- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution


Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Adversity in childhood...
Adversity in childhood is linked to mental and physical health throughout life
Read our collection on toxic stress and ptsd in children.
- Related content
- Peer review
- Charles A Nelson , Richard David Scott chair in pediatric developmental medicine 1 ,
- Zulfiqar A Bhutta , co-director, director of research 2 3 ,
- Nadine Burke Harris , surgeon general 4 ,
- Andrea Danese , professor of child and adolescent psychiatry 5 ,
- Muthanna Samara , professor of psychology 6
- 1 Department of Pediatrics, Boston Children’s Hospital and Harvard Medical School, Harvard Graduate School of Education, Boston, MA, USA
- 2 Centre for Global Child Health, Hospital for Sick Children, Toronto, Canada
- 3 Institute for Global Health and Development, Aga Khan University, South Central Asia, East Africa and UK
- 4 State of California, CA, USA
- 5 Institute of Psychiatry, Psychology and Neuroscience, King’s College London and the National and Specialist CAMHS Clinic for Trauma, Anxiety, and Depression, South London and Maudsley NHS Foundation Trust, London, UK
- 6 Department of Psychology, Kingston University London, London, UK
- Correspondence to: C Nelson charles_nelson{at}harvard.edu
The prevalence of “toxic stress” and huge downstream consequences in disease, suffering, and financial costs make prevention and early intervention crucial, say Charles A Nelson and colleagues
Today’s children face enormous challenges, some unforeseen in previous generations, and the biological and psychological toll is yet to be fully quantified. Climate change, terrorism, and war are associated with displacement and trauma. Economic disparities cleave a chasm between the haves and have nots, and, in the US at least, gun violence has reached epidemic proportions. Children may grow up with a parent with untreated mental illness. Not least, a family member could contract covid-19 or experience financial or psychological hardship associated with the pandemic.
The short and long term consequences of exposure to adversity in childhood are of great public health importance. Children are at heightened risk for stress related health disorders, which in turn may affect adult physical and psychological health and ultimately exert a great financial toll on our healthcare systems.
Growing evidence indicates that in the first three years of life, a host of biological (eg, malnutrition, infectious disease) and psychosocial (eg, maltreatment, witnessing violence, extreme poverty) hazards can affect a child’s developmental trajectory and lead to increased risk of adverse physical and psychological health conditions. Such impacts can be observed across multiple systems, affecting cardiovascular, immune, metabolic, and brain health, and may extend far beyond childhood, affecting life course health. 1 2 3 These effects may be mediated in various direct and indirect ways, presenting opportunities for mitigation and intervention strategies.
Defining toxic stress
It is important to distinguish between adverse events that happen to a child, “stressors,” and the child’s response to these events, the “toxic stress response.” 4 A consensus report published by the US National Academy of Sciences, Engineering, and Medicine (2019) defined the toxic stress response as:
Prolonged activation of the stress response systems that can disrupt the development of brain architecture and other organ systems and increase the risk for stress related disease and cognitive impairment, well into the adult years. The toxic stress response can occur when a child experiences strong, frequent, and/or prolonged adversity—such as physical or emotional abuse, chronic neglect, caregiver substance abuse or mental illness, exposure to violence, and/or the accumulated burdens of family economic hardship—without adequate adult support. Toxic stress is the maladaptive and chronically dysregulated stress response that occurs in relation to prolonged or severe early life adversity. For children, the result is disruption of the development of brain architecture and other organ systems and an increase in lifelong risk for physical and mental disorders.
What is childhood adversity?
A large number of adverse experiences (ie, toxic stressors) in childhood can trigger a toxic stress response. 4 5 6 These range from the commonplace (eg, parental divorce) to the horrific (eg, the 6 year old “soldier” ordered to shoot and kill his mother 7 ).
Adversity can affect development in myriad ways, at different points in time, although early exposures that persist over time likely lead to more lasting impacts. Moreover, adversity can become biologically embedded, increasing the likelihood of long term change. Contextual factors are important.
Type of adversity— Not all adversities exert the same impact or trigger the same response; for example, being physically or sexually abused may have more serious consequences for child development than does parental divorce. 8 9
Duration of adversity— How long the adversity lasts can have an impact on development. However, it is often difficult to disentangle duration of adversity from the type of adversity (eg, children are often born into poverty, whereas maltreatment might begin later in a child’s life).
Developmental status and critical period timing— The child’s developmental status at the time he or she is exposed to adversity will influence the child’s response, as will the timing of when these adversities occur. 10
Number of adversities and the interaction among them—— The Adverse Childhood Experiences (ACE) study 11 12 and subsequent body of ACE research provide compelling evidence that the risk of adverse health consequences increases as a function of the number of categories of adversities adults were exposed to in childhood. Although this seems intuitive, it belies the fact that, when it comes to severe adversity (eg, maltreatment), few children are exposed to only a single form of adversity at a single point in time. In addition, the effects of exposure to multiple adversities is likely more than additive. Thus, multiple forms of adversity may act in complex and synergistic ways over time to affect development.
Exacerbating factors— Children with recurrent morbidities, concurrent malnutrition, key micronutrient deficiencies, or exposure to environmental toxicants may be more sensitive to the adverse effects of other forms of toxic exposures. 13
Supportive family environments— Children develop in an environment of relationships, 14 15 16 and supportive relationships can buffer the response to toxic stress. Safe, stable, and nurturing relationships and environments are associated with reduced neuroendocrine, immunologic, metabolic, and genetic regulatory markers of toxic stress, as well as improved clinical outcomes of physical and mental health. 17 18
Pre-existing characteristics —Many of the adversities being considered are not distributed at random in the population. They may occur more commonly in children and families with pre-existing vulnerabilities linked to genetic or fetal influences that lead to cognitive deficits. 19 20 21 Infants who are more vulnerable to adverse life events (eg, stigma) include those born very early (eg, at 25 weeks’ gestation) or very small (eg, <1500 g), those born with substantial perinatal complications (eg, hypoxic-ischaemic injury), infants exposed prenatally to high levels of alcohol, or those born with greater genetic liability to develop an intellectual or developmental disability (eg, fragile X syndrome) or impairments in social communication (eg, autism).
Individual variation— Finally, children may have different physiological reactions to the same stressor. For example, Boyce, 22 has proposed that by virtue of temperament, some children (such as those who are particularly shy and behaviourally inhibited) are highly sensitive to their environments and unless the environment accommodates such children, the risk of developing serious lifelong psychopathology is greatly increased; conversely, some children thrive under almost any conditions.
Figures 1 and 2 illustrate how duration and type of adversity interact with family environments and pre-existing characteristics to affect development ( fig 1 ), and how early adversity may become biologically embedded ( fig 2 ).

The interplay of adversities, context, and human development
- Download figure
- Open in new tab
- Download powerpoint

Some of the pathways that mediate exposure to early adversity and adult outcomes. Exposure to adversity early in life interacts with a child’s genetic endowment (eg variations in genetic polymorphisms), which in turn leads to a host of biological changes across multiple levels. These changes, in turn, influence adult outcomes (adapted from Berens et al 23 ). HPA axis (SHRP)=hypothalamic pituitary adrenal axis (stress hyporesponsive period)
Consequences of exposure to adversity
Behavioral consequences —Childhood exposure to adversity may result in a variety of behavioral and emotional problems 7 —for example, increased risk taking, aggressive behaviour, involvement in violence (home, school, and neighbourhood), and difficulties in relationships with others. 24 25 Of great concern is the development of post-traumatic stress disorder (PTSD). 9 26
Children experiencing trauma (eg, witnessing the murder of a family member; sexual assault) are also at elevated risk of several other psychiatric disorders, including depression, PTSD, conduct problems, substance abuse, self-harm, and suicidal thoughts and attempts. 8 25 Some forms of physical and psychological abuse in early childhood can be associated with eating disorders and mental health issues affecting typical development and education.
Neurobiological consequences —Many studies have identified structural and functional differences in brain development associated with environmental stressors, such as low socioeconomic status, 27 28 29 30 31 physical abuse, 32 and care giving neglect. 33 34 For example, exposure to maternal stress in infancy has been associated with reduced brain activity, as inferred from electroencephalogram testing 35 , and profound psychosocial deprivation has been associated with differences in overall brain volume along with reductions in white and grey matter volume in several brain areas 36 37 and reduced brain electrical activity. 38 39 Differences in brain development have also been associated with decreases in several cognitive functions, 40 and particularly executive functions, 41 and distally, in educational achievement. 42
Physical consequences —Early exposure to adversities, especially poverty, is associated with linear growth failure and wasting, and has recently been shown to be associated with reduced brain volume 43 and altered functional connectivity. 44 Children exposed to higher psychological stress have been shown to have higher cortisol levels and greater risk of common diseases of childhood, including otitis media, viral infections, asthma, dermatitis, urticaria, intestinal infectious diseases, and urinary tract infections. 45
Childhood adversities have also been associated with greater risk of adult chronic conditions, including cardiovascular disease, stroke, cancer (excluding skin cancer), asthma, chronic obstructive pulmonary disease, kidney disease, diabetes, overweight or obesity, and depression, as well as increased health risk behaviours. 46 47
Tables 1 and 2 show many of the physical and psychological harms observed among children and adults exposed to adversity early in life.
Health conditions in children associated with adverse childhood experiences (ACE)
- View inline
ACE-associated health conditions in adults associated with adverse childhood experiences (ACE)
What mediates the effects of adversity?
The link between exposure to adversity early in life and physical and psychological development are thought to be mediated through several direct and indirect pathways. We first talk about the effects on physical development, then turn our attention to psychological development.
Effects mediated directly may include altering the regulation of stress-signalling pathways and immune system function 48 ; changing brain structure and function 49 ; and changing the expression of DNA and by accelerating cellular ageing. 50 51 For example, abuse or neglect might directly lead to physical injury or undernutrition or malnutrition. Similarly, stress can directly lead to dysregulation of the hypothalamic-pituitary-adrenal axis and associated neuro-endocrine-immune 19 as well as epigenetic effects. 52
Effects mediated indirectly might include changing the quality of the care giving environment (eg, less responsive care 3 ) or the surrounding distal environment (eg, neighbourhood violence, which in turn will affect child development across several levels 53 ); or building dysfunctional cognitions about the self and the world. 25 54 55 The effects of food insecurity (leading to undernutrition or malnutrition) and unsafe or substandard housing (resulting in exposure to asthmagens or environmental toxicants such as lead) can lead to social disparities in health. 4 Distal effects of adversity include the early adoption of health damaging behaviors (eg, smoking, poor food choices) that later in life lead to diabetes, heart disease, and metabolic syndrome. 47
On the psychological side, early adversity can lead to the development of psychopathology early in life (eg, disruptive behavior) that later in life manifests in more severe forms (eg, antisocial personality). Furthermore, it can lead to the development of dysfunctional cognition about self and others. 54 The interplay of these different mediation mechanisms remains largely unclear.
Modelling the effects of adversity must take into consideration the type of adversity, the duration and timing of the adversity, the synergistic effects of multiple forms of adversity with the child’s genetic endowment ( fig 2 ), and the social supports and interventions on which the child can depend (such as caregivers to whom the child is attached).
What can we do now?
If we wish for today’s youth to inherit a world that is safe and conducive to healthy development, we must do all we can to create such a world, by preventing disorders from developing and intervening once they are apparent.
Even for children living in adverse circumstances, much can be done now to make a difference by preventing such disorders from developing and intervening once they have surfaced. For example, we can screen children experiencing adverse life events, and once screened refer such children to early intervention services, as California is doing (see elsewhere in this collection).
Intervention strategies have been developed to help children manage their toxic stress response 7 56 and to help families cope with adversity. Many children are resilient, and physician-community partnerships can help foster resilience. 26
Recommendations for research
Much of the evidence has depended on the use of self- or parent-report measures, which are relatively easy to score, can be scaled at population level, and can be used (with modification) across cultures. However, such measures are inherently subjective and prone to biases (eg, recall bias). Other measures, such as official court or child protection records, provide a more objective assessment but often underestimate the prevalence of adversity.
Objective and subjective measures of childhood adversity identify largely non-overlapping groups of individuals 57 and, thus, may be associated with health outcomes through different pathways. Subjective experience is particularly important for psychopathology, over and above objective experience. 54
A challenge in examining the effects of adversity on development is how to compare children growing up in different cultures. For example, one study 58 reported that a questionnaire on bullying used in different cultures and countries did not generalize well (eg, how one culture interpreted bullying differed from another). Adversity and trauma should be considered in context, and investigators in different cultures may need to develop different assessments.
To move away from subjective evaluations of toxic stress (eg, self- or other-report), and to gain insight into the neural and biological mechanisms that mediate the toxic stress response, several investigators have started to develop more objective biomarker panels for screening for toxic stress that use markers of neurological, immunological, metabolic, and genetic regulatory derangements. 59 60 61 As this work continues, issues to consider include how much better (eg, as predictors) such measures are than behavior, how early in life they can be used, and whether they are scalable.
The study of toxic stress and the toxic stress response needs to move away from correlational and cross-sectional studies and deploy designs that are amenable to drawing causal inference. This would include longitudinal studies and ideally studies that involve interventions. An advantage of the latter includes the ability to shed light on mechanism.
More attention also needs to be paid to individual differences. Different people respond differently to the same stressors. For example, only a minority of children who experience trauma or maltreatment go on to develop enduring psychiatric disorders; and some children develop physical health disorders such as asthma whereas others will not. 62 In addition, individual differences exist in biological sensitivity to stressors: for example, children identified as shy or inhibited early in life may be more vulnerable to stressors than children with more robust temperaments and who are less fearful of novelty 63 64 65 and are more predisposed to anxiety as adults. 66
Recommendations for policy
Policy is only as good as the underpinning evidence, and these recommendations have sufficient evidence to support them.
Careful consideration should be given to implementing evidence-informed policies for optimizing health, nutrition, and early child development, 67 which in turn can be expanded to include older children and adolescents. Although the first three years of life are generally emphasized, older children exhibit remarkable plasticity in molding their personalities and behaviors. 27 68 Effective interventions exist to treat and possibly prevent psychopathology emerging after childhood trauma, but implementation needs to be scaled up. 7
Linking and optimizing preventive child health and education initiatives early in life are key to successful intervention 69 and need to be done at the appropriate level in the health and education systems. The development of the nurturing care framework 70 has been a welcome step in this direction, engaging platforms such as community health workers and pre-schools . 71
Community, school, and after-school based interventions can reduce the effects of traumatic events among children and adolescents living in adverse circumstances. 25 72
Public health strategies for primary, secondary, and tertiary prevention of childhood maltreatment and adversity include both universal and targeted interventions, ranging from home visiting programs to parent training programs, routine screening for adversity, and cognitive behavioral therapy. 73 74
Key recommendations
Researchers should consider both objective and subjective measures of childhood adversity
Researchers should broaden assessment of interventions beyond mental health measures to more regularly include health outcomes such as asthma, infection, inflammation, and insulin resistance
Adversity and trauma should be considered in context, and investigators in different cultures may need to develop different assessments
Researchers should consider how much better (eg, as predictors) objective biomarker panels are than behavior, how early in life they can be used, and whether they are scalable
Researchers should move towards longitudinal studies and ideally studies that involve interventions
Researchers should pay more attention to individual differences
Governments should implement evidence-informed policies for optimizing health, nutrition, and early child development
Health and education systems should link and optimize preventive child health and education initiatives early in life at the appropriate level
Use community, school, and after-school based interventions
Consider public health strategies for primary, secondary, and tertiary prevention of childhood maltreatment and adversity

Acknowledgments
We thank Lee Anglin and Lily Breen for proofing the manuscript.
Competing interests: We have read and understood BMJ policy on declaration of interests and have no relevant interests to declare.
Provenance and peer review: Commissioned; externally peer reviewed.
This article is part of a series commissioned by The BMJ for the World Innovation Summit for Health (WISH) 2020. The BMJ peer reviewed, edited, and made the decisions to publish. The series, including open access fees, is funded by WISH.
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
- Bellis MA ,
- Ramos Rodriguez G ,
- Nurius PS ,
- Logan-Greene P ,
- ↵ Shonkoff JP, Levitt P, Bunge S, et al. Supportive relationships and active skill-building strengthen the foundations of resilience: working paper 13. 2015. www.developingchild.net
- Shonkoff JP ,
- Garner AS ,
- Siegel BS ,
- Committee on Psychosocial Aspects of Child and Family Health ,
- Committee on Early Childhood, Adoption, and Dependent Care ,
- Section on Developmental and Behavioral Pediatrics
- Burke Harris N
- McLaughlin K ,
- Fleisher W ,
- Arseneault L ,
- Nelson CA 3rd . ,
- Gabard-Durnam LJ
- Felitti VJ ,
- Nordenberg D ,
- Hillis SD ,
- Marchbanks PA
- McDonald CM ,
- Flaxman S ,
- Nutrition Impact Model Study
- Estrada P ,
- Arsenio WF ,
- Holloway SD
- Gunnar MR ,
- Brodersen L ,
- Nachmias M ,
- Boynton-Jarrett R
- van Harmelen A-L
- Moffitt TE ,
- ↵ Boyce, WT. The orchid and the dandelion: why some children struggle and how all can thrive. Knofp Doubleday 2019.
- Berens AE ,
- Jensen SKG ,
- Nelson CA 3rd .
- Taillieu T ,
- El-Khodary B ,
- Hammuda S ,
- Vostanis P ,
- Jenkins LM ,
- Chiang JJ ,
- Johnson SB ,
- Houston SM ,
- Teicher MH ,
- Samson JA ,
- Anderson CM ,
- McLaughlin KA ,
- Sheridan MA ,
- McLaughlin KA
- Pierce LJ ,
- Thompson BL ,
- Zeanah CH ,
- Marshall PJ ,
- Bucharest Early Intervention Project Core Group
- Vanderwert RE ,
- Burneo-Garcés C ,
- Cruz-Quintana F ,
- Pérez-García M ,
- Fernández-Alcántara M ,
- Fasfous A ,
- Pérez-Marfil MN
- Ursache A ,
- Pediatric Imaging, Neurocognition and Genetics Study
- Hanson JL ,
- Turesky TK ,
- Ludvigsson J ,
- Hedmark M ,
- Faresjö Å ,
- Theodorsson E ,
- Merrick MT ,
- Suglia SF ,
- Koenen KC ,
- Boynton-Jarrett R ,
- American Heart Association Council on Epidemiology and Prevention; Council on Cardiovascular Disease in the Young; Council on Functional Genomics and Translational Biology; Council on Cardiovascular and Stroke Nursing; and Council on Quality of Care and Outcomes Research
- Elwenspoek MMC ,
- Muller CP ,
- Stamoulis C ,
- Blackburn EH ,
- Theall KP ,
- Shirtcliff EA ,
- Dismukes AR ,
- Wallace M ,
- Jichlinski A
- Baldwin JR ,
- Newbury JB ,
- Altawil M ,
- Scheithauer H
- Aschbacher K
- Deighton S ,
- Neville A ,
- Shonkoff JP
- Gjelsvik A ,
- Crawford H ,
- Morales S ,
- Degnan KA ,
- Vaivada T ,
- Gaffey MF ,
- Dow-Edwards D ,
- MacMaster FP ,
- Peterson BS ,
- Niesink R ,
- Andersen S ,
- Britto PR ,
- Early Childhood Development Interventions Review Group, for the Lancet Early Childhood Development Series Steering Committee
- ↵ World Health Organization, United Nations Children’s Fund, World Bank Group. Nurturing care for early childhood development. 2018. https://apps.who.int/iris/bitstream/handle/10665/272603/9789241514064-eng.pdf
- Richter LM ,
- Daelmans B ,
- Lombardi J ,
- Paper 3 Working Group and the Lancet Early Childhood Development Series Steering Committee
- El Asam A ,
- Khadaroo A ,
- Macmillan HL ,
- Wathen CN ,
- Fergusson DM ,
- Leventhal JM ,
- National Academies of Sciences Engineering and Medicine
- Search Menu
- Advance articles
- Editor's Choice
- Author Guidelines
- Submission Site
- Open Access
- About The British Journal of Social Work
- About the British Association of Social Workers
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
- Introduction
- Experience of adversities early in life
- Influence of the ACEs narrative
- ACEs-informed policy development in the UK
- Trauma aware
- Resilience aware
- Service development
- < Previous
Adverse Childhood Experiences: Developments in Trauma and Resilience Aware Services
- Article contents
- Figures & tables
- Supplementary Data
Trevor Spratt, Mary Kennedy, Adverse Childhood Experiences: Developments in Trauma and Resilience Aware Services, The British Journal of Social Work , Volume 51, Issue 3, April 2021, Pages 999–1017, https://doi.org/10.1093/bjsw/bcaa080
- Permissions Icon Permissions
Research has demonstrated conclusively that the experience of adversities in childhood increases the risks for poor outcomes in the domains of physical and mental health and economic and social circumstances across the life course. This has produced a wave of interest in the effects of Adverse Childhood Experiences internationally, with developments in policy across the UK nations reflective of this. The translation of such research and policy development has witnessed the growing dominance of the ‘toxic stress model’ as underpinning the early signalling of troubles in children. Such signals are further conceptualised as the presence of ‘trauma’. It is upon these conceptual pillars that therapeutically orientated services are being built. In this article, we describe these developments, offering as they do, challenges to short-term interventions as well as providing opportunities for social workers to appropriate the developing knowledge base so as to inform more effective ways of working.
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1468-263X
- Print ISSN 0045-3102
- Copyright © 2024 British Association of Social Workers
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Adverse Childhood Experiences (ACEs) Research: Implications for practitioners
Research Practice Focus #3 | October 2021
In this Research Practice Focus video, we explain what ACEs are, how they are measured, and the pros and cons of routine screening.
Watch the video

Read the video transcript
About the speakers
Professor Andrea Danese

Andrea Danese is Professor of Child & Adolescent Psychiatry at the Institute of Psychiatry, Psychology and Neuroscience, King’s College London. Research from his team has led to highly-cited publications on the measurement of childhood trauma, risk factors for trauma exposure, biological mechanisms through which trauma affects later health, mechanisms of resilience, modelling of individualised risk prediction for trauma-related psychopathology, and the epidemiology of child trauma and trauma-related psychopathology. Professor Danese is an active clinician working as Consultant Child & Adolescent Psychiatrist at the National & Specialist CAMHS Clinic for Trauma, Anxiety, and Depression, South London & Maudsley NHS Foundation Trust. He is also the Academic Secretary for the Royal College of Psychiatrists’ Faculty of Child & Adolescent Psychiatry.
Professor Helen Minnis
Helen Minnis is Professor of Child and Adolescent Psychiatry at the University of Glasgow. She has had a longstanding clinical and research focus on the psychiatric problems of abused and neglected children. Currently her focus is on intervention research, including a randomised controlled trial of an infant mental health service for young children in foster care and a randomised controlled trial of Dyadic Developmental Psychotherapy for primary school-aged children in adoptive or foster placements. She is also conducting behavioural genetic research focussed on the role of abuse and neglect across the life-course.
David Trickey

