Gene therapy: Comprehensive overview and therapeutic applications
Affiliations.
- 1 Department of Pharmacy, Pravara Rural Education Society's (P.R.E.S.'s) College of Pharmacy, Shreemati Nathibai Damodar Thackersey (SNDT) Women's University, Nashik 400020, Maharashtra, India.
- 2 Department of Biosciences and Bioengineering, Indian Institute of Technology (IIT), Roorkee, Roorkee, Uttarakhand 247667, India.
- 3 Centre for Biomedical Engineering (CBME), Indian Institute of Technology (IIT) Delhi, Hauz Khas, New Delhi 110016, India; Department of Veterinary Pharmacology and Toxicology, College of Veterinary Science (CVSc), PVNRTVU, Rajendranagar, Hyderabad 500030, Telangana, India; Department of Veterinary Pharmacology and Toxicology, College of Veterinary Science (CVSc), PVNRTVU, Mamnoor, Warangal 506166, Telangana, India; Institute of Molecular Pathobiochemistry, Experimental Gene Therapy and Clinical Chemistry (IFMPEGKC), RWTH Aachen University Hospital, Pauwelsstr. 30, D-52074 Aachen, Germany. Electronic address: [email protected].
- 4 Department of Pharmacology, Central University of Punjab, Ghudda, Bathinda 151401, Punjab, India.
- 5 The Business Research Company (TBRC), Jubilee Hills, Hyderabad 500033, Telangana, India.
- 6 Department of Pharmaceutical Chemistry, University Institute of Pharmaceutical Sciences (UIPS), Panjab University, Chandigarh 160014, India.
- 7 Department of Veterinary Pharmacology and Toxicology, College of Veterinary Science (CVSc), PVNRTVU, Rajendranagar, Hyderabad 500030, Telangana, India.
- 8 Institute of Molecular Pathobiochemistry, Experimental Gene Therapy and Clinical Chemistry (IFMPEGKC), RWTH Aachen University Hospital, Pauwelsstr. 30, D-52074 Aachen, Germany. Electronic address: [email protected].
- 9 Department of Veterinary Pharmacology and Toxicology, College of Veterinary Science (CVSc), PVNRTVU, Mamnoor, Warangal 506166, Telangana, India. Electronic address: [email protected].
- PMID: 35123997
- DOI: 10.1016/j.lfs.2022.120375
Gene therapy is the product of man's quest to eliminate diseases. Gene therapy has three facets namely, gene silencing using siRNA, shRNA and miRNA, gene replacement where the desired gene in the form of plasmids and viral vectors, are directly administered and finally gene editing based therapy where mutations are modified using specific nucleases such as zinc-finger nucleases (ZFNs), transcription activator-like effector nucleases (TALENs) and clustered regulatory interspaced short tandem repeats (CRISPR)/CRISPR-associated protein (Cas)-associated nucleases. Transfer of gene is either through transformation where under specific conditions the gene is directly taken up by the bacterial cells, transduction where a bacteriophage is used to transfer the genetic material and lastly transfection that involves forceful delivery of gene using either viral or non-viral vectors. The non-viral transfection methods are subdivided into physical, chemical and biological. The physical methods include electroporation, biolistic, microinjection, laser, elevated temperature, ultrasound and hydrodynamic gene transfer. The chemical methods utilize calcium- phosphate, DAE-dextran, liposomes and nanoparticles for transfection. The biological methods are increasingly using viruses for gene transfer, these viruses could either integrate within the genome of the host cell conferring a stable gene expression, whereas few other non-integrating viruses are episomal and their expression is diluted proportional to the cell division. So far, gene therapy has been wielded in a plethora of diseases. However, coherent and innocuous delivery of genes is among the major hurdles in the use of this promising therapy. Hence this review aims to highlight the current options available for gene transfer along with the advantages and limitations of every method.
Keywords: Gene delivery; Gene therapy; Non-viral vectors; Transfection; Viral vectors.
Copyright © 2022. Published by Elsevier Inc.

Publication types
- CRISPR-Cas Systems*
- Gene Editing*
- Gene Transfer Techniques*
- Genetic Diseases, Inborn / genetics
- Genetic Diseases, Inborn / therapy*
- Genetic Therapy*
- Genetic Vectors / therapeutic use*
More From Forbes
Gene therapy, dna's past, rna's future: a time of promise.
- Share to Facebook
- Share to Twitter
- Share to Linkedin
Artist representation of DNA and genes
This story is part of a series on the current progression in Regenerative Medicine. In 1999, I defined regenerative medicine as the collection of interventions that restore tissues and organs damaged by disease, injured by trauma, or worn by time to normal function. I include a full spectrum of chemical, gene, and protein-based medicines, cell-based therapies, and biomechanical interventions that achieve that goal.
In this subseries, we focus specifically on gene therapies. We explore the current treatments and examine the advances poised to transform healthcare. Each article in this collection delves into a different aspect of gene therapy's role within the larger narrative of Regenerative Medicine.
Gene therapy's history is filled with ingenuity, imagination, and exploration. The 1960s through the 1980s, in particular, were a time of significant progress, marked by breakthroughs and fundamental discoveries. During this period, there was an improved understanding of the nature of genes and their potential for curing diseases.
Today, gene therapy is at the forefront of genetic research, and the possibilities for its use are endless. With continued research and development, gene therapy can transform countless lives.
Development of Gene Therapy Concepts
In the 1960s, the possibility of curing genetic disorders by introducing therapeutic DNA sequences was explored. This idea gained momentum after a discovery in 1961 . This research demonstrated that messenger RNA, known as mRNA, is crucial in transcribing genetic information from DNA to protein factories within cells.
Samsung Releases New Feature Boost To Millions Of Galaxy Phones
Trump again targets judge s daughter in new york criminal case, apple iphone 16 pro new leak reveals updated colors coming this fall.
This discovery resulted from an exhaustive study of the bacteriophage T4, a virus that infects bacteria. The virus's DNA was found to be transcribed into mRNA, a template for synthesizing new virus particles. This mechanism of transcription and translation is now known as the central dogma of molecular biology .
Visual representation of the central dogma of molecular biology.
Also, in 1961, Lorraine Kraus successfully incorporated functional DNA into a mammalian cell . She genetically altered the hemoglobin of cells taken from a sickle-cell anemia patient's bone marrow. This was done by incubating the patient's cells with DNA extracted from a donor with normal hemoglobin in tissue culture. Shortly after this, these concepts were applied practically.
Applying Novel Gene Therapy Concepts
In 1972, two young sisters from West Germany were among the first individuals to receive a pioneering gene therapy treatment for a rare genetic disorder called hyperargininemia. This inherited condition is caused by a deficiency of the arginase enzyme, leading to arginine accumulation in the bloodstream. Any accumulation of arginine can cause brain damage, epilepsy, and other neurological and muscular problems. The treatment was given as a last resort to save the children's lives.
The gene therapy attempted to address the missing enzyme in the sisters' bodies by introducing a modified enzyme. Unfortunately, the therapy did not succeed , and the sisters did not respond to the treatment. However, this early form of gene therapy highlighted the potential of genetic intervention in treating inherited ailments. It paved the way for further investigation and development of the concepts proposed years before, though not everyone was on board with this full-steam-ahead approach.
Around this time, an influential paper on gene therapy's potential for treating human genetic diseases was published. The authors suggested that DNA sequences could be incorporated into patients' cells for breakthrough treatment. However, they warned that the scientific understanding of gene therapies was incomplete and needed to be addressed, making it a challenging and risky treatment option.
Genetic Engineering and Retroviruses
Hot on the heels of this attempt, the field of genetic engineering blossomed and provided some novel tools that could be applied to gene therapies. One of these novel tools was retroviruses. These viruses were a much more efficient way to transfer genes.
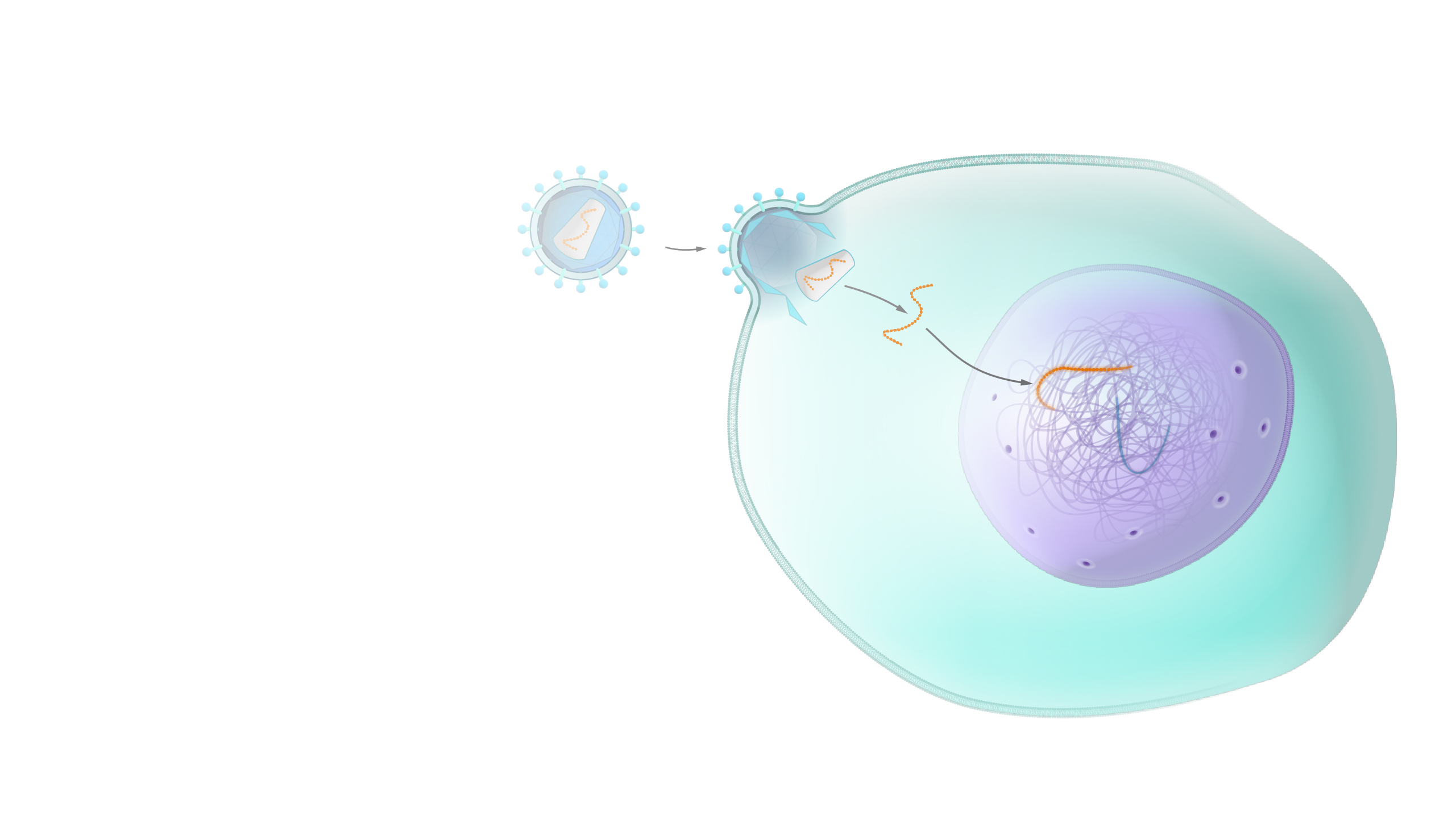
An illustration to show the transfer of a new gene into the nucleus of a cell via a viral vector.
Richard Mulligan , a Massachusetts Institute of Technology researcher, developed the first retroviral vector suitable for gene therapy. In 1983, collaborating with his colleagues, Mulligan genetically modified a mouse leukemia retrovirus . The retrovirus has been modified to deliver desired DNA without reproducing itself in humans. A selective marker, a DNA fragment from Escherichia coli bacteria, has been added to the new vector. This marker helps identify the number of genes that a cell has acquired during gene transfer. Mulligan and his colleagues published works on these retroviruses , how to use them to introduce selectable genes into tissues , and how to efficiently transfer genes . These discoveries allowed the field to progress rapidly with new trials and cases.
Building on Success
During the very late 1980s, French Anderson conducted a groundbreaking experiment to treat patients with ADA-SCID, a severe genetic disorder that compromises the immune system. Anderson's experiment involved inserting a working copy of the defective gene into the patient's cells using a virus as a carrier. This technique marked the first successful clinical demonstration that gene therapy could be used to treat genetic disorders. Anderson's pioneering work unlocked new therapeutic possibilities for treating genetic diseases and made him the "father of gene therapy."
After this came the publications of "the first human gene therapy trial" results . This was a significant milestone in gene therapy research. The trial described involved using a retrovirus to deliver a functional copy of the missing or defective gene into the patient's cells. This technique allowed corrected genes to be inserted into the patient's cells, creating a new source of functional proteins that could combat the genetic disorder. The trial demonstrated the practicality of retroviral gene delivery in humans, paving the way for further progress in gene therapy research and new avenues for treating genetic disorders.
These early experiments' success led to gene therapy research's explosive progression .
A Time of Promise Hits a Snag
From 1960 to 1980, there was much research and development in gene therapy, a significant achievement in genetic medicine. During these two decades, remarkable strides in scientific understanding were made, such as decoding mRNA and conducting the first trials on humans. This period marked a time of real promise.
The following decade was not so kind to gene therapy. In the 1990s, the field faced many challenges and setbacks that threatened to stifle progress. Despite these challenges, the spirit of innovation and improvement that defined the early years of gene therapy never wavered, and we continue to build on its rich legacy.
To learn more about regenerative medicine, read more stories at www.williamhaseltine.com
- Editorial Standards
- Reprints & Permissions
- Introduction to Genomics
- Educational Resources
- Policy Issues in Genomics
- The Human Genome Project
- Funding Opportunities
- Funded Programs & Projects
- Division and Program Directors
- Scientific Program Analysts
- Contact by Research Area
- News & Events
- Research Areas
- Research investigators
- Research Projects
- Clinical Research
- Data Tools & Resources
- Genomics & Medicine
- Family Health History
- For Patients & Families
- For Health Professionals
- Jobs at NHGRI
- Training at NHGRI
- Funding for Research Training
- Professional Development Programs
- NHGRI Culture
- Social Media
- Broadcast Media
- Image Gallery
- Press Resources
- Organization
- NHGRI Director
- Mission & Vision
- Policies & Guidance
- Institute Advisors
- Strategic Vision
- Leadership Initiatives
- Diversity, Equity, and Inclusion
- Partner with NHGRI
- Staff Search
Gene Therapy
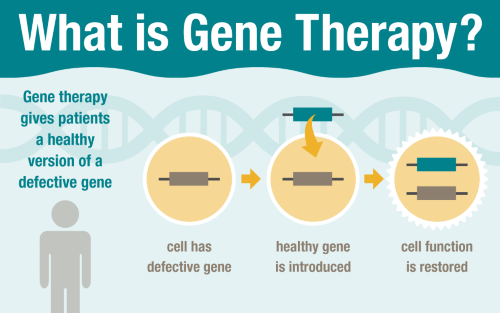
Gene therapy is a technique that uses a gene(s) to treat, prevent or cure a disease or medical disorder. Often, gene therapy works by adding new copies of a gene that is broken, or by replacing a defective or missing gene in a patient’s cells with a healthy version of that gene. Both inherited genetic diseases (e.g., hemophilia and sickle cell disease) and acquired disorders (e.g., leukemia) have been treated with gene therapy.
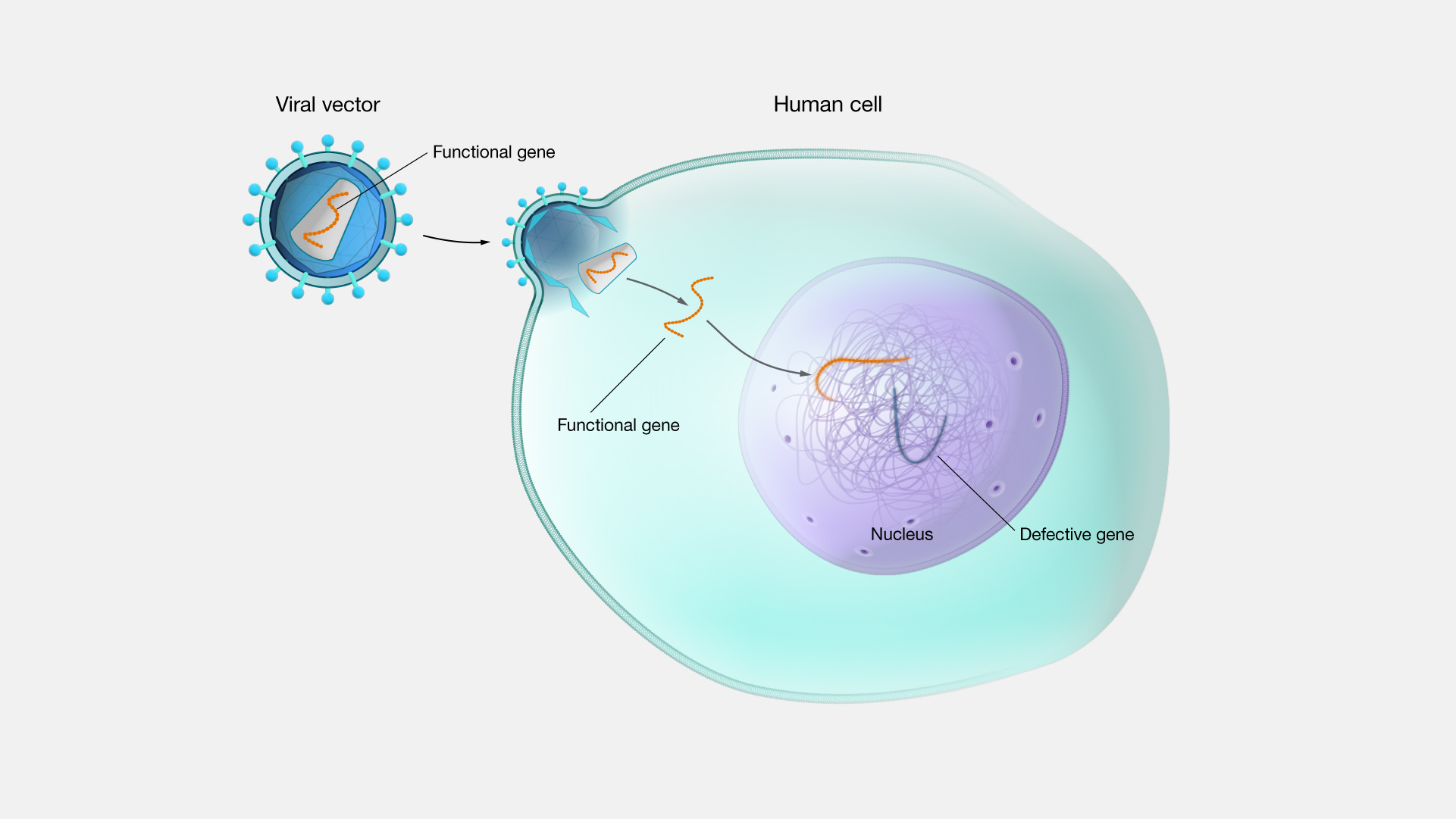
Gene therapy. Gene therapy is a direct way to treat genetic conditions as well as other conditions. There are also other related approaches like gene editing. There are many different versions and approaches to gene therapy and gene editing. It all rests on understanding how genes work and how changes in genes can affect our health. Researchers all over the world are studying many different facets of gene therapy and gene editing.
Clinical Director
Office of the Clinical Director
Gene Therapy News
Top headlines, latest headlines.
- Stronger Immunotherapy Against Lung Cancer
- Genetic Treatments for Vision Loss, CF
- Gene-Editing for Hereditary Disorders
- CAR T Outcomes in Large B Cell Lymphoma
- Toward Safer Gene Therapy
- Mice Possess Natural Gene Therapy System
- Gene Therapy Approach: Genetic Heart Disease
- Treating Spinal Muscular Atrophy
- Achilles Heel of Leukemia Cells Discovered
- Cancer Risk in Gene Therapies
Earlier Headlines
Wednesday, november 1, 2023.
- New Nijmegen Method Reveals Hidden Genetic Variations
Tuesday, October 31, 2023
- Individuals With Severe Sickle Cell Disease Express High Risk Tolerance for Gene Therapies
Tuesday, October 24, 2023
- New Methods for Effective Transport of Large Genes in Gene Therapy
Wednesday, August 30, 2023
- Promising Evidence for Sickle Cell Gene Therapy
Friday, August 11, 2023
- Research Raises Hopes for New Treatment of Fusion-Driven Cancer
Thursday, August 10, 2023
- New Gene Editing Tool Helps Zero in on Small Cancer-Linked Mutations
- Gene Therapy Hope for Children With Kidney Disease
- Scientists Reverse Hearing Loss in Mice
Wednesday, August 9, 2023
- Research Sheds New Light on Gene Therapy for Blood Disorders
Thursday, July 27, 2023
- Researchers Develop 'in Vivo' RNA-Based Gene Editing Model for Blood Disorders
Wednesday, July 12, 2023
- Researchers Pinpoint Protein Tied to Drug Resistance in Patients With Lung Cancer
Tuesday, May 30, 2023
- Researchers Design an Innovative Strategy to Fight Obesity Through Gene Therapy
Tuesday, April 4, 2023
- Peering Into Ocular Waste Recycling
Friday, February 17, 2023
- The Drug Fasudil Is Found to Reverse Key Symptoms of Schizophrenia in Mice
Tuesday, January 24, 2023
- Researchers Circumvent Radiation Resistance in Subtype of Brain Tumors
Wednesday, January 11, 2023
- Researchers Take Key Step Toward New Treatment for Hereditary Blindness
Wednesday, December 7, 2022
- Liver Cancer Study Encourages Caution With Certain Gene Therapies
Wednesday, November 9, 2022
- Silicon Nanochip Could Treat Traumatic Muscle Loss
Thursday, November 3, 2022
- Gene Therapy Targeting Overactive Brain Cells Could Treat Neurological Disorders
Wednesday, October 26, 2022
- New Gene Editing Strategy Could Lead to Treatments for People Born With Inherited Diseases of the Immune System
Thursday, October 20, 2022
- Gene Mutations in Tumors Impact Radiation Sensitivity
Wednesday, October 19, 2022
- Researchers Identify a Gene as a Potential Target in Treatment-Resistant Brain Cancer Glioblastoma Multiforme
Tuesday, October 11, 2022
- Gene Therapy Rapidly Improves Night Vision in Adults With Congenital Blindness
Monday, October 10, 2022
- Researchers Improve Vehicle for Delivering Gene Therapies to the Central Nervous System
Friday, September 23, 2022
- Potential of Precision Genome Editing in Treating Inherited Retinal Diseases
Wednesday, August 24, 2022
- New Gene Therapy Shows Promise for Treating Eye Condition Affecting Millions Across the Globe
Monday, June 6, 2022
- Mouse Study Shows Gene Therapy May Correct Creatine Deficiency Disorder
Tuesday, May 10, 2022
- Gene Therapy Could Treat Pitt-Hopkins Syndrome, Proof-of-Concept Study Suggests
Friday, April 22, 2022
- Establishment of a Pancreatic Cancer Animal Model Using the Pancreas-Targeted Hydrodynamic Gene Delivery Method
Tuesday, April 5, 2022
- DNA Discovery Reveals a Critical 'accordion Effect' For Switching Off Genes
Friday, April 1, 2022
- Novel Nuclear microRNA Is Being Developed for the Treatment of Cardiovascular Disease
Tuesday, March 29, 2022
- An Approach to Treating a Severe Congenital Myopathy
Monday, February 28, 2022
- How a Two-Faced Molecule Can Silence Problematic Genes
Wednesday, February 16, 2022
- A Possible Cure for Sickle Cell?
Monday, January 24, 2022
- My Heart Will Go On: Patient-Derived Heart Cells Mimic Disease in Vitro
Wednesday, January 19, 2022
- Calcium: Important Not Just for Your Bones but Also for Your Heart
- Epilepsy Research Boosts Case for New Gene Therapy for Dravet Syndrome
Tuesday, January 4, 2022
- New Gene Therapy Approach Offers a Potential Long-Term Treatment for Limb-Girdle Muscular Dystrophy 2B
Monday, December 13, 2021
- Experimental Gene Therapy Reverses Sickle Cell Disease for Years
- Gene Network Changes Associated With Cancer Onset and Progression Identify New Treatment Targets
Wednesday, December 8, 2021
- CRISPR/Cas9 Gene Editing Boosts Effectiveness of Ultrasound Cancer Therapy
Thursday, December 2, 2021
- ALS Therapy Should Target Brain, Not Just Spine
Tuesday, October 19, 2021
- Novel Gene Therapy Platform Speeds Search for Ways to Cure Blindness
Monday, October 18, 2021
- Developing a Treatment for Vision Loss Through Transplant of Photoreceptor Precursors
Tuesday, October 12, 2021
- Break Through the Tumor’s Protective Shield
Tuesday, August 31, 2021
- Fighting Brain Cancer at Its Root
Wednesday, August 25, 2021
- Researchers Identify Genetic Cause of Endometriosis and Reveal Potential Drug Target
Tuesday, August 24, 2021
- Teaching an Old Dog New Tricks: An Existing Drug Opens New Possibilities for Treating Childhood Leukemia
Wednesday, July 28, 2021
- Researchers Develop 'dimmer Switch' To Help Control Gene Therapy
Monday, July 12, 2021
- Innovative Gene Therapy 'reprograms' Cells to Reverse Neurological Deficiencies
Thursday, July 8, 2021
- Scientists Show How Light Therapy Treats Depression in Mice Model
Wednesday, June 30, 2021
- Discovery of the Role of a Key Gene in the Development of ALS
Wednesday, June 9, 2021
- New Adaptable Nanoparticle Platform Enables Enhanced Delivery of Gene Therapies
Tuesday, June 1, 2021
- Researchers Develop Proof-of-Concept Treatment That Elevates Adult and Fetal Hemoglobin
Wednesday, May 19, 2021
- Cholesterol Levels Sustainably Lowered Using Base Editing
- Closer to Gene Therapy That Would Restore Hearing for the Congenitally Deaf
Tuesday, May 18, 2021
- Scientists Develop Direct-Acting Antiviral to Treat COVID-19
Tuesday, May 11, 2021
- Gene Therapy Restores Immune Function in Children With Rare Immunodeficiency
- New Genetic Copycatchers Detect Efficient and Precise CRISPR Editing in a Living Organism
Monday, May 10, 2021
- Intense Light May Hold Answer to Dilemma Over Heart Treatment
Tuesday, May 4, 2021
- Gene Therapy in Alzheimer's Disease Mouse Model Preserves Learning and Memory
Wednesday, April 28, 2021
- Cancer-Linked Mutation Accelerates Growth of Abnormal Stroke-Causing Brain Blood Vessels
Wednesday, April 21, 2021
- Bypassing Broken Genes
Monday, April 19, 2021
- Gene Therapy Shows Promise in Initial Trial for Patients With Childhood Blindness
Tuesday, April 13, 2021
- Gene Therapy Shows Promise in Treating Rare Eye Disease in Mice
- Simple Genetic Modification Aims to Stop Mosquitoes Spreading Malaria
Wednesday, April 7, 2021
- PNA-Based Technique an Essential Part of the Gene Editing Toolkit
Wednesday, March 31, 2021
- Turning Back the Clock on a Severe Vision Disorder
- LATEST NEWS
- Health & Medicine
- Diseases & Conditions
- Alzheimer's Research
- Amyotrophic Lateral Sclerosis
- Attention Deficit Disorder
- Back and Neck Pain
- Birth Defects
- Bladder Disorders
- Blood Clots
- COVID and SARS
- Cervical Cancer
- Bladder Cancer
- Multiple Myeloma
- Pancreatic Cancer
- Brain Tumor
- Colon Cancer
- Breast Cancer
- Ovarian Cancer
- Lung Cancer
- Mesothelioma
- Skin Cancer
- Prostate Cancer
- Cerebral Palsy
- Chikungunya
- Chronic Fatigue Syndrome
- Cold and Flu
- Crohn's Disease
- Cystic Fibrosis
- Dengue Fever
- Down Syndrome
- Eating Disorder Research
- Encephalitis
- Epilepsy Research
- Erectile Dysfunction
- Fibromyalgia
- Gastrointestinal Problems
- HIV and AIDS
- Headache Research
- Hearing Loss
- Heart Health
- Cholesterol
- Stroke Prevention
- Heart Disease
- Hormone Disorders
- Hypertension
- Infectious Diseases
- Insomnia Research
- Irritable Bowel Syndrome
- Kidney Disease
- Liver Disease
- Lung Disease
- Lyme Disease
- Mental Health Research
- Multiple Sclerosis Research
- Mumps, Measles, Rubella
- Muscular Dystrophy
- Osteoporosis
- Parkinson's Research
- Prostate Health
- Restless Leg Syndrome
- Sickle Cell Anemia
- Sleep Disorder Research
- Thyroid Disease
- Triglycerides
- Tuberculosis
- Medical Topics
- Accident and Trauma
- Alternative Medicine
- Birth Control
- Bone and Spine
- Chronic Illness
- Controlled Substances
- Dietary Supplements and Minerals
- Epigenetics
- Food Additives
- Foodborne Illness
- Foot Health
- Gene Therapy
- Health Policy
- Human Biology
- Immune System
- Joint Health
- Medical Imaging
- Nervous System
- Pain Control
- Personalized Medicine
- Pharmacology
- Psychology Research
- Wounds and Healing
- PHYSICAL/TECH
- ENVIRONMENT
- SOCIETY & EDUCATION
- Heart Disease Risk: More Than One Drink a Day
- Unlocking Supernova Stardust Secrets
- Why Do Some Memories Become Longterm?
- What Controls Sun's Differential Rotation?
- Robot, Can You Say 'Cheese'?
- Researchers Turn Back the Clock On Cancer Cells
- Making Long-Term Memories: Nerve-Cell Damage
- A Solar Cell You Can Bend and Soak in Water
- 'Cosmic Cannibals': Fast-Moving Jets in Space
- Risk Factors for Faster Brain Aging
Trending Topics
Strange & offbeat.
- Patient Care & Health Information
- Tests & Procedures
- Gene therapy
Gene therapy involves altering the genes inside your body's cells in an effort to treat or stop disease.
Genes contain your DNA — the code that controls much of your body's form and function, from making you grow taller to regulating your body systems. Genes that don't work properly can cause disease.
Gene therapy replaces a faulty gene or adds a new gene in an attempt to cure disease or improve your body's ability to fight disease. Gene therapy holds promise for treating a wide range of diseases, such as cancer, cystic fibrosis, heart disease, diabetes, hemophilia and AIDS.
Researchers are still studying how and when to use gene therapy. Currently, in the United States, gene therapy is available only as part of a clinical trial.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
Gene therapy is used to correct defective genes in order to cure a disease or help your body better fight disease.
Researchers are investigating several ways to do this, including:
- Replacing mutated genes. Some cells become diseased because certain genes work incorrectly or no longer work at all. Replacing the defective genes may help treat certain diseases. For instance, a gene called p53 normally prevents tumor growth. Several types of cancer have been linked to problems with the p53 gene. If doctors could replace the defective p53 gene, that might trigger the cancer cells to die.
- Fixing mutated genes. Mutated genes that cause disease could be turned off so that they no longer promote disease, or healthy genes that help prevent disease could be turned on so that they could inhibit the disease.
- Making diseased cells more evident to the immune system. In some cases, your immune system doesn't attack diseased cells because it doesn't recognize them as intruders. Doctors could use gene therapy to train your immune system to recognize the cells that are a threat.
Gene therapy has some potential risks. A gene can't easily be inserted directly into your cells. Rather, it usually has to be delivered using a carrier, called a vector.
The most common gene therapy vectors are viruses because they can recognize certain cells and carry genetic material into the cells' genes. Researchers remove the original disease-causing genes from the viruses, replacing them with the genes needed to stop disease.
This technique presents the following risks:
- Unwanted immune system reaction. Your body's immune system may see the newly introduced viruses as intruders and attack them. This may cause inflammation and, in severe cases, organ failure.
- Targeting the wrong cells. Because viruses can affect more than one type of cells, it's possible that the altered viruses may infect additional cells — not just the targeted cells containing mutated genes. If this happens, healthy cells may be damaged, causing other illness or diseases, such as cancer.
- Infection caused by the virus. It's possible that once introduced into the body, the viruses may recover their original ability to cause disease.
- Possibility of causing a tumor. If the new genes get inserted in the wrong spot in your DNA, there is a chance that the insertion might lead to tumor formation.
The gene therapy clinical trials underway in the U.S. are closely monitored by the Food and Drug Administration and the National Institutes of Health to ensure that patient safety issues are a top priority during research.
What you can expect
Currently, the only way for you to receive gene therapy is to participate in a clinical trial. Clinical trials are research studies that help doctors determine whether a gene therapy approach is safe for people. They also help doctors understand the effects of gene therapy on the body.
Your specific procedure will depend on the disease you have and the type of gene therapy being used.
For example, in one type of gene therapy:
- You may have blood drawn or you may need bone marrow removed from your hipbone with a large needle.
- Then, in a lab, cells from the blood or bone marrow are exposed to a virus or another type of vector that contains the desired genetic material.
- Once the vector has entered the cells in the lab, those cells are injected back into your body into a vein or into tissue, where your cells take up the vector along with the altered genes.
Viruses aren't the only vectors that can be used to carry altered genes into your body's cells. Other vectors being studied in clinical trials include:
- Stem cells. Stem cells are the cells from which all other cells in your body are created. For gene therapy, stem cells can be trained in a lab to become cells that can help fight disease.
- Liposomes. These fatty particles have the ability to carry the new, therapeutic genes to the target cells and pass the genes into your cells' DNA.
The possibilities of gene therapy hold much promise. Clinical trials of gene therapy in people have shown some success in treating certain diseases, such as:
- Severe combined immune deficiency
- Blindness caused by retinitis pigmentosa
But several significant barriers stand in the way of gene therapy becoming a reliable form of treatment, including:
- Finding a reliable way to get genetic material into cells
- Targeting the correct cells
- Reducing the risk of side effects
Gene therapy continues to be a very important and active area of research aimed at developing new, effective treatments for a variety of diseases.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
- Gene therapy. Genetics Home Reference. http://ghr.nlm.nih.gov/handbook/therapy. Accessed July 21, 2016.
- What is gene therapy? National Cancer Institute. http://cancer.gov/ about-cancer/treatment/types/immunotherapy/bio-therapies-fact-sheet#q8. Accessed July 22, 2016.
- Chuah M, et al. Recent progress in gene therapy for hemophilia. Human Gene Therapy. 2012;23;557.
- FAQs. American Society of Gene & Cell Therapy. http://www.asgct.org/general-public/educational-resources/faqs. Accessed July 22, 2016.
- Cicalese M, et al. Clinical applications of gene therapy for primary immunodeficiencies. Human Gene Therapy. 2015;26:210.
- Ghazi N, et al. Treatment of retinitis pigmentosa due to MERTK mutations by ocular subretinal injection of adeno-associated virus gene vector: Results of a phase I trial. Human Genetics. 2016;135;327.
- Schubert M, et al. Chimeric antigen receptor T cell therapy targeting CD19 positive leukemia and lymphoma in the context of stem cell transplantation. Human Gene Therapy. In press. Accessed Aug. 13, 2016.
- Russell SJ (expert opinion). Mayo Clinic, Rochester, Minn. Aug. 29, 2016.
- Charcot-Marie-Tooth disease
- Epidermolysis bullosa
News from Mayo Clinic
- Science Saturday: Beacon in inner space Oct. 22, 2022, 11:00 a.m. CDT
- Doctors & Departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Let’s celebrate our doctors!
Join us in celebrating and honoring Mayo Clinic physicians on March 30th for National Doctor’s Day.
Advertisement
Current and emerging treatments for hemophilia A and B
Gene therapy: rationale and historical studies, results of recent aav-based gene therapy trials for hemophilia a and b, outcome of gene therapy, limitations of gene therapy, limitations in the possibility of gene therapy, conclusions, gene therapy for hemophilia: a review on clinical benefit, limitations, and remaining issues.
- Split-Screen
- Request Permissions
- Cite Icon Cite
- Search Site
- Open the PDF for in another window
Frank W. G. Leebeek , Wolfgang Miesbach; Gene therapy for hemophilia: a review on clinical benefit, limitations, and remaining issues. Blood 2021; 138 (11): 923–931. doi: https://doi.org/10.1182/blood.2019003777
Download citation file:
- Ris (Zotero)
- Reference Manager
Visual Abstract

