
The Ultimate Guide to Nursing Diagnosis in 2024
What is a nursing diagnosis.
- NANDA Nursing Diagnosis
- Classification
NANDA Nursing Diagnosis List
Writing a nursing diagnosis.
- Nursing Diagnosis vs Medical Diagnosis
- American vs International

A nursing diagnosis is a part of the nursing process and is a clinical judgment that helps nurses determine the plan of care for their patients. These diagnoses drive possible interventions for the patient, family, and community. They are developed with thoughtful consideration of a patient’s physical assessment and can help measure outcomes for the nursing care plan .
In this article, we'll explore the NANDA nursing diagnosis list, examples of nursing diagnoses, and the 4 types.
Some nurses may see nursing diagnoses as outdated and arduous. However, it is an essential tool that promotes patient safety by utilizing evidence-based nursing research.
According to NANDA-I, the official definition of the nursing diagnosis is:
“Nursing diagnosis is a clinical judgment about individual, family, or community responses to actual or potential health problems/life processes. A nursing diagnosis provides the basis for selection of nursing interventions to achieve outcomes for which the nurse is accountable.”
Find Nursing Programs
What is the purpose of a nursing diagnosis.
According to NANDA International , a nursing diagnosis is “a judgment based on a comprehensive nursing assessment.” The nursing diagnosis is based on the patient’s current situation and health assessment, allowing nurses and other healthcare providers to see a patient's care from a holistic perspective.
Proper nursing diagnoses can lead to greater patient safety, quality care, and increased reimbursement from private health insurance, Medicare, and Medicaid.
They are just as beneficial to nurses as they are to patients.
NANDA Nursing Diagnosis
NANDA diagnoses help strengthen a nurse’s awareness, professional role, and professional abilities.
Formed in 1982, NANDA is a professional organization that develops, researches, disseminates, and refines the nursing terminology of nursing diagnosis. Originally an acronym for the North American Nursing Diagnosis Association, NANDA was renamed to NANDA International in 2002 as a response to its broadening worldwide membership.
According to its website, NANDA International’s mission is to:
- Provide the world’s leading evidence-based nursing diagnoses for use in practice and to determine interventions and outcomes
- Contribute to patient safety through the integration of evidence-based terminology into clinical practice and clinical decision-making
- Fund research through the NANDA-I Foundation
- Be a supportive and energetic global network of nurses, who are committed to improving the quality of nursing care and improvement of patient safety through evidence-based practice
NANDA members can be found worldwide, specifically in Brazil, Colombia, Ecuador, Mexico, Peru, Portugal, Germany, Austria, Switzerland, Netherlands, Belgium, and Nigeria-Ghana.
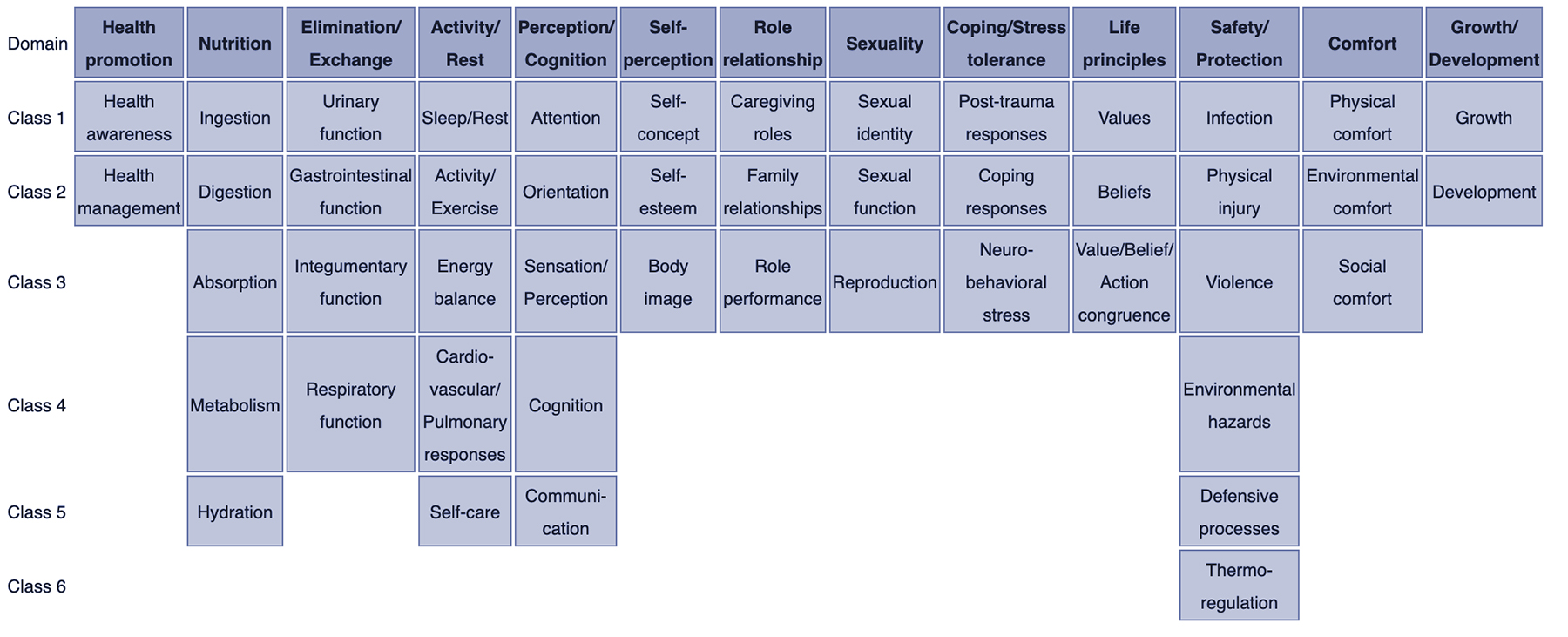
NANDA Classification of Nursing Diagnoses
NANDA-I adopted the Taxonomy II after consideration and collaboration with the National Library of Medicine (NLM) in regards to healthcare terminology codes. Taxonomy II has three levels: domains, classes, and nursing diagnoses.
There are currently 13 domains and 47 classes:
- Health Awareness
- Health Management
- Urinary Function
- Gastrointestinal Function
- Integumentary Function
- Respiratory Function
- Activity/Exercise
- Energy Balance
- Cardiovascular-Pulmonary Responses
- Orientation
- Sensation/Perception
- Communication
- Self-concept
- Self-esteem
- Caregiving Roles
- Family Relationships
- Role Performance
- Sexual Identity
- Sexual Function
- Reproduction
- Post-trauma Responses
- Coping Response
- Neuro-Behavioral Stress
- Value/Belief Action Congruence
- Physical Injury
- Environmental Hazards
- Defensive Processes
- Thermoregulation
- Physical Comfort
- Environmental Comfort
- Social Comfort
- Development
This refined Taxonomy is based on the Functional Health Patterns assessment framework of Dr. Mary Joy Gordon. Furthermore, the NLM suggested changes because the Taxonomy I code structure included information about the location and the level of the diagnosis.
NANDA-I nursing diagnoses and Taxonomy II comply with the International Standards Organization (ISO) terminology model for a nursing diagnosis.
The terminology is also registered with Health Level Seven International (HL7), an international healthcare informatics standard that allows for nursing diagnoses to be identified in specific electronic messages among different clinical information systems.
A full list of NANDA-I-approved nursing diagnoses can be found here .
Additional examples include:
- Dysfunctional ventilatory weaning response
- Impaired transferability
- Activity intolerance
- Situational low self-esteem
- Risk for disturbed maternal-fetal dyad
- Impaired emancipated decision-making
- Risk for impaired skin integrity
- Risk for metabolic imbalance syndrome
- Urge urinary incontinence
- Risk for unstable blood pressure
- Impaired verbal communication
- Acute confusion
- Disturbed body image
- Relocation stress syndrome
- Ineffective role performance
- Readiness for enhanced sleep
Examples of Nursing Diagnoses
The three main components of a nursing diagnosis are as follows.
- Problem and its definition
- Defining characteristics or risk factors
Examples of proper nursing diagnoses may include:
>> Related: What is the Nursing Process?
NANDA Nursing Diagnosis Types
There are 4 types of nursing diagnoses according to NANDA-I. They are:
- Problem-focused
- Health promotion
Popular Online RN-to-BSN Programs

Enrollment: Nationwide

At Purdue Global, discover a faster, more affordable way to earn your Nursing degree. Purdue Global is committed to keeping your tuition costs as low as possible and helping you find the most efficient path to your degree.
Enrollment: Nationwide, but certain programs have state restrictions. Check with Purdue for details.
- RN-to-BSN - ExcelTrack

Pursue Your Dream of Becoming a Nurse! Our 3-Year BSN Program is designed with one goal – to prepare you for a successful career as a BSN-prepared registered nurse. We combine classroom teaching, hands-on simulations, and clinicals in real-world healthcare environments to give you the skills you need.
Enrollment: On-Campus in AZ, FL, MI, MO, NV, OH, TX, UT, VA
- BS in Nursing (RN Not Required)
- RN to BSN - Global Studies

1. Problem-focused diagnosis
A patient problem present during a nursing assessment is known as a problem-focused diagnosis. Generally, the problem is seen throughout several shifts or a patient’s entire hospitalization. However, it may be resolved during a shift depending on the nursing and medical care.
Problem-focused diagnoses have three components.
- Nursing diagnosis
- Related factors
- Defining characteristics
Examples of this type of nursing diagnosis include:
- Decreased cardiac output
- Chronic functional constipation
- Impaired gas exchange
Problem-focused nursing diagnoses are typically based on signs and symptoms present in the patient. They are the most common nursing diagnoses and the easiest to identify.
2. Risk nursing diagnosis
A risk nursing diagnosis applies when risk factors require intervention from the nurse and healthcare team prior to a real problem developing.
- Risk for imbalanced fluid volume
- Risk for ineffective childbearing process
- Risk for impaired oral mucous membrane integrity
This type of diagnosis often requires clinical reasoning and nursing judgment.
3. Health promotion diagnosis
The goal of a health promotion nursing diagnosis is to improve the overall well-being of an individual, family, or community.
- Readiness for enhanced family processes
- Readiness for enhanced hope
- Sedentary lifestyle
4. Syndrome diagnosis
A syndrome diagnosis refers to a cluster of nursing diagnoses that occur in a pattern or can all be addressed through the same or similar nursing interventions.
Examples of this diagnosis include:
- Decreased cardiac output
- Decreased cardiac tissue perfusion
- Ineffective cerebral tissue perfusion
- Ineffective peripheral tissue perfusion
Possible nursing diagnosis
While not an official type of nursing diagnosis, possible nursing diagnosis applies to problems suspected to arise. This occurs when risk factors are present and require additional information to diagnose a potential problem.
Nursing Diagnosis Components
The three main components of a nursing diagnosis are:
- Etiology or risk factors
1. The problem statement explains the patient’s current health problem and the nursing interventions needed to care for the patient.
2. Etiology, or related factors , describes the possible reasons for the problem or the conditions in which it developed. These related factors guide the appropriate nursing interventions.
3. Finally, defining characteristics are signs and symptoms that allow for applying a specific diagnostic label. Risk factors are used in the place of defining characteristics for risk nursing diagnosis. They refer to factors that increase the patient’s vulnerability to health problems.
>> Show Me Online Nursing Programs
Problem-focused and risk diagnoses are the most difficult nursing diagnoses to write because they have multiple parts. According to NANDA-I , the simplest ways to write these nursing diagnoses are as follows:
PROBLEM-FOCUSED DIAGNOSIS
Problem-Focused Diagnosis related to ______________________ (Related Factors) as evidenced by _________________________ (Defining Characteristics).
RISK DIAGNOSIS
The correct statement for a NANDA-I nursing diagnosis would be: Risk for _____________ as evidenced by __________________________ (Risk Factors).
Nursing Diagnosis vs Medical Diagnosis
While all important, the nursing diagnosis is primarily handled through specific nursing interventions while a medical diagnosis is made by a physician or advanced healthcare practitioner.
The nursing diagnosis can be mental, spiritual, psychosocial, and/or physical. It focuses on the overall care of the patient while the medical diagnosis involves the medical aspect of the patient’s condition.
A medical diagnosis does not change if the condition is resolved, and it remains part of the patient’s health history forever. A nursing diagnosis, however, generally refers to a specific period of time.
Examples of medical diagnosis include:
- Congestive Heart Failure
- Diabetes Insipidus
Collaborative problems are ones that can be resolved or worked on through both nursing and medical interventions. Oftentimes, nurses will monitor the problems while the medical providers prescribe medications or obtain diagnostic tests.
History of Nursing Diagnoses
- 1973: The first conference to identify nursing knowledge and a classification system; NANDA was founded
- 1977: First Canadian Conference takes place in Toronto
- 1982: NANDA formed with members from the United States and Canada
- 1984: NANDA established a Diagnosis Review Committee
- 1987: American Nurses Association (ANA) officially recognizes NANDA to govern the development of a classification system for nursing diagnosis
- 1987: International Nursing Conference held in Alberta, Canada
- 1990: 9th NANDA conference and the official definition of the nursing diagnosis established
- 1997: Official journal renamed from “Nursing Diagnosis” to “Nursing Diagnosis: The International Journal of Nursing Terminologies and Classifications”
- 2002: NANDA changes to NANDA International (NANDA-I) and Taxonomy II released
- 2020: 244 NANDA-I approved diagnosis
American vs International Nursing Diagnosis
There is currently no difference between American nursing diagnoses and international nursing diagnoses. Because NANDA-I is an international organization, the approved nursing diagnoses are the same.
Discrepancies may occur when the translation of a nursing diagnosis into another language alters the syntax and structure. However, since there are NANDA-I offices around the world, the non-English nursing diagnoses are essentially the same.
What is an example of a nursing diagnosis?
- A nursing diagnosis is something a nurse can make that does not require an advanced provider’s input. It is not a medical diagnosis. An example of a nursing diagnosis is: Excessive fluid volume related to congestive heart failure as evidenced by symptoms of edema.
What is the most common nursing diagnosis?
- According to NANDA, some of the most common nursing diagnoses include pain, risk of infection, constipation, and body temperature imbalance.
What is a potential nursing diagnosis?
- A potential problem is an issue that could occur with the patient’s medical diagnosis, but there are no current signs and symptoms of it. For instance, skin integrity breakdown could occur in a patient with limited mobility.
How is a nursing diagnosis written?
- Nursing diagnoses are written with a problem or potential problem related to a medical condition, as evidenced by any presenting symptoms. There are 4 types of nursing diagnoses: risk-focused, problem-focused, health promotion-focused, or syndrome-focused.
What is the clinical diagnosis?
- A clinical diagnosis is the official medical diagnosis issued by a physician or other advanced care professional.

Kathleen Gaines (nee Colduvell) is a nationally published writer turned Pediatric ICU nurse from Philadelphia with over 13 years of ICU experience. She has an extensive ICU background having formerly worked in the CICU and NICU at several major hospitals in the Philadelphia region. After earning her MSN in Education from Loyola University of New Orleans, she currently also teaches for several prominent Universities making sure the next generation is ready for the bedside. As a certified breastfeeding counselor and trauma certified nurse, she is always ready for the next nursing challenge.

