Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 23 February 2023

Fetal alcohol spectrum disorders
- Svetlana Popova ORCID: orcid.org/0000-0002-6308-1157 1 ,
- Michael E. Charness 2 , 3 , 4 , 5 ,
- Larry Burd 6 ,
- Andi Crawford 7 ,
- H. Eugene Hoyme 8 ,
- Raja A. S. Mukherjee 9 ,
- Edward P. Riley ORCID: orcid.org/0000-0001-8747-891X 10 &
- Elizabeth J. Elliott 11 , 12
Nature Reviews Disease Primers volume 9 , Article number: 11 ( 2023 ) Cite this article
45k Accesses
71 Citations
158 Altmetric
Metrics details
- Human behaviour
- Neonatal brain damage
Alcohol readily crosses the placenta and may disrupt fetal development. Harm from prenatal alcohol exposure (PAE) is determined by the dose, pattern, timing and duration of exposure, fetal and maternal genetics, maternal nutrition, concurrent substance use, and epigenetic responses. A safe dose of alcohol use during pregnancy has not been established. PAE can cause fetal alcohol spectrum disorders (FASD), which are characterized by neurodevelopmental impairment with or without facial dysmorphology, congenital anomalies and poor growth. FASD are a leading preventable cause of birth defects and developmental disability. The prevalence of FASD in 76 countries is >1% and is high in individuals living in out-of-home care or engaged in justice and mental health systems. The social and economic effects of FASD are profound, but the diagnosis is often missed or delayed and receives little public recognition. Future research should be informed by people living with FASD and be guided by cultural context, seek consensus on diagnostic criteria and evidence-based treatments, and describe the pathophysiology and lifelong effects of FASD. Imperatives include reducing stigma, equitable access to services, improved quality of life for people with FASD and FASD prevention in future generations.
Similar content being viewed by others
Hospitalizations and mortality among patients with fetal alcohol spectrum disorders: a prospective study
Maternal alcohol consumption and risk of offspring with congenital malformation: the Japan Environment and Children’s Study
A data driven approach to identify trajectories of prenatal alcohol consumption in an Australian population-based cohort of pregnant women
Introduction.
Alcohol consumption has occurred for centuries, with harms from prenatal alcohol exposure (PAE) being mentioned in Greek and biblical verses and depicted in the art and literature of the eighteenth and nineteenth centuries 1 , 2 . A French-language publication from 1968, which received little attention at the time, described perinatal death, prematurity, growth retardation, facial features and malformations in the offspring of women who consumed alcohol during pregnancy 3 . Unaware of the French publication, Jones et al. described a similar pattern of altered morphogenesis and function in 11 children of mothers with ‘alcoholism’ in the Lancet in 1973 (ref. 4 ). They reported specific facial features (thin upper lip, smooth philtrum (the vertical groove between the base of the nose and the border of the upper lip) and short palpebral fissures) and coined the term fetal alcohol syndrome (FAS) 5 . By 1977, the US government had issued a warning about the health risks of alcohol use during pregnancy, which was endorsed by professional organizations in the USA 6 , 7 . In 1981, the US Surgeon General issued stronger advice that “women who are pregnant (or considering pregnancy) not drink alcoholic beverages” 8 and other countries subsequently issued similar advice. The teratogenic effects of alcohol were subsequently confirmed in animal studies 9 .
Later studies found that, in addition to FAS, PAE could cause behavioural, cognitive and learning problems, such as attention deficit hyperactivity disorder (ADHD) and speech and language delay, in the absence of facial and other physical features 10 . Recognition of the disconnect between the neurodevelopmental and physical effects (which relate to first-trimester exposure) of PAE and the wide range of outcomes caused by PAE led to the introduction of the term fetal alcohol spectrum disorders (FASD) 11 . Subsequent research identified groups at increased risk of FASD 12 and associations between FASD and metabolic, immunological and cardiovascular diseases in adults 13 , 14 .
FASD occur in all socioeconomic and ethnic groups 15 and are complex, chronic conditions that affect health and family functioning 16 . Individuals with FASD usually require lifelong health care as well as social and vocational support. Some require remedial education and others interact with the justice system. Early diagnosis and a strength-based management approach will optimize health outcomes.
FASD are the most common of the potentially preventable conditions associated with birth anomalies and neurodevelopmental problems 13 , and their global effects, including huge social and economic costs, are substantial 17 . For example, in Canada, the annual cost associated with FASD is an estimated ~CAD$ 1.8 billion (CAD$ 1.3 billion to CAD$ 2.3 billion) 17 , which is attributable in part to productivity loss (41%), correction services (29%) and health care (10%). In North America, the lifetime cost of supporting an individual with FASD is estimated at >CAD$ 1 million 18 . Addressing and preventing alcohol use in pregnancy is a public-health imperative.
This Primer presents the epidemiology of FASD and the latest understanding of its pathophysiology as well as approaches to diagnosis, screening and prevention. The Primer also describes outcomes across the lifespan, management and quality of life (QOL) of people living with FASD, and highlights important areas for future research and clinical practice.
Epidemiology
Alcohol use during pregnancy.
No safe level of PAE has been established 19 , and international guidelines advise against any amount or type of alcohol use during pregnancy 20 , 21 , 22 , 23 . Nevertheless, ~10% of pregnant women worldwide consume alcohol 24 , 25 . The highest prevalence of alcohol use during pregnancy is in the WHO European Region (25.2% 24 ; Fig. 1 ), consistent with the prevalence of heavy alcohol use, heavy episodic drinking and alcohol use disorders in this region 26 .
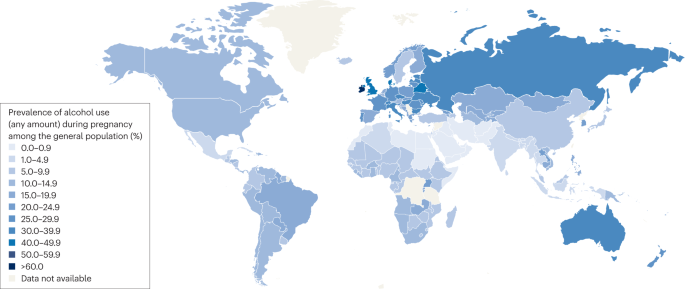
The highest pooled prevalence (%) of alcohol use during pregnancy in the general population is estimated in the WHO European Region (25.2%, 95% CI 21.6–29.6), followed by the Region of the Americas (11.2%, 95% CI 9.4–12.6), the African Region (10.0%, 95% CI 8.5–11.8), the Western Pacific Region (8.6%, 95% CI 4.5–11.6) and the South-East Asia Region (1.8%, 95% CI 0.9–5.1), and the lowest prevalence is estimated in the Eastern Mediterranean Region (0.2%, 95% CI 0.1–0.9), where most of the population is of Muslim faith and the rates of abstinence from alcohol are very high. The pooled global prevalence of alcohol use during pregnancy in the general population is estimated at 9.8% (95% CI 8.9–11.1). Data from ref. 24 .
In 40% of the 162 countries evaluated, >25% of women who consumed any alcohol during pregnancy drank at ‘binge’ levels (defined as ≥4 US standard drinks containing 14 g of pure alcohol per drink on a single occasion). Binge drinking, which increases the risk of FASD, is common in early pregnancy and before pregnancy recognition 25 , 27 . Many fetuses are inadvertently exposed to alcohol because binge drinking is prevalent in young women, millions of women who consume alcohol report having unprotected sex and approximately half of all pregnancies are unplanned 28 , 29 , 30 , 31 . Alcohol use during pregnancy is higher in certain subpopulations, including some Indigenous populations in Australia (55%) 32 , South Africa (37%) 33 and Canada (60%) 34 , often in the context of disadvantage, violence and ongoing traumatic effects of colonization 35 .
Risk factors for maternal alcohol consumption
Various risk factors have been identified for maternal alcohol use in pregnancy, including higher gravidity and parity 36 , delayed pregnancy recognition, inadequate prenatal care or reluctance of health professionals to address alcohol use 37 , 38 , a history of FASD in previous children 38 , alcohol use disorder and other substance use (including tobacco) 39 , mental health disorders (such as depression) 39 , a history of physical or sexual abuse, social isolation (including living in a rural area during pregnancy), intimate partner violence 38 , 40 , alcohol and/or drug use during pregnancy by the mother’s partner 38 , 41 or other family members 38 , 41 , and poverty 42 .
Risk factors for alcohol use during pregnancy vary across countries and throughout the course of pregnancy. For example, in Australia, first-trimester alcohol use was associated with unplanned pregnancy 43 , age <18 years at first intoxication 30 , frequent and binge drinking in adolescence 44 , and current drinking and a tolerant attitude to alcohol use in pregnancy 45 . Women who continued to drink alcohol throughout pregnancy were more likely to be older, have higher socioeconomic status, salary and educational levels, smoke, have a partner who consumes alcohol, and have an unintended pregnancy than those who abstained, and were less likely to agree with guidelines that recommend avoiding alcohol use in pregnancy 30 , 31 , 46 , 47 .
FASD prevalence
The estimated global prevalence of FASD among the general population is 7.7 cases per 1,000 individuals 25 , 48 . Consistent with rates of alcohol use during pregnancy, FASD prevalence (Fig. 2 ) is highest in the WHO European Region (19.8 per 1,000) and lowest in the WHO Eastern Mediterranean Region (0.1 per 1,000) 25 , 48 . In terms of individual countries, South Africa (111.1 per 1,000), Croatia (53.3 per 1,000), Ireland (47.5 per 1,000), Italy (45.0 per 1,000) and Belarus (36.6 per 1,000) have the highest FASD prevalence, whereas Bahrain, Kuwait, Oman, Qatar, Saudi Arabia and the United Arab Emirates have no recorded cases of FASD 25 , 48 . Furthermore, 76 countries have a prevalence of FASD of >1% 25 , 48 , which exceeds the prevalence of neurodevelopmental conditions, including Down syndrome (trisomy 21), Edwards syndrome (trisomy 18), spina bifida and anencephaly in the USA 49 , and is similar to the prevalence of autism spectrum disorders (1.1–2.5%) 50 .
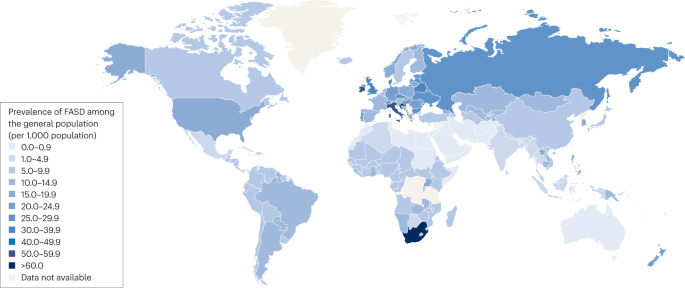
In line with the prevalence of alcohol use during pregnancy, the highest pooled prevalence (per 1,000) of fetal alcohol spectrum disorders (FASD) was in the WHO European Region (19.8 per 1,000 population, 95% CI 14.1–28.0), followed by the Region of the Americas (8.8 per 1,000 population, 95% CI 6.4–13.2), the African Region (7.8 per 1,000 population, 95% CI 5.4–10.7), the Western Pacific Region (6.7 per 1,000 population, 95% CI 4.5–11.7) and the South-East Asia Region (1.4 per 1,000 population, 95% CI 0.6–5.3), and the lowest prevalence was estimated in the Eastern Mediterranean Region (0.1 per 1,000 population, 95% CI 0.1–0.5). The pooled global prevalence of FASD was estimated to be 7.7 (95% CI 4.9–11.7) per 1,000 in the general population. Data from refs. 25 , 48 .
Based on global epidemiological data, an estimated 1 in 13 women who consume alcohol while pregnant will deliver a child with FASD, resulting in the birth of ~630,000 children with FASD globally every year 48 . FASD confers lifelong disability, and an estimated >11 million individuals aged 0–18 years and 25 million aged 0–40 years have FASD 51 .
A systematic review and meta-analysis revealed that FASD prevalence is 10–40 times higher in some subpopulations than in the general population, including in children in out-of-home care and correctional, special education, and specialized clinical settings 12 (Fig. 3 ). The pooled prevalence of FASD among children in out-of-home or foster care is 25.2% in the USA and 31.2% in Chile (32-fold and 40-fold higher than the global prevalence, respectively) 12 . FASD prevalence among adults in the Canadian correctional system (14.7%) is 19-fold higher than in the general population, and the prevalence among special education populations in Chile (8.4%) is over 10-fold higher than in the general population 12 . Moreover, the prevalence of FASD is 62% among children with intellectual disabilities in care in Chile 52 , >50% in adoptees from Eastern Europe 53 , 54 and ~40% among children in Lithuanian orphanages 55 . The prevalence of FASD is 36% in one Australian youth correctional service 56 , >23% in Canadian youth correctional services 57 , >14% among USA populations in psychiatric care 58 and 19% in some remote Australian Indigenous communities 59 . The highest prevalence estimates for FAS (46–68%) are in children with developmental abnormalities in Russian orphanages 60 . The high prevalence of FASD in some subpopulations has prompted calls for targeted screening in these groups.
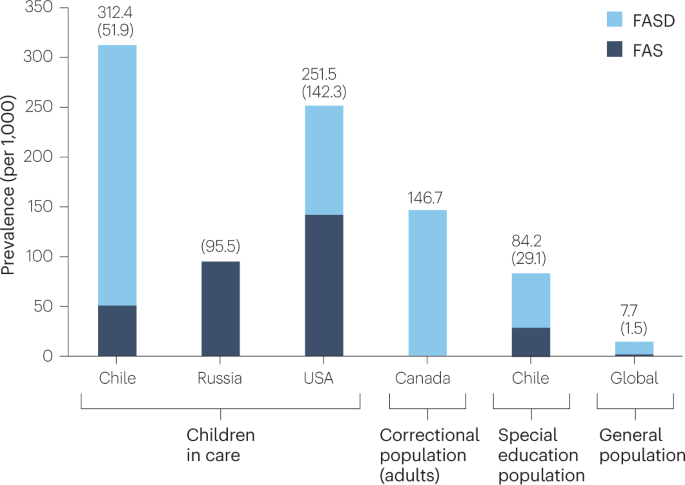
The pooled prevalence (per 1,000) of fetal alcohol spectrum disorders (FASD) is markedly higher in some subpopulations than in the general global population. Subpopulations with a high prevalence of FASD include children in out-of-home care, individuals involved with correctional services and those receiving special education. FAS, fetal alcohol syndrome.
Mechanisms/pathophysiology
Alcohol rapidly equilibrates between the maternal and fetal compartments and is eliminated primarily through maternal metabolism 61 . As previously mentioned, no safe level of PAE has been established 19 . Several developmentally important molecular targets of alcohol, including the L1 neural cell adhesion molecule and GABA A receptors, are disrupted at blood alcohol concentrations attained after one or two US standard drinks 62 , 63 , 64 , 65 , 66 . Hence, repeated exposure to low levels of alcohol or a single exposure at critical periods in gestation could affect development. Indeed, drinking ≤20 g of alcohol per occasion (≤1.5 US standard drinks) or ≤70 g alcohol per week (≤5 US standard drinks) was associated with mild facial dysmorphology (determined via 3D facial imaging) 67 , microstructural brain abnormalities, and externalizing behaviours such as aggression and violation of social norms 68 . The Adolescent Brain Cognitive Development (ABCD) Study, a large, prospective, longitudinal study of child and adolescent development, reported a dose-dependent association between low-level drinking during pregnancy, increased cerebral volume and regional cortical surface area, and a range of adverse cognitive, psychiatric and behavioural outcomes in children aged 9–10 years 69 . There was no inflexion point in the dose–response curves to suggest a cut-off for PAE effects, and significant effects were observed with as little as 1.1 US standard drinks per week throughout pregnancy. Increased brain volume was attributed to impairment of synaptic pruning in the preadolescent brain, consistent with research demonstrating the effect of PAE on trajectories of brain development 70 , 71 .
Genes associated with PAE
Several gene variants confer heightened risk or resilience to PAE 72 , 73 , 74 , and there is higher concordance for FAS among monozygotic than among dizygotic twins 74 . Genetic effects may be exerted through the mother and/or the fetus 72 . ADH1 (encoding alcohol dehydrogenase 1) polymorphisms, such as ADH1B*2 and ADH1B*3 , which increase alcohol metabolism and decrease blood alcohol levels, are associated with reduced risk of FASD 72 . Moreover, zebrafish with pdgfra (encoding platelet-derived growth factor receptor-α) haploinsufficiency have increased susceptibility to craniofacial malformations caused by PAE, which is mirrored in individuals with PDGFRA polymorphisms 75 . Similarly, haploinsufficiency of either Shh or Gli2 (a downstream effector of Shh ) is clinically silent in mice; however, PAE in these mice results in midline craniofacial malformations 76 . Interestingly, hypermethylation of GLI2 (which decreases GLI2 expression) was identified in genome-wide DNA methylation profiling of children with FASD 77 . Prenatal or postnatal choline supplementation improves cognition in animal models and clinical studies 78 and the effect of choline supplementation is modified by polymorphisms in SLC44A1 (encoding choline transporter-like protein 1) 79 .
Timing and quantity of PAE during gestation
The effects of PAE vary according to the quantity, frequency, duration, pattern and timing of exposure 80 . Periconceptional alcohol exposure can adversely affect fetal development and predispose to disease in later life 81 , 82 . PAE at different stages of organogenesis has distinct developmental consequences. PAE during first-trimester organogenesis may cause brain, craniofacial, skeletal and internal organ dysmorphology 80 . In mice, PAE during gastrulation (equivalent to the third week post-fertilization in humans, when an embryo transforms from a bilaminar disc to a multilayered structure comprising the three primary germ layers: ectoderm, mesoderm and endoderm) reproduces the sentinel craniofacial abnormalities of FAS: thin upper lip, smooth philtrum and short palpebral fissures 9 (Fig. 4 ). By contrast, alcohol exposure during neurulation (starting in gestational week three in humans, resulting in the folding of the neural plate to form the neural tube) produces a facial phenotype that resembles DiGeorge syndrome, a chromosomal disorder (22q11.2 deletion) associated with facial anomalies, immune dysfunction, cardiac defects and neurodevelopmental abnormalities 83 .
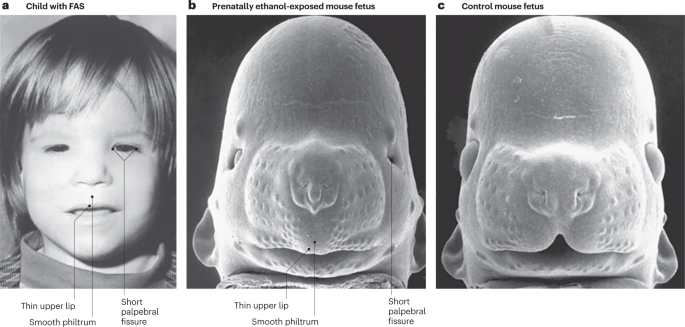
a , b , The facial phenotype of fetal alcohol spectrum disorders can be reproduced in a preclinical model. Comparable to the facial features of the child with fetal alcohol syndrome (FAS) (part a ), the mouse fetus exposed prenatally to alcohol shows a thin upper lip with a smooth philtrum, short palpebral fissures and a small midface (part b ). c , The normal features in a control mouse fetus (not prenatally exposed to alcohol). Part a courtesy of Sterling Clarren. Parts b and c adapted with permission from ref. 9 , AAAS.
The brain is vulnerable to PAE throughout pregnancy 84 , 85 . PAE after 8 weeks of gestation affects neurogenesis, differentiation of neural precursor cells, neuronal migration, pathfinding, synaptogenesis and axon myelination 72 , 85 , 86 but does not cause sentinel craniofacial dysmorphology or major organ defects. Thus, PAE after major organogenesis may result in a FASD phenotype with neurodevelopmental disorder but without physical alterations, making diagnosis difficult 80 . Nutritional deficiency during pregnancy may potentiate the effects of PAE on developmental outcomes, and maternal alcohol intake may further reduce the availability of developmentally important nutrients 87 .
Effects of PAE on the embryo and fetus
Brain development.
As previously mentioned, PAE can affect brain development 88 , 89 . Retrospective examination of 149 brains from individuals with PAE who died between birth and adulthood identified gross abnormalities in brain development causing microcephaly (a smaller than normal head for age and sex using population-based normative data, often associated with a smaller than normal brain (micrencephaly)) in 20.8%. This study found isolated hydrocephalus in 4.0% of individuals with PAE, corpus callosum defects in 4.0%, prenatal ischaemic lesions in 3.4%, minor subarachnoid heterotopias (the presence of normal tissue at an abnormal location, such as an ectopic cluster of neurons within the white matter, often due to abnormal neuronal migration during early brain development) in 2.7%, holoprosencephaly (whereby the embryonic forebrain fails to develop into two discrete hemispheres, often affecting midline brain and craniofacial structures) in 0.7% and lissencephaly (smoothness of the brain surface due to impaired development of cerebral gyri) in 0.7% 88 . Hence, because macroscopic neuropathology is not present in most individuals with FASD, microscopic neuropathology likely underlies many of the associated cognitive and behavioural abnormalities of this disorder. Studies in non-human primates show that first-trimester-equivalent alcohol exposure reduces brainstem and cerebellar volume and disrupts various white matter tracts, including one connecting the putamen and primary sensory cortex 90 . Third-trimester-equivalent alcohol exposure reduced hippocampal neuronal numbers in infant and juvenile Vervet monkeys 86 .
Brain structure
Relatively few macroscopic brain lesions have been identified in clinical neuroimaging studies of children with FASD 80 , 91 . Blind evaluation of clinical MRI studies by neuroradiologists identified clinically significant abnormalities in 3% of individuals with PAE or FASD and in 1% of typically developing controls 91 . Four of 61 patients with FAS had heterotopias 92 . By contrast, quantitative research imaging studies in groups of children with PAE and FASD have revealed region-specific increases or decreases in grey matter thickness, microstructural white matter abnormalities, and neuronal and glial migration defects 69 , 93 , 94 . Volume reduction is disproportionate in the cerebrum, cerebellum, caudate, putamen, basal ganglia, thalamus and hippocampus after accounting for overall reductions in brain volume 94 . Age-dependent decreases in cortical gyrification are also observed 94 , 95 , 96 and the corpus callosum can be hypoplastic, posteriorly displaced or, in rare cases, absent 94 , 97 , 98 , 99 , 100 . Moreover, studies using diffusion tensor imaging reveal reduced integrity of large white matter tracts, including in the corpus callosum, cerebellar peduncles, cingulum and longitudinal fasciculi 101 . Hypoplasia of the corpus callosum in children with FASD is associated with impaired interhemispheric transfer of information 102 .
Imaging studies have also demonstrated the effect of PAE on postnatal grey matter development 99 , 103 . Typical brain development is associated with a large increase in cortical grey matter during early childhood followed by loss of cortical grey matter during late childhood and adolescence via synaptic pruning, a process that reflects cortical plasticity 70 . By contrast, children with FASD show region-specific loss of grey matter and decreased gyrification from early childhood through adolescence 70 , 99 , 102 . This change may partly explain contradictory findings of increased or decreased grey matter volume in various studies, which sampled different brain regions during distinct developmental periods or evaluated populations with different levels of PAE 69 . A relatively small sample size is another source of variation in results among brain imaging studies 104 .
One frequently observed effect of PAE is the disruption of brain plasticity 105 . Animal models and human studies have demonstrated enduring deficits in learning and memory following PAE, associated with abnormal plasticity in hippocampal, thalamic, cortical and cerebellar circuits 105 , 106 , 107 . These deficits are associated with changes in alpha oscillations on magnetoencephalography, fractional anisotropy (a measure of white matter integrity) on diffusion tensor imaging, and functional and resting-state MRI in children with PAE 68 , 94 , 108 , 109 .
Craniofacial development
Brain and craniofacial development are mechanistically linked; therefore, brain and craniofacial abnormalities frequently co-occur 98 , 110 . For example, abnormalities of midline brain structures, such as the corpus callosum, diencephalon and septum, are associated with midline craniofacial abnormalities 98 , 103 , 110 . Craniofacial development relies on the highly choreographed migration of cranial neural crest cells and is most sensitive to PAE during the third week of gestation. Alcohol induces apoptosis of neural crest cells through oxidative injury and disruption of Sonic hedgehog (Shh) signalling 111 . Shh regulates embryonic morphogenesis and organogenesis, including the organization of cells of the central nervous system (CNS), limbs and other body parts. In animal models, diverse antioxidants and inhibitors of apoptosis mitigate the effects of alcohol on neural crest cells 112 , 113 .
Mechanisms of alcohol teratogenesis
Multiple mechanisms of alcohol-induced teratogenesis have been elucidated 9 , 80 , 114 , 115 (Fig. 5 ). Alcohol has protean effects on brain and craniofacial development in part because it is a weak drug that requires millimolar concentrations to produce even mild euphoria 116 . For example, in the USA, legal intoxication is defined as 17.4 mM or 0.08 g/dl; at these high concentrations, alcohol interacts with diverse molecules and signalling pathways that regulate development 117 .
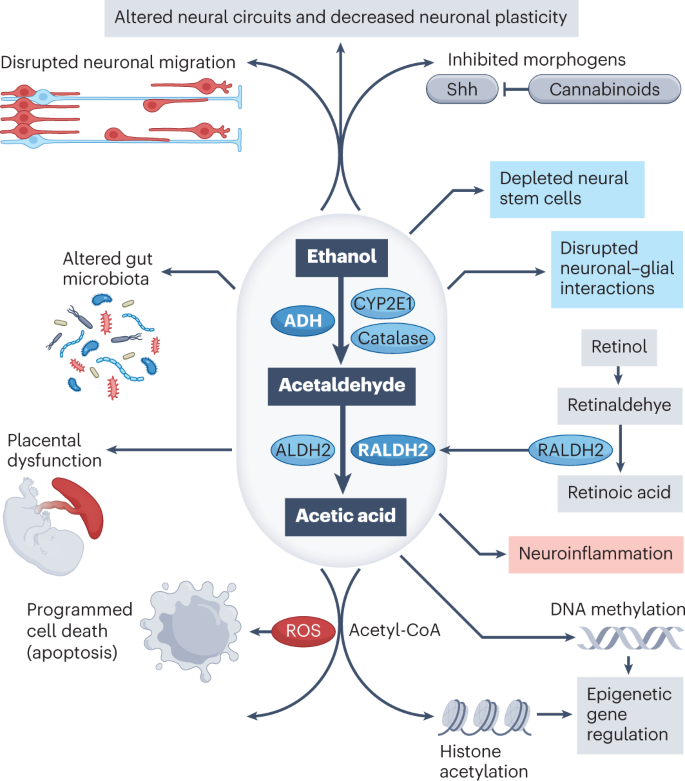
Alcohol (ethanol) metabolism to acetaldehyde and acetic acid generates reactive oxygen species (ROS) that induce programmed cell death. During gastrulation, acetaldehyde competes with retinaldehyde for metabolism by retinaldehyde dehydrogenase 2 (RALDH2), reducing the biosynthesis of retinoic acid, a critical morphogen. Acetyl-CoA, a metabolite of acetic acid, acetylates histones and, therefore, modifies gene expression. Alcohol also alters epigenetic gene regulation through changes in DNA methylation. Moreover, alcohol disrupts neuronal–glial interactions, induces inflammatory changes in the developing brain and causes microencephaly partly by depletion of neural stem cells. Other effects of alcohol include the disruption of Shh signalling (an effect that is potentiated by cannabinoids) and disrupted neuronal migration. The effects of alcohol on the placenta contribute to intrauterine growth retardation and adverse neurodevelopmental outcomes. Modification of gut microbiota by alcohol may influence brain development through the action of circulating microbial by-products. Collectively, these actions of alcohol result in altered neural circuits and decreased neuronal plasticity. ADH, alcohol dehydrogenase; ALDH2, aldehyde dehydrogenase.
Epigenetic changes and disrupted development
Epigenetic changes are chemical modifications (methylation or acetylation) to DNA and surrounding histones that influence gene expression and often occur in response to environmental exposures 118 , 119 . Normal development depends on numerous epigenetic changes in embryonic stem cells that facilitate their transition to fully differentiated and functional cell lineages such as neurons, muscle and fat cells 120 . Alcohol can disrupt development by inducing DNA methylation and histone acetylation in gene clusters and altering gene expression 121 . Epigenetic alterations resulting from PAE have been observed in animal models and humans, and these changes may be lifelong and inherited by future generations 118 , 122 , 123 , 124 . A pattern of DNA methylation in buccal epithelial cells was reasonably accurate (positive predictive value 90%; negative predictive value 78.6%) in discriminating children with FASD from typically developing controls or children with autism spectrum disorders 125 . Large replication studies in different populations are required before this approach might be considered for diagnostic purposes.
Brain injury
Exposure of astrocytes to alcohol and metabolism of alcohol by cytochrome P450 2E1 result in the production of damaging reactive oxygen species 84 , 126 . Alcohol is metabolized to acetaldehyde, a toxin that causes DNA damage, epigenetic gene regulation, mitochondrial and proteosome dysfunction, and altered cellular metabolism 127 , 128 , 129 . Metabolism of acetaldehyde to acetate and then to acetyl-CoA modifies gene expression in the brain via increased histone acetylation 121 (Fig. 5 ).
Disruption of morphogens and growth factors
Retinoic acid is a critical morphogen (a signalling molecule that alters cellular responses to modulate patterns of tissue development), and its deficiency causes craniofacial defects similar to those of FASD 127 , 130 . Retinol is oxidized to retinaldehyde, which is subsequently oxidized by retinaldehyde dehydrogenase 2 (RALDH2) to retinoic acid (Fig. 5 ). During gastrulation, RALDH2 is the predominant enzyme for acetaldehyde metabolism. Therefore, acetaldehyde and retinaldehyde compete for RALDH2, reducing the synthesis of retinoic acid and inducing a state of retinoic acid deficiency, thereby promoting craniofacial defects associated with PAE 127 , 130 .
Another critical morphogen, Shh, is a downstream target of retinoic acid 72 , 130 . Genetic abnormalities of the Shh pathway cause holoprosencephaly syndrome, which is associated with abnormal midline craniofacial and brain development similar to that of FASD 72 , 76 . Alcohol exposure in chick embryos decreases Shh expression and induces craniofacial dysmorphology and cranial neural crest cell death; viral vector-mediated expression of Shh rescues these effects 111 . Alcohol exposure during neurulation of the mouse rostroventral neural tube disrupts the function of cilia, which transduce Shh signals by modulating the expression of genes that regulate ciliogenesis, protein trafficking and stabilization of primary cilia 131 , 132 . The associated dysmorphology in zebrafish can be mitigated by activating downstream elements in the Shh signalling pathway 133 . Alcohol also decreases cellular stores of cholesterol, thereby reducing the covalent binding of cholesterol to Shh (which is necessary for Shh secretion and function) 72 , 134 . These findings suggest that alcohol causes a transient ciliopathy, secondarily disrupting Shh signalling within cilia and producing craniofacial and brain dysmorphology 131 .
Disruption of neuronal and glial migration
PAE is associated with macroscopic and microscopic evidence of impaired neuronal and glial migration, including heterotopias (collections of aberrantly migrated neurons). Heterotopias are associated with seizures, and seizures or abnormal EEG results are reported in up to 25% of individuals with FASD 135 . The L1 neural cell adhesion molecule regulates neuronal migration, axon fasciculation and pathfinding in the developing brain 136 . Mutations in L1CAM (which encodes L1) cause neurodevelopmental abnormalities such as those observed in FASD, including hydrocephalus, hypoplasia or agenesis of the corpus callosum, and dysplasia of the anterior cerebellar vermis 64 . Alcohol inhibits L1-mediated cell adhesion by binding to specific amino acids at a functionally important domain in the extracellular portion of L1 (ref. 137 ). The sensitivity of L1 to alcohol is regulated by phosphorylation, which promotes L1 association with the cytoskeleton 62 , 138 . Importantly, molecules that block alcohol inhibition of L1 adhesion prevent the teratogenic effects of alcohol in mouse embryos 62 , 139 .
GABAergic interneurons comprise the principal inhibitory network of the brain. Alcohol enhances GABA A receptor-mediated depolarization of migrating GABAergic interneurons through activation of L-type voltage-gated calcium channels, thereby accelerating tangential migration 63 . Dysfunction of GABAergic interneurons may impair inhibitory control of brain networks. In mice, PAE during corticogenesis also disrupts radial migration and pyramidal cell development in the somatosensory cortex, which could be linked to decreased tactile sensitivity during adolescence 140 .
Effects on neural stem cells
Effects of PAE on neural stem cells (NSCs) may contribute to reduced brain volume in individuals with FASD. Alcohol causes cell death in differentiated neural cells but not in NSCs; rather, PAE depletes NSCs by blocking their self-renewal and accelerating their transition into more mature neural progenitors and differentiation into astroglial lineages 141 . PAE also selectively upregulates gene expression for the calcium-activated potassium channel Kcnn2 in neural progenitor cells from the motor cortex, and Kcnn2 blockers in adult mice reduced motor learning deficits 142 . Alcohol may trigger the maturation of NSCs by increasing the release of selected microRNAs (miRNAs) from extracellular vesicles in NSCs and activating certain pseudogenes that encode non-protein-coding RNAs 141 , 143 . Proteomic analysis revealed selective enrichment of extracellular vesicles for RNA-binding and chaperone proteins in alcohol-exposed NSCs 144 .
Disruption of neuronal–glial interactions
Brain growth and development are dependent on neuronal–glial interactions 84 , 85 . PAE decreases the proliferation of radial glial cells partly by decreasing Notch1 and fibroblast growth factor 2 receptor signalling 145 . This altered signalling reduces the density and fasciculation of radial glial fibres, which serve as a scaffold for migrating neurons 85 , 145 . PAE perturbs the maturation of oligodendroglia in human fetal brains, increasing the expression of markers of early oligodendroglia progenitors (Oct4 and Nanog) and decreasing the expression of markers of mature oligodendroglia (Olig1, Olig2 and myelin basic protein) 146 . Alcohol also increases apoptosis to a greater extent in oligodendroglia than in neurons 146 , 147 . As myelination is mediated by oligodendroglia, apoptosis of these cells might partly account for the effects of PAE on white matter integrity. The associated upregulation of oligodendroglia-derived chemokines (CXCL1/GRO, IL-8, GCP2/CXCL6, ENA78 and MCP1) could also affect neuronal survival 146 . Astroglial apoptosis is mediated by acetaldehyde toxicity, reactive oxygen species, reductions in the antioxidant glutathione and inflammatory signalling 85 .
Neuroinflammation
PAE activates an inflammatory response in the developing nervous system. Alcohol stimulates the production of reactive oxygen species in microglia and astrocytes, leading to neuronal apoptosis 84 . Moreover, alcohol stimulates the production of pro-inflammatory cytokines (such as IL-1β and TNF) and chemokines (such as CCL2 and CXCL1) through enduring epigenetic modifications that sustain a chronic neuroinflammatory response 119 (Fig. 5 ). Unique networks of pro-inflammatory cytokines in serum from women in the second trimester of pregnancy are markers of PAE and adverse neurodevelopmental outcomes 148 . The persistence of pro-inflammatory cytokines in childhood could predispose to autoimmune and inflammatory conditions later in life 149 . Similarly, PAE may hypersensitize microglia to increased inflammatory signalling, leading to an enduring, heightened neuroinflammatory response 84 .
Gut microbiota alterations
PAE may cause enduring changes in the gut microbiota 150 , and there is increasing recognition of the interplay between gut microbes and nervous system development and function. In a mouse model of PAE, gut microbial metabolites were detected in maternal plasma, fetal liver and fetal brain 151 . Further research is required to determine how effects of PAE on the gut microbiota influence development and later health.
Placental effects
Not all developmental effects of PAE result from the direct actions of alcohol on the developing nervous system. A retrospective autopsy study reported placental abnormalities in 68% of individuals with PAE or FASD 88 . PAE in humans decreases placental weight, epigenetic marks, vasculature and metabolism 81 . PAE during the first 60 of 168 days of gestation in rhesus macaques caused diminished placental perfusion and ischaemic placental injury from middle to late gestation 152 . RNA sequencing analysis revealed activation of inflammatory and extracellular matrix responses. Rats with PAE demonstrate reduced nitric oxide-mediated uterine artery relaxation, potentially contributing to dysregulation of uterine blood flow and intrauterine growth retardation 153 . miRNA act by silencing RNA and modifying post-transcriptional regulation of gene expression. A cluster of 11 extracellular miRNA from serum of women in the second trimester of pregnancy was a marker of PAE and predicted adverse neurodevelopmental outcomes in Ukrainian and South African populations 154 , 155 . Injection of the same 11 miRNAs into pregnant mice decreased placental and fetal growth, suggesting that they mediate the adverse outcomes of PAE 156 .
Synergistic effects of alcohol and other substances
PAE is often associated with prenatal exposure to other drugs. Among 174 individuals with PAE, almost all had prenatal nicotine exposure 88 . Nicotine and alcohol synergistically decrease birthweight and increase the risk of sudden infant death syndrome 157 . The legalization of cannabis has led to increases in the combined use of cannabinoids and alcohol during pregnancy 158 . Alcohol and cannabinoids synergistically increase the frequency of ocular defects in mice by disrupting separate elements in the Shh signalling pathway 132 . PAE and opioids each affect neurodevelopment, raising the possibility of additive or synergistic effects 159 . Alcohol also disrupts the developing blood–brain barrier, exposing the developing CNS to drugs and toxins that are normally excluded 160 .
Diagnosis, screening and prevention
Diagnosis of fasd, principles of diagnosis.
Diagnosis of FASD requires assessment of PAE, neurodevelopmental function and physical features, including facial features (Fig. 6 ). Timely, accurate diagnosis of FASD is crucial to enable early intervention and improve outcomes 161 , but there is no diagnostic test, biomarker or specific neurodevelopmental phenotype for FASD. Ideally, assessment and diagnosis should be conducted by a multidisciplinary team (MDT) comprising paediatricians, neuropsychologists, speech pathologists, occupational therapists, physiotherapists and social workers, with access to psychiatrists and geneticists/dysmorphologists. However, this approach is expensive, time consuming and unavailable to many children worldwide. Often, children present first to family physicians, paediatricians and psychologists who lack sufficient expertise to confidently diagnose FASD. Thus, education and training are urgently needed to increase the capacity for recognition of FASD outside specialist FASD assessment services 51 , 162 and to address its underdiagnosis and misdiagnosis 163 , 164 .
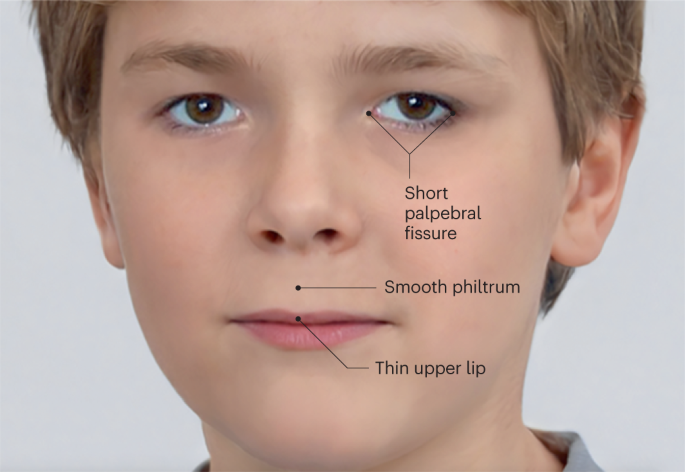
Fetal alcohol syndrome has three characteristic (sentinel) facial features: thin upper lip (with absent cupid bow), smooth philtrum (with absence of the normal midline vertical groove and lateral ridges extending from the base of the nose to the vermilion border of the upper lip) and short palpebral fissures (the space between the medial and lateral canthus of the open eye). Image created by Ria Chockalingam using an image from Generated Photos and modified with Adobe Photoshop.
Approaches to the diagnosis of FASD
The most commonly used diagnostic systems for FASD are the Collaboration on FASD Prevalence (CoFASP) Clinical Diagnostic Guidelines 10 , the University of Washington 4-Digit Diagnostic Code 165 , 166 and the Canadian Guidelines 167 (Table 1 ). The Canadian Guidelines have been adapted for use in Australia 168 and the UK 169 and are also used in New Zealand 170 . Guidelines have also been recommended by the US Centers for Disease Control and Prevention 171 , the State Agency for Prevention of Alcohol-Related Problems (PARPA) in Poland 172 , and The German Federal Ministry of Health 173 .
All diagnostic systems recommend evaluating PAE, facial and non-facial dysmorphology, and CNS structure and function using an MDT approach. Although all these systems recommend assessing otherwise unexplained prenatal and postnatal growth restriction, the Canadian and derivative guidelines exclude growth as a diagnostic criterion. The diagnostic systems differ in their definitions of PAE, thresholds for individual diagnostic elements, required combination of elements to confirm an FASD diagnosis and diagnostic classifications.
Diagnosis of FASD can be challenging. Confirmation of PAE by biological mothers during a diagnostic assessment of children with suspected FASD is often difficult: the topic is sensitive and recall bias is possible 174 . Additionally, many children live in foster or adoptive care, and obstetric records often lack details about PAE 80 . In these situations, clinicians should seek firsthand witness reports and child protection, justice and medical records. A standardized tool 175 , 176 , 177 should be used, when possible, to record the pattern of alcohol intake, either at an interview with the biological mother or using witness reports or records. A challenge in evaluating facial dysmorphology is the unavailability of suitable lip-philtrum guides and standards for palpebral fissure length (PFL) for many racial and ethnic groups, including Indigenous Australians 178 . PFL is the distance between the endocanthion and exocanthion of the eye (the inner (nasal) and outer points, respectively, where the upper and lower eyelids meet) and may be shortened following PAE. Because some domains of cognitive function cannot be evaluated in infants and young children, confirmation of brain dysfunction in this population may be based on global developmental delay, established using a validated tool 10 , 167 . FASD are diagnosed with increasing confidence in children aged 6 years and older, who are more cooperative in physical examinations, and in whom facial dysmorphology and neurocognitive function can be assessed with greater reliability using digital photography and standardized psychometric tests.
In the absence of a ‘gold standard’ for diagnosis of FASD, no diagnostic system may be considered superior. Each system has advantages and disadvantages, including its use in clinical and community settings and the sensitivity and specificity of diagnostic criteria. Diagnosis using these systems shows incomplete agreement 179 , 180 , 181 , confirming the need for a unified approach internationally (Table 1 and Supplementary Boxes 1 and 2 ).
A clinical diagnosis of FASD requires recognition of neurodevelopmental disabilities and a reproducible pattern of minor malformations (dysmorphic features), none of which are pathognomonic, and many of which overlap with other teratogenic or genetic disorders (phenocopies). Thus, a diagnosis of FASD is a diagnosis of exclusion that is made after considering and excluding other causes for the phenotype 10 , 167 . For example, prenatal exposure to teratogens, such as toluene, anticonvulsants or phenylalanine (when the mother has phenylketonuria), can result in dysmorphic features also observed in FASD 10 , 182 , 183 . Additionally, postnatal exposures (such as adverse childhood experiences (ACE)) can contribute to neurodevelopmental impairment, comorbidities (Box 1 ) and adverse ‘secondary’ outcomes (Box 2 ). Genetic conditions with dysmorphic features similar to FASD include Aarskog syndrome, blepharophimosis, ptosis, epicanthus inversus syndrome, CHARGE syndrome, de Lange syndrome, 22q11.2 deletion, Dubowitz syndrome, inverted duplication 15q, Noonan syndrome, Smith–Lemli–Opitz syndrome and Williams syndrome. Patients with intellectual disability without a recognizable pattern of anomalies may also share some dysmorphic features with FASD 10 , 182 . Thus, before establishing a diagnosis of FASD, it is important to ask whether the family history suggests a genetic disorder, whether other teratogenic exposures occurred during pregnancy and whether the patient has features not previously described in FASD. If so, referral to a clinical geneticist/dysmorphologist for evaluation is recommended. When indicated, genetic testing should include chromosome microarray analysis 184 , 185 and exclusion of Fragile X syndrome 186 as a minimum, and whole-exome sequencing should be performed if other genetic pathologies due to point mutations are suspected 10 , 187 . When PAE is confirmed and/or the physical and neurodevelopmental examinations are supportive, the diagnosis can be made by a paediatrician or other health professional familiar with FASD.
Neurobehavioural impairment accounts for the major functional disabilities associated with FASD. Although the Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM-5) 188 criteria for intellectual disability are not always met in patients with FASD, cognitive impairment is often identified and can affect multiple domains, including executive function, memory, mathematical and other academic skills, attention and visuospatial processing 80 , 189 . Poor social skills, inattention and impaired impulse control can adversely affect school and work performance and independent living.
Although no specific constellation of neurobehavioural deficits have been identified in FASD, some groups have attempted to characterize clusters of impairment associated with PAE 190 , 191 . One set of criteria, Neurodevelopmental Disorder associated with PAE, has been proposed as a condition for further study in the DSM-5 (ref. 188 ); it requires deficits in cognition, behaviour and social adaptation. The ICD-11, published in 2022, lists several ‘toxic or drug-related embryofetopathies’ (code LD2F.0) including ‘fetal alcohol syndrome’ (code LD2F.00) 192 . The confounding or potentiating influence of ACE presents a major challenge in identifying a specific neurobehavioural profile 193 .
Box 1 Common comorbidities in patients with fetal alcohol spectrum disorders
More than 400 comorbid conditions have been identified in individuals with fetal alcohol spectrum disorders, which span 18 of the 22 chapters of the ICD-10 (ref. 13 ), the most prevalent coming from the groups of:
Congenital malformations, deformations and chromosomal abnormalities (Chapter XVII) and Mental and behavioural disorders (Chapter V). Shown below are selected comorbid conditions (with codes) from Chapters V and XVII and diseases of the eye (Chapter VII) and ear (Chapter VIII). For more detailed information, see ref. 13 .
Chapter XVII. Congenital malformations, deformations and chromosomal abnormalities
Q02 Microcephaly
Q03 Congenital hydrocephalus
Q04.0 Congenital malformations of corpus callosum
Q04.3 Other reduction deformities of brain
Q04.6 Congenital cerebral cysts
Q04.8 Other specified congenital malformations of brain
Q04.9 Congenital malformation of brain, unspecified
Q05 Spina bifida
Q06.8 Other specified congenital malformations of spinal cord
Chapter V. Mental and behavioural disorders
F10.2 Mental and behavioural disorders due to use of alcohol, dependence syndrome
F19.2 Mental and behavioural disorders due to the use of multiple drugs and use of other psychoactive substances, dependence syndrome
F41.1/F33.8 Anxiety/depression
F80.1 Expressive language disorder
F80.2 Receptive language disorder
F81.9 Developmental disorder of scholastic skills, unspecified
F89 Unspecified disorder of psychological development
F90.0 Disturbance of activity and attention
F91 Conduct disorder
G40 Epilepsy/seizure disorder
Chapter VII. Diseases of the eye
H47.0 Disorders of optic nerve
H52.6 Refractive errors
H54 Visual impairment
Q10.0 Congenital ptosis
Q10.3 Other congenital malformations of eyelid
Q10.6 Other congenital malformations of lacrimal apparatus
Q11.2 Microphthalmos
Q12.0 Congenital cataract
Chapter VIII. Diseases of the ear
H65.0 Acute serous otitis media
H65.2 Chronic serous otitis media
H90.8 Mixed conductive and sensorineural hearing loss, unspecified
Box 2 Challenges for adolescents and adults with fetal alcohol spectrum disorders
Involvement in child welfare services (75%) 309
Disrupted school experiences due to learning and/or behavioural problems (61%) 267
Interaction with the justice system (30% 309 to 60% 267 )
Confinement (detention, prison, or psychiatric or alcohol/drug inpatient setting; 50%) 267
Substance use disorder: alcohol and other drugs (50%) 309
Inappropriate sexual behaviour (49%) 236 , 310
Increased risk of metabolic abnormalities (includes type 2 diabetes, low high-density lipoprotein, high triglycerides, and female-specific overweight and obesity) 311
Difficulties with independent living and trouble gaining and retaining employment (80%) 267
Mean life expectancy (34 years; 95% CI 31–37 years) is considerably lower than in the general population 275 ; leading causes of death are ‘external causes’ (44%), including suicide (15%), accidents (14%), poisoning by illegal drugs or alcohol (7%) and other external causes (7%)
Screening for alcohol use in pregnancy
Early detection of alcohol use during pregnancy can lead to decreased consumption, abstinence or decreased risk of alcohol use in subsequent pregnancies 22 , 194 . The early identification of alcohol use facilitates education about the harms of PAE, delivery of timely, office-based brief interventions, and referral to substance use treatment services if required. Reducing the high prevalence of FASD requires large-scale, population-based screening programmes to ensure that every pregnant woman is asked about alcohol use, with special attention to populations at high risk 22 , 195 , 196 (Table 2 ).
Screening for alcohol use during pregnancy is underused globally 197 , 198 . Barriers to screening include lack of public-health guidelines 199 or screening mandates, insufficient clinician training 200 , 201 , 202 , 203 , competing demands on clinician time, the cost of completing validated alcohol use screening questionnaires 204 , 205 , 206 , and the unavailability of clinically reliable biological markers for PAE. Even a single, clinician-directed question about alcohol use may reduce PAE 207 , 208 ; however, successful screening requires that practitioners understand the importance of preventing PAE and providing non-judgmental screening and brief interventions 196 . Preliminary evidence suggests that web-based or app-based mobile health interventions may mitigate patient stigma and reluctance to report alcohol use and might circumvent barriers related to clinician time constraints, training and motivation 209 . Similarly, mobile health approaches may reduce alcohol and substance use in the preconception, prenatal, and postnatal periods 209 and improve access to interventions for families in rural and remote settings. Empathic, compassionate support of abstinence during pregnancy may improve opportunities for treatment of substance use disorders 22 , 47 , 196 , 202 . Screening for alcohol and substance use should be repeated throughout pregnancy and equally across populations to avoid stigmatizing marginalized populations with selective screening 22 , 196 , 210 , 211 . People who screen positive should be directed to a well-developed management pathway for clinical care.
Prevention (Fig. 7 ) and treatment of alcohol and substance use disorders in pregnancy are central to the 2015 United Nations Sustainable Development Goals (SDG 3.5) 212 . The WHO recommends universal screening and intervention for alcohol use in pregnancy as a primary prevention strategy for FASD 22 , 213 . Prevention programmes should be evidence based and evaluated following implementation. A wide range of approaches has been deployed, including public awareness strategies, preconception interventions (such as preconception clinics and school-based FASD education), holistic support of women with substance use disorders, and postpartum support for new mothers and babies 214 , 215 . These approaches show promise in increasing awareness of FASD and decreasing alcohol use during pregnancy 216 ; however, the quality of supporting evidence is highly variable. Any primary prevention strategy must be underpinned by evidence-based policy and legislation intended to minimize harms from alcohol, including increased alcohol pricing and taxation, restrictions on advertising and promotion of alcohol, and restricted access to alcohol such as by limiting opening hours and the density of liquor outlets 217 . Public-health authorities agree that the alcohol industry should have no involvement in the development of public-health policies owing to their inherent conflict of interest 218 , 219 . The framework in Fig. 7 illustrates one approach that could be linked to national policy to address diverse aspects of population-based prevention of FASD.
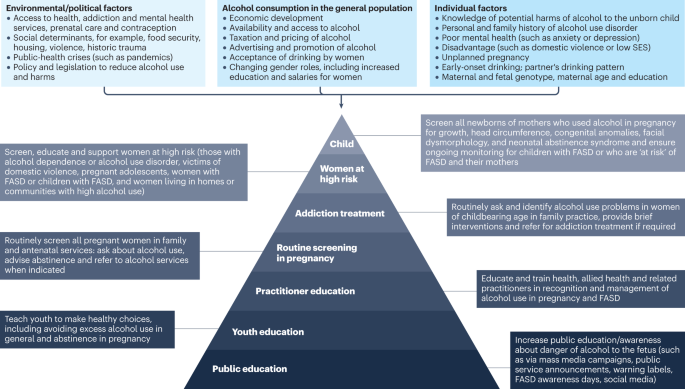
A hierarchy of strategies can be used to prevent fetal alcohol spectrum disorder (FASD), ranging from awareness campaigns for the whole population to health, educational and social support for women and children. The strategies are placed in the context of cultural, political and environmental factors that influence access to, use of and attitudes towards alcohol use in pregnant women. SES, socioeconomic status.
Level 1: raising public awareness through campaigns and other broad strategies
Public-health initiatives that promote and support women’s health, in general, may raise awareness about PAE/FASD. More specific measures include warning signs on alcohol products, pamphlets and public education programmes that encourage healthy, alcohol-free pregnancies 220 , 221 . However, evidence in support of these campaigns is preliminary 216 . Moreover, campaigns that use triggering imagery or blaming/shaming language (such as ‘FASD is 100% preventable’) can stigmatize and isolate pregnant women who use alcohol, particularly when paired with judgmental interventions 196 . Reframing alcohol use in pregnancy as a shared responsibility of women, partners, prenatal health-care providers, treatment programmes for substance use disorder, families, community and government may be helpful 222 .
Level 2: brief counselling with women and girls of reproductive age
Discussing alcohol use and its associated risks with women of childbearing age during preconception conversations about reproductive health is effective in preventing PAE and FASD 215 , primarily by improving contraception use 207 . Screening, Brief Intervention and Referral to Treatment (S-BIRT) for non-pregnant adolescent and adult women reduces the risk of PAE 207 , particularly following multi-session interventions 223 . Preliminary studies suggest that such interventions are also beneficial for Indigenous communities 224 , 225 .
Level 3: specialized prenatal support
Treatment for alcohol use during pregnancy may prevent ongoing PAE and decrease adverse infant outcomes 226 . The combination of case management by a social worker or nurse (including problem identification and preparation, implementation and monitoring of a health-care plan) and motivational interviewing (an evidence-based approach to facilitating behaviour change) reduce drinking by pregnant women at high risk 194 . Moreover, specialized, intensive home-visiting interventions for pregnant women at high risk improve maternal and child outcomes and are cost-effective in preventing new cases of FASD 227 , 228 . Improving maternal nutrition and reducing smoking and family violence may also improve child outcomes in current and future pregnancies 227 , 229 , 230 .
Level 4: specialized postnatal support
In the postpartum period, home-visiting of women at high risk by health professionals or lay supporters improves child outcomes and reduces the risk of PAE in future pregnancies 227 , 231 , 232 . Application of a FASD prevention framework requires consideration of local policy and practices. Best practice programmes support the needs of both the mother and child, recognizing the connections between women’s alcohol use, parenting, family influences and child development. Central to the effective implementation of prevention strategies is the establishment of strong cross-cultural and community partnerships and the embrace of cultural knowledge systems and leadership 233 . Mitigating stigma is vital while addressing the structural and systemic factors that promote prenatal alcohol consumption 35 .
Principles of management of FASD
The complex pathophysiology of FASD (Boxes 1 and 2 ) emphasizes the need for thorough, individualized assessment and treatment. Treatment plans should be culturally appropriate, consider the family and community context, and be developed in partnership with families and individuals with lived experience of FASD 234 , 235 .
Therapeutic approaches must be tailored to individual strengths and needs. For example, an individual who has experienced trauma but has normal intelligence and social and emotional skills requires a trauma-informed, emotion-focused approach. By contrast, an individual with cognitive deficits and poor social and emotional skills may require a more directed, psycho-educational approach or environmental modifications to support and prevent secondary outcomes of FASD such as poor academic performance or inability to obtain/maintain employment 236 .
Management involves multiple service providers and changing interventions across the lifespan. Treatment comprises interventions to anticipate the delivery of a newborn with PAE, prevention of exposure to ACE, home-visiting by a public-health nurse, referral to infant developmental services, vision and hearing screening, preschool speech and language therapy, school-based support for learning disorders, occupational and physical therapy, behavioural and psychological interventions, pharmacotherapy, vocational support, and support for independent living in adolescence and adulthood. Specialized medical or surgical interventions may be required for congenital anomalies and accompanying comorbidities. There remains limited evidence from high-quality trials to support specific interventions for FASD 237 , 238 .
Behaviour support
Several large-scale randomized controlled trials (RCTs) support specific developmental and psychological interventions for FASD in children but few high-quality studies have been conducted in adolescents and adults 237 .
Positive behaviour support 239 is supported by positive results from RCTs and underpins three interventions for FASD: GoFAR 240 , the Math Interactive Learning Experience (MILE) 241 and the Families Moving Forward programme 242 . Positive behaviour support strengthens skills that enhance success and satisfaction in social, academic, work and community settings while proactively preventing problem behaviours; maintaining family involvement is an important element 16 . Where available, these specialized programmes oblige therapists to prioritize treatment for individuals most likely to benefit. The GoFAR intervention (FAR is an acronym for Focus and plan, Act, and Reflect) promotes self-regulation and adaptive function using direct instruction, practice and feedback, and strategies for emotional and behavioural self-regulation 243 . Interventions such as GoFAR, which involve the child and parents in the context of real-life adaptive behavioural problems, improve daily living skills and attention 243 . The MILE intervention provides individualized mathematical instruction through interactive learning and environmental modifications and improves math knowledge and parent report of child behaviour problems 241 , 244 , 245 . Families Moving Forward helps parents reframe their child’s behaviour within a neurodevelopmental paradigm. Adaptation of this approach to an app-based platform may reduce barriers to care 242 .
Self-regulation and executive function
Most children with FASD have significant problems with executive function and self-regulation 189 . The ALERT programme, a 12-week manualized approach using sensory integration and cognitive behavioural strategies, aims to help children regulate their behaviour and address sensory challenges 246 in a home environment 247 , 248 but is less effective when delivered in schools 249 . ALERT programme training is available online but requires adaptation to the family and community context 249 .
Social skills
Interventions to improve social connections in children with FASD include the Children’s Friendship Training (CFT) 250 and the Families on Track programme 251 . CFT involves 12 weeks of social and friendship skill training for children with FASD and their parents; it improves social skills and decreases problem behaviours in children with FASD 250 . Similarly, the Families on Track programme increases emotional regulation and self-esteem and decreases anxiety and disruptive behaviour 251 . However, interventions such as CFT and Families on Track are not widely available, and barriers to their use include the need to adapt to cultural context 252 . International partnerships and sharing of expertise may increase accessibility to these interventions 252 .
Pharmacological interventions
Pharmacological interventions for FASD are widely used and include medications, such as cognitive enhancers, to treat core impairments and medications to treat comorbidities, including ADHD, anxiety, and arousal or sleep disorders 253 . Large RCTs evaluating their effectiveness in FASD are urgently needed.
Children with FASD and ADHD have a different pattern of neurocognitive and behavioural abnormalities than children with ADHD alone 254 , suggesting the need for a tailored therapeutic approach. Expert consensus approaches for the management of ADHD in FASD have been developed. Recommendations in the UK suggest the use of a dexamphetamine-based medication (rather than a methylphenidate-based medicine) for first-line treatment of ADHD in children and adults with FASD; however, research is needed to understand the basis of treatment responses 255 . Guanfacine XL or similar medications can be used in individuals with comorbidities such as autism spectrum disorders 255 . Algorithms have also been developed in Canada for the use of psychotropic medications in FASD 256 . Although based on clinical consensus, these strategies form the basis for future research 256 .
Preclinical trials suggest that choline supplements improve cognitive deficits following PAE but clinical data are limited 257 . A small, placebo-controlled RCT demonstrated that children who received choline supplementation had higher non-verbal intelligence and visual-spatial skills, better working memory and verbal memory, and fewer behavioural symptoms of ADHD at 4-year follow-up than children who received placebo 258 . Despite these positive results, choline supplementation is not routinely recommended for children with FASD due to a lack of strong evidence for its effectiveness.
The role of exposure to adversity
A relationship between PAE and ACE is well established, and both may influence the life course in FASD 193 . Comprehensive neuropsychological assessment and MRI show that PAE accounts for the largest proportion of the variance in regional brain size and brain function in children with both exposures 259 . Furthermore, PAE imparts more risk for adverse outcomes than ACE in individuals with PAE in adoptive care 260 . However, adversity does affect the developmental trajectory and ACE are associated with maladaptive problems in children with FASD 261 . For example, school-age children with FASD and ACE are particularly vulnerable to language and social communication deficits 262 , which are hypothesized to result from the additive effect of prenatal and postnatal environmental exposures. This emphasizes the need for an individualized approach to treatment for individuals with life trauma and FASD.
Attempts have been made to understand the individual and combined effects of PAE and postnatal events on individual behaviours in FASD 263 . One model of complex trauma (Supplementary Fig. 1 ) displays neurodevelopmental variation as a complex interplay between prenatal and postnatal events and improves understanding of their interactions and association with outcomes. Child maltreatment viewed through a neurodevelopmental lens highlights the benefit of a sequential model of therapeutics rather than a focus on specific therapeutic techniques 264 .
Supplementary Fig. 1 highlights how vulnerabilities may present, whereas Supplementary Fig. 2 identifies methods to manage the same vulnerabilities based on understanding the individual and using anticipatory interventions to support development. Box 3 contains some useful resources on FASD for professionals and parents.
Box 3 Resources on alcohol use in pregnancy and fetal alcohol spectrum disorders
Australian guidelines to reduce health risks from drinking alcohol
Canada No. 245 — Alcohol Use and Pregnancy Consensus Clinical Guidelines 312
Centers for Disease Control and Prevention
Collaborative Initiative on Fetal Alcohol Spectrum Disorders (CIFASD)
Fetal Alcohol Spectrum Disorders (FASD) — American Academy of Pediatrics
FASD Hub Australia
FASD United
FASD — Care Action Network
Learning with FASD
National Organization for FASD Australia (NOFASD)
National Institute for Health and Care Excellence UK. Quality Standard QS204. FASD
National Institute on Alcohol Abuse and Alcoholism. Fetal Alcohol Exposure
Pan American Health Organization. Assessment of Fetal Alcohol Spectrum Disorders (2020) 313
The European FASD Alliance
WHO. Guidelines for identification and management of substance use and substance use disorders in pregnancy (2014) 22
Quality of life
Few published studies address QOL in individuals with FASD. One systematic review and meta-analysis identified more than 400 comorbid conditions among individuals with FASD, spanning 18 of 22 chapters of the ICD-10 (ref. 13 ). The most prevalent conditions were within the chapters of “Congenital malformations, deformations, and chromosomal abnormalities” (Chapters Q00–Q99; 43%) and “Mental and behavioural disorders” (Chapters F00–F99; 18%). Comorbid conditions with the highest pooled prevalence (50–91%) included abnormal functional studies of the peripheral nervous system and special senses, conduct disorder, receptive and expressive language disorders, and chronic serous otitis media 13 . Other studies report a high prevalence of vision and hearing problems among people with FASD 265 , 266 . All of these comorbid conditions affect the function and QOL of individuals with FASD and their families (Box 1 ).
Neurodevelopmental impairments may lead to lifelong ‘secondary’ disabilities, including academic failure, substance abuse, mental health problems, contact with law enforcement and inability to live independently or obtain/maintain employment 267 (Box 2 ). These conditions adversely affect QOL and require health, remedial education and correctional, mental health, social, child protection, developmental, vocational and disability services across the lifespan 17 , 268 , 269 . Lack of societal understanding of FASD is a barrier to addressing these secondary disabilities 16 , 270 .
A shift from a deficit-based to a strength-based management approach emphasizes the need to harness the abilities of individuals with FASD to improve their QOL and well-being. A review of 19 studies exploring the lived experience of people with FASD highlighted their strengths, including self-awareness, receptiveness to support, capacity for human connection, perseverance and hope for the future 271 . The lack of accessible, FASD-informed services perpetuates a deficit-based model.
Longitudinal cohort studies of FASD consistently show that adverse outcomes are more likely where support services are lacking. These studies are limited by selection bias and are based on cohorts with severe deficits rather than population-based cohorts receiving adequate support 267 , 270 . Nevertheless, they suggest the potential to modify developmental trajectories by addressing postnatal environmental exposures and opportunities. To address QOL, future studies should better articulate outcomes of interest for individuals and families living with FASD 272 .
FASD is associated with an increased risk of premature death of affected individuals, their siblings and mothers 273 , 274 . One study reported a mean age at death of 34 years for individuals with FASD 275 . Individuals with FASD have nearly fivefold higher mortality risk than people of the same age and year of death, and nearly half of all deaths occur in young adults 276 . In childhood, the leading causes of death in FASD are congenital malformations of the CNS, heart or kidney, sepsis, cancer, and sudden infant death syndrome, and more than half of deaths (54%) occur in the first year of life 277 . In the USA, >29% of adolescent males with FASD reported a serious suicide attempt, which is >19-fold higher than the national average 236 , 278 .
Among children and adolescents with FASD, the mortality rate of siblings with and without FASD is 114 per 1,000, which is approximately sixfold higher than among age-matched controls 273 . Furthermore, mothers of children with FASD have a 44.8-fold increased mortality risk compared with mothers of children without FASD 274 .
Caregiver burden
The complexity of parenting a child with FASD increases across adolescence and young adulthood. Caregivers of children with FASD experience increased burden, levels of stress and feelings of isolation 279 , 280 . The lifelong challenges and unmet needs of caregivers negatively affect family functioning and QOL 281 .
Early recognition of FASD and early emphasis on the prevention of secondary disabilities may decrease demands on families. Moreover, a diagnosis of FASD may indicate the need for specific interventions and parenting supports such as respite care, peer-support groups, treatment for parental alcohol misuse and education of other professionals who care for people with FASD.
FASD are the most common preventable cause of neurodevelopmental impairment and congenital anomalies 164 . These disorders are the legacy of readily available alcohol and societal tolerance to its widespread use, including during pregnancy. FASD affect all strata of society, with enormous personal, social and economic effects across the lifespan.
Diagnostic challenges
The greatest global challenges in the clinical management of FASD are the paucity of resources for diagnosis and treatment and the large number of affected individuals 163 . A substantial increase in resources is required, both for centres of expertise with MDTs and to build diagnostic capacity among non-specialist health services. However, this alone will not bridge the gap in services for children and adults, and a paradigm shift is needed. This might include recognition of the important role of primary care providers and use of new technologies such as app-based screening, diagnostic and treatment tools. Telehealth services will reduce the need for face-to-face care 282 and tele-education could build clinician awareness and skills, especially in rural and remote areas 283 . However, in many low-income and middle-income countries, this technology is not widely available.
