- Find A Doula
- VBAC Resources
- Get Certified
- How to VBAC: The Parents’ Course
- Advanced VBAC Doula Certification
- Skip to right header navigation
- Skip to main content
- Skip to primary sidebar
- Skip to footer

Making birth after Cesarean better


How to Turn a Transverse Baby (and Avoid a C-Section)
If you’ve just found out that your baby is lying transverse, or sideways, in your belly, you likely have a whole bunch of questions. Here at The VBAC Link, we always encourage parents to do activities that will encourage their baby to get in an optimal position. With a transverse lie, this is especially important …
If you’ve just found out that your baby is lying transverse, or sideways, in your belly, you likely have a whole bunch of questions.
Here at The VBAC Link, we always encourage parents to do activities that will encourage their baby to get in an optimal position. With a transverse lie, this is especially important because transverse babies cannot be born vaginally.
In this blog, we dig into what transverse lie looks like. You’ll learn how to tell if you have a transverse baby, when it is a concern, and how to encourage that baby to get into a better position.
Originally written on Oct. 18, 2018, this post was updated and republished on April 13, 2020.
What does transverse lie mean?
Babies move around in all sorts of positions while they are hanging out in a mother’s belly. It is common for them to be constantly changing positions until a few weeks into the third trimester.
Up until 32-34 weeks of pregnancy, a transverse lie position isn’t necessarily a problem or cause for concern. However, after that, if your baby is in a breech or transverse lie position, you will want to start encouraging them to turn head-down.
There are three main fetal positions your baby can be in.
Cephalic/Vertex
A cephalic, or vertex presenting baby is a fancy way of saying that the baby is head-down, with the top of its head pressing against the mother’s pelvic floor.
A breech baby is head-up and bum, or feet down. We have an article dedicated to breech babies if you want to learn more about this position.
Many techniques used to get a breech baby head-down will be helpful to get a transverse baby head-down, too.
Transverse Lie
A transverse baby position means the baby is lying in the womb sideways. It is normal for babies to be in this position in the early weeks and months of pregnancy.
By the early third trimester, especially beyond 34 weeks, providers really want to see the baby in a head-down position. Even a breech position is better than transverse because a breech baby can be born vaginally, and they are easier to turn.
Transverse or shoulder/back presentation occurs in one in 400 births and can cause serious complications for you and your baby.

What causes a baby to be transverse?
There are several reasons that impact what positions a baby decides to rest in and a few important factors impacting the likelihood of a transverse lie.
The second pregnancy (or third, or more!)
After having your first child, your abdominal muscles can remain more pliable, stretchable, and loose, especially if you have diastasis recti which can weaken the abdominal muscles even more.
Looser abdominal muscles mean that your baby has more room to get comfortable in a less than optimal position.
Before 34 weeks
Up until your mid-trimester, it is common for your baby to move into a variety of positions, even several times a day. If your baby is transverse, there is no need to worry or try to maneuver them into a good position until you reach 32-34 weeks gestation.
Too much amniotic fluid (polyhydramnios)
It is common for a parent’s fundal height to measure a few weeks ahead or behind of their due date, and it can vary based on the baby’s position and even how hydrated the mother is. However, if you are measuring ten or more weeks ahead, medical providers typically want to do an ultrasound to check for polyhydramnios or too much amniotic fluid.
Too much fluid can make it very easy for a baby to swim into a transverse lie and stay there, among other potential complications .
Carrying multiples can mean these babies have to puzzle together in different ways to both grow and fit in the uterus. One baby may be head-down or breech, and the other transverse. Typically when baby A is head-down, transverse baby B will turn head-down or breech and then can be born vaginally.
Low-lying placenta/placenta previa
A placenta that is low lying or covering the cervix may take up room that the baby needs to get and stay head-down. With placenta previa, a Cesarean is necessary but, with a low-lying placenta, a transverse baby can still get into a head-down position.
Uterine abnormalities
Uterine abnormalities such as uterine fibroids, a bicornuate or unicornuate uterus, a didelphic womb, septate womb, and arcuate womb, all increase the likelihood of having a transverse baby due to the shape of the uterus.
While having a pelvis too small to birth a baby is incredibly rare, in the case of a misshapen or malformed pelvis, a baby may be forced into a transverse lie.
When a transverse lie position is a concern
It’s perfectly normal for babies to be lying in a transverse (or any other) position in the first and second trimesters of pregnancy. However, midway through the last trimester, especially after 34 weeks gestation, if your baby is still transverse, it is time to get them ready for birth.
Simply put, a transverse baby will not fit into the birth canal and out of the vagina. It is very important to work on getting a transverse baby in a better position before labor starts or your water breaks.
If your water breaks while the baby is still lying sideways the baby’s arm, shoulder, or even more severe, the umbilical cord can prolapse, or come out of, the birth canal. This is very dangerous and can be life-threatening to the baby as blood flow and oxygen flow become restricted. If cord prolapse happens, your baby needs to be delivered as quickly as possible by Cesarean.
You will find that as you approach your due date if your baby is transverse, most medical providers will advocate for a scheduled Cesarean ‘just in case’ your waters rupture prematurely.
A transverse lie presentation can cause very serious complications during labor and birth. Some of the complications are:
- Obstructed labor/labor dystocia — where labor does not move the baby through the pelvis because it is physically blocked in
- Umbilical cord or hand prolapse
- Postpartum hemorrhage
- Birth trauma to the baby
- Increased risk of rupture of the uterus, of particular concern for VBAC parents

How to tell if a baby is transverse
There are several ways you or your medical provider can determine whether your baby is transverse. The most certain way to confirm a baby’s position is by ultrasound. However, a skilled midwife or practitioner should be able to tell by palpating the abdomen to feel for the baby’s position. A vaginal exam may also be able to determine a baby’s position.
Do you want to find out for yourself?
We highly recommend all parents learn belly mapping by Spinning Babies. This is a great way to get comfortable with knowing where your baby is positioned in the womb and determine if additional steps are necessary.
After learning belly mapping, keep practicing so you can get more familiar and confident with it.
Transverse lie baby symptoms:
- Baby’s back is down, facing the birth canal
- Baby’s back is facing up with the hands and feet resting on the birth canal
- Baby has one shoulder down or pressing against the birth canal
In each of these positions, you will be able to distinguish your baby’s head on one side of your belly and bottom on the other side. After that, pay attention to where you feel kicks and wiggles. These movements will tell you where the baby’s hands and feet are to determine which transverse lie your baby is in.

How to turn a transverse baby
If your baby is not in a head-down position by 32 weeks, there are some things you can do to encourage them to flip into a head-down position. As always, make sure to check with your medical provider before doing anything that requires you to be head-down or upside down.
Spinning Babies is a great resource for getting transverse babies to turn, and we encourage you to do the recommended daily activities:
- Forward Leaning Inversion
- Breech Tilt
- Side-Lying Release
- Regular chiropractic care
- The Miles Circuit
- Moxibustion
- ECV (External Cephalic Version) only with a skilled practitioner in a hospital setting
- Myofascial Release
- Pregnancy Belt
If the baby is transverse when you go into labor
If you are in early labor, an external cephalic version (ECV) is a great option to discuss with your provider. Using this technique, the caregiver will attempt to manually turn the baby by pressing on your abdomen and slowly pushing in an attempt to turn the baby head-down.
If successful, and labor is starting, your contractions are likely to both push and keep your baby’s head in this position until the birth. If they can easily be turned into a head-down position, then the waters may be broken by the caregiver to remove some of the fluid that is helping your baby move about. If the baby is still high in your pelvis, breaking the waters can still cause prolapse and is something to consider when making that decision.
Sometimes, an ECV is not successful, or the baby will turn again after the ECV. If they have been transverse for long, keeping them head-down can be tricky. Your provider may suggest induction right away if it is successful and you are at term. Unfortunately, If your baby continues to remain in a transverse position, they will need to be born by Cesarean.
There is only so much space in the uterus, so if you are having twins the second can be transverse because the first twin is engaged in the pelvis. Your transverse lying baby will often turn once the first twin is born as there is more space for your baby to move. If this doesn’t occur naturally, the second twin will generally be able to be turned, so that it can be born vaginally, in either a head-first or breech position.
If a parent goes into labor while the baby is still transverse, it can negatively impact the shoulder of the baby. This is because they are in a folded position that is under pressure to move down the birth canal.
An immediate C-section would be carried out if this happens.
Fortunately, there are many resources available to assist you in encouraging your baby to engage in a head-down position. We highly encourage you to use the resources at Spinning Babies, linked above. We have seen great success using these methods with both our doula clients and in our Facebook Community.
It is always ok to keep trying and ask for more time if your intuition is telling you so.
If you are preparing for labor after Cesarean and your baby is transverse, having a repeat C-section can be devastating, no matter how necessary. Not achieving a VBAC when you have prepared SO much for it is filled with so many emotions. Find out how to cope with and process those emotions and then join our strong and thriving Facebook community to find lots of love and support.
Ready to take your VBAC preparation to the next level? Enroll in our course How to VBAC: The Ultimate Prep Course for parents today.
About Julie Francom
Hi, I'm Julie Francom , and my goal is to help you feel educated and informed about birth after Cesarean. As a doula, birth photographer, and co-founder of The VBAC Link, it is my job to keep you in the know about all the current evidence and information related to VBAC. I am a mom of four, computer geek, Army vet, and a small-town girl just trying to change the world!
Credentials: Certified Labor Doula Certified Birth Photographer VBAC Childbirth Educator Business Owner Bachelor of Science - Information Technology Masters Degree in Business Administration
Related Posts
You may be interested in these posts from the same category.

How to VBAC Parent Course: Unfiltered Customer Reviews

Trying To Conceive: 7 ways to prepare for trying to conceive your VBAC baby

Signs of Uterine Rupture: What You Need to Know as a VBAC Mom

5 Products that *ACTUALLY* Make a Difference in Your VBAC Pregnancy

ECV and VBAC: What You Need to Know

Everything You Need for a Home Birth After Cesarean (HBAC)

5 Healthy Snack Ideas for VBAC Pregnancy

What’s in my doula bag? The 10 Most Essential Items for Supporting VBAC Births

The Best Prenatal for VBAC Moms: Needed vs Ritual

Membrane Sweeps for VBAC: Details Explained

Hospital Bag Checklist: What to Pack When Preparing for Your VBAC

Best Gifts to Show Appreciation for Your VBAC or HBAC Birth Team

Reader Interactions
May 21, 2020 at 4:29 am
My baby was in cephalic position in 30 weeks but in my 34 weeks it has turn into breech position can the baby change position again during birth
June 14, 2020 at 8:52 pm
I’m 25 weeks pregnant now and my ultrasound tells that my baby’s position is transverse is there a chance for her to be in cephalic position on 9th month?
June 15, 2020 at 2:16 pm
Hi! Yes, Baby has plenty of time to turn head down. Check out Spinning Babies, their daily essentials will be very helpful for you!
February 20, 2021 at 12:35 am
Hi I’m in 34 weeks of pregnancy, and my baby was in transverse position, is there any chance to turn my baby in a right position? Thank in advance🥺
January 11, 2022 at 5:21 am
Im in 27 weeks is their a chance my baby to get in position at my tri mester…..
March 18, 2021 at 2:37 pm
Can the baby change position because the baby is 30 weeks already.
March 21, 2021 at 10:49 am
Yes! Baby can move anytime, and at 30 weeks still has plenty of room to change. At 34-36 weeks is where you really want to pay attention to where the baby is and make sure they are head down.
September 22, 2022 at 9:51 am
I’m 31 weeks pregnant now and my baby is transverse. He has been for the past few weeks, at every scan. I have a low-lying front placenta – just half a centimetre from being previa. I’m worried. This is my 3rd pregnancy.
June 18, 2020 at 1:00 am
My baby is in transverse lie and I am 35 weeks today. Getting a bit worried as my baby was head down last week but has turned to transverse this week. Any tips on what I can do? If I take daily walks would this help?
July 2, 2020 at 9:02 pm
I’m in 29 weeks of my pregnancy but my baby is in transverse lie, I’m getting worried . is there any chance my baby can change to cephalic position?
July 3, 2020 at 9:52 pm
Hi! Your baby still has plenty of room to settle into a cephalic position. Do the spinning babies exercises listed above and see a chiropractor if you can. All those things will encourage the baby to get into the best position for birth.
July 10, 2020 at 4:29 pm
Hi I am 34 weeks pregnant and baby has been transverse since 28 weeks. Should I be concerned? Is there still a good chance my baby will go head down? Thank you x
July 13, 2020 at 6:59 am
I am 35 weeks and a scan today showed my baby in a transverse lie. I am very stressed concerned and find it hard to think about a c section after hearing stories. Please help
November 25, 2020 at 4:36 pm
I’m 36 weeks baby has been head down up intel now 😪
July 22, 2020 at 2:19 pm
Am 39 weeks pregnant and my baby is transverse do I still have a hope of giving birth naturally.
July 24, 2020 at 2:07 pm
Yes! Try the things listed above to try and get baby head down, if it is still transverse then a Cesarean will be necessary.
July 24, 2020 at 11:39 am
I’m 38 weeks with cerclage and a transverse baby a bit worried
November 19, 2020 at 2:02 pm
My twins are 36 weeks and in transverse position. I feel so much pain in the waist, what will do
June 6, 2022 at 2:12 pm
Hey ,my baby is transverse at 38weeks ,is there any chance to change to head position or it’s too late no
October 8, 2022 at 9:59 pm
Hi I’m feeling worried my baby is transverse position I’m 32 weeks.
September 22, 2020 at 11:09 am
Hi Im in 35weeks and my baby still in a transverse lie, it posible to turn his head down
December 17, 2020 at 4:42 pm
I’m 34 weeks and my baby is transverse breech. My doctor doesn’t even want to try and flip him because the placenta is infront of him. Is there any way he will still flip into position by himself because I’m really scared to have a cesarean?
April 29, 2021 at 6:28 pm
I’m 36 weeks and my baby is still transverse what are the chances of her turning? I’m getting very worried 😟
September 30, 2021 at 10:01 am
My baby is in right transverse position at 33 weeks 5days of pregnancy and I feel lesser fetal moments… Is this a cause of fetal position or something else.
July 13, 2021 at 4:44 pm
Hi im on 28 weeks 2 days tranverse lie is there a chance to turn into cephalic..thank you
September 21, 2021 at 8:51 pm
My baby is transverse lie at 35 weeks do i have a chance of turning it or is there any other way of doing it myself. thanks
November 4, 2021 at 6:52 am
If a “parent” goes into labor? What is so offensive about saying Mom? We are ruining proper English in exchange to be accepted by those who do not understand basic anatomy. I cannot learn from sites that alter science to appease the foolish.
February 7, 2022 at 12:01 pm
Am in 37 weeks and 6 days and my baby is in transverse and iam feeling less movement. Is there any chance of my baby to turn and what causes lesser movements.
September 22, 2022 at 9:53 am
August 17, 2023 at 10:41 pm
hi im 34 wks pregnant my bps ultrasound sees that it is transverse position, will it be possible that the baby will turn to normal position before my due date . please reply thank you
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
VBACaholics, unite!
Sign up for updates on classes, blogs, and all things VBAC!
- Terms of Service
- Affiliate Disclaimer
- Privacy Policy
- Share Your Story
385-429-2012
Salt Lake City, Utah
United States
Appointments at Mayo Clinic
- Pregnancy week by week
- Fetal presentation before birth
The way a baby is positioned in the uterus just before birth can have a big effect on labor and delivery. This positioning is called fetal presentation.
Babies twist, stretch and tumble quite a bit during pregnancy. Before labor starts, however, they usually come to rest in a way that allows them to be delivered through the birth canal headfirst. This position is called cephalic presentation. But there are other ways a baby may settle just before labor begins.
Following are some of the possible ways a baby may be positioned at the end of pregnancy.
Head down, face down
When a baby is head down, face down, the medical term for it is the cephalic occiput anterior position. This the most common position for a baby to be born in. With the face down and turned slightly to the side, the smallest part of the baby's head leads the way through the birth canal. It is the easiest way for a baby to be born.

Head down, face up
When a baby is head down, face up, the medical term for it is the cephalic occiput posterior position. In this position, it might be harder for a baby's head to go under the pubic bone during delivery. That can make labor take longer.
Most babies who begin labor in this position eventually turn to be face down. If that doesn't happen, and the second stage of labor is taking a long time, a member of the health care team may reach through the vagina to help the baby turn. This is called manual rotation.
In some cases, a baby can be born in the head-down, face-up position. Use of forceps or a vacuum device to help with delivery is more common when a baby is in this position than in the head-down, face-down position. In some cases, a C-section delivery may be needed.

Frank breech
When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head. This is the most common type of breech presentation.
If you are more than 36 weeks into your pregnancy and your baby is in a frank breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Most babies in a frank breech position are born by planned C-section.

Complete and incomplete breech
A complete breech presentation, as shown below, is when the baby has both knees bent and both legs pulled close to the body. In an incomplete breech, one or both of the legs are not pulled close to the body, and one or both of the feet or knees are below the baby's buttocks. If a baby is in either of these positions, you might feel kicking in the lower part of your belly.
If you are more than 36 weeks into your pregnancy and your baby is in a complete or incomplete breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Many babies in a complete or incomplete breech position are born by planned C-section.

When a baby is sideways — lying horizontal across the uterus, rather than vertical — it's called a transverse lie. In this position, the baby's back might be:
- Down, with the back facing the birth canal.
- Sideways, with one shoulder pointing toward the birth canal.
- Up, with the hands and feet facing the birth canal.
Although many babies are sideways early in pregnancy, few stay this way when labor begins.
If your baby is in a transverse lie during week 37 of your pregnancy, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of your health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a transverse lie, talk with a member of your health care team about the choices you have for delivery. Many babies who are in a transverse lie are born by C-section.

If you're pregnant with twins and only the twin that's lower in the uterus is head down, as shown below, your health care provider may first deliver that baby vaginally.
Then, in some cases, your health care team may suggest delivering the second twin in the breech position. Or they may try to move the second twin into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
Your health care team may suggest delivery by C-section for the second twin if:
- An attempt to deliver the baby in the breech position is not successful.
- You do not want to try to have the baby delivered vaginally in the breech position.
- An attempt to move the baby into a head-down position is not successful.
- You do not want to try to move the baby to a head-down position.
In some cases, your health care team may advise that you have both twins delivered by C-section. That might happen if the lower twin is not head down, the second twin has low or high birth weight as compared to the first twin, or if preterm labor starts.