Plus, get exclusive access to discounts for nurses, stay informed on the latest nurse news, and learn how to take the next steps in your career.
By clicking “Join Now”, you agree to receive email newsletters and special offers from Nurse.org. You may unsubscribe at any time by using the unsubscribe link, found at the bottom of every email.
📕 Studying HQ
Writing a nursing diagnosis: a complete guide, rachel r.n..
- October 2, 2023
- How to Guides
Nursing diagnosis is essential to nursing, providing a structured framework for identifying and addressing patients’ health needs. As nursing students, mastering the art of writing nursing diagnoses is crucial for providing quality patient care. In this comprehensive guide, we will walk you through the process of writing a nursing diagnosis , step by step, ensuring you understand the key components and formatting. By the end of this article, you will have the skills and confidence to create effective nursing diagnoses that will benefit you and your patients.
What You'll Learn
Understanding Nursing Diagnosis
1.1 what is a nursing diagnosis.
A nursing diagnosis is a clinical judgment made by a nurse to identify a patient’s health problem, potential health problems, or wellness status. It serves as a basis for developing a care plan to meet the patient’s needs, improve their health outcomes, and provide individualized care.
1.2 Importance of Nursing Diagnosis
- Patient-Centered Care : Nursing diagnoses help nurses focus on patients’ unique needs and provide personalized care plans.
- Clinical Decision Making: They guide nurses in prioritizing interventions and setting achievable goals.
- Documentation: Nursing diagnoses serve as a record of the patient’s health status, which is vital for communication among healthcare providers.
- Evaluation: They provide a basis for evaluating the effectiveness of nursing interventions.
Writing a Nursing Diagnosis
2.1 gathering data.
The first step in writing a nursing diagnosis is to collect comprehensive patient data . This includes:
- Subjective Data: Information provided by the patient, such as their symptoms, feelings, and perceptions.
- Objective Data: Observations and measurements made by the nurse, like vital signs and physical assessments.
- Medical History: Previous medical conditions, surgeries, and medications.
2.2 Formulating Nursing Diagnoses
A nursing diagnosis typically consists of three components:
- Problem: Describes the patient’s health issue or concern.
- Etiology: Identifies the cause or contributing factors of the problem.
- Symptoms or Defining Characteristics: Lists the signs and symptoms that support the diagnosis.
For example:
- Problem: Impaired Gas Exchange
- Etiology: Ineffective breathing pattern related to pneumonia .
- Symptoms: Shortness of breath, decreased oxygen saturation, increased respiratory rate.
2.3 Using the PES Format
To ensure clarity and consistency in your nursing diagnoses, use the PES (Problem-Etiology-Symptoms) format. This format clearly defines the problem, its cause, and the evidence supporting the diagnosis.
- Problem: The “P” in PES; it is the patient’s health issue.
- Etiology: The “E” in PES; it represents the cause or contributing factors.
- Symptoms: The “S” in PES; these are the observed signs and symptoms.
2.4 Avoiding Medical Diagnoses
Nursing diagnoses should focus on the patient’s response to their health condition, not on medical diagnoses. For example, instead of writing “ Diabetes Mellitus ,” write “Risk for Uncontrolled Blood Glucose Levels related to lack of diabetes management knowledge.”
2.5 Prioritizing Nursing Diagnoses
In clinical practice, nurses often encounter multiple nursing diagnoses for one patient. Prioritize these diagnoses based on the patient’s immediate needs and the severity of their conditions. The most urgent issues should take precedence in your care plan .
Formatting Dialogue in an Essay
3.1 the role of dialogue in nursing essays.
In nursing essays, dialogue is often used to illustrate patient-nurse interactions, convey information, or present case studies. Proper formatting of dialogue is essential for clarity and readability.
3.2 Quotation Marks
When including direct speech or dialogue in your essay, enclose the spoken words within double quotation marks. For example:
Nurse Smith asked, “How are you feeling today?”
Patient Jones replied, “I’m experiencing some chest pain .”
3.3 Paragraphing
Each time there is a change in the speaker or topic, start a new paragraph. This helps readers follow the conversation and identify who is speaking. For example:
Patient Jones replied, “I’m experiencing some chest pain.”
Nurse Smith inquired, “Can you describe the pain? Is it sharp or dull?”
3.4 Punctuation
Use commas and periods correctly within dialogue. Commas should be placed inside the quotation marks, while periods should be placed inside if they are part of the quoted text, but outside if they are not. For example:
Incorrect: “I’m not sure if I can do this.” Nurse Smith hesitated.
Correct: “I’m not sure if I can do this,” Nurse Smith hesitated.
3.5 Attribution
Always attribute the dialogue to the appropriate speaker. This helps maintain clarity in your essay. For example:
Patient Jones stated, “I’m feeling very weak today.”
Nurse Smith reassured him, “We’ll take good care of you.”
Mastering the art of writing nursing diagnoses and formatting dialogue in essays is a crucial skill for nursing students. Effective nursing diagnoses are the foundation of patient-centered care, while well-formatted dialogue enhances the quality of your essays and reports. As you continue your nursing education, remember that practice makes perfect. Regularly assess and refine your nursing diagnosis skills, and pay attention to proper dialogue formatting in your written assignments. By doing so, you’ll enhance your nursing practice and excel in your academic pursuits.
If you ever find yourself struggling with nursing assignments, including writing nursing diagnoses or formatting dialogue in essays, don’t hesitate to seek assistance. Our professional writing services are here to support you on your academic journey. Contact us today to discover how we can help you succeed in your nursing studies.
Q1: What is an example of a nursing diagnosis in nursing?
A1: An example of a nursing diagnosis is “Impaired Physical Mobility related to postoperative pain and restricted range of motion,” which addresses a patient’s mobility issues after surgery.
Q2: What is the correct format for writing a nursing diagnosis and what are Nanda approved diagnoses?
A2: The correct format for a nursing diagnosis is the PES format – Problem, Etiology, and Symptoms. NANDA International (formerly known as North American Nursing Diagnosis Association) is a standardized source of approved nursing diagnoses, offering a comprehensive list of diagnoses for nursing practice.
Q3: How do you write a nursing diagnosis goal?
A3: Nursing diagnosis goals should be specific, measurable, achievable, relevant, and time-bound (SMART). For example, if the nursing diagnosis is “ Risk for Falls ,” a SMART goal might be “Patient will demonstrate proper use of assistive devices within one week to reduce fall risk.”
Q4: What is SMART format in nursing?
A4: SMART format is a goal-setting framework used in nursing to make goals Specific, Measurable, Achievable, Relevant, and Time-bound. It helps ensure that nursing interventions are clear, achievable, and focused on improving patient outcomes.
Start by filling this short order form order.studyinghq.com
And then follow the progressive flow.
Having an issue, chat with us here
Cathy, CS.
New Concept ? Let a subject expert write your paper for You
Have a subject expert write for you now, have a subject expert finish your paper for you, edit my paper for me, have an expert write your dissertation's chapter, popular topics.
Business Analysis Examples Essay Topics and Ideas How to Guides Nursing
- Nursing Solutions
- Study Guides
- Cookie Policy
- Free College Essay Examples
- Privacy Policy
- Research Paper Writing Service
- Research Proposal Writing Services
- Writing Service
- Discounts / Offers
Study Hub:
- Studying Blog
- Topic Ideas
- Business Studying
- Nursing Studying
- Literature and English Studying
Writing Tools
- Citation Generator
- Topic Generator
- Paraphrasing Tool
- Conclusion Maker
- Research Title Generator
- Thesis Statement Generator
- Summarizing Tool
- Terms and Conditions
- Confidentiality Policy
- Cookies Policy
- Refund and Revision Policy
Our samples and other types of content are meant for research and reference purposes only. We are strongly against plagiarism and academic dishonesty.
Contact Us:
📧 [email protected]
📞 +15512677917
2012-2024 © studyinghq.com. All rights reserved
Nursing Diagnosis Guide: All You Need to Know to Master Diagnosing
In this ultimate tutorial and nursing diagnosis list, we’ll walk you through the concepts behind writing nursing diagnosis. Learn what a nursing diagnosis is, its history and evolution, the nursing process , the different types and classifications, and how to write nursing diagnoses correctly. Included also in this guide are tips on how you can formulate better nursing diagnoses, plus guides on how you can use them in creating your nursing care plans .
Table of Contents
- What is a Nursing Diagnosis?
Purposes of Nursing Diagnosis
Differentiating nursing diagnoses, medical diagnoses, and collaborative problems, classification of nursing diagnoses (taxonomy ii), nursing process, problem-focused nursing diagnosis, risk nursing diagnosis, health promotion diagnosis, syndrome diagnosis, possible nursing diagnosis, problem and definition.
- Etiology
Risk Factors
Defining characteristics, analyzing data, identifying health problems, risks, and strengths, formulating diagnostic statements, one-part nursing diagnosis statement, two-part nursing diagnosis statement, three-part nursing diagnosis statement, nursing diagnosis for care plans, recommended resources, references and sources, what is a nursing diagnosis.
A nursing diagnosis is a clinical judgment concerning a human response to health conditions/life processes, or a vulnerability to that response, by an individual, family, group, or community. A nursing diagnosis provides the basis for selecting nursing interventions to achieve outcomes for which the nurse has accountability. Nursing diagnoses are developed based on data obtained during the nursing assessment and enable the nurse to develop the care plan.
The purpose of the nursing diagnosis is as follows:
- For nursing students, nursing diagnoses are an effective teaching tool to help sharpen their problem-solving and critical thinking skills.
- Helps identify nursing priorities and helps direct nursing interventions based on identified priorities.
- Helps the formulation of expected outcomes for quality assurance requirements of third-party payers.
- Nursing diagnoses help identify how a client or group responds to actual or potential health and life processes and knowing their available resources of strengths that can be drawn upon to prevent or resolve problems.
- Provides a common language and forms a basis for communication and understanding between nursing professionals and the healthcare team.
- Provides a basis of evaluation to determine if nursing care was beneficial to the client and cost-effective.
The term nursing diagnosis is associated with different concepts. It may refer to the distinct second step in the nursing process , diagnosis (“D” in “ ADPIE “). Also, nursing diagnosis applies to the label when nurses assign meaning to collected data appropriately labeled a nursing diagnosis. For example, during the assessment , the nurse may recognize that the client feels anxious , fearful, and finds it difficult to sleep . Those problems are labeled with nursing diagnoses: respectively, Anxiety , Fear , and Disturbed Sleep Pattern. In this context, a nursing diagnosis is based upon the patient’s response to the medical condition. It is called a ‘nursing diagnosis’ because these are matters that hold a distinct and precise action associated with what nurses have the autonomy to take action about with a specific disease or condition. This includes anything that is a physical, mental, and spiritual type of response. Hence, a nursing diagnosis is focused on care.
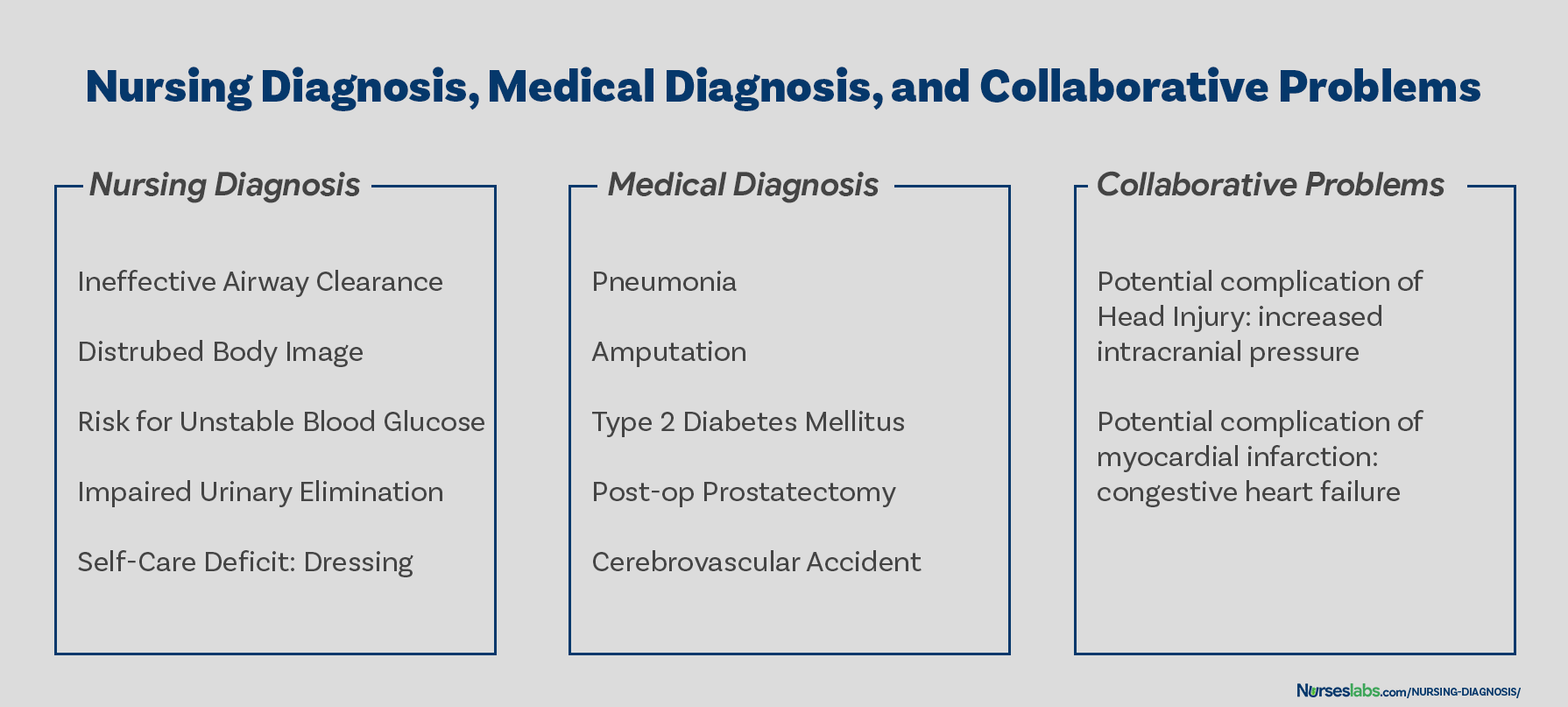
On the other hand, a medical diagnosis is made by the physician or advanced health care practitioner that deals more with the disease, medical condition, or pathological state only a practitioner can treat. Moreover, through experience and know-how, the specific and precise clinical entity that might be the possible cause of the illness will then be undertaken by the doctor, therefore, providing the proper medication that would cure the illness. Examples of medical diagnoses are Diabetes Mellitus , Tuberculosis , Amputation, Hepatitis , and Chronic Kidney Disease. The medical diagnosis normally does not change. Nurses must follow the physician’s orders and carry out prescribed treatments and therapies.
Collaborative problems are potential problems that nurses manage using both independent and physician-prescribed interventions. These are problems or conditions that require both medical and nursing interventions , with the nursing aspect focused on monitoring the client’s condition and preventing the development of the potential complication.
As explained above, now it is easier to distinguish a nursing diagnosis from a medical diagnosis. Nursing diagnosis is directed towards the patient and their physiological and psychological response. On the other hand, a medical diagnosis is particular to the disease or medical condition. Its center is on the illness.
How are nursing diagnoses listed, arranged, or classified? In 2002, Taxonomy II was adopted, which was based on the Functional Health Patterns assessment framework of Dr. Mary Joy Gordon. Taxonomy II has three levels: Domains (13), Classes (47), and nursing diagnoses. Nursing diagnoses are no longer grouped by Gordon’s patterns but coded according to seven axes: diagnostic concept, time, unit of care, age, health status, descriptor, and topology. In addition, diagnoses are now listed alphabetically by their concept, not by the first word.
- Class 1. Health Awareness
- Class 2. Health Management
- Class 1. Ingestion
- Class 2. Digestion
- Class 3. Absorption
- Class 4. Metabolism
- Class 5. Hydration
- Class 1. Urinary function
- Class 2. Gastrointestinal function
- Class 3. Integumentary function
- Class 4. Respiratory function
- Class 1. Sleep/Rest
- Class 2. Activity/Exercise
- Class 3. Energy balance
- Class 4. Cardiovascular/Pulmonary responses
- Class 5. Self-care
- Class 1. Attention
- Class 2. Orientation
- Class 3. Sensation/Perception
- Class 4. Cognition
- Class 5. Communication
- Class 1. Self-concept
- Class 2. Self-esteem
- Class 3. Body image
- Class 1. Caregiving roles
- Class 2. Family relationships
- Class 3. Role performance
- Class 1. Sexual identity
- Class 2. Sexual function
- Class 3. Reproduction
- Class 1. Post-trauma responses
- Class 2. Coping responses
- Class 3. Neurobehavioral stress
- Class 1. Values
- Class 2. Beliefs
- Class 3. Value/Belief/Action congruence
- Class 1. Infection
- Class 2. Physical injury
- Class 3. Violence
- Class 4. Environmental hazards
- Class 5. Defensive processes
- Class 6. Thermoregulation
- Class 1. Physical comfort
- Class 2. Environmental comfort
- Class 3. Social comfort
- Class 1. Growth
- Class 2. Development
The five stages of the nursing process are assessment, diagnosing, planning , implementation , and evaluation . All steps in the nursing process require critical thinking by the nurse. Apart from understanding nursing diagnoses and their definitions, the nurse promotes awareness of defining characteristics and behaviors of the diagnoses, related factors to the selected nursing diagnoses, and the interventions suited for treating the diagnoses.
The steps, importance, purposes, and characteristics of the nursing process are discussed more in detail here: “ The Nursing Process: A Comprehensive Guide “
Types of Nursing Diagnoses
The four types of nursing diagnosis are Actual (Problem-Focused), Risk, Health Promotion , and Syndrome. Here are the four categories of nursing diagnoses:
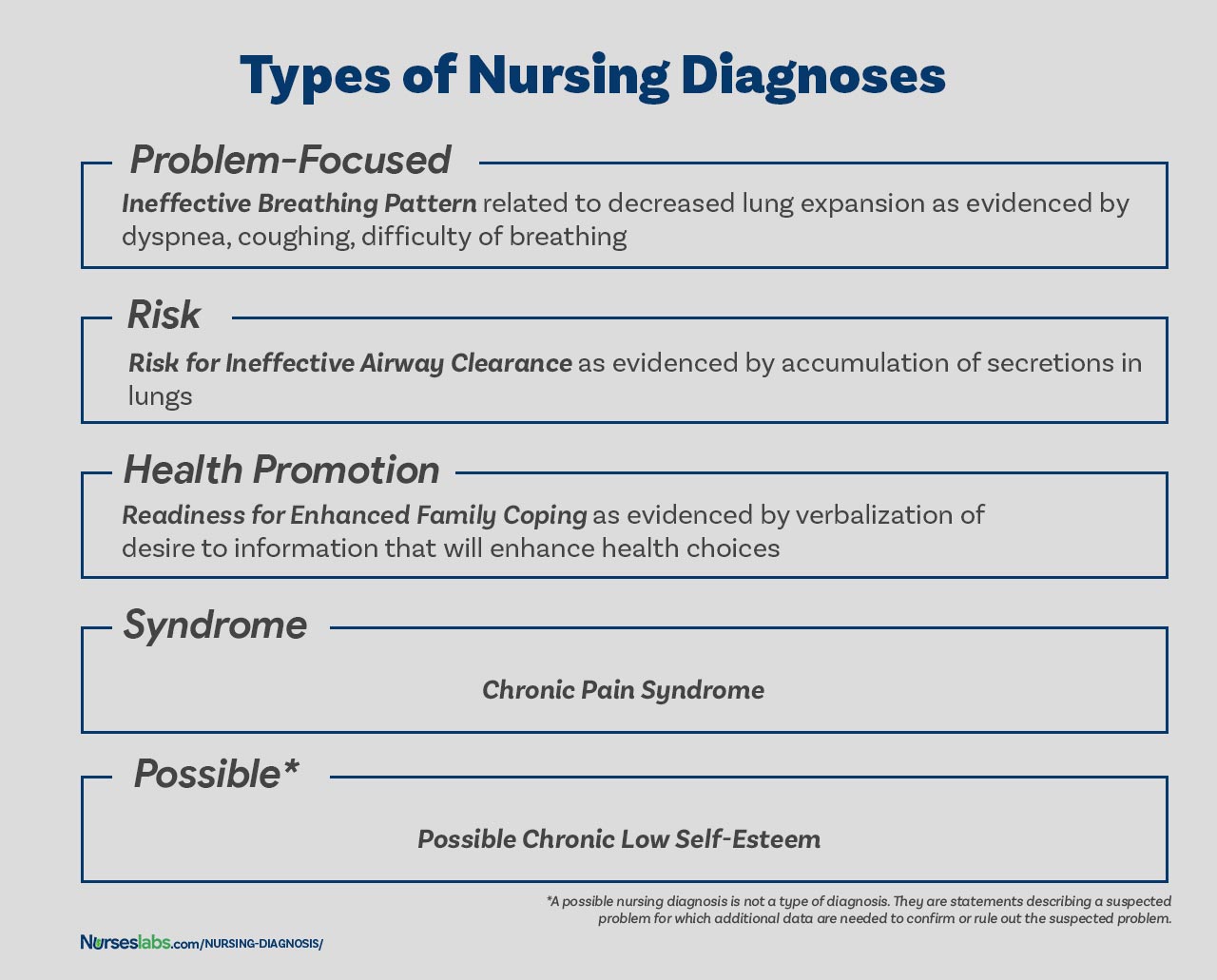
A problem-focused diagnosis (also known as actual diagnosis ) is a client problem present at the time of the nursing assessment . These diagnoses are based on the presence of associated signs and symptoms. Actual nursing diagnosis should not be viewed as more important than risk diagnoses. There are many instances where a risk diagnosis can be the diagnosis with the highest priority for a patient.
Problem-focused nursing diagnoses have three components: (1) nursing diagnosis, (2) related factors, and (3) defining characteristics. Examples of actual nursing diagnoses are:
- Anxiety related to stress as evidenced by increased tension, apprehension, and expression of concern regarding upcoming surgery
- Acute pain related to decreased myocardial flow as evidenced by grimacing, expression of pain , guarding behavior.
The second type of nursing diagnosis is called risk nursing diagnosis. These are clinical judgments that a problem does not exist, but the presence of risk factors indicates that a problem is likely to develop unless nurses intervene. A risk diagnosis is based on the patient’s current health status, past health history , and other risk factors that may increase the patient’s likelihood of experiencing a health problem. These are integral part of nursing care because they help to identify potential problems early on and allows the nurse to take steps to prevent or mitigate the risk.
There are no etiological factors (related factors) for risk diagnoses. The individual (or group) is more susceptible to developing the problem than others in the same or a similar situation because of risk factors. For example, an elderly client with diabetes and vertigo who has difficulty walking refuses to ask for assistance during ambulation may be appropriately diagnosed with risk for injury or risk for falls.
Components of a risk nursing diagnosis include (1) risk diagnostic label, and (2) risk factors. Examples of risk nursing diagnosis are:
- Risk for injury
- Risk for infection
Health promotion diagnosis (also known as wellness diagnosis ) is a clinical judgment about motivation and desire to increase well-being. It is a statement that identifies the patient’s readiness for engaging in activities that promote health and well-being. For example, if a first-time mother shows interest on how to properly breastfeed her baby, a nurse make make a health promotion diagnosis of “Readiness for Enhanced Breastfeeding .” This nursing diagnosis will be then used to guide nursing interventions aimed at supporting the patient in learning about proper breastfeeding.
Additionally, health promotion diagnosis is concerned with the individual, family, or community transition from a specific level of wellness to a higher level of wellness. Components of a health promotion diagnosis generally include only the diagnostic label or a one-part statement. Examples of health promotion diagnosis:
- Readiness for enhanced health literacy
A syndrome diagnosis is a clinical judgment concerning a cluster of problem or risk nursing diagnoses that are predicted to present because of a certain situation or event. They, too, are written as a one-part statement requiring only the diagnostic label. Examples of a syndrome nursing diagnosis are:
- Chronic Pain Syndrome
A possible nursing diagnosis is not a type of diagnosis as are actual, risk, health promotion , and syndrome. Possible nursing diagnoses are statements describing a suspected problem for which additional data are needed to confirm or rule out the suspected problem. It provides the nurse with the ability to communicate with other nurses that a diagnosis may be present but additional data collection is indicated to rule out or confirm the diagnosis. Examples include:
- Possible chronic low self-esteem
- Possible social isolation .
Components of a Nursing Diagnosis
A nursing diagnosis has typically three components: (1) the problem and its definition, (2) the etiology, and (3) the defining characteristics or risk factors (for risk diagnosis).
The problem statement , or the diagnostic label , describes the client’s health problem or response to which nursing therapy is given concisely. A diagnostic label usually has two parts: qualifier and focus of the diagnosis. Qualifiers (also called modifiers ) are words that have been added to some diagnostic labels to give additional meaning, limit, or specify the diagnostic statement. Exempted in this rule are one-word nursing diagnoses (e.g., Anxiety, Constipation , Diarrhea , Nausea , etc.) where their qualifier and focus are inherent in the one term.
| Qualifier | Focus of the Diagnosis |
|---|---|
| Deficient | Fluid volume |
| Imbalanced | Nutrition: Less Than Body Requirements |
| Impaired | Gas Exchange |
| Ineffective | |
| Risk for | Injury |
The etiology , or related factors , component of a nursing diagnosis label identifies one or more probable causes of the health problem, are the conditions involved in the development of the problem, gives direction to the required nursing therapy, and enables the nurse to individualize the client’s care. Nursing interventions should be aimed at etiological factors in order to remove the underlying cause of the nursing diagnosis. Etiology is linked with the problem statement with the phrase “ related to ” for example:
- Activity intolerance related to generalized weakness .
- Decreased cardiac output related to abnormality in blood profile
Risk factors are used instead of etiological factors for risk nursing diagnosis. Risk factors are forces that put an individual (or group) at an increased vulnerability to an unhealthy condition. Risk factors are written following the phrase “as evidenced by” in the diagnostic statement.
- Risk for falls as evidenced by old age and use of walker.
- Risk for infection as evidenced by break in skin integrity .
Defining characteristics are the clusters of signs and symptoms that indicate the presence of a particular diagnostic label. In actual nursing diagnosis, the defining characteristics are the identified signs and symptoms of the client. For risk nursing diagnosis, no signs and symptoms are present therefore the factors that cause the client to be more susceptible to the problem form the etiology of a risk nursing diagnosis. Defining characteristics are written following the phrase “as evidenced by” or “as manifested by” in the diagnostic statement.
Diagnostic Process: How to Diagnose
There are three phases during the diagnostic process: (1) data analysis, (2) identification of the client’s health problems, health risks, and strengths, and (3) formulation of diagnostic statements.
Analysis of data involves comparing patient data against standards, clustering the cues, and identifying gaps and inconsistencies.
In this decision-making step, after data analysis, the nurse and the client identify problems that support tentative actual, risk, and possible diagnoses. It involves determining whether a problem is a nursing diagnosis, medical diagnosis, or a collaborative problem. Also, at this stage, the nurse and the client identify the client’s strengths, resources, and abilities to cope.
Formulation of diagnostic statements is the last step of the diagnostic process wherein the nurse creates diagnostic statements. The process is detailed below.
How to Write a Nursing Diagnosis?
In writing nursing diagnostic statements, describe an individual’s health status and the factors that have contributed to the status. You do not need to include all types of diagnostic indicators. Writing diagnostic statements vary per type of nursing diagnosis (see below).
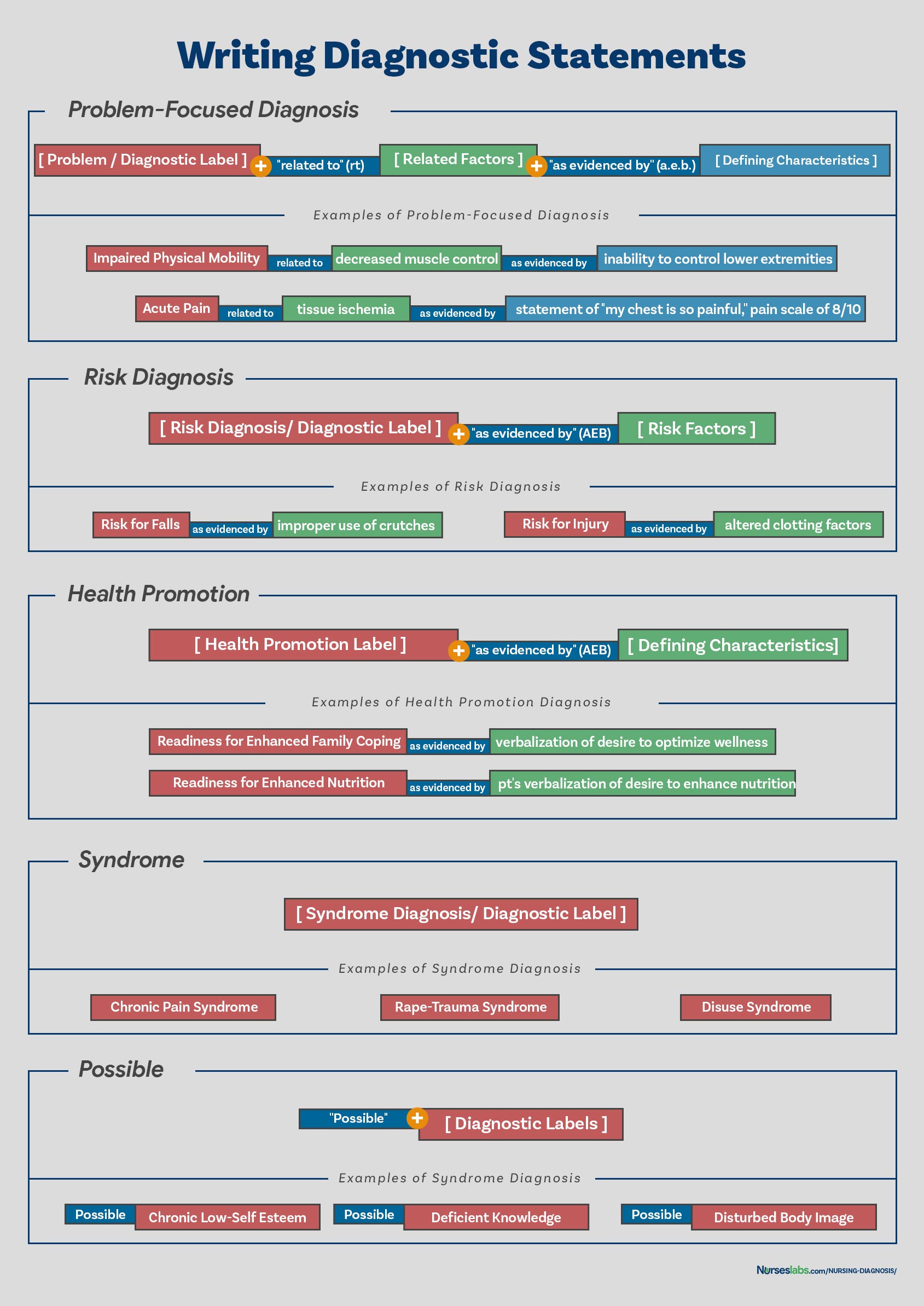
Another way of writing nursing diagnostic statements is by using the PES format, which stands for Problem (diagnostic label), Etiology (related factors), and Signs/Symptoms (defining characteristics). Diagnostic statements can be one-part, two-part, or three-part using the PES format.
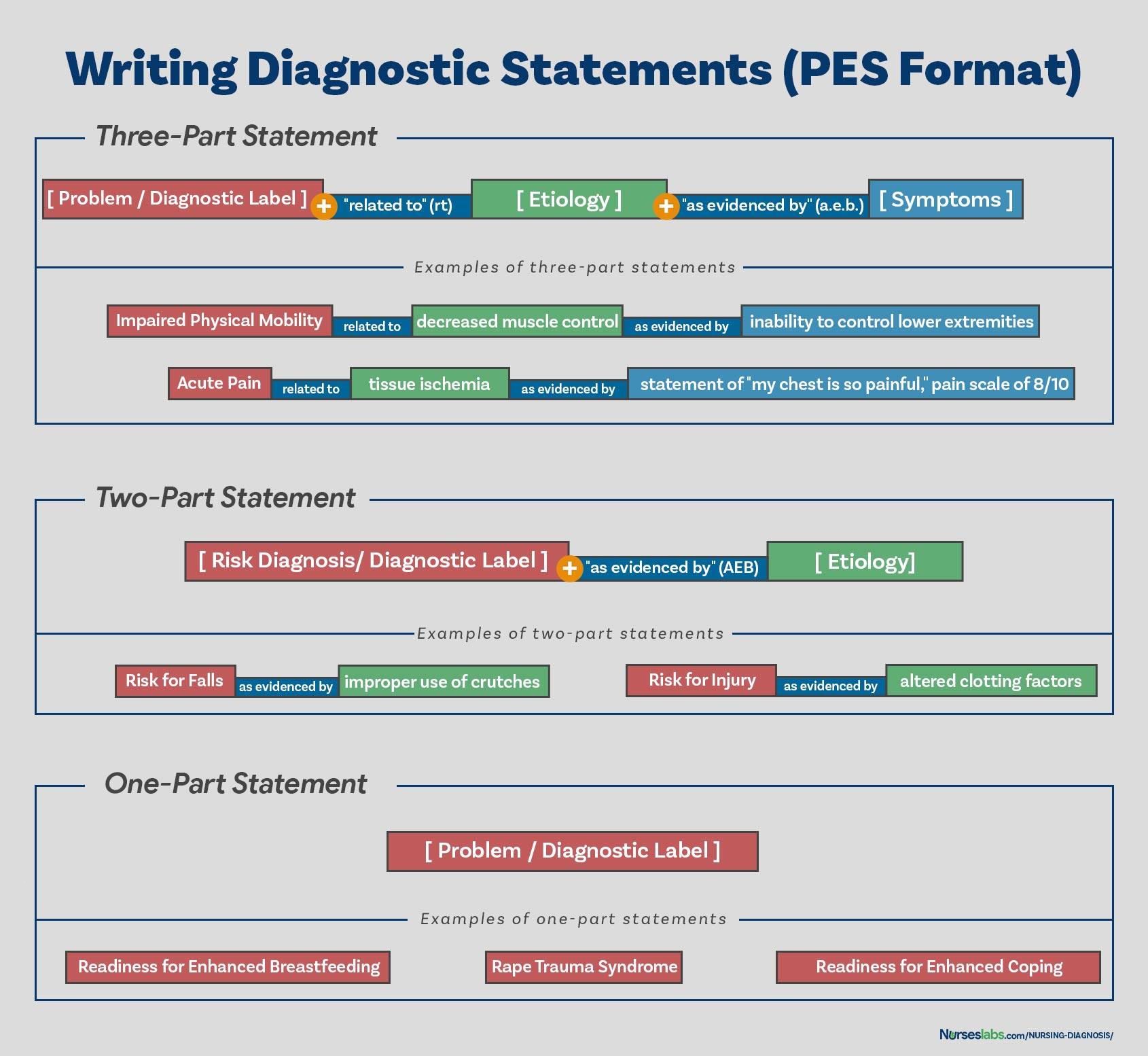
Health promotion nursing diagnoses are usually written as one-part statements because related factors are always the same: motivated to achieve a higher level of wellness through related factors may be used to improve the chosen diagnosis. Syndrome diagnoses also have no related factors. Examples of one-part nursing diagnosis statements include:
- Readiness for enhanced coping
- Rape Trauma Syndrome
Risk and possible nursing diagnoses have two-part statements: the first part is the diagnostic label and the second is the validation for a risk nursing diagnosis or the presence of risk factors. It’s not possible to have a third part for risk or possible diagnoses because signs and symptoms do not exist. Examples of two-part nursing diagnosis statements include:
- Risk for infection as evidenced by weakened immune system response
- Risk for injury as evidenced by unstable hemodynamic profile
An actual or problem-focus nursing diagnosis has three-part statements: diagnostic label, contributing factor (“related to”), and signs and symptoms (“as evidenced by” or “as manifested by”). The three-part nursing diagnosis statement is also called the PES format which includes the Problem, Etiology, and Signs and Symptoms. Example of three-part nursing diagnosis statements include:
- Acute pain related to tissue ischemia as evidenced by statement of “I feel severe pain on my chest!”
Variations on Basic Statement Formats
Variations in writing nursing diagnosis statement formats include the following:
- Using “ secondary to ” to divide the etiology into two parts to make the diagnostic statement more descriptive and useful. Following the “secondary to” is often a pathophysiologic or disease process or a medical diagnosis. For example, Risk for Decreased Cardiac Output related to reduced preload secondary to myocardial infarction .
- Using “ complex factors ” when there are too many etiologic factors or when they are too complex to state in a brief phrase. For example, Chronic Low Self-Esteem related to complex factors.
- Using “ unknown etiology ” when the defining characteristics are present but the nurse does not know the cause or contributing factors. For example, Ineffective Coping related to unknown etiology.
- Specifying a second part of the general response or diagnostic label to make it more precise. For example, Impaired Skin Integrity (Right Anterior Chest) related to disruption of skin surface secondary to burn injury .
This section is the list or database of the common nursing diagnosis examples that you can use to develop your nursing care plans .
See also: Nursing Care Plans (NCP): Ultimate Guide and List
- Chronic Pain
- Constipation
- Decreased Cardiac Output
- Hopelessness
- Hyperthermia
- Hypothermia
Recommended nursing diagnosis and nursing care plan books and resources.
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. For more information, check out our privacy policy .
Ackley and Ladwig’s Nursing Diagnosis Handbook: An Evidence-Based Guide to Planning Care We love this book because of its evidence-based approach to nursing interventions. This care plan handbook uses an easy, three-step system to guide you through client assessment, nursing diagnosis, and care planning. Includes step-by-step instructions showing how to implement care and evaluate outcomes, and help you build skills in diagnostic reasoning and critical thinking.

