- Clinical Trials

About Clinical Studies
Research: it's all about patients.
Mayo's mission is about the patient, the patient comes first. So the mission and research here, is to advance how we can best help the patient, how to make sure the patient comes first in care. So in many ways, it's a cycle. It can start with as simple as an idea, worked on in a laboratory, brought to the patient bedside, and if everything goes right, and let's say it's helpful or beneficial, then brought on as a standard approach. And I think that is one of the unique characteristics of Mayo's approach to research, that patient-centeredness. That really helps to put it in its own spotlight.
At Mayo Clinic, the needs of the patient come first. Part of this commitment involves conducting medical research with the goal of helping patients live longer, healthier lives.
Through clinical studies, which involve people who volunteer to participate in them, researchers can better understand how to diagnose, treat and prevent diseases or conditions.
Types of clinical studies
- Observational study. A type of study in which people are observed or certain outcomes are measured. No attempt is made by the researcher to affect the outcome — for example, no treatment is given by the researcher.
- Clinical trial (interventional study). During clinical trials, researchers learn if a new test or treatment works and is safe. Treatments studied in clinical trials might be new drugs or new combinations of drugs, new surgical procedures or devices, or new ways to use existing treatments. Find out more about the five phases of non-cancer clinical trials on ClinicalTrials.gov or the National Cancer Institute phases of cancer trials .
- Medical records research. Medical records research involves the use of information collected from medical records. By studying the medical records of large groups of people over long periods of time, researchers can see how diseases progress and which treatments and surgeries work best. Find out more about Minnesota research authorization .
Clinical studies may differ from standard medical care
A health care provider diagnoses and treats existing illnesses or conditions based on current clinical practice guidelines and available, approved treatments.
But researchers are constantly looking for new and better ways to prevent and treat disease. In their laboratories, they explore ideas and test hypotheses through discovery science. Some of these ideas move into formal clinical trials.
During clinical studies, researchers formally and scientifically gather new knowledge and possibly translate these findings into improved patient care.
Before clinical trials begin
This video demonstrates how discovery science works, what happens in the research lab before clinical studies begin, and how a discovery is transformed into a potential therapy ready to be tested in trials with human participants:
How clinical trials work
Trace the clinical trial journey from a discovery research idea to a viable translatable treatment for patients:
See a glossary of terms related to clinical studies, clinical trials and medical research on ClinicalTrials.gov.
Watch a video about clinical studies to help you prepare to participate.
Let's Talk About Clinical Research
Narrator: This presentation is a brief introduction to the terms, purposes, benefits and risks of clinical research.
If you have questions about the content of this program, talk with your health care provider.
What is clinical research?
Clinical research is a process to find new and better ways to understand, detect, control and treat health conditions. The scientific method is used to find answers to difficult health-related questions.
Ways to participate
There are many ways to participate in clinical research at Mayo Clinic. Three common ways are by volunteering to be in a study, by giving permission to have your medical record reviewed for research purposes, and by allowing your blood or tissue samples to be studied.
Types of clinical research
There are many types of clinical research:
- Prevention studies look at ways to stop diseases from occurring or from recurring after successful treatment.
- Screening studies compare detection methods for common conditions.
- Diagnostic studies test methods for early identification of disease in those with symptoms.
- Treatment studies test new combinations of drugs and new approaches to surgery, radiation therapy and complementary medicine.
- The role of inheritance or genetic studies may be independent or part of other research.
- Quality of life studies explore ways to manage symptoms of chronic illness or side effects of treatment.
- Medical records studies review information from large groups of people.
Clinical research volunteers
Participants in clinical research volunteer to take part. Participants may be healthy, at high risk for developing a disease, or already diagnosed with a disease or illness. When a study is offered, individuals may choose whether or not to participate. If they choose to participate, they may leave the study at any time.
Research terms
You will hear many terms describing clinical research. These include research study, experiment, medical research and clinical trial.
Clinical trial
A clinical trial is research to answer specific questions about new therapies or new ways of using known treatments. Clinical trials take place in phases. For a treatment to become standard, it usually goes through two or three clinical trial phases. The early phases look at treatment safety. Later phases continue to look at safety and also determine the effectiveness of the treatment.
Phase I clinical trial
A small number of people participate in a phase I clinical trial. The goals are to determine safe dosages and methods of treatment delivery. This may be the first time the drug or intervention is used with people.
Phase II clinical trial
Phase II clinical trials have more participants. The goals are to evaluate the effectiveness of the treatment and to monitor side effects. Side effects are monitored in all the phases, but this is a special focus of phase II.
Phase III clinical trial
Phase III clinical trials have the largest number of participants and may take place in multiple health care centers. The goal of a phase III clinical trial is to compare the new treatment to the standard treatment. Sometimes the standard treatment is no treatment.
Phase IV clinical trial
A phase IV clinical trial may be conducted after U.S. Food and Drug Administration approval. The goal is to further assess the long-term safety and effectiveness of a therapy. Smaller numbers of participants may be enrolled if the disease is rare. Larger numbers will be enrolled for common diseases, such as diabetes or heart disease.
Clinical research sponsors
Mayo Clinic funds clinical research at facilities in Rochester, Minnesota; Jacksonville, Florida; and Arizona, and in the Mayo Clinic Health System. Clinical research is conducted in partnership with other medical centers throughout the world. Other sponsors of research at Mayo Clinic include the National Institutes of Health, device or pharmaceutical companies, foundations and organizations.
Clinical research at Mayo Clinic
Dr. Hugh Smith, former chair of Mayo Clinic Board of Governors, stated, "Our commitment to research is based on our knowledge that medicine must be constantly moving forward, that we need to continue our efforts to better understand disease and bring the latest medical knowledge to our practice and to our patients."
This fits with the term "translational research," meaning what is learned in the laboratory goes quickly to the patient's bedside and what is learned at the bedside is taken back to the laboratory.
Ethics and safety of clinical research
All clinical research conducted at Mayo Clinic is reviewed and approved by Mayo's Institutional Review Board. Multiple specialized committees and colleagues may also provide review of the research. Federal rules help ensure that clinical research is conducted in a safe and ethical manner.
Institutional review board
An institutional review board (IRB) reviews all clinical research proposals. The goal is to protect the welfare and safety of human subjects. The IRB continues its review as research is conducted.
Consent process
Participants sign a consent form to ensure that they understand key facts about a study. Such facts include that participation is voluntary and they may withdraw at any time. The consent form is an informational document, not a contract.
Study activities
Staff from the study team describe the research activities during the consent process. The research may include X-rays, blood tests, counseling or medications.
Study design
During the consent process, you may hear different phrases related to study design. Randomized means you will be assigned to a group by chance, much like a flip of a coin. In a single-blinded study, participants do not know which treatment they are receiving. In a double-blinded study, neither the participant nor the research team knows which treatment is being administered.
Some studies use an inactive substance called a placebo.
Multisite studies allow individuals from many different locations or health care centers to participate.
Remuneration
If the consent form states remuneration is provided, you will be paid for your time and participation in the study.
Some studies may involve additional cost. To address costs in a study, carefully review the consent form and discuss questions with the research team and your insurance company. Medicare may cover routine care costs that are part of clinical trials. Medicaid programs in some states may also provide routine care cost coverage, as well.
When considering participation in a research study, carefully look at the benefits and risks. Benefits may include earlier access to new clinical approaches and regular attention from a research team. Research participation often helps others in the future.
Risks/inconveniences
Risks may include side effects. The research treatment may be no better than the standard treatment. More visits, if required in the study, may be inconvenient.
Weigh your risks and benefits
Consider your situation as you weigh the risks and benefits of participation prior to enrolling and during the study. You may stop participation in the study at any time.
Ask questions
Stay informed while participating in research:
- Write down questions you want answered.
- If you do not understand, say so.
- If you have concerns, speak up.
Website resources are available. The first website lists clinical research at Mayo Clinic. The second website, provided by the National Institutes of Health, lists studies occurring in the United States and throughout the world.
Additional information about clinical research may be found at the Mayo Clinic Barbara Woodward Lips Patient Education Center and the Stephen and Barbara Slaggie Family Cancer Education Center.
Clinical studies questions
- Phone: 800-664-4542 (toll-free)
- Contact form
Cancer-related clinical studies questions
- Phone: 855-776-0015 (toll-free)
International patient clinical studies questions
- Phone: 507-284-8884
- Email: [email protected]
Clinical Studies in Depth
Learning all you can about clinical studies helps you prepare to participate.
- Institutional Review Board
The Institutional Review Board protects the rights, privacy, and welfare of participants in research programs conducted by Mayo Clinic and its associated faculty, professional staff, and students.
More about research at Mayo Clinic
- Research Faculty
- Laboratories
- Core Facilities
- Centers & Programs
- Departments & Divisions
- Postdoctoral Fellowships
- Training Grant Programs
- Publications
Mayo Clinic Footer
- Request Appointment
- About Mayo Clinic
- About This Site
Legal Conditions and Terms
- Terms and Conditions
- Privacy Policy
- Notice of Privacy Practices
- Notice of Nondiscrimination
- Manage Cookies
Advertising
Mayo Clinic is a nonprofit organization and proceeds from Web advertising help support our mission. Mayo Clinic does not endorse any of the third party products and services advertised.
- Advertising and sponsorship policy
- Advertising and sponsorship opportunities
Reprint Permissions
A single copy of these materials may be reprinted for noncommercial personal use only. "Mayo," "Mayo Clinic," "MayoClinic.org," "Mayo Clinic Healthy Living," and the triple-shield Mayo Clinic logo are trademarks of Mayo Foundation for Medical Education and Research.
- En español – ExME
- Em português – EME
An introduction to different types of study design
Posted on 6th April 2021 by Hadi Abbas

Study designs are the set of methods and procedures used to collect and analyze data in a study.
Broadly speaking, there are 2 types of study designs: descriptive studies and analytical studies.
Descriptive studies
- Describes specific characteristics in a population of interest
- The most common forms are case reports and case series
- In a case report, we discuss our experience with the patient’s symptoms, signs, diagnosis, and treatment
- In a case series, several patients with similar experiences are grouped.
Analytical Studies
Analytical studies are of 2 types: observational and experimental.
Observational studies are studies that we conduct without any intervention or experiment. In those studies, we purely observe the outcomes. On the other hand, in experimental studies, we conduct experiments and interventions.
Observational studies
Observational studies include many subtypes. Below, I will discuss the most common designs.
Cross-sectional study:
- This design is transverse where we take a specific sample at a specific time without any follow-up
- It allows us to calculate the frequency of disease ( p revalence ) or the frequency of a risk factor
- This design is easy to conduct
- For example – if we want to know the prevalence of migraine in a population, we can conduct a cross-sectional study whereby we take a sample from the population and calculate the number of patients with migraine headaches.
Cohort study:
- We conduct this study by comparing two samples from the population: one sample with a risk factor while the other lacks this risk factor
- It shows us the risk of developing the disease in individuals with the risk factor compared to those without the risk factor ( RR = relative risk )
- Prospective : we follow the individuals in the future to know who will develop the disease
- Retrospective : we look to the past to know who developed the disease (e.g. using medical records)
- This design is the strongest among the observational studies
- For example – to find out the relative risk of developing chronic obstructive pulmonary disease (COPD) among smokers, we take a sample including smokers and non-smokers. Then, we calculate the number of individuals with COPD among both.
Case-Control Study:
- We conduct this study by comparing 2 groups: one group with the disease (cases) and another group without the disease (controls)
- This design is always retrospective
- We aim to find out the odds of having a risk factor or an exposure if an individual has a specific disease (Odds ratio)
- Relatively easy to conduct
- For example – we want to study the odds of being a smoker among hypertensive patients compared to normotensive ones. To do so, we choose a group of patients diagnosed with hypertension and another group that serves as the control (normal blood pressure). Then we study their smoking history to find out if there is a correlation.
Experimental Studies
- Also known as interventional studies
- Can involve animals and humans
- Pre-clinical trials involve animals
- Clinical trials are experimental studies involving humans
- In clinical trials, we study the effect of an intervention compared to another intervention or placebo. As an example, I have listed the four phases of a drug trial:
I: We aim to assess the safety of the drug ( is it safe ? )
II: We aim to assess the efficacy of the drug ( does it work ? )
III: We want to know if this drug is better than the old treatment ( is it better ? )
IV: We follow-up to detect long-term side effects ( can it stay in the market ? )
- In randomized controlled trials, one group of participants receives the control, while the other receives the tested drug/intervention. Those studies are the best way to evaluate the efficacy of a treatment.
Finally, the figure below will help you with your understanding of different types of study designs.

References (pdf)
You may also be interested in the following blogs for further reading:
An introduction to randomized controlled trials
Case-control and cohort studies: a brief overview
Cohort studies: prospective and retrospective designs
Prevalence vs Incidence: what is the difference?
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
No Comments on An introduction to different types of study design
you are amazing one!! if I get you I’m working with you! I’m student from Ethiopian higher education. health sciences student
Very informative and easy understandable
You are my kind of doctor. Do not lose sight of your objective.
Wow very erll explained and easy to understand
I’m Khamisu Habibu community health officer student from Abubakar Tafawa Balewa university teaching hospital Bauchi, Nigeria, I really appreciate your write up and you have make it clear for the learner. thank you
well understood,thank you so much
Well understood…thanks
Simply explained. Thank You.
Thanks a lot for this nice informative article which help me to understand different study designs that I felt difficult before
That’s lovely to hear, Mona, thank you for letting the author know how useful this was. If there are any other particular topics you think would be useful to you, and are not already on the website, please do let us know.
it is very informative and useful.
thank you statistician
Fabulous to hear, thank you John.
Thanks for this information
Thanks so much for this information….I have clearly known the types of study design Thanks
That’s so good to hear, Mirembe, thank you for letting the author know.
Very helpful article!! U have simplified everything for easy understanding
I’m a health science major currently taking statistics for health care workers…this is a challenging class…thanks for the simified feedback.
That’s good to hear this has helped you. Hopefully you will find some of the other blogs useful too. If you see any topics that are missing from the website, please do let us know!
Hello. I liked your presentation, the fact that you ranked them clearly is very helpful to understand for people like me who is a novelist researcher. However, I was expecting to read much more about the Experimental studies. So please direct me if you already have or will one day. Thank you
Dear Ay. My sincere apologies for not responding to your comment sooner. You may find it useful to filter the blogs by the topic of ‘Study design and research methods’ – here is a link to that filter: https://s4be.cochrane.org/blog/topic/study-design/ This will cover more detail about experimental studies. Or have a look on our library page for further resources there – you’ll find that on the ‘Resources’ drop down from the home page.
However, if there are specific things you feel you would like to learn about experimental studies, that are missing from the website, it would be great if you could let me know too. Thank you, and best of luck. Emma
Great job Mr Hadi. I advise you to prepare and study for the Australian Medical Board Exams as soon as you finish your undergrad study in Lebanon. Good luck and hope we can meet sometime in the future. Regards ;)
You have give a good explaination of what am looking for. However, references am not sure of where to get them from.
Subscribe to our newsletter
You will receive our monthly newsletter and free access to Trip Premium.
Related Articles

Cluster Randomized Trials: Concepts
This blog summarizes the concepts of cluster randomization, and the logistical and statistical considerations while designing a cluster randomized controlled trial.

Expertise-based Randomized Controlled Trials
This blog summarizes the concepts of Expertise-based randomized controlled trials with a focus on the advantages and challenges associated with this type of study.

A well-designed cohort study can provide powerful results. This blog introduces prospective and retrospective cohort studies, discussing the advantages, disadvantages and use of these type of study designs.
- Skip to main content
- Skip to FDA Search
- Skip to in this section menu
- Skip to footer links

The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
U.S. Food and Drug Administration
- Search
- Menu
- For Patients
- Clinical Trials: What Patients Need to Know
Basics About Clinical Trials
What are clinical trials.
Clinical trials are research studies in which people volunteer to help find answers to specific health questions. When carefully conducted, they are the safest and fastest way to find new treatments and ways to improve health.
Clinical trials are conducted according to a plan, called a protocol, which describes:
- the types of patients who may enter the study
- the schedules of tests and procedures
- the drugs involved
- the dosages, or amount of the drug
- the length of the study
- what the researchers hope to learn from the study.
Volunteers who participate in the study must agree to the rules and terms outlined in the protocol. Similarly, researchers, doctors, and other health professionals who manage the clinical trials must follow strict rules set by the FDA. These rules make sure that those who agree to participate are treated as safely as possible.
Learn more about the basics of clinical trial participation, read first hand experiences from actual clinical trial volunteers, and see explanations from researchers at the NIH Clinical Research Trials and You Web site.
Why are clinical trials done?
Clinical trials are conducted for many reasons:
- to determine whether a new drug or device is safe and effective for people to use.
- to study different ways to use standard treatments or current, approved treatments so that they will be more effective, easier to use, or decrease certain side effects.
- to learn how to safely use a treatment in a population for which the treatment was not previously tested, such as children.
Who should consider clinical trials and why?
Some people participate in clinical trials because none of the standard (approved) treatment options have worked, or they are unable to tolerate certain side effects. Clinical trials provide another option when standard therapy has failed. Others participate in trials because they want to contribute to the advancement of medical knowledge.
Ensuring people from diverse backgrounds join clinical trials is key to advancing health equity. Participants in clinical trials should represent the patients that will use the medical products. This is often not the case—people from racial and ethnic minority and other diverse groups are underrepresented in clinical research. This is a concern because people of different ages, races, and ethnicities may react differently to certain medical products. Learn more about the clinical trial diversity initiative from the Office of Minority Health and Health Equity.
All clinical trials have guidelines, called eligibility criteria, about who can participate. The criteria are based on such factors as age, sex, type and stage of disease, previous treatment history, and other medical conditions. This helps to reduce the variation within the study and to ensure that the researchers will be able to answer the questions they plan to study. Therefore, not everyone who applies for a clinical trial will be accepted.
It is important to test drugs and medical products in the people they are meant to help. It is also important to conduct research in a variety of people, because different people may respond differently to treatments. FDA seeks to ensure that people of different ages, races, ethnic groups, and genders are included in clinical trials. Learn more about FDA’s efforts to increase diversity in clinical trials .
Where are clinical trials conducted?
Clinical trials can be sponsored by organizations (such as a pharmaceutical company), Federal offices and agencies (such as the National Institutes of Health or the U.S. Department of Veterans Affairs), or individuals (such as doctors or health care providers). The sponsor determines the location(s) of the trials, which are usually conducted at universities, medical centers, clinics, hospitals, and other Federally or industry-funded research sites.
Are clinical trials safe?
FDA works to protect participants in clinical trials and to ensure that people have reliable information before deciding whether to join a clinical trial. The Federal government has regulations and guidelines for clinical research to protect participants from unreasonable risks. Although efforts are made to control the risks to participants, some may be unavoidable because we are still learning more about the medical treatments in the study.
The government requires researchers to give prospective participants complete and accurate information about what will happen during the trial. Before joining a particular study, you will be given an informed consent document that describes your rights as a participant, as well as details about the study, including potential risks. Signing it indicates that you understand that the trial is research and that you may leave at any time. The informed consent is part of the process that makes sure you understand the known risks associated with the study.
What should I think about before joining a clinical trial?
Before joining a clinical trial, it is important to learn as much as possible. Discuss your questions and concerns with members of the health care team conducting the trial. Also, discuss the trial with your health care provider to determine whether or not the trial is a good option based on your current treatment. Be sure you understand:
- what happens during the trial
- the type of health care you will receive
- any related costs once you are enrolled in the trial
- the benefits and risks associated with participating.
What is FDA’s role in approving new drugs and medical treatments?
FDA makes sure medical treatments are safe and effective for people to use. We do not develop new therapies or conduct clinical trials. Rather, we oversee the people who do. FDA staff meet with researchers and perform inspections of clinical trial study sites to protect the rights of patients and to verify the quality and integrity of the data.
Learn more about the Drug Development Process .
Where can I find clinical trials?
One good way to find out if there are any clinical trials that might help you is to ask your doctor. Other sources of information include:
- FDA Clinical Trials Search. Search a database of Federally and privately supported studies available through clinicaltrials.gov. Learn about each trial’s purpose, who can participate, locations, and who to contact for more information.
- Clinicaltrials.gov. Conduct more advanced searches
- National Cancer Institute or call 1–800–4–CANCER (1–800–422–6237). Learn about clinical trials for people with cancer.
- AIDS Clinical Trials and Information Services (ACTIS) or call 1–800–TRIALS–A (1–800–874–2572). Locate clinical trials for people with HIV.
- AIDSinfo. Search a database of HIV/AIDS trials, sponsored by the National Institutes of Health’s National Library of Medicine.
What is a placebo and how is it related to clinical trials?
A placebo is a pill, liquid, or powder that has no treatment value. It is often called a sugar pill. In clinical trials, experimental drugs are often compared with placebos to evaluate the treatment’s effectiveness.
Is there a chance I might get a placebo?
In clinical trials that include placebos, quite often neither patients nor their doctors know who is receiving the placebo and how is being treated with the experimental drug. Many cancer clinical trials, as well as trials for other serious and life-threatening conditions, do not include placebo control groups. In these cases, all participants receive the experimental drug. Ask the trial coordinator whether there is a chance you may get a placebo rather than the experimental drug. Then, talk with your doctor about what is best for you.
How do I find out what Phase a drug is in as part of the clinical trial?
Talk to the clinical trial coordinator to find out which phase the clinical trial is in. Learn more about the different clinical trial phases and whether they are right for you.
What happens to drugs that don't make it out of clinical trials?
Most drugs that undergo preclinical (animal) research never even make it to human testing and review by the FDA. The drug developers go back to begin the development process using what they learned during with their preclinical research. Learn more about drug development .
Clinical Researcher
Clinical Study Reports 101: Tips and Tricks for the Novice
Clinical Researcher September 15, 2020