David Trickey is a Consultant Clinical Psychologist who has specialised in working with traumatised and bereaved children, young people, and families for more than 20 years. He continues to focus on direct clinical work, as well as the training and supervision of other practitioners. He routinely acts as an expert witness in civil and criminal cases and in 2018 was part of the NICE committee to revise guidelines on PTSD.
Notes on the research
Research links from the video.
ACEs definition
- Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., Koss, M. P., & Marks, J. S. (1998). Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults. American Journal of Preventive Medicine , 14 (4), 245–258. https://doi.org/10.1016/s0749-3797(98)00017-8
Measuring ACEs
- Baldwin, J. R., Caspi, A., Meehan, A. J., Ambler, A., Arseneault, L., Fisher, H. L., Harrington, H., Matthews, T., Odgers, C. L., Poulton, R., Ramrakha, S., Moffitt, T. E., & Danese, A. (2021). Population vs Individual Prediction of Poor Health From Results of Adverse Childhood Experiences Screening. JAMA Pediatrics , 175 (4), 385. https://doi.org/10.1001/jamapediatrics.2020.5602
- Danese, A. (2019). Annual Research Review: Rethinking childhood trauma‐new research directions for measurement, study design and analytical strategies. Journal of Child Psychology and Psychiatry , 61 (3), 236–250. https://doi.org/10.1111/jcpp.13160
- Reuben, A., Moffitt, T. E., Caspi, A., Belsky, D. W., Harrington, H., Schroeder, F., Hogan, S., Ramrakha, S., Poulton, R., & Danese, A. (2016). Lest we forget: comparing retrospective and prospective assessments of adverse childhood experiences in the prediction of adult health. Journal of child psychology and psychiatry, and allied disciplines , 57 (10), 1103–1112. https://doi.org/10.1111/jcpp.12621
Screening ACEs
- Lacey, R. E., & Minnis, H. (2019). Practitioner Review: Twenty years of research with adverse childhood experience scores – Advantages, disadvantages and applications to practice. Journal of Child Psychology and Psychiatry , 61 (2), 116–130. https://doi.org/10.1111/jcpp.13135
Trauma and neurodevelopmental disorders
- Dinkler, L., Lundström, S., Gajwani, R., Lichtenstein, P., Gillberg, C., & Minnis, H. (2017). Maltreatment-associated neurodevelopmental disorders: a co-twin control analysis. Journal of Child Psychology and Psychiatry , 58 (6), 691–701. https://doi.org/10.1111/jcpp.12682
- Gajwani, R., Dinkler, L., Lundström, S., Lichtenstein, P., Gillberg, C., & Minnis, H. (2021). Mania symptoms in a Swedish longitudinal population study: The roles of childhood trauma and neurodevelopmental disorders. Journal of Affective Disorders , 280 , 450–456. https://doi.org/10.1016/j.jad.2020.10.076
Video transcript
David Trickey: Hello, I’m David Trickey. I’m a Consultant Clinical Psychologist and Co-Director of the UK Trauma Council, which brings together the UK’s leading experts in child trauma in order to create resources and guidance for policy-makers and front line professionals working with children and young people following traumatic experiences. Today, in this Research to Practice video, we are going to talk about the implications for practice of the ever-increasing body of research concerning adverse childhood experiences or ACEs. I’m joined by two professors of child and adolescent psychiatry: Professor Helen Minnis from the University of Glasgow and Professor Andrea Danese from King’s College London. So I’m going to ask each of you a few questions if that’s okay. So it’s hard to be a practitioner in child mental health and not have come across the term adverse childhood experiences or ACEs. But, Helen I wonder if we could start by you explaining exactly what ACEs are?
Helen Minnis: So ACEs were defined by an American team, more than two decades ago, as, on the one hand, abuse and neglect and on the other hand, what they called family dysfunction and those family dysfunctions could be uncommon things like having a father in prison or a mother in prison or parent with a severe mental illness or they could be very common things like divorce. And the simplicity of it is that it’s basically a checklist of usually 10 items including that whole range of adversities in childhood.
DT: And Andrea, could you explain to us a bit more exactly how ACEs are measured and are there any problems with that?
Andrea Danese: Sure. So, we typically measure ACEs retrospectively, that is, as in the paper that Helen just mentioned, we ask adults and very rarely children to recall their childhood history. And we don’t assume that those retrospective recalls, those memories, really are exact measures of what could have we could have measured prospectively, for example, from child protection or medical records or asking parents for example. But we have shown in a set of papers that that’s not really the case. So perspective and retrospective measures of ACEs identify two groups that really don’t quite overlap. So, this might be surprising at first to hear, but we have now several consistent observations really showing this very clearly. There is an important implication in this, and that is that it is not just what happened, but what we make of it that really counts. Particularly we know this very well now with regard to psychopathology, but we’re also researching the implication for physical health. So, we may be able to use and improve psychological interventions then to reduce the impact of ACEs on health.
DT: Great thanks very much and Helen, can you tell us a bit more about how do ACEs impact individuals?
HM: Well, that’s really it gets really fascinating because the impact of ACEs is so individual and some individuals seem to get away without any negative effects. And I think that’s because there’s been recent research showing really across the animal kingdom — of course, we are animals — that we are actually adapted to, our physiology is adapted to stress, so you know we rebalance ourselves when we’re stressed, even if the stress is very extreme. But what we don’t know is why and when our stress adaptation system could be overwhelmed. So really the range of impact can be from virtually no impact at all to things like posttraumatic stress disorder if ACES happen in early life, attachment disorders, like reactive attachment disorder for children who don’t want to seek and accept comfort. But that is actually quite rare.
DT: Great. Thank you very much. Andrea, some services started to routinely ask people about their adverse childhood experiences. I just wondered if you could say something about the pros and the cons of such an approach?
AD: Absolutely. So, there are clearly advantages, so some pros, and of course it’s really important to engage in the narrative that people build to explain themselves and others, and therefore also talking about their adverse childhood experiences. It tells us about their worldview, and how they react to it. It can help us build empathy, trust, understanding. So, this discussion and being open in this discussion can be clearly advantageous. However, we have shown in a set of papers and the last one just early this year, that it is dangerous to use simplistic screening methods to make risk prediction for individuals and, therefore, then also allocate resources on intervention, for instance. So, what the research shows is that groups of people with greater ACEs have also greater risk of negative outcomes. However our ACE number is not our destiny, as we have said several times. I mentioned this paper that was led by Jessie Baldwin at UCL now in JAMA Pediatrics earlier this year, where we have highlighted that there is much heterogeneity — many differences within each group determined by ACEs number. So really building again on what Helen was saying right, so there are a lot of differences within groups who have the same ACE number. So, for example, many of those who have four plus ACEs don’t have poor health and those will be false positives. And on the opposite side, many of those with low ACEs can develop poor outcomes and those would be false negatives. Therefore, we cannot simply use ACEs or ACEs count to make individual risk prediction because the individual risk prediction would be really poor. So, we need better computational methods that we are currently trying to develop for it.
DT: Great. Thank you very much, and now my final question to both of you really is, what are the implications of this body of research for practitioners and clinicians. Helen, perhaps I could start with you.
HM: So, I would agree with Andrea that the whole ACES literature should, if anything, help us to be more compassionate and curious about our patients. But for me there’s a really big caveat, so our research has shown that people who have experienced ACEs and also much more likely than the general population to experience other mental health problems which are probably heritable, things like ADHD, for example. And so, what we must be really careful of as clinicians is that a person’s ACE history doesn’t close us off to a holistic view of that individual. If a person has experienced adversity in early life they deserve, in my view, and even more thorough our mental health assessment, and we should also be open-minded to the possibility that they don’t have trauma related problems.
DT: Thank you very much. And Andrea do you have any thoughts about the implications for practitioners?
AD: Absolutely. So, I will start with echoing what Helen just said that ACEs are not randomly distributed in the population. There are many reasons why some children and young adults will have high levels of ACEs, so it’s really important to think about what the pre-existing vulnerabilities and risks are because we need to address those to reduce the impact of ACEs as well. And, more generally, I think that the findings that we just described really warn is that more simple, and perhaps more attractive narratives about childhood trauma may be inaccurate and hide the complexity that we must address to improve the lives of children and adults with high ACEs. And so, we don’t want to just leave it at their count, but we need to develop probably a more complex, but a better description of their needs if we want to help.
DT: Brilliant. Thank you so much, both of you, thank you.
Epigenetics and Mental Health: A brief guide to the research
Research round ups.
A quarterly publication providing short summaries of ten research studies from the field of trauma and childhood maltreatment.
Childhood Trauma and the Brain
- Icon Twitter
- Icon Linkedin
- Icon Facebook
Keep Informed
Join the UKTC’s mailing list to be notified about our conferences and events, and new resources.
- Phone This field is for validation purposes and should be left unchanged.
Feedback on UKTC resources
We welcome feedback on the UKTC resources. Share your thoughts here.
- Help & FAQ
The relationship between adverse childhood experiences and educational disadvantage: A critical perspective
- School of Health in Social Science
- Edinburgh Neuroscience
- Centre for Applied Developmental Psychology (CADP)
Research output : Contribution to journal › Review article › peer-review
Abstract / Description of output
Keywords / materials (for non-textual outputs).
- socioeconomic
Access to Document
- 10.3366/scot.2020.0339
This article has been accepted for publication by Edinburgh University Press in the Scottish Affairs, and can be accessed at https://www.euppublishing.com/doi/full/10.3366/scot.2020.0339.
Fingerprint
- Adverse Childhood Experience Social Sciences 100%
- Perspective Social Sciences 100%
- Childhood Agricultural and Biological Sciences 100%
- Adverse Childhood Experiences Psychology 100%
- Research Social Sciences 33%
- Inequality Social Sciences 22%
- Socioeconomic Position Social Sciences 11%
- Mental Health Social Sciences 11%
T1 - The relationship between adverse childhood experiences and educational disadvantage
T2 - A critical perspective
AU - Goodall, Karen
AU - Robertson, Hannah
AU - Schwannauer, Matthias
PY - 2020/10/29
Y1 - 2020/10/29
N2 - In the last 25 years, converging evidence has supported the view that adverse childhood experiences (ACEs) have long term negative impacts on physical and mental health. More recently, ACEs have been negatively associated with a range of educational measures. As educational attainment is a determining factor in later socioeconomic position, the education system is likely to play a significant role in responding to ACEs. A critical and reflective examination of the available research will be crucial to intervening in evidence based ways. While the ACEs movement has been instrumental in highlighting the educational impact of inequality in childhood, the ACEs research is often difficult to parse due to a reliance on checklists and a cumulative risk model.At present, the mechanisms that link ACEs to educational outcomes are still under-researched. Continued discussion of the concept of ACEs and the strengths and limitations of the current research is warranted.
AB - In the last 25 years, converging evidence has supported the view that adverse childhood experiences (ACEs) have long term negative impacts on physical and mental health. More recently, ACEs have been negatively associated with a range of educational measures. As educational attainment is a determining factor in later socioeconomic position, the education system is likely to play a significant role in responding to ACEs. A critical and reflective examination of the available research will be crucial to intervening in evidence based ways. While the ACEs movement has been instrumental in highlighting the educational impact of inequality in childhood, the ACEs research is often difficult to parse due to a reliance on checklists and a cumulative risk model.At present, the mechanisms that link ACEs to educational outcomes are still under-researched. Continued discussion of the concept of ACEs and the strengths and limitations of the current research is warranted.
KW - education
KW - attainment
KW - engagement
KW - violence
KW - socioeconomic
U2 - 10.3366/scot.2020.0339
DO - 10.3366/scot.2020.0339
M3 - Review article
SN - 0966-0356
JO - Scottish Affairs
JF - Scottish Affairs
- Research article
- Open access
- Published: 03 March 2016
Relationships between adverse childhood experiences and adult mental well-being: results from an English national household survey
- Karen Hughes 1 ,
- Helen Lowey 2 ,
- Zara Quigg 1 &
- Mark A. Bellis 3 , 4
BMC Public Health volume 16 , Article number: 222 ( 2016 ) Cite this article
40k Accesses
124 Citations
34 Altmetric
Metrics details
Individuals’ childhood experiences can strongly influence their future health and well-being. Adverse childhood experiences (ACEs) such as abuse and dysfunctional home environments show strong cumulative relationships with physical and mental illness yet less is known about their effects on mental well-being in the general population.
A nationally representative household survey of English adults ( n = 3,885) measuring current mental well-being (Short Edinburgh-Warwick Mental Well-being Scale SWEMWBS) and life satisfaction and retrospective exposure to nine ACEs.
Almost half of participants (46.4 %) had suffered at least one ACE and 8.3 % had suffered four or more. Adjusted odds ratios (AORs) for low life satisfaction and low mental well-being increased with the number of ACEs. AORs for low ratings of all individual SWEMWBS components also increased with ACE count, particularly never or rarely feeling close to others. Of individual ACEs, growing up in a household affected by mental illness and suffering sexual abuse had the most relationships with markers of mental well-being.
Conclusions
Childhood adversity has a strong cumulative relationship with adult mental well-being. Comprehensive mental health strategies should incorporate interventions to prevent ACEs and moderate their impacts from the very earliest stages of life.
Peer Review reports
Individuals’ childhood experiences are of paramount importance in determining their future outcomes. Research exposing the harmful effects that childhood adversity has on adult physical and mental health has advanced significantly over the past few decades. For instance, the Adverse Childhood Experiences (ACE) framework has provided a mechanism for retrospectively measuring childhood adversities and identifying their impact on health in later life [ 1 ]. ACEs include child maltreatment (e.g. physical, sexual and verbal abuse) and broader experiences of household dysfunction, such as witnessing violence in the home, parental separation and growing up in a household affected by substance misuse, mental illness or criminal behaviour. Studies show a dose-responsive relationship between ACEs and poor outcomes, with the more ACEs a person suffers the greater their risks of developing health harming behaviours (e.g. substance misuse, risky sexual behaviour), suffering poor adult health (e.g. obesity, cancer, heart disease) and ultimately premature mortality [ 1 – 6 ].
Much research on the long-term impacts of ACEs has focused on their relationships with mental illness. Thus, studies have found increasing numbers of ACEs to be associated with increasing risks of conditions including depression, anxiety, panic reactions, hallucinations, psychosis and suicide attempt, along with overall psychopathology, psychotropic medication use and treatment for mental disorders [ 2 , 3 , 7 – 11 ]. However the literature on the impact of ACEs on broader measures of mental health and well-being is less extensive. While definitions vary [ 12 ], mental well-being is widely recognised as being more than just the absence of mental illness; incorporating aspects of mental functioning, feelings and behaviours and having been simply described as feeling good and functioning well [ 13 ]. Positive mental well-being has been associated with better physical and mental health and with reduced mortality in both healthy and ill populations [ 14 , 15 ]. Correspondingly, the promotion of mental well-being has become a public and mental health priority both globally and in countries such as the UK [ 16 , 17 ].
Understanding how different factors impede mental well-being in adults is imperative to investing effectively and efficiently in its promotion. With little longitudinal data available, considerable focus has been placed on the associations between current conditions (e.g. social relationships, residential deprivation, physical exercise, health status) and mental well-being rather than longer-term drivers. However, a US study using the ACE framework found a cumulative relationship between childhood adversity and markers of mental well-being in the general population, including mentally healthy days and life satisfaction [ 18 ]. In England, we conducted a pilot ACE study in a local administrative area which found increased odds of low life satisfaction and low mental well-being in adults with increased ACEs [ 19 ]. Following this pilot, we undertook a national ACE study of adults across England that included validated measurements of mental well-being and life satisfaction. Here we explore relationships between levels of exposure to adversity during childhood and current mental well-being in adults. Finally, we discuss the convergence between the roots of poor physical health and poor mental well-being in early years and consequently, how poor mental well-being in one generation may adversely impact well-being in the next.
A target sample size of 4,000 adult residents of England was established based on the prevalence of ACEs identified in the pilot study [ 19 ]. Study inclusion criteria were: aged 18–69 years; resident in a selected LSOA; and cognitively able to participate in a face-to-face interview. Households were selected through random probability sampling stratified by English region ( n = 10, with inner and outer London treated as two regions) and then by small area deprivation using lower super output areas (LSOAs; geographic areas with a population mean of 1,500) [ 20 ]. Within each region, LSOAs were categorised into deciles of deprivation based on their ranking in the 2010 Index of Multiple Deprivation (IMD; a composite measure including 38 indicators relating to economic, social and housing issues) [ 21 ]. Two LSOAs were then randomly selected from each decile in each region and for each LSOA between 40 and 120 addresses were randomly selected for inclusion from the Postcode Address File ® . Sample sizes in each region were proportionate to their population to provide a sample representative of the English population, with a total of 16,000 households initially sampled to account for ineligibility, non-response and non-compliance.
Sampled households were sent a letter prior to researchers visiting providing information on the study and the opportunity to opt out; 771 (4.8 %) households opted out at this stage. Operating under the direction of the research team, a professional survey company visited households on differing days/times (seven days a week, 9:30 am to 8.30 pm) between April and July 2013. The protocol employed by the survey company was to remove households after four attempted visits with no contact. Where contact was made and more than one household member met the inclusion criteria, the eligible resident with the next birthday was selected for interview. Interviewers explained the purpose of the study, outlined its voluntary and anonymous nature and provided a second opportunity for individuals to opt out, with informed consent obtained verbally at the point of interview. Household visits ceased once the target sample size was achieved. Thus, 9,852 of the sampled households were visited of which 7,773 resulted in contact with a resident. Of these households, 2,719 (35.0 %) opted out, 1,044 (13.4 %) were ineligible and 4,010 completed a study questionnaire. Compliance was 59.6 % across eligible occupied households visited and 53.5 % when including those opting out at the letter stage.
The study used an established questionnaire covering demographics, lifestyle behaviours, health status, mental well-being, life satisfaction and exposure to ACEs before the age of 18 [ 19 ]. Participants were able to complete the questionnaire through a face-to-face interview using a hand held computer (with sensitive questions self-completed; n = 3,852), or to self-complete using paper questionnaires ( n = 158). Mental well-being was measured using the Short Warwick-Edinburgh Mental Well-being Scale (SWEMWBS) [ 22 ], which asks individuals how often over the past two weeks they have been: feeling optimistic about the future; feeling useful; feeling relaxed; dealing with problems well; thinking clearly; feeling close to other people; able to make up their own mind about things . Responses are scored from 1 (none of the time) to 5 (all of the time) and an overall mental well-being score is calculated, ranging from 7 (lowest possible mental well-being) to 35 (highest possible mental well-being). Life satisfaction was measured on a scale of 1–10 using the standard question: All things considered how satisfied are you with your life, with 1 being not at all satisfied and 10 very satisfied [ 23 ]. ACEs were measured using the Centers for Disease Control and Prevention short ACE tool [ 24 ] which comprises eleven questions covering nine ACE types: physical abuse; verbal abuse; sexual abuse (three questions); parental separation; exposure to domestic violence; and growing up in a household with mental illness, alcohol abuse, drug abuse or incarceration (for further information see [ 4 ]). Ethnicity was recorded using standard UK Census categories [ 25 ] and categorised as White, Asian and Other due to small numbers within individual ethnic groups. Respondents were allocated an IMD 2010 quintile of deprivation based on their LSOA of residence. Ethical approval for the study was obtained from Liverpool John Moores University’s Research Ethics Committee and the study adhered to the Declaration of Helsinki.
Analyses were undertaken using SPSS v20. Only individuals with complete data relating to all ACEs, age, sex, ethnicity, and IMD quintile were included in the analysis, resulting in a final sample size of 3,885. Bivariate analyses used chi-squared with backwards conditional logistic regression used to examine independent relationships between ACEs and adult mental well-being and life satisfaction. Consistent with other work including previous ACE studies [ 1 – 3 ] and the World Mental Health Surveys [ 26 – 28 ], the number of ACEs participants reported exposure to was summed into an ACE count (range 0 to 9) and here categorised into four groups for analysis: 0 ACEs ( n = 2,072), 1 ACE ( n = 879), 2–3 ACEs ( n = 594) and 4 + ACEs ( n = 322). We also explored relationships between outcome variables and individual ACEs, with analysis focusing on those with highly significant relationships. The seven individual components of SWEMWBS were each dichotomised to indicate poor ratings (never or rarely in the last two weeks). Overall SWEMWBS scores and life satisfaction (LS) ratings were dichotomised to indicate low scores as >1 standard deviation (SD) below the mean (SWEMWBS, mean 27.5, SD 4.4, low <23; LS, mean 7.7, SD 1.7, low <6).
The demographic breakdown of the sample is shown in Table 1 . Compared with the English population the sample overrepresented females (55.0 % v 50.3 % in England) and individuals aged 60–69 years (20.7 % v 16.1 %) and underrepresented those aged 18–29 (21.0 % v 24.2 %). There were no differences by deprivation quintile or ethnicity. Just under half of participants reported having suffered at least one ACE (46.4 %) with 15.4 % reporting 2–3 ACEs and 8.3 % 4+ ACEs. The proportion of participants with low measures (never or rarely in the last two weeks) for the individual components of SWEMWBS ranged from 2.5 % (able to make up own mind) to 14.5 % (feeling relaxed). Thirteen percent were categorised as having low SWEMWBS scores (<23) and 11.6 % as having low life satisfaction (score <6; Table 1 ).
Low SWEMWBS scores and LS were both associated with age, being most prevalent in the 50–59 year age group (Table 1 ). Significant relationships with age were also seen for all individual SWEMWBS components except feeling useful and dealing with problems. There were no relationships between gender and LS or overall SWEMWBS score, although among the individual SWEMWBS components more females had low scores for feeling relaxed and more males for feeling close to others. There were no significant relationships between ethnicity and either low SWEMWBS score or low LS. However both outcomes increased with deprivation, as did low levels of all individual SWEMWBS components except feeling relaxed.
There were strong associations between ACE count and all markers of low mental well-being. Thus the prevalence of low SWEMWBS score tripled from 9.5 % in those with 0 ACEs to 30.7 % in those with 4+ ACEs, while the prevalence of low LS more than tripled from 7.9 to 26.6 % respectively. These significant relationships remained after controlling for confounders in logistic regression analysis with adjusted odds ratios (AORs) for low SWEMWBS score and low LS increasing with ACE count and reaching 3.9 for both outcomes in those with 4+ ACEs (compared with 0 ACEs; Table 2 ). Importantly, while associations between both outcomes and age also remained in LR, running separate models for each age group showed the relationships between high ACE count and low mental well-being to be consistent across age groups. Thus, compared with individuals with no ACEs, AORs for low SWEBWBS scores in those with 4+ ACEs ranged from 3.08 in both 18–29 year olds (95 % CIs, 1.56–6.07) and 30–39 year olds (95 % CIs 1.66–5.72) to 5.34 (95 % CIs 2.10–13.57) in 60–69 year olds (all p < 0.001) and for low LS from 2.54 (95 % CIs 1.09–5.90, p = 0.030) in 18–29 year olds to 11.20 (95 % CIs 4.43–28.29, p < 0.001) in 60–69 year olds.
Figure 1 presents AORs for low scores for each component of SWEMWBS by increasing ACE count (all ages). All relationships were significant and cumulative with AORs for those with 4+ ACEs (compared with 0 ACEs) ranging from 2.23 (95 % CIs 1.22–4.10) for never or rarely being able to make up one’s own mind to 4.09 (2.70–6.20) for never or rarely feeling close to others.
Relationship between adverse childhood experience count and components of poor adult mental well-being (adjusted odds ratios and 95 % confidence intervals). Variables represent the individual component questions in the SWEMWBS scale. Adjusted odds ratios were calculated using logistic regression analysis. Additional independent variables included in the logistic regression were age, gender, deprivation and ethnicity. All relationships are significant with poor mental well-being components positively related to increasing ACE count ( p < 0.001, except ‘ability to make up own mind where p < 0.05). Ref = reference category
Table 3 shows the relationships between measures of mental well-being and the nine individual ACEs examined. Physical, sexual and emotional abuse, witnessing domestic violence, and living in a household affected by mental illness or drug abuse were significantly associated with low levels of all mental well-being measures and household alcohol misuse and incarceration with low levels of all except the ability to make one’s own mind up about things. However parental separation or divorce was only associated with two of the seven SWEMWBS components (feeling useful, feeling relaxed) and an overall low SWEMWBS score. For each marker of mental well-being, a logistic regression model was run that included individual ACE types significantly related to the marker (in bivariate analysis, see Table 3 ) and demographic variables. Here, household mental illness was found to have independent relationships with the most mental well-being marker, being associated with all except the SWEMWBS component of feeling relaxed (Table 4 ). Childhood sexual abuse was associated with all except the SWEMWBS components of feeling useful and feeling close to others. Emotional and physical abuse each had independent relationships with five of the nine measures and household alcohol problems with four. Feeling close to others (the SWEMWBS component with the strongest relationship with ACE count; Fig. 1 ), was independently associated with household mental illness, emotional abuse and physical abuse.
Promoting mental well-being has become a major public health priority as recognition of the links between well-being and broader health and social outcomes has grown. This has contributed to the emergence of broader policy approaches to mental health, both globally and nationally, that incorporate population-level prevention and promotion activity alongside traditional therapeutic responses to mental illness [ 16 , 17 ]. In England, motivation for increased investment in mental well-being promotion has centred around the notion that interventions to improve mental well-being at a population level could produce greater benefits than those to prevent mental illness in at-risk populations [ 29 , 30 ]. However, the evidence base on which such approaches are based is being questioned as broader measurements and studies of mental well-being emerge [ 12 ]. Thus, existing studies have largely associated mental well-being in adults with factors linked to their current circumstances, such as employment, residential deprivation, social participation, physical exercise, relationship satisfaction and health status [ 31 ]. Correspondingly, interventions have often focused on promoting individual behavioural change through, for example, increasing social connectedness and physical activity [ 32 , 33 ]. A life course perspective that incorporates the longer-term impact of childhood adversity has largely been absent from discussions on mental well-being.
Using a randomly selected national household sample of English adults, our study found a strong cumulative relationship between childhood adversities and two widely used measures of mental well-being. The more ACEs participants reported having suffered during their childhood the more likely they were to report low SWEMWBS scores and low life satisfaction (Table 1 ). These relationships remained after controlling for demographics, with odds of poor outcomes for both measures being elevated in those with even a single ACE and almost four times higher in those with four or more ACEs (compared with those with no ACEs; Table 2 ). We also found ACE count to be independently related to each of the seven individual components of SWEMWBS; individuals with higher ACE counts were more likely to report never or rarely (in the last two weeks) feeling optimistic, useful, relaxed or close to others, dealing with problems well, thinking clearly and being able to make up one’s own mind (Fig. 1 ).
A variety of mechanisms link ACEs to poor adult mental well-being. Critically, maltreatment and other stressors in childhood can affect brain development and have harmful, lasting effects on emotional functioning [ 2 , 34 ]. Children who are maltreated can develop attachment difficulties, including poor emotional regulation, lack of trust and fear of getting close to other people. They can also form negative self-images, lack self-worth and suffer feelings of incompetence, all of which can be retained into adulthood [ 2 , 34 , 35 ]. The relationships between ACEs and factors including poor educational attainment and the development of health-damaging behaviours mean that individuals who suffer ACEs can also face a range of risk factors for poor mental well-being in adulthood, such as poor health, low employment and social deprivation [ 2 , 4 , 36 ]. These effects can contribute to cycles of adversity and poor mental well-being whereby individuals that grew up in adverse conditions are less able to provide optimum childhood environments for their own offspring [ 37 ]. Here, and consistent with previous work [ 38 ], the SWEMWBS component with the strongest relationship with ACE count was never or rarely feeling close to others. Children whose parents show poor relationships with them are at greater risks of ACEs [ 39 ], thus individuals who cannot feel close to others as a result of their own ACE history may subsequently be more likely to expose their own children to ACEs. These relationships may also have implications for the implementation and effectiveness of interventions to improve mental well-being through social connectedness.
While analysis based on ACE count highlights the cumulative impact of childhood adversity on mental well-being, it is also useful to explore which ACEs may have particular effects. All ACE types showed significant bivariate relationships with low SWEMWEBS scores, and all except parental separation/divorce with low life satisfaction and most individual SWEMWBS components. In multivariate analyses, however, the ACEs with the most independent relationships with markers of low mental well-being were growing up in a household with someone affected by mental illness and suffering childhood sexual abuse.
The links between growing up in a household affected by mental illness in childhood and low mental well-being in adulthood may in part reflect genetic risk factors that make the offspring of individuals with mental disorders susceptible to poor mental health themselves [ 40 ]; although genetic explanations for the transmission of mental disorders are disputed [ 41 ]. Thus, parental mental illness can have broader impacts on children’s social and emotional development when parenting practices are affected by factors such as low emotional warmth, reduced responsiveness, impaired attention and unpredictable behavioural patterns [ 42 ]. An extensive body of research provides evidence that exposure to childhood adversity such as parental stress, disrupted care patterns and abuse increases risks of mental illness [ 43 ], while studies are increasingly identifying how exposure to such adversity can trigger epigenetic modifications to gene expressions, altering brain structure, stress reactivity and consequently vulnerability to both mental and physical ill health [ 44 ]. Childhood sexual abuse can have particularly damaging effects on individuals’ emotional development, having been linked to feelings of shame and self-blame, powerlessness, inappropriate sexual beliefs and difficulties forming and maintaining intimate relationships [ 45 , 46 ]. Correspondingly research has identified strong relationships between childhood sexual abuse and adult mental illness [ 11 ]. For example, in England sexual abuse in childhood has been attributed to 11 % of all common mental disorders, along with 7 % of alcohol dependence disorders, 10 % of drug dependence disorders, 15 % of eating disorders and 17 % of post-traumatic stress disorders [ 47 ].