Nursing Care Plans – Nursing Diagnosis & Intervention (10th Edition) Includes over two hundred care plans that reflect the most recent evidence-based guidelines. New to this edition are ICNP diagnoses, care plans on LGBTQ health issues, and on electrolytes and acid-base balance.

Nurse’s Pocket Guide: Diagnoses, Prioritized Interventions, and Rationales Quick-reference tool includes all you need to identify the correct diagnoses for efficient patient care planning. The sixteenth edition includes the most recent nursing diagnoses and interventions and an alphabetized listing of nursing diagnoses covering more than 400 disorders.

Nursing Diagnosis Manual: Planning, Individualizing, and Documenting Client Care Identify interventions to plan, individualize, and document care for more than 800 diseases and disorders. Only in the Nursing Diagnosis Manual will you find for each diagnosis subjectively and objectively – sample clinical applications, prioritized action/interventions with rationales – a documentation section, and much more!

All-in-One Nursing Care Planning Resource – E-Book: Medical-Surgical, Pediatric, Maternity, and Psychiatric-Mental Health Includes over 100 care plans for medical-surgical, maternity/OB, pediatrics, and psychiatric and mental health. Interprofessional “patient problems” focus familiarizes you with how to speak to patients.

Other recommended site resources for this nursing care plan:
- Nursing Care Plans (NCP): Ultimate Guide and Database MUST READ! Over 150+ nursing care plans for different diseases and conditions. Includes our easy-to-follow guide on how to create nursing care plans from scratch.
- Nursing Diagnosis Guide and List: All You Need to Know to Master Diagnosing Our comprehensive guide on how to create and write diagnostic labels. Includes detailed nursing care plan guides for common nursing diagnostic labels.
References for this Nursing Diagnosis guide and recommended resources to further your reading.
- Berman, A., Snyder, S., & Frandsen, G. (2016). Kozier & Erb’s Fundamentals of Nursing: Concepts, process and practice . Boston, MA: Pearson.
- Edel, M. (1982). The nature of nursing diagnosis. In J. Carlson, C. Craft, & A. McGuire (Eds.), Nursing diagnosis (pp. 3-17). Philadelphia: Saunders.
- Fry, V. (1953). The Creative approach to nursing. AJN, 53(3), 301-302.
- Gordon, M. (1982). Nursing diagnosis: Process and application. New York: McGraw-Hill.
- Gordon, M. (2014). Manual of nursing diagnosis . Jones & Bartlett Publishers.
- Gebbie, K., & Lavin, M. (1975.) Classification of nursing diagnoses: Proceedings of the First National Conference. St. Louis, MO: Mosby.
- McManus, R. L. (1951). Assumption of functions in nursing. In Teachers College, Columbia University, Regional planning for nurses and nursing education . New York: Columbia University Press.
- Powers, P. (2002). A discourse analysis of nursing diagnosis . Qualitative health research , 12 (7), 945-965.
87 thoughts on “Nursing Diagnosis Guide: All You Need to Know to Master Diagnosing”
Very useful document indeed.
Thank you Sima! Hope it helps come up with great nursing care plans!
Thank you for this resource material. This is very simple, concise and easy to understand. This would be of great help both for the students and the teacher.
Please make proper table for nursing diagnosis it’ll be easy to read and understand .
This is simple and easy to understand.
Happy to know! Hope you visit our guide on nursing care plans too! Thanks for dropping by Modupe!
I need a complete pdf file
Hi! If you want to save it as a PDF file, simply “Print” this page and “Save as PDF”.
So very happy to stumble upon nurseslabs. Thanks so much
Happy to have helped you. Please do check out our nursing care plans list too! Thanks for visiting, Hussaina!
I want to acknowledge the writer of Understand, Matt Vera for using the initiative in simplifying the nursing notes into simple English that we as upcoming nursing students can understand nursing notes in order to practice them in our clinical. I’ve learned so much from this website and I want to be part of the nurses website so I can gather some more informations. Get me on my email. Thanks so much..
Thank you Lawrencia. Glad to be of help!
VERY NICE EXPLANATION .THANK YOU . DEAR MADAM /SIR PLEASE CAN YOU PROVIDE ME LIST OF NURSING DIAGNOSIS ALONG WITH REVISED ONE TILL DATE . I am Lecturer in college of nursing ,India Thank You
this is so educative thank you
Thank you! Glad you liked it.
really simple and effective, thank you so much.
This is great! Simple and easy to understand for the nursing students.
Comment:nice work, great nurses.
I am a nurse more than 30 yeras and try to teach my team how to used nursing process but it not success. You make me feel it simple and easy to understand . I will use your concept for my team. Thank you somuch
THANK, THANK YOU, THANK YOU FOR THE RESOURCEFUL INFORMATION.
please i want care plan on risk for unstable blood pressure i am a nursing student
@joseph auarshie jnr, can you please send me your care plan if you made it already ? I am a nursing student too. Thank you appreciated
Thanks, I look forward to learning more from you and maybe joining you in writing once am done with school. It’s awesome.
You’re very much welcome! Please feel free to ask further questions. Thank you and goodluck!
I what to check out nursing care plan
Comment: good explanation of health issue pattern
This is great. Thanks for given your time to this. Is so educative. Up thumb
Thanks alot am so interested on this
Great Work!
Thank you for the resourceful information which I was thought in school but almost forgotten until now, brain refresh, thanks
Excellent job done congratulations to all the team worker .
Please is the component of nursing diagnosis the same as type of nursing diagnosis
Each time I research about nursing diagnoses, there is something new to learn. This is a very well written piece giving great insights about nursing. More than ever, I have a better understanding of the unique body of nursing knowledge. Bravo to the Matt and entire Nurseslabs team
Thank you! Be sure to visit also our nursing care plans here .
Sorry madam the risk factors thus the potential problem has the related factors not the sign and symptom because that something has not happed yet so there is no sign and symptoms. Thank you
Excellent work and expertise team work
Usefull information
Nice work Sir/Madam thank you for giving us more hints on Nursing Diagnoses. Excellent team work.
Thank you so much for this nursing diagnosis.
Formulations of the DX has been hectic but thanks to matt vera has been of great help especally answering medsurge quizes just try to expand more on the second part (related to)of actual diagnosis
Hi Mary, Thanks you so much for your comment and endorsement. We welcome your students, thanks again!
Very useful indeed. thank you
I’m practicing nursing diagnosis by using the practice case studies my professor provided but I’m not sure if I’m doing it correctly. Here’s what I’m thinking: Problem:Anxiety Etiology: morning bouts of fear Signs and symptoms: patient stated waking nervous, light headed, agitated, and having a pounding heart Anxiety related to morning bouts of fear as evidenced by patient’s reports of waking light headed, agitated, and having a pounding heart.
In this case study we know to patient has been experiencing anxiety since childhood and was verbally abused by his father. His anxiety is causing difficulties for him to make decisions and he fears he’ll experience misfortunes whenever going to school. We also know about these bouts he has ever morning, which I thought would be a good primary diagnosis because they almost seem like a panic attack which would be extreme anxiety which is a big deal right? Am I thinking about this the right way or not and if not, what should I be concerned about as most important and how should my diagnosis be worded?
The nursing diagnostic statement you made sounds right. For the “as evidenced by” part, I would add the statement of the patient in verbatim since this is a subjective data (place it also under quotation marks) and if possible, do your own assessment and objectively obtain the data.
I would write it this way:
Anxiety related to morning bouts of fear as evidenced by increased in heart rate, apprehensiveness, and patient stating “waking lightheaded, agitated, and having a pounding heart”
well precised and nice to read.
Thanks so much for this readings, am so interested with this website I hope i could use this for my whole time
Hello Professor Matt Vera
I am Mai Ba Hai, from Hue University of Medicine and Pharmacy,faculty of nursing.I found that this content is very useful and helpful to me. I think that this content is really fit to my teaching, so I would like to ask your permission that I can translate this content into my languages (Vietnamese) to teach for my nursing students in Vietnam. I will cite you as author of this document. If you are willing to help in this point I really appreciate about it. I am looking forward to receiving your agreement. Yours sincerely.
This is so fantastic!! Thank you for taking out time to create this wonderful piece
You guys are wonderful. Thanks so much.
Very nice and very interested More ink to your pen I pray
Very useful, thank you so much
Thanks so much for the good job. Nurse Timothy Idachaba (RN, RNE, .MSC in view) from Nigeria
Matt Vera, BSN, R.N, First, I want to thank you for your amazing, short and precise note you provided for us. But I think I’ve got some trouble understanding about 3 components of Nursing diagnosis. This is because there is some variation between defining characteristics among your examples of actual and potential nursing diagnosis. Actual nursing diagnosis -Ineffective breathing pattern related to decreased lung expansion AS EVIDENCED BY dyspnoea, coughing, and difficulty of breathing. Risk diagnosis -Risk for ineffective airway clearance AS EVIDENCED BY accumulation_of_secreations_in_the_Lung. -Risk for fall AS EVIDENCED BY Muscle_weakness ……………………………………………………. As I know before, risk Nursing diagnosis misses Defining characteristics. because, the problem is not happened. but it is to happen.
So, when I compare defining characteristics among actual and risk diagnosis, there is disagreement. Accumulation of secretion in the lung is aetiology for ineffective airway clearance. But you provided it as defining characteristics. So, please make it clear.
Well elaborated, i like using nurseslabs, i always understand easily
Educative I appreciate
Such a beautiful explanation. Thank you
Very comprehensive and understandable. A job Well done by the group
Nice piece, thanks for painstakingly organizing this concise notes, God bless you
Very educative and simple to understand. Thank you for the effort
This is very handy. Your work is appreciated
This is an excellent work . I was having lectures just now on nursing diagnosis and care plan and this note helps me a lot
Its so helpful. Thank you!
Very good content. Happy to learn the Nursing diagnosis. Thanks Nurseslabs
This is a great educative article, kind of review of the nursing diagnosis. Thanks a lot for refreshing my memory.
Sorry, it’s not.
This was so simple and very helpful
So simple, concise and very helpful.
I APPRECIATE THIS WORK, USEFUL AND EASY TO UNDERSTAND.
Beautiful. I love the nursing care plan links. it is just what I have been searching for to assist my students. Thank you
I’ve been a nurse (currently working PRN) since 2015 and not having used nursing diagnosis in my day to day, this source was super helpful and a great refresher! Much thanks to the author!
Thanks for this it was very good and easy to comprehend
Thank you for your opinion; however, I agree with Mebratu. The description shown in your article for statement of “risk for” problem is confusing to me.
My view is as follows: “Actual problem” has 3 parts: nursing diagnosis (client’s problem) related to etiology (pathophysiology of what is causing the problem) as evidenced by defining characteristics (signs and symptoms of the problem)
“Risk for problem” has 2 parts: nursing diagnosis (client’s potential problem) related to etiology (client condition that may cause the problem) There is no “as evidenced by” because there IS no evidence of the problem since the problem does not yet exist.
Very nice and easy explanation, thanku
Please I need the actual manual that’s currently being used or at least a link to it -the NANDA-I document.
For the most current NANDA-I Nursing Diagnosis manual, you might want to check out the latest edition of the “Nursing Diagnosis Handbook” by NANDA International. This handbook is frequently updated with new diagnoses and guidelines.
congratulations MATT VERA, for the very nice and usefully presentation in nursing diagnosis. it has been very usefully for patient care and teaching activities. simple and very nice understandable.
Thanks a lot Matt Vera for the simplicity of the nursing diagnoses. Continue with other pieces of work
You’re welcome! I’m thrilled to hear you found the simplicity of the nursing diagnoses helpful. Your encouragement means a lot, and I’m definitely motivated to keep creating and simplifying more content for you and others in the nursing community.
If there are any specific topics or areas you’d like to see covered next, please let me know. Your feedback is invaluable in guiding the work I do.
Really interesting I thank you
Very impressive step by step explanations
Its good explanation. how to download
Really helpful Thank you
Hi Aneena, You’re welcome! I’m glad to hear you found the nursing diagnosis guide helpful. Is there a particular area or diagnosis you’d like to explore more deeply, or do you have any other questions about nursing diagnoses? Always here to help!
Leave a Comment Cancel reply

Nursing Diagnosis - An Ultimate Guide for Nursing Students

A nursing diagnosis is a critical component of patient care, and it is a powerful tool that helps nurses accurately record the patients' conditions and predict the patient's care outcomes.
Diagnoses appreciate the uniqueness of each patient and are, therefore, different for every patient. A proper nursing diagnosis helps provide patients with patient-centered, evidence-based, safe, and quality-focused care.
Diagnosis is fundamental to nursing: assessment, diagnosis, outcomes and planning, implementation, and evaluation. Student nurses must write diagnoses based on case scenarios, vignettes, and sometimes actual patient data from shadowing experiences or practicum.
If you are a nursing student who wishes to learn how to write a nursing diagnosis either as a stand-alone assignment or as part of a formal nursing care plan, you have come to the right place.
Let's begin by looking at the definition of a nursing diagnosis so that we start from what we know.
What is a Nursing Diagnosis?
A nursing diagnosis is an evidence-based means for nurses to communicate their professional judgments to patients, interprofessional team members, the public, and other healthcare professionals.
The diagnosis is developed based on the assessment of the information gathered in the assessment phase of the nursing process.
After a concrete and comprehensive diagnosis, a nurse student or practitioner develops a nursing care plan to initiate independent nursing interventions, measure outcomes, and evaluate the patient's progress in the continuum of care.
NANDA-I is the custodian of defining, distributing, and integrating standardized diagnoses globally in nursing. And as per NANDA-I, a nursing diagnosis is a clinical judgment relating to the human response to specific health conditions, life processes, or vulnerability to the same response . It offers a basis for selecting plausible nursing interventions that, if implemented well, can achieve better outcomes for accountable nurses. You can write a nursing diagnosis statement for different nursing care plan scenarios for your nursing school assignments or nursing practice.
Components/ Parts of a Nursing Diagnosis
A typical nursing diagnosis has three major components: (1) problem, (2) etiology or risk factors, and (3) defining characteristics.
The problem statement also contains its definition. A problem statement, or diagnostic label, describes the patient's health problem or the response to which nursing intervention is given concisely.
The diagnostic label has two critical parts: the qualifiers and the modifiers. The qualifiers or modifiers are words that are added to the problem statement or diagnostic label to give additional meaning, limit, or specificity to the diagnostic statement, and they are not included in one-word nursing diagnoses. The qualifiers include deficient, ineffective, impaired, risk for, or imbalanced, and they precede the focus of the diagnosis.
Etiology or related factors component of a nursing diagnosis identifies the probable cause or causes of the health problem. It refers to the conditions involved in developing the problem, and they give direction to the required nursing intervention. The nursing interventions should address the etiological or causative factors to remove the underlying cause of the nursing diagnosis. In a nursing diagnosis, the etiology is linked to the problem statement/diagnostic label using the statement " related to."
The risk factors are used instead of the etiological factors when writing a risk nursing diagnosis. The risk factors are the forces or push factors that increase a patient or group's vulnerability to a given unhealthy condition. When writing a diagnostic statement, "as evidenced by" comes before listing all the risk factors.
The defining characteristics are the cluster of signs and symptoms that indicate the presence of a given diagnostic label or patient problem. In a problem-focused nursing diagnosis, these are usually the signs and symptoms of the patient. In a risk nursing diagnosis, they are the factors that cause the patient to be susceptible to the problem. They come after the statements "as evidenced by."
Nursing Diagnosis vs. other types of Diagnoses
In the continuum of care, there exist other diagnoses other than nursing diagnoses. Understanding the difference between these types of diagnosis is vital so that you don't confuse one for the other.
A nursing diagnosis is an evidence-based mechanism nurses use to communicate their professional judgments of patients' problems and issues to fellow nursing professionals, healthcare practitioners, the public, patients, and other healthcare stakeholders. Nurses use it as a label to assign meaning to the patient data collected during the assessment phase.
Let's look at medical and collaborative diagnoses to make things clear.
Unlike a nursing diagnosis, a medical diagnosis is made by a doctor or an advanced healthcare practitioner. The main focus of such a diagnosis is on the patient's medical condition, pathological state, and disease. A medical diagnosis can be informed by a nursing diagnosis, not the other way. A medical diagnosis remains part of a patient's medical history and cannot be altered. Medical diagnoses include jaundice, Type II diabetes mellitus, congestive heart failure, heart attack, diabetes insipidus, meningitis, scoliosis, and stroke.
A third type of diagnosis is collaborative diagnosis , which combines nursing and medical interventions. It is based on working together as part of an interprofessional healthcare team. The nurses can focus on the health problems, whereas the medical practitioners prescribe drugs and order more diagnostic tests to exhaustively address the patient's healthcare needs. A good example is respiratory failure or inefficiency, where doctors and nurses collaborate through different interventions to stabilize the patient's condition.
Related: SOAP notes writing guide for nursing students
Classification of Nursing Diagnosis
Nursing diagnosis has evolved through the years. To track nursing diagnoses, there is a need to follow specific conventions. The NANDA-I has a list, arrangement, and classification of the nursing diagnosis in a register referred to as the Taxonomy II, which has been used for over two decades. Taxonomy Ii has three levels:
- 267 nursing diagnoses
Let's have an overview of each because they are instrumental in formulating a diagnosis when writing a nursing care plan for the patient. Taxonomy II is approved in collaboration with the National Library of Medicine (NMLM), considering the healthcare terminology codes. It is also based on the Functional Health Patterns assessment framework Dr. Mary Joy Gordon developed. It also complies with the Internal Standards Organization (ISO) terminology model for a nursing diagnosis. The terminology is also registered with the Health Level Seven International (HL7), an international healthcare informatics standard that helps identify nursing diagnoses in specific electronic messages among different clinical information systems.
There are currently 13 domains and 47 classes:
Domain 1 - Health Promotion
- Class 1: Health Awareness
- Class 2: Health Management
Domain 2 - Nutrition
- Class 1: Ingestion
- Class 2: Digestion
- Class 3: Absorption
- Class 4: Metabolism
- Class 5: Hydration
Domain 3 - Elimination/Exchange
- Class 1: Urinary Function
- Class 2: Gastrointestinal Function
- Class 3: Integumentary Function
- Class 4: Respiratory Function
Domain 4 - Activity/Rest
- Class 1: Sleep/Rest
- Class 2: Activity/Exercise
- Class 3: Energy Balance
- Class 4: Cardiovascular-Pulmonary Responses
- Class 5: Self-Care
Domain 5 - Perception/Cognition
- Class 1: Attention
- Class 2: Orientation
- Class 3: Sensation/Perception
- Class 4: Cognition
- Class 5: Communication
Domain 6 - Self-Perception
- Class 1: Self-concept
- Class 2: Self-esteem
- Class 3: Body image
Domain 7 - Role Relationship
- Class 1: Caregiving Roles
- Class 2: Family Relationships
- Class 3: Role Performance
Domain 8 - Sexuality
- Class 1: Sexual Identity
- Class 2: Sexual Function
- Class 3: Reproduction
Domain 9 - Coping/Stress Tolerance
- Class 1: Post-trauma Responses
- Class 2: Coping Response
- Class 3: Neuro-Behavioral Stress
Domain 10 - Life Principles
- Class 1: Values
- Class 2: Beliefs
- Class 3: Value/Belief Action Congruence
Domain 11 - Safety/Protection
- Class 1: Infection
- Class 2: Physical Injury
- Class 3: Violence
- Class 4: Environmental Hazards
- Class 5: Defensive Processes
- Class 6: Thermoregulation
Domain 12 - Comfort
- Class 1: Physical Comfort
- Class 2: Environmental Comfort
- Class 3: Social Comfort
Domain 13 - Growth/Development
- Class 1: Growth
- Class 2: Development
Here is a list of potential nursing diagnoses examples that you can consider as you formulate a nursing care plan:
- Risk for injury
- Risk for electrolyte imbalance
- Shortness of breath (apnea)
- Deficient knowledge
- Decreased cardiac output
- Risk for surgical site infection
- Deficient fluid volume
- Ineffective coping
- Ineffective breathing programs
- Ineffective thermoregulation
- Risk for inefficient childbearing process
- Impaired physical mobility
- Ineffective airway clearance
- Impaired comfort
- Disturbed body image
- Risk for vascular trauma
- Risk for neonatal hypothermia
- Risk for obesity
- Risk for kidney failure
- Risk for kidney stones
- Risk for depression
Categories or Types of Nursing Diagnosis
The four main categories of nursing diagnoses recognized by the NANDA-I include problem-focuses (actual), risk, health promotion, and syndrome diagnosis.
Problem-Focused or Actual Nursing Diagnosis
An actual or problem-focused nursing diagnosis is a patient/client problem present during a nursing assessment. The diagnosis is based on the presence of associated signs and symptoms, and it contains three components: (a) Nursing diagnosis, (b) related factors, and (c) defining characteristics. Actual diagnoses can be used throughout the course of a patient�s stay in the hospital or can be solved by the end of a given shift.
The template for a problem-focused diagnosis is
Problem-focused diagnosis related to����. (Related Factors) as evidenced by ��. (defining characteristics).
Examples of problem-focused diagnoses include:
- Anxiety (diagnosis) related to stress and situational crises (related factors) as evidenced by anguish, insomnia, restlessness, and anorexia (defining characteristics)
- Acute pain related to decreased myocardial flow as evidenced by expression of pain, guarding behavior, and grimacing.
- Shortness of breathing related to pain as evidenced by pressure-lip breathing, reports of pain when inhaling, and use of accessory muscles to breathe.
Risk Nursing Diagnosis
The risk nursing diagnosis is also technical as the problem-focused nursing diagnosis. It is a clinical judgment that a problem does not exist. However, the presence of risk factors indicates that the problem will likely develop unless nursing interventions are activated.
A risk diagnosis is based on the current health status of the patient, their past medical or health history, and other risk factors that make a patient vulnerable to experiencing a specific health problem or a set of health problems. It is an important part of nursing care planning as it allows the identification and treatment or management of problems early enough through mitigation measures. When writing a risk diagnosis, the focus is not on the etiological factors, and instead, it is assumed that an individual or a group is more susceptible to developing a health problem than others in the same situation due to the risk factors.
The critical components of a risk nursing diagnosis are the risk diagnostic label and the risk factors. The template for a risk nursing diagnosis is as follows:
Risk diagnosis or diagnostic label (Risk for) �.as evidenced by (AEB)�. (Risk factors)
Examples of risk nursing diagnoses include:
- Risk for infection as evidenced by immunosuppression and missed vaccinations.
- Risk for falls as evidenced by poor bones, osteoporosis, and improper use of crutches
- Risk for injury as evidenced by altered clotting factors
- Risk for kidney stones as evidenced by vigorous dehydration and not drinking enough water
- Risk for adult falls as evidenced by lack of engineering controls at home
- Risk for pressure ulcers as evidenced by lack of ambulation
Health Promotion Diagnosis
The health promotion diagnosis is also known as a wellness diagnosis. Nurses make a clinical judgment about the client's motivation, desire, and need to achieve well-being. It identifies the readiness of the patients to engage in activities that promote their health and well-being. Such diagnoses help guide independent nursing interventions to support the patients in learning and adhering to health promotion patterns and programs. Health promotion diagnoses go beyond the patient to cover family and community transition to attain higher levels of wellness. The components of health promotion diagnosis include the diagnostic label or a one-part statement.
The template for a health promotion diagnosis is as follows:
[Health Promotion Label] as evidenced by (defining characteristics)
Examples of health promotion diagnoses include:
- Readiness for enhanced nutrition as evidenced by the patient�s verbalization of the desire to adhere to enhanced nutrition
- A sedentary lifestyle ad evidenced by insufficient physical activity.
- Reediness to enhanced family coping as evidenced by verbalization of desire to optimize wellness
- Readiness for enhanced self-care as evidenced by an expressed desire to enhance self-care
- Enthusiasm for exclusive breastfeeding as defined by the passion and knowledge of exclusive breastfeeding
Syndromes Diagnosis
A syndrome diagnosis is a clinical judgment relating to a cluster of problems or risk nursing diagnoses predicted to present due to a certain event or situation. Like the health promotion diagnosis, they are also a one-part statement where the diagnostic label is enough, but you can add the defining characteristics.
The template for syndrome diagnosis is:
Syndrome diagnosis or diagnostic label
Examples of syndrome diagnosis include:
- Disuse syndrome
- Rape-trauma syndrome
- Chronic pain syndrome
Steps for Writing a Nursing Diagnosis
As a nursing student, there are specific steps you need to take when writing a nursing diagnosis. Remember, a nursing diagnosis is a short statement that constantly forms the basis of care planning. You must draft hypothetical nursing care plans based on case studies, vignettes, or patient data to hone your clinical judgment, decision-making, problem-solving, and critical thinking. Here are the steps when formulating a nursing diagnosis
Step 1: Assessment
The first step when assigned to write a nursing diagnosis is to observe the presenting symptoms of the patient. Read the case study or vignette or check the patient information/data to describe the patient's problem based on the signs and symptoms.
Step 2: identify the potential diagnosis
Look at what the patient has done to alleviate the symptoms and how they cope with pain, loss of functioning, or discomfort. Look at both the subjective and objective information.
Subjective data is what the patient says about their feelings, whereas objective data comes from measurable and verifiable observations using scientific methods.
Examples of objective information include vital signs and diagnostic/lab results/findings. You should also identify the specific problem you will address in the nursing diagnosis.
It is a matter of prioritizing care to stabilize the patient. You should also look for the source of the problem the patient is experiencing. For instance, if you diagnose a chronic patient, check for injuries or burns related to it.
Check the past medical diagnosis and be open to the fact that the patient can have multiple diagnoses. Your diagnosis should also include the potential problems related to the related factors.
To make an effective clinical judgment, look up the official terminology for your observed problem. For this, you can use the NANDA-I nursing diagnosis categories. You should, at this point, confirm and rule out other diagnoses or create new diagnoses.
Step 3: Write the nursing care plan
Nursing diagnosis helps you implement dependent and interdependent nursing care plans for the patient. You can create measurable and achievable goals and come up with evidence-based interventions.
Step 4: Evaluate
After implementing the nursing care plan, the next step is to constantly evaluate the patient's progress to identify if the current interventions are effective or should be altered. A nursing diagnosis is assessed to ensure the care plan works well.
On a Final Note!
We have done our part as concerns arise about raising all-rounded nurses whose grades reflect skills. Nursing schools are means for you to learn how to become an effective nurse, and knowing how to write nursing diagnoses will boost your grade and enable you to offer patient-centered care.
Related Articles:
- How to write a SOAP Note
- How to Analyze a nursing case study
- How to write a Nursing Concept Map
- How to write a Nursing Care Plan
- Excellent Nursing Theories and Theorists
As part of the care planning process, you will have to conduct a patient assessment (check the vital signs), observe the patient's health, write a nursing diagnosis statement, come up with appropriate health system interventions, develop desired outcomes, and offer holistic care to the patient, whether real or hypothetical.
A proper nursing diagnosis is required for quality care of the patients. As you write the student nursing care plans, you should be able to proceed well, given your understanding of nursing diagnosis writing. Nursing diagnosis is also part of the electronic health record and facilitates evidence-based nursing care.
Many nursing programs will test nursing students' ability to write a good nursing diagnosis. If you are stuck writing a nursing care plan, head-to-toe assessment report, or SOAP Note, you can bank on our affordable nurse writing services . We have the best nurse writing experts you can hire online. You can always pay someone to do your nursing papers and avoid missing deadlines or getting stressed due to lack of time.
Struggling with
Related Articles
How to Make a Great Cover Page for an Essay