In the last decade, enormous progress has been made in the development of gene therapy for hemophilia A and B. After the first encouraging results of intravenously administered adeno-associated virus (AAV)-based liver-directed gene therapy in patients with severe hemophilia B were reported in 2011, many gene therapy studies have been initiated. Most of these studies, using AAV vectors with various gene constructs, showed sufficient factor VIII and IX expression in patients to significantly reduce the number of bleeds and the need for prophylaxis in most patients with severe hemophilia. This resulted in great clinical benefit for nearly all patients. In this review, we will summarize the most recent findings of reported and ongoing gene therapy trials. We will highlight the successful outcome of trials with focus on the results of recently reported phase 1 trials and preliminary results of phase 2b/3 trials for hemophilia A and B. These new reports also reveal the impact of side effects and drawbacks associated with gene therapy. We will therefore also discuss the limitations and remaining issues of the current gene therapy approaches. These issues must be resolved before gene therapy will be widely available for the hemophilia patient population.
Hemophilia is an X-linked hereditary bleeding disorder caused by defects in the F8 or F9 gene, which results in a deficiency of coagulation factor VIII (FVIII) or FIX. Patients with severe hemophilia receive intravenously administered factor concentrate several times per week, thereby reducing joint bleeds and long-term arthropathy. 1 Despite this intensive prophylactic regimen, bleedings may still occur, and eventually arthropathy develops over time in many patients. 2,3 In the last decade, long-acting FVIII and FIX products have been developed requiring less intravenous injections, resulting in higher trough factor levels and a low bleeding rate. 4,5 Other developments are the nonfactor treatments, of which subcutaneously administered emicizumab, a monoclonal antibody mimicking the action of FVIII, is now registered for use in patients with hemophilia A. 6,7 Despite these great improvements, patients still need regular treatment. Also, the risk of bleeding is not completely abolished, and additional treatment is still needed before and after surgical interventions. Gene therapy for hemophilia is another developed treatment modality, and recent studies show long-term factor expression and great clinical benefit for patients. However, with the introduction of extended half-life products and nonfactor treatment, the benefit/risk ratio of gene therapy vs other treatments has to be taken into account and considered for each individual patient. 8-12
Gene therapy is a suitable treatment of hemophilia for various reasons. Hemophilia is caused by a single gene defect, a minimal expression of FVIII or FIX already leads to major improvement of the bleeding phenotype, and gene expression can be evaluated easily by measuring factor levels in plasma. The first studies using an ex vivo approach of gene therapy by gene transfer in autologous fibroblasts or hematopoietic stem cells, resulted in short-lasting low expression of FVIII. 13 Adeno-associated virus (AAV)-based gene therapy was introduced 20 years ago by intramuscular injection of recombinant AAV (rAAV)-FIX in patients with hemophilia B. The procedure was safe, and expression in muscle biopsies lasted for more than 3 years; however, it resulted in a minimal increase of plasma FIX (most patients <1%). 14-16
In 2006, the first AAV2-based liver-directed gene therapy clinical study in patients with hemophilia B showed temporarily expression of FIX. The vector was administered in the hepatic artery, and FIX expression lasted for 2 months. 17 Long-term follow-up revealed no adverse events, no liver toxicity, and no development of hepatocellular carcinoma (HCC) even after a period of 12 to 15 years after vector administration. 18 In 2011, the first study in patients with hemophilia B treated with intravenously administered liver-directed AAV8-based therapy showed expression levels of FIX between 1 and 6 IU/dL, which resulted in a reduction of bleedings without the need for prophylaxis. 19 After 3 years, 6 patients treated with the highest vector dose had median FIX levels of 5 IU/dL, showing long-term stable expression, now even lasting for >8 years. 9,20 These promising results were the basis for further development of gene therapy by several research groups and companies. Currently 47 trials on gene therapy for hemophilia have been carried out or are ongoing (clinical trials.gov; January 2021). For tables summarizing all hemophilia A and B gene therapy trials, we refer to recent reviews. 20,21
Hemophilia A
The first study on intravenously administered AAV-based liver-directed gene therapy for hemophilia A patients was reported in 2017. 10 Because of the size of the full-length FVIII gene, which is too large to be packed in an AAV viral vector, a construct encoding for B-domain deleted FVIII was used. Initial findings of this FVIII gene therapy trial using AAV5 (valoctocogene roxaparvovec) were very encouraging, showing median levels of 77 IU/dL (range, 19-164 IU/dL) at 1 year using a vector dose of 6 × 10 13 vector genomes (vg)/kg. The reported FVIII levels were obtained with a 1-stage clotting assay (OSA), which gives 1.65-fold higher levels than chromogenic assays (CSAs). Long-term data after 3-year follow-up showed a marked reduction of the expression compared with the FVIII levels at 1 year (median CSA, 20 vs 60 IU/dL). 22 According to the recently reported 4-year data from the 6 × 10 13 vg/kg cohort, the decline in FVIII activity continues (median CSA, 16.4 IU/dL). 23 Recently, the 1-year data of the phase 3 study in which 134 patients received 6 × 10 13 vg/kg of valoctocogene roxaparvovec were reported. 24 Median FVIII activity using the CSA was 23.9 IU/dL after 1 year (n = 132; mean, 42.9; standard deviation [SD], 45.5), and the median annualized bleeding rate was 0.0 (mean, 0.8; SD, 3.0). Further details of the study results are awaited, but the large sample size of this study will hopefully allow investigation of several factors that may affect the level and duration of expression of FVIII. Another study on AAV gene therapy in 12 patients with hemophilia A by Spark (SPK8011) showed FVIII levels between 12 and 30 IU/dL (assay type not specified), sufficient to prevent bleeding without the need of prophylaxis. In this study, lower vector doses were infused 0.5 to 2 × 10 12 vg/kg compared with the Biomarin study. 25 Recently, data of a subset of 5 patients who achieved a steady-state FVIII expression after 8 to 12 weeks revealed no decline of FVIII over a period of 2 years (FVIII:C between 5.2% and 19.8%). However, 2 patients of the initial cohort lost expression of FVIII and restarted prophylaxis. 26 Recently, the first data of a phase 1/2 dose-finding study on the use of AAVhu37 capsid vector technology (BAY 2599023, Bayer GET8 study) were presented. In total, 6 patients in 3 dose cohorts showed variable FVIII expression, which was sustained over time up to 16 months. The 2 patients in the highest dose cohort (2 × 10 13 gene copies [gc]/kg) had FVIII levels (CSA) of 12 and 72 IU/dL, but the durability of FVIII response cannot be assessed because of the short follow-up. 27 The study using AAV6-B-domain deleted FVIII (giroctocogene fitelparvovec [SB-525; ALTA study Sangamo/Pfizer]) showed highly variable FVIII expression levels measured with CSA. 28 Five patients in the highest dose cohort (3 × 10 13 vg/kg) achieved FVIII levels within the normal range (mean at 8 weeks, 61.5 IU/dL; SD, 26.1 IU/dL) with no bleeding events and no requirements of FVIII administration at 24 weeks. After a follow-up of 1 year, the median steady-state FVIII activity (CSA) was 50.2 IU/dL (mean, 80.1; SD, 93.3); however, the individual data of most patients show a decline over time 29 ( Table 1 ).
Data of reported results of intravenously administered AAV-based gene therapy phase 1 to 3 trials for hemophilia A and B
Only data for the highest dose of vector administered in the phase 1/2 studies are given. N = number of patients included. n.a., not available.
FVIII or FIX activity levels were obtained by OSAs or CSAs. In case no assay type is specified in the table, this is unknown.
Unfortunately, data of the various phase 1 studies is difficult to compare because of a limited number of observations. There is high variability in FVIII expression not only between the various studies but also within dose cohorts in the various studies. In addition, the reported outcomes in the studies are not uniform regarding measurements of FVIII levels (CSA or OSA). An important observation in 3 of the abovementioned studies, including the preliminary results of the phase 3 study with valoctacogene roxaparvovec, is the decline of FVIII expression over time.
Hemophilia B
Most AAV-based gene therapy studies to date have been performed in patients with hemophilia B ( Table 1 ). As mentioned above, the first study showing long-term expression of FIX using AAV8 liver-directed gene therapy was performed by Nathwani et al. 9,20 Another phase 1 study with AMT-060 (uniQure), a rAAV5 capsid containing the WT-FIX gene showed vector dose-dependent expression of FIX in 2 dose cohorts, with expression levels around 7 IU/dL in the highest dose cohort. 12 Recent data after 5 years of follow-up showed stable and durable expression, with a mean FIX level (OSA) of 5.2 IU/dL (95% confidence interval [CI]: 2.0-8.4) and 7.4 IU/dL (4.2-10.6) in the low dose and high dose cohort, respectively. This was associated with a sustained reduction of factor IX use and ongoing reduction of the number of bleeds. 30 To obtain higher FIX activity levels, fidanacogene elaparvovec (SPK9001; Spark) was developed, an AAV-FIX-Padua (FIX R338L) construct, which contains a FIX variant with a five- to eightfold higher specific activity. The phase 1 study with this Padua variant showed a mean FIX activity of 33.7 ± 18.5 IU/dL. 11 This FIX-Padua variant is now used in all ongoing FIX gene therapy trials. A phase 2b study in 3 patients and a phase 3 study in 54 patients with etranacogene dezaparvovec (AMT-061, uniQure), using the same vector as AMT-060, showed a mean FIX activity (OSA) of 47 and 37.2 IU/dL, respectively, 6 months after gene transfer. 31 In the phase 3 study, this enabled discontinuation of prophylaxis in 96% of patients, and 72% of patients did not report any bleeding during follow-up. 32 This is an important study because patients with preexisting neutralizing antibodies to AAV5 were also included. One patient with the highest titer (3212) did not respond to treatment, but the other patients with titers up to 678 had FIX expression similar to patients without neutralizing antibodies. 33 The phase 1 B-AMAZE study using FLT180a, a AAVS3 capsid carrying a F9 variant with a gain-of-function mutation, included 10 patients, who were treated in 4 cohorts (maximum dose, 1.5 × 10 12 vg/kg). High expression levels of FIX were shown shortly after gene therapy of 24 to 168 IU/dL at 3 weeks, which were stable during follow-up of 1 year. One of the patients with a high expression of FIX (>200 IU/dL) developed a thrombotic occlusion of arteriovenous fistula for which anticoagulant treatment was started. 34 It is still unclear if the obtained FIX levels after gene therapy are sufficient to prevent bleeding during surgery or trauma. Recently, George et al 35 presented data on 2 surgeries in patients with hemophilia B previously treated with fidanacogene elaparvovec. Surgery because of appendicitis and a lumbar discectomy were uneventful without the need for exogenous FIX concentrate in patients with FIX levels of 26.3 and 11.8 IU/dL.
Currently, several phase 3 studies are ongoing for hemophilia A and B. After a lead-in phase of 6 months to record bleeding rates and factor concentrate use on current (prophylactic) treatment, these patients underwent gene therapy and are followed for a period of 1 year and then for an additional 5 years in a separate study, as recommended by the US Food and Drug Administration (FDA). 36 Recently, an updated guide entitled “Human Gene Therapy for Hemophilia; Guidance for Industry” was published by the FDA and contains recommendations for the development of human gene therapy products for hemophilia. 37 The guidance includes recommendations for preclinical studies, the design of clinical trials, and the related development of coagulation FVIII and FIX activity assays, as well as on (surrogate) end points, such as factor levels and bleeding rates. The most advanced hemophilia A gene therapy program, which was expected to be approved in 2020, was rejected by the FDA. BioMarin provided 3-year data from the phase 1/2 trial and requested accelerated approval based on preliminary data in a limited number of patients of the phase 3 trial. The FDA concluded that, because of the differences between the phase 1/2 and phase 3 study, they could not rely on the data of the phase 1/2 to support durability of effect. The FDA recommended completion of the phase 3 study and submission of 2-year follow-up safety and efficacy data on all study participants. Gene therapy will drive a significant development in hemophilia care, and hemophilia centers should be adequately prepared to ensure that patients have an equal chance of being offered gene therapy as a therapeutic option. The recently proposed “hub-and-spoke” model by the European Association for Haemophilia and Allied Disorders–European Haemophilia Consortium will help to differentiate between centers with different experiences and ensure that there is monitoring and transfer of experience and knowledge. 38
Reduction of bleeding and factor use
As mentioned above, most trials in both hemophilia A and B lead to meaningful expression of FVIII and FIX and result in a strong decrease of both the number of bleedings and the need for prophylaxis. 9,12,22 This leads to a tremendous clinical benefit and changes the lives of patients with severe hemophilia.
Achieved levels of FVIII and FIX
For both patients and doctors, the expectations of the achievable factor levels have changed over time. Initially, the aim was to achieve levels of >5 IU/dL to prevent spontaneous joint bleedings. Based on the findings of the phase 1/2 studies, the current desired FVIII and FIX levels after gene therapy are >12 IU/dL and ideally should be above the hemostatic value (>40 IU/dL). 39 Several hemophilia experts have advocated that factor levels should be the main outcome measurement of gene therapy trials. 40 It is important, however, to notice that the reported levels after gene therapy are strongly dependent on the type of assay used. FVIII levels obtained with OSAs provide higher levels than the CSAs. 23 A kinetic bias between OSA and CSA readout times has been suggested, leading to higher OSA levels caused by accelerated early FXa and thrombin formation. 41 In gene therapy for hemophilia B using the full-size FIX gene with the Padua variant OSA yielded ≈1.6 times higher results than CSA. 42 It is still debated whether the levels obtained with OSA or CSA correlate better with the hemostatic potential and bleeding phenotype. Therefore, it is recommended that both tests should be used to quantify FVIII and FIX activity after gene therapy and that the possibly more accurate lower values measured by the CSA test be relied on. 41
Changes in health-related quality of life and loss of identity
Recently, core outcomes have been identified such as the frequency of bleeds, factor activity level, duration of expression, chronic pain, health care resource use, and mental health to evaluate the comparative value of gene therapy. 43 The potential impact of gene therapy on patient reported outcomes (PROs) and quality of life has not yet been determined. Significant improvements were reported for Haemophilia Quality of Life Questionnaire for Adults domains Future, Treatment, View, Sport, Feeling, and Total Score at 1 year after treatment. 44 Further research will be important to understand the appropriateness of already validated hemophilia-specific PRO instruments to assess health-related quality of life after gene therapy, including ensuring that these validated instruments allow the collection of data to compare gene therapy with traditional treatments. It could be expected that these domains would also show improvements in the long term. However, it is still unclear how the need for frequent visits during the first 2 years and the possible treatment with immunosuppressive drugs, as well as the unknown question of the durability of factor expression and long-term safety will influence PRO. In addition, a sense of loss of identity as a person with hemophilia and member of the hemophilia community may have an emotionally negative impact on gene therapy outcomes and counteract the potential cumulative benefits of gene therapy. Three patients with hemophilia B from the AMT-060 study were interviewed about their experiences with conventional and gene therapy and the effects of the therapy on everyday life. All 3 participants have become more active and participate more in sports. However, they expressed the fear that they did not know how long the effect would last and felt that psychologic support would be necessary if the FIX level was to drop again. No patient expressed concern about possible negative long-term consequences of gene therapy. 45
Immunologic response, liver function abnormalities, and liver toxicity
Thus far, limited side effects after intravenous infusion of AAV-based gene therapy have been reported; however, mild infusion-related complaints and, in some studies, even more severe reactions with hypotension and fever were encountered. 12,29 Administration of AAV vectors will induce innate immune response, followed by adaptive immune responses leading to the development of neutralizing antibodies in all individuals, that will be present long term. 46,47 In addition cytotoxic T-cell responses against the vector capsid may occur in 30% to 60% of patients. 46 This immune response may be associated with liver function abnormalities (alanine transaminase [ALT] elevations). This risk of developing this response seems to be vector dose dependent. 19 It may also be associated with loss of factor expression if not treated immediately with corticosteroids. 17,19,48 Remarkably, in several studies, liver function abnormalities occurred without a measurable immunologic cytotoxic T-cell response in the peripheral blood as determined by enzyme-linked immunospot assays; however, this assay is not well standardized and has several limitations. Detailed studies on clinical immunogenicity of AAV5 gene therapy using various humoral and cellular immune response assays showed no clear association between these responses and safety or efficacy measures. 49 In recent studies in patients treated for hemophilia A, liver function abnormalities persist over a longer time span, and it is still unknown what the cause of these persistent transaminitis is, but it may be of different origin than the immune response–related liver function abnormalities observed mainly early after gene therapy. It seems to occur more often after gene therapy in patients with hemophilia A. It has been suggested that this may, besides immunologic responses, be caused by cellular stress because hepatocytes physiologically do not synthesize FVIII; cell death caused by high amounts of viral capsids has also been considered. 50,51 In the highest dose cohort of the SPK8011 study, 5 of 7 patients required corticosteroid treatment for ALT elevations, immune response, or FVIII decline. 25 In the ALTA study, 4 patients receiving giroctocogene fitelparvovec had ALT elevations, responding to corticosteroid treatment, of which 3 had recurrent ALT elevations. 29 Also 2 patients treated with high-dose (2 × 10 13 gc/kg) BAY2599023 experienced recurrent ALT elevations, requiring long-term corticosteroids for >6 months. 52 Because of these observations in many currently initiated trials, corticosteroids with or without additional immunosuppressive drugs are given immediately after vector infusion to prevent liver function abnormalities. The importance of obtaining more insights into the cause of liver function abnormalities is emphasized by the recent reports of 3 children with X-linked myotubular myopathy who experienced severe hepatotoxicity after high-dose (3 × 10 14 gc/kg) AAV6 gene therapy. Eventually this resulted in death caused by sepsis and a bleeding event. 53,54 The precise mechanism of the hepatotoxicity in these cases is not yet known.
Failure of gene therapy
Some gene therapy approaches resulted in only temporary expression of FVIII and FIX and were considered unsuccesful. 8 This was mainly because of immunologic responses and initial low levels of expression measured in the circulation. 55-57 In a dose-ascending AAV8-based study using the FIX Padua variant, 7 of 8 participants with severe and moderate hemophilia B achieved transient, dose-dependent measurable FIX activity (peak FIX, 32-58.5 IU/dL) in the highest dose cohort. However, FIX activity was maintained in only 1 of 7 patients 55 ( Table 1 ). The cause of the loss of transgene expression in the other 6 patients is not known; however, this might have been caused by immune responses by CpG oligodeoxynucleotides introduced in BAX335 by codon optimization. In another study using AAVrh10, only short-term expression of FIX was observed, with peaks between 12 and 20 IU/dL and subsequent loss of expression in 5 of 6 individuals. This may be related to AAVrh10 capsid-induced immune responses, because these patients developed ALT elevations, and despite treatment with corticosteroids, FIX expression was not preserved. 57 In studies that are considered successful, several individual patients did not have expression or very low expression of factor, which should also be considered a failure of this therapy. The mechanism behind these failures and the large variability of expression in general should be further investigated. 12,23,26,29
Integration and oncogenesis after AAV gene therapy?
It is assumed that rAAV remain mainly episomal after hepatocyte transduction. However, integration occurs in the host genome, and the possible implications for oncogenesis have been widely discussed. 58-60 Given the fact that very high AAV vector loads (>10 15 ) are being delivered, even a low percentage of integration may still be important. In mice, intravenous injection of genome-containing particles of an AAV vector resulted in the development of HCC in 33% of the animals, which was linked to AAV vector integration resulting in clonal expansion of transformed cells. 61 Long-term results of gene transfer studies in dogs revealed integration at a low frequency, mainly in intergenic regions of the dog genome, without development of malignancy. 47,60 In another study, which confirmed stable and sustained FVIII expression for up to 10 years, 2 of 9 dogs experienced a gradual increase in FVIII activity that was 4 times the steady-state level, and clonal expansions with integration near genes previously associated with growth control and cancer, however, without any evidence of tumorigenesis. 62,63 In liver biopsies of clinical study participants, a dose-dependent increase of vector DNA corresponding with FVIII expression levels has been detected. 64 None of the 4 patients treated 12 to 15 years ago with AAV2-based intravascular gene therapy developed HCC. 18 Despite these reassuring (pre)clinical data in dogs and humans, recently, HCC developed in a hemophilia B patient 1 year after treatment with etranacogene dezaparvovec gene therapy. 65 Investigations of tumor biopsies have shown no evidence of clonal expansion or any dominant integration event. Additionally, whole genome sequencing confirmed that the HCC had genetic mutations that are independent of vector integration. 65 This event also shows the importance of collecting long-term data on safety and efficacy in a global registry for patients with gene therapy. 66
Preexisting neutralizing AAV antibodies
Preexisting neutralizing antibodies against AAV are widely distributed in the general population. 67 In patients with hemophilia A from the United Kingdom, 21% and 23% had antibodies to AAV 5 and AAV8, respectively, with a high degree of cross-reactivity. Seroprevalence increased with age and exposure to plasma products. 68 A major problem with regard to the importance of detection of these antibodies in circulation is the fact that various assays are in use, and these are not standardized. Preclinical studies demonstrated the capacity of humoral immunity to prevent successful transduction of AAV into hepatocytes. 69,70 Therefore, preexisting neutralizing antibodies are still an exclusion criteria in studies, and it is expected that these patients will also be ineligible in the future. However, in the uniQure AMT-060 studies, 3 patients were included that, on hindsight, turned out to have AAV5 neutralizing antibodies, using a more sensitive luciferase-based assay. These 3 patients had expression and benefit of treatment, and FIX levels were not related to the titer of the neutralizing antibodies. 71 Therefore, in the phase 3 study, individuals with preexistent AAV5 neutralizing antibodies were also included, and preliminary data show that neutralizing antibodies titers up to 678 do not seem to affect FIX expression. 33 It has been demonstrated in nonhuman primates with preexisting high-titer neutralizing antibodies against AAV5 that immune adsorption is effective to reduce the titer of neutralizing antibodies before gene therapy, which resulted in therapeutic levels of FIX expression. 72 Preclinical studies have demonstrated that the immune response induced by AAV antibodies could be inhibited by an endopeptidase (imlifidase) able to degrade circulating immunoglobulin G, which would provide the prospect of treatment of a larger patient population. 73 It is important to note that, after treatment with AAV-based gene therapy, high-titer neutralizing antibodies circulate, which thus far makes it unlikely that patients can be retreated with AAV, although imlifidase may overcome this problem by degrading the anti-AAV immunoglobulin G. 73
Great clinical benefit has been achieved in patients with hemophilia A and B with intravenously administered AAV-based liver-directed gene therapy. The expectations to be able to transform patients with severe hemophilia into patients with mild hemophilia using gene therapy have been met, and FVIII and FIX levels even in the normal range have been achieved. In most patients, prophylaxis could be discontinued, and limited or no bleedings occurred. Unfortunately, several open questions and issues still remain, which are addressed in Table 2 : the variability in expression levels, occurrence of immunologic responses, and the need for immunosuppressive therapy because of the occurrence of liver function abnormalities, of which the nature is yet unresolved. Also, safety issues regarding integration and potential development of malignancy need further research. A major issue has emerged given the observed decline of FVIII expression levels within 3 to 4 years after gene therapy. Therefore, long-term results of ongoing phase 3 studies are needed before gene therapy may become widely available.
Main findings on clinical benefit and remaining issues in hemophilia gene therapy
Contribution: F.W.G.L. and W.M. wrote the manuscript and approved the final manuscript.
Conflict-of-interest disclosure: F.W.G.L. received unrestricted research grants from CSL Behring, Shire/Takeda, and uniQure; is a consultant for CSL Behring, Shire/Takeda, Biomarin, and uniQure, of which the fees go to the University; has received travel support from SOBI; and is a Data Safety Monitoring Board member of a study sponsored by Roche. W.M. received unrestricted research grants from Amgen, Bayer, Biotest, CSL, LFB, Novo Nordisk, Octapharma, Pfizer, Shire, and Sobi; is a consultant for Ablynx, Amgen, Aventis, Bayer, Biomarin, Freeline, Leo, LFB, Octapharma, Sobi, Novartis, Novo Nordisk, Octapharma, Pfizer, Roche, Sanofi, Sobi, and UniQure; and is a DSMB member of a study sponsored by Octapharma.
Correspondence: Frank W. G. Leebeek, Erasmus MC, University Medical Center Rotterdam, Department of Hematology, Dr Molewaterplein 40, 3015 GD Rotterdam, The Netherlands; e-mail: [email protected] .
This feature is available to Subscribers Only
- Previous Article
- Next Article
Email alerts
Affiliations.
- Current Issue
- First edition
- Collections
- Submit to Blood
- About Blood
- Subscriptions
- Public Access
- Permissions
- Blood Classifieds
- Advertising in Blood
- Terms and Conditions
American Society of Hematology
- 2021 L Street NW, Suite 900
- Washington, DC 20036
- TEL +1 202-776-0544
- FAX +1 202-776-0545
ASH Publications
- Blood Advances
- Hematology, ASH Education Program
- ASH Clinical News
- The Hematologist
- Publications
- Privacy Policy
- Cookie Policy
- Terms of Use
This Feature Is Available To Subscribers Only
Sign In or Create an Account
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
What Is Gene Therapy?
A New Type of Therapy for Genetic Diseases
- Why It's Done
- What to Expect
Frequently Asked Questions
Gene therapy is a type of treatment being developed to fight diseases that are caused by genetic defects. This is a relatively new medical intervention that is mainly in the experimental phase, including human trials and animal trials, for the treatment of some conditions, such as cystic fibrosis .
Gene therapy aims to change the unhealthy proteins that are produced as a result of disease-causing genes.
KATERYNA KON / SCIENCE PHOTO LIBRARY / Getty Images
What Is Gene Therapy?
Some diseases are caused by a known genetic defect or a gene mutation. This means that there is a hereditary or acquired error in the DNA molecule that codes for producing a specific protein in the body. The altered protein doesn’t function as it should, resulting in a disease.
The idea behind gene therapy is to direct the body to produce healthy proteins that do not cause disease.
This therapy involves the delivery of DNA or RNA. The RNA molecule is an intermediate molecule that is formed in the process of protein production. The genetic defect for some diseases has been identified, but many genetic mutations haven’t been identified (they might be in the future).
Research is ongoing into ways to correct genetic defects that have been associated with certain diseases. There are different types and methods of gene therapy that are being investigated.
Types of Gene Therapy
Genetic mutations can be hereditary, which means that they are inherited from parents. Genetic defects can also be acquired, sometimes due to environmental factors, like smoking.
Gene therapy is being evaluated as a potential treatment for both types of mutations. There are several ways of delivering the corrected DNA or RNA into a person’s body.
Most cells in your body are somatic cells. The only cells that are not somatic cells are the germline cells, which create the egg and sperm cells that can produce offspring.
Somatic gene therapy : Somatic gene therapy aims to correct a defect in the DNA of a somatic cell or to provide an RNA molecule to treat or prevent a genetic disease in the person who is undergoing the therapy. This treatment may be used if you have an inherited mutation or if the mutation developed due to environmental factors.
Germline gene therapy : Germline gene therapy aims to correct a defect in an egg or a sperm cell to prevent a hereditary disease from eventually affecting future offspring.
Bone Marrow
Sometimes a person’s own cells can be removed from the bone marrow , genetically modified in a laboratory, and then reinserted into the body.
Viral Vector
A viral vector is a virus that has been altered so that it will not cause a viral infection. It is then infused with the correct DNA or RNA sequence. The viral vector containing the correct gene may be injected into a person for delivery of gene therapy.
Stem Cells
Stem cells are immature cells that have the potential to develop into different types of cells. Sometimes stem cells that have been genetically modified are transplanted into a person’s body to replace the defective cells as a way to treat disease.
This technique uses a lipid (fat) to deliver the genetic DNA or RNA material.
Why Is Gene Therapy Done?
Some gene mutations direct the body to make disease-causing proteins. And some genetic mutations are not functional—they cause disease because the body lacks the healthy proteins that should be normally produced by the gene.
Gene therapy aims to direct the body to produce healthy proteins or to inhibit the production of defective proteins. This depends on the type of mutation that is causing the disease.
Gene Augmentation Therapy: Replacing Mutated Genes
With gene augmentation, the goal is to help the body make a healthy protein.
Sometimes the DNA molecule can have a gene inserted into it. This is intended to permanently alter the DNA so that the body can make new cells with the correct DNA code. The new cells will then also make healthy products.
Some research using gene augmentation therapy involves the insertion of a healthy DNA molecule or an RNA sequence into a cell, but not into the DNA of the recipient. This has been shown in experimental studies to trigger the production of healthy proteins, but future copies of the cell are not expected to contain the healthy gene.
Gene Inhibition Therapy: Inactivating Mutated Genes
Sometimes gene therapy aims to cancel out the activity of a mutated gene to prevent the production of a disease-causing protein. This is done by the insertion of a non-mutated gene DNA sequence into a DNA molecule.
Making Diseases Cells Apparent to the Immune System
Another type of gene therapy involves the body’s immune system . An example of this therapy is the use of checkpoint inhibitors. With this therapy, the immune system is modified to recognize material in the body that is produced by the mutated genes in order to destroy them and to prevent the illnesses they cause.
Risks of Gene Therapy
There are some known risks of gene therapy. So far, the most common problem associated with gene therapy is a lack of effectiveness. However, there are also adverse effects that may occur.