- Landon MB, et al., eds. Normal labor and delivery. In: Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 19, 2023.
- Holcroft Argani C, et al. Occiput posterior position. https://www.updtodate.com/contents/search. Accessed May 19, 2023.
- Frequently asked questions: If your baby is breech. American College of Obstetricians and Gynecologists https://www.acog.org/womens-health/faqs/if-your-baby-is-breech. Accessed May 22, 2023.
- Hofmeyr GJ. Overview of breech presentation. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Strauss RA, et al. Transverse fetal lie. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Chasen ST, et al. Twin pregnancy: Labor and delivery. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Cohen R, et al. Is vaginal delivery of a breech second twin safe? A comparison between delivery of vertex and non-vertex second twins. The Journal of Maternal-Fetal & Neonatal Medicine. 2021; doi:10.1080/14767058.2021.2005569.
- Marnach ML (expert opinion). Mayo Clinic. May 31, 2023.
Products and Services
- A Book: Obstetricks
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- 3rd trimester pregnancy
- Fetal development: The 3rd trimester
- Overdue pregnancy
- Pregnancy due date calculator
- Prenatal care: 3rd trimester
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
- Search Please fill out this field.
- Newsletters
- Sweepstakes
What Is a Transverse Baby?
Although rare, a baby can be in a transverse lie position in the third trimester. Here's what that means and how it impacts delivery.
What Does Transverse Lie Mean?
What are the causes of a transverse lie position, what are the possible risks and complications, how can the transverse lie position affect pregnancy, what about delivery, can you turn a transverse baby.
Getty Images
During pregnancy, the fetus moves around into different fetal positions , but most end up in the optimal head down, face down (cephalic occiput anterior) position in the last few weeks. When the fetus doesn’t move into the cephalic position for birth, it’s called fetal malpresentation.
One of the rarest positions is the transverse lie, where the fetus lies horizontally, often with one shoulder down or pressing against the birth canal. If you have a transverse baby at term, the provider will intervene because a vaginal delivery is not possible.
Here’s all you need to know about transverse lie causes and how it may affect pregnancy and delivery.
The transverse lie position is when the fetus lies across the pregnant person’s abdomen horizontally. Because the shoulder is often in the pelvic inlet, it is also sometimes called shoulder presentation. But the fetus can also have its back facing the birth canal or with feet and hands facing it.
The chances of the baby being in the sideways position at term are only around 1 in 300. But before term, at 32 weeks gestation, it’s as high as 1 in 50.
“Transverse lie is normal in the first trimester, common in the second, unusual in the third, and it’s not a position where vaginal birth is possible,” says Gail Tully, CPM, creator of Spinning Babies, a website which offers ways to ease a baby’s rotation through the pelvis based on its position.
Often, a clear cause or risk factor for a transverse lie position is unknown. “But two of the most common risk factors for transverse lie at term include having extra amniotic fluid —often associated with diabetes but can be found on its own—and multiple gestation , such as twins or triplets,” says Layan Alrahmani, MD , maternal and fetal medicine specialist and assistant professor in obstetrics and gynecology at Loyola University Medical Center.
Other possible risk factors for transverse lie include:
- Multiparity (previous births may lead to lax abdominal muscles)
- Premature labor
- Low amniotic fluid
- Placenta previa (placenta is covering the pregnant person’s cervix)
- Pelvic, uterine, or fetal abnormalities (the latter is more common in primiparity, or first time births)
“Sometimes the baby is in the position for a reason,” says Karolyn Zambrotta, CNM , an obstetrics and gynecology specialist. “And after the doctor does the C-section you’ll find the problem, like a short or tight umbilical cord.”
Transverse lie at term can be risky for both the pregnant person and baby.
“The transverse lie is frequently found early in the pregnancy. But if the baby does not change position, then a vaginal delivery cannot occur and we have to plan differently,” says Carolina Bibbo, MD , maternal-fetal medicine specialist at Brigham and Women’s Hospital. “If the water were to break when the baby is in a transverse lie position, the cord could prolapse which is an obstetrical emergency.”
Other possible complications include:
- Obstructed labor
- Uterine rupture
- Birth trauma
- Postpartum hemorrhage
- Birth defects
Some pregnant people feel abdominal and back pain during pregnancy when the fetus is in the sideways position. This is related to the uterus being stretched in different ways and can cause tightening in the ribs and cramping lungs. If your health care provider approves, you can try deep breathing and gentle yoga exercises at home to help relieve pain and encourage the fetus to turn.
If the health care provider still suspects the fetus is lying horizontal at 36 weeks, an ultrasound will be performed to confirm. Because a baby in the transverse lie position cannot be delivered vaginally, your providers will develop an alternate birth plan which can include a procedure called external cephalic version (ECV) to try and turn the fetus for vaginal delivery, or a C-section.
In the case of multiples, triplets are almost always delivered via C-section. But for twins, if the first is head down, the second may drop into the cephalic position for normal delivery having more room after the first one comes out. “You could also try ECV or internal podalic version (IPV) on the second twin if needed,” says Dr. Alrahmani. “It’s really case by case and depends on the provider’s experience and preference too.”
After 34 weeks, it is very unlikely for a fetus in transverse lie to spontaneously change to the optimal head down position. But, in some cases, it is possible to turn a transverse baby.
Natural methods
If the fetus is not head down by 32 weeks, and there are no health concerns, midwives like Zambrotta might first recommend trying some natural techniques. As Dr. Bibbo notes, the data is limited for different approaches but yoga positions can help in some cases.
Low-risk methods to encourage transverse babies to turn include sound or light (putting music or a bright light near the bottom of the uterus), temperature (placing something cold like frozen peas behind the head and something warm like a rice-filled sock at the bottom of the stomach), and Traditional Chinese Medicine (TCM) like moxibustion , which involves heating acupuncture points with a stick of mugwort.
Small studies have shown that the Webster technique, a gentle chiropractic approach that aligns the pelvis, can help correct fetal malpresentation. And the forward leaning inversion, also developed by a chiropractor, is the most effective position for transverse lie babies, according to Tully, who trains labor and delivery nurses on body balance techniques.
Always speak with your health care professional before trying any methods to turn the fetus.
Intervention
If natural methods have not helped by 36 weeks, your provider will likely want to try an ECV in which they use their hands to put pressure on your belly to try and turn the fetus head down. This procedure should be done in a hospital setting to monitor the fetal heart rate, and for the rare case where an emergency C-section is needed. Possible complications include placental abruption, fetal heart rate abnormalities (FHR), premature rupture of the membranes , preterm labor, fetal distress, and vaginal bleeding.
ECV may not be safe if you have placenta previa, a low amount of amniotic fluid, a significant uterine abnormality, vaginal bleeding, high blood pressure, multiples (before delivery of the first twin), or fetal distress.
“In general, the success rate for external cephalic version is 60% of babies,” explains Dr. Bibbo. “But there’s a greater chance for ECV to turn a fetus in transverse lie than in a breech position.”
A baby in the transverse lie position cannot fit through the pregnant person’s pelvis. If gentle exercises, chiropractic techniques, or other natural methods don’t help your baby turn by 36 weeks, you may be a candidate for ECV to move the baby into the optimal head down position for birth. But if ECV doesn’t work, then the health care provider will schedule a C-section.
Whatever ends up being needed to ensure the safety of both parent and fetus, it's always important to ask any questions you may have. That includes information on postpartum recovery should you need a C-section.
Chapter 26: Transverse Lie . Oxorn-Foote Human Labor & Birth, 7e . 2023.
Effectiveness and Safety of Acupuncture and Moxibustion in Pregnant Women with Noncephalic Presentation: An Overview of Systematic Reviews . Evidence-Based Complementary and Alternative Medicine . 2019.
The Webster Technique: a chiropractic technique with obstetric implications . J Manipulative Physiol Ther . 2002.
External Cephalic Version . StatPearls. 2022.
External Cephalic Version . Obstetrics: Normal and Problem Pregnancies (Seventh Edition) , 2017.
External Cephalic Version: A Dying Art Worth Reviving . J Obstet Gynaecol India . 2018.
Related Articles
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Key Points |
Abnormal fetal lie or presentation may occur due to fetal size, fetal anomalies, uterine structural abnormalities, multiple gestation, or other factors. Diagnosis is by examination or ultrasonography. Management is with physical maneuvers to reposition the fetus, operative vaginal delivery , or cesarean delivery .
Terms that describe the fetus in relation to the uterus, cervix, and maternal pelvis are
Fetal presentation: Fetal part that overlies the maternal pelvic inlet; vertex (cephalic), face, brow, breech, shoulder, funic (umbilical cord), or compound (more than one part, eg, shoulder and hand)
Fetal position: Relation of the presenting part to an anatomic axis; for transverse presentation, occiput anterior, occiput posterior, occiput transverse
Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse
Normal fetal lie is longitudinal, normal presentation is vertex, and occiput anterior is the most common position.
Abnormal fetal lie, presentation, or position may occur with
Fetopelvic disproportion (fetus too large for the pelvic inlet)
Fetal congenital anomalies
Uterine structural abnormalities (eg, fibroids, synechiae)
Multiple gestation
Several common types of abnormal lie or presentation are discussed here.

Transverse lie
Fetal position is transverse, with the fetal long axis oblique or perpendicular rather than parallel to the maternal long axis. Transverse lie is often accompanied by shoulder presentation, which requires cesarean delivery.
Breech presentation
There are several types of breech presentation.
Frank breech: The fetal hips are flexed, and the knees extended (pike position).
Complete breech: The fetus seems to be sitting with hips and knees flexed.
Single or double footling presentation: One or both legs are completely extended and present before the buttocks.
Types of breech presentations
Breech presentation makes delivery difficult ,primarily because the presenting part is a poor dilating wedge. Having a poor dilating wedge can lead to incomplete cervical dilation, because the presenting part is narrower than the head that follows. The head, which is the part with the largest diameter, can then be trapped during delivery.
Additionally, the trapped fetal head can compress the umbilical cord if the fetal umbilicus is visible at the introitus, particularly in primiparas whose pelvic tissues have not been dilated by previous deliveries. Umbilical cord compression may cause fetal hypoxemia.

Predisposing factors for breech presentation include
Preterm labor
Uterine abnormalities
Fetal anomalies
If delivery is vaginal, breech presentation may increase risk of
Umbilical cord prolapse
Birth trauma
Perinatal death

Face or brow presentation
In face presentation, the head is hyperextended, and position is designated by the position of the chin (mentum). When the chin is posterior, the head is less likely to rotate and less likely to deliver vaginally, necessitating cesarean delivery.
Brow presentation usually converts spontaneously to vertex or face presentation.
Occiput posterior position
The most common abnormal position is occiput posterior.
The fetal neck is usually somewhat deflexed; thus, a larger diameter of the head must pass through the pelvis.
Progress may arrest in the second phase of labor. Operative vaginal delivery or cesarean delivery is often required.
Position and Presentation of the Fetus
If a fetus is in the occiput posterior position, operative vaginal delivery or cesarean delivery is often required.
In breech presentation, the presenting part is a poor dilating wedge, which can cause the head to be trapped during delivery, often compressing the umbilical cord.
For breech presentation, usually do cesarean delivery at 39 weeks or during labor, but external cephalic version is sometimes successful before labor, usually at 37 or 38 weeks.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
What Is a Transverse Baby Position?
Why It Happens, How to Turn Your Baby, and Tips for a Safe Delivery
Causes and Risk Factors
Turning the fetus, complications, frequently asked questions.
A transverse baby position, also called transverse fetal lie, is when the fetus is sideways—at a 90-degree angle to your spine—instead of head up or head down. This development means that a vaginal delivery poses major risks to both you and the fetus.
Sometimes, a transverse fetus will turn itself into the head-down position before you go into labor. Other times, a healthcare provider may be able to turn the position.
If a transverse fetus can't be turned to the right position before birth, you're likely to have a cesarean section (C-section).
This article looks at causes and risk factors for a transverse baby position. It also covers how it's diagnosed and treated, the possible complications, and how you can plan ahead for delivery.
Marko Geber / Getty Images
How Common Is Transverse Baby Position?
An estimated 2% to 13% of babies are in an unfavorable position at delivery —meaning they're not in the head-down position .
Certain physiological issues can lead to a transverse fetal lie. These include:
- A bicornuate uterus : The uterus has a deep V in the top that separates the uterus into two sides; it may only be able to hold a near-term fetus sideways.
- Oligohydramnios or polyhydramnios : Abnormally low or high amniotic fluid volume (respectively).
Several risk factors can make it more likely for the fetus to be in a transverse lie, such as:
- The placenta being in an unusual position, such as blocking the opening to the cervix ( placenta previa ), which doesn't allow the fetus to reach the head-down position
- Going into labor early, before the fetus has had a chance to get into the right position
- Being pregnant with twins or other multiples, as the uterus is crowded and may not allow for much movement
- An abnormal pelvic structure that limits fetal movement
- Having a cyst or fibroid tumor blocking the cervix
Transverse fetal positioning is also more common after your first pregnancy.
It’s not uncommon for a fetus to be in a transverse position during the earlier stages of pregnancy. In most cases, though, they shift on their own well before labor begins. The transverse fetal position doesn't cause any signs or symptoms.
Healthcare professionals diagnose a transverse lie through an examination called Leopold’s Maneuvers. That involves feeling your abdomen to determine the fetal position. It's usually confirmed by an ultrasound.
You may also discover a transverse fetal lie during a routine ultrasound.
Timing of Transverse Position Diagnosis
The ultrasound done at your 36-week checkup lets your healthcare provider see the fetal position as you get closer to labor and delivery. If it's still a transverse lie at that time, your medical team will look at options for the safest labor and delivery.
Approximately 97% of deliveries involve a fetus positioned with the head down, in the best position to slide out. That makes a vaginal delivery easier and safer.
A transverse position only happens in about 1% of deliveries. In that position, the shoulder, arm, or trunk of the fetus may present first. This isn't a good scenario for either of you because a vaginal delivery is nearly impossible.
In these cases, you have two options:
- Turning the fetal position
- Having a C-section
If the fetus is in a transverse lie late in pregnancy, you or your healthcare provider may be able to change the position. Turning into the proper head-down position may help you avoid a C-section.
Medical Options
A healthcare provider can use one of the following techniques to attempt re-positioning a fetus:
- External cephalic version (ECV) : This procedure typically is performed at or after 36 weeks of pregnancy; involves using pressure on your abdomen where the fetal head and buttocks are.
- Webster technique : This is a chiropractic method in which a healthcare professional moves your hips to allow your uterus to relax and make more room for the fetus to move itself. (Note: No evidence supports this method.)
A 2020 study reported a 100% success rate for trained practitioners who used turning to change a transverse fetal lie. Real-world success rates are closer to 60%.
At-Home Options
You may be able to encourage a move out of the transverse position at home. You can try:
- Getting on your hands and knees and gently rocking back and forth
- Lying on your back with your knees bent and feet flat on the floor, then pushing your hips up in the air (bridge pose)
- Talking or playing music to stimulate the fetus to become more active
- Applying some cold to your abdomen where the fetal head is, which may make them want to move away from it
These methods may or may not work for you. While there's anecdotal evidence that they sometimes work, they haven't been researched.
Talk to your healthcare provider before attempting any of these techniques to ensure you're not doing anything unsafe.
Can Babies Go Back to Transverse After Being Turned?
Even if the fetus does change position or is successfully moved, it is possible that it could return to a transverse position prior to delivery.
Whether your child is born via C-section or is successfully moved so you can have a vaginal delivery, potential complications remain.
Cesarean Sections
C-sections are extremely common and are generally safe for both you and the fetus. Still, some inherent risks are associated with the procedure, as there are with any surgery.
The transverse position can force the surgeon to make a different type of incision, as the fetal lie may be right where they'd usually cut. Possible C-section complications for you can include:
- Increased bleeding
- Bladder or bowel injury
- Reactions to medicines
- Blood clots
- Death (very rare)
In rare cases, a C-section can result in potential complications for the baby , including:
- Breathing problems, if fluid needs to be cleared from their lungs
Most C-sections are safe and result in a healthy baby and parent. In some situations, a surgical delivery is the safest option available.
Vaginal Delivery
If the fetus is successfully moved out of the transverse lie position, you'll likely be able to deliver it vaginally. However, a few complications are possible even after the fetus has been moved:
- Labor typically takes longer.
- Your baby’s face may be swollen and appear bruised for a few days.
- The umbilical cord may be compressed, potentially causing distress and leading to a C-section.
Studies suggest that ECV is safe, effective, and may help lower the C-section rate.
Planning Ahead
As with any birth, if you experience a transverse fetal position, you should work with your healthcare provider to develop a delivery plan. If the transverse position has been maintained throughout the pregnancy, the medical team will evaluate the position at about 36 weeks and make plans accordingly.
Remember that even if the fetal head is down late in pregnancy, things can change quickly during labor and delivery. That means it's worthwhile to discuss options for different types of delivery in case they become necessary.
A transverse baby position, or transverse fetal lie, is the term for a fetus that's lying sideways in the uterus. Vaginal delivery usually isn't possible in these cases.
If the fetus is in this position near the time of delivery, the options are to turn it to make vaginal delivery possible or to have a C-section. A trained healthcare provider can use turning techniques. You may also be able to get the fetus to turn at home with some simple techniques.
Both C-section and vaginal delivery pose a risk of certain complications. However, these problems are rare and the vast majority of deliveries end with a healthy baby and parent.
A Word From Verywell
Pregnancy comes with many unknowns, and the surprises can continue up through labor and delivery.
Talking to your healthcare provider early on about possible scenarios can give you time to think about possible outcomes. This helps to avoid a situation where you’re considering risks and benefits during labor when quick decisions need to be made.
Ideally, a baby should be in the cephalic position (head down) at 32 weeks. If not, a doctor will examine the fetal position at around the 36-week mark and determine what should happen next to ensure a smooth delivery. Whether this involves a cesarian section will depend on the specific case.
Less than 1% of babies are born in the transverse position. In many cases, a doctor might recommend a cesarian delivery to ensure a more safe delivery. The risk of giving birth in the transverse lie position is greater before a due date or if twins or triplets are also born.
A planned cesarian section , or C-section, is typically performed in the 39th week of gestation. This is done so the fetus is given enough time to grow and develop so that it is healthy.
In some cases, a doctor may perform an external cephalic version (ECV) to change a transverse fetal lie. This involves the doctor using their hands to apply firm pressure to the abdomen so the fetus is moved into the cephalic (head-down) position.
Most attempts of ECV are successful, but there is a chance the fetus can move back to its previous position; in these cases, a doctor can attempt ECV again.
The American College of Obstetricians and Gynecologists. If your baby is breech .
Tempest N, Lane S, Hapangama D. Babies in occiput posterior position are significantly more likely to require an emergency cesarean birth compared with babies in occiput transverse position in the second stage of labor: a prospective observational study . Acta Obstet Gynecol Scand . 2020;99(4):537-545. doi:10.1111/aogs.13765
National Institutes of Health, U.S. National Library of Medicine: MedlinePlus. Congenital uterine anomalies .
Figueroa L, McClure EM, Swanson J, et al. Oligohydramnios: a prospective study of fetal, neonatal and maternal outcomes in low-middle income countries . Reprod Health. 2020;17 (article 19). doi:10.1186/s12978-020-0854-y
National Institutes of Health, U.S. National Library of Medicine: MedlinePlus. Placenta previa .
National Institutes of Health, U.S. National Library of Medicine: MedlinePlus. Your baby in the birth canal .
Van der Kaay DC, Horsch S, Duvekot JJ. Severe neonatal complication of transverse lie after preterm premature rupture of membranes . BMJ Case Rep . 2013;bcr2012008399. doi:10.1136/bcr-2012-008399
Oyinloye OI, Okoyomo AA. Longitudinal evaluation of foetal transverse lie using ultrasonography . Afr J Reprod Health ; 14(1):129-133.
Nishikawa M, Sakakibara H. Effect of nursing intervention program using abdominal palpation of Leopold’s maneuvers on maternal-fetal attachment . Reprod Health 2013;10 (article 12). doi.org/10.1186/1742-4755-10-12
National Institutes of Health, U.S. National Library of Medicine: MedlinePlus. Delivery presentations .
Dalvi SA. Difficult deliveries in Cesarean section . J Obstet Gynaecol India . 2018;68(5):344-348. doi:10.1007/s13224-017-1052-x
Zhi Z, Xi L. Clinical analysis of 40 cases of external cephalic version without anesthesia . J Int Med Res . 2021;49(1):300060520986699. doi:10.1177/0300060520986699
National Institutes of Health, U.S. National Library of Medicine: MedlinePlus. Questions to ask your doctor about labor and delivery .
Nemours KidsHealth. Cesarean sections .
By Elizabeth Yuko, PhD Yuko has a doctorate in bioethics and medical ethics and is a freelance journalist based in New York.
Fetal Presentation, Position, and Lie (Including Breech Presentation)
- Variations in Fetal Position and Presentation |
During pregnancy, the fetus can be positioned in many different ways inside the mother's uterus. The fetus may be head up or down or facing the mother's back or front. At first, the fetus can move around easily or shift position as the mother moves. Toward the end of the pregnancy the fetus is larger, has less room to move, and stays in one position. How the fetus is positioned has an important effect on delivery and, for certain positions, a cesarean delivery is necessary. There are medical terms that describe precisely how the fetus is positioned, and identifying the fetal position helps doctors to anticipate potential difficulties during labor and delivery.
Presentation refers to the part of the fetus’s body that leads the way out through the birth canal (called the presenting part). Usually, the head leads the way, but sometimes the buttocks (breech presentation), shoulder, or face leads the way.
Position refers to whether the fetus is facing backward (occiput anterior) or forward (occiput posterior). The occiput is a bone at the back of the baby's head. Therefore, facing backward is called occiput anterior (facing the mother’s back and facing down when the mother lies on her back). Facing forward is called occiput posterior (facing toward the mother's pubic bone and facing up when the mother lies on her back).
Lie refers to the angle of the fetus in relation to the mother and the uterus. Up-and-down (with the baby's spine parallel to mother's spine, called longitudinal) is normal, but sometimes the lie is sideways (transverse) or at an angle (oblique).
For these aspects of fetal positioning, the combination that is the most common, safest, and easiest for the mother to deliver is the following:
Head first (called vertex or cephalic presentation)
Facing backward (occiput anterior position)
Spine parallel to mother's spine (longitudinal lie)
Neck bent forward with chin tucked
Arms folded across the chest
If the fetus is in a different position, lie, or presentation, labor may be more difficult, and a normal vaginal delivery may not be possible.
Variations in fetal presentation, position, or lie may occur when
The fetus is too large for the mother's pelvis (fetopelvic disproportion).
The uterus is abnormally shaped or contains growths such as fibroids .
The fetus has a birth defect .
There is more than one fetus (multiple gestation).