A Review of the WGU RN to BSN Nursing Program (Expert Insights)

Middle-Range Nursing Theories
NurseMyGrades is being relied upon by thousands of students worldwide to ace their nursing studies. We offer high quality sample papers that help students in their revision as well as helping them remain abreast of what is expected of them.
Nursing Diagnosis Guide: All You Need to Know

The term “diagnosis” is defined as an agreed-upon clinical judgment. When we think of a diagnosis, it is often thought of as a medical diagnosis, such as high blood pressure. In its simplest form, a nursing diagnosis is determined by nurses based on their scope and clinical judgment to guide patient care. Nursing diagnoses encompass individuals, families, and communities and relate to health conditions and life processes. Nursing diagnoses reflect the knowledge that is fundamental to nursing practice. Nurses’ diagnoses also reflect the systematic and scientific method of nursing. 1
In this article:
- The Nursing Process
- Purpose of a Nursing Diagnosis
- Nursing Diagnoses vs. Medical Diagnoses
Purpose and Mission of NANDA-I
Related factors, defining characteristics, risk factors, problem focused, health promotion, risk focused, writing a problem-focused nursing diagnosis, writing a risk-focused diagnosis, writing a health promotion-based diagnosis, writing a syndrome diagnosis.
- List of Current Nursing Diagnoses and Domains
- List of Common Nursing Diagnoses
A nursing diagnosis cannot exist without the nursing process; the foundation of nursing practice. It includes five steps:
Assessment: The nurse collects subjective and objective data about the patient which may include their physical, emotional, and psychological health as well as lifestyle factors, socioeconomic status, and culture. Information obtained during the assessment phase may include vital signs, pain, medication use, medical history, and more.
Diagnosis: After the nurse collects and analyzes this data, they can begin to identify actual or potential health problems. This is where nursing diagnoses come into play. The nurse can create a clinical picture to understand possible causes and associations in the patient’s assessment which will become a part of the patient’s care plan.
Planning: The nurse can now develop a plan and interventions along with short and long-term goals that are individualized to the patient’s needs.
Implementation: The nurse puts their plan to action and carries out interventions set in the care plan. Actions are documented for continuity of care.
Evaluation: In the final step of the nursing process, the nurse evaluates the effectiveness of interventions. Goals may be met or may need to be modified. By going through the nursing process again, the care plan can be revised based on changes in the patient’s health.
Nursing diagnoses are the foundation of care plans. Nursing diagnoses drive actions and allow for continued assessment, prioritization, organization, and effective health outcomes.
Nursing diagnoses are used in all care settings and support high-quality, evidence-based care. Here are a few ways nursing diagnoses support nursing practice.
- Nursing diagnoses improve collaboration between team members. Nursing diagnoses improve consistency and clarity of communication between nurses and other members of the care team. Nursing diagnoses can be revised, added, or removed based on the patient’s outcomes.
- Nursing diagnoses are a teaching tool. For new graduate nurses, familiarity with nursing diagnoses helps to improve critical thinking and confidence in practice. Nursing diagnoses and supporting educational material can guide novice nurses to direct interventions and goals for their patients. Understanding how nursing diagnoses contribute to the nursing process allows new nurses to become familiar with possible interventions and care pathways for their patients.
- Nursing diagnoses may improve risk identification. Many nursing diagnoses include diagnoses that alert the care team to avoid a potential risk through intervention. For instance, the nursing diagnosis “risk for bleeding” alerts a nurse that the patient may be receiving an anticoagulant and to monitor for signs of bleeding.
- Nursing diagnoses can help establish care goals. Nursing diagnoses illuminate care priorities, including current issues, future risks, and health promotion opportunities. Once the nursing diagnosis is identified, priorities, interventions, and goals can be created in collaboration with the patient.
- Nursing diagnoses promote patient education. Many nursing diagnoses incorporate teaching and opportunities for learning. The nurse may identify knowledge deficits, including medication adherence, health management, nutrition, coping, etc. The nurse utilizes these nursing diagnoses to help patients reach their health and wellness goals.
- Nursing diagnoses serve as documentation. Documentation is crucial in healthcare. If nursing care is not documented, there is no proof it was completed. Documentation of interventions and outcomes provides continuity of care between staff and protects the nurse.
Nursing diagnoses are the foundation of nursing care plans . Nursing diagnoses drive actions and allow for continued assessment, prioritization, organization, and effective health outcomes.
Although there are some similarities between medical and nursing diagnoses, such as clinical judgment and shared terminology, they are distinct. 2 The most apparent difference between nursing and medical diagnoses is the healthcare practitioner deciding the diagnosis. All nursing designations share nursing diagnoses, while physicians create medical diagnoses. The exception is that nurse practitioners in most states can also determine medical diagnoses and prescribe medication. Therefore, a nurse practitioner could determine both nursing and medical diagnoses.
There are also differences in each type of diagnosis. For example, medical diagnoses focus on the disease or pathology that affects the patient. In contrast, nursing diagnoses concentrate on the patient’s response to the illness or life circumstance, which can be either a physiological or psychological response. By focusing on the client’s response, a nurse applies interventions to address or alter that response.
To clarify this distinction, here are two examples of how medical and nursing diagnoses can work together.
A patient with a medical diagnosis of cerebrovascular accident (stroke) may lead to the complementary nursing diagnosis of unilateral neglect. Without the medical diagnosis, the nurse would not know what was causing unilateral neglect. The nursing diagnosis is a jumping-off point to create goals to manage the deficit and improve patient safety and quality of life.
With the medical diagnosis of dehydration, the nurse knows that the patient is experiencing deficient fluid volume (nursing diagnosis). Therefore, the nurse may implement interventions such as administering IV fluids and recording intake and output for this patient.
Nursing and medical diagnoses are complementary and guide each other to create a holistic clinical story.
What is NANDA-I?
The name NANDA originated as the acronym for the North American Nursing Diagnosis Association. However, with the organization’s global expansion, they no longer use NANDA as an acronym but as a recognizable organizational name. If using the organization’s full name, the correct use is NANDA International, Inc. (no hyphen), and the abbreviation is NANDA-I (with a hyphen). The organization offers networking and education and holds task forces on topics such as diagnosis development, informatics, and nursing research.
NANDA International is an organization that supports the use and development of standardized nursing terminology throughout clinical settings. 3 The organization’s mission is to use nursing diagnoses to promote high-quality patient care through evidence-based research and consistent terminology. Standardized nursing diagnoses inform evidence-based terminology that improves clinical practice by providing clear guidelines for communication and documentation. NANDA International continually releases new editions with revised, added, or retired nursing diagnoses and updates to criteria and classifications.
- Components of a Nursing Diagnosis
Formulating a nursing diagnosis is the second step of the nursing process after assessment. 6 First, the nurse analyzes the assessment data they collect from the patient and through observation or diagnostic testing. The nurse will use that data and create clusters of pertinent information to form hypotheses about the appropriate nursing diagnoses. At this stage, the nurse will either write the nursing diagnosis or decide they need additional information to confirm or update their hypothesized diagnosis.
Related factors are the etiology or cause of the nursing diagnosis. 4 Related factors are used in problem-focused, syndrome, and sometimes health promotion nursing diagnoses. Related factors are the underlying or contributing conditions or circumstances associated with the patient’s health problem. While the cause may not always be known, the nurse aims to understand the root cause to develop appropriate interventions.
Characteristics and risk factors are the evidence behind the nursing diagnosis. 4 However, they should not be used interchangeably. Defining characteristics are observable characteristics that support a problem-focused health promotion diagnosis or syndrome. Defining characteristics are the signs or symptoms of clinical pathology.
Risk factors are used primarily for risk-focused nursing diagnoses. Risk factors replace the defining characteristics of problem-focused nursing diagnoses. Similarly, they provide supporting evidence for the nursing diagnosis. Unlike defining characteristics, risk factors describe why the patient has an increased chance of acquiring the undesirable health outcome identified by the nurse. Risk factors can be biological, psychological, family, or community-related. Patients may have one or multiple risk factors supporting a risk diagnosis.
- Types of Nursing Diagnoses
A problem-focused nursing diagnosis is a nursing diagnosis that addresses a current health challenge. 4 In contrast to other nursing diagnoses that address potential problems or opportunities for health improvement, a problem-focused diagnosis deals with a current, known health challenge. To make this type of diagnosis, the defining characteristics of the diagnosis must be present at the time of evaluation. The defining characteristics include signs, symptoms, and patient health history. Defining characteristics act as clues for the nurse and, when grouped together, form patterns that allow a diagnosis to be assigned. Related factors should also be described as part of a problem-focused nursing diagnosis.
Problem-focused nursing diagnosis example: The nurse notices that the patient has a negative balance between their fluid intake and output. The patient also has dry mucous membranes and weight loss. The nurse makes the problem-based nursing diagnosis of “deficient fluid volume.” The NANDA-I definition is “Decreased intravascular, interstitial, and/or intracellular fluid. This refers to dehydration, water loss alone without change in sodium.” 5 Depending on the etiology and the patient’s health condition, the care plan and interventions will aim to increase fluid intake, identify the cause of the fluid deficit, and maintain evidence of normovolemia.
In contrast to problem-focused nursing diagnoses, health promotion diagnoses require that the individual/family/community is already functioning effectively in the health area, but there is an opportunity to increase well-being. Another requirement of a health promotion nursing diagnosis is that there is an expressed desire for improvement. This is often expressed at the beginning of the nursing diagnosis statement as “Readiness for enhanced…”. Therefore, the defining characteristic of a health promotion diagnosis is the client/family or community expressing a desire to improve or change health behaviors. There is some similarity to risk-focused nursing diagnoses; however, health promotion diagnoses are further upstream than risk-focused nursing diagnoses, as they aim to improve and actualize health potential instead of preventing an undesirable outcome.
Health promotion nursing diagnosis example: A patient expresses the desire to breastfeed exclusively during a prenatal screening visit with a nurse. The nurse recognizes the opportunity for health promotion with the nursing diagnosis of “Readiness for Enhanced Breastfeeding.” The NANDA-I definition is “A pattern of providing milk to an infant or young child directly from the breasts which may be strengthened.” 5 Based on this assessment, the nurse may refer the client to trusted online sources of information or refer them to group education sessions if available.
In a risk-based diagnosis, the nurse uses their clinical judgment to determine that the patient is at risk for health consequences if preventative measures are not implemented. Otherwise stated, the problem has not yet manifested for the client/family/community, but there is a vulnerability related to risk factors that the nurse identifies. Care plans will focus on preventing undesirable health outcomes.
Risk-focused nursing diagnosis example: In an inpatient surgical unit, a nurse is assigned to a patient postoperative day 3 for Whipple surgery. This nurse immediately recognizes that the patient meets the criteria for the nursing diagnosis of “Risk for Infection.” The NANDA-I definition is “At risk for being invaded by pathogenic organisms.” This patient is at risk due to their diagnosis of pancreatic cancer and recent surgery. One intervention the nurse may invoke is patient teaching on handwashing and providing the patient with alcohol-based antiseptic hand rub on their bedside table.
Nursing diagnosis syndromes are created when two or more concurrent nursing diagnoses are related and can be treated using similar interventions. Nursing syndrome diagnoses also cluster problem and risk-focused nursing diagnoses that often accompany specific health processes or life events.
Syndrome nursing diagnosis example: A patient shares that they recently witnessed a motor vehicle accident resulting in multiple injuries, including deaths. While not injured, they report difficulties sleeping, increased alcohol use, and irritability, which are now beginning to impact their ability to work. The nurse recognizes this cluster of symptoms as consistent with the nursing diagnosis of “post-trauma syndrome.” The NANDA-I definition of Post-Trauma Syndrome is “Sustained maladaptive response to a traumatic, overwhelming event.” 5 Other nursing diagnoses that may cluster to form this syndrome include nursing diagnoses related to sleep, anxiety, hope, depression, substance use, and relationships. The nurse discusses the goal of acknowledging the trauma and discusses options to connect the patient to support resources.
- How to Write a Nursing Diagnosis
Standardized methods of writing nursing diagnoses allow for clear communication of their purpose and driving factors. Writing a complete nursing diagnosis helps the nurse clarify their reasoning for potential interventions and care goals.
Problem-focused nursing diagnoses are three-part statements that include the problem, etiology, and symptoms (PES framework).
P roblem (Diagnostic Label) + E tiology (Cause or Related Factors) + S igns/Symptoms (Defining Characteristics)
[Diagnostic Label] + “related to” + [Etiology] + “as evidenced by” + [Defining Characteristics]
Examples of Problem-Focused Diagnosis:
Deficient Fluid Volume related to prolonged vomiting as evidenced by increased pulse rate and poor skin turgor.
Acute Confusion related to alcohol abuse as evidenced by hallucinations and increased agitation.
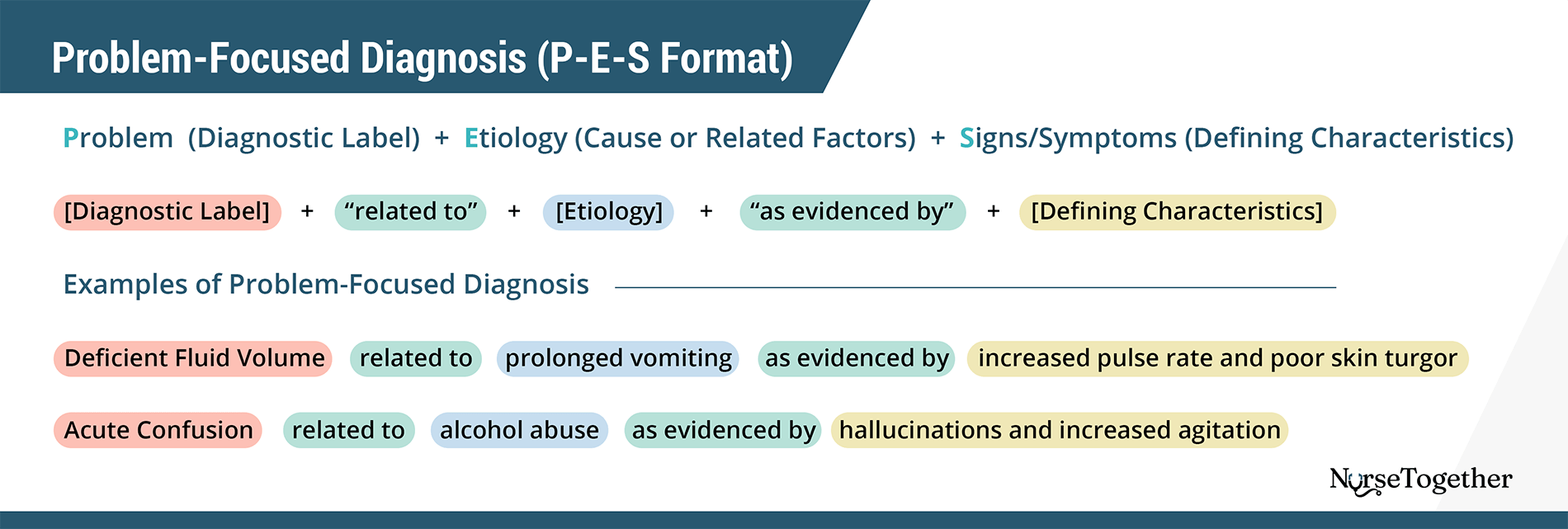
Problem (Nursing Diagnosis)
Nurses should use a NANDA-I label whenever possible to describe the identified problem to ensure consistency in diagnoses. However, if no NANDA-I label adequately represents the problem, the nurse needs to describe the problem in a clear, concise, and useful way to the care team. It is important to avoid judgmental language in the problem statement.
Etiology (Related Factors)
The second part of the problem-focused nursing diagnosis is the etiology or the underlying cause or causes of the nursing diagnosis. The etiology of the diagnosis is key to choosing appropriate interventions, so the nurse should describe the etiology as precisely as possible. For instance, what was the event’s timing, or how long has the client had the disease? When describing an etiology linked to a known pathophysiology or disease, the etiology should be stated as “secondary to.” Otherwise, the etiology should be stated as “related to” (R/T). “Related to” does not necessarily specify a direct cause-and-effect relationship, which is preferred because there may be other factors related to the nursing diagnosis that have not yet been identified.
When various factors contribute to a nursing diagnosis that cannot be summarized into a one-sentence statement, the etiology may be written as “related to complex factors.” This should not be used as a shortcut to finding the appropriate etiology, but when there is no clear primary etiology for the nursing diagnosis.
Signs/Symptoms (Defining Characteristics)
For a problem-focused nursing diagnosis, the described signs and symptoms are the defining characteristics of the nursing diagnosis. The nurse should link the etiology to the signs and symptoms by stating “as manifested by” (AMB) or “as evidenced by” (AEB).
The risk-focused diagnosis is a two-part statement that includes statements of the problem and risk factors.
Risk (Diagnostic Label) + Risk Factors
[Diagnostic Label] + “as evidenced by” + [Risk Factors]
Examples of Risk Diagnosis:
Risk for Infection as evidenced by a history of cancer and recent surgery.
Risk for Falls as evidenced by a history of falls, use of an assistive device, and visual difficulties.
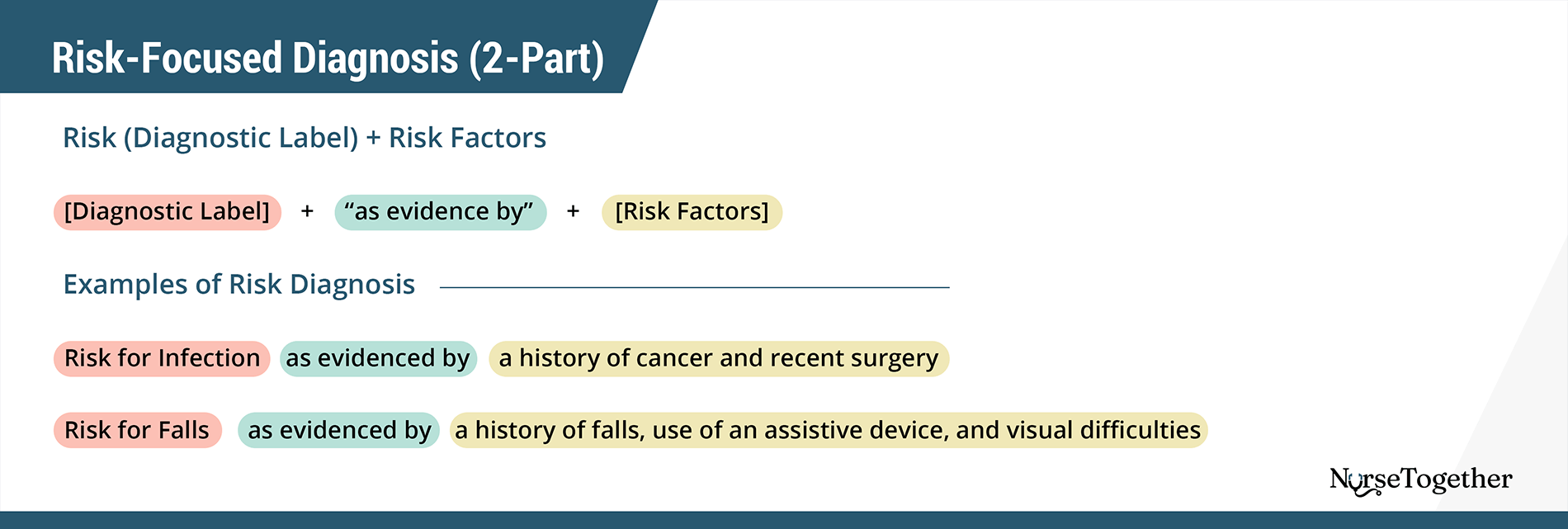
Like a problem-focused diagnosis, the risk-focused statement should also use a NANDA-I approved diagnosis starting with “Risk for…”. If a NANDA-I nursing diagnosis does not adequately describe the vulnerability, the nurse should still begin their problem statement with “Risk for…”.
Rather than describing the etiology or related factors, risk-focused diagnoses are supported by describing the risk factors related to the diagnosis. The risk factor statement should follow the problem statement with the nurse describing the problem “as evidenced by” and then listing the risk factors.
Defining characteristics are not possible because they haven’t actually occurred yet.
A health promotion diagnosis is also described using a two-part statement.
Health Promotion (Diagnostic Label) + Signs & Symptoms (Defining Characteristics)
[Diagnostic Label] + “as evidenced by” + [Defining Characteristics]
Health Promotion-Based Diagnosis Examples:
Readiness for Enhanced Breastfeeding as evidenced by the patient stating their desire to exclusively breastfeed and requesting information on how to achieve this.
Readiness for Enhanced Coping as evidenced by the patient expressing a desire to enhance social support and spiritual resources.
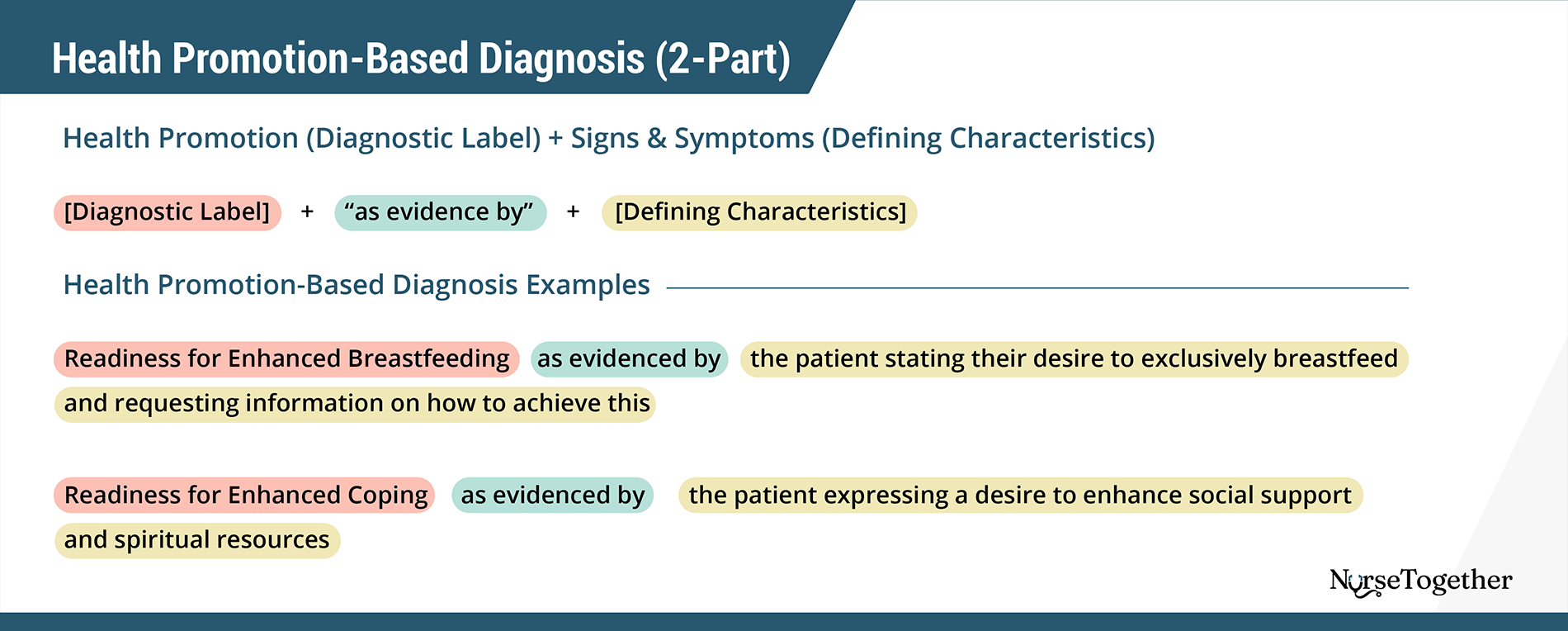
Rather than identifying a health problem, the problem when following the PES framework here is an opportunity for health improvement. When possible, the nurse should use an approved NANDA-I health promotion diagnosis. If the nurse is formulating their own problem statement for a health promotion diagnosis, they should start the statement with “readiness for enhanced…”.
The signs and symptoms used to describe a health promotion diagnosis are related to the patient, family, or community expressing readiness or desire for health improvement. This may be a verbal expression, actions, or other cues that alert the nurse to readiness for health promotion.
The syndrome diagnosis is a group of related nursing diagnoses and should be written as a two-part statement. 7
Syndrome (Diagnostic Label) + 2 or more supporting Nursing Diagnoses
[Diagnostic Label] + “as evidenced by” + [Nursing Diagnosis] + [Nursing Diagnosis]
Syndrome Diagnosis Examples:
Post-Trauma Syndrome as evidenced by Disturbed Sleep Pattern and Hopelessness.
Frail elderly syndrome as evidenced by Social Isolation and Chronic Confusion.
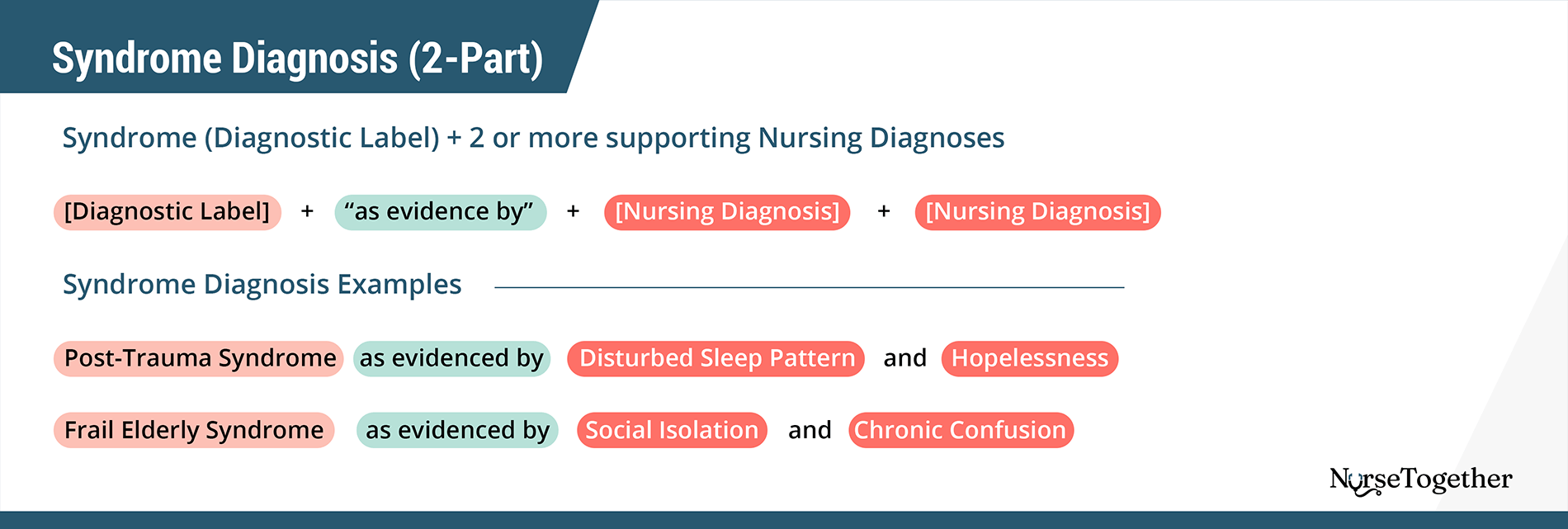
The nurse should use a recognized NANDA-I syndrome to diagnose a nursing syndrome.
Etiology (Additional Nursing Diagnoses)
For a syndrome diagnosis, the etiology is described as two or more nursing diagnoses that form the evidence for the syndrome diagnosis. There should be a minimum of two diagnoses, with no maximum of nursing diagnoses to support a syndrome diagnosis. Each nursing diagnosis should be written in its complete, appropriate form, either including etiology, signs and symptoms, or risk factors.
In the 2020 to 2023 edition of NANDA-I, there are 13 domains of nursing diagnoses. Each domain has between three and six classes of nursing diagnoses that are then broken down into individual diagnoses. Here we list all 13 domains, related classes, and an example nursing diagnosis. Please see NANDA International- Nursing Diagnoses Definitions and Classification, 12th Edition, for the complete list of diagnoses.
Domain 1: Health Promotion Class 1: Health Awareness Class 2: Health Management Diagnosis: Risk for frail elderly syndrome
Domain 2: Nutrition Class 1: Ingestion Class 2: Digestion Class 3: Absorption Class 4: Metabolism Class 5: Hydration Diagnosis: Risk for unstable blood glucose level
Domain 3: Elimination and exchange Class 1: Urinary function Class 2: Gastrointestinal function Class 3: Integumentary function Class 4: Respiratory function Diagnosis: Urinary retention
Domain 4: Activity/rest Class 1: Sleep/Rest Class 2: Activity/Exercise Class 3: Energy balance Class 4: Cardiovascular/pulmonary responses Class 5: Self-care Diagnosis: Bathing self-care deficit
Domain 5: Perception/cognition Class 1: Attention Class 2: Orientation Class 3: Sensation/perception Class 4: Cognition Class 5: Communication Diagnosis: Impaired memory
Domain 6: Self-perception Class 1: Self-concept Class 2: Self-esteem Class 3: Body image Diagnosis: Chronic low self-esteem
Domain 7: Role relationship Class 1: Caregiving roles Class 2: Family relationships Class 3: Role performance Diagnosis: Impaired social interaction
Domain 8: Sexuality Class 1: Sexual identity Class 2: Sexual function Class 3: Reproduction Diagnosis: Risk for disturbed maternal-fetal dyad
Domain 9: Coping/stress tolerance Class 1: Post-trauma responses Class 2: Coping responses Class 3: Neurobehavioral stress Diagnosis: Risk for post-trauma syndrome
Domain 10: Life principles Class 1: Values Class 2: Beliefs Class 3: Value/belief/action congruence Diagnosis: Moral distress
Domain 11: Safety/protection Class 1: Infection Class 2: Physical injury Class 3: Violence Class 4: Environmental hazards Class 5: Defensive processes Class 6: Thermoregulation Diagnosis: Risk of surgical site infection
Domain 12: Comfort Class 1: Physical comfort Class 2: Environmental comfort Class 3: Social comfort Diagnosis: Impaired comfort
Domain 13: Growth/development Class 1: Growth Class 2: Development Diagnosis: Delayed infant motor development
In this section, you will find common NANDA-I nursing diagnoses you can use to create care plans.
- Activity Intolerance
- Acute Confusion
- Chronic Pain
- Constipation
- Decreased Cardiac Output
- Disturbed Body Image
- Excess Fluid Volume
- Fluid Volume Deficit (Dehydration)
- Hopelessness
- Hyperthermia
- Imbalanced Nutrition
- Impaired Comfort
- Impaired Gas Exchange
- Impaired Physical Mobility
- Impaired Skin Integrity
- Impaired Urinary Elimination
- Impaired Verbal Communication
- Ineffective Airway Clearance
- Ineffective Breathing Pattern
- Ineffective Coping
- Ineffective Health Maintenance
- Ineffective Tissue Perfusion
- Knowledge Deficit
- Noncompliance (Ineffective Adherence)
- Risk For Aspiration
- Risk for Bleeding
- Risk for Electrolyte Imbalance
- Risk for Falls
- Risk for Infection
- Risk for Injury
- Risk For Unstable Blood Glucose
- Self-Care Deficit
- Social Isolation
- Stress Overload
- Urinary Retention
- Karaca T, Aslan S. Effect of ‘nursing terminologies and classifications’ course on nursing students’ perception of nursing diagnosis. Nurse education today. 2018;67(Journal Article):114-117. doi:10.1016/j.nedt.2018.05.011
- NANDA Internatioal. What is the difference between a medical diagnosis and a nursing diagnosis? Accessed January 7, 2023. http://nanda.host4kb.com/article/AA-00266/0/What-is-the-difference-between-a-medical-diagnosis-and-a-nursing-diagnosis-.html
- NANDA Internatioal. Our Story. Accessed January 7, 2023. https://nanda.org/who-we-are/our-story/
- NANDA Internatioal. Glossary of Terms. Accessed January 3, 2023. https://nanda.org/publications-resources/resources/glossary-of-terms/
- Carpenito LJ, Books@Ovid Purchased eBooks. Handbook of Nursing Diagnosis. 15th ed. Wolters Kluwer; 2017.
- Open Resources for Nursing. DIAGNOSIS. In: Nursing Fundamentals.
- NANDA Internatioal. The Structure and Development of Syndrome Diagnoses. Accessed January 7, 2023. https://nanda.org/publications-resources/resources/position-statement/


