An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.


StatPearls [Internet].
Gestational diabetes.
Bryan S. Quintanilla Rodriguez ; Heba Mahdy .
Affiliations
Last Update: August 8, 2023 .
- Continuing Education Activity
The definition of gestational diabetes mellitus (GDM) is any degree of glucose intolerance with onset or first recognition during pregnancy. GDM can classify as A1GDM and A2GDM. The classification of gestational diabetes managed without medication and responsive to nutritional therapy is as diet-controlled gestational diabetes (GDM) or A1GDM. Conversely, gestational diabetes managed with medication to achieve adequate glycemic control classifies as A2GDM. Gestational diabetes is a disease developed during the second and third trimester of pregnancy, characterized by a marked insulin resistance secondary to placental hormonal release. This activity highlights the etiology, epidemiology, pathophysiology, treatment, complications, and prognosis for members of the interprofessional team that manage patients with gestational diabetes.
- Identify the etiology of gestational diabetes.
- Review the evaluation of gestational diabetes.
- Outline the treatment and management options available for gestational diabetes.
- Summarize the interprofessional team strategies for improving care coordination and communication to advance gestational diabetes and improve outcomes.
- Introduction
The definition of gestational diabetes mellitus (GDM) is any degree of glucose intolerance with onset or first recognition during pregnancy. GDM can classify as A1GDM and A2GDM. Gestational diabetes managed without medication and responsive to nutritional therapy is diet-controlled gestational diabetes (GDM) or A1GDM. On the other side, gestational diabetes managed with medication to achieve adequate glycemic control is A2GDM.
Historically, the screening for gestational diabetes consisted of assessing patients history, past medical obstetric outcomes, and family history of type 2 diabetes mellitus. Even though it was useful, it was not appropriate. This screening method failed to identify approximately one-half of pregnant women with GDM. In 1973 a significant study suggested the use of the 50 g 1-hour oral glucose tolerance test as a screening for gestational diabetes; this is a very reliable method for screening, and it is used for approximately 95% of obstetricians in the united states of America as a method for screening GDM during pregnancy. In 2014, the U.S preventive service task force recommended screening all pregnant women for GDM at 24 weeks of gestation. [1] [2] [3] [4]
Gestational diabetes etiology is apparently related to 1) the pancreatic beta-cell dysfunction or the delayed response of the beta cells to the glycemic levels, and 2) the marked insulin resistance secondary to placental hormonal release. The human placental lactogen is the main hormone related to increased insulin resistance in GDM. Other hormones related to the development of this disease are growth hormone, prolactin, corticotropin-releasing hormone, and progesterone, these hormones contribute to the stimulation of insulin resistance and hyperglycemia in the pregnancy.
It has been reported some clinical risk factors for developing gestational diabetes. Those clinical factors include [3] :
- Increased body weight (a body mass index greater than 25)
- Decreased physical activity
- A first degree relative with diabetes mellitus
- Prior history of gestational diabetes or a newborn with macrosomia, metabolic comorbidities like hypertension
- Triglycerides greater than 250
- Polycystic ovarian syndrome
- Hemoglobin A1C greater than 5.7
- Abnormal oral glucose tolerance test
- Any significant marker of insulin resistance (acanthosis nigricans)
- Past medical history of cardiovascular diseases
- Epidemiology
Gestational diabetes affects around 2 to 10% of pregnancies in the United States of America.
Women with gestational diabetes (GDM) have an increased 35 to 60% risk of developing diabetes mellitus over 10 to 20 years after pregnancy. [3] [4]
- Pathophysiology
The human placental lactogen is a hormone released by the placenta during the pregnancy. It holds a comparable composition to growth hormone and induces important metabolic changes during pregnancy to support the maintenance of fetal nutritional status. This hormone is capable of provoking alterations and modifications in the insulin receptors. The following molecular variations appear to have links to diminishing glucose uptake at peripheral tissues:1) molecular alteration of the beta-subunit insulin receptor, 2) diminished phosphorylation of tyrosine kinase, 3) remodelings in the insulin receptor substrate-1 and phosphatidylinositol 3-kinase.
Maternal high glucose levels cross the placenta and produce fetal hyperglycemia. The fetal pancreas gets stimulated in response to the hyperglycemia. Insulin anabolic properties induce fetal tissues to growth at an increased rate. [3]
There are reports that a higher body mass index and obesity can lead to low-grade inflammation. Chronic inflammation induces the synthesis of xanthurenic acid, which is associated with the development of pre-diabetes and gestational diabetes mellitus. [5]
- History and Physical
The past medical obstetric outcomes and family history of type 2 diabetes mellitus are important components of the history taking in GDM. The clinical features of gestational diabetes mellitus can be varied. The disproportionate weight gain, obesity, and elevated BMI can be suggestive features. The diagnosis is established by the laboratory screening method at the 24 to 28 weeks of pregnancy.
Reports exist that the gestational age when DSM develops influences pregnancy outcome.
Recommendations are for screening for gestational diabetes at 24 to 28 weeks of pregnancy with a 50-g, 1-hour oral glucose challenge test. If the values are abnormal, greater than or equal to 130 mg/dL (7.22 mmol/L), or greater than or equal to 140 mg/dL (7.77 mmol/L), a confirmatory test is necessary with a 100-g, 3-hour oral glucose tolerance test, with the following values: first hour over 180 mg/dL, second hour over 155 mg/dL, third hour more than 140 mg/dL. The presence of two or more abnormal results establishes the diagnosis of gestational diabetes.
The ADA recommends to consider screening strategy for detecting pregestational diabetes or early gestational diabetes mellitus in all women who are overweight or obese and have one or more of the following risk factors:
- Physical inactivity,
- First degree relative with diabetes
- High-risk race or ethnicity
- Have previously birthed an infant weighing 4000 grams or more
- Previously gestational diabetes, hypertension
- HDL level less than 35mg/dL
- Triglyceride level greater than 250 mg/dL
- Women with polycystic ovarian syndrome
- Hemoglobin A1c greater than 5.7%
- Impaired glucose tolerance test
- Impaired fasting glucose
- History of cardiovascular disease
- Other clinical conditions associated with insulin resistance
The American Diabetes Association (ADA) has noted that measurement of hemoglobin A1C is usable, but it may not be suitable to use alone, due to decreased sensitivity compared to oral glucose tolerance test.
The ACOG recommended levels of blood glucose in pregnancy is fasting plasma glucose under 95 mg/dL, 1 hour postprandial under 130-140 mg/dL, 2 hours postprandial below 120mg/dL.
In the postpartum period, 24 to 72 hours after the delivery, it is recommended to monitor glucose levels. After removing the placenta insulin resistance tends to improve, this can help escalate down insulin or hypoglycemic agents. Glycemic therapy will point towards achieving a euglycemic glucose level. At 4 to 12 weeks post-partum, it is recommended to perform a 75g oral glucose tolerance test to rule out the possibility of development of type 2 diabetes. [1] [6] [4] [6]
- Treatment / Management
Gestational diabetes management begins with nonpharmacologic measurements like diet modifications, exercise, and glucose monitoring. The ADA recommends nutritional counseling by a registered dietitian and development of a personalized plan based on the patients BMI. In some settings, in which dietitians are not able, the physician can provide recommendations based on the three major nutritional concepts: caloric allotment, caloric distribution, and carbohydrate intake.
The amount of exercise recommended in GDM is 30 minutes of moderate-intensity aerobic exercise at least five days a week or a minimum of 150 minutes per week.
If the patient glycemic control is not adequate despite optimal adherence to diet and exercise, it is recommended to begin pharmacologic treatment. The ADA first line of treatment for GDM is insulin. The therapy with insulin has been considered the standard therapy for gestational diabetes management when adequate glucose levels are unachievable with diet and exercise.
Insulin can help achieve an appropriate metabolic control, and it is added to the management if fasting blood glucose is greater or equal to 95 mg/dL, if 1-hour glucose level is greater or equal to 140 mg/dL, or if 2-hour glucose level is greater than 120 mg/dL.
The oral hypoglycemic agents, metformin and glyburide, are increasingly being used among women with gestational diabetes, despite the lack of FDA approval. Glyburide can initiate at a dose of 2.5 mg, and the maximum dose is 20mg. Metformin therapy should start at a dose of 500 mg, and the maximum dose is 2500 mg.
Basal insulin dose can be calculated using the patient’s weight formula, 0.2 units/kg/day. If the blood glucose level becomes elevated following a meal, rapid-acting insulin, or regular insulin can be prescribed before the meal, starting the dose with 2 to 4 units.
In the first trimester, the total daily insulin requirement is 0.7 units/kg/day, in the second trimester it is 0.8 units/kg/day, and in the third trimester, it is 0.9 to 1.0 units/kg/day.
The patient should divide the total daily dose of insulin into two halves; one half given as basal insulin at bedtime, and the other half divided between three meals and given as rapid-acting, or regular insulin before meals.
Lispro and aspart have approval for usage in pregnancy. The short-acting insulin is associated with less hypoglycemia.
The long-acting insulin detemir has received approval for the usage in pregnancy. Long-acting insulin causes less nocturnal hypoglycemia. [6] [7] [8] [9] [10] [4]
- Differential Diagnosis
Many women do not receive the appropriate screening for diabetes mellitus before pregnancy, so in some cases, it is challenging to distinguish gestational diabetes from preexisting diabetes. [7] [9]
At 4 to 12 weeks post-partum, the recommendation is to perform a 75g oral glucose tolerance test to rule out the possibility of the development of type 2 diabetes, impaired fasting glucose or impaired glucose tolerance test. [11]
ADA and ACOG recommend repeating testing every 1 to 3 years for women who developed GDM and had normal postpartum screening results. [12] [13]
- Complications
The complications of developing gestational diabetes categorize as maternal and fetal. The fetal complications include macrosomia, neonatal hypoglycemia, polycythemia, shoulder dystocia, hyperbilirubinemia, neonatal respiratory distress syndrome, increased perinatal mortality, and hypocalcemia. Maternal complications include hypertension, preeclampsia, increased risk of developing diabetes mellitus, and increased risk of cesarean delivery. [12] [13]
- Consultations
OB/GYN physicians best manage gestational diabetes. However, it can include consultations with the endocrinology department to suggest recommendations for cases of hyperglycemia refractory to treatment. [14] [13] [14]
- Deterrence and Patient Education
Patient education is necessary. Education regarding appropriate diet changes, exercise, and lifestyle modifications can help to improve outcomes in patient with gestational diabetes. [14] [13]
- Enhancing Healthcare Team Outcomes
The management and treatment of women with gestational diabetes is an emerging challenge for health care providers and teams. Thus, today, gestational diabetes requires an interprofessional team approach, including physicians, specialists, specialty-trained nurses, and pharmacists, all collaborating across disciplines to achieve optimal patient results and prevent further complications. Efforts and strategies are necessary to recognize them effectively. The development of prevention strategies would facilitate the treatment of gestational diabetes and would help improve health outcomes. Women with gestational diabetes have an increased risk of developing type 2 diabetes over 10 to 20 years after pregnancy. [14] [13] [11] [4]
Many pregnant women who develop diabetes are not diagnosed until very late, which significantly increases the morbidity of the disease.
Many healthcare institutions are now operating pharmacy or nurse practitioner diabetic clinics that offer diabetic education to pregnant females. These clinics regularly monitor blood glucose and refer patients to an endocrinologist. This practice reduces the burden of the obstetrician, lowers healthcare costs, and helps the delivery of optimal care for those who need it.
All members of the interprofessional healthcare team need to collaborate and work together to manage gestational diabetes. Nursing stands at the forefront of patient encounters to determine adherence to therapeutic choices, and monitor for therapy efficacy as well as being alert for potential adverse effects, which they will communicate to other team members. Pharmacists need to perform medication reconciliation, verify the dosing of insulin or other antihyperglycemic drugs, and assist with patient counseling about medication and lifestyle adherence. In this cooperative paradigm, the interprofessional team can guide outcomes most successfully. [Level 5]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Overview of the most significant possible symptoms of diabetes Contributed by Wikimedia Commons (Public Domain)
The process of clinical islet transplantation for the treatment of diabetes Contributed by Wikimedia Commons, Giovanni Maki (CC by 2.5) https://creativecommons.org/licenses/by/2.5/deed.en
Disclosure: Bryan Quintanilla Rodriguez declares no relevant financial relationships with ineligible companies.
Disclosure: Heba Mahdy declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Quintanilla Rodriguez BS, Mahdy H. Gestational Diabetes. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Similar articles in PubMed
- Association between retinol-binding protein 4 concentrations and gestational diabetes mellitus (A1GDM and A2GDM) in different pregnancy and postpartum periods. [Ann Transl Med. 2019] Association between retinol-binding protein 4 concentrations and gestational diabetes mellitus (A1GDM and A2GDM) in different pregnancy and postpartum periods. Du X, Dong Y, Xiao L, Liu GH, Qin W, Yu H. Ann Transl Med. 2019 Sep; 7(18):479.
- Review Screening and diagnosing gestational diabetes mellitus. [Evid Rep Technol Assess (Full ...] Review Screening and diagnosing gestational diabetes mellitus. Hartling L, Dryden DM, Guthrie A, Muise M, Vandermeer B, Aktary WM, Pasichnyk D, Seida JC, Donovan L. Evid Rep Technol Assess (Full Rep). 2012 Oct; (210):1-327.
- [Gestational diabetes mellitus. Experience at a third level hospital]. [Ginecol Obstet Mex. 2005] [Gestational diabetes mellitus. Experience at a third level hospital]. Ramírez Torres MA. Ginecol Obstet Mex. 2005 Sep; 73(9):484-91.
- Review [Gestational diabetes mellitus (Update 2019)]. [Wien Klin Wochenschr. 2019] Review [Gestational diabetes mellitus (Update 2019)]. Kautzky-Willer A, Harreiter J, Winhofer-Stöckl Y, Bancher-Todesca D, Berger A, Repa A, Lechleitner M, Weitgasser R. Wien Klin Wochenschr. 2019 May; 131(Suppl 1):91-102.
- [Gestational diabetes mellitus (Update 2023)]. [Wien Klin Wochenschr. 2023] [Gestational diabetes mellitus (Update 2023)]. Kautzky-Willer A, Winhofer Y, Kiss H, Falcone V, Berger A, Lechleitner M, Weitgasser R, Harreiter J. Wien Klin Wochenschr. 2023 Jan; 135(Suppl 1):115-128. Epub 2023 Apr 20.
Recent Activity
- Gestational Diabetes - StatPearls Gestational Diabetes - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Gestational diabetes...
Gestational diabetes mellitus and adverse pregnancy outcomes: systematic review and meta-analysis
- Related content
- Peer review
- Wenrui Ye , doctoral student 1 2 ,
- Cong Luo , doctoral student 3 ,
- Jing Huang , assistant professor 4 5 ,
- Chenglong Li , doctoral student 1 ,
- Zhixiong Liu , professor 1 2 ,
- Fangkun Liu , assistant professor 1 2
- 1 Department of Neurosurgery, Xiangya Hospital, Central South University, Changsha, Hunan, China
- 2 Hypothalamic Pituitary Research Centre, Xiangya Hospital, Central South University, Changsha, China
- 3 Department of Urology, Xiangya Hospital, Central South University, Changsha, Hunan, China
- 4 National Clinical Research Centre for Mental Disorders, Second Xiangya Hospital, Central South University, Changsha, Hunan, China
- 5 Department of Psychiatry, Second Xiangya Hospital, Central South University, Changsha, Hunan, China
- Correspondence to: F Liu liufangkun{at}csu.edu.cn
- Accepted 18 April 2022
Objective To investigate the association between gestational diabetes mellitus and adverse outcomes of pregnancy after adjustment for at least minimal confounding factors.
Design Systematic review and meta-analysis.
Data sources Web of Science, PubMed, Medline, and Cochrane Database of Systematic Reviews, from 1 January 1990 to 1 November 2021.
Review methods Cohort studies and control arms of trials reporting complications of pregnancy in women with gestational diabetes mellitus were eligible for inclusion. Based on the use of insulin, studies were divided into three subgroups: no insulin use (patients never used insulin during the course of the disease), insulin use (different proportions of patients were treated with insulin), and insulin use not reported. Subgroup analyses were performed based on the status of the country (developed or developing), quality of the study, diagnostic criteria, and screening method. Meta-regression models were applied based on the proportion of patients who had received insulin.
Results 156 studies with 7 506 061 pregnancies were included, and 50 (32.1%) showed a low or medium risk of bias. In studies with no insulin use, when adjusted for confounders, women with gestational diabetes mellitus had increased odds of caesarean section (odds ratio 1.16, 95% confidence interval 1.03 to 1.32), preterm delivery (1.51, 1.26 to 1.80), low one minute Apgar score (1.43, 1.01 to 2.03), macrosomia (1.70, 1.23 to 2.36), and infant born large for gestational age (1.57, 1.25 to 1.97). In studies with insulin use, when adjusted for confounders, the odds of having an infant large for gestational age (odds ratio 1.61, 1.09 to 2.37), or with respiratory distress syndrome (1.57, 1.19 to 2.08) or neonatal jaundice (1.28, 1.02 to 1.62), or requiring admission to the neonatal intensive care unit (2.29, 1.59 to 3.31), were higher in women with gestational diabetes mellitus than in those without diabetes. No clear evidence was found for differences in the odds of instrumental delivery, shoulder dystocia, postpartum haemorrhage, stillbirth, neonatal death, low five minute Apgar score, low birth weight, and small for gestational age between women with and without gestational diabetes mellitus after adjusting for confounders. Country status, adjustment for body mass index, and screening methods significantly contributed to heterogeneity between studies for several adverse outcomes of pregnancy.
Conclusions When adjusted for confounders, gestational diabetes mellitus was significantly associated with pregnancy complications. The findings contribute to a more comprehensive understanding of the adverse outcomes of pregnancy related to gestational diabetes mellitus. Future primary studies should routinely consider adjusting for a more complete set of prognostic factors.
Review registration PROSPERO CRD42021265837.

- Download figure
- Open in new tab
- Download powerpoint
Introduction
Gestational diabetes mellitus is a common chronic disease in pregnancy that impairs the health of several million women worldwide. 1 2 Formally recognised by O’Sullivan and Mahan in 1964, 3 gestational diabetes mellitus is defined as hyperglycaemia first detected during pregnancy. 4 With the incidence of obesity worldwide reaching epidemic levels, the number of pregnant women diagnosed as having gestational diabetes mellitus is growing, and these women have an increased risk of a range of complications of pregnancy. 5 Quantification of the risk or odds of possible adverse outcomes of pregnancy is needed for prevention, risk assessment, and patient education.
In 2008, the Hyperglycaemia and Adverse Pregnancy Outcome (HAPO) study recruited a large multinational cohort and clarified the risks of adverse outcomes associated with hyperglycaemia. The findings of the study showed that maternal hyperglycaemia independently increased the risk of preterm delivery, caesarean delivery, infants born large for gestational age, admission to a neonatal intensive care unit, neonatal hypoglycaemia, and hyperbilirubinaemia. 6 The obstetric risks associated with diabetes, such as pregnancy induced hypertension, macrosomia, congenital malformations, and neonatal hypoglycaemia, have been reported in several large scale studies. 7 8 9 10 11 12 The HAPO study did not adjust for some confounders, however, such as maternal body mass index, and did not report on stillbirths and neonatal respiratory distress syndrome, raising uncertainty about these outcomes. Other important pregnancy outcomes, such as preterm delivery, neonatal death, and low Apgar score in gestational diabetes mellitus, were poorly reported. No comprehensive study has assessed the relation between gestational diabetes mellitus and various maternal and fetal adverse outcomes after adjustment for confounders. Also, some cohort studies were restricted to specific clinical centres and regions, limiting their generalisation to more diverse populations.
By collating the available evidence, we conducted a systematic review and meta-analysis to quantify the short term outcomes in pregnancies complicated by gestational diabetes mellitus. We evaluated adjusted associations between gestational diabetes mellitus and various adverse outcomes of pregnancy.
This meta-analysis was conducted according to the recommendations of Cochrane Systematic Reviews, and our findings are reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (table S16). The study was prospectively registered in the international database of prospectively registered systematic reviews (PROSPERO CRD42021265837).
