ORIGINAL RESEARCH article
The importance of understanding covid-19: the role of knowledge in promoting adherence to protective behaviors.

- 1 Department of Human Ecology, University of California, Davis, Davis, CA, United States
- 2 Intermountain Healthcare, Clinical Operations, Salt Lake City, UT, United States
Background: Past research suggests that knowledge supports- but strong illness expectations thwart- adoption of protective behaviors (e.g., handwashing). Strong illness expectations may place COVID-19 essential workers at risk. It is unclear, however, whether knowledge can moderate the negative effects of pessimistic illness expectations on protective behaviors. We test COVID-19 knowledge as a moderator of the effects of (1) pessimistic illness expectations and (2) essential worker status on adherence to protective behaviors.
Methods: Participants ( n = 350) completed measures of knowledge, illness expectations, and protective behaviors. We used chi-square tests to examine associations between variables and logistic regressions to test the moderation models predicting adherence (low, high) while controlling for demographics.
Results: Knowledge, illness expectations, and adherence were significantly associated with each other ( p < 0.05). Essential workers had stronger illness expectations and lower knowledge than did non-essential workers ( p < 0.001). Logistic regressions showed a non-significant Worker Status × Knowledge interaction ( p = 0.59) but a significant Knowledge × Illness Expectations interaction ( p < 0.05) indicating that those with strong illness expectations and low knowledge were disproportionately at risk of failing to adhere to recommended behaviors.
Conclusions: Knowledge promotes protective behaviors by buffering the negative effects of pessimistic illness expectations. Essential workers are more likely to have low levels of knowledge with strong illness expectations, suggesting that educational policies may be warranted.