University Administration
- Careers @ USA
- For Current Students
- Request Information
- Master of Occupational Therapy (MOT)
- Doctor of Occupational Therapy (OTD)
- Post-Professional Doctor of Occupational Therapy (PPOTD)
- Master of Health Administration (MHA)
- Doctor of Education (EdD)
- Graduate Certificates
- Clinical Orthopedic Residency (OCS)
- Orthopaedic Manual Physical Therapy Fellowship (OMPT)
- Continuing Professional Education (CPE)
- Doctor of Physical Therapy (DPT)
- Non-Degree Physical Therapy Online Courses
- Master of Science in Speech-Language Pathology (MS-SLP)
- Post-Graduate Nursing Certificates
- Master of Science in Nursing (MSN)
- Doctor of Nursing Practice (DNP)
- Browse All Degree-Programs
- Admissions & Aid Home
- Scholarships & Grants
- How to Apply
- Cost of Attendance
- Financial Aid
- Application Deadlines
- Academic Calendar
- Financial Aid FAQ
- Admissions FAQs
- Catalog/Handbook
- Our History
- Accreditation
- B Corp Certified
- Student Achievement Data
- Institutional Learning Outcomes (ILOs)
- Diversity & Inclusion
- San Marcos, California
- St. Augustine, Florida
- Miami, Florida
- Austin, Texas
- Dallas, Texas
- Our Faculty
- Board of Directors

How to Write a Care Plan: A Guide for Nurses

Care plans are a way to strategically approach and streamline the nursing process. They also enable effective communication in a nursing team. This guide will help you understand the fundamentals of nursing care plans and how to create them, step by step. We’ll also outline best practices to keep in mind and provide you with a nursing care plan sample that you can download and print.
Table of Contents
What Is a Nursing Care Plan?
What are the components of a care plan, care plan fundamentals, sample nursing care plan.
A nursing care plan documents the process of identifying a patient’s needs and facilitating holistic care, typically according to a five-step framework. A care plan ensures collaboration among nurses, patients, and other healthcare providers. ((M. Vera., “Nursing Care Plans (NCP): Ultimate Guide and Database”, July 5, 2021: https://nurseslabs.com/nursing-care-plans/ )) ((Medical Dictionary for the Health Professions and Nursing, Farlex, “nursing care plan”, 2012: https://medical-dictionary.thefreedictionary.com/nursing+care+plan )) ((Health Navigator, “Care planning”, April 6, 2021: https://www.healthnavigator.org.nz/clinicians/c/care-planning/ )) ((Tammy J. Toney-Butler and Jennifer M. Thayer, “Nursing Process,” StatsPearls, July 10, 2020: https://www.ncbi.nlm.nih.gov/books/NBK499937/ ))
Key Reasons to Have a Care Plan
The purpose of a nursing care plan is to document the patient’s needs and wants, as well as the nursing interventions (or implementations) planned to meet these needs. As part of the patient’s health record, the care plan is used to establish continuity of care. ((C. Björvell et al., “Development of an audit instrument for nursing care plans in the patient record,” Quality in Health Care , March 1, 2000: https://qualitysafety.bmj.com/content/qhc/9/1/6.full.pdf )) These are the main reasons to write a care plan:
- Patient-centered care
A care plan helps nurses and other care team members organize aspects of patient care according to a timeline. It’s also a tool for them to think critically and holistically in a way that supports the patient’s physical, psychological, social, and spiritual care. Sometimes a patient should be assigned to a nurse with specific skills and experience; a care plan makes that process easier. For patients, having clear goals to achieve will make them more involved in their treatment and recovery. ((Health Navigator, “Care planning”, April 6, 2021: https://www.healthnavigator.org.nz/clinicians/c/care-planning/ ))
- Nursing team collaboration
Writing a care plan allows a team of nurses (as well as physicians, assistants, and other care providers) to access the same information, share opinions, and collaborate to provide the best possible care for the patient.
- Documentation and compliance
A well-written care plan allows nurses to measure the effectiveness of care and to record evidence that the care was given. This is important both to maximize care efficiency and to provide documentation for healthcare providers.
Care plans are structured as a five-step framework: assessment, diagnosis, outcomes and planning, implementation, and evaluation. ((Tammy J. Toney-Butler and Jennifer M. Thayer, “Nursing Process,” StatsPearls, July 10, 2020: https://www.ncbi.nlm.nih.gov/books/NBK499937/ ))

Step 1: Assessment
The first step of writing a care plan requires critical thinking skills and data collection. Different healthcare organizations use different formats for the assessment phase. In general, the data you will collect here is both subjective (e.g., verbal statements) and objective (e.g., height and weight, intake/output). The source of the subjective data could be the patients or their caretakers, family members, or friends.
Nurses can gather data about the patient’s vital signs, physical complaints, visible body conditions, medical history, and current neurological functioning. Digital health records may help in the assessment process by populating some of this information automatically from previous records.
Step 2: Diagnosis
Using the collected data, you will develop a nursing diagnosis—which the North American Nursing Diagnosis Association (NANDA) defines as “a clinical judgment about the human response to health conditions/life processes, or a vulnerability for that response, by an individual, family, group or community.” ((NANDA, “Glossary of Terms”: https://nanda.org/publications-resources/resources/glossary-of-terms/ ))
A nursing diagnosis sets the basis for choosing nursing actions to achieve specific outcomes. A nursing diagnosis is based on Maslow’s Hierarchy of Needs pyramid ((Saul McLeod, “Maslow’s Hierarchy of Needs,” Simply Psychology , Dec. 29, 2020: https://www.simplypsychology.org/maslow.html )) (which identifies and ranks human needs) and helps prioritize treatments. For example, physiological needs (such as food, water, and sleep) are more fundamental to survival than love and belonging, self-esteem, and self-actualization, so they have the priority when it comes to nursing actions. ((Chiung-Yu Shih et al, “The association of sociodemographic factors and needs of haemodialysis patients according to Maslow’s hierarchy of needs,” Journal of Clinical Nursing , July 30, 2018: https://pubmed.ncbi.nlm.nih.gov/29777561/ ))
Based on the diagnosis, you’ll set goals (Step 3) to resolve the patient’s problems through nursing implementations (Step 4).
Step 3: Outcomes and Planning
After the diagnosis is the planning stage. Here, you will prepare SMART goals (more detail on this later) based on evidence-based practice (EBP) guidelines. You will consider the patient’s overall condition, along with their diagnosis and other relevant information, as you set goals for them to achieve desired and realistic health outcomes for the short and long term.
Step 4: Implementation
Once you’ve set goals for the patient, it’s time to implement the actions that will support the patient in achieving these goals. The implementation stage consists of performing the nursing interventions outlined in the care plan. As a nurse, you will either follow doctors’ orders for nursing interventions or develop them yourself using evidence-based practice guidelines.
Interventions are classified into the following seven domains: family, behavioral, physiological, complex physiological, community, safety, and health system interventions. There are several basic interventions that you need to implement during each shift: pain assessment, changing the resting position, listening, cluster care, preventing falls, and fluid consumption.
Step 5: Evaluation
In the final step of a care plan, the health professional (who can be either a doctor or a nurse) will evaluate whether the desired outcome has been met. You will then adjust the care plan based on this information.
In a simple but useful way, Nurse.org explains the core questions your care plan should answer: what, why, and how. ((Mariam Yazdi, “4 Steps to Writing a Nursing Care Plan,” Nurse.org, March 23, 2018: https://nurse.org/articles/nursing-care-plan-how-to/ )) A nursing care plan should include:
- The What : What does the patient suffer from? What do they risk suffering from?
- The Why : Why does your patient suffer from this? Why do they risk suffering from this?
- The How : How can you make this better?
Successful care plans use the fundamental principles of critical thinking, client-centered techniques, goal-oriented strategies, evidence-based practice (EBP) recommendations, and nursing intuition. ((Tammy J. Toney-Butler and Jennifer M. Thayer, “Nursing Process,” StatsPearls, July 10, 2020: https://www.ncbi.nlm.nih.gov/books/NBK499937/ ))
SMART Goals
In the planning phase of writing a care plan, it’s important that you use goal-oriented strategies. A SMART goals template can help in this process:
- Specific : Your goals for the patient must be well-defined and unambiguous.
- Measurable : You need to set certain metrics to measure the patient’s progress toward these goals.
- Achievable : Their goal should be possible to achieve.
- Realistic : Their goals must be within reach and relevant to the overall care plan.
- Time-bound : The patient’s goals should have a clear starting time and end date (which can be flexible).
Effective Communication
Unless your care plan is communicated effectively to all relevant stakeholders, it will only be a plan. Remember that the purpose of a nursing care plan is not to be a static document, but to guide the entire nursing process and enable teamwork, with the goal of improving care. Writing skills are crucially important for nurses—you’ll need to be as accurate and current as possible in your descriptions. For effective communication, keep in mind the following best practices when writing a care plan:
- Write down everything immediately so you don’t forget the details.
- Write clearly and concisely, using terms that your team will understand.
- Include dates and times.
Although you will learn communication skills in an undergraduate or graduate nursing program , you will also develop them over time and with practical experience. ((TigerConnect, “How to Develop a Nursing Care Plan for Your Hospital”: https://tigerconnect.com/blog/how-to-develop-a-nursing-care-plan-for-your-hospital/ ))
Shareable and Easy to Access
Care plans also need to be easy to share with the relevant stakeholders—patients, doctors, other members of the nursing team, insurance companies, etc. The documentation format will vary according to hospital policy , but, in general, care plans are created in electronic format and integrated into the electronic health record (EHR) for easy access to everyone. ((TigerConnect, “How to Develop a Nursing Care Plan for Your Hospital”: https://tigerconnect.com/blog/how-to-develop-a-nursing-care-plan-for-your-hospital/ ))
Finally, you will need to update your care plans often with the latest information. That implies checking in with patients frequently and recording data about how the patient is progressing toward their goals, which will be important in the evaluation stage of the care plan. ((TigerConnect, “How to Develop a Nursing Care Plan for Your Hospital”: https://tigerconnect.com/blog/how-to-develop-a-nursing-care-plan-for-your-hospital/ ))
Despite the overall general objective, nursing care plans written by students are not the same as those created by registered nurses in clinical settings. The student version is much longer, has a greater level of detail, and is exhaustively thorough. On the other hand, nurses often assume some basic concepts and note some of the steps in the care plan only mentally. ((M. Vera., “Nursing Care Plans (NCP): Ultimate Guide and Database”, July 5, 2021: https://nurseslabs.com/nursing-care-plans/ ))
For example, in the interventions section, a student would write: “vital signs recorded every four hours: blood pressure, heart rate, three- or five-lead electrocardiograms, functional oxygen saturation, respiratory rate, and skin temperature,” while an experienced registered nurse might just write “Q4 vital signs.”
Why this difference? As a student or recent graduate, including all the information in your care plan will help you solidify your training. While writing care plans in school can be a very time-consuming task, mastering this information in nursing school will improve your competency and confidence. Most of the information that you’ll have to look up while you’re still in school will become second nature in the future. Here’s what a care plan written by a student looks like:
- Assessment : “heart rate 100 bpm, dyspnea, restlessness, guarding behavior.”
- Diagnosis : “impaired gas exchange RT collection of mucus in airway.”
- Outcomes and planning : “patient must maintain optimal gas exchange.”
- Implementations : “assess respiration; encourage breathing and position changes.”
- Rationale : “respiration will indicate the level of lung involvement, as the patient will adjust their breathing to facilitate gas exchange; these will improve ventilation and allow for chest expansion.”
- Evaluation : “the patient maintained good gas exchange, normal respiratory rate.”
Note that student care plans often have an additional column—rationale—where students note the scientific explanation for the implementations they chose. To help you get started with a care plan writing practice, we’ve created a printable nursing care plan, which you can use to practice writing all the steps outlined in this article.

Wrapping Up: Writing an Effective Nursing Care Plan
To be successful, a nursing plan needs effective communication, goal-oriented tasks, accessibility and shareability, and evidence-based practice.
When it meets these qualities and is supported by the nurse’s intuition, critical thinking, and a general focus on the patient, a nursing care plan becomes a go-to resource for nurses to record and access all the information they need. A care plan is your roadmap for effective nursing care, and a collaboration tool that improves the entire healthcare process.
While all nursing programs teach the basics of writing a care plan, your communication, goal setting, and critical thinking skills will be shaped by the program you attend.
For example, one of the benefits of writing care plans is that it will allow you to develop professionalism , along with important values like accountability, respect, and integrity. Key results of professionalism include better overall care, improved team communication, and a more positive work environment. ((Nursco, “Professionalism in Nursing – 5 Tips for Nurses,” July 13, 2018: https://www.nursco.com/professionalism-nursing-5-tips-nurses/ ))
That’s why it’s important that you choose the right program for your needs—one that will help you develop communication and critical thinking skills, as well as professionalism, to be ready for the day-to-day nursing life.
The University of St. Augustine for Health Sciences (USAHS) offers a Master of Science in Nursing degree (MSN), a Doctor of Nursing Practice degree (DNP), and Post-Graduate Nursing Certificates designed for working nurses. Our degrees are offered online, with optional on-campus immersions.* Role specialties include Family Nurse Practitioner (FNP), Nurse Educator ,** and Nurse Executive . The MSN has several options to accelerate your time to degree completion. Earn your advanced nursing degree while keeping your work and life in balance.
*The FNP role specialty includes two required hands-on clinical intensives as part of the curriculum.
**The Nurse Educator role specialty is not available for the DNP program.
Take charge of your own life-story
More Articles
85 Nursing Quotes: Words of Wisdom for Nurses

How To Study Effectively? 10 Best Study Techniques | USAHS

The Importance of Effective Communication in Nursing
Upcoming events.

Post Professional Doctor of Occupational Therapy (OTD) Webinar - July 9 | USAHS

Doctor of Education (EdD) Webinar - July 10 | USAHS

Doctor of Physical Therapy (DPT) Academic Webinar - July 15| USAHS
Nursing Diagnosis Guide

NurseJournal.org is committed to delivering content that is objective and actionable. To that end, we have built a network of industry professionals across higher education to review our content and ensure we are providing the most helpful information to our readers.
Drawing on their firsthand industry expertise, our Integrity Network members serve as an additional step in our editing process, helping us confirm our content is accurate and up to date. These contributors:
- Suggest changes to inaccurate or misleading information.
- Provide specific, corrective feedback.
- Identify critical information that writers may have missed.
Integrity Network members typically work full time in their industry profession and review content for NurseJournal.org as a side project. All Integrity Network members are paid members of the Red Ventures Education Integrity Network.
Explore our full list of Integrity Network members.
Are you ready to earn your online nursing degree?

Creating a nursing diagnosis is a critical part of providing patient care and is a vital step of the nursing process.
By understanding how to create a nursing diagnosis, you can help improve patient outcomes, improve communication among the medical health team, and organize your day. Both the nursing process and nursing diagnoses help ensure and promote evidence-based, safe practices.
In this guide, you will learn what a nursing diagnosis is, why it is important, and a general overview of how to perform a nursing diagnosis.
The Nursing Process
You can’t discuss a nursing diagnosis without discussing the nursing process. The nursing process has five steps:
Assessment is a thorough and holistic evaluation of a patient. It includes the collection of both subjective and objective patient data such as vital signs, a health history, head-to-toe physical, and a psychological, socioeconomic, and spiritual evaluation.
Diagnosis is formed by the nurse and is based on the data collected during the assessment. The nursing diagnosis directs nursing-specific patient care.
In this step, the nurse forms a diagnosis based on the patient’s specific medical and/or social needs. The diagnosis leads to the creation of goals with measurable outcomes.
The diagnosis must be one that has been approved by NANDA International (NANDA-I), formerly known as North American Nursing Diagnosis Association. NANDA-I is responsible for developing and standardizing nursing diagnoses. Used internationally, the NANDA-I vision and mission is to use evidence-based, universal nursing terminology to promote safe patient care.
NANDA-I defines a nursing diagnosis as follows:
- “a clinical judgment concerning a human response to health conditions/life processes, or a vulnerability for that response, by an individual, family, group or community. A nursing diagnosis provides the basis for selection of nursing interventions to achieve outcomes for which the nurse has accountability.”
- A nursing diagnosis generally has three components: a diagnosis approved by NANDA-I, a related to statement which defines the cause of the NANDA-I diagnosis, and an as evidenced by statement that uses specific patient data to provide a reason for the NANDA-I diagnosis and related to statement.
- Risk-related diagnoses only contain a NANDA-I diagnosis and an as evidenced by statement because it is describing a vulnerability, not a cause. For example, a nurse may use a nursing diagnosis such as “risk for pressure ulcer as evidenced by lack of movement, poor nutrition, and hydration.”

