

Systematic Reviews
- The Research Question
- Inclusion and Exclusion Criteria
- Original Studies
- Translating
- Deduplication
- Project Management Tools
- Useful Resources
- What is not a systematic review?
Inclusion/Exclusion Criteria
Inclusion criteria.
Identify the criteria that will be used to determine which research studies will be included. The inclusion and exclusion criteria must be decided before you start the review. Inclusion criteria is everything a study must have to be included. Exclusion criteria are the factors that would make a study ineligible to be included. Criteria that should be considered include:
Type of studies: It is important to select articles with an appropriate study design for the research question. Dates for the studies and a timeline of the problem/issue being examined may need to be identified.
Type of participants: Identify the target population characteristics. It is important to define the target population's age, sex/gender, diagnosis, as well as any other relevant factors.
Types of intervention: Describe the intervention being investigated. Consider whether to include interventions carried out globally or just in the United States. Eligibility criteria for interventions should include things such as the dose, delivery method, and duration of the investigated intervention. The interventions that are to be excluded may also need to be described here.
Types of outcome measures: Outcome measures usually refer to measurable outcomes or ‘clinical changes in health’. For example, these could include body structures and functions like pain and fatigue, activities as in functional abilities, and participation or quality of life questionnaires.
Read Chapter 3 of the Cochrane Handbook
Exclusion criteria.
A balance of specific inclusion and exclusion criteria is paramount. For some systematic reviews, there may already be a large pre-existing body of literature. The search strategy may retrieve thousands of results that must be screened. Having explicit exclusion criteria from the beginning allows those conducting the screening process, an efficient workflow. For the final product there should be a section in the review dedicated to 'Characteristics of excluded studies.' It is important to summarize why studies were excluded, especially if to a reader the study would appear to be eligible for the systematic review.
For example, a team is conducting a systematic review regarding intervention options for the treatment of opioid addiction. The research team may want to exclude studies that also involve alcohol addiction to isolate the conditions for treatment interventions solely for opioid addiction.
- << Previous: Planning and Protocols
- Next: Searching >>
- Last Updated: Oct 12, 2023 12:30 PM
- URL: https://libguides.sph.uth.tmc.edu/SystematicReviews

Evidence-Based Practice (EBP)
- The EBP Process
- Forming a Clinical Question
- Inclusion & Exclusion Criteria
- Acquiring Evidence
- Appraising the Quality of the Evidence
- Writing a Literature Review
- Finding Psychological Tests & Assessment Instruments
Selection Criteria

Inclusion and exclusion criteria are determined after formulating the research question but usually before the search is conducted (although preliminary scoping searches may need to be undertaken to determine appropriate criteria). It may be helpful to determine the inclusion criteria and exclusion criteria for each PICO component.
Be aware that you may introduce bias into the final review if these are not used thoughtfully.
Inclusion and exclusion are two sides of the same coin, so—depending on your perspective—a single database filter can be said to either include or exclude. For instance, if articles must be published within the last 3 years, that is inclusion. If articles cannot be more than 3 years old, that is exclusion.
The most straightforward way to include or exclude results is to use database limiters (filters), usually found on the left side of the search results page.
Inclusion Criteria
Inclusion criteria are the elements of an article that must be present in order for it to be eligible for inclusion in a literature review. Some examples are:
- Included studies must have compared certain treatments
- Included studies must be a certain type (e.g., only Randomized Controlled Trials)
- Included studies must be located in a certain geographic area
- Included studies must have been published in the last 5 years
Exclusion Criteria
Exclusion criteria are the elements of an article that disqualify the study from inclusion in a literature review. Some examples are:
- Study used an observational design
- Study used a qualitative methodology
- Study was published more than 5 years ago
- Study was published in a language other than English
- << Previous: Forming a Clinical Question
- Next: Acquiring Evidence >>
- Last Updated: Nov 15, 2023 11:47 AM
- URL: https://libguides.umsl.edu/ebp

Systematic Reviews for Health Sciences and Medicine
- Systematic Reviews
- The research question
- Common search errors
- Search translation
- Managing results
- Inclusion and exclusion criteria
- Critical appraisal
- Updating a Review
- Resources by Review Stage
Inclusion and Exclusion Criteria
Inclusion and exclusion criteria set the boundaries for the systematic review. They are determined after setting the research question usually before the search is conducted, however scoping searches may need to be undertaken to determine appropriate criteria. Many different factors can be used as inclusion or exclusion criteria. Information about the inclusion and exclusion criteria is usually recorded as a paragraph or table within the methods section of the systematic review. It may also be necessary to give the definitions, and source of the definition, used for particular concepts in the research question (e.g. adolescence, depression).

Other inclusion/exclusion criteria can include the sample size, method of sampling or availability of a relevant comparison group in the study. Where a single study is reported across multiple papers the findings from the papers may be merged or only the latest data may be included.
- << Previous: Managing results
- Next: Critical appraisal >>
- Last Updated: Apr 17, 2024 12:42 PM
- URL: https://unimelb.libguides.com/sysrev
- Library guides
- Book study rooms
- Library Workshops
- Library Account

Library Services
- Library Services Home
Literature searching and finding evidence
- Literature searching or literature review?
- Use the PICO or PEO frameworks
Establish your Inclusion and Exclusion criteria
- Find related search terms
- Subject Heading/MeSH Searching
- Select databases to search
- Structure your search
- Search techniques
- Search key databases
- Manage results in EBSCOhost and Ovid
- Analyse your search results
- Document your search results
- Training and support
These criteria help you decide which studies will/will not be included in your work. This will help make sure your work is as unbiased, transparent and ethical as possible.
How to establish your Inclusion and Exclusion criteria
To establish your criteria you need to define each aspect of your question to clarify what you are focusing on, and consider if there are any variations you also wish to explore. This is where using frameworks like PICO help:
Example: Alternatives to drugs for controlling headaches in children
Using the PICO structure you clarify what aspects you are most interested in. Here are some examples to consider:
The aspects of the topic you decide to focus on are the Inclusion criteria.
The aspects you don't wish to include are the Exclusion criteria.
- << Previous: Use the PICO or PEO frameworks
- Next: Find related search terms >>
- Last Updated: Apr 24, 2024 11:04 AM
- URL: https://libguides.city.ac.uk/SHS-Litsearchguide
Systematic Reviews: Inclusion and Exclusion Criteria
- What Type of Review is Right for You?
- What is in a Systematic Review
- Finding and Appraising Systematic Reviews
- Formulating Your Research Question
- Inclusion and Exclusion Criteria
- Creating a Protocol
- Results and PRISMA Flow Diagram
- Searching the Published Literature
- Searching the Gray Literature
- Methodology and Documentation
- Managing the Process
- Scoping Reviews
Defining Inclusion/Exclusion Criteria
An important part of the SR process is defining what will and will not be included in your review.
Inclusion and exclusion criteria are developed after a research question is finalized but before a search is carried out. They determine the limits for the evidence synthesis and are typically reported in the methods section of the publication. For unfamiliar or unclear concepts, a definition may be necessary to adequately describe the criterion for readers.
Some examples of common inclusion/exclusion criteria might be:
- Date of publication : only articles published in the last ten years
- Exposure to intervention/ or specific health condition : only people who have participated in the DASH diet
- Language of Publication* : only looking at English articles
- Settings : Hospitals, nursing homes, schools
- Geography : specific locations such as states, countries, or specific populations
*note of caution: research is published all over the world and in multiple languages. Limiting to just English can be considered a bias to your research.
- Common Inclusion/Exclusion Criteria from the University of Melbourne
What happens if no study meets my inclusion/exclusion criteria?
Empty reviews are when no studies meet the inclusion criteria for a SR. Empty reviews are more likely to subject to publication bias, however, they are important in identifying gaps in the literature.
- Unanswered questions implications of an empty review Slyer, Jason T. Unanswered questions, JBI Database of Systematic Reviews and Implementation Reports: June 2016 - Volume 14 - Issue 6 - p 1-2 doi: 10.11124/JBISRIR-2016-002934
- Rapid Prompting Method and Autism Spectrum Disorder: Systematic Review Exposes Lack of Evidence Schlosser, R.W., Hemsley, B., Shane, H. et al. Rapid Prompting Method and Autism Spectrum Disorder: Systematic Review Exposes Lack of Evidence. Rev J Autism Dev Disord 6, 403–412 (2019).
- << Previous: Formulating Your Research Question
- Next: Creating a Protocol >>
- Last Updated: Apr 23, 2024 8:18 AM
- URL: https://guides.lib.lsu.edu/Systematic_Reviews
Provide Website Feedback Accessibility Statement
- Reserve a study room
- Library Account
- Undergraduate Students
- Graduate Students
- Faculty & Staff
How to Conduct a Literature Review (Health Sciences and Beyond)
- What is a Literature Review?
- Developing a Research Question
Selection Criteria
Inclusion criteria, exclusion criteria.
- Database Search
- Documenting Your Search
- Organize Key Findings
- Reference Management
You may want to think about criteria that will be used to select articles for your literature review based on your research question. These are commonly known as inclusion criteria and exclusion criteria . Be aware that you may introduce bias into the final review if these are not used thoughtfully.
Inclusion criteria are the elements of an article that must be present in order for it to be eligible for inclusion in a literature review. Some examples are:
- Included studies must have compared certain treatments
- Included studies must be experimental
- Included studies must have been published in the last 5 years
Exclusion criteria are the elements of an article that disqualify the study from inclusion in a literature review. Some examples are:
- Study used an observational design
- Study used a qualitative methodology
- Study was published more than 5 years ago
- Study was published in a language other than English
- << Previous: Developing a Research Question
- Next: Databases >>
- Last Updated: Mar 15, 2024 12:22 PM
- URL: https://guides.library.vcu.edu/health-sciences-lit-review
USF Libraries Hours by campus
Libraries locations.
- Libraries Hours
- Outages & Maintenance Alerts
RESEARCH TOOLS
- Subject & Course Guides
- USF Libraries Catalog
- Quicksearch All-in-one-search
- Citing Sources
- Find my Librarian
GUIDES / HOW-TO
- Tutorials & Workshops
- Finding Books and Articles
- Finding Reserves
- Checking Out & Renewing
- Reserve a Study Room
- Additional Help Topics
- star Other Services
- For Faculty
- For Graduate Students
- For Undergrads
- Requesting Books & Articles (ILL)
- Textbook Affordability (TAP)
- Library Instruction
- Laptop Checkout
- Schedule Research Help
- Geographic Information Systems
- Data Management Planning
- Copyright & Intellectual Property
- Scholarly Publishing
- Other Services
COLLECTIONS
- What are Collections?
- Special Collections
- Digital Collections
- Digital Heritage & Humanities
- Digital Commons @ USF
- Oral Histories
- Online Exhibitions
- Printing in the Library
- IT Help Desk
- Digital Media Commons (DMC)
- Writing Studio
- Office of Development
- Office for Undergraduate Research
- Directions to the Library
- Library Info & Floor Maps
- Connect From Off Campus
- Renew Materials Online
- Check UBorrow Status
- Printing Help
- Report a Problem
- About the USF Libraries
Systematic Reviews for Social Sciences
- Systematic Reviews
- Mapping Review
- Mixed Methods Review
- Rapid Review
- Scoping Review
- Develop the Question
Define Inclusion/Exclusion Criteria
- Develop A Review Protocol
- Create Search Strategies
- Select Studies
- Extract Data
- Assess the Quality of Studies
- Synthesize Data and Write the Report
- Review Tools
- Librarian Involvement
- Grey Literature
One of the features that distinguishes a systematic review from a narrative review is the pre-specification of criteria for including and excluding studies in the review (eligibility criteria). Explicit criteria, based on the review’s scope and question(s), are used to include and exclude studies.
A large number of references (study titles and abstracts) will have been found at the searching stage of the review. A proportion of these will look as though they are relevant to the review's research questions. So, having explicit criteria against which to assess studies makes the process more efficient in terms of time.
More importantly, it also helps to avoid hidden bias by having clear consistent rules about which studies are being used to answer the review's specific research questions.
Each study needs to be compared against same criteria. To be included in the review, a study needs to meet all inclusion criteria and not meet any exclusion criteria. Inclusion/eligibility criteria include participants, interventions and comparisons and often study design. Outcomes are usually not part of the criteria, though some reviews do legitimately restrict eligibility to specific outcomes.
For example, a systematic review include criteria may be determined using ECLIPSE.
- Expectation - identify best practices for information literacy instruction
- Client Group - Higher education students
- Location - United States
- Impact -Best practices for information literacy instruction
- Professionals - Librarians
- SErvice - Information literacy instruction
Exclusion criteria may include non-peer-reviewed articles, articles not in English, articles before a specified date, and in this case, articles about theory rather than actual practice.
- << Previous: Develop the Question
- Next: Develop A Review Protocol >>
- Last Updated: Aug 31, 2023 4:34 PM
- URL: https://guides.lib.usf.edu/systematicreviews

Systematic Reviews
- Introduction to Systematic Reviews
- Systematic review
- Systematic literature review
- Scoping review
- Rapid evidence assessment / review
- Evidence and gap mapping exercise
- Meta-analysis
- Systematic Reviews in Science and Engineering
- Timescales and processes
- Question frameworks (e.g PICO)
Inclusion and exclusion criteria
- Using grey literature
- Search Strategy This link opens in a new window
- Subject heading searching (e.g MeSH)
- Database video & help guides This link opens in a new window
- Documenting your search and results
- Data management
- How the library can help
- Systematic reviews A to Z

Inclusion and exclusion criteria are a list of pre-defined characteristics to which literature must adhere to be included in a study. They are vital for the decision-making progress on what to review when undertaking a systematic review and will also help with systematic literature reviews.
You should be able to establish your inclusion/exclusion criteria during the process of defining your question. These criteria clearly demonstrate the scope of the study and provide justification for the exclusion of any information that does not meet these characteristics.
Example criteria
- Intervention, treatment, process or experience
- Reported outcomes
- Research methodology
- Participants
- Age of study
- Sample size
- Place of study
- Type of publication
E.g. stage 4 lung disease patients
E.g. whether the study's reported outcomes are relevant to your study and have been presented objectively
E.g. randomised control trial
E.g. age, sex ethnicity etc.
E.g. last 5 years
E.g. over 100 participants
E.g. UK based
E.g. primary research, peer-reviewed
E.g. community-based care
E.g. English
Precision vs Sensitivity
You should aim to be as extensive as possible when conducting searches for systematic reviews. However, it may be necessary to strike a balance between the sensitivity and precision of your search.
- Sensitivity – the number of relevant results identified divided by the total number of relevant results in existence
- Precision - the number of relevant results identified divided by the total number of results identified.
Increasing the comprehensiveness of a search will reduce its precision and will retrieve more non-relevant results. However,
... at a conservatively-estimated reading rate of two abstracts per minute, the results of a database search can be ‘scanread’ at the rate of 120 per hour (or approximately 1000 over an 8-hour period), so the high yield and low precision associated with systematic review searching is not as daunting as it might at first appear in comparison with the total time to be invested in the review. ( Cochrane Handbook for Systematic Reviews of Interventions, 2008, Section 6.4.4 )
- << Previous: Question frameworks (e.g PICO)
- Next: Where to search >>
- Last Updated: Jan 23, 2024 10:52 AM
- URL: https://plymouth.libguides.com/systematicreviews

- JABSOM Library
Literature Review Basics and Searching Skills
- Selecting Criteria
- Getting Started
- Developing Research Questions
- Selecting Databases
- Searching Databases
- Documenting Searches
- Organizing Findings
- Managing Citations & References
- Submitting Your Manuscript
- Finding Help
Selection Criteria
You may want to think about criteria that will be used to select articles for your literature review based on your research question. These are commonly known as inclusion criteria and exclusion criteria . Be aware that you may introduce bias into the final review if these are not used thoughtfully.
Inclusion Criteria
Inclusion criteria are the elements of an article that must be present in order for it to be eligible for inclusion in a literature review. Some examples are:
- Included studies must have compared certain treatments
- Included studies must be experimental
- Included studies must have been published in the last 5 years
Exclusion Criteria
Exclusion criteria are the elements of an article that disqualify the study from inclusion in a literature review. Some examples are:
- Study used an observational design
- Study used a qualitative methodology
- Study was published more than 5 years ago
- Study was published in a language other than English
- << Previous: Developing Research Questions
- Next: Selecting Databases >>
- Last Updated: Mar 20, 2024 11:38 AM
- URL: https://hslib.jabsom.hawaii.edu/lit_review
Health Sciences Library, John A. Burns School of Medicine, University of Hawai‘i at Mānoa, 651 Ilalo Street, MEB 101, Honolulu, HI 96813 - Phone: 808-692-0810, Fax: 808-692-1244
Copyright © 2004-2024. All rights reserved. Library Staff Page - Other UH Libraries


- Collections
- Research Help
- Teaching & Learning
- Library Home
Systematic Reviews
- Getting Started
- Additional Frameworks
- More Types of Reviews
- Timeline & Resources
- Inclusion/Exclusion Criteria
- Resources & More
Inclusion Criteria
Inclusion criteria are elements of an article that must be present in order for it to be eligible for inclusion in a review or analysis. Here are some examples:
- include studies with human subjects only
- include studies published within the last five years
- included studies must be randomized controlled studies or cohort studies
- included studies must have compared certain treatments
Exclusion Criteria
Exclusion criteria are the elements of an article that disqualify the study from inclusion in a review or analysis. Here are some examples:
- the study uses an observational design
- the study was published more than five years ago
- the study uses animal subjects
Why Have Inclusion/Exclusion Criteria?
After developing your PICO question, it is critically important for you and your team to establish a set of "rules" for selecting, then screening the articles located during your database and internet searches. These rules are called the inclusion/exclusion criteria. Be aware that you may introduce bias into the final review if these are not used thoughtfully and adhered to regardless of outcome. The purpose of using inclusions/exclusion criteria "is to minimize ambiguity and reduce the possibility of poor reproducibility". This criteria should not be too narrow or too loose.
McDonagh M, Peterson K, Raina P, et al. Avoiding Bias in Selecting Studies. 2013 Feb 20. In: Methods Guide for Effectiveness and Comparative Effectiveness Reviews [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK126701/
A Visual Representation

Ghezzi-Kopel, Kate. (2019, September 16). Developing your research question. (research guide). Retrieved from https://guides.library.cornell.edu/systematic_reviews/research_question
- << Previous: Timeline & Resources
- Next: Resources & More >>
- Last Updated: Apr 25, 2024 11:37 AM
- URL: https://libguides.wvu.edu/SystematicReviews

