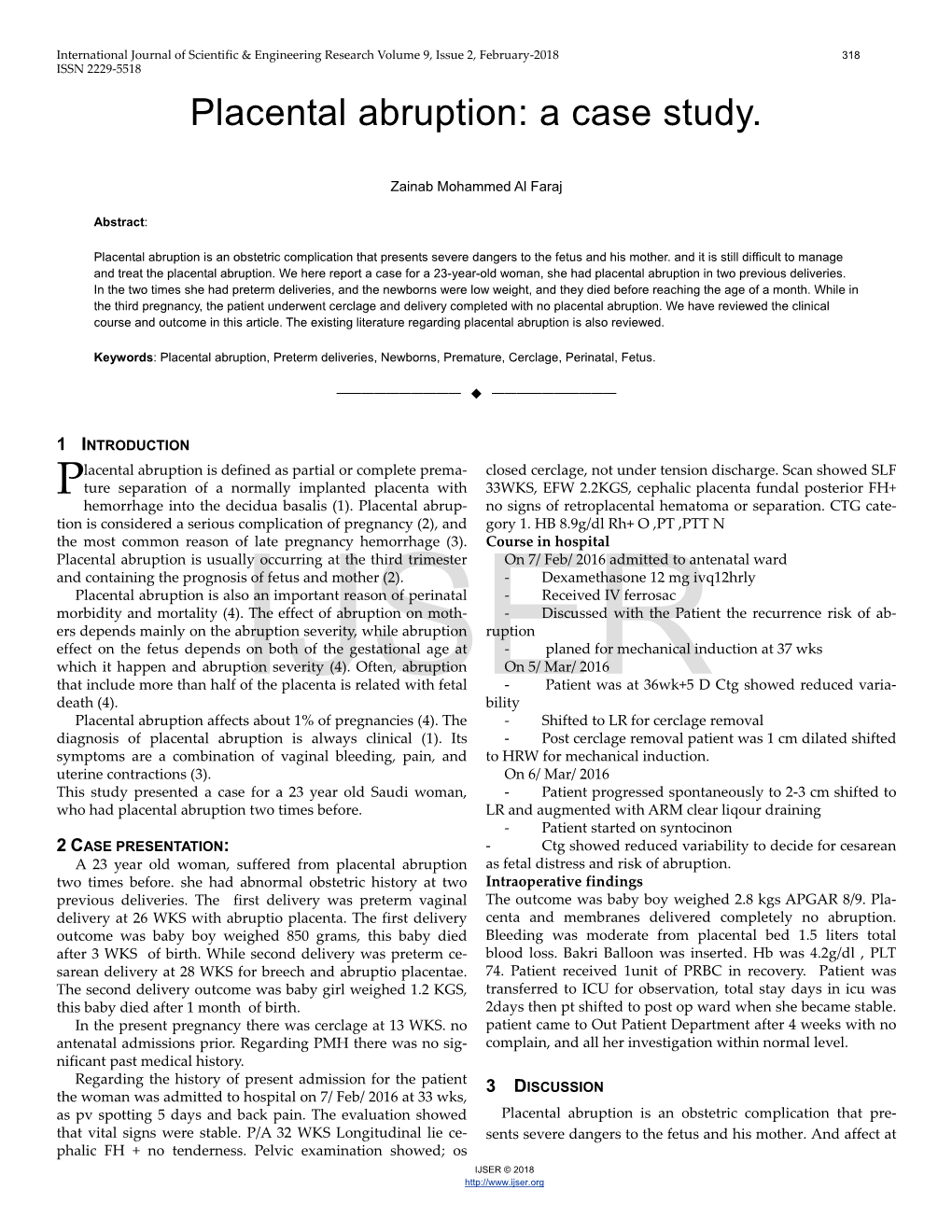
Placental abruption: a case study.
Zainab Mohammed Al Faraj
Placental abruption is an obstetric complication that presents severe dangers to the fetus and his mother. and it is still difficult to manage and treat the placental abruption. We here report a case for a 23-year-old woman, she had placental abruption in two previous deliveries. In the two times she had preterm deliveries, and the newborns were low weight, and they died before reaching the age of a month. While in the third pregnancy , the patient underwent cerclage and delivery completed with no placental abruption. We have reviewed the clinical course and outcome in this article. The existing literature regarding placental abruption is also reviewed.
Keywords: Placental abruption, Preterm deliveries, Newborns, Premature, Cerclage, Perinatal, Fetus.
—————————— ——————————
1 INTRODUCTION lacental abruption is defined as partial or complete prema- closed cerclage, not under tension discharge. Scan showed SLF P ture separation of a normally implanted placenta with 33WKS, EFW 2.2KGS, cephalic placenta fundal posterior FH+ hemorrhage into the decidua basalis (1). Placental abrup- no signs of retroplacental hematoma or separation. CTG cate- tion is considered a serious complication of pregnancy (2), and gory 1. HB 8.9g/dl Rh+ O ,PT ,PTT N the most common reason of late pregnancy hemorrhage (3). Course in hospital Placental abruption is usually occurring at the third trimester On 7/ Feb/ 2016 admitted to antenatal ward and containing the prognosis of fetus and mother (2). - Dexamethasone 12 mg ivq12hrly Placental abruption is also an important reason of perinatal - Received IV ferrosac morbidity and mortality (4). The effect of abruption on moth- - Discussed with the Patient the recurrence risk of ab- ers depends mainly on the abruption severity, while abruption ruption effect on the fetus depends on both of the gestational age at - planed for mechanical induction at 37 wks which it happen and abruption severity (4). Often, abruption On 5/ Mar/ 2016 that include more than half of the placenta is related with fetal - Patient was at 36wk+5 D Ctg showed reduced varia- death (4). IJSERbility Placental abruption affects about 1% of pregnancies (4). The - Shifted to LR for cerclage removal diagnosis of placental abruption is always clinical (1). Its - Post cerclage removal patient was 1 cm dilated shifted symptoms are a combination of vaginal bleeding , pain, and to HRW for mechanical induction. uterine contractions (3). On 6/ Mar/ 2016 This study presented a case for a 23 year old Saudi woman, - Patient progressed spontaneously to 2-3 cm shifted to who had placental abruption two times before. LR and augmented with ARM clear liqour draining - Patient started on syntocinon 2 CASE PRESENTATION: - Ctg showed reduced variability to decide for cesarean A 23 year old woman, suffered from placental abruption as fetal distress and risk of abruption. two times before. she had abnormal obstetric history at two Intraoperative findings previous deliveries. The first delivery was preterm vaginal The outcome was baby boy weighed 2.8 kgs APGAR 8/9. Pla- delivery at 26 WKS with abruptio placenta. The first delivery centa and membranes delivered completely no abruption. outcome was baby boy weighed 850 grams, this baby died Bleeding was moderate from placental bed 1.5 liters total after 3 WKS of birth. While second delivery was preterm ce- blood loss. Bakri Balloon was inserted. Hb was 4.2g/dl , PLT sarean delivery at 28 WKS for breech and abruptio placentae. 74. Patient received 1unit of PRBC in recovery. Patient was The second delivery outcome was baby girl weighed 1.2 KGS, transferred to ICU for observation, total stay days in icu was this baby died after 1 month of birth. 2days then pt shifted to post op ward when she became stable. In the present pregnancy there was cerclage at 13 WKS. no patient came to Out Patient Department after 4 weeks with no antenatal admissions prior. Regarding PMH there was no sig- complain, and all her investigation within normal level. nificant past medical history. Regarding the history of present admission for the patient ISCUSSION the woman was admitted to hospital on 7/ Feb/ 2016 at 33 wks, 3 D as pv spotting 5 days and back pain. The evaluation showed Placental abruption is an obstetric complication that pre- that vital signs were stable. P/A 32 WKS Longitudinal lie ce- sents severe dangers to the fetus and his mother. And affect at phalic FH + no tenderness. Pelvic examination showed; os IJSER © 2018 http://www.ijser.org International Journal of Scientific & Engineering Research Volume 9, Issue 2, February-2018 319 ISSN 2229-5518 about 0.5-1% of the pregnancies (1). The etiology of placental of women represent a risk factor of placental abruption(2). But abruption is unknown, but placental abruption it happens in the current study the patient was 23 year old. more for among smokers, in pregnancies with intra uterine In this study, the patient underwent cerclage in her third growth restriction (IUGR), in hypertensive pregnancies, in pregnancy at 13 weeks, and she succeeded in exceeding 37 trauma instances, with male fetuses , with advancing women weeks of pregnancy. The delivery was completed without pla- age, and among women with a prior placental abruption. cental abruption. Doctors resort to the use of cerclage in cases Many factors are Known to be correlated with increased risk of patients with past obstetrical histories of recurrent mid tri- of placental abruption such as; cocaine use, alcohol and smok- mester miscarriages or preterm delivery (9). ing(3,5). Regarding the management of patients with placental ab- Pathological studies found that placental abruption is asso- ruption, this process is complicated by the fact there has never ciated with abnormal placenta blood vessels, blood clotting, been a randomized control trial examining treatment modali- and decreased placental perfusion. Genetic differences may be ties. So, management is performed on an individual depend- predisposed to these problems (6). The risk of placental abrup- ing on a variety of variables including abruption severity ges- tion varies depending on race, Where it was found that pla- tational age, and maternal and fetal status (8). Most placental centa abruption is more likely to occur among African- abruption cases are unpredictable and cannot be prevented. . American women (1 in 595) than among Latin-American (1 in However, in some cases, the outcomes of mothers and infants 1423) women or White (1 in 876) (5). In the end, both environ- can be improved through awareness to the benefits and risks mental and genetic factors contribute to placental abruption of conservative management, continuous assessment of fetal (5). and maternal well-being, and expeditious delivery where ap- The diagnosis of placental abruption commonly determined propriate (4). by clinical manifestations, placental detachment is confirmed after delivery. Clinical symptoms of placental abruption in- 4 CONCLUSION clude bleeding of vagina, uterine pain, and continuous stiffen- Placental abruption remains a health problem that is diffi- ing of uterine (4). The ultrasonography usefulness have been cult to manage, especially in developing countries. It presents considered as the adjunctive diagnosis, and it is used widely severe dangers to the fetus and his mother. It associated with used for this aim. The findings of ultrasound involve preterm delivery, hypoxia, low birth weight , stillbirth and retroplacental hematoma and placental thickness (7). perinatal death. Placental abruption in previous delivery in- In this study, we presented a case of a woman who had suf- creases the likelihood of recurrence of it. Continuous follow- fered from placental abruption in two previous deliveries. Her up during pregnancy will help to improve the maternal and first delivery was preterm delivery at 26 weeks, while the se- IJSERfetal prognosis. cond was at 28 weeks. Generally, The occurrence of abruption peaks at 24 to 26 weeks of gestation (5). REFERENCES Placental abruption is associated with preterm delivery, hy- [1] Tikkanen, Minna. "Placental abruption: Studies on incidence, risk poxia, low birth weight, stillbirth and perinatal death (1). In- factors and potential predictive biomarkers." (2008). deed, both deliveries of our patient were preterm deliveries. [2] Ouédraogo, Issa, et al. "Placental Abruption in the Obstetrics and The first delivery outcome was weighed 850 grams, this baby Gynecology Service of Regional Hospital Center of Ouahigouya: Ep- died after 3 weeks of birth. While, the second delivery out- idemiological, Clinical Ant and Therapeutic Aspects about 89 Cases come weighed 1.2 KGS, this baby died after 1 month of birth. Collected from 1st January 2013 to 31st December 2015." Open Jour- Abruption associated with perinatal mortality as high as 60 nal of Obstetrics and Gynecology 7.01 (2016): 86. [3] Ghaheh, Hooria Seyedhosseini, et al. "Risk factors of placental abrup- percent (6). In the case of placental abruption, the fetal surviv- tion." Journal of research in medical sciences: the official journal of Is- al depends on the gestational age and the severity of the ab- fahan University of Medical Sciences 18.5 (2013): 422. ruption (1). If abruption of placenta included more than 50% [4] Oyelese, Yinka, and Cande V. Ananth. "Placental abruption." Obstet- of placental surface, it often associated with fetal death (1). rics & Gynecology 108.4 (2006): 1005-1016. Our patient has suffered from placental abruption twice in a [5] Shen, Tammy T., et al. "A population-based study of race-specific row, and this repetition in the abruption is expected. Becausee, risk for placental abruption." BMC pregnancy and childbirth 8.1 (2008): 43. the presence of a prior abruption is the strongest risk factor for [6] Ananth, Cande V., and Allen J. Wilcox. "Placental abruption and repeating the event (5). Whereas, placental abruption from a perinatal mortality in the United States." American journal of epide- previous pregnancy increases the placental abruption risk ten- miology 153.4 (2001): 332-337. fold in a subsequent pregnancy (8). [7] Glantz, Chris, and Leslie Purnell. "Clinical utility of sonography in Many worldwide studies have shown that the advanced age the diagnosis and treatment of placental abruption." Journal of ultra- sound in medicine 21.8 (2002): 837-840. IJSER © 2018 http://www.ijser.org International Journal of Scientific & Engineering Research Volume 9, Issue 2, February-2018 320 ISSN 2229-5518 [8] Wagner, Stephen M., and Serdar H. Ural. "An examination of The Causes, Diagnosis and Management Placental Abruption." Milton S. Hersey Medical Center (2015). [9] Khan, Zakkia, Radhia Khan, and Fauzia Aitazaz. "SUCCESS RATE OF CERVICAL CERCLAGE IN PREVENTING PRETERM LA- BOUR." Pak J Physiol 12.3 (2016): 33-6.
IJSER © 2018 http://www.ijser.org
- DOI: 10.7759/cureus.64793
- Corpus ID: 271306622
Navigating Pregnancy With Uterine Fibroids: A Case Study
- Dharmesh J Patel , Kamlesh Chaudhari , +3 authors Archan Patel
- Published in Cureus 18 July 2024
21 References
Uterine fibroids and pregnancy: a review of the challenges, myoma and myomectomy: poor evidence concern in pregnancy, number and size of uterine fibroids and obstetric outcomes, knowledge of, perception of, and attitude towards uterine fibroids among women with fibroids in lagos, nigeria, the impact and management of fibroids for fertility: an evidence-based approach., complications of uterine fibroids and their management, surgical management of fibroids, laparoscopy and hysteroscopy versus hysterectomy, haemorrhage, adhesions, and complications, uterine myomas during pregnancy: a longitudinal sonographic study, leiomyoma simultaneously impair endometrial bmp-2-mediated decidualization and anticoagulant expression through secretion of tgf-β3., leiomyomas at routine second-trimester ultrasound examination and adverse obstetric outcomes, the impact of uterine leiomyomas on reproductive outcomes., related papers.
Showing 1 through 3 of 0 Related Papers

Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
How the mode of delivery is influenced by patient’s opinions and risk-informed consent in women with a history of caesarean section is vaginal delivery a real option after caesarean section.

