Advertisement

Recent Findings on the Effectiveness of Peer Support for Patients with Type 2 Diabetes
- Open access
- Published: 21 May 2024
- Volume 18 , pages 65–79, ( 2024 )
Cite this article
You have full access to this open access article

- James J. Werner 1 , 2 , 3 , 4 , 5 ,
- Kelsey Ufholz 1 , 2 &
- Prashant Yamajala 1 , 2
306 Accesses
Explore all metrics
Purpose of Review
To review randomized controlled trials (RCTs) published from 2021–2023 that reported the effects of peer support interventions on outcomes in patients with type 2 diabetes (T2DM).
Recent Findings
Literature searches yielded 137 articles and nine RCTs were ultimately reviewed. The reviewed trials involved in-person support groups, peer coach/mentor support, cultural peer support by community health workers, peer support during shared medical appointments (SMAs) including virtual reality-based SMAs, telehealth-facilitated programs, and telephone peer support. Most interventions combined two or more peer support strategies.
Peer support was associated with significant decreases in HbA1c in 6 of the 9 reviewed studies. The largest statistically significant improvements in HbA1c were reported in a study of community health workers in Asia (-2.7% at 12 months) and a Canadian study in which trained volunteer peer coaches with T2DM met with participants once and subsequently made weekly or biweekly phone calls to them (-1.35% at 12 months). Systolic blood pressure was significantly improved in 3 of 9 studies.
The findings suggest that peer support can be beneficial to glycemic control and blood pressure in T2DM patients. Studies of peer support embedded within SMAs resulted in significant reductions in HbA1c and suggest that linkages between healthcare systems, providers, and peer support programs may enhance T2DM outcomes.
Similar content being viewed by others

Enhancing Peer Support Interventions in Diabetes Care
Mobile-Enhanced Peer Support for African Americans with Type 2 Diabetes: a Randomized Controlled Trial
Peer support of complex health behaviors in prevention and disease management with special reference to diabetes: systematic reviews.
Avoid common mistakes on your manuscript.
Introduction
Diabetes is one of the fastest growing global health crises and is a major cause of blindness, kidney failure, heart attacks, stroke, lower limb amputation, and mortality [ 1 ]. In 2021, approximately 537 million people had diabetes worldwide and the number is projected to reach 643 million by 2030 and 783 million by 2045 [ 2 ].
Type 2 diabetes (T2DM) accounts for more than 90% of diabetes cases. Increasing rates are driven by socio-economic, demographic, environmental, and genetic factors [ 3 ]. Much of diabetes care needs to be carried out by patients, including monitoring blood glucose, taking medication, getting regular physical activity and maintaining a healthy diet [ 4 ••, 5 ]. Although complications are often preventable through improved metabolic control and implementation of self-care and lifestyle behaviors, patients face numerous self-management barriers [ 6 , 7 ]. These include inadequate diabetes knowledge, lack of resources for exercise and healthy eating, discomfort from diabetes-related health problems, negative emotions, and lack of social support [ 8 ].
Clinical guidelines recommend that individuals with T2DM participate in a lifestyle management program that includes diabetes self-management education and support (DSMES) comprising medical nutrition therapy, physical activity, smoking cessation counseling, and psychosocial care [ 4 ••, 9 ••]. Peer support is not a specified component of DSMES programs, although diabetes education is often conducted in groups of peers with T2DM [ 10 ]. The utilization, reach, and effectiveness of DSMES programs can be improved through peer support, which may help to overcome barriers and compensate for limited resources [ 11 ]. DSMES programs have proven to be effective in lowering HbA1c, reducing diabetes complications, lowering rates of all-cause mortality, increasing self-efficacy, improving coping skills, and reducing diabetes distress [ 10 ].
Ongoing support from family and peers can be beneficial as patients endeavor to implement and sustain the behaviors needed to effectively self-manage T2DM [ 12 ]. Peer support has been defined as “the provision of emotional, appraisal and informational assistance by a created social network member who possesses experiential knowledge of a specific behavior or stressor and similar characteristics as the target population”. [ 13 ] Peer support typically involves emotional support and informational support. When both peers have diabetes, mutual reciprocity takes place when individuals take turns sharing their personal experiences and providing emotional and informational support to the other person. Through these mechanisms, peer support can improve understanding, motivation, self-efficacy, and mood, and reduce perceived barriers in individuals with T2DM [ 14 ]. Diabetes distress, which is the negative emotional experience resulting from the challenge of living with the demands of diabetes, can also be reduced through peer support. [ 15 ] A classification of diabetes peer support models based on the work of Heisler [ 5 ] is provided in Table 1 titled, Types of Peer Support Models Used in Type 2 Diabetes.
Different types of peers are used across the spectrum of interventions used in diabetes peer support programs. Fellow T2DM patients are peers on the basis of sharing the experience of living with diabetes. Peer support specialists employed by health clinics are peers because they too have been diagnosed with T2DM and live with the condition. Community health workers supporting patients with T2DM are considered to be “cultural peers” because they also live in the same communities, share patients’ racial and ethnic identities and cultural backgrounds, and may have similar life situations including caring for family members with T2DM, although they do not necessarily have a diagnosis of T2DM [ 16 ].
During the COVID-19 pandemic, patients with T2DM were at increased risk of severe infections and mortality and many experienced disruptions to their social support networks [ 12 ]. These were significant psychological stressors and increased diabetes self-management challenges [ 11 ]. The findings of several diabetes peer support interventions conducted during the pandemic are reported in this review.
Peer support interventions have the potential to positively affect outcomes for individuals with T2DM [ 17 •, 18 ]. Though they have shown promise, the type and overall effectiveness of peer support programs is highly variable. Our purpose was to identify peer support studies to better understand the breadth of strategies used and their relative effectiveness on diabetes self-management and cardiometabolic outcomes.
PubMed, the Cochrane Library, and the PsycInfo and PsycArticles databases were searched for articles published between January 1, 2021 and December 31, 2023. This timeframe was selected based on T2DM patients’ increased needs for social and emotional support around the time of the COVID-19 pandemic [ 19 , 20 ]. The included search terms were type 2 diabetes, diabetes mellitus, peer support, social support, support group, self-help group, group support, community support, group education, group visits, and shared medical appointments. Search terms for outcome variables included HbA1c, glycemic control, obesity, body mass index, and weight loss. Studies reporting only survey data or qualitative findings, or that otherwise lacked physiologic outcomes were excluded. Studies of other forms of diabetes (e.g., type 1, gestational) were excluded as were studies of children and non-English language articles.
The searches yielded 137 articles for which 129 abstracts were reviewed against inclusion and exclusion criteria, yielding 41 articles that were examined in full text format. After the exclusion of non-RCTs, pilot studies, and studies with incomplete data or low rates of completion, 9 articles were utilized in this review. A flowchart based on PRISMA guidelines is provided in Fig. 1 , titled Flow Diagram for Review [ 21 ].
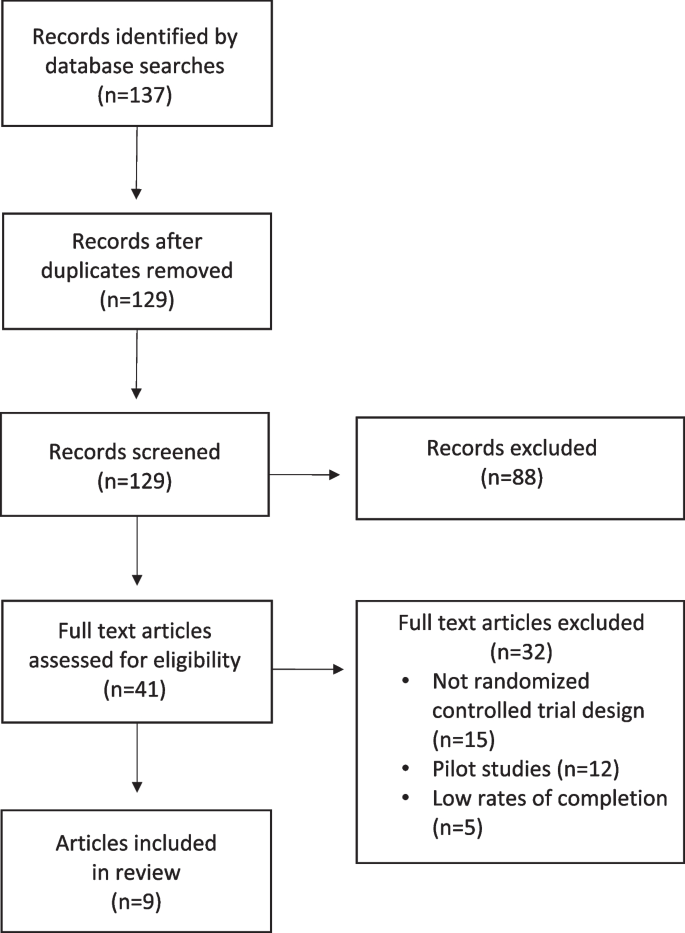
Flow diagram for review
Key findings from the review are discussed in this section and are summarized in Table 2 titled, Characteristics and Key Outcomes of Reviewed Studies.
In-Person Peer Support
There is significant evidence for the effectiveness of in-person (IP) support in diabetes education programs [ 17 •, 18 , 22 ]. IP support allows direct verbal and non-verbal communication, enables social interactions and facilitates the exchange of peer-to-peer information, support, and goal setting.
Shared Medical Appointments
Shared medical appointments (SMAs) are typically IP doctor-patient visits in which groups of patients are seen by one or more healthcare providers. Patients interact with both providers and with peers during SMAs [ 23 ]. Heisler and colleagues compared the effectiveness of diabetes SMAs to usual care in improving HbA1c [ 24 •]. Patients with T2DM and elevated HbA1c who had been prescribed medication were recruited from 5 U.S. Veterans Affairs (VA) health systems. Participants engaged in IP SMAs of 60–120 min totaling 6–8 h over 12 months where they received education, engaged in goal setting, and shared their experiences with peers. A SMA plus reciprocal peer support intervention arm was available in which participants had the option to be connected to another participant for mutual support, but uptake was low resulting in data being combined with the SMA-only group data. The control group received usual care.
At 6 months, the intervention group’s mean HbA1c was reduced by 0.35% compared to usual care ( p = 0.001) and was lower than usual care by 0.53% in participants attending at least half of the sessions ( p = 0.001), however, these differences were not significant at 12 months. Insulin starts were significantly greater in the intervention group at both 6 and 12 months. Significant mean differences were not observed for systolic blood pressure, statin starts, or HTN med class changes.
Health Clinic Staff-facilitated Support Groups
Mexico is among countries with the highest prevalence of diabetes, with more than 24% of adults over age 50 being diagnosed with T2DM [ 25 ]. The Mexican Ministry of Health’s primary care services include diabetes support groups known as Grupos de Ayuda Mutua (GAM), which provide a supportive group environment, glucose self-monitoring and health information via monthly meetings. Rosales and colleagues sought to complement the GAM program with Meta Salud Diabetes (MSD), a secondary prevention curriculum designed to operate within the framework of the GAM and evaluated its effects on Framingham CVD risk in a cluster-randomized trial [ 26 ]. The objective was for the MSD to improve the existing GAM by providing educational information, group discussions, and interactive workshops to promote a healthier diet, increased physical activity and reduced disease complications.
The GAM + MSD intervention consisted of 2-h IP participatory educational sessions and group-based interactive activities facilitated by trained health center staff that engaged GAM support groups at 22 government health clinics over 13 consecutive weeks. The following items were on the agenda at each session: blood pressure and glucose monitoring; readings, discussions and games related to the day’s topic of focus; implementation of a physical activity, and a follow-up goal setting exercise. The usual care group participated in standard GAM support groups.
Mean Framingham CVD risk score was significantly reduced by 3.17% points in the MSD arm versus GAM usual care at 3 months ( p = 0.013), however, the between groups difference was not significant at 12 months. Greater reduction in mean Framingham CVD risk was observed in men than women and in those whose HbA1c was < 8% at baseline. No significant effects were observed for HbA1c, blood pressure, or blood lipids. Compared to baseline, diabetes distress in the GAM + MSD group was significantly lower at the 3- and 12-month follow-up assessments.
IP Diet & Lifestyle Intervention with Telephone Support
Sampson and colleagues implemented an IP diet and lifestyle intervention with and without additional telephone support provided by trained peers in the UK for individuals with newly diagnosed “screen detected” type 2 diabetes [ 27 ]. Participants were randomized into three arms. Those in the intervention arm (INT) received six 2-h group educational sessions over 12 weeks and up to fifteen 2.5-h group maintenance sessions 8 weeks apart; maximum possible contact time was 49.5 h over 30 months. Individuals randomized to the second arm received the INT intervention plus monthly telephone support from peer volunteers who themselves had T2DM and who had received training as diabetes peer mentors (INT-DPM). Telephone contacts were monthly for 3 months and then every 2 months thereafter for up to 46 months. Those in the control arm (CON) received no intervention.
At 12 months, mean HbA1c significantly decreased in the telephone peer support INT-DPM group compared to the control group (CON) (-0.3%; p = 0.007), however, differences were not significant between the INT-DPM and INT groups, or between the INT and control groups. Days of resistance exercise per week significantly increased compared to the control group in both the INT and INT-DPM groups (INT: 4.22 days, p = 0.01; INT-DPM: 3.32 days, p = 0.02). Glycemic control was significantly lower in INT-DPM group vs. the CON group for participants < 65 years of age compared to those > 65 years (INT-DPM -2.7% vs. CON -2.2%; interaction p = 0.007). No significant differences were observed between any of the groups for body weight, body fat %, or waist circumference.
Family- and Friend-focused Peer Intervention
Positive support by family and friends of individuals with T2DM is strongly associated with more consistent self-care and lower glycemic control [ 28 ]. However, it is possible for both helpful and harmful interactions to co-occur within families and friendships. As cultural peers, family members and friends can support or undermine an individual’s diabetes self-care behaviors, which affects the likelihood of them continuing to implement the behaviors [ 29 ].
Nelson and colleagues implemented an intervention entitled, Family/friend Activation to Motivate Self-care (FAMS) to assist patients with T2DM in pursuing self-care goals and in effectively responding to both helpful and harmful input from family and friends [ 30 ]. In this RCT, FAMS provided monthly health coaching phone calls by behavioral health providers that were subsequently reinforced by text messaging over the 9-month intervention period. Each FAMS participant had the option to designate a cultural peer support person (family member or friend) and invite them to receive the text messages sent by their health coach, potentially prompting peer interactions about the participant’s health behaviors and diabetes self-management goals. Monthly coaching calls to FAMS participants focused on building the following skills: improving the ability to recognize and manage both helpful and harmful messages from friends or family members, SMART goal setting, assertive communication, obtaining social support, collaborative problem-solving, and cognitive behavioral coping skills. Participants in the control group received usual care. Participants and support persons in both study arms received print materials on managing diabetes and providing support to individuals with diabetes, and participants received text messages advising how to access their HbA1c results.
At 6 months, mean HbA1c decreased by 0.25% compared to controls but did not reach statistical significance ( p = 0.09). Effects on HbA1c vs. controls were also non-significant at 9 months (-0.05%; p = 0.9) and at 12 months (-0.02%; p = 0.9). Interestingly, participants who were not cohabitating with their support person had significantly lower HbA1c at 6 months (-0.64%; p = 0.033) but not at other time points. The investigators suggested that out-of-home support is likely to strengthen one’s support network, especially for those living alone, and may result in fewer instances of harmful social interactions than can occur with a cohabitating support person. At both 6 and 9 months, significant improvements were observed in intermediate targets of the FAMS intervention compared to controls including diabetes self-efficacy, problem eating behaviors, summative physical activity, helpful family/friend involvement, and autonomy support, although the study did not attempt to measure the relative contributions made by health coaches and cultural peer support persons to these outcomes. Another recent trial of a family and friend cultural peer support intervention for patients with diabetes yielded similar findings, with improvements in intermediate targets but non-significant effects on HbA1c [ 31 ].
Peer Coaches and Peer Mentors
Peer leader supported self-care intervention.
Although large numbers of patients with T2DM receive diabetes care in primary care settings, patients at the highest risk are often managed in subspecialty settings. Tang and colleagues conducted a peer-led intervention for adult T2DM patients presenting to endocrinology and diabetes education centers in British Columbia, Canada [ 32 ] and compared it to a usual care control group. Peer leaders completed 30 h of knowledge and skills training in T2DM self-management, providing emotional support, and linking patients to clinical resources. It is important to note that the peer leaders themselves had T2DM and a mean self-reported HbA1c ≤ 8.0% [ 33 ]. Individuals in the usual care control group received all services normally available to them at the diabetes education centers, including access to a nurse, dietician and social worker.
Intervention group participants received 30 h of T2DM self-management education and were subsequently matched with a peer leader based on gender and geographic proximity. After an initial IP educational meeting between peer leader and participant, peer leaders made 12 weekly telephone contacts with their partners over the first 3 months of the 48-month intervention to discuss self-management challenges, solve problems, and set self-management goals. During the final 36 weeks, peer leaders made 18 biweekly telephone support calls to intervention group participants.
At 3 months and 12 months post-intervention, HbA1c was not significantly different either from baseline within the intervention group or between the intervention and control groups. Significant between group improvements in systolic blood pressure were observed in the intervention group compared to controls at 12 months (-4.1 points; p = 0.023). Overall distress and emotional distress scores in the intervention group were significantly lower at 3 months and 12 months than at baseline but neither were significantly different than controls at any time point.
Community Health Workers
Community health workers (CHWs) are cultural peers in that they typically share cultural, racial, ethnic, community, and socioeconomic backgrounds with the individuals they serve and they may have direct experience with target health conditions as a patient or in support of a family member [ 34 ]. With education and training in diabetes self-management and health behavior change skills, CHWs have the potential to positively affect diabetes outcomes [ 35 ].
Home-based Diabetes Education and Counseling by Trained Volunteers
In Nepal, the healthcare system has traditionally focused on communicable diseases rather than chronic conditions and has struggled to adapt to rapidly increasing rates of T2DM [ 36 ]. A national initiative to address this need involves the mobilization of more than 50,000 Female Community Health Volunteers (FCHVs) in communities across the country. In this study, these locally-based cultural peers delivered a 12-month IP community-based diabetes intervention to adults in semi-urban settings in Western Nepal with the goal of reducing mean blood glucose [ 37 ]. This cluster randomized trial enrolled community residents with a current diagnosis of T2DM or mean blood glucose levels of 126 mg/dL or higher. FCHVs provided home-based diabetes education and counseling, measured blood glucose, blood pressure, height, and weight, and referred patients for clinic visits as needed. Home visits by FCHVs took place once every 4 months (3 visits) for one year. Participants randomized to the control group received usual care in which they managed their T2DM as usual and were placed on a wait list with the option to receive the intervention after 12 months.
Mean fasting blood glucose in the intervention group significantly decreased by 2.7% in the FCHV intervention group while it increased by 2.2% in the usual care group ( p < 0.001). Systolic blood pressure significantly decreased (-7.86 points; p = 0.002) in the intervention group vs. controls. Significant improvements were not observed in diastolic blood pressure, physical activity, BMI, alcohol consumption, smoking, fruit and vegetable intake, or medication adherence.
CHW-led Diabetes Education and Support
In a Houston, TX-based study (USA), Spanish-fluent CHWs served as cultural peers to Spanish-speaking low-income Latino(a) adults with T2DM [ 38 ]. In the intervention group, CHWs led monthly IP diabetes education group visits for 6 months and engaged in weekly m-Health communication (phone call or text) with study participants. To increase the CHWs’ knowledge of T2DM, they received quarterly diabetes training from physicians via telehealth . Participants randomized to the control group received usual care and placed on a wait list to receive the intervention after 6 months.
At 6 months, mean HbA1c in the intervention group was significantly lower (-0.98%) than controls ( p = 0.002) and decreased to a significantly greater extent among intervention group participants with uncontrolled diabetes (-1.31%) compared to control group participants with uncontrolled diabetes ( p = 0.007). Mean systolic blood pressure decreased significantly more in the intervention group than control group (-6.89 vs. + 0.03 points; p = 0.023) and the intervention group was also had a significantly greater reduction in mean diastolic blood pressure vs. the control group (-3.36 vs. + 0.2 points; p = 0.046). No significant between group differences were observed for body weight. Significantly more patients in the intervention group started insulin and statin medications compared to controls. Preventive care measures (B12 screening, foot and eye exams, immunizations, urine microalbumin) occurred significantly more often in the intervention group than the control group ( p < 0.001).
Peer Coaching Supported DVD Education
The personal stories of peers with T2DM were leveraged in an intervention based on social cognitive theory that aimed to improve medication adherence among low-income African American adults with T2DM [ 39 ]. The study took place in a rural Alabama region predominantly populated by African Americans that includes some of the poorest counties in the US, with a prevalence of diabetes of roughly twice the national average [ 40 ]. Medical resources are scarce and age-adjusted mortality rates are 39% higher for African Americans compared to the US average. Study participants were taking diabetes oral medications and who reported medication non-adherence or wanted help taking their medications. Peer coaches were community residents who had diabetes or took care of family members with diabetes.
Intervention participants were provided with DVDs that featured diabetes education and personal stories about how community members accepted their diagnosis of T2DM and overcame barriers to medication adherence during a six-month, 11-session behavioral diabetes self-care program delivered by peer coaches over the phone. During a 6-week intensive phase, intervention participants watched a 15–30 min DVD each week about the challenges and successes experienced by patients with diabetes and afterwards discussed the video’s content with a peer coach in a 30–60 min telephone call. After 6 weeks, peer coaches made biweekly or monthly telephone calls over the remaining 4.5 months to monitor participants’ progress, review information, provide education, and develop self-management strategies. Control participants received a self-paced general health program on topics that were independent of study outcomes.
After 6 months, the study’s primary outcome, medication adherence, significantly improved in the intervention group vs. controls (-0.25; p < 0.0001), however the study arms did not differ in mean HbA1c, blood pressure, body weight, or LDL cholesterol. Intervention participants’ beliefs in the necessity of medications, their medication use self-efficacy, and their diabetes self-efficacy significantly increased, although participants’ self-rated quality of life was not significantly improved. The authors speculated that improvements in medication adherence may not have been substantial enough to affect the physiological measures after 6 months. A limitation that potentially attenuated outcomes was that follow-up blood draws for some participants were delayed for a significant period of time after completion of the intervention.
SMAs Utilizing Telehealth and Virtual Environments
Telehealth became heavily-utilized during the COVID-19 pandemic and has proven comparable to IP consultations in clinical effectiveness [ 41 ]. In Boston, MA (USA) a two-arm trial was implemented to compare conventional IP diabetes SMAs to virtual reality-augmented diabetes SMAs conducted via telehealth for African American or Black and Hispanic or Latina adult women with uncontrolled HbA1c (≥ 8.0%) [ 42 ].
A 3D computer-based simulated environment was used to engage study participants in SMAs and DSME using a telehealth platform with “immersive, experiential learning with animated educational content” [ 42 ]. Virtual world (VW) participants used personal avatars to represent themselves and engage with peers to carry out behavioral changes. They used the avatars to engage in SMAs and to practice the use of positive health behaviors such as dance and social support. Those in the VW group were provided with laptops and wireless internet access.
Both IP and virtual SMAs lasted 120 min including taking vital signs, documenting acute and chronic illness symptoms, health system visits, and self-management activities. All participants received the same 8-module DSME curriculum on topics including diabetes self-monitoring, preventive care, healthy eating, exercise, and stress management.
English- and Spanish-language cohorts of 6–12 individuals met in IP or VW settings for 8 weekly diabetes SMAs of 2-h duration. A healthcare provider met individually with each participant in a separate physical space or via a private telehealth session or telephone call for a one-on-one consult during every SMA. After 8 weeks, participants entered a 16-week maintenance phase when no formal SMAs occurred.
An intention-to-treat (ITT) analysis showed significant mean improvements in HbA1c from baseline to 6 months in the IP group (-0.8%; 10.2% to 9.4%) and in the VW group (-0.5%; 9.7% to 9.2%); between group differences were not statistically significant suggesting that the VW-based SMAs were no less effective than the traditional IP SMAs. Changes in HbA1c in a subset of participants completing at least 6 SMAs per protocol (PP) were similar to the results of the ITT analysis in that between group means were not significantly different.
Significant improvements in levels of physical activity were not observed in either the ITT or PP analyses. The investigators reported that participants had difficulties using the equipment to measure physical activity. Changes in depression scores within the IP and VM groups were non-significant, although substantial within group improvements were observed for diabetes distress in both groups.
Mechanisms of Peer Support
Peer support can play an important role in improving patients’ glycemic outcomes in T2DM [ 43 ]. Conceptually, peer support can be grounded in social cognitive theory [ 44 ] and self-determination theory [ 45 ]. Social cognitive theory proposes that learning can occur by observing the behavior of others and its consequences. Without the necessity of direct personal experience for learning, the volume of knowledge and skills that can be quickly learned by patients with T2DM is greatly expanded compared to experiential learning. Further, by observing peers as “social models,” self-efficacy and mastery of diabetes self-care behaviors may increase [ 44 ].
Self-determination theory posits that individuals are influenced by three factors: their capacity to exert control over their life and their future, their sense of competence (which increases with positive peer feedback which in turn increases motivation), and their connectedness to others [ 46 ]. Peer support can reinforce all 3 of these factors, particularly by providing positive feedback on behaviors, increasing self-efficacy, and leading to satisfying interpersonal connections [ 45 ].
The mechanisms of peer support relationships include having a shared lived experience, the identification of individual strengths, the provision of social and practical support, and the unique position of the peer as fellow patient, peer support specialist, or CHW cultural peer rather than a medical provider [ 47 ]. The mutual sharing of personal difficulties and experiences of suffering have been shown to increase feelings of normalization, connectedness and shared humanity [ 48 , 49 ]. Because peers have faced many of the same problems, peer support is a practical way to learn ways to overcome barriers to diabetes self-management [ 6 ].
Diabetes peer support interventions were associated with significant decreases in HbA1c in 6 of the 9 reviewed studies, and these findings align with those of older reviews. A 2021 systematic review and meta-analysis of 12 studies showed that diabetes self-management education with integrated peer support reduced HbA1c levels, (SMD, -0.41; 95% confidence interval [ 50 ], -0.69 to -0.13; p < 0.001) [ 17 •]. A scoping review by Lu et. al. found that a wide range of peer support models used as complements to primary care were associated with favorable improvements in HbA1c [ 51 ]. Further, a meta-analysis by Liang and colleagues found that peer support significantly improved self-efficacy compared with controls receiving usual care or usual diabetes education [SMD = 0.41, 95% CI = (0.20, 0.62), p = 0.0001], and self-management behaviors were significantly improved versus controls [SMD = 1.21, 95% CI = (0.58, 1.84), p = 0.0002] [ 18 ].
A sizeable decrease in HbA1c (-2.7%) was observed in a Nepal-based intervention study in which trained FCHVs held IP visits with the households of participants to provide diabetes education once every 4 months [ 37 ]. Although intervention contacts were infrequent and the FCHV interventionists were volunteers, it should be noted that FCHVs served as extenders of healthcare providers with whom they work closely at local clinics. As cultural peers to study participants, they were often regarded as integral, trusted member of their communities with whom a relationship had been established, often over many years. In addition, this was the only reviewed study that featured a household-based intervention, involving families in participants’ adoption of diet and lifestyle behaviors, attendance at clinic appointments, and modifications to medication adherence practices.
Mobile phones are nearly ubiquitous and can increase the number of contacts among peers. Six of the nine reviewed studies used mobile phones to support the intervention and four of these studies resulted in significant improvements in glycemic control. Several studies used both telephone calls and text messaging between peers and participants, providing more frequent opportunities for diabetes education, goal setting, problem-solving, trust-building, and strengthening of connections.
Healthcare system-sponsored diabetes education and peer support programs may have advantages compared to stand-alone peer support programs. Study participants were recruited at health clinics for 7 of the reviewed studies, 5 of which resulted in significant reductions in HbA1c. All three of the reviewed studies involving SMAs resulted in significant decreases in HbA1c, suggesting that directly integrating primary care providers and diabetes clinical services into diabetes education and peer support programs yields impactful benefits.
A study comparing VW SMAs to IP SMAs to found them to be comparable in effectiveness. The significant health risks posed by the COVID-19 pandemic to individuals with T2DM were reduced in the VW group as participants’ engaged in the intervention from their homes in comparison. In contrast, IP group visits were implemented in healthcare clinics in proximity to other patients and clinic staff. The VW intervention presents a potentially safer and more convenient way for T2DM patients to participate in SMAs and peer support programs while receiving benefits that are on par with IP SMAs.
Limitations
There are several limitations to this review. The review focuses on diabetes peer support interventions published over a relatively short 3-year time period. The review captured only studies published from 2021–2023 and does not include research published outside of this time frame.
Two of the included studies had modest sample sizes. Small samples have numerous disadvantages including increased risk of bias, increased variability, limited generalizability, and reduced statistical power, all of which can threaten the validity and reliability of a study’s findings.
The follow-up periods were only 6 months in duration for 2 of the 9 studies, which does not permit an evaluation of the longer-term durability of the treatment effect in diabetes, a long-term chronic disease. Due to the short time frames involved, caution should be exercised in drawing conclusions from these studies.
This review was intended to include a number of peer support interventions conducted during the period of the COVID-19 pandemic, which is recognized by the World Health Organization (WHO) to have started in March 2020 and ended in May 2023 [ 52 ]. However, it was difficult to determine the temporal overlap of the study periods with the pandemic. Although most of the included articles specified a date for the initiation of recruitment, they did not indicate an end date for the peer support intervention, which would have allowed it to be determined if the intervention extended into the pandemic period.
The pandemic was an event unrelated to study interventions but that may have influenced outcomes, and is a type of history bias. Interestingly, none of the articles discussed the possible influence of the pandemic on study participants’ experiences and study outcomes. Because there was no assessment of the effects of the pandemic on participants’ experiences in the reviewed studies, it is not possible to estimate its influence on outcomes. Additional research is needed to more closely examine the influence of the pandemic and other types of widespread disruptive events on patients with T2DM and the effects on peer support and outcomes.
It is important to note that diabetes peer support interventions are rarely studied in isolation. In the studies in the present review, peer support was part of a multifaceted intervention involving diabetes self-management education and sometimes clinical care. This makes it difficult to separate and isolate the effects of peer support from other aspects of the interventions. More research is needed to study the effects of peer support both alone and as part of multidimensional diabetes interventions.
Conclusions
Our findings suggest that diabetes education and peer support interventions can be effective for improving control of HbA1c and blood pressure, however, they were not associated with significant improvements in body weight. Studies of peer support groups embedded within SMAs resulted in significant reductions in HbA1c, suggesting that the engagement of clinicians in diabetes peer interventions enhances outcomes. In the design of peer support programs, it may be advantageous to engage households, healthcare providers, and clinics in program implementation.
Data Availability
No datasets were generated or analysed during the current study.
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
World health organization (WHO). Diabetes fact sheet. 2023. https://www.who.int/news-room/fact-sheets/detail/diabetes . Accessed 17 May 2024.
International Diabetes Federation. IDF Diabetes Atlas, 10th Edition. 2021.
Aceves B, Denman CA, Ingram M, Torres JF, Nuño T, Garcia DO, et al. Testing Scalability of a Diabetes Self-Management Intervention in Northern Mexico: An Ecological Approach. Front Public Health. 2021;9:617468. https://doi.org/10.3389/fpubh.2021.617468 .
Article PubMed PubMed Central Google Scholar
•• American Diabetes A. 5. Lifestyle Management: Standards of Medical Care in Diabetes-2019. Diabetes Care. 2019;42(Suppl 1):S46-S60. https://doi.org/10.2337/dc19-S005 . Provides current clinical practice recommendations for lifestyle management of diabetes that provides the general treatment goals and guidelines, components of diabetes care, and tools to evaluate quality of care.
Heisler M. Different models to mobilize peer support to improve diabetes self-management and clinical outcomes: evidence, logistics, evaluation considerations and needs for future research. Fam Pract. 2010;27 Suppl 1(Suppl 1):i23–32. https://doi.org/10.1093/fampra/cmp003 .
Simmons D, Cohn S, Bunn C, Birch K, Donald S, Paddison C, et al. Testing a peer support intervention for people with type 2 diabetes: a pilot for a randomised controlled trial. BMC Fam Pract. 2013;14:5. https://doi.org/10.1186/1471-2296-14-5 .
ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. 3. Prevention or Delay of Type 2 Diabetes and Associated Comorbidities: Standards of Care in Diabetes-2023. Diabetes Care. 2023;46(Suppl 1):S41-S8. https://doi.org/10.2337/dc23-S003 .
Shi C, Zhu H, Liu J, Zhou J, Tang W. Barriers to self-management of Type 2 diabetes during COVID-19 medical isolation: a qualitative study. Diabetes Metab Syndr Obes: Targets Ther. 2020;13:3713–25. https://doi.org/10.2147/DMSO.S268481 .
Article Google Scholar
•• American Diabetes Association Professional Practice. A.5. Facilitating Behavior Change and Well-being to Improve Health Outcomes: Standards of Medical Care in Diabetes-2021. Diabetes Care. 2021;44(Suppl 1):S53-S72. https://doi.org/10.2337/dc21-S005 . Discusses key recommendations for improving outcomes in T2DM through behavior change and evaluates the evidence supporting each recommendation.
Powers MA, Bardsley JK, Cypress M, Funnell MM, Harms D, Hess-Fischl A, et al. Diabetes self-management education and support in adults with type 2 diabetes: a consensus report of the american diabetes association, the association of diabetes care & education specialists, the academy of nutrition and dietetics, the american academy of family physicians, the American academy of PAs, the American association of nurse practitioners, and the American pharmacists association. Diabetes Educ. 2020;46(4):350–69. https://doi.org/10.1177/0145721720930959 .
Article PubMed Google Scholar
Rose KJ, Scibilia R. The COVID19 pandemic - perspectives from people living with diabetes. Diabetes Res Clin Pract. 2021;173:108343. https://doi.org/10.1016/j.diabres.2020.108343 .
Article CAS PubMed Google Scholar
Singh AK, Khunti K. COVID-19 and diabetes. Annu Rev Med. 2022;73:129–47. https://doi.org/10.1146/annurev-med-042220-011857 .
Dennis CL. Peer support within a health care context: a concept analysis. Int J Nurs Stud. 2003;40(3):321–32. https://doi.org/10.1016/s0020-7489(02)00092-5 .
Heisler M, Halasyamani L, Resnicow K, Neaton M, Shanahan J, Brown S, et al. “I am not alone”: the feasibility and acceptability of interactive voice response-facilitated telephone peer support among older adults with heart failure. Congest Heart Fail. 2007;13(3):149–57. https://doi.org/10.1111/j.1527-5299.2007.06412.x .
Skinner TC, Joensen L, Parkin T. Twenty-five years of diabetes distress research. Diabet Med. 2020;37(3):393–400. https://doi.org/10.1111/dme.14157 .
Daniels AS, Bergeson S, Myrick KJ. Defining Peer Roles and Status Among Community Health Workers and Peer Support Specialists in Integrated Systems of Care. Psychiatr Serv. 2017;68(12):1296–8. https://doi.org/10.1176/appi.ps.201600378 .
• Azmiardi A, Murti B, Febrinasari RP, Tamtomo DG. The effect of peer support in diabetes self-management education on glycemic control in patients with type 2 diabetes: a systematic review and meta-analysis. Epidemiology and health. 2021;43:e2021090. https://doi.org/10.4178/epih.e2021090 . A review of the effectiveness of diabetes self-management education interventions with integrated peer support on glycemic control in patients with T2DM.
Liang D, Jia R, Zhou X, Lu G, Wu Z, Yu J, et al. The effectiveness of peer support on self-efficacy and self-management in people with type 2 diabetes: A meta-analysis. Patient Educ Couns. 2021;104(4):760–9. https://doi.org/10.1016/j.pec.2020.11.011 .
Izzo R, Pacella D, Trimarco V, Manzi MV, Lombardi A, Piccinocchi R, et al. Incidence of type 2 diabetes before and during the COVID-19 pandemic in Naples, Italy: a longitudinal cohort study. EClinicalMedicine. 2023;66:102345. https://doi.org/10.1016/j.eclinm.2023.102345 .
Sujan MSH, Tasnim R, Islam MS, Ferdous MZ, Apu MAR, Musfique MM, et al. COVID-19-specific diabetes worries amongst diabetic patients: The role of social support and other co-variates. Prim Care Diabetes. 2021;15(5):778–85. https://doi.org/10.1016/j.pcd.2021.06.009 .
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906. https://doi.org/10.1016/j.ijsu.2021.105906 .
Dale JR, Williams SM, Bowyer V. What is the effect of peer support on diabetes outcomes in adults? Syst Rev Diabet Med. 2012;29(11):1361–77. https://doi.org/10.1111/j.1464-5491.2012.03749.x .
Article CAS Google Scholar
Kirsh SR, Aron DC, Johnson KD, Santurri LE, Stevenson LD, Jones KR, et al. A realist review of shared medical appointments: How, for whom, and under what circumstances do they work? BMC Health Serv Res. 2017;17(1):113. https://doi.org/10.1186/s12913-017-2064-z .
• Heisler M, Burgess J, Cass J, Chardos JF, Guirguis AB, Strohecker LA, et al. Evaluating the Effectiveness of Diabetes Shared Medical Appointments (SMAs) as Implemented in Five Veterans Affairs Health Systems: a Multi-site Cluster Randomized Pragmatic Trial. Journal of general internal medicine. 2021;36(6):1648–55. https://doi.org/10.1007/s11606-020-06570-y . Multi-site RCT that examined the effects of implementing SMAs on glycemic control and other metabolic outcomes in more than 1500 patients with T2DM.
Lopez Sanchez GF, Lopez-Bueno R, Villasenor-Mora C, Pardhan S. Comparison of diabetes mellitus risk factors in Mexico in 2003 and 2014. Front Nutr. 2022;9:894904. https://doi.org/10.3389/fnut.2022.894904 .
Rosales CB, Denman CA, Bell ML, Cornejo E, Ingram M, Del Carmen Castro Vasquez M, et al. Meta Salud Diabetes for cardiovascular disease prevention in Mexico: a cluster-randomized behavioural clinical trial. Int J Epidemiol. 2021;50(4):1272–82. https://doi.org/10.1093/ije/dyab072 .
Sampson M, Clark A, Bachmann M, Garner N, Irvine L, Howe A, et al. Effects of the Norfolk diabetes prevention lifestyle intervention (NDPS) on glycaemic control in screen-detected type 2 diabetes: a randomised controlled trial. BMC Med. 2021;19(1):183. https://doi.org/10.1186/s12916-021-02053-x .
Article CAS PubMed PubMed Central Google Scholar
Vongmany J, Luckett T, Lam L, Phillips JL. Family behaviours that have an impact on the self-management activities of adults living with Type 2 diabetes: a systematic review and meta-synthesis. Diabet Med. 2018;35(2):184–94. https://doi.org/10.1111/dme.13547 .
Bennich BB, Roder ME, Overgaard D, Egerod I, Munch L, Knop FK, et al. Supportive and non-supportive interactions in families with a type 2 diabetes patient: an integrative review. Diabetol Metab Syndr. 2017;9:57. https://doi.org/10.1186/s13098-017-0256-7 .
Nelson LA, Spieker AJ, Greevy RA Jr, Roddy MK, LeStourgeon LM, Bergner EM, et al. Glycemic outcomes of a family-focused intervention for adults with type 2 diabetes: Main, mediated, and subgroup effects from the FAMS 2.0 RCT. Diabetes Res Clin Pract. 2023;206:110991. https://doi.org/10.1016/j.diabres.2023.110991 .
Rosland AM, Piette JD, Trivedi R, Lee A, Stoll S, Youk AO, et al. Effectiveness of a Health Coaching Intervention for Patient-Family Dyads to Improve Outcomes Among Adults With Diabetes: A Randomized Clinical Trial. JAMA Netw Open. 2022;5(11):e2237960. https://doi.org/10.1001/jamanetworkopen.2022.37960 .
Tang TS, Afshar R, Elliott T, Kong J, Gill S. From clinic to community: a randomized controlled trial of a peer support model for adults with type 2 diabetes from specialty care settings in British Columbia. Diabet Med. 2022;39(11):e14931. https://doi.org/10.1111/dme.14931 .
Tang TS, Sidhu R, Halani K, Elliott T, Sohal P, Garg A. Participant-directed intervention tailoring is associated with improvements in glycemic control for South Asian adults with type 2 diabetes. Can J Diabetes. 2022;46(3):287–93. https://doi.org/10.1016/j.jcjd.2021.11.003 .
Jeet G, Thakur JS, Prinja S, Singh M. Community health workers for non-communicable diseases prevention and control in developing countries: Evidence and implications. PLoS ONE. 2017;12(7):e0180640. https://doi.org/10.1371/journal.pone.0180640 .
Hunt CW, Grant JS, Appel SJ. An integrative review of community health advisors in type 2 diabetes. J Community Health. 2011;36(5):883–93. https://doi.org/10.1007/s10900-011-9381-7 .
Gyawali B, Neupane D, Vaidya A, Sandbaek A, Kallestrup P. Community-based intervention for management of diabetes in Nepal (COBIN-D trial): study protocol for a cluster-randomized controlled trial. Trials. 2018;19(1):579. https://doi.org/10.1186/s13063-018-2954-3 .
Gyawali B, Sharma R, Mishra SR, Neupane D, Vaidya A, Sandbæk A, et al. Effectiveness of a female community health volunteer-delivered intervention in reducing blood glucose among adults with type 2 diabetes: an open-label, cluster randomized clinical trial. JAMA Netw Open. 2021;4(2):e2035799. https://doi.org/10.1001/jamanetworkopen.2020.35799 .
Vaughan EM, Hyman DJ, Naik AD, Samson SL, Razjouyan J, Foreyt JP. A Telehealth-supported, Integrated care with CHWs, and MEdication-access (TIME) Program for Diabetes Improves HbA1c: a Randomized Clinical Trial. J Gen int med. 2021;36(2):455–63. https://doi.org/10.1007/s11606-020-06017-4 .
Andreae SJ, Andreae LJ, Cherrington AL, Richman JS, Johnson E, Clark D, et al. Peer coach delivered storytelling program improved diabetes medication adherence: a cluster randomized trial. Contemp Clin Trials. 2021;104:106358. https://doi.org/10.1016/j.cct.2021.106358 .
Andreae SJ, Andreae LJ, Cherrington A, Richman J, Safford M. Peer coach delivered storytelling program for diabetes medication adherence: Intervention development and process outcomes. Contemp Clin Trials Commun. 2020;20:100653. https://doi.org/10.1016/j.conctc.2020.100653 .
Carrillo de Albornoz S, Sia KL, Harris A. The effectiveness of teleconsultations in primary care: systematic review. Fam Pract. 2022;39(1):168–82. https://doi.org/10.1093/fampra/cmab077 .
Mitchell SE, Bragg A, De La Cruz BA, Winter MR, Reichert MJ, Laird LD, et al. Effectiveness of an immersive telemedicine platform for delivering diabetes medical group visits for African American, black and hispanic, or latina women with uncontrolled diabetes: the women in control 20 noninferiority randomized clinical trial. J Med Internet Res. 2023;25:e43669. https://doi.org/10.2196/43669 .
Peimani M, Monjazebi F, Ghodssi-Ghassemabadi R, Nasli-Esfahani E. A peer support intervention in improving glycemic control in patients with type 2 diabetes. Patient Educ Couns. 2018;101(3):460–6. https://doi.org/10.1016/j.pec.2017.10.007 .
Bandura A. Health promotion by social cognitive means. Health Educ Behavior. 2004;31(2):143–64. https://doi.org/10.1177/1090198104263660 .
Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55(1):68–78. https://doi.org/10.1037//0003-066x.55.1.68 .
Ryan RM, Patrick H, Deci EL, Williams GC. Facilitating health behaviour change and its maintenance: Interventions based on Self-Determination Theory. Eur Health Psychol. 2008;10(March):2–5.
Google Scholar
Watson E. The mechanisms underpinning peer support: a literature review. J Ment Health. 2019;28(6):677–88. https://doi.org/10.1080/09638237.2017.1417559 .
Kotera Y, Llewellyn‑Beardsley J, Charles A, Slade M. Common Humanity as an Under‑acknowledged Mechanism for Mental Health Peer Support. International Journal of Mental Health and Addiction. First published online September 19, 2022. https://doi.org/10.1007/s11469-022-00916-9 .
Alasiri E, Bast D, Kolts RL. Using the implicit relational assessment procedure (IRAP) to explore common humanity as a dimension of self-compassion. J Contextual Behav Sci. 2019;14:65–72. https://doi.org/10.1016/j.jcbs.2019.09.004 .
Horigan G, Davies M, Findlay-White F, Chaney D, Coates V. Reasons why patients referred to diabetes education programmes choose not to attend: a systematic review. Diabet Med. 2017;34(1):14–26. https://doi.org/10.1111/dme.13120 .
Lu S, Leduc N, Moullec G. Type 2 diabetes peer support interventions as a complement to primary care settings in high-income nations: a scoping review. Patient Educ Couns. 2022;105(11):3267–78. https://doi.org/10.1016/j.pec.2022.08.010 .
World Health Organization (WHO). Coronavirus disease (COVID-19) pandemic: Overview 2024 [4/14/24]. Available from: https://www.who.int/europe/emergencies/situations/covid-19 . Accessed 17 May 2024.
Download references
No funding was received to assist with the preparation of this manuscript.
Author information
Authors and affiliations.
Department of Family Medicine and Community Health, Case Western Reserve University, Cleveland, OH, 44106, USA
James J. Werner, Kelsey Ufholz & Prashant Yamajala
Department of Family Medicine and Community Health, University Hospitals Cleveland Medical Center, Cleveland, OH, 44106, USA
Department of Psychiatry, Case Western Reserve University, Cleveland, OH, 44106, USA
James J. Werner
Center for Community Health Integration, Case Western Reserve University, Cleveland, OH, 44106, USA
Mandel School of Applied Social Sciences, Case Western Reserve University, Cleveland, OH, 44106, USA
You can also search for this author in PubMed Google Scholar
Contributions
JJW wrote the main manuscript. KU and PY provided editing and feedback and reviewed the final manuscript.
Corresponding author
Correspondence to James J. Werner .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Werner, J.J., Ufholz, K. & Yamajala, P. Recent Findings on the Effectiveness of Peer Support for Patients with Type 2 Diabetes. Curr Cardiovasc Risk Rep 18 , 65–79 (2024). https://doi.org/10.1007/s12170-024-00737-6
Download citation
Accepted : 22 April 2024
Published : 21 May 2024
Issue Date : May 2024
DOI : https://doi.org/10.1007/s12170-024-00737-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Peer support
- Type 2 diabetes
- Peer coaches
- Community health workers
- Find a journal
- Publish with us
- Track your research
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Augmenting Traditional Support Groups for Adolescents With Type 1 Diabetes Using Instagram: Mixed Methods Feasibility Study
Affiliations.
- 1 Department of Pediatrics, University of Washington, Seattle, WA, United States.
- 2 Seattle Children's Research Institute, Seattle, WA, United States.
- PMID: 34673527
- PMCID: PMC8569531
- DOI: 10.2196/21405
Background: In-person support groups have been shown to benefit adolescents with type 1 diabetes (T1D) by helping to decrease perceived diabetes burden and improving knowledge related to chronic disease management. However, barriers exist to participation in traditional support groups, including the timing and location of meetings and resources needed to attend. Adolescents are increasingly utilizing online support groups, which may provide solutions to some of the challenges faced when implementing in-person support groups.
Objective: The purpose of this study was to assess the feasibility and acceptability of a hybrid support group model where traditional in-person support groups were augmented with Instagram participation between monthly support group sessions for adolescents with T1D.
Methods: Participants (13-18 years old with T1D for ≥6 months) were asked to post photos each week for 3 months based on predetermined topics related to diabetes management. At the end of each month, participants attended an in-person support group to discuss their photos using the Photovoice method. Feasibility was assessed through enrollment and retention, number of Instagram posts, poststudy questionnaire, and a template analysis of the focus groups.
Results: Of 24 eligible participants, 16 (67%) enrolled in the study, with 3 dropping out prior to support group participation. The number of photos posted over 3 months ranged from 14 to 41. Among the 11 participants who completed a follow-up questionnaire, the majority of participants (6/11, 55%) reported that they very much enjoyed participating in the hybrid support group, and more than three-quarters (9/11, 82%) of participants reported that they "related to the photos posted." Over half of participants (8/11, 73%) reported "learning something new from the photos posted," which arose from sharing knowledge and experiences related to navigating the common challenges of diabetes management. Additionally, the use of Instagram posts helped facilitate peer discussions during the in-person support groups.
Conclusions: The novel combination of using Instagram to augment traditional in-person support groups was feasible and acceptable to adolescents with T1D. The overall satisfaction with the hybrid support group model, combined with the observed engagement with peers between support group sessions over social media, suggests that a hybrid support group model may have the potential to provide more pronounced benefits to adolescents than in-person meetings alone. Future research should investigate the use of social media as part of the support group model and examine the potential improvement of self-esteem, benefit-finding, and social support using validated tools in adolescents with diabetes.
Keywords: adolescent; diabetes mellitus, type 1; self-help groups; social media.
©Faisal S Malik, Cara Lind, Sarah Duncan, Connor Mitrovich, Michael Pascual, Joyce P Yi-Frazier. Originally published in JMIR Diabetes (https://diabetes.jmir.org), 21.10.2021.
PubMed Disclaimer
Conflict of interest statement
Conflicts of Interest: None declared.
Number of Instagram posts between…
Number of Instagram posts between support groups.
Example post of a participant…
Example post of a participant “relating to the Instagram post” at a support…
Example post of a participant “learning something new from the photos posted” at…
Example post with text caption…
Example post with text caption facilitating peer discussions at a support group.
Similar articles
- Feedback on Instagram posts for a gestational weight gain intervention. Waring ME, Pagoto SL, Moore Simas TA, Heersping G, Rudin LR, Arcangel K. Waring ME, et al. Transl Behav Med. 2022 May 25;12(4):568-575. doi: 10.1093/tbm/ibac001. Transl Behav Med. 2022. PMID: 35191497 Free PMC article.
- An intervention to improve the quality of life in children of parents with serious mental illness: the Young SMILES feasibility RCT. Abel KM, Bee P, Gega L, Gellatly J, Kolade A, Hunter D, Callender C, Carter LA, Meacock R, Bower P, Stanley N, Calam R, Wolpert M, Stewart P, Emsley R, Holt K, Linklater H, Douglas S, Stokes-Crossley B, Green J. Abel KM, et al. Health Technol Assess. 2020 Nov;24(59):1-136. doi: 10.3310/hta24590. Health Technol Assess. 2020. PMID: 33196410 Free PMC article. Clinical Trial.
- Can Instagram be used to deliver an evidence-based exercise program for young women? A process evaluation. Curtis RG, Ryan JC, Edney SM, Maher CA. Curtis RG, et al. BMC Public Health. 2020 Oct 6;20(1):1506. doi: 10.1186/s12889-020-09563-y. BMC Public Health. 2020. PMID: 33023559 Free PMC article. Clinical Trial.
- Behavioral and Pharmacotherapy Weight Loss Interventions to Prevent Obesity-Related Morbidity and Mortality in Adults: An Updated Systematic Review for the U.S. Preventive Services Task Force [Internet]. LeBlanc EL, Patnode CD, Webber EM, Redmond N, Rushkin M, O’Connor EA. LeBlanc EL, et al. Rockville (MD): Agency for Healthcare Research and Quality (US); 2018 Sep. Report No.: 18-05239-EF-1. Rockville (MD): Agency for Healthcare Research and Quality (US); 2018 Sep. Report No.: 18-05239-EF-1. PMID: 30354042 Free Books & Documents. Review.
- [A group cognitive behavioral intervention for people registered in supported employment programs: CBT-SE]. Lecomte T, Corbière M, Lysaker PH. Lecomte T, et al. Encephale. 2014 Jun;40 Suppl 2:S81-90. doi: 10.1016/j.encep.2014.04.005. Epub 2014 Jun 16. Encephale. 2014. PMID: 24948482 Review. French.
- Contrasting Social Media Use Between Young Adults With Inflammatory Bowel Disease and Type 1 Diabetes: Cross-sectional Study. Rajanala S, Wilson JK, Mitchell PD, Garvey KC, Fishman LN. Rajanala S, et al. JMIR Pediatr Parent. 2022 Apr 25;5(2):e34466. doi: 10.2196/34466. JMIR Pediatr Parent. 2022. PMID: 35139484 Free PMC article.
- Borus J, Laffel L. Adherence challenges in the management of type 1 diabetes in adolescents: prevention and intervention. Curr Opin Pediatr. 2010;22(4):405–41. doi: 10.1097/mop.0b013e32833a46a7. - DOI - PMC - PubMed
- Palladino DK, Helgeson VS. Friends or foes? A review of peer influence on self-care and glycemic control in adolescents with type 1 diabetes. Journal of Pediatric Psychology. 2012 Mar 29;37(5):591–603. doi: 10.1093/jpepsy/jss009. - DOI - PMC - PubMed
- Foster NC, Beck RW, Miller KM, Clements MA, Rickels MR, DiMeglio LA, Maahs DM, Tamborlane WV, Bergenstal R, Smith E, Olson BA, Garg SK. State of type 1 diabetes management and outcomes from the T1D exchange in 2016–2018. Diabetes Technology and Therapeutics. 2019 Feb;21(2):66–72. doi: 10.1089/dia.2018.0384. - DOI - PMC - PubMed
- Diabetes Control and Complications Trial Research Group Effect of intensive diabetes treatment on the development and progression of long-term complications in adolescents with insulin-dependent diabetes mellitus: Diabetes Control and Complications Trial. The Journal of Pediatrics. 1994 Aug;125(2):177–188. doi: 10.1016/s0022-3476(94)70190-3. - DOI - PubMed
- White NH, Cleary PA, Dahms W, Goldstein D, Malone J, Tamborlane WV. Beneficial effects of intensive therapy of diabetes during adolescence: outcomes after the conclusion of the Diabetes Control and Complications Trial (DCCT) J Pediatr. 2001 Dec;139(6):804–12. doi: 10.1067/mpd.2001.118887.S0022347601604542 - DOI - PubMed
Related information
Grants and funding.
- K23 DK119465/DK/NIDDK NIH HHS/United States
- UL1 TR000423/TR/NCATS NIH HHS/United States
LinkOut - more resources
Full text sources.
- Europe PubMed Central
- JMIR Publications
- PubMed Central
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

