Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
Methodology
- Ethical Considerations in Research | Types & Examples

Ethical Considerations in Research | Types & Examples
Published on October 18, 2021 by Pritha Bhandari . Revised on May 9, 2024.
Ethical considerations in research are a set of principles that guide your research designs and practices. Scientists and researchers must always adhere to a certain code of conduct when collecting data from people.
The goals of human research often include understanding real-life phenomena, studying effective treatments, investigating behaviors, and improving lives in other ways. What you decide to research and how you conduct that research involve key ethical considerations.
These considerations work to
- protect the rights of research participants
- enhance research validity
- maintain scientific or academic integrity
Table of contents
Why do research ethics matter, getting ethical approval for your study, types of ethical issues, voluntary participation, informed consent, confidentiality, potential for harm, results communication, examples of ethical failures, other interesting articles, frequently asked questions about research ethics.
Research ethics matter for scientific integrity, human rights and dignity, and collaboration between science and society. These principles make sure that participation in studies is voluntary, informed, and safe for research subjects.
You’ll balance pursuing important research objectives with using ethical research methods and procedures. It’s always necessary to prevent permanent or excessive harm to participants, whether inadvertent or not.
Defying research ethics will also lower the credibility of your research because it’s hard for others to trust your data if your methods are morally questionable.
Even if a research idea is valuable to society, it doesn’t justify violating the human rights or dignity of your study participants.
Receive feedback on language, structure, and formatting
Professional editors proofread and edit your paper by focusing on:
- Academic style
- Vague sentences
- Style consistency
See an example

Before you start any study involving data collection with people, you’ll submit your research proposal to an institutional review board (IRB) .
An IRB is a committee that checks whether your research aims and research design are ethically acceptable and follow your institution’s code of conduct. They check that your research materials and procedures are up to code.
If successful, you’ll receive IRB approval, and you can begin collecting data according to the approved procedures. If you want to make any changes to your procedures or materials, you’ll need to submit a modification application to the IRB for approval.
If unsuccessful, you may be asked to re-submit with modifications or your research proposal may receive a rejection. To get IRB approval, it’s important to explicitly note how you’ll tackle each of the ethical issues that may arise in your study.
There are several ethical issues you should always pay attention to in your research design, and these issues can overlap with each other.
You’ll usually outline ways you’ll deal with each issue in your research proposal if you plan to collect data from participants.
| Voluntary participation | Your participants are free to opt in or out of the study at any point in time. |
|---|---|
| Informed consent | Participants know the purpose, benefits, risks, and funding behind the study before they agree or decline to join. |
| Anonymity | You don’t know the identities of the participants. Personally identifiable data is not collected. |
| Confidentiality | You know who the participants are but you keep that information hidden from everyone else. You anonymize personally identifiable data so that it can’t be linked to other data by anyone else. |
| Potential for harm | Physical, social, psychological and all other types of harm are kept to an absolute minimum. |
| Results communication | You ensure your work is free of or research misconduct, and you accurately represent your results. |
Voluntary participation means that all research subjects are free to choose to participate without any pressure or coercion.
All participants are able to withdraw from, or leave, the study at any point without feeling an obligation to continue. Your participants don’t need to provide a reason for leaving the study.
It’s important to make it clear to participants that there are no negative consequences or repercussions to their refusal to participate. After all, they’re taking the time to help you in the research process , so you should respect their decisions without trying to change their minds.
Voluntary participation is an ethical principle protected by international law and many scientific codes of conduct.
Take special care to ensure there’s no pressure on participants when you’re working with vulnerable groups of people who may find it hard to stop the study even when they want to.
Prevent plagiarism. Run a free check.
Informed consent refers to a situation in which all potential participants receive and understand all the information they need to decide whether they want to participate. This includes information about the study’s benefits, risks, funding, and institutional approval.
You make sure to provide all potential participants with all the relevant information about
- what the study is about
- the risks and benefits of taking part
- how long the study will take
- your supervisor’s contact information and the institution’s approval number
Usually, you’ll provide participants with a text for them to read and ask them if they have any questions. If they agree to participate, they can sign or initial the consent form. Note that this may not be sufficient for informed consent when you work with particularly vulnerable groups of people.
If you’re collecting data from people with low literacy, make sure to verbally explain the consent form to them before they agree to participate.
For participants with very limited English proficiency, you should always translate the study materials or work with an interpreter so they have all the information in their first language.
In research with children, you’ll often need informed permission for their participation from their parents or guardians. Although children cannot give informed consent, it’s best to also ask for their assent (agreement) to participate, depending on their age and maturity level.
Anonymity means that you don’t know who the participants are and you can’t link any individual participant to their data.
You can only guarantee anonymity by not collecting any personally identifying information—for example, names, phone numbers, email addresses, IP addresses, physical characteristics, photos, and videos.
In many cases, it may be impossible to truly anonymize data collection . For example, data collected in person or by phone cannot be considered fully anonymous because some personal identifiers (demographic information or phone numbers) are impossible to hide.
You’ll also need to collect some identifying information if you give your participants the option to withdraw their data at a later stage.
Data pseudonymization is an alternative method where you replace identifying information about participants with pseudonymous, or fake, identifiers. The data can still be linked to participants but it’s harder to do so because you separate personal information from the study data.
Confidentiality means that you know who the participants are, but you remove all identifying information from your report.
All participants have a right to privacy, so you should protect their personal data for as long as you store or use it. Even when you can’t collect data anonymously, you should secure confidentiality whenever you can.
Some research designs aren’t conducive to confidentiality, but it’s important to make all attempts and inform participants of the risks involved.
As a researcher, you have to consider all possible sources of harm to participants. Harm can come in many different forms.
- Psychological harm: Sensitive questions or tasks may trigger negative emotions such as shame or anxiety.
- Social harm: Participation can involve social risks, public embarrassment, or stigma.
- Physical harm: Pain or injury can result from the study procedures.
- Legal harm: Reporting sensitive data could lead to legal risks or a breach of privacy.
It’s best to consider every possible source of harm in your study as well as concrete ways to mitigate them. Involve your supervisor to discuss steps for harm reduction.
Make sure to disclose all possible risks of harm to participants before the study to get informed consent. If there is a risk of harm, prepare to provide participants with resources or counseling or medical services if needed.
Some of these questions may bring up negative emotions, so you inform participants about the sensitive nature of the survey and assure them that their responses will be confidential.
The way you communicate your research results can sometimes involve ethical issues. Good science communication is honest, reliable, and credible. It’s best to make your results as transparent as possible.
Take steps to actively avoid plagiarism and research misconduct wherever possible.
Plagiarism means submitting others’ works as your own. Although it can be unintentional, copying someone else’s work without proper credit amounts to stealing. It’s an ethical problem in research communication because you may benefit by harming other researchers.
Self-plagiarism is when you republish or re-submit parts of your own papers or reports without properly citing your original work.
This is problematic because you may benefit from presenting your ideas as new and original even though they’ve already been published elsewhere in the past. You may also be infringing on your previous publisher’s copyright, violating an ethical code, or wasting time and resources by doing so.
In extreme cases of self-plagiarism, entire datasets or papers are sometimes duplicated. These are major ethical violations because they can skew research findings if taken as original data.
You notice that two published studies have similar characteristics even though they are from different years. Their sample sizes, locations, treatments, and results are highly similar, and the studies share one author in common.
Research misconduct
Research misconduct means making up or falsifying data, manipulating data analyses, or misrepresenting results in research reports. It’s a form of academic fraud.
These actions are committed intentionally and can have serious consequences; research misconduct is not a simple mistake or a point of disagreement about data analyses.
Research misconduct is a serious ethical issue because it can undermine academic integrity and institutional credibility. It leads to a waste of funding and resources that could have been used for alternative research.
Later investigations revealed that they fabricated and manipulated their data to show a nonexistent link between vaccines and autism. Wakefield also neglected to disclose important conflicts of interest, and his medical license was taken away.
This fraudulent work sparked vaccine hesitancy among parents and caregivers. The rate of MMR vaccinations in children fell sharply, and measles outbreaks became more common due to a lack of herd immunity.
Research scandals with ethical failures are littered throughout history, but some took place not that long ago.
Some scientists in positions of power have historically mistreated or even abused research participants to investigate research problems at any cost. These participants were prisoners, under their care, or otherwise trusted them to treat them with dignity.
To demonstrate the importance of research ethics, we’ll briefly review two research studies that violated human rights in modern history.
These experiments were inhumane and resulted in trauma, permanent disabilities, or death in many cases.
After some Nazi doctors were put on trial for their crimes, the Nuremberg Code of research ethics for human experimentation was developed in 1947 to establish a new standard for human experimentation in medical research.
In reality, the actual goal was to study the effects of the disease when left untreated, and the researchers never informed participants about their diagnoses or the research aims.
Although participants experienced severe health problems, including blindness and other complications, the researchers only pretended to provide medical care.
When treatment became possible in 1943, 11 years after the study began, none of the participants were offered it, despite their health conditions and high risk of death.
Ethical failures like these resulted in severe harm to participants, wasted resources, and lower trust in science and scientists. This is why all research institutions have strict ethical guidelines for performing research.
If you want to know more about statistics , methodology , or research bias , make sure to check out some of our other articles with explanations and examples.
- Normal distribution
- Measures of central tendency
- Chi square tests
- Confidence interval
- Quartiles & Quantiles
- Cluster sampling
- Stratified sampling
- Thematic analysis
- Cohort study
- Peer review
- Ethnography
Research bias
- Implicit bias
- Cognitive bias
- Conformity bias
- Hawthorne effect
- Availability heuristic
- Attrition bias
- Social desirability bias
Ethical considerations in research are a set of principles that guide your research designs and practices. These principles include voluntary participation, informed consent, anonymity, confidentiality, potential for harm, and results communication.
Scientists and researchers must always adhere to a certain code of conduct when collecting data from others .
These considerations protect the rights of research participants, enhance research validity , and maintain scientific integrity.
Research ethics matter for scientific integrity, human rights and dignity, and collaboration between science and society. These principles make sure that participation in studies is voluntary, informed, and safe.
Anonymity means you don’t know who the participants are, while confidentiality means you know who they are but remove identifying information from your research report. Both are important ethical considerations .
You can only guarantee anonymity by not collecting any personally identifying information—for example, names, phone numbers, email addresses, IP addresses, physical characteristics, photos, or videos.
You can keep data confidential by using aggregate information in your research report, so that you only refer to groups of participants rather than individuals.
These actions are committed intentionally and can have serious consequences; research misconduct is not a simple mistake or a point of disagreement but a serious ethical failure.
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
Bhandari, P. (2024, May 09). Ethical Considerations in Research | Types & Examples. Scribbr. Retrieved June 7, 2024, from https://www.scribbr.com/methodology/research-ethics/
Is this article helpful?

Pritha Bhandari
Other students also liked, data collection | definition, methods & examples, what is self-plagiarism | definition & how to avoid it, how to avoid plagiarism | tips on citing sources, what is your plagiarism score.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
National Institute of Environmental Health Sciences
Your environment. your health., what is ethics in research & why is it important, by david b. resnik, j.d., ph.d..
December 23, 2020
The ideas and opinions expressed in this essay are the author’s own and do not necessarily represent those of the NIH, NIEHS, or US government.

When most people think of ethics (or morals), they think of rules for distinguishing between right and wrong, such as the Golden Rule ("Do unto others as you would have them do unto you"), a code of professional conduct like the Hippocratic Oath ("First of all, do no harm"), a religious creed like the Ten Commandments ("Thou Shalt not kill..."), or a wise aphorisms like the sayings of Confucius. This is the most common way of defining "ethics": norms for conduct that distinguish between acceptable and unacceptable behavior.
Most people learn ethical norms at home, at school, in church, or in other social settings. Although most people acquire their sense of right and wrong during childhood, moral development occurs throughout life and human beings pass through different stages of growth as they mature. Ethical norms are so ubiquitous that one might be tempted to regard them as simple commonsense. On the other hand, if morality were nothing more than commonsense, then why are there so many ethical disputes and issues in our society?
Alternatives to Animal Testing

Alternative test methods are methods that replace, reduce, or refine animal use in research and testing
Learn more about Environmental science Basics
One plausible explanation of these disagreements is that all people recognize some common ethical norms but interpret, apply, and balance them in different ways in light of their own values and life experiences. For example, two people could agree that murder is wrong but disagree about the morality of abortion because they have different understandings of what it means to be a human being.
Most societies also have legal rules that govern behavior, but ethical norms tend to be broader and more informal than laws. Although most societies use laws to enforce widely accepted moral standards and ethical and legal rules use similar concepts, ethics and law are not the same. An action may be legal but unethical or illegal but ethical. We can also use ethical concepts and principles to criticize, evaluate, propose, or interpret laws. Indeed, in the last century, many social reformers have urged citizens to disobey laws they regarded as immoral or unjust laws. Peaceful civil disobedience is an ethical way of protesting laws or expressing political viewpoints.
Another way of defining 'ethics' focuses on the disciplines that study standards of conduct, such as philosophy, theology, law, psychology, or sociology. For example, a "medical ethicist" is someone who studies ethical standards in medicine. One may also define ethics as a method, procedure, or perspective for deciding how to act and for analyzing complex problems and issues. For instance, in considering a complex issue like global warming , one may take an economic, ecological, political, or ethical perspective on the problem. While an economist might examine the cost and benefits of various policies related to global warming, an environmental ethicist could examine the ethical values and principles at stake.
See ethics in practice at NIEHS
Read latest updates in our monthly Global Environmental Health Newsletter

Many different disciplines, institutions , and professions have standards for behavior that suit their particular aims and goals. These standards also help members of the discipline to coordinate their actions or activities and to establish the public's trust of the discipline. For instance, ethical standards govern conduct in medicine, law, engineering, and business. Ethical norms also serve the aims or goals of research and apply to people who conduct scientific research or other scholarly or creative activities. There is even a specialized discipline, research ethics, which studies these norms. See Glossary of Commonly Used Terms in Research Ethics and Research Ethics Timeline .
There are several reasons why it is important to adhere to ethical norms in research. First, norms promote the aims of research , such as knowledge, truth, and avoidance of error. For example, prohibitions against fabricating , falsifying, or misrepresenting research data promote the truth and minimize error.
Join an NIEHS Study
See how we put research Ethics to practice.
Visit Joinastudy.niehs.nih.gov to see the various studies NIEHS perform.

Second, since research often involves a great deal of cooperation and coordination among many different people in different disciplines and institutions, ethical standards promote the values that are essential to collaborative work , such as trust, accountability, mutual respect, and fairness. For example, many ethical norms in research, such as guidelines for authorship , copyright and patenting policies , data sharing policies, and confidentiality rules in peer review, are designed to protect intellectual property interests while encouraging collaboration. Most researchers want to receive credit for their contributions and do not want to have their ideas stolen or disclosed prematurely.
Third, many of the ethical norms help to ensure that researchers can be held accountable to the public . For instance, federal policies on research misconduct, conflicts of interest, the human subjects protections, and animal care and use are necessary in order to make sure that researchers who are funded by public money can be held accountable to the public.
Fourth, ethical norms in research also help to build public support for research. People are more likely to fund a research project if they can trust the quality and integrity of research.
Finally, many of the norms of research promote a variety of other important moral and social values , such as social responsibility, human rights, animal welfare, compliance with the law, and public health and safety. Ethical lapses in research can significantly harm human and animal subjects, students, and the public. For example, a researcher who fabricates data in a clinical trial may harm or even kill patients, and a researcher who fails to abide by regulations and guidelines relating to radiation or biological safety may jeopardize his health and safety or the health and safety of staff and students.
Codes and Policies for Research Ethics
Given the importance of ethics for the conduct of research, it should come as no surprise that many different professional associations, government agencies, and universities have adopted specific codes, rules, and policies relating to research ethics. Many government agencies have ethics rules for funded researchers.
- National Institutes of Health (NIH)
- National Science Foundation (NSF)
- Food and Drug Administration (FDA)
- Environmental Protection Agency (EPA)
- US Department of Agriculture (USDA)
- Singapore Statement on Research Integrity
- American Chemical Society, The Chemist Professional’s Code of Conduct
- Code of Ethics (American Society for Clinical Laboratory Science)
- American Psychological Association, Ethical Principles of Psychologists and Code of Conduct
- Statement on Professional Ethics (American Association of University Professors)
- Nuremberg Code
- World Medical Association's Declaration of Helsinki
Ethical Principles
The following is a rough and general summary of some ethical principles that various codes address*:

Strive for honesty in all scientific communications. Honestly report data, results, methods and procedures, and publication status. Do not fabricate, falsify, or misrepresent data. Do not deceive colleagues, research sponsors, or the public.

Objectivity
Strive to avoid bias in experimental design, data analysis, data interpretation, peer review, personnel decisions, grant writing, expert testimony, and other aspects of research where objectivity is expected or required. Avoid or minimize bias or self-deception. Disclose personal or financial interests that may affect research.

Keep your promises and agreements; act with sincerity; strive for consistency of thought and action.

Carefulness
Avoid careless errors and negligence; carefully and critically examine your own work and the work of your peers. Keep good records of research activities, such as data collection, research design, and correspondence with agencies or journals.

Share data, results, ideas, tools, resources. Be open to criticism and new ideas.
Transparency
Disclose methods, materials, assumptions, analyses, and other information needed to evaluate your research.

Accountability
Take responsibility for your part in research and be prepared to give an account (i.e. an explanation or justification) of what you did on a research project and why.

Intellectual Property
Honor patents, copyrights, and other forms of intellectual property. Do not use unpublished data, methods, or results without permission. Give proper acknowledgement or credit for all contributions to research. Never plagiarize.

Confidentiality
Protect confidential communications, such as papers or grants submitted for publication, personnel records, trade or military secrets, and patient records.

Responsible Publication
Publish in order to advance research and scholarship, not to advance just your own career. Avoid wasteful and duplicative publication.

Responsible Mentoring
Help to educate, mentor, and advise students. Promote their welfare and allow them to make their own decisions.

Respect for Colleagues
Respect your colleagues and treat them fairly.

Social Responsibility
Strive to promote social good and prevent or mitigate social harms through research, public education, and advocacy.

Non-Discrimination
Avoid discrimination against colleagues or students on the basis of sex, race, ethnicity, or other factors not related to scientific competence and integrity.
Maintain and improve your own professional competence and expertise through lifelong education and learning; take steps to promote competence in science as a whole.

Know and obey relevant laws and institutional and governmental policies.

Animal Care
Show proper respect and care for animals when using them in research. Do not conduct unnecessary or poorly designed animal experiments.

Human Subjects protection
When conducting research on human subjects, minimize harms and risks and maximize benefits; respect human dignity, privacy, and autonomy; take special precautions with vulnerable populations; and strive to distribute the benefits and burdens of research fairly.
* Adapted from Shamoo A and Resnik D. 2015. Responsible Conduct of Research, 3rd ed. (New York: Oxford University Press).
Ethical Decision Making in Research
Although codes, policies, and principles are very important and useful, like any set of rules, they do not cover every situation, they often conflict, and they require interpretation. It is therefore important for researchers to learn how to interpret, assess, and apply various research rules and how to make decisions and act ethically in various situations. The vast majority of decisions involve the straightforward application of ethical rules. For example, consider the following case:
The research protocol for a study of a drug on hypertension requires the administration of the drug at different doses to 50 laboratory mice, with chemical and behavioral tests to determine toxic effects. Tom has almost finished the experiment for Dr. Q. He has only 5 mice left to test. However, he really wants to finish his work in time to go to Florida on spring break with his friends, who are leaving tonight. He has injected the drug in all 50 mice but has not completed all of the tests. He therefore decides to extrapolate from the 45 completed results to produce the 5 additional results.
Many different research ethics policies would hold that Tom has acted unethically by fabricating data. If this study were sponsored by a federal agency, such as the NIH, his actions would constitute a form of research misconduct , which the government defines as "fabrication, falsification, or plagiarism" (or FFP). Actions that nearly all researchers classify as unethical are viewed as misconduct. It is important to remember, however, that misconduct occurs only when researchers intend to deceive : honest errors related to sloppiness, poor record keeping, miscalculations, bias, self-deception, and even negligence do not constitute misconduct. Also, reasonable disagreements about research methods, procedures, and interpretations do not constitute research misconduct. Consider the following case:
Dr. T has just discovered a mathematical error in his paper that has been accepted for publication in a journal. The error does not affect the overall results of his research, but it is potentially misleading. The journal has just gone to press, so it is too late to catch the error before it appears in print. In order to avoid embarrassment, Dr. T decides to ignore the error.
Dr. T's error is not misconduct nor is his decision to take no action to correct the error. Most researchers, as well as many different policies and codes would say that Dr. T should tell the journal (and any coauthors) about the error and consider publishing a correction or errata. Failing to publish a correction would be unethical because it would violate norms relating to honesty and objectivity in research.
There are many other activities that the government does not define as "misconduct" but which are still regarded by most researchers as unethical. These are sometimes referred to as " other deviations " from acceptable research practices and include:
- Publishing the same paper in two different journals without telling the editors
- Submitting the same paper to different journals without telling the editors
- Not informing a collaborator of your intent to file a patent in order to make sure that you are the sole inventor
- Including a colleague as an author on a paper in return for a favor even though the colleague did not make a serious contribution to the paper
- Discussing with your colleagues confidential data from a paper that you are reviewing for a journal
- Using data, ideas, or methods you learn about while reviewing a grant or a papers without permission
- Trimming outliers from a data set without discussing your reasons in paper
- Using an inappropriate statistical technique in order to enhance the significance of your research
- Bypassing the peer review process and announcing your results through a press conference without giving peers adequate information to review your work
- Conducting a review of the literature that fails to acknowledge the contributions of other people in the field or relevant prior work
- Stretching the truth on a grant application in order to convince reviewers that your project will make a significant contribution to the field
- Stretching the truth on a job application or curriculum vita
- Giving the same research project to two graduate students in order to see who can do it the fastest
- Overworking, neglecting, or exploiting graduate or post-doctoral students
- Failing to keep good research records
- Failing to maintain research data for a reasonable period of time
- Making derogatory comments and personal attacks in your review of author's submission
- Promising a student a better grade for sexual favors
- Using a racist epithet in the laboratory
- Making significant deviations from the research protocol approved by your institution's Animal Care and Use Committee or Institutional Review Board for Human Subjects Research without telling the committee or the board
- Not reporting an adverse event in a human research experiment
- Wasting animals in research
- Exposing students and staff to biological risks in violation of your institution's biosafety rules
- Sabotaging someone's work
- Stealing supplies, books, or data
- Rigging an experiment so you know how it will turn out
- Making unauthorized copies of data, papers, or computer programs
- Owning over $10,000 in stock in a company that sponsors your research and not disclosing this financial interest
- Deliberately overestimating the clinical significance of a new drug in order to obtain economic benefits
These actions would be regarded as unethical by most scientists and some might even be illegal in some cases. Most of these would also violate different professional ethics codes or institutional policies. However, they do not fall into the narrow category of actions that the government classifies as research misconduct. Indeed, there has been considerable debate about the definition of "research misconduct" and many researchers and policy makers are not satisfied with the government's narrow definition that focuses on FFP. However, given the huge list of potential offenses that might fall into the category "other serious deviations," and the practical problems with defining and policing these other deviations, it is understandable why government officials have chosen to limit their focus.
Finally, situations frequently arise in research in which different people disagree about the proper course of action and there is no broad consensus about what should be done. In these situations, there may be good arguments on both sides of the issue and different ethical principles may conflict. These situations create difficult decisions for research known as ethical or moral dilemmas . Consider the following case:
Dr. Wexford is the principal investigator of a large, epidemiological study on the health of 10,000 agricultural workers. She has an impressive dataset that includes information on demographics, environmental exposures, diet, genetics, and various disease outcomes such as cancer, Parkinson’s disease (PD), and ALS. She has just published a paper on the relationship between pesticide exposure and PD in a prestigious journal. She is planning to publish many other papers from her dataset. She receives a request from another research team that wants access to her complete dataset. They are interested in examining the relationship between pesticide exposures and skin cancer. Dr. Wexford was planning to conduct a study on this topic.
Dr. Wexford faces a difficult choice. On the one hand, the ethical norm of openness obliges her to share data with the other research team. Her funding agency may also have rules that obligate her to share data. On the other hand, if she shares data with the other team, they may publish results that she was planning to publish, thus depriving her (and her team) of recognition and priority. It seems that there are good arguments on both sides of this issue and Dr. Wexford needs to take some time to think about what she should do. One possible option is to share data, provided that the investigators sign a data use agreement. The agreement could define allowable uses of the data, publication plans, authorship, etc. Another option would be to offer to collaborate with the researchers.
The following are some step that researchers, such as Dr. Wexford, can take to deal with ethical dilemmas in research:
What is the problem or issue?
It is always important to get a clear statement of the problem. In this case, the issue is whether to share information with the other research team.
What is the relevant information?
Many bad decisions are made as a result of poor information. To know what to do, Dr. Wexford needs to have more information concerning such matters as university or funding agency or journal policies that may apply to this situation, the team's intellectual property interests, the possibility of negotiating some kind of agreement with the other team, whether the other team also has some information it is willing to share, the impact of the potential publications, etc.
What are the different options?
People may fail to see different options due to a limited imagination, bias, ignorance, or fear. In this case, there may be other choices besides 'share' or 'don't share,' such as 'negotiate an agreement' or 'offer to collaborate with the researchers.'
How do ethical codes or policies as well as legal rules apply to these different options?
The university or funding agency may have policies on data management that apply to this case. Broader ethical rules, such as openness and respect for credit and intellectual property, may also apply to this case. Laws relating to intellectual property may be relevant.
Are there any people who can offer ethical advice?
It may be useful to seek advice from a colleague, a senior researcher, your department chair, an ethics or compliance officer, or anyone else you can trust. In the case, Dr. Wexford might want to talk to her supervisor and research team before making a decision.
After considering these questions, a person facing an ethical dilemma may decide to ask more questions, gather more information, explore different options, or consider other ethical rules. However, at some point he or she will have to make a decision and then take action. Ideally, a person who makes a decision in an ethical dilemma should be able to justify his or her decision to himself or herself, as well as colleagues, administrators, and other people who might be affected by the decision. He or she should be able to articulate reasons for his or her conduct and should consider the following questions in order to explain how he or she arrived at his or her decision:
- Which choice will probably have the best overall consequences for science and society?
- Which choice could stand up to further publicity and scrutiny?
- Which choice could you not live with?
- Think of the wisest person you know. What would he or she do in this situation?
- Which choice would be the most just, fair, or responsible?
After considering all of these questions, one still might find it difficult to decide what to do. If this is the case, then it may be appropriate to consider others ways of making the decision, such as going with a gut feeling or intuition, seeking guidance through prayer or meditation, or even flipping a coin. Endorsing these methods in this context need not imply that ethical decisions are irrational, however. The main point is that human reasoning plays a pivotal role in ethical decision-making but there are limits to its ability to solve all ethical dilemmas in a finite amount of time.
Promoting Ethical Conduct in Science
Do U.S. research institutions meet or exceed federal mandates for instruction in responsible conduct of research? A national survey
Read about U.S. research instutuins follow federal manadates for ethics in research
Learn more about NIEHS Research
Most academic institutions in the US require undergraduate, graduate, or postgraduate students to have some education in the responsible conduct of research (RCR) . The NIH and NSF have both mandated training in research ethics for students and trainees. Many academic institutions outside of the US have also developed educational curricula in research ethics
Those of you who are taking or have taken courses in research ethics may be wondering why you are required to have education in research ethics. You may believe that you are highly ethical and know the difference between right and wrong. You would never fabricate or falsify data or plagiarize. Indeed, you also may believe that most of your colleagues are highly ethical and that there is no ethics problem in research..
If you feel this way, relax. No one is accusing you of acting unethically. Indeed, the evidence produced so far shows that misconduct is a very rare occurrence in research, although there is considerable variation among various estimates. The rate of misconduct has been estimated to be as low as 0.01% of researchers per year (based on confirmed cases of misconduct in federally funded research) to as high as 1% of researchers per year (based on self-reports of misconduct on anonymous surveys). See Shamoo and Resnik (2015), cited above.
Clearly, it would be useful to have more data on this topic, but so far there is no evidence that science has become ethically corrupt, despite some highly publicized scandals. Even if misconduct is only a rare occurrence, it can still have a tremendous impact on science and society because it can compromise the integrity of research, erode the public’s trust in science, and waste time and resources. Will education in research ethics help reduce the rate of misconduct in science? It is too early to tell. The answer to this question depends, in part, on how one understands the causes of misconduct. There are two main theories about why researchers commit misconduct. According to the "bad apple" theory, most scientists are highly ethical. Only researchers who are morally corrupt, economically desperate, or psychologically disturbed commit misconduct. Moreover, only a fool would commit misconduct because science's peer review system and self-correcting mechanisms will eventually catch those who try to cheat the system. In any case, a course in research ethics will have little impact on "bad apples," one might argue.
According to the "stressful" or "imperfect" environment theory, misconduct occurs because various institutional pressures, incentives, and constraints encourage people to commit misconduct, such as pressures to publish or obtain grants or contracts, career ambitions, the pursuit of profit or fame, poor supervision of students and trainees, and poor oversight of researchers (see Shamoo and Resnik 2015). Moreover, defenders of the stressful environment theory point out that science's peer review system is far from perfect and that it is relatively easy to cheat the system. Erroneous or fraudulent research often enters the public record without being detected for years. Misconduct probably results from environmental and individual causes, i.e. when people who are morally weak, ignorant, or insensitive are placed in stressful or imperfect environments. In any case, a course in research ethics can be useful in helping to prevent deviations from norms even if it does not prevent misconduct. Education in research ethics is can help people get a better understanding of ethical standards, policies, and issues and improve ethical judgment and decision making. Many of the deviations that occur in research may occur because researchers simply do not know or have never thought seriously about some of the ethical norms of research. For example, some unethical authorship practices probably reflect traditions and practices that have not been questioned seriously until recently. If the director of a lab is named as an author on every paper that comes from his lab, even if he does not make a significant contribution, what could be wrong with that? That's just the way it's done, one might argue. Another example where there may be some ignorance or mistaken traditions is conflicts of interest in research. A researcher may think that a "normal" or "traditional" financial relationship, such as accepting stock or a consulting fee from a drug company that sponsors her research, raises no serious ethical issues. Or perhaps a university administrator sees no ethical problem in taking a large gift with strings attached from a pharmaceutical company. Maybe a physician thinks that it is perfectly appropriate to receive a $300 finder’s fee for referring patients into a clinical trial.
If "deviations" from ethical conduct occur in research as a result of ignorance or a failure to reflect critically on problematic traditions, then a course in research ethics may help reduce the rate of serious deviations by improving the researcher's understanding of ethics and by sensitizing him or her to the issues.
Finally, education in research ethics should be able to help researchers grapple with the ethical dilemmas they are likely to encounter by introducing them to important concepts, tools, principles, and methods that can be useful in resolving these dilemmas. Scientists must deal with a number of different controversial topics, such as human embryonic stem cell research, cloning, genetic engineering, and research involving animal or human subjects, which require ethical reflection and deliberation.
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
Nih clinical research trials and you, guiding principles for ethical research.
Pursuing Potential Research Participants Protections