Introduction
The COVID-19 pandemic is having devastating effects on human health and well-being and will likely continue to do so through its negative impact on the economy and poverty ( 1 ). The magnitude of the crisis can make it difficult to recognize the fact that individuals play an important role in slowing the spread of infection. Protective behaviors, sometimes called non-pharmaceutical interventions (NPIs), such as social distancing and handwashing, are critical to limiting the spread of infectious diseases ( 2 – 4 ). Essential workers, those who provide critical goods and services during the pandemic, often occupy low-wage positions in public transportation, food production, retail of food and health supplies, and healthcare. Protective of essential workers is particularly important given they are likely to have greater exposure to the virus and are at greater risk of financial strain if they do become infected ( 5 – 7 ).
The Common-Sense Model of Self-Regulation argues that the processes underlying individuals' conceptualization of an illness, referred to as an illness-related memory schema or mental model, include perceptions surrounding the threat posed by the illness and inform potential responses to the threat ( 8 – 11 ). The framework is typically applied to situations in which the patient has experienced a symptom of the illness but is also applicable to self-regulation of prevention-related behaviors during a pandemic. Specifically, illness-related memory schema are based on knowledge and beliefs about the illness and play an important role in the adoption of protective behaviors.
Past research on communicable diseases supports this notion by showing that knowledge and beliefs are important predictors of behaviors that impact the spread of the disease. For example, prior knowledge of a disease has been shown to increase handwashing, which in turn limited the spread of disease ( 12 ) and increase willingness to forgo public activities ( 11 ). In addition, misunderstandings (i.e., knowledge deficits) about influenza reduced adoption of protective behaviors ( 13 – 15 ). A recent study on COVID-19, on the other hand, reported no effects of knowledge on NPI, which as the authors noted, could be due to overall high knowledge scores ( 16 ) Another study, conducted when physical distancing but not mask-wearing was highly recommended ( 17 , 18 ), found that higher levels of COVID-19 knowledge were associated with attending fewer large gatherings and not wearing a mask when leaving home ( 19 ).
In general, the research above suggests that knowledge supports effective health-related decision making. This is consistent with the expression “knowledge is power,” which has appeared in cognitive sciences for decades to illustrate the importance of knowledge in human and artificial intelligence ( 20 ). Theories, such as the Long-term Working Memory theory ( 21 ), propose that the advantages are due to knowledge structures that facilitate comprehension of- and memory for—information that is germane to the knowledge domain ( 22 – 24 ).
In contrast to the beneficial effects of knowledge on NPIs, research indicates that some types of illness-related beliefs can interfere with the adoption of protective behaviors. Specifically, a high level of certainty that one will become infected is associated with lower adherence to health-protective behaviors ( 25 – 28 ). Strong illness expectations may represent the belief that fate, rather than the individual, controls whether the individual contracts the illness, making protective behaviors relatively unimportant ( 25 , 26 ). This is consistent with the notion that pessimistic, or why bother , beliefs increase avoidance behaviors ( 11 , 29 – 31 ). On the other hand beliefs, such as perceived vulnerability, are positively associated with protective behaviors, which presumably help to reduce discomfort associated with feeling vulnerable ( 32 , 33 ).
We are not aware of any studies on protective behaviors that have assessed both knowledge and beliefs as well as the relationship between knowledge and beliefs. However, a recent study that took place prior to an outbreak of COVID-19 in Australia included both knowledge and beliefs as predictors of NPI and vaccine intentions ( 34 ). Results showed that beliefs, including self-protection efficacy and perceived vulnerability, were positively associated with NPI but neither predicted vaccination intentions. Knowledge (symptoms, transmission, and general knowledge) was negatively associated with NPI but positively associated with vaccination intentions ( 34 ). Given the timing of the study, it could be that knowledgeable individuals understood that the threat had not yet reached a critical level so NPIs were not prioritized. Another challenge with interpreting the knowledge findings is many of the items were in areas that were rapidly evolving, making it difficult to know whether an individual knew more or less than what had been released to the public at that time ( 34 ). In another recent COVID-19 study, researchers showed that providing expert information about coronavirus infectiousness reduced fatalistic beliefs ( 35 ). Although NPIs were not assessed in that study, the findings suggest that providing knowledge can reduce maladaptive beliefs. Thus, despite theoretical work supporting the notion that mental models of one's illness, comprised of knowledge and beliefs, play an important role in health behaviors ( 8 – 11 ), there is little direct evidence regarding the extent to which knowledge mitigates the negative effects of illness expectations on the adoption of protective behaviors.
In the present study, we examined the extent to which COVID-19 knowledge and illness expectations predicted adherence to protective behaviors (handwashing, wearing a mask, avoiding crowded areas, 6-foot distance between individuals). We anticipated that knowledge would be positively associated with—but that illness expectations would be negatively associated with—protective-behavior adherence. The current pandemic differs from many past outbreaks in the US in that most individuals were ordered to stay-at-home at the time this study took place ( 18 ), while essential workers were not, providing an opportunity to compare knowledge and beliefs of essential and non-essential workers. We expected that essential workers may have stronger illness expectations than non-essential workers. It is unclear, however, whether knowledge would differ between essential and non-essential workers. Finally, the extent to which knowledge protects against disruptive beliefs, knowledge would be expected to moderate the relationship between beliefs and adherence to protective behaviors, and possibly, between essential-worker status and protective behaviors.
Participants
Participants ( n = 350) from across the United States were recruited through Amazon Mechanical Turk (MTurk) during the 2nd week of April 2020. Stay-at-home mandates were in place for the majority of states at that time (six states had recommendations only, one state had neither a mandate nor recommendation) ( 18 ). MTurk is a crowdsourcing platform that is appearing with increasing frequency in behavioral and medical research ( 36 , 37 ). This method allows individuals to participate from home at any time of day, which may have been particularly advantageous during the pandemic. The study was approved by the university's IRB.
To assess knowledge related to COVID-19, we created 15 True/False questions from public-facing information provided on Johns Hopkins Medicine website on basic definitions and common myths about COVID-19. We developed this measure because no knowledge tests existed at the time of the study. We included items that assessed general information about the virus relative to other infectious diseases, virus transmission, and prevention ( 38 ). Items and correct answers are presented in Table 1 . With one exception ( There is no vaccine to protect against the virus ), answers to the knowledge questions did not change between the time the study took place and the publication of this paper. A vaccine was developed roughly 7 months following the study. The total number of correct responses was used in the logistic regression analyses; however, for consistency with other predictors, a categorical variable (based on a median split) was used to examine unadjusted relationships. Pessimistic illness expectations were assessed using two items: To what extent do you expect to become – infected with COVID-19/– very sick if infected on a scale of 1 (Definitely will not) to 5 (Definitely will) ( 39 ). Because we were interested in pessimistic illness expectations, we considered high scores (ratings of 4 or 5) on either or both items to indicate strong illness expectations and low scores (ratings of 1–3, which included neutral expectations) on both items to indicate weak expectations.
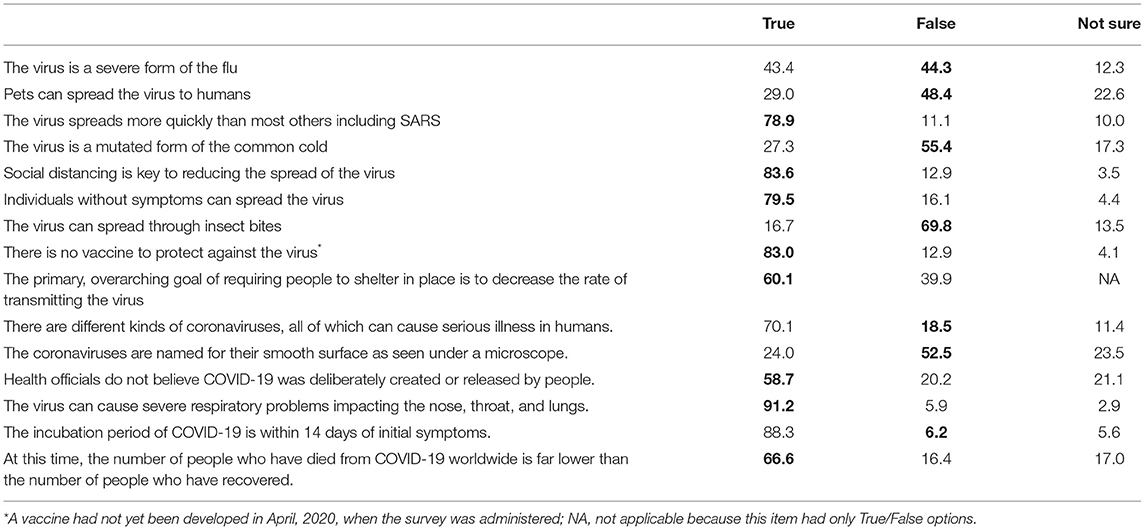
Table 1 . Knowledge items by response type percentage and correct responses shown in bold.
Protective behaviors were assessed by asking participants how frequently they followed 9 recommendations put forth by CDC (e.g., washing hands, social distancing) on a scale of 1 (Not Often) to 4 (Always) to reduce their risk of getting or spreading COVID-19 ( 2 ). Adoption to a protective behavior was considered Yes for scores of “often” or “always” with high adherence defined as the adoption of all nine behaviors. The items, shown in Table 2 , created a reliable assessment of overall protective behaviors as reflected in a Cronbach's alpha coefficient of 0.80. To assess essential worker status, we asked individuals to indicate whether they were an essential worker, non-essential worker, or not working. Finally, we asked participants whether they had tested positive for COVID-19 as a covariate.
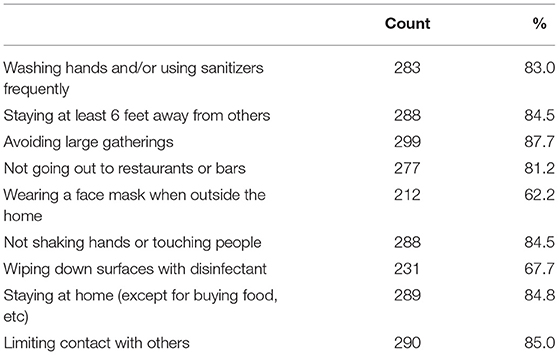
Table 2 . Adherence to protective behaviors.
Analytic Strategy
Unadjusted associations among essential worker status (yes/no), knowledge (low, high), illness expectations (weak/strong pessimism), and protective behavior adherence (low, high) were examined using Chi-square and Spearman's rho. We conducted logistic regressions to test two moderation models on adherence after controlling for age, sex, race, ethnicity, education, and income. The first model tested illness expectations as a possible moderator of the effects of knowledge on prevention behaviors and the second model tested worker status as a possible moderator. In both models, knowledge scores (i.e., total number of questions correctly answered) were mean-centered prior to creating the interaction term.
Of those enrolled in the study ( n = 350), 9 failed to pass the attention check and were excluded from analyses. As shown in Table 3 , the final sample ( n = 341) was 40.2% female, 78.6% Caucasian, and generally well-educated with 62.5% having 2 or more years of college. Close to one-third of the sample (36.7%) were essential workers; only six participants indicated they were not working and these individuals were included in the non-essential worker group. Essential workers were more likely to be Hispanic ( p < 0.001), but did not differ in terms of age ( χ 1 2 < 1), sex ( χ 1 2 = 1.30, p = 0.28), race ( χ 1 2 = 5.01, p = 0.08), education level ( χ 1 2 = 1.62, p = 0.20), or income ( χ 1 2 < 1). The null finding for income is contrary to the suggestion that non-essential workers earn less than other workers ( 5 ), and could be due to the relatively well-educated individuals who tend to participate in research through online panels.
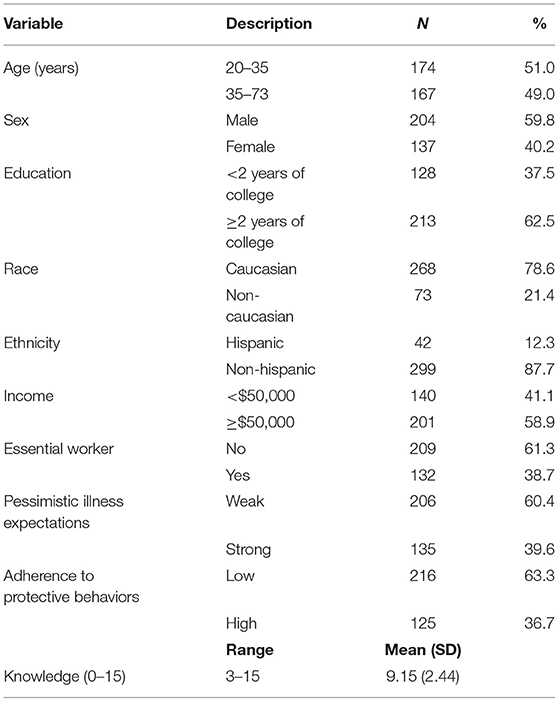
Table 3 . Participant characteristics ( n = 341).
Overall, adherence to protective behaviors was high as indicated by adherence rate of 80% across the nine NPI behaviors. Close to two-thirds of the sample (63%) reported adherence to eight or fewer behaviors. The distribution was highly skewed to the left (skewness = −1.45), leading us to dichotomize the distribution into partial adherence (low) and complete (high) adherence, which represented the top third of the distribution with adherence to all nine behaviors ( 40 ). As shown in Table 2 , the behavior with the lowest adherence was wearing a face mask when outside the home (62%) and the behavior with the highest adherence was avoiding large gatherings (87%).
Unadjusted Associations
Essential worker status was associated with lower knowledge and more pessimistic illness expectations ( p < 0.001 for both). Higher knowledge was associated with less pessimistic illness expectations ( p = 0.02). Adherence was associated with higher knowledge ( p = 0.04), non-essential worker status ( p < 0.01), and less pessimistic illness expectations ( p < 0.01). Although not a key variable, it is interesting to note that only 14 participants (4.1%) indicated that they had tested positive for COVID-19; all of these individuals were essential workers and 13 (92.8%) were in the low-adherence group.
Logistic Regressions
We tested the fit of two moderation models using logistic regressions. For both models, demographic variables (age, sex, race, ethnicity, education, and income) were added in block 1, main effects of key variables (essential worker status, illness expectations, and knowledge) and virus test results were added in block 2, and the interaction effect Knowledge x Illness Expectations (Model 1) or Knowledge x Worker Status (Model 2) was entered in block 3 (see Table 4 ).
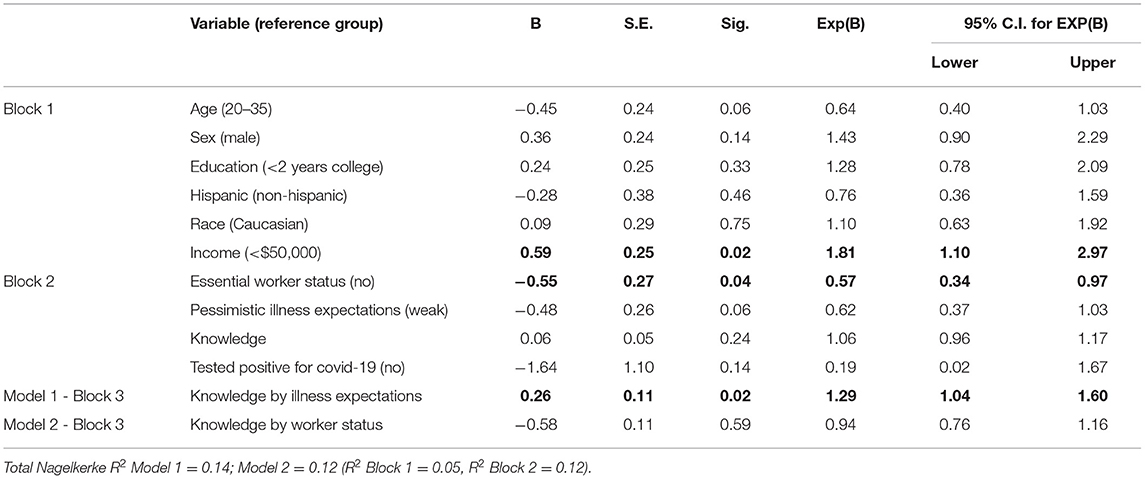
Table 4 . Tests of model effects predicting adherence to protective behaviors (significant effects shown in bold).
Data from Block 2 reflect the effects of predictors after controlling for demographic variables. Results showed Essential Worker Status was negatively associated with adherence (OR 0.58, 95% CI 0.34–0.97, p = 0.04) but the effects of illness expectations (OR 0.62, 95% CI 0.37–1.03, p = 0.06) and knowledge ( p = 0.24) were not significant. Because the zero-order associations were significant, the non-significant effects are likely due to variance shared with the variables entered in blocks 1 and 2. Block 3 differed for each model. In Model 1, the Knowledge × Illness Expectations interaction was significant ( p = 0.02). Figure 1 shows the predicted values from the model indicating that the negative association between pessimistic illness expectations and adherence was evident for those with lower levels of knowledge only. The Essential Worker Status × Knowledge interaction was not significant ( p = 0.59), indicating that knowledge moderates the effects of illness expectations, but not essential worker status per se .
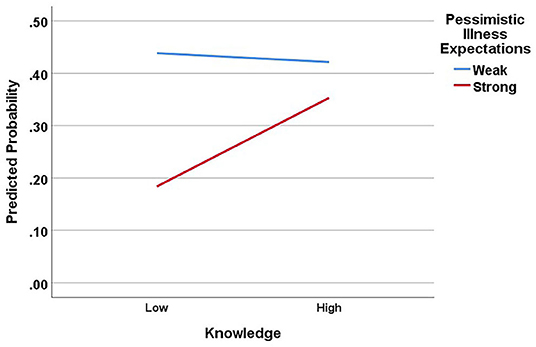
Figure 1 . Moderating effects of knowledge on the relationship between pessimistic illness expectations and adherence to protective behaviors. Note, knowledge scores were entered as a continuous variable in regression analyses but are shown here as a dichotomous variable (median split) for illustration purposes.
Findings from the present study are consistent with past research on NPIs indicating that knowledge is positively—and pessimistic illness expectations are negatively—associated with protective behaviors ( 12 – 14 , 25 , 26 ). We add to the literature by showing that knowledge and illness expectations are negatively associated with each other and suggest that the two predictors have opposing effects on adherence to protective behaviors. We further specify the nature of the relationships by showing that knowledge moderates the effects of illness expectations on adherence such that the negative effects of high levels of illness expectations as mitigated by high levels of knowledge. We cannot determine from this cross-sectional study whether illness expectations lead to adherence failure or knowledge leads to adherence success. Nor can we determine how knowledge impacts the relationship between illness expectations and adherence. Although it seems plausible that understanding the virus tempers the certainty that one will become infected if some precautions are taken, additional research is needed to examine causal links.
The findings are consistent with the Common-Sense Model of Self-Regulation arguing that knowledge and beliefs play a critical role in illness representations (or schema), which in turn drive behavior ( 9 ). Illness expectations that are constructed from knowledge about the virus, how it is transmitted, and what limits transmission may protect against potentially harmful beliefs based on misunderstandings and mistrust of credible sources. For example, understanding that a rapid rate of transmission could overwhelm the healthcare system and in turn limit care for everyone, not just those with COVID-19, may prevent individuals from believing that personal choice should dictate adherence to protective behaviors ( 41 ). Thus, knowledge-based illness representations may serve as a comprehensive navigation tool for making effective health-related decisions during the pandemic ( 38 ).
An important question to consider in future research is how rapidly changing scientific knowledge of an infectious disease impacts the acquisition of laypersons' knowledge of effective NPIs. With many unknowns about the novel coronavirus, particularly at the start of the pandemic, scientific evidence and therefore NPI recommendations were in flux. For example, recommendations to use face covering, broadly defined, appeared at the end of March, 2020; whereas the more precise recommendation to use of multi-layer cloth masks appeared in November, 2020 ( 17 ). State and county mandates surrounding masks and other NPIs have also shifted over time, potentially affecting acceptance of NPIs among the public, and subsequently, COVID-19 growth rates ( 42 ). The flow of information between public health officials and the public is also influenced by social media, which includes information that extends beyond geo-political boundaries ( 43 , 44 ).
Still, even under stay-at-home orders, individuals have many opportunities to be around others inside and outside the home (e.g., visit others, grocery store) requiring the use of protective behaviors. The abundance of misinformation that occurred during COVID-19 has made the question of protection against incorrect information more salient. Future research is needed to examine the extent to which science literacy could serve as a buffer against misinformation that threatens the public's health and well-being.
The rapid spread of COVID-19 in the spring of 2020 likely increased fear and confusion surrounding safety and may have decreased the opportunity to acquire factual information about the virus, for example, its incubation period and transmission process. Layered on top of this, the coronavirus has a relatively wide window of time, potentially 2 weeks, in which those who are infected with COVID-19 can transmit the virus without being aware that they are infectious ( 45 ). Thus, targeted strategies to increase individuals' understanding of COVID-19 may be a necessary component of an organization's safety plan as well as public health outreach more generally.
The data showing that (1) essential workers had strong illness expectations and low levels of knowledge and (2) both patterns predicted reduced adherence to protective behaviors suggest an additional layer of vulnerability. When essential workers—and those they serve—fail to adhere to protective behaviors, risk increases for all. It is unclear what should be done when essential workers or the public fail to adhere to orders requiring protective behaviors. However, an equally important question may be how do we promote learning about COVID-19 and other infectious diseases as a way to prevent adherence failures. Research is needed to examine the extent to which knowledge reduces the impact of maladaptive beliefs on NPIs as well as pharmaceutical interventions such as vaccinations, which are being avoided by a growing number of individuals ( 46 , 47 ).
Limitations
Limitations of this study include the use of crowdsourcing panel that is predominantly white and relatively well-educated and the majority of participants had some college education. Given that education would be expected to increase adherence, the findings may provide a more optimistic view of adherence than is warranted. However, the lack of ethnic and racial diversity limits the generalizability of the findings. Additionally, the study assessed knowledge, illness expectations, and protective behaviors at only one point in time and it could be that these factors change as the crisis evolves. Another limitation is that the study did not differentiate among types of essential workers, such as healthcare or food service, or consider official designations of essential worker categories at the time of data collection. It seems likely, for example, that healthcare workers who interacted with a volume of patients could have greater illness expectations or higher knowledge than other essential workers. Finally, it is important to recognize that the sample size of the study was small relative to epidemiological studies and was not representative of the population. The study was intended to provide an exploration of the dynamics between knowledge and beliefs within a context of a growing pandemic to consider how these factors could potentially impact NPIs. Replication with a larger, representative sample is needed to build on these findings, further specify mechanisms underlying adherence to protective behaviors, and inform the development of interventions that seek to empower individuals through increased knowledge and decrease pessimistic illness expectations.
Conclusions
This study indicates that pessimistic illness expectations increase the risk of failing to adhere to protective behaviors but that knowledge protects against the negative effects of these expectations. The findings have implications for practice and policy, particularly related to essential workers and their environment. Additional work is needed to identify optimal approaches to increasing individuals' knowledge to the point where it reduces or eliminates maladaptive beliefs. By helping to specify the predictors associated with protective behaviors during the pandemic, this line of inquiry may help to fill important gaps in our understanding of how to help slow the transmission of COVID-19 from individual to individual.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by IRB University of California, Davis. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
LM conceptualized the study and collected and analyzed the data. All authors contributed to drafting and revising the manuscript.
Conflict of Interest
PG and RK were employed by the company Intermountain Healthcare.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Parolin Z, Wimer C. Forecasting Estimates of Poverty During the COVID-19 Crisis . New York, NY: Center on Poverty and Social Policy at Columbia University; Columbia University (2020).
Google Scholar
2. Centers for Disease Control and Prevention. Public Health Communicators: Get Your Community Ready: Interim guidance for COVID-19 . (2020). Available online at: https://www.cdc.gov/healthcommunication/phcomm-get-your-community-ready.html (accessed October 3, 2020).
3. Moran KR, Del Valle SY. A meta-analysis of the association between gender and protective behaviors in response to respiratory epidemics and pandemics. PLoS ONE. (2016) 11:e0164541. doi: 10.1371/journal.pone.0164541
PubMed Abstract | CrossRef Full Text | Google Scholar
4. SteelFisher GK, Blendon RJ, Kang M, Ward JR, Kahn EB, Maddox KE, et al. Adoption of preventive behaviors in response to the 2009 H1N1 influenza pandemic: a multiethnic perspective. Influenza Respiratory Viruses. (2015) 9:131–42. doi: 10.1111/irv.12306
5. Ingraham C. Why Many “Essential” Workers Get Paid So Little, According to experts . The Washington Post (2020). Available online at: https://www.washingtonpost.com/business/2020/04/06/whydo-so-many-essential-workers-get-paid-so-little-heres-what-economistshave-say/ (accessed April 15, 2020).
6. Tomer A, Kane JW. How to Protect Essential Workers During COVID-19 . Washington, DC: Brookings Institution (2020).
7. Dennerlein JT, Burke L, Sabbath EL, Williams JAR, Peters SE, Wallace L, et al. An integrative total worker health framework for keeping workers safe and healthy during the COVID-19 pandemic. Hum Factors. (2020) 62:689–96. doi: 10.1177/0018720820932699
8. Benyamini Y, Karademas EC. Introduction to the special issue on the common sense model of self-regulation. Health Psychol Rev. (2019) 13:373–7. doi: 10.1080/17437199.2019.1644189
9. Leventhal H, Phillips LA, Burns E. The Common-Sense Model of Self-Regulation (CSM): a dynamic framework for understanding illness self-management. J Behav Med. (2016) 39:935–46. doi: 10.1007/s10865-016-9782-2
10. Petrie K, Weinman J. Why illness perceptions matter. Clin Med. (2006) 6:536. doi: 10.7861/clinmedicine.6-6-536
CrossRef Full Text | Google Scholar
11. Petrie KJ, Faasse K, Thomas MG. Public perceptions and knowledge of the Ebola virus, willingness to vaccinate, and likely behavioral responses to an outbreak. Disaster Med Public Health Preparedness. (2016) 10:674–80. doi: 10.1017/dmp.2016.67
12. Suen LKP, So ZYY, Yeung SKW, Lo KYK, Lam SC. Epidemiological investigation on hand hygiene knowledge and behaviour: a cross-sectional study on gender disparity. BMC Public Health. (2019) 19:401. doi: 10.1186/s12889-019-6705-5
13. Bults M, Beaujean DJ, Richardus JH, Voeten HA. Perceptions and behavioral responses of the general public during the 2009 influenza A (H1N1) pandemic: a systematic review. Disaster Med Public Health Preparedness. (2015) 9:207–19. doi: 10.1017/dmp.2014.160
14. Lin L, McCloud RF, Jung M, Viswanath K. Facing a health threat in a complex information environment: a national representative survey examining American adults' behavioral responses to the 2009/2010 A(H1N1) pandemic. Health Educ Behav. (2018) 45:77–89. doi: 10.1177/1090198117708011
15. Akmatov MK, Rübsamen N, Deyneko IV, Karch A, Mikolajczyk RT. Poor knowledge of vaccination recommendations and negative attitudes towards vaccinations are independently associated with poor vaccination uptake among adults—Findings of a population-based panel study in Lower Saxony, Germany. Vaccine. (2018) 36:2417–26. doi: 10.1016/j.vaccine.2018.03.050
16. Zickfeld JH, Schubert TW, Herting AK, Grahe J, Faasse K. Correlates of health-protective behavior during the initial days of the COVID-19 outbreak in Norway. Front Psychol. (2020) 11:564083. doi: 10.3389/fpsyg.2020.564083
17. Centers for Disease Control and Prevention. Scientific Brief: Community Use of Cloth Masks to Control the Spread of SARS-CoV-2 . (2020). Available online at: https://www.cdc.gov/coronavirus/2019-ncov/more/masking-science-sars-cov2.html (accessed December 11, 2020).
18. Moreland A, Herlihy C, Tynan MA, Sunshine G, McCord RF, Hilton C, et al. Timing of state and territorial COVID-19 stay-at-home orders and changes in population movement - United States, March 1-May 31, 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:1198–203. doi: 10.15585/mmwr.mm6935a2
19. Clements JM. Knowledge and behaviors toward COVID-19 among US residents during the early days of the pandemic: cross-sectional online questionnaire. JMIR Public Health Surveillance. (2020) 6:e19161. doi: 10.2196/19161
20. Feigenbaum EA. What hath Simon wrought? In: Klahr D, Kotovsky K, editors, Complex information processing: The impact of Herbert A. Simon . Hillsdale, NJ: Erlbaum. p. 165–82.
21. Ericsson KA, Kintsch W. Long-term working memory. Psychol Rev. (1995) 102:211–45. doi: 10.1037/0033-295X.102.2.211
22. Anderson JA. Effects of prior knowledge on memory for new information. Memory Cogn. (1981) 9:237–46. doi: 10.3758/BF03196958
23. Braasch JLG, Goldman SR. The role of prior knowledge in learning from analogies in science texts. Discourse Processes. (2010) 47:447–79. doi: 10.1080/01638530903420960
24. Guida A, Gobet F, Tardieu H, Nicolas S. How chunks, long-term working memory and templates offer a cognitive explanation for neuroimaging data on expertise acquisition: a two-stage framework. Brain Cogn. (2012) 79:221–44. doi: 10.1016/j.bandc.2012.01.010
25. Jimenez T, Restar A, Helm PJ, Cross RI, Barath D, Arndt J. Fatalism in the context of COVID-19: perceiving coronavirus as a death sentence predicts reluctance to perform recommended preventive behaviors. SSM Popul Health. (2020) 11:100615. doi: 10.1016/j.ssmph.2020.100615
26. Shahnazi H, Ahmadi-Livani M, Pahlavanzadeh B, Rajabi A, Hamrah MS, Charkazi A. Assessing preventive health behaviors from COVID-19: a cross sectional study with health belief model in Golestan Province, Northern of Iran. Infect Dis Poverty. (2020) 9:157. doi: 10.1186/s40249-020-00776-2
27. Auld MC. Choices, beliefs, and infectious disease dynamics. J Health Econ. (2003) 22:361–77. doi: 10.1016/S0167-6296(02)00103-0
28. Renner B, Gamp M, Schmälzle R, Schupp HT. Health risk perception. In: Wright JD, editor, International Encyclopedia of the Social & Behavioral Sciences . 2nd ed. Oxford: Elsevier. p. 702–9. doi: 10.1016/B978-0-08-097086-8.14138-8
29. Hagger MS, Orbell S. A meta-analytic review of the common-sense model of illness representations. Psychol Health. (2003) 18:141–84. doi: 10.1080/088704403100081321
30. Pagnini F. The potential role of illness expectations in the progression of medical diseases. BMC Psychol. (2019) 7:70. doi: 10.1186/s40359-019-0346-4
31. van der Velde FW, Hooykaas C, van der Joop P. Risk perception and behavior: pessimism, realism, and optimism about aids-related health behavior. Psychol Health. (1992) 6:23–38. doi: 10.1080/08870449208402018
32. Bish A, Michie S. Demographic and attitudinal determinants of protective behaviours during a pandemic: a review. Br J Health Psychol. (2010) 15:797–824. doi: 10.1348/135910710X485826
33. De Coninck D, d'Haenens L, Matthijs K. Perceived vulnerability to disease and attitudes towards public health measures: COVID-19 in Flanders, Belgium. Pers Individ Dif. (2020) 166:110220. doi: 10.1016/j.paid.2020.110220
34. Faasse K, Newby J. Public perceptions of COVID-19 in Australia: perceived risk, knowledge, health-protective behaviors, and vaccine intentions. Front Psychol. (2020) 11:2553. doi: 10.3389/fpsyg.2020.551004
35. Akesson J, Ashworth-Hayes S, Hahn R, Metcalfe RD, Rasooly I. Fatalism, Beliefs, and Behaviors During the COVID-19 Pandemic . National Bureau of Economic Research, Inc (2020). Available online at: https://ideas.repec.org/p/nbr/nberwo/27245.html (accessed June 18, 2020).
36. Litman L, Robinson J, Abberbock T. TurkPrime.com: a versatile crowdsourcing data acquisition platform for the behavioral sciences. Behav Res Methods. (2017) 49:433–42. doi: 10.3758/s13428-016-0727-z
37. Ranard BL, Ha YP, Meisel ZF, Asch DA, Hill SS, Becker LB, et al. Crowdsourcing–harnessing the masses to advance health and medicine, a systematic review. J General Internal Med. (2014) 29:187–203. doi: 10.1007/s11606-013-2536-8
38. Michie S, West R, Amlot R, Rubin J. Slowing down the covid-19 outbreak: changing behaviour by understanding it. BMJ Opin. (2020). Available online at: https://blogs.bmj.com/bmj/2020/03/11/slowingdown-the-covid-19-outbreak-changing-behaviour-by-understanding-it (accessed March 12, 2020).
39. Atchison CJ, Bowman L, Vrinten C, Redd R, Pristera P, Eaton JW, Ward H. Perceptions and behavioural responses of the general public during the COVID-19 pandemic: a cross-sectional survey of UK Adults. medRxiv. (2020) 2020.04.01.20050039. doi: 10.1101/2020.04.01.20050039
40. DeCoster J, Iselin A-MR, Gallucci M. A conceptual and empirical examination of justifications for dichotomization. Psychol Methods. (2009) 14:349–66. doi: 10.1037/a0016956
41. Ball P, Maxmen A. The epic battle against coronavirus misinformation and conspiracy theories. Nature. (2020) 581:371–4. doi: 10.1038/d41586-020-01452-z
42. Lyu W, Wehby GL. Community use of face masks and COVID-19: evidence from a natural experiment of state mandates in the US. Health Affairs. (2020) 39:1419–25. doi: 10.1377/hlthaff.2020.00818
43. Islam MS, Sarkar T, Khan SH, Mostofa Kamal A-H, Hasan SMM, Kabir A, et al. COVID-19–related infodemic and its impact on public health: a global social media analysis. Am J Trop Med Hygiene. (2020) 103:1621–9. doi: 10.4269/ajtmh.20-0812
44. Yousuf H, Corbin J, Sweep G, Hofstra M, Scherder E, van Gorp E, et al. Association of a public health campaign about coronavirus disease 2019 promoted by news media and a social influencer with self-reported personal hygiene and physical distancing in the Netherlands. JAMA Network Open. (2020) 3:e2014323. doi: 10.1001/jamanetworkopen.2020.14323
45. Lai X, Wang M, Qin C, Tan L, Ran L, Chen D, et al. Coronavirus disease 2019 (COVID-2019) infection among health care workers and implications for prevention measures in a tertiary hospital in Wuhan, China. JAMA Network Open. (2020) 3:e209666. doi: 10.1001/jamanetworkopen.2020.9666
46. Gunaratne K, Coomes EA, Haghbayan H. Temporal trends in anti-vaccine discourse on Twitter. Vaccine. (2019) 37:4867–71. doi: 10.1016/j.vaccine.2019.06.086
47. Madlon-Kay DJ, Smith ER. Interpreters' knowledge and perceptions of childhood vaccines: effect of an educational session. Vaccine. (2020) 38:1216–9. doi: 10.1016/j.vaccine.2019.11.010
Keywords: COVID-19, protective behavior, prior knowledge, essential workers, pessimistic illness expectations
Citation: Miller LMS, Gee PM and Katz RA (2021) The Importance of Understanding COVID-19: The Role of Knowledge in Promoting Adherence to Protective Behaviors. Front. Public Health 9:581497. doi: 10.3389/fpubh.2021.581497
Received: 08 July 2020; Accepted: 10 March 2021; Published: 06 April 2021.
Reviewed by:
Copyright © 2021 Miller, Gee and Katz. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lisa M. Soederberg Miller, lmsmiller@ucdavis.edu
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
How COVID-19 highlighted the importance of research

Professor Tania Sorrell AM
As the University’s Professor of Clinical Infectious Diseases , Professor Tania Sorrell AM has certainly had a challenging year.
While Professor Sorrell has worked for many years on infectious diseases as Director of the Sydney Institute for Infectious Diseases (formally known as Marie Bashir Institute for Infectious Diseases and Biosecurity), the impact of COVID-19 has brought her work squarely into the public spotlight.
High-quality research and open channels of communication with policymakers have been fundamental for the NSW response to COVID-19. Professor Sorrell and her team at Westmead Hospital produced a new diagnostic test specific to the disease within two weeks of seeing their first case. Her team were also able to sequence the entire length of the virus, which has driven a significant amount of the response across the State.

