- Open access
- Published: 24 January 2011

Weight Science: Evaluating the Evidence for a Paradigm Shift
- Linda Bacon 1 &
- Lucy Aphramor 2 , 3
Nutrition Journal volume 10 , Article number: 9 ( 2011 ) Cite this article
511k Accesses
434 Citations
1255 Altmetric
Metrics details
Current guidelines recommend that "overweight" and "obese" individuals lose weight through engaging in lifestyle modification involving diet, exercise and other behavior change. This approach reliably induces short term weight loss, but the majority of individuals are unable to maintain weight loss over the long term and do not achieve the putative benefits of improved morbidity and mortality. Concern has arisen that this weight focus is not only ineffective at producing thinner, healthier bodies, but may also have unintended consequences, contributing to food and body preoccupation, repeated cycles of weight loss and regain, distraction from other personal health goals and wider health determinants, reduced self-esteem, eating disorders, other health decrement, and weight stigmatization and discrimination. This concern has drawn increased attention to the ethical implications of recommending treatment that may be ineffective or damaging. A growing trans-disciplinary movement called Health at Every Size (HAES) challenges the value of promoting weight loss and dieting behavior and argues for a shift in focus to weight-neutral outcomes. Randomized controlled clinical trials indicate that a HAES approach is associated with statistically and clinically relevant improvements in physiological measures (e.g., blood pressure, blood lipids), health behaviors (e.g., eating and activity habits, dietary quality), and psychosocial outcomes (such as self-esteem and body image), and that HAES achieves these health outcomes more successfully than weight loss treatment and without the contraindications associated with a weight focus. This paper evaluates the evidence and rationale that justifies shifting the health care paradigm from a conventional weight focus to HAES.
Peer Review reports
Introduction
Concern regarding "overweight" and "obesity" is reflected in a diverse range of policy measures aimed at helping individuals reduce their body mass index (BMI) 1 . Despite attention from the public health establishment, a private weight loss industry estimated at $58.6 billion annually in the United States [ 1 ], unprecedented levels of body dissatisfaction [ 2 ] and repeated attempts to lose weight [ 3 , 4 ], the majority of individuals are unable to maintain weight loss over the long term and do not achieve the putative benefits of improved morbidity and mortality [ 5 ]. Concern has arisen that this weight focused paradigm is not only ineffective at producing thinner, healthier bodies, but also damaging, contributing to food and body preoccupation, repeated cycles of weight loss and regain, distraction from other personal health goals and wider health determinants, reduced self-esteem, eating disorders, other health decrement, and weight stigmatization and discrimination [ 6 – 8 ]. As evidence-based competencies are more firmly embedded in health practitioner standards, attention has been given to the ethical implications of recommending treatment that may be ineffective or damaging [ 5 , 9 ].
A growing trans-disciplinary movement called Health at Every Size SM (HAES) 2 shifts the focus from weight management to health promotion. The primary intent of HAES is to support improved health behaviors for people of all sizes without using weight as a mediator; weight loss may or may not be a side effect.
HAES is emerging as standard practice in the eating disorders field: The Academy for Eating Disorders, Binge Eating Disorder Association, Eating Disorder Coalition, International Association for Eating Disorder Professionals, and National Eating Disorder Association explicitly support this approach [ 10 ]. Civil rights groups including the National Association to Advance Fat Acceptance and the Council on Size and Weight Discrimination also encourage HAES. An international professional organization, the Association for Size Diversity and Health, has developed, composed of individual members across a wide span of professions who are committed to HAES principles.
Health at Every Size: A Review of Randomized Controlled Trials
Several clinical trials comparing HAES to conventional obesity treatment have been conducted. Some investigations were conducted before the name "Health at Every Size" came into common usage; these earlier studies typically used the terms "non-diet" or "intuitive eating" and included an explicit focus on size acceptance (as opposed to weight loss or weight maintenance). A Pub Med search for "Health at Every Size" or "intuitive eating" or "non-diet" or "nondiet" revealed 57 publications. Randomized controlled trials (RCTs) were vetted from these publications, and additional RCTs were vetted from their references. Only studies with an explicit focus on size acceptance were included.
Evidence from these six RCTs indicates that a HAES approach is associated with statistically and clinically relevant improvements in physiological measures (e.g. blood pressure, blood lipids), health behaviors (e.g. physical activity, eating disorder pathology) and psychosocial outcomes (e.g, mood, self-esteem, body image) [ 11 – 20 ]. (See Table 1 .) All studies indicate significant improvements in psychological and behavioral outcomes; improvements in self-esteem and eating behaviors were particularly noteworthy [ 11 – 14 , 16 , 17 , 19 , 20 ]. Four studies additionally measured metabolic risk factors and three of these studies indicated significant improvement in at least some of these parameters, including blood pressure and blood lipids [ 11 , 12 , 16 , 17 , 19 , 20 ]. No studies found adverse changes in any variables.
A seventh RCT reported at a conference also found significantly positive results [ 18 ], as did a non-randomized controlled study [ 21 ] and five studies conducted without a control [ 22 – 26 ].
All of the controlled studies showed retention rates substantially higher than, or, in one instance, as high, as the control group, and all of the uncontrolled studies also showed high retention rates. Given the well-documented recidivism typical of weight loss programs [ 5 , 27 , 28 ] and the potential harm that may arise[ 29 , 30 ], this aspect is particularly noteworthy.
Assumptions underlying the conventional (weight-focused) paradigm
Dieting and other weight loss behaviors are popular in the general population and widely encouraged in public health policy and health care practice as a solution for the "problem" of obesity. There is increasing concern about the endemic misrepresentation of evidence in these weight management policies [ 5 , 8 ]. Researchers have demonstrated ways in which bias and convention interfere with robust scientific reasoning such that obesity research seems to "enjoy special immunity from accepted standards in clinical practice and publishing ethics" [ 5 , 8 , 31 ]. This section discusses the assumptions that underlie the current weight-focused paradigm, presenting evidence that contests their scientific merit and challenges the value of promoting weight management as a public health measure.
Assumption: Adiposity poses significant mortality risk
Evidence: Except at statistical extremes, body mass index (BMI) - or amount of body fat - only weakly predicts longevity [ 32 ]. Most epidemiological studies find that people who are overweight or moderately obese live at least as long as normal weight people, and often longer [ 32 – 35 ]. Analysis of the National Health and Nutrition Examination Surveys I, II, and III, which followed the largest nationally representative cohort of United States adults, determined that greatest longevity was in the overweight category [ 32 ]. As per the report, published in the Journal of the American Medical Association and reviewed and approved by the Centers for Disease Control and Prevention and the National Cancer Institute, "[this] finding is consistent with other results reported in the literature." Indeed, the most comprehensive review of the research pooled data for over 350,000 subjects from 26 studies and found overweight to be associated with greater longevity than normal weight [ 36 ]. More recently, Janssen analyzed data in the elderly (among whom more than 70 percent of all deaths occur) - also from 26 published studies - and similarly found no evidence of excess mortality associated with overweight [ 37 ]. The Americans' Changing Lives study came to a similar conclusion, indicating that "when socioeconomic and other risk factors are controlled for, obesity is not a significant risk factor for mortality; and... for those 55 or older, both overweight and obesity confer a significant decreased risk of mortality." [ 38 ] The most recent analysis, published in the New England Journal of Medicine, concluded that overweight was associated with increased risk, but only arrived at this conclusion after restricting the analysis by excluding 78 percent of the deaths [ 39 ]. They also used a reference category much narrower than the entire "normal weight" category used by most other studies, which also contributed to making the relative risk for overweight higher.
There is a robust pattern in the epidemiological literature that has been named the "obesity paradox" [ 40 , 41 ]: obesity is associated with longer survival in many diseases. For example, obese persons with type 2 diabetes [ 42 ], hypertension [ 43 , 44 ], cardiovascular disease[ 41 , 45 ], and chronic kidney disease [ 46 ] all have greater longevity than thinner people with these conditions [ 47 – 49 ]. Also, obese people who have had heart attacks, coronary bypass[ 50 ], angioplasty[ 51 ] or hemodialysis [ 52 ] live longer than thinner people with these histories [ 49 ]. In addition, obese senior citizens live longer than thinner senior citizens [ 53 ].
The idea that "this is the first generation of children that may have a shorter life expectancy than their parents" is commonly expressed in scientific journals [ 54 ] and popular press articles [ 55 ], even appearing in Congressional testimony by former Surgeon General Richard Carmona [ 56 ] and a 2010 report from the White House Task Force on Childhood Obesity[ 57 ]. When citation is provided, it refers to an opinion paper published in the New England Journal of Medicine [ 54 ], which offered no statistical evidence to support the claim. Life expectancy increased dramatically during the same time period in which weight rose (from 70.8 years in 1970 to 77.8 years in 2005) [ 58 ]. Both the World Health Organization and the Social Security Administration project life expectancy will continue to rise in coming decades [ 59 , 60 ].
Assumption: Adiposity poses significant morbidity risk
Evidence: While it is well established that obesity is associated with increased risk for many diseases, causation is less well-established. Epidemiological studies rarely acknowledge factors like fitness, activity, nutrient intake, weight cycling or socioeconomic status when considering connections between weight and disease. Yet all play a role in determining health risk. When studies do control for these factors, increased risk of disease disappears or is significantly reduced [ 61 ]. (This is less true at statistical extremes.) It is likely that these other factors increase disease risk at the same time they increase the risk of weight gain.
Consider weight cycling as an example. Attempts to lose weight typically result in weight cycling, and such attempts are more common among obese individuals [ 62 ]. Weight cycling results in increased inflammation, which in turn is known to increase risk for many obesity-associated diseases [ 63 ]. Other potential mechanisms by which weight cycling contributes to morbidity include hypertension, insulin resistance and dyslipidemia [ 64 ]. Research also indicates that weight fluctuation is associated with poorer cardiovascular outcomes and increased mortality risk [ 64 – 68 ]. Weight cycling can account for all of the excess mortality associated with obesity in both the Framingham Heart Study [ 69 ] and the National Health and Nutrition Examination Survey (NHANES) [ 70 ]. It may be, therefore, that the association between weight and health risk can be better attributed to weight cycling than adiposity itself [ 63 ].
As another example, consider type 2 diabetes, the disease most highly associated with weight and fat distribution. There is increasing evidence that poverty and marginalization are more strongly associated with type 2 diabetes than conventionally-accepted risk factors such as weight, diet or activity habits [ 30 , 71 – 73 ]. A large Canadian report produced in 2010, for example, found that low income was strongly associated with diabetes even when BMI (and physical activity) was accounted for [ 73 ]. Also, much evidence suggests that insulin resistance is a product of an underlying metabolic disturbance that predisposes the individual to increased fat storage due to compensatory insulin secretion [ 61 , 74 – 78 ]. In other words, obesity may be an early symptom of diabetes as opposed to its primary underlying cause.
Hypertension provides another example of a condition highly associated with weight; research suggests that it is two to three times more common among obese people than lean people [ 79 ]. To what extent hypertension is caused by adiposity, however, is unclear. That BMI correlates more strongly with blood pressure than percent body fat [ 80 ] indicates that the association between BMI and blood pressure results from higher lean mass as opposed to fat mass. Also, the association may have more to do with the weight cycling that results from trying to control weight than the actual weight itself [ 48 , 81 , 82 ]. One study conducted with obese individuals determined that weight cycling was strongly positively associated with incident hypertension [ 82 ]. Another study showed that obese women who had dieted had high blood pressure, while those who had never been on a diet had normal blood pressure [ 67 ]. Rat studies also show that obese rats that have weight cycled have very high blood pressures compared to obese rats that have not weight cycled [ 83 , 84 ]. This finding could also explain the weak association between obesity and hypertension in cultures where dieting is uncommon[ 48 , 85 ]. Additionally, it is well documented that obese people with hypertension live significantly longer than thinner people with hypertension [ 43 , 86 – 88 ] and have a lower risk of heart attack, stroke, or early death [ 45 ]. Rather than identifying health risk, as it does in thinner people, hypertension in heavier people may simply be a requirement for pumping blood through their larger bodies [ 89 ].
It is also notable that the prevalence of hypertension dropped by half between 1960 and 2000, a time when average weight sharply increased, declining much more steeply among those deemed overweight and obese than among thinner individuals [ 90 ]. Incidence of cardiovascular disease also plummeted during this time period and many common diseases now emerge at older ages and are less severe [ 90 ]. (The notable exception is diabetes, which showed a small, non-significant increase during this time period [ 90 ].) While the decreased morbidity can at least in part be attributed to improvements in medical care, the point remains that we are simply not seeing the catastrophic disease consequences predicted to result from the "obesity epidemic."
Assumption: Weight loss will prolong life
Evidence: Most prospective observational studies suggest that weight loss increases the risk of premature death among obese individuals, even when the weight loss is intentional and the studies are well controlled with regard to known confounding factors, including hazardous behavior and underlying diseases [ 91 – 96 ]. Recent review of NHANES, for example, a nationally representative sample of ethnically diverse people over the age of fifty, shows that mortality increased among those who lost weight [ 97 ].
While many short-term weight loss intervention studies do indicate improvements in health measures, because the weight loss is always accompanied by a change in behavior, it is not known whether or to what extent the improvements can be attributed to the weight loss itself. Liposuction studies that control for behavior change provide additional information about the effects of weight (fat) loss itself. One study which explicitly monitored that there were no changes in diet and activity for 10-12 weeks post abdominal liposuction is a case in point. Participants lost an average of 10.5 kgs but saw no improvements in obesity-associated metabolic abnormalities, including blood pressure, triglycerides, cholesterol, or insulin sensitivity [ 98 ]. (Note that liposuction removes subcutaneous fat, not the visceral fat that is more highly associated with disease, and these results should be interpreted carefully.)
In most studies on type 2 diabetes, the improvement in glycemic control is seen within days, before significant weight or fat is lost. Evidence also challenges the assumption that weight loss is associated with improvement in long-term glycemic control, as reflected in HbA1c values [ 99 , 100 ]. One review of controlled weight-loss studies for people with type 2 diabetes showed that initial improvements were followed by a deterioration back to starting values six to eighteen months after treatment, even when the weight loss was maintained [ 101 ].
Furthermore, health benefits associated with weight loss rarely show a dose response (in other words, people who lose small amounts of weight generally get as much health benefit from the intervention as those who lose larger amounts).
These data suggest that the behavior change as opposed to the weight loss itself may play a greater role in health improvement.
Assumption: Anyone who is determined can lose weight and keep it off through appropriate diet and exercise
Evidence: Long-term follow-up studies document that the majority of individuals regain virtually all of the weight that was lost during treatment, regardless of whether they maintain their diet or exercise program [ 5 , 27 ]. Consider the Women's Health Initiative, the largest and longest randomized, controlled dietary intervention clinical trial, designed to test the current recommendations. More than 20,000 women maintained a low-fat diet, reportedly reducing their calorie intake by an average of 360 calories per day [ 102 ] and significantly increasing their activity [ 103 ]. After almost eight years on this diet, there was almost no change in weight from starting point (a loss of 0.1 kg), and average waist circumference, which is a measure of abdominal fat, had increased (0.3 cm) [ 102 ].
A panel of experts convened by the National Institutes of Health determined that "one third to two thirds of the weight is regained within one year [after weight loss], and almost all is regained within five years." [ 28 ] More recent review finds one-third to two-thirds of dieters regain more weight than was lost on their diets; "In sum," the authors report, "there is little support for the notion that diets lead to lasting weight loss or health benefits [ 5 ]." Other reviews demonstrate the unreliability of conventional claims of sustained weight loss [ 104 , 105 ]. There is a paucity of long term data regarding surgical studies, but emerging data indicates gradual post-surgery weight regain as well [ 106 , 107 ]. Weight loss peaks about one year postoperative, after which gradual weight regain is the norm.
Assumption: The pursuit of weight loss is a practical and positive goal
Evidence: As discussed earlier, weight cycling is the most common result of engaging in conventional dieting practices and is known to increase morbidity and mortality risk. Research identifies many other contraindications to the pursuit of weight loss. For example, dieting is known to reduce bone mass, increasing risk for osteoporosis [ 108 – 111 ]; this is true even in an obese population, though obesity is typically associated with reduced risk for osteoporosis[ 108 ]. Research also suggests that dieting is associated with increased chronic psychological stress and cortisol production, two factors known to increase disease risk [ 112 ]. Also, there is emerging evidence that persistent organic pollutants (POPs), which bioaccumulate in adipose tissue and are released during its breakdown, can increase risk of various chronic diseases including type 2 diabetes [ 113 , 114 ], cardiovascular disease [ 115 ] and rheumatoid arthritis [ 116 ]; two studies document that people who have lost weight have higher concentration of POPs in their blood [ 117 , 118 ]. One review of the diabetes literature indicates "that obese persons that (sic) do not have elevated POPs are not at elevated risk of diabetes, suggesting that the POPs rather than the obesity per se is responsible for the association" [ 114 ].
Positing the value of weight loss also supports widespread anxiety about weight [ 119 , 120 ]. Evidence from the eating disorder literature indicates an emphasis on weight control can promote eating disordered behaviors [ 7 ]. Prospective studies show that body dissatisfaction is associated with binge eating and other eating disordered behaviors, lower levels of physical activity and increased weight gain over time [ 121 , 122 ]. Many studies also show that dieting is a strong predictor of future weight gain [ 66 , 123 – 128 ].
Another unintended consequence of the weight loss imperative is an increase in stigmatization and discrimination against fat individuals. Discrimination based on weight now equals or exceeds that based on race or gender [ 129 ]. Extensive research indicates that stigmatizing fat demotivates, rather than encourages, health behavior change [ 130 ]. Adults who face weight stigmatization and discrimination report consuming increased quantities of food [ 131 – 134 ], avoiding exercise [ 133 , 135 – 137 ], and postponing or avoiding medical care (for fear of experiencing stigmatization) [ 138 ]. Stigmatization and bias on the part of health care practitioners is well-documented, resulting in lower quality care [ 139 , 140 ].
Assumption: The only way for overweight and obese people to improve health is to lose weight
Evidence: That weight loss will improve health over the long-term for obese people is, in fact, an untested hypothesis. One reason the hypothesis is untested is because no methods have proven to reduce weight long-term for a significant number of people. Also, while normal weight people have lower disease incidence than obese individuals, it is unknown if weight loss in individuals already obese reduces disease risk to the same level as that observed in those who were never obese [ 91 , 93 ].
As indicated by research conducted by one of the authors and many other investigators, most health indicators can be improved through changing health behaviors, regardless of whether weight is lost [ 11 ]. For example, lifestyle changes can reduce blood pressure, largely or completely independent of changes in body weight [ 11 , 141 – 143 ]. The same can be said for blood lipids [ 11 , 143 – 145 ]. Improvements in insulin sensitivity and blood lipids as a result of aerobic exercise training have been documented even in individuals who gained body fat during the intervention [ 145 , 146 ].
Assumption: Obesity-related costs place a large burden on the economy, and this can be corrected by focused attention to obesity treatment and prevention
Evidence: The health cost attributed to obesity in the United States is currently estimated to be $147 billion annually [ 147 ] and this cost estimate has been used to justify efforts at obesity treatment and prevention. Although this estimate has been granted credence by health experts, the word "estimate" is important to note: as the authors state, most of the cost changes are not "statistically different from zero." Also, the estimate fails to account for many potentially confounding variables, among them physical activity, nutrient intake, history of weight cycling, degree of discrimination, access to (quality) medical care, etc. All are independently correlated with both weight and health and could play a role in explaining the costs associated with having a BMI over 30. Nor does it account for costs associated with unintended consequences of positing the value of a weight focus, which may include eating disorders, diet attempts, weight cycling, reduced self-esteem, depression, and discrimination.
Because BMI is considered a risk factor for many diseases, obese persons are automatically relegated to greater testing and treatment, which means that positing BMI as a risk factor results in increased costs, regardless of whether BMI itself is problematic. Yet using BMI as a proxy for health may be more costly than addressing health directly. Consider, for example, the findings of a study which examined the "healthy obese" and the "unhealthy normal weight" populations [ 148 ]. The study identified six different risk factors for cardiometabolic health and included subjects in the "unhealthy" group if they had two or more risk factors, making it a more stringent threshold of health than that used in categorizing metabolic syndrome or diabetes. The study found a substantial proportion of the overweight and obese population, at every age, who were healthy and a substantial proportion of the "normal weight" group who were unhealthy. Psychologist Deb Burgard examined the costs of overlooking the normal weight people who need treatment and over-treating the obese people who do not (personal communication, March 2010). She found that BMI profiling overlooks 16.3 million "normal weight" individuals who are not healthy and identifies 55.4 million overweight and obese people who are not ill as being in need of treatment (see Table 2 ). When the total population is considered, this means that 31 percent of the population is mis-identified when BMI is used as a proxy for health.
The weight bias inherent in BMI profiling may actually result in higher costs and sicker people. As an example, consider a 2009 study published in the American Journal of Public Health (96). The authors compared people of similar age, gender, education level, and rates of diabetes and hypertension, and examined how often they reported feeling sick over a 30-day period. Results indicated that body image had a much bigger impact on health than body size. In other words, two equally fat women would have very different health outcomes, depending on how they felt about their bodies. Likewise, two women with similar body insecurities would have similar health outcomes, even if one were fat and the other thin. These results suggest that the stigma associated with being fat is a major contributor to obesity-associated disease. BMI and health are only weakly related in cultures where obesity is not stigmatized, such as in the South Pacific [ 48 , 149 ].
Health at every size: shifting the paradigm from weight to health
This section explains the rationale supporting some of the significant ways in which the HAES paradigm differs from the conventional weight-focused paradigm. The following topics are addressed:
HAES encourages body acceptance as opposed to weight loss or weight maintenance;
HAES supports reliance on internal regulatory processes, such as hunger and satiety, as opposed to encouraging cognitively-imposed dietary restriction; and
HAES supports active embodiment as opposed to encouraging structured exercise.
Encouraging Body Acceptance
Conventional thought suggests that body discontent helps motivate beneficial lifestyle change [ 150 , 151 ]. However, as discussed previously in the section on the pursuit of weight loss, evidence suggests the opposite: promoting body discontent instead induces harm [ 122 , 133 , 134 , 152 ], resulting in less favorable lifestyle choices. A common aphorism expressed in the HAES community is that "if shame were effective motivation, there wouldn't be many fat people." Mounting evidence suggests this belief is unfounded and detrimental[ 8 , 152 ]. Promoting one body size as more favorable than another also has ethical consequences [ 120 ], contributing to shaming and discrimination.
Compassion-focused behavior change theory emerging from the eating disorders field suggests that self-acceptance is a cornerstone of self-care, meaning that people with strong self-esteem are more likely to adopt positive health behaviors [ 153 , 154 ]. The theory is borne out in practice: HAES research shows that by learning to value their bodies as they are right now, even when this differs from a desired weight or shape or generates ambivalent feelings, people strengthen their ability to take care of themselves and sustain improvements in health behaviors [ 8 , 11 ].
Critics of HAES express concern that encouraging body acceptance will lead individuals to eat with abandon and disregard dietary considerations, resulting in weight gain. This has been disproven by the evidence; no randomized controlled HAES study has resulted in weight gain, and all studies that report on dietary quality or eating behavior indicate improvement or at least maintenance [ 11 , 14 – 23 ]. This is in direct contrast to dieting behavior, which is associated with weight gain over time [ 66 , 123 – 128 ].
Supporting Intuitive Eating
Conventional recommendations view conscious efforts to monitor and restrict food choices as a necessary aspect of eating for health or weight control [ 155 ]. The underlying belief is that cognitive monitoring is essential for keeping appetite under control and that without these injunctions people would make nutritionally inadvisable choices, including eating to excess. The evidence, however, disputes the value of encouraging external regulation and restraint as a means for weight control: several large scale studies demonstrate that eating restraint is actually associated with weight gain over time [ 66 , 123 – 126 ].
In contrast, HAES teaches people to rely on internal regulation, a process dubbed intuitive eating [ 156 ], which encourages them to increase awareness of their body's response to food and learn how to make food choices that reflect this "body knowledge." Food is valued for nutritional, psychological, sensual, cultural and other reasons. HAES teaches people to make connections between what they eat and how they feel in the short- and medium-term, paying attention to food and mood, concentration, energy levels, fullness, ease of bowel movements, comfort eating, appetite, satiety, hunger and pleasure as guiding principles.
The journey towards adopting intuitive eating is typically a process one engages in over time. Particularly for people with a long history of dieting, other self-imposed dietary restriction, or body image concerns, it can feel very precarious to let go of old habits and attitudes and risk trying new ways of relating to food and self. Coming to eat intuitively happens gradually as old beliefs about food, nutrition and eating are challenged, unlearned and replaced with new ones.
A large popular literature has accumulated that supports individuals in developing intuitive eating skills [ 8 , 156 – 160 ]. (Intuitive eating is also known in the literature as "attuned eating" or "mindful eating." Note that intuitive eating is sometimes promoted as a means to weight loss and in that context is inconsistent with a HAES approach.)
There is considerable evidence that intuitive eating skills can be learned [ 11 , 18 , 161 ], and that intuitive eating is associated with improved nutrient intake [ 162 ], reduced eating disorder symptomatology [ 17 , 18 , 163 – 165 ] - and not with weight gain [ 11 , 13 , 16 – 18 ]. Several studies have found intuitive eating to be associated with lower body mass [ 162 , 163 , 166 , 167 ].
Supporting Active Embodiment
HAES encourages people to build activity into their day-to-day routines and focuses on helping people find enjoyable ways of being active. The goal is to promote well-being and self-care rather than advising individuals to meet set guidelines for frequency and intensity of exercise. Active living is promoted for a range of physical, psychological and other synergistic benefits which are independent of weight loss. Myths around weight control and exercise are explicitly challenged. Physical activity is also used in HAES as a way of healing a sense of body distrust and alienation from physicality that may be experienced when people are taught to over-ride embodied internal signals in pursuit of externally derived goals, such as commonly occurs in dieting. In addition, some HAES programs have used physical activity sessions, along with other activities such as art and relaxation, to further a community development agenda, creating volunteer, training and employment opportunities and addressing issues of isolation, poor self-esteem and depression among course participants.
Clinical Ethics
There are serious ethical concerns regarding the continued use of a weight-centered paradigm in current practice in relation to beneficence and nonmaleficence. Beneficence concerns the requirement to effect treatment benefit. There is a paucity of literature to substantiate that the pursuit of weight control is beneficial, and a similar lack of evidence to support that weight loss is maintained over the long term or that programs aimed at prevention of weight gain are successful. Nonmaleficence refers to the requirement to do no harm. Much research suggests damage results from a weight-centered focus, such as weight cycling and stigmatization. Consideration of several dimensions of ethical practice - veracity, fidelity, justice and a compassionate response - suggests that the HAES paradigm shift may be required for professional ethical accountability [ 168 ].
Public Health Ethics
The new public health ethics advocates scrutiny of the values and structure of medical care, recognizing that the remedy to poor health and health inequalities does not lie solely in individual choices.
This ethicality has been adopted by HAES in several ways. HAES academics have highlighted the inherent limitations of an individualistic approach to conceptualizing health. Individual self-care is taken as a starting point for HAES programs, but, unlike more conventional interventions, the HAES ethos recognizes the structural basis of health inequities and understands empowerment as a process that effects collective change in advancing social justice [ 169 ]. HAES advocates have also stressed the need for action to challenge the thinness privilege and to better enable fat people's voices to be heard in and beyond health care [ 8 , 170 ].
The hallmark theme of the new public health agenda is that it emphasizes the complexity of health determinants and the need to address systemic health inequities in order to improve population-wide health outcomes and reduce health disparities, making use of the evidence on the strong relationship between a person's social positioning and their health. For example, research since the 1950s has documented huge differences in cardiac health between and across socioeconomic gradients which has come to be recognized as arising from disparities in social standing and is articulated as the status syndrome [ 171 ]. Since weight tracks closely with socioeconomic class, obesity is a particularly potent marker of social disparity [ 172 ].
There is extensive research documenting the role of chronic stress in conditions conventionally described as obesity-associated, such as hypertension, diabetes and coronary heart disease [ 173 ]. These conditions are mediated through increased metabolic risk seen as raised cholesterol, raised blood pressure, raised triglycerides and insulin resistance. The increase in metabolic risk can in part be explained by a change in eating, exercise and drinking patterns attendant on coping with stress. However, changes in health behaviors do not fully account for the metabolic disturbances. Instead, stress itself alters metabolism independent of a person's lifestyle habits [ 174 ]. Thus, it has been suggested that psychological distress is the antecedent of high metabolic risk [ 175 ], which indicates the need to ensure health promotion policies utilize strategies known to reduce, rather than increase, psychological stress. In addition to the impact of chronic stress on health, an increasing body of international research, discussed earlier, recognizes particular pathways through which weight stigmatization and discrimination impact on health, health-seeking behaviors, and quality of health care [ 125 – 133 ].
Policies which promote weight loss as feasible and beneficial not only perpetuate misinformation and damaging stereotypes [ 176 ], but also contribute to a healthist, moralizing discourse which mitigates against socially-integrated approaches to health [ 155 , 168 , 177 , 178 ]. While access to size acceptance practitioners can ameliorate the harmful effects of discrimination in health care for individuals, systemic change is required to address the iatrogenic consequences of institutional size discrimination in and beyond health care, discrimination that impacts on people's opportunities and health.
Quite aside from the ethical arguments underscoring inclusive, non-discriminatory health care and civil rights, there are plausible metabolic pathways through which reducing weight stigma, by reducing inequitable social processes, can help alleviate the burden of poor health.
From the perspective of efficacy as well as ethics, body weight is a poor target for public health intervention. There is sufficient evidence to recommend a paradigm shift from conventional weight management to Health at Every Size. More research that considers the unintended consequences of a weight focus can help to clarify the associated costs and will better allow practitioners to challenge the current paradigm. Continued research that includes larger sample sizes and more diverse populations and examines how best to deliver a Health at Every Size intervention, customized to specific populations, is called for.
We propose the following guidelines, which are supported by the Association for Size Diversity and Health (ASDAH), to assist professionals in implementing HAES. Our proposed guidelines are modified, with permission, from guidelines developed by the Academy for Eating Disorders for working with children [ 7 ].
Interventions should meet ethical standards. They should focus on health, not weight, and should be referred to as "health promotion" and not marketed as "obesity prevention." Interventions should be careful to avoid weight-biased stigma, such as using language like "overweight" and "obesity."
Interventions should seek to change major determinants of health that reside in inequitable social, economic and environmental factors, including all forms of stigma and oppression.
Interventions should be constructed from a holistic perspective, where consideration is given to physical, emotional, social, occupational, intellectual, spiritual, and ecological aspects of health.
Interventions should promote self-esteem, body satisfaction, and respect for body size diversity.
Interventions should accurately convey the limited impact that lifestyle behaviors have on overall health outcomes.
Lifestyle-oriented elements of interventions that focus on physical activity and eating should be delivered from a compassion-centered approach that encourages self-care rather than as prescriptive injunctions to meet expert guidelines.
Interventions should focus only on modifiable behaviors where there is evidence that such modification will improve health. Weight is not a behavior and therefore not an appropriate target for behavior modification.
Lay experience should inform practice, and the political dimensions of health research and policy should be articulated.
These guidelines outline ways in which health practitioners can shift their practice towards a HAES approach and, in so doing, uphold the tenets of their profession in providing inclusive, effective, and ethical care consistent with the evidence base.
1 Critics challenge the value of using BMI terminology, suggesting that BMI is a poor determinant of health and the categories medicalize and pathologize having a certain body. We accept this argument; we have used "overweight" and "obese" throughout this paper when necessary to report research where these categories were used. We recognize, however, that "normal" does not reflect a normative or optimal value; that "overweight" falsely implies a weight over which one is unhealthy; and that the etymology of the word "obese" mistakenly implies that a large appetite is the cause.
2 Health at Every Size/HAES is a pending trademark of the Association for Size Diversity and Health.
Conflict of interests Disclosure
Linda Bacon and Lucy Aphramor are HAES practitioners. Both also speak and write on the topic of Health at Every Size and sometimes receive financial remuneration for this work.