Systematic Reviews
- The Research Question
- Basic Service
- Full Service
- Inclusion and Exclusion Criteria
- Translating
- Deduplication
- Project Management Tools
- Useful Resources
- Other Review Types
Inclusion Criteria
Read chapter 3 of the cochrane handbook.
Identify the criteria that will be used to determine which research studies will be included. The inclusion and exclusion criteria must be decided before you start the review. Inclusion criteria is everything a study must have to be included. Exclusion criteria are the factors that would make a study ineligible to be included. Criteria that should be considered include:
Type of studies: It is important to select articles with an appropriate study design for the research question. Dates for the studies and a timeline of the problem/issue being examined may need to be identified.
Type of participants: Identify the target population characteristics. It is important to define the target population's age, sex/gender, diagnosis, as well as any other relevant factors.
Types of intervention: Describe the intervention being investigated. Consider whether to include interventions carried out globally or just in the United States. Eligibility criteria for interventions should include things such as the dose, delivery method, and duration of the investigated intervention. The interventions that are to be excluded may also need to be described here.
Types of outcome measures: Outcome measures usually refer to measurable outcomes or ‘clinical changes in health’. For example, these could include body structures and functions like pain and fatigue, activities as in functional abilities, and participation or quality of life questionnaires.
Exclusion Criteria
A balance of specific inclusion and exclusion criteria is paramount. For some systematic reviews, there may already be a large pre-existing body of literature. The search strategy may retrieve thousands of results that must be screened. Having explicit exclusion criteria from the beginning allows those conducting the screening process, an efficient workflow. For the final product there should be a section in the review dedicated to 'Characteristics of excluded studies.' It is important to summarize why studies were excluded, especially if to a reader the study would appear to be eligible for the systematic review.
For example, a team is conducting a systematic review regarding intervention options for the treatment of opioid addiction. The research team may want to exclude studies that also involve alcohol addiction to isolate the conditions for treatment interventions solely for opioid addiction.
Exercise for Developing Inclusion/Exclusion
Before developing your inclusion/exclusion criteria, please read Chapter Three of the Cochrane Handbook that reviews considerations for developing this criteria.
You must have a selection of relevant articles (a max of 5). Review the articles and make a bullet point list for each study of why that study would be either included or excluded from the review. This exercise can help jump start your predefined inclusion and exclusion criteria. This should be done before you start the review.
Types of Study Design
There are different study types used for the evidence base in systematic reviews. Below are some definitions of the different study types that may be used.
- Randomized controlled trials (RCT) A group of patients is randomized into an experimental group and a control group to test the efficacy of a treatment/intervention.
- Cohort study Involves the identification of two groups (cohorts) of patients, one which did receive the exposure of interest, and one which did not, and following these cohorts forward for the outcome of interest.
- Case-control study Involves identifying patients who have the outcome of interest (cases) and control patients without the same outcome, and looking to see if they had the exposure of interest. Just like cohort studies, case-control studies are observational.
- Cross-sectional study Typically involves the surveying of a randomly selected group to find out their opinions or facts. These studies can answer questions such as how common a particular disease is, but cause and treatment of the disease cannot be gleaned.
- Qualitative study Collects information on patients with diseases and those close to them. Requires specialized tools for analyzation and interpretation. These studies typically want to access a person's experience .
- Meta-analysis A statistical analysis, which can either be a study in itself or a component of another study type. It uses quantitative methods to summarize the results of scientific studies.
For further reading
Check out the Institute for Quality and Efficiency in Health Care (IQWiG) article What types of studies are there? offered through the National Center for Biotechnology Information, U.S. National Library of Medicine.
- << Previous: Planning and Protocols
- Next: Searching >>
- Last Updated: Mar 27, 2024 2:50 PM
- URL: https://libguides.library.tmc.edu/Systematic_Reviews
- University of Texas Libraries
Literature Reviews
Determine inclusion and exclusion criteria.
- What is a literature review?
- Steps in the Literature Review Process
- Define your research question
- Choose databases and search
- Review Results
- Synthesize Results
- Analyze Results
- Librarian Support
Once you have a clearly defined research question, make sure you are getting precisely the right search results from searching the databases by making decisions about these items:
- Would the most recent five years be appropriate?
- Is your research from a more historical perspective?
- Where has this type of research taken place?
- Will you confine your results to the United States?
- To English speaking countries?
- Will you translate works if needed?
- Is there a particular methodology, or population that you are focused on?
- Are there adjacent fields in which this type of research has been conducted that you would like to include?
- Is there a controversy or debate in your research field that you want to highlight
- Are you creating a historical overview? Is this background reading for your research?
- Is there new technology that can shed light on an old problem or an old technology that can be used in a new way?
- Last Updated: Oct 26, 2022 2:49 PM
- URL: https://guides.lib.utexas.edu/literaturereviews


Literature Reviews: Systematic, Scoping, Integrative
- Introduction to Literature Reviews
- Creating a Search Strategy
Using Limits and Inclusion/Exclusion Criteria
Filters and Limits
Inclusion and Exclusion Criteria
Limits and Inclusion Criteria
- Review Protocols
- Elements of a Systematic Review
- Review Tools and Applications
Ask A Librarian
Once you have some search results, you will need to decide which articles you will actually use in your literature review. This can be done using filters/limits in the databases, applying inclusion/exclusion criteria, and appraising the articles.
Filters and limits (the name varies by database) are tools the database provides to help you narrow your search results. Different databases offer different filters, but these are some of the more common ones you'll find.
- Publication year
- Language of the article
- Age of study subjects
- Study design
Your search terms and the filters/limits you apply are generally not enough to narrow your results to the most relevant and highest quality studies for your project. The final step to selecting these studies is to apply your inclusion and exclusion criteria. Basically, these are the reasons why you keep (include) or reject (exclude) articles as you look through the results, reading titles and abstracts (and sometimes the whole article)
Examples of types of Inclusion/Exclusion Criteria
- PICO(T) elements - if one of the main elements of your topic does not match those of the study, you may need to exclude it
- Age - if you can't use a filter/limit to exclude studies that do not focus on the age group you require, you may need to exclude those studies yourself.
- Setting - i.e. home, acute care, assisted living facility
- Study Design - sometimes a filter/limit doesn't exist for the study design you're interested in; in that case you'll need to look through articles to find that detail yourself.
- Number of subjects - do you have a minimum study group size?
- Study drop-out rate
- << Previous: Creating a Search Strategy
- Next: Review Protocols >>
- Last Updated: Apr 11, 2024 9:51 AM
- URL: https://libguides.massgeneral.org/reviews


Writing your thesis and conducting a literature review
- Writing your thesis
- Your literature review
- Defining a research question
- Choosing where to search
- Search strings
- Limiters and filters
Developing inclusion/exclusion criteria
- Managing your search results
- Screening, evaluating and recording
- Snowballing and grey literature
- Further information and resources
A feature of the systematic literature review is using pre-specified criteria to include/exclude studies. Through searching the literature and formulating your review questions, for example by using PICO, PEO , etc., you will be able to define the specific attributes that research studies must have to be eligible for inclusion in your review, along with other attributes that will exclude them. These attributes will form your inclusion and exclusion criteria, which you will use to assess the relevance and quality of the studies to be included in your final analysis.
Examples of inclusion/exclusion criteria could be:
- Language, e.g., only include articles published in English.
- Timeframe, e.g., papers published after a certain date.
- Geographic location, e.g., UK only.
- Format, e.g., peer reviewed journal articles.
- Type of research, e.g., case studies, empirical papers, qualitative research.
To justify their use, you will need to provide a rationale for each of your inclusion/exclusion criteria.
You will find examples of inclusion/exclusion criteria in research theses on CERES, Cranfield’s repository. Simply keyword search for “systematic review”.
- << Previous: Running your search and reporting search terms
- Next: Managing your search results >>
- Last Updated: Apr 11, 2024 10:52 AM
- URL: https://library.cranfield.ac.uk/writing-your-thesis
Cookie Acknowledgement
This website uses cookies to collect information to improve your browsing experience. Please review our Privacy Statement for more information.
- Administration
- Toggle Search
- Find People

