Get smartphone savvy the easy way: Join our 7-day email challenge to receive helpful tips each day.

Popular Searches
AARP daily Crossword Puzzle
Hotels with AARP discounts
Life Insurance
AARP Dental Insurance Plans
Suggested Links
AARP MEMBERSHIP — $12 FOR YOUR FIRST YEAR WHEN YOU SIGN UP FOR AUTOMATIC RENEWAL
Get instant access to members-only products and hundreds of discounts, a free second membership, and a subscription to AARP the Magazine.
- right_container
Work & Jobs
Social Security
AARP en Español
- Membership & Benefits
AARP Rewards
- AARP Rewards %{points}%
Conditions & Treatments
Drugs & Supplements
Health Care & Coverage
Health Benefits

Staying Fit
Your Personalized Guide to Fitness

AARP Hearing Center
Ways To Improve Your Hearing

Brain Health Resources
Tools and Explainers on Brain Health
How to Save Your Own Life
Scams & Fraud
Personal Finance
Money Benefits

View and Report Scams in Your Area

AARP Foundation Tax-Aide
Free Tax Preparation Assistance

AARP Money Map
Get Your Finances Back on Track

Budget & Savings
Make Your Appliances Last Longer
Small Business
Age Discrimination

Flexible Work
Freelance Jobs You Can Do From Home

AARP Skills Builder
Online Courses to Boost Your Career

31 Great Ways to Boost Your Career

ON-DEMAND WEBINARS
Tips to Enhance Your Job Search

Get More out of Your Benefits

When to Start Taking Social Security

10 Top Social Security FAQs

Social Security Benefits Calculator

Medicare Made Easy
Original vs. Medicare Advantage

Enrollment Guide
Step-by-Step Tool for First-Timers

Prescription Drugs
9 Biggest Changes Under New Rx Law

Medicare FAQs
Quick Answers to Your Top Questions
Care at Home
Financial & Legal
Life Balance

LONG-TERM CARE
Understanding Basics of LTC Insurance

State Guides
Assistance and Services in Your Area

Prepare to Care Guides
How to Develop a Caregiving Plan

End of Life
How to Cope With Grief, Loss
Recently Played
Word & Trivia
Atari® & Retro
Members Only
Staying Sharp
Mobile Apps
More About Games

Right Again! Trivia

Right Again! Trivia – Sports

Atari® Video Games

Throwback Thursday Crossword
Travel Tips
Vacation Ideas
Destinations
Travel Benefits

Beach vacation ideas
Vacations for Sun and Fun

Plan Ahead for Tourist Taxes

AARP City Guide
Discover Seattle

How to Pick the Right Cruise for You
Entertainment & Style
Family & Relationships
Personal Tech
Home & Living
Celebrities
Beauty & Style

TV for Grownups
Best Reality TV Shows for Grownups

Robert De Niro Reflects on His Life
Free Online Novel
Read 'Chase'

Sex & Dating
Spice Up Your Love Life

Navigate All Kinds of Connections

How to Create a Home Gym

Store Medical Records on Your Phone?

Maximize the Life of Your Phone Battery

Virtual Community Center
Join Free Tech Help Events

Create a Hygge Haven

Soups to Comfort Your Soul

AARP Smart Guide
Spring Clean All of Your Spaces
Driver Safety
Maintenance & Safety
Trends & Technology

How to Keep Your Car Running

We Need To Talk
Assess Your Loved One's Driving Skills

AARP Smart Driver Course

Building Resilience in Difficult Times

Tips for Finding Your Calm

Weight Loss After 50 Challenge

Cautionary Tales of Today's Biggest Scams

7 Top Podcasts for Armchair Travelers

Jean Chatzky: ‘Closing the Savings Gap’

Quick Digest of Today's Top News

AARP Top Tips for Navigating Life

Get Moving With Our Workout Series
You are now leaving AARP.org and going to a website that is not operated by AARP. A different privacy policy and terms of service will apply.
Go to Series Main Page
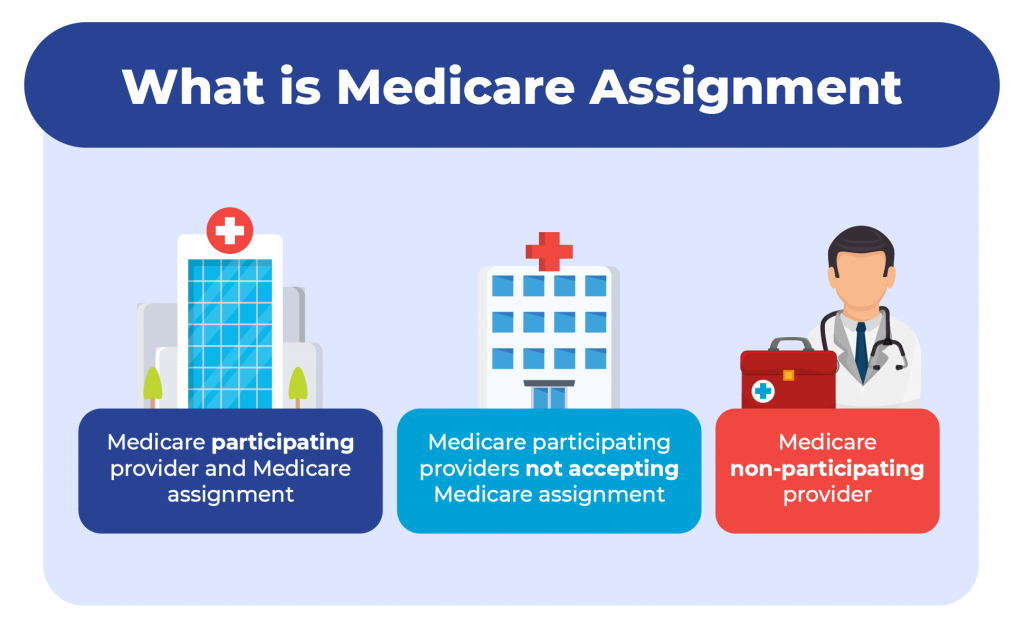
What is Medicare assignment and how does it work?
Kimberly Lankford,
Because Medicare decides how much to pay providers for covered services, if the provider agrees to the Medicare-approved amount, even if it is less than they usually charge, they’re accepting assignment.
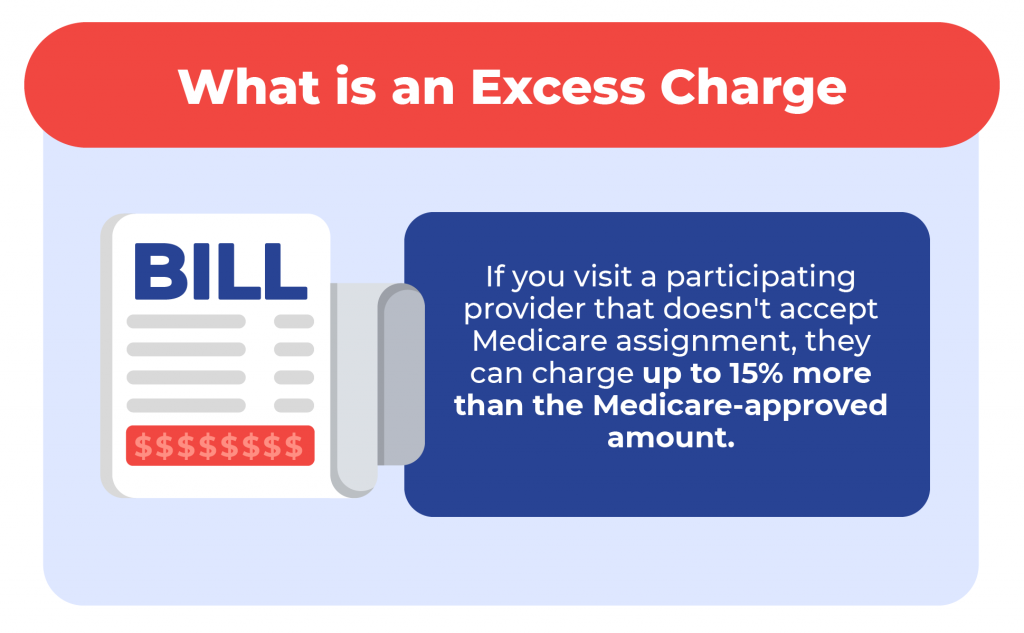
A doctor who accepts assignment agrees to charge you no more than the amount Medicare has approved for that service. By comparison, a doctor who participates in Medicare but doesn’t accept assignment can potentially charge you up to 15 percent more than the Medicare-approved amount.
That’s why it’s important to ask if a provider accepts assignment before you receive care, even if they accept Medicare patients. If a doctor doesn’t accept assignment, you will pay more for that physician’s services compared with one who does.

AARP Membership — $12 for your first year when you sign up for Automatic Renewal
How much do I pay if my doctor accepts assignment?
If your doctor accepts assignment, you will usually pay 20 percent of the Medicare-approved amount for the service, called coinsurance, after you’ve paid the annual deductible. Because Medicare Part B covers doctor and outpatient services, your $240 deductible for Part B in 2024 applies before most coverage begins.
All providers who accept assignment must submit claims directly to Medicare, which pays 80 percent of the approved cost for the service and will bill you the remaining 20 percent. You can get some preventive services and screenings, such as mammograms and colonoscopies , without paying a deductible or coinsurance if the provider accepts assignment.
What if my doctor doesn’t accept assignment?
A doctor who takes Medicare but doesn’t accept assignment can still treat Medicare patients but won’t always accept the Medicare-approved amount as payment in full.
This means they can charge you up to a maximum of 15 percent more than Medicare pays for the service you receive, called “balance billing.” In this case, you’re responsible for the additional charge, plus the regular 20 percent coinsurance, as your share of the cost.
How to cover the extra cost? If you have a Medicare supplement policy , better known as Medigap, it may cover the extra 15 percent, called Medicare Part B excess charges.
All Medigap policies cover Part B’s 20 percent coinsurance in full or in part. The F and G policies cover the 15 percent excess charges from doctors who don’t accept assignment, but Plan F is no longer available to new enrollees, only those eligible for Medicare before Jan. 1, 2020, even if they haven’t enrolled in Medicare yet. However, anyone who is enrolled in original Medicare can apply for Plan G.
Remember that Medigap policies only cover excess charges for doctors who accept Medicare but don’t accept assignment, and they won’t cover costs for doctors who opt out of Medicare entirely.
Good to know. A few states limit the amount of excess fees a doctor can charge Medicare patients. For example, Massachusetts and Ohio prohibit balance billing, requiring doctors who accept Medicare to take the Medicare-approved amount. New York limits excess charges to 5 percent over the Medicare-approved amount for most services, rather than 15 percent.

AARP NEWSLETTERS

%{ newsLetterPromoText }%
%{ description }%
Privacy Policy
ARTICLE CONTINUES AFTER ADVERTISEMENT
How do I find doctors who accept assignment?
Before you start working with a new doctor, ask whether he or she accepts assignment. About 98 percent of providers billing Medicare are participating providers, which means they accept assignment on all Medicare claims, according to KFF.
You can get help finding doctors and other providers in your area who accept assignment by zip code using Medicare’s Physician Compare tool .
Those who accept assignment have this note under the name: “Charges the Medicare-approved amount (so you pay less out of pocket).” However, not all doctors who accept assignment are accepting new Medicare patients.
AARP® Vision Plans from VSP™
Exclusive vision insurance plans designed for members and their families
What does it mean if a doctor opts out of Medicare?
Doctors who opt out of Medicare can’t bill Medicare for services you receive. They also aren’t bound by Medicare’s limitations on charges.
In this case, you enter into a private contract with the provider and agree to pay the full bill. Be aware that neither Medicare nor your Medigap plan will reimburse you for these charges.
In 2023, only 1 percent of physicians who aren’t pediatricians opted out of the Medicare program, according to KFF. The percentage is larger for some specialties — 7.7 percent of psychiatrists and 4.2 percent of plastic and reconstructive surgeons have opted out of Medicare.
Keep in mind
These rules apply to original Medicare. Other factors determine costs if you choose to get coverage through a private Medicare Advantage plan . Most Medicare Advantage plans have provider networks, and they may charge more or not cover services from out-of-network providers.
Before choosing a Medicare Advantage plan, find out whether your chosen doctor or provider is covered and identify how much you’ll pay. You can use the Medicare Plan Finder to compare the Medicare Advantage plans and their out-of-pocket costs in your area.
Return to Medicare Q&A main page
Kimberly Lankford is a contributing writer who covers Medicare and personal finance. She wrote about insurance, Medicare, retirement and taxes for more than 20 years at Kiplinger’s Personal Finance and has written for The Washington Post and Boston Globe . She received the personal finance Best in Business award from the Society of American Business Editors and Writers and the New York State Society of CPAs’ excellence in financial journalism award for her guide to Medicare.
Discover AARP Members Only Access
Already a Member? Login

More on Medicare

How Do I Create a Personal Online Medicare Account?
You can do a lot when you decide to look electronically

I Got a Medicare Summary Notice in the Mail. What Is It?
This statement shows what was billed, paid in past 3 months
Understanding Medicare’s Options: Parts A, B, C and D
Making sense of the alphabet soup of health care choices
Recommended for You
AARP Value & Member Benefits

Learn, earn and redeem points for rewards with our free loyalty program

AARP® Dental Insurance Plan administered by Delta Dental Insurance Company
Dental insurance plans for members and their families