1. Introduction
2. materials and methods, 3.1. questionnaire response analysis, 3.2. actual mode of delivery, 3.3. cs indications: past and present, 3.4. challenges and complications of vd, 3.5. neonatal outcomes, 4. discussion, 5. conclusions, author contributions, institutional review board statement, informed consent statement, data availability statement, conflicts of interest.
- Ayachi, A.; Derouich, S.; Morjene, I.; Mkaouer, L.; Mnaser, D.; Mourali, M. Facteurs prédictifs de l’issue de l’accouchement sur utérus unicicatriciel, expérience du centre de Maternité de Bizerte [Predictors of birth outcomes related to women with a previous caesarean section: Experience of a Motherhood Center, Bizerte]. Pan. Afr. Med. J. 2016 , 25 , 76. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Cobec, I.M.; Varzaru, V.B.; Kövendy, T.; Kuban, L.; Eftenoiu, A.E.; Moatar, A.E.; Rempen, A. External Cephalic Version—A Chance for Vaginal Delivery at Breech Presentation. Medicina 2022 , 58 , 1619. [ Google Scholar ] [ CrossRef ]
- Zhang, H.; Liu, H.; Luo, S.; Gu, W. Oxytocin use in trial of labour after cesarean and its relationship with risk of uterine rupture in women with one previous cesarean section: A meta-analysis of observational studies. BMC Pregnancy Childbirth 2021 , 21 , 11. [ Google Scholar ] [ CrossRef ]
- Son, M.; Roy, A.; Grobman, W.A.; Miller, E.S. Association Between Attempted External Cephalic Version and Perinatal Morbidity and Mortality. Obstet. Gynecol. 2018 , 132 , 365–370. [ Google Scholar ] [ CrossRef ]
- Pan, X.; Sha, S.; Xu, S.; Zhan, B.; Guan, X.; Ling, F. Analysis of Maternal and Infant Outcomes and Related Factors of Vaginal Delivery of Second Pregnancy after Cesarean Section. Comput. Math. Methods Med. 2022 , 2022 , 4243174. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Curtin, S.C.; Gregory, K.D.; Korst, L.M.; Uddin, S.F.G. Maternal morbidity for vaginal and cesarean deliveries, according to previous cesarean history: New data from the birth certificate, 2013. Natl. Cent. Health Stat. Natl. Vital. Stat. Rep. 2015 , 64 , 1–13. [ Google Scholar ]
- Hill, M.G.; Reed, K.L. External Cephalic Version in Cases of Imminent Delivery at Preterm Gestational Ages: A Prospective Series. AJP Rep. 2019 , 9 , e384–e388. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Memon, H.; Handa, V.L. Pelvic floor disorders following vaginal or cesarean delivery. Curr. Opin. Obstet. Gynecol. 2012 , 24 , 349–354. [ Google Scholar ] [ CrossRef ]
- Jansen, C.; de Mooij, Y.M.; Blomaard, C.M.; Derks, J.B.; van Leeuwen, E.; Limpens, J.; Schuit, E.; Mol, B.W.; Pajkrt, E. Vaginal delivery in women with a low-lying placenta: A systematic review and meta-analysis. BJOG 2019 , 126 , 1118–1126. [ Google Scholar ] [ CrossRef ]
- Cobec, I.M.; Rempen, A. Couvelaire-Uterus: Literature review and case report. Rom. J. Mil. Med. 2021 , 124 , 244–246. [ Google Scholar ] [ CrossRef ]
- Wen, J.; Song, X.; Ding, H.; Shen, X.; Shen, R.; Hu, L.Q.; Long, W. Prediction of vaginal birth after cesarean delivery in Chinese parturients. Sci. Rep. 2018 , 8 , 3084. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sentilhes, L.; Vayssière, C.; Beucher, G.; Deneux-Tharaux, C.; Deruelle, P.; Diemunsch, P.; Gallot, D.; Haumonté, J.B.; Heimann, S.; Kayem, G.; et al. Delivery for women with a previous cesarean: Guidelines for clinical practice from the French College of Gynecologists and Obstetricians (CNGOF). Eur. J. Obstet. Gynecol. Reprod. Biol. 2013 , 170 , 25–32. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Colais, P.; Bontempi, K.; Pinnarelli, L.; Piscicelli, C.; Mappa, I.; Fusco, D.; Davoli, M. Vaginal birth after caesarean birth in Italy: Variations among areas of residence and hospitals. BMC Pregnancy Childbirth 2018 , 18 , 383. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Cobec, I.M.; Seropian, P.; Rempen, A. Pregnancy in a non-communicating rudimentary horn of a unicornuate uterus. Hippokratia 2019 , 23 , 92–94. [ Google Scholar ] [ PubMed ]
- German Society for Obstetrics and Gynecology (DGGG) Board for Prenatal Medicine and Obstetrics. Board for Materno-Fetal Medicine (AGMFM) The Caesarean Section. AWMF-Registernummer 015-084 (S3). Available online: https://www.awmf.org/uploads/tx_szleitlinien/015-084l_S3_Sectio-caesarea_2020-06_1_02.pdf (accessed on 11 June 2024).
- Lundgren, I.; Smith, V.; Nilsson, C.; Vehvilainen-Julkunen, K.; Nicoletti, J.; Devane, D.; Bernloehr, A.; van Limbeek, E.; Lalor, J.; Begley, C. Clinician-centred interventions to increase vaginal birth after caesarean section (VBAC): A systematic review. BMC Pregnancy Childbirth 2015 , 15 , 16. [ Google Scholar ] [ CrossRef ]
- Nilsson, C.; Lundgren, I.; Smith, V.; Vehvilainen-Julkunen, K.; Nicoletti, J.; Devane, D.; Bernloehr, A.; van Limbeek, E.; Lalor, J.; Begley, C. Women-centred interventions to increase vaginal birth after caesarean section (VBAC): A systematic review. Midwifery 2015 , 31 , 657–663. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Betrán, A.P.; Temmerman, M.; Kingdon, C.; Mohiddin, A.; Opiyo, N.; Torloni, M.R.; Zhang, J.; Musana, O.; Wanyonyi, S.Z.; Gülmezoglu, A.M.; et al. Interventions to reduce unnecessary caesarean sections in healthy women and babies. Lancet 2018 , 392 , 1358–1368. [ Google Scholar ] [ CrossRef ]
- Chen, I.; Opiyo, N.; Tavender, E.; Mortazhejri, S.; Rader, T.; Petkovic, J.; Yogasingam, S.; Taljaard, M.; Agarwal, S.; Laopaiboon, M.; et al. Non-clinical interventions for reducing unnecessary caesarean section. Cochrane Database Syst. Rev. 2018 , 9 , CD005528. [ Google Scholar ] [ CrossRef ]
- Smith, V.; Gallagher, L.; Carroll, M.; Hannon, K.; Begley, C. Antenatal and intrapartum interventions for reducing caesarean section, promoting vaginal birth, and reducing fear of childbirth: An overview of systematic reviews. PLoS ONE 2019 , 14 , e0224313. [ Google Scholar ] [ CrossRef ]
- Smith, V.; Hannon, K.; Begley, C. Clinician’s attitudes towards caesarean section: A cross-sectional survey in two tertiary level maternity units in Ireland. Women Birth 2022 , 35 , 423–428. [ Google Scholar ] [ CrossRef ]
- Mazzoni, A.; Althabe, F.; Liu, N.H.; Bonotti, A.M.; Gibbons, L.; Sánchez, A.J.; Belizán, J.M. Women’s preference for caesarean section: A systematic review and meta-analysis of observational studies. BJOG 2011 , 118 , 391–399. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Fuglenes, D.; Oian, P.; Kristiansen, I.S. Obstetricians’ choice of cesarean delivery in ambiguous cases: Is it influenced by risk attitude or fear of complaints and litigation? Am. J. Obstet. Gynecol. 2009 , 200 , 48.e1–48.e8. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Zwecker, P.; Azoulay, L.; Abenhaim, H.A. Effect of fear of litigation on obstetric care: A nationwide analysis on obstetric practice. Am. J. Perinatol. 2011 , 28 , 277–284. [ Google Scholar ] [ CrossRef ]
- Panda, S.; Begley, C.; Daly, D. Influence of women’s request and preference on the rising rate of caesarean section—A comparison of reviews. Midwifery 2020 , 88 , 102765. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kornelsen, J.; Hutton, E.; Munro, S. Influences on decision making among primiparous women choosing elective caesarean section in the absence of medical indications: Findings from a qualitative investigation. J. Obstet. Gynaecol. Can. 2010 , 32 , 962–969. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Liang, H.; Fan, Y.; Zhang, N.; Chongsuvivatwong, V.; Wang, Q.; Gong, J.; Sriplung, H. Women’s cesarean section preferences and influencing factors in relation to China’s two-child policy: A cross-sectional study. Patient Prefer. Adherence 2018 , 12 , 2093–2101. [ Google Scholar ] [ CrossRef ]
- Jiang, Q.; Li, Y.; Sanchez-Barricarte, J.J. Fertility Intention, Son Preference, and Second Childbirth: Survey Findings from Shaanxi Province of China. Soc. Indic. Res. 2016 , 125 , 935–953. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Paré, E.; Quiñones, J.N.; Macones, G.A. Vaginal birth after caesarean section versus elective repeat caesarean section: Assessment of maternal downstream health outcomes. BJOG 2006 , 113 , 75–85. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ryan, G.A.; Nicholson, S.M.; Morrison, J.J. Vaginal birth after caesarean section: Current status and where to from here? Eur. J. Obstet. Gynecol. Reprod. Biol. 2018 , 224 , 52–57. [ Google Scholar ] [ CrossRef ]
- Tolmacheva, L. Vaginal birth after caesarean or elective caesarean—What factors influence women’s decisions? Br. J. Midwifery 2015 , 23 , 470–475. [ Google Scholar ] [ CrossRef ]
- Fitzpatrick, K.E.; Kurinczuk, J.J.; Alfirevic, Z.; Spark, P.; Brocklehurst, P.; Knight, M. Uterine rupture by intended mode of delivery in the UK: A national case-control study. PLoS Med. 2012 , 9 , e1001184. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Silver, R.M.; Landon, M.B.; Rouse, D.J.; Leveno, K.J.; Spong, C.Y.; Thom, E.A.; Moawad, A.H.; Caritis, S.N.; Harper, M.; Wapner, R.J.; et al. Maternal morbidity associated with multiple repeat cesarean deliveries. Obstet. Gynecol. 2006 , 107 , 1226–1232. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Guise, J.M.; Denman, M.A.; Emeis, C.; Marshall, N.; Walker, M.; Fu, R.; Janik, R.; Nygren, P.; Eden, K.B.; McDonagh, M. Vaginal birth after cesarean: New insights on maternal and neonatal outcomes. Obstet. Gynecol. 2010 , 115 , 1267–1278. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Emmett, C.L.; Montgomery, A.A.; Murphy, D.J.; DiAMOND Study Group. Preferences for mode of delivery after previous caesarean section: What do women want, what do they get and how do they value outcomes? Health Expect. 2011 , 14 , 397–404. [ Google Scholar ] [ CrossRef ]
- Antoine, C.; Young, B.K. Cesarean section one hundred years 1920–2020: The Good, the Bad and the Ugly. J. Perinat. Med. 2020 , 49 , 5–16. [ Google Scholar ] [ CrossRef ]
- Chen, Y.T.; Hsieh, Y.C.; Shen, H.; Cheng, C.H.; Lee, K.H.; Torng, P.L. Vaginal birth after cesarean section: Experience from a regional hospital. Taiwan J. Obstet. Gynecol. 2022 , 61 , 422–426. [ Google Scholar ] [ CrossRef ]
- Guidelines Programm of the German/Austrian/Swiss Society for Obstetrics and Gynecology (DGGG/OEGGG/SGGG). Induction of Labour. AWMF-Registernummer 015-088 (S2k). Available online: https://register.awmf.org/assets/guidelines/015-088ladd_S2k_Geburtseinleitung_2021-04.pdf (accessed on 11 June 2024).
- Darmian, M.E.; Yousefzadeh, S.; Najafi, T.F.; Javadi, S.V. Comparative study of teaching natural delivery benefits and optimism training on mothers’ attitude and intention to select a type of delivery: An educational experiment. Electron. Physician 2018 , 10 , 7038–7045. [ Google Scholar ] [ CrossRef ]
Click here to enlarge figure
| Preferred Mode of Delivery after Birth Planning | Total | |||
|---|---|---|---|---|
| VD | CS | |||
| Preferred mode of delivery before birth planning | VD | 72 | 2 | 74 |
| CS | 0 | 51 | 51 | |
| Total | 72 | 53 | 125 | |
| Preferred Mode of Delivery after Birth Planning | Actual Mode of Delivery | Total | |||
|---|---|---|---|---|---|
| VD | CS | ||||
| Natural | Vacuum Extraction | Planned CS | CS Performed during Labour by Medical Necessity | ||
| VD | 40 | 5 | 7 | 20 | 72 |
| CS | 2 | 0 | 43 | 8 | 53 |
| Total | 42 | 5 | 50 | 28 | 125 |
| Indication for Current CS | Planned CS | CS Performed during Labour by Medical Necessity | Total |
|---|---|---|---|
| At the request of the patient with a history of CS | 44 | 10 | 54 |
| Pathological CTG | 0 | 7 | 7 |
| Stalled active labour phase | 0 | 5 | 5 |
| Stalled early labour phase | 0 | 1 | 1 |
| Macrosomia | 2 | 0 | 2 |
| Breech presentation | 2 | 0 | 2 |
| Occiput posterior position | 0 | 1 | 1 |
| Intra-amniotic infection | 0 | 1 | 1 |
| Unsuccessful labour induction | 0 | 1 | 1 |
| Inguinal pain | 0 | 1 | 1 |
| Suspicion of uterine rupture | 0 | 1 | 1 |
| History of myoma enucleation | 1 | 0 | 1 |
| Epilepsy | 1 | 0 | 1 |
| Total | 50 | 28 | 78 |
| Indication for the Actual Mode of Delivery in CS Patients Who Preferred CS | Planned CS | CS Performed during Labour by Medical Necessity | Total |
|---|---|---|---|
| At the request of the patient with a history of CS | 38 | 7 | 45 |
| Breech presentation | 2 | 0 | 2 |
| Macrosomia | 1 | 0 | 1 |
| Inguinal pain | 0 | 1 | 1 |
| History of myoma enucleation | 1 | 0 | 1 |
| Epilepsy | 1 | 0 | 1 |
| Total | 43 | 8 | 51 |
| Indication for Actual Mode of Delivery in CS Patients Who Preferred VD | Planned CS | CS Performed during Labour by Medical Necessity | Total |
|---|---|---|---|
| At the request of the patient with a history of CS | 6 | 3 | 9 |
| Pathological CTG | 0 | 7 | 7 |
| Stalled active labour phase | 0 | 5 | 5 |
| Stalled early labour phase | 0 | 1 | 1 |
| Occiput posterior position | 0 | 1 | 1 |
| Intra-amniotic infection | 0 | 1 | 1 |
| Macrosomia | 1 | 0 | 1 |
| Unsuccessful labour induction | 0 | 1 | 1 |
| Suspicion of uterine rupture | 0 | 1 | 1 |
| Total | 7 | 20 | 27 |
| Indication for Current CS Performed due to Medical Necessity | Total | |||||
|---|---|---|---|---|---|---|
| Pathological CTG | Failure to Progress in Labour | Patient’s Preference | Other | |||
| Indication for Prior CS | Pathological CTG | 3 | 4 | 0 | 1 | 8 |
| Failure to progress in labour | 3 | 1 | 0 | 2 | 6 | |
| Patient’s preference | 0 | 0 | 2 | 0 | 2 | |
| Other | 1 | 1 | 1 | 1 | 4 | |
| Total | 7 | 6 | 3 | 4 | 20 | |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Cobec, I.M.; Rempen, A.; Anastasiu-Popov, D.-M.; Eftenoiu, A.-E.; Moatar, A.E.; Vlad, T.; Sas, I.; Varzaru, V.B. How the Mode of Delivery Is Influenced by Patient’s Opinions and Risk-Informed Consent in Women with a History of Caesarean Section? Is Vaginal Delivery a Real Option after Caesarean Section? J. Clin. Med. 2024 , 13 , 4393. https://doi.org/10.3390/jcm13154393
Cobec IM, Rempen A, Anastasiu-Popov D-M, Eftenoiu A-E, Moatar AE, Vlad T, Sas I, Varzaru VB. How the Mode of Delivery Is Influenced by Patient’s Opinions and Risk-Informed Consent in Women with a History of Caesarean Section? Is Vaginal Delivery a Real Option after Caesarean Section? Journal of Clinical Medicine . 2024; 13(15):4393. https://doi.org/10.3390/jcm13154393
Cobec, Ionut Marcel, Andreas Rempen, Diana-Maria Anastasiu-Popov, Anca-Elena Eftenoiu, Aurica Elisabeta Moatar, Tania Vlad, Ioan Sas, and Vlad Bogdan Varzaru. 2024. "How the Mode of Delivery Is Influenced by Patient’s Opinions and Risk-Informed Consent in Women with a History of Caesarean Section? Is Vaginal Delivery a Real Option after Caesarean Section?" Journal of Clinical Medicine 13, no. 15: 4393. https://doi.org/10.3390/jcm13154393
Article Metrics
Further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
Cannabis in pregnancy linked to some maternal health problems
- July 22, 2024

Large Kaiser Permanente study finds greater risk of pregnancy complications
Cannabis use during pregnancy is linked with health problems such as high blood pressure, preeclampsia, and weight issues, according to a large new Kaiser Permanente study published in JAMA Internal Medicine.
The findings were consistent with some previous studies of prenatal cannabis use but differed from others. The study authors said the findings are concerning and underscore the need for more research.

“These findings are worrisome, as they add to a growing body of evidence that cannabis is not safe to use during pregnancy,” said lead author Kelly Young-Wolff , PhD, MPH, a research scientist with the Kaiser Permanente Division of Research (DOR). “Previous research has focused on the health of the baby, and the relative lack of research on how prenatal cannabis use impacts maternal health is notable. Our study was designed to address this research gap with the goal of providing better data for clinicians to use when working with their patients to make more informed decisions about prenatal cannabis use.”
The researchers studied 316,722 pregnancies among more than 250,000 individual patients of Kaiser Permanente Northern California (KPNC) between 2011 and 2019. Cannabis use was measured by urine toxicology tests and a self-administered questionnaire, which are both given routinely at the entrance to prenatal care in KPNC.
The analysis found an increased risk of several health concerns among those who used cannabis during early pregnancy: gestational hypertension, or high blood pressure; preeclampsia , a serious complication of pregnancy; weight gain above or below guidelines for pregnancy; and placental abruption , the early separation of the placenta from the lining of the uterus during labor. For gestational hypertension, the researchers found the risk increased with more frequent reported cannabis use.
Patients using cannabis had a decreased risk of gestational diabetes. The authors said previous studies have been mixed on this question, and more research is needed to explore the impact of frequency of use and mode of administration – whether cannabis is smoked or taken in an edible form.
The study did not find increased risk of some other maternal health issues, such as eclampsia (a serious hypertensive condition that can cause seizures), placenta previa or placenta accreta (abnormalities in where the placenta grows in the uterus), or severe maternal morbidity.

The results were consistent with another large study that found people with cannabis use disorder had higher risk of gestational hypertension and preeclampsia. This suggests greater health risk with more frequent use, the authors said.
“The findings related to the frequency of use offer an important message for harm reduction,” said study senior author Lyndsay Avalos , PhD, MPH, a DOR research scientist. “For patients who are not willing to stop using cannabis during pregnancy, decreasing use may pose lower risk of pregnancy complications.”
“Also, if our findings are replicated by other researchers, this could lead to interventions to reduce their risk of poor health outcomes,” Avalos added. “For example, patients who use cannabis in pregnancy might benefit from medical interventions to prevent preeclampsia, such as low-dose aspirin.”
More information helps women
The DOR study team has also examined prenatal cannabis use and infant health outcomes, and reported in the journal Obstetrics & Gynecology an increased likelihood of low birth weight and admission to the neonatal intensive care unit (NICU) for babies whose mothers used cannabis during pregnancy.
“Women may come across conflicting information about whether they can use cannabis safely during pregnancy, or if it is a good choice to manage pregnancy-related symptoms such as nausea,” said co-author Deborah Ansley , MD, regional medical director for KPNC’s Early Start prenatal health program. “Increasingly, research is suggesting the answer may be ‘no.’”

At the same time, Ansley said, patients need realistic and empathetic advice from their health care team, and to know they can discuss their substance use without stigma or fear of being reported to child protective officials. In California, prenatal cannabis use is not reportable to child welfare authorities.
The study was funded by the National Institute on Drug Abuse. It is part of an ongoing body of NIDA-funded work exploring prenatal cannabis use trends, adverse obstetrical and neonatal outcomes, maternal health outcomes, modes of cannabis administration, and effects of legalization in California.
Additional co-authors were Sara R. Adams, MPH, Stacey E. Alexeeff , PhD, Yeyi Zhu , PhD, Natalie E. Slama, MPH, and Monique B. Does, MPH, of the Division of Research; Lynn D. Silver, MD, MPH, of the Public Health Institute; and Carley Castellanos, LMFT, of Kaiser Permanente Northern California.
About the Kaiser Permanente Division of Research
The Kaiser Permanente Division of Research conducts, publishes and disseminates epidemiologic and health services research to improve the health and medical care of Kaiser Permanente members and society at large. It seeks to understand the determinants of illness and well-being, and to improve the quality and cost-effectiveness of health care. Currently, DOR’s 600-plus staff is working on more than 450 epidemiological and health services research projects. For more information, visit divisionofresearch.kaiserpermanente.org or follow us @KPDOR.
This Post Has One Comment
Such incredible work Kelly, Lyndsey, and Deb!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Related Stories

Parents benefit from virtual group prenatal care, study suggests

Comparison of fibroid treatment finds surgical removal has fewest follow-up procedures

Prenatal detection rates for congenital heart disease can be achieved with fewer fetal echocardiograms

Childhood adversity and low resilience may increase odds of depression, anxiety in pregnancy
Division of Research 4480 Hacienda Drive Pleasanton, CA 94588
Privacy Policy | Terms and Conditions
Follow us on these external social media sites that will open in a new browser window.
© 2024 Kaiser Permanente Division of Research
Partial Placental Abruption 33 weeks