Position and Presentation of the Fetus
Variations in fetal position and presentation.
Some variations in position and presentation that make delivery difficult occur frequently.
Occiput posterior position
In occiput posterior position (sometimes called sunny-side up), the fetus is head first (vertex presentation) but is facing forward (toward the mother's pubic bone—that is, facing up when the mother lies on her back). This is a very common position that is not abnormal, but it makes delivery more difficult than when the fetus is in the occiput anterior position (facing toward the mother's spine—that is facing down when the mother lies on her back).
When a fetus faces up, the neck is often straightened rather than bent,which requires more room for the head to pass through the birth canal. Delivery assisted by a vacuum device or forceps or cesarean delivery may be necessary.
Breech presentation
In breech presentation, the baby's buttocks or sometimes the feet are positioned to deliver first (before the head).
When delivered vaginally, babies that present buttocks first are more at risk of injury or even death than those that present head first.
The reason for the risks to babies in breech presentation is that the baby's hips and buttocks are not as wide as the head. Therefore, when the hips and buttocks pass through the cervix first, the passageway may not be wide enough for the head to pass through. In addition, when the head follows the buttocks, the neck may be bent slightly backwards. The neck being bent backward increases the width required for delivery as compared to when the head is angled forward with the chin tucked, which is the position that is easiest for delivery. Thus, the baby’s body may be delivered and then the head may get caught and not be able to pass through the birth canal. When the baby’s head is caught, this puts pressure on the umbilical cord in the birth canal, so that very little oxygen can reach the baby. Brain damage due to lack of oxygen is more common among breech babies than among those presenting head first.
In a first delivery, these problems may occur more frequently because a woman’s tissues have not been stretched by previous deliveries. Because of risk of injury or even death to the baby, cesarean delivery is preferred when the fetus is in breech presentation, unless the doctor is very experienced with and skilled at delivering breech babies or there is not an adequate facility or equipment to safely perform a cesarean delivery.
Breech presentation is more likely to occur in the following circumstances:
Labor starts too soon (preterm labor).
The uterus is abnormally shaped or contains abnormal growths such as fibroids .
Other presentations
In face presentation, the baby's neck arches back so that the face presents first rather than the top of the head.
In brow presentation, the neck is moderately arched so that the brow presents first.
Usually, fetuses do not stay in a face or brow presentation. These presentations often change to a vertex (top of the head) presentation before or during labor. If they do not, a cesarean delivery is usually recommended.
In transverse lie, the fetus lies horizontally across the birth canal and presents shoulder first. A cesarean delivery is done, unless the fetus is the second in a set of twins. In such a case, the fetus may be turned to be delivered through the vagina.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
7.6 Transverse lie and shoulder presentation
A transverse lie constitutes an absolute foeto-pelvic disproportion, and vaginal delivery is impossible.
This is an obstetric emergency, because labour is obstructed and there is a risk of uterine rupture and foetal distress.
7.6.1 Diagnosis
- The uterus is very wide: the transverse axis is virtually equivalent to the longitudinal axis; fundal height is less than 30 cm near term.
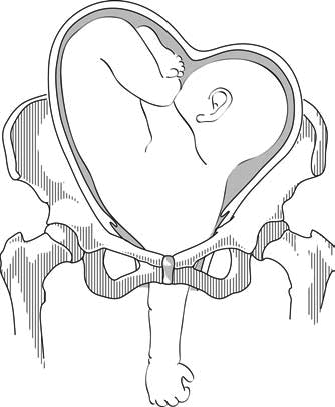
- On examination: head in one side, breech in the other (Figures 7.1a and 7.1b). Vaginal examination reveals a nearly empty true pelvis or a shoulder with—sometimes—an arm prolapsing from the vagina (Figure 7.1c).
Figures 7.1 - Transverse lie and shoulder presentation
7.6.2 Possible causes
- Grand multiparity (5 deliveries or more)
- Uterine malformation
Twin pregnancy
- Prematurity
- Placenta praevia
- Foeto-pelvic disproportion
7.6.3 Management
This diagnosis should be made before labour begins, at the last prenatal visit before the birth.

At the end of pregnancy
Singleton pregnancy.
- External version 4 to 6 weeks before delivery, in a CEmONC facility ( Section 7.7 ).
- If this fails, delivery should be carried out by caesarean section, either planned or at the beginning of labour (Chapter 6, Section 6.4.1 ).
- External version is contra-indicated.
- If the first twin is in a transverse lie (unusual): schedule a caesarean section.
- If the second twin is in a transverse lie: there is no indication for caesarean section, but plan delivery in a CEmONC facility so that it can be performed if necessary. Deliver the first twin and then, assess the foetal position and give a few minutes for the second twin to adopt a longitudinal lie. If the second twin stays in a transverse lie, and depending on the experience of the operator, perform external version ( Section 7.7 ) and/or internal version ( Section 7.8 ) on the second twin.
During labour, in a CEmONC facility
Foetus alive and membranes intact.
- Gentle external version, between two contractions, as early as possible, then proceed as with normal delivery.
- If this fails: caesarean section.
Foetus alive and membranes ruptured
- Multipara with relaxed uterus and mobile foetus, and an experienced operator: internal version and total breech extraction.
- Primipara, or tight uterus, or immobile foetus, or engaged arm, or scarred uterus or insufficiently-experienced operator: caesarean section.
- Incomplete dilation: caesarean section.
Caesarean section can be difficult due to uterine retraction. Vertical hysterotomy is preferable. To perform extraction, grasp a foot in the fundus (equivalent to a total breech extraction, but by caesarean section).
Foetus dead
Embryotomy for transverse lie (Chapter 9, Section 9.7.7 ).
During labour, in remote settings where surgery is not available
Try to refer the patient to a CEmONC facility. If not feasible:
- Attempt external version as early as possible.
- If this fails, wait for complete dilation.
- Perform an external version ( Section 7.7 ) combined with an internal version ( Section 7.8 ), possibly placing the woman in various positions (Trendelenburg or knee-chest).
- Put the woman into the knee-chest position.
- Between contractions, push the foetus back and try to engage his head.
- Vacuum extraction (Chapter 5, Section 5.6.1 ) and symphysiotomy (Chapter 5, Section 5.7 ) at the slightest difficulty.
- Incomplete dilation: Trendelenburg position and watchful waiting until complete dilation.
Try to refer the patient, even if referral takes some time. If not feasible, embryotomy for transverse lie (Chapter 9, Section 9.7.7 ).
Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic
RELATED TOPICS
INTRODUCTION
This topic will discuss the diagnosis, clinical course, and management of OT position. OT position is unrelated to transverse lie, in which the long axis of the fetal body is perpendicular to the long axis of the mother. (See "Transverse fetal lie" .)
If an obstetrical provider uses ultrasound to determine fetal position in labor, the provider should receive specialized training for this type of sonographic examination and undergo supervision by a more experienced diagnostician until they develop proficiency. The International Society of Ultrasound in Obstetrics and Gynecology (ISUOG) has an online video that provides guidance on techniques and sonographic findings.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Delivery, face and brow presentation.
Julija Makajeva ; Mohsina Ashraf .
Affiliations
Last Update: January 9, 2023 .
- Continuing Education Activity
Face and brow presentation is a malpresentation during labor when the presenting part is either the face or, in the case of brow presentation, it is the area between the orbital ridge and the anterior fontanelle. This activity reviews the evaluation and management of these two presentations and explains the role of the interprofessional team in managing delivery safely for both the mother and the baby.
- Describe the mechanism of labor in the face and brow presentation.
- Summarize potential maternal and fetal complications during the face and brow presentations.
- Review different management approaches for the face and brow presentation.
- Outline some interprofessional strategies that will improve patient outcomes in delivery cases with face and brow presentation issues.
- Introduction
The term presentation describes the leading part of the fetus or the anatomical structure closest to the maternal pelvic inlet during labor. The presentation can roughly be divided into the following classifications: cephalic, breech, shoulder, and compound. Cephalic presentation is the most common and can be further subclassified as vertex, sinciput, brow, face, and chin. The most common presentation in term labor is the vertex, where the fetal neck is flexed to the chin, minimizing the head circumference.
Face presentation – an abnormal form of cephalic presentation where the presenting part is mentum. This typically occurs because of hyperextension of the neck and the occiput touching the fetal back. Incidence of face presentation is rare, accounting for approximately 1 in 600 of all presentations. [1] [2] [3]
In brow presentation, the neck is not extended as much as in face presentation, and the leading part is the area between the anterior fontanelle and the orbital ridges. Brow presentation is considered the rarest of all malpresentation with a prevalence of 1 in 500 to 1 in 4000 deliveries. [3]
Both face and brow presentations occur due to extension of the fetal neck instead of flexion; therefore, conditions that would lead to hyperextension or prevent flexion of the fetal neck can all contribute to face or brow presentation. These risk factors may be related to either the mother or the fetus. Maternal risk factors are preterm delivery, contracted maternal pelvis, platypelloid pelvis, multiparity, previous cesarean section, black race. Fetal risk factors include anencephaly, multiple loops of cord around the neck, masses of the neck, macrosomia, polyhydramnios. [2] [4] [5]
These malpresentations are usually diagnosed during the second stage of labor when performing a digital examination. It is possible to palpate orbital ridges, nose, malar eminences, mentum, mouth, gums, and chin in face presentation. Based on the position of the chin, face presentation can be further divided into mentum anterior, posterior, or transverse. In brow presentation, anterior fontanelle and face can be palpated except for the mouth and the chin. Brow presentation can then be further described based on the position of the anterior fontanelle as frontal anterior, posterior, or transverse.
Diagnosing the exact presentation can be challenging, and face presentation may be misdiagnosed as frank breech. To avoid any confusion, a bedside ultrasound scan can be performed. [6] The ultrasound imaging can show a reduced angle between the occiput and the spine or, the chin is separated from the chest. However, ultrasound does not provide much predicting value in the outcome of the labor. [7]
- Anatomy and Physiology
Before discussing the mechanism of labor in the face or brow presentation, it is crucial to highlight some anatomical landmarks and their measurements.
Planes and Diameters of the Pelvis
The three most important planes in the female pelvis are the pelvic inlet, mid pelvis, and pelvic outlet.
Four diameters can describe the pelvic inlet: anteroposterior, transverse, and two obliques. Furthermore, based on the different landmarks on the pelvic inlet, there are three different anteroposterior diameters, named conjugates: true conjugate, obstetrical conjugate, and diagonal conjugate. Only the latter can be measured directly during the obstetric examination. The shortest of these three diameters is obstetrical conjugate, which measures approximately 10.5 cm and is a distance between the sacral promontory and 1 cm below the upper border of the symphysis pubis. This measurement is clinically significant as the fetal head must pass through this diameter during the engagement phase. The transverse diameter measures about 13.5cm and is the widest distance between the innominate line on both sides.
The shortest distance in the mid pelvis is the interspinous diameter and usually is only about 10 cm.
Fetal Skull Diameters
There are six distinguished longitudinal fetal skull diameters:
- Suboccipito-bregmatic: from the center of anterior fontanelle (bregma) to the occipital protuberance, measuring 9.5 cm. This is the presenting diameter in vertex presentation.
- Suboccipito-frontal: from the anterior part of bregma to the occipital protuberance, measuring 10 cm
- Occipito-frontal: from the root of the nose to the most prominent part of the occiput, measuring 11.5cm
- Submento-bregmatic: from the center of the bregma to the angle of the mandible, measuring 9.5 cm. This is the presenting diameter in face presentation where the neck is hyperextended.
- Submento-vertical: from the midpoint between fontanelles and the angle of the mandible, measuring 11.5cm
- Occipito-mental: from the midpoint between fontanelles and the tip of the chin, measuring 13.5 cm. It is the presenting diameter in brow presentation.
Cardinal Movements of Normal Labor
- Neck flexion
- Internal rotation
- Extension (delivers head)
- External rotation (Restitution)
- Expulsion (delivery of anterior and posterior shoulders)
Some of the key movements are not possible in the face or brow presentations.
Based on the information provided above, it is obvious that labor will be arrested in brow presentation unless it spontaneously changes to face or vertex, as the occipito-mental diameter of the fetal head is significantly wider than the smallest diameter of the female pelvis. Face presentation can, however, be delivered vaginally, and further mechanisms of face delivery will be explained in later sections.
- Indications
As mentioned previously, spontaneous vaginal delivery can be successful in face presentation. However, the main indication for vaginal delivery in such circumstances would be a maternal choice. It is crucial to have a thorough conversation with a mother, explaining the risks and benefits of vaginal delivery with face presentation and a cesarean section. Informed consent and creating a rapport with the mother is an essential aspect of safe and successful labor.
- Contraindications
Vaginal delivery of face presentation is contraindicated if the mentum is lying posteriorly or is in a transverse position. In such a scenario, the fetal brow is pressing against the maternal symphysis pubis, and the short fetal neck, which is already maximally extended, cannot span the surface of the maternal sacrum. In this position, the diameter of the head is larger than the maternal pelvis, and it cannot descend through the birth canal. Therefore the cesarean section is recommended as the safest mode of delivery for mentum posterior face presentations.
Attempts to manually convert face presentation to vertex, manual or forceps rotation of the persistent posterior chin to anterior are contraindicated as they can be dangerous.
Persistent brow presentation itself is a contraindication for vaginal delivery unless the fetus is significantly small or the maternal pelvis is large.
Continuous electronic fetal heart rate monitoring is recommended for face and brow presentations, as heart rate abnormalities are common in these scenarios. One study found that only 14% of the cases with face presentation had no abnormal traces on the cardiotocograph. [8] It is advised to use external transducer devices to prevent damage to the eyes. When internal monitoring is inevitable, it is suggested to place monitoring devices on bony parts carefully.
People who are usually involved in the delivery of face/ brow presentation are:
- Experienced midwife, preferably looking after laboring woman 1:1
- Senior obstetrician
- Neonatal team - in case of need for resuscitation
- Anesthetic team - to provide necessary pain control (e.g., epidural)
- Theatre team - in case of failure to progress and an emergency cesarean section will be required.
- Preparation
No specific preparation is required for face or brow presentation. However, it is essential to discuss the labor options with the mother and birthing partner and inform members of the neonatal, anesthetic, and theatre co-ordinating teams.
- Technique or Treatment
Mechanism of Labor in Face Presentation
During contractions, the pressure exerted by the fundus of the uterus on the fetus and pressure of amniotic fluid initiate descent. During this descent, the fetal neck extends instead of flexing. The internal rotation determines the outcome of delivery, if the fetal chin rotates posteriorly, vaginal delivery would not be possible, and cesarean section is permitted. The approach towards mentum-posterior delivery should be individualized, as the cases are rare. Expectant management is acceptable in multiparous women with small fetuses, as a spontaneous mentum-anterior rotation can occur. However, there should be a low threshold for cesarean section in primigravida women or women with large fetuses.
When the fetal chin is rotated towards maternal symphysis pubis as described as mentum-anterior; in these cases further descend through the vaginal canal continues with approximately 73% cases deliver spontaneously. [9] Fetal mentum presses on the maternal symphysis pubis, and the head is delivered by flexion. The occiput is pointing towards the maternal back, and external rotation happens. Shoulders are delivered in the same manner as in vertex delivery.
Mechanism of Labor in Brow Presentation
As this presentation is considered unstable, it is usually converted into a face or an occiput presentation. Due to the cephalic diameter being wider than the maternal pelvis, the fetal head cannot engage; thus, brow delivery cannot take place. Unless the fetus is small or the pelvis is very wide, the prognosis for vaginal delivery is poor. With persistent brow presentation, a cesarean section is required for safe delivery.
- Complications
As the cesarean section is becoming a more accessible mode of delivery in malpresentations, the incidence of maternal and fetal morbidity and mortality during face presentation has dropped significantly. [10]
However, there are still some complications associated with the nature of labor in face presentation. Due to the fetal head position, it is more challenging for the head to engage in the birth canal and descend, resulting in prolonged labor.
Prolonged labor itself can provoke foetal distress and arrhythmias. If the labor arrests or signs of fetal distress appear on CTG, the recommended next step in management is an emergency cesarean section, which in itself carries a myriad of operative and post-operative complications.
Finally, due to the nature of the fetal position and prolonged duration of labor in face presentation, neonates develop significant edema of the skull and face. Swelling of the fetal airway may also be present, resulting in respiratory distress after birth and possible intubation.
- Clinical Significance
During vertex presentation, the fetal head flexes, bringing the chin to the chest, forming the smallest possible fetal head diameter, measuring approximately 9.5cm. With face and brow presentation, the neck hyperextends, resulting in greater cephalic diameters. As a result, the fetal head will engage later, and labor will progress more slowly. Failure to progress in labor is also more common in both presentations compared to vertex presentation.
Furthermore, when the fetal chin is in a posterior position, this prevents further flexion of the fetal neck, as browns are pressing on the symphysis pubis. As a result, descend through the birth canal is impossible. Such presentation is considered undeliverable vaginally and requires an emergency cesarean section.
Manual attempts to change face presentation to vertex, manual or forceps rotation to mentum anterior are considered dangerous and are discouraged.
- Enhancing Healthcare Team Outcomes
A multidisciplinary team of healthcare experts supports the woman and her child during labor and the perinatal period. For a face or brow presentation to be appropriately diagnosed, an experienced midwife and obstetrician must be involved in the vaginal examination and labor monitoring. As fetal anomalies, such as anencephaly or goiter, can contribute to face presentation, sonographers experienced in antenatal scanning should also be involved in the care. It is advised to inform the anesthetic and neonatal teams in advance of the possible need for emergency cesarean section and resuscitation of the neonate. [11] [12]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Julija Makajeva declares no relevant financial relationships with ineligible companies.
Disclosure: Mohsina Ashraf declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Makajeva J, Ashraf M. Delivery, Face and Brow Presentation. [Updated 2023 Jan 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PubMed Links to PubMed
Similar articles in PubMed
- Sonographic diagnosis of fetal head deflexion and the risk of cesarean delivery. [Am J Obstet Gynecol MFM. 2020] Sonographic diagnosis of fetal head deflexion and the risk of cesarean delivery. Bellussi F, Livi A, Cataneo I, Salsi G, Lenzi J, Pilu G. Am J Obstet Gynecol MFM. 2020 Nov; 2(4):100217. Epub 2020 Aug 18.
- Review Sonographic evaluation of the fetal head position and attitude during labor. [Am J Obstet Gynecol. 2022] Review Sonographic evaluation of the fetal head position and attitude during labor. Ghi T, Dall'Asta A. Am J Obstet Gynecol. 2022 Jul 6; . Epub 2022 Jul 6.
- Stages of Labor. [StatPearls. 2024] Stages of Labor. Hutchison J, Mahdy H, Hutchison J. StatPearls. 2024 Jan
- Leopold Maneuvers. [StatPearls. 2024] Leopold Maneuvers. Superville SS, Siccardi MA. StatPearls. 2024 Jan
- Review Labor with abnormal presentation and position. [Obstet Gynecol Clin North Am. ...] Review Labor with abnormal presentation and position. Stitely ML, Gherman RB. Obstet Gynecol Clin North Am. 2005 Jun; 32(2):165-79.
Recent Activity
- Delivery, Face and Brow Presentation - StatPearls Delivery, Face and Brow Presentation - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