Search strategy and selection criteria
We searched the electronic databases PubMed, Web of Science, Medline, and the Cochrane Database of Systematic Reviews with the keywords: “pregnan*,” “gestatio*” or “matern*” together with “diabete*,” “hyperglycaemia,” “insulin,” “glucose,” or “glucose tolerance test*” to represent the exposed populations, and combined them with terms related to outcomes, such as “pregnan* outcome*,” “obstetric* complicat*,” “pregnan* disorder*,” “obstetric* outcome*,” “haemorrhage,” “induc*,” “instrumental,” “caesarean section,” “dystocia,” “hypertensi*,” “eclampsia,” “premature rupture of membrane,” “PROM,” “preter*,” “macrosomia,” and “malformation,” as well as some abbreviated diagnostic criteria, such as “IADPSG,” “DIPSI,” and “ADIPS” (table S1). The search strategy was appropriately translated for the other databases. We included observational cohort studies and control arms of trials, conducted after 1990, that strictly defined non-gestational diabetes mellitus (control) and gestational diabetes mellitus (exposed) populations and had definite diagnostic criteria for gestational diabetes mellitus (table S2) and various adverse outcomes of pregnancy.
Exclusion criteria were: studies published in languages other than English; studies with no diagnostic criteria for gestational diabetes mellitus (eg, self-reported gestational diabetes mellitus, gestational diabetes mellitus identified by codes from the International Classification of Diseases or questionnaires); studies published after 1990 that recorded pregnancy outcomes before 1990; studies of specific populations (eg, only pregnant women aged 30-34 years, 13 only twin pregnancies 14 15 16 ); studies with a sample size <300, because we postulated that these studies might not be adequate to detect outcomes within each group; and studies published in the form of an abstract, letter, or case report.
We also manually retrieved reference lists of relevant reviews or meta-analyses. Three reviewers (WY, CL, and JH) independently searched and assessed the literature for inclusion in our meta-analysis. The reviewers screened the titles and abstracts to exclude ineligible studies. The full texts of relevant records were then retrieved and assessed. Any discrepancies were resolved after discussion with another author (FL).
Data extraction
Three independent researchers (WY, CL, and JH) extracted data from the included studies with a predesigned form. If the data were not presented, we contacted the corresponding authors to request access to the data. We extracted data from the most recent study or the one with the largest sample size when a cohort was reported twice or more. Sociodemographic and clinical data were extracted based on: year of publication, location of the study (country and continent), design of the study (prospective or retrospective cohort), screening method and diagnostic criteria for gestational diabetes mellitus, adjustment for conventional prognostic factors (defined as maternal age, pregestational body mass index, gestational weight gain, gravidity, parity, smoking history, and chronic hypertension), and the proportion of patients with gestational diabetes mellitus who were receiving insulin. For studies that adopted various diagnostic criteria for gestational diabetes mellitus, we extracted the most recent or most widely accepted one for subsequent analysis. For studies adopting multivariate logistic regression for adjustment of confounders, we extracted adjusted odds ratios and synthesised them in subsequent analyses. For unadjusted studies, we calculated risk ratios and 95% confidence intervals based on the extracted data.
Studies of women with gestational diabetes mellitus that evaluated the risk or odds of maternal or neonatal complications were included. We assessed the maternal outcomes pre-eclampsia, induction of labour, instrumental delivery, caesarean section, shoulder dystocia, premature rupture of membrane, and postpartum haemorrhage. Fetal or neonatal outcomes assessed were stillbirth, neonatal death, congenital malformation, preterm birth, macrosomia, low birth weight, large for gestational age, small for gestational age, neonatal hypoglycaemia, neonatal jaundice, respiratory distress syndrome, low Apgar score, and admission to the neonatal intensive care unit. Table S3 provides detailed definitions of these adverse outcomes of pregnancy.
Risk-of-bias assessment
A modified Newcastle-Ottawa scale was used to assess the methodological quality of the selection, comparability, and outcome of the included studies (table S4). Three independent reviewers (WY, CL, and JH) performed the quality assessment and scored the studies for adherence to the prespecified criteria. A study that scored one for selection or outcome, or zero for any of the three domains, was considered to have a high risk of bias. Studies that scored two or three for selection, one for comparability, and two for outcome were regarded as having a medium risk of bias. Studies that scored four for selection, two for comparability, and three for outcome were considered to have a low risk of bias. A lower risk of bias denotes higher quality.
Data synthesis and analysis
Pregnant women were divided into two groups (gestational diabetes mellitus and non-gestational diabetes mellitus) based on the diagnostic criteria in each study. Studies were considered adjusted if they adjusted for at least one of seven confounding factors (maternal age, pregestational body mass index, gestational weight gain, gravidity, parity, smoking history, and chronic hypertension). For each adjusted study, we transformed the odds ratio estimate and its corresponding standard error to natural logarithms to stabilise the variance and normalise their distributions. Summary odds ratio estimates and their 95% confidence intervals were estimated by a random effects model with the inverse variance method. We reported the results as odds ratio with 95% confidence intervals to reflect the uncertainty of point estimates. Unadjusted associations between gestational diabetes mellitus and adverse outcomes of pregnancy were quantified and summarised (table S6 and table S14). Thereafter, heterogeneity across the studies was evaluated with the τ 2 statistics and Cochran’s Q test. 17 18 Cochran’s Q test assessed interactions between subgroups. 18
We performed preplanned subgroup analyses for factors that could potentially affect gestational diabetes mellitus or adverse outcomes of pregnancy: country status (developing or developed country according to the International Monetary Fund ( www.imf.org/external/pubs/ft/weo/2020/01/weodata/groups.htm ), risk of bias (low, medium, or high), screening method (universal one step, universal glucose challenge test, or selective screening based on risk factors), diagnostic criteria for gestational diabetes mellitus (World Health Organization 1999, Carpenter-Coustan criteria, International Association of Diabetes and Pregnancy Study Groups (IADPSG), or other), and control for body mass index. We assessed small study effects with funnel plots by plotting the natural logarithm of the odds ratios against the inverse of the standard errors, and asymmetry was assessed with Egger’s test. 19 A meta-regression model was used to investigate the associations between study effect size and proportion of patients who received insulin in the gestational diabetes mellitus population. Next, we performed sensitivity analyses by omitting each study individually and recalculating the pooled effect size estimates for the remaining studies to assess the effect of individual studies on the pooled results. All analyses were performed with R language (version 4.1.2, www.r-project.org ) and meta package (version 5.1-0). We adopted the treatment arm continuity correction to deal with a zero cell count 20 and the Hartung-Knapp adjustment for random effects meta models. 21 22
Patient and public involvement
The experience in residency training in the department of obstetrics and the concerns about the association between gestational diabetes mellitus and health outcomes inspired the author team to perform this study. We also asked advice from the obstetrician and patients with gestational diabetes mellitus about which outcomes could be included. The covid-19 restrictions meant that we sought opinions from only a limited number of patients in outpatient settings.
Characteristics of included studies
Of the 44 993 studies identified, 156 studies, 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 61 62 63 64 65 66 67 68 69 70 71 72 73 74 75 76 77 78 79 80 81 82 83 84 85 86 87 88 89 90 91 92 93 94 95 96 97 98 99 100 101 102 103 104 105 106 107 108 109 110 111 112 113 114 115 116 117 118 119 120 121 122 123 124 125 126 127 128 129 130 131 132 133 134 135 136 137 138 139 140 141 142 143 144 145 146 147 148 149 150 151 152 153 154 155 156 157 158 159 160 161 162 163 164 165 166 167 168 169 170 171 172 173 174 175 176 177 178 involving 7 506 061 pregnancies, were eligible for the analysis of adverse outcomes in pregnancy ( fig 1 ). Of the 156 primary studies, 133 (85.3%) reported maternal outcomes and 151 (96.8%) reported neonatal outcomes. Most studies were conducted in Asia (39.5%), Europe (25.5%), and North America (15.4%). Eighty four (53.8%) studies were performed in developed countries. Based on the Newcastle-Ottawa scale, 50 (32.1%) of the 156 included studies showed a low or medium risk of bias and 106 (67.9%) had a high risk of bias. Patients in 35 (22.4%) of the 156 studies never used insulin during the course of the disease and 63 studies (40.4%) reported treatment with insulin in different proportions of patients. The remaining 58 studies did not report information about the use of insulin. Table 1 summarises the characteristics of the study population, including continent or region, country, screening methods, and diagnostic criteria for the included studies. Table S5 lists the key excluded studies.

Search and selection of studies for inclusion
Characteristics of study population
- View inline
Associations between gestational diabetes mellitus and adverse outcomes of pregnancy
Based on the use of insulin in each study, we classified the studies into three subgroups: no insulin use (patients never used insulin during the course of the disease), insulin use (different proportions of patients were treated with insulin), and insulin use not reported. We reported odds ratios with 95% confidence intervals after controlling for at least minimal confounding factors. In studies with no insulin use, women with gestational diabetes mellitus had increased odds of caesarean section (odds ratio 1.16, 95% confidence interval 1.03 to 1.32), preterm delivery (1.51, 1.26 to 1.80), low one minute Apgar score (1.43, 1.01 to 2.03), macrosomia (1.70, 1.23 to 2.36), and an infant born large for gestational age (1.57, 1.25 to 1.97) ( fig 2 and fig S1). In studies with insulin use, adjusted for confounders, the odds of an infant born large for gestational age (odds ratio 1.61, 95% confidence interval 1.09 to 2.37), or with respiratory distress syndrome (1.57, 1.19 to 2.08) or neonatal jaundice (1.28, 1.02 to 1.62), or requiring admission to the neonatal intensive care unit (2.29, 1.59 to 3.31) were higher in women with than in those without gestational diabetes mellitus ( fig 3) . In studies that did not report the use of insulin, women with gestational diabetes mellitus had increased odds ratio for pre-eclampsia (1.46, 1.21 to 1.78), induction of labour (1.88, 1.16 to 3.04), caesarean section (1.38, 1.20 to 1.58), premature rupture of membrane (1.13, 1.06 to 1.20), congenital malformation (1.18, 1.10 to 1.26), preterm delivery (1.51, 1.19 to 1.93), macrosomia (1.48, 1.13 to 1.95), neonatal hypoglycaemia (11.71, 7.49 to 18.30), and admission to the neonatal intensive care unit (2.28, 1.26 to 4.13) (figs S3 and S4). We found no clear evidence for differences in the odds of instrumental delivery, shoulder dystocia, postpartum haemorrhage, stillbirth, neonatal death, low five minute Apgar score, low birth weight, and infant born small for gestational age between women with and without gestational diabetes mellitus in all three subgroups ( fig 2, fig 3, and figs S1-S4). Table S6 shows the unadjusted associations between gestational diabetes mellitus and adverse outcomes of pregnancy.

Findings of meta-analysis of association between gestational diabetes mellitus and adverse outcomes of pregnancy after adjusting for at least minimal confounding factors, in studies in patients who never used insulin during the course of the disease (no insulin use). NA=not applicable

Findings of meta-analysis of association between gestational diabetes mellitus and adverse outcomes of pregnancy after adjusting for at least minimal confounding factors, in studies where different proportions of patients were treated with insulin (insulin use). NA=not applicable
Subgroup, meta-regression, and sensitivity analyses
Subgroup analyses, based on risk of bias, did not show significant heterogeneity between the subgroups of women with and without gestational diabetes mellitus for most adverse outcomes of pregnancy ( table 2 and table 3 ), except for admission to the neonatal intensive care unit in studies where insulin use was not reported (table S7). Significant differences between subgroups were reported for country status and macrosomia in studies with (P<0.001) and without (P=0.001) insulin use ( table 2 and table 3 ), and for macrosomia (P=0.02) and infants born large for gestational age (P<0.001) based on adjustment for body mass index in studies with insulin use (table S8). Screening methods contributed significantly to the heterogeneity between studies for caesarean section (P<0.001) and admission to the neonatal intensive care unit (P<0.001) in studies where insulin use was not reported (table S7). In most outcomes, the estimated odds were lower in studies that used universal one step screening than those that adopted the universal glucose challenge test or selective screening methods ( table 2 and table 3 ). Diagnostic criteria were not related to heterogeneity between the studies for all of the study subgroups (no insulin use, insulin use, insulin use not reported). The subgroup analysis was performed only for outcomes including ≥6 studies.
Subgroup analysis according to country status, diagnostic criteria, screening method, and risk of bias for adverse outcomes of pregnancy in women with gestational diabetes mellitus compared with women without gestational diabetes mellitus in studies with no insulin use
Subgroup analysis according to country status, diagnostic criteria, screening method, and risk of bias for adverse outcomes of pregnancy in women with gestational diabetes mellitus compared with women without gestational diabetes mellitus in studies with insulin use
We applied meta-regression models to evaluate the modification power of the proportion of patients with insulin use when sufficient data were available. Significant associations were found between effect size estimate and proportion of patients who had received insulin for the adverse outcomes caesarean section (estimate=0.0068, P=0.04) and preterm delivery (estimate=−0.0069, P=0.04) (table S9).
In sensitivity analyses, most pooled estimates were not significantly different when a study was omitted, suggesting that no one study had a large effect on the pooled estimate. The pooled estimate effect became significant (P=0.005) for low birth weight when the study of Lu et al 99 was omitted, however (fig S5). We found evidence of a small study effect only for caesarean section (Egger’s P=0.01, table S10). Figure S6 shows the funnel plots of the included studies for various adverse outcomes (≥10 studies).
Principal findings
We have provided quantitative estimates for the associations between gestational diabetes mellitus and adverse outcomes of pregnancy after adjustment for confounding factors, through a systematic search and comprehensive meta-analysis. Compared with patients with normoglycaemia during pregnancy, patients with gestational diabetes mellitus had increased odds of caesarean section, preterm delivery, low one minute Apgar score, macrosomia, and an infant born large for gestational age in studies where insulin was not used. In studies with insulin use, patients with gestational diabetes mellitus had an increased odds of an infant born large for gestational age, or with respiratory distress syndrome or neonatal jaundice, or requiring admission to the neonatal intensive care unit. Our study was a comprehensive analysis, quantifying the adjusted associations between gestational diabetes mellitus and adverse outcomes of pregnancy. The study provides updated critical information on gestational diabetes mellitus and adverse outcomes of pregnancy and would facilitate counselling of women with gestational diabetes mellitus before delivery.
To examine the heterogeneity conferred by different severities of gestational diabetes mellitus, we categorised the studies by use of insulin. Insulin is considered the standard treatment for the management of gestational diabetes mellitus when adequate glucose levels are not achieved with nutrition and exercise. 179 Our meta-regression showed that the proportion of patients who had received insulin was significantly associated with the effect size estimate of adverse outcomes, including caesarean section (P=0.04) and preterm delivery (P=0.04). This finding might be the result of a positive linear association between glucose concentrations and adverse outcomes of pregnancy, as previously reported. 180 However, the proportion of patients who were receiving insulin indicates the percentage of patients with poor glycaemic control in the population and cannot reflect glycaemic control at the individual level.
Screening methods for gestational diabetes mellitus have changed over time, from the earliest selective screening (based on risk factors) to universal screening by the glucose challenge test or the oral glucose tolerance test, recommended by the US Preventive Services Task Force (2014) 181 and the American Diabetes Association (2020). 182 The diagnostic accuracy of these screening methods varied, contributing to heterogeneity in the analysis.
Several studies have tried to pool the effects of gestational diabetes mellitus on pregnancy outcomes, but most focused on one outcome, such as congenital malformations, 183 184 macrosomia, 185 186 or respiratory distress syndrome. 187 Our findings of increased odds of macrosomia in gestational diabetes mellitus in studies where insulin was not used, and respiratory distress syndrome in studies with insulin use, were similar to the results of previous meta-analyses. 188 189 The increased odds of neonatal respiratory distress syndrome, along with low Apgar scores, might be attributed to disruption of the integrity and composition of fetal pulmonary surfactant because gestational diabetes mellitus can delay the secretion of phosphatidylglycerol, an essential lipid component of surfactants. 190
Although we detected no significant association between gestational diabetes mellitus and mortality events, the observed increase in the odds of neonatal death (odds ratio 1.59 in studies that did not report the use of insulin) should be emphasised to obstetricians and pregnant women because its incidence was low (eg, 3.75% 87 ). The increased odds of neonatal death could result from several lethal complications, such as respiratory distress syndrome, neonatal hypoglycaemia (3.94-11.71-fold greater odds), and jaundice. These respiratory and metabolic disorders might increase the likelihood of admission to the neonatal intensive care unit.
For the maternal adverse outcomes, women with gestational diabetes mellitus had increased odds of pre-eclampsia, induction of labour, and caesarean section, consistent with findings in previous studies. 126 Our study identified a 1.24-1.46-fold greater odds of pre-eclampsia between patients with and without gestational diabetes mellitus, which was similar to previous results. 191
Strengths and limitations of the study
Our study included more studies than previous meta-analyses and covered a range of maternal and fetal outcomes, allowing more comprehensive comparisons among these outcomes based on the use of insulin and different subgroup analyses. The odds of adverse fetal outcomes, including respiratory distress syndrome (P=0.002), neonatal jaundice (P=0.05), and admission to the neonatal intensive care unit (P=0.005), were significantly increased in studies with insulin use, implicating their close relation with glycaemic control. The findings of this meta-analysis support the need for an improved understanding of the pathophysiology of gestational diabetes mellitus to inform the prediction of risk and for precautions to be taken to reduce adverse outcomes of pregnancy.
The study had some limitations. Firstly, adjustment for at least one confounder had limited power to deal with potential confounding effects. The set of adjustment factors was different across studies, however, and defining a broader set of multiple adjustment variables was difficult. This major concern should be looked at in future well designed prospective cohort studies, where important prognostic factors are controlled. Secondly, overt diabetes was not clearly defined until the IADPSG diagnostic criteria were proposed in 2010. Therefore, overt diabetes or pre-existing diabetes might have been included in the gestational diabetes mellitus groups if studies were conducted before 2010 or adopted earlier diagnostic criteria. Hence we cannot rule out that some adverse effects in newborns were related to prolonged maternal hyperglycaemia. Thirdly, we divided and analysed the subgroups based on insulin use because insulin is considered the standard treatment for the management of gestational diabetes mellitus and can reflect the level of glycaemic control. Accurately determining the degree of diabetic control in patients with gestational diabetes mellitus was difficult, however. Finally, a few pregnancy outcomes were not accurately defined in studies included in our analysis. Stillbirth, for example, was defined as death after the 20th or 28th week of pregnancy, based on different criteria, but some studies did not clearly state the definition of stillbirth used in their methods. Therefore, we considered stillbirth as an outcome based on the clinical diagnosis in the studies, which might have caused potential bias in the analysis.
Conclusions
We performed a meta-analysis of the association between gestational diabetes mellitus and adverse outcomes of pregnancy in more than seven million women. Gestational diabetes mellitus was significantly associated with a range of pregnancy complications when adjusted for confounders. Our findings contribute to a more comprehensive understanding of adverse outcomes of pregnancy related to gestational diabetes mellitus. Future primary studies should routinely consider adjusting for a more complete set of prognostic factors.
What is already known on this topic
The incidence of gestational diabetes mellitus is gradually increasing and is associated with a range of complications for the mother and fetus or neonate
Pregnancy outcomes in gestational diabetes mellitus, such as neonatal death and low Apgar score, have not been considered in large cohort studies
Comprehensive systematic reviews and meta-analyses assessing the association between gestational diabetes mellitus and adverse pregnancy outcomes are lacking
What this study adds
This systematic review and meta-analysis showed that in studies where insulin was not used, when adjusted for confounders, women with gestational diabetes mellitus had increased odds of caesarean delivery, preterm delivery, low one minute Apgar score, macrosomia, and an infant large for gestational age in the pregnancy outcomes
In studies with insulin use, when adjusted for confounders, women with gestational diabetes mellitus had increased odds of an infant large for gestational age, or with respiratory distress syndrome or neonatal jaundice, or requiring admission to the neonatal intensive care unit
Future primary studies should routinely consider adjusting for a more complete set of prognostic factors
Ethics statements
Ethical approval.
Not required.
Data availability statement
Table S11 provides details of adjustment for core confounders. Supplementary data files contain all of the raw tabulated data for the systematic review (table S12). Tables S13-15 provide the raw data and R language codes used for the meta-analysis.