Has anyone else experienced a partial placental abruption? I’m 33 weeks and was admitted to the hospital on Saturday after an episode of bleeding. The bleeding has stopped and my baby is active and healthy. Needing some positive thoughts and advice if anyone has had this happen. I am alone as my husband went to Texas (13 hours away) to help clean up from the hurricane to make the money we need for me to stay home with our son. Trying not to think of the worst possible outcome like i always do. ��
I have received two steroid injections to ensure baby’s lungs are developed in case he has to come prematurely. Labs and cervical exam were good, dilated to 0.5. I had contractions the monitor was picking up but they stopped over 24 hours ago. They believe the contractions were from two different cervical exams.
I just posted about this a couple days ago. I had a partial abruption at 26 weeks and was admitted to the hospital for 5 days. It lightened up and I went home. Unfortunately I’ve had light to moderate bleeding on/ off since but but I am bleeding free for 2 weeks now. I’m 32+3 and I go to weekly appointments where they do an US and NST. Baby has been totally happy and fine this entire time even when I was in the hospital and I’ve never registered any contractions on the monitor. They have no idea why this happened. They can’t see the abruption on the US so they think it is small… even a small abruption can cause a lot of blood. Once it separates they say it can be a “sensitive spot” the entire rest of the pregnancy…
I did exactly what you did though- steroid shot, monitoring in hospital. Did they mention whether you can go home since the bleeding has resolved? When I was sent home they advised modified bedrest and basically taking it as easy as possible. The big things are no lifting, bending over, etc.
same experience as other mama here.
Since my 26 weeks I went from placenta prévia and vasa previa to chronic abruption. Both placenta prévia and vasa resolved by the 29 week, however they found out that I have the chronic abruption. I had in total 6 bleeding (went admitted all the time I had a bleeding) and two ultrasound showed oligohydramnios. Being monitored 1-2 times a week, low fluid and is possible that the cause is the placenta abruption.
Try not to google and panic. It’s hard but we can do it!
The contractions can be also from the bleeding. The blood can irritate the uterus making you more susceptible to contractions. Drink a lot of water and that should help it cease or decrease.
You May Also Like
Planning Visitors During Hospital Stay
You’re pregnant how these moms reacted, help keep our community safe, to create a safe place, please, on our end, we will, about what to expect, popular articles, tools & registry.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Maternal, Labor, Delivery, and Perinatal Outcomes Associated with Placental Abruption: A Systematic Review
Katheryne l. downes.
1 Division of Intramural Population Health Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, Bethesda, Maryland
2 Maternal and Child Health Program, University of Maryland, College Park, Maryland
3 Department of Obstetrics and Gynecology, Center for Research in Reproduction and Women’s Health, University of Pennsylvania, Philadelphia, Pennsylvania
Katherine L. Grantz
Edmond d. shenassa.
4 Department of Epidemiology and Biostatistics, University of Maryland, College Park, Maryland
5 Department of Epidemiology and Biostatistics, University of Maryland, Baltimore, Maryland
Risk factors for placental abruption have changed, but there has not been an updated systematic review investigating outcomes.
We searched PubMed, EMBASE, Web of Science, SCOPUS, and CINAHL for publications from January 1, 2005 through December 31, 2016. We reviewed English-language publications reporting estimated incidence and/or risk factors for maternal, labor, delivery, and perinatal outcomes associated with abruption. We excluded case studies, conference abstracts, and studies that lacked a referent/comparison group or did not clearly characterize placental abruption.
A total of 123 studies were included. Abruption was associated with elevated risk of cesarean delivery, postpartum hemorrhage and transfusion, preterm birth, intrauterine growth restriction or low birth weight, perinatal mortality, and cerebral palsy. Additional maternal outcomes included relaparotomy, hysterectomy, sepsis, amniotic fluid embolism, venous thromboembolism, acute kidney injury, and maternal intensive care unit admission. Additional perinatal outcomes included acidosis, encephalopathy, severe respiratory disorders, necrotizing enterocolitis, acute kidney injury, need for resuscitation, chronic lung disease, infant death, and epilepsy.
Few studies examined outcomes beyond the initial birth period, but there is evidence that both mother and child are at risk of additional adverse outcomes. There was also considerable variation in, or absence of, the reporting of abruption definitions.
Placental abruption, the premature detachment of the placenta from the uterine wall, before birth and after 20 weeks of gestation, is one of the most significant determinants of maternal morbidity as well as perinatal morbidity and mortality. 1 – 4 It is estimated to occur in 0.6 to 1% of pregnancies in the United States, 5 but the reported incidence is lower (0.4–0.5%) in Nordic countries 5 and higher (3.5–3.8%) among some south Asian countries. 3 , 6 It typically presents with maternal symptoms of vaginal bleeding, abdominal pain and contractions, and/or abnormal fetal heart rate tracings. 2 , 7 , 8 The disorder is also characterized by chronic placental dysfunction and separation from the uterine wall, which, with progression, can lead to a corresponding decrease in the placental surface area available for oxygen exchange and nutrient supply for the fetus. 9 This process can lead to an elevated risk of low birth weight, prematurity, and perinatal mortality. 5 Severe cases of abruption can rapidly progress to significant maternal blood loss, fetal hypoxia, and fetal death and necessitate emergent cesarean delivery. 5
With the recent creation of the National Institute of Health’s Human Placenta project, placental functioning and dysfunction has come to the forefront of research priorities in the United States. 10 However, the only two extant systematic reviews that included outcomes associated with abruption were based on studies that are all over a decade old. 5 , 11 In the past 10 years, there have been changes in several key risk factors for abruption, including increasing maternal age and body mass index and increasing use of assisted fertility methods. Furthermore, considerable new evidence has emerged on maternal, labor, delivery, and perinatal outcomes associated with placental abruption since that time. Finally, changes in medical and diagnostic technology over the past decade may mean that risk estimates in systematic reviews of studies prior to 2005 no longer accurately represent the risk associated with today’s cases. Therefore, the aim of this study was to provide a comprehensive, systematic review of the scientific literature examining outcomes associated with placental abruption published between January 1, 2005, and December 31, 2016.
Data Sources
A systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement guidelines. 12 We searched PubMed (includes MEDLINE), Embase, Science Citation Index, SCOPUS, and CINAHL databases from January 2005 through December 2016 using the following key words: “abruption,” “abruption placentae,” “premature separation of the placenta,” “retroplacental hemorrhage,” and “retroplacental hematoma.” To identify outcomes, the key words “maternal,” “neonatal,” “perinatal,” and “fetal” were used in conjunction with the outcome terms “outcomes,” “morbidity,” “mortality,” “hemorrhage,” “intensive care unit,” “transfusion,” “hysterectomy,” “disseminated intravascular coagulopathy,” “premature rupture of membranes,” “mode of delivery,” “cesarean,” “labor,” “preterm birth,” “low birth weight,” “small for gestational age (SGA),” “intrauterine growth restriction (IUGR),” “neonatal intensive care unit,” “respiratory,” “respiratory distress syndrome,” “apnea,” “anemia,” “asphyxia,” “need for transfusion,” “anomalies,” “cerebral palsy,” “death,” and “sudden infant death syndrome.”
Only English-language, peer-reviewed, original research publications were reviewed. We excluded clinical case studies, animal studies, conference abstracts, and studies that lacked a referent/comparison group. Studies in which abruption was combined with other disorders to form a composite risk factor without provision of a separate risk estimate for abruption in particular were also excluded. Studies reporting risk of congenital anomalies 13 associated with abruption were not formally included in this review, but are included in the references. After excluding duplicate publications and applying the aforementioned exclusion criteria, 123 articles were selected for this review. The summary tables in this review include outcome incidence among pregnancies with abruption versus those without abruption, as well as any available risk estimates, with preference given to adjusted risk estimates. Studies are organized first by type (cohort, followed by case–control), then by year of publication, and then alphabetical by first author. The term “mild” or “severe” abruption is used in the descriptive text of this review if the original authors described their results in that language, but it should be noted that there is substantial variation in how this is defined. Overall, the reported incidence of abruption in the reviewed literature ranged from 0.01 to 5.1%, but the majority of studies had an incidence ranging from 0.5 to 1.0% ( Table 1 – 7 ).
Obstetrical morbidity incidence and risk estimates a
| Authors, location (year) | Inclusion criteria and dates; data source | Sample size (abruptions) | Cesarean | Relaparotomy | Hysterectomy |
|---|---|---|---|---|---|
| Gedikbasi et al, Turkey (2008) | All cesarean deliveries, 2002–2006; single site | 28,799 (547) | NR | 1.5% vs. NR; OR: 15.3 (6.9–33.8) | NR |
| Tucker Edmonds et al, Multistate (2011) | All deliveries, 23–24 wk, 1995–2005; registry | 8,290 (1,197) | 48.0 vs. NR; aOR: 2.4 (2.1–2.8) | NR | NR |
| Pariente et al, Israel (2011) | All deliveries 1988–2008; single site | 185,476 (1,365) | 67.7 vs. 12.8%; OR: 14.3 (12.7–16.0) | NR | 0.4 vs. 0.1%; OR: 7.9 (3.4–18.1) |
| Chen et al, China (2013) | All deliveries ≥20 wk, 2009–2010; registry | 34,014 (NR) | NR | NR | Peripartum: NR; aOR: 3.0 (0.7–13.1) NS |
| Boisramé et al, France (2014) | All deliveries >24 wk, 2003–2012; single site | 55,926 (247) | 90.3 vs. 19.8%; NR | NR | NR |
| do Nascimento et al, Brazil (2014) | All stillbirths, 2005–2008; single site | 163 (2) | NR; aHR: 45.0 (3.1–654.0) | NR | NR |
| Morikawa et al, Japan (2014) | Singleton deliveries ≥30 wk, 2005–2009; multisite | 293,899 (2,649) | 71.7 vs. 27.7%; NR | NR | NR |
| Räisänen et al, Finland (2014) | Singleton deliveries >22 wk, >500 g, 2000–2010; registry | 620,463 (NR) | Nonplanned, nulliparous: NR; aOR: 29.4 (24.2–35.7) nonplanned, multiparous: NR; aOR: 61.8 (52.9–72.2) | NR | NR |
| Janoudi et al, Canada (2015) | All deliveries >20 wk, >500 g, live birth, maternal age ≥20, 2011–2012; single site | 134,088 (805) | NR; RR: 2.31 (2.18–2.45) | NR | NR |
| Macheku et al, Tanzania (2015) | All deliveries ≥28 wk, 2000–2010; registry | 39,993 (112) | 75.9 vs. 32.4%; aOR: 5.6 (3.6–8.8) | NR | NR |
| Spiegel et al, Israel (2015) | All twin deliveries with vaginal delivery of first twin, 1988–2010; single site | 1966 (25) | Emergent delivery of second twin: NR; OR: 3.6 (1.5–8.9) | NR | NR |
| Friedman et al, United States (2016) | All deliveries among women with low to moderate risk for peripartum hysterectomy, 1998–2011; registry | 55,214,208 (573,723) | NR | NR | Peripartum: 0.3 vs. NR; aRR: 2.8 (2.5–3.2) |
| Gul et al, Pakistan (2016) | All deliveries presenting with antepartum hemorrhage>28 wk, 2011–2013; single site | 334 (69) | 36.2 vs. 23.8%; NR | NR | NR |
| Lindqvist and Happach, Sweden (2006) | All deliveries, 1992–1999; single site | 2,483 (112) | 81.3 vs. 9.4%; NR | NR | NR |
| Tikkanen et al, Finland (2006) | All deliveries >22 wk, >500 g, 1997–2001; single site | 594 (198) | 91 vs. 24%; OR: 34.7 (20.0–60.1) | NR | NR |
| Bodelon et al, Washington (2009) | All deliveries with cases defined as peripartum hysterectomy, 1987–2006; registry | 4,451 (126) | NR | NR | Peripartum: NR; aOR: 3.2 (1.8–5.8) |
| Kessous et al, Israel (2012) | All cesarean deliveries, 1989–2009; single site | 34,469 (1284) | NA | NR; aOR: 3.5 (1.8–6.8) | NR |
| Levin et al, Israel (2012) | All cesarean deliveries, 2000–2010; single site | 177 (6) | NA | NR; OR: 31.1 (3.2–1531) | NR |
| Hasegawa et al, Japan (2014) | Singleton deliveries >24 wk, 2005–2012; single site | 738 (123) | Emergent: 33.3 vs. 5.5%; NR | NR | NR |
| Furukawa et al, Japan (2015) | All deliveries 22–26 wk, admitted to perinatal center, 2000–2010; single site | 101 (32) | 56 vs. 67% NS; NR | NR | NR |
Abbreviations: aOR, adjusted odds ratio; CD, cesarean delivery; NR, not reported; NS, not significant; OR, odds ratio.
Note: Studies are organized first by type (cohort, followed by case–control), then by year of publication, and then alphabetically by first author.
Long-term maternal morbidity and mortality incidence and risk estimates a
| Authors, location (year) | Inclusion criteria and dates; data source | Sample size (abruptions) | Morbidity | Mortality |
|---|---|---|---|---|
| Lykke et al, Denmark (2010) | Women aged 15–50 y with a first singleton delivery and no history of preceding cardiovascular diagnosis, 1978–2007; registry | 796,915 (7,684) | NR | Noncardiovascular: 1.4 vs. NR; aHR: 1.56 (1.29–1.89) Cardiovascular: 0.2 vs. NR; aHR: 1.23 (0.78–1.93) NS |
| Ray et al, Canada (2012) | Women aged 14–50 y delivering at ≥20 wk who were disease free at least a year prior to delivery, 1992–2009; registry | 1,130,764 (10,935) | Hospitalization for heart failure or an atrial or ventricular dysrhythmia: NR; aHR:1.51 (0.97–2.35) NS | NR |
| Pariente et al, Israel (2014) | All deliveries, 1988–1998; Registry | 47,585 (653) | NR | Cardiovascular: 0.6 vs. 0.1%; aHR: 4.3 (1.1–18.6) |
| Arazi et al, Israel (2015) | All deliveries without known renal disease before or during pregnancy, 1988–2012; registry | 99,354 (1,807) | Renal morbidity: 0.2 vs. 0.1%; aOR: 1.8 (0.6–4.8) NS; Renal-related hospitalization: 0.2 vs. 0.1%; aHR: 1.6 (0.6–4.2) NS | NR |
| DeRoo et al, Norway and Sweden (2016) | Women with singleton deliveries, 1967–2002 (Norway), 1973–2003 (Sweden); registry | 2,117,797 (10,981) | NR | Noncardiovascular: Abruption in first pregnancy: 2.5 vs. 1.9%; aHR: 1.2 (1.0–1.3); Abruption in any pregnancy: 2.4 vs. 1.9%; aHR: 1.2 (1.1–1.3) Cardiovascular: Abruption in first pregnancy:0.5 vs. 0.3%; aHR: 1.8 (1.3–2.4); Abruption in any pregnancy: 0.5 vs. 0.3%; aHR: 1.8 (1.5–2.2) |
| Ray et al, Canada (2016) | Women ≥20 y undergoing a first percutaneous coronary intervention or artery bypass with a history of ≥1 deliveries, 1993–2012; registry | 1,985 (48) | NR | Death after coronary artery revascularization: NR; aHR: 2.79 (1.31–5.96) |
Abbreviations: aHR, adjusted hazard ratio; aOR, adjusted odds ratio; aRR, adjusted relative risk; CP, cerebral palsy; NR, not reported; NS, not significant; OR, odds ratio; SIDS, sudden infant death syndrome.
Obstetrical Morbidity
Cesarean delivery risk ranged from 2.4 to 61.8 (incidence range: 33.3–91%) and was the most frequently reported labor and delivery outcome associated with abruption ( Table 1 ). 2 , 8 , 14 – 24 The variation in risk estimates is likely attributable to the specification of subpopulations or types of cesarean, as the lowest risk was seen in a cohort study of periviable neonates 14 and the highest risk was seen in non-planned cesareans among multiparous women. 18 A single study did not find elevated risk of cesarean associated with abruption, but it was limited to deliveries 22 to 26 weeks and the nonabruption cesarean delivery rate was unusually high at 67%. 25 Abruption was also associated with 3.5 to 31.1 times elevated risk of relaparotomy following cesarean, 26 – 28 as well as need for hysterectomy. 15 , 29 , 30 One study that did not find an association with hysterectomy may have been underpowered, as they only had two cases of abruption among the hysterectomy group, but it was unclear how many cases of abruption presented in the overall study population. 31 We classify cesarean delivery, relaparotomy, and hysterectomy as obstetric morbidities, but it is important to note that cesarean delivery is often necessary in the setting of placental abruption to limit further oxygen deprivation to the fetus; to reduce blood loss for the mother; and, in extreme cases, to prevent the death of the fetus, the mother, or both. 2 Similarly, relaparotomy and hysterectomy are often necessary and life-saving measures when they are performed. The risks of performing these interventions must be weighed against the potential benefits of reduction in maternal and fetal morbidity and mortality.
Short-Term Maternal Morbidity and Mortality
Postpartum hemorrhage (PPH) was the most frequently reported maternal morbidity associated with abruption, but there was a lack of consensus in the literature as to whether the risk was truly elevated ( Table 2 ). Estimates of PPH risk ranged from 1.62 to 17.9 (incidence: 0.4–50%) and five of eight studies reported a significantly elevated risk in the setting of abruption. 2 , 20 , 32 – 34 Of the three studies reporting nonsignificant associations, one did not provide a definition of hemorrhage 15 and the other two were examining risk of severe hemorrhage versus nonsevere hemorrhage, 35 , 36 which likely explains the conflicting findings. Variation in risk estimates in the remaining studies is likely due to specification of subpopulations (only cesarean deliveries, only emergent cesareans, etc.), as well as the different definitions for PPH (>500 mL, >1,000 mL, 500–1,500 mL, and >2,000 mL).
Maternal morbidity and mortality incidence and risk estimates a
| Authors, location (year) | Inclusion criteria and dates; data source | Sample size (abruptions) | PPH | Transfusion | Other morbidity | Mortality |
|---|---|---|---|---|---|---|
| Abenhaim et al, United States (2008) | All deliveries, 1999–2003; registry | 2,940,362 (14,702) | NR | NR | AFE: NR; aOR: 8.0 (4.0–15.9) | AFE: NR; aOR: 2.8 (0.6–13.6) NS |
| Jacobsen et al, Multicountry (2008) | All deliveries, 1990–2003; registry | 613,533 (3,481) | NR | NR | VTE: NR; aOR: 2.5 (1.4–4.6) | NR |
| Madan et al, New Jersey (2009) | All deliveries, 1997–2005; registry | 1,004,116 (NR) | NR | NR | ICU admission: NR; aOR: 8.9 (8.3–9.6) | NR |
| Spiliopoulos et al, New Jersey (2009) | All deliveries, 1997–2005; registry | 1,004,116 (NR) | NR | NR | AFE: NR; aOR: 4.0 (1.5–10.9) | NR |
| Fong et al, California (2010) | All deliveries with PPH, 1991–2000; registry | 138,316 (NR) | NA | NR | NR | PPH: NR; OR: 2.4 (1.4–4.2) |
| Kolås et al, Norway (2010) | All cesarean deliveries >23 wk, 1998–1999; multisite | 2,536 (81) | >1,000 mL: 7.4 vs. 2.7%; aOR: 5.4 (2.0–14.5) | NR | NR | NR |
| Pariente et al, Israel (2011) | All deliveries, 1988–2008; single site | 185,476 (1,365) | 0.8 vs. 0.5%; OR: 1.5 (0.8–2.7) NS | 14.9 vs. 1.2%; OR: 14.3 (12.2–16.7) | Sepsis: 0.3 vs. 0%; OR: 17.4 (6.1–49.5) | NR |
| Bentata et al, Morocco (2012) | All deliveries >20 wk, admitted or transferred to ICU during pregnancy or immediately postpartum, 2008–2011; single site | 137 (17) | NR | NR | AKI: NR; aOR: 6.3 (1.4–27.6) | ICU: NR; OR: 2.5 (0.7–8.9) NS |
| Ehrenthal et al, Delaware (2012) | All deliveries ≥ 20 wk, ≥350 g, single 2000–2008; site | 59,282 (35) | NR | All deliveries: 11.4 vs. 1.0%; OR: 12.4 (4.37–35.24); vaginal deliveries: NR; aOR: 10.4 (0.9–117.5) NS; Cesarean deliveries: NR; aOR: 2.37 (0.6–9.7) NS | NR | NR |
| Skjeldestad and Oian, Norway (2012) | All cesarean deliveries, singleton or twins, 1999–2008; registry | 80,658 (1,918) | 500–1,500 mL after emergent CD: NR; aOR: 2.3 (2.1–2.6); >1,500 mL after emergent CD:NR; aOR: 4.8 (4.0–5.8) | NR | NR | NR |
| Suzuki et al, Japan (2012) | All deliveries >22 wk, 2003–2011; single site | 17,405 (91) | NR | Singletons, cesarean deliveries: NR; OR: 13.5 (6.7–27.0) | NR | NR |
| Mehrabadi et al, Canada (2013) | All deliveries, 2001–2009; registry | 371,193 (NR) | Atonic: NR; aOR: 1.6 (1.4–1.9) | NR | NR | NR |
| Mhyre et al, New York (2013) | All deliveries, 1998–2007; registry | 690,742 (NR) | NR | ≥10 units red blood cells <24 h: NR;aOR: 14.6 (11.2–19.0) | NR | NR |
| Boisramé et al, France (2014) | All deliveries >24 wk, 2003–2012; single site | 55,926 (247) | 12.2 vs. 5.5%; NR | 16.6 vs. NR; NR | NR | 0% |
| Wikkelsø et al, Denmark (2014) | All deliveries among women with a first and second pregnancy, 2001–2009; registry | 96, 545 (374) | NR | Vaginal delivery: NR; OR: 14.4 (7.6–27.5); cesarean: NR; OR: 3.1 (2.0–4.8) | NR | NR |
| Cortet et al, France (2015) | All deliveries with PPH, 2004–2006; multisite | 7,236 (20) | >2000mL: 50 vs. 18.7%; aOR: 3.1 (1.0–9.4) NS | NR | NR | NR |
| Ekin et al, Turkey (2015) | All deliveries with PPH <24 hrs after delivery, 2011–2014; single site | 536 (90) | Severe PPH: NR; aOR: 0.5 (0.2–1.3) NS | NR | NR | NR |
