REVIEW article
Twenty years of research on borderline personality disorder: a scientometric analysis of hotspots, bursts, and research trends.

- 1 Department of Psychology, School of Humanities and Social Sciences, Anhui Agricultural University, Hefei, China
- 2 College of Computing & Informatics, Drexel University, Philadelphia, PA, United States
- 3 Department of Psychology, School of Education, China University of Geosciences, Wuhan, China
- 4 Department of Information Management, Anhui Vocational College of Police Officers, Hefei, China
Borderline personality disorder (BPD), a complex and severe psychiatric disorder, has become a topic of considerable interest to current researchers due to its high incidence and severity of consequences. There is a lack of a bibliometric analysis to visualize the history and developmental trends of researches in BPD. We retrieved 7919 relevant publications on the Web of Science platform and analyzed them using software CiteSpace (6.2.R4). The results showed that there has been an overall upward trend in research interest in BPD over the past two decades. Current research trends in BPD include neuroimaging, biological mechanisms, and cognitive, behavioral, and pathological studies. Recent trends have been identified as “prevention and early intervention”, “non-pharmacological treatment” and “pathogenesis”. The results are like a reference program that will help determine future research directions and priorities.

1 Introduction
Borderline personality disorder (BPD) is a complex and severe psychiatric disorder characterized by mood dysregulation, interpersonal instability, self-image disturbance, and markedly impulsive behavior (e.g., aggression, self-injury, suicide) ( 1 ). In addition, people with BPD may have chronic, frequent, random feelings of emptiness, fear, and so on. These symptoms often lead them to use unhealthy coping mechanisms in response to negative emotions, such as alcohol abuse ( 2 ). BPD has a long course, which makes treatment difficult and may have a negative impact on patients’ quality of life ( 3 ). Due to its clinical challenge, BPD is by far the most studied category of personality disorder ( 4 ). This disorder is present in 1−3% of the general population as well as in 10% of outpatients, 15−20% of inpatients, and 30−60% of patients with a diagnosed personality disorder, and has a suicide rate of up to 10% ( 5 , 6 ). Families of individuals with serious mental illness often experience distress, and those with relatives diagnosed with BPD tend to carry a heavier burden compared to other mental illnesses ( 7 , 8 ). As early as the 20th century, scholars began describing BPD and summarizing its symptoms. However, there was some debate regarding the precise definition of BPD.
In the past few decades, the research community has made remarkable progress in the study of BPD, equipping us with a wider range of perspectives and tools for understanding this intricate condition. However, numerous challenges still remain to be tackled by researchers. Diagnosing BPD is inherently challenging and often more difficult than anticipated. The symptoms of BPD are complex, diverse, and often overlap with those of other mental health conditions. For example, individuals with BPD may experience extreme mood swings similar to those observed in individuals with bipolar disorder ( 9 ); At the same time, they may also be entrenched in long-term depression, making it easy for doctors to initially misdiagnose them with depression ( 10 ). Because these symptoms overlap and interfere with each other, doctors often face the risk of misdiagnosing or overlooking the condition during initial diagnosis. Therefore, researchers are working to develop more accurate and comprehensive diagnostic tools and methods.
According to the “Neuro-behavioral Model” proposed by Lieb ( 1 ), the process of BPD formation is very complex and is determined by the interaction of several factors. The interaction between different factors can be complex and dynamic. Genetic factors and adverse childhood experiences may contribute to emotional disorders and impulsivity, leading to dysfunctional behaviors and inner conflicts. These, in turn, can reinforce emotional dysregulation and impulsivity, exacerbating the preexisting conditions. Genetic factors are an important factor in the development of BPD ( 11 ). Psychosocial factors, including adverse childhood experiences, have also been strongly associated with the development of BPD ( 12 ). Emotional instability and impulsive behavior are even more common in patients with BPD ( 13 ). The current study is based on the “Neuro-behavioral Model” and conducts a literature review of previous scientific research on BPD through bibliometric analysis to reorganize the influencing factors. Through large-sample data analysis, the association between BPD and other diseases is explored, which contributes to further refining this theory’s explanation of the common neurobiological mechanisms among various mental illnesses.
It is worth noting that with the development of BPD, some scholars have conducted bibliometrics studies on BPD to provide insights into this academic field. To date, the current study has identified two published bibliometric studies on the field: One is Ilaria M. A. Benzi and her colleagues’ 2020 metrological analysis of the literature in the field of BPD pathology for the period 1985−2020 ( 14 ). The other is a bibliometric analysis by Taylor Reis and his colleagues of the growth and development of research on personality disorders between 1980 and 2019 ( 15 ). Ilaria M. A. Benzi and her colleagues integrated and sorted out the research results of borderline personality pathology, and revealed the research results and development stages in this field through the method of network and cluster analysis. The results of the study clearly demonstrate that the United States and European countries are the main contributors, that institutional citations are more consistent, and that BPD research is well developed in psychiatry and psychology. At the same time, the development of research in borderline personality pathology is demonstrated from the initial development of the construct, through studies of treatment effects, to the results of longitudinal studies. Taylor Reis and his colleagues used a time series autoregressive moving average model to analyze publishing trends for different personality disorders to reveal their historical development patterns, and projected the number of publications for the period 2024 to 2029. The study finds a trend towards diversity in the research and development of personality disorders, with differences in publication rates for different types of personality disorders, and summarizes the reasons that influence these differences. This may ultimately determine which personality disorders will remain in future psychiatric classifications. These studies have provided valuable insights into the evolution of BPD, focusing primarily on its pathology or a broader personality disorder perspective. While basic bibliometric analyses of these studies have been conducted, there is a need for more in-depth investigations of specific trends in the evolution of BPD and a clearer delineation of emerging research foci. Therefore, in order to enhance the current study, this study extends the analysis to 2022 and utilizes a comprehensive structural variation analysis of the literature using scientometric methods. Building on previous bibliometric studies, we expect to provide new insights and additions to research in this area. At the same time, the research trends and hot topics in the field of BPD are further explored. In addition, several cocitation-based analyses are also carried out in order to better understand citation performance.
2.1 Objectives
One of our goals was to understand the current status and progress of researches on BPD, and to summarize the latest developments and research findings in BPD, such as new treatment methods and disease mechanisms. Through the intuitive presentation of knowledge graphs and other images or data, we aimed to provide clinical practice and research guidance for clinicians, researchers, and policymakers.
Our second goal was to help identify future research directions and priorities, and provide more scientific and systematic research guidance for researchers. For example, by identifying hotspots and associations in certain research areas, we can determine the fields and issues that require further investigations, thus providing clearer directions and focus for researches. Additionally, through bibliometric analysis, we can provide researchers with more targeted and practical research strategies and methods, improving research efficiency and the quality of research outcomes.
2.2 Search strategy and data collection
The selection of appropriate methods and tools in the process of analyzing research information is crucial. Web of Science (WOS) is a popular database for bibliometric analysis that includes numerous respectable and high-impact academic journals. In addition, data information, such as references and citations, is more extensive than other academic databases ( 16 ). Data collection took place on the date of May 10, 2023. The search strategy included the following: topic=“Neuro-behavioral Model” or “borderline characteristics” or “borderline etiology” or “borderline personality disorder”, database selected=WOS Core Collection, time span=2003−2022, index=Science Citation Index Expanded (SCI-EXPENDED) and Social Sciences Citation Index (SSCI). The “Neuro-behavioral Model” serves as a theoretical framework that is useful for explaining the development and pathophysiology of BPD; “borderline characteristics” can describe the related symptoms and features of BPD; “borderline etiology” helps to understand the factors that contribute to the development of BPD; “borderline personality disorder” is the most commonly used terms in relevant research. Using these as keywords in title searches can help researchers find researches related to BPD more accurately, facilitating deeper understanding of the characteristics, pathophysiology, etiology, and other aspects of BPD. In the current study, we focused only on two types of literature: articles and review articles, and limited the language to English. After removing all literature unrelated to BPD, a total of 7919 records met the criteria. They were exported in record and reference formats, and saved in plain text file format.
2.3 Data analysis and tools
Bibliometrics was first proposed by Alan Pritchard in 1969, as a method that combines data visualization to analyze publications statistically and quantitatively in specific fields and journals ( 17 ). Bibliometric analysis is a good way to analyze the trend of knowledge structure and research activities in scientific fields over time, and has been widely used in various fields since it was first used ( 18 ). Scientometrics is the application of bibliometrics in scientific fields, and it focuses on the quantitative characteristics and features of science and scientific researches ( 19 ). Compared to traditional literature review studies, visualized knowledge graphs can accurately identify key articles from many publications, comprehensively and systematically combing existing research in a field ( 20 ).
Currently, two important academic indicators are included in research. The impact factor (IF) is used as an indicator of a publication’s impact to assess the quality and importance of the publication ( 21 ). However, some researchers believe that IF has defects such as inaccuracy and misuse ( 22 ). Although many researchers have proposed to replace the impact factor with other indicators, IF is still one of the most effective ways to measure the impact of a journal ( 23 ). The IF published in the 2021 Journal Citation Reports were used. Another indicator is the H-index, which is an important measure of a scholar’s academic achievements. Some researchers consider it as a correction or supplement to the traditional IF ( 24 ).
All data were imported into CiteSpace (6.2.R4) and Scimago Graphica (1.0.30) for analysis. CiteSpace was used to obtain collaboration networks and impact networks. Scimago Graphica was used to construct a network graph of country collaboration. CiteSpace is a Java-based software developed in the context of scientometrics and data visualization ( 25 ). It combines scientific knowledge mapping with bibliometric analysis to determine the progress and current research frontiers in a particular field, as well as predict the development trends in that field ( 26 ). Scimago Graphica is a no-code tool. It can not only perform visualization analysis on communication data but also explore exploratory data ( 27 ). Currently, it is used for visual analysis of national cooperation relationships, displaying the geographic distribution of countries and publication trends.
3.1 Analysis of publication outputs, and growth trend prediction
Annual publications can provide an overview of the evolution of a research area and its progress ( 28 ). We retrieved 7919 articles from the WOS database on BPD between 2003 and 2022, including 6834 research articles and 1085 reviews ( Figure 1 ). As of the search date, these articles had received a total of 289,958 citations, equating to an average of 14,498 citations per year. Over the past two decades, the number of research articles published on BPD has shown a fluctuating upward trend. In addition, citations to these publications have increased significantly. A polynomial curve fit of the literature on BPD clearly indicates a strong correlation between the year of publication and the number of publications ( R 2 = 0.973). The number of research articles on BPD has indeed fluctuated and increased over the past two decades. This observation does, to some extent, indicate an upward trend, probably due to increasing interest in BPD. However, there are other factors to consider as well. For example, the accumulation of data or technological advances, government policies and corporate investment may also affect the direction of BPD research development.
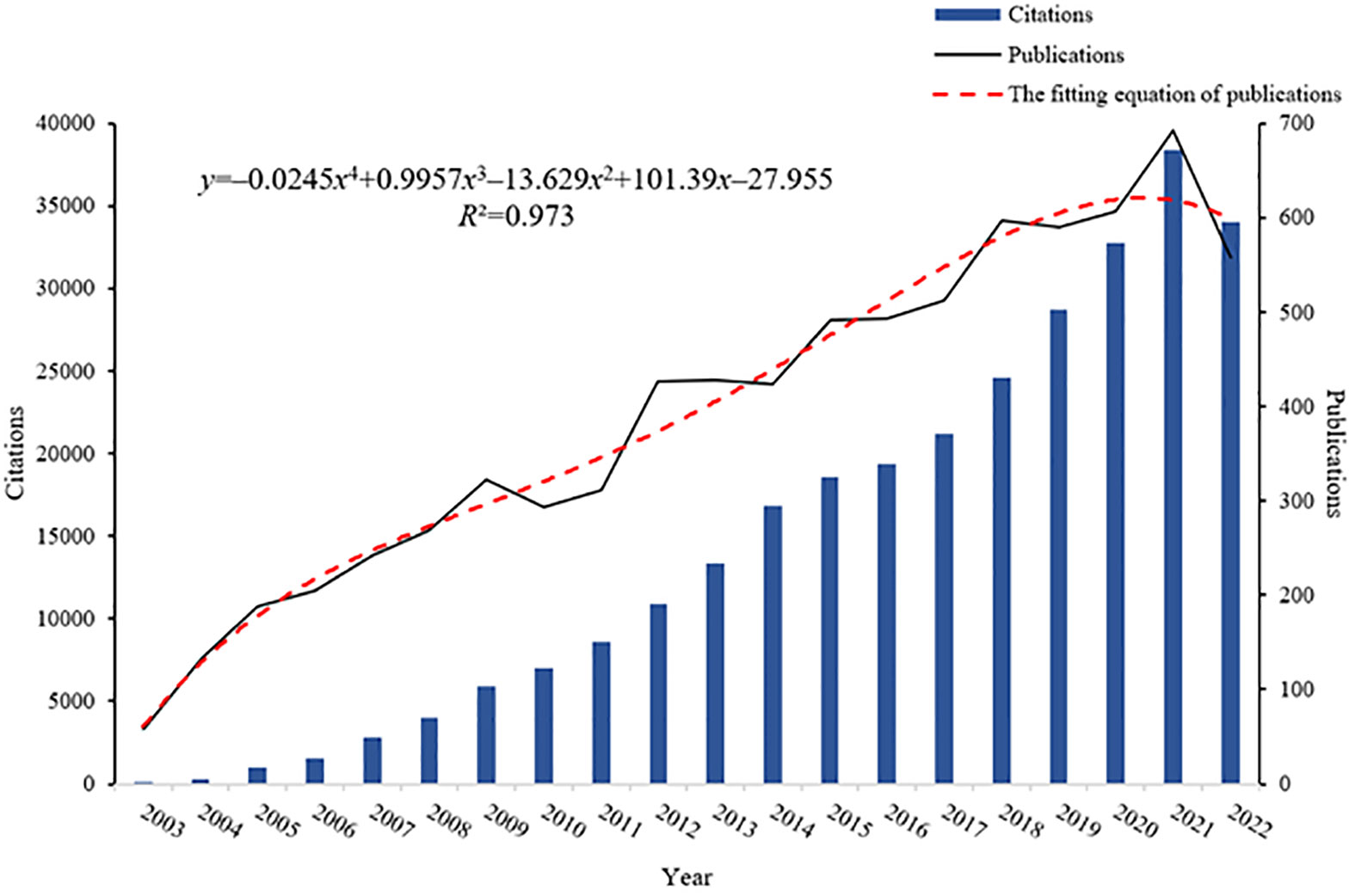
Figure 1 Annual publications, citation counts, and the fitting equation for annual publications in BPD.
3.2 Analysis of co-citation references: clusters and timeline of research
Co-cited references, which are cited by multiple papers concurrently, are considered a crucial knowledge base in any given field ( 28 ). In the current study, CiteSpace clustering was utilized to identify common themes within BPD-related literature. Figure 2 presented a co-citation network of highly cited references between 2003 and 2022, comprising 1163 references. A time slice of 1 was used, with the g -index was set at k =25, which resulted in the identification of 14 clusters representing distinct research themes in BPD. The significant cluster structure is denoted by a modularity value ( Q value) of 0.7974, and the high confidence level in the clusters by an average profile value ( S value) of 0.9176.
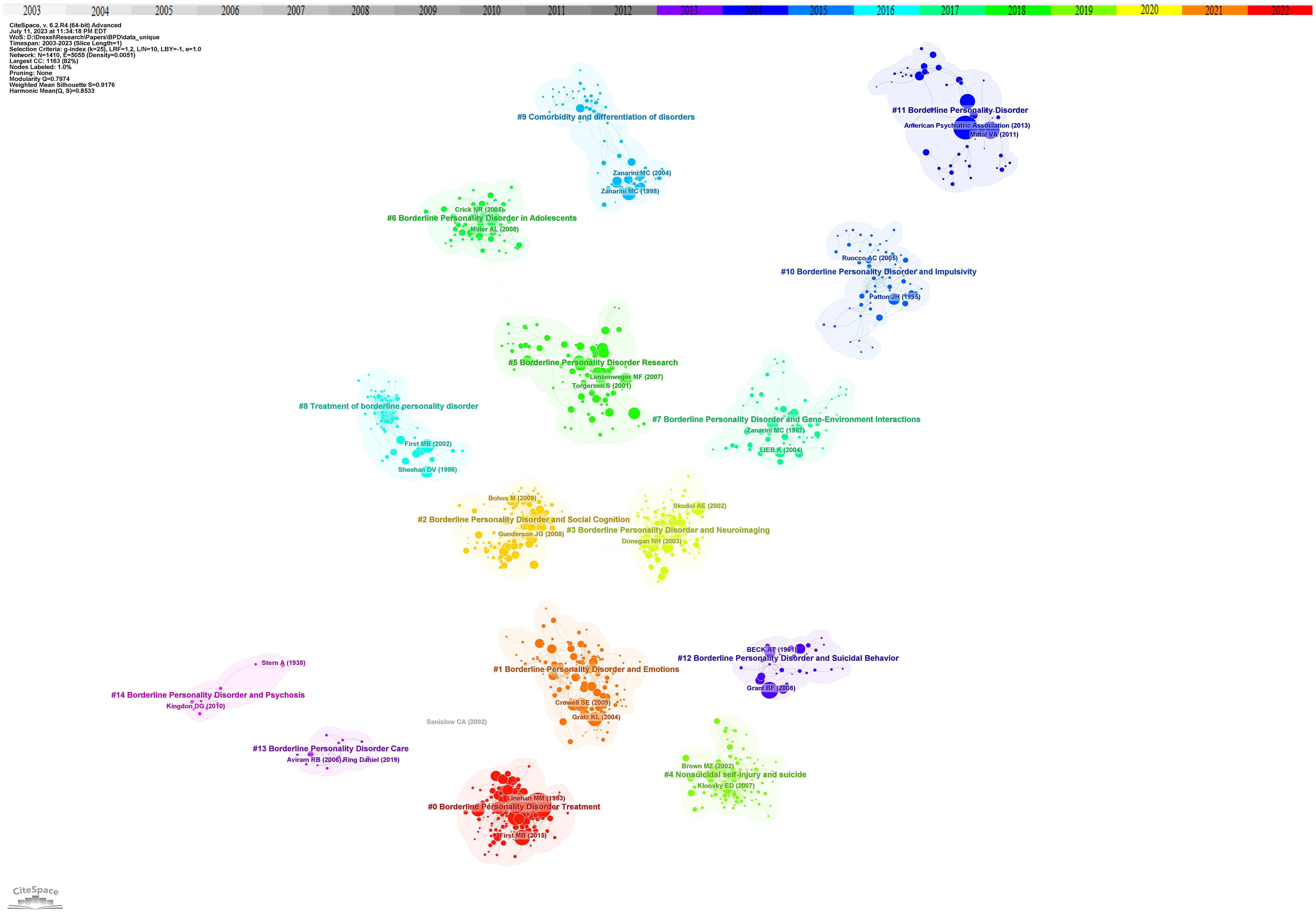
Figure 2 Reference co-citation network with cluster visualization in BPD. Trend 1 clinical researches, sub-trend clinical characteristics includes clusters #1, #2, #4, #10, #12; biological mechanisms include clusters #3, #7; nursing treatments includes clusters #0, #8, #13. Trend 2 associations and complications includes clusters #5, #6, #9, #11, #14.
Cluster analysis is performed through CiteSpace. Related clusters are classified into the same trend based on the knowledge of related fields and whether the clusters show similar trends. At the same time, based on the analysis of time series, to identify the movement of one cluster to another. Based on the cluster map of co-cited references on BPD, several different research trends were identified. The first major research trend is clinical research on BPD, which in turn consists of three sub-trends: clinical characterization of BPD, biological mechanisms, and nursing treatment. Of the data obtained, the earliest research on the clinical characterization of BPD began in 1992 with cluster #12, “borderline personality disorder and suicidal behavior” ( S =0.979; 1992). Paul H. Soloff and his colleagues conducted a comparative study of suicide attempts between major depressives and patients with BPD. The aim of this study was to develop more effective intervention strategies for suicide prevention ( 29 ). This cluster was further developed in cluster #4, “nonsuicidal self-injury and suicide” ( S =0.96; 2004). Thomas A. Widiger and Timothy J. Trull proposed a more flexible dimension-based categorization model to overcome the previous drawbacks of personality disorder categorization ( 30 ). Next in cluster #10 “borderline personality disorder and impulsivity” ( S =0.93; 2000), Jim H. Patton and his colleagues revised the Barratt Impulsivity Scale to measure impulsivity to facilitate practical clinical research ( 31 ). Related research continues to evolve into cluster #1 “borderline personality disorder and emotions” ( S =0.87; 2007) and cluster #2 “borderline personality disorder and social cognition” ( S =0.911; 2009), researchers have focused on understanding the causal relationship between BPD traits and factors such as social environment, emotion regulation, and interpersonal evaluative bias, as well as their potential impact ( 32 , 33 ). In the sub-trend of biological mechanisms, two main clusters are involved: cluster #7 “borderline personality disorder and gene-environment interactions” ( S =0.871; 2002) and cluster #3 “borderline personality disorder and neuroimaging” ( S =0.938; 2007). In the related cluster, researchers have found a relationship between BPD and genetic and environmental factors ( 34 ). Researchers have also utilized various external techniques to explore the degree of correlation between the risk of developing BPD and its biological mechanisms, aiming to reveal the complex mechanisms that influence the emergence and development of BPD ( 35 ). In nursing treatment, cluster #8 “treatment of borderline personality disorder “ ( S =0.968; 2001), Silvio Bellino and his colleagues systematically analyzed the current publications on BPD pharmacotherapy research and summarized relevant clinical trials and findings ( 36 ). However, due to the complexity of BPD, there is still a lack of information on the exact efficacy of pharmacotherapy in BPD, and therefore pharmacotherapy remains an area of ongoing development and research. This trend continues to be developed in cluster #0 “borderline personality disorder treatment” ( S =0.887; 2006), which emphasizes the development of novel pharmacotherapies for BPD. Cluster #13 “borderline personality disorder care” ( S =0.997; 2013) mainly focuses on the comprehensive care of people with borderline personality disorder and the education of patients and families. The goal is to improve patients’ quality of life, reduce self-injury and suicidal behavior, and promote full recovery.
The second major research trend is association and comorbidity. This trend first began in cluster #9 “comorbidity and differentiation of disorders” ( S =0.946; 1999). Mary C Zanarini and his colleagues explored the comorbidity of BPD with other psychiatric disorders on Axis I ( 37 ). Cluster #14 “borderline personality disorder and psychosis” ( S =0.966; 2003) also explored symptoms associated with BPD ( 38 ). This trend continues, with researchers studying BPD research in cluster #11 “borderline personality disorder” ( S =0.935; 2004) and cluster #5 “borderline personality disorder research” ( S =0.881; 2007) ( 39 , 40 ). In addition, cluster #6 “borderline personality disorder in adolescents” ( S =0.894; 2011) points out that the focus of BPD research is increasingly shifting towards adolescents ( 41 ).
Figure 3 showed the time span and research process of the developmental evolution of these different research themes. The temporal view reveals the newest and most active clusters, namely #0 “dialectical behavior therapy”, #1 “daily life”, and #2 “social cognition”, which have been consistently researched for almost a decade. Cluster #0 “dialectical behavior therapy” has the largest number and the longest duration, lasting almost 10 years. Similarly, this article by Rebekah Bradley and Drew Westen on understanding the psychodynamic mechanisms of BPD from the perspective of developmental psychopathology has the largest node ( 34 ).