Outcomes and Planning
Outcome and planning involves developing a patient care plan based on the nursing diagnosis. Planning should be measurable and goal-oriented for the patient and/or their family members.
Implementation
Implementation is when nurses initiate the care plan and put it into action. This step provides the continuation of care during hospitalization until discharge.
Evaluation is the final step of the nursing process. A patient care plan is evaluated based on specific goals and desired outcomes and may be adjusted based on the patient’s needs.
Popular Nursing Programs
Learn about start dates, transferring credits, availability of financial aid, and more by contacting the universities below.
How Do Nursing Diagnoses Differ From Medical Diagnoses?
To best understand a nursing diagnosis, it may help to first understand how it differs from a medical diagnosis.
A nursing diagnosis is initiated by a nurse and describes a response to the medical diagnosis. A medical diagnosis is given by a doctor to a patient to define a medical condition/disease or injury.
Nursing Diagnosis
- Based on the patient’s immediate situation
- Initiated to resolve a health problem
- Improves communication among the healthcare teams
- A holistic approach to caring for patients
Example: Ineffective breathing pattern related to impaired inhalation and exhalation as evidenced by the use of accessory muscles
Medical Diagnosis
- Initiated by a medical doctor or specialist
- Defines a medical condition, disease, or injury
- Explains the signs and symptoms of the disease
Example: Asthma
4 Categories of Nursing Diagnoses
The need for standardized language, respecting nurses’ clinical judgment, and providing care for patients with measurable results defines the use of a nursing diagnosis. The nursing diagnosis can be divided into four main categories. Please note all examples are taken from the Nursing Diagnoses Definitions and Classification 2015-2017.
Problem-focused Diagnosis
A nursing diagnosis related to a patient’s problem. It can be used throughout the course of the patient’s hospitalization or be resolved by the end of the shift.
Example: Anxiety related to situational crises and stress (related factors) as evidenced by restlessness, insomnia, anguish, and anorexia (defining characteristics)
Risk Diagnosis
A nursing diagnosis that identifies when the patient is at risk for developing a problem. NANDA-I describes it as a vulnerability the patient has encountered.
Example: Risk for infection as evidenced by inadequate vaccination and immunosuppression (risk factors)
Health-promotion Diagnosis
A nursing diagnosis used to identify how to help improve the health of a patient. Health-promotion diagnosis includes the patient and their family/community members.
Example: Readiness for enhanced self-care as evidenced by expressed desire to enhance self-care
Syndrome Diagnosis
A nursing diagnosis identifying a cluster of diagnoses for a patient. These nursing diagnoses are best described together. The patient may be experiencing a number of health problems forming a pattern.
Example: Chronic pain syndrome
Nursing Diagnosis Classification
NANDA-I created Taxonomy II after collaborating with the National Library of Medicine. By definition, taxonomy is the “practice and science of categorization and classification.” The NANDA-I Taxonomy currently has 235 nursing diagnoses with 13 categories of nursing practice:
- Health promotion
- Elimination and exchange
- Activity/rest
- Perception/cognition
- Self-perception
- Role relationships
- Coping/stress tolerance
- Life principles
- Safety/protection
- Growth/development
They also have 47 classes related to each category.
How to Perform a Nursing Diagnosis
Nurses complete five steps to carry out a strong, accurate nursing diagnosis. All nurses should follow the nursing process:
Nursing Science
Having a solid understanding of nursing science and theory provides a strong foundation for patient care. It is also the first step in initiating a nursing diagnosis and care plan that is holistic and patient-centered.
During the assessment, nurses gather medical, surgical, and social history. They also perform a physical on the patient. Nurses then ask themselves: What is the current and priority health problem(s) the patient is experiencing? This information is applied to creating a nursing diagnosis.
Identifying Potential Diagnoses
Once the health problem or human response(s) to the health problem is identified, nurses ask another question: What important information is relevant to the health problem and what’s unrelated?
The answer to this question helps create a potential nursing diagnosis. Nurses will then:
- Determine the category of the nursing diagnosis
- Confirm and rule out other diagnoses
- Create new diagnoses
The nursing diagnosis must be validated and critically thought out. NANDA-I advises using an in-depth assessment. This will confirm or rule out a diagnosis.
NANDA-I recommends structuring a nursing diagnosis in “related factors” and “defining characteristics” format, as first published by Marjory Gordon, Ph.D. This can highlight the strength and accuracy of the nursing diagnosis.
Implementing a Care Plan
A nursing diagnosis determines the care plan. Nurses create measurable, achievable goals and related interventions. They then take action, administering the planned interventions.
Nurses are constantly evaluating their patients. A nursing diagnosis is often evaluated to make sure the care plan is working. If it is not, nurses must think about what else can be done to improve the patient’s health.
A Critical Component of Care
Nurses are the eyes and ears of the patient. They are the liaison between the medical health team and the patient and their family. Understanding the power and usefulness of a nursing diagnosis is a critical aspect of patient care. Each patient is unique and complex. The nursing process and nursing diagnosis can help provide safe, individualized, and evidence-based care.
Whether you’re looking to get your pre-licensure degree or taking the next step in your career, the education you need could be more affordable than you think. Find the right nursing program for you.
You might be interested in

HESI vs. TEAS Exam: The Differences Explained
Nursing schools use entrance exams to make admissions decisions. Learn about the differences between the HESI vs. TEAS exams.

10 Nursing Schools That Don’t Require TEAS or HESI Exam

For Chiefs’ RB Clyde Edwards-Helaire, Nursing Runs in the Family

The Complete Guide to Writing Nursing Diagnoses: Techniques and Examples
- Dr. Huey Logan
- December 8, 2023
- Study Guides
Welcome to our comprehensive guide on developing accurate nursing diagnoses . In this series of articles, we will provide you with the essential techniques, examples, and guidelines to excel in healthcare writing , specifically in nursing care plans and diagnosis formulation. We understand the critical role nursing diagnoses play in delivering optimal patient care, and our aim is to equip you with the knowledge and tools to develop precise and effective nursing diagnoses in your practice.
Here's What You'll Learn
Before we dive into the specifics, let’s first establish the importance of nursing diagnoses and their differentiation from medical diagnoses. Nursing diagnoses are essential for identifying and addressing actual or potential health problems, promoting health, and improving patient outcomes. While medical diagnoses focus on disease pathology, nursing diagnoses center on identifying patient responses to health conditions and providing personalized care plans.
Throughout this series, we will explore the classification of nursing diagnoses according to Taxonomy II . This classification system organizes nursing diagnoses into various categories, including problem-focused nursing diagnoses, risk nursing diagnoses, health promotion diagnoses, and syndrome diagnoses. Understanding these classifications will aid in creating accurate and individualized care plans that address specific patient needs.
Key Takeaways:
- Nursing diagnoses play a crucial role in delivering effective patient care.
- Nursing diagnoses differ from medical diagnoses, focusing on patient responses and personalized care plans.
- Taxonomy II classifies nursing diagnoses into problem-focused, risk, health promotion, and syndrome diagnoses.
- Understanding these classifications enables the development of accurate and individualized nursing care plans.
- Stay tuned for our upcoming articles where we will delve into the definition, classification, and guidelines for writing precise nursing diagnoses.
Understanding Nursing Diagnoses: Definition and Classification
In this section, we will discuss the definition and classification of nursing diagnoses, providing a comprehensive understanding of their role in healthcare. Nursing diagnoses are essential in guiding the nursing process and developing effective care plans for patients. They complement medical diagnoses by focusing on the unique nursing perspective of patient care.
Nursing diagnoses are standardized statements that identify actual or potential health problems and provide the basis for nursing interventions. They are classified according to Taxonomy II , which categorizes nursing diagnoses into different types. These types include problem-focused nursing diagnoses, risk nursing diagnoses, health promotion diagnoses, and syndrome diagnoses.
Problem-focused nursing diagnoses address existing health issues or concerns and guide the selection of nursing interventions. Risk nursing diagnoses, on the other hand, identify potential health problems that the patient may be at risk for developing. Health promotion diagnoses focus on enhancing the patient’s well-being and preventing future health problems. Lastly, syndrome diagnoses identify related clusters of nursing diagnoses that occur together in certain conditions or situations.
Understanding the classification of nursing diagnoses is crucial for healthcare professionals as it aids in accurate assessment, planning, implementation, and evaluation of nursing care. By utilizing the appropriate nursing diagnosis classification, nurses can provide individualized care that meets the unique needs of each patient.
Now, let’s take a closer look at the different types of nursing diagnoses and their application in clinical practice through real-life examples and case studies.
Guidelines for Writing Accurate Nursing Diagnoses
In this final section, we will provide practical guidelines for writing accurate nursing diagnoses. As healthcare professionals, it is crucial that we have a clear understanding of the diagnostic process and the steps involved in formulating precise nursing diagnoses. This knowledge enables us to develop effective nursing care plans and provide optimal patient care.
The diagnostic process begins with a comprehensive analysis of patient data, including medical history, physical assessments, laboratory results, and patient interviews. By carefully examining this information, we can identify health problems and determine their underlying causes.
Once we have identified the health problems, we can formulate a nursing diagnosis using the Problem-Etiology-Symptom (PES) format. The PES format consists of three components: the problem, the etiology or cause of the problem, and the defining characteristics or symptoms. This format provides a clear and concise structure for articulating nursing diagnoses.
Nursing diagnoses are not only essential for individualized patient care but also play a significant role in the development of nursing care plans. By incorporating accurate nursing diagnoses into care plans, we can effectively address the identified health problems and establish goals and interventions to promote patient well-being and recovery.
What is a nursing diagnosis?
A nursing diagnosis is a clinical judgment about a patient’s response to actual or potential health problems. It identifies the patient’s health problem and describes what the nurse can do to address it.
What is the difference between a nursing diagnosis and a medical diagnosis?
A medical diagnosis focuses on the disease or condition itself, while a nursing diagnosis focuses on the patient’s response to the disease or condition. Medical diagnoses are typically made by doctors, while nursing diagnoses are made by nurses as part of the nursing process .
How are nursing diagnoses classified?
Nursing diagnoses are classified according to Taxonomy II , which categorizes them into different domains and classes. This classification system helps nurses identify the specific needs of their patients and develop appropriate care plans.
What are the different types of nursing diagnoses?
There are four main types of nursing diagnoses: problem-focused, risk, health promotion, and syndrome diagnoses. Problem-focused diagnoses address existing health problems, risk diagnoses identify potential health problems, health promotion diagnoses focus on improving overall health and wellness, and syndrome diagnoses are related to a specific cluster of signs and symptoms.
How do I write an accurate nursing diagnosis?
To write an accurate nursing diagnosis, you need to analyze the patient’s data, identify the health problem, and formulate a diagnostic statement. This statement should follow the PES format , which includes the problem, etiology (cause), and signs and symptoms. Nursing diagnoses are then used in the development of nursing care plans.
Source Links
- https://nurseslabs.com/nursing-diagnosis/
- https://nursejournal.org/resources/nursing-diagnosis-guide/
- https://www.nursetogether.com/nursing-diagnosis/
Does this Look Like Your Assignment? We Can do an Original Paper for you!
Have no time to write let a subject expert write your paper for you, have a subject expert write for you, have a subject expert finish your paper for you, edit my paper for me, have an expert write your dissertation's chapter, popular searches.
- Company Overview
- How it Works
- Client Reviews
- Discount Codes
- Privacy Policy
- Frequently Asked Questions
Knowledge Base
- All Writing Guides
- Nursing Essay Writing Guides
- Topics Ideas
- Nursing Guides
- Business Analysis Guides
- Literature Guides
- Write My Essay
- Do My Essay
- Pay For Essay
- Buy Research Paper
- Buy Essays
- Get Nursing Papers
- Online Nursing Papers
Writing Tools
- Citation Generator
- Topic Generator
- Thesis Generator
- Sentence Rewriter
- Title Page Generator
- Research Paper Title Generator
Use our resources and guides to write perfect papers. You can use our writing service and order customized sample papers without plagiarism!
Thestudycorp.com helps students cope with college assignments and write papers on various topics. We deal with academic writing, creative writing, and non-word assignments.
All the materials from our website should be used with proper references. All the work should be used per the appropriate policies and applicable laws.
Our samples and other types of content are meant for research and reference purposes only. We are strongly against plagiarism and academic dishonesty.

Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Nursing Diagnosis Handbook: An Evidence-Based Guide to Planning Care

Related Papers
International Journal of Nursing Terminologies and Classifications
Doris Kowalski
Nursing diagnosis is increasingly recognized as an integral component of professional nursing practice. Implementation of nursing diagnosis impacts on all elements of professional practice: the philosophy, purpose, and objectives of an organization; care planning; quality assurance; staff education; performance standards; the nursing care delivery system; documentation; and patient classification. A guide organized around these elements has been developed to assist with the implementation of nursing diagnosis. This guide can be used to gather information to plan for the implementation of nursing diagnosis or as a post-test to judge the success of the implementation process.
Texila International Journal
Meenakshi Gijare , Vikram Padbidri
Anggi L Wicaksana
Zyarif Malingi
Nurilign Abebe
Journal of Clinical Nursing
Matthew Leach
Joel Gonzales Patalagsa
Nursing education is beset with challenges brought about by increasing complexities in providing health care as well as changing needs of stakeholders and consumers. The need to equip nurse graduates with basic patient care competencies necessitates that theoretical and clinical learning experiences be updated in order to keep abreast with these challenges. This book offers a solution to the difficulties encountered by nursing students in formulating and implementing their nursing care plans. An enhanced model is presented in order to provide direct to the point guides in developing and improving critical thinking and clinical decision making skills in each component of the nursing care plan. Holistic approach in providing safe and quality patient care is integrated. The nursing care plan scoring model should facilitate review by instructors and students on the completeness, appropriateness, relevance, use of evidence, and relatedness of the information presented by students in each...
Rofiat Omolara Amidu
Onesimus Jappah
Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
RELATED PAPERS
International Journal of Nursing Knowledge
ercole vellone , Fabio D'Agostino , Maria Grazia De Marinis
Nursing Forum
kelvin M Mutegi
Revista Brasileira de Enfermagem
Paulino Sousa
Journal of advanced nursing
Mary A Lavin
Liz Hernandez
Yudha Anugrah
Rahmad Gurusinga
Amanda Henderson
Andi Ali Mukti Pratama
Eastern-European Journal of Medical Humanities and Bioethics
Fatjona Kamberi
Florianus Situ
Alfonso Miguel García Hernández
Siniša Franjić
Janet Schnall
Gregory T Papanikos
Jurnal Ners
International journal of nursing knowledge
Heather Herdman
Clinical Journal of Oncology Nursing
Wendy Stiver
Journal of Advanced Nursing
Hrund Thorsteinsson
International Nursing Review
Maud Heinen
Meherun Nesa
Wolter Paans
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
Concept of Nursing Diagnosis Essay (Critical Writing)
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment
Sickle Cell Anemia is a disorder that normally increases blood thickness hence affects the smooth flow of blood. This is caused by the destruction of red cells where the normal shape of red cell becomes a stiff sickle shape. As a result, sufficient oxygen does not reach the vital organs.
A vaso-occlusive crisis arises from hindrance of blood circulation by sickle shaped blood cells. It is characterized by sturdy pains and in some cases; it may cause permanent organ damage. This paper seeks to formulate a nursing diagnosis, as well as a plan of care that includes nursing interventions and the methods to be used to evaluate whether the interventions are successful (American Sickle Cell Anemia Association, 2010).
Nursing diagnosis is a clinical assessment of health problems experienced by a family or an individual and their response to this health problem. It helps in determination of interventions that are to be put in place so as to realize the desired outcome. This diagnosis enables the nurse to come up with a care plan for the patient (National Institute of Health, 2002).
In this case, the nursing diagnosis is probably a sickle cell crisis and the possibility of shift in self perception that is linked to the notion of being different from peers. Outlined herein, are some of the interventions with their rationale and outcomes. Firstly, Maya and the family should be encouraged and helped to alternate the intervals of resting and activity. The rationale is that this could help their bodies reduce the demand for oxygen and hence reduce their hypoxia level.
Maya should also be assisted in taking deep breath movements and mild body turning exercises. The rationale behind procedure is that it promotes chest expansion, which boosts the circulations of secretions thus reducing the risks of blood clotting (Sickle Cell Disease Association of America, n.d.). The outcome is that the patient’s family will know the precautions to be taken and the strenuous activities to be avoided for them to keep fit.
Another intervention is to encourage Maya and her family to take sufficient fluids, like eight glasses per day. The rationale is to keep the body well hydrated to prevent or reduce viscosity of blood so as to have proper circulation. Here the outcome is that the concerned people will know the amount and the exact fluids to be taken (Hockenberry & Wilson, 2007, p. 648).
Another intervention is to monitor Maya’s respiratory rate, the rationale being indicators of sufficient respiratory process. There is also need for the nurse to be around several times in a day in order to monitor the patient’s cardiac regularity. Rationale: changes of cardiac rhythm could imply the effects of hypoxia on cardiovascular.
Also the nurse should analyze reports of chest pains and occurrence of fatigue. The rationale is the possibility of severe chest syndrome development. The outcome is that the people concerned will be given specialized treatment as it may be required (Hockenberry & Wilson, 2007, p. 658). More important, there is need for counseling as an intervention. This will help patient realize that he/she is not different from other children.
Having put up the necessary interventions, the next step is to evaluate whether they are successful. This could be done by observing and recording how the patient is responding to treatment. The question in mind should be, is the patient improving or deteriorating? If the patient is improving, then the nursing diagnosis should continue until full recovery.
In conclusion, nursing diagnosis coupled with medical diagnosis is an effective treatment of patients with sickle cell anemia. However, the choice of interventions should be done carefully so as to realize the desired outcome otherwise it may not be successful. Key among the interventions listed here, is counseling. This may help the patients to have hope and this may aid in quick recovery.
American Sickle Cell Anemia Association. (2010). Research . Web.
Hockenberry, M.J., & Wilson, D. (2007). Wong’s nursing care of infants and children (8th.ed.). New York: Mosby publishing group.
National Institute of Health. (2002). The management of sickle cell disease. Web.
Sickle Cell Disease Association of America. (n.d). Research and screening . Web.
- The Sickle Cell Disease Concept
- Hypoxia in Pilots at Higher Altitudes
- Sickle cell and Anemia
- How to Become a Registered Nurse
- Areas of Potential Liability for the Advanced Practice Nurse
- Nursing and Philosophy
- The Overview of Nursing Association in the US
- Reduce Hospitalization of Nursing Home Residents
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2018, October 12). Concept of Nursing Diagnosis. https://ivypanda.com/essays/nursing-diagnosis/
"Concept of Nursing Diagnosis." IvyPanda , 12 Oct. 2018, ivypanda.com/essays/nursing-diagnosis/.
IvyPanda . (2018) 'Concept of Nursing Diagnosis'. 12 October.
IvyPanda . 2018. "Concept of Nursing Diagnosis." October 12, 2018. https://ivypanda.com/essays/nursing-diagnosis/.
1. IvyPanda . "Concept of Nursing Diagnosis." October 12, 2018. https://ivypanda.com/essays/nursing-diagnosis/.
Bibliography
IvyPanda . "Concept of Nursing Diagnosis." October 12, 2018. https://ivypanda.com/essays/nursing-diagnosis/.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health