| Fong et al, California (2015) | All deliveries, 2001–2007; registry | 2,770,781 (NR) | NR | NR | AFE: 0.05 vs. 0.004%; aOR: 7.6 (4.2–13.9) | NR |
| Macheku et al, Tanzania (2015) | All deliveries ≥28 wk, 2000–2010; registry | 39,993 (112) | 8.9 vs. 0.4%; aOR: 17.9 (8.8–36.4) | 38.4 vs. 5.6%; aOR: 9.6 (6.5–14.1) | Altered liver function: 1.8 vs. 0.3%; aOR:5.3 (1.3–21.6); Acute renal failure: 0.9 vs. 0.4%; aOR: 2.2 (0.3–15.5) NS Prolonged hospital stay: 16.1 vs. 3.5%; aOR:3.5 (1.8–9.6) | 3.6% vs. NR; aOR: 1.6 (1.5–1.8) |
| Ananth et al, United States (2016) | Singleton deliveries, 2006–2012; registry | 27,796,465 (268,050) | NR | NR | Severe abruption: AFE: 0.05% vs. 0.004%; aRR: 10.6 (8.4–13.2) | NR |
Abbreviations: AFE, amniotic fluid embolism; AKI, acute kidney injury; aOR, adjusted odds ratio; CD, cesarean delivery; ICU, intensive care unit; NR, not reported; NS, not significant; OR, odds ratio; PPH, postpartum hemorrhage; RR, relative risk; VTE, venous thromboembolism.
In what is likely a secondary consequence to PPH, abruption was also associated with elevated risk of transfusion, which varied from 2.37 to 14.6. 15 , 20 , 37 – 40 The one study which reported results separately by delivery mode found that the estimated risk of transfusion was higher among vaginal deliveries (odds ratio [OR]: 14.4) than cesarean delivery (OR: 3.1), but there was no direct comparison of modes reported. 40 The difference by delivery mode may be due to either a more rapid delivery or the ability to directly access the uterus for control of the bleeding. Additionally, risk of sepsis, 15 amniotic fluid embolism (AFE), 41 – 44 venous thromboembolism (VTE), 45 acute kidney injury (AKI), 46 intensive care unit (ICU) admission, 47 and maternal mortality attributed to abruption 4 , 20 , 41 , 46 have also been reported. A recent report examining outcomes associated with mild and severe abruption found elevated risk of several additional serious maternal complications, including pulmonary edema, puerperal cerebrovascular disorders, acute heart failure, acute myocardial infarction, cardiomyopathy, acute respiratory failure, and coma. 44 The degree of PPH associated with abruption is the likely explanation behind many of these serious maternal complications.
Preterm Birth and Fetal or Neonatal Size
Preterm birth (<37 weeks) was one of the most frequently reported outcomes associated with abruption ( Table 3 ). Estimated risk ranged from 1.2 to 31.7 with incidence ranging from 5.8 to 80.1%, but the majority of studies reported between 40 and 60%. 1 , 2 , 8 , 15 , 17 , 48 – 63 Approximately 50 to 80% of preterm births in the setting of abruption are spontaneous (preterm labor or membrane rupture), but abruption is also considered the fourth most common cause of medically indicated preterm birth. 50 , 64 Spontaneous preterm birth due to abruption is thought to be the result of bleeding from the separation of the placental which irritates the uterine lining and stimulates contractions which progress into preterm labor. 65 Similar to cesarean delivery, medically indicated preterm birth can be necessary in the setting of abruption to reduce the risk of maternal and perinatal morbidity and mortality. 50 , 66
Neonatal morbidity and mortality incidence and risk estimates a
| Authors, location (year) | Inclusion criteria and dates; data source | Sample size (abruptions) | GA <37 wk | IUGR/SGA | Birthweight <2,500 g | IUFD | Neonatal death | Perinatal death |
|---|---|---|---|---|---|---|---|---|
| Ananth et al, United States (2005) | Twin deliveries, ≥22 wk and ≥ 500 g, live birth, 1989–2000; registry | 1,073,743 (13,527) | 80.1 vs. 51.9%; aRR: 1.5 (1.4–1.6) | 11.7 vs. 9.2%; aRR: 1.3 (1.2–1.4) | NR | NR | NR | NR |
| Levy et al, Israel (2005) | All deliveries 1988–2002; single site | 153,396 (1,152) | NR; aOR: 1.2 (1.0–1.4) | NR | NR; aOR: 1.4 (1.1–1.6) | NR | NR | NR |
| Salihu et al, United States (2005) | All deliveries, 1995–1998; registry | Singletons: 15,051,87 (93,968) Twins: 413,619 (5,051) Triplets: 22,585 (353) | NR | NR | NR | Singletons: 8.3 vs. 0.5%; aOR: 18.9 (16.9–20.8) Twins: 6.8 vs. 1.7%; aOR: 3.6 (3.6–4.9) Triplets: 10.2 vs. 2.2%; aOR: 5.7 (3.2–10.2) | Singletons: 4.2 vs. 0.3%; aOR: 11.1 (10.0–12.3) Twins: 9.0 vs. 2.3%; aOR: 4.2 (3.7–4.8) Triplets: 9.8 vs. 5.2%; aOR: 2.0 (1.1–3.5) | Singletons: NR; aOR: 14.3 (13.2–15.4) Twins: NR; aOR: 4.4 (3.9–4.9) Triplets: NR; aOR: 3.0 (2.0–4.6) |
| Ticconi et al, Zimbabwe (2005) | All deliveries, 2000–2001; single site | 1,768 (NR) | NR | NR | NR; aOR: 5.49 (1.28–23.52) | NR | NR | NR |
| Ananth and Vintzileos, Missouri (2006) | Singleton deliveries >19 wk, live birth, 1989–1997; multisite | 684,711 (1,812) | <35 wk: 5.8 vs. 0.5%; aRR: 8.8 (8.3–9.3) | NR | NR | NR | NR | NR |
| Ananth et al, United States (2006) | Singleton deliveries ≥22 wk ≥ 500 g, 1995–2002; registry | 30,378,902 (179,204) | NA | Preterm: 16.5 vs. 9.4%; aRR: 1.93 (1.90–1.97) Term: 22.5 vs. 9.2%; aRR: 2.95 (2.91–3.00) | Preterm: 77.5 vs. 37.7%; NR Term: 12.0 vs. 2.6%; NR | Preterm: 9.8 vs. 2.0%; NR Term: 3.4 vs. 0.1%; NR | NR | NR |
| Getahun et al, Missouri (2007) | Singleton deliveries ≥21 wk, 1989–1997; registry | 626, 883 (NR) | NR | NR | NR | White: 4.7 vs. NR; aHR: 10.2 (8.1–12.9) Black: 6.8 vs. NR; aHR: 10.9 (7.4–15.9) | NR | NR |
| Lo et al, Taiwan (2007) | Singleton deliveries >20 wk, structurally and chromosomally normal, 1990–2003; single site | 36,453 (295) | Spontaneous <34 wk: NR; aOR: 13.4 (9.4–19.2) | NR | NR | NR | NR | NR |
| McDonald et al, Canada (2007) | All deliveries, 1995–2001; registry | 1,854,463 (24,492) | NR | NR | NR | NR; aOR: 11.4 (10.6–12.2) | NR | NR |
| De Lange et al, Australia (2008) | All deliveries with cases defined as perinatal deaths, 2001–2005; registry | 87,231 (668) | NR | NR | NR | NR | NR | NR; aOR: 6.40 (4.80–8.55) |
| Engel et al, Australia (2008) | Singleton deliveries, 1995–1999; registry | 16,445 (42) | NR | NR | NR | NR; OR: 25.1 (11.44–55.25) | NR | NR |
| Hossain et al, Pakistan (2009) | All vaginal deliveries, cases defined as stillbirths >28 wk, 2008; single site | 1,011 (NR) | NR | NR | NR | NR; OR: 137 (52.7–356.3) | NR | NR |
| Bhattacharya et al, Scotland (2010) | All deliveries >24 wk, with first and second pregnancies recorded, 1981–2000; registry | 309,304 (2,031) | NR | NR | NR | NR; aOR: 1.96 (1.63–2.35) | NR | NR |
| Burton and Ananth, United States (2010) | Twin deliveries, 20–44 wk, 1995–2004; registry | 1,105,666 (10,225) | NR; aHR: 2.73 (2.67–2.78) | NR | NR | NR | NR | NR |
| Gargano et al, Michigan (2010) | Singleton deliveries, POUCH study, 1998–2004; multisite | 996 (31) | NR; aOR: 3.8 (1.5–9.5) | NR | NR | NR | NR | NR |
| Ananth and VanderWeele, United States (2011) | Singleton deliveries, 1995–2002; registry | 26,364,462 (170,068) | 48.7 vs. 8.2%; NR | NR | NR | NR: aRR: 16.91 (16.45–17.36) | Early neonatal: NR; aRR: 8.98 (8.58–9.37); Late neonatal: NR; aRR: 5.86 (5.44–6.28) | NR: aRR: 13.76 (13.45–14.08) |
| Auger et al, Canada (2011) | Singleton deliveries, 1989–2006; multisite | 1,329,737 (22,278) | 31.9 vs. NR; aOR: 7.9 (7.7–8.2) | NR | NR | NR | NR | NR |
| Ohana et al, Israel (2011) | All deliveries ≥22 wk, ≥500 g, 1988–2009; single site | 228,239 (NR) | NR | NR | NR | NR; aOR: 2.9 (2.4–3.5) | NR | NR |
| Pariente et al, Israel (2011) | All deliveries, 1988–2008; single site | 185,476 (1,365) | 56 vs. 7.5%; NR | 8.1 vs. 2.1%; OR: 4.2 (3.4–5.1) | 54.9 vs. 7.6%; NR | NR | NR | 19.4 vs. 1.1%; aOR: 2.7 (2.2–3.3) |
| Stringer et al, Zambia (2011) | All deliveries ≥1,000 g, 2006–2009; registry | 100,454 (95) | NR | NR | NR | NR; aOR: 5.21 (2.93–9.29) | NR | NR |
| Crippa et al, Italy (2012) | All deliveries <1500 g, live-born, 2004–2007; single site | 240 (17) | NR | NR; OR: 0.17 (0.04–0.69) | NR | NR | Composite neonatal death or adverse neurodevelopmental: NR; aOR: 1.6 (0.4–5.9) NS | NR |
| Faiz et al, New Jersey (2012) | Singleton deliveries, ≥20 wk, >500 g, 1997–2005; registry | 933,258 (NR) | NR | NR | NR | NR; aHR: 40.2 (36.9–43.9) | NR | NR |
| Hu et al, Taiwan (2012) | All deliveries ≥20 wk, >500 g, 2001–2004; registry | 940,978 (NR) | NR | NR | NR | NR; aOR: 6.20 (5.35–7.19) | NR | NR |
| Sarkar et al, Michigan (2012) | All deliveries ≥36 wk with asphyxia and receipt of hypothermia for HIE, single site | 68 (15) | NR | NR | NR | NR | Composite death or abnormal brain MRI: NR; aOR: 10.3 (1.4–76.7) | NR |
| Tikkanen et al, Finland (2012) | All deliveries, ≥22 wk OR >500 g, 1980–2005; registry | 1,582,282 (6,231) | 48.6 vs. 6.3%; NR | 9.4 vs. 2.3%; NR | 38.4 vs. 4.5%; NR | NR | NR | NR |
| Anderson et al, New Zealand (2013) | Singleton deliveries, 2006–2009; single site | 26,254 (134) | NR | NR; aOR: 2.57 (1.74–3.78) | NR | NR | NR | NR |
| Ogawa et al, Japan (2013) | Singleton deliveries, 22–36 wk, <1,000 g, 2001–2002; registry | 1,713 (95) | NR | NR | NR | NR | NR | 38.9 vs. 20.3%; aOR: 2.5 (1.2–5.0) |
| Oliveira and Costa, Brazil (2013) | All deliveries admitted to obstetric ICU and maternal near miss, 2007–2010; single site | 20,195 (26) | NR | NR | NR | NR | NR | NR; aOR: 8.86 (3.03–25.91) |
| Räisänen et al, Finland (2013) | Singleton deliveries ≥22 wk OR >500 g, 1987–2010; registry | 1,390,742 (2,634) | <28 wk: NR; aOR: 23.41 (18.87–29.04); 28–31 wk: NR; aOR: 31.69 (29.92–37.32); 31–36 wk: NR; aOR: 12.18 (11.04–13.44) | NR | NR | NR | NR | NR |
| Tikkanen et al, Finland (2013) | All deliveries ≥22 wk, >500 g, 1987–2005; registry | 1,137,466 (4,336) | NR | NR | NR | NR | NR | Singletons: 12.4 vs. 0.6%; aOR: 25.8 (23.5–28.4) Multiples:4 vs. 3.1%; aOR: 1.3 (0.7–2.3) NS |
| Bassil et al, Canada (2014) | All deliveries, 34–40 wk, >500 g, 2005–2012; registry | 458,384 (2,606) | 34–36 wk: 21.6 vs. 5.2%; aRR: 2.3 (2.0–2.7) | NR | NR | NR | NR | NR |
| Boisramé et al, France (2014) | All deliveries >24 wk, 2003–2012; single site | 55,926 (247) | 69.2 vs. 10.7%; NR | 15.1 vs. 5.9%; NR | NR | 12.3 vs. 0.4%; NR | 6.1 vs. 0.5%; aOR: 0.9 (0.5–1.7)NS | 18.4 vs. 0.9%; NR |
| Kobayashi et al, Japan (2014) | Singleton deliveries with suspected risk of abortion with recurrent bleeding 5–21 wk and exposed defined as chronic abruption-oligohydramnios sequence, 2005–2011; single site | 30 (15) | NR | 40 vs. 6.7%; | NR | NR | NR | 26.7 vs. 0%; |
| Morikawa et al, Japan (2014) | Singleton deliveries >30 wk, 2005–2009; multisite | 293,899 (2,649) | 60.1 vs. 11.0%; NR | NR | 61.6 vs. 15.8%; NR | 12.4 vs. 0.4%; NR | Early neonatal death: 1.1 vs. 0.2%; NR | NR |
| Patel et al, Utah (2014) | Singleton deliveries <30 wk admitted to NICU, 2010–2013; single site | 342 (57) | NR | NR | NR | NR | NR | Composite death, severe IVH or NEC: NR; AOR: 1.95 (1.03–3.69) |
| Trønnes et al, Norway (2014) | All deliveries 23–43 wk, 1967–2001; registry | 1,764,509 (7,736) | NR; aOR: 13.5 (12.8–14.2) | NR | NR | NR | NR | NR |
| Vogel et al, World (2014) | Singleton deliveries ≥22 wk, >500 g, 2010–2011; multisite | 308,392 (1045) | NR | NR | NR | Macerated late fetal death: NR; aOR: 9.44 (6.22–14.34); Fresh late fetal death: NR; aOR: 12.4 (8.17–18.75) | Early neonatal death: NR; aOR: 4.00 (2.74–5.86) | NR |
| Cetinkaya et al, Turkey (2015) | All deliveries, ≤1,500 g, live-born, 2008–2012; single site | 241 (NR) | NR | NR | NR | NR | NR | NR; OR: 3.4 (0.8–14.1) NS |
| Fallahi et al, Iran (2015) | All deliveries >20 wk, 2012–2013; single site | 1,700 (83) | NR; RR: 4.30 (2.44–7.59) | NR | NR | NR | NR | NR |
| Kidanto et al, Tanzania (2015) | All deliveries, 2013; multisite | 15,305 (NR) | NR | NR | NR | NR; OR: 40.96 (28.97–57.91) | NR | NR |
| Kurtyka et al, New Jersey (2015) | Singleton deliveries >21 wk among Asian Indian and non-Hispanic White women, 2008–2011; registry | 192,556 (748) | NR | Asian Indian: NR; aRR: 1.63 (1.18–2.26) Non-Hispanic White: NR; aRR: 1.99 (1.73–2.30) | NR | NR | NR | NR |
| Macheku et al, Tanzania (2015) | All deliveries ≥28 wk, 2000–2010; registry | 39,993 (112) | 26.8 vs. 11.2%; aOR: 0.4 (0.1–7.1) NS | NR | 50 vs. 13.2%; aOR: 5.9 (3.9–8.7) | 51.8 vs. 3.7%; aOR: 23.7 (15.6–35.9) | Early neonatal death: 4.5 vs. 0.8%; aOR: 4.3 (1.8–9.9) | 56.3 vs. 4.4%; aOR: 17.6 (11.3–27.3) |
| Chibwesha et al, Zambia (2016) | Singleton and first-born twin deliveries ≥28 wk, ≥1,000 g, 2006–2012; registry | 200,557 (122) | NR | NR | 41 vs. 10.5%; aOR: 5.2 (2.8–9.4) | NR | NR | NR |
| Delorme et al, France (2016) | Singleton live births 24–34 wk, 2011; registry | 3,138 (92) | NR | NR | NR | NR | NR | 13 vs. NR; aOR: 1.6 (0.7–3.7) NS |
| Leal et al, Brazil (2016) | All deliveries, 2011–2012; multisite | 23,448 (291) | NR; aOR: 2.38 (1.27–4.47) | NR | NR | NR | NR | NR |
| Aagaard-Tillery et al, Utah (2006) | All deliveries ≥20 wk, non-anomalous, 1992–2002; registry | 4,286 (NR) | NR | NR | NR | NR; aOR: 8.67 (4.92–15.27) | NR | NR |
| Lindqvist and Happach, Sweden (2006) | All deliveries, 1992–1999; single site | 2,483 (112) | NR | 14.3 vs. 5%; NR | NR | 4.5 vs. 0.1%; NR | NR | NR |
| Shaaban et al, Saudi Arabia (2006) | Singleton deliveries, ≥1,500 g, 2001–2002; single site | 16,562 (24) | NR | NR | NR | NR; OR: 23.4 (4.6–119.3) | NR | NR |
| Tikkanen et al, Finland (2006) | All deliveries >22 wk, >500 g, 1997–2001; single site | 594 (198) | 59 vs. 10%; OR: 12.9 (8.3–19.8) | 25 vs. 4%; OR: 7.9 (4.4–14.3) | NR | 4.8 vs. 0.5%; NR | NR | 9.2 vs. 1%; OR: 10.1 (3.4–30.1) |
| Nath et al, New Jersey (2008) | Singleton deliveries ≥20 wk, 2002-NR; multisite | 326 (156) | SGA: 10.3 vs. 1.8%; aOR: 17.4 (4.6–64.9) Non-SGA: 57.1 vs. 12.4%; aOR: 15.8 (8.4–29.8) | ≥37 wk: 5.1 vs. 8.9%; aOR: 1.7 (0.6–4.3) NS <37 wk: 10.3 vs. 1.8%; aOR: 17.4 (4.6–64.9) | 60.3 vs. 11.2%; aOR: 13.7 (7.4–25.2) | NR | NR | NR |
| Ofori et al, Quebec (2008) | All deliveries, 1997–2003; registry | 70,207 (2,080) | Singleton: 25.8 vs. 5.9%; aOR: 4.9 (4.3–5.5);Multiple: 42.9 vs. 27.9%; aOR: 2.0 (0.8–5.2) NS <28 wk: NR; aOR: 18.0 (12.9–25.0);28–32 wk: NR; aOR: 11.0 (8.9–13.7);33–36 wk: NR; aOR: 3.4 (3.0–3.9) | NR | NR | NR | NR | NR |
| Helgadottir et al, Norway (2011) | All deliveries ≥23 wk, >500 g, 1990–2003; multisite | 88,987 (491) | NR | NR | NR | NR; aOR: 22.0 (15.8–30.8) | NR | NR |
| Al-Kadri and Tamim, Saudi Arabia (2012) | Singleton deliveries ≥24 wk, single site >500 g, 2008–2009; | 375 (26) | NR | NR | NR | NR; aOR: 25.81 (5.84–114.13) | NR | NR |
| Brailovschi et al, Israel (2012) | All deliveries ≥24 wk, >500 g, alive at start of labor, 1988–2008; single site | 204,102 (1,221) | NR | NR | NR | NR; aOR: 3.24 (1.74–6.05) | NR | NR |
| Hasegawa et al, Japan (2014) | Singleton deliveries >24 wk, 2005–2012; single site | 738 (123) | NR | Intrapartum: 31.2 vs. 15.9%; NR; Antepartum: 28.9 vs. 15.9%; NR | NR | 4.9 vs. 2.1% NS; NR | NR | NR |
| Joseph et al, Nova Scotia (2014) | Singleton deliveries, ≥21 wk, ≥500 g, 1988–2003; registry | 132,714 (NR) | sPTB: NR; aRR: 9.15 (7.78–10.8); Iatrogenic: NR; aRR: 12.6 (9.14–17.5) | NR | NR | NR | NR | NR |
| Furukawa et al, Japan (2015) | All deliveries 22–26 wk, admitted to perinatal center, 2000–2010; single site | 101 (32) | NA | 2 vs. 14% NS; NR | NR | NR | 19 vs. 12% NS; NR | NR |
Abbreviations: aHR, adjusted hazard rate; aOR, adjusted odds ratio; aRR, adjusted relative risk; GA, gestational age; HIE, hypoxic-ischemic encephalopathy; IUFD, intrauterine fetal demise; IUGR, intrauterine growth restriction; IVH, intraventricular hemorrhage; NEC, necrotizing enterocolitis; NICU, neonatal intensive care unit; NR, not reported; NS, not significant; OR, odds ratio; RR, relative risk; SGA, small for gestational age; sPTB, spontaneous preterm birth.
Abruption is also frequently reported as a risk factor for low birth weight, which is primarily related to the corresponding incidence of preterm birth described previously ( Table 3 ). 15 , 17 , 20 , 49 , 55 , 60 , 67 , 68 However, abruption has also been associated with IUGR and SGA. Depending on the population specified (singletons vs. twins, preterm vs. term, intrapartum vs. antepartum abruption), IUGR/SGA was reported to occur in 2 to 40% of abruption cases ( Table 3 ). 2 , 8 , 15 , 22 , 23 , 25 , 48 , 55 , 60 , 68 – 72 The majority of studies reported an elevated risk of IUGR/SGA ranging between 1.3 and 17.4 associated with abruption. The two studies reporting null findings may have been underpowered, as each had fewer than 200 cases of abruption, compared with the other studies which included several hundred to several thousand cases. 25 , 60 The association between abruption and fetal growth is likely to be a reflection of underlying chronic placental ischemic disease, which reduces the oxygen and nutrient availability to the fetus, thereby stunting fetal growth. It is also possible that a milder, partial separation of the placental could occur earlier in gestation, thereby directly reducing supply to the fetus, while not triggering a preterm birth.
Intrauterine Fetal Demise, Neonatal Death, and Perinatal Death
Abruption was most frequently reported as a risk factor for stillbirth (range: 3.4–51.8%), 1 , 2 , 8 , 17 , 20 , 22 , 23 , 68 , 73 – 89 neonatal death (range: 1.1–19%), 1 , 2 , 17 , 20 , 25 , 69 , 73 , 79 , 90 and overall perinatal mortality (range: 4–56.3%; Table 3 ). 1 , 2 , 8 , 15 , 20 , 71 , 73 , 91 – 96 Although more than half (55%) of excess perinatal deaths associated with abruption are attributed to preterm birth, the elevated risk of perinatal mortality remains significant even after adjusting for preterm delivery and growth restriction. 1 It is plausible that perinatal deaths that are not due to preterm birth are attributable to asphyxia in the setting of abruption (see discussion later).
While none of the studies that met inclusion criteria reported on the location of the abruption or the degree of separation, one case series of abruptions has reported that detachment ≥45%, central location, and concealed bleeding more frequently resulted in stillbirth and lesser detachment, marginal separation, and revealed bleeding were more often associated with neonatal asphyxia. 97 Overall, the results indicate that the characteristics of the abruption are likely important factors for determining likelihood of fetal survival.
Other Short-Term Neonatal Morbidities
The majority of the studies of neonatal outcomes associated with abruption have focused on low birth weight, preterm birth, and perinatal morality. A small number of publications have linked abruption and elevated risk of acidosis (a marker for exposure to hypoxia), 2 , 25 , 98 , 99 as well as brain-related injuries such as neonatal encephalopathy (NE)/hypoxic-ischemic encephalopathy (HIE). 100 – 102 The three studies examining risk of intraventricular and periventricular hemorrhage found no association with placental abruption ( Table 4 ). 25 , 103 , 104 However, all three studies examined preterm neonates only; therefore, it remains unclear whether there is elevated risk in the setting of term birth. There were also single reports of abruption-associated elevated risk of respiratory distress syndrome (RDS), 105 necrotizing enterocolitis (NEC), 106 retinopathy of prematurity (ROP), 107 fetomaternal hemorrhage, 108 AKI, 109 and nosocomial infections ( Table 4 ). 110 In a small number of studies, abruption was also associated with elevated need for resuscitation, 2 , 71 , 111 but not with risk of neonatal ICU admission. 20 , 23 These morbidities can largely be attributed to the associations between abruption and risk of preterm birth (RDS, NEC, ROP, AKI), hypoxia (acidosis, HIE), and blood loss (fetomaternal hemorrhage).
Other short-term neonatal morbidities
| Authors, location (year) | Inclusion criteria and dates; data source | Sample size (abruptions) | Prematurity-related morbidity | Hypoxia-related morbidity | Other morbidity |
|---|---|---|---|---|---|
| Luig et al, Australia (2005) | All deliveries 24–31 wk, admitted to NICU, 1994–1999; multisite | 4,649 (108) | NEC: NR; aOR: 2.09 (1.30–3.35) | NR | NR |
| Andreani et al, Italy (2007) | Singleton deliveries 24–33.6 wk, 1993–2005; single site | 786 (60) | NR | Acidosis: NR; OR: 6.9 (2.9–15.8) | NR |
| Gouyon et al, France (2008) | All deliveries ≥37 wk, live births, 2000–2003; registry | 65,000 (112) | RDS: NR; aOR: 5.0 (1.2–20.5) | NR | NR |
| Távora et al, Brazil (2008) | All deliveries, admitted to NICU, 2003; single site | 948 (59) | NR | NR | Nosocomial infection: 45.8 vs. 25.5%; aOR: 2.7 (1.4–5.4) |
| Dani et al, Italy (2010) | All deliveries ≤28 wk, admitted to NICU, 1999–2007; single site | 218 (19) | IVH: 32 vs. 30%; aRR: 0.94 (0.47–1.88) NS | NR | NR |
| Stroustrup and Trasande, United States (2012) | Singleton deliveries, 1993–2008; registry | 65,516,569 (55,274) | NR | NR | FMH: NR; aOR: 9.77 (7.18–13.31) |
| Chen et al, China (2013) | All deliveries ≤34 wk, 2005–2006; multisite | 1,792 (NR) | IVH or PVL: NR; OR: 1.30 (0.25–6.87) NS | NR | NR |
| Lee et al, Multistate (2013) | All deliveries ≤28 wk, 2002–2004; multisite | 1,199 (126) | ROP: Stage 3–5: NR; aOR: 0.6 (0.3–1.0) NS; Plus disease: NR; aOR: 0.5 (0.2–1.1) NS; Zone I: NR; aOR: 0.2 (0.1–0.8); Prethreshold/threshold: NR; aOR: 0.3 (0.1–0.7); ET-ROP treatable: NR; aOR: 0.6 (0.3–1.2) NS | NR | NR |
| Akinloye et al, Canada (2014) | All deliveries ≥35 wk, requiring positive pressure ventilation at birth, 1994–2013; single site | 3,305 (91) | NR | NR | Prolonged PPV: NR; OR: 2.5 (1.5–4.1) |
| Boisramé et al, France (2014) | All deliveries >24 wk, 2003–2012; single site | 55,926 (247) | NR | Acidosis: 12.4 vs. 0.6%; aOR: 14.9 (9.2–23.9) | Resuscitation: 63.4 vs. 9.1%; aOR: 4.6 (3.1–6.8) |