Contributors: WY and FL developed the initial idea for the study, designed the scope, planned the methodological approach, wrote the computer code and performed the meta-analysis. WY and CL coordinated the systematic review process, wrote the systematic review protocol, completed the PROSPERO registration, and extracted the data for further analysis. ZL coordinated the systematic review update. WY, JH, and FL defined the search strings, executed the search, exported the results, and removed duplicate records. WY, CL, ZL, and FL screened the abstracts and texts for the systematic review, extracted relevant data from the systematic review articles, and performed quality assessment. WY, ZL, and FL wrote the first draft of the manuscript and all authors contributed to critically revising the manuscript. ZL and FL are the study guarantors. ZL and FL are senior and corresponding authors who contributed equally to this study. All authors had full access to all the data in the study, and the corresponding authors had final responsibility for the decision to submit for publication. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: The research was funded by the National Natural Science Foundation of China (grants 82001223 and 81901401), and the Natural Science Foundation for Young Scientist of Hunan Province, China (grant 2019JJ50952). The funders had no role in considering the study design or in the collection, analysis, interpretation of data, writing of the report, or decision to submit the article for publication.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/disclosure-of-interest/ and declare: support from the National Natural Science Foundation of China and the Natural Science Foundation for Young Scientist of Hunan Province, China for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
The lead author (the manuscript’s guarantor) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Dissemination to participants and related patient and public communities: The dissemination plan targets a wide audience, including members of the public, patients, patient and public communities, health professionals, and experts in the specialty through various channels: written communication, events and conferences, networks, and social media.
Provenance and peer review: Not commissioned; externally peer reviewed.
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
- Saravanan P ,
- Diabetes in Pregnancy Working Group ,
- Maternal Medicine Clinical Study Group ,
- Royal College of Obstetricians and Gynaecologists, UK
- O’Sullivan JB ,
- Hartling L ,
- Dryden DM ,
- Guthrie A ,
- Vandermeer B ,
- McIntyre HD ,
- Catalano P ,
- Mathiesen ER ,
- Metzger BE ,
- HAPO Study Cooperative Research Group
- Persson M ,
- Balsells M ,
- García-Patterson A ,
- Simmonds M ,
- Murphy HR ,
- Roland JM ,
- East Anglia Study Group for Improving Pregnancy Outcomes in Women with Diabetes (EASIPOD)
- Magnuson A ,
- Simmons D ,
- Sumeksri P ,
- Wongyai S ,
- González González NL ,
- Bellart J ,
- Guillén MA ,
- Herranz L ,
- Barquiel B ,
- Hillman N ,
- Burgos MA ,
- Pallardo LF
- Higgins JP ,
- Thompson SG ,
- Davey Smith G ,
- Schneider M ,
- Sweeting MJ ,
- Sutton AJ ,
- Hartung J ,
- IntHout J ,
- Ioannidis JP ,
- Alberico S ,
- Montico M ,
- Barresi V ,
- Multicentre Study Group on Mode of Delivery in Friuli Venezia Giulia
- Alfadhli EM ,
- Anderberg E ,
- Ardawi MS ,
- Nasrat HA ,
- Al-Sagaaf HM ,
- Kenealy T ,
- Barakat MN ,
- Youssef RM ,
- Al-Lawati JA
- Ibrahim I ,
- Eltaher F ,
- Benhalima K ,
- Hanssens M ,
- Devlieger R ,
- Verhaeghe J ,
- Berggren EK ,
- Boggess KA ,
- Stuebe AM ,
- Jonsson Funk M
- Korucuoglu U ,
- Aksakal N ,
- Himmetoglu O
- Bodmer-Roy S ,
- Cousineau J ,
- Broekman BFP ,
- GUSTO study group
- Catalano PM ,
- Cruickshank JK ,
- Chanprapaph P ,
- Cheung NW ,
- Lopez-Rodo V ,
- Rodriguez-Vaca D ,
- Benchimol M ,
- Carbillon L ,
- Benbara A ,
- Pharisien I ,
- Scifres CM ,
- Gorban de Lapertosa S ,
- Salzberg S ,
- DPSG-SAD Group
- Zijlmans AB ,
- Rademaker D ,
- Djelmis J ,
- Mulliqi Kotori V ,
- Pavlić Renar I ,
- Ivanisevic M ,
- Oreskovic S
- Domanski G ,
- Ittermann T ,
- Donovan LE ,
- Edwards AL ,
- Torrejón MJ ,
- Ekeroma AJ ,
- Chandran GS ,
- McCowan L ,
- Eagleton C ,
- Erjavec K ,
- Poljičanin T ,
- Matijević R
- Ethridge JK Jr . ,
- Feleke BE ,
- Feleke TE ,
- Forsbach G ,
- Cantú-Diaz C ,
- Vázquez-Lara J ,
- Villanueva-Cuellar MA ,
- Alvarez y García C ,
- Rodríguez-Ramírez E
- Gonçalves E ,
- Gortazar L ,
- Flores-Le Roux JA ,
- Benaiges D ,
- Gruendhammer M ,
- Brezinka C ,
- Lechleitner M
- Hedderson MM ,
- Ferrara A ,
- Hillier TA ,
- Pedula KL ,
- Morris JM ,
- Hossein-Nezhad A ,
- Maghbooli Z ,
- Vassigh AR ,
- Massaro N ,
- Streckeisen S ,
- Ikenoue S ,
- Miyakoshi K ,
- Raghav SK ,
- Jensen DM ,
- Sørensen B ,
- Rich-Edwards JW ,
- Kreisman S ,
- Tildesley H
- Kachhwaha CP ,
- Kautzky-Willer A ,
- Bancher-Todesca D ,
- Weitgasser R ,
- Keikkala E ,
- Mustaniemi S ,
- Koivunen S ,
- Keshavarz M ,
- Babaee GR ,
- Moghadam HK ,
- Kgosidialwa O ,
- Carmody L ,
- Gunning P ,
- Kieffer EC ,
- Carman WJ ,
- Sanborn CZ ,
- Viljakainen M ,
- Männistö T ,
- Kachhawa G ,
- Laafira A ,
- Griffin CJ ,
- Johnson JA ,
- Lapolla A ,
- Dalfrà MG ,
- Ragazzi E ,
- De Cata AP ,
- Norwitz E ,
- Leybovitz-Haleluya N ,
- Wainstock T ,
- Hinkle SN ,
- Grantz KL ,
- Lopez-de-Andres A ,
- Carrasco-Garrido P ,
- Gil-de-Miguel A ,
- Hernandez-Barrera V ,
- Jiménez-García R
- Luengmettakul J ,
- Sunsaneevithayakul P ,
- Talungchit P
- Macaulay S ,
- Munthali RJ ,
- Dunger DB ,
- Makwana M ,
- Bhimwal RK ,
- El Mallah KO ,
- Kulaylat NA ,
- Melamed N ,
- Vandenberghe H ,
- Jensen RC ,
- Kibusi SM ,
- Munyogwa MJ ,
- Patient C ,
- Miailhe G ,
- Legardeur H ,
- Mandelbrot L
- Minsart AF ,
- N’guyen TS ,
- Ratsimandresy R ,
- Ali Hadji R
- Matsumoto T ,
- Morikawa M ,
- Sugiyama T ,
- Knights SJ ,
- Olayemi OO ,
- Mwanri AW ,
- Ramaiya K ,
- Abalkhail B ,
- Nguyen TH ,
- Nguyen CL ,
- Minh Pham N ,
- Nicolosi BF ,
- Vernini JM ,
- Kragelund Nielsen K ,
- Andersen GS ,
- Nybo Andersen AM
- Ogonowski J ,
- Miazgowski T ,
- Czeszyńska MB ,
- Kuczyńska M ,
- Miazgowski T
- Morrish DW ,
- O’Sullivan EP ,
- O’Reilly M ,
- Dennedy MC ,
- Gaffney G ,
- Atlantic DIP collaborators
- Ovesen PG ,
- Rasmussen S ,
- Kesmodel US
- Ozumba BC ,
- Premuzic V ,
- Zovak Pavic A ,
- Bevanda M ,
- Mihaljevic S ,
- Ramachandran A ,
- Snehalatha C ,
- Clementina M ,
- Sasikala R ,
- Redman LM ,
- LIFE-Moms Research Group
- Spanish Group for the Study of the Impact of Carpenter and Coustan GDM thresholds
- Bowker SL ,
- Montoro MN ,
- Lawrence JM
- Kamalanathan S ,
- Saldana TM ,
- Siega-Riz AM ,
- Savitz DA ,
- Thorp JM Jr .
- Savona-Ventura C ,
- Schwartz ML ,
- Lubarsky SL
- Segregur J ,
- Buković D ,
- Milinović D ,
- Cavkaytar S ,
- Shahbazian H ,
- Nouhjah S ,
- Shahbazian N ,
- McElduff A ,
- Sheffield JS ,
- Butler-Koster EL ,
- McIntire DD ,
- Saigusa Y ,
- Nakanishi S ,
- Templeton A ,
- Sirimarco MP ,
- Guerra HM ,
- Lisboa EG ,
- Sletner L ,
- Yajnik CS ,
- Soliman A ,
- Al Rifai H ,
- Soonthornpun S ,
- Soonthornpun K ,
- Aksonteing J ,
- Thamprasit A
- Srichumchit S ,
- Sugiyama MS ,
- Roseveare C ,
- Basilius K ,
- Madraisau S
- Hansen BB ,
- Mølsted-Pedersen L
- Caswell A ,
- Holliday E ,
- Petrović O ,
- Crnčević Orlić Ž ,
- Vambergue A ,
- Nuttens MC ,
- Goeusse P ,
- Biausque S ,
- van Hoorn J ,
- von Katterfeld B ,
- McNamara B ,
- Langridge AT
- Wahabi HA ,
- Esmaeil SA ,
- Alzeidan RA
- Esmaeil S ,
- Mamdouh H ,
- Wahlberg J ,
- Nyström L ,
- Persson B ,
- Arnqvist HJ
- Nankervis A ,
- Weijers RN ,
- Bekedam DJ ,
- Smulders YM
- Bleicher K ,
- Saunders LD ,
- Demianczuk NN
- Homer CSE ,
- Sullivan EA
- American Diabetes Association
- U.S. Preventive Services Task Force
- Tabrizi R ,
- Lankarani KB ,
- Leung-Pineda V ,
- Gronowski AM
- Bryson CL ,
- Ioannou GN ,
- Rulyak SJ ,
- Critchlow C
Gestational Diabetes Mellitus: Review Essay
Gestational diabetes mellitus (GDM) is a very serious condition that affects the health of the mother, as well as her baby in varying time periods: immediate, short-term, or long-term. It is a type of diabetes that affects pregnant mothers and has the potential to recur despite the fact that it mainly disappears after birth. This paper is aimed at enhancing the understanding of GDM among Australian pregnant mothers with a focus on its prevalence, causes, health implications, established policies and public initiates aimed at addressing it, as well as future strategies and approaches that could help reduce its incidence and prevalence.
The prevalence of gestational diabetes worldwide has shown a general increasing trend in the last 20 years across race/ethnicity groups. According to recent data by Ferrara (2007), an increase of approximately 10 to 100% has been reported in various race/ethnicity groups. In Australia, the prevalence of GDM is estimated to range between 5.2 and 8.8% (Cheung & Byth 2003). The 2005-6 gestational diabetes mellitus in Australia report gave a figure of 4.6% to represent the fraction of pregnant women aged 15-49 years with GDM. This was a 20% increase compared with what had been recorded in 2000-1 (Templeton & Pieris-Cladwell 2008). According to this report, the incidence of gestational diabetes was increasing. This is seconded by Ferrara’s (2007) in his research work, in which he showed increasing trends in the prevalence of GDM in various geographical regions where South Australia was part. On an annual basis, 16,500 women are diagnosed with GDM (Dodd et al. 2007). Unfortunately, this is expected to continue growing.
There is no definite known cause for GDM but there are different facts and theories presented to guide this. One version is that during pregnancy, the hormones responsible for foetal growth and development impede the action of insulin hence insulin resistance (Australian Government and Diabetes Australia 2010). Based on this theory, it is automatically presumed that when the release of the blocking hormones stops, then the insulin levels go back to normal. As a result, it lacks a definite cause. Alternatively, risk factors are used to explain the cause of GDM as stated by Jovanovic & Pettitt (2001). These risk factors among others include obesity, maternal age, and a family history of diabetes. The fact that a pregnant woman gets GDM for the first time during their pregnancy is a risk factor in itself because histories of GDM are associated with high chances of developing the disease in subsequent pregnancies (Hall 2001).
Racial differences are also very imperative in determining the occurrence of GDM. This can be supported by the fact that the prevalence of GDM was reported to be higher in Chinese and Indian women residing in Australia compared with the women of European or Northern African descent, who were residing in Australia as well (State Government of Victoria 2012). In addition, the Aboriginal women rather than the non-Aboriginal women were more exposed to this type of diabetes (Ishak & Petocz 2003). The 2005-6 GDM report simply states that the incidence of GDM among women who had been born from other countries was twice as large as the incidence of those women born in Australia. Those born in Southern Asia were 3.4 times more at risk of getting the disease compared with those born in Australia (Templeton & Pieris-Caldwell 2008).
Gestational diabetes mellitus is a public health issue with serious implications. As stated earlier, its implications are felt almost immediately, in the short-term, or long-term. The implications of GDM are mainly felt by the infants in the newborn period. This is because of the current patterns that show an increase in the prevalence of diabetes in offspring born to mothers with GDM (Ferrara, 2007). Short-term-effects mainly include those that are observable or detectable during pregnancy, labour and a short time after birth and inexhaustibly include outcome of pregnancy, intensive care admissions, duration of pregnancy, need for resuscitation, method of delivery, foetal growth characteristics, and type of labour (Australian Institute of Health and Welfare 2010).
Neonates born to mothers with GDM experience the implications of GDM in the following ways: increased exposure to stillbirth, respiratory distress syndrome, caesarean section, shoulder dystocia, and macrosomia (Gonzalez-Quintero et al. 2007). Stone et al. (2002) implies that babies born to mothers with GDM are more at risk of going through the effects of this disease compared with babies of non-GDM mothers. This is due to the facts presented; whereas 17% of neonates from mothers with GDM were macrosomic, only 10% of the neonates from mothers without GDM had the condition, 13% of the newborns from mothers with GDM had neonatal jaundice compared with 7% of non-GDM mothers, and 32% of the newborns from mothers with GDM were delivered by caesarean compared with 19% of newborns belonging to mothers without GDM. Suhenon & Teramo (1993) indicate that GDM exposes pregnant mothers to pregnancy-induced hypertension and pre-eclampsia, operation during delivery, and induced labour. According to a study carried out in Victoria in 1996, 37% of women with GDM compared with 23% of women without GDM had induced labour. In addition, 41% of the women with GDM underwent operative delivery by means of vacuum extraction, forceps, or caesarean as opposed to 29% of women without GDM (Stone et al. 2002).
The long term implications of GDM to the mothers include increased risk of recurrent GDM in subsequent pregnancies. In addition, it results in progression to type 2 in these mothers and a general resultant effect of high prevalence of type 2 diabetes in general. It is has been estimated that 17% of Australian women with GDM are later diagnosed with type 2 diabetes within 10 years. These figures can go up as high as 50% when the timeframe changes to 30 years (Lee, et al., 2007; Metzger 2007). The explanation behind this is that the prevalence of GDM has been indicated as a reflection of the prevalence of type 2 diabetes in the larger population. In addition, it is the attributive risk factor for type 2 diabetes among the pregnant mothers with GDM (Kim, Newton & Knopp, 2002).
GDM posses as a serious health risk for pregnant mothers because it also exposes them to heart diseases according to Retnakaran & Baiju (2009). Women with GDM have an increased risk of neonatal hypoglycaemia, and hyperbilirubinaemia. The babies are also affected in the long term because they tend to have congenital anomalies. They also have an increased risk of obesity, impaired glucose tolerance, and are also susceptible to type II diabetes in early adulthood (Fetita et al. 2007).
As a result of the need to reduce associated co-morbidities and death, there have been initiatives put in place to ensure that GDM is reduced and lives are saved. The government has been involved in funding Diabetes Australia for the successful development and execution of effective mechanisms to reduce the incidence and prevalence of GDM (Australian government 2012). The National Diabetes Services Scheme (NDSS) is a project that was initiated by the Australian government through Diabetes Australia, and its role has been greatly recognized in as far as reduction and prevention efforts of GDM are concerned. Within the National Diabetes Services Scheme, there is the National Gestational Diabetes Register that was set up to enable women with GDM to gain control over their conditions and ensure that their health conditions do not worsen (Diabetes Australia, 2012).
Pregnant women are required to register with this body, the National Gestational Diabetes Register, and in return they are to receive some benefits. Their doctors and they are sent consistent reminders of the need to engage in diabetes checks. In addition, this body is involved in sensitizing and providing information in printed form to the women on the need of, and how they should adopt a healthy lifestyle. However, this does not guarantee that the women will actually read and understand the information. Therefore, it could be a reason for the continued increase because even though there is sensitization, the manner in which it is carried out matters a lot.
As indicated earlier, one’s lifestyle is a great determinant to one’s health and especially diabetes including GDM. Sometimes, individuals are not knowledgeable in as far as healthy diets are concerned, or they may not realize the essence of such diets. Consistent provision and distribution of printed materials on GDM and how it can be controlled is assumed to act as consistent reminders on the need to ensure that one adopts and practices healthy feeding habits. But this medium of passing information is questionable. This registration has been made free and therefore every pregnant woman is not restricted by money to get the reading materials, and engage in medical check-ups. Regardless of this free service, thoroughness in terms of follow-ups should be observed because the women act out of their own will and it might not be consistent. Such free services deserve more emphasis and should not be viewed as opportunities for only the less privileged because they are equally important to everyone.
Registration with NDSS also enhances one’s access to various products such as testing strips, insulin syringes and pen needles, and insulin pump consumables. These devices are very important in the management of GDM through monitoring of one’s glucose levels. It should not just be a matter of distributing these devices because if someone does not know how to effectively and properly use and take of this equipment, it would be a goalless venture. Ensuring that there is available data on the incidence and prevalence rates of pregnant women with GDM is another initiative. This data has been made available in the Gestational diabetes mellitus in Australia report. The first one was developed in 2005-6 and it aimed at providing researchers, scholars or related academicians with information on the incidence of GDM among women giving birth in hospitals. This report also provided information on high-risk sub-groups, which are defined on the basis of their orientation towards the condition. Factors mentioned in this report that determine inclination towards the disease include age and genes (Templeton & Pieris-Caldwell 2008).
A realization is that despite the strategies in place currently, the prevalence of GDM is still increasing. This could mean several things but in future, there is need to carry out researches and establish the effect of each strategy in reducing GDM and therefore establish their effectiveness, as well as what is not addressed by the various strategies. The world is constantly changing and therefore, there is need to constantly review and update data. Researchers should exercise validity because there lacks consistency in the levels of incidence and prevalence of GDM. Yet, this is very important in planning and allocating resources to address GDM in the future. Accurate figures enable the government and various bodies addressing diabetes to focus. I second Lancaster (1996) on the essence of enhancing the research area so as to give consistent and reliable results.
The main challenge is usually maintenance. Once the glucose levels have gone down, there is a tendency for women to assume that they are okay and therefore tend to ignore the monitoring bit. This is a reflection of the NDSS scheme where follow-up lacks and therefore, this element should be given full attention. There is need to clearly point out the essence and ways of maintaining a normal glucose level and especially for those mothers who have experienced GDM before so as to avoid its recurrence. Lack of follow-up is an indication of lack of seriousness. The notion by health care workers that diabetes is just like any other disease, and that they do not put much seriousness are elements that may have certain effects on the patients. As a result, the women may miss out on some fundamental practices that can affect their prognosis and road to recovery.
A lot of emphasis is mainly placed on the pharmacological dimension of GDM yet behavioural interventions such as healthy eating, engagement in healthy physical activity and proper stress coping mechanisms are more effective in reducing the recurrence of the disease but are not accorded the required attention and emphasis (Australian Government and Diabetes Australia 2010). There should therefore be a shift in emphasis where women should be really encouraged to change their lifestyles and adopt healthier ones, or maintain the healthy ones. Counselling services should be offered affordably, or as part of the NDSS package to ensure that all mothers benefit. To enable such utilization of services to enhance behaviour change, there is need to evaluate the accessibility of health care services among the GDM mothers and thereby figure out if there is a way that accessibility could be enhanced. Examples here would include subsidizing health care costs with a focus on the individual’s background financial position.