Show simple item record
A Systematic Review of Inclusion and Exclusion Criteria in Healthy Occupational Voice Users in Human Research
Files in this item.
- Open access
- Published: 26 April 2024
Shining a spotlight on the inclusion of disabled participants in clinical trials: a mixed methods study
- Yoshiko Sakuma ORCID: orcid.org/0009-0004-3751-0837 1 ,
- Marie L. E. Miller 2 ,
- Daphne S. Babalis 2 ,
- Alex Baker 3 ,
- Meena Reddi 3 ,
- Aisha Anjum 2 ,
- Jane Bruton 4 ,
- Kathryn N Jones 4 ,
- Umm Zeinab Mulla 5 &
- Henock Taddese 5
Trials volume 25 , Article number: 281 ( 2024 ) Cite this article
95 Accesses
3 Altmetric
Metrics details
It is crucial to include a wide range of the population in clinical trials for the outcome to be applicable in real-world settings. Existing literature indicates that under-served groups, including disabled people, have been excluded from participating in clinical trials without justification. Exclusion from clinical trials exacerbates disparities in healthcare and diminishes the benefits for excluded populations. Therefore, this study was conducted to investigate potential obstacles that prevent disabled people from participating in clinical trials in the United Kingdom (UK).
The study was carried out through an explanatory sequential mixed methods design. The Imperial Clinical Trials Unit devised and implemented an online questionnaire-based survey (with open/closed-ended questions) and an online focus group discussion. The target population were disabled people, family members/carers of disabled people and staff involved in clinical trials, whereupon the sample was recruited by convenience sampling methods via posters and emails through various networks. The Qualtrics XM survey system was used as the host platform for the online survey, and Microsoft Teams was used for an online focus group discussion. The focus group discussion was conducted to gain a deeper understanding of the themes identified from the survey responses. We analysed responses to the survey via descriptive analysis and used thematic analysis to synthesise the free-text answers from the survey and focus group discussion.
We received 45 responses to the survey questionnaire and 5 disabled people took part in a focus group discussion. Our findings highlighted the differences between the perspectives of researchers and those “being researched” and different types of barriers experienced by disabled people: opportunity barriers (inadequate recruitment strategy and ambiguous eligibility criteria), awareness barriers (perception of disability) and acceptance/refusal barriers (available support and adjustment, and sharing of trial results).
Our findings support perspectives drawn from the Ford Framework regarding the need to consider all barriers, not just up to the point of enrolment into trials but also beyond the point of inclusion in clinical trials. We support calls for the introduction of legislation on including disabled people in clinical trials, implementation of industry/community-wide participatory approaches and the development of guidelines, a combined public–private approach.
Peer Review reports
Clinical trials are conducted to assess the clinical effectiveness and safety of medical, surgical or behavioural interventions [ 1 ]. The efficacy and safety of interventions are influenced by intrinsic/extrinsic factors such as gender, race, age, ethnicity, medical history and genetic background. Outcomes may widely vary between populations [ 2 ]. Therefore, clinical trials should include a wide range of populations to enhance their generalisability [ 3 ].
However, research has highlighted that specific demographic groups have been excluded from clinical trials, and such exclusions would limit the generalisability of the results of clinical trials to real-world practice [ 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 ]. The population groups predominantly excluded from clinical trials, collectively referred to as “under-served groups”, include disabled people [ 12 ]. Such exclusions might be because of the lack of cultural competency of under-served groups, and better evidence that differences in genetics, implied by gender and ethnicity, significantly impact the response to interventions tested in clinical trials [ 13 , 14 ].
This long-standing lack of inclusion of under-served groups in clinical trials risks widening health inequalities in the population and increasing the number of people left out of the benefits of healthcare advancement [ 15 , 16 , 17 , 18 , 19 , 20 , 21 ]. To date, disabled people have faced many obstacles that prevent them from participating in clinical trials. These barriers encompass a spectrum of issues, from the physical inaccessibility of clinical facilities, informed consent process, lack of disability awareness among healthcare professionals, and lack of clarity and justification on eligibility criteria [ 22 , 23 , 24 ]. It is especially worth noting the paradoxical scenario where disabled individuals may be excluded from clinical trials in research focusing on conditions that could lead to disability, such as neurological disorders [ 23 , 24 ]. These multifaceted barriers underscore the need for comprehensive strategies to enhance accessibility and equity in clinical trial participation.
In response to this issue within the UK, in 2017, the National Institute for Health and Care Research (NIHR) launched the NIHR-INCLUDE initiative, which aims to bring a paradigm shift in attitudes surrounding inclusion in clinical trials [ 25 ]. Furthermore, in 2020, NIHR updated the guidance for applicants on Equality, Diversity and Inclusion (EDI) for study participants [ 26 ]. The new statement adds emphasis that all eligible participants should be offered the same opportunity for participate in clinical trials, regardless of geographical location, age, disability, gender reassignment, marriage and civil partnership, pregnancy and maternity, ethnicity, religion or belief, sex, sexual orientation, socioeconomic status, or access to health or social care [ 27 ]. In 2022, the NIHR also developed the INCLUDE Impaired Capacity to Consent Framework. This initiative is designed to enable the inclusion of individuals with impaired capacity due to conditions like dementia, stroke or learning disabilities to consent to clinical research [ 28 ].
Despite all the efforts made by NIHR towards inclusiveness and integration of disabled people into clinical trials in the UK [ 25 , 26 , 28 ], there are still no comprehensive guidelines for researchers to take into account various types of disability. This reflects a significant policy gap as disabled people account for 15% of the global population [ 29 ], 10.4 million people in the UK [ 30 ] and are more likely to have unmet medical needs compared to non-disabled people [ 31 ]. Although the challenges faced by under-served groups participating in clinical trials have been investigated internationally, research focusing on disabled people in this context is still limited. Most of the evidence currently available is from researcher perspectives, literature reviews or primary quantitative studies [ 22 , 23 , 24 , 32 , 33 , 34 ]. The perspectives of carers and disabled people themselves are rarely represented in the research outputs.
In light of the above, this study aimed to explore the potential obstacles faced by people with various disabilities in participating in clinical trials. The study provides further insight into the inclusion of disabled people in clinical trials, as well as improving accessibility to clinical trials in the UK.
Theoretical framework
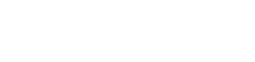
We adopted a guiding conceptual framework, the Ford framework, developed by Jean G. Ford et al. [ 35 ]. This framework categorises barriers to participate in clinical trials based on their predicted effects on awareness, opportunity and the acceptance/refusal of participation. We used the Ford framework to guide the development of the online survey, topic guide and analysis of results (Fig. 1 ).
The conceptual framework categorises barriers to participate in clinical trials [ 35 ] (source: Jean G Ford. 2007. p.229)
Study design
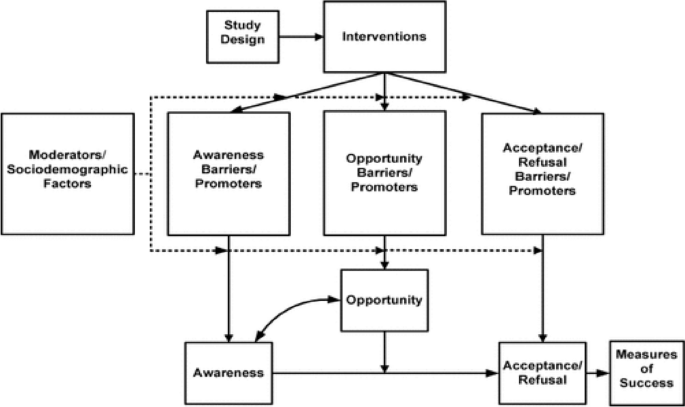
We employed an explanatory sequential mixed methods design (see Fig. 2 ) to generate a deeper understanding of the potential obstacles that disabled people may face when participating in clinical trials in the UK [ 36 , 37 ]. An online survey with open- and close-ended questions was followed by an online focus group discussion devised and implemented by the Imperial Clinical Trials Unit (ICTU).
Explanatory sequential mixed methods design adopted in this study [ 36 ]
The Qualtrics XM survey system was the host platform for the online surveys and was open for approximately 2 weeks, from 28th June, 2022, to 15th July, 2022. The surveys consisted of multiple choice and free-text questions. The survey questions for disabled people and carers/families covered aspects of lived experiences of being disabled, experiences of participating in clinical trials and barriers and enablers to trial participation. The questions for trial staff were comprised of understanding of disability, clinical trials administration for disabled people and barriers and enablers for participation. The survey was limited to one completion per person with Qualtrics’s prevent multiple submission function, but carers/family members who cared for more than one person were encouraged to complete the survey more than once.
The consent question was included at the start of the survey form, and participants could not begin the survey unless they fully understood the purpose of the study and agreed to participate. If participants wished to participate in the focus group discussion, they were asked to contact the ICTU research team at the end of the survey. The participants received an invitation text and a participant information sheet detailing the focus group, which was sent by the project team. Additionally, they were requested to complete a consent form and a registration form to authorise the use of their data and to confirm their participation.
The preliminary survey results were used to elaborate and revise the topic guide (Additional file 1 ). The topic guide explored different factors based on the Ford framework. The focus group was conducted on Microsoft Teams and lasted approximately 2 h, including a break. The focus group participants were nominally reimbursed for their time and the Internet connection.
Participant recruitment and selection
We followed convenience sampling to recruit participants for this study. The target populations were disabled people, carers/family members of disabled people and clinical trial staff. The adverts were distributed electronically and in paper via various distribution networks (Additional file 2 ). The inclusion and exclusion criteria of the study were:
Inclusion criteria
A person with long-term disabilities and willing to disclose their disabilities.
Carer/family member of a disabled person—willing to discuss the disability/relevant medical history of the person they care for.
Staff involved in clinical trials—irrespective of their position/role, at any stage.
Exclusion criteria
Disabled people and their carers/family members unwilling to disclose their disability.
Non-disabled persons.
Data analysis
All data and results were analysed and presented in accordance with the Good Reporting of a Mixed Methods Study (GRAMMS) guidance [ 38 ]. The quantitative data from the survey was descriptively analysed first. The qualitative data from the survey and focus group were thematically analysed guided by the Ford framework [ 35 , 36 , 37 , 38 , 39 , 40 , 41 ]. At the end of the analysis, the findings from the open-ended questions in the survey and focus group data were integrated to aid interpretation.
Public involvement
According to the Ladder of Citizen Participation proposed by Arnstein [ 42 ], the study centred on partnerships and recruited five public partners with a range of disabilities, and one person who previously partnered with the ICTU. Public partners reviewed the participant information sheet, survey questions, images used in the surveys and materials for disseminating results, providing recommendations to enhance inclusivity. The recommendations included incorporating a text-to-read function into the survey, using images, providing videos with subtitles and increasing the text size.
Researcher’s positionality
The study was conducted, analysed and integrated by an international student studying for a Master of Public Health at Imperial College London. The student is Asian, has a healthcare background and has experience conducting research with disabled people. The philosophical position adopted in the study, namely pragmatism, guided the project to utilise quantitative and qualitative findings to answer questions instrumental to the inclusion of disabled people in clinical trials.
Available support/adjustment
To make the survey as accessible as possible, the study adverts informed participants that they could complete the survey online, paper or verbally if they wished by contacting the project team by email or telephone. All documents used in the study were compliant with the university accessibility guidelines. In addition, for the focus group, if participants were unfamiliar with Microsoft Teams, they were offered guidance beforehand. The results were developed in multiple formats, including a written report with lay terms, infographics and a video (with subtitles).
Research team training
In this study, facilitators and staff involved in the focus group had completed safeguarding training on vulnerable people, Good Clinical Practice training, and underwent a Disclosure and Barring Service check.
Demographic characteristics
A total of 45 people completed the survey. Of these, 26 (58%) were disabled people, 8 (18%) were carers/family members and 11 (24%) were trial staff. To tabulate results, numeric characters were assigned for disabled people (Disabled person 1–26), carers (Carer 1–Carer 8) and clinical trial staff (Staff 1–Staff 11). A focus group was conducted with five disabled people. To ensure anonymity, participants were assigned random alphanumeric characters (Participant 1–Participant 5). Table 1 explains the number of responses we received and the detailed characteristics of the survey respondents. Detailed demographic characteristics of focus group participants are available in Additional File 3 .
The following sections discuss the results from the survey and focus group in an integrated manner. Tables 2 and Table 3 provide the summary statistics derived from the survey’s closed-ended questions. The results for each of these elements are elaborated upon in the following section. Additional file 4 provides supplementary information on the frequencies of themes derived from the focus group discussion.
Theme 1: Opportunity barrier—inadequate recruitment strategy and ambiguous eligibility criteria
Inadequate recruitment strategy
Survey closed-ended questions
There were gaps in participants’ and researchers’ awareness and perceptions regarding clinical trial recruitment. The survey results show that 47% of disabled people and carers/family members said that advertisements were not fully accessible and understandable. In contrast, 55% of the staff involved in clinical trials reported that the trial venue was accessible to participants, while a higher percentage, 64%, reported that the advertisement for the trial call was accessible to participants.
Survey open-ended questions
A response from one disabled person pointed out that the current recruitment strategy for clinical trials is predominantly led by clinicians. This approach tends to limit inclusivity for people outside of the clinic, as the target population is often too selectively chosen. To reach disabled people, different recruitment tactics should be employed, such as approaching local communities, local media and pharmacies and using relatable promotional materials. For example, disabled people described what they thought would be an effective approach for enhancing recruitment.
“Use ‘real’ case examples of disabled people with different impairments and ‘conditions’ to recruit” [Disabled person 19].
Focus group discussion
Focus group participants highlighted how information tends to be less accessible to disabled people. They mentioned that clinical trial participants are mainly recruited directly from clinics or hospitals and trials are often not openly advertised. They underscored a need for broader access to information on how people can participate and which clinical trials are currently ongoing. Additionally, they highlighted that disabled people are more likely to be overlooked as part of the target audience for clinical trials.
Ambiguous eligibility criteria
Sixty-four of staff perceived that certain groups of disabled people are excluded from participating in clinical trials. Eight-two percent of staff indicated that eligibility criteria for disabled people are sometimes ambiguous and lead disabled people to be unnecessarily excluded from participating in clinical trials.
It was reported, mainly by clinical trial staff, that the eligibility criteria for disabled people largely depend on the discretion of the principal investigators and co-investigators. Clinical trial staff who responded to the survey questionnaire described the eligibility criteria of many clinical trials as a “grey area” for recruiting disabled people.
“This is ambiguous and leaves it up to the Investigator to interpret, they may be over cautious and exclude people ‘to be on the safe side’ when in fact these people are eligible” [Staff 2].
To improve this, respondents suggested that tailored inclusion and exclusion criteria for disabled people should be used, and disability and capacity to consent should be assessed at the individual level. However, it was also mentioned that implementing such adjustments takes time and financial consideration.
“To allow for patients with fluctuating capacity; however, they may then not be able to give informed consent if it is a more complex trial. The patients would have to be assessed individually to ensure they can retain and understand the information to give consent” [Staff 3].
The focus group highlighted that the current eligibility criteria of clinical trial designs are not grounded in “realistic expectations” of disabled people. Disabled people also mentioned that researchers feared that by including a small number of disabled people would hamper statistics and potentially introduce confounding factors in the model.
“Funders, e.g., NIHR, need to recognise the requirements for inclusivity can be unrealistic” [Participant 2].
Theme 2: Awareness barrier—perception of disabilities
Ninety-four percent of disabled people and carers/family members stated that their disability interfered with their activities of daily living, and 88% of them said it affected their communication. Of these, 26% of disabled people and carers/family members said their daily tasks were always affected.
Disabled people who responded to the open-ended questions in the survey stated that the perception of disability that clinical trial staff have remains superficial and sometimes over-medicalised, thereby highlighting the need to understand better how having a disability affects peoples’ daily lives in different ways. It is often challenging to fully understand the extent of disability, particularly in individuals with invisible disabilities (conditions that are not immediately obvious, e.g., chronic pain, hearing loss, mental health conditions). These individuals run the risk of not being perceived as disabled.
“People think that I’m lazy, that losing weight and exercise would solve all my problems. They do not understand the pain with every single task” [Disabled person 10].
In addition to the survey respondents, focus group participants highlighted that invisible disabilities and multiple conditions are often not recognised in the research. Participant 5 described the importance of invisible and multiple disabilities being recognised, along with her experience of having a visual impairment but not being recognised by others as having a disability. Thus, understanding different dimensions of disability by staff and sponsors involved in clinical trials is essential; this also relates to whether support and adjustments are available to disabled people.
“Visual impairments fall off the radar, disabilities aren’t necessarily declared. And having multiple conditions is not always recognised in surveys or trials” [Participant 5].
Theme 3: Acceptance/refusal barrier—available support and adjustment, sharing results
Available support and adjustment
Although 82% of staff were aware that the assessments and site visits could be burdensome for disabled people, only 42% of disabled people had been asked about the need for support/adjustment when participating in clinical trials.
Survey respondents highlighted that having a disability had several consequences in the lives of disabled people and their participation in clinical trials — these burdens on disabled people include time and financial, physical and mental constraints. Twenty-one percent of survey respondents stated that they were not asked in advance about the support and help they would need when taking part. Although the need for support is recognised among staff, staff responses revealed that this is subject to resources and financial constraints, such as whether funders are willing to support such as sign language interpreters and cover travel expenses.
“For me, length of travel, accessibility to trial rooms, and how long the trial might take would all be factors, and I understand these factors may well be outside the researchers’ scope” [Disabled person 12].
Similarly, disabled people who participated in the focus group discussed the need for providers to recognise that participating in clinical trials, in addition to their usual care and treatment, is not easy and that they would need to make considerable preparation to participate, such as transport, whether the venue clinic has soft seating, and whether there are places for refreshments and breaks. They highlighted that support and adjustment for participation in clinical trials need to reflect the realities and needs of people with disabilities more accurately.
“I would like to ‘do my bit’, I might be in a unique position because of my disability but also can’t do much because of my disability” [Participant 4].
“It is hard work, you always have to plan, plan, plan. If I need to go to the shops, how far is it, can I get there, will I need the bathroom. All these worries make it difficult before you even leave the house” [Disabled person 5].
Sharing results
Interesting data on the sharing of clinical trial results were obtained. Out of the 19 participants in the study who indicated they had participated in clinical trials, only seven (37%) of the carers/family members and disabled individuals were informed about the trial results.