Without a definitive diagnostic test, a clinical diagnosis of FASD must be made. Diagnosis is facilitated by identification of PAE in association with neurodevelopmental impairment, with or without specific craniofacial dysmorphology, and exclusion of alternative diagnoses. Many clinicians fail to document alcohol use in pregnancy or PAE in children, highlighting the need for enhanced training, standardized tools to document PAE and, especially, routine screening for alcohol use before and during pregnancy. Biomarkers for PAE are urgently needed because many children with FASD live in out-of-home care and reliable PAE histories are frequently unavailable. Although biomarkers for PAE (such as fatty acid ethyl esters, ethyl glucuronide and phosphatidylethanol) are identifiable in maternal hair, blood and meconium, their clinical use is limited, and testing may be costly or unavailable 284 . Identification of miRNAs from women in the second trimester and epigenetic signatures in placental and infant tissue hold promise as biomarkers for PAE and hence for risk of abnormal neurodevelopment 154 , 155 , 156 , 187 ; however, further research is required before their use becomes routine in clinical practice 81 , 125 .
Accessible e-health technologies to facilitate the diagnosis of FASD are under development. For example, 3D facial imaging may facilitate diagnosis by automatically quantifying the three sentinel facial features of FASD and identifying more subtle facial dysmorphology that reflects PAE after gastrulation 67 , 285 . The use and availability of 3D imaging will increase as more sophisticated and cheaper 3D cameras evolve and image capture on smartphones combined with cloud-based image analysis become available. Similarly, web-based tools are in development for identification of neurocognitive impairments associated with FASD. BRAIN-online enables screening for cognitive and behavioural features of PAE or FASD 286 . Decision trees simplify neurocognitive testing by including only tests that contribute most to the diagnosis of FASD 287 . Porting this software to tablets or online websites will broaden access to relevant neurocognitive testing. For example, the FASD-Tree 288 provides a dichotomous indication and a risk score for FASD, considering both neurobehaviour and dysmorphology, and successfully discriminates between children with and without PAE with a high predictive value 289 .
The lack of internationally agreed diagnostic criteria for FASD is challenging and hinders the comparison of prevalence and clinical outcomes between studies. In response, the National Institute on Alcohol Abuse and Alcoholism (NIAAA) has convened an international consensus committee to analyse data derived from existing diagnostic systems and develop a consensus research classification for FASD 290 . The field would also benefit from improved, population-based, normative data for growth and PFL as well as internationally accepted definitions of a standard drink and of the ‘low, moderate and high’ levels of risk of PAE. Additionally, the range and aetiology of adult outcomes require clarification to inform assessment and prognosis in FASD 291 . A research initiative for elderly people with FASD is urgently needed as there is virtually no information about the diagnostic criteria or neuropsychological outcomes of FASD in this age group.
Understanding pathophysiology
Functional MRI can be used to elucidate brain growth trajectories and disruptions to neuronal pathways after PAE (including low-level PAE), thereby assisting our understanding of CNS dysfunction in FASD 68 . Advances in our understanding of the genetics of rare neurodevelopmental disorders may identify genes that govern susceptibility or resilience to PAE and provide additional insights into the pathogenesis of FASD 187 . Advances in neuroscience research, including novel preclinical studies, may help elucidate the relationship between PAE-induced brain dysfunction and the FASD phenotype and inform therapeutics and prevention 292 .
Prevention and management
Preclinical studies suggest that epigenetic changes induced by PAE underpin metabolic, immunological, renal and cardiac disorders in FASD 13 , but further studies in patients are required to confirm this. The paucity of high-quality evidence to inform the treatment of neurodevelopmental impairments and comorbidities associated with FASD across the lifespan requires urgent redress 237 , 238 . Behavioural, family-based, school-based and pharmacological treatments require evaluation through multicentre RCTs. Moreover, little attention has been paid to preventing and managing the secondary outcomes of FASD in adults: substance use, mental health disorders, contact with the justice system, and issues with sleep, sexuality and violence. These must be prioritized to improve the QOL of individuals and reduce the societal and economic effects of FASD.
The COVID-19 pandemic demonstrated the use of telemedicine for virtual neuropsychiatric assessment and delivery of therapy 282 . Telemedicine approaches may also partly fill the need to increase health professionals’ capacity for FASD-informed care and to help education, child protection and justice professionals to recognize and understand FASD 283 .
Improving the primary prevention of alcohol use in pregnancy and hence FASD is also warranted 237 , 238 . Alcohol consumption and binge drinking are increasing among women of childbearing age in many countries, particularly in the most populous countries such as China and India 26 . This rise reflects increased availability of alcohol, societal acceptance of drinking among women, shifting gender roles, increasing income of women, and targeted marketing of alcohol to women and predicts a future global increase in FASD prevalence. Alcohol use in adolescence predicts subsequent use during pregnancy, and family physicians can play a role in identifying young women at risk 293 .
Another concern is that a large proportion of pregnancies globally are unplanned 29 , which can result in unintentional exposure of the embryo to PAE in the earliest stages of pregnancy. Accordingly, effective and cost-effective population-based preventive strategies should be adapted such as those promoted by the WHO in their Global Action Plan for the Prevention and Control of NCDs 294 and their Global Strategy to Reduce the Harmful Use of Alcohol 295 .
Although the role of national guidelines, community education and family support is important, these efforts must be underpinned by strategies proven to drive behavioural change and reduce alcohol harm, including legislated restrictions on the advertising and promotion of alcohol, appropriate taxation and pricing, and limited access to alcohol through restricted liquor outlets and opening hours and community-initiated alcohol restrictions 26 , 295 .
In pregnant women with ongoing alcohol consumption, food supplementation with folic acid, selenium, DHA, L-glutamine, boric acid or choline may reduce the effects of PAE 87 , 296 . However, research is required to define optimal levels of nutritional supplementation for pregnancy. Women who consume large amounts of alcohol often have iron deficiency, which increases the risk of FASD, and iron supplementation may be valuable 297 . Although novel in utero therapies with potential to prevent harm from PAE have been explored in preclinical models, none have been proven safe or effective in human RCTs 298 , 299 , 300 , 301 , 302 , 303 , 304 , 305 , 306 , 307 . Candidate therapies include agents that reduce ethanol-induced oxidative stress, cerebral neuronal apoptosis, growth deficits and structural anomalies caused by PAE 308 .
Future research should be collaborative and informed by people living with FASD and their families. FASD is a lifelong condition and information must be sought about adult patients, including the elderly. Further understanding of the pathophysiology underpinning the teratogenic and neurotoxic effects of PAE is required to inform prevention and management. Moreover, novel diagnostic tools and treatments must be rigorously tested, and new approaches are needed to reduce stigma, improve the QOL of people with FASD and prevent FASD in future generations.
Gellius, A. & Beloe, W. The Attic Nights of Aulus Gellius (Johnson, J., 1795).
Goodwin, W. W. (ed.) Plutarch’s Morals (Little & Brown, 1871).
Lemoine, P., Harousseau, H., Borteyru, J. P. & Menuet, J. C. Children of alcoholic parents: observed anomalies: discussion of 127 cases. Ouest Med. 8 , 476–482 (1968). This article describes FAS, beginning the modern era of understanding of the impact of PAE on development.
Google Scholar
Jones, K., Smith, D., Ulleland, C. & Streissguth, A. Pattern of malformation in offspring of chronic alcoholic mothers. Lancet 301 , 1267–1271 (1973). This article describes FAS, beginning the modern era of understanding of the impact of PAE on development.
Article Google Scholar
Jones, K. & Smith, D. Recognition of the fetal alcohol syndrome in early infancy. Lancet 302 , 999–1001 (1973). This article describes FAS, beginning the modern era of understanding of the impact of PAE on development.
Article CAS PubMed Google Scholar
Warren, K. R. & Hewitt, B. G. Fetal alcohol spectrum disorders: when science, medicine, public policy, and laws collide. Dev. Disabil. Res. Rev. 15 , 174 (2009).
Brown, J. M., Bland, R., Jonsson, E. & Greenshaw, A. J. A brief history of awareness of the link between alcohol and fetal alcohol spectrum disorder. Can. J. Psychiatr. 64 , 164–168 (2019).
Armstrong, E. M. & Abel, E. L. Fetal alcohol syndrome: the origins of a moral panic. Alcohol Alcohol. 35 , 276–282 (2000).
Sulik, K. K., Johnston, M. C. & Webb, M. A. Fetal alcohol syndrome: embryogenesis in a mouse model. Science 214 , 936–938 (1981). This article demonstrates the replicability of the sentinel facial characteristics of FASD in a mouse model of PAE and the importance of the timing of PAE in determining dysmorphology.
Hoyme, H. E. et al. Updated clinical guidelines for diagnosing fetal alcohol spectrum disorders. Pediatrics 138 , e20154256 (2016).
Article PubMed PubMed Central Google Scholar
Bertrand, J. et al. Fetal Alcohol Syndrome: Guidelines for Referral and Diagnosis. Report by National Task Force on FAS & FAE (Centers for Disease Control and Prevention, 2004).
Popova, S., Lange, S., Shield, K., Burd, L. & Rehm, J. Prevalence of fetal alcohol spectrum disorder among special subpopulations: a systematic review and meta‐analysis. Addiction 114 , 1150–1172 (2019).
Popova, S. et al. Comorbidity of fetal alcohol spectrum disorder: a systematic review and meta-analysis. Lancet 387 , 978–987 (2016).
Article PubMed Google Scholar
Cook, J. C., Lynch, M. E. & Coles, C. D. Association analysis: fetal alcohol spectrum disorder and hypertension status in children and adolescents. Alcohol Clin. Exp. Res. 43 , 1727–1733 (2019).
Popova, S. et al. Population-based prevalence of fetal alcohol spectrum disorder in Canada. BMC Public Health https://doi.org/10.1186/s12889-019-7213-3 (2019).
Phillips, N. L. et al. Impact of fetal alcohol spectrum disorder on families. Arch. Dis. Child. 107 , 755–757 (2022).
Popova, S., Lange, S., Burd, L. & Rehm, J. The economic burden of fetal alcohol spectrum disorder in Canada in 2013. Alcohol Alcohol. 51 , 367–375 (2016).
Popova, S., Stade, B., Bekmuradov, D., Lange, S. & Rehm, J. What do we know about the economic impact of fetal alcohol spectrum disorder? A systematic literature review. Alcohol Alcohol. 46 , 490–497 (2011).
Charness, M. E., Riley, E. P. & Sowell, E. R. Drinking during pregnancy and the developing brain: Is any amount safe? Trends Cogn. Sci. 20 , 80–82 (2016).
Centers for Disease Control and Prevention. Advisory on Alcohol Use During Pregnancy. A 2005 Message to women from the US Surgeon General (CDC, 2005).
Graves, L. et al. Guideline no. 405: Screening and counselling for alcohol consumption during pregnancy. J. Obstet. Gynaecol. Can. 42 , 1158–1173.e1 (2020).
World Health Organization. Guidelines for the Identification and Management of Substance Use and Substance Use Disorders in Pregnancy (World Health Organization, 2014).
National Health and Medical Research Council. Australian Guidelines to Reduce Health Risks from Drinking Alcohol (Australian Research Council and Universities Australia, Commonwealth of Australia, 2020).
Popova, S., Lange, S., Probst, C., Gmel, G. & Rehm, J. Estimation of national, regional, and global prevalence of alcohol use during pregnancy and fetal alcohol syndrome: a systematic review and meta-analysis. Lancet Glob. Health 5 , e290–e299 (2017). Presents the epidemiology of PAE and FAS.
Popova, S., Lange, S., Probst, C., Gmel, G. & Rehm, J. Global prevalence of alcohol use and binge drinking during pregnancy, and fetal alcohol spectrum disorder. Biochem. Cell Biol. 96 , 237–240 (2018).
World Health Organization. Global Status Report on Alcohol and Health, 2018 (World Health Organization, 2018).
Lange, S., Probst, C., Rehm, J. & Popova, S. Prevalence of binge drinking during pregnancy by country and World Health Organization region: systematic review and meta-analysis. Reprod. Toxicol. 73 , 214–221 (2017).
Green, P. P., McKnight-Eily, L. R., Tan, C. H., Mejia, R. & Denny, C. H. Vital signs: alcohol-exposed pregnancies — United States, 2011-2013. MMWR Morb. Mortal. Wkly Rep. 65 , 91–97 (2016).
Sedgh, G., Singh, S. & Hussain, R. Intended and unintended pregnancies worldwide in 2012 and recent trends. Stud. Fam. Plann. 45 , 301–314 (2014).
Muggli, E. et al. “Did you ever drink more?” A detailed description of pregnant women’s drinking patterns. BMC Public Health 16 , 683 (2016).
McCormack, C. et al. Prenatal alcohol consumption between conception and recognition of pregnancy. Alcohol Clin. Exp. Res. 41 , 369–378 (2017).
Fitzpatrick, J. P. et al. Prevalence and patterns of alcohol use in pregnancy in remote western Australian communities: the Lililwan project. Drug Alcohol Rev. 34 , 329–339 (2015).
Petersen Williams, P., Jordaan, E., Mathews, C., Lombard, C. & Parry, C. D. Alcohol and other drug use during pregnancy among women attending midwife obstetric units in the cape metropole, South Africa. Adv. Prev. Med. 2014 , 871427 (2014).
Allen, L. et al. Pregnant and early parenting Indigenous women who use substances in Canada: a scoping review of health and social issues, supports, and strategies. J. Ethn. Subst. Abus. https://doi.org/10.1080/15332640.2022.2043799 (2022).
Gonzales, K. L. et al. An indigenous framework of the cycle of fetal alcohol spectrum disorder risk and prevention across the generations: historical trauma, harm and healing. Ethn. Health 26 , 280–298 (2021).
Mulat, B., Alemnew, W. & Shitu, K. Alcohol use during pregnancy and associated factors among pregnant women in sub-Saharan Africa: further analysis of the recent demographic and health survey data. BMC Pregnancy Childbirth 22 , 361 (2022).
Singal, D. et al. Prenatal care of women who give birth to children with fetal alcohol spectrum disorder in a universal health care system: a case–control study using linked administrative data. CMAJ Open 7 , E63 (2019).
Esper, L. H. & Furtado, E. F. Identifying maternal risk factors associated with fetal alcohol spectrum disorders: a systematic review. Eur. Child Adolesc. Psychiatry 23 , 877–889 (2014).
Popova, S., Dozet, D., O’Hanlon, G., Temple, V. & Rehm, J. Maternal alcohol use, adverse neonatal outcomes and pregnancy complications in British Columbia, Canada: a population-based study. BMC Pregnancy Childbirth 21 , 74 (2021).
Poole, N. in Fetal Alcohol Spectrum Disorder: Management and Policy Perspectives of FASD Ch. 9 (eds Riley, E. P., Clarren, S., Weinberg, J. & Jonsson, E.) 161–173 (Weily, 2010).
May, P. A. et al. Prevalence and characteristics of fetal alcohol spectrum disorders. Pediatrics 134 , 855–866 (2014).
Skagerstróm, J., Chang, G. & Nilsen, P. Predictors of drinking during pregnancy: a systematic review. J. Womens Health 20 , 91–913 (2011).
Colvin, L., Payne, J., Parsons, D., Kurinczuk, J. J. & Bower, C. Alcohol consumption during pregnancy in nonindigenous west Australian women. Alcohol Clin. Exp. Res. 31 , 276–284 (2007).
Hutchinson, D. et al. Longitudinal prediction of periconception alcohol use: a 20-year prospective cohort study across adolescence, young adulthood and pregnancy. Addiction 117 , 343–353 (2022).
Peadon, E. et al. Attitudes and behaviour predict women’s intention to drink alcohol during pregnancy: the challenge for health professionals. BMC Public Health 11 , 584 (2011).
Australian Institute of Health and Welfare. National Drug Strategy Household Survey 2016: Detailed Findings (Australian Institute of Health and Welfare, 2017).
Tsang, T. W. et al. Predictors of alcohol use during pregnancy in Australian women. Drug Alcohol Rev. 41 , 171–181 (2022).
Lange, S. et al. Global prevalence of fetal alcohol spectrum disorder among children and youth: a systematic review and meta-analysis. JAMA Pediatr. 171 , 948–956 (2017). Presents the epidemiology of FASD.
Parker, S. E. et al. Updated national birth prevalence estimates for selected birth defects in the United States, 2004-2006. Birth Defects Res. A Clin. Mol. Teratol. 88 , 1008–1016 (2010).
Zablotsky, B. et al. Prevalence and trends of developmental disabilities among children in the United States: 2009-2017. Pediatrics https://doi.org/10.1542/peds.2019-0811 (2019).
Popova, S., Dozet, D. & Burd, L. Fetal alcohol spectrum disorder: can we change the future? Alcohol Clin. Exp. Res. 44 , 815–819 (2020).
Mena, M., Navarrete, P., Avila, P., Bedregal, P. & Berríos, X. Alcohol drinking in parents and its relation with intellectual score of their children. Rev. Med. Chile 121 , 98–105 (1993).
CAS PubMed Google Scholar
Landgren, M., Svensson, L., Strömland, K. & Grönlund, M. A. Prenatal alcohol exposure and neurodevelopmental disorders in children adopted from eastern Europe. Pediatrics 125 , e1178–e1185 (2010).
Colom, J. et al. Prevalence of fetal alcohol spectrum disorders (FASD) among children adopted from eastern European countries: Russia and Ukraine. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph18041388 (2021).
Kuzmenkovienė, E., Prasauskienė, A. & Endzinienė, M. The prevalence of fetal alcohol spectrum disorders and concomitant disorders among orphanage children in Lithuania. J. Popul. Ther. Clin. Pharmacol. 19 , e423 (2012).
Bower, C. et al. Fetal alcohol spectrum disorder and youth justice: a prevalence study among young people sentenced to detention in Western Australia. BMJ Open 8 , e019605 (2018).
Fast, D. K., Conry, J. & Loock, C. A. Identifying fetal alcohol syndrome among youth in the criminal justice system. J. Dev. Behav. Pediatr. 20 , 370–372 (1999).
Bell, C. & Chimata, R. Prevalence of neurodevelopmental disorders among low-income African Americans at a clinic on Chicago’s south side. Psychiatr. Serv. 66 , 539–542 (2015).
Fitzpatrick, J. P. et al. Prevalence and profile of neurodevelopment and fetal alcohol spectrum disorder (FASD) amongst Australian aboriginal children living in remote communities. Res. Dev. Disabil. 65 , 114–126 (2017).
Legonkova, S. V. Clinical and Functional Characteristics of Fetal Alcohol Syndrome in Early Childhood [Russian] Thesis, St. Peterburg’s State Paediatric Medical Academy (2011).
Heller, M. & Burd, L. Review of ethanol dispersion, distribution, and elimination from the fetal compartment. Birth Defects Res. A Clin. Mol. Teratol. 100 , 277–283 (2014).
Dou, X., Lee, J. Y. & Charness, M. E. Neuroprotective peptide NAPVSIPQ antagonizes ethanol inhibition of L1 adhesion by promoting the dissociation of L1 and Ankyrin-G. Biol. Psychiatry 87 , 656–665 (2020).
Lee, S. M., Yeh, P. W. L. & Yeh, H. H. L-type calcium channels contribute to ethanol-induced aberrant tangential migration of primordial cortical GABAergic interneurons in the embryonic medial prefrontal cortex. eNeuro https://doi.org/10.1523/eneuro.0359-21.2021 (2022).
Ramanathan, R., Wilkemeyer, M. F., Mittal, B., Perides, G. & Charness, M. E. Alcohol inhibits cell-cell adhesion mediated by human L1. J. Cell Biol. 133 , 381–390 (1996).
Kalinowski, A. & Humphreys, K. Governmental standard drink definitions and low-risk alcohol consumption guidelines in 37 countries. Addiction 111 , 1293–1298 (2016).
Cuzon, V. C., Yeh, P. W., Yanagawa, Y., Obata, K. & Yeh, H. H. Ethanol consumption during early pregnancy alters the disposition of tangentially migrating GABAergic interneurons in the fetal cortex. J. Neurosci. 28 , 1854–1864 (2008).
Article CAS PubMed PubMed Central Google Scholar
Muggli, E. et al. Association between prenatal alcohol exposure and craniofacial shape of children at 12 months of age. JAMA Pediatr. 171 , 771–780 (2017). Shows the potential of 3D imaging in identifying individuals with FASD and PAE.
Long, X. & Lebel, C. Evaluation of brain alterations and behavior in children with low levels of prenatal alcohol exposure. JAMA Netw. Open 5 , e225972 (2022).
Lees, B. et al. Association of prenatal alcohol exposure with psychological, behavioral, and neurodevelopmental outcomes in children from the adolescent brain cognitive development study. Am. J. Psychiatry 177 , 1060–1072 (2020).
Lebel, C. et al. A longitudinal study of the long-term consequences of drinking during pregnancy: heavy in utero alcohol exposure disrupts the normal processes of brain development. J. Neurosci. 32 , 15243–15251 (2012).
Kar, P. et al. Trajectories of brain white matter development in young children with prenatal alcohol exposure. Hum. Brain Mapp. https://doi.org/10.1002/hbm.25944 (2022).
Eberhart, J. K. & Parnell, S. E. The genetics of fetal alcohol spectrum disorders. Alcohol Clin. Exp. Res. 40 , 1154–1165 (2016).
Kaminen-Ahola, N. Fetal alcohol spectrum disorders: genetic and epigenetic mechanisms. Prenat. Diagn. 40 , 1185–1192 (2020).
Astley Hemingway, S. J. et al. Twin study confirms virtually identical prenatal alcohol exposures can lead to markedly different fetal alcohol spectrum disorder outcomes-fetal genetics influences fetal vulnerability. Adv. Pediatr. Res. https://doi.org/10.24105/apr.2019.5.23 (2018).
McCarthy, N. et al. Pdgfra protects against ethanol-induced craniofacial defects in a zebrafish model of FASD. Development 140 , 3254–3265 (2013).
Kietzman, H. W., Everson, J. L., Sulik, K. K. & Lipinski, R. J. The teratogenic effects of prenatal ethanol exposure are exacerbated by sonic hedgehog or GLI2 haploinsufficiency in the mouse. PLoS ONE 9 , e89448 (2014).
Cobben, J. M. et al. DNA methylation abundantly associates with fetal alcohol spectrum disorder and its subphenotypes. Epigenomics 11 , 767–785 (2019).
Ernst, A. M. et al. Prenatal and postnatal choline supplementation in fetal alcohol spectrum disorder. Nutrients https://doi.org/10.3390/nu14030688 (2022).
Smith, S. M. et al. Polymorphisms in SLC44A1 are associated with cognitive improvement in children diagnosed with fetal alcohol spectrum disorder: an exploratory study of oral choline supplementation. Am. J. Clin. Nutr. 114 , 617–627 (2021).
Wozniak, J. R., Riley, E. P. & Charness, M. E. Clinical presentation, diagnosis, and management of fetal alcohol spectrum disorder. Lancet Neurol. 18 , 760–770 (2019). Outlines the key neurodevelopmental characteristics in children with PAE and FASD.
Steane, S. E. et al. Prenatal alcohol consumption and placental outcomes: a systematic review and meta-analysis of clinical studies. Am. J. Obstet. Gynecol. 225 , 607.e1–607.e22 (2021).
Gårdebjer, E. M. et al. Effects of periconceptional maternal alcohol intake and a postnatal high-fat diet on obesity and liver disease in male and female rat offspring. Am. J. Physiol. Endocrinol. Metab. 315 , E694–E704 (2018).
Lipinski, R. J. et al. Ethanol-induced face-brain dysmorphology patterns are correlative and exposure-stage dependent. PLoS ONE 7 , e43067 (2012).
Kane, C. J. M. & Drew, P. D. Neuroinflammatory contribution of microglia and astrocytes in fetal alcohol spectrum disorders. J. Neurosci. Res. 99 , 1973–1985 (2021).
Wilhelm, C. J. & Guizzetti, M. Fetal alcohol spectrum disorders: an overview from the glia perspective. Front. Integr. Neurosci. 9 , 65 (2015).
PubMed Google Scholar
Burke, M. W., Ptito, M., Ervin, F. R. & Palmour, R. M. Hippocampal neuron populations are reduced in vervet monkeys with fetal alcohol exposure. Dev. Psychobiol. 57 , 470–485 (2015).
Young, J. K., Giesbrecht, H. E., Eskin, M. N., Aliani, M. & Suh, M. Nutrition implications for fetal alcohol spectrum disorder. Adv. Nutr. 5 , 675–692 (2014).
Jarmasz, J. S., Basalah, D. A., Chudley, A. E. & Del Bigio, M. R. Human brain abnormalities associated with prenatal alcohol exposure and fetal alcohol spectrum disorder. J. Neuropathol. Exp. Neurol. 76 , 813–833 (2017).
Marguet, F. et al. Prenatal alcohol exposure is a leading cause of interneuronopathy in humans. Acta Neuropathol. Commun. 8 , 208 (2020).
Wang, X. et al. In utero MRI identifies consequences of early-gestation alcohol drinking on fetal brain development in rhesus macaques. Proc. Natl Acad. Sci. USA 117 , 10035–10044 (2020).
Treit, S., Jeffery, D., Beaulieu, C. & Emery, D. Radiological findings on structural magnetic resonance imaging in fetal alcohol spectrum disorders and healthy controls. Alcohol Clin. Exp. Res. 44 , 455–462 (2020).
Sullivan, E. V. et al. Graded cerebellar lobular volume deficits in adolescents and young adults with fetal alcohol spectrum disorders (FASD). Cereb. Cortex 30 , 4729–4746 (2020).
Lebel, C., Roussotte, F. & Sowell, E. R. Imaging the impact of prenatal alcohol exposure on the structure of the developing human brain. Neuropsychol. Rev. 21 , 102–118 (2011).
Nguyen, V. T. et al. Radiological studies of fetal alcohol spectrum disorders in humans and animal models: an updated comprehensive review. Magn. Reson. Imaging 43 , 10–26 (2017).
De Guio, F. et al. A study of cortical morphology in children with fetal alcohol spectrum disorders. Hum. Brain Mapp. 35 , 2285–2296 (2014).
Infante, M. A. et al. Atypical cortical gyrification in adolescents with histories of heavy prenatal alcohol exposure. Brain Res. 1624 , 446–454 (2015).
Boronat, S. et al. Correlation between morphological MRI findings and specific diagnostic categories in fetal alcohol spectrum disorders. Eur. J. Med. Genet. 60 , 65–71 (2017).
Yang, Y. et al. Callosal thickness reductions relate to facial dysmorphology in fetal alcohol spectrum disorders. Alcohol Clin. Exp. Res. 36 , 798–806 (2012).
Yang, Y. et al. Abnormal cortical thickness alterations in fetal alcohol spectrum disorders and their relationships with facial dysmorphology. Cereb. Cortex 22 , 1170–1179 (2012).
Donald, K. A. et al. Neuroimaging effects of prenatal alcohol exposure on the developing human brain: a magnetic resonance imaging review. Acta Neuropsychiatr. 27 , 251–269 (2015).
Ghazi Sherbaf, F., Aarabi, M. H., Hosein Yazdi, M. & Haghshomar, M. White matter microstructure in fetal alcohol spectrum disorders: a systematic review of diffusion tensor imaging studies. Hum. Brain Mapp. 40 , 1017–1036 (2019).
Biffen, S. C. et al. Compromised interhemispheric transfer of information partially mediates cognitive function deficits in adolescents with fetal alcohol syndrome. Alcohol Clin. Exp. Res. 46 , 517–529 (2022).
Roussotte, F. F. et al. Regional brain volume reductions relate to facial dysmorphology and neurocognitive function in fetal alcohol spectrum disorders. Hum. Brain Mapp. 33 , 920–937 (2012).
Marek, S. et al. Reproducible brain-wide association studies require thousands of individuals. Nature 603 , 654–660 (2022).
Medina, A. E. Fetal alcohol spectrum disorders and abnormal neuronal plasticity. Neuroscientist 17 , 274–287 (2011).
Marquardt, K. & Brigman, J. L. The impact of prenatal alcohol exposure on social, cognitive and affective behavioral domains: insights from rodent models. Alcohol 51 , 1–15 (2016).
Harvey, R. E., Berkowitz, L. E., Hamilton, D. A. & Clark, B. J. The effects of developmental alcohol exposure on the neurobiology of spatial processing. Neurosci. Biobehav. Rev. 107 , 775–794 (2019).
Stephen, J. M., Hill, D. E. & Candelaria-Cook, F. T. Examining the effects of prenatal alcohol exposure on corticothalamic connectivity: a multimodal neuroimaging study in children. Dev. Cogn. Neurosci. 52 , 101019 (2021).
Candelaria-Cook, F. T., Schendel, M. E., Flynn, L., Hill, D. E. & Stephen, J. M. Altered resting-state neural oscillations and spectral power in children with fetal alcohol spectrum disorder. Alcohol Clin. Exp. Res. 45 , 117–130 (2021).
Suttie, M. et al. Combined face-brain morphology and associated neurocognitive correlates in fetal alcohol spectrum disorders. Alcohol Clin. Exp. Res. 42 , 1769–1782 (2018). Shows the potential of 3D imaging in identifying individuals with FASD and PAE.
Ahlgren, S. C., Thakur, V. & Bronner-Fraser, M. Sonic hedgehog rescues cranial neural crest from cell death induced by ethanol exposure. Proc. Natl Acad. Sci. USA 99 , 10476–10481 (2002).
Li, Y. et al. Sulforaphane protects against ethanol-induced apoptosis in human neural crest cells through diminishing ethanol-induced hypermethylation at the promoters of the genes encoding the inhibitor of apoptosis proteins. Front. Cell Dev. Biol. 9 , 622152 (2021).
Chen, S.-Y. & Sulik, K. K. Free radicals and ethanol-induced cytotoxicity in neural crest cells. Alcohol Clin. Exp. Res. 20 , 1071–1076 (1996).
Chung, D. D. et al. Toxic and teratogenic effects of prenatal alcohol exposure on fetal development, adolescence, and adulthood. Int. J. Mol. Sci. 22 , 8785 (2021).
Mitoma, H., Manto, M. & Shaikh, A. G. Mechanisms of ethanol-induced cerebellar ataxia: underpinnings of neuronal death in the cerebellum. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph18168678 (2021).
Charness, M. E., Simon, R. P. & Greenberg, D. A. Ethanol and the nervous system. N. Engl. J. Med. 321 , 442–454 (1989).
Harris, R. A., Trudell, J. R. & Mihic, S. J. Ethanol’s molecular targets. Sci. Signal. 1 , re7 (2008).
Gutherz, O. R. et al. Potential roles of imprinted genes in the teratogenic effects of alcohol on the placenta, somatic growth, and the developing brain. Exp. Neurol. 347 , 113919 (2022).
Lussier, A. A., Bodnar, T. S. & Weinberg, J. Intersection of epigenetic and immune alterations: implications for fetal alcohol spectrum disorder and mental health. Front. Neurosci. 15 , 788630 (2021).
Cheedipudi, S., Genolet, O. & Dobreva, G. Epigenetic inheritance of cell fates during embryonic development. Front. Genet. https://doi.org/10.3389/fgene.2014.00019 (2014).
Mews, P. et al. Alcohol metabolism contributes to brain histone acetylation. Nature 574 , 717–721 (2019).
Cantacorps, L., Alfonso-Loeches, S., Guerri, C. & Valverde, O. Long-term epigenetic changes in offspring mice exposed to alcohol during gestation and lactation. J. Psychopharmacol. 33 , 1562–1572 (2019).
Gangisetty, O., Chaudhary, S., Palagani, A. & Sarkar, D. K. Transgenerational inheritance of fetal alcohol effects on proopiomelanocortin gene expression and methylation, cortisol response to stress, and anxiety-like behaviors in offspring for three generations in rats: evidence for male germline transmission. PLoS ONE 17 , e0263340 (2022).
Jarmasz, J. S. et al. Global DNA Methylation and histone posttranslational modifications in human and nonhuman primate brain in association with prenatal alcohol exposure. Alcohol Clin. Exp. Res. 43 , 1145–1162 (2019).
CAS PubMed PubMed Central Google Scholar
Lussier, A. A. et al. DNA methylation as a predictor of fetal alcohol spectrum disorder. Clin. Epigenetics 10 , 5 (2018).
Ehrhart, F. et al. Review and gap analysis: molecular pathways leading to fetal alcohol spectrum disorders. Mol. Psychiatry 24 , 10–17 (2019).
Shabtai, Y., Bendelac, L., Jubran, H., Hirschberg, J. & Fainsod, A. Acetaldehyde inhibits retinoic acid biosynthesis to mediate alcohol teratogenicity. Sci. Rep. 8 , 347 (2018).
Yan, T., Zhao, Y., Jiang, Z. & Chen, J. Acetaldehyde induces cytotoxicity via triggering mitochondrial dysfunction and overactive mitophagy. Mol. Neurobiol. 59 , 3933–3946 (2022).
Weeks, O. et al. Embryonic alcohol exposure disrupts the ubiquitin-proteasome system. JCI Insight https://doi.org/10.1172/jci.insight.156914 (2022).
Petrelli, B., Bendelac, L., Hicks, G. G. & Fainsod, A. Insights into retinoic acid deficiency and the induction of craniofacial malformations and microcephaly in fetal alcohol spectrum disorder. Genesis 57 , e23278 (2019).
Boschen, K. E., Fish, E. W. & Parnell, S. E. Prenatal alcohol exposure disrupts sonic hedgehog pathway and primary cilia genes in the mouse neural tube. Reprod. Toxicol. 105 , 136–147 (2021).
Fish, E. W. et al. Cannabinoids exacerbate alcohol teratogenesis by a CB1-hedgehog interaction. Sci. Rep. 9 , 16057 (2019).
Burton, D. F. et al. Pharmacological activation of the sonic hedgehog pathway with a Smoothened small molecule agonist ameliorates the severity of alcohol-induced morphological and behavioral birth defects in a zebrafish model of fetal alcohol spectrum disorder. J. Neurosci. Res. 100 , 1585–1601 (2022).
Li, Y. X. et al. Fetal alcohol exposure impairs hedgehog cholesterol modification and signaling. Lab. Invest. 87 , 231–240 (2007).
Boronat, S. et al. Seizures and electroencephalography findings in 61 patients with fetal alcohol spectrum disorders. Eur. J. Med. Genet. 60 , 72–78 (2017).
Maness, P. F. & Schachner, M. Neural recognition molecules of the immunoglobulin superfamily: signaling transducers of axon guidance and neuronal migration. Nat. Neurosci. 10 , 19–26 (2007).
Arevalo, E. et al. An alcohol binding site on the neural cell adhesion molecule L1. Proc. Natl Acad. Sci. USA 105 , 371–375 (2008).
Dou, X. et al. L1 coupling to ankyrin and the spectrin-actin cytoskeleton modulates ethanol inhibition of L1 adhesion and ethanol teratogenesis. FASEB J. 32 , 1364–1374 (2018).
Wilkemeyer, M. F. et al. Differential effects of ethanol antagonism and neuroprotection in peptide fragment NAPVSIPQ prevention of ethanol-induced developmental toxicity. Proc. Natl Acad. Sci. USA 100 , 8543–8548 (2003).
Delatour, L. C., Yeh, P. W. & Yeh, H. H. Ethanol exposure in utero disrupts radial migration and pyramidal cell development in the somatosensory cortex. Cereb. Cortex 29 , 2125–2139 (2019).
Salem, N. A. et al. A novel Oct4/Pou5f1-like non-coding RNA controls neural maturation and mediates developmental effects of ethanol. Neurotoxicol. Teratol. 83 , 106943 (2021).
Mohammad, S. et al. Kcnn2 blockade reverses learning deficits in a mouse model of fetal alcohol spectrum disorders. Nat. Neurosci. 23 , 533–543 (2020).
Tseng, A. M. et al. Ethanol exposure increases miR-140 in extracellular vesicles: implications for fetal neural stem cell proliferation and maturation. Alcohol Clin. Exp. Res. 43 , 1414–1426 (2019).
Chung, D. D. et al. Dose-related shifts in proteome and function of extracellular vesicles secreted by fetal neural stem cells following chronic alcohol exposure. Heliyon 8 , e11348 (2022).
Rubert, G., Miñana, R., Pascual, M. & Guerri, C. Ethanol exposure during embryogenesis decreases the radial glial progenitorpool and affects the generation of neurons and astrocytes. J. Neurosci. Res. 84 , 483–496 (2006).
Darbinian, N. et al. Ethanol-mediated alterations in oligodendrocyte differentiation in the developing brain. Neurobiol. Dis. 148 , 105181 (2021).
Creeley, C. E., Dikranian, K. T., Johnson, S. A., Farber, N. B. & Olney, J. W. Alcohol-induced apoptosis of oligodendrocytes in the fetal macaque brain. Acta Neuropathol. Commun. 1 , 23 (2013).
Bodnar, T. S. et al. Immune network dysregulation associated with child neurodevelopmental delay: modulatory role of prenatal alcohol exposure. J. Neuroinflammation 17 , 39 (2020).
Bodnar, T. S. et al. Modulatory role of prenatal alcohol exposure and adolescent stress on the response to arthritis challenge in adult female rats. EBioMedicine 77 , 103876 (2022).
Bodnar, T. S. et al. Evidence for long-lasting alterations in the fecal microbiota following prenatal alcohol exposure. Alcohol Clin. Exp. Res. 46 , 542–555 (2022).
Virdee, M. S. et al. An enriched biosignature of gut microbiota-dependent metabolites characterizes maternal plasma in a mouse model of fetal alcohol spectrum disorder. Sci. Rep. 11 , 248 (2021).
Lo, J. O. et al. Effects of early daily alcohol exposure on placental function and fetal growth in a rhesus macaque model. Am. J. Obstet. Gynecol. 226 , 130.e1–130.e11 (2022).
Naik, V. D. et al. Mechanisms underlying chronic binge alcohol exposure-induced uterine artery dysfunction in pregnant rat. Alcohol Clin. Exp. Res. 42 , 682–690 (2018).
Balaraman, S. et al. Plasma miRNA profiles in pregnant women predict infant outcomes following prenatal alcohol exposure. PLoS ONE 11 , e0165081 (2016).
Mahnke, A. H. et al. Infant circulating microRNAs as biomarkers of effect in fetal alcohol spectrum disorders. Sci. Rep. 11 , 1429 (2021).
Tseng, A. M. et al. Maternal circulating miRNAs that predict infant FASD outcomes influence placental maturation. Life Sci. Alliance https://doi.org/10.26508/lsa.201800252 (2019).
Elliott, A. J. et al. Concurrent prenatal drinking and smoking increases risk for SIDS: safe passage study report. EClinicalMedicine 19 , 100247–100247 (2020).
Page, K. et al. Prevalence of marijuana use in pregnant women with concurrent opioid use disorder or alcohol use in pregnancy. Addict. Sci. Clin. Pract. 17 , 3 (2022).
Lowe, J. R. et al. Early developmental trajectory of children with prenatal alcohol and opioid exposure. Pediatr. Res. https://doi.org/10.1038/s41390-022-02252-z (2022).
Siqueira, M. & Stipursky, J. Blood brain barrier as an interface for alcohol induced neurotoxicity during development. Neurotoxicology 90 , 145–157 (2022).
Chudley, A. E. & Longstaffe, S. E. in Management of Genetic Syndromes Ch. 25 (eds Cassidy, S. B. & Allanson, J. E.) 363–380 (Wiley, 2010).
Clarren, S. K., Lutke, J. & Sherbuck, M. The Canadian guidelines and the interdisciplinary clinical capacity of Canada to diagnose fetal alcohol spectrum disorder. J. Popul. Ther. Clin. Pharmacol. 18 , e494–e499 (2011).
Chasnoff, I. J., Wells, A. M. & King, L. Misdiagnosis and missed diagnoses in foster and adopted children with prenatal alcohol exposure. Pediatrics 135 , 264–270 (2015).
May, P. A. et al. Prevalence of fetal alcohol spectrum disorders in 4 US communities. JAMA 319 , 474–482 (2018).
Astley, S. J. Validation of the fetal alcohol spectrum disorder (FASD) 4-digit diagnostic code. J. Popul. Ther. Clin. Pharmacol. 20 , e416–e467 (2013).
Astley, S. J. Diagnostic Guide for Fetal Alcohol Spectrum Disorders: The 4-Digit Diagnostic Code (Univ. Washington, 2004).
Cook, J. L. et al. Fetal alcohol spectrum disorder: a guideline for diagnosis across the lifespan. CMAJ Open 188 , 191–197 (2016).
Bower, C. & Elliott, E. J. Australian Guide to the Diagnosis of FASD (Australian Government Department of Health, 2020).
Scottish Intercollegiate Guidelines Network. Children and Young People Exposed Prenatally to Alcohol (SIGN publication no. 156) (SIGN, 2019).
Gibbs, A. & Sherwood, K. Putting fetal alcohol spectrum disorder (FASD) on the map in New Zealand: a review of health, social, political, justice and cultural developments. Psychiatr. Psychol. Law 24 , 825–842 (2017).
Centres for Disease Control. Fetal Alcohol Syndrome: Guidelines for Referral and Diagnosis (US Department of Health and Human Services, 2004).
Okulicz-Kozaryn, K., Maryniak, A., Borkowska, M., Śmigiel, R. & Dylag, K. A. Diagnosis of fetal alcohol spectrum disorders (FASDs): guidelines of interdisciplinary group of Polish professionals. Int. J. Environ. Res. Public Health 18 , 7526 (2021).
Landgraf, M. N., Nothacker, M. & Heinen, F. Diagnosis of fetal alcohol syndrome (FAS): German guideline version 2013. Eur. J. Paediatr. Neurol. 17 , 437–446 (2013).
Chudley, A. E. et al. Fetal alcohol spectrum disorder: Canadian guidelines for diagnosis. Can. Med. Assoc. J. 172 (Suppl. 5), S1–S21 (2005).
Bush, K., Kivlahan, D. R., McDonell, M. B., Fihn, S. D. & Bradley, K. A. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Arch. Intern. Med. 158 , 1789–1795 (1998).
Sokol, R. J., Martier, S. S. & Ager, J. W. The T-ACE questions: practical prenatal detection of risk-drinking. Am. J. Obstet. Gynecol. 160 , 863–870 (1989).
Chiodo, L. M. et al. Increased cut-point of the TACER-3 screen reduces false positives without losing sensitivity in predicting risk alcohol drinking in pregnancy. Alcohol Clin. Exp. Res. 38 , 1401–1408 (2014).
Tsang, T. W. et al. Digital assessment of the fetal alcohol syndrome facial phenotype: reliability and agreement study. BMJ Paediatr. 1 , e000137 (2017).
Hemingway, S. J. A. et al. Comparison of the 4-digit code, Canadian 2015, Australian 2016 and Hoyme 2016 fetal alcohol spectrum disorder diagnostic guidelines. Adv. Pediatr. Res. https://doi.org/10.35248/2385-4529.19.6.31 (2019).
Coles, C. D. et al. A comparison among 5 methods for the clinical diagnosis of fetal alcohol spectrum disorders. Alcohol Clin. Exp. Res. 40 , 1000–1009 (2016).
Coles, C. D. et al. Comparison of three systems for the diagnosis of fetal alcohol spectrum disorders in a community sample. Alcohol Clin. Exp. Res. https://doi.org/10.1111/acer.14999 (2022).
Leibson, T., Neuman, G., Chudley, A. E. & Koren, G. The differential diagnosis of fetal alcohol spectrum disorder. J. Popul. Ther. Clin. Pharmacol. 21 , e1–e30 (2014).
Pearson, M. A., Hoyme, H. E., Seaver, L. H. & Rimsza, M. E. Toluene embryopathy: delineation of the phenotype and comparison with fetal alcohol syndrome. Pediatrics 93 , 211–215 (1994).
Abdelmalik, N. et al. Diagnostic outcomes of 27 children referred by pediatricians to a genetics clinic in the Netherlands with suspicion of fetal alcohol spectrum disorders. Am. J. Med. Genet. A 161A , 254–260 (2013).
Douzgou, S. et al. Diagnosing fetal alcohol syndrome: new insights from newer genetic technologies. Arch. Dis. Child. 97 , 812 (2012).
Malinowski, J. et al. Systematic evidence-based review: outcomes from exome and genome sequencing for pediatric patients with congenital anomalies or intellectual disability. Genet. Med. 22 , 986–1004 (2020).
McKay, L., Petrelli, B., Chudley, A. E. & Hicks, G. G. In Fetal Alcohol Spectrum Disorder: Advances in Research and Practice Vol. 188 (eds Chudley, A. E. & Hicks, G. G.) 77–117 (Springer USA, 2022).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5 5th edn (American Psychiatric Association, 2013).
Mattson, S. N., Bernes, G. A. & Doyle, L. R. Fetal alcohol spectrum disorders: a review of the neurobehavioral deficits associated with prenatal alcohol exposure. Alcohol Clin. Exp. Res. 43 , 1046–1062 (2019). This article outlines the key neurodevelopmental characteristics in children with PAE and FASD.
PubMed PubMed Central Google Scholar
Klug, M. G., O’Connell, A. M., Palme, A., Kobrinsky, N. & Burd, L. A validation study of the alcohol related neurodevelopmental disorders behavioral checklist. Alcohol Clin. Exp. Res. 45 , 765–772 (2021).
Kable, J. A. et al. Characteristics of the symptoms of the proposed ND-PAE disorder in first grade children in a community sample. Child Psychiatry Hum. Dev. https://doi.org/10.1007/s10578-022-01414-8 (2022).
World Health Organization. International Classification of Diseases, Eleventh Revision (ICD-11), for mortality and morbidity statistics. WHO https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/362980699-11 (2022).
Kambeitz, C., Klug, M. G., Greenmyer, J., Popova, S. & Burd, L. Association of adverse childhood experiences and neurodevelopmental disorders in people with fetal alcohol spectrum disorders (FASD) and non-FASD controls. BMC Pediatrics 19 , 498 (2019).
May, P. A. et al. Case management reduces drinking during pregnancy among high risk women. Int. J. Alcohol Drug Res. 2 , 61–70 (2013).
Poole, N., Schmidt, R. A., Bocking, A., Bergeron, J. & Fortier, I. The potential for fetal alcohol spectrum disorder prevention of a harmonized approach to data collection about alcohol use in pregnancy cohort studies. Int. J. Environ. Res. Public Health 16 , 2019 (2019).
Dozet, D., Burd, L. & Popova, S. Screening for alcohol use in pregnancy: a review of current practices and perspectives. Int. J. Ment. Health Addict. https://doi.org/10.1007/s11469-021-00655-3 (2021).
Arnold, K. et al. Fetal alcohol spectrum disorders: knowledge and screening practices of university hospital medical students and residents. J. Popul. Ther. Clin. Pharmacol. 20 , e18–e25 (2013).
Payne, J. et al. Health professionals’ knowledge, practice and opinions about fetal alcohol syndrome and alcohol consumption in pregnancy. Aust. NZ J. Public Health 29 , 558–564 (2005).
Furtwængler, N. A. F. F. & de Visser, R. O. Lack of international consensus in low-risk drinking guidelines. Drug Alcohol Rev. 32 , 11–18 (2013).
Wangberg, S. C. Norwegian midwives’ use of screening for and brief interventions on alcohol use in pregnancy. Sex. Reprod. Healthc. 6 , 186–190 (2015).
France, K. et al. Health professionals addressing alcohol use with pregnant women in western Australia: Barriers and strategies for communication. Subst. Use Misuse 45 , 1474–1490 (2010).
Doi, L., Cheyne, H. & Jepson, R. Alcohol brief interventions in Scottish antenatal care: a qualitative study of midwives’ attitudes and practices. BMC Pregnancy Childbirth 14 , 170 (2014).
Doi, L., Jepson, R. & Cheyne, H. A realist evaluation of an antenatal programme to change drinking behaviour of pregnant women. Midwifery 31 , 965–972 (2015).
Oni, H. T. et al. Barriers and facilitators in antenatal settings to screening and referral of pregnant women who use alcohol or other drugs: a qualitative study of midwives’ experience. Midwifery 81 , 102595 (2020).
Lange, S., Shield, K., Koren, G., Rehm, J. & Popova, S. A comparison of the prevalence of prenatal alcohol exposure obtained via maternal self-reports versus meconium testing: a systematic literature review and meta-analysis. BMC Pregnancy Childbirth 14 , 127 (2014).
Szewczyk, Z. et al. Cost, cost-consequence and cost-effectiveness evaluation of a practice change intervention to increase routine provision of antenatal care addressing maternal alcohol consumption. Implement. Sci. 17 , 14 (2022).
Floyd, R. L. et al. Preventing alcohol-exposed pregnancies: a randomized controlled trial. Am. J. Prev. Med. 32 , 1–10 (2007).
Tzilos, G. K., Sokol, R. J. & Ondersma, S. J. A randomized phase I trial of a brief computer-delivered intervention for alcohol use during pregnancy. J. Womens Health 20 , 1517–1524 (2011).
Wouldes, T. A., Crawford, A., Stevens, S. & Stasiak, K. Evidence for the effectiveness and acceptability of e-SBI or e-SBIRT in the management of alcohol and illicit substance use in pregnant and post-partum women. Front. Psychiatr. 12 , 634805 (2021).
Coons, K. D., Watson, S. L., Yantzi, N. M., Lightfoot, N. E. & Larocque, S. Health care students’ attitudes about alcohol consumption during pregnancy: responses to narrative vignettes. Glob. Qual. Nurs. Res. 4 , 2333393617740463 (2017).
Greenmyer, J. R. et al. Pregnancy status is associated with screening for alcohol and other substance use in the emergency department. J. Addict. Med. 14 , e64–e69 (2020).
United Nations. The UN Sustainable Development Goals (United Nations, 2015).
Schölin, L. Prevention of Harm Caused by Alcohol Exposure in Pregnancy: Rapid Review and Case Studies from Member States (World Health Organization, Regional Office for Europe, 2016).
Poole, N., Schmidt, R. A., Green, C. & Hemsing, N. Prevention of fetal alcohol spectrum disorder: current Canadian efforts and analysis of gaps. J. Subst. Abus. Treat. 2016 , 1–11 (2016).
Poole, N. Fetal alcohol spectrum disorder (FASD) prevention: Canadian perspectives. Public Health Agency of Canada https://www.phac-aspc.gc.ca/hp-ps/dca-dea/prog-ini/fasd-etcaf/publications/cp-pc/pdf/cp-pc-eng.pdf (2008).
Jacobsen, B., Lindemann, C., Petzina, R. & Verthein, U. The universal and primary prevention of foetal alcohol spectrum disorders (FASD): a systematic review. J. Prev. 43 , 297–316 (2022).
Centers for Disease Control and Prevention. Alcohol & public health — preventing excessive alcohol use . CDC https://www.cdc.gov/alcohol/fact-sheets/prevention.htm (2022).
Jernigan, D. H. & Trangenstein, P. J. What’s next for WHO’s global strategy to reduce the harmful use of alcohol? Bull. World Health Organ. 98 , 222–223 (2020).
Babor, T. et al. Who is responsible for the public’s health? The role of the alcohol industry in the WHO global strategy to reduce the harmful use of alcohol. Addiction 108 , 2045–2047 (2013).
Driscoll, D. L., Barnes, V. R., Johnston, J. M., Windsor, R. & Ray, R. A formative evaluation of two FASD prevention communication strategies. Alcohol Alcohol. 53 , 461–469 (2018).
Thomas, G., Gonneau, G., Poole, N. & Cook, J. The effectiveness of alcohol warning labels in the prevention of fetal alcohol spectrum disorder: a brief review. Int. J. Alcohol Drug Res. 3 , 91–103 (2014).
Choate, P., Badry, D., MacLaurin, B., Ariyo, K. & Sobhani, D. Fetal alcohol spectrum disorder: what does public awareness tell us about prevention programming? Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph16214229 (2019).
Reid, N. et al. Preconception interventions to reduce the risk of alcohol‐exposed pregnancies: a systematic review. Alcohol Clin. Exp. Res. 45 , 2414–2429 (2021).
Symons, M., Pedruzzi, R. A., Bruce, K. & Milne, E. A systematic review of prevention interventions to reduce prenatal alcohol exposure and fetal alcohol spectrum disorder in indigenous communities. BMC Public Health 18 , 1227 (2018).
Montag, A., Clapp, J. D., Calac, D., Gorman, J. & Chambers, C. A review of evidence-based approaches for reduction of alcohol consumption in Native women who are pregnant or of reproductive age. Am. J. Drug Alcohol Abuse 38 , 436–443 (2012).
O’Connor, E. A. et al. Screening and behavioral counseling interventions to reduce unhealthy alcohol use in adolescents and adults: updated evidence report and systematic review for the US preventive services task force. JAMA 320 , 1910–1928 (2018).
Erng, M. N., Smirnov, A. & Reid, N. Prevention of alcohol‐exposed pregnancies and fetal alcohol spectrum disorder among pregnant and postpartum women: a systematic review. Alcohol Clin. Exp. Res. 44 , 2431–2448 (2020).
Thanh, N. X. et al. An economic evaluation of the parent–child assistance program for preventing fetal alcohol spectrum disorder in Alberta, Canada. Adm. Policy Ment. Health 42 , 10–18 (2015).
Keen, C. L. et al. The plausibility of maternal nutritional status being a contributing factor to the risk for fetal alcohol spectrum disorders: the potential influence of zinc status as an example. BioFactors 36 , 125–135 (2010).
McQuire, C., Daniel, R., Hurt, L., Kemp, A. & Paranjothy, S. The causal web of foetal alcohol spectrum disorders: a review and causal diagram. Eur. Child Adolesc. Psychiatr. 29 , 575–594 (2020).
Samawi, L., Williams, P. P., Myers, B. & Fuhr, D. C. Effectiveness of psychological interventions to reduce alcohol consumption among pregnant and postpartum women: a systematic review. Arch. Womens Ment. Health 24 , 557–568 (2021).
Greenmyer, J. R., Popova, S., Klug, M. G. & Burd, L. Fetal alcohol spectrum disorder: a systematic review of the cost of and savings from prevention in the United States and Canada. Addiction 115 , 409–417 (2020).
Wolfson, L. et al. Collaborative action on fetal alcohol spectrum disorder prevention: Principles for enacting the truth and reconciliation commission call to action #33. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph16091589 (2019).
Reid, N., Crawford, A., Petrenko, C., Kable, J. & Olson, H. C. A family-directed approach for supporting individuals with fetal alcohol spectrum disorders. Curr. Dev. Disord. Rep. 9 , 9–18 (2022).
Bertrand, J. Interventions for children with fetal alcohol spectrum disorders (FASDs): overview of findings for five innovative research projects. Res. Dev. Disabil. 30 , 986–1006 (2009).
Streissguth, A. P., Barr, H. M., Kogan, J. & Bookstein, F. L. Understanding the Occurrence of Secondary Disabilities in Clients with Fetal Alcohol Syndrome (FAS) and Fetal Alcohol Effects (FAE). Final Report to the Centers for Disease Control and Prevention (CDC). Report No. 96-06 (Univ. Washington, Fetal Alcohol & Drug Unit, 1996).
Reid, N. et al. Systematic review of fetal alcohol spectrum disorder interventions across the life span. Alcohol Clin. Exp. Res. 39 , 2283–2295 (2015).
Ordenewitz, L. K. et al. Evidence-based interventions for children and adolescents with fetal alcohol spectrum disorders — a systematic review. Eur. J. Paediatr. Neurol. 33 , 50–60 (2021).
Carr, E. G. et al. Positive behavior support: evolution of an applied science. J. Posit. Behav. Inter. 4 , 4–16 (2002).
Kable, J. A., Taddeo, E., Strickland, D. & Coles, C. D. Improving FASD children’s self-regulation: piloting phase 1 of the GoFAR intervention. Child Fam. Behav. Ther. 38 , 124–141 (2016).
Kable, J. A., Coles, C. D. & Taddeo, E. Socio-cognitive habilitation using the math interactive learning experience program for alcohol-affected children. Alcohol Clin. Exp. Res. 31 , 1425–1434 (2007).
Petrenko, C. L., Parr, J., Kautz, C., Tapparello, C. & Olson, H. C. A mobile health intervention for fetal alcohol spectrum disorders (families moving forward connect): development and qualitative evaluation of design and functionalities. JMIR mHealth uHealth 8 , e14721 (2020).
Coles, C. D., Kable, J. A., Taddeo, E. & Strickland, D. GoFAR: improving attention, behavior and adaptive functioning in children with fetal alcohol spectrum disorders: brief report. Dev. Neurorehabil. 21 , 345–349 (2018).
Coles, C. D., Kable, J. A. & Taddeo, E. Math performance and behavior problems in children affected by prenatal alcohol exposure: intervention and follow-up. J. Dev. Behav. Pediatr. 30 , 7–15 (2009).
Kully-Martens, K. et al. Mathematics intervention for children with fetal alcohol spectrum disorder: a replication and extension of the math interactive learning experience (MILE) program. Res. Dev. Disabil. 78 , 55–65 (2018).
Williams, M. S. & Shellenberger, S. How Does Your Engine Run?: A Leader’s Guide to the Alert Program for Self-Regulation (TherapyWorks, Inc., 1996).
Soh, D. W. et al. Self-regulation therapy increases frontal gray matter in children with fetal alcohol spectrum disorder: evaluation by voxel-based morphometry. Front. Hum. Neurosci. 9 , 108 (2015).
Wells, A. M., Chasnoff, I. J., Schmidt, C. A., Telford, E. & Schwartz, L. D. Neurocognitive habilitation therapy for children with fetal alcohol spectrum disorders: an adaptation of the Alert Program ® . Am. J. Occup. Ther. 66 , 24–34 (2012).
Wagner, B. et al. School-based intervention to address self-regulation and executive functioning in children attending primary schools in remote Australian Aboriginal communities. PLoS ONE 15 , e0234895 (2020).
Frankel, F. D. & Myatt, R. J. Children’s Friendship Training (Routledge, 2013).
Petrenko, C. L. M., Pandolfino, M. E. & Robinson, L. K. Findings from the families on track intervention pilot trial for children with fetal alcohol spectrum disorders and their families. Alcohol Clin. Exp. Res. 41 , 1340–1351 (2017).
Petrenko, C. L. M. & Alto, M. E. Interventions in fetal alcohol spectrum disorders: an international perspective. Eur. J. Med. Genet. 60 , 79–91 (2017).
Ritfeld, G. J., Kable, J. A., Holton, J. E. & Coles, C. D. Psychopharmacological treatments in children with fetal alcohol spectrum disorders: a review. Child Psychiatry Hum. Dev. 53 , 268–277 (2022).
Coles, C. D. et al. A comparison of children affected by prenatal alcohol exposure and attention deficit, hyperactivity disorder. Alcohol Clin. Exp. Res. 21 , 150–161 (1997).
Young, S. et al. Guidelines for identification and treatment of individuals with attention deficit/hyperactivity disorder and associated fetal alcohol spectrum disorders based upon expert consensus. BMC Psychiatry 16 , 324 (2016).
Mela, M. et al. Treatment algorithm for the use of psychopharmacological agents in individuals prenatally exposed to alcohol and/or with diagnosis of fetal alcohol spectrum disorder (FASD). J. Popul. Ther. Clin. Pharmacol. 27 , e1–e13 (2020).
Akison, L. K., Kuo, J., Reid, N., Boyd, R. N. & Moritz, K. M. Effect of choline supplementation on neurological, cognitive, and behavioral outcomes in offspring arising from alcohol exposure during development: a quantitative systematic review of clinical and preclinical studies. Alcohol Clin. Exp. Res. 42 , 1591–1611 (2018).
Wozniak, J. R. et al. Four-year follow-up of a randomized controlled trial of choline for neurodevelopment in fetal alcohol spectrum disorder. J. Neurodev. Disord. 12 , 9 (2020).
Hemingway, S. J. A., Davies, J. K., Jirikowic, T. & Olson, E. M. What proportion of the brain structural and functional abnormalities observed among children with fetal alcohol spectrum disorder is explained by their prenatal alcohol exposure and their other prenatal and postnatal risks? Adv. Pediatr. Res. 7 , 41 (2020).
McSherry, D. & McAnee, G. Exploring the relationship between adoption and psychological trauma for children who are adopted from care: a longitudinal case study perspective. Child Abus. Negl. 130 , 105623 (2022).
Koponen, A. M., Kalland, M. & Autti-Rämö, I. Caregiving environment and socio-emotional development of foster-placed FASD-children. Child. Youth Serv. Rev. 31 , 1049–1056 (2009).
Coggins, T. E., Timler, G. R. & Olswang, L. B. A state of double jeopardy: impact of prenatal alcohol exposure and adverse environments on the social communicative abilities of school-age children with fetal alcohol spectrum disorder. Lang. Speech Hear. Serv. Sch. 38 , 117–127 (2007).
Joseph, J. J., Mela, M. & Pei, J. Aggressive behaviour and violence in children and adolescents with FASD: a synthesizing review. Clin. Psychol. Rev. 94 , 102155 (2022).
Perry, B. D. Examining child maltreatment through a neurodevelopmental lens: clinical applications of the neurosequential model of therapeutics. J. Loss Trauma 14 , 240–255 (2009).
Cheung, M. M. Y. et al. Ear abnormalities among children with fetal alcohol spectrum disorder: a systematic review and meta-analysis. J. Pediatr. 242 , 113–120.e16 (2022).
Tsang, T. W. et al. Eye abnormalities in children with fetal alcohol spectrum disorders: a systematic review. Ophthalmic Epidemiol. https://doi.org/10.1080/09286586.2022.2123004 (2022).
Streissguth, A. P. et al. Risk factors for adverse life outcomes in fetal alcohol syndrome and fetal alcohol effects. J. Dev. Behav. Pediatr. 25 , 228–238 (2004).
Oh, S. S. et al. Hospitalizations and mortality among patients with fetal alcohol spectrum disorders: a prospective study. Sci. Rep. 10 , 19512 (2020).
Greenmyer, J. R., Klug, M. G., Kambeitz, C., Popova, S. & Burd, L. A multicountry updated assessment of the economic impact of fetal alcohol spectrum disorder: costs for children and adults. J. Addict. Med. 12 , 466–473 (2018).
Petrenko, C., Tahir, N., Mahoney, E. & Chin, N. Prevention of secondary conditions in fetal alcohol spectrum disorders: identification of systems-level barriers. Matern. Child Health J. 18 , 1496–1505 (2014).
Flannigan, K. et al. Balancing the story of fetal alcohol spectrum disorder: a narrative review of the literature on strengths. Alcohol Clin. Exp. Res. 45 , 2448–2464 (2021).
Mukherjee, R., Wray, E., Commers, M., Hollins, S. & Curfs, L. The impact of raising a child with FASD upon carers: findings from a mixed methodology study in the UK. Adopt. Foster. 37 , 43–56 (2013).
Burd, L., Klug, M. & Martsolf, J. Increased sibling mortality in children with fetal alcohol syndrome. Addict. Biol. 9 , 179–186 (2004).
Li, Q., Fisher, W. W., Peng, C.-Z., Williams, A. D. & Burd, L. Fetal alcohol spectrum disorders: a population based study of premature mortality rates in the mothers. Matern. Child Health J. 16 , 1332–1337 (2012).
Thanh, N. X. & Jonsson, E. Life expectancy of people with fetal alcohol syndrome. J. Popul. Ther. Clin. Pharmacol. 23 , e53–e59 (2016).
Burd, L. et al. Mortality rates in subjects with fetal alcohol spectrum disorders and their siblings. Birth Defects Res. Part. A Clin. Mol. Teratol. 82 , 217–223 (2008).
Article CAS Google Scholar
Thompson, A., Hackman, D. & Burd, L. Mortality in fetal alcohol spectrum disorders. Open J. Pediatr. 4 , 21–33 (2014).
O’Connor, M. J., Portnoff, L. C., Lebsack-Coleman, M. & Dipple, K. M. Suicide risk in adolescents with fetal alcohol spectrum disorders. Birth Defects Res. 111 , 822–828 (2019).
Bobbitt, S. A. et al. Caregiver needs and stress in caring for individuals with fetal alcohol spectrum disorder. Res. Dev. Disabil. 55 , 100–113 (2016).
Domeij, H. et al. Experiences of living with fetal alcohol spectrum disorders: a systematic review and synthesis of qualitative data. Dev. Med. Child Neurol. 60 , 741–752 (2018).
Reid, N. & Moritz, K. M. Caregiver and family quality of life for children with fetal alcohol spectrum disorder. Res. Dev. Disabil. 94 , 103478 (2019).
Connolly, S. L., Miller, C. J., Gifford, A. L. & Charness, M. E. Perceptions and use of telehealth among mental health, primary, and specialty care clinicians during the COVID-19 pandemic. JAMA Netw. Open https://doi.org/10.1001/jamanetworkopen.2022.16401 (2022).
Petrenko, C. L. A review of intervention programs to prevent and treat behavioral problems in young children with developmental disabilities. J. Dev. Phys. Disabil. https://doi.org/10.1007/s10882-013-9336-2 (2013).
Bager, H., Christensen, L. P., Husby, S. & Bjerregaard, L. Biomarkers for the detection of prenatal alcohol exposure: a review. Alcohol Clin. Exp. Res. 41 , 251–261 (2017).
Suttie, M. et al. Facial dysmorphism across the fetal alcohol spectrum. Pediatrics 131 , e779–e788 (2013).
Indiana Alliance on Prenatal Substance Exposure. BRAIN-online. Indiana Alliance on Prenatal Substance Exposure https://inalliancepse.org/brain-online/ (2023).
Goh, P. K. et al. A decision tree to identify children affected by prenatal alcohol exposure. J. Pediatr. 177 , 121–127.e1 (2016).
Mattson, S. N. et al. Validation of the FASD-Tree as a screening tool for fetal alcohol spectrum disorders. Alcohol Clin. Exp. Res. 1-10 https://doi.org/10.1111/acer.14987 the CIFASD (2022).
Bernes, G. A. et al. Development and validation of a postnatal risk score that identifies children with prenatal alcohol exposure. Alcohol Clin. Exp. Res. 46 , 52–65 (2022).
Mooney, S. M., Petrenko, C. L. M., Hamre, K. M. & Brigman, J. Proceedings of the 2021 annual meeting of the fetal alcohol spectrum disorders study group. Alcohol 102 , 23–33 (2022).
Himmelreich, M., Lutke, C., Hargrove, E., Begun, A. & Murray, M. in The Routledge Handbook of Social Work and Addictive Behaviors (eds Begun, A. L. & Murray, M. M.) (Routledge, 2020).
Altimus, C. M. et al. The next 50 years of neuroscience. J. Neurosci. 40 , 101–106 (2020).
Brown, S. A. & Tapert, S. F. Adolescence and the trajectory of alcohol use: basic to clinical studies. Ann. NY Acad. Sci. 1021 , 234–244 (2004).
World Health Organization. Global Action Plan for the Prevention and Control of NCDs 2013–2020 (World Health Organization, 2013).
World Health Organization. Global Strategy to Reduce the Harmful Use of Alcohol (World Health Organization, 2010).
Yanaguita, M. Y. et al. Pregnancy outcome in ethanol-treated mice with folic acid supplementation in saccharose. Childs Nerv. Syst. 24 , 99–104 (2008).
Helfrich, K. K., Saini, N., Kling, P. J. & Smith, S. M. Maternal iron nutriture as a critical modulator of fetal alcohol spectrum disorder risk in alcohol-exposed pregnancies. Biochem. Cell Biol. 96 , 204–212 (2018).
Joya, X., Garcia-Algar, O., Salat-Batlle, J., Pujades, C. & Vall, O. Advances in the development of novel antioxidant therapies as an approach for fetal alcohol syndrome prevention. Birth Defects Res. A Clin. Mol. Teratol. 103 , 163–177 (2015).
Zhang, Y., Wang, H., Li, Y. & Peng, Y. A review of interventions against fetal alcohol spectrum disorder targeting oxidative stress. Int. J. Dev. Neurosci. 71 , 140–145 (2018).
Zheng, D. et al. The protective effect of astaxanthin on fetal alcohol spectrum disorder in mice. Neuropharmacology 84 , 13–18 (2014).
Peng, Y. et al. Ascorbic acid inhibits ROS production, NF-κB activation and prevents ethanol-induced growth retardation and microencephaly. Neuropharmacology 48 , 426–434 (2005).
Shirpoor, A., Nemati, S., Ansari, M. H. K. & Ilkhanizadeh, B. The protective effect of vitamin E against prenatal and early postnatal ethanol treatment-induced heart abnormality in rats: a 3-month follow-up study. Int. Immunopharmacol. 26 , 72–79 (2015).
Wentzel, P., Rydberg, U. & Eriksson, U. J. Antioxidative treatment diminishes ethanol-induced congenital malformations in the rat. Alcohol Clin. Exp. Res. 30 , 1752–1760 (2006).
Luo, G. et al. Resveratrol attenuates excessive ethanol exposure induced insulin resistance in rats via improving NAD + /NADH ratio. Mol. Nutr. Food Res. 61 , 1700087 (2017).
Yuan, H. et al. Neuroprotective effects of resveratrol on embryonic dorsal root ganglion neurons with neurotoxicity induced by ethanol. Food Chem. Toxicol. 55 , 192–201 (2013).
Cantacorps, L., Montagud-Romero, S. & Valverde, O. Curcumin treatment attenuates alcohol-induced alterations in a mouse model of foetal alcohol spectrum disorders. Prog. Neuropsychopharmacol. Biol. Psychiatry 100 , 109899 (2020).
Tiwari, V. & Chopra, K. Protective effect of curcumin against chronic alcohol-induced cognitive deficits and neuroinflammation in the adult rat brain. Neuroscience 244 , 147–158 (2013).
Gupta, K. K., Gupta, V. K. & Shirasaka, T. An update on fetal alcohol syndrome-pathogenesis, risks, and treatment. Alcohol Clin. Exp. Res. 40 , 1594–1602 (2016).
Popova, S. et al. Health, social and legal outcomes of individuals with diagnosed or at risk for fetal alcohol spectrum disorder: Canadian example. Drug Alcohol Depend. 219 , 108487 (2021).
Popova, S., Lange, S., Bekmuradov, D., Mihic, A. & Rehm, J. Fetal alcohol spectrum disorder prevalence estimates in correctional systems: a systematic literature review. Can. J. Public Health 102 , 336–340 (2011).
Weeks, O. et al. Fetal alcohol spectrum disorder predisposes to metabolic abnormalities in adulthood. J. Clin. Invest. 130 , 2252–2269 (2020).
Carson, G. et al. No. 245-Alcohol use and pregnancy consensus clinical guidelines. J. Obstet. Gynaecol. Can. 39 , e220–e254 (2017).
Gomez, D., Petrenko, C., Monteiro, M. & Rahman, O. Assessment of Fetal Alcohol Spectrum Disorders. Report No. 978-92-75-12224-2 (Pan American Health Organization, 2020).
Download references
Acknowledgements
M.E.C. and E.P.R.: part of the work on mechanisms of alcohol harm was done in conjunction with the Collaborative Initiative on Fetal Alcohol Spectrum Disorders (CIFASD), which is funded by grants from the National Institute on Alcohol Abuse and Alcoholism (NIAAA). Support was provided by U24 AA014811 (E.P.R. and M.E.C.). Additional information about CIFASD, including information on how to request data, can be found at www.cifasd.org . H.E.H.: the section on diagnostic guidelines was partially supported by the National Institute on Alcohol Abuse and Alcoholism grants R01 AA11685, R01/U01 AA01115134, and U01 AA019879-01/NIH-NIAAA (Collaboration on Fetal Alcohol Spectrum Disorders Prevalence (CoFASP)), and by the Oxnard Foundation, Newport Beach, CA, USA. E.J.E. is supported by an Australian Medical Research Futures Fund Next Generation Fellowship (#MRF1135959) and National Health and Medical Research Council of Australia funding for a Centre of Research Excellence in FASD (#GNT1110341).
Author information
Authors and affiliations.
Institute for Mental Health Policy Research, Centre for Addiction and Mental Health, University of Toronto, Toronto, Ontario, Canada
Svetlana Popova
VA Boston Healthcare System, West Roxbury, MA, USA
Michael E. Charness
Department of Neurology, Harvard Medical School, Boston, MA, USA
Department of Neurology, Boston University Chobanian & Avedisian School of Medicine, Boston, MA, USA
Department of Neurology, Brigham and Women’s Hospital, Boston, MA, USA
North Dakota Fetal Alcohol Syndrome Center, Department of Pediatrics, University of North Dakota School of Medicine and Health Sciences, Pediatric Therapy Services, Altru Health System, Grand Forks, ND, USA
Faculty of Medical and Health Sciences, University of Auckland, Auckland, New Zealand
Andi Crawford
Sanford Children’s Genomic Medicine Consortium, Sanford Health, and University of South Dakota Sanford School of Medicine, Sioux Falls, SD, USA
H. Eugene Hoyme
National UK FASD Clinic, Surrey and Borders Partnership NHS Foundation Trust, Redhill, Surrey, UK
Raja A. S. Mukherjee
Center for Behavioral Teratology, San Diego State University, San Diego, CA, USA
Edward P. Riley
Faculty of Medicine and Health, University of Sydney, Sydney, New South Wales, Australia
Elizabeth J. Elliott
New South Wales FASD Assessment Service, CICADA Centre for Care and Intervention for Children and Adolescents affected by Drugs and Alcohol, Sydney Children’s Hospitals Network, Westmead, Sydney, New South Wales, Australia
You can also search for this author in PubMed Google Scholar
Contributions
Introduction (E.P.R. and E.J.E.); Epidemiology (S.P.); Mechanisms/pathophysiology (M.E.C.); Diagnosis, screening and prevention (E.J.E., M.E.C., H.E.H., E.P.R., S.P., A.C. and L.B.); Management (R.A.S.M., A.C. and E.J.E.); Quality of life (S.P., L.B. and R.A.S.M.); Outlook (E.J.E. and M.E.C.); Overview of Primer (S.P. and E.J.E.).
Corresponding author
Correspondence to Svetlana Popova .
Ethics declarations
Competing interests.
The authors declare no competing interests
Peer review
Peer review information.
Nature Reviews Disease Primers thanks C. Chambers, O. Garcia-Algar, J. Kable, C. Valenzuela and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Informed consent.
The authors affirm that human research participants provided informed consent, for publication of the images in Figure 4 .
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information, rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Popova, S., Charness, M.E., Burd, L. et al. Fetal alcohol spectrum disorders. Nat Rev Dis Primers 9 , 11 (2023). https://doi.org/10.1038/s41572-023-00420-x
Download citation
Accepted : 16 January 2023
Published : 23 February 2023
DOI : https://doi.org/10.1038/s41572-023-00420-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
An overview of current advances in perinatal alcohol exposure and pathogenesis of fetal alcohol spectrum disorders.
- Xingdong Zeng
Journal of Neurodevelopmental Disorders (2024)
Prevention of alcohol exposed pregnancies in Europe: the FAR SEAS guidelines
- Carla Bruguera
- Lidia Segura-García
BMC Pregnancy and Childbirth (2024)
Sexually dimorphic effects of prenatal alcohol exposure on the murine skeleton
- Lucie E. Bourne
- Soher N. Jayash
- Katherine A. Staines
Biology of Sex Differences (2024)
Scoping review on the role of the family doctor in the prevention and care of patients with foetal alcohol spectrum disorder
- Sébastien Leruste
- Bérénice Doray
- Michel Spodenkiewicz
BMC Primary Care (2024)
Fetal alcohol spectrum disorders prevention and clinical guidelines research - workshop report
- Tracey Pérez Koehlmoos
- Elizabeth Lee
- Tom Donaldson
BMC Proceedings (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