- Previous Article
- Next Article
Findings from a Diabetes Support Group—A Pilot Study
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Cite Icon Cite
- Get Permissions
LORI MCLEER MALONEY , JEREMY FLOOD , NAJI ALAMUDDIN , MONA AL MUKADDAM; Findings from a Diabetes Support Group—A Pilot Study. Diabetes 1 July 2018; 67 (Supplement_1): 720–P. https://doi.org/10.2337/db18-720-P
Download citation file:
- Ris (Zotero)
- Reference Manager
Purpose: Diabetes Self-Management Education (DSME) is a crucial aspect of treating type 2 diabetes mellitus (T2DM). Daily individual decisions affect patient health, well-being, and long term outcomes. This pilot study evaluated what best educates and motivates patients to improve glucose control.
Method: 17 participants with T2DM were recruited from Penn Rodebaugh Diabetes Center to attend 3 monthly diabetes support group meetings, and receive American Association of Diabetes Educators education. Weight and hemoglobin A1C (A1C) were measured at baseline and completion. Fitbit Activity Trackers were provided, as well as bi-weekly communication to reinforce behavior change. Pre and post-study surveys assessed nutrition, activity, monitoring blood glucose, and taking medication. Two sided paired t-test was performed to compare change in A1C and weight. A type I error rate of 0.was used for statistical significance.
Results: 15 participants completed the study. DSME interventions resulted in a statistically significant decrease in mean A1C from 8.5% to 7.7% with a mean A1C reduction of 0.8% in 3 months (p-value=0.01). Mean weight decreased 4.80 lb (p-value=0.0001). 11 remained on same medications, and 1 required reduced insulin. 3 added a glucagon-like peptide receptor agonist (GLP-1RA), with 1 adding a sodium-glucose cotransporter-2 inhibitor. 7 increased daily steps wearing Fitbit, while 8 reported no motivation. 10 increased weekly exercise, and 11 increased daily activity. All benefited from bi-weekly reinforcement, and reported improved nutrition. Food replica models aided visual reinforcement.
Conclusion: DSME in a group setting can motivate self-care and reduce both A1C and weight, however, the study met challenges. Time per patient spent coordinating was substantial. Food models and phone communication to reinforce lifestyle modification were useful. Research is needed to determine what provides long-term sustainability in a busy clinical practice.
L. McLeer Maloney: None. J. Flood: None. N. Alamuddin: Consultant; Self; Novo Nordisk Inc.. M. Al Mukaddam: None.
Email alerts
- Online ISSN 1939-327X
- Print ISSN 0012-1797
- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Thanks for visiting! GoodRx is not available outside of the United States. If you are trying to access this site from the United States and believe you have received this message in error, please reach out to [email protected] and let us know.
Diabetes Support Resources
Diabetes Support provides ongoing support to people with diabetes to maintain and reinforce upon the skills knowledge, and lifestyle changes gained from Recognized Diabetes Self-Management Education and Support (DSMES) services . Diabetes Support is a great way for patients to connect with resources in their community. We hope the resources below will be useful to both you and your patients/clients.
Education Recognition Programs
The ADA’s recognized DSMES programs help individuals gain the knowledge, skills, and confidence to thrive with diabetes. The program’s certified educators are ready to work with you to find practical solutions that fit your personal needs. Visit www.diabetes.org/findaprogram to find a location near you.
Diabetes Support Toolkit
The purpose of this Diabetes Support toolkit is to provide information and guidance that will help providers and educators meet the National Standards for Diabetes Self-Management Education and Support (DSMES), specifically Standard 8, Ongoing Support.
Diabetes Support Plan
This Diabetes Support Plan can be used by providers and educators to personalize and identify local resources and activities as part of ongoing diabetes support.
Ask the Experts
Ask the Experts is a free Q&A series created to help tackle issues commonly faced by people living with diabetes and wondering about the relationship between diabetes, heart disease and stroke. Individuals can ask their questions—online or on the phone—in a live Q&A with ADA diabetes experts.
Diabetes Food Hub
Diabetes Food Hub is a cooking and recipe destination made for people living with diabetes and their families. The Diabetes Food Hub includes an interactive Meal Planner, editable Grocery List tool and Healthy Tips from ADA food and nutrition experts.
Diabetes Placemats Our Diabetes Placemats provide a simple guide to planning meals and managing portions. The diabetes placemats are a great resource for health educators and patients. The sample pack of seven different diabetes placemats include: Classic, Southern, Hispanic, Vegetarian, Asian, Indian, and Pacific Islander.
Living with Type 2 Diabetes Program
Through this free year-long program available in English and Spanish, participants receive guidance on emotional well-being, healthy eating, getting active, and more. Participants receive six informational digital packages, a monthly e-newsletter with tips and resources and opportunities to find support from others living with diabetes.
Patient Education Library
Our Patient Education Library has more than 170 free downloadable or printable PDF materials on a range of diabetes-related topics. We encourage you to share these with your patients/clients. Materials are available in Arabic, Chinese, English, French, Haitian Creole, Korean, Portuguese, Russian, Spanish, Tagalog, and Vietnamese.
All information on this website is provided for information purposes only. The information was updated and current as of January 2022, and is subject to future changes without prior notice.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Diabetes Support Groups
Defeat diabetes foundation, american diabetes association, beyond type 2, carenity: type 2 diabetes community, diabetessisters, diabetes daily, frequently asked questions.
By 2030, it is estimated that globally over 500 million people will be living with type 2 diabetes .
Receiving a diagnosis of type 2 diabetes and learning to manage your condition can be overwhelming and confusing. People with diabetes spend an estimated 8,000 hours per year self-managing their condition in addition to the time they spend within a medical setting. Support groups can be a helpful addition to your diabetes management team, along with guidance and care from your healthcare providers.
Read on to find information on select online and in-person support groups.
photography by Kate Hiscock / Getty Images
Support groups for diabetes are not a replacement for professional medical care. It is important to research groups before joining them and always verify information received from support groups and their members.
- Membership fee : Free
- Structure : Search tool
- Details : Allows you to look for contact information by state
- Things to consider : It isn't a support group itself, but rather a tool to find a support group
Defeat Diabetes Foundation (DDF) has been in existence for more than 30 years. Its mission is to find sustainable solutions to help prevent , identify , and manage type 2 diabetes. It raises awareness of diabetes by providing research-based information to communities and individuals. DDF offers action-oriented steps everyone can take to help prevent the development of type 2 diabetes, including providing information on nutrition and exercise and sharing comprehensive resources on their website.
DDF provides outreach and helps people connect with community-based impact programs. In addition to information found on their website, they offer a sign-up newsletter and a search tool to find support groups.
- Membership fee : Varies by program
- Structure : Individual programs, online information, diabetes education
- Details : Extensive resource offering the opportunity for connecting with professionals and with peers
- Things to consider : Covers a broad scope of aspects surrounding diabetes, including education, research, legal rights, and more
The American Diabetes Association (ADA) is a large organization consisting of a network of over 565,000 volunteers (as well as families and caregivers ), more than 250 staff members, and a professional society of almost 16,000 healthcare providers.
ADA aims to prevent diabetes and improve the lives of those who are affected by diabetes. They fund research, provide services to communities, offer credible information, and advocate for the rights of those with diabetes.
The ADA runs a recognized diabetes education program facilitated by certified educators, which helps people with diabetes learn practical information about their condition and gain skills and confidence as they navigate living with diabetes. A referral from the healthcare provider managing your diabetes is needed to enter the program.
The ADA also offers an afterschool program for kids ages 5 to 12 called Project Power . The program promotes healthy lifestyle choices that can help prevent type 2 diabetes and empower children to develop healthy lifelong habits .
The program is free and offered in person or virtually. Check the website for available dates and times.
- Structure : Online community
- Details : An online platform that allows you to connect with other people affected by type 2 diabetes, find resources, ask questions, have discussions, etc. Available in English and Spanish.
- Things to consider : You request to join by answering two questions (why you want to join and where you heard about them), then wait for approval
Beyond Type 2 is a program that stems from the nonprofit organization Beyond Type 1. Beyond Type 1 was founded in 2015 and launched Beyond Type 2 in 2019.
Beyond Type 2 provides a platform for people with type 2 diabetes to connect online with a community in which they can ask questions, share experiences, exchange ideas and resources, and more. The program is available in both English and Spanish.
Beyond Type 2 is supported by a partnership between The American Diabetes Association and Beyond Type 1.
- Structure : Online forum
- Details : An online forum where members can ask for advice, seek and give support, and discuss topics surrounding diagnosis, treatment, and diet
- Things to consider : Carenity is a general site for many health conditions. The type 2 diabetes forum is one community within the greater site
Carenity is an online community that offers a social network through a newsfeed, discussion forums, private messaging, and more.
Under the Carenity umbrella, there is a section specifically for people with type 2 diabetes .
- Structure : Online forum, online and in-person meet-ups
- Details : Peer support and education for individuals with all forms of diabetes
- Things to consider : This resource is for women only
Founded in 2008, DiabetesSisters is an organization managed by women with diabetes that offers education and support services to help women living with diabetes thrive. Peer support is a core component of the organization.
DiabetesSisters has an online forum through which women with diabetes can connect with each other.
DiabetesSisters also has a program called Part of DiabetesSisters (PODS) Meetups for women age 18 and up who are living with any type of diabetes, including prediabetes . You can look at the spotlight list on their meetups page, check their event calendar , or complete a PODS interest form to connect with a meetup.
- Details : A collection of discussion boards separated by category
- Things to consider : This site consists of discussions between members only, not expert advice
TuDiabetes is an online community for people with all types of diabetes . It is a program through the nonprofit organization Beyond Type 1 and is sponsored by the Diabetes Hands Foundation. As of 2014, it had more than 35,000 registered members.
Content on the message boards is curated by members and should not be used as a primary source of information but as a place to start your search or as a complement to expert advice.
- Details : Discussion boards separated by topic
- Things to consider : The website and its forums address all types of diabetes, so you will need to look specifically for topics and information that pertain to type 2 diabetes
Diabetes Daily was founded in 2005 after one of its founders was diagnosed with type 1 diabetes and saw a need for community-based support for people living with diabetes.
Diabetes Daily has online forums through its website and also helps people connect through Facebook, Twitter, and email. Their online community is made up of almost 1 million members.
The Diabetes Daily website posts information about diabetes , including recipes .
Online vs. Local Groups
Both online and in-person local diabetes groups foster a community that includes aspects such as:
- Peer support
- Self-expression
- Sharing information
- Seeking and giving advice
Some benefits of an online support group include:
- Easier access
- More flexibility in terms of when and how the community is accessed
- An opportunity for anonymity for those who want it
- The ability to quietly observe without participating for those not ready to share
- Cost-effectiveness
There can be downsides to online support groups as well, such as:
- High access to misinformation, some of which can be harmful
- Potential privacy and security risks
- Less personal
- Greater potential for harassment and bad behavior due to “the online disinhibition effect"
In-person support groups can be more difficult to plan as they require a venue (such as places of worship, classrooms, or community centers) and occur on a schedule that must be worked into the participants' calendars.
While less convenient, some people may prefer in-person groups as they allow for a more personal face-to-face connection. They can also foster relationships with local people who may have common interests outside of their condition. In-person groups also provide the opportunity for social activities and guest speakers.
Support groups can help people with type 2 diabetes connect with others who have the same condition. These groups allow for peer support, sharing information and resources, venting frustration, offering encouragement, and more.
Support groups can exist in-person or online (such as on online forums or social media).
Information found in support groups is not always accurate and should be verified. Support groups are not a substitute for professional medical care.
A Word From Verywell
Whether you have just received a diagnosis, or have been living with type 2 diabetes for a while, you may find a support group beneficial.
Do your research before joining an in-person or online group to make sure they are a credible resource, and talk to your healthcare provider before applying the medical advice you receive from other members.
Looking at credible diabetes organizations such as the American Diabetes Association and Beyond Type 1/Beyond Type 2 is a good start. Check the community links on these websites for online forums or links to support groups.
There are a number of ways you can help support someone with diabetes, including:
- Educating yourself on their condition
- Seeing them as an individual with unique needs
- Attending their appointments (if they want you to)
- Asking what they need and listening to what they say
- Recognizing that managing diabetes can be time-consuming and allowing time for checking blood sugar and other necessary procedures during your plans together
- Respecting their boundaries and not expecting them to share everything about their condition or experience with you
- Understanding that changes in blood sugar can cause mood shifts
- Engaging in the same lifestyle choices and activities they are, such as a healthful diet and physical activity
- Knowing how to recognize the signs of low blood sugar and what to do about it
Beyond Type 2. Home .
Litchman ML, Walker HR, Ng AH, et al. State of the science: a scoping review and gap analysis of diabetes online communities . J Diabetes Sci Technol . 2019;13(3):466-492. doi:10.1177/1932296819831042
Hilliard ME, Sparling KM, Hitchcock J, Oser TK, Hood KK. The emerging diabetes online community . Curr Diabetes Rev. 2015;11(4):261-272. doi:10.2174/1573399811666150421123448
Defeat Diabetes Foundation. The tools you need to win the fight to defeat diabetes .
American Diabetes Association. Home .
Carenity. Diabetes (type 2) forum .
DiabetesSisters. Home .
TuDiabetes. Home .
Diabetes Daily. Welcome to Diabetes Daily!
Herrero N, Guerrero-Solé F, Mas-Manchón L. Participation of patients with type 2 diabetes in online support groups is correlated to lower levels of diabetes self-management . J Diabetes Sci Technol . 2021;15(1):121-126. doi:10.1177/1932296820909830
diaTribe. How and where to find in-person support groups and social activities for young adults with diabetes .
Centers For Disease Control and Prevention. Friends, family & diabetes .
By Heather Jones Jones is a freelance writer with a strong focus on health, parenting, disability, and feminism.

