Featured Topics
Featured series.
A series of random questions answered by Harvard experts.

Explore the Gazette
Read the latest.

Weight-loss drug linked to fewer COVID deaths

Billions worldwide deficient in essential micronutrients

Smokers are less likely to develop Parkinson’s. Why?
‘Dramatic’ inroads against aggressive brain cancer
Cutting-edge therapy shrinks tumors in early glioblastoma trial
Haley Bridger
Mass General Communications
A collaborative project to bring the promise of cell therapy to patients with a deadly form of brain cancer has shown dramatic results among the first patients to receive the novel treatment.
In a paper published Wednesday in The New England Journal of Medicine, researchers from Mass General Cancer Center shared the results for the first three patient cases from a Phase 1 clinical trial evaluating a new approach to CAR-T therapy for glioblastoma.
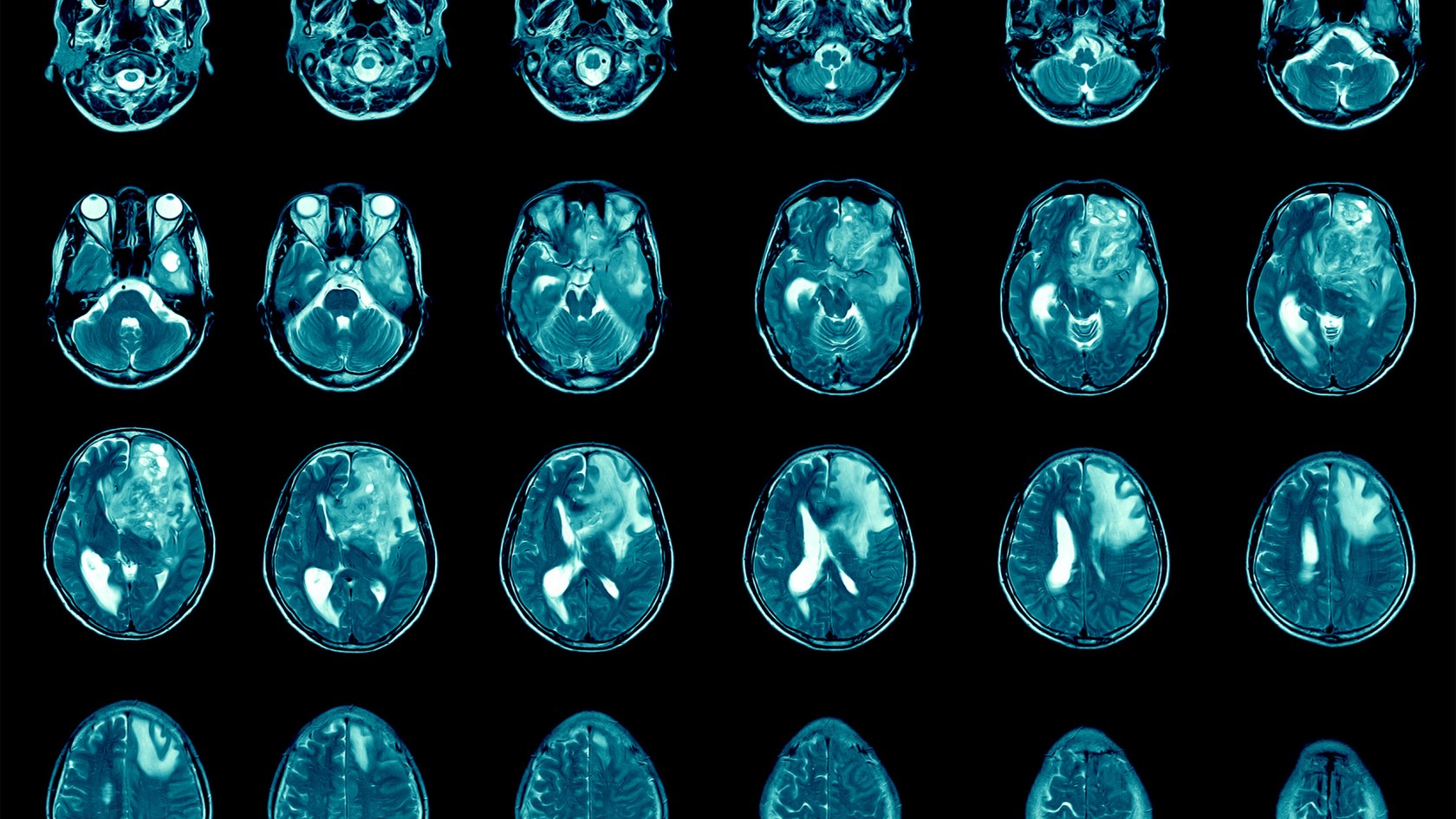
Just days after a single treatment, patients experienced dramatic reductions in their tumors, with one patient achieving near-complete tumor regression. In time, the researchers observed tumor progression in these patients, but given the strategy’s promising preliminary results, the team will pursue strategies to extend the durability of response.

Left: MRI in Participant 3 before infusion. Right: After infusion on day five.
Image courtesy of The New England Journal of Medicine
“This is a story of bench-to-bedside therapy, with a novel cell therapy designed in the laboratories of Massachusetts General Hospital and translated for patient use within five years, to meet an urgent need,” said co-author Bryan Choi , a neurosurgeon at Harvard-affiliated Mass General and an assistant professor at Harvard Medical School. “The CAR-T platform has revolutionized how we think about treating patients with cancer, but solid tumors like glioblastoma have remained challenging to treat because not all cancer cells are exactly alike and cells within the tumor vary. Our approach combines two forms of therapy, allowing us to treat glioblastoma in a broader, potentially more effective way.”
The new approach is a result of years of collaboration and innovation springing from the lab of Marcela Maus , director of the Cellular Immunotherapy Program and an associate professor at the Medical School. Maus’ lab has set up a team of collaborating scientists and expert personnel to rapidly bring next-generation genetically modified T cells from the bench to clinical trials in patients with cancer.
“We’ve made an investment in developing the team to enable translation of our innovations in immunotherapy from our lab to the clinic, to transform care for patients with cancer,” said Maus. “These results are exciting, but they are also just the beginning — they tell us that we are on the right track in pursuing a therapy that has the potential to change the outlook for this intractable disease. We haven’t cured patients yet, but that is our audacious goal.”
CAR-T (chimeric antigen receptor T-cell) therapy works by using a patient’s own cells to fight cancer — it is known as the most personalized way to treat the disease. A patient’s cells are extracted, modified to produce proteins on their surface called chimeric antigen receptors, and then injected back into the body to target the tumor directly. Cells used in this study were manufactured by the Connell and O’Reilly Families Cell Manipulation Core Facility of the Dana-Farber/Harvard Cancer Center.
CAR-T therapies have been approved for the treatment of blood cancers, but the therapy’s use for solid tumors is limited. Solid tumors contain mixed populations of cells, allowing some malignant cells to continue to evade the immune system’s detection even after treatment with CAR-T. Maus’ team is working to overcome this challenge by combining two previously separate strategies: CAR-T and bispecific antibodies, known as T-cell engaging antibody molecules. The version of CAR-TEAM for glioblastoma is designed to be directly injected into a patient’s brain.
In the new study, the three patients’ T cells were collected and transformed into the new version of CAR-TEAM cells, which were then infused back into each patient. Patients were monitored for toxicity throughout the duration of the study. All patients had been treated with standard-of-care radiation and temozolomide chemotherapy and were enrolled in the trial after disease recurrence.
- A 74-year-old man had his tumor regress rapidly but transiently after a single infusion of the new CAR-TEAM cells.
- A 72-year-old man was treated with a single infusion of CAR-TEAM cells. Two days after receiving the cells, an MRI showed a decrease in the tumor’s size by 18 percent. By day 69, the tumor had decreased by 60 percent, and the response was sustained for more than six months.
- A 57-year-old woman was treated with CAR-TEAM cells. An MRI five days after the infusion showed near-complete tumor regression.
The authors note that despite the remarkable responses among the first three patients, they observed eventual tumor progression in all the cases, though in one case, there was no progression for over six months. Progression corresponded in part with the limited persistence of the CAR-TEAM cells over the weeks following infusion. As a next step, the team is considering serial infusions or preconditioning with chemotherapy to prolong the response.
“We report a dramatic and rapid response in these three patients. Our work to date shows signs that we are making progress, but there is more to do,” said co-author Elizabeth Gerstner, a Mass General neuro-oncologist.
In addition to Choi, Maus, and Gerstner, other authors are Matthew J. Frigault, Mark B. Leick. Christopher W. Mount, Leonora Balaj, Sarah Nikiforow, Bob S. Carter, William T. Curry, and Kathleen Gallagher.
The study was supported in part by the National Gene Vector Biorepository at Indiana University, which is funded under a National Cancer Institute contract.
Share this article
You might like.
Large-scale study finds Wegovy reduces risk of heart attack, stroke

Inadequate levels carry risk of adverse pregnancy outcomes, blindness

Researchers test theory explaining medical mystery and identify potential new treatment
You want to be boss. You probably won’t be good at it.
Study pinpoints two measures that predict effective managers
Your kid can’t name three branches of government? He’s not alone.
Efforts launched to turn around plummeting student scores in U.S. history, civics, amid declining citizen engagement across nation
Good genes are nice, but joy is better
Harvard study, almost 80 years old, has proved that embracing community helps us live longer, and be happier
News Center
New glioblastoma treatment reaches human brain tumor and helps immune cells recognize cancer cells, novel immunotherapy is first-in-human treatment for this brain cancer.