National Institute on Alcohol Abuse and Alcoholism (NIAAA)
Fetal alcohol spectrum disorders.
Updated: 2023
The National Institute on Alcohol Abuse and Alcoholism (NIAAA)—part of the National Institutes of Health, the Nation’s medical research agency— funds research on fetal alcohol spectrum disorders (FASD) with projects on preventing prenatal alcohol exposure, treating women with alcohol use disorder, improving the diagnosis of FASD, establishing more precise prevalence estimates of FASD in the United States, increasing our understanding of the effects of alcohol on the unborn child, and developing effective interventions to mitigate the health effects on individuals prenatally exposed to alcohol.
Prenatal alcohol exposure is a leading preventable cause of birth defects and neurodevelopmental deficits in the United States. It can cause a range of intellectual and behavioral problems, which appear at any time during childhood and last a lifetime. FASD is an umbrella term for a range of physical, cognitive, and behavioral disorders caused by prenatal alcohol exposure. Depending on the features identified, the medical disorders labeled as FASD include: Fetal Alcohol Syndrome (FAS), partial FAS (pFAS), alcohol-related neurodevelopmental disorder (ARND), alcohol-related birth defects (ARBD), and neurobehavioral disorder associated with prenatal alcohol exposure (ND-PAE). Recent prevalence studies estimate that approximately 1 to 5 percent of U.S. first-grade children have FASD.
Historically, medical professionals did not recognize the risks posed by alcohol use during pregnancy. In 1973, responding to Jones and Smith’s publication on the original syndrome FAS, NIAAA initiated several epidemiological and animal studies on prenatal alcohol exposure. By 1977, this research facilitated NIAAA issuing the first government health advisory to limit alcohol use during pregnancy. Now, after 50 years, NIAAA continues to provide leadership and support as the largest funder of biomedical research on FASD in the United States.
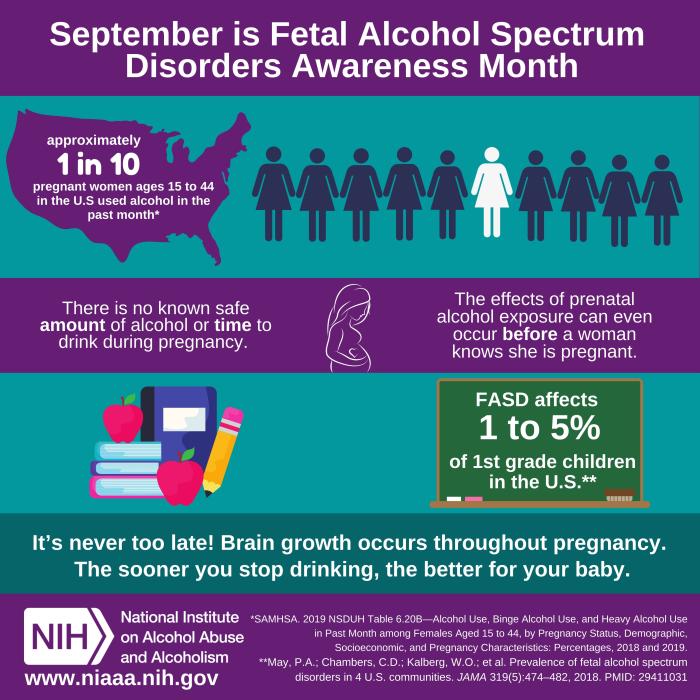
NIAAA’s FASD Grant Portfolio
In FY2023, NIAAA allocated approximately 7% of its extramural research and training budget, or roughly $30 million, for its portfolio of FASD-related grants. This portfolio currently comprises approximately 96 grants, including research project grants, cooperative agreements, training grants, center grants, fellowships, and career development awards, that collectively address FASD prevention, diagnosis, treatment, and etiology. In addition, NIAAA funds conference grants that support the annual meeting of the FASD Study Group ( www.fasdsg.org ) and the International Research Conference on FASD in Vancouver. A list of NIH funded FASD-related projects may be found at NIH RePORTER , selecting FASD under the NIH Spending Category of the Advanced Project Search.
Research Centers and Consortia working on FASD
- The Collaborative Initiative on Fetal Alcohol Spectrum Disorders (CIFASD) is a multidisciplinary consortium of domestic and international projects established by NIAAA in 2003 to address prevention of FASD, diagnosis of the full range of birth defects associated with prenatal alcohol exposure, and ameliorative interventions for affected individuals. CIFASD aims to accelerate the translation of key research findings by fostering collaboration and by coordinating clinical, basic, and translational research. Learn more about the CIFASD at www.cifasd.org .
- New Mexico Alcohol Research Center (NMARC) is a NIAAA-designated specialized Alcohol Research Center located at the University of New Mexico Health Sciences Center. NMARC is one of just twenty Alcohol Research Centers in the United States, and the only such center focused solely on Fetal Alcohol Spectrum Disorders (FASD). NMARC’s central focus is on understanding the neurobiological mechanisms underlying the behavioral problems associated with FASD and how to use this knowledge to help develop better methods of early diagnoses and more effective interventions for patients with FASD. Learn more about the NMARC at https://hsc.unm.edu/nmarc/ .
- Developmental Exposure Alcohol Research Center (DEARC) is a NIAAA-designated specialized Alcohol Research Center located at Binghamton University. The research of the DEARC focuses on the two primary developmental periods during which alcohol exposure occurs: prenatally/postnatally through maternal use and during adolescence. Learn more about the DEARC at https://www.binghamton.edu/centers/dearc/ .
- Native Center for Alcohol Research and Education (NCARE) is a NIAAA-designated comprehensive Alcohol Research Center located at Washington State University. Among its research projects is Native CHOICES, a study implementing a culturally adapted intervention with American Indian women of reproductive age to reduce their risk for an alcohol-exposed pregnancy. Learn more about NCARE at https://ireach.wsu.edu/ncare/ .
Program Directors to contact with FASD-related inquiries
- Tatiana Balachova, Ph.D. [email protected] Program Director – Division of Epidemiology and Prevention Research (DEPR) Focus areas: Reproductive and perinatal epidemiology; Prevention among women of child-bearing age; Family-based prevention
- Bill Dunty, Ph.D. [email protected] NIAAA FASD Research Coordinator Program Director – Division of Metabolism and Health Effects (DMHE) Focus areas: Basic and clinical research on the consequences of prenatal alcohol exposure; Animal models of FASD
- Elizabeth Powell, Ph.D. [email protected] Program Director – Division of Neuroscience and Behavior (DNB) Focus areas: Developmental neurobiology; FASD, Bioengineering
- Deidra Roach, M.D. [email protected] Program Director – Division of Treatment and Recovery Research (DTRR) Focus areas: AUD and co-occurring medical conditions; alcohol and women; Interventions for FASD
New FASD-related Initiatives
Notice of funding opportunities
PAR-24-067: Prevention and Intervention Approaches for Fetal Alcohol Spectrum Disorders (R34 Clinical Trial Optional) Open Date: January 16, 2024 Expiration Date: January 08, 2027
PAR-24-068: Prevention and Intervention Approaches for Fetal Alcohol Spectrum Disorders (R61/R33 Clinical Trial Optional) Open Date: January 16, 2024 Expiration Date: November 17, 2026
PAR-23-270: Screening, Brief Intervention and Referral to Treatment or Prevention (SBIRT/P) for alcohol, tobacco, and other drugs (ATOD) use and misuse in adult populations that experience health disparities (R01 Clinical Trial Required) Open Date: January 05, 2024 Expiration Date: May 08, 2027
NOT-OD-22-179: Addressing Evidence Gaps in Screening Open Date: October 04, 2022 Expiration Date: May 08, 2025
NOT-OD-22-178: Increasing Uptake of Evidence-Based Screening in Diverse Populations Across the Lifespan Open Date: July 14, 2022 Expiration Date: May 08, 2025
Consensus Conference on Research Classification of FASD
In October 2019, the National Institute on Alcohol Abuse and Alcoholism (NIAAA), part of the US National Institutes of Health (NIH), convened a 1.5-day meeting to explore the possibility of developing an international consensus classification system for research on FASD. We believe that a single classification system will harmonize research efforts across the globe and accelerate progress in understanding the epidemiology, pathogenesis, diagnosis, and treatment of FASD. A major goal of the conference was to build consensus among participants who subsequently agreed to test a few draft classification systems in their own research databases to inform the process going forward. A summary of the meeting can be found here .
Latest News & Research
September 9 is International Fetal Alcohol Spectrum Disorders Awareness Day (September 2023) NIAAA is bringing attention to the range of cognitive and behavioral problems associated with fetal alcohol spectrum disorders (FASDs) that may appear at various times during childhood or early adolescence and that last a lifetime by recognizing September 9 th as International FASD Awareness Day—part of FASD Awareness Month.
Drinking and smoking during pregnancy linked with stillbirth (August 2021) The NIH-funded Safe Passage Study elucidates how stillbirth risk is influenced by the timing and amount of prenatal exposure to the combination of tobacco and alcohol. A report of the study appears in JAMA Network Open.
Advances in Research on Fetal Alcohol Spectrum Disorders (September 2020) This feature article from the Fall 2020 issue of the NIAAA Spectrum webzine highlights recent advances in research on Fetal alcohol spectrum disorders (FASD).
Choline supplements in young children with fetal alcohol spectrum disorder have lasting cognitive benefits (July 20, 2020) NIAAA-funded scientists report that early life dietary choline supplements improve some of the cognitive and behavioral symptoms associated with fetal alcohol spectrum disorders (FASD) four years after treatment ended. The results of this study suggest that choline treatment during an important time window during early childhood can alter brain development in a way that produces lasting therapeutic behavioral effects for children with FASD. The findings were published in the Journal of Neurodevelopmental Disorders.
Fetal Alcohol Spectrum Disorders May Increase the Risk of Type 2 Diabetes and Other Metabolic Issues (June 9, 2020) Adults with fetal alcohol spectrum disorders (FASD) may have an increased risk of type 2 diabetes, and other metabolic abnormalities such as low HDL cholesterol and elevated levels of triglycerides compared to people without FASD. The research team confirmed their findings in a zebrafish model of FASD and gained insight into the mechanisms that may play a role in these metabolic issues. The study was published in The Journal of Clinical Investigations
Combined prenatal smoking and drinking greatly increases SIDS risk (January 20, 2020) SIDS is the sudden, unexplained, death of an infant under one year of age. Many studies have shown that the risk of SIDS is increased by maternal smoking during pregnancy. Some studies have also found that prenatal alcohol exposure, particularly from heavy drinking during pregnancy, can increase SIDS risk. The NIH-funded Safe Passage Study elucidates how SIDS risk is influenced by the timing and amount of prenatal exposure to tobacco and alcohol. A report of the study appears in EclinicalMedicine, an online journal published by The Lancet.
Using both marijuana and alcohol during early pregnancy may increase the likelihood of disrupting fetal development (November 8, 2019) New preclinical research reported in animal models shows that exposure to compounds found in marijuana called cannabinoids (CBs), which include cannabidiol (CBD) and tetrahydrocannabinol (THC), during early pregnancy can cause malformations in the developing embryo. The research also demonstrated that co-exposure to CBs and alcohol increased the likelihood of birth defects involving the face and brain. The study was published in Scientific Reports.
Study of first-graders shows fetal alcohol spectrum disorders prevalent in US communities (February 6, 2019) A study of more than 6,000 first graders across four U.S. communities has found that a significant number of the children have fetal alcohol spectrum disorders (FASD), with conservative rates ranging from 1 to 5 percent in community samples. The new findings represent more accurate prevalence estimates of FASD among general U.S. communities than prior research. Previous FASD estimates were based on smaller study populations and did not reflect the overall U.S. population. The study was published in JAMA.
Director's Blog: Why September is Especially Important to Alcohol Research (September 2019) September is a significant month for the alcohol field for two reasons: it is the month dedicated to raising awareness about fetal alcohol spectrum disorders (FASD) and to celebrating recovery from alcohol and other substance use disorders.
Director's Blog: Raising Awareness about Fetal Alcohol Spectrum Disorders (September 2018) Fetal alcohol spectrum disorders, also known as FASD, is a term that refers to the broad range of lifelong birth defects and neurodevelopmental abnormalities that occur as a result of prenatal alcohol exposure. In this edition of Dr. Koob’s blog, he wants to remind everyone that there is no known safe level of alcohol, or time to drink, during pregnancy.
FASD-related Brochures and Fact Sheets
- Fetal Alcohol Exposure [ PDF - 346.92 KB]
- Alcohol and Your Pregnancy [ PDF - 184.65 KB l Español ]
- Women and Alcohol [ PDF - 1.41 MB | Español ]
Federal and Professional Partners
- The Interagency Coordinating Committee on Fetal Alcohol Spectrum Disorders ( ICCFASD )
- Centers for Disease Control and Prevention ( CDC )
- American Academy of Pediatrics ( AAP )
- American College of Obstetricians and Gynecologists ( ACOG )
- FASD United (formerly NOFAS)
- PROOF Alliance
niaaa.nih.gov
An official website of the National Institutes of Health and the National Institute on Alcohol Abuse and Alcoholism
- Research article
- Open access
- Published: 28 October 2019
Fetal alcohol spectrum disorder: neurodevelopmentally and behaviorally indistinguishable from other neurodevelopmental disorders
- Shannon Lange ORCID: orcid.org/0000-0002-8067-8932 1 , 2 ,
- Kevin Shield 1 , 4 ,
- Jürgen Rehm 1 , 2 , 4 , 5 , 6 ,
- Evdokia Anagnostou 2 , 7 , 8 &
- Svetlana Popova 1 , 2 , 3 , 4
BMC Psychiatry volume 19 , Article number: 322 ( 2019 ) Cite this article
8286 Accesses
22 Citations
10 Altmetric
Metrics details
The lack of universally accepted diagnostic criteria and the high rate of psychiatric comorbidity make it difficult to diagnose Fetal Alcohol Spectrum Disorder (FASD). In an effort to improve the diagnosis of FASD, the current study aimed to identify a neurodevelopmental profile that is both sensitive and specific to FASD.
A secondary analysis was conducted on data obtained from the Canadian component of the World Health Organization International Study on the Prevalence of FASD. Data on neurodevelopmental status and behavior were derived from a battery of standardized tests and the Child Behavior Checklist for 21 children with FASD, 28 children with other neurodevelopmental disorders, and 37 typically developing control children, aged 7 to 11 years. Two latent profile analyses were performed to derive discriminative profiles: i) children with FASD compared with typically developing control children, and ii) children with FASD compared with typically developing control children and children with other neurodevelopmental disorders. The classification function of the resulting profiles was evaluated using the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV). Confidence intervals (CIs) were approximated using 10,000 bootstrapped samples.
The neurodevelopmental profile of FASD tested consisted of impairments in perceptual reasoning, verbal comprehension, visual-motor speed and motor coordination, processing speed (nonverbal information), attention and executive function, visuospatial processing, and language, in combination with rule-breaking behavior and attention problems. When children with FASD were compared with typically developing control children, a 2-class model fit the data best and resulted in a sensitivity of 95.2% (95% CI: 84.2–100.0%), specificity of 89.2% (95% CI: 78.4–97.5%), PPV of 83.3% (95% CI: 66.7–96.2%), and NPV of 97.1% (95% CI: 90.3–100.0%). When children with FASD were compared with typically developing control children and children with other neurodevelopmental disorders, the neurodevelopmental profile correctly identified only 56.9% (95% CI: 45.1–69.2%) of typically developing children and children with other neurodevelopmental disorders as not having FASD, and thus the profile was found not to be specific to children with FASD.
The findings question the uniqueness of children with FASD with respect to their neurodevelopmental impairments and behavioral manifestations.
Peer Review reports
Exposure to alcohol prenatally is the etiological cause of Fetal Alcohol Spectrum Disorder (FASD) – a term that is used to cover a range of diagnoses, including: Fetal Alcohol Syndrome (FAS), Partial FAS (pFAS), Alcohol-Related Neurodevelopmental Disorder (ARND), and depending on the diagnostic guideline, Alcohol-Related Birth Defects [ 1 , 2 ]. Although historically used as a non-diagnostic umbrella term, it has recently been proposed that FASD be used as a diagnostic term with the specification of the presence or absence of sentinel facial features [ 3 ]. This is in agreement with the newly proposed diagnosis of Neurobehavioral Disorder Associated with Prenatal Alcohol Exposure (ND-PAE) in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) [ 4 ]. ND-PAE encompasses a range of neurobehavioral effects associated with prenatal alcohol exposure, and can be diagnosed independent of any physical findings [ 5 ].
It is well documented that individuals with FASD exhibit a broad array of neurodevelopmental impairments, such as deficits in adaptive function, attention, executive function, motor function, social cognition, verbal and nonverbal learning, as well as externalizing behaviors [ 6 , 7 ]. It is also commonly reported that children with FASD have diminished intellectual functioning [ 8 ]; however, when compared with IQ-matched control children, differences in their neurodevelopmental presentation have been noted [ 9 ]. Although it is widely accepted that the neurodevelopmental and behavioral effects of prenatal alcohol exposure are far-reaching [ 7 ], the current diagnostic guidelines tend to focus on the severity of the neurodevelopmental impairments rather than on the specific impairments.
Early and accurate diagnosis of FASD is crucial to providing timely developmental interventions, which are key to altering the developmental trajectory of affected individuals with respect to social functioning, improving their quality of life, and preventing subsequent adverse outcomes common among individuals with FASD, such as school failure and dropping out, addiction, mental health problems, dependent living, as well as involvement with the law and incarceration [ 10 ]. However, even in clinical settings where FASD is an important area of emphasis, individuals who have been affected by prenatal alcohol exposure often go undiagnosed or are misdiagnosed [ 11 ]. This can likely be attributed to the fact that the diagnosis of FASD is complicated due to difficulties in obtaining confirmation of prenatal alcohol exposure, a high rate of psychiatric comorbidity [ 12 , 13 ], and the existence of signs and symptoms that overlap with those of other neurodevelopmental disorders [ 14 ].
Thus, with the aim of improving screening and diagnostic efforts, the concept of a unique neurodevelopmental profile of FASD, defined as the outward expression (behavioral and developmental) of the central nervous system damage caused by prenatal alcohol exposure, has received some attention in recent years. A distinct neurodevelopmental profile of FASD could assist in accurately identifying individuals with FASD, distinguishing between FASD and other conditions that present similar clinical features, improving clinical services for individuals with FASD, and triaging of individuals most in need of a full multidisciplinary FASD diagnostic assessment. Further, a unique neurodevelopmental profile of FASD could aid in the ascertainment of accurate prevalence estimates, as well as the planning and development of appropriate targeted interventions for individuals with FASD. Therefore, the objective of the current study was to identify a neurodevelopmental profile that is both sensitive and specific to FASD.
As discussed above, FASD includes several distinct diagnoses. As such, there is the possibility that individuals with FASD exhibit more than one neurodevelopmental profile (i.e., a unique profile could exist for each diagnostic category). In order to explore this possibility, the current study utilized a methodology that allows for the empirical determination of the number of distinct profiles.
Participants
This study was a secondary analysis of data for 37 typically developing children (70.3% male; mean [standard deviation (SD)] age: 9.0 [1.0] years), 21 children with FASD (52.4% male; mean [SD] age: 9.7 [0.8] years), and 28 children with other neurodevelopmental disorders (Attention Deficit Hyperactivity Disorder [ADHD] and/or Autism Spectrum Disorder [ASD]; 75.0% male; mean [SD] age: 9.3 [1.0] years) from the Canadian component of the World Health Organization (WHO) International Study on the Prevalence of FASD [ 15 ]. The Canadian FASD prevalence study employed a cross-sectional, observational design using active case ascertainment, along with retrospective collection of prenatal alcohol exposure information, to identify cases of suspected FASD among elementary school students in grades 2, 3, and 4 attending public school in the Greater Toronto Area in Ontario, Canada. The study procedures followed a step-wise approach, where only those students meeting predetermined criteria proceeded to the subsequent phase. Phase I involved: 1) taking growth measurements, 2) identifying learning and/or behavioral problems, and 3) a dysmorphology examination. Phase II involved: 1) a neurodevelopmental assessment, 2) maternal interview, and 3) behavioral observations/ratings by parents, obtained via the Child Behavior Checklist (CBCL) [ 15 ]. In addition, a group of typically developing control children was randomly selected from a list of all students who completed Phase I and who did not meet the criteria for Phase II using a systematic sampling technique; these students underwent a complete assessment in Phase II. Final diagnostic screening conclusions were made, by consensus, by a team of experienced multidisciplinary experts, using the 2005 Canadian diagnostic guidelines [ 1 ]. A detailed description of the methodology of the Canadian FASD prevalence study is presented in Popova et al. [ 16 ].
Neurodevelopmental assessment
Neurodevelopmental assessments were conducted by qualified psychometrists using the WHO International Study on the Prevalence of FASD test battery, which included: Wechsler Abbreviated Scales of Intelligence, Second Edition (WASI-II [ 17 ]; subtests administered included block design, matrix reasoning, similarities, and vocabulary); Wechsler Intelligence Scale for Children, Fourth Edition (WISC-IV [ 18 ]; subtests administered included coding, digit span, symbol search, and letter-number sequencing); and NEPSY, Second Edition (NEPSY-II [ 19 ]; subtests administered included arrows, auditory attention, fingertip tapping, response set, and word generation). This test battery was devised based on the minimum measurements necessary to screen children for FASD, as per expert opinion. All tests were administered and scored by the examiner according to published test manuals and rechecked by a second examiner. Raw scores were converted to scaled scores according to age and sex norms. Canadian norms were used for the WISC-IV, and US norms were used for the WASI-II and NEPSY-II (as Canadian norms are not available for the respective instruments).
Behavioral observations/ratings by parents
Parents were asked to complete the CBCL to evaluate their child’s social competencies and identify any behavioral problems. The CBCL is a widely used, standardized questionnaire to assess emotional and behavioral problems in children aged 6–18 years [ 15 ]. T-scores were computed for 23 composite scales using 113 behavioral descriptors, scored on a three-point Likert scale (0 = not true, 1 = somewhat or sometimes true, 2 = very true or often true), according to age and sex norms.
Latent profile analysis
Analysis 1: children with FASD vs. typically developing control children
Latent profile analysis (LPA) [ 20 ] was first performed on a sample of children with FASD and typically developing control children in order to identify the measures that best differentiate the two groups of participants. A step-wise approach was used to select indicator variables for the LPA. A total of 42 variables were available for consideration (22 derived from the subtests of the neurodevelopmental test battery and 20 derived from the composite scales of the CBCL). Variables were initially selected based on standardized differences in means between children with FASD and typically developing control children (measured through Cohen’s d ) [ 21 ]; variables with a large effect size ( d ≥ 0.8) were retained. Pearson’s correlation coefficients ( r ) were calculated to avoid the inclusion of redundant variables. For strongly correlated variables ( r ≤ − 0.7 or r ≥ 0.7), the variable with the larger effect size was retained. If the effect sizes were equal, Student’s unpaired t-tests were performed (to test differences in the means between children with FASD and typically developing control children), and the variable with the larger t-score was retained.
Post-hoc analysis
High levels of prenatal alcohol exposure have been found to be associated with an increased risk of impaired intellectual functioning [ 8 ]. In order to determine if children with FASD are distinguishable from typically developing control children by IQ alone, LPA was performed using IQ (i.e., the WISC-IV, FSIQ-4 score) only.
Analysis 2: children with FASD vs. typically developing control children and children with other neurodevelopmental disorders
To determine whether the neurodevelopmental profile identified in analysis 1 is specific to FASD, LPA was performed on the complete sample (i.e., children with FASD, children with other neurodevelopmental disorders, and typically developing children). In addition to the class solution selected based on model fit, as described below, a 4-class model was also explored as there were four diagnostically distinct groups included in the sample (FASD, ADHD, ASD, and typically developing children).
Sensitivity analysis
Given the small number of children with ASD in the group of children with other neurodevelopmental disorders and the shared characteristics of FASD and ASD [ 22 ], LPA was performed on a sample of children with FASD ( n = 21), children with ADHD ( n = 22), and typically developing control children ( n = 37) to determine the influence that the inclusion of children with ASD had on the ability of the neurodevelopmental profile to differentiate the respective groups of children.
Model selection
The number of subgroups in the sample was tested iteratively based on the following model fit statistics: Akaike Information Criterion (AIC) [ 23 ], Bayesian Information Criterion (BIC) [ 24 ], log likelihood, and the Lo-Mendell-Rubin adjusted log likelihood ratio test [ 25 ]. Optimal model fit was defined by lower relative AIC and BIC values and higher log likelihood values. Further, an entropy value > 0.8 was used as an indicator of highly discriminating latent classes (i.e., an indicator of low classification uncertainty) [ 26 ].
Model evaluation
In LPA, following the determination of the likely number of classes, participants were subsequently assigned to a subgroup based on the probability of membership as indicated by the model. This assignment allows for the model’s classification function, as a binary classification test, to be evaluated. This evaluation was achieved through the calculation of the resulting model’s sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV). The 95% confidence interval (CI) for each measure of interest was approximated using the 2.5th and 97.5th percentiles of 10,000 bootstrap generated estimates. Further, Cohen’s d and unpaired Student’s t-test for normally distributed data were used to compare the resulting subgroups on each of the observed indicator variables.
Missing data imputation
Little’s missing completely at random (MCAR) test [ 27 ] was performed to test the assumption that missing data were missing completely at random ( X 2 (3) = 2.575, p = 0.462); this was confirmed. As such, missing data (0.5% of the data were missing) were replaced by the mean score of the complete cases in the study sample (i.e., mean imputation).
Statistical software
Variable selection and the MCAR test were performed using Stata version 15.1 [ 28 ], the LPA was conducted using Mplus version 8.0 [ 29 ], and CIs were computed in R version 3.4.4 [ 30 ]. Statistical significance was based on an acceptable type-I error rate (α) of 0.05.
The three groups of children differed from one another with respect to ethnicity ( p = 0.020), height ≤ 10th percentile ( p = 0.041), and occipitofrontal circumference ≤ 10th percentile ( p = 0.011). With respect to mean IQ, both children with FASD (mean = 87.2 [SD = 10.2]) and children with other neurodevelopmental disorders (mean = 95.6 [SD = 14.1]) differed from typically developing control children (mean = 106.4 [SD = 12.9]; p = < 0.001 and p = 0.003, respectively), but were not significantly different from one another ( p = 0.064). The groups did not significantly differ from one another on age, sex, handedness, weight ≤ 10th percentile, or the three characteristic facial features that discriminate individuals with and without FAS or pFAS (i.e., palpebral fissure length 2 standard deviations below the mean, smooth philtrum, and thin vermillion border). Demographic and descriptive data for study participants are presented in Table 1 .
Based on the variable selection process, described above, ten observed indicator variables were retained. Eight variables were derived from the neurodevelopmental test battery (WASI-II - block design, similarities, and vocabulary; WISC-IV - coding and symbol search; and NEPSY-II - response set, arrows, and word generation (letters)), and two variables were derived from the CBCL (attention problems and rule breaking behavior). Based on the model fit statistics, a 2-class model best fit the data (see Table 2 for the model fit statistics).
In this model, 24 participants (41.4% of the sample) were assigned to subgroup 1, and 34 participants (58.6% of the sample) were assigned to subgroup 2. Participants in subgroup 1 performed worse than participants in subgroup 2 for each of the above eight observed variables derived from the subtests of the neurodevelopmental test battery and scored higher on the above two observed variables derived from the composite scales of the CBCL (Table 3 ).
The final 2-class model resulted in 91.4% of participants being classified correctly overall, with almost all (20 out of 21; 95.2% [sensitivity], 95% CI: 84.2–100.0%) children with FASD assigned to subgroup 1, and notably more (33 out of 37; 89.2% [specificity], 95% CI: 78.4–97.5%) typically developing control children assigned to subgroup 2 (Table 4 ).
Post-hoc analysis: latent profile analysis based on IQ only
When IQ was included as the only indicator variable, a 1-class model fit better than a 2-class model (Table 2 ). As such, the respective model was not explored further. Although the mean IQs for children with FASD and for typically developing control children were found to be significantly different (87.2 [SD = 10.2] vs. 106.4 [SD = 12.9], respectively; p < 0.001), the post-hoc analysis demonstrated that these two groups of children could not be differentiated based on IQ only.
A 2-class model best described the overall sample (Table 2 ), and correctly identified 83.8% (31 out of 37 [specificity]; 95% CI: 71.0–94.3%) of typically developing children as not having either FASD or other neurodevelopmental disorders (Table 5 ). However, the 2-class model was only able to correctly identify 56.9% (37 out of 65 [specificity]; 95% CI: 45.1–69.2%) of children with other neurodevelopmental disorders and typically developing children as not having FASD. The 2-class model resulted in almost all children with FASD (20 out of 21) and considerably more children with other neurodevelopmental disorders (22 out of 28) being assigned to subgroup 1, and significantly more typically developing children (31 out of 37) being assigned to subgroup 2 (Table 5 ). As would be expected, participants in subgroup 1 performed worse than participants in subgroup 2 for each of the eight observed variables derived from the neurodevelopmental subtests and scored higher on the two observed variables derived from the CBCL (Table 3 and Fig. 1 ).
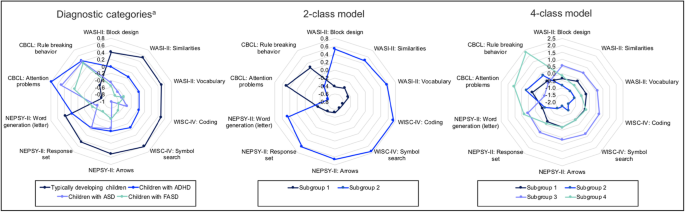
Mean scores for each diagnostic category and subgroup in the 2- and 4-class models in analysis 2. ADHD: Attention Deficit Hyperactivity Disorder; ASD: Autism Spectrum Disorder; CBCL: Child Behavior Checklist; FASD: Fetal Alcohol Spectrum Disorder; NEPSY-II: NEPSY, Second Edition; WASI-II: Wechsler Abbreviated Scales of Intelligence, Second Edition; WISC-IV: Wechsler Intelligence Scale for Children, Fourth Edition. a Children with comorbid diagnoses are not included. Note. All scores are presented as z-scores. In the 2-class model, subgroup 1 is comprised of 20 children with FASD, 22 children with other neurodevelopmental disorders, and six typically developing children; and subgroup 2 is comprised of one child with FASD, six children with other neurodevelopmental disorders, and 31 typically developing children. In the 4-class model, subgroup 1 is comprised of 13 children with FASD, 15 children with other neurodevelopmental disorders, and six typically developing children; subgroup 2 is comprised of five children with FASD and four children with other neurodevelopmental disorders; subgroup 3 is comprised of five children with other neurodevelopmental disorders and 31 typically developing children; and subgroup 4 is comprised of three children with FASD and four children with other neurodevelopmental disorders
The 4-class model resulted in all 21 children with FASD and most children with other neurodevelopmental disorders (23 out of 28) being assigned to subgroup 1, 2, or 4, and the majority of typically developing children (31 out of 37) being assigned to subgroup 3. However, the 4-class model did not produce subgroups that were reflective of the diagnostic constructs represented in the sample (see Fig. 1 ); the model correctly identified only 55.4% (36 out of 65 [specificity]; 95% CI: 43.5–67.2%) of children with other neurodevelopmental disorders and typically developing children as not having FASD.
A 2-class model best fit the data (Table 2 ). However, the 2-class model was only able to correctly identify 62.7% (37 out of 59 [specificity]; 95% CI: 50.0–74.6%) of children with ADHD and typically developing children as not having FASD (Table 5 ). Thus, although children with FASD performed most similarly to children with ASD on the neurodevelopmental subtest included in the profile (Fig. 1 ), including a small number of children with ASD did not appear to negatively influence the ability of the neurodevelopmental profile to differentiate children with FASD from children with other neurodevelopmental disorders.
Although the neurodevelopmental profile identified was sensitive to FASD, it was not specific to FASD, suggesting that a neurodevelopmental profile that can differentiate children with FASD from children with other neurodevelopmental disorders may not exist. However, the findings are limited by the measures used in the analyses, as the inclusion of additional measures may have resulted in a more specific FASD neurodevelopmental profile. Also, data on the use of psychotropic medications were not available. Given that such medications are intended to alter brain function, their use could have impacted the results of the current study. Despite the relatively small sample size, albeit sufficient [ 31 ], the latent profile analyses did produce statistically and clinically significant results. Given the few cases of ASD, it was not possible to provide classification results for ASD specifically. Even though the 4-class model did result in children with neurodevelopmental disorders (including FASD) being broken down into subgroups, they were not grouped according to their diagnostic categories. It should be acknowledged that it is possible that the subgroupings could have been an artifact of the methodology used, as the primary goal of LPA is to maximize the homogeneity within subgroups and the heterogeneity between them.
The findings of the current study are in line with those of Mattson and colleagues [ 32 ], who were able to demonstrate that a set of neurodevelopmental tests measuring executive function, attention, and visual and spatial memory could differentiate between individuals with FASD and individuals not exposed to alcohol prenatally; however, when using a clinical comparative group, the profile was more accurate at identifying individuals with ADHD than individuals with FASD. Unlike previous studies seeking to identify a unique neurodevelopmental profile of FASD, the current study used a population-based sample of children with FASD – the sample was drawn from a cross-sectional, population-based study that utilized active case ascertainment (the gold standard [ 33 ]) to identify cases of FASD. This is also the first study to analyze and incorporate both behavioral observations/ratings of parents and performance-based measures of neurodevelopment when seeking to identify a neurodevelopmental profile of FASD.
Although prenatal alcohol exposure is a necessary cause of FASD, the genetic etiology of FASD remains unknown. Advances in the understanding of genetics and its role in neurodevelopmental disorder risk have created a paradigm shift, such that neurodevelopmental disorders are no longer viewed as having a psychogenic etiology but rather a genetic etiology (see for example, Glessner et al. [ 34 ]). Prenatal alcohol exposure leads to epigenetic changes (i.e., altered gene expression) [ 35 ]. These changes may contribute to the spectrum of effects and different phenotypes observed in children with FASD [ 35 ]. The discovery of reliable genetic and epigenetic markers for FASD would have significant implications for its diagnosis. Such investigations should not be restricted to FASD, but rather include all neurodevelopmental disorders, as this may lead to current categorical classifications of neurodevelopmental disorders being redefined to be more reflective of biologically homogeneous groups [ 36 ]. Accordingly, future studies should explore whether neurodevelopmental data combined with genetic and epigenetic data would produce a profile able to diagnose and differentiate FASD from other neurodevelopmental disorders.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Attention Deficit Hyperactivity Disorder
Akaike Information Criterion
Alcohol-Related Neurodevelopmental Disorder
Autism Spectrum Disorder
Bayesian Information Criterion
Child Behavior Checklist
Confidence interval
Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition
Fetal Alcohol Syndrome
Fetal Alcohol Spectrum Disorder
Log-Likelihood Value
Neurobehavioral Disorder Associated with Prenatal Alcohol Exposure
NEPSY, Second Edition
Negative predictive value
Occipitofrontal circumference
Partial Fetal Alcohol Syndrome
Palpebral fissure length
Positive predictive value
Standard deviation
Wechsler Abbreviated Scales of Intelligence, Second Edition
Wechsler Intelligence Scale for Children, Fourth Edition
Chudley AE, Conry J, Cook JL, Loock C, Rosales T. N. L: Fetal alcohol spectrum disorder: Canadian guidelines for diagnosis. Can Med Assoc J. 2005;172(5 suppl):S1–S21.
Article Google Scholar
Hoyme HE, Kalberg WO, Elliott AJ, Blankenship J, Buckley D, Marais A-S, Manning MA, Robinson LK, Adam MP, Abdul-Rahman O, et al. Updated clinical guidelines for diagnosing fetal alcohol spectrum disorders. Pediatrics. 2016;138(2):e20154256.
Cook JL, Green CR, Lilley CM, Anderson SM, Baldwin ME, Chudley AE, Conry JL, LeBlanc N, Loock CA, Lutke J, et al. Fetal alcohol spectrum disorder: a guideline for diagnosis across the lifespan. CMAJ. 2016;188(3):191–7.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 5th edition (DSM-5). Arlington: American Psychiatric Association; 2013.
Book Google Scholar
Kable JA, O'Connor MJ, Olson HC, Paley B, Mattson SN, Anderson SM, Riley EP. Neurobehavioral disorder associated with prenatal alcohol exposure (ND-PAE): proposed DSM-5 diagnosis. Child Psychiatry Hum Dev. 2016;47(2):335–46.
Kodituwakku PW. Neurocognitive profile in children with fetal alcohol spectrum disorders. Dev Disabil Res Rev. 2009;15(3):218–24.
Mattson SN, Crocker N, Nguyen TT. Fetal alcohol spectrum disorders: neuropsychological and behavioral features. Neuropsychol Rev. 2011;21(2):81–101.
Mattson SN, Riley EP, Gramling L, Delis DC, Jones KL. Heavy prenatal alcohol exposure with or without physical features of fetal alcohol syndrome leads to IQ deficits. J Pediatr. 1997;131(5):718–21.
Article CAS Google Scholar
Vaurio L, Riley EP, Mattson SN. Neuropsychological comparison of children with heavy prenatal alcohol exposure and an IQ-matched comparison group. J Int Neuropsychol Soc. 2011;17(3):463–73.
Streissguth A, Barr H, Kogan J, Bookstein FL. Understanding the occurrence of secondary disabilities in clients with fetal alcohol syndrome (FAS) and fetal alcohol effects (FAE). In: Final report edn. Seattle: University of Washington, School of Medicine; 1996.
Google Scholar
Chasnoff IJ, Wells AM, King L. Misdiagnosis and missed diagnoses in foster and adopted children with prenatal alcohol exposure. Pediatrics. 2015;135(2):264–70.
Lange S, Rehm J, Anagnostou E, Popova S. Prevalence of externalizing disorders and autism Spectrum disorders among children with fetal alcohol spectrum disorder: systematic review and meta-analysis. Biochem Cell Biol. 2018;96(2):241–51.
Popova S, Lange S, Shield K, Mihic A, Chudley AE, Mukherjee RAS, Bekmuradov D, Rehm J. Comorbidity of fetal alcohol spectrum disorder: a systematic review and meta-analysis. Lancet. 2016;387(10022):978–87.
McLennan JD. Misattributions and potential consequences: the case of child mental health problems and fetal alcohol spectrum disorders. Can J Psychiatr. 2015;60(12):587–90.
Achenbach T, Rescorla L. Manual for the ASEBA school-age forms and profiles. Burlington: University of Vermont, Research Center for Children Youth & Families; 2001.
Popova S, Lange S, Poznyak V, Chudley A, Shield KD, Reynolds JN, Murray M, Rehm J. Population-based prevalence of fetal alcohol spectrum disorder in Canada. BMC Public Health. 2019;19(1):845.
Wechsler D. Wechsler abbreviated scale of intelligence–second edition (WASI-II). San Antonio: PsychCorp; 2011.
Wechsler D. Wechsler intelligence scale for children–fourth edition (WISC-IV). San Antonio: PsychCorp; 2008.
Korkman M, Kirk U, Kemp S. NEPSY-II: a developmental neuropsychological assessment. San Antonio: PsychCorp; 2007.
Loehlin JC. Latent variable models, 3rd edition. Mahwah: Lawrence Erlbaum; 1998.
Cohen J. Statistical power analysis for the behavioral sciences, 2nd edition. Hillsdale: Lawrence Earlbaum Associates; 1988.
Stevens SA, Nash K, Koren G, Rovet J. Autism characteristics in children with fetal alcohol spectrum disorders. Child Neuropsychol. 2013;19(6):579–87.
Akaike H. A new look at the statistical model identification. IEEE Trans Autom Control. 1974;19:716–23.
Sclove S. Application of model-selection criteria to some problems in multivariate analysis. Psychometrika. 1987;52(3):333–43.
Lo Y, Mendell N, Rubin D. Testing the number of components in a normal mixture. Biometrika. 2001;88:767–78.
Celeux G, Soromenho G. An entropy criterion for assessing the number of clusters in a mixture model. J Classif. 1996;13:195–212.
Little R. A test of missing completely at random for multivariate data with missing values. J Am Stat Assoc. 1988;83:1198–202.
Stata Corporation. Statistical software: release 15. College Station: Stata Corporation; 2017.
Muthén L, Muthén B. Mplus user’s guide. 8th ed. Los Angeles: Muthén & Muthén; 2017.
R Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2016.
Wurpts IC, Geiser C. Is adding more indicators to a latent class analysis beneficial or detrimental? Results of a Monte-Carlo study. Front Psychol. 2014;5:920.
Mattson SN, Roesch SC, Glass L, Deweese BN, Coles CD, Kable JA, May PA, Kalberg WO, Sowell ER, Adnams CM, et al. Further development of a neurobehavioral profile of fetal alcohol spectrum disorders. Alcohol Clin Exp Res. 2013;37(3):517–28.
May PA, Gossage JP. Estimating the prevalence of fetal alcohol syndrome. A summary. Alcohol Res Health. 2001;25(3):159–67.
CAS PubMed PubMed Central Google Scholar
Glessner JT, Li J, Wang D, March M, Lima L, Desai A, Hadley D, Kao C, Gur RE, Cohen N, et al. Copy number variation meta-analysis reveals a novel duplication at 9p24 associated with multiple neurodevelopmental disorders. Genome Med. 2017;9(1):106.
Liyanage VR, Curtis K, Zachariah RM, Chudley AE, Rastegar M. Overview of the genetic basis and epigenetic mechanisms that contribute to FASD pathobiology. Curr Top Med Chem. 2017;17(7):808–28.
Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, Sanislow C, Wang P. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry. 2010;167(7):748–51.
Download references
Acknowledgements
Not applicable.
No external funding was sought.
Author information
Authors and affiliations.
Institute for Mental Health Policy Research, Centre for Addiction and Mental Health, 33 Russell Street, Toronto, ON, M5S 2S1, Canada
Shannon Lange, Kevin Shield, Jürgen Rehm & Svetlana Popova
Institute of Medical Science, University of Toronto, 1 King’s College Circle, Toronto, ON, M5S 1A8, Canada
Shannon Lange, Jürgen Rehm, Evdokia Anagnostou & Svetlana Popova
Factor-Inwentash Faculty of Social Work, University of Toronto, 246 Bloor Street, West, Toronto, ON, M5S 1V4, Canada
Svetlana Popova
Dalla Lana School of Public Health, University of Toronto, 155 College Street, Toronto, ON, M5T 3M7, Canada
Kevin Shield, Jürgen Rehm & Svetlana Popova
Institute of Clinical Psychology and Psychotherapy & Center for Clinical Epidemiology and Longitudinal Studies, Technische Universität Dresden, Chemnitzer Str. 46, 01187, Dresden, Germany
Jürgen Rehm
Department of Psychiatry, University of Toronto, 250 College Street, Toronto, ON, M5T 1R8, Canada
Holland Bloorview Kids Rehabilitation Hospital, Bloorview Research Institute, 150 Kilgour Rd., East York, ON, M4G 1R8, Canada
Evdokia Anagnostou
Department of Pediatrics, University of Toronto, 555 University Avenue, Toronto, ON, M5G 1X8, Canada
You can also search for this author in PubMed Google Scholar
Contributions
SL led the conception and design of the study, acquired the data, performed the statistical analysis, interpreted the data, and wrote the manuscript; KS contributed to the statistical analysis, data interpretation, and writing of the manuscript; EA contributed to data interpretation and to revising the manuscript; SP and JR contributed to the conception and design of the study, data interpretation, and writing of the manuscript. All authors approved the final manuscript.
Corresponding author
Correspondence to Shannon Lange .
Ethics declarations
Ethics approval and consent to participate.
The current study was approved by the Research Ethics Board at the Centre for Addiction and Mental Health (Protocol #116/2016).
Consent for publication
Not applicable. The current study utilized secondary, de-identified, anonymized data.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Lange, S., Shield, K., Rehm, J. et al. Fetal alcohol spectrum disorder: neurodevelopmentally and behaviorally indistinguishable from other neurodevelopmental disorders. BMC Psychiatry 19 , 322 (2019). https://doi.org/10.1186/s12888-019-2289-y
Download citation
Received : 29 May 2019
Accepted : 12 September 2019
Published : 28 October 2019
DOI : https://doi.org/10.1186/s12888-019-2289-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Classification function
- Fetal alcohol spectrum disorder
- Neurodevelopmental profile
BMC Psychiatry
ISSN: 1471-244X
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection

Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Fetal Alcohol Syndrome and Fetal Alcohol Spectrum Disorders
Affiliation.
- 1 University of Arizona College of Medicine, Phoenix, AZ, USA.
- PMID: 29094891
Fetal alcohol syndrome (FAS) and fetal alcohol spectrum disorders (FASD) result from intrauterine exposure to alcohol and are the most common nonheritable causes of intellectual disability. The percentage of women who drink or binge drink during pregnancy has increased since 2012. FAS is commonly missed or misdiagnosed, preventing affected children from receiving needed services in a timely fashion. Diagnosis is based on the presence of the following clinical features, all of which must be present: prenatal and/or postnatal growth retardation, facial dysmorphology, central nervous system dysfunction, and neurobehavioral disabilities. FASD is a broader diagnosis that encompasses patients with FAS and others who are affected by prenatal alcohol exposure but do not meet the full criteria for FAS. Management is multidisciplinary and includes managing comorbid conditions, providing nutritional support, managing behavioral problems and educational difficulties, referring patients for habilitative therapies, and educating parents. The Centers for Disease Control and Prevention and other organizations recognize no safe amount of alcohol consumption during pregnancy and recommend complete abstinence from alcohol. All women should be screened for alcohol use during preconception counseling and prenatal care, and alcohol use should be addressed with brief interventions.
PubMed Disclaimer
Similar articles
- Fetal alcohol spectrum disorders in Finland: clinical delineation of 77 older children and adolescents. Autti-Rämö I, Fagerlund A, Ervalahti N, Loimu L, Korkman M, Hoyme HE. Autti-Rämö I, et al. Am J Med Genet A. 2006 Jan 15;140(2):137-43. doi: 10.1002/ajmg.a.31037. Am J Med Genet A. 2006. PMID: 16353236
- Multifaceted case management during pregnancy is associated with better child outcomes and less fetal alcohol syndrome. May PA, Marais AS, Kalberg WO, de Vries MM, Buckley D, Hasken JM, Snell CL, Barnard Röhrs R, Hedrick DM, Bezuidenhout H, Anthonissen L, Bröcker E, Robinson LK, Manning MA, Hoyme HE, Seedat S, Parry CDH. May PA, et al. Ann Med. 2023 Dec;55(1):926-945. doi: 10.1080/07853890.2023.2185808. Ann Med. 2023. PMID: 36919586 Free PMC article.
- Prenatal effects of alcohol. Abel EL. Abel EL. Drug Alcohol Depend. 1984 Sep;14(1):1-10. doi: 10.1016/0376-8716(84)90012-7. Drug Alcohol Depend. 1984. PMID: 6386408 Review.
- Global prevalence of alcohol use and binge drinking during pregnancy, and fetal alcohol spectrum disorder. Popova S, Lange S, Probst C, Gmel G, Rehm J. Popova S, et al. Biochem Cell Biol. 2018 Apr;96(2):237-240. doi: 10.1139/bcb-2017-0077. Epub 2017 Aug 23. Biochem Cell Biol. 2018. PMID: 28834683
- Fetal Alcohol Spectrum Disorders: Characteristics, Complications, and Treatment. Wilhoit LF, Scott DA, Simecka BA. Wilhoit LF, et al. Community Ment Health J. 2017 Aug;53(6):711-718. doi: 10.1007/s10597-017-0104-0. Epub 2017 Feb 6. Community Ment Health J. 2017. PMID: 28168434 Review.
- The Impact of Oxidative Stress on the Epigenetics of Fetal Alcohol Spectrum Disorders. Terracina S, Tarani L, Ceccanti M, Vitali M, Francati S, Lucarelli M, Venditti S, Verdone L, Ferraguti G, Fiore M. Terracina S, et al. Antioxidants (Basel). 2024 Mar 28;13(4):410. doi: 10.3390/antiox13040410. Antioxidants (Basel). 2024. PMID: 38671857 Free PMC article. Review.
- Oxidative Effects in Early Stages of Embryo Development Due to Alcohol Consumption. González-Flores D, Márquez A, Casimiro I. González-Flores D, et al. Int J Mol Sci. 2024 Apr 7;25(7):4100. doi: 10.3390/ijms25074100. Int J Mol Sci. 2024. PMID: 38612908 Free PMC article. Review.
- Prenatal Alcohol Exposure and Metabolic Disorders in Pediatrics: The Role of the Oxidative Stress-A Review of the Literature. Derme M, Briante M, Ceccanti M, Giannini G, Vitali M, Messina MP, Piccioni MG, Mattia A, Nicotera S, Crognale A. Derme M, et al. Children (Basel). 2024 Feb 21;11(3):269. doi: 10.3390/children11030269. Children (Basel). 2024. PMID: 38539304 Free PMC article. Review.
- Fetal Alcohol Spectrum Disorders and Inadequacy of Care: Importance of Raising Awareness in Clinical Practice. Lesinskienė S, Žilinskas E, Utkus A, Marčiukaitytė R, Vasiliauskaitė G, Stankevičiūtė R, Kinčinienė O. Lesinskienė S, et al. Children (Basel). 2023 Dec 20;11(1):5. doi: 10.3390/children11010005. Children (Basel). 2023. PMID: 38275426 Free PMC article. Review.
- Clinical Diagnosis and Management of Fetal Alcohol Spectrum Disorder and Sensory Processing Disorder in Children. Breuer L, Greenmyer JR, Wilson T. Breuer L, et al. Children (Basel). 2024 Jan 16;11(1):108. doi: 10.3390/children11010108. Children (Basel). 2024. PMID: 38255421 Free PMC article. Review.
- Search in MeSH
Related information
- Cited in Books
LinkOut - more resources
Full text sources.
- American Academy of Family Physicians
- MedlinePlus Health Information
Research Materials
- NCI CPTC Antibody Characterization Program
Miscellaneous
- NCI CPTAC Assay Portal
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- For authors
- BMJ Journals
You are here
- Volume 106, Issue 7
- Fetal alcohol spectrum disorders: an overview of current evidence and activities in the UK
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
This article has a correction. Please see:
- Correction: Fetal alcohol spectrum disorders: an overview of current evidence and activities in the UK - November 01, 2021
- http://orcid.org/0000-0002-1348-672X Lisa Schölin 1 ,
- http://orcid.org/0000-0002-2171-928X Raja A S Mukherjee 2 ,
- Neil Aiton 3 ,
- Carolyn Blackburn 4 ,
- Sarah Brown 5 ,
- Kate M Flemming 6 , 7 ,
- Paul R Gard 8 ,
- Helen Howlett 9 ,
- Moira Plant 10 ,
- Alan D Price 11 ,
- Jennifer Shields 5 ,
- Lesley A Smith 12 ,
- Michael Suttie 13 ,
- David C Zammitt 5 ,
- Penny A Cook 14
- The UK FASD Research Collaboration
- 1 School of Health in Social Science , The University of Edinburgh , Edinburgh , UK
- 2 Fetal Alcohol Syndrome Specialist Behaviour Clinic , Surrey and Borders Partnership NHS Foundation Trust , Surrey , UK
- 3 One Stop Clinic , Royal Sussex County Hospital , Brighton , Brighton and Hove , UK
- 4 Centre for the Study of Practice and Culture in Education , Birmingham City University , Birmingham , West Midlands , UK
- 5 Fetal Alcohol Advisory and Support Team , NHS Ayrshire and Arran , Ayr , South Ayrshire , UK
- 6 Department of Public Health, Policy and Systems, Institute of Population Health , University of Liverpool , Liverpool , Merseyside , UK
- 7 Liverpool Centre for Alcohol Research , Liverpool , UK
- 8 School of Pharmacy and Biomolecular Science , University of Brighton , Brighton , East Sussex , UK
- 9 Faculty of Health and Life Science , Northumbria University , Newcastle upon Tyne , Tyne and Wear , UK
- 10 Faculty of Health and Applied Sciences , University of the West of England Bristol , Bristol , UK
- 11 School of Health and Society , University of Salford , Salford , Greater Manchester , UK
- 12 Institute of Clinical and Applied Health Research , University of Hull , Hull , Kingston upon Hull , UK
- 13 Nuffield Department of Women's and Reproductive Health , Oxford University , Oxford , Oxfordshire , UK
- 14 School of Health Sciences , University of Salford , Salford , UK
- Correspondence to Dr Raja A S Mukherjee, Fetal Alcohol Syndrome Specialist Behaviour Clinic, Surrey and Borders Partnership NHS Foundation Trust, Surrey, UK; raja.mukherjee{at}sabp.nhs.uk
Estimates for the UK suggest that alcohol consumption during pregnancy and prevalence of fetal alcohol spectrum disorder (FASD)—the most common neurodevelopmental condition—are high. Considering the significant health and social impacts of FASD, there is a public health imperative to prioritise prevention, interventions and support. In this article, we outline the current state of play regarding FASD knowledge and research in the UK, which is characterised by a lack of evidence, a lack of dedicated funding and services, and consequently little policy formulation and strategic direction. We highlight progress made to date, as well as current knowledge and service gaps to propose a way forward for UK research.
- adolescent health
- neonatology
Data availability statement
No data are available. Not applicable.
https://doi.org/10.1136/archdischild-2020-320435
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Twitter @lesaangelica, @rajamukherjee10, @blackbu5, @mykiesutt
Correction notice This article has been corrected since it first published. The provenance and peer review statement has been included.
Contributors RM and PC convened the first meeting of the UK FASD Research Collaboration, where the authors of this paper met to establish research priorities and create an outline of this paper, led by LS. All authors contributed writing sections of the paper, which was edited and coordinated by LS. All authors reviewed the final manuscript before submission.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests RM is an unpaid voluntary Medical advisor to various UK and international FASD charities and has received occasional honoraria for academic talks related to FASD. JS, SB and DZ have funding from a Scottish Government grant to expand training, research and clinical knowledge of FASD. Remaining authors have no conflict of interest to report.
Provenance and peer review Not commissioned; externally peer reviewed.
Linked Articles
- Original research Genetic testing in patients with possible foetal alcohol spectrum disorder Zena Lam Kathryn Johnson Rosalyn Jewell Archives of Disease in Childhood 2020; 106 653-655 Published Online First: 23 Nov 2020. doi: 10.1136/archdischild-2020-319572
- Atoms Highlights from this issue Nick Brown Archives of Disease in Childhood 2021; 106 i-i Published Online First: 18 Jun 2021. doi: 10.1136/archdischild-2021-322579
- Miscellaneous Correction: Fetal alcohol spectrum disorders: an overview of current evidence and activities in the UK BMJ Publishing Group Ltd and Royal College of Paediatrics and Child Health Archives of Disease in Childhood 2021; 106 e46-e46 Published Online First: 20 Oct 2021. doi: 10.1136/archdischild-2020-320435corr1
Read the full text or download the PDF:
Association of Prenatal Alcohol Exposure With Psychological, Behavioral, and Neurodevelopmental Outcomes in Children From the Adolescent Brain Cognitive Development Study
Information & authors, metrics & citations, view options, conclusions:, study population.
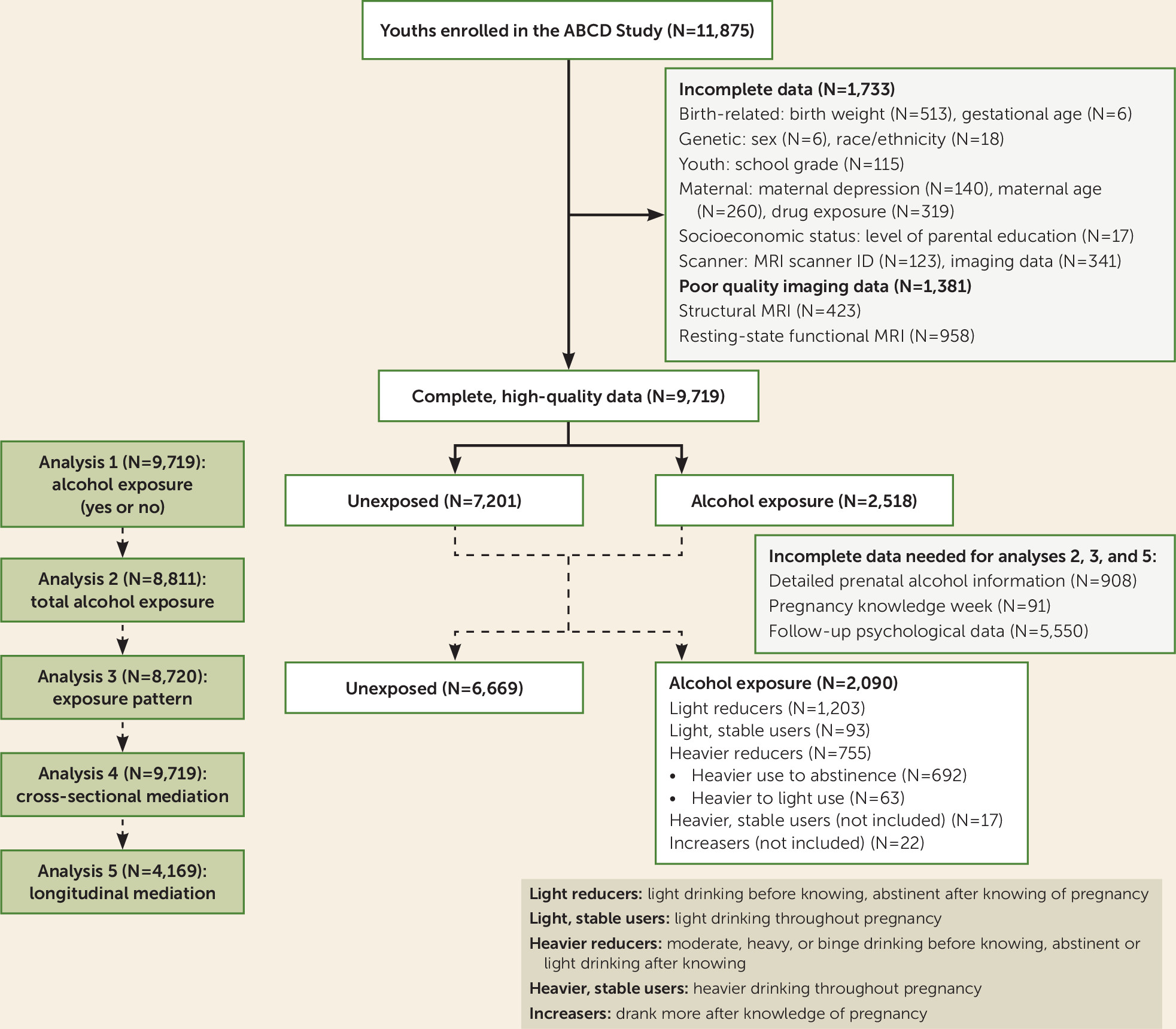
- Prenatal Alcohol Exposure
Psychological and Behavioral Variables
Cognitive variables.
| Characteristic | Unexposed Youths (N=7,201) | Youths With Prenatal Alcohol Exposure (N=2,518) | p | ||
|---|---|---|---|---|---|
| Sex | 0.32 | ||||
| Male | 3,776 | 52.4 | 1,291 | 51.3 | |
| Female | 3,425 | 47.6 | 1,227 | 48.7 | |
| Race/ethnicity | <0.001 | ||||
| White | 3,631 | 50.4 | 1,630 | 64.7 | |
| Black | 1,126 | 15.6 | 216 | 8.6 | |
| Hispanic | 1,574 | 21.9 | 407 | 16.2 | |
| Asian | 139 | 1.9 | 27 | 1.1 | |
| Other | 731 | 10.2 | 238 | 9.5 | |
| Born premature | 0.07 | ||||
| Yes | 1,417 | 19.7 | 443 | 17.6 | |
| No | 5,757 | 79.9 | 2,065 | 82.0 | |
| Unknown | 27 | 0.4 | 10 | 0.4 | |
| Prenatal tobacco exposure | <0.001 | ||||
| Yes | 637 | 8.8 | 628 | 24.9 | |
| No | 6,551 | 91.0 | 1,865 | 74.1 | |
| Unknown | 13 | 0.2 | 25 | 1.0 | |
| Prenatal cannabis exposure | <0.001 | ||||
| Yes | 204 | 2.8 | 325 | 12.9 | |
| No | 6,987 | 97.0 | 2,150 | 85.4 | |
| Unknown | 10 | 0.1 | 43 | 1.7 | |
| Prenatal cocaine exposure | <0.001 | ||||
| Yes | 9 | 0.1 | 44 | 1.7 | |
| No | 7,187 | 99.8 | 2,446 | 97.1 | |
| Unknown | 5 | 0.1 | 28 | 1.1 | |
| Prenatal heroin exposure | <0.001 | ||||
| Yes | 7 | 0.1 | 8 | 0.3 | |
| No | 7,190 | 99.8 | 2,482 | 98.6 | |
| Unknown | 4 | 0.1 | 28 | 1.1 | |
| School grade performance | <0.001 | ||||
| A | 3,233 | 44.9 | 1,190 | 47.3 | |
| B | 2,408 | 33.4 | 788 | 31.3 | |
| C | 776 | 10.8 | 226 | 9.0 | |
| D | 130 | 1.8 | 43 | 1.7 | |
| F | 28 | 0.4 | 7 | 0.3 | |
| Ungraded | 626 | 8.7 | 264 | 10.5 | |
| Consumed full drink of alcohol | 10 | 0.1 | 6 | 0.2 | 0.44 |
| Age (years) | 9.9 | 0.6 | 9.9 | 0.6 | 0.89 |
| Birth weight (lb) | 6.6 | 1.5 | 6.7 | 1.4 | <0.001 |
| Highest level of education | <0.001 | ||||
| Less than high school diploma | 547 | 7.6 | 59 | 2.3 | |
| High school diploma or General Equivalency Diploma | 838 | 11.6 | 155 | 6.2 | |
| Some college | 2,191 | 30.4 | 687 | 27.3 | |
| Bachelor’s degree | 1,999 | 27.8 | 809 | 32.1 | |
| Postgraduate degree | 1,626 | 22.6 | 808 | 32.1 | |
| Maternal depression | <0.001 | ||||
| Yes | 1,530 | 21.2 | 656 | 26.1 | |
| No | 5,495 | 76.3 | 1,763 | 70.0 | |
| Unknown | 176 | 2.4 | 99 | 3.9 | |
| Maternal age at delivery (years) | 29.2 | 6.3 | 30.1 | 5.9 | <0.001 |
| Week of pregnancy knowledge | 6.9 | 7.0 | 6.9 | 5.7 | 0.93 |
Imaging Procedure
Statistical analysis, associations with prenatal alcohol exposure., mediation analysis., study sample, associations with prenatal alcohol exposure, dichotomous prenatal alcohol exposure associations..
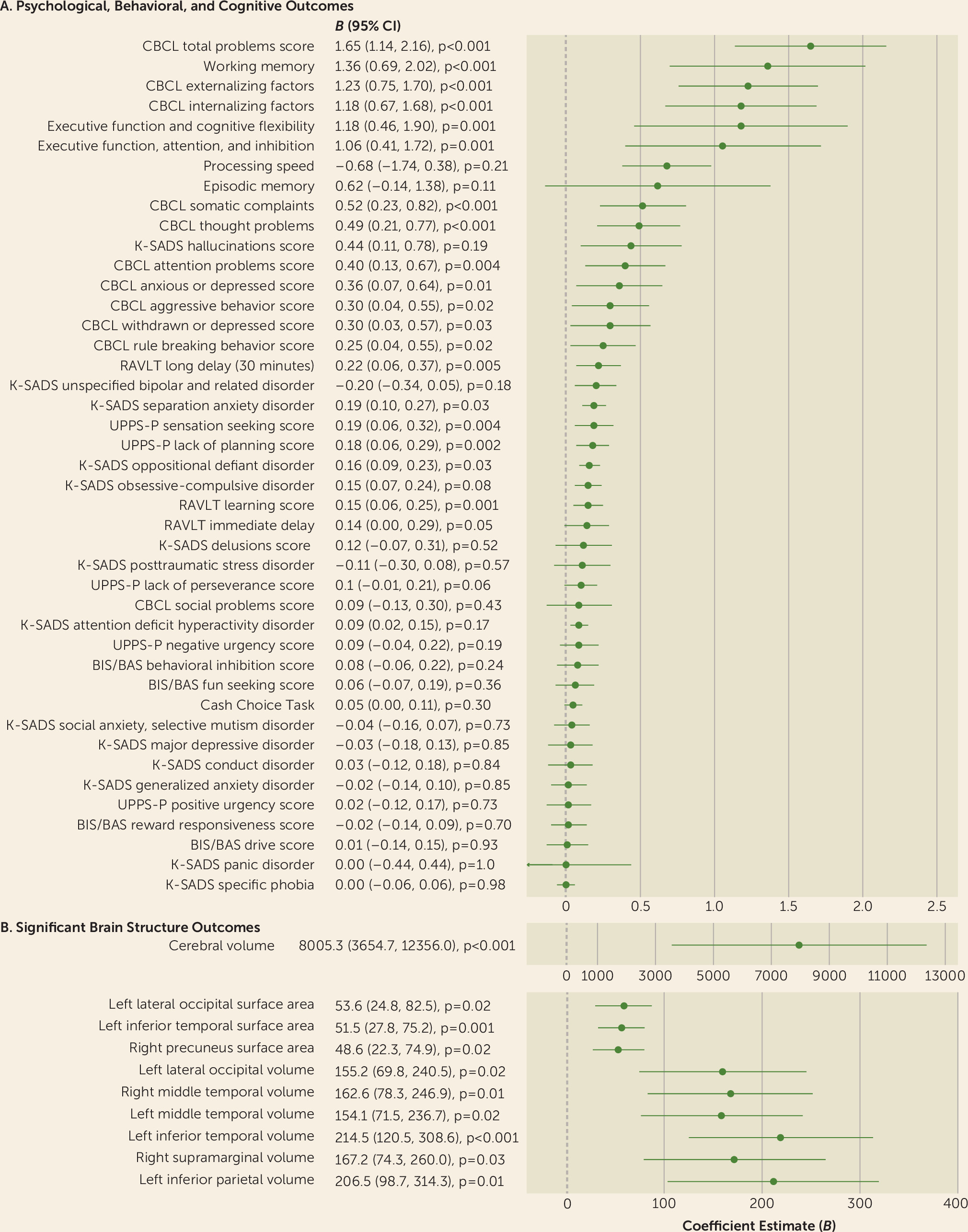
Dose-dependent associations.
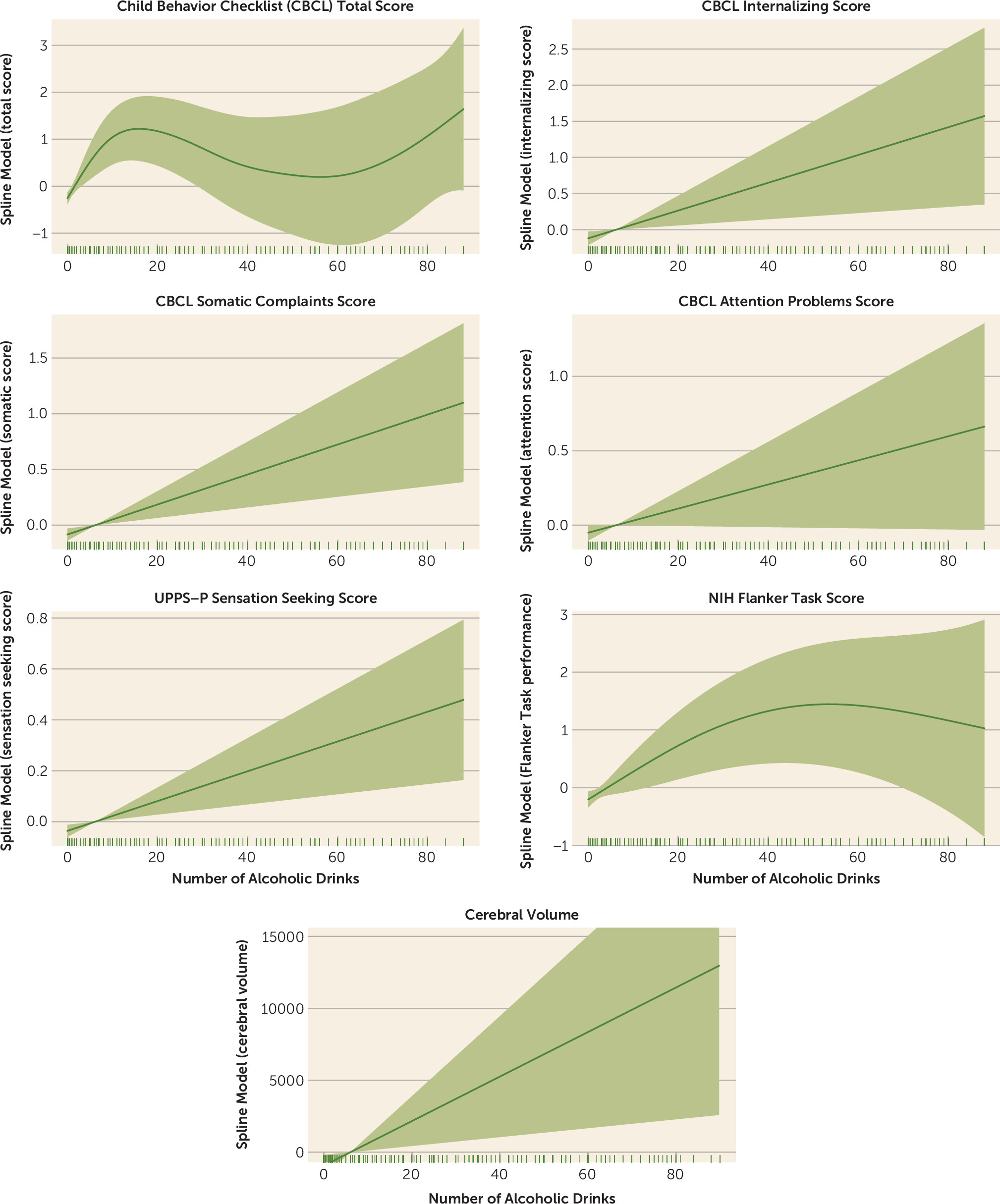
Exposure pattern associations.
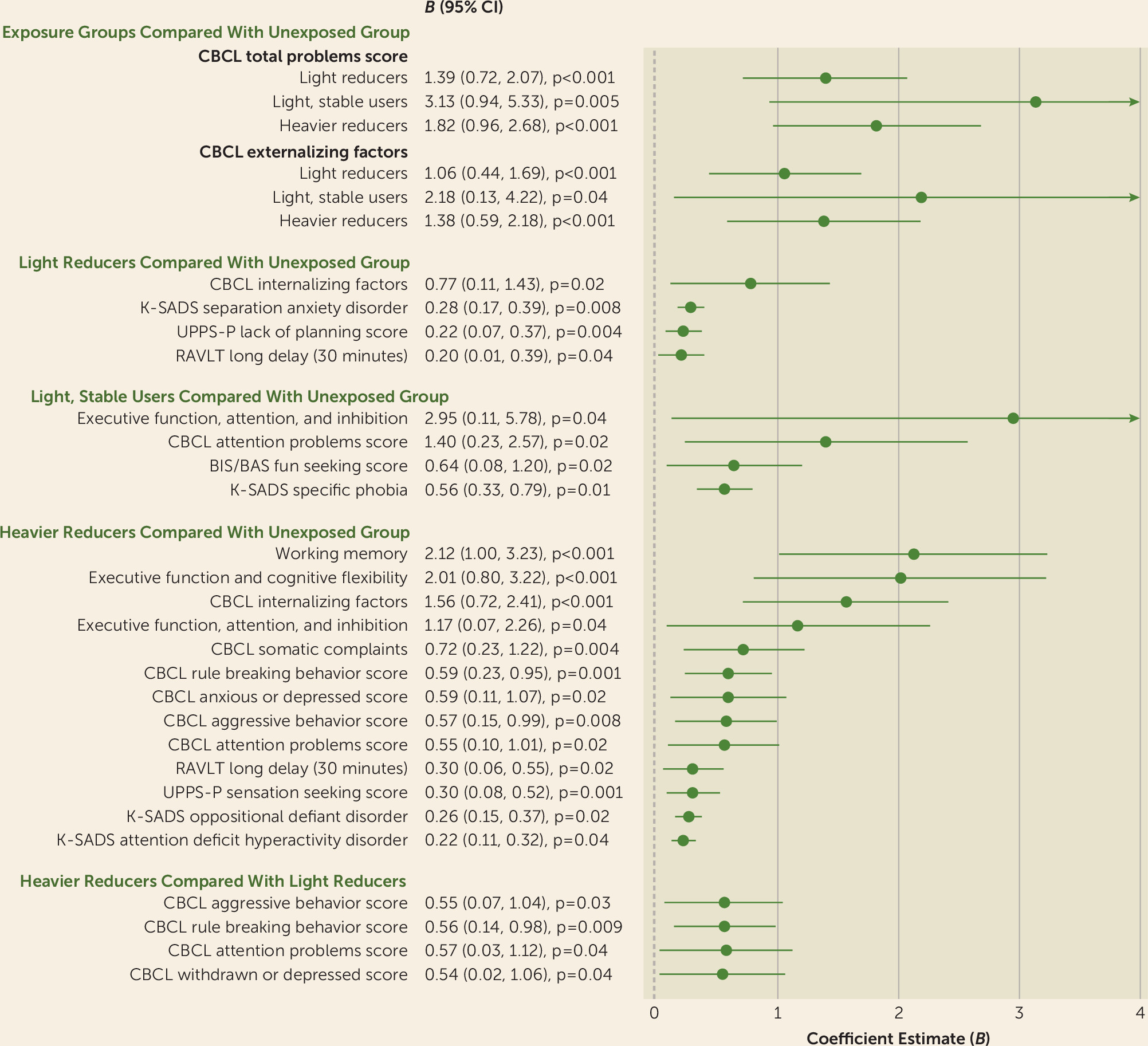
Sensitivity analysis.
Mediation analysis, alcohol exposure findings, comparison with other studies, interpretation and potential biological mechanisms underlying neurobehavioral outcomes, acknowledgments, supplementary material.
- View/Download
Information
Published in.
- Brain Development
- Psychopathology
- Child/Adolescent Psychiatry
Funding Information
Export citations.
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download. For more information or tips please see 'Downloading to a citation manager' in the Help menu .
| Format | |
|---|---|
| Citation style | |
| Style | |
To download the citation to this article, select your reference manager software.
There are no citations for this item
View options
Login options.
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Purchase Options
Purchase this article to access the full text.
PPV Articles - American Journal of Psychiatry
Not a subscriber?
Subscribe Now / Learn More
PsychiatryOnline subscription options offer access to the DSM-5-TR ® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).
Share article link
Copying failed.
PREVIOUS ARTICLE
Next article, request username.
Can't sign in? Forgot your username? Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username
Create a new account
Change password, password changed successfully.
Your password has been changed
Reset password
Can't sign in? Forgot your password?
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password.
Your Phone has been verified
As described within the American Psychiatric Association (APA)'s Privacy Policy and Terms of Use , this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences. Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.

