- How it works


Useful Links
How much will your dissertation cost?
Have an expert academic write your dissertation paper!
Dissertation Services
Get unlimited topic ideas and a dissertation plan for just £45.00
Order topics and plan
Get 1 free topic in your area of study with aim and justification
Yes I want the free topic
Latest List of Best Diabetes Dissertation Topics
Published by Owen Ingram at January 2nd, 2023 , Revised On May 17, 2024
The prevalence of diabetes among the world’s population has been increasing steadily over the last few decades, thanks to the growing consumption of fast food and an increasingly comfortable lifestyle. With the field of diabetes evolving rapidly, it is essential to base your dissertation on a trending diabetes dissertation topic that fills a gap in research.
Finding a perfect research topic is one of the most challenging aspects of dissertation writing in any discipline . Several resources are available to students on the internet to help them conduct research and brainstorm to develop their topic selection, but this can take a significant amount of time. So, we decided to provide a list of well-researched, unique and intriguing diabetes research topics and ideas to help you get started.
Other Subject Links:
- Evidence-based Practice Nursing Dissertation Topics
- Child Health Nursing Dissertation Topics
- Adult Nursing Dissertation Topics
- Critical Care Nursing Dissertation Topics
- Palliative Care Nursing Dissertation Topics
- Mental Health Nursing Dissertation Topics
- Nursing Dissertation Topics
- Coronavirus (COVID-19) Nursing Dissertation Topics
List of Diabetes Dissertation Topics
- Why do people recently diagnosed with diabetes have such difficulty accepting reality and controlling their health?
- What are the reactions of children who have recently been diagnosed with diabetes? What can be done to improve their grasp of how to treat the disease?
- In long-term research, people getting intensive therapy for the condition had a worse quality of life. What role should health professionals have in mitigating this effect?
- Why do so many individuals experience severe depression the months after their diagnosis despite displaying no other signs of deteriorating health?
- Discuss some of the advantages of a low-carbohydrate, high-fat diet for people with diabetes
- Discuss the notion of diabetes in paediatrics and why it is necessary to do this research regularly.
- Explain the current threat and difficulty of childhood obesity and diabetes, stressing some areas where parents are failing in their position as guardians to avoid the situation
- Explain some of the difficulties that persons with diabetes have, particularly when obtaining the necessary information and medical treatment
- Explain some of the most frequent problems that people with diabetes face, as well as how they affect the prevalence of the disease. Put out steps that can be implemented to help the problem.
- Discuss the diabetes problem among Asian American teens
- Even though it is a worldwide disease, particular ethnic groups are more likely to be diagnosed as a function of nutrition and culture. What can be done to improve their health literacy?
- Explain how self-management may be beneficial in coping with diabetes, particularly for people unable to get prompt treatment for their illness
- Discuss the possibility of better management for those with diabetes who are hospitalised
- What current therapies have had the most influence on reducing the number of short-term problems in patients’ bodies?
- How have various types of steroids altered the way the body responds in people with hypoglycemia more frequently than usual?
- What effects do type 1, and type 2 diabetes have on the kidneys? How do the most widely used monitoring approaches influence this?
- Is it true that people from specific ethnic groups are more likely to acquire heart disease or eye illness due to their diabetes diagnosis?
- How has the new a1c test helped to reduce the detrimental consequences of diabetes on the body by detecting the condition early?
- Explain the difficulty of uncontrolled diabetes and how it can eventually harm the kidneys and the heart
- Discuss how the diabetic genetic strain may be handed down from generation to generation
- What difficulties do diabetic people have while attempting to check their glucose levels and keep a balanced food plan?
- How have some individuals with type 1 or type 2 diabetes managed to live better lives than others with the disease?
- Is it true that eating too much sugar causes diabetes, cavities, acne, hyperactivity, and weight gain?
- What effect does insulin treatment have on type 2 diabetes?
- How does diabetes contribute to depression?
- What impact does snap participation have on diabetes rates?
- Why has the number of persons who perform blood glucose self-tests decreased? Could other variables, such as social or environmental, have contributed to this decrease?
- Why do patients in the United States struggle to obtain the treatment they require to monitor and maintain appropriate glucose levels? Is this due to increased healthcare costs?
- Nutrition is critical to a healthy lifestyle, yet many diabetic patients are unaware of what they should consume. Discuss
- Why have injuries and diabetes been designated as national health priorities?
- What factors contribute to the growing prevalence of type II diabetes in adolescents?
- Does socioeconomic status influence the prevalence of diabetes?
- Alzheimer’s disease and type 2 diabetes: a critical assessment of the shared pathological traits
- What are the effects and consequences of diabetes on peripheral blood vessels?
- What is the link between genetic predisposition, obesity, and type 2 diabetes development?
- Diabetes modifies the activation and repression of pro- and anti-inflammatory signalling pathways in the vascular system.
- Understanding autoimmune diabetes through the tri-molecular complex prism
- Does economic status influence the regional variation of diabetes caused by malnutrition?
- What evidence is there for using traditional Chinese medicine and natural products to treat depression in people who also have diabetes?
- Why was the qualitative method used to evaluate diabetes programs?
- Investigate the most common symptoms of undiagnosed diabetes
- How can artificial intelligence help diabetes patients?
- What effect does the palaeolithic diet have on type 2 diabetes?
- What are the most common causes of diabetes and what are the treatments?
- What causes diabetes mellitus, and how does it affect the United Kingdom?
- The impact of sociodemographic factors on the development of type II diabetes
- An examination of the link between gut microbiome and diabetes risk
- The effectiveness of lifestyle interventions in preventing type II diabetes
- The role of maternal diabetes in offspring’s risk of developing diabetes
- Artificial intelligence in diabetes diagnosis and management
- Continuous glucose monitoring
- Telehealth interventions for improving diabetes self-management
- The role of wearable technology in diabetes management
- Personalised medicine approaches for diabetes treatment
- The impact of diabetes on mental health and well-being
- The link between diabetes and cognitive decline
- The potential of stem cell therapy for diabetes treatment
- Advances in closed-loop insulin delivery systems
- The use of glucagon-like peptide-1 (GLP-1) receptor agonists in diabetes treatment
- Investigating the efficacy of new oral medications for type II diabetes
- The role of bariatric surgery in the management of type II diabetes
- Improving patient adherence to diabetes treatment regimens
- The role of social support in diabetes management
- Developing culturally sensitive diabetes education programs
- The role of dietary patterns in diabetes prevention and management
- Low-carbohydrate vs. Mediterranean diet for diabetes: A comparative study
- The use of artificial sweeteners in diabetes management: Benefits and risks
- The impact of the gut microbiome on dietary interventions for diabetes
- The role of exercise in improving glycemic control
- Developing effective exercise programs for individuals with diabetes
- The impact of physical activity on diabetic complications
- Promoting physical activity adherence in people with diabetes
- The use of exercise gamification to increase physical activity in diabetes
- The potential of CRISPR gene editing for diabetes treatment
- The role of the microbiome in the development and treatment of diabetes
- An analysis of the artificial Pancreas systems
- The use of big data analytics in diabetes research
- The impact of environmental factors on diabetes risk
- Cost-effectiveness of different diabetes treatment strategies
- Developing effective diabetes prevention programs for communities
- The role of government policies in addressing the diabetes epidemic
- Improving access to diabetes care in underserved populations
- The impact of social determinants of health on diabetes risk
- Management of diabetes in children and adolescents
- The unique challenges of diabetes management in older adults
- Diabetes in ethnic minorities: Disparities in prevalence and care
- The impact of diabetes on LGBTQ+ populations
Hire an Expert Writer
Orders completed by our expert writers are
- Formally drafted in an academic style
- Free Amendments and 100% Plagiarism Free – or your money back!
- 100% Confidential and Timely Delivery!
- Free anti-plagiarism report
- Appreciated by thousands of clients. Check client reviews
You can contact our 24/7 customer service for a bespoke list of customised diabetes dissertation topics , proposals, or essays written by our experienced writers . Each of our professionals is accredited and well-trained to provide excellent content on a wide range of topics. Getting a good grade on your dissertation course is our priority, and we make sure that happens. Find out more here .
Free Dissertation Topic
Phone Number
Academic Level Select Academic Level Undergraduate Graduate PHD
Academic Subject
Area of Research
Frequently Asked Questions
How to find diabetes dissertation topics.
To find diabetes dissertation topics:
- Study recent research in diabetes.
- Focus on emerging trends.
- Explore prevention, treatment, tech, etc.
- Consider cultural or demographic aspects.
- Consult experts or professors.
- Select a niche that resonates with you.
You May Also Like
The study of cognitive psychology focuses on how the brain processes and stores information. The underlying mechanisms are investigated using experimental methods, computer modeling, and neuropsychology.
Family law dissertation topics are included in a section of UK law. This topic is more of a minor category in terms of your broader research. Family law dissertations are challenging.
Need interesting and manageable sociology dissertation topics? Here are the trending sociology dissertation titles so you can choose the most suitable one.
USEFUL LINKS
LEARNING RESOURCES

COMPANY DETAILS

- How It Works
- Open access
- Published: 28 March 2023
Nurses’ knowledge, attitudes, and practice with regards to nutritional management of diabetes mellitus
- Mahsa Farzaei 1 ,
- Shahla Shahbazi 2 ,
- Neda Gilani 3 ,
- Alireza Ostadrahimi 4 &
- Leila Gholizadeh 5
BMC Medical Education volume 23 , Article number: 192 ( 2023 ) Cite this article
4804 Accesses
1 Citations
2 Altmetric
Metrics details
The prevalence of diabetes is increasing rapidly worldwide. Nurses work collaboratively with multidisciplinary teams to improve diabetes management. Yet, little is known about nurses’ role in nutritional management of diabetes. This study aimed to evaluate nurses’ knowledge, attitudes, and practice (KAP) toward nutritional management of diabetes.
This cross-sectional study was conducted with 160 nurses, who were recruited between July 4 and July 18, 2021 from two referral tertiary teaching hospitals in Iran. A validated paper-based self-reported questionnaire was used to assess nurses’ KAP. Data were analyzed using descriptive statistics and multiple linear regression analysis.
The mean knowledge score of nurses about nutritional management of diabetes was 12.16 ± 2.83, and 61.2% showing a moderate knowledge level on nutritional management of diabetes. The mean attitudes score was 60.68 ± 6.11, with 86.92% of participants demonstrating positive attitudes. The mean practice score of study participants was 44.74 ± 7.81, with 51.9% having a moderate level of practice. Higher knowledge scores were observed among male nurses (B = -7.55, p = 0.009) and those with blended learning as a preferred learning method (B = 7.28, p = 0.029). Having an opportunity to provide education to patients with diabetes during shifts affected nurses’ attitudes positively (B = -7.59, p = 0.017). Practice scores were higher among nurses who perceived themselves competent in the nutritional management of diabetes (B = -18.05, p = 0.008).
Nurses’ knowledge and practice in the nutritional management of diabetes should be increased to help improve the quality of the dietary care and patient education they provide these patients. Further studies are needed to confirm the results of this study both in Iran and internationally.
Peer Review reports
Diabetes mellitus is one of the fastest growing chronic diseases globally, with a significant burden on individuals and societies [ 1 ]. Management of diabetes includes nutritional therapy, exercise, monitoring, pharmacologic therapy, and patient education. Nutritional management is a key element of diabetes care. An effective nutritional management helps achieve and maintain glycemic control and contributes to the well-being and quality of life of patients [ 2 ]. While registered dietitians or nutritionists take the main responsibility in nutritional assessment and management of patients with diabetes, nurses and other members of the health care team must be knowledgeable about diabetes nutrition therapy and support patients in implementation of nutritional and lifestyle changes [ 3 ].
Nurses are more likely to encounter patients with diabetes as the number of associated hospital admissions rises. Further, they are in unique position to improve the outcomes for patients with diabetes due to the length of time they spend with patients. The holistic nature of the nursing profession requires nurses to be informal nutrition advisors [ 4 ], and ensure that patients in hospital receive an appropriate diet. They assist patients at meal times, during which patients may seek dietary advice [ 5 ]. Thus, nurses should be aware of the guidelines for the nutritional management of diabetes [ 6 ].
Yet, results of previous studies suggest significant knowledge gap among nurses with regards to nutritional management of patients with diabetes [ 7 , 8 ]. Poor knowledge of health care providers of dietary requirements of patients with diabetes can lead to a poor glycemic control and increase the risk of diabetes-associated complications [ 9 ]. Further, nurses had the lowest attitudes towards diabetes management among healthcare professionals in the study by Babelgaith et al. [ 10 ]. Nurses’ negative attitudes can affect their practice on nutritional management of diabetes. Other factors include time, nutrition education, organizational support, and resource availability [ 11 , 12 , 13 ].
Strategies to reduce the incidence of hypoglycemia and hyperglycemia are imperative to patient safety, and effective nutritional management can help achieve and maintain target glycemic control. Therefore, it is important that nurses have adequate knowledge and positive attitudes toward nutritional management in patients with diabetes to improve their practice [ 14 , 15 ]. The healthcare system in Iran has recently mandated a comprehensive assessment of all patients on their hospital admission. As part of this program, nurses assess the nutritional status of patients and report those with a poor nutritional status, including those with poorly controlled diabetes, to the physician to request a nutritional consultation. Adequate knowledge, positive attitudes, and good practice of nurses are important to achievement of therapeutic goals for patients in diabetes and supporting patients in their self-care practice [15,16 ].
This study was underpinned by the KAP model, which considers using a structured standardized questionnaire to quantify and analyze what is known (knowledge), believed (attitudes), and done (practices) by a target population with regard to a topic of interest. Specific to this study, we aimed to develop an understanding of the knowledge level of nurse regarding of nutritional management of diabetes, and how the knowledge affected nurses’ attitudes and practice toward nutritional management of diabetes. Overall, studies investigating nurses’ KAP with regards to nutritional management of diabetes are limited, and to the best of our knowledge, there is no such a study in Iran. This study aimed to examine nurses’ KAP with regards to nutritional management of diabetes in Iran. Understanding nurses’ KAP about nutritional management of diabetes can generate evidence to inform the development of nutritional management programs. The specific objectives were to:
identify nurses’ knowledge about nutritional management of diabetes.
identify nurses’ attitudes toward nutritional management of diabetes.
identify nurses’ practice on nutritional management of diabetes.
identify relationships between nurses’ KAP about nutritional management of diabetes.
Identify multiple factors that affect nurses’ KAP about nutritional management of diabetes.
This study applied a descriptive cross-sectional design. Participants were recruited from 35 medical and surgical wards of two teaching tertiary referral hospitals in the Northwest of Iran using random sampling method. In the first step, all eligible nurses were identified from the 35 wards and their names were written on pieces of papers and folded and put in a box. The researchers then mixed the box before drawing out the required number of sample. To be eligible for the study, participants needed to have a minimum of a bachelor’s degree in nursing and be working as a fixed term registered nurse in a medical or surgical ward for at least one month. Information from a pilot study was used to calculate the sample size in this study. The required sample size increased to 156 participants when a possible dropout rate of 20% was considered. One hundred sixty participants were recruited to the study.
There is no diabetes educator position in Iran [ 17 ]. During data collection for this study, none of the participating hospitals had a designated diabetes educator or diabetes link nurse. However, both hospitals had a nutrition unit, which was responsible for providing general nutrition care for all forms of health conditions, including nutritional consultation to patients with diabetes.
Data collection tools
Data were collected using a self-report paper-based survey package containing four sections: The first section included questions about the socio-demographic and professional characteristics of nurses. The second section included the Nutritional Management of Diabetes Knowledge Test (NMDKT), designed and validated by Mogre et al. [ 5 ]. Its original version contains 21 questions; correct answers are scored 1, and others scored 0. Higher scores on the NMDKT represent higher level of knowledge about nutritional management of diabetes mellitus. A permission to modify and use the questionnaire for the current study was obtained from the designers (personal communication, November 3, 2019). The third section was the Nurses’ Attitudes about Nutritional Management of Diabetes Questionnaire, which developed by the researchers specifically for this study based on the WHO and the American Diabetes Association nutrition guidelines and the review of the relevant literature [ 2 , 16 , 18 ]. It contained 15 questions and used a five-point Likert scale, with responses ranging from strongly disagree (1) to strongly agree (5). Total scores could range from 15 to 75. The scores were then standardized between 0 to100 and categorized to three categories of high (66.6–100), moderate (33.3–66.6), and poor attitudes (0-33.3).
The final section included the Nurses’ Practice on Nutritional Management of Diabetes Questionnaire. This questionnaire was also developed by the researchers. It contained 15 questions and used a four-point Likert scale, with responses ranging from never (1) to always. Total practice scores could range from 15 to 60. The scores on practice about nutritional management of diabetes mellitus were then standardized between 0 to100 and categorized to three categories of good (66.6–100), moderate (33.3–66.6) and poor practice (0-33.3).
Validity and reliability
The survey package was submitted to a panel of 13 experts, 4 in nutrition and 9 in nursing, for evaluation of the face and content validity. The questionnaire was revised based on the comments of the review panel and resubmitted for further evaluation. For example, question 12 was removed for a cultural reason. The panel approved all the items as appropriate, assuring good content validity. In addition, the Content Validity Ratio (CVR) and content validity index (CVI) of all questionnaires were assessed and the results supported the content validity of the used tools. The CVR and CVI for were 0.99 and 0.98, respectively. The Nurses’ Attitudes about Nutritional Management of Diabetes Questionnaire had the CVR and the CVI of 0.99 and 1.00, respectively, and the Nurses’ Practice on Nutritional Management of Diabetes Questionnaire demonstrated the CVR and the CVI of 0.99 and 1.00, respectively. Using Cronbach’s alpha to measure internal consistency, a reliability coefficient of 0.65 was attained for the NMDKT, 0.83 for the Nurses’ Attitudes on Nutritional Management of Diabetes Questionnaire, and 0.90 for the Nurses’ Practice on Nutritional Management of Diabetes Questionnaire. The questionnaire took an average 17.88 ± 9.40 min to complete.
Thus, we used the NMDKT containing 20 questions in this study. Total row scores ranged from 0 to 20. The NMDKT scores were then standardized between 0 to100 and categorized to three categories of high (66.6–100), moderate (33.3–66.6) and poor knowledge (0-33.3).
Ethical considerations
The study received ethical approval from the Regional Research Ethics Committee of Tabriz University of Medical Sciences (Approval ID: IR.TBZMED.REC.1399.844), was carried out in accordance with the Declaration of Helsinki. Potential nurses were informed about the study and what participation would entail, and all provided informed consent before participating in the study. Permission to have access to the hospitals was obtained from hospital mangers. The survey was anonymous, and participants were ensured that the data could not be traced back to individual participants or hospitals.
Data analysis
Data were analyzed using descriptive statistics to characterize respondents’ profiles. This included reporting mean values and standard deviations for continuous variables and frequency and percentages for categorical and ordinal variables. Relationship between KAP concepts was assessed by Pearson’s correlation coefficient, and multiple linear regression analysis was used to identify the significant associates of KAP. Analyses were conducted using the IBM SPSS for Windows, Version 24.0 statistical software package. A p-value of < 0.05 was considered statistically significant.
Characteristics of the participants
Demographic characteristics and professional and educational background of the study nurses were summarized in Table 1 . All potential participants, who were invited to participate, accepted the invitations except three nurses (acceptance rate of 98.16%). Two nurses rejected the study of due to heavy workload due and one nurse due to sickness. The mean age of participants was 30.31 ± 6.32 years; the majority were female (n = 110, 68.75%), and had a Bachelor’s degree in Nursing (n = 158, 98.8%) while the remaining (n = 2, 1.2%) had a Master’s degree in Nursing in addition to a Bachelor of Nursing degree. Above half of the participants (n = 90, 56.3%) were working in medical wards and the remaining (n = 70, 43.8%) in the surgical wards. Only small number of nurses (n = 34, 21.3%) were satisfied with nutrition education they had received during university training. The majority of nurses in this study (n = 147, 91.9%) did not have a refresher training on diabetes (Table 1 ).
The first objective of this study was to identify nurses’ knowledge about nutritional management of diabetes. The result showed that the mean knowledge score was 12.16 ± 2.83, with minimum score of 4 and maximum score of 18. Based on standardized scores, 93(61.2%) participants demonstrated a moderate level of knowledge (Table 2 ).
The second objective was to identify nurses’ attitudes toward nutritional management of diabetes. The mean attitudes score was 60.68 ± 6.11. Based on standardized scores, 133(86.92%) participants demonstrated positive attitudes toward nutritional management of diabetes (Table 3 ).
The third objective was to identify nurses’ practice on nutritional management of diabetes. The mean practice score was 44.74 ± 7.8. Based on standardized scores 82(51.9%) of participants demonstrated a moderate level practice (Table 4 ).
The forth objective of this study was to identify relationships between nurses’ KAP about nutritional management of diabetes. The correlation between knowledge, attitudes, and practice was evaluated using the Pearson’s correlation analysis. There was a statistically significant correlation between both knowledge (r= -0.164, p = 0.045) and attitudes (r = 0.361, p < 0.001) with practice scores. However, the correlation between knowledge and attitudes was not statistically significant (r=-0.067, p = 0.423) (Table 5 ).
In the multiple linear regression analysis, gender and preferred method of learning were statistically significant correlates of participants’ knowledge of nutritional management of diabetes (Table 6 ). Higher knowledge was reported among male nurses (B = -7.55, p = 0.009), and those reported blended learning as their preferred learning method (B = 7.28, p = 0.029).
Only provision of diabetes education during working shifts was the statistically significant correlate of attitudes toward nutritional management of diabetes (Table 7 ). Positive attitudes scores were reported by nurses who provided diabetes education for patients during their work shifts (B = -7.59, p = 0.017).
The multiple linear regression analysis showed statistically significant relationships between hospital and feeling competent and practice on nutritional management of diabetes (Table 8 ). Higher practice scores were observed among nurses who were employed in hospital 2 and those who perceived themselves competent in the nutritional management of diabetes (B = -18.05, p = 0.008).
The findings of this study provide insights into nurses’ KAP about the nutritional management of diabetes. Overall, participants demonstrated a moderate level of knowledge on the nutritional management of diabetes. Knowledge forms the basis of professional practice. Knowledge deficits of diabetes care, including nutritional management of diabetes, imposes a significant risk to delivery of safe practice [ 7 ]. The results of a review study revealed a significant knowledge deficit in the core aspects of diabetes care among nurses globally [ 7 ]. Comparing our findings with the past research, the mean knowledge score in our study was higher than the overall 44% correct responses reported by Mogre et al. [ 5 ]. Also, Naz et al. reported that half nurses in their study had an unsatisfactory level of knowledge about diabetes and diabetes meal planning [ 6 ]. Badshah et al. found that the majority of nurses had poor knowledge regarding diabetic diet [ 19 ]. Likewise, the study by Oyewole et al. revealed nurses’ knowledge deficiency in some critical areas, such as diabetes diet [ 20 ]. Inadequate nutritional knowledge of nurses could lead to inaccurate information provided to diabetic patients, which may lead to poor diabetes management and an increase in the rate of diabetes-related complications and treatment costs [ 19 ].
The moderate level of knowledge found among the nurses in our study could be due the fact that nurses mostly had not received any diabetes education after graduation from university. Similar to the present study results, Samancioglu et al. reported that only 3.9% of the nurses had a certificate as a ‘diabetes educator’ in Turkey [ 21 ]. Likewise, Alhaiti et al. reported that most nurses in Saudi Arabia in their study (78.4%) had not received any refreshing training on diabetes [ 22 ]. Like many other countries [ 23 ], nurses in Iran receive 26 h of education on nutrition during their bachelor of nursing degree. Considering the dramatic rise in the prevalence of diabetes worldwide, educational curriculums in health-related fields should better focus on training health care professionals about diabetes care, including the nutritional management of diabetes [ 24 ].
The majority of nurses in our study demonstrated positive attitudes toward the nutritional management of diabetes mellitus, which is a promising finding. Similar to the present study, a study by Kim and Choue showed that most Korean nurses possessed positive attitudes about attending to nutritional needs of patients and showed a high desire to receive further training on patient nutrition [ 14 ]. In contrast to the current study, Oyewole et al. in Nigeria reported that 48.9% of nurses in their study exhibited negative attitudes toward diabetes care in general [ 20 ]. Positive attitudes can be considered as an opportunity to improve the knowledge and practice of nurses on the nutritional management of diabetes mellitus.
Overall nurses in the current study reported a moderate level of practice on the nutritional management of diabetes. Direct comparison to other studies is difficult due to limited studies assessing nurses’ practice with regards to nutritional management of diabetes. The available studies mostly assessed nurses’ practice in relation to diabetes in general or addressed nutritional management in hospitalized patients in general, with a few questions targeted on diabetes. Comparing our findings with available evidence, the mean practice score achieved by the nurses in this study was higher than scores reported by Emami et al. in Iran [ 18 ]. In the Emami et al.’s study, nurses acted poorly on nutritional screening and the subsequent referral to a dietician for professional assessment. Initial nutritional assessment of chronically ill patients, including those with poorly controlled diabetes can have a significant effect on patient outcomes. A reason for the suboptimal practice of nurses in our study could be due to time constraint, making the process of initial nutritional assessment of patients and their referral to a dietitian unrealistic in the clinical settings.
The current study found a positive correlation between knowledge and attitudes with practice. The research team could not find any study that attempted to find the correlation between KAP about nutrition management of diabetes among nurses in Iran. The knowledge scores of nurses about nutritional management of diabetes were significantly higher among male nurses and nurses who selected blended learning as their preferred learning method. Similar to this finding, in the study conducted by Mogre et al. in Ghana, male nurses scored higher than female nurses on the NMDKT [ 5 ].
Furthermore, the present study revealed an association between attitude scores and involvement in diabetes education. Nurses who provided education to diabetic patients during their work possessed more positive attitudes toward nutritional management of diabetes. Higher practice scores were observed among nurses who were employed in hospital 2. One reasonable explanation to this finding could be that hospital 1 had an endocrine ward, admitting most patients with diabetes. This might have caused the nurses of other wards in hospital 1 have less exposure to patients with diabetes, and develop competency in managing the nutritional care needs of patients with diabetes. Supporting this explanation, practice scores in this study were positively associated with nurses’ perceived competency in nutritional management of diabetes.
Limitations
The results of this study contributed to our understanding of nurses’ KAP on the nutritional management of diabetes in Iran. Using random sampling method and recruiting participants from two tertiary referral teaching hospitals increase the generalizability of the findings. However the self-report nature of the data is a limitation. Also, this study was conducted in hospital settings, it should be noted that only small percentage of patients with diabetes are admitted to hospitals, and the main part of diabetes care is provided in primary care settings or outpatient clinics. Thus, the results of this study are applicable to hospital settings only.
Conclusions
Nurses in this study demonstrated a moderate level of knowledge and practice in relation to the nutritional management of diabetes mellitus, although their attitude toward this aspect of patient care was positive. Being a male nurse, having a preference for blended learning, having opportunities to get involved in providing education to diabetes patients during work, hospital where employed, and perceive competency in the nutritional management of diabetes affected nurses’ knowledge, attitudes, and practice. Given the growing trend of diabetes worldwide and the role of nutrition in diabetes management, it is necessary to improve the knowledge, attitudes, and practice of nurses about the nutritional management of diabetes. The educational curriculums should be examined for adequate education of nurses about diabetes care.
Data Availability
The datasets generated and/or analyzed during the current study are not publicly available due to agreements with participants who restricted data sharing but are available from the corresponding author on reasonable request.
Sørensen H, Toft. Prevention of diabetes mortality at ages younger than 25 years: access to medications and high-quality health care. Lancet Diabets Endocrionol. 2022;10(3):151–2.
Article Google Scholar
Middelbeek RJ, Hafida S, Schrager C. Medical nutrition therapy for the treatment of diabetes: prioritizing recommendations based on evidence. nutrition guide for physicians and related healthcare professions.Springer; 2022:pp. 109–119.
Brunner L, Sholtis SCO, Smeltzer. Suddarth. Brunner & Suddarth’s textbook of medical-surgical nursing. Volume 2. Lippincott Williams & Wilkins; 2010.
Henning M. Nursing’s role in nutrition. CIN: Computers Informatics Nursing. 2009;27(5):301–6.
Google Scholar
Mogre V, Ansah GA, Marfo DN, Garti HA. Assessing nurses’ knowledge levels in the nutritional management of diabetes. Int J Afr Nurs Sci. 2015;3:40–3.
Naz S, Jan A, Muhammad D. Assessment of nurses ’knowledge regarding nutritional management of diabetic patients in public and private sector tertiary care hospital, Peshawar. Rehman J Health Sci. 2021;3(2):68–71.