Clinical Researcher—September 2020 (Volume 34, Issue 8)
PEER REVIEWED
Sheryl Stewart, MCR, CCRP
The tenets of Good Clinical Practice (GCP), promulgated by the International Council for Harmonization (ICH), require that investigator-initiated trials (IITs), especially those involving an Investigational New Drug application to the U.S. Food and Drug Administration (FDA), have the principal investigator (PI), the institution, and the study team assume roles of both the sponsor (ICH GCP E6(R2), Section 5) and of the PI (ICH GCP E6(R2), Section 4).{1} If you are part of an IIT team, whether you are the investigator, a clinical research coordinator, or someone working in any of the many other important roles within the team, you may be tasked with authoring a clinical study report (CSR) at one time or another within the course of the study. At the very least, you may be asked to contribute to, or provide peer review of the document before it is submitted for its intended purpose.
The purpose of this review is to provide a framework for study team members, whether it’s for a large team that includes regulatory and administrative support or for smaller teams with only one or two members, for writing and organizing the CSR.
First, is important to understand the definition, requirements, and potential uses of a CSR. The report is a comprehensive look at all the data produced in a clinical study, presented in text, tables, and figure formats. It will often include discussions and conclusions that provide context to the findings regarding the drug, device, biological product, surgical method, counseling practice, or any other type of therapeutic product or practice under study and where it may contribute to an improvement on the state of the art for treating or preventing a particular health condition.
If a study has prespecified endpoints or parameters, the CSR will report the current outcomes and statistical parameters for these endpoints. Key messages will be referred to and highlighted throughout. Key messages are important study findings that support the prespecified endpoints, supply proof of the justification of clinical benefit, or differentiate the study product from others in the therapeutic space.
Most likely you already appreciate the ethical responsibility a clinical study team has to clinical study data transparency, which for that reason alone would make the production of some sort of CSR necessary. Indeed, the preparation and representation of study progress is prescribed in the aforementioned ICH GCP E6(R2) guideline,{1} which states that study sponsors should ensure that clinical trial reports are prepared and provided to regulatory agencies as they are required.
Further, the guideline recommends study sponsors to rely on a subsequent guideline on Structure and Content of Clinical Study Reports (ICH E3).{2} Lastly, adhering to this ethical responsibility and following GCP have become mandated both in the U.S. and in Europe, where study data are expected to be recorded on ClinicalTrials.gov and the EudraCT database, respectively, for the sake of transparency and in support of further scientific inquiry, thus making the organization and preparation of study data in a prespecified format necessary.{3,4}
There are a few different uses for a CSR, though primarily it is utilized either to summarize the data and outcomes at the end of the study, or for marketing authorization. Those two purposes are specifically outlined in ICH E3 and ICH E6.{1,2} However, a CSR may also be written for third-party payer reimbursement purposes, providing details in support of clinical benefit. Because in most cases CSRs will ultimately have a regulatory reviewer, authoring a report that is consistent in formatting and content with what is expected will hopefully not only enable a smooth review, but also will facilitate proper data cleaning, presentation, and timeliness that make the document fit for purpose.
ICH E3 offers a CSR template to guide you in terms of providing the proper data and content in a specified order and format. This guideline can be found either on the ICH website or the FDA website.{2,5}
It is important to note that there are no requirements to follow the template precisely. Not every section is appropriate for every study, and because the overarching purpose of a CSR is to provide proper representation of the study data and any key messages you want to report, flexibility is allowed and encouraged in order to meet those important goals. However, for anyone new to the process of crafting a CSR, this template is a helpful starting point.
Transcelerate Biopharma, a nonprofit organization involved in researching means to increase efficiency and innovation in the pharmaceutical research sciences, also has interpreted the ICH template and has produced a useful tool to improve this reporting.{6} If the instruction and guidance in the ICH or Transcelerate templates do not meet your needs, or you have further questions as to how to properly represent the study data, the CORE reference manual (Clarity and Openness in Reporting E3-based) is another resource. It was produced in 2016 in response to regulatory changes for public disclosure of clinical study data, and can provide direction and interpretation of the ICH E3 template.{7}
For the novice author of a CSR, however, the ICH E3 template, coupled with the Transcelerate template, should provide a strong starting point for the project planning of the report, as well as the document formatting.
Sidebar: Tips and Tricks for Getting Started
Determining Stakeholders
Once you’ve reviewed the template and created a draft outline of the project, determine the key stakeholders with whom you’ll need to partner to complete this project. Likely you will need input from your clinical study management team, teammates responsible for data entering and cleaning, a biostatistician, any teammate or organization member able to perform literature reviews, those staff qualified to compose patient or adverse event narratives, and those team members who can help determine key messaging in this report. Lastly you will want to determine the group of key stakeholders who will be your final review team for the document—those who will help you finalize the document prior to submission.
Sidebar: Tips and Tricks for Stakeholder and Project Management
Determining Timelines
Once you have determined your key stakeholders, you will want to determine timelines to ensure steady progress continues to be made on the document. If you’ve chosen to utilize a scope document, you’ll want to include these timelines in it, so the entire team is aware of the project process, the timing requirements, and each gating item (key gating items are summarized in Figure 1).
Figure 1: Preparing, Writing, and Review of the Clinical Study Report—Key Gating Items
Time management is paramount for clinical trial submissions to regulatory authorities. Attendees at medical writing conferences over the course of a five-year period (2008 to 2013, n=78) were surveyed to determine to how long each step of the CSR process can typically require.{8}
To complete a “moderately complex” CSR for a Phase III study with 200 to 400 participants, the surveyed medical writers responded with a mean answer of 16.9 days from the receipt of the final tables, listings, and figures (TLFs) to delivery of the first draft of the CSR. They estimated a mean of 25.7 days from the first draft to the final draft routed for review. The time from database lock to completion was reported to be on average 83 days.
While there was a wide range for the timelines reported, these data provide the novice CSR author a basic reference point for how long the individual processes can expect to take with experienced medical writers. Fortunately, while TLFs are being crafted, multiple other “Writing and Document Review” tasks from Table 1 can be performed simultaneously.
At Last…the Writing!
Typically, the flow of your CSR will progress under six primary headings or sections, not unlike those used in a research manuscript. On the front end, even before the background and introduction, the document will include a title page, synopsis, table of contents, list of abbreviations, ethics statements, and details on the study’s administrative structure. The primary sections to come after that are highlighted in Figure 2 and summarized in turn below.
Figure 2: Primary Sections
Background, Intro. > Non-Results > Results > Discussion > Conclusion > Exec. Summary
Background and Introduction
When available, utilize any state-of-the-art analysis of the product/therapy from the protocol for your CSR introduction. If not available, you can briefly summarize the study design, objectives, and population and then you’ll need to craft a novel but brief state-of-the-art analysis based on literature review.
Be sure to align with the key messaging of your study and the indications of your study drug, device, or other type of therapeutic product or method. Utilize good literature review practices, such as choosing peer-reviewed publications, editorials from key opinion leaders in the therapeutic area, and studies with large or randomized cohorts, for support. This section will likely be no longer than one page.
Non-Results Section
Whether to cut and paste the procedures and assessments, primary and secondary endpoints, parameters or hypotheses, planned statistical analyses, monitoring plans, adverse event definitions, and assessment rules directly from the protocol or to simply refer to the protocol and the other study documents in an appendix is a topic of debate amongst medical writers of CSRs. Keep in mind that the CSR should be able to stand alone as a document, and thus while it is important to keep the document concise, it must be comprehensive enough for the reader to understand the study design, objectives, endpoints, processes, and intended analyses without having to refer constantly to the protocol. Regardless, in any summary of the study design, processes, and endpoints, be sure to align with any previously utilized language for consistency across study documents.
Results Section
Using the template and your tables as your structure, summarize the data and pull out any signals and trends, aligning with key messaging where possible. Start with patient disposition and demographics as per the template. Note any protocol deviations that may or may not have impacted patient safety or the evaluation of the outcomes.
Assess and evaluate the study outcome results against primary endpoints and secondary endpoints before discussing any additional secondary outcomes. You should not simply restate the data in the tables; however, refer to specifics in the tables when summarizing.
If you find that you cannot make a statement or conclusion given the TLFs you have, or you are consistently having to perform your own math to support your statements, consider asking your biostatistician to create the tables that will represent the data in a way that will better support your statement. For instance, it is acceptable to state that “most” of the patients responded to the study drug if more than 50% did so; however, if you are having to consistently add up percentages in a table to be able to state, for example, that 77% of the patients responded in a certain way and 33% responded in another, then you should have the biostatistician reformat the data output so it represents the percentages you want to report.
Patient narratives are an important source of context for the reader of the CSR. Depending on your study, you may need to collaborate with either your teammates responsible for assessment of adverse events or the study database administrator to help generate patient and/or event narratives for the CSR. If tasked with compiling or editing patient narratives yourself, the ICH E3 guideline prescribes the necessary components of a comprehensive patient safety narrative (Section 12).{2}
Narrative writing advice has also been previously published and would be a helpful source of direction for the novice narrative writer.{9,10} Narratives are suggested for every patient who experienced a safety endpoint event or death during the course of the study. Tie in patient narratives where appropriate when discussing safety events or refer to the patient narrative section when highlighting a particular patient’s data.
Discussions and Conclusions
Discussion and conclusion sections can either be placed after each section or placed at the end of the document. They should not simply restate the previous table summaries, but provide context and align the results with key messaging. Use an evidence-based approach, including literature references to provide more context as to the nature of the study outcomes with respect to the state of the art for the product/therapy, outcomes from alternate approaches, or further justification of clinical benefit with regard to potential disease progression. The conclusion section at the end of the document is often in bulleted format—not only for ease of the reader, but also to clearly highlight the key messaging and important outcomes you wish to impart.
Executive Summary
The executive summary, while placed at the front of the document prior to the introduction, is often easiest to construct last, as an overall summary of the entire document. The key elements of this summary should briefly recap the study design and objectives. Most likely only the primary and secondary endpoints should be included, unless additional outcomes proved compelling and important within the course of the study. Refer to any important literature comparisons as they relate to any conclusions made about the success or outcomes of the trials. Conclude the executive summary in a similar fashion to the overall study conclusion.
Sidebar: Tips and Tricks for the CSR Writing Process
Review Process
The review process can either facilitate a better document or it can slow down the entire process. The purpose of a cross functional review of a CSR is to confirm accurate key study messaging and data; allow medical review of the patient narratives, outcomes, and conclusionary statements; review the logical flow of ideas; and ensure that the CSR language is consistent across any other study document (i.e., the protocol, statistical analysis plan, etc.).
Sidebar: Tips and Tricks for an Efficient Review Process
CSRs are required by regulatory authorities to report and summarize the outcomes of a clinical study. Pre-project stakeholder determination and timeline planning can help with project management. Templates contained with the ICH E3 guideline can help organize the project as well as help create and finalize a document that is fit for purpose and meets the content expectations of the regulatory reviewer.
- ICH Working Group. 2016. ICH HARMONISED GUIDELINE INTEGRATED ADDENDUM TO ICH E6(R1): GUIDELINE FOR GOOD CLINICAL PRACTICE E6(R2).
- ICH Working Group. 1995. ICH HARMONISED TRIPARTITE GUIDELINE: Structure and Content of Clinical Study Reports E3 .
- U.S. Department of Health and Human Services. 2016. Clinical Trials Registration and Results Information Submission, 42 CFR Part 11. https://www.federalregister.gov/documents/2016/09/21/2016-22129/clinical-trials-registration-and-results-information-submission
- European Commission. 2001. Letter to Stakeholders Regarding the Requirements to provide results for Authortied clinical trials in EUDRACT. In: Article 57(2) Regulation (EC) No 726/2004 and Article 41(2) of Regulation (EC) No 1901/2006. https://eudract.ema.europa.eu/
- U.S. Food and Drug Administration. 2018. ICH Guidance Documents . https://www.fda.gov/science-research/guidance-documents-including-information-sheets-and-notices/ich-guidance-documents
- Transcelerate Biopharma Inc. Clinical Template Suite (CTS), Template, Resources, and Use Guidance. https://transceleratebiopharmainc.com/assets/clinical-content-reuse-assets/
- Hamilton S, Bernstein AB, Blakey G, et al. 2016. Developing the Clarity and Openness in Reporting: E3-based (CORE) Reference user manual for creation of clinical study reports in the era of clinical trial transparency. Research integrity and peer review. 1:4.
- Hamilton S. 2014. Effective authoring of clinical study reports. Medical Writing 23(2).
- Nambiar I. 2018. Analysis of serious adverse event: Writing a narrative. Perspect Clin Res 9(2):103–6.
- Ledade SD, Jain SN, Darji AA, Gupta VH. 2017. Narrative writing: Effective ways and best practices. Perspect Clin Res 8(2):58–62.

Sheryl Stewart, MCR, CCRP, ( [email protected] ) is a Medical Writer working in the medical device industry in southern California.
Sorry, we couldn't find any jobs that match your criteria.

Embracing the Future: Opportunities and Challenges of AI Integration in Healthcare

Utilizing Cultural Humility as a Tool to Support Diversity in Clinical Research

Looking at Clinical Trial Technology Through a Site Lens
Study record managers: refer to the Data Element Definitions if submitting registration or results information.
Search for terms

- Advanced Search
- See Studies by Topic
- See Studies on Map
- How to Search
- How to Use Search Results
- How to Find Results of Studies
- How to Read a Study Record

- Learn About Studies
- Other Sites About Studies
- Glossary of Common Site Terms

- Submit Studies to ClinicalTrials.gov PRS
- Why Should I Register and Submit Results?
- FDAAA 801 and the Final Rule
- How to Apply for a PRS Account
- How to Register Your Study
- How to Edit Your Study Record
- How to Submit Your Results
- Frequently Asked Questions
- Support Materials
- Training Materials

- Selected Publications
- Clinical Alerts and Advisories
- Trends, Charts, and Maps
- Downloading Content for Analysis

- ClinicalTrials.gov Background
- About the Results Database
- History, Policies, and Laws
- ClinicalTrials.gov Modernization
- Media/Press Resources
- Linking to This Site
- Terms and Conditions
About Studies
Learn About Clinical Studies
- Other Sites About Clinical Studies
Clinical Trials
Observational studies, who conducts clinical studies, where are clinical studies conducted, how long do clinical studies last, reasons for conducting clinical studies, who can participate in a clinical study, how are participants protected, relationship to usual health care, considerations for participation, questions to ask, what is a clinical study.
A clinical study involves research using human volunteers (also called participants) that is intended to add to medical knowledge. There are two main types of clinical studies: clinical trials (also called interventional studies) and observational studies. ClinicalTrials.gov includes both interventional and observational studies.
In a clinical trial, participants receive specific interventions according to the research plan or protocol created by the investigators. These interventions may be medical products, such as drugs or devices; procedures; or changes to participants' behavior, such as diet. Clinical trials may compare a new medical approach to a standard one that is already available, to a placebo that contains no active ingredients, or to no intervention. Some clinical trials compare interventions that are already available to each other. When a new product or approach is being studied, it is not usually known whether it will be helpful, harmful, or no different than available alternatives (including no intervention). The investigators try to determine the safety and efficacy of the intervention by measuring certain outcomes in the participants. For example, investigators may give a drug or treatment to participants who have high blood pressure to see whether their blood pressure decreases.
Clinical trials used in drug development are sometimes described by phase. These phases are defined by the Food and Drug Administration (FDA).
Some people who are not eligible to participate in a clinical trial may be able to get experimental drugs or devices outside of a clinical trial through expanded access. See more information on expanded access from the FDA .
In an observational study, investigators assess health outcomes in groups of participants according to a research plan or protocol. Participants may receive interventions (which can include medical products such as drugs or devices) or procedures as part of their routine medical care, but participants are not assigned to specific interventions by the investigator (as in a clinical trial). For example, investigators may observe a group of older adults to learn more about the effects of different lifestyles on cardiac health.
Every clinical study is led by a principal investigator, who is often a medical doctor. Clinical studies also have a research team that may include doctors, nurses, social workers, and other health care professionals.
Clinical studies can be sponsored, or funded, by pharmaceutical companies, academic medical centers, voluntary groups, and other organizations, in addition to Federal agencies such as the National Institutes of Health, the U.S. Department of Defense, and the U.S. Department of Veterans Affairs. Doctors, other health care providers, and other individuals can also sponsor clinical research.
Clinical studies can take place in many locations, including hospitals, universities, doctors' offices, and community clinics. The location depends on who is conducting the study.
The length of a clinical study varies, depending on what is being studied. Participants are told how long the study will last before they enroll.
In general, clinical studies are designed to add to medical knowledge related to the treatment, diagnosis, and prevention of diseases or conditions. Some common reasons for conducting clinical studies include:
- Evaluating one or more interventions (for example, drugs, medical devices, approaches to surgery or radiation therapy) for treating a disease, syndrome, or condition
- Finding ways to prevent the initial development or recurrence of a disease or condition. These can include medicines, vaccines, or lifestyle changes, among other approaches.
- Evaluating one or more interventions aimed at identifying or diagnosing a particular disease or condition
- Examining methods for identifying a condition or the risk factors for that condition
- Exploring and measuring ways to improve the comfort and quality of life through supportive care for people with a chronic illness
Participating in Clinical Studies
A clinical study is conducted according to a research plan known as the protocol. The protocol is designed to answer specific research questions and safeguard the health of participants. It contains the following information:
- The reason for conducting the study
- Who may participate in the study (the eligibility criteria)
- The number of participants needed
- The schedule of tests, procedures, or drugs and their dosages
- The length of the study
- What information will be gathered about the participants
Clinical studies have standards outlining who can participate. These standards are called eligibility criteria and are listed in the protocol. Some research studies seek participants who have the illnesses or conditions that will be studied, other studies are looking for healthy participants, and some studies are limited to a predetermined group of people who are asked by researchers to enroll.
Eligibility. The factors that allow someone to participate in a clinical study are called inclusion criteria, and the factors that disqualify someone from participating are called exclusion criteria. They are based on characteristics such as age, gender, the type and stage of a disease, previous treatment history, and other medical conditions.
Informed consent is a process used by researchers to provide potential and enrolled participants with information about a clinical study. This information helps people decide whether they want to enroll or continue to participate in the study. The informed consent process is intended to protect participants and should provide enough information for a person to understand the risks of, potential benefits of, and alternatives to the study. In addition to the informed consent document, the process may involve recruitment materials, verbal instructions, question-and-answer sessions, and activities to measure participant understanding. In general, a person must sign an informed consent document before joining a study to show that he or she was given information on the risks, potential benefits, and alternatives and that he or she understands it. Signing the document and providing consent is not a contract. Participants may withdraw from a study at any time, even if the study is not over. See the Questions to Ask section on this page for questions to ask a health care provider or researcher about participating in a clinical study.
Institutional review boards. Each federally supported or conducted clinical study and each study of a drug, biological product, or medical device regulated by FDA must be reviewed, approved, and monitored by an institutional review board (IRB). An IRB is made up of doctors, researchers, and members of the community. Its role is to make sure that the study is ethical and that the rights and welfare of participants are protected. This includes making sure that research risks are minimized and are reasonable in relation to any potential benefits, among other responsibilities. The IRB also reviews the informed consent document.
In addition to being monitored by an IRB, some clinical studies are also monitored by data monitoring committees (also called data safety and monitoring boards).
Various Federal agencies, including the Office of Human Subjects Research Protection and FDA, have the authority to determine whether sponsors of certain clinical studies are adequately protecting research participants.
Typically, participants continue to see their usual health care providers while enrolled in a clinical study. While most clinical studies provide participants with medical products or interventions related to the illness or condition being studied, they do not provide extended or complete health care. By having his or her usual health care provider work with the research team, a participant can make sure that the study protocol will not conflict with other medications or treatments that he or she receives.
Participating in a clinical study contributes to medical knowledge. The results of these studies can make a difference in the care of future patients by providing information about the benefits and risks of therapeutic, preventative, or diagnostic products or interventions.
Clinical trials provide the basis for the development and marketing of new drugs, biological products, and medical devices. Sometimes, the safety and the effectiveness of the experimental approach or use may not be fully known at the time of the trial. Some trials may provide participants with the prospect of receiving direct medical benefits, while others do not. Most trials involve some risk of harm or injury to the participant, although it may not be greater than the risks related to routine medical care or disease progression. (For trials approved by IRBs, the IRB has decided that the risks of participation have been minimized and are reasonable in relation to anticipated benefits.) Many trials require participants to undergo additional procedures, tests, and assessments based on the study protocol. These requirements will be described in the informed consent document. A potential participant should also discuss these issues with members of the research team and with his or her usual health care provider.
Anyone interested in participating in a clinical study should know as much as possible about the study and feel comfortable asking the research team questions about the study, the related procedures, and any expenses. The following questions may be helpful during such a discussion. Answers to some of these questions are provided in the informed consent document. Many of the questions are specific to clinical trials, but some also apply to observational studies.
- What is being studied?
- Why do researchers believe the intervention being tested might be effective? Why might it not be effective? Has it been tested before?
- What are the possible interventions that I might receive during the trial?
- How will it be determined which interventions I receive (for example, by chance)?
- Who will know which intervention I receive during the trial? Will I know? Will members of the research team know?
- How do the possible risks, side effects, and benefits of this trial compare with those of my current treatment?
- What will I have to do?
- What tests and procedures are involved?
- How often will I have to visit the hospital or clinic?
- Will hospitalization be required?
- How long will the study last?
- Who will pay for my participation?
- Will I be reimbursed for other expenses?
- What type of long-term follow-up care is part of this trial?
- If I benefit from the intervention, will I be allowed to continue receiving it after the trial ends?
- Will results of the study be provided to me?
- Who will oversee my medical care while I am participating in the trial?
- What are my options if I am injured during the study?
- For Patients and Families
- For Researchers
- For Study Record Managers
- Customer Support
- Accessibility
- Viewers and Players
- Freedom of Information Act
- HHS Vulnerability Disclosure
- U.S. National Library of Medicine
- U.S. National Institutes of Health
- U.S. Department of Health and Human Services