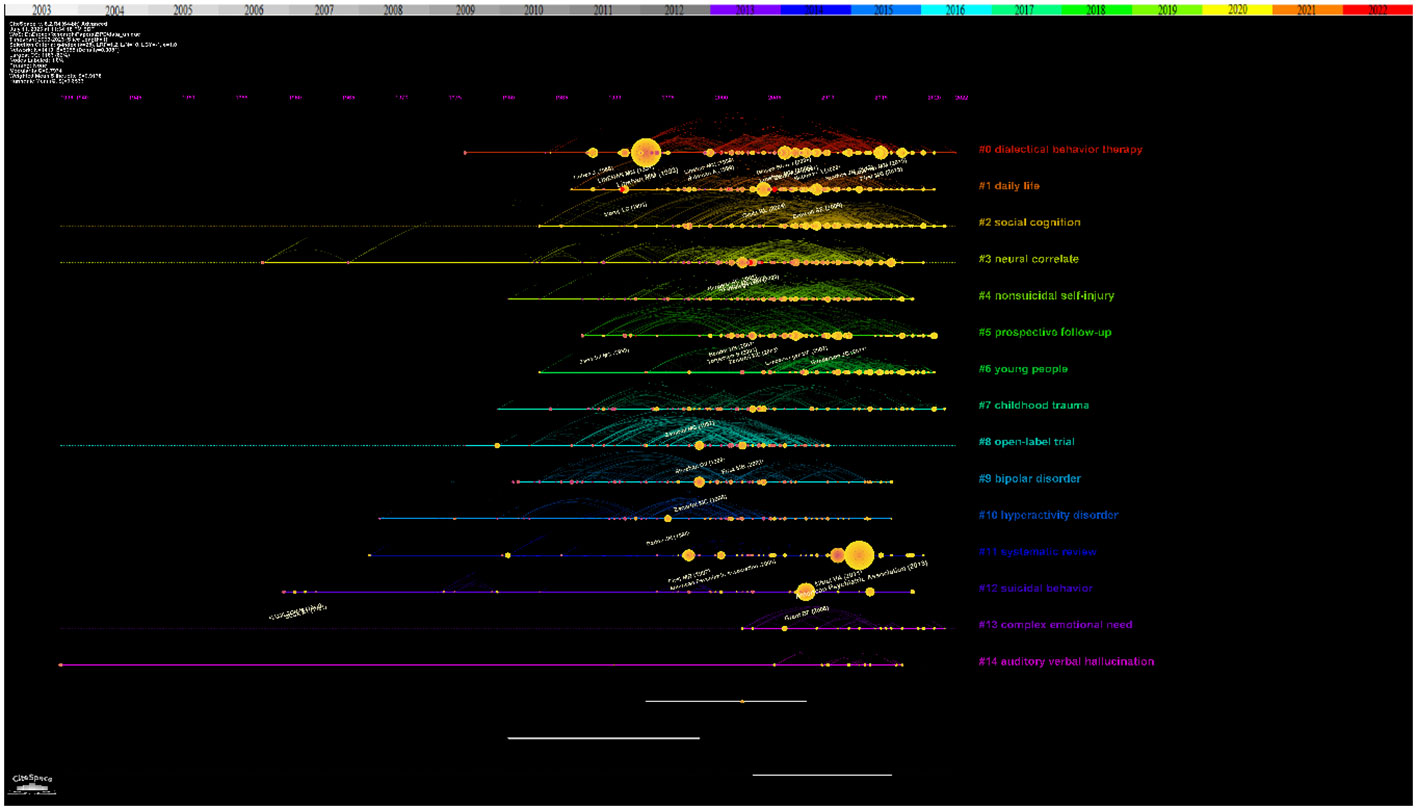
Figure 3 Reference co-citation network with timeline visualization in BPD.
3.3 Most cited papers
The top 10 highly cited papers on BPD research were presented in Table 1 . The most cited paper, by Marsha M. Linehan and colleagues, focus on the treatment of suicidal behavior in BPD ( 42 ). The transition between suicidal and non-suicidal self-injurious behavior in individuals with BPD has attracted researchers’s attention, mainly in cluster #4 “nonsuicidal self-injury and suicide” ( 52 ). The second is the experimental study by Josephine Giesen-Bloo and his colleagues on the psychotherapy of BPD ( 43 ). In cluster #0 “borderline personality disorder treatment” and Cluster #8 “treatment of borderline personality disorder”, researchers strive to find non-pharmacological approaches with comparable or enhanced therapeutic effects. This was followed by Sheila E. Crowell and her colleagues’ study of the biological developmental patterns of BPD ( 44 ). Research on the biological mechanisms and other contributing factors of BPD, including #7 “borderline personality disorder and gene-environment interactions” have been closely associated with the development of BPD ( 53 ).
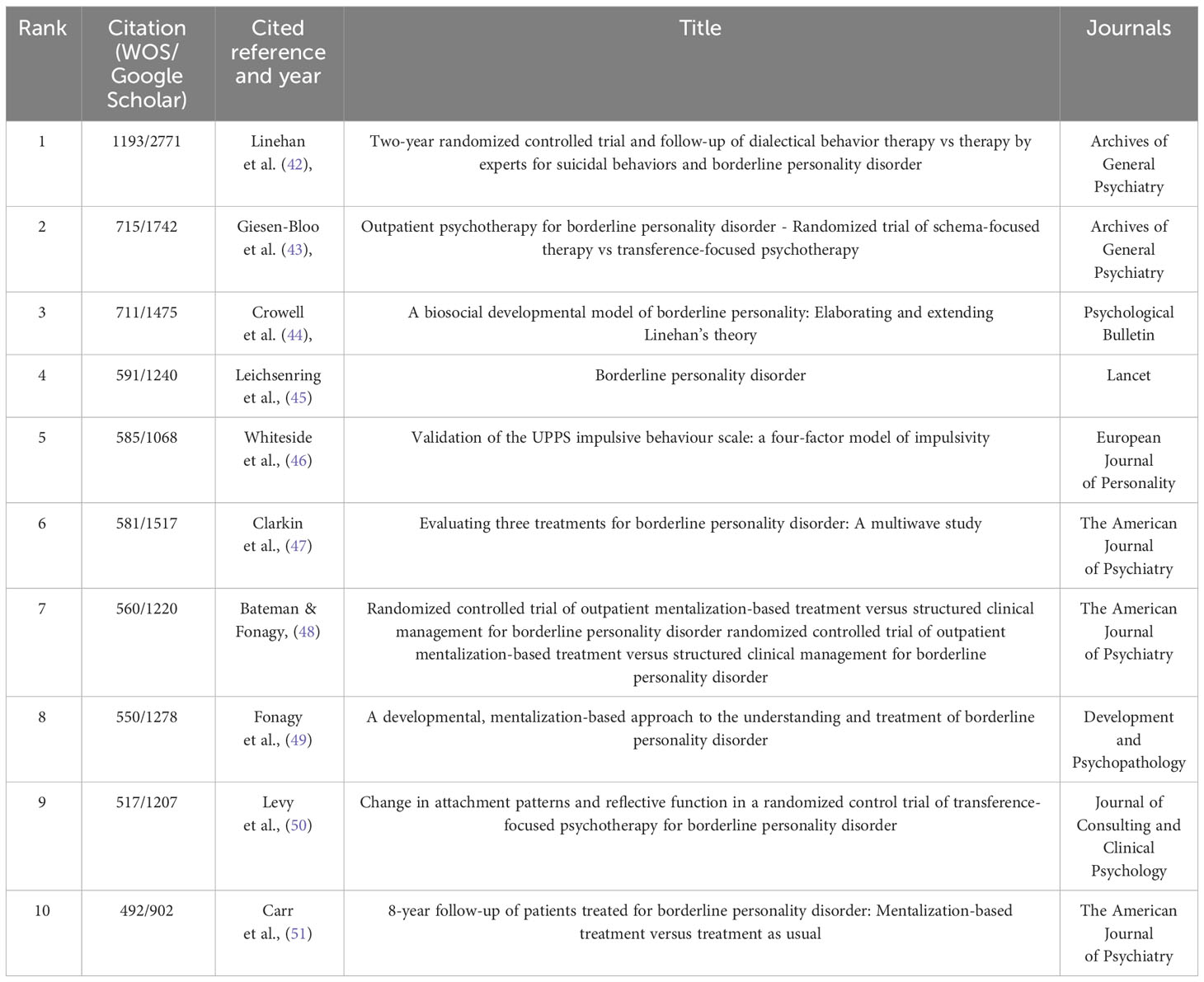
Table 1 Top 10 cited references that published BPD researches.
3.4 Burst analysis and transformative papers
The “citation explosion” reflects the changing research focus of a field over time and indicates that certain literature has been frequently cited over time. Figure 4 showed the top 9 references with the highest citation intensity. The three papers with the greatest intensity of outbursts during the period 2003−2022 are: The first is the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders ( 54 ). In the second article, Vijay A. Mittal and Elaine F. Walker discuss key issues surrounding dyspraxia, tics, and psychosis that are likely to appear in an upcoming edition of the Diagnostic and Statistical Manual of Mental Disorders ( 39 ). In addition, Ioana A. Cristea and colleagues conducted a systematic review and meta-analysis to evaluate the effectiveness of psychotherapy for borderline personality disorder ( 55 ).
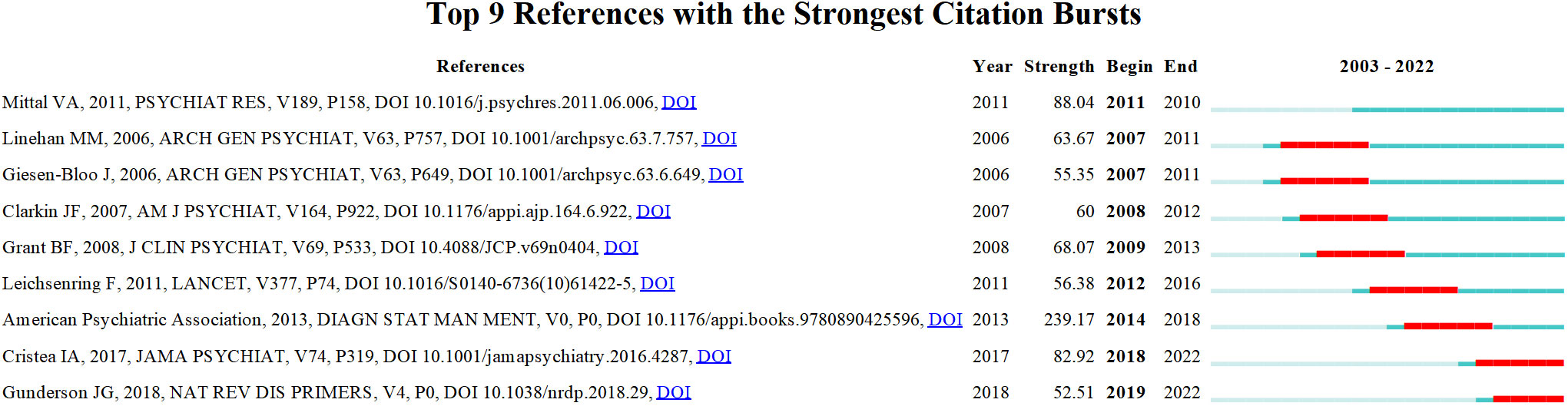
Figure 4 References with the strongest occurrence burst on BPD researches. Article titles correspond from top to bottom: Mittal VA et al. Diagnostic and Statistical Manuel of Mental Disorders; Linehan MM et al. Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder; Giesen-Bloo J et al. Outpatient psychotherapy for borderline personality disorder: Randomized trial of schema-focused therapy vs transference-focused psychotherapy; Clarkin Jf et al. Evaluating three treatments for borderline personality disorder: A multiwave study; Grant BF et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: Results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions; Leichsenring F et al. Borderline personality disorder; American Psychiatric Association, DSM-5 Task Force. Diagnostic and statistical manual of mental disorders: DSM-5™ (5th ed.); Cristea IA et al. Efficacy of psychotherapies for borderline personality disorder: A systematic review and meta-analysis; Gunderson JG et al. Borderline personality disorder.
Structural variation analysis can be understood as a method of measuring and studying structural changes in the field, mainly reflecting the betweenness centrality and sigma of the references. The high centrality of the reference plays an important role in the connection between the preceding and following references and may help to identify critical points of transformation, or intellectual turning points. Sigma values, on the other hand, are used to measure the novelty of a study, combining a combination of citation burst and structural centrality ( 56 ). Table 2 listed the top 10 structural change references that can be considered as landmark studies connecting different clusters. The top three articles with high centrality are the studies conducted by Milton Z. Brown and his colleagues on the reasons for suicide attempts and non-suicidal self-injury in BPD women ( 57 ); the research by Nelson H. Donegan and his colleagues on the impact of amygdala on emotional dysregulation in BPD patients ( 59 ); and the fMRI study by Sabine C. Herpertz and her colleagues on abnormal amygdala function in BPD patients ( 61 ). In addition, publications with high sigma values are listed. They are Larry J. Siever and Kenneth L. Davis on psychobiological perspectives on personality disorders ( 58 ); Ludger Tebartz van Elst and his colleagues on abnormalities in frontolimbic brain functioning ( 60 ); and Marsha M. Linehan on therapeutic approaches in BPD research ( 62 ). These works are recognized as having transformative potential and may generate some new ideas.
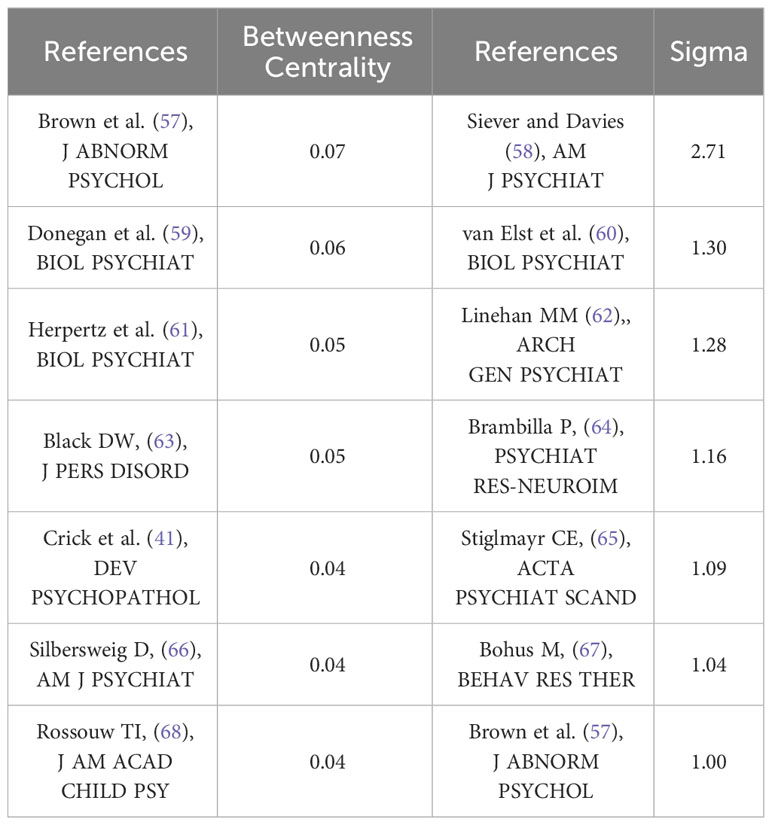
Table 2 Top 7 betweenness centrality and stigma references.
3.5 Analysis of authors and co-authors
Figure 5 showed a map of the co-authorship network over the last two decades. In total, 10 different clusters are shown, each of which gathers co-authors around the same research topic. For example, the main co-authors of cluster #0 “remission” are Christian Schmahl, Martin Bohus, Sabine C. Herpertz, Timothy J. Trull and Stefan Roepke. More recently, the three authors with the greatest bursts of research have been Mary C. Zanarini, Erik Simonsen, and Carla Sharp. As shown in Table 3 , the three most published authors are Martin Bohus (145 publications; 1.83%; H-index=61), Mary C. Zanarini (144 publications; 1.82%; H-index=80) and Christian Schmahl (142 publications; 1.79%; H-index=54).
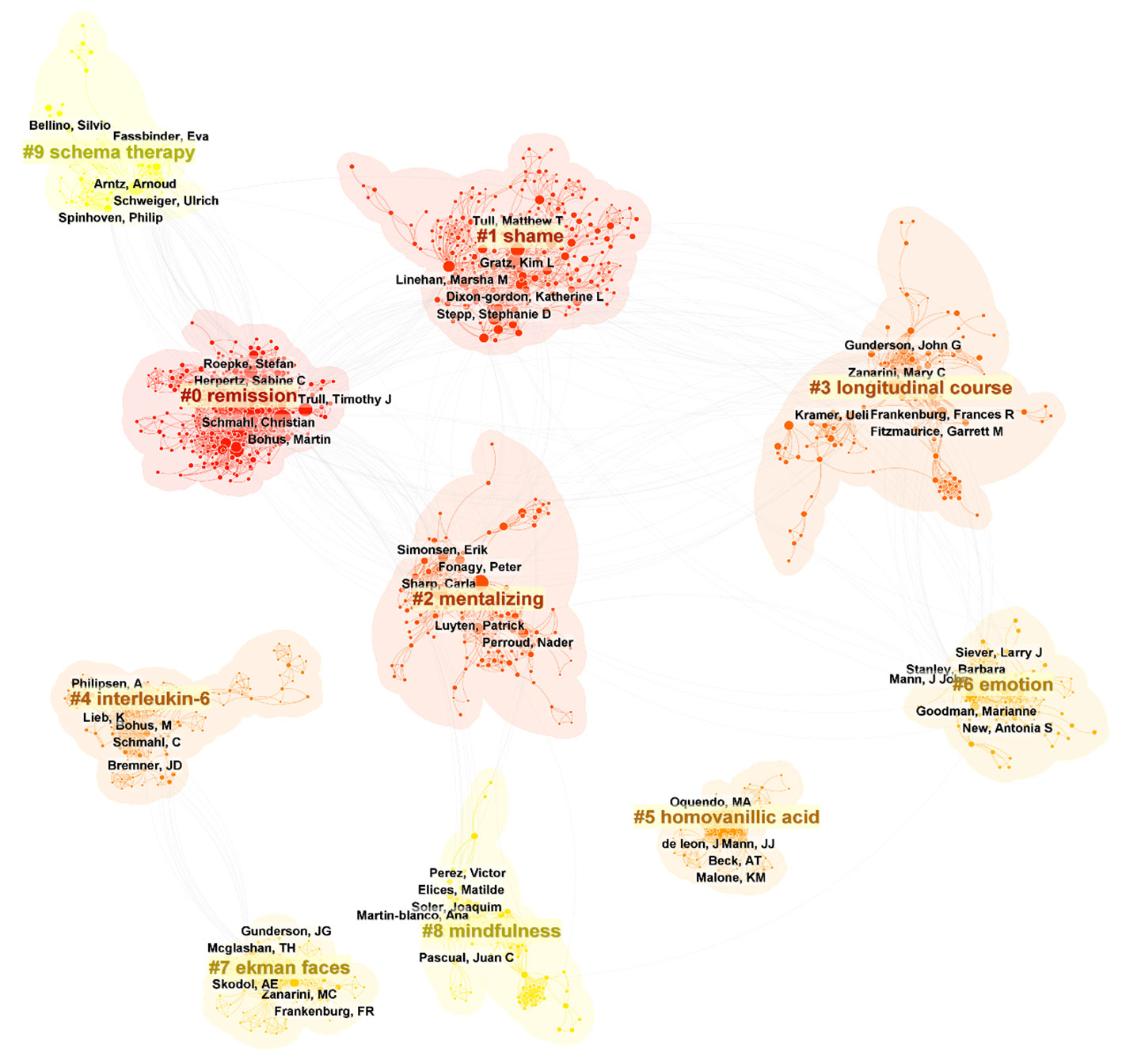
Figure 5 Top 10 clusters of coauthors in BPD (2003–2023). Selection Criteria: Top 10 per slice. Clusters labeled by keywords. The five authors with the highest number of publications in each cluster were labeled.
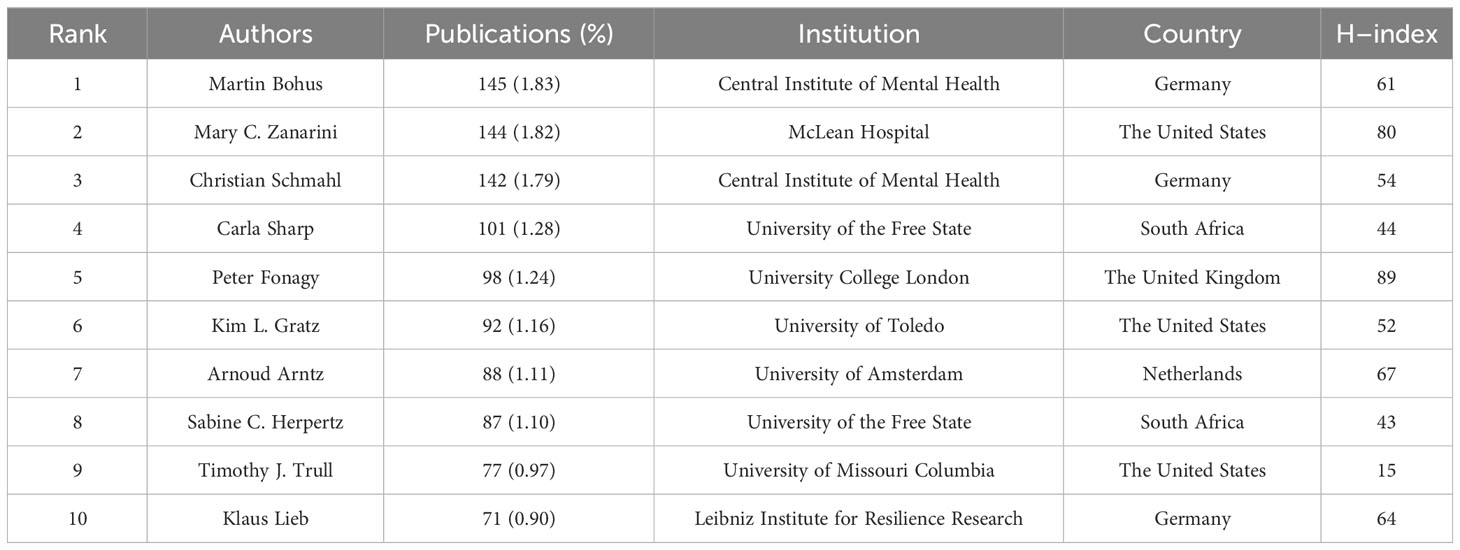
Table 3 Top 10 authors that published BPD researches.
3.6 Analysis of cooperation networks across countries
The top 10 countries in terms of number of publications in the BPD are added in Table 4 . With 3,440 published papers, or nearly 43% of all BPD research papers, the United States is the leading contributor to BPD research. This is followed by Germany (1196 publications; 15.10%) and the United Kingdom (1020 publications; 9.32%). Centrality refers to the degree of importance or centrality of a node in a network and is a measure of the importance of a node in a network ( 69 ). In Table 4 the United States is also has the highest centrality (0.43). Figure 6 shows the geographic collaboration network of countries in this field, with 83 countries contributing to BPD research, primarily from the United States and Europe.
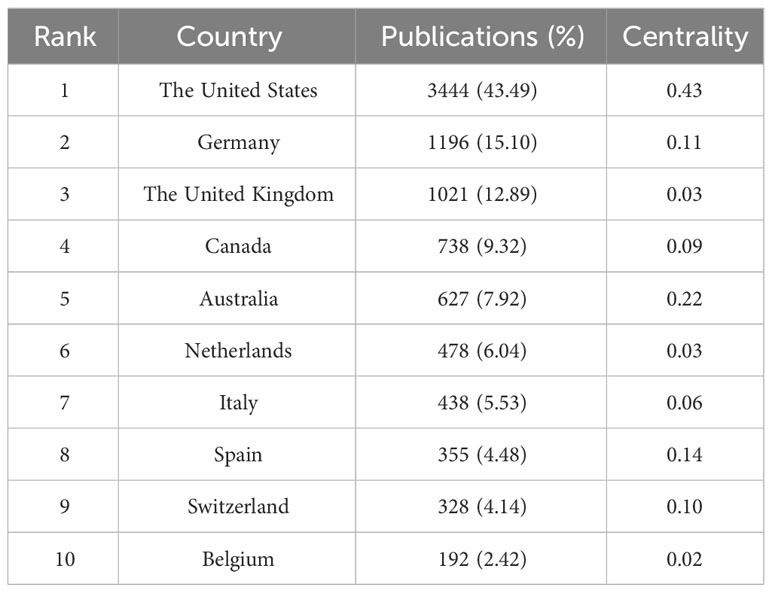
Table 4 Top 10 countries that published BPD researches.