Unwanted Immune System Reaction
Gene therapy that involves the immune system may cause excess immune reactivity to healthy cells that resemble the disease cells, potentially causing damage to healthy cells.
Wrong Target Cell
Potentially, the immune reaction that is mediated by gene therapy can affect the wrong cell type, instead of the intended target cells.
Infection Caused by Viral Vector
When a viral vector is used, there may be a risk that the virus could cause an infection. Depending on the primary disease that is being treated, a person receiving gene therapy may have a weak immune system and, therefore, could have difficulty fighting the virus.
Possible Tumor
A new DNA sequence that’s inserted into a person’s genes could potentially lead to a mutation that could cause cancer to form.
What to Expect From Gene Therapy
If you are considering gene therapy, you will go through a process of diagnosis, treatment, and medical surveillance to assess the effects.
This step will determine whether you have a medical condition that can be treated with gene therapy. This means that you would have a blood sample sent to a laboratory to identify treatable gene mutations that are associated with your medical condition.
Examples of conditions that may be treatable with gene therapy include:
- Cystic fibrosis : An inherited disorder in which thick mucus is produced, clogging the airways and blocking the secretion of digestive enzymes
- Sickle cell disease : An inherited disorder that results in abnormal hemoglobin production (the protein that carries oxygen in the red blood cells)
- Leber's hereditary optic neuropathy (LHON) : An inherited disorder that causes the death of cells in the optic nerve , resulting in damage to central vision
- Inherited or acquired retinal disease : Conditions that damage to the retina , the light-sensing layer in the back of the eye
- WW domain-containing oxidoreductase (WWOX) epileptic encephalopathy syndrome : A genetic condition resulting in severe epilepsy, developmental delays, and early death
- Spinocerebellar ataxia and autosomal recessive 12 (SCAR12) : An inherited disorder resulting in seizures in infancy, developmental delays, and inability to coordinate movement
- Cancer : Many types of cancer
Your treatment may involve collection of your cells and delivery of the genes into your cells with a viral vector or liposome. The modified cells will be restored to your body after the treatment.
Surveillance
The effects of your treatment will be assessed, and you will be monitored for adverse events (side effects). If this occurs, you may be treated again.
Clinical Trials
You can find clinical trials for gene therapy by talking to your doctor or by searching for organizations that support your medical condition, such as the Cystic Fibrosis Foundation.
Gene therapy is a relatively new treatment designed to alleviate disease by modifying defective genes or altering the production of proteins by faulty genes. There are several ways that healthy genes can be inserted into the body, such as inside a deactivated virus or inside a fat particle.
Sometimes immature and healthy cells are transplanted to replace cells that have a disease-causing mutation. This type of therapy can cause side effects, and there is also a risk that it might not work.
A Word From Verywell
If you have a genetic disease with a known and identified gene mutation, you might be a candidate for gene therapy treatment in a clinical trial. This type of treatment is not a standard therapy, and you would need to be monitored closely so that you and your doctors would know if the therapy is working and whether you are having any side effects.
You can talk to your doctor about gene therapy. This treatment is not widespread, so there is a possibility that you may need to travel to be able to participate in a clinical trial if there is not a research study near you.
This therapy is considered safe, but there are risks and side effects. You may have an opportunity to participate in a clinical trial, and side effects and adverse effects would be monitored.
One example of this therapy is the use of a deactivated virus to insert a portion of a DNA molecule into the body’s cells so that the healthy DNA sequence can provide a blueprint for healthy proteins.
The main goal of gene therapy is to provide DNA or RNA to code for healthy proteins so the body will not be affected by a genetic disease.
Cystic Fibrosis Foundation. Gene therapy for cystic fibrosis .
Food and Drug Administration. What is gene therapy?
Jiang J, Sun G, Miao Q, Li B, Wang D, Yuan J, Chen C. Observation of peripapillary choroidal vascularity in natural disease course and after gene therapy for Leber's hereditary optic neuropathy. Front Med (Lausanne) . 2021;8:770069. doi:10.3389/fmed.2021.770069
Repudi S, Kustanovich I, Abu-Swai S, Stern S, Aqeilan RI. Neonatal neuronal WWOX gene therapy rescues Wwox null phenotypes . EMBO Mol Med. 2021;13(12):e14599. doi:10.15252/emmm.202114599
Tan TE, Fenner BJ, Barathi VA, Tun SBB, Wey YS, Tsai ASH, Su X, Lee SY, Cheung CMG, Wong TY, Mehta JS, Teo KYC. Gene-based therapeutics for acquired retinal disease: Opportunities and progress . Front Genet. 2021;12:795010. doi:10.3389/fgene.2021.795010
Lu Z, Chen H, Jiao X, et. al. Germline HLA-B evolutionary divergence influences the efficacy of immune checkpoint blockade therapy in gastrointestinal cancer . Genome Med . 2021;13(1):175. doi:10.1186/s13073-021-00997-6
By Heidi Moawad, MD Heidi Moawad is a neurologist and expert in the field of brain health and neurological disorders. Dr. Moawad regularly writes and edits health and career content for medical books and publications.
Gene therapy at St. Jude
Gene therapy treats genetic diseases by giving patients a healthy version of a defective gene. St. Jude is developing innovative gene therapy approaches for patients with blood diseases, immune disorders and other conditions.
Potential for a cure
A baby is born with a defective gene, leading to a life-threatening disease. Standard therapies are limited; the child is faced with battling a chronic condition for life.
But perhaps there is an alternative — one that may lead to a permanent cure.
Gene therapy is designed to restore the function of a patient’s defective gene by introducing a healthy copy, with the potential to permanently correct a genetic disease. This compelling concept has intrigued the medical community for more than 20 years. While still primarily performed as part of research studies, gene therapy is becoming more widely adopted for clinical treatment of some conditions.
Bubble boy disease
For children born with severe combined immunodeficiency (SCID), a parent’s touch can be life-threatening. Often called “bubble boy disease,” SCID devastates the immune system and leaves patients vulnerable to lethal infections. Early death is common, even with existing therapies.
X-linked SCID, the most common form of SCID, is caused by defects in a gene encoding a critical protein called the common gamma chain. Without it, immune system cells called T cells, B cells and natural killer cells do not develop normally.
With the aim of pioneering a safe, effective gene therapy approach, St. Jude scientists have spent years developing an innovative vector for X-linked SCID. The vector is manufactured in the on-site Good Manufacturing Practice (GMP) facility using a process developed at St. Jude. The process, which uses stable cultured cell lines to produce the vector, addresses the challenge of manufacturing large quantities of clinical-grade vector in a reproducible manner.
The vector has been designed with features to reduce the risk of activating cancer-causing genes. It has also been subjected to extensive laboratory testing to ensure it does not readily insert into chromosomes near such genes.
Clinical trials led by St. Jude and the National Institute of Allergy and Infectious Diseases (NIAID) have recently confirmed that this vector can safely provide long-lasting health benefits to patients with X-linked SCID.
Read about the St. Jude trial: LVXSCID-ND: Gene Transfer for X-Linked Severe Combined Immunodeficiency in Newly Diagnosed Infants
Featured research: Gene therapy provides cure for SCID
St. Jude researchers have cured X-linked SCID in eight infants treated at St. Jude and UCSF Benioff Children’s Hospital San Francisco. As of early 2019, eight infants have received the novel combination therapy and have not shown any immediate side effects. The patients have begun developing healthy immune systems and have started responding to vaccinations. This study also demonstrated that the gene-corrected cells could be produced reliably and in significant quantities to treat a large number of patients.
Read full results published in the New England Journal of Medicine .
Learn more about the study .
Gene therapy offers hope of a cure
Scientists at St. Jude developed a novel gene therapy for children born with a rare immune disease
Gene therapy for hemophilia and other blood disorders
In 2014, St. Jude investigators and colleagues published historic results from a gene therapy trial for hemophilia B. A vector developed and manufactured at St. Jude had transformed the lives of young men with this inherited bleeding disorder.
Andrew M. Davidoff, MD, St. Jude Children's Research Hospital
Hemophilia B is caused by defects in the gene for factor IX, a blood clotting protein. Hemophilia B can be managed with lifelong regular injections of factor IX protein, which can cost $250,000 per year.
Years after receiving a single dose of gene therapy, patients on the hemophilia B trial continued to produce their own clotting factor from the normal transferred gene with minimal side effects. The treatment dramatically decreased their need for protein replacement injections, and some were able to participate in sports without worrying about bleeding.
The trial stemmed from a decade-long collaboration between St. Jude and University College London to discover effective gene therapies for this blood disorder. The St. Jude team was led by Andrew Davidoff, MD , chair of St. Jude Surgery and Arthur Nienhuis, MD, of St. Jude Hematology. Vector development was a critical aspect of the project, with years of careful improvements required to produce sufficient levels of factor IX to relieve symptoms.
Read about the hemophilia B study.
St. Jude and University College London are currently collaborating on another Phase I/II gene therapy clinical trial for adult men with hemophilia B, scheduled to launch in the U.S. in early 2019.
Designing better gene therapy vectors
A major step forward has been the development of safer approaches following lessons learned from early clinical trials. In gene therapy, new genetic material (DNA or RNA) is introduced into a patient’s cells, most often via a disabled virus called a vector. The new genetic material either floats free in the cells or is inserted into the patient’s chromosomes, depending on the type of vector.
St. Jude has played a key role in vector development, pioneering innovative vector designs for patients with hemophilia and the devastating immune disorder X-linked severe combined immunodeficiency (SCID). Other vectors are in development. St. Jude has also developed exclusive manufacturing processes to produce large amounts of clinical-grade genetic material for clinical trials.
Vectors designed and manufactured at St. Jude have already helped transform the lives of patients participating in gene therapy clinical trials for immune and blood disorders.
Challenges and opportunities
To date, results from clinical studies of gene therapies pioneered at St. Jude have been promising. It will be important to follow patients for many years to confirm the therapy’s long-lasting safety and health benefits.
St. Jude researchers are now focused on applying investigational gene therapy approaches to treat X-linked SCID, hemophilia B and a related disorder, hemophilia A. The long-term vision is to apply these technologies to other genetic diseases, such as sickle cell disease, and to explore applications in developing effective immune therapies for cancer.