In a major advance for the treatment of the deadly brain cancer glioblastoma, Northwestern Medicine scientists used ultrasound technology to penetrate the blood-brain barrier and provide a small dose of a chemotherapy and immunotherapy drug cocktail. The study, published in Nature Communications, found that this treatment boosted the immune system’s recognition of the cancer cells and could lead to a new treatment approach.
The scientists made several breakthroughs reported in a new study, including showing for the first time that a skull-implantable ultrasound device can enhance the penetration of the chemotherapy drug doxorubicin and immune checkpoint blockade antibodies — a novel immunotherapy treatment combination — into the human brain. The device produces microbubbles that temporarily open the blood-brain barrier, allowing the immunotherapy to enter the brain.
The scientists also showed for the first time that a small dose of doxorubicin (smaller than the dose used for traditional chemotherapy regimens) delivered with the immune checkpoint antibodies can boost the recognition of malignant glioblastoma cells by the immune system and reinvigorate the lymphocytes (immune cells) that are in charge of attacking the cancer cells.
An immune checkpoint blockade antibody blocks the deactivation of the immune system by the cancer cells. The immune system has built-in brakes — called immune checkpoints — so it doesn’t overdo it and injure the body when attacking cancer and infections. Glioblastoma evolves to activate the brakes, and therefore, the immune system (i.e., lymphocytes) won’t attack it.
In addition to the tumor cells, glioblastoma contains other cell populations called macrophages and microglia. These are the most abundant components of the tumor microenvironment and the cells that glioblastoma modulates to inhibit lymphocytes. The study showed that the chemo and antibody cocktail altered these cells, enabling the lymphocytes to recognize and kill the cancer cells.
“This is the first report in humans where an ultrasound device has been used to deliver drugs and antibodies to glioblastoma to change the immune system, so it can recognize and attack the brain cancer,” said co-corresponding author Adam Sonabend, MD , associate professor of Neurological Surgery and a Northwestern Medicine neurosurgeon. “This could be a major advance for the treatment of glioblastoma, which has been a frustratingly difficult cancer to treat, in part due to poor penetration of circulating drugs and antibodies into the brain.”
The study was conducted in four patients who had advanced progression of their tumors. They had already been treated with conventional chemotherapy for their tumors as well as an experimental treatment in a clinical trial, but both times, the tumors returned.
“This is a great example of translational bench-to-bedside-back-to-bench research, which sets an exceptional scenario to learn about the ability of the immune system to kill brain tumors in real-time upon treatment,” said co-corresponding author Catalina Lee-Chang, PhD , assistant professor of Neurological Surgery. “Given the lack of effective immune response against these deadly tumors, these findings encourage us to envision a potential new treatment approach.”
Clinical trial launched with new treatment
These new findings are the basis for a novel clinical trial that was just launched at Northwestern using ultrasound to deliver immunotherapy for glioblastoma. The trial will initially enroll 10 participants to determine the safety of the treatment, followed by 15 additional to measure whether the treatment can prolong survival.
Previous large clinical trials have failed to show that this type of immunotherapy can prolong survival in glioblastoma patients. Sonabend, however, believes that by enhancing the delivery of these antibodies and drugs into the brain and relying on biomarkers that indicate which tumors are most susceptible to immunotherapy, this treatment might be shown to be effective for some glioblastoma patients.
“Here we show in a small cohort of patients that when you use this technology, you can enhance the delivery of the chemotherapy and the antibodies, and change the tumor’s microenvironment, so the immune system can recognize the tumor,” Sonabend said.
Sonabend and Lee-Chang are members of the Robert H. Lurie Comprehensive Cancer Center of Northwestern University and the Malnati Brain Tumor Institute . Sonaband is also director of translational neuro-oncology at Feinberg.
Other Northwestern authors include first author Víctor A. Arrieta, PhD; Andrew Gould; Kwang-Soo Kim, PhD; Karl J. Habashy, PhD; Crismita Dmello, PhD , research assistant professor of Neurological Surgery; Gustavo I. Vázquez-Cervantes, PhD; Irina Palacín-Aliana, PhD; Graysen McManus; Christina Amidei, PhD, research assistant professor of Neurological Surgery; Cristal G. Gomez, MS; Silpol Dhiantravan; Li Chen, PhD; Daniel Y. Zhang; Ruth Saganty; Meghan E. Cholak; Surya Pandey, PhD , research assistant professor of Medicine in the Division of Hematology and Oncology ; Matthew McCord, PhD; Kathleen McCortney, MS; Rachel Ward, RN; Bin Zhang, MD, PhD ; the Johanna Dobe Professor of Cancer Immunology in the Department of Medicine; Jason M. Miska, PhD , assistant professor of Neurological Surgery; Maciej S. Lesniak, MD , the chair and Michael J. Marchese Professor of Neurosurgery; Craig M. Horbinski, MD, PhD , the Director of Neuropathology in the Department of Pathology ; Rimas V. Lukas, MD , associate professor of Neurology in the Division of Neuro-oncology ; and Roger Stupp, MD , chief of Neuro-oncology in the Department of Neurology and the Paul C. Bucy Professor of Neurological Surgery.
The research was supported in part by the National Cancer Institute grants 1R01NS110703-01A1, 1U19CA264338-01 and 1R01CA245969-01A1 of the National Institutes of Health, grant P50CA221747 SPORE for Translational Approaches to Brain Cancer and the Moceri Family Foundation and the Panattoni family. Sonabend and Stupp have received funding support for research from Agenus, BMS, and Carthera. Sonabend, Arrieta, Kim, Amidei, and Stupp are co-authors of an IP filed by Northwestern University related to the content of this manuscript. (PCT/US2023/034299). Sonabend has served as a consultant for Carthera and EnClear Therapies. Stupp has acted or is acting as a scientific advisor or has served on advisory boards for the following companies: Alpheus Medical, AstraZeneca, Boston Scientific, Carthera, Celularity, GT Medical, Insightec, Lockwood (BlackDiamond), Northwest Biotherapeutics, Novocure, Inc., Syneos Health (Boston Biomedical), TriAct Therapeutics, Varian Medical Systems. Other co-authors C. Desseaux, G. Bouchoux, and M. Canney are employees and hold an ownership interest in Carthera. M. Canney, G. Bouchoux, and A. Carpentier have patents related to the ultrasound technology described herein. Stupp is an advisory member and consultant for Carthera. Carpentier is a consultant for Carthera. Lee-Chang is a co-founder and consultant for Sera BioPharma.
Related Posts
Non-neuron brain cells produce a third of amyloid plaque in alzheimer’s disease, northwestern receives $55 million to advance health research, oncoprotein activity increases prostate cancer progression.
Comments are closed.
Type above and press Enter to search. Press Esc to cancel.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Neurosci
Editorial: Brain Cancers: New Perspectives and Therapies
1 Toxicology Unit, Laboratory of Clinical and Experimental Toxicology, Pavia Poison Centre, National Toxicology Information Centre, Istituti Clinici Scientifici Maugeri IRCCS, Pavia, Italy
Maria Grazia Bottone
2 Department of Biology and Biotechnology “L. Spallanzani, ” University of Pavia, Pavia, Italy
Brain diseases come in many different forms. It is estimated that these pathologies affect the lives of 1 in 6 people, and cost over a trillion dollars in annual treatment. The major categories of brain diseases include diverse brain cancers. Brain tumors are the most primitive, invasive and malignant in humans with poor survival after diagnosis (Mckinney, 2004 ; Laquintana et al., 2009 ). Although in recent years, numerous studies have been carried out to identify novel therapeutic protocols and tumor molecular markers capable to predict survival and response to treatment, the life expectancy of neuro-oncological patients is still very limited (24–36 months) (Aldape et al., 2019 ; Liang et al., 2020 ).
About 33% of all brain tumors are gliomas, accounting for about 80% of the total malignant central nervous system (CNS) tumors in adults (Hanif et al., 2017 ). Glioma is a broad category of glial brain and spinal cord tumors which originate in the glial cells that surround and support neurons in the brain, including astrocytes, oligodendrocytes, and ependymal cells. Among these, glioblastoma (GBM) is one of the most common and aggressive primary brain tumors (van Tellingen et al., 2015 ; Davis, 2016 ; Taylor et al., 2019 ; Birzu et al., 2021 ), characterized by diffuse infiltration of the adjacent brain parenchyma and development of drug resistance to standard treatment (Chen et al., 2018 ; Shergalis et al., 2018 ). So far, GBM remains associated with an extremely aggressive clinical course, and only 0.05–4.7% of patients survive 5 years from diagnosis (Ostrom et al., 2018 ). Cellular pleomorphism with nuclear atypia, high mitotic activity, and microvascular proliferation distinguish GBM from other lower-grade gliomas (Hambardzumyan and Bergers, 2015 ). In addition, the inter- and intra-patient tumor heterogeneity causes several obstacles, limiting the improvement of an early diagnosis and treatment protocols.
The tumor microenvironment (TME) plays a crucial role in mediating tumor progression and invasiveness, contributing to brain tumor aggression and poor prognosis ( Di Cintio et al. ; Yekula et al., 2020 ). Recent studies showed that differentiated tumor cells may have the ability to dedifferentiate acquiring a stem-like phenotype in response to microenvironment stresses such as hypoxia. Acidic extracellular pH and nitric oxide were also shown to be involved in stemness preservation (Dahan et al., 2014 ). Currently, the standard of care consists of surgical resection followed by radiotherapy (RT) and concomitant and adjuvant chemotherapy. Despite this aggressive treatment regimen, the median survival is only around 15 months, and the 2-year survival rate is only 26.5% (von Neubeck et al., 2015 ; Chen et al., 2018 ). Indeed, due to the location of gliomas origin and infiltrative growth (Urbańska et al., 2014 ), complete surgical resection of the tumor is often not possible other than with a high risk of neurological damages for the patient (Goldbrunner et al., 2018 ). Treating patients with primary brain tumors and brain metastases can be challenging. This is primarily due to the presence of the blood–brain barrier (BBB), posing an obstacle to overcome for most systemic treatments (van Tellingen et al., 2015 ; Brahm et al., 2020 ). Despite initial benefits, chemotherapy, using conventional agents, e.g., alkylating agents such as temozolomide, platinum-based drugs, or VEGF inhibitors (Dasari and Tchounwou, 2014 ; Pérez et al., 2019 ; Senbabaoglu et al. ; Strobel et al., 2019 ), is often associated with severe systemic toxicity, which occurs especially after long-term treatment (Karasawa and Steyger, 2015 ; Chovanec et al., 2017 ). Among these adverse side effects, neurotoxicity assumed increasing clinical importance as it is dose-cumulative and becomes limiting in long-lasting therapies, and also to the severe side effects (Chovanec et al., 2017 ; Staff et al., 2019 ). Therefore, high-grade gliomas or GBM are currently considered incurable and all patients inevitably experience and succumb to tumor recurrence, highlighting the urgent need to identify, validate and apply new therapeutic options (Ravanpay et al., 2019 ; Taylor et al., 2019 ; Maggs et al. ; Ghouzlani et al., 2021 ).
This Frontiers Research Topic Proposal on “ Brain Cancers: New Perspectives and Therapies ” joined contributions from scientists and physicians who investigate on etiopathogenesis and treatment of brain cancers. In fact, studies exploiting the existing link between enhancing the knowledge of cellular and molecular pathways involved in the onset/progression of these pathologies and the development of innovative therapies, improving patient prognosis and quality of life, need further in-depth investigations.
The published articles are based on neuro-oncological research and deal with proposing novel effective therapeutic strategies, focusing on different targets and aspects typical of brain tumors: tumor heterogeneity and microenvironment, cancer cell response to new chemotherapeutics and innovative radiotherapy treatments settings (often tested in combined protocols), immune-mediated gene therapies, which may involve blockade of immune checkpoint inhibitors, and other targeted therapies such virotherapy, CAR-T cells, dendritic cells' vaccines, or nanoparticle-mediated vaccination technologies ( Alghamri et al. ; Brandalise et al. ; Chen et al. ; Di Cintio et al. ; Ferrari et al. ; Lange et al. ; Maggs et al. ; Pasi et al. ; Senbabaoglu et al. ).
The joint mechanisms of neuro-inflammation, tumor microenvironment and BBB leakage status, which have been shown to trigger the tumor onset, invasion and progression, often mediated by the deregulation of a number of channel proteins and ion pumps ( Brandalise et al. ), have been also explored as promising targets for personalized pharmacological interventions ( Alghamri et al. ; Di Cintio et al. ; Lee et al., 2020 ). Another exploited key mechanism is cell death, a crucial multifaceted process dependent on signal transduction pathways, in which several Hsp90 client proteins, frequently abnormally expressed, may be involved ( Cao et al. ; Chen et al. ). It widely accepted that in cancer cells, particularly in gliomas cells, cell death pathways can be deactivated or defective for various causes, thus promoting cancer formation, proliferation, invasiveness, and even the induction of resistance to the drugs treatment. Particular effort has been devoted to the repositioning of old drugs as potent therapeutics for GMB and/or to exploit the combined effects of novel drugs in synergism with different irradiation protocols ( Chen et al. ; Lange et al. ; Ferrari et al. ; Pasi et al. ).
In summary, clinical evidences highlights the urgent medical need to further comprehend and delineate the complex mechanisms/interactions between cancer cells, immune cells, tumor stroma, resident healthy brain cells, and tumor vasculature, to develop innovative effective treatment strategies through the identification of novel targets. A multidisciplinary approach, taking into consideration all brain tumors aspects, including the modulation of the communication processes between cancer niche and tumor microenvironment and also the potential reactivation of defective cell death mechanisms, can currently be considered as a promising strategy.
This Frontiers Research Topic had the ultimate goal to apply new knowledges coming from multitiered approaches, to identify novel effective therapeutic strategies to be used in the field of clinical neuro-oncology, to improve the patient prognosis and quality of life, also reducing adverse side effects due to conventional treatments, in view of a focused, personalized medicine. The published contributions may play a crucial role, laying the groundwork to translate the experimental findings to clinical setting, turning them into new clinical therapeutic protocols, facing the challenges in this field and developing new healing perspectives.
Author Contributions
Both authors equally contributed to the work, giving a substantial, direct, and intellectual contribution, and they both approved the work for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
- Aldape K., Brindle K. M., Chesler L., Chopra R., Gajjar A., Gilbert M. R., et al.. (2019). Challenges to curing primary brain tumours . Nat. Rev. Clin. Oncol . 16 , 509–520. 10.1038/s41571-019-0177-5 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Birzu C., French P., Caccese M., Cerretti G., Idbaih A., Zagonel V., et al.. (2021). Recurrent glioblastoma: from molecular landscape to new treatment perspectives . Cancers 13 :47. 10.3390/cancers13010047 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brahm C. G., van Linde M. E. H, Enting R. H., Schuur M., Otten R. H. J., et al.. (2020). The current status of immune checkpoint inhibitors in neuro-oncology: a systematic review. Cancers 12 :586. 10.3390/cancers12030586 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chen X., Zhang M., Gan H., Wang H., Lee J. H., Fang D., et al.. (2018). A novel enhancer regulates MGMT expression and promotes temozolomide resistance in glioblastoma . Nat. Commun . 9 :2949. 10.1038/s41467-018-05373-4 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chovanec M., Abu Zaid M., Hanna N., El-Kouri N., Einhorn L. H., Albany C. (2017). Long-term toxicity of cisplatin in germ-cell tumor survivors . Ann.Oncol . 28 , 2670–2679. 10.1093/annonc/mdx360 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dahan P., Martinez Gala J., Delmas C., Monferran S., Malric L. (2014). Ionizing radiations sustain glioblastoma cell dedifferentiation to a stem-like phenotype through survivin: possible involvement in radioresistance . Cell. Death Dis . 5 :e1543. 10.1038/cddis.2014.509 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dasari S., Tchounwou P. B. (2014). Cisplatin in cancer therapy: molecular mechanisms of action . Eur. J. Pharmacol . 5 , 364–378. 10.1016/j.ejphar.2014.07.025 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Davis M. E. (2016). Glioblastoma: overview of disease and treatment . Clin. J. Oncol. Nurs . 20 , 2–8. 10.1188/16.CJON.S1.2-8 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ghouzlani A., Kandoussi S., Tall M., Reddy K. P., Rafii S., Badou A. (2021). Immune checkpoint inhibitors in human glioma microenvironment . Front. Immunol . 12 :679425. 10.3389/fimmu.2021.679425 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Goldbrunner R., Rug M., Kocher M., Lucas C. W., Galldiks N., Grau S. (2018). The treatment of gliomas in adulthood . Dtsch. Arztebl. Int . 115 , 356–364. 10.3238/arztebl.2018.0356 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hambardzumyan D., Bergers G. (2015). Glioblastoma: defining tumor niches . Trends Cancer 1 , 252–265. 10.1016/j.trecan.2015.10.009 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hanif F., Muzaffar K., Perveen K., Malhi S. M., Simjee S. U. (2017). Glioblastoma multiforme: a review of its epidemiology and pathogenesis through clinical presentation and treatment . Asian Pac. J. Cancer. Prev . 18 , 3–9. 10.22034/APJCP.2017.18.1.3 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Karasawa T., Steyger P. S. (2015). An integrated view of cisplatin-induced nephrotoxicity and ototoxicity . Toxicol. Lett . 237 , 219–227. 10.1016/j.toxlet.2015.06.012 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Laquintana V., Trapani A., Denora N., Wang F., Gallo J. M., Trapani G. (2009). New strategies to deliver anticancer drugs to brain tumors . Exp. Opin. Drug Deliv. 6 , 1017–1032. 10.1517/17425240903167942 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lee C. H., Cho J., Lee K. (2020). Tumour regression via integrative regulation of neurological, inflammatory, and hypoxic tumour microenvironment . Biomol. Ther . 28 , 119–130. 10.4062/biomolther.2019.135 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Liang J., Lv X., Lu C., Ye X., Chen X., Fu J., et al.. (2020). Prognostic factors of patients with gliomas - an analysis on 335 patients with glioblastoma and other forms of gliomas . BMC Cancer 20 :35. 10.1186/s12885-019-6511-6 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mckinney P. A. (2004). Brain tumours: incidence, survival, and aetiology . J. Neurol. Neurosurg. Psychiatry 75 ( Suppl. II ), ii12–ii17. 10.1136/jnnp.2004.040741 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ostrom Q. T., Cote D. J., Ascha M., Kruchko C., Barnholtz-Sloan J. S. (2018). Adult glioma incidence and survival by race or ethnicity in the United States from 2000 to 2014 . JAMA Oncol . 4 , 1254–1262. 10.1001/jamaoncol.2018.1789 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pérez J. E., Fritzell S., Kopecky J., Visse E., Darabi A., Siesjö P. (2019). The effect of locally delivered cisplatin is dependent on an intact immune function in an experimental glioma model . Sci. Rep . 9 :5632. 10.1038/s41598-019-42001-7 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ravanpay A. C., Gust J., Johnson A. J., Rolczynski L. S., Cecchini M., Chang C. A., et al.. (2019). EGFR806-CAR T cells selectively target a tumour-restricted EGFR epitope in glioblastoma . Oncotarget 10 , 7080–7095. 10.18632/oncotarget.27389 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shergalis A., Bankhead A., 3rd, Luesakul U., Muangsin N., Neamati N. (2018). Current challenges and opportunities in treating glioblastoma . Pharmacol. Rev . 70 , 412–445. 10.1124/pr.117.014944 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Staff N. P., Cavaletti G., Islam B., Lustberg M., Psimaras D., Tamburin S. (2019). Platinum-induced peripheral neurotoxicity: from pathogenesis to treatment . J. Peripher. Nerv. Syst . 24 , S26–S39. 10.1111/jns.12335 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Strobel H., Baisch T., Fitzel R., Schilberg K., Siegelin M. D., Karpel-Massler G., et al.. (2019). Temozolomide and other alkylating agents in glioblastoma therapy . Biomedicines 7 :69. 10.3390/biomedicines7030069 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Taylor O. G., Brzozowski J. S., Skelding K. A. (2019). Glioblastoma multiforme: an overview of emerging therapeutic targets . Front. Oncol. 9 :963. 10.3389/fonc.2019.00963 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Urbańska K., Sokołowska J., Szmidt M., Sysa P. (2014). Glioblastoma multiforme - an overview . Contemp. Oncol. 18 , 307–312. 10.5114/wo.2014.40559 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- van Tellingen O., Yetkin-Arik B., de Gooijer M. C., Wesseling P., Wurdinger T., de Vries H. E. (2015). Overcoming the blood-brain tumor barrier for effective glioblastoma treatment . Drug Resist. Updat . 19 , 1–12. 10.1016/j.drup.2015.02.002 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- von Neubeck C., Seidlitz A., Kitzler H. H., Beuthien-Baumann B., Krause M. (2015). Glioblastoma multiforme: emerging treatments and stratification markers beyond new drugs . Br. J. Radiol . 88 :20150354. 10.1259/bjr.20150354 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yekula A., Yekula A., Muralidharan K., Kang K., Carter B., Balaj L. (2020). Extracellular vesicles in glioblastoma tumor microenvironment . Front. Immunol . 10 :3137. 10.3389/fimmu.2019.03137 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Advances in Brain Tumor Clinical Care and Research
April 29, 2020 , by Brittany Cordeiro, NCI-CONNECT Program Manager
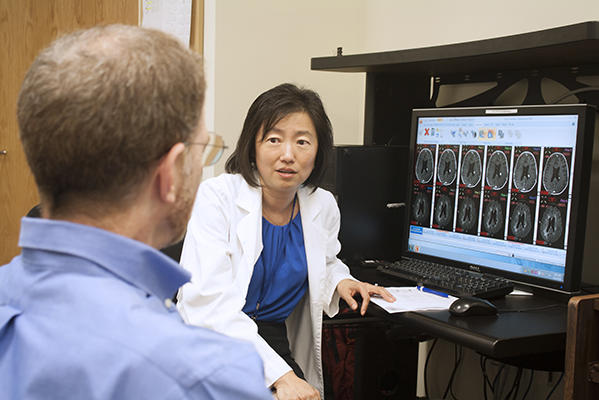
Dr. Jing Wu
The NCI Center for Cancer Research's Neuro-Oncology Branch is advancing care and treatment for people with brain tumors through collaborative scientific workshops, research discoveries, and successful clinical trials.
At the NCI Center for Cancer Research's Neuro-Oncology Branch (NOB), our neuro-oncology providers care for people with brain tumors. They also work with other specialists to improve treatments to help patients live longer and with a better quality of life.
Our neuro-oncology scientists work behind-the-scenes in labs to understand the biology of brain tumors. Their discoveries often lead to studies in people, or clinical trials. And a successful clinical trial can set a new treatment standard.
Together, our health care providers and scientists have made significant progress in clinical care and research for people with brain tumors. Read about our most recent accomplishments.
Collaborative Scientific Workshops and Meetings
NCI-CONNECT scientific workshops bring together brain cancer experts from around the world and across specialties—neuro-oncology, neuropathology, neurosurgery, and scientific research—with patient advocates to discuss the biology of a specific disease and find ways to collaborate to improve therapies and develop new clinical trials.
In 2018 and 2019, we successfully brought together health care providers, scientists, and advocates to discuss histone mutated (midline) gliomas, oligodendrogliomas, medulloblastomas, and ependymomas—and hosted a Clinical Outcomes Assessment Meeting. We also co-hosted the Fourth Biennial World Summit of Brain Tumor Patient Advocates.
Experts at the Histone Mutated Glioma Workshop identified the need for diagnostic and treatment standards, disease biology and biological targets, and disease-specific clinical trial designs. Their recommendations and action plan were published in Neuro-Oncology Advances in January 2020.
Participants at the Oligodendroglioma Workshop recognized the need to combine data, resources, and samples to develop better treatments for patients with oligodendrogliomas. Their recommendations and action plans were published in Neuro-Oncology Advances in December 2019 and include a multifaceted and interrelated approach that covers: biology and preclinical models, data sharing, advanced molecular diagnosis and imaging, clinical trial design, and patient outreach and engagement.
At the Medulloblastoma Workshop , participants reviewed advances in research and shared insights related to scientific and clinical challenges in studying and treating patients. Working groups identified unmet needs in clinical trial design, tissue acquisition and testing, tumor modeling, and measurement of clinical outcomes. Participants also identified opportunities for collaboration; discussed plans to create a working group of clinicians, researchers, and patient advocates; and developed specific action items and next steps to expedite progress in adult medulloblastoma.
The Fourth Biennial Ependymoma Consensus determined areas of research for ependymoma, including grading and diagnosing ependymoma, molecular and genetic testing , and clinical care and treatments to make progress in patient outcomes. With these goals and strategies, participants will collaborate to more effectively address these issues.
Participants at the Clinical Outcomes Assessment Meeting discussed the importance of incorporating—in both clinical care and clinical research—how a person with a brain tumor feels and functions. People with brain and spine tumors often struggle with many functional limitations and experience symptoms that negatively impact their daily lives. This group, representing clinical care experts, advocates, and clinical trial experts, developed core symptoms and functions that should be assessed. Input from the meeting was used to publish a paper in Lancet Oncology .
The Fourth Biennial World Summit of Brain Tumour Patient Advocates was co-hosted with the International Brain Tumour Alliance. It brought together 96 patient advocates from 25 countries around the world and leaders in neuro-oncology for three days. It was focused on the most important topics for the patient advocacy community, including treatment advances, quality of life measures, support and education resources, and more.
The success of our scientific workshops shows the importance of community collaborations. It encourages and motivates the development of partnerships and networks for the care of people with brain tumors.
Discoveries in Tumor Biology
In brain tumor research, NOB Investigators Orieta Celiku, Ph.D., Mark Gilbert, M.D. (NOB chief), and Orit Lavi, Ph.D., studied how glioblastoma cells can evolve over time through exploratory adaptation. This concept explains how organisms, including cancer cells, adapt and survive in stressful or new conditions. Being able to predict how these changes occur is a crucial step to increasing patient survival. The findings were published in Nature Communications in December 2019. This is an important step to understanding various parts of the tumor and how cells change or regrow after surgery, which is the first and best treatment option to increase patient survival in glioblastoma.
Another NOB investigator, Chunzhang Yang, Ph.D. , discovered a new strategy for treating brain tumors with mutations in metabolic enzymes. He found that cancers with mutations in key metabolic enzymes , called isocitrate dehydrogenases (IDHs), disrupt normal oxygen metabolism. This leads to a buildup of a byproduct known as reactive oxygen species .
Using a preclinical model, Dr. Yang showed that a small molecule could inhibit the action of a protein that allows mutated cancer cells to survive. His findings were published in the Journal of the National Cancer Institute in February 2019 and introduce conceptual advances in the understanding of IDH-related malignancies.
Progress in Clinical Care and Outcomes
NOB Deputy Chief Terri Armstrong, Ph.D., studies how patients feel and function during clinical trials. This includes what symptoms they experience, as well as when and how these symptoms impact their daily activities.
In a new study published in Lancet Oncology in February 2020, Dr. Armstrong showed how including specific data on how patients function and their symptoms in clinical trials can help determine the benefit of a trial. The study combined input from patients and their families, literature, and clinical groups to develop a standard list of recommended outcomes. The next steps are to formally establish these outcomes in all clinical trials.
Another remarkable feat was led by NOB Investigator Jing Wu, M.D., Ph.D . In December 2019, the U.S. Food and Drug Administration granted orphan drug status to zotiraciclib for use in patients with glioma. Gliomas comprise about 30 percent of all brain and central nervous system (CNS) tumors and 80 percent of all cancerous brain tumors. The types of gliomas include astrocytoma, ependymoma, glioblastoma, and oligodendroglioma.
This designation is based on results from Dr. Wu’s phase 1 clinical trial to evaluate zotiraciclib plus temozolomide for the treatment of recurrent anaplastic astrocytoma and glioblastoma. Dr. Wu’s team is now working with Dr. Gilbert to open a phase 2 study of zotiraciclib plus temozolomide versus temozolomide alone in recurrent high grade glioma patients.
Importantly, Dr. Armstrong, Dr. Gilbert and NOB Neuro-Oncologist Marta Penas-Prado, M.D., reviewed the recent progress in the molecular understanding and therapeutic options of select rare CNS tumors. The paper , published in Current Opinions in Neurology in December 2019, was designed to present an overview of the current state of the science related to patient care and tumor treatment. They concluded there is a need for dedicated clinical trials with a strong correlative component in patients of all ages with rare CNS tumors. Critical research questions include relevance of the selected target for specific tumor types, persistence of the actionable biomarker at recurrence, blood-brain barrier penetration, and analysis of mechanisms of primary and acquired resistance.
Improving Ependymoma Treatment Guidelines
Ependymoma is a rare tumor for which the role of chemotherapy has not been established—either for newly diagnosed or recurrent disease. Dr. Gilbert led the first prospective adult clinical trial of chemotherapy for recurrent ependymoma. The trial treated 50 adult patients with temozolomide and lapatinib.
Results from this study, published in Neuro-Oncology in November 2018, demonstrated evidence of clinical activity, including objective responses and a nearly 40 percent stable disease rate at one year. Importantly, even in those with stable disease, patients undergoing this treatment had improvement in disease-related symptoms and stable-to-improved functional status. This combination regimen was so well tolerated that it has been endorsed by the National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines in Oncology as a standard treatment for adult patients with recurrent ependymoma. "This is a major step to providing hope for ependymoma and other rare brain and spine tumors," says Dr. Gilbert.
Our scientific and clinical care progress exemplifies the impact doctors, nurses, and researchers across the world can make when they come together. Brain tumors are challenging to understand and treat, but with focused collaborations we can continue to improve care and treatment.