Marketdata Enterprises: The U.S. Weight Loss & Diet Control Market (10th Edition). Lynbrook. 2009
Google Scholar
Monteath SA, McCabe MP: The influence of societal factors on female body image. J Soc Psychol. 1997, 137: 708-727. 10.1080/00224549709595493.
CAS PubMed Google Scholar
Neumark-Sztainer D, Rock CL, Thornquist MD, Cheskin LJ, Neuhouser ML, Barnett MJ: Weight-control behaviors among adults and adolescents: Associations with dietary intake. Prev Med. 2000, 30: 381-391. 10.1006/pmed.2000.0653.
Jeffery RW, Adlis SA, Forster JL: Prevalence of dieting among working men and women: The Healthy Worker Project. Health Psychol. 1991, 10: 274-281. 10.1037/0278-6133.10.4.274.
Mann T, Tomiyama AJ, Westling E, Lew AM, Samuels B, Chatman J: Medicare's Search for Effective Obesity Treatments: Diets Are Not the Answer. Am Psychol. 2007, 62: 220-233. 10.1037/0003-066X.62.3.220.
PubMed Google Scholar
Neumark-Sztainer D: Preventing obesity and eating disorders in adolescents: what can health care providers do?. J Adolesc Health. 2009, 44: 206-213. 10.1016/j.jadohealth.2008.11.005.
Daníelsdóttir S, Burgard D, Oliver-Pyatt W: AED Guidelines for Childhood Obesity Prevention Programs. 2009, Academy of Eating Disorders
Bacon L: Health at Every Size: The Surprising Truth About Your Weight. 2010, Dallas: BenBella Books, Second
Schmidt H, Voigt K, Wikler D: Carrots, Sticks, and Health Care Reform -- Problems with Wellness Incentives. N Engl J Med. 2009, 362: e3-
Medical News Today: Eating Disorder Organizations Join Forces To Urge Focus On Health And Lifestyle Rather Than Weight. 2009
Bacon L, Stern J, Van Loan M, Keim N: Size acceptance and intuitive eating improve health for obese, female chronic dieters. J Am Diet Assoc. 2005, 105: 929-936. 10.1016/j.jada.2005.03.011.
Ciliska D: Evaluation of two nondieting interventions for obese women. West J Nurs Res. 1998, 20: 119-135. 10.1177/019394599802000108.
Goodrick GK, Poston WSC, Kimball KT, Reeves RS, Foreyt JP: Nondieting versus dieting treatment for overweight binge-eating women. J Consult Clin Psychol. 1998, 66: 363-368. 10.1037/0022-006X.66.2.363.
Tanco S, Linden W, Earle T: Well-being and morbid obesity in women: A controlled therapy evaluation. Int J Eat Disord. 1998, 23: 325-339. 10.1002/(SICI)1098-108X(199804)23:3<325::AID-EAT10>3.0.CO;2-X.
Miller WC, Wallace JP, Eggert KE, Lindeman AK: Cardiovascular risk reduction in a self-taught, self-administered weight loss program called the nondiet diet. Med Exerc Nutr Health. 1993, 2: 218-223.
Rapoport L, Clark M, Wardle J: Evaluation of a modified cognitive-behavioural programme for weight management. Int J Obes. 2000, 24: 1726-1737. 10.1038/sj.ijo.0801465.
CAS Google Scholar
Provencher V, Begin C, Tremblay A, Mongeau L, Corneau L, Dodin S, Boivin S, Lemieux S: Health-at-every-size and eating behaviors: 1-year follow-up results of a size acceptance intervention. J Am Diet Assoc. 2009, 109: 1854-1861. 10.1016/j.jada.2009.08.017.
Mensinger J, Close H, Ku J: Intuitive eating: A novel health promotion strategy for obese women. Paper presented at American Public Health Association. Philadelphia, PA. 2009
Bacon L, Keim N, Van Loan M, Derricote M, Gale B, Kazaks A, Stern J: Evaluating a "Non-diet" Wellness Intervention for Improvement of Metabolic Fitness, Psychological Well-Being and Eating and Activity Behaviors. Int J Obes. 2002, 26: 854-865. 10.1038/sj.ijo.0802012.
Provencher V, Bégin C, Tremblay A, Mongeau L, Boivin S, Lemieux S: Short-term effects of a "health-at-every-size" approach on eating behaviors and appetite ratings. Obesity (Silver Spring). 2007, 15: 957-966. 10.1038/oby.2007.638.
Steinhardt M, Bezner J, Adams T: Outcomes of a traditional weight control program and a nondiet alternative: a one-year comparison. J Psychol. 1999, 133: 495-513. 10.1080/00223989909599758.
Carrier KM, Steinhardt MA, Bowman S: Rethinking traditional weight management programs: A 3-year follow-up evaluation of a new approach. J Psychol. 1993, 128: 517-535.
Omichinski L, Harrison KR: Reduction of dieting attitudes and practices after participation in a non-diet lifestyle program. J Can Diet Assoc. 1995, 56: 81-85.
Polivy J, Herman CP: Undieting: A program to help people stop dieting. Int J Eat Disord. 1992, 11: 261-268. 10.1002/1098-108X(199204)11:3<261::AID-EAT2260110309>3.0.CO;2-F.
Roughan P, Seddon E, Vernon-Roberts J: Long-term effects of a psychologically based group programme for women preoccupied with body weight and eating behaviour. Int J Obes. 1990, 14: 135-147.
Higgins L, Gray W: Changing the body image concern and eating behaviour of chronic dieters: the effects of a psychoeducational intervention. Psychol and Health. 1998, 13: 1045-1060. 10.1080/08870449808407449.
Miller WC: How effective are traditional dietary and exercise interventions for weight loss?. Med Sci Sports Exerc. 1999, 31: 1129-1134. 10.1097/00005768-199908000-00008.
National Institutes of Health (NIH): Methods for voluntary weight loss and control (Technology Assessment Conference Panel). Ann Intern Med. 1992, 116: 942-949.
Gregg EW, Gerzoff RB, Thompson TJ, Williamson DF: Intentional weight loss and death in overweight and obese U.S. adults 35 years of age and older. Ann Intern Med. 2003, 138: 383-389.
Wamala S, Lynch J, Horsten M: Education and the Metabolic Syndrome in Women. Diabetes Care. 1999, 22: 1999-2003. 10.2337/diacare.22.12.1999.
Aphramor L: Validity of claims made in weight management research: a narrative review of dietetic articles. Nutr J. 2010, 9: 30-10.1186/1475-2891-9-30.
PubMed PubMed Central Google Scholar
Flegal KM, Graubard BI, Williamson DF, Gail MH: Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005, 293: 1861-1867. 10.1001/jama.293.15.1861.
Durazo-Arvizu R, McGee D, Cooper R, Liao Y, Luke A: Mortality and optimal body mass index in a sample of the US population. Am J Epidemiol. 1998, 147: 739-749.
Troiano R, Frongillo E, Sobal J, Levitsky D: The relationship between body weight and mortality: A quantitative analysis of combined information from existing studies. Int J Obes Relat Metab Disord. 1996, 20: 63-75.
Flegal K, Graubard B, Williamson D, Gail M: Supplement: Response to "Can Fat Be Fit". Sci Am. 2008, 297: 5-6.
McGee DL: Body mass index and mortality: a meta-analysis based on person-level data from twenty-six observational studies. Ann Epidemiol. 2005, 15: 87-97. 10.1016/j.annepidem.2004.05.012.
Janssen I, Mark AE: Elevated body mass index and mortality risk in the elderly. Obes Rev. 2007, 8: 41-59. 10.1111/j.1467-789X.2006.00248.x.
Lantz PM, Golberstein E, House JS, Morenoff J: Socioeconomic and behavioral risk factors for mortality in a national 19-year prospective study of U.S. adults. Soc Sci Med. 2010, 70: 1558-1566. 10.1016/j.socscimed.2010.02.003.
Berrington de Gonzalez A, Hartge P, Cerhan JR, Flint AJ, Hannan L, MacInnis RJ, Moore SC, Tobias GS, Anton-Culver H, Freeman LB, et al: Body-mass index and mortality among 1.46 million white adults. N Engl J Med. 2010, 363: 2211-2219. 10.1056/NEJMoa1000367.
Childers D, Allison D: The 'obesity paradox': a parsimonious explanation for relations among obesity, mortality rate and aging?. Int J Obes (Lond). 2010, 34: 1231-1238. 10.1038/ijo.2010.71.
Morse S, Gulati R, Reisin E: The obesity paradox and cardiovascular disease. Curr Hypertens Rep. 2010, 12: 120-126. 10.1007/s11906-010-0099-1.
Ross C, Langer RD, Barrett-Connor E: Given diabetes, is fat better than thin?. Diabetes Care. 1997, 20: 650-652. 10.2337/diacare.20.4.650.
Barrett-Connor E, Khaw K: Is hypertension more benign when associated with obesity?. Circulation. 1985, 72: 53-60.
Barrett-Connor EL: Obesity, atherosclerosis and coronary artery disease. Ann Intern Med. 1985, 103: 1010-1019.
Kang X, Shaw LJ, Hayes SW, Hachamovitch R, Abidov A, Cohen I, Friedman JD, Thomson LE, Polk D, Germano G, Berman DS: Impact of body mass index on cardiac mortality in patients with known or suspected coronary artery disease undergoing myocardial perfusion single-photon emission computed tomography. J Am Coll Cardiol. 2006, 47: 1418-1426. 10.1016/j.jacc.2005.11.062.
Beddhu S: The body mass index paradox and an obesity, inflammation, and atherosclerosis syndrome in chronic kidney disease. Seminars in Dialysis. 2004, 17: 229-232. 10.1111/j.0894-0959.2004.17311.x.
Ernsberger P, Haskew P: Health implications of obesity: An alternative view. J of Obesity and Weight Regulation. 1987, 9: 39-40.
Ernsberger P, Koletsky RJ: Biomedical rationale for a wellness approach to obesity: An alternative to a focus on weight loss. J Soc Issues. 1999, 55: 221-260. 10.1111/0022-4537.00114.
Lavie CJ, Milani RV, Ventura HO: Obesity, heart disease, and favorable prognosis--truth or paradox?. Am J Med. 2007, 120: 825-826. 10.1016/j.amjmed.2007.06.023.
Gruberg L, Mercado N, Milo S, Boersma E, Disco C, van Es GA, Lemos PA, Ben Tzvi M, Wijns W, Unger F, et al: Impact of body mass index on the outcome of patients with multivessel disease randomized to either coronary artery bypass grafting or stenting in the ARTS trial: The obesity paradox II?. Am J Cardiol. 2005, 95: 439-444. 10.1016/j.amjcard.2004.10.007.
Lavie CJ, Osman AF, Milani RV, Mehra MR: Body composition and prognosis in chronic systolic heart failure: the obesity paradox. Am J Cardiol. 2003, 91: 891-894. 10.1016/S0002-9149(03)00031-6.
Schmidt DS, Salahudeen AK: Obesity-survival paradox-still a controversy?. Semin Dial. 2007, 20: 486-492. 10.1111/j.1525-139X.2007.00349.x.
Kulminski AM, Arbeev KG, Kulminskaya IV, Ukraintseva SV, Land K, Akushevich I, Yashin AI: Body mass index and nine-year mortality in disabled and nondisabled older U.S. individuals. J Am Geriatr Soc. 2008, 56: 105-110. 10.1111/j.1532-5415.2007.01494.x.
Olshansky SJ, Passaro DJ, Hershow RC, Layden J, Carnes BA, Brody J, Hayflick L, Butler RN, Allison DB, Ludwig DS: A potential decline in life expectancy in the United States in the 21st century. N Engl J Med. 2005, 352: 1138-1145. 10.1056/NEJMsr043743.
Belluck P: Children's Life Expectancy Being Cut Short by Obesity. 2005, New York Times. New York City
Carmona R: Testimony Before the Subcommittee on Competition, Infrastructure, and Foreign Commerce Committee on Commerce, Science, and Transportation. United States Senate. 2004
White House Task Force on Childhood Obesity: Solving the Problem of Childhood Obesity Within a Generation. Report to the White House. 2010
National Center for Health Statistics: Health, United States, 2007. With Chartbook on Trends in the Health of Americans. Hyattsville, MD. 2007
Mathers C, Loncar D: Projections of Global Mortality and Burden of Disease from 2002 to 2030. PLoS Med. 2006, 3: 2011-2029. 10.1371/journal.pmed.0030442.
Social Security Administration: Periodic Life Table. 2007, (updated 7/9/07)
Campos P, Saguy A, Ernsberger P, Oliver E, Gaesser G: The epidemiology of overweight and obesity: public health crisis or moral panic?. Int J Epidemiol. 2005, 35: 55-60. 10.1093/ije/dyi254.
Kruger J, Galuska DA, Serdula MK, Jones DA: Attempting to lose weight: specific practices among U.S. adults. Am J Prev Med. 2004, 26: 402-406. 10.1016/j.amepre.2004.02.001.
Strohacker K, McFarlin B: Influence of obesity, physical inactivity, and weight cycling on chronic inflammation. Front Biosci. 2010, E2: 98-104. 10.2741/e70.
Montani JP, Viecelli AK, Prevot A, Dulloo AG: Weight cycling during growth and beyond as a risk factor for later cardiovascular diseases: the 'repeated overshoot' theory. Int J Obes (Lond). 2006, 30 (Suppl 4): S58-66. 10.1038/sj.ijo.0803520.
Olson MB, Kelsey SF, Bittner V, Reis SE, Reichek N, Handberg EM, Merz CN: Weight cycling and high-density lipoprotein cholesterol in women: evidence of an adverse effect: a report from the NHLBI-sponsored WISE study. Women's Ischemia Syndrome Evaluation Study Group. J Am Coll Cardiol. 2000, 36: 1565-1571. 10.1016/S0735-1097(00)00901-3.
French SA, Jeffrey RW, Forster JL, McGovern PG, Kelder SH, Baxter J: Predictors of weight change over two years among a population of working adults: The Healthy Worker Project. Int J Obes. 1994, 18: 145-154.
Guagnano MT, Pace-Palitti V, Carrabs C, Merlitti D, Sensi S: Weight fluctuations could increase blood pressure in android obese women. Clinical Sciences (London). 1999, 96: 677-680. 10.1042/CS19990050.
Rzehak P, Meisinger C, Woelke G, Brasche S, Strube G, Heinrich J: Weight change, weight cycling and mortality in the ERFORT Male Cohort Study. Eur J Epidemiol. 2007, 22: 665-673. 10.1007/s10654-007-9167-5.
Lissner L, Odell PM, D'Agostino RB, Stokes J, Kreger BE, Belanger AJ, Brownell KD: Variability of body weight and health outcomes in the Framingham population. N Engl J Med. 1991, 324: 1839-1844. 10.1056/NEJM199106273242602.
Diaz VA, Mainous AG, Everett CJ: The association between weight fluctuation and mortality: results from a population-based cohort study. J Community Health. 2005, 30: 153-165. 10.1007/s10900-004-1955-1.
McDermott R: Ethics, Epidemiology, and the Thrifty Gene: Biological Determinism as a Health Hazard. Soc Sci Med. 1998, 47: 1189-1195. 10.1016/S0277-9536(98)00191-9.
Brunner E, Marmot M: Social Organization, Stress, and Health. Social Determinants of Health. Edited by: Marmot M, Wilkinson RG. 2006, New York: Oxford University Press, 17-43. 2
Raphael D, Lines E, Bryant T, Daiski I, Pilkington B, Dinca-Panaitescu S, Dinca-Panaitescu M: Type 2 Diabetes: Poverty, Priorities and Policy. The Social Determinants of the Incidence and Management of Type 2 Diabetes. 2010, Toronto: York University School of Health Policy and Management and School of Nursing
Charles MA, Pettitt DJ, Saad MF, Nelson RG, Bennett PH, Knowler WC: Development of impaired glucose tolerance with or without weight gain. Diabetes Care. 1993, 16: 593-596. 10.2337/diacare.16.4.593.
Odeleye OE, de Courten M, Pettitt DJ, Ravussin E: Fasting hyperinsulinemia is a predictor of increased body weight gain and obesity in Pima Indian children. Diabetes. 1997, 46: 1341-1345. 10.2337/diabetes.46.8.1341.
Sigal RJ, El-Hashimy M, Martin BC, Soeldner JS, Krolewski AS, Warram JH: Acute postchallenge hyperinsulinemia predicts weight gain: a prospective study. Diabetes. 1997, 46: 1025-1029. 10.2337/diabetes.46.6.1025.
Yost TJ, Jensen DR, Eckel RH: Weight regain following sustained weight reduction is predicted by relative insulin sensitivity. Obes Res. 1995, 3: 583-587.
Halberg N, Henriksen M, Söderhamn N, Stallknecht B, Ploug T, Schjerling P, Dela F: Effect of intermittent fasting and refeeding on insulin action in healthy men. J Appl Physiol. 2005, 99: 2128-2136. 10.1152/japplphysiol.00683.2005.
Akram DS, Astrup AV, Atinmo T, Boisson JL, Bray GA, Carroll KK, Chunming C, Chitson P, Dietz WH, Hill JO, et al: Obesity: Preventing and managing the global epidemic. Report of a WHO consultation on obesity. 1997, Geneva, Switzerland: World Health Organization
Weinsier RL, Norris DJ, Birch R, Bernstein RS, Wang J, Yang MU, Pierson RN, Van Itallie TB: The relative contribution of body fat and fat pattern to blood pressure level. Hypertension. 1985, 7: 578-585.
Ernsberger P, Nelson DO: Effects of fasting and refeeding on blood pressure are determined by nutritional state, not by body weight change. Am J Hypertens. 1988, 153S-157S.
Schulz M, Liese A, Boeing H, Cunningham J, Moore C, Kroke A: Associations of short-term weight changes and weight cycling with incidence of essential hypertension in the EPIC-Potsdam Study. J Hum Hypertens. 2005, 19: 61-67. 10.1038/sj.jhh.1001776.
Ernsberger P, Koletsky RJ, Baskin JZ, Collins LA: Consequences of weight cycling in obese spontaneously hypertensive rats. Am J Physiol. 1996, 270: R864-R872.
Ernsberger P, Koletsky RJ, Baskin JZ, Foley M: Refeeding hypertension in obese spontaneously hypertensive rats. Hypertension. 1994, 24: 699-705.
Chernin K: The Obsession: Reflections on the tyranny of slenderness. 1981, New York: Harper & Row
Cambien F, Chretien J, Ducimetiere L, Guize L, Richard J: Is the relationship between blood pressure and cardiovascular risk dependent on body mass index?. Am J Epidemiol. 1985, 122: 434-442.
Weinsier R, James L, Darnell B, Dustan H, Birch R, Hunter G: Body fat: Its relationship to coronary heart disease, blood pressure, lipids, and other risk factors measured in a large male population. Am J Med. 1976, 61: 815-824. 10.1016/0002-9343(76)90405-8.
Uretsky S, Messerli FH, Bangalore S, Champion A, Cooper-Dehoff RM, Zhou Q, Pepine CJ: Obesity paradox in patients with hypertension and coronary artery disease. Am J Med. 2007, 120: 863-870. 10.1016/j.amjmed.2007.05.011.
Messerli FH: Cardiovascular adaptations to obesity and arterial hypertension: detrimental or beneficial?. Int J Cardiol. 1983, 3: 94-97. 10.1016/0167-5273(83)90069-4.
Gregg EW, Cheng YJ, Cadwell BL, Imperatore G, Williams DE, Flegal KM, Narayan KM, Williamson DF: Secular trends in cardiovascular disease risk factors according to body mass index in US adults. JAMA. 2005, 293: 1868-1874. 10.1001/jama.293.15.1868.
Williamson DF, Pamuk E, Thun M, Flanders D, Byers T, Heath C: Prospective study of intentional weight loss and mortality in never-smoking overweight U.S. white women aged 40-64 years. Am J Epidemiol. 1995, 141: 1128-1141.
Williamson DF, Pamuk E, Thun M, Flanders D, Byers T, Heath C: Prospective study of intentional weight loss and mortality in overweight white men aged 40-64 years. Am J Epidemiol. 1999, 149: 491-503.
Andres R, Muller DC, Sorkin JD: Long-term effects of change in body weight on all-cause mortality. A review. Ann Intern Med. 1993, 119: 737-743.
Yaari S, Goldbourt U: Voluntary and involuntary weight loss: associations with long term mortality in 9,228 middle-aged and elderly men. Am J Epidemiol. 1998, 148: 546-555.
Sørensen T, Rissanen A, Korkeila M, Kaprio J: Intention to lose weight, weight changes, and 18-y mortality in overweight individuals without co- morbidities. PLoS Med. 2005, 2: E171-
Simonsen MK, Hundrup YA, Obel EB, Gronbaek M, Heitmann BL: Intentional weight loss and mortality among initially healthy men and women. Nutr Rev. 2008, 66: 375-386. 10.1111/j.1753-4887.2008.00047.x.
Ingram DD, Mussolino ME: Weight loss from maximum body weight and mortality: the Third National Health and Nutrition Examination Survey Linked Mortality File. Int J Obes. 2010, 34: 1044-1050. 10.1038/ijo.2010.41.
Klein S, Fontana L, Young VL, Coggan AR, Kilo C, Patterson BW, Mohammed BS: Absence of an effect of liposuction on insulin action and risk factors for coronary heart disease. N Engl J Med. 2004, 350: 2549-2557. 10.1056/NEJMoa033179.
Manning RM, Jung RT, Leese GP, Newton RW: The comparison of four weight reduction strategies aimed at overweight patients with diabetes mellitus: four-year follow-up. Diabet Med. 1998, 15: 497-502. 10.1002/(SICI)1096-9136(199806)15:6<497::AID-DIA599>3.0.CO;2-W.
Wing RR, Anglin K: Effectiveness of a behavioral weight control program for blacks and whites with NIDDM. Diabetes Care. 1996, 19: 409-413. 10.2337/diacare.19.5.409.
Ciliska D, Kelly C, Petrov N, Chalmers J: A review of weight loss interventions for obese people with non-insulin dependent diabetes mellitus. Can J of Diabetes Care. 1995, 19: 10-15.
Howard BV, Manson JE, Stefanick ML, Beresford SA, Frank G, Jones B, Rodabough RJ, Snetselaar L, Thomson C, Tinker L, et al: Low-fat dietary pattern and weight change over 7 years: the Women's Health Initiative Dietary Modification Trial. JAMA. 2006, 295: 39-49. 10.1001/jama.295.1.39.
Howard BV, Van Horn L, Hsia J, Manson JE, Stefanick ML, Wassertheil-Smoller S, Kuller LH, LaCroix AZ, Langer RD, Lasser NL, et al: Low-fat dietary pattern and risk of cardiovascular disease: the Women's Health Initiative Randomized Controlled Dietary Modification Trial. JAMA. 2006, 295: 655-666. 10.1001/jama.295.6.655.
Aphramor L: Is A Weight-Centred Health Framework Salutogenic? Some Thoughts on Unhinging Certain Dietary Ideologies. Social Theory and Health. 2005, 3: 315-340. 10.1057/palgrave.sth.8700059.
Aphramor L: Weight management as a cardioprotective intervention raises issues for nutritional scientists regarding clinical ethics. Proc Nut Soc. 2009, 67: E401-10.1017/S002966510800075X.
Sjostrom L, Lindroos AK, Peltonen M, Torgerson J, Bouchard C, Carlsson B, Dahlgren S, Larsson B, Narbro K, Sjostrom CD, et al: Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004, 351: 2683-2693. 10.1056/NEJMoa035622.
Christou NV, Look D, Maclean LD: Weight gain after short- and long-limb gastric bypass in patients followed for longer than 10 years. Ann Surg. 2006, 244: 734-740. 10.1097/01.sla.0000217592.04061.d5.
Bacon L, Stern JS, Keim NL, Van Loan MD: Low bone mass in premenopausal chronic dieting obese women. Eur J Clin Nutr. 2004, 58: 966-971. 10.1038/sj.ejcn.1601922.
Van Loan MD, Keim NL: Influence of cognitive eating restraint on total-body measurements of bone mineral density and bone mineral content in premenopausal women 18-45 y: a cross-sectional study. Am J Clin Nutr. 2000, 72: 837-843.
Van Loan MD, Bachrach LK, Wang MC, Crawford PB: Effect of drive for thinness during adolescence on adult bone mass. J Bone Miner Res. 2000, 15: S412-
Barr SI, Prior JC, Vigna YM: Restrained eating and ovulatory disturbances: Possible implications for bone health. Am J Clin Nutr. 1994, 59: 92-97.
Tomiyama AJ, Mann T, Vinas D, Hunger JM, Dejager J, Taylor SE: Low calorie dieting increases cortisol. Psychosom Med. 2010, 72: 357-364. 10.1097/PSY.0b013e3181d9523c.
CAS PubMed PubMed Central Google Scholar
Lee DH, Lee IK, Song K, Steffes M, Toscano W, Baker BA, Jacobs DR: A strong dose-response relation between serum concentrations of persistent organic pollutants and diabetes: results from the National Health and Examination Survey 1999-2002. Diabetes Care. 2006, 29: 1638-1644. 10.2337/dc06-0543.
Carpenter DO: Environmental contaminants as risk factors for developing diabetes. Rev Environ Health. 2008, 23: 59-74.
Ha MH, Lee DH, Jacobs DR: Association between serum concentrations of persistent organic pollutants and self-reported cardiovascular disease prevalence: results from the National Health and Nutrition Examination Survey, 1999-2002. Environ Health Perspect. 2007, 115: 1204-1209. 10.1289/ehp.10184.
Lee DH, Steffes M, Jacobs DR: Positive associations of serum concentration of polychlorinated biphenyls or organochlorine pesticides with self-reported arthritis, especially rheumatoid type, in women. Environ Health Perspect. 2007, 115: 883-888. 10.1289/ehp.9887.
Chevrier J, Dewailly E, Ayotte P, Mauriege P, Despres JP, Tremblay A: Body weight loss increases plasma and adipose tissue concentrations of potentially toxic pollutants in obese individuals. Int J Obes Relat Metab Disord. 2000, 24: 1272-1278. 10.1038/sj.ijo.0801380.
Lim JS, Son HK, Park SK, Jacobs DR, Lee DH: Inverse associations between long-term weight change and serum concentrations of persistent organic pollutants. Int J Obes (Lond). 2010.
Davison KK, Markey CN, Birch LL: A longitudinal examination of patterns in girls' weight concerns and body dissatisfaction from ages 5 to 9 years. Int J Eat Disord. 2003, 33: 320-332. 10.1002/eat.10142.
Holm S: Obesity interventions and ethics. Obes Rev. 2007, 8 (Suppl 1): 207-210. 10.1111/j.1467-789X.2007.00343.x.
Neumark-Sztainer D, Levine MP, Paxton SJ, Smolak L, Piran N, Wertheim EH: Prevention of body dissatisfaction and disordered eating: What next?. Eat Disord. 2006, 14: 265-285. 10.1080/10640260600796184.
van den Berg P, Neumark-Sztainer D: Fat 'n happy 5 years later: is it bad for overweight girls to like their bodies?. J Adolesc Health. 2007, 41: 415-417. 10.1016/j.jadohealth.2007.06.001.
Stice E, Cameron RP, Killen JD, Hayward C, Taylor CB: Naturalistic weight-reduction efforts prospectively predict growth in relative weight and onset of obesity among female adolescents. J Consult Clin Psychol. 1999, 67: 967-974. 10.1037/0022-006X.67.6.967.
Coakley EH, Rimm EB, Colditz G, Kawachi I, Willett W: Predictors of weight change in men: Results from the Health Professionals Follow-Up Study. Int J Obes Relat Metab Disord. 1998, 22: 89-96. 10.1038/sj.ijo.0800549.
Bild DE, Sholinksy P, Smith DE, Lewis CE, Hardin JM, Burke GL: Correlates and predictors of weight loss in young adults: The CARDIA study. Int J Obes Relat Metab Disord. 1996, 20: 47-55.
Korkeila M, Rissanen A, Kapriio J, Sorensen TIA, Koskenvuo M: Weight-loss attempts and risk of major weight gain. Am J Clin Nutr. 1999, 70: 965-973.
Neumark-Sztainer D, Wall M, Guo J, Story M, Haines J, Eisenberg M: Obesity, disordered eating, and eating disorders in a longitudinal study of adolescents: how do dieters fare 5 years later?. J Am Diet Assoc. 2006, 106: 559-568. 10.1016/j.jada.2006.01.003.
Field AE, Austin SB, Taylor CB, Malspeis S, Rosner B, Rockett HR, Gillman MW, Colditz GA: Relation between dieting and weight change among preadolescents and adolescents. Pediatrics. 2003, 112: 900-906. 10.1542/peds.112.4.900.
Puhl RM, Andreyeva T, Brownell KD: Perceptions of weight discrimination: prevalence and comparison to race and gender discrimination in America. Int J Obes (Lond). 2008, 32: 992-1000. 10.1038/ijo.2008.22.
Brownell K, Puhl R, Schwartz M, Rudd LE: Weight bias: Nature, consequences, and remedies. 2005, New York: Guilford
Puhl RM, Brownell KD: Confronting and coping with weight stigma: an investigation of overweight and obese adults. Obesity (Silver Spring). 2006, 14: 1802-1815. 10.1038/oby.2006.208.
Haines J, Neumark-Sztainer D, Eisenberg ME, Hannan PJ: Weight teasing and disordered eating behaviors in adolescents: longitudinal findings from Project EAT (Eating Among Teens). Pediatrics. 2006, 117: e209-215. 10.1542/peds.2005-1242.
Neumark-Sztainer D, Falkner N, Story M, Perry C, Hannan PJ, Mulert S: Weight-teasing among adolescents: correlations with weight status and disordered eating behaviors. Int J Obes Relat Metab Disord. 2002, 26: 123-131. 10.1038/sj.ijo.0801853.
Puhl RM, Moss-Racusin CA, Schwartz MB: Internalization of weight bias: Implications for binge eating and emotional well-being. Obesity (Silver Spring). 2007, 15: 19-23. 10.1038/oby.2007.521.
Faith MS, Leone MA, Ayers TS, Heo M, Pietrobelli A: Weight criticism during physical activity, coping skills, and reported physical activity in children. Pediatrics. 2002, 110: e23-10.1542/peds.110.2.e23.
Storch EA, Milsom VA, Debraganza N, Lewin AB, Geffken GR, Silverstein JH: Peer victimization, psychosocial adjustment, and physical activity in overweight and at-risk-for-overweight youth. J Pediatr Psychol. 2007, 32: 80-89. 10.1093/jpepsy/jsj113.
Vartanian LR, Shaprow JG: Effects of weight stigma on exercise motivation and behavior: a preliminary investigation among college-aged females. J Health Psychol. 2008, 13: 131-138. 10.1177/1359105307084318.
Amy N, Aalborg A, Lyons P, Keranen L: Barriers to routine gynecological cancer screening for White and African-American obese women. Int J Obes Relat Metab Disord. 2006, 30: 147-155. 10.1038/sj.ijo.0803105.
Puhl R, Brownell K: Bias, discrimination and obesity. Obes Res. 2001, 9: 788-805. 10.1038/oby.2001.108.
Puhl RM, Heuer CA: The stigma of obesity: a review and update. Obesity (Silver Spring). 2009, 17: 941-964. 10.1038/oby.2008.636.
Fagard RH: Physical activity in the prevention and treatment of hypertension in the obese. Med Sci Sports Exerc. 1999, 31: S624-630. 10.1097/00005768-199911001-00022.
Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM, et al: A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med. 1997, 33: 1117-1124. 10.1056/NEJM199704173361601.
Gaesser GA: Exercise for prevention and treatment of cardiovascular disease, type 2 diabetes, and metabolic syndrome. Curr Diab Rep. 2007, 7: 14-19. 10.1007/s11892-007-0004-8.
Kraus WE, Houmard JA, Duscha BD, Knetzger KJ, Wharton MB, McCartney JS, Bales CW, Henes S, Samsa GP, Otvos JD, et al: Effects of the amount and intensity of exercise on plasma lipoproteins. N Engl J Med. 2002, 347: 1483-1492. 10.1056/NEJMoa020194.