“When people are invited to participate in research, there is a strong belief that it should be their choice based on their understanding of what the study is about, and what the risks and benefits of the study are,” said Dr. Christine Grady, chief of the NIH Clinical Center Department of Bioethics, to Clinical Center Radio in a podcast.
Clinical research advances the understanding of science and promotes human health. However, it is important to remember the individuals who volunteer to participate in research. There are precautions researchers can take – in the planning, implementation and follow-up of studies – to protect these participants in research. Ethical guidelines are established for clinical research to protect patient volunteers and to preserve the integrity of the science.
NIH Clinical Center researchers published seven main principles to guide the conduct of ethical research:
Social and clinical value
Scientific validity, fair subject selection, favorable risk-benefit ratio, independent review, informed consent.
- Respect for potential and enrolled subjects
Every research study is designed to answer a specific question. The answer should be important enough to justify asking people to accept some risk or inconvenience for others. In other words, answers to the research question should contribute to scientific understanding of health or improve our ways of preventing, treating, or caring for people with a given disease to justify exposing participants to the risk and burden of research.
A study should be designed in a way that will get an understandable answer to the important research question. This includes considering whether the question asked is answerable, whether the research methods are valid and feasible, and whether the study is designed with accepted principles, clear methods, and reliable practices. Invalid research is unethical because it is a waste of resources and exposes people to risk for no purpose
The primary basis for recruiting participants should be the scientific goals of the study — not vulnerability, privilege, or other unrelated factors. Participants who accept the risks of research should be in a position to enjoy its benefits. Specific groups of participants (for example, women or children) should not be excluded from the research opportunities without a good scientific reason or a particular susceptibility to risk.
Uncertainty about the degree of risks and benefits associated with a clinical research study is inherent. Research risks may be trivial or serious, transient or long-term. Risks can be physical, psychological, economic, or social. Everything should be done to minimize the risks and inconvenience to research participants to maximize the potential benefits, and to determine that the potential benefits are proportionate to, or outweigh, the risks.
To minimize potential conflicts of interest and make sure a study is ethically acceptable before it starts, an independent review panel should review the proposal and ask important questions, including: Are those conducting the trial sufficiently free of bias? Is the study doing all it can to protect research participants? Has the trial been ethically designed and is the risk–benefit ratio favorable? The panel also monitors a study while it is ongoing.
Potential participants should make their own decision about whether they want to participate or continue participating in research. This is done through a process of informed consent in which individuals (1) are accurately informed of the purpose, methods, risks, benefits, and alternatives to the research, (2) understand this information and how it relates to their own clinical situation or interests, and (3) make a voluntary decision about whether to participate.
Respect for potential and enrolled participants
Individuals should be treated with respect from the time they are approached for possible participation — even if they refuse enrollment in a study — throughout their participation and after their participation ends. This includes:
- respecting their privacy and keeping their private information confidential
- respecting their right to change their mind, to decide that the research does not match their interests, and to withdraw without a penalty
- informing them of new information that might emerge in the course of research, which might change their assessment of the risks and benefits of participating
- monitoring their welfare and, if they experience adverse reactions, unexpected effects, or changes in clinical status, ensuring appropriate treatment and, when necessary, removal from the study
- informing them about what was learned from the research
More information on these seven guiding principles and on bioethics in general
This page last reviewed on March 16, 2016
Connect with Us
- More Social Media from NIH
When you choose to publish with PLOS, your research makes an impact. Make your work accessible to all, without restrictions, and accelerate scientific discovery with options like preprints and published peer review that make your work more Open.
- PLOS Biology
- PLOS Climate
- PLOS Complex Systems
- PLOS Computational Biology
- PLOS Digital Health
- PLOS Genetics
- PLOS Global Public Health
- PLOS Medicine
- PLOS Mental Health
- PLOS Neglected Tropical Diseases
- PLOS Pathogens
- PLOS Sustainability and Transformation
- PLOS Collections
Understanding Scientific and Research Ethics

How to pass journal ethics checks to ensure a smooth submission and publication process
Reputable journals screen for ethics at submission—and inability to pass ethics checks is one of the most common reasons for rejection. Unfortunately, once a study has begun, it’s often too late to secure the requisite ethical reviews and clearances. Learn how to prepare for publication success by ensuring your study meets all ethical requirements before work begins.
The underlying principles of scientific and research ethics
Scientific and research ethics exist to safeguard human rights, ensure that we treat animals respectfully and humanely, and protect the natural environment.
The specific details may vary widely depending on the type of research you’re conducting, but there are clear themes running through all research and reporting ethical requirements:
Documented 3rd party oversight
- Consent and anonymity
- Full transparency
If you fulfill each of these broad requirements, your manuscript should sail through any journal’s ethics check.

If your research is 100% theoretical, you might be able to skip this one. But if you work with living organisms in any capacity—whether you’re administering a survey, collecting data from medical records, culturing cells, working with zebrafish, or counting plant species in a ring—oversight and approval by an ethics committee is a prerequisite for publication. This oversight can take many different forms:
For human studies and studies using human tissue or cells, obtain approval from your institutional review board (IRB). Register clinical trials with the World Health Organization (WHO) or International Committee of Medical Journal Editors (ICMJE). For animal research consult with your institutional animal care and use committee (IACUC). Note that there may be special requirements for non-human primates, cephalopods, and other specific species, as well as for wild animals. For field studies , anthropology and paleontology , the type of permission required will depend on many factors, like the location of the study, whether the site is publicly or privately owned, possible impacts on endangered or protected species, and local permit requirements.
TIP: You’re not exempt until your committee tells you so
Even if you think your study probably doesn’t require approval, submit it to the review board anyway. Many journals won’t consider retrospective approvals. Obtaining formal approval or an exemption up front is worth it to ensure your research is eligible for publication in the future.
TIP: Keep your committee records close
Clearly label your IRB/IACUC paperwork, permit numbers, and any participant permission forms (including blank copies), and keep them in a safe place. You will need them when you submit to a journal. Providing these details proactively as part of your initial submission can minimize delays and get your manuscript through journal checks and into the hands of reviewers sooner.
Consent & anonymity
Obtaining consent from human subjects.
You may not conduct research on human beings unless the subjects understand what you are doing and agree to be a part of your study. If you work with human subjects, you must obtain informed written consent from the participants or their legal guardians.
There are many circumstances where extra care may be required in order to obtain consent. The more vulnerable the population you are working with the stricter these guidelines will be. For example, your IRB may have special requirements for working with minors, the elderly, or developmentally delayed participants. Remember that these rules may vary from country to country. Providing a link to the relevant legal reference in your area can help speed the screening and approval process.
TIP: What if you are working with a population where reading and writing aren’t common?
Alternatives to written consent (such as verbal consent or a thumbprint) are acceptable in some cases, but consent still has to be clearly documented. To ensure eligibility for publication, be sure to:
- Get IRB approval for obtaining verbal rather than written consent
- Be prepared to explain why written consent could not be obtained
- Keep a copy of the script you used to obtain this consent, and record when consent was obtained for your own records
Consent and reporting for human tissue and cell lines
Consent from the participant or their next-of-kin is also required for the use of human tissue and cell lines. This includes discarded tissue, for example the by-products of surgery.
When working with cell lines transparency and good record keeping are essential. Here are some basic guidelines to bear in mind:
- When working with established cell lines , cite the published article where the cell line was first described.
- If you’re using repository or commercial cell lines , explain exactly which ones, and provide the catalog or repository number.
- If you received a cell line from a colleague , rather than directly from a repository or company, be sure to mention it. Explain who gifted the cells and when.
- For a new cell line obtained from a colleague there may not be a published article to cite yet, but the work to generate the cell line must meet the usual requirements of consent—even if it was carried out by another research group. You’ll need to provide a copy of your colleagues’ IRB approval and details about the consent procedures in order to publish the work.
Finally, you’re obliged to keep your human subjects anonymous and to protect any identifying information in photos and raw data. Remove all names, birth dates, detailed addresses, or job information from files you plan to share. Blur faces and tattoos in any images. Details such as geography (city/country), gender, age, or profession may be shared at a generalized level and in aggregate. Read more about standards for de-identifying datasets in The BMJ .
TIP: Anonymity can be important in field work too
Be careful about revealing geographic data in fieldwork. You don’t want to tip poachers off to the location of the endangered elephant population you studied, or expose petroglyphs to vandalism.
Full Transparency
No matter the discipline, transparent reporting of methods, results, data, software and code is essential to ethical research practice. Transparency is also key to the future reproducibility of your work.
When you submit your study to a journal, you’ll be asked to provide a variety of statements certifying that you’ve obtained the appropriate permissions and clearances, and explaining how you conducted the work. You may also be asked to provide supporting documentation, including field records and raw data. Provide as much detail as you can at this stage. Clear and complete disclosure statements will minimize back-and-forth with the journal, helping your submission to clear ethics checks and move on to the assessment stage sooner.
TIP: Save that data
As you work, be sure to clearly label and organize your data files in a way that will make sense to you later. As close as you are to the work as you conduct your study, remember that two years could easily pass between capturing your data and publishing an article reporting the results. You don’t want to be stuck piecing together confusing records in order to create figures and data files for repositories.
Read our full guide to preparing data for submission .
Keep in mind that scientific and research ethics are always evolving. As laws change and as we learn more about influence, implicit bias and animal sentience, the scientific community continues to strive to elevate our research practice.
A checklist to ensure you’re ethics-check ready
Before you begin your research
Obtain approval from your IRB, IACUC or other approving body
Obtain written informed consent from human participants, guardians or next-of-kin
Obtain permits or permission from property owners, or confirm that permits are not required
Label and save all of records
As you work
Adhere strictly to the protocols approved by your committee
Clearly label your data, and store it in a way that will make sense to your future self
As you write, submit and deposit your results
Be ready to cite specific approval organizations, permit numbers, cell lines, and other details in your ethics statement and in the methods section of your manuscript
Anonymize all participant data (including human and in some cases animal or geographic data)
If a figure does include identifying information (e.g. a participant’s face) obtain special consent
The contents of the Peer Review Center are also available as a live, interactive training session, complete with slides, talking points, and activities. …
The contents of the Writing Center are also available as a live, interactive training session, complete with slides, talking points, and activities. …
There’s a lot to consider when deciding where to submit your work. Learn how to choose a journal that will help your study reach its audience, while reflecting your values as a researcher…
Table of Contents
Ai, ethics & human agency, collaboration, information literacy, writing process, research ethics.
As an investigator be sure to protect your research subjects and follow ethical standards. As a consumer of research, be mindful of when investigators may be exaggerating results, making claims that exceed the authority of a research method, misrepresenting findings, or plagiarizing.

Research ethics are the moral principles and practices that guide how researchers work with information (especially data/texts), human subjects, and animals.
Since 1947, following the publication of the Nuremberg Code , governments (e.g., see Canada ) and professional organizations (e.g., see American Psychological Association) have created ethical codes of conduct to protect research subjects and society.
Since 1964, following the publication of the Declaration of Helsinki , investigators working with human subjects have been required to write an IRB Board in the U.S. or an Ethics Committee in the European Union before any research is conducted.
Research ethics and moral principles are a major concern across academic disciplines, professions, and consumers. Governments, hospitals, universities, and professional organizations have robust policies that guide how investigators work with texts, other humans, and animals, including
- policies for conducting research, such as prohibitions against plagiarism, misrepresentation of data, or fabrication of data
- policies for collaboration, authorship, peer review
- policies for protecting human subjects or animals involved in studies
- policies to account for, avoid, or ameliorate conflicts of interest
- policies for illustrating the value of funded research from governments, foundations, think tanks, and other organizations.
Even so, problems with research ethics endure.
Sometimes investigators cheat and engage in unethical behavior. Politics, economic interests, corporate interests, personal interests — these factors and more are associated with unethical behavior.
And sometimes investigators may not even be conscious that they are acting unethically. People can be unaware of their own confirmation bias, their tendency to ignore disconfirming evidence and selectively seek out evidence that confirms their thesis or research question .
Consumers of research are wise to consider ethics when weighing a study’s truth claims .
[ The CRAAP Test (Currency, Relevance, Authority, Accuracy, Purpose) ]
In 2009, Dr. Daniele Fanelli, a professor at The University of Edinburgh, conducted a meta analysis of 21 surveys that explored how frequently scientists fabricate, falsify or cook data. Remarkably, she discovered that 33.7% of the scientists surveyed admitted to questionable research practices. When discussing the work of colleagues they assumed 14.12% of scientists falsified data and 72% engaged in questionable research practices:
it is likely that, if on average 2% of scientists admit to have falsified research at least once and up to 34% admit other questionable research practices, the actual frequencies of misconduct could be higher than this. Fanelli, Daniele (5/29/09). How Many Scientists Fabricate and Falsify Research? A Systematic Review and Meta-Analysis of Survey Data . PLOS ONE, https://doi.org/10.1371/journal.pone.0005738
For researchers, research ethics and moral principles are not an ornamental feature, an afterthought. Rather, ethical considerations form the foundation of research protocols , guiding the selection of research methods, the techniques used to gather and interpret data, and the ways data are interpreted and represented in research reports.
Examples of Research Ethics
To learn more about research ethics and moral principles, review the following ethical codes:
- National Science Foundation (NSF)
- Food and Drug Administration (FDA)
- Environmental Protection Agency (EPA)
- US Department of Agriculture (USDA)
- Singapore Statement on Research Integrity
- American Chemical Society, The Chemist Professional’s Code of Conduct
- Code of Ethics (American Society for Clinical Laboratory Science)
- American Psychological Association, Ethical Principles of Psychologists and Code of Conduct
- Statement on Professional Ethics (American Association of University Professors)
- World Medical Association’s Declaration of Helsinki
- International ethical guidelines for biomedical research involving human subjects
- International ethical guidelines for epidemiological studies
- European Group on Ethics
- Directive 2001/20/ec of the European Parliament and of the Council
- Council of Europe (Oviedo Convention – Protocol on biomedical research)
- National Institutes of Health (NIH)
Fanelli, Daniele (5/29/09). How Many Scientists Fabricate and Falsify Research? A Systematic Review and Meta-Analysis of Survey Data . PLOS ONE, https://doi.org/10.1371/journal.pone.0005738
Related Articles:
Human subjects research, informed consent, irb (institutional review board), ethics committee, suggested edits.
- Please select the purpose of your message. * - Corrections, Typos, or Edits Technical Support/Problems using the site Advertising with Writing Commons Copyright Issues I am contacting you about something else
- Your full name
- Your email address *
- Page URL needing edits *
- Phone This field is for validation purposes and should be left unchanged.
Be aware of the moral principles and practices that inform research with human subjects.
Informed Consent is a legal and ethical requirement for research studies engaged in human subjects research.
Prior to conducting research involving human subjects, be sure to seek approval from an IRB (Institional Review Board) or Ethics Committee.
Featured Articles

Academic Writing – How to Write for the Academic Community

Professional Writing – How to Write for the Professional World
Credibility & Authority – How to Be Credible & Authoritative in Speech & Writing

Site Search
- How to Search
- Advisory Group
- Editorial Board
- OEC Fellows
- History and Funding
- Using OEC Materials
- Collections
- Research Ethics Resources
- Ethics Projects
- Communities of Practice
- Get Involved
- Submit Content
- Open Access Membership
- Become a Partner
Introduction: What is Research Ethics?
Research Ethics is defined here to be the ethics of the planning, conduct, and reporting of research. This introduction covers what research ethics is, its ethical distinctions, approaches to teaching research ethics, and other resources on this topic.
What is Research Ethics
Why Teach Research Ethics
Animal Subjects
Biosecurity
Collaboration
Conflicts of Interest
Data Management
Human Subjects
Peer Review
Publication
Research Misconduct
Social Responsibility
Stem Cell Research
Whistleblowing
Descriptions of educational settings , including in the classroom, and in research contexts.
Case Studies
Other Discussion Tools
Information about the history and authors of the Resources for Research Ethics Collection
What is Research Ethics?
Research Ethics is defined here to be the ethics of the planning, conduct, and reporting of research. It is clear that research ethics should include:
- Protections of human and animal subjects
However, not all researchers use human or animal subjects, nor are the ethical dimensions of research confined solely to protections for research subjects. Other ethical challenges are rooted in many dimensions of research, including the:
- Collection, use, and interpretation of research data
- Methods for reporting and reviewing research plans or findings
- Relationships among researchers with one another
- Relationships between researchers and those that will be affected by their research
- Means for responding to misunderstandings, disputes, or misconduct
- Options for promoting ethical conduct in research
The domain of research ethics is intended to include nothing less than the fostering of research that protects the interests of the public, the subjects of research, and the researchers themselves.
Ethical Distinctions
In discussing or teaching research ethics, it is important to keep some basic distinctions in mind.
- It is important not to confuse moral claims about how people ought to behave with descriptive claims about how they in fact do behave. From the fact that gift authorship or signing off on un-reviewed data may be "common practice" in some contexts, it doesn't follow that they are morally or professionally justified. Nor is morality to be confused with the moral beliefs or ethical codes that a given group or society holds (how some group thinks people should live). A belief in segregation is not morally justified simply because it is widely held by a group of people or given society. Philosophers term this distinction between prescriptive and descriptive claims the 'is-ought distinction.'
- A second important distinction is that between morality and the law. The law may or may not conform to the demands of ethics (Kagan, 1998). To take a contemporary example: many believe that the law prohibiting federally funded stem cell research is objectionable on moral (as well as scientific) grounds, i.e., that such research can save lives and prevent much human misery. History is full of examples of bad laws, that is laws now regarded as morally unjustifiable, e.g., the laws of apartheid, laws prohibiting women from voting or inter-racial couples from marrying.
- It is also helpful to distinguish between two different levels of discussion (or two different kinds of ethical questions): first-order or "ground-level" questions and second-order questions.
- First-order moral questions concern what we should do. Such questions may be very general or quite specific. One might ask whether the tradition of 'senior' authorship should be defended and preserved or, more generally, what are the principles that should go into deciding the issue of 'senior' authorship. Such questions and the substantive proposals regarding how to answer them belong to the domain of what moral philosophers call 'normative ethics.'
- Second-order moral questions concern the nature and purpose of morality itself. When someone claims that falsifying data is wrong, what exactly is the standing of this claim? What exactly does the word 'wrong' mean in the conduct of scientific research? And what are we doing when we make claims about right and wrong, scientific integrity and research misconduct? These second-order questions are quite different from the ground-level questions about how to conduct one's private or professional life raised above. They concern the nature of morality rather than its content, i.e., what acts are required, permitted or prohibited. This is the domain of what moral philosophers call 'metaethics' (Kagan, 1998).
Ethical Approaches
Each of these approaches provides moral principles and ways of thinking about the responsibilities, duties and obligations of moral life. Individually and jointly, they can provide practical guidance in ethical decision-making.
- One of the most influential and familiar approaches to ethics is deontological ethics, associated with Immanuel Kant (1742-1804). Deontological ethics hold certain acts as right or wrong in themselves, e.g., promise breaking or lying. So, for example, in the context of research, fraud, plagiarism and misrepresentation are regarded as morally wrong in themselves, not simply because they (tend to) have bad consequences. The deontological approach is generally grounded in a single fundamental principle: Act as you would wish others to act towards you OR always treat persons as an end, never as a means to an end.
- From such central principles are derived rules or guidelines for what is permitted, required and prohibited. Objections to principle-based or deontological ethics include the difficulty of applying highly general principles to specific cases, e.g.: Does treating persons as ends rule out physician-assisted suicide, or require it? Deontological ethics is generally contrasted to consequentialist ethics (Honderich, 1995).
- According to consequentialist approaches, the rightness or wrongness of an action depends solely on its consequences. One should act in such a way as to bring about the best state of affairs, where the best state of affairs may be understood in various ways, e.g., as the greatest happiness for the greatest number of people, maximizing pleasure and minimizing pain or maximizing the satisfaction of preferences. A theory such as Utilitarianism (with its roots in the work of Jeremy Bentham and John Stuart Mill) is generally taken as the paradigm example of consequentialism. Objections to consequentialist ethics tend to focus on its willingness to regard individual rights and values as "negotiable." So, for example, most people would regard murder as wrong independently of the fact that killing one person might allow several others to be saved (the infamous sacrifice of an ailing patient to provide organs for several other needy patients). Similarly, widespread moral opinion holds certain values important (integrity, justice) not only because they generally lead to good outcomes, but in and of themselves.
- Virtue ethics focuses on moral character rather than action and behavior considered in isolation. Central to this approach is the question what ought we (as individuals, as scientists, as physicians) to be rather than simply what we ought to do. The emphasis here is on inner states, that is, moral dispositions and habits such as courage or a developed sense of personal integrity. Virtue ethics can be a useful approach in the context of RCR and professional ethics, emphasizing the importance of moral virtues such as compassion, honesty, and respect. This approach has also a great deal to offer in discussions of bioethical issues where a traditional emphasis on rights and abstract principles frequently results in polarized, stalled discussions (e.g., abortion debates contrasting the rights of the mother against the rights of the fetus).
- The term 'an ethics of care' grows out of the work of Carol Gilligan, whose empirical work in moral psychology claimed to discover a "different voice," a mode of moral thinking distinct from principle-based moral thinking (e.g., the theories of Kant and Mill). An ethics of care stresses compassion and empathetic understanding, virtues Gilligan associated with traditional care-giving roles, especially those of women.
- This approach differs from traditional moral theories in two important ways. First, it assumes that it is the connections between persons, e.g., lab teams, colleagues, parents and children, student and mentor, not merely the rights and obligations of discrete individuals that matter. The moral world, on this view, is best seen not as the interaction of discrete individuals, each with his or her own interests and rights, but as an interrelated web of obligations and commitment. We interact, much of the time, not as private individuals, but as members of families, couples, institutions, research groups, a given profession and so on. Second, these human relationships, including relationships of dependency, play a crucial role on this account in determining what our moral obligations and responsibilities are. So, for example, individuals have special responsibilities to care for their children, students, patients, and research subjects.
- An ethics of care is thus particularly useful in discussing human and animal subjects research, issues of informed consent, and the treatment of vulnerable populations such as children, the infirm or the ill.
- The case study approach begins from real or hypothetical cases. Its objective is to identify the intuitively plausible principles that should be taken into account in resolving the issues at hand. The case study approach then proceeds to critically evaluate those principles. In discussing whistle-blowing, for example, a good starting point is with recent cases of research misconduct, seeking to identify and evaluate principles such as a commitment to the integrity of science, protecting privacy, or avoiding false or unsubstantiated charges. In the context of RCR instruction, case studies provide one of the most interesting and effective approaches to developing sensitivity to ethical issues and to honing ethical decision-making skills.
- Strictly speaking, casuistry is more properly understood as a method for doing ethics rather than as itself an ethical theory. However, casuistry is not wholly unconnected to ethical theory. The need for a basis upon which to evaluate competing principles, e.g., the importance of the well-being of an individual patient vs. a concern for just allocation of scarce medical resources, makes ethical theory relevant even with case study approaches.
- Applied ethics is a branch of normative ethics. It deals with practical questions particularly in relation to the professions. Perhaps the best known area of applied ethics is bioethics, which deals with ethical questions arising in medicine and the biological sciences, e.g., questions concerning the application of new areas of technology (stem cells, cloning, genetic screening, nanotechnology, etc.), end of life issues, organ transplants, and just distribution of healthcare. Training in responsible conduct of research or "research ethics" is merely one among various forms of professional ethics that have come to prominence since the 1960s. Worth noting, however, is that concern with professional ethics is not new, as ancient codes such as the Hippocratic Oath and guild standards attest (Singer, 1986).
- Adams D, Pimple KD (2005): Research Misconduct and Crime: Lessons from Criminal Science on Preventing Misconduct and Promoting Integrity. Accountability in Research 12(3):225-240.
- Anderson MS, Horn AS, Risbey KR, Ronning EA, De Vries R, Martinson BC (2007): What Do Mentoring and Training in the Responsible Conduct of Research Have To Do with Scientists' Misbehavior? Findings from a National Survey of NIH-Funded Scientists . Academic Medicine 82(9):853-860.
- Bulger RE, Heitman E (2007): Expanding Responsible Conduct of Research Instruction across the University. Academic Medicine. 82(9):876-878.
- Kalichman MW (2006): Ethics and Science: A 0.1% solution. Issues in Science and Technology 23:34-36.
- Kalichman MW (2007): Responding to Challenges in Educating for the Responsible Conduct of Research, Academic Medicine. 82(9):870-875.
- Kalichman MW, Plemmons DK (2007): Reported Goals for Responsible Conduct of Research Courses. Academic Medicine. 82(9):846-852.
- Kalichman MW (2009): Evidence-based research ethics. The American Journal of Bioethics 9(6&7): 85-87.
- Pimple KD (2002): Six Domains of Research Ethics: A Heuristic Framework for the Responsible Conduct of Research. Science and Engineering Ethics 8(2):191-205.
- Steneck NH (2006): Fostering Integrity in Research: Definitions, Current Knowledge, and Future Directions. Science and Engineering Ethics 12:53-74.
- Steneck NH, Bulger RE (2007): The History, Purpose, and Future of Instruction in the Responsible Conduct of Research. Academic Medicine. 82(9):829-834.
- Vasgird DR (2007): Prevention over Cure: The Administrative Rationale for Education in the Responsible Conduct of Research. Academic Medicine. 82(9):835-837.
- Aristotle. The Nichomachean Ethics.
- Beauchamp RL, Childress JF (2001): Principles of Biomedical Ethics, 5th edition, NY: Oxford University Press.
- Bentham, J (1781): An Introduction to the Principles of Morals and Legislation.
- Gilligan C (1993): In a Different Voice: Psychological Theory and Women's Development. Cambridge: Harvard University Press.
- Glover, Jonathan (1977): Penguin Books.
- Honderich T, ed. (1995): The Oxford Companion to Philosophy, Oxford and New York: Oxford University Press.
- Kagan S (1998): Normative Ethics. Westview Press.
- Kant I (1785): Groundwork of the Metaphysics of Morals.
- Kant I (1788): Critique of Practical Reason.
- Kant I (1797): The Metaphysics of Morals.
- Kant I (1797): On a Supposed right to Lie from Benevolent Motives.
- Kuhse H, Singer P (1999): Bioethics: An Anthology. Blackwell Publishers.
- Mill JS (1861): Utilitarianism.
- Rachels J (1999): The Elements of Moral Philosophy, 3rd edition, Boston: McGraw-Hill.
- Regan T (1993): Matters of Life and Death: New Introductory Essays in Moral Philosophy, 3rd edition. New York: McGraw-Hill. The history of ethics.
- Singer P (1993): Practical Ethics, 2nd ed. Cambridge University Press.
The Resources for Research Ethics Education site was originally developed and maintained by Dr. Michael Kalichman, Director of the Research Ethics Program at the University of California San Diego. The site was transferred to the Online Ethics Center in 2021 with the permission of the author.
Related Resources
Submit Content to the OEC Donate

This material is based upon work supported by the National Science Foundation under Award No. 2055332. Any opinions, findings, and conclusions or recommendations expressed in this material are those of the author(s) and do not necessarily reflect the views of the National Science Foundation.
An Introduction to Research Ethics and Scientific Integrity
- Living reference work entry
- First Online: 30 May 2019
- Cite this living reference work entry