- Mammary Glands
- Fallopian Tubes
- Supporting Ligaments
- Reproductive System
- Gametogenesis
- Placental Development
- Maternal Adaptations
- Menstrual Cycle
- Antenatal Care
- Small for Gestational Age
- Large for Gestational Age
- RBC Isoimmunisation
- Prematurity
- Prolonged Pregnancy
- Multiple Pregnancy
- Miscarriage
- Recurrent Miscarriage
- Ectopic Pregnancy
- Hyperemesis Gravidarum
- Gestational Trophoblastic Disease
- Breech Presentation
- Abnormal lie, Malpresentation and Malposition
- Oligohydramnios
- Polyhydramnios
- Placenta Praevia
- Placental Abruption
- Pre-Eclampsia
- Gestational Diabetes
- Headaches in Pregnancy
- Haematological
- Obstetric Cholestasis
- Thyroid Disease in Pregnancy
- Epilepsy in Pregnancy
- Induction of Labour
- Operative Vaginal Delivery
- Prelabour Rupture of Membranes
- Caesarean Section
- Shoulder Dystocia
- Cord Prolapse
- Uterine Rupture
- Amniotic Fluid Embolism
- Primary PPH
- Secondary PPH
- Psychiatric Disease
- Postpartum Contraception
- Breastfeeding Problems
- Primary Dysmenorrhoea
- Amenorrhoea and Oligomenorrhoea
- Heavy Menstrual Bleeding
- Endometriosis
- Endometrial Cancer
- Adenomyosis
- Cervical Polyps
- Cervical Ectropion
- Cervical Intraepithelial Neoplasia + Cervical Screening
- Cervical Cancer
- Polycystic Ovary Syndrome (PCOS)
- Ovarian Cysts & Tumours
- Urinary Incontinence
- Genitourinary Prolapses
- Bartholin's Cyst
- Lichen Sclerosus
- Vulval Carcinoma
- Introduction to Infertility
- Female Factor Infertility
- Male Factor Infertility
- Female Genital Mutilation
- Barrier Contraception
- Combined Hormonal
- Progesterone Only Hormonal
- Intrauterine System & Device
- Emergency Contraception
- Pelvic Inflammatory Disease
- Genital Warts
- Genital Herpes
- Trichomonas Vaginalis
- Bacterial Vaginosis
- Vulvovaginal Candidiasis
- Obstetric History
- Gynaecological History
- Sexual History
- Obstetric Examination
- Speculum Examination
- Bimanual Examination
- Amniocentesis
- Chorionic Villus Sampling
- Hysterectomy
- Endometrial Ablation
- Tension-Free Vaginal Tape
- Contraceptive Implant
- Fitting an IUS or IUD
Abnormal Fetal lie, Malpresentation and Malposition
Original Author(s): Anna Mcclune Last updated: 1st December 2018 Revisions: 12
- 1 Definitions
- 2 Risk Factors
- 3.2 Presentation
- 3.3 Position
- 4 Investigations
- 5.1 Abnormal Fetal Lie
- 5.2 Malpresentation
- 5.3 Malposition
The lie, presentation and position of a fetus are important during labour and delivery.
In this article, we will look at the risk factors, examination and management of abnormal fetal lie, malpresentation and malposition.
Definitions
- Longitudinal, transverse or oblique
- Cephalic vertex presentation is the most common and is considered the safest
- Other presentations include breech, shoulder, face and brow
- Usually the fetal head engages in the occipito-anterior position (the fetal occiput facing anteriorly) – this is ideal for birth
- Other positions include occipito-posterior and occipito-transverse.
Note: Breech presentation is the most common malpresentation, and is covered in detail here .
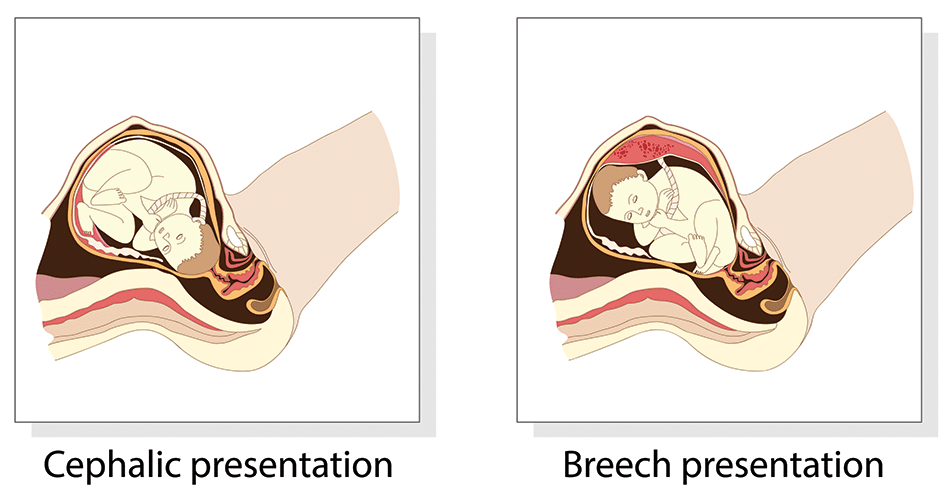
Fig 1 – The two most common fetal presentations: cephalic and breech.
Risk Factors
The risk factors for abnormal fetal lie, malpresentation and malposition include:
- Multiple pregnancy
- Uterine abnormalities (e.g fibroids, partial septate uterus)
- Fetal abnormalities
- Placenta praevia
- Primiparity
Identifying Fetal Lie, Presentation and Position
The fetal lie and presentation can usually be identified via abdominal examination. The fetal position is ascertained by vaginal examination.
For more information on the obstetric examination, see here .
- Face the patient’s head
- Place your hands on either side of the uterus and gently apply pressure; one side will feel fuller and firmer – this is the back, and fetal limbs may feel ‘knobbly’ on the opposite side
Presentation
- Palpate the lower uterus (above the symphysis pubis) with the fingers of both hands; the head feels hard and round (cephalic) and the bottom feels soft and triangular (breech)
- You may be able to gently push the fetal head from side to side
The fetal lie and presentation may not be possible to identify if the mother has a high BMI, if she has not emptied her bladder, if the fetus is small or if there is polyhydramnios .
During labour, vaginal examination is used to assess the position of the fetal head (in a cephalic vertex presentation). The landmarks of the fetal head, including the anterior and posterior fontanelles, indicate the position.
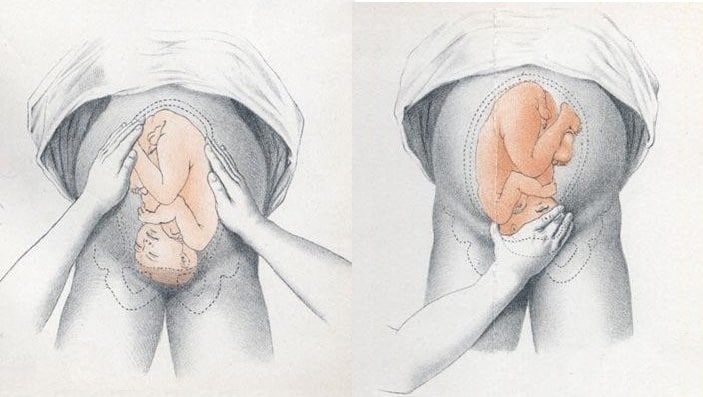
Fig 2 – Assessing fetal lie and presentation.
Investigations
Any suspected abnormal fetal lie or malpresentation should be confirmed by an ultrasound scan . This could also demonstrate predisposing uterine or fetal abnormalities.
Abnormal Fetal Lie
If the fetal lie is abnormal, an external cephalic version (ECV) can be attempted – ideally between 36 and 38 weeks gestation.
ECV is the manipulation of the fetus to a cephalic presentation through the maternal abdomen.
It has an approximate success rate of 50% in primiparous women and 60% in multiparous women. Only 8% of breech presentations will spontaneously revert to cephalic in primiparous women over 36 weeks gestation.
Complications of ECV are rare but include fetal distress , premature rupture of membranes, antepartum haemorrhage (APH) and placental abruption. The risk of an emergency caesarean section (C-section) within 24 hours is around 1 in 200.
ECV is contraindicated in women with a recent APH, ruptured membranes, uterine abnormalities or a previous C-section .
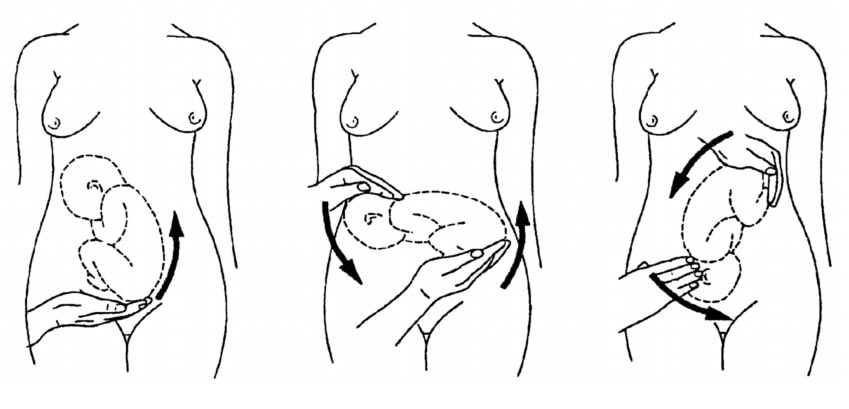
Fig 3 – External cephalic version.
Malpresentation
The management of malpresentation is dependent on the presentation.
- Breech – attempt ECV before labour, vaginal breech delivery or C-section
- Brow – a C-section is necessary
- If the chin is anterior (mento-anterior) a normal labour is possible; however, it is likely to be prolonged and there is an increased risk of a C-section being required
- If the chin is posterior (mento-posterior) then a C-section is necessary
- Shoulder – a C-section is necessary
Malposition
90% of malpositions spontaneously rotate to occipito-anterior as labour progresses. If the fetal head does not rotate, rotation and operative vaginal delivery can be attempted. Alternatively a C-section can be performed.
- Usually the fetal head engages in the occipito-anterior position (the fetal occiput facing anteriorly) - this is ideal for birth
If the fetal lie is abnormal, an external cephalic version (ECV) can be attempted - ideally between 36 and 38 weeks gestation.
- Breech - attempt ECV before labour, vaginal breech delivery or C-section
Found an error? Is our article missing some key information? Make the changes yourself here!
Once you've finished editing, click 'Submit for Review', and your changes will be reviewed by our team before publishing on the site.
We use cookies to improve your experience on our site and to show you relevant advertising. To find out more, read our privacy policy .
Privacy Overview
Achieve Mastery of Medical Concepts
Study for medical school and boards with lecturio.
USMLE Step 1 | USMLE Step 2 | COMLEX Level 1 | COMLEX Level 2 | ENARM | NEET
Fetal Malpresentation and Malposition
Fetal presentation describes which part of the fetus will enter through the cervix Cervix The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Externally, the cervix is lined by stratified squamous cells; however, the cervical canal is lined by columnar epithelium. Uterus, Cervix, and Fallopian Tubes: Anatomy first, while position is the orientation Orientation Awareness of oneself in relation to time, place and person. Psychiatric Assessment of the fetus compared to the maternal bony pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 "hip" bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy . Presentations include vertex (the fetal occiput will present through the cervix Cervix The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Externally, the cervix is lined by stratified squamous cells; however, the cervical canal is lined by columnar epithelium. Uterus, Cervix, and Fallopian Tubes: Anatomy first), face, brow, shoulder, and breech. If a fetal limb is presenting next to the presenting part (e.g., the hand Hand The hand constitutes the distal part of the upper limb and provides the fine, precise movements needed in activities of daily living. It consists of 5 metacarpal bones and 14 phalanges, as well as numerous muscles innervated by the median and ulnar nerves. Hand: Anatomy is next to the head), this is known as a compound presentation. Malpresentation refers to any presentation other than vertex, with the most common being breech presentations. Vaginal delivery of a breech infant increases the risk for head entrapment and hypoxia Hypoxia Sub-optimal oxygen levels in the ambient air of living organisms. Ischemic Cell Damage , so, especially in the United States, mothers are generally offered a procedure to help manually rotate the baby to a head-down position instead (known as an external cephalic version) or a planned cesarean delivery Cesarean Delivery Cesarean delivery (CD) is the operative delivery of ≥ 1 infants through a surgical incision in the maternal abdomen and uterus. Cesarean deliveries may be indicated for a number of either maternal or fetal reasons, most commonly including fetal intolerance to labor, arrest of labor, a history of prior uterine surgery, fetal malpresentation, and placental abnormalities. Cesarean Delivery .
Last updated: Feb 14, 2023
Fetal Lie and Presentation
Presenting diameter, management of cephalic and compound presentations, risks and management of breech and transverse presentations.
Share this concept:
- The “presenting part” refers to the part of the baby that will come through the cervix Cervix The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Externally, the cervix is lined by stratified squamous cells; however, the cervical canal is lined by columnar epithelium. Uterus, Cervix, and Fallopian Tubes: Anatomy first.
- The position refers to how that body part (and thus the baby) is oriented within the maternal pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 “hip” bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy .
- The uterine fundus Fundus The superior portion of the body of the stomach above the level of the cardiac notch. Stomach: Anatomy is typically roomier, so babies tend to orient themselves head down so that their body and limbs occupy the larger portion of the uterus Uterus The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The uterus has a thick wall made of smooth muscle (the myometrium) and an inner mucosal layer (the endometrium). The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Uterus, Cervix, and Fallopian Tubes: Anatomy .
Clinical relevance
- The maternal pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 “hip” bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy has a diameter of about 10 cm, through which the fetus must pass.
- The presentation and position of the fetus will determine how wide the fetus is (known as the “presenting fetal diameter”) as it attempts to pass through the maternal pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 “hip” bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy .
- Certain presentation/positions are more difficult (or even impossible) to pass through the pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 “hip” bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy because of their large presenting diameter.
- Knowledge of the presentation and position are required to safely manage labor and delivery.
Risk factors for fetal malpresentation
- Multiparity (which can result in lax abdominal walls)
- Multiple gestations (e.g., twins)
- Prematurity Prematurity Neonatal Respiratory Distress Syndrome
- Uterine abnormalities (e.g., leiomyomas, uterine septa)
- Narrow pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 “hip” bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy shapes
- Fetal anomalies (e.g., hydrocephalus Hydrocephalus Excessive accumulation of cerebrospinal fluid within the cranium which may be associated with dilation of cerebral ventricles, intracranial. Subarachnoid Hemorrhage )
- Placental anomalies (e.g., placenta previa Placenta Previa Abnormal placentation in which the placenta implants in the lower segment of the uterus (the zone of dilation) and may cover part or all of the opening of the cervix. It is often associated with serious antepartum bleeding and premature labor. Placental Abnormalities , in which the placenta Placenta A highly vascularized mammalian fetal-maternal organ and major site of transport of oxygen, nutrients, and fetal waste products. It includes a fetal portion (chorionic villi) derived from trophoblasts and a maternal portion (decidua) derived from the uterine endometrium. The placenta produces an array of steroid, protein and peptide hormones (placental hormones). Placenta, Umbilical Cord, and Amniotic Cavity covers the internal cervical os)
- Polyhydramnios Polyhydramnios Polyhydramnios is a pathological excess of amniotic fluid. Common causes of polyhydramnios include fetal anomalies, gestational diabetes, multiple gestations, and congenital infections. Patients are often asymptomatic but may present with dyspnea, extremity swelling, or abdominal distention. Polyhydramnios (too much fluid)
- Oligohydramnios Oligohydramnios Oligohydramnios refers to amniotic fluid volume less than expected for the current gestational age. Oligohydramnios is diagnosed by ultrasound and defined as an amniotic fluid index (AFI) of ‰¤ 5 cm or a single deep pocket (SDP) of Oligohydramnios (not enough fluid)
- Malpresentation in a previous pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care
Epidemiology
Prevalence Prevalence The total number of cases of a given disease in a specified population at a designated time. It is differentiated from incidence, which refers to the number of new cases in the population at a given time. Measures of Disease Frequency rates for different malpresentations at term:
- Vertex presentation, occiput posterior position: 1 in 19 deliveries
- Breech presentation: 1 in 33 deliveries
- Face presentation: 1 in 600–800 deliveries
- Transverse lie: 1 in 833 deliveries
- Compound presentation: 1 in 1500 deliveries
Related videos
Fetal lie is how the long axis of the fetus is oriented in relation to the mother. Possible lies include:
- Longitudinal: fetus and mother have the same vertical axis (their spines are parallel).
- Transverse: fetal vertical axis is at a 90-degree angle to mother’s vertical axis (their spines are perpendicular).
- Oblique: fetal vertical axis is at a 45-degree angle to mother’s vertical axis (unstable, and will resolve to longitudinal or transverse during labor).
Presentation
Presentation describes which body part of the fetus will pass through the cervix Cervix The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Externally, the cervix is lined by stratified squamous cells; however, the cervical canal is lined by columnar epithelium. Uterus, Cervix, and Fallopian Tubes: Anatomy first. Presentations include:
- Cephalic: head down
- Breech: bottom/feet down
- Transverse presentation: shoulder
- Compound presentation: an extremity presents alongside the primary presenting part
Cephalic presentations
Cephalic presentations can be categorized as:
- Vertex presentation: chin Chin The anatomical frontal portion of the mandible, also known as the mentum, that contains the line of fusion of the two separate halves of the mandible (symphysis menti). This line of fusion divides inferiorly to enclose a triangular area called the mental protuberance. On each side, inferior to the second premolar tooth, is the mental foramen for the passage of blood vessels and a nerve. Melasma flexed, with the occipital Occipital Part of the back and base of the cranium that encloses the foramen magnum. Skull: Anatomy fontanel as the presenting part