Lamarche B, Despres JP, Pouliot MC, Moorjani S, Lupien PJ, Theriault G, Tremblay A, Nadeau A, Bouchard C: Is body fat loss a determinant factor in the improvement of carbohydrate and lipid metabolism following aerobic exercise training in obese women?. Metabolism. 1992, 41: 1249-1256. 10.1016/0026-0495(92)90017-5.
Bjorntorp P, DeJounge K, Sjostrom L, Sullivan L: The effect of physical training on insulin production in obesity. Metabolism. 1970, 19: 631-638. 10.1016/0026-0495(70)90020-X.
Finkelstein EA, Trogdon JG, Cohen JW, Dietz W: Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff (Millwood). 2009, 28: w822-831. 10.1377/hlthaff.28.5.w822.
Wildman RP, Muntner P, Reynolds K, McGinn AP, Rajpathak S, Wylie-Rosett J, Sowers MR: The obese without cardiometabolic risk factor clustering and the normal weight with cardiometabolic risk factor clustering: prevalence and correlates of 2 phenotypes among the US population (NHANES 1999-2004). Arch Intern Med. 2008, 168: 1617-1624. 10.1001/archinte.168.15.1617.
Beaglehole R, Prior IA, Foulkes MA, Eyles EF: Death in the South Pacific. N Z Med J. 1980, 91: 375-378.
Crister G: Fat Land: How Americans Became the Fattest People in the World. 2004, New York: Houghton Mifflin
Heinberg L, Matzon J: Body image dissatisfaction as a motivator for healthy lifestyle change: Is some distress beneficial?. Eating disorders: Innovative directions for research and practice. Edited by: Striegel-Moore R, Smolak L. 2001, Washington, DC: American Psychological Association, 215-232.
Puhl R, Heuer C: Obesity Stigma: Important Considerations for Public Health. Am J Public Health. 2010, 100: 1019-1028. 10.2105/AJPH.2009.159491.
Leary MR, Tate EB, Adams CE, Allen AB, Hancock J: Self-compassion and reactions to unpleasant self-relevant events: the implications of treating oneself kindly. J Pers Soc Psychol. 2007, 92: 887-904. 10.1037/0022-3514.92.5.887.
Goss K, Allen S: Compassion focused therapy for eating disorders. Int J of Cognitive Therapy. 2010, 3: 141-158. 10.1521/ijct.2010.3.2.141.
Aphramor L, Gingras J: That remains to be seen: Disappeared feminist discourses on fat in dietetic theory and practice. The Fat Studies Reader. Edited by: Rothblum E, Solovay S. 2009, New York: New York University Press, 97-105.
Tribole E, Resch E: Intuitive eating: a revolutionary program that works. 2010, New York: St. Martin's Griffin, 2
Hirschmann JR, Munter CH: When women stop hating their bodies: freeing yourself from food and weight obsession. 1995, New York: Fawcett Columbine, 1
Matz J, Frankel E: The Diet Survivor's Handbook: 60 Lessons in Eating, Acceptance and Self-care. 2006, Naperville, IL: Sourcebooks
May M: Eat What You Love, Love What You Eat: How to Break Your Eat-Repent-Repeat Cycle. 2009, Greenleaf Book Group Press
Satter E: Secrets of Feeding a Healthy Family: How to Eat, How to Raise Good Eaters and How to Cook. 2008, Madison, WI: Kelcy Press
Cole R, Horacek T: Effectiveness of the "My Body Knows When" intuitive-eating pilot program. Am J Health Behav. 2010, 34: 286-297.
Smith T, Hawks S: Intuitive eating, diet composition and the meaning of food in healthy weight promotion. Am J Health Educ. 2006, 37: 130-136.
Tylka T: Development and psychometric evaluation of a measure of intuitive eating. J Couns Psychol. 2006, 53: 226-240. 10.1037/0022-0167.53.2.226.
Kristeller J, Hallett C: An exploratory study of a meditation-based intervention for binge eating disorder. J Health Psychol. 1999, 4: 357-363. 10.1177/135910539900400305.
Smitham L: Evaluating an intuitive eating program for binge eating disorder: A benchmarking study [dissertation]. 2008, South Bend, IN: University of Notre Dame
Hawks S, Madanat H, Hawks J, Harris A: The relationship between intuitive eating and health indicators among college women. Am J Health Educ. 2005, 36: 331-336.
Weigensberg M, Shoar Z, Lane C, Spruijt-Metz D: Intuitive eating (IE) Is associated with decreased adiposity and increased insulin sensitivity (Si) in obese Latina female adolescents. 2009, DiabetesPro
Aphramor L, Gingras J: Helping People Change: Promoting Politicised Practice in the Healthcare Professions. Debating Obesity: Critical Perspectives. Edited by: Rich E, Monaghan L, Aphramor L. 2010, U.K.: Palgrave/Macmillan
Aphramor L, Gingras J: Weight in Practice, Health in Perspective. Critical Bodies. Edited by: Riley S, Burns M, Frith H, Wiggins S, Markula P. 2007, Palgrave/Macmillan, 155-117.
Bacon L: Reflections on Fat Acceptance: Lessons Learned from Privilege. Keynote Speech, National Association to Advance Fat Acceptance conference; Washington, DC. 2009, [ http://www.lindabacon.org/Bacon_ThinPrivilege080109.pdf ]
Marmot MG: Status syndrome: a challenge to medicine. JAMA. 2006, 295: 1304-1307. 10.1001/jama.295.11.1304.
Clarke P, O'Malley PM, Johnston LD, Schulenberg JE: Social disparities in BMI trajectories across adulthood by gender, race/ethnicity and lifetime socio-economic position: 1986-2004. Int J Epidemiol. 2009, 38: 499-509. 10.1093/ije/dyn214.
Chandola T, Brunner E, Marmot M: Chronic stress at work and the metabolic syndrome: prospective study. BMJ. 2006, 332: 521-525. 10.1136/bmj.38693.435301.80.
Vitaliano PP, Scanlan JM, Zhang J, Savage MV, Hirsch IB, Siegler IC: A path model of chronic stress, the metabolic syndrome, and coronary heart disease. Psychosom Med. 2002, 64: 418-435.
Raikkonen K, Matthews KA, Kuller LH: The relationship between psychological risk attributes and the metabolic syndrome in healthy women: antecedent or consequence?. Metabolism. 2002, 51: 1573-1577. 10.1053/meta.2002.36301.
Aphramor L: Disability and the Anti-Obesity Offensive. Disability & Society. 2009, 24: 897-909.
Lebesco K: Fat Panic and the New Morality. Against Health: How Health Became the New Morality. Edited by: Metzl J, Kirkland A. 2010, New York: New York University Press, 72-82.
Klein R: What is Health and How Do You Get It?. Against Health: How Health Became the New Morality. Edited by: Metzl J, Kirkland A. 2010, New York: New York University Press, 15-25.
Download references
Acknowledgements
Deb Burgard conceptualized the obesity cost analysis. The authors thank Deb Burgard, Sigrún Daníelsdóttir, Paul Ernsberger, Janell Mensinger, Elise Paradis, Jon Robison, Camerin Ross, Abigail Saguy, and Evelyn Tribole for their contributions and critical review. Lucy Aphramor thanks the WM NMAHP Research Training Awards for financial support.
Author information
Authors and affiliations.
Davis, and City College of San Francisco, University of California, Box S-80, City College of San Francisco, 50 Phelan Avenue, San Francisco, CA, 94112, USA
Linda Bacon
Applied Research Centre in Health and Lifestyle Interventions, Coventry University, Priory Street, Coventry, CV1 1FB, UK
Lucy Aphramor
Cardiac Rehab, University Hospitals Coventry and Warwickshire NHS Trust, Cardiology Suite, 1st Floor, East Wing, Walsgrave Hospital, Clifford Bridge Road, Coventry, CV2 2DX, UK
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Linda Bacon .
Additional information
Authors' contributions.
LB initiated the collaboration. Both authors contributed to conceptualizing and drafting the review. LB was lead researcher and undertook the systematic review and designed and completed the tables. Both authors approved the final manuscript.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Bacon, L., Aphramor, L. Weight Science: Evaluating the Evidence for a Paradigm Shift. Nutr J 10 , 9 (2011). https://doi.org/10.1186/1475-2891-10-9
Download citation
Received : 01 October 2010
Accepted : 24 January 2011
Published : 24 January 2011
DOI : https://doi.org/10.1186/1475-2891-10-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Eating Disorder
- Binge Eating
- Body Dissatisfaction
- Obese People
- Weight Cycling
Nutrition Journal
ISSN: 1475-2891
- General enquiries: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 22 February 2022
Clinical application of intermittent fasting for weight loss: progress and future directions
- Krista A. Varady ORCID: orcid.org/0000-0002-9279-9934 1 ,
- Sofia Cienfuegos 1 ,
- Mark Ezpeleta 1 &
- Kelsey Gabel ORCID: orcid.org/0000-0003-4613-8892 1
Nature Reviews Endocrinology volume 18 , pages 309–321 ( 2022 ) Cite this article
19k Accesses
112 Citations
1327 Altmetric
Metrics details
- Endocrine system and metabolic diseases
- Medical research
Intermittent fasting diets have become very popular in the past few years, as they can produce clinically significant weight loss. These diets can be defined, in the simplest of terms, as periods of fasting alternating with periods of eating. The most studied forms of intermittent fasting include: alternate day fasting (0–500 kcal per ‘fast day’ alternating with ad libitum intake on ‘feast days’); the 5:2 diet (two fast days and five feast days per week) and time-restricted eating (only eating within a prescribed window of time each day). Despite the recent surge in the popularity of fasting, only a few studies have examined the health benefits of these diets in humans. The goal of this Review is to summarize these preliminary findings and give insights into the effects of intermittent fasting on body weight and risk factors for cardiometabolic diseases in humans. This Review also assesses the safety of these regimens, and offers some practical advice for how to incorporate intermittent fasting diets into everyday life. Recommendations for future research are also presented.
The three main forms of intermittent fasting (alternate day fasting, the 5:2 diet and time-restricted eating) produce mild to moderate weight loss (3–8% loss from baseline) over short durations (8–12 weeks).
The degree of weight loss achieved with intermittent fasting is on a par with that achieved with traditional dieting approaches (daily calorie restriction).
The ability of these intermittent fasting protocols to help to manage weight long-term is still poorly understood, as the majority of studies to date have run for short durations.
Some studies demonstrate that intermittent fasting improves cardiometabolic risk factors such as blood pressure, levels of LDL cholesterol and triglycerides, insulin resistance and HbA 1c , while others show no benefit on these parameters.
Intermittent fasting is generally safe and produces few gastrointestinal, neurological, hormonal or metabolic adverse effects.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
195,33 € per year
only 16,28 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
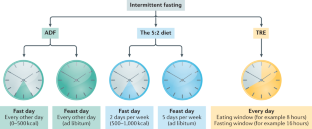
Similar content being viewed by others
Intermittent fasting plus early time-restricted eating versus calorie restriction and standard care in adults at risk of type 2 diabetes: a randomized controlled trial
Randomized controlled trial for time-restricted eating in healthy volunteers without obesity
Impact of intermittent vs. continuous energy restriction on weight and cardiometabolic factors: a 12-month follow-up
Williamson, D. A., Bray, G. A. & Ryan, D. H. Is 5% weight loss a satisfactory criterion to define clinically significant weight loss? Obesity 23 , 2319–2320 (2015).
Article PubMed Google Scholar
Brody, J. E. The benefits of intermittent fasting. The New York Times (23 Feb 2020).
Kohik, S. Why is intermittent fasting so popular? BBC News (3 Jun 2019).
de Cabo, R. & Mattson, M. P. Effects of intermittent fasting on health, aging, and disease. N. Engl. J. Med. 381 , 2541–2551 (2019).
Brandhorst, S. & Longo, V. D. Dietary restrictions and nutrition in the prevention and treatment of cardiovascular disease. Circ. Res. 124 , 952–965 (2019).
Article CAS PubMed Google Scholar
Longo, V. D. & Panda, S. Fasting, circadian rhythms, and time-restricted feeding in healthy lifespan. Cell Metab. 23 , 1048–1059 (2016).
Article CAS PubMed PubMed Central Google Scholar
Mattson, M. P., Longo, V. D. & Harvie, M. Impact of intermittent fasting on health and disease processes. Ageing Res. Rev. 39 , 46–58 (2017).
Paoli, A., Tinsley, G., Bianco, A. & Moro, T. The influence of meal frequency and timing on health in humans: the role of fasting. Nutrients 11 , 719 (2019).
Article CAS PubMed Central Google Scholar
St-Onge, M. P. et al. Meal timing and frequency: implications for cardiovascular disease prevention: a scientific statement from the American Heart Association. Circulation 135 , e96–e121 (2017).
Article PubMed PubMed Central Google Scholar
Harvie, M. & Howell, A. Potential benefits and harms of intermittent energy restriction and intermittent fasting amongst obese, overweight and normal weight subjects–a narrative review of human and animal evidence. Behav. Sci. 7 , 4 (2017).
Article PubMed Central Google Scholar
Patterson, R. E. & Sears, D. D. Metabolic effects of intermittent fasting. Annu. Rev. Nutr. 37 , 371–393 (2017).
Tinsley, G. M. & La Bounty, P. M. Effects of intermittent fasting on body composition and clinical health markers in humans. Nutr. Rev. 73 , 661–674 (2015).
Stekovic, S. et al. Alternate day fasting improves physiological and molecular markers of aging in healthy, non-obese humans. Cell Metab. 31 , 878–881 (2020).
Catenacci, V. A. et al. A randomized pilot study comparing zero-calorie alternate-day fasting to daily caloric restriction in adults with obesity. Obesity 24 , 1874–1883 (2016).
Johnson, J. B. et al. Alternate day calorie restriction improves clinical findings and reduces markers of oxidative stress and inflammation in overweight adults with moderate asthma. Free Radic. Biol. Med. 42 , 665–674 (2007).
Cho, A. R. et al. Effects of alternate day fasting and exercise on cholesterol metabolism in overweight or obese adults: a pilot randomized controlled trial. Metabolism 93 , 52–60 (2019).
Trepanowski, J. F. et al. Effect of alternate-day fasting on weight loss, weight maintenance, and cardioprotection among metabolically healthy obese adults: a randomized clinical trial. JAMA Intern. Med. 177 , 930–938 (2017).
Hoddy, K. K. et al. Meal timing during alternate day fasting: impact on body weight and cardiovascular disease risk in obese adults. Obesity 22 , 2524–2531 (2014).
Antoni, R., Johnston, K. L., Collins, A. L. & Robertson, M. D. Investigation into the acute effects of total and partial energy restriction on postprandial metabolism among overweight/obese participants. Br. J. Nutr. 115 , 951–959 (2016).
Harvie, M. N. et al. The effects of intermittent or continuous energy restriction on weight loss and metabolic disease risk markers: a randomized trial in young overweight women. Int. J. Obes. 35 , 714–727 (2011).
Article CAS Google Scholar
Schubel, R. et al. Effects of intermittent and continuous calorie restriction on body weight and metabolism over 50 wk: a randomized controlled trial. Am. J. Clin. Nutr. 108 , 933–945 (2018).
Carter, S., Clifton, P. M. & Keogh, J. B. Effect of intermittent compared with continuous energy restricted diet on glycemic control in patients with type 2 diabetes: a randomized noninferiority trial. JAMA Netw. Open 1 , e180756 (2018).
Cienfuegos, S. et al. Effects of 4- and 6-h time-restricted feeding on weight and cardiometabolic health: a randomized controlled trial in adults with obesity. Cell Metab. 32 , 366–378 (2020).
Tinsley, G. M. et al. Time-restricted feeding in young men performing resistance training: a randomized controlled trial. Eur. J. Sport. Sci. 17 , 200–207 (2017).
Tinsley, G. M. et al. Time-restricted feeding plus resistance training in active females: a randomized trial. Am. J. Clin. Nutr. 110 , 628–640 (2019).
Chow, L. S. et al. Time-restricted eating effects on body composition and metabolic measures in humans who are overweight: a feasibility study. Obesity 28 , 860–869 (2020).
Wilkinson, M. J. et al. Ten-hour time-restricted eating reduces weight, blood pressure, and atherogenic lipids in patients with metabolic syndrome. Cell Metab. 31 , 92–104.e5 (2020).
Parvaresh, A. et al. Modified alternate-day fasting vs. calorie restriction in the treatment of patients with metabolic syndrome: a randomized clinical trial. Complement. Ther. Med. 47 , 102187 (2019).
Bhutani, S., Klempel, M. C., Kroeger, C. M., Trepanowski, J. F. & Varady, K. A. Alternate day fasting and endurance exercise combine to reduce body weight and favorably alter plasma lipids in obese humans. Obesity 21 , 1370–1379 (2013).
Bhutani, S. et al. Effect of exercising while fasting on eating behaviors and food intake. J. Int. Soc. Sports Nutr. 10 , 50 (2013).
Varady, K. A. et al. Alternate day fasting for weight loss in normal weight and overweight subjects: a randomized controlled trial. Nutr. J. 12 , 146 (2013).
Fitzgerald, K. C. et al. Effect of intermittent vs. daily calorie restriction on changes in weight and patient-reported outcomes in people with multiple sclerosis. Mult. Scler. Relat. Disord. 23 , 33–39 (2018).
Harvie, M. et al. The effect of intermittent energy and carbohydrate restriction v. daily energy restriction on weight loss and metabolic disease risk markers in overweight women. Br. J. Nutr. 110 , 1534–1547 (2013).
Sundfor, T. M., Svendsen, M. & Tonstad, S. Effect of intermittent versus continuous energy restriction on weight loss, maintenance and cardiometabolic risk: a randomized 1-year trial. Nutr. Metab. Cardiovasc. Dis. 28 , 698–706 (2018).
Overland, J. et al. The safety and efficacy of weight loss via intermittent fasting or standard daily energy restriction in adults with type 1 diabetes and overweight or obesity: a pilot study. Obes. Med. 12 , 13–17 (2018).
Article Google Scholar
Gabel, K. et al. Effects of 8-hour time restricted feeding on body weight and metabolic disease risk factors in obese adults: a pilot study. Nutr. Healthy Aging 4 , 345–353 (2018).
Lin, S. et al. Does the weight loss efficacy of alternate day fasting differ according to sex and menopausal status? Nutr. Metab. Cardiovasc. Dis. 31 , 641–649 (2020).
Article PubMed PubMed Central CAS Google Scholar
Gabel, K. et al. Differential effects of alternate-day fasting versus daily calorie restriction on insulin resistance. Obesity 27 , 1443–1450 (2019).
CAS PubMed Google Scholar
Cioffi, I. et al. Intermittent versus continuous energy restriction on weight loss and cardiometabolic outcomes: a systematic review and meta-analysis of randomized controlled trials. J. Transl. Med. 16 , 371 (2018).
Harris, L., McGarty, A., Hutchison, L., Ells, L. & Hankey, C. Short-term intermittent energy restriction interventions for weight management: a systematic review and meta-analysis. Obes. Rev. 19 , 1–13 (2018).
Headland, M., Clifton, P. M., Carter, S. & Keogh, J. B. Weight-loss outcomes: a systematic review and meta-analysis of intermittent energy restriction trials lasting a minimum of 6 months. Nutrients 8 , 354 (2016).
Article PubMed Central CAS Google Scholar
Willoughby, D., Hewlings, S. & Kalman, D. Body composition changes in weight loss: strategies and supplementation for maintaining lean body mass, a brief review. Nutrients 10 , 1876 (2018).
Heymsfield, S. B., Gonzalez, M. C., Shen, W., Redman, L. & Thomas, D. Weight loss composition is one-fourth fat-free mass: a critical review and critique of this widely cited rule. Obes. Rev. 15 , 310–321 (2014).
Pownall, H. J. et al. Changes in body composition over 8 years in a randomized trial of a lifestyle intervention: the look AHEAD study. Obesity 23 , 565–572 (2015).
Ravussin, E. et al. A 2-year randomized controlled trial of human caloric restriction: feasibility and effects on predictors of health span and longevity. J. Gerontol. A Biol. Sci. Med. Sci. 70 , 1097–1104 (2015).
Moro, T. et al. Effects of eight weeks of time-restricted feeding (16/8) on basal metabolism, maximal strength, body composition, inflammation, and cardiovascular risk factors in resistance-trained males. J. Transl. Med. 14 , 290 (2016).
Klempel, M. C., Bhutani, S., Fitzgibbon, M., Freels, S. & Varady, K. A. Dietary and physical activity adaptations to alternate day modified fasting: implications for optimal weight loss. Nutr. J. 9 , 35 (2010).
Harvey, J., Howell, A., Morris, J. & Harvie, M. Intermittent energy restriction for weight loss: spontaneous reduction of energy intake on unrestricted days. Food Sci. Nutr. 6 , 674–680 (2018).
Dansinger, M. L., Gleason, J. A., Griffith, J. L., Selker, H. P. & Schaefer, E. J. Comparison of the Atkins, Ornish, Weight Watchers, and Zone diets for weight loss and heart disease risk reduction: a randomized trial. JAMA 293 , 43–53 (2005).
Das, S. K. et al. Long-term effects of 2 energy-restricted diets differing in glycemic load on dietary adherence, body composition, and metabolism in CALERIE: a 1-y randomized controlled trial. Am. J. Clin. Nutr. 85 , 1023–1030 (2007).
Jospe, M. R. et al. Intermittent fasting, Paleolithic, or Mediterranean diets in the real world: exploratory secondary analyses of a weight-loss trial that included choice of diet and exercise. Am. J. Clin. Nutr. 111 , 503–514 (2020).
Kalam, F. et al. Beverage intake during alternate-day fasting: relationship to energy intake and body weight. Nutr. Health 25 , 167–171 (2019).
Sutton, E. F. et al. Early time-restricted feeding improves insulin sensitivity, blood pressure, and oxidative stress even without weight loss in men with prediabetes. Cell Metab. 27 , 1212–1221.e3 (2018).
Lowe, D. A. et al. Effects of time-restricted eating on weight loss and other metabolic parameters in women and men with overweight and obesity: the TREAT randomized clinical trial. JAMA Intern. Med. 180 , 1491–1499 (2020).
Andersson, B., Wallin, G., Hedner, T., Ahlberg, A. C. & Andersson, O. K. Acute effects of short-term fasting on blood pressure, circulating noradrenaline and efferent sympathetic nerve activity. Acta Med. Scand. 223 , 485–490 (1988).
Johnston, J. G., Speed, J. S., Jin, C. & Pollock, D. M. Loss of endothelin B receptor function impairs sodium excretion in a time- and sex-dependent manner. Am. J. Physiol. Ren. Physiol. 311 , F991–F998 (2016).
Rolland, C. & Broom, I. The effects of very-low-calorie diets on HDL: a review. Cholesterol 2011 , 306278 (2011).
Article PubMed CAS Google Scholar
Kodama, S. et al. Effect of aerobic exercise training on serum levels of high-density lipoprotein cholesterol: a meta-analysis. Arch. Intern. Med. 167 , 999–1008 (2007).
Leon, A. S. & Sanchez, O. A. Response of blood lipids to exercise training alone or combined with dietary intervention. Med. Sci. Sports Exerc. 33 , S502–S515 (2001).
Browning, J. D., Baxter, J., Satapati, S. & Burgess, S. C. The effect of short-term fasting on liver and skeletal muscle lipid, glucose, and energy metabolism in healthy women and men. J. Lipid Res. 53 , 577–586 (2012).
Halberg, N. et al. Effect of intermittent fasting and refeeding on insulin action in healthy men. J. Appl. Physiol. 99 , 2128–2136 (2005).
Salgin, B. et al. Effects of prolonged fasting and sustained lipolysis on insulin secretion and insulin sensitivity in normal subjects. Am. J. Physiol. Endocrinol. Metab. 296 , E454–E461 (2009).
Freckmann, G. et al. Continuous glucose profiles in healthy subjects under everyday life conditions and after different meals. J. Diabetes Sci. Technol. 1 , 695–703 (2007).
Cervantes Gracia, K., Llanas-Cornejo, D. & Husi, H. CVD and oxidative stress. J. Clin. Med. 6 , 22 (2017).
Donath, M. Y. & Shoelson, S. E. Type 2 diabetes as an inflammatory disease. Nat. Rev. Immunol. 11 , 98–107 (2011).
Maritim, A. C., Sanders, R. A. & Watkins, J. B. 3rd Diabetes, oxidative stress, and antioxidants: a review. J. Biochem. Mol. Toxicol. 17 , 24–38 (2003).
Siti, H. N., Kamisah, Y. & Kamsiah, J. The role of oxidative stress, antioxidants and vascular inflammation in cardiovascular disease (a review). Vasc. Pharmacol. 71 , 40–56 (2015).
Tsalamandris, S. et al. The role of inflammation in diabetes: current concepts and future perspectives. Eur. Cardiol. 14 , 50–59 (2019).
Wellen, K. E. & Hotamisligil, G. S. Inflammation, stress, and diabetes. J. Clin. Invest. 115 , 1111–1119 (2005).
Houstis, N., Rosen, E. D. & Lander, E. S. Reactive oxygen species have a causal role in multiple forms of insulin resistance. Nature 440 , 944–948 (2006).
Rains, J. L. & Jain, S. K. Oxidative stress, insulin signaling, and diabetes. Free Radic. Biol. Med. 50 , 567–575 (2011).
Zaulkffali, A. S. et al. Vitamins D and E stimulate the PI3K-AKT signalling pathway in insulin-resistant SK-N-SH neuronal cells. Nutrients 11 , 2525 (2019).
Manning, P. J. et al. Effect of high-dose vitamin E on insulin resistance and associated parameters in overweight subjects. Diabetes Care 27 , 2166–2171 (2004).
Gabel, K., Hoddy, K. K. & Varady, K. A. Safety of 8-h time restricted feeding in adults with obesity. Appl. Physiol. Nutr. Metab. 44 , 107–109 (2019).
Hoddy, K. K. et al. Safety of alternate day fasting and effect on disordered eating behaviors. Nutr. J. 14 , 44 (2015).
Blau, J. N., Kell, C. A. & Sperling, J. M. Water-deprivation headache: a new headache with two variants. Headache 44 , 79–83 (2004).
Spigt, M. G. et al. Increasing the daily water intake for the prophylactic treatment of headache: a pilot trial. Eur. J. Neurol. 12 , 715–718 (2005).
Akasheh, R. T. et al. Weight loss efficacy of alternate day fasting versus daily calorie restriction in subjects with subclinical hypothyroidism: a secondary analysis. Appl. Physiol. Nutr. Metab. 45 , 340–343 (2020).
Heilbronn, L. K., Smith, S. R., Martin, C. K., Anton, S. D. & Ravussin, E. Alternate-day fasting in nonobese subjects: effects on body weight, body composition, and energy metabolism. Am. J. Clin. Nutr. 81 , 69–73 (2005).
Jebeile, H. et al. Intermittent energy restriction is a feasible, effective, and acceptable intervention to treat adolescents with obesity. J. Nutr. 149 , 1189–1197 (2019).
Lister, N. B. et al. Fast track to health – intermittent energy restriction in adolescents with obesity. A randomised controlled trial study protocol. Obes. Res. Clin. Pract. 14 , 80–90 (2020).
Vidmar, A. P., Goran, M. I. & Raymond, J. K. Time-limited eating in pediatric patients with obesity: a case series. J. Food Sci. Nutr. Res. 2 , 236–244 (2019).
PubMed PubMed Central Google Scholar
Culbert, K. M., Racine, S. E. & Klump, K. L. The influence of gender and puberty on the heritability of disordered eating symptoms. Curr. Top. Behav. Neurosci. 6 , 177–185 (2011).
Klump, K. L. Puberty as a critical risk period for eating disorders: a review of human and animal studies. Horm. Behav. 64 , 399–410 (2013).
Klump, K. L., Culbert, K. M., O’Connor, S., Fowler, N. & Burt, S. A. The significant effects of puberty on the genetic diathesis of binge eating in girls. Int. J. Eat. Disord. 50 , 984–989 (2017).
Jebeile, H. et al. Treatment of obesity, with a dietary component, and eating disorder risk in children and adolescents: a systematic review with meta-analysis. Obes. Rev. 20 , 1287–1298 (2019).
Antoni, R., Johnston, K. L., Collins, A. L. & Robertson, M. D. Intermittent v. continuous energy restriction: differential effects on postprandial glucose and lipid metabolism following matched weight loss in overweight/obese participants. Br. J. Nutr. 119 , 507–516 (2018).
Chaix, A., Manoogian, E. N. C., Melkani, G. C. & Panda, S. Time-restricted eating to prevent and manage chronic metabolic diseases. Annu. Rev. Nutr. 39 , 291–315 (2019).
Wegman, M. P. et al. Practicality of intermittent fasting in humans and its effect on oxidative stress and genes related to aging and metabolism. Rejuvenation Res. 18 , 162–172 (2015).
Apolzan, J. W., Carnell, N. S., Mattes, R. D. & Campbell, W. W. Inadequate dietary protein increases hunger and desire to eat in younger and older men. J. Nutr. 137 , 1478–1482 (2007).
Leidy, H. J., Tang, M., Armstrong, C. L., Martin, C. B. & Campbell, W. W. The effects of consuming frequent, higher protein meals on appetite and satiety during weight loss in overweight/obese men. Obesity 19 , 818–824 (2011).
Weigle, D. S. et al. A high-protein diet induces sustained reductions in appetite, ad libitum caloric intake, and body weight despite compensatory changes in diurnal plasma leptin and ghrelin concentrations. Am. J. Clin. Nutr. 82 , 41–48 (2005).
Cava, E., Yeat, N. C. & Mittendorfer, B. Preserving healthy muscle during weight loss. Adv. Nutr. 8 , 511–519 (2017).
Mettler, S., Mitchell, N. & Tipton, K. D. Increased protein intake reduces lean body mass loss during weight loss in athletes. Med. Sci. Sports Exerc. 42 , 326–337 (2010).
Swithers, S. E. Artificial sweeteners produce the counterintuitive effect of inducing metabolic derangements. Trends Endocrinol. Metab. 24 , 431–441 (2013).
Hartmann-Boyce, J. et al. Cognitive and behavioural strategies for weight management in overweight adults: results from the Oxford Food and Activity Behaviours (OxFAB) cohort study. PLoS ONE 13 , e0202072 (2018).
Kelley, C. P., Sbrocco, G. & Sbrocco, T. Behavioral modification for the management of obesity. Prim. Care 43 , 159–175 (2016).
Teixeira, P. J. et al. Successful behavior change in obesity interventions in adults: a systematic review of self-regulation mediators. BMC Med. 13 , 84 (2015).
Ghelani, D. P., Moran, L. J., Johnson, C., Mousa, A. & Naderpoor, N. Mobile apps for weight management: a review of the latest evidence to inform practice. Front. Endocrinol. 11 , 412 (2020).
Carter, S., Clifton, P. M. & Keogh, J. B. Intermittent energy restriction in type 2 diabetes: a short discussion of medication management. World J. Diabetes 7 , 627–630 (2016).
Grajower, M. M. & Horne, B. D. Clinical management of intermittent fasting in patients with diabetes mellitus. Nutrients 11 , 873 (2019).
Varady, K. A., Bhutani, S., Church, E. C. & Klempel, M. C. Short-term modified alternate-day fasting: a novel dietary strategy for weight loss and cardioprotection in obese adults. Am. J. Clin. Nutr. 90 , 1138–1143 (2009).
Carlson, O. et al. Impact of reduced meal frequency without caloric restriction on glucose regulation in healthy, normal-weight middle-aged men and women. Metabolism 56 , 1729–1734 (2007).
Higgins, J. P. et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343 , d5928 (2011).
Download references
Acknowledgements
The authors thank the participants in the trials discussed in this Review for their time and effort. The authors acknowledge support from the National Institute of Diabetes and Digestive and Kidney Diseases (grant no. R01DK119783). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and affiliations.
Department of Kinesiology and Nutrition, University of Illinois at Chicago, Chicago, IL, USA
Krista A. Varady, Sofia Cienfuegos, Mark Ezpeleta & Kelsey Gabel
You can also search for this author in PubMed Google Scholar
Contributions
K.A.V., S.C., M.E. and K.G. contributed to all aspects of the preparation and writing of this Review.