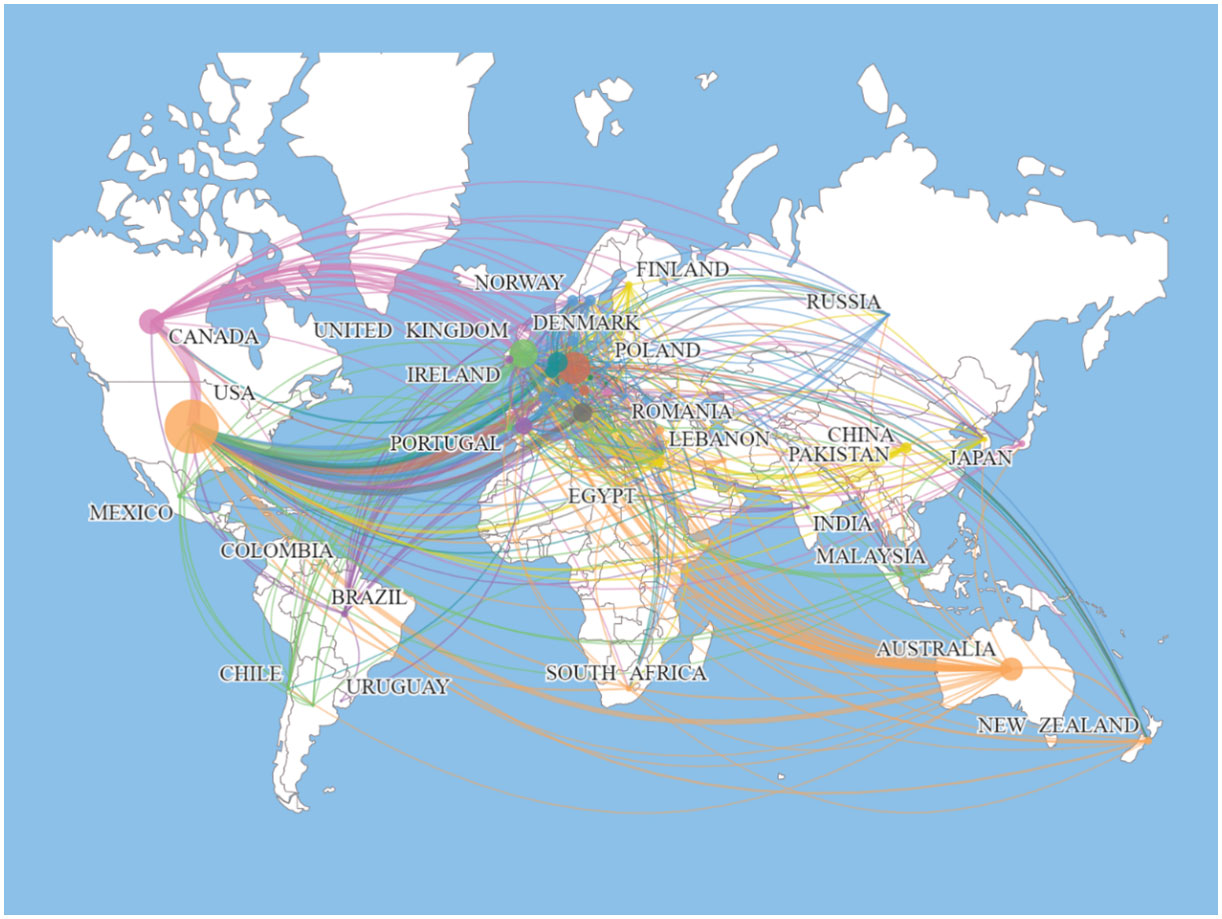
Figure 6 Map of the distribution of countries/regions engaged in BPD researches.
3.7 Analysis of the co-author’s institutions network
Table 5 listed the top 10 institutions ranked by the number of publications. The current study shows that Research Libraries Uk is the institution with the highest number of publications, with 766 publications (9.67%). The subsequent institutions are Harvard University and Ruprecht Karls University Heidelberg with 425 (5.37%) and 389 (4.91%) publications respectively. As can be seen from Table 4 , six of the top 10 institutions in terms of number of publications are from the United States. In part, this reflects the fact that the United States institutions are at the forefront of the BPD field and play a key role in it.
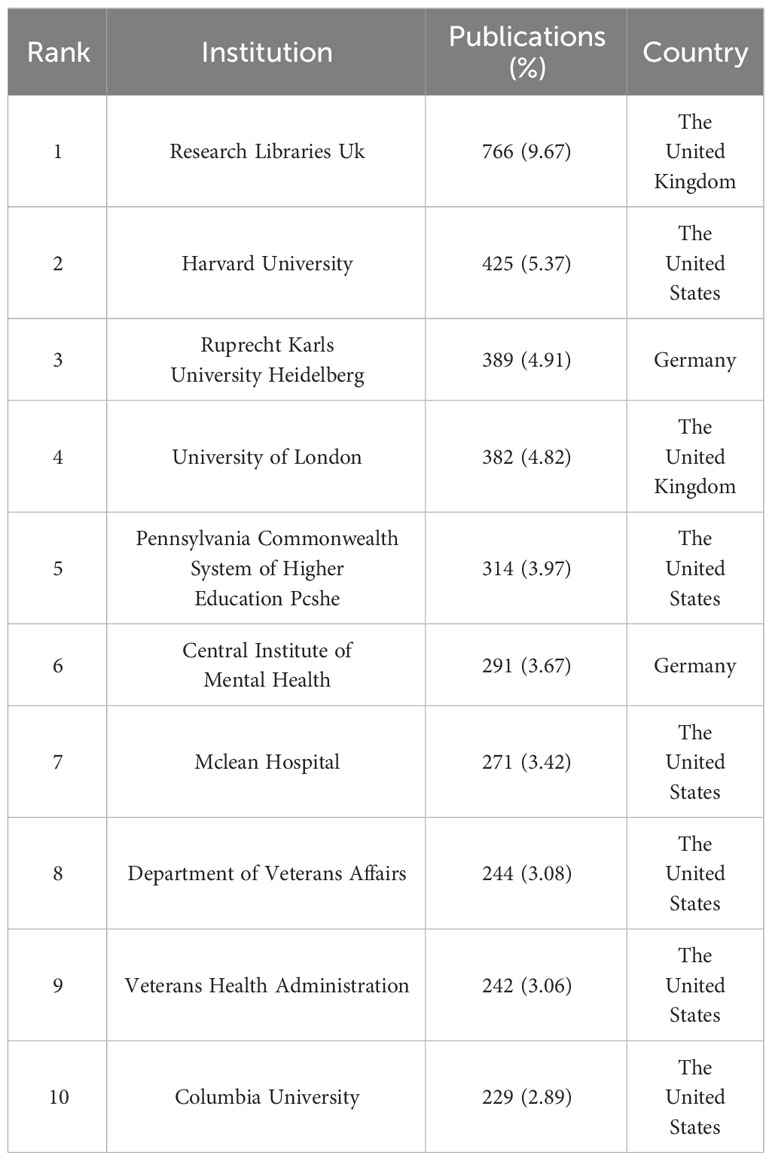
Table 5 Top 10 institutions that published BPD researches.
3.8 Analysis of journals and cited journals
If the more papers are published in a particular journal and at the same time it has a high number of citations, then it can be considered that the journal is influential ( 70 ). The top 10 journals in the field of BPD in terms of number of publications are listed in Table 6 . Journal of Personality Disorders from the Netherlands published the most literature on BPD with 438 (5.53%; IF=3.367) publications. This was followed by two journals from the United States: Psychiatry Research and Personality Disorders Theory Research and Treatment , with 269 (3.40%, IF=11.225) and 232 (2.93%; IF=4.627) publications, respectively. Among the top 10 journals in terms of number of publications published, Psychiatry Research has the highest impact factor.
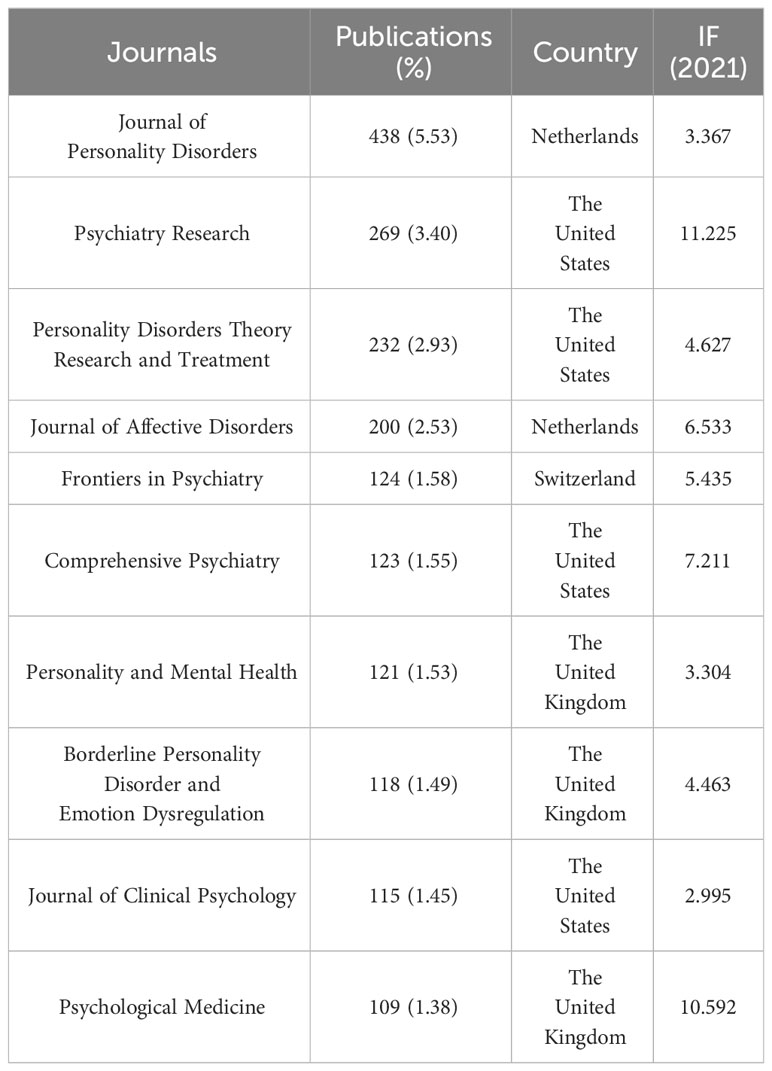
Table 6 Top 10 journals that published BPD researches.
3.9 Analysis of keywords and keywords co-occurrence
Keyword co-occurrence analysis can help researchers to understand the research hotspots in a certain field and the connection between different research topics. As shown in Figure 7 , all keywords can be categorized into 9 clusters: cluster #0 “diagnostic interview”, cluster #1 “diagnostic behavior therapy”, cluster #3 “social cognition”, cluster #4 “emotional regulation”, cluster #5 “substance use disorders “, cluster #6 “posttraumatic stress disorder”, cluster #7 “suicide” and cluster #8 “double blind”. These keywords have all been important themes in BPD research during the last 20 years.
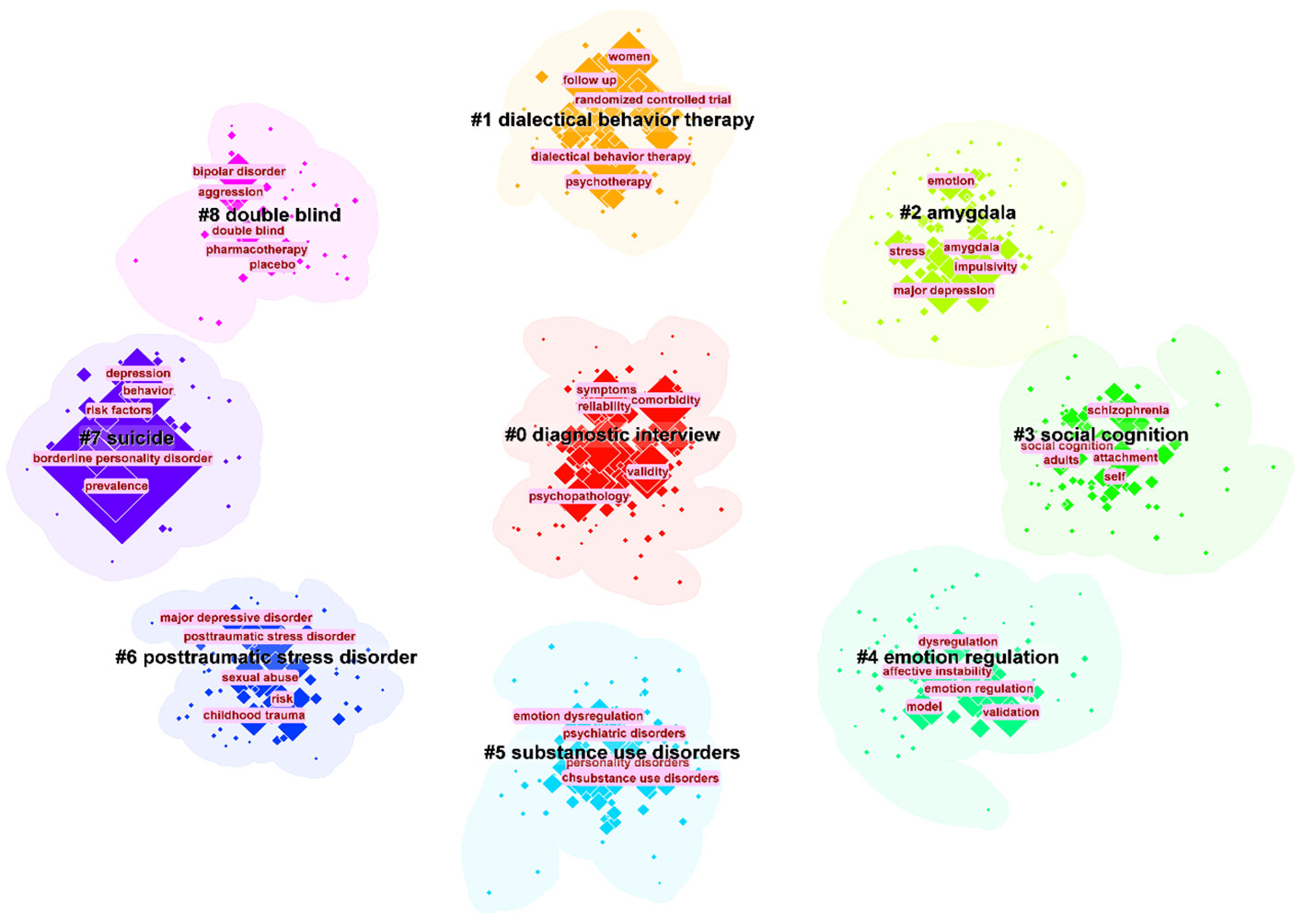
Figure 7 The largest 9 clusters of co-occurring keywords. The top 5 most frequent keywords in each cluster are highlighted.
Keyword burst is used to identify keywords with a significant increase in the frequency of occurrence in a topic or domain, helping to identify emerging concepts, research hotspots or keyword evolutions in a specific domain ( 71 ). Figure 8 presented the top 32 keywords with the strongest citation bursts in BPD from 2003−2023. Significantly, the keywords “positron emission tomography” (29.63), “major depression” (27.93), and “partial hospitalization” (27.1) had the highest intensity of outbreaks.
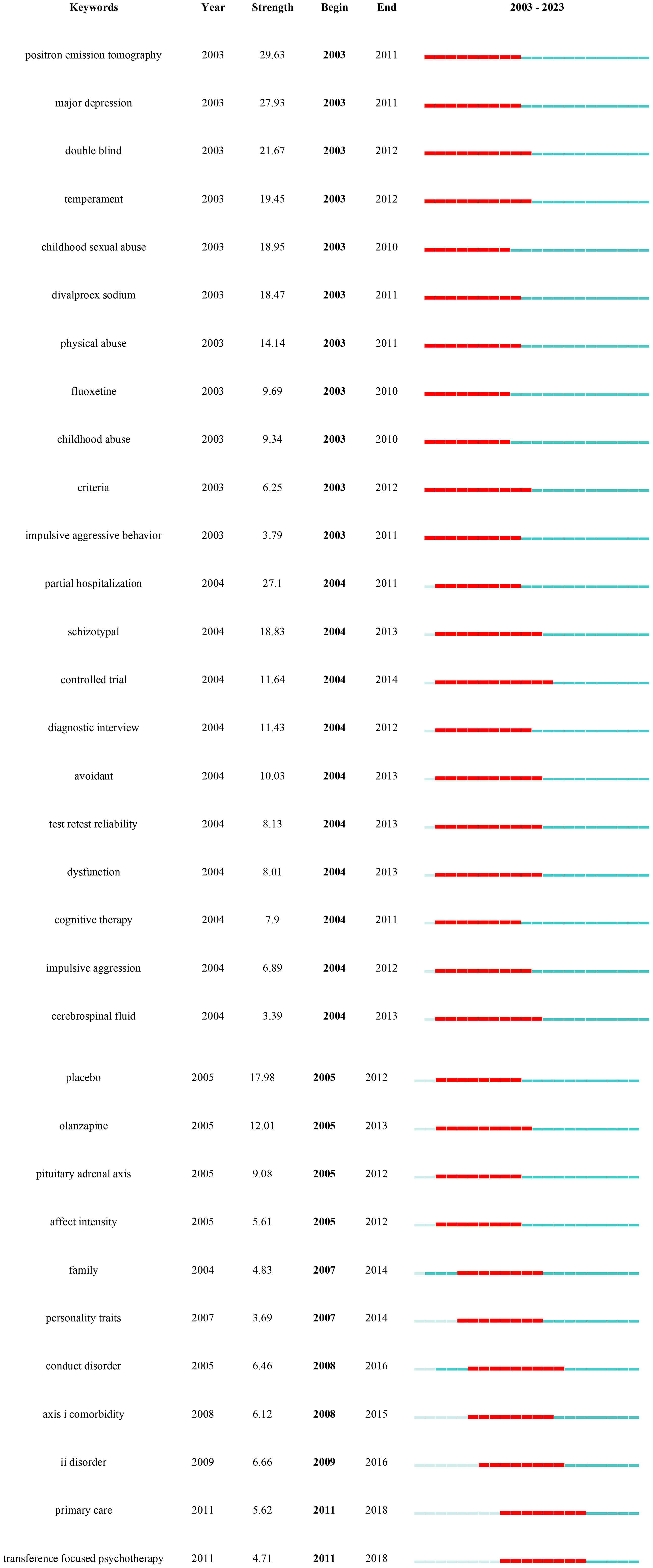
Figure 8 Keywords with the strongest occurrence burst on BPD researches.
4 Discussion
4.1 application of the “neuro-behavioral model” to bpd research.
In this study, we chose specific search terms, particularly “Neuro-behavioral Model”, to efficiently collect and analyze BPD research literature related to this emerging framework. This choice of keyword helped narrow the research scope and ensure its relevance to our objectives. However, it may have excluded some studies using different terminology, thus limiting comprehensiveness. In addition, the ‘Neuro-behavioral Model’, as an interdisciplinary field, encompasses a wide range of connotations and extensions, which also poses challenges to our research. This undoubtedly adds to the complexity of the study, yet it enhances our understanding of the field’s diversity.
4.2 Summary of the main findings
This current study utilized CiteSpace and Scimago Graphic software to conduct a comprehensive bibliometric analysis of the research literature on BPD. The study presented the current status of research, research hotspots, and research frontiers in BPD over the past 20 years (2003–2022) through knowledge mapping. The scientific predictions of future trends in BPD provided by this study can guide researchers interested in this field. This study also uses bibliometrics analysis method to show the knowledge structure and research results in the field of BPD, as well as the scientific prediction of the future trend of BPD research.
4.3 Identification of research hotspots
Previous studies have indicated an increasing trend in the number of papers focused on BPD, with the field gradually expanding into various areas. The first major research trend involves clinical studies on BPD. This includes focusing on emotional recognition difficulties in BPD patients, as well as studying features related to suicide attempts and non-suicidal self-injury. Clinical recognition and confirmation of BPD remains low, mainly related to the lack of clarity of its biological mechanisms ( 72 ). The nursing environment for BPD patients plays an important role in the development of the condition, which has become a focus of research. Researchers are also exploring the expansion of treatment options from conventional medication to non-pharmacological approaches, particularly cognitive-behavioral therapy. Another major research trend involves the associations and complications of BPD, including a greater focus on the adolescent population to reduce the occurrence of BPD starting from adolescence. Additionally, many researchers are interested in the comorbidity of BPD with various clinical mental disorders.
4.4 Potential trends of future research on BPD
Based on the results of the above studies and the results of the research trends in the table of details of the co-citation network clusters in 2022 ( Table 7 ), several predictions are made for the future trends in the field of BPD. In Table 7 , there were some trends related to previous studies, including #1”dialectical behavior therapy”, #7 “dialectical behavior therapy” ( 73 ), #5 “mentalization” ( 74 ), and #9 “non-suicidal self-injury” ( 75 ). The persistence of these research trends is evidence that they have been a complex issue in this field and a focus of researchers. The recently emerged turning point paper provides a comprehensive assessment about BPD, offering practical information and treatment recommendations ( 76 ). New research is needed to improve standards and suggest more targeted and cost-effective treatments.
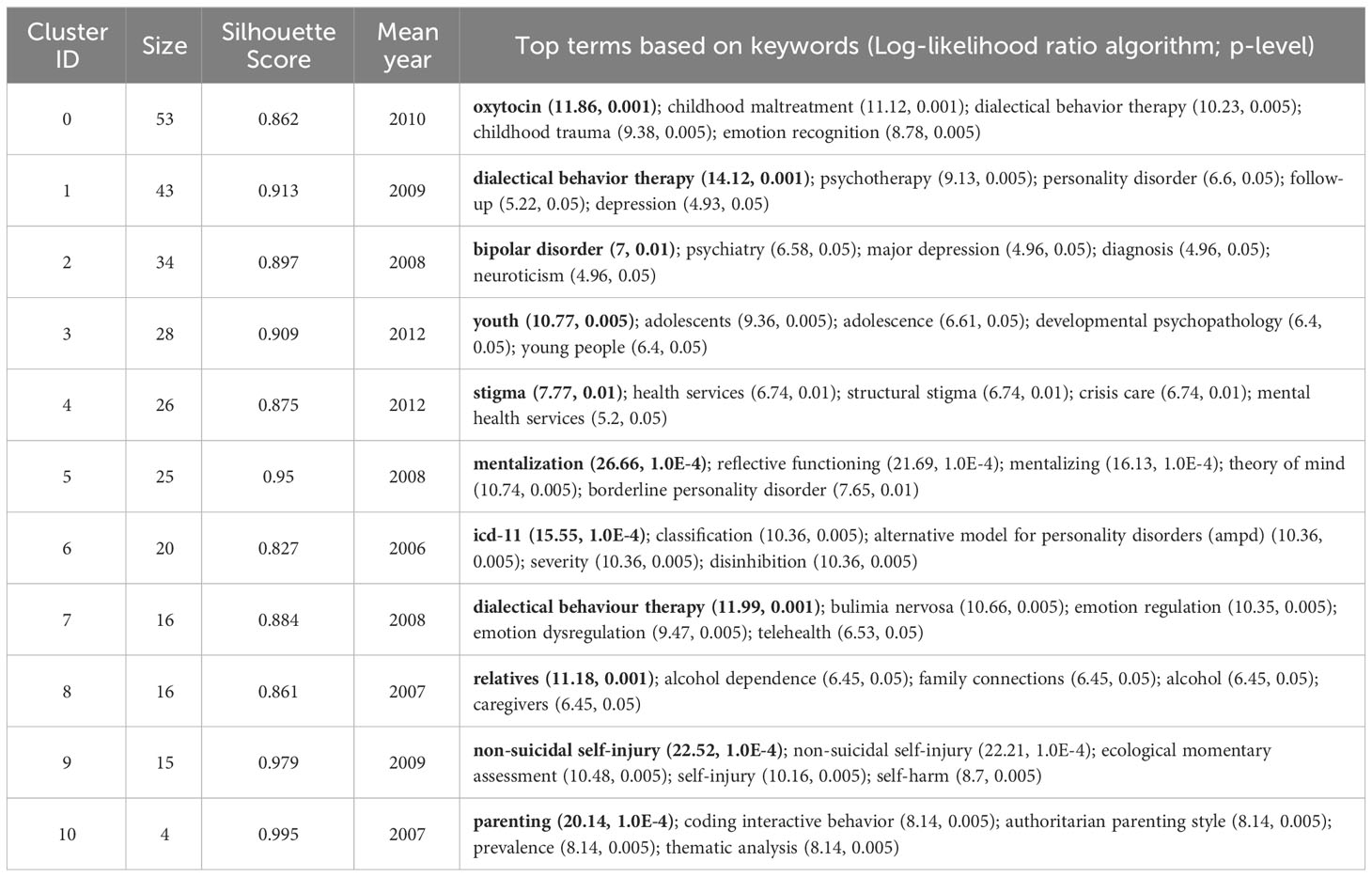
Table 7 The references co-citation network cluster detail (2022).