Stanford Cancer Institute
Search stanford cancer institute, clinical trials, search clinical trials, what are clinical trials.
Clinical trials are scientific studies that involve people in research and are the only way to advance cancer treatment. Before people are given a new intervention, it is carefully studied in the laboratory. Studies with the most promising results are then moved into clinical trials with people. Clinical trials are used to evaluate new and better ways to treat, prevent, detect, diagnose, and manage symptoms of cancer.
How do I know if I am eligible for a trial?
Once you locate a trial/s of interest through our search engine (via conditions or eligibility), or mobile app ( iOS | Android ), click through to the trial’s detail page. Scroll down and review the “Eligibility” section. All clinical trials have guidelines about who can take part. Anyone who wants to take part must fit the guidelines to be in the study (called the inclusion and exclusion criteria). These usually relate to age and gender, cancer type and stage, other medical conditions you may have and the types of treatments already undergone.
Once you have located a study in which you feel you reasonably meet the eligibility criteria, contact the study team directly. On the trial’s detail page you will find “contact information” listed on the right hand side of the page.
After contacting the study team you may be pre-screened prior to an in-person consultation with a study physician who determines if you are eligible for the trial.
· The study team may ask you questions over the phone though their pre-screening process.
· You may be asked to set up an appointment through New Patient Coordinator for an in-person consultation with a study physician to determine eligibility and treatment options. The New Patient Coordinator phone number is (650) 498-6000.
If after reading study descriptions you find it difficult to decide which study is appropriate, discuss the study with your oncologist or make an appointment for a second opinion at Stanford to find out about all potential treatment options. To make an appointment, please call the Stanford Cancer Center New Patient Coordinator at 650-498-6000.
What questions should I ask before joining a cancer clinical trial?
You should ask many questions so you can best decide if joining a trial is right for you. Here are some questions you may want to consider… More
What does it cost to participate in a trial?
There are two types of costs:
1) Routine care costs
2) Research costs. Health insurance typically covers the cost of the routine care.
These are costs that would incur whether or not you were in a clinical trial. However, you will still be responsible for any co-payments and/or deductibles. Research costs for the research portion of a trial are paid for by the trial itself at no cost to you. However, there may be additional costs, such as personal time and travel expenses, which may or may not be covered by a clinical trial. Please be aware that each trial is unique. The study team will go over the costs of participation with you before you agree to participate.
Sign up for trial Alerts
Receive email alerts when trials open to patients. Simply choose a condition and enter your email address and we will send new trial notices directly to your email account.
The Email & Condition fields are required. Please validate the input
Your request has been sent. Please check your email to confirm this subscription.
Need help finding a trial?
If you are interested in applying for a clinical trial or have questions, an associate is available to provide information and assist you with the application process. Feel free to reach out for further guidance and support.

Patient Care
Health equity, shared resources, stanford medicine, health care.

©2024 Stanford Medicine
An official website of the United States government
Here’s how you know
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.

U.S. Dept. of Health & Human Services
Clinical Research Study Investigator's Toolbox
The purpose of the NIA Clinical Research Toolbox is to provide a Web-based informational repository for investigators and staff involved in clinical research. The Toolbox contains templates, sample forms, guidelines, regulations and informational materials to assist investigators in the development and conduct of high quality clinical research studies.
Issued by: National Institutes of Health (NIH)
NIA Clinical Research Investigator's Toolbox
Supporting clinical research, study startup.
- NIA Guidance on Clinical Trials
Forms and Templates
- Glossary of Terms
Data Safety and Monitoring
As depicted in the NIA Guidance on Clinical Trials , NIA is responsible for overseeing the data and safety monitoring of the clinical research it supports. Data and safety monitoring of a clinical trial is commensurate with the risks posed to the study participants and with the size and complexity of the study.
Applicants requesting support for any intervention study must complete "PHS Human Subjects and Clinical Trials Information" form of the SF424 (R&R), describe a data and safety monitoring plan (DSMP), which discusses the need for an independent data and safety monitoring body or justifies why such a body is not needed to monitor the study and proposes an alternative safety monitoring mechanism. For example, for a single-site, low risk study, the PI may propose a local safety monitor, while a multi-site, higher risk study might propose a Data and Safety Monitoring Board (DSMB).
- Data and Safety Monitoring Plan (DSMP) Template and Guidelines (MS Word, 37K) and DSMP Checklist (MS Word, 43K) were developed to assist investigators in preparation of a sound data and safety monitoring plan. All clinical trials require study-specific monitoring procedures to ensure participant safety and data integrity. The DSMP outlines procedures that investigators and study staff will follow when implementing a clinical trial. Investigators submitting grant applications for clinical trials are required to include a general description of the DSMP as part of the research grant application.
- Guideline for Budgeting for Data and Safety Monitoring Activities (MS Word, 25K) aids investigators in budgeting for an independent DSMB or a Safety Officer when preparing the budget section of a grant application.
Data Sharing
The National Institutes of Health (NIH) advocates making available to the public the results and accomplishments of the activities that it funds. NIH assures that research resources developed with public funds become readily available to the broader research community in a timely manner for further research, development, application, and secondary data analysis. The expectation is that this will lead to products and knowledge of benefit to public health. To ensure that future research can build on previous efforts and discoveries, the National Institutes of Health (NIH) has developed a data sharing policy effective October 1, 2003, for applicants seeking NIH funding of $500,000 or more in direct costs in any one year. The policy expects final research data, especially unique data, from NIH-supported research efforts be made available to the investigators. The NIH policy on data sharing applies to:
- Basic research, clinical studies, surveys, and other types of research supported by the NIH.
- Human subjects and laboratory research.
- Data not produced with NIH funding but used in an NIH-supported activity in some instances.
Investigators are expected to include in their grant application a brief description of how final research data will be shared, or explain why data-sharing is not possible (for example: human subject protection concerns). Please see NIH’s Example Plan (MS Word, 55K) for a template you may modify to fit the data you plan to share.
Initial Proposal Concept Form (MS Word, 39K) - This form should be used to advocate for an initiative by the Division of Geriatrics and Clinical Gerontology (DGCG) for a clinical trial or trials that exceed $2 million in direct costs in any year of funding. DGCG Clinical Trials Advisory Panel, a task force of the National Advisory Council on Aging (NACA), will evaluate the concept proposals in October – November of each Fiscal Year and will provide its recommendations to DGCG, NACA, and to the NIA Director on initiatives for large clinical trials.
Back to top
The clinical protocol is a document that describes how a clinical study will be conducted by detailing the objective(s), design, methodology, statistical considerations and organization of a clinical study, and describes methods used to ensure the safety of the study participants and integrity of the data collected.
Protocol (MS Word, 93K) - The Clinical Intervention Study Protocol Template outlines a clinical study protocol and provides guidance on important content to include in each section. The template can be downloaded as an MS Word file for adaptation by the study investigator.
Manual of Procedures
A Manual of Procedures (MOP) is a handbook that details a study’s conduct and operations as well as facilitates consistency in protocol implementation and data collection across study participants and sites. It operationalizes the study protocol and describes each step of the study and how it is to be executed. A copy of the MOP should be provided to each member of the Study Team. Ideally, the MOP would contain an adequate amount of detail that any individual(s) at any site(s) could run the study consistently with only the information contained in the MOP and its appendices.
Get resources to support your study recruitment
Visit NIA’s ADORE (Alzheimer’s and Dementia Outreach, Recruitment, and Engagement) Resources for a searchable collection of materials for clinical trials recruitment and retention.
The NIA recognizes the importance of a MOP and has developed documents to assist principal investigators in writing their study MOP. Investigators with a multi-site study are required to submit a MOP, while single-site study investigators are strongly encouraged to review the MOP and determine which sections are necessary in order to ensure the study procedures are performed as intended. The Guidelines below provide details on each section of the MOP, while the MOP Outlines are an overview listing the sections that are most relevant in those types of studies.
- Manual of Procedures (MOP) Outline – Multi-Site (MS Word, 30K)
- Manual of Procedures (MOP) Guidelines – Multi-Site (MS Word, 179K)
- Manual of Procedures (MOP) Outline – Single-Site (MS Word, 27K)
- Manual of Procedures (MOP) Guidelines - Single-Site (MS Word, 170K)
The following documents can also be found within the MOP template:
- Screening Log provides documentation of all individuals who were evaluated for participation in a research study. The log typically contains a unique identification number for each person screened along with individuals’ initials, age, gender, race and ethnicity, screening date, and eligibility status.
- Schedule of Events presents the activities that take place at each contact with the participant.
- Protocol Deviation Log provides participant-specific documentation of missed visits and other actions that deviate from the protocol.
Informed Consent
The consent process provides individuals with sufficient information for making informed decisions about participation in a clinical research study. The following documents are provided as a tool to assist NIA investigators for developing a comprehensive informed consent:
- Informed Consent Template (MS Word, 115K) provides a general outline of a study specific informed consent form (ICF). It is critical that investigators consult with their local IRB for any institution-specific templates and/or requirements regarding the format and content of the consent form.
- Informed Consent Checklist (MS Word, 55K) presents required and additional elements of the consent forms as set forth in Code of Federal Regulations.
- Informed Consent Version Tracker (MS Excel, 20K) provides a template with two examples of tools that sites may use to track informed consent versions; this helps minimize the use of expired versions and the occurrence of consent deviations.
Data Safety and Monitoring Boards
The Data and Safety Monitoring Board (DSMB) is an independent group of experts that advises the NIA Director and the study investigators. The members of the DSMB serve in an individual capacity and provide their expertise and recommendations. The need for DSMB oversight is based on assessment of the study’s overall risk. Investigators may propose a DSMB in their grant application, or NIA may require that a DSMB be established following consideration of review panel’s comments, NIA’s National Advisory Council on Aging (NACA) advice, and/or input from NIA staff.
- Sample Data and Safety Monitoring Board Charter (MS Word, 24K) The DSMB Charter describes the responsibilities of the DSMB to ensure ongoing, independent study review and assure the study is conducted according to the highest scientific and ethical standards.
- DSMB Conflict of Interest and Confidentiality Statement (MS Word, 20K) - All members of the DSMB are required to be independent of the studies being reviewed and need to certify this by signing a DSMB Conflict of Interest and Confidentiality statement.
- DSMB Report - Single Site Open (MS Word, 323K)
- DSMB Report - Single Site Closed (MS Word, 342K)
- DSMB Report - Multi Site Open (MS Word, 449K)
- DSMB Report - Multi Site Closed (MS Word, 348K)
Additional Startup Tools
- Recruitment and Retention Tips (MS Word, 33K) describe approaches to recruitment and retention of older individuals from diverse ethnic and racial groups in clinical research studies.
- Data Management Tips (MS Word, 30K) help to ensure adequate data management processes and procedures in a clinical study. Investigators are encouraged to use Data Management Tips to describe how data will be handled in the study.
- Best Practices for Data Coordinating Centers – This Compendium, developed by the National Heart Lung and Blood Institute (NHLBI) provides helpful tips for clinical researchers and other stakeholders for developing large, multisite clinical trial programs.
Investigators must include in their application proposed adverse event (AE) and serious adverse event (SAE) definitions and discuss their monitoring and reporting. All clinical trials of drugs and biological products conducted under an Investigational New Drug Application (IND) must use definitions of adverse events and adverse reactions and follow the reporting requirements established by 21 Code of Federal Regulations (CFR) Part 312.32. Trials of medical devices conducted under an Investigational Device Exemption (IDE) must use the definitions and reporting requirements established by 21 CFR 812. All other interventional studies must propose their definitions of adverse events and their reporting procedures. See the NIA Guidance on Clinical Trials for additional information .
- Adverse Event Form ( MS Word , 38K or screen-readable PDF , 69K) provides a template for a study form for collecting information about adverse events that is reviewed by safety monitoring bodies.
- Serious Adverse Event Form ( MS Word , 31K or screen-readable PDF , 769K) provides a template for a study form for collecting information about serious adverse events. The form includes major components of the Food and Drug Administration (FDA) Form 3500.
- AE/SAE Process Flow ( MS Word , 79K or screen-readable plain text file , 4K) illustrates how adverse events and serious adverse events are handled within a study.
The NIA Safety Training Course (available below), an online training venue, provides an overview of human subject safety surveillance and reporting requirements in clinical research studies. The intent of the course is to help clinical study investigators and staff understand and implement NIA and regulatory requirements for safe, high quality clinical research. The topics covered include Good Clinical Practice (GCP), Human Subject Protections, Adverse Events and Unanticipated Problems, Safety Monitoring and Reporting Requirements, Safety Monitoring and Oversight: Data and Safety Monitoring Boards (DSMBs) and Safety Officers, Regulatory Requirements and Responsibilities of Principal Investigators, and Data and Safety Monitoring Plans. The course requires about 40 minutes to complete.
Administrative Forms
Site Signature Log - Delegation of Authority Log ( MS Excel, 47K or screen-readable PDF, 294K ) A record of all study personnel and their specific responsibilities, signatures, and dates of involvement during the conduct of a clinical research study.
Note to File Template (MS Word, 20K) - Used by clinical site staff to document protocol deviations or other discrepancies identified during the conduct of the clinical research study and plans for resolution/prevention.
Sample Visit Flow and Schedule (MS Word, 25K) – The visit schedule tracks an individual participant’s progress through the study and helps to ensure that visits take place during the protocol-specified timeframe. The visit flow provides an overview of the activities that take place at each study visit, and may be customized for each study site.
Study Drug/Investigational Product Tracker (MS Excel, 12K) - Used to track study drug/investigational product disposition and accountability by the clinical research site. For multi-site studies under an investigational new drug (IND) application, this tracker could be used by coordinating centers to track the overall distribution of investigational product.
Study Drug/Investigational Product Compliance Log (MS Word, 30K) - Used to track study drug/investigational product disposition and accountability for each individual participant. This form may be used to track protocol adherence via amount dispensed and returned and is designed to be used in conjunction with the Study Drug/Investigational Product Tracker. May also be used to track study drug/investigational return or destruction.
Study-wide Forms
Adverse Events Form ( MS Word, 38K or screen-readable PDF, 68K )
Prior and Concomitant Medications ( MS Word, 34K or screen-readable PDF, 58K )
Protocol Deviations Form ( MS Word, 46K or screen-readable PDF, 80K )
Serious Adverse Events Form ( MS Word, 31K or screen-readable PDF, 769K )
Study Disposition Form ( MS Word, 32K or screen-readable PDF, 56K )
Baseline Visit Forms
Visit Checklist ( MS Word, 34K or screen-readable PDF, 53K )
Eligibility Form ( MS Word, 29K or screen-readable PDF, 184K )
Demographics Form ( MS Word, 32K or screen-readable PDF, 661K )
Medical History Form ( MS Word, 50K or screen-readable PDF, 87K )
Medical History Conventional ( MS Word, 54K or screen-readable PDF,184 K )
Vital Signs Form ( MS Word, 33K or screen-readable PDF, 101K )
Physical Exam Form ( MS Word, 73K or screen-readable PDF, 193K )
Randomization and Enrollment Form ( MS Word, 32K or screen-readable PDF, 806K )
HHS is committed to making its websites and documents accessible to the widest possible audience, including individuals with disabilities. We are in the process of retroactively making some documents accessible. If you need assistance accessing an accessible version of this document, please reach out to the [email protected] .
DISCLAIMER: The contents of this database lack the force and effect of law, except as authorized by law (including Medicare Advantage Rate Announcements and Advance Notices) or as specifically incorporated into a contract. The Department may not cite, use, or rely on any guidance that is not posted on the guidance repository, except to establish historical facts.
- Current Trials We are currently recruiting participants for over 250 active studies. Click here to see if you are eligible.
- The Recruitment Guaranteed Method Discover our unique process that has helped to guarantee recruitment for over 600 studies.
- Articles Discover how to optimize your recruitment with our approachable article library.
Clinical Trial Advertising: Everything You Need to Know in 2021 (with examples)
- Facebook Messenger
Getting the green light to pull the trigger on your clinical trial is worth celebrating. After all, it can take months of back and forth before you receive the go-ahead and even longer to secure enough funding.
But after the excitement wears off, a new worry looms: Clinical trial marketing and participant recruitment.
Clinical trial marketing has changed a lot over the last decade.

With social media platforms like Facebook, Instagram, and YouTube along with online search tools like Google eating up advertising market share, patient recruitment advertising needs to keep pace.
Let’s take a deeper look into how successful research teams are using digital patient recruitment strategies to their advantage and meeting their study recruitment goals.
Table of Contents
Why traditional media isn’t as effective for clinical trial ads
Harnessing mobile technology and social media
Factoring for age and disease type, the “facebook dilemma”: understanding new privacy rules and “app tracking transparency”.
- IRB/Ethics approval is needed for everything
Platform advertising policy and requirement changes
What you really need to think about to successfully recruit patients for your study, the real deal about digital patient recruitment in the 21st century.
Google “How do I advertise on Facebook?” and you’ll get back 1.47 billion results.
Once upon a time, newspapers, radio and television ruled the advertising world. The keys to successful advertising were relatively straightforward and consistent.
The average clinical trial could get away with recruiting patients through traditional means like patient databases and by posting flyers in high traffic areas. Likewise, studies with a budget could run a few newspaper ads, take out a page in a community newsletter or order some radio spots to make up for a recruitment shortfall.
These approaches to a clinical trial advertisement would bring in interested participants, though without any way to predict their eligibility or how consistently they’d show up.
The market share held by traditional media has continued to shrink over the last 10 years and in its place, digital marketing has taken over.

In 2020, spending on online advertising in the United States grew by 12.2% year-over-year despite the pandemic, hitting almost $356 billion dollars . Ad spending for traditional media, meanwhile, has been steadily falling since as early as 2012 .
That’s a significant difference, and it’s estimated that spending on digital advertising will account for $645 billion advertising dollars by 2024.
It should come as no surprise why traditional advertising doesn’t work very well anymore.
Even before COVID-19 restrictions were in place in 2020, people weren’t engaging in the same old mediums anymore. Instead of watching local TV, we spend our time on Netflix, Apple TV, and YouTube.Instead of listening to the radio, we’re listening to podcasts, Spotify and other digital shows. Instead of reading newspapers, we’re now getting the news from our Facebook news feed, Twitter, Reddit or directly from news apps.
With so much change to digital information in such a quick period of time, it can be hard to keep up with what works and what doesn’t. It’s safe to say that digital advertising is here to stay and will continue to eat up market share.
When done correctly, digital advertising can outperform traditional media because of the reach of online platforms and audience targeting features they use.
Fuelled by the adoption of mobile technology like smarphones and tablet PCs, digital media is a regular part of the lives of billions of people around the world.
For example, Facebook boasts over two billion user accounts. (As of 2020 the global population sits at 7.8 billion people.) According to Pew Research , almost 70% of adults in the United States used Facebook in 2019. With a population of 328 million people, this means that close to 230 million Americans are connected to the social media giant.
Aside from the sheer volume of people accessing information online and through social media, these platforms have advanced demographic targeting features available to advertisers that no traditional media source can compete with.
The trick is to use these tools effectively and to understand what kind of information the computer algorithms must be fed in order to get your ad in front of the right people at the right time. Without the understanding of the back-end set up and the way that digital advertising works across each platform, you can easily spend your entire advertising budget and have nothing to show for it.
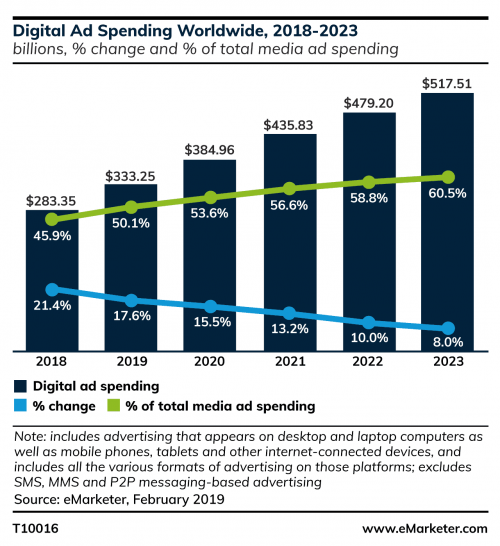
Here’s some good (and maybe surprising) news: The 65+ demographic is the fastest growing group adopting digital technology. Older populations are on social media and many of them have smartphones This target demographic may not be who you immediately assume uses social media, but don’t count someone out because of their age.
In a nutshell, this means digital marketing can be just as effective for older demographics and unique populations because of the reach and advanced targeting features.In fact, these tools could make recruitment easier because of how specific you can design advertisements and the post-click experience for your target population.
In fact, these tools can make recruitment easier because of how specific you can design advertisements and the post-click experience for your target population.
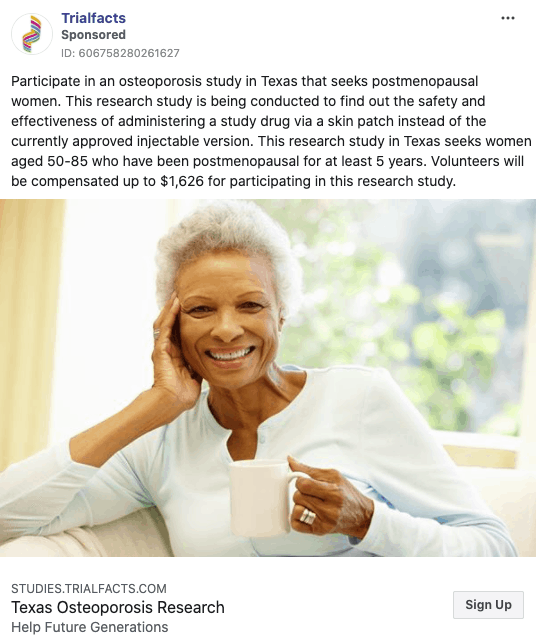
Social media advertising can reach more than just your target audience. In addition to these individuals themselves, patient recruitment ads can be targeted towards partners, caregivers or friends of older individuals or unique populations, who then see the ad and respond on their behalf.
In some disease areas, especially those that can be incredibly isolating, the online world is a lifeline for these patients.
The key to successful recruitment is knowing what platforms and search tools these groups use, and optimizing your advertising to reach them.
Related: Does Social Media Make Sense for My Clinical Trial?
Digital marketing has made advertising more complex than ever.
While running an ad in a newspaper or putting together a radio spot is relatively straightforward, the sheer number of platforms, options, requirements and limitations of each digital marketing method has added a lot of additional complexity that’s often overlooked.
When you think about online advertising options it’s likely that Facebook , Google , and YouTube are the first that come to mind because of their proliferation of the online advertising space. But there are a lot of other options available to savvy marketers to get their message in front of the right audience.
These include platforms and services like Instagram (owned by Facebook), Twitter , Reddit , TikTok , Spotify , podcasts , banner ads and a host of others.