The WHO Mental Health Action Plan 2013–2020 incorporates the promotion of mental well-being as part of its overarching goal: highlighting the need for a life course approach that intervenes early to prevent mental health difficulties; recognising the importance of reducing violence; and emphasising the importance of services being responsive to the needs of survivors of violence [ 17 ]. Interventions that seek to reduce ACEs, develop parenting skills and promote resilience in children should thus be considered essential elements in comprehensive mental health strategies. Starting at the very earliest stages of life, these can include measures to train midwives, health visitors and other early years professionals to enquire about parental mental well-being and identify and treat post-natal depression and other mental health concerns [ 48 ]. The ante- and post-natal periods also offer the opportunity to identify and address a broader range of ACEs including parental substance use and domestic violence as well as to increase parenting skills and knowledge. Effective interventions include home visiting and parenting programmes that promote parent-child bonding and develop parenting skills, along with social and emotional development programmes that strengthen life skills and thus resilience in children [ 49 , 50 ]. Measures should also be taken to ensure service providers across a broad range of disciplines are cognisant of the lasting damage that ACEs place on mental well-being and wider health and social outcomes, and are trained to recognise and respond appropriately to clients with adverse backgrounds [ 51 ]. In particular, professionals in mental health services should be trained to routinely enquire about childhood experiences during client assessments. Studies suggest such enquiry is often lacking, with mental health treatment typically based on a medical model that focuses on biological factors and ignores the profound influence of socio-environmental experiences on brain development and functioning [ 52 , 53 ].
While the ACE methodology has been widely employed [ 54 ] it remains vulnerable to issues associated with any cross-sectional and retrospective survey with, for example, results relying on accurate recall and willingness to report ACEs. While adults with low mental well-being may have more negative perceptions of their childhoods, studies suggest false-positive reports of ACEs are rare [ 55 ]. Measures of current mental well-being and life satisfaction were also self-reported and therefore vulnerable to subjectivity, while the exclusion of individuals cognitively unable to participate in a face-to-face survey may have created bias in our sample. The dichotomisation of well-being scales may also have resulted in loss of information, although we used a consistent method to identify low mental well-being of greater than one SD from the sample mean. We used a recognised tool to measure nine important ACEs yet other common adversities such as neglect, bullying and parental death were not recorded. We explored the independent associations between outcome variables and both ACE counts and individual ACEs. However, we had insufficient sample size to look at how interactions between the individual ACE types, different combinations of ACEs and demographics may have resulted in different relationships with mental wellbeing. Such limitations aside our analyses did include multiple statistical analyses potentially increasing risks of type I errors. Consequently, while we have presented all figures for transparency, discussion has focused on highly significant results [ 56 ]. Finally, our study did not measure resilience resources [ 57 ], and developing understanding of factors that promote resiliency in those affected by ACEs would be an important future research priority.
While the high prevalence of mental disorders in the most vulnerable children (e.g. those in child protection systems) and the continued risks of mental illness in adults who suffered ACEs are widely recognised, data linking childhood adversity to the development and persistence of low mental well-being in the broader population is scarce. Our study suggests that almost half of the general English population have experienced at least one ACE and over one in twelve have suffered four or more ACEs. Such childhood adversity places individuals at significantly increased risk of low mental well-being and may have implications for the implementation and success of interventions that seek to promote mental well-being in the general population. The strong links between ACEs and adult mental well-being emphasise the need for a life course approach to mental health with the drivers of poor mental and physical health outcomes rooted together in childhood issues. Many of the ACEs that impact on children’s long term health and well-being are linked to familial behaviours and mental health (e.g. mental illness, substance abuse, violent and aggressive behaviour) suggesting that the mental health impacts of ACEs are what pushes much of their cyclical nature. A life course approach suggests that preventing ACEs would contribute to better physical and mental health from childhood through to old age and thus improve mental well-being in future generations.
Availability of data and materials
Data sets and other materials used in this article can be accessed by request to Professor Karen Hughes.
Abbreviations
adverse childhood experience
adjusted odds ratio
confidence interval
Index of Multiple Deprivation
life satisfaction
lower super output area
Short Warwick and Edinburgh Mental Well-being Scale
Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14:245–58.
Article CAS PubMed Google Scholar
Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, et al. The enduring effects of abuse and related adverse experiences in childhood. A convergence of evidence from neurobiology and epidemiology. Eur Arch Psychiatry Clin Neurosci. 2006;256:174–86.
Article PubMed PubMed Central Google Scholar
Bellis MA, Hughes K, Leckenby N, Jones L, Baban A, Kachaeva M, et al. Adverse childhood experiences and associations with health-harming behaviours in young adults: surveys in eight eastern European countries. Bull World Health Organ. 2014;92:641–55.
Bellis MA, Hughes K, Leckenby N, Perkins C, Lowey H. National household survey of adverse childhood experiences and their relationship with resilience to health-harming behaviors in England. BMC Med. 2014;12:72.
Bellis MA, Hughes K, Leckenby N, Hardcastle KA, Perkins C, Lowey H. Measuring mortality and the burden of adult disease associated with adverse childhood experiences in England: a national survey. J Public Health (Oxf). 2014;37:445–54.
Article Google Scholar
Brown DW, Anda RF, Tiemeier H, Felitti VJ, Edwards VJ, Croft JB, Giles WH. Adverse childhood experiences and the risk of premature mortality. Am J Prev Med. 2009;37:389–96.
Article PubMed Google Scholar
Anda RF, Brown DW, Felitti VJ, Bremner JD, Dube SR, Giles WH. Adverse childhood experiences and prescribed psychotropic medications in adults. Am J Prev Med. 2007;32:389–94.
Clark C, Caldwell T, Power C, Stansfeld SA. Does the influence of childhood adversity on psychopathology persist across the lifecourse? A 45-year prospective epidemiologic study. Ann Epidemiol. 2010;20:385–94.
Koskenvuo K, Koskenvuo M. Childhood adversities predict strongly the use of psychotropic drugs in adulthood: a population-based cohort study of 24 284 Finns. J Epidemiol Community Health. 2015;69:354–60.
Pirkola S, Isometsä E, Aro H, Kestilä L, Hämäläinen J, Veijola J, et al. Childhood adversities as risk factors for adult mental disorders: Results from the health 2000 study. Soc Psychiatry Psychiatri Epidemiol. 2005;40:769–77.
Varese F, Smeets F, Drukker M, Lieverse R, Lataster T, Viechtbauer W, et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull. 2012;38:661–71.
Davies SC, Mehta N, Murphy O, Lillford-Wildman C. Annual report of the Chief Medical Officer 2013, Public mental health priorities: investing in the evidence. London: Department of Health; 2014.
Google Scholar
Keyes CL. The mental health continuum: from languishing to flourishing in life. J Health Soc Behav. 2002;43:207–22.
Chida Y, Steptoe A. Positive psychological well-being and mortality: a quantitative review of prospective observational studies. Psychosom Med. 2008;70:741–56.
Diener E, Chan MY. Happy people live longer: subjective wellbeing contributes to health and longevity. Appl Psychol: Health and Well-Being. 2010;3:1–43.
Department of Health. Closing the gap: priorities for essential change in mental health. London: Department of Health; 2014.
World Health Organization. Mental health action plan 2013–2020. Geneva: World Health Organization; 2013.
Nurius PS, Logan-Greene P, Green S. Adverse Childhood Experiences (ACE) within a social disadvantage framework: distinguishing unique, cumulative, and moderated contributions to adult mental health. J Prev Interv Community. 2012;40:278–90.
Bellis MA, Lowey H, Leckenby N, Hughes K, Harrison D. Adverse childhood experiences: retrospective study to determine their impact on adult health behaviours and health outcomes in a UK population. J Public Health (Oxf). 2013;36:81–91.
Bates A. Methodology used for producing ONS’s small area population estimates. Popul Trends. 2006;12:30–6.
Department for Communities and Local Government. English indices of deprivation. 2010. London: https://www.gov.uk/government/statistics/english-indices-of-deprivation-2010 . Accessed 18 Aug 2015.
Stewart-Brown S, Tennant A, Tennant R, Platt S, Parkinson J, Weich S. Internal construct validity of the Warwick-Edinburgh Mental Well-being Scale (WEMWBS): a Rasch analysis using data from the Scottish Health Education Population Survey. Health Qual Life Outcomes. 2009;7:15.
Waldron S. Measuring subjective wellbeing in the UK. Newport: Office for National Statistics; 2010.
Bynum L, Griffin T, Ridings DL, Wynkoop KS, Anda RF, Edwards VJ, et al. Adverse childhood experiences reported by adults --- five states, 2009. MMWR Morb Mortal Wkly Rep. 2010;59:1609–13.
Office for National Statistics. Population estimates by ethnic group 2002–2009. http://www.ons.gov.uk/ons/rel/peeg/population-estimates-by-ethnic-group--experimental-/current-estimates/population-density--change-and-concentration-in-great-britain.pdf . Accessed 18 Aug 2015.
Scott KM, Von Korff M, Angermeyer MC, Benjet C, Bruffaerts R, de Girolamo G, et al. The association of childhood adversities and early onset mental disorders with adult onset chronic physical conditions. Arch Gen Psychiatry. 2011;68:838–44.
Bruffaerts R, Demyttenaere K, Borges G, Haro JM, Chiu WT, Hwang I, et al. Childhood adversities as risk factors for onset and persistence of suicidal behavior. Br J Psychiatry. 2010;197:20–7.
Kessler RC, McLaughln KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, et al. Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. Br J Psychiatry. 2010;197:378–85.
Foresight Mental Capital and Wellbeing Project. Mental capital and wellbeing: making the most of ourselves in the 21st century. London: The Government Office for Science; 2008.
Huppert FA. A new approach to reducing disorder and improving well-being. Psychol Sci. 2009;4:108–11.
Chanfreau J, Lloyd C, Byron C, Roberts C, Craig R, De Feo D, McManus S. Predicting wellbeing. London: NatCen Social Research; 2013.
Aked J, Marks N, Cordon C, Thompson S. Five ways to wellbeing: the evidence. London: New Economics Foundation; 2008.
Aked J, Thompson S. Five ways to wellbeing: new applications, new ways of thinking. London: New Economics Foundations and NHS Confederation; 2011.
Danese A, McEwen BS. Adverse childhood experiences, allostatis, allostatic load, and age-related disease. Physiol Behav. 2012;106:29–39.
Riggs SA. Childhood emotional abuse and the attachment system across the life cycle: what theory and research tell us. J Aggress Maltreat Trauma. 2010;19:5–51.
Currie J, Widom CS. Long-term consequences of child abuse and neglect on adult economic well-being. Child Maltreat. 2010;15:111–20.
Read J, Bentall RP. Childhood experiences and mental health: theoretical, clinical and primary prevention implications. Br J Psychiatry. 2012;200:89–91.
Bellis MA, Hughes K, Jones A, Perkins C, McHale P. Childhood happiness and violence: a retrospective study of their impacts on adult well-being. BMJ Open. 2013;3:e003427.
Stith SM, Liu T, Davies LC, Boykin EL, Alder MC, Harris JM, et al. Risk factors in child maltreatment: a meta-analytical review of the literature. Aggress Violent Behav. 2009;14:13–29.
Cross-Disorder Group of the Psychiatric Genomics Consortium. Identification of risk loci with shared effects on five major psychiatric disorders: a genome-wide analysis. Lancet. 2013;381:1371–9.
Article PubMed Central Google Scholar
Joseph J. Why the emporer (still) has no genes. In: Read J, Dillon J, editors. Models of madness: psychological, social and biological approaches to psychosis. Hove: Routledge; 2013.
Manning C, Gregoire A. Effect of parental mental illness on children. Psychiatry. 2008;8:7–9.
Read J, Fosse R, Moskowitz A, Perry B. The traumagenic neurodevelopmental model of psychosis revisited. Neuropsychiatry. 2014;4:65–79.
Vaiserman AM. Epigenetic programming by early-life stress: evidence from human populations. Dev Dyn. 2015;244:254–65.
Finkelhor D, Browne A. The traumatic impact of child sexual abuse: a conceptualization. Am J Orthopsych. 1985;4:530–41.
Lalor K, McElvaney R. Child sexual abuse, links to later sexual exploitation/high-risk sexual behavior, and prevention/treatment programs. Trauma Violence Abuse. 2010;11:159–77.
Jonas S, Bebbington P, McManus S, Meltzer H, Jenkins R, Kuipers E, et al. Sexual abuse and psychiatric disorder in England: results from the 2007 Adult Psychiatric Morbidity Survey. Psychol Med. 2011;41:709–19.
Morrell CJ, Warner R, Slade P, Dixon S, Walters S, Paley G, et al. Psychological interventions for postnatal depression: cluster randomised trial and economic evaluation. The PoNDER trial. Health Technol Assess. 2009;13:30.
Sethi D, Bellis MA, Hughes K, Gilbert R, Mitis F, Galea G. European report on preventing child maltreatment. Copenhagen: World Health Organization Regional Office for Europe; 2013.
World Health Organization. Violence prevention: the evidence. Geneva: World Health Organization; 2010.
Kagi R, Regala D. Translating the Adverse Childhood Experiences (ACE) study into public policy: progress and possibility in Washington State. J Prev Interv Community. 2012;40:271–7.
Hepworth I, McGowan L. Do mental health professionals enquire about childhood sexual abuse during routine mental health assessment in acute mental health settings? A substantive literature review. J Psychiatr Ment Health Nurs. 2013;20:473–83.
Read J, Bentall RP, Fosse R. Time to abandon the bio-bio-bio model of psychosis: exploring the epigenetic and psychological mechanisms by which adverse life events lead to psychotic symptoms. Epidemiol Psichiatr Soc. 2009;18:299–310.
PubMed Google Scholar
Anda RF, Butchart A, Felitti VJ, Brown DW. Building a framework for global surveillance of the public health implications of adverse childhood experiences. Am J Prev Med. 2010;39:93–8.
Hardt J, Rutter M. Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. J Child Psychol Psychiatry. 2004;45:260–73.
Perneger TV. What’s wrong with Bonferroni adjustments. BMJ. 1998;316:1236–8.
Article CAS PubMed PubMed Central Google Scholar
Logan-Greene P, Green S, Nurius PS, Longhi D. Distinct contributions of adverse childhood experiences and resilience resources: a cohort analysis of adult physical and mental health. Soc Work Health Care. 2014;53:776–97.
Download references
Acknowledgments
We thank Nicola Leckenby for coordinating the study and preparing data for analysis, and Katie Hardcastle and Olivia Sharples for supporting study implementation. We are grateful to all the surveyors for their time and commitment to the project and to all the individuals who participated in the study.
Author information
Authors and affiliations.
Centre for Public health, Liverpool John Moores University, 15-21 Webster Street, Liverpool, L3 2ET, UK
Karen Hughes & Zara Quigg
Blackburn with Darwen Borough Council, Public Health Department, 10 Duke Street, Blackburn, BB2 1DH, UK
Helen Lowey
Bangor University, Normal Site, Bangor, LL57 2PZ, UK
Mark A. Bellis
Director of Policy, Research and International Development, Public Health Wales, Hadyn Ellis Building, Maindy Road, Cardiff, CF24 4HQ, UK
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Karen Hughes .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors’ contributions
KH supported study development and implementation, analysed the data and wrote the manuscript. HL supported study development and contributed to data analysis and manuscript writing. ZQ edited the manuscript. MAB designed the study, supported data analysis and contributed to manuscript writing. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Hughes, K., Lowey, H., Quigg, Z. et al. Relationships between adverse childhood experiences and adult mental well-being: results from an English national household survey. BMC Public Health 16 , 222 (2016). https://doi.org/10.1186/s12889-016-2906-3
Download citation
Received : 21 August 2015
Accepted : 22 February 2016
Published : 03 March 2016
DOI : https://doi.org/10.1186/s12889-016-2906-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Adverse childhood experiences
- Child maltreatment
- Mental well-being
- Life satisfaction
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Adverse Childhood Experiences (ACEs): educational interventions
Introduction.
This evidence summary seeks to address the following questions relating to adverse childhood experiences (ACEs) and interventions within the education system:
- How may ACEs impact young people’s educational experiences?
- How can schools best support young people with ACEs?
- What kinds of approaches have been effective in creating the conditions for positive educational outcomes?
About the evidence presented below
We drew on a wide range of evidence, including academic research in the fields of social work, healthcare, psychology, early years and education in relevant databases (e.g. ASSIA, ProQuest Public Health, SCIE Social Care Online, Social Services Abstracts) and recommendations from specialist organisations (e.g. CELCIS, Scottish Adverse Childhood Experiences Hub). We searched the academic databases, Google Scholar, search engines and key websites using a broad range of terms including variations on concepts including adverse childhood experiences, child behaviour, early life adversity, educational attainment, mental health, outcomes, wellbeing, and trauma informed approaches.
There is relatively little robust research into what works to support attainment, wellbeing and other educational outcomes for young people with ACEs. In an evidence summary of the role of health and wellbeing interventions in schools for NHS Health Scotland, White (2017) found a lack of research studies, conducted in the UK and Ireland, examining health and wellbeing interventions in a school setting that report educational outcomes. The research that has been conducted tends to focus on what works under particular circumstances, rather than what will reliably work anywhere ( Dyson et al. 2010 ). Howarth et al. (2016) go further, suggesting that in relation to psychoeducational interventions, “there is a need to pause the development of new interventions and to focus on the systematic evaluation of existing programmes” and to “explicitly identify and address the structural, practical and cultural barriers that may have hampered the development of the UK evidence base to date”.
The focus of this review was to identify evidence around ACEs and trauma-informed approaches to education and how ACEs can impact educational outcomes. Although we were unable to identify many studies that specifically identified ACEs as a reason for poor attainment and other educational outcomes, this may be due to the methodological difficulties associated with controlling for a wide range of variables in this context.
In our evaluation of the evidence we found that papers reporting on the impact of interventions tended not to rigorously establish causality between activities to support young people with ACEs and any positive outcomes identified. In some instances claims were made about the degree of confidence that researchers had in this connection, but overall there is a lack of ability to determine that existing programmes and activities based around ACEs and trauma-informed practice definitely do result in positive educational outcomes. However, we found qualitative studies that discussed positive student and teacher perceptions of interventions and evidence to suggest activities are well-regarded and do have an impact on the perceptions of the overall school environment.
Despite the limitations of the evidence presented below, a better understanding of what impact ACEs may have on children’s behaviour, social and emotional development, and physical and mental health can help people working with children in an educational context to address challenges appropriately and lead to more positive educational outcomes, regardless of whether or not individual children can be identified as ‘having’ ACEs.
Accessing resources
We have provided links to the materials referenced in the summary. Some of these materials are published in academic journals and are only available with a subscription through the The Knowledge Network with a NHSScotland OpenAthens username. The Knowledge Network offers accounts to everyone who helps provide health and social care in Scotland in conjunction with the NHS and Scottish Local Authorities, including many in the third and independent sectors. You can register here .
There has been a recent interest in approaches to education that support young people with Adverse Childhood Experiences (ACEs), including trauma informed and attachment approaches. For example, the Welsh Government has recently announced that training to help children who face early childhood trauma is to be offered to all schools in Wales. Teachers will be taught how to support pupils who have adverse experiences such as family breakdown, bereavement or physical, sexual or substance abuse. Public Health Wales worked with Cymru Well Wales, Barnardo's Cymru and the NSPCC will create the training package. ( BBC News 12 March 2018 ). Web of Science analytics indicate that between 2010 and 2017, references to adverse childhood experiences have increased tenfold at a steady pace, suggesting a significant growth in discourse around the concept.
Scottish context
Concerns around ACEs have been picked up by policymakers across education and social care in Scotland. The University of Glasgow Adverse Childhood Experiences Research Centre suggests that children who suffer difficult early experiences, such as illness, neurodevelopmental problems, neglect or abuse can develop mental health problems that can burden them throughout their lives, holding them back in social development, family life, education, the workplace, and even their physical health. Similarly, Health Scotland argues that when children are exposed to adverse and stressful experiences, it can have long-lasting impact on their ability to think, interact with others and on their learning. Dodds (2017) provides a set of slides giving the context to the ‘ACEs journey’ in Scotland so far linking to key policy documents.
There is currently an evidence gap in the Scottish context, with a lack of clarity around the prevalence specifically of ACEs among the general population ( Fabiani 2018 ) and a lack of evidence about the efficacy of interventions, the relationship between ACEs and poverty, and the social justice implications of applying the ACEs lens to individual and social disadvantage.
Scottish Government: Getting It Right For Every Child (GIRFEC)
A key policy or approach relating to ACEs in Scotland is Getting It Right For Every Child (GIRFEC) ( Scottish Government 2018 ). It connects ACEs like parental drug and alcohol abuse, parental incarceration, physical or sexual abuse or neglect, to poorer physical and mental health in adulthood, risky health behaviours, violence and homelessness.
The document states that the Scottish Government will “embed a focus on preventing ACEs and supporting the resilience of children and adults in overcoming early life adversity across all areas of public service, including education, health, justice and social work”. There is a heavy emphasis on prevention of ACEs and mitigation of their impact. Interventions include:
- Measures to reduce parental incarceration by moving to a presumption against short sentences
- More support for children and families in the very earliest years, through expansion in Health Visitor numbers and roll-out of Family Nurse Partnerships
- The expansion of high quality early learning and childcare, including action to increase take-up of provision for 2 year olds
- Investment in projects and services which support parents and families to cope better, keep children safe and prevent children going into care
- Providing funding direct to schools to tackle the attainment gap
- Scottish Adverse Childhood Experiences Hub (2017) Tackling the attainment gap by preventing and responding to Adverse Childhood Experiences (ACEs) ( pdf )
In this document, the Scottish ACEs Hub directly connects ACEs to the school context and argues that tackling ACEs will support educational attainment through improving the mental health and wellbeing of young people through schools’ improved understanding of the behavioural outcomes of early adversity and resulting developments around learning to be a supportive and inclusive environment for learning. It emphasises the importance of understanding child development and how early childhood adversity can impact on biology, relationships and the ability to learn.
This review draws together some evidence around effective school-based interventions that have demonstrable impact on outcomes for children with ACEs.
- Dartington Social Research Unit (2016) Transforming Children’s Services Conference ( set of YouTube videos )
In this set of videos from the Transforming Children’s Services Conference in 2016, several speakers provide their perspectives around and insights and lessons from case studies across Scotland. Speakers include John Swinney, Louise Morpeth, Michael Little, Kenneth Ferguson, Ian Miller and John Fyffe.
The origin of ACEs
The original ACE Study was conducted at Kaiser Permanente from 1995 to 1997. Around 17,000 mostly white, middle class college-educated people in Southern California completed surveys about their childhood experiences and current health status and behaviours, and received physical exams ( Centers for Disease Control and Prevention (CDC) 2016 ). The findings of this research resulted in the development of the ‘ACE Pyramid’, which represents the conceptual framework for the ACE Study and the study’s findings identify a link between childhood experiences, and adult health and wellbeing outcomes:
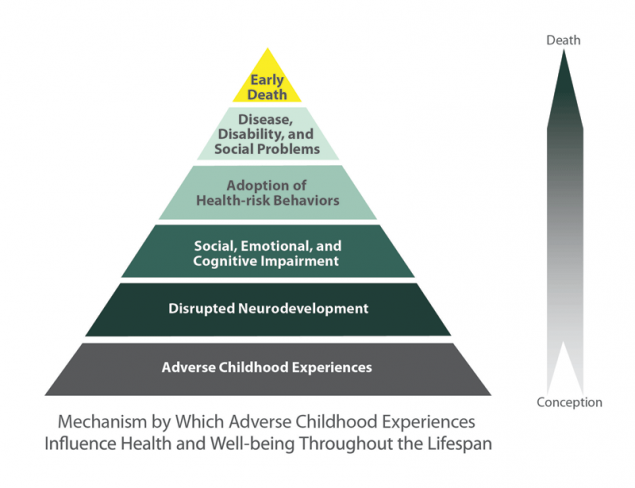
Image from CDC (2016)
Defining ACEs and trauma
According to Corcoran and McNulty (2018) , adverse childhood experiences are “traumatic events (e.g., sexual abuse, physical abuse, emotional abuse) or chronic stressors (e.g., neglect, parental separation) that are uncontrollable to the child”.
The original ACE questionnaire used the following categories and refer to the respondent’s first 18 years of life, which fall under the wider categories of abuse, neglect, and household challenges:
- Emotional abuse: A parent, stepparent, or adult living in your home swore at you, insulted you, put you down, or acted in a way that made you afraid that you might be physically hurt.
- Physical abuse: A parent, stepparent, or adult living in your home pushed, grabbed, slapped, threw something at you, or hit you so hard that you had marks or were injured.
- Sexual abuse: An adult, relative, family friend, or stranger who was at least 5 years older than you ever touched or fondled your body in a sexual way, made you touch his/her body in a sexual way, attempted to have any type of sexual intercourse with you.
Household Challenges
- Mother treated violently: Your mother or stepmother was pushed, grabbed, slapped, had something thrown at her, kicked, bitten, hit with a fist, hit with something hard, repeatedly hit for over at least a few minutes, or ever threatened or hurt by a knife or gun by your father (or stepfather) or mother’s boyfriend.
- Household substance abuse: A household member was a problem drinker or alcoholic or a household member used street drugs.
- Mental illness in household: A household member was depressed or mentally ill or a household member attempted suicide.
- Parental separation or divorce: Your parents were ever separated or divorced.
- Criminal household member: A household member went to prison.
Neglect (Collected during Wave 2 only)
- Emotional neglect: Someone in your family helped you feel important or special, you felt loved, people in your family looked out for each other and felt close to each other, and your family was a source of strength and support (Items were reverse-scored to reflect the framing of the question).
- Physical neglect: There was someone to take care of you, protect you, and take you to the doctor if you needed it (items were reverse-scored to reflect the framing of the question), you didn’t have enough to eat, your parents were too drunk or too high to take care of you, and you had to wear dirty clothes.
A distinction is made between stressful life events and adverse childhood experiences. The former is associated with undesirable life events such as parental divorce or illness of a loved one whist the latter to the experience of more severe very traumatic life events, such as being or seeing someone else physically or sexually abused or being caught in a fire, that can be associated with post traumatic stress disorder ( Parkinson 2012 ).
However, there are some concerns with the categories selected for ACEs criteria, and authors such as Mersky et al. (2017) suggest the need for a more systematic approach to conceptualising and measuring ACEs. Similarly, there is no consensus on the use of terms associated with trauma in childhood, which makes efforts to both implement and study trauma-informed approaches to care challenging ( Maynard et al. 2017 ). Some researchers have also challenged the validity of retrospective adult reporting of ACEs ( Hardt and Rutter 2004 ), which is the method the original studies and many others since have been based on.
Impact of ACEs
The original ACE study ( CDC 2016 ) found the following:
The ACE score, a total sum of the different categories of ACEs reported by participants, is used to assess cumulative childhood stress. Study findings repeatedly reveal a graded dose-response relationship between ACEs and negative health and well-being outcomes across the life course. As the number of ACEs increases so does the risk for the following: Alcoholism and alcohol abuse Chronic obstructive pulmonary disease Depression Fetal death Health-related quality of life Illicit drug use Ischemic heart disease Liver disease Poor work performance Financial stress Risk for intimate partner violence Multiple sexual partners Sexually transmitted diseases Smoking Suicide attempts Unintended pregnancies Early initiation of smoking Early initiation of sexual activity Adolescent pregnancy Risk for sexual violence Poor academic achievement
The theory behind ACEs is that adverse childhood experiences lead to neurobiological impacts and health risks, which in turn lead to long-term social and health problems. The greater the neurobiological impacts and health risks, the more serious the lifelong consequences to health and wellbeing. ( Kahn and Vezzuto 2015 )
Impact of trauma on educational outcomes
In a systematic review of the effects of trauma-informed approaches in schools, Maynard et al. (2017) outline existing evidence of the impact of trauma on educational outcomes:
In a systematic review specifically examining school-related outcomes of traumatic event exposure, Perfect and colleagues (2016) identified 44 studies that examined cognitive functioning, 34 that examined academic functioning and 24 that examined social-emotional-behavioural functioning. Their findings suggest that youth who have experienced trauma are at significant risk for impairments across various cognitive functions, including IQ, memory, attention and language/verbal ability; poorer academic performance and school-related behaviours such as discipline, dropout and attendance; and higher rates of behavioural problems and internalizing symptoms.
Other studies suggest that ACEs increase the risk of behaviour and learning problems in children ( Burke et al. 2011 ; Freeman 2014 ; Hunt et al. 2017 ; Iachini et al. 2016 ), as well as physical and mental health outcomes in later life ( Crouch et al. 2018 ).
Limitations and concerns
As discussed above, Mersky et al. (2017) and others have expressed concern about the definition of ACEs and the items identified within the ACEs framework. Coyne (2017) argues that the ACE checklist is “a collection of very diverse and ambiguous items that cannot be presumed to necessarily represent traumatic experiences”. He also argues that the methods used to research the impact of interventions are limited, suggesting that “claims about the efficacy of trauma-focused treatment are not borne out in actually examining effects observed in randomized controlled trials”.
Other researchers have raised the issue that the impact of ACEs is not necessarily the same across all young people. Although some research suggests that the higher the number of ACEs experienced, the worse the life outcomes, some researchers suggest that this data is not reliable due to evidence to suggest, for example, that young BME people are less likely to report mental health problems than young white people ( Garland et al. 2005 ). Additionally, girls are more likely to demonstrate mental health problems than boys ( Cauffman et al. 2007 ). Furthermore, there is a lack of clarity around the specific impacts of specific ACE categories on young people. For example, Murray et al. (2012) found that “[t]he most rigorous studies showed that parental incarceration is associated with higher risk for children's antisocial behavior, but not for mental health problems, drug use, or poor educational performance.” This indicates a potential need for a better understanding of what challenges young people with different ACEs are more likely to experience in order to effectively design programmes of support in schools.
A significant body of research exists causally connecting adverse childhood experiences to poor educational outcomes. For example, Cook et al (2005) suggest:
By early elementary school, maltreated children are more frequently referred for special education services. A history of maltreatment is associated with lower grades and poorer scores on standardized tests and other indices of academic achievement. Maltreated children have three times the dropout rate of the general population. These findings have been demonstrated across a variety of trauma exposures (eg, physical abuse, sexual abuse, neglect, exposure to domestic violence) and cannot be accounted for by the effects of other psychosocial stressors such as poverty.
Recent doctoral research by McDowell (2017) identified that young people who had multiple ACEs were less likely to care about doing well in school and less likely to do all required homework than children who had no ACEs.
However, a significant amount of research fails to demonstrate that ACEs are the cause of negative educational outcomes and therefore are not able to demonstrate that these experiences are not confounders of an underlying causal element such as poverty. The studies presented below demonstrate a causal link between ACEs and impacts including educational outcomes.
Studies measuring the effectiveness of interventions to mitigate against ACEs
The interventions summarised below include trauma-informed, attachment aware and ACE approaches to interventions to support young people in the school environment and with educational attainment.