- Face presentation
- Brow presentation: forehead Forehead The part of the face above the eyes. Melasma is the presenting part
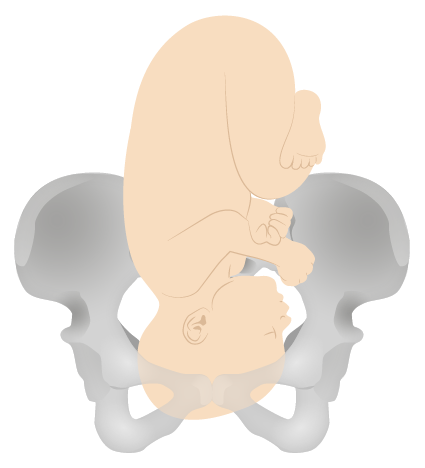
Vertex presentation
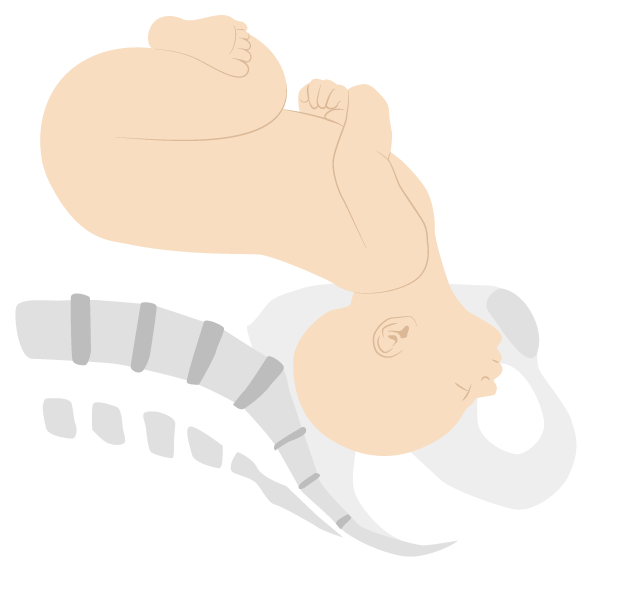
Face presentation (mentum anterior position)
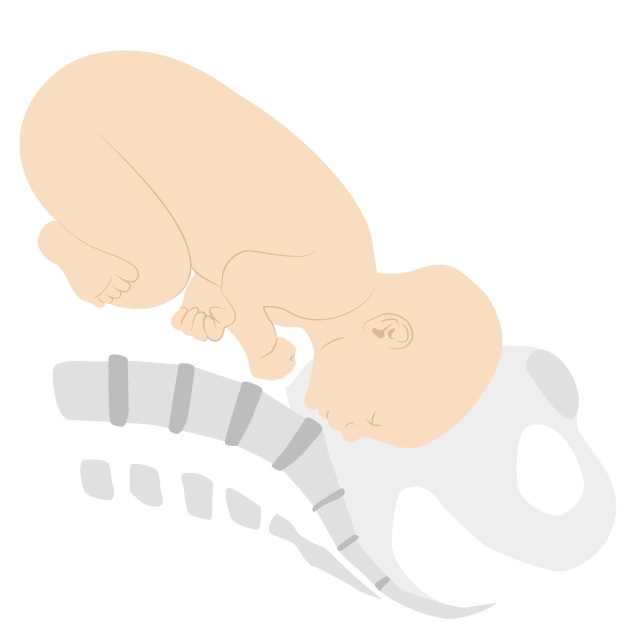
Brow presentation (mentum posterior position)
Breech presentations
Breech presentations can be categorized as:
- Frank breech: bottom down, legs extended (50%–70%)
- Complete breech: bottom down, hips and knees both flexed
- Incomplete breech: 1 or both hips not completely flexed
- Footling breech: feet down
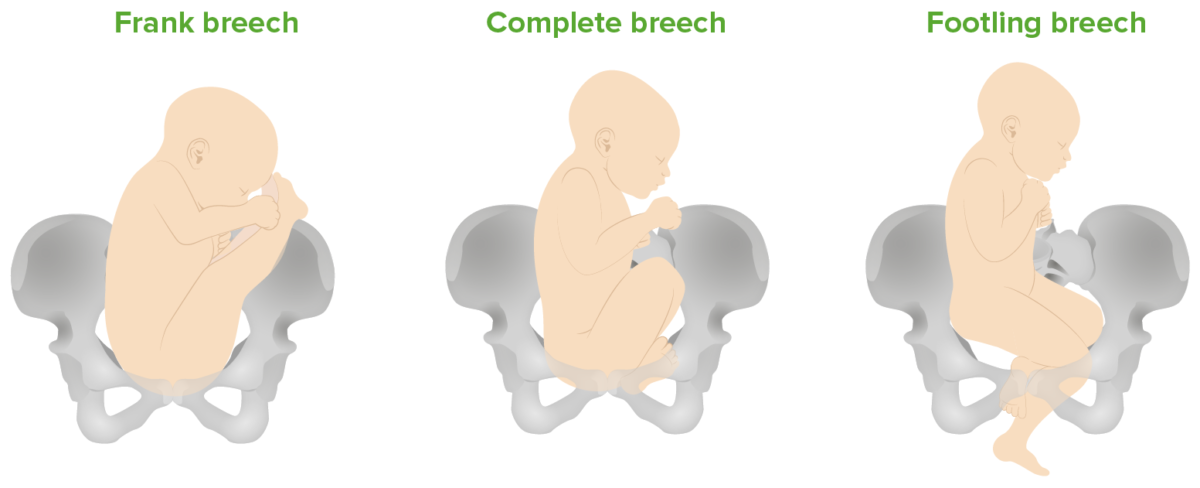
Breech presentations: Frank (bottom down, legs extended), complete (bottom down, hips and knees both flexed), and footling (feet down) breech presentations
Transverse and compound presentations
- Uncommon, but when they occur, the presenting fetal part is the shoulder.
- If the cervix Cervix The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Externally, the cervix is lined by stratified squamous cells; however, the cervical canal is lined by columnar epithelium. Uterus, Cervix, and Fallopian Tubes: Anatomy begins dilating, the arm Arm The arm, or “upper arm” in common usage, is the region of the upper limb that extends from the shoulder to the elbow joint and connects inferiorly to the forearm through the cubital fossa. It is divided into 2 fascial compartments (anterior and posterior). Arm: Anatomy may prolapse through the cervix Cervix The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Externally, the cervix is lined by stratified squamous cells; however, the cervical canal is lined by columnar epithelium. Uterus, Cervix, and Fallopian Tubes: Anatomy .
- In compound presentations, the most common situation is a hand Hand The hand constitutes the distal part of the upper limb and provides the fine, precise movements needed in activities of daily living. It consists of 5 metacarpal bones and 14 phalanges, as well as numerous muscles innervated by the median and ulnar nerves. Hand: Anatomy or arm Arm The arm, or “upper arm” in common usage, is the region of the upper limb that extends from the shoulder to the elbow joint and connects inferiorly to the forearm through the cubital fossa. It is divided into 2 fascial compartments (anterior and posterior). Arm: Anatomy presenting with the head.
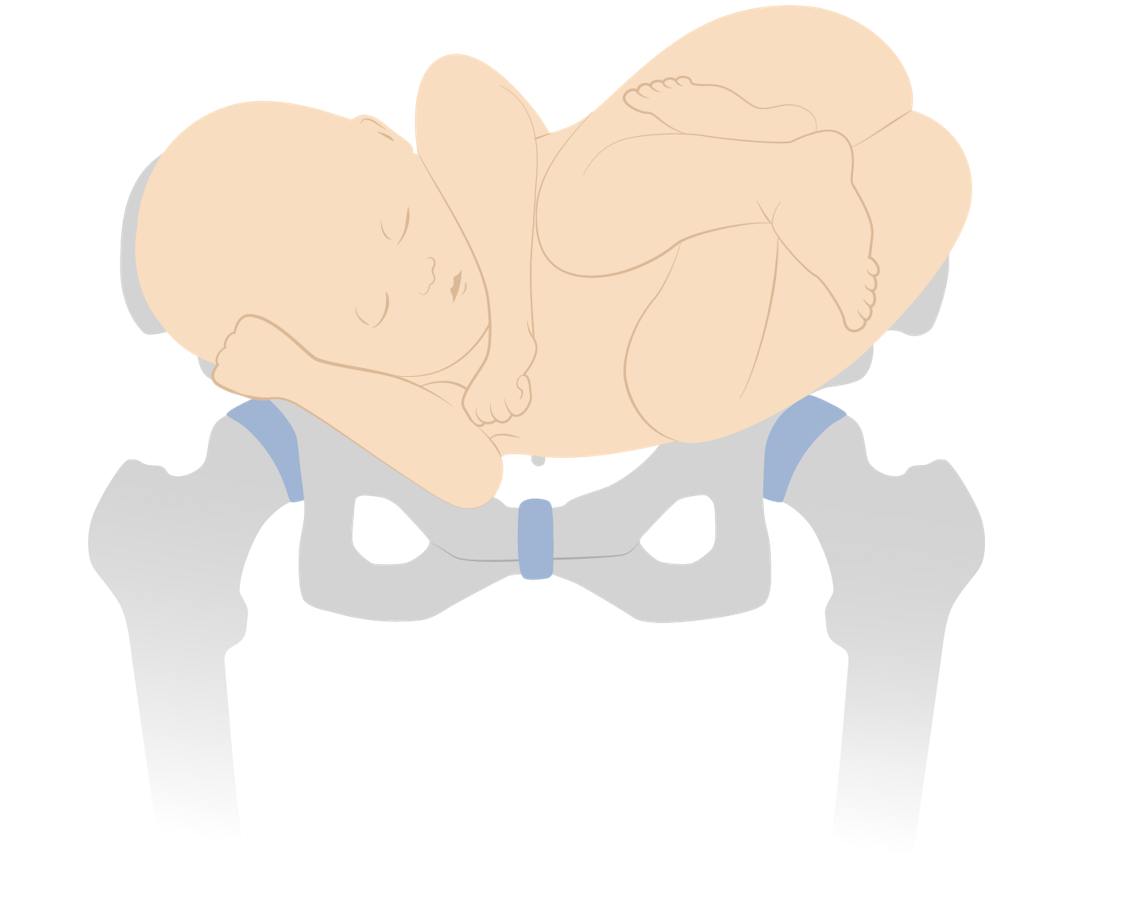
Shoulder presentation (transverse lie)
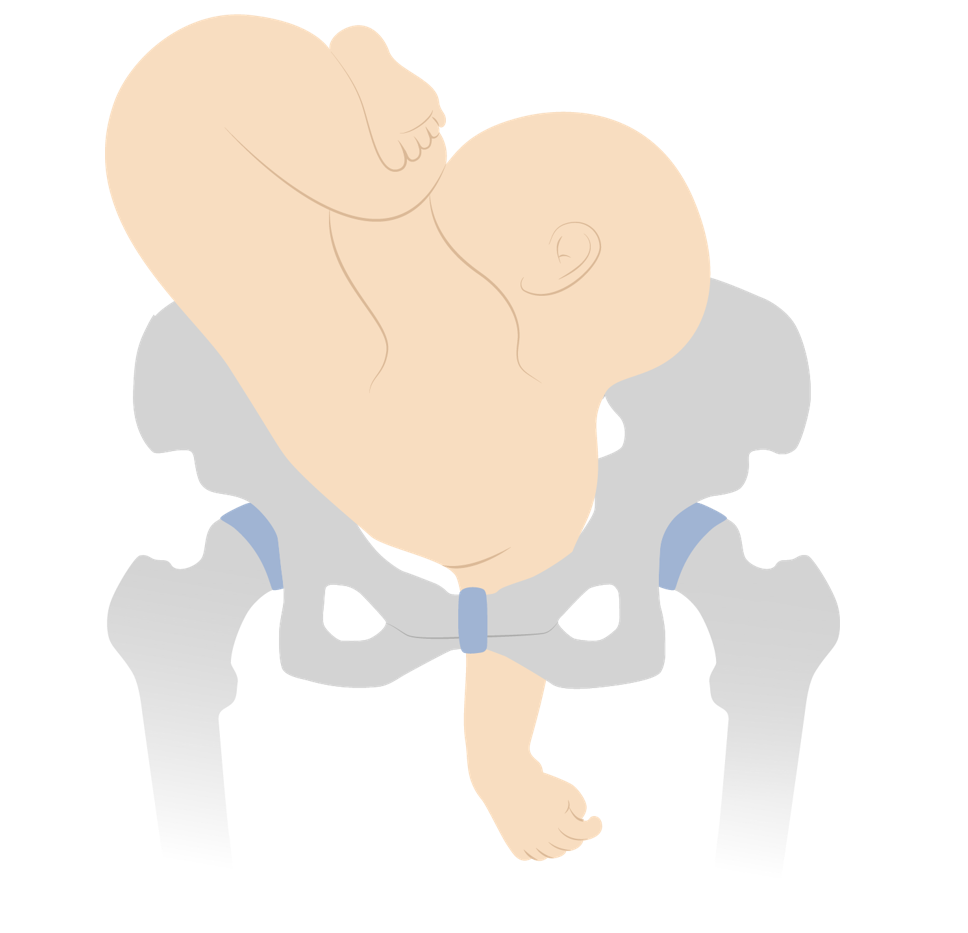
Neglected shoulder presentation resulting in arm prolapse during labor
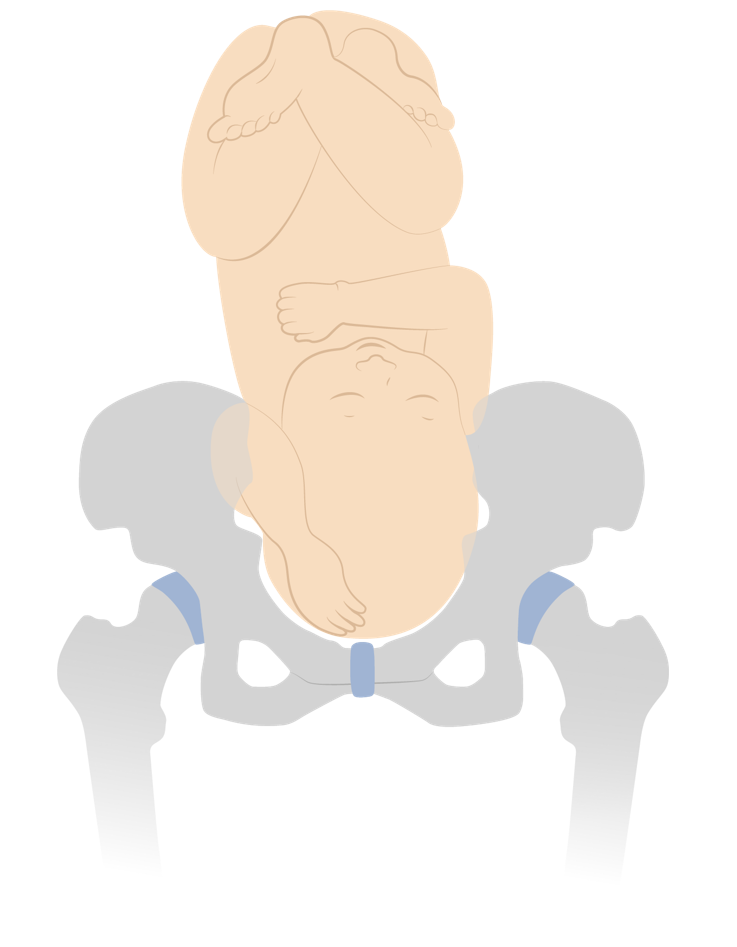
Vertex presentation with a compound hand
Fetal malpresentation
- Any presentation other than vertex
- Clinically, this means breech, face, brow, and shoulder presentations.
Position describes the relation of the fetal presenting part to the maternal bony pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 “hip” bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy .
Vertex positions
Positions for vertex presentations describe the position of the fetal occiput .
- Identified on cervical exam as the area in the midline between the anterior and posterior fontanelles Fontanelles Physical Examination of the Newborn
- Anterior, posterior, or transverse in relation to the maternal pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 “hip” bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy
- Being on the maternal right or left
- Right or left occiput anterior
- Right or left occiput posterior
- Right or left occiput transverse
- Direct occiput anterior or posterior
- The most common positions (and easiest for vaginal delivery) are occiput anterior.
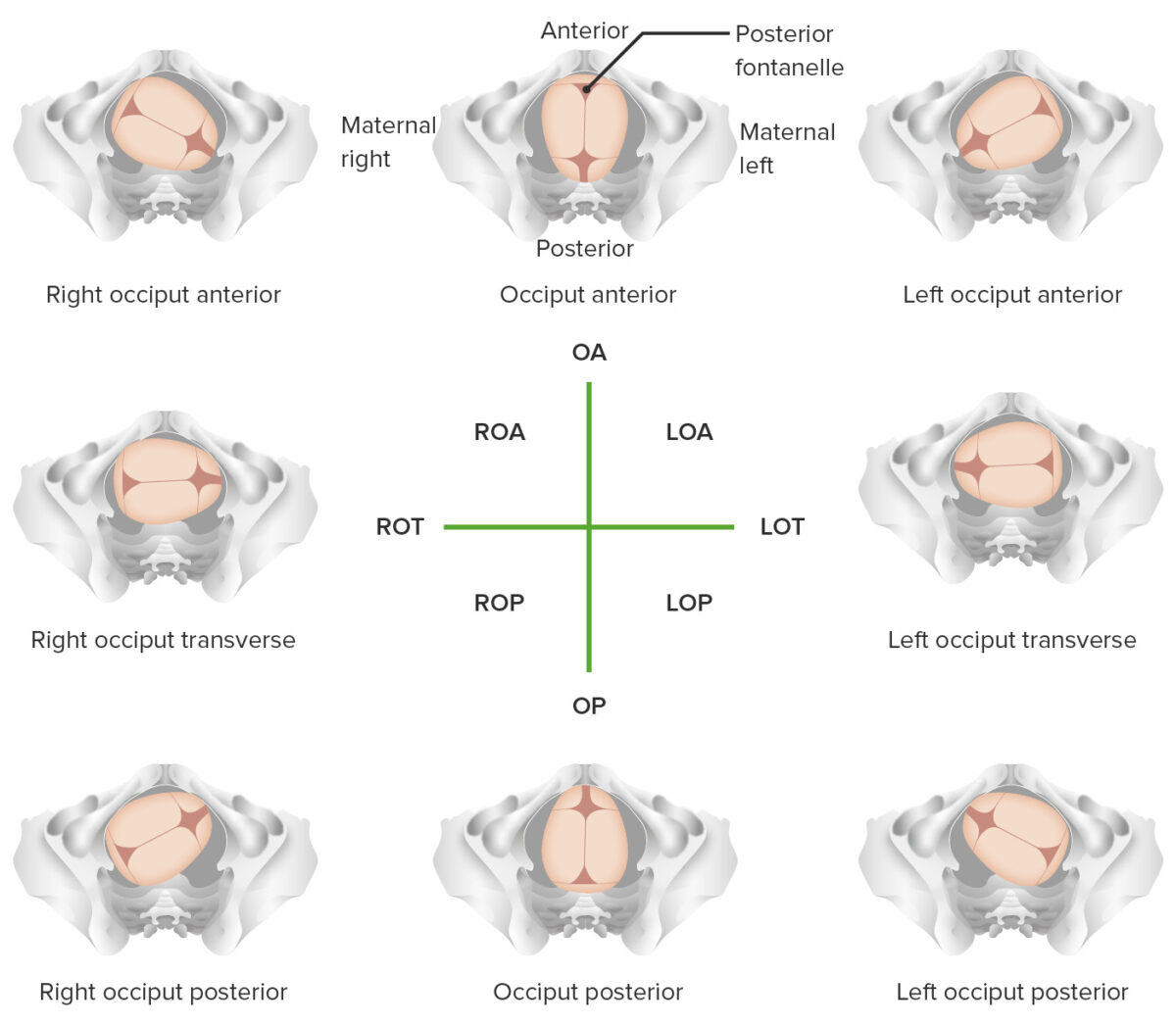
Overview of different vertex positions LOA: left occiput anterior LOP: left occiput posterior LOT: left occiput transverse OA occiput anterior OP: occiput posterior ROA: right occiput anterior ROP: right occiput posterior ROT: right occiput transverse
Face and brow positions
Positions for face and brow presentations describe the position of the chin Chin The anatomical frontal portion of the mandible, also known as the mentum, that contains the line of fusion of the two separate halves of the mandible (symphysis menti). This line of fusion divides inferiorly to enclose a triangular area called the mental protuberance. On each side, inferior to the second premolar tooth, is the mental foramen for the passage of blood vessels and a nerve. Melasma .
- The chin Chin The anatomical frontal portion of the mandible, also known as the mentum, that contains the line of fusion of the two separate halves of the mandible (symphysis menti). This line of fusion divides inferiorly to enclose a triangular area called the mental protuberance. On each side, inferior to the second premolar tooth, is the mental foramen for the passage of blood vessels and a nerve. Melasma is referred to as the mentum.
- Right or left mentum anterior
- Right or left mentum posterior
- Right or left mentum transverse
- Direct mentum anterior or posterior
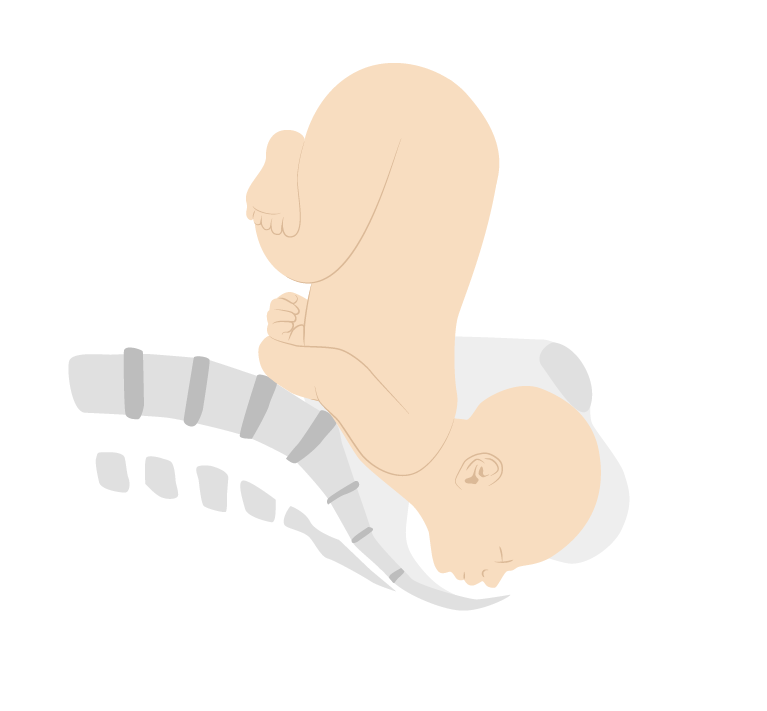
Face presentation (mentum posterior position)
Breech and shoulder positions
- Positions for breech presentations describe the position of the sacrum Sacrum Five fused vertebrae forming a triangle-shaped structure at the back of the pelvis. It articulates superiorly with the lumbar vertebrae, inferiorly with the coccyx, and anteriorly with the ilium of the pelvis. The sacrum strengthens and stabilizes the pelvis. Vertebral Column: Anatomy . Similar to other presentations, they include anterior, posterior, and transverse and right, left, and direct.
- Dorso-superior (back up)
- Dorso-inferior (back down)
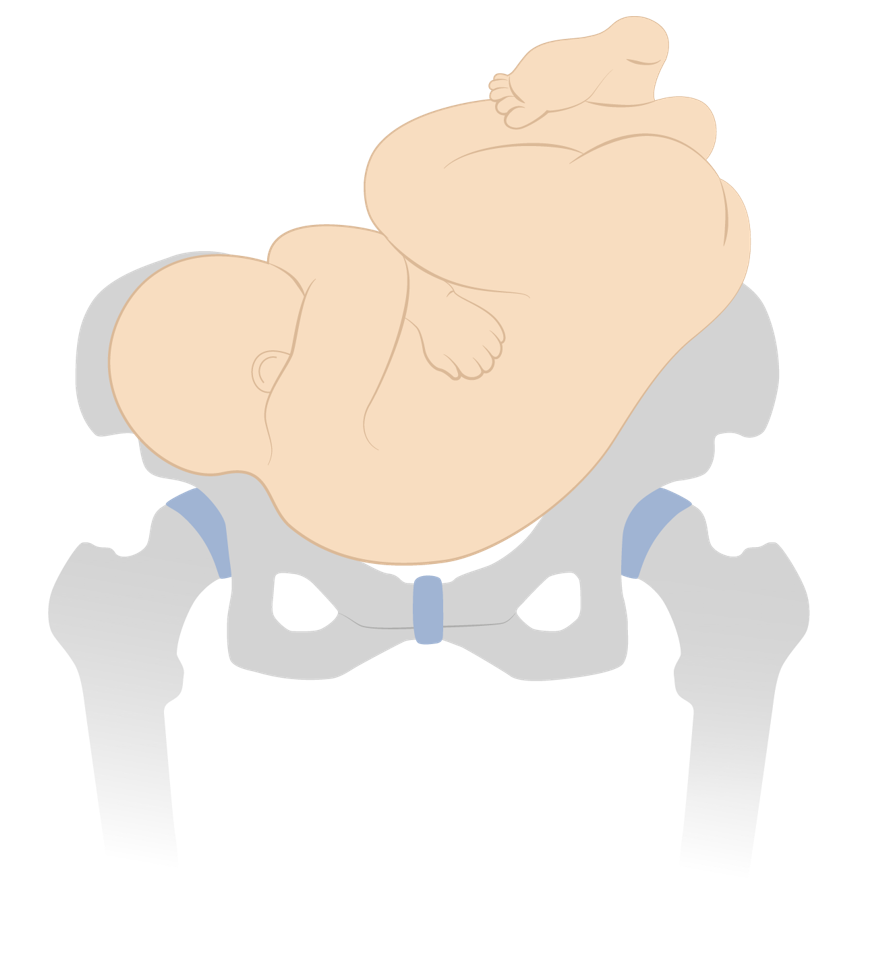
Dorso-inferior shoulder presentation
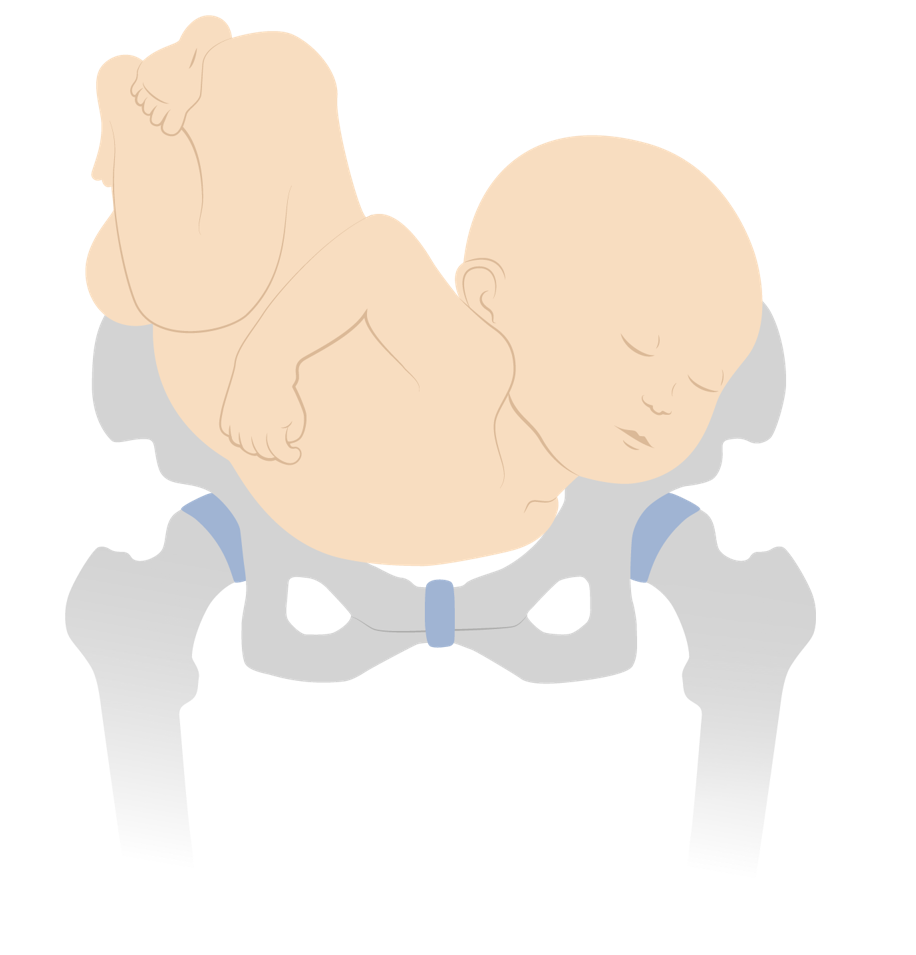
Dorso-superior shoulder presentation
Attitude and asynclitism
- Attitude: amount of flexion Flexion Examination of the Upper Limbs or extension Extension Examination of the Upper Limbs of the fetal head
- Lateral deflection of the sagittal Sagittal Computed Tomography (CT) suture to 1 side or the other
- Mild degrees of asynclitism are normal.
- More severe asynclitism increases the presenting fetal diameter and makes it more difficult for the fetal head to pass through the maternal pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 “hip” bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy .
Fetal malposition
- Commonly refers to any position other than right occiput anterior, left occiput anterior, or direct occiput anterior
- All nonvertex presentations are also malpositioned.
- The terms fetal malpresentation and fetal malposition are often used interchangeably.
- The presenting diameter refers to the width of the presenting part.
- The maternal pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 “hip” bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy is about 10 cm at its narrowest point; the infant must orient itself so that it can fit through.
- Most commonly, the infant will move into a cephalic, vertex presentation, in 1 of the occiput anterior positions → presents the narrowest diameter
- Vertex presentation: suboccipitobregmatic diameter, approximately 9.5 cm
- Vertex presentation with deflexed head: occipitofrontal diameter, approximately 11.5 cm
- Brow presentation: occipitomental diameter, approximately 13 cm
- Face presentation: submentobregmatic diameter, approximately 9.5 cm
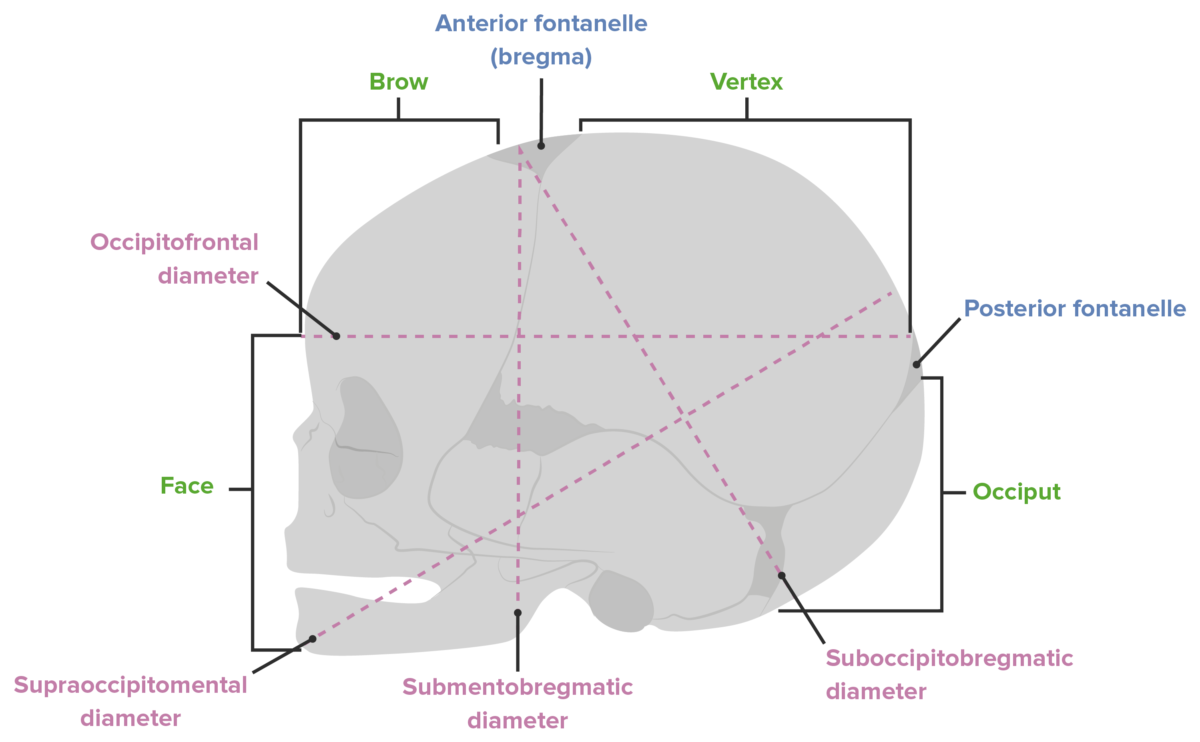
Diameters of the fetal head
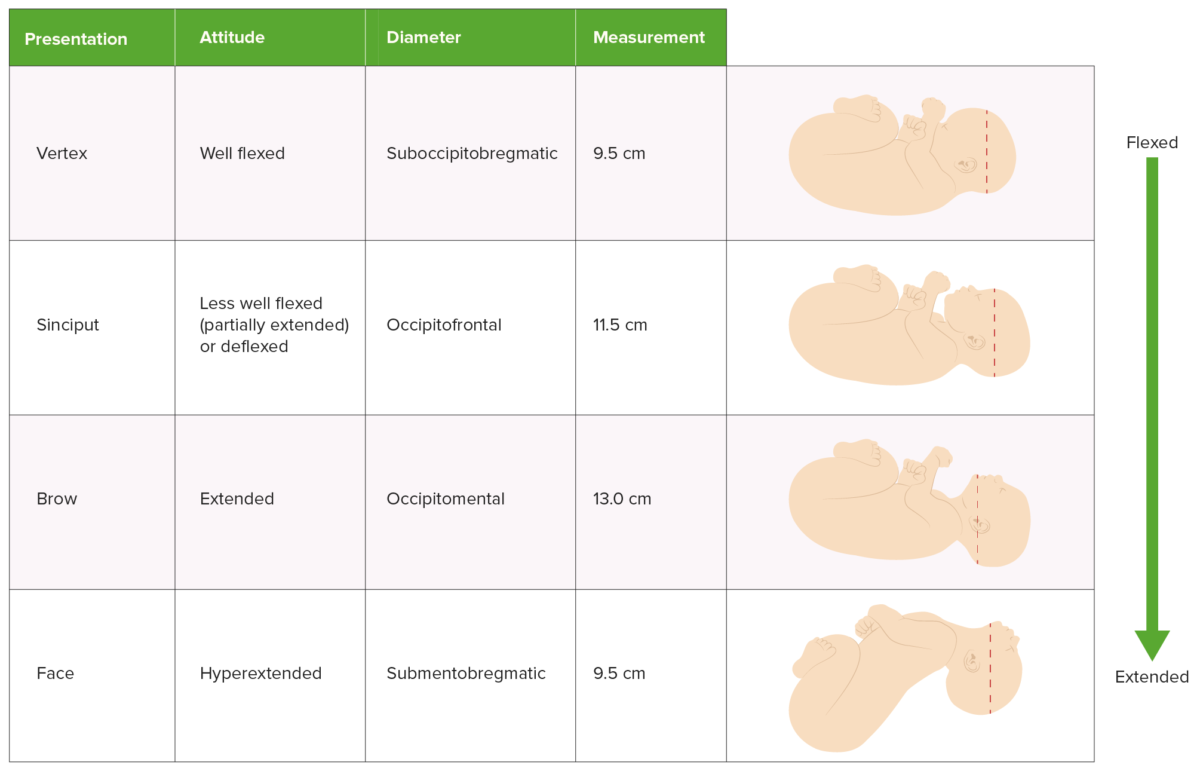
Comparison of presentation, attitude, and presenting diameter
How to establish lie, presentation, and position
Delivery is managed differently depending on the presentation and position of the infant. This information can be established in several different ways:
Leopold’s maneuvers
Ultrasonography.
- Cervical examination
- Techniques using abdominal palpation Abdominal Palpation Abdominal Examination to determine the presentation of the fetus
- The fetal head will be hard and round.
- The lower body will be bulkier, nodular, and mobile.
- The back will be hard and smooth.
- The other side (anterior surface of the fetus) will be filled with irregular, mobile fetal parts.
- Experienced providers can also estimate the fetal weight using these maneuvers.
- Bedside abdominal ultrasonography can easily identify the fetal head and its orientation Orientation Awareness of oneself in relation to time, place and person. Psychiatric Assessment .
- Quick bedside ultrasonography Bedside Ultrasonography ACES and RUSH: Resuscitation Ultrasound Protocols on admission to labor and delivery to assess fetal presentation is considered standard of care Standard of care The minimum acceptable patient care, based on statutes, court decisions, policies, or professional guidelines. Malpractice .
- The fetal head will typically encompass the entire window and appear like a large white circle (the fetal skull Skull The skull (cranium) is the skeletal structure of the head supporting the face and forming a protective cavity for the brain. The skull consists of 22 bones divided into the viscerocranium (facial skeleton) and the neurocranium. Skull: Anatomy ).
- Identification Identification Defense Mechanisms of the eyes can help determine position.
- It is quick and easy to perform and presents minimal risk to mother and infant.
- Allowing mothers to labor with infants in a noncephalic presentation significantly increases the risks to both of them.
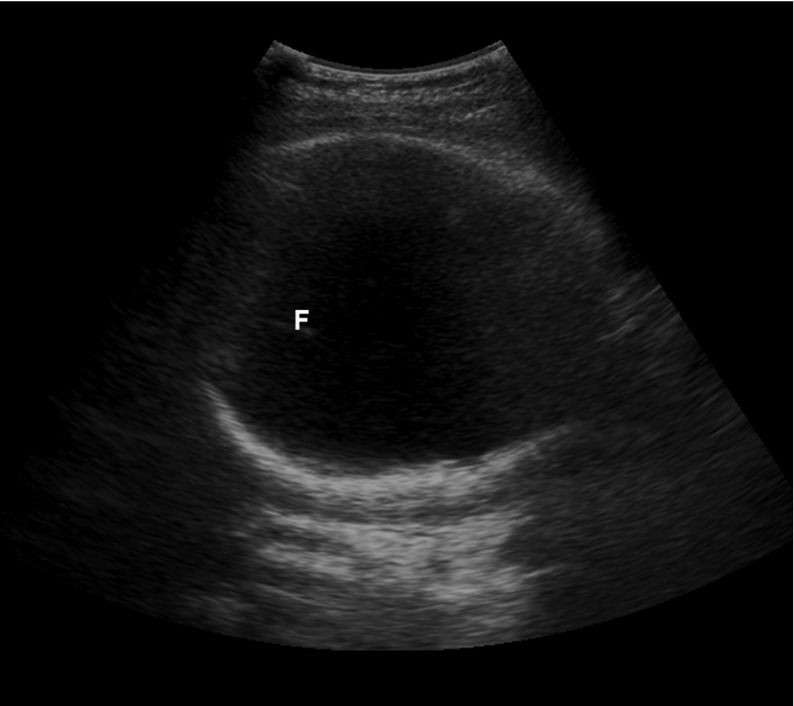
Suprapubic bedside ultrasound showing the large white circle of the fetal skull, confirming a cephalic presentation F: fetal falx
Vaginal and cervical examination
- As the cervix Cervix The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Externally, the cervix is lined by stratified squamous cells; however, the cervical canal is lined by columnar epithelium. Uterus, Cervix, and Fallopian Tubes: Anatomy dilates, the fetal fontanelles Fontanelles Physical Examination of the Newborn can be directly palpated.
- Identifying the location of the fetal fontanelles Fontanelles Physical Examination of the Newborn allows the practitioner to establish the position.
- Insert 1–2 fingers through the cervix Cervix The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Externally, the cervix is lined by stratified squamous cells; however, the cervical canal is lined by columnar epithelium. Uterus, Cervix, and Fallopian Tubes: Anatomy posteriorly.
- Sweep fingers along the fetal head moving anteriorly.
- This maneuver allows for identification Identification Defense Mechanisms of the sagittal Sagittal Computed Tomography (CT) suture.
- The fontanelles Fontanelles Physical Examination of the Newborn are then identified by moving along the sagittal Sagittal Computed Tomography (CT) suture.
Vertex presentations
- Expectant management
- All have high chances of successful vaginal delivery.
Compound presentations
- Observation when labor is progressing normally (many compound presentations will resolve spontaneously intrapartum).
- Can attempt to gently pinch the compound extremity trying to provoke the fetus into withdrawing the part (no good quality Quality Activities and programs intended to assure or improve the quality of care in either a defined medical setting or a program. The concept includes the assessment or evaluation of the quality of care; identification of problems or shortcomings in the delivery of care; designing activities to overcome these deficiencies; and follow-up monitoring to ensure effectiveness of corrective steps. Quality Measurement and Improvement evidence, but unlikely to be harmful)
- Can attempt to manually replace the compound extremity
- If labor is prolonged and the compound part remains, cesarean delivery Cesarean Delivery Cesarean delivery (CD) is the operative delivery of ≥ 1 infants through a surgical incision in the maternal abdomen and uterus. Cesarean deliveries may be indicated for a number of either maternal or fetal reasons, most commonly including fetal intolerance to labor, arrest of labor, a history of prior uterine surgery, fetal malpresentation, and placental abnormalities. Cesarean Delivery (CD) should be performed.
- Prolonged labor
- Umbilical cord Umbilical cord The flexible rope-like structure that connects a developing fetus to the placenta in mammals. The cord contains blood vessels which carry oxygen and nutrients from the mother to the fetus and waste products away from the fetus. Placenta, Umbilical Cord, and Amniotic Cavity prolapse
- Increased maternal morbidity Morbidity The proportion of patients with a particular disease during a given year per given unit of population. Measures of Health Status from lacerations
- Ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage of the compound part
Brow presentations
- The majority spontaneously convert to a vertex presentation.
- Cesarean delivery Cesarean Delivery Cesarean delivery (CD) is the operative delivery of ≥ 1 infants through a surgical incision in the maternal abdomen and uterus. Cesarean deliveries may be indicated for a number of either maternal or fetal reasons, most commonly including fetal intolerance to labor, arrest of labor, a history of prior uterine surgery, fetal malpresentation, and placental abnormalities. Cesarean Delivery may be required if labor is prolonged.
Face presentations
- Management depends on the position.
- Can be delivered vaginally by an experienced provider
- Cesarean delivery Cesarean Delivery Cesarean delivery (CD) is the operative delivery of ≥ 1 infants through a surgical incision in the maternal abdomen and uterus. Cesarean deliveries may be indicated for a number of either maternal or fetal reasons, most commonly including fetal intolerance to labor, arrest of labor, a history of prior uterine surgery, fetal malpresentation, and placental abnormalities. Cesarean Delivery may be required.
- Head is fully extended and unable to pass through the birth canal Birth canal Pelvis: Anatomy .
- Normally, the fetal head flexes as it passes under the pubic bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types ; however, this is impossible in an MP position.
- Cesarean delivery Cesarean Delivery Cesarean delivery (CD) is the operative delivery of ≥ 1 infants through a surgical incision in the maternal abdomen and uterus. Cesarean deliveries may be indicated for a number of either maternal or fetal reasons, most commonly including fetal intolerance to labor, arrest of labor, a history of prior uterine surgery, fetal malpresentation, and placental abnormalities. Cesarean Delivery is always required (unless the infant spontaneously rotates to a mentum anterior (MA) position).
There are 3 primary options for managing breech presentations: performing CD, attempting an external cephalic version to manually rotate the baby into a vertex presentation for attempted vaginal delivery, or a planned vaginal breech delivery (which is generally not done in the United States).
Natural history of breech presentations
Most infants will spontaneously rotate to a vertex presentation as the pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care progresses. At different gestational ages, the prevalence Prevalence The total number of cases of a given disease in a specified population at a designated time. It is differentiated from incidence, which refers to the number of new cases in the population at a given time. Measures of Disease Frequency of breech presentations is:
- < 28 weeks: 20%–25%
- 32 weeks: 10%–15%
- Term (> 37 weeks): 3%
- Spontaneous version is possible even at > 40 weeks.
- Flexed fetal legs
- Polyhydramnios Polyhydramnios Polyhydramnios is a pathological excess of amniotic fluid. Common causes of polyhydramnios include fetal anomalies, gestational diabetes, multiple gestations, and congenital infections. Patients are often asymptomatic but may present with dyspnea, extremity swelling, or abdominal distention. Polyhydramnios