Again, the important thing to remember is to consider where your target participants spend time. If you’re looking to recruit young, healthy individuals as part of a control group, TikTok may be a great place to advertise. However, if you’re looking for older adults who suffer from rheumatoid arthritis, it may not be.
Further complicating things are the specific, nuanced ways that advertisements must be written and designed in order to be effective. For example, image sizes and format requirements for each platform are different. Additionally, you’ll need to consider how your ad is presented – it’s placement and overall goal on the site – and follow the social company’s policies. All these factors impact how your ad will be viewed.
As nice as it would be, there isn’t a “one size fits all” approach that can be used across all platforms.
Related: Beginner’s Guide to Using Facebook Advertising for Patient Recruitment
Before the update even hit iPhone users’ systems, both Facebook and marketers alike were in an uproar about how the iOS 14.5 update would hinder their shared ability to reach target audiences in digital marketing campaigns if they were using an iPhone.
The belief (rightly so) was that when given the option to “opt out” of application tracking, consumers would do just that. It didn’t take long for the numbers to reflect Mark Zuckerberg’s worst fear: Just a few weeks after its release, only 5% of iPhone users opted to allow tracking on their devices .
And it’s not just Apple users – Google announced in mid-2021 that Android phones would also begin limiting some application tracking features . However, their changes will be less challenging for businesses.
As a researcher embarking on a new digital patient recruitment campaign, the implications are clear – you, like anyone else running ads across digital platforms, will have to contend with these new changes.
While it may seem like online clinical trial marketing is a lost cause, that’s far from the truth. In reality, your clinical trial advertisement will still reach the masses, though it make take a little more time to reach the right kind of participants that will fit your eligibility criteria.
At the end of the day, yes, this change in individual user privacy settings may slightly affect your recruitment campaign. However, your overall experience depends greatly on a number of factors, including how well-developed your ad is and whether it speaks to your target participant audience and what kind of campaign you choose to run .
All is not yet lost when it comes to privacy hurdles and digital trial recruitment.
The Ultimate Swipe File For Clinical Trial Recruitment Ads

→ Take a sneak peek at the top ads that are working for clinical trials
→ Discover the underlying marketing principles behind the best-performing clinical trial recruitment ads
→ Learn how to tailor your message for each platform
How do clinical trials advertise to recruit participants?
If the complexity behind designing and publishing online advertisements wasn’t enough for you to think about calling in the experts, it’s entirely possible that the next two points will be all you need. Digital patient recruitment comes with its own set of hurdles.
IRB/Ethics approval is needed for everything. Every. Single. Thing.
The need for IRB/Ethics approval won’t come as a surprise to anyone that’s been involved in a clinical trial before. But the scope and scale of necessary approvals for a digital marketing campaign is enormous.
Many researchers make the mistake of thinking they only need to make one or two ads and have these approved before running them on their platform of choice.
In reality, you must create hundreds of ads in order to test them effectively with online audiences.
Ad testing is a critical step in creating an effective clinical trial marketing campaign and your IRB/Ethics committee must approve every version of each ad – even if it’s a small change to your text.
To make things even more maddening, approval is also required for responses to comments that may be left behind on ads. If an ad generates a strong response with a lot of comments left by users, you’ll find yourself with your hands tied if you want to respond in real time.
What this looks like in reality is having several generic responses that are approved in advance. While it’s a helpful fix, it limits your ability to actively engage with participants in a meaningful way and can cause you a lot of frustration, as social media is supposed to foster discussion.
In the digital marketing industry, it’s no secret that platform specific advertising policies and requirements change all the time. We also know that these specs can change on a whim and that they’re proprietary algorithms, exclusive to each platform that impact what is approved and what is effective.
No one, aside from the company that owns the platform, really knows what words, phrases, and images may be banned at any given time. Changes are often made without any advance notice, so an ad strategy that worked yesterday could suddenly be irrelevant today.
Without the expertise to know what information in your adis the source of a failed campaign, you might find yourself running in circles.

There are many things that go into a successful recruitment campaign that most researchers and trial sponsors don’t realize are important or consider until things aren’t going well.
Consider these 7 points as effective clinical trial marketing guidelines.

It’s about more than writing a great clinical trial ad.
What is trial advertising at its core? Writing an effective clinical trial ad is one of the easy and less time consuming parts of the process.
Instead, you should also be thinking about nuances of each platform, their advertising policies and back-end reporting setup along with audience targeting features, among a host of other factors.
Related: Creating Effective Social Media Posts for Clinical Trial Recruitment
For example, the entire post-click experience – where your ad takes people to after they click – plays an essential role in attracting and retaining qualified patient leads, and is often overlooked by researchers.
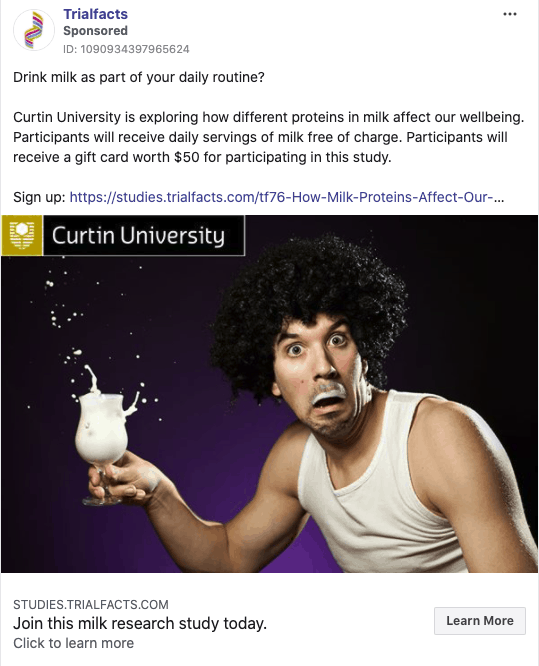
Creation of effective landing pages or websites can make or break you.
Consider your own experience when you click on an ad on social media. You expect to be redirected to a clear, consise webpage. But how do you feel when the opposite happens and you’re taken to a poorly functioning, outdated or unprofessional landing page?
You’re probably not very invested in looking at the rest of the page. It could be unclear text, bad stock images or other elements that immediately turn you off. In many of these cases, you’re likely to give up before even starting to scroll through the content.
Your potential participants are no different.
A good landing page for digital patient recruitmentneeds to strike a balance between being descriptive and detailed without getting bogged down in medical jargon. It also needs to be optimized for mobile browsing and consider the entire user experience.
Another thing to remember is that the people clicking on your ad and finding their way to your landing page don’t know you.
Effective landing pages shape the participant experience and set the tone for your study.
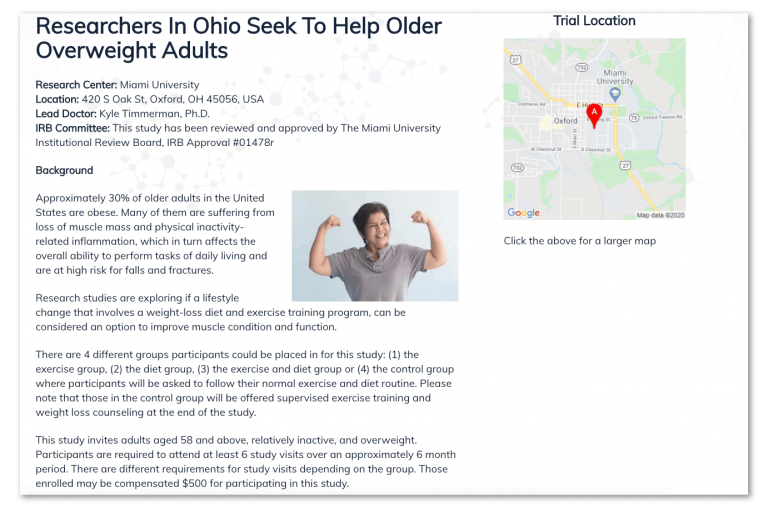
They have no context about your study or why it may be important to them. Without this clearly spelled out right away, they’re likely to leave the page.
It’s your job to talk about the potential benefits of participating without going overboard and staying within the principles of GCP and the content that has been approved by your IRB/Ethics committee.
Think of your landing page as a profile page on social media or a dating app. What you convey on your landing page is the first step in building trust and rapport with a potential participant and you don’t want to ruin your first impression.
Proper back-end set up is a key to success.
There are many back-end considerations that go into running a clinical trial marketing campaign. As a researcher, it’s not part of your day-to-day job and you don’t really need to know in the grand scheme of your work.

These include things like having the expertise to know how computer algorithms operate and the type of information they need to properly distribute your ad. It also includes having the proper reporting infrastructure in place to measure the cost per enrollment of each participant.
Sure, it might look nice to have 1,000 people “like” your ad on Facebook. But if none of them have signed up for your study, you really have nothing to show for your efforts (or your diminishing ad budget).
A lot of the measurements and data to which you have access – things like cost per click, cost per thousand impressions, click through rate, and cost per conversion – are relatively meaningless to clinical trial recruitment.
For example, there are many situations where an ad might have low engagement rates but is highly successful in converting potential recruits into enrolled participants.
What matters is cost per enrolled participant into your study and the rate of participants flowing through your funnel. Anything else is an interim measure which can help indicate how things are going, but they’re nowhere near as important.
Without ongoing measurement and review of your data, you’re flying blind and hoping that whatever you’re doing sticks.
Platform-specific advertising policies and requirements are hard to navigate.
You can be forgiven for thinking that if your advertisement has been approved by your IRB/Ethics committee that it will be approved by your chosen platform. However, this isn’t always the case.
The rules around word count, image size, banned or inappropriate language/terminology, and even how ads are reviewed prior to posting are also all fair game.
If you take a closer look at the screenshot below, you’ll see there are specific policies related to prohibited and restricted content, video ads, targeting, positioning, and the use of text in ad images.
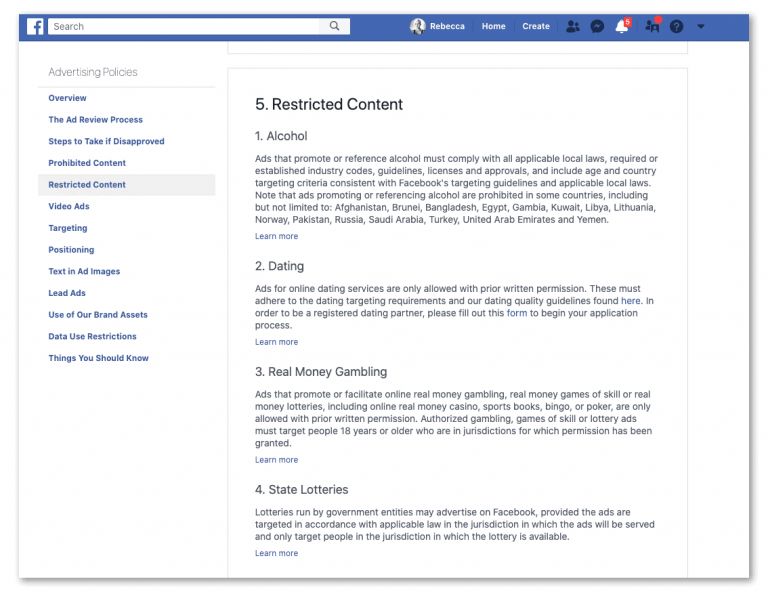
Facebook, in particular, has pages of advertising policies to sift through. Without the background expertise to navigate this potential minefield, you’re likely to find yourself frustrated with lackluster results from your online advertising efforts.
You’ll also not understand why your ads are being rejected or underperforming.
Online prescreening can save you time and money.
As you’ve probably already seen with other parts of digital marketing and online patient recruitment, when something is done properly it can save you a lot of hassle…
…and online prescreening is no different.
Imagine the ease of having an interested patient immediately directed from your study landing page to an online prescreening survey. From here, their eligibility can be determined in as short as 5-10 minutes without your staff having to lift a finger.
Potential participants can complete screening from their desk or smartphone when it works for them. You can weed out ineligible patients and quickly move those who do qualify along your pipeline to the next step.
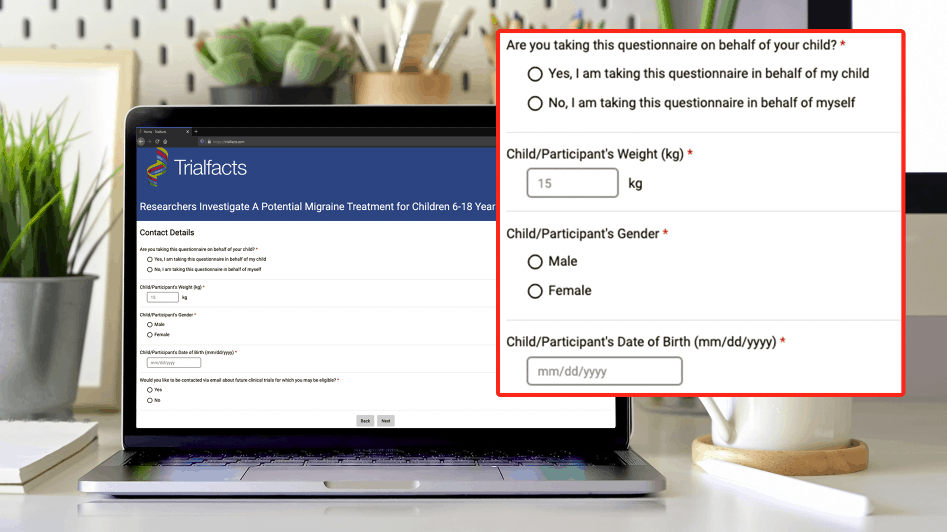
This has the potential to save you countless hours and dollars from your budget. With an eye to the patient experience from start to finish, a properly executed prescreening process can help set expectations for the rest of your enrollment process.
A well designed and executed screening process will let your participants know that they’re in good hands.
Ignoring the behind-the-scenes targeting of your advertisements will lead to recruitment failure.
Online digital advertising platforms will happily take your money and share your ad to the masses, but this is a surefire way to fail to meet your recruitment goals.
There is considerable expertise that goes into developing and executing a strategy that gets your ad in front of the right audience. Not only is demographic and socioeconomic data important, but also understanding the online habits of your ideal participant is essential. This can be anything from the type of websites they visit to the amount of time they spend on their mobile devices.
You can also think about their social media browsing habits and even specific likes and dislikes.
The more complete picture you can pull together of your ideal participant, the better designed your clinical trial marketing campaign can be.
Without giving the details extra thought or even consideration, you’re setting your campaign up for what is likely to be a disappointment.
Interpreting analytical data and campaign optimization is ongoing.
Digital marketing is driven by analytical data that can and should be used for constant and ongoing refinement of your campaign.
But there’s a catch.
What we see and equate with success are often referred to as “ vanity metrics .” These are things like engagement – the number of likes, clicks, and shares – that a particular advertisement gets.
What most people don’t realize is that a post can get a lot of engagement, but it translates into few people actually following through with sign-up.
Focus on the metrics that matter, like the number of questionnaires passed.
The important numbers are related to actual conversions of interested patients into enrolled participants. It’s these data sets that need to be reviewed daily and used to adjust campaigns accordingly.
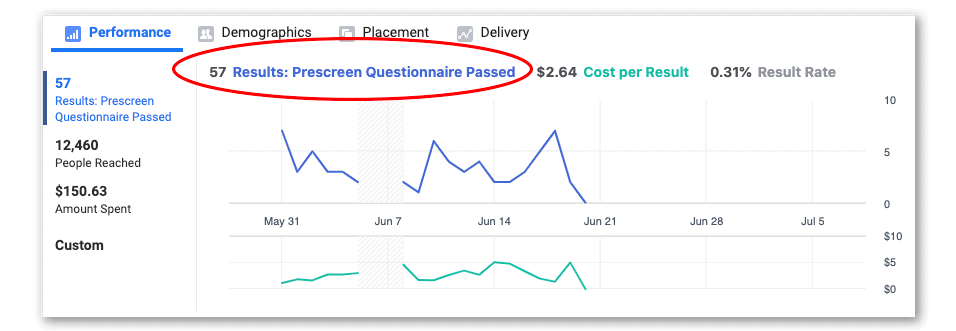
Unfortunately, with digital patient recruitment advertising, there is no “set it and forget it” strategy that’s going to get you the results you’re after.
If you fail to have the right reporting infrastructure in place that includes regular data review and reporting, you’re likely to be wasting your money.
There is a small chance that you could do the recruitment yourself and it might go well, it might not cost you too much, and it might all work out… What’s much more likely is that you’ll start recruitment and it won’t just immediately work and you won’t know what to do next.
There’s no doubt that clinical trial recruitment has become more complex than ever as digital marketing and social media platforms outpace and outperform traditional patient recruitment advertising methods.
However, with a little bit of advanced planning and knowing when to get external help from the experts, you can launch your study recruitment with relative ease.

Which Social Media Platform Should I Use to Recruit for My Clinical Trial?

Does Social Media Recruitment Make Sense for My Clinical Trial?

Beginner’s Guide to Using Facebook Advertising for Patient Recruitment
Get a free, no obligation recruitment plan:.
We’ll undergo our due diligence process and determine how many patients we can provide for your study (guaranteed).
CTA Get Your Free Recruitment Plan
Together we are beating cancer
About cancer
Cancer types
- Breast cancer
- Bowel cancer
- Lung cancer
- Prostate cancer
Cancers in general
- Clinical trials
Causes of cancer
Coping with cancer
- Managing symptoms and side effects
- Mental health and cancer
- Money and travel
- Death and dying
- Cancer Chat forum
Health Professionals
- Cancer Statistics
- Cancer Screening
- Learning and Support
- NICE suspected cancer referral guidelines
Get involved
- Make a donation
By cancer type
- Leave a legacy gift
- Donate in Memory
Find an event
- Race for Life
- Charity runs
- Charity walks
- Search events
- Relay For Life
- Volunteer in our shops
- Help at an event
- Help us raise money
- Campaign for us
Do your own fundraising
- Fundraising ideas
- Get a fundraising pack
- Return fundraising money
- Fundraise by cancer type
- Set up a Cancer Research UK Giving Page
- Find a shop or superstore
- Become a partner
- Cancer Research UK for Children & Young People
- Our We Are campaign
Our research
- Brain tumours
- Skin cancer
- All cancer types
By cancer topic
- New treatments
- Cancer biology
- Cancer drugs
- All cancer subjects
- All locations
By Researcher
- Professor Duncan Baird
- Professor Fran Balkwill
- Professor Andrew Biankin
- See all researchers
- Our achievements timeline
- Our research strategy
- Involving animals in research
Funding for researchers
Research opportunities
- For discovery researchers
- For clinical researchers
- For population researchers
- In drug discovery & development
- In early detection & diagnosis
- For students & postdocs
Our funding schemes
- Career Development Fellowship
- Discovery Programme Awards
- Clinical Trial Award
- Biology to Prevention Award
- View all schemes and deadlines
Applying for funding
- Start your application online
- How to make a successful application
- Funding committees
- Successful applicant case studies
How we deliver research
- Our research infrastructure
- Events and conferences
- Our research partnerships
- Facts & figures about our funding
- Develop your research career
- Recently funded awards
- Manage your research grant
- Notify us of new publications
Find a shop
- Volunteer in a shop
- Donate goods to a shop
- Our superstores
Shop online
- Wedding favours
- Cancer Care
- Flower Shop
Our eBay store
- Shoes and boots
- Bags and purses
- We beat cancer
- We fundraise
- We develop policy
- Our global role
Our organisation
- Our strategy
- Our Trustees
- CEO and Executive Board
- How we spend your money
- Early careers
Cancer news
- Cancer News
- For Researchers
- For Supporters
- Press office
- Publications
- Update your contact preferences
ABOUT CANCER
GET INVOLVED
NEWS & RESOURCES
FUNDING & RESEARCH
You are here

A study using a blood sample to diagnose cancer (PREVAILctDNA)
Cancer type:.