Defeat Diabetes Foundation
Diabetes Support Groups
Facing a diabetes diagnosis, whether it’s you, a cherished individual, or a family member, can lead to feelings of being swamped. Engaging in a diabetes support group represents a proactive strategy for discovering assistance, guidance, insights, and resources, forming an integral component of managing diabetes holistically.
If you’re seeking a diabetes support group in the United States to assist you in handling your diabetes, we encourage you to commence your search with the details provided below. Just click one of the buttons to locate a diabetes support group within your state.
Have a diabetes support group you would like to list on our directory? Please send your information to: [email protected]
Knowledge is power, and action taken from that knowledge produces results. We invite you to explore our site and arm yourself with the important knowledge and support you need to prevent diabetes, manage the disease, and better understand the connection diabetes has to the health of our planet.
Understanding Diabetes
Diabetes risk factors, healthful eating, active and mindful lifestyle, global awareness and responsibility, research explained.
- Overview & Types
- Symptoms & Diagnosis
- Understanding Blood Sugar
- Diet & Exercise
- Better Living
- Complications
- Related Conditions
- Symptoms & Causes
- Diagnosis & Tests
- Prevention & Treatment
- Living & Managing
- Complications & Related Diseases
- Treating & Managing
- Complications & Related Conditions
- Gestational Diabetes
- Appointment Prep
- View Full Guide
Where to Find More Diabetes Resources

Looking for organizations that provide information that can help you manage your diabetes? You may want to start with these groups.
Health Organizations
Academy of Nutrition and Dietetics (formerly the American Dietetic Association) 120 South Riverside Plaza, Suite 2000 Chicago, IL 60606-6995 800-877-1600 www.eatright.org
American Association of Clinical Endocrinologists (AACE) 245 Riverside Avenue, Suite 200 Jacksonville, FL 32202 (904) 353-7878 www.aace.com
American Diabetes Association (ADA) 2451 Crystal Drive, Suite 900 Arlington, VA 22202 800-342-2383 www.diabetes.org
American Association of Diabetes Educators (AADE) 125 S. Wacker, Suite 600 Chicago, IL 60606 800-338-3633 www.diabeteseducator.org
Juvenile Diabetes Research Foundation International (JDRF) 200 Vesey St New York, NY 10281 800-533-2873 www.jdrf.org
National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) 9000 Rockville Pike Bethesda, MD 20892 (301) 496-3583 https://www2.niddk.nih.gov/
Diabetes Journals/Newsletters/Social Networks
TypeOneNation
Juvenile Diabetes Research Foundation International
typeonenation.org
Diabetes Forecast: The Healthy Living Magazine
from the American Diabetes Association https://www.diabetesforecast.org/
MyFoodAdvisor: Recipes for Healthy Living
from the American Diabetes Association
https://www.diabetes.org/food-and-fitness/food/myfoodadvisor.html

Top doctors in ,
Find more top doctors on, related links.
- Diabetes Health Center News
- Diabetes Health Center Reference
- Diabetes Health Center Slideshows
- Diabetes Health Center Quizzes
- Diabetes Blogs
- Diabetes Health Center Videos
- Diabetes Health Center Medications
- Find an Endocrinologist
- Book: Take Control of Your Diabetes Risk
- General Diabetes
- Type 1 Diabetes
- Type 2 Diabetes
- Prediabetes
- Blood Glucose Tracker
- Blood Sugar Control
- Diabetic Neuropathy
- Eye Problems Assessment
- Heart Disease
- Living Healthy
- Metabolic Syndrome
- More Related Topics

- Message from the Chair
- Faculty & Staff Resources
- Diversity, Equity and Inclusion
- Recruitment
- How To Apply
- Coming for an Interview?
- Living in Tucson
- Facts & Figures
- Accolades & Awards
- Photo Galleries
- Media Mentions
- DOM News Archive
- Maps & Directions
- Ways to Give
- Dermatology
- Endocrinology
- Gastroenterology and Hepatology
- General Internal Medicine, Geriatrics and Palliative Medicine
- Hematology and Oncology
- Infectious Diseases
- Inpatient Medicine
- Pulmonary, Allergy, Critical Care and Sleep Medicine
- Rheumatology
- Message from the Vice Chair
- Medical Student Education
- Residency Programs
- Fellowships
- Applicant Recruitment Notice
- Where We Teach And Train
- Core & Key Clinical Faculty Guide
- Tools for Teaching
- Academic Activity Log
- Teaching Resources
- Statistical Support Initial Request Form
- Proteomics Lab
- Featured Spotlights
- Researcher Spotlights
- Research Projects
- DOM Research Seminar Series
- Publications
- Top Doctors In The News
- DOM Blog Posts
- Where We Practice
- UA Arthritis Center
- UA Asthma & Airway Disease Research Center
- UA Cancer Center
- UA Center on Aging
- UA Center for Applied Genetics & Genomic Medicine
- UA Center for Biomedical Informatics & Biostatistics
- UA Center for Disparities in Diabetes, Obesity & Metabolism
- UA Center for Integrative Medicine
- UA Center for Sleep, Circadian & Neuroscience Research
- UA Petersen HIV Clinics
- Pacific AIDS Education & Training Center – Arizona
- UA Sarver Heart Center
- UA Skin Cancer Institute
- UA Thomas D. Boyer Liver Institute
- UA Valley Fever Center for Excellence
You are here
Advancing diabetes research and serving an at-risk community.
![(From left) Teran’s family: mother Sandra Teran; nephews and nieces Johnny Gonzales, Rene Teran, Neveah Teran, Aminna Teran and Andrea Teran; Teran; and niece Amaya Teran. (Photo by Kris Hanning, UArizona Health Sciences Office of Communications) [An image of Teran with family members gathered around a table]](https://deptmedicine.arizona.edu/sites/default/files/styles/story_slide_680/public/06072024-tina_teran_family_klh2294_1200x450px.jpg?itok=yInWJ72n×tamp=1719596744)
Preparing healthy meals with her family, including niece Amaya Teran, is one of the ways Tina Teran (in red polka dot apron) manages her Type 2 diabetes. (Photo by Kris Hanning, UArizona Health Sciences Office of Communications)
Tina Teran worked in the Pima County Health Department for 10 years. She knew being overweight could damage her health, but like many people, her attempts at dieting ultimately failed. Then, a medical emergency put things in perspective.
![Tina Teran visited Universal Studios in California in 2015, before her 155 pound weight loss journey. (Photo courtesy of Tina Teran) [Candid photo of Tina Teran standing next to a minion statue at a theme park]](https://deptmedicine.arizona.edu/sites/default/files/tina_before-inline.jpg)
At the emergency department, Teran was told she was diabetic and needed an insulin shot to reduce dangerously high sugar levels. For Teran, this was the beginning of a journey to get her health under control.
More than 38 million Americans have diabetes, and 90% to 95% of them have Type 2 diabetes, according to the Centers for Disease Control and Prevention. Research shows that Hispanic people are at a higher risk of developing Type 2 diabetes than many other racial and ethnic groups.
Lawrence Mandarino, PhD , director of the Center for Disparities in Diabetes, Obesity and Metabolism at the University of Arizona Health Sciences , has been researching this condition for decades. The mission of the Center for Disparities in Diabetes, Obesity and Metabolism is to improve the health and well-being of the Hispanic and Latino population while advancing research into diabetes and other metabolic conditions
The center’s Wellness Bank, or El Banco por Salud , is central to this mission.
Using data to improve health
Type 2 diabetes involves unusually high blood sugar levels and an inability of the body to use that sugar for fuel. If left untreated, complications can include heart disease, vision loss and kidney disease.
Risk factors for Type 2 diabetes include being overweight and inactive, in addition to socio-economic, demographic, environmental and genetic influences. That’s where the Wellness Bank comes in. Its biorepository of blood, DNA specimens and patient data serves as a resource to connect academic researchers and the community.
![Preparing healthy meals with her family, including niece Amaya Teran, is one of the ways Tina Teran manages her Type 2 diabetes. (Photo by Kris Hanning, UArizona Health Sciences Office of Communications) [A Hispanic family in a kitchen preparing a healthy meal together]](https://deptmedicine.arizona.edu/sites/default/files/styles/small_image/public/06072024-tina_teran_family_klh2259-herocard_0.jpg?itok=6qF7bmih)
Teran was one of those patients.
“I was not the first person to ignore their health in my family. My mom has a very similar story to how she found out she was diabetic. I lost my sister three years ago, and she had previously suffered a heart attack before finding out she was diabetic,” she said. “I decided right there that I needed to do this. I needed to be an example for nieces, nephews, children and grandchildren. They've lost too much already.”
Teran underwent gastric bypass surgery and lost 155 pounds. She started eating a healthy diet and being more active. When she signed up for a study through the Wellness Bank, she learned another potentially lifesaving piece of information about her health.
“They would monitor my blood pressure, blood sugar and heart rate before and after walking on the treadmill. That’s where I found out I also have an irregular heartbeat,” Teran said. “I had to get a procedure done to make sure I didn’t have any blood clots. I take medication for it now.”
For people with Type 2 diabetes, or metabolic conditions that frequently lead to Type 2 diabetes, participating in the Wellness Bank offers a unique opportunity to explore their health at zero cost to them.
“Participants get all of their lab tests for free, including things like their dietary sugar control, cholesterol control, kidney function, liver function and electrolyte levels,” said Dr. Soltani. “I review each of these lab tests and it is not infrequent that I find that they do have diabetes, or out-of-control blood pressure or kidney failure. This partnership allows us to immediately follow up with them.”
Researchers and doctors benefit from increased knowledge of social and biological factors leading to poor glucose control with an emphasis on the implementation of pharmacogenomics clinical decision support.
Tracking diabetes through time
Dr. Mandarino, who also is a professor and chief of the Division Endocrinology, Diabetes and Metabolism in the Department of Medicine at the UArizona College of Medicine – Tucson , created the Arizona Insulin Resistance Registry, a precursor to the Wellness Bank, in the Phoenix area in the early 2000s.
“We were able to collect biospecimens and data from hundreds of people in the community that are still being used by researchers today, but we also learned some valuable lessons about things we wanted to do differently,” Dr. Mandarino said. “Many of our participants did not have health insurance or a primary care doctor. We realized we needed a community partner that could explain the results of different lab tests and follow up with a treatment plan if needed.”
![(From left) Lisa Soltani, MD, and Lawrence Mandarino, PhD, are collaborating to advance diabetes research and improve Latino community health through the Wellness Bank biorepository. (Photos by Kris Hanning & Noelle Haro-Gomez, UArizona Health Sciences Office of Communications) [Portrait images of Drs. Lisa Soltani and Lawrence Mandarino]](https://deptmedicine.arizona.edu/sites/default/files/soltani_mandarino_inline.jpg)
The Wellness Bank and its stores of data have helped facilitate dozens of studies. Researchers can access participant blood samples and also retrieve details about lifestyle and eating habits. Study objectives range from searching for a link between mental health and diabetes, to assessing the association between breastfeeding and metabolic syndrome, to exploring diet interventions for food insecure adults.
“In one study, we asked participants on three different days if they had eaten any fruit or vegetables that day and scored them on a healthy-eating index,” Dr. Mandarino said. “We found that low scores were associated with people who also noted that they sometimes did not have enough money to buy food. This is one example of how someone could have a genetic risk factor for Type 2 diabetes, and then socio-economic factors can have an additive effect.”
Teran says the Wellness Bank was a key part of her path to better health, and she is happy her participation might advance science and research geared to help her community.
“I am so proud of my heritage, and I have always stood up for my family and community,” she said. “I am honored to do this for them.”
Experts Lawrence Mandarino, PhD Director, Center for Disparities in Diabetes, Obesity and Metabolism, University of Arizona Health Sciences Professor, Department of Medicine, College of Medicine – Tucson Chief, Division of Endocrinology, Diabetes and Metabolism , College of Medicine – Tucson
Contact: Brian Brennan UArizona Health Sciences Office of Communications 520-621-3510, [email protected]
Original story link .
ALSO SEE: “Dr. Lawrence Mandarino Recognized with College of Medicine – Tucson Mentoring Award” | Posted July 21, 2020 “UA Health Sciences Centers Collaborate to Present Discovering New Medicines at Arizona Summit” | Posted Sept. 30, 2019 “DOM Continues to Lead U.S. News ‘Best Hospital’ List for Banner – UMC Tucson” | Posted Aug. 15, 2018 “DOM Faculty Turn Out in Force for 50th Anniversary UA College of Medicine Research Fair” | Posted Oct. 23, 2017 “UA-Led Study on How Insulin Controls Glucose Uptake Picked for Cover of Proteomics Journal” | Posted Oct. 3, 2017 “Dr. Lawrence J. Mandarino to Head new UA Center for Disparities in Diabetes, Obesity and Metabolism” | Posted April 12, 2016
- Study protocol
- Open access
- Published: 03 July 2024
A holistic lifestyle mobile health intervention for the prevention of type 2 diabetes and common mental disorders in Asian women with a history of gestational diabetes: a randomised control trial with 3-year follow-up protocol
- Alicia Salamanca-Sanabria ORCID: orcid.org/0000-0002-2756-5592 1 ,
- Seaw Jia Liew 2 ,
- Jacqueline Mair 3 , 4 , 5 ,
- Maria De Iorio 1 , 6 ,
- Young Doris Yee Ling 7 ,
- Mya Thway Tint 1 , 2 ,
- Yew Tong Wei 6 , 8 ,
- Karen Lim 9 ,
- Desmond Ong 10 ,
- Yu Chung Chooi 1 ,
- Vicky Tay 1 &
- Johan Gunnar Eriksson 1 , 2 , 11 , 12
Trials volume 25 , Article number: 443 ( 2024 ) Cite this article
121 Accesses
1 Altmetric
Metrics details
Women with a history of gestational diabetes mellitus (GDM) are 12-fold more likely to develop type 2 diabetes (T2D) 4–6 years after delivery than women without GDM. Similarly, GDM is associated with the development of common mental disorders (CMDs) (e.g. anxiety and depression). Evidence shows that holistic lifestyle interventions focusing on physical activity (PA), dietary intake, sleep, and mental well-being strategies can prevent T2D and CMDs. This study aims to assess the effectiveness of a holistic lifestyle mobile health intervention (mHealth) with post-GDM women in preventing T2D and CMDs in a community setting in Singapore.
The study consists of a 1-year randomised controlled trial (RCT) with a 3-year follow-up period. Post-GDM women with no current diabetes diagnosis and not planning to become pregnant will be eligible for the study. In addition, participants will complete mental well-being questionnaires (e.g. depression, anxiety, sleep) and their child’s socio-emotional and cognitive development. The participants will be randomised to either Group 1 (Intervention) or Group 2 (comparison). The intervention group will receive the “LVL UP App”, a smartphone-based, conversational agent-delivered holistic lifestyle intervention focused on three pillars: Move More (PA), Eat Well (Diet), and Stress Less (mental wellbeing). The intervention consists of health literacy and psychoeducational coaching sessions, daily “Life Hacks” (healthy activity suggestions), slow-paced breathing exercises, a step tracker (including brisk steps), a low-burden food diary, and a journaling tool. Women from both groups will be provided with an Oura ring for tracking physical activity, sleep, and heart rate variability (a proxy for stress), and the “HAPPY App”, a mHealth app which provides health promotion information about PA, diet, sleep, and mental wellbeing, as well as display body mass index, blood pressure, and results from the oral glucose tolerance tests. Short-term aggregate effects will be assessed at 26/27 weeks (midpoint) and a 1-year visit, followed by a 2, 3, and 4-year follow-up period.
High rates of progression of T2D and CMDs in women with post-GDM suggest an urgent need to promote a healthy lifestyle, including diet, PA, sleep, and mental well-being. Preventive interventions through a holistic, healthy lifestyle may be the solution, considering the inextricable relationship between physical and psychological health. We expect that holistic lifestyle mHealth may effectively support behavioural changes among women with a history of GDM to prevent T2D and CMDs.
Trial status
The protocol study was approved by the National Healthcare Group in Singapore, Domain Specific Review Board (DSRB) [2023/00178]; June 2023. Recruitment began on October 18, 2023.
Trial registration
ClinicalTrials.gov NCT05949957. The first submission date is June 08, 2023.
Peer Review reports
Introduction
Background and rationale {6a}.
Individuals, families, and societies worldwide are affected by diabetes. According to recent reports, one in ten adults has diabetes worldwide, accounting for 10.5% of the global population [ 1 , 2 ]. Globally, it is projected to be 700 million people with diabetes, with women being 343 million by 2045 [ 2 ]. Diabetes ranks ninth for women and eighth for men in the global ranking of disability-adjusted life years (DALYs) [ 3 , 4 ]. There is a parallel increase in obesity and type 2 diabetes (T2D) in the general population, as well as a rise in gestational diabetes mellitus (GDM) incidence [ 5 ]. GDM affects between 1 and 30% of pregnancies worldwide [ 6 ] and is particularly prevalent among Asian women [ 7 ], showing distribution in the Middle East (8.8–20.0%), Southeast (9.6–18.3) and Western Pacific (4.5–20.3%), respectively [ 6 ]. A recent report in Singapore shows that GDM prevalence is 23.5% [ 8 ]. GDM can cause pregnancy and birth complications and long-term chronic conditions such as cardiometabolic disorders and T2D in both mother and offspring [ 9 , 10 ]. Compared to women with a normoglycemic pregnancy, women with a history of GDM are more likely to develop T2D [ 11 ]. The prospective birth cohort study in Singapore, Growing Up in Singapore Towards Healthy Outcomes (GUSTO), showed that the risk of developing T2D is 12-fold higher in Singaporean women 4–6 years after their GDM diagnosis [ 12 ].
Risk factors for T2D among those with a history of GDM included greater pre-pregnancy Body Mass Index (BMI), excessive weight gain, unhealthy dietary patterns, physical inactivity, and a short period of lactation [ 13 ]. Post-natal risk, such as missing medical assistance in the continuum of GDM care after delivery, could be another risk for progression to T2D among Asian mothers with a history of GDM [ 7 ]. In terms of the pathophysiology, GDM has several similarities to T2D, namely impaired insulin sensitivity and dysfunction of the β-cell caused by the metabolic stress of pregnancy [ 5 , 14 ].
Besides T2D and cardiometabolic diseases, current literature suggests that women with a history of GDM also have a higher risk of developing common mental disorders (CMDs) (depression, anxiety) [ 15 , 16 ]. CMDs are the most common morbidity in the peripartum (during pregnancy and up to 1 year following delivery). Approximately one in five women develop CMDs during pregnancy or in the year following delivery [ 17 ], which is associated with adverse maternal and foetal outcomes as well as emotional and behavioural difficulties in the offspring [ 18 ]. Likewise, poor quality of sleep associated with gestational diabetes can pose significant health risks to both mothers and their newborns [ 19 , 20 , 21 ]. Previous studies have shown that women with GDM have shorter sleep time, less efficient sleep, and more sleep disorders and daytime dysfunction [ 19 ]. The evidence has been demonstrated that sleep disturbances can impair glucose metabolism by affecting insulin sensitivity and β-cell function, which is also associated with obesity and depression [ 20 ]. Thus, women with a history of GDM also may present poor sleep quality and CMDs. However, effective interventions that aim to improve these women’s mental well-being and sleep quality remain scarce.
A systematic review and meta-analysis about the prevention of T2D in women with previous GDM has shown that lifestyle interventions produced only a borderline reduction in T2D risk (RR 0.75, 95% CI: 0.55–1.03) [ 22 ]. The interventions did not focus on modifiable risk factors like sleep and mental well-being, which could have been addressed to improve the outcome. Observational studies suggest that approximately 45% of GDM cases might be preventable by the adoption of a healthy diet and increased physical activity (PA), including psychosocial factors (stress, anxiety, depression interventions) [ 6 , 23 , 24 , 25 ]. However, most preventative studies are undertaken in Western countries [ 21 ], and it is challenging to directly apply these strategies in Asian countries due to differences in demographics, socioeconomics, ethnicity, and cultural factors [ 7 ]. A recent systematic review study concluded that in most of the studies, the evidence-based intervention might not be culturally appropriate for the prevention of T2D in women with a history of GDM [ 13 ].
Postpartum women often report difficulty engaging with lifestyle management interventions due to several barriers [ 26 , 27 ], including multiple face-to-face sessions, travel distances, time constraints, and cost are some factors [ 26 , 28 ] that may be alleviated by technological advancements [ 29 ]. Thus, lifestyle interventions delivered through mobile health (mHealth) interventions represent a feasible, affordable and scalable solution for the prevention of T2D and CMDs among women with a history of GDM [ 30 ]. While several mHealth lifestyle intervention studies have been conducted to prevent NCDs [ 31 , 32 ] and CMDs [ 33 ] few have taken a holistic approach to improving health and mental wellbeing. The inextricable link between physical and psychological health [ 2 , 4 , 22 , 23 , 24 ] highlights the combined effects of holistic interventions integrating body and mind may have a greater total effect than any single intervention in preventing T2D and CMD [ 34 ]. The LvL UP is a scalable holistic mHealth intervention to prevent NCDs and CMDs in Asian populations [ 35 ]. The intervention has been informed by leading evidence- and theory-based frameworks in mental health [ 36 ] and behaviour change [ 36 ] to deliver motivational interviewing-inspired digital coaching via conversational agent and behavioural tools centred around three core pillars: Move More, Eat Well, Stress Less. The intervention has undergone rigorous development and refinement, including feasibility and user-centred design studies (unpublished data) to assess its technical feasibility and acceptability, but has not yet been tested for effectiveness.
Objectives {7}
This study aims to assess the effectiveness of a scalable smartphone-delivered holistic lifestyle coaching intervention for the prevention of T2D and CMDs with post-GDM Asian women from the community setting in Singapore. We have five specific objectives:
Objective 1: To carry out a 1-year randomised control trial (RCT) followed by a 3-year follow-up period with post-GDM women from the community setting in Singapore.
Objective 2: To examine the potential impacts of the proposed intervention on the health and mental well-being of women and their children.
Objective 3: To determine the diabetes risk of the participants over a 3-year follow-up period.
Objective 4: To explore the potential economic impacts of the proposed intervention (e.g. healthcare expenditures)
Objective 5: To study the importance of gut microbiota and epigenetic factors in changes in glucose metabolism.
Trial design {8}
This study is a 1-year randomised controlled trial (RCT) with 3 years of follow-up. We will conduct a two-arm single parallel assignment individually randomised equal allocation control trial on n = 400 women with a history of GDM. It will compare the aggregate effects of the Intervention group (receiving a holistic lifestyle mHealth intervention (LvLUP App), Sleep tracker, Oura ring/Oura App and psychoeducation to promote healthy lifestyle (Happy App)) and (comparison group (Happy App (psychoeducation only), Oura ring and Oura App) at 26/27 weeks, and 1-year visit. After completing the 1-year RCT period, both groups will be followed up in years 2, 3, and 4. We hypothesise that the intervention will reduce the risk of T2D/pre-diabetes and CMDs in post-GDM women.
Methods: participants, Interventions, and outcomes
Study settings {9}.
Participants are women with a history of GDM from a large community setting in Singapore.
Eligibility criteria {10}
All eligible females in this study will be (a) women between 21 and 45 years old; (b) with a history of GDM (at least 1 year and no more than 10 years); (c) Chinese, Malay, or Indian ethnicity; (d) BMI between 18.5 and 35 kg/m 2 ; (e) not planning to conceive in the next 1 year; (f) not performing exclusive breastfeeding during the study period; (g) owners of a smartphone compatible with the study mobile Apps; (h) proficient in the English language; (j)willing to comply with study protocol; and (k) able to provide written informed consent.
Exclusion criteria include (a) current or previous diagnosis of diabetes (type 1 or 2), except GDM; (b) currently pregnant; (c)given birth within the last 12 weeks; (d) severely limited mobility (e.g. wheelchair-bound, require long-term walking aid, etc.); (e) diagnosed with malnutrition or eating disorder; (f) diagnosed with cancers, unstable heart diseases, severe kidney disease, severe liver disease; (g) diagnosed with severe insomnia, unstable mental conditions, dementia, or cognitive impairment; (h) experienced alcohol or drug abuse; (i) currently having medications known to influence glucose metabolism (e.g. peroral corticosteroids); and (j) currently participating in a concurrent clinical trial or lifestyle intervention study.
Who will solicit informed consent? {26a}
Consent procedures were approved by the Domain Specific Review Board (DSRB) of the National Healthcare Group in Singapore. All potential subjects are required to sign the informed consent in order to participate in the study.
Additional consent provisions for collection and use of participant data and biological specimens in ancillary studies {26b}
There are no additional consent provisions for collecting or using biological samples. If we decide to do an ancillary study in the future, we will seek prior consent of participants to be re-contacted and re-consent for the ancillary study following DSRB approval.
Interventions
Explanation for choice of comparators {6b}.
mHealth may provide practical and scalable support to women adopting and maintaining a healthy lifestyle. The effectiveness of mHealth interventions targeting lifestyle behaviours has been demonstrated [ 31 , 34 , 37 ]. More recently, studies have supported that prevention and promotion request more than one pillar, meaning that holistic lifestyle behaviours, such as PA, diet, sleep, and mental well-being, are more effective in parallel [ 34 ]. Studies have shown that education alone is insufficient to support individuals in changing their lifestyles, and it is important to incorporate techniques and behavioural strategies that facilitate and measure the effectiveness of the interventions [ 31 , 34 , 37 ]. Therefore, we propose to compare two mHealth interventions, the intervention group (LvL UP App, Happy App, and Oura Ring) and the comparison group (HAPPY App and Oura Ring). The LvL UP App is based on evidence-based strategies and interactive tools developed in Singapore [ 35 ]. The HAPPY App is available to every eligible participant (both groups) in the trial; it provides public holistic health recommendations and displays participants’ health data measured during study visits over time. Also, the Oura ring is a sleep tracker that includes heart rate variability, and a step tracker will be provided to both groups.
Intervention description {11a}
The comparison and intervention group will be assigned to holistic lifestyle mHealth interventions. The comparison group (Happy App and Oura ring) will receive only psychoeducation to promote a healthy lifestyle through the HAPPY App and sleep tracking using an Oura ring and associated App. The Happy App was developed by the Singapore Institute for Clinical Sciences (SICS); it encompasses only educational content on lifestyles based on resources from the Singapore Health Promotion Board, including information about diet intake, physical activity, sleep, and mental well-being. The HAPPY app also displays health outcome data collected during the study visits (e.g. body weight, blood pressure, fasting glucose, and 2-h 75 g OGTT). The Oura Ring is an activity-tracking wearable that monitors physical activity, sleep, and heart rate variability, which can be synced with the Oura App.
The intervention group (LvL UP App, Happy App, and Oura Ring) will receive the same Happy App, Oura Ring and Oura App, with the additional LvL UP App version 2.0. The LvL UP App has been developed by the Future Health Technologies Programme at the Singapore ETH-Centre (SEC) for iOS and Android. It is designed to be culturally relevant in Singapore and is based on evidence-based behavioural strategies [ 35 ]. A separate paper[ 35 ] describes the conceptual model, development process, and characteristics of LvLUP version 1.0. In this study, we will use an updated 2.0. version. The LvL UP App 2.0 is a smartphone-delivered holistic lifestyle intervention focusing on three core pillars: eat well (diet), move more (PA), and stress less (mental well-being), including sleep content in each pillar delivered through a coaching health and tools paradigm.
LvL UP App: coaching health
The participants assigned to LvL UP will receive weekly motivational interview-inspired coaching sessions from a digital coach (conversational agent; CA) on topics related to the core intervention pillars. Coaching sessions are text-based dialogues between the participant and the CA based on predefined rules, and each session lasts between pillars, which are recommended in a predefined order, although participants can choose the order and topic if they wish. There are eight coaching sessions per pillar, which are recommended in a predefined order, although participants can choose the order and topic if they wish. The participant starts the intervention with a welcome dialogue, which introduces the LvL UP App and assesses the participant’s needs in each of the core pillars using the Patient Health Questionnaire-4 (PHQ-4) [ 38 ], a Modified Food Frequency Questionnaire (FFQ) based on dietary recommendations, and the International Physical Activity Questionnaire-Short Form (IPAQ-SF) [ 39 ]. Based on the participant’s needs, a starting pillar is recommended, but the participant can still choose the pillar they wish to focus on. Following the welcome dialogue, the participants complete two short sessions to identify their perceived values and strengths, which are later reflected to the participant by the CA during coaching sessions.
LvL UP App: tools
Additionally, the LvL UP App includes different tools that complement each pillar, including a set of self-regulatory behaviour change techniques, actionable habit-forming suggestions, and a slow-paced breathing training mini-game. The self-regulatory tools include a low-burden image tracking food diary ( MakanMemo ), a step tracker ( StepLah! ) that displays steps collected by Apple Health (iOS) or GoogleFit (Android) and allows users to set and track step goals, including brisk steps (120 steps/min or higher), and a Journal with different templates inspired by cognitive behavioural therapy to support mental well-being. Life Hacks are actionable tips for improving healthy habits and are designed to be easily executed during the daily routine. They operate on the premise that taking small, concrete actions can accumulate and lead to noticeable changes over time. Finally, Breeze is a slow-paced breathing training mini-game that uses breathing data collected by the smartphone microphone to move a sailboat along a river in real time [ 40 ].
The intended use of the LvL UP intervention is to complete weekly coaching sessions and use the tools daily. Gamification is built into the App whereby a puzzle piece is awarded for completed activities to fill up the LvL UP Shield. Once the shield is filled, the participant progresses to the next level and the shield resets. There are three levels in total. The LvL UP App delivers reminders and prompts (push notifications) related to intervention actions to encourage the participant to complete the intervention as intended.
Criteria for discontinuing or modifying allocated interventions {11b}
The participant will be withdrawn from the study if she becomes pregnant during the 1-year intervention period. If a participant becomes pregnant during the 3-year follow-up period, she will skip the follow-up visit for the year and return to the subsequent follow-up visit(s) post-pregnancy. In the same way, if a participant is diagnosed with T2D by her doctor during the 1-year intervention period, she will be invited to complete the endpoint study visit measures before being withdrawn from the study. If the participant is diagnosed with T2D by the study team during the follow-up visits, she will be removed after completing that visit.
Strategies to assess and improve adherence to interventions {11c}
User adherence in mHealth interventions varied based on user-related, content-related, and technology (personalise remainders, user-friendly, technically stable App, personal support, and gamification features) related barriers and facilitators of engagement [ 41 , 42 ]. The intervention group [LvL UP] will receive notifications and reminders about the coaching session’s date and time, daily random lifehack, and motivational messages to engage with the LvL UP App. Additionally, a dashboard link to monitor the participant’s live activity regarding last-time interaction, tools used, and the current level is considered to reach up to support adherence with the participants. Thus, the following three strategies will be implemented: calling participants who have not interacted for 2 weeks with the LvL UP App after baseline; texting the participants who have low interaction (e.g. using the App once/twice for 2 weeks), and sending automatic SMS 3, 5 and 7 weeks after the baseline visit to encourage them to use the App.
The HAPPY App will detect the number of logged entries and the last interaction with the app. A manual schedule reminder will be sent by the App if the participant has not read the suggested articles or documents.
Relevant concomitant care permitted or prohibited during the trial {11d}
The participants will be excluded if they have enrolled in a concurrent lifestyle intervention research study during the study. However, trial participants can receive concomitant treatment (e.g. psychotherapy, pharmacology), which will be assessed during the follow-up period.
Provisions for post-trial care {30}
Access to the Happy App will continue for the 3-year follow-up period after the trial for all the participants.
Outcomes {12}
Table 1 shows the outcomes and timeline of the study. The primary outcome will be the onset of T2D/confirmed by a 2-h 75 g oral glucose tolerance test (OGTT) over a 4-year study period. OGTT will be done at the screening visit, year 1 visit, and follow-up visits in years 2, 3, and 4. Secondary outcomes include (a) onset of impaired fasting glucose and impaired glucose tolerance; (b) changes in cardiometabolic variables (body weight, HbA 1c , insulin, blood lipids, blood pressure), and (c) changes in women’s body composition as assessed by bioelectrical impedance analysis (BIA). Secondary measures will be taken at baseline visits, middle point, year 1, and 2, 3, and 4-year follow-up period.
Additionally, we will assess changes in women’s mental well-being by completing the following questionnaires at all study visits:
Beck Depression Inventory (BDI-II): A 21-item self-reported rating inventory using a 3-point Likert scale that measures symptoms and severity of depression, classified as follows: minimal (0–13); mild (14–19); moderate (20–28); and severe (29–63). The BDI-II internal consistency as measured by Cronbach’s alpha ranges from 0.87 to 0.93 [ 43 ].
State-Trait Anxiety Inventory (STAI): A 40-item self-report questionnaire using a 4-point Likert scale. The STAI measures two types of anxiety — state anxiety and trait anxiety, which are classified as no or low anxiety (20–37), moderate anxiety (38–44), and high anxiety (45–80). Internal consistency coefficients for the scale have ranged from 0.86 to 0.95 [ 44 ].
Cognitive Emotion Regulation Questionnaire ( CERQ ): A 36-item self-report measure designed to identify the cognitive emotion regulation strategies (or cognitive coping strategies) someone uses after having experienced adverse events or situations. It is commonly used to assess individual differences in the cognitive regulation of emotions in response to stressful, threatening, or traumatic life events. Internal consistency ranges from 0.72 and 0.83 [ 45 ].
Subjective Happiness Scale (SHS): A 4-item self-report measure to assess an individual’s overall happiness. Internal consistency ranges from 0.79 to 0.94 [ 46 ].
WHO-5 Wellbeing Index ( WHO-5 ): A 5-item self-reported questionnaire that aims to assess mental wellbeing over the last 2 weeks. The WHO-5 shows reliability across countries between 0.86 and 0.96 [ 47 ].
Perceived Stress Scale ( PSS-4 ): A brief self-report measure of the extent to which recent life events are considered stressful. The PSS-4 has demonstrated acceptable criterion validity and internal consistency ( α = 0.72) [ 48 ].
The short Form Health Survey ( SF-36 ): Indicates overall health status; it aims to assess the impact of clinical and social interventions on quality of life in several domains. The SF-36 has shown a reliability of 0.90 [ 49 ].
Health Literacy Questionnaire ( HLQ ): The HLQ examines an individual’s understanding, access and engagement with health information and health services. The HLQ Cronbach’s alpha has shown an internal consistency of 0.87 [ 50 ].
Moreover, changes in women’s sleep will be assessed using the following measurements:
Morningness-Eveningness Questionnaire ( MEQ ): A 19-item MEQ aims to assess morningness and eveningness where questions are asked preferentially, i.e. asking respondents to indicate when, for example, they would prefer to wake up or start sleep, rather than when they do. MEQ internal consistency is 0.82 [ 51 ].
Pittsburgh Sleep Quality Index ( PSQI ): Measures the quality and patterns of sleep-in adults. It differentiates “poor” from “good” sleep quality by measuring seven areas (components): subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medications, and daytime dysfunction over the last month. The PSQI Cronbach’s alpha has shown good internal consistency ranging from 0.64 to 0.83 [ 52 ].
Furthermore, changes in the health and well-being of the women’s children will be collected. Only children born during a GDM pregnancy will be considered in this study. The following measurements will be used:
Cognitive Home Environment Questionnaire ( StimQ ): The StimQ-toddler (age 12–35 months)/StimQ-pre-school (for age 36 – 72 months) is designed to identify the different types of toys and games that children have in the home and the kinds of activities that mother and child do together [ 53 ]. The StimQ has demonstrated good internal and external reliability ( α = 0.85) [ 54 ].
Ages & Stages Questionnaires-3 ( ASQ-3 ) (1–66 months): The ASQ-3 development screening tool assesses children’s communication, autonomy, compliance, adaptive functioning, affect, and interaction with people. ASQ-3 is a reliable and valid instrument with a test–retest reliability of 92%, a sensitivity of 87.4% and a specificity of 95.7% [ 55 ].
Behaviour Rating Inventory of Executive Functions-2 (BRIEF-2) parent form : BRIEF-2 is designed for use in medical and educational settings to estimate the global executive function of children/youth and determine whether a comprehensive assessment is appropriate (age 5–18 years). BRIEF-2 has shown reliability coefficients ranging between 0.8 and 0.9 [ 56 ].
Behavioural and Emotional Screening System (BASC-3-BESS) Parent Form : This screens children and adolescents’ behavioural and emotional strengths and weaknesses (age 3–18 years 11 months). BASC-3 BESS has high internal consistency at 0.80 [ 57 ].
Changes in the child’s sleep will be assessed at the baseline visit and the first-year visit. The following is a description of child sleep questionnaires:
The Brief Infant Sleep Questionnaire-Revised Short Form ( BISQ-R-SF ): A parent-reported toddler (0–3 years) sleep over the prior 1 week, assessing sleep patterns, ecology, and parental perceptions of sleep. The BISQ-R indicates excellent reliability at 0.80 [ 58 ].
Children’s Sleep Habits Questionnaire (CSHQ) Short Form (SF)version : The SF-CSHQ assesses the frequency of children’s behaviours associated with common paediatric sleep difficulties for children between 48 and 72 months. The SF-CSHQ has been validated, showing Internal consistency coefficients ranging from 0.90 to 0.94 [ 59 ].
After completing the 1-year RCT period, both groups will be followed up for 3 years. During the follow-up visits, body measurements, OGTT, bio-sampling, and data collection will be conducted, and the questionnaires listed above.
Additionally, the intervention group will also complete the following questionnaires through the LvL UP App:
Patient Health Questionnaire-4 ( PHQ-4 ): A 4-item self-report measure that assesses anxiety and depression symptoms. Each item is scored on a 4-point scale (0–3), and scores range from 0 to 27. The score can be used to describe a patient’s symptoms in one of the five categories: none (0–2), mild (3–5), moderate (6–8), and severe (9–12), The PHQ-4 has been shown to have good internal reliability (Cronbach alpha = 0.82) [ 38 ].
Modified Food Frequency Questionnaire ( MFFQ ): A 7-item self-report checklist of food and beverages with a frequency response section based on My Healthy Plate Singapore[ 60 ].
The International Physical Activity Questionnaire-Short Form ( IPAQ-SF ): A self-report measure assesses the type of intensity of physical activity and sitting time[ 39 ]. The IPAQ-SF has shown a moderate internal consistency of 0.647 [ 61 , 62 ].
Screening survey overview and follow-up
The screening surveys will include questions of 8 types: (i) socio-demographics, (ii) GDM and family history of diabetes, (iii) medical history, (iv) lifestyle, (v) dietary, (vi) diabetes awareness, (vii) paternal demographics and health and (viii) child demographics and health (see Table 2 ). Those surveys will also be completed in baseline and 1-year visits (see Table 1 ).
Participants timeline {13}
The participants’ flow for the trial is outlined in Fig. 1 . Once participants are identified through one of the recruiting methods, they will be invited to the SICS clinic for screening, in which a consent form will be explained and signed, and OGTT test, height, weight, blood pressure measures, HbA1c (finger proc test) and sociodemographic survey will be completed. Those who are eligible will be randomised to one of the two arms (comparison or intervention group) and will subsequently be asked to take follow-up height, weight and blood pressure measurements, BIA, report the child’s height and weight, fasting blood draw, collection of the buccal swab, saliva, and stool sample, and complete questionnaires for the mother and their child at midpoint (26/27 weeks) visit, and year one visit after randomisation. After the midpoint assessments, additional interventions will be delivered via the HAPPY App to subjects in the intervention group who require further recommendations to improve their BMI or manage their body weight. During the 3 year-followed-up periods, participants will be asked to complete the following: (a) OGTT test; (b) height, weight and blood pressure measurements; (c) BIA; (d) fasting blood draw; (e) collection of the buccal swab, saliva and stool samples; (f) reported child’s height and weight; (g) complete mother and child questionnaires; (h) issue of Oura Ring (8 weeks); and (i) 14-day e-Diary recording in year 2, 3 and 4 visit. The schedule of enrolment, intervention, and assessments for the trial is outlined in Fig. 2 .