BPD symptoms in adolescents have been shown to respond to interventions with good results, so prevention and intervention for BPD is warranted ( 77 ). This trend can be observed in #3 “youth” ( 78 ). Mark F. Lenzenweger and Dante Cicchetti summarized the developmental psychopathology approach to BPD, one of the aims of which is to provide information for the prevention of BPD ( 79 ). Prevention and early intervention of BPD has been shown to provide many benefits, including reduced occurrence of secondary disorders, improved psychosocial functioning, and reduced risk of interpersonal conflict ( 80 ). However, there are differences between individuals, and different prevention goals are recommended for adolescents at risk for BPD. Therefore, prevention and early intervention for BPD has good prospects for the future.
The etiology of BPD is closely related to many factors, and its pathogenesis is often ignored by clinicians. The exploration of risk factors has been an important research direction in the study. Some studies have found that BPD is largely the product of traumatic childhood experiences, which may lead to negative psychological effects on children growing up ( 81 ). It has also been found that the severity of borderline symptoms in parents is positively associated with poor parenting practices ( 82 ). Future researches need to know more about the biological-behavioral processes of parents in order to provide targeted parenting support and create a good childhood environment.
Because pharmacotherapy is only indicated for comorbid conditions that require medication, psychotherapy has become one of the main approaches to treating BPD. The increasingly advanced performance and availability of contemporary mobile devices can help to take advantage of them more effectively in the context of optimizing the treatment of psychiatric disorders. The explosion of COVID-19 is forcing people to adapt to online rather than face-to-face offline treatment ( 83 ). The development of this new technology will effectively advance the treatment of patients with BPD. Although telemedicine has gained some level of acceptance by the general public, there are some challenges that have been reported, so further research on the broader utility of telemedicine is needed in the future.
4.5 The current study compares with a previous bibliometric review of BPD
As mentioned earlier, there have been previous bibliometric studies conducted by scholars in the field of BPD. This paper focuses more on BPD in personality disorders than the extensive study of personality disorders as a category by Taylor Reis et al. ( 15 ). The results of both studies show an increasing trend in the number of publications in the field of BPD, suggesting positive developments in the field. Taylor Reis et al. focused primarily on quantifying publications on personality disorders and did not delve into other specific aspects of BPD. Ilaria M.A. Benzi et al. focused on a bibliometric analysis of the pathology of BPD ( 14 ). They give three trends for the future development of BPD pathology: first, the growing importance of self-injurious behavior research; second, the association of attention deficit hyperactivity disorder with BPD and the influence of genetics and heritability on BPD; and third, the new focus on the overlap between fragile narcissism and BPD. The study in this paper also concludes that there are three future development directions for BPD: first, the prevention and early intervention of BPD; second, the non-pharmacological treatment of BPD; and third, research into the pathogenesis of BPD. Owing to variations in research backgrounds and data sources, the outcomes presented in the two studies diverge significantly. Nevertheless, both contributions hold merit in advancing the understanding of BPD. In addition to this, this paper also identifies trends in BPD over the past 20 years: the first trend is the clinical research of BPD, which is specifically subdivided into three sub-trends; the second trend is association and comorbidity. The identification of these trends is important for understanding the disorder, improving diagnosis and treatment, etc. Structural variant analysis also features prominently in the study. The impact of literature in terms of innovativeness is detected through in-depth mining and analysis of large amounts of literature data. This analysis is based on research in the area of scientific creativity, especially the role and impact of novel reorganizations in creative thinking. Structural variation analysis is precisely designed to find and reveal embodiments of such innovative thinking in scientific literature, enabling researchers to more intuitively grasp the dynamics and cutting-edge advances in the field of science.
5 Limitations
However, it must be admitted that our study has some limitations. The first is the limited nature of data resources. The data source for our study came from only one database, WOS. Second, the limitation of article type. Search criteria are limited to papers and reviews in SCI and SSCI databases. Third, the effect of language type. In the current study, only English-language literature could be included in the analysis, which may lead us to miss some important studies published in other languages. Fourth, limitations of research software. Although this study used well-established and specialized software, the results obtained by choosing different calculation methods may vary. Finally, the diversity of results interpretation. The results analyzed by the software are objective, but there is also some subjectivity in the interpretation and analysis of the research results. While we endeavor to be comprehensive and accurate in our research, the choice of search terms inevitably introduces certain limitations. Using “Neuro-behavioral Model” as the search term enhances the study’s relevance, but it may also cause us to miss significant studies in related areas. This limits the generalizability and replicability of our results. Furthermore, the inherent complexity and diversity of neurobehavioral models might introduce subjectivity and bias in our interpretation and application of the literature. Although we endeavored to reduce bias via multi-channel validation and cross-referencing, we cannot entirely eliminate its potential impact on our findings.
6 Conclusion
Overall, a comprehensive scientometrics analysis of BPD provides a comprehensive picture of the development of this field over the past 20 years. This in-depth examination not only reveals research trends, but also allows us to understand which areas are currently hot and points the way for future research efforts. In addition, this method provides us with a framework to evaluate the value of our own research results, which helps us to more precisely adjust the direction and strategy of research. More importantly, this in-depth analysis reveals the depth and breadth of BPD research, which undoubtedly provides valuable references for researchers to have a deeper understanding of BPD, and also provides a reference for us to set future research goals. In short, this scientometrics approach gives us a window into the full scope of BPD research and provides valuable guidance for future research.
Author contributions
YL: Data curation, Formal analysis, Investigation, Methodology, Software, Visualization, Writing – original draft, Writing – review & editing. CC: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. YZ: Validation, Visualization, Writing – review & editing. NZ: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. SL: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. SL is supported by the Outstanding Youth Program of Philosophy and Social Sciences in Anhui Province (2022AH030089) and the Starting Fund for Scientific Research of High-Level Talents at Anhui Agricultural University (rc432206).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Lieb K, Zanarini MC, Schmahl C, Linehan MM, Bohus M. Borderline personality disorder. Lancet (2004) 364:453–61. doi: 10.1016/S0140-6736(04)16770-6
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Chugani CD, Byrd AL, Pedersen SL, Chung T, Hipwell AE, Stepp SD. Affective and sensation-seeking pathways linking borderline personality disorder symptoms and alcohol-related problems in young women. J Pers Disord . (2020) 34:420–31. doi: 10.1521/pedi_2018_32_389
3. Bagge CL, Stepp SD, Trull TJ. Borderline personality disorder features and utilization of treatment over two years. J Pers Disord . (2005) 19:420–39. doi: 10.1521/pedi.2005.19.4.420
4. Paris J. Suicidality in borderline personality disorder. Medicina . (2019) 55:223. doi: 10.3390/medicina55060223
5. Lenzenweger MF, Lane MC, Loranger AW, Kessler RC. DSM-IV personality disorders in the National Comorbidity Survey Replication. Biol Psychiatry . (2007) 62:553–64. doi: 10.1016/j.biopsych.2006.09.019
6. Skodol AE, Gunderson JG, Pfohl B, Widiger TA, Livesley WJ, Siever LJ. The borderline diagnosis I: Psychopathology, comorbidity, and personality structure. Biol Psychiatry . (2002) 51:936–50. doi: 10.1016/s0006-3223(02)01324-0
7. Bailey RC, Grenyer BF. Burden and support needs of carers of persons with borderline personality disorder: A systematic review. Harvard Rev Psychiatry . (2013) 21:248–58. doi: 10.1097/HRP.0b013e3182a75c2c
CrossRef Full Text | Google Scholar
8. Weimand BM, Hedelin B, Sällström C, Hall-Lord M-L. Burden and health in relatives of persons with severe mental illness: A Norwegian cross-sectional study. Issues Ment Health Nursing . (2010) 31:804–15. doi: 10.3109/01612840.2010.520819
9. Saccaro LF, Schilliger Z, Dayer A, Perroud N, Piguet C. Inflammation, anxiety, and stress in bipolar disorder and borderline personality disorder: A narrative review. Neurosci Biobehav Rev . (2021) 127:184−192. doi: 10.1016/j.neubiorev.2021.04.017
10. Dixon-Gordon KL, Laws H. Emotional variability and inertia in daily life: Links to borderline personality and depressive symptoms. J Pers Disord . (2021) 35:162−171. doi: 10.1521/pedi_2021_35_504
11. Torgersen S. Genetics of patients with borderline personality disorder. Psychiatr Clinics North A . (2000) 23:1–9. doi: 10.1016/S0193-953X(05)70139-8
12. Quenneville AF, Kalogeropoulou E, Küng AL, Hasler R, Nicastro R, Prada P, et al. Childhood maltreatment, anxiety disorders and outcome in borderline personality disorder. Psychiatry Res . (2020) 284:112688. doi: 10.1016/j.psychres.2019.112688
13. Antoine SM, Fredborg BK, Streiner D, Guimond T, Dixon-Gordon KL, Chapman AL, et al. Subgroups of borderline personality disorder: A latent class analysis. Psychiatry Res . (2023) 323:115131. doi: 10.1016/j.psychres.2023.115131
14. Benzi IMA, Di Pierro R, De Carli P, Cristea IA, Cipresso P. All the faces of research on borderline personality pathology: Drawing future trajectories through a network and cluster analysis of the literature. J Evidence-Based Psychotherapies . (2020) 20:3–30. doi: 10.24193/jebp.2020.2.9
15. Reis T, Gekker M, Land MGP, Mendlowicz MV, Berger W, Luz MP, et al. The growth and development of research on personality disorders: A bibliometric study. Pers Ment Health . (2022) 16:290–9. doi: 10.1002/pmh.1540
16. Singh VK, Singh P, Karmakar M, Leta J, Mayr P. The journal coverage of Web of Science, Scopus and Dimensions: A comparative analysis. Scientometrics . (2021) 126:5113–42. doi: 10.1007/s11192-021-03948-5
17. Pritchard A. Statistical bibliography or bibliometrics. J Documentation . (1969) 25:348.
Google Scholar
18. Price DJ. Networks of scientific papers. Science . (1965) 149:510–5. doi: 10.1126/science.149.3683.510
19. Sabe M, Chen C, Perez N, Solmi M, Mucci A, Galderisi S, et al. Thirty years of research on negative symptoms of schizophrenia: A scientometric analysis of hotspots, bursts, and research trends. Neurosci Biobehav Rev . (2023) 144:104979. doi: 10.1016/j.neubiorev.2022.104979
20. Shen Z, Ji W, Yu S, Cheng G, Yuan Q, Han Z, et al. Mapping the knowledge of traffic collision reconstruction: A scientometric analysis in CiteSpace, VOSviewer, and SciMAT. Sci Justice . (2023) 63:19–37. doi: 10.1016/j.scijus.2022.10.005
21. Wu H, Wang Y, Tong L, Yan H, Sun Z. Global research trends of ferroptosis: A rapidly evolving field with enormous potential. Front Cell Dev Biol . (2021) 9:646311. doi: 10.3389/fcell.2021.646311
22. Brody S. Impact factor: Imperfect but not yet replaceable. Scientometrics . (2013) 96:255–7. doi: 10.1007/s11192-012-0863-x
23. Kaldas M, Michael S, Hanna J, Yousef GM. Journal impact factor: A bumpy ride in an open space. J Invest Med . (2020) 68:83–7. doi: 10.1136/jim-2019-001009
24. Schubert A, Glänzel W. A systematic analysis of Hirsch-type indices for journals. J Informetrics . (2007) 1:179–84. doi: 10.1016/j.joi.2006.12.002
25. Chen C. CiteSpace II: Detecting and visualizing emerging trends and transient patterns in scientific literature. J Am Soc Inf Sci Technol . (2006) 57:359–77. doi: 10.1002/asi.20317
26. Cheng K, Guo Q, Shen Z. Bibliometric analysis of global research on cancer photodynamic therapy: Focus on nano-related research. Front Pharmacol . (2022) 13:927219. doi: 10.3389/fphar.2022.927219
27. Hassan-Montero Y, De-Moya-Anegón F, Guerrero-Bote VP. SCImago Graphica: A new tool for exploring and visually communicating data. Profesional la Información . (2022) 31:e310502. doi: 10.3145/EPI
28. Wang Y, Li D, Jia Z, Hui J, Xin Q, Zhou Q, et al. A bibliometric analysis of research on the links between gut microbiota and atherosclerosis. Front Cardiovasc Med . (2022) 9:941607. doi: 10.3389/fcvm.2022.941607
29. Soloff PH, Lynch KG, Kelly TM, Malone KM, Mann JJ. Characteristics of suicide attempts of patients with major depressive episode and borderline personality disorder: a comparative study. Am J Psychiatry . (2000) 157:601–8. doi: 10.1176/appi.ajp.157.4.601
30. Widiger TA, Trull TJ. Plate tectonics in the classification of personality disorder: shifting to a dimensional model. Am Psychol . (2007) 62:71–83. doi: 10.1037/0003-066X.62.2.71
31. Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol . (1995) 51:768–74. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1
32. Bartow S, Stopsack M, Grabe HJ, Meinke C, Spitzer C, Kronmüller K, et al. Interpersonal evaluation bias in borderline personality disorder. Behav Res Ther . (20092009) 47:359–65. doi: 10.1016/j.brat.2009.02.003
33. Cheavens JS, Rosenthal MZ, Daughters SB, Nowak J, Kosson D, Lynch TR, et al. An analogue investigation of the relationships among perceived parental criticism, negative affect, and borderline personality disorder features: The role of thought suppression. Behav Res Ther . (2005) 43:257–68. doi: 10.1016/j.brat.2004.01.006
34. Bradley R, Westen D. The psychodynamics of borderline personality disorder: a view from developmental psychopathology. Dev Psychopathol . (2005) 17:927–57. doi: 10.1017/s0954579405050443
35. Tzourio-Mazoyer N, Landeau B, Papathanassiou D, Crivello F, Etard O, Delcroix N, et al. Automated anatomical labeling of activations in SPM using a macroscopic anatomical parcellation of the MNI MRI single-subject brain. NeuroImage . (2002) 15:273–89. doi: 10.1006/nimg.2001.0978
36. Bellino S, Rinaldi C, Bozzatello P, Bogetto F. Pharmacotherapy of borderline personality disorder: a systematic review for publication purpose. Curr Medicinal Chem . (2011) 18:3322–9. doi: 10.2174/092986711796504682
37. Zanarini MC, Frankenburg FR, Dubo ED, Sickel AE, Trikha A, Levin A. Axis I comorbidity of borderline personality disorder. Am J Psychiatry . (1998) 155:1733–9. doi: 10.1176/ajp.155.12.1733
38. Yee L, Korner AJ, McSwiggan S, Meares RA, Stevenson J. Persistent hallucinosis in borderline personality disorder. Compr Psychiatry . (2005) 46:147–54. doi: 10.1016/j.comppsych.2004.07.032
39. Mittal VA, Walker EF. Diagnostic and statistical manual of mental disorders. Psychiatry Res . (2011) 189:158–9. doi: 10.1016/j.psychres.2011.06.006
40. Torgersen S, Kringlen E, Cramer V. The prevalence of personality disorders in a community sample. Arch Gen Psychiatry . (2001) 58:590–6. doi: 10.1001/archpsyc.58.6.590
41. Crick NR, Murray-Close D, Woods K. Borderline personality features in childhood: A short-term longitudinal study. Dev Psychopathol . (2005) 17:1051–70. doi: 10.1017/S0954579405050492
42. Linehan MM, Comtois KA, Murray AM, Brown MZ, Gallop RJ, Heard HL, et al. Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Arch Gen Psychiatry . (2006) 63:757–66. doi: 10.1001/archpsyc.63.7.757
43. Giesen-Bloo J, van Dyck R, Spinhoven P, van Tilburg W, Dirksen C, van Asselt T, et al. Outpatient psychotherapy for borderline personality disorder: Randomized trial of schema-focused therapy vs transference-focused psychotherapy. Arch Gen Psychiatry . (2006) 63:649–58. doi: 10.1001/archpsyc.63.6.649
44. Crowell SE, Beauchaine TP, Linehan MM. A biosocial developmental model of borderline personality: Elaborating and extending Linehan's theory. psychol Bulletin . (2009) 135:495–510. doi: 10.1037/a0015616
45. Leichsenring F, Leibing E, Kruse J, New AS, Leweke F. Borderline personality disorder. Lancet (2011) 377(9759):74–84. doi: 10.1016/S0140-6736(10)61422-5
46. Whiteside SP, Lynam DR, Miller JD, Reynolds SK. Validation of the UPPS impulsive behaviour scale: A four-factor model of impulsivity. Eur J Pers (2005) 19(7):559–74. doi: 10.1002/per.556
47. Clarkin JF, Levy KN, Lenzenweger MF, Kernberg OF. Evaluating three treatments for borderline personality disorder: A multiwave study. Am J Psychiatry (2007) 164(6):922–8. doi: 10.1176/ajp.2007.164.6.922
48. Bateman A, Fonagy P. Randomized controlled trial of outpatient mentalization-based treatment versus structured clinical management for borderline personality disorder. Am J Psychiatry (2009) 166(12):1355–64. doi: 10.1176/appi.ajp.2009.09040539
49. Fonagy P, Luyten P. A developmental, mentalization-based approach to the understanding and treatment of borderline personality disorder. Dev Psychopathol (2009) 21(4):1355–81. doi: 10.1017/S0954579409990198
50. Levy KN, Meehan KB, Kelly KM, Reynoso JS, Weber M, Clarkin JF, et al. Change in attachment patterns and reflective function in a randomized control trial of transference-focused psychotherapy for borderline personality disorder. J Consulting Clin Psychol (2006) 74(6):1027–40. doi: 10.1037/0022-006X.74.6.1027
51. Carr DS, Francis A. Childhood familial environment, maltreatment and borderline personality disorder symptoms in a non-clinical sample: A cognitive behavioural perspective. Clin Psychol (2009) 13(1):28–37. doi: 10.1080/13284200802680476
52. Selby EA, Kranzler A, Fehling KB, Panza E. Nonsuicidal self-injury disorder: The path to diagnostic validity and final obstacles. Clin Psychol Review . (2015) 38:79–91. doi: 10.1016/j.cpr.2015.03.003
53. Skoglund C, Tiger A, Rück C, Petrovic P, Asherson P, Hellner C, et al. Familial risk and heritability of diagnosed borderline personality disorder: A register study of the Swedish population. Mol Psychiatry . (2021) 26:999–1008. doi: 10.1038/s41380-019-0442-0
54. American Psychiatric Association, DSM-5 Task Force. Diagnostic and statistical manual of mental disorders: DSM-5™ . 5th ed. Washington: American Psychiatric Publishing, Inc., (2013). doi: 10.1176/appi.books.9780890425596
55. Cristea IA, Gentili C, Cotet CD, Palomba D, Barbui C, Cuijpers P. Efficacy of psychotherapies for borderline personality disorder: A systematic review and meta-analysis. JAMA Psychiatry . (2017) 74:319–28. doi: 10.1001/jamapsychiatry.2016.4287
56. Chen C. Predictive effects of structural variation on citation counts. J Am Soc Inf Sci Technol . (2012) 63:431–49. doi: 10.1002/asi.21694
57. Brown MZ, Comtois KA, Linehan MM. Reasons for suicide attempts and non-suicidal self-injury in women with borderline personality disorder. J Abnormal Psychol . (2002) 111:198–202. doi: 10.1037//0021-843x.111.1.198
58. Siever LJ, Davis KL. A psychobiological perspective on the personality disorders. Am J Psychiatry . (1991) 148:1647–58. doi: 10.1176/ajp.148.12.1647
59. Donegan NH, Sanislow CA, Blumberg HP. Amygdala hyperreactivity in borderline personality disorder: Implications for emotional dysregulation. Biol Psychiatry . (2003) 54:1284–93. doi: 10.1016/S0006-3223(03)00636-X
60. Tebartz van Elst L, Hesslinger B, Thiel T, Geiger E, Haegele K, Lemieux L, et al. Frontolimbic brain abnormalities in patients with borderline personality disorder: A volumetric magnetic resonance imaging study. Biol Psychiatry . (2003) 54:163–71. doi: 10.1016/s0006-3223(02)01743-2
61. Herpertz SC, Dietrich TM, Wenning B, Krings T, Erberich SG, Willmes K, et al. Evidence of abnormal amygdala functioning in borderline personality disorder: A functional MRI study. Biol Psychiatry . (2001) 50:292–8. doi: 10.1016/S0006-3223(01)01075-7
62. Linehan MM. Cognitive-behavioral treatment of borderline personality disorder . New York: Guilford Press (1993).
63. Black DW, Blum N, Pfohl B, Hale N. Suicidal behavior in borderline personality disorder: Prevalence, risk factors, prediction, and prevention. J Pers Disord (2004) 18(3):226–39. doi: 10.1521/pedi.18.3.226.35445
64. Brambilla P, Soloff PH, Sala M, Nicoletti MA, Keshavan MS, Soares JC. Anatomical MRI study of borderline personality disorder patients. Psychiatry Res (2004) 131(2):125–33. doi: 10.1016/j.pscychresns.2004.04.003
65. Stiglmayr CE, Grathwol T, Linehan MM, Ihorst G, Fahrenberg J, Bohus M. Aversive tension in patients with borderline personality disorder: A computer-based controlled field study. Acta Psychiatrica Scandinavica (2005) 111(5):372–9. doi: 10.1111/j.1600-0447.2004.00466.x
66. Silbersweig D, Clarkin JF, Goldstein M, Kernberg OF, Tuescher O, Levy KN, et al. Failure of frontolimbic inhibitory function in the context of negative emotion in borderline personality disorder. Am J Psychiatry (2007) 164(12):18321841. doi: 10.1176/appi.ajp.2007.06010126
67. Bohus M, Haaf B, Stiglmayr C, Pohl U, Böhme R, Linehan M. Evaluation of inpatient dialectical-behavioral therapy for borderline personality disorder–a prospective study. Behav Res Ther (2000) 38(9):875887. doi: 10.1016/s0005-7967(99)00103-5
68. Rossouw TI, Fonagy P. Mentalization-based treatment for self-harm in adolescents: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry (2012) 51(12):13041313. doi: 10.1016/j.jaac.2012.09.018
69. Zhang S, Wang S, Liu R. A bibliometric analysis of research trends of artificial intelligence in the treatment of autistic spectrum disorders. Front Psychiatry . (2022) 13:967074. doi: 10.3389/fpsyt.2022.967074
70. Dzikowski P. A bibliometric analysis of born global firms. J Business Res . (2018) 85:281–94. doi: 10.1016/j.jbusres.2017.12.054
71. Chen C, Ibekwe-SanJuan F, Hou J. The structure and dynamics of cocitation clusters: A multiple-perspective cocitation analysis. J Am Soc Inf Sci Technol . (2010) 61:1386–409. doi: 10.1002/asi.21309
72. Gunderson JG, Herpertz SC, Skodol AE, Torgersen S, Zanarini MC. Borderline personality disorder. Nat Rev Dis Primers . (2018) 4:18029. doi: 10.1038/nrdp.2018.29
73. Tan MYL, McConnell B, Barlas J. Application of Dialectical Behaviour Therapy in treating common psychiatric disorders: Study protocol for a scoping review. BMJ Open . (2002) 12:e058565. doi: 10.1136/bmjopen–2021–058565
74. Quevedo Y, Booij L, Herrera L, Hernández C, Jiménez JP. Potential epigenetic mechanisms in psychotherapy: A pilot study on DNA methylation and mentalization change in borderline personality disorder. Front Hum Neurosci . (2022) 16:955005. doi: 10.3389/fnhum.2022.955005
75. Uhlmann C, Tschöke S, Steinert T, Schmid P. Can you see and hear how bad I feel right now? Self–injury and suicidal communication in borderline personality disorder-A secondary analysis. Psychiatrische Praxis . (2022) 49:329–33. doi: 10.1055/a–1820–0438
76. Bohus M, Stoffers-Winterling J, Sharp C, Krause-Utz A, Schmahl C, Lieb K. Borderline personality disorder. Lancet (2022) 398:1528–40. doi: 10.1016/S0140–6736(21)00476–1
77. Schuppert HM, Giesen-Bloo J, van Gemert TG, Wiersema HM, Minderaa RB, Emmelkamp PMG, et al. Effectiveness of an emotion regulation group training for adolescents—A randomized controlled pilot study. Clin Psychol Psychother . (2009) 16:467–78. doi: 10.1002/cpp.637
78. American Psychiatric Association. Diagnostic and statistical manual of mental disorders, text revision . 4th ed. Washington: American Psychiatric Association (2000).