Professor Sorrell says Australia is uniquely positioned as a global leader in medical research. She says that we can strongly contribute to the fight against serious infectious diseases like COVID-19 in the future, but the key is continued funding of vital research.
That is one of the reasons Professor Sorrell has generously decided to create a legacy beyond her working lifetime. She will be leaving a significant portion of her estate towards research into, and prevention of, infectious diseases.
"I very much have wanted, from the time of my appointment, to build up infectious diseases and potentially leave it as a legacy of excellent research and education and student support within the University of Sydney," said Professor Sorrell.
Professor Sorrell says she also wants to support early career researchers. New researchers often struggle to turn promising starts into fully-fledged careers with a long-term impact in their disciplines, due to funding shortages.
“I think we’re all aware that government is funding medical research to a lesser extent than it used to. That’s why philanthropic funding is becoming a really important mechanism by which emerging young researchers can be assisted in achieving their aims.”
A better world is one without COVID-19, or other infectious diseases – and it is one which Professor Sorrell is working hard to create, now and well into the future.
“We’ve been very fortunate to have donors contribute in the past,” she says. “We’re just giving back to those who’ve given so much – that’s very much part of the ethos.”
Postgraduate research
Related articles, sotrovimab shown to cause covid-19 treatment-resistant mutations.
Australian researchers have uncovered resistance mutations to Sotrovimab - a monoclonal antibody treatment developed to minimise the risk of severe COVID-19 in patients who have underlying health conditions.
COVID-19 Delta & Omicron variant in education settings: new report
Living in the new ‘normal’.
Coronavirus experts discuss importance of research investments, lessons learned from COVID-19 at Chancellor’s Lecture Series
Media inquiries.
- 615-322-6397 Email
Latest Stories
- WATCH: FBI Director Christopher Wray gives keynote address at Vanderbilt’s Summit on Modern Conflict and Emerging Threats
- Vanderbilt University transitions benefits administration starting July 1
- Rites of Spring music festival is April 20
Mar 24, 2021, 10:18 AM
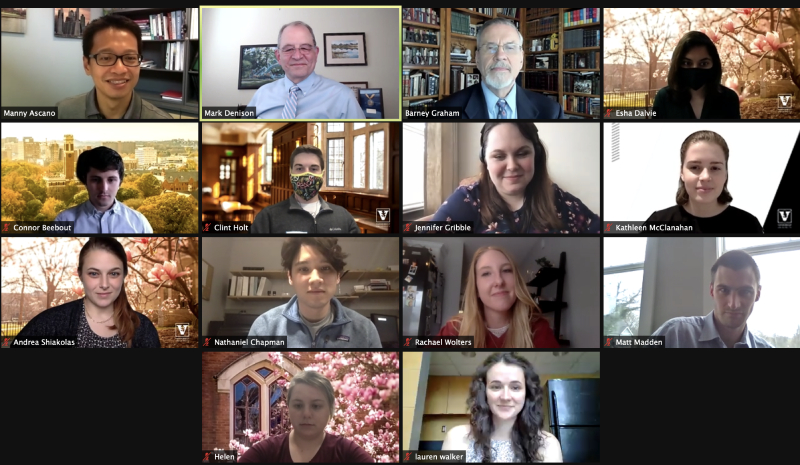
Vanderbilt’s role in shaping each step of the medical response to the pandemic caused by SARS-CoV-2 began three decades ago and is grounded in the determination of a small group of scientists to understand coronaviruses. The research, and the faculty and alumni who helped lead it, was the topic of the March 23 Vanderbilt Chancellor’s Lecture Series virtual event, “Vanderbilt in the Vanguard: The Decades-Long Journey to a Coronavirus Vaccine.”
The conversation outlined the path to the development of therapeutics for COVID-19 and what is expected to come next. The three panelists— Dr. Mark R. Denison , Dr. Barney S. Graham and Dr. Kathleen Neuzil —emphasized the importance of collaborative thinking and of scientific research with long-term horizons in solving the world’s greatest modern challenge. Provost and Vice Chancellor for Academic Affairs Susan R. Wente , a distinguished biomedical scientist and professor of cell and developmental biology who holds a Cornelius Vanderbilt Chair, moderated the event, which was hosted by Chancellor Daniel Diermeier.
Denison is the Edward Claiborne Stahlman Professor of Pediatrics, professor of pathology, microbiology and immunology, and director of the Division of Pediatric Infectious Diseases at Vanderbilt University Medical Center. Graham is the deputy director of the Vaccine Research Center, NIAID, NIH; and chief, Viral Pathogenesis Laboratory. Neuzil is the Myron M. Levine Professor in Vaccinology, professor of medicine and pediatrics, and director of the Center for Vaccine Development and Global Health at the University of Maryland School of Medicine.
Now spread out across the U.S., Denison, Graham and Neuzil once lived in the same Nashville neighborhood. They have never seen so much of each other as they have in the past year, however, as they have regularly joined infectious disease experts at the virtual table to share data, strategies and ideas to tackle the global pandemic.
To Denison, Graham and Neuzil, the most important lessons for the next pandemic center on investment in scientific discovery and creating pathways that reward collaboration. Graham called for a 194-country accord, similar to the Paris Agreement on climate change, focused on how to effectively manage emerging infectious diseases that know no borders. He also noted that there are 250 global vaccine groups working to develop a vaccine for SARS-CoV-2—a single virus. Instead, Graham thinks, groups should consolidate and tackle each of the 26 virus families that can infect humans and keep experts like him awake at night. “We need to harness our capabilities to more of a global approach to this problem,” he said.
COVID-19 therapeutics, including the Moderna vaccine and the antiviral remdesivir, were developed by the panelists, who shed light on the choices that were made. “The reason we chose [mRNA for this project] is because it is fast,” Graham said. “We wanted to pair our precision antigen design, or the atomic-level structure-guided antigens that we thought were the right thing for the immune system to see, with something that could have rapid delivery.”
The group confirmed that the successful development, substantial clinical trials and subsequent distribution of multiple mRNA vaccines will have a strong ripple effect on how other virus vaccines are developed, including those for emerging SARS-CoV-2 variants. Recent FDA guidance now clarifies that less grandiose clinical trials would be required for variant strains, with a process similar to those conducted for influenza strain changes.
“It is absolutely appropriate while we continue to improve and move forward with these highly effective [SARS-CoV-2] vaccines, that we do start to think about coronaviruses as a whole, as a family, and how we might target them,” Neuzil said of a pan-coronavirus vaccine. Denison shared his optimism that mRNA vaccines—which themselves are not viruses—will soon be used across many different viruses.
Looking back on the advances made throughout his career, Graham agreed. “The technologies we have [now] are so stunning—I couldn’t have imagined what we could do 30 years ago,” he said. “I think we have the tools to deal with these things. It’s a matter of investment.”
This investment is no more clearly understood anywhere than by this group, and by Denison in particular. Today he is recognized as a leading global expert in coronaviruses, but not long ago he struggled to continue research on a virus that no one knew or cared much about.
Funding research for non-obvious public health concerns may take decades to pay off, but all three researchers are hopeful that the past year has made the case for continued science and public-health-driven investments that don’t necessarily fit in an election cycle.
The work must be “predicated on a long-term biological understanding of the research,” Denison said. “I think of our work as being like an index mutual fund—it rises slowly, and not very many people find it interesting. But I think it’s better than a growth stock sometimes.”
Explore Story Topics
- Barney Graham
- Chancellor’s Lecture Series
- COVID-19 Research and Innovation
- covid-19-experts
- covid-19-featured
- Dr. Barney Graham
- Dr. Mark Denison
- featured myvu
- Kathleen Neuzil
- Mark Denison
- Susan Wente
The role of the health research system during the COVID-19 epidemic: experiences, challenges and future vision
Health research systems were already under strain when COVID-19 brought significant challenges, as well as making the existing challenges in health research systems more visible and significant [1].
In this context, the global, national and local health research system is expected to be able to answer the following questions:
- How to manage and control the current epidemic,
- How to prevent future epidemics,
- How to be more prepared in the event of the outbreak of such crises.
To control and manage the COVID-19 epidemic, and to effectively prevent and respond to future epidemics there are knowledge gaps that need to be addressed in various fields, and a wide range of research in basic sciences, clinical sciences, public health sciences, implementation science, and policy and system studies is needed to fill these gaps.
There are different systems, structures and processes for health research in different countries. In some countries the research system is fragmented, and since a wide range of interdisciplinary research is needed to control and manage the COVID-19 epidemic [2], the way these separate parts interact together is very important.
Recognising this, HARPS is dedicating a thematic issue to the role of health research systems in the control and management of COVID-19, so that the experiences of countries can be shared with each other and the lessons learned are accessible to all. Although the role of research systems in the control and management of crisis can be examined from different perspectives and by different frameworks, the following topics are particularly valuable:
o The building blocks of the health research system[3]: What was the status of each of these elements alone and in relation to each other, and what effect did the status have on the effective performance of the health research system? What interventions and innovations were made in each of the blocks to strengthen its status and what effect did it have?
These building blocks and operational components are: Stewardship : define and articulate vision for a health research system, identify appropriate health research priorities and coordinate adherence to them, set and monitor ethical standards for health research and research partnerships, monitor and evaluate of the health research system, Financing : Secure research funds and allocate them accountably, Creating and sustaining resources : Build, strengthen and sustain the human and physical capacity to conduct, absorb and utilize health research), Producing and using research : Produce scientifically valid research output, Translate and communicate research to inform health policy, strategies, practices and public opinion, Promote the use of research to develop new tools to improve health.
o The effectiveness, efficiency and equity of the health research system in facing the COVID-19 epidemic [4]: Effectiveness : Dose it produce any outputs, outcomes or broader impact? Efficiency : Compared to the cost spent on conducting research, how acceptable are its outputs (e.g investigating and reducing research waste)? Equity : Fair distribution of research resources and distribution of research benefits in target groups in connection to personal needs
The Editors declare no competing interests.
References: 1. Turner T, El-Jardali F. The crucible of COVID-19: what the pandemic is teaching us about health research systems. Health Research Policy and Systems . 2020; 18 :52. 2. Interdisciplinary research in epidemic preparedness and response, Workshop report , UK Academy of Medical Sciences , Medical Research Council, InterAcademy Partnership for Health; October 2019. 3. Hanney S KL, Pokhrel S, Jones T, Boaz A. What is the evidence on policies, interventions and tools for establishing and/or strengthening national health research systems and their effectiveness? Copenhagen: WHO Regional Office for Europe; 2020 (Health Evidence Network (HEN) synthesis report 69). 4. Hinrichs-Krapels.S, Jonathan.G. Exploring the effectiveness, efficiency and equity (3e’s) of research and research impact assessment. Palcomms 2016; 2 :16090.
A novel methodological approach to participant engagement and policy relevance for community-based primary medical care research during the COVID-19 pandemic in Australia and New Zealand
Community-based primary care, such as general practice (GP) or urgent care, serves as the primary point of access to healthcare for most Australians and New Zealanders. Coronavirus disease 2019 (COVID-19) has ...
- View Full Text
Connections between health research systems and decision-making spaces: lessons from the COVID-19 pandemic in the province of Québec, Canada
The coronavirus 2019 (COVID-19) pandemic allowed for exceptional decision-making power to be placed in the hands of public health departments. Data and information were widely disseminated in the media and on ...
Lessons learnt while designing and conducting a longitudinal study from the first Italian COVID-19 pandemic wave up to 3 years
Several scientific contributions have summarized the “lessons learnt” during the coronavirus disease 2019 (COVID-19) pandemic, but only a few authors have discussed what we have learnt on how to design and con...
A framework for seroepidemiologic investigations in future pandemics: insights from an evaluation of WHO’s Unity Studies initiative
The WHO Unity Studies initiative supports countries, especially low- and middle-income countries (LMICs), in conducting seroepidemiologic studies for rapidly informing responses to the COVID-19 pandemic. Ten g...
Online Health Communities: an alternative feasible data registry tool for developing countries
Given the many challenges facing healthcare access in many developing countries and the added limitations observed in emergencies like COVID-19 pandemic, the authors here discuss an alternative and feasible ap...
Tracking health system performance in times of crisis using routine health data: lessons learned from a multicountry consortium
COVID-19 has prompted the use of readily available administrative data to track health system performance in times of crisis and to monitor disruptions in essential healthcare services. In this commentary we d...
Limitations of COVID-19 testing and case data for evidence-informed health policy and practice
Coronavirus disease 2019 (COVID-19) became a pandemic within a matter of months. Analysing the first year of the pandemic, data and surveillance gaps have subsequently surfaced. Yet, policy decisions and publi...
Standardising policy and technology responses in the immediate aftermath of a pandemic: a comparative and conceptual framework
The initial policy response to the COVID-19 pandemic has differed widely across countries. Such variability in government interventions has made it difficult for policymakers and health research systems to com...
The whole-of-society approach of mass COVID-19 vaccination in China: a qualitative study
Many countries have an inefficient vaccination system, which hinders global exit from the COVID-19 pandemic. It is vital to summarize COVID-19 vaccination practices in countries with high vaccination coverage ...
Strengthening research ethics governance and regulatory oversight in Central America and the Dominican Republic in response to the COVID-19 pandemic: a qualitative study
Good governance and regulatory supervision are required to conduct research in an international public health emergency context and to ensure compliance with ethical standards. The “Strengthening research ethi...
How can health technology assessment support our response to public health emergencies?
Public health emergencies (PHEs), such as the COVID-19 crisis, are threats to global health and public order. We recommend that countries bolster their PHE responses by investing in health technology assessmen...
Building capacity for integrated knowledge translation: a description of what we can learn from trainees’ experiences during the COVID-19 pandemic
The use of collaborative health research approaches, such as integrated knowledge translation (IKT), was challenged during the COVID-19 pandemic due to physical distancing measures and transition to virtual pl...
Saving millions of lives but some resources squandered: emerging lessons from health research system pandemic achievements and challenges
During the SARS-CoV-2 pandemic, astonishingly rapid research averted millions of deaths worldwide through new vaccines and repurposed and new drugs. Evidence use informed life-saving national policies includin...
The collaborative research and service delivery partnership between the United States healthcare system and the U.S. Military Health System during the COVID-19 pandemic
To examine the military-civilian collaborative efforts which addressed the unprecedented challenges of the COVID-19 pandemic, particularly in areas including provision of supplies, patient and provider support...
The organization and impacts of clinical research delivery workforce redeployment during the COVID-19 pandemic: a qualitative case study of one research-intensive acute hospital trust
COVID-19 has tested healthcare and research systems around the world, forcing the large-scale reorganization of hospitals, research infrastructure and resources. The United Kingdom has been singled out for the...
Knowledge gaps and national research priorities for COVID-19 in Iran
In the present COVID-19 crisis, one of the greatest challenges for research funding at both the international and national level is selecting the best research topic to achieve efficiency and equity in health ...
Rapid research response to the COVID-19 pandemic: perspectives from a National Institute for Health Biomedical Research Centre
With over 5 million COVID-19 deaths at the time of writing, the response of research leaders was and is critical to developing treatments to control the global pandemic. As clinical research leaders urgently r...
The qualitative experience of telehealth access and clinical encounters in Australian healthcare during COVID-19: implications for policy
Adaptive models of healthcare delivery, such as telehealth consultations, have rapidly been adopted to ensure ongoing delivery of essential healthcare services during the COVID-19 pandemic. However, there rema...
Challenges encountered in comparing international policy responses to COVID-19 and their effects
A variety of policies have been implemented around the world in response to the COVID-19 pandemic. This study originally aimed to identify and compare policy responses of different countries and their effects ...
Rethinking approaches of science, technology, and innovation in healthcare during the COVID-19 pandemic: the challenge of translating knowledge infrastructures to public needs
The coronavirus disease 2019 (COVID-19) outbreak made it clear that despite the potential of science, technology, and innovation (ST&I) to positively impact healthcare systems worldwide, as shown by the rapid ...
Lessons from the pandemic on the value of research infrastructure
The COVID-19 pandemic has shed a spotlight on the resilience of healthcare systems, and their ability to cope efficiently and effectively with unexpected crises. If we are to learn one economic lesson from the...
Direct from the COVID-19 crisis: research and innovation sparks in Brazil
The coronavirus disease 2019 (COVID-19) pandemic has spread throughout more than 160 countries, infecting millions of people worldwide. To address this health emergency, countries have organized the flow of pr...
Health research system resilience: lesson learned from the COVID-19 crisis
Producing evidence in epidemics is crucial to control the current epidemic and prevent its recurrence in the future. Data must be collected and analyzed rapidly to recognize the most efficient and feasible met...

Preparing for the next health crisis: COVID-19 showed the importance of community-engaged research
Research Associate, Health Sciences, Simon Fraser University
Assistant Professor, Faculty of Health Sciences, Simon Fraser University
Disclosure statement
Julia Smith receives funding from the Canadian Institutes of Health Research and Health Research BC.
Simran Purewal does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
Simon Fraser University provides funding as a member of The Conversation CA.
Simon Fraser University provides funding as a member of The Conversation CA-FR.
View all partners
Community-engaged research involves the active and meaningful involvement of people directly affected by a research problem. Like most activities that require personal interaction, this type of research was disrupted by the restrictions of the COVID-19 pandemic.
This research approach is intended to build trustworthy relationships and yield mutual benefits. Community-engaged projects have garnered attention over the past two decades as they focus on tackling inequities , which often arise during public health crises.
Conducting community-engaged research has several benefits, like increasing the relevancy of studies , incorporating lived experience , and supporting the sharing of findings back to affected communities. Community engagement also plays an important role in emergency responses. Community-engaged emergency responses can promote the uptake of public health interventions and bolster advocacy efforts.
Community-engaged research during the pandemic
Researchers’ ability to engage with communities was impacted by the COVID-19 pandemic. Public health measures focused on preventing the spread of COVID-19 (such as limits on in-person gatherings) halted traditional forms of fieldwork. For example, researchers could not safely host in-person interviews. They were forced to quickly adapt to unfamiliar virtual teaching and learning platforms.
At the same time, civil society organizations (CSOs), non-profit agencies operating separately from government and business, were stretched thin as their demand soared. These organizations are sought after as community research partners since they are embedded in the communities they serve and provide crucial services to community members. Examples include the United Way BC and Sources Community Resource Centre , which provide direct services, support and relief to communities across B.C.
In 2023, the Pacific Institute on Pathogens, Pandemics, and Society ( PIPPS ) hosted a roundtable with community-engaged researchers at Simon Fraser University to learn about their experiences engaging with communities amid the pandemic. Findings from our roundtable, supplementing this article, have also been included in our Community-Engaged Research during Health Crises: Engaging with Civil Society Organizations handbook published by PIPPS and SFU Community Engaged Research Initiative .
Barriers to conducting community-engaged research
Roundtable attendees first discussed the challenges of conducting research remotely, with one noting how their research plans were put on pause for more than three months because of pandemic-related restrictions. Attendees also highlighted how managing multiple forms of online communication disrupted their work-life balance.
Several attendees found it difficult to recruit research participants; they discussed the challenges of the digital divide , referring to the gap between communities’ access to information and communication technologies.
Researchers faced challenges with ethics review boards, which did not consider the risks and unique considerations of engaging communities in a public health crisis. While ethics applications were expedited, researchers felt they lacked guidance for community-engaged research during the pandemic.
Researchers also found it hard to maintain relationships with communities amidst the pandemic. Some key ways researchers connect with communities are through sharing findings and hosting food-sharing events, such as lunch and learns. These opportunities were not available during the pandemic. In addition, many of their long-standing relationships with CSOs were strained as they experienced layoffs and increased demand. Researchers did not want to impede on CSOs’ frontline pandemic-related efforts.
Opportunities emerging from the pandemic

Despite the challenges they faced, researchers identified a range of opportunities that emerged as a result of the pandemic. They noted how they could increase the scope of their projects since virtual tools, like Zoom, allowed them to reach rural and remote communities. These platforms also provided low-barrier forms of participation for participants with accommodation needs.
Researchers also discussed how the pandemic forced the “professional veneers to slip away.” Over time, researchers connected on a more vulnerable level with their community partners, as they all attempted to get through the pandemic. Collectively, they showed up in their most authentic way and practised humility in their partnerships. Moreover, research teams emphasized the importance of building community, which reinforced their commitment to mutual benefit .
Through their community-engaged work, some researchers hired people with lived experience of the research problem of interest. This opportunity emerged during the pandemic. Compensating members of the research team for their knowledge strengthened the relevancy of their findings as they directly learned how the pandemic was impacting distinct groups.
Lessons learned: Conducting community-engaged research in future crises
Participants were asked what they would do differently in future health crises. Some discussed the significance of holding informal check-ins with their teams to openly discuss professional and personal challenges. Others pointed to the need for knowledge and resource sharing with other community-engaged researchers, to break down silos.
Additionally, attendees underscored the benefits of interdisciplinary research teams , bringing together diverse skills and expertise. In health crises, they aim to work collaboratively with academics and service providers from CSOs.