Alotaibi A, Al-Ganmi A, Gholizadeh L, Perry L. Diabetes knowledge of nurses in different countries: an integrative review. Nurse Educ Today. 2016;39:32–49.
Alotaibi A, Gholizadeh L, Al-Ganmi AHA, Perry L. Factors influencing nurses’ knowledge acquisition of diabetes care and its management: a qualitative study. J Clin Nurs. 2018;27(23–24):4340–52.
Mian SI, Brauer PM. Dietary education tools for South Asians with diabetes. Can J Diet Pract Res. 2009;70(1):28–35.
Babelgaith SD, Alfadly S, Baidi M. Assessment of the attitude of health care professionals towards diabetes care in Mukalla, Yemen. Int J Public Health Sciences. 2013;2(4):159–64.
Boocock RC, Lake AA, Haste A, Moore HJ. Clinicians’ perceived barriers and enablers to the dietary management of adults with type 2 diabetes in primary care: a systematic review. J Hum Nutr Dietetics. 2021;34(6):1042–52.
Gianfrancesco C, Johnson M. Exploring the provision of diabetes nutrition education by practice nurses in primary care settings. J Hum Nutr Dietetics. 2020;33(2):263–73.
Hulbert LR, Zhang X, Ng BP, Nhim K, Khan T, Cannon MJ. Health Care Providers’ knowledge, attitudes, and Practices and the Association with Referrals to the National Diabetes Prevention Program Lifestyle Change Program. Am J Health Promotion. 2022;36(2):236–47.
Kim H, Choue R. Nurses’ positive attitudes to nutritional management but limited knowledge of nutritional assessment in Korea. Int Nurs Rev. 2009;56(3):333–9.
Al-Mugheed K, Bayraktar N, Al-Bsheish M, AlSyouf A, Jarrar Mt, AlBaker W, Aldhmadi BK. Patient safety attitudes among doctors and nurses: associations with workload, adverse events, experience. Healthcare. Vol.10. No.4. MDPI. 2022: 631.
RPHN EYORR. Primary Health Care Nurses’ Competencies and Resources availability for diabetes Mellitus Care at Local Government Areas of Ibadan. Int J Caring Sci. 2020;13(1):368–80.
Yazdani F, Abazari P, Haghani F, Iraj B. The most prominent problems of diabetes education in Iran: A qualitative content analysis.Journal of Education and Health Promotion. 2021;10.
Emami M, Zarezadeh M, Sharifzadeh M, Fazelifarsani Z, Khorshidi M. Evaluation of nutritional assessment quality and rate of referral to dietitian in Shariati hospital, Tehran-Iran: a clinical audit. J Nutritional Sci Dietetics. 2019;5(1):8–13.
Badshah S, Naz S, ullah S, Aziz F, Bibi K, Wahab N, Akhtar R, Akhtar T, uddin N. Knowledge of Nurses regarding Nutritional management of Diabetes mellitus Patients in Tertiary Care Hospitals, Peshawar. IJRDO -Journal of Health Sciences and Nursing. 2020; 5(1).
Oyewole EY, Ojewale LY, Abimbola OO. Primary Health Care Nurses’ Competencies and Resources availability for diabetes Mellitus Care at Local Government Areas of Ibadan. Int J Caring Sci. 2020;13(1):368–80.
Samancioglu S, Ozturk Donmez R, Arda Surucu H, Bayindir Cevik A. Experiences of clinic nurses regarding diabetes education in Turkey’health system. Health Syst Policy Res. 2017;4(3):1–5.
Alhaiti AH, Senitan M, Shanmuganathan S, Dacosta C, Jones LK, Lenon GB. Nurses’ attitudes towards diabetes in tertiary care: a cross-sectional study. Nurs Open. 2019;6(4):1381–7.
Al-Shwaiyat NM, Sinjillawi AB, Al-Rethaiaa AS, Fahmy A-EA, Al-Saraireh RM, Aqel MM, Al-Hajjaj SM, Al-Sbou AS. Assessment of therapeutic nutritional knowledge of jordanian nurses. Int J Nutr Food Sci. 2013;2(3):142–8.
Kobos E, Imiela J, Kryczka T, Szewczyk A, Knoff B. Actual and perceived knowledge of type 1 diabetes mellitus among school nurses. Nurse Educ Today. 2020;87:104304.
Download references
Acknowledgements
The present study is a part of a master of nursing thesis. The research proposal was approved and supported by Tabriz University of Medical Sciences. Hence, the researchers feel obliged to thank Tabriz University of Medical Sciences for their support. In addition, the authors would like to thank the nurses who participated in this study. We would also like to thank Dr. Victor Mogre for the permission to use the Nutritional Management of Diabetes Knowledge Test (NMDKT) in this study. Finally, we would like to thank the Clinical Research Development Unit, Sina Educational, Research, and Treatment Center, Tabriz University of Medical Sciences, for their assistance in this research.
Not applicable.
Author information
Authors and affiliations.
Department of Medical-Surgical Nursing, Faculty of Nursing and Midwifery, Tabriz University of Medical Sciences, P.O. Box 51745347, Tabriz, Iran
Mahsa Farzaei
Department of Medical- Surgical Nursing, Faculty of Nursing and Midwifery& Clinical Research Development Unit, Sina Educational, Research and Treatment Center, Tabriz University of Medical Sciences, P.O. Box 51745347, Tabriz, Iran
Shahla Shahbazi
Department of Statistics and Epidemiology, Faculty of Health, Tabriz University of Medical Sciences, Tabriz, Postal code: 166614711, Iran
Neda Gilani
Nutrition Research Center, Department of Clinical Nutrition, School of Nutrition & Food Sciences, Tabriz University of Medical Sciences, Tabriz, Postal code: 5166614711, Iran
Alireza Ostadrahimi
Faculty of Health, University of Technology, PO Box 123, Broadway, Sydney, NSW, 2007, Australia
Leila Gholizadeh
You can also search for this author in PubMed Google Scholar
Contributions
Study design: ShSh, MF, NG, AOR; Acquisition of data: MF; Analysis and interpretation of data: NG, MF; Drafting of the article: ShSh, LG; All authors read and approved the final manuscript.
Corresponding author
Correspondence to Shahla Shahbazi .
Ethics declarations
Ethics approval and consent to participate.
The study received ethical approval from the Regional Research Ethics Committee of Tabriz University of Medical Sciences. (Approval ID: IR.TBZMED.REC.1399.844). The Declaration of Helsinki was followed in conducting the study. Participants received information about the objectives of the study and provided informed consent before participating in the research. Permission to access the hospitals was obtained from hospital administrators. The study was anonymous and collected data could not trace back to individual respondents or hospitals.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Farzaei, M., Shahbazi, S., Gilani, N. et al. Nurses’ knowledge, attitudes, and practice with regards to nutritional management of diabetes mellitus. BMC Med Educ 23 , 192 (2023). https://doi.org/10.1186/s12909-023-04178-4
Download citation
Received : 18 April 2022
Accepted : 20 March 2023
Published : 28 March 2023
DOI : https://doi.org/10.1186/s12909-023-04178-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Nutritional
- Diabetes mellitus
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Open access
- Published: 24 May 2022
The experiences of patients with diabetes and strategies for their management during the first COVID-19 lockdown: a qualitative study
- Mireia Vilafranca Cartagena ORCID: orcid.org/0000-0003-2953-3196 1 , 2 ,
- Glòria Tort-Nasarre ORCID: orcid.org/0000-0001-5270-821X 3 , 4 , 5 ,
- Maria Romeu-Labayen ORCID: orcid.org/0000-0001-9482-9474 5 , 6 &
- Josep Vidal-Alaball ORCID: orcid.org/0000-0002-3527-4242 7 , 8
BMC Nursing volume 21 , Article number: 124 ( 2022 ) Cite this article
3406 Accesses
6 Citations
3 Altmetric
Metrics details
During the pandemic, primary care systems prioritised attention to COVID-19 patients; chronically ill patients, such as people with Type 2 Diabetes were obliged to take more responsibility for their own care. We aimed to analyse the experiences of patients with Type 2 Diabetes Mellitus during the stay-at-home order that was in place during the first wave of the COVID-19 pandemic and identify the strategies and resources used in managing their care.
We conducted a qualitative descriptive study. The participants were ten patients with type 2 Diabetes Mellitus who experienced strict lockdown during the first wave of the COVID-19 pandemic in Catalonia, Spain, selected using intentional sampling. We recorded semi-structured interviews with the participants and conducted thematic analysis.
We identified 14 subthemes, which we then grouped into three overarching themes: 1) anxiety, fear, and vulnerability (anxiety, fear, vulnerability, rethinking life, loneliness, sadness), 2) insufficient diabetes monitoring by the health system (health care received, glycaemic control, view of treatment by health providers) and proactive self-care (changes in daily routine, diet, physical activity, medication, personal protective equipment & social distancing).
Despite the exceptional nature of the situation and the stress, worry, and changes in their daily lives, many respondents reported that they had successfully modified their lifestyles. Self-care was effective during confinement and was based on a process of adaptation using the resources available, without face-to-face contact with primary care health staff.
Relevance to clinical practice
These results can help to guide the design and implementation of self-care-focused strategies and also to explore new ways of empowering patients without access to health care personnel.
Peer Review reports
Introduction
Novel coronavirus disease (COVID-19) is a highly transmissible, rapidly spreading disease which has had a dramatic impact all over the globe. Although the overall mortality rate due to COVID-19 is relatively low [ 1 ], diabetes has emerged as a prominent comorbidity, associated with a severe and acute picture of respiratory distress and increased mortality. Thus, patients with chronic diseases such as type 2 diabetes (T2D) appear to be particularly vulnerable to the effects of the virus, and T2D is a major risk factor for poor prognosis in COVID-19 infection [ 2 ].
With the outbreak of the pandemic, governments imposed policies to reduce the transmission of the virus, including quarantine, isolation, social distancing and stay-at-home orders. These exceptional measures had a direct effect on the health behaviours of patients with chronic pathologies such as T2D [ 3 ]. Many patients with diabetes have encountered barriers to care due to the policies introduced to combat COVID-19, although maintaining good blood glucose control in these patients has proved to be an effective measure in preventing the transmission of the virus [ 4 ].
Type 2 diabetes cannot be cured, but lifestyle changes such as following a healthy diet, regular physical activity, and maintaining normal body weight can slow the progression of the disease and reverse its effects [ 5 ]. However, previous studies have shown that long-term maintenance of weight loss and complete adherence to diet and physical exercise recommendations is rare, especially in the adult population. Understandably, during the pandemic, many patients with T2D have found it particularly difficult to adhere to these lifestyle recommendations due to the restrictions on their access to health services and the problems in obtaining fresh food and in exercising [ 6 ].
In Catalonia (Spain), a stay-at-home order took place during the first wave of COVID-19, March 14 to May 2, 2020, at which time the measures were progressively relaxed. Stay-at-home orders (or “lockdown”) are implemented when quarantine for exposed patients and isolation for infected patients are insufficient to contain the spread of a disease [ 7 ]. During the seven weeks of strict lockdown in Spain, people were only allowed to leave home to receive medical treatment, buy food or work as an essential worker. Leaving home for exercise was prohibited, and non-essential businesses were shuttered.
Early research shows mixed effects of COVID-19 lockdowns on patients with diabetes. [ 8 ]) show that while glucose levels for type 1 diabetes patients improved significantly, those for T2D worsened in the short term. Makki et al. [ 9 ] show that patients with T2D had better glycaemic control during lockdown, but they do not specify whether the lockdown conditions were as strict as those in Spain.
Nursing professionals have a vital role to play in educating patients about the need to adapt their lifestyles and in helping them to modify their behaviour with respect to their health [ 10 ]. During the pandemic, primary care nurses have been obliged to prioritise care for COVID-19 patients [ 11 ], and as a result they have had to postpone the care of the chronically ill [ 12 ]. In this scenario, innovative strategies are needed to monitor and motivate diabetic patients who have had to take on more responsibility for their care [ 13 ].
Qualitative research on the experience of patients with COVID-19 has provided valuable information [ 4 ]. However, few qualitative studies have addressed the experiences of patients with chronic pathologies during the pandemic, and even fewer in patients with T2D. People with chronic conditions experienced a confluence of the COVID-19 pandemic and chronic diseases in the context of difficulty in accessing healthcare, sedentary lifestyle and increased stress and anxiety [ 14 ]. Shi et al. describes the perceived barriers to diabetes self-management of people with T2D during the pandemic: inadequate knowledge and behavioural beliefs, shortage of resources, health problems, negative emotions and lack of support [ 15 ]. A structured analysis of the experiences of these patients would provide a valuable tool for organising the community and human resources needed in similar situations.
The aim of the present study is to analyse the experiences of patients with T2D that were under a stay-at-home order during the first wave of the COVID-19 pandemic and to identify the strategies and resources used in the management of T2D in this new situation.
We conducted a qualitative descriptive study, a design that is suited to arriving at a deeper understanding of practice in applied disciplines and is especially pertinent when the goal is to understand participants’ perspective and experience [ 16 ]. We began with a deductive approach to develop the interview guide and then conducted an inductive analysis of the resulting data. The study is part of an ongoing project about diabetes and physical activity, which was underway when the pandemic began (Authors, in progress).
Participants
Sampling was intentional [ 17 ]. The participants were the ten patients with T2D from four different primary health centres in central Catalonia (Spain) that were participating in our ongoing study about diabetes and physical activity. The inclusion criteria were adults aged 55 to 79 years diagnosed with T2D at least two years previously. We chose this age range because 55 is the age at which the prevalence of T2D begins to increase rapidly in the population, and a cut-off at 79 allowed us to ensure that participants were young enough to conduct physical activity [ 18 ]). Additional inclusion criteria were having no complications associated with T2D, having good metabolic control (hbA1c < 7), and showing good adherence to T2D treatment (defined as adherence to prescribed medication for T2D, physical activity > 150 min/week, and healthy diet). The exclusion criteria were gestational diabetes or type 1 diabetes, cognitive impairment, or admission to hospital during confinement. All ten participants from our initial study agreed to a follow-up interview about their experiences of COVID-19. Data saturation [ 19 ] was reached by the tenth interview, when we detected that no relevant new information was emerging.
Data collection
Data were collected through a semi-structured interview. The research team developed a set of interview questions relevant to the study objectives, based on the researchers’ clinical experience and a review of the scarce existing literature about patients with chronic illness during the pandemic: How is the COVID-19 pandemic affecting you as a person with diabetes? Can you describe the effect of the stay-at-home order on you at a personal, family, and professional level? Describe to me the care you received for your T2D during the stay-at-home order. How did your lifestyle change (In what sense? Can you tell me?). During the interview, follow-up questions were asked to encourage participants to provide additional details about their perspective.
The interviews were conducted by the principal investigator (PI) between July 2020 and January 2021. In the initial interviews for the ongoing study about T2D and physical activity, the PI had conducted interviews with the participants lasting approximately 45 min. When the pandemic broke out, the team devised a second phase of the study, and the PI invited the participants to a follow-up interview about their COVID-19 experiences. All ten agreed to participate and gave their informed consent. We opted for telephone interviews because we thought it would be easier for participants than video conferencing. We suggested that participants conduct the interview from a quiet place in which they wouldn’t be interrupted. This second interview lasted between 15 and 35 min, meaning that for each participant we have a total of between 60 and 80 min of recorded data. Participants’ confidentiality was protected by giving them pseudonyms. The voice files and transcriptions were encrypted and stored on a computer protected with an encrypted password. The interviews were performed and transcribed in Catalan or Spanish, depending on the preference of the participant. Later, the transcribed interviews were returned to participants for their approval. All participants accepted their transcribed interviews without changes.
Data analysis
Data were analysed using thematic analysis [ 20 ] by ATLAS ti ®vs 9 support. We identified and reported patterns that emerged from the data and arranged them systematically to shed light on the research questions, while trying to keep faithful to the perspectives expressed by participants [ 16 ]. We conducted the analysis in the following phases:
Phase 1 Become familiar with the data by listening to recordings, transcribing them, and reading and rereading the transcripts. Entering transcripts into software Atlas-ti vs 9. Author 1 (MCV) participated in this phase.
Phase 2: Segmenting the meaning units in the transcripts and inductively grouped them to create subthemes and identify relationships among them. Author 1 participated in this phase.
Phase 3: Group the meaning units and abstracted the subthemes. Define the parameters of each subtopic. 14 subtopics have been tagged. Author 1 participated in this phase.
Phase 4: Group the subthemes into overarching themes (which became the primary structure for our analysis). Which in turn we grouped into three themes. Devise a glossary of themes. Author 1 participated in this phase.
Phase 5: Revised, discussed and agreed upon the subthemes and themes while returning to the data to verify the analysis. Authors 1, 2 (MRL) and 4 (GTN) participated in this phase.
Phase 6: Write the research report. Authors 1, 2 and 4 participated in this phase. Author 3 (JVA) examined both the processing and product of the research study.
Rigour, reflexivity and quality criteria
The trustworthiness of data was determined by Credibility, Dependability, Conformability, Transferability [ 21 ].
Credibility has been achieved thanks to the analyst triangulation, to undertook constant revisions of the themes, subthemes and units of analysis and evaluation, ensuring qualitative validity by authors 1, 2 and 4. Transferability has been achieved by describing a phenomenon in sufficient detail to transferable to other settings and people. Dependability was ensured in this study thanks to the review by the third researcher who examined both the processing and product of the research study. Confirmability was achieved through the reflective effort of each researcher to be aware of and try to limit the influence of their own positionality on their analysis. As well as a transparent description of the research steps taken from the start of a research project. All methods were carried out by relevant guidelines and regulations.
The research team have experience with qualitative research and resolved disagreements by consensus, and complied with the Consolidated Criteria for Reporting Qualitative Research [ 22 ].
Ten patients with T2D from four primary care centres in central Catalonia (Spain) participated in the study. Table 1 displays the participants’ main sociodemographic characteristics. Ages ranged from 58 to 79 years, and 60% of participants had had T2D for more than 10 years; most also had a past history of pathology other than T2D.
In our inductive analysis, we identified 14 subthemes, which we grouped into three themes: 1) anxiety, fear and vulnerability, 2) insufficient diabetes monitoring by the health system, and 3) proactive self-care. Table 2 shows an example of the final themes, the codes from which they are built, and an example of a meaning unit from each code.
Anxiety, fear and vulnerability
The context of pandemic and confinement had a strong emotional impact on participants, and the most-expressed emotions were anxiety, fear, and vulnerability. Participants described the lockdown during first wave of the pandemic as something that was totally abnormal and hard to believe; they were shocked to hear the news of the number of deaths in Spain every day:
I thought I was dreaming. I thought this shouldn’t be happening in this day and age 3: 1 (P3).
One issue that respondents mentioned was the fear of infecting others, despite all the protective measures they used. For example, one participant, a health centre worker, was afraid of contagion in spite of the measures she took with her family:
In fact, at first I was worried that I might pass it on to them; I was working, I think the worst time was before [the state of emergency] (…). I got a room ready in case I had to isolate 5:13 (P5).
They also reported negative emotions, such as anxiety and worry:
I have anxiety problems, what`s been getting me down is the fact that I’m feeling a little agoraphobic 8:10 (P8).
It was the anguish of being locked away, of thinking you couldn’t see my 5-year-old granddaughter. My brother …. the family … my daughter and my son… 4:3 (P4).
Others felt fear at seeing so many COVID-19 infections at close range:
We’re all a bit scared. My children have all been through it, three of my four grandchildren. My daughter-in-law has had some awful aftereffects 3: 8 (P3).
Or at living close to death:
Scared. Because you see that the people who started to fall ill were mainly over 55 years old and it really hits you … 6: 1 (P6).
It was made worse by the experience of the loss of friends and family, or by news of acquaintances being admitted to the ICU:
I felt very sad to think of all the people who … I have relatives who have died and … it affected me a lot … not being able to be there … not being able to be with them 3.3 (P3).
On the other hand, some of them managed to keep these feelings of sadness at bay, thanks to their contacts with family, mainly through social media and video conferencing.
I saw them on the phone … and that kept me happy 7:16 (P7).
This feeling of social isolation was extremely negative:
I took it badly because I couldn’t leave the house, I couldn’t see my friends… 9.1 (P9).
For some, it was a negative experience because it disrupted their everyday routines and their self-care.
I felt terrible, it disrupted everything for me. I go to the pool for my water aerobics class, and everything was closed (…). I felt really bad having to spend all day at home 1: 1 (P1).
I used to walk two hours a day, when I was confined because I stayed at home, and I started to put on weight again … 6.4 (P6).
On the other hand, some respondents reported that the confinement and the change in their daily routines was an opportunity for reflection and thinking about their lives:
Three months, locked up at home without singing, without walking, without exercising … I mean, it practically gives you a vision of yourself, the experience of being alone for so many days, it’s a bit like being in a monastery (…). From this point of view the confinement was quite interesting 10.5 (P10).
Insufficient diabetes monitoring by the health system
During the pandemic, health centres prioritised attention to COVID-19 patients, and on-site care of chronic diseases was postponed. Patients reported that their analyses and tests were cancelled:
During the pandemic no diabetes care was available. And even now, there are people who are being told over the phone that it isn’t important … they’re told not to come because no tests are being done 5.6 (P5).
Nonetheless, medication and supplies for diabetics were provided:
At the beginning of the pandemic, I went to look for supplies for diabetes and they gave me enough for three or four months 7.9 (P7).
Some respondents felt abandoned by the health staff who normally cared for them:
Abandoned… (silence) … The normal monthly check-up with the nurse to look at everything (…) didn’t happen. I also have blood tests every three or six months to check my sugar level… (…) but they didn’t happen either 8.2 (P8).
Some participants expressed not understanding the reason for the restriction:
Why can children go to school in a group, in a class, but a doctor can’t see you, they can only talk to you by phone … even though when you go for an appointment there’s a separation between you, the desk, you’re at least a yard away … and wearing their masks … and it turns out they can’t see you … well, a lack of personal protection … yes, you really notice it, because there has been a lot of neglect 8.5 (P8).
But others expressed more understanding of the situation even though they were not seen by health staff:
If you put yourself in their shoes, you realise they couldn't have done any more … 3.5 (P3).
Some patients realised that they had to take control of their disease, because no one else could help them; they ended up accepting the situation:
Well, you realise you’ve got to take care of yourself. And in all, a little self-discipline. Because I didn’t have anyone else to depend on, it was only me, there was no one else (P8).
Others stated that this situation did not affect them because they were already used to a patient-centred model and that the maximum responsibility for their care lay with them:
What sort of care do you expect? We have to care for ourselves … no matter how much they call me and ask me if I’m following my diet, if I’m eating properly, if I’m walking … no matter how much they call … it's up to you …. it's not an injury that you need someone to come and treat you, this is something that’s your own decision 4.5 (P4).
Most participants monitored their blood glucose:
Because I knew I had to check my glucose, I checked it every day and no problem 7.11 (P7).
Proactive self-care
In the management of their disease during lockdown, patients with T2D introduced changes in terms of their physical activity, diet, and medication. Given the impossibility of going outside to exercise, many adapted their physical activity to their home space:
Well, being at home, I coped quite well. I went out onto the rooftop, where I was able to move around and pass the time. I walked up the stairs two or three times. So, I coped quite well 2.2 (P2).
Many participants established routines and did their regular activities, at different levels of intensity:
Every day, every day, every day, and it started … first I started 15 min a day, and then went up to 45 min every day and more intense; I walked fast, then I ran, faster and faster until I got a sore back 4.4 (P4).
This change in physical activity was regarded as a problem by some, but not by others:
I would open all the doors of the apartment and go around until I got tired, and when I got tired, I stopped. It was very boring 1: 5 (P1).
As there was time for everything (…), establishing a routine of walking one hour in the morning and one in the afternoon was not too hard 10: 7 (P10).
However, others abruptly stopped taking exercise:
I didn't do any physical activity while the stay-at-home order lasted 6.6 (P6).
All participants had access to fresh food and their normal diet, since the food shops stayed open during lockdown.
The shops where I go have got everything, fish, meat, chicken, everything 11.9 (P1).
Most reported good adherence to their regular diet:
Well, I saw that I couldn’t … do anything else, or go out … well, it's better to take care of yourself a little, isn’t it? This is also unconscious because I don't think about being diabetic … it’s something I’ve just accepted …. 13.7 (P4).
Others ate between meals, out of stress or boredom:
When I’m nervous, when I’m anxious … there are people whose stomachs close up, but I’m the opposite. I have snacks even though I’m not hungry 12.2 (P3).
None of the respondents had trouble getting their usual medication, and they followed their prescriptions, although they stressed that they were taking the medication without any medical supervision:
What I did is what I always did, there was no change. I went to the pharmacy every month to get my medication 11.9 (P1).
Most participants complied with the recommendations regarding personal protective equipment, hand washing, disinfection, ventilation of the home, and social distancing.
I was careful with my mask, I washed my hands a lot, and cleaned the flat 3.11 (P3).
Some participants applied specific protective measures in their homes:
At the door everyone took off their shoes, and they left their coats in a separate room, they sprayed their hands continuously, and every other day I changed the bed linen, ventilated the flat, cleaned everything. (…). Every time I went to the bathroom I pulled the chain with the lid down, and then cleaned my hands with disinfectant and the toilet as well 4:14 (P4).
Others reported taking particularly strict protective measures, due to their condition:
I took much more care (than other people) because I’m diabetic 8:12 (P8).
Some participants reported that they kept their distance from others, due to their diabetes:
I kept away because I thought I was much more likely to infect them than they were to infect me … so to avoid contagion I kept away from them 8:17 (P8).
Or that their families imposed this distancing on them, in order to protect them:
I asked her [the participant’s granddaughter] to give me a kiss because I needed one, but she said, “No, grandma, I have to go to school, and I don't want to” … And I said, “I’ll just give you a little kiss on your head” and she said “No, no, no!” She wouldn’t let me … 3: 9 (P3).
We have analysed the experiences of patients with T2D in lockdown during the first wave of the COVID-19 pandemic in Catalonia, Spain, and their strategies for managing their disease. Patients with diabetes felt especially vulnerable to infection, and presented emotional difficulties similar to those recorded in patients with COVID-19 at home or with other chronic conditions [ 6 ]. However, despite the changes they experienced in their daily lives and the barriers to accessing chronic care follow-up in primary care centres, they were able to establish routines for self-care.
Fear, anxiety, and vulnerability
Global guidelines on containment measures for the prevention of COVID-19 place special emphasis on vulnerable populations, including people with diabetes [ 23 ]. Our results show that when patients were aware of the risk of contracting COVID-19 due to their T2D status they felt particularly vulnerable and fearful of falling ill. Our data are in line studies showing that having a chronic illness (including T2D), belonging to a risk group, or the death of a family member due to COVID-19 are positively associated with fear of COVID-19 [ 24 ]. The emotional impact of the pandemic was considerable, as the necessary lifestyle changes caused feelings of anxiety among many patients. Elsewhere, the pandemic has been associated with increased stress in general populations, and external stress may reduce physical activity and lead to a poorer diet [ 25 ].
The participants engaged in social distancing due to their fear of infecting others but found the experience to be emotionally challenging. Indeed, due to the high mortality related to COVID and the frequency of near-death experiences, an increased awareness of mortality has been reported during lockdown [ 25 ]. Not only diabetic patients have this perception: other patients with chronic and immunocompromised diseases such as cancer, rheumatoid arthritis, asthma, Crohn’s disease, hypertension, and cardiovascular disease also felt anxiety and fear during the pandemic [ 26 ].
Despite the negative emotional experience of most, for some participants, the suspension of everyday life routines represented an opportunity for reflecting on what was most important to them.
In contrast to reports in other countries [ 27 ], our participants had no difficulty accessing medication or blood glucose control equipment such as glucose strips, needles, or glucometers. However, all of them encountered barriers to accessing primary care. Although they expressed understanding of the pandemic situation, many felt abandoned by the health care system, as other researchers have reported [ 28 ].
Our data suggest that the use of telemedicine and an e-Health model could achieve satisfactory levels of self-care especially in patients with an hb1Ac greater than 6. The popularisation of the Internet and the use of smartphones and emerging fifth-generation networks have allowed patients to attend medical appointments remotely instead of coming to the hospital during the COVID-19 outbreak.