- Ron Iphofen 2
489 Accesses
1 Citations
This chapter outlines the aims for the handbook. A main aim is to be a first point of contact for contemporary information, issues, and challenges in the fields of research ethics and scientific integrity. It is aimed at researchers, reviewers, and policymakers to help them pursue the best ways forward in seeking ethics and integrity in all research across disciplines, methods, subjects, participants, and contexts. The authors form a global network of scholars, practitioners, and researchers with a range of experience and insights that scope a challenging field but one that is vital to the maintenance of research standards and public confidence in science. Fact-based policymaking remains under threat from political and ideological pressures. Scientists and researchers in all disciplines and professions hold a clear responsibility to protect their subjects, research participants, and society from pressures, interests, and prejudices that risk undermining the value of their work. This overview outlines how the handbook is constructed and how readers might gain from it.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Institutional subscriptions
Cadwalladr C (2018) Our Cambridge Analytica scoop shocked the world. But the whole truth remains elusive, The Guardian , 23rd December Accessed at: https://www.theguardian.com/uk-news/2018/dec/23/cambridge-analytica-facebook-scoop-carole-cadwalladr-shocked-world-truth-still-elusive
Cadwalladr C (2019) Cambridge Analytica a year on: ‘a lesson in institutional failure’, The Guardian, 17 March, accessed at: https://www.theguardian.com/uk-news/2019/mar/17/cambridge-analytica-year-on-lesson-in-institutional-failure-christopher-wylie
Cohen S, Young J (1973) The manufacture of news: a reader. Sage, London
Google Scholar
Collingridge D (1980) The social control of technology. Frances Pinter, London
ESOMAR (2016) https://www.esomar.org/what-we-do/code-guidelines
Evans RJ (2002) Telling lies about Hitler: the holocaust, history and the David Irving trial. Verso, London
Fuhrman J (2013) Super immunity. HarperCollins, London
Goldacre B (2001) Bad pharma. HarperCollins, London
Gross J (2018) Poland’s death camp law is designed to falsify history, Financial Times, February 6, accessed at: https://www.ft.com/content/1c183f56-0a6a-11e8-bacb-2958fde95e5e
Hutton W, Adonis A (2018) Saving Britain: how we must change to prosper in Europe. Abacus, London
Ioris AAR (2015) Cracking the nut of agribusiness and global food insecurity: in search of a critical agenda of research. Geoforum 63:1–4. https://doi.org/10.1016/j.geoforum.2015.05.004
Article Google Scholar
Iphofen R (2017) Epistemological metaphors: orders of knowledge and control in the Encyclopedist myths of cyberspace. International Journal of Humanities and Cultural Studies. (ISSN 2356-5926) 4(2):122–141. https://www.ijhcs.com/index.php/ijhcs/article/view/3128
Levitt SD, Dubner SJ (2005) Freakonomics: a rogue economist explores the hidden side of everything. Allen Lane, London
Levitt SD, Dubner SJ (2009) SuperFreakonomics: global cooling, patriotic prostitutes, and why suicide bombers should buy life insurance. Harper Collins, New York
Portes R (2017) Who needs experts? The London Business Review, 9th May. Accessed at: https://www.london.edu/faculty-and-research/lbsr/who-needs-experts
Posner M (2006) Social sciences under attack in the UK (1981–1983), La revue pour l’histoire du CNRS [], 7|2002, 20 October 2006, 09 January 2017. http://histoire-cnrs.revues.org/547 ; https://doi.org/10.4000/histoire-cnrs.547
Schrag Z (2010) Ethical Imperialism: Institutional Review Boards and the Social Sciences, 1965–2009. The John Hopkins University Press, Baltimore
Download references
Author information
Authors and affiliations.
Independent Research Consultant, Chatelaillon Plage, France
Ron Iphofen
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Ron Iphofen .
Editor information
Editors and affiliations.
Chatelaillon Plage, France
Rights and permissions
Reprints and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this entry
Cite this entry.
Iphofen, R. (2019). An Introduction to Research Ethics and Scientific Integrity. In: Iphofen, R. (eds) Handbook of Research Ethics and Scientific Integrity. Springer, Cham. https://doi.org/10.1007/978-3-319-76040-7_62-1
Download citation
DOI : https://doi.org/10.1007/978-3-319-76040-7_62-1
Received : 17 March 2019
Accepted : 01 May 2019
Published : 30 May 2019
Publisher Name : Springer, Cham
Print ISBN : 978-3-319-76040-7
Online ISBN : 978-3-319-76040-7
eBook Packages : Springer Reference Religion and Philosophy Reference Module Humanities and Social Sciences Reference Module Humanities
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Ethical Considerations In Psychology Research
Saul Mcleod, PhD
Editor-in-Chief for Simply Psychology
BSc (Hons) Psychology, MRes, PhD, University of Manchester
Saul Mcleod, PhD., is a qualified psychology teacher with over 18 years of experience in further and higher education. He has been published in peer-reviewed journals, including the Journal of Clinical Psychology.
Learn about our Editorial Process
Olivia Guy-Evans, MSc
Associate Editor for Simply Psychology
BSc (Hons) Psychology, MSc Psychology of Education
Olivia Guy-Evans is a writer and associate editor for Simply Psychology. She has previously worked in healthcare and educational sectors.
On This Page:
Ethics refers to the correct rules of conduct necessary when carrying out research. We have a moral responsibility to protect research participants from harm.
However important the issue under investigation, psychologists must remember that they have a duty to respect the rights and dignity of research participants. This means that they must abide by certain moral principles and rules of conduct.
What are Ethical Guidelines?
In Britain, ethical guidelines for research are published by the British Psychological Society, and in America, by the American Psychological Association. The purpose of these codes of conduct is to protect research participants, the reputation of psychology, and psychologists themselves.
Moral issues rarely yield a simple, unambiguous, right or wrong answer. It is, therefore, often a matter of judgment whether the research is justified or not.
For example, it might be that a study causes psychological or physical discomfort to participants; maybe they suffer pain or perhaps even come to serious harm.
On the other hand, the investigation could lead to discoveries that benefit the participants themselves or even have the potential to increase the sum of human happiness.
Rosenthal and Rosnow (1984) also discuss the potential costs of failing to carry out certain research. Who is to weigh up these costs and benefits? Who is to judge whether the ends justify the means?
Finally, if you are ever in doubt as to whether research is ethical or not, it is worthwhile remembering that if there is a conflict of interest between the participants and the researcher, it is the interests of the subjects that should take priority.
Studies must now undergo an extensive review by an institutional review board (US) or ethics committee (UK) before they are implemented. All UK research requires ethical approval by one or more of the following:
- Department Ethics Committee (DEC) : for most routine research.
- Institutional Ethics Committee (IEC) : for non-routine research.
- External Ethics Committee (EEC) : for research that s externally regulated (e.g., NHS research).
Committees review proposals to assess if the potential benefits of the research are justifiable in light of the possible risk of physical or psychological harm.
These committees may request researchers make changes to the study’s design or procedure or, in extreme cases, deny approval of the study altogether.
The British Psychological Society (BPS) and American Psychological Association (APA) have issued a code of ethics in psychology that provides guidelines for conducting research. Some of the more important ethical issues are as follows:
Informed Consent
Before the study begins, the researcher must outline to the participants what the research is about and then ask for their consent (i.e., permission) to participate.
An adult (18 years +) capable of being permitted to participate in a study can provide consent. Parents/legal guardians of minors can also provide consent to allow their children to participate in a study.
Whenever possible, investigators should obtain the consent of participants. In practice, this means it is not sufficient to get potential participants to say “Yes.”
They also need to know what it is that they agree to. In other words, the psychologist should, so far as is practicable, explain what is involved in advance and obtain the informed consent of participants.
Informed consent must be informed, voluntary, and rational. Participants must be given relevant details to make an informed decision, including the purpose, procedures, risks, and benefits. Consent must be given voluntarily without undue coercion. And participants must have the capacity to rationally weigh the decision.
Components of informed consent include clearly explaining the risks and expected benefits, addressing potential therapeutic misconceptions about experimental treatments, allowing participants to ask questions, and describing methods to minimize risks like emotional distress.
Investigators should tailor the consent language and process appropriately for the study population. Obtaining meaningful informed consent is an ethical imperative for human subjects research.
The voluntary nature of participation should not be compromised through coercion or undue influence. Inducements should be fair and not excessive/inappropriate.
However, it is not always possible to gain informed consent. Where the researcher can’t ask the actual participants, a similar group of people can be asked how they would feel about participating.
If they think it would be OK, then it can be assumed that the real participants will also find it acceptable. This is known as presumptive consent.
However, a problem with this method is that there might be a mismatch between how people think they would feel/behave and how they actually feel and behave during a study.
In order for consent to be ‘informed,’ consent forms may need to be accompanied by an information sheet for participants’ setting out information about the proposed study (in lay terms), along with details about the investigators and how they can be contacted.
Special considerations exist when obtaining consent from vulnerable populations with decisional impairments, such as psychiatric patients, intellectually disabled persons, and children/adolescents. Capacity can vary widely so should be assessed individually, but interventions to improve comprehension may help. Legally authorized representatives usually must provide consent for children.
Participants must be given information relating to the following:
- A statement that participation is voluntary and that refusal to participate will not result in any consequences or any loss of benefits that the person is otherwise entitled to receive.
- Purpose of the research.
- All foreseeable risks and discomforts to the participant (if there are any). These include not only physical injury but also possible psychological.
- Procedures involved in the research.
- Benefits of the research to society and possibly to the individual human subject.
- Length of time the subject is expected to participate.
- Person to contact for answers to questions or in the event of injury or emergency.
- Subjects” right to confidentiality and the right to withdraw from the study at any time without any consequences.
Debriefing after a study involves informing participants about the purpose, providing an opportunity to ask questions, and addressing any harm from participation. Debriefing serves an educational function and allows researchers to correct misconceptions. It is an ethical imperative.
After the research is over, the participant should be able to discuss the procedure and the findings with the psychologist. They must be given a general idea of what the researcher was investigating and why, and their part in the research should be explained.
Participants must be told if they have been deceived and given reasons why. They must be asked if they have any questions, which should be answered honestly and as fully as possible.
Debriefing should occur as soon as possible and be as full as possible; experimenters should take reasonable steps to ensure that participants understand debriefing.
“The purpose of debriefing is to remove any misconceptions and anxieties that the participants have about the research and to leave them with a sense of dignity, knowledge, and a perception of time not wasted” (Harris, 1998).
The debriefing aims to provide information and help the participant leave the experimental situation in a similar frame of mind as when he/she entered it (Aronson, 1988).
Exceptions may exist if debriefing seriously compromises study validity or causes harm itself, like negative emotions in children. Consultation with an institutional review board guides exceptions.
Debriefing indicates investigators’ commitment to participant welfare. Harms may not be raised in the debriefing itself, so responsibility continues after data collection. Following up demonstrates respect and protects persons in human subjects research.
Protection of Participants
Researchers must ensure that those participating in research will not be caused distress. They must be protected from physical and mental harm. This means you must not embarrass, frighten, offend or harm participants.
Normally, the risk of harm must be no greater than in ordinary life, i.e., participants should not be exposed to risks greater than or additional to those encountered in their normal lifestyles.
The researcher must also ensure that if vulnerable groups are to be used (elderly, disabled, children, etc.), they must receive special care. For example, if studying children, ensure their participation is brief as they get tired easily and have a limited attention span.
Researchers are not always accurately able to predict the risks of taking part in a study, and in some cases, a therapeutic debriefing may be necessary if participants have become disturbed during the research (as happened to some participants in Zimbardo’s prisoners/guards study ).
Deception research involves purposely misleading participants or withholding information that could influence their participation decision. This method is controversial because it limits informed consent and autonomy, but can provide otherwise unobtainable valuable knowledge.
Types of deception include (i) deliberate misleading, e.g. using confederates, staged manipulations in field settings, deceptive instructions; (ii) deception by omission, e.g., failure to disclose full information about the study, or creating ambiguity.
The researcher should avoid deceiving participants about the nature of the research unless there is no alternative – and even then, this would need to be judged acceptable by an independent expert. However, some types of research cannot be carried out without at least some element of deception.
For example, in Milgram’s study of obedience , the participants thought they were giving electric shocks to a learner when they answered a question wrongly. In reality, no shocks were given, and the learners were confederates of Milgram.
This is sometimes necessary to avoid demand characteristics (i.e., the clues in an experiment that lead participants to think they know what the researcher is looking for).
Another common example is when a stooge or confederate of the experimenter is used (this was the case in both the experiments carried out by Asch ).
According to ethics codes, deception must have strong scientific justification, and non-deceptive alternatives should not be feasible. Deception that causes significant harm is prohibited. Investigators should carefully weigh whether deception is necessary and ethical for their research.
However, participants must be deceived as little as possible, and any deception must not cause distress. Researchers can determine whether participants are likely distressed when deception is disclosed by consulting culturally relevant groups.
Participants should immediately be informed of the deception without compromising the study’s integrity. Reactions to learning of deception can range from understanding to anger. Debriefing should explain the scientific rationale and social benefits to minimize negative reactions.
If the participant is likely to object or be distressed once they discover the true nature of the research at debriefing, then the study is unacceptable.
If you have gained participants’ informed consent by deception, then they will have agreed to take part without actually knowing what they were consenting to. The true nature of the research should be revealed at the earliest possible opportunity or at least during debriefing.
Some researchers argue that deception can never be justified and object to this practice as it (i) violates an individual’s right to choose to participate; (ii) is a questionable basis on which to build a discipline; and (iii) leads to distrust of psychology in the community.
Confidentiality
Protecting participant confidentiality is an ethical imperative that demonstrates respect, ensures honest participation, and prevents harms like embarrassment or legal issues. Methods like data encryption, coding systems, and secure storage should match the research methodology.
Participants and the data gained from them must be kept anonymous unless they give their full consent. No names must be used in a lab report .
Researchers must clearly describe to participants the limits of confidentiality and methods to protect privacy. With internet research, threats exist like third-party data access; security measures like encryption should be explained. For non-internet research, other protections should be noted too, like coding systems and restricted data access.
High-profile data breaches have eroded public trust. Methods that minimize identifiable information can further guard confidentiality. For example, researchers can consider whether birthdates are necessary or just ages.
Generally, reducing personal details collected and limiting accessibility safeguards participants. Following strong confidentiality protections demonstrates respect for persons in human subjects research.
What do we do if we discover something that should be disclosed (e.g., a criminal act)? Researchers have no legal obligation to disclose criminal acts and must determine the most important consideration: their duty to the participant vs. their duty to the wider community.
Ultimately, decisions to disclose information must be set in the context of the research aims.
Withdrawal from an Investigation
Participants should be able to leave a study anytime if they feel uncomfortable. They should also be allowed to withdraw their data. They should be told at the start of the study that they have the right to withdraw.
They should not have pressure placed upon them to continue if they do not want to (a guideline flouted in Milgram’s research).
Participants may feel they shouldn’t withdraw as this may ‘spoil’ the study. Many participants are paid or receive course credits; they may worry they won’t get this if they withdraw.
Even at the end of the study, the participant has a final opportunity to withdraw the data they have provided for the research.
Ethical Issues in Psychology & Socially Sensitive Research
There has been an assumption over the years by many psychologists that provided they follow the BPS or APA guidelines when using human participants and that all leave in a similar state of mind to how they turned up, not having been deceived or humiliated, given a debrief, and not having had their confidentiality breached, that there are no ethical concerns with their research.
But consider the following examples:
a) Caughy et al. 1994 found that middle-class children in daycare at an early age generally score less on cognitive tests than children from similar families reared in the home.
Assuming all guidelines were followed, neither the parents nor the children participating would have been unduly affected by this research. Nobody would have been deceived, consent would have been obtained, and no harm would have been caused.
However, consider the wider implications of this study when the results are published, particularly for parents of middle-class infants who are considering placing their young children in daycare or those who recently have!
b) IQ tests administered to black Americans show that they typically score 15 points below the average white score.
When black Americans are given these tests, they presumably complete them willingly and are not harmed as individuals. However, when published, findings of this sort seek to reinforce racial stereotypes and are used to discriminate against the black population in the job market, etc.
Sieber & Stanley (1988) (the main names for Socially Sensitive Research (SSR) outline 4 groups that may be affected by psychological research: It is the first group of people that we are most concerned with!
- Members of the social group being studied, such as racial or ethnic group. For example, early research on IQ was used to discriminate against US Blacks.
- Friends and relatives of those participating in the study, particularly in case studies, where individuals may become famous or infamous. Cases that spring to mind would include Genie’s mother.
- The research team. There are examples of researchers being intimidated because of the line of research they are in.
- The institution in which the research is conducted.
salso suggest there are 4 main ethical concerns when conducting SSR:
- The research question or hypothesis.
- The treatment of individual participants.
- The institutional context.
- How the findings of the research are interpreted and applied.
Ethical Guidelines For Carrying Out SSR
Sieber and Stanley suggest the following ethical guidelines for carrying out SSR. There is some overlap between these and research on human participants in general.
Privacy : This refers to people rather than data. Asking people questions of a personal nature (e.g., about sexuality) could offend.
Confidentiality: This refers to data. Information (e.g., about H.I.V. status) leaked to others may affect the participant’s life.
Sound & valid methodology : This is even more vital when the research topic is socially sensitive. Academics can detect flaws in methods, but the lay public and the media often don’t.
When research findings are publicized, people are likely to consider them fact, and policies may be based on them. Examples are Bowlby’s maternal deprivation studies and intelligence testing.
Deception : Causing the wider public to believe something, which isn’t true by the findings, you report (e.g., that parents are responsible for how their children turn out).
Informed consent : Participants should be made aware of how participating in the research may affect them.
Justice & equitable treatment : Examples of unjust treatment are (i) publicizing an idea, which creates a prejudice against a group, & (ii) withholding a treatment, which you believe is beneficial, from some participants so that you can use them as controls.
Scientific freedom : Science should not be censored, but there should be some monitoring of sensitive research. The researcher should weigh their responsibilities against their rights to do the research.
Ownership of data : When research findings could be used to make social policies, which affect people’s lives, should they be publicly accessible? Sometimes, a party commissions research with their interests in mind (e.g., an industry, an advertising agency, a political party, or the military).
Some people argue that scientists should be compelled to disclose their results so that other scientists can re-analyze them. If this had happened in Burt’s day, there might not have been such widespread belief in the genetic transmission of intelligence. George Miller (Miller’s Magic 7) famously argued that we should give psychology away.
The values of social scientists : Psychologists can be divided into two main groups: those who advocate a humanistic approach (individuals are important and worthy of study, quality of life is important, intuition is useful) and those advocating a scientific approach (rigorous methodology, objective data).
The researcher’s values may conflict with those of the participant/institution. For example, if someone with a scientific approach was evaluating a counseling technique based on a humanistic approach, they would judge it on criteria that those giving & receiving the therapy may not consider important.
Cost/benefit analysis : It is unethical if the costs outweigh the potential/actual benefits. However, it isn’t easy to assess costs & benefits accurately & the participants themselves rarely benefit from research.
Sieber & Stanley advise that researchers should not avoid researching socially sensitive issues. Scientists have a responsibility to society to find useful knowledge.
- They need to take more care over consent, debriefing, etc. when the issue is sensitive.
- They should be aware of how their findings may be interpreted & used by others.
- They should make explicit the assumptions underlying their research so that the public can consider whether they agree with these.
- They should make the limitations of their research explicit (e.g., ‘the study was only carried out on white middle-class American male students,’ ‘the study is based on questionnaire data, which may be inaccurate,’ etc.
- They should be careful how they communicate with the media and policymakers.
- They should be aware of the balance between their obligations to participants and those to society (e.g. if the participant tells them something which they feel they should tell the police/social services).
- They should be aware of their own values and biases and those of the participants.
Arguments for SSR
- Psychologists have devised methods to resolve the issues raised.
- SSR is the most scrutinized research in psychology. Ethical committees reject more SSR than any other form of research.
- By gaining a better understanding of issues such as gender, race, and sexuality, we are able to gain greater acceptance and reduce prejudice.
- SSR has been of benefit to society, for example, EWT. This has made us aware that EWT can be flawed and should not be used without corroboration. It has also made us aware that the EWT of children is every bit as reliable as that of adults.
- Most research is still on white middle-class Americans (about 90% of research is quoted in texts!). SSR is helping to redress the balance and make us more aware of other cultures and outlooks.
Arguments against SSR
- Flawed research has been used to dictate social policy and put certain groups at a disadvantage.
- Research has been used to discriminate against groups in society, such as the sterilization of people in the USA between 1910 and 1920 because they were of low intelligence, criminal, or suffered from psychological illness.
- The guidelines used by psychologists to control SSR lack power and, as a result, are unable to prevent indefensible research from being carried out.
American Psychological Association. (2002). American Psychological Association ethical principles of psychologists and code of conduct. www.apa.org/ethics/code2002.html
Baumrind, D. (1964). Some thoughts on ethics of research: After reading Milgram’s” Behavioral study of obedience.”. American Psychologist , 19 (6), 421.
Caughy, M. O. B., DiPietro, J. A., & Strobino, D. M. (1994). Day‐care participation as a protective factor in the cognitive development of low‐income children. Child development , 65 (2), 457-471.
Harris, B. (1988). Key words: A history of debriefing in social psychology. In J. Morawski (Ed.), The rise of experimentation in American psychology (pp. 188-212). New York: Oxford University Press.
Rosenthal, R., & Rosnow, R. L. (1984). Applying Hamlet’s question to the ethical conduct of research: A conceptual addendum. American Psychologist, 39(5) , 561.
Sieber, J. E., & Stanley, B. (1988). Ethical and professional dimensions of socially sensitive research. American psychologist , 43 (1), 49.
The British Psychological Society. (2010). Code of Human Research Ethics. www.bps.org.uk/sites/default/files/documents/code_of_human_research_ethics.pdf
Further Information
- MIT Psychology Ethics Lecture Slides
BPS Documents
- Code of Ethics and Conduct (2018)
- Good Practice Guidelines for the Conduct of Psychological Research within the NHS
- Guidelines for Psychologists Working with Animals
- Guidelines for ethical practice in psychological research online
APA Documents
APA Ethical Principles of Psychologists and Code of Conduct
Related Articles
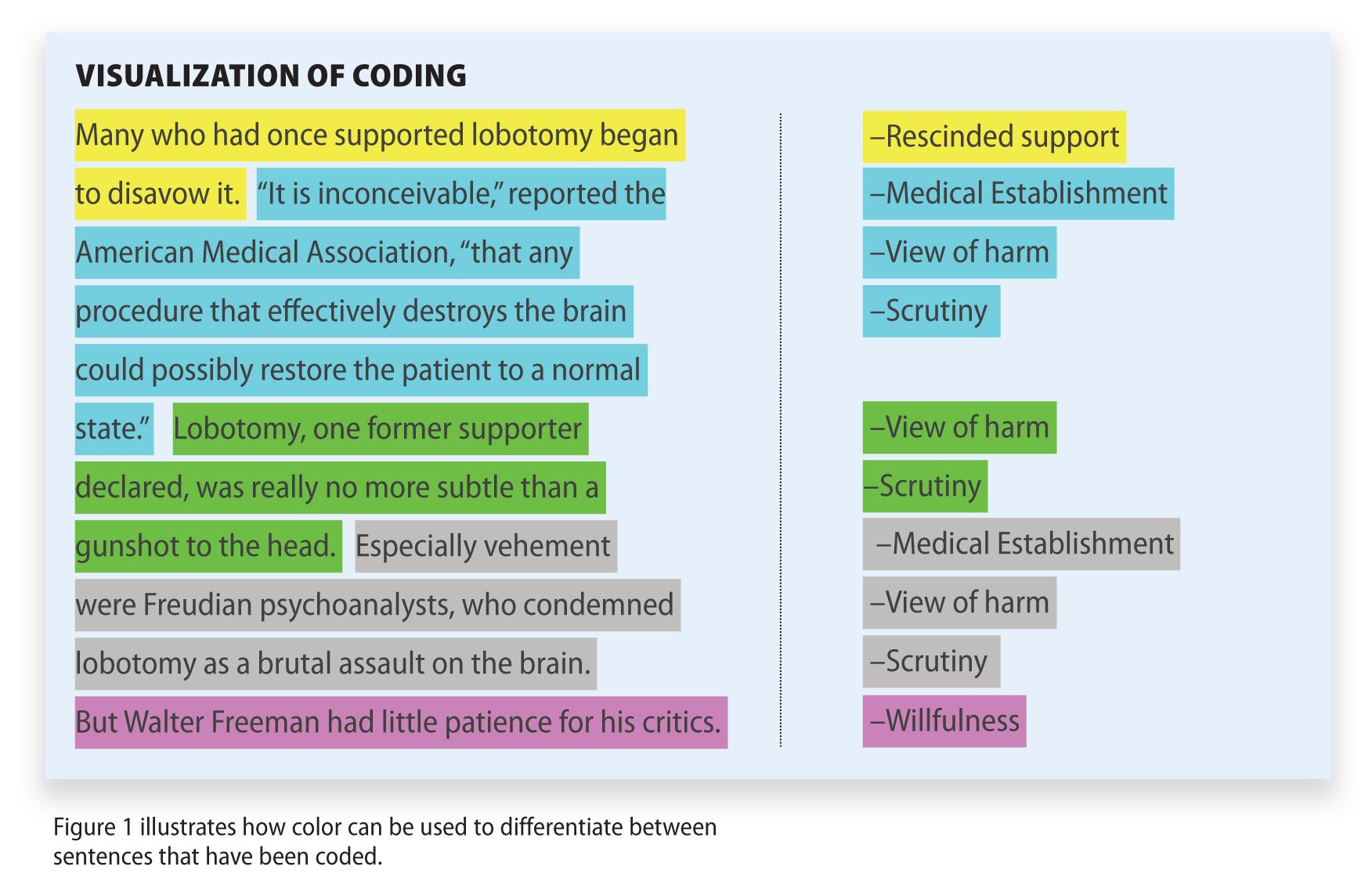
Research Methodology
Qualitative Data Coding

What Is a Focus Group?
Cross-Cultural Research Methodology In Psychology

What Is Internal Validity In Research?

Research Methodology , Statistics
What Is Face Validity In Research? Importance & How To Measure

Criterion Validity: Definition & Examples
Child Care and Early Education Research Connections
Ethics of research.
Researchers are expected to adhere to the principles of ethical research. The Belmont Report provides a broad framework for the ethics of research involving human subjects. Three basic ethical principles are identified:
- Respect for persons—requires that research subjects are not coerced into participating in a study and requires the protection of research subjects who have diminished autonomy.
- Beneficence—requires that research does not harm research subjects, and that researchers minimize the risks for subjects while maximizing the benefits for them.
Justice—requires that all forms of differential treatment among research subjects be justified.
Applications of these principles lead to considerations of the following:
- The researcher must inform the participants of the study's purpose, content, duration, and potential risks and benefits.
- The researcher must inform the participants that they can stop participating in the study at any point.
- In the event of survey research, the researcher must inform the participants that they do not have to answer all the survey questions.
- If the participants are children under legal age, the researcher must seek consent from their parents or guardians.
- Confidentiality Unless consent is given otherwise, it is absolutely imperative that researchers keep participants' identities confidential. Confidentiality means that participants cannot be identified in any way. In survey research, this includes but is not limited to making sure that participants' identifiers are not linked to their survey responses. Common identifiers include names, social security numbers, addresses, and telephone numbers. Such Personal Identifying Information or PII must be safeguarded. When analyzing data collected from small groups or samples with small n's and when reporting the findings from these analyses, the researchers must be extra mindful of not revealing participants' identities. Cell sizes with fewer than three cases should not be reported because information about the individuals in this group could be obtained by subtraction.
- Anonymity Anonymity is an even stronger safeguard of participant privacy. If a researcher assures anonymity, it means that the researcher is unable to link participants' names to the information they provide.
In addition to the above principles, considerations of specific ethical issues are often required depending on the form and context of research. For example, when using administrative data, the researcher must keep in mind that there are many legal protections set by the federal and state governments that require the privacy of program applicant information. For instance, in 1977, the Privacy Protection Study Commission determined that records or information used for statistical research could not be used in an individually identifiable form and that researchers could not take any action that would affect the individual to whom the information pertains.
A main ethical issue confronting researchers engaged in participant observation research is deciding when and how to inform those being observed that they are part of a research study. In theory, a researcher should identify himself or herself as a researcher at the onset of participant observation. However, in reality this may not be feasible without inherently changing the interactions at the outset. If the researcher decides to do so, a general but forthright description of the aims of the research should be sufficient. As relationships with members deepen, any controversial aspects of the study should be revealed. A researcher must obtain informed consent from any member who agrees to a formal, in-depth interview.
Institutional Review Board (IRB) Review
In order to assure that research subject and participant rights and welfare are protected, all researchers should have their project reviewed by an IRB or comparable bodies. The National Institutes of Health supplies strict guidelines for project approval. Many of these guidelines are based on the Belmont Report .
See the following for additional information about research ethics and protecting the rights of study participants and their data:
- CASRO Code of Standards and Ethics for Survey Research (PDF)
- AAPOR Code of Ethics
- National Center for Education Statistical Standards
- Tips on Informed Consent
The content on this page was prepared by Jerry West. It was last modified March 2019.
How To Apply Ethics to Your Research
Applying ethics to your research is super important! It’s how you show the readers that you’ve researched morality and your participants in mind rather than going against important rules or regulations. There are many different principles you should follow to make sure your research is ethical and they’re all as equally important. Without applying ethics to your research, you could find yourself in trouble. So, if you want to find out exactly what ethics is and how to apply it to your work, keep reading!
What is research ethics?
The research ethics definition is to follow moral and professional codes throughout any research conducted, which can be in the collection of the research, the publication of the research, interviews, analysis and more. To break it down, it basically means being moral and professional throughout any research that you do. It helps to protect both yourself and your participants from harm, so it’s super important to make sure you utilise ethics to ensure you’re working in the right way.
One important thing to note is that research ethics can actually differ with the university that you attend. That’s why you must check out your universities website to find out exactly what their rules and regulations are.
So, what should you do?
Make sure you have consent, keep anonymity, keep confidentiality, maintain integrity, respect the views of others, avoid causing any harm.
Something extremely crucial is making sure that the participants don’t come to any harm during the research process. It won’t come as any surprise that this another principle regularly featured on universities websites. It’s your responsibility that no harm is caused and that can be anything like psychological harm, emotional harm to even physical harm. You need to know from the outset that your research is safe to conduct for everyone involved.
You may also like

Purdue Online Writing Lab Purdue OWL® College of Liberal Arts
Ethical Considerations in Primary Research

Welcome to the Purdue OWL
This page is brought to you by the OWL at Purdue University. When printing this page, you must include the entire legal notice.
Copyright ©1995-2018 by The Writing Lab & The OWL at Purdue and Purdue University. All rights reserved. This material may not be published, reproduced, broadcast, rewritten, or redistributed without permission. Use of this site constitutes acceptance of our terms and conditions of fair use.
Primary research is conducted all of the time--journalists use it as their primary means of reporting news and events; national polls and surveys discover what the population thinks about a particular political figure or proposal; and companies collect data on their consumer base and market trends. When conducting research in an academic or professional setting, you need to be aware of the ethics behind your research activity.
Here are some specific points to consider:
- You should have the permission of the people who you will be studying to conduct research involving them.
- Not all types of research require permission—for example, if you are interested in analyzing something that is available publicly (such as in the case of commercials, public message boards, etc) you do not necessarily need the permission of the authors.
- You don’t want to do anything that would cause physical or emotional harm to your subjects. This could be something as simple as being careful how you word sensitive or difficult questions during your interviews.
- Objectivity vs. subjectivity in your research is another important consideration. Be sure your own personal biases and opinions do not get in the way of your research and that you give both sides fair consideration.
- Many types of research, such as surveys or observations, should be conducted under the assumption that you will keep your findings anonymous. Many interviews, however, are not done under the condition of anonymity. You should let your subjects know whether your research results will be anonymous or not.
- When you are doing research, be sure you are not taking advantage of easy-to-access groups of people (such as children at a daycare) simply because they are easy to access. You should choose your subjects based on what would most benefit your research.
- Some types of research done in a university setting require Institutional Board Approval. This means that your research has to be approved by an ethics review committee to make sure you are not violating any of the above considerations.
- When reporting your results be sure that you accurately represent what you observed or what you were told. Do not take interview responses out of context and do not discuss small parts of observations without putting them into the appropriate context.