Based on the key themes of the roundtable, three recommendations emerged to support community-engaged research in future public health crises:
1) Post-secondary institutions should develop guidance for community-engaged research in health emergencies
Since post-secondary institutions increasingly recognize the importance of community-university partnerships , institutions should create protocols to support community-engaged research in public health crises. Attention should be paid to crisis-related considerations, including funding sources, resource challenges and ethics.
2) Develop targeted funding opportunities for community-engaged research partnerships
During the pandemic, research unrelated to COVID-19 faced funding drawbacks and resource constraints . This may have secondary effects in the “ post-pandemic era ,” especially for projects addressing health inequities. To avoid these unintended consequences, partnerships should be proactively supported by post-secondary institutions and funding agencies, to provide research partners with honoraria for their time and insights shared, and to help academic researchers build networks for engagement.
3) Prioritize capacity-building in partnerships
Mutual benefit is a guiding principle of community-engaged research . In partnerships, academic researchers often benefit through career advancement and a sense of fulfillment . Yet, community partners are not always assured the same benefits. To ensure mutual benefit, capacity building , referring to the process of building skills, abilities and resources, should guide community-engaged research partnerships. Both academic researchers and community partners bring significant assets to projects; these assets and training gaps should be uncovered at the outset of projects and considered throughout the partnership.
In addition to these recommendations, a repeated theme for participants was how community-engaged research should be viewed as a fundamental component of their work, as opposed to an afterthought. Rather than treating community-engaged research as a “ peripheral activity ,” the principles of community engagement should be embedded in research, teaching and learning.
- Public health
- Online communication
- Community engagement
- Public health crisis
- Civil society organizations
- Pandemic restrictions

Deputy Social Media Producer

Research Fellow /Senior Research Fellow – Implementation Science

Associate Professor, Occupational Therapy

GRAINS RESEARCH AND DEVELOPMENT CORPORATION CHAIRPERSON

Faculty of Law - Academic Appointment Opportunities
- Our Mission and Values
- Annual Reports
- Diversity and Inclusion
- Message from the Director
- Public Programs
- Careers, Culture and Benefits
- Whitehead Fellows Program
- Campus and Innovation Centers
- Cell Dynamics
- Regeneration, Rejuvenation and Aging
- Genes and Genomes
- Infectious Disease
- Nervous System
- Plant Biology
- Members and Fellows
- Postdoctoral Scholars
- For Journalists
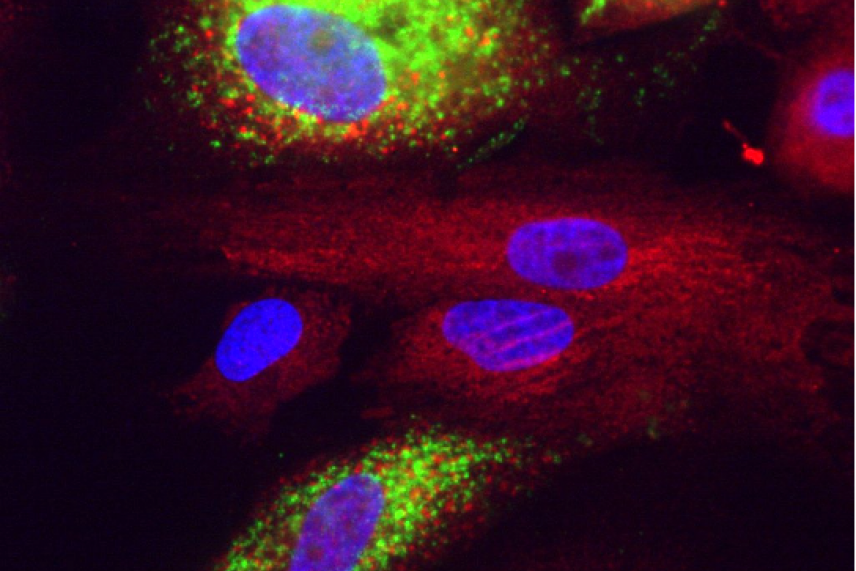
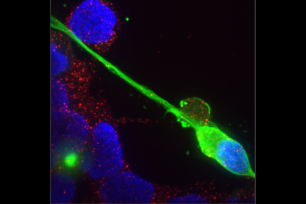
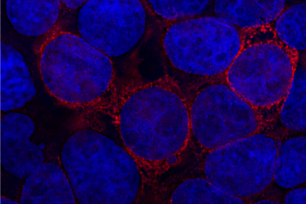
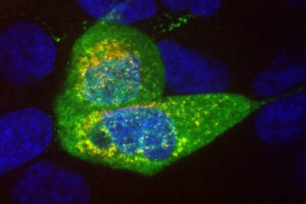
Covid in liver cells. Green is dsRNA, red is calreticulin, blue is nuclei stained with DAPI.
Courtesy of Rudolf Jaenisch

Why RNA research has been critical during the COVID19 pandemic
This story is part of our series, Sculptors of the Cell: RNA research at Whitehead Institute: RNA Research at Whitehead Institute. Click here to see all stories in this collection.
Until the past year, RNA was a molecule mostly relegated to research labs and biology textbooks — an unsung cellular hero. Now, anyone who reads the news can’t help but have it on their mind. The molecule comprises the genetic information of SARS-Cov-2, the virus that causes the COVID19 disease, as well as two of the first vaccines being used to provide immunity against the virus.
Since early in 2020, researchers at Whitehead Institute and around the world have been applying their RNA knowledge to the COVID19 pandemic. In this article, we will explore their research and how advances in RNA biology have helped uncover a light at the end of the pandemic tunnel.
What is an RNA virus, anyway?
The human genome — and that of most other living organisms — is encoded in DNA. But not all living things use DNA as the template for their bodies. “The top 12 deadliest viruses, as classified by the World Health Organization, are all RNA viruses,” says Whitehead Fellow Silvi Rouskin. “That just means that they store their genomes as RNA instead of DNA.”
RNA viruses make up about half of all known viruses. These viruses need to infect hosts with DNA in order to replicate. When an RNA virus like SARS-CoV-2 enters the human body, it attaches itself to the outside of human cells using specialized proteins, and injects the cell with its RNA. The infected cell then treats the RNA like its own, producing proteins from it which are then used to create new viruses. After many viruses have been produced this way, the cell ruptures, unleashing a new generation of viruses to infect other cells.
RNA viruses share some common characteristics beyond their genetic material. For one thing, they usually have a high rate of mutation, meaning that they change often and easily adapt to new conditions. For another, they usually have very small genomes.
“RNA viruses have this challenge that they have to pack so much information in this really small space,” Rouskin says. “So they’ve evolved, and they’ve gotten really creative in optimizing and layering information on top of their primary sequence [the order of the nucleotides that make up the RNA].”
But Rouskin’s previous work on the HIV genome led her to look at other characteristics of the SARS-CoV-2 virus for clues to its function.
“For HIV, there’s only a handful of genes: it actually just has 9 genes — really small,” Rouskin says. “But it needs to express genes from the exact same molecule that is both the genetic material and the thing that gets translated into protein. One way it does this is by folding into certain shapes.”
Using a technique previously developed in her lab, Rouskin and her colleagues were able to discover the secondary structure of SARS-CoV-2’s RNA genome.
Scientists are now studying the different regions of the genome for clues to what the different shapes do throughout the virus’ life cycle, and how this knowledge could be applied to create drugs. “Because those shapes are so important for the function of the molecule, the idea is that by interfering with the shape, then you can cripple the virus in that sense,” Rouskin says. “So it’s a therapeutic-based approach, versus a vaccine.”
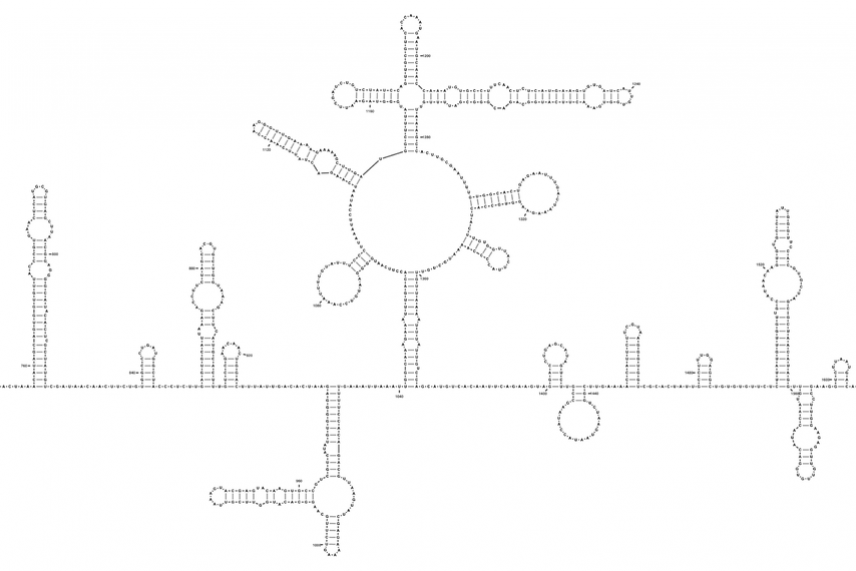
Part of the SARS-CoV-2 genome.
Tammy C. T. Lan et al., bioRxiv
All about RNA vaccines
While Whitehead Institute researchers have been studying possible therapeutic approaches for the virus, other scientists have been tackling the other side of the issue — how to prevent infection by administering a vaccine. As the vaccine rollout reaches more and more people across the country, it’s a good time to reflect on just what a huge step forward these new vaccines are. Traditional vaccines are composed of weakened or inactivated virus proteins. These virus parts act as what are called antigens, provoking the body to develop an immune response without any risk of infection.
The initial vaccines developed for COVID-19 such as those made by Pfizer-BioNTech and Moderna took this method a step further. Instead of providing the body with an antigen, they supply the body with the “recipe” to make the antigen itself in the form of messenger RNA, or mRNA, which is common in the body as an intermediary between DNA and proteins. These two vaccines made history as the world’s first examples of a vaccine approved for human use that used mRNA to confer immunity.
The Pfizer and Moderna vaccines are composed of the messenger RNA that the coronavirus needs to make its spike proteins, proteins on the outside of the virus that help it infect healthy cells. When the mRNA is injected into a person, the person’s cells read the mRNA transcript and create spike protein. Then, the body recognizes the protein as foreign and mounts an immune response, crafting antibodies to find and destroy the spike protein — and whatever it’s attached to. This primes the body for when it encounters a real coronavirus, so it will not have to scramble to throw together an immune response at the last minute.
Drugs that didn’t work — and how we could change that
Throughout the pandemic, there were several examples of drugs that should work against SARS-CoV-2, but for one reason or another, don’t work so well. (One famous example was the broad-spectrum antiviral drug remdesivir).
Whitehead Institute Member Richard Young is investigating how these drugs could be made more effective by building off his past research on small cellular droplets called biomolecular condensates. Condensates bring together the necessary molecules for functions such as transcription, the process of reading DNA into RNA, and previous work from the Young Lab has shown that condensate formation can affect the behavior of drugs in cells.
The Young lab was able to demonstrate in the lab that SARS-CoV-2 proteins form condensates with RNA molecules, and are now working on ways to harness this property to help fight the virus. “We’re figuring out the chemistry that would allow drugs to concentrate in the condensate where [viral RNA] replication is occurring,” Young says.
If their experiments prove fruitful, they could provide another tool in the arsenal scientists have been assembling to tackle SARS-CoV-2 in the future.
Communications and Public Affairs Phone: 617-452-4630 Email: [email protected]
Related News
Whitehead Institute Founding Member Rudolf Jaenisch and colleagues found that SARS-Cov-2 can infect sensory neurons and alter their gene expression. This may help to explain the peripheral nervous system symptoms associated with Covid-19, such as loss of smell.
New research from Whitehead Institute Founding Member Rudolf Jaenisch’s lab adds evidence to their finding that SARS-CoV-2 can integrate into the human genome, but finds that a model of the mRNA vaccine does not integrate.
A paper from the lab of Whitehead Institute Member Rudolf Jaenisch suggests that the genetic material of SARS-CoV-2 can integrate into the host cell genome and be expressed in some patient-derived tissues.
Disclaimer: This translation was last updated on August 2, 2022. For up-to-date content, please visit the English version of this page.
Disclaimer: The Spanish COVID-19 site is currently undergoing significant updates which may lead to a delay in translated content. We apologize for any inconvenience.
About COVID-19
What is covid-19.
COVID-19 (coronavirus disease 2019) is a disease caused by a virus named SARS-CoV-2. It can be very contagious and spreads quickly. Over one million people have died from COVID-19 in the United States.
COVID-19 most often causes respiratory symptoms that can feel much like a cold, the flu, or pneumonia. COVID-19 may attack more than your lungs and respiratory system. Other parts of your body may also be affected by the disease. Most people with COVID-19 have mild symptoms, but some people become severely ill.
Some people including those with minor or no symptoms will develop Post-COVID Conditions – also called “Long COVID.”
How does COVID-19 spread?
COVID-19 spreads when an infected person breathes out droplets and very small particles that contain the virus. Other people can breathe in these droplets and particles, or these droplets and particles can land on their eyes, nose, or mouth. In some circumstances, these droplets may contaminate surfaces they touch.
Anyone infected with COVID-19 can spread it, even if they do NOT have symptoms.
The risk of animals spreading the virus that causes COVID-19 to people is low. The virus can spread from people to animals during close contact. People with suspected or confirmed COVID-19 should avoid contact with animals.
What are antibodies and how do they help protect me?
Antibodies are proteins your immune system makes to help fight infection and protect you from getting sick in the future. A positive antibody test result can help identify someone who has had COVID-19 in the past or has been vaccinated against COVID-19. Studies show that people who have antibodies from an infection with the virus that causes COVID-19 can improve their level of protection by getting vaccinated.
Who is at risk of severe illness from COVID-19?
Some people are more likely than others to get very sick if they get COVID-19. This includes people who are older , are immunocompromised (have a weakened immune system), have certain disabilities , or have underlying health conditions . Understanding your COVID-19 risk and the risks that might affect others can help you make decisions to protect yourself and others .
What are ways to prevent COVID-19?
There are many actions you can take to help protect you, your household, and your community from COVID-19. CDC’s Respiratory Virus Guidance provides actions you can take to help protect yourself and others from health risks caused by respiratory viruses, including COVID-19. These actions include steps you can take to lower the risk of COVID-19 transmission (catching and spreading COVID-19) and lower the risk of severe illness if you get sick.
CDC recommends that you
- Stay up to date with COVID-19 vaccines
- Practice good hygiene (practices that improve cleanliness)
- Take steps for cleaner air
- Stay home when sick
- Seek health care promptly for testing and treatment when you are sick if you have risk factors for severe illness . Treatment may help lower your risk of severe illness.
Masks , physical distancing , and tests can provide additional layers of protection.
What are variants of COVID-19?
Viruses are constantly changing, including the virus that causes COVID-19. These changes occur over time and can lead to new strains of the virus or variants of COVID-19 . Slowing the spread of the virus, by protecting yourself and others , can help slow new variants from developing. CDC is working with state and local public health officials to monitor the spread of all variants, including Omicron.
- COVID-19 Testing
- COVID-19 Vaccines
- Preventing Respiratory Viruses
- Reinfection
- Difference Between Flu and COVID-19
- COVID Data Tracker
Search for and find historical COVID-19 pages and files. Please note the content on these pages and files is no longer being updated and may be out of date.
- Visit archive.cdc.gov for a historical snapshot of the COVID-19 website, capturing the end of the Federal Public Health Emergency on June 28, 2023.
- Visit the dynamic COVID-19 collection to search the COVID-19 website as far back as July 30, 2021.
To receive email updates about COVID-19, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
What Is Long COVID? Understanding the Pandemic’s Mysterious Fallout
BY BROOKS LEITNER April 15, 2024
Just weeks after the first cases of COVID-19 hit U.S. shores, an op-ed appeared in The New York Times titled “We Need to Talk About What Coronavirus Recoveries Look Like: They're a lot more complicated than most people realize.” The author, Fiona Lowenstein, is a writer and yoga teacher living in New York City, who wrote about her own illness and the symptoms she was left with once she was released from the hospital. “In the weeks since I was hospitalized for the coronavirus , the same question has flooded my email inbox, texts and direct messages: Are you better yet? I don’t yet know how to answer.”
She was better, she wrote on April 13, 2020 , but she wasn’t well. And others she was in touch with were having the same issue. Unlike most diseases, Long COVID was first described not by doctors, but by the patients themselves. Even the term “Long COVID” was coined by a patient. Dr. Elisa Perego, an honorary research fellow at University College in London, came up with the hashtag #LongCOVID when tweeting about her own experience with the post-COVID syndrome. The term went viral and suddenly social media, and then the media itself, was full of these stories.
Complaints like "I can't seem to concentrate anymore" or "I'm constantly fatigued throughout the day" became increasingly common, seemingly appearing out of nowhere. With nothing abnormal turning up from their many thorough lab tests, patients and their physicians were left feeling helpless and frustrated.
The World Health Organization (WHO) has defined Long COVID as the "continuation or development of new symptoms three months after the initial SARS-CoV-2 infection, with these symptoms lasting for at least two months with no other explanation." This deliberately broad definition reflects the complex nature of this syndrome. We now understand that these symptoms are wide-ranging, including heart palpitations, cough, nausea, fatigue, cognitive impairment (commonly referred to as "brain fog"), and more. Also, many who experience Long COVID following an acute infection face an elevated risk of such medical complications as blood clots and (type 2) diabetes.
As of March 2024 , it’s estimated that about 17% of patients who get COVID-19 will go on to develop post-acute COVID-19 syndrome, the medical term for Long COVID. Data from the Centers for Disease Control and Prevention (CDC) suggest that Long COVID disproportionately affects women, and individuals between the ages of 40 and 49 have the highest reported rates of developing this post-acute infection syndrome.
Long COVID represents a new clinical challenge
Ebony Dix, MD , a Yale School of Medicine (YSM) assistant professor of psychiatry and the medical director of the geriatric psychiatry inpatient unit at Yale New Haven Hospital, said: "Unfortunately, it is not easy to say who is going to get Long COVID and who isn't." She also emphasized that "it can be overlooked and attributed to a preexisting condition. Sometimes the only thing that patients have in their history is a positive COVID test."
Dr. Dix recalled a patient she treated in the COVID psychiatry unit whose unanticipated clinical decline began with increasing fatigue during physical therapy sessions, ultimately necessitating more care over several weeks. Dr. Dix noted, "Long COVID requires time for things to settle down. It might take several months to get back to baseline." Making timely changes to a patient’s treatment plans was essential to helping her patients get back to good health, she said.
A major challenge with Long COVID is how difficult it can be to diagnose. Determining whether new-onset symptoms, such as fatigue or weakness, are related to an underlying condition or entirely attributed to a prior COVID infection is the greatest challenge for those who care for these patients. This is, in large part, due to the lack of research surrounding the topic.
Defining a basis for Long COVID with clinical research
Inderjit Singh, MBChB , a YSM assistant professor specializing in pulmonary, critical care, and sleep medicine, and director of the Pulmonary Vascular Program, is actively engaged in clinical trials aimed at uncovering the fundamental underpinnings of Long COVID. In one research study, patients suffering from unexplained fatigue and shortness of breath undergo exhaustive exercise testing. In order to be enrolled in this study, patients need to have already completed a substantial work-up, including an echocardiogram, pulmonary function testing, chest CT scans, and more, all which result in no alternative diagnosis.
Through this work, a significant revelation emerged. They observed that patients grappling with Long COVID and facing exercise difficulties were unable to efficiently extract oxygen from their bloodstream during physical exertion. This discovery identifies a specific cause underlying the biological underpinnings of Long COVID.
Recognizing the impracticality of conducting comprehensive exercise tests for every Long COVID patient, Dr. Singh, along with other researchers, is focused on the identification of blood-based markers to assess the severity of Long COVID. For example, a research group, led by Akiko Iwasaki, PhD , Sterling Professor of Immunobiology and Molecular, Cellular, and Developmental Biology, and director of the Center for Infection & Immunity at YSM, most recently created a new method to classify Long COVID severity with circulating immune markers.
Further investigations conducted by Dr. Singh's team identified distinctive protein signatures in the blood of Long COVID patients, which correlated with the degree of Long COVID severity. Researchers identified two major and distinct blood profiles among the patients. Some of them exhibited blood profiles indicating that excessive inflammation played a prominent role in their condition, while others displayed profiles indicative of impaired metabolism. Dr. Singh raises a pressing question: "Do we prioritize treating the inflammation or addressing the metabolic defects?"
Although his research findings and those of his peers are progressively unraveling the mysteries of Long COVID, he acknowledges that "significant challenges persist in defining this syndrome.”
Why does Long COVID happen?
The symptoms of Long COVID can vary significantly from one patient to another. Some individuals may be so fatigued that they find it difficult to get out of bed each morning. Others experience heart palpitations, lightheadedness, nausea, vomiting, diarrhea, or brain fog. This broad spectrum of symptoms—more than 200 documented—has led to various hypotheses about the underlying mechanisms at play.
Researchers currently believe that the impairment of a spectrum of key bodily functions may contribute to these diverse symptoms. These potential mechanisms include compromised immune system function, damage to blood vessels, and direct harm to the brain and nervous system. Importantly, it's likely that most patients experience symptoms arising from multiple underlying causes, which complicates both the diagnosis and treatment of Long COVID.
How can Long COVID be treated?
While the diagnosis and treatment of Long COVID remain challenging, the landscape of treatment options is evolving. At Yale’s Multidisciplinary Long COVID Care Center, a team, including respiratory therapists, physical therapists, and clinical social workers, along with an internist, work together to provide a comprehensive evaluation of each patient. Treatment approaches can vary widely and may encompass medications, supplements, physical therapy, or other interventions. Each regimen is designed to meet the specific presentation of Long COVID in each patient.
Dr. Singh’s apt summarization of the situation? "I don't think there's a magic bullet for it." Effective management of Long COVID necessitates a multidisciplinary approach that harnesses the expertise of a wide variety of specialists, working together to provide tailored care and support for these patients.
Brooks Leitner is an MD/PhD candidate at Yale School of Medicine.
The last word from Lisa Sanders, MD:
I’m the internist who sees patients at Yale New Haven Health’s Multidisciplinary Long COVID Care Center. In our clinic, patients are examined by a variety of specialists to determine the best next steps for these complex patients. Sometimes that entails more testing. Often patients have had extensive testing even before they arrive, and far too often—when all the tests are normal—both doctors and patients worry that their symptoms are “all in their head.”
One of our first tasks is to reassure patients that many parts of Long COVID don’t show up on tests. We don’t know enough about the cause of many of these symptoms to create a test for them. The problem is not with the patient with the symptoms, but of the science surrounding them.
If any good can be said to come out of this pandemic, it will be a better understanding of Long COVID and many of the other post-acute infection syndromes that have existed as long as the infections themselves.
If you’d like to share your experience with Long COVID for possible use in a future post (under a pseudonym), write to us at: LongCovid [email protected]
Information provided in Yale Medicine content is for general informational purposes only. It should never be used as a substitute for medical advice from your doctor or other qualified clinician. Always seek the individual advice of your health care provider for any questions you have regarding a medical condition.
More news from Yale Medicine
COVID infections are causing drops in IQ and years of brain aging, studies suggest
Researchers are trying to explain covid's profound effects on the brain.