Our results also provide relevant data regarding blood glucose control during the COVID-19 pandemic. Although diabetes is a primary risk factor for the development of severe and septic pneumonia due to infection, patients do not generally intensify their metabolic controls [ 29 ]. This may be due to a lack of information received from professionals monitoring the chronicity of primary pare or due to the lack of protocols or clinical practice guidelines adapted to the situation. In the study by [ 30 ], medication intake was significantly reduced during the pandemic, although in our study compliance with medication intake remained good.
Changes in the provision of health care due to the pandemic have created the need for greater attention to emotional and psychosocial health of patients with T2D. [ 31 ].
The measures imposed by the authorities affected the daily life of the general population as well as that of patients with T2D. In general, this situation was experienced negatively, given that it caused social and family isolation.
The restrictions introduced by the authorities to prevent or reduce the risk of virus transmission led to significant changes in diabetes control. One of the nursing strategies applied to address the needs of patients with T2D in primary care was to promote self-care. Self-care-focused nursing interventions can achieve significant improvements in responsibility for health, physical activity, nutrition, and stress management [ 32 ].
All patients had access to fresh food, since food shops remained open during the lockdown and most patients continued with their usual diets. Most already had a good adherence to diet, although some reported eating between meals out of boredom. Although our participants had access to medication and food, the pandemic made it more difficult to manage their diabetes [ 31 ].
The results show that the stay-at-home order forced patients with T2D to limit their activities, including physical activity. Barone et al. [ 33 ] found that physical activity in diabetic patients fell by 59.5% during the COVID-19 pandemic and suggested that this variable be closely monitored due to its potential negative consequences on metabolic and cardiovascular health. As regards physical exercise, some patients reported decreased activity; others adapted their routines at home to be able to carry out physical activities recommended for a healthy lifestyle, such as walking, running, and going up and down stairs. A few participants performed no physical activity during lockdown, and some achieved optimal T2D risk prevention values, by brisk walking or by observing the current recommendation of 150 min/week of moderate aerobic activity or 30 min/day for 5 days/week [ 34 ]. Despite these changes in behaviour, however, the amount of time devoted to exercise was not optimal for preventing the risks caused by diabetes. The emotional and social impact on certain patients may also be related to the reduction in physical activity, as regular exercise is acknowledged to improve the mental and social health of patients with T2D [ 35 ].
Limitations
This study has several limitations. The first is that the results can only be extrapolated to similar clinical contexts and similar users. The sample is small, and therefore is not representative of all T2D patients with a similar profile. This study can be a launch point, useful for comparison with larger studies in other contexts, to identify best practices in caring for people with T2D during a health crisis.
Second, the context in which the study was carried out was limited to primary care centres in Catalonia with specific sociodemographic characteristics and with good adherence to their prescribed T2D care. Including other types of patients from other geographic areas could provide different results.
Finally, our study includes only the perspective of patients. A fuller picture would emerge if the perspective of nurses monitoring diabetic patients were also included.
Conclusions
This study has provided information on the experiences and emotional responses of patients with T2D during home confinement and on the adaptation of the management of their pathology in Catalonia, Spain. All participants were diabetic patients with good adherence to treatment prior to the pandemic. Due to their health status, patients reported feeling highly vulnerable and fearful of infection. Despite this, patients with T2D were able to establish self-care routines for physical activity and nutrition. In some cases, the lack of access to their normal care at primary care centres made them feel abandoned, although the fact that they were well and that their blood sugar levels were within the recommended levels meant that they did not feel particularly anxious; in general, they were sympathetic to the situation of the health workers. A silver lining of the pandemic may be the way it allowed patients to take control of their disease. This pro-activity on the part of patients should be considered in preparation for future health crises.
Availability of data and materials
The interviews were conducted by the lead author and she is the only researcher who knew the identity of the participants. Her record of interviewees’ names and other personal information will be deleted after publication. Data will be provided upon reasonable request.
Ioannidis JPA. OMS | Tasa de letalidad por la infección de la COVID-19 calculada a partir de los datos de seroprevalencia. WHO [Internet]. World Health Organization; 2021 [Cited 2021 May 26]; Available from: http://www.who.int/bulletin/volumes/99/1/20-265892-ab/es/
Bellido V, Pérez A. Consequences of COVID-19 on people with diabetes. Endocrinol Diabetes y Nutr [Internet]. Elsevier Doyma; 2020 [cited 2021 May 26];67:355–6. Available from: https://www.elsevier.es/es-revista-endocrinologia-diabetes-nutricion-13-articulo-consecuencias-covid-19-sobre-personas-con-S253001642030104X
International Diabetes Federation. COVID-19: Perspectives from people with diabetes. Diabetes Res Clin Pract. 2020;163:108201. https://doi.org/10.1016/j.diabres.2020.108201 .
Banerjee M, Chakraborty S, Rimesh P. Diabetes self-management amid COVID-19 pandemic | Elsevier Enhanced Reader. Diabetes Metab Syndr [Internet]. 2020;14:351–4. [Cited 2021 May 26]. Available from: https://reader.elsevier.com/reader/sd/pii/S1871402120300783?token=FB54D3A227BBCC2E2790E384834A32E17A24F9748CDB1F68563AA3F7178AD32A01D7F49F8B1A42EF80BD4D2E9DEB83B3&originRegion=eu-west-1&originCreation=20210526105736 .
Schmidt SK, Hemmestad L, Macdonald CS, Langberg H, Valentiner LS. Motivation and barriers to maintaining lifestyle changes in patients with type 2 diabetes after an intensive lifestyle intervention (The U-TURN trial): A longitudinal qualitative study. Int J Env Res Public Heal. 2020;17:1–16 MDPI AG.
Google Scholar
Musche V, Kohler H, Bäuerle A, Schweda A, Weismüller B, Fink M, et al. Covid-19-related fear, risk perception, and safety behavior in individuals with diabetes. Healthc [Internet]. 2021;9:480. MDPI AG; [Cited 2021 Jul 19]. Available from: https://doi.org/10.3390/healthcare9040480 .
Sánchez-Villena AR, de La Fuente-Figuerola V. COVID-19: cuarentena, aislamiento, distanciamiento social y confinamiento, ¿son lo mismo? An Pediatr [Internet]. 2020;93:73–4. Elsevier; [Cited 2022 Mar 1]. Available from: https://www.analesdepediatria.org/es-covid-19-cuarentena-aislamiento-distanciamiento-social-articulo-S1695403320301776 .
Eberle C, Stichling S. Impact of COVID-19 lockdown on glycemic control in patients with type 1 and type 2 diabetes mellitus: a systematic review. Diabetol Metab Syndr [Internet]. BioMed Central Ltd. 2021;13:1–8. [Cited 2022 Mar 5]. Available from: https://doi.org/10.1186/s13098-021-00705-9 .
Makki I, Alnoon N, Rahmani N, Almulla J, Alamiri A, Alfalasi A, et al. Impact of COVID 19 Lockdown on Glycemic Control in Patients with Type 2 Diabetes Mellitus in Dubai. Curr Diabetes Rev [Internet]. Curr Diabetes Rev; 2021 [cited 2022 Mar 5];18. Available from: https://pubmed.ncbi.nlm.nih.gov/34879807/
Kemppainen V, Tossavainen K, Turunen H. Nurses’ roles in health promotion practice: An integrative review. Heal Promot Int. 2013;28:490–501.
Article Google Scholar
Agencia de SalutPública de Catalunya. INFORME-TECNIC-1-COVID-19–19032020. 2020.
Ojeda Ibáñez MF. Telemedicina como estrategia para el control de los pacientes con diabetes mellitus tipo ll en el contexto de pandemia por la COVID-19. Estado del arte [Internet]. Universidad Peruana Cayetano Heredia; 2021. Available from: https://repositorio.upch.edu.pe/handle/20.500.12866/9262
Zhai YK, Zhu WJ, Cai YL, Sun DX, Zhao J. Clinical- and cost-effectiveness of telemedicine in type 2 diabetes mellitus: a systematic review and meta-analysis. Medicine (Baltimore) [Internet]. Medicine (Baltimore); 2014 [cited 2022 Mar 1];93:e312. Available from: https://pubmed.ncbi.nlm.nih.gov/25526482/
Singh K, Kaushik A, Johnson L, Jaganathan S, Jarhyan P, Deepa M, et al. Patient experiences and perceptions of chronic disease care during the COVID-19 pandemic in India: a qualitative study. BMJ Open [Internet]. BMJ Open; 2021 [cited 2022 Mar 2];11. Available from: https://pubmed.ncbi.nlm.nih.gov/34145019/
Shi C, Zhu H, Liu J, Zhou J, Tang W. Barriers to self-management of type 2 diabetes during covid-19 medical isolation: A qualitative study. Diabetes Metab Syndr Obes [Internet]. 2020;13:3713–25. Dove Medical Press Ltd; [Cited 2021 Jul 22]. Available from: https://pubmed.ncbi.nlm.nih.gov/33116721/ .
Colorafi KJ, Evans B. Qualitative Descriptive Methods in Health Science Research. HERD [Internet]. 2016;9:16–25. HERD; [Cited 2022 Mar 7]. Available from: https://pubmed.ncbi.nlm.nih.gov/26791375/ .
Morse JM. Molding qualitative health research. Qual Heal Res [Internet]. SAGE PublicationsSage CA: Los Angeles, CA; 2011 [cited 2022 Mar 7];21:1019–21. Available from: https://journals.sagepub.com/doi/ https://doi.org/10.1177/1049732311404706
Tulloch H, Sweet S, Fortier M, Capstick G, Kenny G, Sigal R. Exercise facilitators and barriers from adoption to maintenance in the diabetes aerobic and resistance exercise trial. Can J Diabetes [Internet]. 2013;37:367–74. [Cited 2014 Dec 17]. Available from: http://www.sciencedirect.com/science/article/pii/S1499267113012744 .
Saunders B, Sim J, Kingstone T, Baker S, Waterfield J, Bartlam B, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant [Internet]. 2018;52:1893–907. Qual Quant; [Cited 2022 Mar 15]. Available from: https://pubmed.ncbi.nlm.nih.gov/29937585/ .
Braun V, Clarke V. What can ‘thematic analysis’ offer health and wellbeing researchers? Int J Qual Stud Health Well-being. 2014;9:20–2.
Guba E, Lincoln Y. Competing paradigms in qualitative research. In: Denzin N, Lincoln Y, editors. Handb Qual Res. Thousands Oaks, California: Sage; 1994. p. 105–17.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int J Qual Heal Care. 2007;19:349–57.
Beran D, Aebischer Perone S, Castellsague Perolini M, Chappuis F, Chopard P, Haller DM, et al. Beyond the virus: Ensuring continuity of care for people with diabetes during COVID-19. Prim Care Diabetes. 2021;15:16–7.
TzurBitan D, Grossman-Giron A, Bloch Y, Mayer Y, Shiffman N, Mendlovic S. Fear of COVID-19 scale: Psychometric characteristics, reliability and validity in the Israeli population. Psychiatry Res. 2020;289:113100 Elsevier Ireland Ltd.
Article CAS Google Scholar
Munekawa C, Hosomi Y, Hashimoto Y, Okamura T, Takahashi F, Kawano R, et al. Effect of coronavirus disease 2019 pandemic on the lifestyle and glycemic control in patients with type 2 diabetes: A cross-section and retrospective cohort study. Endocr J [Internet]. 2021;68:201–10. Japan Endocrine Society; [Cited 2021 Jul 21]. Available from: https://pubmed.ncbi.nlm.nih.gov/32999133/ .
Al-Rahimi JS, Nass NM, Hassoubah SA, Wazqar DY, Alamoudi SA. Levels and predictors of fear and health anxiety during the current outbreak of COVID-19 in immunocompromised and chronic disease patients in Saudi Arabia: A cross-sectional correlational study. PLoS One [Internet]. Public Library of Science; 2021 [cited 2021 Jul 22];16. Available from: https://pubmed.ncbi.nlm.nih.gov/33901260/
Wicaksana AL, Hertanti NS, Ferdiana A, Pramono RB. Diabetes management and specific considerations for patients with diabetes during coronavirus diseases pandemic: A scoping review. Diabetes Metab Syndr. 2020;14(5):1109–20. https://doi.org/10.1016/j.dsx.2020.06.070 .
Jeong IK, Yoon KH, Lee MK. Diabetes and COVID-19: Global and regional perspectives. Diabetes Res Clin Pr. 2020;166:108303 Elsevier Ireland Ltd.
Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL, et al. Practical recommendations for the management of diabetes in patients with COVID-19. Lancet Diabetes Endocrinol Elsevier Ltd. 2020;8:546–50.
Alshareef R, Zahrani A Al, Alzahrani A, Ghandoura L. Impact of the COVID-19 lockdown on diabetes patients in Jeddah, Saudi Arabia. Diabetes Metab Syndr Clin Res Rev [Internet]. 2020;14:1583–7. Elsevier Ltd; [Cited 2021 May 26]. Available from: https://pubmed.ncbi.nlm.nih.gov/32947759/
Fisher L, Polonsky W, Asuni A, Jolly Y, Hessler D. The early impact of the COVID-19 pandemic on adults with type 1 or type 2 diabetes: A national cohort study. J Diabetes Complicat [Internet]. J Diabetes Complications; 2020 [cited 2022 Mar 15];34. Available from: https://pubmed.ncbi.nlm.nih.gov/33059981/
Spoorenberg S, Wynia K, Uittenbroek RJ, Kremer H, Reijneveld SA. Effects of a population-based, person-centred and integrated care service on health, wellbeing and self-management of community-living older adults: A randomised controlled trial on Embrace. PLoS One. 2018;13. https://doi.org/10.1371/journal.pone .
Barone MTU, Harnik SB, de Luca PV, Lima BL de S, Wieselberg RJP, Ngongo B, et al. The impact of COVID-19 on people with diabetes in Brazil. Diabetes Res Clin Pr. 2020;166:108304. https://doi.org/10.1016/j.diabres.2020.108304 .
Colberg SR, Sigal RJ, Fernhall B, Regensteiner JG, Blissmer BJ, Rubin RR, et al. Exercise and type 2 diabetes: The American College of Sports Medicine and the American Diabetes Association: Joint position statement. Diabetes Care. 2010;33(12):e147–67. https://doi.org/10.2337/dc10-9990 .
Wylie TAF, Shah C, Connor R, Farmer AJ, Ismail K, Millar B, et al. Transforming mental well-being for people with diabetes: research recommendations from Diabetes UK’s 2019 Diabetes and Mental Well-Being Workshop. Diabet Med. 2019;36:1532–8.
Download references
Acknowledgements
The research team would like to thank all participants for their collaboration. We would also like to thank the expert Dr. Susan Frekko.
This research received no external funding.
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
Department of Nursing, Faculty of Health Science and Welfare, University of Vic-Central University of Catalonia (UVIC-UCC), Av. Universitaria 4-6, 08242, Manresa, Spain
Mireia Vilafranca Cartagena
Althaia Fundation, C/Dr Joan Soler 1-3, 08243, Manresa, Spain
Department of Nursing, Faculty of Nursing and Physiotherapy, University of Lleida, C/Montserrat Roig, 25198, Lleida, Spain
Glòria Tort-Nasarre
SAP ANOIA. Gerencia Territorial Catalunya Central. Institut Català de La Salut, 087272, Sant Fruitós del Bages, Spain
AFIN Research Group and Outreach Centre, Autonomous University of Barcelona. Campus Bellaterra, Cerdanyola del Vallès, Spain
Glòria Tort-Nasarre & Maria Romeu-Labayen
Department of Public Health, Mental Health and Mother-Infant Nursing, Faculty of Medicine and Health Sciences, University of Barcelona, L’Hospitalet del Llobregat, Spain
Maria Romeu-Labayen
Health Promotion in Rural Areas Research Group, Gerència Territorial de La Catalunya Central, Institut Català de La Salut, 08272, Sant Fruitós de Bages, Spain
Josep Vidal-Alaball
Unitat de Suport a La Recerca de La Catalunya Central, Fundació Institut Universitari Per a La Recerca a L’Atenció Primària de Salut Jordi Gol I Gurina, 08272, Sant Fruitós de Bages, Spain
You can also search for this author in PubMed Google Scholar
Contributions
The research team was formed by three nurses (authors 1, 2 and 4) and a medical doctor (author 3). All the authors have experience with qualitative research, but authors 2 and 4 have long experience. Author 4 proposed the study, contributed to its design and to data analysis and supervised the project. Author 2 contributed to analysis. Author 3 examined both the processing and product of the research study. Author 1, who is also the PI, conducted the interviews and contributed to the analysis and to writing the discussion. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Mireia Vilafranca Cartagena .
Ethics declarations
Ethics approval and consent to participate.
The study was approved by the ethics and research committee “Fundació Unió Catalana d'Hospitals” (code nº 19/45) and also complied with the principles of the Helsinki Declaration. Participants received verbal and written information explaining that their participation was voluntary and that they could withdraw from the project at any time. All participants provided informed consent. All interviews were anonymised by assigning an alphanumeric code in observance of the Spanish legislation on personal data protection of 2018.
Consent for publication
All the authors gave their consent for publication.
Competing interests
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Vilafranca Cartagena , M., Tort-Nasarre, G., Romeu-Labayen, M. et al. The experiences of patients with diabetes and strategies for their management during the first COVID-19 lockdown: a qualitative study. BMC Nurs 21 , 124 (2022). https://doi.org/10.1186/s12912-022-00911-4
Download citation
Received : 09 November 2021
Accepted : 09 May 2022
Published : 24 May 2022
DOI : https://doi.org/10.1186/s12912-022-00911-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Type 2 diabetes mellitus
- Patient isolation
- Primary health care
- Qualitative Research
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
Diabetes Mellitus

The major sources of the glucose that circulates in the blood are through the absorption of ingested food in the gastrointestinal tract and formation of glucose by the liver from food substances.
- Diabetes mellitus is a group of metabolic diseases that occurs with increased levels of glucose in the blood.
- Diabetes mellitus most often results in defects in insulin secretion, insulin action, or even both.
Classification
The classification system of diabetes mellitus is unique because research findings suggest many differences among individuals within each category, and patients can even move from one category to another, except for patients with type 1 diabetes .
- Diabetes has major classifications that include type 1 diabetes , type 2 diabetes , gestational diabete s, and diabetes mellitus associated with other conditions.
- The two types of diabetes mellitus are differentiated based on their causative factors, clinical course, and management.
Pathophysiology
Diabetes Mellitus has different courses of pathophysiology because of it has several types
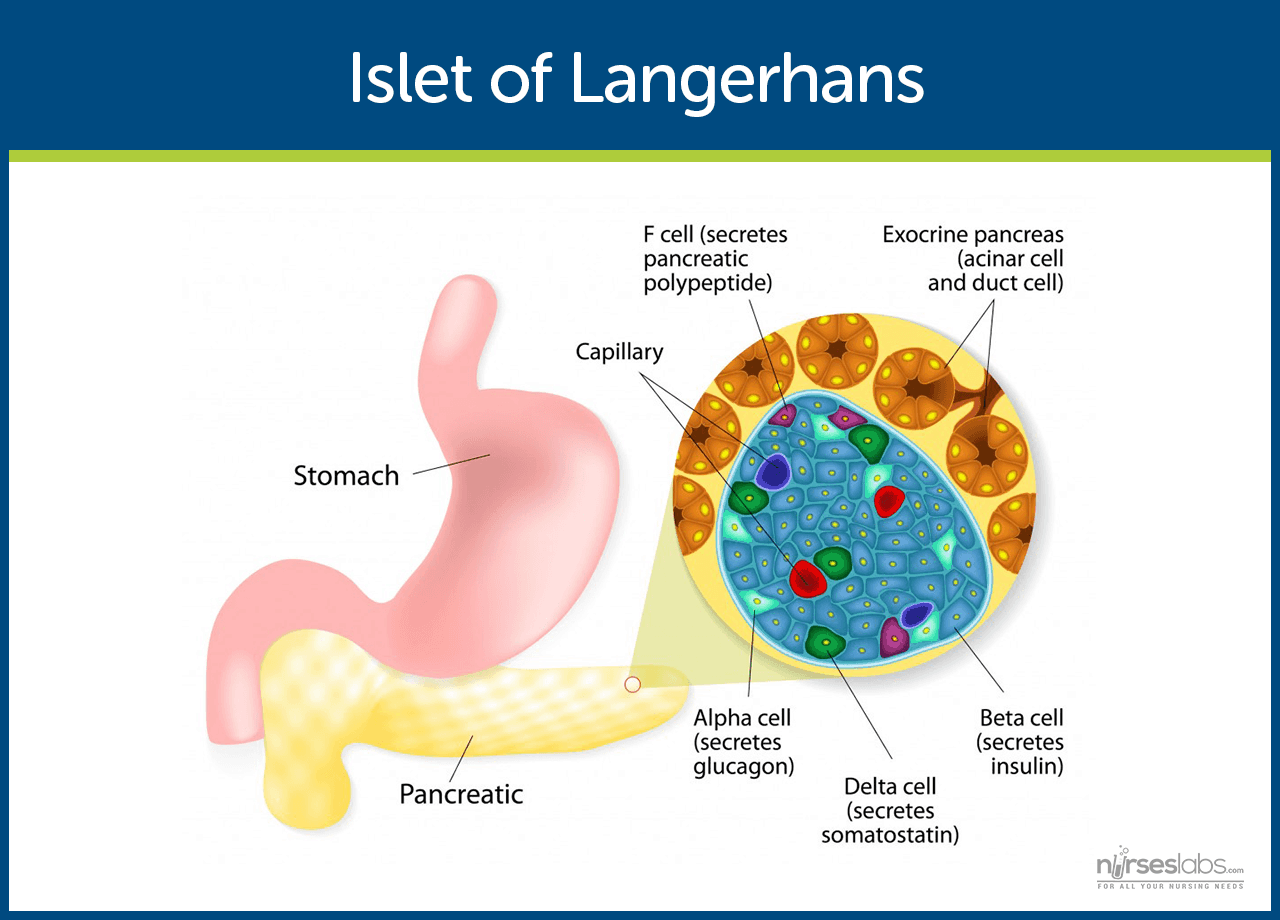
- Insulin is secreted by beta cells in the pancreas and it is an anabolic hormone.
- When we consume food, insulin moves glucose from blood to muscle , liver, and fat cells as insulin level increases.
- The functions of insulin include the transport and metabolism of glucose for energy, stimulation of storage of glucose in the liver and muscle, serves as the signal of the liver to stop releasing glucose, enhancement of the storage of dietary fat in adipose tissue, and acceleration of the transport of amino acid into cells.
- Insulin and glucagon maintain a constant level of glucose in the blood by stimulating the release of glucose from the liver.
Type 1 Diabetes Mellitus
- Type 1 diabetes mellitus is characterized by destruction of the pancreatic beta cel ls.
- A common underlying factor in the development of type 1 diabetes is a genetic susceptibility .
- Destruction of beta cells leads to a decrease in insulin production, unchecked glucose production by the liver and fasting hyperglycemia .
- Glucose taken from food cannot be stored in the liver anymore but remains in the blood stream.
- The kidneys will not reabsorb the glucose once it has exceeded the renal threshold, so it will appear in the urine and be called glycosuria .
- Excessive loss of fluids is accompanied by excessive excretion of glucose in the urine leading to osmotic diuresis .
- There is fat breakdown which results in ketone production , the by-product of fat breakdown.
Type 2 Diabetes Mellitus
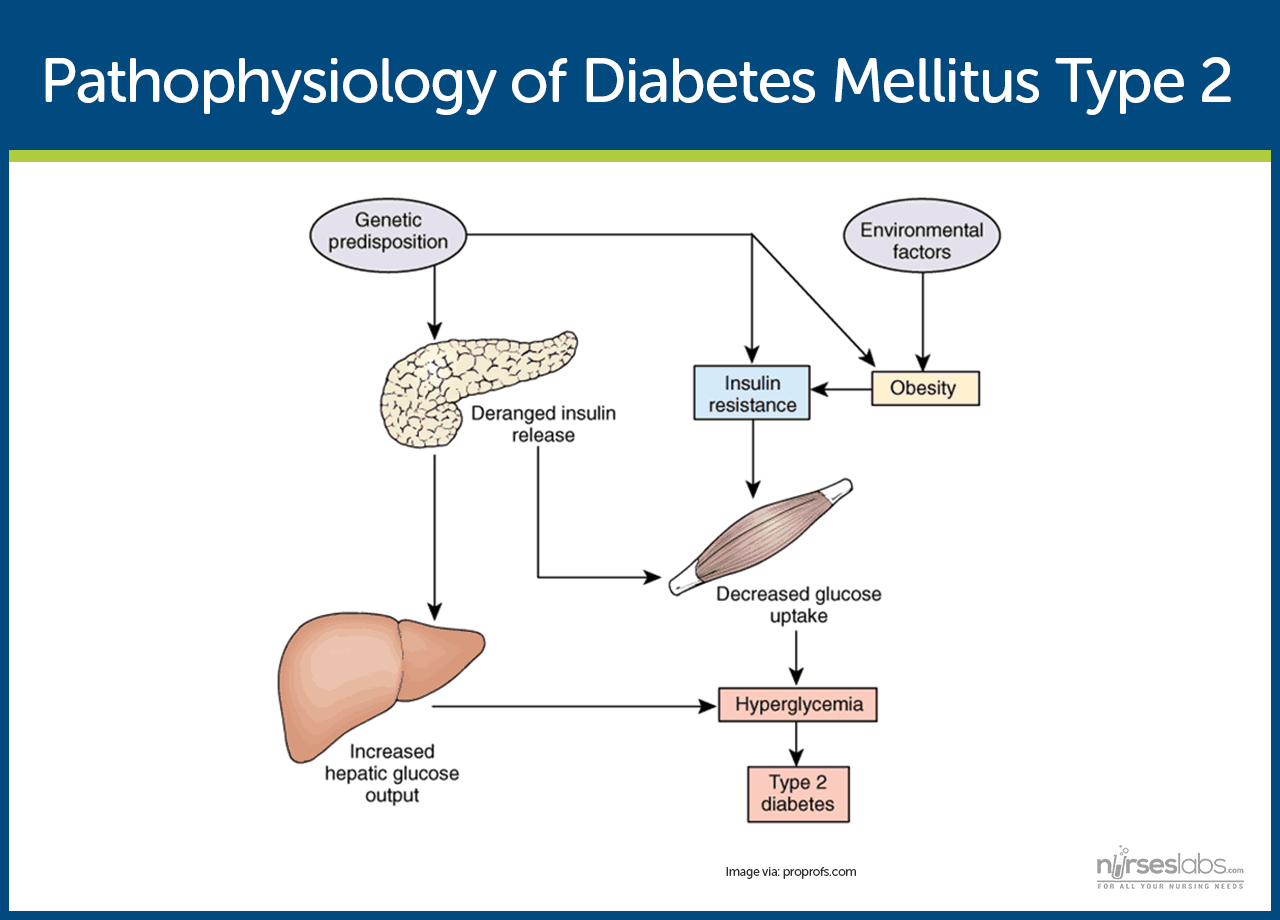
- Type 2 diabetes mellitus has major problems of insulin resistance and impaired insulin secretion .
- Insulin could not bind with the special receptors so insulin becomes less effective at stimulating glucose uptake and at regulating the glucose release.
- There must be increased amounts of insulin to maintain glucose level at a normal or slightly elevated level.
- However, there is enough insulin to prevent the breakdown of fats and production of ketones.
- Uncontrolled type 2 diabetes could lead to hyperglycemic, hyperosmolar nonketotic syndrome .
- The usual symptoms that the patient may feel are polyuria, polydipsia, polyphagia, fatigue , irritability, poorly healing skin wounds, vaginal infections, or blurred vision .
Gestational Diabetes Mellitus
- With gestational diabetes mellitus ( GDM ) , the pregnant woman experiences any degree of glucose intolerance with the onset of pregnancy.
- The secretion of placental hormones causes insulin resistance , leading to hyperglycemia.
- After delivery, blood glucose levels in women with GDM usually return to normal or later on develop type 2 diabetes.
Epidemiology
Diabetes mellitus is now one of the most common disease all over the world. Here are some quick facts and numbers on diabetes mellitus.
- More than 23 million people in the United States have diabetes, yet almost one-third are undiagnosed.
- By 2030, the number of cases is expected to increase more than 30 million.
- Diabetes is especially prevalent in the elderly ; 50% of people older than 65 years old have some degree of glucose intolerance.
- People who are 65 years and older account for 40% of people with diabetes.
- African-Americans and members of other racial and ethnic groups are more likely to develop diabetes.
- In the United States, diabetes is the leading cause of non-traumatic amputations, blindness in working-age adults, and end-stage renal disease .
- Diabetes is the third leading cause of death from disease.