The clinical trial staff did not raise any issues regarding sharing results and content. However, the disabled people and carers who responded to the questionnaire highlighted this issue. The following quote stated that the results were unacceptable as the participants felt they had been misrepresented. This highlights the unpicked issue of “how” and “when” results should be shared with disabled people/carers.
“I received information on the study results but not before I had read about it in the national press, and the way that the results were presented made me feel that I had been an inadequate mother….” [Carer 8].
This study explored potential obstacles that influence the participation of disabled people in clinical trials in the UK from the perspective of disabled people, carers and clinical trial staff, using an explanatory sequential mixed methods design. Guided by The Ford framework [ 35 ], we specified multiple factors across different dimensions: “opportunity barriers” (inadequate recruitment strategy, ambiguous eligibility criteria), “awareness barriers” (perception of disability) and “acceptance/refusal barriers” (available support and adjustment, sharing results). There was a general sentiment among all participant groups that disabled people are often unnecessarily excluded from participating in clinical trials. Additionally, we note key differences between the “being researched” and the “researcher” perspectives and, specifically, highlight a key topic that had not been signalled by the guiding framework: issues/problems related to “sharing of clinical trial findings”.
The most frequently reported barrier in this study was related to the opportunity to participate, such as inadequate recruitment strategies and ambiguous eligibility criteria for clinical trial participation. Opportunities for recruitment into clinical trials with disabled people are very limited; there is a strong desire for more openly publicised advertising and recruitment methods. This can be improved by using public involvement with various public partners with lived experience of disability at all stages of clinical trials [ 43 ].
Another barrier to participation is the presence of ambiguous eligibility criteria, such as the lack of clearly justified criteria for individuals with conditions that may put participants at risk during the trial. This ambiguity may not adequately account for the diverse range of disabilities among participants in clinical trials [ 44 ]. This has been discussed in many previous studies and is a very complex topic that has not yet reached a consensus on the implementation of standardised practice [ 45 , 46 , 47 ]. However, the very high rate of ambiguous exclusion criteria and inadequate exclusion of persons with disabilities in clinical trials has been highlighted by Camanni et al. [ 44 ]; their study revealed that, in 44.5% of the trials, the discretion of the investigators regarding the exclusion of study participants was considered implicit exclusion criteria [ 44 ]. Although some studies have proposed the consideration of alternative methods, such as proxy consent or the use of disability assessment tools at the individual level, there are still only a few reports of their actual implementation in clinical trials [ 48 , 49 , 50 ]. No clear measures on this topic have yet been presented, however, employing a tool like the Impaired Capacity to Consent Framework, explicitly designed for individuals with impaired capacity to consent, could be implemented to assist researchers in determining the necessary actions and resources, potentially guiding interventions for patients with diverse disabilities [ 28 ].
The importance of the perception of disability, identified as an awareness barrier, has also been discussed by Marjanovic et al. [ 51 ]. Lack of appropriate knowledge and awareness among stakeholders affects the quality of trial outcomes and retention of participants [ 51 ]. Stakeholders in clinical trials should recognise that participants may have visible as well as invisible disabilities and seek to understand how their disabilities impact their lives and what support they need.
We also underscore the importance of readily available help and adjustments, which are key elements for the acceptability of participation. We recommend training staff and incorporating planning and guidance into the Standard Operating Procedure guidelines for centres running clinical trials, as well as considering the physical, mental, financial and time constraints of trial participants. In this study, disabled people and their carers said they would have been able to participate in clinical trials if they had received appropriate support, which is in line with the findings of a previous study by Feldman et al. [ 52 ]. Our findings reaffirm the need for better awareness regarding critical support and adjustment needs.
The one theme identified in this study that did not fall in the Ford framework was the factor related to sharing clinical trial results. In clinical trial participation, it should be an ethical norm for participants to receive ongoing progress updates and study results, which are significant aspects of clinical trial inclusion [ 53 ]. The importance and effectiveness of sharing the results of clinical trials, as well as approaches to sharing results, have been described in prior literature [ 54 ]. This practice can increase potential participation in future clinical trials and foster trust in research [ 54 ]. The specific needs of people with disabilities and carers, obtained in this study (e.g., appropriate language, timing, methods), add future insight concerns regarding this crucial step in the research process. However, there is still a notable gap in the evidence regarding the best practices for sharing research results with people with disabilities and their carers, particularly concerning the optimal timing, mode and content of such communication. It is clear that more detailed research is required to address this evidence gap.
Strengths and limitations
This study adds valuable evidence to the topic with actual voices from disabled people, carers/families and trial staff. This study was conducted in partnership with public partners with disabilities at different stages of the research. This process has helped make the study more inclusive [ 55 ]. In addition, the study was designed to be accessible to as many participants as possible, whereby we offered a range of survey formats to accommodate the different preferences of survey respondents.
However, in this study, the participants were recruited without specific criteria regarding the types/degree of disability. Therefore, the present study cannot comprehensively consider all disabilities. Second, due to time and resource constraints, we were not able to include carers/families and trial staff in focus groups nor conduct semi-structured interviews. To some extent, we have overcome this limitation by combining qualitative data from the survey with findings from the focus group. Third, this study was unable to collect sociodemographic information in the online questionnaire. Disability status has intersectionality with other sociodemographic backgrounds such as gender, age, sexuality and ethnicity. Future studies should collect disability status as sociodemographic information and conduct sub-analyses to provide additional insights into the inclusion of other under-served population groups.
We recommend the introduction of legislation on the inclusion of under-served groups in clinical trials, the implementation of an industry/community-wide participatory approach, such as guidance or training for stakeholders, and the development of guidelines specific to disability. These measures will go a long way towards ensuring optimal participation of disabled people and other under-served populations and enhance the validity and generalisability of clinical trial results.
Availability of data and materials
Other data is available upon reasonable request.
Abbreviations
Biomedical Research Centre
Equality, Diversity and Inclusion
The Imperial Clinical Trials Unit
National Institute for Health and Care Research
The NIHR-Innovations in Clinical Trial Design and Delivery for the Under-served
United Kingdom
World Health Organization. Clinical trials. 2024. https://www.who.int/health-topics/clinical-trials#tab=tab_1 . Accessed 9 Mar 2024.
Clark LT, Watkins L, Piña IL, Elmer M, Akinboboye O, Gorham M, Jamerson B, McCullough C, Pierre C, Polis AB, Puckrein G, Regnante JM. Increasing Diversity in Clinical Trials: Overcoming Critical Barriers. Curr Probl Cardiol. 2019;44(5):148–72. https://doi.org/10.1016/j.cpcardiol.2018.11.002 .
Article PubMed Google Scholar
Bodicoat DH, Routen AC, Willis A, et al. Promoting inclusion in clinical trials - a rapid review of the literature and recommendations for action. Trials. 2021;22:880. https://doi.org/10.1186/s13063-021-05849-7 .
Article PubMed PubMed Central Google Scholar
Bierer BE, Meloney LG, Ahmed HR, White SA. Advancing the inclusion of underrepresented women in clinical research. Cell Report Med. 2022;3(4). https://doi.org/10.1016/j.xcrm.2022.100553 .
Larson E. Exclusion of certain groups from clinical research. Image--the journal of nursing scholarship. 1994;26(3):185–190. https://doi.org/10.1111/j.1547-5069.1994.tb00311.x .
Hussain-Gambles M, Atkin K, Leese B. Why ethnic minority groups are under- represented in clinical trials: a review of the literature. Health Soc Care Community. 2004;12(5):382–8. https://doi.org/10.1111/j.1365-2524.2004.00507.x .
Heiat A, Gross CP, Krumholz HM. Representation of the elderly, women, and minorities in heart failure clinical trials. Arch Intern Med. 2002;162(15):1682–8. https://doi.org/10.1001/archinte.162.15.1682 .
Jabson JM, Blosnich JR. Representation of lesbian, gay, and bisexual people in clinical cancer trials. Ann Epidemiol. 2012;22(11):821–3. https://doi.org/10.1016/j.annepidem.2012.08.006 .
Hein I, Troost P, de Vries M, et al. Why do children decide not to participate in clinical research: a quantitative and qualitative study. Pediatr Res. 2015;103–108. https://doi.org/10.1038/pr.2015.74 .
Witham MD, Anderson E, Carroll CB On behalf of the NIHR CRN INCLUDE Steering Group, et al. Ensuring that COVID-19 research is inclusive: guidance from the NIHR INCLUDE project. BMJ Open.2020;10:e043634. https://doi.org/10.1136/bmjopen-2020-043634 .
Treweek S, Forouhi NG, Venkat Narayan KM, Khunti K. COVID-19 and ethnicity: who will research result apply to? Lancet. 2020;395(10242):1955–7. https://doi.org/10.1016/S0140-6736(20)31380-5 .
Article CAS PubMed PubMed Central Google Scholar
National Institute for Health and Care Research. Improving inclusion of under-served groups in clinical research: Guidance from INCLUDE project. 2022. https://www.nihr.ac.uk/documents/improving-inclusion-of-under-served-groups-in-clinical-research-guidance-from-include-project/25435 . Accessed 11 Jan 2024.
Gross AS, Harry AC, Clifton CS, Della Pasqua O. Clinical trial diversity: An opportunity for improved insight into the determinants of variability in drug response. Br J Clin Pharmacol. 2022;88(6):2700–17. https://doi.org/10.1111/bcp.15242 .
Bodicoat DH, Routen AC, Willis A, Ekezie W, Gillies C, Lawson C, Yates T, Zaccardi F, Davies MJ, Khunti K. Promoting inclusion in clinical trials-a rapid review of the literature and recommendations for action. Trials. 2021;22(1):880. https://doi.org/10.1186/s13063-021-05849-7 .
Cavazzoni P, Anagnostiadis E, Lolic M. Drug trials snapshots: summary report. The U.S Food & Drug Administration. 2021. https://www.fda.gov/media/145718/download . Accessed 11 Jan 2024.
Goodson N, Wicks P, Morgan J, et al. Opportunities and counterintuitive challenges for decentralised clinical trials to broaden participant inclusion. NPJ Digit Med. 2022;5(58). https://doi.org/10.1038/s41746-022-00603-y .
Rubin R. Pregnant People’s Paradox—Excluded From Vaccine Trials Despite Having a Higher Risk of COVID-19 Complications. JAMA. 2021;325(11):1027–8. https://doi.org/10.1001/jama.2021.2264 .
Article CAS PubMed Google Scholar
Treweek S., Banister K., Bower P. et al. Developing the INCLUDE Ethnicity Framework—a tool to help trialists design trials that better reflect the communities they serve. Trials. 2021;22(337). https://doi.org/10.1186/s13063-021-05276-8 .
U.S Food and Drug Administration. Collection of Race and Ethnicity data in clinical trials: guidance for industry and food and drug administration staff. 2016. https://www.fda.gov/media/75453/download . Accessed 11 Jan 2024.
Eliasson E. Ethnicity and adverse drug reactions BMJ (Clinical research ed). 2006;332(7551):1163–4. https://doi.org/10.1136/bmj.332.7551.1163 .
Williams LK, Padhukasahasram B, Ahmedani BK, Peterson EL, Wells KE, González Burchard E, Lanfear DE. Differing effects of metformin on glycemic control by race- ethnicity. J Clin Endocrinol Metab. 2014;99(9):3160–8. https://doi.org/10.1210/jc.2014-1539 .
DeCormier Plosky W, Ne’eman A, Silverman BC, Strauss DH, Francis LP, Stein MA, Bierer BE. Excluding People With Disabilities From Clinical Research: Eligibility Criteria Lack Clarity And Justification. Health affairs (Project Hope). 2022;41(10):1423–32. https://doi.org/10.1377/hlthaff.2022.00520 .
Trivedi RB, Humphreys K. Participant exclusion criteria in treatment research on neurological disorders: Are unrepresentative study samples problematic?, Contemporary Clinical Trials, Volume 44. ISSN. 2015;20–25:1551–7144. https://doi.org/10.1016/j.cct.2015.07.009 .
Article Google Scholar
Inchai P, Tsai WC, Chiu LT, Kung PT. Incidence, risk, and associated risk factors of stroke among people with different disability types and severities: A national population-based cohort study in Taiwan. Disabil Health J. 2021;14(4):101165. https://doi.org/10.1016/j.dhjo.2021.101165 .
National Institute for Health and Care Research. The NIHR-INCLUDE project. 2021. https://sites.google.com/nihr.ac.uk/include/home . Accessed 11 Jan 2024.
National Institute for Health and Care Research. Equality, diversity and inclusion. 2022. https://www.nihr.ac.uk/about-us/our-key-priorities/equality-diversity-and-inclusion/ . Accessed 11 Jan 2024.
National Institute for Health and Care Research. Strengthening our commitment to equality, diversity, inclusion and patient and public involvement and engagement (PPIE). 2022. https://www.nihr.ac.uk/documents/strengthening-our-commitment-to-equality-diversity-inclusion-and-patient-and-public-involvement-and-engagement-ppie/24697 . Accessed 11 Jan 2024.
Trial Forge. The include Impaired Capacity to Consent Framework. 2023. https://www.trialforge.org/trial-forge-centre/impaired-capacity/#:~:text=The%20NIHR%20INCLUDE%20Impaired%20Capacity,trial%20design%20and%20funding%20application . Accessed 11 Jan 2024.
World Health Organization. World Report on Disabilities 2011. 2011. https://www.who.int/teams/noncommunicable-diseases/sensory-functions-disability-and-rehabilitation/world-report-on-disability . Accessed 11 Jan 2024.
Office for National Statistic. Disability, England and Wales: Census 2021. 2021. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandwellbeing/bulletins/disabilityenglandandwales/census2021#:~:text=does%20it%20matter%3F-,Disability%20in%20England%20and%20Wales,19.5%25%20(10.0%20million) . Accessed 11 Jan 2024.
Alwadi M.A, Baker S.R, Owens J. The inclusion of children with disabilities in oral health research: A systematic review. Community Dentistry Oral Epidemiol. 2018;46(3):238–244. ISSN 0301–5661. https://doi.org/10.1111/cdoe.12374 .
McDonald K. E., Conroy N. E., Olick R. S., Project ETHICS Expert Panel. A quantitative study of attitudes toward the research participation of adults with intellectual disability: Do stakeholders agree? Disabil Health J. 2018;11(3):345–50. https://doi.org/10.1016/j.dhjo.2017.12.004 .
Mulhall P, Taggart L, Coates V, McAloon T, Hassiotis A. A systematic review of the methodological and practical challenges of undertaking randomised-controlled trials with cognitive disability populations. Soc Sci Med. 2018;200:114–28. https://doi.org/10.1016/j.socscimed.2018.01.032 .
Shariq S, Cardoso Pinto AM, Budhathoki SS, et al. Barriers and facilitators to the recruitment of disabled people to clinical trials: a scoping review. Trials. 2023;24:171. https://doi.org/10.1186/s13063-023-07142-1 .
Ford JG, Howerton MW, Lai GY, et al. Barriers to recruiting underrepresented populations to cancer clinical trials: A systematic review. Cancer. 2007;112(2):228–42. https://doi.org/10.1002/cncr.23157 .
Johnson RB, Onwuegbuzie AJ, Turner LA. Toward a Definition of Mixed Methods Research. J Mixed Methods Res. 2007;1(2):112–33. https://doi.org/10.1177/1558689806298224 .
Shorten A, Smith J. Mixed methods research: expanding the evidence base. Evidence- Based Nursing. 2017;20(3):74–5. https://doi.org/10.1136/eb-2017-102699 .
O’Cathain A, Murphy E, Nicholl J. The Quality of Mixed Methods Studies in Health Services Research. Journal of Health Service Research & Policy. 2017;13:2. https://doi.org/10.1258/jhsrp.2007.007074 .
Michelle E. Kiger, Lara Varpio. Thematic analysis of qualitative data: AMEE Guide No. 131. Med Teacher. 2020. https://doi.org/10.1080/0142159X.2020.1755030 .
Jane Ritchie, Jane Lewis, Carol Mcnaughton Nicholls, Rachel Ormston. Qualitative Research Practice: A guide for social science students and researchers (2nd Ed). London, SAGE publication Ltd. 2014. https://uk.sagepub.com/en-gb/eur/qualitative-research-practice/book237434 . Accessed 11 Jan 2024.
Virginia Braun & Victoria Clarke. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. https://doi.org/10.1191/1478088706qp063oa .
Arnstein SR. A Ladder Of Citizen Participation. J Am Inst Plann. 1969;35(4):216–24. https://doi.org/10.1080/01944366908977225 .
Selman LE, Clement C, Douglas M, et al. Patient and public involvement in randomised clinical trials: a mixed-methods study of a clinical trials unit to identify good practice, barriers and facilitators. Trials. 2021;22:735. https://doi.org/10.1186/s13063-021-05701-y .
Shariq S, Cardoso Pinto AM, Budhathoki SS, Miller M, Cro S. Barriers and facilitators to the recruitment of disabled people to clinical trials: a scoping review. Trials. 2023;24(1):171. https://doi.org/10.1186/s13063-023-07142-1 .
Schwartz J. Inclusion of people with disabilities in drug development research. Arch Phys Med Rehabil. 2017;98(10):E75–6. https://doi.org/10.1016/j.apmr.2017.08.237 .
Spaul SW, Hudson R, Harvey C, et al. Exclusion criterion: learning disability. The Lancet. 2020;395(10223):E29. https://doi.org/10.1016/S0140-6736(20)30051-9 .
Schwartz JK, Unni E. Inclusion of People with Disabilities in Research to Improve Medication Adherence: A Systematic Review. Patient Prefer Adherence. 2021;15:1671–7. https://doi.org/10.2147/PPA.S314135] .
Biesecker B., Raspa M., Rupert D., Moultrie R., Furberg R., McCormack L. A. Making Clinical Trials More Patient-Centered Using Digital Interactive E-Consent Tools. RTI Press. 2019. https://www.ncbi.nlm.nih.gov/books/NBK558162/ . Accessed 11 Jan 2024.
Horner-Johnson W., Bailey D. Assessing Understanding and Obtaining Consent from Adults with Intellectual Disabilities for a Health Promotion Study. J Policy Pract Intellectual Disabilities. 2013;10(3). https://doi.org/10.1111/jppi.12048 .
Shepherd V., Wood F., Griffith R. et al. Protection by exclusion? The (lack of) inclusion of adults who lack capacity to consent to research in clinical trials in the UK. Trials. 2019;20, 474. https://doi.org/10.1186/s13063-019-3603-1 .
THIS institute. Involving NHS staff in research. 2019. https://www.thisinstitute.cam.ac.uk/research-articles/involving-nhs-staff-in-research/ . Accessed 11 Jan 2024.
Feldman MA, Bosett J, Collet C, Burnham-Riosa P. Where are persons with intellectual disabilities in medical research? A survey of published clinical trials. Journal of intellectual disability research: JIDR. 2014;58(9):800–9. https://doi.org/10.1111/jir.12091 .
Partridge AH, Winer EP. Informing clinical trial participants about study results. JAMA. 2002;288(3):363–5. https://doi.org/10.1001/jama.288.3.363 .
South A, Joharatnam-Hogan N, Purvis C, James EC, Diaz-Montana C, Cragg WJ, Tweed C, Macnair A, Sydes MR, Snowdon C, Gillies K, Isaacs T, Bierer BE, Copas AJ. Testing approaches to sharing trial results with participants: The Show RESPECT cluster randomised, factorial, mixed methods trial. PLoS Med. 2021;18(10): e1003798. https://doi.org/10.1371/journal.pmed.1003798 .
Blackburn S, McLachlan S, Jowett S, et al. The extent, quality and impact of patient and public involvement in primary care research: a mixed methods study. Research Involvement and Engagement. 2018;4:16. https://doi.org/10.1186/s40900-018-0100-8 .
Download references
Acknowledgements
We would like to take this opportunity to express our deepest gratitude to the public partners who helped us enhance the study by reviewing the research design and outcomes, as well as to all who participated in the survey and focus group discussion.
This study received an award from the Imperial College London, Equality, Diversity and Inclusion Seed Fund from Imperial College London. ICTU staff are supported by the NIHR Imperial Biomedical Research Centre (BRC).
Author information
Authors and affiliations.
Faculty of Medicine, School of Public Health, Imperial College London, South Kensington Campus, London, SW7 2AZ, UK
Yoshiko Sakuma
Imperial Clinical Trials Unit, School of Public Health, Imperial College London, Stadium House, 68 Wood Ln, London, W12 7RH, UK
Marie L. E. Miller, Daphne S. Babalis & Aisha Anjum
Imperial Clinical Trials Unit - Cancer, Department of Surgery and Cancer, Convergence Science Centre, Imperial College London, South Kensington Campus, London, Cancer Research, SW7 2AZ, UK
Alex Baker & Meena Reddi
Patient Experience Research Centre, Imperial College London, South Kensington Campus, London, SW7 2AZ, UK
Jane Bruton & Kathryn N Jones
Faculty of Medicine, School of Public Health, Medical School, Imperial College London, St Mary’s Campus, 167, Praed Street, London, W2 1NY, UK
Umm Zeinab Mulla & Henock Taddese
You can also search for this author in PubMed Google Scholar
Contributions
All authors were involved in the design, development and conduct of the study. MM, AA, AW, DB, JB, KJ and MR initiated the project’s design, created documentation for funding and ethical approval and drafted the survey questionnaire. YS was primarily responsible for developing the qualitative component, such as creating the documents for participants, ethical approval and the topic guide. YS, JB and KJ conducted data analysis and result integration for this study. ZM and HT were the primary supervisors of the design/analysis of the quantitative/qualitative results interpretation and academic writing.
Corresponding author
Correspondence to Yoshiko Sakuma .
Ethics declarations
Ethics approval and consent to participate.
This study has been approved by the Imperial College Research Ethics Committee and the Imperial College London, Faculty of Medicine, Data Protection Assessment Team (ICREC No.22IC768). Participants were asked to read a Participant Information Sheet and privacy policy and consent to participate in this study.
Consent for publication
All participants were fully informed and gave their consent for their pseudonymised data to be published and presented at conferences.
Competing interests
The authors declare that they have no competing interests.

Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Topic guide. Questions were used in focus group.
Additional file 2.
Survey distribution network. Table of dissemination network for the project.
Additional file 3.
Demographic characteristics of focus group participants. Table of demographic characteristics of focus group participants.
Additional file 4.
Frequency of identified themes. Frequency table of thematic analysis.
Additional file 5.
Survey for disabled people. Survey questions for disabled people.
Additional file 6.
Survey for carers/family members. Survey questions for carers/family members.
Additional file 7.
Survey for trial staff. Survey questions for trial staff.
Additional file 8.
Good Reporting of A Mixed Methods Study (GRAMMS) Guidelines.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Sakuma, Y., Miller, M.L.E., Babalis, D.S. et al. Shining a spotlight on the inclusion of disabled participants in clinical trials: a mixed methods study. Trials 25 , 281 (2024). https://doi.org/10.1186/s13063-024-08108-7
Download citation
Received : 01 August 2023
Accepted : 12 April 2024
Published : 26 April 2024
DOI : https://doi.org/10.1186/s13063-024-08108-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Clinical trials
- Mixed methods study
- Under-served groups
- Disabled people
ISSN: 1745-6215
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Open access
- Published: 27 April 2024
Association of the TRIM family protein with survival outcomes and clinicopathological features in colorectal cancer: a systematic review and meta-analysis
- Ying Wu 1 ,
- Chen Chen 1 ,
- Xian Hua 1 ,
- Chunhua Zhao 2 &
- Han Min 1
BMC Cancer volume 24 , Article number: 537 ( 2024 ) Cite this article
155 Accesses
1 Altmetric
Metrics details
The tripartite motif (TRIM) proteins have been reported to play crucial roles in various malignancies. However, the clinical significance of TRIM proteins in colorectal cancer (CRC) remains controversial. This study aimed to evaluate the association between TRIM proteins and the clinicopathological features and survival outcomes in patients with CRC.
We performed a meta-analysis to investigate whether TRIM is a prognostic factor in CRC. PubMed, Embase, Web of Science, CNKI and Weipu databases were searched to identify eligible studies that evaluated the association between TRIM proteins and overall survival (OS), as well as the clinicopathological features of patients with CRC. Hazard ratios (HR) or odds ratios (OR) with 95% confidence interval (CI) were derived and pooled using a fixed-effects model.
From inception to March 2023, we extracted study characteristics and prognostic data for each identified study. Twelve studies enrolling 1608 patients were eligible for inclusion. Data on OS and recurrence-free survival (RFS) were available for 12 and 2 studies, respectively. The pooled analysis results showed a significant correlation between the elevated TRIM proteins and shorter OS (HR = 2.42, 95% CI: 1.96–2.99) and worse RFS (HR = 2.51, 95% CI: 1.78–3.54) in patients with CRC. The combined ORs indicated that TRIM protein over-expression was significantly associated with advanced TNM stage (OR = 2.26, 95% CI: 1.25–4.10), deep tumor invasion (OR = 2.01, 95% CI: 1.04–3.88), lymph node metastasis (OR = 2.99, 95% CI: 2.19–4.09) and perineural invasion (OR = 1.95, 95% CI: 1.18–3.23).
Conclusions
Our findings suggest that TRIM proteins can predict tumor progression and poor prognosis in CRC. Therefore, TRIM proteins may be promising therapeutic targets for patients with CRC.
Graphical Abstract
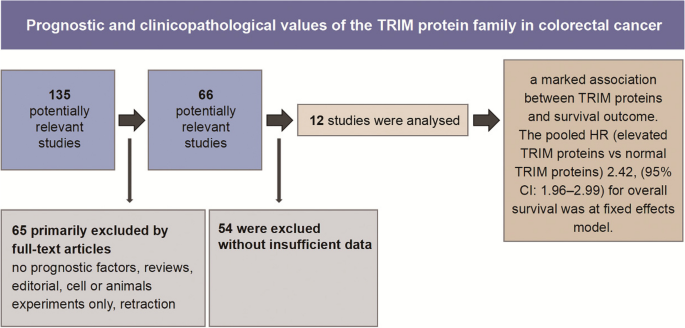
Peer Review reports
Introduction
Colorectal cancer (CRC) is a common malignant cancer in both males and females and is the second leading cause of cancer-related deaths worldwide [ 1 ]. Despite a slight decrease in mortality due to enhanced detection techniques and ever-improving therapeutic approaches, patients with CRC still exhibit poor survival owing to the rising metastatic capacity of primary tumors and high recurrence rate [ 2 , 3 ]. Recently, numerous studies have concentrated on novel biomarkers for the clinicopathological characteristics and prognosis of patients with CRC, with the aim of identifying new therapeutic targets [ 4 , 5 ].
The tripartite motif (TRIM) family of proteins is characterized by an N-terminal TRIM containing a RING-finger domain, one or two zinc-finger domains known as a B-box and a coiled-coil region [ 6 ]. Owing to the RING-finger domain, TRIM proteins possess E3 ligase activity and participate in the degradation of a series of proteins. TRIM proteins have been reported to play crucial roles in various biological behaviors, and their dysregulation contributes to oncogenesis and tumor progression [ 7 , 8 ]. Several studies have examined the prognostic role of different TRIM proteins in various malignancies [ 9 , 10 , 11 ]. However, the prognostic role of the TRIM protein family in CRC remains unclear.
Therefore, we conducted a systematic review and meta-analysis to evaluate the association between TRIM proteins and the clinical outcomes in patients with CRC. Understanding TRIM proteins can considerably contribute to their validations as promising novel biomarkers and potential therapeutic targets for CRC.
Materials and methods
The present study was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses [ 12 ]. We registered on PROSPERO (CRD42023417799) before conducting the literature search.
Search strategy
Two independent researchers systematically searched the Web of Science, PubMed, Embase, CNKI and Weipu electronic databases from their inception to March 1, 2023. No language restrictions were imposed. The following medical subject headings or keywords were adopted according to the retrieval strategy: ‘trim’ OR ‘trim family’ OR ‘trim proteins’ OR ‘tripartite motif’ OR ‘tripartite motif proteins’; ‘cancer’ OR ‘tumor’ OR ‘carcinoma’ OR ‘neoplasm’; ‘colon’ OR ‘rectum’ OR ‘colorectal’. To avoid ignoring qualified studies, all references of the selected primary studies were screened.
Inclusion and exclusion criteria
First, based on the pre-specified selection criteria, two independent researchers screened titles and abstracts to exclude irrelevant studies. Duplicate studies were also excluded from analysis. Next, the full text of all potentially pertinent studies were assessed according to the following inclusion criteria: (1) the expression of TRIM proteins was detected in primary tumor tissues after surgical resection; (2) all patients included were divided into two or more groups based on the TRIM expression levels; (3) the hazard ratio (HR) of survival outcomes or clinicopathological features related to high and low levels of TRIM expressions were available; and (4) the survival curves or sufficient data were available to calculate the HR with 95% confidence interval (CI).
The exclusion criteria were as follows: (1) studies without prognostic outcomes; (2) studies with insufficient data for analysis; and (3) study designs of reviews, case reports, conference abstracts, editorials and letters.
Data extraction
The following data were independently collected by two investigators from eligible studies: first author, year of publication, country, sample capacity, duration of follow-up, overexpression rate, detection method and outcome measures. The data were extracted into a predefined table. Additionally, information was collected on the clinicopathological parameters related to tumor progression. For survival outcome extraction, the HRs and 95% CIs were directly collected from the multivariate and univariate analysis calculated by Cox proportional hazards regression model. We extracted the crude HR and 95% CIs from the univariate analysis and the adjusted HR and 95% CIs after adjustment for potential confounders from the multivariate analysis. Engauge Digitizer version 4.0. was used to estimate survival statistics if Kaplan–Meier curves were only provided. Disagreements between the two reviewers were verified after a discussion and review of the trial information.
Quality assessment
The quality of the enrolled studies was assessed using the Newcastle–Ottawa quality assessment scale, which consists of three main aspects: (1) selection of the research groups, (2) comparability of the groups and (3) ascertainment of the exposure or outcome [ 13 ].
Statistical analysis
The relationship between the expression of TRIM proteins and prognosis, as well as the clinicopathological features of CRCs, was analyzed using STATA/SE 17. To estimate the potential heterogeneity among the included studies, I 2 statistics and the Chi-square Q test were employed. A fixed-effects model was applied to pool the HR of each eligible study into a summary HR if there was no obvious heterogeneity (I 2 < 50% or P Q ≥ 0.10). In contrast, when heterogeneity was considered significant (I 2 ≥ 50% or P Q < 0.10), the random-effects model was adopted. The sources of heterogeneity were explored using subgroup or meta-regression analyses to examine all possible factors. Funnel plots and Egger’s and Begg’s tests were performed to assess the risk of publication bias [ 14 ]. Sensitivity analysis was performed to ensure the stability of the summarized results. In the present study, * P < 0.05 indicated a significant difference.
Characteristics of eligible studies
Details of the meta-analysis search process are shown in Fig. 1 . Using a database search, 135 articles were initially identified, after removing duplicates. Following the removal of reviews and articles focusing on cellular or animal experiments, 66 studies remained for further reading. Finally, 12 articles with 1608 patients in total were included in the present meta-analysis based on the bias of the inclusion and exclusion criteria abovementioned [ 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 ]. The lack of sufficient data for analysis was the most common reason for exclusion during the full-text review process.
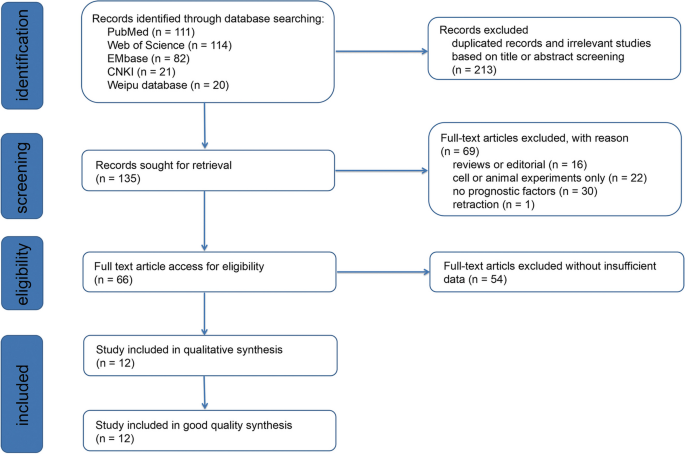
Flow-process diagram of the study selection process
The characteristics of the included 12 studies are summarized in Table 1 . Among the 12 eligible studies published from 2013 to 2020, one was from Ireland and the remaining 11 were conducted in China. Seven of 12 studies didn’t report the follow-up duration. Two study’s follow-up time were at least 40 months and 60 months respectively. The median follow-up duration is 54 months (range 1–122 months) in Seán Fitzgerald’s research, 60 months in Zhang Y’s study and 43.6± 38.4 months (range, 4–132 months) in Li CG’s work. Twelve studies reported the overall survival (OS) of patients with CRC, whereas two studies reported an association between recurrence-free survival (RFS) and TRIM proteins. The expression of TRIM proteins in tissue samples and adjacent non-tumor tissues was detected by immunohistochemistry. Most of the enrolled studies performed univariate and multivariate Cox regression analyses; otherwise, Kaplan–Meier Curves were provided. The crude and adjusted HR values reported by univariate and multivariate analysis and HR extracted by Kaplan-Meier curves are listed in Supplementary Table 1 .
All enrolled articles, ranging from six to nine, were assessed to be of high quality based on the Newcastle–Ottawa quality assessment scale.
Correlation between increased TRIM expression and OS
As is shown in Fig. 2 , the summary HR for the OS comparing TRIM proteins over-expression versus low-expression is 2.42 (95% CI: 1.96–2.99, *** P ≤ 0.0001), and moderate heterogeneity between studies (I 2 = 40.9%, P = 0.069) is observed. Elevated TRIM expressions in CRC tissues are strongly associated with poor OS, indicating that elevated TRIM protein levels could serve as a poor prognostic indicator in CRC. In addition, considering the presence of heterogeneity, subgroup analyses were performed according to the following three parameters: cut-off value (final staining scores, percentage of positive cells and others), sample size of studies (≥ 100 and < 100) and analysis type (multivariate and survival curves). Pooled analysis results demonstrated that all subgroups were in accordance with the OS as abovementioned (Supplementary Table 2 ); however, a possible interaction was noted between the analysis type and sample size subgroups. The heterogeneity was clearly decreased in the analysis type (I 2 = 0.0%) and sample size (I 2 = 27.1%) subgroups, suggesting that different types of analyses and sample capacity may result in the main heterogeneity among the correlations between the overexpression and OS.
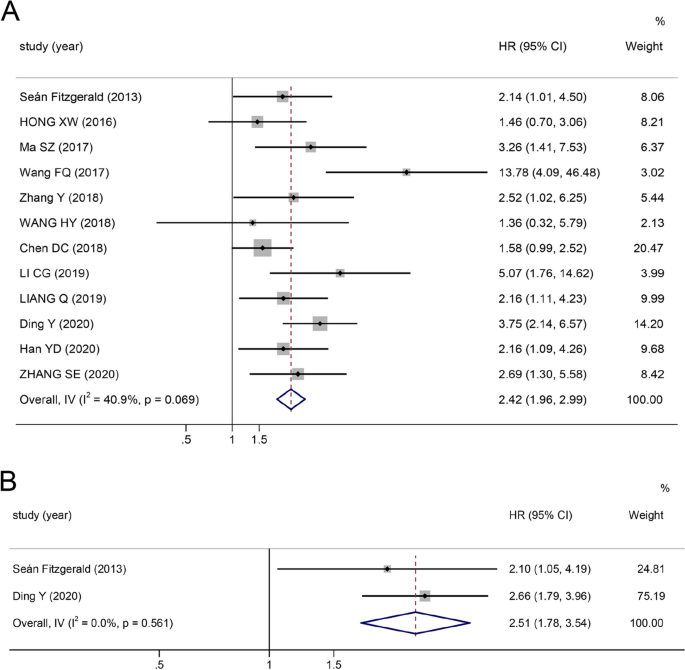
Forest plot of HR for the relationship between increased TRIM family expressions and OS and RFS
Correlation between increased TRIM expression and RFS
As shown in Fig. 2 , the pooled HR demonstrates that a high level of TRIM expression is associated with poor RFS (HR 2.51, 95% CI: 1.78–3.54, *** P ≤ 0.0001). No heterogeneity was observed among the studies (I 2 = 0.0%, P = 0.561).
Correlation between increased TRIM expression and clinicopathological features
To assess the risk of TRIM overexpression under different clinicopathological features, the pooled odds ratios (ORs) were calculated (Table 2 ). The results revealed that a high-level expression of TRIM was associated with an advanced TNM stage (OR = 2.26, 95% CI: 1.25–4.10), deeper depth of tumor invasion (OR = 2.01, 95% CI: 1.04–3.88), poor tumor differentiation (OR = 0.63, 95% CI: 0.44–0.90), lymph node metastasis (OR = 2.99, 95% CI: 2.19–4.09) and perineural invasion (OR = 1.95, 95% CI: 1.18–3.23). Conversely, no significant association was observed between up-regulated TRIM expressions and gender (OR = 1.04, 95% CI: 0.82–1.33, P = 0.725), tumor location (OR = 0.93, 95% CI: 0.65–1.33, P = 0.673) or distant metastasis (OR = 0.92, 95% CI: 0.39–2.19, P = 0.855).
Publication bias and sensitivity analysis
Funnel plot and Begg’s and Egger’s tests were used to test for publication bias. The funnel plot for OS did not show any obvious publication bias (Fig. 3 ). The results of Begg’s ( P = 0.244) and Egger’s ( P = 0.184) tests were not significantly different (Supplementary Figure S 1 ); therefore, no significant publication bias occurred in the present meta-analysis. In addition, sensitivity analysis (Fig. 4 ) showed that even after sequentially omitting the included articles, the pooled results of the meta-analysis were still relatively robust.
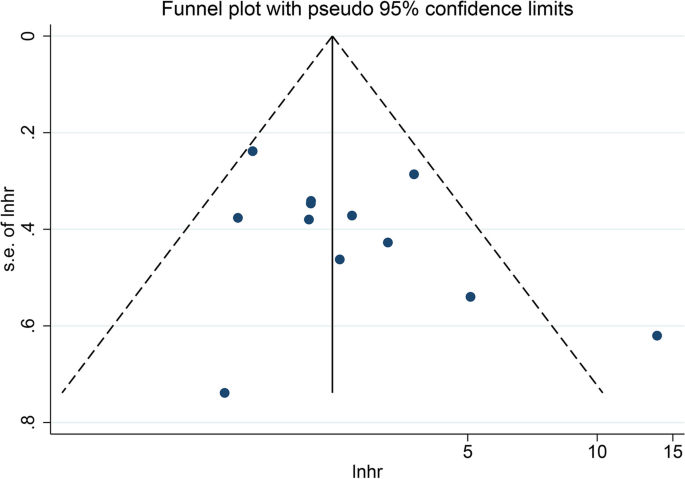
Funnel plot of TRIM family expressions and OS
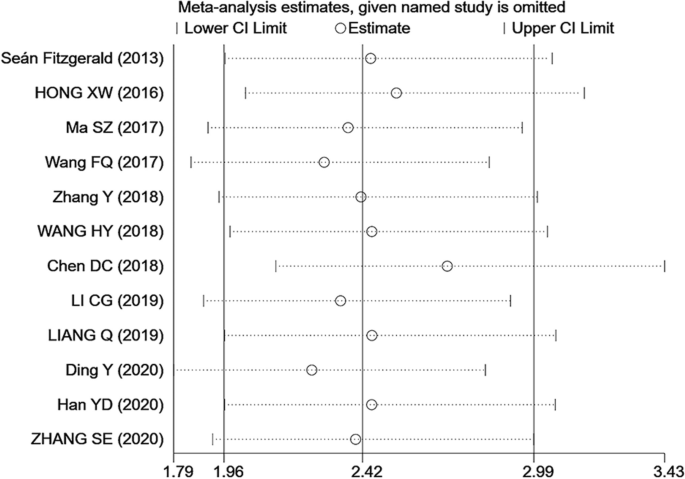
Sensitivity analysis of TRIM family expressions and OS
Thus far, more than 80 TRIM proteins have been discovered and shown to be involved in the tumor progression of various malignancies [ 27 ]. Numerous TRIM proteins are implicated in the ubiquitination–proteasome system as E3-ubiquitin ligases. Therefore, they regulate diverse cellular processes, including proliferation, differentiation, signal transduction, autophagy and protein stability, which can result in tumorigenesis in an increasingly specific and important manner [ 8 ]. Numerous TRIM family members have been reported to be overexpressed in one or more cancers, such as hepatocellular carcinoma, gastric, lung and pancreatic cancers and breast carcinoma [ 28 , 29 , 30 ]. In contrast to non-tumor tissues, CRC tissues show higher levels of TRIM52 expression, and elevated TRIM52 levels are significantly correlated with the proliferation, migration and invasion of CRC cells [ 31 ]. TRIM59 is also upregulated and associated with tumor size and lymph node metastasis, indicating poor prognosis in CRC [ 32 ]. The upregulation of distinct TRIM family members is correlated with poor overall survival outcomes among cancer patients; therefore, TRIM proteins have excellent potential as biomarkers for cancer prognosis.
Recent studies have aggregated the functions of certain TRIM family members in cancer prognosis according to diverse tumor types. For instance, Hu et al. estimated the mortality risk in a relatively large population composed of 7239 participants in 17 studies, which showed that high expression of TRIM21 was significantly correlated with improved OS and progression-free survival in various cancers [ 33 ]. A meta-analysis by Xiao et al. reported that overexpression of TRIM44 was significantly correlated with not only shorter over-survival and worse disease-free survival, but also tumor metastasis, poor tumor differentiation, deeper tumor invasion and advanced clinical stage [ 34 ]. Both Xue et al. and Yuan et al. reported that upregulated TRIM24 expression significantly predicts poor overall survival in different types of malignancies [ 35 , 36 ]. Whether the overexpression of TRIM proteins could be useful in predicting the prognosis of patients with CRC remains unclear.
To our knowledge, our meta-analysis is the first systematic review and meta-analysis to assess the prognostic and clinicopathological values of TRIM proteins for patients with CRC. Herein, the pooled results of 1608 participants with CRC from 12 eligible studies indicated that patients with CRC with elevated TRIM protein expressions had significantly shorter OS and worse RFS than those with normal TRIM expressions. In the meta-analysis of OS, moderate heterogeneity was observed (I 2 =40.9%, P = 0.069). However, subsequent subgroup analyses further confirmed that the cut-off value, sample size and type of analysis did not significantly affect the results. Moreover, sensitivity analyses were performed by omitting one study at a time, and publication bias tests did not significantly influence the results. Therefore, the overexpression of TRIM proteins may be positively correlated with poor prognosis. TRIM28, which is highly expressed in patients with CRC, is an independent prognostic marker for OS, with a pooled HR of 2.57 in two different prospective studies by Fitzgerald et al. and Ma et al., with a total of 202 patients with CRC (Supplementary Figure S 2 ) [ 15 , 17 ].
Because the clinicopathological features in different groups of patients affect their outcomes, eight major factors between patients with upregulated and normal TRIM expressions were compared. The overexpression of TRIM proteins was markedly associated with higher TNM stage, deeper invasion, lymph node metastasis and perineural invasion. Notably, patients with higher levels of TRIM proteins exhibited an enhanced degree of tumor histological differentiation, which contradicts previous studies [ 34 ]. Thus, more studies with larger populations should be conducted in the future to confirm these conflicting results. However, TRIM protein expression was not significantly associated with gender, tumor site or distant metastasis. In the present study, overexpression of TRIM proteins was associated with CRC progression and poor clinical outcomes. An increasing number of studies have demonstrated that TRIM proteins contribute to the diverse malignant biological behaviors of CRC cells. Hence, TRIM proteins have excellent potential to serve as biomarkers for CRC prognosis, and further research should be conducted to investigate the molecular mechanisms and to verify the clinical application of TRIM proteins.
Our systematic review has some limitations. First, most of the studies we chose were conducted in the Chinese population, to the extent that the statistical analysis of publication bias lacked sufficient power. Notably, one study with a high HR was responsible for almost all the observed heterogeneity. However, sensitivity analyses showed that removing this article did not significantly influence the pooled results. Therefore, additional samples from other countries or races should be included to confirm the reliability of these results. Second, we were unable to contact the authors of certain studies to retrieve data. In some articles, HRs and 95% CI were extracted from additional data, such as Kaplan–Meier curves, which might have resulted in an uncertain bias for the pooled estimates. And unfortunately, some studies lack of detailed information, which might result in a lack of control for potential confounding factors. Third, owing to the limited number of studies, heterogeneity still existed in some results of clinicopathological characteristics.
In summary, our current study demonstrates that TRIM proteins are correlated with cancer progression and prognosis in patients with CRC. The TRIM family may be a reliable biomarker for determining the clinicopathological characteristics and prognosis of malignancies. With further understanding of the regulatory mechanisms, TRIM proteins are promising new therapeutic targets for CRC.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its Supplementary information files.
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209–49.
Article PubMed Google Scholar
Siegel RL, Wagle NS, Cercek A, Smith RA, Jemal A. Colorectal cancer statistics, 2023. CA Cancer J Clin. 2023;73(3):233–54.
Brenner H, Kloor M, Pox CP. Colorectal cancer. Lancet Lond Engl. 2014;383(9927):1490–502.
Article Google Scholar
De Sousa E, Melo F, Colak S, Buikhuisen J, Koster J, Cameron K, de Jong JH, et al. Methylation of cancer-stem-cell-associated Wnt target genes predicts poor prognosis in colorectal cancer patients. Cell Stem Cell. 2011;9(5):476–85.
Giovannetti E, Backus HHJ, Wouters D, Ferreira CG, van Houten VMM, Brakenhoff RH, et al. Changes in the status of p53 affect drug sensitivity to thymidylate synthase (TS) inhibitors by altering TS levels. Br J Cancer. 2007;96(5):769–75.
Article CAS PubMed PubMed Central Google Scholar
Vunjak M, Versteeg GA. TRIM proteins. Curr Biol CB. 2019;29(2):R42-4.
Article CAS PubMed Google Scholar
Hatakeyama S. TRIM Family Proteins: Roles in Autophagy, Immunity, and Carcinogenesis. Trends Biochem Sci. 2017;42(4):297–311.
Mohammadi A, Pour Abbasi MS, Khorrami S, Khodamoradi S, Mohammadi Goldar Z, Ebrahimzadeh F. The TRIM proteins in cancer: from expression to emerging regulatory mechanisms. Clin Transl Oncol. 2022;24(3):460–70.
Marzano F, Caratozzolo MF, Pesole G, Sbisà E, Tullo A. TRIM Proteins in Colorectal Cancer: TRIM8 as a Promising Therapeutic Target in Chemo Resistance. Biomedicines. 2021;9(3):241.
Lu K, Pan Y, Huang Z, Liang H, Ding ZY, Zhang B. TRIM proteins in hepatocellular carcinoma. J Biomed Sci. 2022;29(1):69.
Zhan W, Zhang S. TRIM proteins in lung cancer: Mechanisms, biomarkers and therapeutic targets. Life Sci. 2021;1(268): 118985.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;29(372): n71.
Wells G, Shea B, O'Connell J. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. Ottawa Health Research Institute Web site. 2014;7(1).
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Fitzgerald S, Sheehan KM, O’Grady A, Kenny D, O’Kennedy R, Kay EW, et al. Relationship between epithelial and stromal TRIM28 expression predicts survival in colorectal cancer patients: TRIM28 predicts survival in colorectal cancer. J Gastroenterol Hepatol. 2013;28(6):967–74.
Xu W, Xu B, Yao Y, Yu X, Cao H, Zhang J, et al. RNA interference against TRIM29 inhibits migration and invasion of colorectal cancer cells. Oncol Rep. 2016;36(3):1411–8.
Ma SZ, et al. Expression of TRIM28 in colorectal cancer tissues and its effect on the proliferation and migration of cancer cells. Shandong Medical Journal. 2017;57:28–30.
Google Scholar
Fengqin Wang. Prognostic relevance of tripartite motif containing 24 expression in colorectal cancer. Pathol - Res Pract. 2017;213(10):1271–5.
Haiyu Wang Lu, Yao Yuda Gong, Zhang Bo. TRIM31 regulates chronic inflammation via NF-κB signal pathway to promote invasion and metastasis in colorectal cancer. Am J Transl Res. 2018;10(4):1247.
PubMed PubMed Central Google Scholar
Zhang Y, Feng Y, Ji D, Wang Q, Qian W, Wang S, et al. TRIM27 functions as an oncogene by activating epithelial-mesenchymal transition and p-AKT in colorectal cancer. Int J Oncol. 2018;53(2):620–32.
CAS PubMed PubMed Central Google Scholar
Chen Daici, Li Yichen, Zhang Xiaowen, Haiyong Wu, Wang Qian, Cai Jian, et al. Ubiquitin ligase TRIM65 promotes colorectal cancer metastasis by targeting ARHGAP35 for protein degradation. Oncogene. 2019;38(37):6429–44.
Li CG, Hu H, Yang XJ, Huang CQ, Yu XQ. TRIM44 Promotes Colorectal Cancer Proliferation, Migration, and Invasion Through the Akt/mTOR Signaling Pathway. OncoTargets Ther. 2019;12:10693–701.
Article CAS Google Scholar
Liang Q, Tang C, Tang M, Zhang Q, Gao Y, Ge Z. TRIM47 is up-regulated in colorectal cancer, promoting ubiquitination and degradation of SMAD4. J Exp Clin Cancer Res CR. 2019;12(38):159.
Ding Y, et al. expression of TRIM14 in Colorectal Cancer and Its Clinical Significance. Acta Med Univ Sci Technol Huazhong. 2020;49(3):323–7.
Zheng Shuier, Zhou Chenliang, Wang Yonggang, Li Hongtao, Sun Yong, Shen Zan. TRIM6 promotes colorectal cancer cells proliferation and response to thiostrepton by TIS21/FoxM1. J Exp Clin Cancer Res CR. 2020;28(39):23.
Han Y, Tan Y, Zhao Y, Zhang Y, He X, Yu L, et al. TRIM23 overexpression is a poor prognostic factor and contributes to carcinogenesis in colorectal cancer. J Cell Mol Med. 2020;24(10):5491–500.
Gu J, Chen J, Xiang S, Zhou X, Li J. Intricate confrontation: Research progress and application potential of TRIM family proteins in tumor immune escape. J Adv Res. 2023;S2090–1232(23):00024–3.
Yang X, Zhang Y, Xue Z, Hu Y, Zhou W, Xue Z, et al. TRIM56 promotes malignant progression of glioblastoma by stabilizing cIAP1 protein. J Exp Clin Cancer Res CR. 2022;41(1):336.
Ji J, Ding K, Luo T, Zhang X, Chen A, Zhang D, et al. TRIM22 activates NF-κB signaling in glioblastoma by accelerating the degradation of IκBα. Cell Death Differ. 2021;28(1):367–81.
Liu Y, Tao S, Liao L, Li Y, Li H, Li Z, et al. TRIM25 promotes the cell survival and growth of hepatocellular carcinoma through targeting Keap1-Nrf2 pathway. Nat Commun. 2020;11(1):348.
Article PubMed PubMed Central Google Scholar
Guo Y, Zhou Y, Gu X, Xiang J. Tripartite motif 52 (TRIM52) promotes proliferation, migration, and regulation of colon cancer cells associated with the NF-κB signaling pathway. J Gastrointest Oncol. 2022;13(3):1097–111.
Dahpy MA, Salama RHM, Kamal AA, El-Deek HE, Abdel Motaleb AA, Abd-El-Rehim AS, et al. Evaluation of tripartite motif 59 and its diagnostic utility in benign bowel diseases and colorectal cancer. J Biochem Mol Toxicol. 2022;36(7):e23065.
Hu F, Liu Y, Wang F, Fu X, Liu X, Zou Z, et al. Prognostic and clinicopathological significance of TRIM21 in various cancers: A meta and bioinformatic analysis. Medicine (Baltimore). 2023;102(23): e34012.
Xiao G, Yang Q, Bao Z, Mao H, Zhang Y, Lin S. Expression of tripartite motif-containing 44 and its prognostic and clinicopathological value in human malignancies:a meta-analysis. BMC Cancer. 2020;20(1):525.
Xue Y, Ge W, Shi W, Huang W, Wang R. Prognostic role of tripartite motif containing 24 in various human solid malignant neoplasms: An updated meta-analysis and systematic review. Medicine (Baltimore). 2021;100(51): e28383.
He Y, Peng KW, Tang T, Deng L, Ye ZL, Luo MJ, et al. Prognostic Implications of Tripartite Motif Containing 24 Expression Levels in Patients with Solid Tumors: A Systematic Review and Meta-Analysis. Genet Test Mol Biomark. 2019;23(7):473–9.
Download references
Acknowledgements
I really appreciate for what Chen Chen, Hua Xian, Chunhua Zhao and Han Min contributed to the study, as well as Editage edited my manuscript.
This work was supported by the Suzhou Municipal Health Commission (GSWS2021041) and the Postgraduate Research and Innovation Program, Jiangsu Province (KYCX22_1781).
Author information
Authors and affiliations.
Department of Gastroenterology, The Affiliated Suzhou Hospital of Nanjing Medical University, Suzhou Municipal Hospital, Gusu School, Nanjing Medical University, Suzhou, Jiangsu, China
Ying Wu, Chen Chen, Xian Hua & Han Min
Department of General Medicine, Big Data Center, The Affiliated Suzhou Hospital of Nanjing Medical University, Suzhou Municipal Hospital, Nanjing Medical University, Suzhou, China
Chunhua Zhao
You can also search for this author in PubMed Google Scholar
Contributions
Ying Wu and Chun-Hua Zhao generated the research question, designed the study and approved the final manuscript. Xian Hua made critical appraisals. Chen Chen, Han Min and Chun-Hua Zhao contributed to critically reviewing and editing of the manuscript with regard to important intellectual content. All authors approved of this final version of the manuscript to be submitted.
Corresponding authors
Correspondence to Chunhua Zhao or Han Min .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Wu, Y., Chen, C., Hua, X. et al. Association of the TRIM family protein with survival outcomes and clinicopathological features in colorectal cancer: a systematic review and meta-analysis. BMC Cancer 24 , 537 (2024). https://doi.org/10.1186/s12885-024-12280-z
Download citation
Received : 21 September 2023
Accepted : 17 April 2024
Published : 27 April 2024
DOI : https://doi.org/10.1186/s12885-024-12280-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Colorectal cancer
- TRIM family proteins
- Clinicopathological features
ISSN: 1471-2407
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Comparison of the perioperative outcomes of robot-assisted laparoscopic transperitoneal versus retraperitoneal partial nephrectomy for posterior-lateral renal tumors: a systematic review and meta-analysis
- Published: 29 April 2024
- Volume 18 , article number 186 , ( 2024 )
Cite this article