Research Methods
- Introduction
- Key Resources
- Books, Articles & Videos
What is Research Ethics?
Research misconducts, responsible conduct of research, youtube video.
- Methods by Subject
Research ethics provides guidelines for the responsible conduct of research. In addition, it educates and monitors scientists conducting research to ensure a high ethical standard. The following is a general summary of some ethical principles:
Honestly report data, results, methods and procedures, and publication status. Do not fabricate, falsify, or misrepresent data.
Objectivity:
Strive to avoid bias in experimental design, data analysis, data interpretation, peer review, personnel decisions, grant writing, expert testimony, and other aspects of research.
Keep your promises and agreements; act with sincerity; strive for consistency of thought and action.
Carefulness:
Avoid careless errors and negligence; carefully and critically examine your own work and the work of your peers. Keep good records of research activities.
Share data, results, ideas, tools, resources. Be open to criticism and new ideas.
Respect for Intellectual Property:
Honor patents, copyrights, and other forms of intellectual property. Do not use unpublished data, methods, or results without permission. Give credit where credit is due. Never plagiarize.
Confidentiality:
Protect confidential communications, such as papers or grants submitted for publication, personnel records, trade or military secrets, and patient records.
Responsible Publication:
Publish in order to advance research and scholarship, not to advance just your own career. Avoid wasteful and duplicative publication.
Responsible Mentoring:
Help to educate, mentor, and advise students. Promote their welfare and allow them to make their own decisions.
Respect for Colleagues:
Respect your colleagues and treat them fairly.
Social Responsibility:
Strive to promote social good and prevent or mitigate social harms through research, public education, and advocacy.
Non-Discrimination:
Avoid discrimination against colleagues or students on the basis of sex, race, ethnicity, or other factors that are not related to their scientific competence and integrity.
Competence:
Maintain and improve your own professional competence and expertise through lifelong education and learning; take steps to promote competence in science as a whole.
Know and obey relevant laws and institutional and governmental policies.
Animal Care:
Show proper respect and care for animals when using them in research. Do not conduct unnecessary or poorly designed animal experiments.
Human Subjects Protection:
When conducting research on human subjects, minimize harms and risks and maximize benefits; respect human dignity, privacy, and autonomy.
Source: What is Ethics in Research & Why is it Important? U.S. National Institute of Environmental Health Sciences
- Five Principles for Research Ethics (American Psychological Association)
- Ethical Guidelines for Good Research Practice (Association of Social Anthropologists, UK)
- Australian Code for the Responsible Conduct of Research, 2018 (Australian Government)
- ESRC Framework for Research Ethics 2015 (The Economic and Social Research Council, UK)
How different aspects of your research relate to the six ethics principles set out in the ESRC Framework for Research Ethics? Click the image below to find out.
http://www.ethicsguidebook.ac.uk/EthicsPrinciples
What are research misconducts?
(a) Fabrication - making up data or results and recording or reporting them.
(b) Falsification - manipulating research materials, or changing or omitting data or results such that the research is not accurately represented in the research record.
(c) Plagiarism - the appropriation of another person's ideas, processes, results, or words without giving appropriate credit.
(d) Research misconduct does not include honest error or differences of opinion.
Source: Definition of Research Misconduct The Office of Research Integrity, U.S. Department of Health & Human Services
ORI Introduction to the Responsible Conduct of Research
Yale School of Medicine Professor Robert Levine spoke on guidelines for human subjects protection.
Video from: https://www.youtube.com/watch?v=jD-YCDE_5yw
- << Previous: Books, Articles & Videos
- Next: Methods by Subject >>
- Last Updated: Jun 7, 2024 11:37 AM
- URL: https://libguides.library.cityu.edu.hk/researchmethods
© City University of Hong Kong | Copyright | Disclaimer
- History and Mission
- University Leadership and Offices
- Strategic Plan – FDU Will Soar
- Faculty and Staff Directory
- Accreditations
- 2024-2025 Self-Study
- Rankings and Distinctions
- Community Outreach
- Program Finder
- Undergraduate Programs
- Graduate Programs
- Vancouver Academics
- Online Programs
- Colleges and Schools
- Academic Calendar
- Core Curriculum
- Academic Advising and Support
- Special Academic Opportunities
- University Bulletins
- Centers and Institutes
- Community College Partnership
- Honors at FDU
- Global Education and Study Abroad
- Adult and Continuing Education
- Freshman/First-Year Admissions
- Apply Now to FDU
- Tuition and Fees
- Transfer Student Admissions
- Apply to Online Programs
- Adult/Nontraditional/Part-time Admissions
- International Admissions
- Summer Sessions 2024
- Graduate Admissions
- Vancouver Admissions Services
- Financial Aid
- Florham Campus
- Metropolitan Campus
- Vancouver Campus
- Wroxton College
- Off-Campus Sites
- Dean of Students
- Housing and Residence Life
- Student Wellness Services
- Disability Support Services
- Student Community
- Student Clubs and Organizations
- Policies and Procedures
- Computer Facilities
- Student Publications
- Career Support
- New Student Checklists
- Division I FDU Knights
- Division III FDU Devils
- Giving to FDU
- Student Life Calendar Metropolitan
- Metro Campus This Month
- Student Life Calendar Florham
- Florham Campus This Month
- Vancouver Academic Calendar
- Vancouver Campus This Month
- Information Technology
- Office 365 and Email
- Self-Service
- SAMI Support
- myFDU Connect
- Coursefinder
- Up to Research Ethics and Compliance
Do I need IRB Review?
- Research with Humans/IRB
As stated in the FDU policy, research involving human subjects conducted by an agent of FDU must be submitted to the Institutional Review Board for review. This applies to all research, unfunded or funded by an extramural agency (government, foundation, or private sources). Faculty, students, and other investigators are encouraged to consult with the IRB months before submitting a project for review to discuss IRB-related issues that may affect the design or conduct of the investigation.
The following are activities that typically do NOT represent human subjects research requiring IRB review:
Case report: the project consists of a case report or a retrospective analysis of one, two, or three medical or educational activities/cases. If more than three cases are involved in the analytical activity, the activity WILL constitute research and will require IRB review.
Course-Related Activities: the project is limited to course-related activities designed specifically for educational or teaching purposes where data is collected from and about the students as part of a routine class exercise or assignment and is NOT intended for use outside the classroom. Note: IRB approval may be required if an instructor or department has an academic interest in pedagogy, and the classroom is used to test hypotheses/innovations with the goal of contributing to or changing generalizable knowledge about pedagogy.
Research on Decedents: research that uses only human cadavers, cadaveric tissue, decedent medical/educational record information, or discarded decedent specimens from clinical use is not subject to prior review and approval by the IRB UNLESS the research study includes BOTH living and deceased individuals.
If the project involves the use/and or collection of PHI (protected health information)HIPAA regulations apply to decedent research. Please contact the Human Research Compliance Manager for more information.
Oral History: The project is limited to oral history activities, such as open-ended interviews, that only document a specific historical event or the experiences of individuals without the intent to draw conclusions or generalize findings. Note: IRB approval is required when the oral history activities are intended to produce generalizable conclusions (e.g., that serve as a data collection intended to test economic, sociological, or anthropological models/theories).
Program evaluation/Quality Improvement/Quality Assurance Activities: the project is limited to program evaluation, quality improvement, or quality assurance activities designed specifically to assess or improve performance within the department, organization, or other specified setting. The intention of the project is not to generate conclusions that may be applied universally, outside of the immediate environment where the project occurred.
Public Use Datasets: The project is limited to analyzing de-identified data contained within a publicly available dataset. Some examples of data sources that do not qualify as research with human subjects, UNLESS the researcher has received restricted-use data, include data files from the Center for Disease Control, Bureau of Economic Analysis, FBI Uniform Crime Reporting Program, Global Health Observatory data repository, etc.
Coded Private Information and/or Human Biological specimens: The project is LIMITED to the use of existing and/or prospectively collected coded private information and/or human biological specimens. IRB approval is not required if ALL the following conditions apply:
The private information or specimens were/are not collected specifically for the currently proposed research project through intervention or interaction with living individuals, and,
The investigators cannot readily ascertain the identity of the individual(s) to whom the coded private information or specimens pertain because, for example:
the investigators and the holder of the code key enter into an agreement prohibiting the release of the key to investigators under any circumstances until the individuals are deceased.
there are IRB-approved written policies and operating procedures for a repository or data management center that prohibits the release of the key to investigators under any circumstances, until the individuals are deceased; or
there are other legal requirements prohibiting the release of the key to investigators are deceased, and
specimens are NOT being used to test effectiveness of a medical device or as a control in an investigation of an investigational device and the results of the activity are to be submitted to the FDA.
De-identified private information or Human Biological Specimens: The project is limited to the use of existing and/or prospectively collected de-identified private information and/or human bio specimens. IRB approval is not required if you confirm and show evidence of the following:
The private information or specimens were/are not collected specifically for the currently proposed research project through an intervention or interaction with living individuals; and
the investigator can confirm that the use of the private information and specimens is not in violation of the terms of use under which the information or specimens were/will be collected; and
the investigator will only receive information or specimens that are fully de-identified. De-identified means that the materials to be studied are devoid of any of the 18 Protected Health Information elements set forth in the Privacy Rule, as well as any codes that would enable linkage of the information or specimens to individual identifiers. Note: To be considered de-identified (unidentifiable), nobody, including individuals who are not involved in the conduct of the project, should be able to link the information or specimens back to identifiers; and
Specimens are not being used to test the effectiveness of a medical device or as a control on an investigation of investigational device and the results of the activity are to be submitted to the FDA or held for inspection by the FDA; and
The records/images/charts that being collected for this study are NOT from individuals who are or will become recipients of an FDA regulated product (approved or experimental) or act as a control as directed by a research protocol and not by medical practice, and the results of the activity are to be submitted to the FDA or held for inspection by the FDA.
Please note: a Data Use Agreement (DUA) may be required depending on the type of data being provided to FDU by another entity. A DUA is a written agreement used to govern the transfer of research data between institutions. It describes the data being transferred or shared and addresses the ownership of the data, the permitted use of the data, publication of results, development of inventions, disposal of the data and any liability.
If data is coming from another Institution or being collected at another Institution, that Institution must know and approve the use of the data for research purposes. IRB review may be required by the data providing Institution.
If it is a transfer of biological materials, a Material Transfer Agreement (MTA) may be needed. An MTA is a contract that governs the transfer of materials between institutions for use in research. These agreements address issues such as ownership of the transferred material and modifications and derivatives made by the recipient. They also may limit the use and further dissemination of the material by the recipient, address publication rights and confidentiality and rights to inventions and research results.
Please contact the HRCM for the operating procedure for DUAs and MTAs.
If you are unsure if your project is human subjects research or want confirmation, you may complete the Human Research Determination Form found here and on the IRB Forms and Templates page. Your form will be reviewed, and a determination made.

American Psychological Association


The impact of transgender legislation
Psychological science points to an increased risk of suicide and poor mental health amid a record number of bills aimed at restricting the rights of the LGBTQ+ population
APA policy supporting transgender, gender diverse, nonbinary individuals
Membership in APA

APA Community
A new exclusive destination tailored for APA members

Membership benefits
Unlock the tools, discounts, and services included with your membership

Renew your membership
Keep your benefits and access to leading psychological information
Psychology topics spotlight

Misinformation and disinformation

Resources to navigate trauma

Tips to foster a healthy workplace
Science and practice of psychology

Ethics Code

Continuing Education

Grants, Awards, and Funding

Standards and Guidelines
Networks and communities

Network with peers, enhance your professional development, expand your personal growth, and more

APA Divisions

High school teachers

Undergraduate educators

Graduate students

Early career psychologists

Managing your career
Resources to help you throughout your career in psychology, including finding a job, salary data, finances and money management, mentoring and supervision, and training and professional development

Explore career paths

Psychologist profiles

How did you get that job?

Events and training
Featured jobs
Apa publications and products.

Write with clarity, precision, and inclusion
Children’s books
Monitor on Psychology
Newsletters
Reports and surveys
Continuing education
Merchandise

Real Siblings

Jacob's Missing Book

Harper Becomes a Big Sister
Attachment-Based Family Therapy for Sexual and Gender Minority Young Adults and Their Non-Accepting Parents
Dismantling Everyday Discrimination
APA Services

Learn how you can help APA advocate for psychology-informed federal policy and legislation, and support psychological research

APA Services, Inc.
A companion professional organization to APA, serving all members and advocating for psychology
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Springer Nature - PMC COVID-19 Collection

Ethical Issues in Research: Perceptions of Researchers, Research Ethics Board Members and Research Ethics Experts
Marie-josée drolet.
1 Department of Occupational Therapy (OT), Université du Québec à Trois-Rivières (UQTR), Trois-Rivières (Québec), Canada
Eugénie Rose-Derouin
2 Bachelor OT program, Université du Québec à Trois-Rivières (UQTR), Trois-Rivières (Québec), Canada
Julie-Claude Leblanc
Mélanie ruest, bryn williams-jones.
3 Department of Social and Preventive Medicine, School of Public Health, Université de Montréal, Montréal (Québec), Canada
In the context of academic research, a diversity of ethical issues, conditioned by the different roles of members within these institutions, arise. Previous studies on this topic addressed mainly the perceptions of researchers. However, to our knowledge, no studies have explored the transversal ethical issues from a wider spectrum, including other members of academic institutions as the research ethics board (REB) members, and the research ethics experts. The present study used a descriptive phenomenological approach to document the ethical issues experienced by a heterogeneous group of Canadian researchers, REB members, and research ethics experts. Data collection involved socio-demographic questionnaires and individual semi-structured interviews. Following the triangulation of different perspectives (researchers, REB members and ethics experts), emerging ethical issues were synthesized in ten units of meaning: (1) research integrity, (2) conflicts of interest, (3) respect for research participants, (4) lack of supervision and power imbalances, (5) individualism and performance, (6) inadequate ethical guidance, (7) social injustices, (8) distributive injustices, (9) epistemic injustices, and (10) ethical distress. This study highlighted several problematic elements that can support the identification of future solutions to resolve transversal ethical issues in research that affect the heterogeneous members of the academic community.
Introduction
Research includes a set of activities in which researchers use various structured methods to contribute to the development of knowledge, whether this knowledge is theoretical, fundamental, or applied (Drolet & Ruest, accepted ). University research is carried out in a highly competitive environment that is characterized by ever-increasing demands (i.e., on time, productivity), insufficient access to research funds, and within a market economy that values productivity and speed often to the detriment of quality or rigour – this research context creates a perfect recipe for breaches in research ethics, like research misbehaviour or misconduct (i.e., conduct that is ethically questionable or unacceptable because it contravenes the accepted norms of responsible conduct of research or compromises the respect of core ethical values that are widely held by the research community) (Drolet & Girard, 2020 ; Sieber, 2004 ). Problematic ethics and integrity issues – e.g., conflicts of interest, falsification of data, non-respect of participants’ rights, and plagiarism, to name but a few – have the potential to both undermine the credibility of research and lead to negative consequences for many stakeholders, including researchers, research assistants and personnel, research participants, academic institutions, and society as a whole (Drolet & Girard, 2020 ). It is thus evident that the academic community should be able to identify these different ethical issues in order to evaluate the nature of the risks that they pose (and for whom), and then work towards their prevention or management (i.e., education, enhanced policies and procedures, risk mitigation strategies).
In this article, we define an “ethical issue” as any situation that may compromise, in whole or in part, the respect of at least one moral value (Swisher et al., 2005 ) that is considered socially legitimate and should thus be respected. In general, ethical issues occur at three key moments or stages of the research process: (1) research design (i.e., conception, project planning), (2) research conduct (i.e., data collection, data analysis) and (3) knowledge translation or communication (e.g., publications of results, conferences, press releases) (Drolet & Ruest, accepted ). According to Sieber ( 2004 ), ethical issues in research can be classified into five categories, related to: (a) communication with participants and the community, (b) acquisition and use of research data, (c) external influence on research, (d) risks and benefits of the research, and (e) selection and use of research theories and methods. Many of these issues are related to breaches of research ethics norms, misbehaviour or research misconduct. Bruhn et al., ( 2002 ) developed a typology of misbehaviour and misconduct in academia that can be used to judge the seriousness of different cases. This typology takes into consideration two axes of reflection: (a) the origin of the situation (i.e., is it the researcher’s own fault or due to the organizational context?), and (b) the scope and severity (i.e., is this the first instance or a recurrent behaviour? What is the nature of the situation? What are the consequences, for whom, for how many people, and for which organizations?).
A previous detailed review of the international literature on ethical issues in research revealed several interesting findings (Beauchemin et al., 2021 ). Indeed, the current literature is dominated by descriptive ethics, i.e., the sharing by researchers from various disciplines of the ethical issues they have personally experienced. While such anecdotal documentation is relevant, it is insufficient because it does not provide a global view of the situation. Among the reviewed literature, empirical studies were in the minority (Table 1 ) – only about one fifth of the sample (n = 19) presented empirical research findings on ethical issues in research. The first of these studies was conducted almost 50 years ago (Hunt et al., 1984 ), with the remainder conducted in the 1990s. Eight studies were conducted in the United States (n = 8), five in Canada (n = 5), three in England (n = 3), two in Sweden (n = 2) and one in Ghana (n = 1).
Summary of Empirical Studies on Ethical Issues in Research by the year of publication
| References | Country | Types of research participants | Study design |
|---|---|---|---|
| Hunt et al., ( ) | USA | marketing researchers | mixed-methods |
| Pope & Vetter ( ) | USA | members of the American psychological association | quantitative |
| Swazey et al., ( ) | USA | doctoral candidates and faculty members | quantitative |
| Balk ( ) | USA | study participants | mixed-methods |
| Sigmon ( ) | USA | psychopathology researchers | quantitative |
| Fraser ( ) | UK | education researchers | qualitative |
| Lynöe et al., ( ) | Sweden | research ethics board members, researchers, healthcare politicians and district nurses | quantitative |
| Bouffard ( ) | Canada | researchers, health professionals and patients | qualitative |
| Davison ( ) | UK | social work researchers | qualitative |
| Miyazaki & Taylor ( ) | USA | non-traditional undergraduate students | quantitative |
| Mondain & Bologo ( ) | Ghana | researcher participants and other stakeholders | qualitative |
| Wiegand & Funk ( ) | Canada | nurses | quantitative |
| McGinn ( ) | USA | nanotechnology researchers | quantitative |
| Colnerud ( ) | Sweden | researchers | qualitative |
| Lierville et al., ( ) | Canada | Managers, Researchers, Unit Leaders and Practitioners | Qualitative |
| Giorgini et al., ( ) | USA | researchers | mixed-methods |
| Birchley et al., ( ) | UK | smart-home researchers | qualitative |
| Jarvis ( ) | Canada | research participants (women and their family members), health care providers and key stakeholders | qualitative |
| Drolet & Girard ( ) | Canada | occupational therapist researchers | qualitative |
Further, the majority of studies in our sample (n = 12) collected the perceptions of a homogeneous group of participants, usually researchers (n = 14) and sometimes health professionals (n = 6). A minority of studies (n = 7) triangulated the perceptions of diverse research stakeholders (i.e., researchers and research participants, or students). To our knowledge, only one study has examined perceptions of ethical issues in research by research ethics board members (REB; Institutional Review Boards [IRB] in the USA), and none to date have documented the perceptions of research ethics experts. Finally, nine studies (n = 9) adopted a qualitative design, seven studies (n = 7) a quantitative design, and three (n = 3) a mixed-methods design.
More studies using empirical research methods are needed to better identify broader trends, to enrich discussions on the values that should govern responsible conduct of research in the academic community, and to evaluate the means by which these values can be supported in practice (Bahn, 2012 ; Beauchemin et al., 2021 ; Bruhn et al., 2002 ; Henderson et al., 2013 ; Resnik & Elliot, 2016; Sieber 2004 ). To this end, we conducted an empirical qualitative study to document the perceptions and experiences of a heterogeneous group of Canadian researchers, REB members, and research ethics experts, to answer the following broad question: What are the ethical issues in research?
Research Methods
Research design.
A qualitative research approach involving individual semi-structured interviews was used to systematically document ethical issues (De Poy & Gitlin, 2010 ; Hammell et al., 2000 ). Specifically, a descriptive phenomenological approach inspired by the philosophy of Husserl was used (Husserl, 1970 , 1999 ), as it is recommended for documenting the perceptions of ethical issues raised by various practices (Hunt & Carnavale, 2011 ).
Ethical considerations
The principal investigator obtained ethics approval for this project from the Research Ethics Board of the Université du Québec à Trois-Rivières (UQTR). All members of the research team signed a confidentiality agreement, and research participants signed the consent form after reading an information letter explaining the nature of the research project.
Sampling and recruitment
As indicated above, three types of participants were sought: (1) researchers from different academic disciplines conducting research (i.e., theoretical, fundamental or empirical) in Canadian universities; (2) REB members working in Canadian organizations responsible for the ethical review, oversight or regulation of research; and (3) research ethics experts, i.e., academics or ethicists who teach research ethics, conduct research in research ethics, or are scholars who have acquired a specialization in research ethics. To be included in the study, participants had to work in Canada, speak and understand English or French, and be willing to participate in the study. Following Thomas and Polio’s (2002) recommendation to recruit between six and twelve participants (for a homogeneous sample) to ensure data saturation, for our heterogeneous sample, we aimed to recruit approximately twelve participants in order to obtain data saturation. Having used this method several times in related projects in professional ethics, data saturation is usually achieved with 10 to 15 participants (Drolet & Goulet, 2018 ; Drolet & Girard, 2020 ; Drolet et al., 2020 ). From experience, larger samples only serve to increase the degree of data saturation, especially in heterogeneous samples (Drolet et al., 2017 , 2019 ; Drolet & Maclure, 2016 ).
Purposive sampling facilitated the identification of participants relevant to documenting the phenomenon in question (Fortin, 2010 ). To ensure a rich and most complete representation of perceptions, we sought participants with varied and complementary characteristics with regards to the social roles they occupy in research practice (Drolet & Girard, 2020 ). A triangulation of sources was used for the recruitment (Bogdan & Biklen, 2006 ). The websites of Canadian universities and Canadian health institution REBs, as well as those of major Canadian granting agencies (i.e., the Canadian Institutes of Health Research, the Natural Sciences and Engineering Research Council of Canada, and the Social Sciences and Humanities Research Council of Canada, Fonds de recherche du Quebec), were searched to identify individuals who might be interested in participating in the study. Further, people known by the research team for their knowledge and sensitivity to ethical issues in research were asked to participate. Research participants were also asked to suggest other individuals who met the study criteria.
Data Collection
Two tools were used for data collecton: (a) a socio-demographic questionnaire, and (b) a semi-structured individual interview guide. English and French versions of these two documents were used and made available, depending on participant preferences. In addition, although the interview guide contained the same questions, they were adapted to participants’ specific roles (i.e., researcher, REB member, research ethics expert). When contacted by email by the research assistant, participants were asked to confirm under which role they wished to participate (because some participants might have multiple, overlapping responsibilities) and they were sent the appropriate interview guide.
The interview guides each had two parts: an introduction and a section on ethical issues. The introduction consisted of general questions to put the participant at ease (i.e., “Tell me what a typical day at work is like for you”). The section on ethical issues was designed to capture the participant’s perceptions through questions such as: “Tell me three stories you have experienced at work that involve an ethical issue?” and “Do you feel that your organization is doing enough to address, manage, and resolve ethical issues in your work?”. Although some interviews were conducted in person, the majority were conducted by videoconference to promote accessibility and because of the COVID-19 pandemic. Interviews were digitally recorded so that the verbatim could be transcribed in full, and varied between 40 and 120 min in duration, with an average of 90 min. Research assistants conducted the interviews and transcribed the verbatim.
Data Analysis
The socio-demographic questionnaires were subjected to simple descriptive statistical analyses (i.e., means and totals), and the semi-structured interviews were subjected to qualitative analysis. The steps proposed by Giorgi ( 1997 ) for a Husserlian phenomenological reduction of the data were used. After collecting, recording, and transcribing the interviews, all verbatim were analyzed by at least two analysts: a research assistant (2nd author of this article) and the principal investigator (1st author) or a postdoctoral fellow (3rd author). The repeated reading of the verbatim allowed the first analyst to write a synopsis, i.e., an initial extraction of units of meaning. The second analyst then read the synopses, which were commented and improved if necessary. Agreement between analysts allowed the final drafting of the interview synopses, which were then analyzed by three analysts to generate and organize the units of meaning that emerged from the qualitative data.
Participants
Sixteen individuals (n = 16) participated in the study, of whom nine (9) identified as female and seven (7) as male (Table 2 ). Participants ranged in age from 22 to 72 years, with a mean age of 47.5 years. Participants had between one (1) and 26 years of experience in the research setting, with an average of 14.3 years of experience. Participants held a variety of roles, including: REB members (n = 11), researchers (n = 10), research ethics experts (n = 4), and research assistant (n = 1). As mentioned previously, seven (7) participants held more than one role, i.e., REB member, research ethics expert, and researcher. The majority (87.5%) of participants were working in Quebec, with the remaining working in other Canadian provinces. Although all participants considered themselves to be francophone, one quarter (n = 4) identified themselves as belonging to a cultural minority group.
Description of Participants
| Participant number | Gender | Age | Year(s) of experience | Participant’s role(s) |
|---|---|---|---|---|
| P1 | F | 20–25 | 1–5 | REB member, and research assistant |
| P2 | F | 45–50 | 10–15 | REB member |
| P3 | F | 35–40 | 20–25 | Researcher |
| P4 | H | 55–60 | 20–25 | REB member, research ethics expert, and researcher |
| P5 | H | 70–75 | 20–25 | REB member and researcher |
| P6 | H | 45–50 | 5–10 | REB member |
| P7 | H | 40–45 | 5–10 | REB member, research ethics expert, and researcher |
| P8 | H | 45–50 | 15–20 | REB member, research ethics expert, and researcher |
| P9 | F | 35–40 | 5–10 | REB member |
| P10 | F | 65–70 | 25–30 | Researcher and research ethics expert |
| P11 | F | 60–65 | 20–25 | REB member |
| P12 | F | 45 − 40 | 20–25 | Researcher |
| P13 | F | 40–45 | 5–10 | REB member |
| P14 | H | 30–35 | 1–15 | Researcher |
| P15 | F | 40–45 | 5–10 | REB member and researcher |
| P16 | H | 50–55 | 20–25 | Researcher |
With respect to their academic background, most participants (n = 9) had a PhD, three (3) had a post-doctorate, two (2) had a master’s degree, and two (2) had a bachelor’s degree. Participants came from a variety of disciplines: nine (9) had a specialty in the humanities or social sciences, four (4) in the health sciences and three (3) in the natural sciences. In terms of their knowledge of ethics, five (5) participants reported having taken one university course entirely dedicated to ethics, four (4) reported having taken several university courses entirely dedicated to ethics, three (3) had a university degree dedicated to ethics, while two (2) only had a few hours or days of training in ethics and two (2) reported having no knowledge of ethics.
Ethical issues
As Fig. 1 illustrates, ten units of meaning emerge from the data analysis, namely: (1) research integrity, (2) conflicts of interest, (3) respect for research participants, (4) lack of supervision and power imbalances, (5) individualism and performance, (6) inadequate ethical guidance, (7) social injustices, (8) distributive injustices, (9) epistemic injustices, and (10) ethical distress. To illustrate the results, excerpts from verbatim interviews are presented in the following sub-sections. Most of the excerpts have been translated into English as the majority of interviews were conducted with French-speaking participants.