- Bartlett, JD et al. (2018) The impact of a statewide trauma-informed care initiative in child welfare on the well-being of children and youth with complex trauma. Children and Youth Services Review, 84(1), pp.110-117 ( Open Access )
This study examines the effectiveness of three community-based trauma treatments with 842 child welfare involved children and young people to assess whether participation in treatment predicted positive child outcomes for the different models. Key findings include that trauma treatment was associated with significant improvements in child behaviour problems, post-traumatic stress symptoms, strengths and needs; results differed by treatment model, with optimal outcomes for children receiving Attachment, Self-Regulation and Competency (ARC) and Trauma-Focused Cognitive Behavioural Therapy (TF-CBT).
- Dingwall, N and Sebba, J (2018) Evaluation of the attachment aware schools programme: final report. Rees Centre, University of Oxford ( pdf )
This mixed-methods study looks at the impact of an Attachment Aware Schools Programme run by Bath and NE Somerset Council, Bath Spa University and Kate Cairns Associates between October 2015-July 2016. The training included part-time continuing professional development with sessions at Bath Spa University, e-learning, consultant support for planning and evaluation and completing a practical project. Participants in the training were 25 participants from 16 schools (6 secondary, 7 primary, 1 middle and two special schools), who were mainly teachers, with two teaching assistants and two family support workers (with a social work background). In addition to impacts on the recipients of the training, the study aimed to identify any improvement in children’s educational progress, well-being, and attendance (including exclusions).
Using surveys, documentary analysis, data analysis, observation and interviews, the researchers found evidence to suggest that the training had an impact on whole staff understanding of attachment, the meaning behind behaviour and emotional well-being.
The authors report that attainment in the schools for the ‘vulnerable students’ targeted by the scheme increased in the year since the programme ended. However, only six of the ten schools provided attainment data for these students which means the extent of the impact is unclear. Additionally, it is not clear if the change in attainment can be attributed to this specific programme or if these six schools were also investing in other activities that may have supported student attainment, for example. The authors argue that the general attainment data for all the schools in the programme supports a positive trend in increasing attainment. However, due to changes in measuring attainment across the years included in the data, it is not clear whether the schools have seen an increase in attainment, and if this potential impact is due to the Attachment Aware Schools programme. The authors identify several other Programmes running alongside the Attachment Aware Programme, such as Thrive, Place 2B, ELSA and Mindfulness.
Students and teachers reported positive changes to the school environment, student behaviour and student well-being, which were viewed as interconnected. The pre- and post-intervention surveys of teachers from the six out of 16 returned sets of data indicated reductions in emotional problems, conduct problems, hyperactivity and peer problems. Pro-social behaviour scores increased.
Attendance data indicates a reduction in attendance across 10 of the 16 schools. However, the authors suggest some schools also saw reductions in persistent absences. There is also a lack of a clear picture about attendance of looked after children, and the proportion of unauthorised absences within the attendance data.
Despite the limitations of the methodology and analysis of the data available, this report is an example of the potential impact of attachment informed schools in the UK and connects qualitative evidence from participants to quantitative findings which may provide useful insights.
- Fancourt, N and Sebba, J (2018) The Leicestershire virtual school’s Attachment Aware Schools Programme: evaluation report ( pdf )
This evaluation aims to: provide an independent assessment of the outcomes of the Attachment Aware Schools Programme in developing knowledge and understanding of the effects of trauma and neglect on attachment and learning and attitudes towards practices for vulnerable pupils in schools. Findings indicate that the programme contributed to staff understanding of attachment theory and emotion coaching. As with Dingwall and Sebba’s report described above, any improvements in educational outcomes and pupil attendance cannot definitely be attributed to the programme under study. However, the report includes feedback from pupils about their perceptions of the school environment following intervention that may be of relevance.
- Howarth, E et al. (2016) IMPRoving Outcomes for children exposed to domestic ViolencE (IMPROVE): an evidence synthesis. Public Health Research, 4(10) ( Open Access )
This evidence synthesis focuses on programmes or intervention with the aim of improving behavioural, mental health or social and educational outcomes for children exposed to domestic violence and abuse. The authors state:
The evidence for clinical effectiveness of the studies included in the review was limited, and where an effect was found there were improvements in behavioural or mental health outcomes, with modest effect sizes but significant heterogeneity and high or unclear risk of bias. Psychoeducational group-based interventions delivered to the child were found to be more effective for improving mental health outcomes than other types of intervention. Interventions delivered to (non-abusive) parents and to children were most likely to be effective for improving behavioural outcomes. However, there is a large degree of uncertainty around comparisons, particularly with regard to mental health outcomes...
There is limited evidence for the acceptability of other types of intervention. In terms of the UK evidence base and service delivery landscape, there were no UK-based trials, few qualitative studies and little widespread service evaluation. Most programmes are group-based psychoeducational interventions. However, the funding crisis in the DVA sector is significantly undermining programme delivery.
Larkin, H et al. (2014) Social work and adverse childhood experiences research: implications for practice and health policy. Journal of Prevention & Intervention in the Community, 40(4), pp.263-70 ( Author manuscript )
This article explores the relationship between the extent of childhood adversity, adult health risk behaviors, and principal causes of death in the United States. It provides a selective review of the ACE Study and related social science research to describe how effective social work practice that prevents ACEs and mobilizes resilience and recovery from childhood adversity could support the achievement of national health policy goals.
The authors argue that social work responses to adverse childhood experiences may contribute to improvement in overall health. They outline prevention and intervention response strategies with individuals, families, communities, and the larger society.
Rose, J et al. (2015) Emotion coaching - a strategy for promoting behavioural self-regulation in children/young people in schools: a pilot study. The European Journal of Social and Behavioural Sciences, 13(1), pp.1767-1790 ( Open Access )
This study explores the effectiveness of using emotion coaching in professional practice within community settings. emotion coaching techniques to promote a more relational and skills-based approach to supporting children’s behaviour.
Two year pilot used mixed methods. Participating institutions included 1 secondary, 4 primary schools, 4 children’s centres and 1 youth centre for Part 1 of the pilot (year 1) and 1 secondary school and 5 primary schools for Part 2 of the pilot (year 2).
Participants included senior and junior teaching staff, teaching assistants, school support staff, Children’s Service staff including health and social care services, early years practitioners, youth workers and youth mentors, and some parents. Participants were trained in emotion coaching techniques (the training phase) and supported via four network/booster meetings (the action research phase) to adopt, adapt and sustain emotion coaching into their practice over a period of one year for each setting pre- and post-impact psychometric questionnaires with all participants, exit questionnaires with all participants, pre- and post- training behaviour indices and oral recordings of the network/booster meetings and focus group discussions.
Findings focus on the emotion coaching in schools and report changes in behavioural and socialisation practices. Quantitative analysis identifies a reduction in the number of call-outs (incidents where children are called out of the classroom), exclusions (external exclusion from school), and consequences (sanction applied), and an increase in rewards for pro-social behaviour. Results indicate a positive impact on professional practice, adult self-regulation and improvements in children/young people’s self-regulation and behaviour. The authors suggest that emotion coaching promotes children’s self-awareness of their emotions, positive self-regulation of their behaviour and generates nurturing relationships. However, the paper does not indicate that children’s perspectives were included in analysis and findings are therefore limited to teachers’ self-reporting of their behaviour before and after the training. It is also not clear if the training was the causal factor for the improved quantitative outcome measures.
- Verbitsky-Savitz, N (2016) Preventing and mitigating the effects of ACEs by building community capacity and resilience: APPI cross-site evaluation findings. Mathematica Policy Research ( pdf )
This report summarizes the final findings of an evaluation of community-based initiatives in Washington State that were intended to prevent child maltreatment and exposure to toxic stress, mitigate their effects, and improve several child and youth development outcomes.
The study focused on outcomes identified by the initiatives that were believed to be successful, and sought to validate sites’ perceptions of effectiveness by examining changes in related outcomes with rigorous evaluation methods.
The study found that 6 (of the 11) evaluated activities were associated with positive and statistically significant changes in targeted outcomes. The remaining five activities either had inconsistent findings or had limited or no outcomes data available. Where positive changes were identified, these related to the following outcomes:
- Resolving barriers to regular school attendance
- Reduction of in-school suspension
- Increase of school rewards for pro-social involvement
- Decrease in student reporting of low commitment to school
- Improvements in reading proficiency in some year groups
- Reducing teenage drinking
- Reduction in “negative maternal behaviors”
Examples and recommended practice
This section focuses on examples of trauma, attachment and ACEs informed approaches to education and documents that make good practice recommendations.
The quality of school attended is important for young people’s health and wellbeing, and schools play a critical role in the development of children and young people’s social networks and their experiences of social relationships ( Dodds 2016 ). Research indicates that the school setting can offer protection against adversities ( McPherson 2013 in Dodds 2016 ).
The six key principles of a trauma-informed approach include safety; trustworthiness and transparency; peer support; collaboration and mutuality; empowerment, voice and choice; and cultural, historical and gender issues ( SAMHSA, 2014 in Maynard et al. 2017 ). Maynard et al. (2017) emphasise that A trauma-informed approach “can include trauma-specific interventions, but trauma-specific interventions alone are not seen as sufficient for achieving optimal outcomes or to influence service systems”.
The ACEs lens can be applied in different ways, including primary prevention and through ‘ACE-aware/informed’ services. In the context of this review, educational interventions are conceptualised as secondary interventions rather than primary prevention.
Depending on the severity of ACEs they could be conceptualised as traumatic. We have therefore also provided resources relevant to trauma-informed education.
- Bath Spa University (no date) Attachment aware schools project ( website )
This website has a list of resources including videos and journal articles that may have useful information.
The attachment aware approach is based on the idea that “[e]ducators must establish attachment-like relationships with their students, particularly with challenging and vulnerable children and young people, in order to improve their chances of learning and achieving.” The Bath Spa website provides information about how the approach has been used in schools, including its use by teachers dealing with behavioural, academic and truancy issues, case reports.
Key research findings from the project include:
- Nurturing adult attachments provide children with protective, safe havens and secure bases from which to explore and engage with others and their environment (Bowlby 1988)
- Early care-giving has a long-lasting impact on development, the ability to learn, capacity to regulate emotions and form satisfying relationships (Siegel 2012)
- Attachment is crucial to children’s psychological welfare and forms the basis of personality development and socialisation (Bowlby 1988)
- Teachers, youth workers and significant adults in a child’s life can provide important attachments for children (Bergin and Bergin 2009, Riley 2010)
- The National Institute for Health and Care Excellence (NICE) 2015 guidelines on children's attachment indicate the importance of attachment issues in schools.
Potentially relevant videos about attachment aware schools include:
Why do we need attachment aware schools?
- Introduction - A scripted piece which can be used from early years to secondary settings, showing an early years aged child/children
- Maggie Atkinson (Children's Commissioner for England) - Outlines why it is important for teachers to know about attachment issues
- Robin Balbernie (Clinical Psychologist) - Introduction to attachment theory and spectrum of needs
- Mike Gorman - Outlines why it is important for teachers to know about attachment issues
- Louise Bomber (Attachment disorder specialist) - Impact of trauma on children in schools, why schools need to be attachment aware
- Jeremy Holmes - The neuroscience of attachment (including the amygdala/frontal lobe development, mirror neurons and vagal tone)
How do we create an attachment aware school?
- Keith Ford (Primary Head Teacher) - A whole school approach - the nurturing school
- Peter Elfer - Early Years attachment and the Key Adult, including why nursery and early years settings need to be attachment aware
- Louise Bomber - Key features of an attachment aware school
- Felicia Wood (Secondary School Teacher) - The importance of consistency in the school's approach
Making a difference through everyday practice
- Clare Langhorn (Head teacher of Special Educational Needs school) - A whole school approach, the difference in her school when it became attachment aware for her staff and students
- Adam Crockett - The child/young person's insights (the need for attachment-like relationships)
- Paul and Caroline Hicks - How parents and carers can be involved and supported
- Felicia Wood - The Key Adult/Attachment Lead
- Peter Elfer - The Key Adult approach, an overview of how it promotes attachment
- James Beattie (Play specialist) - How specialist agencies can work with schools
- Heidi Limbert (Health Visitor/Children's Centre Manager, Somer Valley) - How can partner agencies work with schools, particularly Health Visitors and Children's Centres
- Niki Smith (Senior Social Work Practitioner) - How specialist agencies can work with schools
Department for Education (2016) Mental health and behaviour in schools: departmental advice for school staff ( pdf )
This non-statutory advice clarifies the responsibility of the school, outlines what they can do and how to support a child or young person whose behaviour - whether it is disruptive, withdrawn, anxious, depressed or otherwise - may be related to an unmet mental health need. It includes recommendations for practice including positive classroom management and small group work, social skills development, peer mentoring and support from external bodies.
Forster, M et al. (2017) Associations between adverse childhood experiences, student-teacher relationships, and non-medical use of prescription medications among adolescents. Addictive Behaviors, 68(1), pp.30-34 ( Available with NHS Scotland OpenAthens username or author copy )
This study explores whether student-teacher relationships can help prevent the use of nonmedical use of prescription medication by young people with ACEs. Using a survey of 104,332 8th, 9th and 11th grade students in Minnesota in 2013, the research suggests that cultivating strong student-teacher relationships are important considerations for future school-based substance use prevention initiatives. However, this is not based on a causal relationship between student-teacher relationships and drug (non)use. Although there is evidence to suggest that caring bonds with adults support healthy development, the authors acknowledge that there is “scant research investigating whether positive, caring student-teacher relationships have compensatory effects for youth raised in dysfunctional familial environments”.
- Holmes, P and Farnfield, S (2014) The Routledge handbook of attachment: implications and interventions ( ebook available through NHS Scotland )
This book offers an introduction to therapies produced as a result of the popularity of attachment studies. These therapies can be divided into two categories: those that are 'attachment-based', in that they use evidence-based attachment assessments in their development, or 'attachment-informed', in that the theories of attachment have been integrated into the practice of existing schools of therapy. The book reviews the field and provides a range of interventions for children, adults and parents.
Kahn, P and Vezzuto, L (2015) Understanding and responding to adverse childhood experiences in the school setting. Orange County Department of Education Center for Healthy Kids and Schools ( pdf )
This presentation provides a clear overview of the types of childhood trauma and the background theory to the recommendations around how educators can create a trauma-informed school with a multi-tiered system of support services.
- Maynard, BR et al. (2017) Effects of trauma-informed approaches in schools. Campbell Collaboration review ( pdf )
This background and plan for a systematic review into the impact of trauma-informed approaches in schools includes several excerpts that may be of relevance, including:
A trauma-informed approach in schools is designed to create a systematic model for schools to decrease the impact of trauma on students (Wiest-Stevenson & Lee, 2016) and more appropriately address academic, behavioral and socio-emotional problems by recognizing and responding to student behavior from a trauma-informed perspective. This is done through a multi-level approach intended to improve the school environment through implementing trauma-informed policies and procedures; increase the ability of school staff to recognize and more effectively respond to students through professional development; and prevent, mitigate and reduce trauma-associated symptoms through evidence-informed practices, leading to improved student academic, behavioral, and socio-emotional outcomes. While schools may be implementing trauma-informed approaches, it is unclear to what extent or how much variation there is in what schools are implementing, how much emphasis they are putting on various components (e.g., workforce development versus organizational change versus practice changes) and whether schools may implement trauma-informed approaches differently based on the characteristics of their students, neighbourhood, country or other contextual factors.
The results of this systematic review have not yet been published, but will be shared on the Campbell Collaboration webpage for the study when they are available.
A limitation of the systematic review is that it does not intend to include qualitative research, which means that impact that cannot be recorded using quantitative measures will not be captured.
Mendelson, T et al. (2015) Brief report: Moving prevention into schools: the impact of a trauma-informed school-based intervention ( Available with NHS Scotland OpenAthens username )
This study of 29 students in seventh and eighth grade in the US examined the impact of the RAP Club, sessions led by teachers that incorporate psychoeducation, cognitive behavioral (CBT), and mindfulness strategies to focus on several areas:
- Identifying stress
- Awareness of emotional states
- Using a mindful approach
- Communication skills
- Problem solving skills
- Distress tolerance skills
The research found that the trauma-informed group activity improved teacher-rated emotion regulation, social and academic competence, classroom behavior, and discipline, but that student self-report outcomes did not differ between students who attended the sessions and the control group.
Methodological limitations of this pilot study include small sample size, a volunteer sample, limitations to the randomization process, and no long-term follow-ups. The teachers who rated the children’s changed behaviour were also aware of the intervention taking place (but had limited knowledge of what the programme entailed).
- National Institute for Health and Care Excellence (2015) Children’s attachment: attachment in children and young people who are adopted from care, in care or at high risk of going into care. NICE Guideline 26 ( pdf )
This guideline covers the identification, assessment and treatment of attachment difficulties in children and young people up to age 18 who are adopted from care, in special guardianship, looked after by local authorities in foster homes (including kinship foster care), residential settings and other accommodation, or on the edge of care. It aims to address the many emotional and psychological needs of children and young people in these situations, including those resulting from maltreatment.
Recommendations include:
- Schools and other education providers should ensure that all staff who may come into contact with children and young people with attachment difficulties receive appropriate training on attachment difficulties
- Recognising and assessing attachment difficulties and parenting quality, including parental sensitivity
- Recognising and assessing multiple socioeconomic factors (for example, low income, single or teenage parents) that together are associated with an increased risk of attachment difficulties
- Recognising and assessing other difficulties, including coexisting mental health problems and the consequences of maltreatment, including trauma
- Knowing when and how to refer for evidence-based interventions for attachment difficulties
The guidelines also provide recommendations for attachment-focused interventions and effective methodologies for designing and evaluating the impact of these interventions. Specific recommendations are provided for designing and evaluating interventions in a school setting.
- Nead, K (2016) Adverse Childhood Experiences (ACEs) and Trauma-Informed Care (TIC): critical insights for navigating school health. Thriving Schools ( website )
This website discusses the role of schools and strategies for trauma-informed care in schools. It provides examples, including UCSF Healthy Environments and Response to Trauma in Schools (HEARTS) project, which recommends the following strategies for teachers:
- Recognize that a child is going into survival mode and respond in a kind, compassionate way. When you notice that a child might be having a difficult time, start by asking yourself, “What’s happening here?” rather than “What’s wrong with this child?” This simple mental switch can help you realize that the student has been triggered into a fear response, which can take many forms.
- Create calm, predictable transitions. Transitions between activities can easily trigger a student into survival mode. Some teachers will play music, ring a meditation bell or blow a harmonica to signal it’s time to transition. The important thing is to build a routine around transitions so that children know: a) what the transition is going to look like, b) what they’re supposed to be doing, and c) what’s next.
- Praise publicly and criticize privately. For children who have experienced complex trauma, getting in trouble can sometimes mean either they or a parent will get hit. And for others, “I made a mistake” can mean “I’m entirely unlovable.” Hence, teachers need to be particularly sensitive when reprimanding these students.
- Adapt your classroom’s mindfulness practice. Mindfulness is a fabulous tool for counteracting the impact of trauma. However, it can also be threatening for children who have experienced trauma, as the practice may bring up scary and painful emotions and body sensations.
NYSUT and Co-Ordinated Care Services Inc (2015) Webinar: Trauma Sensitive Schools: transformational school climate change ( YouTube video )
This 1-hour webinar produced by NYSUT looks at the latest research on trauma among school children, exploring trauma's prevalence and impact on childrens' behavior, relationships, and learning. Elements of a trauma sensitive school approach are offered along with resources for implementation.
- Public Health Wales (2018) Sources of resilience and their moderating relationships with harms from adverse childhood experiences. Report 1: mental illness ( pdf )
Findings in this report aim to inform the potential benefits to mental health in Wales of developing resilience both in children and adults to mitigate at least some of the detrimental impacts of experiencing ACEs. It includes recommendations of actions that can be taken to support young people to develop resilience.
- Rossen, E and Cowan, KC (2013) The role of schools in supporting traumatized students. Principal’s Research Review, 8(6), pp.1–7 ( pdf )
This short report provides a potentially useful and clear outline defining trauma, identifying the potential impact of trauma and considering the benefits of multilayered systems of support (MTSS). The authors emphasise the potential benefits of an MTSS approach for all students:
Schools have an opportunity to provide a range of supports to students who experience stress or trauma through an MTSS approach. More specifically, these approaches can help all students feel safe, supported, and connected, including those with undisclosed trauma histories.
This paper has been produced to inform thinking about the impact of adverse childhood experiences and how to use the Pupil Equity Funding to reduce the attainment gap. It highlights key factors that play a role in children achieving their potential.
- Steele, H and Steele, M (2018) Handbook of attachment-based interventions. London: Guilford Press
This book examines science-based interventions that have been effective in promoting attachment security. Focuses on strengthening caregiving relationships in early childhood and working with children and parents who have been exposed to trauma and other adverse experiences. Includes interventions for school-age children, at-risk adolescents and couples, with an emphasis on father involvement in parenting. Describes the approaches and how they are informed by attachment theory and research, how sessions are structured and conducted, special techniques used, the empirical evidence base for the approach, and training requirements. Includes illustrative case material. (Summary from NSPCC)
- Trauma and Learning Policy Initiative (no date) Trauma sensitive schools ( website )
The Trauma and Learning Policy Initiative argues that trauma-sensitive schools help children feel safe to learn. They define the core attributes of a trauma sensitive school to include:
- A shared understanding among all staff
- The school supports all children to feel safe physically, socially, emotionally, and academically
- The school addresses students needs in holistic ways, taking into account their relationships, self-regulation, academic competence, and physical and emotional well-being
- The school explicitly connects students to the school community and provides multiple opportunities to practice newly developing skills
- The school embraces teamwork and staff share responsibility for all students
- Leadership and staff anticipate and adapt to the ever-changing needs of students
The website provides several reports, research outputs and other potentially relevant resources.
White, J (2017) Rapid evidence review: reducing the attainment gap – the role of health and wellbeing interventions in schools ( pdf )
This evidence briefing conducted for NHS Health Scotland and Education Scotland examines the effectiveness of health and wellbeing interventions in a school setting to potentially reduce inequalities in educational outcomes.
Several potentially effective types of intervention are identified and the methods of delivery that have been found to work well are highlighted. Key findings include:
- Programmes that fit the needs and context of the class or school and are easy to carry out are more likely to be implemented well
- The quality of implementation of social and emotional learning programmes was important for positive outcomes
- International review-level evidence suggests that universal social and emotional learning programmes can have positive impacts on wellbeing and educational outcomes. However, findings from studies conducted in the UK and Ireland were mixed.
- Offering healthy, nutritious lunches at school tended to have beneficial effects on educational outcomes.
- There was inconsistent evidence that breakfast clubs, where children were provided with a nutritious breakfast at school, have an impact on educational outcomes.
- A number of studies reported beneficial effects such as lower anxiety levels and improved concentration which have been linked to positive learning-related behaviours
However, a limitation of the studies included in the review is that there is a lack of evidence around the effect of interventions on children and young people from different socio-economic or ethnic backgrounds. There is also a general lack of longitudinal research so it is not clear if the effectiveness of the interventions is long-lasting.
- Burke, N et al. (2011) The impact of adverse childhood experiences on an urban pediatric population. Child Abuse & Neglect, 35(6), pp.408-413 ( paywalled and author manuscript )
- Cauffman, E et al. (2007) Gender differences in mental health symptoms among delinquent and community youths. Youth Violence and Juvenile Justice, 5(3) , pp.287-307 ( paywalled )
- Centers for Disease Control and Prevention (2016) About the CDC-Kaiser ACE Study ( website )
- Corcoran, M and McNulty, M (2018) Examining the role of attachment in the relationship between childhood adversity, psychological distress and subjective wellbeing. Child Abuse & Neglect, 76(1), pp.297–309 ( paywalled )
- Crouch, E et al. (2018) Examining exposure to adverse childhood experiences and later outcomes of poor physical and mental health among South Carolina adults. Children and Youth Services Review, 84, pp.193-197 ( Open Access )
- Department for Education (2016) Mental health and behaviour in schools
- Departmental advice for school staff ( pdf )
- Department for Education (2015) Promoting the health and well-being of looked-after children: statutory guidance for local authorities, clinical commissioning groups and NHS England ( pdf )
- Dodds, S (2016) Health and early years, children and young people: a GCPH synthesis ( pdf )
- Dyson, A (2010) Narrowing the gap in educational achievement and improving emotional resilience for children and young people with additional needs. Centre for Excellence and Outcomes in Children and Young People’s Services (C4EO) ( pdf )
- Forster, M et al. (2017) Associations between adverse childhood experiences, student-teacher relationships, and non-medical use of prescription medications among adolescents. Addictive Behaviors, 68(1), pp.30-34 ( paywalled or author copy )
- Freeman, PC (2014) Prevalence and relationship between adverse childhood experiences and child behavior among young children. Infant Mental Health Journal 35(6), pp. 544-554 ( Open Access )
- Garland, A et al. (2005) Racial and ethnic differences in utilization of mental health services among high-risk youths. American Journal of Psychiatry, 162(7), pp.1336–1343 ( author manuscript ).
- Hardt, J and Rutter, M (2004) Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. The Journal of Child Psychology and Psychiatry, 45(2), pp.260–273 ( paywalled )
- Hunt, T et al. (2017) Adverse childhood experiences and behavioral problems in middle childhood. Child Abuse & Neglect, 67(1), pp.391-40 ( paywalled )
- Iachini, A et al. (2016) Examining adverse childhood experiences among students repeating the ninth grade: Implications for school dropout prevention. Children & Schools, 38(4), pp. 218-226 ( paywalled )
- Kahn, P and Vezzuto, L (2015) Understanding and responding to Adverse Childhood Experiences in the school setting. Orange County Department of Education, Center for Healthy Kids & Schools ( pdf )
- Kalmakis, K and Chandler, G (2015) Health consequences of adverse childhood experiences: a systematic review. Journal Of The American Association Of Nurse Practitioners, 27(8) pp.457-465 ( Open Access )
- Larkin, H et al. (2014) Social work and adverse childhood experiences research: implications for practice and health policy. Journal of Prevention & Intervention in the Community, 40(4), pp.263-70 ( author manuscript )
- Larkin, H et al. (2012) Mobilizing resilience and recovery in response to Adverse Childhood Experiences (ACE): a restorative integral support (RIS) case study. Journal Of Prevention & Intervention in the Community, 40(4) pp.335-346 ( paywalled )
- McDowell, N (2017) The association between adverse childhood experiences and educational outcomes among children ages 6-17. Thesis, Georgia State University ( pdf )
- McPherson K et al. (2013) The role and impact of social capital on the health and wellbeing of children and adolescents: a systematic review. Glasgow Centre for Population Health ( pdf )
- Mendelson, T et al. (2015) Brief report: Moving prevention into schools: The impact of a trauma-informed school-based intervention. Journal of Adolescence, 43(1) pp.142-147 ( paywalled )
- Mersky, J et al (2017) Rethinking the measurement of adversity: moving toward second-generation research on Adverse Childhood Experiences. Child Maltreatment, 22(1), pp.58-68 ( paywalled )
- Murphy, A, Steele, H, Bate, J, Nikitiades, A, Allman, B, Bonuck, K, Meissner, P, & Steele, M (2015) Group attachment-based intervention: Trauma-informed care for families with adverse childhood experiences. Family & Community Health: The Journal Of Health Promotion & Maintenance, 38(3), pp.268-279 ( paywalled )
- Murray, J et al. (2012) Children's antisocial behavior, mental health, drug use, and educational performance after parental incarceration: A systematic review and meta-analysis. Psychological Bulletin, 138(2), pp.175-210 ( Open Access )
- NYSUT and Co-Ordinated Care Services Inc. (2015) Webinar: Trauma Sensitive Schools: transformational school climate change ( YouTube video )
- Parkinson, J (2012) Establishing a core set of national, sustainable mental health indicators for children and young people in Scotland: final report. NHS Health Scotland ( pdf )
- Rose, J et al. (2015) Emotion coaching - a strategy for promoting behavioural self-regulation in children/young people in schools: a pilot study. The European Journal of Social and Behavioural Sciences, 13(1) pp.1767-1790 ( Open Access )
- Scottish Government (2018) Getting it right for every child (GIRFEC) ( website )
- White, J (2017) Evidence summary: reducing the attainment gap – the role of health and wellbeing interventions in schools. Edinburgh: NHS Health Scotland ( pdf )
Featured in the collection: Trauma
Covid-19: Stress, anxiety, and social care worker's mental health
ESSS Outline