- Pengjun Xu 1 ,
- Jia Luo 1 ,
- Hui Shuai 1 ,
- Tao Cai 1 ,
- Shu Cui 1 ,
- Lin Zhou 1 ,
- Qian Xu 1 ,
- Yuxin Zhao 1 ,
- Tao Chen 1 ,
- Wang Shan 2 &
- Tao Wu 1 , 3
The study aims to assess the available literature and compare the perioperative outcomes of robotic-assisted partial nephrectomy (RAPN) for posterior-lateral renal tumors using transperitoneal (TP) and retroperitoneal (RP) approaches. Systematically searched the Embase, PubMed, and Cochrane Library databases for literature. Eligible studies were those that compared TP-RAPN and RP-RAPN for posterior-lateral renal tumors. The data from the included studies were analyzed and summarized using Review Manager 5.3, which involved comparing baseline patient and tumor characteristics, intraoperative and postoperative outcomes, and oncological outcomes. The analysis included five studies meeting the inclusion criteria, with a total of 1440 patients (814 undergoing RP-RAPN and 626 undergoing TP-RAPN). Both groups showed no significant differences in age, gender, BMI, R.E.N.A.L. score, and tumor size. Notably, compared to TP-RAPN, the RP-RAPN group demonstrated shorter operative time (OT) (MD: 17.25, P = 0.01), length of hospital stay (LOS) (MD: 0.37, P < 0.01), and lower estimated blood loss (EBL) (MD: 15.29, P < 0.01). However, no significant differences were found between the two groups in terms of warm ischemia time (WIT) (MD: -0.34, P = 0.69), overall complications (RR: 1.25, P = 0.09), major complications (the Clavien-Dindo classification ≥ 3) (RR: 0.97, P = 0.93), and positive surgical margin (PSM) (RR: 1.06, P = 0.87). The systematic review and meta-analysis suggests RP-RAPN may be more advantageous for posterior-lateral renal tumors in terms of OT, EBL, and LOS, but no significant differences were found in WIT, overall complications, major complications, and PSM. Both surgical approaches are safe, but a definitive advantage remains uncertain.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Data availability
All data generated or analyzed during this study are included in the article. Further inquiries can be directed to the corresponding author.
Siegel RL, Miller KD, Wagle NS, Jemal A (2023) Cancer statistics. CA Cancer J Clin 73(1):17–48. https://doi.org/10.3322/caac.21763
Article PubMed Google Scholar
Schaeffer EM, Srinivas S, Adra N et al (2023) Prostate cancer, version 4.2023, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw 21(10):1067–1096. https://doi.org/10.6004/jnccn.2023.0050
Article CAS PubMed Google Scholar
Carbonara U, Simone G, Minervini A et al (2021) Robotic-assisted partial nephrectomy for “very small” (<2 cm) renal mass: results of a multicenter contemporary cohort. Eur Urol Focus 7(5):1115–1120. https://doi.org/10.1016/j.euf.2020.10.001
Ghani KR, Porter J, Menon M, Rogers C (2014) Robotic retroperitoneal partial nephrectomy: a step-by-step guide. BJU Int 114(2):311–313. https://doi.org/10.1111/bju.12709
Fan X, Xu K, Lin T et al (2013) Comparison of transperitoneal and retroperitoneal laparoscopic nephrectomy for renal cell carcinoma: a systematic review and meta-analysis. BJU Int 111(4):611–621. https://doi.org/10.1111/j.1464-410X.2012.11598.x
Bourgi A, Ayoub E, Merhej S et al (2023) A comparison of perioperative outcomes of transperitoneal versus retroperitoneal robot-assisted partial nephrectomy: a systematic review. J Robot Surg 17(6):2563–2574. https://doi.org/10.1007/s11701-023-01685-w
Xia L, Zhang X, Wang X et al (2016) Transperitoneal versus retroperitoneal robot-assisted partial nephrectomy: a systematic review and meta-analysis. Int J Surg 30:109–115. https://doi.org/10.1016/j.ijsu.2016.04.023
Luo D, Wan X, Liu J, Tong T (2018) Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res 27(6):1785–1805. https://doi.org/10.1177/0962280216669183
Wan X, Wang W, Liu J, Tong T (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 19(14):135. https://doi.org/10.1186/1471-2288-14-135
Article Google Scholar
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–605. https://doi.org/10.1007/s10654-010-9491-z
Harke NN, Darr C, Radtke JP et al (2021) Retroperitoneal versus transperitoneal robotic partial nephrectomy: a multicenter matched-pair analysis. Eur Urol Focus 7(6):1363–1370. https://doi.org/10.1016/j.euf.2020.08.012
Maurice MJ, Kaouk JH, Ramirez D et al (2017) robotic partial nephrectomy for posterior tumors through a retroperitoneal approach offers decreased length of stay compared with the transperitoneal approach: a propensity-matched analysis. J Endourol 31(2):158–162. https://doi.org/10.1089/end.2016.0603
Paulucci DJ, Beksac AT, Porter J et al (2019) A Multi-institutional propensity score matched comparison of transperitoneal and retroperitoneal partial nephrectomy for cT1 posterior tumors. J Laparoendosc Adv Surg Tech A 29(1):29–34. https://doi.org/10.1089/lap.2018.0313
Takagi T, Yoshida K, Kondo T et al (2021) Comparisons of surgical outcomes between transperitoneal and retroperitoneal approaches in robot-assisted laparoscopic partial nephrectomy for lateral renal tumors: a propensity score-matched comparative analysis. J Robot Surg 15(1):99–104. https://doi.org/10.1007/s11701-020-01086-3
Carbonara U, Eun D, Derweesh I et al (2021) Retroperitoneal versus transepritoneal robot-assisted partial nephrectomy for postero-lateral renal masses: an international multicenter analysis. World J Urol 39(11):4175–4182. https://doi.org/10.1007/s00345-021-03741-2
Kim EH, Larson JA, Potretzke AM et al (2015) Retroperitoneal robot-assisted partial nephrectomy for posterior renal masses is associated with earlier hospital discharge: a single-institution retrospective comparison. J Endourol 29(10):1137–1142. https://doi.org/10.1089/end.2015.0076
Wang L, Li KP, Liu Y et al (2023) Perioperative and oncologic outcomes of transperitoneal versus retroperitoneal laparoscopic radical nephrectomy for large-volume renal carcinoma (> 7 cm): a systematic review and pooled analysis of comparative outcomes. World J Surg Oncol. https://doi.org/10.1186/s12957-023-02967-1
Article PubMed PubMed Central Google Scholar
Marconi L, Challacombe B (2018) Robotic partial nephrectomy for posterior renal tumours: retro or transperitoneal approach? Eur Urol Focus 4(5):632–635. https://doi.org/10.1016/j.euf.2018.08.003
Xiong L, Nguyen JK, Peng Y et al (2022) What happens to the preserved renal parenchyma after clamped partial nephrectomy? Eur Urol 81(5):492–500. https://doi.org/10.1016/j.eururo.2021.12.036
Ge S, Chen L, Tai S (2020) Comparison of therapeutic effects among different surgical approaches in robot-assisted partial nephrectomy: a systematic review and meta-analysis. J Endourol 35(5):623–632. https://doi.org/10.1089/end.2020.0432
McLean A, Mukherjee A, Phukan C et al (2020) Trans-peritoneal vs. retroperitoneal robotic assisted partial nephrectomy in posterior renal tumours: need for a risk-stratified patient individualised approach. A systematic review and meta-analysis. J Robot Surg. https://doi.org/10.1007/s11701-019-00973-8
Download references
This work was supported by the City of Nanchong Strategic Cooperation with the Local Universities Foundation of Technology (20SXQT0305 and 18SXHZ0321), the Application and Basic Research Program of the Sichuan Science and Technology Department (2020YJ0185 and 2022NSFSC0804), the Primary Health Development Research Center of Sichuan Province Program (SWFZ21-C-98), and the Medical Research Project of the Sichuan Medical Association (S21061).
Author information
Authors and affiliations.
Department of Urology, Affiliated Hospital of North Sichuan Medical College, No. 1 Maoyuan South Road,Shunqing, Nanchong, 637000, Sichuan, People’s Republic of China
Pengjun Xu, Jia Luo, Hui Shuai, Tao Cai, Shu Cui, Lin Zhou, Qian Xu, Yuxin Zhao, Tao Chen & Tao Wu
Department of Biomedical Engineering, Faculty of Engineering, The Hong Kong Polytechnic University, Hong Kong, China
Department of Urology, Affiliated Hospital of North Sichuan Medical College, Wenhua Road 57, Shunqing District, Nanchong, 637000, Sichuan, People’s Republic of China
You can also search for this author in PubMed Google Scholar
Contributions
XPJ: project development; data analysis; manuscript writing. LJ: project development; data collection; manuscript writing. SH: data collection; manuscript writing. Cai Tao: manuscript editing. CS: manuscript editing. ZL: data analysis. XQ: data analysis. ZYX: data analysis. Tao chen: data analysis. WT: project development; supervision. All authors read and approved the final version of the manuscript.
Corresponding author
Correspondence to Tao Wu .
Ethics declarations
Conflict of interest.
The authors declare that there is no conflict of interest.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (DOCX 17 KB)
Rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Xu, P., Luo, J., Shuai, H. et al. Comparison of the perioperative outcomes of robot-assisted laparoscopic transperitoneal versus retraperitoneal partial nephrectomy for posterior-lateral renal tumors: a systematic review and meta-analysis. J Robotic Surg 18 , 186 (2024). https://doi.org/10.1007/s11701-024-01963-1
Download citation
Received : 08 March 2024
Accepted : 21 April 2024
Published : 29 April 2024
DOI : https://doi.org/10.1007/s11701-024-01963-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Kidney neoplasms
- Robotic Surgical Procedures
- Patient Outcome Assessment
- Posterior-lateral tumors
- Robot-assisted partial nephrectomy
- Find a journal
- Publish with us
- Track your research
- Open access
- Published: 24 April 2024
Breast cancer screening motivation and behaviours of women aged over 75 years: a scoping review
- Virginia Dickson-Swift 1 ,
- Joanne Adams 1 ,
- Evelien Spelten 1 ,
- Irene Blackberry 2 ,
- Carlene Wilson 3 , 4 , 5 &
- Eva Yuen 3 , 6 , 7 , 8
BMC Women's Health volume 24 , Article number: 256 ( 2024 ) Cite this article
198 Accesses
Metrics details
This scoping review aimed to identify and present the evidence describing key motivations for breast cancer screening among women aged ≥ 75 years. Few of the internationally available guidelines recommend continued biennial screening for this age group. Some suggest ongoing screening is unnecessary or should be determined on individual health status and life expectancy. Recent research has shown that despite recommendations regarding screening, older women continue to hold positive attitudes to breast screening and participate when the opportunity is available.
All original research articles that address motivation, intention and/or participation in screening for breast cancer among women aged ≥ 75 years were considered for inclusion. These included articles reporting on women who use public and private breast cancer screening services and those who do not use screening services (i.e., non-screeners).
The Joanna Briggs Institute (JBI) methodology for scoping reviews was used to guide this review. A comprehensive search strategy was developed with the assistance of a specialist librarian to access selected databases including: the Cumulative Index to Nursing and Allied Health Literature (CINAHL), Medline, Web of Science and PsychInfo. The review was restricted to original research studies published since 2009, available in English and focusing on high-income countries (as defined by the World Bank). Title and abstract screening, followed by an assessment of full-text studies against the inclusion criteria was completed by at least two reviewers. Data relating to key motivations, screening intention and behaviour were extracted, and a thematic analysis of study findings undertaken.
A total of fourteen (14) studies were included in the review. Thematic analysis resulted in identification of three themes from included studies highlighting that decisions about screening were influenced by: knowledge of the benefits and harms of screening and their relationship to age; underlying attitudes to the importance of cancer screening in women's lives; and use of decision aids to improve knowledge and guide decision-making.
The results of this review provide a comprehensive overview of current knowledge regarding the motivations and screening behaviour of older women about breast cancer screening which may inform policy development.
Peer Review reports
Introduction
Breast cancer is now the most commonly diagnosed cancer in the world overtaking lung cancer in 2021 [ 1 ]. Across the globe, breast cancer contributed to 25.8% of the total number of new cases of cancer diagnosed in 2020 [ 2 ] and accounts for a high disease burden for women [ 3 ]. Screening for breast cancer is an effective means of detecting early-stage cancer and has been shown to significantly improve survival rates [ 4 ]. A recent systematic review of international screening guidelines found that most countries recommend that women have biennial mammograms between the ages of 40–70 years [ 5 ] with some recommending that there should be no upper age limit [ 6 , 7 , 8 , 9 , 10 , 11 , 12 ] and others suggesting that benefits of continued screening for women over 75 are not clear [ 13 , 14 , 15 ].
Some guidelines suggest that the decision to end screening should be determined based on the individual health status of the woman, their life expectancy and current health issues [ 5 , 16 , 17 ]. This is because the benefits of mammography screening may be limited after 7 years due to existing comorbidities and limited life expectancy [ 18 , 19 , 20 , 21 ], with some jurisdictions recommending breast cancer screening for women ≥ 75 years only when life expectancy is estimated as at least 7–10 years [ 22 ]. Others have argued that decisions about continuing with screening mammography should depend on individual patient risk and health management preferences [ 23 ]. This decision is likely facilitated by a discussion between a health care provider and patient about the harms and benefits of screening outside the recommended ages [ 24 , 25 ]. While mammography may enable early detection of breast cancer, it is clear that false-positive results and overdiagnosis Footnote 1 may occur. Studies have estimated that up to 25% of breast cancer cases in the general population may be over diagnosed [ 26 , 27 , 28 ].
The risk of being diagnosed with breast cancer increases with age and approximately 80% of new cases of breast cancer in high-income countries are in women over the age of 50 [ 29 ]. The average age of first diagnosis of breast cancer in high income countries is comparable to that of Australian women which is now 61 years [ 2 , 4 , 29 ]. Studies show that women aged ≥ 75 years generally have positive attitudes to mammography screening and report high levels of perceived benefits including early detection of breast cancer and a desire to stay healthy as they age [ 21 , 30 , 31 , 32 ]. Some women aged over 74 participate, or plan to participate, in screening despite recommendations from health professionals and government guidelines advising against it [ 33 ]. Results of a recent review found that knowledge of the recommended guidelines and the potential harms of screening are limited and many older women believed that the benefits of continued screening outweighed the risks [ 30 ].
Very few studies have been undertaken to understand the motivations of women to screen or to establish screening participation rates among women aged ≥ 75 and older. This is surprising given that increasing age is recognised as a key risk factor for the development of breast cancer, and that screening is offered in many locations around the world every two years up until 74 years. The importance of this topic is high given the ambiguity around best practice for participation beyond 74 years. A preliminary search of Open Science Framework, PROSPERO, Cochrane Database of Systematic Reviews and JBI Evidence Synthesis in May 2022 did not locate any reviews on this topic.
This scoping review has allowed for the mapping of a broad range of research to explore the breadth and depth of the literature, summarize the evidence and identify knowledge gaps [ 34 , 35 ]. This information has supported the development of a comprehensive overview of current knowledge of motivations of women to screen and screening participation rates among women outside the targeted age of many international screening programs.
Materials and methods
Research question.
The research question for this scoping review was developed by applying the Population—Concept—Context (PCC) framework [ 36 ]. The current review addresses the research question “What research has been undertaken in high-income countries (context) exploring the key motivations to screen for breast cancer and screening participation (concepts) among women ≥ 75 years of age (population)?
Eligibility criteria
Participants.
Women aged ≥ 75 years were the key population. Specifically, motivations to screen and screening intention and behaviour and the variables that discriminate those who screen from those who do not (non-screeners) were utilised as the key predictors and outcomes respectively.
From a conceptual perspective it was considered that motivation led to behaviour, therefore articles that described motivation and corresponding behaviour were considered. These included articles reporting on women who use public (government funded) and private (fee for service) breast cancer screening services and those who do not use screening services (i.e., non-screeners).
The scope included high-income countries using the World Bank definition [ 37 ]. These countries have broadly similar health systems and opportunities for breast cancer screening in both public and private settings.
Types of sources
All studies reporting original research in peer-reviewed journals from January 2009 were eligible for inclusion, regardless of design. This date was selected due to an evaluation undertaken for BreastScreen Australia recommending expansion of the age group to include 70–74-year-old women [ 38 ]. This date was also indicative of international debate regarding breast cancer screening effectiveness at this time [ 39 , 40 ]. Reviews were also included, regardless of type—scoping, systematic, or narrative. Only sources published in English and available through the University’s extensive research holdings were eligible for inclusion. Ineligible materials were conference abstracts, letters to the editor, editorials, opinion pieces, commentaries, newspaper articles, dissertations and theses.
This scoping review was registered with the Open Science Framework database ( https://osf.io/fd3eh ) and followed Joanna Briggs Institute (JBI) methodology for scoping reviews [ 35 , 36 ]. Although ethics approval is not required for scoping reviews the broader study was approved by the University Ethics Committee (approval number HEC 21249).
Search strategy
A pilot search strategy was developed in consultation with an expert health librarian and tested in MEDLINE (OVID) and conducted on 3 June 2022. Articles from this pilot search were compared with seminal articles previously identified by the members of the team and used to refine the search terms. The search terms were then searched as both keywords and subject headings (e.g., MeSH) in the titles and abstracts and Boolean operators employed. A full MEDLINE search was then carried out by the librarian (see Table 1 ). This search strategy was adapted for use in each of the following databases: Cumulative Index to Nursing and Allied Health Literature (CINAHL), Medical Literature Analysis and Retrieval System Online (MEDLINE), Web of Science and PsychInfo databases. The references of included studies have been hand-searched to identify any additional evidence sources.
Study/source of evidence selection
Following the search, all identified citations were collated and uploaded into EndNote v.X20 (Clarivate Analytics, PA, USA) and duplicates removed. The resulting articles were then imported into Covidence – Cochrane’s systematic review management software [ 41 ]. Duplicates were removed once importation was complete, and title and abstract screening was undertaken against the eligibility criteria. A sample of 25 articles were assessed by all reviewers to ensure reliability in the application of the inclusion and exclusion criteria. Team discussion was used to ensure consistent application. The Covidence software supports blind reviewing with two reviewers required at each screening phase. Potentially relevant sources were retrieved in full text and were assessed against the inclusion criteria by two independent reviewers. Conflicts were flagged within the software which allows the team to discuss those that have disagreements until a consensus was reached. Reasons for exclusion of studies at full text were recorded and reported in the scoping review. The Preferred Reporting Items of Systematic Reviews extension for scoping reviews (PRISMA-ScR) checklist was used to guide the reporting of the review [ 42 ] and all stages were documented using the PRISMA-ScR flow chart [ 42 ].
Data extraction