| Kobayashi et al, Japan (2014) | Singleton deliveries with suspected risk of abortion with recurrent bleeding 5–21 wk and exposed defined as chronic abruption-oligohydramnios sequence, 2005–2011; single site | 30 (15) | NR | NR | Mechanical ventilation: 86.7 vs. 13.3% NR; High-frequency oscillation: 46.7% vs. 6.7%; NR; Home oxygen therapy: 45.5 vs. 6.7%; NR |
| Nelson et al, Texas (2014) | Singleton deliveries ≥36 wk, live-born, 2005–2011; single site | 86,371 (171) | NR | Whole-body cooling: NR; aOR: 17.4 (6.9–43.6) | NR |
| Macheku et al, Tanzania (2015) | All deliveries ≥28 wk, 2000–2010; registry | 39,993 (112) | NR | NR | NICU admission: 20.5% vs. 14.2%; aOR: 1.5 (0.9–2.4) NS |
| Zhao et al, China (2015) | All deliveries ≥37 wk and Apgar ≥7, 2012; single site | 1,199 (4) | NR | NR | Retinal hemorrhage: NR; OR: 1.03 (0.11–9.89) NS |
| Sabol and Caughey, Oregon (2016) | Singleton deliveries ≥37 wk, nonanomalous with 5-min Apgar ≥7, 1990–2009; single site | 26,669 (NR) | NR | pH ≤7.0: 13.2 3.4%; vs. NR | NR |
| Locatelli et al, Italy (2010) | All deliveries ≥37 wk, live births with cases defined as neonatal encephalopathy, 1993–2003; single site | 127 (5) | NR | NE: NR; OR: 17.2 (2.4–118.9) | NR |
| Hasegawa et al, Japan (2014) | Singleton deliveries >24 wk, 2005–2012; single site | 738 (123) | NR | NR | NICU admission: 38.2 vs. 35.1% NS; NR |
| Arcinue et al, Ohio (2015) | All deliveries with cases defined as neonates with AKI and either ELW or birth weight <750 g who were admitted to NICU,1998–2008; single site | 211 (NR) | AKI: NR; OR: 2.26 (1.30–3.94) | NR | NR |
| Furukawa et al, Japan (2015) | All deliveries 22–26 wk, admitted to perinatal center, 2000–2010; single site | 101 (32) | IVH: 22 vs. 23% NS; NR | Acidosis: 0 vs. 4.3% NS; NR | NR |
| Nasiell et al, Sweden (2016) | All deliveries with cases defined as infants receiving hypothermia for treatment of HIE, 2007–2010; multisite | 141 (8) | NR | HIE: NR; OR: 20.31 (1.99–207.53) | NR |
Abbreviations: AKI, acute kidney injury; aOR, adjusted odds ratio; aRR, adjusted relative risk; CD, cesarean delivery; ELBW, extremely low birth weight; FMH, fetomaternal hemorrhage; HIE, hypoxic-ischemic encephalopathy; IVH, intraventricular hemorrhage; NEC, necrotizing enterocolitis; NICU, neonatal intensive care unit; NR, not reported; NS, not significant; PPV, positive pressure ventilation; OR, odds ratio; RDS, respiratory distress syndrome; ROP, retinopathy of prematurity; RR, relative risk.
Neonatal Long-Term Morbidity and Mortality
Finally, there were also long-term risks for the neonate associated with abruption, most of which were likely attributed to the in utero exposure to hypoxia ( Table 5 ). The most frequently described long-term outcome among surviving neonates was elevated risk of cerebral palsy, 58 , 112 – 116 but there have also been reports of elevated risk of chronic lung disease, 25 , 71 infant mortality, 48 cognitive deficits, 117 and epilepsy. 118 It is worth noting that the association between abruption and cerebral palsy was not universal. In three reports, there was no difference in risk between neonates in pregnancies with and without abruption, but all three focused on particular subpopulations (women without chronic hypertension, spastic cerebral palsy only, and deliveries between 22 and 26 weeks). 25 , 119 , 120
Long-term infant morbidity and mortality incidence and risk estimates a
| Authors, location (year) | Inclusion criteria and dates; data source | Sample size (abruptions) | Cerebral palsy | Chronic lung disease | Infant mortality | Epilepsy | Cognitive deficit |
|---|---|---|---|---|---|---|---|
| Ananth et al, United States (2005) | Twin deliveries, ≥22 wk and ≥500 g, live birth, 1989–2000; registry | 1,073,743 (13,527) | NR | NR | Non-SGA, term: 1.3 vs. 3.1%; aRR: 2.0 (1.0–3.9) NS; SGA only: 3.5 vs. 3.1%; aRR: 9.9 (5.4–14.5); Preterm only: 7.9 vs. 3.1%; aRR: 25.0 (22.3–28.1); SGA and preterm: 5.9 vs. 3.1%; aRR: 36.2 (28.4–44.1) | NR | NR |
| Whitehead et al, Canada (2006) | All deliveries with live births, 1986–2001; registry | 124,207 (1,054) | NR | NR | NR | NR; aRR: 2.3 (1.5–3.6) | NR |
| Hjern and Thorngren-Jerneck, Sweden (2008) | All deliveries, neonates surviving first year, 1987–1993; registry | 805,543 (3,778) | NR; OR: 10.9 (8.4–14.1) | NR | NR | NR | NR |
| Love et al, United Kingdom (2012) | All deliveries among primigravidae women without hypertension, 1995–2008; registry | 28,967 (172) | NR; aOR: 2.46 (0.65–9.24) NS | NR | NR | NR | NR |
| Kobayashi et al, Japan (2014) | Singleton deliveries with suspected risk of abortion with recurrent bleeding 5–21 wk and exposed defined as chronic abruption-oligohydramnios sequence, 2005–2011; single site | 30 (15) | NR | 73.3 vs. 6.7%; NR | NR | NR | NR |
| Trønnes et al, Norway (2014) | All deliveries 23–43 wk, 1967–2001; registry | 1,764,509 (7,736) | NR; aOR: 8.0 (6.6–9.6) | NR | NR | NR | NR |
| Ananth et al, United States (2016) | Singleton deliveries ≥24 wk, 1959–1966; registry | 40,539 (635) | NR | NR | NR | NR | 8 mo abnormal Bayley motor: 3.3 vs. 0.9%; aRR: 2.35 (1.39–3.98); 8 mo abnormal Bayley mental: 2.5 vs. 0.9%; aRR: 2.03 (1.13–3.64); 4 y IQ <70: 5.3 vs. 4.1%; aRR: 1.77 (1.23–2.55); 7 y IQ <70: 3.7 vs. 3.1%; aRR: 1.59 (0.97–2.60) NS |
| Hasegawa et al, Japan (2016) Case–Control | Singleton deliveries ≥33 wk, ≥2,000 g, live birth, no major congenital anomalies, 2009–2011; registry | 144,339 (161) | NR; aRR: 20.89 (11.82–36.9) | NR | NR | NR | NR |
| Stelmach et al, Estonia (2005) | All cases with CP <16 years old, 2000; registry | 421 (17) | NR; OR: 13.1 (2.99–57.7) | NR | NR | NR | NR |
| Thorngren-Jerneck and Herbst, Sweden (2006) | All cases of CP ≥4 years old, 1984–1998; registry | 1,602,303 (NR) | NR; OR: 8.58 (5.63–13.3) | NR | NR | NR | NR |
| Nielsen et al, Denmark (2008) | Singleton deliveries with cases defined as spastic cerebral palsy, 1982–1990; registry | 434 (45) | NR; OR: 1.1 (0.56–1.99) NS | NR | NR | NR | NR |
| Kułak et al, Poland (2010) | All deliveries >36 wk, live birth, 1990–2005; single site | 493 (34) | NR; OR: 2.41 (1.16–4.97) | NR | NR | NR | NR |
| Furukawa et al, Japan (2015) | All deliveries 22–26 wk, admitted to perinatal center, 2000–2010; single site | 101 (32) | 28 vs. 33% NS;NR | 66 vs. 43%;NR | NR | NR | NR |
Abbreviations: aOR, adjusted odds ratio; aRR, adjusted relative risk; NR, not reported; NS, not significant; OR, odds ratio; SGA, small for gestational age; SIDS, sudden infant death syndrome.
Subsequent Pregnancy Morbidity
Although there is comparatively less research on the topic, placental abruption in a previous pregnancy is associated with elevated risks in subsequent pregnancies ( Table 6 ). In particular, repeat abruption, preeclampsia, and small for gestational age are the most frequently reported risks in subsequent pregnancies. 20 , 22 , 121 – 128 These three conditions have been collectively termed “ischemic placental disease” and it has been suggested that all three have an origin based in uteroplacental ischemia and it is plausible that they are different manifestations of the same disease. 121 , 129 , 130 With that understanding, rather than a cause and effect, abruption in a previous pregnancy may be a marker of underlying disease which also makes preeclampsia and growth restriction more likely to occur.
Subsequent pregnancy maternal and perinatal morbidity and mortality incidence and risk estimates a
| Authors, location (year) | Inclusion criteria and dates; data source | Sample size (abruptions) | Preeclampsia | Repeat abruption | Other maternal morbidity | Perinatal morbidity and mortality |
|---|---|---|---|---|---|---|
| Ananth et al, Missouri (2007) | Singleton delivery pairs, live births, 1989–1997; registry | 154,810 pairs (2,167) | 15.0 vs. 8.2%; aOR: 1.91 (1.52–2.40) | 2.8 vs. 0.7%; aOR: 3.16 (2.18–4.58) | NR | SGA: 15.0 vs. 8.2%; aOR: 1.6 (1.4–1.9) |
| Ananth et al, Sweden (2007) | Singleton delivery pairs, 1983–2001; registry | 526,690 pairs (2,673) | NR | 4.4 vs. 0.4%; aOR: 11.6 (9.5–14.1) | NR | NR |
| Lo et al, Taiwan (2007) | Singleton deliveries >20 wk, structurally and chromosomally normal, 1990–2003; single site | 36,453 (295) | NR | NR | NR | sPTB <34 wk: NR; aOR: 7.9 (2.4–26.0) |
| Rasmussen, Norway (2007) | Delivery pairs ≥16 wk, 1967–2005; registry | 119,518 pairs (990) | Mild: 4.5 vs. 1.8%; aOR: 2.4 (1.6–3.6); Severe: 1.8 vs. 0.6%; aOR: 2.7 (1.4–5.1); Early onset: 1.6 vs. 0.3%; aOR: 5.3 (2.7–10.4) | 3.9 vs. 0.4%; aOR: 8.3 (5.1–13.5) | NR | SGA: 14.3 vs. 8.3%; aOR: 1.7 (1.4–2.2) |
| Rasmussen et al, Norway (2009) | Singleton delivery pairs 16–44 wk, 1967–2005; registry | 611,957 pairs (3,295) | NR | NR | NR | Stillbirth: NR; Overall: aOR: 2.8 (2.2–3.5); mild abruption: aOR: 1.4 (0.8–2.4) NS; severe abruption: aOR: 3.4 (2.6–4.5) |
| Ananth et al, Norway (2015) | Singleton delivery pairs, 1967–2009; registry | 747,566 pairs (4,218) | NR | Overall:3.9 vs. 0.5%; NR | NR | NR |
| Macheku et al, Tanzania (2015) | All deliveries ≥28 wk, 2000–2010; registry | 39,993 (112) | NR | 0.7 vs. 0.2%; aOR: 2.3 (1.8–3.4) | NR | NR |
| Ruiter et al, the Netherlands (2015) | Singleton delivery pairs, 1999–2007; registry | 264,424 pairs (709) | NR | 5.8 vs. 0.1%; aOR: 93 (62–139) | NR | NR |
| Lindqvist and Happach, Sweden (2006) | All deliveries, 1992–1999; single site | 2,483 (112) | NR | NR; OR: 25.8 (9.8–68.3) | NR | NR |
| Matsaseng et al, South Africa (2006) | Deliveries >24 wk; NR; single site | 108 (63) | NR | 35.5 vs. 3.1%; NR | Thrombocytopenia: 26 vs. 14% NS; NR; DIC: 15.6 vs. 0%; NR; Renal impairment: 11.1 vs. 3.0% NS; NR; High-care admit >3 d: 13.0 vs. 1.5% NS; NR | NR |
| Tikkanen et al, Finland (2006) | All deliveries >22 wk, >500 g, 1997–2001; single site | 594 (198) | NR | NR; OR: 4.5 (1.1–18.0) | NR | NR |
| Parker et al, Finland (2015) | Singleton deliveries ≥22 wk, ≥500 g, multiparous; 1996–2010; registry | 32,435 (207) | NR; aOR: 1.7 (1.2–2.3) <34 wk: NR; aOR: 3.0 (1.6–5.4); ≥34 wk: NR; aOR: 1.5 (1.1–2.2) | NR | NR | NR |
Abbreviations: aOR, adjusted odds ratio; aRR, adjusted relative risk; CP, cerebral palsy; DIC, disseminated intravascular coagulopathy; NR, not reported; NS, not significant; OR, odds ratio; SGA, small for gestational age; SIDS, sudden infant death syndrome; sPTB, spontaneous preterm birth.
A history of placental abruption has also been linked with thrombocytopenia, disseminated intravascular coagulopathy, renal impairment, and high-care admission >3 days among mothers, as well as spontaneous preterm birth <34 weeks and stillbirth among neonates, in subsequent pregnancies. 51 , 126 , 131 This risk is likely attributed, in part, to the tendency for abruption to reoccur, but in at least one analysis, history of severe abruption (defined as <37 weeks of gestational, with either birth weight <2,500 g or perinatal death) was associated with elevated risk of stillbirth (adjusted OR [aOR] = 2.7, 95% confidence interval [CI]: 1.8–3.9) that was not attributed to preeclampsia, small for gestational age, or repeat placental abruption.
Long-Term Maternal Morbidity and Mortality
Finally, abruption has also been associated with long-term maternal renal and cardiovascular morbidity and mortality; notably, the risk of mortality is elevated for both cardiovascular and noncardiovascular causes ( Table 7 ). 132 – 137 The elevated risk of cardiovascular-related morbidity and mortality may be a reflection of shared underlying pathophysiology that causes both the abruption and the future cardiovascular events. However, it is less clear how abruption increases risk of noncardiovascular deaths.
In this systematic review, we examined the labor, delivery, maternal, and neonatal outcomes associated with placental abruption in more recent publications when known risk factors have changed. Placental abruption was associated with significant maternal morbidity and perinatal morbidity and mortality. There is preliminary evidence that abruption may increase the risk of several poor outcomes independently of preterm birth and that there may also be long-term risks for mothers as well as surviving neonates.
There were several methodological issues in the abruption literature identified in the process of this review. After excluding selection errors and articles in which abruption was an outcome, approximately half of remaining articles were excluded from the review because they lacked a comparison group of any type. Without a referent group, it becomes impossible to determine whether the reported outcomes are occurring more or less frequently than would be observed without placental abruption. Other prominent issues were the lack of, or inconsistency in, definitions of abruption as well as the absence of type and severity information. There is evidence that the percentage of detachment and specific location of the separation are important factors for perinatal outcomes, yet that information is rarely reported. Additionally, as there is no gold standard for diagnosis, there is considerable heterogeneity in what is classified as an “abruption.” When the method of identification was reported, clinical diagnosis of abruption by examination of the placenta in the delivery room was most common, but depending on the study, use of ICD-9-CM or ICD-10 discharge codes, or additional clinical criteria, such as abdominal pain or vaginal bleeding, was sometimes specified. Other studies relied on pathological examination of the placenta which, at present, has uncertain reliability and validity. 138 The lack of standardization of both definitions and reporting requirements alike makes it difficult to interpret and compare risk estimates from various populations. There was also substantial variability in the estimated incidence of abruption, which likely depended on the modality used to identify cases (clinical inspection vs. ultrasound vs. pathological inspection) as well as the particular definition used. At present, little is known about differences in outcomes associated with antepartum versus intrapartum abruptions as well as the latency period for delivery in mild cases. The few studies that did report timing associated with abruption reported the gestational age at delivery, which may or may not be the same as the gestational age at the time the abruption initially occurred. Therefore, we were unable to determine how frequently mild cases of abruption spontaneously resolved or the amount of time that passed between when the abruption occurred and the onset of labor contractions. The lack of information about the specific timing of the abruption itself also makes it more difficult to identify instances of chronic versus acute abruption. Certain outcomes could be used as proxy indicators, such as IUGR for chronic abruption and fetal distress for acute abruption. However, it is entirely possible that IUGR could have resulted from underlying placental dysfunction, which culminated with an acute abruption or that a chronic abruption suddenly worsened, leading to fetal distress. It is certainly likely that chronic and acute abruptions are associated with different patterns of maternal and fetal-neonatal complications, but it remains difficult to clearly distinguish the two with the current state of the science of placental monitoring.
Beyond these issues, little is known about the effect of abruption on labor. It is possible that the hypertonic uterine activity that is frequently associated with abruption contributes to the development of labor contractions and may act in a synergetic manner, effectively shortening the duration of labor. Conversely, it could also be that the contraction pattern associated with abruption disrupts or interferes with labor contractions, which could then result in dysfunctional labor.
The optimal mode of delivery in the setting of abruption is also uncertain. Most countries report higher usage of cesarean delivery in the setting of abruption, but again, it is unclear whether these studies were including mild or severe cases (or both). 2 , 8 , 22 Case studies (not included in this review) in countries that reported low usage of cesarean in this setting (25–40%) also typically reported higher perinatal mortality (40.4–67.9%), indicating possibly low resource settings. 139 – 142 It is difficult to determine whether vaginal delivery resulted in more intrapartum fetal deaths, or whether the mother had a vaginal delivery because there was an antepartum fetal death. It may be that cesarean delivery is associated with better birth outcomes in certain circumstances, but these circumstances remain to be identified. Surprisingly, little has been published on delivery practices with abruption in the United States. In one study that met the criteria for this review, 48% of abruption cases were delivered by cesarean, but this study was based on deliveries occurring prior to 2005 and focused exclusively on periviable neonates. 14 Current estimates in a general, representative population remain unknown.
Finally, as a broader methodological issue, there was considerable variation in both the reporting and analysis of related conditions (preeclampsia, IUGR) when estimating risk attributed to abruption specifically. In some instances, these conditions were analyzed as covariates 20 , 127 ; in others, the presence of these disorders was an exclusion criteria 136 or the conditions (and whether they were present or absent) were not mentioned at all. 1 , 2 , 73 The optimal methods for accounting for the relative contribution of these related conditions to maternal and neonatal outcomes is not established, but standardizing the reporting of the incidence and how frequently they co-occur with abruption would be advisable. Likewise, it is not clear how frequently other placental disorders (abnormal cord insertion, single umbilical artery, etc.) co-occur with abruption and how such combinations may impact the outcomes.
Beyond elevated risk of low birth weight, preterm birth, and perinatal mortality, little is known about the short-term or long-term perinatal/neonatal morbidity associated with abruption. Only a handful of studies have examined other outcomes and those have yielded conflicting results. It is also unknown whether these outcomes are found only in severe cases or if mild cases of abruption are also associated with elevated risks.
Despite these limitations, it is clear that placental abruption is associated with significant maternal morbidity and perinatal morbidity and mortality. There is preliminary evidence that abruption may increase the risk of several poor outcomes independently of preterm birth and that there may also be long-term risks for surviving neonates. Our findings underscore the growing recognition for need of standardized definitions of both placental abruption and morbidities in obstetrics to improve comparison of outcomes across research studies and populations. 143 Future studies should include more detailed information about the abruption location, percentage of detachment, and, preferably, the timing and severity of the abruption.
Acknowledgments
K.L. Grantz is an employee of the federal government. This research was supported in part by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
Conflict of Interest
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 24 July 2024
Prenatal exposure to Benzo[a]pyrene affects maternal–fetal outcomes via placental apoptosis
- Nan Zhao ORCID: orcid.org/0000-0001-5358-866X 1 na1 ,
- Jun Chu 2 na1 ,
- Jieying Liu 1 ,
- Liangkun Ma 3 ,
- Ning Ma 4 ,
- Wei Song 1 &
- Tianshu Sun 1
Scientific Reports volume 14 , Article number: 17002 ( 2024 ) Cite this article
104 Accesses
Metrics details
- Environmental sciences
Prenatal exposure to Benzo[a]pyrene (BaP) has been suggested to increase the risk of adverse pregnancy outcomes. However, the role of placental apoptosis on BaP reproductive toxicity is poorly understood. We conducted a maternal animal model of C57BL/6 wild-type (WT) and transformation-related protein 53 (Trp53) heterozygous knockout (p53KO) mice, as well as a nested case–control study involving 83 women with PB and 82 term birth from a birth cohort on prenatal exposure to BaP and preterm birth (PB). Pregnant WT and p53KO mice were randomly allocated to BaP treatment and control groups, intraperitoneally injected of low (7.8 mg/kg), medium (35 mg/kg), and high (78 mg/kg) doses of 3,4-BaP per day and equal volume of vegetable oil, from gestational day 10.5 until delivery. Results show that high-dose BaP treatment increased the incidence of preterm birth in WT mice. The number of fetal deaths and resorptions increased with increasing doses of BaP exposure in mice. Notably, significant reductions in maternal and birth weights, increases in placental weights, and decrease in the number of livebirths were observed in higher-dose BaP groups in dose-dependent manner. We additionally observed elevated p53-mediated placental apoptosis in higher BaP exposure groups, with altered expression levels of p53 and Bax/Bcl-2. In case–control study, the expression level of MMP2 was increased among women with high BaP exposure and associated with the increased risk of all PB and moderate PB. Our study provides the first evidence of BaP-induced reproductive toxicity and its adverse effects on maternal–fetal outcomes in both animal and population studies.
Similar content being viewed by others