It was open to people with a number of different cancer types. It is now open to people with a coupe of cancer types. To find out which cancer types these are look in 'who can enter’.
More about this trial
- gastroscopy
- bronchoscopy
- colonoscopy
- cystoscopy
Taking the biopsy this way increases the likelihood that body fluids from these openings can spray out as fine droplets. For example saliva from the mouth when you have the procedure. This is a natural and uncontrollable reflex. And sometimes this can be a concern. For example during the COVID-19 pandemic.
It may also be that some cancers are in a position in the body that makes it very difficult to get a biopsy.
So researchers are looking for a way to diagnose cancer without having to do these procedures.
They will try to find this out by taking blood samples and testing them for ctDNA. The team will compare the results of the ctDNA test with the standard tests and scans you have.
This study is in 2 parts. In the 1st part the team will look at using ctDNA in the everyone who takes part. In the 2nd part the team will look at whether ctDNA can help with the diagnosis and treatment for pancreatic and bile duct cancer.
The aims of part 1 of the study are to find out:
- the number of people that ctDNA shows up in people who might have cancer
- whether ctDNA can help diagnose cancer
The aims of part 2 of the study are to find out whether ctDNA can help to:
- diagnose and treat suspected pancreatic cancer and bile duct cancer
- improve the waiting times for people with pancreatic cancer and bile duct cancer
Who can enter
The following bullet points are a summary of the entry conditions for this study. Talk to your doctor or the study team if you are unsure about any of these. They will be able to advise you.
Who can take part
For part 1 You may be able to join part 1 of the study if you have had a tissue sample taken (biopsy). And you are waiting for a diagnosis of one of the following:
- bowel cancer that has spread to a new area of the body (metastatic)
- gastrointestinal stromal tumours (GIST)
You might be able to join if you have a diagnosis of one of the following cancers. And you are waiting for a gene test result or there wasn’t enough of the tissue sample taken to do a gene test. The cancers are:
- bowel cancer that has spread
For part 2 You may be able to join part 2 of the study if you have pancreatic cancer or bile duct cancer and all the following apply.
- You are in the ACCESS implementation programme. Your doctor will know this.
- The Guardant360 test detected ctDNA. Your doctor will know this.
- The ctDNA is consistent or diagnostic with a diagnosis of pancreatic cancer or bile duct cancer. Your doctor will know this.
For both parts Both of following must apply. You:
- are well enough to have treatment
- are at least 18 years old
Who can’t take part
Trial design
The team need 144 people to join part 1. And 150 people to join part 2.
You have the standard tests and scans to diagnose your cancer.
You give blood samples for the study. The team take all the samples they need at one time. They use the samples to look for small pieces of cancer DNA (ctDNA) in the blood.
Your doctor will get the results of the ctDNA. They will discuss them with you.
If you have surgery or a tissue sample (biopsy) taken the team will look in your medical records for the results. They want to see if those results match the ctDNA results.
You stay in the study until you have a treatment plan. You and your doctor decide your treatment plan.
Hospital visits
There are no extra hospital visits in this study.
Side effects
There is a small risk that the results of the ctDNA test are not accurate. You will have the standard tests and scans to help with diagnosing whether you have cancer or not.
Recruitment start:
Recruitment end:.
- How to join a clinical trial
Please note: In order to join a trial you will need to discuss it with your doctor, unless otherwise specified.
Chief Investigator
Dr Naureen Starling
Supported by
The Royal Marsden NHS Foundation Trust
If you have questions about the trial please contact our cancer information nurses
Freephone 0808 800 4040
Last review date
Cruk internal database number:, around 1 in 5 people take part in clinical trials.

Around 1 in 5 people diagnosed with cancer in the UK take part in a clinical trial.
Last reviewed:
- What clinical trials are
- How to find a clinical trial
- What you should be told about a clinical trial
- How clinical trials are planned and organised
- Clinical trial results
- What to ask your doctor about clinical trials
- Clinical trial organisations

Rate this page:

- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Quantifying possible...
Quantifying possible bias in clinical and epidemiological studies with quantitative bias analysis: common approaches and limitations
- Related content
- Peer review
- Jeremy P Brown , doctoral researcher 1 ,
- Jacob N Hunnicutt , director 2 ,
- M Sanni Ali , assistant professor 1 ,
- Krishnan Bhaskaran , professor 1 ,
- Ashley Cole , director 3 ,
- Sinead M Langan , professor 1 ,
- Dorothea Nitsch , professor 1 ,
- Christopher T Rentsch , associate professor 1 ,
- Nicholas W Galwey , statistics leader 4 ,
- Kevin Wing , assistant professor 1 ,
- Ian J Douglas , professor 1
- 1 Department of Non-Communicable Disease Epidemiology, London School of Hygiene and Tropical Medicine, London, UK
- 2 Epidemiology, Value Evidence and Outcomes, R&D Global Medical, GSK, Collegeville, PA, USA
- 3 Real World Analytics, Value Evidence and Outcomes, R&D Global Medical, GSK, Collegeville, PA, USA
- 4 R&D, GSK Medicines Research Centre, GSK, Stevenage, UK
- Correspondence to: J P Brown jeremy.brown{at}lshtm.ac.uk (or @jeremy_pbrown on X)
- Accepted 12 February 2024
Bias in epidemiological studies can adversely affect the validity of study findings. Sensitivity analyses, known as quantitative bias analyses, are available to quantify potential residual bias arising from measurement error, confounding, and selection into the study. Effective application of these methods benefits from the input of multiple parties including clinicians, epidemiologists, and statisticians. This article provides an overview of a few common methods to facilitate both the use of these methods and critical interpretation of applications in the published literature. Examples are given to describe and illustrate methods of quantitative bias analysis. This article also outlines considerations to be made when choosing between methods and discusses the limitations of quantitative bias analysis.
Bias in epidemiological studies is a major concern. Biased studies have the potential to mislead, and as a result to negatively affect clinical practice and public health. The potential for residual systematic error due to measurement bias, confounding, or selection bias is often acknowledged in publications but is seldom quantified. 1 Therefore, for many studies it is difficult to judge the extent to which residual bias could affect study findings, and how confident we should be about their conclusions. Increasingly large datasets with millions of patients are available for research, such as insurance claims data and electronic health records. With increasing dataset size, random error decreases but bias remains, potentially leading to incorrect conclusions.
Sensitivity analyses to quantify potential residual bias are available. 2 3 4 5 6 7 However, use of these methods is limited. Effective use typically requires input from multiple parties (including clinicians, epidemiologists, and statisticians) to bring together clinical and domain area knowledge, epidemiological expertise, and a statistical understanding of the methods. Improved awareness of these methods and their pitfalls will enable more frequent and effective implementation, as well as critical interpretation of their application in the medical literature.
In this article, we aim to provide an accessible introduction, description, and demonstration of three common approaches of quantitative bias analysis, and to describe their potential limitations. We briefly review bias in epidemiological studies due to measurement error, confounding, and selection. We then introduce quantitative bias analyses, methods to quantify the potential impact of residual bias (ie, bias that has not been accounted for through study design or statistical analysis). Finally, we discuss limitations and pitfalls in the application and interpretation of these methods.
Summary points
Quantitative bias analysis methods allow investigators to quantify potential residual bias and to objectively assess the sensitivity of study findings to this potential bias
Bias formulas, bounding methods, and probabilistic bias analysis can be used to assess sensitivity of results to potential residual bias; each of these approaches has strengths and limitations
Quantitative bias analysis relies on assumptions about bias parameters (eg, the strength of association between unmeasured confounder and outcome), which can be informed by substudies, secondary studies, the literature, or expert opinion
When applying, interpreting, and reporting quantitative bias analysis, it is important to transparently report assumptions, to consider multiple biases if relevant, and to account for random error
Types of bias
All clinical studies, both interventional and non-interventional, are potentially vulnerable to bias. Bias is ideally prevented or minimised through careful study design and the choice of appropriate statistical methods. In non-interventional studies, three major biases that can affect findings are measurement bias (also known as information bias) due to measurement error (referred to as misclassification for categorical variables), confounding, and selection bias.
Misclassification occurs when one or more categorical variables (such as the exposure, outcome, or covariates) are mismeasured or misreported. 8 Continuous variables might also be mismeasured leading to measurement error. As one example, misclassification occurs in some studies of alcohol consumption owing to misreporting by study participants of their alcohol intake. 9 10 As another example, studies using electronic health records or insurance claims data could have outcome misclassification if the outcome is not always reported to, or recorded by, the individual’s healthcare professional. 11 Measurement error is said to be differential when the probability of error depends on another variable (eg, differential participant recall of exposure status depending on the outcome). Errors in measurement of multiple variables could be dependent (ie, associated with each other), particularly when data are collected from one source (eg, electronic health records). Measurement error can lead to biased study findings in both descriptive and aetiological (ie, cause-effect) non-interventional studies. 12
Confounding arises in aetiological studies when the association between exposure and outcome is not solely due to the causal effect of the exposure, but rather is partly or wholly due to one or more other causes of the outcome associated with the exposure. For example, researchers have found that greater adherence to statins is associated with a reduction in motor vehicle accidents and an increase in the use of screening services. 13 However, this association is almost certainly not due to a causal effect of statins on these outcomes, but more probably because attitudes to precaution and risk that are associated with these outcomes are also associated with adherence to statins.
Selection bias occurs when non-random selection of people or person time into the study results in systematic differences between results obtained in the study population and results that would have been obtained in the population of interest. 14 15 This bias can be due to selection at study entry or due to differential loss to follow-up. For example, in a cohort study where the patients selected are those admitted to hospital in respiratory distress, covid-19 and chronic obstructive pulmonary disease might be negatively associated, even if there was no association in the overall population, because if you do not have one condition it is more likely you have the other condition in order to be admitted. 16 Selection bias can affect both descriptive and aetiological non-interventional studies.
Handling bias in practice
All three biases should ideally be minimised through study design and analysis. For example, misclassification can be reduced by the use of a more accurate measure, confounding through measurement of all relevant potential confounders and their subsequent adjustment, and selection bias through appropriate sampling from the population of interest and accounting for loss to follow-up. Other biases should also be considered, for example, immortal time bias through the appropriate choice of time zero, and sparse data bias through collection of a sample of sufficient size or by the use of penalised estimation. 17 18
Even with the best available study design and most appropriate statistical analysis, we typically cannot guarantee that residual bias will be absent. For instance, it is often not possible to perfectly measure all required variables, or it might be either impossible or impractical to collect or obtain data on every possible potential confounder. For instance, studies conducted using data collected for non-research purposes, such as insurance claims and electronic health records, are often limited to the variables previously recorded. Randomly sampling from the population of interest might also not be practically feasible, especially if individuals are not willing to participate.
To ignore potential residual biases can lead to misleading results and erroneous conclusions. Often the potential for residual bias is acknowledged qualitatively in the discussion, but these qualitative arguments are typically subjective and often downplay the impact of any bias. Heuristics are frequently relied on, but these can lead to an misestimation of the potential for residual bias. 19 Quantitative bias analysis allows both authors and readers to assess robustness of study findings to potential residual bias rigorously and quantitatively.
Quantitative bias analysis
When designing or appraising a study, several key questions related to bias should be considered ( box 1 ). 20 If, on the basis of the answers to these questions, there is potential for residual bias(es), then quantitative bias analysis methods can be considered to estimate the robustness of findings.
Key questions related to bias when designing and appraising non-interventional studies
Misclassification and measurement error: Are the exposure, outcome, and covariates likely to be measured and recorded accurately?
Confounding: Are there potential causes of the outcome, or proxies for these causes, which might differ in prevalence between exposure groups? Are these potential confounders measured and controlled through study design or analysis?
Selection bias: What is the target population? Are individuals in the study representative of this target population?
Many methods for quantitative bias analysis exist, although only a few of these are regularly applied in practice. In this article, we will introduce three straightforward, commonly applied, and general approaches 1 : bias formulas, bounding methods, and probabilistic bias analysis. Alternative methods are also available, including methods for bias adjustment of linear regression with a continuous outcome. 7 21 22 Methods for dealing with misclassification of categorical variables are outlined in this article. Corresponding methods for sensitivity analysis to deal with mismeasurement of continuous variables are available and are described in depth in the literature. 23 24
Bias formulas
We can use simple mathematical formulas to estimate the bias in a study and to estimate what the results would be in the absence of that bias. 4 25 26 27 28 Commonly applied formulas, along with details of available software to implement methods listed, are provided in the appendices. Some of these methods can be applied to the summary results (eg, risk ratio), whereas other methods require access to 2×2 tables or participant level data.
These formulas require us to specify additional information, typically not obtainable from the study data itself, in the form of bias parameters. Values for these parameters quantify the extent of bias present due to confounding, misclassification, or selection.
Bias formulas for unmeasured confounding generally require us to specify the following bias parameters: prevalence of the unmeasured confounder in the unexposed individuals, prevalence of the unmeasured confounder in the exposed individuals (or alternatively the association between exposure and unmeasured confounder), and the association between unmeasured confounder and outcome. 4 28 29
These bias formulas can be applied to the summary results (eg, risk ratios, odds ratios, risk differences, hazard ratios) and to 2×2 tables, and they produce corrected results assuming the specified bias parameters are correct. Generally, the exact bias parameters are unknown so a range of parameters can be entered into the formula, producing a range of possible bias adjusted results under more or less extreme confounding scenarios.
Bias formulas for misclassification work in a similar way, but typically require us to specify positive predictive value and negative predictive value (or sensitivity and specificity) of classification, stratified by exposure or outcome. These formulas typically require study data in the form of 2×2 tables. 7 30
Bias formulas for selection bias are applicable to the summary results (eg, risk ratios, odds ratios) or to 2×2 tables, and normally require us to specify probabilities of selection into the study for different levels of exposure and outcome. 25 When participant level data are available, a general method of bias analysis is to weight each individual by the inverse of their probability of selection. 31 Box 2 describes an example of the application of bias formulas for selection bias.
Application of bias formulas for selection bias
In a cohort study of pregnant women investigating the association between lithium use (relative to non-use) and cardiac malformations in liveborn infants, the observed covariate adjusted risk ratio was 1.65 (95% confidence interval 1.02 to 2.68). 32 Only liveborn infants were selected into the study; therefore, there was potential for selection bias if differences in the termination probabilities of fetuses with cardiac malformations existed between exposure groups.
Because the outcome is rare, the odds ratio approximates the risk ratio, and we can apply a bias formula for the odds ratio to the risk ratio. The bias parameters are selection probabilities for the unexposed group with outcome S 01 , exposed group with outcome S 11 , unexposed group without outcome S 00 , and exposed group without outcome S 10 :
OR BiasAdj = OR Obs × ((S 01 ×S 10 ) ÷ (S 00 ×S 11 ))
(Where OR BiasAdj is the bias adjusted odds ratio and OR Obs is the observed odds ratio.)
For example, if we assume that the probability of terminations is 30% among the unexposed group (ie, pregnancies with no lithium dispensation in first trimester or three months earlier) with malformations, 35% among the exposed group (ie, pregnancies with lithium dispensation in first trimester) with malformations, 20% among the unexposed group without malformations, and 25% among the exposed group without malformations, then the bias adjusted odds ratio is 1.67.
OR BiasAdj = 1.65 × ((0.7×0.75) ÷ (0.65×0.8)) = 1.67
In the study, a range of selection probabilities (stratified by exposure and outcome status) were specified, informed by the literature. Depending on assumed selection probabilities, the bias adjusted estimates of the risk ratio ranged from 1.65 to 1.80 ( fig 1 ), indicating that the estimate was robust to this selection bias under given assumptions.

Bias adjusted risk ratio for different assumed selection probabilities in cohort study investigating association between lithium use (relative to non-use) and cardiac malformations in liveborn infants. Redrawn and adapted from reference 32 with permission from Massachusetts Medical Society. Selection probability of the unexposed group without cardiac malformations was assumed to be 0.8 (ie, 20% probability of termination). Selection probabilities in the exposed group were defined relative to the unexposed group by outcome status (ie, −0%, −5%, and −10%)
- Download figure
- Open in new tab
- Download powerpoint
It is possible to incorporate measured covariates in these formulas, but specification then generally becomes more difficult because we typically have to specify bias parameters (such as the prevalence of the unmeasured confounder) within stratums of measured covariates.
Although we might not be able to estimate these unknowns from the main study itself, we can specify plausible ranges based on the published literature, clinical knowledge, or a secondary study or substudy. Secondary studies or substudies, in which additional information from a subset of study participants or from a representative external group are collected, are particularly valuable because they are more likely to accurately capture unknown values. 33 However, depending on the particular situation, they could be infeasible for a given study owing to data access limitations and resource constraints.
The published literature can be informative if there are relevant published studies and the study populations in the published studies are sufficiently similar to the population under investigation. Subjective judgments of plausible values for unknowns are vulnerable to the viewpoint of the investigator, and as a result might not accurately reflect the true unknown values. The validity of quantitative bias analysis depends critically on the validity of the assumed values. When implementing quantitative bias analysis, or appraising quantitative bias analysis in a published study, study investigators should question the choices made for these unknowns, and report these choices with transparency.
Bounding methods
Bounding methods are mathematical formulas, similar to bias formulas, that we can apply to study results to quantify sensitivity to bias due to confounding, selection, and misclassification. 5 34 35 36 However, unlike bias formulas, they require only a subset of the unknown values to be specified. While this requirement seems advantageous, one important disadvantage is that bounding methods generate a bound on the maximum possible bias, rather than an estimate of the association adjusted for bias. When values for all unknown parameters (eg, prevalence of an unmeasured confounder) can be specified and there is reasonable confidence in their validity, bias formulas or probabilistic bias analysis can generally be applied and can provide more information than bounding methods. 37
One commonly used bounding method for unmeasured confounding is the E-value. 5 35 By using E-value formulas, study investigators can calculate a bound on the bias adjusted estimate by specifying the association (eg, risk ratio) between exposure and unmeasured confounder and between unmeasured confounder and outcome, while leaving the prevalence of the unmeasured confounder unspecified. The E-value itself is the minimum value on the risk ratio scale that the association between exposure and unmeasured confounder or the association between unmeasured confounder and outcome must exceed to potentially reduce the bias adjusted findings to the null (or alternatively to some specified value, such as a protective risk ratio of 0.8). If the plausible strength of association between the unmeasured confounder and both exposure and outcome is smaller than the E-value, then that one confounder could not fully explain the observed association, providing support to the study findings. If the strength of association between the unmeasured confounder and either exposure or outcome is plausibly larger than the E-value, then we can only conclude that residual confounding might explain the observed association, but it is not possible to say whether such confounding is in truth sufficient, because we have not specified the prevalence of the unmeasured confounder. Box 3 illustrates the use of bounding methods for unmeasured confounding. Although popular, the application of E-values has been criticised, because these values have been commonly misinterpreted and have been used frequently without careful consideration of a specific unmeasured confounder or the possibility of multiple unmeasured confounders or other biases. 38
Application of bounding methods
In a cohort study investigating the association between use of proton pump inhibitors (relative to H2 receptor antagonists) and all cause mortality, investigators found evidence that individuals prescribed proton pump inhibitors were at higher risk of death after adjusting for several measured covariates including age, sex, and comorbidities (covariate adjusted hazard ratio 1.38, 95% confidence interval (CI) 1.33 to 1.44). 39 However, unmeasured differences in frailty between users of H2 receptor antagonists and users of proton pump inhibitors could bias findings. Because the prevalence of the unmeasured confounder in the different exposure groups was unclear, the E-value was calculated. Because the outcome was rare at the end of follow-up, and therefore the risk ratio approximates the hazard ratio given proportional hazards, 40 the E-value formula, which applies to the risk ratio, was applied to the hazard ratio.
E-value = RR Obs + √(RR Obs ×(RR Obs −1))
= 1.38 + √(1.38×(1.38−1))
(Where RR Obs is the observed risk ratio.)
The E-value for the point estimate of the adjusted hazard (1.38) was 2.10. Hence either the adjusted risk ratio between exposure and unmeasured confounder, or the adjusted risk ratio between unmeasured confounder and outcome, must be greater than 2.10 to potentially explain the observed association of 1.38. The E-value can be applied to the bounds of the CI to account for random error. The calculated E-value for the lower bound of the 95% CI (ie, covariate adjusted hazard ratio=1.33) was 1.99. We can plot a curve to show the values of risk ratios necessary to potentially reduce the observed association, as estimated by the point estimate and the lower bound of the CI, to the null ( fig 2 ). An unmeasured confounder with strengths of associations below the blue line could not fully explain the point estimate, and below the yellow line could not fully explain the lower bound of the confidence interval.