The National Hearing Test
Members can take a free hearing test by phone

AARP® Staying Sharp®
Activities, recipes, challenges and more with full access to AARP Staying Sharp®
SAVE MONEY WITH THESE LIMITED-TIME OFFERS
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Medicare Assignment: Everything You Need to Know
Medicare assignment.
- Providers Accepting Assignment
- Providers Who Do Not
- Billing Options
- Assignment of Benefits
- How to Choose
Frequently Asked Questions
Medicare assignment is an agreement between Medicare and medical providers (doctors, hospitals, medical equipment suppliers, etc.) in which the provider agrees to accept Medicare’s fee schedule as payment in full when Medicare patients are treated.
This article will explain how Medicare assignment works, and what you need to know in order to ensure that you won’t receive unexpected bills.
fizkes / Getty Images
There are 35 million Americans who have Original Medicare. Medicare is a federal program and most medical providers throughout the country accept assignment with Medicare. As a result, these enrollees have a lot more options for medical providers than most of the rest of the population.
They can see any provider who accepts assignment, anywhere in the country. They can be assured that they will only have to pay their expected Medicare cost-sharing (deductible and coinsurance, some or all of which may be paid by a Medigap plan , Medicaid, or supplemental coverage provided by an employer or former employer).
It’s important to note here that the rules are different for the 29 million Americans who have Medicare Advantage plans. These beneficiaries cannot simply use any medical provider who accepts Medicare assignment.
Instead, each Medicare Advantage plan has its own network of providers —much like the health insurance plans that many Americans are accustomed to obtaining from employers or purchasing in the exchange/marketplace .
A provider who accepts assignment with Medicare may or may not be in-network with some or all of the Medicare Advantage plans that offer coverage in a given area. Some Medicare Advantage plans— health maintenance organizations (HMOs) , in particular—will only cover an enrollee’s claims if they use providers who are in the plan's network.
Other Medicare Advantage plans— preferred provider organizations (PPOs) , in particular—will cover out-of-network care but the enrollee will pay more than they would have paid had they seen an in-network provider.
Original Medicare
The bottom line is that Medicare assignment only determines provider accessibility and costs for people who have Original Medicare. People with Medicare Advantage need to understand their own plan’s provider network and coverage rules.
When discussing Medicare assignment and access to providers in this article, keep in mind that it is referring to people who have Original Medicare.
How to Make Sure Your Provider Accepts Assignment
Most doctors, hospitals, and other medical providers in the United States do accept Medicare assignment.
Provider Participation Stats
According to the Centers for Medicare and Medicaid Services, 98% of providers participate in Medicare, which means they accept assignment.
You can ask the provider directly about their participation with Medicare. But Medicare also has a tool that you can use to find participating doctors, hospitals, home health care services, and other providers.
There’s a filter on that tool labeled “Medicare-approved payment.” If you turn on that filter, you will only see providers who accept Medicare assignment. Under each provider’s information, it will say “Charges the Medicare-approved amount (so you pay less out-of-pocket).”
What If Your Provider Doesn’t Accept Assignment?
If your medical provider or equipment supplier doesn’t accept assignment, it means they haven’t agreed to accept Medicare’s approved amounts as payment in full for all of the services.
These providers can still choose to accept assignment on a case-by-case basis. But because they haven’t agreed to accept Medicare assignment for all services, they are considered nonparticipating providers.
Note that "nonparticipating" does not mean that a provider has opted out of Medicare altogether. Medicare will still pay claims for services received from a nonparticipating provider (i.e., one who does not accept Medicare assignment), whereas Medicare does not cover any of the cost of services obtained from a provider who has officially opted out of Medicare.
If a Medicare beneficiary uses a provider who has opted out of Medicare, that person will pay the provider directly and Medicare will not be involved in any way.
Physicians Who Have Opted Out
Only about 1% of all non-pediatric physicians have opted out of Medicare.
For providers who have not opted out of Medicare but who also don’t accept assignment, Medicare will still pay nearly as much as it would have paid if you had used a provider who accepts assignment. Here’s how it works:
- Medicare will pay the provider 95% of the amount they would pay if the provider accepted assignment.
- The provider can charge the person receiving care more than the Medicare-approved amount, but only up to 15% more (some states limit this further). This extra amount, which the patient has to pay out-of-pocket, is known as the limiting charge . But the 15% cap does not apply to medical equipment suppliers; if they do not accept assignment with Medicare, there is no limit on how much they can charge the person receiving care. This is why it’s particularly important to make sure that the supplier accepts Medicare assignment if you need medical equipment.
- The nonparticipating provider may require the person receiving care to pay the entire bill up front and seek reimbursement from Medicare (using Form CMS 1490-S ). Alternatively, they may submit a claim to Medicare on behalf of the person receiving care (using Form CMS-1500 ).
- A nonparticipating provider can choose to accept assignment on a case-by-case basis. They can indicate this on Form CMS-1500 in box 27. The vast majority of nonparticipating providers who bill Medicare choose to accept assignment for the claim being billed.
- Nonparticipating providers do not have to bill your Medigap plan on your behalf.
Billing Options for Providers Who Accept Medicare
When a medical provider accepts assignment with Medicare, part of the agreement is that they will submit bills to Medicare on behalf of the person receiving care. So if you only see providers who accept assignment, you will never need to submit your own bills to Medicare for reimbursement.
If you have a Medigap plan that supplements your Original Medicare coverage, you should present the Medigap coverage information to the provider at the time of service. Medicare will forward the claim information to your Medigap insurer, reducing administrative work on your part.
Depending on the Medigap plan you have, the services that you receive, and the amount you’ve already spent in out-of-pocket costs, the Medigap plan may pay some or all of the out-of-pocket costs that you would otherwise have after Medicare pays its share.
(Note that if you have a type of Medigap plan called Medicare SELECT, you will have to stay within the plan’s network of providers in order to receive benefits. But this is not the case with other Medigap plans.)
After the claim is processed, you’ll be able to see details in your MyMedicare.gov account . Medicare will also send you a Medicare Summary Notice. This is Medicare’s version of an explanation of benefits (EOB) , which is sent out every three months.
If you have a Medigap plan, it should also send you an EOB or something similar, explaining the claim and whether the policy paid any part of it.
What Is Medicare Assignment of Benefits?
For Medicare beneficiaries, assignment of benefits means that the person receiving care agrees to allow a nonparticipating provider to bill Medicare directly (as opposed to having the person receiving care pay the bill up front and seek reimbursement from Medicare). Assignment of benefits is authorized by the person receiving care in Box 13 of Form CMS-1500 .
If the person receiving care refuses to assign benefits, Medicare can only reimburse the person receiving care instead of paying the nonparticipating provider directly.
Things to Consider Before Choosing a Provider
If you’re enrolled in Original Medicare, you have a wide range of options in terms of the providers you can use—far more than most other Americans. In most cases, your preferred doctor and other medical providers will accept assignment with Medicare, keeping your out-of-pocket costs lower than they would otherwise be, and reducing administrative hassle.
There may be circumstances, however, when the best option is a nonparticipating provider or even a provider who has opted out of Medicare altogether. If you choose one of these options, be sure you discuss the details with the provider before proceeding with the treatment.
You’ll want to understand how much is going to be billed and whether the provider will bill Medicare on your behalf if you agree to assign benefits (note that this is not possible if the provider has opted out of Medicare).
If you have supplemental coverage, you’ll also want to check with that plan to see whether it will still pick up some of the cost and, if so, how much you should expect to pay out of your own pocket.
A medical provider who accepts Medicare assignment is considered a participating provider. These providers have agreed to accept Medicare’s fee schedule as payment in full for services they provide to Medicare beneficiaries. Most doctors, hospitals, and other medical providers do accept Medicare assignment.
Nonparticipating providers are those who have not signed an agreement with Medicare to accept Medicare’s rates as payment in full. However, they can agree to accept assignment on a case-by-case basis, as long as they haven’t opted out of Medicare altogether. If they do not accept assignment, they can bill the patient up to 15% more than the Medicare-approved rate.
Providers who opt out of Medicare cannot bill Medicare and Medicare will not pay them or reimburse beneficiaries for their services. But there is no limit on how much they can bill for their services.
A Word From Verywell
It’s in your best interest to choose a provider who accepts Medicare assignment. This will keep your costs as low as possible, streamline the billing and claims process, and ensure that your Medigap plan picks up its share of the costs.
If you feel like you need help navigating the provider options or seeking care from a provider who doesn’t accept assignment, the Medicare State Health Insurance Assistance Program (SHIP) in your state may be able to help.
A doctor who does not accept Medicare assignment has not agreed to accept Medicare’s fee schedule as payment in full for their services. These doctors are considered nonparticipating with Medicare and can bill Medicare beneficiaries up to 15% more than the Medicare-approved amount.
They also have the option to accept assignment (i.e., accept Medicare’s rate as payment in full) on a case-by-case basis.
There are certain circumstances in which a provider is required by law to accept assignment. This includes situations in which the person receiving care has both Medicare and Medicaid. And it also applies to certain medical services, including lab tests, ambulance services, and drugs that are covered under Medicare Part B (as opposed to Part D).
In 2021, 98% of American physicians had participation agreements with Medicare, leaving only about 2% who did not accept assignment (either as a nonparticipating provider, or a provider who had opted out of Medicare altogether).
Accepting assignment is something that the medical provider does, whereas assignment of benefits is something that the patient (the Medicare beneficiary) does. To accept assignment means that the medical provider has agreed to accept Medicare’s approved fee as payment in full for services they provide.
Assignment of benefits means that the person receiving care agrees to allow a medical provider to bill Medicare directly, as opposed to having the person receiving care pay the provider and then seek reimbursement from Medicare.
Centers for Medicare and Medicaid Services. Medicare monthly enrollment .
Centers for Medicare and Medicaid Services. Annual Medicare participation announcement .
Centers for Medicare and Medicaid Services. Lower costs with assignment .
Centers for Medicare and Medicaid Services. Find providers who have opted out of Medicare .
Kaiser Family Foundation. How many physicians have opted-out of the Medicare program ?
Center for Medicare Advocacy. Durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS) updates .
Centers for Medicare and Medicaid Services. Check the status of a claim .
Centers for Medicare and Medicaid Services. Medicare claims processing manual. Chapter 26 - completing and processing form CMS-1500 data set .
Centers for Medicare and Medicaid Services. Ambulance fee schedule .
Centers for Medicare and Medicaid Services. Prescription drugs (outpatient) .
By Louise Norris Louise Norris has been a licensed health insurance agent since 2003 after graduating magna cum laude from Colorado State with a BS in psychology.
Medicare Interactive Medicare answers at your fingertips -->
Participating, non-participating, and opt-out providers, outpatient provider services.
You must be logged in to bookmark pages.
Email Address * Required
Password * Required
Lost your password?
If you have Original Medicare , your Part B costs once you have met your deductible can vary depending on the type of provider you see. For cost purposes, there are three types of provider, meaning three different relationships a provider can have with Medicare . A provider’s type determines how much you will pay for Part B -covered services.
- These providers are required to submit a bill (file a claim ) to Medicare for care you receive. Medicare will process the bill and pay your provider directly for your care. If your provider does not file a claim for your care, there are troubleshooting steps to help resolve the problem .
- If you see a participating provider , you are responsible for paying a 20% coinsurance for Medicare-covered services.
- Certain providers, such as clinical social workers and physician assistants, must always take assignment if they accept Medicare.
- Non-participating providers can charge up to 15% more than Medicare’s approved amount for the cost of services you receive (known as the limiting charge ). This means you are responsible for up to 35% (20% coinsurance + 15% limiting charge) of Medicare’s approved amount for covered services.
- Some states may restrict the limiting charge when you see non-participating providers. For example, New York State’s limiting charge is set at 5%, instead of 15%, for most services. For more information, contact your State Health Insurance Assistance Program (SHIP) .
- If you pay the full cost of your care up front, your provider should still submit a bill to Medicare. Afterward, you should receive from Medicare a Medicare Summary Notice (MSN) and reimbursement for 80% of the Medicare-approved amount .
- The limiting charge rules do not apply to durable medical equipment (DME) suppliers . Be sure to learn about the different rules that apply when receiving services from a DME supplier .
- Medicare will not pay for care you receive from an opt-out provider (except in emergencies). You are responsible for the entire cost of your care.
- The provider must give you a private contract describing their charges and confirming that you understand you are responsible for the full cost of your care and that Medicare will not reimburse you.
- Opt-out providers do not bill Medicare for services you receive.
- Many psychiatrists opt out of Medicare.
Providers who take assignment should submit a bill to a Medicare Administrative Contractor (MAC) within one calendar year of the date you received care. If your provider misses the filing deadline, they cannot bill Medicare for the care they provided to you. However, they can still charge you a 20% coinsurance and any applicable deductible amount.
Be sure to ask your provider if they are participating, non-participating, or opt-out. You can also check by using Medicare’s Physician Compare tool .
Update your browser to view this website correctly. Update my browser now

Physician Acceptance of Medicare Assignment

- Medicare assignment pertains to an agreement between Medicare and participating doctors. Learn more about the physicians that accept Medicare assignment.
Medicare assignment, or Medicare assignment of benefits, is the process in which a Medicare beneficiary authorizes Medicare to directly reimburse health care providers for services. To ensure all services are charged at Medicare-determined rates, recipients should verify whether their primary physicians fall under the accept assignment definition prior to scheduling services.
What Is the Medicare Accept Assignment Definition?
The Medicare accept assignment definition pertains to physicians, medical suppliers and medical providers that agree to accept Medicare-approved charges as total and full payment for all covered services without adding extra charges. These providers also agree to charge only the allowed Medicare deductible and coinsurance charges to patients. Medicare-approved providers who accept Medicare assignment are referred to as participating providers.
Non-participating providers may accept Medicare and provide Medicare-covered services. However, as non-participating providers, they are not required to accept Medicare's pre-determined costs for procedures and office visits. Additionally, non-participating providers are legally allowed to charge up to 15% above Medicare-approved amounts. That extra amount is billed to the patient.
In addition to participating and non-participating providers, some providers choose not to accept Medicare in any capacity. These providers are referred to as opt-out providers. Only a small percentage (under 2%) of providers choose to completely opt out.
What Are Some Benefits of Medicare Assignment?
Medicare recipients who receive primary care through Medicare assignment providers may have lower out-of-pocket costs than recipients who utilize the services of non-participating providers. Providers who accept Medicare assignment must submit all claims directly to Medicare, so recipients can't be charged anything for claim submission. In most cases, Medicare assignment providers wait to charge recipients for their share in costs (when applicable) until after Medicare pays its share, which may help make medical expenses more manageable.
What May Happen When a Provider Doesn't Accept Assignment?
In addition to possibly being charged up to an additional 15% for procedures and services, individuals who use non-participating providers may be required to pay full costs for services upfront. Recipients may also need to submit their own insurance claims to Medicare to receive reimbursements. Medicare recipients who receive services through providers who are completely opted out are generally required to pay for all services and procedures, even if they would normally be covered by Medicare. Recipients who prefer to use opt-out providers may be able to set up payment plans through private contracts.
What Is Part B Medicare Assignment?
Medicare assignment Part B pertains to outpatient services. Recipients who work with participating providers are generally required to pay 20% of allowed amounts out of pocket. Those who choose providers defined as non-participating may be required to pay excess charges of up to 15%. Recipients with health care providers who are completely opted out may be responsible for 100% of costs for services and procedures.