A hidden epidemic of fetal alcohol syndrome
New legislation could help bring awareness and resources to prevention, diagnosis, and treatment of fetal alcohol spectrum disorders
Vol. 53 No. 5 Print version: page 24
- Substance Use, Abuse, and Addiction
- Infants and Toddlers

Stress and alcohol use often go hand in hand, a concerning pattern on the heels of the Covid -19 pandemic. Researchers have found that alcohol use increased sharply during the pandemic, and there is some evidence that those patterns were present among pregnant women as well, said Ira Chasnoff, MD, a pediatrician and fetal alcohol spectrum disorder (FASD) researcher at the University of Illinois College of Medicine in Chicago. Experts worry that the trend could result in more babies being born with damage from prenatal alcohol exposure.
Even before the pandemic, FASD was a significant problem. Experts estimate that 2% to 5% of U.S. schoolchildren—as many as 1 in 20—may be affected by prenatal alcohol exposure, which can cause complications with growth, behavior, and learning. The effects on individuals and families, as well as the economic costs, are substantial.
Yet support for FASD research and services is limited. The National Institute on Alcohol Abuse and Alcoholism funds innovative research on FASD, said Christie Petrenko, PhD, a clinical psychologist and research associate professor at Mt. Hope Family Center, University of Rochester, and codirector of the FASD Diagnostic and Evaluation Clinic there. But a Substance Abuse and Mental Health Services Administration (SAMHSA)–funded FASD Center for Excellence program was shuttered in 2016, leaving a big gap between the research being done and practical solutions for children and families affected by FASD, she said. Now, there’s a bipartisan bill before Congress, the FASD Respect Act, which would support FASD research, surveillance, and activities related to diagnosis, prevention, and treatment. (APA has endorsed this bill.)
Such attention is sorely needed, and psychologists have a significant role to play in diagnosis, prevention, and treatment, Petrenko said. “Families are desperate for support.” Yet many people with FASD haven’t even received an accurate diagnosis, let alone appropriate treatments.
Clinicians should be aware that FASD often overlaps with mental health symptoms. These problems begin in early childhood and exist through adulthood, as described by Mary O’Connor, PhD, ABPP, founder of the UCLA Fetal Alcohol Spectrum Disorders Clinic ( Current Developmental Disorders Reports , Vol. 1, No. 1, 2014 ). Her research has also found a higher incidence of suicidal ideation and behavior in adolescents with FASD ( Birth Defects Research , Vol. 111, No. 12, 2019 ). And many adults with FASD who have mental health disorders aren’t getting treatment, said Susan Stoner, PhD, a research associate professor at the University of Washington School of Medicine and director of the Washington State Parent-Child Assistance Program, a program for pregnant and parenting women with substance use disorders ( Alcoholism: Clinical and Experimental Research , Vol. 46, No. 2, 2022 ). “We found those with less severe FASD tend to have worse mental health than those with more severe FASD, which might be because those with more severe FASD are more likely to have a diagnosis and more likely to get support,” she said.
Understanding FASD
Many variables determine whether an infant will be born with FASD and how severe the disorder will be. Such factors include how much a pregnant person drinks, the rate at which they metabolize alcohol, and the stage of fetal development during alcohol exposure. “There are too many variables at play to estimate a safe level of drinking during pregnancy,” Stoner said. “The safest amount of alcohol during pregnancy is zero.”
Prenatal alcohol exposure can result in several conditions that fall under the FASD umbrella. These include fetal alcohol syndrome (FAS) and partial FAS, both of which can cause growth problems, central nervous system problems, and characteristic facial features (including small eye openings, flattening of the ridge between the nose and lip, and a thin upper lip), in addition to problems with learning and behavior. People with alcohol-related neurodevelopmental disorder (ARND) don’t have the characteristic facial features or growth deficiency of FAS, but they may have wide-ranging neurocognitive disabilities and problems with behavior and learning. These diagnoses overlap with a newer term—neurobehavioral disorder associated with prenatal alcohol exposure (ND-PAE)—a classification first included in the Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition) as a condition requiring further study (Kable, J. A., et al., Child Psychiatry & Human Development , Vol. 47, No. 2, 2016 ).
Each of the disorders in the fetal alcohol spectrum can cause problems with self-regulation, executive functioning, social skills, and math skills. These deficits often interfere with children’s performance in school and their ability to make friends. Yet while FASD often causes learning difficulties, the symptoms can be unpredictable. “FASD is the most common preventable cause of intellectual disability in the world. But the majority of alcohol-exposed children have a normal IQ,” Chasnoff said. One notable feature of FASD is a gap between intelligence and adaptive functioning, he added. One of his teen patients, for example, has above average intelligence but is unable to read clocks or count money. “In children affected by alcohol exposure, adaptive functioning is significantly lower than IQ,” he said.
Behavioral problems associated with FASD are common, and often misunderstood, said Petrenko. “So many of the symptoms of FASD can look like intentionally willful or oppositional behavior, when really there are underlying neurodevelopmental explanations,” she said. An accurate diagnosis is the first step toward putting supports in place to address those neurodevelopmental challenges and help people with FASD thrive.
Diagnosis and treatment of FASD
The gold standard for FASD diagnosis is a multidisciplinary evaluation looking at physical features, neurobehavioral impairments, and any known history of prenatal alcohol exposure. The assessment typically involves a variety of specialists such as physicians, speech/language pathologists, psychologists, and geneticists. But those comprehensive evaluations are hard to come by. “There are very few FASD clinics that provide full-service diagnosis,” O’Connor said. “It’s estimated that about only 1% of people with prenatal alcohol exposure can get a diagnosis in that type of situation.”
As a result, many children with FASD are falling through the cracks. Chasnoff and colleagues collected data from 547 foster and adopted children and found that within this group 86.5% of youth with FASD had never been diagnosed or had been misdiagnosed ( Pediatrics , Vol. 135, No. 2, 2015 ). “The great majority of children that are affected by alcohol are misdiagnosed and taking inappropriate medications or receiving ineffective therapy,” Chasnoff said. “FASD should be in the differential diagnosis for any child who presents with behavior problems. And while no single discipline can diagnose FASD, psychologists have a major role to play in the diagnosis.”
Psychologists are also instrumental in designing treatments for children with FASD. To date, only a handful of evidence-based interventions have been developed, each targeting different aspects of FASD. Parents and Children Together (PACT), developed by Chasnoff and colleagues, is a 12-week family intervention that works with children ages 6 to 12 years old and their parents or caregivers to improve self-regulation and executive function. PACT builds on techniques learned from treating traumatic brain injury and sensory processing disorders. The research has found that the intervention improves executive functioning and emotional problem-solving in children with FAS and ARND (Wells, A. M., et al., American Journal of Occupational Therapy , Vol. 66, No. 1, 2012 ).
The Math Interactive Learning Experience (MILE) program, developed by clinical psychologist Claire Coles, PhD, at Emory University, is a tutoring intervention designed to improve math knowledge and skills, a common area of struggle for children with FASD. A study showed that the 6-week intervention improved both math skills and behavior in alcohol-affected children ages 3 to 10 ( Journal of Developmental & Behavioral Pediatrics , Vol. 30, No. 1, 2009 ).
Children with FASD often have trouble learning social skills as well. The Good Buddies program, developed by O’Connor and colleagues, is designed to teach those skills in a group format over 12 weeks to children ages 6 to 12. The program is derived from an evidence-based treatment for improving children’s friendships, adapted for the specific behavioral and cognitive deficits common in children with FASD (Laugeson, E. A., et al., Child and Family Behavior Therapy , Vol. 29, No. 3, 2007 ).
The Families Moving Forward Program, created by Heather Carmichael Olson, PhD, and colleagues at Seattle Children’s Research Institute, provides support for families of children with FASD and significant behavioral challenges. The program targets caregivers rather than children themselves and typically lasts about 9 months, in person or by telehealth. Studies have shown the efficacy of the program (Bertrand, J., Research in Developmental Disabilities , Vol. 30, No. 5, 2009 ), which is now used in multiple states and Canada. Petrenko is collaborating with Olson and colleagues to develop a mobile app, Families Moving Forward (FMF) Connect, to help more families access resources and support ( JMIR Formative Research , Vol. 5, No. 12, 2021 ). The researchers are also adapting the program for children from birth to age 3.
With the right tools, children and adults with FASD can lead successful lives. “The biggest thing we’ve learned is the idea of reframing—looking at behavioral symptoms in a new way,” Petrenko said. Instead of treating a child as oppositional, for instance, reframing helps providers and parents understand that the child may be unable to do what they’re asked because of working memory deficits or other cognitive impairments. “By reframing these interpretations, you can put supports in place to help people be more successful,” she said.
Preventing FASD, attacking stigma
Efforts are also underway to prevent babies from being born with FASD. The Centers for Disease Control and Prevention promotes two strategies to reduce alcohol-exposed pregnancies. Choices is an evidence-based program that helps women make decisions around drinking and contraception (Floyd, R. L., et al., American Journal of Preventive Medicine , Vol. 32, No. 1, 2007 ). The other strategy, alcohol screening and brief intervention (SBI), is a preventive service that involves screening questions about drinking patterns, a short conversation with patients who drink more than recommended amounts, and referral to treatment when appropriate ( Planning and Implementing Screening and Brief Intervention for Risky Alcohol Use [PDF, 2.11MB] , Centers for Disease Control and Prevention, 2014). “These interventions could easily be incorporated as part of a psychologist’s practice,” O’Connor said. (See more on brief screening interventions .)
Other efforts are underway to reduce the number of children born with FASD. Stoner directs the Washington State Parent-Child Assistance Program (PCAP), a 3-year intensive case management program for mothers who have used alcohol or drugs during pregnancy. PCAP works with pregnant women to stop drinking and also continues to provide support after they give birth. The program connects mothers to social and health services to reduce the likelihood that their future children will be exposed to alcohol or drugs prenatally by reducing substance use or deferring pregnancy. PCAP has 15 sites in Washington covering 19 counties and 90% of the state population, Stoner said. While the program has had success, it was developed several decades ago, and its wide dissemination across the state makes it difficult to do a modern trial to evaluate its effectiveness. To develop that evidence base, Stoner and colleagues have launched a randomized controlled trial in Oklahoma, where they will compare outcomes for women in PCAP with those who receive services as usual.
While education and awareness of FASD have increased among physicians and mental health providers, many are still reluctant to speak with pregnant women about substance use, O’Connor said. Clinical psychologists can and should raise the topic with women in their care who are or might become pregnant. “Prevention can begin in the therapy room,” Stoner said. But it’s important to ask a woman about pregnancy and substance use in ways that encourage honesty and reduce stigma, O’Connor added. “So, for example, instead of asking, ‘Did you drink during pregnancy?’, it’s better to ask, ‘How often did you drink before you found out you were pregnant? And how much did you drink after?’” she said.
While careful conversation can help, stigma continues to be a challenge. Discomfort around the subject often prevents medical providers from asking women about alcohol use during pregnancy at all. Stigma also prevents women from seeking help for alcohol dependence and may prevent them from pursuing a FASD diagnosis for their child. Addressing negative perceptions about alcohol use during pregnancy is an important step toward reducing rates of FASD and improving lives for people with these conditions, Petrenko said. “People with FASD and their families are capable. They can thrive if we recognize their strengths and provide appropriate services and supports.”
Additional resources
Updated clinical guidelines for diagnosing fetal alcohol spectrum disorders Hoyme, H. E., et al., Pediatrics , 2016
Treatment improvement protocol (TIP) series 58: Addressing fetal alcohol spectrum disorders (FASD) Substance Abuse and Mental Health Services Administration, 2013
Fetal alcohol spectrum disorders training and resources Centers for Disease Control and Prevention, 2022
Fetal alcohol spectrum disorders national resource directory University of Washington Fetal Alcohol and Drug Unit, 2022
FASD intervention, training, and research Families Moving Forward Program, 2022
Recommended Reading
Contact apa, you may also like.
- Research article
- Open access
- Published: 23 June 2017
Neurodevelopmental profile of Fetal Alcohol Spectrum Disorder: A systematic review
- Shannon Lange 1 , 2 ,
- Joanne Rovet 3 , 4 ,
- Jürgen Rehm 1 , 2 , 5 , 6 &
- Svetlana Popova 1 , 2 , 5 , 7
BMC Psychology volume 5 , Article number: 22 ( 2017 ) Cite this article
15k Accesses
61 Citations
13 Altmetric
Metrics details
In an effort to improve the screening and diagnosis of individuals with Fetal Alcohol Spectrum Disorder (FASD), research has focused on the identification of a unique neurodevelopmental profile characteristic of this population. The objective of this review was to identify any existing neurodevelopmental profiles of FASD and review their classification function in order to identify gaps and limitations of the current literature.
A systematic search for studies published up to the end of December 2016 reporting an identified neurodevelopmental profile of FASD was conducted using multiple electronic bibliographic databases. The search was not limited geographically or by language of publication. Original research published in a peer-reviewed journal that involved the evaluation of the classification function of an identified neurodevelopmental profile of FASD was included.
Two approaches have been taken to determine the pathognomonic neurodevelopmental features of FASD, namely the utilization of i) behavioral observations/ratings by parents/caregivers and ii) subtest scores from standardized test batteries assessing a variety of neurodevelopmental domains. Both approaches show some promise, with the former approach (which is dominated by research on the Neurobehavioral Screening Tool) having good sensitivity (63% to 98%), but varying specificity (42% to 100%), and the latter approach having good specificity (72% to 96%), but varying sensitivity (60% to 88%).
Conclusions
The current review revealed that research in this area remains limited and a definitive neurodevelopmental profile of FASD has not been established. However, the identification of a neurodevelopmental profile will aid in the accurate identification of individuals with FASD, by adding to the armamentarium of clinicians. The full review protocol is available in PROSPERO ( http://www.crd.york.ac.uk/PROSPERO/ ); registration number CRD42016039326; registered 20 May 2016.
Peer Review reports
Fetal Alcohol Spectrum Disorder (FASD) is a term that encompasses a range of disorders, all of which involve prenatal alcohol exposure as the etiological cause. The effects of prenatal alcohol exposure can vary from mild to severe, and can include a broad array of cognitive, behavioral, emotional, adaptive functioning deficits, as well as congenital anomalies. FASD includes the following alcohol-related diagnoses: Fetal Alcohol Syndrome (FAS), Partial FAS (pFAS), Alcohol-Related Neurodevelopmental Disorder (ARND), and depending on the diagnostic guideline, Alcohol-Related Birth Defects (ARBD; [ 1 , 2 ]). Recently, it has been proposed that FASD be used as a diagnostic term with the specification of the presence or absence of the sentinel facial features, rather than simply a non-diagnostic umbrella term [ 3 ]. This is in line with the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5; [ 4 ]) where Neurobehavioral Disorder Associated with Prenatal Alcohol Exposure (ND-PAE) was included as a condition that warrants further research and also as one specifier for the broader diagnostic term of Other Specified Neurodevelopmental Disorder. ND-PAE is intended to encompass the behavioral, developmental and mental health symptoms associated with prenatal alcohol exposure and is appropriate for individuals with or without physical findings [ 5 ].
With the exception of ARBD, all of the disorders within the spectrum are associated with a broad array of neurodevelopmental deficits [ 6 , 7 , 8 , 9 ]. Specifically, individuals with FASD exhibit relative deficits in adaptive function, attention, executive function, externalizing behaviors, motor function, social cognition, and verbal and nonverbal learning [ 10 , 11 ].
Until very recently, the specific domains of function to be evaluated during the neurodevelopmental assessment have been relatively undefined and have lacked consensus [ 12 ]. The diagnostic guidelines have had a tendency to focus on the severity of the neurodevelopmental impairments rather than the specificity of the impairments. This weakness of the former diagnostic guidelines mainly impacted the diagnosis of ARND, given that diagnosis is based primarily on the neurodevelopmental impairments the child exhibits as the characteristic facial traits and growth deficits associated with FAS and pFAS are often absent with ARND. Yet, ARND is recognized to be the largest category of affected individuals, representing as many as 80–90% of FASD cases [ 13 ]. In addition to the ambiguity surrounding the diagnosis of FASD, the neurodevelopmental assessment is thought to be the lengthiest and most cumbersome component of the diagnostic evaluation [ 14 ]. Following the revised clinical guidelines of Hoyme and colleagues [ 2 ] and the proposed criteria for ND-PAE [ 5 ], three primary domains of functional impairment have been identified, namely neurocognition, self-regulation and adaptive functioning. Nevertheless, more information is needed regarding the validity of the available diagnostic approaches and the suggested cut-points.
Further, coupled with the fact that the signs of such conditions as traumatic head injury and intellectual disability where the etiological cause is not prenatal alcohol exposure are similar to FASD, the diagnostic criteria of FASD may also overlap with other neurodevelopmental disorders such as Attention Deficit Hyperactivity Disorder (ADHD), Oppositional Defiant Disorder (ODD), and Conduct Disorder (CD) [ 15 ]. As a result, individuals with FASD often receive multiple diagnoses before actually being assessed for and diagnosed with FASD [ 16 ]. It is important to note that diagnostic misclassification can have a number of untoward consequences, particularly inappropriate treatments and interventions, mismanagement of behavioral symptoms, inaccurate incidence and prevalence estimates, and reduced ability to detect a significant difference between diagnostic groups in clinical research studies [ 16 , 17 ].
Therefore, in an effort to improve the screening and diagnosis of individuals with FASD, most research to date has focused on the identification of a distinct neurodevelopmental profile of FASD – defined as the outward expression (behavioral and developmental) of the central nervous system damage caused by prenatal alcohol exposure. The notion that a distinctive neurodevelopmental profile exists in individuals with FASD first emerged in the late 1990s by Stressiguth and colleagues [ 18 ]. However, identifying a neurodevelopmental profile remains to be a challenge given the wide range of deficits individuals with FASD exhibit, as well as the fact that their deficits may overlap with other neurodevelopmental disorders. Moreover, in order to determine how well a profile can accurately identify individuals with FASD, it must be tested in a diverse population and also be both sensitive and specific. Footnote 1
In order to identify gaps and limitations of the existing literature, the current review aimed to i) identify existing neurodevelopmental profiles of FASD and ii) review the classification function (the ability of a profile to determine to which group each case most likely belongs – i.e., the sensitivity and specificity) of the respective profiles. As such, the current review is limited to those profiles for which their classification function, as a binary classification test, has been evaluated.
Comprehensive systematic literature search
The systematic literature search was conducted and reported according to the standards set out in Preferred Reporting Items for Systematic Reviews and Meta-Analyses [ 19 ]. A systematic literature search was performed to identify all studies that have identified a neurodevelopmental profile of FASD and were published between November 1, 1973, when FAS was first described [ 20 ], and December 30, 2016. The search was conducted in multiple electronic bibliographic databases, which included: CINAHL, Embase, ERIC, Medline, Medline in process, PsychINFO, Scopus and Web of Science (including Arts and Humanities Citation Index, Science Citation Index, and Social Sciences Citation Index). The following key words were used: 1) alcohol* embryopath*, alcohol* related* neurodevelopmental* disorder*, alcohol* related* birth defect*, arnd, arbd, fetal* alcohol* effect*, fae, fas, fasd, fetal alcohol syndrome*, fetal alcohol spectrum disorder*, foetal* alcohol* effect, foetal* alcohol syndrome*, foetal* alcohol spectrum disorder*, pfas, partial fetal alcohol syndrome, partial foetal alcohol syndrome, prenatal* alcohol expos*, OR pre-natal* alcohol expos*; AND 2) behavio*, cogniti*, development*, neurobehavio*, neurocogniti*, neurodevelopment*, neuropsycholog*, OR psycholog*; AND 3) profile*, phenotype*, OR profile analysis. The search was not limited geographically or by language of publication. Manual reviews of the content pages of the major journals in the field of neurodevelopmental disorders were conducted, as well as citations in any of the relevant articles. The full review protocol is available in PROSPERO ( http://www.crd.york.ac.uk/PROSPERO/ ), registration number CRD42016039326.
Inclusion and exclusion criteria
Articles were included if they were full-text articles (i.e., conference abstracts were excluded) consisting of original, quantitative research published in a peer-reviewed journal that identified a neurodevelopmental profile of FASD. Articles were excluded if they did not involve an evaluation of the classification function of the identified neurodevelopmental profile of FASD.
Data selection and extraction
Study selection began by screening titles and abstracts for inclusion. Then, full-text articles of all studies screened as potentially relevant were considered. All data were extracted by one investigator and then independently crosschecked by a second investigator for accuracy against the original studies. All discrepancies were reconciled by team discussion.
Uncertainty
In order to estimate the level of uncertainty surrounding the classification estimates, exact 95% confidence intervals (CI) were estimated using a binomial distribution.
Initially, the search strategy yielded a total of 768 records. After removing 325 duplicates, a total of 443 records were screened using titles and abstracts. Forty-six full-text articles were retrieved for further consideration, 37 of which were subsequently excluded. This left a total of nine studies, all in English, that met the inclusion criteria and were retained for review. A schematic diagram of the search strategy is depicted in Fig. 1 .
Schematic diagram depicting the search strategy employed
Based on the identified studies, two general approaches were observed for determining the pathognomonic neurodevelopmental features of FASD, namely: i) behavioral observations/ratings by parents/caregivers (six studies), and ii) subtest scores from standardized test batteries assessing a variety of neurodevelopmental domains (three studies).
Neurodevelopmental profiles of FASD based on behavioral observations/ratings by parents/caregivers
The Child Behavior Checklist (CBCL; five studies) and the Behavior Rating Inventory of Executive Function (BRIEF; one study) have been used to identify a neurodevelopmental profile characteristic of FASD.
Child Behavioral Checklist (CBCL)
Nash and colleagues [ 21 ] sought to determine if a behavioral profile distinguishes children with FASD (diagnosed according to the 2005 Canadian diagnostic guidelines; [ 1 ]) from typically developing children and children with ADHD. The CBCL is a well-established standardized parent/caregiver questionnaire utilized for evaluating social competencies and behavioral problems in children 6 to 18 years of age, and is comprised of a series of open ended questions and a rating scale of 113 behavioral descriptors. The authors utilized discriminant function analysis and Receiver Operating Characteristics curve analyses to determine sensitivity and specificity of different item combinations. Findings revealed ten specific behavioral characteristics captured by the CBCL (Table 1 ) had the potential to differentiate between children with FASD from children with ADHD and typically developing control children, all 6 to 16 years of age. Specific item combinations (Table 2 ) resulted in 86% (95% CI: 77%–95%) sensitivity and 82% (95% CI: 72%–92%) specificity when children with FAS where compared to typically developing control children, and 70% (95% CI: 58%–82%) to 81% (95% CI: 71%–91%) sensitivity and 72% (95% CI: 61%–83%) to 80% (95% CI: 70%–90%) specificity when children with FAS where compared to children with ADHD.
Nash, Koren, and Rovet [ 22 ] replicated their earlier study [ 21 ] using a larger sample and comparing children with FASD (diagnosed according to the 2005 Canadian Guidelines; [ 1 ]) to children with ODD/CD, as well as children with ADHD and typically developing control children in order to establish the specificity of the 10-item screening tool. All children ranged in age from 6 to 18 years of age. Findings revealed the tool differentiated children with FASD from control children with 98% (95% CI: 95%–100%) sensitivity and 42% (95% CI: 33%–51%) specificity, and from children with ADHD with 89% (95% CI: 83%–95%) sensitivity and 42% (95% CI: 33%–51%) specificity. However, sensitivity and specificity could not be determined for discriminating children with FASD from children with ODD/CD since only one item significantly differentiated these groups, namely “acts young”.
From their preliminary investigations showing that certain behaviors had the potential to identify children with a high likelihood of having FASD, Nash and colleagues [ 21 , 22 ] proposed using this 10-item questionnaire as a screening tool and coined it the “Neurobehavioral Screening Tool (NST)”. Based on the two studies discussed above [ 21 , 22 ], it was discerned that the NST has the potential to delineate children with FASD from children with ADHD and normally developing children. However, these two studies were limited in that they retrospectively extracted items from the fully administered CBCL, and their samples consisted of children aged 6 to 18 only. The former limitation is noteworthy given that the CBCL is scored on a three-point scale (i.e., “not true”, “somewhat or sometimes true”, and “very true or often true”); the authors of the NST collapsed the responses “somewhat or sometimes true” and “very true or often true” and this can affect the classification accuracy. The latter limitation means that the behaviors noted in the NST cannot be assumed to be reflective of children with FASD outside this age range (i.e., less than 6 and over 18 years of age).
Accordingly, Breiner, Nulman, and Koren [ 23 ] conducted a study in order to determine if the NST could be validated among a sample of children diagnosed with FASD (according to the 2005 Canadian Guidelines; [ 1 ]), children with either a deferred diagnosis or for whom a diagnosis could not be confirmed, and normally developing control children, all 4 to 6 years of age. Three items (lie/cheat, steal at home, and steal outside the home) were excluded from the analysis due to the inability to verify these items in most young children. Using the seven remaining items, the authors found that the NST had 94% (95% CI: 88%–100%) sensitivity and 96% (95% CI: 91%-100%) specificity in identifying children with FASD (Table 2 ). However, it is unclear from which group children with FASD were discriminated (i.e., if the non-diagnosed group was combined with the control children), as the methods and results sections describing it are inadequate. Further, this study retrospectively extracted items from the CBCL in its entirety.
More recently, LaFrance et al. [ 24 ] administered the NST as a stand-alone instrument to parents/caregivers of children 6 to 17 years of age and thus, addressed the limitation of collapsing items originally scored on a three-point scale [ 21 , 22 , 23 ]. Using the scoring approach published by Nash and associates [ 21 ], compared with normally developing control children, the NST yielded 63% (95% CI: 52%–74%) sensitivity and 100% (not possible to estimate 95% CI) specificity for children with FASD (diagnosed according to the 4-Digit Diagnostic Code; [ 25 ]) and 50% (95% CI: 37%–63%) sensitivity and 100% (not possible to estimate 95% CI) specificity for children prenatally exposed to alcohol who did not meet the diagnostic threshold when assessed (Table 2 ). This study also assessed possible age- and sex-related differences on the NST, by comparing 6–to 11-year old children with 12–to 17-year old adolescents, and boys versus girls. For both the FASD group and the group of children prenatally exposed to alcohol who did not meet the diagnostic threshold, the NST showed higher sensitivity among adolescents (71% [95% CI: 61%–81%] and 71% [95% CI: 59%–83%], respectively) when compared with children (54% [95% CI: 43%–65%] and 40% [95% CI: 27%–53%], respectively). For the FASD group only, the NST also had higher sensitivity among boys when compared with girls (71% [95% CI: 61%–81%] and 56% [95% CI: 45%–67%], respectively). Specificity was found not to differ with respect to age and sex, as it was 100% (not possible to estimate 95% CI) in all of the comparisons. Lastly, the authors explored an alternative cumulative scoring option, with the endorsement of at least four items resulting in 90% (95% CI: 83%–97%) sensitivity and 91% (95% CI: 85%–97%) specificity. This study is not only the first to administer the NST as a stand-alone instrument, but is also the first to differentiate children prenatally exposed to alcohol who do not meet the criteria for an FASD diagnosis from typically developing control children. The discrimination of children prenatally exposed to alcohol who did not meet the criteria for an FASD diagnosis helps to further establish the specificity and discriminate validity of the NST. Nonetheless, it must be noted that this study involved the retrospective administration of the NST in a sample of children that had had already undergone a full diagnostic evaluation, thereby limiting the degree to which the results can be said to establish the validity of the NST as a “screening” tool per se.
In order to further establish the specificity of the NST, Haynes, Nulman, and Koren [ 26 ] recently evaluated the influence of maternal depression – the most prevalent psychiatric morbidity among women with difficulties inhibiting their consumption of alcohol during pregnancy [ 27 ] – on the previously identified behavioral presentation of children with FASD [ 21 , 22 , 24 ] (diagnosed according to either the 2005 Canadian diagnostic guidelines [ 1 ] or the 4-Digit Diagnostic Code [ 25 ]). Specifically, the investigators sought to determine if the NST resulted in any false positives among a sample of children born to and reared by mothers with clinical depression and typically developing control children. None of the children with mothers suffering from depression scored positive on the NST (100% specificity, not possible to estimate 95% CI; Table 2 ). In fact, only one item (hyperactive) was found to be significantly higher in the group of children with mothers suffering from depression, compared with the control children.
In summary, the NST has demonstrated good sensitivity (63% to 98%), but varying specificity (42% to 100%, with some estimates being unfavorably low), and thus should still be considered in the validation stage. It is important to note that the NST is intended for screening purposes only [ 21 , 22 ], and given it is limited to overt behaviors only, its ability as a diagnostic tool is questionable since it does not fully capture all neurodevelopmental impairments seen among individuals with FASD. However, there are few limitations of the available studies on the NST that should be noted. First, all of the studies evaluating the psychometric utility of the NST are plagued by small or modest at best, clinically-referred Canadian samples, thus limiting generalizability of the above findings. Second, the NST has the inherent problem of providing the behavioral observations of parent or parent substitutes, who by definition are not masked to the child’s history and thus may convey observations distorted by positive intent. Third, although a few of the studies investigating the NST specified whether the participants that made up the comparison groups were screened for prenatal alcohol exposure, and subsequently excluded [ 21 , 22 ], others did not [ 23 , 24 , 26 ].
Behavior Rating Inventory of Executive Function (BRIEF)
Recently, Nguyen and colleagues [ 28 ] sought to determine whether the BRIEF clinical scales, a parent/caregiver questionnaire that consists of 86-items and eight empirically derived clinical scales assessing executive function and self-regulation in children 5 to 18 years of age, can distinguish among the following four groups of children: 79 children prenatally alcohol-exposed with ADHD; 36 children prenatally alcohol-exposed without ADHD; 90 children with idiopathic ADHD (without prenatal alcohol exposure); and 168 typically developing control children. Prenatal alcohol exposure was defined as at least four drinks per occasion at least once per week or at least 14 drinks per week during pregnancy. A discriminant function analysis revealed that the following four clinical scales best distinguished the groups: i) Inhibit, which describes a child’s ability to tune out irrelevant stimuli; ii) Emotional Control, which describes a child’s ability to modulate emotional responses; iii) Working Memory, which describes a child’s ability to hold information in mind for the purpose of completing a task; and iv) Organization of Materials, which describes a child’s orderliness of work, play, and storage spaces. Classification accuracy was 71% (95% CI: 66%–76%) overall, with 67% (95% CI: 62%–72%) of children prenatally alcohol-exposed with ADHD, 43% (95% CI: 38%–48%) children prenatally alcohol-exposed without ADHD, 51% (95% CI: 46%–56%) of children with idiopathic ADHD, and 92% (95% CI: 89%–95%) of typically developing control children classified correctly.
Although its use as tool to discriminate individuals with FASD from other clinical populations is still in the exploratory stages, the BRIEF appears to distinguish alcohol-exposed children with ADHD from those with idiopathic ADHD, and thus may be useful as a screening tool. However, based on the results presented above, the ability of the BRIEF to identify children prenatally alcohol-exposed without ADHD is limited.
Neurodevelopmental profiles of FASD based on subtest scores from a battery of standardized tests
Mattson and colleagues [ 29 ] sought to identify a neurodevelopmental profile of FASD using subtest scores from a battery of neurodevelopmental tests administered to individuals heavily exposed to alcohol prenatally, defined as four or more drinks per occasion at least once per week or 13 or more drinks per week, and individuals with no prenatal alcohol exposure or minimal exposure, defined as no more than one drink per week on average and a maximum of two drinks per occasion. All participants were between 7 and 21 years of age and subsequently categorized based only on physical features, regardless of their exposure status. Classifications included “FAS”, defined as the presence of at least two of the three key facial features (short palpebral fissures, smooth philtrum, and thin vermillion boarder) and either microcephaly (head circumference ≤10 th percentile) or growth deficiency (weight and/or height ≤10 th percentile) or both; “Not FAS”; or “Deferred”, defined as the presence of at least one key facial feature, or microcephaly and growth deficiency, or microcephaly or growth deficiency and at least one additional specified feature documented to be prevalent among those with FASD such as ptosis, and camptodactyly. Twenty-two variables, derived from the subtests of a battery of standardized tests, were selected based on their effect size in detecting the difference between exposed and unexposed individuals.
Two latent profile analyses were performed in order to derive a discriminative profile. In both analyses, a two-class solution fit better than a one-class solution – meaning that, based on the response means, it was more likely that there were two unobserved groups in the sample used in each analysis. In the first analysis, exposed individuals who met the study criteria for FAS ( n = 41) were compared with unexposed individuals categorized as Not FAS ( n = 46); the resulting profile had an overall classification accuracy of 92% (95% CI: 86%–98%), with 88% (95% CI: 81%–95%) sensitivity and 96% (95% CI: 92%–100%) specificity. In the second analysis, exposed individuals categorized as Not FAS or Deferred ( n = 38) were compared with unexposed individuals categorized as Not FAS or Deferred ( n = 60); the resulting profile had an overall classification accuracy of 85% (95% CI:78%–92%), with 68% (95% CI: 59%–77%) sensitivity and 95% (95% CI: 91%–99%) specificity. The discriminative profile consisted of deficits in executive function, attention, spatial reasoning and memory, fine motor speed, and visual motor integration (Table 3 ). In both analyses, individuals categorized as belonging to “Group 1” performed more poorly than those belonging to “Group 2”, with significantly more alcohol-exposed individuals in “Group 1” and significantly more unexposed individuals in “Group 2”. See Table 3 for the measures included in the profile and neurodevelopmental domains assessed.
In a subsequent study, Mattson and colleagues [ 30 ] attempted to further refine their initial neurodevelopmental profile [ 29 ] by i) reducing the number of variables included, ii) using a larger sample between 8 and 17 years of age, and iii) including a clinical contrast group. The same definitions of “heavily exposed to alcohol prenatally” and “no prenatal alcohol exposure or minimal exposure” were used as before [ 29 ]. Based on clinical judgment and expertise, researchers selected 11 variables from the large test battery, four of which overlapped with those selected in the previous study [ 29 ] (Note: overlapping measures are indicated with an asterisk in Table 4 ).
Three latent profile analyses were conducted. In all three analyses, a two-class solution fit better than a one-class solution. In the first analysis, exposed individuals who met the study criteria for FAS (same criteria as the authors previous study [ 29 ]; n = 79) were compared with unexposed individuals ( n = 185) and the resulting profile yielded an overall classification accuracy of 76% (95% CI: 71%–81%), with 77% (95% CI: 72%–82%) sensitivity and 76% (95% CI: 71%–81%) specificity. In the second analysis, exposed individuals who did not meet the criteria for FAS ( n = 117) were compared with unexposed individuals ( n = 185); the resulting profile had an overall classification accuracy of 72% (95% CI:67%–77%), with 70% (95% CI: 65%–75%) sensitivity and 72% (95% CI: 67%–77%) specificity. The third analysis comparing exposed individuals with and without FAS ( n = 209) and individuals with ADHD who were not exposed to alcohol prenatally (as per the definition of prenatal alcohol exposure used by the authors; n = 74) led to a profile with an overall classification accuracy of 74% (95% CI: 69%–79%), with 60% (95% CI: 54%–66%) sensitivity and 76% (95% CI: 71%–81%) specificity. The discriminative profile consisted of deficits in executive function, attention, and visual and spatial memory, with measures of executive function most effectively distinguishing individuals prenatally alcohol-exposed from those not exposed (Table 4 ). In all three analyses, significantly more alcohol-exposed individuals belonged to “Group 1” and significantly more unexposed individuals to “Group 2” (see Table 4 for the measures included in the profile and neurodevelopmental domains assessed).
From a clinical perspective, the psychometric utility of the profile of Mattson and colleagues [ 30 ] was not optimal in discriminating those with FASD from those with ADHD – it was more accurate at identifying individuals with ADHD than individuals with FASD. Further, it appears that a more limited test battery is not equally as useful at distinguishing between individuals with FASD and unexposed individuals as a larger test battery, as the sensitivity was reduced from 88% in the first study [ 29 ] to 77% in the second study [ 30 ]. Lastly, although the classification rates were significant, a number of subjects were misclassified. Further, the two studies by Mattson et al. [ 29 , 30 ] have a few limitations to note. First, coupled with the fact that the authors utilized test batteries that accommodated the large age range and language variations of their samples, the batteries used do not constitute a full clinical assessment battery typically used in an FASD diagnostic clinics. As such, the test batteries lacked clinical sensitivity and likely excluded other measures that may have been useful in distinguishing individuals with FASD from unexposed controls and other clinical populations. Second, the samples were made up of participants clinically referred for suspected problems or exposures and thus, prone to sampling bias, undermining the external validity of the findings. Third, the investigators only included weaknesses in their neurodevelopmental profile and did not include relative strengths. Fourth, the classification of individuals as having FAS was based on physical traits only, and is not reflective of how FAS is classified elsewhere (see for example, the Canadian guidelines for diagnosis; [ 1 ]).
Recently, Enns and Taylor [ 31 ] used logistic regression to determine which neurodevelopmental variables are most predictive of an FASD diagnosis. Studied were 180 children and adolescents (5 to 17 years of age) prenatally exposed to alcohol, 107 of whom received a diagnosis of FASD according to the 2005 Canadian diagnostic guidelines [ 1 ] and 73 who did not. The authors identified a model that incorporated specific intelligence indices (verbal intelligence and working memory), academic achievements (spelling and math calculations), auditory working memory, and spatial planning correctly classified 75% (95% CI: 70%–80%) of cases (sensitivity and specificity were not reported). However, it was not clear if scaled scores were used in the model, and the most obvious limitation of the study is that data was retrospectively collected via a chart review of a clinically referred sample. Further, given the retrospective nature of the study, the number of children and adolescents assessed using each measure varied – however, the sample size was not specified for the final profile. Although the identified profile was able to differentiate individuals diagnosed with FASD from those who were prenatally exposed to alcohol but whom did not receive a diagnosis of FASD, the ability to differentiate individuals with FASD from unexposed individuals and individuals with other clinical populations remains unclear. See Table 5 for the measures included in the profile and neurodevelopmental domains assessed by Enns and Taylor [ 31 ].
Based on the studies reviewed above, it is clear that a definitive neurodevelopmental profile of FASD has yet to be identified. However, the current literature has notable clinical implications. First, behavioral ratings by primary caregivers have the potential to be used in the development of a screening tool, which can be used to identify those children most in need of a full multi-disciplinary diagnostic assessment. Second, a battery of neurodevelopmental tests can be used to distinguish between children with FASD and typically developing children, children prenatally exposed to alcohol but who do not meet the criteria for a diagnosis of FASD, as well as children with ADHD. Overall, the results of the current review support a stepwise approach the diagnosis of FASD. A diagnosis of FASD has a number of important benefits namely, participation in developmental interventions, improved quality of life and a more prosperous developmental trajectory in terms of social functioning.
Although a biomarker would be the most ideal method for diagnosing cases of FASD, at this time observational data and neurodevelopmental testing are the most appropriate tools. Thus, the identification of a distinct neurodevelopmental profile that is pathognomonic of FASD will assist in the: i) accurate identification of individuals with FASD, by adding to the resources available to clinicians; ii) discrimination of FASD from other clinical populations (i.e., differential diagnosis); iii) ascertainment of accurate prevalence estimates; iv) planning/development of appropriate targeted interventions for individuals with FASD; and v) enhancement of clinical services to this population. Coupled with the fact that the neurodevelopmental assessment is both time consuming and costly [ 14 ], the current capacity of diagnostic services is also limited [ 32 ]. Thus, delineating the specific neurodevelopmental profile of FASD will not only reduce the time it takes to fully assess an individual, but it will also assist in triaging children most in need of a full clinical assessment [ 21 , 22 ].
Nevertheless, studies utilizing observational and/or neurodevelopmental data to identify the presence of a unique neurodevelopmental profile of FASD are not without their limitations (e.g., confounding, and a lack of normative data with respect to FASD and mixed racial groups). In addition to the inherent data limitations, the two approaches currently used in determining the neurodevelopmental profile of FASD are both limited in scope. For instance, the approach involving observations/ratings of parents/caregivers (i.e., the NST) is solely based on problem behaviors. However, individuals with FASD have a number of other developmental impairments and behavioral manifestations that could be useful when delineating FASD from other clinical populations. Further, the neurodevelopmental profiles based on the subtest scores from a battery of standardized tests do not consider the relative strengths of individuals with FASD [ 11 , 33 ].
It should also be recognized that the studies reviewed used different diagnostic guidelines for ascertaining cases of FASD. Given that it was recently reported that existing FASD diagnostic guidelines lack convergent validity and are limited in their concordance with respect to the specific diagnostic entities [ 34 ], the consequence of this variation is that the profiles are essentially classifying different groups of affected individuals. Thus, the only conceivable way to resolve this issue is for a standardized common diagnostic approach to be developed and widely accepted. Only then will we be able to identify whether a neurodevelopmental profile of FASD exists, and truly assess its classification function.
Further, given the stigmatization associated with alcohol use during pregnancy and the increased likelihood of underreporting [ 35 ], it is possible that the comparison groups of typically developing control children used in the studies reviewed may contain some children prenatally exposed to alcohol, which is possible for example in studies of Mattson and colleagues [ 29 , 30 ] given their definition of prenatal alcohol exposure. Consequently, the classification function of a particular profile could in fact be more robust than observed.
Although it is clear that the identification of a neurodevelopmental profile of FASD has a number of notable benefits, at least eight areas of future research need to be addressed before a neurodevelopmental profile is defined and put into practice. The first concerns testing the profile on larger, more diverse samples, as well as in general population screening settings (i.e., among population-based samples). Second, the profile’s ability to differentiate children with FASD from other clinical populations (e.g., other than idiopathic ADHD, without prenatal alcohol exposure) needs to be determined. Third, potential gender and age differences need to be explored, and the cross-cultural utility of the profile needs to be established. Fourth, a broader, more comprehensive array of neurodevelopmental domains needs to be evaluated. Fifth is the possibility that individuals with FASD exhibit more than one neurodevelopmental profile should be explored. For example, a distinct profile could exist for each diagnostic category. Sixth, future studies need to control for adverse prenatal exposures such as maternal smoking and drug use during pregnancy, maternal and paternal psychopathologies, and postnatal experiences including abuse and neglect. Seventh is the possibility that some of the associated neurodevelopmental symptoms were inherited from parents (e.g., a math disability) and not strictly attributable to the prenatal alcohol exposure. Eighth, it is possible that individual differences in factors that influence the consequences of prenatal alcohol exposure may interfere with the identification a unique neurodevelopmental profile of FASD given that susceptibility to prenatal alcohol exposure depends on the genotype of the fetus [ 36 ] and the developmental stage at the time of exposure, and that the manifestations of abnormal development increase in frequency and degree as dosage increases (as per the principles of teratogenesis; [ 37 , 38 ]). Accordingly, genetic factors/differences in fetal susceptibility to alcohol and information on dosage and timing of exposure should also be taken into consideration when identifying and validating a neurodevelopmental profile of FASD. It is likely that many of these areas of future research will only be achievable if and when large detailed datasets are developed containing data on individuals with FASD diagnosed using a common diagnostic guideline, which will allow for certain variables (e.g., experience of postnatal adversities) to be controlled for.
However, given that the outcomes of prenatal alcohol exposure depend on a number of factors (e.g., genetics, health, alcohol metabolism, polysubstance exposure, timing of exposure [ 39 , 40 , 41 ]), as well as the fact that FASD is associated with multiple comorbid mental disorders [ 42 , 43 , 44 ], it should be acknowledged that FASD may in fact have a complex phenotype and a pathognomonic neurodevelopmental profile of FASD may not exist. It is possible that FASD has a pleiotropic phenotype (i.e., one cause (prenatal alcohol exposure) results in many outcomes); if this is the case it will negate the existence of a neurodevelopmental profile unique to those with FASD.
Strengths and limitations
The current literature review has a number of notable strengths, namely the comprehensive search strategies, strict inclusion and exclusion criteria, and the critical approach to presenting the existing neurodevelopmental profiles of FASD. However, it is important to acknowledge that this review is limited to those profiles that were accompanied by an evaluation of their classification function. Nevertheless, there are profiles that show some promise that were not eligible for inclusion in the current review (e.g., Nash et al. [ 8 ] and Stevens et al. [ 45 ]).
This systematic review elucidates the need for additional well-conducted research investigating the existence of a neurodevelopmental profile of FASD. Although research in this area is limited and a definitive neurodevelopmental profile of FASD remains to be established, the benefits of identifying a pathognomonic neurodevelopmental profile are noteworthy. It is likely that a neurodevelopmental profile of FASD that includes both behavioral observations/ratings and performance-based measures of neurodevelopment will be the most comprehensive and as such, future studies should include measures covering a broad array of neurodevelopmental and behavioral domains.
Sensitivity and specificity are measures of a binary classification test’s accuracy. Sensitivity is the probability of a positive test result among those with the condition (i.e., the percentage of individuals who are correctly identified as having the condition), while specificity is the probability of a negative test result among those without the condition (i.e., the percentage of individuals who are correctly identified as not having the condition).
Abbreviations
Attention Deficit Hyperactivity Disorder
Alcohol-Related Birth Defects
Alcohol-Related Neurodevelopmental Disorder
Cambridge Neuropsychological Test Automated Battery
Conduct Disorder
Children’s Memory Scale
Delis-Kaplan Executive Function System
Fetal Alcohol Syndrome
- Fetal Alcohol Spectrum Disorder
Morris Virtual Water Maze
Neurobehavioral Disorder Associated with Prenatal Alcohol Exposure
Neurobehavioral Evaluation System 3
Neurobehavioral Screening Tool
Oppositional Defiant Disorder
Partial Fetal Alcohol Syndrome
Wechsler Intelligence Scale for Children, Fourth Edition
Wechsler Memory Scale, Fourth Edition
Wide Range Achievement Test, Fourth Edition
Chudley AE, Conry J, Cook JL, Loock C, Rosales T, LeBlanc N. Fetal alcohol spectrum disorder: Canadian guidelines for diagnosis. CMAJ. 2005;172 Suppl 5:S1–21.
Article PubMed PubMed Central Google Scholar
Hoyme HE, Kalberg WO, Elliott AJ, Blankenship J, Buckley D, Marais AS, et al. Updated clinical guidelines for diagnosing fetal alcohol spectrum disorders. Pediatrics. 2016;138:e20154256.
Article PubMed Google Scholar
Cook JL, Green CR, Lilley CM, Anderson SM, Baldwin ME, Chudley AE, et al. Fetal alcohol spectrum disorder: a guideline for diagnosis across the lifespan. CMAJ. 2016;188(3):191–7.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 5 th edition: DSM-5. Washington, DC: American Psychiatric Association; 2013.
Book Google Scholar
Kable JA, O’Connor MJ, Olson HC, Paley B, Mattson SN, Anderson SM, et al. Neurobehavioral disorder associated with prenatal alcohol exposure (ND-PAE): Proposed DSM-5 diagnosis. Child Psychiatry Hum Dev. 2016;47(2):335–46.
Aragón AS, Coriale G, Fiorentino D, Kalberg WO, Buckley D, Gossage JP, et al. Neuropsychological characteristics of Italian children with fetal alcohol spectrum disorders. Alcohol Clin Exp Res. 2008;32(11):1909–19.
PubMed PubMed Central Google Scholar
Kodituwakku PW, Handmaker NS, Cutler SK, Weathersby EK, Handmaker SD. Specific impairments in self-regulation in children exposed to alcohol prenatally. Alcohol Clin Exp Res. 1995;19(6):1558–64.
Nash K, Stevens S, Rovet J, Fantus E, Nulman I, Sobara D, et al. Towards identifying a characteristic neuropsychological profile for fetal alcohol spectrum disorders: 1. Analysis of the Motherisk FASD Clinic. J Popul Ther Clin Pharmacol. 2013;20(1):e44–52.
PubMed Google Scholar
Rasmussen C, Horne K, Witol A. Neurobehavioral functioning in children with fetal alcohol spectrum disorder. Child Neuropsychol. 2006;12(6):453–68.
Kodituwakku PW. Neurocognitive profile in children with fetal alcohol spectrum disorders. Dev Disabil Res Rev. 2009;15:218–24.
Mattson SN, Crocker N, Nguyen TT. Fetal alcohol spectrum disorders: Neuropsychological and behavioral features. Neuropsychol Rev. 2011;21(2):81–101.
Bastons-Compta A, Astals M, Garcia-Algar O. Foetal alcohol spectrum disorder (FASD) diagnostic guidelines: A neuropsychological diagnostic criteria review proposal. J Neuropsychopharmacol Ment Health. 2016;1(2):e104.
Article Google Scholar
Chudley AE. Fetal alcohol spectrum disorder: Counting the invisible – mission impossible? Arch Dis Child. 2008;93(9):721–2.
Popova S, Lange S, Burd L, Chudley AE, Clarren SK, Rehm J. Cost of fetal alcohol spectrum disorder diagnosis in Canada. PLoS One. 2013;8(4):e60434.
McLennan JD. Misattributions and potential consequences: The case of child mental health problems and fetal alcohol spectrum disorders. Can J Psychitry. 2015;60(12):587–90.
Chasnoff IJ, Wells AM, King L. Misdiagnosis and missed diagnoses in foster and adopted children with prenatal alcohol exposure. Pediatrics. 2015;135(2):264–70.
Astley SJ, Clarren SK. Diagnosing the full spectrum of fetal alcohol-exposed individuals: Introducing the 4-digit diagnostic code. Alcohol Alcohol. 2000;35(4):400–10.
Streissguth AP, Bookstein FL, Barr HM, Press S, Sampson PD. A fetal alcohol behavior scale. Alcohol Clin Exp Res. 1998;22(2):325–33.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100.
Jones KL, Smith DW. Recognition of the fetal alcohol syndrome in early infancy. Lancet. 1973;2:999–1001.
Nash K, Rovet J, Greenbaum R, Fantus E, Nulman I, Koren G. Identifying the behavioural phenotype in fetal alcohol spectrum disorder: sensitivity, specificity and screening potential. Arch Womens Ment Health. 2006;9(4):181–6.
Nash K, Koren G, Rovet J. A differential approach for examining the behavioral phenotype of fetal alcohol spectrum disorders. J Popul Ther Clin Pharmacol. 2011;18(3):e440–53.
Breiner P, Nulman I, Koren G. Identifying the neurobehavioral phenotype of fetal alcohol spectrum disorder in young children. J Popul Ther Clin Pharmacol. 2013;20(3):e334–9.
LeFrance MA, McLachlan K, Nash K, Andrew G, Loock C, Oberlander TF, et al. Evaluation of the Neurobehavioral Screening Tool in children with fetal alcohol spectrum disorders (FASD). J Popul Ther Clin Pharmacol. 2014;21(2):e197–210.
Google Scholar
Astley S. Diagnostic Guide for Fetal Alcohol Spectrum Disorders: The 4-Digit Diagnostic Code. 3rd ed. Seattle, Washington, DC: University of Washington Publication Services; 2004.
Haynes K, Nulman I, Koren G. Fetal alcohol spectrum disorder and the neurobehavioural screening tool: evaluating the effect of maternal depression. J Popul Ther Clin Pharmacol. 2014;21(3):e387–94.
Procopio DO, Saba L, Walter H, Lesch O, Skala K, Schlaff G, et al. (2013). Genetic markers of comorbid depression and alcoholism in women. Alcohol Clin Exp Res. 2013;37(6):894–904.
Nguyen TT, Glass L, Coles CD, Kable JA, May PA, Kalberg WO, et al. The clinical utility and specificity of parent report of executive function among children with prenatal alcohol exposure. J Int Neuropsychol Soc. 2014;20(7):704–16.
Mattson SN, Roesch SC, Fagerlund A, Autti-Rämö I, Jones KL, May PA, et al. Toward a neurobehavioral profile of fetal alcohol spectrum disorders. Alcohol Clin Exp Res. 2010;34(9):1640–50.
Mattson SN, Roesch SC, Glass L, Deweese BN, Coles CD, Kable JA, et al. Further development of a neurobehavioral profile of fetal alcohol spectrum disorders. Alcohol Clin Exp Res. 2013;37(3):517–28.
Enns LN, Taylor NM. Factors predictive of a fetal alcohol spectrum disorder: Neuropsychological assessment. Child Neuropsychol. 2016. [Epub ahead of print].
Clarren SK, Lutke J, Sherbuck M. (2011). The Canadian Guidelines and the Interdisciplinary Clinical Capacity of Canada to Diagnose Fetal Alcohol Spectrum Disorder. J Popul Ther Clin Pharmacol. 2011;18(3):e494–9.
Greenbaum R, Nulman I, Rovet J, Koren G. The Toronto experience in diagnosing alcohol-related neurodevelopmental disorder: a unique profile of deficits and assets. Can J Clin Pharmacol. 2002;9(4):215–25.
Coles CD, Gailey AR, Mulle JG, Kable JA, Lynch ME, Jones KL. A Comparison Among 5 Methods for the Clinical Diagnosis of Fetal Alcohol Spectrum Disorders. Alcohol Clin Exp Res. 2016;40(5):1000–9.
Lange S, Shield K, Koren G, Rehm J, Popova S. A comparison of the prevalence of prenatal alcohol exposure obtained via maternal self-reports versus meconium testing: a systematic literature review and meta-analysis. BMC Pregnancy Childbirth. 2014;14:127.
Eberhart JK, Parnell SE. The genetics of fetal alcohol spectrum disorders. Alcohol Clin Exp Res. 2016;40(6):1154–65.
O’Leary-Moore SK, Parnell SE, Lipinski RJ, Sulik KK. Magnetic resonance-based imaging in animal models of fetal alcohol spectrum disorder. Neuropsychol Rev. 2011;21(2):167–85.
Sulik KK. Fetal alcohol spectrum disorder: pathogenesis and mechanisms. Handb Clin Neurol. 2014;125:463–75.
Day J, Savani S, Krempley BD, Nguyen M, Kitlinska JB. Influence of paternal preconception exposures on their offspring: through epigenetics to phenotype. Am J Stem Cells. 2016;5(1):11–8.
Eberhart JK, Parnell SE. The Genetics of Fetal Alcohol Spectrum Disorders. Alcohol Clin Exp Res. 2016;40(6):1154–65.
May PA, Gossage JP. Maternal risk factors for fetal alcohol spectrum disorders: Not as simple as it might seem. Alcohol Res Health. 2011;34(1):15–26.
Burd L, Klug MG, Martsolf JT. Fetal alcohol syndrome: neuropsychiatric phenomics. Neurotoxicol Teratol. 2003;25(6):697–705.
Lange S, Rehm J, Anagnostou E, Popova S. Prevalence of externalizing disorders and autism spectrum disorder among children with fetal alcohol spectrum disorder: systematic review and meta-analysis. Biochem Cell Biol. 2017; [Epub ahead of print].
Popova S, Lange S, Shield K, Mihic A, Chudley AE, Mukherjee RAS, et al. Comorbidity of fetal alcohol spectrum disorder: a systematic review and meta-analysis. Lancet. 2016;387(10022):978–87.
Stevens SA, Nash K, Fantus E, Nulman I, Rovet J, Koren G. Towards identifying a characteristic neuropsychological profile for fetal alcohol spectrum disorders – 2. Specific caregiver- and teacher-rating. J Popul Ther Clin Pharmacol. 2013;20(1):e53–62.
Download references
Acknowledgements
Not applicable.
No external funding was sought for the current study.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Author information
Authors and affiliations.
Institute for Mental Health Policy Research, Centre for Addiction and Mental Health , Toronto, ON, Canada
Shannon Lange, Jürgen Rehm & Svetlana Popova
Institute of Medical Science, University of Toronto, Toronto, ON, Canada
Neuroscience and Mental Health Program, The Hospital for Sick Children, Toronto, ON, Canada
Joanne Rovet
Department of Pediatrics, University of Toronto, Toronto, ON, Canada
Dalla Lana School of Public Health, University of Toronto, Toronto, ON, Canada
Jürgen Rehm & Svetlana Popova
Institute of Clinical Psychology and Psychotherapy & Center of Clinical Epidemiology and Longitudinal Studies, Technische Universität Dresden, Dresden, Germany
Jürgen Rehm
Factor-Inwentash Faculty of Social Work, University of Toronto, Toronto, ON, Canada
Svetlana Popova
You can also search for this author in PubMed Google Scholar
Contributions
Ms. Lange led the conception and design of the study, acquired the data, analyzed and interpreted the data, wrote the first draft of the manuscript, and revised the manuscript; Drs. Rovet and Rehm contributed to data interpretation, and have revised the manuscript critically for important intellectual content; and Dr. Popova contributed to the conception and design of the study, supervised the analysis and interpretation of the data, and revised the manuscript critically for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Shannon Lange .
Ethics declarations
Consent for publication, competing interests.
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Lange, S., Rovet, J., Rehm, J. et al. Neurodevelopmental profile of Fetal Alcohol Spectrum Disorder: A systematic review. BMC Psychol 5 , 22 (2017). https://doi.org/10.1186/s40359-017-0191-2
Download citation
Received : 01 February 2017
Accepted : 15 June 2017
Published : 23 June 2017
DOI : https://doi.org/10.1186/s40359-017-0191-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Classification accuracy
- Neurodevelopmental profile
- Prenatal alcohol exposure
- Systematic review
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]