- University News
- Faculty & Research
- Health & Medicine
- Science & Technology
- Social Sciences
- Humanities & Arts
- Students & Alumni
- Arts & Culture
- Sports & Athletics
- The Professions
- International
- New England Guide
The Magazine
- Current Issue
- Past Issues
Class Notes & Obituaries
- Browse Class Notes
- Browse Obituaries
Collections
- Commencement
- The Context
Harvard Squared
- Harvard in the Headlines
Support Harvard Magazine
- Why We Need Your Support
- How We Are Funded
- Ways to Support the Magazine
- Special Gifts
- Behind the Scenes
Classifieds
- Vacation Rentals & Travel
- Real Estate
- Products & Services
- Harvard Authors’ Bookshelf
- Education & Enrichment Resource
- Ad Prices & Information
- Place An Ad
Follow Harvard Magazine:
Right Now | Tumor Tumescence
The Brain-Cancer Link
November-December 2023
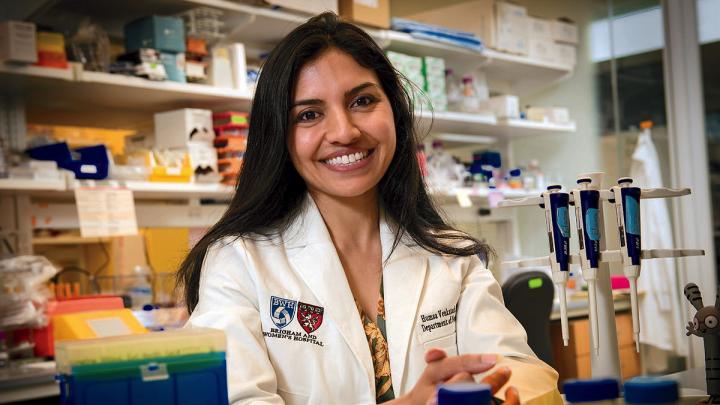
Humsa Venkatesh | Photograph by Stu Rosner
Humsa Venkatesh website
During the past two decades, the number of annual cancer deaths in the United States has fallen by 27 percent, a remarkable improvement driven by new precision diagnoses and treatments tailored to individual patients. Today, oncologists can detect cancer in its earliest stages and deliver drugs that enlist the patient’s own immune system to improve their odds of survival. Yet cancer remains the second deadliest disease in the United States, claiming more than 600,000 lives every year. Its persistence underscores the urgent need for a deeper understanding of how cancer interacts with the body. Assistant professor of neurology Humsa Venkatesh believes she may have found a promising new pathway for highly effective cancer treatments in the most unexpected of places: the human brain.
Venkatesh and her colleagues have been pioneering a new approach to oncology that she calls “cancer neuroscience,” focused on understanding the bidirectional relationship between cancer and the brain. Although researchers first observed that nerves are numerous around cancer tumors nearly a century ago, Venkatesh says this link was “largely ignored” as oncologists focused instead on the molecular and genetic features of cancer that could be targeted with precision drugs.
“Cancer biologists and neuroscientists were just in completely different worlds and never really crossed paths,” she says. “But over the past few decades, science has become extraordinarily interdisciplinary as communication and technology barriers began to fall.”
While pursuing a Ph.D. in cancer biology from Stanford, Venkatesh launched a series of experiments that applied neuroscientific tools and techniques to brain tumors for the first time. It was a high-risk gamble for an early career scientist entering a field that was largely focused on personalized cancer treatments, but what she found out about the link between cancer and the nervous system launched a new field of cancer research.
About a decade ago, she and her collaborators sought to determine whether increased neural activity promotes or inhibits the growth of gliomas, a type of cancer that originates in the brain. They used optogenetics—a method for precisely stimulating neural circuits using light and genetic engineering—to activate brain regions around a glioma and found that increased neural activity resulted in robust growth of brain tumors. “It was really the first evidence ever that neural activity can drive tumor growth, and we were really excited by those results,” Venkatesh said. “The next big question was, why does this occur?”
To resolve this mystery, she needed to think like a detective, using neuroscience tools to “wiretap” the communication channels between neurons and cancer cells to eavesdrop on their cryptic communications. After a few years of detailed observation, she had her answer. The heightened neural activity Venkatesh had induced in previous experiments caused the brain to produce a protein called neuroligin-3. When this protein interacted with glioma cells, it stimulated cell division, causing the tumor to grow.
This alone wasn’t particularly surprising. Proteins that stimulate cell growth are known as mitogens, and researchers have identified hundreds that play a role in tumor growth. But given the strong link between heightened neural activity and tumor growth, it didn’t seem far-fetched that this particular mitogen—neuroligin-3—might be the linchpin driving glioma growth. If true, reducing the amount of neuroligin-3 produced in the brain might stop the growth of the tumor altogether. When Venkatesh and her colleagues tested this theory in mice genetically modified not to produce neuroligin-3, “We found that the lack of this single protein completely abrogates the tumor’s ability to grow,” she said. “For those of us who work in cancer research, that’s really, really astounding. We know there are several mitogens at play that promote tumor growth, so if we take one away, we might expect some growth inhibition, but not something this stark.”
As Venkatesh dug deeper into neuroligin-3’s role in the brain, she realized that, beyond its known role of stimulating cell growth, this protein also helps neurons communicate. When it interacts with a cancer cell, neuroligin-3 enables that cell to communicate with other neurons as if it were a healthy cell. Even more surprising was the discovery that this communication was bidirectional: increased neural activity led to faster tumor growth, and faster tumor growth caused more electrical activity in healthy neurons.
“These tumors are essentially hijacking our normal brain mechanisms for abnormal neuroplasticity,” said Venkatesh. “This was the first time we had seen these bursts of electrical activity in malignant tumor tissue.This was a characteristic of tumor pathophysiology we had been missing.”
How to translate these exciting results in mice into a clinical treatment wasn’t obvious. Although several drugs—including antiepileptics and antidepressants—change the way neurons communicate, they target the entire nervous system and may have significant “off-target” effects. To treat gliomas, Venkatesh wanted a drug that would specifically target cancer by reducing the production of neuroligin-3. After a long search, she and her colleagues found one that appeared perfect for the job; it is being tested in a Phase I clinical trial in children with recurrent aggressive brain cancers.
“We’ve tested it in preclinical models in the lab, and we seem to have some really positive results,” Venkatesh said. “I don’t think that it’s going to be a silver bullet, but I think it could perhaps ameliorate the effects by lessening the overall amount of neuroligin-3 in the brain.”
As the researchers wait for the clinical trial’s results next summer, they’re exploring whether their results can be generalized to cancers outside the brain. Their first target is small-cell lung cancers, the most aggressive form of the deadliest type of cancer. It’s a natural next step, given that these malignancies tend to arise from “pulmonary neuroendocrine cells,” which have many features similar to neurons. This may explain why small-cell lung cancers have very high odds of metastasizing to the brain—a longstanding mystery in oncology—and makes them a promising starting place for understanding how neural activity affects cancers elsewhere in the body.
Venkatesh says it’s too early to tell how widely her results will translate to other tumors outside the brain, but the growing body of evidence she and her colleagues have accumulated has made her optimistic that cancer neuroscience will have an important role to play in developing new therapies that could save the lives of countless patients. Cancer researchers are, by nature, cautious of hyping novel therapies given the field’s long history of would-be cures falling short of their promise. Cancers, like the brain, are remarkably complex and no single approach is likely to rid the world of these deadly diseases. But after a decade of breakthrough after breakthrough, Venkatesh seems hardly able to contain her excitement about the future of cancer neuroscience. “The more I think about it, the more I appreciate how wild it is that we hadn’t gone down this path yet,” she says. “The field has been gaining so much momentum, and that’s just so exciting to see as one of the people who was lucky enough to be a pioneer in this space.”
You might also like

Harvard Reiterates Campus Rules
As fall semester begins, the University executive vice president underscores the limits to protest.

Rakesh Khurana To Step Down
The College dean will retire next June.

Alan Garber’s Opening Words
Harvard president welcomes students, foresees conflict in the year ahead.
Most popular
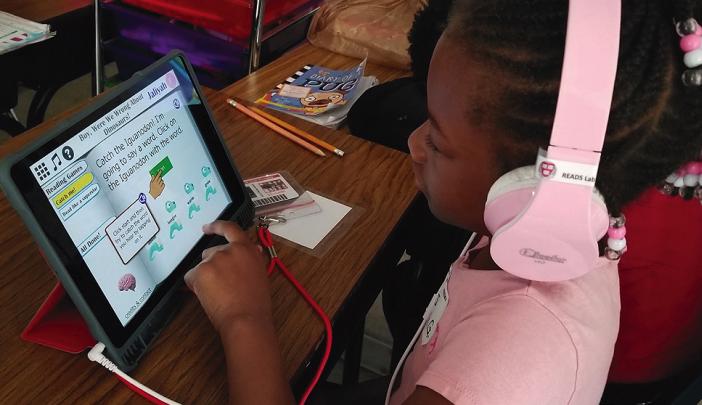
A Right Way to Read?
The science, art, and politics of teaching an essential skill

In Search of the Social Microbiome
The microbiome may be socially exchanged, modulating both health and metabolism.

The Power of Patience
Teaching students the value of deceleration and immersive attention
More to explore

What is the Economic Impact of Climate Change on Global GDP?
The impact on global GDP is likely six times greater than previously estimated.
Art Made Out of Buttons
Works by Harlem-based artist Beau McCall at Brockton's Fuller Craft Museum

John Harvard's Journal
Susan Farbstein on Human Rights Law
Human rights lawyer on law’s ability to promote justice—and shape public understanding
- See us on facebook
- See us on twitter
- See us on youtube
- See us on linkedin
- See us on instagram
A new branch of oncology, cancer neuroscience, offers hope for hard-to-treat brain tumors
To drive their growth, many tumors hijack nervous system signals, including those needed for brain plasticity. Stanford Medicine discoveries are opening a promising new branch of oncology research.
November 1, 2023 - By Erin Digitale

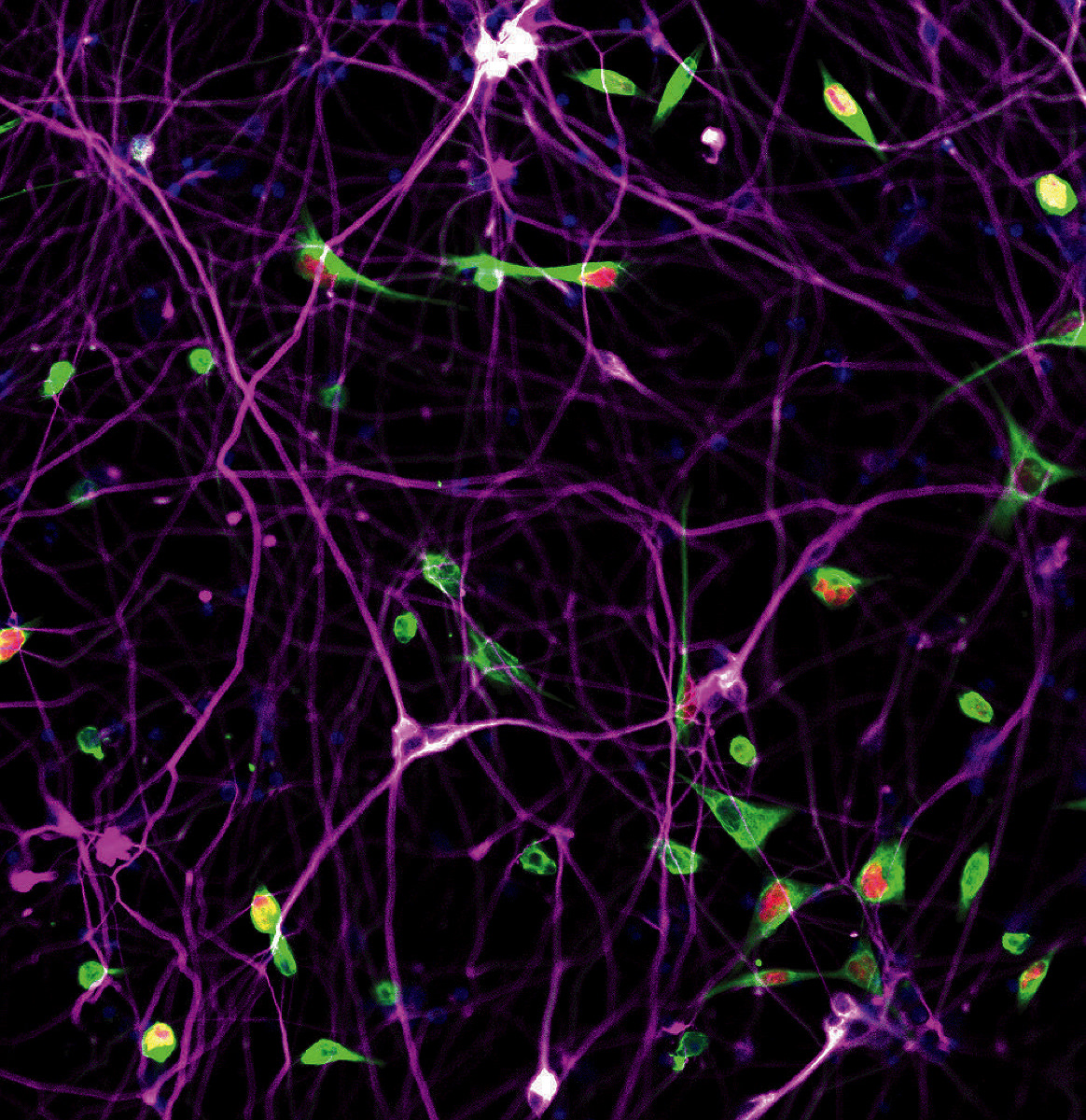
Michelle Monje's team has found that brain tumors can exploit the biological machinery of brain plasticity to drive their own growth. Timothy Archibald
Cancer cells hijack normal biological processes, allowing them to multiply. For example, tumors spur construction of new blood vessels, building themselves “highways” to supply nutrients.
Researchers have known about cancer’s blood vessel infiltration for decades, but it was only in the past few years that Stanford Medicine scientists and their colleagues discovered that tumors don’t just tap the body’s highway system; they can also infiltrate and exploit its “telecommunications.”
To put it in physiologic terms, tumors don’t just grow blood vessels; they also wire themselves into the nervous system. Certain brain cancers form working electrical connections with nearby nerves, then use the nerves’ electrical signals for their own purposes, the research has shown. The latest findings , published Nov. 1 in Nature , demonstrate that these tumors can even hijack the biological machinery of brain plasticity — which enables learning — to drive their own growth.
The discoveries have opened a novel field of medicine called cancer neuroscience. It offers new opportunities to target some of the deadliest forms of cancer, including brain tumors that are almost always lethal. Scientists are especially intrigued by the cancer treatment potential of FDA-approved drugs developed for other neurological disorders, such as epilepsy. It turns out that several such medications interrupt neural signals now understood to fuel certain cancers.
“Since 2015, when we first published that neuronal activity actually drives the growth of cancer in multiple brain tumor types, there has been a very exciting explosion of studies on these interactions,” said Michelle Monje , MD, PhD, a professor of neurology and neurological sciences and senior author of the new Nature study, whose team’s discoveries form the foundation of cancer neuroscience. “This is clearly a major set of interactions crucial to tumor biology that we had missed.”
Tumors’ hidden talent
Why did cancer’s ability to twine into the nervous system stay hidden from researchers for so long? A focus on how malignant and healthy cells differ may provide an explanation.
“People tend to think of cancer as more like an infectious disease, something that’s occurring but has nothing really to do with our body,” said Kathryn Taylor , PhD, lead author of the Nature study and a postdoctoral scholar in neurology and neurological sciences. “Whereas really, particularly in pediatric tumors, it’s a developmental disease.”