Christian Worstell is a senior Medicare and health insurance writer with HelpAdivsor.com. He is also a licensed health insurance agent. Christian is well-known in the insurance industry for the thousands of educational articles he’s written, helping Americans better understand their health insurance and Medicare coverage.
Christian’s work as a Medicare expert has appeared in several top-tier and trade news outlets including Forbes, MarketWatch, WebMD and Yahoo! Finance.
While at HelpAdvisor, Christian has written hundreds of articles that teach Medicare beneficiaries the best practices for navigating Medicare. His articles are read by thousands of older Americans each month. By better understanding their health care coverage, readers may hopefully learn how to limit their out-of-pocket Medicare spending and access quality medical care.
Christian’s passion for his role stems from his desire to make a difference in the senior community. He strongly believes that the more beneficiaries know about their Medicare coverage, the better their overall health and wellness is as a result.
A current resident of Raleigh, Christian is a graduate of Shippensburg University with a bachelor’s degree in journalism. You can find Christian’s most recent articles in our blog .
If you’re a member of the media looking to connect with Christian, please don’t hesitate to email our public relations team at [email protected] .
- Does Medicare Cover Physical Therapy?
- What is the Medicare Wellness Exam?
- What Is the Welcome to Medicare Visit?
- Does Medicaid Cover Physical Therapy?
- Medicare Part B Medical Insurance: Costs, Coverage and Benefits

What Does It Mean for a Doctor to Accept Medicare Assignment?
Written by: Malini Ghoshal, RPh, MS
Reviewed by: Malinda Cannon, Licensed Insurance Agent
Key Takeaways
Doctors who accept Medicare assignment are paid agreed-upon rates for services.
It’s important to verify that your doctor accepts assignment before receiving services to avoid high out-of-pocket costs.
A doctor or clinician may be “non-participating” but can still agree to accept Medicare assignment for some services.
If you visit a doctor or clinician who has opted out (doesn’t accept Medicare), you may have to pay for your entire visit cost unless it’s a medical emergency.
Medigap Supplemental insurance (Medigap) plans won’t pay for service costs from doctors who don’t accept assignment.
One of the things that Original Medicare beneficiaries often enjoy about their coverage is that they can use it anywhere in the country. Unlike plans with provider networks, they can visit doctors either at home or on the road; both are covered the same.
But do all doctors accept Medicare patients?
Truth is, this wide-ranging coverage area only applies to doctors who accept Medicare assignment. Fortunately, most do. If you’re eligible for Medicare, it’s important to visit doctors and clinicians who accept Medicare assignment. This will help keep your out-of-pocket costs within your control. Doctors who agree to accept Medicare assignment sign an agreement that they’re willing to accept payment from Medicare for their services.
If you’re a current beneficiary or nearing enrollment, you may have other questions. Do all doctors accept Medicare Advantage plans? What about Medicare Supplement insurance (Medigap)? Read on to learn how to find doctors that accept Medicare assignment and how this keeps your healthcare costs down.
Let’s find your ideal Medicare Advantage plan.
What Is Medicare Assignment of Benefits?
When you’re eligible for Medicare, you have the option to visit doctors and clinicians who accept assignment. This means they are Medicare-approved providers who agree to receive Medicare reimbursement rates for covered services. This helps save you money.
If you have Original Medicare (Part A and B), your doctor visits are covered by your Part B plan. Inpatient services such as hospital stays and some skilled nursing care are covered by Part A .
In order for a participating doctor (or facility) to bill Medicare and be reimbursed, you must authorize Medicare to reimburse your doctor directly for your covered services. This is called the Medicare assignment of benefits. You transfer your right to receive Medicare payment for a covered service to your doctor or other provider.
Note: If you have a Medicare Supplement insurance ( Medigap ) plan to pay for out-of-pocket costs, you may also need to sign a separate assignment of benefits form for Medigap reimbursement. More on Medigap below.
How Can I Find Doctors Near Me That Accept Medicare?
There are several ways to find doctors and other clinicians who accept Medicare assignment close to you.
First, let’s take a look at the different types of Medicare providers.
They include:
Participating providers: Medicare-participating doctors and providers sign a participation agreement stating they will accept Medicare reimbursement rates for their services.
Non-participating providers: Doctors or providers who are non-participating providers are eligible to accept Medicare assignment but haven’t signed a Medicare agreement. They may choose to accept assignment on a case-by-case basis. If you visit a non-participating provider, make sure to ask if they accept assignment for your particular service. Also get a copy of their fees. They will need to select “yes” on Centers for Medicare & Medicaid Services CMS Form 1500 to accept assignment for the service.
Opt-out providers: Some doctors and other providers choose not to accept Medicare. If they choose to opt out, the period is two years (based on Medicare guidelines). The opt-out automatically renews if the provider doesn’t request a change in their status. You would be responsible for paying all costs for services received from an opt-out provider. You cannot bill Medicare for reimbursement unless the service was an urgent or emergency medical need. According to a report from KFF , roughly 1% of non-pediatric physicians opted out of Medicare in 2023.
Visiting a doctor who doesn’t accept assignment may cost you more. These providers can charge you up to 15% more than the Medicare-approved rate for a given service. This 15% charge is called the limiting charge. Some states limit this extra charge to a certain percent. This may also be called the Part B excess charge.
Here are some tips for finding doctors and providers who accept Medicare assignment:
- The easiest way to find a doctor who accepts Medicare assignment is to contact their office and ask them directly.
- If you’re looking for a new doctor, you can use the Medicare search tool to find clinicians and doctors that accept Medicare assignment.
- You can also ask a state health insurance assistance program (SHIP) representative for help in locating a doctor that accepts Medicare assignment.
- Don’t assume that having a longstanding relationship with your doctor means nothing will ever change. Check in with them to make sure they still accept Medicare assignment and whether they’re planning to opt out.
Note: Your doctor can choose to become a non-participating provider or opt out of participating in Medicare. It’s important to verify they accept Medicare assignment before receiving any services.
My Medicare coverage doesn’t address all of my needs.
Do Doctors Who Accept Medicare Have to Accept Supplement Plans?
If your doctor accepts Medicare assignment and you have Original Medicare (Medicare Part A and Part B) with a Medicare Supplement (Medigap) plan, they will accept the supplemental insurance. Depending on your Medigap plan coverage , it may pay all or part of your out-of-pocket costs such as deductibles, copayments and coinsurance.
However, if you have a Medicare Advantage plan (Part C), you may have a network of covered doctors under the plan. If you visit an out-of-network doctor, you may need to pay all or part of the cost for your services.
Keep in mind that you can’t have a Medigap supplemental plan if you have a Medicare Advantage plan.
If you have questions or want to learn more about different Medicare plans like Original Medicare with Medigap versus Medicare Advantage, GoHealth has licensed insurance agents ready to help. They can shop your different options and offer impartial guidance where you need it.
Do Most Doctors Accept Medicare Advantage Plans?
Many doctors accept Medicare Advantage (Part C) plans, but these plans often use provider networks. These networks are groups of doctors and providers in an area that have agreed to treat an insurance company’s customers. If you have a Part C plan, you may be required to see in-network doctors with few exceptions. However, these types of plans are popular options for all-in-one coverage for your health needs. Plans must offer Part A and B coverage, plus a majority also include Part D , or prescription drug coverage. But whether a doctor accepts a Medicare Advantage plan may depend on where you live and the type of Medicare Advantage plan you have.
There are several types of Medicare Advantage plans including:
- Health Maintenance Organization (HMO): These plans have a network of covered providers, as well as a primary care physician to manage your care. If you visit a doctor outside your plan network, you may have to pay the full cost of your visit.
- Preferred Provider Organization (PPO): You’ll probably still have a primary care physician, but these are more flexible plans that allow you to go out of network in some cases. But you may have to pay more.
- Private Fee for Service (PFFS): You may be able to visit any doctor or provider with these plans, but your costs may be higher.
- Special Needs Plan (SNP): This type of plan is only for certain qualified individuals who either have a specific health condition ( C-SNP ) or who qualify for both Medicaid and Medicare insurance ( D-SNP ).
Can I bundle multiple benefits into one plan?
What Are Medicare Assignment Codes?
Medicare assignment codes help Medicare pay for covered services. If your doctor or other provider accepts assignment and is a participating provider, they will file for reimbursement for services with a CMS-1500 form and the code will be “assigned.”
But non-participating providers can select “not assigned.” This means they are not accepting Medicare-assigned rates for a given service. They can charge up to 15% over the full Medicare rate for the service.
If you go to a doctor or provider who accepts assignment, you don’t need to file your own claim. Your doctor’s office will directly file with Medicare. Always check to make sure your doctor accepts assignment to avoid excess charges from your visit.
Health Insurance Claim Form . CMS.gov.
Lower costs with assignment . Medicare.gov.
How Many Physicians Have Opted-Out of the Medicare Program? KFF.org.
Joining a plan . Medicare.gov.
This website is operated by GoHealth, LLC., a licensed health insurance company. The website and its contents are for informational and educational purposes; helping people understand Medicare in a simple way. The purpose of this website is the solicitation of insurance. Contact will be made by a licensed insurance agent/producer or insurance company. Medicare Supplement insurance plans are not connected with or endorsed by the U.S. government or the federal Medicare program. Our mission is to help every American get better health insurance and save money. Any information we provide is limited to those plans we do offer in your area. Please contact Medicare.gov or 1-800-MEDICARE to get information on all of your options.
Let's see if you're missing out on Medicare savings.
We just need a few details.
Related Articles

What Is Medicare IRMAA?
What Is an IRMAA in Medicare?

How to Report Medicare Fraud
Medicare Fraud Examples & How to Report Abuse

How to Change Your Address with Medicare
Reporting a Change of Address to Medicare

Can I Get Medicare if I’ve Never Worked?
Can You Get Medicare if You've Never Worked?

Why Are Some Medicare Advantage Plans Free?
Why Are Some Medicare Advantage Plans Free? $0 Premium Plans Explained

What Is Medicare Assignment?

Am I Enrolled in Medicare?

When and How Do I Enroll?
When and How Do I Enroll in Medicare?

Medicare Frequently Asked Questions
Let’s see if you qualify for Medicare savings today!
Everything PTs Need to Know About Accepting Medicare Assignment
There's no one-size-fits-all answer as to whether or not a PT should accept Medicare assignment, but you can better understand your options.
There's no one-size-fits-all all answer as to whether or not a PT should accept Medicare assignment, but you can better understand your options.

Get the latest news and tips directly in your inbox by subscribing to our monthly newsletter
Discuss any topic within rehab therapy, and chances are that Medicare will come up at some point. Whether it’s talking about Medicare and direct access or Medicare supervision requirements , it’s hard to avoid discussing the ins and outs of the program, given its prominence in healthcare at large. However, there’s one question that probably doesn't get asked enough: do providers have to participate in Medicare? We’re going to dive into the specifics of what rehab therapists can and can’t do when it comes to accepting Medicare assignment, and the pros and cons of each.
What it means to “accept Medicare assignment”
In short, accepting Medicare assignment means signing a contract to accept whatever Medicare pays for a covered service as full payment. Participating and non-participating status only applies to Medicare Part B; Medicare Advantage plans operate with contracts similar to commercial insurance with in-network and out-of-network providers.
Participating Providers
If you’re accepting Medicare assignment for all covered services, you are considered to be a participating provider under Medicare and may not charge patients above and beyond what Medicare agrees to pay. In this case, you can charge 100% of the Medicare Physician Fee Schedule (MPFS) and are paid at 80% of that rate, minus the Multiple Procedure Payment Reduction (MPPR) and the 2% sequestration adjustment.
You may, however, collect patient deductibles and coinsurances—although, as explained in the Medicare payer guide , these providers typically ask Medicare to pay its share before collecting anything from the patient. Per the same resource, these providers are required to submit claims directly to Medicare for reimbursement and cannot charge patients for the claim submission. As Dr. Jarod Carter, PT, DPT, MTC, writes in Medicare and Cash-Pay PT Services , “This is the most common and best-understood relationship that physical therapists have with Medicare.”
Because Medicare beneficiaries often pay less out-of-pocket costs when receiving care from a provider who accepts assignment, patients may be more willing to work with these providers. Thus, if you accept assignment, you may have access to not only more Medicare patients but also more potential referral partners who only work with assignment-accepting providers.
You must accept whatever Medicare deems appropriate compensation, and as we know, that’s below market value more often than not. Given the recently announced cuts to assistant-provided services and the 8% cut to all physical therapy services , accepting assignment may be increasingly less appealing to physical therapists. That said, if you serve a large Medicare population, the volume of patients you see may make it financially beneficial for you to continue playing by Medicare’s rules.
If you don’t want to accept Medicare assignment, what are your other options?
Non-participating providers.
As Meredith Castin explains in 4 Things to Know About Billing for Cash-Pay PT , Medicare also allows physical therapists to be non-participating providers (a.k.a. non-enrolled providers), which simply means that, while they are still in a contractual relationship with Medicare (and thus, are eligible to provide covered services to Medicare beneficiaries), they have not agreed to accept assignment across the board.
If a non-participating provider opts to accept assignment for a case, they can charge 95%.
If they do not accept assignment but still treat the patient, these providers may charge up to what Medicare calls “the limiting charge” for a service—which is 15% above the Medicare allowed amount. Non-participating providers may choose to accept assignment for some services, but not others —or no services at all. For services that are not under assignment, the provider may collect payment directly from the patient; however, he or she must still bill Medicare, so that Medicare may reimburse the patient.
Non-participating providers are still eligible to serve Medicare beneficiaries, but they maintain some degree of freedom when it comes to pricing their services. In other words, if you are a non-participating provider, you are less beholden to what Medicare deems as appropriate payment than you are as a participating provider.
That said, you do still have to charge within Medicare’s limit, which means your freedom is far from total. Additionally, because patients may have to pay more out of pocket for your services and/or pay and wait for reimbursement from Medicare, you may have to work harder to convince them that you’re worth the financial investment. With the right data and marketing , it’s definitely doable; it may just require more effort.
No Relationship with Medicare
Physicians are eligible to “opt-out” of Medicare, which means that even if they are neither participating nor non-participating providers, they can still see Medicare beneficiaries on a cash-pay basis. Physical therapists do not enjoy the same privilege. So, if you decide not to be a Medicare participating provider or non-participating provider, then you effectively have no relationship with Medicare. Thus, you are not able to provide Medicare-covered services to Medicare beneficiaries.
That said, all physical therapists, regardless of their relationship with Medicare, may provide never-covered services to Medicare beneficiaries, including wellness services. According to Castin, though, providers who go down that route, “need to be very clear about Medicare’s definition of ‘wellness services’ versus ‘physical therapy services.’” According to cash-pay PT Jarod Carter , it’s imperative for your documentation to clearly support that the services were indeed wellness as opposed to therapy.
As a provider with no relationship with Medicare, you’re not required to play by Medicare’s rules when it comes to reporting requirements or (lowball) payments. You’re also not at all affected by Medicare’s most recent cuts, which, quite frankly, is a big bonus.
However, as of 2007 , 15% of the US population was enrolled in Medicare; that’s 44 million people—most of whom could benefit from seeing a physical therapist to improve function and mobility and decrease pain. And that number is projected to grow to 79 million people by 2030. As such, choosing not to play ball with Medicare means you’re walking away from a very large market of patients who need your services.
It’s your decision.
Deciding on accepting Medicare assignment—and what type of relationship you’d like to have with Medicare—is not an easy decision to make, and there are a lot of factors to take into consideration before getting involved or breaking it off with this substantial federal payer. That said, it is important to know that you have options. Have more questions about what it means to accept assignment as a PT? Ask them below, and we’ll do our best to find you an answer.
Related posts

How to Document and Bill for Home-Based Physical Therapy Services

How to Pick the Right ICD-10 Code for Depression

What You Need to Know About the Change Healthcare Cyberattack

Medicare and Cash-Pay PT Services, Part 1: The Must-Know Concepts to Avoid Legal Issues and Capitalize on Opportunities

Medicare and Direct Access

The Medicare Maintenance Care Myth

Learn how WebPT’s PXM platform can catapult your practice to new heights.