A data extraction form was created in Covidence and used to extract study characteristics and to confirm the study’s relevance. This included specific details such as article author/s, title, year of publication, country, aim, population, setting, data collection methods and key findings relevant to the review question. The draft extraction form was modified as needed during the data extraction process.
Data analysis and presentation
Extracted data were summarised in tabular format (see Table 2 ). Consistent with the guidelines for the effective reporting of scoping reviews [ 43 ] and the JBI framework [ 35 ] the final stage of the review included thematic analysis of the key findings of the included studies. Study findings were imported into QSR NVivo with coding of each line of text. Descriptive codes reflected key aspects of the included studies related to the motivations and behaviours of women > 75 years about breast cancer screening.
In line with the reporting requirements for scoping reviews the search results for this review are presented in Fig. 1 [ 44 ].
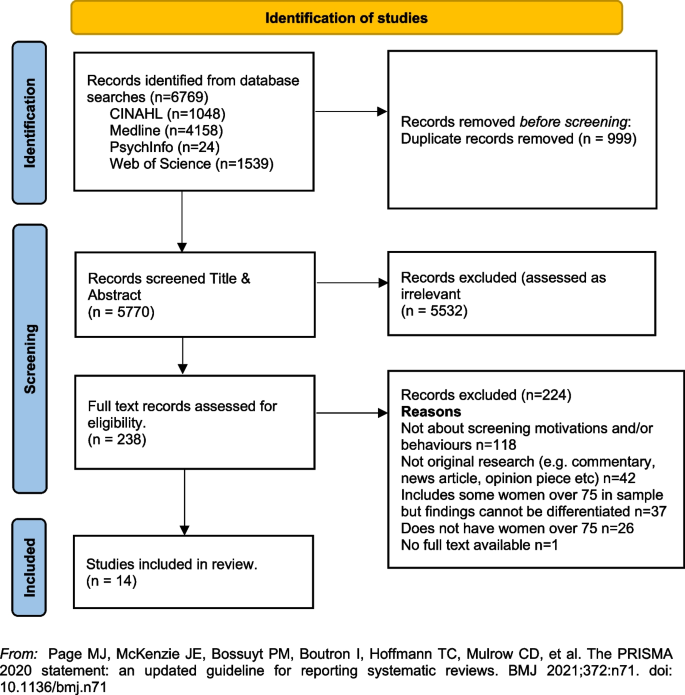
PRISMA Flowchart. From: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. https://doi.org/10.1136/bmj.n71
A total of fourteen [ 14 ] studies were included in the review with studies from the following countries, US n = 12 [ 33 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 ], UK n = 1 [ 23 ] and France n = 1 [ 56 ]. Sample sizes varied, with most containing fewer than 50 women ( n = 8) [ 33 , 45 , 46 , 48 , 51 , 52 , 55 ]. Two had larger samples including a French study with 136 women (a sub-set of a larger sample) [ 56 ], and one mixed method study in the UK with a sample of 26 women undertaking interviews and 479 women completing surveys [ 23 ]. One study did not report exact numbers [ 50 ]. Three studies [ 47 , 53 , 54 ] were undertaken by a group of researchers based in the US utilising the same sample of women, however each of the papers focused on different primary outcomes. The samples in the included studies were recruited from a range of locations including primary medical care clinics, specialist medical clinics, University affiliated medical clinics, community-based health centres and community outreach clinics [ 47 , 53 , 54 ].
Data collection methods varied and included: quantitative ( n = 8), qualitative ( n = 5) and mixed methods ( n = 1). A range of data collection tools and research designs were utilised; pre/post, pilot and cross-sectional surveys, interviews, and secondary analysis of existing data sets. Seven studies focused on the use of a Decision Aids (DAs), either in original or modified form, developed by Schonberg et al. [ 55 ] as a tool to increase knowledge about the harms and benefits of screening for older women [ 45 , 47 , 48 , 49 , 52 , 54 , 55 ]. Three studies focused on intention to screen [ 33 , 53 , 56 ], two on knowledge of, and attitudes to, screening [ 23 , 46 ], one on information needs relating to risks and benefits of screening discontinuation [ 51 ], and one on perceptions about discontinuation of screening and impact of social interactions on screening [ 50 ].
The three themes developed from the analysis of the included studies highlighted that decisions about screening were primarily influenced by: (1) knowledge of the benefits and harms of screening and their relationship to age; (2) underlying attitudes to the importance of cancer screening in women's lives; and (3) exposure to decision aids designed to facilitate informed decision-making. Each of these themes will be presented below drawing on the key findings of the appropriate studies. The full dataset of extracted data can be found in Table 2 .
Knowledge of the benefits and harms of screening ≥ 75 years
The decision to participate in routine mammography is influenced by individual differences in cognition and affect, interpersonal relationships, provider characteristics, and healthcare system variables. Women typically perceive mammograms as a positive, beneficial and routine component of care [ 46 ] and an important aspect of taking care of themselves [ 23 , 46 , 49 ]. One qualitative study undertaken in the US showed that few women had discussed mammography cessation or the potential harms of screening with their health care providers and some women reported they would insist on receiving mammography even without a provider recommendation to continue screening [ 46 ].
Studies suggested that ageing itself, and even poor health, were not seen as reasonable reasons for screening cessation. For many women, guidance from a health care provider was deemed the most important influence on decision-making [ 46 ]. Preferences for communication about risk and benefits were varied with one study reporting women would like to learn more about harms and risks and recommended that this information be communicated via physicians or other healthcare providers, included in brochures/pamphlets, and presented outside of clinical settings (e.g., in community-based seniors groups) [ 51 ]. Others reported that women were sometimes sceptical of expert and government recommendations [ 33 ] although some were happy to participate in discussions with health educators or care providers about breast cancer screening harms and benefits and potential cessation [ 52 ].
Underlying attitudes to the importance of cancer screening at and beyond 75 years
Included studies varied in describing the importance of screening, with some attitudes based on past attendance and some based on future intentions to screen. Three studies reported findings indicating that some women intended to continue screening after 75 years of age [ 23 , 45 , 46 ], with one study in the UK reporting that women supported an extension of the automatic recall indefinitely, regardless of age or health status. In this study, failure to invite older women to screen was interpreted as age discrimination [ 23 ]. The desire to continue screening beyond 75 was also highlighted in a study from France that found that 60% of the women ( n = 136 aged ≥ 75) intended to pursue screening in the future, and 27 women aged ≥ 75, who had never undergone mammography previously (36%), intended to do so in the future [ 56 ]. In this same study, intentions to screen varied significantly [ 56 ]. There were no sociodemographic differences observed between screened and unscreened women with regard to level of education, income, health risk behaviour (smoking, alcohol consumption), knowledge about the importance and the process of screening, or psychological features (fear of the test, fear of the results, fear of the disease, trust in screening impact) [ 56 ]. Further analysis showed that three items were statistically correlated with a higher rate of attendance at screening: (1) screening was initiated by a physician; (2) the women had a consultation with a gynaecologist during the past 12 months; and (3) the women had already undergone at least five screening mammograms. Analysis highlighted that although average income, level of education, psychological features or other types of health risk behaviours did not impact screening intention, having a mammogram previously impacted likelihood of ongoing screening. There was no information provided that explained why women who had not previously undergone screening might do so in the future.
A mixed methods study in the UK reported similar findings [ 23 ]. Utilising interviews ( n = 26) and questionnaires ( n = 479) with women ≥ 70 years (median age 75 years) the overwhelming result (90.1%) was that breast screening should be offered to all women indefinitely regardless of age, health status or fitness [ 23 ], and that many older women were keen to continue screening. Both the interview and survey data confirmed women were uncertain about eligibility for breast screening. The survey data showed that just over half the women (52.9%) were unaware that they could request mammography or knew how to access it. Key reasons for screening discontinuation were not being invited for screening (52.1%) and not knowing about self-referral (35.1%).
Women reported that not being invited to continue screening sent messages that screening was no longer important or required for this age group [ 23 ]. Almost two thirds of the women completing the survey (61.6%) said they would forget to attend screening without an invitation. Other reasons for screening discontinuation included transport difficulties (25%) and not wishing to burden family members (24.7%). By contrast, other studies have reported that women do not endorse discontinuation of screening mammography due to advancing age or poor health, but some may be receptive to reducing screening frequency on recommendation from their health care provider [ 46 , 51 ].
Use of Decision Aids (DAs) to improve knowledge and guide screening decision-making
Many women reported poor knowledge about the harms and benefits of screening with studies identifying an important role for DAs. These aids have been shown to be effective in improving knowledge of the harms and benefits of screening [ 45 , 54 , 55 ] including for women with low educational attainment; as compared to women with high educational attainment [ 47 ]. DAs can increase knowledge about screening [ 47 , 49 ] and may decrease the intention to continue screening after the recommended age [ 45 , 52 , 54 ]. They can be used by primary care providers to support a conversation about breast screening intention and reasons for discontinuing screening. In one pilot study undertaken in the US using a DA, 5 of the 8 women (62.5%) indicated they intended to continue to receive mammography; however, 3 participants planned to get them less often [ 45 ]. When asked whether they thought their physician would want them to get a mammogram, 80% said “yes” on pre-test; this figure decreased to 62.5% after exposure to the DA. This pilot study suggests that the use of a decision-aid may result in fewer women ≥ 75 years old continuing to screen for breast cancer [ 45 ].
Similar findings were evident in two studies drawing on the same data undertaken in the US [ 48 , 53 ]. Using a larger sample ( n = 283), women’s intentions to screen prior to a visit with their primary care provider and then again after exposure to the DA were compared. Results showed that 21.7% of women reduced their intention to be screened, 7.9% increased their intentions to be screened, and 70.4% did not change. Compared to those who had no change or increased their screening intentions, women who had a decrease in screening intention were significantly less likely to receive screening after 18 months. Generally, studies have shown that women aged 75 and older find DAs acceptable and helpful [ 47 , 48 , 49 , 55 ] and using them had the potential to impact on a women’s intention to screen [ 55 ].
Cadet and colleagues [ 49 ] explored the impact of educational attainment on the use of DAs. Results highlight that education moderates the utility of these aids; women with lower educational attainment were less likely to understand all the DA’s content (46.3% vs 67.5%; P < 0.001); had less knowledge of the benefits and harms of mammography (adjusted mean ± standard error knowledge score, 7.1 ± 0.3 vs 8.1 ± 0.3; p < 0.001); and were less likely to have their screening intentions impacted (adjusted percentage, 11.4% vs 19.4%; p = 0.01).
This scoping review summarises current knowledge regarding motivations and screening behaviours of women over 75 years. The findings suggest that awareness of the importance of breast cancer screening among women aged ≥ 75 years is high [ 23 , 46 , 49 ] and that many women wish to continue screening regardless of perceived health status or age. This highlights the importance of focusing on motivation and screening behaviours and the multiple factors that influence ongoing participation in breast screening programs.
The generally high regard attributed to screening among women aged ≥ 75 years presents a complex challenge for health professionals who are focused on potential harm (from available national and international guidelines) in ongoing screening for women beyond age 75 [ 18 , 20 , 57 ]. Included studies highlight that many women relied on the advice of health care providers regarding the benefits and harms when making the decision to continue breast screening [ 46 , 51 , 52 ], however there were some that did not [ 33 ]. Having a previous pattern of screening was noted as being more significant to ongoing intention than any other identified socio-demographic feature [ 56 ]. This is perhaps because women will not readily forgo health care practices that they have always considered important and that retain ongoing importance for the broader population.
For those women who had discontinued screening after the age of 74 it was apparent that the rationale for doing so was not often based on choice or receipt of information, but rather on factors that impact decision-making in relation to screening. These included no longer receiving an invitation to attend, transport difficulties and not wanting to be a burden on relatives or friends [ 23 , 46 , 51 ]. Ongoing receipt of invitations to screen was an important aspect of maintaining a capacity to choose [ 23 ]. This was particularly important for those women who had been regular screeners.
Women over 75 require more information to make decisions regarding screening [ 23 , 52 , 54 , 55 ], however health care providers must also be aware that the element of choice is important for older women. Having a capacity to choose avoids any notion of discrimination based on age, health status, gender or sociodemographic difference and acknowledges the importance of women retaining control over their health [ 23 ]. It was apparent that some women would choose to continue screening at a reduced frequency if this option was available and that women should have access to information facilitating self-referral [ 23 , 45 , 46 , 51 , 56 ].
Decision-making regarding ongoing breast cancer screening has been facilitated via the use of Decision Aids (DAs) within clinical settings [ 54 , 55 ]. While some studies suggest that women will make a decision regardless of health status, the use of DAs has impacted women’s decision to screen. While this may have limited benefit for those of lower educational attainment [ 48 ] they have been effective in improving knowledge relating to harms and benefits of screening particularly where they have been used to support a conversation with women about the value of screening [ 54 , 55 , 56 ].
Women have identified challenges in engaging in conversations with health care providers regarding ongoing screening, because providers frequently draw on projections of life expectancy and over-diagnosis [ 17 , 51 ]. As a result, these conversations about screening after age 75 years often do not occur [ 46 ]. It is likely that health providers may need more support and guidance in leading these conversations. This may be through the use of DAs or standardised checklists. It may be possible to incorporate these within existing health preventive measures for this age group. The potential for advice regarding ongoing breast cancer screening to be available outside of clinical settings may provide important pathways for conversations with women regarding health choices. Provision of information and advice in settings such as community based seniors groups [ 51 ] offers a potential platform to broaden conversations and align sources of information, not only with health professionals but amongst women themselves. This may help to address any misconception regarding eligibility and access to services [ 23 ]. It may also be aligned with other health promotion and lifestyle messages provided to this age group.
Limitations of the review
The searches that formed the basis of this review were carried in June 2022. Although the search was comprehensive, we have only captured those studies that were published in the included databases from 2009. There may have been other studies published outside of these periods. We also limited the search to studies published in English with full-text availability.
The emphasis of a scoping review is on comprehensive coverage and synthesis of the key findings, rather than on a particular standard of evidence and, consequently a quality assessment of the included studies was not undertaken. This has resulted in the inclusion of a wide range of study designs and data collection methods. It is important to note that three studies included in the review drew on the same sample of women (283 over > 75)[ 49 , 53 , 54 ]. The results of this review provide valuable insights into motivations and behaviours for breast cancer screening for older women, however they should be interpreted with caution given the specific methodological and geographical limitations.
Conclusion and recommendations
This scoping review highlighted a range of key motivations and behaviours in relation to breast cancer screening for women ≥ 75 years of age. The results provide some insight into how decisions about screening continuation after 74 are made and how informed decision-making can be supported. Specifically, this review supports the following suggestions for further research and policy direction:
Further research regarding breast cancer screening motivations and behaviours for women over 75 would provide valuable insight for health providers delivering services to women in this age group.
Health providers may benefit from the broader use of decision aids or structured checklists to guide conversations with women over 75 regarding ongoing health promotion/preventive measures.
Providing health-based information in non-clinical settings frequented by women in this age group may provide a broader reach of information and facilitate choices. This may help to reduce any perception of discrimination based on age, health status or socio-demographic factors.
Availability of data and materials
All data generated or analysed during this study is included in this published article (see Table 2 above).
Cancer Australia, in their 2014 position statement, define “overdiagnosis” in the following way. ‘’Overdiagnosis’ from breast screening does not refer to error or misdiagnosis, but rather refers to breast cancer diagnosed by screening that would not otherwise have been diagnosed during a woman’s lifetime. “Overdiagnosis” includes all instances where cancers detected through screening (ductal carcinoma in situ or invasive breast cancer) might never have progressed to become symptomatic during a woman’s life, i.e., cancer that would not have been detected in the absence of screening. It is not possible to precisely predict at diagnosis, to which cancers overdiagnosis would apply.” (accessed 22. nd August 2022; https://www.canceraustralia.gov.au/resources/position-statements/overdiagnosis-mammographic-screening ).
World Health Organization. Breast Cancer Geneva: WHO; 2021 [Available from: https://www.who.int/news-room/fact-sheets/detail/breast-cancer#:~:text=Reducing%20global%20breast%20cancer%20mortality,and%20comprehensive%20breast%20cancer%20management .
International Agency for Research on Cancer (IARC). IARC Handbooks on Cancer Screening: Volume 15 Breast Cancer Geneva: IARC; 2016 [Available from: https://publications.iarc.fr/Book-And-Report-Series/Iarc-Handbooks-Of-Cancer-Prevention/Breast-Cancer-Screening-2016 .
Australian Institute of Health and Welfare. Cancer in Australia 2021 [Available from: https://www.canceraustralia.gov.au/cancer-types/breast-cancer/statistics .
Breast Cancer Network Australia. Current breast cancer statistics in Australia 2020 [Available from: https://www.bcna.org.au/media/7111/bcna-2019-current-breast-cancer-statistics-in-australia-11jan2019.pdf .
Ren W, Chen M, Qiao Y, Zhao F. Global guidelines for breast cancer screening: A systematic review. The Breast. 2022;64:85–99.
Article PubMed PubMed Central Google Scholar
Cardoso F, Kyriakides S, Ohno S, Penault-Llorca F, Poortmans P, Rubio IT, et al. Early breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2019;30(8):1194–220.
Article CAS PubMed Google Scholar
Hamashima C, Hattori M, Honjo S, Kasahara Y, Katayama T, Nakai M, et al. The Japanese guidelines for breast cancer screening. Jpn J Clin Oncol. 2016;46(5):482–92.
Article PubMed Google Scholar
Bevers TB, Helvie M, Bonaccio E, Calhoun KE, Daly MB, Farrar WB, et al. Breast cancer screening and diagnosis, version 3.2018, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Net. 2018;16(11):1362–89.
Article Google Scholar
He J, Chen W, Li N, Shen H, Li J, Wang Y, et al. China guideline for the screening and early detection of female breast cancer (2021, Beijing). Zhonghua Zhong liu za zhi [Chinese Journal of Oncology]. 2021;43(4):357–82.
CAS PubMed Google Scholar
Cancer Australia. Early detection of breast cancer 2021 [cited 2022 25 July]. Available from: https://www.canceraustralia.gov.au/resources/position-statements/early-detection-breast-cancer .