- Costs related to diabetes are estimated to be almost $174 billion annually.
The exact cause of diabetes mellitus is actually unknown, yet there are factors that contribute to the development of the disease.
- Genetics. Genetics may have played a role in the destruction of the beta cells in type 1 DM.
- Environmental factors. Exposure to some environmental factors like viruses can cause the destruction of the beta cells.
- Weight. Excessive weight or obesity is one of the factors that contribute to type 2 DM because it causes insulin resistance.
- Inactivity. Lack of exercise and a sedentary lifestyle can also cause insulin resistance and impaired insulin secretion.
- Weight. If you are overweight before pregnancy and added extra weight, it makes it hard for the body to use insulin.
- Genetics. If you have a parent or a sibling who has type 2 DM, you are most likely predisposed to GDM.
Clinical Manifestations
Clinical manifestations depend on the level of the patient’s hyperglycemia.
- Polyuria or increased urination . Polyuria occurs because the kidneys remove excess sugar from the blood, resulting in a higher urine production.
- Polydipsia or increased thirst. Polydipsia is present because the body loses more water as polyuria happens, triggering an increase in the patient’s thirst.
- Polyphagia or increased appetite. Although the patient may consume a lot of food but glucose could not enter the cells because of insulin resistance or lack of insulin production.
- Fatigue and weakness . The body does not receive enough energy from the food that the patient is ingesting.
- Sudden vision changes. The body pulls away fluid from the eye in an attempt to compensate the loss of fluid in the blood, resulting in trouble in focusing the vision.
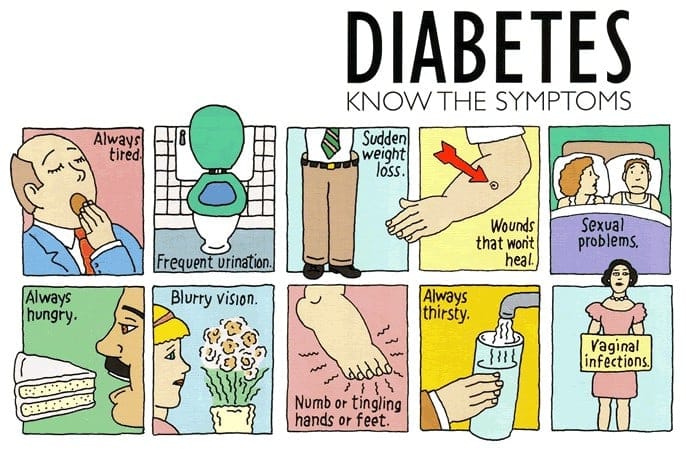
- Tingling or numbness in hands or feet. Tingling and numbness occur due to a decrease in glucose in the cells.
- Dry skin. Because of polyuria, the skin becomes dehydrated.
- Skin lesions or wounds that are slow to heal. Instead of entering the cells, glucose crowds inside blood vessels, hindering the passage of white blood cells which are needed for wound healing .
- Recurrent infections. Due to the high concentration of glucose, bacteria thrives easily.
Appropriate management of lifestyle can effectively prevent the development of diabetes mellitus.
- Standard lifestyle recommendations, metformin , and placebo are given to people who are at high risk for type 2 diabetes.
- The 16-lesson curriculum of the intensive program of lifestyle modifications focused on weight reduction of greater than 7% of initial body weight and physical activity of moderate intensity.
- It also included behavior modification strategies that can help patients achieve their weight reduction goals and participate in exercise.
Complications
If diabetes mellitus is left untreated, several complications may arise from the disease
- Hypoglycemia. Hypoglycemia occurs when the blood glucose falls to less than 50 to 60 mg/dL because of too much insulin or oral hypoglycemic agents, too little food, or excessive physical activity .
- Diabetic Ketoacidosis . DKA is caused by an absence or markedly inadequate amounts of insulin and has three major features of hyperglycemia, dehydration and electrolyte loss, and acidosis.
- Hyperglycemic Hyperosmolar Nonketotic Syndrome . HHNS is a serious condition in which hyperosmolarity and hyperglycemia predominate with alteration in the sense of awareness.

Assessment and Diagnostic Findings
Hypoglycemia may occur suddenly in a patient considered hyperglycemic because their blood glucose levels may fall rapidly to 120 mg/dL or even less.
- Serum glucose: Increased 200–1000 mg/dL or more.
- Serum acetone ( ketones ): Strongly positive.
- Fatty acids: Lipids, triglycerides , and cholesterol level elevated.
- Serum osmolality: Elevated but usually less than 330 mOsm/L.
- Glucagon: Elevated level is associated with conditions that produce (1) actual hypoglycemia , (2) relative lack of glucose (e.g., trauma , infection ), or (3) lack of insulin. Therefore, glucagon may be elevated with severe DKA despite hyperglycemia.
- Glycosylated hemoglobin ( HbA 1C ): Evaluates glucose control during past 8–12 wk with the previous 2 wk most heavily weighted. Useful in differentiating inadequate control versus incident-related DKA (e.g., current upper respiratory infection [URI]). A result greater than 8% represents an average blood glucose of 200 mg/dL and signals a need for changes in treatment.
- Serum insulin: May be decreased/absent (type 1) or normal to high (type 2), indicating insulin insufficiency/improper utilization (endogenous/exogenous). Insulin resistance may develop secondary to formation of antibodies.
- Electrolytes :
- Sodium : May be normal, elevated, or decreased.
- Potassium : Normal or falsely elevated (cellular shifts), then markedly decreased.
- Phosphorus: Frequently decreased.
- Arterial blood gases ( ABGs ): Usually reflects low pH and decreased HCO 3 (metabolic acidosis) with compensatory respiratory alkalosis.
- CBC: Hct may be elevated ( dehydration ); leukocytosis suggest hemoconcentration, response to stress or infection.
- BUN: May be normal or elevated ( dehydration /decreased renal perfusion).
- Serum amylase: May be elevated, indicating acute pancreatitis as cause of DKA.
- Thyroid function tests: Increased thyroid activity can increase blood glucose and insulin needs.
- Urine: Positive for glucose and ketones; specific gravity and osmolality may be elevated.
- Cultures and sensitivities: Possible UTI, respiratory or wound infections.
Medical Management
Here are some medical interventions that are performed to manage diabetes mellitus.
- Normalize insulin activity . This is the main goal of diabetes treatment — normalization of blood glucose levels to reduce the development of vascular and neuropathic complications.
- Intensive treatment. Intensive treatment is three to four insulin injections per day or continuous subcutaneous insulin infusion, insulin pump therapy plus frequent blood glucose monitoring and weekly contacts with diabetes educators.
- Exercise caution with intensive treatment. Intensive therapy must be done with caution and must be accompanied by thorough education of the patient and family and by responsible behavior of patient.
- Diabetes management has five components and involves constant assessment and modification of the treatment plan by healthcare professionals and daily adjustments in therapy by the patient.
Nutritional Management
- The foundations. Nutrition, meal planning , and weight control are the foundations of diabetes management.
- Consult a professional. A registered dietitian who understands diabetes management has the major responsibility for designing and teaching this aspect of the therapeutic plan.
- Healthcare team should have the knowledge. Nurses and other health care members of the team must be knowledgeable about nutritional therapy and supportive of patients who need to implement nutritional and lifestyle changes.
- Weight loss. This is the key treatment for obese patients with type 2 diabetes.
- How much weight to lose? A weight loss of as small as 5% to 10% of the total body weight may significantly improve blood glucose levels.
- Other options for diabetes management. Diet education, behavioral therapy, group support, and ongoing nutritional counselling should be encouraged.
Meal Planning
- Criteria in meal planning . The meal plan must consider the patient’s food preferences, lifestyle, usual eating times, and ethnic and cultural background.
- Managing hypoglycemia through meals. To help prevent hypoglycemic reactions and maintain overall blood glucose control, there should be consistency in the approximate time intervals between meals with the addition of snacks as needed.
- Assessment is still necessary. The patient’s diet history should be thoroughly reviewed to identify his or her eating habits and lifestyle.
- Educate the patient. Health education should include the importance of consistent eating habits, the relationship of food and insulin, and the provision of an individualized meal plan.
- The nurse ‘s role. The nurse plays an important role in communicating pertinent information to the dietitian and reinforcing the patients for better understanding .
Other Dietary Concerns
- Alcohol consumption. Patients with diabetes do not need to give up alcoholic beverages entirely, but they must be aware of the potential adverse of alcohol specific to diabetes.
- If a patient with diabetes consumes alcohol on an empty stomach , there is an increased likelihood of hypoglycemia .
- Reducing hypoglycemia . The patient must be cautioned to consume food along with alcohol, however, carbohydrate consumed with alcohol may raise blood glucose.
- How much alcohol intake? Moderate intake is considered to be one alcoholic beverage per day for women and two alcoholic beverages per day for men.
- Artificial sweeteners. Use of artificial sweeteners is acceptable, and there are two types of sweeteners: nutritive and nonnutritive.
- Types of sweeteners. Nutritive sweeteners include all of which provides calories in amounts similar to sucrose while nonnutritive have minimal or no calories.
- Exercise. Exercise lowers blood glucose levels by increasing the uptake of glucose by body muscles and by improving insulin utilization.
- A person with diabetes should exercise at the same time and for the same amount each day or regularly.
- A slow, gradual increase in the exercise period is encouraged.
Using a Continuous Glucose Monitoring System
- A continuous glucose monitoring system is inserted subcutaneously in the abdomen and connected to the device worn on a belt.
- This can be used to determine whether treatment is adequate over a 24-hour period.
- Blood glucose readings are analyzed after 72 hours when the data has been downloaded from the device.
Testing for Glycated Hemoglobin
- Glycated hemoglobin or glycosylated hemoglobin, HgbA1C, or A1C reflects the average blood glucose levels over a period of approximately 2 to 3 months.
- The longer the amount of glucose in the blood remains above normal, the more glucose binds to hemoglobin and the higher the glycated hemoglobin becomes.
- Normal values typically range from 4% to 6% and indicate consistently near-normal blood glucose concentrations.
Pharmacologic Therapy
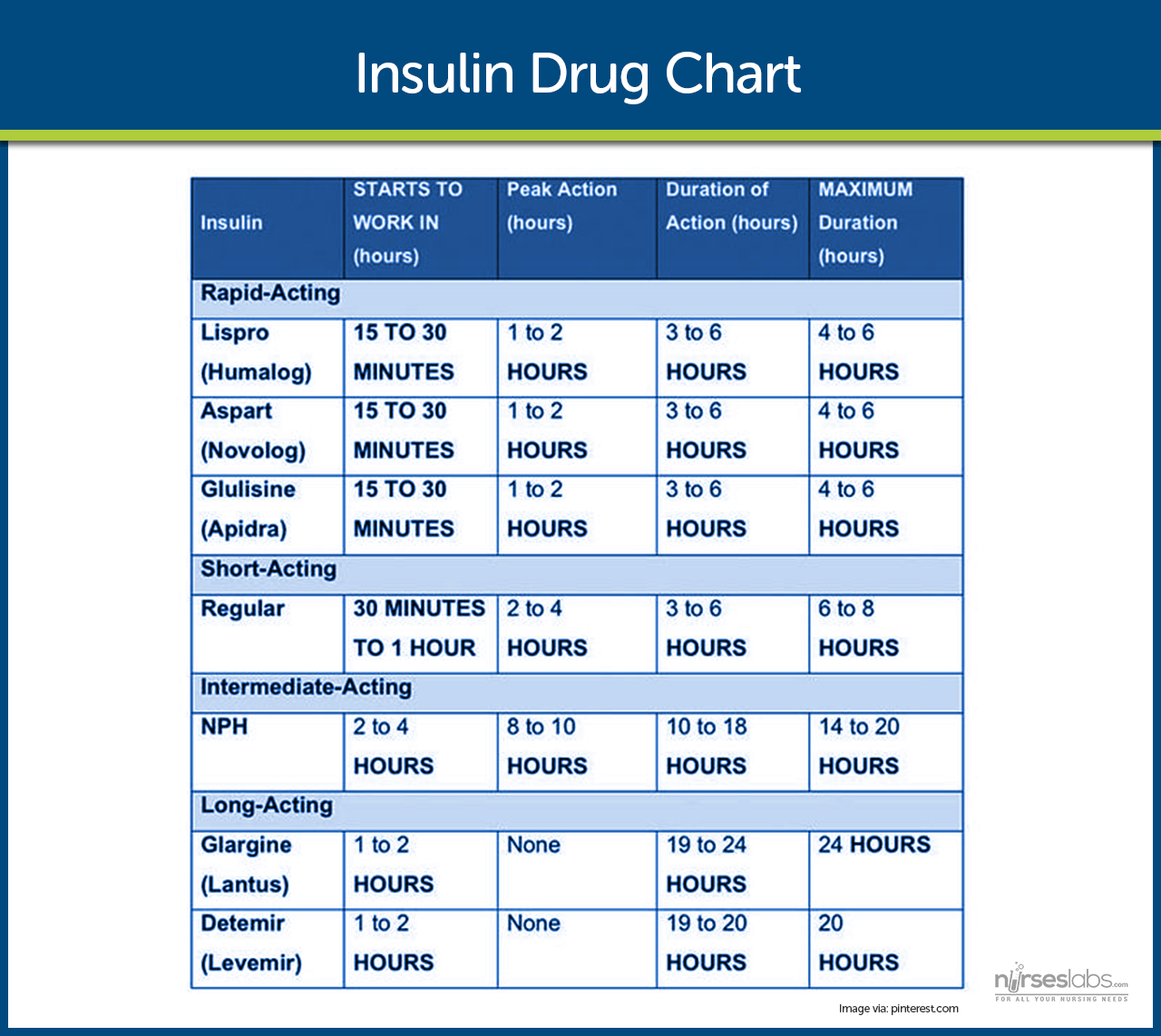
- Exogenous insulin. In type 1 diabetes, exogenous insulin must be administered for life because the body loses the ability to produce insulin.
- Insulin in type 2 diabetes. In type 2 diabetes, insulin may be necessary on a long-term basis to control glucose levels if meal planning and oral agents are ineffective.
- Self-Monitoring Blood Glucose (SMBG). This is the cornerstone of insulin therapy because accurate monitoring is essential.
- Human insulin. Human insulin preparations have a shorter duration of action because the presence of animal proteins triggers an immune response that results in the binding of animal insulin.
- Rapid-acting insulin. Rapid-acting insulins produce a more rapid effect that is of shorter duration than regular insulin.
- Short-acting insulin. Short-acting insulins or regular insulin should be administered 20-30 minutes before a meal , either alone or in combination with a longer-acting insulin.
- Intermediate-acting insulin. Intermediate-acting insulins or NPH or Lente insulin appear white and cloudy and should be administered with food around the time of the onset and peak of these insulins.
- The rapid-acting and short-acting insulins are expected to cover the increase in blood glucose levels after meals; immediately after the injection.
- Intermediate-acting insulins are expected to cover subsequent meals, and long-acting insulins provide a relatively constant level of insulin and act as a basal insulin.
- Approaches to insulin therapy. There are two general approaches to insulin therapy: conventional and intensive.
- Conventional regimen. Conventional regimen is a simplified regimen wherein the patient should not vary meal patterns and activity levels.
- Intensive regimen. Intensive regimen uses a more complex insulin regimen to achieve as much control over blood glucose levels as is safe and practical.
- A more complex insulin regimen allows the patient more flexibility to change the insulin doses from day to day in accordance with changes in eating and activity patterns.
- Methods of insulin delivery. Methods of insulin delivery include traditional subcutaneous injections, insulin pens, jet injectors, and insulin pumps.
- Insulin pens use small prefilled insulin cartridges that are loaded into a pen-like holder.
- Insulin is delivered by dialing in a dose or pushing a button for every 1- or 2-unit increment administered.
- Jet injectors deliver insulin through the skin under pressure in an extremely fine stream.
- Insulin pumps involve continuous subcutaneous insulin infusion with the use of small, externally worn devices that closely mimic the function of the pancreas.
- Oral antidiabetic agents may be effective for patients who have type 2 diabetes that cannot be treated by MNT and exercise alone.
- Oral antidiabetic agents . Oral antidiabetic agents include sulfonylureas , biguanides, alpha-glucosidase inhibitors, thiazolidinediones , and dipeptidyl-peptidase-4.
- Half of all the patients who used oral antidiabetic agents eventually require insulin, and this is called secondary failure .
- Primary failure occurs when the blood glucose level remains high 1 month after initial medication use.
Nursing Management
Nurses should provide accurate and up-to-date information about the patient’s condition so that the healthcare team can come up with appropriate interventions and management.
For the complete and comprehensive nursing care plan and management of patients with diabetes, please visit 20 Diabetes Mellitus Nursing Care Plans
Practice Quiz: Diabetes Mellitus
For our diabetes mellitus practice quiz, please do visit our nursing test bank for diabetes:
- Diabetes Mellitus Reviewer and NCLEX Questions (100 Items)
7 thoughts on “Diabetes Mellitus”
Humbled by the content I read here.. this is absolutely exceptional..work made easier
please can you give me your opinion on this weather is “Diabetes- only progression or can be regressed”
Perfect notes
Lesson is extremely explicit and easy to grasp
Hi Jennifer, Awesome to hear the lesson on diabetes mellitus was clear and easy to get! 😊 Anything in particular you found really helpful or any other topics you’re keen to explore?
Very effective
Leave a Comment Cancel reply
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Effect of a Nurse-Led Diabetes Self-Management Education Program on Glycosylated Hemoglobin among Adults with Type 2 Diabetes
Affiliations.
- 1 Department of Nursing and Rehabilitations, Faculty of Medicine and Health Sciences, University Putra Malaysia (UPM), 43400 Serdang, Selangor, Malaysia.
- 2 Department of Nursing, Faculty of Nursing and Midwifery, Ilam University of Medical Sciences, Ilam 693917714, Iran.
- 3 Department of Family Medicine, Faculty of Medicine and Health Sciences, University Putra Malaysia (UPM), 43400 Serdang, Selangor, Malaysia.
- 4 Department of Community Health, Faculty of Medicine and Health Sciences, University Putra Malaysia (UPM), 43400 Serdang, Selangor, Malaysia.
- PMID: 30225268
- PMCID: PMC6129337
- DOI: 10.1155/2018/4930157
In recent years, great emphasis has been placed on the role of nonpharmacological self-management in the care of patients with diabetes. Studies have reported that nurses, compared to other healthcare professionals, are more likely to promote preventive healthcare seeking behaviors. The aim of this study was to investigate the effectiveness of a nurse-led diabetes self-management education on glycosylated hemoglobin. A two-arm parallel-group randomized controlled trial with the blinded outcome assessors was designed. One hundred forty-two adults with type 2 diabetes were randomized to receive either usual diabetes care (control group) or usual care plus a nurse-led diabetes self-management education (intervention group). Duration of the intervention was 12 weeks. The primary outcome was glycosylated hemoglobin (HbA1c values). Secondary outcomes were changes in blood pressure, body weight, lipid profiles, self-efficacy (efficacy expectation and outcome expectation), self-management behaviors, quality of life, social support, and depression. Outcome measures were assessed at baseline and at 12-week and 24-week postrandomizations. Patients in the intervention group showed significant improvement in HbA1c, blood pressure, body weight, efficacy expectation, outcome expectation, and diabetes self-management behaviors. The beneficial effect of a nurse-led intervention continued to accrue beyond the end of the trial resulting in sustained improvements in clinical, lifestyle, and psychosocial outcomes. This trial is registered with IRCT2016062528627N1.
PubMed Disclaimer
Consort flow diagram of study…
Consort flow diagram of study participation.
Similar articles
- BetaMe: impact of a comprehensive digital health programme on HbA1c and weight at 12 months for people with diabetes and pre-diabetes: study protocol for a randomised controlled trial. Sarfati D, McLeod M, Stanley J, Signal V, Stairmand J, Krebs J, Dowell A, Leung W, Davies C, Grainger R. Sarfati D, et al. Trials. 2018 Mar 5;19(1):161. doi: 10.1186/s13063-018-2528-4. Trials. 2018. PMID: 29506562 Free PMC article.
- Technology-Intensified Diabetes Education Study (TIDES) in African Americans with type 2 diabetes: study protocol for a randomized controlled trial. Williams JS, Lynch CP, Knapp RG, Egede LE. Williams JS, et al. Trials. 2014 Nov 25;15:460. doi: 10.1186/1745-6215-15-460. Trials. 2014. PMID: 25425504 Free PMC article. Clinical Trial.
- Efficacy of a self-management education programme on patients with type 2 diabetes in primary care: A randomised controlled trial. Gamboa Moreno E, Mateo-Abad M, Ochoa de Retana García L, Vrotsou K, Del Campo Pena E, Sánchez Perez Á, Martínez Carazo C, Arbonies Ortiz JC, Rúa Portu MÁ, Piñera Elorriaga K, Zenarutzabeitia Pikatza A, Urquiza Bengoa MN, Méndez Sanpedro T, Oses Portu A, Aguirre Sorondo MB, Rotaeche Del Campo R; Osakidetza Active Patient Research Group. Gamboa Moreno E, et al. Prim Care Diabetes. 2019 Apr;13(2):122-133. doi: 10.1016/j.pcd.2018.10.001. Epub 2018 Nov 6. Prim Care Diabetes. 2019. PMID: 30409669 Clinical Trial.
- The effect of nurse-led diabetes self-management education on glycosylated hemoglobin and cardiovascular risk factors: a meta-analysis. Tshiananga JK, Kocher S, Weber C, Erny-Albrecht K, Berndt K, Neeser K. Tshiananga JK, et al. Diabetes Educ. 2012 Jan-Feb;38(1):108-23. doi: 10.1177/0145721711423978. Epub 2011 Nov 23. Diabetes Educ. 2012. PMID: 22116473 Review.
- Psychological interventions for diabetes-related distress in adults with type 2 diabetes mellitus. Chew BH, Vos RC, Metzendorf MI, Scholten RJ, Rutten GE. Chew BH, et al. Cochrane Database Syst Rev. 2017 Sep 27;9(9):CD011469. doi: 10.1002/14651858.CD011469.pub2. Cochrane Database Syst Rev. 2017. PMID: 28954185 Free PMC article. Review.
- The Implication of Diabetes-Specialized Nurses in Aiming for the Better Treatment and Management of Patients with Diabetes Mellitus: A Brief Narrative Review. Zhu Y, Zhang H, Xi Y, Zhu H, Lu Y, Luo X, Tang Z, Lei H. Zhu Y, et al. Diabetes Ther. 2024 May;15(5):917-927. doi: 10.1007/s13300-024-01558-x. Epub 2024 Mar 12. Diabetes Ther. 2024. PMID: 38472627 Free PMC article. Review.
- The Influence of Nurse-Led Interventions on Diseases Management in Patients with Diabetes Mellitus: A Narrative Review. Dailah HG. Dailah HG. Healthcare (Basel). 2024 Jan 30;12(3):352. doi: 10.3390/healthcare12030352. Healthcare (Basel). 2024. PMID: 38338237 Free PMC article. Review.
- The effectiveness of diabetes self-management education intervention on glycaemic control and cardiometabolic risk in adults with type 2 diabetes in low- and middle-income countries: A systematic review and meta-analysis. Chowdhury HA, Harrison CL, Siddiquea BN, Tissera S, Afroz A, Ali L, Joham AE, Billah B. Chowdhury HA, et al. PLoS One. 2024 Feb 2;19(2):e0297328. doi: 10.1371/journal.pone.0297328. eCollection 2024. PLoS One. 2024. PMID: 38306363 Free PMC article.
- The role of the nurse in meeting the educational needs for self-care in cachectic cancer patients and their family caregivers: A scoping review. Hopkinson JB. Hopkinson JB. Asia Pac J Oncol Nurs. 2023 Aug 23;10(Suppl 1):100294. doi: 10.1016/j.apjon.2023.100294. eCollection 2023 Nov. Asia Pac J Oncol Nurs. 2023. PMID: 38197042 Free PMC article. Review.
- Effects of family-based diabetes self-management education and support programme on support behaviour amongst adults with type 2 diabetes in Western Ethiopia. Diriba DC, Leung DYP, Suen LKP. Diriba DC, et al. Sci Rep. 2023 Nov 27;13(1):20867. doi: 10.1038/s41598-023-48049-w. Sci Rep. 2023. PMID: 38012247 Free PMC article. Clinical Trial.
- United Nations. Most Populous Cities of the World. 2014. http://www.infoplease.com/ipa/A0762524.html .
- Mehrdad R. Health system in Iran. JMAJ. 2009;52:69–73.
- Owlia P., Eftekhari M. B., Forouzan A. S., Bahreini F., Farahani M., Ghanei M. Health research priority setting in Iran: introduction to a bottom up approach. Journal of Research in Medical Sciences: the Official Journal of Isfahan University of Medical Sciences. 2011;16(5):691–698. - PMC - PubMed
- Boutayeb A. The double burden of communicable and non-communicable diseases in developing countries. Transactions of the Royal Society of Tropical Medicine and Hygiene. 2006;100(3):191–199. doi: 10.1016/j.trstmh.2005.07.021. - DOI - PubMed
- Lopez A. D., Mathers C. D. Measuring the global burden of disease and epidemiological transitions: 2002–2030. Annals of Tropical Medicine & Parasitology. 2006;100(5-6):481–499. doi: 10.1179/136485906X97417. - DOI - PubMed
Publication types
- Search in MeSH
Related information
- Cited in Books
LinkOut - more resources
Full text sources.
- Europe PubMed Central
- Hindawi Limited
- PubMed Central
Other Literature Sources
- scite Smart Citations
- Genetic Alliance
- MedlinePlus Health Information
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Call to +1 844 889-9952
188 Diabetes Research Topics & Essay Examples
📝 diabetes research papers examples, 💡 essay ideas on diabetes, 👍 good diabetes essay topics to write about, 🏆 best diabetes essay titles, 🎓 simple research topics about diabetes, ❓ diabetes research questions.
| Definition | The term “diabetes mellitus” refers to a whole group of endocrine diseases, united by a common feature: they are based on disorders of carbohydrate metabolism. |
|---|---|
| Specialty | Endocrinology |
| History | The first descriptions of diabetes singled out its most recognizable symptoms – fluid loss (polyuria) and unquenchable thirst (polydipsia). In 1889, Joseph von Mering and Oskar Minkowski showed that a dog develops symptoms of diabetes after pancreatectomy. And in 1910, Sir Edward Albert Sharpay-Schafer suggested that diabetes was caused by a deficiency of a chemical secreted by the islets of Langerhans in the pancreas. |
| Symptoms | In the initial stage, diabetes mellitus has practically no pronounced symptoms. The main signs of diabetes are constant dryness of the mouth, intense thirst with sufficient or excessive fluid intake, and frequent urination. Dry skin, itching sensation in the feet, elbows, legs are also potential symptoms of diabetes. Moreover, sudden and rapid weight gain or loss combined with constant hunger, fatigue, drowsiness, and decreased performance, too, point out to the presence of diabetes. |
| Causes | Today, diabetes is considered polyetiological – there are several theories for the occurrence of carbohydrate metabolism disorders and problems with insulin. A special role is assigned to unfavorable heredity if close relatives suffer from diabetes. In addition, certain factors can trigger the disease, such as poor nutrition with an excess of light carbohydrates, refined foods, fast food, saturated and trans fats, a lack of dietary fiber. Overweight and obesity are also considered potential causes of diabetes. |
| Prevention | In order to maintain health and reduce the risk of developing the disease, it is necessary to control weight, regularly evaluate carbohydrate and lipid metabolism, and undergo medical examination. Moderate physical activity, drinking enough fluids and a balanced diet with a decrease in carbohydrates, saturated fats, fast food, refined foods are also important. |
| Diagnostic Method | The main laboratory tests confirming diabetes are a blood test for glucose levels, load test to determine glucose tolerance, and biochemical studies (level of protein, lipids, electrolytes). |
| Treatment | The basis of treatment is a combination of non-drug approaches, lifestyle changes with an individual selection of drugs that control the level of glycaemia in diabetes mellitus. Approaches to therapy differ depending on the type of disease. |
| Duration | Diabetes is a chronic disease that remains with the patient till the end of their life. |
| Prognosis | The life expectancy of type 1 diabetics has increased significantly in recent years with the introduction of modern insulins and self-monitoring devices. The prognosis for life in people with type 2 diabetes mellitus strongly correlates with the degree of disease control, and also depends on gender, age, and the presence of complications. |
| Complications | The disease can be complicated by serious pathologies and changes in the body that threaten disability and even threaten life. Severe visual impairment, damage to structures inside the eyeball and its vessels, the formation of persistent hypertension, and lipid metabolism disorders which lead to atherosclerosis are the most common complications of diabetes. Against the background of metabolic disorders, life-threatening conditions such as coma can occur. |
| Frequency in Population | Among all endocrine diseases, diabetes mellitus in women and men is the most common. There are more than 250 million people in the world with different types of this pathology. |
| Deaths | Every year, 3.8 million people die from complications of diabetes, including cardiovascular diseases. |
| Society | Nowadays, diabetes is no longer considered a terrible disease, but a special way of life, provided that the necessary therapy is received. |
- Healthcare Concern: High Rate of Diabetes The primary health concern for Eatonville’s diverse population is a high rate of diabetes. Approximately 24% of residents are suffering from the condition.