Use and Significance of Nursing Diagnosis in Hospital Emergencies: A Phenomenological Approach
Jose miguel cachón-pérez.
1 Department of Nursing, European University, 28670 Madrid, Spain; [email protected] (M.R.-G.); [email protected] (O.O.-F.); [email protected] (E.G.-G.)
Purificación Gonzalez-Villanueva
2 Department of Nursing and Physiotherapy, Alcala University, 28801 Alcala de Henares, Spain; moc.liamg@75zelaznogirup (P.G.-V.); [email protected] (J.C.F.-G.)
Marta Rodriguez-Garcia
Oscar oliva-fernandez, esther garcia-garcia, juan carlos fernandez-gonzalo.
Background: Professional nursing organizations recommend the use of nursing diagnosis to enhance and facilitate the standardization of care and the development of a common language used by nursing practitioners. In the clinical reality of hospital emergency departments, however, its use is controversial. The objectives of the research are (a) to explore the use of nursing diagnosis in hospital emergency departments, and (b) to describe the meaning of nursing diagnosis for hospital emergency nurses. Methods: A qualitative phenomenological study was conducted. A purposeful sampling and snowball technique were used. Data were collected using in-depth interviews, researchers’ field notes, and documental analysis. An inductive analysis based on Giorgi´s proposal was used to identify significant emerging themes from interviews and field notes. Seventeen participants with a mean age of 40 were recruited. Results: Three themes were identified. The results showed how the use of nursing diagnosis in hospital emergency departments depends on nurses to apply a working methodology in their practice, along with other dimensions such as the characteristics of emergency care, the type of health problems, and the complexity of care. Conclusions: The use of standardized language in emergency departments is complex due to the overcrowded nature of care in these settings.
1. Introduction
The nursing process and the use of nursing diagnosis in favor of a homogenization and standardization of the care we provide to patients and the use of a common and universal language used by nursing professionals are recommended by NANDA International and previous studies and other national associations in Spain, such as the Spanish Association of Nomenclature, Taxonomy, and Nursing Diagnosis (AENTDE) and the Spanish Society of Emergency Nursing (SEEUE) [ 1 , 2 , 3 ].
The nursing diagnosis is a clinical judgment that identifies a health problem and is the basis for the nurse to describe the objectives and interventions to be performed [ 4 , 5 ]. In Spain, in the field of emergency care, the SEEUE recommends that it is necessary to use the nursing process along with nursing diagnoses to maintain scientific, professional, and quality assurance [ 6 ] in order for a nursing language with a high degree of consensus and standardization to be achieved, thanks to the different international taxonomies and classifications which reflect the stages of the nursing practice process, understanding the nursing diagnosis and its language as a development opportunity for the nursing profession [ 5 ]. Nursing diagnosis in the emergency department facilitates the resolution of ethical and social conflicts by the nursing staff [ 7 ]. Nursing diagnoses allow to organize the work of nurses in the emergency services, structuring through nursing objectives and interventions. Emergency department nurses find nursing diagnoses to be a difficulty rather than a facilitating tool for nursing care. Diagnoses are a work methodology that may not be applicable to the emergency department.
Nursing classification systems are used to report nursing practices and maintain a unified documentation language. Nursing interventions classification (NIC) and nursing outcomes classification (NOC) are among the recognized terminology systems [ 7 ].
The objectives of the present study were (a) to describe the experiences of hospital emergency nurses in the use of nursing diagnoses; and (b) to describe the meaning of nursing diagnoses in nurses working in hospital emergency departments.
2. Materials and Methods
The guidelines for conducting qualitative studies established by the Consolidated Criteria for Reporting Qualitative Research (COREQ) [ 8 ] and the Standards for Reporting Qualitative Research (SRQR) [ 9 ] were followed.
2.1. Design
The choice of design is determined by the research question [ 9 , 10 ]. In the present study, the question aimed at describing the participants’ experiences in the hospital emergency context and the use and meaning given to nursing diagnoses. A qualitative descriptive phenomenological study was applied.
2.2. Research Team
The research team was made up of six nurses, all of whom belong to the university environment (J.M.C.-P., P.G.-V., M.R.-G.) and three of whom share teaching and clinical activity (J.C.F.-G., E.G.G., O.O.-F.). Prior to the study, the positioning of the researchers was established in terms of their theoretical framework, beliefs, and their motivations for conducting this research Table 1 shows the readiness of the researchers on the subject to be investigated.
The readiness of research.
| Theoretical framework | Research is based on an interpretative framework, where the experience of a phenomenon may vary individually. There is no single, objectifiable reality; experience can modify the meaning given to a lived event or phenomenon. |
| Beliefs | Nursing diagnoses are a theoretical expression of nursing knowledge that, in some contexts, such as emergency services, can present difficulties in their application because they do not reflect the reality of the healthcare activity. |
| Motivation for the research | The aim is to give a voice to nurses in emergency departments in order to describe their experience with nursing diagnoses and NANDA language. |
2.3. Setting and Participants
The emergency departments analyzed have an average of 30 emergency beds. The nursing professionals are responsible for the initial triage of patients and initial care until discharge or referral of patients to hospitalization units, as well as for the discharge or admission reports to the different hospital units.
A non-probabilistic sampling strategy was used in this study, with an initial strategy of purposive sampling for the recruitment of supervisors of the emergency unit, later continued with snowball sampling. It was the participants themselves who pointed out other potential informants as relevant informants due to their experience and knowledge [ 11 ].
Inclusion criteria were (a) nurses who were actively working in the emergency department, (b) with at least one year of experience working in hospital emergency departments, and (c) who voluntarily participated and signed the informed consent form.
We contacted the nursing directors in the hospitals, who were responsible for searching within the participating emergency departments for nurses interested in participating in our study. We obtained an initial list of 25 nurses, 18 of whom volunteered to participate in the study.
2.4. Data Collection
An unstructured in-depth interview was used, aimed at understanding the participants’ perspectives on the phenomenon under study. A question guide was used with the topics to be discussed, but not closed, to allow the flow of information between researcher and informant. Table 2 shows the questions used by the researchers to interview the participants.
Unstructured in-depth interview guide.
| Investigated Theme | Questions |
|---|---|
| What is the nursing methodology used in the emergency department where you work? | |
| How many patients usually come to the emergency department on a typical day? | |
| What are the professional development opportunities for nurses in the emergency department? | |
| What communication system is used in your emergency department to interact with other healthcare professionals? |
Interviews were stopped when data redundancy was reached, that is, when no new information or relevant data were incorporated in successive interviews [ 12 ].
All interviews were recorded and field notes were made. The recordings of these interviews were transcribed verbatim. Subsequently, each informant was sent the transcript of his or her interview so that he or she had the opportunity to modify or eliminate any fragment of the interview or to make any clarification that the informant had in mind, without having to give any explanation or justification.
The interviews were conducted in the participating hospitals in a room attached to the emergency departments.
2.5. Data Analysis
Amadeus Giorgi’s proposal was applied. In the first stage/phase, the researcher identifies units of meaning and then groups these units into sub-themes and topics by common meanings, identifying main themes [ 13 , 14 ]. Two researchers with experience in qualitative studies performed the analysis of the interview data. First, an analysis of each interview was performed. Afterwards, the results of the initial analysis were subsequently merged in joint sessions, during which the data collection and analysis procedures were discussed. In the case of differences of opinion, theme identification was decided by consensus. No qualitative software was used on the data.
2.6. Rigour
The quality criteria enunciated by Leininger were followed, such as credibility, confirmability, context significance, recurrent patterns, data saturation, and transferability [ 10 , 11 ]. In order to guarantee methodological rigor, information triangulation was used, both with the participants and with the literature found in reference to the phenomenon studied.
2.7. Ethical Considerations
The research has followed the propositions contained in the Helsinki declaration in reference to the ethical principles for medical research involving human subjects [ 15 ]. The study was approved by the Research Ethics Committee of the Hospital U. de Getafe (Code 28062017119912), Hospital U. Fundación Alcorcon (Code 11.13), and the Universidad European de Madrid (Code CIPI/21/040).
The participants’ data were processed according to the criteria of Law 15/1999, of 13 December on the Protection of Personal Data, removing their personal data and assigning a pseudonym to each informant. On agreeing to participate in the study, the participant signed an informed consent document with explanations regarding the study. At any time, the informant could withdraw or refuse to participate in the study without having to provide any justification.
A total of 18 nurses working in emergency departments were recruited, the mean age of the participants was 40 years (SD 8.2). See Table 3 for characteristics of the participants.
Characteristics of the participants.
| Age | Media: 40 |
| SD: 8.2 | |
| Sex | Male: 4 |
| Female: 14 | |
| Time of Working | Media:19 |
| SD: 6.3 |
Three themes were obtained: (a) experience of difficulties for use of nursing diagnosis; (b) experience of opportunity—professional development?, and (c) dilemmas and conflicts—a labor or professional labyrinth?. The results of the study describe the difficulties experienced by nurses in emergency departments in using nursing diagnoses, the opportunity to work under a nursing methodology, and the dilemmas and conflicts involved in providing care in services saturated by the demand for care and the management of nursing taxonomy. See Table 4 for the themes identified.
Themes identified.
| Themes | Description |
|---|---|
| Experience of difficulties for use of nursing diagnosis | Nurses believe that nursing diagnoses implement the complexity of nursing care. |
| Experience of opportunity—professional development? | This topic refers to the possibility of improving the nursing profession through the use of nursing diagnostics. |
| Dilemmas and conflicts—a labor or professional labyrinth? | The discussion on working methodology is a boost to clinical care in the emergency department for nurses. |
3.1. Experience of Difficulties for Use of Nursing Diagnosis
This makes reference to those aspects that nurses report as a difficulty for the use of nursing diagnosis in the emergency department.
The nurses noted how in the emergency department, time takes on a highly relevant importance, care is on demand, without any planning, with multiple reasons for consultation with different prognoses that make it difficult to create a care plan using nursing diagnosis as a methodological tool.
DP4: “Emergency times do not allow for this type of analysis. What we always try to do in the short term is to solve acute problems at first, then the rest is a posteriori”.
DP2: “Because it does not adapt to the work, nor to the rhythm of work in the emergency department. Diagnoses need a period of time, that is to say, a period of time” .
Another of the difficulties identified is that nurses experience nursing diagnoses as something strange and difficult to understand, alien to their daily care activity. They perceive it negatively. It was even pointed out that nursing diagnosis is imported from another culture and they feel forced to implement it.
DP12: “Well, one of the first points is that it is cumbersome to the point of satiety, we can look for any word we want. Cumbersome, petulant and pedantic. Possibly because you want to escape, you don’t want to look for the point of union in the diagnosis of all life” .
DP5: “All this is very American, the problem is how we have it implanted and how we have inherited it from another type of culture, more American style; if you get into NANDA, NIC, NOC you either handle it a lot or you are incapable of knowing what you are talking about… And in the ER” .
A final difficulty is the use of nursing diagnosis as a working tool to apply care. Participants relate how using nursing diagnostics does not add value. They do not find a relationship between the actual work in an emergency department and the theorization of nursing diagnoses.
DP6: “To give names to things that no one understands and if we called things by their basic name, when you say it, identify what you mean, without having to go to a dictionary of diagnoses...”
DP10: “…using those diagnostic labels, the patient would not understand what we are saying” .
3.2. Opportunity Experience. Professional Development?
This theme describes opportunities to improve the professional position of nurses in emergency departments by using and applying nursing diagnosis. It highlights what the nurses interviewed define as “patient assessment in practice”.
DP10: “...you can give them a nursing assessment, an emergency nursing assessment, always an emergency nursing assessment, the four things of risk and vital...”
However, they also refer to positive meanings of the use of nursing diagnosis in emergency departments. It is striking that these accounts are expressed or described with verbs in the conditional tense; the participants describe them as possible meanings if they were able to use nursing diagnosis. They observe how they would be able to use their own professional language, which would help them to identify the specific care in these services and which they consider would contribute to the development of the professional figure as an emergency nurse.
DP4: “It would be like establishing a...Or a language or whatever of communication, which in the end might be the nursing diagnosis, but which would give real continuity to what we do”.
DP11: “To give it a name, I think it could be to give it a name. If we have considered it, giving it a name with a diagnosis” .
DP1: “I think it could help us to organize ourselves mentally, it would help us not to forget things, we would have a similar way of working, we would all be more unified”.
3.3. Dilemmas and Conflicts. A Labor or Professional Labyrinth?
Emergency nurses are often faced with dilemmas in relation to the use of nursing diagnoses. On the one hand, they receive input on what is correct to do, using nursing diagnoses defined with recognized taxonomies (corresponding to what they are told they have to do in their daily practice). On the other hand, the professionals describe how this diagnosis uses a somewhat sumptuous terminology, which requires a laborious process in practice, which labels the patient and does not give them a sense of professional development. What the theory says is far removed from their usual practice. They are at a crossroads between what they are told is the right thing to do, what they believe they could do, and what they actually do on a daily basis.
DP11: “So far NANDA and all its diagnoses are so general that they cannot be applied to emergency care. At least today, it is so theoretical and so... that it cannot be applied to these services(…)I know what happens is that we put everything very bombastic”.
DP1: “Right now, in the day-to-day running of this emergency department, someone is talking about nursing diagnoses and we would say, ‘What are you telling me?”
DP11: “I would say theoretical, there are many that are not even understood, I read some and I say, but what is this”.
DP7: “We don’t use it among ourselves, neither to change the report, nor to count the patients on the floor. Look, we are now talking about nursing diagnoses and I see it as something, I don’t know it is not real, it is theoretical”.
However, they spoke of how they perform activities called “emergency care”, which could correspond to what the theory states or dictates, but they do it in an undefined, intuitive way, without being truly aware of how they are doing it.
DP: “We are using it, but we are not naming it or saying let’s see what diagnosis does not come out”.
DP8: “Yes, it is done, but then when it comes to writing it down, it is not done in a standardized way”.
DP11: “We make many nursing assessments that we are not aware of, we are making nursing assessments and diagnoses to patients, what happens is that we don’t, we don’t have it in writing, it’s a little bit like that, isn’t it?”
DP2: “You make a mental diagram of what is happening to the patient or what could happen to him/her” .
4. Discussion
Our results reflect how emergency nurses relate to the use of nursing diagnoses during their work in the emergency department.
Experience of difficulties for use of nursing diagnosis. We can observe how Pourhosseini et al. [ 16 ] describe the emergency department as one of the units that receive the greatest care pressure, based on the high occupancy and the structural and functional characteristics of the service. This could condition the application of methodologies for the development and application of nursing care in this context.
Previous studies show how the application of standardized language in nursing and the enunciation of nursing diagnoses present difficulties in the nurses’ perception of them. This occurs because nurses believe that this language does not adequately represent clinical practice or the health status of patients [ 17 ].
In addition, Rifà Ros et al. [ 18 ] pointed out that the terminology of nursing diagnoses is not the true language of nurses when talking about care. The same authors [ 18 ] reported that they did not capture the true essence of nursing work and are difficult to use in all contexts and may even become irrelevant. Rifà Ros et al. [ 18 ] showed that the terminology of these diagnoses creates difficulties for nurses to communicate effectively with each other, with other professionals and with patients and families.
Experience of difficulties for use of nursing diagnosis. Rivera et al. [ 19 ], in their review, call nursing diagnoses and the taxonomy used ‘academic language’, characterized by abstract, impractical, ineffective, time-consuming terminology that offers little benefit to patient care. It delves into how taxonomies are static tools and the static hardly brings advances in knowledge.
Gonzalez and Monroy [ 4 ] and NANDA [ 20 ], in the different definitions they put forward about the nursing process and in the identification of the stages of this process, always have nursing assessment first; as an essential step to give continuity to the following stages of the nursing care process. According to the results of the research, emergency nurses express a series of positive traits or distinctions in reference to the use of nursing diagnosis; specifically, if they had the opportunity to use it.
Brito [ 21 ] described how the nursing discipline, from the university, tries to strengthen and gain autonomy with its own body of knowledge and the use of clinical judgment. However, Brito [ 21 ] reported how there has been a problem with the practical application of nursing theories. The nursing care process was the ideal formula to carry out the objective, but the application of this process has not been viable in the face of the vortex and the excessive daily workload of the nursing units, and where sometimes nurses continue to work applying techniques.
Castner [ 22 ] described a series of difficulties in working with nursing diagnosis in the ED, highlighting the special characteristics of this type of service where nurses develop their care activity: different nursing actions and interventions, collaborative or not, that occur in short periods of time, and high responsibility decisions that limit the development and use of nursing diagnosis in the ED. However, it was proposed as an alternative to investigate and develop a specific work system for the ED, based on a methodology of nursing thinking, since it does show the need for standardization both in language and in nursing procedures in these EDs.
Dilemmas and conflicts—a labor or professional labyrinth? The nurses in their narratives speak of carrying out actions and activities in their usual practice, under the protection of a nursing care process, including some use of diagnosis. However, they express that this is done in a non-formal way; they refer to doing it in a non-defined or standardized way. Analyzing the aspect of clinical expertise and experience of nurses, Taghavi Larijani and Saatchi [ 23 ] showed that these condition their diagnostic capacity. She indicates that novice nurses focus especially on what they are able to observe, on clinical manifestations, signs, and symptoms; they are more comfortable performing the different stages of the diagnostic process until they reach the identification of a label. On the other hand, competent nurses are more able to grasp the globality of patients’ situations, incorporating patterns of knowledge and previous experiences that they synthesize until obtaining the possible identification of the problem, from a more precise clinical judgment.
Matney et al. [ 24 ] suggests a model where the expert nurse develops after having lived considerable experiences, which allow the professional to use intuition in decision making and does not depend on explicit knowledge. Specifically, Edwards [ 25 ] reported nursing science as a practical knowledge, a "know-how", and how environments are of vital importance and contribute to the daily learning of the professional in direct contact with the patient.
The authors of the present manuscript believed that the use of nursing diagnostics in the emergency department can serve to unify the way nursing professionals work and communicate, as well as an opportunity for professional development.
Strengths and Limitations
Among the strengths of this study, to the best of our knowledge, this study described the experiences of emergency nurses regarding NANDA diagnoses and their use in clinical scenarios. Moreover, non-structured interviews and descriptions of researchers’ field notes were used to collect qualitative data. It is important to note that this study has certain constraints on the generalizability of findings, which limit the extrapolation of our results to the entire population of emergency nurses. Although the results cannot be extrapolated to the entire population, they can help nurse managers better understand the NANDA diagnoses use in emergency unit.
5. Conclusions
Based on the results obtained, we observed that standardized nomenclatures and taxonomies such as NANDA, NIC, NOC are not the methodological tool used by nurses in hospital emergency departments; we found that it is a language that is difficult to use and is not adapted to the practice and casuistry of patients attending these hospital emergency departments. Regarding its applicability or implementation, we noted a series of conditions such as simplifying the definitions of diagnostic labels to improve the adaptability of this process to clinical practice; the possibility of dedicating more time to standardized records; and increasing training in standardized nomenclature. We emphasize as an alternative the use of a clinical language that is not specific to nursing professionals but is shared with other health professionals working in hospital emergency departments.
Acknowledgments
The authors would like to thank all those who participated in this study.
Author Contributions
Conceptualization, J.M.C.-P. and P.G.-V.; methodology, J.M.C.-P. and J.C.F.-G.; software, J.C.F.-G.; validation, E.G.-G., O.O.-F., and M.R.-G.; formal analysis, J.M.C.-P. investigation, J.C.F.-G.; resources, J.C.F.-G.; data curation, J.C.F.-G.; writing—original draft preparation, J.M.C.-P.; writing—review and editing, E.G.-G.; visualization, J.M.C.-P.; supervision, J.C.F.-G.; project administration, J.C.F.-G.; funding acquisition, none. All authors have read and agreed to the published version of the manuscript.
This research received no external funding.
Institutional Review Board Statement
The study was approved by the Research Ethics Committee of the Hospital U. de Getafe (Code 28062017119912), Hospital U. Fundación Alcorcon (Code 11.13), and the Universidad European de Madrid (Code CIPI/21/040).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Conflicts of Interest
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Make an Appoinment
How to write a nursing diagnosis essay paper.
As a nursing student, you must learn how to write a nursing diagnosis paper before you complete your academic program. That is because a nursing diagnosis guides nurses in determining appropriate patient care plans. A nurse writes nursing diagnoses based on the patient’s assessment. It must include the problem and its description, the etiology, and the identified risk factors.
Writing a nursing diagnosis helps students to learn how to prepare for their careers. Mastering this art will help you to communicate your judgment based on the information you gathered after assessment to the physicians, other nurses, patients, families, and the public. A nursing diagnosis is an important part of the nursing process. It’s a fundamental tool for nurses and, even, for a lot of healthcare providers.
In our article, you can read everything you need about nursing diagnosis. Besides learning and being able to answer the question,” What is Nanda’s nursing diagnosis?” You will understand the different types and differences between various nursing diagnoses, definitions, formats, and comparisons and get nursing diagnosis examples, among others. If you need help writing a nursing diagnosis, contact us.
How to Understand Nursing Diagnosis
A nursing diagnosis is an integral section of the nursing process that helps nurses assess the patient’s health condition and develop care plans based on their thoughtful consideration and judgment. It determines the possible interventions for the family, patients, and community if it is a community nursing diagnosis.
Nursing diagnosis is usually determined based on the patient’s current situation; hence, interventions are based on evidence-based nursing research. From there, the health care providers, among nurses, consider the kind of care to provide to patients from a holistic poin t of view.
Nanda Approved Nursing Diagnosis
Nanda-approved nursing diagnoses include;
Actual/problem-focused diagnosis
This diagnosis focuses on specific signs and symptoms that are observable and present during the assessment stage. A nurse prepares a problem statement based on related stressors, complications, or concerns and explains the patient’s current health problem and the nursing interventions needed to develop the patient care plan.
One example of problem-focused nursing diagnosis is recognizing the symptoms of mental distress. The nurse will note behaviors like the patient’s struggle to concentrate, confused thinking, extreme mood changes, and struggle to sleep. The nurse shares this information with other healthcare providers to assist in making a diagnosis that further guides them in making decisions, such as passing it along to the medical provider to assist in making the diagnosis. The nursing diagnosis guides further decisions.
Risk nursing diagnosis
The risk nursing diagnosis identifies the nursing interventions needed to lower the risk related to a patient’s developing problem. It mainly requires nursing judgment and clinical reasoning because there are no etiological factors for risk diagnoses. A risk nursing diagnosis includes risk factors and diagnostic risk labels.
An example of a risk diagnosis would be the risk of imbalanced body fluid volume.
Health promotion diagnosis
This nursing diagnosis aims to improve the well-being of the patient, community, or family. This diagnosis only consists of a diagnostic label. Examples include readiness for enhanced family survival.
Syndrome diagnosis
A syndrome diagnosis refers to a group of nursing diagnoses that can be addressed through the same interventions and occurs in the same pattern. An example of this diagnosis is decreased peripheral tissue perfusion.
How Can I Write My Nursing Diagnosis
For consistency and safe nursing practices, there are standardized ways that you need to pay attention to as you write your nursing diagnosis. Unlike a medical diagnosis that addresses a specific medical condition, a nursing diagnosis addresses patient needs. That is why a nurse needs to personalize a nursing diagnosis to fit the patient’s status and health situation. Ensure it addresses the problem, linked signs and symptoms, and any other related factor that could affect patient care. You can achieve that by:
Data gathering and analyzing
Take time to observe the patient’s symptoms and note their condition. Come up with a description of the critical problem based on the symptoms observed. You can use non-specialist language to write your observations at this point.
Discuss with the patient and relatives about their feeling
As you formulate a nursing diagnosis, remember that you will be using information from the patient and their loved ones. Ask them about the notable changes in patient behavior and how it has affected them and their relationship.
Evaluate the patient’s response to their condition
Understand what the patient has done to eliminate or cope with their situation. Consider the patient, healthcare provider, and relative attitude toward the symptoms. Also, note the behavioral change and patient attitude when these parties are around.
Distinguish between subjective and objective data
Subjective data is acquired from the patient’s complaints about their condition. This kind of data is unverified. On the other hand, objective data is gathered from measurable and verifiable observations using scientific methods. Objective data is crucial in forming a basis for your nursing diagnosis. Subjective data can be used to create a patient care plan.
Identify the problem
Check for patterns in the data you collected. Symptoms and signs that may lead you to get a proper diagnosis for the patient. Focus on the patient’s experience. Nursing diagnosis is never the same for patients, even those suffering from the same condition. Each problem identified is diagnosed separately.
Identify related factors
Identify the source of the problem and then figure out why the patient is facing such an issue. Once you have an answer, you can develop nursing interventions that will help eliminate or prevent the problem.
Evaluate the patient’s history and overall health
Assess the patient’s past medical records to learn about the factors that could be associated with their current situation. You can share with other healthcare providers to help you learn about the patient’s overall health.
Find the most appropriate nursing diagnosis
At this point, you must research an appropriate term for your observation. You can use your coursebook or Nanda-approved nursing diagnosis list to help you find a word that best fits the condition and needs of the patient. After developing a nursing diagnosis, find potential outcomes and interventions that will work for the patients. Consider how they apply to a specific patient.
ORDER A PLAGIARISM-FREE PAPER HERE
Bring the related factors together for your diagnosis .
List all the causes of the patient’s problem and the related factors. Search for the standardized terms for these factors in your coursebook or other scholarly materials available. Identifying the associated factors helps the nurse in the second section of their diagnosis.
Summarize the data in an “As Evidenced By” statement
Ensure you separate the collected data from the characteristics that indicate the diagnosed problem. Only include the observed features in your AEB statement. Indicate whether the data is objective or subjective.
Difference between Medical Diagnosis and Nursing Diagnosis
In the medical field, there are a lot of terminologies that are used for simple illnesses, such as running noses. Understanding these terms and what they mean helps nursing students to be able to appropriately apply them in their careers in the future.
Let’s discuss the diagnosis. Medical diagnosis vs nursing diagnosis.
Differences by Definitions and Purpose
What is a medical diagnosis?
A medical diagnosis focuses on a patient’s medical condition, physiological and psychological response. The physician makes this kind of diagnosis based on the illness itself. The sickness is determined through knowledge, experience, and examination of all other possible causes. The doctor then prescribes proper medication that would help cure the disease.
What is a nursing diagnosis?
This diagnosis is based on the patient’s response to the medical condition. A nursing diagnosis is more focused on patient care. Nurses have the autonomy to provide care and treatment using everything linked to human reaction to a specific illness. That could be a spiritual, mental, or physical kind of reaction.
It is essential to understand how each of these diagnoses works to help the patient and other healthcare providers and relatives know how nursing and medical diagnoses complement each other.
Examples of medical diagnoses include:
- Congestive Heart Failure
- Diabetes Mellitus
Community Nursing Diagnosis
You can conduct a community nursing diagnosis after identifying the problem and analyzing the data gathered. Nursing diagnosis for community health may be formulated concerning the following issues
- Heath hazards
- Airborne diseases
- Covid-19 pandemic
- Inaccessible health services
- Community dysfunction
- Morbidity and mortality rates
- Inaccessible and unavailable services
- Mortality and morbidity rates
- Physical or emotional problems for specific demographics
- Health promotion needs for specific demographics
Below are some community health nursing diagnosis examples that will help you develop a successful nursing care plan.
- Reduced Activity Tolerance
- Hyperthermia
- Chronic Pain
- Risk for electrolyte imbalance
- Bathing/dressing/feeding self-care deficit
- Risk for ineffective childbearing process
- Hypothermia
- Decreased Cardiac activity
- Deficient Body Fluid
- Ineffective Thermoregulation
- Ineffective Breathing Pattern
- Surplus fluid volume
- Hopelessness
- Less Nutrient Than Body Requirements
- Impaired Gas Exchange
- Impaired Skin Integrity
- Impaired Urinary Elimination
- Ineffective Airway Clearance
- Ineffective Respiratory Pattern
- Ineffective Tissue Perfusion
Risk for Falls
- Risk for Impaired Skin Integrity
- Risk for Infection
Risk for Injury
- Risk for Imbalanced Glucose Level
- Dysfunctional ventilatory weaning response
- Impaired transferability
- Activity intolerance
- Situational low self-esteem
- Risk for disturbed maternal-fetal dyad
- Impaired emancipated decision-making
- Risk for poor skin integrity
- Risk for metabolic imbalance syndrome
- Urge urinary incontinence
- Risk for unstable blood pressure
- Impaired verbal communication
- Acute confusion
- Disturbed body image
- Relocation stress syndrome
- Ineffective role performance
- Readiness for enhanced sleep
Safety Nursing Diagnosis
Accidents and injuries resulting from burns, motor vehicle accidents, falls, drowning, overdoses and poisoning are some of the common cases in health care. When providing care to the victims of accidents and injuries, you are expected to write a safety nursing diagnosis to guide you in developing a plan.
Some of the risk factors that can increase the chances of patient injury are:
Risk for falls may occur due to
- Patients’ cognitive
- Physiological state
As evidenced by : Muscle weakness
The patient’s vulnerability to injury can result from internal and external causes.
Nursing Diagnosis : Risk for Injury
Related to :
- Side effects of medication
- Vision impairment
- Mobility impairment
- Hearing impairment
- Amputated/loss of limbs
As evidenced by:
There are no ‘evidenced by’ symptoms and signs as the issue has not happened. Prevention is the only aim of nursing intervention.
Expected outcomes :
- The patient will be able to identify possible exposures to risk of injury
- The patient will apply safety tips and measure to prevent injury
- The patient will remain uninjured
Assessment :
- Evaluate emotional and physical factors such as amnesia, grief, and recent traumatic experiences, among others, that could affect patient safety.
- Identify possible socioeconomic factors. Inaccessible resources such as housing and transportation can increase the chances of injuries.
- Evaluate for any abuse. It is the role of the nurse to report any form of abuse. Whether it is physical, emotional, or verbal abuse.
Interventions :
Refer to resources as necessary
Help to prevent injuries by educating patients in self-care and basic safety measures. Such as putting on safety belts to reduce the chances of injury if a motor vehicle accident occurs. For patients with dementia and developmental delays, a nurse should consider providing care in nursing homes and at home.
Administer medications
Ensure you give the right patient the right medication, in proper dosage and at the right time. Double-check the details to make sure everything is clear.
Educate the patient and family on first-aid strategies
This helps them act immediately after the accident to facilitate swift, professional intervention and reduce the risk of complications after the injury.
Do You Need Help with Your Nursing Diagnosis?
Nursing diagnosis is a valuable tool that helps nurses provide quality, safe and evidence-based patient care. Every nurse must learn how a nursing diagnosis template works and master every aspect of health care provision.
You can contact us to hire a tutor that will help you learn a simple nursing diagnosis format and give you a simple step-by-step guide that will aid in formulating and writing a nursing diagnosis seamlessly. Contact us today!

Have Any Questions !
Phone number
+1 (315) 636-5071
- Personal Statement
- College Essay
- Nursing Report Writing Service
- Course Work
- Nursing Homework Help
- Assignments
- Entrance Essays
- Essay Writing
- Presentations
- Term Papers
- Dissertation
- Case Studies
- Shadow Health Assessment Help
- Annotated Bibliography
- Research Papers
- Grant Proposals
Community Health Nursing Diagnosis Statement
This essay about community health nursing diagnosis statements highlights their vital role in understanding and addressing the multifaceted nature of community health. Unlike individual diagnoses, these statements consider the broader social, economic, and environmental factors influencing health outcomes. They emphasize holistic assessment, community engagement, and collaborative interventions tailored to each community’s unique needs. Furthermore, these statements serve as advocacy tools, empowering nurses to address health disparities and promote health equity. Overall, they represent a dynamic approach to community health that prioritizes partnership, empathy, and social justice.
How it works
Community health nursing diagnosis statements serve as dynamic blueprints, guiding nurses in decoding the complex tapestry of community health. Unlike traditional medical diagnoses, which focus on individual ailments, these statements illuminate the interconnected web of social, economic, and environmental factors influencing the health of entire populations.
At the heart of community health nursing diagnosis statements lies a commitment to holistic assessment. Nurses don their detective hats, probing not only physical symptoms but also delving into the emotional, mental, and social landscapes of communities.
This panoramic view reveals underlying health determinants, from access to fresh foods and safe housing to the strength of social support networks, guiding nurses towards targeted interventions that address root causes rather than mere symptoms.
Moreover, these diagnostic statements are not stagnant declarations but living documents shaped by community voices. Nurses become co-creators with community members, weaving together narratives of lived experiences, cultural nuances, and local wisdom. This collaborative approach ensures that interventions resonate authentically with the community’s values, fostering trust and empowerment among its members.
Furthermore, community health nursing diagnosis statements serve as compasses in the vast sea of public health initiatives. Nurses navigate through a myriad of options, charting courses towards impactful interventions that promote wellness and prevent disease. Whether it’s launching community-wide health education campaigns, spearheading initiatives to improve access to healthcare services, or advocating for policies that address social inequalities, these statements provide a roadmap for action tailored to the unique needs of each community.
Beyond their practical utility, community health nursing diagnosis statements carry a potent message of advocacy and social justice. Nurses wield them as powerful tools to shine a spotlight on health disparities and structural inequities, challenging policymakers and stakeholders to dismantle systemic barriers to health. Through their tireless advocacy efforts, nurses champion the cause of health equity, striving to ensure that every individual, regardless of background or circumstance, has the opportunity to thrive.
In essence, community health nursing diagnosis statements are not mere bureaucratic documents but catalysts for transformation. They embody the spirit of collaboration, empathy, and resilience that defines the nursing profession. As nurses harness their expertise and passion to uplift communities, they pave the way towards a future where health is not just a privilege but a fundamental human right
Cite this page
Community Health Nursing Diagnosis Statement. (2024, Apr 29). Retrieved from https://papersowl.com/examples/community-health-nursing-diagnosis-statement/
"Community Health Nursing Diagnosis Statement." PapersOwl.com , 29 Apr 2024, https://papersowl.com/examples/community-health-nursing-diagnosis-statement/
PapersOwl.com. (2024). Community Health Nursing Diagnosis Statement . [Online]. Available at: https://papersowl.com/examples/community-health-nursing-diagnosis-statement/ [Accessed: 8 Jul. 2024]
"Community Health Nursing Diagnosis Statement." PapersOwl.com, Apr 29, 2024. Accessed July 8, 2024. https://papersowl.com/examples/community-health-nursing-diagnosis-statement/
"Community Health Nursing Diagnosis Statement," PapersOwl.com , 29-Apr-2024. [Online]. Available: https://papersowl.com/examples/community-health-nursing-diagnosis-statement/. [Accessed: 8-Jul-2024]
PapersOwl.com. (2024). Community Health Nursing Diagnosis Statement . [Online]. Available at: https://papersowl.com/examples/community-health-nursing-diagnosis-statement/ [Accessed: 8-Jul-2024]
Don't let plagiarism ruin your grade
Hire a writer to get a unique paper crafted to your needs.