Kathryn Taylor
Small missteps in development underlie some of the worst childhood tumors, Monje’s team has shown.
This is true of one especially horrible type of brain cancer, diffuse intrinsic pontine glioma. Known as a high-grade glioma, DIPG arises in the brainstem that controls essential body functions such as breathing and heartbeat. It entwines with healthy cells, meaning it can’t be removed surgically. The five-year survival rate is 1%.
In 2011, Monje showed that DIPG arises from a type of healthy brain cells called oligodendrocyte precursor cells. Normally, OPCs develop into brain cells that produce insulating myelin, a substance that coats nerves and speeds up their electrical signals. This “neuron maintenance” job requires the healthy cells to stay in close communication with adjacent neurons, receiving and responding to neurons’ electrical and chemical signals.
DIPG cells respond to the same signals, but use them to fuel malignant growth, Monje’s team has demonstrated.
“The cancer is diffusely and widely invading the nervous system because that’s advantageous for it,” Monje said. “It integrates into neural circuits.”
Hardwired into the brain
In 2019, Monje’s team published a groundbreaking study showing that DIPG and similar cancers form working synapses with neurons. Synapses are the nervous-system widgets that allow electrical signals to cross the gaps between one cell and the next. Via these connections and additional means of electrical signaling, about half of all glioma cells in a given tumor have some type of electrical response to signals from healthy neurons, the research showed.
Adjacent brain cells also signal to each other with proteins that cross the space between cells to trigger complex intracellular responses. Such responses include molecular signals that underlie the neural plasticity needed for learning and memory. (The brain physically changes as we learn; these signals are part of that change.)
The new study investigates tumor responses to brain-derived neurotrophic factor, or BDNF, a protein that helps enable brain plasticity. With BDNF, the brain can strengthen synaptic connections between cells, enforcing a neural circuit that’s built as we learn.
The tumors use BDNF the same way healthy brain cells do, the researchers showed: BDNF travels from neurons to tumor cells to trigger a chain reaction inside the tumor that ultimately helps the tumor form more and stronger synapses.
During the studies of BDNF, which Taylor led, one key experiment showed that when the cell machinery triggered by BDNF was activated more strongly, the tumor cells responded with stronger electrical currents, which then fueled their growth. In other words, cancer uses the brain’s learning machinery to grow.
“We looked at the electrophysiological recordings and seeing this increase was … I will never forget that. It was pretty incredible,” Taylor said. “What was so striking about that finding was that not only can the cells connect, they also dynamically respond to input from healthy brain cells. The tumor cell is not only plugging into the network, it’s increasing its connection to that plug.”
Prior research by Monje’s team showed that another mechanism involved in neural plasticity, driven by a signaling molecule called neuroligin 3, works independently of BDNF to also increase neuron-to-glioma synapses.
It’s unsettling that tumors use brain activity to grow, Taylor admits. “It’s the same electrical activity that helps us think, move, feel, touch and see,” she said. “Cancer is plugging into that and using that to grow, invade and even occur in the first place.”
Hope for treatment
But understanding these unsettling interactions between tumors and the healthy nervous system presents new options for cancer treatment.
In the Nature study, Taylor, Monje and their team showed that medications aimed at the BDNF receptor, which were developed for other forms of cancer that have mutations affecting the receptor, work surprisingly well at slowing the growth of DIPG and other gliomas that do not typically have genetic alterations in that receptor.
We understand enough about this disease now to have lots of really rational ways to try to fight it.
Other drugs, including certain painkillers, anti-seizure medications and blood pressure medications also have potential as cancer fighters. A detailed understanding of how the tumors tap nerve signals to grow provides a huge leg up in cancer treatment research, as scientists can match what’s in the “medicine cabinet” of FDA-approved neuroactive drugs with their new knowledge of how cancers operate.
Stopping the worst gliomas, including DIPG, will require a mixture of tactics, from cancer neuroscience and from other oncology specialties, Monje said. Perhaps doctors can start treatment with neurological medications that slow the tumors’ growth, then give immunotherapies — such as specially engineered immune cells called CAR-T cells, which her team is also studying as a treatment for DIPG — as a second line of attack. Such a strategy might give immunotherapy treatments enough of a head start to enable them to outpace the rapidly growing tumors.
Monje’s team also plans to learn more about how electrical currents prompt tumor growth. “As we uncover granular details of those voltage-sensitive mechanisms, that will open up a whole additional realm of potential therapeutic targets,” she said.
Cancer neuroscience is also offering clues about how to tackle tumors outside the brain. Nerves normally send signals to stem cells that help regulate healthy organ development and repair, and research is increasingly documenting that these signals can fuel cancer. “There are critically important roles for the nervous system in pancreas, prostate, breast, colon, gastric, skin, and head and neck cancers — a very long list,” Monje said, adding that there’s also evidence that tumors that began outside the nervous system can piggyback on normal nerve signals once they invade the brain.
Hope for the future
For Monje, who was inspired to study DIPG more than 20 years ago, at a time when the biology of the disease was completely unknown, the new options are heartening. The old way of trying to treat the deadly tumor — a sort of throw-the-spaghetti-at-the-wall approach, using drugs not fitted to how the tumor grows — is obsolete, she said.
“This is a connected tumor; it’s connecting to the entire nervous system. We have to disconnect it,” she said. “We understand enough about this disease now to have lots of really rational ways to try to fight it.”
Researchers contributed to the new study from the Weizmann Institute of Science in Rehovot, Israel; Massachusetts General Hospital; Harvard Medical School; and the Broad Institute, a collaboration of the Massachusetts Institute of Technology and Harvard.
The study was funded by grants from the National Institute of Neurological Disorders and Stroke (grant R01NS092597), the NIH Director’s Pioneer Award (DP1NS111132), the National Cancer Institute (P50CA165962, R01CA258384 and U19CA265404), Abbie’s Army, the Robert J. Kleberg Jr. and Helen C. Kleberg Foundation, the Gatsby Charitable Foundation, Cancer Research UK, Damon Runyon Cancer Research, ChadTough Defeat DIPG, the Stanford Maternal and Child Health Research Institute, N8 Foundation, the McKenna Claire Foundation, the Kyle O’Connell Foundation, the Virginia and D.K. Ludwig Fund for Cancer Research, the Waxman Family Research Fun, and the Will Irwin Research Fund.

About Stanford Medicine
Stanford Medicine is an integrated academic health system comprising the Stanford School of Medicine and adult and pediatric health care delivery systems. Together, they harness the full potential of biomedicine through collaborative research, education and clinical care for patients. For more information, please visit med.stanford.edu .
The majestic cell
How the smallest units of life determine our health


- Adolescent and Young Adult Cancer
- Bile Duct Cancer
- Bladder Cancer
- Brain Cancer
- Breast Cancer
- Cervical Cancer
- Childhood Cancer
- Colorectal Cancer
- Endometrial Cancer
- Esophageal Cancer
- Head and Neck Cancer
- Kidney Cancer
- Liver Cancer
- Lung Cancer
- Mouth Cancer
- Mesothelioma
- Multiple Myeloma
- Neuroendocrine Tumors
- Ovarian Cancer
- Pancreatic Cancer
- Prostate Cancer
- Skin Cancer/Melanoma
- Stomach Cancer
- Testicular Cancer
- Throat Cancer
- Thyroid Cancer
- Prevention and Screening
- Diagnosis and Treatment
- Research and Clinical Trials
- Survivorship

Request an appointment at Mayo Clinic

Brain tumors: What you should know
Share this:.
Primary brain tumors originate in the brain or tissues close to the brain, such as in brain-covering membranes, cranial nerves, or the pituitary or pineal glands. There are many types of primary brain tumors, and over 84,000 people will receive a primary brain tumor diagnosis in 2021, according to the National Brain Tumor Society. The median age for these diagnoses is 60.
The most common cancerous, or malignant, brain tumor is the glioblastoma , a type of glioma that begins in the brain or spinal cord. The most common primary noncancerous, or benign, brain tumor is the meningioma , which arises from the membranes that surround the brain and spinal cord.
On this "Mayo Clinic Q&A" podcast, Dr. Alyx Porter , co-chair of the Central Nervous System Tumor Disease Group at Mayo Clinic Cancer Center , discusses the various types of brain tumors and how they are diagnosed and treated:
_________________________________________
For the safety of its patients, staff and visitors, Mayo Clinic has strict masking policies in place. Anyone shown without a mask was either recorded prior to COVID-19 or recorded in a nonpatient care area where social distancing and other safety protocols were followed.
A version of this article originally appeared on the Mayo Clinic News Network .
Learn more about brain tumors and find a brain tumor clinical trial at Mayo Clinic.
Join the Brain Tumor Group on Mayo Clinic Connect.
Also read these articles:
- " Glioblastoma in older adults: improving survival and quality of life "
- " Complex brain surgery gives woman more time with family "
- " New therapies, holistic modalities and hope help photographer see future "
Related Posts

A former gymnast and a cancer survivor, Dr. Allison Rosenthal has a history of helping athletes return to sports after cancer.

Study results showed significantly higher survival rates when blinatumomab was added to chemotherapy for people with B-cell acute lymphoblastic leukemia.

Dr. Collin Costello explains how to spot the most common nonmelanoma skin cancers: basal cell carcinoma and squamous cell carcinoma.

New Technique Shows Promise in Fighting Brain Cancer
Summary: Researchers developed a new method, burst sine wave electroporation (B-SWE), to treat glioblastoma, a fast-growing brain tumor. B-SWE disrupts the blood-brain barrier more effectively than traditional methods, allowing cancer drugs better access to the brain.
This technique could enhance treatment by minimizing damage to healthy brain tissue while targeting cancer cells. The study highlights a promising advance in brain cancer therapy.
- B-SWE disrupts the blood-brain barrier more effectively than conventional methods.
- The technique may allow more cancer-fighting drugs to enter the brain.
- B-SWE minimizes damage to healthy brain tissue while targeting cancer cells.
Source: Virginia Tech
Tackling brain cancer is complicated, but groundbreaking new research could help add another tool to the cancer-fighting arsenal.
A team from Georgia Tech and Virginia Tech published a paper in APL Bioengineering in May that explores a new option that could one day be used to target glioblastoma, a deadly and fast-growing brain tumor.
Supported by National Institutes of Health grants, this work stems from past research on high frequency irreversible electroporation, better known as H-FIRE. H-FIRE is a minimally invasive process that uses non-thermal electrical pulses to break down cancer cells.

Treating any type of cancer isn’t easy, but when it comes to brain cancers, the blood-brain barrier adds an extra challenge. The barrier defends the brain against toxic material — but that’s not always a positive thing.
“Mother Nature designed it to prevent us from poisoning ourselves, but unfortunately, the way that works, it also excludes about 99 percent of all small-molecule drugs from entering the brain and achieving adequate concentrations to elucidate their therapeutic effect. That’s particularly true for chemotherapeutics, biologics, or immunotherapies,” said John Rossmeisl, the Dr. and Mrs. Dorsey Taylor Mahin Professor of Neurology and Neurosurgery at the Virginia-Maryland College of Veterinary Medicine. Rossmeisl is one of the paper’s coauthors.
The square-shaped wave typically used with H-FIRE performs double dut: It disrupts the blood-brain barrier around the tumor site while destroying cancer cells. However, this was the first study to use a sinusoidal wave to disrupt the barrier. This new modality is called burst sine wave electroporation (B-SWE).
The researchers used a rodent model to study the effects of the sinusoidal wave versus the more conventional, square-shaped wave. They found that B-SWE resulted in less damage to cells and tissue but more disruption of the blood-brain barrier.
In some clinical cases, both ablation and blood-brain barrier disruption would be ideal, but in others, blood-brain barrier disruption may be more important than destroying cells.
For example, if a neurosurgeon removed the visible tumor mass, the sinusoidal waveform could potentially be used to disrupt the blood-brain barrier around the site, allowing drugs to enter the brain and eliminate the last of the cancer cells. B-SWE could result in minimal damage to the healthy brain tissue.
Research indicates that the conventional square waveforms show good blood-brain barrier disruption, but this study finds even better blood-brain barrier disruption with B-SWE. This could allow more cancer-fighting drugs to access the brain.
“We thought we had that problem solved, but this shows you that with some forward thinking, there’s always potentially better solutions,” said Rossmeisl, who also serves as associate head of the Department of Small Animal Clinical Sciences.
During the study, the researchers hit a snag: In addition to more blood-brain barrier disruption, they found that the sinusoidal wave also caused more neuromuscular contractions.
These muscle contractions run the risk of damaging the organ. However, by tweaking the dose of B-SWE, they were able to reduce the contractions while providing a level of blood-brain barrier disruption similar to that of a higher dose.
The next step in this research is to study the effects of B-SWE using an animal model of brain cancer to see how the sinusoidal waveform stands up against the conventional H-FIRE technique.
The project was spearheaded by first author Sabrina Campelo while she completed her Ph.D. at the Virginia Tech-Wake Forest University School of Biomedical Engineering and Sciences. Campelo is now a postdoctoral fellow at the Wallace H. Coulter Department of Biomedical Engineering at Georgia Tech and Emory University.
About this brain cancer research news
Author: Andrew Mann Source: Virginia Tech Contact: Andrew Mann – Virginia Tech Image: The image is credited to Neuroscience News
Original Research: Open access. “ Burst sine wave electroporation (B-SWE) for expansive blood–brain barrier disruption and controlled non-thermal tissue ablation for neurological disease ” by John Rossmeisl et al. ALP Bioengineering
Burst sine wave electroporation (B-SWE) for expansive blood–brain barrier disruption and controlled non-thermal tissue ablation for neurological disease
The blood–brain barrier (BBB) limits the efficacy of treatments for malignant brain tumors, necessitating innovative approaches to breach the barrier.
This study introduces burst sine wave electroporation (B-SWE) as a strategic modality for controlled BBB disruption without extensive tissue ablation and compares it against conventional pulsed square wave electroporation-based technologies such as high-frequency irreversible electroporation (H-FIRE).
Using an in vivo rodent model, B-SWE and H-FIRE effects on BBB disruption, tissue ablation, and neuromuscular contractions are compared.
Equivalent waveforms were designed for direct comparison between the two pulsing schemes, revealing that B-SWE induces larger BBB disruption volumes while minimizing tissue ablation.
While B-SWE exhibited heightened neuromuscular contractions when compared to equivalent H-FIRE waveforms, an additional low-dose B-SWE group demonstrated that a reduced potential can achieve similar levels of BBB disruption while minimizing neuromuscular contractions.
Repair kinetics indicated faster closure post B-SWE-induced BBB disruption when compared to equivalent H-FIRE protocols, emphasizing B-SWE’s transient and controllable nature.
Additionally, finite element modeling illustrated the potential for extensive BBB disruption while reducing ablation using B-SWE.
B-SWE presents a promising avenue for tailored BBB disruption with minimal tissue ablation, offering a nuanced approach for glioblastoma treatment and beyond.
Tau May Protect Brain Cells from Oxidative Damage

Morphine’s Pain Relief Mechanism Unveiled

Dogs Using Soundboard Buttons Understand Words

How We Recognize Words in Real-Time
Masks Strongly Recommended but Not Required in Maryland, Starting Immediately
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines

Brain Tumors and Brain Cancer
There are over 120 brain tumor types, based on the brain tissues they affect. not all brain tumors are brain cancer, but even benign (or noncancerous) tumors can be dangerous because of their size or location..
What is a brain tumor? | What is brain cancer? | Symptoms | Causes | Locations and Types | Brain Tumors in Children | Diagnosis | Treatment | Prognosis
What is a brain tumor?
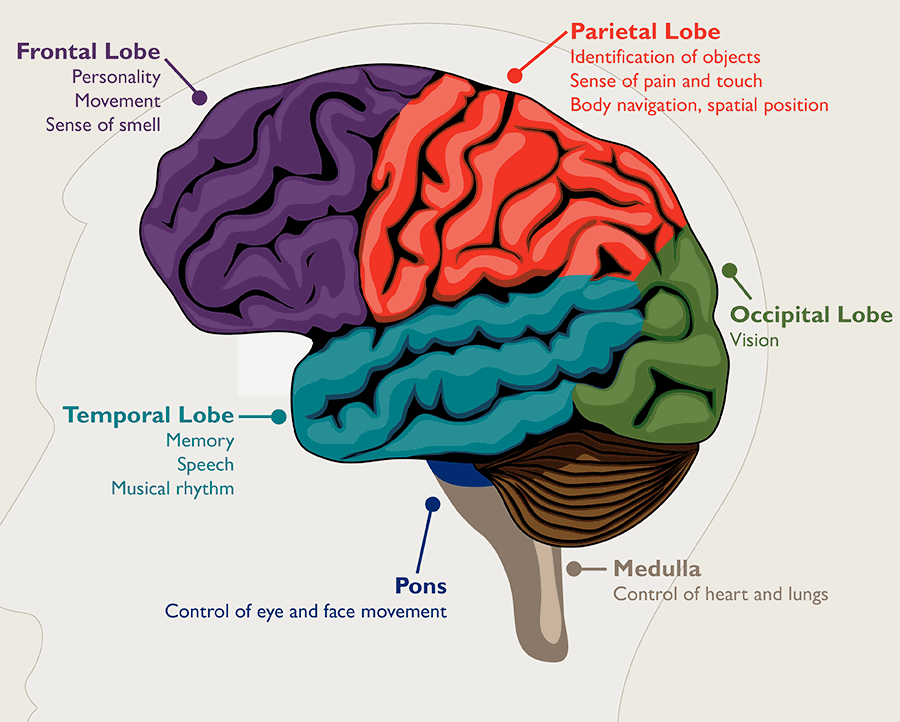
A brain tumor is a growth of abnormal cells in the brain. The anatomy of the brain is very complex, with different parts responsible for different nervous system functions. Brain tumors can develop in any part of the brain or skull, including its protective lining, the underside of the brain ( skull base ), the brainstem, the sinuses and the nasal cavity, and many other areas. There are more than 120 different types of tumors that can develop in the brain , depending on what tissue they arise from.
How common are brain tumors, and are they dangerous?
In the United States, brain and nervous system tumors affect about 30 adults out of 100,000. Brain tumors are dangerous because they can put pressure on healthy parts of the brain or spread into those areas. Some brain tumors can also be cancerous or become cancerous. They can cause problems if they block the flow of fluid around the brain, which can lead to an increase in pressure inside the skull. Some types of tumors can spread through the spinal fluid to distant areas of the brain or the spine.
Related Video

Brain Tumors: Frequently Asked Questions | Jon Weingart, M.D.
How is a tumor different from a brain lesion.
A brain tumor is a specific type of brain lesion. A lesion describes any area of damaged tissue. All tumors are lesions, but not all lesions are tumors. Other brain lesions can be caused by stroke , injury , encephalitis and arteriovenous malformation .
Brain Tumor vs. Brain Cancer
All brain cancers are tumors, but not all brain tumors are cancerous. Noncancerous brain tumors are called benign brain tumors.
Benign brain tumors typically grow slowly, have distinct borders and rarely spread. Benign tumors can still be dangerous. They can damage and compress parts of the brain, causing severe dysfunction. Benign brain tumors located in a vital area of the brain can be life-threatening. Very rarely, a benign tumor can become malignant. Examples of typically benign tumors include meningioma , vestibular schwannoma and pituitary adenoma.
Malignant brain tumors are cancerous. They typically grow rapidly and invade surrounding healthy brain structures. Brain cancer can be life-threatening due to the changes it causes to the vital structures of the brain. Some examples of malignant tumors that originate in or near the brain include olfactory neuroblastoma , chondrosarcoma and medulloblastoma .
Primary vs. Metastatic Brain Tumors
Primary brain tumors are tumors that start in the brain. Examples of tumors that most often originate in the brain include meningioma and glioma. Very rarely, these tumors can break away and spread to other parts of the brain and spinal cord. More commonly, tumors spread to the brain from other parts of the body.
Metastatic brain tumors , also called secondary brain tumors, are malignant tumors that originate as cancer elsewhere in the body and then metastasize (spread) to the brain. Metastatic brain tumors are about four times more common than primary brain tumors. They can grow rapidly, crowding or invading nearby brain tissue.
Common cancers that can spread to the brain are:
- Breast cancer
- Colon cancer
- Kidney cancer
- Lung cancer
- Skin cancer (melanoma)
Brain Tumor Locations
Brain tumors can form in any part of the brain , but there are certain regions where specific tumors form:
- Meningiomas form in the meninges, the protective lining of the brain.
- Pituitary tumors develop in the pituitary gland.
- Medulloblastoma tumors arise from the cerebellum or brainstem.
- Skull base tumors grow on the underside of the brain, called the skull base.
Other brain tumors are described by the kinds of cells they are made of. For instance, gliomas are composed of glial cells.
Learn more about these and other brain tumor types.
Brain Tumors in Children
Brain tumors are the most common solid tumor in children and adolescents, affecting about 5,000 children in the U.S. each year. Several different types of brain tumors can occur in children, including astrocytomas (e.g., glioblastoma multiforme), gliomas, ependymomas and medulloblastomas.
Learn more about brain tumors in children .
Brain Tumor Symptoms
Different parts of the brain control different functions, so brain tumor symptoms will vary depending on the tumor’s location. For example, a brain tumor located in the cerebellum at the back of the head may cause trouble with movement, walking, balance and coordination. If the tumor affects the optic pathway, which is responsible for sight, vision changes may occur.
The tumor’s size and how fast it’s growing also affect which symptoms a person will experience.
In general, the most common symptoms of a brain tumor may include:
- Seizures or convulsions
- Difficulty thinking, speaking or finding words
- Personality or behavior changes
- Weakness, numbness or paralysis in one part or one side of the body
- Loss of balance, dizziness or unsteadiness
- Loss of hearing
- Vision changes
- Confusion and disorientation
- Memory loss
Can you have a brain tumor with no symptoms?
Brain tumors don’t always cause symptoms. In fact, the most common brain tumor in adults, meningioma, often grows so slowly that it goes unnoticed. Tumors may not start causing symptoms until they become large enough to interfere with healthy tissues inside the brain.