Social work with unaccompanied asylum seeking children in Scotland
Healing environments for children who have experienced trauma
Experiential therapies for children who have experienced trauma

How early years trauma affects the brain
The child who mistrusts good care
Trauma sensitive practice with children in care
Related resources.
Room 130, Spaces 1 West Regent Street Glasgow G2 1RW
- Hannah Martin
- Ian Phillip
- Jeanette Sutton
- Jon Dimmick
- Kerry Musselbrook
- Louise Bowen
- Stuart Muirhead
- Our governance
- Be an associate
- Job vacancies
- Our priority areas
- Our innovation model
- Partner with us
- Current work
- Iriss podcast
- Case studies
- Learning materials
- Student research

- Publications
Adverse childhood experiences in context
Briefing paper
First published on 23 August 2019
Description
This paper has been produced by the Scottish Adverse Childhood Experiences (ACEs) Hub to help shape the public health approach to adverse childhood experiences. This paper, written in August 2019, outlines a number of principles that could underpin cross-sectoral work in Scotland to prevent and respond to childhood adversity.
Adverse childhood experiences in context (PDF, 236.0KB)
English language version
Other formats
If you require publications or documents in other formats please email the Public Health Scotland Other Formats team .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Glob Pediatr Health
The Impact of Adverse Childhood Experiences on Health and Development in Young Children
Erica m. webster.
1 SUNY Cortland, Cortland, NY, USA
In recent years, there have been advances in research regarding the prevalence of Adverse Childhood Experiences (ACEs) and resulting poor outcomes for children who have experiences ACES. ACE exposure has been connected with poor academic performance, poor health outcomes, and certain diseases. However, there is still relatively little known about the prevalence and impact of ACE exposure in early childhood. Using the 2016 National Survey of Children’s Health, this study assessed the prevalence of adverse childhood experiences for children under the age of six years. This research measured the impact of individual ACEs on health and developmental outcomes and found that financial hardship and parental mental illness both had increased odds of having health and developmental difficulties. Furthermore, this work finds that there is a dose-response relationship between ACE count and increased risk of health and developmental difficulties. Conversely, children who were reported as affectionate with their parent had decreased risk for health and developmental problems. Programs supporting families with young children should focus efforts on enhancing quality of attachment, especially for children experiencing ACEs.
The study of Adverse Childhood Experiences (ACEs) is helpful in demonstrating how adversity is often associated with negative outcomes. The ACE questionnaire measures traumatic events in childhood, like abuse, neglect, and family dysfunction, that present a risk for future medical, academic, and social problems. High ACE scores have been determined to predict adult risky behavior and are associated with health and disability in childhood. 1 - 4 Studying the impact of ACEs in childhood is important for developing interventions to help mitigate additional risks associated with ACE exposure. 5
This study aims to add to the existing literature on ACEs by examining the impact of ACEs on development in early childhood. Due to the rapid brain development in young children, ACE exposure early in childhood may impact children’s health, learning, and behavior. 6 Using a developmental cascade framework to examine risk in early childhood, this study aims to examine developmental risk factors associated with individual and cumulative ACEs. 7 This research will supplement the body of literature on the achievement gap by including an in-depth analysis of multiple adversities, in addition to income, and examine the odds of additional associated medical and developmental risks. Understanding the prevalence of ACEs and the risks associated with ACEs in early childhood is critical for creating interventions that promote positive development for youth and inform parental education to minimize future ACE exposure.
Specifically, this study aims to examine the relationship of each individual ACE and the number of special health needs that represent chronic health conditions and developmental risk factors in young children (such as having emotional or behavioral problems). Furthermore, this study examines the likelihood of developmental risk factors with the increase in cumulative ACE score, examining a dose-response relationship to multiple developmental adversities. I hypothesized that children with higher ACE scores will have more health and developmental difficulties. Zero-inflated negative binominal regression was used to determine the likelihood of health and developmental problems in relation to the number of ACEs a child has experienced. Additionally, this relationship was examined for differences between children who demonstrate affection to their caregiver and those who rarely or never do.
Prior Literature
The ACE study measures traumatic events in childhood, like abuse, neglect and family dysfunction, that present a risk for future problems. The original 10 item ACE questionnaire includes questions regarding household dysfunction: parental separation, incidents of domestic violence, substance abuse, mental illness, and criminal behavior; abuse: psychological, physical, and emotional; and neglect: physical and emotional. 4
The initial ACE study found a strong relationship between exposure to abuse or household dysfunction during childhood and multiple health risk factors for the leading causes of death in adulthood. In their research Felitti et al 4 found that adults who had experienced 4 or more ACEs showed a 12 times higher prevalence of health risks such as alcoholism, drug use, depression, and suicide attempts. These findings raised awareness about the connection between childhood experiences and outcomes as an adult.
The study of ACEs demonstrates the many interconnected implications of risk. Traumatic events that occur within a child’s immediate environment impact the child’s development. Recent studies on ACEs have shown an increase in health and disability diagnosis associated with higher ACE scores. 2 , 3 Due to this field of research, adversity is no longer perceived as solely a social issue, as it effects health and development also. Interventions such as the Center for Youth Wellness, 5 are targeting the medical, social, and psychological effects of adversities through a multidisciplinary approach. Supporting this complex relationship between ACEs and health other research found that children with special health care needs were more likely to have been reported as having experienced each individual ACE and had a higher average ACE score. 8
The study of adverse experiences focuses on the objective events but is not fully able to include the subjective interpretation of life events. Resilience, or positive adaptation, is evident from participants with high ACE scores in the initial ACE study given that the population examined was adults who were employed and insured, this signifies that even those adults who experienced significant adversity as a child were able to successfully meet social standards by obtaining employment. 4 This study represents the complex nature of risk and resilience since the participants were engaging in some maladaptive behaviors, while showing competence in other areas. While there was a strong correlation between ACEs and risky behavior such as addiction and obesity there is still variation in social outcomes.
A more recent study examined over 700 medical records of youth receiving medical services at an inner-city pediatric clinic. Researchers found a 30-fold increase in learning or behavior problems (as reported by parents) between children with high ACE scores (4 or more) compared to children with no ACEs. This work helps to connect the dots between social risk factors and educational outcomes.
Bower and Baldwin 2 studied the prevalence of ACEs among high school aged children in an urban school district. They found that the prevalence and specific type of adversities varied from different socioeconomic groups. Parental put downs were more common among children from higher socio-economic status (SES) and neighborhood violence was more common in children from lower SES backgrounds. The authors used multiple regression models to control for poverty when measuring the impact of ACEs on individual and school performance. Overall, higher ACE scores were significant in predicting grades, school achievement, and drug abuse. Average ACE scores for schools were associated with state test scores, graduation rates, and college attendance rates.
In a nationally representative study, children with higher ACE exposure were less likely to be engaged in school and more likely to repeat a grade. Furthermore, children with more than 2 aces were more likely to have attention deficit hyperactivity disorder (ADHD), behavior problems, and to bully others. 1 The ACE studies have been helpful in connecting cumulative risks with academic, health, and social outcomes.
Additional research shows that having a trusting adult present in childhood can serve as a buffer for the negative impact of ACEs. A study in the United Kingdom studied the impact of ACEs on health harming behaviors in adulthood and the mitigating effect of having an always available adult present in childhood. The increase of ACEs without the support of a trusted adult was associated with a higher ratio of harmful health behaviors. Even in participants with zero ACEs there were higher rates of smoking and poor diet in those without a trusting adult available during childhood. 9 This research signifies the importance of having available adults as a mitigating factor for adversities including economic deprivation as well as other ACEs. This study is significant in that is suggests that even while many of the ACE questions are directly related to parental stressors, there is still variation in adult outcomes based on having the support of a trusting adult in childhood. This could help inform perspective interventions aimed at mitigating the impact of ACEs in early childhood.
Furthermore, the role of attachment has previously been established as critical during the early childhood years. Masten, 10 states:
“The attachment relationship, in the elaborated theory, serves as a template for future relationships. A secure early attachment bond cascades to foster close relationships in subsequent years with friends, mentors, and romantic partners, serving protective functions for human adaptation over the life course. Research has demonstrated that sensitive, consistent caregiving enhances the quality of the attachment relationships, forecasting better social and emotional development.” (p. 20)
Thus, in early childhood, secure attachment can be preventative in nature, promote positive relational development, or protective in nature, depending on the context.
Developmental Opportunities
Furthermore, there are 3 natural periods in development where youth are especially susceptible to change. The first critical period of development is in early childhood years where brain development is rapidly occurring, and children are in a state of neural plasticity. Any exposure to adversity, or ACEs, during this period of development may hinder healthy development. 6 Prior research on early exposure of abuse and neglect has established the consequences on the developing brain altering normative development. 11 Additionally, another critical period of development occurs in adolescents, where the brain is experiencing neural pruning and individuals are seeking a sense of identity. And finally, the transition into adulthood is a crucial period for developing self-efficacy, pursuing meaning, and exposure to opportunities for success. 12 These developmental transitions are periods of vulnerability and opportunity. Research measures for resilience in youth need to consider developmental timing for determining potential risks, protective factors, and outcome measures. Parents are particularly important in raising young children as they pass along genes, impact the environment and provide experiences; all of which has the potential for both positive and negative impact on development. 13 Prior research associated exposure to ACEs in early childhood with academic and behavioral difficulties in kindergarten. 14 This study considers the role of parental stressors and other ACEs, in early childhood when children are especially reliant on their parents in connection to the child’s developmental outcomes.
Developmental Cascades
This study of risk and development is fitting with the framework of developmental cascades. Masten and Cicchetti 7 define developmental cascades as “the cumulative consequences for development of the many interactions and transactions occurring in developing systems that result in spreading effects across levels, among domains at the same level, and across different systems or generations.” (p. 491). This framework can be used to explain the impact of family systems on individual child development and the relationship between one area of development on another. The study of developmental cascades encompasses the impact of one system on another area of development, such as the connection between ACE exposure in childhood and health outcomes in adulthood. 4 This negative type of developmental cascade is also referred to as a risk cascade. 12 Conversely, a positive developmental cascade may be triggered by the impact of an intervention that promotes a healthy developmental trajectory that has lasting effects. This type of cascade is evident in the research on the effectiveness of interventions in early childhood that promote skills for school readiness and parental education that alter the predicted course of development and have a lasting impact. 15 Likewise, Masten and Cicchetti, 7 state:
“Well-times and targeted interventions could interrupt negative or promote positive cascades; these efforts may work by counteracting negative cascades, by targeting the reduction of problems, or by targeting improvements in competence in domains that increase the probability of better function in other domains.” (p. 491)
Understanding the impact of developmental risk cascades in early childhood is especially important for tailoring interventions that can promote a positive developmental trajectory given that the return on investment is greater during early childhood. 16 Therefore, the study of ACEs on the developing child could provide information for interventions to prevent future ACEs and reduce the negative impact of ACEs on development.
Research Questions:
- (1) Is there a difference between individual ACEs in predicting the increased likelihood for health and developmental problems?
- (2) What predictive power does ACE count have in determining the likelihood of cumulative health and developmental problems in early childhood?
- (3) Does the relative risk of ACE score on health and developmental outcomes differ for children who are affectionate with their parent?
For this study data from the 2016 National Survey for Children’s Health (NSCH) will be used. This dataset, developed by the Health Resources and Service Administration (HRSA) and Maternal and Child Health Bureau (MCHB), provides data on multiple aspects of children’s health and development. The participant sample includes a nationally representative sample of noninstitutionalized children between the ages of newborn and 17 years. Initially, 139 923 households were screened for age eligible children and then one child was selected at random for an interview regarding health and wellbeing. Surveys were administered both by mail and via the internet. A total of 50 212 surveys were completed by parents or guardians. 17 The 2016 NSCH data also includes information on children with special health care needs. Data collection instruments can be found at https://www.childhealthdata.org/learn-about-the-nsch/survey-instruments .
Participants
For this analysis only information using the topical questionnaire for children who were 5 years old or younger are included. Data are weighted to represent the population of noninstitutionalized children nationally and in each state. This analysis includes a subpopulation of children under the age of 6—the age most heavily relying on parents for protection and educational opportunities. There is a total of 14 494 survey responses for children under the age of 6 (29% of the total surveyed sample).
Demographic characteristics. For this analysis, I have included age (in years), gender, and race/ethnicity (Hispanic, white, Black, other/multi-racial) as control variables. Additionally, a ratio of the household poverty provided by NSCH is included in the descriptive demographic table, but not controlled for in the analysis due to the overlap with the ACE question “How often has it been hard to get by on your family’s income—hard to cover basics like food or housing?”
Adverse Childhood Experiences (ACEs)
The NSCH measure for ACEs is based on parent report and are measured as being either present or absent. The wording of the NSCH ACE questionnaire was modified from the original screener used by the Center for Disease Control (CDC) to minimize under-reporting. 18 The 9 ACE questions were included based on the observable nature of items on which parents can report. The ACE scale included one question for each of the following: economic hardship, parental divorce, death of a parent, parental incarceration, mental illness of a family member, drug/alcohol abuse of family member, domestic violence, neighborhood violence, and racial discrimination. The 9 questions used to measure ACEs are listed in Table 4 . The low non-response rate (1.4%) for the ACE questions signifies that the measures were acceptable for respondents. The NSCH-ACE measure is determined to collectively measure overall adversity (Cronbach’s alpha = .66). This is consistent with the findings of Bethell et al 19 confirmatory factor analysis and latent class analysis supporting the usage of the NSCH-ACE measure for assessing cumulative risk.
Survey Question and Prevalence of Each NSCH-ACEs.
Special health care needs
Five questions were asked in the initial screener regarding special health care needs of children, representing overall problems with health and development. In determining the special health care needs (SHCN) status, NSCH combined several health risks including (1) taking prescription medication, (2) requiring more medical/mental health/educational services than usual for the child’s age, (3) having a condition that limits ability to do age-appropriate tasks, (4) needing special therapies (physical, occupational, or speech), or (5) having ongoing emotional, developmental, or behavioral concerns. If respondents answered yes to any condition a follow up question was asked regarding if the condition is expected to last 12 months or longer. SHCN status is determined based on the presence of a qualifying factor and the anticipated duration of more than 12 months. NSCH also included a total count of qualifying factors that determine whether a child is considered to have special health care needs. 18 An additional variable is available for children who have 2 or more qualifying factors signifying a greater developmental impact of one condition or the presence of multiple comorbid conditions. This analysis includes the total count of all qualifying factors.
To investigate the impact of individual ACE predictive power and cumulative ACE count on children’s overall health and development, 2 separate zero inflated negative binomial regression models were used. One model was used measuring the individual impact of each ACE ( Figure 1 ). This model will be helpful to measure the direct impact of specific adversities in order to plan targeted interventions. A second model was measured to examine the cumulative impact of ACE count on health and developmental outcomes ( Figure 2 ). This model examines the total cumulative impact of adversities in early childhood.

Relationship of individual ACEs to the relative risk of cumulative health and developmental impairments.
Abbreviations: ACEs, Adverse Childhood Experiences; CSHCN, Child with Special Health Care Needs.

Relationship of total ACE score to the relative risk of total health and developmental impairments.
In preparation for data analysis, I examined all variable distribution for normality. Distribution of the continuous independent variable and missing data patterns were assessed. Regarding the ACE count, the skew (3.07) and kurtosis (15.26) fell outside the acceptable range (<3), for this reason and to enhance readability, ACE score will be categorized as (1) 0 ACEs, (2) 1 ACE, (3) 2 or 3 ACEs, or (4) 4 or more ACEs. These categories are consistent with previous research on ACEs. 2 , 4 , 9
There is no missing data for factors considered as special health needs as these questions were asked in the screener administered before the full questionnaire was completed. As seen in Table 4 , missing data for the ACE questions are relatively low (less than 5% for all measures). I found no significant predictors of missingness relative to the variables in my dataset. Therefore, complete case analysis will be used. This decision is supported by the notion that it would be inappropriate to impute sensitive information such as ACE scores or diagnosis.
Variance inflation factors for all variables were <3.0, suggesting no multicollinearity of the data. 20 To determine the best fitting model Poisson regression model (PRM), negative binomial regression model (NBRM), zero inflated Poisson (ZIP), and zero inflated negative binomial (ZINB) models were compared. Zero inflated negative binomial model was preferred over other models based on the AIC and BIC (shown in Table 1 ). The α (IRR = 0.64, se = 0.16, 95% CI = 0.4, 1.03) is not equal to zero signifying over dispersion of the data, justifying the appropriate use of the zero inflated negative binomial model. In this data having zero qualifying health care needs could be due to lack of qualifying factors or could be lack of health care access to evaluate special health needs. In this data there were a significant percent of children without health care needs. Having no qualifying health needs was associated with younger children, with 95% of children under the age of 1 having zero special health care factors, whereas 84% of children 5 years old had zero qualifying special health care needs (shown in Table 2 ).
Model Fit Comparisons.
Percent of Special Health Care Needs by Age.
Descriptive statistics for the early childhood population are shown in Table 3 . The greatest proportion of sample participants were white (70%), followed by other or mixed-racial (14%). The population of this study had slightly more males (51.8%) than females. Children’s age ranged between 1 month and 5 years old with the mean age of 2.6 years old (SD = 1.64). The majority of respondents reported their family income to be above 400% of the federal poverty level with about 10% falling at or below the poverty level.
Sample Characteristics and Prevalence of Special Health Care Needs by ACE count category: Children Ages 0-5 National Survey for Children’s Health 2016.
This table also includes the percent of children with each qualifying special health need for children with 2 or more ACEs in comparison with those with less than 2 ACEs. A higher proportion of children with 2 or more ACEs experience each of the individual health and developmental conditions. This cut off was used because the overall prevalence of ACEs was fairly low for the early childhood population and this gives an idea of differences on health factors between the group with low adversity and those with moderate or high levels of adversity. Children with special health care needs comprised 11.6% of the sample (shown in Table 3 ). Taking prescription medication was the most common qualifying factor (7.2%), followed by elevated use of medical or educational services (6.1%), and the fewest number of children (3.3%) qualified based on emotional, behavioral, or developmental needs.
Special health care needs were considered for children with less than 2 ACEs and for children with 2 or more ACEs, this showed differences in the proportion of children within each group who had qualifying special health care needs. 24.1% of children with 2 or more ACEs qualified as having special health care needs, whereas only 10.4% of children with less than 2 ACEs qualified. A greater proportion of children with 2 or more ACEs was found for each of the qualifying factors when compared to children with less ACEs. Additionally, 15% of children with 2 or more ACES also had 2 or more special health care needs, whereas only 5% of children with less than 2 ACEs had multiple health needs. This signifies a difference in the prevalence of special health care needs for young children with ACEs.
Table 4 shows the prevalence of the sample having experienced each individual ACE and broken down by ACE count categories. Of the children in this sample 70.9% had experienced zero ACEs with the average ACE score of 0.44 (SD = 0.92). As represented in Table 4 the prevalence of each individual adversity is low with the most common adversities being financial hardship (18.6%) and parental separation (9.4%).
In the first model, the relative risk of special health needs was determined for each of the ACE questions individually. The model controls for race and sex. Significant findings showed the expected special health needs count increase by 84% for children whose families reported financial hardship (IRR = 1.84, se = 0.12, z = 9.30, P < .001, 95% CI = 1.62, 2.10) and increased by 42% for children who lived with someone who had a mental illness (IRR = 1.42, se = 0.16, z = 3.18, P < .001, 95% CI = 1.14, 1.76). Model results are displayed in Table 5 .
Incidence-Rate Ratio for Increased Health and Developmental Difficulties by Individual ACE Exposure and by Cumulative ACE Score.
Models controls for age, sex, and race.
*** P < .001. ** P < .01. * P < .05.
A zero inflated negative binominal model was used to determine the predictive power of ACE count on cumulative health care needs. In the second model, after controlling for race and sex, the relative risk of special health care needs was determined based on the cumulative ACE count category and by attachment to caregiver. Overall, there was a strong positive relationship between the number of ACEs a child had experienced and the count of special health care needs (displayed in Table 5 ). Compared to those with zero ACEs, children with one ACE have 68% higher odds of having special health care needs (IRR = 1.68, se = 0.11, z = 7.69, P < .001, 95% CI = 1.48, 1.91). Children with 2 or 3 ACEs have 83% higher odds of having special health care needs relative to those with no ACEs (IRR = 1.83, se = 0.16, z = 6.98, P < .001, 95% CI = 1.55, 2.18). Lastly, children who experienced 4 or more ACEs had 137% increase odds when compared to those with no ACEs (IRR = 2.37, se = 0.30, z = 6.87, P < .001, 95% CI = 1.85, 3.03).
Alternatively, there was a 33% decrease in odds of special health care needs for children who were reported as being affectionate with their caregiver relative to those who were not (IRR = 0.67, se = 0.06, z = −4.57, P < .001, 95% CI = 1.77, 3.08). This relationship is depicted in Figure 3 . An ANOVA was used to test the significance of the difference in mean qualifying factors by affection at each ACE count category. Findings indicated a statistically significant ( P < .001) difference for children with less than 4 ACEs (results not shown). For children with 4 or more ACEs, being affectionate with a parent was not significant in predicting mean number of special health care factors.