E-value plot for unmeasured confounding of association between use of proton pump inhibitors and all cause mortality. Curves show the values of risk ratios necessary to potentially reduce the observed association, as estimated by the point estimate and the lower bound of the confidence interval, to the null
Given risk ratios of >2 observed in the literature between frailty and mortality, unmeasured confounding could not be ruled out as a possible explanation for observed findings. However, given that we used a bounding method, and did not specify unmeasured confounder prevalence, we could not say with certainty whether such confounding was likely to explain the observed result. Additional unmeasured or partially measured confounders might have also contributed to the observed association.
Probabilistic bias analysis
Probabilistic bias analysis takes a different approach to handling uncertainty around the unknown values. Rather than specifying one value or a range of values for an unknown, a probability distribution (eg, a normal distribution) is specified for each of the unknown quantities. This distribution represents the uncertainty about the unknown values, and values are sampled repeatedly from this distribution before applying bias formulas using the sampled values. This approach can be applied to either summary or participant level data. The result is a distribution of bias adjusted estimates. Resampling should be performed a sufficient number of times (eg, 10 000 times), although this requirement can become computationally burdensome when performing corrections at the patient record level. 41
Probabilistic bias analysis can readily handle many unknowns, which makes it particularly useful for handling multiple biases simultaneously. 42 However, it can be difficult to specify a realistic distribution if little information on the unknowns is available from published studies or from additional data collection. Commonly chosen distributions include uniform, trapezoidal, triangular, beta, normal, and log-normal distributions. 7 Sensitivity analyses can be conducted by varying the distribution and assessing the sensitivity of findings to distribution chosen. When performing corrections at the patient record level, analytical methods such as regression can be applied after correction to adjust associations for measured covariates. 43 Box 4 gives an example of probabilistic bias analysis for misclassification.
Application of probabilistic bias analysis
In a cohort study of pregnant women conducted in insurance claims data, the observed covariate adjusted risk ratio for the association between antidepressant use and congenital cardiac defects among women with depression was 1.02 (95% confidence interval 0.90 to 1.15). 44
Some misclassification of the outcome, congenital cardiac defects, was expected, and therefore probabilistic bias analysis was conducted. A validation study was conducted to assess the accuracy of classification. In this validation study, full medical records were obtained and used to verify diagnoses for a subset of pregnancies with congenital cardiac defects recorded in the insurance claims data. Based on positive predictive values estimated in this validation study, triangular distributions of plausible values for sensitivity ( fig 3 ) and of specificity of outcome classification were specified and were used for probabilistic bias analysis.

Specified distribution of values for sensitivity of outcome ascertainment
Values were sampled at random 1000 times from these distributions and were used to calculate a distribution of bias adjusted estimates incorporating random error. The median bias adjusted estimate was 1.06, and the 95% simulation interval was 0.92 to 1.22. 44 This finding indicates that under the given assumptions, the results were robust to outcome misclassification, because the bias adjusted results were similar to the initial estimates. Both sets of estimates suggested no evidence of association between antidepressant use and congenital cardiac defects.
Pitfalls of methods
Incorrect assumptions.
Study investigators and readers of published research should be aware that the outputs of quantitative bias analyses are only as good as the assumptions made. These assumptions include both assumptions about the values chosen for the bias parameters ( table 1 ), and assumptions inherent to the methods. For example, applying the E-value formula directly to a hazard ratio rather than a risk ratio is an approximation, and only a good approximation when the outcome is rare. 45
Common bias parameters for bias formulas and probabilistic bias analysis
- View inline
Simplifying assumptions are required by many methods of quantitative bias analysis. For example, it is often assumed that the exposure does not modify the unmeasured confounder-outcome association. 4 If these assumptions are not met then the findings of quantitative bias analysis might be inaccurate.
Ideally, assumptions would be based on supplemental data collected in a subset of the study population (eg, internal validation studies to estimate predictive values of misclassification) or, in the case of selection bias, in the source population from which the sample was selected, but additional data collection is not always feasible. 7 Validation studies can be an important source of evidence on misclassification, although proper design is important to obtain valid estimates. 33
Multiple biases
If the results are robust to one source of bias, it is a mistake to assume that they must necessarily reflect the causal effect. Depending on the particular study, multiple residual biases could exist, and jointly quantifying the impact of all of these biases is necessary to properly assess robustness of results. 34 Bias formulas and probabilistic bias analyses can be applied for multiple biases, but specification is more complicated, and the biases should typically be accounted for in the reverse order from which they arise (appendices 2 and 3 show an applied example). 7 46 47 Bounding methods are available for multiple biases. 34
Prespecification
Prespecification of quantitative bias analysis in the study protocol is valuable so that choice of unknown values and choice to report bias analysis is not influenced by whether the results of bias analysis are in line with the investigators expectations. Clearly a large range of analyses is possible, although we would encourage judicious application of these methods to deal with biases judged to be of specific importance given the limitations of the specific study being conducted.
Accounting for random and systematic error
Both systematic errors, such as bias due to misclassification and random error due to sampling, affect study results. To accurately reflect this issue, quantitative bias analysis should jointly account for random error as well as systematic bias. 48 Bias formulas, bounding methods, and probabilistic bias analysis approaches can be adapted to account for random error (appendix 1).
Deficiencies in the reporting of quantitative bias analysis have been previously noted. 1 48 49 50 When reporting quantitative bias analysis, study investigators should state:
The method used and how it has been implemented
Details of the residual bias anticipated (eg, which specific potential confounder was unmeasured)
Any estimates for unknown values that have been used, with justification for the chosen values or distribution for these unknowns
Which simplifying assumptions (if any) have been made
Quantitative bias analysis is a valuable addition to a study, but as with any aspect of a study, should be interpreted critically and reported in sufficient detail to allow for critical interpretation.
Alternative methods
Commonly applied and broadly applicable methods have been described in this article. Other methods are available and include modified likelihood and predictive value weighting with regression analyses, 51 52 53 propensity score calibration using validation data, 54 55 multiple imputation using validation data, 56 methods for matched studies, 3 and bayesian bias analysis if a fully bayesian approach is desired. 57 58
Conclusions
Quantitative bias methods provide a means to quantitatively and rigorously assess the potential for residual bias in non-interventional studies. Increasing the appropriate use, understanding, and reporting of these methods has the potential to improve the robustness of clinical epidemiological research and reduce the likelihood of erroneous conclusions.
Contributors: This article is the product of a working group on quantitative bias analysis between the London School of Hygiene and Tropical Medicine and GSK. An iterative process of online workshops and email correspondence was used to decide by consensus the content of the manuscript. Based on these decisions, a manuscript was drafted by JPB before further comment and reviewed by all group members. JPB and IJD are the guarantors. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: No specific funding was given for this work. JPB was supported by a GSK PhD studentship.
Competing interests: All authors have completed the ICMJE uniform disclosure form at https://www.icmje.org/disclosure-of-interest/ and declare: AC, NWG, and JNH were paid employees of GSK at the time of the submitted work; AC, IJD, NWG, and JNH own shares in GSK; AC is currently a paid employee of McKesson Corporation in a role unrelated to the submitted work; JNH is currently a paid employee of Boehringer Ingelheim in a role unrelated to this work; DN is UK Kidney Association Director of Informatics Research; JPB was funded by a GSK studentship received by IJD and reports unrelated consultancy work for WHO Europe and CorEvitas; SML has received unrelated grants with industry collaborators from IMI Horizon, but no direct industry funding; all authors report no other relationships or activities that could appear to have influenced the submitted work.
Provenance and peer review: Not commissioned; externally peer reviewed.
- Petersen JM ,
- Ranker LR ,
- Barnard-Mayers R ,
- MacLehose RF ,
- Rosenbaum PR ,
- Rosenbaum PR
- Vanderweele TJ ,
- VanderWeele TJ
- Greenland S
- Hernán MA ,
- Zaridze D ,
- Brennan P ,
- Boreham J ,
- Gomez-Roig MD ,
- Marchei E ,
- Herrett E ,
- Thomas SL ,
- Schoonen WM ,
- Murray EJ ,
- Sealy-Jefferson S
- Dormuth CR ,
- Patrick AR ,
- Shrank WH ,
- Westreich D
- Greenland S ,
- Mansournia MA ,
- Lévesque LE ,
- Hanley JA ,
- Sterne JA ,
- Reeves BC ,
- Cinelli C ,
- D’Agostino McGowan L
- Gustafson P ,
- Carroll RJ ,
- Marshall RJ
- Schlesselman JJ
- Schmidt M ,
- Jensen AO ,
- Engebjerg MC
- Hernández-Díaz S ,
- Patorno E ,
- Huybrechts KF ,
- Bateman BT ,
- Mathur MB ,
- VanderWeele TJ ,
- Ioannidis JPA ,
- Tazare JR ,
- Williamson E ,
- Maldonado G ,
- McCandless LC ,
- Palmsten K ,
- Brendel P ,
- Collin LJ ,
- MacLehose RF
- Ioannidis JPA
- Hunnicutt JN ,
- Ulbricht CM ,
- Chrysanthopoulou SA ,
- Superak HM ,
- Stürmer T ,
- Schneeweiss S ,
- Rothman KJ ,
- Edwards JK ,
- Troester MA ,
- Richardson DB
- Shields PG ,

“It’s not about the money, money” - Well, actually it is. Divergent views on drivers of early phase clinical trial participation among ethnically diverse potential trial participants in the United Kingdom: A Mixed Methods Study
- Find this author on Google Scholar
- Find this author on PubMed
- Search for this author on this site
- For correspondence: [email protected]
- Info/History
- Preview PDF
Background Novel therapeutics should always be tested in a sample representative of the population in need of treatment. Initial efforts of drug development take place in early phase trials (phase-I and -II), setting the direction for late-stage studies (phase-III and -IV). However, study samples in early phase trials typically fail to recruit Black, Asian and minority ethnic groups, which might produce results which don’t generalise to a broader population in later trials, and ultimately, clinical practice. Focusing on early phase clinical trials the present study (1) explored the barriers and incentives that determine participation of ethnic minorities in clinical research, and (2) proposes strategies that mitigate such barriers.
Methods A systematic literature review explored barriers affecting participation rates from individuals from diverse ethnic backgrounds. An exploratory phase involved two online surveys (researchers and general population) and focus groups (general population) analysed using thematic analysis.
Results The systematic review found little published evidence, with most studies undertaken in the USA and focused on specific clinical areas. The exploratory phase showed a discordance between researchers’ and general public’s perspectives on both drivers and barriers to early phase trial participation.
Discussion These findings were synthesised into a Clinical Trials Participatory Framework , which contextualises reasons for reduced trial participation, while providing mechanisms/strategies to increase uptake among minority ethnic participants. This may guide researchers when implementing strategies to aid under-representation in their samples. Further research should evaluate the framework by actively implementing, testing, and iterating upon the strategies.
Competing Interest Statement
The authors have declared no competing interest.
Funding Statement
This study did not receive any funding
Author Declarations
I confirm all relevant ethical guidelines have been followed, and any necessary IRB and/or ethics committee approvals have been obtained.
The details of the IRB/oversight body that provided approval or exemption for the research described are given below:
North Star Review Board, nonprofit IRB. Determined to not require ethical review, likely would have been exempt if under jurisdiction of the Common Rule
I confirm that all necessary patient/participant consent has been obtained and the appropriate institutional forms have been archived, and that any patient/participant/sample identifiers included were not known to anyone (e.g., hospital staff, patients or participants themselves) outside the research group so cannot be used to identify individuals.
I understand that all clinical trials and any other prospective interventional studies must be registered with an ICMJE-approved registry, such as ClinicalTrials.gov. I confirm that any such study reported in the manuscript has been registered and the trial registration ID is provided (note: if posting a prospective study registered retrospectively, please provide a statement in the trial ID field explaining why the study was not registered in advance).
I have followed all appropriate research reporting guidelines, such as any relevant EQUATOR Network research reporting checklist(s) and other pertinent material, if applicable.
Data Availability
All data produced in the present work are contained in the manuscript
View the discussion thread.
Thank you for your interest in spreading the word about medRxiv.
NOTE: Your email address is requested solely to identify you as the sender of this article.