Mamcarz E, Zhou S, Lockey T, Abdelsamed H, Cross S, Kang G, Ma Z, Condori J, Dowdy J, Triplett B, Li C, Maron G, Sorrentino B, et al. Lentiviral Gene Therapy Combined with Low-Dose Busulfan in Infants with SCID-X1 . N Engl J Med 380:1525-1534, 2019. doi: 10.1056/NEJMoa1815408.
De Ravin SS, Wu X, Moir S, Kardava L, O’Brien SA, Ulrick J, Kwatemaa N, Little P, Theobald N, Choi U, Su L, Marquesen M, Hilligoss D, Lee J, Buckner CM, Zarember KA, O’Connor G, McVicar D, Kuhns D, Throm RE, Zhou S, Notarangelo LD, Hanson IC, Cowan MJ, Kang E, Hadigan C, Meagher M, Gray JT, Sorrentino BP, Malech HL. Lentiviral hematopoietic stem cell gene therapy for X-linked severe combined immunodeficiency. Sci Transl Med 8(335):335ra57, 2016. doi: 10.1126/scitranslmed.aad8856
Zhou S, Fatima S, Ma Z, Wang YD, Lu T, Janke LJ, Du Y, Sorrentino BP. Evaluating the Safety of Retroviral Vectors Based on Insertional Oncogene Activation and Blocked Differentiation in Cultured Thymocytes. Mol Ther March 9, 2016. Epub ahead of print. doi: 10.1038/mt.2016.55. PMID: 26957223.
Nathwani AC, Reiss UM, Tuddenham EG, Rosales C, Chowdary P, McIntosh J, Della Peruta M, Lheriteau E, Patel N, Raj D, Riddell A, Pie J, Rangarajan S, Bevan D, Recht M, Shen YM, Halka KG, Basner-Tschakarjan E, Mingozzi F, High KA, Allay J, Kay MA, Ng CY, Zhou J, Cancio M, Morton CL, Gray JT, Srivastava D, Nienhuis AW, Davidoff AM. Long-term safety and efficacy of factor IX gene therapy in hemophilia B . N Engl J Med 371(21):1994-2004, 2014. doi: 10.1056/NEJMoa1407309. PMID: 25409372. PMCID: PMC4278802.
Nathwani AC, Tuddenham EG, Rangarajan S, Rosales C, McIntosh J, Linch DC, Chowdary P, Riddell A, Pie AJ, Harrington C, O'Beirne J, Smith K, Pasi J, Glader B, Rustagi P, Ng CY, Kay MA, Zhou J, Spence Y, Morton CL, Allay J, Coleman J, Sleep S, Cunningham JM, Srivastava D, Basner-Tschakarjan E, Mingozzi F, High KA, Gray JT, Reiss UM, Nienhuis AW, Davidoff AM. Adenovirus-associated virus vector-mediated gene transfer in hemophilia B. N Engl J Med 365(25):2357-65, 2011. doi: 10.1056/NEJMoa1108046. PMID: 22149959. PMCID: PMC3265081.
Fischer A, Hacein-Bey-Abina S, Cavazzana-Calvo M. 20 years of gene therapy for SCID . Nat Immunol 11(6):457-60, 2010. doi: 10.1038/ni0610-457. PMID: 20485269.
Throm RE, Ouma AA, Zhou S, Chandrasekaran A, Lockey T, Greene M, De Ravin SS, Moayeri M, Malech HL, Sorrentino BP, Gray JT. Efficient construction of producer cell lines for a SIN lentiviral vector for SCID-X1 gene therapy by concatemeric array transfection. Blood 113(21):5104-10, 2009. doi: 10.1182/blood-2008-11-191049. PMID: 19286997. PMCID: PMC2686181.
There’s a powerful story behind every headline at Ohio State Health & Discovery. As one of the largest academic health centers and health sciences campuses in the nation, we are uniquely positioned with renowned experts covering all aspects of health, wellness, science, research and education. Ohio State Health & Discovery brings this expertise together to deliver today’s most important health news and the deeper story behind the most powerful topics that affect the health of people, animals, society and the world. Like the science and discovery news you find here? You can support more innovations fueling advances across medicine, science, health and wellness by giving today.
BROUGHT TO YOU BY
- The Ohio State University
- College of Dentistry
- College of Medicine
- College of Nursing
- College of Optometry
- College of Pharmacy
- College of Public Health
- College of Veterinary Medicine
- Ohio State Wexner Medical Center
- Ohio State's Comprehensive Cancer Center – James Cancer Hospital and Solove Research Institute
Subscribe. The latest from Ohio State Health & Discovery delivered right to your inbox.

How gene therapy changed everything for child born with AADC deficiency
Ohio state researchers deliver life-changing treatment for genetic disorder.
- Share on Facebook
- Share on Linkedin
- Share via Email
- Share this page
Soon after Rian was born , her parents noticed she wasn’t developing at the same pace that her older sibling had. She didn’t move or bat at toys. Her hands remained in tiny fists long after babies typically become more dexterous.
After countless tests — MRIs, blood samples, biopsies and more — and screening for well over a thousand diseases, she was diagnosed at 11 months old with aromatic L-amino acid decarboxylase (AADC) deficiency.
Meanwhile, Krystof Bankiewicz, MD, PhD , and Russell Lonser, MD , had been helping developing a gene therapy for AADC . Drs. Bankiewicz and Lonser invented a surgical technique to deliver the gene therapy to the right spot in the brain, so that the body could begin properly producing dopamine and serotonin.
At 5, Rian was able to receive this surgery, and her mother says she was reborn. She was soon able to hold up her head. Reach for toys. Sit. Roll. Walk.
Dr. Bankiewicz, director of the Brain Health and Performance Center at The Ohio State Unviersity Wexner Medical Center and a professor at The Ohio State University College of Medicine , and Dr. Lonser, a neurosurgeon at the Ohio State Wexner Medical Center and chair of the Department of Neurosurgery at the Ohio State College of Medicine, continue to treat children with AADC through their work at the Neurological Institute at Ohio State.
Their clinical trials underway in gene therapy research aim to develop similar treatments for people with muscle movement and brain disorders such as Parkinson’s , Alzheimer’s and Huntington’s diseases.
See Rian's progress in the video above .
When you give to The Ohio State University Wexner Medical Center, you’re helping improve lives
We’re committed to making advancements in research, education and patient care that will have an impact throughout Ohio and the world.
- AADC Deficiency ,
- Brain Disorders ,
- College of Medicine ,
- Gene Therapy ,
- Movement Disorders ,
- Neurological Disorders ,
- Neurology ,
- Discovery & Innovation
- Treatment Advances
Related websites
Recent videos.