Maternal high-fat diet during pregnancy with concurrent phthalate exposure leads to abnormal placentation

Sex-specific difference in placental inflammatory transcriptional biomarkers of maternal phthalate exposure: a prospective cohort study

Oxidative stress increases in liver of lactating rats after BPF-low-dose exposure: perinatal effects in the offspring
Introduction.
Polycyclic aromatic hydrocarbons (PAHs) are ubiquitous environmental contaminants generated by combustion of cigarette smoking, fossil fuels, industrial or domestic coal, and during cooking foods 1 , 2 , and belong to group 1 carcinogenic to humans according to the International Agency for Research on Cancer 3 . Studies, including ours 2 , have suggested that exposure to PAHs during pregnancy is associated with adverse pregnancy outcomes, including early embryo mortality, stillbirths, intrauterine growth restriction (IUGR), preterm birth (PB), and low birth weight (LBW) 2 , 4 , 5 , 6 , 7 . A plausible mechanism is that PAHs exposure affect embryonic development by destroying nucleotides, as they can directly alter cell function at the molecular level by forming DNA adducts, which result in DNA mutation and transcription factors activation 8 . As a representative marker of exposure to total carcinogenic PAHs, Benzo[a]pyrene (BaP) is systematically distributed to form DNA adducts in numerous tissues after exposure to PAHs. In Chinese birth cohorts, we previously observed an increased risk of PB in relation to interquartile increase in maternal BaP-DNA adducts level (3.56 ± 1.46 μg/gDNA in PB) 2 . Tang et al. have found that high levels of BaP-DNA adduct (0.29 ± 0.13 adducts/10 8 nucleotides) are associated with reduced fetal growth 9 . Moreover, the presence of BaP–DNA adducts (0.32 ± 1.04 adducts/10 8 nucleotides) is adequate to alter global genomic DNA methylation in cord blood 10 . A recent Chinese cohort study reported that prenatal exposure to PAHs (mean BaP levels in 55 subjects: 0.75 ng/mL) might increase the risk of LBW by modulating the DNA methylation status of genomic DNA and growth-related genes in the umbilical cord blood 11 . However, the variations in study populations, regions, and the samples and measures used for detection across different studies cannot be ignored, the associations between BaP exposure and adverse maternal–fetal outcomes are still inconclusive. In addition, the mechanisms underlying the associations remain unclear.
Apoptosis is recognized as a critical mechanism underlying cytotoxic effects and teratogenicity 12 . Growing evidence supports its role in fetal development and reproductive health 13 . During embryogenesis, apoptosis is pivotal for cell elimination, which is essential for shaping tissues and body formation. p53 can interact with and regulate various components of the apoptotic signaling pathways, and has been suggested to inhibit the expression of anti-apoptotic proteins, such as Bcl-2 protein family (Bax, Bak) 14 , 15 . Apoptosis might lead to the activation or increased expression of matrix metallopeptidase (MMP), MMP family is involved in the breakdown of the extracellular matrix in embryonic development and reproduction 16 . On the other hand, when apoptosis is triggered by exposure to exogenous substances such as bacteria, viruses, and parasites, it can disrupt placental and fetal growth, potentially leading to fetal death, organ injury, or subsequent limited sequelae 17 . Therefore, altered expression patterns of MMPs and pro-apoptotic elements may be associated with adverse pregnancy outcomes 18 .
Few studies have investigated the role of apoptosis in the association between prenatal BaP exposure and reproductive health. A previous study has shown that BaP disrupts genomic DNA stability and increased cell apoptosis in mouse embryonic stem cells 19 . An important gene in the apoptosis pathway, Bax (Bcl-2-associated X protein) was activated in PAHs-exposed embryos, and embryonic loss was diminished in Bax-deficient mice 20 . After PAHs exposure, Bax were found to be downregulated in aryl hydrocarbon receptor-deficient mouse fetuses, with less placental cell death observed compared to wild-type (WT) fetuses 21 . However, increased proliferative activity in trophoblast and complete inhibition of apoptosis were detected in afterbirths exposed to aromatic hydrocarbons 22 . Consequently, whether apoptosis in placenta is activated or inhibited remains controversial.
In light of literature gap regarding the relationship between prenatal exposure to BaP and adverse maternal–fetal outcomes, as well as the role of placental apoptosis in this association, we conducted an intervention study in mice exposed to BaP and a nested case–control study from a birth cohort. We aimed to investigate association between BaP exposure and maternal–fetal outcomes, and the underlying mechanism potentially involving placental apoptosis.
Prenatal exposure to BaP and adverse maternal–fetal outcomes
As presented in Fig. 1 , compared to pregnant mice in control group, maternal and birth weights were lower in BaP treatment groups. Higher doses of BaP were associated with decreases in maternal and birth weights as compared to low doses of BaP (Fig. 1 D, WT-C vs WT-L: p = 0.64, WT-C vs WT-M: p = 0.24, WT-C vs WT-H: p = 0.034, WT-C vs p53KO-C: p = 0.06, p trend = 0.16; Fig. 1 C, WT-C vs WT-M: p = 0.0006, WT-C vs WT-H: p = 0.0018, p trend < 0.0001) (Tables S1 , 2 ). We also observed higher placental weights in BaP-exposed mice as compared to those in non-exposed group (WT-C vs WT-L: p = 0.028, WT-C vs WT-H: p = 0.0072, p trend = 0.017) (Fig. 1 E, Table S3 ). PB was observed in WT-H group (n = 2, p = 0.14) at day 11 and 15 of gestation and WT-M group (n = 1, p = 0.32) at day 13 of gestation (Fig. 1 F). There were fewer living fetuses in WT-M (4.50 ± 1.35) and WT-H (1.00 ± 0.78) groups than in WT-C (5.50 ± 1.31) and WT-L (5.38 ± 1.32) groups with no statistical significance. Higher doses of BaP were associated with decreases in number of livebirths as compared to low doses of BaP (WT-C vs WT-M: p = 0.60, WT-C vs WT-H: p = 0.0084, p trend (between groups) = 0.034). However, we observed only one livebirth in both p53KO-C and p53KO-L groups, corresponding to one of six and one of eight livebirth rates, respectively (WT-C vs p53KO-C: p = 0.017) (Fig. 1 G, Table S4 ). As seen in Fig. 1 H (Table S5 ), pregnant mice administered with higher doses of BaP were more likely to have stillbirth and resorbed fetuses (2.00 ± 0.63 in WT-M and 3.25 ± 1.32 in WT-H group), compared with those treated with vegetable oil and low dose of BaP (1.40 ± 0.51 in WT-C and 0.60 ± 0.24 in WT-L group, p trend = 0.12). Those associations between levels of BaP exposure and pregnancy outcomes, such as placental and birth weights, and the number of livebirths, showed significant dose-dependent manners. Additionally, we observed that interaction terms of different dosages and mouse genotype was significantly associated with placental weights (p = 0.017, Fig. 1 E) and the number of death and resorbed fetuses (p = 0.016, Fig. 1 H), respectively.