79. Lenzenweger MF, Cicchetti D. Toward a developmental psychopathology approach to borderline personality disorder. Dev Psychopathol . (2005) 17:893–8. doi: 10.1017/S095457940505042X
80. Chanen AM, Jovev M, McCutcheon LK, Jackson HJ, McGorry PD. Borderline personality disorder in young people and the prospects for prevention and early intervention. Curr Psychiatry Rev . (2008) 4:48–57. doi: 10.2174/157340008783743820
81. Pohl S, Steuwe C, Mainz V, Driessen M, Beblo T. Borderline personality disorder and childhood trauma: Exploring the buffering role of self-compassion and self-esteem. J Clin Psychol . (2021) 77:837–45. doi: 10.1002/jclp.23070
82. Bartsch DR, Roberts R, Proeve M. Relationships between parental borderline symptom severity, empathy, parenting styles and child psychopathology. Clin Psychol . (2022) 26:211–21. doi: 10.1080/13284207.2022.2031947
83. Lakeman R, Hurley J, Campbell K, Hererra C, Leggett A, Tranter R, et al. High fidelity dialectical behaviour therapy online: Learning from experienced practitioners. Int J Ment Health Nursing . (20222022) 31:1405–16. doi: 10.1111/inm.13039
Keywords: neuro-behavioral model, borderline personality disorder, BPD, bibliometric, Scimago Graphica
Citation: Liu Y, Chen C, Zhou Y, Zhang N and Liu S (2024) Twenty years of research on borderline personality disorder: a scientometric analysis of hotspots, bursts, and research trends. Front. Psychiatry 15:1361535. doi: 10.3389/fpsyt.2024.1361535
Received: 12 January 2024; Accepted: 19 February 2024; Published: 01 March 2024.
Reviewed by:
Copyright © 2024 Liu, Chen, Zhou, Zhang and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shen Liu, [email protected] ; Chaomei Chen, [email protected] ; Na Zhang, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 30 July 2024
Overlapping genetic influences between creativity and borderline personality symptoms in a large Dutch sample
- Natalia Azcona-Granada 1 , 2 ,
- Gonneke Willemsen 1 , 3 ,
- Dorret I. Boomsma 1 , 2 &
- Bruno Sauce 1
Scientific Reports volume 14 , Article number: 17589 ( 2024 ) Cite this article
363 Accesses
6 Altmetric
Metrics details
- Behavioural genetics
- Human behaviour
- Psychiatric disorders
Creativity and mental disorders are sometimes seen as intertwined, but research is still unclear on whether, how much, and why. Here we explore the potential role of shared genetic factors behind creativity and symptoms of borderline personality disorder (BPD, characterized by mood swings and randomness of thoughts). Data were collected from 6745 twins (2378 complete pairs) by the Netherlands Twin Register on BPD scores (PAI-BOR questionnaire) and working in a creative profession (proxy for creativity). First, we tested whether there is an association between BPD symptoms and creative professions. Results confirmed that individuals scoring higher on the BPD spectrum are more likely to have a creative profession (Cohen’s d = 0.16). Next, we modeled how much of this association reflects underlying genetic and/or environmental correlations—by using a bivariate classical twin design. We found that creativity and BPD were each influenced by genetic factors (heritability = 0.45 for BPD and 0.67 for creativity) and that these traits are genetically correlated rG = 0.17. Environmental influences were not correlated. This is evidence for a common genetic mechanism between borderline personality scores and creativity which may reflect causal effects and shed light on mechanisms.
Similar content being viewed by others
Borderline personality disorder and the big five: molecular genetic analyses indicate shared genetic architecture with neuroticism and openness

Multivariate genetic analysis of personality and cognitive traits reveals abundant pleiotropy

Associating broad and clinically defined polygenic scores for depression with depression-related phenotypes
Introduction.
“ It pays to keep an open mind, but not so open your brains fall out ”. - Carl Sagan.
There is an ancient, almost proverbial intuition that links creativity with psychiatric vulnerability and mental disorders. Millennia ago, Aristotle already epitomized: “No great genius has ever existed without a strain of madness” 1 . Some famous anecdotes lend weight to this statement. The artist Salvador Dalí had been diagnosed with psychotic illnesses 2 , interlinked with both his unusual persona and masterpieces of hallucination-like qualities (like his late painting “La persistencia de la memoria (1931)”). The musician, Odette, was diagnosed with Borderline Personality Disorder giving the lyrics of her personal album a deeper sense. Vincent van Gogh had severe mood swings that could get him “absorbed in the moment […] in a fury of work” or “lying in a deep, dark pit, powerless to do anything”—probably due to bipolar disorder and borderline personality disorder 3 .
A connection between creativity and mental disorders has been the subject of theoretical as well as empirical investigations 4 . Empirical studies and meta-analyses show the existence of discrepancies: some confirm a connection (with a variety of proposed causal mechanisms), while others refute this association (for an in-depth look into these discrepancies, see 5 , 6 , 7 , 8 ). This lack of consensus could be due to methodology issues. Previous studies are generally hampered by small cohorts, lack of standardized tools to assess creativity, or the use of retrospective biographies to establish diagnoses 8 , 9 . Here, our goal is to: (1) test the association between being in a creative profession and symptoms of borderline personality disorder (BPD); (2) test whether this association shares some of the same genetic predispositions and environmental experiences.
Creativity is defined as the ability to generate ideas or products that are both original and, in some way, useful 10 . It is considered a positive trait that may have helped humans survive and adapt to a changing environment. As with many other complex traits, creativity is considered a continuum that varies among people. Some individuals have hardly any creative capacity and others are highly creative, with most of the population somewhere in between 11 .
Borderline personality disorder (BPD)
Borderline personality disorder (BPD) is a severe mood and personality disorder. The lifetime prevalence of a clinical diagnosis in 2018 was estimated to be 5.9 percent in the general population in the USA 12 . In a study based on the Netherlands Mental Health survey, it was found that 25.2% of the population had 1 to 2 symptoms, 3.8% had 3 to 4 symptoms, and 1.1% had 5 or more BPD symptoms 13 . BPD symptoms include symptoms in common with other disorders such as schizophrenia or bipolar disorder—disorders that have previously been associated with creativity, but not always 5 , 6 , 7 , 8 , 14 (more on this later). Individuals diagnosed with BPD may experience intense and highly variable moods as well as distorted and unstable self-image or sense of self. They also tend to view things in extremes. Their interests and values can vary quickly (leading to impulsive behavior) and their feelings for others can change from one extreme to the other (leading to unstable relationships and emotional pain) 15 . Additional symptoms may include feelings of dissociation or feelings of unreality 16 , self-harm, suicidal thoughts, and other less common symptoms like acoustic hallucinations 17 . Milder symptoms of BPD are also common in the general population and this supports the concept of a vulnerability model, where an increasing number and severity of symptoms leads to a higher probability of a clinical diagnosis. In other words, BPD is a spectrum.
Association between creativity and BPD
When addressing the association between mental disorders and creativity, initial studies focused on schizophrenia. More recently, a relationship has been found between creativity and bipolar disease and other mood disorders 5 , 6 , 7 , 8 , 14 . Therefore, some results claim creativity and psychopathology to be positively associated, others show no association, and others still show a negative association 8 , 9 . However, such studies have reached contradictory conclusions—in part due to the complexities of assessing creativity and issues with statistical power 8 , 9 . Much less is known on the association of creativity with borderline personality disorder (BPD)—there are almost no studies on its potential association with creativity 18 , and much remains inconclusive.
But even if we grant that creativity and mental disorders—and specifically BPD—are connected, what can be the cause of that? Given that both mental disorders and creativity have strong genetic influences, perhaps their association could have genetic sources in common.
Genetics of the association
Previous studies found that creativity has a high heritability—in other words, the differences in creativity between people are to a large extent due to genetic variation. In a twin study, Piffer & Hur (2014) estimated the heritability of creative achievement to range from 43 to 63%, depending on the type of assessment 19 . Roeling et al. (2017) measured “being in a creative profession” as an approximation of creativity and found a heritability estimate of 70% in a Dutch twin-sibling study 20 .
As far as we know, there are a few inconclusive studies on borderline personality and creativity specifically, and the closest approach is the study about the association between mood disorders and artistic creativity. Research into this area has suggested that subjects with cyclothymia and first‑degree relatives of subjects with manic depression had higher creativity scores than controls 21 . Carson et al. (2011) concluded that prominent creative people incurred a greater risk for mood disorders than their less creative counterparts. And compared with the general population, creative people in all professional categories demonstrated higher rates of undifferentiated mood disorder 22 . The authors suggested that mild forms of bipolar pathology or genetic risk for bipolar disorder are more beneficial to creative output than more severe forms of the illness. In a different study, Andreasen also found that both mood disorders and creative interests tended to run in families, concluding that “affective disorder may be both a ‘hereditary taint’ and a hereditary gift” 7 .
Considering the lack of studies on both creativity and BPD, here we describe results from other mental disorders with similar symptoms. For example, for schizophrenia, empirical findings implicate a relationship between creativity and familial risk of schizophrenia in adopted children 23 , 24 . In a different study, Higier et al. (2014) examined individuals with bipolar disorder and their healthy co-twins and found an increased sharing of positive temperament traits, schizotypy, impulsivity, and sensation seeking. These personality features were correlated with increased verbal learning and fluency in the co-twins. These data provided further evidence to suggest that creativity may result from the combined effects of bipolar spectrum traits and enhanced cognition 25 .
Genome-wide association studies (GWAS, where estimates of an association between DNA variants and a phenotype are obtained) have confirmed the genetic association between creativity and schizophrenia 26 , 27 and also bipolar 26 . Furthermore, Li et al. (2020) revealed that a diagnosis of schizophrenia, depression, and risky behaviors, but not bipolar disorder, was significantly correlated with creativity through shared DNA variants (a DNA variant is a change in the DNA sequence of a gene so that it differs among individuals in a population). Rajagopal et al. (2023) found that having an increased risk for psychiatric disorders, language ability, and creativity might have overlapping genetic roots 28 .
By combining multiple GWASs, genetic correlations can be estimated, but with the caveat that accuracy depends on how many of the relevant genetic variants have been found/included. And such analysis cannot assess environmental correlations among two traits (which represent all the life experiences in common that might underlie both traits) 29 . In contrast, research designs based on twin, adoption, and family data can provide an estimate of non-genetic (environmental) correlations underlying an association between traits, as well as a potentially more complete and accurate estimate of genetic correlations.
Using a genetic epidemiological approach with twins can be an important, and complementary method to elucidate the link between creativity and psychopathology. Because environmental/experiential factors are also critical for mental health and creativity, classical twin studies are a powerful study design 30 . Of note, however, no previous studies tried to estimate such influences between creativity and borderline personality disorder. This is a pity, because BPD is a promising avenue of research on creativity—with many symptoms in common with better studied traits such as schizophrenia and bipolar disorder.
In addition to being a good candidate symptoms-wise, borderline personality disorder also has, like schizophrenia and biopolar, multiple genetic, environmental, and social factors behind it, like family history, genetic vulnerability, and traumatic life events 31 . Distel et al. (2009) showed that genetic factors play a role in BPD, increasing risk among relatives 32 . Lubke et al. (2014) showed a SNP heritability of 23% 33 while Carpenter et al. (2013) concluded that the best evidence to date supports a gene-environment correlation (rGE) model for borderline personality traits, indicating that those with a genetic risk for BPD are also at increased risk for exposure to environments that may trigger BPD 34 .
Given the background of previous findings described above, our study here aims to test two main hypotheses in the Netherlands Twin Register: 1) creativity and borderline personality disorder score are associated, so the higher the score for borderline personality, the higher the chances to be in a creative profession; 2) The BPD-creativity association is in part explained by overlapping genetic factors (genetic correlations) and overlapping environments/experiences (environmental correlations).
Materials and methods
Participants.
Participants included in this study were part of the Netherlands Twin Register (NTR), a national register with extensive data collection on mental health, personality, lifestyle, demographics, etc. The only inclusion criteria for being part of the NTR is to be a Dutch-literacy twin or a relative of a twin. The representativeness of the general population has been assessed previously 35 with positive results. Our study included data from two surveys completed in 2004–2008 (called here “survey 7” 36 ) and 2009–2012 (“survey 8” 37 ) as described in 38 , 39 . The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration. Data collection was approved by the Central Ethics Committee on Research Involving Human Subjects of the University Medical Centers Amsterdam. Informed consent was obtained from all individual participants included in the study. Ethical approval numbers are as follows: ANTR7 (IRB00002991/03-181), ANTR8 (NL25220.029.08/2008-244.
Data were available for 12,939 twins (4610 complete twin pairs). Data from triplets or second twins in the same family were excluded. We removed data from twins with missing zygosity (N = 344). We kept only the individuals who completed surveys that included the PAI-BOR (see below) and questions about their profession, which were coded to reflect if a person worked in a creative profession. There were 4326 families in which one or two twins participated, with 6745 individual twins, with 2378 pairs with data for both twins. These twins were either identical twins (aka, monozygotic twins, MZ, who share nearly all the same DNA) or fraternal twins (aka, dizygotic twins, DZ, who share on average half of their DNA). Of the 6745 individuals, 990 were monozygotic males, 555 dizygotic males, 2569 monozygotic females, 1255 dizygotic females, and 1367 dizygotic opposite-sex. The mean age for the twins was 41.51 [standard deviation ( SD ) 12.41, range 19–90 years].
Zygosity (whether twins are monozygotic or dizygotic) was determined either by genotyping or from self- and parental report answers to survey questions on physical resemblance. DNA and survey zygosity agreement reached more than 96% 39 .
Creative occupation
As described in Roeling et al., individuals were asked to report a detailed description of their profession 20 . Creative professionals were defined as those having positions in the fields of dance, film, music, theater, visual arts, architecture, or writing (coded as yes/no). Individuals not working at the moment of the survey (e.g. retirement, illness, housewives/housemen) were asked for their past occupation to determine their creative profession status. Housewives or housemen who had not worked in any occupation before were coded as non-creative. When full-time or part-time education was reported, creative profession was coded as missing 20 .
BPD symptoms score
Scores for borderline personality have been previously analyzed in the NTR 40 , 41 . The BPD characteristics/symptoms were assessed by the Personality Assessment Inventory-Borderline Features scale (PAI-BOR) 42 . The 24 items of this scale include stability of mood and affects, anger control, self-image, feelings of emptiness, intense and unstable relationships, and self-harm and are rated on a four-point scale (0–3; false, slightly true, mainly true, very true). Previous studies using multigroup confirmatory factor analysis showed that the PAI-BOR is measurement invariant across sex and age 43 , 44 .
Statistical analyses
Descriptive analyses were done in R v.4.1.0. We performed all modeling and testing in Rstudio, notably with the packages “OpenMx” v2.19.8, "psych" v2.1.6, "ggplot2" v3.3.5, "foreign" 0.8–81, "gee" v4.13–20.
To determine the association between creativity and BP symptoms, we performed a logistic regression analysis on creativity by borderline scale, correcting for familial clustering in a Generalized Estimating Equation (GEE) model.
As suggested by the reviewers, post hoc GEE regression analyses were performed to assess the role of possible confounders—sex, age, IQ, educational attainment, and the big 5 of personality—for creativity, borderline, and its association. These GEE models allow to correct for the cluster of families.
To decompose the phenotypic variances and covariance into genetic and environmental components and to estimate genetic and environmental correlations between creativity and BPD, we conducted univariate and bivariate twin models. The identification of genetic and non-genetic parameters in the classical twin models is based on the different degrees of genetic relatedness between monozygotic (MZ) and dizygotic (DZ) twins. MZ twins are (nearly) 100% genetically similar, while DZ twins share ~ 50% of their segregating genes. Because both types of twins are born at the same time and grow up in the same household, MZ and DZ twins share features of their environment and experiences—called the common environment (C), which might affect their trait resemblance. Unique environmental factors and experiences (E) cause differences within MZ and DZ pairs and include all influences associated with “unique” environments (aspects of the environment that differ among siblings), and all forms of error and random noise. E factors are correlated zero by definition in MZ and DZ pairs. When there is a higher resemblance between MZ twins than between DZ twins for a trait, this indicates an influence of genetic factors. Twin resemblance can be a function of additive genetic influences, or an influence from interactions between alleles at the same locus (dominance) or between alleles at different loci (epistasis). We modeled additive genetic influences, based on the earlier analyses of these data 20 , 26 , 32 .
We estimated first phenotypic correlations between creativity and BPD, and then univariate twin correlations for these two traits, and cross-trait correlations, i.e. BPD in one twin with creativity in the cotwin. Tetrachoric correlations were estimated for the dichotomous traits (creativity). These are based on modeling a continuous liability distribution of the observed creativity variable, for MZ twins and DZ twin pairs 45 (for more detail see explanation of the ‘liability’ model below). For the continuous borderline scores, Pearson correlations were estimated for MZ and DZ twin pairs 46 . To evaluate the correlation cross-trait between a dichotomous and continuous trait, a point-biserial correlation was estimated, with a total of 4 correlations, within-person in MZ and in DZ twins, cross-trait within-twin in MZ twins, cross-trait cross-twin in DZ twins 47 .
Genetic structural equation modelling 48 to estimate genetic and environmental influences was performed in OpenMx 49 , first in a univariate classical twin model for each trait separately. For the creativity data, we assumed an underlying ‘liability’ model 50 , in which the variable was assumed to reflect an imprecise measurement of an underlying normal distribution of liability, with zero mean and unit variance. A threshold acts as a reference for the prevalence of the different categories in the population 51 . On the observed scale, creativity was coded as 0 (never worked in a creative profession) and 1 (worked in a creative profession). The estimated threshold divides individuals into a creative and non-creative group and depends on the prevalence in the population 51 , 52 .
The bivariate twin model estimates the correlated influences of additive genetic effects (A), common environmental effects shared by twins from the same family (C), and unique environmental effects (E) on creativity and borderline personality score. These models are based on the comparison of cross-trait cross-twin correlations in MZ and DZ pairs. When these are higher in MZ than in DZ pairs, the correlation between traits is due to correlated genetic effects. For a description of twin model methodology and comparable bivariate twin designs, please see the Supplementary material and publications, e.g. 53 , 54 , 55 . As noted previously in the participants section, we included incomplete pairs, but not participants who had BPD scores but lacked creativity data. Possible sex differences in genetic architecture were assessed in previous NTR studies and showed no differences in heritability for BPD 44 or for creativity 20 .
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration. Data collection was approved by the Central Ethics Committee on Research Involving Human Subjects of the University Medical Centers Amsterdam. Informed consent was obtained from all individual participants included in the study. Ethical approval numbers are as follows: ANTR7 (IRB00002991/03-181), ANTR8 (NL25220.029.08/2008-244).
In our sample, 6569 individuals never worked in a creative profession (97.39%), while 176 (2.61%) worked in a creative profession. For the BPD score, the mean of the full sample was 14.88 ( SD = 8.14). The mean BPD symptoms score of the non-creative group was 14.81 ( SD = 8.12) while the mean of the creative group was 17.45 ( SD = 8.65) (T = −4.0021, df = 183.36, p < 0.001). The distributions of this variable are shown in Table 1 and Supplementary Fig. 1 for the full whole sample and for the creative and non-creative groups separately.
We first tested whether borderline personality symptom score and creativity are related. The logistic regression analyses showed a significant association between borderline personality symptoms score and creativity (z = 4.64, β = 0.29, p < 0.001; OR = 1.34 (1.18–1.51)).
Phenotypic correlations between twins were calculated within traits and cross-traits. Tetrachoric correlations for the creativity variable were r = 0.68 (CI = 0.50–0.80) in MZ twins and r = 0.34 (CI = 0.02–0.59) in DZ twins. The correlation for the borderline variable in MZ was estimated at r = 0.43 (CI = 0.38–0.47) and in DZ was r = 0.18 (CI = 0.12–0.24). The point-biserial cross-trait correlation for creativity in twin 1 vs borderline in twin 2 had an estimate for the MZ correlation of r = 0.06 (CI = 0.01–0.11) and for the DZ correlation of r = −0.02 (CI = −0.07–0.04). The phenotypic correlation between the traits was r = 0.13 (CI = 0.07–0.19).
Univariate genetic models
The best-fitting model for the borderline variable was an AE model with a heritability estimate for borderline personality score of 0.46. The parameters of the model are specified in Fig. 1 A. The details of the likelihood ratio test for every model performed are specified in Table 2 .
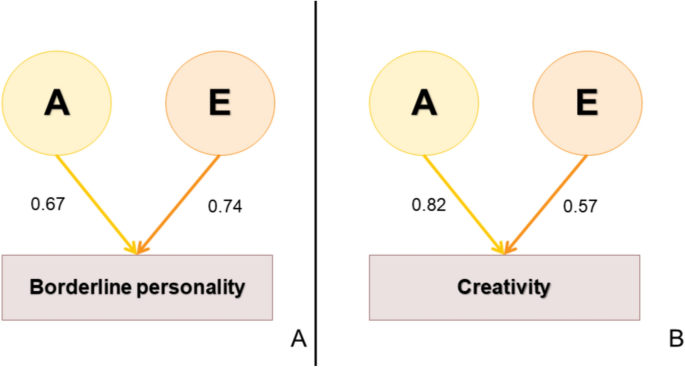
Univariate best-fitting models with parameter specification for borderline ( A ) and for creativity ( B ). The parameters in model A (borderline) and in model B (creativity) are the path values, therefore the sqrt of the standardized variance. A is the additive genetic component and E is the non-shared environment component for each trait.
For creativity, the heritability estimate was 0.68 (CI = 0.52–0.80) and an E parameter of 0.32 (CI = 0.20–0.48). The parameters of the model are specified in Fig. 1 B. The details of the likelihood ratio test for all the models performed are specified in Table 3 .
1. The negative log-likelihood subtracted for the more general model from the -2LL of the more restricted model. 2. Degrees of freedom (df) of the model. 3. The Akaike information criterion (AIC) is an estimator of prediction error and thereby relative quality of statistical models for a given set of data. 4. Χ 2 test given in the −2LL test. 5. Difference of degrees of freedom equal to the difference in the number of estimated parameters in the two models. 6. P represents the p -value of the test performed. In bold are the models with no difference from the original model, therefore, the best fitting models.
Bivariate model
The best-fitting model was an AE model with a heritability estimate of 0.45 (CI = 0.41–0.49) for borderline personality symptom score and 0.67 (CI = 0.57–0.80) for creativity. The genetic correlation between borderline personality score and working in a creative profession was estimated at rG = 0.17 (CI = 0.01–0.33). This additive genetic effect explained 72% of the phenotypic correlation of 0.13. The non-shared environmental correlation was estimated at rE = 0.09 (CI = −0.10–0.27), with the CI indicating this is a non-significant estimate. The specifications of this AE model and the details of the -2LL tests for every model performed are explained in detail in Supplementary Fig. 2, Tables 1 and 2 . The representation of the best-fitting model is shown in Fig. 2 .