Convexity Meningioma | A Hollywood Stuntwoman's Story
Brain tumor causes and risk factors.
Doctors don’t know why some cells begin to form into tumor cells. It may have something to do with a person’s genes or his or her environment, or both. Some potential brain tumor causes and risk factors may include:
- Cancers that spread from other parts of the body
- Certain genetic conditions that predispose a person to overproduction of certain cells
- Exposure to some forms of radiation
Are brain tumors hereditary?
Genetics are to blame for a small number (fewer than 5%) of brain tumors. Some inherited conditions put individuals at greater risk of developing tumors, including:
- Neurofibromatosis
- Von Hippel-Lindau disease
- Li-Fraumeni syndrome
- Familial adenomatous polyposis
- Lynch syndrome
- Basal cell nevus syndrome (Gorlin syndrome)
- Tuberous sclerosis
- Cowden syndrome
Find a Doctor
Specializing IN:
- Brain Tumors
- Brain Cancer
- Metastatic Brain Tumors
- Pediatric Brain Cancer
- Pediatric Brain Tumors
At Another Johns Hopkins Member Hospital:
- Howard County Medical Center
- Sibley Memorial Hospital
- Suburban Hospital
Brain Tumor Diagnosis
Diagnosing a brain tumor usually involves a neurological exam, brain scans and a biopsy, if it can be done safely.
- A neurological exam may include a variety of tests to evaluate neurological functions such as balance, hearing, vision and reflexes.
- A variety of imaging techniques, including CT (or CAT) scan , MRI, occasionally an angiogram or X-rays can be used to identify the tumor, pinpoint its location and/or assess the function of your brain.
- If doctors cannot safely perform a biopsy (tissue sample collection and analysis), they will diagnose the brain tumor and plan the treatment based on other test results. If a biopsy was possible, doctors can use it to determine the tumor grade (how aggressive it is), as well as study the tumor tissue for any biomarkers that can help personalize the treatment approach.
Depending on your symptoms, doctors may also perform these tests to help confirm the diagnosis and rule out other conditions:
- Lumbar puncture to collect a sample of cerebrospinal fluid and see if it contains traces of the tumor cells.
- Evoked potentials studies to measure electrical activity in the nerves and/or electroencephalography (EEG) to measure electrical activity in the brain.
- Neurocognitive assessment to evaluate any changes in cognition and well-being.
- Neuro-ophthalmological examination to assess for signs of tumor affecting the eyes.
- Endocrinological evaluation to assess hormone function.
Proper diagnosis is essential in determining the best course of treatment.
Brain Tumor Grading
The grade of a brain tumor defines how serious it is. Using the biopsy sample, a pathologist will examine the tumor under a microscope to determine its grade. Brain tumor grading is a category system that describes the brain tumor cells and indicates how likely the tumor is to grow and spread.
Brain tumor grading uses a scale from 1 (least aggressive) to 4 (most aggressive).
(World Health Organization tumor grading system)
Grade I brain tumor
- Benign (noncancerous)
- Slow-growing
- Cells look almost normal under a microscope
- Usually associated with long-term survival
- Rare in adults
Grade II brain tumor
- Relatively slow-growing
- Sometimes spreads to nearby normal tissue and comes back (recurs)
- Cells look slightly abnormal under a microscope
- Sometimes comes back as a higher grade tumor
Grade III brain tumor
- Malignant (cancerous)
- Actively reproduces abnormal cells
- Tumor spreads into nearby normal parts of the brain
- Cells look abnormal under a microscope
- Tends to come back, often as a higher grade tumor
Grade IV brain tumor
- Most aggressive
- Easily spreads into nearby normal parts of the brain
- Cells look very abnormal under a microscope
- Tumor forms new blood vessels to maintain rapid growth
- Tumors have areas of dead cells in their center (called necrosis)
A changing diagnosis
The grade of a brain tumor might change, usually to a higher grade, often without a cause. It’s also possible that the biopsy sample might not represent the entire tumor, giving an inaccurate initial data for the grade.
A change from a low-grade tumor to a high-grade tumor happens more often in adults than in children.
Brain Tumor Staging
Staging refers to how far a tumor has spread. If a tumor has migrated to other parts of the body, it has metastasized. Staging is often done for other types of tumors but not primary brain tumors. This is because brain tumors are unlikely to spread beyond the nervous system.
Conversely, other types of tumors (e.g., lung cancer) can spread to the brain. Tumors that have spread to the brain are advanced stage.
What does the size of a brain tumor mean?
Because larger tumors are more likely to interfere with normal brain function, they more often cause symptoms and complications.
Brain Tumor Treatment
The most common treatment for brain tumors is surgery. For some tumors, surgical removal and continued monitoring may be the only treatment needed. Common surgical approaches to brain tumor removal include craniotomy , neuroendoscopy , laser ablation and laser interstitial thermal therapy .
Chemotherapy and radiation therapy can be used to treat brain cancer by helping shrink the tumor, slowing down its growth and/or preventing it from coming back. External beam radiation therapy , stereotactic radiosurgery and proton therapy are some of the radiation treatments for brain tumor.
Learn more about these and other brain tumor treatment options.
The Johns Hopkins Brain Tumor Center

The Johns Hopkins Comprehensive Brain Tumor Center is one of the largest brain tumor treatment and research centers in the world. We tailor each patient's treatment using an array of advanced approaches, including emerging treatments such as tumor-treating fields and MRI-guided laser ablation.
Brain Tumor Prognosis
Brain tumor can be a frightening diagnosis. It’s important to partner with a medical team you trust to determine the best next steps, whether it’s observation, surgery, radiation therapy or another treatment. How successful your personal outcome will be depends on many factors, including:
- The type of brain tumor, its size, grade and location
- Whether the tumor has spread within the brain or to other parts of the body
- Your age and overall health
- How long you had symptoms before you were diagnosed with a brain tumor
- How much the brain tumor affects your ability to function
- Your treatment preferences
- The expertise of your treatment team
There is no projected survival rate for those diagnosed with a brain tumor, as individual circumstances play a big role. For example, some malignant tumors can be successfully controlled by radiation therapy. Others, because of their location, may be life-threatening even if they are benign. Doctors have to look at thousands of patients with similar characteristics to see a trend in how certain tumors progress and how different treatments affect them.
Your overall outlook and prognosis are likely to change as you undergo various treatments. If you have surgery, how much of the tumor the neurosurgeon can remove will impact what will happen next. Other brain tumor treatments will determine future steps as well.
Request an Appointment
Related topics.
- Brain, Nerves and Spine
Cookie Policy
This website uses cookies that help the website function and that help us understand how you interact with it. Please read our privacy policy for more information.
Brain Tumors
Brain tumor facts.
- Brain Tumor Types
- Informed in 30 Videos
- Pediatric Brain Tumors
- Signs & Symptoms
- Treatment Options
- Stages of Treatment
- Clinical Trial Finder
- Survivorship
- End of Life
- Share Your Story
- Community Publications

Join NBTS’s campaign to raise awareness about the importance of biomarker testing and clinical trials for patients with brain tumors.
Support Services
- Personalized Support
- Brain Tumor Support Conversations
- Grief Support
- Key Questions
- Patient & Care Partner Resources
- Meditation Mondays
- DNA Damage Response (DDR) Consortium
- Immunotherapy
- Precision Medicine
- Tumor Metabolism
- Collaborative Ependymoma Research Network (CERN)
- Brain Tumor Investment Fund
- Quality of Life Research
- Research Roundtable
- Past Workshops
- Funding Opportunities
- Become an Advocate
- Policy Agenda
- Head to the Hill
- Advocate From Your State
- Action Alerts
- Tools & Trainings
- Walks, Races & Activities
- Find an Event
- Fundraise Your Way
- Gray Nation Endurance®️
- Brain Tumor Awareness Month
- Glioblastoma Awareness Day
Childhood Cancer Awareness Month
- #NBTSConnect
- Facebook Challenges

For every child with a brain tumor, it’s time for a better chance. This September, join us as we work together to conquer and cure brain tumors — once and for all.
Take Action
- Memorial Giving
- Planned Giving
- Become Our Partner
- Our Current Partners
- 2023 Annual Report
- Press Releases
- Mission, Vision & Values
- Leadership & Staff
There are more than 100 distinct types of primary brain tumors, each with its own spectrum of presentations, treatments, and outcomes. More than any other cancer, brain tumors can have lasting and life-altering physical, cognitive, and psychological impacts on a patient’s life. And, despite years of research, brain cancer survival rates have remained little-changed in recent years, even while survival rates for many other cancers have been significantly improved.
The following statistics and facts provide a snapshot of the burden primary brain tumors cause to Americans of all walks of life. Additional references are noted at the bottom of the page, but for a majority of the information listed below the figures stem from population statistics sampled during the 2015-2019 time period and analyzed in 2022, and reflect the latest available data at that time.
1 million Americans
are living with a brain tumor
94,390 Americans
will receive a primary brain tumor diagnosis in 2023
35.7% Relative Survival Rate
for all patients with a malignant brain tumor

18,990 Americans
will die from a malignant brain tumor in 2023
Brain Tumor Quick Facts
- An estimated 1 million Americans are living with a primary brain tumor [1]
- Approximately 72% of all brain tumors are benign
- Approximately 28% of all brain tumors are malignant
- Approximately 59% of all brain tumors occur in females
- Approximately 41% of all brain tumors occur in males
- Non-malignant meningiomas are the most commonly occurring primary non-malignant brain tumors, accounting for 39.7% of all tumors and 55.4% of all non-malignant tumors
- Glioblastoma is the most commonly occurring primary malignant brain tumor, accounting for 14.2% of all tumors and 50.1% of all malignant tumors
- The median age at diagnosis for a primary brain tumor is 61 years
- Survival rates vary by age at diagnosis and tumor type and generally decrease with age
- The most common primary non-malignant brain tumor, meningioma, has a average five-year survival of 88.2% after diagnosis
- For patients with malignant brain tumors, the five-year relative survival rate following diagnosis is 35.7%
- For the most common form of primary malignant brain tumors, glioblastoma, the five-year relative survival rate is only 6.9% and median survival is only 8 months
- And estimated 18,990 people will die because of a malignant brain tumor (brain cancer) in 2023 [2]
- Brain cancer is estimated to be the 10th leading cause of cancer death in 2023 for both males and females in all age groups [2]
Brain Tumors in Children (0-14)
- Approximately 3.9% of all brain tumors cases diagnosed occur in children ages 0-14 years
- An estimated 3,920 new cases of primary childhood brain tumors are expected to be diagnosed in 2023
- Brain tumors are the most commonly diagnosed solid cancer in children ages 0-14 years, as well as the leading cause of childhood cancer-related death
- 13,657 children were estimated to be living with a primary brain tumor in the U.S. in 2010 [3]
- For primary malignant childhood tumors, the five-year relative survival rate is 75.6% [4]
- Pilocytic astrocytomas (18.7%)
- Other gliomas (15.3%)
- Medulloblastomas make up the largest percentage of embryonal tumors (68.3%)
- Atypical teratoid/rhabdoid tumors (AT/RT) make up the second largest percentage of embryonal tumors (17.2%)
- Gliomas account for approximately 49.4% of tumors diagnosed in this age group
Brain Tumors in All Pediatric Populations (0-19)
- Approximately 1.7% of all brain tumors occur in the adolescent (15-19) population
- Infants less than one year of age have the highest incidence of brain tumors of all children and adolescents 0-19 [3]
- An estimated 5,230 new cases of primary brain tumors in children and adolescents will be diagnosed in the U.S. in 2023
- Brain tumors are the most common cancer overall in adolescents ages 15-19 years in the U.S. [2]
- For malignant tumors, the five-year relative survival rate is 75.6%
- High-grade gliomas cause the greatest proportion of deaths (44.2%), followed by medulloblastoma and AT/RT [3]
- Pilocytic astrocytoma has the highest survival rates after diagnosis
- Relative survival rates generally improve with increasing age at diagnosis in this population group, with poorest survival in those less than a year old at diagnosis [3]
- Pilocytic astrocytoma (15.3%)
- Other gliomas (12.6%)
- Medulloblastoma account for the latest percentage of embryonal tumors in this population (69.5%)
- Gliomas account for approximately 44.6% of tumors in this age group (27.9% in ages 15-19 years)
- Tumors of the pituitary are the most common in the 15-19 age group (33.5%)
- In children and adolescents, incidence is higher in females than males
- Incidence rates are highest among children and adolescents who are White compared to children and adolescents who are Black, Asian or Pacific Islander (APIA), or American Indian and Alaskan Native (AIAN)
- Incidence rates are highest among children and adolescents who are non-Hispanic compared to children and adolescents who are Hispanic
- It was estimated in 2009, that a total of 47,631.5 years of potential life were lost due to brain tumors in children and adolescents in the US [3]
Brain Tumors in Adolescents and Young Adults (15-39)
- Approximately 14.3% of all primary brain tumors occur in the AYA population
- An estimated 11,660 new cases of primary brain tumors will be diagnosed in AYA patients in 2023
- Brain tumors are the second most common cancer overall in individuals ages 15-39 and the second leading cause of cancer related death in those 15-39 years of age
- The rate is 71.7% for malignant tumors and 98.3% for non-malignant tumors
- Tumors of pituitary (36.0%)
- Meningiomas (15.9%)
- Nerve sheath tumors (8.6%)
- Gliomas account for approximately 24.8% of all primary AYA brain tumors and 82.4% of all malignant tumors in this group
- AYA had higher rates of relative survival than adults greater than 40 years old for all histopathologic types. Though one-year relative survival for most tumor types was higher for AYA than children, five- and ten-year survival were usually higher for children as compared to AYA.
Brain Tumors in Adults (40+)
- Approximately 81.7% of all primary brain tumors occur in the adult population
- An estimated 79,340 adults age 40+ will be diagnosed with a primary brain tumor in 2023 in the U.S.
- Brain tumors are the seventh most common tumor type overall and the sixth most common cause of cancer related death among persons ages 40+ years
- For adults ages 20+ years, age-specific incidence rates for primary brain tumors are highest among those age 85+
- The five-year relative survival rate for those ages 40+ years is 21% for malignant tumors and 90.3% for non-malignant tumors
- Meningiomas (46.1%)
- Glioblastoma (16.4%)
- Tumors of the pituitary (14.5%)
- For 2023, the highest number of new cases is predicted in those age 65+ years
- Older adults (40+ years old) had poorer survival than children (0-14 years) in nearly all primary brain tumor types
Brain Tumors by Race/Ethnicity*
- Incidence rates of non-malignant brain tumors are highest in people who are Black, followed by people who are White, APIA, and AIAN
- Incidence rates of malignant brain tumors are highest in people who are White, followed by people who are Black, AIAN, and APIA
- Individual who are White have significantly higher incidence rates for glioblastoma, all other astrocytomas, embryonal tumors, and nerve sheath tumors compared to people who are Black
- Individual who are Black have higher rates of meningioma and pituitary tumors compared to people who are White
- Overall incidence rates of brain tumors are higher in people who are non-Hispanic than people who are Hispanic
- Individuals who are Black, non-Hispanic have poorer survival outcomes compared to people who are White, non-Hispanic with the exception of glioblastoma, unique astrocytoma variants, other neuroepithelial tumors, other hemopoietic neoplasms, germ cell tumors, and neoplasms unspecified
- Individuals who are AIAN, non-Hispanic have poorer overall survival as compared to individuals who are White, non-Hispanic in many tumor types, though the small size of this population means that many of these associations are not biologically significant
- Individuals who are APIA, non-Hispanic have improved survival in many tumor types compared to White, not Hispanic, though many of these associations were non-significant
- Hispanic ethnicity was associated with improved survival in most brain tumor types
*The U.S. Census Bureau defines race as a person’s self-identification with one or more social groups, which can include white, Black or African American, Asian, American Indian, Alaska Native, Native Hawaiian, and/or Other Pacific Islander. Federal statistical standards used by the Census and the National Center for Education Statistics, conceptualize a person’s ethnicity into one of two categories: Hispanic (or Latino/a/x) or Not Hispanic (Latino/a/x). A Hispanic (or Latino/a/x) person can self-report as any race.
**While there are several tumor types where significant differences in incidence were observed by race and/or ethnicity, in most cases the actual difference in incidence rates is small and may not be significant.
Brain Tumors by Sex
- Overall, incidence rates for all primary brain tumors are higher in females (58.7% of diagnoses) than in males (41.3%)
- Non-malignant primary brain tumors occur more often in females (64.4%) than in males (35.6%)
- Malignant primary brain tumors occur more often in males (55.8%) than in females (44.2%)
- Incidence rates for specific brain tumor types vary by sex. For example, glioblastoma is more common in males, while meningioma is more common in females
- Overall, males have higher mortality rates from malignant brain tumors than females, and generally worse survival outcomes with the exception of glioblastoma, malignant gliomas, embryonal tumors, other hematopoietic neoplasms, and germ cell tumors
Additional Information
- Grade 1 tumors, such as some meningiomas, are the lowest and typically least aggressive grade. Grade 4 tumors, such as glioblastoma, are the highest and most aggressive grade of tumors
- For many tumor types, surgery and radiation remain the standard of care, and national guidelines suggest that clinical trials remain the best place to care for patients
- Survival rates for adult and pediatric patients with brain tumors have not changed significantly over the past 45 years despite major improvements made in the treatment of other cancers.
- The incidence of brain metastases appears to be increasing [7]
- Several studies have cited that the percentage of patients with cancer who will develop brain metastases is anywhere from approximately 10% to 30% [8] [9]
- These include melanoma (where it’s been estimated that most cases will metastasize to the brain), lung, breast, renal, and colorectal cancers [10] [11] [12]
- Metastatic brain tumors are five times more common than primary brain tumors (those that originate in the brain). [9]
- Quinn T Ostrom, Ph.D., M.P.H, Mackenzie Price, M.P.H, Corey Neff, M.P.H, Gino Cioffi, M.P.H, Kristin A Waite, Ph.D, Carol Kruchko, B.A, Jill S Barnholtz-Sloan, Ph.D, CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2015–2019, Neuro-Oncology, Volume 24, Issue Supplement_5, October 2022, Pages v1–v95, https://doi.org/10.1093/neuonc/noac202
- Brain tumor statistics are typically classified as “brain and other central nervous system (CNS) tumors” in research reports. For ease and clarity, in this document we use “brain tumors” as shorthand to include both tumors occurring in the brain and other central nervous system locations, such as the spine.
- Unless otherwise noted, all references on this page refer to primary brain tumors, and all stats refer to U.S. populations.
[1] Porter KR, McCarthy BJ, Freels S, Kim Y, Davis FG. Prevalence Estimates for Primary Brain Tumors in the United States by Age, Gender, Behavior, and Histology. Neuro Oncol. 2010.; 12(60):520-527.
[2] Siegel, RL, Miller, KD, Wagle, NS, Jemal, A. Cancer statistics, 2023. CA Cancer J Clin. 2023; 73( 1): 17- 48. doi: 10.3322/caac.21763
[3] Central Brain Tumor Registry of the United States Fact Sheet for Pediatric Brain Tumors 2022
[4] Quinn T Ostrom, Mackenzie Price, Katherine Ryan, Jacob Edelson, Corey Neff, Gino Cioffi, Kristin A Waite, Carol Kruchko, Jill S Barnholtz-Sloan, CBTRUS Statistical Report: Pediatric Brain Tumor Foundation Childhood and Adolescent Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2014–2018, Neuro-Oncology, Volume 24, Issue Supplement_3, September 2022, Pages iii1–iii38, https://doi.org/10.1093/neuonc/noac161
[5] National Brain Tumor Society analysis
[6] Workshop on Product Development for Central Nervous System Metastases
[7] https://www.ncbi.nlm.nih.gov/books/NBK470246/
[8] Nayak L, Lee EQ, Wen PY. Epidemiology of brain metastases. Curr Oncol Rep. 2012 Feb;14(1):48-54.
[9] https://www.hopkinsmedicine.org/health/conditions-and-diseases/metastatic-brain-tumors
[10] https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Metastatic-Brain-Tumors
[11] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6064184/
[12] Lamba N, Wen PY, Aizer AA. Epidemiology of brain metastases and leptomeningeal disease. Neuro Oncol. 2021 Sep 1;23(9):1447-1456. doi: 10.1093/neuonc/noab101. PMID: 33908612; PMCID: PMC8408881.
Stay Informed & Connected
University of Notre Dame
Notre Dame News
- Home ›
- News ›
Researchers develop affordable, rapid blood test for brain cancer
Published: August 27, 2024
Author: Brandi Wampler