Ethical issues in research according to the participants
Research Integrity
The research environment is highly competitive and performance-based. Several participants, in particular researchers and research ethics experts, felt that this environment can lead both researchers and research teams to engage in unethical behaviour that reflects a lack of research integrity. For example, as some participants indicated, competition for grants and scientific publications is sometimes so intense that researchers falsify research results or plagiarize from colleagues to achieve their goals.
Some people will lie or exaggerate their research findings in order to get funding. Then, you see it afterwards, you realize: “ah well, it didn’t work, but they exaggerated what they found and what they did” (participant 14). Another problem in research is the identification of authors when there is a publication. Very often, there are authors who don’t even know what the publication is about and that their name is on it. (…) The time that it surprised me the most was just a few months ago when I saw someone I knew who applied for a teaching position. He got it I was super happy for him. Then I looked at his publications and … there was one that caught my attention much more than the others, because I was in it and I didn’t know what that publication was. I was the second author of a publication that I had never read (participant 14). I saw a colleague who had plagiarized another colleague. [When the colleague] found out about it, he complained. So, plagiarism is a serious [ethical breach]. I would also say that there is a certain amount of competition in the university faculties, especially for grants (…). There are people who want to win at all costs or get as much as possible. They are not necessarily going to consider their colleagues. They don’t have much of a collegial spirit (participant 10).
These examples of research misbehaviour or misconduct are sometimes due to or associated with situations of conflicts of interest, which may be poorly managed by certain researchers or research teams, as noted by many participants.
Conflict of interest
The actors and institutions involved in research have diverse interests, like all humans and institutions. As noted in Chap. 7 of the Canadian Tri-Council Policy Statement: Ethical Conduct for Research Involving Humans (TCPS2, 2018),
“researchers and research students hold trust relationships, either directly or indirectly, with participants, research sponsors, institutions, their professional bodies and society. These trust relationships can be put at risk by conflicts of interest that may compromise independence, objectivity or ethical duties of loyalty. Although the potential for such conflicts has always existed, pressures on researchers (i.e., to delay or withhold dissemination of research outcomes or to use inappropriate recruitment strategies) heighten concerns that conflicts of interest may affect ethical behaviour” (p. 92).
The sources of these conflicts are varied and can include interpersonal conflicts, financial partnerships, third-party pressures, academic or economic interests, a researcher holding multiple roles within an institution, or any other incentive that may compromise a researcher’s independence, integrity, and neutrality (TCPS2, 2018). While it is not possible to eliminate all conflicts of interest, it is important to manage them properly and to avoid temptations to behave unethically.
Ethical temptations correspond to situations in which people are tempted to prioritize their own interests to the detriment of the ethical goods that should, in their own context, govern their actions (Swisher et al., 2005 ). In the case of researchers, this refers to situations that undermine independence, integrity, neutrality, or even the set of principles that govern research ethics (TCPS2, 2018) or the responsible conduct of research. According to study participants, these types of ethical issues frequently occur in research. Many participants, especially researchers and REB members, reported that conflicts of interest can arise when members of an organization make decisions to obtain large financial rewards or to increase their academic profile, often at the expense of the interests of members of their research team, research participants, or even the populations affected by their research.
A company that puts money into making its drug work wants its drug to work. So, homeopathy is a good example, because there are not really any consequences of homeopathy, there are not very many side effects, because there are no effects at all. So, it’s not dangerous, but it’s not a good treatment either. But some people will want to make it work. And that’s a big issue when you’re sitting at a table and there are eight researchers, and there are two or three who are like that, and then there are four others who are neutral, and I say to myself, this is not science. I think that this is a very big ethical issue (participant 14). There are also times in some research where there will be more links with pharmaceutical companies. Obviously, there are then large amounts of money that will be very interesting for the health-care institutions because they still receive money for clinical trials. They’re still getting some compensation because its time consuming for the people involved and all that. The pharmaceutical companies have money, so they will compensate, and that is sometimes interesting for the institutions, and since we are a bit caught up in this, in the sense that we have no choice but to accept it. (…) It may not be the best research in the world, there may be a lot of side effects due to the drugs, but it’s good to accept it, we’re going to be part of the clinical trial (participant 3). It is integrity, what we believe should be done or said. Often by the pressure of the environment, integrity is in tension with the pressures of the environment, so it takes resistance, it takes courage in research. (…) There were all the debates there about the problems of research that was funded and then the companies kept control over what was written. That was really troubling for a lot of researchers (participant 5).
Further, these situations sometimes have negative consequences for research participants as reported by some participants.
Respect for research participants
Many research projects, whether they are psychosocial or biomedical in nature, involve human participants. Relationships between the members of research teams and their research participants raise ethical issues that can be complex. Research projects must always be designed to respect the rights and interests of research participants, and not just those of researchers. However, participants in our study – i.e., REB members, researchers, and research ethics experts – noted that some research teams seem to put their own interests ahead of those of research participants. They also emphasized the importance of ensuring the respect, well-being, and safety of research participants. The ethical issues related to this unit of meaning are: respect for free, informed and ongoing consent of research participants; respect for and the well-being of participants; data protection and confidentiality; over-solicitation of participants; ownership of the data collected on participants; the sometimes high cost of scientific innovations and their accessibility; balance between the social benefits of research and the risks to participants (particularly in terms of safety); balance between collective well-being (development of knowledge) and the individual rights of participants; exploitation of participants; paternalism when working with populations in vulnerable situations; and the social acceptability of certain types of research. The following excerpts present some of these issues.
Where it disturbs me ethically is in the medical field – because it’s more in the medical field that we’re going to see this – when consent forms are presented to patients to solicit them as participants, and then [these forms] have an average of 40 pages. That annoys me. When they say that it has to be easy to understand and all that, adapted to the language, and then the hyper-technical language plus there are 40 pages to read, I don’t understand how you’re going to get informed consent after reading 40 pages. (…) For me, it doesn’t work. I read them to evaluate them and I have a certain level of education and experience in ethics, and there are times when I don’t understand anything (participant 2). There is a lot of pressure from researchers who want to recruit research participants (…). The idea that when you enter a health care institution, you become a potential research participant, when you say “yes to a research, you check yes to all research”, then everyone can ask you. I think that researchers really have this fantasy of saying to themselves: “as soon as people walk through the door of our institution, they become potential participants with whom we can communicate and get them involved in all projects”. There’s a kind of idea that, yes, it can be done, but it has to be somewhat supervised to avoid over-solicitation (…). Researchers are very interested in facilitating recruitment and making it more fluid, but perhaps to the detriment of confidentiality, privacy, and respect; sometimes that’s what it is, to think about what type of data you’re going to have in your bank of potential participants? Is it just name and phone number or are you getting into more sensitive information? (participant 9).
In addition, one participant reported that their university does not provide the resources required to respect the confidentiality of research participants.
The issue is as follows: researchers, of course, commit to protecting data with passwords and all that, but we realize that in practice, it is more difficult. It is not always as protected as one might think, because professor-researchers will run out of space. Will the universities make rooms available to researchers, places where they can store these things, especially when they have paper documentation, and is there indeed a guarantee of confidentiality? Some researchers have told me: “Listen; there are even filing cabinets in the corridors”. So, that certainly poses a concrete challenge. How do we go about challenging the administrative authorities? Tell them it’s all very well to have an ethics committee, but you have to help us, you also have to make sure that the necessary infrastructures are in place so that what we are proposing is really put into practice (participant 4).
If the relationships with research participants are likely to raise ethical issues, so too are the relationships with students, notably research assistants. On this topic, several participants discussed the lack of supervision or recognition offered to research assistants by researchers as well as the power imbalances between members of the research team.
Lack of Supervision and Power Imbalances
Many research teams are composed not only of researchers, but also of students who work as research assistants. The relationship between research assistants and other members of research teams can sometimes be problematic and raise ethical issues, particularly because of the inevitable power asymmetries. In the context of this study, several participants – including a research assistant, REB members, and researchers – discussed the lack of supervision or recognition of the work carried out by students, psychological pressure, and the more or less well-founded promises that are sometimes made to students. Participants also mentioned the exploitation of students by certain research teams, which manifest when students are inadequately paid, i.e., not reflective of the number of hours actually worked, not a fair wage, or even a wage at all.
[As a research assistant], it was more of a feeling of distress that I felt then because I didn’t know what to do. (…) I was supposed to get coaching or be supported, but I didn’t get anything in the end. It was like, “fix it by yourself”. (…) All research assistants were supposed to be supervised, but in practice they were not (participant 1). Very often, we have a master’s or doctoral student that we put on a subject and we consider that the project will be well done, while the student is learning. So, it happens that the student will do a lot of work and then we realize that the work is poorly done, and it is not necessarily the student’s fault. He wasn’t necessarily well supervised. There are directors who have 25 students, and they just don’t supervise them (participant 14). I think it’s really the power relationship. I thought to myself, how I saw my doctorate, the beginning of my research career, I really wanted to be in that laboratory, but they are the ones who are going to accept me or not, so what do I do to be accepted? I finally accept their conditions [which was to work for free]. If these are the conditions that are required to enter this lab, I want to go there. So, what do I do, well I accepted. It doesn’t make sense, but I tell myself that I’m still privileged, because I don’t have so many financial worries, one more reason to work for free, even though it doesn’t make sense (participant 1). In research, we have research assistants. (…). The fact of using people… so that’s it, you have to take into account where they are, respect them, but at the same time they have to show that they are there for the research. In English, we say “carry” or take care of people. With research assistants, this is often a problem that I have observed: for grant machines, the person is the last to be found there. Researchers, who will take, use student data, without giving them the recognition for it (participant 5). The problem at our university is that they reserve funding for Canadian students. The doctoral clientele in my field is mostly foreign students. So, our students are poorly funded. I saw one student end up in the shelter, in a situation of poverty. It ended very badly for him because he lacked financial resources. Once you get into that dynamic, it’s very hard to get out. I was made aware of it because the director at the time had taken him under her wing and wanted to try to find a way to get him out of it. So, most of my students didn’t get funded (participant 16). There I wrote “manipulation”, but it’s kind of all promises all the time. I, for example, was promised a lot of advancement, like when I got into the lab as a graduate student, it was said that I had an interest in [this particular area of research]. I think there are a lot of graduate students who must have gone through that, but it is like, “Well, your CV has to be really good, if you want to do a lot of things and big things. If you do this, if you do this research contract, the next year you could be the coordinator of this part of the lab and supervise this person, get more contracts, be paid more. Let’s say: you’ll be invited to go to this conference, this big event”. They were always dangling something, but you have to do that first to get there. But now, when you’ve done that, you have to do this business. It’s like a bit of manipulation, I think. That was very hard to know who is telling the truth and who is not (participant 1).
These ethical issues have significant negative consequences for students. Indeed, they sometimes find themselves at the mercy of researchers, for whom they work, struggling to be recognized and included as authors of an article, for example, or to receive the salary that they are due. For their part, researchers also sometimes find themselves trapped in research structures that can negatively affect their well-being. As many participants reported, researchers work in organizations that set very high productivity standards and in highly competitive contexts, all within a general culture characterized by individualism.
Individualism and performance
Participants, especially researchers, discussed the culture of individualism and performance that characterizes the academic environment. In glorifying excellence, some universities value performance and productivity, often at the expense of psychological well-being and work-life balance (i.e., work overload and burnout). Participants noted that there are ethical silences in their organizations on this issue, and that the culture of individualism and performance is not challenged for fear of retribution or simply to survive, i.e., to perform as expected. Participants felt that this culture can have a significant negative impact on the quality of the research conducted, as research teams try to maximize the quantity of their work (instead of quality) in a highly competitive context, which is then exacerbated by a lack of resources and support, and where everything must be done too quickly.
The work-life balance with the professional ethics related to work in a context where you have too much and you have to do a lot, it is difficult to balance all that and there is a lot of pressure to perform. If you don’t produce enough, that’s it; after that, you can’t get any more funds, so that puts pressure on you to do more and more and more (participant 3). There is a culture, I don’t know where it comes from, and that is extremely bureaucratic. If you dare to raise something, you’re going to have many, many problems. They’re going to make you understand it. So, I don’t talk. It is better: your life will be easier. I think there are times when you have to talk (…) because there are going to be irreparable consequences. (…) I’m not talking about a climate of terror, because that’s exaggerated, it’s not true, people are not afraid. But people close their office door and say nothing because it’s going to make their work impossible and they’re not going to lose their job, they’re not going to lose money, but researchers need time to be focused, so they close their office door and say nothing (participant 16).
Researchers must produce more and more, and they feel little support in terms of how to do such production, ethically, and how much exactly they are expected to produce. As this participant reports, the expectation is an unspoken rule: more is always better.
It’s sometimes the lack of a clear line on what the expectations are as a researcher, like, “ah, we don’t have any specific expectations, but produce, produce, produce, produce.” So, in that context, it’s hard to be able to put the line precisely: “have I done enough for my work?” (participant 3).
Inadequate ethical Guidance
While the productivity expectation is not clear, some participants – including researchers, research ethics experts, and REB members – also felt that the ethical expectations of some REBs were unclear. The issue of the inadequate ethical guidance of research includes the administrative mechanisms to ensure that research projects respect the principles of research ethics. According to those participants, the forms required for both researchers and REB members are increasingly long and numerous, and one participant noted that the standards to be met are sometimes outdated and disconnected from the reality of the field. Multicentre ethics review (by several REBs) was also critiqued by a participant as an inefficient method that encumbers the processes for reviewing research projects. Bureaucratization imposes an ever-increasing number of forms and ethics guidelines that actually hinder researchers’ ethical reflection on the issues at stake, leading the ethics review process to be perceived as purely bureaucratic in nature.
The ethical dimension and the ethical review of projects have become increasingly bureaucratized. (…) When I first started working (…) it was less bureaucratic, less strict then. I would say [there are now] tons of forms to fill out. Of course, we can’t do without it, it’s one of the ways of marking out ethics and ensuring that there are ethical considerations in research, but I wonder if it hasn’t become too bureaucratized, so that it’s become a kind of technical reflex to fill out these forms, and I don’t know if people really do ethical reflection as such anymore (participant 10). The fundamental structural issue, I would say, is the mismatch between the normative requirements and the real risks posed by the research, i.e., we have many, many requirements to meet; we have very long forms to fill out but the research projects we evaluate often pose few risks (participant 8). People [in vulnerable situations] were previously unable to participate because of overly strict research ethics rules that were to protect them, but in the end [these rules] did not protect them. There was a perverse effect, because in the end there was very little research done with these people and that’s why we have very few results, very little evidence [to support practices with these populations] so it didn’t improve the quality of services. (…) We all understand that we have to be careful with that, but when the research is not too risky, we say to ourselves that it would be good because for once a researcher who is interested in that population, because it is not a very popular population, it would be interesting to have results, but often we are blocked by the norms, and then we can’t accept [the project] (participant 2).
Moreover, as one participant noted, accessing ethics training can be a challenge.
There is no course on research ethics. […] Then, I find that it’s boring because you go through university and you come to do your research and you know how to do quantitative and qualitative research, but all the research ethics, where do you get this? I don’t really know (participant 13).
Yet, such training could provide relevant tools to resolve, to some extent, the ethical issues that commonly arise in research. That said, and as noted by many participants, many ethical issues in research are related to social injustices over which research actors have little influence.
Social Injustices
For many participants, notably researchers, the issues that concern social injustices are those related to power asymmetries, stigma, or issues of equity, diversity, and inclusion, i.e., social injustices related to people’s identities (Blais & Drolet, 2022 ). Participants reported experiencing or witnessing discrimination from peers, administration, or lab managers. Such oppression is sometimes cross-sectional and related to a person’s age, cultural background, gender or social status.
I have my African colleague who was quite successful when he arrived but had a backlash from colleagues in the department. I think it’s unconscious, nobody is overtly racist. But I have a young person right now who is the same, who has the same success, who got exactly the same early career award and I don’t see the same backlash. He’s just as happy with what he’s doing. It’s normal, they’re young and they have a lot of success starting out. So, I think there is discrimination. Is it because he is African? Is it because he is black? I think it’s on a subconscious level (participant 16).
Social injustices were experienced or reported by many participants, and included issues related to difficulties in obtaining grants or disseminating research results in one’s native language (i.e., even when there is official bilingualism) or being considered credible and fundable in research when one researcher is a woman.
If you do international research, there are things you can’t talk about (…). It is really a barrier to research to not be able to (…) address this question [i.e. the question of inequalities between men and women]. Women’s inequality is going to be addressed [but not within the country where the research takes place as if this inequality exists elsewhere but not here]. There are a lot of women working on inequality issues, doing work and it’s funny because I was talking to a young woman who works at Cairo University and she said to me: “Listen, I saw what you had written, you’re right. I’m willing to work on this but guarantee me a position at your university with a ticket to go”. So yes, there are still many barriers [for women in research] (participant 16).
Because of the varied contextual characteristics that intervene in their occurrence, these social injustices are also related to distributive injustices, as discussed by many participants.
Distributive Injustices
Although there are several views of distributive justice, a classical definition such as that of Aristotle ( 2012 ), describes distributive justice as consisting in distributing honours, wealth, and other social resources or benefits among the members of a community in proportion to their alleged merit. Justice, then, is about determining an equitable distribution of common goods. Contemporary theories of distributive justice are numerous and varied. Indeed, many authors (e.g., Fraser 2011 ; Mills, 2017 ; Sen, 2011 ; Young, 2011 ) have, since Rawls ( 1971 ), proposed different visions of how social burdens and benefits should be shared within a community to ensure equal respect, fairness, and distribution. In our study, what emerges from participants’ narratives is a definite concern for this type of justice. Women researchers, francophone researchers, early career researchers or researchers belonging to racialized groups all discussed inequities in the distribution of research grants and awards, and the extra work they need to do to somehow prove their worth. These inequities are related to how granting agencies determine which projects will be funded.
These situations make me work 2–3 times harder to prove myself and to show people in power that I have a place as a woman in research (participant 12). Number one: it’s conservative thinking. The older ones control what comes in. So, the younger people have to adapt or they don’t get funded (participant 14).
Whether it is discrimination against stigmatized or marginalized populations or interest in certain hot topics, granting agencies judge research projects according to criteria that are sometimes questionable, according to those participants. Faced with difficulties in obtaining funding for their projects, several strategies – some of which are unethical – are used by researchers in order to cope with these situations.
Sometimes there are subjects that everyone goes to, such as nanotechnology (…), artificial intelligence or (…) the therapeutic use of cannabis, which are very fashionable, and this is sometimes to the detriment of other research that is just as relevant, but which is (…), less sexy, less in the spirit of the time. (…) Sometimes this can lead to inequities in the funding of certain research sectors (participant 9). When we use our funds, we get them given to us, we pretty much say what we think we’re going to do with them, but things change… So, when these things change, sometimes it’s an ethical decision, but by force of circumstances I’m obliged to change the project a little bit (…). Is it ethical to make these changes or should I just let the money go because I couldn’t use it the way I said I would? (participant 3).
Moreover, these distributional injustices are not only linked to social injustices, but also epistemic injustices. Indeed, the way in which research honours and grants are distributed within the academic community depends on the epistemic authority of the researchers, which seems to vary notably according to their language of use, their age or their gender, but also to the research design used (inductive versus deductive), their decision to use (or not use) animals in research, or to conduct activist research.
Epistemic injustices
The philosopher Fricker ( 2007 ) conceptualized the notions of epistemic justice and injustice. Epistemic injustice refers to a form of social inequality that manifests itself in the access, recognition, and production of knowledge as well as the various forms of ignorance that arise (Godrie & Dos Santos, 2017 ). Addressing epistemic injustice necessitates acknowledging the iniquitous wrongs suffered by certain groups of socially stigmatized individuals who have been excluded from knowledge, thus limiting their abilities to interpret, understand, or be heard and account for their experiences. In this study, epistemic injustices were experienced or reported by some participants, notably those related to difficulties in obtaining grants or disseminating research results in one’s native language (i.e., even when there is official bilingualism) or being considered credible and fundable in research when a researcher is a woman or an early career researcher.
I have never sent a grant application to the federal government in English. I have always done it in French, even though I know that when you receive the review, you can see that reviewers didn’t understand anything because they are English-speaking. I didn’t want to get in the boat. It’s not my job to translate, because let’s be honest, I’m not as good in English as I am in French. So, I do them in my first language, which is the language I’m most used to. Then, technically at the administrative level, they are supposed to be able to do it, but they are not good in French. (…) Then, it’s a very big Canadian ethical issue, because basically there are technically two official languages, but Canada is not a bilingual country, it’s a country with two languages, either one or the other. (…) So I was not funded (participant 14).
Researchers who use inductive (or qualitative) methods observed that their projects are sometimes less well reviewed or understood, while research that adopts a hypothetical-deductive (or quantitative) or mixed methods design is better perceived, considered more credible and therefore more easily funded. Of course, regardless of whether a research project adopts an inductive, deductive or mixed-methods scientific design, or whether it deals with qualitative or quantitative data, it must respect a set of scientific criteria. A research project should achieve its objectives by using proven methods that, in the case of inductive research, are credible, reliable, and transferable or, in the case of deductive research, generalizable, objective, representative, and valid (Drolet & Ruest, accepted ). Participants discussing these issues noted that researchers who adopt a qualitative design or those who question the relevance of animal experimentation or are not militant have sometimes been unfairly devalued in their epistemic authority.
There is a mini war between quantitative versus qualitative methods, which I think is silly because science is a method. If you apply the method well, it doesn’t matter what the field is, it’s done well and it’s perfect ” (participant 14). There is also the issue of the place of animals in our lives, because for me, ethics is human ethics, but also animal ethics. Then, there is a great evolution in society on the role of the animal… with the new law that came out in Quebec on the fact that animals are sensitive beings. Then, with the rise of the vegan movement, [we must ask ourselves]: “Do animals still have a place in research?” That’s a big question and it also means that there are practices that need to evolve, but sometimes there’s a disconnection between what’s expected by research ethics boards versus what’s expected in the field (participant 15). In research today, we have more and more research that is militant from an ideological point of view. And so, we have researchers, because they defend values that seem important to them, we’ll talk for example about the fight for equality and social justice. They have pressure to defend a form of moral truth and have the impression that everyone thinks like them or should do so, because they are defending a moral truth. This is something that we see more and more, namely the lack of distance between ideology and science (participant 8).
The combination or intersectionality of these inequities, which seems to be characterized by a lack of ethical support and guidance, is experienced in the highly competitive and individualistic context of research; it provides therefore the perfect recipe for researchers to experience ethical distress.
Ethical distress