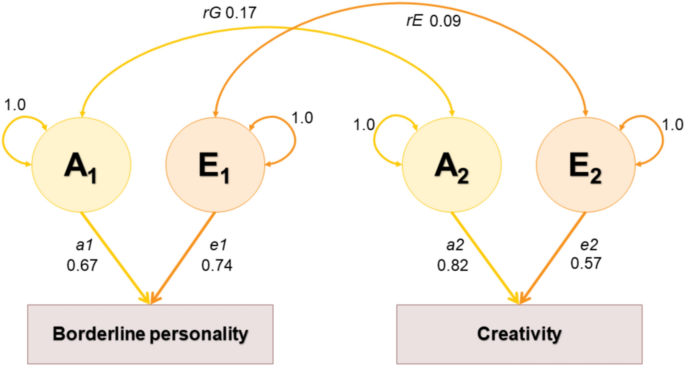
Model specification of the best fitting model (AE). The parameters are shown as path values, therefore the sqrt of the standardized variance. A 1 is the additive genetic component and E 1 is the non-shared environment component for borderline personality; A 2 is the additive genetic component and E 2 is the non-shared environment component for creativity. a1 is the unique genetic contribution for borderline; rG is the genetic correlation between both traits and a2 is the unique genetic contribution for creativity. e1 is the unique non-shared environment contribution for borderline; rE is the non-shared environment correlation between both traits and e2 is the unique non-shared environment contribution for creativity.
The results of the post hoc analyses for the possible confounders showed that the original genetic correlation between the proxy of the creative profession and the PAI-BOR score of borderline that we found seems to be really about BPD symptoms and creativity. For more detail, see Supplementary analyses.
Here we studied the relationship between borderline personality disorder (BPD) and creativity. In a large sample of twins drawn from the general population in the Netherlands, our results confirmed our first hypothesis: borderline personality scores indeed predicted creativity (proxied here as the status of working in a creative profession), with a small effect size. But what could be the sources of this relationship? Are there common genetic predispositions or life experiences that are driving this connection? Our second (and main) hypothesis in this study was that BPD-creativity association is, in part, due to these traits sharing some of the same genetic and environmental/experiential influences. Our models showed that there is indeed a significant genetic overlap between both traits, however (contrary to our expectation) no overlap for the environmental factors. As far as we know, this is the first study to show a genetic influence on the relationship between borderline personality score and creativity.
We think it's worthwhile to first discuss the separate, univariate models. For BPD symptoms, an AE model was confirmed to be the best-fitting model. That means that additive genetic effects (A) and unique environmental effects (E) played a role in the variation of borderline symptoms in our sample, but there are no shared environmental effects (in other words, experiences shared in common between pairs of twins do not make their BPD symptoms more alike). On genetic effects, BPD symptoms showed a heritability of 0.46. These results are in line with previous results published by Distel et al. (2008) in the same cohort, where they also concluded no variance explained by shared environmental factors 44 , 56 . As for creativity, the best-fitting model resulted in an AE model, without a role of shared environment (C). Working in a creative profession had a high heritability of 0.68. Those results are in line with a previous study in the NTR focused solely on creativity 20 .
We note the lack of shared environmental effects (C) that we found for creativity and for BPD (in the univariate as well as the bivariate models). A small C is fairly common in many psychological traits 57 , 58 . A possible explanation is that interactions of C with additive genetic effects are counted as “A” in the classical twin design 59 .
Now onto the bivariate models—the models that have data of both creativity and borderline symptoms together and test the potential overlap in sources of influences. The bivariate model with creativity and borderline personality symptoms showed a small genetic overlap between the traits, but enough to have a significant effect on the model if we remove it. For other, related mental disorders, molecular studies suggest a small overlap with polygenic risk scores for schizophrenia or bipolar disease predicting creativity 26 , 27 (a polygenic risk score is an index derived from the associations of a GWAS that represents, for each individual, the genetic risk/predisposition for the trait). Note that no past genetic study existed that combines borderline personality and creativity (neither molecular nor familial/twin).
As for environmental effects, we did not find any overlap between borderline symptoms and creativity. The absence of previous studies similar to this approach prevents us from comparing results. The lack of significance in the environmental correlation could mean that “environmental” factors people usually associate with both traits (disorders and creativity)—like for example lifestyle or drug use (selection bias)—are not purely environmental. These factors might (speculatively) be led by their genetic component.
In light of our main results on the shared genetic predispositions between BPD symptoms and creativity: what could be driving such a genetic overlap? There are multiple potential (and non-exclusive) explanations. It could be, for example, that genes which are influencing the creative process are the same that are connected to being prone to mental problems. At the same time, given the genetic correlation and the possible pleiotropism, a molecular approach should be considered in future research to provide additional evidence for the genetic etiology of covariation on borderline personality disorder and creativity. Or it could be because these genes make people more likely to both gravitate towards a creative profession (for non-creative reasons, like personality) and gravitate towards friend groups/profiles that makes them more vulnerable to BPD. Here we favor another explanation inspired by empirical findings from other fields (on the role of mania/obsession and randomness in creativity, described below 60 , 61 ) as well as famous anecdotes (of disturbed creative geniuses). We believe our results show a genetic overlap because there is a potential causal role from mood swings, random thoughts, and hallucinations (all BPD symptoms and genetically influenced) on creativity. How could this causal mechanism work?
For mood swings (mania/depression): Research in Psychology and Psychiatry shows that mood disorder patients who have manic and mixed states have higher creativity than depressive individuals 60 . And a different study found that in healthy, non-clinical subjects, mania risk was related to lifetime creativity and creative personality 61 . (Although not related to performance on a laboratory task of creative insight; which, speculatively, could also mean that our current findings using a measure of creative profession might tie it better with BPD than if we had used creative lab tasks).
For randomness of thoughts and hallucinations: Research in Computer Science suggests that machine learning models and neural networks can perform better and find more solutions to problems if they are given (during training) elements of randomness—which effectively moves the algorithm out of stuck situations/suboptimal solutions 62 , 63 . Randomness in the algorithm improve the likelihood of locating the global optima or a better local optima 64 . In Psychology, it has been hypothesized that elements of randomness might be the key to human creativity—adding something that no one else could or has added before 65 . This randomness may open the floodgates of the mind and let our imagination run wild. During sleep, for example, randomness is enhanced and helps us solve problems 66 . In an experimental study by Lacaux et al. (2021), they found that participants who slept after seeing a mathematical problem tripled the chance of discovering the hidden rule to solve it compared to participants who remained awake 66 . Similarly (and in a more extreme sense), mental illness could be a factor that would help in the creative process, because sometimes the most bizarre and distant associations (as seen in some mental disorders) can turn into the most brilliant creative ideas in our minds 21 .
Given our results of a positive, linear association between BPD and creativity, does that mean that mood swings, random thoughts, and hallucinations are always positively correlated with creativity? Very likely not—at some point, too much mania and randomness will obviously be dysfunctional even to basic day-to-day activities. And remember that in our sample, most participants were healthy, and the average score of BPD was below the clinical threshold. Some authors 22 , 67 have proposed that creativity relates to psychopathology in an inverted U model. Increasing symptom severity results in increased creativity to a certain point beyond which it starts to diminish—as represented in Fig. 3 .
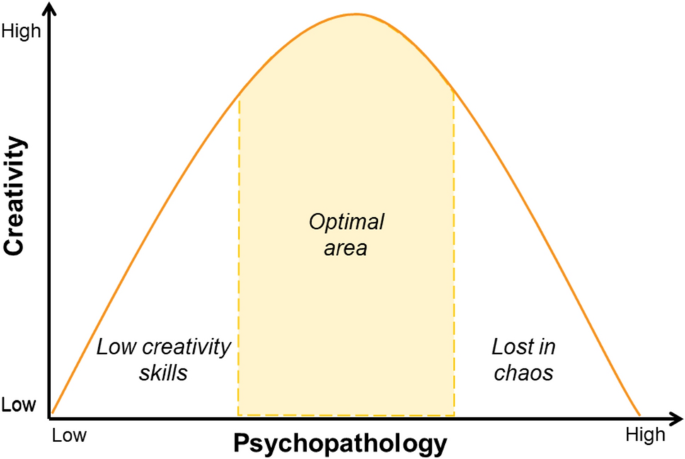
Inverted U model relating psychopathology and creativity. The hypothesis considers people with low psychopathology characteristics would also have low creative capacity. When this psychopathology increases, there is an optimal area where creativity is considerably increased to a certain point beyond which it starts to diminish again.
The inverted-U model may be the key to understanding why studies with clinical and non-clinical samples report different conclusions. Studies done with clinical samples frequently conclude that psychopathology and creativity are not related 5 , 68 , or even that these traits are negatively related 69 . But note that, in the inverted-U model, clinical samples are at the extreme end of the distribution and therefore, the expected creativity capacity is low because the harm from too many psychopathology symptoms overcomes the creativity capacity. Results from non-clinical studies are also controversial, but some authors like Csikszentmihalyi 70 , Runco 71 , 72 and Hofmann 9 concluded that slight forms of mental disorders (e.g., mild depressive or hypomanic states) are compatible with creative work, as long as the person has sufficient cognitive capacities, affective energies, and supportive environments.
Under the inverted U model, our study has a special advantage because the BPD questionnaire (PAI-BOR) does not diagnose BPD per se, but scores features related to the BPD syndrome 73 . The mean score for borderline personality in our creative sample was 17.45, meaning that they are not in the extreme to be diagnosed as BPD, and therefore those creative participants could be in the optimal area of creative functioning. Reddy et al. (2018) emphasized that eminent creators may lie on the same spectrum of psychopathological syndromes, but may display a less severe form of it, and hence, use it to their benefit 21 . However, with the present methodology, we cannot directly test if we are indeed seeing an inverted U distribution.
Another feature worth mentioning from our study is the large sample size. The final number of twins used in the twin models was 6745. To our knowledge, that’s the largest empirical sample size in any study of creativity and any study of borderline personality (combined and in isolation as well).
In our current study, we cannot conclude if the effects we found are due to something unique about borderline personality or because of comorbidity and/or common features that BPD shares with other disorders. BPD often co-occurs with other mental illnesses, so a person with borderline personality disorder also may be more likely to experience symptoms of major depression, PTSD, bipolar disorder, anxiety disorders, substance abuse, or eating disorders 74 , 75 . Patients with borderline personality disorder have been shown to have high rates of comorbid disorders: mood disorders 80% to 96%, anxiety disorders 88%, substance abuse disorders 64%, eating disorders 53%, attention deficit hyperactivity disorder (ADHD) 10% to 30%, bipolar disorder 15%, somatoform disorders 10% 76 . Not only that, but BPD is genetically correlated with other disorders as stated by Witt et al. (2017). Significant genetic correlations with BPD were found for bipolar disorder (rg = 0.28; s.e. = 0.094; P = 2.99 × 10 − 3), major depressive disorder (rg = 0.57; s.e. = 0.18; P = 1.04 × 10 − 3) and schizophrenia (rg = 0.34; s.e. = 0.082; P = 4.37 × 10 − 5) 77 . Then, it's likely that analyses on those disorders might show some genetic correlations with creativity as well. Future studies should also look at these comorbidities to further clarify how much the association between creativity and borderline overlaps with (or is partly driven by) other traits. Given past research, we think that some features and comorbidities of borderline would be positively associated with higher creativity- like the mania and mood swings characteristics of bipolar disorder, and the randomness of thought and hallucinations related to schizophrenia. While other features, like eating disorders, PTSD, and anxiety will probably not be.
Our study is limited in using only self-report data on professions (categorized by us as creative or non-creative), and in the low prevalence of creative professions. Possibly, the focus on creative professions provides a flawed reflection of creativity. Sometimes the typical categorization of “creative professions” can overestimate the creativity involved in the work, like, for example, in the case of musicians who don’t compose their own songs. And sometimes such categorization can underestimate creativity, like in professions not typically seen as “creative” but that can involve a considerable amount of creative work, such as in the STEM professions. For example, the mathematician John Nash suffered hallucinations from schizophrenia and these possibly inspired his revolutionary theorems in decision-making 78 . The physicist J. Robert Oppenheimer was also initially diagnosed with schizophrenia (called dementia praecox at that time). Or in cases when participants are still creative in their own time (e.g., in hobbies) which is not captured by this study.
Besides, someone deciding to follow a “creative profession” may not always be due to creative inspiration, but because of the lifestyle (socially) connected to such professions. In other words, the causation from borderline personality to creativity may not be direct but indirect: Mood disorders may cause people to gravitate toward particular subcultures and lifestyles (like a bohemian life) that would make them more likely to be artists. Actually, it may be that lifestyle causes both creativity and BPD, and there is no causal connection between borderline personality and creativity. These possibilities should be studied in further studies.
This study brings new insights to society. If it turns out that Borderline symptoms and creativity are causally connected, a creative therapy could help individuals with mild-symptoms of mental disorders, channeling these symptoms in a hurtless way and helping patients to have a more normal life. In addition, these results could give the general public a better understanding of borderline disorder and give it a less negative perception.
In short, this study provides empirical evidence on the relationship between borderline personality and creativity, adding new knowledge about the shared genetic contributions to this relationship. However, our knowledge of the genetic influence and the causation of this relationship is rather limited, and further studies are needed. Nonetheless, the saying that geniuses are mad, as in Dalí’s, van Gogh’s, and Nash’s examples, may perhaps not be so far from reality—at least in moderate doses of madness.
Data availability
Being part of a national prospective cohort study, Netherlands Twin Registerdata cannot be made publicly available for privacy reasons,but they are available for legitimate researchers via the data access procedure ( https://ntr-data-request.psy.vu.nl/ ). The research data collected by the Netherlands Twin Registry (NTR) are pseudonimized, annotated and stored in the NTR Repository. This is a secure database that is only accessible to our data managers. Metadata (i.e. variable names, labels, counts etc.) can be consulted by researchers in the NTR Data Showcase ( https://ntr-data-request.psy.vu.nl/data-showcase.html ). The Data Showcase allows researchers to create a list of variables and export it for use in a Data Sharing Request ( https://ntr-data-request.psy.vu.nl/submitting-a-data-sharing-request.html ). Researchers with an approved data sharing request who abide by the rules of the European General Data Protection Regulation will receive temporary access to the NTR data for their own research projects. More information on our data sharing procedures and associated costs can be found https://ntr-data-request.psy.vu.nl/data-sharing-procedures.html . The datasets used and/or analysed during the current study available from the corresponding author on reasonable request. To reproduce this study, the variables "BOR_7", "bor_8", and the creative profession (not included in the data showcase) “creatief7” and “creatief8” should be requested.
Code availability
https://github.com/NataliaAG99/CreativityBorderlineBivariateTwin .
Motto, A. L. & Clark, J. R. The Paradox of Genius and madness: Seneca and his influence. Cuad. Filol. Clásica Estud. Lat. 189–200 (1992).
Murphy, C. The link between artistic creativity and psychopathology: Salvador Dalí. Personal. Individ. Differ. 46 , 765–774 (2009).
Article CAS Google Scholar
Nolen, W. A., van Meekeren, E., Voskuil, P. & van Tilburg, W. New vision on the mental problems of Vincent van Gogh; results from a bottom-up approach using (semi-)structured diagnostic interviews. Int. J. Bipolar Disord. 8 , 1–9 (2020).
Article Google Scholar
Carson, S. H. Creativity and mental illness. Camb. Handb. Creat. https://doi.org/10.1017/9781316979839.016 (2019).
Kyaga, S. et al. Mental illness, suicide and creativity: 40-Year prospective total population study. J. Psychiatr. Res. 47 , 83–90 (2013).
Article PubMed Google Scholar
Kyaga, S. et al. Creativity and mental disorder: Family study of 300 000 people with severe mental disorder. Br. J. Psychiatry 199 , 373–379 (2011).
Andreasen, N. C. Creativity and mental illness: Prevalence rates in writers and their first-degree relatives. Am. J. Psychiatry 144 , 1288–1292 (1987).
Article CAS PubMed Google Scholar
Thys, E., Sabbe, B. & De Hert, M. Creativity and psychopathology: A systematic review. Psychopathology 47 , 141–147 (2014).
Holm-Hadulla, R. M., Hofmann, F. H., Sperth, M. & Mayer, C. H. Creativity and psychopathology: An interdisciplinary view. Psychopathology 54 , 39–46 (2021).
Barron, F. Creative Person and Creative Process . (Holt, Rinehart, & Winston, 1969).
Lloyd, P. & Jones, D. Everyday creativity in design process. Art Des. Commun. High. Educ. 12 , 247–263 (2013).
Borderline personality disorder. Nat. Rev. Dis. Primer 4 , 18030 (2018).
Ten Have, M. et al. Prevalence rates of borderline personality disorder symptoms: A study based on the Netherlands Mental Health Survey and Incidence Study-2. BMC Psychiatry 16 , (2016).
Zhao, R., Tang, Z., Lu, F., Xing, Q. & Shen, W. An updated evaluation of the dichotomous link between creativity and mental health. Front. Psychiatry 12 , 2472 (2022).
Koenigsberg, H. W. & Siever, L. J. Borderline personality disorder. Encycl. Stress No. QF 17- , 348–350 (2007).
Diagnostic and statistical manual of mental disorders. DSM Library https://doi.org/10.1176/appi.books.9780890425596 .
Kingdon, D. G. et al. Schizophrenia and borderline personality disorder: similarities and differences in the experience of auditory hallucinations, paranoia, and childhood trauma. J. Nerv. Ment. Dis. 198 , 399–403 (2010).
Leutgeb, V. et al. Creativity and borderline personality disorder: evidence from a voxel-based morphometry study. Cognit. Neuropsychiatry 21 , 242–255 (2016).
Piffer, D. & Hur, Y. M. Heritability of creative achievement. Creat. Res. J. 26 , 151–157 (2014).
Roeling, M. P., Willemsen, G. & Boomsma, D. I. Heritability of working in a creative profession. Behav. Genet. 47 , 298–304 (2017).
Reddy, I., Ukrani, J., Indla, V. & Ukrani, V. Creativity and psychopathology: Two sides of the same coin?. Indian J. Psychiatry 60 , 168–174 (2018).
Article PubMed PubMed Central Google Scholar
Carson, S. H. Creativity and psychopathology: A shared vulnerability model. Can. J. Psychiatry 56 , 144–153 (2011).
McNeil, T. F. Prebirth and postbirth influence on the relationship between creative ability and recorded mental illness. J. Pers. 39 , 391–406 (1971).
Kinney, D. K. et al. Creativity in offspring of schizophrenic and control parents: An adoption study. Creat. Res. J. 13 , 17–25 (2010).
Higier, R. G. et al. Enhanced neurocognitive functioning and positive temperament in twins discordant for bipolar disorder. Am. J. Psychiatry 171 , 1191–1198 (2014).
Power, R. A. et al. Polygenic risk scores for schizophrenia and bipolar disorder predict creativity. Nat. Neurosci. 18 , 953–955 (2015).
Li, H. et al. Genome-wide association study of creativity reveals genetic overlap with psychiatric disorders, risk tolerance, and risky behaviors. Schizophr. Bull. 46 , 1317–1326 (2020).
Rajagopal, V. M. et al. Genome-wide association study of school grades identifies genetic overlap between language ability, psychopathology and creativity. Sci. Rep. 13 , 429 (2023).
Article ADS CAS PubMed PubMed Central Google Scholar
Hagenbeek, F. A. et al. Maximizing the value of twin studies in health and behaviour. Nat. Hum. Behav. 7 , 849–860 (2023).
Boomsma, D., Busjahn, A. & Peltonen, L. Classical twin studies and beyond. Nat. Rev. Genet. 3 , 872–882 (2002).
Chapman, J., Jamil, R. T. & Fleisher, C. Borderline Personality Disorder. in StatPearls (StatPearls Publishing, Treasure Island (FL), 2023).
Distel, M. A. et al. Familial resemblance of borderline personality disorder features: Genetic or cultural transmission?. PloS One 4 , e5334 (2009).
Article ADS PubMed PubMed Central Google Scholar
Lubke, G. H. et al. Genome-wide analyses of borderline personality features. Mol. Psychiatry 19 , 923–929 (2014).
Carpenter, R. W., Tomko, R. L., Trull, T. J. & Boomsma, D. I. Gene-environment studies and borderline personality disorder: A review. Curr. Psychiatry Rep. 15 , 336 (2013).
Vink, J. M. et al. Estimating non-response bias in family studies: Application to mental health and lifestyle. Eur. J. Epidemiol. 19 , 623–630 (2004).
Distel, M. A. et al. Personality, health and lifestyle in a questionnaire family study: A comparison between highly cooperative and less cooperative families. Twin Res. Hum. Genet. Off. J. Int. Soc. Twin. Stud. 10 , 348–353 (2007).
van Beek, J. H. D. A., de Moor, M. H. M., Geels, L. M., Willemsen, G. & Boomsma, D. I. Explaining individual differences in alcohol intake in adults: Evidence for genetic and cultural transmission?. J. Stud. Alcohol Drugs 75 , 201–210 (2014).
Willemsen, G. et al. The Adult Netherlands twin register: Twenty-five years of survey and biological data collection. Twin Res. Hum. Genet. Off. J. Int. Soc. Twin Stud. 16 , 271–281 (2013).
Ligthart, L. et al. The Netherlands twin register: Longitudinal research based on twin and twin-family designs. Twin Res. Hum. Genet. https://doi.org/10.1017/thg.2019.93 (2019).
Distel, M. A. et al. Life events and borderline personality features: the influence of gene-environment interaction and gene-environment correlation. Psychol. Med. 41 , 849–860 (2011).
Lubke, G. H. et al. Genome-wide analyses of borderline personality features. Mol. Psychiatry 19 , 923 (2014).
Morey, L. C. & Ambwani, S. The personality assessment inventory. SAGE Handb. Personal. Theory Assess. Vol. 2 - Personal. Meas. Test. 626–645 (2008) https://doi.org/10.4135/9781849200479.N30 .
De Moor, M. H. M., Distel, M. A., Trull, T. J. & Boomsma, D. I. Assessment of borderline personality features in population samples: Is the personality assessment inventory-borderline features scale measurement invariant across sex and age?. Psychol. Assess. 21 , 125–130 (2009).
Distel, M. A. et al. Heritability of borderline personality disorder features is similar across three countries. Psychol. Med. 38 , 1219–1229 (2008).
Bonett, D. G. & Price, R. M. Inferential methods for the tetrachoric correlation coefficient. Sour.: J. Educ. Behav. Stat. 30 (2005).
Schober, P. & Schwarte, L. A. Correlation coefficients: Appropriate use and interpretation. Anesth. Analg. 126 , 1763–1768 (2018).
Glass, G.V, H., K. D. Statistical Methods in Education and Psychology . (Englewood Cliffs, 1984).
Bruins, S., Franic, S., Borsboom, D., Dolan, C. & Boomsma, D. Structural Equation Modeling in Genetics. in Handbook of Structural Equation Modeling (ed. Hoyle, R. H.) 646–663 (Guilford Press, 2023).
Boker, S. et al. OpenMx: An open source extended structural equation modeling framework. Psychometrika 76 , 306–317 (2011).
Article MathSciNet PubMed PubMed Central Google Scholar
Falconer, D. S. The inheritance of liability to certain diseases, estimated from the incidence among relatives. Ann. Hum. Genet. 29 , 51–76 (1965).
Hill, W. G. & Mackay, T. F. C. D. S. Falconer and introduction to quantitative genetics. Genetics 167 , 1529–1536 (2004).
Wray, N. R. & Visscher, P. M. Quantitative genetics of disease traits. J. Anim. Breed. Genet. Z. Tierzuchtung Zuchtungsbiologie 132 , 198–203 (2015).
Kiecolt, K. J., Aggen, S. H. & Kendler, K. S. Genetic and environmental influences on the relationship between mastery and alcohol dependence. Alcohol. Clin. Exp. Res. 37 , 905–913 (2013).
Article CAS PubMed PubMed Central Google Scholar
Posthuma, D. et al. Theory and practice in quantitative genetics. Twin Res. Off. J. Int. Soc. Twin Stud. 6 , 361–376 (2003).
Poelen, E. A. P. et al. The relative contribution of genes and environment to alcohol use in early adolescents: Are similar factors related to initiation of alcohol use and frequency of drinking?. Alcohol. Clin. Exp. Res. 32 , 975–982 (2008).
Torgersen, S. et al. The heritability of cluster B personality disorders assessed both by personal interview and questionnaire. J. Personal. Disord. 26 , 848–866 (2012).
Turkheimer, E. Three laws of behavior genetics and what they mean. Curr. Dir. Psychol. Sci. 9 , 160–164 (2000).
Bouchard, T. J. & McGue, M. Genetic and environmental influences on human psychological differences. J. Neurobiol. 54 , 4–45 (2003).
Purcell, S. Variance components models for gene-environment interaction in twin analysis. Twin Res. Hum. Genet. 5 , 554–571 (2002).