Corresponding author
Correspondence to Krista A. Varady .
Ethics declarations
Competing interests.
K.A.V. received author fees from Hachette Book Group for the book, The Every Other Day Diet . The other authors declare no competing interests.
Peer review
Peer review information.
Nature Reviews Endocrinology thanks M. Harvie, K. Petersen and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information, rights and permissions.
Reprints and permissions
About this article
Cite this article.
Varady, K.A., Cienfuegos, S., Ezpeleta, M. et al. Clinical application of intermittent fasting for weight loss: progress and future directions. Nat Rev Endocrinol 18 , 309–321 (2022). https://doi.org/10.1038/s41574-022-00638-x
Download citation
Accepted : 24 January 2022
Published : 22 February 2022
Issue Date : May 2022
DOI : https://doi.org/10.1038/s41574-022-00638-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Effects of dash diet with or without time-restricted eating in the management of stage 1 primary hypertension: a randomized controlled trial.
- Xiaoxin Zhou
- Xiaoqian Lin
Nutrition Journal (2024)
Network meta-analysis of three different forms of intermittent energy restrictions for overweight or obese adults
International Journal of Obesity (2024)
Role of dietary interventions on microvascular health in South-Asian Surinamese people with type 2 diabetes in the Netherlands: A randomized controlled trial
- Anouk I. M. van der Velden
- Daphne H. T. IJpelaar
- Bernard M. van den Berg
Nutrition & Diabetes (2024)
Systemic proteome adaptions to 7-day complete caloric restriction in humans
- Maik Pietzner
- Burulça Uluvar
- Claudia Langenberg
Nature Metabolism (2024)
Intermittent Fasting Regulates Metabolic Homeostasis and Improves Cardiovascular Health
- Lina Dimachkie
Cell Biochemistry and Biophysics (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- - Google Chrome
Intended for healthcare professionals
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Dietary sugars and...
Dietary sugars and body weight: systematic review and meta-analyses of randomised controlled trials and cohort studies
- Related content
- Peer review
- Lisa Te Morenga , research fellow 1 2 ,
- Simonette Mallard , research assistant 1 ,
- Jim Mann , professor 1 2 3
- 1 Departments of Human Nutrition and Medicine, University of Otago, PO Box 56, Dunedin 9054, New Zealand
- 2 Riddet Institute, University of Otago
- 3 Edgar National Centre for Diabetes and Obesity Research, University of Otago
- Correspondence to: J Mann jim.mann{at}otago.ac.nz
- Accepted 28 October 2012
Objective To summarise evidence on the association between intake of dietary sugars and body weight in adults and children.
Design Systematic review and meta-analysis of randomised controlled trials and prospective cohort studies.
Data sources OVID Medline, Embase, PubMed, Cumulative Index to Nursing and Allied Health Literature, Scopus, and Web of Science (up to December 2011).
Review methods Eligible studies reported the intake of total sugars, intake of a component of total sugars, or intake of sugar containing foods or beverages; and at least one measure of body fatness. Minimum duration was two weeks for trials and one year for cohort studies. Trials of weight loss or confounded by additional medical or lifestyle interventions were excluded. Study selection, assessment, validity, data extraction, and analysis were undertaken as specified by the Cochrane Collaboration and the GRADE working group. For trials, we pooled data for weight change using inverse variance models with random effects. We pooled cohort study data where possible to estimate effect sizes, expressed as odds ratios for risk of obesity or β coefficients for change in adiposity per unit of intake.
Results 30 of 7895 trials and 38 of 9445 cohort studies were eligible. In trials of adults with ad libitum diets (that is, with no strict control of food intake), reduced intake of dietary sugars was associated with a decrease in body weight (0.80 kg, 95% confidence interval 0.39 to 1.21; P<0.001); increased sugars intake was associated with a comparable weight increase (0.75 kg, 0.30 to 1.19; P=0.001). Isoenergetic exchange of dietary sugars with other carbohydrates showed no change in body weight (0.04 kg, −0.04 to 0.13). Trials in children, which involved recommendations to reduce intake of sugar sweetened foods and beverages, had low participant compliance to dietary advice; these trials showed no overall change in body weight. However, in relation to intakes of sugar sweetened beverages after one year follow-up in prospective studies, the odds ratio for being overweight or obese increased was 1.55 (1.32 to 1.82) among groups with the highest intake compared with those with the lowest intake. Despite significant heterogeneity in one meta-analysis and potential bias in some trials, sensitivity analyses showed that the trends were consistent and associations remained after these studies were excluded.
Conclusions Among free living people involving ad libitum diets, intake of free sugars or sugar sweetened beverages is a determinant of body weight. The change in body fatness that occurs with modifying intakes seems to be mediated via changes in energy intakes, since isoenergetic exchange of sugars with other carbohydrates was not associated with weight change.
Introduction
Sugar has been a component of human diets since ancient times, with earliest reports of consumption coming from China and India, and much later from Europe after the Crusades in the 11th century. 1 The suggestion that sugar might have adverse health effects has been a recurring theme for decades, with claims that high intake may be associated with an increased risk of conditions as diverse as dental caries, obesity, cardiovascular disease, diabetes, gout, fatty liver disease, some cancers, and hyperactivity. 2 3 4 5 6 However, inadequate study design, differences in assessing dietary intake, inconsistent findings, and varying definitions of “sugars” have precluded definitive conclusions regarding these associations.
The most consistent association has been between a high intake of sugar sweetened beverages and the development of obesity, 7 8 9 10 11 12 but not all published meta-analyses have reported a statistically significant link. 7 11 The expert consultations organised by the World Health Organization and the Food and Agriculture Organization of the United Nations and the scientific updates undertaken by WHO 13 14 15 have adopted a classification of carbohydrates and clarified definitions of various groups of sugars including the category of “free sugars” (table 1 ⇓ ). This classification enables a more standardised approach to examining potential adverse health effects.
Classification of dietary carbohydrates
- View inline
To update the recommendations through the guideline’s development process that was launched in January 2009, WHO commissioned a systematic literature review to answer a series of questions 16 relating to the effects of sugars on excess adiposity. These questions asked whether reducing or increasing intake of dietary sugars influences measures of body fatness in adults and children, and whether the existing evidence provides support for the recommendation to reduce intake of free sugars to less than 10% total energy (box). 15 Body fatness was selected as an outcome in view of the extent to which comorbidities of obesity contribute to the global burden of non-communicable disease.
Questions posed by the WHO Nutrition Guidance Expert Advisory Group-Subgroup on Diet and Health, to develop recommendations regarding sugars intakes
What is the effect of a reduction in free sugars intakes in adults?
What is the effect of an increase in free sugars intakes in adults?
What is the effect of a reduction in free sugars intakes in children?
What is the effect of an increase in free sugars intakes in children?
(Where “free sugars” are defined as all monosaccharides and disaccharides added to foods by the manufacturer, cook, or consumer; plus sugars naturally present in honey, syrups, and fruit juices.)
Since the answers to the questions posed (box) were designed to inform population based dietary guidelines rather than advise individual patients, it was deemed appropriate to include cohort studies and randomised controlled trials of free living people consuming ad libitum diets (that is, with no strict control of food intake). The interventions mainly involved advice to increase or decrease intake of sugars, or of sugar containing foods or beverages, without emphasising the need to achieve weight loss.
We also examined randomised controlled trials comparing higher and lower intakes of sugars, but where energy intake was strictly controlled. Trials specifically designed to achieve weight loss were excluded. We acknowledged that the studies identified by this approach would inevitably be heterogeneous, that it would be difficult to disentangle the effects of a range of dietary changes that might occur after altering the intake of sugars, and that it might be difficult to identify a dose response. However, the findings from such an approach were expected to provide an indication of what might be achieved by population changes in intake of dietary sugars.
In accordance with the WHO guideline’s development process, 17 systematic reviews and meta-analyses were conducted according to the methods of the Cochrane Collaboration. 18 We prepared tables summarising quality assessment, effect size, and importance of findings, from which recommendations may be derived, in the format required by the Grading of Recommendations Assessment, Development and Evaluation (GRADE) working group. Ethical approval was not required for this research.
Search strategy
Two separate electronic searches were conducted to identify randomised trials and prospective cohort studies relating intake of dietary sugars to measures or changes of body fatness (web appendix 1). OVID Medline, Embase, PubMed, Cumulative Index to Nursing and Allied Health Literature, Scopus, and Web of Science electronic databases were searched for clinical trials and cohort studies, published up to December 2011, which met the inclusion criteria. In OVID Medline, we used the highly sensitive Cochrane search strategy to limit the first search to clinical trials, meta-analyses, and randomised controlled trials. We hand searched meta-analyses and reviews to identify studies that might have been missed.
Study selection
Two reviewers assessed titles and abstracts of all identified English language studies. Discrepancies in opinion as to whether studies should be selected for full review were resolved by discussion. A similar approach was used to determine which of these studies should be included in the formal analysis. Animal studies, cross sectional studies, and case-control studies were excluded. Studies were required to report intake of total sugars, intake of a component of total sugars (expressed in absolute amounts or as a percentage of total energy), or intake of sugar containing foods or beverages, assessed by continuous or categorical variables; and at least one measure of body fatness.
Participants were adults and children free from acute illness, but those with diabetes or other non-communicable diseases in whom conditions were regarded as stable could be included. Randomised trials were required to be of at least two weeks’ duration, and prospective cohort studies were required to be of at least one year’s duration. We included trials comparing diets differing in sugars intakes and in which the effect of sugars could be separated from the effects of other lifestyle or medical interventions.
Two groups of trials were identified. One group included studies in which participants in the intervention arm were advised to decrease or increase sugars, or foods and drinks containing sugars. Although such advice was generally accompanied by the recommendation to increase or decrease other forms of carbohydrate, there was no strict attempt at weight control. These trials are referred to as ad libitum studies. The other group of trials attempted to achieve isoenergetic replacement of sugars with other forms of carbohydrate. Interventions designed to achieve weight loss were excluded because the ultimate aim of the review was to facilitate the development of population based recommendations rather than nutritional recommendations for the management of obesity.
Data extraction and quality assessment
Data extraction and validity assessment were carried out independently by two reviewers, and any discrepancies resolved by discussion. For both randomised trials and cohort studies, outcomes, data relating to participants, exposure or interventions, potential effect modifiers, and study quality were extracted by use of piloted data extraction forms. In the cohort studies, we aimed to extract the least and most adjusted relative risk, odds ratio, or mean difference when comparing the most exposed group of participants with the least exposed group, or a β coefficient for the continuous effect of a one unit change in sugars intake. We extracted these statistics separately for sugars exposures reported as baseline values or as values for change over time.
Cochrane criteria 18 were used to examine validity of each randomised trial, including sequence generation, allocation concealment, blinding of participants, personnel and outcome assessors, incomplete outcome data, and selective outcome reporting. Additional review specific criteria included similarity, or not, of type and intensity of intervention in both arms, and whether the studies were funded by industries with potentially vested interests. We examined the effect of bias on the pooled effect estimates by excluding studies that had a high risk of bias for two or more validity criteria in sensitivity analyses.
Statistical analysis
Studies were grouped to answer the major questions that had been posed (box). We considered data for adults and children separately. Studies of isoenergetic exchange of sugars with other carbohydrates were examined to help explain possible mechanisms through which sugars might exert their effects.
Randomised trials
The effects of decreasing or increasing dietary sugars in adults were examined principally by meta-analysing the randomised trials in which participants were required to consume different amounts of sugar (sucrose) or other sugars (which would now be classified as “free sugars”). Terminology varied among trials. The term “free sugars” refers to all monosaccharides and disaccharides added to foods by the manufacturer, cook, or consumer, plus sugars naturally present in honey, syrups, and fruit juices (table 1). 14 The term “added sugar” is sometimes used interchangeably with “free sugar” but is considered to include sugars and syrups added to foods during processing, food preparation, or at the table—but does not include honey, syrups, or fruit juice. 19 “Sugar” is generally assumed to be purified sucrose. 14
Data for each group of studies were pooled using Review Manager 5.1 software. 20 In trials involving adult participants, we used generic inverse variance of analysis for mean differences in body weight between intervention and control groups to compare the parallel and crossover experimental designs reporting change in body weight. In the studies involving children and adolescents, we used standardised mean differences because studies reported differences in either body mass index (BMI) or standardised BMI units.
Heterogeneity was assessed with the I 2 test and Q statistics. We considered an I 2 value greater than 50% and P<0.05 as indicative of heterogeneity. 18 We used random effects models because significant heterogeneity was associated with trial design and duration in some analyses.
Estimates for the standard error of the difference in means for treatment groups in crossover studies were derived from reported P values when the standard error of the mean difference was not reported. 18 If P values for the differences were reported simply as non-significant, then P=0.2 was assumed. 18
We did sensitivity analyses to explore the differences between studies in the short term (<eight weeks) and longer term (>eight weeks). We also tested the effects of removing those studies that achieved a difference in sugars intakes of less than 5% of total energy intake between intervention and control groups. Metaregression (using Stata/IC 11.2 software for Mac (StataCorp)) was used to test for a dose-response effect of sugars on weight change, and for associations between weight change and study duration, study design (that is, crossover or parallel), and whether sugars intake changed in the intervention arm.
Publication bias among the randomised controlled trials of adults was examined by visual inspection of a funnel plot and Egger’s test for bias. 21 Publication bias is suspected when the funnel plot is asymmetrical. We combined the 15 ad libitum studies for this analysis because it is generally accepted that asymmetry cannot readily be assessed with 10 or fewer studies. 18 Sensitivity analyses examined the influence of small study effects, by comparing the estimates derived from random and fixed effects models 22 and by using the Duval and Tweedie 23 “trim and fill” method in Stata 12 (Metatrim). There were insufficient studies in children to conduct a meaningful examination of publication bias.
Prospective cohort studies
Cohort studies in adults provided limited additional information. Data from cohort studies in children were necessary to determine the effect of increasing sugars intake on adiposity, owing to a lack of suitable randomised trials. We grouped individual studies for meta-analysis on the basis of the methods used for reporting adiposity outcomes and sugars exposure variables.
We used four main methods of reporting outcomes:
β coefficients for the continuous association between sugars exposure at baseline and adiposity outcome.
Odds ratios for the risk of overweight or obesity comparing participants who had the highest intakes of sugars with those who had the lowest intakes of sugars (groups or frequency of servings).
Mean differences in change in measures of adiposity over time between participants with the highest intakes of sugars and those with the lowest intakes (groups or frequency of servings).
β coefficients for the continuous association between increases in sugars exposure over time and adiposity outcome.
Sugars exposures included sugar sweetened beverages, fruit juice, sweets (including jams, syrups, cakes, and desserts), sucrose, or total sugars. Exposures were reported as servings per time period and were converted to servings per day, volume of beverage consumed per day, percentage of energy intake, frequency of consumption, or grams per day. Where possible, we scaled exposures to comparable units to allow data to be pooled. We assumed that one serving of sugar sweetened beverage was equivalent to 240 mL or 8 fluid ounces, and contained 26 g of sucrose. 24 This portion equated to about 5% of daily total energy intake in adults.
Measures of body fatness included weight change, change in BMI or BMI z score, waist circumference, body fat (%), fat mass, and trunk fat (%). If studies reported more than one measure of sugars intake, we derived an average effect size. We ranked adiposity outcomes in terms of importance for pooling, from highest to lowest: BMI z score, BMI, body weight, waist circumference, percentage body fat, fat mass, and percentage trunk fat. If studies reported outcomes for more than one measure of adiposity, we used the highest ranked adiposity outcome. We generated pooled estimates for the various subgroups using metan commands with random effects in Stata. Two sided P<0.05 was considered significant for all analyses.
GRADE assessment
GRADE assessment 25 was carried out to assess the totality of the evidence by the authors and then refined by the WHO Nutrition Guidance Expert Advisory Group (NUGAG) Subgroup on Diet and Health ( www.who.int/nutrition/topics/advisory_group/en/index.html ) to fulfil the required process for developing WHO guidelines. 17 GRADE assessment took into account study design limitations, consistency of results across the available studies, precision of the results, directness, and likelihood of publication bias when assessing the quality of the evidence from the randomised trials. 17 25 Further criteria were considered for the cohort studies. These criteria included magnitude of the effect, evidence of a dose-response gradient, and the direction of plausible biases. The quality of the evidence was categorised as high, moderate, low, or very low. Web appendix 2 shows the relevant GRADE tables.
Figures 1 ⇓ and 2 ⇓ show the process by which the included studies were identified. We identified 7895 potential randomised trials from the electronic search and a further 10 studies through hand searches of relevant review articles and on recommendation from NUGAG panel members. Removing duplicates left 6634 articles, of which 6557 were assessed to be irrelevant. Abstracts and full text articles for the remaining 77 studies were judged as requiring full review and were reviewed by three independent reviewers. Of these remaining studies, 19 met the inclusion criteria for ad libitum studies 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 and 11 were identified for the comparative analysis of isoenergetic studies. 48 49 50 51 52 53 54 55 56 57 58 For cohort studies, we identified 9445 potential studies from the electronic search and an additional 10 studies through hand searches of relevant review articles. Of 69 studies selected for full review, 38 were considered to meet the inclusion criteria. 59 60 61 62 63 64 65 66 67 68 69 70 71 72 73 74 The 47 excluded randomised trials and 31 excluded cohort studies are described in web appendices 3 and 4.
Fig 1 PRISMA flow diagram for randomised controlled trials
- Download figure
- Open in new tab
- Download powerpoint
Fig 2 PRISMA flow diagram for cohort studies
Assessment of study quality
Risk of bias varied among the randomised trials (web figs 1 and 2, web appendix 5). Failure to conceal treatment allocation (almost impossible to achieve in dietary trials involving free living participants) was the major potential source of bias (performance bias). In many trials, it was unclear as to whether outcome measures had been assessed by observers unaware of treatment allocation (detection bias) and whether there had been selection bias. Three trials, in which there was evidence of differences between dropouts and completers, reported data only for those who completed the intervention. 28 34 39
Our analysis included 38 prospective studies lasting at least 12 months, and in which data relating to an association between sugars and a measure of adiposity could be extracted; none was excluded on the basis of study quality. Of these 38 studies, 15 used self reported estimates of adiposity outcomes 59 64 65 66 67 68 70 71 73 74 75 76 77 78 79 80 ; seven collected exposure data from questionnaires where the validity for assessing sugars intake was not stated or not assessed 60 61 67 79 81 82 ; 19 involved convenience sampling 59 61 62 67 71 73 78 83 84 85 86 87 88 89 90 91 92 93 ; and 18 provided estimates that were adjusted for total energy intake. 59 60 64 66 69 72 75 76 86 88 90 91 92 93 94 95 96 97 There was a lack of consistency in the covariates used to adjust analyses and a wide range of methods of assessing sugars exposures and adiposity outcomes, which made pooling studies difficult.
Effect of reducing dietary sugars on measures of body fatness in adults
Table 2 ⇓ describes the five studies identified for this analysis, 28 30 31 33 41 49 and figure 3 ⇓ shows the quantitative meta-analysis (forest plot). Reduction in dietary sugars intake was associated with significantly reduced weight (−0.80 kg (95% confidence interval −1.21 to −0.39); P<0.001) at the end of the intervention period by comparison with no reduction or an increase in sugars intake. The trials all involved a reduction in intake of sugars (classified as free sugars) in the intervention arm compared with the control arm. 28 31 33 39 41 Study durations ranged from 10 weeks to eight months. In four studies, participants were advised to limit sugar containing foods, 31 33 39 41 and in one study, participants were asked to substitute usual sugar rich foods with low sugar alternatives. 28 Three of the five trials reported data for completers only. 28 39 41 However, only two of these studies considered this to be a potential source of bias. 28 41 Exclusion of these two studies from the meta-analysis slightly attenuated the effect, although the effect estimate remained significant (−0.81 kg, −1.41 to −0.21). After excluding three studies 28 39 41 that had a high risk of bias for two or more validity criteria, the effect estimate was no longer significant although the difference in weight was similar (−0.81 kg, −1.69 to 0.07).
Characteristics of trials examining the effect of reducing intake of free sugars on measures of body fatness in adults
Fig 3 Effect of reducing intake of free sugars on measures of body fatness in adults. Pooled effects for difference in body weight (kg) shown for studies comparing reduced intakes (lower sugars) with usual or increased intakes (higher sugars). Overall effect shows increased body weight after intervention in the higher sugars groups. Data are expressed as weighted mean difference (95% confidence interval), using generic inverse variance models with random effects
Differences in sugar intakes between intervention and control groups ranged from less than 1% 33 to 14% of total energy intake. 39 Two studies achieved a difference in reported sugars intake of less than 5% of total energy intake at the end of the intervention. 28 33 Paineau and colleagues 33 reported a difference in sugars intake between groups of 2.2 g/day, and Gatenby and colleagues 28 reported a difference of about 3% of energy intake (15 g/day). Exclusion of these studies from the meta-analysis strengthened the overall effect of lowered sugar intakes on body weight change (−1.22 kg, 95% confidence interval −1.81 to −0.63). We saw no evidence of heterogeneity (I 2 =17%, P=0.3), and the test for overall effect showing an association between sugar reduction and increased weight loss was highly significant.
Effects of increasing dietary sugars on measures of body fatness in adults
Table 3 ⇓ describes the 10 studies identified for this analysis, and figure 4 ⇓ shows the quantitative meta-analysis (forest plot). 26 32 34 36 37 38 43 44 45 47 Because there was statistical evidence for significant heterogeneity among the studies (I 2 =82%, P<0.001), we used a random effects model to derive the pooled estimates. Increased intake in dietary sugars was associated with significantly greater weight (0.75 kg (95% confidence interval 0.30 to 1.19); P=0.001) at the end of the intervention period by comparison with no increase in sugars intake. The studies involved an increase in dietary sugars; mostly sugar sweetened beverages, in the intervention arm of the randomised trial. Only two studies lasted longer than eight weeks. 34 36 Subgroup analysis for these two longer term studies resulted in a significantly greater effect size (2.73 kg, 1.68 to 3.78) than the pooled effect for the shorter term studies (0.52 kg, 0.14 to 0.89). The difference between these subgroups was highly significant (P<0.001).
Characteristics of randomised trials examining the effect of increasing intake of free sugars on measures of body fatness in adults
Fig 4 Effect of increasing free sugars on measures of body fatness in adults. Pooled effects for difference in body weight (kg) shown for studies comparing increased intake (higher sugars) with usual intake (lower sugars). Overall effect shows increased body weight after intervention in the higher sugars groups. Data are expressed as weighted mean difference (95% confidence interval), using generic inverse variance models with random effects
One trial reported a higher rate of participant dropout in the high sugars group than in the low sugars group and presented results for only participants who completed the whole study. 37 Exclusion of this study from the meta-analysis increased the overall effect size slightly (0.83 kg, 95% confidence interval 0.31 to 1.35). The association also remained significant after excluding from the meta-analysis five studies 26 32 34 37 43 that had a high risk of bias for two or more validity criteria (0.96 kg, 0.06 to 1.85).
Isoenergetic exchanges of dietary sugars with other carbohydrates or other macronutrient sources
We identified 12 studies that involved isoenergetic exchange of dietary sugars with other macronutrients (table 4 ⇓ ). 48 49 50 51 52 53 54 55 56 57 58 Interventions ranged from two weeks to six months, and sugars were in the form of either sucrose or fructose used to sweeten foods or liquids. We saw no evidence of difference in weight change as a result of differences in sugars intakes when energy intakes were equivalent (0.04 kg (95% confidence interval −0.04 to 0.13); fig 5 ⇓ ).
Characteristics of trials comparing the effect on body weight change in adults of isocaloric diets high in free sugars with diets relatively low in free sugars
Fig 5 Isoenergetic exchanges of free sugars with other carbohydrates or other macronutrient sources. Pooled effects for difference in body weight (kg) for studies comparing isoenergetic exchange of free sugars (higher sugars) with other carbohydrates (lower sugars). Data are expressed as weighted mean difference (95% confidence interval), using generic inverse variance models with random effects
Findings of cohort studies
Table 5 ⇓ describes 16 cohort studies in adults that provided analyses of the relation between sugars exposures and measures of adiposity. 59 60 61 62 64 65 66 67 68 69 70 71 72 73 74 76 With a vote counting approach, 11 studies reported one or more significantly positive associations between a sugars exposure and a measure of adiposity, 59 60 61 62 64 65 68 69 70 71 73 74 and one study reported a significantly negative association. 73 Two studies reporting changes in intake of sugar sweetened beverages during follow-up showed a significantly greater increase in weight change among participants with the highest intake than in those with the lowest intake. 71 74 Web table 1 summarises pooled estimates for the relation between sugars intakes and various measures of adiposity from all other prospective studies in adults that met the inclusion criteria. Forest plots for these comparisons are provided in web figures 3-5 (web appendix 5).
Summary of prospective cohort studies examining association between free sugars exposures and adiposity in adults

Effects of reducing dietary sugars on measures of body fatness in children
Table 6 ⇓ describes the five intervention trials identified for this analysis, and figure 6 ⇓ shows the forest plot. 27 29 33 40 46 Interventions generally included advice to reduce sugar sweetened beverages and other foods containing (free) sugars. We saw no association between such advice to reduce intake of dietary sugars and change in standardised BMI or BMI z score in children (0.09, 95% confidence interval −0.14 to 0.32). The studies included in this meta-analysis involved advice to reduce the intake of sugar sweetened beverages alone, 27 29 40 or together with a further reduction in other sugar rich foods and an increase in dietary fibre. 33 46 Poor compliance with the intervention advice was reported in three of the five studies, 29 33 46 and the effect of the intervention was a reduction of 51 mL/day in another study. 40 Significant heterogeneity was observed and a random effects model was used for the meta-analysis. Excluding the study by Davis and colleagues, 46 which had a high risk of bias for two or more validity criteria, did not alter the effect estimate.
Fig 6 Effect of reducing free sugars on measures of body fatness in children. Pooled effects for standardised mean difference in body mass index for studies comparing advice to reduce intake of free sugars with no advice regarding free sugars. Data are expressed as weighted, standardised mean difference (95% confidence interval), using generic inverse variance models with random effects
Characteristics of intervention studies measuring the effect of advice to reduce intakes free sugars on change in BMI in children and adolescents
Effects of increasing dietary sugars on measures of body fatness in children
There were no randomised trials available in children, thus we used data from 21 cohort studies in children (reported in 22 articles) to assess the effect of increasing sugars intakes on body fatness (table 7 ⇓ ). Most studies related to intake of sugar sweetened beverages. A quantitative meta-analysis (fig 7 ⇓ ) was based on five cohort studies, with seven comparisons. These studies reported data for the odds of being overweight at follow-up in children consuming about one daily serving of sugar sweetened beverages at baseline compared with children consuming none or very little. 80 94 95 96 97 Comparison of the higher intakes with lower intakes suggested a significantly increased risk of being overweight associated with higher intakes (odds ratio 1.55, 95% confidence interval 1.32 to 1.82). We saw no evidence of heterogeneity, and all the studies reported a positive association. When assessing the 23 cohort studies in children using a “vote counting” approach, 15 reported a positive association between increased sugars intake and a measure of adiposity. 75 79 80 81 82 86 88 89 91 92 94 95 96 97 98 Fourteen of these 15 studies reported the sugars exposure as a sugar sweetened beverage. By contrast, only four studies reported a negative association, 87 90 93 98 of which two reported fruit juice as the sugars exposure. 90 98
Fig 7 Association between free sugars intakes and measures of body fatness in children. Pooled estimates for odd ratios for incident overweight or obesity in children consuming one or more servings of sugar sweetened beverages per day at baseline compared with children who consumed none or very little at baseline. Overall estimate shows higher odds of overweight or obesity at follow-up in those who consumed one or more servings of sugar sweetened beverages at baseline. Data are expressed as odds ratio (95% confidence interval), using generic inverse variance models with random effects
Summary of prospective cohort studies examining associations between free sugars exposures and adiposity in children
Web table 2 summarises pooled and unpooled estimates for the association between sugars intakes and measures of adiposity from all other prospective studies in children that met the inclusion criteria. Because of the wide variation in how the study effects were reported, it was not always possible to pool studies reporting similar outcomes, and there was no evidence of association between increased sugars and adiposity. Web figures 6 and 7 (web appendix 5) show forest plots.
Sensitivity analyses
The overall meta-regression of randomised trials examining the effect of sugars on adiposity in adults showed no evidence of a dose-response association between sugar as a percentage of total energy intake and body weight (0.02 kg (95% confidence interval −0.03 to 0.08); P=0.392). The difference in weight changes associated with differing intakes of sugars was unrelated to study design (crossover or parallel design trials; 0.30 kg (−0.44 to 1.05); P=0.393), study duration (0.01 kg per week (−0.02 to 0.05); P=0.460), or whether sugars intakes were reduced or increased in the intervention arm relative to the control arm (0.12 kg (−0.73 to 0.96); P=0.817).
Publication bias
The funnel plot of all 15 randomised ad libitum trials conducted in adults was asymmetrical and the Egger’s test for bias was significant (P=0.001), which suggested possible publication bias (fig 8 ⇓ ). The pooled effect size for all 15 trials was 0.78 kg (95% confidence interval 0.43 to 1.12), based on a random effects model which accounted for significant heterogeneity (I 2 =77%, P<0.001) seen between the relatively short term crossover trials with small variances and the longer term parallel trials with larger variances. Use of fixed effects models attenuated the overall effect (0.42 kg, 0.28 to 0.56), but it remained significant. Excluding the studies with the largest study variances 34 41 from the analysis had little effect (0.72, 0.37 to 1.06). Trim and fill analysis showed a somewhat attenuated but significant effect size (0.50, 0.18 to 0.21). Visual inspection of the funnel plot and the Egger’s test for bias (P=0.248) did not suggest publication bias among the isoenergetic trials.
Fig 8 Funnel plot of randomised ad libitum trials in adults
The meta-analyses based on controlled trials provide consistent evidence that increasing or decreasing intake of dietary sugars from current levels of intake is associated with corresponding changes in body weight in adults. Although some evidence of potential publication bias existed, this did not seem to have an important effect on the findings. Results from cohort studies were generally comparable with the trial findings. The reviewed studies largely related to the manipulation or observation of intake of sugars which, using current terminology, would be described as “free sugars.” Two six month trials, 99 100 published subsequent to the census date for this systematic review, involved different intakes of sugar sweetened beverages in adults. The trials also showed a trend towards increased body weight in participants with raised intake, but the difference between groups was not significant, perhaps owing to small number of participants.
Poor compliance with dietary advice could explain why the data from trials in children were equivocal. This was confirmed by two controlled trials published after our systematic review’s census date. 101 102 De Ruyter and colleagues 101 showed a smaller increase in BMI z score after 18 months among trial completers who were provided with sugar free, artificially sweetened beverages, compared with participants who received equal quantities of sugar sweetened beverages. Ebbeling and colleagues 102 showed the potential of an intervention designed to decrease the consumption of sugar sweetened beverages in overweight and obese adolescents. BMI and body weight were significantly reduced after one year in the intervention group compared with the control group. However, after a further year’s follow-up with no further intervention, the difference between the groups was no longer significant.
Cohort studies in children confirmed a link between intake of sugar sweetened beverages and the risk of becoming overweight, but showed no consistent associations between other measures of sugars intake and adiposity. Although comparison of groups with the highest versus lowest intakes in cohort studies was compatible with a recommendation to restrict intake to below 10% total energy, currently available data did not allow formal dose-response analysis.
Strengths and limitation
An important strength of this in depth review of the literature lay in the overall quality and consistency of the data, especially those derived from adult populations. Although the trials were published over a long timeframe and used different experimental approaches, the results were consistent. Evidence was derived principally from randomised trials, but data from cohort studies that compared higher and lower groups of intake were also confirmatory. Criteria from both GRADE 25 and the World Cancer Research Fund 103 for judging strength of evidence of association specify randomised controlled trials as the highest level of evidence, but evidence from another study type is recognised as providing important confirmation.