Does epilepsy always cause seizures, and do they affect everyone the same?
By Danielle Becker, MD, MS
What is dilated cardiomyopathy and who does it affect?
Articles on discovery & innovation.

Why join a clinical trial?
By John L Hays, MD, PhD
Clinical trials make new medications and treatments available. Find out how clinical trials work from an Ohio State cancer researcher.

New ultra-high-frequency ultrasound improves lymphedema treatment
By Roman Skoracki, MD
The James at Ohio State is one of few institutions able to treat lymphedema (debilitating swelling) with a new ultrasound technology that’s more precise than ever.
Studying the intersection of obesity and pancreatic cancer to unlock early warning signs
By Wendy Margolin
How clinical trials work
By Julie Johnson, PharmD
Accelerating the pace of heart and lung research and discovery
By Beth Harvilla
Get articles and stories about health, wellness, medicine, science and education delivered right to your inbox from the experts at Ohio State.
Required fields
Tell us more about yourself
By clicking "Subscribe" you agree to our Terms of Use . Learn more about how we use your information by reading our Privacy Policy .
Stealing Strategies from Cancerous T Cells May Boost Immunotherapy
March 20, 2024 , by Sharon Reynolds
CAR T cells (yellow) may get a boost in cancer-killing abilities from the addition of mutations found in blood-cancer cells.
For some people with blood cancers like leukemia and lymphoma, CAR T-cell therapies have proven to be a transformative treatment. But for solid tumors like breast, colorectal, or pancreatic cancer, which make up about 90% of cancer cases, success with T-cell therapies has been harder to come by.
One big reason for these failures is that T cells , the immune system’s primary defense against infected and diseased cells, often become weakened and incapacitated in the toxic environment found within and around solid tumors. Researchers have been exploring many ways to help CAR T cells and other experimental T-cell therapies survive within these hostile surroundings, known as the tumor microenvironment .
In a new study, an NCI-funded research team showed the promise of one such tactic: looking to the genetic changes that cancerous T cells themselves use to stay alive and grow. Incorporating those genetic changes into T-cell therapies, the team found, may make them better cancer killers .
When tested in mice, T cells engineered to have one specific genetic alteration the team discovered in cancerous T cells gave the engineered cells “superpowers,” said Jaehyuk Choi, M.D., Ph.D., of Northwestern University, who co-led the study.
Adding the genetic change, a fusion of parts of two genes, helped the engineered T cells divide faster, kill more tumor cells, and survive for more than a year in the treated mice. And, importantly, it didn’t make the T cells behave like cancer cells, the researchers reported February 7 in Nature .
“When we added [this] single mutation, we didn’t see the sort of unrestrained [T-cell] growth [you see in cancer], but it gave [the engineered] T cells capabilities that they don’t naturally have,” explained the study’s other leader, Kole Roybal, Ph.D., of the University of California San Francisco.
The first two decades of T-cell therapy research focused on the basics, explained Rosa Nguyen, M.D., Ph.D., who studies cellular therapies in NCI’s Center for Cancer Research but was not involved in this study. That work included figuring out what molecules on cancer cells can be targeted by T cells and how to change T cells to better identify such targets, as is done in CAR T-cell therapies .
“Now people are getting super creative in coming up with different things [to add] to these cells to make them work better,” Dr. Nguyen said. “That’s what the field is moving toward now.”
Harnessing nature’s survival strategies
Any type of cell in the body has the potential to turn cancerous, even immune cells. As its name implies, the blood cancer called T-cell lymphoma starts in T cells.
These cancerous T cells have something many normal T cells often lack: the ability to thrive in the hostile environment of a tumor. That environment can include other immune cells that actually work to slow down or disable T cells, as well as other cells and molecules that make it hard for T cells to function.

First Cancer TIL Therapy Gets FDA Approval for Advanced Melanoma
The new treatment, lifileucel, was originally developed by NCI researchers and is the first cell therapy approved for a solid tumor.
Dr. Choi’s lab has been studying the survival traits of T-cell lymphomas for over a decade. “It’s … amazing how these T-cell cancers have developed ways to protect themselves,” he explained.
From the perspective of developing a T cell – based therapy, many of the mutations found in cancerous T cells provide an additional advantage, Dr. Choi explained: Any one of them, on its own, is not likely to direct a cell to become cancerous.
Their years of research clearly showed that “nature has already done this massive experiment to make [cancerous] T cells stronger,” he explained. So “we thought maybe [nature] can show us the way” to improve T-cell therapies.
Better, faster-acting, and safe T cells
Joining forces with Dr. Roybal’s lab, which specializes in T-cell engineering, the researchers first carefully analyzed a wide range of cancerous T cells from T-cell lymphomas, looking for genetic alterations that appeared to help them survive in that tumor microenvironment.
They initially found 71 candidate alterations. In further laboratory experiments, they engineered CAR T cells to have some of the most promising candidate alterations, and this achieved what the researchers had hoped: They increased the CAR T cells’ ability to kill cancer cells and keep creating more CAR T cells.
Additional work revealed what appeared to be the most promising alteration: a fusion of parts of two genes, CARD11 and PIK3R3.
“This single [fusion] activated many things that people have predicted would help [improve] T-cell therapies,” Dr. Choi explained. In experiments in mice, treating them with CAR T cells engineered to express this fusion gene increased the production of molecules that T cells need to survive and function.
And these improvements only occurred when the specific protein recognized by the T cells’ specialized receptor, their chimeric antigen receptor , was present. That is, these extra-engineered CAR T cells would only become supercharged where and when needed inside a tumor.
Improved T cell survival and persistence in solid tumors
The team tested the CAR T cells engineered to express the gene fusion in mouse models of different cancers, including solid tumors like mesothelioma and melanoma. Across those experiments, they found that the treatment was much more effective at shrinking tumors—and keeping them under control for longer—than CAR T cells without the fusion.
“Persistence, the ability to stick around in the tumor microenvironment, is the biggest problem [these cells] solved,” Dr. Choi said. While T cells without the fusion died within a few days, the ones with the fusion “seem to stick around for as long as needed,” he said.
The treatment was very effective even though the mice didn’t also get chemotherapy, Dr. Choi pointed out. That is important because currently, “almost everyone who gets treated with [T-cell therapies] needs to have what’s called conditioning chemotherapy beforehand,” Dr. Choi explained. But this chemotherapy can cause side effects, often severe enough that patients have to wait longer to get the T-cell treatment or possibly preventing them from doing so at all.
“If we ever want these sorts of therapies to be given in less specialized centers, or even in the outpatient setting, we need to get rid of these cumbersome techniques [like conditioning chemotherapy] that are toxic to patients,” added Dr. Roybal.
The researchers also engineered the fusion into a different type of T cell – based immunotherapy, called TCRs, and saw similar results.
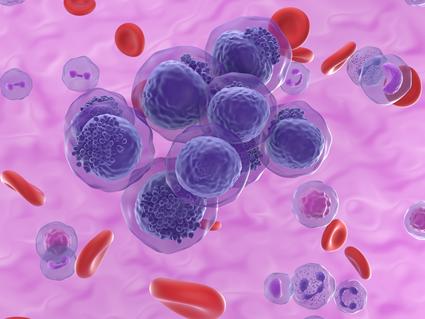
One CAR T-Cell Therapy for Blood Cancers?
Using CRISPR, researchers have developed a potential “universal” immunotherapy for blood cancers like leukemia and lymphoma.
In a mouse model of melanoma, for example, TCR T cells with the fusion gene flowed into tumors in much greater numbers and killed tumor cells much more effectively than TCR T cells without the fusion gene. The TCR T cells with the fusion even showed this advantage at starting doses 20 to 100 times lower than TCR T cells without the fusion.
Being able to give a lower dose of a T-cell therapy would provide another safety advantage for patients, Dr. Roybal explained. Current CAR T-cell therapies, which are given in large doses, have the potential to cause a dangerous—or even fatal—immune system overreaction called cytokine release syndrome . That risk would likely be lower with a smaller dose that ramps up its activity over time, he added.
The researchers also tracked the T cells in the mice for more than 400 days after treatment. Though they initially multiplied rapidly to kill the tumors, their numbers then shrank back down and showed no signs of becoming cancerous themselves.
Testing supercharged T cells in people
The researchers have launched a biotechnology startup to move their CAR T-cell therapy with this gene fusion into human trials, although they are likely 2 to 3 years away from launching these studies, Dr. Roybal explained.
Eventually, researchers may want to try mixing and matching different ways to soup up T cells, Dr. Nguyen said. But these approaches first need to be tested one at a time to better understand how each one works. “We have to use a stepwise approach,” she said.
Drs. Roybal and Choi also want to keep exploring the dozens of other promising mutations their screen initially uncovered.
“We found a lot of different mutations … that could [potentially] be used” in T-cell therapies to treat “a variety of different types of cancer,” said Dr. Roybal.
“Maybe the [CARD11–PIK3R3] fusion protein will be good for [fighting] some subset of solid cancers. And one of the other [mutations] we found will be important for another subset,” he said. “This is the beginning [of this research], not the end.”
Featured Posts
February 22, 2024, by Carmen Phillips
January 23, 2024, by Elia Ben-Ari
January 12, 2024, by Shana Spindler
- Biology of Cancer
- Cancer Risk
- Childhood Cancer
- Clinical Trial Results
- Disparities
- FDA Approvals
- Global Health
- Leadership & Expert Views
- Screening & Early Detection
- Survivorship & Supportive Care
- February (6)
- January (6)
- December (7)
- November (6)
- October (7)
- September (7)
- February (7)
- November (7)
- October (5)
- September (6)
- November (4)
- September (9)
- February (5)
- October (8)
- January (7)
- December (6)
- September (8)
- February (9)
- December (9)
- November (9)
- October (9)
- September (11)
- February (11)
- January (10)

- News & Publications
This Pitt program is leveling up the gene therapy workforce in Pittsburgh

Translational Research Office (TRO)
- For Researchers
- For Industry
- Funding Opportunities
- Translational Education
- UCL Advanced Therapies Symposium

Creating new business links at the largest Advanced Therapies Congress
21 March 2024
The UCL Translational Research Office (TRO) partnered with UCL Business (UCLB), our technology transfer office, to exhibit at this year’s Advanced Therapies Congress at ExCel, London, engaging with experts in cell and gene therapy from around the world.

Photo 1: Dr. Pamela Tranter, Head of the Translational Research Group within the UCL Translational Research Office, spoke at a panel discussion addressing the educational and training needs for the future.
The two-day Advanced Therapies Congress concluded on 20 March 2024, with a record-breaking number of over 2,000 attendees from across the ATMP space exchanging ideas on cell and gene therapy. The TRO was pleased joined hands with UCLB to participate in the event by hosting an exhibition booth, introducing delegates to UCL's extensive translational biomedical network and its partner hospitals, with the aim of fostering connections within the wider ATMP community.
UCL has one of the most extensive Advanced Therapy Medicinal Products (ATMP) pipelines in the world, with over 100 projects in development. Its extensive experimental know-how spans across disciplines, highlighting specialisms in Rare Diseases, Ophthalmology, Haematology/Oncology, Neurology, and Immunology. Twelve successful spinouts in advanced therapeutics, five of which have received collective external investment of over £2bn.
Statistics* also show that 54% of all UK academic-sponsored clinical trials and 43% of all UK commercial-sponsored clinical trials are conducted by UCL partner hospitals, demonstrating UCL’s leading position in delivering these complex therapies.
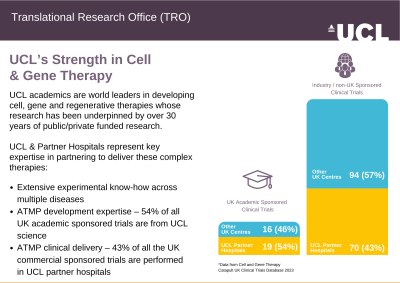
At TRO, our mission is to support and nurture key partnerships in the ecosystem to advance the biomedical therapy pipeline and deliver biomedical impact. We eagerly anticipate continuing conversations with the ATMP community and extend our gratitude to everyone who connected with us at the event, paving the way for potential collaborations.
Contact us: If you are a UCL researcher looking for translational research consultation or funding application support, please contact: Pamela Tranter, [email protected]
If you are an industry partner looking for collaboration opportunities with UCL, please contact: Basma Jeelani , [email protected]

Photo 3 – 4: The event has generated numerous discussions about UCL’s ATMP capabilities and collaboration potential among colleagues from the UCL Translational Research Office, UCL Business, and other ATMP experts attending the event.
Interested to stay informed of upcoming news, events and funding calls?
Subscribe to our newsletter and you would automatically become a member of UCL TINs (Therapeutic Innovation Networks) and be the first to receive our event invitations
Follow us on social media ( LinkedIn , Twitter ) and stay tuned to our news and updates.
Related News
We use cookies to understand how you use our site and to improve your experience. This includes personalizing content and advertising. To learn more, click here . By continuing to use our site, you accept our use of cookies, revised Privacy Policy and Terms of Service .

New to Zacks? Get started here.
Member Sign In
Don't Know Your Password?

- Zacks #1 Rank
- Zacks Industry Rank
- Zacks Sector Rank
- Equity Research
- Mutual Funds
- Mutual Fund Screener
- ETF Screener
- Earnings Calendar
- Earnings Releases
- Earnings ESP
- Earnings ESP Filter
- Stock Screener
- Premium Screens
- Basic Screens
- Research Wizard
- Personal Finance
- Money Managing
- Real Estate
- Retirement Planning
- Tax Information
- My Portfolio
- Create Portfolio
- Style Scores
- Testimonials
- Zacks.com Tutorial
Services Overview
- Zacks Ultimate
- Zacks Investor Collection
- Zacks Premium
Investor Services
- ETF Investor
- Home Run Investor
- Income Investor
- Stocks Under $10
- Value Investor
- Top 10 Stocks
Other Services
- Method for Trading
- Zacks Confidential
Trading Services
- Black Box Trader
- Counterstrike
- Headline Trader
- Insider Trader
- Large-Cap Trader
- Options Trader
- Short Sell List
- Surprise Trader
- Alternative Energy

You are being directed to ZacksTrade, a division of LBMZ Securities and licensed broker-dealer. ZacksTrade and Zacks.com are separate companies. The web link between the two companies is not a solicitation or offer to invest in a particular security or type of security. ZacksTrade does not endorse or adopt any particular investment strategy, any analyst opinion/rating/report or any approach to evaluating individual securities.
If you wish to go to ZacksTrade, click OK . If you do not, click Cancel.
Image: Bigstock
Charles River (CRL) Extends Gene Therapy Deal With NUS Medicine
Charles River Laboratories International, Inc. ( CRL Quick Quote CRL - Free Report ) recently announced a high-quality (HQ) plasmid DNA development and manufacturing agreement with the National University of Singapore’s (“NUS”) Yong Loo Lin School of Medicine (NUS Medicine). The collaboration provides phase-appropriate plasmid DNA to support the development of engineered stem cells for cancer therapy.
The latest development will strongly boost the company’s Biologics Solutions business under the Manufacturing segment.
News in Detail
The prestigious medical education institution, NUS Medicine, has a world-renowned medical research field of stem cell biology and therapy. The collaboration will utilize Charles River’s market-leading contract development and manufacturing organization expertise in HQ and GMP-compliant plasmid DNA, which serves as a critical starting material for its engineered stem cell cancer therapy and builds on a historic provision of research-grade plasmid.

Moreover, NUS Medicine will leverage this collaboration to access Charles River’s center of excellence and established manufacturing platform, eXpDNA. The company is excited to extend its partnership with NUS Medicine and contribute to their groundbreaking efforts in advancing engineered stem cells for cancer therapy. With decades of experience in manufacturing and consistently delivering plasmid DNA, both as a vital starting material and finished drug product, Charles River is dedicated to ensuring the success of customers' programs.
In recent years, the company has significantly expanded its cell and gene therapy portfolio to streamline complex supply chains and meet the growing demand for plasmid DNA, viral vector and cell therapy services. Combined with its legacy testing capabilities, Charles River offers an industry-leading “concept to cure” advanced therapeutic solution, helping developers navigate the path to the clinic and beyond.
Industry Prospects
Per a Research report , the global cell and gene therapy market was valued at $15.46 billion in 2022 and is expected to grow at a compound annual growth rate of 18.3% by 2032.
Other Developments in the Manufacturing Segment
In March, Charles River entered into a comprehensive gene therapy manufacturing collaboration with Navega Therapeutics, Inc. — a preclinical stage company developing epigenetic-regulation gene therapies. As part of Charles River’s Cell and Gene Therapy Accelerator Program, Navega will have access to established CDMO capabilities and advisory services to produce an adeno-associated virus (AAV)-based gene therapy, NT-Z001, for Phase I clinical trials.
Earlier in January 2024, the company expanded its robust bacterial endotoxin testing (BET) portfolio with the addition of a new animal-free testing solution. Building on Charles River’s existing Trillium rCR (recombinant cascade reagent) vial product, the Endosafe Trillium rCR cartridge offering enhances testing efficiency and accelerates manufacturing timelines while simultaneously contributing to the company’s 4Rs imperatives (Replacement, Reduction, Refinement and Responsibility) and further progress the client’s goals on sustainability and animal welfare.
Price Performance
In the past six months, Charles River has mostly outperformed its industry. Shares of the company have rallied 36.3% compared with the industry ’s rise of 13.8%.
Zacks Rank and Key Picks
Charles River carries a Zacks Rank #3 (Hold).
Some better-ranked stocks in the broader medical space are Cardinal Health ( CAH Quick Quote CAH - Free Report ) , Stryker ( SYK Quick Quote SYK - Free Report ) and DaVita ( DVA Quick Quote DVA - Free Report ) . While Cardinal Health and Stryker each carry a Zacks Rank #2 (Buy), DaVita sports a Zacks Rank #1 (Strong Buy) at present. You can see the complete list of today’s Zacks #1 Rank stocks here .
Cardinal Health’s stock has surged 55.8% in the past year. Earnings estimates for Cardinal Health have risen from $7.28 to $7.29 in fiscal 2024 and from $8.02 to $8.04 in fiscal 2025 in the past 30 days.
CAH’s earnings beat estimates in each of the trailing four quarters, delivering an average surprise of 15.6%. In the last reported quarter, it posted an earnings surprise of 16.67%.
Estimates for Stryker’s 2024 earnings per share have remained constant at $11.86 in the past 30 days. Shares of the company have moved 26.2% upward in the past year compared with the industry’s rise of 5.2%.
SYK’s earnings surpassed estimates in each of the trailing four quarters, the average surprise being 5.09%. In the last reported quarter, it delivered an average earnings surprise of 5.81%.
Estimates for DaVita’s 2024 earnings per share have moved up from $8.97 to $9.23 in the past 30 days. Shares of the company have surged 74.7% in the past year compared with the industry’s 22% rise.
DVA’s earnings surpassed estimates in each of the trailing four quarters, the average surprise being 35.57%. In the last reported quarter, it delivered an average earnings surprise of 22.22%.
See More Zacks Research for These Tickers
Normally $25 each - click below to receive one report free:.
Stryker Corporation (SYK) - free report >>
DaVita Inc. (DVA) - free report >>
Cardinal Health, Inc. (CAH) - free report >>
Charles River Laboratories International, Inc. (CRL) - free report >>
Published in
This file is used for Yahoo remarketing pixel add
Due to inactivity, you will be signed out in approximately:
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
Research articles
Adeno-associated virus genome quantification with amplification-free CRISPR-Cas12a
- Zach Hetzler
- Stella M. Marinakos
- Qingshan Wei
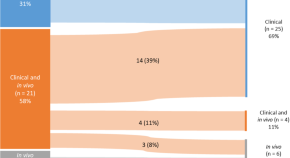
Advancing rare disease treatment: EMA’s decade-long insights into engineered adoptive cell therapy for rare cancers and orphan designation
- Maria Elisabeth Kalland
- Tomas Pose-Boirazian
- Segundo Mariz
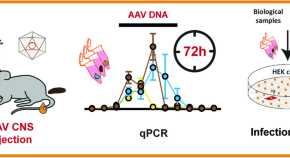
A shedding analysis after AAV8 CNS injection revealed fragmented viral DNA without evidence of functional AAV particles in mice
- Felix Krause
- Katja Schmidtke
- Max O. Rybarski
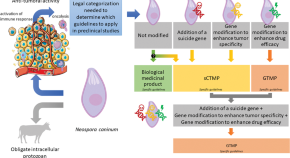
Are genetically modified protozoa eligible for ATMP status? Concerning the legal categorization of an oncolytic protozoan drug candidate
- Mathieu Guerriaud
- Cyril Poupet
- Nathalie Moiré
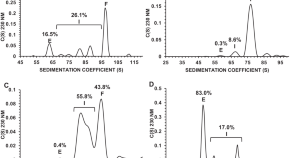
Analytical characterization of full, intermediate, and empty AAV capsids
- Aisleen McColl-Carboni
- Serena Dollive
- James B. McGivney IV
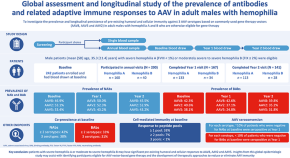
Multicenter assessment and longitudinal study of the prevalence of antibodies and related adaptive immune responses to AAV in adult males with hemophilia
- Ingrid Pabinger
- Mila Ayash-Rashkovsky
- John Chapin