Soeiro-de-Souza, M. G., Dias, V. V., Bio, D. S., Post, R. M. & Moreno, R. A. Creativity and executive function across manic, mixed and depressive episodes in bipolar I disorder. J. Affect. Disord. 135 , 292–297 (2011).
Ruiter, M. & Johnson, S. L. Mania risk and creativity: A multi-method study of the role of motivation. J. Affect. Disord. 170 , 52–58 (2015).
Dalessandro, B. Bring the noise: Embracing randomness is the key to scaling up machine learning algorithms. Big Data 1 , 110–112 (2013).
Scardapane, S. & Wang, D. Randomness in neural networks: an overview. WIREs Data Min. Knowl. Discov. 7 , e1200 (2017).
Asi, H. & Duchi, J. C. The importance of better models in stochastic optimization. Proc. Natl. Acad. Sci. 116 , 22924–22930 (2019).
Article ADS MathSciNet CAS PubMed PubMed Central Google Scholar
Lehrer, J. Imagine: How Creativitty Works . (Hougton Mifflin Harcourt, 2012).
Lacaux, C. et al. Sleep onset is a creative sweet spot. Sci. Adv. 7 , 5866 (2021).
Article ADS Google Scholar
Richards, R., Kinney, D., Lunde, I., Benet, M. & Merzel, A. Creativity in manic-depressives, cyclothymes, their normal relatives, and control subjects. J. Abnorm. Psychol. 97 , 281–288 (1988).
Acar, S., Chen, X. & Cayirdag, N. Schizophrenia and creativity: A meta-analytic review. Schizophr. Res. 195 , 23–31 (2018).
Eisenman, R. Creativity, Preference for Complexity, and Physical and Mental Illness . vol. 3 (Taylor & Francis Group, 2009).
Csikszentmihalyi, M. Creativity: Flow and the Psychology of Discovery and Invention . (New York, 1996).
Mark A. Runco. Creativity: Theories and Themes: Research, Development, and Practice . (Elsevier, 2014).
Runco, M. A. Creativity. Annu. Rev. 55 , 657–687 (2004).
Google Scholar
Morey, L. C. The Personality Assessment Inventory Professional Manual. (Odessa, 1991).
Shah, R. & Zanarini, M. C. Comorbidity of borderline personality disorder: Current status and future directions. Psychiatr. Clin. North Am. 41 , 583–593 (2018).
Slotema, C. W., Blom, J. D., Niemantsverdriet, M. B. A., Deen, M. & Sommer, I. E. C. Comorbid diagnosis of psychotic disorders in borderline personality disorder: Prevalence and influence on outcome. Front. Psychiatry 9 , 84 (2018).
Chapman, J., Jamil, R. T. & Fleisher, C. Borderline Personality Disorder. Cult. Sociol. Ment. Illn. Z Guide https://doi.org/10.4135/9781483346342.n230 (2022).
Witt, S. H. et al. Genome-wide association study of borderline personality disorder reveals genetic overlap with bipolar disorder, major depression and schizophrenia. Transl. Psychiatry 7 , e1155–e1155 (2017).
Funaki, T. Nash: Genius with schizophrenia or vice versa?. Pac. Health Dialog 15 , 129–137 (2009).
PubMed Google Scholar
Download references
Acknowledgements
We warmly thank all participating twins in the Netherlands Twin Register who dedicated part of their time to make research possible as well as everyone involved in the collection of the data and data management. NAG would like to thank her grandmother Amelia A.I. for her constant support; grandma, it is not a Nobel Prize but it tastes like one, it's for you. Funding for the surveys whose data we analyzed: ANTR Survey 8: Genetic determinants of risk behavior in relation to alcohol use and alcohol use disorder: a developmental perspective. ZonMW (Addiction) Project nr: 31160008; PI Boomsma; METC: 2008/244; ANTR Survey 7: Borderline Personality Disorder in a Dutch Twin Cohort. Borderline Foundation; PI Boomsma; METC: 03/181.
Author information
Authors and affiliations.
Department of Biological Psychology, Vrije Universiteit Amsterdam, Van Der Boechorststraat 7, 1081 BT, Amsterdam, The Netherlands
Natalia Azcona-Granada, Gonneke Willemsen, Dorret I. Boomsma & Bruno Sauce
Amsterdam Public Health Research Institute, Amsterdam University Medical Centre, Amsterdam, The Netherlands
Natalia Azcona-Granada & Dorret I. Boomsma
Faculty of Health, Sports and Wellbeing, Inholland University of Applied Sciences, Haarlem, The Netherlands
Gonneke Willemsen
You can also search for this author in PubMed Google Scholar
Contributions
NAG conceived and designed the work; performed the analysis, interpreted the data; drafted the paper; and substantively revised the paper. GW acquired the data, interpreted the data; and substantively revised the paper. DIB acquired the data, interpreted the data; and substantively revised the paper. BS conceived and designed the work; interpreted the data; and substantively revised the paper. All authors have approved the submitted version and have agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Corresponding authors
Correspondence to Natalia Azcona-Granada or Bruno Sauce .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary information., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Azcona-Granada, N., Willemsen, G., Boomsma, D.I. et al. Overlapping genetic influences between creativity and borderline personality symptoms in a large Dutch sample. Sci Rep 14 , 17589 (2024). https://doi.org/10.1038/s41598-024-68146-8
Download citation
Received : 19 February 2024
Accepted : 19 July 2024
Published : 30 July 2024
DOI : https://doi.org/10.1038/s41598-024-68146-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Sweepstakes
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
50+ Research Topics for Psychology Papers
How to Find Psychology Research Topics for Your Student Paper
- Specific Branches of Psychology
- Topics Involving a Disorder or Type of Therapy
- Human Cognition
- Human Development
- Critique of Publications
- Famous Experiments
- Historical Figures
- Specific Careers
- Case Studies
- Literature Reviews
- Your Own Study/Experiment
Are you searching for a great topic for your psychology paper ? Sometimes it seems like coming up with topics of psychology research is more challenging than the actual research and writing. Fortunately, there are plenty of great places to find inspiration and the following list contains just a few ideas to help get you started.
Finding a solid topic is one of the most important steps when writing any type of paper. It can be particularly important when you are writing a psychology research paper or essay. Psychology is such a broad topic, so you want to find a topic that allows you to adequately cover the subject without becoming overwhelmed with information.
I can always tell when a student really cares about the topic they chose; it comes through in the writing. My advice is to choose a topic that genuinely interests you, so you’ll be more motivated to do thorough research.
In some cases, such as in a general psychology class, you might have the option to select any topic from within psychology's broad reach. Other instances, such as in an abnormal psychology course, might require you to write your paper on a specific subject such as a psychological disorder.
As you begin your search for a topic for your psychology paper, it is first important to consider the guidelines established by your instructor.
Research Topics Within Specific Branches of Psychology
The key to selecting a good topic for your psychology paper is to select something that is narrow enough to allow you to really focus on the subject, but not so narrow that it is difficult to find sources or information to write about.
One approach is to narrow your focus down to a subject within a specific branch of psychology. For example, you might start by deciding that you want to write a paper on some sort of social psychology topic. Next, you might narrow your focus down to how persuasion can be used to influence behavior .
Other social psychology topics you might consider include:
- Prejudice and discrimination (i.e., homophobia, sexism, racism)
- Social cognition
- Person perception
- Social control and cults
- Persuasion, propaganda, and marketing
- Attraction, romance, and love
- Nonverbal communication
- Prosocial behavior
Psychology Research Topics Involving a Disorder or Type of Therapy
Exploring a psychological disorder or a specific treatment modality can also be a good topic for a psychology paper. Some potential abnormal psychology topics include specific psychological disorders or particular treatment modalities, including:
- Eating disorders
- Borderline personality disorder
- Seasonal affective disorder
- Schizophrenia
- Antisocial personality disorder
- Profile a type of therapy (i.e., cognitive-behavioral therapy, group therapy, psychoanalytic therapy)
Topics of Psychology Research Related to Human Cognition
Some of the possible topics you might explore in this area include thinking, language, intelligence, and decision-making. Other ideas might include:
- False memories
- Speech disorders
- Problem-solving
Topics of Psychology Research Related to Human Development
In this area, you might opt to focus on issues pertinent to early childhood such as language development, social learning, or childhood attachment or you might instead opt to concentrate on issues that affect older adults such as dementia or Alzheimer's disease.
Some other topics you might consider include:
- Language acquisition
- Media violence and children
- Learning disabilities
- Gender roles
- Child abuse
- Prenatal development
- Parenting styles
- Aspects of the aging process
Do a Critique of Publications Involving Psychology Research Topics
One option is to consider writing a critique paper of a published psychology book or academic journal article. For example, you might write a critical analysis of Sigmund Freud's Interpretation of Dreams or you might evaluate a more recent book such as Philip Zimbardo's The Lucifer Effect: Understanding How Good People Turn Evil .
Professional and academic journals are also great places to find materials for a critique paper. Browse through the collection at your university library to find titles devoted to the subject that you are most interested in, then look through recent articles until you find one that grabs your attention.
Topics of Psychology Research Related to Famous Experiments
There have been many fascinating and groundbreaking experiments throughout the history of psychology, providing ample material for students looking for an interesting term paper topic. In your paper, you might choose to summarize the experiment, analyze the ethics of the research, or evaluate the implications of the study. Possible experiments that you might consider include:
- The Milgram Obedience Experiment
- The Stanford Prison Experiment
- The Little Albert Experiment
- Pavlov's Conditioning Experiments
- The Asch Conformity Experiment
- Harlow's Rhesus Monkey Experiments
Topics of Psychology Research About Historical Figures
One of the simplest ways to find a great topic is to choose an interesting person in the history of psychology and write a paper about them. Your paper might focus on many different elements of the individual's life, such as their biography, professional history, theories, or influence on psychology.
While this type of paper may be historical in nature, there is no need for this assignment to be dry or boring. Psychology is full of fascinating figures rife with intriguing stories and anecdotes. Consider such famous individuals as Sigmund Freud, B.F. Skinner, Harry Harlow, or one of the many other eminent psychologists .
Psychology Research Topics About a Specific Career
Another possible topic, depending on the course in which you are enrolled, is to write about specific career paths within the field of psychology . This type of paper is especially appropriate if you are exploring different subtopics or considering which area interests you the most.
In your paper, you might opt to explore the typical duties of a psychologist, how much people working in these fields typically earn, and the different employment options that are available.
Topics of Psychology Research Involving Case Studies
One potentially interesting idea is to write a psychology case study of a particular individual or group of people. In this type of paper, you will provide an in-depth analysis of your subject, including a thorough biography.
Generally, you will also assess the person, often using a major psychological theory such as Piaget's stages of cognitive development or Erikson's eight-stage theory of human development . It is also important to note that your paper doesn't necessarily have to be about someone you know personally.
In fact, many professors encourage students to write case studies on historical figures or fictional characters from books, television programs, or films.
Psychology Research Topics Involving Literature Reviews
Another possibility that would work well for a number of psychology courses is to do a literature review of a specific topic within psychology. A literature review involves finding a variety of sources on a particular subject, then summarizing and reporting on what these sources have to say about the topic.
Literature reviews are generally found in the introduction of journal articles and other psychology papers , but this type of analysis also works well for a full-scale psychology term paper.
Topics of Psychology Research Based on Your Own Study or Experiment
Many psychology courses require students to design an actual psychological study or perform some type of experiment. In some cases, students simply devise the study and then imagine the possible results that might occur. In other situations, you may actually have the opportunity to collect data, analyze your findings, and write up your results.
Finding a topic for your study can be difficult, but there are plenty of great ways to come up with intriguing ideas. Start by considering your own interests as well as subjects you have studied in the past.
Online sources, newspaper articles, books , journal articles, and even your own class textbook are all great places to start searching for topics for your experiments and psychology term papers. Before you begin, learn more about how to conduct a psychology experiment .
What This Means For You
After looking at this brief list of possible topics for psychology papers, it is easy to see that psychology is a very broad and diverse subject. While this variety makes it possible to find a topic that really catches your interest, it can sometimes make it very difficult for some students to select a good topic.
If you are still stumped by your assignment, ask your instructor for suggestions and consider a few from this list for inspiration.
- Hockenbury, SE & Nolan, SA. Psychology. New York: Worth Publishers; 2014.
- Santrock, JW. A Topical Approach to Lifespan Development. New York: McGraw-Hill Education; 2016.
By Kendra Cherry, MSEd Kendra Cherry, MS, is a psychosocial rehabilitation specialist, psychology educator, and author of the "Everything Psychology Book."

General call for papers
Personality Disorders: Theory, Research, and Treatment ( PD:TRT ), the official journal of the North American Society for the Study of Personality Disorders, welcomes manuscripts from research psychologists, as well as researchers from other disciplines such as psychiatry, social work, and public health.
PD:TRT seeks the following types of submissions:
- Full-Length Articles: Manuscripts presenting empirical findings may be submitted as full-length articles, not to exceed 36 pages.
- Brief Reports: Brief reports of empirical findings, not to exceed 18 pages.
- Registered Reports: Initial submissions consist of a detailed research proposal, including an abstract, introduction, hypotheses (if applicable), power analyses, method, and planned analyses. Manuscripts are then peer reviewed solely on the basis of this information; in most cases, researchers collect the data (or access it, if using archival data) only after receiving a stage 1 acceptance. Please visit the Center for Open Science for more details on this mechanism.
- Target Conceptual Articles: Manuscripts that evaluate and synthesize the research literature and/or make important theoretical contributions, not to exceed 40 pages. Four commentaries invited by the journal will be published on the PD:TRT homepage, along with the author's response to the commentaries.
- Practice Reviews: Practice reviews present an issue from clinical practice, review relevant research, and provide a practical recommendation informed by the reviewed research. They must be coauthored by at least one individual with a primary focus in clinical practice and at least one individual with a primary focus in research. This partnering of individuals with a different professional emphasis is crucial for practice reviews to provide a credible bridge between research and practice. When submitting a practice review, provide a description of each individual's primary professional focus in the cover letter. Practice reviews should not exceed 30 pages.
- PD:TRT is substantially invested in open science practices and encourages submissions that involve preregistration and the sharing of data, code, and materials, etc. when possible. The journal has adopted the Transparency and Openness Promotion (TOP) Level 2 Guidelines in support of these principles and awards several open science badges for which authors of accepted manuscripts can apply.

Manuscript submission
Manuscripts should be submitted electronically to the PD:TRT submission portal .
All submissions will undergo rigorous peer review.
Additional information about the journal and guidance for authors is available on the PD:TRT homepage .
For questions or further information, please contact the Editor, Joshua D. Miller , PhD.
Other calls for papers

Calls for papers for journal manuscripts
More about this journal
- Personality Disorders: Theory, Research, and Treatment
- Pricing and subscription info
- Read sample articles
Contact Journals
- Open access
- Published: 08 July 2024
Towards an informed research agenda for the field of personality disorders by experts with lived and living experience and researchers
- Babette Renneberg 1 , 2 ,
- Joost Hutsebaut 3 ,
- Ann Berens 4 , 5 ,
- Chiara De Panfilis 6 ,
- Katja Bertsch 7 ,
- Andres Kaera 8 ,
- Ueli Kramer 9 ,
- Christian Schmahl 10 , 11 ,
- Michaela Swales 12 ,
- Svenja Taubner 13 ,
- Mariana Mendoza Alvarez 4 , 5 , 14 ,
- Julia Sieg 1 &
30 experts with lived experience – clients, relatives, significant others - from 10 European countries
Borderline Personality Disorder and Emotion Dysregulation volume 11 , Article number: 14 ( 2024 ) Cite this article
529 Accesses
Metrics details
We describe a collection of themes for a research agenda for personality disorders that was originally formulated for the ESSPD Borderline Congress in 2022.
Experts with lived and living experience (EE), researchers and clinicians met virtually, exchanged ideas and discussed research topics for the field of personality disorders. The experts - patients, relatives, significant others - named the topics they thought most relevant for further research in the field. These topics were presented at the ESPPD conference in October 2022.
The five top themes were: 1. Prevention, early detection and intervention, 2. Recovery beyond symptom improvement, 3. Involvement of relatives in treatment, 4. Gender dysphoria, and 5. Stigma.
Conclusions
In general, the topics reflect current issues and changes in societal values. Overarching aims of research on these topics are the improvement of social participation and integration in society, better dissemination of research, and better information of the general public and political stakeholders.
Introduction
The importance of the perspectives of service users in research on mental health has been increasingly recognized over the last decades. While historically, experts with lived and living experience and their significant others (EE) were primarily seen as the object of clinical and research endeavors, there is a growing number of projects and attempts to create collaborations and partnership between experts by profession and EE. This participatory approach is also called public and patient involvement [ 11 ]. To improve this situation, many research funding agencies now require EE to be involved in research. Ideally, this should be the case in every step of the research. As Lloyd and White [ 32 ] pointed out: Research priorities are rarely set democratically. Priorities for research of academic researchers differ from those of EE.
An exemplary approach in this field is established by the James Lind Alliance (JLA https://www.jla.nihr.ac.uk/ ) Priority Setting Partnerships in Oxford, UK. The JLA was established in 2004 and is funded by the UK Medical Research Council and National Institute for Health Research (NIHR). This non-profit initiative brings together patients, carers and clinicians to identify and prioritize research questions that should be further explored and funded for a given disease or disorder. The aim of such initiatives (see also e.g., [ 2 ]) is to integrate patients and relatives as co-creators in all stages of the research process. Ethical and legal reasons form the base for this participatory process which also ensures that research becomes more relevant and more credible for those affected by the disease or the disorder.
However, PPI has hardly been realized in mainstream psychological/psychiatric research in many countries, especially when it is accompanied by actual decision-making power of EE. The reasons for this include that PPI is cost- and time-intensive, sometimes it is difficult to find EE partners, and that power over the research process is reluctantly shared [ 11 ]. Furthermore, in many countries an organized structure for PPI does not exist. Thus, it is difficult to find EEs for researchers if structures from funding agencies are not yet established and no funds exist to pay the effort and the participation of EE.
Recently, a growing body of research involving EE has emerged. Here, a distinction should be made between research that seeks to explore the experiences and perspectives of EE (e.g., [ 3 , 48 ]), and research that is planned and conducted in collaboration with EE (e.g., [ 14 ], see below). While the former reinforces the patient – practitioner dichotomy, the latter creates the potential for new forms of equal partnership. One example of such collaborative research is a qualitative study on understandings of recovery [ 14 ]. In this study, the research team consisted of one service user researcher, one university researcher and a clinical researcher. In an additional article, the authors reflect upon their work process and the way their different perspectives enhanced and challenged the collaboration [ 13 ]. Obviously, an equal partnership does not happen easily and different perspectives demand more reflection and dialogue than traditional research teams might face. But the approach also holds the potential for the team to widen the perspective, yielding in more relevant research and results.
Involvement of EE matters for multiple reasons and at different levels. Priorities change depending on whether the priorities of EE and experts by profession tend to differ. A vivid example is provided by Adebajo who reflected upon his experience of participating in two James Lind partnerships – first as a stroke patient and then as a medical professional [ 1 ]. He himself seemed surprised how his priorities differed in the two partnership settings. As a medical professional, he was favoring pathogenetic, diagnostic and treatment priorities. When he participated as a patient, however, he chose support and rehabilitation priorities instead – a pattern that has been observed before [ 1 ].
Another reason for the involvement of experts with lived experience (EE) in research is the empowerment and the potential reduction of stigma that comes through the process of being actively engaged in research. It should be noted that in research on personality disorders it is sometimes difficult to engage EE in the process for various reasons, among them the fear of speaking openly in public. Often, people with a personality disorder and their family members have experienced a long history of discrimination and have difficult treatment experiences within the mental health system (e.g., [ 34 ], for family members see [ 30 ]). This issue is reported across various professions (e.g. [ 26 ]) and is paralleled by the finding that mental health professionals often report rather pessimistic attitudes toward patients with personality disorders, who might still today be regarded as “the patients psychiatrists dislike” [ 28 ]. The process of being actively engaged in research could be an experience that is empowering and has the potential to reduce stigma.
In line with the experience of Adebajo [ 1 ], a first step to involve EE might be to collect research priorities from EE and their relatives. Thus, we set out to identify which research questions EE prioritize with the aim to create a starting ground for more collaborative research in the field of personality disorders. Here, we report on the outcomes of this initiative and complement with some additional comments that were raised during the subsequent discussion during the presidential debate of the 2022 ESSPD congress, where the findings were presented.
Aim of the study was to identify research questions of EE to create a starting point for more collaborative research in the field of personality disorders.
The research agenda was developed in two rounds. In the first round, we collected input from several Dutch and Belgian EE and family associations. These countries were chosen as the starting point, because originally the plan was to have the ESSPD congress in Antwerp, Belgium. EE and representatives of EE associations were asked what topics for research they considered to be the most important in the field of PDs and what specific research questions they would like to see addressed by the research field. Input was received in two ways: by sending out a survey to all major patient and family societies in Belgium and the Netherlands (in the field of PDs and broader) and by organizing a focus group with representatives of these societies. EE were encouraged to 1) formulate research topics and questions they considered to be of interest from their perspectives and 2) to argue why they found these topics and questions to be important to them. Based on their input, overarching themes were identified by two authors (J.H. and A.B.), including a large number of specific questions. The resulting proposal including research themes, their description, and their rationale were sent by email to the Belgian and Dutch participants to obtain agreement. In a second round, participants from various European countries provided additional comments and suggestions to this proposal, in different ways (i.e., some of them wrote extensive comments, others marked the various themes / questions in order or relevance). The input of these international participants was then added in the definitive proposal, with the goal to be as inclusive as possible in representing the perspective of people with lived experience across all Europe. No specific consensus scores were calculated.
Participants
Participants for the first round were recruited through Belgian and Dutch patient and family societies. We contacted them, explained our goal related to the upcoming conference and asked for their participation. Representatives from five societies were involved in the inventory, and most of them retrieved ideas from peer-EE within their societies. Participants for the second round were recruited through the ESSPD board. Board members reached out to EE societies or individual EE from various European countries, either personally or by asking colleagues in their professional networks to spread the notice of this initiative among EE they were in contact with. Both, individual consumers or carers/family members with lived/living experience and representatives of EE societies were invited to participate. This was accomplished by sending them an email detailing the background and scope of the initiative. Participants were asked to provide their ideas and feedback upon the input from the first round, indicate their priorities and suggest additional themes or edits / rephrase some research questions. Potential respondents were informed that this inventory represented a first effort to present the input and expertise of EE to the research community at the Opening Ceremony of the 2022 ESSPD Conference. In total, more than 30 persons with lived experience and relatives from nine European countries, including Belgium, Sweden, Denmark, Norway, Spain, Germany, Italy, the Netherlands and Switzerland, provided input for the research agenda. Overall, the idea of involving clients and relatives in research was very well received. Some respondents expressed their hope to continue this work.
In Table 1 questions as submitted by EE are listed. These questions were grouped into topics and summarized by professional experts (J.H. and B.R.).
The final consensus proposal consisted of five research topics for personality disorders that were considered most important by 30 EE:
Prevention, early detection and intervention
Recovery beyond symptom improvement
Involving relatives in treatment
Gender dysphoria
In the following, we will briefly summarize the reasons why each theme was considered important according to and approved by participants and which specific research questions arose (see Table 1 ). The first three themes were mentioned as the most important ones, in this order. In the discussion section of this paper, each theme is elaborated further.
Prevention and early detection and intervention
Almost all EE recognize that they or their affected family members were diagnosed and treated for their personality disorder at a late stage. Many EE live their daily lives for years with symptoms that severely impair their functioning. EE think that a delayed diagnosis conditioned their life and their decisions. Notably, many EE explicitly mention that they personally do not consider a personality disorder diagnosis stigmatizing (see also 5. Stigma). Rather, they report that receiving a diagnosis not only grants them access to appropriate care, but also provides an explanation about the way they feel, they deal with the world, and ultimately makes them feel less alone – “there are others like us”. Furthermore, calling the personality disorder “by its name” gives meaning to the suffering of the affected individuals, and lowers their feelings of inadequacy. EE also pointed out the need for the mental health system to communicate and to collaborate with other services, e.g., community services in order to facilitate early diagnosis (i.e., schools, GPs…). Regarding preventive measures, the question was raised: What protective elements in early development help a personality develop in a healthy way and can be delivered through schools, for example? For other specific research questions see Table 1 .