We found less consistent findings from the trials conducted in children, which can be attributed to several factors. These trials tended to last longer than adult trials, and where compliance was assessed, it was clear that adherence to dietary advice (typically advice to reduce sugar sweetened beverages) was poor. For example, in a trial by Davis and colleagues, 46 children receiving nutrition education to improve carbohydrate quality achieved a reduction in added sugars intake of only 8 g/day, compared with control children. However, in children (as in adults), comparison of the highest intakes with the lowest intakes (usually of sugar sweetened beverages) suggested that those participants consuming the largest quantities had a higher body weight or other measure of adiposity.
The limitations of these findings are those inherent to the primary research on which they are based, notably inadequacy of dietary intake data, and variation in the nature and quality of the dietary intervention. Most cohort studies and some trials reported effects largely or solely related to the consumption of sugar sweetened beverages. Most trials involved different levels of intake of sugar (sucrose) and other monosaccharides and disaccharides in the control and intervention arms. These compounds have been described as “free sugars,” as defined by WHO (all monosaccharides and disaccharides added to foods by the manufacturer, cook, or consumer, plus sugars naturally present in honey, syrups, and fruit juices). 14 We had originally intended to report separately on the effects of total sugars as well as the various subcategories of sugars, but presentation of data in the studies precluded such analyses.
Assessment of dietary intake of sugars, whether by some method of recall as used in the trials, or by food frequency questionnaires as in cohort studies, was associated with a considerable degree of measurement error even when using validated methods. This is probably one explanation why a dose-response effect could not be shown between change in dietary intake and magnitude of weight change. Nevertheless, even crude estimates of intake provided assistance in interpreting potentially inconsistent findings. The studies of long term intervention in children 27 29 33 40 46 and two studies of interventions reducing dietary sugars in adults 28 33 found little difference in intakes between intervention and control groups, and no meaningful change in weight.
The heterogeneity of the studies, especially in terms of the consequences of altering intake of sugars in ad libitum diets, resulted in difficulties in fully explaining the effects of different dietary changes. Nevertheless, the changes in weight observed in studies of adults provided some indication of what might be achieved by the implementation of a dietary guideline relating to sugar, and conversely what might occur if consumption continued to increase.
The potential problem of residual confounding to explain some or all of an effect is inherent to all cohort studies. However, the overall consistency of our findings, regardless of study type, is reassuring. The only potential major source of bias identified in the trials was that four trials in adults reported data for completers. These data could have overestimated the effect, but we saw no meaningful difference in the magnitude of the effect between these trials and the other studies. Both participants and researchers in many of the trials were not blinded to intervention allocation. Studies providing beverages as a means of manipulating sugars intakes were blinded, but blinding was clearly not possible in studies relying on the provision of dietary advice to manipulate sugars intake. However, we do not believe that a lack of blinding altered our findings substantially. Measurement of body weight did not involve judgment that was subject to bias.
Potential mechanisms
The most obvious mechanism by which increasing sugars might promote weight gain is by increasing energy consumption to an extent that exceeds energy output and distorts energy balance. For sugar sweetened beverages, it has been suggested that energy in liquid form could be less satiating than when derived from solid foods, resulting in increased consumption. 104 Solid foods containing sugars are typically (although not invariably) energy dense, and frequent and substantial consumption of energy dense foods is associated with excessive weight gain and other measures of excess adiposity. We observed that isoenergetic replacement of dietary sugars with other macronutrients resulted in no change in weight (fig 5). This finding strongly suggested that energy imbalance is a major determinant of the potential for dietary sugars to influence measures of body fatness. However, other less direct mechanisms independent of energy balance have been proposed.
Sugars (particularly table sugar, sucrose, and high fructose corn syrup) contribute to the intake of fructose, which in turn can, at least in some people, increase levels of uric acid and hyperinsulinaemia. 105 Hyperuricaemia has been identified as a potentially important and independent predictor of obesity and the metabolic syndrome. 2 Sugar sweetened beverages and other sources of dietary fructose have been suggested to promote the deposition of liver, skeletal, and visceral fat and an increase in serum lipids independently of an effect on body weight. 106 Although this issue is relevant to any overarching discussion regarding the health consequences of dietary sugars and the extent to which they should be restricted, it is beyond the scope of this review.
Results in the context of existing knowledge
Most of the relevant published studies, reviews, and meta-analyses related to the association between intake of sugar sweetened beverages and body weight, weight gain, or other measures of adiposity. Widely discrepant conclusions have emerged, ranging from strong or convincing evidence for an association 8 107 to evidence described as inconclusive or equivocal. 3 7 11 108 109 110 This variance is hardly surprising, owing to the poor compliance in most intervention trials, the insensitive instruments used for assessing dietary intakes in cohort studies, and that in such studies, intakes might have changed between initial dietary assessment and measurement of outcome. One meta-analysis combined data for adults and children. 11 We found no evidence for an association between intake and weight in children when considering the intervention trials, nor were the data sufficient to examine for a dose-response effect when considering β coefficients for the continuous association between baseline sugars exposure and adiposity outcome. Nevertheless, we were able to show a consistent effect when comparing groups with the highest intakes of sugars with those with the lowest intakes.
There have been fewer reviews and meta-analyses relating to sugars or sugar rather than sugar sweetened beverages. In a systematic review and meta-analysis, Sievenpiper and colleagues concluded that isoenergetic substitution of fructose for other carbohydrates was not associated with weight gain. 110 However, free fructose at high doses that provided excess calories modestly increased body weight to an extent probably due to the extra calories rather than any particular metabolic attributes of fructose. Dolan and colleagues 111 drew similar conclusions when reviewing studies in which fructose was fed at “normal levels of intake.” Van Baak and Astrup 3 and Ruxton 104 recently concluded that there was insufficient evidence to indicate that replacing sugars with other carbohydrates resulted in a reduction in body weight. However, by limiting analyses to ad libitum trials, and considering studies in adults and children separately, our systematic review showed a clear positive association between higher intake of sugars and body fatness in adults, and provided an explanation as to why the findings in children were less conclusive.
Conclusions
This series of meta-analyses provides evidence that intake of sugars is a determinant of body weight in free living people consuming ad libitum diets. The data suggest that the change in body fatness that occurs with modifying intake of sugars results from an alteration in energy balance rather than a physiological or metabolic consequence of monosaccharides or disaccharides. Owing to the multifactorial causes of obesity, it is unsurprising that the effect of reducing intake is relatively small. The extent to which population based advice to reduce sugars might reduce risk of obesity cannot be extrapolated from the present findings, because few data from the studies lasted longer than ten weeks. However, when considering the rapid weight gain that occurs after an increased intake of sugars, it seems reasonable to conclude that advice relating to sugars intake is a relevant component of a strategy to reduce the high risk of overweight and obesity in most countries.
What is already known on this topic
Excessive intakes of dietary sugars have been linked to obesity, and a higher risk of chronic diseases, but the link with obesity is tenuous
The most consistent association has been between a high intake of sugar sweetened beverages and the development of obesity
No upper safe limit of intake has been agreed universally, but WHO has suggested that intakes of free sugars should be less than 10% of the total energy intake
What this study adds
Among free living people, advice to reduce free sugars was associated with an average 0.80 kg reduction in weight; advice to increase intake was associated with a corresponding 0.75 kg increase
This parallel effect seems to be due to an altered energy intake; isoenergetic replacement of sugars with other carbohydrates did not result in any change in body weight
Evidence was less consistent in children than in adults
Cite this as: BMJ 2012;345:e7492
We thank Carolyn Summerbell and Bernard Venn for their help on the initial development of this research; Melissa Butt and Sarah Harvey, who contributed to the data search for the randomised controlled trials; Marcus Du, who contributed to the data search and extraction for the cohort studies; and the members of the WHO NUGAG Subgroup on Diet and Health for their contribution to this work.
WHO agreed to the publication of this systematic review in a scientific journal, because it serves as the background evidence review for updating WHO guidelines on total sugars intake and should therefore, be available widely.
Contributors: The questions for the review were discussed and developed by the WHO NUGAG Subgroup on Diet and Health in February 2010, and the protocol was approved by the NUGAG Subgroup on Diet and Health. LT and SM supervised study searches. LT, SM, and JIM assessed inclusion, extracted data, and assessed validity. LT did the meta-analyses. LT and JM wrote the manuscript. The NUGAG Subgroup on Diet and Health reviewed the first draft of the report and contributed to the GRADE assessment. All authors read and approved the final draft of the report.
Funding: The authors were supported by the University of Otago and the Riddet Institute, a New Zealand National Centre of Research Excellence. The research was supported by the University of Otago, Riddet Institute, and WHO. The authors undertook the submitted work for WHO for the purposes of updating WHO guidelines on sugars intake, and WHO provided some funding to the University of Otago towards the cost of carrying out the review.
Competing interests: All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: support from the University of Otago, Riddet Institute, and WHO; no other financial relationships with any organisations that might have an interest in the submitted work in the previous 3 years; and no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: Not required.
Data sharing: No additional data available.
This is an open-access article distributed under the terms of the Creative Commons Attribution Non-commercial License, which permits use, distribution, and reproduction in any medium, provided the original work is properly cited, the use is non commercial and is otherwise in compliance with the license. See: http://creativecommons.org/licenses/by-nc/2.0/ and http://creativecommons.org/licenses/by-nc/2.0/legalcode .
- ↵ Kiple KF, Ornelas KC. The Cambridge world history of food. Cambridge University Press, 2000.
- ↵ Johnson RJ, Segal MS, Sautin Y, Nakagawa T, Feig DI, Kang DH, et al. Potential role of sugar (fructose) in the epidemic of hypertension, obesity and the metabolic syndrome, diabetes, kidney disease, and cardiovascular disease. Am J Clin Nutr 2007 ; 86 : 899 -906. OpenUrl Abstract / FREE Full Text
- ↵ van Baak MA, Astrup A. Consumption of sugars and body weight. Obes Rev 2009 ; 10 (suppl 1): 9 -23. OpenUrl CrossRef PubMed
- ↵ Burt BA, Pai S. Sugar consumption and caries risk: a systematic review. J Dent Educ 2001 ; 65 : 1017 -23. OpenUrl Abstract
- ↵ Bristol JB, Emmett PM, Heaton KW, Williamson RC. Sugar, fat, and the risk of colorectal cancer. BMJ Clin Res Ed 1985 ; 291 : 1467 -70. OpenUrl Abstract / FREE Full Text
- ↵ Milich R, Wolraich M, Lindgren S. Sugar and hyperactivity: a critical review of empirical findings. Clin Psychol Rev 1986 ; 6 : 493 -513. OpenUrl CrossRef Web of Science
- ↵ Forshee RA, Anderson PA, Storey ML. Sugar-sweetened beverages and body mass index in children and adolescents: a meta-analysis [correction in Am J Clin Nutr 2009;89:441-2]. Am J Clin Nutr 2008 ; 87 : 1662 -71. OpenUrl Abstract / FREE Full Text
- ↵ Vartanian LR, Schwartz MB, Brownell KD. Effects of soft drink consumption on nutrition and health: a systematic review and meta-analysis. Am J Public Health 2007 ; 97 : 667 -75. OpenUrl CrossRef PubMed Web of Science
- ↵ Malik VS, Schulze MB, Hu FB. Intake of sugar-sweetened beverages and weight gain: a systematic review. Am J Clin Nutr 2006 ; 84 : 274 -88. OpenUrl Abstract / FREE Full Text
- ↵ Drewnowski A, Bellisle F. Liquid calories, sugar, and body weight. Am J Clin Nutr 2007 ; 85 : 651 -61. OpenUrl Abstract / FREE Full Text
- ↵ Mattes RD, Shikany JM, Kaiser KA, Allison DB. Nutritively sweetened beverage consumption and body weight: a systematic review and meta-analysis of randomized experiments. Obes Rev 2011 ; 12 : 346 -65. OpenUrl CrossRef PubMed
- ↵ Gibson S. Sugar-sweetened soft drinks and obesity: a systematic review of the evidence from observational studies and interventions. Nutr Res Rev 2008 ; 21 : 134 -47. OpenUrl CrossRef PubMed
- ↵ Mann J, Cummings JH, Englyst HN, Key T, Liu S, Riccardi G, et al. FAO/WHO Scientific Update on carbohydrates in human nutrition: conclusions. Eur J Clin Nutr 2007 ; 61 : S132 -7. OpenUrl CrossRef PubMed Web of Science
- ↵ Food and Agricultural Organization of the United Nations/WHO. Carbohydrates in human nutrition. Report of a Joint FAO/WHO Expert Consultation. FAO Food Nutr Pap 1998 ; 66 : 1 -140. OpenUrl PubMed
- ↵ WHO. Diet, nutrition and the prevention of chronic diseases. World Health Organ Tech Rep Ser 2003 ; 916 : i -viii,1-149,backcover. OpenUrl PubMed
- ↵ WHO. First meeting of the WHO Nutrition Guidance Expert Advisory Group (NUGAG). 2012. www.who.int/nutrition/topics/NUGAG_meeting/en/index.html .
- ↵ WHO. WHO handbook for guideline development. 2010. www.who.int/hiv/topics/mtct/grc_handbook_mar2010_1.pdf .
- ↵ Higgins JPT, Green S. Cochrane Handbook for systematic reviews of interventions version 5.0.2. www.cochrane-handbook.org .
- ↵ Johnson RK, Appel LJ, Brands M, Howard BV, Lefevre M, Lustig RH, et al. Dietary sugars intake and cardiovascular health: a scientific statement from the American Heart Association. Circulation 2009 ; 120 : 1011 -20. OpenUrl Abstract / FREE Full Text
- ↵ Cochrane Collaboration. Review Manager (RevMan). Version 5.1. Nordic Cochrane Centre, 2011.
- ↵ Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997 ; 315 : 629 -34. OpenUrl Abstract / FREE Full Text
- ↵ Sterne JA, Sutton AJ, Ioannidis JP, Terrin N, Jones DR, Lau J, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 2011 ; 343 : d4002 . OpenUrl FREE Full Text
- ↵ Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000 ; 56 : 455 -63. OpenUrl CrossRef PubMed Web of Science
- ↵ United States Department of Agriculture. USDA National Nutrient Database for standard reference, release 24. 2012. www.ars.usda.gov/nutrientdata .
- ↵ Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008 ; 336 : 924 -6. OpenUrl FREE Full Text
- ↵ Brynes AE, Edwards CM, Ghatei MA, Dornhorst A, Morgan LM, Bloom SR, et al. A randomised four-intervention crossover study investigating the effect of carbohydrates on daytime profiles of insulin, glucose, non-esterified fatty acids and triacylglycerols in middle-aged men. Br J Nutr 2003 ; 89 : 207 -18. OpenUrl CrossRef PubMed Web of Science
- ↵ Ebbeling CB, Feldman HA, Osganian SK, Chomitz VR, Ellenbogen SJ, Ludwig DS. Effects of decreasing sugar-sweetened beverage consumption on body weight in adolescents: A randomized, controlled pilot study. Pediatrics 2006 ; 117 : 673 -80. OpenUrl Abstract / FREE Full Text
- ↵ Gatenby SJ, Aaron JI, Jack VA, Mela DJ. Extended use of foods modified in fat and sugar content: nutritional implications in a free-living female population. Am J Clin Nutr 1997 ; 65 : 1867 -73. OpenUrl Abstract / FREE Full Text
- ↵ James J, Thomas P, Cavan D, Kerr D. Preventing childhood obesity by reducing consumption of carbonated drinks: cluster randomised controlled trial. BMJ 2004 ; 328 : 1237 . OpenUrl Abstract / FREE Full Text
- ↵ Mann JI, Hendricks DA, Truswell AS, Manning E. Effects on serum-lipids in normal men of reducing dietary sucrose or starch for five months. Lancet 1970 ; 1 : 870 -2. OpenUrl PubMed Web of Science
- ↵ Mann JI, Truswell AS, Manning EB. Effects on serum lipids of reducing dietary sucrose or starch for 22 weeks in normal men. S Afr Med J 1972 ; 46 : 827 -34. OpenUrl PubMed
- ↵ Marckmann P, Raben A, Astrup A. Ad libitum intake of low-fat diets rich in either starchy foods or sucrose: effects on blood lipids, factor VII coagulant activity, and fibrinogen. Metabolism 2000 ; 49 : 731 -5. OpenUrl CrossRef PubMed Web of Science
- ↵ Paineau DL, Beaufils F, Boulier A, Cassuto DA, Chwalow J, Combris P, et al. Family dietary coaching to improve nutritional intakes and body weight control: a randomized controlled trial. Arch Pediatr Adolesc Med 2008 ; 162 : 34 -43. OpenUrl CrossRef PubMed Web of Science
- ↵ Poppitt SD, Keogh GF, Prentice AM, Williams DEM, Sonnemans HMW, Valk EEJ, et al. Long-term effects of ad libitum low-fat, high-carbohydrate diets on body weight and serum lipids in overweight subjects with metabolic syndrome. Am J Clin Nutr 2002 ; 75 : 11 -20. OpenUrl Abstract / FREE Full Text
- ↵ Raben A, Macdonald I, Astrup A. Replacement of dietary fat by sucrose or starch: effects on 14 d ad libitum energy intake, energy expenditure and body weight in formerly obese and never-obese subjects. Int J Obes Relat Metab Disord 1997 ; 21 : 846 -59. OpenUrl CrossRef PubMed Web of Science
- ↵ Raben A, Vasilaras TH, Moller AC, Astrup A. Sucrose compared with artificial sweeteners: different effects on ad libitum food intake and body weight after 10 wk of supplementation in overweight subjects. Am J Clin Nutr 2002 ; 76 : 721 -9. OpenUrl Abstract / FREE Full Text
- ↵ Reid M, Hammersley R, Duffy M. Effects of sucrose drinks on macronutrient intake, body weight, and mood state in overweight women over 4 weeks. Appetite 2010 ; 55 : 130 -6. OpenUrl CrossRef PubMed Web of Science
- ↵ Reid M, Hammersley R, Hill AJ, Skidmore P. Long-term dietary compensation for added sugar: effects of supplementary sucrose drinks over a 4-week period. Br J Nutr 2007 ; 97 : 193 -203. OpenUrl CrossRef PubMed
- ↵ Saris WHM, Astrup A, Prentice AM, Zunft HJF, Formiguera X, Verboeket-van de Venne WPHG, et al. Randomized controlled trial of changes in dietary carbohydrate/fat ratio and simple vs complex carbohydrates on body weight and blood lipids: the CARMEN study. Int J Obes 2000 ; 24 : 1310 -8. OpenUrl CrossRef PubMed Web of Science
- ↵ Sichieri R, Trotte AP, de Souza RA, Veiga GV. School randomised trial on prevention of excessive weight gain by discouraging students from drinking sodas. Public Health Nutr 2009 ; 12 : 197 -202. OpenUrl CrossRef PubMed Web of Science
- ↵ Smith JB, Niven BE, Mann JI. The effect of reduced extrinsic sucrose intake on plasma triglyceride levels. Eur J Clin Nutr 1996 ; 50 : 498 -504. OpenUrl PubMed Web of Science
- ↵ Sorensen LB, Raben A, Stender S, Astrup A. Effect of sucrose on inflammatory markers in overweight humans. Am J Clin Nutr 2005 ; 82 : 421 -7. OpenUrl Abstract / FREE Full Text
- ↵ Szanto S, Yudkin J. The effect of dietary sucrose on blood lipids, serum insulin, platelet adhesiveness and body weight in human volunteers. Postgrad Med J 1969 ; 45 : 602 -7. OpenUrl Abstract / FREE Full Text
- ↵ Tordoff M, Alleva A. Effect of drinking soda sweetened with aspartame or high-fructose corn syrup on food intake and body weight. Am J Clin Nutr 1990 ; 51 : 963 -9. OpenUrl Abstract / FREE Full Text
- ↵ Werner D, Emmett PM, Heaton KW. Effects of dietary sucrose on factors influencing cholesterol gall stone formation. Gut 1984 ; 25 : 269 -74. OpenUrl Abstract / FREE Full Text
- ↵ Davis JN, Kelly LA, Lane CJ, Ventura EE, Byrd-Williams CE, Alexandar KA, et al. Randomized control trial to improve adiposity and insulin resistance in overweight Latino adolescents. Obesity 2009 ; 17 : 1542 -8. OpenUrl CrossRef PubMed Web of Science
- ↵ Aeberli I, Gerber PA, Hochuli M, Kohler S, Haile SR, Gouni-Berthold I, et al. Low to moderate sugar-sweetened beverage consumption impairs glucose and lipid metabolism and promotes inflammation in healthy young men: a randomized controlled trial. Am J Clin Nutr 2011 ; 94 : 479 -85. OpenUrl Abstract / FREE Full Text
- ↵ Bantle JP, Swanson JE, Thomas W, Laine DC. Metabolic effects of dietary fructose in diabetic subjects. Diabetes Care 1992 ; 15 : 1468 -76. OpenUrl Abstract / FREE Full Text
- ↵ Bantle JP, Swanson JE, Thomas W, Laine DC. Metabolic effects of dietary sucrose in type II diabetic subjects. Diabetes Care 1993 ; 16 : 1301 -5. OpenUrl Abstract / FREE Full Text
- ↵ Grigoresco C, Rizkalla SW, Halfon P, Bornet F, Fontvieille AM, Bros M, et al. Lack of detectable deleterious effects on metabolic control of daily fructose ingestion for 2 mo in NIDDM patients. Diabetes Care 1988 ; 11 : 546 -50. OpenUrl Abstract / FREE Full Text
- ↵ Koivisto VA, Yki-Jarvinen H. Fructose and insulin sensitivity in patients with type 2 diabetes. J Intern Med 1993 ; 233 : 145 -53. OpenUrl CrossRef PubMed
- ↵ Malerbi DA, Paiva ES, Duarte AL, Wajchenberg BL. Metabolic effects of dietary sucrose and fructose in type II diabetic subjects. Diabetes Care 1996 ; 19 : 1249 -56. OpenUrl Abstract / FREE Full Text
- ↵ Mann JI, Truswell AS. Effects of isocaloric exchange of dietary sucrose and starch on fasting serum lipids, postprandial insulin secretion and alimentary lipaemia in human subjects. Br J Nutr 1972 ; 27 : 395 -405. OpenUrl CrossRef PubMed Web of Science
- ↵ Mann JI, Truswell AS. Sucrose-free diet and serum-lipid levels. Lancet 1973 ; 2 : 153 -4. OpenUrl PubMed
- ↵ Osei K, Bossetti B. Dietary fructose as a natural sweetener in poorly controlled type 2 diabetes: a 12-month crossover study of effects on glucose, lipoprotein and apolipoprotein metabolism. Diabet Med 1989 ; 6 : 506 -11. OpenUrl CrossRef PubMed
- ↵ Peterson DB, Lambert J, Gerring S, Darling P, Carter RD, Jelfs R, et al. Sucrose in the diet of diabetic patients--just another carbohydrate? Diabetologia 1986 ; 29 : 216 -20. OpenUrl CrossRef PubMed Web of Science
- ↵ Santacroce G, Forlani G, Giangiulio S, Galuppi V, Pagani M, Vannini P. Long-term effects of eating sucrose on metabolic control of type 1 (insulin-dependent) diabetic outpatients. Acta Diabetol Lat 1990 ; 27 : 365 -70. OpenUrl CrossRef PubMed Web of Science
- ↵ Swanson JE, Laine DC, Thomas W, Bantle JP. Metabolic effects of dietary fructose in healthy subjects. Am J Clin Nutr 1992 ; 55 : 851 -6. OpenUrl Abstract / FREE Full Text
- ↵ Bes-Rastrollo M, Sanchez-Villegas A, Basterra-Gortari FJ, Nunez-Cordoba JM, Toledo E, Serrano-Martinez M. Prospective study of self-reported usual snacking and weight gain in a Mediterranean cohort: the SUN project. Clin Nutr 2010 ; 29 : 323 -30. OpenUrl CrossRef PubMed
- ↵ Dhingra R, Sullivan L, Jacques PF, Wang TJ, Fox CS, Meigs JB, et al. Soft drink consumption and risk of developing cardiometabolic risk factors and the metabolic syndrome in middle-aged adults in the community. Circulation 2007 ; 116 : 480 -8. OpenUrl Abstract / FREE Full Text
- ↵ Drapeau V, Despres JP, Bouchard C, Allard L, Fournier G, Leblanc C, et al. Modifications in food-group consumption are related to long-term body-weight changes. Am J Clin Nutr 2004 ; 80 : 29 -37. OpenUrl Abstract / FREE Full Text
- ↵ French SA, Jeffery RW, Forster JL, McGovern PG, Kelder SH, Baxter JE. Predictors of weight change over two years among a population of working adults: the Healthy Worker Project. Int J Obes Relat Metab Disord 1994 ; 18 : 145 -54. OpenUrl PubMed Web of Science
- ↵ Halkjaer J, Sorensen TI, Tjonneland A, Togo P, Holst C, Heitmann BL. Food and drinking patterns as predictors of 6-year BMI-adjusted changes in waist circumference. Br J Nutr 2004 ; 92 : 735 -48. OpenUrl CrossRef PubMed
- ↵ Halkjaer J, Tjonneland A, Overvad K, Sorensen TI. Dietary predictors of 5-year changes in waist circumference. J Am Diet Assoc 2009 ; 109 : 1356 -66. OpenUrl CrossRef PubMed
- ↵ Halkjaer J, Tjonneland A, Thomsen BL, Overvad K, Sorensen TI. Intake of macronutrients as predictors of 5-y changes in waist circumference. Am J Clin Nutr 2006 ; 84 : 789 -97. OpenUrl Abstract / FREE Full Text
- ↵ Hendriksen MA, Boer JM, Du H, Feskens EJ, van der AD. No consistent association between consumption of energy-dense snack foods and annual weight and waist circumference changes in Dutch adults. Am J Clin Nutr 2011 ; 94 : 19 -25. OpenUrl Abstract / FREE Full Text
- ↵ Kvaavik E, Andersen LF, Klepp KI. The stability of soft drinks intake from adolescence to adult age and the association between long-term consumption of soft drinks and lifestyle factors and body weight. Public Health Nutr 2005 ; 8 : 149 -57. OpenUrl CrossRef PubMed Web of Science
- ↵ Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB. Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med 2011 ; 364 : 2392 -404. OpenUrl CrossRef PubMed Web of Science
- ↵ Nooyens AC, Visscher TL, Schuit AJ, van Rossum CT, Verschuren WM, van Mechelen W, et al. Effects of retirement on lifestyle in relation to changes in weight and waist circumference in Dutch men: a prospective study. Public Health Nutr 2005 ; 8 : 1266 -74. OpenUrl CrossRef PubMed Web of Science
- ↵ Odegaard AO, Koh WP, Arakawa K, Yu MC, Pereira MA. Soft drink and juice consumption and risk of physician-diagnosed incident type 2 diabetes: the Singapore Chinese Health Study. Am J Epidemiol 2010 ; 171 : 701 -8. OpenUrl Abstract / FREE Full Text
- ↵ Palmer JR, Boggs DA, Krishnan S, Hu FB, Singer M, Rosenberg L, et al. Sugar-sweetened beverages and incidence of type 2 diabetes mellitus in African American women. Arch Intern Med 2008 ; 168 : 1487 -92. OpenUrl CrossRef PubMed Web of Science
- ↵ Parker DR, Gonzalez S, Derby CA, Gans KM, Lasater TM, Carleton RA. Dietary factors in relation to weight change among men and women from two southeastern New England communities. Int J Obes Relat Metab Disord 1997 ; 21 : 103 -9. OpenUrl CrossRef PubMed Web of Science
- ↵ Schulz M, Kroke A, Liese AD, Hoffmann K, Bergmann MM, Boeing H. Food groups as predictors for short-term weight changes in men and women of the EPIC-Potsdam cohort. J Nutr 2002 ; 132 : 1335 -40. OpenUrl Abstract / FREE Full Text
- ↵ Schulze MB, Manson JE, Ludwig DS, Colditz GA, Stampfer MJ, Willett WC, et al. Sugar-sweetened beverages, weight gain, and incidence of type 2 diabetes in young and middle-aged women. JAMA 2004 ; 292 : 927 -34. OpenUrl CrossRef PubMed Web of Science
- ↵ Berkey CS, Rockett HR, Field AE, Gillman MW, Colditz GA. Sugar-added beverages and adolescent weight change. Obes Res 2004 ; 12 : 778 -88. OpenUrl CrossRef PubMed Web of Science
- ↵ Colditz GA, Willett WC, Stampfer MJ, London SJ, Segal MR, Speizer FE. Patterns of weight change and their relation to diet in a cohort of healthy women. Am J Clin Nutr 1990 ; 51 : 1100 -5. OpenUrl Abstract / FREE Full Text
- ↵ Haerens L, Vereecken C, Maes L, De Bourdeaudhuij I. Relationship of physical activity and dietary habits with body mass index in the transition from childhood to adolescence: a 4-year longitudinal study. Public Health Nutr 2010 ; 13 : 1722 -8. OpenUrl CrossRef PubMed Web of Science
- ↵ Vanselow MS, Pereira MA, Neumark-Sztainer D, Raatz SK. Adolescent beverage habits and changes in weight over time: findings from Project EAT. Am J Clin Nutr 2009 ; 90 : 1489 -95. Epub 2009/10/30. OpenUrl Abstract / FREE Full Text
- ↵ Viner RM, Cole TJ. Who changes body mass between adolescence and adulthood? Factors predicting change in BMI between 16 year and 30 years in the 1970 British Birth Cohort. Int J Obes 2006 ; 30 : 1368 -74. OpenUrl CrossRef PubMed Web of Science
- ↵ Weijs PJ, Kool LM, van Baar NM, van der Zee SC. High beverage sugar as well as high animal protein intake at infancy may increase overweight risk at 8 years: a prospective longitudinal pilot study. Nutr J 2011 ; 10 : 95 . OpenUrl CrossRef PubMed
- ↵ Faith MS, Dennison BA, Edmunds LS, Stratton HH. Fruit juice intake predicts increased adiposity gain in children from low-income families: weight status-by-environment interaction. Pediatrics 2006 ; 118 : 2066 -75. OpenUrl Abstract / FREE Full Text
- ↵ Nissinen K, Mikkila V, Mannisto S, Lahti-Koski M, Rasanen L, Viikari J, et al. Sweets and sugar-sweetened soft drink intake in childhood in relation to adult BMI and overweight. The Cardiovascular Risk in Young Finns Study. Public Health Nutr 2009 ; 12 : 2018 -26. OpenUrl CrossRef PubMed Web of Science
- ↵ Blum JW, Jacobsen DJ, Donnelly JE. Beverage consumption patterns in elementary school aged children across a two-year period. J Am Coll Nutr 2005 ; 24 : 93 -8. OpenUrl CrossRef PubMed Web of Science
- ↵ Butte NF, Cai G, Cole SA, Wilson TA, Fisher JO, Zakeri IF, et al. Metabolic and behavioral predictors of weight gain in Hispanic children: the Viva la Familia Study. Am J Clin Nutr 2007 ; 85 : 1478 -85. OpenUrl Abstract / FREE Full Text
- ↵ Buyken AE, Cheng G, Gunther AL, Liese AD, Remer T, Karaolis-Danckert N. Relation of dietary glycemic index, glycemic load, added sugar intake, or fiber intake to the development of body composition between ages 2 and 7 y. Am J Clin Nutr 2008 ; 88 : 755 -62. OpenUrl Abstract / FREE Full Text
- ↵ Fiorito LM, Marini M, Francis LA, Smiciklas-Wright H, Birch LL. Beverage intake of girls at age 5 y predicts adiposity and weight status in childhood and adolescence. Am J Clin Nutr 2009 ; 90 : 935 -42. OpenUrl Abstract / FREE Full Text
- ↵ Herbst A, Diethelm K, Cheng G, Alexy U, Icks A, Buyken AE. Direction of associations between added sugar intake in early childhood and body mass index at age 7 years may depend on intake levels. J Nutr 2011 ; 141 : 1348 -54. OpenUrl Abstract / FREE Full Text
- ↵ Libuda L, Alexy L, Sichert-Hellert W, Stehle P, Karaolis-Danckert N, Buyken AE, et al. Pattern of beverage consumption and long-term association with body-weight status in German adolescents—results from the DONALD study. Brit J Nutr 2008 ; 99 : 13970 -9. OpenUrl
- ↵ Phillips SM, Bandini LG, Naumova EN, Cyr H, Colclough S, Dietz WH, et al. Energy-dense snack food intake in adolescence: longitudinal relationship to weight and fatness. Obes Res 2004 ; 12 : 461 -72. OpenUrl CrossRef PubMed Web of Science
- ↵ Skinner JD, Carruth BR. A longitudinal study of children’s juice intake and growth: the juice controversy revisited. J Am Diet Assoc 2001 ; 101 : 432 -7. OpenUrl CrossRef PubMed Web of Science
- ↵ Stoof SP, Twisk JW, Olthof MR. Is the intake of sugar-containing beverages during adolescence related to adult weight status? Public Health Nutr 2011 :1-6.