Medicare Assignment: Understanding How It Works

Medicare assignment is a term used to describe how a healthcare provider agrees to accept the Medicare-approved amount. Depending on how you get your Medicare coverage, it could be essential to understand what it means and how it can affect you.
What is Medicare assignment?
Medicare sets a fixed cost to pay for every benefit they cover. This amount is called Medicare assignment.
You have the largest healthcare provider network with over 800,000 providers nationwide on Original Medicare . You can see any doctor nationwide that accepts Medicare.
Understanding the differences between your cost and the difference between accepting Medicare and accepting Medicare assignment could be worth thousands of dollars.
Doctors that accept Medicare
Your healthcare provider can fall into one of three categories:
Medicare participating provider and Medicare assignment
Medicare participating providers not accepting medicare assignment, medicare non-participating provider.
More than 97% of healthcare providers nationwide accept Medicare. Because of this, you can see almost any provider throughout the United States without needing referrals.
Let’s discuss the three categories the healthcare providers fall into.
Participating providers are doctors or healthcare providers who accept assignment. This means they will never charge more than the Medicare-approved amount.
Some non-participating providers accept Medicare but not Medicare assignment. This means you can see them the same way a provider accepts assignment.
You need to understand that since they don’t take the assigned amount, they can charge up to 15% more than the Medicare-approved amount.
Since Medicare will only pay the Medicare-approved amount, you’ll be responsible for these charges. The 15% overcharge is called an excess charge. A few states don’t allow or limit the amount or services of the excess charges. Only about 5% of providers charge excess charges.
Opt-out providers don’t accept Original Medicare, and these healthcare providers are in the minority in the United States. If healthcare providers don’t accept Medicare, they won’t be paid by Medicare.
This means choosing to see a provider that doesn’t accept Medicare will leave you responsible for 100% of what they charge you. These providers may be in-network for a Medicare Advantage plan in some cases.
Avoiding excess charges
Excess charges could be large or small depending on the service and the Medicare-approved amount. Avoiding these is easy. The simplest way is to ask your provider if they accept assignment before service.
If they say yes, they don’t issue excess charges. Or, on Medicare.gov , a provider search tool will allow you to look up your healthcare provider and show if they accept Medicare assignment or not.
Medicare Supplement and Medicare assignment
Medigap plans are additional insurance that helps cover your Medicare cost-share . If you are on specific plans, they’ll pay any extra costs from healthcare providers that accept Medicare but not Medicare assigned amount. Most Medicare Supplement plans don’t cover the excess charges.
The top three Medicare Supplement plans cover excess charges if you use a provider that accepts Medicare but not Medicare assignment.
Medicare Advantage and Medicare assignment
Medicare assignment does not affect Medicare Advantage plans since Medicare Advantage is just another way to receive your Medicare benefits. Since your Medicare Advantage plan handles your healthcare benefits, they set the terms.
Most Medicare Advantage plans require you to use network providers. If you go out of the network, you may pay more. If you’re on an HMO, you’d be responsible for the entire charge of the provider not being in the network.
Do all doctors accept Medicare Supplement plans?
All doctors that accept Original Medicare accept Medicare Supplement plans. Some doctors don’t accept Medicare. In this case, those doctors won’t accept Medicare Supplements.
Where can I find doctors who accept Medicare assignment?
Medicare has a physician finder tool that will show if a healthcare provider participates in Medicare and accepts Medicare assignments. Most doctors nationwide do accept assignment and therefore don’t charge the Part B excess charges.
Why do some doctors not accept Medicare?
Some doctors are called concierge doctors. These doctors don’t accept any insurance and require cash payments.
What is a Medicare assignment?
Accepting Medicare assignment means that the healthcare provider has agreed only to charge the approved amount for procedures and services.
What does it mean if a doctor does not accept Medicare assignment?
The doctor can change more than the Medicare-approved amount for procedures and services. You could be responsible for up to a 15% excess charge.
How many doctors accept Medicare assignment?
About 97% of doctors agree to accept assignment nationwide.
Is accepting Medicare the same as accepting Medicare assignment?
No. If a doctor accepts Medicare and accepts Medicare assigned amount, they’ll take what Medicare approves as payment in full.
If they accept Medicare but not Medicare assignment, they can charge an excess charge of up to 15% above the Medicare-approved amount. You could be responsible for this excess charge.
What is the Medicare-approved amount?
The Medicare-approved amount is Medicare’s charge as the maximum for any given medical service or procedure. Medicare has set forth an approved amount for every covered item or service.
Can doctors balance bill patients?
Yes, if that doctor is a Medicare participating provider not accepting Medicare assigned amount. The provider may bill up to 15% more than the Medicare-approved amount.
What happens if a doctor does not accept Medicare?
Doctors that don’t accept Medicare will require you to pay their full cost when using their services. Since these providers are non-participating, Medicare will not pay or reimburse for any services rendered.
Get help avoiding Medicare Part B excess charges
Whether it’s Medicare assignment, or anything related to Medicare, we have licensed agents that specialize in this field standing by to assist.
Give us a call, or fill out our online request form . We are happy to help answer questions, review options, and guide you through the process.
Related Articles
- What are Medicare Part B Excess Charges?
- How to File a Medicare Reimbursement Claim?
- Medicare Defined Coinsurance: How it Works?
- Welcome to Medicare Visit
- Guide to the Medicare Program

CALL NOW (833) 972-1339

What Is Medicare Assignment?
Some people have been with the same family doctor for years. Now that you’re on Medicare, you’ll need to find out if your long-time doctor accepts Medicare assignment.
When it comes to Medicare, providers agree to be participating providers, non-participating providers, or they opt-out altogether. Knowing and understanding where your doctors fall in these categories will help you make educated choices about your care.
Sign up for our newsletter for weekly emails about senior interest topics like Medicare, health and fitness, gardening, retirement planning, and more!
When a doctor accepts Medicare assignment , it simply means they agree to take Medicare. Medicare has their own long list of approved charges, or what they will pay for every service under the sun. It’s usually far less than the “retail” cost of care, so when a doctor agrees to take Medicare, they agree to accept those rates.
You’ll see or hear the term “Medicare assignment” when you look up Medicare coverage for different procedures or doctor visits. It may also come up in conversations with your insurance agent about Medicare and supplemental coverage.

As of 2020, approximately 96% of health care providers accept Medicare assignment . So in reality, you don’t need to be too concerned about your doctor not taking Medicare. However, even though most providers accept Medicare assignment, a quick call to make sure they accept it is always a good idea.
Rest assured that if a provider does not take Medicare, they are required to give you a form stating this, and you have to sign it saying you understand Medicare will not pay for the services. If you don’t sign that form, they cannot continue care.
If you’re looking for a new physician or for one that specializes in a medical area, you can use Medicare’s physician compare tool . It's easy to navigate by simply entering your location and a doctor's name or any condition or body part; then, it'll tell you who accepts Medicare assignment in your area. That’ll ensure you don’t waste any time, or possibly money, on a provider that doesn’t accept your Medicare insurance.
Related: How to Find a Good Doctor: 18 Steps to Help You Choose the Right Physician
Participating Providers
Participating providers agree to accept Medicare assignment and will only charge you the Medicare-approved amount for any covered services. The provider doesn’t charge you upfront but will bill Medicare for the cost of services.

This doesn’t mean you won’t owe any money, though. Medicare will pay 80% of the cost, and if you don’t have a Medicare Supplement, you may still be responsible for your 20% copay.
For example, if you have Medicare and Medigap Plan F* or Plan G – and use a doctor or provider that accepts Medicare assignment – you won’t pay any coinsurance at all. With Plan F, you have zero out-of-pocket costs, and with Plan G, you only have to meet a very low deductible of $198 as of 2020.
*Plan F was phased out at the beginning of 2020 for new Medicare enrollees. However, if you’re already enrolled in Plan F, you can keep it. If you were eligible for Medicare before January 1, 2020, you can still purchase it.
Related reading:
- A Shopper’s Guide to Comparing Medicare Supplement Prices
- Medigap Plan F Is Officially Phasing Out: What to Do Now
Non-Participating Providers
Non-participating providers have not signed an agreement to accept the Medicare-approved amount for Medicare-covered services, but they can choose to do so. Since they haven’t agreed to the Medicare-approved amount, they can charge more for their services than participating providers.
However, there is a limiting charge on how much doctors who don’t accept Medicare's approved amount can charge people on Medicare. Federal law sets the limit at no more than 15% of the Medicare-approved amount, but some states limit it even further. That 15% charge is called an excess charge .

So, if you went to the doctor and the Medicare-approved rate for an office visit was $100, the excess charge could make your new total $115.
Depending on how your doctor handles payment, you may have to pay the total amount before leaving. If this is the case, Medicare will reimburse you 80% of the Medicare-approved charge, leaving you with the 20% copay plus the 15% upcharge. Using our same example, you would owe $20 for the copay and $15 for the excess charge making your total portion $35.
Here again, the Medicare Supplemental Plans F and G not only cover your coinsurance, but they also cover that 15% excess charge. You would still have zero out-of-pocket expenses except for Plan G’s $198 deductible in 2020.
Opt-Out Providers
Opt-Out Providers are those that prefer not to participate in the Medicare program at all. That 15% charge limit we just talked about doesn’t apply to these providers. They can charge whatever they want for services, and they won’t be sending any of the bills to Medicare.

A doctor who opts-out of accepting Medicare requires a private contract between patient and provider, agreeing that neither will receive reimbursement from Medicare for services provided.

Popular Providers that Don’t Accept Medicare Assignment
Even though only 4% of healthcare providers don’t accept Medicare assignment, there are a few popular ones you may be interested to know.
Mayo Clinic is top-ranked for quality more often than any other health care organization. Their care is commonly referred to as world-class, but interestingly enough, they don’t accept Medicare assignment.
Another area of medical service that doesn’t accept Medicare assignment is Concierge Medicine . This type of practice, also known as direct primary care, is an alternative to the typical “fee-for-service” doctor’s office. Rather than pay a fee each time you visit your physician, concierge services require a membership fee.
What makes Concierge Medicine stand out from your typical doctor’s office is they are there to serve you – the practice is set up to serve the patient, not the physician.
David Winter, MD, a concierge medicine physician in Dallas explains to HealthLeaders Media that patients get valet parking, coffee and soft drinks when they arrive, 24/7 access to service, lengthier and unrushed appointments, and no idle time in the waiting room. In fact, they don’t call it a waiting room – they call it a greeting room.
Many have chosen to pay for this top-of-the-line service rather than utilize their Medicare benefits. To find a Concierge Medicine provider in your area, we recommend doing an online search for “concierge medicine in [city].” If there are any providers near you, they should come up right away.
Each person and medical need is different. There is nothing wrong with a provider that doesn’t accept Medicare assignment, and depending on your situation, the Mayo Clinic or Concierge Medicine might be the right choice for you.
The Lasso Healthcare Medicare MSA Is Unique
The Lasso Healthcare MSA is a $0 premium, high-deductible health insurance plan paired with a special deposit that you can use for qualified medical expenses. In 2020, Lasso Healthcare deposits $3,240 in a savings account, and you can use that money to pay for doctor visits, hospital stays, lab work, and the list goes on.
The Lasso Healthcare MSA does not have networks, which means you can see any doctor that accepts Medicare. However, you can also see doctors who don’t accept Medicare – it just works a little differently.

So, let’s say the doctor is non-participating. They aren’t required to see you, but they can bill you up to that limiting charge, which is typically 15% more than the Medicare-approved rate. While this won’t count towards your plan deductible, you can use your deposit to pay for it!
The same goes for providers who opt-out of Medicare completely. This becomes a private contract between you and that provider. While this won’t count toward your plan deductible – and the plan won’t pay them if you’ve reached your deductible – you can use your annual deposit to pay for it.
As long as the item or service is a qualified medical expense (these are outlined in IRS Publication 502 ), you can use any funds left in your medical savings account.
The Lasso Healthcare MSA provides flexibility.
Benefits of Using Health Care Providers Who Accept Medicare Assignment
When you choose a doctor or physician who accepts Medicare assignment, you’re sure about several things:
- You’ll know what charges to expect
- You may pay less out-of-pocket
- Usually, you won’t have to pay anything until Medicare has been billed and pays their part
- Your doctor will submit all the claims to Medicare for you
Downfalls of Using a Non-Participating Health Care Provider or One Who Opts-Out
If you choose a doctor who either opts-out of Medicare or does not participate in Medicare assignment, you can expect to encounter the following:
- You will typically pay out-of-pocket for all charges up-front, and then be reimbursed by Medicare
- Your doctor may or may not file claims for you – you may have to do that yourself
- You can be charged an excess charge of up to 15% on top of your copay which is 20%
Rest assured that if you have a Medicare Supplement Plan F or G, you don’t have to worry about excess charges.
In the case that you choose to see a health care provider that has opted-out of Medicare assignment, you’ll find:
- Your provider doesn’t have to stick with the Medicare-approved amount or the limiting charge – they can charge you whatever they choose
- You’ll pay the entire amount for all services – Medicare won’t reimburse you
This doesn’t mean that any of these categories of doctors is better than the other. They are simply going to cost you different amounts.
It's essential to understand what Medicare assignment means, as well as the different options available to you when it comes to your health care.
Medicare assignment gives you peace of mind knowing what to expect financially, but that doesn’t always mean it’s the right choice.

Before making any decisions, take a good look at your finances, know your medical needs, and talk with your insurance agent to make an educated decision on what is best for you.
You are ultimately responsible for your healthcare. Making well-informed decisions is a significant first step.

Related Reading
- Medicare 101: What You Need to Know About Medicare
- Medicare and Social Security: How They Work Together
- When Does Medicare Start?
Get Your Free Medicare Planner
At the end of the day, your Medicare Planner will give you clarity and peace of mind knowing that your financial future is in great hands.

Our team of dedicated, licensed agents can help you as little or as much as you need. Whether it’s answering a few questions about Medicare or creating a comprehensive Medicare Planner with you, we are your Senior Allies.
122 W. Prairie Avenue Decatur, Illinois 62523 Toll-Free: 833-801-7999
Not connected with or endorsed by the United States government or the federal Medicare program.
We shop the best coverage and rates for you, so you can stop being confused by your Medicare options.
Site Navigation
- New to Medicare
- Coverage Types
- Get a Quote
Get Weekly Articles & Announcements
What Is Medicare Reimbursement?