Gene therapy corrects the neurological deficits of mice with sialidosis
- Wuh-Liang Hwu
- Karine Chang
- Yin-Hsiu Chien

Development of a stable Sf9 insect cell line to produce VSV-G pseudotyped baculoviruses
- María del Pilar Plastine
- Sabrina Amalfi
- Victoria Alfonso

Preclinical dose response study shows NR2E3 can attenuate retinal degeneration in the retinitis pigmentosa mouse model Rho P23H+/ −
- Shannon M. McNamee
- Natalie P. Chan
- Neena B. Haider

Analysis and comparative evaluation of expedited programs for gene therapy products: insights from the United States, the European Union, Japan, and South Korea
- Hyeokgyo Jeong
- Sujata Purja
- Eunyoung Kim
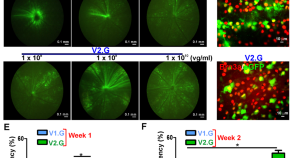
AAV2 vector optimization for retinal ganglion cell-targeted delivery of therapeutic genes
- Brahim Chaqour
- Thu T. Duong
- Ahmara G. Ross
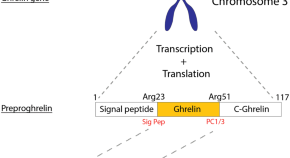
Ghrelin mediated cardioprotection using in vitro models of oxidative stress
- Cindy Y. Kok
- George Ghossein
- Eddy Kizana
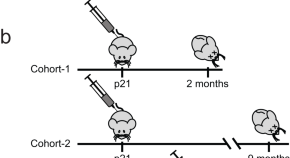
CSTB gene replacement improves neuroinflammation, neurodegeneration and ataxia in murine type 1 progressive myoclonus epilepsy
- Emrah Gumusgoz
- Sahba Kasiri
- Berge A. Minassian

Distributional comparison of different AAV vectors after unilateral cochlear administration

Engineered compact pan-neuronal promoter from Alphaherpesvirus LAP2 enhances target gene expression in the mouse brain and reduces tropism in the liver
- Carola J. Maturana

Modeling Glutaric Aciduria Type I in human neuroblastoma cells recapitulates neuronal damage that can be rescued by gene replacement
- A. Mateu-Bosch
- E. Segur-Bailach

Overexpression of KCNN4 channels in principal neurons produces an anti-seizure effect without reducing their coding ability
- Evgeny S. Nikitin
- Tatiana Y. Postnikova
- Aleksey V. Zaitsev
Approval and therapeutic value of gene therapies in the US and Europe
- Kerstin N. Vokinger
- Camille E. G. Glaus
- Aaron S. Kesselheim
Successes and challenges in clinical gene therapy
- Donald B. Kohn
- Yvonne Y. Chen
- Melissa J. Spencer
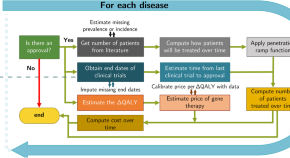
The estimated annual financial impact of gene therapy in the United States
- Chi Heem Wong
- Rena M. Conti
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Asian J Pharm Sci
- v.16(6); 2021 Nov
Applications and developments of gene therapy drug delivery systems for genetic diseases
Genetic diseases seriously threaten human health and have always been one of the refractory conditions facing humanity. Currently, gene therapy drugs such as siRNA, shRNA, antisense oligonucleotide, CRISPR/Cas9 system, plasmid DNA and miRNA have shown great potential in biomedical applications. To avoid the degradation of gene therapy drugs in the body and effectively deliver them to target tissues, cells and organelles, the development of excellent drug delivery vehicles is of utmost importance. Viral vectors are the most widely used delivery vehicles for gene therapy in vivo and in vitro due to their high transfection efficiency and stable transgene expression. With the development of nanotechnology, novel nanocarriers are gradually replacing viral vectors, emerging superior performance. This review mainly illuminates the current widely used gene therapy drugs, summarizes the viral vectors and non-viral vectors that deliver gene therapy drugs, and sums up the application of gene therapy to treat genetic diseases. Additionally, the challenges and opportunities of the field are discussed from the perspective of developing an effective nano-delivery system.
Graphical abstract
Types of gene therapy drugs, viral and non-viral delivery strategies, and disease treatment status of gene therapy drugs.

1. Introduction
Typically, the deepened knowledge of genetic materials offers an innovative perspective for understanding disease occurrence and treatment. Genetic diseases are caused by genetic material changes or controlled by disease-causing genes, which are wholly or partly determined by genetic factors. Genetic diseases are classified into monogenic diseases and polygenic diseases. Monogenic diseases are caused by a pair of essential genes in accordance with Mendelian laws of inheritance, such as hemophilia and huntington's disease [ [1] , [2] , [3] – 4 ]. Polygenic diseases are controlled by two or more pairs of genes affected by the environment, such as diabetes and malignant tumors [ 5 , 6 ]. Although drugs can suppress the symptoms of genetic diseases, they cannot achieve the fundamental effect of treatment. On the grounds that the complexity of the pathogenesis and the lack of medicines, genetic diseases have imposed a heavy burden on families and society, so the treatment of genetic diseases has always been a concern of biomedical scientists. Researchers have been exploring the solution to genetic diseases by modifying and repairing the disease-causing gene, that is, gene therapy.
Gene therapy is one of the most revolutionary medical technologies developed with DNA recombination technology and gene cloning technology [7] . It is a biomedical treatment method based on changing human genetic material. For genetic diseases, gene therapy can directly repair or even replace the disease-causing genes at the molecular level, restoring defective protein. After decades of development, gene therapy has shown great potential in treating significant diseases caused by genetic defects and genetic abnormalities such as malignant tumors, acquired immunodeficiency syndrome, and cardiovascular diseases.
At present, gene therapy drugs mainly include plasmids DNA, small interfering RNA (siRNA) [8] , microRNA (miRNA), short hairpin RNA (shRNA), antisense oligonucleotide (ASO), and CRISPR/Cas9 system. With the development of gene therapy and the improvement of innovative vectors, gene therapy drug products have been resoundingly approved by the Food and Drug Administration (FDA), such as Kynamro, Imlygic, Spinraza, Exondys51, Yescarta, Kymriah, Zolgensma, and so on ( Table 1 ) [9] . Despite the dawn of gene therapy, its delivery systems still face many difficulties, limiting the widespread clinical application. Usually, the target site of activity for gene therapy drugs is a specific organelle or intracellular location. Thus, one of the main challenges of gene therapy is to deliver gene therapy drugs to working sites, but naked gene therapy drugs have the following disadvantages: (1) Easily degraded by RNase in serum; (2) Recognized by serum immunologically active factors and phagocytosed by mononuclear macrophages; (3) Interact with serum proteins; (4) Renal Clearance; (5) Poor tissue targeting and cell uptake capacity; (6) Low endosomal escape and intracellular release efficiency [10] . However, with the development of materials science and nanotechnology, numerous novel viral vectors and non-viral vectors are used for gene therapy drug delivery to solve above obstacles.
Gene therapy drugs approved by the FDA and in clinical trials.
Currently, the main gene delivery systems are viral vectors and non-viral vectors [ [11] , [12] – 13 ]. Viral vector systems include retroviruses [14] , adenoviruses (AdV) [15] , adenovirus-associated viruses (AAV) [ 16 , 17 ], lentiviruses (LV) [18] , bacteriophages and the like. Most of the gene therapy drugs currently on the market use viruses as vectors. Although viral vectors have the disadvantages of high immunogenicity, safety hazards, and production difficulties, their higher transfection efficiency is the unique advantage for gene delivery. Non-viral vectors are favored by researchers profiting from large gene load, low immunogenicity, and high safety for large-scale production. Commonly used non-viral carriers include cationic liposomes, micelles [19] , polymers, and inorganic nanoparticles. With the rise of biomaterials, innovative nanocarriers have been reported, such as DNA nanoclews [20] , metal organic frameworks [21] , cell membrane, and so on [22] . With the deepening of research, the modified nanocarriers have better performance, which can not only improve the drug loading and gene therapy effect, but also induce higher biological safety and higher targeting characteristics than viral vectors. Therefore, it is necessary to find a suitable carrier loaded with gene therapy drugs to overcome the bottleneck encountered during the delivery process.
In this review, we first introduce the gene therapy drugs and their current application progress. Then we narrate the delivery systems of gene therapy drugs, including virus delivery and non-virus delivery. Next, we systematically summarize the research progress of gene therapy drugs in the field of genetic disease treatment. Finally, the challenges and opportunities associated with gene therapy are discussed from multiple perspectives.
2. Gene therapy drugs
At present, most of the targets of conventional drugs are proteins expressed by disease-causing genes, such as enzyme inhibitors and antibodies. In contrast, gene therapy drugs can correct gene transcription and translation processes at the DNA or mRNA level and occupy a far-reaching clinical treatment position. This section shall discuss several of the most commonly studied gene therapy drugs, including siRNA, miRNA, plasmid DNA (pDNA), ASO, CRISPR/Cas9, and the like. Table 2 illustrates some advances in the use of gene therapy drugs for genetic diseases in recent years.
Summary of gene therapy drugs for genetic diseases.
2.1. Small interfering RNA (siRNA)
RNA interference (RNAi) is a new technology developed in recent years that can block the expression of specific genes and has excellent potential in gene therapy [45] . When the endogenous or exogenous double-stranded RNA enters the cell, it is processed into 21–23 nucleotide siRNA by Dicer enzyme in the cytoplasm. The antisense strand binds to the RNA-induced silencing complex (RISC) containing various nucleases [46] . Next, the siRNA is untwisted and the siRNA targeting sequence on the RISC complex is used as a guide to digest mRNA. The digested fragments are non-specifically degraded by nucleases in the cytoplasm, which silences the gene and prevents specific protein expression. The therapeutic effect of siRNA is through interaction with mRNA rather than protein, which reduces harmful proteins produced before synthesis. Moreover, the regulation of different target genes by changing the sequence of siRNA can be applied to many major human diseases [47] .
SiRNA is easily degraded by enzymes, filtered by the kidneys, and engulfed by host cells. Besides, its immunogenicity and membrane passing capacities are insufficient, limiting its clinical transformation [48] . Nanocarriers have gradually become a potential tool for siRNA system gene therapy to deliver siRNA to specific cells efficiently. Non-viral carriers of siRNA include cationic lipid polymers, polypeptides, polyethyleneimine (PEI) and nucleic acid self-assembly carriers [49] . The nucleic acid self-assembly carrier can overcome the rigid structure of siRNA, increase the negative charge of siRNA to increase the loading of siRNA, and significantly improve gene silencing efficiency. Bujold et al. assembled a prismatic DNA nanocage and wrapped siRNA in a responsive gated DNA strand structure to avoid nuclease degradation. The anti-apoptotic factors Bcl-2 and Bcl-xl antisense nucleotide chains were used to control the release of siRNA. The FRET method at the molecular level proved that the assembled DNA nanocage could effectively release therapeutic genes such as siRNA ( Fig. 1 ) [50] .

Schematic illustrations of the siRNA-encapsulating prism and release mechanism. Reprinted with permission from [50] . Copyright 2016 American Chemical Society.
2.2. MicroRNA (miRNA)
MiRNA is a non-coding small RNA of about 19–22 nt encoded by the cell genome of eukaryotic organisms. It regulates gene expression by promoting the degradation of target mRNA or inhibiting mRNA translation, ultimately affecting the development, proliferation, differentiation, and apoptosis of cells [51] . The mechanism of miRNA is to combine with miRNA-induced silencing complex(miRISC) on the target mRNA to form an asymmetric RISC. Studies have shown that miRNA recognizes the 3′ untranslated region (3′UTRs) of target mRNA, and binds to miRISC under the catalysis of RISC endonuclease, thereby inhibiting the translation of target mRNA [52] .
MiRNA plays a vital role in the treatment of genetic diseases, especially tumors. Zhao et al. sequenced the miRNAs involved in the pathogenesis of hepatoma carcinoma cells and found that miR-451a expression was significantly down-regulated in hepatoma carcinoma cells. As a tumor suppressor, miR-451a acts on the downstream essential target lipoprotein 1 (lpin1) and promotes the apoptosis of hepatoma carcinoma cells and endothelial cells [53] . Li et al. found that the overexpression of miRNA-218 reduced the kidney damage and the levels of IL-6, TNF-α, IL-1β, and MCP-1 in the mouse podocyte model of diabetic nephropathy [44] . The dual-luciferase reporter gene assay confirmed that miR-218 targeted the mRNA encoding IKK-β and regulated NF-κB-mediated inflammation. Furthermore, miRNA can treat cardiovascular diseases by regulating heart development, remodeling and regeneration, endothelial function, and angiogenesis [54] . Samanta et al. reported that miR-124 and miR-135a are involved in regulating blood pressure by weakening the signal transduction of the renin-angiotensin-testosterone system [55] . Many miRNAs, including miR-17-3p, miR-31, and miR-126, regulate vascular inflammation by regulating E-selectin expression, intercellular cell adhesion factor 1, and vascular cell adhesion factor 1 [56] . Moreover, Dwivedi reported that specific miRNAs (miR-941, miR-589) in the blood could be used as clinical biomarkers to diagnose major depression [57] .
2.3. Antisense oligonucleotide (ASO)
ASO is a molecular drug that inhibits gene expression by specifically binding to the target gene DNA or mRNA, and regulates it at the gene level. The mechanism of ASO is through complementary binding to the target mRNA nucleotide sequence, and part of the DNA sequence from synthetic antisense oligonucleotides binds to the target mRNA to form a DNA-RNA hybrid. Finally, it attracts endogenous RNase H to this site, shears and degrades the target mRNA, thereby reducing the expression of the target gene. Up to now, there are four antisense oligonucleotide drugs approved by the FDA for marketing: fomivirsen sodium, mipomersen sodium, eteplirsen and nusinersen sodium. Eteplirsen became the first phosphoramidite morpholino oligonucleotide approved for the treatment of duchenne muscular dystrophy (DMD). Subsequently, nusinersen sodium is approved by the FDA for the treatment of spinal muscular atrophy (SMA). ASO lays the foundation for the rapid development of the nucleic acid drug market, and promotes nucleic acid to become the third promising drug after small molecule drugs and protein drugs.
ASO drugs have a place in clinical applications and studies are continuing and making progress. Yang et al. studied biodegradable lipid nanoparticles to deliver ASO to cultured human cells and animal models. The proprotein convertase subtilisin/kexin type 9 (PCSK9) was selected as the therapeutic target, and the results showed that the delivery system had a high gene knockout efficiency. This bioreducible lipid is a valuable candidate for ASO delivery and provides new ideas for the development of ASO-based therapies [43] . Leitner et al. prepared a positively charged ethyl cellulose nanoemulsion and successfully complexed with ASO. In vitro transfection tests showed that transfection efficiency of 40% could be obtained when the N/P ratio in serum-free medium was 28. The complexes are expected to take effect in vitro diagnostic tests and in vivo gene therapy [44] .
2.4. CRISPR/Cas9
CRISPR/Cas9 system is mainly composed of Cas9 protein and single-stranded guide RNA (sgRNA). In the presence of protospacer adjacent motif (PAM), Cas9 protein can reach different target sites through base complementary pairing under the guidance of sgRNA, and cleave the target gene to achieve DNA double strand break (DSB) [58] . At present, the delivery of CRISPR/Cas9 system can be divided into three levels based on plasmid, RNA and protein. Delivery of plasmids encoding Cas9 protein and sgRNA does not require multiple transfections, which is convenient and stable; delivery of mRNA encoding Cas9 protein has lower off-target rate than delivery plasmid; direct delivery of Cas9 protein has low immunogenicity. The pDNA-based CRISPR/Cas9 system has become an extremely attractive tool due to its simple operation and low cost. However, the size of the encoded pDNA and the transcription process will significantly hinder the delivery of the system and reduce the efficiency of gene editing. For the CRISPR/Cas9 system, the most efficient way is to skip pDNA or mRNA expression on Cas9 protein and sgRNA and directly deliver the Cas9/sgRNA ribonucleoprotein (RNP) to minimize off-target effects. Viral vectors are most commonly used to deliver the CRISPR/Cas9 system, followed by physical methods such as electroporation, microinjection, and tail vein high pressure injection. Ghassemi et al. constructed plasmids encoding Cas9 protein and double sgRNA, aiming to target the exon 2 and 3 sites of the broken Hbb-bs gene. The recombinant plasmid was delivered to the fertilized eggs by microinjection, and then the fertilized eggs were implanted into pregnant mice for progeny screening and genotyping. Finally, a β-thalassemia mouse model with Hbb-bs gene knockout was established ( Fig. 2 ) [59] .