Social Sharing

When COVID-19 first reared its head back in 2019, it brought with it a slew of strange symptoms beyond just respiratory problems. One of the most puzzling symptoms in those early days was something called "brain fog" — cognitive issues like confusion, forgetfulness, and trouble focusing.
And while other symptoms have changed as the virus mutated, brain fog is still a common complaint of COVID sufferers not only during the initial illness, but extending for months or even years afterwards. Several recent studies have been trying to understand exactly what this virus is doing to our brains — and how to stop it. Dr. Ziyad Al-Aly, the chief of research and development at the VA St. Louis Health Care System, spoke with Quirks & Quarks host Bob McDonald about what he's seeing in his research on COVID and the brain. Here is part of their conversation.
Take me through some of these effects that COVID has had on the brain. What have you seen?
One of the key manifestations that people experience after SARS-CoV-2 infection is what we call colloquially as brain fog. That's the mental haziness, the inability to remember things, to connect the dots, to really think clearly.

In addition to brain fog, we see people coming back to the clinics with mini strokes. We see a lot of people with headache disorders, sleep disturbances, sleep problems. A lot of people come back to the clinic with tingling of the extremities, tingling in the legs or sometimes in the arms. In rare cases, seizure disorders. So really a variety of health problems in the brain.
Is COVID actually affecting the way the brain functions?
There are studies that have been done comparing people who had COVID-19, versus people who didn't, and then gave them cognitive testing to measure their ability to cognitively process information and test their IQ. And there's very clear differences in the IQ of people who had been infected with COVID-19 versus people who did not. Even mild COVID can give people about a three-point loss of IQ.

The key caveat to those studies is that most of these were done from the original phase of the pandemic when we didn't have vaccination, when the virus was very different and we didn't have antivirals. And we also don't really know whether those cognitive losses that I just described, that three-point IQ loss, we don't really know how permanent that is.
What about brain aging?
It's very, very clear that in some individuals they do experience structural abnormalities and some other abnormalities of imaging that are commensurate with what normal people experience with about seven years of brain aging .
Now the hope is that those effects are not are not long lasting and then the brain with neuroplasticity and other other sort of mechanisms will be able to restore itself back to normal health. But I think that really remains to be characterized and seen in studies.
How is the virus that comes in through the lungs affecting the brain so much?
It induces inflammation of the brain . One of the clear signals from the studies that we've done and a lot of other people have done over the past several years is that clearly in some people it can provoke inflammatory reactions in the brain or neuroinflammation and that may explain some of the symptoms that are experienced by some individuals.

It can affect multiple substances on which the brain really depends to function normally. One of them is cortisol. So people have studied this out of Yale University and have shown that people with long COVID or people after SARS-CoV-2 infection can experience inappropriately low level of cortisol and that's actually an important hormone for a lot of certain normal physiologic processes, including cognitive performance, and a lower cortisol level than where it should be can explain some of the cognitive dysfunction that is seen in some people after SARS-CoV-2 infection. There are some studies also done on showing low serotonin levels and that can also explain some of the symptoms.
But doesn't the brain have a protective mechanism, the so-called blood brain barrier?
By inducing that inflammation of the brain, that actually makes that barrier leaky , so it starts leaking things into the brain that shouldn't be there. And things from the brain to outside the brain that also should not exit outside the brain. So a leaky blood brain barrier can also explain, you know, some of the manifestations that we see after COVID-19 infection.
How is this changing over time as the virus mutates?
We're in a different phase of the pandemic now than what we all experienced in March 2020. We have a different virus. We have availability of vaccines now. We have antivirals. So all of these drivers have now sort of reduced overall the burden of long COVID.

That doesn't mean that SARS-CoV-2 infection is benign, is inconsequential. We still see people in the hospital with SARS-CoV-2 infection, we still see people with strokes and heart attacks and, you know, brain fog and all other manifestations. But overall, I think the risk has sort of declined over the course of the pandemic.
How unique are these other effects on the body and the brain and the heart to COVID?
The big revelation or the big aha moment in this pandemic was the realization that SARS-CoV-2 infection can produce this really large basket of long-term adverse health effects. When we went back and started thinking about what happened to people after the Spanish flu, we found historical accounts that sort of resemble, to a large degree, what we described now after SARS-CoV-2 infection, people having increased risk of Parkinson's disease, headaches, brain fog etcetera.
I think one of the major lessons that I learned from this pandemic is that there are long tails to pandemics. And yes, we can focus all we want on the acute phase, or the tip of the iceberg, but the reality is that there is a really much larger chunk of disability and disease beneath that tip of the iceberg.
Q&A edited for length and clarity.
ABOUT THE AUTHOR

Amanda Buckiewicz is an award-winning science journalist with CBC Radio's legendary science show, Quirks & Quarks. Her work can be found on Discovery Channel, BBC Earth, Smithsonian, and Amazon Prime.
Ranking technologies for managing indoor pathogen transmission
JRC foresight expert exercise: what are the most promising current and emerging technologies for being up to the task when the next airborne disease like COVID-19 hits?
In a JRC-HERA study published today, well-established filtration and ventilation topped the list of the highest-impact current technologies for capturing and cleansing germs that spread through the air indoors. UV radiation and nucleic acid amplification came next in the impact ranking.
The foresight study also pinpointed other promising technologies, which require more development or are expected to appear in the future. From these, the impact of plasma-based inactivation, aerosol samplers, biosensors, and direct identification through physico-chemical properties came out on top.
Which technology should we prioritise? A balancing act
The study is the result of a foresight process designed and managed by the JRC and implemented by the JRC and HERA .
The more than 50 experts involved in the process emphasised that, despite the ranking, there is no one-size-fits-all technology for fighting airborne pathogens indoors and decision-makers should carefully weigh solutions based on their needs and the means at their disposal.
Filtration/ventilation, for example, although is time-tested and efficient, has the drawback of using high amounts of electricity. UV radiation can sterilise objects and surfaces, but has limitations in terms of deployment since, depending on the wavelength, it can damage human skin and eyes.
Similarly, plasma discharges – for example when using ozone – can damage cell membranes, inactivating pathogens this way. Yet these are rather expensive to generate and might irritate the respiratory tract and the lungs.
Another technology, aerosol samplers, both the cyclonic/impactor and the condensation type, are efficient at collecting microorganisms and viral particles. Yet, similarly to some alternative detection technologies, they cannot identify what exactly the particles are, so they must be coupled with other technologies.
One such detection technology, biosensors, widely known and used in lateral flow antigen tests (also known as rapid antigen tests), are affordable and require little skill for use. However, their detection level usually lags behind polymerase chain reaction (PCR) tests and they can only be used with condensation-type aerosol samplers.
PCR tests rely on nucleic acid amplification, which is highly efficient in detecting pathogens with known genomic sequences, even if they have lost structural integrity. Unfortunately, it is expensive and time-consuming, so it might not be the most suitable solution in cash-strapped and urgent circumstances.
On the more sophisticated end, spectroscopic and spectrometric techniques can spot pathogens by looking at their physico-chemical properties, but require enhanced Artificial Intelligence for automated deployment and becoming truly disruptive.
- Supplementary information
- 16 April 2024
JRC science helps you make sense of technologies against diseases that spread through the air.
Scenario planning: three possible health crises
Other analysed detection (particle counters, cell cultures, next-generation sequencing) and decontamination technologies (electrostatic capture, thermal inactivation, chemical aerosolization, microwave radiation, photocatalytic oxidation) present similar trade-offs to those explained above.
To illustrate that the technology of the choice can depend on the situation, the authors of the study drew up three hypothetical health crises scenarios.
In the first scenario, a tuberculosis endemic broke out in a country ravished by conflict. In this case, detection was considered less important, as tuberculosis requires close contact to spread.
The second scenario, an avian influenza pandemic, meant that more research & development, as well as resources, were available. In such conditions, the experts favoured pairing up cyclonic and impactor aerosol samplers with nucleic acid amplification and biosensors for best detection.
A yearlong burden from diseases such as the flu, COVID-19 or respiratory syncytial virus (RSV), the third scenario, would require filters for sampling and nucleic acid amplification for detection, according to the study participants.
In all scenarios, however, ventilation/filtration was one of the favoured decontamination technologies, building the first line of defence.
Why is this important?
The COVID-19 pandemic demonstrated the damage that airborne pathogens can cause. Other airborne diseases, such as the flu or RSV are also a threat to patients and health systems.
Preparedness for the next wave of infections is crucial. Knowing which technologies are the most impactful can help policymakers and the health industry channel funding the most efficiently.
Indeed, the authors identified investment/funding as the primary driver of change influencing such technologies, followed by regulatory guidance.
Harmonised standards, building codes, and trained personnel were named among the drivers and enablers that shape development and adaption.
Furthermore, in a detailed set of recommendations, the authors stressed the need to come up with a comprehensive strategy for indoor air quality. For this, multisector communities, healthcare workers, building architects, scientists, regulators and civil society representatives should cooperate.
This strategy should provide guidance on healthy concentration limits for pathogens in indoor air. Too many disease-causing agents would harm individuals and communities exposed, but completely stamping out pathogens could harm the human microbiome and immune system.
What is JRC foresight?
Foresight is a crucial tool for future preparedness and resilience. While it does not predict the future, or make projections, through the use of scenarios it can help identify (potential) future developments, emerging risks, and issues decision-makers need to take into account when designing policies.
By incorporating strategic foresight into policymaking, policies can be made more future-proof and resilient to shocks.
This particular study is the result of an inclusive and participatory foresight exercise. More than 50 experts from academia, research and technology organisations, businesses, business associations, non-governmental organisations, consultancies, and public entities filled in a survey and more than 30 participated in workshop discussions.
What is HERA?
The Health Emergency Preparedness and Response Authority (HERA) is a Commission service set up to strengthen Europe’s ability to prevent, detect, and rapidly respond to cross-border health emergencies by ensuring the development, manufacturing, procurement, and equitable distribution of key medical countermeasures. HERA prepares for future emergencies by analysing, identifying and prioritising possible health threats in view of ensuring the development, production and distribution of medicines, vaccines and other crisis-related medical countermeasures, such as gloves and masks.
Upcoming JRC foresight activity
The JRC publishes regular reports and bulletins that use foresight thinking.
Horizon scanning bulletins focus on detecting emerging “game changers” or trends with major impact on society and policy, at an early stage.
The upcoming Global Trends Report, informed by the discussions at the European Strategy and Policy Analysis System (ESPAS) conference in November will delve into the EU’s strategic choices ahead of the next electoral cycle and beyond.
The Future Risks Report, expected to be published this spring, presents a foresight approach to increase preparedness for unexpected developments and the risks they could create, based on ten snapshots of the future. In this study, the EU Policy Lab analyses different potential risks across these snapshots of the future, grouping them into ten wider risk clusters.
Futures Garden showcases pioneering policy innovation through speculative design, creativity, empathy, and analytical insight. It is a visionary journey into emerging trends and the issues shaping the EU’s future.
- Health crises responses
- Life and health sciences
More news on a similar topic

- News announcement
- 20 March 2024
- General publications
- 12 March 2024
- 9 February 2024
Share this page
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