LEEANNE DENNY, MD, SARAH COLES, MD, AND ROBIN BLITZ, MD
This is a corrected version of the article that appeared in print. Figure 2 has been updated.
Am Fam Physician. 2017;96(8):515-522A
AAFP Resource: See related resources from the American Academy of Family Physicians on alcohol misuse.
Patient information: A handout on this topic is available at https://familydoctor.org/condition/fetal-alcohol-syndrome .
Author disclosure: No relevant financial affiliations.
Fetal alcohol syndrome (FAS) and fetal alcohol spectrum disorders (FASD) result from intrauterine exposure to alcohol and are the most common nonheritable causes of intellectual disability. The percentage of women who drink or binge drink during pregnancy has increased since 2012. FAS is commonly missed or misdiagnosed, preventing affected children from receiving needed services in a timely fashion. Diagnosis is based on the presence of the following clinical features, all of which must be present: prenatal and/or postnatal growth retardation, facial dysmorphology, central nervous system dysfunction, and neurobehavioral disabilities. FASD is a broader diagnosis that encompasses patients with FAS and others who are affected by prenatal alcohol exposure but do not meet the full criteria for FAS. Management is multidisciplinary and includes managing comorbid conditions, providing nutritional support, managing behavioral problems and educational difficulties, referring patients for habilitative therapies, and educating parents. The Centers for Disease Control and Prevention and other organizations recognize no safe amount of alcohol consumption during pregnancy and recommend complete abstinence from alcohol. All women should be screened for alcohol use during preconception counseling and prenatal care, and alcohol use should be addressed with brief interventions.
Fetal alcohol spectrum disorders (FASD) result from prenatal exposure to alcohol and include fetal alcohol syndrome (FAS), partial fetal alcohol syndrome (PFAS), alcohol-related neurodevelopmental disorder, and alcohol-related birth defects. 1 FAS is the most severe form of FASD. 2
WHAT IS NEW ON THIS TOPIC: FETAL ALCOHOL SPECTRUM DISORDERS
According to the Centers for Disease Control and Prevention, the percentage of pregnant women who consume alcohol increased from 7.6% in 2012 to 10.2% in 2015, and the number of pregnant women reporting binge drinking (at least four alcoholic beverages at once) increased from 1.4% to 3.1%.
A study demonstrated that more than one-half of children with fetal alcohol spectrum disorders do not consume the recommended dietary allowance of fiber, calcium, or vitamins D, E, and K.
| The diagnosis of fetal alcohol syndrome and partial fetal alcohol syndrome is based on defined clinical characteristics and does not require confirmed alcohol use during pregnancy. | C | |
| Neurobehavioral testing should be conducted in all children with suspected fetal alcohol spectrum disorders when feasible. Comprehensive evaluation may not be possible using conventional assessment tools until after three years of age. | C | |
| Contraception should be offered to women of childbearing age who drink. If they desire pregnancy, abstinence from alcohol should be recommended. | C | |
| Pregnant women should be screened for alcohol use. This can be done using the TACER-3 tool. | C | , , |
According to the Centers for Disease Control and Prevention, the percentage of pregnant women who consume alcohol increased from 7.6% in 2012 to 10.2% in 2015, and the number of pregnant women reporting binge drinking (four or more alcoholic beverages at once) increased from 1.4% to 3.1%. 3 , 4 These trends are concerning because alcohol is the most common teratogen, and FASD is the most common cause of nonheritable intellectual disability. 5 Binge drinking is associated with the development of behavioral problems and physical deformities. 6
Although there is wide variation in the estimated prevalence of FAS/FASD, FAS is thought to occur in 0.3 to 0.8 per 1,000 children in the United States and in 2.9 per 1,000 globally. 7 , 8 The prevalence of FASD is estimated at 33.5 per 1,000 children in the United States and 22.8 per 1,000 globally. 8 In the United States, FASD is least prevalent in Hispanic children and most prevalent in Native Americans and Alaska Natives. 4 FAS is diagnosed at an average age of 48.3 months 9 ; however, it is commonly missed or misdiagnosed, preventing affected children from receiving needed services in a timely fashion.
FASD carries a significant economic burden. Children with FAS who are enrolled in Medicaid have annual mean medical expenses nine times higher than those for children without FAS, equating to a median annual expenditure of $6,670 per child (vs. $518 for those without FAS). 10
Any child who was exposed to alcohol pre-natally or presents with growth retardation, facial dysmorphology, central nervous system dysfunction, or neurobehavioral disabilities—the key manifestations of FASD—should prompt consideration of FASD. 11 The assessment and diagnosis require a multidisciplinary team ( Table 1 1 , 12 ) and should include neuropsychological assessment. 1
| Audiologist |
| Cardiologist |
| Developmental pediatrician |
| Developmental therapist |
| Family therapist |
| Nephrologist |
| Neurologist |
| Occupational therapist |
| Ophthalmologist |
| Physical therapist |
| Play therapist |
| Primary care physician |
| Psychiatrist |
| Psychotherapist |
| Sensory integration therapist |
| Social worker |
| Special education teachers |
| Speech-language pathologist |
Diagnosis begins with assessment of prenatal alcohol exposure, including quantity of alcohol consumed per occasion, frequency of use, and timing of consumption during pregnancy. Prenatal alcohol exposure is defined as at least one of the following documented findings: (1) six or more drinks per week for two or more weeks during pregnancy; (2) three or more drinks per occasion on two or more occasions during pregnancy; (3) alcohol-related social or legal problems around the time of pregnancy; (4) intoxication during pregnancy documented by blood, breath, or urinary alcohol testing; (5) positive test for alcohol exposure biomarkers during pregnancy (fatty acid ethyl esters, phosphatidylethanol, and ethyl glucuronide in maternal hair, fingernails, urine, or blood, or in placenta or meconium); (6) increased prenatal risk associated with alcohol use during pregnancy as assessed by a validated screening tool. Documentation includes drinking levels reported by the mother three months before pregnancy recognition or at the time of a positive pregnancy test. Information must be obtained by the mother or a reliable source, such as family member, social service agency, or medical record. 1
Exposure to other teratogens should also be assessed, because women who consume alcohol during pregnancy are more likely to use other drugs. 1 The diagnostic criteria for FAS or PFAS do not require confirmed alcohol use if characteristic findings are present. 1 , 11 However, a confirmed absence of alcohol exposure rules out the diagnoses. Confirmation of alcohol exposure is required for diagnosis of alcohol-related neurodevelopmental disorder and alcohol-related birth defects. 1
KEY DIAGNOSTIC CRITERIA
As previously noted, FASD comprises four distinct categories: FAS, PFAS, alcohol-related neurodevelopmental disorder, and alcohol-related birth defects. Each category is distinguished by the presence or absence of characteristic facial dysmorphology, growth retardation, central nervous system dysfunction, and neurobehavioral disabilities ( Table 2 ) . 1
| + | + | + | + | + | Fetal alcohol syndrome |
| – | + | + | + | + | Fetal alcohol syndrome |
| + | + | + | – | + | Partial fetal alcohol syndrome |
| + | + | – | + | + | Partial fetal alcohol syndrome |
| + | + | – | – | + | Partial fetal alcohol syndrome |
| – | + | + | – | + | Partial fetal alcohol syndrome |
| – | + | – | + | + | Partial fetal alcohol syndrome |
| + | – | – | – | + | Alcohol-related neurodevelopmental disorder |
Characteristic facial dysmorphology associated with FASD includes short palpebral fissures (10th percentile or less for age and racial norms), a thin vermilion border of the upper lip, and a smooth philtrum 1 ( Figure 1 13 ) . Two of the three characteristic features are required for the diagnosis of FAS or PFAS. Palpebral fissures can be measured using a small plastic ruler, noting the distance between the endocanthion (where the eyelids meet medially) and exocanthion (where they meet laterally). The ruler should be angled to follow the curve of the zygoma. 1 The presence of a thin vermilion border and smooth philtrum is scored objectively using the lip-philtrum scoring guide ( Figure 2 ) . 14 Scores of 4 or 5 are consistent with FAS or PFAS.
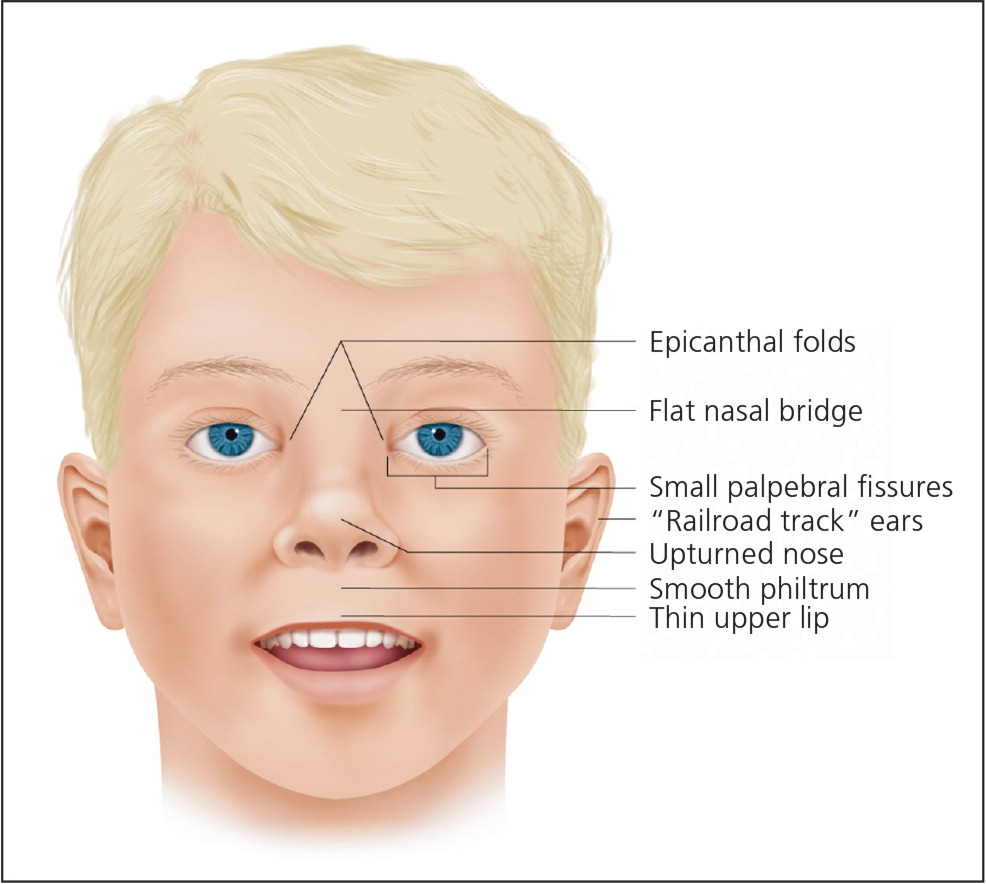
Growth retardation is defined as the 10th percentile or less using height and weight measurements on standard growth curves. 1 For central nervous system dysfunction to qualify as consistent with FASD, it must include deficient brain growth, abnormal structure, or abnormal neurophysiology. This can be documented as a head circumference in the 10th percentile or less on appropriate growth curves, structural brain abnormalities, or recurrent nonfebrile seizures with no other identifiable cause. 1 Magnetic resonance imaging has identified structural brain abnormalities in children with FASD (e.g., temporal lobe asymmetry, change in size or shape of corpus callosum, cerebellum, or basal ganglia), and it may be used in the evaluation of suspected FASD; it can also be helpful if there is a question about the differential diagnosis. 1 , 15 – 17
Neurobehavioral disabilities in FASD include deficient global intellectual ability and cognition, and poor behavior, self-regulation, and adaptive skills. These domains should be measured using standardized testing, which often cannot be administered until after three years of age. A deficiency on these tests is characterized by scores of at least 1.5 standard deviations below the mean. 1 Alcohol-related neurodevelopmental disorder is diagnosed with documented prenatal alcohol exposure and neurobehavioral impairment in at least two domains in the absence of other defining characteristics for FAS.
Although they are not included in the diagnostic criteria for FAS or PFAS, multiple congenital abnormalities associated with prenatal alcohol exposure have been described for nearly every organ system ( Table 3 ) . 15 , 18 – 21 In the absence of defining criteria for FAS or PFAS, documented prenatal alcohol exposure and the presence of one or more major malformations known to result from prenatal alcohol exposure are diagnostic for alcohol-related birth defects 1 ( eTable A , Figure 3 13 ).
| Auditory | Chronic serous otitis media, conductive and/or neurosensory hearing loss |
| Cardiac | Aberrant great vessels, atrial septal defects, ventricular septal defects |
| Gastrointestinal | Enteric neuropathy |
| Musculoskeletal | Camptodactyly, clinodactyly ( ), flexion contractures, hypoplastic nails, radioulnar synostosis, scoliosis, spinal malformations |
| Neurologic | Microcephaly, seizure disorder, spinal cord abnormalities, structural brain abnormalities (including corpus callosum, cerebellum, caudate, and hippocampus) |
| Ophthalmologic | Ptosis, retinal malformation, strabismus, visual impairment |
| Orofacial | Cleft lip, cleft palate |
| Psychiatric/ neurobehavioral | Attention-deficit/hyperactivity disorder, conduct disorder, intellectual disability, language disorders, learning disabilities, mood disorders, oppositional defiant disorder, substance use disorders |
| Renal | Aplastic/dysplastic/hypoplastic kidneys, horseshoe kidney, hydronephrosis, ureteral duplications |
| Documented prenatal alcohol exposure | |
| At least 1 of the following specific major malformations known to be the result of prenatal alcohol exposure: | |
| Auditory: conductive and/or neurosensory hearing loss | |
| Cardiac: aberrant great vessels, atrial septal defect, conotruncal heart defects, ventricular septal defect | |
| Musculoskeletal: flexion contractures, radioulnar synostosis, scoliosis, vertebral segmentation defects | |
| Ophthalmologic: optic nerve hypoplasia, ptosis, retinal vascular anomalies, strabismus | |
| Renal: aplastic/dysplastic/hypoplastic kidneys, horseshoe kidney, ureteral duplications | |

Differential Diagnosis
The differential diagnosis for FASD includes a variety of chromosomal abnormalities, exposure to other teratogens, and behavioral and psychiatric diagnoses ( Table 4 ) . 2 , 22 – 28 If the diagnosis is uncertain, the workup should include referral to a developmental pediatrician or geneticist for further evaluation, which may involve a chromosomal microarray, cranial neuroimaging, and cardiac/abdominal ultrasonography. 2
| Aarskog syndrome | X-linked recessive, often mutations in , although others unknown | Broad philtrum, intellectual and neurobehavioral disabilities, small nose with anteverted nares, wide-spaced eyes | Brachydactyly, crease below lower lip, dental eruption problems, downward-slanting palpebral fissures, shawl scrotum (scrotum folds around penis), short stature that resolves with puberty, widow's peak |
| Bloom syndrome | Autosomal recessive chromosomal instability caused by mutation in | Short stature with mild microcephaly, variably impaired intellectual ability | Café au lait spots; facial telangiectasia erythema; keel-shaped face; predisposition to early cancer, infertility, and immunodeficiency; sparse subcutaneous adipose tissue |
| Cornelia de Lange (Brachmann-de Lange) syndrome | Autosomal dominant from spontaneous mutations in , and , or X-linked dominant with mutations in or | Anteverted nares, depressed nasal bridge, growth impairment, hearing loss, intellectual disability, microcephaly, short stature, smooth philtrum, thin vermilion border | Arched eyebrows that meet in the middle (synophrys), downturned mouth, high arched palate, hypertrichosis, long eyelashes, short limbs |
| Dubowitz syndrome | Unknown; suspected autosomal recessive | Neurobehavioral disabilities (hyperactivity, impulsivity, and inattentiveness), epicanthal folds, intellectual disability, microcephaly, short palpebral fissures, short stature, wide-spaced eyes | Broad nasal tip, cryptorchidism, eczema-like skin disorder, high-pitched voice, shallow supraorbital ridge with nasal bridge near level of forehead |
| Fetal hydantoin syndrome | Prenatal exposure to phenytoin (Dilantin) | Depressed nasal bridge, growth deficits, occasional intellectual disability, wide-spaced eyes | Genitourinary defects, hirsutism, hypoplastic fingertips, low hairline, orofacial clefts, short neck, short nose with bowed upper lip |
| Fetal valproate syndrome | Prenatal exposure to valproate (Depacon) | Anteverted nares, epicanthal folds, long philtrum, thin vermilion border, wide-spaced eyes | Cardiac malformations, high forehead, infraorbital crease, neural tube defects, small mouth |
| Noonan syndrome | Autosomal dominant, often mutation in | Epicanthal folds, intellectual disability, low nasal bridge, short stature, wide-spaced eyes | Bleeding diathesis, cryptorchidism, downward-slanting palpebral fissures, hypertrophic cardiomyopathy, keratoconus, low posterior hairline, pectus excavatum, protruding upper lip, pulmonary stenosis, webbed neck, wide mouth |
| Phenylalanine embryopathy | Maternal phenylketonuria | Epicanthal folds, growth impairment, intellectual disability, long philtrum, microcephaly, short palpebral fissures, small nose with anteverted nares, thin vermilion border | Cardiac malformations, hypertonia, prominent glabella, round facies |
| Toluene embryopathy | Prenatal exposure to toluene | Growth deficits, midface hypoplasia, short palpebral fissures, smooth philtrum, thin vermilion border | Bifrontal narrowing of the skull, downturned mouth, ear abnormalities, hair pattern abnormalities, large anterior fontanelle, micrognathia |
| Velocardiofacial syndrome | Autosomal dominant with microdeletion in chromosome 22q11 | Intellectual disabilities, psychiatric disorders, small palpebral fissures | Cardiac malformations, cleft palate, long face with prominent nose, transient neonatal hypocalcemia, weak pharyngeal muscles resulting in hypernasal speech |
| Williams syndrome | Heterozygous 7q11.23 deletion, including elastin gene | Anteverted nares, depressed nasal bridge, epicanthal folds, growth impairment, intellectual disability, long philtrum, short nose, short palpebral fissures | Aortic and pulmonary stenosis, connective tissue disorders, endocrine abnormalities, full lips, hoarse voice, hypertension, periorbital fullness, poor to near-normal language skills, renal abnormalities, stellate pattern of iris, systemic arterial stenosis, wide mouth |
There is no cure for FASD. 5 There is a lack of evidence on which to base recommendations for optimal management; therefore, much of the management is based on expert opinion. Treatment consists of providing a medical home for the patient and family, managing comorbid conditions, providing nutritional support, addressing behavioral and emotional problems, arranging referrals for habilitative therapies (therapeutic intervention for those who have never developed a specific skill), coordinating care with a multidisciplinary team, and educating parents ( Table 5 ) . Early intervention is necessary to optimize health outcomes. 11 , 29
| and |
MANAGING COMORBID CONDITIONS
Children with FASD can have a range of comorbid conditions ( Table 3 ) 15 , 18 – 21 ; referrals to members of the multidisciplinary team are based on the specific needs identified. Because hearing and vision impairments are correlated with prenatal alcohol exposure, all children with suspected FASD should have hearing and vision screening. 30 , 31
NUTRITIONAL SUPPORT
Children with FASD are nutritionally and socially vulnerable and may benefit from nutritional education and support. By midchildhood, most of these children have spent, on average, one-fourth of their life with unmet basic needs and one-third of their life with someone who abuses alcohol or drugs. 29 One study showed that more than 50% of children with FASD do not consume the recommended dietary allowance of fiber, calcium, or vitamins D, E, and K. 32 It is important to regularly assess the child's height, weight, and body mass index and refer for support (e.g., nutritionist, social worker) when nutritional problems are identified. 33 Some children will require high-calorie foods and supplements.
MANAGING BEHAVIORAL PROBLEMS
Children with FASD should be monitored and screened for behavioral problems. They have an increased risk of attention-deficit/hyperactivity disorder (40% to 95%), 34 , 35 mood disorders (50%), 36 and oppositional defiant disorder (38%). 35 Medications can improve hyperactivity and impulsivity, but not symptoms of inattention. 37 , 38 Children with FASD and attention-deficit/hyperactivity disorder or other disruptive behaviors should be referred to a developmental pediatrician, psychologist, and/or psychiatrist. Behavioral interventions such as play therapy, children's friendship training, and specially trained case managers have reasonable evidence of effectiveness, but these resources have variable availability. 37
FAMILY SUPPORT
Children with FASD are at increased risk of physical and sexual violence, with 61% experiencing physical or sexual abuse or witnessing domestic violence by 12 years of age. 29 , 39 Sexual abuse should be considered in children who present with inappropriate sexual behaviors. Children with FASD who remain in the care of their biologic mother are more likely to experience family dysfunction and instability (e.g., divorce, unemployment, drug and alcohol use). 25 , 29 Those who are raised in stable homes have improved outcomes and are less likely to be expelled from or drop out of school, be arrested, or develop substance use problems. 29 Interventions should be aimed at stabilizing the home environment and improving parent-child interactions. 11 Such interventions include parental substance abuse referrals, child discipline courses, parent support groups, and child protective services.
Prognosis varies with the degree of impairment. Persons with FASD are more likely to require special education, receive disability pensions, and be unemployed. 40 Those who receive early diagnosis and intervention (before 12 years of age) have significantly better outcomes, including a two- to fourfold reduction in rates of imprisonment and substance abuse. 29
The Centers for Disease Control and Prevention, the American Academy of Family Physicians, the American Academy of Pediatrics, and the American Congress of Obstetricians and Gynecologists recognize no safe amount of alcohol consumption during pregnancy and recommend complete abstinence. 26 , 41 – 43 Although many women abstain from alcohol when they learn they are pregnant, some consume alcohol before they find out. Contraception should be offered to women of child-bearing age who drink; if they desire pregnancy, abstinence from alcohol should be recommended. 44 The American Congress of Obstetricians and Gynecologists recommends screening women in the first trimester for alcohol use, and Canadian guidelines recommend screening all pregnant women for alcohol use. 42 , 45 A useful screening tool is the TACER-3, which identifies women whose drinking may put their fetus at risk of FASD ( Table 6 ) . 46
| Tolerance | ≥ 2 drinks | 2 | How many drinks does it take to make you feel high? |
| Annoyance | Yes | 1 | Has anybody ever annoyed you by complaining about your drinking? |
| Cut down | Yes | 1 | Have you ever felt you ought to cut down on your drinking? |
| Eye-opener | Yes | 1 | Have you ever needed a drink first thing in the morning to get going? |
If alcohol use in pregnancy is identified, physicians should recommend cessation and offer group-based interventions such as Alcoholics Anonymous and alcohol rehabilitation centers. 47 Brief interventions that include the patient's partner improve FASD-related birth outcomes and should include assessing maternal understanding of healthy pregnancy behaviors, assisting the mother in setting the goal of abstinence from alcohol, planning alternative behaviors for when the temptation to drink arises, and inviting the partner to find methods to support the mother's abstinence from alcohol. 48 , 49
This article updates a previous article on this topic by Wattendorf and Muenke . 13
Data Sources: Sources searched include PubMed (OVID), Evidence Summary from the AFP 's editors, Essential Evidence Plus, Cochrane database, and the Agency for Healthcare Research and Quality. Search terms included: fetal alcohol syndrome, fetal alcohol spectrum disorder, alcohol-related birth defects, maternal alcohol consumption, prenatal alcohol exposure. Search dates: February 2016, April 2016, May 2016, June 2016, July 2016, November 2016, and December 2016.
Figures 1 and 3 courtesy of Darryl Leja, National Human Genome Research Institute, National Institutes of Health, Bethesda, Md.
Hoyme HE, Kalberg WO, Elliott AJ, et al. Updated clinical guidelines for diagnosing fetal alcohol spectrum disorders. Pediatrics. 2016;138(2):e20154256.
de Sanctis L, Memo L, Pichini S, Tarani L, Vagnarelli F. Fetal alcohol syndrome: new perspectives for an ancient and underestimated problem. J Matern Fetal Neonatal Med. 2011;24(suppl 1):34-37.
Tan CH, Denny CH, Cheal NE, Sniezek JE, Kanny D. Alcohol use and binge drinking among women of childbearing age—United States, 2011–2013. MMWR Morb Mortal Wkly Rep. 2015;64(37):1042-1046.
Centers for Disease Control and Prevention (CDC). Alcohol use and binge drinking among women of childbearing age—United States, 2006–2010. MMWR Morb Mortal Wkly Rep. 2012;61(28):534-538.
Joya X, Garcia-Algar O, Salat-Batlle J, Pujades C, Vall O. Advances in the development of novel antioxidant therapies as an approach for fetal alcohol syndrome prevention. Birth Defects Res A Clin Mol Teratol. 2015;103(3):163-177.
Alvik A, Aalen OO, Lindemann R. Early fetal binge alcohol exposure predicts high behavioral symptom scores in 5.5-year-old children. Alcohol Clin Exp Res. 2013;37(11):1954-1962.
Fox DJ, Pettygrove S, Cunniff C, et al.; Centers for Disease Control and Prevention (CDC). Fetal alcohol syndrome among children aged 7–9 years—Arizona, Colorado, and New York, 2010. MMWR Morb Mortal Wkly Rep. 2015;64(3):54-57.
Roozen S, Peters GJ, Kok G, Townend D, Nijhuis J, Curfs L. Worldwide prevalence of fetal alcohol spectrum disorders: a systematic literature review including meta-analysis [published correction appears in Alcohol Clin Exp Res . 2016;40(7):1587]. Alcohol Clin Exp Res. 2016;40(1):18-32.
Moberg DP, Bowser J, Burd L, Elliott AJ, Punyko J, Wilton G Fetal Alcohol Syndrome Surveillance Program-FASSLink Team. Fetal alcohol syndrome surveillance: age of syndrome manifestation in case ascertainment. Birth Defects Res. 2014;100(9):663-669.
Amendah DD, Grosse SD, Bertrand J. Medical expenditures of children in the United States with fetal alcohol syndrome. Neurotoxicol Teratol. 2011;33(2):322-324.
Bertrand J, Floyd LL, Weber MK Fetal Alcohol Syndrome Prevention Team, Division of Birth Defects and Developmental Disabilities, National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention (CDC). Guidelines for identifying and referring persons with fetal alcohol syndrome [published correction appears in MMWR Morb Mortal Wkly Rep . 2006;55(20):568]. MMWR Recomm Rep. 2005;54(RR-11):1-14.
Chasnoff IJ, Wells AM, King L. Misdiagnosis and missed diagnoses in foster and adopted children with prenatal alcohol exposure. Pediatrics. 2015;135(2):264-270.
Wattendorf DJ, Muenke M. Fetal alcohol spectrum disorders. Am Fam Physician. 2005;72(2):279-282.
FAS Diagnostic & Prevention Network. Lip-philtrum guides. http://depts.washington.edu/fasdpn/htmls/lip-philtrum-guides.htm . Accessed January 30, 2017.
Norman AL, Crocker N, Mattson SN, Riley EP. Neuroimaging and fetal alcohol spectrum disorders. Dev Disabil Res Rev. 2009;15(3):209-217.
Stoos C, Nelsen L, Schissler KA, Elliot AJ, Kinney HC. Fetal alcohol syndrome and secondary schizophrenia: a unique neuropathological study. J Child Neurol. 2015;30(5):601-605.
Cook JL, Green CR, Lilley CM, et al.; Canada Fetal Alcohol Spectrum Disorder Research Network. Fetal alcohol spectrum disorder: a guideline for diagnosis across the lifespan. CMAJ. 2016;188(3):191-197.
Popova S, Lange S, Shield K, et al. Comorbidity of fetal alcohol spectrum disorder: a systematic review and meta-analysis. Lancet. 2016;387(10022):978-987.
American Academy of Pediatrics Committee on Substance Abuse and Committee on Children with Disabilities. Fetal alcohol syndrome and alcohol-related neurodevelopmental disorders. Pediatrics. 2000;106(2 pt 1):358-361.
Caputo C, Wood E, Jabbour L. Impact of fetal alcohol exposure on body systems: a systematic review. Birth Defects Res C Embryo Today. 2016;108(2):174-180.
Gummel K, Ygge J. Ophthalmologic findings in Russian children with fetal alcohol syndrome. Eur J Ophthalmol. 2013;23(6):823-830.
Douzgou S, Breen C, Crow YJ, et al. Diagnosing fetal alcohol syndrome: new insights from newer genetic technologies. Arch Dis Child. 2012;97(9):812-817.
Burd L, Cotsonas-Hassler TM, Martsolf JT, Kerbeshian J. Recognition and management of fetal alcohol syndrome. Neurotoxicol Teratol. 2003;25(6):681-688.
Jones KL. Fetal alcohol syndrome. In: Smith's Recognizable Patterns of Human Malformation . 6th ed. Philadelphia, Pa.: Elsevier Saunders; 2006:646.
Toutain S, Lejeune C. Family management of infants with fetal alcohol syndrome or fetal alcohol spectrum disorders. J Dev Phys Disabil. 2008;20(5):425-436.
National Center on Birth Defects and Developmental Disabilities; Centers for Disease Control and Prevention; U.S. Department of Health and Human Services; National Task Force on Fetal Alcohol Syndrome and Fetal Alcohol Effect. Fetal alcohol syndrome: guidelines for referral and diagnosis. July 2004. http://www.cdc.gov/ncbddd/fasd/documents/FAS_guidelines_accessible.pdf . Accessed July 23, 2016.
Thackray H, Tifft C. Fetal alcohol syndrome. Pediatr Rev. 2001;22(2):47-55.
Adams DJ, Clark DA. Common genetic and epigenetic syndromes. Pediatr Clin North Am. 2015;62(2):411-426.
Streissguth AP, Bookstein FL, Barr HM, Sampson PD, O'Malley K, Young JK. Risk factors for adverse life outcomes in fetal alcohol syndrome and fetal alcohol effects. J Dev Behav Pediatr. 2004;25(4):228-238.
Pruett D, Waterman EH, Caughey AB. Fetal alcohol exposure: consequences, diagnosis, and treatment. Obstet Gynecol Surv. 2013;68(1):62-69.
Carter RC, Jacobson SW, Molteno CD, Chiodo LM, Viljoen D, Jacobson JL. Effects of prenatal alcohol exposure on infant visual acuity. J Pediatr. 2005;147(4):473-479.
Fuglestad AJ, Fink BA, Eckerle JK, et al. Inadequate intake of nutrients essential for neurodevelopment in children with fetal alcohol spectrum disorders (FASD). Neurotoxicol Teratol. 2013;39:128-132.
Young JK, Giesbrecht HE, Eskin MN, Aliani M, Suh M. Nutrition implications for fetal alcohol spectrum disorder. Adv Nutr. 2014;5(6):675-692.
Fryer SL, McGee CL, Matt GE, Riley EP, Mattson SN. Evaluation of psychopathological conditions in children with heavy prenatal alcohol exposure. Pediatrics. 2007;119(3):e733-e741.
O'Connor MJ, Shah B, Whaley S, Cronin P, Gunderson B, Graham J. Psychiatric illness in a clinical sample of children with prenatal alcohol exposure. Am J Drug Alcohol Abuse. 2002;28(4):743-754.
Davis K, Desrocher M, Moore T. Fetal alcohol spectrum disorder: a review of neurodevelopmental findings and interventions. J Dev Phys Disabil. 2011;23(2):143-167.
Oesterheld JR, Kofoed L, Tervo R, Fogas B, Wilson A, Fiechtner H. Effectiveness of methylphenidate in Native American children with fetal alcohol syndrome and attention deficit/hyperactivity disorder: a controlled pilot study. J Child Adolesc Psychopharmacol. 1998;8(1):39-48.
Freunscht I, Feldmann R. Young adults with fetal alcohol syndrome (FAS): social, emotional and occupational development. Klin Padiatr. 2011;223(1):33-37.
Rangmar J, Hjern A, Vinnerljung B, Strömland K, Aronson M, Fahlke C. Psychosocial outcomes of fetal alcohol syndrome in adulthood. Pediatrics. 2015;135(1):e52-e58.
Williams JF, Smith VC Committee on Substance Abuse. Fetal alcohol spectrum disorders. Pediatrics. 2015;136(5):e1395-e1406.
American College of Obstetricians and Gynecologists; Committee on Health Care for Underserved Women. Committee opinion no. 496: at-risk drinking and alcohol dependence: obstetric and gynecologic implications. Obstet Gynecol. 2011;118(2 pt 1):383-388.
American Academy of Family Physicians. Substance abuse and addiction. https://www.aafp.org/about/policies/all/substance-abuse.html . Accessed December 9, 2016.
Green P, McKnight-Eily L, Tan C, Mejia R, Denny C. Vital signs: alcohol-exposed pregnancies—United States, 2011–2013. MMWR Morb Mortal Wkly Rep. 2016;65(4):91-97.
Carson G, Cox LV, Crane J, et al.; Society of Obstetricians and Gynaecologists of Canada. Alcohol use and pregnancy consensus clinical guidelines. J Obstet Gynaecol Can. 2010;32(8 suppl 3):S1-S31.
Chiodo LM, Delaney-Black V, Sokol RJ, Janisse J, Pardo Y, Hannigan JH. Increased cut-point of the TACER-3 screen reduces false positives without losing sensitivity in predicting risk alcohol drinking in pregnancy. Alcohol Clin Exp Res. 2014;38(5):1401-1408.
Committee opinion no. 633: alcohol abuse and other substance use disorders: ethical issues in obstetric and gynecologic practice. Obstet Gynecol. 2015;125(6):1529-1537.
Chang G, McNamara TK, Orav EJ, et al. Brief intervention for prenatal alcohol use: a randomized trial. Obstet Gynecol. 2005;105(5 pt 1):991-998.
O'Connor MJ, Whaley SE. Brief intervention for alcohol use by pregnant women. Am J Public Health. 2007;97(2):252-258.
Continue Reading

More in AFP
More in pubmed.
Copyright © 2017 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.

An official website of the United States government
Here's how you know
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.