Predictive margins by ACE score for increased health and developmental difficulties sorted by affectionate children.
During the period of early childhood, children are rapidly developing neurological connections; thus, development during these crucial years is also associated with success in later years. 6 In this nationally representative sample of young children, experiencing ACEs was associated with poor health and developmental outcomes. Similar to prior ACE research, this study finds significant predictive power in cumulative ACE count and increased odds for worse overall outcomes with high ACE scores. 1 - 4 This phenomenon of ACE count predicting poor health and developmental outcomes, which is in turn predictive of difficulties later in life, is considered a risk cascade 7 . Conversely, children with no or low ACEs were less likely to experience health and developmental difficulties, and are therefore, likely to continue experiencing success on age salient tasks, this represents a positive developmental trajectory or success cascade. The desired outcome of interventions would be to alter the developmental trajectory for those youth who have experienced adversity and put into place factors which will promote future successes.
In this study individual ACEs were measured for predictive power and it was found that many of the ACEs when measured individually did not have significant predictive power in determining the odds for increase health and developmental difficulties. The 2 ACEs that were statistically significant (financial hardship and living with someone with a mental illness) both had slightly larger confidence intervals indicating that there is variance in outcome for children who have experienced those ACEs. Financial hardship has been determined to be associated with many additional risk factors, such as poor health and development, so this finding aligns with prior research on the impacts of poverty. 21 Prior research on parental depression and mental illness has noted the impact of depression on the social-emotional development of children. Furthermore, there is notable differences in the parent-child attachment for children whose parent has a mental illness. 22 Additionally, parental mental illness may be associated with increased odds for special health needs based on the genetic risk of passing down emotional difficulties to the child.
The second model used in this study confirmed that higher ACE scores are associated with increased risk for health and developmental factors. These findings confirm the suggestions from Bethell et al 19 to use an ACE score to measure cumulative risk. Relative to children with no ACEs, children who have experienced ACEs had an increased risk for taking prescription medication, requiring more medical/educational services than typical for their age, have limitations that impact their daily functioning, receiving special services, or having emotional, behavioral, or developmental difficulties. This study adds to the growing body of literature around ACEs in that it links adversity to health and developmental difficulties in childhood. 1 - 3 These special health and developmental needs in early childhood have implications for future developmental trajectories. 6
These findings also add to the literature connecting childhood adversity to adult health outcomes. Comple-menting prior work focusing on adult health behaviors, this study provides information connecting ACE exposure to health and developmental outcomes during childhood that may influence the health disparities observed in adulthood. 4 Recent research predicts that prevention of ACEs would lead to a significant decrease in depression, kidney disease, stroke, coronary heart disease, cancer, diabetes, and obesity in America. 23 Furthermore, ACE prevention was associated with predictive decreases in health risk behaviors (smoking and drinking) in adulthood and in socioeconomic challenges such as unemployment.
This study highlights the risk cascade associated with early childhood exposure to ACEs and health and developmental outcomes. Given the connection between health and development for young children, this work has implications for both pediatricians and early childhood educators. Given the frequent contact with families and length of time working with a family, these professionals are uniquely positioned to identify ACEs and developmental outcomes. Additionally, they can provide resources or referrals for families in order to promote positive developmental trajectories. Programs such as Head Start, Nurse Home Visiting, Universal Pre-Kindergarten and other preventative programs may help reduce the achievement gap and health disparities noted in other studies. 2 , 3 , 24 Guidance from the National Center for Injury Prevention and Control echoes this need in emphasizing the role of quality care and education in early childhood in preventing future ACE exposure. 25
Lastly, this study contributes to the growing body of literature around resilience in examining the role of secure attachment in altering the impact of ACEs on health and development. Children who were reported showing affection to their parent had a decreased risk for health and developmental difficulties when compared to children with the same number of ACEs who did not frequently show affection toward their parent. This finding contributes to the work of Bellis et al 9 in confirming the role of a secure attachment in undermining the negative impact of ACEs. This confirms the notion that parents can serve as protective factors in mitigating the impact of risks and promoting resilience in youth. 12
Limitations and Recommendations
While this study adds to the growing body of literature regarding ACEs and ACE resilience, it is not without limitations. The dataset used for this analysis was a convenient nationally representative sample, yet the NSCH data may not be fully representative of children experiencing ACEs since the majority of the sample had experienced none. Additionally, the sample was composed of majority white and affluent respondents. Furthermore, the nature of the NSCH questionnaire was self-report which may have been biased by social desirability. 26
One limitation in measuring developmental cascades is that it does not measure developmental changes over time. The data being used takes into consideration the parents’ perspective in health conditions expected to last at least 12 months, but this does not give a complete picture of the relationship between ACEs and children’s developmental trajectories. The nature of the NSCH data provides rich data from a single time point, but there is currently no publicly available longitudinal data measuring ACEs in childhood.
While the difference in predictive power of ACEs on cumulative health outcomes were examined both for children with and without an affectionate relationship with their parent, the analysis used does not measure a moderating effect. Additionally, research on resilience includes many parental characteristics that serve as protective factors. 12 In this analysis the only parent level measures were the ACEs. It is recommended that further research be conducted to look at the positive impact that families can have in lessening the impact of ACEs.
This study enriches the rapidly expanding literature on adverse childhood experiences and developmental implications, by narrowing the focus to early childhood where children are most reliant on their families and therefore may be most susceptible to family dysfunction and other ACEs. This study uses a nationally representative sample to confirm the risk cascade relationship between increased ACEs and risk for health and developmental difficulties. Furthermore, this study begins to examine the role parent-child attachment can play in promoting resilience in the face of adversity. The findings from this study underscore the importance of tailored interventions to prevent further risks and promote positive developmental trajectories during early childhood.
Author Contributions: The author confirm contribution to the paper as follows: study conception and design; analysis and interpretation of results; draft manuscript preparation and review.
Declaration of Conflicting Interests: The author declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author received no financial support for the research, authorship, and/or publication of this article.