The concept of “ethical distress” refers to situations in which people know what they should do to act ethically, but encounter barriers, generally of an organizational or systemic nature, limiting their power to act according to their moral or ethical values (Drolet & Ruest, 2021 ; Jameton, 1984 ; Swisher et al., 2005 ). People then run the risk of finding themselves in a situation where they do not act as their ethical conscience dictates, which in the long term has the potential for exhaustion and distress. The examples reported by participants in this study point to the fact that researchers in particular may be experiencing significant ethical distress. This distress takes place in a context of extreme competition, constant injunctions to perform, and where administrative demands are increasingly numerous and complex to complete, while paradoxically, they lack the time to accomplish all their tasks and responsibilities. Added to these demands are a lack of resources (human, ethical, and financial), a lack of support and recognition, and interpersonal conflicts.
We are in an environment, an elite one, you are part of it, you know what it is: “publish or perish” is the motto. Grants, there is a high level of performance required, to do a lot, to publish, to supervise students, to supervise them well, so yes, it is clear that we are in an environment that is conducive to distress. (…). Overwork, definitely, can lead to distress and eventually to exhaustion. When you know that you should take the time to read the projects before sharing them, but you don’t have the time to do that because you have eight that came in the same day, and then you have others waiting… Then someone rings a bell and says: “ah but there, the protocol is a bit incomplete”. Oh yes, look at that, you’re right. You make up for it, but at the same time it’s a bit because we’re in a hurry, we don’t necessarily have the resources or are able to take the time to do things well from the start, we have to make up for it later. So yes, it can cause distress (participant 9). My organization wanted me to apply in English, and I said no, and everyone in the administration wanted me to apply in English, and I always said no. Some people said: “Listen, I give you the choice”, then some people said: “Listen, I agree with you, but if you’re not [submitting] in English, you won’t be funded”. Then the fact that I am young too, because very often they will look at the CV, they will not look at the project: “ah, his CV is not impressive, we will not finance him”. This is complete nonsense. The person is capable of doing the project, the project is fabulous: we fund the project. So, that happened, organizational barriers: that happened a lot. I was not eligible for Quebec research funds (…). I had big organizational barriers unfortunately (participant 14). At the time of my promotion, some colleagues were not happy with the type of research I was conducting. I learned – you learn this over time when you become friends with people after you enter the university – that someone was against me. He had another candidate in mind, and he was angry about the selection. I was under pressure for the first three years until my contract was renewed. I almost quit at one point, but another colleague told me, “No, stay, nothing will happen”. Nothing happened, but these issues kept me awake at night (participant 16).
This difficult context for many researchers affects not only the conduct of their own research, but also their participation in research. We faced this problem in our study, despite the use of multiple recruitment methods, including more than 200 emails – of which 191 were individual solicitations – sent to potential participants by the two research assistants. REB members and organizations overseeing or supporting research (n = 17) were also approached to see if some of their employees would consider participating. While it was relatively easy to recruit REB members and research ethics experts, our team received a high number of non-responses to emails (n = 175) and some refusals (n = 5), especially by researchers. The reasons given by those who replied were threefold: (a) fear of being easily identified should they take part in the research, (b) being overloaded and lacking time, and (c) the intrusive aspect of certain questions (i.e., “Have you experienced a burnout episode? If so, have you been followed up medically or psychologically?”). In light of these difficulties and concerns, some questions in the socio-demographic questionnaire were removed or modified. Talking about burnout in research remains a taboo for many researchers, which paradoxically can only contribute to the unresolved problem of unhealthy research environments.
Returning to the research question and objective
The question that prompted this research was: What are the ethical issues in research? The purpose of the study was to describe these issues from the perspective of researchers (from different disciplines), research ethics board (REB) members, and research ethics experts. The previous section provided a detailed portrait of the ethical issues experienced by different research stakeholders: these issues are numerous, diverse and were recounted by a range of stakeholders.
The results of the study are generally consistent with the literature. For example, as in our study, the literature discusses the lack of research integrity on the part of some researchers (Al-Hidabi et al., 2018 ; Swazey et al., 1993 ), the numerous conflicts of interest experienced in research (Williams-Jones et al., 2013 ), the issues of recruiting and obtaining the free and informed consent of research participants (Provencher et al., 2014 ; Keogh & Daly, 2009 ), the sometimes difficult relations between researchers and REBs (Drolet & Girard, 2020 ), the epistemological issues experienced in research (Drolet & Ruest, accepted; Sieber 2004 ), as well as the harmful academic context in which researchers evolve, insofar as this is linked to a culture of performance, an overload of work in a context of accountability (Berg & Seeber, 2016 ; FQPPU; 2019 ) that is conducive to ethical distress and even burnout.
If the results of the study are generally in line with those of previous publications on the subject, our findings also bring new elements to the discussion while complementing those already documented. In particular, our results highlight the role of systemic injustices – be they social, distributive or epistemic – within the environments in which research is carried out, at least in Canada. To summarize, the results of our study point to the fact that the relationships between researchers and research participants are likely still to raise worrying ethical issues, despite widely accepted research ethics norms and institutionalized review processes. Further, the context in which research is carried out is not only conducive to breaches of ethical norms and instances of misbehaviour or misconduct, but also likely to be significantly detrimental to the health and well-being of researchers, as well as research assistants. Another element that our research also highlighted is the instrumentalization and even exploitation of students and research assistants, which is another important and worrying social injustice given the inevitable power imbalances between students and researchers.
Moreover, in a context in which ethical issues are often discussed from a micro perspective, our study helps shed light on both the micro- and macro-level ethical dimensions of research (Bronfenbrenner, 1979 ; Glaser 1994 ). However, given that ethical issues in research are not only diverse, but also and above all complex, a broader perspective that encompasses the interplay between the micro and macro dimensions can enable a better understanding of these issues and thereby support the identification of the multiple factors that may be at their origin. Triangulating the perspectives of researchers with those of REB members and research ethics experts enabled us to bring these elements to light, and thus to step back from and critique the way that research is currently conducted. To this end, attention to socio-political elements such as the performance culture in academia or how research funds are distributed, and according to what explicit and implicit criteria, can contribute to identifying the sources of the ethical issues described above.
Contemporary culture characterized by the social acceleration
The German sociologist and philosopher Rosa (2010) argues that late modernity – that is, the period between the 1980s and today – is characterized by a phenomenon of social acceleration that causes various forms of alienation in our relationship to time, space, actions, things, others and ourselves. Rosa distinguishes three types of acceleration: technical acceleration , the acceleration of social changes and the acceleration of the rhythm of life . According to Rosa, social acceleration is the main problem of late modernity, in that the invisible social norm of doing more and faster to supposedly save time operates unchallenged at all levels of individual and collective life, as well as organizational and social life. Although we all, researchers and non-researchers alike, perceive this unspoken pressure to be ever more productive, the process of social acceleration as a new invisible social norm is our blind spot, a kind of tyrant over which we have little control. This conceptualization of the contemporary culture can help us to understand the context in which research is conducted (like other professional practices). To this end, Berg & Seeber ( 2016 ) invite faculty researchers to slow down in order to better reflect and, in the process, take care of their health and their relationships with their colleagues and students. Many women professors encourage their fellow researchers, especially young women researchers, to learn to “say No” in order to protect their mental and physical health and to remain in their academic careers (Allaire & Descheneux, 2022 ). These authors also remind us of the relevance of Kahneman’s ( 2012 ) work which demonstrates that it takes time to think analytically, thoroughly, and logically. Conversely, thinking quickly exposes humans to cognitive and implicit biases that then lead to errors in thinking (e.g., in the analysis of one’s own research data or in the evaluation of grant applications or student curriculum vitae). The phenomenon of social acceleration, which pushes the researcher to think faster and faster, is likely to lead to unethical bad science that can potentially harm humankind. In sum, Rosa’s invitation to contemporary critical theorists to seriously consider the problem of social acceleration is particularly insightful to better understand the ethical issues of research. It provides a lens through which to view the toxic context in which research is conducted today, and one that was shared by the participants in our study.
Clark & Sousa ( 2022 ) note, it is important that other criteria than the volume of researchers’ contributions be valued in research, notably quality. Ultimately, it is the value of the knowledge produced and its influence on the concrete lives of humans and other living beings that matters, not the quantity of publications. An interesting articulation of this view in research governance is seen in a change in practice by Australia’s national health research funder: they now restrict researchers to listing on their curriculum vitae only the top ten publications from the past ten years (rather than all of their publications), in order to evaluate the quality of contributions rather than their quantity. To create environments conducive to the development of quality research, it is important to challenge the phenomenon of social acceleration, which insidiously imposes a quantitative normativity that is both alienating and detrimental to the quality and ethical conduct of research. Based on our experience, we observe that the social norm of acceleration actively disfavours the conduct of empirical research on ethics in research. The fact is that researchers are so busy that it is almost impossible for them to find time to participate in such studies. Further, operating in highly competitive environments, while trying to respect the values and ethical principles of research, creates ethical paradoxes for members of the research community. According to Malherbe ( 1999 ), an ethical paradox is a situation where an individual is confronted by contradictory injunctions (i.e., do more, faster, and better). And eventually, ethical paradoxes lead individuals to situations of distress and burnout, or even to ethical failures (i.e., misbehaviour or misconduct) in the face of the impossibility of responding to contradictory injunctions.
Strengths and Limitations of the study
The triangulation of perceptions and experiences of different actors involved in research is a strength of our study. While there are many studies on the experiences of researchers, rarely are members of REBs and experts in research ethics given the space to discuss their views of what are ethical issues. Giving each of these stakeholders a voice and comparing their different points of view helped shed a different and complementary light on the ethical issues that occur in research. That said, it would have been helpful to also give more space to issues experienced by students or research assistants, as the relationships between researchers and research assistants are at times very worrying, as noted by a participant, and much work still needs to be done to eliminate the exploitative situations that seem to prevail in certain research settings. In addition, no Indigenous or gender diverse researchers participated in the study. Given the ethical issues and systemic injustices that many people from these groups face in Canada (Drolet & Goulet, 2018 ; Nicole & Drolet, in press ), research that gives voice to these researchers would be relevant and contribute to knowledge development, and hopefully also to change in research culture.
Further, although most of the ethical issues discussed in this article may be transferable to the realities experienced by researchers in other countries, the epistemic injustice reported by Francophone researchers who persist in doing research in French in Canada – which is an officially bilingual country but in practice is predominantly English – is likely specific to the Canadian reality. In addition, and as mentioned above, recruitment proved exceedingly difficult, particularly amongst researchers. Despite this difficulty, we obtained data saturation for all but two themes – i.e., exploitation of students and ethical issues of research that uses animals. It follows that further empirical research is needed to improve our understanding of these specific issues, as they may diverge to some extent from those documented here and will likely vary across countries and academic research contexts.
Conclusions
This study, which gave voice to researchers, REB members, and ethics experts, reveals that the ethical issues in research are related to several problematic elements as power imbalances and authority relations. Researchers and research assistants are subject to external pressures that give rise to integrity issues, among others ethical issues. Moreover, the current context of social acceleration influences the definition of the performance indicators valued in academic institutions and has led their members to face several ethical issues, including social, distributive, and epistemic injustices, at different steps of the research process. In this study, ten categories of ethical issues were identified, described and illustrated: (1) research integrity, (2) conflicts of interest, (3) respect for research participants, (4) lack of supervision and power imbalances, (5) individualism and performance, (6) inadequate ethical guidance, (7) social injustices, (8) distributive injustices, (9) epistemic injustices, and (10) ethical distress. The triangulation of the perspectives of different members (i.e., researchers from different disciplines, REB members, research ethics experts, and one research assistant) involved in the research process made it possible to lift the veil on some of these ethical issues. Further, it enabled the identification of additional ethical issues, especially systemic injustices experienced in research. To our knowledge, this is the first time that these injustices (social, distributive, and epistemic injustices) have been clearly identified.
Finally, this study brought to the fore several problematic elements that are important to address if the research community is to develop and implement the solutions needed to resolve the diverse and transversal ethical issues that arise in research institutions. A good starting point is the rejection of the corollary norms of “publish or perish” and “do more, faster, and better” and their replacement with “publish quality instead of quantity”, which necessarily entails “do less, slower, and better”. It is also important to pay more attention to the systemic injustices within which researchers work, because these have the potential to significantly harm the academic careers of many researchers, including women researchers, early career researchers, and those belonging to racialized groups as well as the health, well-being, and respect of students and research participants.
Acknowledgements
The team warmly thanks the participants who took part in the research and who made this study possible. Marie-Josée Drolet thanks the five research assistants who participated in the data collection and analysis: Julie-Claude Leblanc, Élie Beauchemin, Pénéloppe Bernier, Louis-Pierre Côté, and Eugénie Rose-Derouin, all students at the Université du Québec à Trois-Rivières (UQTR), two of whom were active in the writing of this article. MJ Drolet and Bryn Williams-Jones also acknowledge the financial contribution of the Social Sciences and Humanities Research Council of Canada (SSHRC), which supported this research through a grant. We would also like to thank the reviewers of this article who helped us improve it, especially by clarifying and refining our ideas.
Competing Interests and Funding
As noted in the Acknowledgements, this research was supported financially by the Social Sciences and Humanities Research Council of Canada (SSHRC).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
- Al-Hidabi, Abdulmalek, M. D., & The, P. L. (2018). Multiple Publications: The Main Reason for the Retraction of Papers in Computer Science. In K. Arai, S. Kapoor, & R. Bhatia (eds), Future of Information and Communication Conference (FICC): Advances in Information and Communication, Advances in Intelligent Systems and Computing (AISC), Springer, vol. 886, pp. 511–526
- Allaire, S., & Deschenaux, F. (2022). Récits de professeurs d’université à mi-carrière. Si c’était à refaire… . Presses de l’Université du Québec
- Aristotle . Aristotle’s Nicomachean Ethics. Chicago: The University of Chicago Press; 2012. [ Google Scholar ]
- Bahn S. Keeping Academic Field Researchers Safe: Ethical Safeguards. Journal of Academic Ethics. 2012; 10 :83–91. doi: 10.1007/s10805-012-9159-2. [ CrossRef ] [ Google Scholar ]
- Balk DE. Bereavement Research Using Control Groups: Ethical Obligations and Questions. Death Studies. 1995; 19 :123–138. doi: 10.1080/07481189508252720. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Beauchemin, É., Côté, L. P., Drolet, M. J., & Williams-Jones, B. (2021). Conceptualizing Ethical Issues in the Conduct of Research: Results from a Critical and Systematic Literature Review. Journal of Academic Ethics , Early Online. 10.1007/s10805-021-09411-7
- Berg, M., & Seeber, B. K. (2016). The Slow Professor . University of Toronto Press
- Birchley G, Huxtable R, Murtagh M, Meulen RT, Flach P, Gooberman-Hill R. Smart homes, private homes? An empirical study of technology researchers’ perceptions of ethical issues in developing smart-home health technologies. BMC Medical Ethics. 2017; 18 (23):1–13. doi: 10.1186/s12910-017-0183-z. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Blais, J., & Drolet, M. J. (2022). Les injustices sociales vécues en camp de réfugiés: les comprendre pour mieux intervenir auprès de personnes ayant séjourné dans un camp de réfugiés. Recueil annuel belge d’ergothérapie , 14, 37–48
- Bogdan, R. C., & Biklen, S. K. (2006). Qualitative research in education: An introduction to theory and methods . Allyn & Bacon
- Bouffard C. Le développement des pratiques de la génétique médicale et la construction des normes bioéthiques. Anthropologie et Sociétés. 2000; 24 (2):73–90. doi: 10.7202/015650ar. [ CrossRef ] [ Google Scholar ]
- Bronfenbrenner, U. (1979). The Ecology of Human development. Experiments by nature and design . Harvard University Press
- Bruhn JG, Zajac G, Al-Kazemi AA, Prescott LD. Moral positions and academic conduct: Parameters of tolerance for ethics failure. Journal of Higher Education. 2002; 73 (4):461–493. doi: 10.1353/jhe.2002.0033. [ CrossRef ] [ Google Scholar ]
- Clark, A., & Sousa (2022). It’s time to end Canada’s obsession with research quantity. University Affairs/Affaires universitaires , February 14th. https://www.universityaffairs.ca/career-advice/effective-successfull-happy-academic/its-time-to-end-canadas-obsession-with-research-quantity/?utm_source=University+Affairs+e-newsletter&utm_campaign=276a847f 70-EMAIL_CAMPAIGN_2022_02_16&utm_medium=email&utm_term=0_314bc2ee29-276a847f70-425259989
- Colnerud G. Ethical dilemmas in research in relation to ethical review: An empirical study. Research Ethics. 2015; 10 (4):238–253. doi: 10.1177/1747016114552339. [ CrossRef ] [ Google Scholar ]
- Davison J. Dilemmas in Research: Issues of Vulnerability and Disempowerment for the Social Workers/Researcher. Journal of Social Work Practice. 2004; 18 (3):379–393. doi: 10.1080/0265053042000314447. [ CrossRef ] [ Google Scholar ]
- DePoy E, Gitlin LN. Introduction to Research. St. Louis: Elsevier Mosby; 2010. [ Google Scholar ]
- Drolet, M. J., & Goulet, M. (2018). Travailler avec des patients autochtones du Canada ? Perceptions d’ergothérapeutes du Québec des enjeux éthiques de cette pratique. Recueil annuel belge francophone d’ergothérapie , 10 , 25–56
- Drolet MJ, Girard K. Les enjeux éthiques de la recherche en ergothérapie: un portrait préoccupant. Revue canadienne de bioéthique. 2020; 3 (3):21–40. doi: 10.7202/1073779ar. [ CrossRef ] [ Google Scholar ]
- Drolet MJ, Girard K, Gaudet R. Les enjeux éthiques de l’enseignement en ergothérapie: des injustices au sein des départements universitaires. Revue canadienne de bioéthique. 2020; 3 (1):22–36. [ Google Scholar ]
- Drolet MJ, Maclure J. Les enjeux éthiques de la pratique de l’ergothérapie: perceptions d’ergothérapeutes. Revue Approches inductives. 2016; 3 (2):166–196. doi: 10.7202/1037918ar. [ CrossRef ] [ Google Scholar ]
- Drolet MJ, Pinard C, Gaudet R. Les enjeux éthiques de la pratique privée: des ergothérapeutes du Québec lancent un cri d’alarme. Ethica – Revue interdisciplinaire de recherche en éthique. 2017; 21 (2):173–209. [ Google Scholar ]
- Drolet MJ, Ruest M. De l’éthique à l’ergothérapie: un cadre théorique et une méthode pour soutenir la pratique professionnelle. Québec: Presses de l’Université du Québec; 2021. [ Google Scholar ]
- Drolet, M. J., & Ruest, M. (accepted). Quels sont les enjeux éthiques soulevés par la recherche scientifique? In M. Lalancette & J. Luckerhoff (dir). Initiation au travail intellectuel et à la recherche . Québec: Presses de l’Université du Québec, 18 p
- Drolet MJ, Sauvageau A, Baril N, Gaudet R. Les enjeux éthiques de la formation clinique en ergothérapie. Revue Approches inductives. 2019; 6 (1):148–179. doi: 10.7202/1060048ar. [ CrossRef ] [ Google Scholar ]
- Fédération québécoise des professeures et des professeurs d’université (FQPPU) Enquête nationale sur la surcharge administrative du corps professoral universitaire québécois. Principaux résultats et pistes d’action. Montréal: FQPPU; 2019. [ Google Scholar ]
- Fortin MH. Fondements et étapes du processus de recherche. Méthodes quantitatives et qualitatives. Montréal, QC: Chenelière éducation; 2010. [ Google Scholar ]
- Fraser DM. Ethical dilemmas and practical problems for the practitioner researcher. Educational Action Research. 1997; 5 (1):161–171. doi: 10.1080/09650799700200014. [ CrossRef ] [ Google Scholar ]
- Fraser, N. (2011). Qu’est-ce que la justice sociale? Reconnaissance et redistribution . La Découverte
- Fricker, M. (2007). Epistemic Injustice: Power and the Ethics of Knowing . Oxford University Press
- Giorgi A, et al. De la méthode phénoménologique utilisée comme mode de recherche qualitative en sciences humaines: théories, pratique et évaluation. In: Poupart J, Groulx LH, Deslauriers JP, et al., editors. La recherche qualitative: enjeux épistémologiques et méthodologiques. Boucherville, QC: Gaëtan Morin; 1997. pp. 341–364. [ Google Scholar ]
- Giorgini V, Mecca JT, Gibson C, Medeiros K, Mumford MD, Connelly S, Devenport LD. Researcher Perceptions of Ethical Guidelines and Codes of Conduct. Accountability in Research. 2016; 22 (3):123–138. doi: 10.1080/08989621.2014.955607. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Glaser, J. W. (1994). Three realms of ethics: Individual, institutional, societal. Theoretical model and case studies . Kansas Cuty, Sheed & Ward
- Godrie B, Dos Santos M. Présentation: inégalités sociales, production des savoirs et de l’ignorance. Sociologie et sociétés. 2017; 49 (1):7. doi: 10.7202/1042804ar. [ CrossRef ] [ Google Scholar ]
- Hammell KW, Carpenter C, Dyck I. Using Qualitative Research: A Practical Introduction for Occupational and Physical Therapists. Edinburgh: Churchill Livingstone; 2000. [ Google Scholar ]
- Henderson M, Johnson NF, Auld G. Silences of ethical practice: dilemmas for researchers using social media. Educational Research and Evaluation. 2013; 19 (6):546–560. doi: 10.1080/13803611.2013.805656. [ CrossRef ] [ Google Scholar ]
- Husserl E. The crisis of European sciences and transcendental phenomenology. Evanston, IL: Northwestern University Press; 1970. [ Google Scholar ]
- Husserl E. The train of thoughts in the lectures. In: Polifroni EC, Welch M, editors. Perspectives on Philosophy of Science in Nursing. Philadelphia, PA: Lippincott; 1999. [ Google Scholar ]
- Hunt SD, Chonko LB, Wilcox JB. Ethical problems of marketing researchers. Journal of Marketing Research. 1984; 21 :309–324. doi: 10.1177/002224378402100308. [ CrossRef ] [ Google Scholar ]
- Hunt MR, Carnevale FA. Moral experience: A framework for bioethics research. Journal of Medical Ethics. 2011; 37 (11):658–662. doi: 10.1136/jme.2010.039008. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jameton, A. (1984). Nursing practice: The ethical issues . Englewood Cliffs, Prentice-Hall
- Jarvis K. Dilemmas in International Research and the Value of Practical Wisdom. Developing World Bioethics. 2017; 17 (1):50–58. doi: 10.1111/dewb.12121. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kahneman D. Système 1, système 2: les deux vitesses de la pensée. Paris: Flammarion; 2012. [ Google Scholar ]
- Keogh B, Daly L. The ethics of conducting research with mental health service users. British Journal of Nursing. 2009; 18 (5):277–281. doi: 10.12968/bjon.2009.18.5.40539. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lierville AL, Grou C, Pelletier JF. Enjeux éthiques potentiels liés aux partenariats patients en psychiatrie: État de situation à l’Institut universitaire en santé mentale de Montréal. Santé mentale au Québec. 2015; 40 (1):119–134. doi: 10.7202/1032386ar. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lynöe N, Sandlund M, Jacobsson L. Research ethics committees: A comparative study of assessment of ethical dilemmas. Scandinavian Journal of Public Health. 1999; 27 (2):152–159. doi: 10.1177/14034948990270020401. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Malherbe JF. Compromis, dilemmes et paradoxes en éthique clinique. Anjou: Éditions Fides; 1999. [ Google Scholar ]
- McGinn R. Discernment and denial: Nanotechnology researchers’ recognition of ethical responsibilities related to their work. NanoEthics. 2013; 7 :93–105. doi: 10.1007/s11569-013-0174-6. [ CrossRef ] [ Google Scholar ]
- Mills, C. W. (2017). Black Rights / White rongs. The Critique of Racial Liberalism . Oxford University Press
- Miyazaki AD, Taylor KA. Researcher interaction biases and business ethics research: Respondent reactions to researcher characteristics. Journal of Business Ethics. 2008; 81 (4):779–795. doi: 10.1007/s10551-007-9547-5. [ CrossRef ] [ Google Scholar ]
- Mondain N, Bologo E. L’intentionnalité du chercheur dans ses pratiques de production des connaissances: les enjeux soulevés par la construction des données en démographie et santé en Afrique. Cahiers de recherche sociologique. 2009; 48 :175–204. doi: 10.7202/039772ar. [ CrossRef ] [ Google Scholar ]
- Nicole, M., & Drolet, M. J. (in press). Fitting transphobia and cisgenderism in occupational therapy, Occupational Therapy Now
- Pope KS, Vetter VA. Ethical dilemmas encountered by members of the American Psychological Association: A national survey. The American Psychologist. 1992; 47 (3):397–411. doi: 10.1037/0003-066X.47.3.397. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Provencher V, Mortenson WB, Tanguay-Garneau L, Bélanger K, Dagenais M. Challenges and strategies pertaining to recruitment and retention of frail elderly in research studies: A systematic review. Archives of Gerontology and Geriatrics. 2014; 59 (1):18–24. doi: 10.1016/j.archger.2014.03.006. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rawls, J. (1971). A Theory of Justice . Harvard University Press
- Resnik DB, Elliott KC. The Ethical Challenges of Socially Responsible Science. Accountability in Research. 2016; 23 (1):31–46. doi: 10.1080/08989621.2014.1002608. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rosa, H. (2010). Accélération et aliénation. Vers une théorie critique de la modernité tardive . Paris, Découverte
- Sen, A. K. (2011). The Idea of Justice . The Belknap Press of Harvard University Press
- Sen, A. K. (1995). Inegality Reexaminated . Oxford University Press
- Sieber JE. Empirical Research on Research Ethics. Ethics & Behavior. 2004; 14 (4):397–412. doi: 10.1207/s15327019eb1404_9. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sigmon ST. Ethical practices and beliefs of psychopathology researchers. Ethics & Behavior. 1995; 5 (4):295–309. doi: 10.1207/s15327019eb0504_1. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Swazey JP, Anderson MS, Lewis KS. Ethical Problems in Academic Research. American Scientist. 1993; 81 (6):542–553. [ Google Scholar ]
- Swisher LL, Arsalanian LE, Davis CM. The realm-individual-process-situation (RIPS) model of ethical decision-making. HPA Resource. 2005; 5 (3):3–8. [ Google Scholar ]
- Tri-Council Policy Statement (TCPS2) (2018). Ethical Conduct for Research Involving Humans . Government of Canada, Secretariat on Responsible Conduct of Research. https://ethics.gc.ca/eng/documents/tcps2-2018-en-interactive-final.pdf
- Thomas SP, Pollio HR. Listening to Patients: A Phenomenological Approach to Nursing Research and Practice. New York: Springer Publishing Company; 2002. [ Google Scholar ]
- Wiegand DL, Funk M. Consequences of clinical situations that cause critical care nurses to experience moral distress. Nursing Ethics. 2012; 19 (4):479–487. doi: 10.1177/0969733011429342. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Williams-Jones B, Potvin MJ, Mathieu G, Smith E. Barriers to research on research ethics review and conflicts of interest. IRB: Ethics & Human Research. 2013; 35 (5):14–20. [ PubMed ] [ Google Scholar ]
- Young, I. M. (2011). Justice and the Politics of difference . Princeton University Press
Get the Reddit app
A place for researchers to interact. Ask questions, tell stories, share tips, and anything in between!
How people outside academia can get approval of their independent research from an ethics committee?
There are some people who likes to do research out of pure curiosity. But these people need to be in academia. Their employer might not be having any ethics board (think of someone working in a small company). Or they could be unemployed people.
My question is... if I have a research question... I have resources and knowledge to conduct the research... but I am not from academia... how can I get approval of an external ethics committee? are there any private companies which offers this service i.e. providing ethics approval?
Why not ask your employer to set up an ethics committee? Ans: Employer doesn't care.
Why not collaborate with someone from academia? Ans: I tried. The subject is controversial so nobody would touch it.
Ethics and Human Rights
Life and death decisions are a part of nursing, and ethics are therefore fundamental to the integrity of the nursing profession. Every day, nurses support each other to fulfill their ethical obligations to patients and the public, but in an ever-changing world – there are increased challenges.