Citation Manager Formats
- EndNote (tagged)
- EndNote 8 (xml)
- RefWorks Tagged
- Ref Manager
- Tweet Widget
- Facebook Like
- Google Plus One
Subject Area
- Health Systems and Quality Improvement
- Addiction Medicine (316)
- Allergy and Immunology (618)
- Anesthesia (160)
- Cardiovascular Medicine (2277)
- Dentistry and Oral Medicine (279)
- Dermatology (201)
- Emergency Medicine (370)
- Endocrinology (including Diabetes Mellitus and Metabolic Disease) (801)
- Epidemiology (11581)
- Forensic Medicine (10)
- Gastroenterology (679)
- Genetic and Genomic Medicine (3586)
- Geriatric Medicine (337)
- Health Economics (618)
- Health Informatics (2307)
- Health Policy (914)
- Health Systems and Quality Improvement (864)
- Hematology (335)
- HIV/AIDS (753)
- Infectious Diseases (except HIV/AIDS) (13159)
- Intensive Care and Critical Care Medicine (757)
- Medical Education (359)
- Medical Ethics (100)
- Nephrology (389)
- Neurology (3351)
- Nursing (191)
- Nutrition (507)
- Obstetrics and Gynecology (651)
- Occupational and Environmental Health (646)
- Oncology (1759)
- Ophthalmology (525)
- Orthopedics (209)
- Otolaryngology (284)
- Pain Medicine (223)
- Palliative Medicine (66)
- Pathology (438)
- Pediatrics (1005)
- Pharmacology and Therapeutics (422)
- Primary Care Research (406)
- Psychiatry and Clinical Psychology (3063)
- Public and Global Health (5993)
- Radiology and Imaging (1224)
- Rehabilitation Medicine and Physical Therapy (715)
- Respiratory Medicine (811)
- Rheumatology (367)
- Sexual and Reproductive Health (353)
- Sports Medicine (316)
- Surgery (386)
- Toxicology (50)
- Transplantation (171)
- Urology (142)
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- Topic Collection
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 7, Issue 3
- Attributes, skills and actions of clinical leadership in nursing as reported by hospital nurses: a cross-sectional study
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0001-8401-4976 Majd T Mrayyan 1 ,
- http://orcid.org/0000-0002-6393-3022 Abdullah Algunmeeyn 2 ,
- http://orcid.org/0000-0002-2639-9991 Hamzeh Y Abunab 3 ,
- Ola A Kutah 2 ,
- Imad Alfayoumi 3 ,
- Abdallah Abu Khait 1
- 1 Department of Community and Mental Health Nursing, Faculty of Nursing , The Hashemite University , Zarqa , Jordan
- 2 Advanced Nursing Department, Faculty of Nursing , Isra University , Amman , Jordan
- 3 Basic Nursing Department, Faculty of Nursing , Isra University , Amman , Jordan
- Correspondence to Dr Majd T Mrayyan, Department of Community and Mental Health Nursing, Faculty of Nursing, The Hashemite University, Zarqa 13133, Jordan; mmrayyan{at}hu.edu.jo
Background Research shows a significant growth in clinical leadership from a nursing perspective; however, clinical leadership is still misunderstood in all clinical environments. Until now, clinical leaders were rarely seen in hospitals’ top management and leadership roles.
Purpose This study surveyed the attributes and skills of clinical nursing leadership and the actions that effective clinical nursing leaders can do.
Methods In 2020, a cross-sectional design was used in the current study using an online survey, with a non-random purposive sample of 296 registered nurses from teaching, public and private hospitals and areas of work in Jordan, yielding a 66% response rate. Data were analysed using descriptive analysis of frequency and central tendency measures, and comparisons were performed using independent t-tests.
Results The sample consists mostly of junior nurses. The ‘most common’ attributes associated with clinical nursing leadership were effective communication, clinical competence, approachability, role model and support. The ‘least common’ attribute associated with clinical nursing leadership was ‘controlling’. The top-rated skills of clinical leaders were having a strong moral character, knowing right and wrong and acting appropriately. Leading change and service improvement were clinical leaders’ top-rated actions. An independent t-test on key variables revealed substantial differences between male and female nurses regarding the actions and skills of effective clinical nursing leadership.
Conclusions The current study looked at clinical leadership in Jordan’s healthcare system, focusing on the role of gender in clinical nursing leadership. The findings advocate for clinical leadership by nurses as an essential element of value-based practice, and they influence innovation and change. As clinical leaders in various hospitals and healthcare settings, more empirical work is needed to build on clinical nursing in general and the attributes, skills and actions of clinical nursing leadership of nursing leaders and nurses.
- clinical leadership
- health system
- leadership assessment
Data availability statement
Data are available on request due to privacy/ethical restrictions. https://authorservices.taylorandfrancis.com/data-sharing/share-your-data/data-availability-statements/
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/leader-2022-000672
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
WHAT IS ALREADY KNOWN ON THIS TOPIC
Clinical leadership was limited to service managers; however, currently, all clinicians are invited to participate in leadership practices. Clinical leaders are needed in various healthcare settings to produce positive outcomes.
WHAT THIS STUDY ADDS
This study outlined clinical leadership attributes, skills and actions to understand clinical nursing leadership better. The current study highlighted the role of gender in clinical nursing leadership, and it asserts that effective clinical nursing leadership is warranted to improve the efficiency and effectiveness of care. The results call for nurses’ clinical leadership as essential in today’s turbulent work environment.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Nurses and clinical leaders need additional attributes, skills and actions. Clinical nursing leaders should use innovative interventions and have skills or actions to manage current work environments. Further work is needed to build on clinical nursing in general and the attributes, skills and actions of clinical nursing leadership. Clinical leadership programmes must be integrated into the nursing curricula.
Introduction
Clinical leadership is a matter of global importance. Currently, all clinicians are invited to participate in leadership practices. 1 This invitation is based on the fact that people deliver healthcare within complex systems. Effective clinicians must understand systems of care to function effectively. 1 2 Engaging in clinical leadership is an obligation, not a choice, for all clinicians at all levels. This obligation is more critical in nursing with many e merging global health issues , 2 such as the COVID-19 pandemic.
The systematic literature review of Cummings et al 3 shows the differences in leadership literature. In early 2000, clinical leadership emerged in scientific literature. 4 It is about having the knowledge, skills and competencies needed to effectively balance the needs of patients and team members within resource constraints. 4 Clinical leadership is vital in nursing as nurses face complex challenges in clinical settings, especially in acute care settings. 4 Although developed from the management domain, leadership and management are two concepts used interchangeably, 5–9 leading to further misunderstanding of the relationship between clinical leadership and management. While different types of leadership have been evident in nursing and health industry literature, clinical leadership is still misunderstood in clinical environments. 8 Clinical leadership is not fully understood among health professionals trained to care for patients, as clinical leadership is a management concept, leaving the concept open to different interpretations. 10 For example, Gauld 10 reported that clinical leaders might be professionals (such as doctors and nurses) who are no longer clinically active, mandating that clinical leaders should also be involved in delivering care. 10
There is no clear definition of ‘clinical leadership’. However, effective clinical leadership involves individuals with the appropriate clinical leadership skills and attributes at different levels of an organisation, focusing on multidisciplinary and interdisciplinary work. 10 The main skills associated with clinical leadership were having values and beliefs consistent with their actions and interventions, being supportive of colleagues, communicating effectively, serving as a role model and engaging in reflective practice. 4–9 The main attributes associated with clinical leadership were using effective communication, clinical competence, being a role model, supportive and approachability. 4–9 Stanley and colleagues reported that clinical leaders are found across health organisations and are presented in all clinical environments. Clinical leaders are often found at the highest level for clinical interaction but not commonly found at the highest management level in wards or units. 4–9
With the increasing urgency to improve the efficiency and effectiveness of care, effective nursing leadership is warranted. 4 11–17 Clinical leaders can be found in various healthcare settings, 4 most often at the highest clinical level, but they are uncommon at the top executive level. 6–9 18–24 In the UK, the National Health Service (NHS) 25 empowers clinicians and front-line staff to build their decision-making capabilities, which is required for clinical leadership. This empowerment encourages a broader practice of clinical leadership without being limited to top executives alone. 25 26
Purpose and significance
This study assesses clinical nursing leadership in Jordan. More specifically, it answers the following research questions: (1) What attributes are associated with clinical nursing leadership in Jordanian hospitals? (2) What skills are important for effective clinical nursing leadership? (3) What actions are important for effective clinical nursing leadership? (4) What are the differences in skills critical to effective clinical nursing leadership based on the sample’s characteristics? (5) What are the differences in effective clinical nursing leaders’ actions based on the sample’s characteristics?
Nursing leadership studies are abundant; however, clinical leadership research is not well established. 8 27 Until fairly recently, clinical leadership in nursing has tended to focus on nursing leaders in senior leadership positions, ignoring nurse managers in clinical positions. 8 There has been significant growth in research exploring clinical leadership from a nursing perspective. 4 8 9 14–17 24 26–32 A new leadership theory, ‘congruent leadership’, has emerged, claiming that clinical leaders acted on their values and beliefs about care and thus were followed. 6–9 20 This study is the first in Jordan’s nursing and health-related research about clinical leadership. Clarifying this concept from nurses’ perspectives will support greater healthcare delivery efficiencies.
Search methods
The initial search was done using ‘clinical nursing leadership’ at the Clarivate database and Google Scholar database from 2017 to 2021, yielded 35 studies, of which, after abstracting, 14 studies were selected. However, Stanley’s work (12 studies), including those before 2017, was included because we followed the researcher’s passion and methodology of studying clinical leadership; also, some classical models of clinical leadership because they were essential for the conceptualisation of the study as well as the discussion, such as the NHS Leadership Academy (three studies; ref 25 33 34 ).
Another search was run using the words ‘attributes’, ‘skills’ or ‘actions’ using the same time frame; most of the yielded studies were not relevant, this search year was expanded to 2013–2021 because the years 2013–2015 were the glorious time of studying these concepts. Using ‘clinical leadership’ rather than ‘leadership studies’, 15 studies were yielded; however, Stanley’s above work was excluded to avoid repetition, resulting in using three studies (ref 29 30 35 ). A relevant reference of 2022 similar to our study (ref 36 ) was added at the stages of revisions. The remaining 16 of 49 references were related to the methodology and explanation of some results, such as those related to gender differences in leadership. The following limits were set: the language was English; and the year of publication was basically the last 5 years to ensure that the search was current.
Clinical leadership
Clinical leadership ensures quality patient care by providing safe and efficient care and creating a healthy clinical work environment. 4 10–17 27 31 32 It also decreases the high costs of clinical litigation settlements and improves the safety of service delivery to consumers. 4 11–17 32 For these reasons, healthcare organisations should initiate interventions to develop clinical leadership among front-line clinicians, including nurses. 8 9
Literature was scarce on clinical leadership in nursing. 4 8–10 14–17 27 28 31 Stanley and Stanley 8 defined clinical leadership as developing a culture and leading a set of tasks to improve the quality and safety of service delivery to consumers.
Clinical leadership is about focusing on direct patient care, delivering high-quality direct patient care, motivating members of the team to provide effective, safe and satisfying care, promoting staff retention, providing organisational support and improving patient outcomes. 31 Clinical leadership roles include providing the vision, setting the direction, promoting professionalism, teamwork, interprofessional collaborations, good practice and continued medical education, contributing to patient care and performing tasks effectively. 31 Moreover, the researchers added that clinical leadership is having the approachability and the ability to communicate effectively, the ability to gain support and influence others, role modelling, visibility and availability to support, the ability to promote change, advise and guide. 31 Clinical leadership competencies include demonstrating clinical expertise, remaining clinically focused and engaged and comprehending clinical leadership roles and decision-making. In addition, clinical leadership was not associated with a position within the management and organisational structure, unlike health service management. 31 33
Clinical leadership is hindered by many barriers that include the lack of time and the high clinical/client demand on their time. 8 9 Clinical leadership is limited because of the deficit in intrapersonal and interpersonal capabilities among team members and interdisciplinary and organisational factors, such as a lack of influence in interdisciplinary care planning and policy. 37 Other barriers include limited organisational leadership opportunities, the perceived need for leadership development before serving in leadership roles and a lack of funding for advancement. 38
This paper aligns with the theory of congruent leadership proposed by Stanley. 19 This theory is best suited for understanding clinical leadership because it defines leadership as a congruence between the activities and actions of the leader and the leader’s values, beliefs and principles, and those of the organisation and team.
Attributes of clinical leadership
The clinical leadership attributes needed for nurses 8 28 to perform their roles effectively are: (1) personal attributes: nurses are confident in their abilities to provide best practice, communicate effectively and have emotional intelligence; (2) team attributes: encouraging trust and commitment to others, team focus and valuing others’ skills and expertise; and (3) capabilities: encouraging contribution from others, building and maintaining relationships, creating clear direction and being a role model. 8 28 Clinical leadership attributes are linked to communicating effectively, role modelling, promoting change, providing advice and guidance, gaining support and influencing others. 28–30 Other attributes to include are clinical leaders’ engagement in reflective practice, 29 provision of the vision; setting direction, having the resources to perform tasks effectively and promoting professionalism, teamwork, interprofessional collaborations, effective practice and continued education. 27 28 31
Skills of clinical leadership
Clinical leadership skills include (1) a ‘clinical focus’: being expert knowledge, providing evidence-based rationale and systematic thinking, understanding clinical leadership, understanding clinical decision-making, being clinically focused, remaining clinically engaged and demonstrating clinical expertise; (2) a ‘follower/team focus’: being supportive of colleagues, effectively communicating communication skills, serving as a role model and empowering the team; and (3) a ‘personal qualities focus’: engaging in reflective practice, initiating change and challenging the status quo. 17 30 32 Clinical leaders have advocacy skills, facilitate and maintain healthier workplaces by driving changes in cultural issues among all health professionals. 17 29 Moreover, the overlap between the attributes and skills of clinical leaders includes being credible to colleagues because of clinical competence and the skills and capacity to support multidisciplinary teams effectively. 17 29 32
Actions of clinical leadership
A clinical leader is anyone in a clinical position exercising leadership. 26 The clinical leader’s role is to continuously instil in clinicians the capability to improve healthcare on small and large scales. 26 Furthermore, Stanley et al 9 demonstrated that clinical leaders are not always managers or higher-ups in organisations. Clinical leaders act following their values and beliefs, are approachable and provide superior service to their clients. 9 Clinical leaders define and delegate safety and quality responsibilities and roles. 14 32 39 They also ensure safety and quality of care, manage the operation of the clinical governance system, implement strategic plans and implement the organisation’s safety culture. 14 32 39 The Australian Commission on Safety and Quality in Health Care 39 also reported that clinical leaders might support other clinicians by reviewing safety and quality performance data, supervising the clinical workforce, conducting performance appraisals and ensuring that the team understands the clinical governance system.
In summary, clinical leadership attributes, skills and actions were outlined to understand clinical nursing leadership. The literature shows limited nursing research on clinical leadership, calling for clinical leadership that paves the road for nurses in the current turbulent work environment.
Study design
A descriptive quantitative analysis was developed to collect data about the attributes and skills of clinical nursing leadership and the actions that effective nursing clinical leaders can take. A cross-sectional design was employed to measure clinical leadership using an online survey in 2020. This design was appropriate for such a study as it allows the researchers to measure the outcome and the exposures of the study participants at the same time. 40
Sample and settings
The general population was registered nurses in medical centres in Jordan. The target population was registered nurses in teaching, public and private hospitals. Most nurses in Jordan are females working at different shifts on a full-time basis in different types of healthcare services. The baccalaureate degree is the minimum entry into the clinical practice of registered nurses. As previous nurses, we would like to attest that nurses in Jordanian hospitals commonly use team nursing care delivery models with different decision-making styles. The size of the sample was calculated by using Thorndike’s rule as follows: N≥10(k)+50 (where N was the sample size, k is the number of independent variables) (attributes, skills, actions), the minimum sample size should be 80 participants. 40 From experience, the researcher considers the sample’s demographics and subscales as independent variables (k=17); the overall sample should not be less than 220.
Research participants were recruited through a ‘direct recruitment strategy’ from the hospitals where the nursing students were trained. A survey was used to collect data using non-random purposive sampling; of possible 450 Jordanian nurses, 296 were recruited from different types of hospitals: teaching (51 of possible 120 nurses), public (180 of possible 210 nurses) and private (65 of possible 120 nurses), with a response rate of 66%, which is adequate for an online survey. The inclusion criteria were that nurses should work in hospital settings, and any nurses who work in non-hospital settings were excluded. No incentives were applied.
Using a direct measurement method, Stanley’s Clinical Leadership Scale ( online supplemental file 1 ) was used to collect the data using the English version of the scale because English is the official education language of nursing in Jordan. 8 9 The original questionnaire consists of 24 questions: 12 quantitative and qualitative questions relevant to clinical leadership, and 12 related to the sample’s demographics. Several studies about clinical leadership among nurses and paramedics in the UK and Australia used modified versions of a survey tool 5 8 9 18–24 ; construct validity was ensured using exploratory factor analysis or triangulation of validation. Cronbach’s alpha measures the homogeneity in the survey, and it was reported to be 0.87 8 9 and 0.88 in the current study.
Supplemental material
Several questions were measured on a 5-point Likert scale in the original scale, and others were qualitative. The survey for the current study consists of 12 quantitative and qualitative questions related to clinical leadership and 14 questions related to the sample’s demographics. However, the qualitative data obtained were scattered and incomplete; thus, only the quantitative questions were analysed and reported, and another qualitative study about clinical leadership was planned. For the current study, three quantitative questions only focused on clinical leadership, leadership skills and the actions of clinical leaders, and 14 questions focused on the sample’s characteristics relevant to the Jordanian healthcare system developed by the first author. The sample characteristics were gender, marital status, shift worked, time commitment, level of education, age, years of experience in nursing, years of experience in leadership and the number of employees directly supervised. Other characteristics include the type of unit/ward, model of nursing care, ward/unit’s decision-making style, formal leadership-related education (yes/no) and formal management-related education (yes/no). Before data collection, permission to use the tool was granted.
Ethical considerations
Nurses were invited to answer the survey while assuring the voluntary nature of their participation. The participants were told that their participation in the survey was their consent form. Participants’ anonymity and confidentiality of information were assured; all questionnaires were numerically coded, and the overall results were shared with nursing and hospital administrators. 40
Patient and public involvement
There was no patient or public involvement in this research’s design, conduct, reporting or dissemination.
Data collection procedures
After a pilot study on 12 December 2020, which checked for the suitability of the questionnaire for the Jordanian healthcare settings, data were collected over a month on 23 December 2020. Data were collected through Google Forms; the survey was posted on various WhatsApp groups and Facebook pages. Using purposive snowball sampling, nurses were asked to invite their contacts and to submit the survey once. To assure one submission, the Google Forms was designed to allow for one submission only.
No problem was encountered during data collection. The two attrition prevention techniques used were effective communication and asserting to the participants that the study was relevant to them.
The researchers controlled for all possible extraneous and confounding variables by including them in the study. A possible non-accounted extraneous variable is the organisational structure; a centralised organisational structure may hinder the use of clinical nursing leadership.
Data analyses
After data cleaning and checking wild codes and outliers, all coded variables were entered into the Statistical Package for Social Sciences (SPSS) (V.25), 35 which was used to generate statistics according to the level of measurement. A descriptive analysis focused on frequency and central tendency measures. 40 Part 1 of the scale comprises 54 qualities or characteristics to answer the first research question. Responses related to skills were measured on a 1–5 Likert scale; thus, means and SDs were reported to answer the second research question. Eight actions were rated on a 1–5 Likert scale; thus, means and SDs were reported to answer the third research question. Independent t-tests using all sample characteristics were performed to answer the fourth and fifth research questions.
The preanalysis phase of data analysis was performed; data were eligible and complete as few missing data were found; thus, they were left without intervention. The assumption of normality was met; both samples are approximately normally distributed, and there were no extreme differences in the sample’s SDs.
Characteristics of the sample
There were 296 nurses in the current study from different types of hospitals: teaching (51 nurses), public (180 nurses) and private (65 nurses), with a response rate of 66%. Most nurses were females (209, 70.6%), single (87, 29.4%), working a day shift (143, 48.3%) or rotating shifts (92, 31.1%), on a full-time basis (218, 73.6%), with a baccalaureate degree (236, 79.7%), aged less than 25 years (229, 77.4%) and 25–34 years (45, 15.2%), respectively. Also, 65.1% (166) of nurses reported having less than 1 year of experience in nursing; thus, they have few nurses under them to supervise (145, 49% supervise one to two nurses), and 23.3% (69) of nurses reported having 1–9 years of experience in leadership. Nurses reported that their unit or ward has a primary (81, 27.4%) or team nursing care delivery model (162, 54.7%), with a mixed (94, 31.8%) or participatory decision-making style (113, 38.2%), and had formal leadership-related education (191, 64.5%), and had no formal management-related education (210, 70.9%) ( table 1 ).
- View inline
Sample’s characteristics (N=296*)
Attributes of clinical nursing leadership
Nurses were asked to think about the attributes and features of clinical leadership. Based on Stanley’s Clinical Leadership Scale, 8 9 nurses were given a list of 54 qualities and characteristics and asked to select the most strongly associated with clinical leadership, followed by those least strongly associated with clinical leadership. Table 2 shows the respondents’ ‘top ten’ selected qualities in ranked order.
'Most’ and ‘Least’ important attributes associated with clinical nursing leadership (N=296)
Skills of effective clinical nursing leaders
On a Likert scale of 1–5, respondents were asked to rank the skills of effective clinical leaders from ‘not relevant’ or ‘not important’ to 5=‘very relevant’ or ‘very important’. The top skills were having a strong moral character, knowing right and wrong and acting appropriately which received a high rating, with a mean of 4.17 out of 5 (0.92). Being in a management position to be effective was ranked as the least skill of an effective leader, with a mean value of 3.78 out of 5 (1.00). As indicated by respondents, other skills of effective clinical leaders are shown in table 3 .
Skills of effective clinical nursing leaders (N=296)
Actions of effective clinical nursing leaders
On a Likert scale of 1–5, respondents were asked to rank the actions of effective clinical leaders. Leading change and service management achieved a high rating of 4.07 out of 5 points (0.90). Influencing organisational policy was rated last, with a mean score of 3.95 out of 5 (1.01), which may reflect the very junior nature of the majority of the sample. As described by respondents, some of the other actions of effective leaders are shown in table 4 .
Actions effective clinical nursing leaders can do (N=296)
Significant differences in skills of effective clinical nursing leaders based on gender
Independent t-tests using all sample’s characteristics were performed to answer the fourth research question. Gender was the only characteristic variable that differentiated clinical leadership skills. An independent t-test demonstrates that males and females have distinct perspectives on 3 out of 10 items measuring clinical leadership skills. Female participants outperform male participants in terms of ‘working within the team (p value=0.021)’, ‘being visible in the clinical environment (p value=0.004)’ and ‘recognizing optimal performance and expressing appreciation promptly (p value=0.042) ( table 5 )’.
Significant differences in skills and actions of effective clinical nursing leaders based on gender (n=296)
Significant differences in actions of effective clinical nursing leaders based on gender
Independent t-tests using all sample’s characteristics were performed to answer the fifth research question. Gender was the only characteristic variable that differentiated clinical leadership actions, and it was discovered that five of the eight propositions varied in their actions: the way clinical care is administered (p=0.010); participating in staff development education (p=0.006); providing valuable staff support (p=0.033); leading change and service improvement (p=0.014); and encouraging and leading service management (p=0.019). The independent t-test results revealed that female participants scored higher in those acts, corresponding to effective leaders’ competencies. The mean values of participants’ responses to the actions of effective clinical leaders are shown in table 5 .
The characteristics of the current sample are similar to those of the structure of the task force in Jordan. The remaining question is how men in Jordan be supported in nursing to develop clinical leadership skills on par with females. Al-Motlaq et al 41 proposed using a part-time nurses policy to address nurses’ gender imbalances. Although this is necessary for both genders, we propose to develop a clinical leadership training package to promote working male nurses’ clinical leadership. In Jordan, we apply the modern trend of using leadership in nursing rather than management. About 65% of the nurses reported having formal leadership-related education, while around 71% reported no formal management-related education.
The findings clearly showed what nurses seek in a clinical leader. They appear to refer to a good communicator who values relationships and encouragement, is flexible, approachable and compassionate, can set goals and plans, resource allocation, is clinically competent and visible and has integrity. They necessitate clinical nursing leaders who can be role models for others in practice and deal with change. They should be supportive decision-makers, mentors and motivators. They should be emphatic; otherwise, they should not be in a position of control. These findings align with other research on clinical leadership. 7–9 21 Clinical leaders should be visible and participate in team activities. They should be highly skilled clinicians who instil trust and set an example, and their values should guide them in providing excellent patient care. 8 9
Participants chose other terms or functions associated with leadership roles less frequently or perceived as unrelated to clinical leadership functions. Management, creativity and vision were among the terms and functions mentioned. The absence of the word ‘visionary’ from the list of the most important characteristics suggests that traditional leadership theories, as transformational leadership and situational leadership, do not provide a solid foundation for understanding clinical leadership approaches in the clinical setting. This result can also be influenced by the junior level of the majority of the sample.
Skills of clinical nursing leadership
Numerous studies have documented the characteristics and skills of clinical leaders. 27 29 31 Clinical leaders’ skills include advocacy, facilitation and healthier workplaces. 27 29 31 Our participants were rated as having high morals (similar to other studies) 27 29 31 and worked within teams. 29 In turn, they were flexible and expressed appreciation promptly. 7–9 21 They were clinically competent; thus, they improvised and responded to various situations with appropriate skills and interventions. They recognised optimal performance, initiated interventions, led actions and procedures and had the skills and resources necessary to perform their tasks.
The lowest mean was ‘ being in a management position to be effective ’. This lowest meaning ‘ somehow ’ makes sense; all nurses can be effective leaders rather than managers, assuming effective clinical leadership roles without having management positions. 28 42
Actions of clinical nursing leadership
Influential nursing leaders are clinically competent and can initiate interventions and lead actions; these skills translate to actions. Clinical leaders are qualified to lead and manage the service improvement change (similar to Major). 42 This role will not suddenly happen; it requires clinical nursing leaders who encourage and participate in staff development education (consistent with Major). 42 This is an essential milestone and an example of providing valuable staff support. As these were the lowest reported actions, clinical nursing leaders should initiate and lead improvement initiatives in their clinical settings, 42 resulting in service improvement. They also have to influence evidence-based policies to improve work–life integration 43 and enhance patients, nurses and organisational outcomes. These outcomes include quality of care, nurses’ empowerment, job satisfaction, quality of life and work engagement. 4 11–17 32
Female nurses had more clinical leadership skills. Because the findings of this study have never been reported in the previous clinical leadership research literature, they are considered novel. This finding indicates that one possible explanation is that the overwhelming majority of respondents were females, with the proportion of females in favour (70.6%) exceeding that of males (29.4%). Furthermore, the current findings could be explained because the study was conducted in Jordan, a traditionally female-dominated gender nursing career.
This study discovered that there are gender differences in the characteristics of nurses and their clinical leadership skills, with female clinical nursing leaders scoring higher on the t-test than male clinical nursing leaders in the following areas: this is contrary to Masanotti et al , 43 who reported that male nurses have a greater sense of coherence and, in turn, more teamwork than female nurses, who commonly have job dissatisfaction and less teamwork. These could apply to female clinical nursing leaders. These female nurses had more ‘visibility in the clinical environment’, as expected in female-dominated gender nursing careers. As they were commonly dissatisfied as nurses, 43 clinical nursing leaders would be competent in caring for their nurses’ psychological status. These leaders know that even ‘thank you’ is the simplest way to show appreciation and recognition; however, this should be given promptly.
In Arab and developing countries, the perception that females have more skills with effective clinical leadership characteristics than males is consistent with Alghamdi et al 44 and Yaseen. 45 They found that females outperform males on leadership scales, which may also apply to clinical leadership. This study shows consistency between female and male clinical nursing leaders’ general perceptions of clinical leadership skills in female-dominated gender nursing careers but not in male-dominated, gender-segregated countries, including Jordan.
Female nurses had more clinical leadership actions, which differed in five out of eight actions. Female clinical nursing leaders were better at impacting clinical care delivery, participating in staff development education, providing valuable staff support, leading change and improving service.
It is aware that the nursing profession has a difficult context in some Arab and developing countries. For example, a study conducted in Saudi Arabia could explain the current findings that male nurses face various challenges, including a lack of respect and discrimination, resulting in fewer opportunities for professional growth and development. 46 The researchers reported that female clinical nursing leaders are preferred over male nurses because nursing is a nurturing and caring profession; it has been dubbed a ‘female profession’. 46 Additionally, this study corroborates a study that found many males avoid the nursing profession entirely due to its negative connotations 47 ; the profession is geared towards females. These and other stereotypes have influenced male nurses to pursue masculine nursing roles.
The study’s findings are unique because they have never been published in the previous clinical leadership research literature. However, these results can be explained indirectly based on non-clinical leadership literature. Consistent with Khammar et al , 48 as it is a female-dominated profession, it is apparent that female clinical nursing leaders are better at delivering clinical care. This result could also be related to female clinical nursing leaders having a better attitude towards clinical conditions and managing different conditions. 48 Female clinical nursing leaders, in turn, are better at influencing patient care and improving patient safety 36 and overall care and services. This improvement will not happen suddenly; it should be accompanied by paying more attention to providing continuous support, especially during induced change.
The current study reported that female clinical nursing leaders supported staff development and education because it is a female-oriented sample. Yet, Khammar et al 48 reported that men had more opportunities to educate themselves in nursing; this is true in a male-dominated country like Jordan. They also noted that males could communicate better during nursing duties. Regardless of gender, all of us should pay attention to our staff’s working environment and related issues, including promoting open communication, providing support, encouraging continuing education, managing change and improving the overall outcomes.
Limitations
Even though the study’s findings are intriguing, further investigation is needed to comprehend them. Because of the cross-sectional design used in the current study, we cannot establish causality. For this reason, the results should be interpreted with caution. Also, the purposive sample limits the generalisability; thus, this research should be carried out again with a broader selection of nursing candidates and clinical settings. Moreover, the sample consists mostly of nurses with minimal experience compared with nurses in other international countries such as Canada, the UK and the USA. 5 The current study also included nurses in their 40s and above, with male nurses less represented, and this causes misunderstanding of the true clinical leadership in nursing.
Implications
For practice, our sample consists of nurses with minimal experience compared with nurses in other developed counties. Our sample reported ‘influencing organizational policy’ as the last clinical leadership skill, which reflects the very junior nature of the sample. Unlike our study, in their systematic review, Guibert-Lacasa and Vázquez-Calatayud 36 reported that the profiles of the care clinical nurses’ experience usually varied, ranging from recent graduates to senior nurses. If our nurses were more experienced, it might lead to different results. More nurses’ clinical experience would increase nurses’ abilities at the bedside, especially in areas related to reasoning and problem solving. 36 More experienced nurses tend to work collaboratively within the team with greater competency and autonomy. 36 More experienced nurses would provide high-quality care, 36 resulting in patient satisfaction. To generate positive outcomes of clinical nursing leadership, such early-career nurses should be qualified. Guibert-Lacasa and Vázquez-Calatayud 36 suggested using the nursing clinical leadership programme based on the American Organization for Nursing Leadership 34 competency model, pending the presence of organisational support for such an initiative. 36
‘Most’ important clinical nursing leadership attributes should be promoted at all organisational and clinical levels. Clinical nursing leadership’s ‘least’ important attributes should be defeated to achieve better outcomes. Clinical nursing leaders should use innovative interventions and have skills or actions conducive to a healthy work environment. These interventions include being approachable to enable their staff to cope with change, 28 using open and consistent communication, 28–30 being visible and consistently available as role models and mentors and taking risks. 28 Hospital administrators must help their clinical leaders, including nursing leaders, to effectively use their authority, responsibility and accountability; clinical leadership is not only about complying with the job description. A good intervention to start with to promote the culture of clinical leadership is setting an award for the ‘ideal nursing leaders’. This award will bring innovative attributes, skills and actions.
Moreover, as they are in the front line of communication, nurses and clinical nursing leaders should be involved in policy-related matters and committees. 49 An interventional programme that gives nurses more autonomy in making decisions is warranted. In turn, various patient, nurse and organisational outcomes will be improved. 13–17 32
The study’s findings revealed statistically significant differences in the skills and actions of effective clinical leaders, with female nurses scoring higher in many skills and actions. Hence, healthcare organisations must re-evaluate current leadership and staff development policies and prioritise professional development for nurses while also introducing new modes of evaluation and assessment that are explicitly geared at improving clinical leadership among nurses, particularly males.
For education, this study outlined clinical leadership attributes, skills and actions to understand clinical nursing leadership in Jordan better. Nevertheless, nurses and clinical leaders need additional attributes, skills and actions. Consequently, undergraduate nursing students might benefit from clinical leadership programmes integrated into the academic curriculum to teach them the fundamentals of clinical leadership. A master’s degree programme in ‘Clinical Nursing Leadership’ would prepare nurses for this pioneering role and today and tomorrow’s clinical nursing leaders. However, all nurses are clinical leaders regardless of their degrees and experience. Conducting presentations, convening meetings, overseeing organisational transformation and settling disagreements are common ways to hone these abilities.
For research purposes, it is worth exploring the concept of clinical leadership from a practice nurse’s perspective to provide insight into practice nurses’ feelings and perceptions. Thus, a longitudinal quantitative design or a phenomenological qualitative design might be adopted to assess the subjective experience of the nurses involved. It is better in future research to focus on both young and veteran clinical leaders; some of our nurses were aged 45 years and above, and those nurses may not be clinically focused.
Summary and conclusion
The current study put clinical leadership into the context of the healthcare system in Jordan. This study highlighted the role of gender in clinical nursing leadership. Nurses’ clinical leadership is a milestone for influencing innovation and change. The current study identified the ‘most’ and ‘least’ important attributes, skills and actions associated with clinical leadership. However, the male and female nurses found substantial differences in effective clinical nursing leadership skills and actions. This study is unique; little is known about the collective concepts of attributes, skills and actions necessary for clinical nursing leadership.
Nurses need leadership attributes, skills and actions to influence policy development and change in their work environments. Leadership attributes can help develop programmes that give nurses more autonomy in making decisions. As a result, nurses will be more active as clinical leaders.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
This study involves human participants and was approved by The Hashemite University, Jordan (IRB number: 1/1/2020/2021) on 18 October 2020. Participants gave informed consent to participate in the study before taking part.
Acknowledgments
The researchers thank the subjects who participated in the study, and Mrs Othman and Mr Sayaheen who collected the data.
- Folaron I ,
- Colburn JA , et al
- Edmonson C ,
- McCarthy C ,
- Trent-Adams S , et al
- Cummings GG ,
- Tate K , et al
- Connolly M ,
- Stanley D ,
- Blanchard D ,
- Hohol A , et al
- Cao T , et al
- Cordeiro R ,
- Rengel-Diaz C ,
- Duignan M ,
- Drennan J ,
- McCarthy VJC
- Tao Z , et al
- Cuthbertson J ,
- Metcalfe H , et al
- Latimer K ,
- NHS Leadership Academy
- Loewenthal L , et al
- Claus S , et al
- Jackson D ,
- Mannix J , et al
- Siegel EO ,
- American Organization for Nursing Leadership
- Guibert-Lacasa C ,
- Vázquez-Calatayud M
- McNamara MS ,
- Casey M , et al
- Peltzer JN ,
- Shen Q , et al
- Australian Commission on Safety and Quality in Health Care
- Al-Motlaq M ,
- Masanotti GM ,
- Paolucci S ,
- Abbafati E , et al
- Alghamdi MG ,
- Abdelkader MA ,
- Abdelrahman S
- Abushaikha L ,
- Mahadeen A ,
- AbdelKader R , et al
- Khammar A ,
- Poursadeghiyan M ,
- Marioryad H , et al
- Kitson AL ,
- Gifford W , et al
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
Contributors MTM developed the study conception, abstract, introduction, literature review and methods; collected the data and wrote the first draft of this research paper and the final proofreading. HAN analysed the data and wrote the results. AA wrote the discussion and updated the literature review. OK wrote the limitations, implications, and summary and conclusion. IAF and AAK did the critical revisions and the final proofreading. All authors contributed to the current work.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
Appointments at Mayo Clinic
- Consumer health
- Mindfulness exercises
See how mindfulness helps you live in the moment.
If you've heard of or read about mindfulness meditation — also known as mindfulness — you might be curious about how to practice it. Find out how to do mindfulness exercises and how they might benefit you.
What is mindfulness?
Mindfulness is a type of meditation in which you focus on being intensely aware of what you're sensing and feeling in the moment, without interpretation or judgment. Practicing mindfulness involves breathing methods, guided imagery, and other practices to relax the body and mind and help reduce stress.
Spending too much time planning, problem-solving, daydreaming, or thinking negative or random thoughts can be draining. It can also make you more likely to experience stress, anxiety and symptoms of depression. Practicing mindfulness exercises can help you direct your attention away from this kind of thinking and engage with the world around you.
What are the benefits of meditation?
Meditation has been studied in many clinical trials. The overall evidence supports the effectiveness of meditation for various conditions, including:
- High blood pressure (hypertension)
Preliminary research indicates that meditation can also help people with asthma and fibromyalgia.
Meditation can help you experience thoughts and emotions with greater balance and acceptance. Meditation also has been shown to:
- Improve attention
- Decrease job burnout
- Improve sleep
- Improve diabetes control
What are some examples of mindfulness exercises?
There are many simple ways to practice mindfulness. Some examples include:
- Pay attention. It's hard to slow down and notice things in a busy world. Try to take the time to experience your environment with all of your senses — touch, sound, sight, smell and taste. For example, when you eat a favorite food, take the time to smell, taste and truly enjoy it.
- Live in the moment. Try to intentionally bring an open, accepting and discerning attention to everything you do. Find joy in simple pleasures.
- Accept yourself. Treat yourself the way you would treat a good friend.
- Focus on your breathing. When you have negative thoughts, try to sit down, take a deep breath and close your eyes. Focus on your breath as it moves in and out of your body. Sitting and breathing for even just a minute can help.
You can also try more structured mindfulness exercises, such as:
- Body scan meditation. Lie on your back with your legs extended and arms at your sides, palms facing up. Focus your attention slowly and deliberately on each part of your body, in order, from toe to head or head to toe. Be aware of any sensations, emotions or thoughts associated with each part of your body.
- Sitting meditation. Sit comfortably with your back straight, feet flat on the floor and hands in your lap. Breathing through your nose, focus on your breath moving in and out of your body. If physical sensations or thoughts interrupt your meditation, note the experience and then return your focus to your breath.
- Walking meditation. Find a quiet place 10 to 20 feet in length, and begin to walk slowly. Focus on the experience of walking, being aware of the sensations of standing and the subtle movements that keep your balance. When you reach the end of your path, turn and continue walking, maintaining awareness of your sensations.
When and how often should I practice mindfulness exercises?
It depends on what kind of mindfulness exercise you plan to do.
Simple mindfulness exercises can be practiced anywhere and anytime. Research indicates that engaging your senses outdoors is especially beneficial.
For more structured mindfulness exercises, such as body scan meditation or sitting meditation, you'll need to set aside time when you can be in a quiet place without distractions or interruptions. You might choose to practice this type of exercise early in the morning before you begin your daily routine.
Aim to practice mindfulness every day for about six months. Over time, you might find that mindfulness becomes effortless. Think of it as a commitment to reconnecting with and nurturing yourself.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Bystritsky A. Complementary and alternative treatments for anxiety symptoms and disorders: Physical, cognitive, and spiritual interventions. https://uptodate.com/contents/search. Accessed June 14, 2018.
- Seaward BL. Meditation and mindfulness. In: Managing Stress: Principles and Strategies for Health and Well-being. 9th ed. Burlington, Mass.: Jones & Bartlett Learning; 2018.
- Shapiro SL, et al. The Art and Science of Mindfulness: Integrating Mindfulness into Psychology and the Helping Professions. 2nd ed. Washington, D.C.: American Psychological Association; 2017.
- Lymeus F, et al. Building mindfulness bottom-up: Meditation in natural settings supports open monitoring and attention restoration. Consciousness and Cognition. 2018;59:40.
- Blanck P, et al. Effects of mindfulness exercises as stand-alone interventions on symptoms of anxiety and depression: Systematic review and meta-analysis. Behaviour Research and Therapy. 2018;102:25.
- AskMayoExpert. Meditation. Rochester, Minn.: Mayo Foundation for Medical Education and Research; 2018.
- Khoury B, et al. Mindfulness-based stress reduction for healthy individuals: A meta-analysis. Journal of Psychosomatic Research. 2015;78:519.
- Practice mindfulness and relaxation. Springboard Beyond Cancer. https://survivorship.cancer.gov/springboard/stress-mood/practice-mindfulness. Accessed June 14, 2018.
Products and Services
- A Book: The Mayo Clinic Diet Bundle
- The Mayo Clinic Diet Online
- A Book: Mayo Clinic Guide to Pain Relief
- A very happy brain
- Alternative cancer treatments: 11 options to consider
- Candida cleanse diet
- Colloidal silver supplements
- Colon cleansing
- Detox foot pads
- Diabetes treatment: Can cinnamon lower blood sugar?
- Do infrared saunas have any health benefits?
- Prickly pear cactus
- Herbal supplements and heart drugs
- Kombucha tea
- Kratom: Unsafe and ineffective
- Kratom for opioid withdrawal
- Learn to reduce stress through mindful living
- Medical marijuana
- Meditation 2.0: A new way to meditate
- Natural remedies for depression: Are they effective?
- Tai Chi and Cardiac Rehab
- Valerian: A safe and effective herbal sleep aid?
- Alternative psoriasis treatments
- Do zinc supplements shorten colds?
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Emerg (Tehran)
- v.5(1); 2017