- Research Article
- Open access
- Published: 12 June 2020
Adverse childhood experiences: a retrospective study to understand their associations with lifetime mental health diagnosis, self-harm or suicide attempt, and current low mental wellbeing in a male Welsh prison population
- Kat Ford ORCID: orcid.org/0000-0002-2984-5838 1 ,
- Mark A. Bellis 1 , 2 ,
- Karen Hughes 1 , 2 ,
- Emma R. Barton 2 &
- Annemarie Newbury 2
Health & Justice volume 8 , Article number: 13 ( 2020 ) Cite this article
14k Accesses
25 Citations
3 Altmetric
Metrics details
Prisoners are at increased risk of poor mental health and self-harming behaviours, with suicide being the leading cause of death in custody. Adverse childhood experiences (ACEs) such as child maltreatment are strong predictors of poor mental health and wellbeing yet despite high levels of ACEs in offender populations, relatively few studies have explored the relationships between ACEs and prisoners’ mental health and wellbeing. We conducted an ACE survey with 468 male adult prisoners in a Welsh prison who were not currently considered to be at risk of self-harm and suicide and explored relationships between ACEs, lifetime mental illness diagnosis, self-harm (lifetime and lifetime in prison) or suicide attempt (lifetime and lifetime in prison), and current low mental wellbeing.
Most participants (84.2%) had suffered at least one ACE and 45.5% had suffered ≥4 ACEs. Prevalence of lifetime mental illness diagnosis, self-harm (lifetime and lifetime in prison) or suicide attempt (lifetime and lifetime in prison), and current low mental wellbeing increased with exposure to ACEs. For example, 2.7% of those with no ACEs reported lifetime self-harm or suicide attempt in prison compared with 31.0% (self-harm in prison) and 18.3% (suicide attempt in prison) of those with ≥4 ACEs. Compared with participants with no ACEs, those with ≥4 ACEs were four times more likely to report lifetime mental illness diagnosis and suicide attempt, and over 10 times more likely to report lifetime self-harm than those with no ACEs. Independent of lifetime mental illness diagnosis, self-harm or suicide attempt, participants with ≥4 ACEs were almost three times more likely to have current low mental wellbeing than those with no ACEs.
Conclusions
Male prisoners that have suffered multiple ACEs are substantially more likely to have lifetime mental illness diagnosis, self-harm or suicide attempt, and to have current low mental wellbeing whilst in prison. Findings suggest that trauma-informed approaches are needed in prisons to support prisoner mental health and wellbeing.
Prisoner mental health is a worldwide public health concern (Borschmann et al. 2018 ; Jack et al. 2018 ). Individuals who are incarcerated are often characterised by complex and multiple health needs and the experience of imprisonment, including isolation, insecurity, and a lack of privacy, can negatively impact an individual’s mental health and wellbeing (Konrad et al. 2007 ). Mental wellbeing (MWB) relates to how people feel and how well they can cope with day to day life, and has been described as feeling good and functioning well (Regan et al. 2016 ). Although correlated to mental illness, MWB is an independent concept - individuals may have low MWB in the absence of mental illness, and conversely can have mental illness but high MWB (Taggart et al. 2015 ). However, low MWB is associated with vulnerability to mental illness alongside poorer health outcomes and behaviours (Howell et al. 2007 ; Stranges et al. 2014 ). Studies evidence a higher prevalence of current low MWB, mental illness and self-harm amongst those incarcerated than the general population (Fazel et al. 2016 ; Kariminia et al. 2007 ; Tweed et al. 2018 , 2019 ), whilst suicide is the leading cause of death in custody globally (Butler et al. 2018 ). In England and Wales, rates of self-harm in the male adult prison population have been increasing, with over 43,000 incidents reported in the year ending September 2018; a rate of 540 incidents per 1000 prisoners (Ministry of Justice 2019 ). There were 89 self-inflicted deaths among male prisoners in 2018; a rate of 1.1 per 1000 prisoners (Ministry of Justice 2019 ). An investigation into deaths in prison found that while 70% of individuals with a self-inflicted death had been identified as having mental health needs, less than half had had these needs flagged on entry to prison (Prisons and Probation Ombudsman 2016 ).
While poor mental health is a known risk factor for self-harm and suicidal behaviour in male prisoners, a range of other risk factors have also been identified, such as low educational attainment, homelessness, and being on remand/unsentenced or serving a life sentence (Jenkins et al. 2005 ; Pope 2018 ). Further, a growing body of evidence is suggesting that a history of adverse childhood experiences (ACEs) is also a key risk factor (Clements-Nolle et al. 2009 ; Marzano et al. 2011 ). The term ACEs is used to describe a range of stressful and potentially traumatic events that children can be exposed to whilst growing up, such as child maltreatment, witnessing domestic violence, parental substance abuse or having a household member incarcerated. Such experiences can impact children’s neurobiological, social and emotional development and increase their risks of health and social harms throughout the life course (Berens et al. 2017 ). Further, risks of poor life course health outcomes increase along with the number of ACE types suffered, and particularly strong relationships are identified between ACEs and mental illness, self-harm and suicide attempt, as well as behaviours conducive to criminal justice involvement such as violence, problematic drug use, and youth and prolific offending (Baglivio and Epps 2016 ; Baglivio et al. 2014 ; Hughes et al. 2017 ). Accordingly, the prevalence of ACEs has been shown to be substantially higher in justice-involved populations than general populations (Skarupski et al. 2016 ) and poorer mental health and greater suicidality (Godet-Mardirossian et al. 2011 ) has been found among prisoners with ACEs. For example, studies with incarcerated males have found increased levels of depression, psychological distress, and personality disorders among those with specific ACE types, such as childhood physical and sexual abuse (Roberts et al. 2008 ; Sergentanis et al. 2014 ; Skarupski et al. 2016 ; Wolff and Caravaca Sánchez 2019 ; Wolff and Shi 2012 ; Zhang and Zheng 2018 ). However, to our knowledge no previous studies have explored associations between exposure to cumulative ACEs and prisoner MWB, while most studies exploring relationships between cumulative ACEs and prisoner mental illness have focused on women. Research in female prison populations has identified that a mental illness diagnosis and suicide attempt are associated with increasing numbers of ACEs (Friestad et al. 2014 ; Messina and Grella 2006 ).
Imprisonment provides a unique opportunity to identify and support individuals who may be at risk of mental illness, self-harm and suicide attempt. Developing a better understanding of the association between ACEs, current low MWB and lifetime mental illness diagnosis, self-harm or suicide attempt in the prison population can help to identify where preventative work can be directed. The detection of prisoners at high-risk of these negative outcomes and delivery of appropriate care may also provide an important step in reducing wider health disparities in this population (Borschmann et al. 2018 ).
We use primary data collected in a Welsh male prison population (Ford et al. 2019 ) to explore associations between ACEs and lifetime mental illness diagnosis, self-harm (lifetime and lifetime in prison) or suicide attempt (lifetime and lifetime in prison), and whether ACEs predict current low MWB in prisoners.
Data collection
A convenience sampling method was used to recruit a sample of incarcerated males in Wales. Her Majesties Prison (HMP) Parc Footnote 1 was selected as the research site due to it housing the largest prison population in Wales at the time of data collection (approximately 1700 in January 2018; Ministry of Justice 2018 ). Study inclusion criteria were: aged 18–69 years; cognitively able to participate; and not being managed under the care planning process for being at risk of suicide or self-harm (Assessment, Care in Custody & Teamwork [ACCT] procedures; Ministry of Justice 2013 ). This latter criteria was included as individuals managed under ACCT were considered too vulnerable to participate in the study. To provide an adequate sample size with high ACEs for analyses, we aimed to survey a third of the eligible prison population (estimated to be 1448 at the time of data collection).
The study was advertised through electronic information points on each prison unit in advance of fieldwork and through the distribution of leaflets advertising the study during data collection (February to June 2018). Trained researchers approached potential participants on the prison units during free time, outlining the study aims and methodology. Names and prison identification numbers were taken for study volunteers and a suitable time/date was arranged for them to complete the interview (Monday-Thursday, 8:00 am-6:30 pm). At the point of interview, the researcher verbally summarised and provided participants with a study information sheet outlining: the study purpose and voluntary, anonymous, and confidential nature; their right to withdraw; that participation or a decline to participate would not affect their care; and a contact within the prison for any issues or complaints. Participants were given the opportunity to ask questions and provided written informed consent before proceeding with the survey. Face-to-face interviews were undertaken by researchers who completed questionnaires using pen and paper, with participants given the opportunity to self-complete the more sensitive questions (e.g. ACE questions). Following survey completion, participants were provided with a thank you leaflet including contact details for a designated lead within the prison and information on available help and support accessible within the prison. No personal identifiable data were collected during the interview, with the exception of the written record of consent, which was stored separately to the study questionnaire. All study materials were available in English and Welsh and respondents could complete the survey in either language.
During the study period, contact was made with 696 individuals, of whom 188 (27.0%) declined participation and 508 volunteered to take part. Of the individuals who opted to participate in the study, 12 (2.4%) were ineligible and 26 (5.2%) left the prison before they were able to participate. Of the 658 eligible individuals remaining in prison that were approached for participation, 470 individuals completed the questionnaire, resulting in a study participation rate of 71.4%. However, any individuals who did not provide all ACE data required for analysis ( n = 2) were removed from the sample, resulting in a final sample of 468.
Questionnaire / measures
All questionnaire measures were self-reported. Standardised ACE survey questions from the US Centers for Disease Control and Prevention short ACE tool (Centers for Disease Control and Prevention n.d. ) and the World Health Organization’s Short Child Maltreatment Questionnaire (Meinck et al. 2016 ) were used to measure exposure to 11 categories of ACE (before 18 years of age: 1) physical abuse, 2) verbal abuse, 3) sexual abuse, 4) emotional neglect, 5) physical neglect, 6) parental separation, 7) witnessing domestic violence, and living with a household member who was 8) a problem alcohol user, 9) a drug user, 10) mentally ill, or 11) incarcerated; see Additional file 1 : Table S1). The ACE tool has been validated as a reliable tool for the retrospective assessment of ACEs (Meinck et al. 2016 ). In line with previous studies (Bellis et al. 2015 ; Felitti et al. 1998 ), the number of ACEs reported by participants was summed (possible range 0–11 ACEs) and categorised into an ACE count variable (0 ACEs, 1 ACE, 2–3 ACEs, and ≥ 4 ACEs).
To measure lifetime mental illness diagnosis, participants were asked if they had ever been diagnosed by a doctor or nurse with any mental health condition (e.g. depression, anxiety or other mental illness), using a question adapted from the national Welsh ACE survey (Hughes et al. 2018 ).
Using questions taken from the Measuring the Quality of Prison Life (MQPL) questionnaire routinely used in UK prisons (Liebling et al. 2011 ), participants were asked to report lifetime (1) self-harm or (2) suicide attempt, with response options: no, never attempted; yes, outside of prison only; yes, in prison only; and, yes, outside and in prison, Responses to self-harm and suicide attempt questions were dichotomised ‘no’ and ‘yes’ for four outcomes: ‘lifetime self-harm’, ‘lifetime suicide attempt’, ‘lifetime self-harm in prison’ and ‘lifetime suicide attempt in prison’.
Current MWB was measured using the validated Short Warwick-Edinburgh Mental Wellbeing Scale (SWEMWBS; Stewart-Brown et al. 2009 ), which asks individuals how often over the past 2 weeks they have been: feeling optimistic about the future; feeling useful; feeling relaxed; dealing with problems well; thinking clearly; feeling close to other people; able to make up their own mind about things . Responses are scored using a Likert scale: 1, none of the time; 2, rarely; 3, some of the time; 4, often; 5, all of the time). An overall MWB score was calculated by summing response scores for the seven questions and transforming total raw scores to metric score in line with guidelines (possible range 7 [lowest] to 35 [highest]; Stewart-Brown et al. 2009 ). Current low MWB was categorised as scores ≤19.59 based on cut offs from general population level data in Wales (Davies et al. 2019 ; low scores > 1 standard deviation [SD] below the mean). Responses to the seven individual components of SWEMWBS were also dichotomised to indicate low ratings (never or rarely in the last 2 weeks; yes or no).
Participant demographic information collected included age, ethnicity (self-identified using UK census categories) and education qualifications attained (none; secondary school or equivalent [level 2]; college or equivalent [level 3]; university or equivalent [≥level 4]; based on the National Qualifications Framework/Qualification and Credit Framework). Age was categorised into four groups (18–20; 21–29; 30–39; and ≥ 40 years) and ethnicity was re-categorised into White and other due to low numbers in individual non-White ethnic groups.
Statistical analysis
Data entry and statistical analyses were completed using SPSS v24. Analyses employed cross-tabulations and chi-square tests to initially examine bivariate associations between ACEs, demographic characteristics, and the study outcomes of interest: lifetime mental illness diagnosis, self-harm (lifetime and lifetime in prison) or suicide attempt (lifetime and lifetime in prison), current low MWB, and low ratings for the seven individual SWEMWBS components. Logistic regression was then employed to examine the independent contributions of ACEs on each outcome of interest, controlling for demographics (i.e. adjusted for age, ethnicity and qualifications). A further logistic regression model was used to explore the associations between ACEs and current low MWB controlling for demographics, lifetime mental illness diagnosis, self-harm or suicide attempt.
Sample characteristics
Over half (54.9%) of the men in the sample were aged 30 years and over, with less than one in ten (9.2%) aged 18–20 (Table 1 ). The majority (84.2%) reported White ethnicity and almost a third (31.0%) reported having no educational qualifications. Most participants (84.2%) reported having been exposed to at least one ACE, with just under half (45.5%) reporting exposure to ≥4 ACEs.
Nearly half (48.7%) of participants reported having lifetime mental illness diagnosis, and almost a third reported lifetime self-harm (33.1%) or suicide attempt (32.1%; Table 1 ). In total 40.4% of the sample reported lifetime self-harm or suicide attempt, and 21.4% lifetime self-harm or suicide attempt whilst in prison. Of individuals reporting self-harm, 60.0% reported lifetime self-harm in prison (19.9% of all participants) and 28.4% had only ever self-harmed in prison (9.4% of all participants). Of those reporting suicide attempt, 33.3% reported lifetime suicide attempt in prison (10.7% of all participants) and 18.0% had only ever attempted-suicide in prison (5.8% of all participants).
Three in ten (29.6%) participants were categorised as having current low MWB. The proportion responding low ratings (i.e. ‘never’ or ‘rarely’ in the last 2 weeks) to the seven individual components of SWEMWBS ranged from 7.1% for able to make up my own mind about things , to 33.6% for feeling close to others (Table 2 ).
Bivariate analysis
In chi-squared analysis, levels of lifetime mental illness diagnosis, self-harm or suicide attempt (lifetime and lifetime in prison), and current low MWB were significantly higher in White participants (Table 1 ). Lifetime self-harm (lifetime and lifetime in prison) and current low MWB were associated with low levels of educational attainment (Table 1 ). The prevalence of lifetime mental illness diagnosis increased with age ( p = 0.013), whilst lifetime self-harm in prison was highest amongst those aged 21–24 ( p = 0.036).
All outcomes explored were strongly associated with ACE count ( p < 0.001, Table 1 ). Lifetime mental illness diagnosis almost doubled from 35.1% in those with no ACEs to 64.3% in those with ≥4 ACEs. Similar increases were seen for all self-harm and suicide attempt outcomes, with levels of lifetime self-harm in prison increasing from 2.7% in those with no ACEs to 31.0% in those with ≥4 ACEs and levels of lifetime suicide attempt in prison increasing from 2.7% to 18.3% respectively. The proportion of respondents with current low MWB tripled from 13.5% in those with no ACEs to 40.8% in those with ≥4 ACEs (Table 1 ).
The proportions reporting low ratings for the individual SWEMWBS components: feeling relaxed, dealing with problems well, thinking clearly and feeling close to others also increased significantly with ACE count (Table 2 ).
Multivariate analysis
Logistic regression analyses explored the independent relationships between ACEs and lifetime mental illness diagnosis, self-harm (lifetime and lifetime in prison) or suicide attempt (lifetime and lifetime in prison), controlling for relationships with demographics. High ACEs remained strongly related to each of these outcomes (Table 3 ). Compared with those with no ACEs, those with ≥4 ACEs were around four times more likely to have lifetime mental illness diagnosis (adjusted odds ratio [AOR] 3.96, p < 0.001) and to have lifetime suicide attempt (AOR 4.36, p < 0.001), and eight times (AOR 7.98, p = 0.005) more likely to have lifetime suicide attempt in prison. There were no associations between lower levels of ACEs and the outcomes: lifetime mental illness diagnosis and suicide attempt. However, odds of lifetime self-harm (lifetime and lifetime in prison) were substantially elevated in those with both ≥4 ACEs and 2–3 ACEs. Compared with those with no ACEs, those with ≥4 ACEs were over ten times (AOR 10.7, p < 0.001) more likely to have lifetime self-harm and 15 times (AOR 15.1, p < 0.001) more likely to have lifetime self-harm in prison. Independent relationships were also found between White ethnicity and lifetime mental illness diagnosis, self-harm (lifetime and lifetime in prison) or suicide attempt (lifetime and lifetime in prison); between lifetime self-harm in prison and lower education qualifications; and between lifetime mental illness diagnosis and older age (Table 3 ).
Logistic regression analysis was also used to explore relationships between ACEs and current low MWB (Table 4 ). A first model controlling for demographics found that individuals with ≥4 ACEs were four times (AOR 4.35, p < 0.001) more likely to have current low MWB than those with no ACEs. There were no associations at lower ACE counts.
Given the strong relationships identified between ACEs and lifetime mental illness diagnosis, self-harm or suicide attempt (Table 3 ), a second model was run to explore the association between ACEs and current low MWB controlling for demographics, lifetime mental illness diagnosis, self-harm or suicide attempt. Independent of these lifetime outcomes, having ≥4 ACEs remained predictive of experiencing current low MWB, with participants almost three times more likely to have current low MWB than those with no ACEs (AOR 2.75, p = 0.010; Table 4 ). In this model, participants with lifetime mental illness diagnoses were twice as likely to have current low MWB (AOR 2.21, p = 0.002). However, lifetime self-harm or suicide attempt was not found to significantly increase the risk of current low MWB.
Logistic regression was also run to explore relationships between ACEs and low ratings for the seven individual components of SWEMWBS, controlling for demographics. ACEs were associated with low ratings for all individual SWEMWBS components except feeling optimistic or being able to make up my own mind about things (Table 5 ).
Improving the mental health and wellbeing of prisoners is a complex task and it is essential that the risk factors for poor mental health and wellbeing in prison are understood (Phillips et al. 2018 ). This study has aimed to identify associations between ACEs and lifetime mental illness diagnosis, self-harm or suicide attempt in incarcerated males, and to explore if ACEs predict current low MWB in prison. Levels of ACE exposure reported by participants were substantially higher than those measured in the Welsh general population, with 84.4% of male prisoners reporting at least one of the 11 ACEs measured and 45.5% reporting ≥4 ACEs; compared with 46.3% (at least one ACE) and 11.9% (≥4 ACEs) respectively in males in the general population (Hughes et al. 2018 ). Consistent with other international studies (Butler et al. 2018 ), reported levels of lifetime mental illness diagnoses, self-harm or suicide attempt among prisoners were also elevated compared to general population levels (Hughes et al. 2018 ). Despite our study excluding those that were currently being managed due to risk of self-harm or suicide attempt, one in five participants reported lifetime self-harm whilst in prison and one in ten reported lifetime suicide attempt.
Prisoners that reported multiple ACEs had substantially higher odds of having a history of poor mental health. For lifetime mental illness diagnosis and suicide attempt (lifetime and lifetime in prison), increased risks were seen in those with ≥4 ACEs, while for lifetime self-harm (lifetime and lifetime in prison), odds were higher and elevated even in those with ≥2 ACEs. Critically, individuals with ≥4 ACEs were 15 times more likely to have lifetime self-harm and eight times more likely to have lifetime suicide attempt in prison. An increasing body of evidence is identifying how chronic early life stress can lead to lasting structural changes in the developing brain that can embed vulnerability to poor mental health, affecting aspects including stress responses, coping skills, attachment, and emotional regulation and functioning (Pechtel and Pizzagalli 2011 ; Teicher et al. 2016 ). These effects may not only increase offenders’ vulnerability to developing poor mental health in prison, but also their ability to adapt to the prison environment (Skarupski et al. 2016 ). For example, the reduction of privacy or restrained movement; uncertainty and lack of personal control; social isolation; and aggression or threat of violence in prison may pose additional risk for vulnerable populations, and individuals that have suffered ACEs may suffer re-traumatisation (Crisanti and Frueh 2011 ; Krammer et al. 2018 ; Marzano et al. 2011 ; Welfare and Hollin 2015 ). Thus the experience of entering prison may compound the effect of ACEs on mental health and wellbeing.
Though widely explored at the population level, few studies have measured MWB in prisoners (Tweed et al. 2018 , 2019 ) and there is a limited evidence base on the factors associated with current low MWB in this group. We found multiple ACEs to be predictive of current low MWB in incarcerated males, even after controlling for lifetime mental illness diagnosis, self-harm or suicide attempt. For the seven individual components of SWEMWBS measured, having ≥4 ACEs was associated with never or rarely (in the last 2 weeks) feeling useful, relaxed, thinking clearly or dealing with problems well, while having one ACE was associated with never or rarely feeling close to others. In particular, this latter component of MWB may impact on prisoners’ ability to form supportive relationships and seek help in the prison setting. Elsewhere, increased ACE count has been shown to be associated with lower levels of perceived social support among offender populations (Krammer et al. 2018 ) while in the general population, ACEs have been associated with perceiving services as less supportive (Hughes et al. 2018 ).
Here, primary data collection has generated a novel dataset to examine a number of mental health and wellbeing outcomes in a male English and Welsh prisoner population. Previous work exploring the relationship between exposure to cumulative ACEs, mental illness and suicide attempt has predominantly been conducted within female prison populations (Friestad et al. 2014 ; Messina and Grella 2006 ). Although in this manuscript we do not aim to provide a gender comparison, this would be a useful focus for future research to explore.
Attention is increasingly being drawn to the importance of the provision of trauma-informed services and the need for staff to be understanding of the underlying causes behind current low MWB, self-harm and suicidal behaviour (Baglivio and Epps 2016 ; Krammer et al. 2018 ; Marzano et al. 2011 ). Such examples of trauma-informed interventions in the prison setting are starting to emerge (see Biddle et al. 2018 ). Recent years have also seen an increase in calls for the implementation of routine enquiry to proactively identify ACEs in a variety of health and other settings. Existing screening procedures in prisons are thought to fail to adequately assess and record individuals’ risk of self-harm and suicide (House of Commons Library 2017 ) and understanding prisoners’ childhood experiences might help identify those who are more vulnerable to low MWB, self-harm, and suicide attempt and direct support services to those at risk of harm. However, the evidence base for routine ACE enquiry is still in its infancy (Ford et al. 2019 ) and its place within the criminal justice system has yet to be fully explored, Further, consideration of the implementation of enquiry for ACEs within the criminal justice service requires further exploration of the support systems needed to appropriately respond to any disclosures without re-traumatising the individual (Leitch 2017 ). The potential to use existing personal data held on prisoners to understand risks of low MWB, self-harm or suicide attempt following exposure to ACEs for this purpose also needs exploration.
With projections for further growth of an already high prison rate in England and Wales (House of Commons Library 2019 ; Walmsley 2018 ), the burden on prison health care systems placed by self-harm and suicide attempt is likely to also increase (Borschmann et al. 2018 ). Incarceration has been thought of as a time to focus interventions (Friestad et al. 2014 ), and work to address the specific mental health and other needs of prisoners with ACEs is likely to not only benefit prison mental health but also support prisoners’ rehabilitation, help build their trust in support services and have broader societal and public health benefits. Thus ACEs have been associated with recidivism in offender populations (Craig et al. 2017 ), while levels of self-harm and suicide after release from prison are also markedly higher than rates found in the general population (Binswanger et al. 2007 ; Borschmann et al. 2016 ). The identification of interventions that can work to support mental health and wellbeing in prisoners affected by ACEs, and of factors that can protect against mental health difficulties in this vulnerable population, are important areas for future research. A focus should also remain on the primary prevention of ACEs. Preventing future generations from being exposed to ACEs and supporting children affected by them, including the families of prisoners, should help reduce risks of offending and criminal justice system involvement in future generations.
Limitations
There are a number of study limitations which should be recognised in the interpretation of findings. First, a convenience sample was used and therefore the sample cannot be considered to be representative of the prisoners in the prison studied, nor the wider prison population in England and Wales. However, recruitment aimed to maximise the inclusion of all eligible prisoners, and achieved a high participation rate (71.4%). Our definition of suicide attempt did not rely on suicidal intent and no qualitative data was explored on motivations for either of the self-harm or suicide outcomes explored here. However, self-harm and suicide attempt are commonly used as proxies for suicide (Marzano et al. 2009 ). Self-harm may not be indicative of suicide attempt and therefore self-harm and suicide attempt were examined as distinct behaviours. Equally, medical diagnosis of depression or other mental health conditions is not necessarily an accurate measure of need for services (Martin et al. 2015 ), and is likely to provide an under-estimate of lifetime mental illness. Further, we explored lifetime measures for mental illness diagnosis, self-harm and suicide attempt, and we did not collect information on the timing of individual outcomes, and consequently could not explore temporal relationships between ACE exposure, the development of mental illness and timings of self-harm and suicide attempt within or outside the prison setting. This is an important area for future research.
As no information was recorded on the individuals who declined participation in the study, we are unable to identify any bias through self-selection to participate. In line with the ACE methodology, ACE data are retrospective and therefore subject to recall-bias. All data were self-reported and due to the sensitive nature of the ACE, self-harm and suicide attempt questions the responses to these items could be subject to reporting accuracy as disclosure of these issues can be stigmatising. The under-reporting of self-harm and suicidal behaviours could contribute to more conservative findings. Further, prisoners who were on an ACCT, by definition those being at risk of self-harm or suicide at the time of interview, were excluded from participation. Nonetheless, the prevalence of both ACEs, self-harm, and suicide as identified here are similar to those identified in other research studies within the prisoner population (Reavis et al. 2013 ; Skarupski et al. 2016 ). Finally, while White ethnicity was associated with most outcomes explored here (see Results ), there were too few individuals from other ethnicities to explore whether relationships between ACEs and these outcomes varied by ethnicity, and this would be a useful area for further study.
International evidence has highlighted the detrimental impact that ACEs can have on mental health across the life course (Bellis et al. 2015 ; Felitti et al. 1998 ; Hughes et al. 2017 ). Our study evidences this effect in a UK prison population, showing that prisoners with multiple ACEs are substantially more likely to have a history of mental illness and self-harming behaviour, including self-harm and suicide attempt within prison settings. It also shows that prisoners with multiple ACEs are at risk of current low MWB whilst in prison. Thus findings suggest that prisoners with multiple ACEs may be particularly vulnerable to poor mental health whilst incarcerated, and that prisons may provide a critical opportunity for providing support to this vulnerable population. Thus, policy and interventions to support mental health and wellbeing within prisons should include ensuring that prison staff are trauma-informed and have an understanding of the underlying causes behind these behaviours (Baglivio and Epps 2016 ; Krammer et al. 2018 ; Marzano et al. 2011 ; Ramluggun 2013 ). Improving the mental health and wellbeing of prisoners is a complex task, but one which is essential to reducing reoffending, improving the health of prisoners and is also likely to benefit wider population public health.
Availability of data and materials
The datasets analysed during the current study are available from the corresponding author on reasonable request.
HMP Parc is a Category B Male Prison, for prisoners for whom escape must be made very difficult but the very highest conditions of security are not necessary (House of Commons Library 2015 ).
Abbreviations
Assessment, Care in Custody and Teamwork
- Adverse childhood experiences
Adjusted odds ratio
Confidence interval
Her Majesties Prison
- Mental wellbeing
Measuring the Quality of Prison Life
Reference category
Standard deviation
Short Warwick-Edinburgh Mental Wellbeing Scale
Baglivio, M. T., & Epps, N. (2016). The interrelatedness of adverse childhood experiences among high-risk juvenile offenders. Youth Violence and Juvenile Justice, 14 (3), 179–198. https://doi.org/10.1177/1541204014566286 .
Article Google Scholar
Baglivio, M. T., Jackowski, K., Greenwald, M. A., & Howell, J. (2014). Serious, violent, and chronic juvenile offenders: a statewide analysis of prevalence and prediction of subsequent recidivism using risk and protective factors. Criminology & Public Policy, 13 (1), 83–116. https://doi.org/10.1111/1745-9133.12064 .
Bellis, M. A., Ashton, K., Hughes, K., Ford, K., Bishop, J., & Paranjothy, S. (2015). Adverse childhood experiences and their impact on health-harming behaviours in the Welsh adult population . Cardiff: Public Health Wales http://www.wales.nhs.uk/sitesplus/888/page/88504 . Accessed 22 Oct 2019.
Google Scholar
Berens, A. E., Jensen, S. K. G., & Nelson, C. A. (2017). Biological embedding of childhood adversity: from physiological mechanisms to clinical implications. BMC Medicine, 15 , 135. https://doi.org/10.1186/s12916-017-0895-4 .
Biddle, P., Dyer, W., Hand, R., & Strinati, C. (2018). Reflections on a project to prevent suicide and self-harm among prisoners identified as high risk in two prisons in northern England. Health & Justice, 6 (1), 22. https://doi.org/10.1186/s40352-018-0080-7 .
Binswanger, I. A., Stern, M. F., Deyo, R. A., Heagerty, P. J., Cheadle, A., Elmore, J. G., & Koepsell, T. D. (2007). Release from prison - a high risk of death for former inmates. New England Journal of Medicine, 356 (2), 157–165. https://doi.org/10.1056/nejmsa064115 .
Borschmann, R., Thomas, E., Moran, P., Carroll, M., Heffernan, E., Spittal, M. J., et al. (2016). Self-harm following release from prison: a prospective data linkage study. Australian & New Zealand Journal of Psychiatry, 51 (3), 250–259. https://doi.org/10.1177/0004867416640090 .
Borschmann, R., Young, J. T., Moran, P. A., Spittal, M. J., & Kinner, S. A. (2018). Self-harm in the criminal justice system: a public health opportunity. The Lancet Public Health, 3 (1), e10–e11. https://doi.org/10.1016/S2468-2667(17)30243-8 .
Butler, A., Young, J. T., Kinner, S. A., & Borschmann, R. (2018). Self-harm and suicidal behaviour among incarcerated adults in the Australian Capital Territory. BMC Health & Justice, 6 (1), 13. https://doi.org/10.1186/s40352-018-0071-8 .
Centers for Disease Control and Prevention. (n.d.). Behavioral Risk Factor Surveillance System ACE Data. Retrieved from https://www.cdc.gov/violenceprevention/childabuseandneglect/acestudy/ace-brfss.html . Accessed 20 Feb 2020.
Clements-Nolle, K., Wolden, M., & Bargmann-Losche, J. (2009). Childhood trauma and risk for past and future suicide attempts among women in prison. Women's Health Issues, 19 (3), 185–192. https://doi.org/10.1016/j.whi.2009.02.002 .
Craig, J. M., Baglivio, M. T., Wolff, K. T., Piquero, A. R., & Epps, N. (2017). Do social bonds buffer the impact of adverse childhood experiences on reoffending? Youth Violence and Juvenile Justice, 15 (1), 3–20. https://doi.org/10.1177/1541204016630033 .
Crisanti, A. S., & Frueh, B. C. (2011). Risk of trauma exposure among persons with mental illness in jails and prisons: what do we really know? Current Opinion in Psychiatry, 24 (5), 431–435. https://doi.org/10.1097/YCO.0b013e328349bbb8 .
Davies, A. R., Sharp, C. A., Homolova, L., & Bellis, M. A. (2019). Population health in a digital age: the use of digital technology to support and monitor health in Wales . Cardiff: Public Health Wales & Bangor University https://phw.nhs.wales/files/research/population-health-in-a-digital-age/ . Accessed 22 Oct 2019.
Fazel, S., Hayes, A. J., Bartellas, K., Clerici, M., & Trestman, R. (2016). Mental health of prisoners: prevalence, adverse outcomes, and interventions. The Lancet Psychiatry, 3 (9), 871–881. https://doi.org/10.1016/S2215-0366(16)30142-0 .
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., et al. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. American Journal of Preventive Medicine, 14 (4), 245–258. https://doi.org/10.1016/S0749-3797(98)00017-8 .
Ford, K., Barton, E. R., Newbury, A., Hughes, K., Bezeczky, Z., Roderick, J., & Bellis, M. A. (2019). Understanding the prevalence of adverse childhood experiences (ACEs) in a male offender population in Wales: the prisoner ACE survey . Wrexham: Public Health Wales NHS Trust, Bangor University https://www.bangor.ac.uk/news/documents/PHW-Prisoner-ACE-Survey-Report-E.pdf . Accessed 10 Oct 2019.
Friestad, C., Ase-Bente, R., & Kjelsberg, E. (2014). Adverse childhood experiences among women prisoners: relationships to suicide attempts and drug abuse. The International Journal of Social Psychiatry, 61 (1), 40–46. https://doi.org/10.1177/0020764012461235 .
Godet-Mardirossian, H., Jehel, L., & Falissard, B. (2011). Suicidality in male prisoners: influence of childhood adversity mediated by dimensions of personality. Journal of Forensic Sciences, 56 , 942–949. https://doi.org/10.1111/j.1556-4029.2011.01754.x .
House of Commons Library. (2015). Categorisation of prisoners in the UK: Briefing paper. Number 07437. https://researchbriefings.parliament.uk/ResearchBriefing/Summary/CBP-7437 . Accessed 1 Oct 2019.
House of Commons Library. (2017). Mental health in prisons: Eighth Report of Session 2017–19. https://publications.parliament.uk/pa/cm201719/cmselect/cmpubacc/400/400.pdf . Accessed 28 Oct 2019.
House of Commons Library. (2019). UK Prison Population Statistics. Briefing paper. Number CBP-04334, www.gov.uk/government/collections/prison-population-statistics . Accessed 1 Oct 2019.
Howell, R. T., Kern, M. L., & Lyubomirksy, S. (2007). Health benefits: meta-analytically determining the impact of well-being on objective health outcomes. Health Psychology Review, 1 , 83–136. https://doi.org/10.1080/17437190701492486 .
Hughes, K., Bellis, M. A., Hardcastle, K. A., Sethi, D., Butchart, A., Mikton, C., et al. (2017). The impact of multiple adverse childhood experiences on health: a systematic review and meta-analysis. The Lancet Public Health, 2 (8), e356–e366. https://doi.org/10.1016/S2468-2667(17)30118-4 .
Hughes, K., Ford, K., Davies, A. R., Homolova, L., & Bellis, M. A. (2018). Sources of resilience and their moderating relationships with harms from adverse childhood experiences . Cardiff: Public Health Wales https://www.wales.nhs.uk/sitesplus/documents/888/ACE%20&%20Resilience%20Report%20(Eng_final2).pdf . Accessed 1 Oct 2019.
Jack, H. E., Fricchione, G., Chibanda, D., Thornicroft, G., Machando, D., & Kidia, K. (2018). Mental health of incarcerated people: a global call to action. The Lancet Psychiatry, 5 (5), 391–392. https://doi.org/10.1016/S2215-0366(18)30127-5 .
Jenkins, R., Bhugra, D., Meltzer, H., Singleton, N., Bebbington, P., Brugha, T., et al. (2005). Psychiatric and social aspects of suicidal behaviour in prisons. Psychological Medicine, 35 (2), 257–269. https://doi.org/10.1017/S0033291704002958 .
Kariminia, A., Butler, T. G., Corben, S. P., Levy, M. H., Grant, L., Kaldor, J. M., & Law, M. G. (2007). Extreme cause-specific mortality in a cohort of adult prisoners - 1988 to 2002: a data-linkage study. International Journal of Epidemiology, 36 (2), 310–316. https://doi.org/10.1093/ije/dyl225 .
Konrad, N., Daigle, M. S., Daniel, A. E., Dear, G. E., Frottier, P., Hayes, L. M., et al. (2007). Preventing suicide in prisons, part I. Crisis, 28 , 113–121. https://doi.org/10.1027/0227-5910.28.3.113 .
Krammer, S., Eisenbarth, H., Hügli, D., Liebrenz, M., & Kuwert, P. (2018). The relationship between childhood traumatic events, social support, and mental health problems in prisoners. The Journal of Forensic Psychiatry & Psychology, 29 (1), 72–85. https://doi.org/10.1080/14789949.2017.1337802 .
Leitch, L. (2017). Action steps using ACEs and trauma-informed care: a resilience model. BMC Health & Justice, 5 (1), 5. https://doi.org/10.1186/s40352-017-0050-5 .
Liebling, A., Hulley, S., & Crewe, B. (2011). Conceptualising and measuring the quality of prison life. In D. Gadd, S. Karstedt, & S. Messner (Eds.), The sage handbook of criminological research methods (pp. 358–372). London: Sage.
Martin, M. S., Eljdupovic, G., McKenzie, K., & Colman, I. (2015). Risk of violence by inmates with childhood trauma and mental health needs. Law and Human Behavior, 39 (6), 614–623. https://doi.org/10.1037/lhb0000149 .
Marzano, L., Hawton, K., Rivline, A., & Fazel, S. (2011). Psychosocial influences on prisoner suicide: a case-control study of near-lethal self-harm in women prisoners. Social Science & Medicine, 72 , 874–883. https://doi.org/10.1016/j.socscimed.2010.12.028 .
Marzano, L., Rivlin, A., Fazel, S., & Hawton, K. (2009). Interviewing survivors of near-lethal self-harm: a novel approach for investigating suicide amongst prisoners. Journal of Forensic and Legal Medicine, 16 , 152–155. https://doi.org/10.1016/j.jflm.2008.08.011 .
Meinck, F., Steinert, J. I., Sethi, D., Gilbert, R., Bellis, M. A., Mikton, C., et al. (2016). Measuring and monitoring national prevalence of child maltreatment: a practical handbook . Copenhagen: World Health Organization.
Messina, N., & Grella, C. (2006). Childhood trauma and women’s health outcomes in a California prison population. American Journal of Public Health, 96 (10), 1842–1848. https://doi.org/10.2105/AJPH.2005.082016 .
Ministry of Justice. (2013). Management of prisoners at risk of harm to self, to others and from others (Safer Custody). https://www.justice.gov.uk/offenders/psis/prison-service-instructions-2011 . Accessed 4 Nov 2019.
Ministry of Justice. (2018). Population bulletin: monthly January 2018. https://www.gov.uk/government/statistics/prison-population-figures-2018 . Accessed 24 Feb 2020.
Ministry of Justice. (2019). Safety in custody statistics, England and Wales: deaths in prison custody to December 2018, assaults and self-harm to September 2018. https://www.gov.uk/government/statistics/safety-in-custody-quarterly-update-to-september-2018 . Accessed 4 Nov 2019.
Pechtel, P., & Pizzagalli, D. A. (2011). Effects of early life stress on cognitive and affective function: an integrated review of human literature. Psychopharmacology, 214 (1), 55–70. https://doi.org/10.1007/s00213-010-2009-2 .
Phillips, J., Padfield, N., & Gelsthorpe, L. (2018). Suicide and community justice. BMC Health & Justice, 6 (1), 14. https://doi.org/10.1186/s40352-018-0072-7 .
Pope, L. (2018). Self-harm by adult men in prison: a rapid evidence assessment (REA). Her majesty’s prison and probation service . London: Ministry of Justice Analytical Series.
Prisons and Probation Ombudsman. (2016). Learning from PPO investigations: prisoner mental health . London: Prisons and Probation Ombudsman.
Ramluggun, P. (2013). A critical exploration of the management of self-harm in a male custodial setting: qualitative findings of a comparative analysis of prison staff views on self-harm. Journal of Forensic Nursing, 9 (1), 23–34. https://doi.org/10.1097/JFN.0b013e31827a5984 .
Reavis, J. A., Looman, J., Franco, K. A., & Rojas, B. (2013). Adverse childhood experiences and adult criminality: how long must we live before we possess our own lives? The Permanente Journal, 17 (2), 44–48. https://doi.org/10.7812/tpp/12-072 .
Regan, M., Elliott, I., & Goldie, I. (2016). Better mental health for all: a public health approach to mental health improvement . London: Faculty of Public Health, Mental Health Foundation.
Roberts, A., Yang, M., Zhang, T., & Coid, J. (2008). Personality disorder, temperament, and childhood adversity: findings from a cohort of prisoners in England and Wales. The Journal of Forensic Psychiatry & Psychology, 19 (4), 460–483. https://doi.org/10.1080/14789940801936597 .
Sergentanis, T. N., Sakelliadis, E. I., Vlachodimitropoulos, D., Goutas, N., Sergentanis, I. N., Spiliopoulou, C. A., & Papadodima, S. A. (2014). Does history of childhood maltreatment make a difference in prison? A hierarchical approach on early family events and personality traits. Psychiatry Research, 220 (3), 1064–1070. https://doi.org/10.1016/j.psychres.2014.10.019 .
Skarupski, K. A., Parisi, J. M., Thorpe, R., Tanner, E., & Gross, D. (2016). The association of adverse childhood experiences with mid-life depressive symptoms and quality of life among incarcerated males: exploring multiple mediation. Aging & Mental Health, 20 (6), 655–666. https://doi.org/10.1080/13607863.2015.1033681 .
Stewart-Brown, S., Tennant, A., Tennant, R., Platt, S., Parkinson, J., & Weich, S. (2009). Internal construct validity of the Warwick-Edinburgh Mental Well-being Scale (WEMWBS): a Rasch analysis using data from the Scottish Health Education Population Survey. Health and Quality of Life Outcomes, 7 (1), 15. https://doi.org/10.1186/1477-7525-7-15 .
Stranges, S., Samaraweera, P. C., Taggart, F., Kandala, N., & Stewart-Brown, S. (2014). Major health-related behaviours and mental well-being in the general population: the health survey for England. BMJ Open, 4 (9), e005878. https://doi.org/10.1136/bmjopen-2014-005878 .
Taggart, F., Stewart-Brown, S., & Parkinson, J. (2015). Warwick-Edinburgh Mental Well-being Scale (WEMWBS). User Guide – Version 2 . Warwick and Edinburgh: University of Warwick and NHS Health Scotland.
Teicher, M. H., Samson, J. A., Anderson, C. M., & Ohashi, K. (2016). The effects of childhood maltreatment on brain structure, function and connectivity. Nature Reviews Neuroscience, 17 (10), 652–666. https://doi.org/10.1038/nrn.2016.111 .
Tweed, E. J., Gounari, X., & Graham, L. (2018). Mental wellbeing in prisoners in Scotland: an analysis of repeat cross-sectional surveys. Lancet, 392 (2), S11. https://doi.org/10.1016/S0140-6736(18)32151-2 .
Tweed, E. J., Gounari, X., & Graham, L. (2019). Mental wellbeing among people in prison in Scotland: an analysis of repeat cross-sectional surveys. Journal of Public Health , fdz106. https://doi.org/10.1093/pubmed/fdz106 .
Walmsley, R. (2018). World prison population list (12th ed.). London: International centre for Prison Studies.
Welfare, H. R., & Hollin, C. R. (2015). Childhood and offense-related trauma in young people imprisoned in England and Wales for murder and other acts of serious violence: a descriptive study. Journal of Aggression, Maltreatment & Trauma, 24 (8), 955–969. https://doi.org/10.1080/10926771.2015.1070230 .
Wolff, N., & Caravaca Sánchez, F. (2019). Associations among psychological distress, adverse childhood experiences, social support, and resilience in incarcerate men. Criminal Justice and Behavior, 46 (11), 1630–1649. https://doi.org/10.1177/0093854819876008 .
Wolff, N., & Shi, J. (2012). Childhood and adult trauma experiences of incarcerated persons and their relationship to adult behavioral health problems and treatment. International Journal of Environmental Research and Public Health, 9 (5), 1908–1926. https://doi.org/10.3390/ijerph9051908 .
Zhang, J., & Zheng, Y. (2018). Childhood maltreatment profiles among incarcerated Chinese males and their associations with personality disorder symptoms and criminal behaviors. Psychiatry Research, 268 , 272–278. https://doi.org/10.1016/j.psychres.2018.06.063 .
Download references
Acknowledgements
We are very grateful to the all the individuals who kindly participated in the survey and to the staff of HMP Parc and the Parc Intervention and Research Panel for assisting the research team with their data collection. We are grateful to Zoe Bezeczky for assisting with data collection. We would also like to thank Janine Roderick, Jessica Evans, Eleanor Worthington and other colleagues at Public Health Wales who supported the development of the study.
This work was funded through the Early Action Together (EAT) programme by the Home Office Police Innovation Fund, the South Wales Police and Crime Commissioner and Public Health Wales (Reference 2016–039). KF and MAB designed the study. The funders had no role in study design, analysis, interpretation of data, or writing of the manuscript.
Author information
Authors and affiliations.
Public Health Collaborating Unit, School of Health Sciences, College of Human Sciences, Bangor University, Wrexham, LL13 7YP, UK
Kat Ford, Mark A. Bellis & Karen Hughes
World Health Organization Collaborating Centre on Investment for Health and Wellbeing, Policy and International Health Directorate, Public Health Wales, Wrexham, LL13 7YP, UK
Mark A. Bellis, Karen Hughes, Emma R. Barton & Annemarie Newbury
You can also search for this author in PubMed Google Scholar
Contributions
KF and MAB designed study. KF directed the study, undertook data collection, management, analyses and wrote the first draft of this manuscript. EB and AN collected data and contributed to manuscript editing. MAB and KH advised on statistical analyses and contributed to manuscript editing. All authors contributed to the editing of the manuscript and approved the final text.
Corresponding author
Correspondence to Kat Ford .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was obtained for the study from Bangor University’s Health Sciences and Medical Sciences Ethics Committee (2017–16210), the National Health Service (NHS) Research Ethics Committee (Reference 17/WA/0249), and Her Majesty’s Prison and Probation Service. Research and development approval was also granted by the Public Health Wales Research and Development Office. Consistent with our ethical approval, informed written consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1:.
Table S1. Questions used to identify ACEs with qualifying responses.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ford, K., Bellis, M.A., Hughes, K. et al. Adverse childhood experiences: a retrospective study to understand their associations with lifetime mental health diagnosis, self-harm or suicide attempt, and current low mental wellbeing in a male Welsh prison population. Health Justice 8 , 13 (2020). https://doi.org/10.1186/s40352-020-00115-5
Download citation
Received : 06 November 2019
Accepted : 31 May 2020
Published : 12 June 2020
DOI : https://doi.org/10.1186/s40352-020-00115-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Incarceration
- Mental illness
- Mental health
Health & Justice
ISSN: 2194-7899
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Verywell Mind Insights
- 2023 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
What Are Adverse Childhood Experiences (ACEs)?
Wendy Wisner is a health and parenting writer, lactation consultant (IBCLC), and mom to two awesome sons.
:max_bytes(150000):strip_icc():format(webp)/28685632_10156312296594515_9028950978590849197_n-815354ed2f8e44be900fda9060a465f5.jpg)
Ann-Louise T. Lockhart, PsyD, ABPP, is a board-certified pediatric psychologist, parent coach, author, speaker, and owner of A New Day Pediatric Psychology, PLLC.
:max_bytes(150000):strip_icc():format(webp)/Ann-Louise-1000-601bd9ba1f744bd0a2a4a6f722bd1553.jpg)
Mixetto / Getty Images
Childhood is a vulnerable time, and what happens to us then has long deep impacts. Adverse childhood experiences (ACEs) describe traumatic experiences that can have lasting effects into adulthood. The more ACEs someone experiences, the more challenging they may be to overcome.
Let’s take a look at what adverse childhood experiences are, what impacts they may have, how to prevent them—and most importantly, how you can cope if you are someone who endured traumatic experiences in childhood.
Adverse Childhood Experiences (ACEs) are traumatic experiences that children experience before the age of 18 that can have lasting impacts on their mental health, physical health, and general well-being.
Many kinds of traumas in childhood can be ACEs. Some examples of ACEs include:
- Experiencing physical or emotional abuse
- Abandonment or neglect
- Losing a family member to suicide
- Growing up in a household with substance abuse or alcoholism
- Having a mentally ill parent
- Having an incarcerated parent
- Being a child of divorce or parental separation
Between 1995 to 1997, the Centers for Disease Control and Prevention (CDC), in conjunction with Kaiser Permanente, began the first study of ACEs with the goal of coming up with a framework for this concept.
In the study, roughly 17,000 people were interviewed about various traumatic experiences they experienced in childhood, including abuse, violence, neglect, and abandonment.
An estimated 66% of responders revealed that they’d experienced at least one ACE; 20% had experienced three ACEs. The researchers noted connections between experiencing ACEs and detriments to one’s physical health years later, including heart disease and cancer.
Risk Factors For Adverse Childhood Experiences
ACEs don’t happen randomly. A child’s economic status, family history, and the kind of community they grow up in all come into play.
Here are some of the factors that may make a child more likely to experience an ACE:
- Coming from a low income family
- Coming from a family with a low level of education
- Growing up with high levels of family stress
- Growing up with high levels of economic stress
- Growing in a family that is not close knit and doesn’t speak openly about feelings
- Having parents who used spanking or corporal punishment
- Having parents who themselves had been abused or neglected
- Living in a community with high rates of violence
- Living in an economically disadvantaged community
- Living in a community with high levels of substance abuse
- Living in a community with few resources for youth
How Common Are ACEs?
Unfortunately, ACEs are not rare. According to the CDC, about 61% of adults experienced an ACE, and 1 in 6 adults have experienced four or more different ACEs.
It’s important to note that there are racial disparities when it comes to ACEs, with children of color experiencing more ACEs than White children. As per the National Conference of State Legislatures, about 61% of Black children have experienced an ACE and about 51% of Hispanic children have.
On the other hand, 40% of white children had experienced an ACE, and 23% of Asian children had.
What Impacts Do Adverse Childhood Experiences Have?
All children live through difficult experiences at times, but with the right tools, they can learn from their experiences and become stronger. ACEs are traumas that are more difficult to overcome and that can leave lasting scars on a child, especially if the child is not supported through.
ACEs can cause what is called “toxic stress,” which is where the stress that floods the body is so intense that it can cause changes to one’s metabolism, immune system, cardiovascular system, as well as brain and nervous system. There is a cumulative effect when it comes to toxic stress, and the more ACEs a child experiences, the greater impact it can have on their mental and physical health.
Children who experience ACEs and toxic stress may:
- Have difficulty forming close relationships with others
- Have trouble keeping a job
- Have difficulty with finances
- Experience depression
- Be more likely to be involved in violence
- Experience early, unwanted pregnancies
- Be more likely to be incarcerated
- Experience higher levels of unemployment
- Be more likely to also expose their children to ACEs
- Have a higher risk of alcohol or substance abuse
- Have a higher risk of suicide attempts
- Have a higher risk of health issues such as heart disease cancer, lung disease, and liver disease
How to Prevent Adverse Childhood Experiences
The good news here is that not every child is fated to experience multiple ACEs. Parents, community members, physicians, policy makers, and anyone who works with children have an obligation to prevent ACEs.
According to the CDC, preventing ACEs in children includes several steps and is truly a group effort. Here are some of the top ways we can prevent ACEs in children:
- Policy makers can work toward increasing financial security for families and preventing food and housing insecurity
- Workplaces can make their institutions more family-friendly and establish family leave policies
- Communities and policy makers can protect against violence by promoting anti-violence campaigns and education
- Professionals who work with families can teach positive parenting skills and teach socio-emotional learning
- Policy makers can promote a strong start for children by expanding childcare, preschool, and early childhood education options
- Communities can prioritize youth services, mentors for youth, and substance abuse recovery programs
Coping With Adverse Childhood Experiences
Again, having experienced an ACE is common, and if you are someone who experienced one, you are not alone. You are also not alone in feeling the impacts of that trauma even years later.
If you are experiencing anxiety, depression, or PTSD related to ACEs, a trauma-focused therapist or social worker can help you work through this, and get to the other side. If you are also experiencing physical effects that you think are linked to this trauma, speaking to a healthcare provider is another important step.
Lifestyle changes can also help you cope with and work through your trauma. Consider adding in mediation, breathing exercises, and physical activity and exercise. Journaling is another wonderful tool that can help you unpack your feelings.
If you are recovering from a trauma like abuse, abandonment , growing up with mentally ill parents, or parents who abused alcohol or drugs, you may want to join a support group specific to that experience. Speaking with other grown-ups who experienced similar ACEs as you did can be invaluable to your recovery.
Press Play for Advice On Healing Childhood Wounds
Hosted by therapist Amy Morin, LCSW, this episode of The Verywell Mind Podcast , featuring award-winning actress Chrissy Metz, shares how to heal childhood trauma, safeguard your mental health, and how to get comfortable when faced with difficult emotions. Click below to listen now.
Follow Now : Apple Podcasts / Spotify / Google Podcasts
A Word From Verywell
If you or someone you love has experienced an adverse childhood experience, it can be difficult to talk about, think about, or even read about. Childhood traumas can live in our psyches and our bodies for years to come, and it’s common to feel triggered easily at their mere mention.
Please remember that even someone who experienced several ACEs can heal and recover from the experience. Help is out there, and it’s possible to live a full life even if you have endured trauma in childhood.
Harvard University. ACEs and Toxic Stress: Frequently Asked Questions .
Centers for Disease Control and Prevention. Preventing Adverse Childhood Experiences .
Centers for Disease Control and Prevention. About the CDC-Kaiser ACE Study .
Felitti V, Anda R, Nordenberg D. Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults . American Journal of Preventative Medicine. 1998;14(4):P245-258. doi:10.1016/S0749-3797(98)00017-8
Centers for Disease Control and Prevention. Risk and Protective Factors .
National Conference of State Legislatures. Adverse Childhood Experiences .
Bellis M, Lowey H, Leckenby N, Hughes K, Harrison D. Adverse childhood experiences: retrospective study to determine their impact on adult health behaviours and health outcomes in a UK population . Journal of Public Health . 2014;36(1):81–91. doi:10.1093/pubmed/fdt038
Merrick M, Ford D, Ports K, Guinn A. Prevalence of Adverse Childhood Experiences From the 2011-2014 Behavioral Risk Factor Surveillance System in 23 States . JAMA Pediatrics. 2018;172(11):1038–1044. doi:10.1001/jamapediatrics.2018.2537
By Wendy Wisner Wendy Wisner is a health and parenting writer, lactation consultant (IBCLC), and mom to two awesome sons.
- Skip to content
- Skip to navigation
- Adverse Childhood Experiences (ACEs) and Attachment
- Child and Adolescent Mental Health Service (CAMHS)
- Young People