Participant flow consort

Schedule for enrolment, intervention, and assessments for the trial. OGTT, 2-h 75 g Oral Glucose Tolerance Test; BIA, Bioelectrical impedance analysis, SF-36, short-form health survey; STAI, The Stare-Trait Anxiety Inventory; BDI-II, Beck Depression Inventory; CERQ, Cognitive Emotion Regulation Questionnaire; MEQ, Morningness-Eveningness Questionnaire; PSQI, The Pittsburgh Sleep Quality Index; SHS, Subjective Happiness Scale; HLQ, Health Literacy Questionnaire; PSS-4, Perceived Stress Scale 4; WHO-5, World Health Organization Wellbeing Index; BISQ-R-SF, Brief Infant Sleep Questionnaire-Revised Short Form; CSHQ, Children’s Sleep Habits Questionnaire; StimQ toddler/preschool, Cognitive Home Environment Questionnaire; ASQ-3, Ages & Stages Questionnaires-3; BRIEF-2, Behaviour Rating Inventory of Execute Functions-2; BASC-3-BESS Parent Form, Behavioral and Emotional Screening System; PHQ-4, Patient Health Questionnaire; IPAQ-SF, The International Physical Activity Questionnaire- Short Form; MFFQ, Modified Food Frequency Questionnaire
Sample size {14}
Expected number of participants.
The sample size is estimated based on the cumulative diabetes risk identified from the GUSTO study [ 12 ]. We assume groups of equal size, with a significance level of 0.05% and a power of 80%. Additionally, we consider a median survival time of 6 years for the non-intervention group (based on GUSTO data), a follow-up period of 3 years, and an expected 50% reduction in the risk of developing T2D for the intervention group (hazard ratio = 0.5). These assumptions yield a cumulative event rate of 0.22 for the comparison group and 0.12 for the intervention group. Considering a 20% censoring rate, we calculate a sample size of 189 for the intervention group and 188 for the comparison group, aiming for a total of 65 events over the study period[ 63 ].
Recruitment {15}
The study protocol was approved by the National Healthcare Group in Singapore, Domain Specific Review Board. There are four avenues of recruitment. The first is contacting participants from a previous pilot study conducted by the same research team in this protocol [ 64 ]. The second avenue is recruiting participants using snowball sampling (e.g. friends, family), the third is via electronic flyer invitation through corporate e-mails (National University Healthcare System (NUHS) and Agency for Science, Technology and Research (A*STAR)), and the fourth is advertising on social media (e.g. LinkedIn, Instagram, Facebook advertisements). Interested individuals will contact the study team via phone or e-mail. The study team will explain the study and answer any questions raised . Potential participants will be invited to attend a screening visit for informed consent and screening procedures. Those who are screened passed will be scheduled to attend baseline and midpoint visits (26/27 weeks), year 1, and follow-up visit periods in years 2, 3, and 4. All the participants will be able to provide written informed consent.
Assignment intervention: allocation
Sequence generation {16a}.
A total of 400 women will be stratified and randomised based on prognosis factors to either group 1 (intervention) or group 2 (control) based on 1:1 allocation using R statistical software.
Concealment mechanism {16b}
The allocation is concealed in that the allocation sequence is automatically generated in R software and simultaneous with the assignment.
Implementation {16c}
The allocation sequence will automatically be generated in the Block Rand R software at the end of the baseline, and a screen will show participants to which group she has been assigned.
Assignment of interventions: blinding
Who will be blinded {17a}.
Given the nature of the study design, blinding of participants and research personnel will not be possible. The study team will instruct the participants in the intervention and comparison groups to download the Apps, and each participant will be provided with a unique identification code.
Procedure for unblinding if needed {17b}
In the case of high depression scores on the BDI, including item 9 (suicidal ideation) and anxiety on the STAI, the participant will be flagged and reported to research coordinators, who will contact the participant to provide additional referral and helpline resources in Singapore. Similarly, scores that reveal a potential developmental delay in the child measured by the ASQ-3 will be notified to the mother, and a referral will be made for further evaluation.
Data collection and management
Plans for assessment and collection of outcomes{18a}.
The baseline, midpoint visit (26/27 weeks), 1-year visit, and 3-year follow-up assessments will be administered on-site through the Recap platform assisted by research coordinators. The REDCap will be used for all the measurements and will follow complex skip logic developed for this study, based on participants’ responses to reduce respondent burden and increase the completeness and accuracy of responses.
The intervention group randomised to the LvL UP App will collect objective and self-reported scales from the mHealth App throughout the intervention.
Plans to promote participant retention and complete follow-up {18b}
Participants will be reimbursed for their time, inconvenience and transportation costs as follows: (a) screening visit — S$20; (b) completion of baseline study visit — S$80; (c) completion of midpoint study visit — S$40; (d) completion of year 1 study visit — S$80; (e) completion of level 1 to level 3 digital coaching sessions via LvL UP App (applicable to participants in intervention group) will be a total of S$120 and S$40 per level of completion; (f) completions for all three study visits, participants will be given an additional S$80 as bonus; and (g) completion of year 2, 3 and 4 yearly visit the participants will receive S$80 per visit. The research team will call the participants to remind them to attend the visits.
Additionally, the intervention group will receive reminders from the LvL UP App regarding the day and time of the coaching session and daily random lifehack from any of the pillars.
Data management {19}
The Singapore Institute for Clinical Sciences (SICS) team will maintain a master dataset for all participants who were referred to the project for recruitment, along with a record of whether they withdrew before or after completing the screening and baseline measurements or after initiating the intervention, were considered ineligible for participation, or were terminated from the study or conducted the study. Protection of participant privacy concerning biological samples and questionnaire data will be achieved by assigning each participant a study identification number and then creating a separate de-identified file. Anonymised data from the participants will be shared between SEC and SICS through a secure AWS server. All data analyses will be carried out with the de-identified data file.
Confidentiality {27}
Identifiable individual participant information obtained from this study is confidential, and disclosure to non-relevant third parties is prohibited. Participant confidentiality will be further ensured by assigning each participant a unique participant identification code for anonymised data entry and sample identification. All computer entry and networking programs will be done with coded numbers only.
Statistical methods
Statistical methods for primary and secondary outcomes {20a}, analysis of aggregate intervention effects.
The primary continuous outcome for the onset of diabetes will be analyzed with linear mixed models (LMM) with outcome measurement (at the three follow-up time points) as the dependent variable and based on the intention-to-treatment (ITT) principle.
Multiple linear regressions will determine the relationship between outcome measures and predictors, adjusting for potential confounders. Multiple linear regression analyses will estimate the effects between groups at the end point follow-up. Generalised estimating equations and mixed effect models will be used for longitudinal data analysis. A p -value of < 0.05 will be considered statistically significant. Correction for multiple tests will be performed. All statistical analyses will be conducted using the R program or STATA for Windows (Stata Corporation). The treatment effect within and between the two groups will be assessed using the Cohen d statistics [ 65 ].
Interim analyses {21b}
Interim analyses will be conducted to examine initial trial efficacy and safety outcomes. Frequencies (percentages), means (standard deviations), or medians (interquartile ranges) will be used to summarise the data collected from questionnaires and surveys. Statistical tests will be performed, e.g. Chi-square or Fisher’s exact test for categorical variables, and two independent sample t -tests or ANOVA for continuous variables. Nonparametric tests will be used as deemed fit. For binary outcomes, the strength of associations between independent and dependent variables will be assessed by odds ratio estimated in logistic regression models. Crude associations will be evaluated using univariate models. Subsequently, associations will be evaluated using multivariable models adjusted for potential confounders.
Methods for additional analyses (e.g. subgroup analyses) {20b}
We will carry out additional analyses that evaluate the effect of the intervention on the children born to the women during the GDM pregnancy with a focus on cognitive and socio-emotional development (ASQ-3, BASC-3-BESS, BRIEF, StimQ) and sleep (BISQ-R-SF, CSHQ) using linear mixed models (LMM) with outcome measurements (baseline and the three follow-up time points) based on intention-to-treat (ITT).
Descriptive statistics will be used to establish the intervention response rate based on the number of coaching sessions completed, logins into the App, and estimated time spent.
Methods in analysis to handle protocol non-adherence and any statistical methods to handle missing data {20c}
Intention-to-treat analysis will be used to examine trial efficacy. Total scores will be modelled using fixed effects of time, intervention group, interaction between time and intervention group, and a random effect of individual.
Plans to give access to the full protocol, participant-level data and statistical code {31c}
The anonymized datasets analysed during the current study and statistical code are available from the corresponding author on reasonable request, as is the full protocol.
Oversight and monitoring
Composition of the coordinating centre and trial steering committee {5d}.
The study team will have overall responsibility for monitoring the integrity of the study and participant safety. The study team will monitor consent procedures, and safety plans prior to study initiation, amendments thereafter, and monitoring study progress, in terms of recruitment and retention of participants, adverse events, and protocol deviations.
Composition of the data monitoring committee, its role and reporting structure {21a}
The committee comprises research coordinators (RCs), a data manager, co-investigators, and the principal investigator (JGE). RCs are responsible for electronic data capture following the standard operating procedure, and the data manager monitors data collection. The data manager will raise queries with RCs during data monitoring. The data manager prepares data exports for monthly review and reports to the principal investigator and co-investigators.
Adverse event reporting and harms {22}
The Principal Investigator (PI) (JGE) will manage the data and safety monitoring after participant enrolment. In the event of any adverse events or safety issues, appropriate reporting will be made to DSRB accordingly. Regarding the questionnaires, we have the following monitoring plan: (a)BDI-II: participants who exhibit suicidality ideation (item 9) or have scored 29 or above (severe depression) will be offered a clinical referral. If the participant declines the referral, she will be provided with local helpline contact numbers (Samaritans of Singapore and Institute of Mental Health); (b) STAI: for participants who exhibit high anxiety with a score of 45 or above in the STAI, the study team will provide a local helpline contact number (Singapore Association for Mental Health). Additionally, the PHQ-4 will be completed by the LvL UP App participants (intervention group) with a score of 9 or higher (severe anxiety depression); the LvL UP App will provide information regarding mental health services in Singapore, including local helplines. The study team will follow up with the participant if she wishes to get a clinical referral. Finally, based on the ASQ-3, if a child shows scores suggesting developmental delay, we will discuss with the participant if she has any concerns and would like a referral for clinical follow-up.
Biological samples will be collected through blood tests, which will be analyzed by an accredited lab providing the normal reference range of the lab results. The PI (JGE) will review blood test results. For all abnormal blood test results and incidental findings discovered during the study period, the study PI will determine if the findings are clinically significant and actionable. The study PI will sign a referral letter to seek primary healthcare. Subsequently, a delegated study team member will contact the participant to relay the internal findings on behalf of the study PI. Participants who agree to be re-identified and notified of the internal findings will be contacted at their primary contact number provided in the consent form. The referral letter will be emailed to her. If the participant is uncontactable on her direct contact number, her next of kin listed on the consent form will be contacted. If the participant and next of kin are not contactable after 1 month, the referral letter will be sent directly to the participant’s home address. In the case incidental findings meet the study exclusion criteria, the affected participant will be informed and withdrawn from the study.
For the rest of the study measures/questionnaires, there is no clinical validation available. Hence no applicable management plan will be carried out.
Frequency and plans for monitoring trial conduct {23}
Study activities, including those related to consent, randomisation, data collection, and intervention, will be monitored on an ongoing basis . The data management team will monitor the data on the Amazon Web Services (AWS) server and REDCap platform. The study team will upload outcome data by the participants at the AWS server monthly.
Plans for communicating necessary protocol amendments to relevant parties (e.g. trial participants, ethical committees) {25}
Changes to the study protocol will be communicated to the DSRB when required. Deviations from the protocol will be fully documented using a breach report form and it will be updated to the protocol in the clinical trial registry.