Volume 37 Issue 1 January 1, 2015
Advances in Diagnosis and Treatment of Fetal Alcohol Spectrum Disorders: From Animal Models to Human Studies
Part of the Topic Series: Improving Health Through Translational Alcohol Research
Nathen J. Murawski, Ph.D.; Eileen M. Moore, Ph.D.; Jennifer D. Thomas, Ph.D.; and Edward P. Riley, Ph.D.
Nathen J. Murawski, Ph.D., is a postdoctoral fellow at the Center for Behavioral Teratology; Eileen M. Moore, Ph.D., is a research assistant professor in the Department of Psychology; Jennifer D. Thomas, Ph.D., is associate director at the Center for Behavioral Teratology and a professor in the Department of Psychology; and Edward P. Riley, Ph.D., is director of the Center for Behavioral Teratology and a distinguished professor in the Department of Psychology, all at San Diego State University, San Diego, California.
Prenatal alcohol exposure can cause a number of physical, behavioral, cognitive, and neural impairments, collectively known as fetal alcohol spectrum disorders (FASD). This article examines basic research that has been or could be translated into practical applications for the diagnosis or treatment of FASD. Diagnosing FASD continues to be a challenge, but advances are being made at both basic science and clinical levels. These include identification of biomarkers, recognition of subtle facial characteristics of exposure, and examination of the relation between face, brain, and behavior. Basic research also is pointing toward potential new interventions for FASD involving pharmacotherapies, nutritional therapies, and exercise interventions. Although researchers have assessed the majority of these treatments in animal models of FASD, a limited number of recent clinical studies exist. An assessment of this literature suggests that targeted interventions can improve some impairments resulting from developmental alcohol exposure. However, combining interventions may prove more efficacious. Ultimately, advances in basic and clinical sciences may translate to clinical care, improving both diagnosis and treatment.
Alcohol consumption during preg nancy can interfere with both embryonic and fetal development, producing a wide range of outcomes that fall under the rubric of fetal alcohol spectrum disorders (FASD). FASD is the nondiagnostic umbrella term used to refer to the full range of effects that can occur following prenatal alcohol exposure. Such exposure can produce a variety of effects, including physical birth defects, growth retardation, and facial dysmorphism, but the most profound effects are on the developing brain and accompanying cognition and behavior. The disabilities associated with prenatal alcohol are variable, influenced by numerous factors, and can have a lifelong impact. Therefore, early diagnosis and intervention are essential for improved clinical outcomes (Streissguth et al. 2004).
Animal models have played a critical role in research on FASD, including studies confirming that alcohol is indeed a teratogen and those providing insights into the mechanisms by which alcohol exerts its teratogenic effect. Researchers have used a wide variety of organisms to model the effects of prenatal alcohol exposure, which mimic both the physical and the behavioral alterations seen in human FASD (Wilson and Cudd 2011). These models allow researchers to experimentally control factors, including alcohol dose, pattern and timing of exposure, nutritional status, maternal factors, and genetics, that are known to influence and contribute to variability in clinical outcomes. Animal models also can help identify better strategies for diagnosing and treating FASD. This review will not directly compare the animal and human data because previous reviews have done this (Schneider et al. 2011). Rather, it will highlight and integrate translational research that might lead to advancements in the diagnosis and treatment of FASD. Furthermore, several psychosocial, academic, and behavioral interventions for FASD that recently have been discussed elsewhere (Paley and O’Connor 2011) are difficult to model in animals and thus will not be reviewed here. Instead, this review focuses on recent pharmacological, nutritional, and exercise interventions that have shown promise in preclinical studies and are progressing toward translation to the clinic.
Identification and Diagnosis
To obtain an accurate estimate of FASD prevalence and provide early intervention for affected individuals, it is critical to identify infants prenatally exposed to alcohol. Identification is less problematic on the severe end of the spectrum—where fetal alcohol syndrome (FAS) lies—because it is characterized by obvious growth retardation, central nervous system (CNS) dysfunction, and a specific pattern of craniofacial anomalies (see figure 1A). However, many, if not the majority, of individuals affected by prenatal alcohol exposure do not meet criteria for FAS (Bertrand et al. 2005), yet have significant neurobehavioral impairments (Mattson et al. 2013). These cases are referred to as alcohol-related neurodevelopmental disorders (ARND) and are often difficult to identify because they lack the characteristic facial features and growth retardation seen in FAS. In fact, an ARND diagnosis requires confirmation of prenatal alcohol exposure, which often is unavailable or unreliable (see Riley et al. 2011 for a comparison of various diagnostic schemas for FAS and ARND). Finding novel ways to identify at-risk individuals for disabilities along the spectrum is critical, as is identifying effective interventions to mitigate these cognitive and behavioral effects.
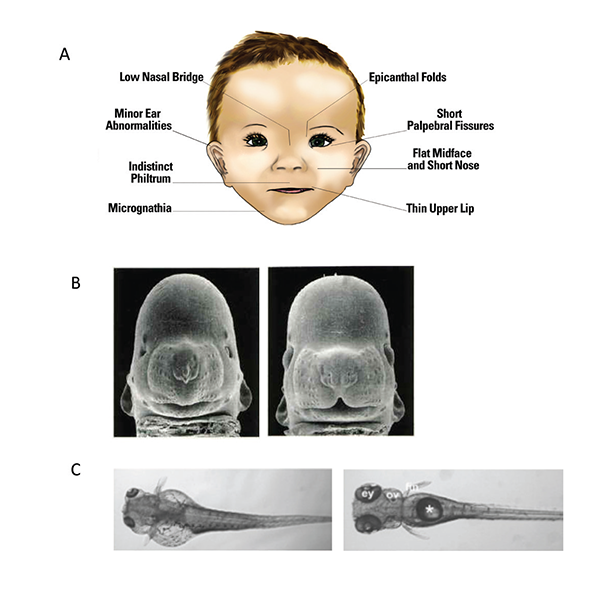
The routine use of objective, validated, and highly specific markers of prenatal alcohol exposure would help improve FASD identification, which currently is hampered by a lack of good information. For example, a recent study (May et al. 2014 a ) found that only 33 percent of the mothers of children given a diagnosis of FAS provided information about their alcohol consumption. In addition, a large number of children with FASD are in adoptive situations or foster care, and there may be little knowledge of their alcohol exposure. Several indirect and direct markers of alcohol exposure (see figure 2A) exist and have been described at length elsewhere (Bakhireva and Savage 2011). Fatty acid ethyl esters, ethyl glucuronide, ethyl sulphate, and the alcohol-derived phospholipid phosphatidylethanol are among several promising metabolic biomarkers. All of these are byproducts of alcohol metabolism, and each is limited by how long after alcohol exposure they are detectable. Another newly identified marker may persist longer than these metabolic markers. As shown in a sheep model, unique circulating microRNAs (miRNA) may help identify individuals consuming alcohol and, importantly, those exposed to alcohol in utero. An initial study suggests that several microRNAs (miRNAs), including miR-9, -15b, -19b, and -20a, are potentially sensitive indices of alcohol exposure in both the pregnant ewe and newborn lamb (Balaraman et al. 2014) (see figure 2B). Researchers are conducting miRNA studies in humans to confirm the sheep findings. If they succeed, miRNAs may provide a new tool to identify alcohol-exposed pregnancies/infants, similar to their use as diagnostic biomarkers in a variety of other disease states (Weiland et al. 2012).
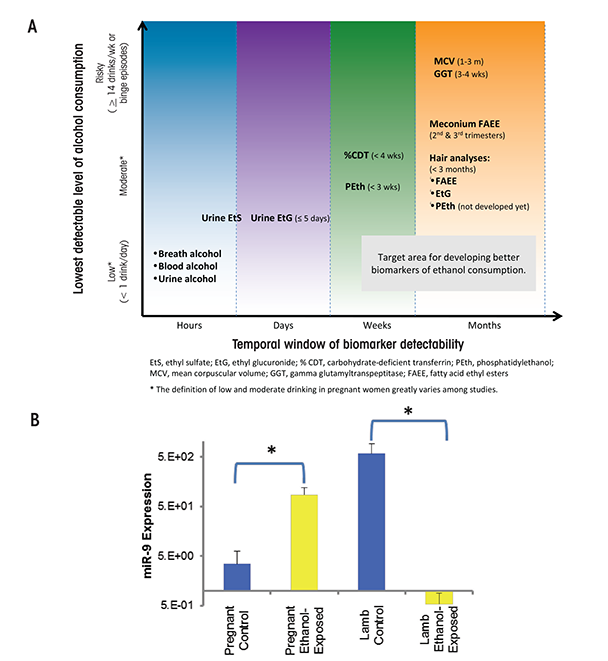
Other novel FASD diagnostic techniques include ways to identify potential at-risk individuals based upon subtle, subclinical facial features. In particular, researchers have developed a computerized method for detecting facial features using three-dimensional facial imaging and computer-based dense-surface modeling (see figure 3). Hammond and colleagues (Suttie et al. 2013) compared this approach with a standard dysmorphology exam for diagnosing FAS and found a high degree of agreement. The researchers used sophisticated mathematical tech niques to characterize the facial features of heavily exposed individuals who did not have facial features that would have led to a diagnosis of FAS using traditional measures. They categorized participants as having facial features that were either “more similar to those with FAS” or “more similar to unex posed controls.” Importantly, the heavily exposed children with FAS-like faces performed at a level similar to the FAS group on neurobehavioral tests, whereas those with more control-like faces exhibited behavioral profiles similar to control subjects. These data were collected on a homogenous ethnic group in South Africa and therefore need to be replicated in other populations. Still, they provide preliminary evidence that this approach may constitute a means to identify at-risk individuals based upon subtle, sub-clinical facial features.
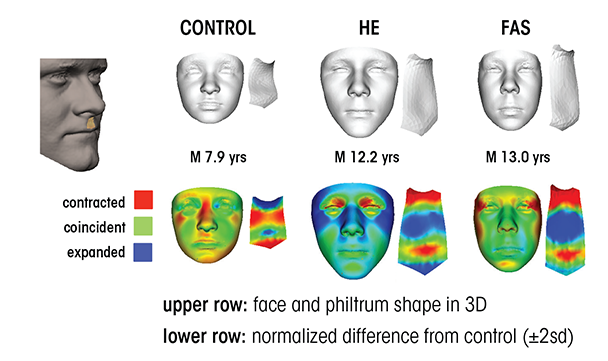
Developing truly accurate and specific methods for identifying individuals with FASD requires an understanding of the full spectrum of alcohol-related consequences and clarification of the various factors, both protective and permissive, that influence outcome variability. Animal models have provided information on the mechanisms by which alcohol affects facial development and the factors that may make a fetus more susceptible to these facial changes (see figure 1B and C for examples of craniofacial defects in the mouse and zebrafish). In the mouse, for example, alcohol administration on gestational day (GD) 7, equivalent to approximately week 3 postfertilization in a human pregnancy, produces a constellation of facial malformations similar to those seen in FAS. Defects include severe midfacial hypoplasia, shortening of the palpebral fissures, an elongated upper lip, and deficient philtrum (Godin et al. 2010). However, alcohol exposure delayed a day and a half to GD 8.5 produces a distinctly different pattern of malformations, with mild hypoplasia and shortening of the palpebral fissures and upper lip but a preserved philtrum (Lipinski et al. 2012) (see figure 4A and B). These data suggest that maternal alcohol consumption, even before many women are aware that they are pregnant, can cause significant and selective facial alterations in their offspring. The distinctive facial phenotype of FAS depends on the timing of exposure, and other facial characteristics resulting from alcohol exposure during different critical periods are possible.
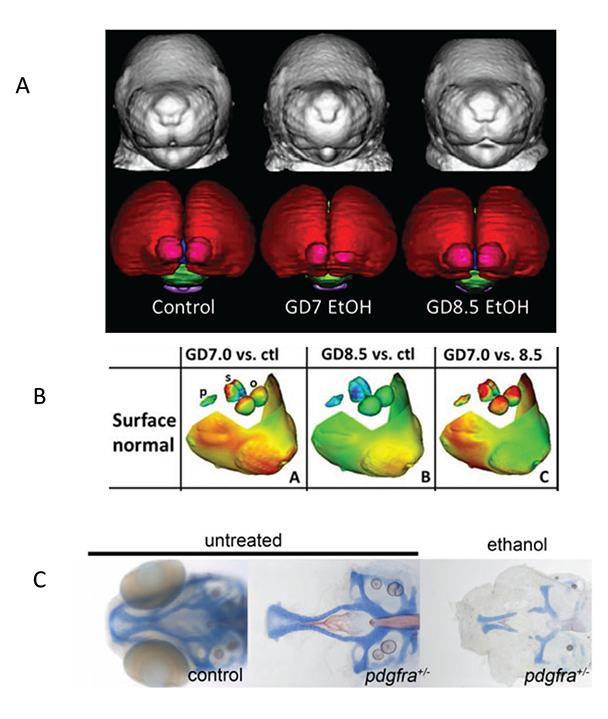
As with facial dysmorphology, basic science models illustrate that the timing of alcohol administration also produces differing patterns of brain malformations, which again may account for the variability in outcomes. O’Leary-Moore and colleagues (2011) recently reviewed the different brain changes following a single day of alcohol exposure during early fetal development in the mouse using magnetic resonance imaging (MRI). Alcohol exposure on GD 7 was particularly damaging to medial forebrain regions, with relative sparing of mesencephalic and rhomb encephalic regions (Godin et al. 2010). The morphological changes induced by alcohol exposure on GD 8 included disproportionate volume reductions in the olfactory bulbs, hippocampus, and cerebellum and relative sparring of the pituitary and septal regions (Parnell et al. 2009). GD 9 exposure produced reductions in cerebellar volume, ventricle enlargement, and shape deviations in the cerebral cortex, hippocampus, and right striatum (Parnell et al. 2013). In contrast, offspring exposed to alcohol on GD 10 displayed enlarged ventricles and disproportionate reductions in cortical volume (O’Leary-Moore et al. 2010). Brain-imaging studies in humans with FASD also find morpho logical alterations in many of these brain structures (see Moore et al. 2014 for review), which may vary depending on the specific timing of alcohol exposure. These exposure timing– dependent brain changes likely produce different behavioral outcomes, contributing to the variability in impairment seen clinically. Ultimately, understanding the relationship between alcohol exposure parameters and variability in outcome, including different behavioral phenotypes, may improve detection of individuals with FASD.
Recent studies also suggest that the interaction of alcohol with specific genes involved in brain development and the development of facial features may affect the FASD phenotype. A study in zebrafish, for example, examined the interaction of alcohol with the gene for platelet-derived growth factor receptor alpha (Pdgfra) (McCarthy et al. 2013). This gene is involved in cellular migration and proliferation and is necessary for proper migration of neural crest cells, which contribute to the formation of diverse structures, including the face. The researchers found that pdgfra interacts with alcohol to protect against severe craniofacial defects. Specifically, more than 60 percent of zebrafish heterozygous for the pdgfra gene showed cranial facial defects after alcohol exposure compared with only about 10 percent of the alcohol-treated wild-type embryos (figure 4C). A genome-wide genetic scan, using single nucleotide polymor phisms (SNPs), in humans with FASD supports these findings, showing that craniofacial phenotypes seen in FASD are linked to the PDGFRA gene (McCarthy et al. 2013). A more recent study in zebrafish found that a gene involved in the development of the embryonic axis, vangl2, interacts strongly with alcohol (Swartz et al. 2014). This finding provides another potential gene target to help identify significant sources of variance in terms of susceptibility to the facial characteristics and perhaps changes in brain seen in FASD (see McCarthy and Eberhart 2014 for a recent review of genetic factors involved in FASD).
Basic research in people with FASD also is providing new methods for assessing alcohol’s clinical effects. Studies have identified several relationships between facial measurements and brain structure in FASD (reviewed in Moore et al. 2014). For example, shorter palpebral fissures predict volume reductions in the bilateral ventral diencephalon, a thinner anterior corpus callosum, and a thicker right inferior frontal cortex. The smoothness of the philtrum predicts volumetric reductions in the thalamus and the left pallidum. Facial measures also predict brain maturation patterns: Children with greater facial dysmorphia displayed a linear pattern of cerebral cortex growth, at least from childhood through adolescence, rather than the developmentally appropriate inverted U-shaped trajectory. Continued research examining the relationship between face, brain, and behavioral outcomes resulting from prenatal alcohol eventually may lead to the identification of specific patterns of anomalies that can be used to better identify FASD and improve diagnosis. Moreover, patterns of outcomes may illuminate mechanisms by which alcohol disrupts developmental processes, which can inform treatment strategies. It must be cautioned, however, that the utility of these findings will largely depend on their sensitivity and specificity to alcohol .
Treatment Strategies
Although no specific treatments exist that are unique for FASD, the similarity between the cognitive and behavioral characteristics of FASD and other disorders provides a framework for treatment development. For example, estimates indicate that anywhere from around 50 percent to over 90 percent of individuals with FASD who have been clinically referred meet diagnostic criteria for attention deficit/hyperactivity disorder (ADHD) (Bhatara et al. 2006; Fryer et al. 2007). One approach would be to treat individuals with FASD with medications, such as stimulants, that have been successful in treating ADHD. However, mixed results have been found with stimulant treatment in clinical studies on FASD. For example, treatment with stimulant medications may reduce hyperactivity, with little evidence for beneficial effects on attention (e.g., Doig et al. 2008). Other studies have noted variable and unpredictable effects (O’Malley and Nanson 2002) or even poorer outcomes (Frankel et al. 2006) in FASD. Animal studies find that perinatal alcohol exposure leads to hyperactivity and that treatment with stimulants later in life increases, rather than attenuates, animals’ spontaneous locomotor behaviors (Hannigan and Berman 2000). Atomoxetine (Strattera), a nonstimulant medication for ADHD, also is often used in the treatment of attention problems in FASD and a clinical trial of its effectiveness in FASD is under way.
Researchers are using their knowledge of the mechanisms underlying alcohol’s toxic effect on the fetus to design preclinical models that test the efficacy of a number of pharmaceutical agents to mitigate alcohol-related impair ments (Idrus and Thomas 2011). For example, prenatal alcohol exposure results in deficient activation of cyclic-AMP response element–binding protein (CREB), which can impair brain plasticity, a process of neural change important for brain development, learning, and memory. The pharmaceutical vinpocetine, a vasodilator and anti-inflammatory agent, inhibits the enzyme phosphodiesterase type 1, an action that prolongs CREB activation and thereby strengthens synaptic connections. Studies in animal models find that vinpocetine attenuates alcohol-related impairments in cortical plasticity and reduces learning and memory deficits associated with developmental alcohol exposure (Medina 2011). Clinical trials in humans with dementia have shown some promise and no serious adverse consequences, although results with other disorders, such as ischemic stroke remain incon clusive (Medina 2011). Clinical studies to evaluate this drug in humans with FASD are an important next step.
Preclinical models of FASD also have used neuroprotective peptides to mitigate neuropathologies and behavioral impairments resulting from developmental alcohol exposure. Originally, researchers administered the neuroactive peptides NAP and SAL concurrently with alcohol to pregnant rodents in an attempt to prevent alcohol-induced damage in the offspring. Subsequently, researchers have administered the peptides to adolescent rodents exposed to alcohol prenatally and found that they can reduce deficits in behavioral tasks, such as a T-maze and a Morris water maze (Incerti et al. 2010). The peptides also reversed alcohol-related changes in NMDA receptors in the hippocampus and cortex. These peptides are being developed to treat a number of neurodegenerative diseases and may prove useful in the treatment of FASD.
Nutritional Interventions
Research clearly shows that nutritional factors influence alcohol’s damaging effects on the fetus. Moreover, it is possible that postnatal nutrition also might influence physical and behavioral outcomes in individuals with FASD.
Prenatal Nutritional Interventions
Some studies suggest that women who drink during pregnancy have nutritional deficits relative to control subjects. In one study, for example, May and colleagues (2014 b ) examined the nutritional status of a group of South African mothers who gave birth to children with FASD compared with a group of mothers who gave birth to children without FASD. The mothers of children with FASD were more likely to be deficient in several vitamins, including vitamins A, B6, choline, C, D, and E; minerals, including calcium, iron, and zinc; and omega-3 fatty acids. Deficiencies in these micronutrients during pregnancy can contribute to abnormal fetal development (Nyaradi et al. 2013) and may further exacerbate the damaging effects of alcohol on the developing embryo and fetus. In animal models, maternal nutritional deficiencies (e.g., zinc or iron) during pregnancy increase the detrimental effects of prenatal ethanol on brain development and subsequent behavior in offspring. For example, the combined insults of prenatal alcohol exposure and iron deficiency resulted in increased cerebellar apoptosis (cell death), reduced myelin content, and greater impairments in cerebellar-dependent classical eyeblink conditioning compared with either insult alone (Rufer et al. 2012).
Research also finds that nutritional supplementation during pregnancy may attenuate ethanol’s teratogenic effects. In one relatively small study (Avalos et al. 2011), low to moderate alcohol consumption during pregnancy resulted in a twofold increase in small-for-gestational-age infants relative to mothers who abstained. However, the offspring of women who consumed alcohol and reported taking nutritional supplements during pregnancy were no different on these measures than the offspring of abstainers ( Avalos et al. 2011). The study reported similar results for preterm births. In a study of pregnant women currently being conducted in the Ukraine, r esearchers compared the birth outcomes of women given vitamin supplements with those not given supplements. Both groups included women who were consuming alcohol. Although the researchers still are analyzing the results, preliminary reports indicate that the women consuming alcohol and taking micronutrient supplements have a lower rate of babies with FASD than women in the nonsupplement group (Chambers et al. 2013).
Other nutritional interventions target oxidative stress. Alcohol increases oxidative stress, which in turn can initiate a cascade of events that eventually lead to widespread CNS cell loss during development (Brocardo et al. 2011). In rodent models of FASD, pregnant females given nutrients high in antioxidant properties (e.g., vitamin C, vitamin E, omega-3 fatty acids) during the time they also are given alcohol, give birth to offspring with reduced oxidative stress and cell loss, and fewer behavioral impairments (Brocardo et al. 2011; Patten et al. 2013 a ). Although antioxidant treatments in animal models are encouraging, researchers prematurely terminated a clinical trial utilizing high doses of vitamins C and E in women with alcohol-exposed pregnancies because of safety concerns (Goh et al. 2007).
Other studies are examining the role of nutritional supplements on gene transcription. Animal models of FASD demonstrate that prenatal alcohol exposure significantly affects gene transcription through epigenetic modifications (Ungerer et al. 2013). Specifically, alcohol-induced changes in DNA methylation, histone modification, and noncoding RNAs may alter the expression patterns of numerous genes important for neurodevelopment and behavior. Nutrients such as choline, betaine, folic acid, methionine, and zinc can influence these epigenetic profiles and can potentially attenuate alcohol-induced changes to the epigenome. For example, supplemental choline in rats exposed to alcohol during development alters alcohol-related changes in global DNA methylation in the hippocampus and prefrontal cortex (Otero et al. 2012) and significantly attenuates ethanol-induced hypermethylation of genes in the hypothalamus (Bekdash et al. 2013). Additionally, access to a diet supple mented with nutrients that act as methyl donors normalized changes to DNA methylation patterns in embryonic tissue following a single binge exposure to alcohol in early gestation (Downing et al. 2011). These nutrient- induced changes to the epigenome may contribute to the behavioral and cognitive improve- ments seen in alcohol-exposed rodents following supplementation (see below).
Additional preclinical research indicates that supplementation with beta- carotene (provitamin A), nicotinamide (the amide of vitamin B3), and zinc all may reduce alcohol’s effects on fetal development, including cell loss, fetal dysmorphology, and cognitive impairments (reviewed in Idrus and Thomas 2011). These animal studies highlight the protective effects that nutrient supplementation can have on development during alcohol exposure. Improving the nutritional status of pregnant women, especially those who consume alcohol, will likely result in improved outcomes in offspring.
Postnatal Nutrient Interventions
Nutritional status also can affect cognitive development throughout childhood (Bryan et al. 2004). Recent studies have examined the nutritional intake of children with FASD. Based on their dietary habits, many children with FASD are not consuming adequate or daily-recommended amounts of omega-3 fatty acids, vitamin D, and choline (figure 5A) (Fuglestad et al 2013; Werts et al. 2014). Although these studies have some limitations—including low sample sizes, comparison with national data rather than a local control group, and relying on self-reports—they do indicate that individuals with FASD ingest inadequate levels of certain nutrients and therefore may benefit from nutrient supplementation. In rodent models, administering these micronutrients during or shortly following developmental alcohol exposure significantly mitigated ethanol-induced impairments on brain and behavior (figure 5B) (Idrus and Thomas 2011; Patten et al. 2013 b ). For example, animal models have shown that choline can attenuate ethanol’s adverse effects on both brain and behavioral development when administered postnatally, long after alcohol exposure has ceased (Ryan et al. 2008).
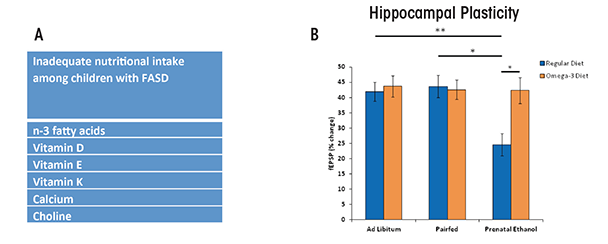
Clinical studies currently are under- way to examine the effectiveness of choline supplementation in children with FASD. Preliminary results from a study examining choline supplementation in children with FASD aged 2.5–4.9 years suggest that supplemental choline is both feasible and tolerable, with few side effects being reported (Wozniak et al. 2013). The results on behavioral measures should be available soon. In addition to nutrient supplementation, at-risk populations may benefit from better access to food naturally high in nutrients found to improve outcomes in animal studies.
Exercise Interventions
Exercise has many beneficial effects on brain and behavior outcomes. Reports in both human and rodents indicate that exercise improves learning and memory; increases circulating proteins that support brain function, such as brain-derived neurotrophic factor (BDNF); and, in rodents, increases generation of new neurons in the adult hippocampus (Voss et al. 2013). In addition, clinical studies show beneficial cognitive effects following exercise in normal aging, Alzheimer’s disease, and Parkinson’s disease (reviewed in Yau et al. 2014). No published studies to date have implemented an exercise intervention to improve cognitive and behavioral outcomes in individuals with FASD, but preliminary data and preclinical results are promising, as described below.
Studies suggest that running may enhance learning and memory in rodents prenatally exposed to alcohol. Rodents will run multiple kilometers per day when they have access to a running wheel, making it ideal for an exercise intervention. Indeed, access to a running wheel significantly attenuates spatial learning and memory impairments in adult rats exposed to alcohol during development (Christie et al. 2005; Thomas et al. 2008). In addition, these improvements in cognitive function following exercise are associated with exercise-induced enhancements in BDNF and adult hippocampal neurogenesis, both of which are influenced by developmental alcohol exposure (Gil-Mohapel et al. 2010).
However, the long-term effects of short periods of exercise may be limited. For example, increases in BDNF return to normal levels within 2 weeks following exercise (Gil-Mohapel et al. 2010). That said, the benefits of exercise may be prolonged through additional environmental experiences, such as those provided by raising animals in an enriched, stimulating environment. In fact, Hamilton and colleagues (2014) have found that the combination of wheel running followed by enrichment significantly increases adult neurogenesis relative to wheel running alone in alcohol-exposed rats. Similarly, exercise plus enrichment mitigates alcohol-induced impairments on behavioral tasks, such as trace eyeblink condi tioning and contextual fear conditioning. Behavioral improvement was associated with increases in adult neurogenesis (Hamilton et al. 2014). In addition, specific motor training can have beneficial effects on the structure and function of the cerebellum among rodents exposed to alcohol prenatally (Klintsova et al. 2000).
In translating these preclinical findings to human studies, researchers may need to tailor their exercise interventions to accommodate some of the motor impairments evident in FASD. A recent meta-analysis of motor skills in children and adolescents with FASD reported impairments in balance, motor coordination, and ball skills (Lucas et al. 2014).
A number of clinical research programs are using these findings to develop motor training and/or exercise interventions and investigate their efficacy in individuals with FASD. None have published results yet, except in abstract form. The following are two promising examples:
- Researchers at the University of Washington are using sensorimotor training via a virtual-reality system to try to improve motor deficits. Participants stand on a moveable surface, wearing virtual-reality goggles as the program attempts to train them to use sensory information for balance (Jirkowic et al. 2014) .
- Researchers at the University of the Fraser Valley are using strength-based interventions in an attempt to improve motor skills and cognitive function in FASD. In this intervention, clinicians create a physical activity and motor skills program based on an individual child’s strengths, with the hope that such training may generalize to some aspects of executive functioning, attention, and visuospatial processing in children with FASD (Keiver et al. 2014).
FASD can be difficult to treat for a number of reasons. First, identifying individuals with prenatal alcohol exposure can be a challenge. Although the characteristics of FAS are well defined, alcohol-affected children who do not meet the criteria for FAS or for whom exposure histories are unknown are more difficult to ascertain. Children who are diagnosed earlier have improved clinical outcomes (Streissguth et al. 2004), highlighting the need for early identification. Although there are methodological and ethical concerns that must be addressed, sensitive and specific biomarkers of exposure or effect would improve identification. Continued research examining the interrelations among alcohol-induced face and brain malformations and neurocognitive outcomes using both human and animal models may yield novel means for identification and/or novel specific targets for interventions.
Overall, studies with animal models of FASD demonstrate a wide array of benefits of pharmacological, nutritional, and environmental interventions to both brain structure/function and behavior. However, relatively few clinical studies have evaluated such treatments in FASD. There are some important potential limitations to these treatments. First, many of the treatments have very specific targets and consequences, whereas the range of deficits in FASD is quite varied. For example, in animal models of FASD, nutritional supplementation with choline has a greater positive effect on hippocampal function compared with cerebellar function; in contrast, motor training may be better able to target cerebellar effects in this population. Interventions that use multiple intervention strategies (e.g., nutrition and exercise) as well as more traditional interventions (educational, speech, occupational and/or physical therapies) may mitigate a wider range of cognitive impairments when translated to clinical cases of FASD. Given the numerous successes in identifying potential interventions in preclinical research, the upcoming years should increase translation of these findings to clinical research and eventually to health care settings.
Apoptosis : A process of programmed cell death.
Brain-derived neurotrophic factor (BDNF) : A protein secreted in the brain to support the survival of neurons; it plays a role in the growth, differentiation, and maintenance of these cells.
Cerebellum : An area of the brain important for coordinating motor function, as well as playing a role in simple learning and attention.
Corpus callosum : A wide bundle of fibers that connects the left and right hemispheres of the brain.
Cortex : The outer layer of the brain that is composed of folded gray matter and associated with perception, voluntary movement, and integration of information to support cognitive functions such as memory, language, and abstract thinking, among others.
cAMP response element–binding protein (CREB) : A protein that binds to certain stretches of DNA and influences activation of genes.
Epigenetics : The study of factors that affect gene expression without directly changing the DNA.
Epigenome : Chemical changes to the DNA and histone proteins that affect gene expression.
Ethyl glucuronide : A byproduct of alcohol metabolism formed in the body after alcohol consumption.
Ethyl sulphate : A byproduct of alcohol metabolism formed in the body after alcohol consumption.
Fatty acid ethyl esters : The products of a reaction between ethanol and fatty acid cells.
NMDA receptors : A receptor in the brain activated by the neurotrans-mitter glutamate. Among its many roles, NMDA receptors help control synaptic plasticity (the ability of the brain to change and evolve), learning and memory.
Oxidative stress : When there is an imbalance between the body’s production of reactive oxygen species (free radicals), and antioxidants, which defend against reactive oxygen species.
Pallidum : Refers to the globus pallidus, a subcortical brain structure involved in the regulation of voluntary movement.
Palpebral fissures : The opening between the upper and lower eyelids; length is measured as the distance between the inner to outer eye corners.
Peptide : Chains of 10 to 50 amino acids.
Philtrum : The typically vertical groove between the upper lip and nose.
Phosphatidylethanol : A metabolite of alcohol, created when phospholipase D interacts with alcohol.
Teratogen : A substance that interferes with development and causes birth defects.
Thalamus : A part of the vertebrate brain made up of two symmetrical halves deep in the middle of the brain. Among other roles, it is involved in relaying sensory and motor signals to the cerebral cortex, and regulating consciousness, sleep, and alertness.
Disclosures
The authors declare that they have no competing financial interests.
Avalos, L.A.; Kaskutas, L.; Block, G.; et al. Does lack of multinutrient supplementation during early pregnancy increase vulnerability to alcohol-related preterm or small-for-gestational-age births? Maternal and Child Health Journal 15(8):1324–1332, 2011. PMID: 20949322
Bakhireva, L.N., and Savage, D.D. Focus on: Biomarkers of fetal alcohol exposure and fetal alcohol effects. Alcohol Research & Health 34(1):56–63, 2011. PMID: 23580042
Balaraman, S.; Lunde, E.R.; Sawant, O.; et al. Maternal and neonatal plasma microRNA biomarkers for fetal alcohol exposure in an ovine model. Alcoholism: Clinical and Experimental Research 38(5):1390–1400, 2014. PMID: 24588274
Bekdash, R.A.; Zhang, C.; and Sarkar, D.K. Gestational choline supplementation normalized fetal alcohol-induced alterations in histone modifications, DNA methylation, and proopiomelanocortin (POMC) gene expression in β -endorphin-producing POMC neurons of the hypothalamus. Alcoholism: Clinical and Experimental Research 37(7):1133–1142, 2013. PMID: 23413810
Bertrand, J.; Floyd, L.L.; and Weber, M.K. Guidelines for identifying and referring persons with fetal alcohol syndrome. Morbidity and Mortality Weekly Report (MMWR) Recommendations and Reports 54(RR–11):1–14, 2005. PMID: 16251866
Bhatara, V.; Loudenberg, R.; and Ellis, R. Association of attention deficit hyperactivity disorder and gestational alcohol exposure: An exploratory study. Journal of Attention Disorders 9(3):515–522, 2006. PMID: 16481668
Brocardo, P.S.; Gil-Mohapel, J.; and Christie, B.R. The role of oxidative stress in fetal alcohol spectrum disorders. Brain Research Reviews 67(1–2):209–225, 2011. PMID: 21315761
Bryan, J.; Osendarp, S.; Hughes, D.; et al. Nutrients for cognitive development in school-aged children. Nutrition Reviews 62(8):295–306, 2004. PMID: 15478684
Chambers, C.; Yevtushok, L.; Zymak-Zakutnya, N.; et al.Maternal alcohol consumption during pregnancy, nutritional status, and impact on infant outcomes [abstract]. Alcohol and Alcoholism 48(S1):S21.2, 2013
Christie, B.R.; Swann, S.E.; Fox, C.J.; et al. Voluntary exercise rescues deficits in spatial memory and long-term potentiation in prenatal ethanol-exposed male rats. European Journal of Neuroscience 21(6):1719–1726, 2005. PMID: 15845099
Doig, J.; McLennan, J.D.; and Gibbard, W.B. Medication effects on symptoms of attention-deficit/hyperactivity disorder in children with fetal alcohol spectrum disorder. Journal of Child and Adolescent Psychopharmacology 18(4):365–371, 2008. PMID: 18759646
Downing, C.; Johnson, T.E.; Larson, C.; et al. Subtle decreases in DNA methylation and gene expression at the mouse Igf2 locus following prenatal alcohol exposure: Effects of a methyl-supplemented diet. Alcohol 45(1):65–71, 2011. PMID: 20705422
Frankel, F.; Paley, B.; Marquardt, R.; and O’Connor. Stimulants, neuroleptics, and children’s friendship training for children with fetal alcohol spectrum disorders. Journal of Child and Adolescent Psychopharm- acology 16(6):777–789, 2006. PMID: 17201621
Fryer, S.L.; McGee, C.L.; Matt, G.E.; et al. Evaluation of psychopathological conditions in children with heavy prenatal alcohol exposure. Pediatrics 119(3):e733–e741, 2007. PMID: 17332190
Fuglestad, A.J.; Fink, B.A.; Eckerle, J.K.; et al. Inadequate intake of nutrients essential for neurodevelopment in children with fetal alcohol spectrum disorders (FASD). Neurotoxicology and Teratology 39:128–132, 2013. PMID: 23871794
Gil-Mohapel, J.; Boehme, F.; Kainer, L.; and Christie, B.R. Hippocampal cell loss and neurogenesis after fetal alcohol exposure: Insights from different rodent models. Brain Research Reviews 64(2):283–303, 2010. PMID: 20471420
Godin, E.A.; O’Leary-Moore, S.K.; Khan, A.A.; et al. Magnetic resonance microscopy defines ethanol-induced brain abnormalities in prenatal mice: Effects of acute insult on gestational day 7. Alcoholism: Clinical and Experimental Research 34(1):98–111, 2010. PMID: 19860813
Goh, Y.I.; Ungar, W.; Rover, J.; et al. Mega-dose vitamin C and E in preventing FASD: The decision to terminate the study prematurely. Journal of FAS International 5(e3):1–3, 2007.
Hamilton, G.F.; Jablonski, S.A.; Schiffino, F.L.; et al. Exercise and environment as an intervention for neonatal alcohol effects on hippocampal adult neurogenesis and learning. Neuroscience 265:274–290, 2014. PMID: 24513389
Hannigan, J.H., and Berman, R.F. Amelioration of fetal alcohol-related neurodevelopmental disorders in rats: Exploring pharmacological and environmental treatments. Neurotoxicology and Teratology 22(1):103–111, 2000. PMID: 10642119
Idrus, N.M., and Thomas, J.D. Fetal alcohol spectrum disorders: Experimental treatments and strategies for intervention. Alcohol Research & Health 34(1):76–85, 2011. PMID: 23580044
Incerti, M.; Vink, J.; Roberson, R.; et al. Reversal of alcohol-induced learning deficits in the young adult in a model of fetal alcohol syndrome. Obstetrics and Gynecology 115(2 Pt. 1):350–356, 2010. PMID: 20093910
Jirkowic, T.; Hsu, L.Y.; McCoy, S.W.; et al. Clinical balance responses to sensorimotor training to affect balance for children with fetal alcohol spectrum disorders [abstract]. Alcoholism: Clinical and Experimental Research 38(S1):179A, 2014.
Keiver, K.; Pritchard Orr, A.; Bertram, C.; et al. Effects of a motor skill development program on neurocognitive function (NEPSY-II) in children with fetal alcohol spectrum disorder [abstract]. Alcoholism: Clinical and Experimental Research 38(S1):180A, 2014.
Klintsova, A.Y.; Goodlett, C.R.; and Greenough, W.T. Therapeutic motor training ameliorates cerebellar effects of postnatal binge alcohol. Neurotoxicology and Teratology 22(1):125–132, 2000. PMID: 10642121
Lipinski, R.J.; Hammond, P.; O’Leary-Moore, S.K.; et al. Ethanol-induced face-brain dysmorphology patterns are correlative and exposure-stage dependent. PLoS One 7(8):e43067, 2012. PMID: 22937012
Lucas, B.R.; Latimer, J.; Pinto, R.Z.; et al. Gross motor deficits in children prenatally exposed to alcohol: A meta-analysis. Pediatrics 134(1):e192–e209, 2014. PMID: 24913787
Marrs, J.A.; Clendenon, S.G.; Ratcliffe, D.R.; et al. Zebrafish fetal alcohol syndrome model: Effects of ethanol are rescued by retinoic acid supplement. Alcohol 44(7-8):707–715, 2010. PMID: 20036484
May, P.A.; Baete, A.; Russo, J.; et al. Prevalence and characteristics of fetal alcohol spectrum disorders. Pediatrics 134(5):855–866, 2014 a . PMID: 25349310
May, P.A.; Hamrick, K.J.; Corbin, K.D.; et al. Dietary intake, nutrition, and fetal alcohol spectrum disorders in the Western Cape Province of South Africa. Reproductive Toxicology 46:31–39, 2014 b . PMID: 24568797
Mattson, S.N.; Roesch, S.C.; Glass, L.; et al. Further development of a neurobehavioral profile of fetal alcohol spectrum disorders. Alcoholism: Clinical and Experimental Research 37(3):517–528, 2013. PMID: 22974253
McCarthy, N., and Eberhart, J.K. Gene-ethanol interactions underlying fetal alcohol spectrum disorders. Cellular and Molecular Life Sciences 71(14):2699–2706, 2014. PMID: 24554057
McCarthy, N.; Wetherill, L.; Lovely, C.B.; et al. Pdgfra protects against ethanol-induced craniofacial defects in a zebrafish model of FASD. Development 140(15): 3254–3265, 2013. PMID: 23861062
Medina, A.E. Therapeutic utility of phosphodiesterase type 1 inhibitors in neurological conditions. Frontiers in Neuroscience 5:21, 2011. PMID: 21373359
Moore, E.M.; Migliorini, R.; Infante, M.A.; and Riley, E.P. Fetal alcohol spectrum disorders: Recent neuroimaging findings. Current Developmental Disorders Reports 1(3):161–172, 2014 . PMID: 25346882
Nyaradi, A.; Li, J.; Hickling, S.; et al. The role of nutrition in children’s neurocognitive development, from pregnancy through childhood. Frontiers in Human Neuroscience 7:97, 2013. PMID: 23532379
O’Leary-Moore, S.K.; Parnell, S.E.; Godin, E.A.; et al. Magnetic resonance microscopy-based analyses of the brains of normal and ethanol-exposed fetal mice. Birth Defects Research. Part A, Clinical and Molecular Teratology 88(11):953–964, 2010. PMID: 20842647
O’Leary-Moore, S.K.; Parnell, S.E.; Lipinski, R.J.; and Sulik, K.K. Magnetic resonance-based imaging in animal models of fetal alcohol spectrum disorder. Neuropsychology Review 21(2):167–185, 2011. PMID: 21445552
O’Malley, K.D., and Nanson, J. Clinical implications of a link between fetal alcohol spectrum disorder and attention-deficit hyperactivity disorder. Canadian Journal of Psychiatry 47(4):349–354, 2002. PMID: 12025433
Otero, N.K.; Thomas, J.D.; Saski, C.A.; et al. Choline supplementation and DNA methylation in the hippocampus and prefrontal cortex of rats exposed to alcohol during development. Alcoholism: Clinical and Experimental Research 36(10):1701 – 1709, 2012. PMID: 22509990
Paley, B., and O’Connor, M.J. Behavioral interventions for children and adolescents with fetal alcohol spectrum disorders. Alcohol Research & Health 34(1):64–75, 2011. https://pubs.niaaa.nih.gov/publications/arh341/64-75.htm
Parnell, S.E.; Holloway, H.T.; O’Leary-Moore, S.K.; et al. Magnetic resonance microscopy-based analyses of the neuroanatomical effects of gestational day 9 ethanol exposure in mice. Neurotoxicology and Teratology 39:77–83, 2013. PMID: 23911654
Parnell, S.E.; O’Leary-Moore, S.K.; Godin, E.A.; et al. Magnetic resonance microscopy defines ethanol-induced brain abnormalities in prenatal mice: Effects of acute insult on gestational day 8. Alcoholism: Clinical and Experimental Research 33(6):1001–1011, 2009. PMID: 19302087
Patten, A.R.; Brocardo, P.S.; and Christie, B.R. Omega-3 supplementation can restore glutathione levels and prevent oxidative damage caused by prenatal ethanol exposure. Journal of Nutritional Biochemistry 24(5):760–769, 2013 a . PMID: 22841392
Patten, A.R.; Sickmann, H.M.; Dyer, R.A.; et al. Omega-3 fatty acids can reverse the long-term deficits in hippocampal synaptic plasticity caused by prenatal ethanol exposure. Neuroscience Letters 551:7–11, 2013 b . PMID: 23872044
Riley, E.P.; Infante, M.A.; and Warren, K.R. Fetal alcohol spectrum disorders: An overview. Neuropsychology Review 21(2):73–80, 2011. PMID: 21499711
Rufer, E.S.; Tran, T.D.; Attridge, M.M.; et al. Adequacy of maternal iron status protects against behavioral, neuroanatomical, and growth deficits in fetal alcohol spectrum disorders. PLoS One 7(10):e47499, 2012. PMID: 23094056
Ryan, S.H.; Williams, J.K.; and Thomas, J.D. Choline supplementation attenuates learning deficits associated with neonatal alcohol exposure in the rat: Effects of varying the timing of choline administration. Brain Research 1237:91–100, 2008. PMID: 18786517
Schneider, M.L.; Moore, C.F.; and Adkins, M.M. The effects of prenatal alcohol exposure on behavior: Rodent and primate studies. Neuropsychology Review 21(2):186–203, 2011. PMID: 21499982
Streissguth, A.P.; Bookstein, F.L.; Barr, H.M., et al. Risk factors for adverse life outcomes in fetal alcohol syndrome and fetal alcohol effects. Journal of Developmental and Behavioral Pediatrics 25(4):228–238, 2004. PMID: 15308923
Suttie, M.; Foroud, T.; Wetherill, L.; et al. Facial dysmorphism across the fetal alcohol spectrum. Pediatrics 131(3):e779–e788, 2013. PMID: 23439907
Swartz, M.E.; Wells, M.B.; Griffin, M.; et al. A screen of zebrafish mutants identifies ethanol-sensitive genetic loci. Alcoholism: Clinical and Experimental Research 38(3):694–703, 2014. PMID: 24164477
Thomas, J.D.; Sather, T.M.; and Whinery, L.A. Voluntary exercise influences behavioral development in rats exposed to alcohol during the neonatal brain growth spurt. Behavioral Neuroscience 122(6):1264–1273, 2008. PMID: 19045946
Ungerer, M.; Knezovich, J.; and Ramsay, M. In utero alcohol exposure, epigenetic changes, and their consequences. Alcohol Research: Current Reviews 35(1):37–46, 2013. PMID: 24313163
Voss, M.W.; Vivar, C.; Kramer, A.F.; and van Praag, H. Bridging animal and human models of exercise-induced brain plasticity. Trends in Cognitive Sciences 17(10):525–544, 2013. PMID: 24029446
Warren, K.R.; Hewitt, B.G.; and Thomas, J.D. Fetal alcohol spectrum disorders: Research challenges and opportunities. Alcohol Research & Health 34(1):4–14, 2011. https://pubs.niaaa.nih.gov/publications/arh341/4-14.htm
Weiland, M.; Gao, X-H.; Zhou, L.; and Mi, Q-S. Small RNAs have a large impact: Circulating microRNAs as biomarkers for human diseases. RNA Biology 9(6):850–859, 2012. PMID: 22699556
Werts, R.L.; Van Calcar, S.C.; Wargowski, D.S.; and Smith, S.M. Inappropriate feeding behaviors and dietary intakes in children with fetal alcohol spectrum disorder or probable prenatal alcohol exposure. Alcoholism: Clinical and Experimental Research 38(3):871–878, 2014. PMID: 24164456
Wilson, S. E., and Cudd, T. A. Focus on: The use of animal models for the study of fetal alcohol spectrum disorders. Alcohol Research & Health 34(1):92–98, 2011. PMID: 23580046
Wozniak, J.R.; Fuglestad, A.J.; Eckerle, J.K.; et al. Choline supplementation in children with fetal alcohol spectrum disorders has high feasibility and tolerability. Nutrition Research 33(11):897 – 904, 2013. PMID: 24176229
Yau, S.Y.; Gil-Mohapel, J.; Christie, B.R.; and So, K.F. Physical exercise-induced adult neurogenesis: A good strategy to prevent cognitive decline in neurodegenerative diseases? BioMed Research International 2014: 403120, 2014. PMID: 24818140
- Business News
- Michigan News
- National News
- International News
- Real Estate
- Local Sports
- Michigan Sports
- National Sports
- Local columns
- Letters to the Editor
- Engagements
- Special Sections
- Classifieds
- Garage Sales
- Statement of Values
- Terms of Service
- Submit News
- Browse Notices
- Place a Notice

- Today's Paper
Subscribe Today
Drinking alcohol before conceiving a child could accelerate their aging.
Editor’s note: The Conversation is an independent and nonprofit source of news, analysis and commentary from academic experts. Today’s piece is by Michael Golding, Texas A&M University.
(THE CONVERSATION) — The conditions within a person’s home, family and community affect their ability to stay healthy. Scientists studying these social determinants of health are trying to understand whether nature or nurture has a stronger effect on a person’s ability to fight disease.
I am a developmental physiologist studying the ways that drinking affects fetal development and lifelong health. Although researchers have long recognized that a father’s alcohol abuse negatively affects his children’s mental health and social development, it hasn’t been clear if paternal drinking has any lasting biological effects on his offspring’s physical health.
My lab’s recently published research shows that chronic alcohol use from both parents has an enduring effect on the next generation by causing their offspring to age faster and become more susceptible to disease.
Fetal alcohol spectrum disorders
According to the National Institutes of Health, nearly 11% of adults in the U.S. have an alcohol use disorder. Heavy drinking causes multiple health issues, including liver disease, heart problems, declining cognitive function and accelerated aging.
Parents may pass these health problems on to their children. Fetal alcohol spectrum disorders refer to a wide range of alcohol-related physical, developmental and behavioral deficits that affect as many as 1 in 20 U.S. schoolchildren.
Children with fetal alcohol spectrum disorders experience an early onset of adult diseases, including type 2 diabetes and heart disease. Cardiovascular disease first appears during adolescence for people with these disorders, while the rest of the population is affected typically in their 40s and 50s. Children with fetal alcohol spectrum disorders are also more likely to be hospitalized and have lifespans that are 40% shorter than children without these conditions.
However, it has been unclear whether these health problems are because of life circumstances – people with fetal alcohol spectrum disorders have high rates of psychiatric disorders, which cause stress that makes them more susceptible to aging and disease – or if their parents’ substance use directly causes lasting negative effects to their health. In other words, can a parent’s alcohol abuse before conception directly influence their offspring’s physical health and lifespan?
Mom and dad drinking
In our study, my colleagues and I used a mouse model to measure the effects that alcohol use by mom, dad or both parents around the time of conception have on their offspring aging and chronic disease. The mice chose when and how much alcohol to drink.
We found that paternal and maternal drinking both cause harmful changes to their offspring’s mitochondria. Mitochondria – often called the battery of the cell – control many aspects of aging and health. Like a cellphone battery, mitochondria deteriorate over time and cause cells to lose their ability to repair damage and control metabolism.
Our experiments in mice show that dad’s drinking causes a defect in mitochondrial function that first emerges during fetal development and persists into adult life, causing the offspring to age faster. For example, paternal alcohol exposure caused a twofold increase in age-related liver disease, suggesting that parental alcohol use – particularly by the father – could have significant implications on aging and age-related diseases.
Importantly, we found that when both parents drank, the effects on their offspring were worse than when only one parent consumed alcohol. For example, we observed a threefold increase in age-related liver scarring when both parents consumed alcohol.
Treating fetal alcohol syndrome
People with fetal alcohol syndrome face lifelong challenges, including problems with hand-eye coordination and difficulties with memory and attention.
Early educational interventions for children with fetal alcohol spectrum disorders, like using visual and auditory materials instead of print, can provide additional structure to help facilitate learning.
Although my team and I examined chronic alcohol exposure, we do not know if moderate alcohol use also causes mitochondrial problems. We also don’t know if these same effects emerge in people who haven’t been diagnosed with fetal alcohol spectrum disorders but whose parents drank heavily. Whether paternal drinking influences human embryonic development is still unclear, although emerging studies are beginning to suggest it does.
The next step is to explore if interventions that focus on mitochondrial health, such as exercise and specific diets, can improve health outcomes for people with fetal alcohol spectrum disorders.
— — —
This article is republished from The Conversation under a Creative Commons license. Read the original article here: https://theconversation.com/drinking-alcohol-before-conceiving-a-child-could-accelerate-their-aging-new-research-in-mice-235762.
Today's breaking news and more in your inbox
- Daily Newsletter
- Breaking News
Gifted furniture sparks family wedding fallout
Dear Annie: This is a long story, but I will try to keep it short. I gave my mother a couch and chair as she was in ...
Autumn’s adventures
Autumn is quietly making its presence known, with cool nights, complemented by warm, somewhat-sunny days and ...

Retirement can mean feeling unmoored and irrelevant
Editor’s note: The Conversation is an independent and nonprofit source of news, analysis and commentary from ...
Animal shelters burst at the seams
Dear Heloise: I’m a volunteer at a local shelter for animals. We are bursting at the seams with cats, dogs, ...