- ↵ Striegel-Moore RH, Thompson D, Affenito SG, Franko DL, Obarzanek E, Barton BA, et al. Correlates of beverage intake in adolescent girls: the National Heart, Lung, and Blood Institute Growth and Health Study. J Pediatr 2006 ; 148 : 183 -7. OpenUrl CrossRef PubMed Web of Science
- ↵ Williams CL, Strobino BA. Childhood diet, overweight, and CVD risk factors: the Healthy Start project. Prev Cardiol 2008 ; 11 : 11 -20. OpenUrl CrossRef PubMed
- ↵ Dubois L, Farmer A, Girard M, Peterson K. Regular sugar-sweetened beverage consumption between meals increases risk of overweight among preschool-aged children. J Am Diet Assoc 2007 ; 107 : 924 -34; discussion 34-5. OpenUrl CrossRef PubMed
- ↵ Ludwig DS, Peterson KE, Gortmaker SL. Relation between consumption of sugar-sweetened drinks and childhood obesity: a prospective, observational analysis. Lancet 2001 ; 357 : 505 -8. OpenUrl CrossRef PubMed Web of Science
- ↵ Welsh JA, Cogswell ME, Rogers S, Rockett H, Mei Z, Grummer-Strawn LM. Overweight among low-income preschool children associated with the consumption of sweet drinks: Missouri, 1999-2002. Pediatrics 2005 ; 115 : e223 -9. OpenUrl Abstract / FREE Full Text
- ↵ Lim S, Zoellner JM, Lee JM, Burt BA, Sandretto AM, Sohn W, et al. Obesity and sugar-sweetened beverages in African-American preschool children: a longitudinal study. Obesity (Silver Spring) 2009 ; 17 : 1262 -8. OpenUrl PubMed
- ↵ Johnson L, Mander AP, Jones LR, Emmett PM, Jebb SA. Is sugar-sweetened beverage consumption associated with increased fatness in children? Nutrition 2007 ; 23 : 557 -63. OpenUrl CrossRef PubMed Web of Science
- ↵ Maersk M, Belza A, Stodkilde-Jorgensen H, Ringgaard S, Chabanova E, Thomsen H, et al. Sucrose-sweetened beverages increase fat storage in the liver, muscle, and visceral fat depot: a 6-mo randomized intervention study. Am J Clin Nutr. 2012;95(2):283-9. Epub 2011/12/30.
- ↵ Tate DF, Turner-McGrievy G, Lyons E, Stevens J, Erickson K, Polzien K, et al. Replacing caloric beverages with water or diet beverages for weight loss in adults: main results of the Choose Healthy Options Consciously Everyday (CHOICE) randomized clinical trial. Am J Clin Nutr. 2012;95(3):555-63. Epub 2012/02/04.
- ↵ de Ruyter JC, Olthof MR, Seidell JC, Katan MB. A trial of sugar-free or sugar-sweetened beverages and body weight in children. N Engl J Med. 2012;367(15):1397-406. Epub 2012/09/25.
- ↵ Ebbeling CB, Feldman HA, Chomitz VR, Antonelli TA, Gortmaker SL, Osganian SK, et al. A randomized trial of sugar-sweetened beverages and adolescent body weight. N Engl J Med. 2012;367(15):1407-16. Epub 2012/09/25.
- ↵ World Cancer Research Fund/American Institute for Cancer Research. Food, nutrition, physical activity, and the prevention of cancer: a global perspective. AICR, 2007.
- ↵ DiMeglio DP, Mattes RD. Liquid versus solid carbohydrate: effects on food intake and body weight. Int J Obes Relat Metab Disord 2000 ; 24 : 794 -800. OpenUrl CrossRef PubMed Web of Science
- ↵ Johnson RJ, Perez-Pozo SE, Sautin YY, Manitius J, Sanchez-Lozada LG, Feig DI, et al. Hypothesis: could excessive fructose intake and uric acid cause type 2 diabetes? Endocr Rev 2009 ; 30 : 96 -116. OpenUrl CrossRef PubMed Web of Science
- ↵ Silbernagel G, Machann J, Unmuth S, Schick F, Stefan N, Haring HU, et al. Effects of 4-week very-high-fructose/glucose diets on insulin sensitivity, visceral fat and intrahepatic lipids: an exploratory trial. Br J Nutr 2011 ; 106 : 79 -86. OpenUrl CrossRef PubMed
- ↵ Hu FB, Malik VS, Schulze MB. Intake of sugar-sweetened beverages and weight gain: a systematic review. Am J Clin Nutr 2006 ; 84 : 274 -88. OpenUrl Abstract / FREE Full Text
- ↵ Ruxton CH, Gardner EJ, McNulty HM, Ruxton CHS. Is sugar consumption detrimental to health? A review of the evidence 1995-2006. Crit Rev Food Sci Nutr 2010 ; 50 : 1 -19. OpenUrl CrossRef PubMed
- ↵ Livesey G, Taylor R. Fructose consumption and consequences for glycation, plasma triacylglycerol, and body weight: meta-analyses and meta-regression models of intervention studies; but reports on isocaloric comparisons. Am J Clin Nutr 2008 ; 88 : 1419 -37. OpenUrl Abstract / FREE Full Text
- ↵ Sievenpiper JL, de Souza RJ, Mirrahimi A, Yu ME, Carleton AJ, Beyene J, et al. Effect of fructose on body weight in controlled feeding trials: a systematic review and meta-analysis. Ann Intern Med 2012 ; 156 : 291 -304. OpenUrl CrossRef PubMed Web of Science
- ↵ Dolan LC, Potter SM, Burdock GA. Evidence-based review on the effect of normal dietary consumption of fructose on development of hyperlipidemia and obesity in healthy, normal weight individuals. Crit Rev Food Sci Nutr 2010 ; 50 : 53 -84. OpenUrl CrossRef PubMed
- Get new issue alerts Get alerts
Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
Study on body composition and its correlation with obesity
A cohort study in 5121 chinese han participants.
Editor(s): Tarantino., Giovanni
a Department of Cardiothoracic Surgery, the Second Xiangya Hospital of Central South University, Changsha
b Central South University Xiangya School of Medicine Affiliate Haikou Hospital, Haikou, Hainan
c Key Laboratory of Resource Biology and Biotechnology in Western China (Northwest University), Ministry of Education, Northwest University, Xi’an, Shaanxi, China.
Correspondence: Yifeng Yang, #139 Renmin Middle Road, Furong District, Changsha 410011, Hunan, China (e-mail: [email protected] ).
Abbreviations: BFP = body fat percentage, BIA = bioelectrical impedance analysis, BMI = body mass index, VFA = visceral fat area, WC = waist circumference, WHR = waist-hip ratio of fat.
This work is supported by Hainan Natural Science Foundation Project (No. 20168318).
The authors have no conflicts of interest to disclose.
This is an open access article distributed under the terms of the Creative Commons Attribution-Non Commercial-No Derivatives License 4.0 (CCBY-NC-ND), where it is permissible to download and share the work provided it is properly cited. The work cannot be changed in any way or used commercially without permission from the journal. http://creativecommons.org/licenses/by-nc-nd/4.0
Received November 10, 2017
Accepted April 23, 2018
Rare reports can be found about sex- and age-specific body composition survey among Chinese population. The aim of this study is to explore the change of body composition with aging in Chinese males and females respectively.
The present cross-sectional study was carried out in Central South University Xiangya School of Medicine Affiliate Haikou Hospital, on a random sample consisting of 5121 participants. Inbody720 body composition analyzer was used to detect the human body composition. Data collection was based on the assessment of anthropometric body composition measurements done with the help of bioelectric impedance. And the data were analyzed with SPSS19.0.
We selected 5121 participants, 3276 males and 1845 females. A significant trend ( P < 0 .05) for all anthropometric indices was observed with age for both genders. Body fat in men and women were 18.33 kg and 19.82 kg, respectively. Body fat percentage in men and women were 25.74% and 34.01%, respectively. Visceral fat area in men and women were 91.98 cm 2 and 77 cm 2 , respectively And, with the increase of age, body fat, body fat percentages and visceral fat area also increased, both in men and in women. Meanwhile, with the increase of BMI, the body fat, body fat percentages, and visceral fat area also increased, both in men and in women.
Significant trends were observed for body fat, body fat percentages and visceral fat area for both genders with age and both genders with BMI. Focusing on obesity-related lifestyle and prevent weight gain.
1 Introduction
At present, obesity is well recognized as one of the major public health issues worldwide. Prior to the 1980s, the prevalence of obesity has been very stable, but has since increased dramatically throughout the world. [1] According to the 2014 World Health Organization (WHO), a rough estimate of 600 million obese adults worldwide. A Chinese nutrition survey shows that the prevalence of overweight and obesity was 19.2% and 15.0%, respectively. [2] Obesity is a serious problem because of the increasing possibility of a wide range of health consequences, including hypertension, insulin insensitivity, diabetes mellitus, cardiovascular disease, and distinct types of cancers. [3] The cost of medical care for obese patients is 30% higher than that of the normal weight peers. [4]
Human body composition is one of the branches of human biology, mainly to study the change rule of the number of body composition in human body, the influence of various factors in vivo and in vitro on the quantitative relationship between components, as well as in vivo determination of human components. [5] Body composition measurements not only indicate systemic nutritional status and health status, but also provide valuable information for the diagnosis and treatment of various diseases, whose quality and distribution are closely related to the health status of people at all ages. [6] The human body consists of 4 components: fat, protein, water and inorganic salts, the proportion of its composition is an important measure of physical health standards, the proportion of dysplasia is the root cause of the development of many diseases, to maintain the proportion of body composition is normal to achieve body composition balance, and maintain the health status of a basic condition, [7,8] at the same time, its composition to a certain extent, also reflects the gender, age, geographical, genetic, growth and development, nutrition, socioeconomic level, and disease and other factors.
Obesity in Saudi Arabia is a major public health concern, which is one of the fastest growing countries in the world. Azzeh and his colleague [9] found that along with the increase of age, body mass index, waist circumference, body fat, visceral fat and muscle mass also increase, whether in men or women. Mott et al [10] reported that at the age of <70 years old, with the increase of age, the amount of body fat mass also increased in 4 ethnic groups (Asian, Black, Puerto Rican, White); when the age was >70, the body fat mass decreased slightly. In the Xinjiang region of China, Liu et al [11] analysis the body composition characteristics in different nationalities in Urumqi overweight obesity and analysis the component change trend, the results shown that among overweight people, Han ethnicity males, and Uighur men had statistically significant differences in visceral fat are. In the obesity group, Uygur adults had a significantly difference in body fat percentage (BFP), waist-hip ratio of fat (WHR), and visceral fat area (VFA) than that in Han men and women. So, the body composition exist racial differences and regional differences.
Therefore, with the increase of age, systematic assessment of the changes in human body components is important for human health and nutritional status. Therefore, the main purpose of this study is to explore the relationship between human body composition and age and obesity in Hainan population.
2 Materials and methods
All subjects declared their written informed consent and were familiar with the aims, methods and risks of participating in the study in accordance with the Helsinki Declaration and rules of Good Clinical Practice, as the study was approved by the Ethics Committee of the Central South University Xiangya School of Medicine Affiliate Haikou Hospital. The ethics number for the study is 2015-039.
We recruited 5121 participants in physical examination center of Central South University Xiangya School of Medicine Affiliate Haikou Hospital from December 2015 to April 2017, which including 3276 males (aged 9–88 years) and 1845 females (aged 7–90 years). When participants have the following diseases or tumors, we will be excluded, such as cardiovascular diseases, metabolic diseases, chronic diseases, etc., pregnant women are also excluded.
Inbody720 body composition analyzer (Biospace Co., Korea) was used to detect the human body composition based on the recommendation provided in the user manual (according to the principle of bioelectrical impedance, the size of the different components in the body through current is different, have different electrical impedance). The subjects were tested in the quiet state after fasting emptying in the morning. When the test subjects barefoot standing on the pedal plate electrode, hands naturally hang down, hold the hand electrode gently, and the angle between the trunk and upper limbs is maintained at 15°, the subject is in a relaxed state, the test indexes including basal metabolic rate, lean body weight, intracellular fluid, extracellular fluid, protein content, mineral content, body water content, skeletal muscle, body fat, abdominal obesity, etc. Weight in kilograms with no shoes in a minimal clothing state by a digital scale (Beurer, Germany), height in centimeters was measured. BMI was calculated as the weight in kilograms divided by the square of the height in meters (kg/m 2 ). According to the working group on obesity (WGOC) recommended BMI classification criteria: underweight (<18.5 kg/m 2 ), normal weight (18.5 to 24 kg/m 2 ), overweight (24 to 28 kg/m 2 ), and obesity (≥28 kg/m 2 ).
Descriptive anthropometry and body composition are presented as the means and standard deviation for men and women separately. Student's t test analysis was performed to investigate differences in mean values of anthropometric measures between men and women. According to the age criteria of WHO, young people are subdivided into those under 30 and 30 to 45, so, the subjects were divided into one of the following 4 age groups: <30 years old, 30 to 45, 45 to 60, > 60 years old. Use l<30 years old as a reference, to analysis the trends of baseline characteristics of both genders with age brackets in male and female. According to the working group on obesity (WGOC) recommended BMI classification criteria: underweight (<18.5 kg/m 2 ), normal weight (18.5 to 24 kg/m 2 ), overweight (24 to 28 kg/m 2 ), and obesity (≥28 kg/m 2 ). Use normal weight (18.5 to 24 kg/m 2 ) as a reference, we used variance analysis to analysis the relationship between the body composition and BMI in male and female. Data analysis was performed using the Statistical Package for Social Sciences (SPSS) software version 19. A P -value < .05 was considered statistically significant.
3.1 Baseline characteristics of study sample stratified by gender
From Table 1 , the mean of BMI was calculated in males and females, 24.48±3.37 for males and 23.18±3.33 for females. The basal metabolic rate of males and females were 1480 ± 142.88 kcal and 1181.92 ± 109.65 kcal, respectively. Body fat in men and women were 18.33 ± 6.49 and 19.82 ± 5.97. The body fat percentage in men and women were 25.74% and 34.01%. Visceral fat area in men and women were 91.98 ± 34.95 cm 2 and 77 ± 33.77 cm 2 , respectively.

3.2 Trends of baseline characteristics of both genders with age brackets
According to WHO's age criteria, the subjects were divided into one of the following 4 age groups: <30 years old, 30 to 45, 45 to 60, >60 years old. Use <30 years old as a reference, to analysis the trends of baseline characteristics of both genders with age brackets in male and female. From Table 2 , with age, the body composition will follow the change.

According to the age group, under 30 years, 30 to 45 years old, 45 to 60 and 60 years, in men, the mean value of BMI were 23.11 ± 3.58, 24.88 ± 3.29, 25.4 ± 3.03, and 24.35 ± 3.05 kg/m 2 . In women, the mean value of BMI were 20.85 ± 2.95, 22.65 ± 2.84, 24.31 ± 3.01, 24.31 ± 3.43 kg/m 2 ; In men, the mean value of body fat were 15.56 ± 6.82, 18.57 ± 6.18, 20.1 ± 5.81, and 19.32 ± 5.86; while in women, the mean value of body fat were 16.49 ± 5.35, 19.08 ± 5.33, 21.66 ± 5.33, 21.48 ± 6.17 kg. In men, the mean value of body fat percentage were 21.17%, 25.58%, 27.60%, and 28.51%; In women, the mean value of body fat percentage were 30.65%, 32.99%, 35.76%, and 36.72%.
According to the age group, under 30 years, 30 to 45 years old, 45 to 60 and 60 years, in men, the mean of protein were 10.4, 10.44, 10.21 and 9.26 kg; the mean of intracellular fluid were 24.06, 24.16, 23.63, and 21.41 kg; the mean of extracellular fluid were 14.32, 14.4, 14.39, and 13.48 kg. While in women, the mean of protein were 7.13, 7.43, 7.48, and 7.01 kg; the mean of intracellular fluid were 16.5, 17.19, 17.31, and 16.21 kg; the mean of extracellular fluid were 10.21, 10.66, 10.85, and 10.37 kg.
3.3 Correlation between body composition and BMI
According to BMI stratification, the differences of different components and indexes in different sex groups were analyzed. Table 3 shows the analysis of variance ANOVA for the correlated variables and BMI. It is clear from Table 3 that with the increase of BMI, the mean of protein content, body fat and basal metabolic rate also increased, both in men and in women.

According to BMI stratification (BMI < 18.5, 18.5≤BMI < 24, 24≤BMI < 28, and BMI≥28), for body fat, in men, 7.69 ± 2.31, 13.87 ± 3.62, 20.62 ± 3.43, and 28.15 ± 5.11 kg, respectively; in women group, in order, 10.97 ± 2.08, 17.55 ± 3.35, 23.7 ± 3.25, and 31.15 ± 4.79 kg. For body fat percentage, in men, 22.11%, 15.16%, 28.09%, and 32.97%, respectively; in women, in order, 32.33%, 25.12%, 37.63%, and 42.89%.
4 Discussion
In 2014, WHO declared that the worldwide prevalence of overweight and obesity affected about 1.9 billion adults aged 18 years or elder. This study is the first directly comparative study of body composition and obesity-related in Hainan population. Our results showed that with the increase of age, body fat, body fat percentages and visceral fat area also increased, both in men and in women. Meanwhile, with the increase of BMI, the body fat, body fat percentages and visceral fat area also increased, both in men and in women. Significant trends were observed for body fat, body fat percentages, and visceral fat area for both genders with age and both genders with BMI.
In our study, body fat in men and women were 18.33 and 19.82. The body fat percentage in men and women were 25.74% and 34.01%. Visceral fat area in men and women were 91.98 and 77 cm 2 . And, with the increase of age, body fat, body fat percentages and visceral fat area also increased, both in men and in women. Meanwhile, with the increase of BMI, the body fat, body fat percentages and visceral fat area also increased, both in men and in women. Studies by Yusuf et al [12] showed that after middle age, body fat accumulation began to increase with age and tended to accumulate in certain areas of the body. In general, the fat accumulation of males is “Apple type,” and their fat mainly accumulates in the abdomen of the trunk. The fat accumulation of females is “pear type,” and their fat mainly accumulates below the waist to the thigh part. The “Apple type” is more dangerous than “pear type” in the heart disease. Using InBody 720 body composition analyzer to measure 1121 obese adults overweight body mass index, body fat percentage, waist-hip ratio of fat and visceral fat area, and compare the body composition changes in different groups. The results suggested that Han ethnicity males and Uighur men had significantly difference in BFP, WHR, and VFA than that in Han men and women. [11] Heo et al [13] analysis the trend of percentage of body fat in 3 race-ethnicity groups (non-Hispanic whites, non-Hispanic blacks, and Mexican Americans), and the results shown that as the body mass index increases, the percentage of body fat also increases no matter in male group and female group. One research in Kuwait people revealed that the body fat percentages of males and females are 23.3% and 37.7%, respectively, females were greater than that for males, and males have a significantly higher proportion of obesity than women. [14] This result is consistent with the findings of other studies in other countries. Although the trend of body fat rate is similar in different countries, there are still some differences. Body fat percentages differ among countries depending on genetic factors, eating patterns, regular exercise, and other life-style habits. Studies revealed that obesity is associated with the occurrence of various diseases, such as insulin resistance, T2DM, stroke_, CVD, MetS, non alcoholic fatty liver disease. The accumulation of visceral fat also related to T2DM, CVD, insulin resistance. [15] Some research found that weight gain in adulthood appears to increase the risk for colon cancer. [16] Valdes et al [17] pointed that obesity is not only related to shortened life expectancy, but also related to accelerated aging. So, focusing on obesity-related lifestyle and prevent weight gain is very important.
Extracellular fluid refers to exist in the extracellular fluids, including plasma, tissue fluid and lymph, is the internal environment of the body; Intracellular fluid is a kind of body fluids, which can directly affect cell metabolism and physiological function. Determination of the internal and external fluid amount to the cells of our bodies can not only reflect the status of the function of the body's tissues, can also display cell physiology. In our research, we found that under 30 years, 30 to 45 years old, 45 to 60 and 60 years, in men, mean of intracellular fluid were 24.06, 24.16, 23.63, and 21.41 kg; the mean of extracellular fluid were 14.32, 14.4, 14.39, and 13.48 kg. While in women, the mean of intracellular fluid were 16.5, 17.19, 17.31, and 16.21 kg; the mean of extracellular fluid were 10.21, 10.66, 10.85, and 10.37 kg. The research shows that after the age of 45, intracellular fluid has a tendency to decline, and the extracellular fluid has a tendency to rise. One research revealed that the middle-aged male group had the highest intracellular fluid and extracellular fluid volume, and the middle-aged group had significant differences with the young group and the elderly group. The middle-aged women also showed the highest level of intracellular and extracellular fluid, but there was no significant difference in the intracellular fluid between the young and middle-aged women. The mean intracellular fluid was the lowest in the elderly group, which was significantly different from the middle-aged group. The physiological state of the elderly cells are greatly reduced, while large differences between individuals. [18] At the same time, in our study found that as the growth of the age, with lower protein content. The study found that the volume change of extracellular fluid and intracellular fluid can reflect the conditions of nutrition metabolism of the body, poor nutrition can lead to the abnormal distribution of extracellular and intracellular fluid, shown that extracellular fluid increases, intracellular fluid decreases, and more serious the degree of malnutrition. [19] And to a certain extent, the decrease of intracellular fluid is associated with an increased protein catabolism. For obese people, with the increase of body fat, extracellular fluid volume also increased. [20] Several other studies have examined extracellular water volume in relation to BMI. Brochner-Mortensen et al [21] matched obese and nonobese patients for height and age and found higher extracellular water volume in the obese, while Visser et al [22] recorded a positive correlation between BMI and the increase in extracellular water volume.
Bioelectrical impedance analysis (BIA) was first proposed by Lukaski, [23] and it assumes that the body is composed of fat and nonfatty substances, to use the conductive differences of human body fat, water and other components of the body to determine the content of body composition. The study shows that bioelectrical impedance method is one of the important methods of body composition measurement, which can reflect the weight and distribution of body fat and can be evaluated nutritionally, has the advantages of simple operation, fast detection, safe, noninvasive, economy, reliability, and validity, etc., suitable for large-scale research group, has an important value in the diagnosis obesity or malnutrition. [24–26]
There are several potential limitations of the present study: Firstly, we used the Inbody 720 body composition analyzer, which originally developed and validated only in the Korean population. There are genetic differences in the Korean and the Chinese population; there may be significant differences in body fat composition. This may create a systematic bias in the analysis. Secondly, in order to get more accurate and reliable results, the sample size is still not big enough, and the sample size needs to be adjusted according to the occurrence probability of Type 1 and Type II errors. Thirdly, this study inevitably has a certain bias in the selection of the respondents. In order to strengthen the strength of its argument and verify its conclusion, large-scale, multi-category research is still needed.
5 Conclusions
In our research, we found that significant trends were observed for body fat, body fat percentages and visceral fat area for both genders with age and both genders with BMI. Focusing on obesity-related lifestyle and prevent weight gain. In recent years, studies have showed that the body composition anomalies is closely related to lipid metabolic disorder diseases, such as obesity, diabetes and other disease, these may be a risk factor for cardiovascular disease. According to the results of body composition analysis, can be found the body composition change and adipose accumulation as early as possible, in order to change lifestyle of each age overweight and obese people, improve the subhealth.
Acknowledgments
We are grateful to individuals who participated in the study. We would also like to thank the clinicians and other hospital staff who contributed to the data collection for this study.
Author contributions
Conceptualization: Yi feng Yang.
Data curation: Xian hua Chen, Jing Li, Meng dan Yan.
Formal analysis: Xiong fei Liang, Xian hua Chen, Jing Li, Meng dan Yan.
Funding acquisition: Yi feng Yang.
Methodology: Jing Li, Meng dan Yan.
Project administration: Yi feng Yang.
Software: Xian hua Chen.
Writing – original draft: Xiong fei Liang.
Writing – review & editing: Yi feng Yang.
body composition; body mass index; Hainan population; inbody720 body composition analyzer; obesity
- + Favorites
- View in Gallery
Readers Of this Article Also Read
Associations of anthropometric adiposity indexes with hypertension risk: a..., waist-hip ratio as a predictor of myocardial infarction risk: a systematic....
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Examining the Role of Exercise Timing in Weight Management: A Review
Jennifer m. blankenship.
1 Division of Endocrinology, Metabolism, and Diabetes, Department of Medicine, University of Colorado Anschutz Medical Campus, Aurora, CO
Rebecca C. Rosenberg
2 Department of Medicine, Saint Joseph Hospital, Denver, CO
Corey A. Rynders
Edward l. melanson.
3 Department of Geriatrics, VA Eastern Colorado Health Care System, Aurora, CO
Victoria A. Catenacci
4 Anschutz Health and Wellness Center, University of Colorado Anschutz Medical Campus, Aurora, CO
Seth A. Creasy
Many adults cite exercise as a primary strategy for losing weight yet exercise alone is modestly effective for weight loss and results in variable weight loss responses. It is possible that some of the variability in weight loss may be explained by the time of day that exercise is performed. Few studies have directly compared the effects of exercise performed at different times of the day (i.e., morning versus evening exercise). Results from these existing studies are mixed with some studies demonstrating superior weight and fat mass loss from morning exercise, while other studies have found that evening exercise may be better for weight management. Exercise timing may alter modifiable lifestyle behaviors involved in weight management, such as non-exercise physical activity, energy intake, and sleep. The purpose of this review is to summarize evidence for and against time-of-day dependent effects of exercise on weight management. Although limited, we also review studies that have examined the effect of exercise timing on other lifestyle behaviors linked to body weight regulation. While exercise at any time of day is beneficial for health, understanding whether there is an optimal time of day to exercise may advance personalized treatment paradigms for weight management.
INTRODUCTION
Despite significant efforts to thwart the increasing prevalence of overweight and obesity (BMI ≥25.0 kg/m 2 ), rates have continued to increase amongst U.S. adults [ 1 – 3 ]. It has been projected that by 2030 nearly 50% of US adults will have obesity (BMI ≥30 kg/m 2 ) and nearly 25% will have severe obesity (BMI ≥35 kg/m 2 ) [ 4 ]. Obesity is associated with increased risk of cardiovascular disease [ 5 , 6 ], type 2 diabetes [ 7 , 8 ], cancer [ 9 – 11 ], all-cause mortality [ 12 ], and lower quality of life [ 13 ]. Exercise and physical activity (PA) are critically important to prevent and treat overweight and obesity. Current guidelines recommend high levels of PA for weight management [ 14 , 15 ]; however, there is considerable unexplained individual variability in the weight loss response to exercise [ 16 – 19 ].
Recent evidence suggests that circadian rhythms (i.e., endogenous rhythms that occur with near 24h rhythmicity without external stimuli) and timing of lifestyle behaviors influence body weight regulation [ 20 – 23 ]. For example, evidence from observational and experimental studies have suggested that the timing of food intake may influence bodyweight [ 24 – 33 ]. Most evidence in humans suggests that a greater proportion of food intake consumed earlier in the day helps to promote a healthier, lower bodyweight [ 25 , 26 , 31 – 33 ]. There have been far fewer studies examining the effect of exercise timing (i.e., the time of day of exercise) on body weight regulation; however, this is an emerging area of research. The purpose of this review is to provide an overview of the current evidence on the effect of exercise timing on body weight. In addition, we examine three potential areas by which exercise timing may affect body weight: 1) energy intake (EI), 2) energy expenditure (EE) and substrate metabolism, 3) and sleep. The conceptual framework for how exercise timing may affect these factors and ultimately weight management is illustrated in Figure 1 . Finally, we address the strengths and limitations of current studies, recognize research gaps, and identify future areas of research that are needed.

Exercise is a key component of lifestyle changes to promote weight loss and manage healthy body weights. Exercise has systemic impacts on factors related to weight management including energy balance, energy expenditure/substrate oxidation, and sleep. The effect of morning (yellow) vs. evening (blue) exercise on these components is likely different and illustrated in the conceptual framework. Solid lines represent well supported relationships whereas dotted lines represent proposed relationships.
EFFECT OF EXERCISE TYPE ON BODY WEIGHT AND BODY COMPOSITION
Exercise and PA are important behaviors for achieving and maintaining a healthy body weight [ 14 ]. Prior studies have demonstrated that weight loss from exercise without dietary changes results in modest weight loss [ 18 , 34 – 36 ]. However, with high doses of exercise (e.g., >2000 kcal/week), clinically meaningful weight loss is attainable [ 37 – 39 ]. Aerobic exercise training is considered the most effective form of exercise to reduce weight and fat mass [ 14 ]. In contrast, resistance exercise training may be beneficial for retaining lean mass and may elicit modest reductions in fat mass when performed in combination with aerobic exercise or diet restriction [ 14 ]. Current guidelines and recommendations related to weight management primarily focus on aerobic exercise [ 14 , 15 , 40 , 41 ]. Therefore, for the purpose of this review, we focus on the impact of aerobic exercise performed at different times of day on body weight and body composition.
THE VARIOUS DEFINITIONS OF EXERCISE TIMING
To date, there are no standard definitions of exercise timing. This is largely due to the fact that timing of exercise can be anchored to clock time, markers of circadian phase (e.g., dim light melatonin onset, core body temperature), habitual sleep and wake times, and/or eating events (e.g., pre vs. post meal; fasted vs. non-fasted). Mechanistic studies focusing on physiological pathways have traditionally defined exercise timing relative to circadian time and eating events, while secondary analyses and pragmatic clinical trials have defined exercise timing relative to clock times. All of these definitions are relevant to bodyweight regulation and the current review; thus, we will review data from several studies with different definitions of exercise timing. However, the focus of this review will be on morning vs. evening exercise because these are the most common exercise times and are generalizable to most adults. The definitions of morning and evening exercise vary by study and are reported as such below.
EFFECT OF EXERCISE TIMING ON BODY WEIGHT AND BODY COMPOSITION
There is accumulating evidence from observational and clinical studies that the timing of exercise and PA affects body weight regulation [ 42 – 49 ]. Some evidence suggests that morning exercise and PA is associated with more favorable changes in weight and body composition [ 42 , 45 ] and increased ability to prevent weight regain [ 46 , 47 , 49 ]. However, some data suggest that evening exercise may be more beneficial for reducing fat [ 44 , 48 ] ( Table 1 ). Due to a paucity of direct head-to-head comparisons of different exercise times of day, it remains difficult to discern whether there is an optimal time of day for exercise to maximize weight loss benefits. The evidence to date, summarized below, is from observational studies, small randomized trials, and retrospective analyses [ 42 – 50 ].