Mice modeling of BaP exposure and observations on maternal–fetal outcomes. ( A ) Schematic diagram of BaP-treated WT and p53 heterozygous knockout pregnant mice in high (78 mg/kg/d), medium (35 mg/kg/d), low (7.8 mg/kg/d) dose, and blank (corn oil) groups. Time points of female mice impregnation, drug injection to pregnant mice, C-section, and observation of maternal–fetal outcomes were presented in chronological order. ( B ) Photographs of pregnant mice and fetuses at autopsy. ( C ) Maternal weights on day 18.5 of gestation/at delivery (Student’s t -test: **p < 0.01, ***p < 0.001, one-way ANOVA: ### p trend < 0.001). ( D ) Birth weights of maternal mice delivered by C-section (Student’s t -test, *p < 0.05). ( E ) Placental weights (Student’s t -test, *p < 0.05, **p < 0.01, one-way ANOVA: # p trend < 0.05, two-way ANOVA: $ p < 0.05). ( F ) The occurrence of preterm births observed before full term gestational day. The vertical coordinate represents percentage of the numbers of female mice that gave full term birth at the end of observation. The horizontal coordinate represents the birth date of the premature fetuses. ( G ) Number of livebirths per pregnant mice (Student’s t -test: *p < 0.05, **p < 0.01, one-way ANOVA: # p trend < 0.05). ( H ) Number of still births and resorbed fetuses per pregnant mice that gave birth (two-way ANOVA: $ p < 0.05).
Placental apoptosis in BaP-exposed pregnant mice
As shown in Fig. 2 A, the level of BaP-DNA adducts in placenta was increased as BaP doses increased in WT treatment groups (0.0560 ± 0.0258 ng/mL in WT-C, 0.1611 ± 0.0126 ng/mL in WT-L, 0.4832 ± 0.1586 ng/mL in WT-M, 0.1120 ± 0.02810 ng/mL in WT-H; WT-C vs WT-L: p = 0.06, WT-C vs WT-M: p = 0.011, WT-C vs WT-H: p = 0.22, WT-L vs WT-M: p = 0.046) in a significant dose-dependent manner among WT-C, WT-L, and WT-M groups (p trend = 0.0058), as well as in p53 treatment group (0.1821 ± 0.0741 ng/mL in p53KO-C, 0.3221 ± 0.0741 ng/mL in p53KO-L; p53KO-C vs p53KO-L: p = 0.25) (Table S6 ). Except for the BaP-DNA adducts level of placentas in WT-H was lower than that in WT-L and WT-M groups (WT-L vs WT-H: p = 0.48, WT-M vs WT-H: p = 0.11). Cell apoptosis in placentas assessed by TUNEL staining was showed in Fig. 2 B and C. We observed TUNEL staining spots only in placentas of BaP-exposed mice, as well as an increase in the number of brown spots was found in higher doses groups (WT-M and WT-H). In p53KO mice, there were significant less TUNEL staining positive spots observed in p53KO-L group than in WT-L group. Figure 2 D and E presented the placental protein expression levels of genes in apoptosis pathway. Expression levels of p53 and Baxwere up-regulated in placentas of WT mice after exposed to BaP, while Bcl-2 was not detected (data not shown). However, a slight up-regulation in p53 expression was observed in p53KO mice group and no change in other genes.

Apoptosis in placental cells. ( A ) Levels of BaP-DNA adducts in placentas. The vertical coordinate represents the levels of BaP-DNA adducts in placentas dissected from the abdominal cavity of pregnant mice (Student’s t -test: *p < 0.05, one-way ANOVA: ## p trend < 0.01). ( B ) TUNEL immunohistochemical staining of placental apoptosis. The arrow points to the DNA break signal observed under the microscope at 10X magnification. ( C ) The number of positive spots by TUNEL in ( B ) (Student’s t -test: **p < 0.01, ***p < 0.001). ( D ) Protein relative expression levels of apoptosis genes in placenta. The expression of β-actin was regarded as internal standard. ( E ) Relative quantitative level of protein by Western blot in ( D ).
Associations between BaP exposure, MMP2, and preterm birth in pregnant women
In case–control study, we observed that the expression levels of placental MMP2 were higher among pregnant women with high BaP exposure levels (9.49 ± 17.93 ng/ml), compared to those with low BaP levels (8.24 ± 12.12 ng/ml) (Table 1 ). Table 2 showed that, after adjustment for BaP-DNA adducts level and other important confounding factors, there were slight increased risks of PB and moderate PB observed as per unit increase in expression of placental MMP2.
Our study supported that maternal exposure to high levels of BaP was associated with the occurrence of adverse maternal–fetal outcomes in mice. We found a significant decrease in maternal weight and an increased incidence of preterm birth after high dose (78 mg/kg/day) of BaP treatment for 7 days in WT mice. The number of fetal deaths and resorptions increased as the dose of BaP exposure increased. Especially, significant decreases in birth weight, increase in placental weight, and the number of livebirths were observed in higher doses BaP groups with significant dose–response relationships. Additionally, elevated p53-mediated placental apoptosis and MMP2 expression were observed in higher BaP exposure groups in pregnant mice and women, respectively.
Population studies including ours have suggested that PAHs exposure during pregnancy may increase the risk of adverse pregnancy outcomes, such as PB and LBW 1 , 2 , 4 , 5 , 23 . Five previous studies in vivo have investigated the reproductive toxicity of BaP exposure on adverse pregnancy outcomes, including oocyte meiotic arrest and fertilization failure 24 , changes in endometrium receptivity 25 ; endometrial cell apoptosis 26 , defect in embryo implantation and pregnancy maintenance 27 ; and recurrent pregnancy loss 28 . However, the causal effect of prenatal BaP exposure on maternal–fetal outcomes in vivo, and whether this relationship is mediated by placenta apoptosis, remains unclear. By conducting a mouse model of BaP intervention during early pregnancy, our study prospectively observed adverse pregnancy conditions in mice after high-level of BaP exposure. The gestational period in mice is shorter than in humans, with mice typically giving birth 18–21 days after conception, compared to the 9–10 months human gestational period. The specific dosing window from 10.5 to 17.5 days in mice aligns with a critical period in human development, corresponding to the late first trimester to delivery. Consistent with previous evidence from population studies, we observed adverse pregnancy outcomes at a dose of 35 mg/kg BaP and more severe outcomes at a dose of 78 mg/kg, including a decrease in livebirths, an increase in stillbirths and resorbed fetuses, and the occurrence of PB. Additionally, we observed reduced maternal and birth weights with increasing doses of BaP exposure in a significant dose–response relationship, suggesting an important role of BaP toxicity in fetal development.
Previous population study has demonstrated that BaP can be biologically transformed to BPDE across placenta barrier and accumulated as BaP-DNA adducts, resulting in abnormal murine fetuses 28 . Consistently, we observed BaP-DNA adducts accumulated in pregnant women’s whole blood and in mice’s placentas (Table 1 , Fig. 2 A), suggesting that the reproductive toxicity of BaP via the placenta might be initiated 10 , 11 . The induction of placental apoptosis by BaP might be attributed to oxidative stress, systemic inflammation, DNA damage, endocrine disruption 29 . An in vitro study has shown that BaP can interfere with cell growth and genomic DNA stability during mouse embryonic development and increase cell apoptosis 19 . Placental apoptosis has been reported to be accompanied by more macrophage infiltration into the placenta in patients with preeclampsia after nicotine exposure 30 , a high placenta/birth weight ratio has also been suggested to associated with adverse maternal–fetal outcomes 31 , which may be a possible reason for the increase in placental weight observed in our study. However, the variation of placental inflammatory factors after BaP exposure and whether cell apoptosis may trigger placental aseptic inflammation remained unclear. We speculated that BaP exposure may affect the placenta by activating the p53 induced apoptosis pathway. BaP may cause apoptosis by increasing Bax activity and Bax/Bcl-2 ratio in trophoblast cells and endometrial 25 , 28 , 32 . Our study identified the apoptotic signaling proteins in animal models of BaP exposure, and provided evidence that p53-induced apoptosis might be triggered by the upregulation of Bax (Figs. 2 D,E and 3 ), similar results was documented at RNA level by Detmar et al. 20 .