The impact of COVID-19 on research
a Department of Pediatric Urology and Pediatric Surgery, Hopital Pellegrin-Enfants, CHU Bordeaux, France
b Service de chirurgie et urologie pédiatrique, hôpital Lapeyronie, CHU de Montpellier et Université de Montpellier, France
G.M.A. Beckers
c Department of Urology, Section of Pediatric Urology, AmsterdamUMC, Location VUmc, Amsterdam, the Netherlands
d Indiana University, 702 Barnhill Drive, Suite 4230, Indianapolis, IN, USA
A.J. Nieuwhof-Leppink
e Department of Medical Psychology and Social Work, Urology, Wilhelmina Children’s Hospital, University Medical Center Utrecht, PO box 85090, 3508 AB, Utrecht, the Netherlands
Magdalena Fossum
f Department of Pediatric Surgery, Copenhagen University Hospital Rigshospitalet, DK-2100, Denmark
g Department of Women's and Children's Health, Bioclinicum, Floor 10, Karolinska Institutet, SE-171 76, Stockholm, Sweden
K.W. Herbst
h Division of Urology, Department of Research, Connecticut Children's Medical Center, Hartford, CT, USA
i Hospital for Sick Chidlren, Univeristy of Toronto, Canada
Coronavirus disease 2019 (COVID-19) has swept across the globe causing hundreds of thousands of deaths, shutting down economies, closing borders and wreaking havoc on an unprecedented scale. It has strained healthcare services and personnel to the brink in many regions and will certainly deeply mark medical research both in the short and long-term.
Prior to the COVID pandemic, virology research (including influenza) represented less than 2% of all biomedical research. However, the number of laboratories and investigators that have pivoted to address COVID related research questions is astonishing, likely comprising 10–20% of current biomedical investigation, showing the incredible adaptability of the research community [ 1 ]. The multinational support rapidly infused for COVID-19 research is in the billions of euros [ 2 ]. The sharing of research findings and research data has never been as rapid and efficient [ 3 ]. The crisis has also brought disease, health, and healthcare back to the forefront of societal issues, and will have a lasting impact on public spending. However, with all this optimism and focus, there is a downside.
To begin, the COVID-19 crisis has led to a massive influx of publications. Not only are specialty journals being flooded with submissions by authors being unwittingly granted much needed writing time, but publications on COVID have literally inundated us. More than 20,000 papers have been published since December 2019, many in prestigious journals. There are also an increasing number of studies being uploaded to preprint servers, such as BioRxiv, for rapid dissemination prior to any peer review. However, we cannot assume that the time and quality available for peer review is able to keep pace with the explosion of publication. There is need for increased caution in the wake of this massive influx of submissions, especially since we are increasingly seeing these results being picked up by the media and diffused to a less attuned audience. In recent weeks, several prestigious journals, including the Lancet and the New England Journal of Medicine, have published retractions of earlier and potentially major COVID-related findings [ 4 , 5 ]. On June 15, 2020, The New York Times highlighted potential lapses in the peer review process affecting major scientific journals [ 6 ].
We must strive to improve scientific quality always. The current debate over the use of hydroxychloroquine further illustrates the undermining of the scientific process when faced with global desperation for ready-made truths and solutions [ 4 , 7 , 8 ]. Science needs time, and good science needs a lot of it for data to grow and knowledge to evolve, but this process is ill-prepared to handle the rush for solutions to the COVID crises.
Moreover, just as COVID-19 has shown social, racial, and economic health disparities, the pandemic seems also to have accentuated existing gender inequalities within the field of research [ 9 ]. Indeed, early analyses suggest that female academics are publishing less and starting fewer research projects than their male peers. This might be an effect of the lockdown and the fact that more women than are men are juggling caring for families and children despite both “working” from home [ 10 , 11 ].
Travel, social, and funding restrictions will also take a serious toll on scientific research worldwide. Research staff and resources have been purposely and purposefully prioritized to COVID-19 activities above all else. Distancing and transmission issues have caused most non-COVID clinical research to be suspended, causing a reduction in recruitment of research subjects and a delay in data entry into clinical trial databases [ 12 ]. Research-related hiring has been suspended because of travel restrictions and young researchers might soon find themselves out of a job if their subject is not the pandemic. Indeed, though government-funded medical research bodies worldwide say they are committed to maintaining the continuity and breadth of biomedical research, how the economic downfall will influence government spending remains to be seen. Furthermore, research funding that relies on public fundraising is expected to drop substantially and many researchers will see a significant decrease in funding opportunities [ 13 ]. The global impact the crisis will have on the economy makes it hard to imagine that future research funding will not be substantially affected.
During this crisis, many resources were understandably redirected toward preparing for and caring for COVID-19 patients, but the collateral damage to so many patients with non-COVID-19 medical conditions that did not receive, or failed to seek, treatment will surely emerge [ 14 ]. Finally, children have also paid a high price for the redirecting of medical resources, with delays in their medical and surgical management, as well as vaccinations [ 15 , 16 ]. This may be especially problematic when many aspects of pediatric care is based on their developmental clock, which even the pandemic cannot stop. Whether this was the best option will certainly be analyzed in retrospect. Congenital anomalies alone account for over 400,000 deaths worldwide every year, and inflict a considerable burden both on children, families, and healthcare systems [ 17 ]. Thus, it is essential that funding for medical research does not follow the same pattern with a disproportionate decrease in funding for non-COVID research including pediatric and developmental urology.
COVID-19 has already changed the world, not only because of the disease itself, but because of the long-term effects of the world's reaction to the pandemic. While the pandemic may have brought with it some silver linings, it is crucial that the scientific community conduct current and future research broadly and openly, lest future pandemic preparedness in research repeat the hard-fought lessons of today.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 15 April 2024
COVID-19 drug discovery and treatment options
- Jasper Fuk-Woo Chan ORCID: orcid.org/0000-0001-6336-6657 1 , 2 , 3 , 4 ,
- Shuofeng Yuan ORCID: orcid.org/0000-0001-7996-1119 1 , 2 , 3 , 4 ,
- Hin Chu ORCID: orcid.org/0000-0003-2855-9837 1 , 2 , 3 , 4 ,
- Siddharth Sridhar ORCID: orcid.org/0000-0002-2022-8307 1 , 2 , 3 &
- Kwok-Yung Yuen ORCID: orcid.org/0000-0002-2083-1552 1 , 2 , 3 , 4
Nature Reviews Microbiology ( 2024 ) Cite this article
139 Accesses
25 Altmetric
Metrics details
- Antiviral agents
- Viral infection
The coronavirus disease 2019 (COVID-19) pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has caused substantial morbidity and mortality, and serious social and economic disruptions worldwide. Unvaccinated or incompletely vaccinated older individuals with underlying diseases are especially prone to severe disease. In patients with non-fatal disease, long COVID affecting multiple body systems may persist for months. Unlike SARS-CoV and Middle East respiratory syndrome coronavirus, which have either been mitigated or remained geographically restricted, SARS-CoV-2 has disseminated globally and is likely to continue circulating in humans with possible emergence of new variants that may render vaccines less effective. Thus, safe, effective and readily available COVID-19 therapeutics are urgently needed. In this Review, we summarize the major drug discovery approaches, preclinical antiviral evaluation models, representative virus-targeting and host-targeting therapeutic options, and key therapeutics currently in clinical use for COVID-19. Preparedness against future coronavirus pandemics relies not only on effective vaccines but also on broad-spectrum antivirals targeting conserved viral components or universal host targets, and new therapeutics that can precisely modulate the immune response during infection.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
195,33 € per year
only 16,28 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others

Necroptosis blockade prevents lung injury in severe influenza
Avishekh Gautam, David F. Boyd, … Siddharth Balachandran

Long COVID: major findings, mechanisms and recommendations
Hannah E. Davis, Lisa McCorkell, … Eric J. Topol