Future strategies should not focus solely on the GDM but instead, they should also encompass the associated type of diabetes that results. In essence, the strategies to address GDM should be designed in such a manner that also minimizes the occurrence of type II diabetes. The successful implementation of projects and policies is grounded in integration and co-operation among the involved parties. The various health care systems entail various departments and all these should liaise effectively with one another through effective communication to avoid inefficiencies and deficiencies in the system. These inefficiencies and deficiencies are so serious such that regardless of the great advocacy and accessibility to health care, lack of co-ordination results in poor delivery of services and may not produce the desired effect on the patient.
Australian Institute of Health and Welfare 2010, Diabetes in pregnancy: its impact on Australian women and their babies , Diabetes series no. 14. Cat. no. CVD 52, AIHW, Canberra.
Australian Government and Diabetes Australia 2010, Gestational Diabetes: Caring for yourself and your baby , Web.
Cheung, NW & Byth, K 2003, “The population health significance of gestational diabetes”, Diabetes Care, vol. 26 , pp. 2005-9.
Diabetes Australia 2012, Gestational Diabetes , Web.
Dodd, JM, Crowther, CA, Antoniou, G, Baghurst, P & Robinson, JS 2007, “Screening for gestational diabetes: the effect of varying blood glucose definitions in the prediction of adverse maternal and infant health outcomes”, Aust N Z J Obstet Gynaecol , vol. 47, no. 4, pp. 307-312.
Ferrara, A 2007, “Increasing Prevalence of Gestational Diabetes Mellitus: A Public Health Perspective”, Diabetes Care , vol. 30, no. 2, pp. S141-S146.
Fetita, L, Sobngwi, S, Serradas, P, Calvo, F & Gautier, J 2007, “Review: Consequences of fetal exposure to maternal diabetes in offspring”, Journal of Clinical Endocrinology and Metabolism, vol. 91, no. 10, pp. 3718–3724.
Gonzalez-Quintero, VH, Istwan, NB, Rhea, DJ, Rodriguez, LI, Cotter, A, Carter, J, Mueller, A & Stanziano, GJ 2007, “The impact of glycemic control on neonatal outcome in singleton pregnancies complicated by gestational diabetes”, Diabetes Care, vol. 30, no. 3, pp. 467–470.
Hall, LD, Sberna, J & Utermohle, C 2001, “Diabetes in pregnancy, Alaska 1990–1999”, State of Alaska Epidemiology Bulletin, vol. 5, no. 3, pp. 1–9.
Ishak, M & Petocz, P 2003, “Gestational diabetes among Aboriginal Australians: prevalence, time trend, and comparisons with non-Aboriginal Australians”, Ethnicity and Disease, vol. 13, pp. 55–60.
Jovanovic, L, & Pettitt, DJ 2001, “Gestational diabetes mellitus”, JAMA, vol. 286, pp. 2516–2518.
Kim, C, Newton, KM, & Knopp, RH 2002, “Gestational diabetes and the incidence of type 2 diabetes: a systematic review ”, Diabetes Care , vol. 25, pp. 1862-68.
Lancaster, P 1996, “The health of Australia’s mothers and babies—improvements in the collection of perinatal statistics are needed to fill the gaps”, Medical Journal of Australia, vol. 164, pp. 198–199.
Lee, AJ, Hiscock, RJ, Wein, P, Walker, SP & Permezel, M 2007, “Gestational diabetes mellitus: clinical predictors and long-term risk of developing Type 2 diabetes”, Diabetes Care, vol. 30, no. 4, pp. 878–883.
Metzger, BE 2007, “Long-term outcomes in mothers diagnosed with gestational diabetes mellitus and their offspring”, Clinical Obstetrics and Gynecology, vol. 50, no. 4, pp. 972–979.
Retnakaran, R & Baiju, RS 2009, “Mild glucose intolerance in pregnancy and risk of cardiovascular disease: a population-based cohort study”, Canadian Medical Association Journal, vol. 181, no. 6–7, pp. 371–377.
State Government of Victoria 2012, Diabetes-Gestational, Web.
Stone, CA, McLachlan, KA, Halliday, JL, Wein, P &Tippett, C 2002, “Gestational diabetes in Victoria in 1996: incidence, risk factors and outcomes ”, Medical Journal of Australia, vol.177, pp. 486–491.
Suhonen, L & Teramo, K 1993, “Hypertension and pre-eclampsia in women with gestational glucose intolerance”, Acta Obstetricia et Gynecologica Scandinavica, vol. 72, no. 4, pp. 269–272.
Templeton, M & Pieris-Caldwell, I 2008, Gestational diabetes mellitus in Australia , 2005-06. Cat. no. CVD 44, AIHW, Canberra.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2022, May 3). Gestational Diabetes Mellitus: Review. https://ivypanda.com/essays/gestational-diabetes-mellitus-review/
"Gestational Diabetes Mellitus: Review." IvyPanda , 3 May 2022, ivypanda.com/essays/gestational-diabetes-mellitus-review/.
IvyPanda . (2022) 'Gestational Diabetes Mellitus: Review'. 3 May.
IvyPanda . 2022. "Gestational Diabetes Mellitus: Review." May 3, 2022. https://ivypanda.com/essays/gestational-diabetes-mellitus-review/.
1. IvyPanda . "Gestational Diabetes Mellitus: Review." May 3, 2022. https://ivypanda.com/essays/gestational-diabetes-mellitus-review/.
Bibliography
IvyPanda . "Gestational Diabetes Mellitus: Review." May 3, 2022. https://ivypanda.com/essays/gestational-diabetes-mellitus-review/.
- Gestational Diabetes: Child Bearing Experience
- Gestational Diabetes Mellitus - NSW, Australia
- Gestational Diabetes in a Pregnant Woman
- Exploring Glucose Tolerance and Gestational Diabetes Mellitus
- Diabetes Mellitus Epidemiology Statistics
- Control of LDL Cholesterol Levels in Patients, Gestational Diabetes Mellitus
- Women, Heart, and Nursing
- Gestational Diabetes: American Diabetes Association Publishers
- Pathophysiology of Mellitus and Insipidus Diabetes
- Critical Analysis of Policy for Type 2 Diabetes Mellitus in Australia
- Blood Disorder: Disease Analysis
- The Endocrine System Researching
- Endocrine Disruption Through Phthalates/Plasticizers
- 52-Year-Old Female Patient With Type II Diabetes
- R-insulin: Article Critique
- Research article
- Open access
- Published: 07 February 2020
Women’s experiences of a diagnosis of gestational diabetes mellitus: a systematic review
- Louise Craig 1 ,
- Rebecca Sims 1 ,
- Paul Glasziou 1 &
- Rae Thomas ORCID: orcid.org/0000-0002-2165-5917 1
BMC Pregnancy and Childbirth volume 20 , Article number: 76 ( 2020 ) Cite this article
27k Accesses
64 Citations
46 Altmetric
Metrics details
Gestational diabetes mellitus (GDM) - a transitory form of diabetes induced by pregnancy - has potentially important short and long-term health consequences for both the mother and her baby. There is no globally agreed definition of GDM, but definition changes have increased the incidence in some countries in recent years, with some research suggesting minimal clinical improvement in outcomes. The aim of this qualitative systematic review was to identify the psychosocial experiences a diagnosis of GDM has on women during pregnancy and the postpartum period.
We searched CINAHL, EMBASE, MEDLINE and PsycINFO databases for studies that provided qualitative data on the psychosocial experiences of a diagnosis of GDM on women across any stage of pregnancy and/or the postpartum period. We appraised the methodological quality of the included studies using the Critical Appraisal Skills Programme Checklist for Qualitative Studies and used thematic analysis to synthesis the data.
Of 840 studies identified, 41 studies of diverse populations met the selection criteria. The synthesis revealed eight key themes: initial psychological impact; communicating the diagnosis; knowledge of GDM; risk perception; management of GDM; burden of GDM; social support; and gaining control. The identified benefits of a GDM diagnosis were largely behavioural and included an opportunity to make healthy eating changes. The identified harms were emotional, financial and cultural. Women commented about the added responsibility (eating regimens, appointments), financial constraints (expensive food, medical bills) and conflicts with their cultural practices (alternative eating, lack of information about traditional food). Some women reported living in fear of risking the health of their baby and conducted extreme behaviours such as purging and starving themselves.
A diagnosis of GDM has wide reaching consequences that are common to a diverse group of women. Threshold cut-offs for blood glucose levels have been determined using the risk of physiological harms to mother and baby. It may also be advantageous to consider the harms and benefits from a psychosocial and a physiological perspective. This may avoid unnecessary burden to an already vulnerable population.
Peer Review reports
Gestational diabetes mellitus (GDM) is diagnosed by elevated blood glucose in pregnancy though the definition has changed repeatedly since its first description in the 1960’s [ 1 , 2 ]. The most frequently reported perinatal consequence of GDM is macrosomia (usually defined as a neonate weighing over 4 kg) which can increase the risk of caesarean section and shoulder dystocia. For the mother, there are also potential longer-term consequences including an increased risk of type 2 diabetes post-pregnancy and/or in later life [ 3 ]. The investigators of a large international Hyperglycemia and Adverse Pregnancy Outcome (HAPO) study aimed to identify a cut-point in the continuum to decide the blood glucose level (BGL) thresholds that should be used to define GDM [ 4 ]. However, a definitive cut-point was not identified and using the HAPO data the International Association of the Diabetes and Pregnancy Study Groups (IADSPG) consensus panel recommended a BGL threshold associated with the risk of adverse infant outcomes (such as risk of macrosomia, excess infant adiposity and neonatal hyperinsulinemia) [ 5 ]. This change was controversial, and there is currently a lack of an agreed standard for diagnosing high blood glucose in pregnancy.
Pregnancy can be a vulnerable period when a woman is adapting and responding to changes in body perceptions, such as loss of strength or fitness, which can result in reduced self-esteem and depression [ 6 ]. Many women report depression and anxiety during pregnancy which often includes worry for the baby’s wellbeing [ 7 , 8 ]. A diagnosis of a health condition such as GDM could have a detrimental effect on a pregnant woman’s quality of life due to fears that the illness may affect her and/or her baby [ 9 ]. This has potential to convert pregnancy, a natural process, into one associated with risks, ill-health and increased surveillance [ 10 ]. Understanding a women’s response to the GDM diagnosis and its psychological impact has emerged as an important issue [ 11 ]. Some studies report women describing the initial response as one of ‘shock’ [ 12 , 13 ], ‘sadness’ and ‘guilt’ [ 13 ]. A women’s acceptance of risk and fear of complications is likely to influence the acceptability of various interventions. Therefore, it is imperative to amalgamate the findings of these studies to synthesise the array of potential psychosocial consequences of a diagnosis of GDM.
In many countries the prevalence of GDM is rising [ 14 , 15 , 16 ]. Some of this is due to the increasing age at which women are becoming pregnant, an increase in obesity amongst women, more testing during pregnancy, and better recording during pregnancy. However, much of the rise has occurred since 2013 when some countries adopted the new IADPSG criteria and testing regimen for gestational diabetes. This resulted in the anomalous position that two women in two countries with exactly the same glucose levels may or may not be diagnosed with GDM depending on the country’s definition. Caution had been previously raised that the new IADPSG definition would increase prevalence of women diagnosed with GDM by two-to-three-fold [ 17 ].
Despite a significant increase in prevalence of GDM after the introduction of the new IADPSG criteria [ 15 , 16 ], some pre-post studies suggest negligible clinical improvement in the adverse outcomes measured [ 17 , 18 ]. Findings from a qualitative study of 19 women of different cultural backgrounds investigating women’s experiences of a GDM diagnosis reported that the diagnostic criteria itself was viewed as ‘confusing’ by some women and treatment for their ‘borderline’ condition unnecessary [ 19 ].
Although multiple studies have considered the impact of a diagnosis of GDM, a systematic review to synthesise the evidence around the emotional impact of a diagnosis at different stages, i.e. time of diagnosis, after diagnosis, at the delivery of the baby, and post-delivery, is lacking. The findings could inform healthcare clinicians of women’s attitudes and the consequences of a diagnosis and illuminate potential opportunities to provide support and advise. Therefore, in this systematic review, we aim to synthesise the evidence of the psychosocial experiences a diagnosis of GDM has on women during pregnancy and the postpartum period.
We followed the Enhancing Transparency in Reporting the Synthesis of Qualitative Research Guidelines (ENTREQ; Additional file 1 : Table S1) [ 20 ]. We included primary studies published in peer-review journals that:
included pregnant women with a current diagnosis or women with a history of GDM;
provided qualitative data on the psychosocial experiences of a diagnosis of GDM on women across any stage of pregnancy and/or the postpartum period; and
where participants have provided an account of their experience or perspective of living with GDM
No restrictions were placed on country, written language, or year of publication.
Studies were excluded, if:
the primary aim was to identify barriers and/or facilitators to service as these focused on the management of GDM rather than the GDM diagnosis; or
participants were women diagnosed with diabetes before pregnancy
Abstracts, letters, editorials and commentaries were also excluded.
Search methods for identification of studies
The search strategy (MEDLINE version provided in the Additional file 1 ) was developed using a combination of Medical Subject Headings terms centred around three key areas: i) gestational diabetes mellitus ii) diagnostic testing for gestational diabetes mellitus and iii) patient experiences. The Systematic Review Accelerator software was used to translate the search strategy for each of the different databases and to remove duplicated articles [ 21 ]. We searched CINAHL, EMBASE, MEDLINE and PsycINFO databases from inception to April 2018. Forward and backward citation searching of included studies was conducted.
Selection process
A single reviewer (LC) screened the titles and abstracts of retrieved references using Endnote Version X7.7.1. Potentially eligible full-texts were independently reviewed by LC and RS with conflicts resolved via discussion. Two full-text studies published in Portuguese were first translated using Google Translate and then validated by a researcher with both spoken and written Portuguese language skills located within our research network.
Data extraction
All data labelled as results or findings including themes, categories, theories were extracted and imported into NVivo Version 12 by LC. Study characteristics were extracted by LC which included study location, reported research aims, study design, methodology and the analytical approach. Information about the diagnostic criteria used to determine GDM in women was also extracted.
Data synthesis and analysis
To synthesise the findings, we used a thematic synthesis described by Thomas and Harden [ 22 ]. Thematic synthesis has the potential for conclusions to be drawn based on common aspects across otherwise heterogeneous studies and produce findings that directly inform health practitioners [ 22 , 23 ]. Coding was inductive, with codes derived from the data. First, extracted text relevant to patient experiences and perspectives was coded line by line. A subset of studies ( n = 5) were coded independently by LC and RS to develop a coding framework. Disagreements were resolved by discussion. LC and RS coded a further subset ( n = 4) and established an inter-rater reliability of Kappa = 0.87. Following this, LC applied the coding framework to the remaining studies. New codes were iteratively developed as new concepts arose.
Second, relationships between the codes were identified by LC to form the basis of descriptive themes across the studies. Similar codes were grouped to generate themes and less frequently used codes were classified into sub-themes. In the final stage, analytical themes were developed to ‘go beyond’ the primary studies to amalgamate and interpret the findings. The relevant quotes to support each theme were tabulated.
Quality assessment
As recommended by the Cochrane Qualitative Research Methods Group, we assessed the quality of the included studies using the Critical Appraisal Skills Programme Qualitative Checklist (CASP). This tool uses a systematic approach to appraise three key areas: study validity, an evaluation of methodological quality, and an assessment of external validity [ 24 ]. Critical appraisal was conducted by one reviewer (LC) for all studies, with second reviewer appraisal (RS) for a sub-set of included papers. The findings from the two reviewers were compared and any contrasting items were discussed and re-reviewed.
The search identified 840 studies. After deduplication and screening of titles and abstracts 88 full-text articles were assessed (Fig. 1 ). Seven further articles were identified through citation searching. Data were extracted from 41 studies meeting eligibility criteria and were included in the review [ 11 , 12 , 13 , 19 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 ].
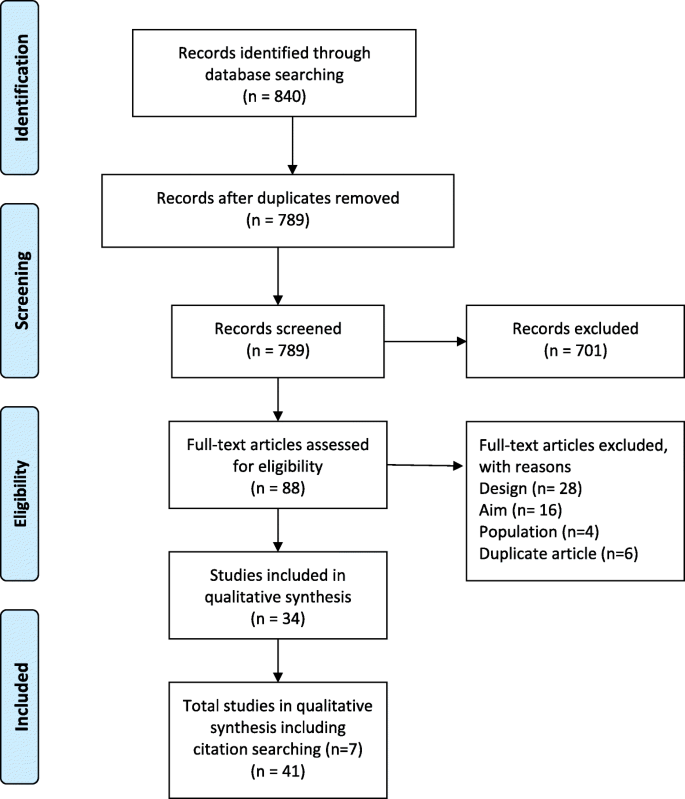
Prima flow diagram
Study characteristics
The studies reflected a variety of sampling methods and data collection methods. For example, interviews were conducted in 34 studies [ 10 , 12 , 13 , 25 , 27 , 28 , 30 , 31 , 32 , 34 , 35 , 36 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 60 , 61 ], focus group methods were used in three [ 19 , 32 , 37 ], and interviews and focus groups were used in two studies [ 29 , 51 ]. Two studies used a mixed method approach [ 26 , 59 ]. The sample sizes ranged from 6 to 57 women. Eighteen studies were conducted in Europe, 10 in Australia, 9 in North America, and 2 studies each in Asia and South America. Table 1 details the characteristics of the included studies.
Quality appraisal
Most studies were assessed as high quality (Additional file 1 : Table S2). Study aims were stated in all but one study [ 47 ]. As the purpose of all included studies was to explore or gain knowledge, opinions or attitudes about GDM, the qualitative methods employed in all the studies were appropriate. Different study designs were used and in some cases the lack of reporting details made judgments of the appropriateness of study methods difficult. Data were collected in a way that addressed the research issue, however, a few authors did not discuss or report details such as saturation of data [ 31 , 47 , 56 , 59 ]. The relationship between researcher and participants was considered in only two studies [ 51 , 61 ]. Appropriateness of data analysis was assessed as “unclear” when there was a lack of details about how themes were derived.
Thematic analyses
Eight themes were generated from the data synthesis: 1. initial psychological impact; 2. communicating the diagnosis; 3. knowledge of GDM; 4. risk perception; 5. management of GDM; 6. burden of GDM; 7. social support; and 8. gaining control. The relevant quotes to support each theme are presented in Table 2 .
Initial psychological impact
When initially diagnosed with GDM, most women reported reactions such as self-blame, failure, fear, sadness, concern and confusion. Women often focused on the uncertainty of diagnostic prognosis and some considered it to be a life-altering experience. Some women felt lost and unsure what to do next. Often women felt an overwhelming sense of vulnerability and guilt. In some cases, the diagnosis was received positively and was viewed as an opportunity for lifestyle improvements. For example, some women viewed the diagnosis as a ‘ wake up’ call and were grateful for the chance to intervene and potentially prevent adverse outcomes for their babies and themselves. Some women viewed gaining less weight than expected during their pregnancy as a benefit of having a GDM diagnosis.
Communicating the diagnosis
Communication with healthcare professionals (HCPs) and their families was a common theme throughout the findings of the included studies. Generally, the level and quality of communication with HCPs was mixed – with some women reporting positive and informative encounters, while others described brief encounters with overly technical language and unsupportive consultations. The main issues were limited time available to spend with the HCP, lack of continuity of care and lack of understanding about the role of the HCP at follow-up. In some instances, women felt that GDM was not a topic that HCPs were keen to discuss - ‘the nurses, they never talked to me about my gestational diabetes’. [ 23 ] The level and quality of information provided was often conflicting, confusing or insufficient. Areas of contention were appropriate foods and the dietary changes that should be made.