- Patient Teaching Plan: Type II Diabetes The patient's genetic history strongly suggests a risk of developing type II diabetes. Hypertension is a common condition among many of its members.
- Diabetes Self-Management Education Evidence suggests that web-based education initiatives positively correlate with self-management outcomes in patients with type 2 diabetes.
- Diabetes Types and Drug Treatments This paper explores the four types of diabetes, medication applied to manage type 1, and the effects that the condition has on individuals' lives.
- Diabetes Education for Hispanic Patients This article discusses the question of is continuing patient education effective in improving HgBA1C in diabetic Hispanic patients.
- Hispanics With Diabetes Mellitus This paper discusses the issue of how effectively does diabetes education improves health outcomes in Hispanics with diabetes mellitus.
- The Church's Diabetes Self-Management Education Program The main goal of this study was to analyze the effectiveness of a multi-faceted church-based diabetes self-management education program. The researchers assessed the impact of this intervention.
- Various Diabetes Management Activities Diabetes management includes different activities. Education and support are basic aspects of any treatment plan because the disease requires daily monitoring and control performed by a patient.
- Educational Programs for Patients With Diabetes The effectiveness of educational programs for patients with diabetes is still a relevant issue. Different specialists claim that diabetes self-management education does not adequately address the problems.
- Diabetes Education Programs for Patients Problems related to diabetes are especially relevant for Latin Americans. There are different methods to address such a problem. One of the most effective approaches is educational programs.
- Silent Myocardial Infarction and Diabetes Mellitus Type 2 Patients who are diagnosed with diabetes mellitus type 2 often die from silent myocardial infarction and heart failure.
- Diabetes Mellitus: Educational Plan This paper will outline an education plan for homebound elderly with diabetes. The plan aims to reinforce the population’s understanding of the condition and improve their self-care behaviors.
- Diabetes and Hypertension Patient's Healthcare Plan This paper presents the healthcare plan of a 49-year-old white woman with a history of type 2 diabetes, obesity, hypertension, and migraine headaches.
- Diabetes Prevention in Hispanic Populations Hispanic people face a considerably higher risk of type 2 diabetes due to the lack of knowledge about the condition and poor access to care.
- Enhancing Diabetes Self-Management The study by George and Thomas was aimed at revealing how the aged (65 years and above) diagnosed with insulin-dependent diabetes and living in rural areas perceive self-management.
- Type 2 Diabetes Patient's Support Needs To reduce the probability of contracting type 2 diabetes, it is strongly advisable for the patient to find more information about the disease and possible ways of its prevention.
- Useful Interventions in Treating Diabetes Diabetes is a chronic disease that mainly affects the older population. This paper discusses useful interventions that have been shown to yield better results.
- Obesity, Hypertension, Diabetes Type 2: Assessment Obesity plays a substantial role in adipocytokine dysregulation which is suggested to be a pathogenic trigger of insulin resistance and other diabetes-related problems.
- Treatment of Patient: Risk of Diabetes and Hypertension The risk of diabetes is to be reduced with the help of a diet. To evaluate the effectiveness, keep track of BMI and blood sugar level.
- Diagnosis and Treatment of Diabetes and Hypertension The advantageous method to evaluate the intervention's efficiency is activity log. This element contains all the information about the patient's activities and progresses.
- Pathophysiology: Diabetes Type 1 and 2 Diabetes is an autoimmune disease; the immune system of the body attacks the beta cells of the pancreas, which results in the elimination of insulin production.
- Measuring the Global Burden of Disease Community members should identify the best sources of statistical information in order to understand the major illnesses affecting them.
- Diabetes Evidence-Based Treatment Outcomes Diabetes is associated with a decline in health-related quality of life, so after the intervention, it is reasonable to expect improvements in several areas.
- Elderly Education on Diabetes: Study Design This paper is meant to study the effect of post-discharge self-management education promotions and techniques for elderly patients with diabetes on health outcomes.
- Managing the Daily Life of Individuals With Diabetes The suggested teaching plan covers the topic of primary prevention and health promotion. The health problem it comprises is diabetes.
- A High Risk Of Type 2 Diabetes The purpose of the paper is to overview the type 2 diabetes , describe an evidence-based intervention related to the modifiable risk factor, and suggest a teaching plan for the patient.
- Hypertension and Type II Diabetes Mellitus Pathophysiology The clinical findings and physical examination of the patient provide evidence that prove the development of right-sided heart failure.
- Diabetes Patient: The Impact of Chronic Illness The interview indicates that the patient has accepted her disease and manages it. She is aware of her condition and controls her blood glucose level regularly.
- The Prevention and Control the Type-2 Diabetes Type 2 diabetes is a widespread health issue that affects many people around the world regardless of age and gender.
- Diabetes: Disease Analysis Diabetes is a chronic metabolic disease. There are three types of diabetes, such as type 1, type 2, and gestational diabetes.
- Teaching Patients to Live with Diabetes The lesson informs patients about possible behavioral changes associated with diabetes and prepares them to live under new conditions, requirements and restrictions.
- Diabetes Management and Pharmacological Effects The research paper provides pharmacological effects of herbal supplements and metformin medication in the management of diabetes and nursing implications.
- Epidemiology Topics for Signature Assignment The topic of diabetic retinopathy is relevant to my future career as I will seek to encourage every patient with diabetes to have an eye examination regularly.
- Cardiovascular Issues in Hispanic Diabetes Patient This paper discusses the disease processes and produces a treatment plan for a 59-year-old Hispanic male with type 2 diabetes and high blood pressure.
- Chronic Renal Failure: Prevention and Treatment in Diabetic Patients Chronic renal failure (CRF), which is the final stage of chronic kidney disease, is a condition when kidneys fail to perform their function and respond to the needs of a body.
- Benefits of the Ketogenic Diet in Diabetic Patients The goal of this study is to verify the benefits of ketogenic diets in diabetic patients. The objectives included searching the literature for recent articles on the use of ketogenic diets in diabetes.
- The Issue of Diabetes in Native Americans The paper contributes to efforts for improving the quality of care for Native American patients diagnosed with or at risk for diabetes.
- Diabetes Documentation for Non-Medical Individuals This essay looks at how diabetes has been documented for non-medical individuals over the decades. Examples will be drawn from the poem Diabetes by James Dickey.
- Effectiveness of Pragmatic Lifestyle Interventions for the Prevention of Type 2 Diabetes The studies show that even small changes in lifestyle and physical activity may significantly facilitate the condition of a patient with diabetes.
- The Management of Diabetes in Children The management of diabetes in children needs comprehensive understanding owing to the age of patients and the complexity that comes with the disease.
- Diabetes Prevention: Plan of Care As a lifestyle and dietary choices are central to diabetes prevention and management, it is critical to develop a plan of care for the use in health delivery to this population.
- Prevention of Type 2 Diabetes Type 2 diabetes is one of the primary health concerns of the American healthcare system. The prevalence of the disorder is likely to remain unchanged or even increase due to population aging.
- Geriatric Diabetes Management: Evidence-Based Project The presence of diabetes may provoke several complications such as an increase in the levels of blood sugar and blood glucose.
- Genetics of Type 2 Diabetes The patient involved in the assessment should pay attention to his diet as a modifiable risk factor associated with type 2 diabetes.
- Patient Education: Prepare to Live with Diabetes Living with diabetes is not an easy task. Unfortunately, no cure can be offered to patients in order to eliminate it completely.
- Diabetes Signs, Screening and Treatment Diabetes is among the most common endocrine disorders among adults. The condition can be successfully managed using a combination of pharmacologic and non-pharmacologic approaches.
- Diabetes Monitor Health Application: Patient Guide The Diabetes Monitor health application records, analyzes, and controls the development of diabetes, reminds of blood glucose tests and the prescribed medicine.
- Nutritional Recommendations for Pediatric Diabetes The issue of children who have diabetes has gained a lot of attention in recent years due to the overwhelming number of consequences that influence their health on a daily basis.
- Diabetes: Causes and Effects Diabetes is the ailment in which there is lack of the production and improper utilization of insulin in the body.
- Diabetic Patient's Education on Insulin Injections The nursing case study is about Juan Duran, a Mexican-American who was prescribed to take insulin injections but was not instructed in how to perform them.
- Diabetes in Adolescents: Research Critique The following topics are discussed in this essay: protection of human participants, data collection, data management and analysis, findings, and interpretation of findings.
- Diabetes Mellitus: Recent Research and Clinical Findings Diabetes mellitus is a chronic disease, so it can not be completely treated; only properly managed, this is why the reliable method of diagnostics is a great tool for fighting it.
- The Negative Impact of Diabetes on Pregnancy This paper aims to raise awareness about the negative impact of diabetes on pregnancy and how this impact can be mitigated.
- Poor Diabetes Control in Miami-Dade County, Florida Diabetes is a chronic disease that affects a patient’s blood sugar level and leads to a range of negative consequences.
- The Family-Based Education for Adult Patients with T2DM: Positive Effects The purpose of this review is to determine whether family-based education improves glycemic control and health-related quality of life in adult patients with T2DM.
- “Depression, Anxiety, and Stress in Diabetes” by Chlebowy In the article, Chlebowy et al. examined one’s ability to manage diabetes type 2 and possible complications in the form of depression, anxiety, and stress.
- The Treatment of Foot Ulcers in Diabetic Patients: Case Study The treatment of foot ulcers in diabetic patients is characterized by several restrictions and precautionary measures.
- Evidence-Based Practice Interventions for Diabetes: CLC Assignment in Nursing Looking for evidence-based practice interventions for diabetes? ➤ Read our project paper example to ✅ learn about mobile health interventions in diabetes care.
- Diabetes and Hypertension Avoiding Recommendations It is vital to develop a system of health recommendations that would promote the prevention of diabetes in Hispanic Americans.
- About Diabetes Treatment The article is a summary of the literature on the most recent findings for effective type 2 diabetes management strategies with a focus on patient engagement.
- Prevalence of Diabetes in Minority Populations This paper examines how nurse specialists could cope with the progression of diabetes in minority populations, such as Hispanics.
- COPD, Heart Failure, Hypertension and Diabetes Mellitus The paper aims to address health problems associated with high blood pressure and diabetes mellitus. It involves analyzing patients’ lifestyles.
- Type 2 Diabetes in Aged Indigenous Australians The prevalence of diabetes 2 is common amongst the indigenous Australian people. The trend can be attributed to the genetic susceptibility amongst these people.
- Resistin and Its Potential Effects on Insulin Resistance The paper explores the physiological effects of the gut hormone Resistin. In the study conducted at The Penn Diabetes Center, resistin was first discovered as a 12 kDa polypeptide.
- The Global Prevalence of Diabetes in the World This document explores diabetes’ occurrence, causes, and the people more affected around the world, discusses symptoms of the disease and corrective measures to deal with it.
- Management of Foot Ulcers for People with Diabetes Diabetes-related complications are responsible for diabetic foot ulceration and amputation. Cases of lower limb amputation have increased because of diabetes.
- Patient Illness Trajectory From Diabetes Diagnosis to Hemodialysis in Taiwan The article reviews a study that examined diabetic patients' perceptions of their health and the importance of such information for nurses in the treatment of the disease.
- Diabetes Prevention Program Review This report aims to review the curriculum for the Diabetes Prevention Program that is offered by the Centers for Disease Control and Prevention in preventing diabetes
- Diabetes Mellitus: The Key Aspects Diabetes mellitus signifies a chronic, lifetime condition that affects the aptitude of the body to consume the glucose in the blood.
- Prevention of Medication Errors in Diabetic Patients in Home Health Services The paper seeks to point out how medical errors can be prevented in-home care and hence lead to improved health outcomes in-home care for diabetic patients.
- Diabetes Risk Factors in Adolescents Diabetes is a common disease among young people in the USA. Dietary practices and a sedentary lifestyle are the main risk factors for the development of type II diabetes.
- How To Protect an Infant Born to a Diabetic Mother This paper evaluates an effective care plan to be given to the baby as a way of mitigating the risks of an infant born of a diabetic mother contracting the disease.
- Care Plan Development: Treating Diabetes Mellitus This study discusses my role as a nurse in the examination of the health of an individual having diabetes and the provision of medical care.
- Diabetes: Obesity in Children This paper will discuss obesity in children and the management strategies that may help to reduce cases of overweight among the kids.
- Type 2 Diabetes Effect on African American Community The paper focuses on an effective learning program that will create awareness about Type 2 diabetes so that members can avoid behavior that may put them at the risk.
- A Study of Juvenile Type 1 Diabetes in the Northwest of England Juvenile type 1 diabetes mellitus is the form of insulin-dependent diabetes mellitus that occurs in children and adolescents.
- Healthy People 2020 Initiative Goals in Miami, FL The three population-based communicable diseases analyzed are HIV/AIDS, STDs, and Diabetes. The community considered is Miami, FL 33155.
- Diabetes Mellitus: Resources Diabetes resource centers provide information that aids in learning the best manner of preventing and managing the illness.
- Support for Diabetes Using Technology by Hunt et al. Although technology applications can be used in the self-management of diabetes, people need to understand the multifaceted treatment plan.
- Critical Analysis: Diabetes Risk Factors in Adolescents The paper is divided into various sections, as follows: protection of human participants; data collection; data management and analysis; problem statement; interpretation of findings.
- Strengthening Adherence in Patients With Diabetes Strengthening adherence in patients with diabetes could be realized via strong social and family support, the involvement of medical personnel, is also of great assistance.
- Diabetes Type-2 Management and Intervention Plan Better management of type-2 diabetes can help make positive changes in lifestyle and delay or avoid the complications related to this disorder.
- The Coping Skills, Treatment, and Support Aspects of Diabetes Mellitus Chronic disease such as diabetes mellitus is a big blow to the patient. The paper analysis the coping skills, treatment, and support aspects of diabetes mellitus.
- The Insulin Pump Therapy for Type 1 Diabetes The purpose of this paper is to discuss Johnson and the group findings in the context of the existing research the insulin pump therapy and its importance for the nursing practice.
- A Diabetes Diagnosis: Insulin Pump Therapy The current article discusses the long-term results of a diabetes diagnosis known as Insulin Pump Therapy. A large population was used to investigate these outcomes.
- Diabetes Mellitus Management Strategy This paper seeks to identify the most current diabetes management strategy, critically analyzing its findings in terms of its relevance to diabetes management.
- Pharmacological Treatment of Hypertension for Elderly Patients With Diabetes This essay discusses the pathophysiology of hypertension in elderly diabetic patients, pharmacological principles in its management, and general nursing care.
- Diabetes Mellitus and Insulin This paper discusses the structure, synthesis, secretion and metabolism of insulin in association with its major function, which is to regulate blood glucose.
- Treatment for Diabetes Analysis Although the new discoveries of antidiabetic drugs appear on the market, diabetic patients still suffer from diseases and side effects of these discoveries.
- Course Project: Lesson Plan for Diabetes Mellitus The main purpose of the lesson plan is to inform and sensitize more people about the issues associated with diabetes mellitus.
- Diabetes Management and Quality Improvement Initiative The purpose of the diabetes management and quality improvement initiative is to enhance the process of the healthcare provider and the outcome of patients.
- Diabetes Mellitus Type II Diabetes mellitus type II is a chronic metabolic syndrome that affects the body’s sugar metabolism by resisting the stimulation and production of insulin.
- Diabetes and Healthy People 2020 Care Plan This project has identified the patient vulnerable to the selected health issue of diabetes and assessed one’s health status from the point of view of Healthy People 2020.
- Diabetes Resources, Control and Prevention The following project will list three helpful resources for this patient and for all those who need help in diabetes prevention and health promotion.
- Diabetic Diet Management: Patient Education Plan A nurse supporting individuals with diabetes should use education plans to produce the best goals, focus on a wide range of issues such as disease management, exercise, and diet.
- Diabetes Prevention Lesson and Teaching Plan In this paper, the teaching plan will be elaborated to help the community people affected by the diabetes problem improve their health status.
- Diabetes Impact on Direct Care Plan Development A diabetes direct care plan for the people in the community should be based on the data obtained during the screening and evaluation procedures.
- Aspirin Usage for Women with Diabetes For women with diabetes, does the use of low-dose aspirin daily reduce the risk of cardiovascular events within several years in comparison with no usage of low-dose aspirin?
- Type 2 Diabetes: The Ways to Prevent or Delay It This paper aims to describe several ways to prevent or delay type 2 diabetes: adequate diet, physical activity, etc.
- Diabetes and Positive Influence of Physical Exercise Continuous physical exercise helps diabetic patients to reduce their daily need for insulin, attain a healthy body mass index, and lower cardiovascular complications.
- Researching Intervention on Diabetes It is emotionally challenging for adolescents to understand why diabetes is a chronic disease that will accompany them throughout their lives
- Indicators in Black Diabetes Mellitus Type II Patients This paper aims to analyze the importance of the variables and their topicality to the chosen PICOT question about black diabetes mellitus type II patients.
- The BlueStar Diabetes Mobile Health Application The mobile health application "BlueStar Diabetes" is advised for the client to help improve his quality of life and prevent any complications.
- Type 2 Diabetes: Age-Related Changes Type 2 diabetes is a disorder commonly caused by blood sugar imbalance in the body when insulin hormone becomes defective, and mainly results from lifestyle implications.
- Type 2 Diabetes Mellitus and Coronary Artery Disease The paper demonstrates that type 2 diabetes mellitus and coronary artery disease (CAD) can cause the symptoms of feeling extremely tired and gaining weight.
- Diabetes and Healthy People 2020 The paper will address diabetes from the point of view of Healthy People 2020 and discuss diabetes' impact on individual health and the overall health of the nation.
- Type 2 Diabetes Prevention: Health Promotion Program The prevention of type 2 diabetes can be accomplished by ensuring that patients exercise, maintain a proper diet, get an annual physical, and participate in lifestyle seminars.
- Diabetes Intervention as Evidence-Based Practice Project The development of artificial pancreas technology provides an opportunity for more effective and safe treatment that is ongoing 24/7.
- Rapid Weight Loss in Elderly Diabetic Patient The paper discusses about measures for diagnostic causes problem of weight loss in diabetic and importance of right diagnostics.
- Quality Healthcare: Measuring NP Performance Out of six domains of care proposed by the National Committee for Quality Assurance, the paper focuses on such domains as the effectiveness of care.
- Diabetes in Children: Policies and Programs Diabetes is a chronic disease, the onset of which is caused due to the lack of insulin produced by the pancreas or organism's inability to use this insulin.
- Reducing Hospital Readmissions Among Diabetes Patients This paper proposes to use several strategies that may not only improve outcomes in patients with diabetes but also reduce related workload and cost burden on the industry.
- Constant Glucose Monitoring in Diabetic Patients The paper discusses the importance of Constant Glucose Monitoring in diabetic patients. It includes that GCM improves treatment satisfaction.
- Health Belief Model in Diabetes Care It is important to note that diabetes is a chronic condition where an individual’s body experiences issues with blood sugar regulations.
- The Type 2 Diabetes Patient Education Knowledge of type 2 diabetes and mortality from this disease will help to raise awareness of patients in this matter.
- A Diabetes Patient's Challenging Experiences The current paper provides one with a better understanding of individuals’ experiences with chronic illnesses and associated vulnerabilities.
- Reducing Hospital Readmissions With Diabetes The current paper will review the ways of reducing frequent hospital readmissions among the population of patients with diabetes.
- Type 2 Diabetes Treatment Plan for Teenager The patient is a female teenager who goes to high school and frequently attends soccer practice, as she is the goalie of the soccer team.
- Factors That Affect the Increase of Type 2 Diabetes Worldwide
- Diabetes Mellitus and Contemporary Naturopathic Medicine
- Glucose Tolerance Tests Accuracy in Diagnosing Diabetes
- Metformin and Biliary Tract Cancer in Patients With Type 2 Diabetes
- Diabetes Among Ethnic Minorities and the Aging Population
- Diabetes, Ethnicity, and Genetics
- Type Two Diabetes Mellitus as a Disease That Discriminates Against Lifes
- Medications Adherence and Associated Factors Among Patients With Type 2 Diabetes Mellitus in the Gaza Strip, Palestine
- Obesity and Diabetes: Implications for Brain-Immunometabolism
- Optimizing Exercise for the Prevention and Treatment of Type 2 Diabetes
- Obesity and Diabetes: Energy Regulation by Free Fatty Acid Receptors
- Living With Diabetes: The Benefits of a High Fat and Low Carbohydrate Diet
- Sex and Gender Aspects in Diabetes
- Childhood Obesity and Its Correlation With Type 2 Diabetes
- Diabetes Mellitus and Erectile Dysfunctions
- Vegetarian and Vegan Diets on Type 2 Diabetes Management
- Genetic Origins and Interventions of Insulin-Dependent Diabetes Mellitus
- Understanding Autoimmune Diabetes Through the Prism of the Tri-Molecular Complex
- Mediterranean Diet and Type 2 Diabetes
- Alzheimer’s Disease and Type 2 Diabetes: A Critical Assessment of the Shared Pathological Traits
- Novel Biomarkers for Type 2 Diabetes
- Family-based Diabetes Intervention for Hispanic Adults and Their Family Members
- Type Two Diabetes Mellitus Among African Americans
- Diabetes Alters Activation and Repression of Pro- And Anti-inflammatory Signaling Pathways in the Vasculature
- Diabetes: All About the Disease, Its Causes, Effects, Treatments, and Possible Future Treatments
- Diabetes Health and Prevention for Asian Americans
- Traditional and Alternative Medicine for Type Two Diabetes
- Camel Milk and Its Effects on People With Type One Diabetes
- Diabetes, Pancreatic Cancer, and Metformin Therapy
- Platelet Measurements and Type 2 Diabetes: Investigations in Two Population-based Cohorts
- Gestational Diabetes and How To Treat the Disease During Pregnancy
- Connecting Alzheimer’s Disease With Diabetes Mellitus Through Amyloidogenic Evolvability
- Phosphatidylserine-liposomes Promote Tolerogenic Features on Dendritic Cells in Human Type 1 Diabetes by Apoptotic Mimicry
- Factors That Affect the Health Condition of Diabetes
- Native Americans and the Effects of Diabetes
- Type 1 Diabetes Symptoms, Causes, Diagnosis, and Treatments
- Asian Indians With Prediabetes Have Similar Skeletal Muscle Mass and Function to Those With Type 2 Diabetes
- Diabetes and Complementary and Alternative Therapies
- Diabetes Disease and Its Effect on the Digestive System
- Type One Diabetes and the Consequences
- What Are the Screening Tools for Type 1 Diabetes?
- How Does Insulin Help Diabetes Be Controlled?
- What Is the Prophylaxis To Prevent Type 2 Diabetes?
- How Does Diabetes Not Cause Depression?
- Why Are Approximately 1,800 New Cases of Diabetes Diagnosed in America Every Day?
- Does Alcohol Decrease the Risk of Diabetes?
- What Is the Relationship Between Excess Iron and Type 2 Diabetes?
- Does Overeating Cause Diabetes, Cavities, Acne, Hyperactivity and Make You Fat?
- How Fat and Obesity Cause Diabetes?
- What Is Nephrogenic Diabetes Insipidus?
- What Are the Effects of Diabetes on the Peripheral Blood Vessels and the Consequences?
- How Diabetes Insipidus Takes Place in the Human Body?
- Cell-Based Therapy for Type 1 Diabetes: Should We Take Hyperglycemia Into Account?
- What Is the Prevalence and Statistics of Diabetes in Australia?
- How Diabetes Mellitus Changes Urine Formation?
- What Is the Public Awareness of Diabetes?
- Can Diabetes Become Preventable?
- What Are the Main Causes and Treatments of Diabetes?
- Can Exercising and Dieting Prevent People From Type 2 Diabetes?
- What Is Pharmacotherapy and How Does It Help in the Treatment of Type 2 Diabetes?
- Can Coffee Reduce the Risk of Diabetes?
- What Factors Are Involved in the Increasing Prevalence of Type II Diabetes in Adolescents Living in Sub-saharan Africa?
- Is It Possible to Manage Diabetes Through Diet and Weight Control?
- What Is the Relationship Between Depression and Diabetes?
- How Does the Treatment With Insulin Affect Type 2 Diabetes?
- What Is the Relationship Between Genetic Predisposition, Obesity, and the Development of Type 2 Diabetes?
- How to Reduce the Likelihood of Rehospitalization of Patients With Diabetes?
- Why Diabetes Mellitus and How It Affects the United States?
- Does Valproic Acid Have Potential in the Treatment of Diabetes Mellitus?
- What Is the Relationship Between Genetics and Diabetes?
Cite this page
Select style
- Chicago (A-D)
- Chicago (N-B)
NursingBird. (2024, May 23). 188 Diabetes Research Topics & Essay Examples. https://nursingbird.com/topics/diabetes-research-topics/
"188 Diabetes Research Topics & Essay Examples." NursingBird , 23 May 2024, nursingbird.com/topics/diabetes-research-topics/.
NursingBird . (2024) '188 Diabetes Research Topics & Essay Examples'. 23 May.
NursingBird . 2024. "188 Diabetes Research Topics & Essay Examples." May 23, 2024. https://nursingbird.com/topics/diabetes-research-topics/.
1. NursingBird . "188 Diabetes Research Topics & Essay Examples." May 23, 2024. https://nursingbird.com/topics/diabetes-research-topics/.
Bibliography
NursingBird . "188 Diabetes Research Topics & Essay Examples." May 23, 2024. https://nursingbird.com/topics/diabetes-research-topics/.
- Human Papillomavirus
- Subscribe to journal Subscribe
- Get new issue alerts Get alerts
Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
Keeping up-to-date with diabetes care and education
Funnell, Martha M. MS, RN, CDE, FAAN; Freehill, Karein BSN, MS, RN, CDE
At the University of Michigan Medical School, Department of Learning Health Sciences, in Ann Arbor, Mich., Martha M. Funnell is an emeritus research scientist and Karein Freehill is an outreach coordinator/diabetes educator. Ms. Funnell is also a member of the Nursing2018 Editorial Board.
Acknowledgment: Supported in part by Grant Number P30DK092926 (MCDTR) from the National Institute of Diabetes and Digestive and Kidney Diseases.
The authors and planners have disclosed no potential conflicts of interest, financial or otherwise.
The American Diabetes Association publishes standards of care that are updated annually by a panel of experts in nursing, education, behavior, psychology, nutrition, pharmacology, and medicine. This article describes current evidence-based approaches to care and education for adults and highlights revisions in the 2018 Standards of Care that are relevant to nurses and patients with type 2 diabetes.
The American Diabetes Association publishes standards of care that are updated annually by a panel of experts. This article describes evidence-based approaches to care and education for adults with diabetes and highlights revisions in the 2018 Standards of Care that are relevant to nurses and patients with type 2 diabetes.

THE CDC ESTIMATES that 30.3 million people in the US have diabetes, and of those, 7.2 million are undiagnosed. 1 In addition, 84.1 million American adults have prediabetes. This means that 114 million people in the US are at risk for developing the complications of diabetes. Because diabetes and its complications are widespread, burdensome, and costly, nurses need to provide care, patient education, and support based on current evidence and recommendations.
Research in the treatment and care of diabetes is a growing and dynamic field. New medications and therapies become available each year. Research is ongoing about how to delay, prevent, and treat diabetes and prevent and treat its complications. New research findings indicate how to implement effective education, support, and healthcare; improve quality of life; and reach diverse communities.
Each year, the American Diabetes Association (ADA) publishes standards of care for patients with diabetes. 2 These standards are updated annually by a panel of experts in nursing, education, behavior, psychology, nutrition, pharmacology, and medicine. This article describes current evidence-based approaches to care and education for adults with diabetes and highlights revisions in the 2018 Standards that are relevant to nurses and patients with type 2 diabetes.