“The Code” is a vital tool for nurses now and in the future. VIEW THE CODE
The ANA Center for Ethics and Human Rights
The Center is committed to addressing the complex ethical and human rights issues confronting nurses and designing activities and programs to increase the ethical competence and human rights sensitivity of nurses. Through the Center, ANA's abiding commitment to the human rights dimensions of health care is demonstrated.
The American Nurses Association (ANA) Center for Ethics and Human Rights was established to help nurses navigate ethical and value conflicts, and life and death decisions, many of which are common to everyday practice. The Center develops policy designed to address issues in ethics and human rights at the state, national, and international levels. Through its highly visible information, activities, and programs, the Center promotes the ethical competence and human rights sensitivity of nurses in all practice settings and demonstrates ANA’s abiding commitment to human rights.
2020 Center for Ethics and Human Rights Annual Report 2019 Center for Ethics and Human Rights Annual Report 2018 Center for Ethics and Human Rights Annual Report 2017 Center for Ethics and Human Rights Annual Report
Contact the Center of Ethics and Human Rights at [email protected]
READ MORE ABOUT THE CENTER FOR ETHICS AND HUMAN RIGHTS
The Code of Ethics for Nurses with Interpretive Statements, or “The Code”, is a vital tool for nurses now and in the future. While the foundational values of nursing do not change, The Code is regularly updated to reflect changes in health care structure, financing, and delivery. It supports nurses in providing consistently respectful, humane, and dignified care. These values are often second nature to nurses’ caregiving but are frequently challenged by the failings in U.S. health care and by negative social determinants of health.
The Code, consisting of nine provisions and their accompanying interpretive statements:
- Provides a succinct statement of the ethical values, obligations, and duties of every individual who enters the nursing profession;
- Serves as the profession’s nonnegotiable ethical standard; and
- Expresses nurses' own understanding of our commitment to society.
The Code is particularly valuable in today’s healthcare environment because it clearly and eloquently reiterates the fundamental values and commitments of the nurse (Provisions 1–3), identifies the boundaries of duty and loyalty (Provisions 4–6), and describes the duties of the nurse that extend beyond individual patient encounters (Provisions 7–9).
To serve as the most useful aid in challenging situations, The Code's interpretive statements provide specific guidance for practice. The statements respond to the contemporary context of nursing and recognize the larger scope of nursing’s concern for societal health.
The Code of Ethics for Nurses with Interpretive Statements is the social contract that nurses have with the U.S. public. It exemplifies our profession's promise to provide and advocate for safe, quality care for all patients and communities. It binds nurses to support each other so that all nurses can fulfill their ethical and professional obligations. This Code is a reflection of the proud ethical heritage of nursing; one which will continue on, whatever challenges the modern health care system presents.
BUY THE CODE OF ETHICS FOR NURSES WITH INTERPRETIVE STATEMENTS ONLINE
Compra Código de Ética para Profesionales de la Enfermería
The ANA Center for Ethics and Human Rights helps nurses navigate complex and every day ethical issues, in all practice settings.
ANA position statements on ethics and human rights
In tandem with The Code, ANA’s position statements support nurses by offering an explanation, a justification, or a recommendation for a course of action in particular situations.
- Capital Punishment and Nurses' Participation in Capital Punishment (Approved 2/24)
- Nurses' Roles and Responsibilities in Providing Care and Support at the End of Life (Approved 2/24)
- Privacy and Confidentiality (Revised 2/24)
- The Ethical Use of Artificial Intelligence in Nursing Practice (Approved 12/20/22)
- The Nurse's Role and Responsibility in Unveiling and Dismantling Racism in Nursing (2022)
- Risk and Responsibility in Providing Nursing Care (Approved 10/6/2022)
- Therapeutic use of Marijuana and Related Cannabinoids (Approved 5/4/2021)
Nurses’ Professional Responsibility to Promote Ethical Practice Environments (Approved 5/4/2021)
- The Ethical Use of Restraints: Balancing Dual Nursing Duties of Patient Safety and Personal Safety (Approved 11/23/2020)
- Nursing Care and Do-not-resuscitate (DNR) Decisions (Approved 2/19/2020)
- Nurse’s Role in Providing Ethically and Developmentally Appropriate Care to People With Intellectual and Developmental Disabilities (Approved 10/10/19)
- Ethical Considerations for Local and Global Volunteerism (Approved 8/2/19) [VIDEO]
- The Nurse’s Role When a Patient Requests Medical Aid in Dying (Approved 6/22/19)
- The Nurse’s Role in Addressing Discrimination: Protecting and Promoting Inclusive Strategies in Practice Settings, Policy, and Advocacy (Approved 10/3/18) [ VIDEO ]
- The Ethical Responsibility to Manage Pain and the Suffering It Causes (Approved 2/23/2018) [VIDEO]
- Interdisciplinary Guidelines for Care of Women Presenting to the Emergency Department with Pregnancy Loss (Endorsed 2/23/2018)
- Nursing Advocacy for LGBTQ+ Populations (Approved 4/19/18)
- Non-Punitive Treatment of Pregnant and Breastfeeding Women with Substance Use Disorders (Approved 3/15/17)
- Nutrition and Hydration at the End of Life (Revised 6/7/17)
- Frequently Asked Questions: ANA Position on Capital Punishment
- The Nurse’s Role in Ethics and Human Rights: Protecting and Promoting Individual Worth, Dignity, and Human Rights in Practice Settings (February 2016)
Retired ANA Position Statements
- Constituent/State Nurses Associations (C/SNAs) as Ethics Resources, Educators, and Advocates (Retired ANA Position Statement - Approved 11/11/11)
- Stem Cell Research (Retired ANA Position Statement - Approved 1/10/07)
Ethics Topics and Resources
For nurses to fulfill their ethical obligations to patients, it is vital to have access to a wide range of information and to keep up-to-date with advances in ethical practices. These articles and links offer context for nurses on difficult issues and best-practice recommendations.
Social Justice
When nurses vow to protect the health and safety of patients, that promise does not end at the bedside. While social justice is a logical extension of the nursing profession, it can be difficult for nurses to navigate these divisive areas and ensure every individual receives timely and high-quality care.
Sign the Pledge Against Torture
Given the importance of ethics and the protection of human rights in nursing practice, the American Nurses Association is urging RNs to join ANA President Pamela F. Cipriano, PhD, RN, NEA-BC, FAAN, and ANA Chief Executive Officer Marla J. Weston, PhD, RN, FAAN, in signing on to the Health Professionals' Pledge Against Torture.
Physicians for Human Rights launched a pledge May 18 for health professionals across the United States to stand together in their rejection of torture, voicing the consensus that torture and cruel, inhuman, or degrading treatment are absolutely prohibited in all circumstances. Already the list of signers includes Nobel laureates in medicine, former surgeons general, prison physicians, leaders of health professional organizations, and medical ethicists who pledge never to collude in torture under any circumstances, in keeping with the ethical codes of their professions.
By uniting in large numbers behind the pledge, nurses and other health care professionals send a strong message to policymakers, health professional associations and the American public that future attempts to enlist health professionals in the design, study or use of practices that result in severe physical or mental abuse will not be tolerated. The pledge also serves as a declaration of support for health professionals who resist orders to torture or inflict harm.
For more than a decade, PHR and its network of partners have led efforts advocating against torture, documented the devastating long-term health consequences of torture, and called attention to the complicity of some health professionals in the post-9/11 U.S. torture program.
“At a time when human rights are increasingly under threat, we’ve launched this pledge to marshal the powerful voices of health professionals across the United States and reaffirm their ethical duties to honor human dignity,” said PHR Executive Director Donna McKay.
ANA’s Code of Ethics for Nurses with Interpretive Statements is essential to nursing practice, and the national association has a long history of human rights advocacy. For example, ANA successfully advocated for the ethical right of a Navy nurse to refuse to force-feed detainees at Guantanamo Bay. In January, ANA released its Ethics and Human Rights Statement emphasizing that nursing “is committed to both the welfare of the sick, injured, and vulnerable in society and to social justice.” To read more visit, Health Professionals' Pledge Against Torture.
More Social Justice Resources
- ANA Releases New Position Statement Opposing Capital Punishment (2/21/17)
- ANA President Responds to Executive Order on Immigration Press Release (Released: January 31, 2017)
- ANA Ethics and Human Rights Statement
Moral Courage, Moral Distress, Moral Resilience
Nurses practicing in today’s health care environment face increasingly complex ethical dilemmas. Upholding our commitment to patients and communities requires significant moral courage and resilience. It involves the willingness to speak out, whether alone or collectively, to do what is right for patients and other nurses
Documentary
The Moral Distress Education Project Core multidisciplinary experts on moral distress from across the country were interviewed in a documentary-style media project. This project is a self-guided web documentary.
A Call To Action Report: Exploring Moral Resilience Toward a Culture of Ethical Practice
Relevant Nursing Journal Articles
- Compassion Fatigue as a Threat to Ethical Practice: Identification, Personal and Workplace Prevention/Management Strategies, MEDSURG Nursing: July-August, 2016
- Moral Resilience: Managing and Preventing Moral Distress and Moral Residue MEDSURG Nursing: March-April, 2016
- Moral Distress References
- Moral Distress in Academia OJIN: The Online Journal of Issues in Nursing
- Moral Courage and the Nurse Leader OJIN: The Online Journal of Issues in Nursing
- Creating Workplace Environments that Support Moral Courage OJIN: The Online Journal of Issues in Nursing
- Strategies Necessary for Moral Courage OJIN: The Online Journal of Issues in Nursing
- Moral Courage in Healthcare: Acting Ethically Even in the Presence of Risk OJIN: The Online Journal of Issues in Nursing
- Understanding and Addressing Moral Distress OJIN: The Online Journal of Issues in Nursing
- Using the AACN Framework to Alleviate Moral Distress OJIN: The Online Journal of Issues in Nursing
- Moral Distress and Moral Courage in Everyday Nursing Practice OJIN: The Online Journal of Issues in Nursing
- Moral Courage in Action: Case Studies MEDSURG Nursing: August, 2007
- Moral Courage: A Virtue in Need of Development? MEDSURG Nursing: April, 2007
End of Life Issues
In an aging population with rapidly increasing technological interventions possible, end of life care is a vital discussion. With multiple perspectives to consider, these resources serve to convey the breadth of opinion that nurses experience, and help nurses respect individual dignity and autonomy.
Advance directives, Education, Professional Organizations, Hospice
Advance directives.
End of life care often starts when a person is healthy. Many people, including nurses, have specific ideas about what health care they want, or do not want, at the end of life. Advance directives are a means to allow people to convey their wishes for end of life care. This includes discussions with those who might be a surrogate decision maker, as well as documents used to express preferences.
The National Hospice & Palliative Care Organization (NHPCO) HHPCO has a directory of advance directives that are acceptable to each statue.
Five Wishes An easy guide for patients and families to discuss preferences for end of life care, as well as for healthcare professionals who might not be comfortable with such discussions. The guide includes prompts for discussions about how you wish to be remembered.
The End-of-Life Nursing Consortium (ELNEC) ELNEC is a series of programs developed by the American Association of Colleges of Nursing. Current ELNEC modules include core curriculum, pediatric palliative care, geriatric, and many others. There are also train-the-trainer modules. After taking a train the trainer course, a nurse can then offer an ELNEC course. The courses are comprehensive and provide all teaching materials needed. The courses are typically offered in a block over two days.
Education in Palliative and End of Life Care (EPEC) EPEC was originally developed as physician education but has expanded. It has both in-seat and online programs. The model includes the training of facilitators. Sessions may be given in day-long formats, or in shorter sessions, such as grand rounds.
Professional Organizations
The Hospice & Palliative Nurses Association (HPNA) HPNA has the mission of advancing expert care in serious illness. HPNA is the professional organization for palliative care nurses and hospice nurses. HPNA provides education and certification for nurses across levels, including Advance Practice Registered Nurses (APRN), Registered Nurses (RN), RN Pediatrics, and more. HPNA has many Special Interest Groups (SIGs) with online discussion groups. The organization has also developed a series of position statements to guide professional practice. With The American Academy of Hospice & Palliative Medicine (AAHPM), HPNA has an annual assembly for professionals.
The American Academy of Hospice & Palliative Medicine (AAHPM) AAHPM is the professional organization for hospice physicians, palliative medicine physicians, and other health care professionals (nurses, social workers, chaplains, etc.) in these fields. Their goal is to improve the care of patients living with serious illness. AAHPM provides certification for physicians in palliative medicine, as well as for hospice medical directors. AAHPM provides many options for education, online discussion groups, special interest groups, and certification. With HPNA, AAHPM has an annual assembly for professionals.
The Center to Advance Palliative Care (CAPC) CAPC is a multidisciplinary organization that supports practice, research, and education. Hospitals can become member organization, and all employees of those organizations have extensive access to continuing education and other resources. Even non-members have access to the myriad resources of CAPC.
The National Hospice & Palliative Care Organization (NHPCO) NHPCO is one of the oldest advocacy organizations in the fields of hospice and palliative care. Their focus is primarily on the care of patients with terminal illness, and their families. They have developed Standards of Practice and have several position statements.
The Schwartz Center The Schwartz Center is another organization whose goal is to improve the care of patients who are dying. One of their best known efforts is Schwartz Center Rounds, which are intended as a regularly scheduled forum for caregivers to discuss the challenges of caring for patients and families. Schwartz Center Rounds are currently held in about 550 centers in the U.S., U.K., and Canada.
Hospice is a model of care for people who are at the end of life. Specifically, hospice care is eligible for people who are estimated to have a prognosis of six months or less. Hospice is tremendously underutilized, with about 50% of patients having a length of stay of less than 18 days, as opposed to the approximately 180 days of the hospice benefit. Misperceptions about hospice are common. A common misunderstanding is that hospice is a place (“She’s going to hospice”), rather than a model of care. Greater than 90% of hospice care occurs in patients’ homes.
The Centers for Medicare and Medicaid Services This resource explaining the hospice guidelines is helpful for patients, families, and providers.
Elder Law Answers This resource from Elder Law Answer is used to make the Medicare Hospice Benefit more comprehensible.
Related Resources
- Do Not Resuscitate Orders: Nurse's Role Requires Moral Courage
- Left Ventricular Assist Device Deactivation: Ethical Issues
- Nurses Role in Increasing Access to Hospice
- Physician-Assisted Suicide
- Voluntary Stopping of Eating and Drinking?: An Ethical Alternative to PAS
Caregiving Resources
Nurses frequently come into contact with caregivers and can provide vital support to individuals who may not come into regular contact with others due to the often all-consuming nature of providing care. It is important for caregivers to realize that they are not alone and that there’s a wealth of information and resources to improve their situation.
Links to tools and support groups for caregivers:
National Association for Home Care & Hospice (NAHC) NAHC is the voice of home care and hospice. NAHC represents the nation’s 33,000 home care and hospice providers, along with the more than two million nurses, therapists, and aides they employ.
Caregiver Action Network (CAN) Education, peer support, and resources for family caregivers. CAN serves a broad spectrum of family caregivers ranging from the parents of children with special needs, to the families and friends of wounded soldiers; from a young couple dealing with a diagnosis of MS, to adult children caring for parents with Alzheimer’s disease.
Help for cancer caregivers Tools and information to improve the quality of life for caregivers.
The American Cancer Society A national website with a tab on finding support for caregivers: what to expect; what you need to know when caring for a loved one at home; and tips of caring for oneself.
The American Association of Critical-Care Nurses You can search for Caregivers and it links you to multiple articles on caring for the chronically critically ill.
Patients’ Action Network Has a tab on advocate resources.
Women's Institute For A Secure Retirement Resource tab for caregivers and their families.
Caregiver support - online caregiver support Caregiver support for people who take care of their elderly loved ones, or have the possibility of being a new caregiver or potential caregiver.
The Conversation Project Contains a toolkit to help people talk about their wishes for end-of-life care. An essential for all caregivers.
VA Caregiver Support Can tell you about assistance available from VA, help you access the services, connect you to the Caregiver Support Coordinator at a VA Medical Center near you, and just listen, if that is what you need. Support line 1.855.260.3274.
Alzheimer’s Association Caregiver Stress Describes caregiver stress and offers tips for managing stress.
American Psychological Association Common Ethical Issues: Supporting the Caregiver .
While the consequences of Bioethics may not be felt by every single nurse, it is vital they are aware of the enormous implications of these issues, in case of crisis. From Ebola to natural disasters, through keeping aware of the very latest threats, nurses can protect patients and themselves in the face of any obstacles.
American Society of Bioethics and Humanities (ASBH) Serves as a resource for anyone interested in bioethics and humanities by providing a group of further online resources and links to aid in finding other related information through the Internet.
Ethics, the law, and a nurse’s duty to respond in a disaster
International Council of Nurses Ethics and Human Rights.
National Center for Ethics in Health Care - Veterans Affairs A resource for addressing complex ethical issues in health care.
The NCSBN National Nursing Guidelines for Medical Marijuana Nursing guidelines for the patient using medical marijuana
National Reference Center for Bioethics Literature Offers extensive searches in Bioethics.
Nursing2015 / Issues in Nursing “A Nurse’s Obligations to Patients with Ebola.”
United Nations Educational, Scientific and Cultural Organization (UNESCO)
You May Also Like