Mechanisms of SARS-CoV-2 entry into cells
Cody B. Jackson, Michael Farzan, … Hyeryun Choe
Zumla, A. et al. Coronaviruses—drug discovery and therapeutic options. Nat. Rev. Drug Discov. 15 , 327–347 (2016).
Article CAS PubMed PubMed Central Google Scholar
Cheng, V. C. et al. Severe acute respiratory syndrome coronavirus as an agent of emerging and reemerging infection. Clin. Microbiol. Rev. 20 , 660–694 (2007).
Chan, J. F. et al. Middle East respiratory syndrome coronavirus: another zoonotic betacoronavirus causing SARS-like disease. Clin. Microbiol. Rev. 28 , 465–522 (2015).
Zhou, P. et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 579 , 270–273 (2020).
Chan, J. F. et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet 395 , 514–523 (2020).
To, K. K. et al. Lessons learned 1 year after SARS-CoV-2 emergence leading to COVID-19 pandemic. Emerg. Microbes Infect. 10 , 507–535 (2021).
Jeon, S. et al. Identification of antiviral drug candidates against SARS-CoV-2 from FDA-approved drugs. Antimicrob. Agents Chemother. 64 , e00819-20 (2020).
Article PubMed PubMed Central Google Scholar
Yuan, S. et al. Broad-spectrum host-based antivirals targeting the interferon and lipogenesis pathways as potential treatment options for the pandemic coronavirus disease 2019 (COVID-19). Viruses 12 , 628 (2020).
Riva, L. et al. Discovery of SARS-CoV-2 antiviral drugs through large-scale compound repurposing. Nature 586 , 113–119 (2020).
Jang, W. D. et al. Drugs repurposed for COVID-19 by virtual screening of 6,218 drugs and cell-based assay. Proc. Natl Acad. Sci. USA 118 , e2024302118 (2021).
Luttens, A. et al. Ultralarge virtual screening identifies SARS-CoV-2 main protease inhibitors with broad-spectrum activity against coronaviruses. J. Am. Chem. Soc. 144 , 2905–2920 (2022).
Gunther, S. et al. X-ray screening identifies active site and allosteric inhibitors of SARS-CoV-2 main protease. Science 372 , 642–646 (2021).
Jin, Z. et al. Structure of M pro from SARS-CoV-2 and discovery of its inhibitors. Nature 582 , 289–293 (2020).
Article CAS PubMed Google Scholar
Chen, C. Z. et al. Drug repurposing screen for compounds inhibiting the cytopathic effect of SARS-CoV-2. Front. Pharmacol. 11 , 592737 (2020).
Yuan, S. et al. Discovery of the FDA-approved drugs bexarotene, cetilistat, diiodohydroxyquinoline, and abiraterone as potential COVID-19 treatments with a robust two-tier screening system. Pharmacol. Res. 159 , 104960 (2020).
Hung, I. F. et al. Triple combination of interferon β-1b, lopinavir-ritonavir, and ribavirin in the treatment of patients admitted to hospital with COVID-19: an open-label, randomised, phase 2 trial. Lancet 395 , 1695–1704 (2020).
Cao, B. et al. A trial of lopinavir-ritonavir in adults hospitalized with severe COVID-19. N. Engl. J. Med. 382 , 1787–1799 (2020).
Article PubMed Google Scholar
Beigel, J. H. et al. Remdesivir for the treatment of COVID-19—final report. N. Engl. J. Med. 383 , 1813–1826 (2020).
Wang, Y. et al. Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet 395 , 1569–1578 (2020).
Gautret, P. et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int. J. Antimicrob. Agents 56 , 105949 (2020).
WHO Solidarity Trial Consortium. Repurposed antiviral drugs for COVID-19 — interim WHO Solidarity Trial results. N. Engl. J. Med. 384 , 497–511 (2021).
Article Google Scholar
Cihlar, T. & Mackman, R. L. Journey of remdesivir from the inhibition of hepatitis C virus to the treatment of COVID-19. Antivir. Ther. 27 , 13596535221082773 (2022).
Masyeni, S. et al. Molnupiravir: a lethal mutagenic drug against rapidly mutating severe acute respiratory syndrome coronavirus 2—a narrative review. J. Med. Virol. 94 , 3006–3016 (2022).
US Food & Drug Administration. Coronavirus (COVID-19) update: FDA authorizes monoclonal antibodies for treatment of COVID-19. US Food & Drug Administration https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-authorizes-monoclonal-antibodies-treatment-covid-19 (2020).
Owen, D. R. et al. An oral SARS-CoV-2 M pro inhibitor clinical candidate for the treatment of COVID-19. Science 374 , 1586–1593 (2021).
Wahl, A. et al. SARS-CoV-2 infection is effectively treated and prevented by EIDD-2801. Nature 591 , 451–457 (2021).
Valero, J. et al. A serum-stable RNA aptamer specific for SARS-CoV-2 neutralizes viral entry. Proc. Natl Acad. Sci. USA 118 , e2112942118 (2021).
de Vries, R. D. et al. Intranasal fusion inhibitory lipopeptide prevents direct-contact SARS-CoV-2 transmission in ferrets. Science 371 , 1379–1382 (2021).
Liu, L. et al. Striking antibody evasion manifested by the Omicron variant of SARS-CoV-2. Nature 602 , 676–681 (2022).
Iketani, S. et al. Antibody evasion properties of SARS-CoV-2 Omicron sublineages. Nature 604 , 553–556 (2022).
Liu, L. et al. An antibody class with a common CDRH3 motif broadly neutralizes sarbecoviruses. Sci. Transl. Med. 14 , eabn6859 (2022).
Tortorici, M. A. et al. Broad sarbecovirus neutralization by a human monoclonal antibody. Nature 597 , 103–108 (2021).
Xiang, Y. et al. Superimmunity by pan-sarbecovirus nanobodies. Cell Rep. 39 , 111004 (2022).
Xia, S. et al. Peptide-based pan-CoV fusion inhibitors maintain high potency against SARS-CoV-2 Omicron variant. Cell Res. 32 , 404–406 (2022).
Zhao, H. et al. Fusion-inhibition peptide broadly inhibits influenza virus and SARS-CoV-2, including Delta and Omicron variants. Emerg. Microbes Infect. 11 , 926–937 (2022).
Yuan, S. et al. Targeting papain-like protease for broad-spectrum coronavirus inhibition. Protein Cell 13 , 940–953 (2022).
Quan, B. X. et al. An orally available M pro inhibitor is effective against wild-type SARS-CoV-2 and variants including Omicron. Nat. Microbiol. 7 , 716–725 (2022).
RECOVERY Collaborative Group et al. Dexamethasone in hospitalized patients with COVID-19. N. Engl. J. Med. 384 , 693–704 (2021).
Stone, J. H. et al. Efficacy of tocilizumab in patients hospitalized with COVID-19. N. Engl. J. Med. 383 , 2333–2344 (2020).
Huet, T. et al. Anakinra for severe forms of COVID-19: a cohort study. Lancet Rheumatol. 2 , e393–e400 (2020).
Bastard, P. et al. Autoantibodies against type I IFNs in patients with life-threatening COVID-19. Science 370 , eabd4585 (2020).
Richardson, P. et al. Baricitinib as potential treatment for 2019-nCoV acute respiratory disease. Lancet 395 , e30–e31 (2020).
Stebbing, J. et al. COVID-19: combining antiviral and anti-inflammatory treatments. Lancet Infect. Dis. 20 , 400–402 (2020).
Gordon, D. E. et al. A SARS-CoV-2 protein interaction map reveals targets for drug repurposing. Nature 583 , 459–468 (2020).
Bojkova, D. et al. Proteomics of SARS-CoV-2-infected host cells reveals therapy targets. Nature 583 , 469–472 (2020).
Yuan, S. et al. SARS-CoV-2 exploits host DGAT and ADRP for efficient replication. Cell Discov. 7 , 100 (2021).
Yuen, T. T. et al. Targeting ACLY efficiently inhibits SARS-CoV-2 replication. Int. J. Biol. Sci. 18 , 4714–4730 (2022).
Stukalov, A. et al. Multilevel proteomics reveals host perturbations by SARS-CoV-2 and SARS-CoV. Nature 594 , 246–252 (2021).
Sadegh, S. et al. Exploring the SARS-CoV-2 virus–host–drug interactome for drug repurposing. Nat. Commun. 11 , 3518 (2020).
Zhu, N. et al. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 382 , 727–733 (2020).
Chu, H. et al. Comparative tropism, replication kinetics, and cell damage profiling of SARS-CoV-2 and SARS-CoV with implications for clinical manifestations, transmissibility, and laboratory studies of COVID-19: an observational study. Lancet Microbe 1 , e14–e23 (2020).
Chu, H. et al. Host and viral determinants for efficient SARS-CoV-2 infection of the human lung. Nat. Commun. 12 , 134 (2021).
Hoffmann, M. et al. Chloroquine does not inhibit infection of human lung cells with SARS-CoV-2. Nature 585 , 588–590 (2020).
Wang, S. et al. AXL is a candidate receptor for SARS-CoV-2 that promotes infection of pulmonary and bronchial epithelial cells. Cell Res. 31 , 126–140 (2021).
Daniloski, Z. et al. Identification of required host factors for SARS-CoV-2 infection in human cells. Cell 184 , 92–105 e16 (2021).
Wang, L. et al. Susceptibility to SARS-CoV-2 of cell lines and substrates commonly used to diagnose and isolate influenza and other viruses. Emerg. Infect. Dis. 27 , 1380–1392 (2021).
Matsuyama, S. et al. Enhanced isolation of SARS-CoV-2 by TMPRSS2-expressing cells. Proc. Natl Acad. Sci. USA 117 , 7001–7003 (2020).
Zhu, N. et al. Morphogenesis and cytopathic effect of SARS-CoV-2 infection in human airway epithelial cells. Nat. Commun. 11 , 3910 (2020).
Sheahan, T. P. et al. An orally bioavailable broad-spectrum antiviral inhibits SARS-CoV-2 in human airway epithelial cell cultures and multiple coronaviruses in mice. Sci. Transl. Med. 12 , eabb5883 (2020).
Hou, Y. J. et al. SARS-CoV-2 reverse genetics reveals a variable infection gradient in the respiratory tract. Cell 182 , 429–446.e14 (2020).
Yuan, S. et al. Clofazimine broadly inhibits coronaviruses including SARS-CoV-2. Nature 593 , 418–423 (2021).
Alfi, O. et al. Human nasal and lung tissues infected ex vivo with SARS-CoV-2 provide insights into differential tissue-specific and virus-specific innate immune responses in the upper and lower respiratory tract. J. Virol. 95 , e0013021 (2021).
Chu, H. et al. Comparative replication and immune activation profiles of SARS-CoV-2 and SARS-CoV in human lungs: an ex vivo study with implications for the pathogenesis of COVID-19. Clin. Infect. Dis. 71 , 1400–1409 (2020).
Chu, H. et al. SARS-CoV-2 induces a more robust innate immune response and replicates less efficiently than SARS-CoV in the human intestines: an ex vivo study with implications on pathogenesis of COVID-19. Cell Mol. Gastroenterol. Hepatol. 11 , 771–781 (2021).
Mykytyn, A. Z. et al. SARS-CoV-2 entry into human airway organoids is serine protease-mediated and facilitated by the multibasic cleavage site. eLife 10 , e64508 (2021).
Salahudeen, A. A. et al. Progenitor identification and SARS-CoV-2 infection in human distal lung organoids. Nature 588 , 670–675 (2020).
Zhou, J. et al. Infection of bat and human intestinal organoids by SARS-CoV-2. Nat. Med. 26 , 1077–1083 (2020).
Kruger, J. et al. Drug inhibition of SARS-CoV-2 replication in human pluripotent stem cell-derived intestinal organoids. Cell Mol. Gastroenterol. Hepatol. 11 , 935–948 (2021).
Zhang, B. Z. et al. SARS-CoV-2 infects human neural progenitor cells and brain organoids. Cell Res. 30 , 928–931 (2020).
Monteil, V. et al. Inhibition of SARS-CoV-2 infections in engineered human tissues using clinical-grade soluble human ACE2. Cell 181 , 905–913.e7 (2020).
Zhao, B. et al. Recapitulation of SARS-CoV-2 infection and cholangiocyte damage with human liver ductal organoids. Protein Cell 11 , 771–775 (2020).
Menuchin-Lasowski, Y. et al. SARS-CoV-2 infects and replicates in photoreceptor and retinal ganglion cells of human retinal organoids. Stem Cell Rep. 17 , 789–803 (2022).
Article CAS Google Scholar
Han, Y. et al. Identification of SARS-CoV-2 inhibitors using lung and colonic organoids. Nature 589 , 270–275 (2021).
Chan, J. F. et al. Simulation of the clinical and pathological manifestations of coronavirus disease 2019 (COVID-19) in a golden Syrian hamster model: implications for disease pathogenesis and transmissibility. Clin. Infect. Dis. 71 , 2428–2446 (2020).
Trimpert, J. et al. The Roborovski dwarf hamster is a highly susceptible model for a rapid and fatal course of SARS-CoV-2 infection. Cell Rep. 33 , 108488 (2020).
Winkler, E. S. et al. SARS-CoV-2 infection of human ACE2-transgenic mice causes severe lung inflammation and impaired function. Nat. Immunol. 21 , 1327–1335 (2020).
Kim, Y. I. et al. Infection and rapid transmission of SARS-CoV-2 in ferrets. Cell Host Microbe 27 , 704–709.e2 (2020).
Munster, V. J. et al. Respiratory disease in rhesus macaques inoculated with SARS-CoV-2. Nature 585 , 268–272 (2020).
Munoz-Fontela, C. et al. Animal models for COVID-19. Nature 586 , 509–515 (2020).
Shuai, H. et al. Attenuated replication and pathogenicity of SARS-CoV-2 B.1.1.529 Omicron. Nature 603 , 693–699 (2022).
Halfmann, P. J. et al. SARS-CoV-2 Omicron virus causes attenuated disease in mice and hamsters. Nature 603 , 687–692 (2022).
Shuai, H. et al. The viral fitness and intrinsic pathogenicity of dominant SARS-CoV-2 Omicron sublineages BA.1, BA.2, and BA.5. EBioMedicine 95 , 104753 (2023).
Hu, B. et al. Divergent trajectory of replication and intrinsic pathogenicity of SARS-CoV-2 Omicron post-BA.2/5 subvariants in the upper and lower respiratory tract. EBioMedicine 99 , 104916 (2023).
Hoffmann, M. et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 181 , 271–280.e8 (2020).
Yeung, M. L. et al. Soluble ACE2-mediated cell entry of SARS-CoV-2 via interaction with proteins related to the renin–angiotensin system. Cell 184 , 2212–2228.e12 (2021).
V’Kovski, P. et al. Coronavirus biology and replication: implications for SARS-CoV-2. Nat. Rev. Microbiol. 19 , 155–170 (2021).
Hassler, L. et al. A novel soluble ACE2 protein provides lung and kidney protection in mice susceptible to lethal SARS-CoV-2 infection. J. Am. Soc. Nephrol. 33 , 1293–1307 (2022).
El-Shennawy, L. et al. Circulating ACE2-expressing extracellular vesicles block broad strains of SARS-CoV-2. Nat. Commun. 13 , 405 (2022).
Ikemura, N. et al. An engineered ACE2 decoy neutralizes the SARS-CoV-2 Omicron variant and confers protection against infection in vivo. Sci. Transl. Med. 14 , eabn7737 (2022).
Chen, Y. et al. Broadly neutralizing antibodies to SARS-CoV-2 and other human coronaviruses. Nat. Rev. Immunol. 23 , 189–199 (2022).
Takamatsu, Y. et al. Highly neutralizing COVID-19 convalescent plasmas potently block SARS-CoV-2 replication and pneumonia in Syrian hamsters. J. Virol. 96 , e0155121 (2022).
McMahan, K. et al. Correlates of protection against SARS-CoV-2 in rhesus macaques. Nature 590 , 630–634 (2021).
Libster, R. et al. Early high-titer plasma therapy to prevent severe COVID-19 in older adults. N. Engl. J. Med. 384 , 610–618 (2021).
Sullivan, D. J. et al. Early outpatient treatment for COVID-19 with convalescent plasma. N. Engl. J. Med. 386 , 1700–1711 (2022).
Rothenberger, S. et al. The trispecific DARPin ensovibep inhibits diverse SARS-CoV-2 variants. Nat. Biotechnol. 40 , 1845–1854 (2022).
Chan, J. F. et al. A molecularly engineered, broad-spectrum anti-coronavirus lectin inhibits SARS-CoV-2 and MERS-CoV infection in vivo. Cell Rep. Med. 3 , 100774 (2022).
Ohashi, H. et al. Potential anti-COVID-19 agents, cepharanthine and nelfinavir, and their usage for combination treatment. iScience 24 , 102367 (2021).
Clausen, T. M. et al. SARS-CoV-2 infection depends on cellular heparan sulfate and ACE2. Cell 183 , 1043–1057.e15 (2020).
Zhang, Q. et al. Heparan sulfate assists SARS-CoV-2 in cell entry and can be targeted by approved drugs in vitro. Cell Discov. 6 , 80 (2020).
Hu, Y. et al. Brilacidin, a COVID-19 drug candidate, demonstrates broad-spectrum antiviral activity against human coronaviruses OC43, 229E, and NL63 through targeting both the virus and the host cell. J. Med. Virol. 94 , 2188–2200 (2022).
Wang, M. et al. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 30 , 269–271 (2020).
Hoffmann, M. et al. Camostat mesylate inhibits SARS-CoV-2 activation by TMPRSS2-related proteases and its metabolite GBPA exerts antiviral activity. EBioMedicine 65 , 103255 (2021).
Li, K. et al. The TMPRSS2 inhibitor nafamostat reduces SARS-CoV-2 pulmonary infection in mouse models of COVID-19. mBio 12 , e0097021 (2021).
Takahashi, W. et al. Potential mechanisms of nafamostat therapy for severe COVID-19 pneumonia with disseminated intravascular coagulation. Int. J. Infect. Dis. 102 , 529–531 (2021).
Hoffmann, M., Kleine-Weber, H. & Pohlmann, S. A multibasic cleavage site in the spike protein of SARS-CoV-2 is essential for infection of human lung cells. Mol. Cell 78 , 779–784.e5 (2020).
Essalmani, R. et al. Distinctive roles of furin and TMPRSS2 in SARS-CoV-2 infectivity. J. Virol. 96 , e0012822 (2022).
Peacock, T. P. et al. The furin cleavage site in the SARS-CoV-2 spike protein is required for transmission in ferrets. Nat. Microbiol. 6 , 899–909 (2021).
Chan, J. F. et al. Altered host protease determinants for SARS-CoV-2 Omicron. Sci. Adv. 9 , eadd3867 (2023).
Wang, G. et al. Dalbavancin binds ACE2 to block its interaction with SARS-CoV-2 spike protein and is effective in inhibiting SARS-CoV-2 infection in animal models. Cell Res. 31 , 17–24 (2021).
Zhao, M. M. et al. Cathepsin L plays a key role in SARS-CoV-2 infection in humans and humanized mice and is a promising target for new drug development. Signal. Transduct. Target. Ther. 6 , 134 (2021).
Shang, C. et al. Inhibitors of endosomal acidification suppress SARS-CoV-2 replication and relieve viral pneumonia in hACE2 transgenic mice. Virol. J. 18 , 46 (2021).
Yuan, S. et al. Viruses harness YxxO motif to interact with host AP2M1 for replication: a vulnerable broad-spectrum antiviral target. Sci. Adv. 6 , eaba7910 (2020).
Rosenke, K. et al. Hydroxychloroquine prophylaxis and treatment is ineffective in macaque and hamster SARS-CoV-2 disease models. JCI Insight 5 , e143174 (2020).
Zhao, H. et al. A broad-spectrum virus- and host-targeting peptide against respiratory viruses including influenza virus and SARS-CoV-2. Nat. Commun. 11 , 4252 (2020).
Zhao, H. et al. Cross-linking peptide and repurposed drugs inhibit both entry pathways of SARS-CoV-2. Nat. Commun. 12 , 1517 (2021).
Braga, L. et al. Drugs that inhibit TMEM16 proteins block SARS-CoV-2 spike-induced syncytia. Nature 594 , 88–93 (2021).
Shin, D. et al. Papain-like protease regulates SARS-CoV-2 viral spread and innate immunity. Nature 587 , 657–662 (2020).
Klemm, T. et al. Mechanism and inhibition of the papain-like protease, PL pro , of SARS-CoV-2. EMBO J. 39 , e106275 (2020).
Fu, Z. et al. The complex structure of GRL0617 and SARS-CoV-2 PL pro reveals a hot spot for antiviral drug discovery. Nat. Commun. 12 , 488 (2021).
Swaim, C. D. et al. 6-Thioguanine blocks SARS-CoV-2 replication by inhibition of PL pro . iScience 24 , 103213 (2021).
Chu, C. M. et al. Role of lopinavir/ritonavir in the treatment of SARS: initial virological and clinical findings. Thorax 59 , 252–256 (2004).
Chan, J. F. et al. Treatment with lopinavir/ritonavir or interferon-β1b improves outcome of MERS-CoV infection in a nonhuman primate model of common marmoset. J. Infect. Dis. 212 , 1904–1913 (2015).
Schoergenhofer, C. et al. Pharmacokinetics of lopinavir and ritonavir in patients hospitalized with coronavirus disease 2019 (COVID-19). Ann. Intern. Med. 173 , 670–672 (2020).
Fintelman-Rodrigues, N. et al. Atazanavir, alone or in combination with ritonavir, inhibits SARS-CoV-2 replication and proinflammatory cytokine production. Antimicrob. Agents Chemother. 64 , e00825-20 (2020).
Chaves, O. A. et al. Atazanavir is a competitive inhibitor of SARS-CoV-2 M pro , impairing variants replication in vitro and in vivo. Pharmaceuticals 15 , 21 (2021).
Ma, C. et al. Boceprevir, GC-376, and calpain inhibitors II, XII inhibit SARS-CoV-2 viral replication by targeting the viral main protease. Cell Res. 30 , 678–692 (2020).
Mahmoud, A. et al. Telaprevir is a potential drug for repurposing against SARS-CoV-2: computational and in vitro studies. Heliyon 7 , e07962 (2021).
Qiao, J. et al. SARS-CoV-2 M pro inhibitors with antiviral activity in a transgenic mouse model. Science 371 , 1374–1378 (2021).
Li, Z. et al. Identify potent SARS-CoV-2 main protease inhibitors via accelerated free energy perturbation-based virtual screening of existing drugs. Proc. Natl Acad. Sci. USA 117 , 27381–27387 (2020).
Ghahremanpour, M. M. et al. Identification of 14 known drugs as inhibitors of the main protease of SARS-CoV-2. ACS Med. Chem. Lett. 11 , 2526–2533 (2020).
Vuong, W. et al. Feline coronavirus drug inhibits the main protease of SARS-CoV-2 and blocks virus replication. Nat. Commun. 11 , 4282 (2020).
Boras, B. et al. Preclinical characterization of an intravenous coronavirus 3CL protease inhibitor for the potential treatment of COVID-19. Nat. Commun. 12 , 6055 (2021).
de Vries, M. et al. A comparative analysis of SARS-CoV-2 antivirals characterizes 3CL pro inhibitor PF-00835231 as a potential new treatment for COVID-19. J. Virol. 95 , e01819-20 (2021).
Wong, C. K. H. et al. Real-world effectiveness of molnupiravir and nirmatrelvir plus ritonavir against mortality, hospitalisation, and in-hospital outcomes among community-dwelling, ambulatory patients with confirmed SARS-CoV-2 infection during the omicron wave in Hong Kong: an observational study. Lancet 400 , 1213–1222 (2022).
Wong, C. K. H. et al. Real-world effectiveness of early molnupiravir or nirmatrelvir–ritonavir in hospitalised patients with COVID-19 without supplemental oxygen requirement on admission during Hong Kong’s omicron BA.2 wave: a retrospective cohort study. Lancet Infect. Dis. 22 , 1681–1693 (2022).
Hammond, J. et al. Oral nirmatrelvir for high-risk, nonhospitalized adults with COVID-19. N. Engl. J. Med. 386 , 1397–1408 (2022).
Chan, J. F. et al. Genomic characterization of the 2019 novel human-pathogenic coronavirus isolated from a patient with atypical pneumonia after visiting Wuhan. Emerg. Microbes Infect. 9 , 221–236 (2020).
Sheahan, T. P. et al. Broad-spectrum antiviral GS-5734 inhibits both epidemic and zoonotic coronaviruses. Sci. Transl. Med. 9 , eaal3653 (2017).
de Wit, E. et al. Prophylactic and therapeutic remdesivir (GS-5734) treatment in the rhesus macaque model of MERS-CoV infection. Proc. Natl Acad. Sci. USA 117 , 6771–6776 (2020).
Williamson, B. N. et al. Clinical benefit of remdesivir in rhesus macaques infected with SARS-CoV-2. Nature 585 , 273–276 (2020).
White, M. A., Lin, W. & Cheng, X. Discovery of COVID-19 inhibitors targeting the SARS-CoV-2 Nsp13 helicase. J. Phys. Chem. Lett. 11 , 9144–9151 (2020).
Yuan, S. et al. Metallodrug ranitidine bismuth citrate suppresses SARS-CoV-2 replication and relieves virus-associated pneumonia in Syrian hamsters. Nat. Microbiol. 5 , 1439–1448 (2020).
Wang, R. et al. Orally administered bismuth drug together with N -acetyl cysteine as a broad-spectrum anti-coronavirus cocktail therapy. Chem. Sci. 13 , 2238–2248 (2022).
Shu, T. et al. SARS-coronavirus-2 Nsp13 possesses NTPase and RNA helicase activities that can be inhibited by bismuth salts. Virol. Sin. 35 , 321–329 (2020).
Zeng, J. et al. Identifying SARS-CoV-2 antiviral compounds by screening for small molecule inhibitors of nsp13 helicase. Biochem. J. 478 , 2405–2423 (2021).
Idris, A. et al. A SARS-CoV-2 targeted siRNA-nanoparticle therapy for COVID-19. Mol. Ther. 29 , 2219–2226 (2021).
Romano, M. et al. A structural view of SARS-CoV-2 RNA replication machinery: RNA synthesis, proofreading and final capping. Cells 9 , 1267 (2020).
Hackbart, M., Deng, X. & Baker, S. C. Coronavirus endoribonuclease targets viral polyuridine sequences to evade activating host sensors. Proc. Natl Acad. Sci. USA 117 , 8094–8103 (2020).
Wang, Y. et al. Coronavirus nsp10/nsp16 methyltransferase can be targeted by nsp10-derived peptide in vitro and in vivo to reduce replication and pathogenesis. J. Virol. 89 , 8416–8427 (2015).
Russ, A. et al. Nsp16 shields SARS-CoV-2 from efficient MDA5 sensing and IFIT1-mediated restriction. EMBO Rep. 23 , e55648 (2022).
Kim, Y. et al. Tipiracil binds to uridine site and inhibits Nsp15 endoribonuclease NendoU from SARS-CoV-2. Commun. Biol. 4 , 193 (2021).
Wang, X. et al. Combination of antiviral drugs inhibits SARS-CoV-2 polymerase and exonuclease and demonstrates COVID-19 therapeutic potential in viral cell culture. Commun. Biol. 5 , 154 (2022).
Yuan, S. et al. SREBP-dependent lipidomic reprogramming as a broad-spectrum antiviral target. Nat. Commun. 10 , 120 (2019).
Wong, L. R. et al. Eicosanoid signalling blockade protects middle-aged mice from severe COVID-19. Nature 605 , 146–151 (2022).
White, K. M. et al. Plitidepsin has potent preclinical efficacy against SARS-CoV-2 by targeting the host protein eEF1A. Science 371 , 926–931 (2021).
Mullen, P. J. et al. SARS-CoV-2 infection rewires host cell metabolism and is potentially susceptible to mTORC1 inhibition. Nat. Commun. 12 , 1876 (2021).
Acharya, A. et al. PI3K-ɑ/mTOR/BRD4 inhibitor alone or in combination with other anti-virals blocks replication of SARS-CoV-2 and its variants of concern including Delta and Omicron. Clin. Transl. Med. 12 , e806 (2022).
Rajasekharan, S. et al. Inhibitors of protein glycosylation are active against the coronavirus severe acute respiratory syndrome coronavirus SARS-CoV-2. Viruses 13 , 808 (2021).
Ambike, S. et al. Targeting genomic SARS-CoV-2 RNA with siRNAs allows efficient inhibition of viral replication and spread. Nucleic Acids Res. 50 , 333–349 (2022).
Zhao, H. et al. A trifunctional peptide broadly inhibits SARS-CoV-2 Delta and Omicron variants in hamsters. Cell Discov. 8 , 62 (2022).
Chu, H. et al. Coronaviruses exploit a host cysteine-aspartic protease for replication. Nature 609 , 785–792 (2022).
CAS PubMed Google Scholar
Chu, H. et al. Targeting highly pathogenic coronavirus-induced apoptosis reduces viral pathogenesis and disease severity. Sci. Adv. 7 , eabf8577 (2021).
Lee, S. et al. Virus-induced senescence is a driver and therapeutic target in COVID-19. Nature 599 , 283–289 (2021).
Merad, M. et al. The immunology and immunopathology of COVID-19. Science 375 , 1122–1127 (2022).
Ye, Z. W. et al. Beneficial effect of combinational methylprednisolone and remdesivir in hamster model of SARS-CoV-2 infection. Emerg. Microbes Infect. 10 , 291–304 (2021).
Yu, L. M. et al. Inhaled budesonide for COVID-19 in people at high risk of complications in the community in the UK (PRINCIPLE): a randomised, controlled, open-label, adaptive platform trial. Lancet 398 , 843–855 (2021).
Ezer, N. et al. Inhaled and intranasal ciclesonide for the treatment of COVID-19 in adult outpatients: CONTAIN phase II randomised controlled trial. BMJ 375 , e068060 (2021).
Bessiere, P. et al. Intranasal type I interferon treatment is beneficial only when administered before clinical signs onset in the SARS-CoV-2 hamster model. PLoS Pathog. 17 , e1009427 (2021).
Ye, F. et al. Novaferon effectively inhibits ancestral SARS-CoV-2 and Omicron variant in vitro, 2022. China CDC Wkly. 4 , 509–512 (2022).
PubMed PubMed Central Google Scholar
Tamir, H. et al. Induction of innate immune response by TLR3 agonist protects mice against SARS-CoV-2 infection. Viruses 14 , 189 (2022).
WHO Solidarity Trial Consortium. Remdesivir and three other drugs for hospitalised patients with COVID-19: final results of the WHO Solidarity randomised trial and updated meta-analyses. Lancet 399 , 1941–1953 (2022).
Article PubMed Central Google Scholar
Tam, A. R. et al. Early treatment of high-risk hospitalized COVID-19 patients with a combination of interferon β-1b and remdesivir: a phase 2 open-label randomized controlled trial. Clin. Infect. Dis. 76 , e216–e226 (2022).
Dinnon, K. H. III et al. A mouse-adapted model of SARS-CoV-2 to test COVID-19 countermeasures. Nature 586 , 560–566 (2020).
Chong, Z. et al. Nasally delivered interferon-λ protects mice against infection by SARS-CoV-2 variants including Omicron. Cell Rep. 39 , 110799 (2022).
Reis, G. et al. Early treatment with pegylated interferon λ for COVID-19. N. Engl. J. Med. 388 , 518–528 (2023).
Hoang, T. N. et al. Baricitinib treatment resolves lower-airway macrophage inflammation and neutrophil recruitment in SARS-CoV-2-infected rhesus macaques. Cell 184 , 460–475.e21 (2021).
Kalil, A. C. et al. Baricitinib plus remdesivir for hospitalized adults with COVID-19. N. Engl. J. Med. 384 , 795–807 (2021).
Afzali, B. et al. The state of complement in COVID-19. Nat. Rev. Immunol. 22 , 77–84 (2022).
Vlaar, A. P. et al. Anti-C5a antibody (vilobelimab) therapy for critically ill, invasively mechanically ventilated patients with COVID-19 (PANAMO): a multicentre, double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Respir. Med. 10 , 1137–1146 (2022).
Ho, J. S. Y. et al. TOP1 inhibition therapy protects against SARS-CoV-2-induced lethal inflammation. Cell 184 , 2618–2632.e17 (2021).
Li, L. et al. Effect of convalescent plasma therapy on time to clinical improvement in patients with severe and life-threatening COVID-19: a randomized clinical trial. JAMA 324 , 460–470 (2020).
WHO Working Group on the Clinical Characterisation and Management of COVID-19 Infection. A minimal common outcome measure set for COVID-19 clinical research. Lancet Infect. Dis. 20 , e192–e197 (2020).
WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group et al. Association between administration of IL-6 antagonists and mortality among patients hospitalized for COVID-19: a meta-analysis. JAMA 326 , 499–518 (2021).
WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group. Association between administration of systemic corticosteroids and mortality among critically ill patients with COVID-19: a meta-analysis. JAMA 324 , 1330–1341 (2020).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/study/NCT04381936 (2024).
US National Library of Medicine. ClinicalTrials.gov https://www.clinicaltrials.gov/study/NCT02735707 (2024).
Sette, A. & Crotty, S. Adaptive immunity to SARS-CoV-2 and COVID-19. Cell 184 , 861–880 (2021).
Jayk Bernal, A. et al. Molnupiravir for oral treatment of COVID-19 in nonhospitalized patients. N. Engl. J. Med. 386 , 509–520 (2022).
Butler, C. C. et al. Molnupiravir plus usual care versus usual care alone as early treatment for adults with COVID-19 at increased risk of adverse outcomes (PANORAMIC): an open-label, platform-adaptive randomised controlled trial. Lancet 401 , 281–293 (2023).
Wang, L. et al. COVID-19 rebound after Paxlovid and molnupiravir during January–June 2022. Preprint at medRxiv https://doi.org/10.1101/2022.06.21.22276724 (2022).
Chen, P. et al. SARS-CoV-2 neutralizing antibody LY-CoV555 in outpatients with COVID-19. N. Engl. J. Med. 384 , 229–237 (2021).
Arabi, Y. M. et al. Interferon β-1b and lopinavir–ritonavir for Middle East respiratory syndrome. N. Engl. J. Med. 383 , 1645–1656 (2020).
Zheng, F. et al. SARS-CoV-2 clearance in COVID-19 patients with Novaferon treatment: a randomized, open-label, parallel-group trial. Int. J. Infect. Dis. 99 , 84–91 (2020).
Monk, P. D. et al. Safety and efficacy of inhaled nebulised interferon β-1a (SNG001) for treatment of SARS-CoV-2 infection: a randomised, double-blind, placebo-controlled, phase 2 trial. Lancet Respir. Med. 9 , 196–206 (2021).
RECOVERY Collaborative Group. Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet 397 , 1637–1645 (2021).
Peng, J. et al. Efficacy and secondary infection risk of tocilizumab, sarilumab and anakinra in COVID-19 patients: a systematic review and meta-analysis. Rev. Med. Virol. 32 , e2295 (2022).
Spinner, C. D. et al. Effect of remdesivir vs standard care on clinical status at 11 days in patients with moderate COVID-19: a randomized clinical trial. JAMA 324 , 1048–1057 (2020).
Skipper, C. P. et al. Hydroxychloroquine in nonhospitalized adults with early COVID-19: a randomized trial. Ann. Intern. Med. 173 , 623–631 (2020).
PRINCIPLE Trial Collaborative Group. Azithromycin for community treatment of suspected COVID-19 in people at increased risk of an adverse clinical course in the UK (PRINCIPLE): a randomised, controlled, open-label, adaptive platform trial. Lancet 397 , 1063–1074 (2021).
Butler, C. C. et al. Doxycycline for community treatment of suspected COVID-19 in people at high risk of adverse outcomes in the UK (PRINCIPLE): a randomised, controlled, open-label, adaptive platform trial. Lancet Respir. Med. 9 , 1010–1020 (2021).
Lopez-Medina, E. et al. Effect of ivermectin on time to resolution of symptoms among adults with mild COVID-19: a randomized clinical trial. JAMA 325 , 1426–1435 (2021).
Weinreich, D. M. et al. REGEN-COV antibody combination and outcomes in outpatients with COVID-19. N. Engl. J. Med. 385 , e81 (2021).
Gottlieb, R. L. et al. Effect of bamlanivimab as monotherapy or in combination with etesevimab on viral load in patients with mild to moderate COVID-19: a randomized clinical trial. JAMA 325 , 632–644 (2021).
Feld, J. J. et al. Peginterferon λ for the treatment of outpatients with COVID-19: a phase 2, placebo-controlled randomised trial. Lancet Respir. Med. 9 , 498–510 (2021).
Jagannathan, P. et al. Peginterferon λ-1a for treatment of outpatients with uncomplicated COVID-19: a randomized placebo-controlled trial. Nat. Commun. 12 , 1967 (2021).
Ramakrishnan, S. et al. Inhaled budesonide in the treatment of early COVID-19 (STOIC): a phase 2, open-label, randomised controlled trial. Lancet Respir. Med. 9 , 763–772 (2021).
Reis, G. et al. Oral fluvoxamine with inhaled budesonide for treatment of early-onset COVID-19: a randomized platform trial. Ann. Intern. Med. 176 , 667–675 (2023).
Salama, C. et al. Tocilizumab in patients hospitalized with COVID-19 pneumonia. N. Engl. J. Med. 384 , 20–30 (2021).
Salvarani, C. et al. Effect of tocilizumab vs standard care on clinical worsening in patients hospitalized with COVID-19 pneumonia: a randomized clinical trial. JAMA Intern. Med. 181 , 24–31 (2021).
Rosas, I. O. et al. Tocilizumab in hospitalized patients with severe COVID-19 pneumonia. N. Engl. J. Med. 384 , 1503–1516 (2021).
Lescure, F. X. et al. Sarilumab in patients admitted to hospital with severe or critical COVID-19: a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Respir. Med. 9 , 522–532 (2021).
Dorward, J. et al. Colchicine for COVID-19 in the community (PRINCIPLE): a randomised, controlled, adaptive platform trial. Br. J. Gen. Pract. 72 , e446–e455 (2022).
Gautret, P. et al. Clinical and microbiological effect of a combination of hydroxychloroquine and azithromycin in 80 COVID-19 patients with at least a 6-day follow up: a pilot observational study. Travel. Med. Infect. Dis. 34 , 101663 (2020).
Rosendaal, F. R. Review of: “Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial Gautret et al. 2010”. Int. J. Antimicrob. Agents 56 , 106063 (2020).
Niburski, K. & Niburski, O. Impact of Trump’s promotion of unproven COVID-19 treatments and subsequent Internet trends: observational study. J. Med. Internet Res. 22 , e20044 (2020).
Rathi, S. et al. Hydroxychloroquine prophylaxis for COVID-19 contacts in India. Lancet Infect. Dis. 20 , 1118–1119 (2020).
Mehra, M. R. et al. Hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: a multinational registry analysis. Lancet 395 , P1820 (2020); retraction 395 , 1820 (2020).
US Food and Drug Administration. Why you should not use ivermectin to treat or prevent COVID-19. US Food and Drug Administration https://nycourts.gov/reporter/webdocs/Why-You-Should-Not-Use-Ivermectin-to-Treat-or-Prevent-COVID-19.pdf (2021).
Tang, C. et al. Caution against corticosteroid-based COVID-19 treatment. Lancet 395 , 1759–1760 (2020).
Download references
Acknowledgements
This study was partly supported by funding by the National Natural Science Foundation of China General Program (82272337); the Health and Medical Research Fund (20190572), Health Bureau, Government of the Hong Kong Special Administrative Region; the General Research Fund (17122322), Collaborative Research Fund (C7060-21G) and Theme-Based Research Scheme (T11-709/21-N), Research Grants Council, Government of the Hong Kong Special Administrative Region; Health@InnoHK, Innovation and Technology Commission, Government of the Hong Kong Special Administrative Region; the Partnership Programme of Enhancing Laboratory Surveillance and Investigation of Emerging Infectious Diseases and Antimicrobial Resistance for the Department of Health of the Hong Kong Special Administrative Region Government; the National Key Research and Development Program of China (projects 2021YFC0866100 and 2023YFC3041600); the Sanming Project of Medicine in Shenzhen, China (SZSM201911014); the High Level-Hospital Program, Health Commission of Guangdong Province, China; the Emergency Collaborative Project of Guangzhou Laboratory (EKPG22-01); the University of Hong Kong Outstanding Young Researcher Award; and the University of Hong Kong Research Output Prize (Li Ka Shing Faculty of Medicine); and by donations from the Shaw Foundation Hong Kong, Richard Yu and Carol Yu, Michael Seak-Kan Tong, May Tam Mak Mei Yin, Providence Foundation Limited (in memory of the late Lui Hac Minh), Lee Wan Keung Charity Foundation Limited, Hong Kong Sanatorium & Hospital, Hui Ming, Hui Hoy and Chow Sin Lan Charity Fund Limited, The Chen Wai Wai Vivien Foundation Limited, Chan Yin Chuen Memorial Charitable Foundation, Tse Kam Ming Laurence, Marina Man-Wai Lee, the Hong Kong Hainan Commercial Association South China Microbiology Research Fund, Pui-Sze Cheng, Perfect Shape Medical Limited, Kai Chong Tong, Tse Kam Ming Laurence, Foo Oi Foundation Limited and Betty Hing-Chu Lee, Ping Cham So, and Lo Ying Shek Chi Wai Foundation. The funding sources had no role in the study design, data collection, analysis, interpretation, or writing of the report.
Author information
Authors and affiliations.
State Key Laboratory of Emerging Infectious Diseases, The University of Hong Kong, Pokfulam, Hong Kong Special Administrative Region, China
Jasper Fuk-Woo Chan, Shuofeng Yuan, Hin Chu, Siddharth Sridhar & Kwok-Yung Yuen
Carol Yu Centre for Infection, Department of Microbiology, School of Clinical Medicine, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Pokfulam, Hong Kong Special Administrative Region, China
Department of Infectious Diseases and Microbiology, The University of Hong Kong-Shenzhen Hospital, Shenzhen, Guangdong Province, China
Centre for Virology, Vaccinology and Therapeutics, Hong Kong Science and Technology Park, Shatin, Hong Kong Special Administrative Region, China
Jasper Fuk-Woo Chan, Shuofeng Yuan, Hin Chu & Kwok-Yung Yuen
You can also search for this author in PubMed Google Scholar
Contributions
All authors researched data for the article, contributed substantially to discussion of the content, wrote the article, and reviewed and edited the manuscript before submission.
Corresponding author
Correspondence to Kwok-Yung Yuen .
Ethics declarations
Competing interests.
J.F.-W.C. has received travel grants from Pfizer Corporation Hong Kong and Astellas Pharma Hong Kong Corporation Ltd, and was an invited speaker for Gilead Sciences Hong Kong Ltd and Luminex Corporation. K.-Y.Y. is a shareholder of Hong Kong Universal Biologicals Company Ltd and Hong Kong Universal Vaccine Ltd, and collaborates with Sinovac Biotech Ltd and China National Pharmaceutical Group Co., Ltd (Sinopharm). J.F.-W.C., S.Y., H.C. and K.-Y.Y. have patent applications on a number of therapeutic candidates included in this article. S.S. declares no competing interests.
Peer review
Peer review information.
Nature Reviews Microbiology thanks Christopher Butler, Shuibing Chen, Stanley Perlman and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information, rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Chan, J.FW., Yuan, S., Chu, H. et al. COVID-19 drug discovery and treatment options. Nat Rev Microbiol (2024). https://doi.org/10.1038/s41579-024-01036-y
Download citation
Accepted : 28 February 2024
Published : 15 April 2024
DOI : https://doi.org/10.1038/s41579-024-01036-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