Patient-centered approaches
Over the past few years, one of the most significant changes in the care of patients with diabetes has been the strong emphasis on tailoring treatment and education to meet the needs of each individual, including patient preferences, prognosis, and comorbidities. 2 The first section of the Standards of Care (Improving Care and Promoting Health in Populations) highlights critical themes to guide this care and address disparities: patient-centered collaborative care, use of evidence-based guidelines to align with the Chronic Care Model, team-based care, community involvement, and referral to needed resources. 2,3
Treatment goals such as hemoglobin A1C (A1C) levels, weight and physical activity, and action plans to reach those goals should be created in collaboration with patients and their families based on their preferences, values, and goals. The burden of treatment and the patient's self-efficacy also should be considered, as well as the patient's social context, by assessing housing stability, food security, language barriers, finances, and community resources. 2
When collaborating with patients, nurses need to assess each patient's:
- work and school schedule and environment
- health beliefs
- support systems
- nutritional and physical activity patterns and preferences
- social situation
- financial concerns
- family, ethnicity, cultural, and religious factors
- literacy and numeracy
- complications and duration of disease
- comorbidities and health priorities. 2
Active listening during the assessment process can be used by the patient and the nurse to develop self-determined metabolic, behavioral, and psychosocial goals that are realistic and personally meaningful. The goals need to match both the patient's lifestyle and improve his or her health outcomes. For example, a low-income working mother may set a goal to prepare more healthful meals at home rather than eating fast food, while an older person who is newly widowed may set a goal to become involved with a diabetes support group.
Screening, prevention, and treatment
The criteria for the diagnosis of diabetes and prediabetes have not changed (see Criteria for the diagnosis of prediabetes and diabetes ). Fasting, 2-hour plasma glucose after a 75-g glucose (oral glucose tolerance test [OGTT]) load, and A1C testing can all be used for screening, and no one test is preferred for diagnosis. However, if A1C is used, it should be done in a lab using a method certified by the NGSP and standardized to the Diabetes Control and Complications Trial assay. Do not use A1C levels for diagnosis if the patient has a condition associated with increased red blood cell turnover (such as sickle cell trait, second or third trimester pregnancy, or chronic kidney disease requiring hemodialysis). Among these patients, only plasma blood glucose testing should be used for diagnosis. 2,4
Because both prediabetes and type 2 diabetes have a long presymptomatic period, nurses can help patients determine their level of risk through an informal assessment or a questionnaire, such as the Type 2 Diabetes Risk test ( www.diabetes.org/are-you-at-risk/diabetes-risk-test ). Screening is recommended for adults of any age who are overweight or obese and have one or more risk factors for type 2 diabetes. 2 (See Risk factors for type 2 diabetes .) All adults should be screened for diabetes starting at age 45. 2 When glucose readings are normal, the screening should be repeated at 3-year intervals. A new recommendation is that screening should also be considered for children and adolescents who are overweight or obese and have one or more risk factors for type 2 diabetes. 2
Prevention or delay of type 2 diabetes
Patients with prediabetes are at risk for diabetes and cardiovascular disease (CVD) and should be referred to an intensive diabetes prevention program that includes follow-up counseling and maintenance. 2,5 They should also be screened and treated for modifiable CVD risk factors.
In-person programs based on the Diabetes Prevention Program (DPP), certified or recognized diabetes self-management education and support (DSMES) programs, and technology-based programs can be useful to achieve and sustain the weight loss (7% of body weight) and exercise (150 min/week of moderate intensity) recommendations needed to lower the risk of diabetes. 2,6 Recent studies support behavioral and content delivery through virtual small groups, internet-driven social networks, cell phones, wireless weight scales, pedometers, and other mobile internet-enabled devices. 7,8 The CDC has begun to certify electronic and mobile health programs as effective DPP interventions. 6
There is no specific “diet” for diabetes prevention; however, weight loss is key. In addition, nutrition plans rich in monounsaturated and polyunsaturated fats (such as the Mediterranean diet) may delay or prevent diabetes. 8,9 A healthful diet incorporating whole grains, nuts, dairy, and berries, as well as limiting red meat, added sugar, and sugar-sweetened beverages, may also be helpful. 2,10-12 Moderate exercise, such as brisk walking, can improve insulin sensitivity and reduce abdominal fat, and is beneficial as part of a prevention program. 13
Metformin should also be considered for patients with prediabetes, especially those with a body mass index (BMI) of 35 or greater, under age 60, and women with a history of gestational diabetes. 5
Treatment of type 2 diabetes
Due to the progressive nature of type 2 diabetes, treatment occurs in stages beginning with lifestyle interventions including referral to a formal DSMES program. Medication therapy begins with monotherapy, most often metformin. Assessing and addressing healthful eating, weight management, physical activity, self-determined behavioral goals, and psychological and social needs are essential elements that should be provided by nurses at each stage of therapy. 2,14 Both drug-specific and patient factors should be considered and discussed as part of patient-provider shared decision-making when prescribing and advancing antihyperglycemic treatment. These factors include efficacy, safety, risk for hypoglycemia and other adverse reactions, weight change, cardiovascular effects, renal effects, costs, and route of administration. 2
Additional medications including insulin or other injectables (alone or in combination) are added as needed to achieve the A1C target chosen in collaboration with the patient. 15 One area that has been given more emphasis in the 2018 ADA Standards of Care is the prevention and management of CVD. Among patients with diabetes and CVD, adding agents that will reduce cardiovascular events and mortality (such as empagliflozin or liraglutide) is recommended. 2,16 The effect of glucose-lowering medications on weight should be considered for overweight and obese patients. Measurement of B12 levels should be considered for patients who take metformin, especially those with anemia or peripheral neuropathy. 2
Although an A1C goal of 7% or less is recommended for most adults, patient-specific and disease factors are used to determine higher or lower personal goals. Optimal target glucose recommendations are a preprandial capillary plasma glucose level of 80 to 130 mg/dL and a peak postprandial plasma glucose level of 180 mg/dL. Personal targets are based on self-management preferences, capacities, and personal goals; available support systems and resources; risk for hypoglycemia; disease duration; life expectancy; severity of comorbidities; and presence of vascular complications. 2,15 For example, an otherwise healthy adult newly diagnosed with diabetes and a strong support system might choose more stringent targets than an older adult with long-standing diabetes, one or more comorbidities, and limited support.
Self-management and psychosocial issues
All patients should be referred for DSMES and medical nutrition therapy (MNT) and receive ongoing assessment of educational, dietary, and psychosocial issues, and the need for support. 2
In accordance with the National Standards for Diabetes Self-Management Education and Support, all patients with diabetes should take part in DSMES to obtain the knowledge, skills, and ability to participate in self-management and ongoing support to implement and sustain these behaviors. 2,17 Four critical times to assess and refer patients for DSMES are at diagnosis, annually, when complicating factors arise, and when transitions in care occur. 2,18
DSMES can be provided in individual or group settings, as well as through internet-based services. 2,17 Regardless of format, it should be patient-centered and patient-driven; address the clinical, behavioral, and emotional aspects of diabetes; and be responsive to individual questions, concerns, preferences, needs, and values. 2,14 This means that both care and education are less directive, and nurses should use patient-centered communication styles (such as open-ended questions, active listening, self-directed goal setting, and assessing emotional concerns) focused on helping patients with diabetes and their family members design a management program that works not only for their diabetes, but also for their lives. 14,17,19 For example, beginning an educational or clinical assessment by asking patients what is hardest for them about managing diabetes, what questions they have, and how they are coping with the demands of diabetes are ways to assess their needs and perceptions so these can be addressed at the beginning of the DSMES or clinical encounter. 14
The ADA does not endorse a standardized or “ideal” meal plan or percentages of macronutrients for patients with diabetes. 2 MNT is instead based on diabetes medications, other therapies, and patient and family preferences, rather than a standard “diabetic” or “ADA diet.” 2,12,20 Modest and sustained weight loss has been shown to improve glycemia among patients with type 2 diabetes and reduce the need for medications. 2,12 Improvements related to weight management are most likely to occur early in the course of diabetes when insulin secretory ability is relatively intact. Reducing calories is the key to weight loss, with similar outcomes for meal plans that reduce fat, carbohydrates, or protein. 2
The ADA 2018 Standards of Care highlight the importance of addressing psychosocial concerns and self-directed goal setting and other behavioral change efforts. 2,14 It is recommended that all patients with diabetes be routinely screened for depression, diabetes distress (a common and significant psychological reaction to diabetes related to the burden of daily self-management demands, the emotional burden of caring for a serious and complex disease, and the anxiety of the potential or actuality of disease progression), anxiety, eating disorders, and cognitive impairment. 2,22 Because it is so common and has an independent negative effect on outcomes among people with diabetes and their family members, diabetes distress needs to be assessed and addressed. 2,20,21 Prevalence rates of diabetes distress range from 18% to 45%, with an incidence of 38% to 48% over 18 months. High levels of distress (such as guilt, anger, frustration, fear, and burnout) have been linked with elevated A1C levels, lower self-efficacy, and poorer dietary, exercise, and medication-taking behaviors. 22
Obesity management
The management of obesity among patients with type 2 diabetes is an important part of diabetes treatment.
- A BMI of less than 25 kg/m 2 is defined as normal (less than 23 kg/m 2 among Asian Americans)
- A BMI of 25 to 29.9 kg/m 2 is defined as overweight (23.0-27.4 kg/m 2 among Asian Americans)
- A BMI of 30 to 40 kg/m 2 is defined as obese (27.5 to 37.4 kg/m 2 among Asian Americans)
- A BMI over 40 kg/m 2 is defined as extremely obese (over 37.5 kg/m 2 among Asian Americans). 2
MNT, physical activity, and behavioral, pharmacologic, and surgical interventions are recommended strategies for obesity management. 2 Patient engagement in meal planning is critical for weight loss. MNT, physical activity planning, and behavioral strategies designed to achieve a 5% weight loss should be offered to all overweight and obese adult patients who indicate a desire and readiness to lose weight. 2 Approved weight loss medications may be offered to patients with a BMI of 27 kg/m 2 or greater. Bariatric surgery may be considered by patients with type 2 diabetes and a BMI of 35 kg/m 2 or greater; this treatment may result in normalization of glucose levels. 23
Diabetes and pregnancy
Recommendations are provided for women with type 1 or type 2 diabetes before pregnancy (pregestational diabetes), gestational diabetes, and general principles for diabetes management in pregnancy. A recommendation of interest to nurses is the importance of assessing the need for and providing preconception counseling at every opportunity for women of childbearing age with type 1 and type 2 diabetes. Areas to address include family planning, discussing pregnancy plans with her provider, and achieving an A1C of 6.5% or less before becoming pregnant. 2
Glycemic targets for pregnant women with type 1, type 2, and pregestational diabetes are:
- Fasting, 95 mg/dL (5.3 mmol/L) or less
- 1-hour postprandial, 130 mg/dL (7.8 mmol/L) or less
- 2-hour postprandial, 120 mg/dL (6.7 mmol/mol) or less. 2,24
A target A1C of 6.0% to 6.5% is recommended, but less than 6% may be optimal if it can be achieved without hypoglycemia. Less stringent targets (less than 7%) may be recommended for women who experience significant hypoglycemia. 2
Insulin is the preferred treatment for management of both type 1 and type 2 diabetes during pregnancy, although metformin and glyburide may also be used. 2 Women with both type 1 and type 2 diabetes should be prescribed low-dose aspirin, unless contraindicated, from the end of the first trimester until the baby is born to lower the risk of preeclampsia. 25
Complications and other comorbidities
Macrovascular complications.
Both the prevention and treatment of acute and long-term complications of diabetes remain a significant focus. The BP recommendation remains at 140/90 mm Hg, although multiple drug therapy may be required to reach this target. It may be appropriate to aim for a BP of 130/80 mm Hg for certain patients (such as younger patients or those with albuminuria or other cardiovascular risk factors) if it can be obtained without significant treatment burden. 2 The recommended first line of treatment for hypertension is either an angiotensin-converting enzyme inhibitor or an angiotensin receptor blocker at the maximally tolerated dose. Because these reduce the effect of the hormone angiotensin II that is most active during sleep, it is preferable to take them at bedtime. 2 Older adults should also be treated for hypertension. A new recommendation is that all patients with hypertension should monitor their BP at home. 26
Lifestyle and moderate statin therapy is recommended for adults with diabetes age 40 or over without atherosclerotic cardiovascular disease (ASCVD), including older adults with an intermediate life expectancy. 2 High-intensity statin therapy should be added to lifestyle therapy for all patients with ASCVD. Patients under age 40 with additional ASCVD risk factors should consider moderate-intensity statin therapy. Lifestyle management and optimal glycemic control are also recommended for patients with serum triglyceride levels of 150 mg/dL and over and/or a low high-density lipoprotein cholesterol level (under 40 mg/dL for men; under 50 mg/dL for women). A recent systematic review indicated that statins do not have an adverse effect on cognition. 27
Aspirin (75 to 162 mg/day) may be considered as a primary prevention for all patients with diabetes who are at increased cardiovascular risk. 2 This includes most adults with diabetes over age 50 who have at least one other risk factor and are not at risk for bleeding.
Microvascular complications
Optimal blood glucose and BP levels are still recommended to lower the risk and slow progression of kidney disease and retinopathy. 2 Either laser retinal photocoagulation or intravitreal antivascular endothelial growth factor injections can be used to protect vision among patients with proliferate diabetic retinopathy. 28 Aspirin therapy does not increase the risk of retinal hemorrhage among patients with retinopathy. 2
Assess signs and symptoms of both diabetic peripheral neuropathy and autonomic neuropathy. Either pregabalin or duloxetine are recommended as initial therapy for neuropathic pain. 2 Provide general preventive foot self-management care to all adults with diabetes.
Acute complications
The alert blood glucose level for hypoglycemia is 70 mg/dL or less. 2,29 The preferred treatment is 15 to 20 g of fast-acting glucose (such as glucose tablets), although any type of fast-acting carbohydrate that contains glucose is acceptable. Treatments that contain fat may delay the glycemic response. Among patients with type 2 diabetes, carbohydrate sources high in protein should not be used to treat or prevent hypoglycemia. 2 Protein can increase insulin production without raising the level of glucose. Once the blood glucose level has returned to normal, a meal or snack may be needed. Teach patients to wear diabetes identification and carry a readily available source of glucose.
Illness or other stressful events may raise glucose levels and lead to diabetic ketoacidosis in patients with type 1 diabetes or to a hyperosmolar hyperglycemic state in patients with type 2 diabetes. 2 Both of these complications are life-threatening and require immediate treatment. Review sick-day strategies with patients and emphasize the need to obtain recommended immunizations.
Hospital and long-term care
The guidelines for hospitalized patients, either newly diagnosed or with long-standing diabetes, have not changed. Insulin therapy should be initiated at a threshold of 180 mg/dL with a target range of 140 to 180 mg/dL. 2 Basal insulin plus a bolus correction dose is the preferred treatment; the sole use of sliding scale insulin is strongly discouraged. Of interest to nurses is the focus on discharge planning: medication reconciliation, transition care, communication, and follow-up. Along with a referral for DSMES and MNT, review blood glucose monitoring; when to contact the healthcare provider; the recognition, treatment, and prevention of hypoglycemia; hyperglycemia and sick-day management; consistent use of medications; and consistent timing of meals. 2,17
Special populations
The sections of the 2018 Standards of Care related to children and adolescents have been expanded to capture the nuances of care and DSMES specific for these populations, such as diabetes management in child-care settings and at school. 2 An A1C goal of less than 7.5% is recommended across all pediatric groups. Nurses, parents, and other healthcare professionals should prepare young adults for the transition to adult healthcare and self-management.
Three recommendations that were added to the 2018 Standards of Care highlight the need to individualize pharmacologic therapy for older adults in order to reduce the risk of hypoglycemia, avoid overtreatment, and simplify complex treatment plans. 2 Older adults who are otherwise healthy with intact cognitive function and functional status should have lower glycemic goals than those with multiple health and functional impairments, especially patients who reside in long-term-care facilities. Meal plans need to be flexible and tailored to personal choices, preferences, culture, and personal goals for patients with diabetes in long-term-care facilities and in end-of-life care.
Patient education is the key
Because of the increasing number of individuals with diabetes in both the US and throughout the world, most nurses are likely to encounter many patients with diabetes regardless of their specialty or work situation. Whether in the community, an outpatient specialty, primary care setting, or hospital, providing quality diabetes education and ongoing support and care is a role that most nurses must be prepared to assume. Although referral to a comprehensive DSMES program is essential, providing information and ongoing support also needs to occur informally using “teachable moments” and answering questions and concerns raised by patients with diabetes and their family members.
Providing self-management education and addressing psychosocial issues are critical elements of both diabetes care and nursing practice. Regardless of technology or new treatments, nurses must never lose sight of their roles as patient advocate and supporter.
Criteria for the diagnosis of prediabetes and diabetes 2
Prediabetes
Fasting plasma glucose 100-125 mg/dL (5.6-6.9 mmol/L)
2-h plasma glucose during 75-OGTT 140-199 mg/dL (7.8-11.0 mmol/L)
A1C 5.7%-6.4% (39-47 mmol/mol)
Fasting plasma glucose ≥126 mg/dL (7.0 mmol/L)
2-h plasma glucose ≥200 mg/dL (11.1 mmol/L)
A1C ≥6.5% (48 mmol/mol)
Classic symptoms of hyperglycemia, hyperglycemic crisis, random plasma glucose ≥200 mg/dL (11.1 mmol/L)
Risk factors for type 2 diabetes 30
Individuals are more likely to develop type 2 diabetes if they:
- have a family history of diabetes (first-degree relative)
- are overweight or obese
- are age 45 or older
- are Black, Alaska Native, Native American, Asian American, Hispanic, Native Hawaiian, or Pacific Islander
- have hypertension
- have a low serum high-density lipoprotein cholesterol level, or a high serum triglyceride level
- have a history of gestational diabetes or gave birth to a baby weighing 9 lb or more
- are not physically active
- have a history of heart disease or stroke
- have a history of depression
- have polycystic ovary syndrome
- have acanthosis nigricans (velvety, hyperpigmented plaques on the skin, especially intertriginous sites such as the neck and axillae).
American Diabetes Association; diabetes; diabetes distress; diabetes self-management; diabetes standards of care; gestational diabetes; hyperglycemia; hypoglycemia; prediabetes; type 1 diabetes; type 2 diabetes
- + Favorites
- View in Gallery
Readers Of this Article Also Read
Caring for people with diabetes: a fresh look at an old disease, diabetes: changing the conversation, communication strategies for patients with dementia, assessing nursing interventions to reduce patient falls, leaders, managers, and followers: working in harmony.
357 Diabetes Essay Topics & Examples
When you write about the science behind nutrition, heart diseases, and alternative medicine, checking titles for diabetes research papers can be quite beneficial. Below, our experts have gathered original ideas and examples for the task.
🏆 Best Diabetes Essay Examples & Topics
⭐ most interesting diabetes research paper topics, ✅ simple & easy diabetes essay topics, 🎓 good research topics about diabetes, 💡 interesting topics to write about diabetes, 👍 good essay topics on diabetes, ❓ diabetes research question examples.
- Type 2 Diabetes The two major types of diabetes are type 1 diabetes and type 2 diabetes. Doctor: The first step in the treatment of type 2 diabetes is consumption of healthy diet.
- Type 2 Diabetes as a Public Health Issue In recent years, a steady increase in the incidence and prevalence of diabetes is observed in almost all countries of the world.
- Adult-Onset Type 2 Diabetes: Patient’s Profile Any immediate care as well as post-discharge treatment should be explained in the best manner possible that is accessible and understandable to the patient.
- Leadership in Diabetes Management Nurses can collaborate and apply evidence-based strategies to empower their diabetic patients. The involvement of all key stakeholders is also necessary.
- Nursing Care Development Plan for Diabetes and Hypertension In addressing the first nursing diagnosis, the main aim of the nursing interventions will be to prevent the development of secondary hypoglycemia by increasing blood glucose levels.
- Evidence Synthesis Assignment: Prevention of Diabetes and Its Complications The purpose of this research is to analyze and synthesize evidence of good quality from three quantitative research and three non-research sources to present the problem of diabetes and justify the intervention to address it.
- Disease Management for Diabetes Mellitus The selection of the appropriate philosophical and theoretical basis for the lesson is essential as it allows for the use of an evidence-based method for learning about a particular disease.
- Intervention Methods for Type 2 Diabetes Mellitus An individual should maintain a regulated glycemic control using the tenets of self-management to reduce the possibility of complications related to diabetes.
- Living With a Chronic Disease: Diabetes and Asthma This paper will look at the main effects of chronic diseases in the lifestyle of the individuals and analyze the causes and the preventive measures of diabetes as a chronic disease.
- Diabetes: Symptoms, Treatment, and Prevention As a consequence, the amount of sugar in the blood is made to rise and this cause discomfort for the affected individuals.
- Diabetes Mellitus Management in the Elderly Diabetes mellitus is a health complication involving an increase in the concentration in the concentration of blood sugar either due to a failure by cells to effectively respond to the production of insulin in the […]
- Relation Between Diabetes And Nutrition Any efforts to lessen and eliminate the risk of developing diabetes must involve the dietary habit of limiting the consumption of carbohydrates, sugar, and fats. According to Belfort-DeAguiar and Dongju, the three factors of obesity, […]
- Diabetes Mellitus: Types, Causes, Presentation, Treatment, and Examination Diabetes mellitus is a chronic endocrinologic disease, which is characterized by increased blood glucose concentration.
- The Nature of Type 1 Diabetes Mellitus Type 1 diabetes mellitus is a chronic autoimmune disease that has an active genetic component, which is identified by increased blood glucose levels, also known as hyperglycemia.
- Health Promotion: Diabetes Mellitus and Comorbidities This offers a unique challenge in the management of diabetes and other chronic diseases; the fragmented healthcare system that is geared towards management of short-term medical emergencies often is not well prepared for the patient […]
- Diabetes Impact on Cardiovascular and Nervous Systems Diabetes is one of the commonest conditions affecting many people in different parts of the world. The first type is also called “juvenile diabetes” and it occurs when the body of an individual is incapable […]
- Ethics of Type 2 Diabetes Prevalence in Minorities The purpose of this article analysis is to dwell on scholarly evidence that raises the question of ethical and cultural aspects of T2DM prevalence in minorities.
- Gestational Diabetes in a 38-Year-Old Woman The concept map, created to meet B.’s needs, considers her educational requirements and cultural and racial hurdles to recognize her risk factors and interventions to increase her adherence to the recommended course of treatment.B.said in […]
- Type 2 Diabetes Mellitus and Its Implications You call an ambulance and she is taken in to the ED. Background: Jean is still very active and works on the farm 3 days a week.
- Development of Comprehensive Inpatient and Outpatient Programs for Diabetes Overcoming the fiscal and resource utilization issues in the development of a comprehensive diabetes program is essential for the improvement of health and the reduction of treatment costs.
- Healthcare Cost Depending on Chronic Disease Management of Diabetes and Hypertension A sufficient level of process optimization and the presence of a professional treating staff in the necessary number will be able to help improve the indicators.
- Improving Glycemic Control in Black Patients with Type 2 Diabetes Information in them is critical for answering the question and supporting them with the data that might help to acquire an enhanced understanding of the issue under research. Finally, answering the PICOT question, it is […]
- Shared Decision-Making That Affects the Management of Diabetes The article by Peek et al.is a qualitative study investigating the phenomenon of shared decision-making that affects the management of diabetes. The researchers demonstrate the racial disparity that can arise in the choice of approaches […]
- Managing Obesity as a Strategy for Addressing Type 2 Diabetes When a patient, as in the case of Amanda, requires a quick solution to the existing problem, it is necessary to effectively evaluate all options in the shortest possible time.
- Tests and Screenings: Diabetes and Chronic Kidney Disease The test is offered to patients regardless of gender, while the age category is usually above 45 years. CDC1 recommends doing the test regardless of gender and is conducted once or twice to check the […]
- Obesity Management for the Treatment of Type 2 Diabetes American Diabetes Association states that for overweight and obese individuals with type 2 diabetes who are ready to lose weight, a 5% weight reduction diet, physical exercise, and behavioral counseling should be provided.
- COVID-19 and Diabetes Mellitus Lim et al, in their article, “COVID-19 and diabetes mellitus: from pathophysiology to clinical management”, explored how COVID-19 can worsen the symptoms of diabetes mellitus.
- The Importance of Physical Exercise in Diabetes II Patients The various activities help to improve blood sugar levels, reduce cardiovascular cases and promote the overall immunity of the patient. Subsequently, the aerobic part will help to promote muscle development and strengthen the bones.
- Diabetes Education Workflow Process Mapping DSN also introduces the patient to the roles of specialists involved in managing the condition, describes the patient’s actions, and offers the necessary educational materials.
- Diabetes: Treatment Complications and Adjustments One of the doctor’s main priorities is to check the compatibility of a patient’s medications. The prescriptions of other doctors need to be thoroughly checked and, if necessary, replaced with more appropriate medication.
- The Type 2 Diabetes Mellitus PICOT (Evidence-Based) Project Blood glucose levels, A1C, weight, and stress management are the parameters to indicate the adequacy of physical exercise in managing T2DM.
- Chronic Disease Cost Calculator (Diabetes) This paper aims at a thorough, detailed, and exhaustive explanation of such a chronic disease as diabetes in terms of the prevalence and cost of treatment in the United States and Maryland.
- Diabetes Mellitus Epidemiology Statistics This study entails a standard established observation order from the established starting time to an endpoint, in this case, the onset of disease, death, or the study’s end. It is crucial to state this value […]
- Epidemiology: Type II Diabetes in Hispanic Americans The prevalence of type II diabetes in Hispanic Americans is well-established, and the search for inexpensive prevention methods is in the limelight.
- Diabetes: Risk Factors and Effects Trends in improved medical care and the development of technology and medicine are certainly contributing to the reduction of the problem. All of the above indicates the seriousness of the problem of diabetes and insufficient […]
- Barriers to Engagement in Collaborative Care Treatment of Uncontrolled Diabetes The primary role of physicians, nurses, and other healthcare team members is to provide patients with medical treatment and coordinate that care while also working to keep costs down and expand access.
- Hereditary Diabetes Prevention With Lifestyle Modification Yeast infections between the fingers and toes, beneath the breast, and in or around the genital organs are the common symptoms of type 2 diabetes.
- Health Equity Regarding Type 2 Diabetes According to Tajkarimi, the number of research reports focusing on T2D’s prevalence and characteristics in underserved minorities in the U. Adapting the program’s toolkits to rural Americans’ eating and self-management habits could also be instrumental […]
- Diabetes Mellitus: Treatment Methods Moreover, according to the multiple findings conducted by Park et al, Billeter et al, and Tsilingiris et al, bariatric surgeries have a positive rate of sending diabetes into remission.
- Diagnosing Patient with Insulin-Dependent Diabetes The possible outcomes of the issues that can be achieved are discussing the violations with the patient’s family and convincing them to follow the medical regulations; convincing the girl’s family to leave her at the […]
- Human Service for Diabetes in Late Adulthood The mission of the Georgia Diabetic Foot Care Program is to make a positive difference in the health of persons living with diabetes.
- Diabetes: Symptoms and Risk Factors In terms of the problem, according to estimates, 415 million individuals worldwide had diabetes mellitus in 2015, and it is expected to rise to 642 million by the year 2040.
- Diabetes: Types and Management Diabetes is one of the most prevalent diseases in the United States caused when the body fails to optimally metabolize food into energy.
- Epidemiology of Diabetes and Forecasted Trends The authors note that urbanization and the rapid development of economies of different countries are the main causes of diabetes. The authors warn that current diabetes strategies are not effective since the rate of the […]
- The Aboriginal Diabetes Initiative in Canada The ADI’s goal in the CDS was to raise type 2 diabetes awareness and lower the incidence of associated consequences among Aboriginal people.
- Communicating the Issue of Diabetes The example with a CGM sensor is meant to show that doctors should focus on educating people with diabetes on how to manage their condition and what to do in extreme situations.
- Obesity and Diabetes Mellitus Type 2 The goal is to define the features of patient information to provide data on the general course of the illness and its manifestations following the criteria of age, sex, BMI, and experimental data.
- The Prevention of Diabetes and Its Consequences on the Population At the same time, these findings can also be included in educational programs for people living with diabetes to warn them of the risks of fractures and prevent them.
- Uncontrolled Type 2 Diabetes and Depression Treatment The data synthesis demonstrates that carefully chosen depression and anxiety treatment is likely to result in better A1C outcomes for the patient on the condition that the treatment is regular and convenient for the patients.