Summary of Studies on the Effect of Exercise Timing on Body Weight
| Reference | Sample Size | Participants | Study Design | Intervention | Study Duration | Weight Outcomes | Related Outcomes |
|---|---|---|---|---|---|---|---|
| Alizadeh [ ] | 48 | Inactive females aged 20–45 y with a BMI ≥25.0–29.9 kg/m | RT | Frequency: 3 d/wk Intensity: at ventilatory threshold Type: Supervised treadmill running Time: 30 min/d AM-Ex: 08:00 – 10:00 PM-Ex: 14:00 – 16:00 | 6 weeks | Δ in Weight: AM-Ex = −1.6 kg PM-Ex = −0.3 kg No differences in change in body composition | Δ in EI: AM-Ex = −362 kcal/d PM-Ex = −28 kcal/d 77% retention; adherence to exercise not reported |
| Willis [ ] | 88 | Inactive males and females aged 20–45 y with a BMI ≥25.0 – 40.0 kg/m | NR | Frequency: 5 d/wk Intensity: 70–80% MHR Type: Primarily supervised treadmill walking/running Time: varied by participant as prescriptions were based on EE; 400 and 500 kcals per session AM-Ex: 07:00 – 11:59 PM-Ex: 15:00 – 19:00 Control: No-exercise | 10 months | Δ in Weight: AM-Ex = −7.2 ± 1.2% PM-Ex = −2.1 ± 1.0% Control = 0.5 ± 1.0% Changes in fat mass followed the same trends at weight loss | Δ in EI: AM-Ex = −63 ± 444 kcal/d PM-Ex = 121 ± 484 kcal/d Δ in Non-Exercise EE: AM-Ex = 28 ± 446 kcal/d PM-Ex = −105 ± 510 kcal/d |
| Creasy [ ] | 90 | Cohort of weight loss maintainers compared to control with and without obesity | OBS | - | - | WLM = BMI of 23.7 ± 2.4 kg/m ; maintaining weight loss for 9.5 ± 10.2 years NC = BMI of 22.7 ± 2.0 kg/m OC = BMI of 33.4 ± 5.1 kg/m | MVPA 0–3 hours after waking up: WLM: 25.1 ± 23.1 min NC: 14.3 ± 12.3 min OC:12.3 ± 14.3 min |
| Schumacher [ ] | 375 | Cohort of weight loss maintainers; mostly white females with a mean age of 53.4 y | OBS | - | - | WLM = Current BMI of 26.5 ± 4.8 kg/m ; maintaining a significant weight loss | WLM with temporally consistent physical activity patterns engaged in the higher amounts of MVPA compared to WLM with temporally inconsistent patterns (350 min/wk vs. 285 min/wk; p=0.03) WLM with temporally consistent patterns predominantly were active in the early mornings (4:00–8:59). |
| Chomistek [ ] | 7,157 | Cohort of women in the Women’s Health Study; mean BMI = 26.1 ± 4.9 kg/m | OBS | - | - | Women in the lowest quartile of accelerometer counts prior to 12:00 (<39% of total counts) have 26% higher odds of having obesity compared to those in the highest quartile (≥54% of total counts). | - |
| Di Blasio [ ] | 42 | Inactive post-menopausal women aged 48–58 y with a BMI ≥25.0 kg/m | NR | Frequency: 4 d/wk Intensity: 55% HRR Type: Walking Time: 50 min/d Morning Exercise: 07:00 – 09:00 Evening Exercise: 18:00 – 20:00 | 3 months | Δ in Weight: AM-Ex: 0.2 ± 2.0 kg PM-Ex: −0.02 ± 1.7 kg Δ in FM: AM-Ex:−0.2 ± 1.5 kg PM-Ex: −1.7 ± 2.4 kg | Adherence to Exercise: AM-Ex: 83.2% PM-Ex: 87% Δ in EI: AM-Ex: −40 ± 209 kcal/d PM-Ex: 101 ± 285 kcal/d Δ in Meal-timing: AM-Ex: 0.4 ± 8.1% increase in AM intake PM-Ex: 6.1 ± 5.7% increase in AM intake |
| Marinac [ ] | 125 | US Adults with a mean age of 35.3±11 y and a mean BMI of 27.6±6.5 kg/m | OBS | - | - | Timing of physical activity (morning=prior to 12:00 vs. evening = after 19:00) was not associated with BMI. | - |
| Mancilla [ ] | 32 | Inactive males age 58±7 y at risk for or diagnosed with type 2 diabetes and a BMI ≥26.0 kg/m | NR | Frequency: 3 d/wk (aerobic=2 days; resistance=1 day) Intensity: aerobic=70% Wmax Resistance=60% of MVC Type: aerobic=cycling resistance=3×10 reps of leg extension, leg press, chest press, lat pull down, tricep and bicep curls, abdominal crunches, horizontal row Time: aerobic=30 min/d; resistance=until completion Morning Exercise: 08:00 – 10:00 Evening Exercise: 15:00 – 18:00 | 12 weeks | Δ in Weight: AM-Ex: 0.7 ± 1.6 kg PM-Ex: −0.6 ± 2.5 kg Δ in FM: AM-Ex: −0.2 ± 1.0 kg PM-Ex: −1.2 ± 1.3 kg | Adherence to Exercise: Overall= 98% compliance Δ in VO : AM-Ex: 1.8 ± 2.2 ml/kg/min PM-Ex: 3.0 ± 2.1 ml/kg/min |
Abbreviations and symbols: BMI: body mass index, y: years, d/wk: days per week, min/d: minutes per day, RT: randomized trial, OBS: observational, NR: not-randomized, AM-EX: morning exercise, PM-Ex: evening exercise, MHR: maximal heart rate, HRR: heart rate reserve, Δ: change, BF: body fat, FM: fat mass, EI: energy intake, EE: energy expenditure, MVPA: moderate to vigorous physical activity, WLM: weight loss maintainers, NC: controls without obesity, OC: controls with obesity, US: United States, Wmax: maximum workload, MVC: maximal voluntary contraction,
Results from observational studies suggest that there may be an effect of time of day of PA on body weight and BMI. Chomistek et al. examined the PA patterns of 7157 women enrolled in the Women’s Health Study. Women who engaged in the highest amount of PA prior to 12:00 had 26% lower odds of having obesity compared to those who engaged in the lowest amount of PA prior to 12:00 [ 47 ]. In contrast, Marinac et al. found that neither engaging in morning PA (prior to 12:00) nor evening PA (after 19:00) was associated with BMI in a convenience sample of 125 US adults [ 50 ]. In addition to timing of PA, the authors also examined the association between two phenotypes (“early bird” vs. “night owl”) and BMI. “Early birds” and “night owls” were defined by a combination of factors including the timing of last outdoor light exposure, last indoor light exposure, first indoor light exposure, bedtime, waketime, and timing of last meal. The “night owl” phenotype was associated with a lower BMI; however, this was not significant after adjustment for covariates. While these studies do not provide congruent results, they highlight the need for further investigation in this area.
There have been very few randomized control trials comparing different exercise times of day on changes in body weight and body composition. Alizadeh et al. [ 42 ] randomized women (age 20–45 years, BMI of 25–30 kg/m 2 ) to six weeks of supervised morning (08:00–10:00) or afternoon (14:00–16:00) exercise of equivalent duration (90 min/wk). While this study was not powered to detect differences in weight change, in a completers analysis, body weight decreased more in morning exercisers compared to afternoon exercisers (−1.6 vs. −0.3 kg, SD not reported, p=0.04 for group*time interaction). This study had several strengths including the randomized design, provision of supervised exercise, and measurement of body composition and EI. However, the sample size was relatively small (n=48), and the population studied was exclusively women with overweight between the ages of 20–45 years. Thus, the results of this study may not be generalizable to other populations such as men, postmenopausal women, and individuals with obesity (BMI ≥30.0 kg/m 2 ). Moreover, the exercise intervention was modest (3 days per week, 30 minutes per session of treadmill running at the individualized ventilatory threshold), exercise adherence was not reported, and the intervention duration was very short (6 weeks). This level of exercise is not expected to result in clinically significant weight loss [ 14 ]; thus, it is not surprising that average weight loss was minimal (<2 kg). Further, it is unlikely that the differences in weight loss observed between morning exercise and evening exercise would result in any clinically meaningful differences in other health-related outcomes.
Willis et al. retrospectively examined the effect of morning exercise vs. evening exercise on weight loss and energy balance in the Midwest Exercise Trial 2 (MET-2) [ 45 ]. MET-2 was a highly controlled 10-month exercise-only intervention which examined the effects of 2000 and 3000 kcal/wk of supervised exercise (5 days per week) in men and women (18–30 years, BMI 25–40 kg/m 2 ). Importantly, only individuals who were >90% adherent to the exercise intervention were retained in MET-2. In this post-hoc analysis, participants were categorized based on the time of day in which they completed most of their exercise sessions: morning exercisers: >50% of sessions completed between 7:00–11:59; ( n = 21, mean ± SD; 70 ± 14% of exercise sessions completed in the morning), evening exercisers: >50% of sessions completed between 15:00–19:00; ( n = 25, 66 ± 12% of exercise sessions completed in the evening), and sporadic exercisers: <50% of sessions completed in any time category; ( n = 24). Morning exercisers lost significantly more weight (−6.5 ± 5.3 kg, −7.2%) compared to evening exercisers (−2.2 ± 4.5 kg, −2.2%) at 10 months despite similar levels of exercise EE and similar baseline characteristics. Sporadic exercisers exhibited weight loss of −5.0 ± 5.3 kg (−5.5%) of bodyweight which was intermediate between morning and evening exercisers. Sensitivity analyses confirmed that morning exercisers achieved superior weight loss compared to evening exercisers regardless of randomization group (2000 kcal/wk group vs. 3000 kcal/wk group) or sex. In addition, morning exercisers lost significantly more fat mass (−6.2 ± 1.1 kg) compared to evening exercisers (−1.6 ± 0.9 kg) as measured using dual-energy x-ray absorptiometry (p=0.008). Strengths of this study include fully supervised exercise with a prescription based on exercise EE measured and adjusted throughout the study, clinically relevant study duration, and inclusion of men and women. However, it is important to note that participants were not randomized to morning or evening exercise in this secondary analysis and as a result, unobserved confounders may have impacted these findings. Additionally, this study utilized arbitrary ranges for morning (07:00–11:59) and evening exercise (15:00–19:00); these defined clock times may not appropriately reflect morning and evening for all people.
Not all studies show a benefit of morning exercise for weight loss. Di Blasio et al. performed an interventional study to examine the effect of morning exercise vs. evening exercise on changes in weight, body composition, and eating behavior [ 44 ]. Forty-two postmenopausal women self-selected either morning (7:00–9:00) or evening exercise (18:00–20:00) for 3 months. The exercise intervention consisted of 4 sessions per week of walking for 50 minutes per session at an intensity equivalent to 55% of heart rate reserve (200 minutes per week). Two sessions per week were supervised by a trainer and two sessions per week were unsupervised. Overall exercise adherence was similar between groups (83.2% for morning and 87.0% for evening exercise). In contrast to the previously described studies, weight change was similar between morning exercise (0.2 ± 2.0 kg) and evening exercise (−0.02 ± 1.7 kg); however, evening exercise exhibited a greater decrease in fat mass (−1.7 ± 2.4 kg) compared to morning exercise (−0.2 ± 1.5 kg), as measured using bioelectrical impedance (p=0.037). There were several strengths of this study including high levels of adherence to the exercise intervention, partial exercise supervision, and well controlled exercise intensity. However, because participants were allowed to self-select the timing of exercise, it is difficult to determine if the differential weight loss was due to time of day or other confounders.
Another recent secondary analysis also found that evening exercise may lead to more favorable effects on body weight, body composition, and insulin sensitivity in men who were at risk for or diagnosed with type 2 diabetes [ 48 ]. Thirty-two men self-selected to exercise in the morning (08:00–10:00) or the early evening (15:00–18:00) for 12 weeks. All exercise was supervised and included two days per week of cycling at 70% of maximum workload for 30 minutes and 1 day per week of resistance training exercises (3 sets of 10 repetitions) at 60% of maximum voluntary contraction. Overall compliance to exercise training was 98%. Changes in body weight were not statistically different between morning exercise (0.7 ± 1.6 kg) and early evening exercise (−0.6 ± 2.5); however, early evening exercise had greater reductions in body fat (−1.2 ± 1.3 kg) compared to morning exercise (−0.2 ± 1.0 kg, p=0.03). In addition, early evening exercise resulted in superior improvements in peripheral insulin sensitivity, insulin-mediated suppression of adipose tissue lipolysis, and morning fasting glucose levels. There were several strengths of this study including high levels of adherence to the exercise intervention, inclusion of aerobic and resistance exercise, exercise supervision, and well controlled exercise intensity. However, the non-randomized design makes it difficult to discern whether the findings were due to time of day of exercise or other potential confounders.
Prescribing exercise based on time of day is a promising future direction of overweight and obesity treatments. A recent rigorously designed randomized control trial by Brooker et al. [ 43 ] assessed the feasibility, safety, and acceptability of prescribing morning versus evening exercise in 20 adults with overweight and obesity (BMI: 25–40 kg/m 2 ). Participants (age 18–60 years) were randomized to 12 weeks of morning exercise (06:00–9:00, n=9), evening exercise (16:00–19:00, n=7), or a no intervention control (n=4). Exercise volume was 250 minutes per week at moderate intensity. The intervention started as fully supervised (5 days per week, 50 minutes per session) and was tapered to two sessions per week of supervision over the intervention. Both morning exercise and evening exercise resulted in favorable changes in BMI and percent body fat compared to control. Because of the limited sample size, direct comparisons of weight outcomes between morning and evening exercise were not performed. The study did report high adherence to supervised exercise sessions at both times of day (94% in morning exercise, 87% in evening exercise). These data indicate that prescribing exercise based on time of day is feasible and acceptable in the setting of overweight and obesity treatments. A future randomized control trial that is powered to detect differences in body composition between morning and evening exercise is warranted.
Timing of exercise and PA may also play a role in the maintenance of weight loss. In the National Weight Control Registry Ostendorf et al. found that weight loss maintainers (individuals who maintained a weight loss of >13.6 kg for >1 year) engaged in higher volumes of moderate to vigorous PA (MVPA) across the week as compared to controls with (OC) and without obesity (LC) [ 51 ]. In a secondary analysis of these data, Creasy et al. found that weight loss maintainers were most active in the morning and averaged 3278 ± 3004 steps and 25.1 ± 23.1 min of MVPA (~27% of daily totals) within 3 hours of waking, significantly higher levels than controls ( Figure 2 ) [ 49 ]. In a separate study, Schumacher et al. also found that weight loss maintainers self-reported engaging in high amounts of MVPA [ 46 ]. In that study, participants who were classified as temporally consistent exercisers (i.e., regularly exercised at the same time of day) engaged in more MVPA (350 min/wk) compared to temporally inconsistent exercisers (285 min/wk). However, the time of day that activity was performed was not associated with amount of MVPA. Thus, in the context of chronic exercise and achieving high levels of PA, consistency of exercise may be more important than time of day. Engaging in PA at the same time of day may help with the habit formation necessary for achieving high levels of MVPA. However, cross-sectional data for which this premise is based on should be interpreted with caution. Prospective research is needed to understand the physiological and behavioral mechanisms through which exercise timing and consistency of PA influences body weight regulation.

24-hour patterns of stepping in weight loss maintainers (WLM), lean control (LC) and control participants with overweight/obesity (OC)
In summary, exercise at any time of the day is beneficial for weight management and several other health outcomes. Some studies suggest that morning exercise may promote superior weight management benefits as compared to evening exercise [ 42 , 45 , 49 ]. The effects appear minimal in one short-term randomized study of 6 weeks [ 42 ]; however, in a 10-month non-randomized study those who performed most of their exercise in the morning achieved 3 times greater weight loss than those who performed most of their exercise in the evening [ 45 ]. The data are equivocal with two non-randomized short-term studies finding no differences in weight loss, and superior fat loss in evening exercise compared to morning exercise [ 44 , 48 ]. However, these collective data come from small studies, secondary analyses, and observational studies. Adequately powered randomized trials are needed to confirm these preliminary findings. A major area of interest is understanding the mechanisms by which exercise timing may generate differences in weight loss. The remainder of the review will focus on 3 major areas which may contribute to the impact of exercise timing on body weight regulation: 1) EI, 2) EE and substrate metabolism 3) and sleep.
EFFECT OF EXERCISE TIMING ON ENERGY INTAKE
In general, acute bouts of exercise have been shown to alter hormonal drives of EI leading to reductions in hunger and short-term EI; however, this effect is not observed in all individuals and may be influenced by sex, adiposity, and the exercise stimulus [ 52 – 54 ]. Some longer-term studies examining the effect of exercise training on EI show that exercise leads to a compensatory increase in EI [ 18 , 55 – 58 ]; however, other studies have found minimal increases in EI in response to exercise training [ 16 , 37 , 59 ]. In these studies, there is substantial inter-individual variability in the EI response to exercise. Time of day of exercise may be an underappreciated factor contributing to this variability. Well-controlled studies have found that hunger and appetite hormones such as leptin, ghrelin, and peptide YY exhibit circadian oscillations [ 60 – 62 ]. Because appetite related hormones exhibit circadian rhythmicity and are influenced by exercise, morning versus evening exercise may differentially impact subsequent EI. However, current evidence from well-controlled studies on time of day of exercise and its effect on hunger, drivers of appetite, and total EI is limited.
Comparison of Morning vs. Evening Exercise – Acute Bouts
In a randomized cross-over study by Alizadeh et al. [ 63 ], 50 women with overweight engaged in a 30 minute bout of exercise at the ventilatory threshold in the morning (08:00–10:00) and the afternoon (14:00–16:00). Visual analog scales were used to measure hunger, satiety, and food cravings before and 15 minutes following exercise. Subsequent EI was measured over the 24 hours following each exercise session using 24-hour food records. Although EI was not different, satiety was higher following morning exercise compared to evening exercise suggesting that participants felt fuller following morning exercise. In a separate study by Maraki et al. [ 64 ], 12 young, normal weight females performed either 1 hour of exercise or 1 hour of seated rest in the morning (08:15–09:15) or evening (19:15–20:15). Both morning and evening exercise induced a similar 24-hour energy deficit, increased hunger and prospective food consumption, and decreased satiety and fullness compared to control conditions, but there were no differences between conditions. Finally, Larsen et al. [ 65 ] compared appetite and appetitive hormones in response to acute morning (06:00–07:00), afternoon (14:00–16:00), and evening (19:00–20:00) exercise. Although ghrelin was higher 30 minutes after afternoon exercise compared to morning and evening exercise, subjective appetite responses after exercise were not different between groups. Additionally, self-reported 24-hour EI following the exercise bout was not different between all three conditions. Thus, timing of an acute exercise bout does not seem to impact subsequent EI.
Comparison of Morning vs. Evening Exercise – Exercise Training
Few studies have investigated the impact of exercise timing on EI and appetite responses in the context of chronic exercise training. Two studies which demonstrated superior weight loss with morning exercise compared to evening exercise have also documented a potential time of day effect on EI and appetite [ 42 , 45 ]. In the study by Willis et al., EI was quantified using digital photography in a school cafeteria setting assessed over 7 days pre- and post-intervention. Food consumed outside of the cafeteria was assessed using multiple-pass recalls. Despite significant differences in weight loss outcomes between morning and evening exercisers, there were no significant within or between group differences in energy intake over 10 months (morning exercisers: −63±444 kcal/d; evening exercisers +121±484 kcal/d) [ 45 ]. However, this study was not powered to detect differences in EI and these small observed differences in EI may have influenced weight loss. Alizadeh et al. found that morning exercise tended to reduce 24-hour self-reported EI by 362 kcal/d compared to evening exercisers who reported a change in EI of −28 kcal/d (p=0.06 for group difference) [ 42 ]. However, neither group reported any consistent changes in hunger, satiety, and other eating behaviors across the exercise intervention. Finally, Di Blasio et al. showed no differences in change of total EI or hunger/satiety following 3 months of morning and evening exercise, but there were significant changes in the timing of EI [ 44 ]. Evening exercise increased the proportion of EI consumed in the morning and decreased the proportion of EI consumed in the evening, while morning exercise did not alter timing of food intake. This study is one of the first to demonstrate that the timing of exercise may naturally shift timing of food intake.
A major and perhaps under recognized challenge in understanding the impact of exercise timing on EI is related to the time of the last EI event. The duration of fasting prior to a morning exercise bout compared to an evening exercise bout can be very different. Bachman et al. found that individuals who performed fasted morning exercise vs. non-fasted morning exercise reported consuming less EI over the next 24h [ 66 ]. These data demonstrate that fasting prior to exercise may affect EI, thus it is important to consider the duration of fasting when examining the effect of exercise timing on appetite and EI responses. Given the logistical challenges of controlling fasting windows prior to exercise at varying times of the day, this may be a complicated area of study. Nonetheless, more research is needed in this area, as it is difficult to draw conclusions from existing literature. Most of the studies to date have relied on self-reported measures of EI, appetite/hunger, and eating behavior. Future controlled studies are needed to understand whether the timing of exercise alters objectively measured food intake over periods longer than 24 hours, appetite-related hormones, and neuronal responses to food cues.
EFFECT OF EXERCISE TIMING ON ENERGY EXPENDITURE AND SUBSTRATE OXIDATION
Exercise likely has differential metabolic effects depending on the time of day it is performed; however, this is an understudied area that needs further exploration. Several studies using circadian protocols (e.g., constant routine, forced desynchrony, simulated shift work) have shown that resting metabolic rate [ 60 , 67 – 69 ], thermic effect of food [ 70 ], and substrate oxidation [ 60 , 67 – 69 , 71 ] vary over 24h; however, the rhythmicity and timing of peaks and nadirs have varied by study. Despite the inconsistency in the rhythmicity of these data across studies, it is clear that whole-body metabolism changes across the day in humans. While research to date has focused on resting metabolism, it is likely that exercise metabolism (i.e., substrate utilization and EE) also varies across the day. It is possible that exercise timing could alter EE during an exercise bout or over the subsequent 24 hours, which would have implications for weight management. In addition to physiological effects, the timing of exercise may alter diurnal behaviors for the rest of the day. For example, morning exercise may invigorate a person to reduce sedentary and sitting behaviors and increase non-exercise PA the rest of the day. In contrast, it is possible that morning exercise results in increased fatigue the rest of day and results in increased sedentary behavior and decreased non-exercise PA. Below, we outline the existing evidence on physiological and behavioral mechanisms through which the timing of exercise may affect whole body metabolism.
Two recent studies in mice found that exercise time of day altered molecular metabolic pathways, fuel utilization, exercise capacity and whole-body EE [ 72 , 73 ]. Interestingly, Ezagouri et al. also found that in 10 adults, evening exercise (performed at 18:00) resulted in lower oxygen consumption, higher respiratory exchange ratio (e.g., more carbohydrate metabolism), and lower perceived exertion compared to morning exercise (performed at 08:00) at the same workload over 60 minutes [ 73 ]. The authors concluded that evening exercise is more metabolically efficient than morning exercise. Whether differences in substrate utilization and metabolic efficiency translate to differences in exercise EE, weight loss or other clinically relevant measures of health is unclear and worthy of future study.
Few studies have examined the effect of the exercise time of day on PA behaviors. Bond et al. [ 74 ] found that in a population of bariatric surgery patients regular morning exercisers (defined as individuals who performed their longest bout of MVPA between 04:00–12:00) had higher levels of adherence to the exercise intervention and higher increases in total PA compared to those who performed most of their exercise after 12:00. The authors concluded that prescribing morning PA may be an effective strategy to increase MVPA in bariatric surgery patients. In the study by Willis et al., compared to evening exercisers, morning exercisers engaged in higher amounts of non-exercise PA and lower amounts of sedentary behavior compared to evening exercisers [ 45 ]. This was associated with higher levels of non-exercise EE. Although these differences were not significant, if they were consistent over many months, they could significantly affect bodyweight. No studies to date have been adequately powered to study the effect of exercise time of day on non-exercise PA and/or changes in EE.
EFFECT OF EXERCISE TIMING ON SLEEP
Current evidence suggests that acute bouts of exercise [ 75 , 76 ] and chronic exercise training [ 75 – 77 ] improve subjective sleep quality and objectively derived measures of sleep. Because both sleep quality and sleep duration have been linked to bodyweight regulation [ 78 – 81 ], it is possible that sleep is a mediator in the relationship between exercise and weight loss. Below we review existing literature on whether the effect of acute and chronic exercise on parameters of sleep is dependent on time of day.
Studies directly comparing aerobic exercise performed at different times of day on measures of sleep (e.g., sleep architecture and sleep quality) are limited. Research on the effect of exercise timing on measures of sleep have primarily focused on the potential sleep disrupting effects of evening exercise. Evening exercise was originally believed to be detrimental to sleep quality, however a recent meta-analysis by Stutz et al. [ 82 ] reported that evening exercise improved sleep quality compared to no exercise. A separate meta-analysis by Kredlow et al. [ 76 ] showed that time of day of moderated the beneficial effects of exercise on wake after sleep onset (WASO) and stage 1 sleep but not total sleep, sleep efficiency, sleep onset latency (SOL), and slow wave sleep. In a few small studies, morning exercise has also shown favorable effects on indices of sleep quality. Fairbrother et al. showed that compared to afternoon exercise (13:00), morning exercise (07:00) reduced sleep latency and increased time slow wave sleep in middle-aged adults with prehypertension [ 83 ]. Similarly, Morita et al. [ 84 ] showed that a group of older adults with insomnia reduced awakenings during the night after an acute bout of morning exercise (09:30) compared to evening exercise (17:30). While some data support a benefit of exercise regardless of time of day, the limited number of head-to-head comparisons of exercise times across the day make it difficult to discern the best time of day for exercise to improve sleep quality.
One factor that may be important in optimizing exercise for improvements in sleep quality is the impact of chronotype. Chronotype describes an individual’s natural propensity for sleep and wake timing [ 85 ]. A recent observational study of sleeping patterns after acute exercise in 909 college students found that chronotype was a moderator of the relationship between exercise timing and bed timing [ 86 ]. Later exercise times were associated with later bedtimes in both morning and evening chronotypes; however, the effect was more pronounced in morning chronotypes. These data demonstrate that the impact of exercise timing on sleep may be dependent on an individual’s natural propensity for wake and sleep. Future studies should include assessments of chronotype when investigating the optimal timing of exercise for sleep.
Thomas et al. studied the effect of exercise timing on an individual’s sleep and circadian rhythm (dim light melatonin onset, DLMO) [ 87 ]. Participants were randomized to perform 5 days of supervised morning exercise (10 hours after DLMO) or evening exercise (20 hours after DLMO) for 30 minutes per day at 70% VO 2 peak. While there were no differences in sleep duration or fragmentation (assessed by actigraphy), there was a shift in the melatonin rhythm with exercise. Regardless of chronotype, morning exercise resulted in a phase advance of the melatonin rhythm (i.e., DLMO occurred at an earlier time); however, the impact of evening exercise was dependent on chronotype. Evening exercise resulted in a similar phase advance of DLMO in evening chronotypes, but a phase delay (i.e., DLMO occurred at a later time) in morning chronotypes. These data highlight emerging evidence that exercise may act as a zeitgeber (time cue) for the central circadian system. Youngstedt et al. performed a rigorous circadian study finding that exercise performed in the morning (07:00) and early afternoon (13:00 and 14:00) led to a phase advance in melatonin rhythms, whereas exercise in the evening (19:00) and at night (22:00) resulted in a phase delay [ 88 ]. Exercise at 02:00 and 16:00 had a minimal impact on the melatonin rhythm. Collectively, these data indicate that there are times of the day that the circadian system may be more sensitive to exercise. Ultimately, alterations to the circadian system will likely have downstream effects on other metabolic processes and may be a mechanism responsible for differential impacts of timed exercise. Future studies should leverage our current understanding of exercise on central circadian rhythms to guide future explorations of the therapeutic potential of exercise timing for sleep, metabolism, and weight management.
In the context of exercise training, much less is known regarding the impact of exercise timing on sleep. Overall, exercise training studies show improvements in sleep quality [ 89 – 94 ]; however, most studies have allowed participants to self-select the time of exercise. Very few studies have randomized participants to perform exercise at different times of day. A short-term training study by Benloucif et al. showed similar improvements in subjective sleep quality with morning and evening exercise training for 2 weeks in older adults [ 95 ]. Küüsmaa-Schildt et al. randomized 70 young men to perform either morning or evening exercise (~2 days per week of combined endurance and strength) training for 24 weeks. Both morning and evening exercise groups experienced small improvements in self reported sleep quality and duration [ 96 ]. Finally, Seol et al. randomized 60 older adults to eight weeks of either a morning or evening exercise training (30 min/day of low intensity stepping). Both exercise groups showed similar improvements in objectively derived measures of sleep quality including sleep efficiency and wakenings after sleep onset [ 97 ]. Together, these data suggest that the sleep quality benefits of chronic exercise training may be more related to consistently performing exercise rather than the time of the exercise bout. Notably, the majority of sleep and exercise research has been conducted in healthy young men, many of whom are highly trained athletes [ 98 – 104 ]. Therefore, a major gap in the current literature is a lack of studies in populations that are translatable to the overall population. Future studies with more diversity of sex and gender, race/ethnicity, BMI, and chronotype are necessary to conclusively determine the impact of exercise timing on sleep within the context of exercise training.
RESEARCH GAPS AND FUTURE DIRECTIONS
Does exercise timing affect weight loss success.
There is a mounting evidence demonstrating that the time at which behaviors are performed confer differential health benefits, particularly related to weight management. As highlighted by this review, most studies that have investigated the impact of exercise timing on weight loss are comprised of small pilot studies, secondary analyses, and observational studies. It is difficult to confer a definitive conclusion from these studies. Adequately powered, prospective, randomized trials in generalizable cohorts of both men and women with overweight and obesity are needed to confirm these preliminary findings. In particular, studies are needed that are longer in duration, prescribe exercise based on EE at a dose that will elicit weight loss, and ensure high adherence to exercise at a dose that will elicit weight loss. Future studies are also needed to examine if sex, gender, race/ethnicity, and baseline BMI moderate the relationship between time of day of exercise and weight loss. By identifying individuals who benefit most from exercise at different times of day, researchers, clinicians, and public health officials can create more tailored treatment paradigms which will result in better overall treatment success.
How does the timing of exercise affect energy balance?
There is lack of understanding of both the behavioral and physiological mechanisms through which time of day of exercise may differentially affect body weight. To better understand the mechanisms by which exercise timing may confer differential effects on energy balance and body weight, both acute and chronic training studies are needed. Acute studies are needed to understand how timing of exercise bouts may affect factors such as eating behavior, appetite-related hormones, meal-timing, overall EI, substrate utilization, exercise EE, overall daily EE and other factors related to energy balance. Training studies are needed to understand how consistent training at the same time of day may elicit differential effects on these parameters as compared to acute exercise. For example, consistent exercise training at the same time of day may lead to shifts in meal timing, sleep timing, and other factors that would not be detectable in short term studies. Moreover, studies are needed which anchor exercise timing to sleep/wake rather than clock time. While using clock time is a practical approach, using habitual sleep/wake time to anchor exercise may help to reduce variability in outcomes of interest.
Does the timing of exercise affect sleep?
Having better sleep quality may affect both sides of the energy balance equation by increasing PA, decreasing sedentary behaviors during the day [ 105 ] and improving dietary behaviors. While exercise is believed to be important for sleep, the importance of exercise timing for sleep remains unknown. Both acute, in-depth sleep studies and exercise training studies are needed to understand if there is an optimal time of day to exercise for improving sleep. Moreover, future studies are needed with more diverse populations, including women, untrained individuals, adults across the age and BMI spectrum, and adults with various health conditions. Specifically, future studies with individuals who have reported sleep disturbances are needed to understand if timed exercise is a potential therapeutic target.
CONCLUSIONS
Exercise at any time of day is important for overall health. Exercise and PA are critically important to treat and prevent overweight and obesity; however, there is considerable individual variability in the weight loss response to exercise. The timing of exercise may be a contributing factor to this observed variability in weight loss. As illustrated in Figure 1 , the timing of exercise may have a differential impact on EE, EI and sleep, with all these factors ultimately affecting body weight regulation. Studies comparing morning versus evening exercise and their effect on body weight regulation are inconclusive. Ultimately, large-scale clinical and translational studies are needed to if altering time of day of exercise can lead to clinically meaningful differences in weight loss and other health outcomes.
CONFLICTS OF INTEREST
Three authors are supported by NIH Career Development Awards: F32 DK121403 (PI: Blankenship), K01 DK113063 (PI: Rynders), K01 HL145023 (PI: Creasy). ELM is supported by resources from the Geriatric Research, Education, and the Clinical Center at the Denver VA Medical Center. The contents do not represent the views of the U.S. Department of Veterans Affairs or the United States Government. Other authors have nothing to disclose. We confirm that this study meets the ethical standards of the International Journal of Sports Medicine [ 106 ].