- Longer umbilical cord Umbilical cord The flexible rope-like structure that connects a developing fetus to the placenta in mammals. The cord contains blood vessels which carry oxygen and nutrients from the mother to the fetus and waste products away from the fetus. Placenta, Umbilical Cord, and Amniotic Cavity
- Lack of fetal/uterine anomalies
- Multiparity
Fetal risks associated with breech presentations
The following risks are associated with breech presentations in utero, regardless of mode of delivery:
- ↑ Association with congenital Congenital Chorioretinitis malformations
- Torticollis Torticollis A symptom, not a disease, of a twisted neck. In most instances, the head is tipped toward one side and the chin rotated toward the other. The involuntary muscle contractions in the neck region of patients with torticollis can be due to congenital defects, trauma, inflammation, tumors, and neurological or other factors. Cranial Nerve Palsies
- Developmental hip dysplasia
Fetal risks associated with vaginal breech delivery
The primary risk of a vaginal breech delivery is fetal head entrapment:
- The fetal body delivers, but the head remains trapped in the uterus Uterus The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The uterus has a thick wall made of smooth muscle (the myometrium) and an inner mucosal layer (the endometrium). The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Uterus, Cervix, and Fallopian Tubes: Anatomy .
- Causes compression Compression Blunt Chest Trauma of the umbilical cord Umbilical cord The flexible rope-like structure that connects a developing fetus to the placenta in mammals. The cord contains blood vessels which carry oxygen and nutrients from the mother to the fetus and waste products away from the fetus. Placenta, Umbilical Cord, and Amniotic Cavity running past the head (between the delivered umbilicus and the undelivered placenta Placenta A highly vascularized mammalian fetal-maternal organ and major site of transport of oxygen, nutrients, and fetal waste products. It includes a fetal portion (chorionic villi) derived from trophoblasts and a maternal portion (decidua) derived from the uterine endometrium. The placenta produces an array of steroid, protein and peptide hormones (placental hormones). Placenta, Umbilical Cord, and Amniotic Cavity )
- Leads to hypoxia Hypoxia Sub-optimal oxygen levels in the ambient air of living organisms. Ischemic Cell Damage until head is delivered → ↑ risk of fetal death
- The cervix Cervix The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Externally, the cervix is lined by stratified squamous cells; however, the cervical canal is lined by columnar epithelium. Uterus, Cervix, and Fallopian Tubes: Anatomy may not be fully dilated enough to accommodate the head.
- The fetal head may not fit through the bony pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 “hip” bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy .
- The mother’s expulsive efforts are unable to quickly deliver the head.
- Umbilical cord Umbilical cord The flexible rope-like structure that connects a developing fetus to the placenta in mammals. The cord contains blood vessels which carry oxygen and nutrients from the mother to the fetus and waste products away from the fetus. Placenta, Umbilical Cord, and Amniotic Cavity prolapse during labor → requires emergent CD
- Birth injuries to the fetus (e.g., brachial plexus Brachial Plexus The large network of nerve fibers which distributes the innervation of the upper extremity. The brachial plexus extends from the neck into the axilla. In humans, the nerves of the plexus usually originate from the lower cervical and the first thoracic spinal cord segments (c5-c8 and T1), but variations are not uncommon. Peripheral Nerve Injuries in the Cervicothoracic Region injury)
Vaginal breech delivery
Vaginal breech deliveries for singleton gestations may be considered for certain low-risk women if vaginal delivery is strongly desired by the mother. In contrast, vaginal breech deliveries are done frequently for breech 2nd twins; the procedure is known as a breech extraction.
- Mothers must be fully counseled on risks.
- Mothers and infants should be monitored throughout labor with continuous electronic fetal heart rate Heart rate The number of times the heart ventricles contract per unit of time, usually per minute. Cardiac Physiology (FHR) and tocometry monitors.
- Mothers should understand that a CD will be recommended if there are signs of fetal distress or prolonged labor.
- Avoid artificial rupture of membranes to ↓ risk of cord prolapse.
- Frank or complete breech presentation with no hyperextension of the fetal head on ultrasonography
- No contraindications Contraindications A condition or factor associated with a recipient that makes the use of a drug, procedure, or physical agent improper or inadvisable. Contraindications may be absolute (life threatening) or relative (higher risk of complications in which benefits may outweigh risks). Noninvasive Ventilation to a vaginal birth
- No prior CDs
- Prior successful vaginal deliveries (i.e., multiparity)
- Gestational age Gestational age The age of the conceptus, beginning from the time of fertilization. In clinical obstetrics, the gestational age is often estimated as the time from the last day of the last menstruation which is about 2 weeks before ovulation and fertilization. Pregnancy: Diagnosis, Physiology, and Care ≥ 36 weeks
- Spontaneous labor
- Normal bony pelvis Pelvis The pelvis consists of the bony pelvic girdle, the muscular and ligamentous pelvic floor, and the pelvic cavity, which contains viscera, vessels, and multiple nerves and muscles. The pelvic girdle, composed of 2 “hip” bones and the sacrum, is a ring-like bony structure of the axial skeleton that links the vertebral column with the lower extremities. Pelvis: Anatomy shown on X-ray X-ray Penetrating electromagnetic radiation emitted when the inner orbital electrons of an atom are excited and release radiant energy. X-ray wavelengths range from 1 pm to 10 nm. Hard x-rays are the higher energy, shorter wavelength x-rays. Soft x-rays or grenz rays are less energetic and longer in wavelength. The short wavelength end of the x-ray spectrum overlaps the gamma rays wavelength range. The distinction between gamma rays and x-rays is based on their radiation source. Pulmonary Function Tests
- Estimated fetal weight Estimated Fetal Weight Obstetric Imaging between approximately 2500 and 3500 grams (exact range varies based on clinician Clinician A physician, nurse practitioner, physician assistant, or another health professional who is directly involved in patient care and has a professional relationship with patients. Clinician–Patient Relationship )
- Immediately after delivery of the 1st twin in the cephalic presentation, the physician reaches up into the uterus Uterus The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The uterus has a thick wall made of smooth muscle (the myometrium) and an inner mucosal layer (the endometrium). The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Uterus, Cervix, and Fallopian Tubes: Anatomy , manually grabs the infant’s legs, and gently guides them down through the birth canal Birth canal Pelvis: Anatomy while the cervix Cervix The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Externally, the cervix is lined by stratified squamous cells; however, the cervical canal is lined by columnar epithelium. Uterus, Cervix, and Fallopian Tubes: Anatomy is still fully dilated.
- ↓ Risk of head entrapment compared to singleton vaginal breech deliveries
External cephalic version
An external cephalic version (ECV) is a procedure in which the physician attempts to manually rotate the fetus from a breech to a cephalic presentation by pushing on the maternal abdomen.
- Approximately 50%–60% (higher in multiparous Multiparous A woman with prior deliveries Normal and Abnormal Labor than in nulliparous women)
- 97% of infants remained cephalic at birth.
- 86% delivered vaginally.
- Women who are candidates for ECV should be counseled on their options to attempt an ECV, or they may simply elect to schedule a CD.
- Infant is full term in case emergent CD is required because of complications from the procedure (e.g., placental abruption Placental Abruption Premature separation of the normally implanted placenta from the uterus. Signs of varying degree of severity include uterine bleeding, uterine muscle hypertonia, and fetal distress or fetal death. Antepartum Hemorrhage ).
- Better ratio of infant size to fluid level than later in pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care
- Allows infant more time for spontaneous version than if the procedure was done earlier
- After a successful version, the mother can await spontaneous labor or be induced immediately, depending on the situation.
- There is still a chance that the infant may spontaneously rotate between the failed ECV and the planned CD date; therefore, presentation should always be checked immediately prior to CD.
- Another contraindication for a vaginal delivery (e.g., placenta previa Placenta Previa Abnormal placentation in which the placenta implants in the lower segment of the uterus (the zone of dilation) and may cover part or all of the opening of the cervix. It is often associated with serious antepartum bleeding and premature labor. Placental Abnormalities )
- Severe oligohydramnios Oligohydramnios Oligohydramnios refers to amniotic fluid volume less than expected for the current gestational age. Oligohydramnios is diagnosed by ultrasound and defined as an amniotic fluid index (AFI) of ‰¤ 5 cm or a single deep pocket (SDP) of Oligohydramnios
- Nonreassuring fetal monitoring Fetal monitoring The primary goals of antepartum testing and monitoring are to assess fetal well-being, identify treatable situations that may cause complications, and evaluate for chromosomal abnormalities. These tests are divided into screening tests (which include cell-free DNA testing, serum analyte testing, and nuchal translucency measurements), and diagnostic tests, which provide a definitive diagnosis of aneuploidy and include chorionic villus sampling (CVS) and amniocentesis. Antepartum Testing and Monitoring prior to the procedure
- A hyperextended fetal head
- Significant fetal or uterine anomalies
- Leads to fetal and maternal hemorrhage
- An immediate CD is required.
- If the version was successful, labor should be induced immediately.
- If the version was unsuccessful, the mother should undergo immediate CD.
- Cord prolapse: can occur with PROM PROM Prelabor rupture of membranes (PROM), previously known as premature rupture of membranes, refers to the rupture of the amniotic sac before the onset of labor. Prelabor rupture of membranes may occur in term or preterm pregnancies. Prelabor Rupture of Membranes and requires immediate/emergent CD.
- Common during the procedure, but typically resolves shortly after pressure on the abdomen is released.
- If distress persists, the mother should undergo an immediate CD.
Cesarean delivery Cesarean Delivery Cesarean delivery (CD) is the operative delivery of ≥ 1 infants through a surgical incision in the maternal abdomen and uterus. Cesarean deliveries may be indicated for a number of either maternal or fetal reasons, most commonly including fetal intolerance to labor, arrest of labor, a history of prior uterine surgery, fetal malpresentation, and placental abnormalities. Cesarean Delivery
- Scheduled at 39 weeks’ gestational age Gestational age The age of the conceptus, beginning from the time of fertilization. In clinical obstetrics, the gestational age is often estimated as the time from the last day of the last menstruation which is about 2 weeks before ovulation and fertilization. Pregnancy: Diagnosis, Physiology, and Care (WGA) if the infant is known to be in the breech presentation.
- Alternative option to attempting ECV
- Postpartum hemorrhage Postpartum hemorrhage Postpartum hemorrhage is one of the most common and deadly obstetric complications. Since 2017, postpartum hemorrhage has been defined as blood loss greater than 1,000 mL for both cesarean and vaginal deliveries, or excessive blood loss with signs of hemodynamic instability. Postpartum Hemorrhage
- Postpartum endomyometritis
- Maternal injury
- Longer recovery time postpartum
- Complications in future pregnancies (e.g., placenta previa Placenta Previa Abnormal placentation in which the placenta implants in the lower segment of the uterus (the zone of dilation) and may cover part or all of the opening of the cervix. It is often associated with serious antepartum bleeding and premature labor. Placental Abnormalities , placenta accreta Placenta Accreta Abnormal placentation in which all or parts of the placenta are attached directly to the myometrium due to a complete or partial absence of decidua. It is associated with postpartum hemorrhage because of the failure of placental separation. Placental Abnormalities , uterine rupture Uterine Rupture A complete separation or tear in the wall of the uterus with or without expulsion of the fetus. It may be due to injuries, multiple pregnancies, large fetus, previous scarring, or obstruction. Antepartum Hemorrhage )
- Maternal request (mother declines ECV attempt)
- ECV contraindicated
- ECV unsuccessful
- Fetal distress during labor
Management of transverse presentations
- As with breech presentations, mothers may be offered an attempt at ECV or a CD.
- Unlike breech presentations, vaginal transverse delivery is always contraindicated.
- Hofmeyr, G.J. (2021). Overview of breech presentation. In Barss, V.A. (Ed.), UpToDate. Retrieved July 14, 2021, from https://www.uptodate.com/contents/overview-of-breech-presentation
- Hofmeyr, G.J. (2021). Delivery of the singleton fetus in breech presentation. In Barss, V.A. (Ed.), UpToDate. Retrieved July 14, 2021, from https://www.uptodate.com/contents/delivery-of-the-singleton-fetus-in-breech-presentation
- Hofmeyr, G.J. (2021). External cephalic version. In Barss, V.A. (Ed.), UpToDate. Retrieved July 14, 2021, from https://www.uptodate.com/contents/external-cephalic-version
- Julien, S., and Galerneau, F. (2021). Face and brow presentations in labor. In Barss, V.A., (Ed.), UpToDate. Retrieved July 14, 2021, from https://www.uptodate.com/contents/face-and-brow-presentations-in-labor
- Strauss, R.A., Herrera, C.A. (2021). Transverse fetal lie. In Barss, V.A., (Ed.), UpToDate. Retrieved July 14, 2021, from https://www.uptodate.com/contents/transverse-fetal-lie
- Barth, W.H. (2021). Compound fetal presentation. In Barss, V.A., (Ed.), UpToDate. Retrieved July 14, 2021, from https://www.uptodate.com/contents/compound-fetal-presentation
- Cunningham, F. G., Leveno, K. J., et al. (2010). Williams Obstetrics, 23rd ed., pp. 374‒382.
Study with Lecturio for
Medical School
Nursing School
- Data Privacy
- Terms and Conditions
- Legal Information
USMLE™ is a joint program of the Federation of State Medical Boards (FSMB®) and National Board of Medical Examiners (NBME®). MCAT is a registered trademark of the Association of American Medical Colleges (AAMC). NCLEX®, NCLEX-RN®, and NCLEX-PN® are registered trademarks of the National Council of State Boards of Nursing, Inc (NCSBN®). None of the trademark holders are endorsed by nor affiliated with Lecturio.
Create your free account or log in to continue reading!
Sign up now and get free access to Lecturio with concept pages, medical videos, and questions for your medical education.
Log in to your account
User Reviews
Get Premium to test your knowledge
Lecturio Premium gives you full access to all content & features
Get Premium to watch all videos
Verify your email now to get a free trial.
Create a free account to test your knowledge
Lecturio Premium gives you full access to all contents and features—including Lecturio’s Qbank with up-to-date board-style questions.
- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games
How your twins’ fetal positions affect labor and delivery