Holy Name students mark start of school year
Starting at $2.99/week..
- Open access
- Published: 05 September 2024
Correction: Analysis of alcohol-metabolizing enzymes genetic variants and RAR/RXR expression in patients diagnosed with fetal alcohol syndrome: a case-control study
- Melina Vieiros 1 , 2 , 3 na1 ,
- Elisabet Navarro-Tapia 2 , 4 na1 ,
- Anna Ramos-Triguero 1 ,
- Àgueda García-Meseguer 1 ,
- Leopoldo Martínez 2 , 5 ,
- Óscar García-Algar 1 , 6 na2 &
- Vicente Andreu-Fernández 1 , 7 na2
BMC Genomics volume 25 , Article number: 835 ( 2024 ) Cite this article
Metrics details
The Original Article was published on 17 June 2024
Correction: BMC Genomics 25, 610 (2024)
https://doi.org/10.1186/s12864-024-10516-7
Following publication of the original article it was reported that Melina Vieiros was missing the following affiliation: Department de Cirurgia i Especialitats Mèdico-Quirúrgiques, Universitat de Barcelona, Barcelona, Spain.
The updated authorship information is available in this Correction article and the original article has been updated.
Author information
Melina Vieiros and Elisabet Navarro-Tapia contributed equally to this work.
Óscar García-Algar and Vicente Andreu-Fernández shared the last position.
Authors and Affiliations
Grup de Recerca Infància i Entorn (GRIE), Institut d’investigacions Biomèdiques August Pi i Sunyer (IDIBAPS), Barcelona, Spain
Melina Vieiros, Anna Ramos-Triguero, Àgueda García-Meseguer, Óscar García-Algar & Vicente Andreu-Fernández
IdiPAZ - Instituto de Investigación Hospital Universitario La Paz, Madrid, Spain
Melina Vieiros, Elisabet Navarro-Tapia & Leopoldo Martínez
Department de Cirurgia i Especialitats Mèdico-Quirúrgiques, Universitat de Barcelona, Barcelona, Spain
Melina Vieiros
Faculty of Health Sciences, Valencian International University, Valencia, Spain
Elisabet Navarro-Tapia
Department of Pediatric Surgery, Hospital Universitario La Paz, Madrid, Spain
Leopoldo Martínez
Department of Neonatology, Hospital Clínic-Maternitat, ICGON, BCNatal, Barcelona, Spain
Óscar García-Algar
Biosanitary Research Institute, Valencian International University, Valencia, Spain
Vicente Andreu-Fernández
You can also search for this author in PubMed Google Scholar
Corresponding authors
Correspondence to Elisabet Navarro-Tapia or Vicente Andreu-Fernández .
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The online version of the original article can be found at https://doi.org/10.1186/s12864-024-10516-7 .
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Vieiros, M., Navarro-Tapia, E., Ramos-Triguero, A. et al. Correction: Analysis of alcohol-metabolizing enzymes genetic variants and RAR/RXR expression in patients diagnosed with fetal alcohol syndrome: a case-control study. BMC Genomics 25 , 835 (2024). https://doi.org/10.1186/s12864-024-10766-5
Download citation
Published : 05 September 2024
DOI : https://doi.org/10.1186/s12864-024-10766-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
BMC Genomics
ISSN: 1471-2164
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Alcohol Res Health
- v.33(1-2); 2010

Fetal Alcohol Spectrum Disorders
Forty years ago, alcohol was not commonly recognized as a teratogen, an agent that can disrupt the development of a fetus. Today, we understand that prenatal alcohol exposure induces a variety of adverse effects on physical, neurological, and behavioral development. Research supported by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) has contributed to the identification of the range and prevalence of fetal alcohol spectrum disorders (FASD), as well as methods for prevention and treatment of FASD. The worldwide prevalence and high personal and societal costs of FASD speak to the importance of this research. This article briefly examines some of the ways that NIAAA has contributed to our understanding of FASD, the challenges that we still face, and how this research is translated into changes in public policy.
Despite centuries of alcohol use, the first two clinical reports of fetal alcohol syndrome (FAS) in English literature did not appear until 1973, published in the journal Lancet by a group of investigators from the University of Washington, Seattle. The first paper ( Jones et al. 1973 ) described the common dysmorphic and developmental problems in eight children of alcoholic women. The second paper ( Jones and Smith 1973 ) characterized an additional three children and introduced the term “fetal alcohol syndrome” to describe the common pattern of observed deficits.
Within 2 years following these publications, the National Institute on Alcohol Abuse and Alcoholism (NIAAA) initiated its first research projects on FAS. The goals of that early research were to confirm alcohol’s ability to disrupt the development of a fetus (i.e., its teratogenicity) and, if confirmed, to further characterize the syndrome. Among the first grants awarded was one to Dr. Ann Streissguth, a coauthor on the first Lancet paper, to begin an investigation of the effects of alcohol across the full spectrum of dose levels on neurodevelopmental outcomes. Subsequently known as the Seattle 500 Study, based on the number of children recruited, this initial project has been an active research program for more than 30 years. Two other epidemiologic studies also were awarded to examine the relationship between alcohol and fetal outcome: one of these was awarded to Dr. Jan Kuzma, an epidemiologist at Loma Linda University, and the other to Dr. Joel Alpert at the Boston University School of Medicine. One of the coleaders of the Boston University project was Dr. Henry Rosett, a psychiatrist and NIAAA Career Teacher who became an important and prominent leader in research and education on FAS.
Concurrent to these investigations, NIAAA initiated a number of research projects involving animal models. These animal models were critical for addressing the early skepticism that alcohol was a teratogenic agent. The argument was made that if alcohol causes birth defects, surely the medical field would have noted this long before, given the thousands of years of alcohol use. In addition, although the initial cases of FAS all were born to women who had significant alcohol use disorders (AUDs), it was not clear if FAS was the direct result of alcohol on the embryo and fetus or it was caused by some other drug, malnutrition, or even “a deviant lifestyle.” The animal studies enabled scientists to control many of these other variables and thereby truly assess whether FAS was indeed the result of alcohol or some other factor. The initial animal models studied rats, mice, and dogs, among other species, and effects of alcohol were similar to those observed in the offspring of women with AUDs ( Abel and Dintcheff 1978 ; Chernoff 1977 ; Ellis and Pick 1980 ; Randall and Taylor 1979 ; Randall et al. 1977 ; Riley et al. 1979 ). Thus, animal studies were critical for the recognition of alcohol as a teratogen.
In February 1977, NIAAA organized the first workshop on FAS. Researchers from epidemiological, clinical, and basic science fields (about 50 in attendance) brought their findings to the forum. Although the intent was primarily to help guide future research directions, the attendees at the meeting were so impressed with the findings that they collectively expressed a need to inform the public that alcohol could be damaging to the developing fetus, potentially resulting in FAS.
NIAAA took responsibility for gaining approval from the Department of Health Education and Welfare (DHEW) for issuing an advisory on alcohol use in pregnancy. After documenting the available evidence in a state-of-the-science report, the Department approved an advisory issuance. It was released on June 1, 1977, in the Food and Drug Administration’s (FDA’s) Drug Bulletin and the Centers for Disease Control and Prevention’s (CDC’s) Morbidity and Mortality Weekly Report , as well as through a press conference at DHEW headquarters. The FDA and CDC bulletins were selected as the appropriate dissemination vehicles because their audiences were physicians and other health care professionals—the primary targets sought at that time. The advisory warned against heavy drinking in pregnancy and recommended a somewhat refrained two-drink-per-day drinking limit.
Following the publication of the advisory in the FDA Drug Bulletin , the Commissioner of the FDA wrote to the Director of the then Bureau of Alcohol Tobacco and Firearms in the Department of the Treasury on the need for warning labels on alcohol-containing beverages to inform drinkers of the potential harm caused by alcohol’s use in pregnancy. The letter, which also was publicly distributed, led to initiation of Senate hearings on FAS and potential beverage alcohol warning labels. Two sets of Senate hearings were held in successive years. The outcome was a legislatively passed requirement for a joint report to be submitted by both the Department of Human Health Services (DHHS; replacing DHEW) and the Department of the Treasury, addressing the health hazards of alcohol, with particular reference to pregnancy and recommendations on what could and should be done to address the problems. In 1980, the joint DHHS and Treasury Report (1980) was sent to Congress. The Report did not immediately call for alcohol beverage labeling but rather requested the Surgeon General to issue a (new) health advisory on FAS. Released in May 1981, the Surgeon General’s advisory went further than the original NIAAA/DHEW 1977 advisory and recommended that both pregnant women and those seeking to become pregnant avoid all alcohol. In 1988, the issue of alcoholic beverage labeling emerged again in Congress. This time, Congress passed legislation requiring all alcohol-containing beverages to carry a warning label. That label addressed both alcohol and pregnancy and other risks associated with alcohol use. The language of the warning label, as well as the size, color, and placement have not been changed since 1989.
Also of note, NIAAA took a lead in developing information on the dangers of alcohol use during pregnancy and disseminated those findings through public information campaigns in both print brochures and radio and television public service announcements, as early as 1978. Thus, NIAAA has been instrumental in affecting public policy and informing the public of the adverse effects of prenatal alcohol exposure. Moreover, over the last 35 years of NIAAA-supported research, our understanding of alcohol’s teratogenic effects has grown substantially, and many questions have been answered in whole or in part. The number of researchers in the field has grown, with more than 400 members of the Fetal Alcohol Spectrum Disorders Study Group and 106 studies currently funded by NIAAA, as important questions surrounding prenatal alcohol exposure continue to be addressed.
The Consequences of Prenatal Alcohol Exposure
FAS is characterized by three diagnostic criteria: a distinct pattern of facial dysmorphology (see figure 1 ), pre- and postnatal growth deficiencies, and central nervous system dysfunction. However, it was readily apparent to all involved in the early days of alcohol and pregnancy research that prenatal alcohol exposure could produce a range of effects that fell short of meeting all of the diagnostic criteria for full-blown FAS. Over the years, a number of terms have been used to describe these alcohol-attributed effects, including partial FAS, fetal alcohol effects, alcohol-related birth defects, and alcohol-related neurodevelopmental disorders, with the Institute of Medicine providing some standardization in their 1996 report ( Stratton et al. 1996 ). Subsequently, a general acceptance emerged that the adverse outcomes fall across a spectrum, and an umbrella term was introduced for this full spectrum: fetal alcohol spectrum disorders (FASD) ( Streissguth and O’Malley 2000 ).

Facial features of FAS.
NIAAA-supported investigations were vital for identifying many of the adverse outcomes of prenatal alcohol exposure, from neurodevelopmental and physical effects to end points such as a heightened risk of miscarriage and stillbirth. Although early research focused only on those individuals most affected by prenatal alcohol exposure, recent research is examining the range of FASD using novel technologies to advance our understanding. For example, early studies of prenatal alcohol-induced neuropathology were derived from postmortem tissue, which showed that prenatal alcohol leads to microencephaly (small brain), as well as neuroglial heterotopias (nerve cells that have migrated to the wrong location) and disrupted development of the corpus callosum and cerebellum ( Clarren et al. 1978 ). However, these reports were derived from cases at the severe end of the FASD continuum.
In the early 1990s, NIAAA funded seminal research by Dr. Edward Riley and colleagues, which used noninvasive imaging to show that multiple areas of the central nervous system are adversely affected by prenatal alcohol exposure. Structural imaging studies confirmed reductions in the volume of overall brain size, with disproportionate reductions in basal ganglia and the anterior vermis of the cerebellum ( Mattson et al. 1992 ). Additional studies have shown alterations in brain shape, changes in cortical thickness, reduced size, and altered shape of the corpus callosum, as well as alterations in the hippocampus (see Norman et al. 2009 ).
Since those early studies, a variety of imaging techniques have been used, including diffusion tensor imaging, magnetic resonance spectroscopy, functional magnetic resonance imaging, positron emission tomography, and single-photon emission computed tomography (for a review, see Norman et al. 2009 ). These studies show that prenatal alcohol exposure disrupts development of both gray and white matter (see figure 2 ) and further illustrate alcohol-related alterations in cerebral blood flow, neurotransmitters, and neuronal activity, even when there are no obvious structural changes. Importantly, it was discovered that individuals exposed to alcohol prenatally could suffer from brain anomalies and dysfunction without exhibiting distinct facial dysmorphology, a finding with significant implications for the identification of children with FASD. More recently, prenatal and neonatal ultrasound are being used to help identify brain anomalies early in development, which may be key for early intervention. NIAAA also is now supporting similar brain-imaging techniques with animal models, in which alcohol exposure parameters can be controlled ( Parnell et al. 2009 ) (see figure 3 ).

Magnetic Resonance Imaging (MRI) scans of four children: (A) shows a typically developing 10-year-old boy who has not been exposed to alcohol (B) features an 11-year-old boy with partial fetal alcohol syndrome (pFAS) (C) shows a 7-year-old girl with FAS, and (D) shows a 14-year-old boy with FAS. Notice the variability in brain structures among the individuals with fetal alcohol syndrome disorders, including alcohol-related changes in areas such as the corpus callosum (red arrow) and cerebellum (yellow arrow).
SOURCE: Sowell, E.; Nunez, S.; Roussotte, F. Structural and functional brain abnormalities in fetal alcohol spectrum disorders, Alcohol Research & Health, in press.

3D reconstruction of the faces and brains of mice at 17 days of gestation. Control mice are shown in a and c, mice exposed to alcohol are shown in b and d. Mouse fetuses in b and d illustrate dysmorphology resulting from exposure to alcohol at 7 days of gestation. Compared to the control (a), the ethanol-exposed fetus (b) has a smaller head size, a small nose, and an elongated/abnormal philtral portion of the upper lip. These facial features are characteristic of fetal alcohol syndrome. The brain of the ethanol-exposed animal also is dysmorphic (d); the olfactory bulbs are absent and the cerebral hemispheres are united rostrally (open arrow). Color codes: red=cerebral cortex, pink=olfactory bulbs, magenta=mesencephalon, light green=diencephalon, dark green=pons and medulla, teal=cerebellum.
SOURCE: O’Leary-Moore, S.K.; Parnell, S.E.; Godin, E.A.; and Sulik, K.K. Magnetic resonance-based studies of FASD in animal models, Alcohol Research & Health , in press. Modified from Godin, E.A.; O’Leary-Moore, S.K.; Khan, A.A.; et al. Magnetic resonance microscopy defines ethanol-induced brain abnormalities in prenatal mice: effects of acute insult on gestational day 7. Alcoholism: Clinical and Experimental Research 34(1):98–111, 2010. PMID: 19860813
The neuropathology associated with FASD leads to a range of behavioral effects. Early studies demonstrated general impairments in intelligence (although there is quite a range of IQ scores among individuals exposed to alcohol prenatally), impaired reflex development, deficits in motor coordination, and hyperactivity. More recent studies suggest that deficits in attention, learning and memory, emotional dysregulation, and executive functioning are core deficits, likely reflecting the dysfunction of the frontal lobe (for reviews, see Kodituwakku 2007 ; Riley and McGee 2005 ). These behavioral domains also are disrupted with animal models of FASD ( Driscoll et al. 1990 ). Moreover, prenatal alcohol-induced alterations in cognitive functioning and stress responses may contribute to secondary disabilities, including psychiatric comorbidities and vulnerability to addiction. One of the challenges is to determine if there is a pattern of neuropathology and behavioral expression that is unique to prenatal alcohol exposure and therefore useful for diagnosis, as described below.
Prenatal alcohol also leads to physical and physiological changes that are not part of an FAS diagnosis, including alterations in skeletal and organ formation as well as immune function (see Zhang et al. 2005 ). Prenatal alcohol exposure also may contribute to other disorders. For example, it may disrupt the development of brain structures that contribute to sudden infant death syndrome. NIAAA is addressing this issue jointly with the National Institute on Child Health and Human Development via a consortium. When considering that 40 years ago it was not commonly recognized that alcohol was a teratogen, remarkable strides have been made in understanding the range of ethanol’s adverse effects on the developing embryo and fetus.
Problems in Identifying Individuals Exposed to Alcohol Prenatally
The identification of individuals who have been exposed to alcohol prenatally can be challenging. Accurate maternal drinking histories may not be available and even if the child exhibits the defining features of FAS, they may be missed if the child is not diagnosed by a trained dysmorphologist. It is even more challenging to identify individuals who have been exposed to alcohol prenatally but who do not meet the diagnostic criteria for FAS (i.e., do not exhibit all of the defining facial features). Thus, there is a need for tools to enhance diagnoses, particularly because diagnoses often are necessary for the individual to receive appropriate services. The possibility that more subtle dysmorphic features could aid in a diagnosis of FAS or partial FAS in the absence of information on alcohol exposure in pregnancy (after eliminating genetic disorders otherwise appearing as phenocopies) currently is being investigated by an international consortium funded by NIAAA. Three-dimensional camera imaging is being explored as a means for identifying facial features that represent the full spectrum of FASD. Such images could serve as a tool for sites that do not have access to a trained dysmorphologist and to detect individuals with partial FAS. Moreover, evaluation of the relationship between the dysmorphic facial features, the neuroanatomic brain features, and the neurodevelopmental alterations may not only elucidate the common embryological processes that are disrupted but also can be used to determine if a pattern of injury exists that can serve as a unique signature of prenatal alcohol exposure.
Identification of FASD also can be improved by better detection of women who are drinking alcohol during pregnancy. Clinical research has shown that it is possible in many situations, both prospectively and retrospectively, to obtain good clinical histories on alcohol exposure during pregnancy ( Chiodo et al. 2009 ; Hannigan et al. 2009 ; Sokol et al. 1989 ). Screening for such alcohol exposure information has been aided by a number of brief questionnaires that have been developed over the years, such as the T-ACE ( Chiodo et al. 2010 ; Sokol et al. 1989 ), TWEAK ( Russell et al. 1994 , 1996 ), the 10-question AUDIT ( Bohn et al. 1995 ), and the more direct and convenient 3-question AUDIT-C ( Dawson et al. 2005 ), among several others ( Chasnoff et al. 2007 ; Chiodo et al. 2009 ). Nonetheless, there are occasions during which the attainment of reliable alcohol exposure information is not possible, for example, when maternal memory is poor, drinking is denied, or biological parents are not available.
Therefore, the identification of biomarkers that can reliably reflect fetal alcohol exposure and/or injury is of high priority, especially because such markers may be useful for early case recognition and thereby early intervention. Although metabolites of tobacco or other drugs often are used as biomarkers of their respective use, the prime oxidative metabolites of alcohol are carbon dioxide and water, both of which are present in such abundance that they cannot serve as a marker of alcohol use. However, there also are less prominent nonoxidative routes by which alcohol is eliminated from the body. This includes the formation of esters with the body’s fatty acids to make fatty acid ethyl esters (FAEEs). The FAEEs, which can accumulate in hair, are a potential marker for prior alcohol use ( Kulaga et al. 2009 ). FAEEs also may be found in the meconium from newborns and can indicate exposure to alcohol in the last few weeks or months of pregnancy ( Bearer et al. 2003 ). Other nonoxidative metabolites of ethanol include ethyl glucuronide, which already has been used as a clinical marker to reflect alcohol exposure within the past 3 days, and phosphatidyl ethanol, a marker that may indicate alcohol use for up to 1 to 2 weeks ( Litten et al. 2010 ). Newer technologies in the fields of proteomics and metabolomics ( Harrigan et al. 2008 ; Hiller-Sturmhöfel et al. 2008 ), and even epigenetic alterations of histone proteins and DNA methylation eventually may provide meaningful indications of alcohol exposure via biological fluids from either maternal or infant sources. Markers that can reliably indicate level and timing of alcohol exposure would greatly improve the ability to identify individuals with FASD.
Defining the Problem
Although the Institute of Medicine (1996) estimates the prevalence of FAS in the United States to be between 0.5 and 2.0 cases per 1,000 live births, this is likely an underestimate. Determining the true prevalence has proven to be a major challenge because children with FASD often are diagnosed with other disorders (such as attention deficit hyperactivity disorder, oppositional defiant disorder, or conduct disorder), or the neurodevelopmental deficits are totally ignored and no educational or clinical diagnosis is given. Obtaining an accurate prevalence of FAS requires the use of an expensive epidemiologic technique called active case ascertainment ( May et al. 2009 ). When this method was applied in South Africa, it revealed an alarmingly high FAS prevalence of 65 to 74 per 1,000 live births ( Viljoen et al. 2005 ). An active case ascertainment study in Italy revealed an FAS prevalence of 3.7 to 7.4 per 1,000 live births ( May et al. 2006 ), a rate similar to a pilot active case ascertainment study in a small western city in the United States ( Clarren et al. 2001 ). Incidence of the full spectrum of FASD is much higher, estimated to affect 1 percent of live births in the United States ( Sampson et al. 1997 ), 2 to 4 percent in Italy ( May et al. 2006 ), and 7 to 9 percent in South Africa ( May et al. 2007 ). Through examination of FASD at various international sites, NIAAA is identifying not only the prevalence of FASD but also the environmental factors that may convey risk or protection against FASD.
The Risk Factors for FASD
Both clinical and preclinical studies have identified a number of risk factors for FASD, including dose, pattern, and timing of alcohol exposure (see Abel and Hannigan 1995 ; May et al. 2008 a ; West 1987 ). For example, using a mouse model, Sulik and colleagues (1981) demonstrated that facial dysmorphology is caused by alcohol exposure during early gestation (i.e., during gastrulation). Heavier drinking and binge drinking increase the likelihood of FASD. But is there a threshold for alcohol’s damaging effects? This is a difficult question and, to date, safe amounts of alcohol during pregnancy have not been established. Moreover, because so many factors influence alcohol’s adverse effects, including polydrug use, prenatal care, nutrition, and genetic factors, it is difficult to predict outcome on an individual basis. In general, low socioeconomic status and education, increased maternal age and number of pregnancies (i.e., gravidity), and poor nutrition are associated with more severe outcomes following prenatal alcohol exposure. One approach to better understanding the relationship between maternal and alcohol exposure factors to fetal outcome is through prospective studies. NIAAA currently is funding several prospective studies to address risk factors in FASD. Understanding protective and provocative factors will allow prevention efforts to be targeted at high-risk populations.
Preventing High-Risk Drinking During Pregnancy
The most desirable route for prevention involves eliminating or significantly reducing alcohol consumption by women during pregnancy. In 1996, the Institute of Medicine report proposed a three-level model for prevention involving components targeted to the general population (universal prevention), to high-risk communities (targeted prevention), and to the specific individuals at greatest risk, which would include women who already have given birth to a child with an FASD or women who meet diagnostic criteria for alcohol dependence (indicated prevention) ( Stratton et al. 1996 ). Whereas universal prevention efforts have failed to provide meaningful success in FASD prevention, targeted and indicated prevention efforts have met with significant success ( May et al. 2008 b ).
One aspect of FASD prevention involves the recognition of high-risk drinking in women in primary-care settings and prenatal clinics. Importantly, research shows that screening and brief interventions in these settings are highly effective in reducing and eliminating risky drinking. Unfortunately, even though such tools are readily available through NIAAA ( http://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/clinicians_guide.htm ), they are not routinely utilized, fostering the need to greatly expand such efforts ( Chang et al. 2000 , 2005 ).
FASD is completely preventable if women would no longer drink alcohol during pregnancy. Recognizing that this ideal goal often may not be met, other efforts are underway to explore the possibility of minimizing the damage caused by prenatal alcohol exposure (see sections below).
How Does Alcohol Disrupt Development?
Understanding the mechanisms by which alcohol disrupts development is important, both for the development of better prevention efforts and of novel interventions. Because alcohol exerts multiple actions on the developing embryo and fetus, it induces damage via many mechanisms ( Goodlett et al. 2005 ). For example, studies show that alcohol can disrupt every step in central nervous system development, from proliferation, migration, and differentiation, to synaptogenesis and myelination; in fact, alcohol can directly lead to apoptotic and necrotic cell death.
Neuropathology can be induced both by alcohol actions on neurons as well as by supportive glial cells. The mechanisms will depend on the dose and developmental timing of alcohol exposure and the characteristics of the various cell populations. Early research demonstrated that both alcohol and its metabolite acetaldehyde are directly teratogenic. Alcohol also can have secondary effects, including interference with placental function and nutrient absorption. More recent research supported by NIAAA demonstrates that alcohol disrupts development via some specific actions, including oxidative stress and mitochondrial dysfunction, inhibition of cell adhesion molecules, reduction of neurotrophic factors, and effects on neurotransmitter systems such as glutamate and γ-aminobutyric acid systems. These mechanisms of action have led to the development of a variety of experimental therapeutics, as described below.
Developmental alcohol exposure also alters gene expression. For example, alcohol may affect a number of early gestational genes, including Pax 6 , Otx 6 , Sox 3 , NCAM , TBX 5 , and Vax 2 ( Peng et al. 2004 ). Recently, NIAAA, recognizing the importance of epigenetic aspects in alcohol’s actions, has marked this as a key area of research in the Institute’s strategic plan. Epigenetic factors refer to factors that regulate gene expression (through DNA methylation, histone modification, or via micro RNAs) without altering the actual DNA. Recent studies indicate that developmental alcohol may lead to epigenetic changes (for reviews, see Ramsay 2010 ; Haycock 2009 ). Such findings may help to explain the results of early studies (Stockard 1913) showing the teratogenic effects of alcohol exposure before conception and on male gametes. Epigenetic effects may contribute to long-lasting changes in physical and behavioral development, including changes in the stress and immune systems that can impact a range of cognitive and emotional effects in offspring.
Intervening With and Treating Individuals With FASD
Despite prevention efforts, many women continue to drink alcohol during pregnancy. Moreover, many countries have yet to acknowledge that FASD occurs in their populations, so policies to reduce alcohol are not in place. Thus, it is vital to identify ways of reducing the severity of effects in children with FASD.
NIAAA began funding studies to examine how nutritional and environmental factors might reduce the severity of FASD within 10 years of the recognition of FAS. To date, NIAAA has funded numerous preclinical and clinical studies that examine methods for protecting against alcohol-related damage at the time of the insult, as well as treatments that may effectively reduce the severity of FASD among individuals who have been exposed to alcohol prenatally.
For example, as noted above, alcohol may lead to oxidative stress. Numerous animal studies have shown that various agents with antioxidant properties, including vitamins C and E, or even the activation of endogenous antioxidants can reduce the adverse physical, neuropathological, and behavioral effects of alcohol. Protection against the physical effects of alcohol exposure also has been observed with administration of a variety of neurotrophic factors, including BDNF, IGF-I, NGF, and neuropeptides derived from activity-dependent neurotrophic factor (ADNF) and activity-dependent neurotrophic peptide (ADNP), as well as their small peptide active fragments SAL and NAP, to name a few. In fact, NAP and SAL, which now are being investigated as a treatment for other disorders such as Alzheimer’s disease, can protect against physical and neuropathological effects of alcohol (i.e., Chen et al. 2005 ). Serotonin agonists also can protect against alcohol-related developmental damage, as serotonin serves not only as a neurotransmitter but also as a neurotrophic factor (i.e., Druse et al. 2006 ). Similarly, drugs that block the over activity of N -methyl- d -aspartic acid receptors, which may contribute to brain damage during alcohol withdrawal, also can reduce neuropathology and behavioral deficits (i.e., Thomas et al. 2001 ). Finally, agents that antagonize alcohol’s blockade of cell adhesion sites are being further refined ( Arevalo et al. 2008 ; Chen et al. 2001 ).
As noted above, another key risk factor for FASD is poor nutrition. Animal studies have shown that some nutrients may attenuate alcohol’s teratogenic effects, including choline, folate, zinc, and nicotinamide, although not all studies have found beneficial effects. This leads to the intriguing question of whether nutritional supplements can reduce FASD in clinical populations. NIAAA currently is funding the first study to examine the effectiveness of micronutrient supplementation among women who have been drinking alcohol during pregnancy.
In the meantime, what can be done after the child is born and already has sustained the alcohol-induced injury? Early reports suggested that the IQs of individuals exposed to alcohol prenatally were stable and little could be done to improve the cognitive and behavioral abilities of those with FASD. More recently, however, it has been recognized that the brain’s ability to recover (i.e., its plasticity) from early alcohol exposure is much greater than previously thought and, although some studies suggest that prenatal alcohol may limit lifespan neuroplasticity, interventions may indeed improve behavioral function and quality of life.
Animal model studies indicate that various pharmacological, nutritional, and behavioral interventions can improve outcome. For example, drugs like cognitive enhancers ( Medina et al. 2006 ) may enhance plasticity and recovery of function. Nutritional factors, such as choline, also have been shown to effectively improve cognitive functioning, even when administered weeks after developmental alcohol exposure. Choline supplementation can reduce the severity of deficits on a variety of cognitive tasks (i.e. Thomas et al. 2007 ). Finally, environmental or behavioral interventions, such as communal rearing, environmental enrichment, motor acrobatic training, and exercise also can improve cognitive and motor function ( Hannigan et al. 2007 ; Klintsova et al. 2000 ; Thomas et al. 2008 ). These studies suggest that if individuals with FASD are given the appropriate experience, whether social, cognitive, or motor in nature, their performance can improve (see Kelly et al. 2009 ).
Consistent with preclinical findings, clinical studies show that stable home environments are associated with a better outcome than unstable, stressful environments ( Streissguth et al. 1996 ). Moreover, based on NIAAA-funded studies showing that environmental factors could influence outcome, an increasing number of studies are demonstrating that educational interventions can reduce the severity of FASD. Such interventions can effectively assist families in creating a stable environment, and train individuals with FASD on targeted skills, such as mathematical abilities, social skills, metacognition, and literacy.
These promising studies indicate that multiple approaches may improve the quality of life of people with FASD. NIAAA continues to support research to identify the most effective neurodevelopmental and educational interventions for FASD.
Forty years ago, alcohol was not commonly recognized as a teratogen. Today, not only has public policy changed, but we also have a better understanding of the consequences of prenatal alcohol exposure and the prevalence and mechanisms of alcohol-related damage. Although we have developed diagnostic, prevention, and treatment strategies, challenges remain. Better identification and diagnosis of the full range of FASD are needed, which could be improved with the development of biomarkers that aid in detection and accurate quantification of prenatal alcohol consumption. Continued development of effective prevention and treatment strategies also is critical. Through support of epidemiological, clinical, and preclinical research; facilitation of scientific exchange through conferences; and by leading public policy, NIAAA will continue to play an important role in understanding the complexities of FASD.
F inancial D isclosure
The authors declare that they have no competing financial interests.
- Abel EL, Dintcheff BA. Effects of prenatal alcohol exposure on growth and development in rats. Journal of Pharmacology and Experimental Therapeutics. 1978; 207 (3):916–921. [ PubMed ] [ Google Scholar ]
- Abel EL, Hannigan JH. Maternal risk factors in fetal alcohol syndrome: Provocative and permissive influences. Neurotoxicology and Teratology. 1995; 17 (4):445–462. [ PubMed ] [ Google Scholar ]
- Arevalo E, Shanmugasundararaj S, Wilkemeyer MF, et al. An alcohol binding site on the neural cell adhesion molecule L1. Proceedings of the National Academy of Sciences of the United States of America. 2008; 105 (1):371–375. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bearer CF, Jacobson JL, Jacobson SW, et al. Validation of a new biomarker of fetal exposure to alcohol. Journal of Pediatrics. 2003; 143 (4):463–469. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bohn MJ, Babor TF, Kranzler HR. The Alcohol Use Disorders Identification Test (AUDIT): Validation of a screening instrument for use in medical settings. Journal of Studies on Alcohol. 1995; 56 (4):423–432. [ PubMed ] [ Google Scholar ]
- Chang G, Goetz MA, Wilkins-Haug L, Berman S. A brief intervention for prenatal alcohol use: An in-depth look. Journal of Substance Abuse Treatment. 2000; 18 (4):365–369. [ PubMed ] [ Google Scholar ]
- Chang G, McNamara TK, Orav EJ, et al. Brief intervention for prenatal alcohol use: A randomized trial. Obstetrics and Gynecology. 2005; 105 (5 Pt. 1):991–998. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Chasnoff IJ, Wells AM, McGourty RF, Bailey LK. Validation of the 4P’s Plus screen for substance use in pregnancy. Journal of Perinatology. 2007; 27 (12):744–748. [ PubMed ] [ Google Scholar ]
- Chen SY, Charness ME, Wilkemeyer MF, Sulik KK. Peptide-mediated protection from ethanol-induced neural tube defects. Developmental Neuroscience. 2005; 27 (1):13–19. [ PubMed ] [ Google Scholar ]
- Chen SY, Wilkemeyer MF, Sulik KK, Charness ME. Octanol antagonism of ethanol teratogenesis. FASEB Journal. 2001; 15 (9):1649–1651. [ PubMed ] [ Google Scholar ]
- Chernoff GF. The fetal alcohol syndrome in mice: An animal model. Teratology. 1977; 15 (3):223–229. [ PubMed ] [ Google Scholar ]
- Chiodo LM, Janisse J, Delaney-Black V, et al. A metric of maternal prenatal risk drinking predicts neurobehavioral outcomes in preschool children. Alcoholism: Clinical and Experimental Research. 2009; 33 (4):634–644. [ PubMed ] [ Google Scholar ]
- Chiodo LM, Sokol RJ, Delaney-Black V, et al. Validity of the T-ACE in pregnancy in predicting child outcome and risk drinking. Alcohol. 2010 [Epub ahead of print]. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Clarren SK, Alvord EC, Jr, Sumi SM, et al. Brain malformations related to prenatal exposure to ethanol. Journal of Pediatrics. 1978; 92 (1):64–67. [ PubMed ] [ Google Scholar ]
- Clarren SK, Randels SP, Sanderson M, Fineman RM. Screening for fetal alcohol syndrome in primary schools: A feasibility study. Teratology. 2001; 63 (1):3–10. [ PubMed ] [ Google Scholar ]
- Dawson DA, Grant BF, Stinson FS, Zhou Y. Effectiveness of the derived Alcohol Use Disorders Identification Test (AUDIT-C) in screening for alcohol use disorders and risk drinking in the US general population. Alcoholism: Clinical and Experimental Research. 2005; 29 (5):844–854. [ PubMed ] [ Google Scholar ]
- Driscoll CD, Streissguth AP, Riley EP. Prenatal alcohol exposure: Comparability of effects in humans and animal models. Neurotoxicology and Teratology. 1990; 12 (3):231–237. [ PubMed ] [ Google Scholar ]
- Druse MJ, Tajuddin NF, Gillespie RA, Le P. The effects of ethanol and the serotonin(1A) agonist ipsapirone on the expression of the serotonin(1A) receptor and several antiapoptotic proteins in fetal rhombencephalic neurons. Brain Research. 2006; 1092 (1):79–86. [ PubMed ] [ Google Scholar ]
- Ellis FW, Pick JR. An animal model of the fetal alcohol syndrome in beagles. Alcoholism: Clinical and Experimental Research. 1980; 4 (2):123–134. [ PubMed ] [ Google Scholar ]
- Goodlett CR, Horn KH, Zhou FC. Alcohol teratogenesis: Mechanisms of damage and strategies for intervention. Experimental Biology and Medicine (Maywood) 2005; 230 (6):394–406. [ PubMed ] [ Google Scholar ]
- Hannigan JH, O’Leary-Moore SK, Berman RF. Postnatal environmental or experiential amelioration of neurobehavioral effects of perinatal alcohol exposure in rats. Neuroscience and Biobehavioral Reviews. 2007; 31 (2):202–211. [ PubMed ] [ Google Scholar ]
- Hannigan JH, Chiodo LM, Sokol RJ, et al. A 14-year retrospective maternal report of alcohol consumption in pregnancy predicts pregnancy and teen outcomes. Alcohol. 2009. [Epub ahead of print]. [ PMC free article ] [ PubMed ]
- Harrigan GG, Maguire G, Boros L. Metabolomics in alcohol research and drug development. Alcohol Research & Health. 2008; 31 (1):26–35. [ PubMed ] [ Google Scholar ]
- Haycock PC. Fetal alcohol spectrum disorders: The epigenetic perspective. Biology of Reproduction. 2009; 81 (4):607–617. [ PubMed ] [ Google Scholar ]
- Hiller-Sturmhöfel S, Sobin J, Mayfield RD. Proteomic approaches for studying alcoholism and alcohol-induced organ damage. Alcohol Research & Health. 2008; 31 (1):36–48. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Jones KL, Smith DW. Recognition of the fetal alcohol syndrome in early infancy. Lancet. 1973; 302 (7836):999–1001. [ PubMed ] [ Google Scholar ]
- Jones KL, Smith DW, Ulleland CN, Streissguth AP. Pattern of malformation in offspring of chronic alcoholic mothers. Lancet. 1973; 1 (7815):1267–1271. [ PubMed ] [ Google Scholar ]
- Kelly SJ, Goodlett CR, Hannigan JH. Animal models of fetal alcohol spectrum disorders: Impact of the social environment. Developmental Disabilities Research Reviews. 2009; 15 (3):200–208. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Klintsova AY, Goodlett CR, Greenough WT. Therapeutic motor training ameliorates cerebellar effects of postnatal binge alcohol. Neurotoxicology and Teratology. 2000; 22 (1):125–132. [ PubMed ] [ Google Scholar ]
- Kodituwakku PW. Defining the behavioral phenotype in children with fetal alcohol spectrum disorders: A review. Neuroscience and Biobehavioral Reviews. 2007; 31 (2):192–201. [ PubMed ] [ Google Scholar ]
- Kulaga V, Pragst F, Fulga N, Koren G. Hair analysis of fatty acid ethyl esters in the detection of excessive drinking in the context of fetal alcohol spectrum disorders. Therapeutic Drug Monitoring. 2009; 31 (2):261–266. [ PubMed ] [ Google Scholar ]
- Litten RZ, Bradley AM, Moss HB. Alcohol biomarkers in applied settings: Recent advances and future research opportunities. Alcoholism: Clinical and Experimental Research. 2010 Apr 5; [Epub ahead of print] [ PubMed ] [ Google Scholar ]
- Mattson SN, Riley EP, Jernigan TL, et al. Fetal alcohol syndrome: A case report of neuropsychological, MRI and EEG assessment of two children. Alcoholism: Clinical and Experimental Research. 1992; 16 (5):1001–1003. [ PubMed ] [ Google Scholar ]
- May PA, Fiorentino D, Gossage JP, et al. Epidemiology of FASD in a province in Italy: Prevalence and characteristics of children in a random sample of schools. Alcoholism: Clinical and Experimental Research. 2006; 30 (9):1562–1575. [ PubMed ] [ Google Scholar ]
- May PA, Gossage JP, Kalberg WO, et al. Prevalence and epidemiologic characteristics of FASD from various research methods with an emphasis on recent in-school studies. Developmental Disabilities Research Reviews. 2009; 15 (3):176–192. [ PubMed ] [ Google Scholar ]
- May PA, Gossage JP, Marais AS, et al. The epidemiology of fetal alcohol syndrome and partial FAS in a South African community. Drug and Alcohol Dependence. 2007; 88 (2–3):259–271. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- May PA, Gossage JP, Marais AS, et al. Maternal risk factors for fetal alcohol syndrome and partial fetal alcohol syndrome in South Africa: A third study. Alcoholism: Clinical and Experimental Research. 2008a; 32 (5):738–753. [ PubMed ] [ Google Scholar ]
- May PA, Miller JH, Goodhart KA, et al. Enhanced case management to prevent fetal alcohol spectrum disorders in Northern Plains communities. Maternal and Child Health Journal. 12 (6):747–759. 2008b. [ PubMed ] [ Google Scholar ]
- Medina AE, Krahe TE, Ramoa AS. Restoration of neuronal plasticity by a phosphodiesterase type 1 inhibitor in a model of fetal alcohol exposure. Journal of Neuroscience. 2006; 26 (3):1057–1060. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Norman AL, Crocker N, Mattson SN, Riley EP. Neuroimaging and fetal alcohol spectrum disorders. Developmental Disabilities Research Reviews. 2009; 15 (3):209–217. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Parnell SE, O’Leary-Moore SK, Godin EA, et al. Magnetic resonance microscopy defines ethanol-induced brain abnormalities in prenatal mice: Effects of acute insult on gestational day 8. Alcoholism: Clinical and Experimental Research. 2009; 33 (6):1001–1011. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Peng Y, Yang PH, Ng SS, et al. A critical role of Pax6 in alcohol-induced fetal microcephaly. Neurobiology of Disease. 2004; 16 (2):370–376. [ PubMed ] [ Google Scholar ]
- Ramsay M. Genetic and epigenetic insights into fetal alcohol spectrum disorders. Genome Medicine. 2010; 2 (4):27. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Randall CL, Taylor J, Walker DW. Ethanol-induced malformations in mice. Alcoholism: Clinical and Experimental Research. 1977; 1 (3):219–224. [ PubMed ] [ Google Scholar ]
- Randall CL, Taylor WJ. Prenatal ethanol exposure in mice: Teratogenic effects. Teratology. 1979; 19 (3):305–311. [ PubMed ] [ Google Scholar ]
- Riley EP, Lochry EA, Shapiro NR, Baldwin J. Response perseveration in rats exposed to alcohol prenatally. Pharmacology, Biochemistry, and Behavior. 1979; 10 (2):255–259. [ PubMed ] [ Google Scholar ]
- Riley EP, McGee CL. Fetal alcohol spectrum disorders: An overview with emphasis on changes in brain and behavior. Experimental Biology and Medicine. 2005; 230 (6):357–365. [ PubMed ] [ Google Scholar ]
- Russell M, Martier SS, Sokol RJ, et al. Screening for pregnancy risk-drinking. Alcoholism: Clinical and Experimental Research. 1994; 18 (5):1156–1161. [ PubMed ] [ Google Scholar ]
- Russell M, Martier SS, Sokol RJ, et al. Detecting risk drinking during pregnancy: A comparison of four screening questionnaires. American Journal of Public Health. 1996; 86 (10):1435–1439. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sampson PD, Streissguth AP, Bookstein FL, et al. Incidence of fetal alcohol syndrome and prevalence of alcohol-related neurodevelopmental disorder. Teratology. 1997; 56 (5):317–326. [ PubMed ] [ Google Scholar ]
- Sokol RJ, Martier SS, Ager JW. The T-ACE questions: Practical prenatal detection of risk-drinking. American Journal of Obstetrics and Gynecology. 1989; 160 (4):863–868. discussion 868–870. [ PubMed ] [ Google Scholar ]
- Stratton KR, Howe CJ, Battaglia FC. Fetal Alcohol Syndrome: Diagnosis, Epidemiology, Prevention, and Treatment. Washington, DC: National Academy Press; 1996. [ Google Scholar ]
- Streissguth AP, Barr HM, Kogan J, Bookstein FL. Final Report to the Centers for Disease Control and Prevention (CDC) Seattle, Washington: University of Washington, Fetal Alcohol & Drug Unit; 1996. Understanding the occurrence of secondary disabilities in clients with fetal alcohol syndrome (FAS) and fetal alcohol effects (FAE) [ Google Scholar ]
- Streissguth AP, O’Malley K. Neuropsychiatric implications and long-term consequences of fetal alcohol spectrum disorders. Seminars in Clinical Neuropsychiatry. 2000; 5 (3):177–190. [ PubMed ] [ Google Scholar ]
- Sulik KK, Johnston MC, Webb MA. Fetal alcohol syndrome: Embryogenesis in a mouse model. Science. 1981; 214 (4523):936–938. [ PubMed ] [ Google Scholar ]
- Thomas JD, Biane JS, O’Bryan KA, et al. Choline supplementation following third-trimester-equivalent alcohol exposure attenuates behavioral alterations in rats. Behavioral Neuroscience. 2007; 121 (1):120–130. [ PubMed ] [ Google Scholar ]
- Thomas JD, Fleming SL, Riley EP. MK-801 can exacerbate or attenuate behavioral alterations associated with neonatal alcohol exposure in the rat, depending on the timing of administration. Alcoholism: Clinical and Experimental Research. 2001; 25 (5):764–773. [ PubMed ] [ Google Scholar ]
- Thomas JD, Sather TM, Whinery LA. Voluntary exercise influences behavioral development in rats exposed to alcohol during the neonatal brain growth spurt. Behavioral Neuroscience. 2008; 122 (6):1264–1273. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- US Department of the Treasury and U.S. Department of Health and Human Services . Report to the President and Congress on Health Hazards Associated With Alcohol and Method to Inform the General Public of these Hazards. Washington, DC: U.S. Government Printing Office; 1980. [ Google Scholar ]
- Viljoen DL, Gossage JP, Brooke L, et al. Fetal alcohol syndrome epidemiology in a South African community: A second study of a very high prevalence area. Journal of Studies on Alcohol. 2005; 66 (5):593–604. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- West JR. Fetal alcohol-induced brain damage and the problem of determining temporal vulnerability: A review. Alcohol and Drug Research. 1987; 7 (5–6):423–441. [ PubMed ] [ Google Scholar ]
- Zhang X, Sliwowska JH, Weinberg J. Prenatal alcohol exposure and fetal programming: Effects on neuroendocrine and immune function. Experimental Biology and Medicine. 2005; 230 (6):376–388. [ PubMed ] [ Google Scholar ]

IMAGES
VIDEO
COMMENTS
Tools. Prenatal exposure to alcohol can damage the developing fetus and is the leading preventable cause of birth defects and intellectual and neurodevelopmental disabilities. In 1973, fetal alcohol syndrome was first described as a specific cluster of birth defects resulting from alcohol exposure in utero. Subsequently, research unequivocally ...
Fetal alcohol syndrome (FAS) is a developmental and congenital disorder characterized by neurocognitive impairment, structural defects, and growth restriction due to prenatal alcohol exposure. ... This has always been cited in basic and clinical research articles that have identified alcohol-related malformations. In 2005, Hoyme et al. ...
Prenatal alcohol exposure can cause a number of physical, behavioral, cognitive, and neural impairments, collectively known as fetal alcohol spectrum disorders (FASD). This article examines basic research that has been or could be translated into practical applications for the diagnosis or treatment of FASD.
Fetal alcohol spectrum disorders (FASD) are the broad range of neurodevelopmental and physical effects that result from prenatal exposure to alcohol. People with FASD may have facial abnormalities and growth impairments, but the most profound effects are cognitive and behavioral deficits.
INTRODUCTION. Since the identification of alcohol as a teratogen in 1973 (Jones and Smith, 1973, Jones et al., 1973), an extensive amount of research focused on the long-term effects of prenatal alcohol exposure indicates that consuming alcoholic beverages during pregnancy can significantly affect fetal development.The physical and neurobehavioral effects of alcohol are collectively known as ...
Fetal alcohol spectrum disorders - Nature
Abstract. Purpose of review: The purpose of this review is to describe recent findings on the clinical presentation, pathogenesis, and management of fetal alcohol spectrum disorders (FASDs). Alcohol causes a range of physical, developmental, and cognitive impairments on the developing fetus. Individuals exposed to alcohol prenatally have a wide ...
Fetal Alcohol Spectrum Disorders
The lack of universally accepted diagnostic criteria and the high rate of psychiatric comorbidity make it difficult to diagnose Fetal Alcohol Spectrum Disorder (FASD). In an effort to improve the diagnosis of FASD, the current study aimed to identify a neurodevelopmental profile that is both sensitive and specific to FASD. A secondary analysis was conducted on data obtained from the Canadian ...
Review of published manuscripts on fetal alcohol exposure on several body systems. Method: Articles in this review were found online using databases such as Medline, Medline Complete, PubMed, and Health Source: Nursing/Academic Edition. The following terms were searched: fetal alcohol spectrum disorders, fetal alcohol syndrome, prenatal alcohol exposure, and alcohol related birth defects.
Fetal alcohol syndrome (FAS) and fetal alcohol spectrum disorders (FASD) result from intrauterine exposure to alcohol and are the most common nonheritable causes of intellectual disability. The percentage of women who drink or binge drink during pregnancy has increased since 2012. FAS is commonly missed or misdiagnosed, preventing affected ...
Estimates for the UK suggest that alcohol consumption during pregnancy and prevalence of fetal alcohol spectrum disorder (FASD)—the most common neurodevelopmental condition—are high. Considering the significant health and social impacts of FASD, there is a public health imperative to prioritise prevention, interventions and support. In this article, we outline the current state of play ...
In this issue of Alcoholism: Clinical and Experimental Research, 3 additional papers examining the prevalence of fetal alcohol spectrum disorders (FASDs; May et al., 2020a, 2020b, 2020c) follow the earlier paper by Chambers and colleagues ().These studies present state‐of‐the‐art FASD active case ascertainment (ACA) of prevalence among school‐age children conducted in the United States ...
One of the most disabling potential outcomes of drinking during pregnancy is fetal alcohol syndrome, which has an estimated global prevalence in the general population of 14.6 per 10,000 people ().Fetal alcohol syndrome is associated with brain anomalies, postnatal growth restriction, and facial dysmorphology, as well as psychological, behavioral, and cognitive deficits ().
A hidden epidemic of fetal alcohol syndrome
In an effort to improve the screening and diagnosis of individuals with Fetal Alcohol Spectrum Disorder (FASD), research has focused on the identification of a unique neurodevelopmental profile characteristic of this population. The objective of this review was to identify any existing neurodevelopmental profiles of FASD and review their classification function in order to identify gaps and ...
Fetal Alcohol Syndrome and Fetal Alcohol Spectrum ...
The Association of Women's Health, Obstetric and Neonatal Nurses (AWHONN) recommends that all patients be screened routinely for alcohol use during the preconception, antepartum, intrapartum, and postpartum periods using a validated tool. Screening should be ongoing during these periods, and when clinically indicated, early referral to intervention and treatment to prevent fetal alcohol ...
Fetal alcohol spectrum disorder (FASD) is an umbrella term used to describe the lifelong neuro-developmental disabilities that may result from prenatal alcohol exposure (Michaud and Temple, 2013). It is the leading non-genetic cause of developmental disability in Canada (Green, et al., 2014).
Diagnosis, epidemiology, assessment, pathophysiology ...
Treating fetal alcohol syndrome People with fetal alcohol syndrome face lifelong challenges , including problems with hand-eye coordination and difficulties with memory and attention.
Alcohol consumption during pregnancy can interfere with both embryonic and fetal development, producing a wide range of outcomes that fall under the rubric of fetal alcohol spectrum disorders (FASD). FASD is the nondiagnostic umbrella term used to refer to the full range of effects that can occur following prenatal alcohol exposure.
People with fetal alcohol syndrome face lifelong challenges, including problems with hand-eye coordination and difficulties with memory and attention. Early educational interventions for children with fetal alcohol spectrum disorders, like using visual and auditory materials instead of print, can provide additional structure to help facilitate ...
The estimated prevalence of fetal alcohol spectrum disorders (FASD) is conservatively around 1%; however, a recent study in North America found rates as high as 4.8% of the school-age population is affected by prenatal alcohol exposure, indicating a significant public health concern (May et al., 2014; May et al., 2015).
Correction: Analysis of alcohol-metabolizing enzymes genetic variants and RAR/RXR expression in patients diagnosed with fetal alcohol syndrome: a case-control study. Melina Vieiros 1,2,3 na1, Elisabet Navarro-Tapia 2,4 na1, Anna Ramos-Triguero 1, Àgueda García-Meseguer 1, Leopoldo Martínez 2,5, Óscar García-Algar 1,6 na2 & …
The epidemiology of fetal alcohol syndrome and partial FAS in a South African community. Drug and Alcohol Dependence. 2007; 88 (2-3):259-271. [PMC free article] [Google Scholar] May PA, Gossage JP, Marais AS, et al. Maternal risk factors for fetal alcohol syndrome and partial fetal alcohol syndrome in South Africa: A third study.