Dissemination plans {31a}
Study results will be disseminated through webinars, written documents, conferences, and research meetings at SICS. We will also prepare scientific reports of the study results for publication in peer-reviewed journals.
This study aims to identify post-GDM women from community settings in Singapore and assess the effectiveness of a holistic lifestyle mHealth intervention for the prevention of T2D and CMDs. It is essential to develop preventative interventions to encourage healthy lifestyle habits, given the high incidence rates of T2D and CMD among women following GDM. This study may provide further support for the effectiveness of preventative interventions that consider the close relationship between physical and psychological health. Holistic lifestyle interventions that promote healthy habits such as maintaining a balanced healthier diet, engaging in regular physical activity, getting adequate sleep, and prioritising mental well-being can work together to produce more effective results [ 34 , 66 , 67 ]. mHealth also offers practical, affordable, and scalable intervention support for individuals adopting and maintaining healthy lifestyles. The evidence has shown that holistic mHealth targeting lifestyle behaviours are available and have shown to be effective [ 31 , 34 , 37 ]. However, few studies have been tested using multicompetent lifestyle using mHealth [ 34 ]. This RCT study represents a pioneer attempt to investigate the effectiveness of a holistic lifestyle mHealth intervention focused on the prevention of T2D and CMDs in women with a history of GDM.
mHealth has the potential to transform preventive healthcare, and particularly support post-GDM women who encounter challenges due to fatigue, child-caring responsibilities, and motivation to change their lifestyles. Additionally, we expect that the holistic mHealth proposed will permit to build capacities to disseminate interventions and could have enormous public health implications for the region and serve as a model for implementing preventative interventions in Asia and globally.
DSRB Approval of Protocol Version 1.0; 1/6/2023. Recruitment began 20/10/2023. Recruitment is tentatively scheduled to be completed on 30/10/2024.
Availability of data and materials {29}
Final de-identified data and trial materials will be publicly available after the trial is concluded.
Abbreviations
Agency for Science, Technology and Research
Amazon Web Services
Behavioral and Emotional Screening System
Behavioural change techniques
Brief Infant Sleep Questionnaire-Revised Short Form
Beck Depression Inventory
Behaviour Rating Inventory of Execute Functions-2
Cognitive behavioural therapy
Cognitive Emotion Regulation Questionnaire
Common mental disorders
Children’s Sleep Habits Questionnaire
Domain-Specific Review Board
Diabetes Prevention Program
Health Literacy Questionnaire
- Gestational diabetes mellitus
Morningness-Eveningness Questionnaire
National University Health System
National University of Singapore
Physical activity
Patient health questionnaire, 4-item
Principal investigator
The Pittsburgh Sleep Quality Index
Perceived Stress Scale 4
Positive psychology
Randomised control trial
Singapore ETH-Centre
Subjective Happiness Scale
Singapore Institute for Clinical Sciences
Short-form health curve
The State-Trait Anxiety Inventory
Cognitive Home Environment Questionnaire toddler/preschool
- Type 2 diabetes
World Health Organization-5 Wellbeing Index
Federation ID. IDF Diabetes Atlas. 10th ed. Brussels; 2021. https://www.diabetesatlas.org .
Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas. Diabetes Res Clin Pract. 2019;157:107843.
Article PubMed Google Scholar
Sun J, Hu W, Ye S, Deng D, Chen M. The description and prediction of incidence, prevalence, mortality, disability-adjusted life years cases, and corresponding age-standardized rates for global diabetes. J Epidemiol Glob Health. 2023;13(3):566–76. https://doi.org/10.1007/s44197-023-00138-9 .
Article PubMed PubMed Central Google Scholar
Collaborators GOD, Bernabe E, Marcenes W, Hernandez C, Bailey J, Abreu L, et al. Global, regional, and national levels and trends in burden of oral conditions from 1990 to 2017: a systematic analysis for the global burden of disease 2017 study. J Dent Res. 2020;99(4):362–73.
Article Google Scholar
Monod C, Kotzaeridi G, Linder T, Eppel D, Rosicky I, Filippi V, et al. Prevalence of gestational diabetes mellitus in women with a family history of type 2 diabetes in first-and second-degree relatives. Acta Diabetol. 2023;60(3):345–51.
Article CAS PubMed Google Scholar
McIntyre HD, Catalano P, Zhang C, Desoye G, Mathiesen ER, Damm P. Gestational diabetes mellitus. Nat Rev Dis Primers. 2019;5(1):47.
Li L-J, Huang L, Tobias DK, Zhang C. Gestational diabetes mellitus among asians–a systematic review from a population health perspective. Front Endocrinol. 2022;13:840331.
Kunasegaran T, Balasubramaniam VR, Arasoo VJ, Palanisamy UD, Ramadas A. Gestational diabetes mellitus in Southeast Asia: a scoping review. Int J Environ Res Public Health. 2021;18(3):1272. https://doi.org/10.3390/ijerph18031272 . https://www.mdpi.com/1660-4601/18/3/1272 .
Hod M, Kapur A, Sacks DA, Hadar E, Agarwal M, Di Renzo GC, et al. The international federation of gynecology and obstetrics (FIGO) Initiative on gestational diabetes mellitus: A pragmatic guide for diagnosis, management, and care. Int J Gynecol Obstet. 2015;131:S173–211.
Kc K, Shakya S, Zhang H. Gestational diabetes mellitus and macrosomia: a literature review. Ann Nutr Metab. 2015;66(Suppl. 2):14–20.
Vounzoulaki E, Khunti K, Abner SC, Tan BK, Davies MJ, Gillies CL. Progression to type 2 diabetes in women with a known history of gestational diabetes: systematic review and meta-analysis. Bmj. 2020;369:m1361.
Chen L-W, Soh SE, Tint M-T, Loy SL, Yap F, Tan KH, et al. Combined analysis of gestational diabetes and maternal weight status from pre-pregnancy through post-delivery in future development of type 2 diabetes. Sci Rep. 2021;11(1):5021.
Article CAS PubMed PubMed Central Google Scholar
Ukke GG, Boyle JA, Reja A, Lee WK, Chen M, Ko MSM, et al. Lifestyle interventions to prevent type 2 diabetes in women with a history of gestational diabetes: a systematic review and meta-analysis through the lens of health equity. Nutrients. 2023;15(21):4666.
Plows JF, Stanley JL, Baker PN, Reynolds CM, Vickers MH. The pathophysiology of gestational diabetes mellitus. Int J Mol Sci. 2018;19(11):3342.
OuYang H, Chen B, Abdulrahman AM, Li L, Wu N. Associations between gestational diabetes and anxiety or depression: a systematic review. J Diabetes Res. 2021;2021(1):9959779. https://doi.org/10.1155/2021/9959779 . https://link.springer.com/article/10.1007/s44197-023-00138-9 .
Wilson CA, Newham J, Rankin J, Ismail K, Simonoff E, Reynolds R, et al. Is there an increased risk of perinatal mental disorder in women with gestational diabetes? A systematic review and meta-analysis. Diabet Med. 2020;37(4):602–22.
O’Hara MW, Wisner KL. Perinatal mental illness: definition, description and aetiology. Best Pract Res Clin Obstet Gynaecol. 2014;28(1):3–12.
Stein A, Pearson RM, Goodman SH, Rapa E, Rahman A, McCallum M, et al. Effects of perinatal mental disorders on the fetus and child. The Lancet. 2014;384(9956):1800–19.
Wu Q, Meng Z, Liu Q, Zhang L, Mao B, Wang C, et al. Sleep quality in women with diabetes in pregnancy: a single-center retrospective study. BMC Pregnancy Childbirth. 2023;23(1):597.
Itani O, Jike M, Watanabe N, Kaneita Y. Short sleep duration and health outcomes: a systematic review, meta-analysis, and meta-regression. Sleep Med. 2017;32:246–56.
Saadati F, Sehhatiei Shafaei F, Mirghafourvand M. Sleep quality and its relationship with quality of life among high-risk pregnant women (gestational diabetes and hypertension). J Matern Fetal Neonatal Med. 2018;31(2):150–7.
Goveia P, Cañon-Montañez W, Santos DdP, Lopes GW, Ma RC, Duncan BB, et al. Lifestyle intervention for the prevention of diabetes in women with previous gestational diabetes mellitus: a systematic review and meta-analysis. Front Endocrinol. 2018;9:583.
Zhang C, Tobias DK, Chavarro JE, Bao W, Wang D, Ley SH, et al. Adherence to healthy lifestyle and risk of gestational diabetes mellitus: prospective cohort study. Bmj. 2014;349:g5450.
Tuomilehto J, Lindström J, Eriksson JG, Valle TT, Hämäläinen H, Ilanne-Parikka P, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344(18):1343–50.
Zakaria H, Abusanana S, Mussa BM, Al Dhaheri AS, Stojanovska L, Mohamad MN, et al. The Role of lifestyle interventions in the prevention and treatment of gestational diabetes mellitus. Medicina. 2023;59(2):287.
Huang S, Magny-Normilus C, McMahon E, Whittemore R. Systematic review of lifestyle interventions for gestational diabetes mellitus in pregnancy and the postpartum period. J Obstet Gynecol Neonatal Nurs. 2022;51(2):115–25.
Lie M, Hayes L, Lewis-Barned N, May C, White M, Bell R. Preventing type 2 diabetes after gestational diabetes: women’s experiences and implications for diabetes prevention interventions. Diabet Med. 2013;30(8):986–93.
Pagoto S. The current state of lifestyle intervention implementation research: where do we go next? Transl Behav Med. 2011;1(3):401–5. https://doi.org/10.1007/s13142-011-0071-x . https://academic.oup.com/tbm/article-abstract/1/3/401/4562980?redirectedFrom=fulltext .
Lim S, Tan A, Madden S, Hill B. Health professionals’ and postpartum women’s perspectives on digital health interventions for lifestyle management in the postpartum period: a systematic review of qualitative studies. Front Endocrinol. 2019;10:767.
Moschonis G, Siopis G, Jung J, Eweka E, Willems R, Kwasnicka D, et al. Effectiveness, reach, uptake, and feasibility of digital health interventions for adults with type 2 diabetes: a systematic review and meta-analysis of randomised controlled trials. The Lancet Digital Health. 2023;5(3):e125–43.
Mair JL, Salamanca-Sanabria A, Augsburger M, Frese BF, Abend S, Jakob R, et al. Effective behavior change techniques in Digital health interventions for the prevention or management of noncommunicable diseases: an umbrella review. Ann Behav Med. 2023;57(10):817–35.
Keller R, Hartmann S, Teepe GW, Lohse K-M, Alattas A, Tudor Car L, et al. Digital behavior change interventions for the prevention and management of type 2 diabetes: systematic market analysis. J Med Internet Res. 2022;24(1):e33348.
Andersson G, Carlbring P, Titov N, Lindefors N. Internet interventions for adults with anxiety and mood disorders: a narrative umbrella review of recent meta-analyses. Can J Psychiatr. 2019;64(7):465–70.
Zheng S, Edney SM, Goh CH, Tai BC, Mair JL, Castro O, et al. Effectiveness of holistic mobile health interventions on diet, and physical, and mental health outcomes: a systematic review and meta-analysis. EClinicalMedicine. 2023;66. https://doi.org/10.1016/j.eclinm.2023.102309 . https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(23)00486-8/fulltext .
Castro O, Mair JL, Salamanca-Sanabria A, Alattas A, Keller R, Zheng S, et al. Development of “LvL UP 1.0”: a smartphone-based, conversational agent-delivered holistic lifestyle intervention for the prevention of non-communicable diseases and common mental disorders. Front Digit Health. 2023;5:1039171.
Hofmann SG, Asnaani A, Vonk IJ, Sawyer AT, Fang A. The efficacy of cognitive behavioral therapy: A review of meta-analyses. Cogn Ther Res. 2012;36(5):427–40.
Zheng S, Edney SM, Mair JL, Kowatsch T, Castro O, Salamanca-Sanabria A, et al. Holistic mHealth interventions for the promotion of healthy ageing: protocol for a systematic review. BMJ Open. 2023;13(5):e066662. https://doi.org/10.1136/bmjopen-2022-066662 .
Löwe B, Wahl I, Rose M, Spitzer C, Glaesmer H, Wingenfeld K, et al. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disord. 2010;122(1–2):86–95.
Craig C, Marshall A, Sjostrom M, Bauman A, Lee P, Macfarlane D, et al. International physical activity questionnaire-short form. J Am Coll Health. 2017;65(7):492–501.
Google Scholar
Lukic YX, Teepe GW, Fleisch E, Kowatsch T. Breathing as an input modality in a gameful breathing training app (breeze 2): development and evaluation study. JMIR Serious Games. 2022;10(3):e39186.
Borghouts J, Eikey E, Mark G, De Leon C, Schueller SM, Schneider M, et al. Barriers to and facilitators of user engagement with digital mental health interventions: systematic review. J Med Internet Res. 2021;23(3):e24387.
Jakob R, Harperink S, Rudolf AM, Fleisch E, Haug S, Mair JL, et al. Factors influencing adherence to mHealth apps for prevention or management of noncommunicable diseases: systematic review. J Med Internet Res. 2022;24(5):e35371.
Wang Y-P, Gorenstein C. Psychometric properties of the beck depression inventory-II: a comprehensive review. Braz J Psychiatr. 2013;35:416–31.
Spielberger CD. State‐trait anxiety inventory. The Corsini Encyclopedia of Psychology. 2010:1. https://doi.org/10.1002/9780470479216.corpsy0943 .
Jermann F, Van der Linden M, d’Acremont M, Zermatten A. Cognitive emotion regulation questionnaire (CERQ). Eur J Psychol Assess. 2006;22(2):126–31.
Lyubomirsky S, Lepper HS. A measure of subjective happiness: Preliminary reliability and construct validation. Soc Indic Res. 1999;46:137–55.
Sischka PE, Costa AP, Steffgen G, Schmidt AF. The WHO-5 well-being index–validation based on item response theory and the analysis of measurement invariance across 35 countries. Journal of Affective Disorders Reports. 2020;1:100020.
Chan SF, La Greca AM. Perceived stress scale (PSS). Encyclopedia of behavioral medicine: Springer; 2020. p. 1646–8.
Ware JE Jr. SF-36 health survey update. Spine. 2000;25(24):3130–9.
Osborne RH, Batterham RW, Elsworth GR, Hawkins M, Buchbinder R. The grounded psychometric development and initial validation of the Health Literacy Questionnaire (HLQ). BMC Public Health. 2013;13(1):1–17.
Adan A, Almirall H. Horne & Östberg morningness-eveningness questionnaire: A reduced scale. Personality Individ Differ. 1991;12(3):241–53.
Smyth C. The Pittsburgh sleep quality index (PSQI). NJ: SLACK Incorporated Thorofare; 1999. p. 10.
Mendelsohn A, Dreyer B, Tamis-LeMonda C, Ahuja P. Validity of StimQ, a scale for assessing the cognitive home environment. J Dev Behav Pediatr. 1999;20(5):399.
Cates CB, Roby E, Canfield CF, Johnson M, Raak C, Weisleder A, et al. Validation of the StimQ2: A parent-report measure of cognitive stimulation in the home. PLoS ONE. 2023;18(7):e0286708.
Squires J, Bricker DD, Twombly E. Ages & stages questionnaires. Baltimore: Paul H. Brookes; 2009. https://aaimsschool.com/uploads/3/5/3/0/35304913/printable_asq_developmental_guide_1month_-5.5years_old.pdf .
LeJeune B, Beebe D, Noll J, Kenealy L, Isquith P, Gioia G. Psychometric support for an abbreviated version of the Behavior Rating Inventory of Executive Function (BRIEF) Parent Form. Child Neuropsychol. 2010;16(2):182–201.
Reynolds CR, Kamphaus RW, Vannest KJ. BASC3: Behavior assessment system for children. San Antonio: PscyhCorp; 2015. https://link.springer.com/referenceworkentry/10.1007/978-3-319-56782-2_1524-2 .
Mindell JA, Gould RA, Tikotzy L, Leichman ES, Walters RM. Norm-referenced scoring system for the brief infant sleep questionnaire–revised (BISQ-R). Sleep Med. 2019;63:106–14.
Bonuck KA, Goodlin-Jones BL, Schechter C, Owens J. Modified Children’s sleep habits questionnaire for behavioral sleep problems: A validation study. Sleep Health. 2017;3(3):136–41.
(HPB) HPB. My healthy plate [Available from: https://www.healthhub.sg/programmes/nutrition-hub/eat-more?utm_source=google&utm_medium=paid-search&utm_campaign=fy23-nl-edsh-ao&utm_content=fy23-nl-edsh-ao_google_paid-search_my-healthy-plate&gclid=Cj0KCQiAm4WsBhCiARIsAEJIEzW-T5XOZPkMBnn5v33wOHwatbKpGVTTx6s-l4_oIW5wrdabjmf4RhoaAjoCEALw_wcB#my-healthy-plate .
Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–95.
Lee PH, Macfarlane DJ, Lam TH, Stewart SM. Validity of the international physical activity questionnaire short form (IPAQ-SF): A systematic review. Int J Behav Nutr Phys Act. 2011;8(1):1–11.
Schoenfeld DA. Sample-size formula for the proportional-hazards regression model. Biometrics. 1983;39:499–503.
Liew SJ, Soon CS, Chooi YC, Tint MT, Eriksson JG. A holistic approach to preventing type 2 diabetes in Asian women with a history of gestational diabetes mellitus: a feasibility study and pilot randomized controlled trial. Front Clin Diabetes Healthc. 2023;4:1251411. https://doi.org/10.3389/fcdhc.2023.1251411 .
Cohen, J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Routledge; 1988. https://doi.org/10.4324/9780203771587 . eBook ISBN 9780203771587.
Wong VW-H, Ho FY-Y, Shi NK, Sarris J, Ng CH, Tam OKY. Lifestyle medicine for anxiety symptoms: A meta-analysis of randomized controlled trials. J Affect Disord. 2022;310:354–68.
Wong VW-H, Ho FY-Y, Shi N-K, Sarris J, Chung K-F, Yeung W-F. Lifestyle medicine for depression: a meta-analysis of randomized controlled trials. J Affect Disord. 2021;284:203–16.
Download references
Acknowledgements
We would like to express our gratitude and acknowledge the research coordinators, biobank team, and data management team at the Singapore Institute for Clinical Sciences (SICS) and National University of Singapore (NUS) who support this study, as well as the Singapore ETH-Centre (SEC) members who support the LvL UP App intervention for this study.
This study is supported by Human Potential- FY21 Prenatal/Early Childhood grant call 2023 (Grant number: H22P0M0004) from the Agency for Science, Technology and Research (A*STAR) Singapore, and Human Potential Translational Research Programme, Yong Loo Lin School of Medicine, National University of Singapore, Singapore.
Author information
Authors and affiliations.
Singapore Institute for Clinical Sciences, Agency for Science, Technology and Research (A*STAR), Singapore, Singapore
Alicia Salamanca-Sanabria, Maria De Iorio, Mya Thway Tint, Yu Chung Chooi, Vicky Tay & Johan Gunnar Eriksson
Human Potential Translational Research Program, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore
Seaw Jia Liew, Mya Thway Tint & Johan Gunnar Eriksson
Campus for Research Excellence and Technological Enterprise (CREATE), Future Health Technologies, Singapore-ETH Centre, Singapore, Singapore
Jacqueline Mair
Saw Swee Hock School of Public Health, National University of Singapore, Singapore, Singapore
Centre for Digital Health Interventions, Department of Management, Technology, and Economics, ETH Zurich, Zurich, Switzerland
Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore
Maria De Iorio & Yew Tong Wei
Division of Family Medicine, Department of Medicine, Yoo Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore
Young Doris Yee Ling
Division of Endocrinology, National University Hospital, Singapore, Singapore
Yew Tong Wei
Division of Maternal-Foetal Medicine, Department of Obstetrics and Gynaecology, National University Hospital, Singapore, Singapore
Family Medicine Residency Programme, National University Hospital, Singapore, Singapore
Desmond Ong
Department of Obstetrics and Gynaecology, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore
Johan Gunnar Eriksson
Folkhälsan Research Centre, Helsinki, Finland
You can also search for this author in PubMed Google Scholar
Contributions
SL and JGE contribute to the study’s conception, design, and development of the study protocol. JM support the intervention design and study protocol. AS-S wrote the initial draft with contributions and revisions from all the authors who read and approved the final manuscript.
Corresponding author
Correspondence to Alicia Salamanca-Sanabria .
Ethics declarations
Ethics approval and consent to participate {24}.
The protocol study was approved by the National Healthcare Group in Singapore, Domain Specific Review Board (DSRB) [2023/00178] in June 2023. All the participants will be required to provide informed consent before enrolling in the study.
Consent for publication {32}
Not applicable.
Competing interests {28}
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: spirit checklist., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Salamanca-Sanabria, A., Liew, S.J., Mair, J. et al. A holistic lifestyle mobile health intervention for the prevention of type 2 diabetes and common mental disorders in Asian women with a history of gestational diabetes: a randomised control trial with 3-year follow-up protocol. Trials 25 , 443 (2024). https://doi.org/10.1186/s13063-024-08247-x
Download citation
Received : 06 January 2024
Accepted : 14 June 2024
Published : 03 July 2024
DOI : https://doi.org/10.1186/s13063-024-08247-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Preventive healthcare
- Digital health
- Behaviour change
ISSN: 1745-6215
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Ann Fam Med
- v.13(Suppl 1); 2015 Aug
Effects of Providing Peer Support on Diabetes Management in People With Type 2 Diabetes
1 Department of Medicine and Therapeutics, The Chinese University of Hong Kong, Shatin, Hong Kong
Rebecca Wong
2 Diabetes and Endocrine Centre, Prince of Wales Hospital, Shatin, Hong Kong
3 Ruttonjee Hospital, Hong Kong
Harriet Chung
4 Asia Diabetes Foundation, Prince of Wales Hospital, Shatin, Hong Kong
5 Hong Kong Institute of Diabetes and Obesity, The Chinese University of Hong Kong, Shatin, Hong Kong
6 Alice Ho Mui Ling Nethersole Hospital, Tai Po, Hong Kong
7 North District Hospital, Fanling, Hong Kong
Chiuchi Tsang
Roseanne yeung.
8 Division of Endocrinology, University of British Columbia, Canada
Juliana C. N. Chan
We examined the effects of participating in a “train-the-trainer” program and being a peer supporter on metabolic and cognitive/psychological/behavioral parameters in Chinese patients with type 2 diabetes.
In response to our invitation, 79 patients with fair glycemic control (HbA 1c <8%) agreed to participate in a “train-the-trainer” program to become peer supporters. Of the 59 who completed the program successfully, 33 agreed to be peer supporters (“agreed trainees”) and were each assigned to support 10 patients for 1 year, with a voluntary extension period of 3 additional years, while 26 trainees declined to be supporters (“refused trainees”). A group of 60 patients with fair glycemic control who did not attend the training program and were under usual care were selected as a comparison group. The primary outcome was the change in average HbA 1c levels for the 3 groups from baseline to 6 months.
At 6 months, HbA 1c was unchanged in the trainees (at baseline, 7.1 ± 0.3%; at 6 months, 7.1 ± 1.1%) but increased in the comparison group (at baseline, 7.1 ± 0.5%; at 6 months, 7.3 ± 1.1%. P = .02 for between-group comparison). Self-reported self-care activities including diet adherence and foot care improved in the trainees but not the comparison group. After 4 years, HbA 1c remained stable among the agreed trainees (at baseline, 7.0 ± 0.2%; at 4 years: 7.2 ± 0.6%), compared with increases in the refused trainees (at baseline, 7.1 ± 0.4%; at 4 years, 7.8 ± 0.8%) and comparison group (at baseline, 7.1 ± 0.5%; at 4 years, 8.1 ± 0.6%. P = .001 for between-group comparison).
CONCLUSIONS
Patients with diabetes who engaged in providing ongoing peer support to other patients with diabetes improved their self-care while maintaining glycemic control over 4 years.
INTRODUCTION
Diabetes self-management is often emotionally and physically taxing, demanding lifelong commitment to medication adherence and lifestyle modification. 1 Health care professionals such as diabetes nurses can effectively deliver diabetes self-management education (DSME), especially for the initial acquisition of knowledge and skills. 2 , 3 In the United States, the Medicare system provides for 10 hours of initial diabetes education in the first year for patients who have diabetes, with 2 hours of follow-up education for each subsequent year. 4 In a meta-analysis of 31 randomized controlled trials, DSME programs decreased HbA 1c by 0.76% more than in the comparison groups at immediate follow-up, and by 0.26% at 1 to 3 months, with a 1% reduction in HbA 1c associated with every additional 23.6 hours of contact. 2 Given the importance of contact time to maintain learned behaviors, peer support has been recommended as a means to improve long-term self-management. 5
Peer support refers to the transfer of experiential knowledge of a specific behavior or coping strategy for a stressor between people who share a particular characteristic. 6 , 7 Thus, people with a common illness can share knowledge and experience in a less hierarchical and more reciprocal relationship than that between patients and health care professionals. 8 , 9 Recent studies support the use of expert patients as peer supporters for patients with chronic diseases. 7 , 10 , 11 To date, most studies have focused on the effects of peer support on the recipients, 12 – 14 while the effects of being a peer supporter have been systematically examined in only a few studies. These studies, which have involved conditions other than diabetes, have reported improvements in health behaviors and self-efficacy, 15 , 16 depression, 16 and even mortality risk among peer supporters. 17 , 18
We previously reported a randomized trial conducted to evaluate the effect of receiving peer support in patients with type 2 diabetes. 19 In an integrated care setting that incorporated specialized diabetes clinics in Hong Kong, receiving peer support did not further improve cardiometabolic well-being within 1 year, but a subgroup of patients with negative emotions benefited from peer support to the extent of having improved psychological health and reduced hospitalization. In this part of the same study, we prospectively evaluated the effects of providing peer support on metabolic, cognitive, and psychological parameters in peer supporters themselves.
Participant Recruitment and Selection
Between February 1 and May 31 of 2009, participants from 3 hospitals (Ruttonjee Hospital, Alice Ho Miu Ling Nethersole Hospital, and Prince of Wales Hospital, all in Hong Kong) were identified and recruited by their nurses during routine medical visits. Patients with type 2 diabetes aged 18 to 75 years with fair glycemic control (HbA 1c <8%), good understanding of living with diabetes, clear communication skills, and a desire to serve were invited to attend a “train-the-trainer” program as potential peer supporters. Exclusion criteria included illiteracy, physical impairment, and mental illness impairing communication with others. Those who completed the training program and passed assessments were invited to be peer supporters. Those who agreed (“agreed trainees”) were compared with those who declined (“refused trainees”). A group of patients from the same sites under usual care who had similar glycemic control but did not attend the training program were selected as comparison group subjects. All patients gave written informed consent for research and publication purposes. The study was approved by the Chinese University of Hong Kong New Territories East Cluster Clinical Research Ethics Committee.
The “Train-the-Trainer” Program
The train-the-trainer program was designed to empower trainees to provide basic knowledge and emotional support to their peers with type 2 diabetes. The program consisted of 4 monthly workshops, each lasting 8 hours, for a total of 32 hours. Health care experts led the workshops, which included both didactic components and interactive components such as role playing and group sharing. The main components of the syllabus were these:
- Effective communication, focusing on positive thinking, empathetic listening, and appropriate questioning, taught by a neurolinguistic programming expert
- Diabetes diet review, with cooking tips, education on common misconceptions of the diabetic diet, and suggestions for weight management, taught by an accredited dietician
- Physical activity training, including precautions to take during exercise, stretching exercises, and sustaining motivation for daily physical activity, delivered by a nurse qualified in fitness training
- Behavioral psychology, with emphasis on positive thinking, goal setting, decision making, and coping with negative emotions, delivered by a qualified psychologist At the end of the training program, all trainees underwent formal evaluation using case scenarios and questionnaires to assess their competency as potential peer supporters.
Peer Support Delivery
Each agreed trainee was assigned 10 patients of the same gender to support. Agreed trainees were introduced to their patient groups in several meetings where the rationale, purpose, and expectations for this study were explained. The meeting was hosted by 1 attending doctor, 1 nurse, and the project coordinator. The peer supporters were asked to provide structured peer support for at least 1 year, with provision for a voluntary extension of 3 more years.
We have described elsewhere how peer support was delivered during the 1-year structured program. 19 Briefly, the peer supporters were asked to give each of their assigned patients a 15- to 20-minute telephone call biweekly for the first 3 months, monthly for the second 3 months, and every 2 months for the last 6 months. Peer supporters were given a checklist to use in reviewing specific self-management skills, including medication adherence, healthy diet, regular exercise, sick day management, foot care, and glucose monitoring. They were also encouraged to provide psychological support based on their own experiences. Peer supporters submitted their phone call checklists every 3 months for documentation of their discussion items, duration of each call, and relevant remarks. Additional electronic communication and group gatherings were left to the discretion of the participants. During the voluntary extension period, the peer supporters were asked to maintain contact with their assigned patients every 1 to 2 months for another 3 years. They were also required to document the calls and return the checklists to the project coordinator every year.
Providing Ongoing Support to Peer Supporters
In the 1-year structured program, peer supporters were reviewed by the doctor-nurse team and a project coordinator in 3 half-day debriefing meetings to share experiences, troubleshoot, and provide mutual support. Peer supporters were given opportunities to express their feelings and frustrations with their patient groups and to develop follow-up actions. Peer supporters anxious about their performance were reminded that, as nonprofessionals, they should not expect themselves to perform at the professional level, and they were reminded to encourage their patients to seek medical advice for uncertain issues. They were also asked to share sensitive information only with the medical team.
In the voluntary 3-year extension period, peer supporters met every 6 months with the project team, including at least 1 nurse, in a less formal group setting, such as hiking or having lunch together. They were encouraged to build a community among themselves and contact each other to share experiences and provide mutual support. They were also reminded to seek help from the project coordinator or the nurses if they encountered any problems.
Outcome Measurements
The primary outcome was change in HbA 1c at 6 months. Secondary outcomes included changes in blood pressure, lipid profile, and cognitive/psychological/behavioral measures. Changes in the latter were assessed using validated instruments in Chinese, including the Depression Anxiety and Stress Scale (DASS) for emotional health, 20 the EuroQol-5D (EQ-5D) for health-related quality of life, 21 the Diabetes Empowerment Scale (DES) for self-efficacy, 22 the Patient Health Questionnaire (PHQ) for depression, 23 the General Health Questionnaire (GHQ) for psychological health in general population, 24 and the Summary of Diabetes Self Care Activities (SDSCA) for self-care activities. 25 At the end of the 3-year extension period, metabolic parameters were retrieved from the Hong Kong Hospital Authority Clinical Management System, which is shared by all public hospitals.
Clinical Care
All 3 groups were managed in the usual care setting of their hospital or community-based clinic. Hong Kong has a heavily subsidized health care system, and all patients have access to medications, investigations, and consultations for a nominal fee (US $10 per clinic visit, US $1.50 per drug for a 3–4–month supply). All individuals had access to professional diabetes education at their hospital and were usually followed up every 3–4 months at their clinics.
Sample Size Estimation and Statistical Analysis
As we said earlier, this training program was part of a trial to evaluate the effect of receiving peer support on glycemic control in patients with type 2 diabetes. 19 Based on power calculations for the main study, we needed 30 peer supporters for a 1:10 ratio of peer supporters to peers. Expecting that one-half of the qualified trainees might agree to become peer supporters, we needed to train 60 subjects. Assuming a 25% attrition rate, we enrolled 79 patients in the training program.
All data were expressed as mean ± SD, median (interquartile range [IQR]), or percentage, as appropriate. Paired t -tests for continuous variables and McNemar tests for categorical variables were used for within-group comparisons. For between-group comparisons at baseline, independent t -tests and chi-square tests were used, while analysis of covariance was used for comparing the change from baseline to the 6th month between groups. We adjusted for gender when comparing the trainees and comparison group. For comparison of metabolic control after 4 years, we compared the entire group of agreed trainees, refused trainees and comparison group members using one-way ANOVA. All statistical analysis was performed using SPSS Statistics, version 20.0 (IBM).
From February through May 2009, 79 eligible patients with fair glycemic control, age 55.6 ± 11.5 years, with disease duration of 11.0 ± 6.7 years, 35% male, consented to attend the train-the-trainer program, and another group of 60 patients with similar HbA 1c levels who did not obtain the training were selected as the comparison group. Of the 59 trainees who completed the training program and passed their assessments, 33 agreed to be peer supporters and 26 refused. Two-thirds (21/33) of the peer supporters continued the 3-year voluntary extension and 17 completed the entire extension period ( Figure 1 ).

Recruitment and assessments of participants.
Comparison Between the Trainees and Comparison Group
At baseline, while the comparison group was more heavily male than the trainee group (65% vs 35%), the 2 groups did not differ in age, disease duration, education, or risk factor control. The trainees had higher SDSCA scores in the domains of glucose monitoring and medication adherence than the comparison group ( Table 1 ).
Clinical, Psychological, and Behavioral Characteristics at Baseline and After 6 Months for Patients With Type 2 Diabetes Who Joined the Training Program (Trainee Group) and Those Under Usual Care (Comparison Group)
| Trainee Group n = 79 | Comparison Group n = 60 | Between Groups Value | |||
|---|---|---|---|---|---|
| Baseline | Month 6 | Baseline | Month 6 | ||
| Age, y, mean ± SD | 55.6 ± 11.5 | 56.5 ± 10.9 | |||
| Male (%) | 35 | 65 | |||
| High school or above (%) | 12.5 | 20.6 | |||
| Disease duration, y, mean ± SD | 11.0 ± 6.7 | 8.3 ± 6.6 | |||
| Non-smoker (%) | 93.6 | 87.9 | |||
| HbA , mean ± SD | 7.1 ± 0.3 | 7.1 ± 1.1 | 7.1 ± 0.5 | 7.3 ± 1.1 | |
| Fasting plasma glucose, mg/dL, mean ± SD | 137 ± 43 | 137 ± 20 | 142 ± 42 | 144 ± 43 | .56 |
| Systolic blood pressure, mmHg, mean ± SD | 127 ± 13.6 | 123 ± 14.8 | 129 ± 29.5 | 122 ± 54.0 | .28 |
| Diastolic blood pressure, mmHg, mean ± SD | 71 ± 7.0 | 72 ± 12.5 | 77 ± 17.0 | 79 ± 11.2 | .15 |
| Total cholesterol, mg/dL, mean ± SD | 180 ± 30 | 170 ± 39 | 170 ± 25 | 170 ± 20 | |
| Triglyceride, mg/dL, mean (IQR) | 124 (70–168) | 124 (53–160) | 124 (62–186) | 132 (88–204) | .39 |
| HDL-cholesterol, mg/dL, mean (IQR) | 58 (31–77) | 58 (35–81) | 46 (31–77 | 46 (31–77) | .20 |
| LDL-cholesterol, mg/dL, mean ± SD | 100 ± 27 | 93 ± 31 | 97 ± 23 | 93 ± 23 | .15 |
| DES total score, mean ± SD | 37.9 ± 6.71 | 37.0 ± 7.38 | 41.0 ± 8.02 | 40.4 ± 9.77 | .42 |
| GHQ total score, mean ± SD | 44.4 ± 3.93 | 43.3 ± 3.67 | 45.5 ± 4.63 | 45.1 ± 4.06 | .09 |
| DASS total score, mean (IQR) | 4 (2–9) | 3 (0–7) | 6 (2–9) | 5 (1–8) | .68 |
| PHQ total score, mean (IQR) | 2 (1–3) | 1 (0–2)c | 2 (0–3) | 1 (0–3) | .21 |
| EQ-5D index, mean (IQR) | 1 (0.80–1) | 1 (0.82–1) | 1 (0.80–1) | 1 (0.81–1) | .34 |
| EQ-5D VAS, mean ± SD | 81.6 ± 11.5 | 81.8 ± 10.7 | 81.6 ± 12.4 | 79.0 ± 11.5 | .25 |
| General diet, mean ± SD | 4.73 ± 1.63 | 5.57 ± 1.32c | 4.6 ± 1.8 | 4.62 ± 1.88 | |
| Special diet, mean ± SD | 4.55 ± 1.27 | 5.32 ± 1.3 | 4.42 ± 1.7 | 4.46 ± 1.5 | |
| Exercise, mean ± SD | 4.55 ± 2.15 | 4.63 ± 2.07 | 3.83 ± 2.32 | 3.65 ± 2.07 | .07 |
| Glucose monitoring, mean ± SD | 2.58 ± 1.81 | 2.89 ± 1.77 | 2.33 ± 2.08 | 2.52 ± 2.21 | .47 |
| Foot care, mean ± SD | 4.97 ± 1.78 | 5.66 ± 1.44 | 4.31 ± 2.18 | 4.27 ± 1.95 | |
| Medication adherence, mean ± SD | 6.81 ± 1.06 | 6.59 ± 1.41 | 5.95 ± 1.84 | 6.3 ± 1.6 | .75 |
Note: These are the score ranges for assessment tools:
DES: 20-item Diabetes Empowerment Scale, range 20–100; higher score means better self-efficacy.
GHQ: 12-item General Health Questionnaire, range 0–36; higher score means poorer psychological health.
DASS: 21-item Depression Anxiety Stress Scale, range 0–63; higher score means more depression, anxiety and stress.
PHQ: 9-item Patient Health Questionnaire, range 0–27; higher score means more depression.
EQ-5D index score: 5-item Euroqol; UK traffic was used; range -0.594 to 1; higher score means better health-related quality of life.
EQ-5D VAS: Visual Analogue Scale of EQ-5D, range 0–100; higher score means better self-rated health status.
SDSCA: (14-item Summary of Diabetes Self Care Assessment, range: 0–98; higher score means better self-care.
After 6 months, HbA 1c had increased in the comparison group from 7.1 ± 0.3% to 7.3 ± 1.1% ( P = .19) while remaining unchanged in the trainee group (7.1 ± 0.3% to 7.1 ± 1.1%, P = .81; between-group P = .02). The trainee group also had reductions in total cholesterol (180 ± 30 mg/dL to 170 ± 39 mg/Dl [4.7 ± 0.9 mmol/L to 4.3 ± 1.0 mmol/L], P = .01), low density-lipoprotein cholesterol (LDL-C) (100 ± 27 mg/dL to 93 ± 31 mg/dL, P = .03), and improvements in self-reported self-care activities, which were not seen in the comparison group.
Comparison Between the Agreed Group and Refused Group
Of the 59 qualified trainees, 26 refused to be peer supporters due to lack of time (50%), lack of interest in the program (19%), feeling unprepared (15%), and other reasons (16%). Among the 33 agreed trainees, 9 (28%) were housewives, 15 (47%) were retirees, and 8 (25%) were non-manual workers. The two groups had similar clinical profiles at baseline except that the agreed trainees had a better self-rated health status based on GHQ and EQ-5D VAS ( Table 2 ).
Clinical, Psychological, and Behavioral Characteristics at Baseline and 6 Months of Patients With Type 2 Diabetes Who Agreed to Become Peer Supporters (Agreed Trainees) And Patients Who Refused (Refused Trainees) After Attending The Training Program
| Agreed Trainees (n = 33) | Refused Trainees (n = 26) | Between Groups Value | |||
|---|---|---|---|---|---|
| Baseline | Month 6 | Baseline | Month 6 | ||
| Age, y, mean ± SD | 55.6 ± 11.5 | 53.8 ± 14.8 | |||
| Male (%) | 35 | 20 | |||
| High school or above (%) | 20.6 | 12.5 | |||
| Disease duration, y, mean ± SD | 11.3 ± 6.7 | 12.6 ± 6.4 | |||
| Non-smoker (%) | 93.8 | 92.9 | |||
| 125.1 | |||||
| HbA , mean ± SD | 7.0 ±2 | 7.0 ± 0.6 | 7.1 ± 0.4 | 7.1 ± 0.5 | .38 |
| Fasting plasma glucose, mg/dL | 135 ± 41 | 117 ± 31 | 140 ± 61 | 137 ± 43 | .04 |
| Systolic blood pressure, mmHg, mean ± SD | 125 ± 12.3 | 123 ± 10. 7 | 127 ± 14.4 | 125 ± 19.9 | .17 |
| Diastolic blood pressure, mmHg, mean ± SD | 72 ± 9.5 | 73 ± 9.9 | 69 ± 6.2 | 72 ± 12.4 | .27 |
| Total cholesterol, mg/dL, mean ± SD | 174 ± 35 | 155 ± 50 | 182 ± 35 | 170 ± 39 | .81 |
| Triglyceride, mg/dL, mean (IQR) | 124 (97–160) | 142 (97–186) | 124 (53–160) | 124 (53–142) | .16 |
| HDL-cholesterol, mg/dL, mean (IQR) | 50 (42–58) | 46 (38–54) | 58 (46–66) | 58 (6–77) | .41 |
| LDL-cholesterol, mg/dL, mean ± SD | 97 ± 31 | 89 ± 35 | 104 ± 22 | 100 ± 23 | .69 |
| DES mean score, mean ± SD | 4.18 ± 0.35 | 4.13 ± 0.27 | 4.02 ± 0.35 | 3.97 ± 0.15 | .20 |
| GHQ total score, mean ± SD | 43.5 ± 3.8 | 43 ± 3.82 | 46.2 ± 4.2 | 44.3 ± 2.76 | .45 |
| DASS total score, mean (IQR) | 4 (2–9) | 3 (0–8) | 6 (3–14) | 3.5 (1.8–11.8) | .67 |
| PHQ total score, mean (IQR) | 2 (1–3) | 0 (0–2) | 2 (0–4) | 2 (1–3) | .33 |
| EQ-5D index, mean (IQR) | 1 (0.80–1) | 1 (0.82–1) | 1 (0.80–1) | 0.80 (0.15–1) | .009 |
| EQ-5D VAS, mean ± SD | 84.6 ± 7.7 | 88.1 ± 8.9 | 74.5 ± 14.2 | 76.1 ± 15.2 | .95 |
| General diet, mean ± SD | 4.59 ± 1.62 | 5.76 ± 0.95 | 4.11 ± 2.01 | 5.3 ± 2.11 | .52 |
| Special diet, mean ± SD | 4.62 ± 1.28 | 5.78 ± 1.30 | 4.39 ± 1.39 | 5.17 ± 1.28 | .39 |
| Exercise, mean ± SD | 4.48 ± 1.95 | 4.76 ± 2.06 | 3.68 ± 2.28 | 4.4 ± 2.12 | .56 |
| Glucose monitoring, mean ± SD | 2.82 ± 1.94 | 3.17 ± 1.89 | 3.23 ± 2.47 | 2.5 ± 1.78 | .63 |
| Foot care, mean ± SD | 4.85 ± 1.82 | 5.79 ± 1.45 | 4.33 ± 1.87 | 5.4 ± 1.43 | .09 |
| Medication adherence, mean ± SD | 6.79 ± 1.11 | 6.54 ± 1.5 | 6.45 ± 1.48 | 7 ± 0.85 | .31 |
After 6 months, fasting plasma glucose had decreased from 135 ± 41 mg/dL to 117 ± 31 mg/dL, ( P = .033) in the agreed trainees while not changing in the refused trainees (140 ± 61 mg/dL to 137 ± 43 mg/dL, P = .61; between-group P = .04). Health-related quality of life decreased in the refused trainees (1[0.8–1.0] vs 0.8[0.5–1.0], P = .35) but remained stable in the agreed trainees (1[0.8–1.0] vs 1[0.8–1.0], P = .57) (between-group P = .009) who also had improvements in total cholesterol, LDL-C, depressive symptoms, and self-care compared with baseline ( Table 2 ).
Metabolic Control After 4 years
HbA 1c remained unchanged in the agreed trainees after they had provided structured peer support for 4 years (baseline, 7.0 ± 0.2%; at 4 years, 7.2 ± 0.6%, P = .07) but increased in both the refused trainees (7.1 ± 0.4% to 7.8 ± 0.8%, P = .02) and the comparison group (7.1 ± 0.5% to 8.1 ± 0.6%, P = .01; among groups, P <.001) ( Figure 2 ). No significant changes in blood pressure or LDL-C were observed in any group during the 4 years (data not shown).