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Effects of cinnamon supplementation on body weight and composition in adults: A systematic review and meta-analysis of controlled clinical trials
Affiliations.
- 1 Nutrition and Food Security Research Center, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
- 2 Department of Nutrition, School of Public Health, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
- PMID: 31800140
- DOI: 10.1002/ptr.6539
Background: This systematic review and meta-analysis aimed to investigate the effect of cinnamon on body weight, body mass index (BMI), waist circumference (WC), waist-hip ratio (WHR), and body fat mass including the maximum number of studies.
Methods: Medline, ISI Web of Science, Scopus, Google Scholar, and Cochrane library were searched with no limitation from inception up to August 2019 for relevant randomized controlled clinical trials (RCTs). The RCTs' risk of bias was assessed using the Cochrane collaboration's tool. Random-effects model was used for meta-analysis.
Results: Twenty-one RCTs with 1,480 participants were included. The meta-analysis showed that cinnamon supplementation significantly reduces BMI [weighted mean difference (WMD) = -0.40 kg/m 2 , 95% confidence interval (CI): -0.57, -0.22 kg/m 2 , p < .001, I 2 = 78.9%], body weight (WMD = -0.92 kg; 95% CI: -1.51, -0.33 kg; p = .002; I 2 = 84.2%), and WHR (WMD = -0.02, 95% CI: -0.038, -0.018; p < 0.001; I 2 = 0%). Cinnamon supplementation did not significantly affect the WC (WMD = -1.76 cm, 95% CI: -3.57, -0.045 cm; p = .056; I 2 = 90.8%) and body fat mass (WMD = -0.87%, 95% CI: -1.87, 0.025%; p = .057; I 2 = 78.6%).
Conclusion: Cinnamon supplementation significantly reduces body weight, BMI, and WHR. Future high-quality long-term RCTs are recommended to confirm these results.
Keywords: anthropometric indices; body composition; body weight; cinnamon; meta-analysis; systematic review.
© 2019 John Wiley & Sons, Ltd.
PubMed Disclaimer
Similar articles
- Cinnamon supplementation positively affects obesity: A systematic review and dose-response meta-analysis of randomized controlled trials. Mousavi SM, Rahmani J, Kord-Varkaneh H, Sheikhi A, Larijani B, Esmaillzadeh A. Mousavi SM, et al. Clin Nutr. 2020 Jan;39(1):123-133. doi: 10.1016/j.clnu.2019.02.017. Epub 2019 Feb 15. Clin Nutr. 2020. PMID: 30799194
- The effects of curcumin supplementation on body mass index, body weight, and waist circumference in patients with nonalcoholic fatty liver disease: A systematic review and dose-response meta-analysis of randomized controlled trials. Baziar N, Parohan M. Baziar N, et al. Phytother Res. 2020 Mar;34(3):464-474. doi: 10.1002/ptr.6542. Epub 2019 Dec 4. Phytother Res. 2020. PMID: 31799714
- The effect of green coffee extract supplementation on anthropometric measures in adults: A comprehensive systematic review and dose-response meta-analysis of randomized clinical trials. Asbaghi O, Sadeghian M, Rahmani S, Mardani M, Khodadost M, Maleki V, Pirouzi A, Talebi S, Sadeghi O. Asbaghi O, et al. Complement Ther Med. 2020 Jun;51:102424. doi: 10.1016/j.ctim.2020.102424. Epub 2020 May 5. Complement Ther Med. 2020. PMID: 32507437
- Beneficial effects of the probiotics and synbiotics supplementation on anthropometric indices and body composition in adults: A systematic review and meta-analysis. Saadati S, Naseri K, Asbaghi O, Yousefi M, Golalipour E, de Courten B. Saadati S, et al. Obes Rev. 2024 Mar;25(3):e13667. doi: 10.1111/obr.13667. Epub 2023 Nov 29. Obes Rev. 2024. PMID: 38030409 Review.
- Almond supplementation on appetite measures, body weight, and body composition in adults: A systematic review and dose-response meta-analysis of 37 randomized controlled trials. Chahibakhsh N, Rafieipour N, Rahimi H, RajabiNezhad S, Momeni SA, Motamedi A, Malekzadeh J, Islam MS, Mohammadi-Sartang M. Chahibakhsh N, et al. Obes Rev. 2024 May;25(5):e13711. doi: 10.1111/obr.13711. Epub 2024 Feb 13. Obes Rev. 2024. PMID: 38351580 Review.
- The effects of cinnamon supplementation on adipokines and appetite-regulating hormones: A systematic review of randomized clinical trials. Gheflati A, Pahlavani N, Nattagh-Eshtivani E, Namkhah Z, Ghazvinikor M, Ranjbar G, Shahraki Jazinaki M, Norouzy A. Gheflati A, et al. Avicenna J Phytomed. 2023 Sep-Oct;13(5):463-474. doi: 10.22038/AJP.2022.21538. Avicenna J Phytomed. 2023. PMID: 38089418 Free PMC article. Review.
- Development of a Functional Acceptable Diabetic and Plant-Based Snack Bar Using Mushroom ( Coprinus comatus ) Powder. Dimopoulou M, Vareltzis P, Floros S, Androutsos O, Bargiota A, Gortzi O. Dimopoulou M, et al. Foods. 2023 Jul 14;12(14):2702. doi: 10.3390/foods12142702. Foods. 2023. PMID: 37509794 Free PMC article.
- Cinnamon: an aromatic condiment applicable to chronic kidney disease. Moreira LSG, Brum ISDC, de Vargas Reis DCM, Trugilho L, Chermut TR, Esgalhado M, Cardozo LFMF, Stenvinkel P, Shiels PG, Mafra D. Moreira LSG, et al. Kidney Res Clin Pract. 2023 Jan;42(1):4-26. doi: 10.23876/j.krcp.22.111. Epub 2023 Jan 31. Kidney Res Clin Pract. 2023. PMID: 36747357 Free PMC article.
- A comparison of the effects of cinnamon, ginger, and metformin consumption on metabolic health, anthropometric indices, and sexual hormone levels in women with poly cystic ovary syndrome: A randomized double-blinded placebo-controlled clinical trial. Dastgheib M, Barati-Boldaji R, Bahrampour N, Taheri R, Borghei M, Amooee S, Mohammadi-Sartang M, Wong A, Babajafari S, Mazloomi SM. Dastgheib M, et al. Front Nutr. 2022 Nov 29;9:1071515. doi: 10.3389/fnut.2022.1071515. eCollection 2022. Front Nutr. 2022. PMID: 36523331 Free PMC article.
- Afshin, A., Forouzanfar, M. H., Reitsma, M. B., Sur, P., Estep, K., Lee, A., … Murray, C. J. L. (2017). Health effects of overweight and obesity in 195 countries over 25 years. The New England Journal of Medicine, 377(1), 13-27. https://doi.org/10.1056/NEJMoa1614362
- Akilen, R., Pimlott, Z., Tsiami, A., & Robinson, N. (2013). Effect of short-term administration of cinnamon on blood pressure in patients with prediabetes and type 2 diabetes. Nutrition, 29(10), 1192-1196. https://doi.org/10.1016/j.nut.2013.03.007
- Akilen, R., Tsiami, A., Devendra, D., & Robinson, N. (2010). Glycated haemoglobin and blood pressure-lowering effect of cinnamon in multi-ethnic Type 2 diabetic patients in the UK: A randomized, placebo-controlled, double-blind clinical trial. Diabetic Medicine, 27(10), 1159-1167. https://doi.org/10.1111/j.1464-5491.2010.03079.x
- Aldayel, T. S. (2016). Health Benefits of Cinnamon Supplement: In Vitro and In Vivo. (Doctoral), University of Surrey, Retrieved from http://epubs.surrey.ac.uk/810443/
- Allen, R. W., Schwartzman, E., Baker, W. L., Coleman, C. I., & Phung, O. J. (2013). Cinnamon use in type 2 diabetes: An updated systematic review and meta-analysis. Annals of Family Medicine, 11(5), 452-459. https://doi.org/10.1370/afm.1517
Publication types
- Search in MeSH
Grants and funding
- Nutrition and Food Security Research Center, Shahid Sadoughi University of Medical Sciences
LinkOut - more resources
Full text sources.
- Ovid Technologies, Inc.
- MedlinePlus Health Information

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Modeling body size information within weight labels using probability distributions
- Published: 22 July 2024
Cite this article

- Thomas Chazelle 1 ,
- Michel Guerraz 1 &
- Richard Palluel-Germain 1
Explore all metrics
What images of bodies do we associate with thinness and fatness? Can our representations of weight-related words be described by simple probability distributions? To answer these questions, the present study examined participants’ perceptions of a set of weight-related words using a pictural scale. 259 French women indicated the thinnest, fattest, and best-fitting figures for 13 words. We then used their responses to construct PERT probability distributions, simple skewed distributions allowing to visualize what body sizes were associated with each word. In particular, the variability of the distributions showed how different weight labels can have more or less precise meanings. We found some evidence that the lowest body mass index associated with a label shifted towards thinner figures as body dissatisfaction increased. Using the same method, we investigated the boundaries of what participants consider the ideal body, and showed that the inclusion of their own body in these boundaries predicted their levels of body dissatisfaction. We argue that PERT distributions can be a useful, easy-to-use tool in body image research for modeling the representations of weight labels in different populations.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or Ebook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
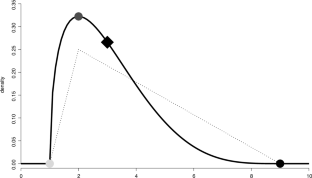
Similar content being viewed by others
Beyond BMI for self-estimates of body size and shape: A new method for developing stimuli correctly calibrated for body composition

The scale matters: assessing body size with figure rating scales in a diverse sample of young adults
Evidence for a perceptual mechanism relating body size misperception and eating disorder symptoms
Data availability.
The datasets collected during the current study are available on the Open Science Framework page of this project, https://osf.io/p74yg/ .
Abbate-Daga, G., Amianto, F., Delsedime, N., De-Bacco, C., & Fassino, S. (2013). Resistance to treatment and change in anorexia nervosa: A clinical overview. BMC Psychiatry, 13 (1), 294. https://doi.org/10.1186/1471-244X-13-294
Article PubMed PubMed Central Google Scholar
Bates, D., Mächler, M., Bolker, B., & Walker, S. (2015). Fitting linear mixed-effects models using lme4. Journal of Statistical Software, 67 (1), 1–48. https://doi.org/10.18637/jss.v067.i01
Article Google Scholar
Befort, C. A., & Rickard, K. M. (2003). Gender similarities in response to figure-size feedback in a selected nonclinical population. Sex Roles, 49 , 71–80. https://doi.org/10.1023/A:1023913720317
Belsley, D. A., Kuh, E., & Welsch, R. E. (1980). Regression diagnostics: Identifying influential data and sources of collinearity (1st ed.). New York: Wiley. https://doi.org/10.1002/0471725153
Book Google Scholar
Brochu, P. M., & Esses, V. M. (2011). What’s in a name? The effects of the labels “fat” versus “overweight” on weight bias. Journal of Applied Social Psychology, 41 (8), 1981–2008. https://doi.org/10.1111/j.1559-1816.2011.00786.x
Centre de Recherches Inter-langues sur la Signification en Contexte. (2019). Dictionnaire électronique des synonymes . https://crisco4.unicaen.fr/des/
Chan, A. W. Y., Noles, D. L., Utkov, N., Akbilgic, O., & Smith, W. (2021). Misalignment between perceptual boundaries and weight categories reflects a new normal for body size perception. Scientific Reports, 11 (1), 10442. https://doi.org/10.1038/s41598-021-89533-5
Clark, C. E. (1962). The PERT model for the distribution of an activity time. Operations Research, 10 (3), 405–406. https://doi.org/10.1287/opre.10.3.405
Cohen, R., Fardouly, J., Newton-John, T., & Slater, A. (2019). #BoPo on Instagram: An experimental investigation of the effects of viewing body positive content on young women’s mood and body image. New Media & Society, 21 (7), 1546–1564. https://doi.org/10.1177/1461444819826530
Cornelissen, K. K., Brokjøb, L. G., Gumančík, J., Lowdon, E., McCarty, K., Irvine, K. R., Tovée, M. J., & Cornelissen, P. L. (2022). The effect of own body concerns on judgments of other women’s body size. Frontiers in Psychology, 13 , 888904. https://doi.org/10.3389/fpsyg.2022.888904
Cornelissen, K. K., Widdrington, H., McCarty, K., Pollet, T. V., Tovée, M. J., & Cornelissen, P. L. (2019). Are attitudinal and perceptual body image the same or different? Evidence from high-level adaptation. Body Image, 31 , 35–47. https://doi.org/10.1016/j.bodyim.2019.08.001
Article PubMed Google Scholar
Corno, G., Serino, S., Cipresso, P., Baños, R. M., & Riva, G. (2018). Assessing the relationship between attitudinal and perceptual component of body image disturbance using virtual reality. Cyberpsychology, Behavior, and Social Networking, 21 (11), 679–686. https://doi.org/10.1089/cyber.2018.0340
Essayli, J. H., Murakami, J. M., Wilson, R. E., & Latner, J. D. (2017). The impact of weight labels on body image, internalized weight stigma, affect, perceived health, and intended weight loss behaviors in normal-weight and overweight college women. American Journal of Health Promotion, 31 (6), 484–490. https://doi.org/10.1177/0890117116661982
Evans, C., & Dolan, B. (1993). Body shape questionnaire: Derivation of shortened “alternate forms.” International Journal of Eating Disorders, 13 (3), 315–321. https://doi.org/10.1002/1098-108X(199304)13:3%3c315::AID-EAT2260130310%3e3.0.CO;2-3
Grabe, S., Ward, L. M., & Hyde, J. S. (2008). The role of the media in body image concerns among women: A meta-analysis of experimental and correlational studies. Psychological Bulletin, 134 (3), 460–476. https://doi.org/10.1037/0033-2909.134.3.460
Greenleaf, C., Starks, M., Gomez, L., Chambliss, H., & Martin, S. (2004). Weight-related words associated with figure silhouettes. Body Image, 1 (4), 373–384. https://doi.org/10.1016/j.bodyim.2004.10.004
Groesz, L. M., Levine, M. P., & Murnen, S. K. (2002). The effect of experimental presentation of thin media images on body satisfaction: A meta-analytic review. International Journal of Eating Disorders, 31 (1), 1–16. https://doi.org/10.1002/eat.10005
Grogan, S. (2010). Promoting positive body image in males and females: Contemporary issues and future directions. Sex Roles, 63 , 757–765. https://doi.org/10.1007/s11199-010-9894-z
Harris, C. V., Bradlyn, A. S., Coffman, J., Gunel, E., & Cottrell, L. (2008). BMI-based body size guides for women and men: Development and validation of a novel pictorial method to assess weight-related concepts. International Journal of Obesity, 32 (2), 336–342. https://doi.org/10.1038/sj.ijo.0803704
Heider, N., Spruyt, A., & De Houwer, J. (2018). Body dissatisfaction revisited: On the importance of implicit beliefs about actual and ideal body image. Psychologica Belgica, 57 (4), 158–173. https://doi.org/10.5334/pb.362
Hunger, J. M., & Tomiyama, A. J. (2014). Weight labeling and obesity: A longitudinal study of girls aged 10 to 19 years. JAMA Pediatrics, 168 (6), 579–580. https://doi.org/10.1001/jamapediatrics.2014.122
Kuznetsova, A., Brockhoff, P. B., & Christensen, R. H. B. (2017). lmerTest package: Tests in linear mixed effects models. Journal of Statistical Software, 82 (13), 1–26. https://doi.org/10.18637/jss.v082.i13
Lazuka, R. F., Wick, M. R., Keel, P. K., & Harriger, J. A. (2020). Are we there yet? Progress in depicting diverse images of beauty in Instagram’s body positivity movement. Body Image, 34 , 85–93. https://doi.org/10.1016/j.bodyim.2020.05.001
Legault, L., & Sago, A. (2022). When body positivity falls flat: Divergent effects of body acceptance messages that support vs. undermine basic psychological needs. Body Image, 41 , 225–238. https://doi.org/10.1016/j.bodyim.2022.02.013
Lentillon-Kaestner, V., Berchtold, A., Rousseau, A., & Ferrand, C. (2014). Validity and reliability of the French versions of the body shape questionnaire. Journal of Personality Assessment, 96 (4), 471–477. https://doi.org/10.1080/00223891.2013.843537
McBride, W. J., & McClelland, C. W. (1967). PERT and the beta distribution. IEEE Transactions on Engineering Management, EM-14 (4), 166–169. https://doi.org/10.1109/TEM.1967.6446985
McFarlane, T., Polivy, J., & Herman, C. P. (1998). Effects of false weight feedback on mood, self-evaluation, and food intake in restrained and unrestrained eaters. Journal of Abnormal Psychology, 107 (2), 312–318. https://doi.org/10.1037/0021-843X.107.2.312
Moussally, J. M., Grynberg, D., Goffinet, S., Simon, Y., & Van der Linden, M. (2017a). Novel assessment of own and ideal body perception among women: Validation of the computer-generated figure rating scale. Cognitive Therapy and Research, 41 (4), 632–644. https://doi.org/10.1007/s10608-016-9827-4
Moussally, J. M., Rochat, L., Posada, A., & Van der Linden, M. (2017b). A database of body-only computer-generated pictures of women for body-image studies: Development and preliminary validation. Behavior Research Methods, 49 (1), 172–183. https://doi.org/10.3758/s13428-016-0703-7
Musher-Eizenman, D. R., Holub, S. C., Edwards-Leeper, L., Persson, A. V., & Goldstein, S. E. (2003). The narrow range of acceptable body types of preschoolers and their mothers. Journal of Applied Developmental Psychology, 24 (2), 259–272. https://doi.org/10.1016/S0193-3973(03)00047-9
Nuttall, F. Q. (2015). Body mass index: Obesity, BMI, and health a critical review. Nutrition Today, 50 (3), 117–128. https://doi.org/10.1097/NT.0000000000000092
Ogden, J., & Evans, C. (1996). The problem with weighing: Effects on mood, self-esteem and body image. International Journal of Obesity and Related Metabolic Disorders, 20 (3), 272–277.
PubMed Google Scholar
Oldham, M., & Robinson, E. (2018). Visual body size norms and the under-detection of overweight and obesity: Visual norms and underestimation of obesity. Obesity Science & Practice, 4 (1), 29–40. https://doi.org/10.1002/osp4.143
Opie, C. A., Glenister, K., & Wright, J. (2019). Is social exposure to obesity associated with weight status misperception? Assessing Australians ability to identify overweight and obesity. BMC Public Health, 19 (1), 1222. https://doi.org/10.1186/s12889-019-7556-9
Paterna, A., Alcaraz-Ibáñez, M., Fuller-Tyszkiewicz, M., & Sicilia, Á. (2021). Internalization of body shape ideals and body dissatisfaction: A systematic review and meta-analysis. International Journal of Eating Disorders, 54 (9), 1575–1600. https://doi.org/10.1002/eat.23568
Pauzé, A., Plouffe-Demers, M.-P., Fiset, D., Saint-Amour, D., Cyr, C., & Blais, C. (2021). The relationship between orthorexia nervosa symptomatology and body image attitudes and distortion. Scientific Reports, 11 (1), 13311. https://doi.org/10.1038/s41598-021-92569-2
Pollet, T. V., Dawson, S., Tovée, M. J., Cornelissen, P. L., & Cornelissen, K. K. (2021). Fat talk is predicted by body dissatisfaction and social comparison with no interaction effect: Evidence from two replication studies. Body Image, 38 , 317–324. https://doi.org/10.1016/j.bodyim.2021.05.005
Pouillot, R., & Delignette-Muller, M. L. (2010). Evaluating variability and uncertainty separately in microbial quantitative risk assessment using two R packages. International Journal of Food Microbiology, 142 (3), 330–340. https://doi.org/10.1016/j.ijfoodmicro.2010.07.011
Puhl, R. M. (2020). What words should we use to talk about weight? A systematic review of quantitative and qualitative studies examining preferences for weight-related terminology. Obesity Reviews . https://doi.org/10.1111/obr.13008
R Core Team. (2022). R: A language and environment for statistical computing. R Foundation for Statistical Computing. https://www.R-project.org/
Rand, C. S. W., Resnick, J. L., & Seldmant, R. S. (1997). Assessment of socially acceptable body sizes by university students. Obesity Research, 5 (5), 425–429. https://doi.org/10.1002/j.1550-8528.1997.tb00665.x
Robinson, E. (2017). Overweight but unseen: A review of the underestimation of weight status and a visual normalization theory. Obesity Reviews, 18 (10), 1200–1209. https://doi.org/10.1111/obr.12570
Romero-Corral, A., Somers, V. K., Sierra-Johnson, J., Thomas, R. J., Collazo-Clavell, M. L., Korinek, J., Allison, T. G., Batsis, J. A., Sert-Kuniyoshi, F. H., & Lopez-Jimenez, F. (2008). Accuracy of body mass index in diagnosing obesity in the adult general population. International Journal of Obesity, 32 (6), 959–966. https://doi.org/10.1038/ijo.2008.11
Rousseau, A., Knotter, A., Barbe, P., Raich, R. M., & Chabrol, H. (2005). Validation of the French version of the body shape questionnaire. L’encéphale, 31 (2), 162–173. https://doi.org/10.1016/S0013-7006(05)82383-8
Smith, C. A., Schmoll, K., Konik, J., & Oberlander, S. (2007). Carrying weight for the world: Influence of weight descriptors on judgments of large-sized women. Journal of Applied Social Psychology, 37 (5), 989–1006. https://doi.org/10.1111/j.1559-1816.2007.00196.x
Stewart, S.-J.F., & Ogden, J. (2021). The role of social exposure in predicting weight bias and weight bias internalisation: An international study. International Journal of Obesity, 45 (6), 1259–1270. https://doi.org/10.1038/s41366-021-00791-9
Stunkard, A. J., Sorensen, T., & Schulsinger, F. (1983). Use of Danish adoption register for the study of obesity and thinness. In S. S. Kety, L. P. Rowland, R. L. Sidman, & S. W. Matthysse (Eds.), Genetics of neurological and psychiatric disorders (pp. 115–120). Raven Press.
Google Scholar
Thompson, J. K., & Heinberg, L. J. (1999). The media’s influence on body image disturbance and eating disorders: We’ve reviled them, now can we rehabilitate them? Journal of Social Issues, 55 (2), 339–353. https://doi.org/10.1111/0022-4537.00119
Thompson, J. K., & Stice, E. (2001). Thin-ideal internalization: Mounting evidence for a new risk factor for body-image disturbance and eating pathology. Current Directions in Psychological Science, 10 (5), 181–183. https://doi.org/10.1111/1467-8721.00144
Thurston, I. B., Decker, K. M., Kamody, R. C., Kaufman, C. C., Maye, C. E., Richmond, T. K., & Sonneville, K. R. (2022). The scale matters: Assessing body size with figure rating scales in a diverse sample of young adults. Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity, 27 , 263–271. https://doi.org/10.1007/s40519-021-01166-9
Tiggemann, M., Anderberg, I., & Brown, Z. (2020). #Loveyourbody: The effect of body positive Instagram captions on women’s body image. Body Image, 33 , 129–136. https://doi.org/10.1016/j.bodyim.2020.02.015
Williamson, G., Osa, M. L., Budd, E., & Kelly, N. R. (2021). Weight-related teasing is associated with body concerns, disordered eating, and health diagnoses in racially and ethnically diverse young men. Body Image, 38 , 37–48. https://doi.org/10.1016/j.bodyim.2021.03.010
Download references
This research received no specific grant from any funding agency. It was funded by the Body and Space team of the Laboratory of Psychology and NeuroCognition (LPNC).
Author information
Authors and affiliations.
Univ. Grenoble Alpes, Univ. Savoie Mont Blanc, CNRS, LPNC, 38000, Grenoble, France
Thomas Chazelle, Michel Guerraz & Richard Palluel-Germain
You can also search for this author in PubMed Google Scholar
Contributions
T.C.: conceptualization, data curation, formal analysis, investigation, methodology, project administration, resources, software, visualization, writing—original draft; M.G.: conceptualization, funding acquisition, methodology, supervision, validation, writing—review and editing; R.P.-G.: conceptualization, funding acquisition, investigation, methodology, project administration, resources, supervision, validation, writing—review and editing. All authors gave final approval for publication and agreed to be held accountable for the work performed therein.
Corresponding author
Correspondence to Richard Palluel-Germain .
Ethics declarations
Conflict of interest.
The authors declare no competing interests.
Ethical approval
This experiment was approved by the Grenoble Alpes Research Ethics Committee (CERGA-Avis-2021-10). All participants consented to participate in the study.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Chazelle, T., Guerraz, M. & Palluel-Germain, R. Modeling body size information within weight labels using probability distributions. Psychological Research (2024). https://doi.org/10.1007/s00426-024-02006-y
Download citation
Received : 15 December 2023
Accepted : 06 July 2024
Published : 22 July 2024
DOI : https://doi.org/10.1007/s00426-024-02006-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Find a journal
- Publish with us
- Track your research

COMMENTS
During the last 25 years, most research on body weight control has been adipocentric. However, since FM accounts for only 10 to 40% of body weight, any control of FM can represent only a similarly sized part of the body weight control. ... The ideas presented in this paper also point to the need for a self-critical view: two generations of ...
However, the focus of the existing body of research on PA and BMD is between structured resistance/weight bearing and aerobic exercise [32,33]. However, the selection of a preference for modality is intuitive, as both forms of exercise elicit similar increases in spine BMD following 12-24 months of structured PA (resistance 0.8-6.8% ...
1. Introduction. Many different diets are proposed for prevention and treatment of overweight and obesity. In several popular diets, the overall strategy is to manipulate macronutrient composition within the whole diet and to focus on limiting or increasing one macronutrient [1,2,3].Classic theories posit that macronutrient composition of a diet or a meal affects appetite via homeostatic ...
Body weight, and its extreme of obesity, has emerged as a major public health concern. Nearly 1/3 of the adult US population is now estimated to be obese, as defined by a body mass index (BMI, the weight in kilograms divided by the square of the height in meters) ≥ 30. 1 The cost of obesity on the healthcare system is substantial; an estimated $147 billion in medical costs were attributed to ...
The body mass index (BMI) is the metric currently in use for defining anthropometric height/weight characteristics in adults and for classifying (categorizing) them into groups. The common interpretation is that it represents an index of an individual's fatness. It also is widely used as a risk factor for the development of or the prevalence of ...
In the United States, overweight and obesity are chronic diseases that contribute to excess morbidity and mortality. Despite public health efforts, these disorders are on the rise, and their consequences are burgeoning. 1 The Centers for Disease Control and Prevention report that during 2017 to 2018, the prevalence of obesity in the United States was 42.4%, which was increased from the ...
The mean change in body weight from baseline to week 68 was −14.9% in the semaglutide group as compared with −2.4% with placebo, for an estimated treatment difference of −12.4 percentage ...
This project aimed to identify the perceptions of body weight that vary by body mass index. First, a qualitative study explored body weight perceptions in 17 individuals with overweight. Second, a questionnaire was developed and completed by a UK sample with body mass index from 16.6 to 59.7 kg/m 2 (N = 328). A higher body mass index was ...
This overview of reviews aimed to summarize the effects of exercise training programs on weight loss, changes in body composition, and weight maintenance in adults with overweight or obesity. A systematic search of systematic reviews and meta-analyses (SR-MAs) published between 2010 and December 201 …
Objective To examine the effectiveness of behavioural weight management interventions for adults with obesity delivered in primary care. Design Systematic review and meta-analysis of randomised controlled trials. Eligibility criteria for selection of studies Randomised controlled trials of behavioural weight management interventions for adults with a body mass index ≥25 delivered in primary ...
Circadian physiology has been linked to body weight regulation and obesity. To date, few studies have assessed the association between exercise timing and weight related outcomes. The aim of this ...
BMI as a Determinant of Body Fat Mass. A particular problem with BMI as an index of obesity is that it does not differentiate between body lean mass and body fat mass; that is, a person can have a high BMI but still have a very low fat mass and vice versa. 39,41-46 From an anatomical and metabolic perspective, the term obesity should refer to an excessive accumulation of body fat ...
Concern regarding "overweight" and "obesity" is reflected in a diverse range of policy measures aimed at helping individuals reduce their body mass index (BMI) 1.Despite attention from the public health establishment, a private weight loss industry estimated at $58.6 billion annually in the United States [], unprecedented levels of body dissatisfaction [] and repeated attempts to lose weight ...
Methods. We conducted a randomized controlled single center trial (ClinicalTrial.gov number, NCT03672903), to evaluate the efficacy of artificially increased weight loading on body weight in subjects with mild obesity (BMI 30-35 kg/m 2).Subjects were either treated with a heavy (=high load; 11% of body weight) or light (=low load; 1% of body weight) weight vest for eight hours per day for ...
As opposed to waist circumference (WC) or body mass index (BMI), weight-adjusted waist index (WWI) is a superior method for assessing obesity. ... All research data for this paper can be found in ...
Introduction. The body mass index (BMI kg/m 2) is an index of weight-for-height that works on the premise that weight increases proportionately to height squared, so that dividing weight by height squared results in an index that is uncorrelated with height.This is an attractive quality for researchers and clinicians who want to analyse or assess body weight while accounting for the fact that ...
The review will help to grasp the complexity of the problem and can lead to novel hypotheses in obesity research. Objective. This paper focuses on the objective to understand historical background on the development of "reference and standard tables" of weight as a platform for normal versus abnormal body weight definition. Methods.
When body weight is reduced as a result of consuming a calorie-restricted diet, approximately 75% of the weight lost is fat mass, and 25% is lean mass 42,43,44,45. Based on the evidence reviewed ...
1. INTRODUCTION. Physical activity is recognized as an integral part of the management of persons with overweight or obesity in combination with diet, behavioral support, and treatment of comorbidities. 1, 2, 3 Expected benefits of physical activity, or exercise, in this setting include positive effects on weight loss, but also fat loss together with preservation of lean mass during weight ...
Objective To summarise evidence on the association between intake of dietary sugars and body weight in adults and children. Design Systematic review and meta-analysis of randomised controlled trials and prospective cohort studies. Data sources OVID Medline, Embase, PubMed, Cumulative Index to Nursing and Allied Health Literature, Scopus, and Web of Science (up to December 2011).
In our study, body fat in men and women were 18.33 and 19.82. The body fat percentage in men and women were 25.74% and 34.01%. Visceral fat area in men and women were 91.98 and 77 cm 2. And, with the increase of age, body fat, body fat percentages and visceral fat area also increased, both in men and in women.
Associations with changes in blood lipids and HbA1c were minor, consistent with previous research showing that body weight is more closely related to blood pressure than lipids ... PAPER Effects of ten year body weight variability on cardiovascular risk factors in Japanese middle-aged men and women [Internet] Int. J. Obes., 25 (2001) ...
Another recent secondary analysis also found that evening exercise may lead to more favorable effects on body weight, body composition, and insulin sensitivity in men who were at risk for or diagnosed with type 2 diabetes . Thirty-two men self-selected to exercise in the morning (08:00-10:00) or the early evening (15:00-18:00) for 12 weeks.
Background: This systematic review and meta-analysis aimed to investigate the effect of cinnamon on body weight, body mass index (BMI), waist circumference (WC), waist-hip ratio (WHR), and body fat mass including the maximum number of studies. Methods: Medline, ISI Web of Science, Scopus, Google Scholar, and Cochrane library were searched with no limitation from inception up to August 2019 for ...
The way we talk about body shape has been extensively studied in clinical and social psychology as a type of interpersonal social influence. The use of weight labels, specific words describing body size and shape, is associated with a wide range of outcomes, including body dissatisfaction (Essayli et al., 2017; Puhl, 2020), social comparison tendencies (Pollet et al., 2021), and health (Hunger ...
This has been evidenced for sports with the weight category. Research has shown that rapid weight loss (RWL) of up to 3% of body mass (BM), which can be accomplished by various means such as short-term fluid restriction or exercise, and has minimal impact on performance, is relatively safe with effective rehydration strategies (Burke et al ...