Medicare reimbursement is when a doctor or healthcare facility receives payment directly from Medicare for providing care to a Medicare enrollee.
Medicare sets reimbursement rates for each of its covered services, so when a provider accepts Medicare assignment, they agree to these rates and may not ask the patients to pay more. A doctor who accepts assignment may only charge the patient for their deductible or coinsurance , filing a claim for reimbursement from Medicare for the remaining charges.
In some cases, however, a doctor who does not accept assignment may still provide care to a Medicare beneficiary and decline to file a claim for Medicare reimbursement. In this scenario, the beneficiary must front the full cost of care, which may exceed Medicare’s set rates, and submit their own claim for reimbursement.
Table of Contents
How does medicare reimbursement work.
If you have Original Medicare and seek a covered service from a provider who does not accept assignment, you may have to file for Medicare reimbursement. Here’s how reimbursement works for each part of Medicare .
Medicare Part A
Medicare Part A provides hospital insurance. If you seek hospital services from a facility that does not accept assignment and declines to file its own reimbursement claim to Medicare, you may have to seek reimbursement yourself.
Medical services covered by Part A include:
- Inpatient hospital care
- Skilled nursing facilities
- Nursing homes
- Home healthcare
If you seek any of the above types of care from a facility that does not accept assignment, you may have to file for Medicare reimbursement. Medicare might reimburse you directly, or the facility might receive the reimbursement from Medicare and issue you a refund accordingly.
Medicare Part B
Medicare Part B covers medically necessary and preventative health services. You may have to seek Medicare reimbursement under Part B if your provider does not accept assignment or file their own reimbursement claim for the following types of services:
- Ambulance transportation
- Bone mass measurement
- Care as part of a clinical research study
- Clinical lab services
- Counseling to quit smoking
- Durable medical equipment
- Emergency department services
- Health screenings and tests
- Home health services
- Inpatient or outpatient care or partial hospitalization for a mental health condition
- Medical nutrition, occupational, or physical therapy
- Preventative healthcare
- Services and supplies for kidney dialysis
- Vaccinations
When Medicare issues your reimbursement, you may receive it directly or receive it in the form of a refund from your provider.
Medicare Advantage
Unlike Original Medicare, which comprises Part A and Part B, Medicare Advantage (also called Part C) plans come from private insurance companies. All Medicare Advantage Plans provide the same coverage as Original Medicare, plus added benefits like prescription drug coverage, vision , and dental.
If you have a Medicare Advantage Plan , you may not file for reimbursement from Medicare since your health coverage comes from a private insurer. If you seek covered health services and the facility or doctor bills you rather than your insurance company for the cost, you may have to seek reimbursement from your insurance provider.
Medicare Advantage Plans vary by provider, so ask your insurance company how to file for reimbursement should this situation occur.
Medicare Part D
Medicare Part D covers prescription drugs. As with Medicare Advantage, Part D plans come from private insurance providers, so their specific benefits and terms of coverage vary from company to company.
Because you receive Part D coverage through a private company, you will never request Medicare reimbursement for products or services covered under Part D.
If you pay out of pocket for services covered under Part D, you might file for reimbursement from your Part D Plan’s insurance provider. However, this process varies among individual providers; contact yours for detailed guidance on how to request reimbursement.
Medicare Part B only pays for 80% of the cost of its covered services. Medigap, also called Medicare supplementary insurance, helps pay for the remaining 20% to reduce the beneficiary’s out-of-pocket expenses .
Medigap plans are only available to Original Medicare enrollees through private insurance companies; if you have a Medicare Advantage Plan, you may not purchase Medigap. If you receive a covered service from a health provider who accepts assignment, Medigap may reimburse you for your portion of the treatment cost.
However, because Medigap plans come from private providers, you will not file claims for Medigap reimbursement to Medicare directly. Contact your Medigap provider to learn about its specific reimbursement process.
How Are Reimbursements Determined?
Medicare revises its established reimbursement rates for covered services on an annual basis. A select committee helps determine these rates each year, with committee members including a mix of medical professionals and other professionals.
The process of determining reimbursement rates is complex and often warrants criticism from the medical community for lacking transparency. Generally, reimbursement rates account for the following factors:
- The type of product or service
- The type of health provider or facility
- How complex the service is
- Where the service takes place
- Adjustments for inflation
The Medicare program is not required to accept the committee’s recommendations for reimbursement rates , but in more than 90% of cases, it has.
What Happens if Medicare Does Not Reimburse You in Full?
Medicare may not provide reimbursement for services that are not medically necessary or covered by Original Medicare. If Medicare denies your request for reimbursement and you disagree with the decision, you may file an appeal .
In some cases, if you file for Medicare reimbursement, you may not receive the full amount you paid out of pocket for your covered service. Remember, Medicare pre-establishes its reimbursement rates. If your health provider does not accept assignment, they did not agree to cap charges at the Medicare-approved rate. For this reason, you may not get all of your money back.
How To Receive Medicare Reimbursement
If you paid out of pocket for a Medicare-covered service from a provider who does not accept assignment, first ask the provider to file the Medicare reimbursement claim. If they decline to do so, it’s up to you to request reimbursement from Medicare. Here’s how to do it:
- Download the Patient’s Request for Medical Payment (Form CMS-1490S) from the Centers for Medicare and Medicaid Services (CMS) website.
- Follow the provided instructions to complete the form, including a detailed explanation of why you are filing the claim instead of your health provider.
- Provide an itemized bill, your provider’s name and address, your diagnosis, details on when and where you received the service, and a description of the service, along with any other information that might support your claim.
- Make a copy of your completed form to keep for your personal record.
- Consult the CMS’s Medicare contractor directory to determine where you should mail your claim.
- Mail a completed Form CMS-1490S to your Medicare contractor.
If you are unable to file the claim yourself, you may designate someone else to do it for you. In this case, make sure to download and complete the Authorization to Disclose Personal Health Information (Form CMS-10106) from CMS’s website.
As a Medicare beneficiary, you may receive covered services from a medical provider who does not accept assignment from Medicare. For you to get coverage for these services, you or your provider must file a claim for reimbursement from Medicare.
If your provider refuses or otherwise declines to file for Medicare reimbursement, it’s up to you to do so, which involves downloading, completing, and mailing in the appropriate form.
If you have a Medicare Advantage Plan, you must file reimbursement through your private insurance provider rather than through Medicare directly. The same applies if you are seeking reimbursement for services covered by Medicare Part D or Medigap.
Frequently Asked Questions
Yes, Medicare does not reimburse enrollees for health services that are not medically necessary or covered by Original Medicare. Such services might include dental care , eye exams , cosmetic surgery , custodial care, and hearing aids . Moreover, Medicare does not provide reimbursements to Medicare Advantage enrollees or for Medigap or Part D claims.
No, Medicare does not reimburse beneficiaries for premium costs. However, some types of Medicare Advantage Plans offer Part B premium reduction benefits, through which the plan pays for some or all of the Part B premium. Moreover, some employers may offer Medicare Part B premium reimbursements.
You’re just a few steps away from seeing your Medicare Advantage plan options.
Call 662-844-3300
What is medicare assignment.
- October 21, 2020

Share this Content
When you have Original Medicare, you should ask your doctor if they accept Medicare assignment before getting services. But there are more than 800,000 doctors who take Medicare. So no matter if you want to see the local specialist or the top doctor in a big city, it’s likely they’re in-network. Today, we’re going to define Medicare assignment and explain what doctors accept it.
Medicare Assignment Defined
It’s an agreement between Medicare and a physician. Accepting assignment means your doc agrees to Medicare’s payment terms for covered services. Did you know that over 93% of all physicians in America accept Medicare assignment?
Before people are eligible for Medicare, most use networks and referrals.
Related Post: Medicare Terms You Should Know
Categories for Medicare Assignment
There are three categories:
- Participating doctors accept Medicare assignment. The doc takes Medicare and only charges up to the Medicare-approved amount.
- Non-Participating doctors decide to accept or not accept Medicare. The doc takes Medicare but can charge an excess fee.
- Doctors that have opted out are the minority. These physicians don’t take Medicare and you pay 100% of the costs.
Again, since MOST doctors accept Medicare assignment, you’ll have more freedom with choosing your doctor (when you get Medicare). BUT you should always confirm first whether or not your doctor accepts the assignment.
Related Post: Should I Be Worried About Medicare Excess Charges?
What Doctors Accept Medicare Assignment?
Not everyone agrees to the terms. Doctors may choose to opt-out or not participate in Medicare.
Doctors who accept Medicare will also accept Medicare Supplement (Medigap) coverage. However, not all doctors that accept Medicare will take a Medicare Advantage plan.
What If a Doctor Doesn’t Accept Medicare Assignment?
This means you pay for medical services out of pocket. You might pay 100%, then wait for reimbursement. Medicare reimbursement isn’t guaranteed.
Medicare Opt-Out Private Contract
Sometimes doctors ask their patients to sign a private contract. This usually occurs with physicians who won’t have an agreement with Medicare. In other words, they’ve opted-out of Medicare payment terms. If you sign a contract, you accept the full amount by yourself, and Medicare can’t repay you.
Does Having Medicaid Affect Your Doctor Network?
This can be a complex situation. If you’re on Medicare and Medicaid, you can visit any doctor that accepts Original Medicare (A and B). The best thing you can do is ensure that the provider takes both. Then, the Medicaid plan will pay your share of the bill.
You Can Lower Costs with Medicare Assignment
By seeing a doctor that accepts Medicare assignment, you’ll have lower costs. Medicare recipients with Medigap insurance pay less out-of-pocket, and they can save money on deductibles, copays, and coinsurance. Just know that Medigap plans have higher premiums than most Medicare Advantage programs.
Whether you’re interested in Medicare Advantage, Medicare Supplements , or prescription drug coverage, we can help. Bobby Brock Insurance will find you the right plan — at the best rate — in your area. Contact an agent online or call (662) 844-3300.
Related Blog Posts

When you turn 65 (or if you are disabled and have been receiving Social Security benefits for 24 months), you…

Hospice care is a type of health care that helps people with a terminal illness and are not likely to…