- Type 2 Diabetes: Prevention and Education Schillinger et al.came to the same conclusion; thus, their findings on the study of the Bigger Picture campaign effectiveness among youth of color are necessary to explore diabetes prevention.
- A Diabetes Quantitative Article Analysis The article “Correlates of accelerometer-assessed physical activity and sedentary time among adults with type 2 diabetes” by Mathe et al.refers to the global issue of the prevention of diabetes and its complications.
- A Type 2 Diabetes Quantitative Article Critique Therefore, the main issue is the prevention of type 2 diabetes and its consequences, and this paper will examine one of the scientific studies that will be used for its exploration.
- The Diabetes Prevention Articles by Ford and Mathe The main goal of the researchers was to measure the baseline MVPA of participants and increase their activity to the recommended 150 minutes per week through their participation in the Diabetes Community Lifestyle Improvement Program.
- Type 2 Diabetes in Hispanic Americans The HP2020 objectives and the “who, where, and when” of the problem highlight the significance of developing new, focused, culturally sensitive T2D prevention programs for Hispanic Americans.
- Diabetes Mellitus as Problem in US Healthcare Simultaneously, insurance companies are interested in decreasing the incidence of diabetes to reduce the costs of testing, treatment, and provision of medicines.
- Diabetes Prevention as a Change Project All of these queries are relevant and demonstrate the importance of including people at high risk of acquiring diabetes in the intervention.
- Diabetes Mellitus: Causes and Health Challenges Second, the nature of this problem is a clear indication of other medical concerns in this country, such as poor health objectives and strategies and absence of resources.
- Diabetes in Adults in Oxfordshire On a national level, Diabetes Research and Wellness Foundation aims to prevent the spread of the decease through research of the causes and effective treatment of diabetes 2 type.
- Diabetes Mellitus (DM) Disorder Case Study Analysis Thus, informing the patient about the importance of regular medication intake, physical activity, and adherence to diet in maintaining diabetes can solve the problem.
- Diabetes Mellitus in Young Adults Thus, programs for young adults should predominantly focus on the features of the transition from adolescence to adulthood. As a consequence, educational programs on diabetes improve the physical and psychological health of young adults.
- A Healthcare Issue of Diabetes Mellitus Diabetes mellitus is seen as a primary healthcare issue that affects populations across the globe and necessitates the combination of a healthy lifestyle and medication to improve the quality of life of people who suffer […]
- Control of LDL Cholesterol Levels in Patients, Gestational Diabetes Mellitus In addition, some patients with hypercholesterolemia may have statin intolerance, which reduces adherence to therapy, limits treatment efficacy, and increases the risk of CVD.
- Exploring Glucose Tolerance and Gestational Diabetes Mellitus In the case of a glucose tolerance test for the purpose of diagnosing GDM type, the interpretation of the test results is carried out according to the norms for the overall population.
- Type 2 Diabetes Health Issue and Exercise This approach will motivate the patient to engage in exercise and achieve better results while reducing the risk of diabetes-related complications.
- Diabetes Interventions in Children The study aims to answer the PICOT Question: In children with obesity, how does the use of m-Health applications for controlling their dieting choices compare to the supervision of their parents affect children’s understanding of […]
- Diabetes Tracker Device and Its Advantages The proposed diabetes tracker is a device that combines the functionality of an electronic BGL tester and a personal assistant to help patients stick to their diet plan.
- Latino People and Type 2 Diabetes The primary aim of the study is to determine the facilitators and barriers to investigating the decision-making process in the Latin population and their values associated with type 2 diabetes.
- Diabetes Self-Management Education and Support Program The choice of this topic and question is based on the fact that despite the high prevalence of diabetes among adolescents in the United States, the use of DSMES among DM patients is relatively low, […]
- Diabetes Mellitus Care Coordination The aim is to establish what medical technologies, care coordination and community resources, and standards of nursing practice contribute to the quality of care and safety of patients with diabetes.
- Healthy Lifestyle Interventions in Comorbid Asthma and Diabetes In most research, the weight loss in cases of comorbid asthma and obesity is reached through a combination of dietary interventions and physical exercise programs.
- Case Study of Patient with DKA and Diabetes Mellitus It is manifested by a sharp increase in glucose levels and the concentration of ketone bodies in the blood, their appearance in the urine, regardless of the degree of violation of the patient’s consciousness.
- PDSA in Diabetes Prevention The second step in the “Do” phase would be to isolate a few members of the community who are affected by diabetes voluntarily.
- Diabetes: Statistics, Disparities, Therapies The inability to produce adequate insulin or the body’s resistance to the hormone is the primary cause of diabetes. Diabetes is a serious health condition in the U.S.and the world.
- Type 2 Diabetes Prescriptions and Interventions The disadvantage is the difficulty of obtaining a universal model due to the complexity of many factors that can affect the implementation of recommendations: from the variety of demographic data to the patient’s medical history.
- Health Education for Female African Americans With Diabetes In order to address and inform the public about the challenges, nurses are required to intervene by educating the population on the issues to enhance their understanding of the risks associated with the conditions they […]
- Diabetes Risk Assessment and Prevention It is one of the factors predisposing patients suffering from diabetes to various cardiovascular diseases. With diabetes, it is important to learn how to determine the presence of carbohydrates in foods.
- Diabetes Mellitus: Preventive Measures In addition to addressing the medical specialists who will be of service in disease prevention, it will emphasize the intervention programs required to help control the spread of the illness.
- “The Diabetes Online Community” by Litchman et al. The researchers applied the method of telephone interviews to determine the results and effectiveness of the program. The study described the value of DOC in providing support and knowledge to older diabetes patients.
- Mobile App for Improved Self-Management of Type 2 Diabetes The central focus of the study was to assess the effectiveness of the BlueStar app in controlling glucose levels among the participants.
- Type 2 Diabetes in Minorities from Cultural Perspective The purpose of this paper is to examine the ethical and cultural perspectives on the issue of T2DM in minorities. Level 2: What are the ethical obstacles to treating T2DM in ethnic and cultural minorities?
- Type 2 Diabetes in Minorities: Research Questions The Level 2 research questions are: What are the pathophysiological implications of T2DM in minorities? What are the statistical implications of T2DM in minorities?
- Improving Adherence to Diabetes Treatment in Primary Care Settings Additionally, the patients from the intervention group will receive a detailed explanation of the negative consequences of low adherence to diabetes treatment.
- An Advocacy Tool for Diabetes Care in the US To ensure the implementation and consideration of my plea, I sent a copy of the letter to the government officials so it could reach the president.
- Diabetes and Allergies: A Statistical Check The current dataset allowed us to test the OR for the relationship between family history of diabetes and the presence of diabetes in a particular patient: all variables were dichotomous and discrete and could take […]
- Type 2 Diabetes in Adolescents According to a National Diabetes Statistics Report released by the Centers for Disease Control and Prevention, the estimated prevalence of the disease was 25 cases per 10,000 adolescents in 2017. A proper understanding of T2D […]
- Analysis of Diabetes and Its Huge Effects In the US, diabetes is costly to treat and has caused much physical, emotional and mental harm to the people and the families of those who have been affected by the disease.
- Nursing: Self-Management of Type II Diabetes Sandra Fernandes and Shobha Naidu’s journal illustrates the authors’ understanding of a significant topic in the nursing profession.”Promoting Participation in self-care management among patients with diabetes mellitus” article exposes readers to Peplau’s theory to understand […]
- The Impact of Vegan and Vegetarian Diets on Diabetes Vegetarian diets are popular for a variety of reasons; according to the National Health Interview Survey in the United States, about 2% of the population reported following a vegetarian dietary pattern for health reasons in […]
- “Diabetes Prevention in U.S. Hispanic Adults” by McCurley et al. This information allows for supposing that face-to-face interventions can be suitable to my practicum project that considers measures to improve access to care among African Americans with heart failure diseases. Finally, it is possible to […]
- Diabetes Disease of the First and Second Types It is a decrease in the biological response of cells to one or more effects of insulin at its average concentration in the blood. During the first type of diabetes, insulin Degludec is required together […]
- Person-Centered Strategy of Diabetes and Dementia Care The population of focus for this study will be Afro-American women aged between sixty and ninety who have diabetes of the second type and dementia or are likely to develop dementia in the future.
- Video Consultations Between Patients and Clinicians in Diabetes, Cancer, and Heart Failure Services For example, during one of my interactions with the patient, I was asked whether the hospital had the policy to avoid face-to-face interaction during the pandemic with the help of video examinations.
- Diets to Prevent Heart Disease, Cancer, and Diabetes In order to prevent heart disease, cancer, and diabetes, people are required to adhere to strict routines, including in terms of diet. Additionally, people wanting to prevent heart disease, cancer, and diabetes also need to […]
- The Centers for Diabetes’ Risks Assessment In general, the business case for the Centers for Diabetes appears to be positive since the project is closely aligned with the needs of the community and the targets set by the Affordable Care Act.
- Diabetes Management Type 1 and Type 2 diabetes contrast based on their definitions, the causes, and the management of the conditions. Since the CDC promotes the avoidance of saturated fat and the increase of fiber intake for […]
- Diabetes Mellitus as Leading Cause of Disability The researchers used data from the Centers for Disease Control and Prevention, where more than 12% of older people in the US live with the condition.
- Depression in Diabetes Patients The presence of depression concomitant to diabetes mellitus prevents the adaptation of the patient and negatively affects the course of the underlying disease.
- The Relationship Between Diabetes and COVID-19 After completing the research and analyzing the articles, it is possible to suggest a best practice that may be helpful and effective in defining the relationship between diabetes and COVID-19 and providing a way to […]
- Pre-diabetes and Urinary Incontinence Most recent reports indicate that a physiotherapy procedure gives a positive result in up to 80% of patients with stage I or SUI and mixed form and 50% of patients with stage II SUI.
- Type 1 Diabetes: Recommendations for Alternative Drug Treatments Then, they have to assess the existing levels of literacy and numeracy a patient has. Tailoring educational initiatives to a person’s unique ethnic and cultural background is the basis of cultural competence in patient education.
- Type 2 Diabetes: A Pharmacologic Update Diabetes presents one of the most common diagnoses in causes of ED visits among adults and one of the leading causes of death in the United States.
- Diabetes: Vulnerability, Resilience, and Care In nursing care, resilience is a critical concept that shows the possibility of a person to continue functioning and meeting objectives despite the existing challenges.
- Diabetes Prevention in the United States The analysis of these policies and the other strategies provides the opportunity to understand what role they might play in the improvement of human health. NDPP policy, on the other hand, emphasizes the role of […]
- Teaching Experience: Diabetes Prevention The primary objective of the seminar is to reduce the annual number of diabetes cases and familiarize the audience with the very first signs of this disease.
- Summary of Type 2 Diabetes: A Pharmacologic Update The authors first emphasize that T2D is one of the most widespread diseases in the United States and the seventh leading cause of death.
- Insulin Effects in a Diabetes Person I will use this source to support my research because the perception of diabetes patients on insulin therapy is essential for understanding the impact they cause on the person.
- Diabetes and Medical Intervention In the research conducted by Moin et al, the authors attempted to define the scope of efficiency of such a tool as an online diabetes prevention program in the prevention of diabetes among obese/overweight population […]
- Diabetes Mellitus Type 2 and a Healthy Lifestyle Relationship The advantage of this study over the first is that the method uses a medical approach to determining the level of fasting glucose, while the dependences in the study of Ugandans were found using a […]
- Diabetes and Its Economic Effect on Healthcare For many years, there has been an active increase in the number of cases of diabetes of all types among the global population, which further aggravates the situation.
- Pathogenesis and Prevention of Diabetes Mellitus and Hypertension The hormone is produced by the cells of the islets of Langerhans found in the pancreas. It is attributed to the variation in the lifestyle of these individuals in these two geographical zones.
- Parental Intervention on Self-Management of an Adolescent With Diabetes Diabetes development and exposure are strongly tied to lifestyle, and the increasing incidents rate emphasizes the severity of the population’s health problem.
- Addressing the Needs of Hispanic Patients With Diabetes Similarly, in the program at hand, the needs of Hispanic patients with diabetes will be considered through the prism of the key specifics of the community, as well as the cultural background of the patients.
- Diabetes Issues: Insulin Price and Unaffordability According to the forecast of researchers from Stanford University, the number of people with type 2 diabetes who need insulin-containing drugs in the world will increase by about 79 million people by 2030, which will […]
- Diabetes: Epidemiologic Study Design For instance, the range of their parents’ involvement in the self-management practices can be a crucial factor in treatment and control.
- What to Know About Diabetes? Type 1 diabetes is caused by autoimmune reaction that prevent realization of insulin in a body. Estimated 5-10% of people who have diabetes have type 1.
- Diabetes in Saudi Arabia It is expected that should this underlying factor be discovered, whether it is cultural, societal, or genetic in nature, this should help policymakers within Saudi Arabia create new governmental initiatives to address the problem of […]
- “Medical Nutrition Therapy: A Key to Diabetes Management and Prevention” Article Analysis In the process of MNT application, the dietitian keeps a record of the changes in the main components of food and other components of the blood such as blood sugars to determine the trend to […]
- Global and Societal Implications of the Diabetes Epidemic The main aim of the authors of this article seems to be alerting the reader on the consequences of diabetes to the society and to the whole world.
- Diabetes and Hypertension Avoiding Recommendations Thus, the promotion of a healthy lifestyle should entail the encouragement of the population to cease smoking and monitor for cholesterol levels.
- Pregnant Women With Type I Diabetes: COVID-19 Disease Management The grounded theory was selected for the given topic, and there are benefits and drawbacks of utilizing it to study the experiences of pregnant women with type I diabetes and COVID-19.
- Current Recommendations for the Glycemic Control in Diabetes Management of blood glucose is one of the critical issues in the care of people with diabetes. Therefore, the interval of the A1C testing should also depend on the condition of the patient, the physician’s […]
- Diabetes Problem at Country Walk Community: Intervention and Evaluation This presentation develops a community health nursing intervention and evaluation tool for the diabetes problem affecting Country Walk community.
- The Minority Diabetes Initiative Act’s Analysis The bill provides the right to the Department of Health and Human Services to generate grants to public and nonprofit private health care institutions with the aim of providing treatment for diabetes in minority communities.
- Communication Challenges Between Nurses and Patients With Type 2 Diabetes According to Pung and Goh, one of the limitations of communication in a multicultural environment is the language barrier that manifests itself in the direct interaction of nurses with patients and in the engagement work […]
- Diabetes Type 2 from Management Viewpoint Demonstrate the effects of type 2 diabetes and provide background information on the disease; Discuss the management plans of diabetes centers and critically analyze the frameworks implemented in the hospitals; Examine the existing methodology models […]
- Nursing Plan for the Patient with Diabetes Type 2, HTN, and CAD The health of the population is the most valuable achievement of society, so the preservation and strengthening of it is an essential task in which everyone should participate without exception.
- Diagnosis and Classification of Diabetes Mellitus Diabetes is a serious public health concern that introduces a group of metabolic disorders caused by changes in the sugar blood level.
- Diabetes Mellitus Type II: A Case of a Female Adult Patient In this presentation, we are going to develop a care plan for a 47-year-old woman with a 3-year-old history of Diabetes Mellitus Type 2 (also known as Type II DM).
- Diabetes Insipidus: Disease Process With Implications for Healthcare Professionals This presentation will consider the topic of Diabetes Insipidus (DI) with a focus on its etiology and progress.
- A Study of Juvenile Type 1 Diabetes in the Northwest of England The total number of children under seventeen years living with type 1 diabetes in North West England by 2009 was 2,630.
- Imperial Diabetes Center Field Study The purpose is to examine the leadership’s practices used to maintain and improve the quality and safety standards of the facility and, using the observations and scholarly research, offer recommendations for improvement.
- Diabetes Risk Assessment After completing the questionnaire, I learned that my risk for the development of diabetes is above average. Modern risk assessment tools allow identifying the current state of health and possibilities of developing the disease.
- The Role of Telenursing in the Management of Diabetes Type 1 Telemedicine is the solution that could potentially increase the coverage and improve the situation for many t1DM patients in the world.
- Health Issues of Heart Failure and Pediatric Diabetes As for the population, which is intended to participate in the research, I am convinced that there is the need to specify the patients who should be examined and monitored.
- Juvenile Diabetes: Demographics, Statistics and Risk Factors Juvenile diabetes, also referred to as Type 2 diabetes or insulin-dependent diabetes, describes a health condition associated with the pancreas’s limited insulin production. The condition is characterized by the destruction of the cells that make […]
- Diabetes Mellitus: Pathophysiologic Processes The main function of insulin produced by cells within the pancreas in response to food intake is to lower blood sugar levels by the facilitation of glucose uptake in the cells of the liver, fat, […]
- Type 2 Diabetes Management in Gulf Countries One such study is the systematic review on the quality of type 2 diabetes management in the countries of the cooperation council for the Arab states of the Gulf, prepared by Alhyas, McKay, Balasanthiran, and […]
- Patient with Ataxia and Diabetes Mellitus Therefore, the therapist prioritizes using the cushion to the client and persuades the patient to accept the product by discussing the merits of the infinity cushion with a low profile in enabling the customer to […]
- Diabetes Evidence-Based Project: Disseminating Results In this presentation, the involvement of mentors and collaboration with administration and other stakeholders are the preferred steps, and the idea to use social networking and web pages has to be removed.
- The Problem of Diabetes Among African Americans Taking into consideration the results of the research and the information found in the articles, the problem of diabetes among African Americans has to be identified and discussed at different levels.
- Childhood Obesity, Diabetes and Heart Problems Based on the data given in the introduction it can be seen that childhood obesity is a real problem within the country and as such it is believed that through proper education children will be […]
- Hypertension and Antihypertensive Therapy and Type 2 Diabetes Mellitus In particular, Acebutolol impairs the functions of epinephrine and norepinephrine, which are neurotransmitters that mediate the functioning of the heart and the sympathetic nervous system.
- Diabetes: Diagnosis and Treatment The disease is characterized by the pancreas almost not producing its own insulin, which leads to an increase in glucose levels in the blood.
- How to Manage Type 2 Diabetes The article is significant to the current research problem as the researchers concluded that the assessment of metabolic processes in diabetic patients was imperative for adjusting in the management of the condition.
- Clinical Trial of Diabetes Mellitus On the other hand, type II diabetes mellitus is caused by the failure of the liver and muscle cells to recognize the insulin produced by the pancreatic cells.
- Diabetes: Diagnosis and Related Prevention & Treatment Measures The information presented on the articles offers an insight in the diagnosis of diabetes among various groups of persons and the related preventive and treatment measures. The study identified 3666 cases of initial stages of […]
- Reinforcing Nutrition in Schools to Reduce Diabetes and Childhood Obesity For example, the 2010 report says that the rates of childhood obesity have peaked greatly compared to the previous decades: “Obesity has doubled in Maryland over the past 20 years, and nearly one-third of youth […]
- The Connection Between Diabetes and Consuming Red Meat In light of reporting the findings of this research, the Times Healthland gave a detailed report on the various aspects of this research.
- Synthesizing the Data From Relative Risk Factors of Type 2 Diabetes Speaking of such demographic factors as race, the white population suffers from it in the majority of cases, unlike the rest of the races, the remaining 0.
- Using Exenatide as Treatment of Type 2 Diabetes Mellitus in Adults Kendal et al.analyzed the effects of exenatide as an adjunct to a combination of metformin and sulfonylurea against the combination of the same drugs without the adjunct.
- Enhancing Health Literacy for People With Type 2 Diabetes Two professionals, Andrew Long, a professor in the school of heath care in the University of Leeds, and Tina Gambling, senior lecturer in the school of health care studies from the University of Cardiff, conducted […]
- The Scientific Method of Understanding if Coffee Can Impact Diabetes The hypothesis of the experiment ought to be straightforward and understandable. The control group and the experiment group for the test are then identified.
- Gestational Diabetes Mellitus: Review This is because of the current patterns that show an increase in the prevalence of diabetes in offspring born to mothers with GDM.
- Health Service Management of Diabetes During the task, Fay makes a countless number of short calls and often takes water irrespective of the time of the day or the prevailing weather conditions.
- Necrotizing Fasciitis: Pathophysiology, Role of Diabetes In the event of such an infection, the body becomes desperate to get rid of the intruders. For WBC, zero is given if the count is below 15cells/mm3, one is given if the count lies […]
- The Benefits of Sharing Knowledge About Diabetes With Physicians In this research, 3600 diabetic patients were surveyed from twelve hospitals, but due to exclusion criterion, only 1,200 were considered for this particular research. The system allocated numbers to the participants out of which 100 […]
- Gestational Diabetes Mellitus – NSW, Australia We had a deeper evaluation of the implications of GDM and we cited the inadequacy of resources and technology as the contributors of GDM.
- Health and Wellness: Stress, Diabetes and Tobacco Related Problems Emotional health and well being refers to our ability to deal with our emotions as well as the emotions of those around us.
- 52-Year-Old Female Patient With Type II Diabetes Diabetes type two is the primary differential diagnosis because the patient presented with: A family history of diabetes, complications of hyperglycemia, blood pressure of 130/92, ingrown toenails, tingling sensation on the feet, fasting blood glucose […]
- Healthy People Project: Personal Review About Diabetes
- Nursing Diagnosis: Type 1 Diabetes & Hypertension
- Nursing Care For the Patient With Diabetes
- Coronary Heart Disease Aggravated by Type 2 Diabetes and Age
- Diabetes as the Scourge of the 21st Century: Locating the Solution
- Psychosocial Implications of Diabetes Management
- Gestational Diabetes in a Pregnant Woman
- Diabetes Mellitus: Prominent Metabolic Disorder
- Holistic Approach to Man’s Health: Diabetes Prevention
- Holistic Image in Prevention of Diabetes
- Educational Strategies for Diabetes to Patients
- Diabetes and Obesity in the United Arab Emirates
- Epidemiological Problem: Diabetes in Illinois
- Diabetes as a Chronic Condition
- Managing Diabetes Through Genetic Engineering
- Diabetes, Functions of Insulin, and Preventive Practices
- Treating of Diabetes in Adults
- Counseling and Education Session in Type II Diabetes
- Diabetes II: Reduction in the Incidence
- Community Health Advocacy Project: Diabetes Among Hispanics
- Community Health Advocacy Project: Hispanics With Diabetes
- Hispanics Are More Susceptible to Diabetes That Non-Hispanics
- Rates Diabetes Between Hispanics Males and Females
- Diabetes Mellitus and HFSON Conceptual Framework
- Prince Georges County Community Health Concern: Diabetes
- Fats and Proteins in Relation to Type 2 Diabetes
- Alcohol Interaction With Medication: Type 2 Diabetes
- Diabetes Management and Evidence-Based Practice
- Critical Analysis of Policy for Type 2 Diabetes Mellitus in Australia
- The Treatment and Management of Diabetes
- Obesity and Diabetes: The Enemies Within
- Impact of Diabetes on the United Arab Emirates’ Economy
- Childhood Obesity and Type 2 Diabetes
- Health Nursing and Managing Diabetes
- Diabetes Management: How Lifestyle, Daily Routine Affect Blood Sugar
- Diabetes Management: Diagnostics and Treatment
- Diabetes Mellitus Type 2: The Family Genetic History
- Diabetes Type II: Hormonal Mechanism and Intracellular Effects of Insulin
- Social, Behavioral, and Psychosocial Causes of Diseases: Type 2 Diabetes
- Supportive Intervention in the Control of Diabetes Mellitus
- Enhancing Foot Care Practices in Patients With Diabetes
- Community Health Promotion: The Fight Against Diabetes in a Community Setting
- Diabetes in Australia and Saudi Arabia
- Diabetes: The Advantages and Disadvantages of Point of Care Testing
- Diabetes Mellitus Type 2 or Non-Insulin-Dependent Diabetes Mellitus
- Qualitative Research in Diabetes Management in Elderly Patient
- Diabetes Prevention Measures in the Republic of the Marshall Islands
- Impact of Diabetes on Healthcare
- Gestational Diabetes: American Diabetes Association Publishers
- Gestational Diabetes: Child Bearing Experience
- Diabetes Mellitus Effects on Periodontal Disease
- Diabetes Type II Disease in the Community
- The Relationship of Type 2 Diabetes and Depression
- Glycemic Control in Individuals With Type 2 Diabetes
- The Diagnosis of Diabetes in Older Adults and Adolescents
- Physical Activity in Managing Type-2 Diabetes
- High Risk of Developing Type 1 and Type 2 Diabetes Mellitus
- Children With Type 1 Diabetes in Clinical Practice
- Type 2 Diabetes Treatment Analysis
- Type 2 Diabetes Mellitus: Revealing the Diagnosis
- The Type 2 Diabetes Prevention: Lifestyle Choices
- Indigenous and Torres Strait Population and Diabetes
- Interpretation of the Diabetes Interview Transcript
- Type 1 Diabetes: Using Glucose Monitoring in Treatment
- Managing Type 2 Diabetes Patients’ Blood Sugar Prior to and After Surgical Procedures
- Diabetes Prevention: The Sanofi-Aventis Leaflet Review
- Canagliflozin and Cardiovascular and Renal Events in Type 2 Diabetes: Medical Terminology Definition
- Modern Diabetes Treatment Tools
- Current Dietary for the Treatment of Diabetes
- Stranahan on Diabetes Impairs Hippocampal Function
- A Clinical-Based Study of Young Adults Who Have Diabetes
- Is There Anu Cure For Diabetes?
- Diabetes Self-Management: Evidence-Based Nursing
- Diabetes Type 2 in Children: Causes and Effects
- Diabetes Prevention in Chinese Elderly in Hunan
- Type 2 Diabetes: Nursing Change Project
- Type 2 Diabetes in Geriatric Patients
- Cultural Empowerment. Diabetes in Afro-Americans
- Diabetes Self-Management: Relationships & Expectations
- Diagnosis and Classification of Diabetes Mellitus
- Side Effects of Metformin in Diabetes Treatment
- Type 2 Diabetes and Drug Treatments
- Diabetes Mellitus and Health Determinants
- Nursing Leadership in Diabetes Management
- Latent Autoimmune Adult Diabetes
- Obesity: Epidemiology and Health Consequences
- Diabetes in Urban Cities of United States
- Diabetes in Australia: Analysis
- Type 2 Diabetes in the Afro-American Bronx Community
- Type 2 Diabetes From Cultural and Genetic Aspects
- Type 2 Diabetes in Bronx: Evidence-Based Practice
- Type 2 Diabetes in Bronx Project for Social Change
- Diabetes as Community Health Issue in the Bronx
- Diabetes Management Plan: Diagnosis and Development
- Diabetes Treatment and Care
- Transition from Pediatric to Adult Diabetes Care
- Diabetes Awareness Program and Strategic Planning
- Diabetes: Disease Control and Investigation
- Perception of Diabetes in the Hispanic Population
- Clinical Studies of Diabetes Mellitus
- Diabetes Mellitus and Problems at Work
- Diabetes in the US: Cost Effectiveness Analysis
- Diabetes Investigation in Space Flight Research
- Diabetes Care Advice by Food and Drug Administration
- Artificial Intelligence for Diabetes: Project Experiences
- Diabetes Patients’ Long-Term Care and Life Quality
- Chronic Care Model for Diabetes Patients in the UAE
- Diabetes Among British Adults and Children
- Endocrine Disorders: Diabetes and Fibromyalgia
- Future Technologies: Diabetes Treatment and Care
- Epidemiology of Type 1 Diabetes
- Diabetes: Treatment Technology and Billing
- Pathophysiology of Mellitus and Insipidus Diabetes
- Cure for Diabetes: The Impossible Takes a Little Longer
- Stem Cell Therapy and Diabetes Medical Research
- Type II Diabetes Susceptibility and Socioeconomic Status
- Diabetes Mellitus Type 2: Pathophysiology and Treatment
- Obesity and Hypertension in Type 2 Diabetes Patients
- Strongyloides Stercoralis Infection and Type 2 Diabetes
- Socioeconomic Status and Susceptibility to Type II Diabetes
- Diabetes Mellitus: Differential Diagnosis
- Diabetes Disease in the USA Adults
- Education for African Americans With Type 2 Diabetes
- Diabetes Treatment and Funding in Fulton County
- Diabetes Care: Leadership and Strategy Plan
- Diabetes Mellitus’ New Treatment: Principles and Process
- Diet and Nutrition: European Diabetes
- Preventing the Proliferation Diabetes
- Diabetes and Cardiovascular Diseases in Medicine
- Ecological Models to Deal with Diabetes in Medicine
- Different Types of Diabetes Found in Different Countries
- Analysis of Program “Prevent Diabetes Live Life Well”
- The Effect of Physical, Social, and Health Variables on Diabetes
- Micro and Macro-Cosmos in Medicine and Care Models for Prevention of Diabetes
- Why Qualitative Method Was Chosen for Diabetes Program Evaluation
- Humanistic Image of Managing Diabetes
- Diabetes mellitus Education and hemoglobin A1C level
- Obesity, Diabetes and Heart Disease
- Illuminate Diabetes Event Design
- Cause and Diagnosis of Type 2 diabetes
- Patient Voices: Type 2 Diabetes. Podcast Review
- Type I Diabetes: Pathogenesis and Treatment
- Human Body Organ Systems Disorders: Diabetes
- Age Influence on Physical Activity: Exercise and Diabetes
- Hemoglobin A1C Test for Diabetes
- Why Injury and Diabetes Have Been Identified as National Health Priority?