Some women formed a dependency on HCPs to know what to do and on the electronic reminders for follow-up appointments and monitoring. Often women reported having no choice in treatment resulting in them feeling threatened and frustrated. Often women were automatically booked in for a caesarean section without consultation or lived in fear of this occurring. One woman referred to GDM as being over medicalised. Receiving limited information also prompted women to independently seek information about the impact and management of GDM from other sources such as the internet. However, some women found the internet limited for specific information or confusing.
Knowledge of GDM
Women had varying levels of understanding of GDM which impacted on their initial reaction to the diagnosis. Those who were able to explain the cause of GDM were able to process and accept the diagnosis more readily than those who had little understanding of GDM, or were confused as to how GDM occurred. Lack of knowledge also extended to and impacted on relatives. Some women stated that they would have preferred to be more prepared to receive the diagnosis by having early knowledge about the testing for diabetes. Women reported being on a steep learning curve, especially the onerous approach of dietary trial and error whereby women learnt what foods would increase their blood glucose level (BGL) and what food to avoid. Women also reported challenges in adopting new habits to manage their GDM, including understanding food labels and nutritional values of food. Often this required a trial and error approach. There was also a lack of understanding about the impact of GDM on their baby with some women believing it would be transmitted to their baby via breastmilk.
Risk perception
Women’s perception of risk were reported before the diagnosis of GDM, after they were diagnosed in pregnancy, and after the delivery. Some women attempted to understand their level of risk in context of family history. Some were very surprised by the diagnosis, especially if they were asymptomatic; and some women found it difficult to come to terms with the diagnosis. There was uncertainty about the severity of the condition. Some women considered the condition to be mild, downplaying the disease and believing that too much ‘ fuss’ was being made about GDM and other women doubted the diagnosis and its seriousness. Women often discussed: the adverse effects that GDM would have on her baby; frustration that the focus was on risks to the baby and less so them; their worry about the consequences for the future; and questioned the impact of insulin on the baby. Women worried that their diet was too restrictive for their growing baby and would not provide the nutrients that the baby required. Some women held the view that GDM was a temporary condition and would disappear once the baby was born, and many women reverted to old eating habits after the baby’s birth. Often women referred to the birth as a ‘ moment of truth ’ or as an endpoint to their GDM. This was also reflected in the level of care that the women received after the birth of their baby.
Managing GDM
Dietary management-related stress was commonly reported amongst interviewed women and was experienced by both insulin and non-insulin users. Stress and frustrations often occurred as a consequence of an unexpected abnormal blood glucose reading following strict adherence to dietary advice. Maintaining stable BGL was an ongoing struggle and in some cases the burden proved too much, with a few women ceasing employment. Insulin users described the process as a ‘ roller coaster ’ as well as the emotional and physical discomfort of injecting, while non-insulin users often became obsessed with a well-controlled diet, with some women viewing this as a way to avoid the use of insulin. Conversely, some women felt relieved when they were transitioned onto insulin, as it reduced the need for dietary restriction.
Making lifestyle changes was considered stringent and restrictive by the majority of women, and for some required ‘ major restructuring’ to their diet and daily routines to incorporate exercise. Some women reported extreme behaviours, including falsifying blood glucose readings, self-starvation and hiding their condition, including from family members. Often the impact of non-adherence to lifestyle changes resulted in guilt and belief that the baby would know they have cheated. Other pregnancy related ailments and the need to care for other children interfered with the ability to make the required changes. Women who had a specific culture-related diet discussed the impact and difficulty of applying or tailoring the dietary recommendations to their diet.
The key motivator to making required lifestyle changes, despite the associated hardships, was to minimise the risks to their unborn baby. Women prioritised the health of the baby over their own health and were willing to do anything to ensure that the health of their baby was not compromised. Over time, management of the GDM became a part of their normal routine for many women. However, some women expressed a desire to have a ‘ normal’ pregnancy similar to their friends, discussing that a diagnosis of GDM made them feel as though their pregnancy was atypical, leading to defining their pregnancy as ‘ abnormal ’ or as an ‘ illness ’. For one woman, it made her feel like an ‘ illegal’ person.
Burden of GDM
Women reported that a diagnosis of GDM came with extra responsibility, which added pressure whilst trying to juggle life commitments such as work, childcare, and daily living responsibilities. Monitoring and treating GDM placed burden on women’s daily routines and most woman agreed that taking BGL measurements was time consuming and disruptive. There was a constant need to prudently plan meals and co-ordinate the attendance at additional hospital appointments, all of which were considered time intensive, especially with travel and wait times. Women expressed that GDM consumed a lot of their thinking time e.g., ‘ I think about diabetes everyday’ and felt that they had to acknowledge GDM all the time and became ‘ super-conscious’ . In some instances, women reported a GDM diagnosis took away some of the ‘ joy of pregnancy ’ . One woman described her pregnancy as a ‘ misfortune’ . Women mentioned the financial burden of buying healthier food – ‘it would take lots of money just because it is so expensive to eat healthy’. [ 25 ] Women also considered the physical burden of GDM such as fatigue and the side effects of treatment such as insulin. There was a longer-term impact on family planning, where in some cases women decided not to have another child because they were fearful of enduring a similar restrictive and stressful pregnancy due to GDM.
Social support
Social support, including family and HCP support, was an important aspect for women during their experience of a GDM diagnosis. Changes in lifestyle often had an overflow effect, with other family members adopting healthier lifestyles. Women not in their country of birth, and without family, often reported feeling isolated and lonely. Disappointment and isolation were also expressed by some women when they perceived a lack of healthcare system support. This often occurred postnatally when the expectations of postpartum care were high, however, in reality, support was absent. In some cases, women were stigmatised by their families and in a few cases received undesirable feedback that they were not doing enough to protect their unborn child.
Gaining control
Control was a frequently used word when women described living with and managing a GDM diagnosis. Initially women reported a lack of control especially over their emotions, however, over time women transitioned from feeling like a victim of diabetes, to being active agents in controlling their GDM. The terms ‘ balance’ and ‘ adjustment’ were used to describe how some women tried to offset the strict compliance and active self-management with reducing their risk to their unborn baby and their own future risk of developing diabetes after pregnancy. Some women reported feeling empowered as their pregnancies progressed, especially when they gained more knowledge about GDM and what action they could take to accept and make sense of the diagnosis. Taking control included realising the changes that were required to their lifestyle, self-initiated care, and self-education. Often investigating alternative options, such as natural remedies outside those recommended by HCPs, provided women with some autonomy in managing their condition and some believed that it was a safer option to medication.
Summary of main findings
This synthesis of the qualitative evidence of women’s experiences of being diagnosed with GDM highlighted the psychosocial consequences a diagnosis of GDM can have on women. The purported benefits of a GDM diagnosis identified from our review, were largely behavioural and included an opportunity to improve health, prevent excessive weight gain, control weight during pregnancy, and prompts to make healthy eating changes. However, the purported harms included the added responsibility (eating regimens, appointments), financial constraints (expensive food, medical bills), and conflicts with their cultural practices (alternative eating, lack of information about traditional food). The psychosocial consequences were wide reaching and often resulted in significant social isolation with women only sharing their diagnosis with partners. Furthermore, there were a few reports of over-medicalisation due to a GDM diagnosis, with the perception that HCPs were often authoritarian, focusing on physiological aspects, with little attempt to involve women in decision making. This is noteworthy considering a non-GDM pregnancy has already come under scrutiny as being over-medicalised with increasing levels of unnecessary intervention [ 62 ].
Women from studies included in our review frequently reported inconsistent information provision. Limited GDM information provision has been identified in another systematic review regarding healthcare seeking for GDM during the postpartum period [ 63 ]. In contrast, findings from another study which aimed to evaluate satisfaction with obtaining a diagnosis of GDM concluded that the majority of women were satisfied with their experience of being diagnosed [ 64 ]. Further, women in the latter study associated poor GDM control with perinatal complications and an increased risk of type 2 diabetes following pregnancy [ 64 ].
Another key finding from this review was low awareness of the potential risks of GDM, particularly in the long-term. Low health literacy levels could be one factor to explain knowledge deficits and understanding of GDM, especially given the sociodemographic diverse population included in this review. One study found that low literacy among disadvantaged women had a significant impact on their understanding of GDM information [ 65 ]. Other research found that women who live in an English-speaking country but primarily speak a non-English language, have lower rates of dietary awareness compared with their English speaking counterparts, and this may affect compliance to dietary interventions [ 66 ]. Therefore, it is important that new educational interventions are developed to target those with lower health literacy as well as cultural factors when diagnosing and managing multi-ethnic populations with GDM [ 66 ].
Interestingly, women with a borderline diagnosis of GDM did not seem as concerned as other women and in some cases were dismissive of the diagnosis and the potential consequences. Similarly, in a study which specifically included women with a borderline diagnosis of GDM, the majority of women reported that they were not worried by the diagnosis [ 67 ]. For some women, the potential transitory nature of GDM was emphasised and some reported that it didn’t seem like a real illness. The diagnostic criteria for GDM has previously been compared with the established criteria used to classify a condition as a disease. This comparison revealed disparity which Goer, in 1996, used to suggest that GDM did not pose a serious health risk, was neither easily nor accurately diagnosed, was not treated effectively and that treatment outweighed the risks of the condition [ 68 ]. Therefore, the levels of heightened psychological distress as reported by the women in our review, may actually be unnecessary and others have gone as far as saying that GDM is an example of ‘obstetric iatrogenesis’ [ 69 ].
The findings of this review did underline a few unmet service needs with recurring themes around the lack of individualised care and its continuity, lack of choice regarding important aspects of care such as birthing options, and the scarcity of comprehensive follow-up. There was a sense of abandonment amongst women after delivery in that they had experienced intensive intervention and then nothing. This could be viewed as a missed opportunity to capitalise on the motivation to make changes during pregnancy. Researchers have previously highlighted that adherence to postpartum screening and continued lifestyle modifications to prevent future diabetes seems to dissipate after birth, possibly because the driver to protect their unborn child is no longer there [ 70 ].
The studies included in our review had participants of varying cultures sampled from countries with different GDM definitions. However, there appeared no difference in the qualitative outcomes between studies/countries. In our review, the experiences of women diagnosed with GDM suggest psychosocial harms appear to outweigh the qualitative benefits. Quantitative studies [ 14 , 15 ] that report prevalence increases in GDM after the IADSPG [ 71 ] definition changed, also report minimal improvements to maternal and infant physical outcomes.
This synthesis of women’s experiences of a GDM diagnosis could be used to inform the content of communication materials both before and after a GDM diagnosis. For example, an awareness of GDM testing and basic information including cultural adaptations to dietary guidelines and addressing misconceptions around breastfeeding. There is also an opportunity for HCPs to use teachable moments with women who have been identified at risk of developing type 2 diabetes post-pregnancy and offer supportive, effective advice about lifestyle changes. This is particularly relevant considering a previous review highlighted a significant time is spent in sedentary behaviour during pregnancy [ 72 ]. A study which examined HCPs views of healthcare provision to women with GDM showed that HCPs themselves perceived that there was a shortfall in GDM education [ 73 ]. There are also signals for service improvement and potential for service redesign, such as increasing community-delivered care for women diagnosed with GDM. This would assist in alleviating the burden on women to attend hospital appointments and potentially offer flexible appointment times. Follow-up appointments post-pregnancy could be made with consideration of other appointments such as maternal and child health milestones and breastfeeding weaning classes, and could also focused on healthy eating for both mother and baby.
Strengths and limitations
This systematic review included studies with women of different demographic characteristics and multicultural samples. The themes identified were represented in the majority of studies which increased the internal validity. The relatively high participation rate in the included studies, and that most studies were conducted during pregnancy or shortly after delivery, contributes to the external validity of our study. Although some participants were interviewed antenatally and some postnatally, this distribution over different gestational stages assists the generalisability of the study findings.
The comparison of coding between authors, discussion of the results and reaching consensus was a robust approach to improve the credibility of the results. Overall, the quality of most studies was good, however, a third of the studies used convenience methods to recruit participants which could contribute to sampling bias and limit the external validity of our findings. Only two studies adequately described the facilitator’s prior experience and the relationship between the participants and the facilitator/researcher. Unfortunately, this review did not capture the perception of HCPs which might be used to explain some of the behaviours and attitudes of the women, particularly in relation to communication of the diagnosis and information provision. Finally, although the data were collected from diverse populations, the majority of the countries in which research were conducted in were high-income countries, which could be considered to have more established and evidence-based healthcare systems than low-income countries.

Further research
A previous study has suggested the need for more research on the benefits and harms of alternative treatment choices for women with GDM [ 33 ]. The findings from this review suggest a need for more investigation around the psychosocial benefits and harms of a diagnosis of GDM. Given some women viewed treatment of ‘borderline GDM’ as unimportant, a new model of care based on stratification or individual level of risk for pregnancy and birth complications could be further explored. This may reduce the need for all women to be labelled as having GDM and negate unnecessary anxiety and burden for those at the lower ‘borderline’ threshold. This would then potentially offer tailored treatment options, improve shared-decision making, and improve women’s knowledge about how a diagnosis of GDM might affect them.
Consequences of a GDM diagnosis are multidimensional and highly contextual. Despite the psychosocial challenges frequently experienced, many women (driven by the innate response to safeguard their unborn baby) were able to gradually adapt to the required lifestyle changes and monitoring regimens. Perhaps a question is whether some of them should have to. There is opportunity to improve lifestyle and to assist the prevention of diabetes after pregnancy, however, this needs to be managed alongside the potential harms of a GDM diagnosis such as the negative psychological impact and social isolation. In the context of rising prevalence [ 14 , 15 , 16 , 17 ], potential minimal clinical [ 14 , 15 , 16 ] improvements, and the wide range of psychosocial experiences identified in this study, the findings of this review highlight the need for HCPs to consider the implications that a GDM diagnosis may have on women. It is essential that women diagnosed with GDM receive consistent evidence-based information and ongoing psychological and social support.
Availability of data and materials
The datasets generated during the current systematic review are available from the lead author upon request.
Abbreviations
Blood glucose level
Critical Appraisal Skills Programme Checklist (Qualitative)
Enhancing Transparency in Reporting the Synthesis of Qualitative Research
- Gestational diabetes mellitus
Hyperglycemia and Adverse Pregnancy Outcomes
Health care professional
International Association of the Diabetes and Pregnancy Study Groups
O'Sullivan JB, Mahan CM. Criteria for the oral glucose tolerance test in pregnancy. Diabetes. 1964;13:278–85.
CAS PubMed Google Scholar
Mishra S, Rao CR, Shetty A. Trends in the diagnosis of gestational diabetes mellitus. Scientifica (Cairo). 2016;2016:5489015.
Google Scholar
Kim C, Newton KM, Knopp RH. Gestational diabetes and the incidence of type 2 diabetes. Syst Rev. 2002;25(10):1862–8. https://doi.org/10.2337/diacare.25.10.1862 .
Article Google Scholar
HAPO Study Cooperative Research Group. Hyperglycaemia and adverse pregnancy outcomes. N Engl J Med. 2008;358:1991–2002.
McIntyre HD, Gibbons KS, Lowe J, Oats JJN. Development of a risk engine relating maternal glycemia and body mass index to pregnancy outcomes. Diabetes Res Clin Pract. 2018;139:331–8.
Article PubMed Google Scholar
Kamysheva E, Skouteris H, Wertheim EH, et al. Examination of a multi-factorial model of body-related experiences during pregnancy: The relationships among physical symptoms, sleep quality, depression, self-esteem, and negative body attitudes. Body Image. 2008;5(2):152–63 https://doi.org/10.1016/j.bodyim.2007.12.005 .
Carolan-Olah M, Barry M. Antenatal stress: an Irish case study. Midwifery. 2014;30(3):310–6. https://doi.org/10.1016/j.midw.2013.03.014 [published Online First: 2013/05/21].
Ferreira CR, Orsini MC, Vieira CR, et al. Prevalence of anxiety symptoms and depression in the third gestational trimester. Arch Gynecol Obstet. 2015;291(5):999–1003. https://doi.org/10.1007/s00404-014-3508-x [published Online First: 2014/10/15].
Dalfra MG, Nicolucci A, Bisson T, et al. Quality of life in pregnancy and post-partum: a study in diabetic patients. Qual Life Res. 2012;21(2):291–8. https://doi.org/10.1007/s11136-011-9940-5 .
Article CAS PubMed Google Scholar
Evans MK, O’Brien B. Gestational diabetes: the meaning of an at-risk pregnancy. Qual Health Res. 2005;15(1):66–81.
Devsam BU, Bogossian FE, Peacock AS. An interpretive review of women's experiences of gestational diabetes mellitus: proposing a framework to enhance midwifery assessment. Women Birth. 2013;26(2):E69–76.
Carolan-Olah M, Duarte-Gardea M, Lechuga J, et al. The experience of gestational diabetes mellitus (GDM) among Hispanic women in a U.S. border region. Sex Reprod Healthc. 2017;12:16–23. https://doi.org/10.1016/j.srhc.2016.11.003 .
Persson M, Winkvist A, Mogren I. ‘From stun to gradual balance’—women’s experiences of living with gestational diabetes mellitus. Scand J Caring Sci. 2010;24(3):454–62. https://doi.org/10.1111/j.1471-6712.2009.00735.x .
Cade TJ, Polyakov A, Brennecke SP. Implications of the introduction of new criteria for the diagnosis of gestational diabetes: a health outcome and cost of care analysis. BMJ Open. 2019;9(1):e023293–e93. https://doi.org/10.1136/bmjopen-2018-023293 .
Article PubMed PubMed Central Google Scholar
Sexton H, Heal C, Banks J, et al. Impact of new diagnostic criteria for gestational diabetes. J Obstet Gynaecol Res. 2018;44(3):425–31. https://doi.org/10.1111/jog.13544 [published Online First: 2018/01/13].
Erjavec K, Poljičanin T, Matijević R. Impact of the implementation of new WHO diagnostic criteria for gestational diabetes mellitus on prevalence and perinatal outcomes: a population-based study. J Pregnancy. 2016;2016:2670912. https://doi.org/10.1155/2016/2670912 .
Feldman RK, Tieu RS, Yasumura L. Gestational diabetes screening the international association of the diabetes and pregnancy study groups compared with carpenter-coustan screening. Obstet Gynecol. 2016;127(1):10–7. https://doi.org/10.1097/aog.0000000000001132 .
Pocobelli G, Yu O, Fuller S, et al. One-step approach to identifying gestational diabetes mellitus: association with perinatal outcomes. Obstet Gynecol. 2018;132(4):859–67. https://doi.org/10.1097/aog.0000000000002780 [published Online First: 2018/08/22].
Draffin CR, Alderdice FA, McCance DR, et al. Exploring the needs, concerns and knowledge of women diagnosed with gestational diabetes: a qualitative study. Midwifery. 2016;40:141–7. https://doi.org/10.1016/j.midw.2016.06.019 .
Tong A, Flemming K, McInnes E, et al. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol. 2012;12(1):181. https://doi.org/10.1186/1471-2288-12-181 .
Rathbone J, Carter M, Hoffmann T, et al. Better duplicate detection for systematic reviewers: evaluation of systematic review assistant-deduplication module. Syst Rev. 2015;4:6. https://doi.org/10.1186/2046-4053-4-6 [published Online First: 2015/01/16].
Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8(1):45. https://doi.org/10.1186/1471-2288-8-45 .
Lucas PJ, Baird J, Arai L, et al. Worked examples of alternative methods for the synthesis of qualitative and quantitative research in systematic reviews. BMC Med Res Methodol. 2007;7(1):4. https://doi.org/10.1186/1471-2288-7-4 .
Group CCQM. Chapter 4: critical appraisal of qualitative research. In: Noyes J, Booth A, Hannes K, Harden A, Harris J, Lewin S, Lockwood C, editors. Supplementary guidance for inclusion of qualitative research in cochrane systematic reviews of interventions. Version 1; 2011.
Abraham K, Wilk N. Living with gestational diabetes in a rural community. MCN Am J Matern Child Nurs. 2014;39(4):239–45.
Araujo MF, Pessoa SM, Damasceno MM, et al. Gestational diabetes from the perspective of hospitalized pregnant women. Rev Bras Enferm. 2013;66(2):222–7.
Bandyopadhyay M, Small R, Davey MA. Attendance for postpartum glucose tolerance testing following gestational diabetes among south Asian women in Australia: a qualitative study. Int J Gynecol Obstet. 2015;131:E149.