What is Attachment?
Attachment refers to the pattern of the relationships we have had with our parents or carers early in our lives. It is the emotional bond that forms between a parent and child from birth and has a huge impact on our development. The way a parent or carer responds to their child will impact on the child’s attachment style. This attachment style becomes a template for how we build future relationships with others in our lives, and also a template of how we feel about ourselves and other people. If we have experienced a relationship with a parent or carer which has been positive, we will develop a positive template for other relationships as well as positive feelings about ourselves and others. But sometimes how children are cared for is not so positive, for various reasons, and this can make it harder for people to make and maintain positive relationships in the future, manage their feelings and behaviour, or feel good about themselves or others. When our early attachments have been negative and these lead us to go on to have difficulties with relationships and our mental wellbeing, this can sometimes be described as attachment difficulties.
What are Adverse Childhood Experiences?
Adverse Childhood Experiences (ACEs) are “highly stressful, and potentially traumatic, events or situations that occur during childhood and/or adolescence. They can be a single event, or prolonged threats to, and breaches of, the young person’s safety, security, trust or bodily integrity.” (Young Minds, 2018).
Examples of ACEs:
- Physical abuse
- Sexual Abuse
- Emotional Abuse
- Living with someone who abused drugs
- Living with someone who abused alcohol
- Exposure to domestic violence
- Living with someone who has gone to prison
- Living with someone with serious mental illness
- Losing a parent through divorce, death or abandonment
How Common are ACEs?
In a 2014 UK study on ACEs, 47% of people experienced at least one ACE with 9% of the population having 4+ ACES (Bellis et al, 2014).
Impact of ACEs
Just like attachment, experiencing ACEs can have an impact on our future physical and mental health, and often ACEs can be barriers to healthy attachment relationships forming for children. Some of the effects of ACEs on our physical and mental health are:
- An increase in the risk of certain health problems in adulthood, such as cancer and heart disease, as well as increasing the risk of mental health difficulties, violence and becoming a victim of violence.
- An increase in the risk of mental health problems, such as anxiety, depression, and post-traumatic stress. 1 in 3 diagnosed mental health conditions in adulthood directly relate to ACEs.
- The longer an individual experiences an ACE and the more ACEs someone experiences, the bigger the impact it will have on their development and their health.
Some of the other things exposure to ACEs can impact, are:
- The ability to recognise and manage different emotions.
- The capacity to make and keep healthy friendships and other relationships.
- The ability to manage behaviour in school settings.
Difficulties coping with emotions safely without causing harm to self or others.
CAMHS support
Not everyone who has experienced ACEs, or has experienced some difficulties in their attachments may need CAMHS support. But, CAMHS can offer advice and support in a number of ways to help children and young people manage some of the impacts of ACEs, or after having difficulties within early attachment relationships.
Because ACEs affect everyone differently, CAMHS professionals will always complete an assessment to try and find out what has happened to you and how it is affecting you so that the right support can be arranged.
Sometimes CAMHS will work with parents or carers to think about how they can support their child to cope with what has happened and provide healthier care to help their child develop. CAMHS may also provide family therapy or other ways of working together with parents and children together. Finally, it can also sometimes be useful for children and young people to have their own support, and CAMHS may offer a range of different types of therapy or support, such as Cognitive Behavioural Therapy (CBT) which helps with anxiety, depression and trauma amongst other things, or Eye Movement Desensitisation and Reprocessing Therapy (EMDR) which also helps with trauma. However, the young person may need other support first to help them learn ways to cope with or manage strong feelings or other difficulties, or to help them spend time building up trust with the CAMHS professional. We can also help link young people up with other local community services, if this is what they want.
What can I / my carers do to help me?
Parents and carers have a responsibility to keep children and young people safe from harm and sometimes need support themselves to protect families from ACEs. Seeking to learn about and adopt healthy caring styles can make a big difference.

Essay on Childhood Experience
Students are often asked to write an essay on Childhood Experience in their schools and colleges. And if you’re also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic.
Let’s take a look…
100 Words Essay on Childhood Experience
Introduction.
Childhood is a special time filled with memories that shape our future. It’s a period of learning, growth, and exploration.
My Childhood
I remember my childhood as a time of freedom. Playing games with friends, exploring nature, and learning new things were part of everyday life.
Impact on Life
These experiences helped me develop skills and values. They taught me about friendship, curiosity, and resilience.
Childhood experiences are precious. They shape our personalities and influence our future. It’s important to cherish these memories and learn from them.
250 Words Essay on Childhood Experience
The essence of childhood.
Childhood experiences shape the contours of our adult life, working as the foundational building blocks of our personality. The impressions we gather during these formative years are often indelible, influencing our behaviors, attitudes, and life choices.
Impact of Positive Experiences
Positive childhood experiences, such as supportive familial relationships or success in school, can foster a sense of security and self-worth. They can instill in us an inherent belief in our capabilities, a crucial trait that propels us to strive for our goals. These experiences often lead to the development of resilience, equipping us to navigate life’s challenges with grace and fortitude.
Consequences of Negative Experiences
Conversely, negative experiences in childhood, such as neglect, abuse, or exposure to violence, can leave deep psychological scars. They can lead to the development of maladaptive coping mechanisms, mental health issues, and even perpetuation of harmful behaviors. However, it is important to note that these experiences do not seal one’s fate. With appropriate support and intervention, individuals can overcome these adversities.
Role of Reflection
Reflecting on our childhood experiences can provide valuable insights into our current behaviors and attitudes. It can help us understand our triggers, strengths, and weaknesses, and guide us in making conscious efforts to evolve and grow.
In conclusion, our childhood experiences, both positive and negative, significantly influence our life trajectory. They shape our worldview, our coping mechanisms, and our interpersonal relationships. Understanding this can help us appreciate the importance of providing a nurturing environment for children and empathize with individuals who have had challenging childhoods.
500 Words Essay on Childhood Experience
Childhood is a pivotal stage in the course of human life, characterized by learning, exploration, and growth. It is a period that shapes our personality, values, and beliefs, often leaving an indelible mark on our lives. This essay delves into the significance of childhood experiences, their impact on adulthood, and the role of socio-cultural factors in shaping these experiences.
The Impact of Childhood Experiences
Childhood experiences, both positive and negative, play a crucial role in molding our future selves. Positive experiences such as supportive family relationships, academic achievements, and social interactions foster self-esteem, resilience, and emotional intelligence. They act as a foundation for a healthy, balanced adulthood.
Conversely, adverse childhood experiences (ACEs) like abuse, neglect, or witnessing violence can lead to lasting psychological, social, and health issues. They can disrupt a child’s cognitive development, leading to difficulties in learning and social interaction. ACEs are also linked with higher risks of mental health disorders, substance abuse, and chronic diseases in adulthood.
Childhood Experiences and Personality Development
Childhood experiences significantly contribute to personality development. For instance, children who grow up in nurturing environments tend to develop secure attachment styles, fostering trust, empathy, and positive interpersonal relationships in their later life. On the other hand, those exposed to inconsistent or harsh parenting may develop insecure attachment styles, leading to trust issues, emotional instability, and difficulties in forming healthy relationships.
Role of Socio-Cultural Factors
Socio-cultural factors like family structure, socio-economic status, and cultural norms significantly influence childhood experiences. Children from affluent backgrounds may have access to better educational resources, healthcare, and opportunities for cognitive stimulation, which can positively influence their development. In contrast, children from low-income families may face challenges like food insecurity, inadequate healthcare, and limited educational opportunities, which can hinder their development.
Cultural norms also shape childhood experiences. For instance, in collectivist cultures, children are often taught to prioritize group harmony over individual needs, which may influence their social interactions, conflict resolution strategies, and self-concept.
In conclusion, childhood experiences are instrumental in shaping our future selves. They influence our personality development, emotional health, and social functioning. Socio-cultural factors also play a significant role in shaping these experiences, highlighting the importance of a supportive, nurturing environment for children. It is crucial to understand and address the impact of adverse childhood experiences to promote healthy development and well-being. The insights gained from studying childhood experiences can inform interventions and policies aimed at fostering positive development and mitigating the effects of adverse experiences.
That’s it! I hope the essay helped you.
If you’re looking for more, here are essays on other interesting topics:
- Essay on Favorite Childhood Memory
- Essay on Role of Parents in Children’s Life
- Essay on A Rainy Day
Apart from these, you can look at all the essays by clicking here .
Happy studying!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.

IMAGES
VIDEO
COMMENTS
Abstract. Adverse childhood experiences (ACEs) are events during childhood that are stressful and may impact upon mental and physical health having effects in childhood and future adulthood. Examples of ACEs include abuse (physical, emotional, sexual); neglect; living in a household with domestic violence, substance or alcohol misuse, or ...
Research into adverse childhood experiences (ACEs) consistently shows that a set of 10 adverse experiences in childhood are associated with an increased risk of poor health and other problems in later life. This consistent and compelling evidence has brought greater focus from a wide range of policymakers and public services on the harm caused ...
What is childhood adversity? A large number of adverse experiences (ie, toxic stressors) in childhood can trigger a toxic stress response.4 5 6 These range from the commonplace (eg, parental divorce) to the horrific (eg, the 6 year old "soldier" ordered to shoot and kill his mother7). Adversity can affect development in myriad ways, at different points in time, although early exposures ...
A child who experiences childhood maltreatment and being neglected from parents have a higher chance of developing social anxiety (Kuo, Goldin, Wernerm, Heimbergm, & Gross, 2011).A study conducted by Simon and colleagues 2009 found that children who experience higher amounts of childhood maltreatment are more likely to have a harder time ...
It has been over 20 years since the publication of seminal research by Felitti et al , highlighting the powerful relationship between adverse childhood experiences (ACEs) and a wide range of health and wellbeing outcomes.1 Since the landmark ACE study was published, a compelling body of research has accumulated confirming the strong and proportionate relationship between experiences of ...
Research into adverse childhood experiences (ACEs) has generated a powerful and accessible narrative which has helpfully increased awareness of the lifetime impact of early adversity on children's outcomes. Research into ACEs consistently shows that a set of 10 adverse experiences in childhood
A focus on the limbic system. In recent decades, the cognitive neuroscience of mental health disorders has shed light on how the brain is shaped by adverse childhood events. In particular, we know much more about how components of the limbic system are altered by early adversity and stress. One of these component structures is the amygdala, the ...
Trevor Spratt, Mary Kennedy, Adverse Childhood Experiences: Developments in Trauma and Resilience Aware Services, The British Journal of Social Work, Volume 51, Issue 3, April 2021, Pages 999-1017, ... with developments in policy across the UK nations reflective of this. The translation of such research and policy development has witnessed ...
Today, in this Research to Practice video, we are going to talk about the implications for practice of the ever-increasing body of research concerning adverse childhood experiences or ACEs. I'm joined by two professors of child and adolescent psychiatry: Professor Helen Minnis from the University of Glasgow and Professor Andrea Danese from ...
In the last 25 years, converging evidence has supported the view that adverse childhood experiences (ACEs) have long term negative impacts on physical and mental health. More recently, ACEs have been negatively associated with a range of educational measures. As educational attainment is a determining factor in later socioeconomic position, the ...
a population level, higher numbers of adverse childhood experiences are associated with a higher risk of adverse outcomes in adulthood. But these experiences do not determine those outcomes, and the risks measured at a population level cannot be applied to individuals as a predictive formula. Positive
Individuals' childhood experiences can strongly influence their future health and well-being. Adverse childhood experiences (ACEs) such as abuse and dysfunctional home environments show strong cumulative relationships with physical and mental illness yet less is known about their effects on mental well-being in the general population. A nationally representative household survey of English ...
However, adverse childhood experiences may have a long term physical effects in adulthood from trauma that occurred years ago (Shonkoff et al, 2011). Scientists have shown that adverses in childhood can cause damage in ways that prematurely age cells and affect life longevity (Franke, 2014).
Defining ACEs and trauma. According to Corcoran and McNulty (2018), adverse childhood experiences are "traumatic events (e.g., sexual abuse, physical abuse, emotional abuse) or chronic stressors (e.g., neglect, parental separation) that are uncontrollable to the child". The original ACE questionnaire used the following categories and refer ...
This paper has been produced by the Scottish Adverse Childhood Experiences (ACEs) Hub to help shape the public health approach to adverse childhood experiences. This paper, written in August 2019, outlines a number of principles that could underpin cross-sectoral work in Scotland to prevent and respond to childhood adversity.
The study of Adverse Childhood Experiences (ACEs) is helpful in demonstrating how adversity is often associated with negative outcomes. The ACE questionnaire measures traumatic events in childhood, like abuse, neglect, and family dysfunction, that present a risk for future medical, academic, and social problems.
This paper sets out a summary of the evidence on the links between childhood adversity and victimisation and criminality in adulthood. It makes a strong case for preventing crime by targeting those most at risk of experiencing adverse childhoods, and supporting people in the Justice System whose lives have been affected by adverse childhood ...
Background Prisoners are at increased risk of poor mental health and self-harming behaviours, with suicide being the leading cause of death in custody. Adverse childhood experiences (ACEs) such as child maltreatment are strong predictors of poor mental health and wellbeing yet despite high levels of ACEs in offender populations, relatively few studies have explored the relationships between ...
Adverse Childhood Experiences (ACEs) are traumatic experiences that children experience before the age of 18 that can have lasting impacts on their mental health, physical health, and general well-being. Many kinds of traumas in childhood can be ACEs. Some examples of ACEs include: Experiencing physical or emotional abuse. Abandonment or neglect.
Serious youth violence and its relationship with adverse childhood experiences . Dr Paul Gray, Professor Hannah Smithson and Dr Deborah Jump . NOVEMBER 2021 . 2 . ... (www.oneeducation.co.uk), and a professional sports coach. Given the sensitive nature of the research topic, the decision was made to use storytelling techniques in the workshops ...
Adverse Childhood Experiences (ACEs) are "highly stressful, and potentially traumatic, events or situations that occur during childhood and/or adolescence. They can be a single event, or prolonged threats to, and breaches of, the young person's safety, security, trust or bodily integrity." (Young Minds, 2018). ... In a 2014 UK study on ...
Essay, Pages 5 (1008 words) Views. 1052. Childhood experiences, are what molds an individual's personality and habits. A study was done on the correlation between Adverse Childhood Experiences and the impact they might have on future violence, victimization, suicide, depression, health, drug abuse, and early death to name a few.
Students are often asked to write an essay on Childhood Experience in their schools and colleges. And if you're also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic. ... Conversely, adverse childhood experiences (ACEs) like abuse, neglect, or witnessing violence can lead to lasting psychological ...