Guide to the Code of Ethics for Nurses with Interpretive Statements: Development, Interpretation, and Application, 2nd Edition

Know the Code Bookmarks
Genetics/Genomics Nursing: Scope and Standards of Practice, 2nd Edition

Know the Code Poster
Code of Ethics for Nurses with Interpretive Statements
Item(s) added to cart.
- Open access
- Published: 03 December 2022
Negative emotions experienced by healthcare staff following medication administration errors: a descriptive study using text-mining and content analysis of incident data
- Sanu Mahat 1 ,
- Anne Marie Rafferty 2 ,
- Katri Vehviläinen-Julkunen 3 , 4 &
- Marja Härkänen 1
BMC Health Services Research volume 22 , Article number: 1474 ( 2022 ) Cite this article
4436 Accesses
4 Citations
73 Altmetric
Metrics details
Medication errors regardless of the degree of patient harm can have a negative emotional impact on the healthcare staff involved. The potential for self-victimization of healthcare staff following medication errors can add to the moral distress of healthcare staff. The stigma associated with errors and their disclosure often haunts healthcare professionals, leading them to question their own professional competence. This paper investigates the negative emotions expressed by healthcare staff in their reported medication administration error incidents along with the immediate responses they received from their seniors and colleagues after the incident.
This is a retrospective study using a qualitative descriptive design and text mining. This study includes free-text descriptions of medication administration error incidents ( n = 72,390) reported to National Reporting & Learning System in 2016 from England and Wales. Text-mining by SAS text miner and content analysis was used to analyse the data.
Analysis of data led to the extraction of 93 initial codes and two categories i.e., 1) negative emotions expressed by healthcare staff which included 4 sub-categories of feelings: (i) fear; (ii) disturbed; (iii) sadness; (iv) guilt and 2) Immediate response from seniors and colleagues which included 2 sub-categories: (i) Reassurance and support and (ii) Guidance on what to do after an error.
Negative emotions expressed by healthcare staff when reporting medication errors could be a catalyst for learning and system change. However, negative emotions when internalized as fear, guilt, or self-blame, could have a negative impact on the mental health of individuals concerned, reporting culture, and opportunities for learning from the error. Findings from this study, hence, call for future research to investigate the impact of negative emotions on healthcare staff well-being and identify ways to mitigate these in practice.
Peer Review reports
Medication Errors (MEs) are recognized by the World Health Organization as the leading cause of injury and avoidable harm in healthcare, costing approximately 42 billion dollars annually, which is nearly 1% of total global health expenditure [ 1 ]. The safety of patients is at the forefront of the healthcare system; however, healthcare staff can also be traumatized by the aftermath of MEs. Although the healthcare mantra is “first do no harm”, healthcare professionals involved in adverse events can feel guilt, shame, anger, fear, and anxiety [ 2 ]. They are often neglected with only a few coping strategies and support systems available to help them [ 3 ]. Negative consequences of an adverse event can reach far beyond the “first victim” i.e., the patient. Thus, affecting healthcare staff psychologically making them “second victims” [ 4 ]. The term “second victim” was first coined by Dr. Albert Wu to explain the emotions of a young resident who committed an error and had experienced ridicule, shame, and lack of support, from his peers [ 2 ]. Although this concept was first applied to physicians, other healthcare staff, including nurses, also experience similar emotions. Scott et al. [ 5 ] described the term second victim as “a healthcare provider involved in an unanticipated adverse patient event, medical error and/or a patient-related injury who has become victimized in the sense that the provider is traumatized by the event. Frequently, second victims feel personally responsible for the unexpected patient outcomes and experience as though they have failed their patient, feeling doubts about their clinical skills and knowledge base”[ 5 ].
The use of the term second victim has been criticized recently [ 6 , 7 ] arguing that it might act as a way in which healthcare providers can evade responsibility and accountability and it might be offensive to affected patients and families [ 6 ]. Laying accountability at the door of an individual, ignoring the wider organizational ramifications of accountability in terms of the conditions which trigger errors in the first place, can let the organization off the hook. Even though the use of the term “victim” may sound spurious and uncomfortable to many healthcare professionals, patients, and families, it is indubitably an advantage in reinforcing the seriousness and urgency of the problem among policymakers and healthcare managers [ 8 ]. Wu et al.[ 8 ] have suggested the importance of the use of the term second victim as it is notable and denotes urgency. These assumptions regarding the use of the term second victim are inherent in both positions. Therefore, our research is designed to take this debate one step further by analyzing the consequences of errors in terms of emotional response and lived experiences of healthcare staff.
Regardless of the degree of patient harm, the mere thought of potential patient injury caused by ME is sufficient to induce the feelings of fear, distress, anger, anxiety, guilt and remorse in healthcare staff [ 9 , 10 , 11 ]. Although evidence suggests multiple system-based causes of MEs, the error-maker still tends to blame themselves i.e., they should have functioned proficiently [ 11 ]. If the seriousness of these issues remains unaddressed, it can negatively affect healthcare workers’ personal and professional well-being causing depression, burnout, Post Traumatic Stress Disorder (PTSD), and even suicidal thoughts [ 4 , 12 , 13 ]. Error prevention has therefore been a focus of major attention for healthcare organizations for years but the impact of MEs on the healthcare professional involved has received less attention. A more nuanced and textured exploration of the impact of the problem upon healthcare workers is required if preventative strategies are to be effective [ 11 ].
Previous studies have shown that often MEs causing harm are reported whereas near misses are often under-reported [ 14 ]. This underestimates the number of healthcare staff going through negative experiences [ 15 ]. Fear of legal consequences, blame, losing patients’ trust, and punishment have been recognized as barriers to ME reporting[ 16 ] leading healthcare staff to suffer in silence, sometimes struggling alone in isolation and burdened with a sense of shame [ 9 ]. Therefore, a system is needed to mitigate these barriers and create a “just culture guide” which helps healthcare managers to treat staff involved in adverse events fairly, support open and fair culture and maximize learning from errors [ 17 ]. However, it is apparent that irrespective of organizational effort in promoting a just and no-blame culture, the stigma persists with respect to speaking up about errors [ 18 ].
Patient safety incident reporting has become a common practice, but little is known about the feelings of those who commit or witness incidents. Despite the recent debate regarding the use of the term second victim, we are adopting this terminology throughout our research to analyse the consequences of MEs in terms of psychological responses from healthcare staff. Previous research into second victims has mainly been carried out in a single setting, but this study uses reported incidents at a national level drawing from a range of settings. Also, no previous studies, as far as we are aware, have focused only on Medication Administration Errors (MAEs). To our knowledge, none of these studies have used free-text descriptions of reported medication incidents to review the feelings and emotional responses associated with reporting nor text mining as an innovative method for such analysis.
The aim of this study was to investigate negative emotions expressed by healthcare staff in their reported MAE incidents along with the immediate responses they received from their seniors and colleagues after the incident.
Study design and setting
A retrospective study using qualitative descriptive method and text-mining with an inductive content analysis of the incident data related to Medication Administration (MA) reported in England and Wales was done.
Description of the data
The data consists of MA incidents ( n = 72,390) retrieved from the National reporting and Learning System (NRLS) database based on inclusion criteria: (1) incidents reported to have occurred in England and Wales between 1 January and 31 December 2016, (2) medication incident, (3) administration/supply of medicine from a clinical area, and (4) acute National Health Services (NHS) trust (either specialist or non-specialist). The data included incident reports from all levels of healthcare staff ranging from student nurses to senior-level health professionals who were involved in and who have witnessed the MAE incidents.
Data were acquired from NHS England and NHS Improvement. NRLS is largely voluntary and is the only database that includes all types of patient safety incidents. This study used free-text descriptions of the incidents i.e., healthcare staffs’ descriptions of “what has happened?” or “when the incident occurred?” during the medication process.
Data analysis
First, negative emotional expressions associated with MAEs were defined using the literature and dictionaries (Oxford Learners’ Dictionary, Merriam-Websters’ Dictionary, and Cambridge Dictionary) to define synonyms of the negative emotional expressions (Table 1 ). Second, those expressions were searched from the free-text descriptions of the incidents which were specifically related to MA. For that, The SAS® Enterprise Miner 13.2 and its Text Miner tool were used. Multiple steps were followed for data analysis as described in Fig. 1 . SAS® Text Miner automatically processes the data using ‘text parsing’ i.e., converting unstructured text into a structured form. Text parsing includes tokenization (breaking text into words/terms), stemming (which chops off the end of words reducing words to their stem or root forms), and part-of text tagging (for each word, the algorithm decides whether it is a noun, verb, adjective, adverb, preposition and so on). ‘Text filtering’ was then used to reduce the total number of parsed terms and check the spellings. The English language was chosen for parsing and filtering the text. Using an interactive filter viewer, negative emotional expressions described in the free text were identified and the number of each expression was collected (See Supplementary file 1 ). For the next phase of the analysis, the most common expressions were chosen which are bolded in online-only material 2 (See Supplementary file 2 ).
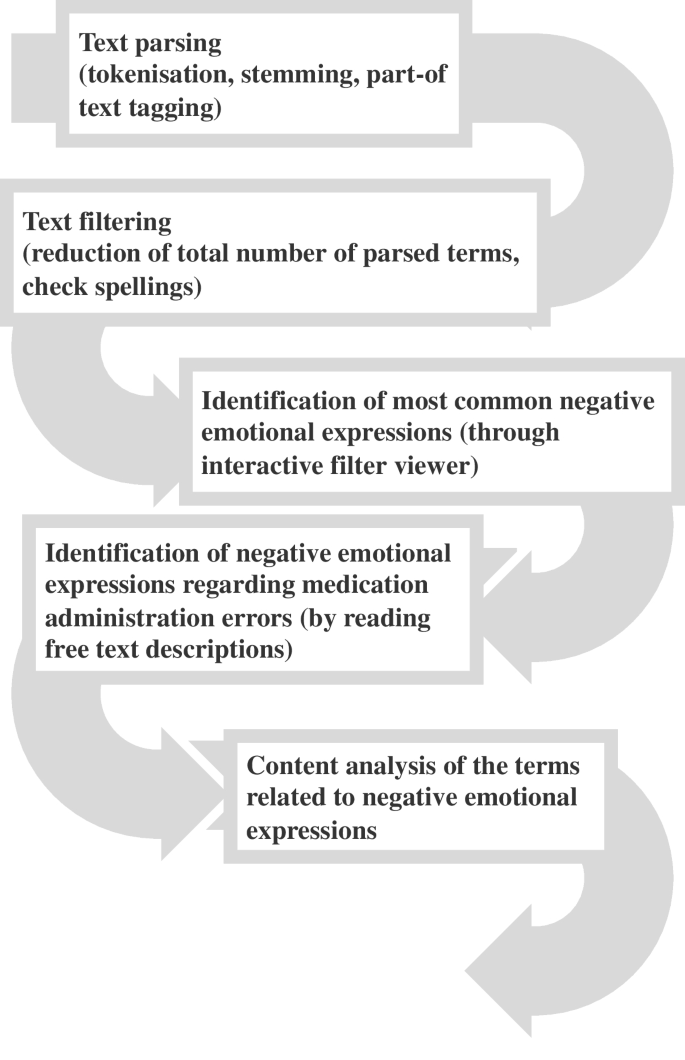
Analysis process of medication administration incident reports’ free text descriptions
Expressions chosen for analysis were used as a search term in an interactive filter viewer. All the descriptions of the incidents that included those expressions (a total of 1861 incident reports) were collected and read through repeatedly. In the first phase of this analysis, the aim was to define who had experienced the emotional feeling. Most of negative emotions were expressed by patients or relatives (See Supplementary file 1 ). Those descriptions of incidents that included negative emotions expressed by healthcare staff and which were expressed in relation to MAEs ( n = 93) were then selected for further analysis.
Content analysis was used to analyze the data. The lead author followed an inductive content analysis where the researchers carefully read, organized, and integrated and formed categories, concepts, and themes by comparing the similarities and differences between the coded data [ 19 ]. The lead author read through the data repeatedly and during this process, identified the main theme which is: Emotional expressions of healthcare staff after MAEs. The data were organized into main themes and sub-themes. After the preliminary classification, a co-coder [the last author of this paper] participated in the analysis and read the classification structure and the related data independently. Once thematic saturation was achieved, both researchers analyzed the entire data corpus according to standard thematic analysis techniques [ 20 ]. All authors contributed to the final form of the analysis. Finally, direct quotes were used to support the findings.
Negative emotional expressions of healthcare staff after MAEs
We found 15 different types of negative emotional expressions used including worry, anxiety, annoyance, agitation, stress, unhappiness, distress, concern, anger, upset, shock, sorry, fault, depression, and frustration. These 15 different types of emotions were expressed 1,861 times in the incident reports (See Supplementary file 1 ).
Among those emotional expressions, 12 were exhibited by the healthcare staff and were mentioned 154 times. Only eight of those 12 expressions: worry, upset, agitation, faulty, sorry, concerned, stressed, and distress were expressed by healthcare staff in direct relation to MAEs, the frequency of expression here was 93 times. The data extraction process in presented as a flowchart in Fig. 2 .
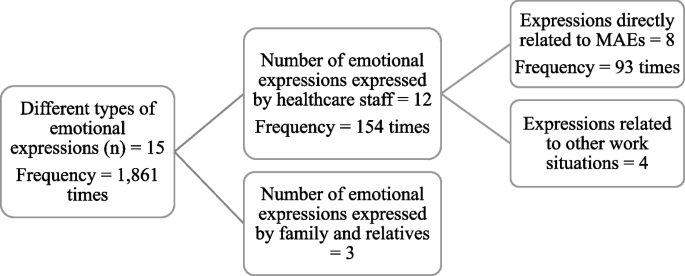
Typology and frequency of emotional expressions
The key emotions revealed were further classified into four categories: (1) feeling of fear, (2) feeling of upset, (3) feeling of sadness, and (4) feeling of guilt (Table 2 ).
Feeling of fear
Healthcare staff described their feeling of fear regarding MAEs using four different synonyms i.e., distressed, concerned, stressed, and worried. Staff mentioned how fearful they were when they discovered their mistakes. Distress was revealed in three of the incident reports as expressions of fear of healthcare staff. Usually, MAE incidents were reported either by the error-makers themselves or by those witnessing their errors. One of the staff described the fear felt by her colleague (staff nurse) by reporting how distressed he was after he administered a medication through wrong route (intravenous instead of oral):
“ I was assessing a patient on Ward X when a staff nurse approached me extremely distressed and agitated. He then ran into the utility without explaining what the problem was. I followed him…nurses were present who proceeded to explain that the nurse who approached me had given a patient 2mls of Oramorph [liquid morphine that has to be given orally] intravenously …"
Healthcare staff also expressed the extreme pressure which acted as an important contextual trigger, driving intense the feelings of fear. Another emotion linked to fear was “concerned” which was expressed in 23 cases by healthcare staff after making an error. One of the healthcare staff reported an error (prescribed wrong strength), which the staff realized two hours later and became concerned about it:
" Prescribed TTA (to take away) of ‘Augmentin [Amoxicillin Clavulanate] Duo’125/31 8 ml TDS [three times a day]. As written, this would be a drug error-there is no 125/31 strength of …This was my error, which I realized and became concerned about 2 hours later …"
Stress was expressed in three cases by healthcare staff while reporting the incident; however, this emotion was expressed by staff not as their feelings after MAEs, but as the reason underlying MAEs. These kinds of explanations were found in many incident reports where healthcare staff accepted the error but eventually pointed towards other hidden causes behind the error:
" Gave Clexane [Enoxaparin] 60 mg to wrong patient. Ward extremely busy- heavy workload and was very stressed due to workload …"
Being “worried” was another expression of fear reported in 11 incident reports by healthcare staff. They were found to be worried about several situations such as the health of patient, degree of harm caused by error, associated legal procedures, and their professional career. One staff nurse was worried about the patients’ condition as he did not administer insulin dosage to one of his patients:
" Staff nurse came to me at the end of the shift and stated that he thought that the patients’ insulin was prescribed prn [whenever necessary] and had not given any…I explained he needed to inform the nurse in charge…he was very sincere and worried that he had not given this insulin …"
Feeling disturbed
The feeling of being disturbed was expressed using two synonyms: upset and agitated. They addressed themselves as being upset in 24 incident reports following MAEs committed either by themselves or by their fellow staff. Healthcare staff reported the error made by fellow staff member and described the emotion of his/her colleague as:
" Nurse called me was very upset to explain that she had given wrong treatment to patient …"
Even near miss situations have caused healthcare staff to get emotionally disturbed. Even after apologizing with patient and family, healthcare staff felt upset thinking that if they were not aware of the near miss situation in time, patients’ condition would have been severe:
" SN asked me to do a syringe driver with her for a palliative patient…on drawing up the ketamine driver, myself and SN made a drug error in which we drew 5 times more ketamine than the required dose…The family and patient have been informed of the drug error we made and we gave our sincere apology for our faults…both myself and SN are very upset with the near miss situation and aware that things could have gone very differently …"
Healthcare staff expressed being agitated in two reports after discovering that they had committed MAEs, except in some situations, where staff though agitated denied their mistake by underestimating the severity of the error they made:
" Patient was discharged off the system by the nurse without confirming with medical team/pharmacy that patient was ready to go… Patient left without anti-sickness medication which the team had told her she could have…Nurse was evidently agitated that the incident was being reported and did not understand that she should check with the team before authorizing …"
Some reports revealed extreme negative emotions associated with feelings of upset such as being devastated and questioning one’s own professional competence. The use of such intense and traumatic language can reflect how much the healthcare staff were impacted and even emotionally wrecked after MAE. One healthcare staff after accidentally administering wrong dosage to the patient, reported that the error was entirely his/her own fault:
" Pt px 120 mg on gentamicin on EOMA, I accidentally gave 210 mg in error. This was entirely my fault …The checker confirmed what I had done. I am so devastated about this and really upset I’d made such a mistake…today was just hectic and I lost concentration ..."
Feeling of sadness
Healthcare staff expressed their feeling of sadness at being sorry for the mistake they had made; it was one of the most common negative emotional expressions expressed in 13 cases. Most staff used this to express a sense of remorse after the error. After missing a dose of insulin for a patient, one healthcare staff expressed his/her sadness by stating that he/she is sorry about the incident:
" I am sorry to say that I missed one dose of insulin (at 22.30…) for one of my patients …"
Along with the feeling of sadness, one healthcare staff also mentioned about learning from the error and how he/she have accepted that she was wrong to assume things:
" I was sitting at the desk, staff nurse handed me a tray with intravenous antibiotics and said, here is one because I had given her patient drug chart, I assume it was patients’ medication. I did not take the drug chart with me to the patient and afterwards when staff nurse came with patients’ drug, I realized I have given the wrong drug. I was very upset as I have never done anything in this form before. I always take the drug chart with me to the patient. I am deeply sorry, and this is a massive learning curve for me, I hold my hand up it was wrong to assume this ."
Healthcare staff who had mentioned learning from the error was quite common in many incident reports. However, there were few cases where the staff did not understand the seriousness of the error she has caused:
"… I spoke to the student nurse about the seriousness of her actions, she said sorry; however, I did not feel she understood the seriousness of what she did …"
Feeling of guilt
In 14 incident reporting cases, healthcare staff were aware of their mistakes and the consequences they might have. They expressed their guilt and identified themselves as being at fault and blaming themselves.
" IV flucloxacillin drawn up and checked by myself and staff nurse…administered drug however in error name band/ allergy band not checked. Realized immediately after administration that I had gone to the wrong patient and given the incorrect medication…conversation with senior staff nurse about error. Explained that the error was my fault completely…patient does not appear to have come to any harm …"
However, this emotion was not just expressed following the error, but also as another reason for error attribution. For example, in the report below, a staff member made an error, and blamed herself and phone reception for being muffled:
" I had to hand over two diabetic patients to the 5–8 pm. I rang Ward sister and confirmed this again later. However, patient was not reallocated, and insulin omitted…Ward sister apologized for yesterday missed patient…she said the reception to her phone was muffled and that it was her fault …"
Immediate response from seniors and colleagues
Some of the healthcare staff while reporting their feelings behind MAE incidents also discussed regarding the immediate responses they received from their seniors and colleagues. Healthcare staff explained how their seniors and colleagues responded after they were informed about MAEs. These responses are categorized into two sub-categories: (1) Reassurance and support and (2) Guidance on what to do after an error.
Reassurance and support
In three incident reports, healthcare staff mentioned about the reassurance and positive support they received from their seniors and colleagues after the disclosure of MAEs, about how they tried to handle the situation very calmly without getting angry. This helped them to cope effectively without undue stress and burden. A nurse mentioned that she reassured one of her colleagues who was very disturbed after she gave the wrong medication to her patient:
" Staff nurse by mistake gave the patient wrong medication…. misread the information by being interrupted by a patient and member of staff…. I reassured the staff nurse as she was very upset …"
Even a little support and reassurance and few kind words during the time of MAEs can help the healthcare staff to cope up with the situation effectively. As one member remarked:
" Medication error – digoxin prescribed in two doses (125mcg and 62.5mcg) did not realize and administered…Immediately alerted sister in-charge of ward and contacted doctor. Doctor did not come to the ward but was happy that observations had been recorded…and told us not to worry …"
Guidance on what to do after error
In 11 incident reports, healthcare staff mentioned about receiving advice from their seniors and colleagues regarding the right thing to do after making an error. They have been guided to observe the situation of the patient to ensure that no serious harm would be caused to them:
"… Administered the oramorph in an unlabeled syringe which was in the same tray as a 10ml flush…I discussed the situation with the medical registrar on call who advised me to monitor observations regularly …" "… I spoke to the nurse in charge after the error from the following shift who said that I should speak to the ward manager at the earliest opportunity which I did …"
Furthermore, in cases where healthcare staff neglected to document the incident, a colleague intervened to guide the staff member to follow the protocol. As one staff member described:
"… I discussed the incident with a colleague shortly afterwards. However, I neglected to escalate and correctly document the incident…The aforementioned colleague has since approached me to discuss the incident, further to this I approached and discussed the incident with my ward manager …"
Our study identified four categories of negative emotions expressed in incident reports: feelings of fear, disturbed, sadness, and guilt with various sub-categories. In addition, this study also captured the immediate responses received by healthcare staff after they informed their seniors and colleagues about MAEs including the reassurance, support, and guidance on what to do after an error. Incident reporting by healthcare staff in this study indicated that unintentional harm caused due to MAEs and even near misses can affect the healthcare staff involved in error emotionally, increasing their risk of becoming the second victim of MAEs, confirming previous research [ 9 , 21 ].
A major finding of this study was the negative emotions experienced by healthcare staff after MAEs. Healthcare staff in this study expressed their fear while reporting incidents by using negative emotions such as stressed, distressed, concerned, and worried. They not only blamed themselves for these mistakes, but also considered other additional explanations which, they perceived as causing the error. These kinds of emotions can be related to staff members’ narration of fear and anxiety for patients’ well-being and for their own professional careers [ 22 ]. Similarly, feelings of being disturbed expressed as being upset and agitated were widely mentioned in incident reports. Identical reasons such as realization of the error and thoughts of the possible seriousness of the error and associated issues lay behind emotions. Further, feeling of sadness expressed as being sorry for the mistake made was another most common emotional expression. Also, healthcare staff felt a deep burden of responsibility for their actions. Feelings of being guilty or at fault is one of the risk factors for healthcare staff for becoming the second victim of MEs. It can also cause loss of self-esteem and inculcate a sense of failure and hopelessness. In a similar study by Treiber & Jones [ 22 ], nurses, upon committing even minor errors, expressed raw and painful emotions, regardless of the degree of harm. Nurses can often recall the details of the error and what they felt at that time [ 22 ]. While the lack of any apparent linkage between emotional response and degree of patient harm might appear counter intuitive, one possible explanation might be that healthcare professionals are not well enough supported by their organizations to cope with any form of negative experience. Thus, those affected might develop strong negative emotion [ 23 ].
Making an error might also have serious consequences for disrupting the personal and professional lives of staff, causing personal and moral distress, and affecting the quality and safety of patient care [ 23 ]. It is crucial to pay attention to these emotional expressions as incidents that are sensitive and make an impact, are often remembered, and reflected in the attempt to prevent recurrence. On the other hand, these incidents can unintentionally impose a mental burden on healthcare staff making them second victim [ 2 ]. Our findings confirms that MAEs can generate negative feelings in healthcare staff associated with it, which can endure long beyond the immediate effect.
Research has confirmed a direct relationship between nurse staffing and missed patient care [ 24 , 25 ], revealing poor nurse staffing as a risk factor for MEs along with other organizational factors such as poor working conditions, distractions, and high workload [ 26 ]. Similarly, in this study, reporters mentioned their own actions as a trigger for MAEs along with the above-mentioned factors whereas some reporters explained organizational and environmental conditions and context surrounding the error as reasons to reduce blame. In the absence of support, self-blame seems to assume greater prominence. This can have long-term repercussions for maintaining emotional health and well-being, a major failure of workforce strategy, especially during the pandemic situations.
The current study also found other healthcare authorities responding in several ways after being informed about MAEs. Sometimes, staff may not know what to do after MEs, they might panic and lose control. Thus, adequate support from colleagues and seniors sensitive to these issues may prevent the error-makers from translating further into second victimhood of MEs. How the organization and related individuals responds is clearly linked to the emotional impact the error can have on the healthcare staff who made the error. Appropriate support and guidance from seniors and colleagues have been found to alleviate the suffering, while lack of support has increased their psychological burden [ 27 ]. Some of the healthcare professionals in our study also opted for consulting with their seniors: doctors, colleagues, and mentors after MAEs and reported about how they have received guidance and suggestions, which helped them to cope effectively. Emotional support plays a vital role in restoring faith and confidence among healthcare professionals in patient safety. Support from co-workers and healthcare institution helps the error-makers to retain a sense of control [ 2 ]. Reassurance from seniors and colleagues can also strengthen healthcare staff’s self-esteem and facilitate the correct reporting of MAEs. As is well known, only a fraction of incidents are reported thus deterring the improvement of patient safety with barriers identified as time pressure, fear of the consequences [ 28 ], poor institutional support, lack of feedback, a blame culture, and inadequate training [ 15 ]. Yet, we can still improve patient safety by identifying these barriers. Moreover, while some staff members perhaps too readily assumed responsibility for errors, as reflected in the prominence of self-blame, others demonstrated reluctance, which could be linked to fear of the consequences of MAEs. Furthermore, little is known about the dynamics and consequences of reporting-what prompts some to report and others not to do so. We demonstrate that the emotional expression of staff can be extremely distressing and negatively impact health and well-being of healthcare staff.
Implications for practice
Our findings indicate that immediate negative feelings experienced by healthcare staff after making MAEs can have long-lasting impacts that stretch far beyond the event itself thus potentially traumatizing them and inducing ruminative thoughts, which trigger the memory. The short, medium, and long-term consequences of errors are unknown as yet but could contribute to burnout and other factors associated with intention to leave the profession. Indeed, a negative memory that will stay with them forever, if not handled accurately. They could potentially become second victims of an error, if unable to confront and deal with negative feelings associated with the error. One source of challenge could be stigma related to this making it difficult to continue to work after MAE. Our findings suggest appropriate guidance and support from fellow staff members could help healthcare staff to handle the situation effectively. Therefore, it should be paramount to tailor appropriate support from persons in-charge and colleagues and to promote an open culture where it is understood. Errors can impair mental health of those who are involved, hence, the system triggers surrounding such errors need to be understood and prevented. In addition, more detailed information about these emotions after incidents and their long-term consequences on emotional well-being should be studied in future.
Implications for research
The negative feelings expressed by healthcare staff after MAEs identified in this study could provide the basis for designing an intervention study to support emotionally affected staff in healthcare institutions. It could be helpful to design a support program which recognizes the importance of expressed emotion and its consequences for internationalizing a sense of self blame and victimhood and the long-term repercussions this might have for the mental health and well-being of the health workforce.
Strengths and Limitations
As far as we are aware, this is the first-time text-mining and content analysis have been used to identify negative emotions reported by healthcare staffs’ MAEs, derived from free text in a large national database. A text-mining approach was used for identifying reports that included emotional expressions, as manual data analysis would have been almost impossible for such a big data set and this approach has been recognized to be time-effective in analysing big-data regarding medication incidents (Härkänen et al., 2019). Further, the emotional expressions identified in this study are relatively rare. These descriptive data of emotional expressions nevertheless cast light on the issues related to MAEs. Furthermore, the researchers adhered to the Standards for Reporting Qualitative Research (SRQR) checklist (see the list in Supplementary file 3 ).
However, while analyzing the free-text descriptions, we may have missed some important expressions as this was a pilot methodology we were testing, subjective decisions were made. Similarly, it was very difficult to combine the synonyms of the word used to express the negative emotions which can give rise to ambiguities. For example, in many cases, one single word could either be a verb, or noun or an adjective i.e., words can have different implication [ 29 ]. On the contrary, this study sheds some light upon how important it is to write incident report and to identify the negative emotions of staff, to prevent further consequences from occurring, encourage reporting and put support mechanisms in place. Patient safety incident data is likely to contain some limitations, more specifically, reporting error and bias which will affect the number, type and temporality of reported incidents and data interpretation [ 30 ]. Since reporting is largely voluntary, there are some potential limitations of NRLS being a reliable indicator of exact number of incidents. Nevertheless, increasing number of incidents may reflect an improved reporting culture. Further, the methodology did not allow for the identification of any positive emotions that might have been expressed by healthcare staff when reporting MAE incidents, as only free-text descriptions which included negative emotions were analyzed .From the free text-descriptions, most of the reports were found to be from nurses, however, staff-specific generalizability and scope is limited due to lack of staff type identification in NRLS data i.e., ST01 [ 31 ]. This makes it difficult to precisely quantify the impact and potential benefits of this research.
A wide range of negative emotions was expressed by healthcare staff after reported MA incidents. However, the associated psychological trauma and low mood expressed by healthcare staff represent significant negative impacts underlying reported negative emotions. It is more likely that MAE incidents are under-reported, therefore problems could be much higher in terms of prevalence and magnitude. There was tremendous variation in reports of healthcare staff encountering with MAEs; some reacted in extremely negative ways, whereas the majority expressed little about their feelings. Although many of the incident reporters did not express their feelings in their reports, there is also the possibility of them being affected by the aftermath of MAEs. Several actions were taken by healthcare staff to help cope with the error: which included, seeking guidance, reassuring, and supporting each other. This calls for further efforts from healthcare organizations to support healthcare staff as a matter of routine when encouraging reporting. Though we do know little about the long-term consequences, from what we see in our data, the scarring effect could potentially be considerable. Therefore, support programs need to be co-designed but incentivize to reward reporting without imposing an emotional burden on already overburdened staff. This is vital for error reporting, safety, and ultimately prevention to flourish in the long run. First and foremost, the system needs to promote psychological safety for its users, which our research currently demonstrates.
Availability of data and materials
Data supporting the findings of this study are made available from NRLS/NHS Improvement. However, restrictions apply to the availability of these data. For this current study, these data were used under license, therefore, are not publicly available. Data are however available if contacted to authors (MH, AMR, SM) upon reasonable request and with permission from NRLS/NHS Improvement.
Abbreviations
Medication Error
Medication Administration Error
Medication Administration
National Reporting and Learning System
National Health Services
Standards for Reporting Qualitative Research
World Health Organization. WHO launches global effort to halve medication-related errors in 5 years [Internet]. 2017 [Cited 2021 Jun 21]. Available from: https://www.who.int/news/item/29-03-2017-who-launches-global-effort-to-halve-medication-related-errors-in-5-years .
Wu AW. Medical error: The second victim. BMJ. 2000;18(7237):726–7. 320.
Article Google Scholar
Wu AW, Steckelberg RC. Medical error, incident investigation and the second victim: Doing better but feeling worse? BMJ Qual Saf. 2012;21(4):267–70.
Article PubMed Google Scholar
Busch IM, Moretti F, Purgato M, Barbui C, Wu AW, Rimondini M. Dealing with Adverse Events: A Meta-analysis on Second Victims’ Coping Strategies. J Patient Saf. 2020;16(2):E51–60.
Scott SD, Hirschinger LE, Cox KR, McCoig M, Hahn-Cover K, Epperly KM, et al. Caring for our own: Deploying a systemwide second victim rapid response team. Jt Comm J Qual Patient Saf. 2010 May;36(5)(1):233–40.
PubMed Google Scholar
Clarkson MD, Haskell H, Hemmelgarn C, Skolnik PJ. Abandon the term “second victim.” BMJ. 2019;27(364):l1233.
Tumelty ME. The second victim: A contested term? J Patient Saf. 2021;17(8):E1488–93.
Wu AW, Shapiro J, Harrison R, Scott SD, Connors C, Kenney L, et al. The Impact of Adverse Events on Clinicians: What’s in a Name? J Patient Saf. 2020;16(1):65–72.
Article PubMed CAS Google Scholar
Seys D, Wu AW, Gerven E, Van, Vleugels A, Euwema M, Panella M, et al. Health Care Professionals as Second Victims after Adverse Events: A Systematic Review. Eval Heal Prof. 2013;36(2):135–62.
Helo S, Moulton CE. Complications: acknowledging, managing, and coping with human error. Transl Androl Urol. 2017;6(6):773–82.
Article PubMed PubMed Central Google Scholar
Jones JH, Treiber LA. More Than 1 Million Potential Second Victims: How Many Could Nursing Education Prevent? Nurse Educ. 2018;43(3):154–7.
Headley M. Are second victims getting the help they need [Internet]. Vol. 15, Patient Safety & Quality Healthcare. 2018 [Cited 2022 May 17]. p. 12–6. Available from: https://www.psqh.com/analysis/are-second-victims-getting-the-help-they-need/ .
Stehman CR, Testo Z. Burnout DO. Suicide : Physician Loss in Emergency Medicine, Part I. West J Emerg Med. 2019;20:485–94.
Cottell M, Wätterbjörk I, Hälleberg Nyman M. Medication-related incidents at 19 hospitals: A retrospective register study using incident reports. Nurs Open. 2020;7(5):1526–35.
Hartnell N, MacKinnon N, Sketris I, Fleming M. Identifying, understanding and overcoming barriers to medication error reporting in hospitals: A focus group study. BMJ Qual Saf. 2012 May;21(5):361–8.
Mahdaviazad H, Askarian M, Kardeh B. Medical Error Reporting: Status Quo and Perceived Barriers in an Orthopedic Center in Iran. Int J Prev Med. 2020;11:14. https://doi.org/10.4103/ijpvm.IJPVM_235_18 .
NHS England. NHS Just Culture Guide [Internet]. 2018 [Cited 2022 May 17]. Available from: https://www.england.nhs.uk/patient-safety/a-just-culture-guide/ .
Edrees HH, Wu AW. Does One Size Fit All? Assessing the Need for Organizational Second Victim Support Programs. J Patient Saf. 2021;17(3):e247–54.
Kyngäs H. Inductive content analysis. In: The application of content analysis in nursing science research. New York (NY): Springer, Cham; 2020. p. 13–21. https://doi.org/10.1007/978-3-030-30199-6_2 .
Saunders B, Sim J, Tom K, Baker S, Waterfield J, Bartlam B, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52(4):1893–907.
Ullström S, Sachs MA, Hansson J, Øvretveit J, Brommels M. Suffering in silence: A qualitative study of second victims of adverse events. BMJ Qual Saf. 2014;23(4):325–31.
Treiber LA, Jones JH. Devastatingly human: An analysis of registered nurses’ medication error accounts. Qual Health Res. 2010;20(10):1327–42.
Harrison R, Lawton R, Perlo J, Gardner P, Armitage G, Shapiro J. Emotion and Coping in the Aftermath of Medical Error: A Cross-Country Exploration. J Patient Saf. 2015;11(1):28–35.
Ball JE, Griffiths P, Rafferty AM, Lindqvist R, Murrells T, Tishelman C. A cross-sectional study of ‘care left undone’ on nursing shifts in hospitals. J Adv Nurs. 2016;72(9):2086–97.
Griffiths P, Recio-Saucedo A, Dall’Ora C, Briggs J, Maruotti A, Meredith P, et al. The association between nurse staffing and omissions in nursing care: A systematic review. J Adv Nurs. 2018;74:1474–87.
Sessions LC, Nemeth LS, Catchpole K, Kelechi TJ. Nurses’ perceptions of high-alert medication administration safety: A qualitative descriptive study. J Adv Nurs. 2019;75(12):3654–67.
Lee W, Pyo J, Jang SG, Choi JE, Ock M. Experiences and responses of second victims of patient safety incidents in Korea: A qualitative study. BMC Health Serv Res. 2019;19(1):1–12.
Mahajan RP. Critical incident reporting and learning. Br J Anaesth [Internet]. 2010;105(1):69–75. Available from: https://doi.org/10.1093/bja/aeq133 .
Härkänen M, Paananen J, Murrells T, Rafferty AM, Franklin BD. Identifying risks areas related to medication administrations - Text mining analysis using free-text descriptions of incident reports. BMC Health Serv Res. 2019;19(1):1–9.
NHS Improvement. NRLS official statistics publications: data quality statement [Internet]. 2018. Available from: https://improvement.nhs.uk/documents/2549/NRLS_Guidance_notes_March_2018.pdf .
NHS England. Patient Safety Alert: improving medication error incident reporting and learning (supporting information) [Internet]. Patient Safety Alert: Stage 3 (directive). 2014. Available from: https://www.england.nhs.uk/2014/03/improving-medication-error-incident-reporting-and-learning/ .
Download references
Acknowledgements
The authors want to thank the NHS England and the NHS Improvement Patient safety team for helping the authors through the data acquisition process and refining the data extraction.
This study has been partially supported from the grant received from Sairaanhoitajien Koulultussäätiö and from early-stage researcher position from the University of Eastern Finland for the first author.
Author information
Authors and affiliations.
Department of Nursing Science, University of Eastern Finland, Yliopistonranta 1c, Kuopio, Finland
Sanu Mahat & Marja Härkänen
King’s College London: Florence Nightingale Faculty of Nursing, Midwifery and Palliative Care, James Clerk Maxwell Building, 57 Waterloo Road, SE1 8WA, London, UK
Anne Marie Rafferty
Department of Nursing Science, University of Eastern Finland, Kuopio, Yliopistonranta 1, 70210, Finland
Katri Vehviläinen-Julkunen
Kuopio University Hospital, Puijonlaaksontie 2, 70210, Kuopio, Finland
You can also search for this author in PubMed Google Scholar
Contributions
SM conducted the analysis, but all authors (SM, AMR, KV-J, and MH) participated in interpretation of data and in drafting and revising the manuscript critically and gave final approval of the version to be submitted.
Corresponding author
Correspondence to Sanu Mahat .
Ethics declarations
Ethics approval and consent to participate.
Data sharing agreement (Ref: 063.DSA.17) between NHS Improvement and King’s College London dated 22.08.2019 allowed us to use this data. As the data used for this study were voluntarily and anonymously submitted incident reports data (a register study), the need for seeking informed consent from the incident reporters was waived from the ethics committee. The King’s College London ethics committee (LRS-17/18-5150) gave ethical approval for this study in October 2017. Incident data used for this study did not comprise any personal or professional identifiers. Therefore, the anonymity and confidentiality of the data and the persons involved were fully ensured. Further, data handling was made confidential and ethical guidelines were followed.
Consent for publication
Not applicable.
Competing interests
No competing interests have been declared by authors.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: supplementary file 1..
Number of incident reports with negative emotional expressions and description about the healthcare staffs’ feeling. Supplementary file 2. Number of negative emotional expressions related specifically to medication administration incident reports ( n =72,390). Supplementary file 3. SRQR checklist for reporting qualitative studies.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Mahat, S., Rafferty, A.M., Vehviläinen-Julkunen, K. et al. Negative emotions experienced by healthcare staff following medication administration errors: a descriptive study using text-mining and content analysis of incident data. BMC Health Serv Res 22 , 1474 (2022). https://doi.org/10.1186/s12913-022-08818-1
Download citation
Received : 29 June 2022
Accepted : 09 November 2022
Published : 03 December 2022
DOI : https://doi.org/10.1186/s12913-022-08818-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Incident report
- Medication error
- Negative emotions
- Second victim
- Healthcare staff
- Text-mining
- Content analysis
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Selecting For Disability: How an Anecdote Can Inspire Regulation of Genetic Reproductive Technologies
Harvard Journal of Law & Technology (forthcoming)
Seton Hall Law School Legal Studies Research Paper Forthcoming
22 Pages Posted:
Doron Dorfman
Seton Hall Law School
Date Written: May 29, 2024
Research on rapid developments in genetic reproductive technologies traditionally deals with the ethics of offspring selection. The scholarly debate mostly explored the "new eugenics" implications of selecting against embryos genetically found to have a disability. However, some have raised concerns about prospective parents with disabilities selecting for an embryo with the same disability. This essay is the first to examine evidence on the existence of selecting for disability and demonstrates that there is lack of evidence for such parental choices. This essay traces discussions on this matter to one single story published in the media in 2002 which reported on an American Deaf couple who chose a deaf sperm donor to have deaf children. The story inspired a moral panic leading to the enactment of legislation in the United Kingdom that bans prospective parents from selecting embryos with disabilities over embryos that do not. Despite the sensationalism of the story, the couple and their children live a happy and full life as part of Washington DC's large Deaf community. By foregrounding the UK legislation and its origin, this essay argues that regulation of genetic reproductive technologies should be based on evidence of an existing problem and not on a moral panic based on speculations. This essay also highlights how the regulation of prospective parents selecting for disability expresses problematic ableist messages about life with a disability. This discussion is a cautionary tale at a time when state legislators and courts are poised to intervene on the issue of reproductive rights.
Keywords: Genetics, Reproductive Technologies, Family Law, Health Law, Disability Law, Reproductive Rights, Bioethics, Comparative Health Law
Suggested Citation: Suggested Citation
Doron Dorfman (Contact Author)
Seton hall law school ( email ).
One Newark Center Newark, NJ 07102-5210 United States
Do you have a job opening that you would like to promote on SSRN?
Paper statistics, related ejournals, family & children's law ejournal.
Subscribe to this fee journal for more curated articles on this topic
Public Health Law & Policy eJournal
Law & society: family law, relations & dispute resolution ejournal, law & culture ejournal, disability law ejournal, reproductive justice, law & policy ejournal, health psychology ejournal.

IMAGES
VIDEO
COMMENTS
Revised on May 9, 2024. Ethical considerations in research are a set of principles that guide your research designs and practices. Scientists and researchers must always adhere to a certain code of conduct when collecting data from people. The goals of human research often include understanding real-life phenomena, studying effective treatments ...
Education in research ethics is can help people get a better understanding of ethical standards, policies, and issues and improve ethical judgment and decision making. Many of the deviations that occur in research may occur because researchers simply do not know or have never thought seriously about some of the ethical norms of research. For ...
NIH Clinical Center researchers published seven main principles to guide the conduct of ethical research: Social and clinical value. Scientific validity. Fair subject selection. Favorable risk-benefit ratio. Independent review. Informed consent. Respect for potential and enrolled subjects.
Reputable journals screen for ethics at submission—and inability to pass ethics checks is one of the most common reasons for rejection. Unfortunately, once a study has begun, it's often too late to secure the requisite ethical reviews and clearances. Learn how to prepare for publication success by ensuring your study meets all ethical requirements before work begins.
1.1 Research Design and Ethical Approval. In this chapter, we aim to guide you through some of the most important ethical issues you may encounter throughout the process of finalizing your research design and preparing it for the process of ethical approval.
Research ethics are the moral principles and practices that guide how researchers work with information (especially data/texts), human subjects, and animals. Since 1947, following the publication of the Nuremberg Code, governments (e.g., see Canada) and professional organizations (e.g., see American Psychological Association) have created ...
Research Ethics is defined here to be the ethics of the planning, conduct, and reporting of research. It is clear that research ethics should include: Protections of human and animal subjects. However, not all researchers use human or animal subjects, nor are the ethical dimensions of research confined solely to protections for research ...
Abstract. Published articles in scientific journals are a key method for knowledge-sharing. Researchers can face the pressures to publish and this can sometimes lead to a breach of ethical values, whether consciously or unconsciously. The prevention of such practices is achieved by the application of strict ethical guidelines applicable to ...
Research ethics are moral principles that need to be adhered to when conducting a research study as well as when writing a scientific article, with the prime aim of avoiding deception or intent to harm study's participants, the scientific community, and society. Practicing and adhering to research ethics is essential for personal integrity as ...
Abstract. This chapter outlines the aims for the handbook. A main aim is to be a first point of contact for contemporary information, issues, and challenges in the fields of research ethics and scientific integrity. It is aimed at researchers, reviewers, and policymakers to help them pursue the best ways forward in seeking ethics and integrity ...
Multiple examples of unethical research studies conducted in the past throughout the world have cast a significant historical shadow on research involving human subjects. Examples include the Tuskegee Syphilis Study from 1932 to 1972, Nazi medical experimentation in the 1930s and 1940s, and research conducted at the Willowbrook State School in the 1950s and 1960s.[1] As the aftermath of these ...
The research team. There are examples of researchers being intimidated because of the line of research they are in. The institution in which the research is conducted. salso suggest there are 4 main ethical concerns when conducting SSR: The research question or hypothesis. The treatment of individual participants.
4. Respect confidentiality and privacy. Upholding individuals' rights to confidentiality and privacy is a central tenet of every psychologist's work. However, many privacy issues are idiosyncratic to the research population, writes Susan Folkman, PhD, in "Ethics in Research with Human Participants" (APA, 2000).
Ethics are a guiding principle that shapes the conduct of researchers. It influences both the process of discovery and the implications and applications of scientific findings 1. Ethical considerations in research include, but are not limited to, the management of data, the responsible use of resources, respect for human rights, the treatment ...
Research using an experiment, a survey or an observational study can be an exciting way of investigating a topic or gathering data to help you answer a question. Anyone who carries out research must consider the ethics of what they are doing, including you as an extended project student. Research is all about exploring questions to which we do not
Researchers are expected to adhere to the principles of ethical research. The Belmont Report provides a broad framework for the ethics of research involving human subjects. Three basic ethical principles are identified: Respect for persons—requires that research subjects are not coerced into participating in a study and requires the protection of research subjects who have diminished autonomy.
What is Ethics in Research & Why is it Important? by David B. Resnik, J.D., Ph.D. When most people think of ethics (or morals), they think of rules for distinguishing between right and wrong, such as the Golden Rule ("Do unto others as you would have them do unto you"), a code of professional conduct like the
studies, typically call our "research participants"). Our field of communication. that refer to the guide-. studies also has its own ethical views, guidelines, and norms that are specific to. lines that are followed to ensure the protection of people (participants) the types of research we conduct, which we will discuss throughout this chapter.
The research ethics definition is to follow moral and professional codes throughout any research conducted, which can be in the collection of the research, the publication of the research, interviews, analysis and more. To break it down, it basically means being moral and professional throughout any research that you do. ...
Primary research involves collecting data about a given subject directly from the real world. This section includes information on what primary research is, how to get started, ethics involved with primary research and different types of research you can do. It includes details about interviews, surveys, observations, and analysis.
Research ethics provides guidelines for the responsible conduct of research. In addition, it educates and monitors scientists conducting research to ensure a high ethical standard. The following is a general summary of some ethical principles: Honesty: Honestly report data, results, methods and procedures, and publication status.
Advancing psychology to benefit society and improve lives. Find resources on research misconduct, publication ethics, protecting research participants, ethics of online research, and guidance from various agencies and organizations, such as the NIH.
If data is coming from another Institution or being collected at another Institution, that Institution must know and approve the use of the data for research purposes. IRB review may be required by the data providing Institution. If it is a transfer of biological materials, a Material Transfer Agreement (MTA) may be needed.
The American Psychological Association (APA) is a scientific and professional organization that represents psychologists in the United States. APA educates the public about psychology, behavioral science and mental health; promotes psychological science and practice; fosters the education and training of psychological scientists, practitioners and educators; advocates for psychological ...
The NASW Code of Ethics is a set of standards that guide the professional conduct of social workers. The 2021 update includes language that addresses the importance of professional self-care. Moreover, revisions to Cultural Competence standard provide more explicit guidance to social workers. All social workers should review the new text and ...
Introduction. Research includes a set of activities in which researchers use various structured methods to contribute to the development of knowledge, whether this knowledge is theoretical, fundamental, or applied (Drolet & Ruest, accepted).University research is carried out in a highly competitive environment that is characterized by ever-increasing demands (i.e., on time, productivity ...
There are some people who likes to do research out of pure curiosity. But these people need to be in academia. Their employer might not be having any ethics board (think of someone working in a small company). Or they could be unemployed people.
The American Nurses Association (ANA) Center for Ethics and Human Rights was established to help nurses navigate ethical and value conflicts, and life and death decisions, many of which are common to everyday practice. The Center develops policy designed to address issues in ethics and human rights at the state, national, and international levels.
Background Medication errors regardless of the degree of patient harm can have a negative emotional impact on the healthcare staff involved. The potential for self-victimization of healthcare staff following medication errors can add to the moral distress of healthcare staff. The stigma associated with errors and their disclosure often haunts healthcare professionals, leading them to question ...
Abstract. Research on rapid developments in genetic reproductive technologies traditionally deals with the ethics of offspring selection. The scholarly debate mostly explored the "new eugenics" implications of selecting against embryos genetically found to have a disability.