Bandyopadhyay M, Small R, Davey MA, et al. Lived experience of gestational diabetes mellitus among immigrant South Asian women in Australia. Aust N Z J Obstet Gynaecol. 2011;51(4):360–4. https://doi.org/10.1111/j.1479-828X.2011.01322.x .
Carolan M. Women’s experiences of gestational diabetes self-management: a qualitative study. Midwifery. 2013;29(6):637–45. https://doi.org/10.1016/j.midw.2012.05.013 .
Doran F. Gestational diabetes mellitus: perspectives on lifestyle changes during pregnancy and post-partum, physical activity and the prevention of future type 2 diabetes. Aust J Prim Health. 2008;14(3):85–92.
Doran F, Davis K. Gestational diabetes mellitus in Tonga: insights from healthcare professionals and women who experienced gestational diabetes mellitus. N Z Med J. 2010;123(1326):59–67.
PubMed Google Scholar
Eades CE, France EF, Evans JMM. Postnatal experiences, knowledge and perceptions of women with gestational diabetes. Diabet Med. 2018;35(4):519–29.
Figueroa Gray M, Hsu C, Kiel L, et al. “It's a very big burden on me”: Women’s experiences using insulin for gestational diabetes. Matern Child Health J. 2017;21(8):1678–85.
Ge L, Albin B, Hadziabdic E, et al. Beliefs about health and illness and health-related behavior among urban women with gestational diabetes mellitus in the south east of China. J Transcult Nurs. 2016;27(6):593–602.
Ge L, Wikby K, Rask M. ‘Is gestational diabetes a severe illness?’ Exploring beliefs and self-care behaviour among women with gestational diabetes living in a rural area of the south east of China. Aust J Rural Health. 2016;24(6):378–84. https://doi.org/10.1111/ajr.12292 .
Han S, Middleton PF, Bubner TK, et al. Women’s views on their diagnosis and management for borderline gestational diabetes mellitus. J Diabetes Res. 2015;2015:209215. https://doi.org/10.1155/2015/209215 .
Article CAS PubMed PubMed Central Google Scholar
Hirst JE, Tran TS, Do MAT, et al. Women with gestational diabetes in Vietnam: a qualitative study to determine attitudes and health behaviours. BMC Pregnancy Childbirth. 2012;12:81.
Hjelm K, Bard K, Apelqvist J. Gestational diabetes: prospective interview-study of the developing beliefs about health, illness and health care in migrant women. J Clin Nurs. 2012;21(21–22):3244–56.
Hjelm K, Bard K, Apelqvist J. A qualitative study of developing beliefs about health, illness and healthcare in migrant African women with gestational diabetes living in Sweden. BMC Womens Health. 2018;18(1):34.
Hjelm K, Bard K, Berntorp K, et al. Beliefs about health and illness postpartum in women born in Sweden and the Middle East. Midwifery. 2009;25(5):564–75.
Hjelm K, Bard K, Nyberg P, et al. Swedish and middle-eastern-born women’s beliefs about gestational diabetes. Midwifery. 2005;21(1):44–60.
Hjelm K, Berntorp K, Apelqvist J. Beliefs about health and illness in Swedish and African-born women with gestational diabetes living in Sweden. J Clin Nurs. 2012;21(9–10):1374–86. https://doi.org/10.1111/j.1365-2702.2011.03834.x .
Hjelm K, Berntorp K, Frid A, et al. Beliefs about health and illness in women managed for gestational diabetes in two organisations. Midwifery. 2008;24(2):168–82.
Hui AL, Sevenhuysen G, Harvey D, et al. Stress and anxiety in women with gestational diabetes during dietary management. Diabetes Educ. 2014;40(5):668–77.
Kaptein S, Evans M, McTavish S, et al. The subjective impact of a diagnosis of gestational diabetes among ethnically diverse pregnant women: a qualitative study. Can. 2015;39(2):117–22. https://doi.org/10.1016/j.jcjd.2014.09.005 .
Kilgour C, Bogossian FE, Callaway L, et al. Postnatal gestational diabetes mellitus follow-up: Australian women’s experiences. Women Birth. 2015;28(4):285–92. https://doi.org/10.1016/j.wombi.2015.06.004 .
Lawson EJ, Rajaram S. A transformed pregnacy – the psychological consequences of gestational diabetes. Sociol Health Illn. 1994;16(4):536–62.
Lie MLS, Hayes L, Lewis-Barned NJ, et al. Preventing type 2 diabetes after gestational diabetes: women’s experiences and implications for diabetes prevention interventions. Diabet Med. 2013;30(8):986–93.
Neufeld HT. Food perceptions and concerns of aboriginal women coping with gestational diabetes in Winnipeg, Manitoba. J Nutr Educ Behav. 2011;43(6):482–91. https://doi.org/10.1016/j.jneb.2011.05.017 .
Nielsen JH, Olesen CR, Kristiansen TM, et al. Reasons for women’s non-participation in follow-up screening after gestational diabetes. Women Birth. 2015;28(4):e157–63. https://doi.org/10.1016/j.wombi.2015.04.006 .
Parsons J, Sparrow K, Ismail K, et al. Experiences of gestational diabetes and gestational diabetes care: a focus group and interview study. BMC Pregnancy Childbirth. 2018;18:25.
Pennington AVR, O’Reilly SL, Young D, et al. Improving follow-up care for women with a history of gestational diabetes: perspectives of GPs and patients. Aust J Prim Health. 2017;23(1):66–74.
Rafii F, Vasegh Rahimparvar SF, Keramat A, et al. Procrastination as a key factor in postpartum screening for diabetes: A qualitative study of Iranian women with recent gestational diabetes. Iran Red Crescent Med J. 2017;19(5). https://doi.org/10.5812/ircmj.44833 .
Razee H, van der Ploeg HP, Blignault I, et al. Beliefs, barriers, social support, and environmental influences related to diabetes risk behaviours among women with a history of gestational diabetes. Health Promot J Austr. 2010;21(2):130–7.
Salomon IMM, Soares SM. Understanding the impact of gestational diabetes diagnosis. Revista Mineira de Enfermagem. 2004;8(3):349–57.
Svensson L, Nielsen KK, Maindal HT. What is the postpartum experience of Danish women following gestational diabetes? A qualitative exploration. Scand J Caring Sci. 2018;32(2):756–64.
Tang JW, Foster KE, Pumarino J, et al. Perspectives on prevention of type 2 diabetes after gestational diabetes: a qualitative study of Hispanic, African-American and White women. Matern Child Health J. 2015;19(7):1526–34. https://doi.org/10.1007/s10995-014-1657-y .
Tierney M, O'Dea A, Danyliv A, et al. Factors influencing lifestyle behaviours during and after a gestational diabetes mellitus pregnancy. Health Psychol Behav Med. 2015;3(1):204–16. https://doi.org/10.1080/21642850.2015.1073111 .
Trutnovsky G, Panzitt T, Magnet E, et al. Gestational diabetes: women's concerns, mood state, quality of life and treatment satisfaction. J Matern Fetal Neonatal Med. 2012;25(11):2464–6. https://doi.org/10.3109/14767058.2012.683900 .
Wah YYE, McGill M, Wong J, et al. Self-management of gestational diabetes among Chinese migrants: a qualitative study. Women Birth. 2019;32(1):e17–e23.
Whitty-Rogers J, Caine V, Cameron B. Aboriginal women’s experiences with gestational diabetes mellitus: a participatory study with mi'kmaq women in Canada. ANS Adv Nurs Sci. 2016;39(2):181–98. https://doi.org/10.1097/ANS.0000000000000115 .
Johanson R, Newburn M, Macfarlane A. Has the medicalisation of childbirth gone too far? BMJ. 2002;324(7342):892–5.
Van Ryswyk E, Middleton P, Shute E, et al. Women's views and knowledge regarding healthcare seeking for gestational diabetes in the postpartum period: a systematic review of qualitative/survey studies. Diabetes Res Clin Pract. 2015;110(2):109–22.
Goldstein RF, Gibson-Helm ME, Boyle JA, et al. Satisfaction with diagnosis process for gestational diabetes mellitus and risk perception among Australian women. Int J Gynaecol Obstet. 2015;129(1):46–9.
Carolan M. Diabetes nurse educators’ experiences of providing care for women, with gestational diabetes mellitus, from disadvantaged backgrounds. J Clin Nurs. 2014;23(9–10):1374–84. https://doi.org/10.1111/jocn.12421 .
Yuen L, Wong VW. Gestational diabetes mellitus: challenges for different ethnic groups. World J Diabetes. 2015;6(8):1024–32. https://doi.org/10.4239/wjd.v6.i8.1024 [published Online First: 2015/07/25].
Carolan M, Steele C, Margetts H. Knowledge of gestational diabetes among a multi-ethnic cohort in Australia. Midwifery. 2010;26(6):579–88. https://doi.org/10.1016/j.midw.2009.01.006 .
Goer H. Gestational diabetes: the emperor has no clothes. The Birth Gazette Summertown: Second Foundation; 1996. p. 32–5.
Han S, Bubner T, Middleton PF, et al. A qualitative study of women's views on diagnosis and management for borderline gestational diabetes. J Paediatr Child Health. 2013;49:128. https://doi.org/10.1111/jpc.12133 .
Nielsen KK, Kapur A, Damm P, et al. From screening to postpartum follow-up - the determinants and barriers for gestational diabetes mellitus (GDM) services, a systematic review. BMC Pregnancy Childbirth. 2014;14:41. https://doi.org/10.1186/1471-2393-14-41 .
International Association of Diabetes and Pregnancy Study Groups Consensus Panel. International Association of Diabetes and Pregnancy Study Groups Recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care. 2010;33(3):676–82.
Article PubMed Central Google Scholar
Fazzi C, Saunders DH, Linton K, et al. Sedentary behaviours during pregnancy: a systematic review. Int J Behav Nutr Phys Act. 2017;14:32. https://doi.org/10.1186/s12966-017-0485-z .
Van Ryswyk E, Middleton P, Hague W, et al. Clinician views and knowledge regarding healthcare provision in the postpartum period for women with recent gestational diabetes: A systematic review of qualitative/survey studies. Diabetes Res Clin Pract. 2014;106(3):401–11 https://doi.org/10.1016/j.diabres.2014.09.001 .
Download references
Acknowledgements
Not applicable.
LC is supported by a National Health and Medical Research Council Partnership Centre for Health System Sustainability grant (#9100002). RS and RT are supported by a National Health and Medical Research Council Program grant (#1106452) and PG is supported by a NHMRC Research Fellowship (#1080042). The funders had no role in design, data collection, analysis, interpretation or writing of the manuscript.
Author information
Authors and affiliations.
Institute for Evidence-Based Healthcare, Bond University, Gold Coast, Australia
Louise Craig, Rebecca Sims, Paul Glasziou & Rae Thomas
You can also search for this author in PubMed Google Scholar
Contributions
PG, LC and RT conceived the project design, LC conducted the search, extracted, analysed and interpreted the data assisted by RS. RT assisted in data interpretation. All authors contributed to the drafting of the manuscript and approve the final version.
Corresponding author
Correspondence to Rae Thomas .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1:.
Table S1. Enhancing Transparency in Reporting the Synthesis of Qualitative Research Guidelines Checklist. Table S2. Assessment of quality of included studies using the CASP tool.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Craig, L., Sims, R., Glasziou, P. et al. Women’s experiences of a diagnosis of gestational diabetes mellitus: a systematic review. BMC Pregnancy Childbirth 20 , 76 (2020). https://doi.org/10.1186/s12884-020-2745-1
Download citation
Received : 24 September 2019
Accepted : 15 January 2020
Published : 07 February 2020
DOI : https://doi.org/10.1186/s12884-020-2745-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Systematic review
- Qualitative
- Diagnostic impacts
BMC Pregnancy and Childbirth
ISSN: 1471-2393
- Submission enquiries: [email protected]
- General enquiries: [email protected]

- Previous Article
- Next Article
Preconception Counseling:
Glycemic management and goals in pregnancy, management of gestational diabetes mellitus (gdm), additional drug considerations during pregnancy, postpartum care, section 15: management of diabetes in pregnancy.
This article is part of a special article collection available at https://diabetesjournals.org/collection/2018/2024-Abridged-Standards-of-Care .
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Cite Icon Cite
- Get Permissions
Section 15: Management of Diabetes in Pregnancy. Clin Diabetes 15 April 2024; 42 (2): 220–221. https://doi.org/10.2337/cd24-a015
Download citation file:
- Ris (Zotero)
- Reference Manager
Incorporate preconception counseling into diabetes care starting at puberty and continuing in all people with diabetes and childbearing potential.
Discuss family planning and prescribe effective contraception to be used until A1C is optimized for pregnancy.
Address the importance of achieving glucose levels as close to normal as is safely possible, ideally A1C <6.5% (<48 mmol/mol) to reduce the risk of congenital anomalies, preeclampsia, macrosomia, preterm birth, and other complications.
Focus on nutrition, diabetes education, and screening for diabetes comorbidities and complications, in addition to achieving glycemic targets.
Counsel on the risk of development and/or progression of diabetic retinopathy. A dilated eye examination should occur before pregnancy or in the first trimester, with continued monitoring every trimester and for 1 year postpartum based on findings.

Individuals without diabetes before or early in pregnancy should be screened for GDM at 24 to 28 weeks of pregnancy.
Lifestyle behavior change is an essential component of GDM management.
Insulin is the preferred medication for treating hyperglycemia in GDM.
Metformin and glyburide should not be used as first-line agents in GDM. Other oral and noninsulin injectable glucose- lowering medications lack long-term safety data for use in GDM.
Postpartum care should include psychosocial assessment and support for self-care.

Email alerts
- Online ISSN 1945-4953
- Print ISSN 0891-8929
- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Home — Essay Samples — Nursing & Health — Diabetes — What is Gestational diabetes
What is Gestational Diabetes
- Categories: Diabetes Pregnancy
About this sample

Words: 409 |
Published: Jan 15, 2019
Words: 409 | Page: 1 | 3 min read
Table of contents
Risk factors, works cited.
- Three or more insulin injections per day
- Difficulty in managing high and low glucose values
- Fear of hypoglycaemia (lows), especially at night
- HbA1c outside the target range
- Difficulty following your prescribed insulin regimen for diabetes management
- Fear of needles
- Seeking more flexibility in your diabetes management
- decreased variability in insulin4
- decreased risk of hypoglycaemia4
- improved control of the dawn phenomenon4
- Using CGM with an insulin pump during pregnancy can improve glycaemic control4
- American Diabetes Association. (2021). Gestational Diabetes. Retrieved from https://www.diabetes.org/diabetes/gestational-diabetes
- Centers for Disease Control and Prevention. (2021). Gestational Diabetes. Retrieved from https://www.cdc.gov/diabetes/basics/gestational.html
- Medtronic Diabetes. (n.d.). Insulin Pump Therapy. Retrieved from https://www.medtronicdiabetes.com/treatments/insulin-pump-therapy
- DeVries, J. H., & Snoek, F. J. (2015). Insulin therapy for pregnant women with diabetes. Diabetes Research and Clinical Practice, 108(2), 184-191. doi:10.1016/j.diabres.2015.02.025
- Kumari, P., Gorthi, R. S., & Gangadhara, P. (2018). Insulin pump therapy in gestational diabetes: A review. International Journal of Medical Science and Clinical Inventions, 5(5), 3921-3925.
- Moses, R. G., Wong, V. C., Lambert, K., Morris, G. J., & San Gil, F. (2017). The impact of gestational diabetes mellitus on postpartum practices and glycemic control in Australian women with type 1 diabetes. Diabetes Care, 40(2), e15-e16. doi:10.2337/dc16-1765
- Rayanagoudar, G., Hashi, A. A., Zamora, J., Khan, K. S., & Hitman, G. A. (2016). Effect of dietary and lifestyle interventions on weight loss during pregnancy and gestational diabetes mellitus: A systematic review and meta-analysis. BMJ Open, 6(6), e010665. doi:10.1136/bmjopen-2015-010665
- Retnakaran, R., Ye, C., Hanley, A. J., & Connelly, P. W. (2018). Prospective association between lactation and insulin resistance and type 2 diabetes in women with prior gestational diabetes mellitus. Diabetologia, 61(5), 972-979. doi:10.1007/s00125-018-4562-y
- Yogev, Y., & Hod, M. (2019). Gestational diabetes mellitus: Treating the patient, not just the numbers. Diabetes Care, 42(3), 442-444. doi:10.2337/dci19-0004
- Ziegler, R., & Heidtmann, B. (2019). Individualized treatment targets for pregnant women with diabetes. Current Diabetes Reports, 19(5), 20. doi:10.1007/s11892-019-1134-5

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Prof Ernest (PhD)
Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
4 pages / 2018 words
6 pages / 2514 words
2 pages / 909 words
2 pages / 1069 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Diabetes
Type 2 diabetes, also known as adult-onset diabetes, is a chronic condition that affects the way the body processes blood sugar (glucose). It is a growing concern worldwide, with approximately 463 million adults living with [...]
Diabetes is a chronic condition that affects millions of people worldwide, leading to serious health complications if not managed properly. This essay aims to delve into the various aspects of diabetes, including its causes, [...]
Type 2 diabetes is a chronic health condition that affects millions of people worldwide. It is characterized by the body's inability to properly utilize insulin, leading to high blood sugar levels. This essay will explore the [...]
Diabetes mellitus is a disease of metabolic dysregulation, most notably abnormal glucose metabolism, accompanied by characteristic long-term complications. The complications that are specific to diabetes include retinopathy, [...]
It should come as no surprise that obesity rates are skyrocketing in the United States. It has become a health crisis within the last decade and there are no signs of slowing down. No matter what experts advise, it seems to be [...]
Diabetes is a general term that refers to any of various disorders that are characterized by excessive urination, also known as polyuria. When used alone it refers to Diabetes Mellitus (DM). There are several types of Diabetes, [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free

ESSAY SAUCE
FOR STUDENTS : ALL THE INGREDIENTS OF A GOOD ESSAY
Essay: Gestational Diabetes Mellitus (GDM)
Essay details and download:.
- Subject area(s): Health essays
- Reading time: 17 minutes
- Price: Free download
- Published: 14 June 2022*
- File format: Text
- Words: 2,082 (approx)
- Number of pages: 9 (approx)
- Tags: Diabetes essays
Text preview of this essay:
This page of the essay has 2,082 words. Download the full version above.
Introduction
Gestational Diabetes Mellitus (GDM) is considered one of the most common conditions that affect women during pregnancy or gestation, where blood glucose levels are increased above normal limits (Baz et al., 2015). Blood glucose levels are controlled normally by insulin hormone (Kinalski et al., 2002). But some pregnant women may have higher levels of glucose that cannot be managed by insulin secreted in their bodies (Kleinwechter et al., 2014).
Diabetes Mellitus, other than GDM , could be one of two types, “type one” in which the body does not secrete insulin hormone at all and mostly called ‘juvenile diabetes’ (Toyoda, 2002), and “type two” in which the body does not secrete enough insulin and/or there is insulin resistance or the cells do not react to insulin) (Toyoda, 2002).
GDM usually arises after 28 weeks, in the third trimester, of pregnancy, and usually disappears after delivery of the baby (Association, 2010). Women with GDM are prone to the risk of preeclampsia and Caesarean section (Ross, 2006) in addition to developing type 2 diabetes later on (Dunne et al., 2003), so they should keep monitoring their blood glucose levels and manage it with their physicians at a regular basis (Kim, 2010). GDM symptoms and signs are very few in general and mostly diagnosed by screening tests blood glucose levels, which are mostly above normal limits, in blood samples withdrawn during pregnancy (Kalelioglu et al., 2007).
Epidemiology
About 3 to 10% of pregnant women are affected with GDM , according to several factors (Chanprapaph and Sutjarit, 2004). If they are not treated, they would deliver infants at high risk of clinical problems, for example being larger than normal (macrosomia) which may cause delivery complications), jaundice and hypoglycemia (Kinalski et al., 2002). This can also lead to seizures or being born dead (stillbirth) (Kinalski et al., 2002).
GDM could be treated and women can decrease these risks effectively by controlling of glucose levels in their blood (Erem et al., 2015). This control could be achieved by following a healthy eating plan and keeping active and physical exercises, and if this does not work, then using anti-diabetic medications (the safest one is insulin), would be necessary (Erem et al., 2015).