Twin fetal presentation – also known as the position of your babies in the womb – dictates whether you'll have a vaginal or c-section birth. Toward the end of pregnancy, most twins will move in the head-down position (vertex), but there's a risk that the second twin will change position after the first twin is born. While there are options to change the second twin's position, this can increase the risk of c-section and other health issues. Learn about the six possible twin fetal presentations: vertex-vertex, vertex-breech, breech-breech, vertex-transverse, breech-transverse, and transverse-transverse – and how they'll impact your delivery and risks for complications.
What is fetal presentation and what does it mean for your twins?
As your due date approaches, you might be wondering how your twins are currently positioned in the womb, also known as the fetal presentation, and what that means for your delivery. Throughout your pregnancy, your twin babies will move in the uterus, but sometime during the third trimester – usually between 32 and 36 weeks – their fetal presentation changes as they prepare to go down the birth canal.
The good news is that at most twin births, both babies are head-down (vertex), which means you can have a vaginal delivery. In fact, nearly 40 percent of twins are delivered vaginally.
But if one baby has feet or bottom first (breech) or is sideways (transverse), your doctor might deliver the lower twin vaginally and then try to rotate the other twin so that they face head-down (also called external cephalic version or internal podalic version) and can be delivered vaginally. But if that doesn't work, there's still a chance that your doctor will be able to deliver the second twin feet first vaginally via breech extraction (delivering the breech baby feet or butt first through the vagina).
That said, a breech extraction depends on a variety of factors – including how experienced your doctor is in the procedure and how much the second twin weighs. Studies show that the higher rate of vaginal births among nonvertex second twins is associated with labor induction and more experienced doctors, suggesting that proper delivery planning may increase your chances of a vaginal birth .
That said, you shouldn't totally rule out a Cesarean delivery with twins . If the first twin is breech or neither of the twins are head-down, then you'll most likely have a Cesarean delivery.
Research also shows that twin babies who are born at less than 34 weeks and have moms with multiple children are associated with intrapartum presentation change (when the fetal presentation of the second twin changes from head-down to feet first after the delivery of the first twin) of the second twin. Women who have intrapartum presentation change are more likely to undergo a Cesarean delivery for their second twin.
Here's a breakdown of the different fetal presentations for twin births and how they will affect your delivery.
Head down, head down (vertex, vertex)
This fetal presentation is the most promising for a vaginal delivery because both twins are head-down. Twins can change positions, but if they're head-down at 28 weeks, they're likely to stay that way.
When delivering twins vaginally, there is a risk that the second twin will change position after the delivery of the first. Research shows that second twins change positions in 20 percent of planned vaginal deliveries. If this happens, your doctor may try to rotate the second twin so it faces head-down or consider a breech extraction. But if neither of these work or are an option, then a Cesarean delivery is likely.
In vertex-vertex pairs, the rate of Cesarean delivery for the second twin after a vaginal delivery of the first one is 16.9 percent.
Like all vaginal deliveries, there's also a chance you'll have an assisted birth, where forceps or a vacuum are needed to help deliver your twins.
Head down, bottom down (vertex, breech)
When the first twin's (the lower one) head is down, but the second twin isn't, your doctor may attempt a vaginal delivery by changing the baby's position or doing breech extraction, which isn't possible if the second twin weighs much more than the first twin.
The rates of emergency C-section deliveries for the second twin after a vaginal delivery of the first twin are higher in second twins who have a very low birth weight. Small babies may not tolerate labor as well.
Head down, sideways (vertex, transverse)
If one twin is lying sideways or diagonally (oblique), there's a chance the baby may shift position as your labor progresses, or your doctor may try to turn the baby head-down via external cephalic version or internal podalic version (changing position in the uterus), which means you may be able to deliver both vaginally.
Bottom down, bottom down (breech, breech)
When both twins are breech, a planned C-section is recommended because your doctor isn't able to turn the fetuses. Studies also show that there are fewer negative neonatal outcomes for planned C-sections than planned vaginal births in breech babies.
As with any C-section, the risks for a planned one with twins include infection, loss of blood, blood clots, injury to the bowel or bladder, a weak uterine wall, placenta abnormalities in future pregnancies and fetal injury.
Bottom down, sideways (breech, transverse)
When the twin lowest in your uterus is breech or transverse (which happens in 25 percent of cases), you'll need to have a c-section.
Sideways, sideways (transverse, transverse)
This fetal presentation is rare with less than 1 percent of cases. If both babies are lying horizontally, you'll almost definitely have a C-section.
Learn more:
- Twin fetal development month by month
- Your likelihood of having twins or more
- When and how to find out if you’re carrying twins or more
Was this article helpful?
32 weeks pregnant with twins