COMMENTS
The COVID-19 pandemic has resulted in unprecedented research worldwide. The impact on research in progress at the time of the pandemic, the importance and challenges of real-time pandemic research ...
The COVID-19 outbreak has posed an unprecedented challenge to humanity and science. On the one side, public and private incentives have been put in place to promptly allocate resources toward research areas strictly related to the COVID-19 emergency. However, research in many fields not directly related to the pandemic has been displaced.
In February 2020, we highlighted the top nine important research questions on SARS-CoV-2 and COVID-19 concerning virus transmission, asymptomatic and presymptomatic virus shedding, diagnosis, treatment, vaccine development, origin of virus and viral pathogenesis. These and related questions are revisited at the end of 2021 to shed light on the ...
COVID-19 pandemic has severely impacted the crude, stock market, gold and metals and almost all areas of the global market [ 1 ]. Large research laboratories and corporate houses are working with a high speed to develop medicines and vaccines for the prevention and treatment of this dreaded disease. To deal with these current health management ...
The WHO Covid-19 Research Database is a resource created in response to the Public Health Emergency of International Concern (PHEIC). Its content remains searchable and spans the time period March 2020 to June 2023. Since June 2023, manual updates to the database have been discontinued. The WHO evidence retrieval sub-group has begun ...
The COVID-19 pandemic has affected a variety of researchers, students and academics. As institutions of higher education have limited in-person activities, research and training have been disrupted. Many graduate students have faced new barriers as a result (Chenneville and Schwartz-Mette, 2020; Thompson, 2020).
The current trial landscape of COVID-19 highlights important issues that illustrate the inefficiencies of clinical trial research. Most COVID-19 trials are small, so they will not provide sufficient statistical power to detect a meaningful treatment effect. Most will never achieve their target recruitment numbers.
Much important research has investigated key public health and clinical issues such as masking, indoor air ventilation, and prone ventilation. But, arguably, no research has been more innovative and impactful than that of the biomedical community around vaccines, therapeutics, and diagnostics. ... COVID-19 has reaffirmed the importance of ...
This article is part of the Research Topic COVID-19 - Social Science Research during a Pandemic View all 75 ... The Importance of Understanding COVID-19: The Role of Knowledge in Promoting Adherence to Protective Behaviors. Front. Public Health 9:581497. doi: 10.3389/fpubh.2021.581497. Received: 08 July 2020; Accepted: 10 March 2021; Published ...
Decades of coronavirus research and intense studies of SARS-CoV-2 since the beginning of the COVID-19 pandemic have led to an unprecedented level of knowledge of coronavirus biology and ...
Yet well into the fourth year of the Covid-19 pandemic, intense political and scientific debates about its origins continue. The two major hypotheses are a natural zoonotic spillover, most likely ...
Professor Sorrell says Australia is uniquely positioned as a global leader in medical research. She says that we can strongly contribute to the fight against serious infectious diseases like COVID-19 in the future, but the key is continued funding of vital research. That is one of the reasons Professor Sorrell has generously decided to create a ...
However, there are important ethical considerations that must be addressed - particularly for a new disease like COVID-19, which we do not yet fully understand and are still learning how to treat; it may be difficult for the medical community and potential volunteers to properly estimate the potential risks of participating in a COVID-19 ...
Vanderbilt's role in shaping each step of the medical response to the COVID-19 pandemic began three decades ago and is grounded in the determination of a small group of scientists to understand ...
Rapid research response to the COVID-19 pandemic: perspectives from a National Institute for Health Biomedical Research Centre. With over 5 million COVID-19 deaths at the time of writing, the response of research leaders was and is critical to developing treatments to control the global pandemic. As clinical research leaders urgently r...
important. Research can: o help doctors and scientists learn if a test or treatment is safe for a particular person, o show if ways to prevent COVID-19 (including vaccines) work and are safe to use, ... COVID-19 research. Special emphasis is placed on inclusion of the following populations: Blacks/African Americans, Hispanics/Latinos, and ...
Community-engaged research was disrupted by COVID-19 restrictions, meaning researchers faced serious challenges when their results were most needed: during a public health crisis.
In my field, tuberculosis (TB) research, many researchers have already pivoted to COVID-19. This is a loss, since TB is the leading infectious killer and is getting even worse because of the pandemic.
The molecule comprises the genetic information of SARS-Cov-2, the virus that causes the COVID19 disease, as well as two of the first vaccines being used to provide immunity against the virus. Since early in 2020, researchers at Whitehead Institute and around the world have been applying their RNA knowledge to the COVID19 pandemic.
Coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is an ongoing global health emergency. Here we highlight nine most important research questions concerning virus transmission, asymptomatic and presymptomatic virus shedding, diagnosis, treatment, vaccine development, origin of virus and ...
COVID-19 (coronavirus disease 2019) is a disease caused by a virus named SARS-CoV-2. It can be very contagious and spreads quickly. Over one million people have died from COVID-19 in the United States. COVID-19 most often causes respiratory symptoms that can feel much like a cold, the flu, or pneumonia. COVID-19 may attack more than your lungs ...
Just weeks after the first cases of COVID-19 hit U.S. shores, an op-ed appeared in The New York Times titled "We Need to Talk About What Coronavirus Recoveries Look Like: They're a lot more complicated than most people realize."The author, Fiona Lowenstein, is a writer and yoga teacher living in New York City, who wrote about her own illness and the symptoms she was left with once she was ...
The role of intersectoral collaboration in responding to COVID-19 is still an under-explored research area. Lessons from the ways in which African countries handled aspects of the COVID-19 pandemic are valuable, especially because African governments face resource and capacity constraints which necessitate an intersectoral collaborative approach.
WASHINGTON — A new report from the National Academies of Sciences, Engineering, and Medicine reviews evidence for 19 potential harms of the COVID-19 vaccines, and for nine potential shoulder injuries from intramuscular administration of vaccines more broadly. The committee that conducted the review identified sufficient evidence to draw 20 conclusions about whether these vaccines could cause ...
Several studies have found evidence that a COVID infection can cause cortisol and serotonin levels to drop in the brain, which could result in 'brain fog.' (Shutterstock) When COVID-19 first ...
In short: A new research study suggests the COVID-19 vaccine campaign prevented 17,760 deaths among NSW residents aged 50 years and over. The study used computer modelling to predict the death ...
Why is this important? The COVID-19 pandemic demonstrated the damage that airborne pathogens can cause. Other airborne diseases, such as the flu or RSV are also a threat to patients and health systems. ... More than 50 experts from academia, research and technology organisations, businesses, business associations, non-governmental organisations ...
WASHINGTON—The Select Subcommittee on the Coronavirus Pandemic held a hearing on "Investigating the Origins of COVID-19" to gather facts about the origination of the virus that has claimed nearly seven million lives globally. At the hearing, several of the witnesses pointed to how the science, facts, and evidence point to a lab leak in Wuhan.
The impact of COVID-19 on research. Coronavirus disease 2019 (COVID-19) has swept across the globe causing hundreds of thousands of deaths, shutting down economies, closing borders and wreaking havoc on an unprecedented scale. It has strained healthcare services and personnel to the brink in many regions and will certainly deeply mark medical ...
Effective treatments are one of the most important components of the armamentarium for emerging infectious diseases. Prior to the coronavirus disease 2019 (COVID-19) pandemic caused by severe ...