Comparison of glycemic control in agreed trainees, refused trainees, and the comparison group during a 4-year observational period.
Data were presented as mean ± SE.
P = .001: Comparison of HbA1c at extension year 2013 among the accepted trainees, refused trainees, and the comparison group.
Patients with type 2 diabetes and fair glycemic control who attended a peer support train-the-trainer program focusing on diet, exercise, psychology, and communication improved their own self-care behaviors and metabolic control. Those who agreed to become peer supporters had higher self-rated health status at baseline with further improvements in glycemic and lipid control as well as self-care behaviors at 6 months. After 4 years, the agreed peer supporters maintained their glycemic control while control deteriorated in the refused and comparison groups.
In a recent meta-analysis of quality improvement strategies within diabetes care, promotion of self-management had the largest positive effect on metabolic control. 26 In our study, people who joined the train-the-trainer program emphasizing DSME improved their self-care behaviors and glycemic control compared with the comparison group at 6 months, lending further support to the effectiveness of self-management training in type 2 diabetes. 3 Moreover, by attending the train-the-trainer program, these patients were empowered with coping skills to address the chronicity of their condition with a focus on positive thinking, goal setting, and stress management, which were associated with reduced depressive symptoms. These findings echo the importance of incorporating coping strategies for dealing with negative emotions in addition to providing medical knowledge and technical skills in a well-designed DSME program. 27 , 28
Compared with patients who attended the train-the-trainer program but refused to be peer supporters, those who agreed to be peer supporters had very similar characteristics at baseline except higher self-rated health status, perhaps reflecting a happier and more optimistic group of individuals. 29 Interestingly, the improvement in self-care behaviors and metabolic control after 6 months appeared to be limited to those who became peer supporters despite the fact thatthe refused group had completed the same training program. Thus, beyond the benefits of the education included in the training, subsequent differences between the agreed and refused trainees suggest benefits of actually providing peer support, not just being trained to do so. Moreover, the volunteer effect and willingness to help among peer supporters might have self-perpetuating and positive benefits. 30 The intention to support others might have engaged the peer supporters to improve their own self-care behaviors and maintain good glycemic control over the long-term. 31 , 32 Additionally, voluntary work has been associated with higher self-esteem, 33 lower psychological distress, better quality of life, 34 and reduced mortality, 18 all findings consistent with the positive changes on emotions and self-management seen in our peer supporters.
Of note, although the refused trainees had a 0.2% lower HbA 1c at 6 months after the training program than the comparison group, HbA 1c had increased by 1% in both these groups after 4 years, in contrast to the observed maintenance of glycemic control of the agreed trainees. These findings underscore the importance of ongoing reinforcement to maintain the short-term improvement after a typical DSME program. 2 , 35 , 36 The mutual learning and ongoing support among peers, peer supporters, and healthcare professionals might have further improved the ability of peer supporters to control their diabetes, solve problems, and cope with negative emotions associated with living with diabetes. 37 , 38
This study had several limitations. Participants in the study group and comparison group were not randomized, but selected based on their having similar glycemic control. The selection process resulted in a mismatch in gender distribution between the groups, for which we adjusted in our statistical comparisons. A self-selection bias in the makeup of the agreed and refused trainee groups is likely. Although we collected reasons for refusal, we did not capture factors like employment status that may have affected patients’ decisions.
Both groups had similar clinical profiles, however, and both received similar clinical care in the same settings. The substantial difference in glycemic control after 4 years supports the hypothesis that engagement as peer supporters, not merely self-selection bias, contributed to the improvements seen in the agreed trainees.
The small sample size in each group precluded more refined analyses such as repeated-measures analysis. We also acknowledge that error may have resulted from multiple comparisons. We did not measure psychosocial status at the end of the 4-year period and were not able to evaluate the longitudinal impact of providing peer support on emotional status. Further, we did not capture detailed information about treatments, such as antidiabetic drug dosage changes, the addition of insulin, etc. Lastly, this study was conducted in hospital-based diabetes clinics and enlisted a multidisciplinary team to train the peer supporters, which might not be generalizable to primary care settings.
This study prospectively reported the long-term effects of providing ongoing peer support to others on patients with type 2 diabetes. It captured multidimensional outcomes and provides longitudinal evidence that by providing ongoing help to others, patients with diabetes benefited in regards to self-care, psychological health, and glycemic control over 4 years. Engaging patients to become peer supporters may be a useful strategy for long-term diabetes management.
Acknowledgments
Special thanks to all staff at the Asia Diabetes Foundation for their support.
Conflicts of interest: authors report none.
Funding support: Funding for this research was provided by the American Academy of Family Physicians Foundation through the Peers for Progress program with support from the Eli Lilly and Company Foundation and by the Asia Diabetes Foundation. The funders had no role in the study design, data collection, data analysis, or preparation of the manuscript.
Previous presentation: The preliminary results of this study were accepted as a poster presentation at the World Diabetes Congress 2011; December 8, 2011; Dubai, United Arab Emirates.
Talk to us about diabetes
0345 123 2399
customer support

Run with Diabetes UK
When you run with us, you get support that’s as relentless as your training. Apply for a place at next year’s London Landmarks Half Marathon.

Type 1 diabetes
All you need to know

Type 2 diabetes

Signs and symptoms
Are you at risk?

Tailored advice
Diabetes and Me
Learning Zone
£ 66 million
We’ve invested millions into diabetes research over the last decade alone, thanks to your donations. With your help, we’re getting closer to a cure.
1,117,010 posts
Join the conversation with 23,268 other people sharing their advice and experiences on our online forum .
2 million checks
Our Know Your Risk tool calculates your risk of diabetes and instantly emails you practical tips and lifestyle advice.
Diabetes UK in your area
Find regional contact information, your local support groups and activities near you.
News & Views

A day in the life as a Diabetes Educator: Amy Mcilhatton

Inhaled insulin and tech for type 2: new research presented from the A...

Omnipod 5 can now connect with the new Freestyle Libre 2 Plus sensor

Different patterns of body fat can protect against, or increase risk o...

Eating well with diabetes
Delicious, healthy recipes and facts about food.
Food and diabetes: need to know
Recipes for every occasion
10 ways to eat well with diabetes

Healthcare professionals
We work with people who contribute to diabetes treatment, care and research.
Diabetes UK's Continuous Professional Development courses
Professionals
Research projects

Here to help
Need to talk call us for answers to your questions and specialist advice.
Newly diagnosed? Let's get started
Diabetes and your emotions
Stories: This is Diabetes
Read inspiring stories from people whose lives have been affected by diabetes. Discover how they have overcome challenges in everyday life, to show you that you're not alone.

Paul's story: The impact of diabetes complications

Khadija's story: Challenges of living with diabetes from a young age

Tom's story - volunteering as a befriender

Reena's story: my experience with gestational diabetes
What is diabetes? Find out in our two-minute video spoken in English. Or choose a version in Urdu, Gujarati, Punjabi or Sylheti from our YouTube playlist

Recipe ideas
All our recipes have been approved by specialist dietitians, so you’ll always know what’s in your food.
© The British Diabetic Association operating as Diabetes UK, a charity registered in England and Wales (no. 215199) and in Scotland (no. SC039136). A company limited by guarantee registered in England and Wales with (no.00339181) and registered office at Wells Lawrence House, 126 Back Church Lane London E1 1FH