28 weeks pregnant with twins

36 weeks pregnant with twins

24 weeks pregnant with twins

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
Cleveland Clinic. Fetal Positions for Birth: https://my.clevelandclinic.org/health/articles/9677-fetal-positions-for-birth Opens a new window [Accessed July 2021]
Mayo Clinic. Fetal Presentation Before Birth: https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/multimedia/fetal-positions/sls-20076615?s=7 Opens a new window [Accessed July 2021]
NHS. Giving Birth to Twins or More: https://pubmed.ncbi.nlm.nih.gov/29016498/ Opens a new window [Accessed July 2021]
Science Direct. Breech Extraction: https://www.sciencedirect.com/topics/medicine-and-dentistry/breech-extraction Opens a new window [Accessed July 2021]
Obstetrics & Gynecology. Clinical Factors Associated With Presentation Change of the Second Twin After Vaginal Delivery of the First Twin https://pubmed.ncbi.nlm.nih.gov/29016498/ Opens a new window [Accessed July 2021]
American Journal of Obstetrics and Gynecology. Fetal presentation and successful twin vaginal delivery: https://www.ajog.org/article/S0002-9378(04)00482-X/fulltext [Accessed July 2021]
The Journal of Maternal-Fetal & Neonatal Medicine. Changes in fetal presentation in twin pregnancies https://www.tandfonline.com/doi/abs/10.1080/14767050400028592 Opens a new window [Accessed July 2021]
Reviews in Obstetrics & Gynecology. An Evidence-Based Approach to Determining Route of Delivery for Twin Gestations https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3252881/ Opens a new window [Accessed July 2021]
Nature. Neonatal mortality and morbidity in vertex–vertex second twins according to mode of delivery and birth weight: https://www.nature.com/articles/7211408 Opens a new window [Accessed July 2021]
Cochrane. Planned cesarean for a twin pregnancy: https://www.cochrane.org/CD006553/PREG_planned-caesarean-section-twin-pregnancy Opens a new window [Accessed July 2021]
Kids Health. What Is the Apgar Score?: https://www.kidshealth.org/Nemours/en/parents/apgar0.html Opens a new window [Accessed July 2021]
American Journal of Obstetrics & Gynecology. Neonatal mortality in second twin according to cause of death, gestational age, and mode of delivery https://pubmed.ncbi.nlm.nih.gov/15467540/ Opens a new window [Accessed July 2021]
Lancet. Planned cesarean section versus planned vaginal birth for breech presentation at term: a randomised multicentre trial. Term Breech Trial Collaborative Group https://pubmed.ncbi.nlm.nih.gov/11052579/ Opens a new window [Accessed July 2021]
Cleveland Clinic. Cesarean Birth (C-Section): https://my.clevelandclinic.org/health/treatments/7246-cesarean-birth-c-section Opens a new window [Accessed July 2021]
St. Jude Medical Staff. Delivery of Twin Gestation: http://www.sjmedstaff.org/documents/Delivery-of-twins.pdf Opens a new window [Accessed July 2021]

Where to go next


- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
How to Make a “Good” Presentation “Great”
- Guy Kawasaki

Remember: Less is more.
A strong presentation is so much more than information pasted onto a series of slides with fancy backgrounds. Whether you’re pitching an idea, reporting market research, or sharing something else, a great presentation can give you a competitive advantage, and be a powerful tool when aiming to persuade, educate, or inspire others. Here are some unique elements that make a presentation stand out.
- Fonts: Sans Serif fonts such as Helvetica or Arial are preferred for their clean lines, which make them easy to digest at various sizes and distances. Limit the number of font styles to two: one for headings and another for body text, to avoid visual confusion or distractions.
- Colors: Colors can evoke emotions and highlight critical points, but their overuse can lead to a cluttered and confusing presentation. A limited palette of two to three main colors, complemented by a simple background, can help you draw attention to key elements without overwhelming the audience.
- Pictures: Pictures can communicate complex ideas quickly and memorably but choosing the right images is key. Images or pictures should be big (perhaps 20-25% of the page), bold, and have a clear purpose that complements the slide’s text.
- Layout: Don’t overcrowd your slides with too much information. When in doubt, adhere to the principle of simplicity, and aim for a clean and uncluttered layout with plenty of white space around text and images. Think phrases and bullets, not sentences.
As an intern or early career professional, chances are that you’ll be tasked with making or giving a presentation in the near future. Whether you’re pitching an idea, reporting market research, or sharing something else, a great presentation can give you a competitive advantage, and be a powerful tool when aiming to persuade, educate, or inspire others.
- Guy Kawasaki is the chief evangelist at Canva and was the former chief evangelist at Apple. Guy is the author of 16 books including Think Remarkable : 9 Paths to Transform Your Life and Make a Difference.
Partner Center

IMAGES
VIDEO
COMMENTS
Transverse or shoulder/back presentation occurs in one in 400 births and can cause serious complications for you and your baby. What causes a baby to be transverse? There are several reasons that impact what positions a baby decides to rest in and a few important factors impacting the likelihood of a transverse lie.
Fetal presentation, or how your baby is situated in your womb at birth, is determined by the body part that's positioned to come out first, and it can affect the way you deliver. ... In a transverse lie, the baby is lying horizontally in your uterus and may be facing up toward your head or down toward your feet. Babies settle this way less than ...
Frank breech. When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head.
Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse. Normal fetal lie is longitudinal, normal presentation is vertex, and occiput anterior is the most common position. Abnormal fetal lie, presentation, or position may occur with. Fetopelvic disproportion (fetus too large for the pelvic inlet)
Transverse lie refers to a fetal presentation in which the fetal longitudinal axis lies perpendicular to the long axis of the uterus. It can occur in either of two configurations: The curvature of the fetal spine is oriented downward (also called "back down" or dorsoinferior), and the fetal shoulder presents at the cervix ( figure 1 ).
Low-risk methods to encourage transverse babies to turn include sound or light (putting music or a bright light near the bottom of the uterus), temperature (placing something cold like frozen peas ...
Fetal position: Relation of the presenting part to an anatomic axis; for transverse presentation, occiput anterior, occiput posterior, occiput transverse. Fetal lie: Relation of the fetus to the long axis of the uterus; longitudinal, oblique, or transverse.
Approximately 97% of deliveries involve a fetus positioned with the head down, in the best position to slide out. That makes a vaginal delivery easier and safer. A transverse position only happens in about 1% of deliveries. In that position, the shoulder, arm, or trunk of the fetus may present first. This isn't a good scenario for either of you ...
Usually, fetuses do not stay in a face or brow presentation. These presentations often change to a vertex (top of the head) presentation before or during labor. If they do not, a cesarean delivery is usually recommended. In transverse lie, the fetus lies horizontally across the birth canal and presents shoulder first. A cesarean delivery is ...
Breech presentation happens when your little one's feet or buttocks are in position to be delivered first, and make up just under 5 percent of all pregnancies. Your provider will likely order an ultrasound toward the end of your pregnancy if they suspect your baby is in a breech position. ... Lying Sideways (Transverse Lie) When baby is ...
These anterior presentations (ROA and LOA) are normal and usually are the easiest way for the fetus to traverse the birth canal. LOT. ROT: Transverse Position This LOT (Left, Occiput, Transverse) position and its' mirror image, ROT, are common in early labor. As labor progresses and the fetal head descends, the occiput usually rotates ...
7.6.1 Diagnosis. The uterus is very wide: the transverse axis is virtually equivalent to the longitudinal axis; fundal height is less than 30 cm near term. On examination: head in one side, breech in the other (Figures 7.1a and 7.1b). Vaginal examination reveals a nearly empty true pelvis or a shoulder with—sometimes—an arm prolapsing from ...
The large majority of fetuses in active labor and the second stage are in the occiput anterior (OA) position, but a small proportion experience malposition with occiput posterior (OP) or occiput transverse (OT). OT position is a fetal cephalic malposition in which the sagittal suture and fontanels align 0 to <15 degrees from the transverse ...
Transverse lie occurs frequently in early pregnancy, when it is of no consequence. At 16 weeks gestation, about half of all pregnancies will be transverse lie. This number steadily falls as pregnancy advances and the incidence of transverse lie by the 28th week is well below 10%. ... Compound presentation means that a fetal hand is coming out ...
It is possible to palpate orbital ridges, nose, malar eminences, mentum, mouth, gums, and chin in face presentation. Based on the position of the chin, face presentation can be further divided into mentum anterior, posterior, or transverse. In brow presentation, anterior fontanelle and face can be palpated except for the mouth and the chin.
Learn how to do external cephalic version to reposition a fetus in breech or transverse presentation: https://www.merckmanuals.com/professional/gynecology-an...
Lie - the relationship between the long axis of the fetus and the mother. Presentation - the fetal part that first enters the maternal pelvis. Position - the position of the fetal head as it exits the birth canal. Other positions include occipito-posterior and occipito-transverse. Note: Breech presentation is the most common ...
A fetus in a transverse lie may present the shoulder or acromion as a point of reference to the examiner. As term approaches, spontaneous conversion to a longitudinal lie is the norm. As seen with breech presentation, there is a rapid decrease in nonaxial lie during the third trimester.
According to studies, this presentation is rare and is found in only 1 in 400 cases. Risk Factors for Transverse Lie Women with the following conditions are at a high risk for transverse presentation:
Transverse presentations: Uncommon, but when they occur, the presenting fetal part is the shoulder. If the cervix Cervix The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Externally, the cervix is ...
When the first twin's (the lower one) head is down, but the second twin isn't, your doctor may attempt a vaginal delivery by changing the baby's position or doing breech extraction, which isn't possible if the second twin weighs much more than the first twin.. The rates of emergency C-section deliveries for the second twin after a vaginal delivery of the first twin are higher in second twins ...
When in doubt, adhere to the principle of simplicity, and aim for a clean and uncluttered layout with plenty of white space around text and images. Think phrases and bullets, not sentences. As an ...