Sampling methods in Clinical Research; an Educational Review
Mohamed elfil.
1 Faculty of Medicine, Alexandria University, Egypt.
Ahmed Negida
2 Faculty of Medicine, Zagazig University, Egypt.
Clinical research usually involves patients with a certain disease or a condition. The generalizability of clinical research findings is based on multiple factors related to the internal and external validity of the research methods. The main methodological issue that influences the generalizability of clinical research findings is the sampling method. In this educational article, we are explaining the different sampling methods in clinical research.
Introduction
In clinical research, we define the population as a group of people who share a common character or a condition, usually the disease. If we are conducting a study on patients with ischemic stroke, it will be difficult to include the whole population of ischemic stroke all over the world. It is difficult to locate the whole population everywhere and to have access to all the population. Therefore, the practical approach in clinical research is to include a part of this population, called “sample population”. The whole population is sometimes called “target population” while the sample population is called “study population. When doing a research study, we should consider the sample to be representative to the target population, as much as possible, with the least possible error and without substitution or incompleteness. The process of selecting a sample population from the target population is called the “sampling method”.
Sampling types
There are two major categories of sampling methods ( figure 1 ): 1; probability sampling methods where all subjects in the target population have equal chances to be selected in the sample [ 1 , 2 ] and 2; non-probability sampling methods where the sample population is selected in a non-systematic process that does not guarantee equal chances for each subject in the target population [ 2 , 3 ]. Samples which were selected using probability sampling methods are more representatives of the target population.

Sampling methods.
Probability sampling method
Simple random sampling
This method is used when the whole population is accessible and the investigators have a list of all subjects in this target population. The list of all subjects in this population is called the “sampling frame”. From this list, we draw a random sample using lottery method or using a computer generated random list [ 4 ].
Stratified random sampling
This method is a modification of the simple random sampling therefore, it requires the condition of sampling frame being available, as well. However, in this method, the whole population is divided into homogeneous strata or subgroups according a demographic factor (e.g. gender, age, religion, socio-economic level, education, or diagnosis etc.). Then, the researchers select draw a random sample from the different strata [ 3 , 4 ]. The advantages of this method are: (1) it allows researchers to obtain an effect size from each strata separately, as if it was a different study. Therefore, the between group differences become apparent, and (2) it allows obtaining samples from minority/under-represented populations. If the researchers used the simple random sampling, the minority population will remain underrepresented in the sample, as well. Simply, because the simple random method usually represents the whole target population. In such case, investigators can better use the stratified random sample to obtain adequate samples from all strata in the population.
Systematic random sampling (Interval sampling)
In this method, the investigators select subjects to be included in the sample based on a systematic rule, using a fixed interval. For example: If the rule is to include the last patient from every 5 patients. We will include patients with these numbers (5, 10, 15, 20, 25, ...etc.). In some situations, it is not necessary to have the sampling frame if there is a specific hospital or center which the patients are visiting regularly. In this case, the researcher can start randomly and then systemically chooses next patients using a fixed interval [ 4 ].
Cluster sampling (Multistage sampling)
It is used when creating a sampling frame is nearly impossible due to the large size of the population. In this method, the population is divided by geographic location into clusters. A list of all clusters is made and investigators draw a random number of clusters to be included. Then, they list all individuals within these clusters, and run another turn of random selection to get a final random sample exactly as simple random sampling. This method is called multistage because the selection passed with two stages: firstly, the selection of eligible clusters, then, the selection of sample from individuals of these clusters. An example for this, if we are conducting a research project on primary school students from Iran. It will be very difficult to get a list of all primary school students all over the country. In this case, a list of primary schools is made and the researcher randomly picks up a number of schools, then pick a random sample from the eligible schools [ 3 ].
Non-probability sampling method
Convenience sampling
Although it is a non-probability sampling method, it is the most applicable and widely used method in clinical research. In this method, the investigators enroll subjects according to their availability and accessibility. Therefore, this method is quick, inexpensive, and convenient. It is called convenient sampling as the researcher selects the sample elements according to their convenient accessibility and proximity [ 3 , 6 ]. For example: assume that we will perform a cohort study on Egyptian patients with Hepatitis C (HCV) virus. The convenience sample here will be confined to the accessible population for the research team. Accessible population are HCV patients attending in Zagazig University Hospital and Cairo University Hospitals. Therefore, within the study period, all patients attending these two hospitals and meet the eligibility criteria will be included in this study.
Judgmental sampling
In this method, the subjects are selected by the choice of the investigators. The researcher assumes specific characteristics for the sample (e.g. male/female ratio = 2/1) and therefore, they judge the sample to be suitable for representing the population. This method is widely criticized due to the likelihood of bias by investigator judgement [ 5 ].
Snow-ball sampling
This method is used when the population cannot be located in a specific place and therefore, it is different to access this population. In this method, the investigator asks each subject to give him access to his colleagues from the same population. This situation is common in social science research, for example, if we running a survey on street children, there will be no list with the homeless children and it will be difficult to locate this population in one place e.g. a school/hospital. Here, the investigators will deliver the survey to one child then, ask him to take them to his colleagues or deliver the surveys to them.
Conflict of interest:

IMAGES
VIDEO
COMMENTS
Introduction. In clinical research, our aim is to design a study, which would be able to derive a valid and meaningful scientific conclusion using appropriate statistical methods that can be translated to the "real world" setting. 1 Before choosing a study design, one must establish aims and objectives of the study, and choose an appropriate target population that is most representative of ...
Clinical research is the comprehensive study of the safety and effectiveness of the most promising advances in patient care. Clinical research is different than laboratory research. It involves people who volunteer to help us better understand medicine and health. Lab research generally does not involve people — although it helps us learn ...
Examples of other kinds of clinical research Many people believe that all clinical research involves testing of new medications or devices. This is not true, however.
Observational study. A type of study in which people are observed or certain outcomes are measured. No attempt is made by the researcher to affect the outcome — for example, no treatment is given by the researcher. Clinical trial (interventional study). During clinical trials, researchers learn if a new test or treatment works and is safe.
For example - we want to study the odds of being a smoker among hypertensive patients compared to normotensive ones. To do so, we choose a group of patients diagnosed with hypertension and another group that serves as the control (normal blood pressure). ... Clinical trials are experimental studies involving humans; In clinical trials, we ...
Clinical trials are conducted for many reasons: to determine whether a new drug or device is safe and effective for people to use. to study different ways to use standard treatments or current ...
Supporting Clinical Research The purpose of the NIA Clinical Research Toolbox is to provide a Web-based informational repository for investigators and staff involved in clinical research. The Toolbox contains templates, sample forms, guidelines, regulations and informational materials to assist investigators in the development and conduct of high quality clinical research studies.
Clinical Researcher—September 2020 (Volume 34, Issue 8) PEER REVIEWED Sheryl Stewart, MCR, CCRP The tenets of Good Clinical Practice (GCP), promulgated by the International Council for Harmonization (ICH), require that investigator-initiated trials (IITs), especially those involving an Investigational New Drug application to the U.S. Food and Drug Administration (FDA), have the principal ...
A clinical study is conducted according to a research plan known as the protocol. The protocol is designed to answer specific research questions and safeguard the health of participants. It contains the following information: The reason for conducting the study. Who may participate in the study (the eligibility criteria)
Chasing WATERFALLs — The Journey from Question to Answer. E. de-MadariaNEJM Evid 2023;2 (7) This clinical trial case study discusses the process that led to the WATERFALL trial — from a question asked by a gastroenterology trainee more than two decades ago about fluid management in acute pancreatitis to the completed clinical trial ...
Clinical trials are scientific studies that involve people in research and are the only way to advance cancer treatment. Before people are given a new intervention, it is carefully studied in the laboratory. Studies with the most promising results are then moved into clinical trials with people. Clinical trials are used to evaluate new and ...
Michigan Institute for Clinical & Health Research (MICHR)1600 Huron Parkway, Building 400 Ann Arbor, MI 48109(734) [email protected]. Cite ItPlease help us continue our support for clinical and translational research by citing our grant number in relevant publications: UL1TR002240.
Clinical Trial Definition. A clinical trial, also known as a clinical study, is a research study conducted using human subjects who are prospectively assigned to one or more interventions. The ...
Back to top. Forms and Templates Administrative Forms. Site Signature Log - Delegation of Authority Log ( MS Excel, 47K or screen-readable PDF, 294K) A record of all study personnel and their specific responsibilities, signatures, and dates of involvement during the conduct of a clinical research study. Note to File Template (MS Word, 20K) - Used by clinical site staff to document protocol ...
For example, Facebook boasts over two billion user accounts. (As of 2020 the global population sits at 7.8 billion people.) According to Pew Research, almost 70% of adults in the United States used Facebook in 2019. With a population of 328 million people, this means that close to 230 million Americans are connected to the social media giant.
The following bullet points are a summary of the entry conditions for this study. Talk to your doctor or the study team if you are unsure about any of these. They will be able to advise you. Who can take part. For part 1 You may be able to join part 1 of the study if you have had a tissue sample taken (biopsy).
Bias in epidemiological studies can adversely affect the validity of study findings. Sensitivity analyses, known as quantitative bias analyses, are available to quantify potential residual bias arising from measurement error, confounding, and selection into the study. Effective application of these methods benefits from the input of multiple parties including clinicians, epidemiologists, and ...
Background: Novel therapeutics should always be tested in a sample representative of the population in need of treatment. Initial efforts of drug development take place in early phase trials (phase-I and -II), setting the direction for late-stage studies (phase-III and -IV). However, study samples in early phase trials typically fail to recruit Black, Asian and minority ethnic groups, which ...
Background Research shows a significant growth in clinical leadership from a nursing perspective; however, clinical leadership is still misunderstood in all clinical environments. Until now, clinical leaders were rarely seen in hospitals' top management and leadership roles. Purpose This study surveyed the attributes and skills of clinical nursing leadership and the actions that effective ...
Similarly, if the sample size is too large, the study will be more difficult and costly, and may even lead to a loss in accuracy. Hence, optimum sample size is an essential component of any research. Careful consideration of sample size and power analysis during the planning and design stages of clinical research is crucial.
Meditation has been studied in many clinical trials. The overall evidence supports the effectiveness of meditation for various conditions, including: ... For example, when you eat a favorite food, take the time to smell, taste and truly enjoy it. Live in the moment. Try to intentionally bring an open, accepting and discerning attention to ...
The generalizability of clinical research findings is based on multiple factors related to the internal and external validity of the research methods. The main methodological issue that influences the generalizability of clinical research findings is the sampling method. ... When doing a research study, we should consider the sample to be ...