Justin Brock
President & CEO of Bobby Brock Insurance
Best Selling
More Search Terms
Looking for something specific?
More From Forbes
Did you know medicare does not cover a physical exam.
- Share to Facebook
- Share to Twitter
- Share to Linkedin
The "Welcome to Medicare" preventive visit is not a physical exam.
A friend, new to Medicare, asked me whether Medicare covered annual physicals. I told him, “No, it doesn’t.” The Social Security act clearly prohibits Medicare from paying for annual physical examinations.
A week later, he told me I was wrong. He found proof that Medicare does indeed cover these examinations. “Physical exams, right there, on the HHS.gov website , in the list of services that Part B covers.” (Health and Human Services is an agency of the federal government that administers health and welfare programs, including Medicare.)
I replied that I wasn’t wrong, HHS just shortened the title for a preventive service that Medicare does cover.
The Affordable Care Act introduced the Initial Preventive Physical Examination. This preventive service for those with Medicare does not resemble a physical exam. There is no palpation (feeling with fingers or hands), no auscultation (listening to body sounds) and no percussion (tapping body parts), all essential components of a physical examination . And, unlike annual physicals, you only get one visit, within the first 12 months of Part B enrollment.
Because “physical examination” is in the regulatory title, there was and still is considerable confusion. Medicare now calls this service a “Welcome to Medicare” preventive visit .
Best High-Yield Savings Accounts Of 2024
Best 5% interest savings accounts of 2024, more about the welcome visit.
The Welcome to Medicare visit is a review of your medical and social history and counseling about preventive services. Specifically, this visit includes :
- Height, weight, and blood pressure measurements
- A calculation of body mass index
- A simple vision test
- A review of risk factors for depression, functional ability and safety level, and current opioid prescriptions
- Screening for visual acuity and potential substance use disorders
- Education, counseling, and referral based on previous components, and
- End-of-life planning (if the patient consents).
Annual Medicare Wellness Visit
Medicare offers a second preventive visit; this one is every 12 months. It may be annual, but this visit is also not a physical exam. The purpose is to update the personalized prevention plan. The components include :
- A review of medical and family history
- Height, weight, blood pressure, and other routine measurements
- Detection of any cognitive impairment
- Personalized health advice
- Updating the list of current providers, suppliers, prescriptions, and health risk factors, and
- Advance care planning.
Both these visits address a plan for screenings, vaccinations, and other preventive services, including:
- Flu and COVID vaccinations
- The RSV (respiratory syncytial virus) vaccine (now covered with no cost sharing under Part D, prescription drug coverage)
- Annual mammogram
- Prostate cancer screening, and
- Colonoscopy.
Medicare covers many more preventive services designed to help beneficiaries stay healthy, most with no cost sharing. Find the list here.
Take-away points
First, here are a few points about the two wellness visits.
- There is no cost for the initial welcome or annual wellness visits.
- However, if the physician addresses a medical issue, such as elevated blood pressure, don’t be surprised if you get a bill. That’s because the visit would be considered diagnostic and cost sharing (deductible and/or copayment) applies.
- If you have Original Medicare, see providers who accept Medicare assignment.
- If you chose a Medicare Advantage plan, schedule your appointments with in-network physicians, most likely with your primary physician.
And here’s what my friend and you need to know about annual physical exams.
- Even though Medicare does not cover them, you can still get a physical exam. But know that you may have to pay for parts or all of it. For example, Part B would cover an EKG or chest x-ray for medical reasons, like an abnormal heart rhythm or severe lung congestion, with the usual cost sharing.
- Some Medicare Advantage plans offer routine physical exams, generally when performed by the primary care physician. Check the plan’s Evidence of Coverage for more information.
- Finally, no matter the issue, know that what you read on a website may not be correct. Double check coverage before you proceed.
- Editorial Standards
- Reprints & Permissions
How does Medicare work? And how is it financed?
Subscribe to the hutchins roundup and newsletter, louise sheiner , louise sheiner the robert s. kerr senior fellow - economic studies , policy director - the hutchins center on fiscal and monetary policy @lsheiner lorae stojanovic , and lorae stojanovic senior research assistant - economic studies , the hutchins center on fiscal and monetary policy david wessel david wessel director - the hutchins center on fiscal and monetary policy , senior fellow - economic studies @davidmwessel.
March 20, 2024
- 11 min read
What is Medicare?
Medicare is a federal health insurance program that covers nearly all Americans aged 65 and over and some younger Americans with disabilities. As of September 2023, 66 million individuals were enrolled in Medicare, with 11% receiving assistance due to disability and 89% due to age. Medicaid, a separate program, covers low-income individuals.
The federal government spent $832 billion on Medicare in fiscal year 2023, a sum equal to 3.1% of GDP. As the size of the population over age 65 grows and healthcare costs rise, Medicare spending will rise; the Congressional Budget Office projects that Medicare will be 4.2% of GDP in 2034. Today, 13.6% of total federal outlays go toward Medicare.
More from Election '24
Wendell Primus, Paris Rich Bingham
February 15, 2024
Wendell Primus, Jack A. Smalligan, Chloe Zilkha
March 6, 2024
Glencora Haskins, Mayu Takeuchi, Julia Bauer, Patrick Rochford
March 15, 2024
What is “traditional” Medicare, and what does it cover?
Traditional Medicare refers to Parts A and B, the programs that Congress created in 1965 .
Beneficiaries choose between traditional Medicare and Medicare Advantage (defined below). Under traditional Medicare, beneficiaries are enrolled in Medicare Part A , which covers inpatient hospital care, some skilled nursing facility care, some home care, and hospice care; and Medicare Part B , which covers physician and other health provider services, outpatient care, preventive care, and some home health visits. Patients who choose traditional Medicare may separately enroll in Medicare Part D , which covers prescription drugs. Traditional Medicare does not cap yearly out-of-pocket payments, but many beneficiaries have supplemental coverage that reduces or eliminates deductibles, copays, and coinsurance and often caps total out-of-pocket expenses. Some beneficiaries purchase supplemental coverage from private insurers, while others receive it through their former or current employer or through Medicaid. Roughly one in ten traditional Medicare patients has no supplemental coverage at all.
What is Medicare Advantage, and what does it cover?
An alternative to traditional Medicare is to enroll in a private plan through Medicare Advantage, also known as Medicare Part C. Beneficiaries in Medicare Advantage pay premiums to private insurance plans. These premiums may be less than or greater than the Part B premium, depending on the plan. Many of these private options include drug coverage comparable to Medicare Part D, plus additional coverage—such as hearing, vision, and dental services—not offered by traditional Medicare. However, Medicare Advantage plans often have less extensive networks of doctors and hospitals than traditional Medicare. And cost-sharing terms dictating copays, coinsurance, premiums, and yearly limits vary between plans. A review of many studies found that Medicare Advantage and traditional Medicare rank similarly when it comes to beneficiary experience, affordability, service utilization, and quality. But Medicare Advantage has been criticized for being more expensive for the government. The Medicare Payment Advisory Commission estimates that the government spends 22% more for a patient enrolled in Medicare Advantage than it would if the same patient enrolled in traditional Medicare.
Medicare Advantage enrollment has surged in recent years. In 2007, one in five eligible Medicare beneficiaries were enrolled in Medicare Advantage. By 2023, half were.
Where does Medicare get its funding?
Each part of Medicare is funded differently. Medicare Part A is funded mainly through the Hospital Insurance (HI) payroll tax, which is levied on both employers and employees. Employees pay a 1.45% tax on wage earnings below a threshold of $200,000 ($250,000 for married couples) and a 2.35% tax on wages exceeding the threshold. Employers pay a tax equal to 1.45% of employees’ earnings. Payroll taxes accounted for 89% of Part A revenues in 2022. An additional 8% of revenues came from income taxes on Social Security benefits received by high-income beneficiaries.
There are no premiums for Part A coverage for most beneficiaries. In contrast, beneficiaries must pay premiums to enroll in Medicare Parts B and D, but premium revenues cover only about one quarter of expenses. Nearly all the remainder is covered by general revenues. Medicare Advantage is paid for by a combination of funds allocated to Medicare Parts A and B. In 2022, Medicare Advantage expenses accounted for 49% of Medicare Part A spending.
Why are Parts A and B of Medicare financed differently?
Medicare’s original financing structure is the result of a political compromise in the 1960s. The Kennedy administration, with the support of many Democrats in Congress, proposed hospital insurance for the elderly that would be covered by a mandatory payroll tax. Many Republicans opposed the idea, favoring instead a voluntary program funded by general revenues and premiums. Some southern Democrats also opposed the plan, fearing that mandatory tax-funded federal healthcare would force racial integration in the still-segregated South.
The compromise, which passed in the wake of Kennedy’s assassination, was a two-part system. Part A, which satisfied Kennedy’s original priorities, funded hospital insurance through a mandatory tax and desegregated hospitals by stipulating they would only receive funding if they admitted Black patients . Part B, which satisfied Republicans’ priorities, expanded insurance beyond hospital care and was funded by general revenues and premiums.
What is the Medicare Hospital Insurance trust fund?
Payroll tax receipts and other Part A revenues are deposited into the Hospital Insurance (HI) trust fund; Part A and some Part C expenses come out of the HI trust fund. The surplus, if any, is invested in interest-earning U.S. Treasury securities.
In recent years, spending has often exceeded revenues. Existing trust fund balances are drawn down to fill the gap. Fueled by increasing per capita healthcare costs and an aging population, Part A Medicare spending is expected to exceed revenues in the coming years, leading to a depletion of trust fund assets. The Centers for Medicare & Medicaid Services project that in 2031, the HI fund will run out of cash, and revenues will be sufficient to cover only 89% of Part A’s expenses.
Parts B and D of Medicare also have a trust fund. However, the gap between spending and premiums is always filled by the Treasury’s general revenues. As a result, this trust fund is never depleted, and it does not face issues of insolvency that the Part A trust fund does.
What happens if the HI trust fund is depleted?
It isn’t clear what will happen if Congress fails to act before the Hospital Insurance trust fund runs dry. On one hand, the law gives Medicare beneficiaries the right to receive services. On the other, the law says that Part A can only be financed by dedicated taxes and the HI trust fund.
In 1997, the HI fund was just four years away from running out of money. To reduce the federal deficit and prevent the HI fund’s impending insolvency, Congress passed the Balanced Budget Act of 1997. It reduced Medicare payments to health care providers and intensified efforts to ensure that payments weren’t fraudulent or inappropriate. It also moved some home health benefits from Part A to Part B (which raised Part B premiums but prevented Part A insolvency). These measures worked: By 2001, the HI fund was projected to stay solvent for 28 years .
Why is Medicare spending projected to grow faster than the economy?
Rising healthcare costs and the aging of the population exert continued pressure on Medicare.
Spending on healthcare has grown faster than the economy for decades. In 1965, when Medicare was inaugurated, national health expenditures (not just Medicare) accounted for 5.6% of GDP. By 2022, national health expenditures accounted for 17.3% of GDP. Many believe this rise reflects increased demand for health care as society gets richer and as new technologies become available. In addition to increased expenditures due to overall health spending growth, Medicare spending is also rising as a share of the economy because of the growing fraction of the population over age 65: In 1966, there were 16 older dependents for every 100 working-age Americans. By 2022, there were 26 older dependents for every 100 working-age Americans.
What options would prevent the Part A trust fund from being depleted?
Trust fund depletion could be prevented by raising revenues or cutting spending. Measures that reshuffle costs out of Medicare Part A and into other parts of Medicare, or that allocate existing government revenues into the HI trust fund, could also extend the fund’s longevity without directly changing overall government revenues or expenses.
What types of revenue increases have been discussed?
The Medicare payroll tax is the main revenue source for the HI trust fund. Raising the tax rate from 2.9% to 3.5% immediately would prevent insolvency of the HI fund for 75 years, according to the Centers for Medicare and Medicaid Services .
Alternatively, Congress could raise revenues from the Net Investment Income Tax (NIIT)—the extra tax that high-income taxpayers pay on their investment income. The Biden administration has proposed raising this tax from 3.8% to 5.0% for taxpayers making over $400,000 per year and expanding the base of the tax so that it includes income generated by certain limited partners and S corporation owners. These additional revenues would be allocated to the HI trust fund. Opponents of raising the NIIT worry that it will deter investment and impose an additional tax burden on successful small-business owners.
Of course, other types of taxes could also be increased, and the resulting revenues dedicated to the HI trust fund.
What about cutting spending?
A 13% immediate cut in Part A expenditures would prevent insolvency of the HI fund for 75 years. There is significant debate on what types of cuts are feasible.
Post-acute care, which helps patients recover from an illness, injury, or surgery, has been one target of possible Medicare spending cuts. Providers of post-acute care tend to have high profit margins . In 2021, for example, skilled nursing facilities had a 17.2% profit margin from Medicare services, home health facilities had a 24.9% profit margin, and inpatient rehabilitation facilities had a 17.0% profit margin. The Trump administration proposed cuts in Medicare payments to post-acute care providers in its fiscal year 2021 budget, claiming it would save $100 billion over a 10-year period. The Obama administration also supported cuts in payments to post-acute care providers.
Spending could also be reduced by increasing premiums that Part A beneficiaries pay for their health insurance, by equalizing payments for similar services performed across different sites, and by expanding competitive bidding for medical equipment.
Part A expenditures could also be indirectly cut through Medicare Part C. (Recall that Medicare Part C receives significant funding through the Part A trust fund.) Because sicker patients are more costly to treat, the government pays each Part C plan based, in part, on the health status of its enrollees. Some argue that this system incentivizes Part C plans to record an excessive number of patient diagnoses. Furthermore, research indicates that available data on Part C enrollees likely overstates their health risks, resulting in overspending on healthcare per patient. More accurate risk profiling could reduce the amount of money that the government pays Part C plans, and Medicare is already phasing in a new system that is expected to take full force in 2026. According to the Centers for Medicare and Medicaid Services, this phase-in will save Medicare (not just Part A) $11.0 billion in 2024 and $9.2 billion in 2025 .
Another way to cut spending is to reduce “benchmarks,” which are the maximum yearly payments the federal government makes to Part C plans. According to the Congressional Budget Office , cutting these benchmarks by 10% beginning in 2025 would save Medicare (not just Part A) nearly $400 billion over the course of a decade. Available research suggests that a reduction in benchmarks would modestly reduce Part C generosity and increase premiums, with the largest impacts on dental, hearing, and vision services. But the Congressional Budget Office predicts that the effects of a 10% reduction in benchmarks would be small, with Part C insurers shielding their enrollees from high-value benefit cuts and only minimally exiting markets as a result of the policy.
What about using general revenues?
Another option is to devote general federal revenues to the HI trust fund. Proponents of the approach—which is already used to fund Medicare Part B and D—argue that it would reduce uncertainty surrounding Part A’s future and avoid the need for sudden tax increases or benefit cuts. Opponents of reallocating general revenues argue that, without this self-imposed limit on spending, Congress will be less likely to adopt reforms to the Medicare program that are needed to address our long-term fiscal imbalances .
There are various ways to use general revenues. One way to delay insolvency would be to move some Medicare Part A costs to other parts of Medicare that are funded by general revenues. For example, one-third of home health services spending is covered by Medicare Part A. Shifting these expenses to Medicare Part B would save the HI fund $6 billion per year. Some detractors of this policy worry that the additional costs placed into Medicare Part B would put upward pressure on the premiums that Part B beneficiaries pay.
The Trump administration’s fiscal year 2021 budget included a proposal to shift some Part A expenses out of the HI trust fund. Under the policy, federal spending on graduate medical education in teaching hospitals through Medicare, Medicaid, and other programs would be consolidated into a single new federal grant program. The expenses of this program would be paid using general revenues, thereby reducing the direct cost burden on the HI fund. Similarly, in 1997, Congress shifted some long-term care services from Medicare Part A to Medicare Part B.
The Brookings Institution is financed through the support of a diverse array of foundations, corporations, governments, individuals, as well as an endowment. A list of donors can be found in our annual reports published online here . The findings, interpretations, and conclusions in this report are solely those of its author(s) and are not influenced by any donation.
Health & Aging Health Insurance Health Care Policy
Economic Studies
The Hutchins Center on Fiscal and Monetary Policy
Election ’24: Issues at Stake
Matthew Fiedler, Loren Adler
March 27, 2024
Matthew Fiedler, Richard G. Frank
March 5, 2024
- Search Search Please fill out this field.
What Is Medicare Supplement Plan G?
- How Plan G Works
Types of Plan G
Plan g vs. plan f.
- Pros & Cons of Plan G
Requirements for Plan G
Frequently asked questions (faqs), the bottom line.
- Health Insurance
- Definitions A - M
:max_bytes(150000):strip_icc():format(webp)/IMG_0589-9327770547f24450bfa8ea00476e5f32.jpeg)
Halfpoint Images / Getty Images
Medicare Supplement Plan G is private health insurance that pays some of the Original Medicare out-of-pocket expenses. According to U.S. government research, Plan G is one of the two most popular Medicare supplement plan options for Medicare recipients.
Like other Medigap plans , Plan G is designed to limit your financial costs and medical expenses as a Medicare beneficiary. Plan G fills cost-sharing gaps, including deductibles, coinsurance, and copayments. It goes the extra mile versus other Medigap plans by paying for excess physician charges and offering a high-deductible option with low premiums.
Key Takeaways
- Plan G is the second most popular Medigap plan.
- Plan G covers more costs than most other Medigap plans, including the entire Part A deductible and 100% of doctor charges Medicare doesn’t pay.
- There are two types of Plan G: Regular and High-Deductible Plan G.
- High-Deductible Plan G charges some of the lowest monthly premiums available.
How Plan G Works
You pay a monthly premium to get Plan G Medigap from a private insurer, the same as any other Medicare supplement plan . Plan G provides the same required benefit package from every insurer. It is also the only Medigap plan available to new enrollees that covers Part B excess charges, which is the difference between a physician’s charges and the Medicare-approved amount.
Plan G was the second-most popular choice for Medicare recipients, with more than 4.5 million enrollees in 2021 (excluding California), according to a 2023 report from the Congressional Research Service.
Here’s what Plan G covers.
Medicare Part A:
- Coinsurance
- Hospital coverage for up to an extra 365 days after using up your Medicare benefits
- Skilled nursing facility coinsurance
- Hospice care coinsurance or copayment
Medicare Part B:
- Coinsurance or copayment for any doctor that accepts Medicare assignment
- Blood (first three pints)
- Excess doctor charges or fees above what Medicare pays
- Lab services
In addition:
- 80% of foreign travel emergency costs
- Durable medical equipment
Plan G doesn’t cover dental, vision, hearing exams or services, or prescription drug services. Medicare Advantage plans may include these benefits on top of health insurance, but Medigap plans do not. You could buy a Part D plan to cover your prescriptions along with Medigap Plan G.
You can buy Medicare supplement Plan G on Medicare.gov, through a private insurance company, from a licensed agent, or possibly with a group plan through your employer.
Some states have approved special benefits for Medigap Plan G on an insurer-by-insurer basis. For example, a Humana Medigap Plan G in Texas was approved to offer drug, hearing, and vision discounts, meal delivery after a hospital stay, and a 24-hour nurse advice line.
Two types of Medigap Plan G exist, with differences in out-of-pocket costs, availability, and coverage. It’s important to compare different providers’ Plan G options to find the best for you.
Plan G is more widely available than High-Deductible Plan G. This plan begins paying costs immediately and may be a better fit for those who think they could have more health expenses in most years, whether now or later. On average, Plan G monthly premiums are higher than the premiums on some Medigap plans (such as Plan A and B), but lower than others, such as Plan C and Plan F.
As an example, 12 insurers in New York offer a regular Plan G, with location-based pricing differences ranging from $199 in Albany, New York to almost $776 in New York City. Plan G also has a higher monthly premium compared to high-deductible Plan G.
Despite Plan G being more or less the same across insurers, prices may differ significantly based on your location or age. Insurers may offer lower rates after discounts for multiple policies, annual or automatic payments, or if you’re female, married, or a non-smoker.
High-Deductible Plan G
A High-Deductible Plan G can be a good fit if you don’t think you’ll have higher health expenses during an average year. It could also be a good fit if you’re concerned about future health costs when you’re older.
With High Deductible Plan G, you must first pay expenses out of pocket until you reach the plan deductible ($2,800 in 2024). Then, your plan begins to pay for costs. The deductible consists of the out-of-pocket expenses (not including premiums) you’ll pay before the private insurer starts paying benefits. Once you meet the deductible, your insurer pays 100% for covered services for the rest of the year.
The High Deductible Plan G counts your Part B deductible payment toward meeting the plan’s overall deductible. You’ll also pay a separate $250 per year deductible for foreign travel emergencies.
Although High-Deductible Plan G typically charges lower premiums, it can be harder to find a High-Deductible Plan G. In contrast to the earlier example, only six insurers in New York State offer a High-Deductible Plan G, with monthly premiums ranging between $52.53 and $103.10, depending on location.
Plan G and Plan F both have a high deductible option that works similarly, with the same 2024 deductible of $2,800.
However, High Deductible Plan F is only available to those who were not new to Medicare before Jan. 1, 2020. In contrast, High Deductible Plan G is available to individuals new to Medicare on or after Jan. 1, 2020. Essentially, Plan G replaced Plan F.
Plan F also covers the Part B deductible of $240. Plan G does not cover this deductible.
Pros & Cons of Plan G
Plan G tends to offer the most cost coverage combined with lower out-of-pocket expenses among the Medicare Supplement options. With Plan G, you can choose between a regular plan and a high-deductible plan, and you can use the plan anywhere in the U.S. with any physician accepting Medicare. Plan G provides some coverage for emergency foreign care, addressing at least one coverage gap.
Plan G also covers excess costs a physician may charge if you don’t live in one of the eight states prohibiting excess charges.
However, if you buy Plan G instead of a Medicare Advantage plan , you’ll need additional coverage for drugs, vision, dental, and hearing services. You must pay the Part B annual deductible before the costs are covered. In addition, your premiums will likely rise with age if your state uses age to set premiums.
Finally, in most states, you have a very short window to enroll in Plan G at a reasonable rate—and trying to get the plan later may be too expensive, as the insurer can factor in your pre-existing conditions when deciding if you qualify and setting your monthly premium.
To qualify for Plan G, you must typically be
- Turning 65 on or after Jan. 1, 2020
- Enrolled in Original Medicare (not Medicare Advantage) Parts A and B
- In the initial enrollment period for Medicare at age 65
- In 33 states, people who qualify for Medicare due to a disability can potentially be eligible for Plan G or other Medicare supplement policies
During the one-time, six-month initial enrollment period for new Medicare beneficiaries, insurers can’t turn away beneficiaries for preexisting health conditions, refuse to sell an individual any Medigap policy offered, or charge more based on health history. If you stay enrolled and pay the premium, the insurer can’t cancel your Medigap Plan G.
States regulate Medigap plans. In some states, Medigap enrollment is extended or occurs at other times beyond the initial six-month period.
It’s wise to familiarize yourself with Medicare plans and prices long before the six-month enrollment window. You want to avoid making a less-than-optimal decision under time pressures.
If you qualify for Plan G and purchase a plan after comparing options, you’ll pay monthly premiums to the insurance company you bought the plan from. Generally, you can expect an increase in the plan premium every year. You can also expect a yearly increase in the Plan G deductible if you purchased a High-Deductible Plan G.
Is Plan G Better Than F?
Unlike Plan F, Plan G does not cover the Part B deductible. That Plan F deductible coverage appealed to many consumers. However, Plan G tends to be less expensive than Plan F. Plan G is more widely available, as Plan F is only available to those who became eligible for Medicare before 2020.
What Is the Cost of Plan G for 2024?
Costs for Plan G vary and depend on your location, age, and whether you enrolled during your guaranteed issue right period . But on average, Medicare Supplement Plan G costs $237 to $409 per month, while High-Deductible Plan G costs $64 to $144 per month.
Can I Still Get Plan G If I Missed the Open Enrollment Window?
Yes, it could still be possible to get Plan G, even if you missed the Open Enrollment Window . At this point, most states would allow insurers to consider your health for the application. If you don’t have serious pre-existing conditions, you could still get plan G. Even if you have health issues, there are other ways to qualify, including living in a state with expanded enrollment, moving away from your Medicare Advantage plan service area, or being within your trial period for a Medicare Advantage plan. Speak with a professional insurance agent to determine whether you qualify.
How Is the Plan G Deductible Calculated?
The deductible for Plan G is based on section 1882(p)(11)(C)(i) of the Social Security Act. For 1998 and 1999, the act prescribed a $1,500 deductible and has increased it since based on increases in the Consumer Price Index for All Urban Consumers (CPI-U ). Since 1998, the Plan G deductible has increased by about 60%, from $1,500 to $2,800.
Plan G can be a good option for people who are enrolled in Medicare Part A and Part B and want more cost coverage than other Medicare Supplement plans can offer. Although you may be healthy and have plenty of extra funds at retirement, Plan G can help contain costs if you face more illness as you age. A High-Deductible Plan G can help split the difference, with low premiums and a cost-assistance plan for a worst-case scenario year or set of years.
Congressional Research Service. “ Medigap: Background and Statistics .”
Medicare.gov. “ Compare Medigap Plan Benefits .”
NY Department of Financial Services. “ Comparison of Year 2024 Community Rated Standardized Medicare Supplement Monthly Premiums .”
Medicare.gov. “ Get Medigap Costs .”
Centers for Medicare and Medicaid Services. “ F, G & J Deductible Announcements .”
Medicare.gov. “ Get Medigap Basics .”
KFF. “ Medigap Enrollment and Consumer Protections Vary Across States .”
:max_bytes(150000):strip_icc():format(webp)/GettyImages-1390654340-5c8ea313008f41c1a79b91ec59c05217.jpg)
- Terms of Service
- Editorial Policy
- Privacy Policy
- Your Privacy Choices
H.R. 7665: ACO Assignment Improvement Act of 2024
Compare this bill to another bill:, react to this bill with an emoji, save your opinion on this bill on a six-point scale from strongly oppose to strongly support.
(Shared on panel .)
Primary Source
Government Publishing Office
Widget for your website
Get a bill status widget »
Follow GovTrack on social media for more updates:
Visit us on Mastodon
- Study Guide
Add a note about this bill. Your note is for you and will not be shared with anyone.
Because you are a member of panel , your positions on legislation and notes below will be shared with the panel administrators. ( More Info )
The text of the bill below is as of Mar 13, 2024 (Introduced).
118th CONGRESS
IN THE HOUSE OF REPRESENTATIVES
March 13, 2024
Mr. Kilmer (for himself, Mr. Smith of Nebraska , Ms. DelBene , and Mr. Gallagher ) introduced the following bill; which was referred to the Committee on Ways and Means , and in addition to the Committee on Energy and Commerce , for a period to be subsequently determined by the Speaker, in each case for consideration of such provisions as fall within the jurisdiction of the committee concerned
To amend title XVIII of the Social Security Act to improve the way beneficiaries are assigned under the Medicare shared savings program by also basing such assignment on primary care services furnished by nurse practitioners, physician assistants, and clinical nurse specialists.
Short title
This Act may be cited as the ACO Assignment Improvement Act of 2024 .
Improvements to the assignment of beneficiaries under the Medicare shared savings program
Section 1899(c)(1) of the Social Security Act ( 42 U.S.C. 1395jjj(c)(1) ) is amended—
in subparagraph (A), by striking and at the end;
in subparagraph (B), by striking the period at the end and inserting ; and ; and
by adding at the end the following new subparagraph:
in the case of performance years beginning on or after January 1, 2025, primary care services provided under this title by an ACO professional described in subsection (h)(1)(B).
[error message]
Text comparison.