General overview and timing. (A) sgRNA design. (B) Vector construction. (C) Microinjection and genotyping. Reprinted with permission from [59] . Copyright 2019 Elsevier.
With the development of nanotechnology in recent years, non-viral vectors of the CRISPR/Cas9 system have effectively delivered to cells and tissues in vivo and in vitro . Mout et al. used arginine gold nanoparticles (ArgNPs) to achieve the co-delivery of Cas9 protein and sgRNA, effectively delivering RNP to the cytoplasm. Subsequently, it was transported to the nucleus, which achieved a delivery efficiency of up to 90% and a gene editing efficiency of 30% [60] . Among organic materials, cationic liposomes are widely used due to their high gene load and transfection ability. Cho et al. designed the sgRNA targeting dipeptidyl peptidase-4 gene (DPP-4) and encapsulated with lecithin cationic liposomes. Intravenous injection into type 2 diabetic mice could significantly destroy the DPP-4 gene, accompanied by normalization of blood glucose levels and reduction of liver and kidney damage [61] .
In order to better achieve the delivery of CRISPR/Cas9 system, the modification of Cas9 protein and sgRNA has also been widely studied. The modified Cas9 protein and sgRNA can reduce the off-target rate and increase stability. Ferdosi et al. combined the hydrophobicity of T cell receptor contact residues with HLA, and identified two immunodominant SpCas9 T cell epitopes of HLA-A* 02:01 through an enhanced prediction algorithm. The study found that SpCas9 protein modification can eliminate immunity dominant epitope while retaining its function and specificity [62] . In addition to modifying Cas9 protein, sgRNA also can be shortened from 20 nt to 17 nt to reduce the off-target rate. After synthesizing 100 nt full-length sgRNA, Hendel et al. performed three different chemical modifications of 2′-O-methyl (M), 2′-O-methyl 3′phosphorothioate (MS), or 2′-O-methyl 3′thioPACE (MSP) at both termini. The results showed that chemical modification of sgRNA could enhance genome editing efficiency of human primary T cells, CD34 + hematopoietic stem cells, and progenitors cells [63] .
2.5. Other gene therapy drugs
ShRNA consists of two short inverted repeats and a stem-loop sequence in the middle to form a hairpin structure. With relatively high viral infection efficiency, shRNA remains stable through virus-mediated transduction. After transduction, the Dicer enzyme in the cell is used to trigger gene silencing in the nucleus. Compared with siRNA, although it has a higher curative effect and a longer lasting effect, the transfection efficiency is low and preparation is time-consuming. Zhang et al. used cationic liposomes to deliver TLR4 shRNA (VA-lip-shRNA-TLR4), induced mitochondrial apoptosis of pancreatic stellate cells, and achieved the purpose of treating pancreatic fibrosis [64] .
Inserting a therapeutic gene into a plasmid and introducing it into a target cell is considered a safer and more convenient treatment method. The gene plasmid containing the foreign antigen is directly introduced into the animal body so that it can express the antigen protein in the host cell and induce the human body to produce an immune response. The pCMFO/DMT complex prepared by Tian et al. resulted in a longer duration of DNA release in the DNA-DMT complex. The results showed that mice vaccinated with pCMFO/DMT caused a biased response to Th1 and a significant increase in CFMO-specific IL2 + T CM cell response in the spleen. pCMFO/DMT is a very promising tuberculosis vaccine and requires further preclinical and clinical trials [65] .
According to the physical properties and mechanism of action, gene therapy drugs vary in drug delivery and gene knockout efficiency in diverse cell lines targeting various genes [66] . Therefore, it is necessary to select suitable gene therapy drugs for specific cell lines and target genes. From the perspective of drug knockout efficacy, the CRISPR/Cas9 system can remove the DNA molecules of the target gene to achieve gene knockout without any mRNA background, while the other gene drugs can only target mRNA molecules interfere at the RNA level with uncertain effects. From the perspective of drug delivery, most gene drugs are negatively charged to hinder drug delivery efficiency, and particle size is an nonnegligible factor. Among gene drugs, nucleic acids of small molecules such as siRNA, miRNA, shRNA, ASO are convenient in terms of drug delivery efficiency thanks to their small size, but the sizeable molecular weight of CRISPR/Cas9 system or pDNA is an urgent problem to be solved in the delivery process. In addition to CRISPR/Cas9 with nuclear localization signals (NLS) to assist the system in entering the nucleus, other free gene drugs based on RNA background cannot achieve target delivery. In short, the current various delivery tools adopt the strategy of maximizing strengths and avoiding weaknesses for each gene therapy drug to accelerate the pace of gene therapy.
3. Viral delivery strategies for gene therapy drugs
In recent years, viral vectors of gene therapy drugs have been widely used in vivo and in vitro due to their high transfection efficiency and stable transgene expression. Commonly used viral vectors include AAVs, AdVs, LVs and bacteriophages. The latest research progress of non-viral vectors is summarized in Table 3 .
Viral delivery strategies for gene therapy drugs.
3.1. Adeno-associated virus (AAV)
AAV is a non-enveloped double-stranded DNA virus with good biological characteristics, genetic stability, high gene transduction efficiency and large-scale ease of use. However, the packaging limit of AAV is only 4.5 kb, the production process is complicated, and the cost is high, so the application of AAV vectors has certain restrictions. In the research of AAV for gene therapy, it is necessary to improve the efficiency of gene therapy and reduce cytotoxicity as much as possible to explore the optimal targeting strategy of AAV vector-mediated gene therapy. There are currently three strategies for optimizing the targeting of AAV infection: genetic modification; targeted regulation at the transcription level; covalent coupling modification on capsid protein.
Genetic modification is the most commonly used method to confer the targeting ability of AAV vectors. Yoon et al. transduced the CRISPR/Cas9 system into mouse embryos by recombinant adeno-associated viruses (rAAVs) to target Tyr locus, resulting in genetically modified mice. rAAVs do not require a lengthy process of embryo isolation, microinjection, embryo culture and transfer to pseudo-pregnant females, thereby facilitating gene editing in mice and other mammals more conveniently [67] . Gene therapy using AAV vectors has broad prospects for treating DMD. Bengtsson et al. used AAV to construct a Cas9 and sgRNA system that can deliver muscle-targeting genes, edit mutations in dystrophic mdx4cv mice, and complete HDR-mediated Duchenne muscle nutrition in vivo . The results indicate that AAV-mediated muscle-specific gene editing has excellent potential for treating neuromuscular diseases ( Fig. 3 ) [68] . Ma et al. studied AAV-mediated TNF-related apoptosis-inducing ligand (TRAIL) and miR-221-Zip co-expressed gene therapy to overcome the drug resistance of TRAIL-induced apoptosis of liver cancer cells. AAV-TRAIL combined with miR-221-Zip combination therapy, has become a new method of therapeutic intervention for liver cancer [69] .

Systemic gene editing results in widespread dystrophin expression. Reprinted with permission from [68] . Copyright 2017 Springer Nature.
3.2. Adenovirus (AdV)
AdV is an unenveloped double-stranded DNA virus with an icosahedral nucleocapsid structure. Due to the wide range of AdV hosts, easy purification, genetic stability, and large foreign gene loading capacity, about 25% of the viral vectors used in clinical gene therapy are AdV vectors. Ehrke-Schulz et al. used high-capacity adenoviral vectors (HCAdV) as vectors, which did not express any viral genes that reduced immunogenicity. This study constructed human papilloma virus (HPV) oncogene E6 , DMD dystrophin-related gene, HIV co-receptor CC chemokine receptor type 5 (CCR5) gene-targeted CRISPR/Cas9 delivery system. The highest gene insertion-deletion can reach 93%, but the HCAdV delivery CRISPR/Cas9 system has not yet been applied in vivo [70] . Tan et al. immunized transgenic mice by constructing a recombinant AdV vector carrying the hepatitis B core antigen (HBcAg) and TPPII genes (Adv-HBcAg-TPPII) to evaluate the specific immune response induced by them and the antiviral ability of the transgenic mice. The results show that Adv-HBcAg-TPPII can break the immune tolerance, stimulate the activity of HBV-specific cytotoxic T lymphocytes, and has a better therapeutic effect in transgenic mice [75] .
3.3. Lentivirus (LV)
LV is a spherical structure composed of single-stranded RNA with an encapsulation volume of about 8 kb and has been widely used to deliver gene therapy drug systems. LVs are the same as AdVs, which delete all genes so as not to activate the immune system. As a delivery vehicle for genetic drugs, LV integration of the host genome may lead to unnecessary non-target insertion mutations, which poses a safety risk. At present, most laboratories cannot prepare non-genomic integrated LV vectors, so LV is used less frequently than AAV and AdV, and it is most commonly used to establish disease models.
Integration-deficient lentiviral vectors (IDLV) retains the high transduction efficiency of LVs and reduces insertion mutations. Ahmed et al. confirmed that IDLVs could efficiently transduce spinal motor neurons, which may provide a new strategy for treating inherited early childhood neurodegenerative diseases ( Fig. 4 ) [71] . Zhao et al. studied the expression of silenced CLDN1 in two breast cancer cells (MDA-MB-231 and MCF7) by LV-mediated RNA interference. The results indicate that CLDN1 RNA interference mediated by lentiviral vectors can control tumor cell growth by inhibiting epithelial-mesenchymal transition (EMT), demonstrating great potential in breast cancer gene therapy [76] . Lu et al. developed a lentivirus-like bionanoparticle (LVLP) vector that can encapsulate up to 100 mRNAs expressing SaCas9 protein. Compared with cells transduced with adeno-associated virus or LV expressing SaCas9, cells that were transduced with LVLP containing SaCas9 mRNA had a lower off-target rate [72] .

Schematic diagram of gene editing of integrated lentiviral vector. Reprinted with permission from [71] . Copyright 2018 Elsevier.
3.4. Bacteriophages
Phage vectors can achieve targeted gene delivery, and can be used for gene therapy target discovery and multi-drug resistance research. However, due to its narrow host selectivity and lower gene delivery efficiency than animal viruses, research applications are relatively few, and most are used in combination with other viral vectors. Suwan et al. modified the viral capsid structure of phage vectors and synthesized a multifunctional mixed adeno-associated virus/phage (AAVP) vector. This directed evolutionary genetic strategy can give the next generation of AAVP particles the ability to neutralize antibodies, escape lysosomal degradation and avoid the pre- and post-internalization barriers of transduction, improving delivery efficiency [73] . Przystal et al. inserted the human AAV single-stranded genome into the M13 phage single-stranded genome to form a bacteriophage capsid (AAVP) containing the AAV genome. This phage vector can double-target therapeutic gene glioma, which provides new ideas for the treatment of glioblastoma multiforme (GBM) [74] .
4. Non-viral delivery strategies for gene therapy drugs
Although viral vectors efficiently deliver gene therapy drugs through cell transduction, their safety issues such as high immunogenicity and high mutation risk also limit their clinical transformation. Generally, to enhance transfection efficiency, the ingenious design of non-viral vectors makes up for the defects of gene therapy drugs. Besides, the ideal gene therapy drug carrier should have the ability to protect the nucleic acid drugs, extend half-life, improve targeting, enhance endosomal escape, and intracellular release. Compared with viral vectors, non-viral vectors are more adaptable, can overcome the problems mentioned above simultaneously and have a broader range of applications. Herein, the delivery strategy is outlined and divided into synthetic nanocarriers and endogenous nanocarriers according to the source of carrier materials ( Table 4 ).
Non-viral vector delivery strategies for gene therapy drugs.
4.1. Synthetic nanocarrier
Synthetic nanocarriers are the most widely used non-viral nano-delivery carriers. Compared to endogenous nanocarriers, raw materials are easy to obtain and can be produced in large quantities at low cost. At present, synthetic nanocarrier technology is relatively mature, and corresponding gene therapy drugs have been launched, such as Patisiran [84] .
4.1.1. Liposome
Liposomes are formed by the orientation of phospholipid biomolecules that can encapsulate fat-soluble and water-soluble drugs, which deliver genetic drugs to the body through fusion with cell membranes. Liposome nanoparticles (LNPs) have the advantages of drug targeting and good biocompatibility, reducing drug toxicity, overcoming drug resistance, and facilitating endosomal escape [85] . Therefore, LNPs have been widely used in the delivery of gene therapy drugs, of which Lipofectamine™, TurboFect™ and Stemfect™ have been commercialized. Cationic liposomes formed by a positively charged amphoteric compound and a neutral lipid are the main force to deliver gene therapy drugs. The positive charge carried by the cationic liposome can interact with the negative charge on the target gene to form a stable complex, increasing the circulation time and enhancing the transfection efficiency. To enhance the delivery efficiency of gene therapy drugs, a large number of ingenious designs of liposomal non-viral vectors have begun to emerge, including exosome-liposome hybrid nanoparticles [86] , DOTAP liposome [87] , hyaluronic acid-modified cationic noisome [88] . Especially, Li et al. developed efficacious LNPs with >25% GFP knockout efficiencies that can load up to 90% of Cas9/sgRNA RNPs, confirming that nanoparticles loaded with the CRISPR/Cas9 system have higher targeted gene knockout capabilities and lower toxicity compared with free CRISPR/Cas9. The cationic liposome delivery system provides a new way to deliver gene editing tools for disease modeling and treatment ( Fig. 5 ) [89] .

(A) Synthetic route employed for lipidoids synthesis. (B) Intracellular delivery of Cas9:sgRNA RNP complex loaded LNPs for gene editing. (C) Chemical structures of amine head (R) groups. Reprinted with permission from [89] . Copyright 2018 Royal Society of Chemistry.
4.1.2. Cationic polymer
The cationic polymer is formed by polymerizing short-chain repeating units with a highly controllable structure and can be precisely designed according to the requirements of the responsiveness of the contained drugs. With its advantages of good biocompatibility, biodegradability and structural controllability, polymers are widely used for gene therapy drug delivery. However, the cytotoxicity of cationic polymers is positively correlated with molecular weight and charge. Common cationic polymer gene carriers include PEI, polyaminoamine, polyaminoesters and natural biocompatible polymer materials. The principle of action is that the positively charged polymer and the negatively charged nucleic acid are combined by electrostatic action to deliver the gene therapy drugs to the target cell to achieve a therapeutic effect. Wang et al. delivered a therapeutic gene encoding human tumor necrosis factor-related apoptosis-inducing ligand (PPR/pTRAIL) with R6dGR peptide-modified PEGylated PEI for breast cancer metastasis treatment, which showed that PEI-PEG-R6dGR /pTRAIL exhibited multiple anti-tumor functions [83] . In addition to PEGylation to enhance transfection efficiency, the functional design of cationic polymer carriers has received attention. Duan et al. reported a highly branched poly(β-amino ester)s (BPAE-NB) with the multivalent arrangement of cationic groups that provides better nucleic acid binding capacity. BPAE-NB exhibited remarkably higher DNA/siRNA transfection, notably outperforming commercial reagents PEI 25k and Lipofectamine 2000 [90] .
Polyamidoamine (PAMAM) is a kind of cationic synthetic dendrimer with high branching degrees, low dispersion, and high functionality. The surface of the dendrimer has a modified amino group that is protonated under physiological conditions to be positively charged. It can be combined with negatively charged DNA, RNA, and mucopolysaccharides on the cell surface through electrostatic interaction. Gu et al. designed a graphene oxide functionalized PAMAM dendrimer (GO-PAMAM) to achieve co-delivery of doxorubicin (DOX) and MMP-9 shRNA plasmids to treat breast cancer. The delivery system has high drug loading, high gene delivery efficiency (14.1% with serum and 29.7% without serum), good biocompatibility, and significantly inhibits the expression of MMP-9 protein in MCF-7 cells ( Fig. 6 ) [81] .

Schematic diagram of gene editing of MMP-9shRNA. Reprinted with permission from [81] . Copyright 2017 Elsevier.
4.1.3. Inorganic nanocarrier
Inorganic nanocarriers have broad application prospects, such as uncomplicated preparation, convenient storage, large specific surface area, good stability, and easy-to-modify features. However, its biosafety is still a controversial topic, which requires long-term and in-depth research. Surface modification can improve the transfection efficiency and reduce the toxicity of nanocarriers. Currently, gold nanoparticles (AuNPs), carbon nanotubes (CNTs) [91] , graphene [92] , quantum dots (QDs) [93] , up-conversion nanoparticles (UCNs) [94] , and silica nanoparticles (MSN) are widely used in gene therapy drugs delivery [95] .
AuNPs are classical inorganic nanomaterials, which have the advantages of low toxicity, high drug loading, customizable size and shape, good chemical stability and biocompatibility, becoming a good platform for gene therapy drug delivery through chemical modification [96] . Kong et al. constructed arginine-glycine-aspartate (Arg-Gly-Asp, RGD) peptide modified dendrimer-trapped gold nanoparticles (Au DENPs), which can efficiently transfect plasmid DNA carrying both the enhanced green fluorescent protein and the luciferase (pEGFPLuc) reporter genes into human mesenchymal stem cells (hMSC). The gene delivery efficiency using K1 (mPEG), K2 (mPEG+AuNPs), K3 (mPEG+RGD), and K4 (mPEG+AuNPs+RGD) was enhanced by 104%, 264%, 180%, and 495%, respectively, indicating that the coexistence of RGD and AuNPs allows the designed carrier to bind stem cells specifically [82] .
With the development of nanomaterials, new types of nanomaterials emerge endlessly and play essential roles in gene delivery. Karim et al. constructed strontium sulfate nanoparticles as new pH-responsive inorganic nanocarriers to effectively transport siRNA into breast cancer cells. The study demonstrated significant binding affinity (ranging from 91% to 94%) towards the siRNA, suggesting that the potential ability of the nanoparticles in carrying siRNAs [78] . Alsaiari et al. used structural carriers (zeolitic imidazole frameworks, ZIFs) prepared with imidazole groups and zinc ions to encapsulate large-diameter Cas9 protein and sgRNA effectively into CC-ZIF nanoparticles. The protonation of the imidazolyl group at pH promoted the escape of CC-ZIF endosomes and transport to the nucleus and finally reduced EGFP protein expression by 37% [97] .
4.2. Endogenous nanocarriers
The endogenous carriers have a perfect natural structure for assembling and isolating the contents, and their inherent biological functions make them have a specific targeting nature delivery. More and more evidence showed that endogenous vectors in drug delivery strategies will become a breakthrough progress, and even have the potential for personalized gene therapy. Compared with synthetic nanocarriers, endogenous nanocarriers have the advantages of low immunogenicity, high stability in blood, and high efficiency of drug delivery.
4.2.1. Exosome
Exosomes are a kind of vesicles secreted by cells at the nanometer scale (40–100 nm), which play an important role in transporting materials and signal communication between cells. Exosomes have the advantages of being similar to the cell membrane, small in size, negatively charged, avoiding phagocytosis, producing immune escape, prolonging circulation time, and penetrating deep tissues. Since the potential biological functions of exosomes from different cell sources are quite different, the source of exosomes is controversial, and there is a risk of promoting tumor growth and immunosuppression. Gyorgy et al. constructed an exosome AAV vector by coupling exosomes with adeno-associated viruses. Strikingly, exo-AAV9 transduced almost 95% of inner hair cells (IHCs) and outer hair cells (OHCs). The conventional AAV1-GFP vector transduced approximately 20% of IHCs and OHCs, whereas exo-AAV1-GFP transduced up to 65% of IHCs and 50% of OHCs, indicating that exo-AAV1-GFP is more effective than conventional AAV1-GFP and it could be a significant transgenic vector for deafness [98] . Exosomes serve as membranes to encapsulate gene drugs allowing high encapsulation efficiency. Zhao et al. constructed cationic bovine serum albumin (CBSA) conjugated siS100A4 and exosome membrane coated nanoparticles with high encapsulation efficiency (EE) of 86.70 ± 1.22% [99] . Even for the CRISPR/Cas9 system with large molecular weight, exosomes also show a better loading advantage. Ye et al. engineered a modified exosome by fusing the exosomal membrane protein CD63 with GFP, which verified that Cas9 proteins were captured and efficiently loaded into exosomes rather than a random package to increase the efficiency of loading [100] .
4.2.2. Ferritin
Ferritin is a protein widely found in various animals and plants, mainly composed of a mineral core and subunit shells. The ferritin that removes the mineral core is called apoferritin (AFn). It is a hollow globular protein shell with an inner diameter of 8 nm and an outer diameter of 12 nm. Its cage-like structure and unique pH-dependent depolymerization/recombination self-assembly properties make it more convenient for drug loading. Furthermore, ferritin can achieve active targeting by specifically recognizing highly expressed transferrin receptors (TfR1) on the surface of various tumor cells. With the above advantages, ferritin has become a recognized and ideal multifunctional nano-drug carrier, which has been used in the delivery of gene therapy drugs in recent years. Our group recently calcified the inner surface of heavy chain ferritin (HFn) for lysosomal escape, carrying siRNA to avoid lysosomal degradation, and finally used for gene silencing. The results showed that the mineralized HFn could be used as a lysosomal escape vector, and the protein expression of HFn@Ca/siEGFR was approximately decreased to 84%, indicating the HFn@Ca can be a potential gene drugs vector [80] . Nevertheless, the in vivo fate of ferritin and its derivatives, the kinetic characteristics of drug release from the nanocage, and the modification of ferritin nanocage to increase its immunogenicity have seriously hindered the development of ferritin nanocage drugs.
4.2.3. Red blood cells membrane
Red blood cells (RBC) are the most abundant blood cells in the blood, and the red blood cell membrane (RBCM) extracted from them can be used as a carrier for gene therapy drug delivery. Hao et al. coated the nano-scale RBCM on the surface of the gene complex through electrostatic interaction to prepare a bionic gene delivery system, thereby prolonging its circulation time in the body and improving its biocompatibility. The phagocytic rate of these biomimetic gene delivery systems reduced by 52% compared with the control group, which will open up a new avenue for gene delivery systems by RBC membrane camouflage ( Fig. 7 ) [101] . Wang et al. reported a nanoworm involving RBCM cloaking of charge-reversible polyplexes of siRNA and polycation. RBCM cloaking charge-reversible polyplexes protected siRNA from RNase A degradation and prolonged blood circulation. The characteristics of charge reversal endow siRNA with the characteristics of loading and releasing, which solves the main problems of delivery process [102] . Due to the outstanding biocompatibility, biodegradability, and half-life extension of RBCM, various studies have achieved good results. However, in some cases, the critical host defense function of phagocytes is hindered, so whether this platform can be used in clinical practice remains considered.