Our writers will help you fix any mistakes and get an A+!
Please check your inbox.
You can order an original essay written according to your instructions.
Trusted by over 1 million students worldwide
1. Tell Us Your Requirements
2. Pick your perfect writer
3. Get Your Paper and Pay
Hi! I'm Amy, your personal assistant!
Don't know where to start? Give me your paper requirements and I connect you to an academic expert.
short deadlines
100% Plagiarism-Free
Certified writers
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Brooker D. Person-centred dementia care.London: Jessica Kingsley; 2007
What is a nursing intervention: a beginner's guide. 2019. https://tinyurl.com/mh2mwhb6 (accessed 1 November 2021)
Butterworth C. How to achieve a person-centred writing style in care plans. Nurs Older People. 2012; 24:(8)21-26 https://doi.org/10.7748/nop2012.10.24.8.21.c9310
Centre for Policy on Ageing. The effectiveness of care pathways in health and social care. 2014. https://tinyurl.com/3t835kfd (accessed 1 November 2021)
Clinical and service integration. The route to improved outcomes. 2010. https://tinyurl.com/whb87xd6 (accessed 1 November 2021)
Department of Health. Refocusing the Care Programme Approach. Policy and positive practice guidance. 2008. https://tinyurl.com/anyrzhy6 (accessed 3 November 2021)
Department of Health. Personalised care planning: improving care for people with Long term conditions. 2011. https://tinyurl.com/uc3u3tkh (accessed 1 November 2021)
Department of Health. Care planning in the treatment of long term conditions: final report of the CAPITOL Project. 2013a. https://tinyurl.com/7399vphc
Department of Health. Mental health payment by results guidance 2013-2014. 2013b. https://tinyurl.com/9zyfmy87 (accessed 1 November 2021)
Dimond B. Exploring the legal status of healthcare documentation in the UK. Br J Nurs. 2005; 14:(9)517-518 https://doi.org/10.12968/bjon.2005.14.9.18078
Foundations of nursing practice: making the difference, 2nd edn. In: Hogston R, Simpson PM (eds). London: Palgrave Macmillan; 2002
Kozier B, Erb G, Berman A, Snyder S, Lake R, Harvey S. Fundamentals of nursing: concepts, process and practice, 8th edn. Harlow: Pearson Education; 2008
Leach M. Clinical decision making in complementary & alternative medicine.Chatswood (NSW, Australia): Elsevier; 2010
Lloyd M. A practical guide to care planning in health and social care.Maidenhead: Open University Press; 2010
Matthews E. Nursing care planning made incredibly easy!.Philadelphia (PA): Lippincott Williams and Wilkins; 2010
Monitor. Delivering better integrated care: A summary of what delivering better integrated care means and how Monitor is supporting the sector. 2015. https://tinyurl.com/825k8kd6 (accessed 1 November 2021)
NHS website. NHS launches accredited suppliers for electronic patient records. 2019. https://tinyurl.com/4fzs4up5 (accessed 1 November 2021)
National Institute for Clinical Excellence. What to expect during assessment and care planning. 2021. https://tinyurl.com/63hm5vvp (accessed 1 November 2021)
NHS England. Personalised care and support planning handbook: the journey to person-centred care: Core information. 2016a. https://tinyurl.com/9fyrtw45 (accessed 1 November 2021)
NHS England. Mental health clustering booklet v5.0 (2016/17). 2016b. https://tinyurl.com/7p6dfnry (accessed 1 November 2021)
NurseChoice. Nursing smart goals: how to set smart goals for Nursing. 2018. https://tinyurl.com/s292baez (accessed 1 November 2021)
Nursing and Midwifery Council. Future nurse: standards of proficiency for registered nurses. 2018a. http://tinyurl.com/yddpadva (accessed 1 November 2021)
Nursing and Midwifery Council. The code: professional standards of practice and behaviour for nurses, midwives and nursing associates. 2018b. https://tinyurl.com/gozgmtm (accessed 1 November 2021)
Nursing and Midwifery Council. Keep records of all evidence and decisions. 2021. https://tinyurl.com/4pcabhms (accessed 1 November 2021)
Revello K, Fields W. An educational intervention to increase nurse adherence in eliciting patient daily goals. Rehabil Nurs. 2015; 40:(5)320-326 https://doi.org/10.1002/rnj.201
Royal College of Nursing. RCN factsheet on nurse prescribing in the UK. 2014. https://tinyurl.com/hkndnbhv (accessed 3 November 2021)
Nursing process. 2021. https://www.ncbi.nlm.nih.gov/books/NBK499937 (accessed 1 November 2021)
Wing JK, Beevor AS, Curtis RH, Park SGB, Hadden J, Burns A. Health of the Nation Outcome Scales (HoNOS). Br J Psychiatry. 1998; 172:(1)11-18 https://doi.org/10.1192/bjp.172.1.11
World Health Organization. Integrated care models: an overview. 2016. https://tinyurl.com/6encn9a5 (accessed 1 November 2021)
Yeomans D. Clustering in mental health payment by results: a critical summary for the clinician. Adv Psychiatr Treat. 2014; 20:(4)227-234 https://doi.org/10.1192/apt.bp.113.011320
Assessing the patient's needs and planning effective care
Benjamin Ajibade
Senior Lecturer, Mental Health Nursing, Northumbria University
View articles · Email Benjamin

Nurses have an essential role to play in the assessment and planning of patient care. This is emphasised in the Nursing and Midwifery Council's 2018Future Nurse proficiency standards. In this article, the author discusses the importance of person-centred care in assessing needs and highlights the need for all nursing interventions to be evidence based. The topics covered include assessing people's needs, care planning, stages of care planning, benefits of care planning, models of care, care pathways, and care clustering in mental health care. The article also highlights the significance of record-keeping.
The central role of nurses in assessing patient needs and planning care is one of the core areas emphasised in Future Nurse, the Nursing and Midwifery Council's (NMC) (2018a) nursing proficiency standards. The document categorises ‘assessing needs and planning care’ as the third of seven areas of proficiency, which are grouped into ‘platforms’. Future Nurse emphasises that the delivery of person-centred care and evidence-based nursing interventions are vital components for effective patient assessment and care planning. The standards further highlight that the nurse should understand the need to assess each patient's capacity to make their own decisions and to allow them the opportunity to give and withdraw consent.
An assessment is a form of a dialogue between client and practitioner, in which they discuss the needs of the former to promote their wellbeing and what they expect to happen in their daily life ( National Institute for Health and Care Excellence (NICE), 2021 ). Nursing assessment involves collecting data from the patient and analysing the information to identify the patient's needs, which are sometimes described as problems.
Register now to continue reading
Thank you for visiting British Journal of Nursing and reading some of our peer-reviewed resources for nurses. To read more, please register today. You’ll enjoy the following great benefits:
What's included
Limited access to clinical or professional articles
Unlimited access to the latest news, blogs and video content
Signing in with your registered email address
Nursing Diagnoses Essays
Analysis of health promotion plan, teaching plan for comprehensive approach to patient education, creating a care plan, popular essay topics.
- American Dream
- Artificial Intelligence
- Black Lives Matter
- Bullying Essay
- Career Goals Essay
- Causes of the Civil War
- Child Abusing
- Civil Rights Movement
- Community Service
- Cultural Identity
- Cyber Bullying
- Death Penalty
- Depression Essay
- Domestic Violence
- Freedom of Speech
- Global Warming
- Gun Control
- Human Trafficking
- I Believe Essay
- Immigration
- Importance of Education
- Israel and Palestine Conflict
- Leadership Essay
- Legalizing Marijuanas
- Mental Health
- National Honor Society
- Police Brutality
- Pollution Essay
- Racism Essay
- Romeo and Juliet
- Same Sex Marriages
- Social Media
- The Great Gatsby
- The Yellow Wallpaper
- Time Management
- To Kill a Mockingbird
- Violent Video Games
- What Makes You Unique
- Why I Want to Be a Nurse
- Send us an e-mail
Diagnosis essays
Tuberculosis, hypertension essay, autism and the diagnosis of autism in the society, mucor – disease description, attention deficit hyperactivity disorder (adhd) teaching plan, precocious puberty, pertussis essay, develop and implementation plan for dnp project.
- Access to Healthcare
- Accountable Care Organizations
- Affordable Care Act (ACA)
- Air Pollution
- Alcohol Abuse
- Alternative Medicine
- Animal Testing

- Log in ▼
- Our Guarantees
- Our Services
- How it Works
NANDA nursing diagnosis essay/ care plan
What is a three-part nursing diagnosis?

ORDER A PLAGIARISM-FREE PAPER HERE
So how does a nursing diagnosis differ from a medical diagnosis ? A doctor diagnoses a disease or a disorder. A nurse offers a diagnosis for a problem present during the nursing assessment which is caused by the disease or disorder. For example, during the nursing assessment, the nurse could diagnose the patient with poor breathing and a cough. A doctor will diagnose a patient with chronic bronchitis and prescribe medication.
A nursing diagnosis is not simply assessing the patient, which is the first step in the nursing process. A nurse will develop a diagnostic statement based on data collected during the nursing assessment. The assessment process involves physically examining a patient. A nurse will monitor a patient’s symptoms, such as nausea, and measure vital signs such as heart rate, temperature, blood pressure and oxygen levels, among many other things. Nurses must often discuss with patients any non-obvious symptoms they may have, such as pain or vertigo, as well as patient history. This is an important part of collecting the data necessary to develop a diagnosis. It may be necessary to perform a psychological exam or a social exam, depending on what field a nurse works in. NANDA nursing diagnosis essay/ care plan.
Developing a three-part nursing diagnosis consists of data analysis, problem identification and the formulation of the nursing diagnosis. There are four different types of nursing diagnosis; actual nursing diagnosis, wellness (or health promotion) nursing diagnosis, risk nursing diagnosis and syndrome diagnosis.
An actual diagnosis identifies a current health problem , such as inadequate airway clearance as evidence by the inability to maintain adequate oxygenation on room air. NANDA nursing diagnosis essay/ care plan.
A wellness or health promotion diagnosis identifies a patient’s readiness to transition to a higher wellness level , such as readiness for enhanced self-care to increase cardiac output related to increased cardiac output due to pacemaker insertion.
A risk diagnosis identifies when a patient could be at risk for additional health problems , such as infection.
A syndrome diagnosis determines symptoms based on certain situations , such as post-trauma syndrome or relocation stress syndrome. NANDA nursing diagnosis essay/ care plan.
So what’s the point of a nursing diagnosis? Ultimately, a nursing diagnosis increases patient safety and means more effective care. You’ll identify every potential syndrome a patient may have and record all important vital signs. This attention to detail could be the difference between the correct treatment and continued illness or injury.
Once you’ve reached your nursing diagnosis, it’s important to write the diagnosis correctly, as established by the North American Nursing Diagnosis Association (NANDA.) Correctly writing the diagnosis helps ensure consistency across communication lines to other health care professionals. The diagnosis can be structured differently depending on the type of diagnosis it is.
An actual nursing diagnosis is written as the problem/diagnosis related to (r/t) x factor/cause as evidenced by data/observations .
A risk nursing diagnosis is written as problem/diagnosis related to (r/t) x factor/cause.
A syndrome nursing diagnosis is written as problem/diagnosis related to (r/t) x factor/cause.
A wellness nursing diagnosis is written as readiness to/for action.
Nursing is an evidence-based practice, and no aspect more so than the three-part nursing diagnosis. Your diagnosis as a nurse can save patients a lot of pain and trouble. NANDA nursing diagnosis essay/ care plan.
The NANDA-I system of nursing diagnosis provides for four categories.
- Actual diagnosis A clinical judgment about human experience/responses to health conditions/life processes that exist in an individual, family, or community. An example of an actual nursing diagnosis is: Sleep deprivation.
- Risk diagnosis Describes human responses to health conditions/life processes that may develop in a vulnerable individual/family/community. It is supported by risk factors that contribute to increased vulnerability. An example of a risk diagnosis is: Risk for shock.
- Health promotion diagnosis A clinical judgment about a person’s, family’s or community’s motivation and desire to increase wellbeing and actualise human health potential as expressed in the readiness to enhance specific health behaviours, and can be used in any health state. An example of a health promotion diagnosis is: Readiness for enhanced nutrition. NANDA nursing diagnosis essay/ care plan.
- Syndrome diagnosis A clinical judgment describing a specific cluster of nursing diagnoses that occur together, and are best addressed together and through similar interventions. An example of a syndrome diagnosis is: Relocation stress syndrome. NANDA nursing diagnosis essay/ care plan.
NANDA nursing diagnosis essay/ care plan Process
The diagnositic process requires a nurse to use critical thinking. In addition to knowing the nursing diagnoses and their definitions, the nurse becomes aware of defining characteristics and behaviors of the diagnoses, related factors to the diagnoses, and the interventions suited for treating the diagnoses.
- Assessment The first step of the nursing process is assessment. During this phase, the nurse gathers information about a patients psychological, physiological, sociological, and spiritual status. This data can be collected in a variety of ways. Generally, nurses will conduct a patient interview. Physical examinations, referencing a patient’s health history, obtaining a patient’s family history, and general observation can also be used to gather assessment data. Patient interaction is generally the heaviest during this evaluative stage. NANDA nursing diagnosis essay/ care plan.
- Diagnosis The diagnosing phase involves a nurse making an educated judgement about a potential or actual health problem with a patient. Multiple diagnoses are sometimes made for a single patient. These assessments not only include a description of the problem or illness (e.g. sleep deprivation) but also whether or not a patient is at risk of developing further problems. These diagnoses are also used to determine a patient’s readiness for health improvement and whether or not they may have developed a syndrome. The diagnoses phase is a critical step as it is used to determine the course of treatment.
- Planning Once a patient and nurse agree of the diagnoses, a plan of action can be developed. If multiple diagnoses need to be addressed, the head nurse will prioritise each assessment and devote attention to severe symptoms and high risk patients. Each problem is assigned a clear, measurable goal for the expected beneficial outcome. For this phase, nurses generally refer to the evidence-based Nursing Outcome Classification, which is a set of standardised terms and measurements for tracking patient wellness. The Nursing Interventions Classification may also be used as a resource for planning. NANDA nursing diagnosis essay/ care plan.
- Implementation The implementing phase is where the nurse follows through on the decided plan of action. This plan is specific to each patient and focuses on achievable outcomes. Actions involved in a nursing care plan include monitoring the patient for signs of change or improvement, directly caring for the patient or performing necessary medical tasks, educating and instructing the patient about further health management, and referring or contacting the patient for a follow-up. Implementation can take place over the course of hours, days, weeks, or even months.
- Evaluation Once all nursing intervention actions have taken place, the nurse completes an evaluation to determine if the goals for patient wellness have been met. The possible patient outcomes are generally described under three terms: patient;s condition improved, patient’s condition stabilised, and patient’s condition deteriorated. In the event where the condition of the patient has shown no improvement, or if the wellness goals were not met, the nursing process begins again from the first step. NANDA nursing diagnosis essay/ care plan.
Why We Are the Best
- 100% non-plagiarized Papers
- Dedicated nursing and healthcare writers
- 24/7 /365 Service Available
- Affordable Prices
- Money-back and Privacy guarantees
- Unlimited Amendments upon request
- Satisfaction guarantee

- Online Nursing Assignment Help
- Nursing Assignment Help
- Nursing Dissertation Writing Services
- Nursing Capstone Project Writing Services
- Best Nursing Essay Writing Company
- Best Online Nursing Assignment Help
- Nursing Term Paper Writing Services
- Nursing Report Writing Services
- Nursing Annotated Bibliography by Professional
- Nursing Essay Assignments
- Nursing Assignment Writing
- Nursing Case Study Writing Services
- Nursing Coursework Writing
- Online Nursing Research Paper writing service
- PICO Question Examples
- Nursing Thesis Writing Services
- Nursing Research Paper Writing Services
- Nursing Presentation Writing
- Terms and Conditions
- Epidemiology assignment help
- Write my nursing dissertation for Me
- Nursing Essay Writing Service
Official websites use .gov
A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
CDC Recommends Updated 2024-2025 COVID-19 and Flu Vaccines for Fall/Winter Virus Season
For Immediate Release: June 27, 2024 Contact: Media Relations (404) 639-3286
Today, CDC recommended the updated 2024-2025 COVID-19 vaccines and the updated 2024-2025 flu vaccines to protect against severe COVID-19 and flu this fall and winter.
It is safe to receive COVID-19 and flu vaccines at the same visit. Data continue to show the importance of vaccination to protect against severe outcomes of COVID-19 and flu, including hospitalization and death. In 2023, more than 916,300 people were hospitalized due to COVID-19 and more than 75,500 people died from COVID-19. During the 2023-2024 flu season, more than 44,900 people are estimated to have died from flu complications.
Updated 2024-2025 COVID-19 Vaccine Recommendation
CDC recommends everyone ages 6 months and older receive an updated 2024-2025 COVID-19 vaccine to protect against the potentially serious outcomes of COVID-19 this fall and winter whether or not they have ever previously been vaccinated with a COVID-19 vaccine. Updated COVID-19 vaccines will be available from Moderna, Novavax, and Pfizer later this year. This recommendation will take effect as soon as the new vaccines are available.
The virus that causes COVID-19, SARS-CoV-2, is always changing and protection from COVID-19 vaccines declines over time. Receiving an updated 2024-2025 COVID-19 vaccine can restore and enhance protection against the virus variants currently responsible for most infections and hospitalizations in the United States. COVID-19 vaccination also reduces the chance of suffering the effects of Long COVID, which can develop during or following acute infection and last for an extended duration.
Last season, people who received a 2023-2024 COVID-19 vaccine saw greater protection against illness and hospitalization than those who did not receive a 2023-2024 vaccine. To date, hundreds of millions of people have safely received a COVID-19 vaccine under the most intense vaccine safety monitoring in United States history.
Updated 2024-2025 Flu Vaccine Recommendation
CDC recommends everyone 6 months of age and older, with rare exceptions, receive an updated 2024-2025 flu vaccine to reduce the risk of influenza and its potentially serious complications this fall and winter. CDC encourages providers to begin their influenza vaccination planning efforts now and to vaccinate patients as indicated once 2024-2025 influenza vaccines become available .
Most people need only one dose of the flu vaccine each season. While CDC recommends flu vaccination as long as influenza viruses are circulating, September and October remain the best times for most people to get vaccinated. Flu vaccination in July and August is not recommended for most people, but there are several considerations regarding vaccination during those months for specific groups:
- Pregnant people who are in their third trimester can get a flu vaccine in July or August to protect their babies from flu after birth, when they are too young to get vaccinated.
- Children who need two doses of the flu vaccine should get their first dose of vaccine as soon as it becomes available. The second dose should be given at least four weeks after the first.
- Vaccination in July or August can be considered for children who have health care visits during those months if there might not be another opportunity to vaccinate them.
- For adults (especially those 65 years old and older) and pregnant people in the first and second trimester, vaccination in July and August should be avoided unless it won’t be possible to vaccinate in September or October.
Updated 2024-2025 flu vaccines will all be trivalent and will protect against an H1N1, H3N2 and a B/Victoria lineage virus. The composition of this season’s vaccine compared to last has been updated with a new influenza A(H3N2) virus .
For more information on updated COVID-19 vaccines visit: Coronavirus Disease 2019 (COVID-19) | CDC . For more information on updated flu vaccines visit: Seasonal Flu Vaccines | CDC .
The following statement is attributable to CDC Director Dr. Mandy Cohen:
“Our top recommendation for protecting yourself and your loved ones from respiratory illness is to get vaccinated,” said Mandy Cohen, M.D., M.P.H. “Make a plan now for you and your family to get both updated flu and COVID vaccines this fall, ahead of the respiratory virus season.”
### U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES
Whether diseases start at home or abroad, are curable or preventable, chronic or acute, or from human activity or deliberate attack, CDC’s world-leading experts protect lives and livelihoods, national security and the U.S. economy by providing timely, commonsense information, and rapidly identifying and responding to diseases, including outbreaks and illnesses. CDC drives science, public health research, and data innovation in communities across the country by investing in local initiatives to protect everyone’s health.
To receive email updates about this page, enter your email address:
- Data & Statistics
- Freedom of Information Act Office
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.

COMMENTS
A medical diagnosis does not change if the condition is resolved, and it remains part of the patient's health history forever. A nursing diagnosis, however, generally refers to a specific period of time. Examples of medical diagnosis include: Arthritis. Congestive Heart Failure. Diabetes Insipidus.
2.3 Using the PES Format. To ensure clarity and consistency in your nursing diagnoses, use the PES (Problem-Etiology-Symptoms) format. This format clearly defines the problem, its cause, and the evidence supporting the diagnosis. Problem: The "P" in PES; it is the patient's health issue. Etiology: The "E" in PES; it represents the ...
Updated on April 29, 2024. By Matt Vera BSN, R.N. In this ultimate tutorial and nursing diagnosis list, we'll walk you through the concepts behind writing nursing diagnosis. Learn what a nursing diagnosis is, its history and evolution, the nursing process, the different types and classifications, and how to write nursing diagnoses correctly.
Step 1: Assessment. The first step when assigned to write a nursing diagnosis is to observe the presenting symptoms of the patient. Read the case study or vignette or check the patient information/data to describe the patient's problem based on the signs and symptoms.
Nursing Diagnoses vs. Medical Diagnoses. Although there are some similarities between medical and nursing diagnoses, such as clinical judgment and shared terminology, they are distinct. 2 The most apparent difference between nursing and medical diagnoses is the healthcare practitioner deciding the diagnosis. All nursing designations share nursing diagnoses, while physicians create medical ...
Nursing team collaboration. Writing a care plan allows a team of nurses (as well as physicians, assistants, and other care providers) to access the same information, share opinions, and collaborate to provide the best possible care for the patient. Documentation and compliance. A well-written care plan allows nurses to measure the effectiveness ...
Diagnosis is formed by the nurse and is based on the data collected during the assessment. The nursing diagnosis directs nursing-specific patient care. In this step, the nurse forms a diagnosis based on the patient's specific medical and/or social needs. The diagnosis leads to the creation of goals with measurable outcomes.
To write an effective nursing diagnosis, start by analyzing data, identifying health problems, risks, and strengths, and then formulate a diagnostic statement. Use formats such as the PES format or one-part, two-part, and three-part statements to accurately document the diagnosis.
To write an accurate nursing diagnosis, you need to analyze the patient's data, identify the health problem, and formulate a diagnostic statement. This statement should follow the PES format, which includes the problem, etiology (cause), and signs and symptoms. Nursing diagnoses are then used in the development of nursing care plans.
Nursing diagnosis is increasingly recognized as an integral component of professional nursing practice. Implementation of nursing diagnosis impacts on all elements of professional practice: the philosophy, purpose, and objectives of an organization; care planning; quality assurance; staff education; performance standards; the nursing care delivery system; documentation; and patient classification.
Here are some tips for writing a risk for nursing diagnosis: - Include all the details about your patient's current health status for the right diagnosis. For example, describe any symptoms or events that led to this particular situation. Be as specific as possible.
Concept of Nursing Diagnosis Essay (Critical Writing) Sickle Cell Anemia is a disorder that normally increases blood thickness hence affects the smooth flow of blood. This is caused by the destruction of red cells where the normal shape of red cell becomes a stiff sickle shape. As a result, sufficient oxygen does not reach the vital organs.
Background: Professional nursing organizations recommend the use of nursing diagnosis to enhance and facilitate the standardization of care and the development of a common language used by nursing practitioners. In the clinical reality of hospital emergency departments, however, its use is controversial. The objectives of the research are (a) to explore the use of nursing diagnosis in hospital ...
That is because a nursing diagnosis guides nurses in determining appropriate patient care plans. A nurse writes nursing diagnoses based on the patient's assessment. It must include the problem and its description, the etiology, and the identified risk factors. Writing a nursing diagnosis helps students to learn how to prepare for their careers.
Nursing Diagnosis Essays. Nursing Theory Application in Practice. Introduction To start with, the existence of nursing theories has helped prove the conceptual framework upon which nursing practice is based. Through the framework, one can understand the interconnectedness of the concepts and constructs, which then aid in understanding and ...
This essay about community health nursing diagnosis statements highlights their vital role in understanding and addressing the multifaceted nature of community health. Unlike individual diagnoses, these statements consider the broader social, economic, and environmental factors influencing health outcomes.
Nursing diagnosis Essays. Examples Of Nursing Diagnosis 892 Words | 4 Pages. A nursing diagnosis may be part of the nursing process . Nursing diagnosis is defined as "a clinical judgment about individual, family, or community experiences/responses to actual or potential health problems/life processes. A nursing diagnosis provides the basis ...
Planning care is essential in the delivery of appropriate nursing care. Following assessment of a patient's needs, the next stage is to 'plan care' to address the actual and potential problems that have been identified. This helps to prioritise the client's needs and assists in setting person-centred goals. Planned care will change as a patient's needs change and as the nurse and/or other ...
Abstract The paper outlines a health promotion plan that addresses three wellness assessment areas. The areas include lack of physical exercise, poor nutrition, adequate sleep, and stress management. The plan will include a detailed analysis of demographics, assessment, nursing diagnoses, interventions, goals, and evaluation methods for each area.
Chase Ty 'Janae Sheria West Virginia Junior College NUR 201 October 8th, 2023 Author Note I will explain 10 nursing diagnosis NANDAs throughout my essay. Summary A nursing diagnosis is a part of the nursing process and is a clinical judgment that helps nurses determine the plan of care for their patients (Gaines, 2023).
Looking for free Diagnosis essay examples? ️ Find high-quality samples in our database. 📚 More than 125 essays on Diagnosis. Don't have time? Order writing help. Search. ... Introduction Nursing is an emerging sector, which is related with the well being of population. The skills, knowledge, and experience in nursing field are the prime ...
A wellness nursing diagnosis is written as readiness to/for action. Nursing is an evidence-based practice, and no aspect more so than the three-part nursing diagnosis. Your diagnosis as a nurse can save patients a lot of pain and trouble. NANDA nursing diagnosis essay/ care plan. The NANDA-I system of nursing diagnosis provides for four categories.
Essay On Nursing Diagnosis. According to NDNA International (Professional Assosiation of Nurses) Nursing Diagnosis is a clinical judgment about individual , family or society responses to real or possible health problems or life process.Nursing diagnosis are developed based on the data obtained during the nursing assessment. A nursing diagnosis ...
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES. Whether diseases start at home or abroad, are curable or preventable, chronic or acute, or from human activity or deliberate attack, CDC's world-leading experts protect lives and livelihoods, national security and the U.S. economy by providing timely, commonsense information, and rapidly identifying and responding to diseases, including outbreaks ...