An official website of the United States government
Here’s how you know
The .gov means it’s official.
Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure.
The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.

Fact Sheets Fiscal Year 2025 Medicare Inpatient Psychiatric Facilities Prospective Payment System (IPF PPS) and Quality Reporting (IPFQR) Updates Proposed Rule (CMS-1806-P)
- Medicare Parts A & B
On March 28, 2024, the Centers for Medicare & Medicaid Services (CMS) issued a proposed rule to update Medicare payment policies and rates for the Inpatient Psychiatric Facilities Prospective Payment System (IPF PPS) for fiscal year (FY) 2025. CMS is publishing this proposed rule consistent with the legal requirements to update Medicare payment policies for IPFs on an annual basis.
Changes included in this proposed rule would support the provision of high-quality behavioral health treatment in inpatient psychiatric facilities, consistent with the Biden Administration’s Unity Agenda and focus on addressing the mental health crisis . This fact sheet discusses the major provisions of the proposed rule, including proposed annual updates to the prospective payment rates, the outlier threshold, the wage index, and associated impact analysis. In addition, the rule includes a proposal to revise patient-level adjustment factors, as well as a proposal to increase the per-treatment amount for Electroconvulsive Therapy (ECT). Additionally, the rule proposes to update the wage index using the Core‑Based Statistical Area (CBSA) Labor Market Areas defined in the Office of Management and Budget (OMB) Bulletin 23-01 . CMS believes these policies will improve or maintain individual access to high-quality care by ensuring that payment rates reflect the best available data on the resources involved in inpatient psychiatric care and the costs of these resources. CMS is proposing a three-year budget-neutral phase-out of the rural adjustment for IPFs located in the 54 rural counties that will become urban under the new OMB delineations. We will also provide a 5% cap on any decrease to the provider’s wage index from its wage index in the prior year, as finalized in previous rulemaking.
In addition, this rule includes a clarification of the eligibility criteria for the option to elect to file an all-inclusive cost report . CMS will issue revised cost reporting guidance and make operational changes to improve the quality of ancillary charge data on IPF claims by enforcing these eligibility criteria, resulting in the appropriate collection of more cost data from IPFs that have been erroneously filing an “all-inclusive” rate cost report. For cost reporting periods beginning on or after October 1, 2024, only government-owned and tribally owned IPFs will be permitted to file an “all-inclusive” rate cost report. CMS believes these operational changes will support its ongoing efforts to analyze variation in costs between patients with different characteristics and will increase the accuracy of future payment refinements to the IPF PPS while also aligning with the President’s Executive Order on Promoting Competition in the American Economy. [1]
This proposed rule also includes two requests for information on future revisions to the IPF PPS facility-level adjustment factors and development of the new standardized IPF Patient Assessment Instrument (IPF-PAI), required by the Consolidated Appropriations Act, 2023 (CAA, 2023), which IPFs participating in the IPF Quality Reporting (IPFQR) Program will be required to report for Rate Year 2028.
For the IPFQR Pro gram, CMS proposes adopting the 30-Day Risk-Standardized All-Cause Emergency Department Visit Following an Inpatient Psychiatric Facility Discharge measure and to require IPFs to submit data on a quarterly basis for patient-level measures.
This fact sheet discusses the provisions of the proposed rule. The FY 2025 Inpatient Psychiatric Facilities Prospective Payment System proposed rule (CMS-1806-P) can be downloaded from the Federal Register at https://www.federalregister.gov/public-inspection/2024-06764/medicare-program-fy-2025-inpatient-psychiatric-facilities-prospective-payment-system---rate-update
Proposed Changes to Payments Under the IPF PPS
Proposed Updates to IPF Payment Rates
For FY 2025, CMS is proposing to update the IPF PPS payment rates by 2.7%, based on the proposed 2021-based IPF market basket increase of 3.1% less a proposed 0.4 percentage point productivity adjustment. CMS is proposing that if more recent data becomes available (for example, a more recent estimate of the market basket update or productivity adjustment), CMS would use this data, if appropriate, to determine the FY 2025 market basket update percentage increase and the productivity adjustment in the final rule. Additionally, CMS proposes to update the outlier threshold so that estimated outlier payments remain at 2.0% of total payments. CMS estimates that this would result in a 0.1% decrease in aggregate payments due to updating the outlier threshold. Total estimated payments to IPFs are estimated to increase by 2.6%, or $70 million, in FY 2025 relative to IPF payments in FY 2024.
Proposed Revisions to IPF PPS Patient-Level Adjustment Factors
CMS is proposing revisions to the methodology for determining the payment rates under the IPF PPS for psychiatric hospitals and psychiatric units based on a review of the data and information collected in prior years in accordance with section 1886(s)(5)(A) of the Social Security Act, as added by the Consolidated Appropriations Act, 2023. CMS is proposing revisions to the IPF patient-level adjustment factors. The patient-level adjustments include Medicare Severity Diagnosis Related Groups (MS–DRGs) assignment of the patient’s principal diagnosis, selected comorbidities, patient age, and the variable per diem adjustments.
The IPF PPS uses the patient and facility-level adjustment factors derived from the regression model implemented in 2005. In this proposed rule, we have updated the regression model used to determine IPF PPS payment adjustments to reflect costs and claims data for 2019, 2020, and 2021. Based on our analysis of the more recent claims and costs data, as well as public comments received in the FY 2022 and FY 2023 IPF PPS rules, we are proposing to change the patient-level adjustments for which we adjust payment. We are proposing to implement these revisions in a budget-neutral manner (that is, estimated payments to IPFs for FY 2025 would be the same with or without the proposed revisions).
Proposed Increase to the Electroconvulsive Therapy Payment per Treatment
In addition, analysis of the latest IPF PPS claims and cost data found that ancillary costs for stays that include electroconvulsive therapy (ECT) treatments have increased since 2005 by a greater amount than the current ECT per treatment payment under the IPF PPS. Therefore, we are proposing to increase the IPF PPS ECT per treatment amount. The current (FY 2024) ECT payment per treatment is $385.58, and the proposed FY 2025 ECT payment per treatment is $660.30. We believe this increase would help ensure that the patients who need ECT are more able to access it.
FY 2025 Wage Index Update for Revised Census Data
IPF regulations require CMS to use the best Medicare data available to estimate the average inpatient operating and capital-related costs per day, including an appropriate wage index to adjust for wage differences. We update the wage index annually based on the most recent available acute care hospital wage index, without any floors or reclassifications applicable under the Medicare Inpatient Prospective Payment System. Historically, we have also updated the Core‑Based Statistical Area (CBSA) delineations in accordance with the latest available Office of Management and Budget (OMB) Bulletin. For FY 2025, we are proposing to adopt the CBSA Labor Market Areas for the IPF PPS wage index as defined in the OMB Bulletin 23-01. We are also proposing that providers transitioning from rural to urban based on these CBSA revisions would receive two-thirds of the rural adjustment in FY 2025, one-third of the rural adjustment in FY 2026, and no rural adjustment in FY 2027. This proposed approach is consistent with how we implemented this policy in previous years.
Clarification of Requirements for Reporting Ancillary Charges and All-Inclusive Status Eligibility Under the IPF PPS
The Consolidated Appropriations Act, 2023 (CAA, 2023) requires the collection of data and information, such as charges related to ancillary services, to revise the IPF PPS. Currently, CMS expects IPFs with a charge structure to report ancillary costs and charges on cost reports, while IPFs without this cost structure have the option to use an alternative method of cost reporting by filing all-inclusive cost reports. All-inclusive cost reporting accommodates these hospitals’ inability to allocate costs to charges and allows them to use an alternative cost allocation method. Historically, there have been a small number of hospitals that file all-inclusive cost reports, which consistently do not include or have very minimal ancillary cost data. These have mostly included Indian Health Service (IHS) hospitals and government-owned psychiatric and acute care hospitals. However, CMS has observed a notable increase in the number of IPFs erroneously filing all-inclusive cost reports.
CMS is clarifying the eligibility criteria for the option to elect to file an all-inclusive cost report and will make operational changes to ensure that only government-owned or tribally owned IPF hospitals are permitted to file an all-inclusive cost report for cost reporting periods beginning on or after October 1, 2024. By improving the reporting of ancillary costs and charges, CMS would be able to increase accuracy of future payment refinements to the IPF PPS, which would further advance behavioral health treatment and support IPFs that provide care to beneficiaries with more complex and costlier conditions.
Request for Information (RFI) about IPF PPS Patient Assessment Instrument Required by the Consolidated Appropriations Act, 2023 (CAA, 2023)
The CAA, 2023, requires IPFs to collect and submit standardized patient assessment data on specified categories. This data will enable CMS to propose future revisions to the IPF PPS that would more accurately pay for care, monitor quality, and assess for disparities in behavioral health care. Therefore, CMS is including an RFI to solicit comments with the goal of engaging the public to identify meaningful data elements for collection that are appropriate for the acute inpatient psychiatric care setting and potential criteria for the development and implementation of the instrument. In addition, we are seeking to understand the burden on IPFs that this additional data collection would impose and soliciting comment on ways we might minimize this burden by evaluating whether any data that is currently collected through one or more existing assessment instruments in other settings, or collected as part of IPFs’ existing processes, could be collected as standardized patient assessment data elements for the IPF-PAI.
Request for Information (RFI) about IPF PPS Facility-Level Adjustment Factors
The CAA, 2023, requires CMS to revise the IPF PPS methodology for determining payment rates for FY 2025 and subsequent years. CMS is seeking input on potential revisions to the IPF PPS facility-level adjustments in the future based on the results of more recent IPF cost and claim analysis. An analysis of 2019 through 2021 IPF claims and costs data identified potential changes in the regression factors for IPFs with a rural location and teaching status and suggested there may be value in including a new facility-level variable for safety net patient population. We also analyzed a potential adjustment based on the Medicare Safety Net Index (MSNI), developed by MedPAC as a recommended alternative to the current statutorily required methodology for disproportionate share payments to IPPS hospitals. In this proposed rule, we discuss considerations related to applicability and modeling that demonstrate the effect of revising the rural and teaching status adjustment factors, as well as the inclusion of a new facility-level variable for safety net patient populations. In future rulemaking, updating these facility-level adjustment factors could more accurately pay for care, support psychiatry residency training, and support IPFs in rural and underserved areas. We welcome feedback on this RFI.
Proposed Updates to the Inpatient Psychiatric Facilities Quality Reporting (IPFQR) Program
The IPFQR Program requires that all IPFs paid under the IPF PPS submit certain specified quality data to CMS in a form and manner and within the timeframes that CMS prescribes. IPFs that do not submit the specified data on quality measures as required by the IPFQR Program receive a 2.0 percentage point reduction to their annual payment update. The IPFQR Program aims to assess and foster improvement in the quality of care provided to patients in IPFs. By requiring IPFs to submit quality data to CMS and by CMS publicly reporting these data under the IPFQR Program, CMS ensures that patients are able to make more informed decisions about their healthcare options.
In this proposed rule, CMS is proposing to adopt one new measure, the 30-Day Risk-Standardized All-Cause Emergency Department Visit Following an Inpatient Psychiatric Facility Discharge measure (also referred to as the IPF ED Visit measure). This claims-based measure would assess the proportion of patients 18 and older with an emergency department visit, including observation stays, within 30 days of discharge from an IPF without subsequent admission. Patients who are subsequently admitted to an acute care hospital or IPF are represented under the Thirty-Day All-Cause Unplanned Readmission Following Psychiatric Hospitalization in an Inpatient Psychiatric Facility measure, which is already in the IPFQR Program. By adopting the IPF ED Visit measure, the IPFQR Program would provide a more complete assessment of post-discharge acute care and encourage improvements in discharge planning and care coordination.
Additionally, CMS is proposing to require IPFs to submit patient-level quality data on a quarterly basis (as opposed to the current annual basis). This would align the IPFQR Program with other quality reporting programs that require patient-level data submission on a quarterly basis and would reduce data strains on IPF systems.
[1] https://www.whitehouse.gov/briefing-room/presidential-actions/2021/07/09/executive-order-on-promoting-competition-in-the-american-economy/
- Previous Newsroom article
- Next Newsroom article
CMS News and Media Group Catherine Howden, Director Media Inquiries Form 202-690-6145
- Committee Assignment
- Tours and Tickets
- Casework & Federal Agency Assistance
- Congressional Art Competition
- Washington DC Visitors
- Internships
- Service Academy Nominations
- Eagle Scout and Gold Award Recipients
- Congressional Veteran Commendation
- Congressional Law Enforcement Award
- Congressional Fire & Rescue EMS Awards
- Congressional Education Awards
- Hurricane Preparedness
- Federal Business Opportunities
- Government Resources
- Kids and Students
- Military Personnel
- Reading Roll Call Votes
- Senior Citizens
- Student Financial Aid
- Additional Resources
- Funding Requests
- Health Care
- Immigration
- Jobs & Economy
- National Security
- Social Security
- Voting Record
- Press Releases
Office Locations
- Newsletter Sign-Up
- Website Problem
- Search Search Go
Buchanan, Soto Lead Bipartisan Letter Urging Biden Admin Not to Undermine Medicare Advantage
March 26 , 2024.
WASHINGTON – Congressman Vern Buchanan, Vice Chairman of the House Ways and Means Committee and Chairman of the Health Subcommittee , and Congressman Darren Soto (D-FL ) announced today that they led a letter with 18 members calling on President Biden’s Centers for Medicare and Medicaid Services (CMS) to reconsider its proposed rate notice to the Medicare Advantage (MA) program that could impact seniors’ access to care and undermine the increasingly popular and successful program. The agency plans to finalize the rule by April 1. According to the Berkeley Research Group (BRG), projected MA medical costs will jump by 4 to 6 percent in 2025, while at the same time, federal government payments to MA plans will decrease by 0.16 percent. Buchanan’s Congressional District, FL-16, has nearly 100,000 seniors enrolled in Medicare Advantage that would be negatively impacted by this proposal. “I am deeply concerned about the administration’s proposed rate notice for Medicare Advantage health plans,” said Congressman Buchanan . “At a time when more than half of the Medicare beneficiary population is enrolled in an MA plan, coupled with still stubbornly high levels of inflation that is pinching the pocketbooks of everyday Americans, the last thing we should be doing is raising health care costs on our nation’s seniors, many of whom are living on fixed incomes.” According to CMS, roughly 33 million seniors and those with disabilities have elected to enroll in MA, with enrollment projected to exceed 34 million by the end of 2024. The proposal could disincentivize benefits if CMS finalizes the rates as is. Seniors choosing MA now make up 52 percent of the Medicare beneficiary population. "Medicare Advantage stands as a cornerstone, offering accessible healthcare to over 30 million seniors and individuals with disabilities across the nation, with a significant 2.7 million in Florida alone. It is imperative to uphold these vital components to preserve the quality and accessibility of healthcare for Medicare Advantage recipients,” said Congressman Darren Soto . “Sustaining stable payments is crucial to guaranteeing reasonable premiums, preserving supplemental benefits, and maintaining competitive provider reimbursements for the millions of seniors and individuals with disabilities who rely on Medicare Advantage." “We recognize the MA program has undergone changes in recent years, including significant growth due to popularity of the program,” the lawmakers wrote in the letter . “However, as we work to improve the overall program, the data and cost assumptions used to project the program’s rates must be grounded in the most recent data available and take into account any increased costs that might occur before the rate notice is finalized, either through rulemaking or Congressional action.” As noted by Grover Norquist, President of Americans for Tax Reform, “it is the free market aspects of MA that have made the program so successful. Efforts should seek to improve this vehicle and capitalize on its success – not push people towards less efficient, less popular alternatives.” In addition to being the Vice Chairman and most senior Republican on the powerful U.S. House Ways and Means Committee, Buchanan is also the Chairman of the Health Subcommittee, which has broad jurisdiction over traditional Medicare, the Medicare prescription drug benefit program, and Medicare Advantage. You can read the full letter HERE or below:
March 25, 2024
The Honorable Xavier Becerra The Honorable Chiquita Brooks-LaSure
Secretary Administrator
Department of Health and Human Services Centers for Medicare & Medicaid Services
200 Independence Avenue, SW 200 Independence Avenue, SW
Washington, DC 20201 Washington, DC 20201
Dear Secretary Becerra and Administrator Brooks-LaSure: We write regarding the Calendar Year (CY) Advance Notice for the Medicare Advantage (MA) program to ensure the final rate announcement accurately reflects growth rates and health care cost increases. It is essential for the over 33 million seniors and individuals with disabilities currently enrolled in MA that the Centers for Medicare & Medicaid Services (CMS) keep payments to the program stable during a time of increased demand for care, as well as the implementation of significant changes stemming from recent rulemaking. Payment stability will ensure that premiums remain affordable, popular supplemental benefits remain intact, and provider reimbursements remain competitive. We recognize the MA program has undergone changes in recent years, including significant growth due to popularity of the program. However, as we work to improve the overall program, the data and cost assumptions used to project the program’s rates must be grounded in the most recent data available and take into account any increased costs that might occur before the rate notice is finalized, either through rulemaking or Congressional action. As you know, the Advance Notice proposes an effective growth rate of 2.44% when calculating the 2025 benchmark, which does not fully account for the increases in utilization over the past year, in part because it does not include utilization data from the fourth quarter of 2023. We are concerned that the proposed MA growth rate, combined with higher-than-expected utilization, could result in providers receiving lower reimbursement rates for their services, as well as increased premiums or reduced supplement benefits provided to beneficiaries. We urge CMS to closely consider all appropriate data and information, including data indicating higher trends in Q4 2023, to ensure that growth rates in the final Rate Notice reflect recent seniors’ expected health care needs in 2025. Through considering Q4 2023 data, CMS would ensure that the MA program maintains its affordability, benefits, and choices for the program – which now serves more than half of those eligible for Medicare – while improving the quality and long-term stability of the program. We look forward to working with you to ensure that the MA program can continue to effectively serve its enrollees and remain an essential contributor to the health and wellness of America's seniors and those with disabilities.
Permalink: https://buchanan.house.gov/2024/3/buchanan-soto-lead-bipartisan-letter-urging-biden-admin-not-to-undermine-medicare-advantage
We look forward to meeting with you and developing lasting relationships that can have a major impact on our district and beyond.
WASHINGTON, DC
2110 Rayburn HOB
Washington, DC 20515
Phone: (202) 225-5015
Fax: (202) 226-0828
510 Vonderburg Drive
Brandon, FL 33511
Phone: (813) 657-1013
Fax: (771) 200-5798
By Appointment Only
8433 Enterprise Circle
Bradenton, FL 34202
Phone: (941) 951-6643
Longboat Key
5370 Gulf of Mexico Drive
Longboat Key, FL 34228