- What Factors Are Involved in the Increasing Prevalence of Type II Diabetes in Adolescents?
- Does the Socioeconomic Position Determine the Incidence of Diabetes?
- What Are the Four Types of Diabetes?
- How Fat and Obesity Cause Diabetes?
- How Exercise Affects Type 2 Diabetes?
- How Does the Treatment With Insulin Affect Type 2 Diabetes?
- How Diabetes Does Cause Depression?
- Does Diabetes Prevention Pay For Itself?
- How Does Snap Participation Affect Rates of Diabetes?
- Does Overeating Sugar Cause Diabetes, Cavities, Acne, Hyperactivity and Make You Fat?
- Why Diabetes Mellitus and How It Affects the United States?
- Does Alcohol Decrease the Risk of Diabetes?
- How Does a Person With Diabetes Feel?
- Does Periodontal Inflammation Affect Type 1 Diabetes in Childhood and Adolescence?
- How Can the Paleolithic Diet Control Type 2 Diabetes?
- How Does Insulin Help Diabetes Be Controlled?
- Does Economic Status Matter for the Regional Variation of Malnutrition-Related Diabetes?
- How Can Artificial Intelligence Technology Be Used to Treat Diabetes?
- What Are the Main Causes and Treatments of Diabetes?
- What Evidence Exists for Treatments Depression With Comorbid Diabetes Using Traditional Chinese Medicine and Natural Products?
- Why Was Qualitative Method Chosen for Diabetes Program Evaluation?
- What Are the Three Types of Diabetes?
- How Does Poverty Affect Diabetes?
- What Is the Leading Cause of Diabetes?
- How Is Diabetes Diagnosed?
- What Are the Main Symptoms of Diabetes?
- How Diabetes Adversely Affects Your Body?
- What Are the Most Common Symptoms of Undiagnosed Diabetes?
- Epigenetics Essay Titles
- Alcohol Abuse Paper Topics
- Pathogenesis Research Ideas
- Therapeutics Research Ideas
- Hypertension Topics
- Osteoarthritis Ideas
- Cardiomyopathy Titles
- Malnutrition Titles
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, February 25). 357 Diabetes Essay Topics & Examples. https://ivypanda.com/essays/topic/diabetes-essay-examples/
"357 Diabetes Essay Topics & Examples." IvyPanda , 25 Feb. 2024, ivypanda.com/essays/topic/diabetes-essay-examples/.
IvyPanda . (2024) '357 Diabetes Essay Topics & Examples'. 25 February.
IvyPanda . 2024. "357 Diabetes Essay Topics & Examples." February 25, 2024. https://ivypanda.com/essays/topic/diabetes-essay-examples/.
1. IvyPanda . "357 Diabetes Essay Topics & Examples." February 25, 2024. https://ivypanda.com/essays/topic/diabetes-essay-examples/.
Bibliography
IvyPanda . "357 Diabetes Essay Topics & Examples." February 25, 2024. https://ivypanda.com/essays/topic/diabetes-essay-examples/.
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Diabetes mellitus and gynecological and inflammation disorders increased the risk of pregnancy loss in a population study.

Share and Cite
Cheng, C.-G.; Su, S.-H.; Chien, W.-C.; Chen, R.; Chung, C.-H.; Cheng, C.-A. Diabetes Mellitus and Gynecological and Inflammation Disorders Increased the Risk of Pregnancy Loss in a Population Study. Life 2024 , 14 , 903. https://doi.org/10.3390/life14070903
Cheng C-G, Su S-H, Chien W-C, Chen R, Chung C-H, Cheng C-A. Diabetes Mellitus and Gynecological and Inflammation Disorders Increased the Risk of Pregnancy Loss in a Population Study. Life . 2024; 14(7):903. https://doi.org/10.3390/life14070903
Cheng, Chun-Gu, Sheng-Hua Su, Wu-Chien Chien, Ryan Chen, Chi-Hsiang Chung, and Chun-An Cheng. 2024. "Diabetes Mellitus and Gynecological and Inflammation Disorders Increased the Risk of Pregnancy Loss in a Population Study" Life 14, no. 7: 903. https://doi.org/10.3390/life14070903
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Healthc Eng
- v.2022; 2022

This article has been retracted.
Study on the nursing effect of diabetes health education nursing methods applied to diabetes patients in the endocrinology department, jianhua wang.
Qingdao Municipal Hospital, Qingdao 266000, China
Associated Data
The simulation experiment data used to support the findings of this study are available from the corresponding author upon request.
The aim of this study was to explore the nursing effect of diabetes education and nursing methods applied to diabetic patients in the endocrinology department. From October 2019 to October 2020, 90 patients with diabetes who were admitted to the Department of Endocrinology in our hospital were selected as the research objects, and the medical records of all patients were retrospectively analyzed. The patients were randomly divided into two groups, 45 patients who were given regular care as the control group and 45 patients who were given the diabetes health education care model as the experimental group. Routine care was given to patients in the routine group; that is, we paid attention to the patients' diet, medication, and blood glucose levels. The experimental group patients were given diabetes health education guidance. The nursing effect, blood sugar level, disease awareness level, occurrence of complications, and compliance of the two groups of patients were evaluated. In this study, diabetes health education was given to the experimental group of patients. The conditions of this group of patients were significantly better than those of the basic group using conventional nursing methods. Therefore, the application of diabetes health education is very effective. The recovery from the disease has positive significance.
1. Introduction
Diabetes is a very common disease in the entire clinic. It belongs to the endocrine system disease. It not only has great harm but also the patient's organs and systems will suffer very serious damage, and sometimes, it may even cause it. Diabetic feet and diabetic kidneys, as well as various diseases such as chloasma of the fundus and peripheral audit damage, directly lead to a continuous decrease in the quality of life of patients [ 1 – 3 ]. In clinical medicine, there is no good method for the treatment of diabetes at this stage, but more attention is paid to the patient's comprehensive life intervention, which can effectively improve the prognosis and prevent the complications of diabetes. The treatment of diabetes is a long process, so it is very important to do a good job of health education during the treatment. Diabetes, as the most common chronic disease, has a very high clinical incidence. The patient's long-term high blood sugar state will cause blood vessels and organs to develop diseases, trigger a variety of complications, and threaten patients' life safety in severe cases. For diabetic patients, long-term medications to control blood sugar are needed, but adverse emotions will also affect the treatment during the treatment of the patient's disease, which will reduce the patient's treatment compliance. If the patient's knowledge of the disease is poor, it will also reduce their treatment compliance [ 4 – 6 ].
2. Materials and Methods
General information: 90 diabetic patients admitted to our hospital's Department of Endocrinology from October 2019 to October 2020 were selected as the research objects, and the medical records of all patients were retrospectively analyzed. The patients were randomly divided into two groups, 45 patients who were given regular care as the control group 45 patients who were given diabetes health education and nursing mode as the experimental group, and the general data such as gender and age of the two groups were compared. There was no statistical difference.
Routine care was given to patients in the routine group; that is, we paid attention to the patient's diet, medication, and blood glucose levels. The experimental group patients were given diabetes health education guidance, and the main operation methods are as follows: Firstly, a diabetes education and nursing research team is built. The director of the endocrinology department, professional diabetes-attending physicians, nursing physicians, head nurses, and key nurses in the department, combined with nutritionists and psychologists, jointly formed a diabetes healthcare research team in the hospital. Secondly, when the patient comes to the hospital for treatment, the nursing staff should enthusiastically and actively communicate with the patient and their family members about the patient's condition, fully grasp the patient's understanding of diabetes, life, eating habits, and physical conditions, and then, build an electronic account of the patient's condition. They should file and continue to improve in the future treatment process. At the same time, it is necessary for the attending physician in the undergraduate room to inform patients on how to control blood sugar so that patients can realize the importance of effective blood sugar control and then effectively control the development of their own disease and complications. Thirdly, during the patient's hospitalization, nursing staff should distribute diabetes health education brochures or leaflets to every patient and appropriately explain the pathogenesis, types, related complications, and correct methods of how to control blood sugar to patients. At the same time, the director of the endocrinology department should regularly organize patients to give lectures on the condition of “diabetes” so that patients can fully understand the correct methods of personal hygiene, diet, exercise, and medication after illness and promote patients in future treatment to eat healthy, exercise rationally, and use scientific medications so that blood sugar can be effectively controlled and patients' self-management ability can be improved so that the continued development of the disease can be controlled and the incidence of complications can be reduced. In addition, the nursing staff should also carry out appropriate education and publicity to the family members of the patients so that the family members can assist the patients in the control of the disease as much as possible and supervise the patients to carry out effective self-management. Finally, nursing staff should patiently instruct patients when they are discharged from the hospital and at the same time, according to the conditions of different patients, formulate relevant care plans and instruct patients to come to the hospital for review on a regular basis. Nursing staff should conduct regular telephone follow-ups after the patients are discharged from the hospital, to grasp the patient's recovery and adjust the care plan in time for the patients' recovery so that the patients can get better care. The department should also set up a consultation hotline to provide convenience for patients' consultation after discharge. It can also establish a patients' WeChat group so that different patients can discuss their conditions together, share treatment experiences, and encourage each other. The nursing effect, blood sugar level, disease awareness level, occurrence of complications, and compliance of the two groups of patients were evaluated. SPSS 22.0 software was used to perform statistics on the data in the text, t and chi-square were regarded as test indicators, and P < 0.05 was regarded as statistically different.
3.1. Comparison of General Information of the Two Groups of Patients
By comparing the general information of the two groups of patients, it was found that there was no significant statistical difference between the patients in terms of gender, age, and time of illness ( P > 0.05). Table 1 shows the comparison of general information of the two groups of patients.
Comparison of general information of the two groups of patients.
| Control group ( = 45) | Test group ( = 45) | T value | value | |
|---|---|---|---|---|
| Gender/male | 21 | 23 | 1.56 | 0.08 |
| Age | 48.98 ± 10.36 | 46.58 ± 9.87 | 1.29 | 0.28 |
| Sick time/year | 5.6 ± 3.5 | 5.8 ± 3.1 | 0.65 | 0.58 |
3.2. Comparison of Nursing Effects between the Two Groups of Patients
After comparing the nursing effect of the two groups of patients, it was found that the nursing effect of the experimental group was better and the total effective rate was higher. The difference between the two groups was statistically significant ( P < 0.05). Table 2 is a comparative analysis of the nursing effect of the two groups of patients.
Comparative analysis of the nursing effect of the two groups of patients (%).
| Group | Markedly effective | Effective | Invalid | Total effective rate |
|---|---|---|---|---|
| Test group ( = 45) | 22 | 18 | 5 | 88.8% |
| Control group ( = 45) | 16 | 17 | 12 | 73.3% |
| X2 | — | — | — | 8.95 |
| value | — | — | — | 0.02 |
3.3. Differences in Blood Glucose Levels and Disease Awareness between the Two Groups
After comparing the blood glucose levels and disease cognition levels of the two groups of patients, it was found that compared with the control group, the fasting blood glucose and the 2 h postmeal blood glucose levels of the experimental group were lower, and the difference was statistically significant. In addition, compared with the control group, the disease cognition level of the experimental group was significantly higher than that of the control group, and the difference was statistically significant ( P < 0.05). Table 3 displays the comparison of blood glucose level and disease awareness level.
Comparison of blood glucose level and disease awareness level ( x ± s ).
| Group | Fasting blood glucose (mmol/L) | 2 h blood glucose after meal (mmol/L) | Disease awareness level (points) |
|---|---|---|---|
| Test group ( = 45) | 6.53 ± 2.56 | 8.16 ± 3.25 | 95.68 ± 4.58 |
| Control group ( = 45) | 9.56 ± 2.64 | 10.26 ± 2.68 | 85.36 ± 3.56 |
| T value | 5.48 | 5.64 | 12.68 |
| value | ≤0.01 | 0.01 | ≤0.01 |
3.4. Comparison of Complications
Comparing the incidence of the two groups of patients, it was found that the complication rate in the experimental group was 6.7%, including 1 case of hypoglycemia and 2 cases of heart failure. The complication rate of the control group was 11%, including 2 cases of hypoglycemia. There were 2 cases of heart failure and 3 cases of angina pectoris. The difference between the two groups was statistically significant ( P < 0.05).
3.5. Compliance Assessment of the Two Groups of Patients
The effective rate of treatment compliance assessment in the experimental group was 91.1%, which was significantly higher than the 75.6% in the control group ( P < 0.05). Table 4 shows the compliance assessment of the two groups of patients.
Compliance assessment of the two groups of patients.
| Group | High compliance | Moderate compliance | Poor compliance | Evaluation efficiency |
|---|---|---|---|---|
| Test group ( = 45) | 30 | 11 | 4 | 91.1% |
| Control group ( = 45) | 26 | 8 | 11 | 75.6% |
| X | — | — | — | 6.54 |
| value | — | — | — | 0.01 |
4. Conclusions
Diabetes patients have higher blood sugar, which is generally caused by autoimmune problems, obesity, environment, genetics, and other factors. Diabetes is caused by a variety of factors. The patients in this study all belong to type 2 diabetes, and diabetes can be controlled by taking medicine. According to related studies, it is difficult to achieve better curative effect if only relying on drugs to treat diabetes, but health education can improve the treatment effect of diabetes. Medical staff should implement health education for patients with diabetes, which can greatly improve patients' compliance with treatment [ 7 , 8 ].
Nursing staff can use various forms to carry out health education. Nursing staff can analyze the patient's condition in detail and formulate a targeted education program based on the patient's condition. The patient's awareness of diabetes can be improved through demonstration, training, and seminars. The content of health education includes blood glucose testing methods, the significance of blood glucose control, and the normal range of blood glucose; the mechanism, symptoms, prognosis, and types of diabetes; methods, goals, and meanings of diet control; the amount of exercise during exercise, the choice of exercise time, etc; the impact of negative emotions on diseases and how to control negative emotions; side effects, indications, dosages, and time of administration of hypoglycemic drugs; and use, storage, injection methods and dosages of insulin. Through health education, patients can actively cooperate with the nursing staff and scientifically control their own behavior and diet, thereby gradually improving the treatment effect. Through this research, we know that the application of diabetes health education in endocrine patients can gradually increase the patient's treatment compliance and improve the patient's diet, behavior, and psychological status, which has a positive significance in improving the treatment effect [ 9 , 10 ].
Diabetes is a metabolic disease. Most diabetic patients are accompanied by endocrine disorders. If not intervened in time, it is likely to lead to metabolic disorders, vascular disease, and serious development of the disease and can even threaten the lives of patients. Relevant studies have shown that endocrine disorders in diabetic patients are mostly related to living habits, work habits, and eating habits. Patients do not have a clear understanding of their own diseases and will not exercise self-control in their daily lives, resulting in poor treatment and prognosis. Therefore, in order to better ensure the treatment effect of diabetic patients, it is necessary to pay attention to health education in clinical practice. Through scientific and effective health education, we should help patients correct their bad living habits and eating habits. At the same time, we should let patients realize the importance of taking medication on time, thereby improving patient compliance with medication and improving treatment effects. Therefore, it is of great significance to do a good job of health education in the endocrine care of diabetic patients [ 11 ].
Nursing staff can use various forms to carry out health education. Nursing staff can analyze the patient's condition in detail and formulate a targeted education program based on the patient's condition. The patient's awareness of diabetes can be improved through demonstration, training, and seminars. The content of health education includes blood glucose testing methods, the significance of blood glucose control, and the normal range of blood glucose; the mechanism, symptoms, prognosis, and types of diabetes; methods, goals, and meanings of diet control; the amount of exercise during exercise, the choice of exercise time, etc.; the impact of negative emotions on diseases and how to control negative emotions; side effects, indications, dosages, and time of administration of hypoglycemic drugs; and use, storage, injection methods and dosages of insulin. Through health education, patients can actively cooperate with the nursing staff and scientifically control their own behavior and diet, thereby gradually improving the treatment effect. Through this study, it is known that the application of diabetes health education in endocrine patients can gradually increase the patient's treatment compliance and improve the patient's diet, behavior, and psychological status, which has a positive significance in improving the treatment effect [ 12 – 14 ].
In this study, by comparing the general information of the two groups of patients, it was found that the patients had no significant statistical differences in gender, age, and time of illness ( P > 0.05). After comparing the nursing effect of the two groups of patients, it was found that the nursing effect of the experimental group was better, and the total effective rate was higher [ 15 – 17 ]. The difference between the two groups was statistically significant ( P < 0.05) [ 18 – 20 ]. By comparing the blood glucose levels and disease cognition levels of the two groups of patients, it was found that compared with the control group, the fasting blood glucose and the 2 h postmeal blood glucose levels of the experimental group were lower, and the difference was statistically significant. In addition, compared with the control group, the disease cognition level of the experimental group was significantly higher than that of the control group, and the difference was statistically significant ( P < 0.05) [ 21 , 22 ]. Comparing the incidence of the two groups of patients, it was found that the complication rate in the experimental group was 6.7%, including 1 case of hypoglycemia and 2 cases of heart failure. The complication rate of the control group was 11%, including 2 cases of hypoglycemia. There were 2 cases of heart failure and 3 cases of angina pectoris. The difference between the two groups was statistically significant ( P < 0.05). The effective rate of treatment compliance assessment in the experimental group was 91.1%, which was significantly higher than the 75.6% in the control group ( P < 0.05).
In summary, in this study, the experimental group of patients was given diabetes health education. The conditions of this group of patients were significantly better than those of the basic group of patients using conventional nursing methods. Therefore, the application of diabetes health education is extremely effective. Also, it has a positive significance for the recovery of the disease.
Data Availability
Conflicts of interest.
The authors declare no conflicts of interest regarding the publication of this paper.
ORIGINAL RESEARCH article
A study of the relationship between social support, depression, alexithymia and glycemic control in patients with type 2 diabetes mellitus:a structural equation modeling approach.

- 1 School of Nursing, Chengdu Medical College, Chengdu, Sichuan Province, China
- 2 First Affiliated Hospital of Chengdu Medical College, Chengdu, Sichuan Province, China
- 3 Department of Rheumatology and Immunology, First Affiliated Hospital of Chengdu Medical College, Chengdu, Sichuan Province, China
The final, formatted version of the article will be published soon.
Select one of your emails
You have multiple emails registered with Frontiers:
Notify me on publication
Please enter your email address:
If you already have an account, please login
You don't have a Frontiers account ? You can register here
The aim of this research was to ascertain the correlations between alexithymia, social support, depression, and glycemic control in patients diagnosed with type 2 diabetes mellitus. Additionally, this study sought to delve into the potential mediating effects of social support and depression in the relationship between alexithymia and glycemic control.Method A purposive sampling methodology was employed to select a cohort of 318 patients afflicted with type 2 diabetes mellitus, hailing from a care establishment situated in Chengdu City.This investigation embraced a cross-sectional framework, wherein instruments such as the General Information Questionnaire, the Toronto Alexithymia Scale 20, the Social Support Rating Scale, and the Hamilton Depression Scale were judiciously administered. The primary objective of this endeavor was to unravel the interplay that exists amongst alexithymia, social support, depression, and glycemic control. The inquiry discerned these interrelationships through both univariate and correlational analyses, subsequently delving into a comprehensive exploration of the mediating ramifications engendered by social support and depression in the nexus between alexithymia and glycemic control.The HbA1c level of patients diagnosed with type 2 diabetes mellitus was recorded as (8.85±2.107), and their current status with regards to alexithymia, social support, and depression were measured as (58.05±4.382), (34.29±4.420), and (7.17±3.367), respectively. Significant correlations were found between HbA1c and alexithymia (R=0.392, P<0.01), social support (R=-0.338, P<0.01), and depression (R=0.509, P<0.01). Moreover, alexithymia correlation with social support (R=-0.357, P<0.01) and with depression (R=0.345, P<0.01). Regarding the mediation analysis, the direct effect of alexithymia on HbA1c was calculated to be 0.158, while the indirect effect through social support and depression were 0.086 and 0.149, respectively. The total effect value was determined to be 0.382, with the mediating effect accounting for 59.95% , and the direct effect accounting for 40.31%.Alexithymia exerts both direct and indirect adverse effects on glycemic control, thereby exacerbating disease outcomes. Hence, it is imperative to prioritize the mental health status of individuals with type 2 diabetes to enhance overall well-being, ameliorate diabetes-related outcomes, elevate patients' quality of life, and alleviate the psychological distress and financial burden associated with the condition.
Keywords: Type 2 diabetes mellitus1, glycemic control2, alexithymia3, social support4, Depression5, structural equation modeling6
Received: 28 Mar 2024; Accepted: 18 Jul 2024.
Copyright: © 2024 Gan, Fan, Wang, Zhou, Tian, Yang and Qi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Hong Qi, First Affiliated Hospital of Chengdu Medical College, Chengdu, Sichuan Province, China
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.

IMAGES
VIDEO
COMMENTS
Education on self- care management has become gold standard for patients with diabetes [ 1 ]. Patients with diabetes require day-to-day knowledge of nutrition, exercise, monitoring, medication to accomplish daily self- care goals [ 2 ]. Evidence have shown that those who were well-equipped with self-care knowledge have become more confident to ...
To find diabetes dissertation topics: Study recent research in diabetes. Focus on emerging trends. Explore prevention, treatment, tech, etc. Consider cultural or demographic aspects. Consult experts or professors. Select a niche that resonates with you.
With the global prevalence of diabetes set to increase over the coming decades from 537 million in 2021 to 783 million in 2045,1 solutions must be found to ensure that both prevention and treatment are guaranteed. A key component to this response will be the strengthening of health systems. Included in the overall health system response is the important role that human resources have in ...
Participants' lack of knowledge about insulin injections sites and etiology of type 1 diabetes mellitus ... • 22% of DSN had a formal role in diabetes research compared with 48% in 2000 (p <0. ... Various studies have explored the topic of nursing care and have found that nurses are greatly involved in educating patients to manage their ...
Diabetes mellitus is taken from the Greek word diabetes, meaning siphon - to pass through and the Latin word mellitus meaning sweet. A review of the history shows that the term "diabetes" was first used by Apollonius of Memphis around 250 to 300 BC. Ancient Greek, Indian, and Egyptian civilizations discovered the sweet nature of urine in this condition, and hence the propagation of the word ...
Abstract. Objectives: To determine the clinical effectiveness (glycemic control, other biological measures, cost-effectiveness and patient satisfaction) of primary care nurse-led interventions for diabetes. Design: A systematic review following methods described for complex interventions and using PRISMA guidelines for reporting was undertaken.
Nurses have a crucial role in monitoring, educating and supporting people with diabetes, as well as their families and significant others. This article provides an overview of the main types and common symptoms of diabetes, its acute and long-term complications and its management. It also outlines the nurse's role in diabetes care, which ...
Diabetes mellitus is a major global threat to public health. Reducing the daily obstacles of coping with the disease for patients with diabetes may improve management. ... Intensive management program to improve glycosylated hemoglobin level and adherence to diet in patients with type 2 diabetes. Applied Nursing Research, 22, 42-47. https ...
Background The prevalence of diabetes is increasing rapidly worldwide. Nurses work collaboratively with multidisciplinary teams to improve diabetes management. Yet, little is known about nurses' role in nutritional management of diabetes. This study aimed to evaluate nurses' knowledge, attitudes, and practice (KAP) toward nutritional management of diabetes. Methods This cross-sectional ...
Background In an acute hospital setting, diabetes can require intensive management with medication modification, monitoring and education. Yet little is known about the experiences and perspectives of nursing/midwifery staff and patients. The aim of this study was to investigate diabetes management and care for patients with diabetes in an acute care setting from the perspectives of nursing ...
A fresh look at an old disease. This article describes current evidence-based approaches to the care and education of adults living with diabetes. It also highlights revisions in the 2022 Standards of Care and evidence-based strategies nurses can use to be more effective. From 2020 through 2022, public health services, health systems, nursing ...
For 2020, World Diabetes Day on Nov 14 is dedicated to promoting the crucial role of nurses in the prevention and management of diabetes. The campaign, Nurses Make the Difference, which is led by the International Diabetes Federation (IDF), highlights that nurses account for almost 60% of the health-care workforce worldwide and play a key part in the care of people with all types of diabetes ...
It focused on clinical effects of individualized nursing and health education (INHE) on patients with diabetes mellitus type 2 (T2DM) and hypertension. 68 patients were randomly rolled into two groups, 34 cases in the control group (group A) received routine nursing and remaining 34 cases in the experimental group (group B) received INHE.
During the pandemic, primary care systems prioritised attention to COVID-19 patients; chronically ill patients, such as people with Type 2 Diabetes were obliged to take more responsibility for their own care. We aimed to analyse the experiences of patients with Type 2 Diabetes Mellitus during the stay-at-home order that was in place during the first wave of the COVID-19 pandemic and identify ...
Diabetes Mellitus is a common and complex condition that affects millions of people worldwide. Learn about the nursing care management, diagnosis, complications, and treatment of this disease with this comprehensive guide from Nurseslabs. Whether you are a student, a nurse, or a patient, this webpage will provide you with valuable information and insights on Diabetes Mellitus.
A two-arm parallel-group randomized controlled trial with the blinded outcome assessors was designed. One hundred forty-two adults with type 2 diabetes were randomized to receive either usual diabetes care (control group) or usual care plus a nurse-led diabetes self-management education (intervention group). Duration of the intervention was 12 ...
Diabetes Documentation for Non-Medical Individuals. This essay looks at how diabetes has been documented for non-medical individuals over the decades. Examples will be drawn from the poem Diabetes by James Dickey. Effectiveness of Pragmatic Lifestyle Interventions for the Prevention of Type 2 Diabetes.
Because diabetes and its complications are widespread, burdensome, and costly, nurses need to provide care, patient education, and support based on current evidence and recommendations. Research in the treatment and care of diabetes is a growing and dynamic field. New medications and therapies become available each year.
generated in relation to the role of nurse in diabetes ca re: 1) Nurses' per-. formed role: the role performed by nurses in diabetes care was regarded as. complex and one that required ...
357 Diabetes Essay Topics & Examples. Updated: Feb 25th, 2024. 25 min. When you write about the science behind nutrition, heart diseases, and alternative medicine, checking titles for diabetes research papers can be quite beneficial. Below, our experts have gathered original ideas and examples for the task.
Part of the Nursing Commons, and the Public Health Education and Promotion Commons ... According to the report from Diabetes Research Institute Foundation (DRIF) (2018) 34.2 million people, or 10.5% of the U.S. population, have diabetes. An estimated ... Thiruvoipati et al. (2015) diabetes mellitus (DM) is a major risk factor for atherosclerotic
The method is advocated as being suitable in the contexts of nursing research and clinical ... MH Diabetes Mellitus+ OR MH Diabetes Mellitus type 1 OR MH Diabetes Mellitus type 2 AND MH Aged+ OR "older people" (keyword) OR MH Frail Elderly AND "self management" (keyword) Limitations: 2007-2018, Peer-review, Swedish, Danish, Norwegian ...
(1) Background: Diabetes mellitus (DM) induces oxidative stress and inflammation with negative effect on pregnancy outcomes. This study aimed to determine whether DM increases the risk of pregnancy loss and to identify other potential risk factors; (2) Methods: We identified female patients diagnosed with DM from 2000-2015 in the Taiwanese National Health Insurance Research Database ...
The aim of this study was to explore the nursing effect of diabetes education and nursing methods applied to diabetic patients in the endocrinology department. From October 2019 to October 2020, 90 patients with diabetes who were admitted to the Department of Endocrinology in our hospital were selected as the research objects, and the medical ...
This article is part of the Research Topic Endocrinology of Obesity, ... 1 School of Nursing, Chengdu Medical College, Chengdu, Sichuan Province, ... control.Method A purposive sampling methodology was employed to select a cohort of 318 patients afflicted with type 2 diabetes mellitus, hailing from a care establishment situated in Chengdu City ...