The plausible mechanism underlying BaP exposure and adverse maternal–fetal outcomes via placental apoptosis.
Apoptosis has been linked to adverse pregnancy outcomes such as preeclampsia, IUGR, and PB 32 , 33 . To initiate apoptosis, cellular stress or injury signals are activated by the release of pro-apoptotic proteins BH3, which can be bound and isolated by pro-survival proteins such as Bcl-2 protein family. When these pro-survival proteins are saturated or absent, Bax and/or Bak (Bcl-2 antagonist/killer) can be activated and cause mitochondrial outer membrane permeabilization, resulting in the release Cytochrome C from the mitochondrial intermembrane space. 34 . The Bcl-2, Bax and Bak were considered as a three-way apoptotic switch as their co-regulation of apoptotic mechanisms 14 . Cells were considered apoptosis-tolerant when Bcl2/Bax was ≥ 50%, and conversely the smaller the Bcl2/Bax ratio the more active the apoptosis 14 . In our western blot results (Fig. 2 D and E), a up-regulated expression of Bax in placentas, which means an up-regulation of Bax/Bcl-2, were observed. A slight increase in expression level of placental p53 was observed in p53KO mice after BaP exposure, but the changes in the expression level of Bax were less pronounced, indicating that BaP induced placenta apoptosis in mice model via the p53-Bax signaling pathway (Fig. 3 ). To the best knowledge, no study has reported the detection of the protein p53 in the placenta, including ours. However, it has been suggested that upregulated p53 induced transcription and expression of the MMP2 gene, resulting in elevated MMP2 enzyme expression. Accordingly, MMP2 induces extensive extracellular matrix (ECM) degradation in the fetal membranes and placenta, leading to rupture of the fetal membranes and placental abruption 15 , inducing preterm labor 35 (Fig. 3 ). Further study regarding this underlying mechanism was warranted.
Our study prospectively conducted a pregnant mice model by different doses of BaP intervention from early pregnancy to delivery, as well as a case–control study on association between prenatal exposure to BaP and risk of PB. The exposure routes in animal study (injection) and population study (inhalation and ingestion) were different, the potential health impacts might not be comparable because of the differences in study design (intervention/observation), study population (animal/human), and exposure assessment methods. However, we observed occurrence of several adverse pregnancy outcomes significantly associated with increased levels of BaP in vivo, which replicated and confirmed the findings in our population study that higher levels of BaP-DNA adduct increase the risk of preterm birth 2 . This study was also the first to suggest that these associations might be mediated by placental apoptosis in mice. The elevated expression of placental MMP2 was found in pregnant women with higher BaP exposure, though p value was not significant. Moreover, this finding from our study cannot provide evidence of intrauterine fetal development with higher BaP exposure, and expression of the protein bcl-2 was not detected in vivo, further studies are warranted. We observed only one pregnant mouse in each p53KO group delivered livebirth due to Trp53 playing a key role in labor and the absence of Trp53 in the uterus causing increased incidence of PB. Together with the reproductive toxicity of high doses of BaP, the fetuses and placentas of p53KO mice exposed to high levels of BaP were more likely to abnormalities and be absorbed during pregnancy as we observed, resulting in no collection at autopsy. Though we employed the low dose of BaP exposure in p53KO mice only, the p53KO mice model provided valuable information to study the activities in apoptotic pathway genes and proteins in placentas. In both WT and p53KO mice, we identified dysregulated expression of related genes and proteins, as well as the activities of BaP-induced placental apoptosis, which have been implicated in adverse pregnancy outcomes.
In conclusion, our study supports the hypothesis that high levels of maternal exposure to BaP was significantly associated with an increased incidence of adverse maternal–fetal outcomes, including fetal death and resorption, reduced maternal and fetal weights, elevated placental weights, and a decrease in livebirths, which replicates and confirmed the observations in our population study. With observations on dysregulation of the signaling pathway genes and their proteins, it is also noteworthy that there are signs of apoptosis in the placentas of mice and pregnant women exposed to BaP. Our study provide evidence for further investigation on BaP reproductive toxicity and the potential causative links between BaP exposure and adverse pregnancy outcomes. Our findings have important public health implications and are relevant to identify policy recommendation for environment management (e.g. wearing a face mask in downtown, healthier cooking method for foods, etc.) regarding pregnant women and newborns. Future transcriptomics and proteomics studies are warranted to investigate the molecular networks of BaP reproductive toxicity in maternal, placental, and fetal outcomes.
Experimental animals
The animal study was conducted with the approval by the Institutional Animal Care and Use Committee of Peking Union Medical College Hospital (No. XHDW-2020-00), and all procedures adhered to the Guidelines of the Care and Use of Laboratory Animals issued by Chinese Council on Animal Research and were reported in accordance with ARRIVE guidelines. C57BL/6 and transformation-related protein 53 (Trp53) heterozygous knockout (p53KO) (C57BL/6- Trp53 tm1Bcgen , BCG-DIS-0001) virgin female mice, aged 6 weeks, were obtained from Biocytogen Pharmaceuticals (Beijing) Co., Ltd. As shown in Fig. 1 A, these female mice were cohabited with C57BL/6 male mice and randomly group-housed in separate cages. Gestational age was determined based on the presence of a vaginal plug, with the morning of detection being designated as embryonic day 0.5 (d 0.5) of gestation. Each cage housed five mice and was provided 12 h of light daily and breeding feeds. Daily observations were performed, abnormalities including nutritional hair, skin and mucous membrane, mental behavior, and convulsive reflex were recorded.
Animal grouping and BaP treatment
Female mice were mated with male mice in the afternoon, a vaginal plug was checked in the early morning of the next day and designated as GD0.5. Conception status of female mice was then confirmed based on their weight gain and abdominal bloating around 10 days post-mating (GD10) by an experienced animal experimenter. According to the preliminary experiment and previous animal studies with BaP treatment 21 , 36 , 37 , 3,4-BaP (B802767, MACKLIN) was dissolved in vegetable oil with volume of 5 mL/kg for administration to pregnant mice. The pregnant mice were randomly allocated to the BaP treatment or control groups. The treatment group received intraperitoneal injection by stepped multiple dosing method of 3,4-BaP at low (7.8 mg/kg), medium (35 mg/kg), and high (78 mg/kg) doses, while the control group received an equivalent volume of vegetable oil, from gestational day 10.5 to day 17.5 (Fig. 1 A) (the delivery date of mice is approximately on GD 18–21). Five to ten biological replicates per group were recommended based on previous literature. To enhance the reliability of the results while minimizing unnecessary animal sacrifice, there were 8 biological replicates per group 36 , except for the WT-H group allocated 9 mice and p53KO C group allocated 6 mice. Our animal study included 63 mice in total.
Previous literature 38 observed significant decreases in embryonic implantation and pregnant rate in p53-/- female mice. Additionally, based on our pre-experiment, p53KO mice were intolerant to medium and high doses of BaP. Thus, there were two groups left for p53KO mice, which were p53KO low (p53KO-L) and p53KO-control (p53KO-C), and four groups for wild type mice, which were wild type low (WT-L), wild type medium (WT-M), wild type high (WT-H), and wild type control (WT-C). Maternal weight and the occurrence of PB was weighted and observed once a day. Pregnant mice were sacrificed by cervical dislocation and dissected on gestational day of 18.5. Data on the number of livebirth and stillbirth, as well as the maternal, fetal, and placental weights were accordingly recorded (Fig. 1 A and B). To ensure the blindness of the experiment, the mouse breeder recorded all data using the ear-labeled numbers without involving the corresponding grouping.
BaP-DNA adducts in placenta
The placentas from each pregnant mouse were collected and washed three times with pre-cold PBS buffer. Genomic DNA of placental tissue was extracted according to the instruction of tissue DNA extraction kit (DP304, TIANGEN). After concentration determination by micro-nucleic acid quantitation instrument, the level of BaP-DNA adducts was measured by Benzo(a)pyrene diolepoxide (BPDE) DNA Adducts ELISA kit (STA-357, Cell Biolabs).
TUNEL staining
The placentas from the mice were fixed with 10% neutral formalin and routinely embedded and sectioned. The apoptosis of placental tissue was assessed by TUNEL (terminal deoxynucleotidyl transferase dUTP nick end labeling) assay kit-HRP-DAB (C1091, Beyotime), which using terminal deoxynucleotidyl transferase (TdT) to catalyze the incorporation of deoxynucleotides at the free 3'-hydroxyl ends of fragmented DNA. The deoxynucleotides were then labeled with streptavidin-HRP and detected using DAB to generate a brown color. Photos were captured using microscope (ZEISS Imager.A2).
Western blotting
Placentas were weighed and lysed with an appropriate volume of Lysis buffer (including protease inhibitor). Total proteins were extracted from placentas by mechanical homogenization method (Minute total protein extraction kit, SD-001/SN-002, Invent biotechnologies). Protein concentration was measured by BCA method, and 30-50 μg protein was separated on SDS-PAGE gel and transferred. Antibodies including anti-p53 (AF1162, Beyotime), anti-Bax (AF1270, Beyotime), anti-Bcl-2 (AF6285, Beyotime) were assessed to represent the expression levels of apoptosis related protein. Anti-β-actin (AF5003, Beyotime) was used to detect internal reference. Images were captured using chemiluminescence analyzer (Tanon 5200).
A nested case–control study
Building upon an existing birth cohort in Taiyuan, China, a nested case–control study was conducted to investigate the relationship between BaP exposure, the expression of apoptosis-related proteins in placenta, and the risk of preterm birth. Details of the study population were described in previous publications 2 . In brief, PB and moderate PB were defined as delivery prior to 37 and between 28 and 32 completed weeks of gestation, respectively. Term birth (control) was defined as delivery at 37 or more completed weeks of gestation. Pregnant women who had maternal blood samples available, who gave singleton live births without birth defects, and who had no chronic hypertension or cardiovascular diseases were included in our study. The estimated sample size with 0.80 power to detect the association of OR = 2.0 was 108 for each group. Of 110 PB randomly selected in this population who met the above criterion, we also excluded medically indicated PB (N = 27) to investigate the association between BaP exposure and PB without considering the effect of maternal complications. Controls from the same population were frequency matched to the cases by age (± 1 years), residence, and season of conception (spring: March to May, summer: June to August, autumn: September to November, winter: December to February). Thus, the final sample size was 83 cases and 82 controls (term births) with additional exclusion of one subject with inadequate amount of DNA isolated. The expression levels of protein p53 and MMP2 in placenta sample were measured according to the protocol of the Ray Biotech Porcine p53 and MMP2 ELISA Kits.
Statistical analysis
Data from animal study were presented as the mean ± standard deviation (SD), plotted by GraphPad Prism 8 and Biorender ( https://app.biorender.com ), and analyzed by the Student’s t -test (two groups), ANOVA (four groups), and log-rank test. In population study, BaP-DNA Adduct levels were treated categorically as low vs. high by a cutoff of 3.21 μg/gDNA (the mean level among controls was a cutoff point) maternal exposure. Descriptive analyses of MMP2 levels between high and low BaP-DNA adduct level groups were performed by using the Student’s t -test. Multivariable unconditional logistic regression was used to examine the relationships between maternal BaP-DNA adducts and risk of PB. Confounding variables included maternal age (≤ 30, ≥ 30 years), education level (< college, ≥ college), family monthly income per capita (< 3000, ≥ 3000RMB), employment status during pregnancy (yes, no), pre-pregnancy body mass index (BMI) (≤ 18.5, 18.5–24, ≥ 24), parity (primiparous, multiparous), C-section (yes, no), newborn’s gender (female, male), passive smoking during pregnancy (yes, no), activities during pregnancy (yes, no), and supplementation status (ever, never). All statistical analyses were performed using SAS software, version 9.4 (SAS Institute, Inc., Cary, North Carolina). A P < 0.05 was considered statistically significant.
Ethics approval and consent to participate
All study procedures were approved by the Human Investigation Committee of Shanxi Medical University and the Institutional Animal Care and Use Committee of Peking Union Medical College Hospital (No. XHDW-2020-00).
Data availability
Data is provided within the manuscript or supplementary information files.
Choi, H., Rauh, V., Garfinkel, R., Tu, Y. & Perera, F. P. Prenatal exposure to airborne polycyclic aromatic hydrocarbons and risk of intrauterine growth restriction. Environ. Health Perspect. 116 (5), 658–665 (2008).
Article CAS PubMed PubMed Central Google Scholar
Zhao, N. et al. Effects of Benzo[a]pyrene-DNA adducts, dietary vitamins, folate, and carotene intakes on preterm birth: A nested case-control study from the birth cohort in China. Environ. Health 21 (1), 48 (2022).
Humans IWGotEoCRt. Chemical agents and related occupations. IARC Monogr. Eval. Carcinog. Risks Hum. 100 (Pt F), 9–562 (2012).
Google Scholar
Padula, A. M. et al. Exposure to airborne polycyclic aromatic hydrocarbons during pregnancy and risk of preterm birth. Environ. Res. 135 , 221–226 (2014).
Agarwal, P., Singh, L., Anand, M. & Taneja, A. Association between placental polycyclic aromatic hydrocarbons (PAHS), oxidative stress, and preterm delivery: A case-control study. Arch. Environ. Contam. Toxicol. 74 (2), 218–227 (2018).
Article CAS PubMed Google Scholar
Cathey, A. L. et al. Polycyclic aromatic hydrocarbon exposure results in altered CRH, reproductive, and thyroid hormone concentrations during human pregnancy. Sci. Total Environ. 749 , 141581 (2020).
Khalili Doroodzani, A. et al. Diet, exposure to polycyclic aromatic hydrocarbons during pregnancy, and fetal growth: A comparative study of mothers and their fetuses in industrial and urban areas in Southwest Iran. Environ. Pollut. 276 , 116668 (2021).
Liu, Y., Ren, X. & He, L. First-principles study of benzo[a]pyrene-7,8-dione and DNA adducts. J. Chem. Phys. 154 (17), 175102 (2021).
Article ADS CAS PubMed Google Scholar
Tang, D. et al. PAH-DNA adducts in cord blood and fetal and child development in a Chinese cohort. Environ. Health Perspect. 114 (8), 1297–1300 (2006).
Herbstman, J. B. et al. Prenatal exposure to polycyclic aromatic hydrocarbons, Benzo[a]pyrene-DNA adducts, and genomic DNA methylation in cord blood. Environ. Health Perspect. 120 (5), 733–738 (2012).
Cao, C. et al. Prenatal exposure to polycyclic aromatic hydrocarbons could increase the risk of low birth weight by affecting the DNA methylation states in a Chinese cohort. Reprod. Biol. 21 (4), 100574 (2021).
Melnik, B. C. Apoptosis may explain the pharmacological mode of action and adverse effects of isotretinoin, including teratogenicity. Acta Derm. Venereol. 97 (2), 173–181 (2017).
Suzanne, M. & Steller, H. Shaping organisms with apoptosis. Cell Death Differ. 20 (5), 669–675 (2013).
Ashkenazi, A., Fairbrother, W. J., Leverson, J. D. & Souers, A. J. From basic apoptosis discoveries to advanced selective BCL-2 family inhibitors. Nat. Rev. Drug Discov. 16 (4), 273–284 (2017).
Fortunato, S. J., Menon, R., Bryant, C. & Lombardi, S. J. Programmed cell death (apoptosis) as a possible pathway to metalloproteinase activation and fetal membrane degradation in premature rupture of membranes. Am. J. Obstet. Gynecol. 182 (6), 1468–1476 (2000).
Kraljevic, D. et al. Proliferation, apoptosis and expression of matrix metalloproteinase-9 in human fetal lung. Acta Histochem. 117 (4–5), 444–450 (2015).
Adams Waldorf, K. M. & McAdams, R. M. Influence of infection during pregnancy on fetal development. Reproduction 146 (5), R151–R162 (2013).
Article PubMed PubMed Central Google Scholar
Menon, R. & Fortunato, S. J. The role of matrix degrading enzymes and apoptosis in rupture of membranes. J. Soc. Gynecol. Investig. 11 (7), 427–437 (2004).
Zhan, S., Zhang, X., Cao, S. & Huang, J. Benzo(a)pyrene disrupts mouse preimplantation embryo development. Fertil. Steril. 103 (3), 815–825 (2015).
Detmar, J. et al. Embryonic loss due to exposure to polycyclic aromatic hydrocarbons is mediated by Bax. Apoptosis 11 (8), 1413–1425 (2006).
Detmar, J. et al. Fetal growth restriction triggered by polycyclic aromatic hydrocarbons is associated with altered placental vasculature and AhR-dependent changes in cell death. Am. J. Physiol. Endocrinol. Metab. 295 (2), E519–E530 (2008).
Wierzba, W., Tyszko, P., Kanecki, K. & Pinkas, J. Proliferation and apoptosis of human placental cells exposed to aromatic hydrocarbons. Ginekol. Pol. 88 (12), 686–691 (2017).
Article PubMed Google Scholar
Ali, M. U. et al. Health impacts of indoor air pollution from household solid fuel on children and women. J. Hazard. Mater. 416 , 126127 (2021).
Zhang, M. et al. BaP exposure causes oocyte meiotic arrest and fertilization failure to weaken female fertility. FASEB J. 32 (1), 342–352 (2018).
Zhao, Y. et al. Exposure of mice to Benzo(a)pyrene impairs endometrial receptivity and reduces the number of implantation sites during early pregnancy. Food Chem. Toxicol. 69 , 244–251 (2014).
Yi, T. et al. Benzo(a)pyrene inhibits endometrial cell apoptosis in early pregnant mice via the WNT5A pathway. J. Cell. Physiol. 234 (7), 11119–11129 (2019).
Li, X. et al. Exposure to Benzo[a]pyrene impairs decidualization and decidual angiogenesis in mice during early pregnancy. Environ. Pollut. 222 , 523–531 (2017).
Ye, Y. et al. Environmental pollutant Benzo[a]pyrene induces recurrent pregnancy loss through promoting apoptosis and suppressing migration of extravillous trophoblast. Biomed. Res. Int. 2020 , 8983494 (2020).
Chen, X. & Li, Z. Research on exposure to polycyclic aromatic hydrocarbons during pregnancy and risk of preterm birth. Zhonghua Yu Fang Yi Xue Za Zhi 49 (7), 665–668 (2015).
CAS PubMed Google Scholar
Li, X., Zhou, B., Han, X. & Liu, H. Effect of nicotine on placental inflammation and apoptosis in preeclampsia-like model. Life Sci. 261 , 118314 (2020).
Shehata, F. et al. Placenta/birthweight ratio and perinatal outcome: A retrospective cohort analysis. BJOG 118 (6), 741–747 (2011).
Wu, F. et al. Role of peroxiredoxin2 downregulation in recurrent miscarriage through regulation of trophoblast proliferation and apoptosis. Cell Death Dis. 8 (6), e2908 (2017).
Saglam, A. et al. The role of apoptosis in preterm premature rupture of the human fetal membranes. Arch. Gynecol. Obstet. 288 (3), 501–505 (2013).
Singh, R., Letai, A. & Sarosiek, K. Regulation of apoptosis in health and disease: The balancing act of BCL-2 family proteins. Nat. Rev. Mol. Cell Biol. 20 (3), 175–193 (2019).
Schatz, F., Guzeloglu-Kayisli, O., Arlier, S., Kayisli, U. A. & Lockwood, C. J. The role of decidual cells in uterine hemostasis, menstruation, inflammation, adverse pregnancy outcomes and abnormal uterine bleeding. Hum. Reprod. Update 22 (4), 497–515 (2016).
Shahid, A. et al. Modulatory effects of catechin hydrate against genotoxicity, oxidative stress, inflammation and apoptosis induced by benzo(a)pyrene in mice. Food Chem. Toxicol. 92 , 64–74 (2016).
Baijie, T. U. & Bin, P. Brain tissue DNA damage in benzo[a]pyrene-poisoned mice. Chin. J. Public Health 22 (1), 82–3 (2006).
Hu, W., Feng, Z., Teresky, A. K. & Levine, A. J. p53 regulates maternal reproduction through LIF. Nature 450 (7170), 721–724 (2007).
Download references
This work was supported by the National Natural Science Foundation of China (82273725), Beijing Nova Program (20230484380), and National High Level Hospital Clinical Research Funding (2022-PUMCH-A-264, 2022-PUMCH-A-204).
Author information
These authors contributed equally: Nan Zhao and Jun Chu.
Authors and Affiliations
Institute of Clinical Medicine, National Infrastructures for Translational Medicine, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, #1 Shuaifuyuan, Dongcheng Dist., Beijing, 100730, China
Nan Zhao, Jieying Liu, Wei Song & Tianshu Sun
College of Animal Science and Technology, Beijing University of Agriculture, Beijing, China
Department of Obstetrics, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China
Liangkun Ma
Department of Echocardiography, Beijing Children’s Hospital, Capital Medical University, Beijing, China
You can also search for this author in PubMed Google Scholar
Contributions
NZ and TS designed the study, JC and NZ conducted the study and investigation process. JC and TS managed and maintained the data. TS and NZ contributed to statistical analysis and prepared figures, NZ and TS wrote the main manuscript text. NZ, TS, JL, LM, and NM reviewed and edited the final manuscript. All authors read and approved the final manuscript.
Corresponding authors
Correspondence to Nan Zhao or Tianshu Sun .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary information., supplementary tables., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Zhao, N., Chu, J., Liu, J. et al. Prenatal exposure to Benzo[a]pyrene affects maternal–fetal outcomes via placental apoptosis. Sci Rep 14 , 17002 (2024). https://doi.org/10.1038/s41598-024-68029-y
Download citation
Received : 18 April 2024
Accepted : 18 July 2024
Published : 24 July 2024
DOI : https://doi.org/10.1038/s41598-024-68029-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Benzo[a]pyrene
- Prenatal exposure
- Adverse maternal–fetal outcomes
- Placental apoptosis
- Matrix metalloproteinases
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

COMMENTS
Background. Placental abruption occurs when the placenta partially or completely separates from the wall of the uterus and complicates ∼1% of pregnancies. It is associated with typical clinical features and a variety of risk factors. It carries significant risk to the fetus due to interruption of placental blood flow and the risk of fetal ...
Placental abruption is the premature separation of the placenta from its uterine attachment before the delivery of a fetus. The clinical manifestations of abruption typically include vaginal bleeding and abdominal pain with a wide variety of abnormal fetal heart rate patterns. Clinical challenges arise when pregnant people with this condition present with profound vaginal bleeding ...
Placental abruption is the early separation of a placenta from the lining of the uterus before the completion of the second stage of labor. It is one of the causes of bleeding during the second half of pregnancy. Placental abruption is a relatively rare but serious complication of pregnancy and places the well-being of both mother and fetus at risk. Placental abruption is also called abruptio ...
Placental abruption is typically defined as the premature separation of the placenta from the decidua at or after 20 weeks gestation. The major clinical findings are vaginal bleeding and abdominal pain, often accompanied by uterine contractions (including tachysystole), uterine tenderness, and a nonreassuring fetal heart rate pattern. ...
Reviewer #1: Changing risk factors for placental abruption: a case crossover study using routinely collected data from Finland, Malta and Aberdeen. This study is a case-crossover study design with records of the two first pregnancies from women who had PA in one pregnancy and not the other.
A 32-year-old multigravid patient at 21 weeks gestation presents with major concealed placental abruption and subsequent fetal demise. During an eventually failed misoprostol regime aiming for vaginal delivery she develops severe disseminated intravascular coagulopathy. Subsequent hysterotomy reveals Couvelaire uterus with major haemorrhage and requires subtotal hysterectomy for haemostasis.
The overwhelming majority of studies were cohort studies, case-control studies or case series examining risk factors associated with placental abruption. ... , chronic hypertension has been a risk factor for placental abruption. In one study, the rate of abruption among women with or without chronic hypertension in singleton pregnancies was 1 ...
Case definition Placental abruption was coded according to the International Classification of Diseases 9th or 10th Revision (ICD—9/10) in all three databases. ICD 10 defines placental abruption as 'The separation of the placenta from the maternal uterine attachment when it occurs after the twen-
Purpose To evaluate changes in the independent contribution of different risk factors for placental abruption over time. Methods In this retrospective nested case-control study, trends of change in ORs for known risk factors for placental abruption occurring in three consecutive 8-year intervals were compared. A univariate assessment of factors associated with placental abruption and two ...
Comparison of risk factors for placental abruption and placenta previa: case-cohort study. J Obstet Gynaecol Res. 2011; 37: 538-546. Crossref; PubMed; Scopus (55) Google Scholar ... Comparison of risk factors for placental abruption and placenta previa: case-cohort study. J Obstet Gynaecol Res. 2011; 37: 538-546. View in Article Scopus (55) ...
Abruptio placentae, also known as placental abruption, is a critical obstetric emergency characterized by the premature detachment of the placenta from the uterine wall before childbirth. This serious condition can result in significant maternal hemorrhage and jeopardize the well-being of the fetus. Early recognition, timely intervention, and skilled nursing care are essential in lessening the ...
The concept of ischemic placental disease, a unifying classification for preeclampsia, IUGR, and abruption, is well supported in the literature. Clinical studies of Doppler findings of both uterine and umbilical arteries, as well as placental histologic findings, confirm the theory that malplacentation is a cause of ischemic placental disease.
Objective: This study aimed to explore the clinical characteristics and outcomes of placental abruption. Materials and methods: A total of 62 placental abruption cases were collected from the Second Hospital of Jilin University between January 2007 and December 2012. A retrospective study was conducted to explore the risk factors for placental abruption, clinical characteristics, and maternal ...
Placental abruption is most likely to occur in the last trimester of pregnancy, especially in the last few weeks before birth. Signs and symptoms of placental abruption include: Vaginal bleeding, although there might not be any. Abdominal pain. Back pain. Uterine tenderness or rigidity. Uterine contractions, often coming one right after another.
Risk factors for placental abruption mainly include preeclampsia (39%) and premature rupture of membrane (10%). Abdominal pain (68%) and bleeding (35%) comprise the classical symptoms of placental abruption but the clinical picture varies from asymptomatic, in which the diagnosis is made by inspection of the placenta at delivery, to massive ...
A case-crossover study design was used; cases were pregnancies with abruption and matched controls were pregnancies without abruption in the same woman. Conditional logistic regression was used to investigate changes in risk factors for placental abruption in pregnancies with and without abruption.
With progress in maternal-fetal monitoring and neonatal resuscitation, we aimed to know the fetal prognosis in the case of PA and if the management of pregnant women diagnosed with placenta abruptio could be improved. ... However, it is a large study on placental abruption and its management and fetal prognosis. Indeed, it included 201 patients ...
Abstract. Placental abruption is a clinical circumstance in which the anesthetist is confronted with a patient who is undergoing a variety of physiological insults. The principles of basic life support, appropriate fluid management, and cooperative gynecological surgeons will aid in the delivery of optimal care to both the mother and the fetus.
In a population-based nested case-control study, cases were defined as women with placental abruption in their second pregnancy, and controls as women without abruption. A total of 43 328 women were included in the study, 0.4% (n = 186) of second pregnancies had placental abruption. Multivariable logistic models were used to study the ...
Placental abruption: a case study. Zainab Mohammed Al Faraj . Abstract: Placental abruption is an obstetric complication that presents severe dangers to the fetus and his mother. and it is still difficult to manage and treat the placental abruption. We here report a case for a 23-year-old woman, she had placental abruption in two previous ...
This study aimed to clarify the maternal and neonatal outcomes based on the presence or absence of a Couvelaire uterus with placental abruption. Methods This single-center retrospective study was conducted at a tertiary perinatal center in Japan, including patients diagnosed with acute placental abruption who delivered live births via cesarean ...
Based on OR estimates obtained from case-control and cohort studies, there was significant association between smoking and placenta abruption (1.80; 95% CI: 1.75, 1.85).
Evidence that uterine fibroids, specifically submucosal and intramural myomas, negatively impact fertility and are associated with adverse obstetrical outcomes such as pain, preterm labor, placental abruption, malpresentation, postpartum hemorrhage, and cesarean section is reviewed. Expand
Here, we report 3 recent cases of a first manifestation of preeclampsia through severe placental abruption. 2. Case Report. A 33-year-old patient 1G0P at 35 + 2 gestation presented to our obstetric unit because of severe abdominal pain that had started a few hours before presentation.
Our study followed patients with a history of CS from the birth planning prenatal check-up to delivery. ... difficult fetal shoulder delivery, placental abruption, and incomplete placenta delivery with curettage and/or bleeding. ... Knight, M. Uterine rupture by intended mode of delivery in the UK: A national case-control study. PLoS Med. 2012 ...
Using at least once a month or more was linked to a greater risk of placental abruption, the study found. In addition, there was an increased risk of eclampsia, a more serious form of preeclampsia ...
Large Kaiser Permanente study finds greater risk of pregnancy complications. Cannabis use during pregnancy is linked with health problems such as ... preeclampsia, a serious complication of pregnancy; weight gain above or below guidelines for pregnancy; and placental abruption, the early separation of the placenta from the lining of the uterus ...
Both placenta prévia and vasa resolved by the 29 week, however they found out that I have the chronic abruption. I had in total 6 bleeding (went admitted all the time I had a bleeding) and two ultrasound showed oligohydramnios. Being monitored 1-2 times a week, low fluid and is possible that the cause is the placenta abruption.
Placental abruption, the premature detachment of the placenta from the uterine wall, before birth and after 20 weeks of gestation, is one of the most significant determinants of maternal morbidity as well as perinatal morbidity and mortality. 1-4 It is estimated to occur in 0.6 to 1% of pregnancies in the United States, 5 but the reported incidence is lower (0.4-0.5%) in Nordic countries 5 ...
In case-control study, we observed that the expression levels of placental MMP2 were higher among pregnant women with high BaP exposure levels (9.49 ± 17.93 ng/ml), compared to those with low ...