IMAGES
VIDEO
COMMENTS
All providers who accept assignment must submit claims directly to Medicare, which pays 80 percent of the approved cost for the service and will bill you the remaining 20 percent. You can get some preventive services and screenings, such as mammograms and colonoscopies, without paying a deductible or coinsurance if the provider accepts assignment.
Medicare assignment is an agreement between Medicare and medical providers (doctors, hospitals, medical equipment suppliers, etc.) in which the provider agrees to accept Medicare's fee schedule as payment in full when Medicare patients are treated.
Medicare assignment is a fee schedule agreement between the federal government's Medicare program and a doctor or facility. When Medicare assignment is accepted, it means your doctor agrees to the payment terms of Medicare. Doctors that accept Medicare assignment fall under one of three designations: a participating doctor, a non ...
You can get the lowest cost if your doctor or other health care provider accepts the. Medicare-approved amount. as full payment for a covered service. This is called "accepting assignment.". If a provider accepts assignment, it's for all Medicare-covered Part A and Part B services.
1. Participating providers, or those who accept Medicare assignment. These providers have an agreement with Medicare to accept the Medicare-approved amount as full payment for their services. You don't have to pay anything other than a copay or coinsurance (depending on your plan) at the time of your visit.
Medicare assignment simply means that your provider has agreed to stick to a Medicare fee schedule when it comes to what they charge for tests and services. Medicare regularly updates fee schedules, setting specific limits for what it will cover for things like office visits and lab testing.
Summary: Medicare Assignment is an agreement between healthcare providers and Medicare, where providers accept the Medicare-approved amount as full payment, preventing them from charging beneficiaries extra. This benefits Medicare beneficiaries by controlling their costs and ensuring they only pay deductibles and copayments.
A Medicare assignment provider agrees to charge no more than the Medicare-approved price for a specific service. The doctor or other provider also agrees to bill Medicare directly, rather than charging the patient on the day of service. This means that if you go to a Medicare-participating provider, you won't usually have to pay anything at the time of service.
Medicare assignment is an agreement by your doctor or other healthcare providers to accept the Medicare-approved amount as the full cost for a covered service. Providers who "accept assignment" bill Medicare directly for Part B-covered services and cannot charge you more than the applicable deductible and coinsurance.
What's assignment for Part B services, and why is it important? Assignment is an agreement by your doctor, provider, or other supplier to be ... Medicare, your prescription drug plan, or your other insurance begins to pay. Medicare-approved amount: In Original Medicare, this is the amount a doctor, provider, or other supplier ...
Participating providers accept Medicare and always take assignment. Taking assignment means that the provider accepts Medicare's approved amount for health care services as full payment. These providers are required to submit a bill (file a claim) to Medicare for care you receive. Medicare will process the bill and pay your provider directly ...
Medicare assignment, or Medicare assignment of benefits, is the process in which a Medicare beneficiary authorizes Medicare to directly reimburse health care providers for services. To ensure all services are charged at Medicare-determined rates, recipients should verify whether their primary physicians fall under the accept assignment ...
Medicare "participation" means you agree to accept claims assignment for all Medicare-covered services to your patients. By accepting assignment, you agree to accept Medicare-allowed amounts as payment in full. You may not collect more from the patient than the Medicare deductible and coinsurance or copayment. Participating Provider or ...
Medicare assignment codes help Medicare pay for covered services. If your doctor or other provider accepts assignment and is a participating provider, they will file for reimbursement for services with a CMS-1500 form and the code will be "assigned.". But non-participating providers can select "not assigned.".
Assignment means that a doctor agrees to accept the Medicare-approved amount as full payment for covered health services and supplies. The majority of doctors accept assignment.
What it means to "accept Medicare assignment". In short, accepting Medicare assignment means signing a contract to accept whatever Medicare pays for a covered service as full payment. Participating and non-participating status only applies to Medicare Part B; Medicare Advantage plans operate with contracts similar to commercial insurance ...
Medicare sets a fixed cost to pay for every benefit they cover. This amount is called Medicare assignment. You have the largest healthcare provider network with over 800,000 providers nationwide on Original Medicare. You can see any doctor nationwide that accepts Medicare. Understanding the differences between your cost and the difference ...
Medicare assignment is an agreement between a doctor and Medicare on a pre-approved amount. This protects you from paying out-of-pocket costs for covered procedures. If a doctor does not accept Medicare assignment then you could be liable for the entire amount of your services.
Nonassignment of Benefits. The second reimbursement method a physician/supplier has is choosing to not accept assignment of benefits. Under this method, a non-participating provider is the only provider that can file a claim as non-assigned. When the provider does not accept assignment, the Medicare payment will be made directly to the beneficiary.
A: If your doctor doesn't "accept assignment," (ie, is a non-participating provider) it means he or she might see Medicare patients but wants to be paid more than the amount that Medicare is willing to pay. As a result, you may end up paying the difference between what Medicare will pay and what your provider charges — up to 15 percent above ...
When a doctor accepts Medicare assignment, it simply means they agree to take Medicare. Medicare has their own long list of approved charges, or what they will pay for every service under the sun. It's usually far less than the "retail" cost of care, so when a doctor agrees to take Medicare, they agree to accept those rates. ...
Medicare reimbursement is when a doctor or healthcare facility receives payment directly from Medicare for providing care to a Medicare enrollee. Medicare sets reimbursement rates for each of its covered services, so when a provider accepts Medicare assignment, they agree to these rates and may not ask the patients to pay more.
Categories for Medicare Assignment. There are three categories: Participating doctors accept Medicare assignment. The doc takes Medicare and only charges up to the Medicare-approved amount. Non-Participating doctors decide to accept or not accept Medicare. The doc takes Medicare but can charge an excess fee. Doctors that have opted out are the ...
Medicare offers a second preventive visit; this one is every 12 months. It may be annual, but this visit is also not a physical exam. The purpose is to update the personalized prevention plan.
Medicare's original financing structure is the result of a political compromise in the 1960s. The Kennedy administration, with the support of many Democrats in Congress, proposed hospital ...
Medicare Advantage, or Medicare Part C, is a type of hospital and medical insurance provided by private companies instead of the federal government. more Related Articles
This Act may be cited as the ACO Assignment Improvement Act of 2024. 2. Improvements to the assignment of beneficiaries under the Medicare shared savings program. Section 1899(c)(1) of the Social Security Act (42 U.S.C. 1395jjj(c)(1)) is amended— (1) in subparagraph (A), by striking and at the end; (2)
On March 28, 2024, the Centers for Medicare & Medicaid Services (CMS) issued a proposed rule to update Medicare payment policies and rates for the Inpatient Psychiatric Facilities Prospective Payment System (IPF PPS) for fiscal year (FY) 2025. CMS is publishing this proposed rule consistent with the legal requirements to update Medicare payment policies for IPFs on an annual basis.
Centers for Medicare and Medicaid Services . 233 North Michigan Ave, Suite 600 . Chicago, IL 60601 . RE: SPA #24-0016 . Non-Institutional Services . Dear Mr. McMillion: The State requests approval of the enclosed amendment #24-0016 to the Title XIX (Medicaid) State Plan for non-institutional services to be effective January 1, 2024 (Appendix I).
WASHINGTON - Congressman Vern Buchanan, Vice Chairman of the House Ways and Means Committee and Chairman of the Health Subcommittee, and Congressman Darren Soto (D-FL) announced today that they led a letter with 18 members calling on President Biden's Centers for Medicare and Medicaid Services (CMS) to reconsider its proposed rate notice to the Medicare Advantage (MA) program that could ...