Health & Environmental Research Online (HERO)
- Learn about HERO
- Search HERO
- Projects in HERO
- Risk Assessment
- Transparency & Integrity
- Study Protocol
- Open access
- Published: 05 July 2024
Strategic use of resources to enhance colorectal cancer screening for patients with diabetes (SURE: CRC4D) in federally qualified health centers: a protocol for hybrid type ii effectiveness-implementation trial
- Denalee M. O’Malley 1 , 2 ,
- Benjamin F. Crabtree 1 , 2 ,
- Srivarsha Kaloth 1 ,
- Pamela Ohman-Strickland 1 , 2 , 3 ,
- Jeanne Ferrante 1 , 2 ,
- Shawna V. Hudson 1 , 2 &
- Anita Y. Kinney 2 , 3
BMC Primary Care volume 25 , Article number: 242 ( 2024 ) Cite this article
Metrics details
Persons with diabetes have 27% elevated risk of developing colorectal cancer (CRC) and are disproportionately from priority health disparities populations. Federally qualified health centers (FQHCs) struggle to implement CRC screening programs for average risk patients. Strategies to effectively prioritize and optimize CRC screening for patients with diabetes in the primary care safety-net are needed.
Guided by the Exploration, Preparation, Implementation and Sustainment Framework, we conducted a stakeholder-engaged process to identify multi-level change objectives for implementing optimized CRC screening for patients with diabetes in FQHCs. To identify change objectives, an implementation planning group of stakeholders from FQHCs, safety-net screening programs, and policy implementers were assembled and met over a 7-month period. Depth interviews ( n = 18–20) with key implementation actors were conducted to identify and refine the materials, methods and strategies needed to support an implementation plan across different FQHC contexts. The planning group endorsed the following multi-component implementation strategies: identifying clinic champions, development/distribution of patient educational materials, developing and implementing quality monitoring systems, and convening clinical meetings. To support clinic champions during the initial implementation phase, two learning collaboratives and bi-weekly virtual facilitation will be provided. In single group, hybrid type 2 effectiveness-implementation trial, we will implement and evaluate these strategies in a in six safety net clinics ( n = 30 patients with diabetes per site). The primary clinical outcomes are: (1) clinic-level colonoscopy uptake and (2) overall CRC screening rates for patients with diabetes assessed at baseline and 12-months post-implementation. Implementation outcomes include provider and staff fidelity to the implementation plan, patient acceptability, and feasibility will be assessed at baseline and 12-months post-implementation.
Study findings are poised to inform development of evidence-based implementation strategies to be tested for scalability and sustainability in a future hybrid 2 effectiveness-implementation clinical trial. The research protocol can be adapted as a model to investigate the development of targeted cancer prevention strategies in additional chronically ill priority populations.
Trial registration
This study was registered in ClinicalTrials.gov (NCT05785780) on March 27, 2023 (last updated October 21, 2023).
Patients with diabetes mellitus have an estimated 27% elevated lifetime risk of developing colorectal cancer (CRC), and are disproportionately from priority health disparities populations (e.g., low-income, Non-Hispanic Black and Hispanic) [ 1 , 2 ]. Nationally, guideline concordant receipt of CRC screening for patients with diabetes is not significantly different for women with diabetes (57% vs. patients without diabetes 58%) and is significantly higher among men with diabetes (63% vs. patients with diabetes 58%) [ 3 ]. CRC screening for patients with diabetes, who do not have other indications of high risk (e.g., family history of CRC, polyp removal during colonoscopy, personal history of CRC, inflammatory bowel disease) are advised to follow the average risk screening recommendations [ 4 ]. Federally qualified health centers (FQHCs) primarily serve as primary care for priority health disparities populations and struggle to sustainably implement CRC screening programs for average-risk patients which includes patients with diabetes. CRC screening uptake in FQHCs populations has been consistently lower (44.1%) than the national average for average risk, age-eligible adults (67.3%) [ 5 ].
Persons receiving diabetes care in FQHCs have elevated health risks overall and higher rates of poverty and low-income status than the general population [ 6 ]. Ten percent of FQHC patients have a diabetes diagnosis and more than a third within this group have uncontrolled diabetes (HbA1c > 9%). Failure to implement preventive CRC screenings translates to an average of 6.5 years of lost life for patients subsequently diagnosed with CRC [ 7 ]. Moreover, this contributes to greater burden for patients with diabetes who are diagnosed with CRC who suffer greater morbidity, all-cause mortality, and cancer-specific mortality compared to CRC patients [ 8 , 9 , 10 ]. Therefore, efforts to prioritize CRC screening for patients with diabetes are needed in primary care safety-net settings.
Multiple evidence-based CRC screening tests are available which complicates implementation. The U.S. Preventive Services Taskforce (USPSTF) recommends CRC screening in adults aged 45–75, with multiple screening options available including non-invasive stool based testing: high sensitivity guaiac fecal occult blood tests (gFOBT), fecal immunochemical test (FIT), FIT plus stool DNA testing (FIT-DNA); and direct visualization tests: colonoscopy, computed tomography (CT) colography, and flexible sigmoidoscopy (FS) (with or without FIT) (see Table 1 for intervals) [ 4 ]. Colonoscopy and FS, have been shown to reduce mortality by (68% and 28%, respectively). FIT and FOBT are associated with 13–33% mortality reductions. Stool-based testing mortality reductions require sustained annual adherence. [ 11 , 12 , 13 , 14 ]. Research has shown that failures to screen at all, to screen at appropriate intervals, and to follow-up on abnormal results are associated with risk of CRC death [ 15 ].
Given major differences in mortality reduction benefits, temporal intervals for retesting, costs, and patient burden, controversies have emerged surrounding the pros and cons of testing methods [ 16 , 17 ]. Colonoscopy and FS allow for polypectomies, which can prevent CRC [ 18 , 19 ]; however, FS is not widely used in the U.S, because colonoscopy evaluates the entire colon, can be done every 10 years, and is associated with a greater mortality reduction [ 20 ]. A re-analysis of the USPSTF data suggest that prevention, through the removal of polyps during colonoscopy, is the sole mechanism of CRC mortality reductions [ 19 ]. Colonoscopy is thus the “gold standard,” despite critiques about the rigor of this evidence (e.g., indirect and observational). [ 21 , 22 , 23 , 24 ]. In FQHCs, non-invasive tests are emphasized and colonoscopies are often a second line-screening based on abnormal gFOBT/FIT findings. [ 25 ]. Non-invasive tests are emphasized because these are less costly, require less time (and time off of work), less complicated to complete, do not require transportation, and are guideline concordant [ 26 ]. Despite stool based testing’s acceptability, US-based trials in FQHCs designed to increase annual adherence to stool-based testing have reported low screening adherence over three years (10.4–16.4%) [ 27 , 28 , 29 ].
Prioritizing colonoscopy with longer testing intervals in under-resourced FQHCs for patients with diabetes introduces fewer opportunities for care breakdowns, is guideline concordant, and prevents CRC by removing premalignant colonic polyps. Guided by the Exploration, Preparation, Implementation and Sustainment [ 30 ]. (EPIS) framework, this research study will develop and evaluate targeted CRCs screening strategies for patients with diabetes in safety-net settings. This study addresses known implementation challenges using a “designing for dissemination” approach [ 31 , 32 , 33 ] that attends to important contextual, organizational capacity and patient complexity factors that impact CRC screening program implementation in clinics and uptake among patients with diabetes.
Conceptual framework
The design of this study was guided by the EPIS framework. EPIS is an evidence-based practice (EBP) implementation framework that includes four defined phases for assessment of inner and outer contextual factors that influence EBP implementation (see Table 2 ). For this study, the EBP is CRC screening uptake among age eligible patients with diabetes. Exploration is the act of identifying patient needs and the availability of EBPs to address identified needs, and the decision to adopt evidence into practice based on fit within the inner clinical context. During this phase, the adaptations to the evidence are based on system, organization, and individual patient factors. Preparation includes planning implementation, inventorying proposed challenges, and developing strategies to overcome anticipated barriers. A critical component of this phase is the planning of implementation strategies to support EBP utilization in the next two phases and to address organizational climate to ensure that EBPs will be supported, expected, and rewarded. During the clinical trial, this study focuses on implementation, the process of assuring and balancing fidelity to the EBP delivered with adaptations needed to assure program success. Sustainment focuses on maintenance and program and factors impacting implementation over the long haul. EPIS considers innovation factors, which are the characteristics of the EBP being implemented. The innovation-EBP fit considers if the EBP fits the patient, provider, and organizational needs. Innovation factors are assessed and can be adapted to maximize the fit of an EBP while maintaining the core elements of the intervention to retain fidelity.
Methods and design
Identifying multi-level change levers: a multi-method stakeholder informed approach.
Earlier phases of this research focused on the Exploration and Preparation phases, while the current protocol describes the intervention implementation and its evaluation. During the exploration phase, a secondary analysis was conducted of a nationally representative data set to identify patient level determinants of CRC screening uptake overall (i.e., with any test) and test-specific uptake among individuals with diabetes. We explored disparities in uptake overall and testing type based on race, ethnicity, income, and educational status. Additionally, a scoping literature review was performed to identify evidence-based interventions and implementation strategies for CRC screening and diabetes management in FQHCs. Based on this scoping review, we identified additional interventions and implementation strategies, using the Expert Recommendations for Implementing Change (ERIC) taxonomy [ 34 ]. A list of interventions and implementation strategies was compiled related to diabetes management processes to expand an existing measure that was developed and used to evaluate the use of evidence-based intervention and implementation for CRC in FQHCs [ 35 ].
For the preparation phase of the formative research, we used implementation mapping, an iterative process that incorporates community based participatory research principles [ 36 , 37 ]. An Implementation Planning Group (IPG) was assembled to represent a diversity of implementation actors (e.g., clinicians, state-level decision makers, screening safety-net programs) who work in and with FQHCs. The goal of the IPG, which met 5 times over a six-month period, was to develop shared understandings of the research problem based on empirical knowledge from the national survey analysis, the scoping review of the literature, and local knowledge of the IPG members about patient population and clinic system capacities. The IPG group identified and prioritized the selection of implementation strategies to improve CRC screening uptake for patients with diabetes. The IPG and research team iterated an implementation plan specifying multi-level change objectives and implementation determinants to develop supports to help prioritize CRC screening implementation for patients with diabetes.
Guided by the insights of the exploration and preparation phases, we developed the Strategic Use of Resources for Enhanced ColoRectal Cancer Screening in Patients with Diabetes (SURE: CRC4D) implementation toolkit, which includes tailorable materials and protocols that will be tested in a single arm, hybrid type 2 effectiveness-implementation single arm clinical trial. The objectives of this trial are to:
Determine the effectiveness of the SURE: CRC4D multi-component implementation strategies to increase CRC screening uptake among patients with diabetes.
Evaluate the fidelity, feasibility, and acceptability of SURE: CRC4D implementation.
Refine the SURE: CRC4D toolkit based on multi-level user feedback and conduct an evaluation to promote scalability and sustainable use.
Study participants and setting
This single arm trial will be conducted in six FQHC clinical sites in New Jersey. Eligibility criteria for the FQHC clinics include: (1) provide care to at least 450 patients aged 50–74 years; (2) 10% of patient population previously diagnosed with diabetes; (3) located in New Jersey; and, 3) clinical and administrative leadership willing to engage in the intervention and research requirements (interviews, data validation, process evaluation). Implementation outcomes will be assessed using mixed methods guided by the EPIS constructs (see Table 2 ). The methods of this study have been reported using Standard Protocol Items: Recommendation for Interventional Trials (SPIRIT) guidelines (Supplemental file 1 ).
During the implementation a clinic-based registry of patients eligible for CRC screening will be developed for each clinic at baseline and updated at six and 12 months post-baseline. Patient eligibility criteria will include: (1) patients not up-to-date or due for CRC screening [ 4 ]. based on electronic health record (EHR) documentation (e.g. FOBT/FIT test in last year, flexible sigmoidoscopy within 4 years, or colonoscopy within 9 years), (2) previous diagnosis of type II diabetes, (3) age-eligible for CRC screening (45–74 years of age) and (4) ) FIT/FOBT that has been ordered for more than 6 months that has not been completed or a sigmoidoscopy or colonoscopy referral that has not been completed for 12 or more months. Patients are excluded if they have EHR documentation medical conditions not concordant with standard CRC screening intervals (e.g. prior CRC diagnosis, inflammatory bowel disease, renal failure, etc.) [ 4 ].
The NJ Primary Care Research Network (NJPCRN) will recruit eligible clinics for participation. The NJPCRN is an Agency for Healthcare Research and Quality recognized practice-based research in primary care practices. The NJPRN will contact FQHCs that participated in previous research and ask IPG members to make introductions with their FQHC leadership networks. Emails with study flyers will be sent to the FQHC with follow-up telephone outreach. This protocol has been approved by the Rutgers University Institutional Review Board (Pro2020002075). All study participants will be asked to provide informed consent prior to participation in all phase of this research. We expect the distribution of patient participants to reflect the racial/ethnic diversity of the FQHCs recruited, who predominantly serve low-income, racial, and ethnic minority populations.
Implementation strategies
The goal of SURE: CRC4D is to enable FQHC clinics to adopt strategies to optimize the use of evidence based colorectal cancer screenings (See Table 1 ) uptake for patients with type II diabetes. To accomplish this, multi-level, multi-component implementation strategies (see Table 3 ) will be utilized. The core components of this implementation effort includes the identification and engagement of 2–3 clinic change champions, who will participate in two virtual learning collaborative events [ 38 , 39 , 40 , 41 ] and lead the change effort in the clinic aided by bi-weekly virtual practice facilitator support [ 38 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 ]. The SURE: CRC4D toolkit will include guidance on pulling data to develop and implement quality monitoring systems to provide regular audit/feedback to the clinic, patient educational materials in English and Spanish and dissemination materials for clinical meetings to orient other clinic members to the change process being implemented to optimize CRC screening for patients with diabetes [ 50 , 51 ]. Clinic champions will tailor toolkit resources as clinics may have different electronic medical records, type and composition of staff, clinical workflows, and standing clinical team meetings.
The implementation will be rolled out over a 12-week period. Initially, clinics will be asked to identify 1–3 clinic champions, with at least one clinician (i.e., physician, advanced practice nurse, physician assistant) per team. Each team will meet with the external practice change facilitator approximately two weeks prior to the initial learning collaborative. This initial facilitation meeting is introductory, with the goal of encouraging clinic champions to reflect about the current clinic CRC screening strategies and diabetes care management processes prior to the 1st virtual learning collaborative. Clinical champions will attend the 1- hour virtual learning collaborative, where the materials in the SURE: CRC4D toolkit will be provided and reviewed, and each clinic team will formulate practice change goals. Teams will decide on how to deploy the toolkit strategies at their FQHC sites over the course of the next ten weeks. The practice facilitator will support the clinic champion team in the development, implementation, and refinement of the local practice change plan. The champions will meet with the practice facilitator every two weeks for 8 weeks (4 times). During this time, the plan will be refined and adjusted based on feedback from clinic leaders and practice staff members and identified strengths and barriers that are encountered during the implementation effort. At week 10, a second learning collaborative will be virtually convened, providing a forum where the different clinic teams can share their successes and obstacles during the development and execution of their plan. This forum will foster cross-team learning and idea generation that can inform the refinement of the SURE: CRC4D toolkit and sustainability of practice change efforts. Two weeks after the second learning collaborative, a final virtual facilitation meeting will be held to reflect and refine the practice plan to support sustainability.
Evaluation of the effectiveness and implementation of SURE: CRC4D
The effectiveness and implementation of SURE: CRC4D will be evaluated using a mixed method learning evaluation strategy, where ongoing data collection and analysis are used to refine implementation to optimize adoption of CRC screening for patients with diabetes [ 52 , 53 ]. This evaluation is designed to address two research questions: (1) are the adapted implementation strategies clinically effective in increasing CRC screening rates for patients with diabetes; and, (2) are the implementation strategies feasible and acceptable to implementers (e.g., clinicians and staff) and patients in FQHCs? This evaluation builds an evidence base about the effectiveness of the implementation strategies in a real-world context and allows for the collection of data that can be used to refine the implementation toolkit for a larger scale, definitive cluster randomized controlled trial. Guided by EPIS, contextual factors were selected based on suggestions from clinical stakeholders, community partners, and previous literature suggesting they may influence implementation success [ 54 , 55 , 56 ] (see Table 4 ). The following assessments and measures will be collected to evaluate the trial:
Organizational assessments
Guided by EPIS, contextual factors will be evaluated at baseline and 1 year-post implementation. Medical Directors or the Chief Operating Officer of each clinic will be asked to complete a web-based survey called the Clinic Organizational Information Form (COIF). This survey assesses Implementation Climate and History of Implementation related to CRC screening and diabetes management [ 35 ]. Additionally, patient demographics, management strategies, and payor mix are collected using this survey for each clinic.
Clinic staff measures and assessments
The Clinic Staff Questionnaire (CSQ) will be administered to all practice clinicians and staff members at baseline and 12-month post-implementation. The clinic team measures include Medical Provider and Staff Background and history with the organization. Additionally, Change Process Capability will be measured, specifically “previous history of change,” and “ability to initiate and sustain change.” [ 57 ]. These two measures have been identified these as key mechanisms for successful organizational change and its wide use in cardiovascular care implementation [ 58 , 59 , 60 ]. Additional practice-based measures will include: Adaptive Reserve a feature of resilient organizations shown to be associated with practice-level implementation of CRC screening, will be measured in the CSQ with the validated 23-item scale [ 57 , 61 ]. The CSQ will also include the Implementation Leadership Scale (ILS), a brief psychometrically strong measure that contains 12-items with four subscales of proactive, knowledgeable, supportive, and perseverant leadership [ 62 ].
Process data outcomes
Learning collaborative and facilitation phone calls will be audio recorded and transcribed to document issues that arose during the implementation process. Additionally, qualitative interviews will be conducted at baseline and beginning at 6 months post implementation. We will select key implementers (3–4 individuals per site) to assess perceptions of organizational readiness to change, leadership style and additional facility characteristics (e.g., assets and deficits of location, satisfaction with ease of access to facility, etc.). Staff and clinician perceptions of the SURE: CRC4D implementations’ feasibility and acceptability will also assessed asking providers and staff to describe their implementation experiences. The interviews will probe stakeholder perceptions of change in their organizations, systems, and factors that they think impacted implementation. Staff or provider fidelity will be assessed based on the clinic-level proportion of eligible patients who were (1) contacted based on implementation protocol and (2) completed any CRC screening at 1 year.
Patient level: clinical effectiveness outcome and implementation assessment
The primary outcome variables to assess clinical effectiveness will be the clinic level proportion of patients with diabetes who: (a) receive any CRC screening and (b) complete a colonoscopy at 12 months from baseline. An exploratory analysis will assess clinic-level CRC screening completion by glucose control (controlled vs. uncontrolled, i.e., HbA1c > 9 at 12 months). Patient level data is collected in aggregate and will include no identified personal health information.
Patient acceptability will be assessed through the assessment of patient rates of opting-out and non-adherence of CRC screening. This rate will be based on the proportion of CRC screening among patients with diabetes compared to overall eligible patient population (without diabetes) in each clinic.
Data analyses
Qualitative analysis.
On a quarterly basis, we will analyze data from each clinic site using a comparative case analysis [ 63 ]. Organizational level data and interview transcripts will be organized, read and coded in ATLAS.ti. Data will be analyzed on an ongoing basis, and a working summary of emergent findings will be updated as incoming data is added. As a validity check of qualitative results, we will check relevant data interpretations against all new data using a constant comparison approach [ 64 ]. We will note similarities and differences of implementation feasibility between practice sites based on clinic characteristics and from data provided in interviews. Each quarter all quantitative and qualitative results will be summarized in brief reports to be shared with the research team for reflections on any changes needed. These analyses represent ongoing monitoring and feedback to inform refinements of the implementation strategy and clinical trial procedures to refine implementation strategy to better fit local needs and contexts.
Quantitative analysis
Descriptive statistics will be used to summarize patient and clinic characteristics. We will declare our intervention a success if at least 25% of those unscreened are screened at 12-month follow-up in this difficult to reach population. We will declare the optimization of screening a success if 15% of those unscreened are screened with a colonoscopy or flexible sigmoidoscopy at 12-months. Overall improvement metrics are comparable to improvements in previous CRC screening implementation studies in FQHCs [ 65 , 66 ]. At baseline, we will calculate average screening rates and their confidence intervals across all practice sites in intent to treat analyses and at 12-months we will assess screening rates and their confidence intervals for all sites. The confidence intervals will be compared to 25%. We will compare differences in CRC screening by glucose control, sex, and race/ethnicity.
Power calculations
The value of information method [ 67 ] was utilized to select a sample size balancing the costs and feasibility goals of the trial. This sample size (e.g., six clinic sites, assuming at least n = 30 patient in each) is sufficient to generate preliminary estimates of the estimated effect (80% confidence interval) of the implementation strategy on CRC screeningrates [ 68 , 69 ]. In developing the power calculation, we assume equal numbers of patients ( n = 50) per clinic (the anticipated number of eligible patients, n = 450 CRC screening eligible, with > 10% diabetes diagnosis). Of those with diabetes, we expect 40% to be up-to-date with screening guidelines based on the average rate of CRC screening in FQHCs [ 70 ]. Thus, the target sample size is n = 30 patients in each FQHC.
This study aims to optimize CRC screening using the engagement of multi-level stakeholders (patients, clinicians, staff in FQHCs) and using an implementation mapping during the exploration and preparation phases prior to implementation [ 37 ]. This project is innovative in several key ways. Regarding conceptual innovation, few studies have included CRC screening as a component of diabetes care prior to CRC diagnosis [ 71 , 72 ], while many have focused on improving CRC screening for average risk adults in FQHCs [ 65 , 66 , 73 , 74 , 75 , 76 , 77 , 78 , 79 ].An EPIS framework systematic review concluded that attention to planning EBP use is “infrequent though critical [ 80 ].” FQHC implementation of CRC screening programs focus on achieving the Uniform Data System (UDS) targets, which do not distinguish patients at greater risk for CRC in the “average-risk” patient population [ 70 , 81 ]. Metrics for UDS CRC screening program are also cross-sectional and collected as separate metrics unrelated to diabetes care or annual stool-based testing adherence. For FIT and FOBT stool-based CRC screening strategies to be clinically effective and for their mortality reductions to be realized sustained annual adherence is required, which has been proven difficult to accomplish in safety-net primary care settings [ 12 , 13 ]. Additionally, few FQHCs formally assess factors related screening prior to implementing improvement interventions [ 82 ]. This study aims to optimize CRC prevention using the engagement of multi-level stakeholders (patients, clinicians, staff in FQHCs) and using an implementation mapping during the exploration and preparation phases prior to implementation [ 37 ].
Despite being the most studied evidence-based cancer screening in the National Institutes of Health implementation science portfolio, no systematic studies have integrated CRC screening and diabetes evidence-based approaches to prioritize preventive care for patients with diabetes in the primary care safety-net. To date, research has focused on overall CRC guideline adherence, relying on an ‘all boats rise’ approach despite the failures of such strategies to achieve improvements in chronic disease targets [ 83 ]. In contrast, this study focuses on optimizing CRC screening using targeted implementation strategies to address disparities among individuals with diabetes to promote health equity.
Study findings are poised to inform the develop scalable, equitable approaches to CRC screening in safety-net primary care settings. If successful, next steps will include testing the scalability and sustainability in federally qualified health centers nationally. Further, this approach can be adapted as a model to investigate the development of targeted cancer prevention strategies in additional chronically ill priority populations.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- Colorectal cancer
Computed tomography
Fecal immunochemical tests
Fecal immunochemical test stool DNA testing
Federally qualified health centers
Flexible sigmoidoscopy
Guaiac fecal occult blood tests
Implementation Planning Group
Electronic health record
Evidence-based practice
Expert Recommendations for Implementing Change
Exploration, Preparation, Implementation, Sustainment
New Jersey Primary Care Research Network
CRC4D: Strategic Use of Resources for Enhanced ColoRectal Cancer Screening in Patients with Diabetes
Standard Protocol Items: Recommendation for Interventional Trials
Uniform Data System
U.S. Preventive Services Taskforce
Spanakis EK, Golden SH. Race/ethnic difference in diabetes and diabetic complications. Curr Diab Rep. 2013;13(6):814–23.
Article PubMed Google Scholar
Karter AJ, Ferrara A, Liu JY, Moffet HH, Ackerson LM, Selby JV. Ethnic disparities in diabetic complications in an insured population. JAMA. 2002;287(19):2519–27.
Miller EA, Tarasenko YN, Parker JD, Schoendorf KC. Diabetes and colorectal cancer screening among men and women in the USA: National Health interview survey: 2008, 2010. Cancer Causes Control. 2014;25(5):553–60. https://doi.org/10.1007/s10552-014-0360-z .
Davidson KW, Barry MJ, Mangione CM, Cabana M, Caughey AB, Davis EM, Donahue KE, Doubeni CA, Krist AH, Kubik M, Li L, Ogedegbe G, Owens DK, Pbert L, Silverstein M, Stevermer J, Tseng CW, Wong JB. Screening for Colorectal Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2021;325(19):1965–77. https://doi.org/10.1001/jama.2021.6238 . PubMed PMID: 34003218.
May FP, Yang L, Corona E, Glenn BA, Bastani R. Disparities in Colorectal Cancer Screening in the United States before and after implementation of the Affordable Care Act. Clinical Gastroenterology and Hepatology; 2019.
Huang ES, Zhang Q, Brown SE, Drum ML, Meltzer DO, Chin MH. The cost-effectiveness of improving diabetes care in U.S. federally qualified community health centers. Health Serv Res. 2007;42(6 Pt 1):2174-93; discussion 294–323. doi: 10.1111/j.1475-6773.2007.00734.x. PubMed PMID: 17995559; PMCID: PMC2151395.
Liu P-H, Wang J-D, Keating NL. Expected years of life lost for six potentially preventable cancers in the United States. Prev Med. 2013;56(5):309–13. https://doi.org/10.1016/j.ypmed.2013.02.003 .
Boakye D, Rillmann B, Walter V, Jansen L, Hoffmeister M, Brenner H. Impact of comorbidity and frailty on prognosis in colorectal cancer patients: A systematic review and meta-analysis. Cancer Treat Rev. 2018;64. https://doi.org/10.1016/j.ctrv.2018.02.003 . Epub 2018/02/10. :30 – 9.
Jiang Y, Ben Q, Shen H, Lu W, Zhang Y, Zhu J. Diabetes mellitus and incidence and mortality of colorectal cancer: a systematic review and meta-analysis of cohort studies. Eur J Epidemiol. 2011;26(11):863–76. https://doi.org/10.1007/s10654-011-9617-y .
Mills KT, Bellows CF, Hoffman AE, Kelly TN, Gagliardi G. Diabetes mellitus and colorectal cancer prognosis: a meta-analysis. Dis Colon Rectum. 2013;56(11):1304–19. https://doi.org/10.1097/DCR.0b013e3182a479f9 .
Article PubMed PubMed Central Google Scholar
Shaukat A, Mongin SJ, Geisser MS, Lederle FA, Bond JH, Mandel JS, Church TR. Long-term mortality after screening for colorectal cancer. N Engl J Med. 2013;369(12):1106–14. https://doi.org/10.1056/NEJMoa1300720 . PubMed PMID: 24047060.
Article CAS PubMed Google Scholar
Jensen CD, Corley DA, Quinn VP, Doubeni CA, Zauber AG, Lee JK, Zhao WK, Marks AR, Schottinger JE, Ghai NR, Lee AT, Contreras R, Klabunde CN, Quesenberry CP, Levin TR, Mysliwiec PA. Fecal immunochemical test program performance over 4 rounds of Annual Screening: a retrospective cohort study. Ann Intern Med. 2016;164(7):456–63. https://doi.org/10.7326/M15-0983 . PubMed PMID: 26811150; PMCID: PMC4973858.
Inadomi JM, Vijan S, Janz NK, Fagerlin A, Thomas JP, Lin YV, Munoz R, Lau C, Somsouk M, El-Nachef N, Hayward RA. Adherence to colorectal cancer screening: a randomized clinical trial of competing strategies. Arch Intern Med. 2012;172(7):575–82. https://doi.org/10.1001/archinternmed.2012.332 . Epub 2012/04/12.
Shroff J, Thosani N, Batra S, Singh H, Guha S. Reduced incidence and mortality from colorectal cancer with flexible-sigmoidoscopy screening: a meta-analysis. World J Gastroenterol. 2014;20(48):18466–76. https://doi.org/10.3748/wjg.v20.i48.18466 . PubMed PMID: 25561818.
Doubeni CA, Fedewa SA, Levin TR, Jensen CD, Saia C, Zebrowski AM, Quinn VP, Rendle KA, Zauber AG, Becerra-Culqui TA, Mehta SJ, Fletcher RH, Schottinger J, Corley DA. Modifiable failures in the colorectal Cancer screening process and their Association with risk of death. Gastroenterology. 2019;156(1):63–e746. https://doi.org/10.1053/j.gastro.2018.09.040 .
Gorin SS. Multilevel approaches to reducing Diagnostic and Treatment Delay in Colorectal Cancer. Annals Family Med. 2019;17(5):386–9.
Article Google Scholar
Breen N, Skinner CS, Zheng Y, Inrig S, Corley DA, Beaber EF, Garcia M, Chubak J, Doubeni C, Quinn VP, Haas JS, Li CI, Wernli KJ, Klabunde CN. Time to follow-up after Colorectal Cancer Screening by Health Insurance Type. Am J Prev Med. 2019;56(5):e143–52. https://doi.org/10.1016/j.amepre.2019.01.005 .
Swartz AW, Eberth JM, Josey MJ, Strayer SM. Ann Intern Med. 2017;167(8):602–3. https://doi.org/10.7326/m17-0859 . Epub 2017/08/23. Reanalysis of All-Cause Mortality in the U.S. Preventive Services Task Force 2016 Evidence Report on Colorectal Cancer Screening.
Swartz AW, Eberth JM, Strayer SM. Preventing colorectal cancer or early diagnosis: Which is best? A re-analysis of the U.S. Preventive Services Task Force Evidence Report. Prev Med. 2019;118. https://doi.org/10.1016/j.ypmed.2018.10.014 . Epub 2018/10/28. :104 – 12.
Lin JS, Piper MA, Perdue LA, Rutter CM, Webber EM, O’Connor E, Smith N, Whitlock EP. Screening for colorectal cancer: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2016;315(23):2576–94.
Atkin WS, Edwards R, Kralj-Hans I, Wooldrage K, Hart AR, Northover JMA, Parkin DM, Wardle J, Duffy SW, Cuzick J. Once-only flexible sigmoidoscopy screening in prevention of colorectal cancer: a multicentre randomised controlled trial. Lancet. 2010;375(9726):1624–33. https://doi.org/10.1016/S0140-6736(10)60551-X .
Schoen RE, Pinsky PF, Weissfeld JL, Yokochi LA, Church T, Laiyemo AO, Bresalier R, Andriole GL, Buys SS, Crawford ED, Fouad MN, Isaacs C, Johnson CC, Reding DJ, O’Brien B, Carrick DM, Wright P, Riley TL, Purdue MP, Izmirlian G, Kramer BS, Miller AB, Gohagan JK, Prorok PC, Berg CD. Colorectal-Cancer incidence and mortality with screening flexible sigmoidoscopy. N Engl J Med. 2012;366(25):2345–57. https://doi.org/10.1056/NEJMoa1114635 . PubMed PMID: 22612596.
Article CAS PubMed PubMed Central Google Scholar
Segnan N, Armaroli P, Bonelli L, Risio M, Sciallero S, Zappa M, Andreoni B, Arrigoni A, Bisanti L, Casella C, Crosta C, Falcini F, Ferrero F, Giacomin A, Giuliani O, Santarelli A, Visioli CB, Zanetti R, Atkin WS, Senore C, Group atSW. Once-only sigmoidoscopy in Colorectal Cancer Screening: follow-up findings of the Italian randomized controlled Trial—SCORE. JNCI: J Natl Cancer Inst. 2011;103(17):1310–22. https://doi.org/10.1093/jnci/djr284 .
Holme Ø, Løberg M, Kalager M, Bretthauer M, Hernán MA, Aas E, Eide TJ, Skovlund E, Schneede J, Tveit KM, Hoff G. Effect of flexible Sigmoidoscopy Screening on Colorectal Cancer incidence and mortality: a Randomized Clinical Trial. JAMA. 2014;312(6):606–15. https://doi.org/10.1001/jama.2014.8266 .
Nishihara R, Wu K, Lochhead P, Morikawa T, Liao X, Qian ZR, Inamura K, Kim SA, Kuchiba A, Yamauchi M, Imamura Y, Willett WC, Rosner BA, Fuchs CS, Giovannucci E, Ogino S, Chan AT. Long-term colorectal-cancer incidence and mortality after lower endoscopy. N Engl J Med. 2013;369(12):1095–105. https://doi.org/10.1056/NEJMoa1301969 . PubMed PMID: 24047059.
Gwede CK, Davis SN, Quinn GP, Koskan AM, Ealey J, Abdulla R, Vadaparampil ST, Elliott G, Lopez D, Shibata D, Roetzheim RG, Meade CD. Tampa Bay Community Cancer Network P. making it work: Health Care Provider perspectives on strategies to increase colorectal Cancer screening in federally qualified Health centers. J Cancer Educ. 2013;28(4):777–83. https://doi.org/10.1007/s13187-013-0531-8 .
Arnold CL, Rademaker A, Wolf MS, Liu D, Lucas G, Hancock J, Davis TC. Final results of a 3-Year literacy-informed intervention to promote Annual Fecal Occult Blood Test Screening. J Community Health. 2016;41(4):724–31. https://doi.org/10.1007/s10900-015-0146-6 . PubMed PMID: 26769026; PMCID: PMC4930386.
Singal AG, Gupta S, Skinner CS, Ahn C, Santini NO, Agrawal D, Mayorga CA, Murphy C, Tiro JA, McCallister K, Sanders JM, Bishop WP, Loewen AC, Halm EA. Effect of Colonoscopy Outreach vs Fecal Immunochemical Test Outreach on Colorectal Cancer Screening Completion: a Randomized Clinical Trial. JAMA. 2017;318(9):806–15. https://doi.org/10.1001/jama.2017.11389 . PubMed PMID: 28873161; PMCID: PMC5648645.
Green BB, Anderson ML, Cook AJ, Chubak J, Fuller S, Meenan RT, Vernon SW. A centralized mailed program with stepped increases of support increases time in compliance with colorectal cancer screening guidelines over 5 years: a randomized trial. Cancer. 2017;123(22):4472–80. https://doi.org/10.1002/cncr.30908 . PubMed PMID: 28753230; PMCID: PMC5673524.
Aarons GA, Hurlburt M, Horwitz SM. Advancing a conceptual model of evidence-based practice implementation in public service sectors. Adm Policy Ment Health. 2011;38(1):4–23. https://doi.org/10.1007/s10488-010-0327-7 . Epub 2011/01/05.
Holtrop JS, Rabin BA, Glasgow RE. Dissemination and implementation science in primary Care Research and Practice: contributions and opportunities. J Am Board Fam Med. 2018;31(3):466–78. https://doi.org/10.3122/jabfm.2018.03 . .170259. PubMed PMID: 29743229.
Dearing JW, Kreuter MW. Designing for diffusion: how can we increase uptake of cancer communication innovations? Patient Educ Couns. 2010;81 Suppl:S100-10. https://doi.org/10.1016/j.pec.2010.10.013 . PubMed PMID: 21067884; PMCID: 3000559.
Brownson RC, Jacobs JA, Tabak RG, Hoehner CM, Stamatakis KA. Designing for dissemination among public health researchers: findings from a national survey in the United States. Am J Public Health. 2013;103(9):1693–9. https://doi.org/10.2105/AJPH.2012.301165 . PubMed PMID: 23865659; PMCID: 3966680.
Powell BJ, Waltz TJ, Chinman MJ, Damschroder LJ, Smith JL, Matthieu MM, Proctor EK, Kirchner JE. A refined compilation of implementation strategies: results from the Expert recommendations for Implementing Change (ERIC) project. Implement Sci. 2015;10(1):21. https://doi.org/10.1186/s13012-015-0209-1 .
Adams SA, Rohweder CL, Leeman J, Friedman DB, Gizlice Z, Vanderpool RC, Askelson N, Best A, Flocke SA, Glanz K, Ko LK, Kegler M. Use of evidence-based interventions and implementation strategies to increase colorectal Cancer screening in federally qualified Health centers. J Community Health. 2018;43(6):1044–52. https://doi.org/10.1007/s10900-018-0520-2 . PubMed PMID: 29770945; PMCID: PMC6239992.
Wallerstein N, Duran B. Community-based participatory research contributions to intervention research: the intersection of science and practice to improve health equity. Am J Public Health. 2010;100(Suppl 1). https://doi.org/10.2105/ajph.2009.184036 . Epub 2010/02/12. :S40-6.
Fernandez ME, Ten Hoor GA, van Lieshout S, Rodriguez SA, Beidas RS, Parcel G, Ruiter RAC, Markham CM, Kok G. Implementation mapping: using intervention mapping to develop implementation strategies. Front Public Health. 2019;7:158. https://doi.org/10.3389/fpubh.2019.00158 . Epub 2019/07/06.
Balasubramanian BA, Chase SM, Nutting PA, Cohen DJ, Strickland PA, Crosson JC, Miller WL, Crabtree BF, Team US. Using learning teams for reflective adaptation (ULTRA): insights from a team-based change management strategy in primary care. Ann Fam Med. 2010;8(5):425–32. https://doi.org/10.1370/afm.1159 . Epub 2010/09/17.
Mittman BS. Creating the evidence base for quality improvement collaboratives. Ann Intern Med. 2004;140(11):897–901. https://doi.org/10.7326/0003-4819-140-11-200406010-00011 . Epub 2004/06/03.
Bate JOV, Cleary P, Cretin P, Gustafson S, McInnes D, McLeod K, Molfenter H, Plsek T, Robert P, Shortell G, Wilson S. Quality collaboratives: lessons from research. Qual Saf Health Care. 2002;11(4):345–51. PubMed PMID: 12468695; PMCID: PMC1757995.
Shaw EK, Chase SM, Howard J, Nutting PA, Crabtree BF. More black box to explore: how quality improvement collaboratives shape practice change. J Am Board Fam Med. 2012;25(2):149–57. https://doi.org/10.3122/jabfm.2012.02.110090 . PubMed PMID: 22403195; PMCID: PMC3362133. Epub 2012/03/10.
Chase SM, Crabtree BF, Stewart EE, Nutting PA, Miller WL, Stange KC, Jaen CR. Coaching strategies for enhancing practice transformation. Fam Pract. 2015;32(1):75–81. https://doi.org/10.1093/fampra/cmu062 . Epub 2014/10/05.
Chase SM, Miller WL, Shaw E, Looney A, Crabtree BF. Meeting the challenge of practice quality improvement: a study of seven family medicine residency training practices. Acad Med. 2011;86(12):1583–9. https://doi.org/10.1097/ACM.0b013e31823674fa . Epub 2011/10/28.
Dickinson WP, Dickinson LM, Nutting PA, Emsermann CB, Tutt B, Crabtree BF, Fisher L, Harbrecht M, Gottsman A, West DR. Practice facilitation to improve diabetes care in primary care: a report from the EPIC randomized clinical trial. Ann Fam Med. 2014;12(1):8–16. https://doi.org/10.1370/afm.1591 . Epub 2014/01/22.
Howard J, Shaw EK, Clark E, Crabtree BF. Up close and (inter)personal: insights from a primary care practice’s efforts to improve office relationships over time, 2003–2009. Qual Manag Health Care. 2011;20(1):49–61. https://doi.org/10.1097/QMH.0b013e31820311e6 . Epub 2010/12/31.
Nutting PA, Crabtree BF, Stewart EE, Miller WL, Palmer RF, Stange KC, Jaen CR. Effect of facilitation on practice outcomes in the National Demonstration Project model of the patient-centered medical home. Ann Fam Med. 2010;8. https://doi.org/10.1370/afm.1119 . PubMed PMID: 20530393; PMCID: PMC2885723. Suppl 1:S33-44; S92Epub 2010/06/16.
Shaw E, Looney A, Chase S, Navalekar R, Stello B, Lontok O, Crabtree B. In the moment’: an analysis of Facilitator Impact during a quality improvement process. Group Facil. 2010;10:4–16. Epub 2010/01/01. PubMed PMID: 22557936; PMCID: PMC3340924.
PubMed PubMed Central Google Scholar
Shaw EK, Ohman-Strickland PA, Piasecki A, Hudson SV, Ferrante JM, McDaniel RR Jr., Nutting PA, Crabtree BF. Effects of facilitated team meetings and learning collaboratives on colorectal cancer screening rates in primary care practices: a cluster randomized trial. Ann Fam Med. 2013;11(3):220–8. https://doi.org/10.1370/afm.1505 . S1-8. Epub 2013/05/22.
Agulnik A, Boykin D, O’Malley DM, Price J, Yang M, McKone M, Curran G, Ritchie MJ. Virtual facilitation best practices and research priorities: a scoping review. Implement Sci Commun. 2024;5(1):16. https://doi.org/10.1186/s43058-024-00551-6 .
Jamtvedt G, Young JM, Kristoffersen DT, O’Brien MA, Oxman AD. Audit and feedback: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2006;2CD000259. https://doi.org/10.1002/14651858.CD000259.pub2 . Epub 2006/04/21.
Hysong SJ, Best RG, Pugh JA. Audit and feedback and clinical practice guideline adherence: making feedback actionable. Implement Sci. 2006;1:9. https://doi.org/10.1186/1748-5908-1-9 . Epub 2006/05/26.
Balasubramanian BA, Cohen DJ, Davis MM, Gunn R, Dickinson LM, Miller WL, Crabtree BF, Stange KC. Learning evaluation: blending quality improvement and implementation research methods to study healthcare innovations. Implement Sci. 2015;10:31. https://doi.org/10.1186/s13012-015-0219-z . Epub 2015/04/19.
Chambers DA, Glasgow RE, Stange KC. The dynamic sustainability framework: addressing the paradox of sustainment amid ongoing change. Implement Sci. 2013;8:117. https://doi.org/10.1186/1748-5908-8-117 . Epub 2013/10/04.
Aarons GA, Green AE, Trott E, Willging CE, Torres EM, Ehrhart MG, Roesch SC. The roles of System and Organizational Leadership in system-wide evidence-based intervention sustainment: a mixed-method study. Adm Policy Ment Health. 2016;43(6):991–1008. PubMed PMID: 27439504; PMCID: 5494253.
Smith JD, Polaha J. Using implementation science to guide the integration of evidence-based family interventions into primary care. Fam Syst Health. 2017;35(2):125–35. https://doi.org/10.1037/fsh0000252 . PubMed PMID: 28617015; PMCID: 5473179.
Stirman SW, Gutner CA, Langdon K, Graham JR. Bridging the Gap between Research and Practice in Mental Health Service settings: an overview of developments in implementation theory and research. Behav Ther. 2016;47(6):920–36. PubMed PMID: 27993341.
Jaen CR, Crabtree BF, Palmer RF, Ferrer RL, Nutting PA, Miller WL, Stewart EE, Wood R, Davila M, Stange KC. Methods for evaluating practice change toward a patient-centered medical home. Ann Fam Med. 2010;8(Suppl 1):S9–20. S92. Epub 2010/06/16. doi: 8/Suppl_1/S9 [pii]. 1370/afm. 1108. PubMed PMID: 20530398; PMCID: 2885721.
Li R, Simon J, Bodenheimer T, Gillies RR, Casalino L, Schmittdiel J, Shortell SM. Organizational factors affecting the adoption of diabetes care management processes in physician organizations. Diabetes Care. 2004;27(10):2312–6. Epub 2004/09/29. doi: 27/10/2312 [pii]. PubMed PMID: 15451893.
Rittenhouse DR, Casalino LP, Gillies RR, Shortell SM, Lau B. Measuring the medical home infrastructure in large medical groups. Health Aff (Millwood). 2008;27(5):1246–58. https://doi.org/10.1377/hlthaff.27.5.1246 . Epub 2008/09/11.
EvidenceNOW: Change Process Capability Questionnaire (CPC-Q). Scoring Guidance. Content last reviewed February 2019. Agency for Healthcare Research and Quality. Rockville, MD. https://www.ahrq.gov/evidencenow/results/research/cpcq-scoring.html .
Nutting PA, Crabtree BF, Miller WL, Stewart EE, Stange KC, Jaén CR. Journey to the patient-centered medical home: a qualitative analysis of the experiences of practices in the National Demonstration Project. Ann Fam Med. 2010;8(Suppl 1). https://doi.org/10.1370/afm.1075 . PubMed PMID: 20530394; PMCID: PMC2885728. S45-56; s92.
Aarons GA, Ehrhart MG, Farahnak LR. The implementation Leadership Scale (ILS): development of a brief measure of unit level implementation leadership. Implement Sci. 2014;9(1):45. https://doi.org/10.1186/1748-5908-9-45 . Epub 20140414.
Yin RK. Case study research and applications. Sage Thousand Oaks, CA; 2018.
Glaser BG. The constant comparative method of qualitative analysis. Soc Probl. 1965;12(4):436–45.
Coronado GD, Petrik AF, Vollmer WM, Taplin SH, Keast EM, Fields S, Green BB. Effectiveness of a Mailed Colorectal Cancer Screening Outreach Program in Community Health clinics: the STOP CRC Cluster Randomized Clinical Trial. JAMA Intern Med. 2018;178(9):1174–81. https://doi.org/10.1001/jamainternmed.2018.3629 .
Coronado GD, Rivelli JS, Fuoco MJ, Vollmer WM, Petrik AF, Keast E, Barker S, Topalanchik E, Jimenez R. Effect of Reminding Patients to Complete Fecal Immunochemical Testing: A Comparative Effectiveness Study of Automated and Live Approaches. Journal of general internal medicine. 2018;33(1):72 – 8. Epub 2017/10/10. https://doi.org/10.1007/s11606-017-4184-x . PubMed PMID: 29019046.
Rothery C, Strong M, Koffijberg HE, Basu A, Ghabri S, Knies S, Murray JF, Schmidler GDS, Steuten L, Fenwick E. Value of information analytical methods: report 2 of the ISPOR value of information analysis emerging good practices task force. Value Health. 2020;23(3):277–86.
Bacchetti P. Current sample size conventions: flaws, harms, and alternatives. BMC Med. 2010;8:17-. https://doi.org/10.1186/1741-7015-8-17 . PubMed PMID: 20307281.
Moore CG, Carter RE, Nietert PJ, Stewart PW. Recommendations for planning pilot studies in clinical and translational research. Clin Transl Sci. 2011;4(5):332–7. https://doi.org/10.1111/j.1752-8062.2011.00347 . .x. PubMed PMID: 22029804.
Administration HRaS. Health Center Program. 2019.
Hong YR, Sonawane KB, Holcomb DR, Deshmukh AA. Effect of multimodal information delivery for diabetes care on colorectal cancer screening uptake among individuals with type 2 diabetes. Prev Med Rep. 2018;11:89–92. https://doi.org/10.1016/j.pmedr.2018.05.008 . Epub 2018/07/10.
Kiran T, Kopp A, Moineddin R, Glazier RH. Longitudinal evaluation of physician payment reform and team-based care for chronic disease management and prevention. CMAJ. 2015;187(17):E494–502. https://doi.org/10.1503/cmaj.150579 . Epub 2015/09/21.
Taplin SH, Haggstrom D, Jacobs T, Determan A, Granger J, Montalvo W, Snyder WM, Lockhart S, Calvo A. Implementing colorectal cancer screening in community health centers: addressing cancer health disparities through a regional cancer collaborative. Med Care. 2008;46(9 Suppl 1):S74–83. https://doi.org/10.1097/MLR.0b013e31817fdf68 . PubMed PMID: 18725837.
Coury J, Schneider JL, Rivelli JS, Petrik AF, Seibel E, D’Agostini B, Taplin SH, Green BB, Coronado GD. Applying the Plan-Do-Study-Act (PDSA) approach to a large pragmatic study involving safety net clinics. BMC Health Serv Res. 2017;17(1):411. https://doi.org/10.1186/s12913-017-2364-3 . Epub 2017/06/21.
Davis T, Arnold C, Rademaker A, Bennett C, Bailey S, Platt D, Reynolds C, Liu D, Carias E, Bass P III. Improving colon cancer screening in community clinics. Cancer. 2013;119(21):3879–86.
Davis SN, Christy SM, Chavarria EA, Abdulla R, Sutton SK, Schmidt AR, Vadaparampil ST, Quinn GP, Simmons VN, Ufondu CB, Ravindra C, Schultz I, Roetzheim RG, Shibata D, Meade CD, Gwede CK. A randomized controlled trial of a multicomponent, targeted, low-literacy educational intervention compared with a nontargeted intervention to boost colorectal cancer screening with fecal immunochemical testing in community clinics. Cancer. 2017;123(8):1390–400. https://doi.org/10.1002/cncr.30481 . Epub 2016/12/01.
Gwede CK, Sutton SK, Chavarria EA, Gutierrez L, Abdulla R, Christy SM, Lopez D, Sanchez J, Meade CD. A culturally and linguistically salient pilot intervention to promote colorectal cancer screening among latinos receiving care in a federally qualified Health Center. Health Educ Res. 2019;34(3):310–20. https://doi.org/10.1093/her/cyz010 . PubMed PMID: 30929015.
Dolan NC, Ramirez-Zohfeld V, Rademaker AW, Ferreira MR, Galanter WL, Radosta J, Eder MM, Cameron KA. The effectiveness of a physician-only and physician-patient intervention on Colorectal Cancer Screening discussions between providers and African American and latino patients. J Gen Intern Med. 2015;30(12):1780–7. https://doi.org/10.1007/s11606-015-3381-8 . Epub 2015/05/19.
Baker DW, Brown T, Buchanan DR, Weil J, Balsley K, Ranalli L, Lee JY, Cameron KA, Ferreira MR, Stephens Q. Comparative effectiveness of a multifaceted intervention to improve adherence to annual colorectal cancer screening in community health centers: a randomized clinical trial. JAMA Intern Med. 2014;174(8):1235–41.
Moullin JC, Dickson KS, Stadnick NA, Rabin B, Aarons GA. Systematic review of the Exploration, Preparation, implementation, sustainment (EPIS) framework. Implement Science: IS. 2019;14(1):1. https://doi.org/10.1186/s13012-018-0842-6 . PubMed PMID: 30611302.
Riehman KS, Stephens RL, Henry-Tanner J, Brooks D. Evaluation of Colorectal Cancer Screening in federally qualified Health centers. Am J Prev Med. 2018;54(2):190–6. https://doi.org/10.1016/j.amepre.2017.10.007 .
Leeman J, Askelson N, Ko LK, Rohweder CL, Avelis J, Best A, Friedman D, Glanz K, Seegmiller L, Stradtman L, Vanderpool RC. Understanding the processes that Federally Qualified Health Centers use to select and implement colorectal cancer screening interventions: a qualitative study. Transl Behav Med. 2019. https://doi.org/10.1093/tbm/ibz023 . PubMed PMID: 30794725. Epub 2019/02/23.
Calman NS, Hauser D, Schussler L, Crump C. A risk-based intervention approach to eliminate diabetes health disparities. Prim Health care Res Dev. 2018;19(5):518–22.
Download references
Acknowledgements
We would like to thank our FQHC participants for informing the intervention and their contributions to this work.
This research is supported by the National Cancer Institute (K99 CA256043/R00CA256043) The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by the funders.
Author information
Authors and affiliations.
Department of Family Medicine and Community Health, Research Division, Rutgers Robert Wood Johnson Medical School, 303 George Street, Rm 309, New Brunswick, NJ, USA
Denalee M. O’Malley, Benjamin F. Crabtree, Srivarsha Kaloth, Pamela Ohman-Strickland, Jeanne Ferrante & Shawna V. Hudson
Rutgers Cancer Institute of New Jersey, New Brunswick, NJ, USA
Denalee M. O’Malley, Benjamin F. Crabtree, Pamela Ohman-Strickland, Jeanne Ferrante, Shawna V. Hudson & Anita Y. Kinney
Department of Biostatistics and Epidemiology, School of Public Health, Rutgers University, New Brunswick, NJ, USA
Pamela Ohman-Strickland & Anita Y. Kinney
You can also search for this author in PubMed Google Scholar
Contributions
D.O. conceptualized study and acquired funding; D.O and S.K. Writing – original draft; BFC, SK, PO, JF, SVH, AK reviewed, edited, and approved the manuscript.
Corresponding author
Correspondence to Denalee M. O’Malley .
Ethics declarations
Ethics approval and consent to participate.
This protocol has been approved by the Rutgers University Institutional. Review Board (Pro2020002075). All study participants will be asked to provide informed consent prior to participation in any phase of this research. All authors have completed ethics training. This research will be performed in accordance with the relevant guidelines and regulations of the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
O’Malley, D.M., Crabtree, B.F., Kaloth, S. et al. Strategic use of resources to enhance colorectal cancer screening for patients with diabetes (SURE: CRC4D) in federally qualified health centers: a protocol for hybrid type ii effectiveness-implementation trial. BMC Prim. Care 25 , 242 (2024). https://doi.org/10.1186/s12875-024-02496-0
Download citation
Received : 18 May 2024
Accepted : 26 June 2024
Published : 05 July 2024
DOI : https://doi.org/10.1186/s12875-024-02496-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Federally qualified health center
- Diabetes mellitus
- Hybrid 2 effectiveness-implementation
- Implementation planning
- Primary care safety-net
BMC Primary Care
ISSN: 2731-4553
- General enquiries: [email protected]

- Advanced Search
Personalized algorithmic pricing decision support tool for health insurance: : The case of stratifying gestational diabetes mellitus into two groups
New citation alert added.
This alert has been successfully added and will be sent to:
You will be notified whenever a record that you have chosen has been cited.
To manage your alert preferences, click on the button below.
New Citation Alert!
Please log in to your account
Information & Contributors
Bibliometrics & citations, view options, recommendations, development of a decision support system for neuro-electrostimulation: diagnosing disorders of the cardiovascular system and evaluation of the treatment efficiency.
The study describes a preliminary stage of the decision support system development for physician performing neuro-electrostimulation of neck neural formations for patients suffering from cardiovascular system disorders. The arterial ...
Display Omitted
- Presents non-intrusive method of arterial hypertension diagnostics.
- Heart rate ...
Incidence of Risk Factors on the Onset of Gestational Diabetes Mellitus: An Empirical Research in Southern Italy
In this study the authors evaluated the prevalence of Gestational Diabetes Mellitus GDM and the incidence in determining the occurrence thereof, given by the following risk factors: age, family history for Diabetes Mellitus DM, Body Mass Index BMI, ...
Gestational diabetes mellitus prediction model: A risk factors analysis of pregnant women with gestational diabetes mellitus but have normal oral glucose tolerance test results in the second trimester of pregnancy
Oral glucose tolerance test (OGTT) is a standard for the diagnosis of gestational diabetes mellitus (GDM). However, clinically, some cases with normal results were diagnosed as GDM in the third trimester.
Information
Published in.
Elsevier Science Publishers B. V.
Netherlands
Publication History
Author tags.
- Algorithmic insurance
- Clinical decision support systems
- Gestational diabetes mellitus
- Feature selection
- Unbalanced data
- Machine learning
- Research-article
Contributors
Other metrics, bibliometrics, article metrics.
- 0 Total Citations
- 0 Total Downloads
- Downloads (Last 12 months) 0
- Downloads (Last 6 weeks) 0
View options
Login options.
Check if you have access through your login credentials or your institution to get full access on this article.
Full Access
Share this publication link.
Copying failed.
Share on social media
Affiliations, export citations.
- Please download or close your previous search result export first before starting a new bulk export. Preview is not available. By clicking download, a status dialog will open to start the export process. The process may take a few minutes but once it finishes a file will be downloadable from your browser. You may continue to browse the DL while the export process is in progress. Download
- Download citation
- Copy citation
We are preparing your search results for download ...
We will inform you here when the file is ready.
Your file of search results citations is now ready.
Your search export query has expired. Please try again.

- Moscow Oblast
- Elektrostal
- Short Term Stay
People Visiting Elektrostal Also Like
About elektrostal short term stay on rent by owner.
Discover more than 32 short term vacation rentals in Elektrostal. We have a huge number of short-term holiday rentals in or near Elektrostal. Whether you are traveling as a whole family, in groups, with friends, or solo, there are rentals that would suit your plans and budget. Short-term rental homes are perfect for those seeking to stay in Elektrostal for a short term or on a temporary basis. RBO short-term stays give you the luxury of enjoying all the benefits attached to having a home. A serene environment, spacious rooms, private pools, indoor/outdoor heated swimming pools, hot tubs, self-catering, spa, and gyms are examples of such benefits. Rent By Owner has plenty of vacation rentals that are available on a weekly or monthly basis in Elektrostal. A furnished short-term rental in Elektrostal comes with great amenities that would make you an unforgettable experience.
These short-term home rentals that are available in Elektrostal come in different sizes and vary according to your needs. Whatever your style or budget is, Rent By Owner has got you covered; all you have to do is use our search and filter tool to find the right rental in a matter of minutes.
Rent By Owner makes it easy to compare, discover and book short-term accommodations, including pet-friendly places to stay, in Elektrostal that is within your budget. RBO helps you save time, and gives you hassle-free booking for your favorite short stay home.
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Sars-cov-2 infection positively correlates with hyperglycemia and inflammatory markers in covid-19 patients: a clinical research study.