Classification
GDM could also be defined as a degree of intolerance of glucose during gestation period (Buchanan and Xiang, 2005). This definition may indicate that pregnant woman has not been diagnosed with diabetes mellitus previously, or she may have developed diabetes mellitus simultaneously with pregnancy (Buchanan and Xiang, 2005). Diabetes Mellitus could be classified into two groups according to this definition, which are Gestational Diabetes Mellitus (type A) and Pregestational Diabetes Mellitus (prior to pregnancy) (Association, 2010).
Furthermore, These two groups are classified according to their related risks and how to manage them (Association, 2010), where Gestational Diabetes Mellitus is divided into type A1 and type A2. Type A1 is diagnosed using oral glucose tolerance test which shows abnormal levels of glucose, however during fasting and after a meal by two hours (postprandial), it shows normal levels of glucose; so following healthy diet and practicing physical activities would be sufficient for management of this type (Mellitus, 2005). Type A2 is diagnosed using oral glucose tolerance test which shows abnormal levels of glucose and during fasting after a meal by two hours (postprandial), it also shows abnormal levels of glucose; so management would necessarily include the use of anti-diabetic medications such as insulin or other oral drugs (Abell et al., 2015).
Pregestational Diabetes Mellitus is also divided into many subtypes, these subtypes may affect different age group and last for different period of time (Table 1), as in subtype B, C and D (Association, 2010). Other may affect different organs of the body, which include subtype E, which is obvious with calcified (rigid) vessels in pelvic region, subtype F which affects the kidney, subtype R which affects the retina, subtype RF which affects both kidney and retina, subtype H which affects the heart, and subtype T which arises before transplantation of kidney (Association, 2010).
Subtype / Period / Age / onset
- B Less than 10 years Equals to or more than age 20
- C Between 10 to 19 years Equals to a range of age 10 to 19
- D More than 20 years Equals to or less than age 10
Table 1 Pregestational Diabetes Mellitus Subtypes
Pathophysiology
GDM develops because of a lot of hormonal changes and otherwise occurring during gestation, when there is not enough insulin secreted to control the rise in blood glucose levels and metabolize such glucose effectively. Insulin is a hormone formed in the pancreas. Insulin helps the body to use glucose for energy and helps control your blood glucose levels (Kinalski et al., 2002). When insulin binds to its receptors, it activates several protein processes necessary for the synthesis of glucose, glycogen and fatty acid synthesis, besides glycolysis process and metabolism of carbs and fats to get energy for cells (Poulakos et al., 2015).
It is unknown yet the exact mechanisms causing GDM (Poulakos et al., 2015). It is thought that pregnancy hormones may interfere with insulin action by binding to its receptors and replacing it, this is called insulin resistance (Kahn, 2003). As insulin activates glucose influx into most cells, then insulin resistance would prevents the occurrence of this action. And so glucose would remain in the bloodstream; this means the rise of glucose levels (Vambergue et al., 2002). As a consequence, more insulin would be needed to resolve this resistance; which could be about 1.5 to 2.5 times more in the normal pregnancy, to ensure enough glucose and nutrients supply to the fetus, so it can grow. This means also that insulin resistance is something normal which arises in the second trimester of pregnancy, but it could further progress to levels equivalent to type 2 diabetes levels (Becquet et al., 2016).
Placental hormones, like cortisol and progesterone, also may control the mechanism of insulin resistance during pregnancy, but estradiol hormone (estrogen sex hormone), prolactin hormone (luteotropin or Milk hormone), placental lactogen hormone (chorionic somatomammotropin), other placental hormones, TNFα (tumor necrosis factor alpha), resistin hormone (adipocyte-specific hormone), and leptin hormone (satiety hormone), are all involved also in decreasing of insulin resistance during pregnancy (Abell et al., 2015).
Complications
GDM risks affect both mother and her baby. These risks are associated and increased with unmanaged glucose levels which exceed normal limits and their effects. Treatment and good control of these levels can reduce many of these risks significantly (Lee et al., 2007). GDM, if not treated or managed, can cause problems for the baby. Babies might be born with a body larger than normal—a condition called macrosomia—as extra glucose in mother’s bloodstream crosses the placenta, which stimulates baby’s pancreas to secrete more insulin, which in turn makes the baby grow too large (Obstetricians and Gynecologists, 2000). Very large babies —of weight › 4 kg — are prone to the risk of being stuck in the birth canal during vaginal delivery, causing problems like shoulder dystocia; when baby’s head passes through the vagina, but baby’s shoulder gets stuck behind pelvic bone. Shoulder dystocia can be dangerous as baby may be unable to breathe easily while stuck (Draycott et al., 2008). These problems make C-section more preferred, or decide early delivery if this happens.
Babies also might be born early (preterm birth) with respiratory distress syndrome. GDM increases the risk of early labor and delivery before the due date. Dysmature babies are prone to this syndrome due to lung immature lung and its surfactant formation which, in turn, affects respiration (breathing) and makes it not easier (Baz et al., 2015). Babies suffering from this syndrome would need respiratory care until their lungs become mature and gets stronger (Brower et al., 2004). Babies also might be born with jaundice, in which the skin and eyes’ whites become yellowish in color. Jaundice usually disappears, when the baby gets enough breastfeeding with the help of phototherapy (Ross, 2006).
Babies also may develop hypoglycemia (Low blood sugar) shortly after birth because their bodies secrete higher amounts of insulin. Severe hypoglycemia may stimulate seizures in the baby, which may need intensive care and quick intervention with good feedings and administration of intravenous glucose solution to return blood sugar to normal levels (Cryer et al., 2003). Babies of mothers who have not treated or managed GDM may be subject to risk of developing Type 2 diabetes and obesity later on in their life (Bellamy et al., 2009). Untreated GDM also could lead to baby death either before birth or after a short time of it (Bellamy et al., 2009). GDM, if not treated or managed, may also increase the mother risk of having high blood pressure (hypertension) and more levels of protein in urine (proteinuria), a condition called preeclampsia (Redman and Sargent, 2005). Preeclampsia usually occurs during the 2nd half or 3rd trimester of pregnancy. If it is not treated, it can cause a lot of problems for both mother and baby and may lead to death. The only way to cure preeclampsia is to give birth or to have a cesarean section to deliver the baby early (preterm birth) (Redman and Sargent, 2005, Sibai, 2003). If preeclampsia develops earlier, the mother may need for bed rest and medicines, which could be achieved by hospitalization for adequate care for both her and the baby (Redman and Sargent, 2005).
It may also increase the mother risk of getting depressed. Depression, in turn, can make her too tired and feel sad, nervous or unable to accommodate with the changes she is facing (Musselman et al., 2003). She may develop diabetes of type 2 and all of its related problems later on (Dunne et al., 2003), check Table 2 for a conclusion of these complications.
Fetal complications / Maternal complications
- Fetal distress/fetal death
- Birth injury due to shoulder dystocia and Macrosomia
- Delayed fetal development Neonatal hypoglycemia
- Neonatal hyperbilirubinemia Neonatal hypocalcemia Neonatal polycythemia
- Respiratory distress syndrome Hypertrophic cardiomyopathy
- Obesity/diabetes later Diabetic retinopathy
- Diabetic nephropathy
- Diabetic ketoacidosis
- Hypoglycemia (when using insulin)
- Spontaneous abortion Premature birth
- Pregnancy-induced hypertension Hydramnios
Table 2 Maternal and fetal complications in pregnancies with carbohydrate intolerance
Risk factors
Every woman should seek health care early, if possible — when she first think about trying to get pregnant — so her doctor can evaluate her risk of developing GDM . If she develops it, then she may need further more screening and checkups. These are most likely to occur during the third trimester (last three months) of pregnancy when the doctor will monitor blood sugar level of mother and baby’s health (MacNeill et al., 2001).
The most common is Polycystic Ovary Syndrome (PCOS), which is a common disorder of endocrine system which develops among women in child-bearing age. It is characterized by enlarged ovaries that contain small collections or follicles of fluid located in each ovary which could be seen during the ultrasound examination. It may lead to infrequent or prolonged menstrual periods, intense hirsutism, increased weight, and developing acne (Toulis et al., 2009). Other factor includes GDM history in the past, intolerance of glucose, previous diabetes, or abnormal fasting levels.
Risk also increase with one of first-degree relatives has a previous history of diabetes type 2, old maternal age which increases as a woman gets older especially for women whose age is over 35 or 45 years (Di Cianni et al., 2003), and ethnicity where non-white race has the highest risk factors including People from Africa, Islands of the Pacific, the Caribbeans, Hispanics, local native Americans, and South Asians (MacNeill et al., 2001). Among the factors also if there is a previous pregnancy which delivered a baby with a macrosomia (weight › 4 kg), if obstetric history is poor (Di Cianni et al., 2003), between smokers and obesity which means that body has excess fats, and body mass index (BMI) is 30 or higher (Mokdad et al., 2003), and other genetic factors where 10 genes at least involved with increased risk of GDM, when a certain polymorphism occurs to them, the most notable one is TCF7L2 gene (Zhang et al., 2013).
Risk factors are not usually demonstrable, nor symptoms in about 40 to 60 percent of women suffering from GDM; so all women must be screened. Some other women may suffer from some of the common symptoms of diabetes, like fatigue, tiredness increase of urination, nasal congestion, thirst, blurred vision, nausea and vomiting, fungal infections and urinary tract infection (MacNeill et al., 2001).
Most women who have well controlled GDM deliver healthy babies. However, GDM that’s not carefully managed can lead to uncontrolled blood sugar levels and cause problems for both the mother and the baby, including an increased potential for C-section delivery (Jensen et al., 2001).
Diagnosis & Screening
Blood tests are commonly used for diagnosing GDM. There are many screening and/or diagnostic tests for detecting high levels of plasma or serum glucose, as per WHO diagnostic criteria, (Table 3).
Condition 2-hour glucose Fasting glucose HbA1c
Unit mg/dl mg/dl mmol/mol DCCT %
Normal <140 <110 <42 <6.0
Impaired fasting glycaemia <140 ≥110 & <126 42-46 6.0–6.4
Impaired glucose tolerance ≥140 <126 42-46 6.0–6.4
Diabetes mellitus ≥200 ≥126 ≥48 ≥6.5
Table 3 WHO diabetes diagnostic criteria
Non-challenge blood glucose tests measure glucose levels in blood samples without challenging or forcing the person to drink a glucose solution, then blood glucose level is determined when fasting or two hours after a meal (postprandial), or at any random time, in contrast, challenge tests measure glucose levels in blood samples after forcing the person to drink a glucose solution (Mellitus, 2005).
Non-challenge blood glucose test, in which diagnosis of GDM is made, when a plasma glucose level is higher than 126 mg/dl after fasting, or over 200 mg/dl at any random time, and then confirmed on the following day, and no further testing is required after that (Nielsen et al., 2012). It is performed usually at the first antenatal visit. It has advantages like simple administration and inexpensive, however disadvantages are low performance, low specificity, moderate sensitivity, and high false positive results (Nielsen et al., 2012).
Screening glucose challenge test (O’Sullivan test) in which diagnosis of GDM is made, when a plasma glucose level is 140 mg/dl after 1 hour of drinking a glucose solution that contains 50 grams of glucose (Palmert et al., 2002). It is done between the gestational weeks 24–28. It has advantages like no previous fasting is required, simple and inexpensive , however disadvantages are glucose solution could cause nausea in some women, so artificial flavors could be added.
Oral glucose tolerance test (OGTT), is done, usually, at morning following fasting overnight (8-14 hours), the person must have unrestricted diet and physical activity during the last 3 days. The person will drink a glucose solution, containing 100 g of glucose, then withdrawing blood samples to measure glucose levels at the beginning and after one, two and three hours thereafter (Stumvoll et al., 2000). Diagnosis of GDM is then made, when fasting blood glucose level is larger than or equals 95 mg/dl, then 1-hour blood glucose level is larger than or equals 180 mg/dl, then 2-hour blood glucose level is larger than or equals 155 mg/dl then 3-hour blood glucose level is larger than or equals 140 mg/dl
Urinary glucose testing measures urine glucose levels which are considered high in women with GDM. Dipstick test, which is a stripe containing a reagent for detecting glucose in urine, is widely used, although it performs poorly; as the sensitivity of glucosuria for GDM in the first 2 trimesters is only around 10% (Goldstein et al., 2004).
Ways that can lower the risk of getting GDM (Ratner et al., 2008) include losing extra weight as pregnancy could lead to a little increase of body weight, which is something good for baby health, but gaining too much weight in a very quick manner may increase the risk of getting GDM (Ratner et al., 2008). Increasing physical activity level before pregnancy is effective also for the prevention of GDM (Sanabria‐Martínez et al., 2015). Stopping smoking also may lower the risk of getting GDM. Monitoring blood glucose levels regularly. Also following a healthy eating plan, eating more grains, fruits, and vegetables, cutting down on fat and calories (Kim et al., 2007).
Healthy Eating Plan is an important factor of managing GDM (Reader et al., 2006). Following a healthy eating regimen or diet will help with controlling blood glucose levels to be within normal limits, providing adequate nutrition for mother and growing fetus, and achieving the convenient necessary changes of weight during pregnancy (Kim et al., 2007). Women with GDM are encouraged to eat small amounts and keep their weight healthy (Reader et al., 2006), eat carbohydrate in every meal, eat foods that provide nutrients especially needed during pregnancy, eat foods with high fiber content, and avoid foods and drinks of large amounts of sugar or high glycemic index ex. Basmati rices.
Carbohydrates are metabolized into glucose which is then used to produce energy. To well control glucose levels, it is necessary to distribute carbohydrate over three small meals and snacks daily (Zhang et al., 2006a). Foods containing carbohydrate include milk, yogurt, cereals, multigrain breads legumes like red kidney and baked beans, rice (Basmati), pasta, noodles, fruits, corn, potato, and sweet potato. Sucrose (table sugar), fruit juices, soft drinks, cakes, and biscuits have low nutritional value (Zhang et al., 2006a). Eating fats, especially saturated fat, should be limited. Healthy fats should be used example, polyunsaturated oils, margarine, canola, olive oil, avocados and unsalted nuts. To avoid or decrease the intake of saturated fat, then low-fat dairy foods, lean meats should be selected and processed and takeaway foods should be avoided (Liang et al., 2010).
Protein should be served two times each day in a small amount, because of its importance for the growth of fetus and maintenance of mother health. It include lean meat, eggs, milk, low fat cheese and fish (Zhang et al., 2006b, Kim et al., 2007). These foods do not affect glucose levels of blood in a direct manner. (Zhang et al., 2006b).
Calcium & iron are increasingly required as pregnancy progresses. So should be served two times daily. (For calcium, one serve is equivalent to 200 g of yogurt, 250 ml milk, or 2 slices of cheese). The iron from red meat, chicken and fish are readily absorbed (Zhang et al., 2006b). In general, any of nutritious foods that do not cause increase of weight or cause glucose levels in blood can be eaten freely. Examples on these foods are fruits and vegetables (except corn, beans, potato, sweet potato, mentioned above) (Zhang et al., 2006b).
Water is considered the best drink for the body – it is recommended with fresh lemon for difference. Sugar-free or diet drinks are preferred for people with diabetes (Gray-Donald et al., 2000). However products containing caffeine and carbonated soft water can increase osteoporosis risk and alter the mood so should have just little of them (Gray-Donald et al., 2000) Alcohols are forbidden as it harms the baby . Alternative sweeteners are more preferred also than to natural sugars, examples are sucralose, aspartame and acesuphame potassium, for sample food plan, check Table 4.
Meal Choose from Plus
Option 1 / Option 2
Breakfast ½ cup untoasted muesli/All Bran®/ rolled oats (raw) 1-2 slices of toast multigrain, soy & linseed, wholemeal, white, heavy fruit bread
- OR 1 slice of toast with ½ cup baked beans 250ml low fat milk
- OR 100g low-fat fruit yoghurt
- OR 200g artificially sweetened yoghurt
Morning tea 4 Vitaweats® with a small amount of reduced fat cheese ½ English muffin
- OR 1 slice toast with a small amount of reduced fat cheese 1 serve of fruit, 1 apple, 1 pear, 1 small banana, 2 kiwi fruits, 4 apricots, ½ cup tinned fruit, 2 tablespoons sultanas
Lunch 2 slices of bread
- OR 1 medium bread roll with tuna, salmon, fresh chicken, egg, roast beef or reduced fat cheese 2/3 cup cooked rice (Basmati/Doongara)
- OR 1 cup pasta/noodles with tuna, salmon, fresh chicken, egg, roast beef or reduced fat cheese Plenty of salad or cooked vegetables (other than potato or corn) PLUS 1 serve of fruit
Afternoon Tea
250mls low fat milk 100g Low fat yoghurt
- OR 200g artificially sweetened yoghurt 1 slice heavy fruit loaf
- OR 1 crumpet
- OR ½ English muffin
Dinner 2/3 cup cooked rice (Basmati)
- OR 1 cup pasta/noodles 1 medium potato and a small corn cob A small serve of lean meat, fish, chicken or tofu, with plenty of salad
- OR cooked vegetables PLUS 1 serve of fruit
Supper ½ cup low fat custard
- OR 2 small scoops of low-fat ice cream 100g low-fat yoghurt
- OR 200g artificially sweetened yoghurt 1 serve of fruit
Table 4 Sample food plan
Moderate intensity physical activity is recommended for women with GDM as it can help to control glucose levels, however, it is more preferred to check that with physician prior to starting any activity during pregnancy. It helps also to lower insulin resistance (Sanabria‐Martínez et al., 2015). Practicing exercise, like walking, regularly will help to increase fitness of mother and be prepared more for delivery of her baby. It also helps to maintain glucose levels of blood under control (Sanabria‐Martínez et al., 2015). Walking as a regular exercise could be achieved by Using a ‘pedometer’ (or a ‘step counter’), standing and moving a lot in the kitchen, taking the stairs not the elevator, walking to faraway stores for shopping instead of using car, making a ‘walking group’ with family or friends at a regular time, and practicing on gardening (Artal et al., 2007).
Glucose levels of pregnant woman usually return to normal limits after delivery, but there is still an increased risk for her to develop type 2 diabetes later in her life (Retnakaran et al., 2007). To decrease this risk or delay it, it is recommended to (Ross, 2006) achieve a healthy weight and maintain it, by eating only balanced, healthy and nutritious foods, as previously mentioned, and practicing physical activities to reduce any extra weight, for at least 30 minutes on most days, keeping checking glucose levels regularly at least every 1-2 years (Vijan, 2010).
Treatment & Management
Recent studies indicate that there is an evidence that good management and treatment of GDM can reduce its complications (Buchanan and Xiang, 2005). Primary complications on the baby included death, fracture of bones, nerve palsy and shoulder dystocia. Primary complications on the mother included the need for premature and/or cesarean delivery. These complications were significantly fewer after treatment, and the need for cesarean deliveries was limited .
The purpose of treatment is to reduce the risks of GDM for both mother and child. Controlling glucose levels can lower fetal complications (such as macrosomia) and increase maternal health (Artal et al., 2007). If a healthy diet, physical exercise, and oral medication are not enough to maintain glucose levels within normal, then treatment with insulin would be necessary (Westermeier et al., 2015).
Counseling before pregnancy is always a good way for a good lifestyle (Artal et al., 2007). Most women can manage their GDM by making healthy dietary changes and exercise activity, as mentioned above. Self-monitoring of glucose levels in blood is an important factor to guide therapy (Saudek et al., 2006). Treatment goals, in the first place, is to achieve normal blood glucose levels (Table 5).
Test Glucose levels (mg per dL)
- Fasting Less than 96
- One-hour after meal Less than 140
- Two-hours after meal Less than 120 to 127
Table 5: Treatment goals for Women with Gestational Diabetes
Some women need anti-diabetic drugs, whereas most commonly need insulin therapy (Artal et al., 2007). Self-monitoring could be achieved using a device called “handheld capillary glucose dosage system” (a device used for measuring blood Glucose levels) (Tang et al., 2000). Testing blood glucose levels is most commonly done once wake up in the morning (fasting) then 2 hours after each meal.
If monitoring indicates failure of maintain of glucose levels within normal limits using these ways, or if there are complications like macrosomia, then treatment with insulin would be necessary (Westermeier et al., 2015). Fast-acting insulin is commonly used just before eating on an empty stomach. Take care to avoid lowering blood sugar levels (hypoglycemia) when injecting excess insulin (Westermeier et al., 2015).