Preparation process of NP/pZNF580/RBCs and their gene delivery by crossing extracellular and intracellular barriers. Reprinted with permission from ref [101] . Copyright 2018Royal Society of Chemistry.
4.3. Innovative delivery strategy
At this stage, the development of new nanocarriers provides new possibilities for the delivery of gene tharapy drugs. Sun et al. prepared DNA nanoclews (DNA NC) by rolling circle replication. The purified Cas9 protein and sgRNA are co-incubated in vitro to form RNP, and the sgRNA in RNP is combined with DNA nanoclews according to the principle of base pairing. After successful loading, the positively charged PEI is coated outside the DNA nanoclews to promote the escape of lysosomes [20] . Recent studies have shown that DNA nanoclews are also used for the successful delivery of siRNA. In vitro experiments have shown that such spherical DNA nanostructures show effective gene knockdown in miRNA and protein levels [33] . Such innovative carriers also include arrestin domain containing protein 1 [ARRDC1]-mediated microvesicles (ARMMs) [103] , multifunctional peptides [104] , cell penetrating peptide modified carriers [105] . From the perspective of enhancing drug transfection efficiency by peptide coupling, Mulholland et al. prepared nanoparticles via condensation of siFKBPL with RALA; a novel, cationic 30 mer amphipathic peptide [106] . Coincidentally, Li et al. conjugated different amounts of REDV-G-TAT-G-NLS-Cys (TP-G) peptide onto PLGA-g-PEI amphiphilic copolymers in which the TP-G peptide and PEI could cooperatively and strongly condense pZNF580. The results showed significantly high internalization efficiency, endosomal/lysosomal escape and nucleus location of pZNF580 through TP-G peptide conjugated gene delivery system [107] .
5. Diseases treated with gene therapy drugs
5.1. cancer therapy.
Cancer is one of the major diseases that endanger human health. Current cancer treatment methods, such as chemotherapy, radiotherapy, and surgical treatment, may reduce body immunity but not satisfactorily achieve restricting tumor growth and spread. With the development of DNA recombination technology, gene therapy has become a new method of treating tumors. RNA interference technology has an apparent silencing effect on endogenous genes and exogenous genes. The treatment of tumors caused by the interaction of stages of disease provides the possibility. Wu et al. used RNAi technology to silence the proto-oncogene PIK3CA and PIK3CB genes to suppress human colon and rectal cancer (CRC). The results show that PIK3CA and PIK3CB can be used as potential therapeutic drug targets for colorectal cancer, alleviating the resistance of cancer cells during chemotherapy, which can provide personalized treatment options for CRC patients [108] .
Gene editing technology can regulate the expression of genes in prostate cancer cells and provides great help for exploring the functions of related genes in prostate cancer. The regulation of the signaling pathway is of great significance to the occurrence and development of cancer. Plant homeodomain finger protein 8 (PHF8) is a histone demethylase that can promote tumor cell mesenchymal transformation and cell cycle progression and inhibit cell apoptosis. Maina et al. found that PHF8 played an important regulatory role in the hypoxia signaling pathway of prostate cancer. They used RNA interference to knock down the expression of PHF8 in LNCa P and knocked out the expression of PHF8 in 293T cells using the CRISPR/Cas9 system. Finally, they found that the hypoxia signaling pathway was significantly suppressed. This work revealed the epigenetic mechanism of the hypoxic signal and laid the foundation for further evaluation of the role of PHF8 inhibitors in the treatment of prostate cancer [109] .
5.2. Duchenne muscular dystrophy
CRISPR/Cas9 system-mediated gene editing can restore the coding frame of the DMD gene by introducing small insertions or deletions and induce exon skipping and correct nonsense mutations through gene recombination. With the continuous development and improvement of the CRISPR/Cas9 gene editing system, the application of this technology for the repair of DMD mutations has rapidly developed. Some researchers have edited and repaired different DMD mutations in pluripotent stem cells (IPSCs) derived from DMD patients. Among them, Young et al. established the CRISPR/Cas9 system to repair the 725 kb mutant fragment between exons 45–55 through non-homologous end joining (NHEJ), which is used to correct 60% of the serious reads in the code mutations of DMD patients. This method is the current CRISPR/Cas9-mediated DMD deletion based on the largest fragment repaired by NHEJ. In vivo studies in mice have shown that cardiomyocytes and skeletal muscles differentiated from IPSC cell clones by this gene editing method have the expression and function of dystrophin, which improves the stability of the membrane and the complexity of glycoproteins ( Fig. 8 ) [110] .

Schematic diagram of CRISPR/Cas9-mediated DMD deletions. Reprinted with permission from ref [110] . Copyright 2016Elsevier.
5.3. Parkinson's disease
The advantage of gene therapy is that it can deliver gene therapy drugs to specific brain regions to change functions and treat Parkinson's disease (PD) while avoiding off-target effects. Currently, there are three main gene therapy strategies for the treatment of PD: (1) restoring the synthesis of striatum dopamine; (2) providing neurotrophic support to promote the survival of neurons in neurodegenerative sites; (3) regulating the subthalamic nucleus excitatory neuron activity [111] . In order to study the mechanism of PARK17 in vivo , Ishizu et al. constructed Vps35 D620N knock-in mice to express homologous mutant proteins with endogenous expression. CRISPR-Cas9 technology knocks out Vps35 in exon 15 of the mouse PARK17 gene, which can significantly reduce the release of midbrain substantia nigra dopamine, and has a specific effect on alleviating PD [112] .
5.4. Other genetic diseases
Hemophilia A (HA) is an X -linked recessive genetic disease. The leading cause is the lack of coagulation factor ( F ) Ⅷ in the body, which leads to coagulation dysfunction. Park et al. used CRISPR/Cas9 technology to genetically edit the F Ⅷ gene of the induced IPSCs to restore the inverted chromosome fragments to the wild state, differentiate the IPSCs into endothelial cells, and transplant the endothelial cells into mice with hemophilia. The mice began to produce F Ⅷ, and bleeding symptoms were also controlled [113] .
Huntington's disease (HD) is an autosomal dominant genetic disease, and the most fundamental treatment is gene therapy. HD is an autosomal dominant genetic disease, and the most fundamental treatment is gene therapy. It currently includes gene editing that directly corrects huntington's gene mutations at the DNA level and inhibits the production of mutant huntinatin (mHTT) proteins at the mRNA level. Merienne et al. introduced a new CRISPR/Cas9 gene editing system containing gRNA targeting the HTT gene (sgHTT) and gRNA targeting the Cas9 gene (sgCas9), making the system excise the Cas9 gene through sgCas9 while excising the HTT gene. This technology can significantly reduce the off-target effect while suppressing the expression of mHTT [114] .
In addition to the above genetic diseases, gene therapy clinical experimental studies including diabetic retinopathy (DR), glaucoma, β-mediterranean anemia, age-related macular degeneration (AMD), and cardiovascular disease (CVD) have made some progress that are not described in detail here.
6. Conclusions and future perspective
In this review, we discussed the current widely used gene therapy drugs and research progress. The delivery methods of gene therapy drugs for viral vectors and non-viral vectors are summarized, which provides a new direction for the delivery of gene therapy drugs. In addition, we also summarized the diseases of gene therapy, providing a reference for the direction of gene therapy. The critical point of gene therapy is to select specific genes that have therapeutic effects on the disease based on understanding the molecular mechanism of disease occurrence. The choice of gene carrier is crucial in the process of gene therapy. Only when gene therapy drugs are used to complement their weaknesses can the progress of gene therapy research go further. The primary problem to be solved for gene therapy drugs is delivery, which is the bottleneck of gene therapy today. Our review summarizes the latest delivery strategies and is committed to the development of effective gene editing strategies.
Gene therapy has become more mature and improved with the emergence of multiple biological technologies, such as second-generation sequencing and gene editing. The genetic diversity of genetic diseases, the complexity of pathogenesis and the innate differences of individuals make it difficult to apply gene therapy in clinical trials and actual treatment. Exploring and studying various targets of genetic diseases has also been the direction of the medical field and scientific researchers. In terms of safety, the use of viral vectors in gene therapy is currently controversial. Although viral vectors are highly efficient and easy to integrate into host cells, the infectivity and parasitism of the virus also need to be focused on, and the problem of off-target has always been gene therapy difficulties. On the other hand, due to the relatively high cost of gene therapy research and development and drug delivery methods, its treatment is expensive. The reform and improvement of gene therapy pricing and payment system are a big challenge, and it is also the only way for gene therapy to enter the market in an all-round way. Taking into account the complexity of human genetic information, gene therapy drugs may also bring unpredictable consequences. Currently, there is no guarantee that such changes in gene structure will never lead to the loss of unknown human functions. Therefore, gene therapy is not only a medical method but also involves ethical issues. Moreover, gene therapy drugs still have obstacles such as lack of efficient delivery systems, lack of sustained and stable expression, and host immune response. In the future, gene therapy research will develop in two directions: one is to deepen basic research, seek more effective drug treatment targets, and solve the delivery problem of gene therapy drugs; the other is to optimize the implementation plan in the clinical trial process, formulate objective evaluation standards and make treatment effects more precise. In short, with the development of molecular biology, molecular genetics, clinical medicine, and emerging nanomaterials, gene therapy will continue to mature and be widely used in clinical practice.
In conclusion, gene therapy drugs have broad application prospects in the treatment of genetic diseases. We believe that with the progress of research and the exploration of new vectors, gene therapy may substantially impact the future treatment of genetic diseases.
Declaration of Competing Interest
The authors declare no competing financial interest.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (No. 51472115) and Double First-class Innovation Team of China Pharmaceutical University (CPU2018GY40).
Cell And Gene Therapy Manufacturing Services Market Set To Grow At A Rate Of More Than 16% Driven By Rising Cancer Cases As Per The Business Research Company's Cell & Gene Therapy Manufacturing Services Global Market Report 2024
The global market reports from the business research company have been updated with the most recent market sizing data for 2024 and projections extended to 2033.
March 28, 2024 11:30 ET | Source: TBRC Business Research PVT LTD TBRC Business Research PVT LTD
LONDON, March 28, 2024 (GLOBE NEWSWIRE) -- As per The Business Research Company’s Cell And Gene Therapy Manufacturing Services Global Market Report 2024, the cell & gene therapy manufacturing services market has experienced rapid growth in recent years, driven by advancements in medical technology and an increasing focus on precision medicine.
Market Growth and Projections
The cell & gene therapy manufacturing services market is witnessing substantial growth, with revenues projected to rise from $7.25 billion in 2023 to $8.55 billion in 2024 , reflecting a robust compound annual growth rate (CAGR) of 17.8%. Looking ahead, the cell & gene therapy manufacturing services market is expected to continue its upward trajectory, reaching $15.77 billion by 2028 , with a CAGR of 16.6%.
Learn More In-Depth On The Cell And Gene Therapy Manufacturing Services Market
https://www.thebusinessresearchcompany.com/report/cell-and-gene-therapy-manufacturing-services-global-market-report
Impact of Cancer Cases
The growing number of cancer cases worldwide is anticipated to be a significant driver of the cell & gene therapy manufacturing services market growth. Cancer remains a pervasive health challenge, with factors such as lifestyle choices, environmental exposures, and an aging population contributing to its prevalence. Cell and gene therapy manufacturing services play a crucial role in cancer treatment by developing personalized cellular products to target and eliminate malignant cells. According to the National Cancer Institute, the number of people living with metastatic cancer in the United States is expected to increase significantly by 2025, underscoring the urgent need for advanced treatment options such as cell and gene therapy.
Innovation in Clinical Trials
Companies in the cell & gene therapy manufacturing services market are actively focusing on innovation to enhance treatment outcomes. For example, Allogene Therapeutics has launched the CAR T Together initiative, aiming to improve CAR T therapies through the development of "off-the-shelf" allogeneic cell therapy options. These therapies, derived from donors, offer the advantage of being readily available and easy to produce in large quantities, potentially revolutionizing cancer treatment approaches.
Cell & Gene Therapy Manufacturing Services Market Segmentation
The cell & gene therapy manufacturing services market is segmented based on several factors, including type, indication, application, and end-user. Key segments include:
- Type : Gene Therapy, Cell Therapy
- Indication : Central Nervous System Disorders, Ophthalmology Diseases, Cardiovascular Diseases, Infectious Diseases, Orthopedic Diseases, Oncology Diseases
- Application : Commercial Manufacturing, Clinical Manufacturing
- End-user : Academic And Research Institutes, Pharmaceutical And Biotechnology Companies, Other End-Users
Market Landscape and Competition
The cell & gene therapy manufacturing services market is characterized by high concentration, with a small number of large players dominating the market. Thermo Fisher Scientific, Inc., Merck KGaA, and F. Hoffmann-La Roche Ltd are among the top competitors, contributing to the the cell & gene therapy manufacturing services market’s dynamism and competitiveness.
Get A Free Sample Of The Global Cell And Gene Therapy Manufacturing Services Market Report
https://www.thebusinessresearchcompany.com/sample_request?id=10035&type=smp
Regional Analysis
North America emerged as the largest region in the cell & gene therapy manufacturing services market, accounting for a significant portion of total market revenues in 2023. This underscores the region's leadership in medical innovation and research.
Cell And Gene Therapy Manufacturing Services Global Market Report 2024 by The Business Research Company provides insights on the cell and gene therapy manufacturing services market size, cell and gene therapy manufacturing services market segments, cell and gene therapy manufacturing services market trends, drivers and restraints, major competitors’ market positioning, revenues and market shares.
The Business Research Company has published over 7,500+ industry reports, covering more than 2,500+ market segments and 60 geographies. The reports draw on 1,500,000 datasets, extensive secondary research, and exclusive insights from interviews with industry leaders.
Check Out Similar Market Intelligence Reports By The Business Research Company:
Cell And Gene Therapy Global Market Report 2024
https://www.thebusinessresearchcompany.com/report/cell-and-genes-therapy-global-market-report
Cell And Gene Therapy Supply Chain/Logistics Global Market Report 2024
https://www.thebusinessresearchcompany.com/report/cell-and-gene-therapy-supply-chain-or-logistics-global-market-report
Nucleic Acid Based Gene Therapy Global Market Report 2024
https://www.thebusinessresearchcompany.com/report/nucleic-acid-based-gene-therapy-global-market-report
Learn More About The Business Research Company
The Business Research Company is a market intelligence firm pioneering in company, market, and consumer research. With offices all around the world, TBRC has specialist consultants in a variety of fields, including manufacturing, healthcare, financial services, chemicals, and technology.
Global Market Model – World’s Most Comprehensive Database
The Business Research Company’s flagship product, Global Market Model , is a market intelligence platform covering various macroeconomic indicators and metrics across 60 geographies and 27 industries. The Global Market Model covers multi-layered datasets which help its users assess supply-demand gaps.

Contact Data

IMAGES
VIDEO
COMMENTS
Gene therapy aims to provide a functional gene copy of the damaged gene(s), ... Besides, the enhanced biological research, cheaper gene vectors will be available in the market, which increases gene therapy accessibility for most cancer patients. This will change the future of cancer treatment, from generalized cancer treatment strategies to ...
Gene therapy involves the introduction of new genes into cells, to restore or add gene expression, for the purpose of treating disease. Most commonly a mutated gene is replaced with DNA encoding a ...
Shi-Kun Zhou. Jun Wang. Nature Communications (2023) Gene therapy is at an inflection point. Recent successes in genetic medicine have paved the path for a broader second wave of therapies and ...
Gene therapy is understood as the capacity for gene improvement by means of the correction of altered (mutated) genes or site-specific modifications that have therapeutic treatment as target. ... Currently, gene therapy is an area that exists predominantly in research laboratories, and its application is still experimental. Most trials are ...
A new gene therapy called Libmeldy has been developed and was approved by the EU FDA in December 2020 to help treat the condition. Libmeldy is an autologous ex vivo lentiviral gene therapy that uses a type of virus called a lentivirus to introduce a healthy copy of the ARSA gene into CD34+ cells extracted from the patient's blood or bone marrow.
Gene therapy has made inroads against cancer, too. An approach known as chimeric antigen receptor (CAR) T cell therapy works by programming a patient's immune cells to recognize and target cells ...
Gene therapy is the product of man's quest to eliminate diseases. Gene therapy has three facets namely, gene silencing using siRNA, shRNA and miRNA, gene replacement where the desired gene in the form of plasmids and viral vectors, are directly administered and finally gene editing based therapy where mutations are modified using specific nucleases such as zinc-finger nucleases (ZFNs ...
In early 2023, there were more than 100 different approved gene, cell, and RNA therapies throughout the world, with over 3,700 more in clinical and preclinical development. This review comprehensively captures the landscape for such advanced therapies, including the different genetic technologies used and diseases targeted in clinical trials.
These early experiments' success led to gene therapy research's explosive progression. A Time of Promise Hits a Snag From 1960 to 1980, there was much research and development in gene therapy, a ...
Gene therapy. Gene therapy is a direct way to treat genetic conditions as well as other conditions. There are also other related approaches like gene editing. There are many different versions and approaches to gene therapy and gene editing. It all rests on understanding how genes work and how changes in genes can affect our health.
Gene Therapy Hope for Children With Kidney Disease; Scientists Reverse Hearing Loss in Mice; Wednesday, August 9, 2023. Research Sheds New Light on Gene Therapy for Blood Disorders; Thursday, July ...
Wave 2, more futuristically, will look at the potential of lentiviruses, which have long-lasting expression. This review will summarize the current status of translational research in CF gene therapy.
To overcome this chokepoint in therapy development, active research focuses on developing non-viral methods of gene delivery, including transposon-mediated gene integration , CRISPR-mediated ...
Clinical trials are research studies that help doctors determine whether a gene therapy approach is safe for people. They also help doctors understand the effects of gene therapy on the body. Your specific procedure will depend on the disease you have and the type of gene therapy being used. For example, in one type of gene therapy:
The first studies using an ex vivo approach of gene therapy by gene transfer in autologous fibroblasts or hematopoietic stem cells, resulted in short-lasting low expression of FVIII. 13 Adeno-associated virus (AAV)-based gene therapy was introduced 20 years ago by intramuscular injection of recombinant AAV (rAAV)-FIX in patients with hemophilia B.
Gene therapy is a type of treatment being developed to fight diseases that are caused by genetic defects. This is a relatively new medical intervention that is mainly in the experimental phase, including human trials and animal trials, for the treatment of some conditions, such as cystic fibrosis. Gene therapy aims to change the unhealthy ...
A Short Overview of Gene Therapy Development. Already back in the 1970s, it was recognized that gene therapy, replacing or supplementing defective disease-causing DNA with exogenous healthy or beneficial DNA, could hold the promise of offering viable treatment options for human genetic diseases (Friedmann and Roblin, 1972).In the 1980s, the concept formed of using a virus vector for gene ...
In 2014, St. Jude investigators and colleagues published historic results from a gene therapy trial for hemophilia B. A vector developed and manufactured at St. Jude had transformed the lives of young men with this inherited bleeding disorder. Andrew M. Davidoff, MD, St. Jude Children's Research Hospital. Hemophilia B is caused by defects in ...
Learn how Ohio State researchers delivered life-changing gene therapy treatment to a child born with AADC deficiency. @OSUWexMed and @OhioStateMed physician-scientists developed a way to deliver gene therapy for children with a rare genetic disorder, leading to dramatic improvements in their ability to make even the most basic movements.
The first two decades of T-cell therapy research focused on the basics, explained Rosa Nguyen, M.D., Ph.D., ... TCR T cells with the fusion gene flowed into tumors in much greater numbers and killed tumor cells much more effectively than TCR T cells without the fusion gene. The TCR T cells with the fusion even showed this advantage at starting ...
At the forefront of medicine, Gene Therapy brings you the latest research into genetic and cell-based technologies to treat disease. It also publishes reviews and articles, which highlight the ...
Today's biotech news includes a potentially major drug approval, an idea to make CAR-T more equitable, and the slow launch of a gene therapy.
Gene therapy enjoyed an initial phase of excitement, until the recognition of immediate and delayed adverse effects resulted in death and caused a major setback. ... The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of ...
This Pitt program is leveling up the gene therapy workforce in Pittsburgh. ... Pitt Med magazine is the flagship publication of the School of Medicine, highlighting research, education, and innovation at the school. Health Sciences. Office of the Senior Vice Chancellor for the Health Sciences. Scaife Hall, Suite 401.
The UCL Translational Research Office (TRO) partnered with UCL Business (UCLB), our technology transfer office, to exhibit at this year's Advanced Therapies Congress at ExCel, London, engaging with experts in cell and gene therapy from around the world. Photo 1: Dr. Pamela Tranter, Head of the ...
Tom Edwards (left), from the Centre for Eye Research Australia, administers a viral-vector-based gene therapy. Credit: Mathew Lynn/CERA. In a landmark 1972 paper 1, physician Theodore Friedmann ...
Per a Research report, the global cell and gene therapy market was valued at $15.46 billion in 2022 and is expected to grow at a compound annual growth rate of 18.3% by 2032. Other Developments in ...
Analysis and comparative evaluation of expedited programs for gene therapy products: insights from the United States, the European Union, Japan, and South Korea. Hyeokgyo Jeong. Sujata Purja ...
The choice of gene carrier is crucial in the process of gene therapy. Only when gene therapy drugs are used to complement their weaknesses can the progress of gene therapy research go further. The primary problem to be solved for gene therapy drugs is delivery, which is the bottleneck of gene therapy today.
Cell And Gene Therapy Manufacturing Services Market Set To Grow At A Rate Of More Than 16% Driven By Rising Cancer Cases As Per The Business Research Company's Cell & Gene Therapy Manufacturing ...