1. Introduction
2. materials and methods, 2.1. study design, ethical considerations, data collection, and case enrollment, 2.2. sample collection and processing, 2.3. estimation of serum ferritin, 2.4. statistical analysis, 3.1. clinical characteristics, 3.2. inflammatory parameters, 3.3. hematological parameters, 4. discussion, 5. conclusions, author contributions, institutional review board statement, informed consent statement, data availability statement, acknowledgments, conflicts of interest.
- Pal, M.; Berhanu, G.; Desalegn, C.; Kandi, V. Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2): An update. Cureus 2020 , 12 , e7423. [ Google Scholar ] [ CrossRef ]
- Care, D. Care in diabetesd2019. Diabetes Care 2019 , 42 , S13–S28. [ Google Scholar ]
- Wu, Z.; McGoogan, J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020 , 323 , 1239–1242. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Deng, S.-Q.; Peng, H.-J. Characteristics of and public health responses to the coronavirus disease 2019 outbreak in China. J. Clin. Med. 2020 , 9 , 575. [ Google Scholar ] [ CrossRef ]
- Guan, W.-J.; Ni, Z.-Y.; Hu, Y.; Liang, W.-H.; Ou, C.-Q.; He, J.-X.; Liu, L.; Shan, H.; Lei, C.-L.; Hui, D.S. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020 , 382 , 1708–1720. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Zhang, J.-J.; Dong, X.; Cao, Y.-Y.; Yuan, Y.-D.; Yang, Y.-B.; Yan, Y.-Q.; Akdis, C.A.; Gao, Y.-D. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy 2020 , 75 , 1730–1741. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Mehraeen, E.; Karimi, A.; Barzegary, A.; Vahedi, F.; Afsahi, A.M.; Dadras, O.; Moradmand-Badie, B.; Alinaghi, S.A.S.; Jahanfar, S. Predictors of mortality in patients with COVID-19—A systematic review. Eur. J. Integr. Med. 2020 , 40 , 101226. [ Google Scholar ] [ CrossRef ]
- Nowotny, K.; Jung, T.; Höhn, A.; Weber, D.; Grune, T. Advanced glycation end products and oxidative stress in type 2 diabetes mellitus. Biomolecules 2015 , 5 , 194–222. [ Google Scholar ] [ CrossRef ]
- Khalid, M.; Petroianu, G.; Adem, A. Advanced glycation end products and diabetes mellitus: Mechanisms and perspectives. Biomolecules 2022 , 12 , 542. [ Google Scholar ] [ CrossRef ]
- Chee, Y.J.; Ng, S.J.H.; Yeoh, E. Diabetic ketoacidosis precipitated by COVID-19 in a patient with newly diagnosed diabetes mellitus. Diabetes Res. Clin. Pract. 2020 , 164 , 108166. [ Google Scholar ] [ CrossRef ]
- Li, J.; Wang, X.; Chen, J.; Zuo, X.; Zhang, H.; Deng, A. COVID-19 infection may cause ketosis and ketoacidosis. Diabetes Obes. Metab. 2020 , 22 , 1935–1941. [ Google Scholar ] [ CrossRef ]
- Ren, H.; Yang, Y.; Wang, F.; Yan, Y.; Shi, X.; Dong, K.; Yu, X.; Zhang, S. Association of the insulin resistance marker TyG index with the severity and mortality of COVID-19. Cardiovasc. Diabetol. 2020 , 19 , 58. [ Google Scholar ] [ CrossRef ]
- Barrett, C.E. Risk for newly diagnosed diabetes 30 days after SARS-CoV-2 infection among persons aged 18 years—United States, March 1, 2020–June 28, 2021. MMWR Morb. Mortal. Wkly. Rep. 2022 , 71 , 59–65. [ Google Scholar ] [ CrossRef ]
- Hamming, I.; Timens, W.; Bulthuis, M.; Lely, A.; Navis, G.v.; van Goor, H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J. Pathol. 2004 , 203 , 631–637. [ Google Scholar ] [ CrossRef ]
- Wang, A.; Zhao, W.; Xu, Z.; Gu, J. Timely blood glucose management for the outbreak of 2019 novel coronavirus disease (COVID-19) is urgently needed. Diabetes Res. Clin. Pract. 2020 , 162 , 108118. [ Google Scholar ] [ CrossRef ]
- Henry, B.M.; De Oliveira, M.H.S.; Benoit, S.; Plebani, M.; Lippi, G. Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): A meta-analysis. Clin. Chem. Lab. Med. (CCLM) 2020 , 58 , 1021–1028. [ Google Scholar ] [ CrossRef ]
- Kumar, A.; Sepolia, S.; Shilpa, R.; Rezayani, G.; Kumari, S.; Gupta, S. Role of hematological and immunological parameters in COVID-19 patients. J. Pharm. Bioallied Sci. 2021 , 13 , 238–243. [ Google Scholar ]
- Usul, E.; Şan, İ.; Bekgöz, B.; Şahin, A. Role of hematological parameters in COVID-19 patients in the emergency room. Biomark. Med. 2020 , 14 , 1207–1215. [ Google Scholar ] [ CrossRef ]
- Elshazli, R.M.; Toraih, E.A.; Elgaml, A.; El-Mowafy, M.; El-Mesery, M.; Amin, M.N.; Hussein, M.H.; Killackey, M.T.; Fawzy, M.S.; Kandil, E. Diagnostic and prognostic value of hematological and immunological markers in COVID-19 infection: A meta-analysis of 6320 patients. PLoS ONE 2020 , 15 , e0238160. [ Google Scholar ] [ CrossRef ]
- Singh, A.K.; Singh, R. Is metformin ahead in the race as a repurposed host-directed therapy for patients with diabetes and COVID-19? Diabetes Res. Clin. Pract. 2020 , 165 , 108268. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Chen, Y.; Gong, X.; Wang, L.; Guo, J. Effects of hypertension, diabetes and coronary heart disease on COVID-19 diseases severity: A systematic review and meta-analysis. MedRxiv 2020 . [ Google Scholar ] [ CrossRef ]
- Ji, D.; Zhang, D.; Xu, J.; Chen, Z.; Yang, T.; Zhao, P.; Chen, G.; Cheng, G.; Wang, Y.; Bi, J. Prediction for progression risk in patients with COVID-19 pneumonia: The CALL score. Clin. Infect. Dis. 2020 , 71 , 1393–1399. [ Google Scholar ] [ CrossRef ]
- Sahu, K.K.; Siddiqui, A.D. From Hematologistʼs desk: The effect of COVID-19 on the blood system. Am. J. Hematol. 2020 , 95 , E213. [ Google Scholar ] [ CrossRef ]
- Wu, C.; Chen, X.; Cai, Y.; Zhou, X.; Xu, S.; Huang, H.; Zhang, L.; Zhou, X.; Du, C.; Zhang, Y. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern. Med. 2020 , 180 , 934–943. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Xu, B.; Kraemer, M.U.; Gutierrez, B.; Mekaru, S.; Sewalk, K.; Loskill, A.; Wang, L.; Cohn, E.; Hill, S.; Zarebski, A.; et al. Open access epidemiological data from the COVID-19 outbreak. Lancet Infect. Dis. 2020 , 20 , 534. [ Google Scholar ] [ CrossRef ]
- Tay, M.Z.; Poh, C.M.; Rénia, L.; MacAry, P.A.; Ng, L.F. The trinity of COVID-19: Immunity, inflammation and intervention. Nat. Rev. Immunol. 2020 , 20 , 363–374. [ Google Scholar ] [ CrossRef ]
- Hu, B.; Guo, H.; Zhou, P.; Shi, Z.-L. Characteristics of SARS-CoV-2 and COVID-19. Nat. Rev. Microbiol. 2021 , 19 , 141–154. [ Google Scholar ] [ CrossRef ]
- Bode, B.; Garrett, V.; Messler, J.; McFarland, R.; Crowe, J.; Booth, R.; Klonoff, D.C. Glycemic characteristics and clinical outcomes of COVID-19 patients hospitalized in the United States. J. Diabetes Sci. Technol. 2020 , 14 , 813–821. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Zhu, L.; She, Z.-G.; Cheng, X.; Qin, J.-J.; Zhang, X.-J.; Cai, J.; Lei, F.; Wang, H.; Xie, J.; Wang, W. Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes. Cell Metab. 2020 , 31 , 1068–1077.e3. [ Google Scholar ] [ CrossRef ]
- Gianchandani, R.; Esfandiari, N.H.; Ang, L.; Iyengar, J.; Knotts, S.; Choksi, P.; Pop-Busui, R. Managing hyperglycemia in the COVID-19 inflammatory storm. Diabetes 2020 , 69 , 2048–2053. [ Google Scholar ] [ CrossRef ]
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F.; Han, Y.; Qiu, Y.; Wang, J.; Liu, Y.; Wei, Y. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020 , 395 , 507–513. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Fadini, G.; Morieri, M.; Longato, E.; Avogaro, D.A. Prevalence and impact of diabetes among people infected with SARS-CoV-2. J. Endocrinol. Investig. 2020 , 43 , 867–869. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Yang, J.; Feng, Y.; Yuan, M.; Yuan, S.; Fu, H.; Wu, B.; Sun, G.; Yang, G.; Zhang, X.; Wang, L.; et al. Plasma glucose levels and diabetes are independent predictors for mortality and morbidity in patients with SARS. Diabet. Med. 2006 , 23 , 623–628. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Yang, J.-K.; Lin, S.-S.; Ji, X.-J.; Guo, L.-M. Binding of SARS coronavirus to its receptor damages islets and causes acute diabetes. Acta Diabetol. 2010 , 47 , 193–199. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Apicella, M.; Campopiano, M.C.; Mantuano, M.; Mazoni, L.; Coppelli, A.; Del Prato, S. COVID-19 in people with diabetes: Understanding the reasons for worse outcomes. Lancet Diabetes Endocrinol. 2020 , 8 , 782–792. [ Google Scholar ] [ CrossRef ]
- Jivanji, C.J.; Asrani, V.M.; Windsor, J.A.; Petrov, M.S. New-onset diabetes after acute and critical illness: A systematic review. In Mayo Clinic Proceedings ; Elsevier: Amsterdam, The Netherlands; pp. 762–773.
- Li, H.; Tian, S.; Chen, T.; Cui, Z.; Shi, N.; Zhong, X.; Qiu, K.; Zhang, J.; Zeng, T.; Chen, L.; et al. Newly diagnosed diabetes is associated with a higher risk of mortality than known diabetes in hospitalized patients with COVID-19. Diabetes Obes. Metab. 2020 , 22 , 1897–1906. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Laursen, J.C.; Jepsen, R.; Bruun-Rasmussen, N.E.; Frimodt-Møller, M.; Jørgensen, M.E.; Rossing, P.; Hansen, C.S. Blood oxygen saturation is lower in persons with pre-diabetes and screen-detected diabetes compared with non-diabetic individuals: A population-based study of the Lolland-Falster Health Study cohort. Front. Epidemiol. 2022 , 2 , 1022342. [ Google Scholar ] [ CrossRef ]
- Vold, M.L.; Aasebø, U.; Wilsgaard, T.; Melbye, H. Low oxygen saturation and mortality in an adult cohort: The Tromsø study. BMC Pulm. Med. 2015 , 15 , 9. [ Google Scholar ] [ CrossRef ]
- Sada, K.; Nishikawa, T.; Kukidome, D.; Yoshinaga, T.; Kajihara, N.; Sonoda, K.; Senokuchi, T.; Motoshima, H.; Matsumura, T.; Araki, E. Hyperglycemia induces cellular hypoxia through production of mitochondrial ROS followed by suppression of aquaporin-1. PLoS ONE 2016 , 11 , e0158619. [ Google Scholar ] [ CrossRef ]
- Vargas-Rodriguez, J.R.; Valdes Aguayo, J.J.; Garza-Veloz, I.; Martinez-Rendon, J.; del Refugio Rocha Pizaña, M.; Cabral-Pacheco, G.A.; Juarez-Alcala, V.; Martinez-Fierro, M.L. Sustained hyperglycemia and its relationship with the outcome of hospitalized patients with severe COVID-19: Potential role of ACE2 upregulation. J. Pers. Med. 2022 , 12 , 805. [ Google Scholar ] [ CrossRef ]
- Kaushal, K.; Kaur, H.; Sarma, P.; Bhattacharyya, A.; Sharma, D.J.; Prajapat, M.; Pathak, M.; Kothari, A.; Kumar, S.; Rana, S.; et al. Serum ferritin as a predictive biomarker in COVID-19. A systematic review, meta-analysis and meta-regression analysis. J. Crit. Care 2022 , 67 , 172–181. [ Google Scholar ] [ CrossRef ]
- Maheshwari, A.V.; Bhoi, B.K.; Sadariya, B.R.; Javia, H.N.; Gusani, J.K.; Sharma, H. Correlation between serum ferritin and glycaemic control in patients of type 2 diabetes mellitus: A case control study. Int. J. Res. Med. Sci. 2015 , 3 , 2327. [ Google Scholar ] [ CrossRef ]
- Lu, J.; Wei, Z.; Jiang, H.; Cheng, L.; Chen, Q.; Chen, M.; Yan, J.; Sun, Z. Lactate dehydrogenase is associated with 28-day mortality in patients with sepsis: A retrospective observational study. J. Surg. Res. 2018 , 228 , 314–321. [ Google Scholar ] [ CrossRef ]
- Kang, H.E.; Park, D.W. Lactate as a biomarker for sepsis prognosis? Infect. Chemother. 2016 , 48 , 252. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Duman, A.; Akoz, A.; Kapci, M.; Ture, M.; Orun, S.; Karaman, K.; Turkdogan, K.A. Prognostic value of neglected biomarker in sepsis patients with the old and new criteria: Predictive role of lactate dehydrogenase. Am. J. Emerg. Med. 2016 , 34 , 2167–2171. [ Google Scholar ] [ CrossRef ]
- Yang, X.; Yu, Y.; Xu, J.; Shu, H.; Liu, H.; Wu, Y.; Zhang, L.; Yu, Z.; Fang, M.; Yu, T. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir. Med. 2020 , 8 , 475–481. [ Google Scholar ] [ CrossRef ]
- Wu, Y.; Hou, B.; Liu, J.; Chen, Y.; Zhong, P. Risk factors associated with long-term hospitalization in patients with COVID-19: A single-centered, retrospective study. Front. Med. 2020 , 7 , 553604. [ Google Scholar ] [ CrossRef ]
- Yuan, X.; Huang, W.; Ye, B.; Chen, C.; Huang, R.; Wu, F.; Wei, Q.; Zhang, W.; Hu, J. Changes of hematological and immunological parameters in COVID-19 patients. Int. J. Hematol. 2020 , 112 , 553–559. [ Google Scholar ] [ CrossRef ]
- Saurabh, A.; Dey, B.; Raphael, V.; Barman, B.; Dev, P.; Tiewsoh, I.; Lyngdoh, B.S.; Dutta, K. Evaluation of hematological parameters in predicting intensive care unit admission in COVID-19 patients. SN Compr. Clin. Med. 2022 , 4 , 39. [ Google Scholar ] [ CrossRef ]
- Matin, S.; Safarzadeh, E.; Rezaei, N.; Negaresh, M.; Salehzadeh, H.; Matin, S.; Sharifiazar, A.H.; Abazari, M.; Dadkhah, M. Hematological parameters as diagnostic factors: Correlation with severity of COVID-19. Acta Bio Medica Atenei Parm. 2022 , 93 , e2022061. [ Google Scholar ]
- Liao, D.; Zhou, F.; Luo, L.; Xu, M.; Wang, H.; Xia, J.; Gao, Y.; Cai, L.; Wang, Z.; Yin, P.; et al. Haematological characteristics and risk factors in the classification and prognosis evaluation of COVID-19: A retrospective cohort study. Lancet Haematol. 2020 , 7 , e671–e678. [ Google Scholar ] [ CrossRef ]
- Anurag, A.; Jha, P.K.; Kumar, A. Differential white blood cell count in the COVID-19: A cross-sectional study of 148 patients. Diabetes Metab. Syndr. Clin. Res. Rev. 2020 , 14 , 2099–2102. [ Google Scholar ] [ CrossRef ]
- Ayalew, G.; Mulugeta, B.; Haimanot, Y.; Adane, T.; Bayleyegn, B.; Abere, A. Neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio can predict the severity in COVID-19 patients from Ethiopia: A retrospective study. Int. J. Gen. Med. 2022 , 15 , 7701. [ Google Scholar ] [ CrossRef ]
- Gujar, R.K.; Meena, A.; Chouhan, S.S.; Likhar, K. Hematological profiles of COVID-19 patients at the Ratlam district, Madhya Pradesh State, India. Bioinformation 2021 , 17 , 686. [ Google Scholar ]
- Gunardi, W.D. Corona Virus Disease 2019 dan Perkembangannya ; PT. Scifintech Andrew Wijaya: South Jakarta, Indonesia, 2022. [ Google Scholar ]
- Zahorec, R.; Hulin, I.; Zahorec, P. Rationale Use of Neutrophil-to-lymphocyte ratio for early diagnosis and stratification of COVID-19. Bratisl. Med. J./Bratisl. Lek. Listy 2020 , 121 , 466–470. [ Google Scholar ] [ CrossRef ]
- Ramesh, J.; Reddy, S.S.; Rajesh, M.; Varghese, J. Evaluation of simple and cost-effective immuno-haematological markers to predict outcome in hospitalized severe COVID-19 patients, with a focus on diabetes mellitus-A retrospective study in Andhra Pradesh, India. Diabetes Metab. Syndr. Clin. Res. Rev. 2021 , 15 , 739–745. [ Google Scholar ] [ CrossRef ]
- Nagareddy, P.R.; Murphy, A.J.; Stirzaker, R.A.; Hu, Y.; Yu, S.; Miller, R.G.; Ramkhelawon, B.; Distel, E.; Westerterp, M.; Huang, L.-S.; et al. Hyperglycemia promotes myelopoiesis and impairs the resolution of atherosclerosis. Cell Metab. 2013 , 17 , 695–708. [ Google Scholar ] [ CrossRef ]
- Cheng, Y.; Yue, L.; Wang, Z.; Zhang, J.; Xiang, G. Hyperglycemia associated with lymphopenia and disease severity of COVID-19 in type 2 diabetes mellitus. J. Diabetes Its Complicat. 2021 , 35 , 107809. [ Google Scholar ] [ CrossRef ]
- Wu, D.; Gao, S. Analysis of the lymphocyte count in type 2 diabetic patients with coronavirus disease (COVID-19): A retrospective study in a centralized treatment center. Diabetes Res. Clin. Pract. 2020 , 166 , 108340. [ Google Scholar ] [ CrossRef ]
- Goel, V.; Raizada, A.; Aggarwal, A.; Madhu, S.; Kar, R.; Agrawal, A.; Mahla, V.; Goel, A. Long-Term Persistence of COVID-Induced Hyperglycemia: A Cohort Study. Am. J. Trop. Med. Hyg. 2024 , 110 , 512. [ Google Scholar ] [ CrossRef ]
- Wang, Y.; Yi, B.; Wang, S.; Chen, X.; Wen, Z. Effect of hyperglycemia on the immune function of COVID-19 patients with type 2 diabetes mellitus: A retrospective study. PeerJ 2022 , 10 , e14570. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Zhou, Y.; Chi, J.; Lv, W.; Wang, Y. Obesity and diabetes as high-risk factors for severe coronavirus disease 2019 (COVID-19). Diabetes/Metab. Res. Rev. 2021 , 37 , e3377. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Esposito, K.; Nappo, F.; Marfella, R.; Giugliano, G.; Giugliano, F.; Ciotola, M.; Quagliaro, L.; Ceriello, A.; Giugliano, D. Inflammatory cytokine concentrations are acutely increased by hyperglycemia in humans: Role of oxidative stress. Circulation 2002 , 106 , 2067–2072. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Nieuwdorp, M.; van Haeften, T.W.; Gouverneur, M.C.; Mooij, H.L.; van Lieshout, M.H.; Levi, M.; Meijers, J.C.; Holleman, F.; Hoekstra, J.B.; Vink, H.; et al. Loss of endothelial glycocalyx during acute hyperglycemia coincides with endothelial dysfunction and coagulation activation in vivo. Diabetes 2006 , 55 , 480–486. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Drucker, D.J. Diabetes, obesity, metabolism, and SARS-CoV-2 infection: The end of the beginning. Cell Metab. 2021 , 33 , 479–498. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Abu-Farha, M.; Al-Mulla, F.; Thanaraj, T.A.; Kavalakatt, S.; Ali, H.; Abdul Ghani, M.; Abubaker, J. Impact of diabetes in patients diagnosed with COVID-19. Front. Immunol. 2020 , 11 , 576818. [ Google Scholar ] [ CrossRef ]
- Zahedi, M.; Kordrostami, S.; Kalantarhormozi, M.; Bagheri, M. A Review of Hyperglycemia in COVID-19. Cureus 2023 , 15 , e37487. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Plummer, M.P.; Bellomo, R.; Cousins, C.E.; Annink, C.E.; Sundararajan, K.; Reddi, B.A.; Raj, J.P.; Chapman, M.J.; Horowitz, M.; Deane, A.M. Dysglycaemia in the critically ill and the interaction of chronic and acute glycaemia with mortality. Intensive Care Med. 2014 , 40 , 973–980. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Mehta, V.K.; Hao, W.; Brooks-Worrell, B.M.; Palmer, J.P. Low-dose interleukin 1 and tumor necrosis factor individually stimulate insulin release but in combination cause suppression. Eur. J. Endocrinol. 1994 , 130 , 208–214. [ Google Scholar ] [ CrossRef ]
- Vedantam, D.; Poman, D.S.; Motwani, L.; Asif, N.; Patel, A.; Anne, K.K. Stress-induced hyperglycemia: Consequences and management. Cureus 2022 , 14 , e26714. [ Google Scholar ] [ CrossRef ]
- Sherwani, S.I.; Khan, H.A.; Ekhzaimy, A.; Masood, A.; Sakharkar, M.K. Significance of HbA1c test in diagnosis and prognosis of diabetic patients. Biomark. Insights 2016 , 11 , 95–104. [ Google Scholar ] [ CrossRef ] [ PubMed ]
Click here to enlarge figure
| Clinical Characteristics | Total | Normoglycemic (RBS < 140 mg/dL) | Hyperglycemic (RBS > 140 mg/dL) |
|---|---|---|---|
| Total number of subjects | n = 550 | n = 202 | n = 348 |
| Gender | |||
| Male | 354 (64.36) | 127 (62.87) | 227 (65.22) |
| Female | 196 (35.63) | 75 (37.12) | 121 (34.77) |
| Age distribution | |||
| <30 | 57 (10.36) | 28 (13.86) | 29 (8.33) |
| 30–60 | 368 (66.90) | 136 (67.32) | 232 (66.66) |
| >60 | 125 (22.72) | 38 (18.81) | 87 (35.08) |
| Vaccination status | |||
| Unvaccinated | 442 (80.36) | 159 (78.71) | 283 (81.32) |
| Vaccinated | 108 (19.63) | 43 (21.28) | 65 (18.67) |
| Single Dose vaccination | 75 (69.44) | 31 (72.09) | 44 (67.69) |
| Double Dose vaccination | 33 (30.55) | 12 (27.90) | 21 (32.30) |
| Clinical features | |||
| Fever | 379 (68.90) | 131 (64.85) | 248 (71.26) |
| Cough | 417 (75.81) | 149 (73.76) | 268 (77.01) |
| Breathlessness | 249 (45.27) | 83 (41.08) | 166 (47.70) |
| Preexisting diabetes | 158 (28.72) | 32 (15.84) | 126 (36.20) |
| New onset hyperglycemia | 225 (40.90) | None | 225 (64.65) |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Chikkahonnaiah, P.; Dallavalasa, S.; Tulimilli, S.V.; Dubey, M.; Byrappa, S.H.; Amachawadi, R.G.; Madhunapantula, S.V.; Veeranna, R.P. SARS-CoV-2 Infection Positively Correlates with Hyperglycemia and Inflammatory Markers in COVID-19 Patients: A Clinical Research Study. Diseases 2024 , 12 , 143. https://doi.org/10.3390/diseases12070143
Chikkahonnaiah P, Dallavalasa S, Tulimilli SV, Dubey M, Byrappa SH, Amachawadi RG, Madhunapantula SV, Veeranna RP. SARS-CoV-2 Infection Positively Correlates with Hyperglycemia and Inflammatory Markers in COVID-19 Patients: A Clinical Research Study. Diseases . 2024; 12(7):143. https://doi.org/10.3390/diseases12070143
Chikkahonnaiah, Prashanth, Siva Dallavalasa, SubbaRao V. Tulimilli, Muskan Dubey, Shashidhar H. Byrappa, Raghavendra G. Amachawadi, SubbaRao V. Madhunapantula, and Ravindra P. Veeranna. 2024. "SARS-CoV-2 Infection Positively Correlates with Hyperglycemia and Inflammatory Markers in COVID-19 Patients: A Clinical Research Study" Diseases 12, no. 7: 143. https://doi.org/10.3390/diseases12070143
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals

IMAGES
COMMENTS
Higher levels of social support—especially illness-specific or regimen-specific support—are associated with better diabetes and other illness self-management. 1,4-8 Moreover, observational studies suggest that providing social support to others may result in health benefits comparable to—or even greater than—receiving support. Individuals who provide social support through ...
Diabetes is one of the most prevalent long-term diseases (LTDs) of this age. Nowadays, people affected by an LTD 1 are increasingly participating in digital communities, 2 often referred to as online support groups (OSGs), to share feelings, gain emotional support, and obtain information about the disease. Diabetes care requires both disease understanding and disease education, as well as ...
Digitalising diabetes peer support groups. Based on calls for support from people with diabetes across the UK, the NIHR Bristol Biomedical Research Centre (University Hospitals of Bristol and Weston NHS Foundation Trust and University of Bristol) partnered with the Diabetes UK South West Team to re‐activate and evaluate peer support group ...
Purpose of Review To review randomized controlled trials (RCTs) published from 2021-2023 that reported the effects of peer support interventions on outcomes in patients with type 2 diabetes (T2DM). Recent Findings Literature searches yielded 137 articles and nine RCTs were ultimately reviewed. The reviewed trials involved in-person support groups, peer coach/mentor support, cultural peer ...
Peer support in diabetes self-management allows patients to engage in mutual knowledge-sharing, collaborative problem-solving, and emotional support for the stresses of dealing with type 2 diabetes. ... This study has significant implications for clinical research and practice in diabetes or public health. ... weekly meetings, and closer group ...
Online support groups. A consistent research finding is that eHealth used with additional support or face-to face-interventions increase the effectiveness compared to stand-alone eHealth interventions [13-15]. Online support groups (OSGs) for people with diabetes have shown to be valuable support in disease management . These groups are run ...
Background: With the growing prevalence of diabetes in Kenya and the complex challenges of managing the disease, individuals with diabetes increasingly turn to social media (SM) support groups ...
Peer support groups are groups of people who share something in common and use their experiences to help each other. As the pandemic persists and health care teams are adjusting to the changing circumstances, facilitating access to peer support groups that can hold meetings via a digital platform can provide a unique source of additional help for diabetes self-management and mental wellbeing.
Background: In-person support groups have been shown to benefit adolescents with type 1 diabetes (T1D) by helping to decrease perceived diabetes burden and improving knowledge related to chronic disease management. However, barriers exist to participation in traditional support groups, including the timing and location of meetings and resources needed to attend.
Background: social support is important for adaptation in chronic diseases, such as diabetes and depression, because it favors recovery and adherence to treatment. Introducing its evaluation in the follow-up of diabetic patients can reduce complications derived from secondary non-adherence. Aims: to establish social support in diabetic patients and its correlation with depressive symptoms.
This pilot study evaluated what best educates and motivates patients to improve glucose control. Method: 17 participants with T2DM were recruited from Penn Rodebaugh Diabetes Center to attend 3 monthly diabetes support group meetings, and receive American Association of Diabetes Educators education. Weight and hemoglobin A1C (A1C) were measured ...
Diabetes support groups can help serve as an invaluable resource for people with diabetes. Peer support groups are readily available both in-person and online. You can tap into the resources and relationships through websites and on social media. You also may want to connect with people and groups in your community.
Like all of Diabetes Foundation's services, our support groups on diabetes-related topics are completely free of charge. Diabetes management is a learning process. If you or a loved one living with diabetes is struggling to create a diabetes healthcare plan, call the Diabetes Foundation at 201-444-0337 or email [email protected].
To locate these groups, just enter "diabetes" in the search field on the platform. You can also start by checking out the Facebook support groups below. Facebook group name and link. Number of members. Type 1 Diabetes Support Group. Over 60,000. Diabetes Support Group. Around 40,000. Diabetes Support.
Diabetes Support Resources. Diabetes Support provides ongoing support to people with diabetes to maintain and reinforce upon the skills knowledge, and lifestyle changes gained from Recognized Diabetes Self-Management Education and Support (DSMES) services. Diabetes Support is a great way for patients to connect with resources in their community.
Support groups can help people with type 2 diabetes connect with others who have the same condition. These groups allow for peer support, sharing information and resources, venting frustration, offering encouragement, and more. Support groups can exist in-person or online (such as on online forums or social media).
Diabetes Support Groups. Facing a diabetes diagnosis, whether it's you, a cherished individual, or a family member, can lead to feelings of being swamped. Engaging in a diabetes support group represents a proactive strategy for discovering assistance, guidance, insights, and resources, forming an integral component of managing diabetes ...
American Association of Clinical Endocrinologists (AACE) 245 Riverside Avenue, Suite 200. Jacksonville, FL 32202. (904) 353-7878. www.aace.com. American Diabetes Association (ADA) 2451 Crystal ...
Research shows that Hispanic people are at a higher risk of developing Type 2 diabetes than many other racial and ethnic groups. Lawrence Mandarino, PhD, director of the Center for Disparities in Diabetes, Obesity and Metabolism at the University of Arizona Health Sciences, has been researching this condition for decades. The mission of the ...
Background Women with a history of gestational diabetes mellitus (GDM) are 12-fold more likely to develop type 2 diabetes (T2D) 4-6 years after delivery than women without GDM. Similarly, GDM is associated with the development of common mental disorders (CMDs) (e.g. anxiety and depression). Evidence shows that holistic lifestyle interventions focusing on physical activity (PA), dietary ...
A team has developed the most comprehensive epidemiological dataset for youth diabetes and prediabetes research, derived from extensive National Health and Nutrition Examination Survey (NHANES ...
DISCUSSION. Patients with type 2 diabetes and fair glycemic control who attended a peer support train-the-trainer program focusing on diet, exercise, psychology, and communication improved their own self-care behaviors and metabolic control. Those who agreed to become peer supporters had higher self-rated health status at baseline with further ...
Donate to support Diabetes UK. Talk to us about diabetes. 0345 123 2399. customer support. Top menu. News and Views; Forum; ... We've invested millions into diabetes research over the last decade alone, thanks to your donations. With your help, we're getting closer to a cure. ... your local support groups and activities near you. Find now ...
METHODS: Support needs were derived from a literature review of relevant journals and interviews of outpatients as well as expert nurses in the field of diabetes to prepare a 45-item questionnaire. Each item was analyzed on a 4-point Likert scale. The study included 634 elderly patients with diabetes who were recruited from 3 hospitals in Japan.
The IPG group identified and prioritized the selection of implementation strategies to improve CRC screening uptake for patients with diabetes. The IPG and research team iterated an implementation plan specifying multi-level change objectives and implementation determinants to develop supports to help prioritize CRC screening implementation for ...
Personalized algorithmic pricing decision support tool for health insurance: : The case of stratifying gestational diabetes mellitus into two groups Authors : Haiyan Yu , Saeed Piri , Hang Qiu , Renying Xu , and Hongxia Miao Authors Info & Claims
Discover the Best Cottage Rentals in or near Elektrostal. With 32 rental cottages near Elektrostal, we are sure to find something for you. Also compare Vacation Rentals, BandBs, Summer Homes, and Holiday Rentals. Get the best prices with Rent By Owner.
Compare Elektrostal Short-Term Rentals and Weekly Vacation Rentals. See large family homes, villas, cottages, and other short stay accommodations in Elektrostal with Rent By Owner™.
Find Support Groups for Children and Young Adults. Free or Affordable Healthcare Facility. Support Groups for Parents. Diabetes management is a learning process. If you or a loved one living with diabetes is struggling to create a diabetes healthcare plan, call the Diabetes Foundation at 201-444-0337 or email [email protected].
Diabetes mellitus (DM) is a common comorbidity in COVID-19 subjects. Hyperglycemia at hospital admission identified as a major risk factor and is responsible for poor prognosis. Hematological and inflammatory parameters have been recognized as predictive markers of severity in COVID-19. In this clinical study, we aimed to assess the impact of hyperglycemia at hospital admission on ...