Certain oral anti-diabetic drugs might be safe or less dangerous in pregnancy on the growing fetus than poorly controlled diabetes (i.e The lesser of two harms) (Zhu et al., 2016). Metformin is better than glyburide. If glucose levels cannot be controlled enough with a single drug, then metformin and insulin combination would be better than insulin alone (Ashoush et al., 2016). Metformin is preferred as oral drug rather than insulin injections. Also, it helps with treatment of polycystic ovarian syndrome during pregnancy one of the risk factors of GDM (Song et al., 2016). Metformin also lowers the need for insulin and help to gain less weight (Song et al., 2016).
Medical Interview
When a pregnant woman is examined for the first time, her doctor should check her history concerning diabetes, and if she had developed it before in a previous pregnancy, and if she is at risk for GDM (Ito et al., 2015). Screening tests are done and if they give positive results, then GDM diagnosis is confirmed. After that she is referred to hospital or care center for further checks. These include measuring blood pressure, weight and heart rate every day during hospitalization, measuring uterine fundus height once every week, examination of pelvis for signs of premature birth, collecting vaginal culture, as well as blood testing and urine analysis (Kilgour, 2013). Pregnant woman with GDM may further be examined for glycoalbumin, HbA1c, once per month, anti- glutamate decarboxylase, anti-insulin, islet cell antibodies, once at early pregnancy, Uric protein, urinary glucose, twice every month, urine ketone bodies and albumin once every month, and measuring creatinine clearance to check for nephropathy in diabetic patients (Kim et al., 2007).
Measurement of baby growth using ultrasound, where the head circumference or biparietal diameter, femur length, and abdominal circumference of the baby are examined at suitable intervals. In case the baby appeared too larger than standard limits, pregnancy termination would be considered and early delivery is decided. Ultrasound is used also for screening for congenital anomalies, spine, nervous system, etc. It helps also to check the amount of amniotic fluid, and overall well-being of the baby (Naylor et al., 1996). When insulin therapy is considered, a special care should be taken for the doses of insulin required during pregnancy, delivery, and after birth as they differs significantly. The need for insulin at the end of pregnancy is increased about two times. But during first-stage of delivery, it is decreased, then increases slightly in the second-stage, and finally decreases rapidly after birth (Itoh et al., 2016).
During delivery, an electrolyte solution containing 5% glucose is administered to the patient at a rate of 100–120 ml/hr, then she is administered intravenous insulin through an infusion pump. Blood glucose is measured at 1–2 hours intervals (Hiden et al., 2012).
GDM generally resolves once the baby is born. According to different studies, the potential of developing GDM in a second pregnancy, if first pregnancy developed GDM, is between 30 and 84%, especially within one year of the previous pregnancy, depending on ethnic background (Nohira et al., 2006).
Women with GDM are subject to an increased risk rate of developing diabetes mellitus in the future, Type 2 (Nohira et al., 2006). This risk is highest in case of women who needed treatment anti- glutamate decarboxylase, anti-insulin, islet cell antibodies and/or insulinoma antigen-2, women who had more than two previous pregnancies, women who were obese, and women who need insulin to treat GDM have a 50 percent risk of getting diabetes within five years (Lee et al., 2007). Also, their children have an increased risk for obesity in childhood and adult phase as well as type 2 diabetes and glucose intolerance later in life (Lee et al., 2007)
Gestational Diabetes Mellitus (GDM) is considered one of the most common conditions that affect women during pregnancy, where blood glucose levels are increased above normal limits (Baz et al., 2015). It usually arises after 28 weeks, in the third trimester, of pregnancy, and usually disappears after delivery of the baby (Association, 2010). GDM develops when there is not enough insulin secreted during pregnancy to control the rise in blood glucose levels (Kinalski et al., 2002), and this comes by several causes including placental hormones, and insulin resistance.
GDM complications, if not treated or managed, affect both mother and her baby, which make C-section or early delivery more preferred. Complications on the baby includes, macrosomia, respiratory distress syndrome, jaundice, hypoglycemia, developing type two diabetes in the future, or baby death (Bellamy et al., 2009). Complications on the mother include hypertension, proteinuria, a condition called preeclampsia, that needs hospitalization to avoid the risk of preterm birth, and may cause depression or diabetes type two in the future and all of its related problems.
Risk factors include Polycystic Ovary Syndrome (Toulis et al., 2009), GDM history in the past, intolerance of glucose, previous diabetes, or abnormal fasting levels. They also increase with first-degree relatives has a previous history of diabetes type two, non-white race, obesity, smoking and genetic factors.
Blood tests are commonly used for diagnosing GDM. They could be either non-challenge blood glucose tests or challenge blood glucose tests. They include non-challenge blood glucose test, screening glucose challenge test (O’Sullivan test), oral glucose tolerance test, and urinary glucose testing (Nielsen et al., 2012).
Prevention of GDM is achieved by losing extra weight, increasing physical activity level, Stopping smoking, and following a healthy eating plan (Ratner et al., 2008).
Finally, For all women who are diagnosed with gestational diabetes, this can be upsetting and frustrating. However, working closely with physician and health care team can maintain glucose levels within the normal limits to provide the best outcomes ever for both the baby and mother.
2016-3-29-1459243434
...(download the rest of the essay above)
Discover more:
- Diabetes essays
Related essays:
- Gestational Diabetes Mellitus (GDM) analysis
- Gestational diabetes mellitus – epidemiology, mechanism, pathogenesis
- Gestational diabetes mellitus
- Gestational diabetes – risk factors, diagnosis, prevention, treatment
- Gestational diabetes – nature, risk factors, screening, treatment
- Diabetes – Type 1 and Type 2 / Gestational
Recommended for you
- Gestational diabetes mellitus – epidemiology, mechanism, pathogenesis
- Gestational Diabetes Mellitus: Overview of Diagnosis, Complications and Treatment
- Type 2 Diabetes (T2DM)
About this essay:
If you use part of this page in your own work, you need to provide a citation, as follows:
Essay Sauce, Gestational Diabetes Mellitus (GDM) . Available from:<https://www.essaysauce.com/health-essays/63524/> [Accessed 13-04-24].
These Health essays have been submitted to us by students in order to help you with your studies.
* This essay may have been previously published on Essay.uk.com at an earlier date.
Essay Categories:
- Accounting essays
- Architecture essays
- Business essays
- Computer science essays
- Criminology essays
- Economics essays
- Education essays
- Engineering essays
- English language essays
- Environmental studies essays
- Essay examples
- Finance essays
- Geography essays
- Health essays
- History essays
- Hospitality and tourism essays
- Human rights essays
- Information technology essays
- International relations
- Leadership essays
- Linguistics essays
- Literature essays
- Management essays
- Marketing essays
- Mathematics essays
- Media essays
- Medicine essays
- Military essays
- Miscellaneous essays
- Music Essays
- Nursing essays
- Philosophy essays
- Photography and arts essays
- Politics essays
- Project management essays
- Psychology essays
- Religious studies and theology essays
- Sample essays
- Science essays
- Social work essays
- Sociology essays
- Sports essays
- Types of essay
- Zoology essays
Gestational Diabetes
Gestational diabetes is a form of diabetes that builds up only in pregnancy. Similar to other diabetes types, it affects the level of sugar in the blood. Patients suffering from this condition have very high glucose levels in their blood. Expectant women should produce more insulin that other women. This is because the hormones from the placenta make the body less responsive to insulin. If the body can not meet the extra demand, then the level of sugar in the blood rises and that might be the root cause of gestational diabetes. Nevertheless, due to hormonal changes that occur in the body during pregnancy some women develop resistance to insulin.
If this sample essay on "Gestational Diabetes" doesn’t help, our writers will!
Gestational diabetes escalates the sugar levels in the blood which affects a womans pregnancy and the health of the baby. If the condition is not managed, the sugar level rises in the blood and crosses the placenta to the baby. This makes the baby grow bigger than normal, which could result in complications during childbirth. The condition also escalates the glucose levels in the blood. Nevertheless, high glucose levels in the blood are bad for the health of the mother and the baby. Gestational diabetes is primarily detected in the late pregnancy. It is a common form of diabetes affects one out of every six women. Fortunately, the condition does not last forever but disappears after the child is born.
Risk Factors
There are several risk factors for gestational diabetes. Although any woman can attain gestational diabetes, some women are at a higher risk than others. There is a high chance of getting gestational diabetes if one is overweight. In such a case, the body mass index (BMI) of a patient must be thirty and above. Because of the extra weight, it becomes hard for the body to use the insulin in the blood. Family health history is also another risk factor for attaining gestational diabetes. If a close family member has diabetes type 2, then there is a risk of a woman developing gestational diabetes.
One might also develop gestational diabetes if she had it during the previous pregnancies, if she delivered a baby weighing more than nine pounds or if she had a stillbirth that could not be explained. Another risk factor for gestational diabetes is polycystic ovary syndrome (PCOS). Women with PCOS miss ovulation and fail to release their ovules. As a result, they become prone to gestational diabetes, disease of the heart, uterine cancer and blood pressure. Family origin is also a contributing factor to gestational diabetes. Past research has indicated that families from South Asia, Middle East or Black Caribbean are at a higher risk of developing gestational diabetes.
Gestational diabetes is treated by ensuring the blood sugar level is in the ideal range. It is important to check and manage the blood sugar levels to protect the health of the unborn baby and also to ensure a safe gestation period and delivery. Gestational diabetes is treated by having a healthy diet, taking the right portion of foods and avoiding gaining of excessive weight. A recommended diet focuses on vegetables, fruits, and whole grains foods which are highly nutritious, with less fat and with low calories. The right diet can vary depending on varying women. For this reason, it is advisable to consult a dietitian.
Exercise is an efficient strategy for controlling gestational diabetes. Exercise stimulates the body to move glucose into the body cells where it is converted to energy hence lowering the blood sugar levels. Through exercises, the sensitivity of cells to insulin is also increased. As a result, less insulin is produced by the body to transport sugar. For extreme cases where exercise and diet are not adequate, having an insulin injection can be essential aimed at lowering the level of sugar in the blood. About ten to twenty percent of those with gestational diabetes require insulin to attain the desired blood sugar level. Some doctors prescribe an oral medication to the control blood sugar levels.
Nevertheless, there are have been medical suggestions in the past suggests that research should be done to confirm the safety and effectiveness of oral drugs in controlling gestational diabetes. Eating regularly is another way of treating gestational diabetes. Pregnant women should ensure that they take all meals in a day without skipping. Such persons should also eat a balanced diet regularly, and mostly consume sufficient starchy carbohydrates. Carbohydrates are absorbed slowly in the blood which stabilizes the glucose level in the blood. Some of the carbohydrates that are highly recommended include rice, pasta or basmati among others. Also, sweet potatoes, yam, porridge oats, pumpernickel are also essential sources of carbohydrates.
It is imperative to regulate the level of sugar in the blood. A blood glucose meter is used to test the level of sugar in the body. This should be done four to five times in a day. Having a blood sugar follow-up checks are important since it reduces the risk of developing diabetes type 2 during pregnancy. A fetus must also be monitored closely when being carried by a woman suffering from this condition. Other tests and ultrasounds are carried out to avoid complications to the mother and the baby. Most women with gestational diabetes deliver their babies normally. However, some doctors will prefer the baby to be delivered before the due date. A cesarean section is recommended if the baby grows bigger than use because of this condition. The risk of complications during delivery is high to the mother and the baby if delivery is done after the due date.
This form of diabetes cannot be prevented in some women. However, one can lower the chances of acquiring the condition by ensuring that the weight is controlled before pregnancy. It is important to lose excessive weight before pregnancy. Gestational diabetes complications can be prevented by controlling the level of sugar in the blood. An obstetrician should closely monitor a pregnant woman during her gestation period. Regular exercise before and during pregnancy reduces the risk of developing gestational diabetes. The persons who have previously suffered from gestational diabetes should avoid insulin resistant medicines such as glucocorticoid medicines and nicotinic acid. Gestational diabetes can also be prevented by having well-balanced diets with a high fiber content. Foods that are low in fat and calories are also highly recommended since they both control the blood sugar levels and are nutritious to the mother and the baby.
In conclusion, gestational diabetes is that type of diabetes that occurs during pregnancy. When one is expectant, extra insulin is made by the body especially during late pregnancy. Extra insulin is needed because the body is rendered less responsive to it by the hormones contained in the placenta. Consequently, failure by the body to meet the extra insulin demand will lead to rising in the blood sugar increasing the probability of attaining gestational diabetes. After pregnancy, gestational diabetes disappears. Nevertheless, women with gestational diabetes are at an elevated risk of acquiring type 2 diabetes in future. Therefore, it is remarkably important for such women to maintain a healthy lifestyle even after their delivery.
If you are the original author of this essay and no longer wish to have it published on the SuperbGrade website, please click below to request its removal:
- Literature Review of New ATP 3 Cholesterol Guidelines
- Potential Risks to the Health and Well-Being in Nursing
- Expository Essay on Providing Whole Person Cares in Health Care
- Collaboration at the Organizational and Personal Level
- Kentucky vs King Case: The Warrant Requirement in Drug Cases
- Case Study Sample on Evidence-Based Practice
- Working Memory and Spatial Relations Skill in Autistic Children: Informative Essay
Submit your request
Sorry, but it's not possible to copy the text due to security reasons.
Would you like to get this essay by email?
Sorry, you can’t copy this text :(
Enter your email to get this essay sample.
Don’t print this from here
Enter your email and we'll send you a properly formatted printable version of this essay right away.
How about making it original at only $7.00/page
Let us edit it for you at only $7.00 to make it 100% original!

IMAGES
VIDEO
COMMENTS
The definition of gestational diabetes mellitus (GDM) is any degree of glucose intolerance with onset or first recognition during pregnancy. GDM can classify as A1GDM and A2GDM. Gestational diabetes managed without medication and responsive to nutritional therapy is diet-controlled gestational diabetes (GDM) or A1GDM. On the other side, gestational diabetes managed with medication to achieve ...
Gestational Diabetes Mellitus ( Gdm ) Essay Gestational Diabetes Mellitus (GDM) is defined as a glucose intolerance that has been diagnosed during pregnancy.1 GDM affects anywhere between 1% to 14% of pregnancies and is on the rise due to the global obesity epidemic.1 Such a large range is due to the differences in screening technique and ...
Introduction. Gestational diabetes mellitus is a common chronic disease in pregnancy that impairs the health of several million women worldwide.1 2 Formally recognised by O'Sullivan and Mahan in 1964,3 gestational diabetes mellitus is defined as hyperglycaemia first detected during pregnancy.4 With the incidence of obesity worldwide reaching epidemic levels, the number of pregnant women ...
Gestational diabetes mellitus (GDM), which has traditionally been defined as glucose intolerance of varying severity with first onset in pregnancy, is rising in prevalence with maternal hyperglycemia currently affecting one in every six pregnancies worldwide. Although often perceived as a medical complication of pregnancy, GDM is actually a chronic cardiometabolic disorder that identifies ...
Gestational diabetes mellitus (GDM) increases type 2 diabetes risk; however, postpartum diabetes screening rates are low. Using semi-structured interviews and focus groups, this study investigates the understanding of GDM and its relationship to future diabetes risk and diabetes prevention among patients with public or no insurance (n = 36), health care providers (n = 21), and clinic staff (n ...
In Australia, the prevalence of GDM is estimated to range between 5.2 and 8.8% (Cheung & Byth 2003). The 2005-6 gestational diabetes mellitus in Australia report gave a figure of 4.6% to represent the fraction of pregnant women aged 15-49 years with GDM. This was a 20% increase compared with what had been recorded in 2000-1 (Templeton & Pieris ...
Gestational diabetes mellitus (GDM) is diagnosed by elevated blood glucose in pregnancy though the definition has changed repeatedly since its first description in the 1960's [1, 2].The most frequently reported perinatal consequence of GDM is macrosomia (usually defined as a neonate weighing over 4 kg) which can increase the risk of caesarean section and shoulder dystocia.
Better Essays. 1850 Words. 8 Pages. Open Document. The prevalence of Gestational Diabetes mellitus (GDM) is growing worldwide. 1-14% of women in pregnancy is affected by DM 1. Due to increased incidence and proposed lower¬ing of the thresholds for diagnosis the health care cost of GDM can be expected to rise proportionately.
Essay on Gestational Diabetes Mellitus (GDM) Gestational diabetes mellitus (GDM) is an intolerance of glucose documented for the first time during pregnancy. It is usually a short-term type of diabetes and the most common health problem with pregnant women. GBM is caused by the way the hormones in pregnancy affect the mother.
Gestational Diabetes Mellitus (GDM) GDM is a state of insulin resistance which disturbs the intrauterine environment and can lead to accelerated fetal growth (Radaelli et al 2003).It effects approximately 7% of pregnant women with approximately 200,000 cases seen each year (Schillan-Koliopoulos and Guadagno 2006).
In conclusion, gestational diabetes mellitus (GDM) is a prevalent complication during pregnancy, affecting approximately 14% of pregnancies globally. The risk factors for GDM include a Westernized diet, advanced maternal age, overweight/obesity, and family history of insulin resistance or diabetes. While GDM often resolves after delivery, it ...
Additional Drug Considerations During Pregnancy. Initiate or titrate blood pressure medication at a threshold of 140/90 mmHg. A target of 110-135/84 mmHg is suggested. Therapy should be reduced if blood pressure is <90/60 mmHg. Stop potentially harmful medications in pregnancy (i.e., ACE inhibitors, angiotensin receptor blockers, and statins ...
What is Gestational Diabetes. Gestational diabetes (also referred to as gestational diabetes mellitus, or GDM), is a form of diabetes occurring during pregnancy. The condition usually goes away after the pregnancy. Gestational diabetes is diagnosed when blood glucose levels appear higher than normal during the pregnancy.
Gestational Diabetes Amongst North American Pregnant Mothers: esponses Crowther, Hiller, Moss et al. (2005) show that "treatment of gestational diabetes reduces serious perinatal morbidity" -- more so than simple routine care, so that was an interesting discovery based on the questions posed by Nelson and isa. The fact that gestational diabetes does affect both the mother and the embryo/fetus ...
1 Introduction. Gestational diabetes mellitus (GDM) is still a major global health concern that has detrimental effects on the health of both the mother and the fetus [].GDM is the most prevalent metabolic disease during pregnancy [], which leads to birth injuries such as shoulder dislocation, fetal metabolic disorders, bone fractures, low birthweight and nerve paralysis.
Bertrand, K.A, et al. Gestational Diabetes and Risk of Breast Cancer Before Age 55 Years. ... Deposit scholarly works such as posters, presentations, research protocols, conference papers or white papers. If you would like to deposit a peer-reviewed article or book chapter, use the "Scholarly Articles and Book Chapters" deposit option. ...
Introduction. Gestational diabetes is a condition that can affect pregnant women, causing their blood glucose levels to become too high during their pregnancy. This can put the mother and baby's health at risk and affect them both later in life. However, only 2-10% of pregnant women suffer from gestational diabetes in the United States each ...
Objectives: Gestational diabetes mellitus (GDM) is the most common pregnancy-related medical complication. It is characterized by the development of hyperglycaemia during pregnancy and is known to lead to higher risk of metabolic disorders and other pathologies in both mothers and offsprings. Some studies probed the impacts of GDM, focusing on specific organs like placenta or adipose tissue ...
Open Document. Gestational diabetes mellitus (GDM) is an intolerance of glucose documented for the first time during pregnancy. It is usually a short-term type of diabetes and the most common health problem with pregnant women. GBM is caused by the way the hormones in pregnancy affect the mother. GDM accounts for 5-7% of all pregnancies ...
The likelihood that gestational diabetes will recur is high, with around 50% of women experiencing it in their first and second pregnancies. The symptoms of gestational diabetes and recurrent ...
Gestational diabetes, a disease that can lead to multiple pregnancy and delivery complications, is the most common pregnancy metabolic complication, affecting 1 in 7 pregnancies.
Gestational Diabetes Mellitus (GDM) is considered one of the most common conditions that affect women during pregnancy, where blood glucose levels are increased above normal limits (Baz et al., 2015). It usually arises after 28 weeks, in the third trimester, of pregnancy, and usually disappears after delivery of the baby (Association, 2010).
Excess insulin resistance contributes to gestational diabetes, prior research has found, but the exact causes of this resistance remains unclear. For this study, researchers conducted genetic ...
Gestational diabetes escalates the sugar levels in the blood which affects a womans pregnancy and the health of the baby. If the condition is not managed, the sugar level rises in the blood and crosses the placenta to the baby. This makes the baby grow bigger than normal, which could result in complications during childbirth.