Researchers at the University of Notre Dame have developed a novel, automated device capable of diagnosing glioblastoma, a fast-growing and incurable brain cancer, in less than an hour. The average glioblastoma patient survives 12-18 months after diagnosis.
The crux of the diagnostic is a biochip that uses electrokinetic technology to detect biomarkers, or active Epidermal Growth Factor Receptors (EGFRs), which are overexpressed in certain cancers such as glioblastoma and found in extracellular vesicles.
“Extracellular vesicles or exosomes are unique nanoparticles secreted by cells. They are big — 10 to 50 times bigger than a molecule — and they have a weak charge. Our technology was specifically designed for these nanoparticles, using their features to our advantage,” said Hsueh-Chia Chang , the Bayer Professor of Chemical and Biomolecular Engineering at Notre Dame and lead author of the study about the diagnostic published in Communications Biology.
The challenge for researchers was two-fold: to develop a process that could distinguish between active and non-active EGFRs, and create a diagnostic technology that was sensitive yet selective in detecting active EGFRs on extracellular vesicles from blood samples.
To do this, researchers created a biochip that uses an inexpensive, electrokinetic sensor about the size of a ball in a ballpoint pen. Due to the size of the extracellular vesicles, antibodies on the sensor can form multiple bonds to the same extracellular vesicle. This method significantly enhances the sensitivity and selectivity of the diagnostic.
Then synthetic silica nanoparticles “report” the presence of active EGFRs on the captured extracellular vesicles, while bringing a high negative charge. When extracellular vesicles with active EGFRs are present, a voltage shift can be seen, indicating the presence of glioblastoma in the patient.
This charge-sensing strategy minimizes interference common in current sensor technologies that use electrochemical reactions or fluorescence.
“Our electrokinetic sensor allows us to do things other diagnostics cannot,” said Satyajyoti Senapati , a research associate professor of chemical and biomolecular engineering at Notre Dame and co-author of the study. “We can directly load blood without any pretreatment to isolate the extracellular vesicles because our sensor is not affected by other particles or molecules. It shows low noise and makes ours more sensitive for disease detection than other technologies.”
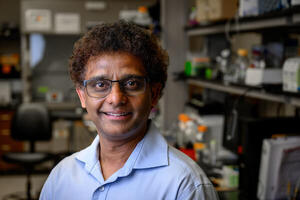
In total, the device includes three parts: an automation interface, a prototype of a portable machine that administers materials to run the test and the biochip. Each test requires a new biochip, but the automation interface and prototype are reusable.
Running one test takes under an hour, requiring only 100 microliters of blood. Each biochip costs less than $2 in materials to manufacture.
Although this diagnostic device was developed for glioblastoma, the researchers say it can be adapted for other types of biological nanoparticles. This opens up the possibility for the technology to detect a number of different biomarkers for other diseases. Chang said the team is exploring the technology for diagnosing pancreatic cancer and potentially other disorders such as cardiovascular disease , dementia and epilepsy.
“Our technique is not specific to glioblastoma, but it was particularly appropriate to start with it because of how deadly it is and the lack of early screening tests available,” Chang said. “Our hope is that if early detection is more feasible, then there is an increased chance of survival.”
Blood samples for testing the device were provided by the Centre for Research in Brain Cancer at the Olivia Newton-John Cancer Research Institute in Melbourne, Australia.
In addition to Chang and Senapati, other collaborators include former postdocs at Notre Dame Nalin Maniya and Sonu Kumar; Jeffrey Franklin, James Higginbotham and Robert Coffey from Vanderbilt University; and Andrew Scott and Hui Gan from the Olivia Newton-John Cancer Research Institute and La Trobe University. The study was funded by the National Institutes of Health Common Fund.
Chang and Senapati are affiliated with Notre Dame’s Berthiaume Institute for Precision Health , the Harper Cancer Research Institute and NDnano .
Contact: Brandi Wampler, associate director of media relations, 574-631-2632, [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Research Briefing
- Published: 23 August 2024
Discovering and targeting vulnerabilities in invasive brain cancer using ROBO1 CAR T cells
Nature Medicine ( 2024 ) Cite this article
427 Accesses
8 Altmetric
Metrics details
- Preclinical research
Despite standard treatment efforts, patients with glioblastoma (GBM), an aggressive form of brain cancer, inevitably succumb to recurrent disease. Integrative genomic analyses reveal that tumor cells hijack normal neurodevelopmental pathways to promote GBM growth and invasion. To target this pathway, we engineer a CAR T cell therapy that blocks the growth of GBM and other invasive brain cancers.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
195,33 € per year
only 16,28 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Brown, C. E. et al. Locoregional delivery of IL-13Rα2-targeting CAR-T cells in recurrent high-grade glioma: a phase 1 trial. Nat. Med. 30 , 1001–1012 (2024). This paper reports clinical trial results for IL-13Rα2-targeting CAR T cells in recurrent GBM.
Article CAS PubMed PubMed Central Google Scholar
Bagley, S. J. et al. Intrathecal bivalent CAR T cells targeting EGFR and IL13Rα2 in recurrent glioblastoma: phase 1 trial interim results. Nat. Med. 30 , 1320–1329 (2024). This paper reports clinical trial results for CAR T cells targeting EGFR and IL-13Rα2 in recurrent GBM.
Article CAS PubMed Google Scholar
Choi, B. D. et al. Intraventricular CARv3-TEAM-E T cells in recurrent glioblastoma. N. Engl. J. Med. 390 , 1290–1298 (2024). This paper reports clinical trial results for a modified CAR T cell modality targeting EGFR in recurrent GBM.
Urwyler, O. et al. Branch-restricted localization of phosphatase Prl-1 specifies axonal synaptogenesis domains. Science 364 , eaau9952 (2019). This paper reports the role of Ptp4a1 (also known as Prl-1 ) in Drosophila axonal guidance processes.
Huang-Hobbs, E. et al. Remote neuronal activity drives glioma progression through SEMA4F. Nature 619 , 844–850 (2023). This paper reports axon guidance genes contributing to glioma infiltration.
Download references
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This is a summary of: Chokshi, C. R. et al. Targeting axonal guidance dependencies in glioblastoma with ROBO1 CAR T cells. Nat. Med . https://doi.org/10.1038/s41591-024-03138-9 (2024).
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Discovering and targeting vulnerabilities in invasive brain cancer using ROBO1 CAR T cells. Nat Med (2024). https://doi.org/10.1038/s41591-024-03229-7
Download citation
Published : 23 August 2024
DOI : https://doi.org/10.1038/s41591-024-03229-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Cancer newsletter — what matters in cancer research, free to your inbox weekly.
- A*STAR Board Members
- Senior Management
- Organisation Structure
- Corporate Social Responsibility
- Diversity at A*STAR
- Annual Reports
- A*STAR Graduate Academy (A*GA)
- Innovation and Enterprise (I&E)
- Research Entities
- About A*STAR Research
- Directory of Researchers
- Funding Opportunities
- Research Focus
- Research Quality Excellence
- Biomedical Research Council
- Science and Engineering Research Council
- Honours and Accolades
- Highly Cited Researchers
- About I&E
- Innovation Offerings
- Innovation Platforms
- Work with I&E
- About A*STAR Scholarships
- A*STAR Research Internship Award (ARIA)
- National Science Scholarship (BS-PhD)
- Singapore International Pre-Graduate Award (SIPGA)
- National Science Scholarship (Masters)
- National Science Scholarship (PhD)
- A*STAR Computing & Information Science Scholarship
- A*STAR Graduate Scholarship
- Singapore International Graduate Award (SINGA)
- A*STAR Research Attachment Programme (ARAP)
- A*STAR International Fellowship
- A*STAR Science Award (Upper Sec)
- A*STAR Science Award (JC)
- A*STAR Science Award (Poly)
- H3 Research Attachment Programme
- A*STAR - MOE Attachment
- Research Attachments at A*STAR RIs
- A*STAR Scholars
- Featured Scholars
- International Awardees
- Developmental Opportunities for A*STAR Scholars
- Scholarship Award Ceremony 2024
- FAQs For Scholarships and Awards
- A*STAR News
- A*STAR Innovate
- Faces of A*STAR
- National Survey of RIE
- Connect with Us
A*STAR NEWS
- Publicity Highlights
- Press Releases
- COVID-19 R&D
Science Is Making Brain Cancer Less Of A Death Sentence
By Professor Hai Yan

For decades, a brain cancer diagnosis has been one of the grimmest prognoses in medicine. Gliomas, the most common malignant primary brain tumours, have long defied our best efforts at treatment. Glioblastoma, the deadliest form, offers patients an average survival time of just 15 months, even with aggressive therapy. But today, science is offering a glimmer of hope on the horizon.
The resistance to treatment stems from the brain's complexity. Its delicate nature makes complete surgical removal of tumours nearly impossible without risking severe harm. Moreover, the blood-brain barrier, while crucial for protection, also prevents many drugs and immune cells from reaching the affected areas. These challenges have led to stagnant survival rates for brain cancer over the past five decades, even as we've made significant strides against other forms of cancer.
Since the risk of these malignancies rises with age, Singapore, with its ageing population, will likely face a growing burden of the disease. In fact, recent studies have projected that brain cancer incidence in Asia will increase significantly over the next two decades , leading to a substantial rise in mortality rates.
Breakthrough Discoveries Paving the Way
Recent scientific breakthroughs are illuminating new paths forward. In 2009, my research identified mutations in genes called isocitrate dehydrogenase (IDH) 1 and 2 as critical drivers in the development of certain brain tumours. These mutations are now recognised as key factors in the progression of low-grade gliomas, which occur mostly in younger adults.
This discovery ignited a flurry of studies and collaborations worldwide, culminating in the recent FDA approval of vorasidenib - the first new treatment for low-grade gliomas in over 20 years. Vorasidenib works by blocking the effects of the mutated IDH 1 and 2 genes, thus slowing down the tumour's growth. In doing so, the oral medication delays patients' need for more toxic treatments such as radiation and chemotherapy, extending their lives and improving their quality of life.
Researchers are now advancing in several key areas. Novel biomarkers for early detection are being identified, and new diagnostic tools for glioblastoma subtypes are being developed to improve treatment outcomes and survival rates. Scientists are also unravelling the secrets of the tumours' micro-environment, pinpointing critical metabolic and immunological pathways that underlie their survival.
Here in Singapore, researchers are also making significant contributions to this global effort. For instance, a team led by Associate Professor Too Heng-Phon at the National University of Singapore's Yong Loo Lin School of Medicine has developed a promising stem cell-based gene therapy to combat aggressive brain tumours . This innovative approach not only kills cancer cells but also activates the patient's own immune system for long-term tumour suppression. Human clinical trials for this therapy are set to begin in 2025, offering new hope for patients with recurrent glioblastoma.
Pushing the Boundaries of Brain Cancer Research
One of the most significant challenges in brain cancer treatment is developing therapeutics that can cross the blood-brain barrier. To address this, a team led by Dr Andrea Pavesi at A*STAR's Institute of Molecular and Cell Biology (IMCB) have designed a groundbreaking microfluidic device that simulates the barrier and human brain tumours . This innovation allows researchers to rapidly screen new chemotherapeutic drugs and evaluate their ability to cross the barrier, a crucial step in developing more effective treatments.
Additionally, the Neuro-Phenomics Laboratory at IMCB is focusing on three key areas: identifying novel biomarkers for early detection, creating drugs that can cross the blood-brain barrier, and understanding the tumours' micro-environment. This research deviates from traditional focus on intrinsic cancer signalling mechanisms, aiming to enhance the body's natural immune response towards glioblastoma. To ensure that its research breakthroughs are quickly and efficiently translated into viable and effective clinical applications, the lab is partnering with an array of leading institutions, including the National Neuroscience Institute, National University Health System and Asian Society of Neuro-Oncology.
We are also exploring personalised medicine approaches that tailor treatments to the profile of individual patients, potentially revolutionising brain cancer treatment. By analysing the unique characteristics of each patient's tumour, we aim to develop tailored strategies that are more effective and have fewer side effects than one-size-fits-all approaches.
From Death Sentence to Curable Condition
As populations age worldwide, the urgency of our work intensifies. With the near-impossibility of totally eradicating brain tumours through surgery, the cure for brain cancer, and glioblastoma in particular, will not be found in the operating theatre but in the laboratory. Our ongoing research and development brings us closer to a long-sought-after goal: transforming brain cancer from a dire prognosis into a manageable, and potentially curable, condition.
As we continue to unravel the complexities of brain cancer, each discovery brings hope to patients and their families. While we still have a long way to go, the progress we've made in recent years suggests that a future where brain cancer is no longer a death sentence is within reach.
With its vibrant clinical research ecosystem, cutting-edge infrastructure, and substantial funding, Singapore is uniquely positioned to lead the fight against glioblastoma in Asia, offering a beacon of hope for patients and families affected by this devastating disease.

Was This Article Helpful ?
A*STAR celebrates International Women's Day

From groundbreaking discoveries to cutting-edge research, our researchers are empowering the next generation of female science, technology, engineering and mathematics (STEM) leaders. Get inspired by our #WomeninSTEM
You must have javascript enabled to use this website.
For the best browsing experience please enable JavaScript. Instructions for Microsoft Edge and Internet Explorer , other browsers

- About cancer
- Get involved
- Our research
- Funding for researchers
- Cancer types
- Cancer in general
- Causes of cancer
- Coping with cancer
- Health professionals
- Do your own fundraising
- By cancer type
- By cancer subject
- Our funding schemes
- Applying for funding
- Managing your research grant
- How we deliver our research
- Find a shop
- Shop online
- Our eBay shop
- Our organisation
- Current jobs
- Cancer news
Brain tumours
Tumours that start in the brain are called primary brain tumours. Tumours can start in any part of the brain or related structures. This section is about primary brain tumours in adults.
Cancers that have spread to the brain from somewhere else in the body are called secondary brain tumours or brain metastases.
- Read about secondary brain cancer
Brain and spinal cord tumours can affect children and adults.
- Find out about brain and spinal cord tumours in children
What are brain tumours?
Primary brain tumours are tumours that start in the brain. They can start anywhere in the brain and there are many different types of tumour.
The brain and spinal cord
To understand brain tumours it helps to know about the different parts of the brain and spinal cord.
Brain tumour symptoms
Common symptoms of brain tumours include headaches, feeling or being sick and seizures (fits).
Getting diagnosed with a brain tumour
You usually start by seeing your GP who might refer you to a specialist. Or you might go to Accident and Emergency (A&E) if you suddenly have severe symptoms.
Survival for brain tumours
Survival depends on different factors such as the type, position and grade of your brain or spinal cord tumour.
Types of brain tumours
There are many different types of brain tumours. They are usually named after the type of cell they develop from.
Grades of brain tumours
The grade of a brain tumour gives doctors an idea of how fast or slow the tumour might grow.
Treatment for brain tumours
Treatment for a brain or spinal cord tumour depends on the type of tumour you have, where it is and your general health.
Research and clinical trials into brain tumours
Researchers in the UK are looking at better ways to diagnose and treat brain tumours and manage treatment side effects.
Living with a brain tumour
Practical and emotional support is available to help you cope with a brain or spinal cord tumour.
Risks and causes of brain tumours
There are some factors that increase your risk of developing a brain tumour. These include being older, and a family history.
It’s a worrying time for many people and we want to be there for you whenever - and wherever - you need us. Cancer Chat is our fully moderated forum where you can talk to others affected by cancer, share experiences, and get support. Cancer Chat is free to join and available 24 hours a day.
Visit the Cancer Chat forum
About Cancer generously supported by Dangoor Education since 2010.