Schünemann HJ, Lerda D, Quinn C, Follmann M, Alonso-Coello P, Rossi PG, et al. Breast Cancer Screening and Diagnosis: A Synopsis of the European Breast Guidelines. Ann Intern Med. 2019;172(1):46–56.
World Health Organization. WHO Position Paper on Mammography Screening Geneva WHO. 2016.
Google Scholar
Lansdorp-Vogelaar I, Gulati R, Mariotto AB. Personalizing age of cancer screening cessation based on comorbid conditions: model estimates of harms and benefits. Ann Intern Med. 2014;161:104.
Lee CS, Moy L, Joe BN, Sickles EA, Niell BL. Screening for Breast Cancer in Women Age 75 Years and Older. Am J Roentgenol. 2017;210(2):256–63.
Broeders M, Moss S, Nystrom L. The impact of mammographic screening on breast cancer mortality in Europe: a review of observational studies. J Med Screen. 2012;19(suppl 1):14.
Oeffinger KC, Fontham ETH, Etzioni R, Herzig A, Michaelson JS, Shih YCT, et al. Breast cancer screening for women at average risk: 2015 Guideline update from the American cancer society. JAMA - Journal of the American Medical Association. 2015;314(15):1599–614.
Walter LC, Schonberg MA. Screening mammography in older women: a review. JAMA. 2014;311:1336.
Article CAS PubMed PubMed Central Google Scholar
Braithwaite D, Walter LC, Izano M, Kerlikowske K. Benefits and harms of screening mammography by comorbidity and age: a qualitative synthesis of observational studies and decision analyses. J Gen Intern Med. 2016;31:561.
Braithwaite D, Mandelblatt JS, Kerlikowske K. To screen or not to screen older women for breast cancer: a conundrum. Future Oncol. 2013;9(6):763–6.
Demb J, Abraham L, Miglioretti DL, Sprague BL, O’Meara ES, Advani S, et al. Screening Mammography Outcomes: Risk of Breast Cancer and Mortality by Comorbidity Score and Age. Jnci-Journal of the National Cancer Institute. 2020;112(6):599–606.
Demb J, Akinyemiju T, Allen I, Onega T, Hiatt RA, Braithwaite D. Screening mammography use in older women according to health status: a systematic review and meta-analysis. Clin Interv Aging. 2018;13:1987–97.
Qaseem A, Lin JS, Mustafa RA, Horwitch CA, Wilt TJ. Screening for Breast Cancer in Average-Risk Women: A Guidance Statement From the American College of Physicians. Ann Intern Med. 2019;170(8):547–60.
Collins K, Winslow M, Reed MW, Walters SJ, Robinson T, Madan J, et al. The views of older women towards mammographic screening: a qualitative and quantitative study. Br J Cancer. 2010;102(10):1461–7.
Welch HG, Black WC. Overdiagnosis in cancer. J Natl Cancer Inst. 2010;102(9):605–13.
Hersch J, Jansen J, Barratt A, Irwig L, Houssami N, Howard K, et al. Women’s views on overdiagnosis in breast cancer screening: a qualitative study. BMJ : British Medical Journal. 2013;346:f158.
De Gelder R, Heijnsdijk EAM, Van Ravesteyn NT, Fracheboud J, Draisma G, De Koning HJ. Interpreting overdiagnosis estimates in population-based mammography screening. Epidemiol Rev. 2011;33(1):111–21.
Monticciolo DL, Helvie MA, Edward HR. Current issues in the overdiagnosis and overtreatment of breast cancer. Am J Roentgenol. 2018;210(2):285–91.
Shepardson LB, Dean L. Current controversies in breast cancer screening. Semin Oncol. 2020;47(4):177–81.
National Cancer Control Centre. Cancer incidence in Australia 2022 [Available from: https://ncci.canceraustralia.gov.au/diagnosis/cancer-incidence/cancer-incidence .
Austin JD, Shelton RC, Lee Argov EJ, Tehranifar P. Older Women’s Perspectives Driving Mammography Screening Use and Overuse: a Narrative Review of Mixed-Methods Studies. Current Epidemiology Reports. 2020;7(4):274–89.
Austin JD, Tehranifar P, Rodriguez CB, Brotzman L, Agovino M, Ziazadeh D, et al. A mixed-methods study of multi-level factors influencing mammography overuse among an older ethnically diverse screening population: implications for de-implementation. Implementation Science Communications. 2021;2(1):110.
Demb J, Allen I, Braithwaite D. Utilization of screening mammography in older women according to comorbidity and age: protocol for a systematic review. Syst Rev. 2016;5(1):168.
Housten AJ, Pappadis MR, Krishnan S, Weller SC, Giordano SH, Bevers TB, et al. Resistance to discontinuing breast cancer screening in older women: A qualitative study. Psychooncology. 2018;27(6):1635–41.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Peters M, Godfrey C, McInerney P, Munn Z, Tricco A, Khalil HAE, et al. Chapter 11: Scoping reviews. JBI Manual for Evidence Synthesis 2020 [Available from: https://jbi-global-wiki.refined.site/space/MANUAL .
Peters MD, Godfrey C, McInerney P, Khalil H, Larsen P, Marnie C, et al. Best practice guidance and reporting items for the development of scoping review protocols. JBI evidence synthesis. 2022;20(4):953–68.
Fantom NJ, Serajuddin U. The World Bank’s classification of countries by income. World Bank Policy Research Working Paper; 2016.
Book Google Scholar
BreastScreen Australia Evaluation Taskforce. BreastScreen Australia Evaluation. Evaluation final report: Screening Monograph No 1/2009. Canberra; Australia Australian Government Department of Health and Ageing; 2009.
Nelson HD, Cantor A, Humphrey L. Screening for breast cancer: a systematic review to update the 2009 U.S. Preventive Services Task Force recommendation2016.
Woolf SH. The 2009 breast cancer screening recommendations of the US Preventive Services Task Force. JAMA. 2010;303(2):162–3.
Covidence systematic review software. [Internet]. Veritas-Health-Innovation 2020. Available from: https://www.covidence.org/ .
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467–73.
Tricco AC, Lillie E, Zarin W, O’Brien K, Colquhoun H, Kastner M, et al. A scoping review on the conduct and reporting of scoping reviews. BMC Med Res Methodol. 2016;16(1):15.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Beckmeyer A, Smith RM, Miles L, Schonberg MA, Toland AE, Hirsch H. Pilot Evaluation of Patient-centered Survey Tools for Breast Cancer Screening Decision-making in Women 75 and Older. Health Behavior and Policy Review. 2020;7(1):13–8.
Brotzman LE, Shelton RC, Austin JD, Rodriguez CB, Agovino M, Moise N, et al. “It’s something I’ll do until I die”: A qualitative examination into why older women in the U.S. continue screening mammography. Canc Med. 2022;11(20):3854–62.
Article CAS Google Scholar
Cadet T, Pinheiro A, Karamourtopoulos M, Jacobson AR, Aliberti GM, Kistler CE, et al. Effects by educational attainment of a mammography screening patient decision aid for women aged 75 years and older. Cancer. 2021;127(23):4455–63.
Cadet T, Aliberti G, Karamourtopoulos M, Jacobson A, Gilliam EA, Primeau S, et al. Evaluation of a mammography decision aid for women 75 and older at risk for lower health literacy in a pretest-posttest trial. Patient Educ Couns. 2021;104(9):2344–50.
Cadet T, Aliberti G, Karamourtopoulos M, Jacobson A, Siska M, Schonberg MA. Modifying a mammography decision aid for older adult women with risk factors for low health literacy. Health Lit Res Prac. 2021;5(2):e78–90.
Gray N, Picone G. Evidence of Large-Scale Social Interactions in Mammography in the United States. Atl Econ J. 2018;46(4):441–57.
Hoover DS, Pappadis MR, Housten AJ, Krishnan S, Weller SC, Giordano SH, et al. Preferences for Communicating about Breast Cancer Screening Among Racially/Ethnically Diverse Older Women. Health Commun. 2019;34(7):702–6.
Salzman B, Bistline A, Cunningham A, Silverio A, Sifri R. Breast Cancer Screening Shared Decision-Making in Older African-American Women. J Natl Med Assoc. 2020;112(5):556–60.
PubMed Google Scholar
Schoenborn NL, Pinheiro A, Kistler CE, Schonberg MA. Association between Breast Cancer Screening Intention and Behavior in the Context of Screening Cessation in Older Women. Med Decis Making. 2021;41(2):240–4.
Schonberg MA, Kistler CE, Pinheiro A, Jacobson AR, Aliberti GM, Karamourtopoulos M, et al. Effect of a Mammography Screening Decision Aid for Women 75 Years and Older: A Cluster Randomized Clinical Trial. JAMA Intern Med. 2020;180(6):831–42.
Schonberg MA, Hamel MB, Davis RB. Development and evaluation of a decision aid on mammography screening for women 75 years and older. JAMA Intern Med. 2014;174:417.
Eisinger F, Viguier J, Blay J-Y, Morère J-F, Coscas Y, Roussel C, et al. Uptake of breast cancer screening in women aged over 75years: a controversy to come? Eur J Cancer Prev. 2011;20(Suppl 1):S13-5.
Schonberg MA, Breslau ES, McCarthy EP. Targeting of Mammography Screening According to Life Expectancy in Women Aged 75 and Older. J Am Geriatr Soc. 2013;61(3):388–95.
Download references
Acknowledgements
We would like to acknowledge Ange Hayden-Johns (expert librarian) who assisted with the development of the search criteria and undertook the relevant searches and Tejashree Kangutkar who assisted with some of the Covidence work.
This work was supported by funding from the Australian Government Department of Health and Aged Care (ID: Health/20–21/E21-10463).
Author information
Authors and affiliations.
Violet Vines Centre for Rural Health Research, La Trobe Rural Health School, La Trobe University, P.O. Box 199, Bendigo, VIC, 3552, Australia
Virginia Dickson-Swift, Joanne Adams & Evelien Spelten
Care Economy Research Institute, La Trobe University, Wodonga, Australia
Irene Blackberry
Olivia Newton-John Cancer Wellness and Research Centre, Austin Health, Melbourne, Australia
Carlene Wilson & Eva Yuen
Melbourne School of Population and Global Health, Melbourne University, Melbourne, Australia
Carlene Wilson
School of Psychology and Public Health, La Trobe University, Bundoora, Australia
Institute for Health Transformation, Deakin University, Burwood, Australia
Centre for Quality and Patient Safety, Monash Health Partnership, Monash Health, Clayton, Australia
You can also search for this author in PubMed Google Scholar
Contributions
VDS conceived and designed the scoping review. VDS & JA developed the search strategy with librarian support, and all authors (VDS, JA, ES, IB, CW, EY) participated in the screening and data extraction stages and assisted with writing the review. All authors provided editorial support and read and approved the final manuscript prior to submission.
Corresponding author
Correspondence to Joanne Adams .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethics approval and consent to participate
Ethics approval and consent to participate was not required for this study.
Consent for publication
Consent for publication was not required for this study.
Competing interest
The authors declare they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Dickson-Swift, V., Adams, J., Spelten, E. et al. Breast cancer screening motivation and behaviours of women aged over 75 years: a scoping review. BMC Women's Health 24 , 256 (2024). https://doi.org/10.1186/s12905-024-03094-z
Download citation
Received : 06 September 2023
Accepted : 15 April 2024
Published : 24 April 2024
DOI : https://doi.org/10.1186/s12905-024-03094-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Breast cancer
- Mammography
- Older women
- Scoping review
BMC Women's Health
ISSN: 1472-6874
- Submission enquiries: [email protected]
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
A type of literature review that uses a systematic and rigorous approach to identify, select, appraise, and synthesize all available evidence on a particular topic. ... The inclusion and exclusion criteria must be decided before you start the review. Inclusion criteria is everything a study must have to be included. Exclusion criteria are the ...
Establishing inclusion and exclusion criteria for study participants is a standard, required practice when designing high-quality research protocols. Inclusion criteria are defined as the key features of the target population that the investigators will use to answer their research question. 2 Typical inclusion criteria include demographic ...
These are commonly known as inclusion criteria and exclusion criteria, and they set the boundaries for the literature review. Inclusion and exclusion criteria are determined after formulating the research question but usually before the search is conducted (although preliminary scoping searches may need to be undertaken to determine appropriate ...
Examples of common inclusion and exclusion criteria are: Demographic characteristics: Age, gender identity, ethnicity. Study-specific variables: Type and stage of disease, previous treatment history, presence of chronic conditions, ability to attend follow-up study appointments, technological requirements (e.g., internet access) Control ...
Step 1: Developing and testing criteria. Developing the inclusion and exclusion criteria may involve an iterative process of refinement during review conceptualization and construction (see Chapter 2).During conceptualization, criteria may be adjusted as reviewers scope the likely literature base, consult stakeholders, and explore what questions may be feasible or relevant.
The EPC should carefully consider whether PICOTS criteria are effect modifiers and how inclusion and exclusion criteria may potentially skew the studies and thus results reported in the review. Table 2 below suggests potential implications or biases that may result from specific hypothetical examples of inclusion and exclusion criteria.
The eligibility criteria are liberally applied in the beginning to ensure that relevant studies are included and no study is excluded without thorough evaluation. At the outset, studies are only excluded if they clearly meet one or more of the exclusion criteria. For example, if the focus of review is children, then studies with adult ...
Inclusion and exclusion criteria set the boundaries for the systematic review. They are determined after setting the research question usually before the search is conducted, however scoping searches may need to be undertaken to determine appropriate criteria. Many different factors can be used as inclusion or exclusion criteria.
Tip: Choose your criteria carefully to avoid bias. For example, if you exclude non-English language articles, you may be ignoring relevant studies. The following 6-minute video explains the relationship between inclusion and exclusion criteria and database searches.
The inclusion and exclusion criteria can be based on research design and methodology (Okoli and Schabram 2010). For instance, studies may be restricted to those carried out in certain geographic areas (e.g., developed vs. developing countries), of certain unit of analyses (e.g., individual business vs. the aggregate economy; individual ...
How to establish your Inclusion and Exclusion criteria. To establish your criteria you need to define each aspect of your question to clarify what you are focusing on, and consider if there are any variations you also wish to explore. This is where using frameworks like PICO help: Example: Alternatives to drugs for controlling headaches in children
Fig. 6.5. Scoping study for setting inclusion and exclusion critera for archetype systematic literature review. Building on the position of the scoping study in Figure 4.6, this figure depicts that a scoping study informs the inclusion and exclusion criteria that should be integrated in the protocol. Full size image.
Inclusion and exclusion criteria. Establishing inclusion and exclusion criteria come after formulating research questions. The concept of inclusion and exclusion of data in a systematic review provides a basis on which the reviewer draws valid and reliable conclusions regarding the effect of the intervention for the disorder under consideration ...
An important part of the SR process is defining what will and will not be included in your review. Inclusion and exclusion criteria are developed after a research question is finalized but before a search is carried out. ... they are important in identifying gaps in the literature. Unanswered questions implications of an empty review. Slyer ...
Exclusion criteria are the elements of an article that disqualify the study from inclusion in a literature review. Some examples are: Study used an observational design; Study used a qualitative methodology; Study was published more than 5 years ago; Study was published in a language other than English
To be included in the review, a study needs to meet all inclusion criteria and not meet any exclusion criteria. Inclusion/eligibility criteria include participants, interventions and comparisons and often study design. Outcomes are usually not part of the criteria, though some reviews do legitimately restrict eligibility to specific outcomes ...
Inclusion and exclusion criteria. Inclusion and exclusion criteria are a list of pre-defined characteristics to which literature must adhere to be included in a study. They are vital for the decision-making progress on what to review when undertaking a systematic review and will also help with systematic literature reviews.
Exclusion criteria are the elements of an article that disqualify the study from inclusion in a literature review. Some examples are: Study used an observational design; Study used a qualitative methodology; Study was published more than 5 years ago; Study was published in a language other than English
The purpose of using inclusions/exclusion criteria "is to minimize ambiguity and reduce the possibility of poor reproducibility". This criteria should not be too narrow or too loose. McDonagh M, Peterson K, Raina P, et al. Avoiding Bias in Selecting Studies. 2013 Feb 20. In: Methods Guide for Effectiveness and Comparative Effectiveness Reviews ...
A balance of specific inclusion and exclusion criteria is paramount. For some systematic reviews, there may already be a large pre-existing body of literature. The search strategy may retrieve thousands of results that must be screened. Having explicit exclusion criteria from the beginning allows those conducting the screening process, an ...
What is a literature review? Steps in the Literature Review Process; Define your research question; Determine inclusion and exclusion criteria; Choose databases and search; Review Results; Synthesize Results; Analyze Results; Write; Librarian Support; Determine inclusion and exclusion criteria. Once you have a clearly defined research question ...
Using Limits and Inclusion/Exclusion Criteria Once you have some search results, you will need to decide which articles you will actually use in your literature review. This can be done using filters/limits in the databases, applying inclusion/exclusion criteria, and appraising the articles.
A feature of the systematic literature review is using pre-specified criteria to include/exclude studies. Through searching the literature and formulating your review questions, for example by using PICO, PEO, etc., you will be able to define the specific attributes that research studies must have to be eligible for inclusion in your review, along with other attributes that will exclude them.
Conclusion: The results of this systematic review highlight the need to consider more expansive inclusion/exclusion criteria as relates to factors that could impact vocal function in participants. Moreover, developing consistent inclusion and exclusion characteristics would provide greater support in the interpretation and generalization of ...
To improve this, respondents suggested that tailored inclusion and exclusion criteria for disabled people should be used, and disability and capacity to consent should be assessed at the individual level. ... Bodicoat DH, Routen AC, Willis A, et al. Promoting inclusion in clinical trials - a rapid review of the literature and recommendations ...
Finally, 12 articles with 1608 patients in total were included in the present meta-analysis based on the bias of the inclusion and exclusion criteria abovementioned [15,16,17,18,19,20,21,22,23,24,25,26]. The lack of sufficient data for analysis was the most common reason for exclusion during the full-text review process.
Inclusion criteria and exclusion criteria. The inclusion criteria for the literature review are as follows: (1) The type of literature should be either a prospective study or a retrospective study. (2) The literature must focus on the comparison between TP-RAPN and RP-RAPN. (3) The study should only include patients with posterior (R.E.N.A.L ...
Resulting libraries from each database were imported to Zotero (version 5.0.96) for the exclusion of duplicates and triplicates. All works from this search strategy were subsequently selected for reading and classification according to the inclusion and exclusion criteria. 2.3 Inclusion and exclusion criteria
Studies will be included in the review if the following criteria are fulfilled: Study designs: register studies, clinical prospective studies and case-control studies. The lower limit for inclusion of a risk factor will be minimum 5 studies that have minimum 10 patients with dislocation(s).
The review was restricted to original research studies published since 2009, available in English and focusing on high-income countries (as defined by the World Bank). Title and abstract screening, followed by an assessment of full-text studies against the inclusion criteria was completed by at least two reviewers.