Find a clinical trial
Search our clinical trials database for all cancer trials and studies recruiting in the UK
Cancer Chat forum
Talk to other people affected by cancer
Nurse helpline 0808 800 4040
Questions about cancer? Call freephone 9 to 5 Monday to Friday or email us
Office of Academic Clinical Affairs
Masonic Cancer Center
- Clinical Trials
- Partners and Locations
- For Patients
- For Researchers Overview
- Grant Program
- Brand Guidelines & Logos

Childhood Cancer Awareness Month: Children & Clinical Research
About childhood cancer.
Childhood Cancer Awareness Month is celebrated each September around the world with the goal of increasing awareness of childhood cancer and advocating for pediatric cancer research and funding. It’s estimated that about 400,000 children and adolescents develop cancer globally each year. The most common types of cancer diagnosed in children are leukemia, brain and other central nervous system (CNS) tumors, and lymphoma. More than 100 different subtypes of childhood cancers exist.
Cancer in children isn’t necessarily the same as cancer in adults. For example, cancer in children is almost never caused by lifestyle choices, behaviors, or exposures. For children, cancer is often caused by genetics and DNA mutations, so it is more likely to be random. Sometimes childhood cancer even begins developing before a child is born. Childhood cancer also can be treated differently, and there are several specific drugs created just for pediatric cancers. While these treatments are effective, they can have long-term side effects and lead to secondary cancers later in life as children grow up and live decades beyond their initial childhood cancer.
In the United States, the five-year survival rate for pediatric cancers is 83-88%. This remarkable rate is due to childhood cancer research that developed successful diagnostic tests and treatments. However, not all pediatric populations have equitable access to cancer diagnosis and treatment, especially in lower or middle-income countries. Childhood cancer organizations work to bring awareness and funding to these populations to close treatment and diagnosis gaps.
Children & Clinical Trials
Overall, childhood cancer treatments have advanced quickly due to clinical research. Treating cancer and conducting research with children have unique considerations. It is important that cancer treatments are given to children of a variety of ages in clinical trials. This is because cancer treatments and drugs affect people differently. A child’s body may not react the same way an adult’s body would. As children grow and develop, their responses to medications also change. All age groups are needed in clinical trials to determine safety, effectiveness, side effects, and appropriate dosage for new treatments. Clinical trials for children might also determine the optimal form of a drug or device, like a liquid instead of a pill since it’s easier for children to swallow.
Children are also considered a vulnerable population. All clinical trials have regulations and safety measures in place. But, there must be even more safeguards and ethical considerations in mind when conducting research with children, especially in balancing benefits and risks of a clinical trial. This typically means that children will be the last population a treatment is given to, and the drug will already have been proven safe and effective in animals, cell models, and adults. Because children are under the age of 18, their participation must ultimately be decided by both the child and by a parent or guardian, who will be involved throughout the entire enrollment, informed consent, and clinical trial processes.
Research into Life Beyond Childhood Cancer
Another area of childhood cancer research that does not necessarily involve children is childhood cancer survivorship research. Because the survival rate for childhood cancer is so high, there are many unique concerns and questions about health outcomes for childhood cancer survivors as they reach adulthood and old age. Common concerns and issues for childhood cancer survivors include mental health issues, accelerated aging, infertility, second cancers, and reduced life expectancy. Research is needed to fully understand the consequences and effects of childhood cancer and treatments. Studies in this area typically occur by following a cohort, or group, of childhood cancer survivors over time to track their health outcomes. This type of research is considered an observational study called a cohort study.
One such study, the Childhood Cancer Survivor Study (CCSS), began in 1994 to better understand childhood cancer survivors and issues they experience, increase survival, and minimize harmful health effects of cancer treatments. The study included more than 14,000 childhood cancer survivors who were diagnosed between 1970 and 1986, as well as 4,000 siblings for comparison. A second group of 10,000 survivors that were diagnosed between 1978 and 1999 and 1,000 of their siblings were later added as well. The study participants were surveyed and followed over the years to monitor their long-term health outcomes. Potential late effects of childhood cancer that have been found from the study include premature menopause, stroke, and subsequent cancers. Data from the study has also been used in many other childhood cancer survivorship studies as well.
Learn More
To learn more about childhood cancer and identify ways to raise awareness and advocate for childhood cancer research, visit the American Childhood Cancer Organization and the Children’s Cancer Research Fund .
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
August 30, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
Potential new drug could target rare childhood brain tumor
by Institute of Cancer Research
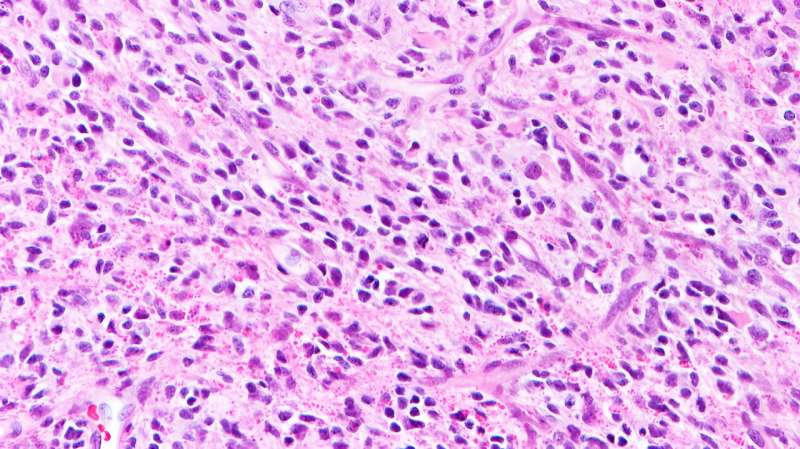
Ribociclib—a drug already used to treat breast cancer—may help slow the growth of diffuse hemispheric glioma (DHG), new research has found.
A team of scientists from The Institute of Cancer Research, London and the Dana-Farber Cancer Institute, Boston, U.S., uncovered clues about the growth of a specific type of DHG—DHG, H3G34-mutant—which allowed them to explore new targeted treatments.
Diffuse hemispheric glioma is a rare, high-grade childhood brain tumor with a prognosis of 18–22 months; there is currently no cure. It is estimated that more than 30% of all pediatric high-grade glioma diagnoses are the DHG-H3G34 variant.
Laboratory tests and pre-clinical models led the researchers to discover that tumor cells disrupt the normal development of neurons, causing them to look like immature early neuron-like cells.
Searching for novel treatments
Exploring what would make these cells vulnerable to novel treatments found that targeting the protein CDK6, which is involved in regulating cell division, could prove promising. Abnormal activity in the CDK6 protein can lead to uncontrolled cell division—a hallmark of cancer.
Ribociclib is a CDK4/6 inhibitor approved to treat breast cancer , but in this study, it was used to treat a child with a brain tumor when other treatments failed. Treatment resulted in stable disease for a further 17 months until it started to grow back.
These very early results are remarkable given the typically poor prognosis for children diagnosed with these aggressive brain tumors.
The child is currently undergoing further treatment , more than four years since her diagnosis.
Clinical trials on the horizon
While ribociclib is not a cure for this devastating brain tumor, these findings are significant because the disease typically progresses within 3.5 months following recurrence.
There are hopes that this research could pave the way for clinical trials, as this was a preliminary test in just one child.
This research also showed that DHG-H3G34 tumors are more responsive to CDK4/CDK6 inhibitors than other high-grade glioma types—opening the door for more targeted treatments for this genetically distinct tumor type.
CDK4/6 inhibitors could be used in a combination treatment strategy
As CDK4/6 inhibitors slow the growth of tumor cells and do not kill them, this would not be a standalone treatment and therefore combination therapies need to be explored.
Professor Chris Jones, Professor of Childhood Brain Tumor Biology at The Institute of Cancer Research, London, said, "This work shows the importance of understanding how brain tumors develop in order to figure out better ways to treat these patients.
"It was a surprise to realize that this type of glioma seemed to arise from developing neurons, but we were able to use this knowledge to find specific vulnerabilities in these cancer cells, which hopefully we can now translate into clinical trials."
Mariella G. Filbin, MD, Ph.D., Co-Director of the Pediatric Neuro-Oncology Program at Dana-Farber Cancer Institute, said, "Our trans-Atlantic collaboration helped tremendously in validating and expanding our results, and I am thrilled to see our work translate into helping a patient so quickly.
"This is the first time we found functional consequences of aberrant lineage specification in tumor cells—a result that was unexpected at first, but is now setting the stage for new therapeutic avenues in this disease."
Dr. Simon Newman, Chief Scientific Officer at The Brain Tumor Charity said, "This research helps us have a better understanding of what is driving this devastating disease in children.
"We know that current treatments are not effective and that finding vulnerabilities in cancer cells could lead to new targeted treatments to help children live longer and better lives. Although this is very early days, we hope that it will provide some data to inform clinical trials in the future."
Explore further
Feedback to editors

Alzheimer's-like brain changes found in long COVID patients
34 minutes ago

Rare genetic variants linked to bicuspid aortic valve disease in young adults identified
44 minutes ago

Blood stem cell research could transform bone marrow transplants

Edoxaban outperforms edoxaban plus antiplatelet agent in patients with a-fib and stable coronary artery disease: Study

Researchers pinpoint key gene mutations, new mechanisms that cause brain bleeding and dementia

Childhood HIV vaccination strategy shows promise in study

Teaching old birds new tricks: Zebra finches defy age-related learning limits

Novel light-based technique shows 90% accuracy in early prostate cancer detection

Proof-of-principle study uncovers promising treatment for incurable prostate cancer

New technique allows comprehensive genetic examination of embryos with a single test
Related stories.

FDA approves new therapy for glioma patients for first time in decades
Aug 7, 2024

FDA approves drug targeting brain cancer gene mutation

Scientists uncover new treatment pathway for rare 'spider web' childhood brain tumors
May 24, 2024

Single set of criteria to assess progression in glioma aims to speed discovery of new medicines
Oct 2, 2023

A new strategy to prevent the most aggressive tumors from generating resistance to chemotherapy
Feb 27, 2020

Using spatial single-cell transcriptomics to visualize diffuse midline glioma
Dec 5, 2022
Recommended for you

Scientists use exosomes secreted by living cells to successfully target TKI-resistant cancer

Blood-based assay shows promise for detecting IDH1.R132H-mutant gliomas
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter

Sign up for the Health News Florida newsletter
This metabolic brain boost revives memory in alzheimer’s mice.

The brain needs a lot of energy — far more than any other organ in the body — to work properly. And aging and Alzheimer’s disease both seem to leave the brain underpowered.
But an experimental cancer drug appeared to re-energize the brains of mice that had a form of Alzheimer’s — and even restore their ability to learn and remember.
The finding, published in the journal Science , suggests that it may eventually be possible to reverse some symptoms of Alzheimer’s in people, using drugs that boost brain metabolism.
The results also offer an approach to treatment that’s unlike anything on the market today. Current drugs for treating Alzheimer’s, such as lecanemab and donanemab, target the sticky amyloid plaques that build up in a patient’s brain. These drugs can remove plaques and slow the disease process, but do not improve memory or thinking.
The result should help “change how we think about targeting this disease,” says Shannon Macauley , an associate professor at the University of Kentucky who was not involved in the study.
A surprise, then a discovery
The new research was prompted by a lab experiment that didn’t go as planned.
A team at Stanford was studying an enzyme called IDO1 that plays a key role in keeping a cell’s metabolism running properly. They suspected that in Alzheimer’s disease, IDO1 was malfunctioning in a way that limited the brain’s ability to turn nutrients into energy.
So the team used genetics to eliminate the enzyme entirely from mice that develop a form of Alzheimer’s. They figured that without any IDO1, brain metabolism would decline.
“We expected to see everything [get] much, much, much worse”, says Dr. Katrin Andreasson , a professor of neurology and neuroscience at Stanford. “But no, it was the complete opposite.”
Without the enzyme, the mouse brains were actually better at turning glucose into energy and didn’t exhibit the memory loss usually associated with Alzheimer’s.
“It was such a profound rescue that we sort of went back to the drawing board and tried to figure out what was going on,” Andreasson says.
Eventually, the team found an explanation.
Getting rid of the enzyme had altered the behavior of cells called astrocytes.
Usually, astrocytes help provide energy to neurons, the cells that allow for learning and memory. But when the toxic plaques and tangles of Alzheimer’s begin to appear in the brain, levels of IDO1 rise and astrocytes stop doing this job.
“They’re kind of put to sleep,” Andreasson says. So “you’ve got to wake them up to get them to help the neurons.”
And that’s what happened when scientists used genetics to remove IDO1.
Their hypothesis was that high levels of IDO1 were limiting the astrocytes’ ability to produce lactate, a chemical that helps brain cells, including neurons, transform food into energy.
To confirm the hypothesis, the team, led by Dr. Paras Minhas , did a series of experiments. One involved placing a mouse in the center of a shiny white disk under a bright light.
“It really wants to get out of there,” Andreasson says. “But it has to learn where the escape hole is” by following visual cues.
Healthy mice learned how to read those cues after a few days of training, and would escape almost instantly.
“But in the Alzheimer mice, the time to find the escape hole really skyrocketed,” Andreasson says.
That changed when the team gave these mice an experimental cancer drug that could block the enzyme much the way genetic engineering had.
The treated mice learned to escape the bright light as quickly as healthy animals. And a look at their brains showed that their astrocytes had woken up and were helping neurons produce the energy needed for memory and thinking.
In the hippocampus, a brain area that’s critical for memory and navigation, tests showed that the drug had restored normal glucose metabolism even though the plaques and tangles of Alzheimer’s were still present.
The team also tested human astrocytes and neurons derived from Alzheimer’s patients. And once again, the drug restored normal function.
Beyond plaques and tangles
The experiments add to the evidence that Alzheimer’s involves a lot more than just the appearance of plaques and tangles.
“We can have these metabolic changes in our brain,” Macaulay says, “but they’re reversible.”
Neurons have long been the focus of Alzheimer’s research. But the new results also show how other kinds of cells in the brain can play an important role in the disease.
The brain is a bit like a beehive, where a neuron is the queen, Macaulay says. But she’s kept alive by worker bees, like astrocytes, which are asked to do more as Alzheimer’s changes the brain.
“Those worker bees are getting unbelievably taxed from all the things they are being asked to do,” Macaulay says. “When that happens, then the whole system doesn’t work well.”
Metabolic treatments that restore astrocytes and other helper cells in the brain could someday augment existing Alzheimer’s drugs that remove amyloid plaques, Macauley says.
And the metabolic approach may be able to improve memory and thinking — something amyloid drugs don’t do.
“Maybe this can make your astrocytes and your neurons work a little bit better, so that you function a little bit better,” Macaulay says.
But first, she says, the promising results will have to be replicated in people.
Copyright 2024 NPR

- Diagnostics
- Health Tech
- Medical Devices

60 minutes! That’s all it takes for this blood test to detect if you have brain cancer or not
The researchers argue that this test could have “great implications” for cancer research, biomarker discovery, and disease monitoring and can be beneficial not just for brain cancer.

A team of scientists has developed a new blood test that can detect brain cancer faster. The researchers claim that this test requires only 100 microliters of blood to run this novel ‘liquid biopsy’, and within an hour, the method can detect biomarkers associated with glioblastoma which the deadliest and most common type of brain tumor.
According to a report by Science Alert, the method seems to be much better than all other existing tests and markers for glioblastoma due to its excellent accuracy. The developers of the prototype say it has “near turn-key functionality”.

A US and Australian team, led by scientists from the University of Notre Dame in the US has achieved this breakthrough. According to the researchers, the test is based on sensing mutated blood biomarkers, called epidermal growth factor receptors (EGFRs), which are overexpressed in certain cancers, like glioblastoma.

Interestingly, these blood biomarkers are found tucked inside extracellular vesicles, which are small packages that contain proteins, lipids, and genetic material from their original cells.
“Extracellular vesicles or exosomes are unique nanoparticles secreted by cells. They are big – 10 to 50 times bigger than a molecule – and they have a weak charge. Our technology was specifically designed for these nanoparticles, using their features to our advantage,” explains biomolecular engineer Hsueh-Chia Chang from Notre Dame as quoted by Science Alert.
The researchers coat a supersensitive biochip in an untreated sample of blood plasma to detect the molecules released from the cells of cancerous tumors.
However, various factors also need to be analysed. The team maintains that to create a more specific test they need to analyse larger cohorts of glioblastoma patients to understand what biomarkers in their blood set them apart.
The findings of the study were published in the Communications Biology journal.
Get live Share Market updates, Stock Market Quotes , and the latest India News … Read More and business news on Financial Express. Download the Financial Express App for the latest finance news.
- Stock Market Stats
Related News
Indian Railways is launching two special trains to connect Chennai and Santragachi in preparation for the festive season. These trains will run on two different routes and will operate weekly until November 2024, offering a total of 13 trips. Advance reservations are now open for these services.
Photo Gallery
21 Anubhuti coaches with aircraft-like features to replace Shatabdi 1st-AC Executive chair cars; 20 amazing facts
11 In Pictures: People stage protests across India as country boils over rape and murder of Kolkata doctor
9 Rs 50, Rs 200, Rs 500 and Rs 2000 notes images: Here are the new currency notes released by RBI
Online Help
Our 24/7 cancer helpline provides information and answers for people dealing with cancer. We can connect you with trained cancer information specialists who will answer questions about a cancer diagnosis and provide guidance and a compassionate ear.
Chat live online
Select the Live Chat button at the bottom of the page
Call us at 1-800-227-2345
Available any time of day or night
Our highly trained specialists are available 24/7 via phone and on weekdays can assist through online chat. We connect patients, caregivers, and family members with essential services and resources at every step of their cancer journey. Ask us how you can get involved and support the fight against cancer. Some of the topics we can assist with include:
- Referrals to patient-related programs or resources
- Donations, website, or event-related assistance
- Tobacco-related topics
- Volunteer opportunities
- Cancer Information
For medical questions, we encourage you to review our information with your doctor.
Brain and Spinal Cord Tumors in Adults
- What Are Adult Brain and Spinal Cord Tumors?
- Types of Brain and Spinal Cord Tumors in Adults
- Key Statistics for Brain and Spinal Cord Tumors
- What’s New in Adult Brain and Spinal Cord Tumor Research?
- Risk Factors for Brain and Spinal Cord Tumors
- What Causes Brain and Spinal Cord Tumors in Adults?
- Can Brain and Spinal Cord Tumors in Adults Be Prevented?
- Can Brain and Spinal Cord Tumors in Adults Be Found Early?
- Signs and Symptoms of Adult Brain and Spinal Cord Tumors
- Tests for Brain and Spinal Cord Tumors in Adults
- Brain and Spinal Cord Tumors in Adults: Prognostic Factors
- Survival Rates for Selected Adult Brain and Spinal Cord Tumors
- Questions to Ask About Adult Brain and Spinal Cord Tumors
- Surgery for Adult Brain and Spinal Cord Tumors
- Radiation Therapy for Adult Brain and Spinal Cord Tumors
- Chemotherapy for Adult Brain and Spinal Cord Tumors
- Targeted Drug Therapy for Adult Brain and Spinal Cord Tumors
- Other Drug Treatments for Adult Brain and Spinal Cord Tumors
- Tumor Treating Fields (TTF) Therapy for Adult Brain and Spinal Cord Tumors
- Treatment of Adult Brain and Spinal Cord Tumors, by Type
- Living as a Brain or Spinal Cord Tumor Survivor
If You're an Adult with a Brain or Spinal Cord Tumor
What are adult brain and spinal cord tumors, are there different kinds of brain and spinal cord tumors, how does the doctor know i have a brain or spinal cord tumor, how serious is my tumor, what kind of treatment will i need, what will happen after treatment.
Brain and spinal cord tumors are masses of cells in the brain or spinal cord that have changed and grown out of control.
Tumors in the brain or spinal cord can press on or spread into nearby normal tissue as they grow. This can make it hard for the brain and spinal cord to work the way they should to control functions in the rest of the body.
The main concerns with brain and spinal cord tumors are how fast they will grow and whether they can be taken out (or destroyed) and not come back.
Some types of brain and spinal cord tumors grow faster and are more likely to spread into nearby parts of the brain or spinal cord than are others. Slow-growing tumors are sometimes called benign . But even benign brain or spinal cord tumors can sometimes cause serious problems.
Many other types of cancer, such as lung cancer or breast cancer, can spread (metastasize) to the brain from another part of the body. These are not the kind of tumors we talk about here. We are talking about tumors that start in cells in the brain or spinal cord. These tumors rarely spread to other parts of the body.
The brain and spinal cord
The brain and spinal cord are called the central nervous system (CNS). They serve as the main “processing center” for all of the nervous system.
The brain and spinal cord are surrounded and protected by a special liquid, called cerebrospinal fluid (CSF). The brain is also protected by the skull. The spinal cord is protected by the stack of spinal bones called vertebrae.
Different parts of the brain control different things, like the way we see, move, feel, or think. The spinal cord connects the brain to nerves all over the body to carry messages back and forth.
There are many kinds of brain and spinal cord tumors . Your doctor can tell you more about the kind you have. Here are some of the more common types and how to say them:
- Glioblastoma (GLEE-o-blast-O-muh)
- Astrocytoma (AS-troh-sy-TOE-muh)
- Oligodendroglioma (AHL-ih-go-DEN-dro-glee-O-muh)
- Ependymoma (eh-PEN-dih-MO-muh)
- Meningioma (meh-NIN-jee-O-muh)
- Medulloblastoma (MED-yew-lo-blas-TOE-muh)
- Schwannoma (shwah-NO-muh)
- Craniopharyngioma (KRAY-nee-o-fuh-RIN-jee-O-muh)
Questions to ask the doctor
- Why do you think I have a brain or spinal cord tumor?
- Is there a chance I don’t have one?
- Would you please write down the kind of tumor you think I might have?
- What will happen next?
The symptoms of brain and spinal cord tumors depend mainly on where the tumor is. Some symptoms may start slowly and get worse over time. Sometimes they happen very fast. Common symptoms are headaches and seizures. Others are blurry vision, feeling sick to your stomach, and changes in the way you feel or act. Of course, these symptoms can have other causes as well.
The doctor will ask you questions about your health and do a physical exam.
If your doctor thinks you might have a tumor, they may send you to a neurologist or a neurosurgeon . These are doctors who treat problems in the nervous system.
Tests that you might have
If signs are pointing to a brain or spinal cord tumor, tests will be done to find out. Here are some of the tests you may need:
MRI scan: This test uses radio waves and strong magnets to make detailed pictures of the inside of the body. MRI is the best way to look for tumors in the brain and spinal cord. Different kinds of MRIs may be used to look at blood vessels, blood flow, and activity in the brain.
CT (CAT) scan: This test uses x-rays to make detailed pictures of the inside of your body. It can be helpful for looking at the bones around the tumor.
MR or CT angiography : These tests use special types of MRI or CT scans to look at the blood vessels inside the brain and around a tumor.
PET scan: For a PET scan, a kind of dye that has sugar is put into your blood. The sugar can be seen inside your body with a special camera. If there is a tumor, this sugar shows up as a “hot spot” where the tumor is found.
Biopsy: In a biopsy, the doctor takes out small pieces of brain or spinal cord tissue to check for tumor cells. This can be done during surgery or with a special hollow needle. A biopsy is often the only way to tell exactly what kind of tumor it is. If tumor cells are found, special lab tests might be done on them to learn more about them.
- What tests will I need?
- Who will do these tests?
- Where will they be done?
- How and when will I get the results?
- Who will explain the results to me?
- What do I need to do next?
For many types of cancer, the stage (extent) of the cancer is used to decide what type of treatment is best and how likely a person is to get better. But brain and spinal cord tumors are not staged like most cancers.
Some of the things that doctors use to decide on treatment and a person’s chances of getting better are:
- The person’s age
- Whether the tumor is affecting normal brain functions
- The type of tumor
- The grade of the tumor (how quickly it’s likely to grow, based on how the cells look)
- If the tumor cells have certain gene (DNA) changes
- The size of the tumor
- Where the tumor is
- How much of the tumor can be taken out with surgery (if it can be done)
- Whether the tumor has spread to other parts of the brain or spinal cord
- Where is the tumor?
- What type of tumor is it?
- How fast is the tumor likely to grow?
- How big is the tumor?
- Can all of the tumor be removed?
- Has the tumor spread to other parts of my brain and spinal cord?
Treatment for brain and spinal cord tumors depends on things like the type of tumor, where it is, and your overall health.
Surgery is the first treatment for most people. Surgery may be used to:
- Get a biopsy sample
- Take out the tumor
- Make the tumor smaller so it can be better treated with radiation or chemo
- Help prevent or treat problems from the tumor (like putting in a tube to drain fluid from around the brain)
There are many kinds of surgery. The type used depends on where the tumor is and how big it is. Radiation may be used with surgery to try to cure the tumor or help keep it from growing.
Ask your doctor what type of surgery you will need. Every type has pros and cons.
Side effects of surgery
Any type of surgery can have risks and side effects, like bleeding or infections. Ask the doctor what you can expect. If you have problems, let your doctors know. Doctors who treat people with brain and spinal cord tumors should be able to help you with any problems that come up.
Radiation treatments
Radiation uses high-energy rays (like x-rays) to kill cancer cells. It may be used:
- After surgery to kill any tumor cells left behind
- As the main treatment if surgery can’t be done
- To help ease or prevent problems from the tumor
There are different ways to give radiation treatments.
Radiation is usually aimed at the tumor from a machine outside the body. This is called external beam radiation. The radiation may be given all at once or in smaller doses given over a few days or weeks.
Radiation can also be given by putting tiny seeds of radiation into or near the tumor. This is called brachytherapy . This kind of radiation is most often given along with external beam radiation.
Side effects of radiation treatments
If your doctor suggests radiation treatment, talk about what side effects might happen. Radiation might cause some people to feel tired, or feel sick and throw up. If large parts of the brain are treated, radiation can change how the brain works.
Most side effects get better after treatment ends. Some might last longer. Talk to your cancer care team about what you can expect during and after treatment. There may be ways to ease side effects.
Chemo is the short word for chemotherapy, the use of drugs to fight cancer. The drugs are often given through a needle into a vein or taken as a pill. These drugs go into the blood and spread through the body.
Chemo can also be put right into the CSF or right into the brain during surgery. Ask your doctor how you will get chemo.
Chemo is often given in cycles or rounds. Each round of treatment is followed by a break. Sometimes more than one chemo drug might be given. Treatment often lasts for many months.
Side effects of chemo
Chemo might make you feel very tired, sick to your stomach, and cause your hair to fall out. But these problems go away after treatment ends.
There are ways to treat most chemo side effects. If you have side effects, talk to your cancer care team so they can help.
Targeted drugs
Targeted drugs are made to work mostly on the changes in cells that make them cancer. These drugs affect mainly tumor cells and not normal cells in the body. They may work even if other treatment doesn’t. They may be given alone or along with chemo to treat certain types of brain and spinal cord tumors.
Side effects of targeted drugs
Side effects depend on which drug is used. These effects usually go away after treatment ends.
There are ways to treat most of the side effects caused by targeted drugs. If you have side effects , talk to your cancer care team so they can help.
Other drugs
Some other drugs don't treat tumors directly, but they can still be helpful. For example:
- S teroid drugs can help reduce swelling in the brain.
- A nti-seizure drugs can help lower the risk of seizures.
- H ormones might be needed if the tumor or its treatment damages the pituitary gland, which sits just under the brain.
Electric field therapy
For some types of brain tumors, sets of electrodes can be placed on the scalp for most of the day. They make mild electric currents that seem to slow the growth of some tumor cells. They can be used along with or instead of chemo. Side effects tend to be mild.
Clinical trials
Clinical trials are research studies that test new drugs or other treatments in people. They compare standard treatments with others that may be better.
If you would like to learn more about clinical trials that might be right for you, start by asking your doctor if your clinic or hospital conducts clinical trials. See Clinical Trials to learn more.
Clinical trials are one way to get the newest treatments. They are the best way for doctors to find better ways to treat tumors. But they might not be right for everyone. If your doctor can find a clinical trial that’s studying the kind of tumor you have, it’s up to you whether to take part. And if you do sign up for a clinical trial, you can always stop at any time.
What about other treatments that I hear about?
When you have a tumor you might hear about other ways to treat it or treat your symptoms. These may not always be standard medical treatments. These treatments may be vitamins, herbs, diets, and other things. You may wonder about these treatments.
Some of these are known to help, but many have not been tested. Some have been shown not to help. A few have even been found to be harmful. Talk to your doctor about anything you’re thinking about using, whether it’s a vitamin, an herb, a diet, or anything else.
- What treatment do you think is best for me?
- What’s the goal of this treatment? Do you think it could cure the tumor?
- Will treatment include surgery? If so, who will do the surgery?
- What will the surgery be like?
- Will I need other types of treatment, too?
- What will these treatments be like?
- What’s the goal of these treatments?
- What side effects could I have from these treatments?
- What can I do about side effects that I might have?
- Is there a clinical trial that might be right for me?
- What about vitamins or diets that friends tell me about? How will I know if they are safe?
- How soon do I need to start treatment?
- What should I do to be ready for treatment?
- Is there anything I can do to help the treatment work better?
- What’s the next step?
Some tumors can be removed (or destroyed) completely, but others might not be. Even if it's gone, it can be hard not to worry about it coming back. Whether the tumor is gone or you are still getting treatment, you will still need to see your doctor.
Be sure to go to all of these follow-up visits. Your doctors will ask about symptoms, do physical exams, and may do tests to see if the tumor has grown or come back. They will also test you to see if treatment has damaged your brain. If needed, they will help you learn to deal with the changes.
Having a brain tumor and dealing with treatment can be hard, but it can also be a time to look at your life in new ways. You might be thinking about how to improve your health. Call us at 1-800-227-2345 or talk to your doctor to find out what you can do to feel better.
You can’t change the fact that you have had a tumor. What you can change is how you live the rest of your life – making healthy choices and feeling as good as you can.
For connecting and sharing during a cancer journey
Anyone with cancer, their caregivers, families, and friends, can benefit from help and support. The American Cancer Society offers the Cancer Survivors Network (CSN) , a safe place to connect with others who share similar interests and experiences. We also partner with CaringBridge , a free online tool that helps people dealing with illnesses like cancer stay in touch with their friends, family members, and support network by creating their own personal page where they share their journey and health updates.
- Words to know
- How can I learn more?

The American Cancer Society medical and editorial content team
Our team is made up of doctors and oncology certified nurses with deep knowledge of cancer care as well as editors and translators with extensive experience in medical writing.
Biopsy (BY-op-see): Taking out a small piece of tissue to see if there are cancer cells in it.
Central nervous system: The brain and the spinal cord, which serve as the main “processing center” for all of the nervous system. Often called the CNS.
Cerebrospinal fluid (suh- REE -bro-SPY-nuhl FLEW-id): The clear liquid that surrounds and cushions the brain and spinal cord. Often called CSF.
Debulking: Removing as much of the tumor as is safely possible. For tumors that can’t be removed completely, this might be done to help with symptoms or to help other treatments like radiation or chemo work better.
Grade: A number given to a tumor based on how quickly a tumor is likely to grow and spread into nearby normal tissue, and on how the tumor cells look. Brain and spinal cord tumors are given a grade from I (1) to IV( 4), with grade IV tumors tending to grow and spread the fastest.
Malignant (mah-LIG-nent) : A tumor that grows quickly and often grows into nearby normal tissues.
Neurologist (nur-AHL-uh-jist): A doctor who specializes in treating nervous system problems or diseases.
Neurosurgeon ( NUR -o-SUR-jun): A doctor who specializes in using surgery to treat nervous system problems or diseases.
Neuroradiologist (NUR-o-ray-dee- AHL -uh-jist): A doctor who specializes in using imaging tests to look at the nervous system.
Ommaya reservoir (o-MY-uh REZ-er-vahr): A plastic, dome-shaped drum that’s put just under the scalp during surgery. A tube attached to it goes into the brain where it reaches the CSF. Doctors and nurses can use a thin needle to give chemo through the drum or to take out CSF for testing.
VP shunt: Also called a ventriculoperitoneal (ven-TRIK-yew-lo-pair-ih-tuh- NEE -ahl) shunt. A thin tube used to drain extra CSF to ease pressure in the brain. Surgery is done to put one end of the shunt in the brain and the other end in the abdomen (belly). The tube runs under the skin of the neck and chest. The flow of CSF is controlled by a valve in the tubing. Shunts may be short-term or permanent.
We have a lot more information for you. You can find it online at www.cancer.org . Or, you can call our toll-free number at 1-800-227-2345 to talk to one of our cancer information specialists.
Last Revised: May 5, 2020
American Cancer Society medical information is copyrighted material. For reprint requests, please see our Content Usage Policy .
American Cancer Society Emails
Sign up to stay up-to-date with news, valuable information, and ways to get involved with the American Cancer Society.
More in Brain And Spinal Cord Tumors In Adults
- About Brain and Spinal Cord Tumors in Adults
- Causes, Risk Factors, and Prevention
- Early Detection, Diagnosis, and Staging
- After Treatment
Help us end cancer as we know it, for everyone.

If this was helpful, donate to help fund patient support services, research, and cancer content updates.

IMAGES
VIDEO
COMMENTS
Find research articles on brain cancer, which may include news stories, clinical trials, blog posts, and descriptions of active studies.
Learn what's new in brain and spinal cord tumor research, including progress in diagnosis, targeted therapies and immunotherapies, and radiation response. Treatment of brain and spinal cord tumors in children and quality of life research is also discussed, along with selected NCI-supported programs.
A collaborative project to bring the promise of cell therapy to patients with a deadly form of brain cancer has shown dramatic results among the first patients to receive the novel treatment. In a paper published Wednesday in The New England Journal of Medicine, researchers from Mass General Cancer Center shared the results for the first three ...
Northwestern Medicine scientists have used ultrasound technology to penetrate the blood-brain barrier and provide a small dose of a chemotherapy and immunotherapy, a major advance for the treatment of this deadly cancer.
Brain cancer. Research on one of the deadliest malignancies is yielding potentially game-changing insights — and treatments. Any type of cancer presents an insidious risk to life. But the ...
This Focus issue highlights current research into the unique biology of brain tumours and brain metastasis and how this research might improve therapy of these often devastating diseases.
This Frontiers Research Topic Proposal on " Brain Cancers: New Perspectives and Therapies " joined contributions from scientists and physicians who investigate on etiopathogenesis and treatment of brain cancers. In fact, studies exploiting the existing link between enhancing the knowledge of cellular and molecular pathways involved in the ...
Brain Tumor Research Studies Johns Hopkins has an unparalleled history of introducing new forms of treatment for the patients affected by malignant brain tumors. For example, the only two new effective surgical treatments for malignant brain tumors approved by FDA (Gliadel and GliaSite) were discovered and developed right here at Johns Hopkins.
NCI's Center for Cancer Research, Neuro-Oncology Branch is advancing care and treatment for people with brain tumors through collaborative scientific workshops, research discoveries, and successful clinical trials.
How cerebral organoids are guiding brain-cancer research and therapies To find better treatments for brain cancer, an important step might be to grow mini-brains in the lab.
Research into causes, prevention, and treatment of brain and spinal cord tumors is ongoing in many medical centers throughout the world. Find out what's new.
Growth-stimulating crosstalk between the brain and cancer tumors presents a new target for therapy.
To drive their growth, many tumors hijack nervous system signals, including those needed for brain plasticity. Stanford Medicine discoveries are opening a promising new branch of oncology research.
Get an overview of brain and spinal cord tumors in adults and the latest key statistics in the US. Find information on cancer types and new research.
The most common primary noncancerous, or benign, brain tumor is the meningioma, which arises from the membranes that surround the brain and spinal cord. On this "Mayo Clinic Q&A" podcast, Dr. Alyx Porter, co-chair of the Central Nervous System Tumor Disease Group at Mayo Clinic Cancer Center, discusses the various types of brain tumors and how ...
Brain Cancer research articles are listed. Brain cancer news covers topics such as diagnosis, brain tumors, chemotherapy, gamma knife technology, brain cancer treatments, glioblastomas, stem cell research, neurosurgery, medicine, genetics, neurology, and other brain research.
The American Cancer Society's estimates for brain and spinal cord tumors in the United States for 2023 include both adults and children. About 25,400 malignant tumors of the brain or spinal cord (14,420 in males and 10,980 in females) will be diagnosed. These numbers would be much higher if benign (non-cancer) tumors were also included.
The study highlights a promising advance in brain cancer therapy. Key Facts: B-SWE disrupts the blood-brain barrier more effectively than conventional methods. The technique may allow more cancer-fighting drugs to enter the brain. B-SWE minimizes damage to healthy brain tissue while targeting cancer cells. Source: Virginia Tech.
Metastatic brain tumors, also called secondary brain tumors, are malignant tumors that originate as cancer elsewhere in the body and then metastasize (spread) to the brain. Metastatic brain tumors are about four times more common than primary brain tumors. They can grow rapidly, crowding or invading nearby brain tissue.
Brain Tumor Facts There are more than 100 distinct types of primary brain tumors, each with its own spectrum of presentations, treatments, and outcomes. More than any other cancer, brain tumors can have lasting and life-altering physical, cognitive, and psychological impacts on a patient's life. And, despite years of research, brain cancer survival rates have remained little-changed in ...
The biochip is used to detect biomarkers for glioblastoma, a fast-growing brain cancer. (Photo by Matt Cashore/University of Notre Dame) Researchers at the University of Notre Dame have developed a novel, automated device capable of diagnosing glioblastoma, a fast-growing and incurable brain cancer, in less than an hour.
Glioblastoma (GBM) is an aggressive form of brain cancer. Despite therapeutic efforts, including surgical resection, radiation and chemotherapy, tumor relapse is inevitable with no standard second ...
Pushing the Boundaries of Brain Cancer Research One of the most significant challenges in brain cancer treatment is developing therapeutics that can cross the blood-brain barrier. To address this, a team led by Dr Andrea Pavesi at A*STAR's Institute of Molecular and Cell Biology (IMCB) have designed a groundbreaking microfluidic device that ...
Discover more about brain cancer including types, symptoms and stages, as well as the treatments and research being pioneered at the OSUCCC - James.
Tumours can start in any part of the brain or related structures. This section is about primary brain tumours in adults. Cancers that have spread to the brain from somewhere else in the body are called secondary brain tumours or brain metastases. Read about secondary brain cancer. Brain and spinal cord tumours can affect children and adults.
About Childhood CancerChildhood Cancer Awareness Month is celebrated each September around the world with the goal of increasing awareness of childhood cancer and advocating for pediatric cancer research and funding. It's estimated that about 400,000 children and adolescents develop cancer globally each year. The most common types of cancer diagnosed in children are leukemia, brain and other ...
A team of scientists from The Institute of Cancer Research, London and the Dana-Farber Cancer Institute, Boston, U.S., uncovered clues about the growth of a specific type of DHG—DHG, H3G34 ...
The brain needs a lot of energy — far more than any other organ in the body — to work properly. And aging and Alzheimer's disease both seem to leave the brain underpowered. But an experimental cancer drug appeared to re-energize the brains of mice that had a form of Alzheimer's — and even restore their ability to learn and remember.
The researchers argue that this test could have "great implications" for cancer research, biomarker discovery, and disease monitoring and can be beneficial not just for brain cancer. 60 minutes!
Find answers to commonly asked questions if you've been diagnosed with a brain or spinal cord tumor as an adult.