Research mainly evaluates whether treatments lead to an improvement of symptoms. For many EE, this does not necessarily imply that patients can actually participate in society (again). Many clients find it difficult to find a new meaning in life and a new identity after treatment. Thus, recovery and integration in social life (i.e., job, relationship) is vital from the perspective of both clients and their relatives. EE think that multiple factors affect recovery, and these factors need to be ascertained on an individual basis. They also think that full recovery implies that an individual is integrated into one’s own social environment, in accordance with his/her attitudes and dispositions. For specific research questions see Table 1 .
Potential benefits of involving relatives in treatment
Personality disorders have an impact on relationships. Family members and friends often find it difficult to assess what they should or should not do. The family/partner relationship can also be inhibitory to the client's recovery. EE have the impression that in many cases it could be positive for treatment if family members were more systematically involved in treatment. This is particularly true when the client him-/herself tends to avoid or reject care or repeatedly terminates treatment prematurely. In addition, there are several other forms of support besides professional care that could be helpful, e.g., self-help groups. For specific research questions on this topic see Table 1 .
This is a specific theme that recurred repeatedly among EE. Questions related to gender identity seem to have become much more common in recent years. It can be unclear whether the experienced gender dysphoria is part of the personality disorder, a comorbid disorder or unrelated. E.g., relatives have the impression that there is a link with autism, but possibly also with personality disorders. Moreover, it raises the question of what the risks or benefits of a medical course of transition might be. For specific research questions on this topic see Table 1 .
The statement of many clients that they personally do not consider a personality disorder diagnosis stigmatizing may be somewhat surprising because there is the assumption that a diagnosis of a personality disorder carries a strong societal stigma. This is particularly true for the diagnosis of borderline personality disorder (BPD). EE struggle with the pros and cons of offering openness about the diagnosis, for example to employers or to other medical doctors. They suggest that, ideally, longitudinal research evaluating the advantages of an early diagnosis in terms of access to and effectiveness of individual and family interventions could clarify whether this approach is superior to the potential harm conveyed by stigma. For specific research questions see Table 1 .
Our aim was to inform which research topics experts with lived experience (EE) regard as important for the field of personality disorders.
Before discussing the results in more depth, we wish to highlight how important it is that researchers and clinicians listen to the EE’s attitudes, preferences, and values and consider them in the research process. To illustrate the point: EE may have a different definition of recovery.
The emergence of early detection and intervention as a number one priority from the perspective of EE is remarkable in the light of a longstanding reluctance to diagnose personality disorders at an early stage [ 6 ]. Whereas most professionals used to delay the diagnosis [ 27 ], based upon a range of misconceptions [ 44 ], EE prioritize the need for early detection and intervention strategies in research. Early intervention approaches for PD, particularly borderline personality disorder (BPD), have been developed, with numerous programs now available for young individuals diagnosed with BPD [ 8 ] . Specifically, at least five early intervention programs have been established in Australia, The Netherlands, and Germany [ 7 , 19 , 22 , 24 , 43 ]. Additionally, programs in Norway and the UK predominantly focus on addressing self-harm behaviors [ 33 , 42 ]. Main critiques of existing literature highlight several key issues, hampering the integration of early intervention for PD within mainstream health services: 1) stigma and discrimination, 2) lack of trials prioritizing adaptive functioning as main outcome, 3) trials have not adequately included emerging adults with early-stage PD, and 4) the need to clarify the complexity of treatments like general community care (GCC) and enhanced usual care (EUC) what makes them efficient and role of individual therapy [ 8 ].
Interestingly, the issue of stigma was also raised by EE in the context of early detection and notably, EE favored research studying the advantages of early detection as opposed to potentially stigmatizing effects. Several EE spontaneously mentioned that they had faced stigmatizing and sometimes punitive reactions from caregivers and a lack of compassionate understanding due to their dysregulated behavior. An early diagnosis that is comprehensively explained [ 31 ] might disrupt trajectories of long-term impairment. Albeit this research is on the rise, there is still much to be done to explore how to best help adolescents with BPD. This emerging field of interventions for adolescents should continue. Research should address this longstanding reluctance by including patients’ perspectives, especially highlighting the advantages of an early diagnosis over those conveyed by potential stigma. According to the EE involved in this research, it may actually be more stigmatizing not to diagnose early. However, note that this issue is discussed very controversially in the field [ 17 ].
The second theme touches upon the core of what it means to recover from a personality disorder. For BPD, most psychotherapeutic treatment studies show promising results [ 45 ], but treatment effectiveness is often restricted to the improvement of symptoms of personality disorders. In a meta-analysis, Zahediabghari et al [ 49 ] summarize that specifically-designed psychotherapies for patients with BPD can improve psychosocial functioning more than unspecific psychotherapies.
However, EE point to the importance of social reintegration and discovering meaningfulness in life [ 36 ]. Several clients mentioned they had followed more than one personality disorder-oriented treatment, which had been very helpful, but who felt they were still struggling with full recovery and satisfactory inclusion in society. Some research is available on this topic and points in the same direction: In a qualitative study, Gillard, Turner & Neffgen [ 14 ] examined the understanding of recovery in the context of lived experience with personality disorders. The authors conclude that key facilitators of recovery were positive personal relationships and wider social interaction. Similarly, self-generated treatment goals by 102 patients with BPD showed that while patients value symptom improvement, 88 % also wanted better psychosocial functioning, including better social relationships and a job [ 34 ]. Patients with BPD also emphasize that personal recovery is represented by practical achievements in the “capacity to work and love”, as indicated by three key themes: 1) love of self and others, 2) making a contribution through work and study, 3) stability in daily life [ 16 ]. These results are comparable to those of qualitative studies focusing on work-related functioning (e.g., [ 29 , 35 ]).
The need for integrative care emerged as the central topic. From her lived experience, one of the participants recalled that not only psychotherapy helped her, but a whole network of people who supported and respected her. It was in the togetherness with others, she said, that she was able to be herself and to feel connected. Although BPD is associated with problems in social connectedness, it remains uncertain if these social challenges reciprocally worsen or trigger BPD symptoms. To clarify this potential bidirectional relationship, further longitudinal studies are necessary [ 10 ]. For further research, we recommend to include measures of recovery of psychosocial functioning next to symptom improvement in treatment outcome studies. Furthermore, the field might benefit from more insight into what “psychosocial (dys)function” means in personality disorders.
Regarding the third theme, a diagnosis of a personality disorder affects not only the individual, but also family members and others at school and at the workplace. The wider network could become a valuable resource for recovery if support and psycho-education about personality disorders are provided. Some psychoeducation programs for carers of patients with BPD have been found to be effective in improving their communication skills toward their affected family member, their psychological well-being and their knowledge of the disorder and in decreasing their subjective burden [ 15 , 20 , 21 , 38 , 39 ]. However, most research is focused on BPD only and evaluates the effects of psychoeducation on family members only. The focus of the research should also include evaluations to reveal if the training, psycho-education or involvement in treatment for family members has a measurable, beneficial impact on their loved ones. For clinical practices, one recommendation could be to include context-based and systemic interventions as part of treatment for personality disorders (e.g., family interventions). While this is usually done in treatment of youth with personality disorders (e.g. [ 42 ]), treatments for adults usually lack a systemic perspective and involvement of families. In the studies that did involve family members in treatment of adults, empirical evidence shows that this was beneficial (e.g. [ 37 ])
Recently, interventions for mothers with BPD to help them raise their children have been designed and are currently evaluated (e.g., [ 41 ]).
It was argued that within the professional field we should not only train specialists in the treatment of BPD but also focus on training generalists such as nurses and general practitioners to better recognize and support people with BPD. Fostering peer support programs might be another solution. Interventions that target the entire social system, including schools, work, family members and partners might be one road towards a future with less stigma and more integration.
The fourth topic, gender dysphoria , may especially reflect current societal changes in many European countries. Issues reflecting the association between personality disorders and gender dysphoria have not been researched enough yet. The lack of systematic research on gender identity and gender incongruence was also addressed in the recently published treatment guidelines for BPD in Germany [ 9 ]. The recommendation was to assess both BPD and gender issues,that both can be present at the same time and should be assessed carefully.
The topic, gender dysphoria, may also reflect an increased awareness of diversity and recognition of minorities. Regarding the relatives' impression that there is a also a possible link with autism and gender dysphoria, there is a lack of research integrating the three domains: autism, gender dysphoria, and personality disorders. According to Van der Miesen and colleagues [ 46 ] numerous hypotheses have been proposed to explain the connection between gender dysphoria and Autism Spectrum Disorder (ASD). However, the majority of these hypotheses are not well-supported by empirical evidence. Meta-analytical results indicate that ASD and GD may be associated, though further research is necessary to determine the magnitude of this relationship [ 25 ].
On the fifth theme, stigma, raised by EE, there is research available emphasizing the stigma associated with a personality disorder diagnosis (especially BPD). However, a question raised like “when to be open about the diagnosis and when not” is very difficult to answer in general, while at the same time, it may be a highly relevant question for the individual. This question is usually dealt with in individual treatment and of course, the answer depends on the individual situation. Van Schie and colleagues [ 47 ] designed a study where users of lived experience and careers provided use of language recommendations for researchers and clinicians with the aim to reduce stigmatization. Participants recommended five ways of reframing language that provides: (1) acceptance, (2) connection, (3) empowerment, (4) gratitude, (5) hope and (6) validation (for details see [ 40 ]).
Although the current study may provide interesting information on specific areas of interest from EE perspective, we want to clarify that initially, the survey was not intended as a scientific study. This initiative originated organically as part of the preparation for EE involvement in the ESSPD conference. It therefore lacks methodological rigor, e.g. the selection of participants was not systematically done, sociodemographic and/or diagnostic information that could characterize the sample of participants were not systematically collected and we did not use specific qualitative research methods for analyzing data. Participating EE came from different European countries, at this point one cannot generalize the results to other countries and cultures.
Involvement of EE in research raises various challenges. In their paper “Designed to Clash?” Beeker et al [ 4 ] provide an excellent insight into the process of conducting truly collaborative research reflecting on the practical, personal, and structural challenges of collaborative research. It has been stated that there is a fundamental conflict in PPI between the researchers' attempt to pursue a scientific career, and the often very personal and idealistic motives of EE to effect change in care [ 12 ]. In addition, professionals may have an implicit desire to maintain a dichotomy between EE and themselves to not be challenged by their own experiences with mental health problems [ 5 ]. The role of emotions is another dividing factor between EE and professionals . The ability to hold a neutral and objective perspective is seen as a goal and sign of maturity in the scientific community – and it is usually a privilege of those who are not personally involved and affected [ 23 ].
We compared the current list of topics in research on personality disorders to the list of the JLA with TOP 10 priorities for research on depression (2016, https://www.jla.nihr.ac.uk/priority-setting-partnerships/depression/top-10-priorities/ ). The JLA list includes questions like: What are the best early interventions for depression? And how early should they be used in order to result in the best patient outcomes? What is the impact on a child of having a parent with depression and can a parent prevent their child from also developing depression? What are the barriers and enablers for people accessing care/treatment when they are depressed, including when feeling suicidal, and how can these be addressed? Does depression impact employment? Interestingly, there is a strong overlap between these questions and the topics raised for personality disorders in this report.
Currently, there are some initiatives to foster collaboration between researchers, clinicians and EE. A more practical initiative in Switzerland, Austria and Germany is the EX-IN program [ 18 ]. The organization trains people with lived experience of mental illness/crisis to become qualified peer supporters in psychiatric settings. On a national level, participation of EE in research differs between countries and, to our knowledge, there are very few initiatives specifically for personality disorders.
Thus, there may be common themes from the perspective of EE with different mental disorders and their relatives. At the same time, initiatives by EE focusing on issues of personality disorders are still rare and may be needed at a national level.
Taken together, we derived five common themes – 1. prevention, early detection and intervention, 2. recovery beyond symptom improvement, 3. gender dysphoria, 4. involvement of relatives in treatment and 5. stigma-, considered to be important by EE and relatives for future research in the field of personality disorders. Of course, the field needs to continue hypotheses driven research. Ideally, from the very first steps, this research is already planned in a dialogue with EE. In our opinion, this report is an important first step to develop a future integrative research agenda, which can then be used to inform researchers, clinicians and experts with lived experience on how to improve PD research so that it matters for those who live with it. Furthermore, the initiative of the ESSPD led to the conclusion that the research field also needs to improve the communication of results to the public.
Availability of data and materials
Not applicable.
Adebajo A. Patients and healthcare professionals in priority setting partnerships: Two very different sides of the same coin. BMJ. 2022;378, o2310. Available from: https://doi.org/10.1136/bmj.o2310 .
Ball S, Harshfield A, Carpenter A, Bertscher A, Marjanovic S. Patient and public involvement in research. Enabling meaningful contributions. RAND Corporation; 2019. Available from: https://www.rand.org/pubs/research_reports/RR2678.html .
Barr KR, Jewell M, Townsend ML, et al. Living with personality disorder and seeking mental health treatment: Patients and family members reflect on their experiences. Bord Personal Disord Emot Dysregul. 2020;7:21. https://doi.org/10.1186/s40479-020-00136-4 .
Article Google Scholar
Beeker T, Glück RK, Ziegenhagen J, Göppert L, Jänchen P, Krispin H, Schwarz J, von Peter S. Designed to clash? Reflecting on the practical, personal, and structural challenges of collaborative research in psychiatry. Front Psychiatry. 2021;12:701312. https://doi.org/10.3389/fpsyt.2021.701312 .
Article PubMed PubMed Central Google Scholar
Cooke S, Daiches A, Hickey E. Narratives of experts by experience: The impact of delivering training in partnership on the subject of personality disorder. J Mental Health Train Educ Pract. 2015;10(4):234–44. https://doi.org/10.1108/JMHTEP-03-2015-0012 .
Chanen AM, McCutcheon LK. Personality disorder in adolescence: The diagnosis that dare not speak its name. Personal Mental Health. 2008;2(1):35–41. https://doi.org/10.1002/pmh.28 .
Chanen AM, McCutcheon L, Kerr IB: HYPE: a cognitive analytic therapy-based prevention and early intervention programme for borderline personality disorder. Handbook of Borderline Personality Disorder in Children and Adolescents. 2014:361-383.
Chanen AM, Thompson KN. Early intervention for personality disorder. Curr Opin Psychol. 2018;21:132–5.
Article PubMed Google Scholar
DGPPN e. V. (Hrsg.) für die Leitliniengruppe: S3-Leitlinie Borderline-Persönlichkeitsstörung. Version 1.0 vom 14.11.2022. https://register.awmf.org/de/leitlinien/detail/038-01 .
Di Bartolomeo, A. A., Siegel, A., Fulham, L., & Fitzpatrick, S. Borderline personality disorder and social connectedness: A systematic review. Personality Disorders: Theory, Research, and Treatment. Advance online publication. 2024. https://doi.org/10.1037/per0000665 .
Dziobek I, Lipinksi S. Partizipative Forschung in Klinischer Psychologie und Psychiatrie in Deutschland – Erreichtes, Gelebtes und ein Blick nach vorne (Participatory Research in Clinical Psychology and Psychiatry in Germany – Achievements, Implementation, and a Look to the Future). Psychiat Praxis. 2021;48:337–40. https://doi.org/10.1055/a-1614-0719 .
Faulkner A. Capturing the experiences of those involved in the TRUE project: A story of colliding worlds. Eastleigh: INVOLVE. 2004. Available from: https://www.invo.org.uk/resource-centre/library-resource/?id=145§ion=invonet .
Gillard S, Turner K, Neffgen M: How does who we are shape the knowledge we produce? Doing collaborative research about personality disorders. Policy Press. 2013. Available from: https://doi.org/10.1332/policypress/9781447307334.003.0005 .
Gillard S, Turner K, Neffgen M. Understanding recovery in the context of lived experience of personality disorders: A collaborative, qualitative research study. BMC Psychiatry. 2015;15:183. https://doi.org/10.1186/s12888-015-0572-0 .
Grenyer BFS, Bailey RC, Lewis KL, Matthias M, Garretty T, Bickerton A. A randomized controlled trial of group psychoeducation for carers of persons with Borderline Personality Disorder. J Pers Disord. 2019;33(2):214–28. https://doi.org/10.1521/pedi_2018_32_340 .
Grenyer BFS, Townsend ML, Lewis KL, Day N. To love and work: a longitudinal study of everyday factors in recovery from borderline personality disorder. Pers Mental Health. 2022;16(2):138–54. https://doi.org/10.1002/pmh.1547 .
Hartley S, Baker C, Birtwhistle M, Burgess JL, Chatburn E, Cobbaert L, Howley M, Huggett C, MacKenzie-Nash C, Newton A, Parry S, Smith J, Taylor CDJ, Taylor PJ, Timoclea R. Commentary: Bringing together lived experience, clinical and research expertise – a commentary on the May 2022 debate (should CAMH professionals be diagnosing personality disorder in adolescence?). Child Adolesc Mental Health. 2022;3:246–9. https://doi.org/10.1111/camh.12586 .
Hegedüs A, Burr C, Pfluger V, Sieg D, Nienaber A, Schulz M. Peer support worker training: results of the evaluation of the Experienced Involvement training programme in Switzerland and Germany. Int J Mental Health Nurs. 2020;30(2):451–60.
Hessels C, van Aken M. HYPE: helping young people early. Kind Adolesc Praktijk. 2014. https://doi.org/10.1007/s12454-014-0009-9 .
Hoffman PD, Fruzzetti AE. Advances in interventions for families with a relative with a personality disorder diagnosis. Curr Psychiatry Rep. 2007;9(1):68–73. https://doi.org/10.1007/s11920-007-0012-z .
Hoffman PD, Fruzzetti AE, Buteau E, Neiditch ER, Penney D, Bruce ML, Hellman F, Struening E. Family connections: a program for relatives of persons with borderline personality disorder. Fam Process. 2005;44(2):217–25. https://doi.org/10.1111/j.1545-5300.2005.00055.x .
Hutsebaut J, Feenstra D, Keur E. Scha¨ fer B, Bales D: Tijdig herkennen en behandelen van borderlineproblematiek bij jongeren met MBT-early. Tijdschrift Voor Psychotherapie. 2017;43:330–44.
Jones N, Cutler E. “The Angry Consumer”: Embracing Difficult Conversations. Mad in America. 2018. Available from: https://www.madinamerica.com/2018/07/angry-consumer-emotions/ .
Kaess M, Ghinea D, Fischer-Waldschmidt G, Resch F. The outpatient clinic for adolescent risk-taking and self-harm behaviors (AtR!Sk) – a pioneering approach of outpatient early detection and intervention of borderline personality disorder. Prax Kinderpsychol Kinderpsychiatr. 2017;66:404–22.
Kallitsounaki A, Williams DM. Autism spectrum disorder and gender dysphoria/incongruence. A systematic literature review and meta-analysis. J Autism Dev Disord. 2023;53(8):3103–17.
Lanfredi M, Elena Ridolfi M, Occhialini G, Pedrini L, Ferrari C, Lasalvia A, Gunderson JG, Black DW, Rossi R, Italian BPD Attitudes Study Group. Attitudes of Mental Health Staff Toward Patients With Borderline Personality Disorder: An Italian Cross-Sectional Multisite Study. J Pers Disord. 2021; 35(1):41-56. https://doi.org/10.1521/pedi_2019_33_421 . Epub 2019 Feb 20. PMID: 30785861.
Laurenssen EM, Hutsebaut J, Feenstra DJ, Van Busschbach JJ, Luyten P. Diagnosis of personality disorders in adolescents: a study among psychologists. Child Adolescent Psychiatr Mental Health. 2013;7:3. https://doi.org/10.1002/pmh.28 .
Lindell-Innes R, Phillips-Hughes AL, Bartsch D, Galletly C, Ludbrook C. Attitudes of psychiatry trainees towards patients with borderline personality disorder: Does the stigma begin during training? Pers Mental Health. 2023;17:387–95. https://doi.org/10.1002/pmh.1587 .
Larivière N, Couture E, Blackburn C, Carbonneau M, Lacombe C, Schinck SA, David P, St-Cyr-Tribble D. Recovery, as experienced by women with borderline personality disorder. Psychiatr Q. 2015;86:555–68. https://doi.org/10.1007/s11126-015-9350-x .
Lawn S, McMahon J. Experiences of family carers of people diagnosed with Borderline Personality Disorder. Psychiatr Mental Health Nurs. 2015;22:234–43. https://doi.org/10.1111/jpm.12193 .
Article CAS Google Scholar
Lester R, Prescott L, McCormack M, Sampson M. North West Boroughs Healthcare, NHS Foundation Trust. Service users’ experiences of receiving a diagnosis of borderline personality disorder: A systematic review. Pers Mental Health. 2020;14(3):263–83. https://doi.org/10.1002/pmh.1478 .
Lloyd K, White J. Democratizing clinical research. Nature. 2011;474(7351):277–8. https://doi.org/10.1038/474277a .
Article CAS PubMed Google Scholar
Mehlum L, Tørmoen AJ, Ramberg M, Haga E, Diep LM, Laberg S, Larsson BS, Stanley BH, Miller AL, Sund AM, Grøholt B. Dialectical behavior therapy for adolescents with repeated suicidal and self-harming behavior: a randomized trial. J Am Acad Child Adolesc Psychiatry. 2014;53:1082–91.
Ng FYY, Carter PE, Bourke ME, Grenyer BFS. What do individuals with Borderline Personality Disorder want from treatment? A study of self-generated treatment and recovery goals. Psychiatr Pract. 2019;25(2):148–55. https://doi.org/10.1097/PRA.0000000000000369 .
Ng FYY, Townsend, ML, Miller, CE, et al. The lived experience of recovery in borderline personality disorder: a qualitative study. Bord Personal Disord Emot Dysregul. 2019;6(10). https://doi.org/10.1186/s40479-019-0107-2 .
Ng FYY, Bourke ME, Grenyer BFS. Recovery from borderline personality disorder: a systematic review of the perspectives of consumers, clinicians family and carers. PLOS One. 2016;11(8):e0160515. https://doi.org/10.1371/journal.pone.0160515 .
Article CAS PubMed PubMed Central Google Scholar
Nguyen, B.A. T Evaluating the fficacy of the family connections program for family members of individuals with borderline personality disorder. Dissertation. 2020. https://rucore.libraries.rutgers.edu/rutgers-lib/64797/PDF/1/play/ .
Pearce J, Jovev M, Hulbert C, McKechnie B, McCutcheon L, Betts M, Chanen AM. Evaluation of a psychoeducational group intervention for family and friends of youth with borderline personality disorder. Bord Personal Disord Emot Dysregul. 2017;24:4(5). https://doi.org/10.1186/s40479-017-0056-6 .
Pitschel-Walz G, Spatzl A, Rentrop M. Psychoeducational groups for close relatives of patients with borderline personality disorder. Eur Arch Psychiatry Clin Neurosci. 2023;273(4):853–64. https://doi.org/10.1007/s00406-022-01395-8 .
Project Air Strategy for Personality Disorders. Talking about personality disorder [Fact Sheet]. Wollongong: University of Wollongong, Illawarra Health and Medical Research Institute. 2019. Available from: https://documents.uow.edu.au/content/groups/public/@web/@project-air/documents/doc/uow263246.pdf .
Rosenbach C, Heinrichs N, Kumsta R, Schneider S, Renneberg B. Study protocol for a multi-center RCT testing a group-based parenting intervention tailored to mothers with borderline personality disorder against a waiting control group (ProChild*-SP1). Trials. 2022;23:589. https://doi.org/10.1186/s13063-022-06531-2 .
Rossouw TI, Fonagy P. Mentalization-based treatment for self-harm in adolescents: A randomized controlled trial. Americ Acad Child Adolescent Psychiatr. 2012;51(12):1304–13. https://doi.org/10.1016/j.jaac.2012.09.018 .
Schuppert HM, Timmerman ME, Bloo J, van Gemert TG, Wiersema HM, Minderaa RB, Emmelkamp PMG, Nauta MH. Emotion regulation training for adolescents with borderline personality disorder traits: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry. 2012;51:1314-1323.e2.
Sharp C. Bridging the gap: The assessment and treatment of adolescent personality disorder in routine clinical care. Arch Dis Childhood. 2017;102(1):103–8. https://doi.org/10.1136/archdischild-2015-310072 .
Storebø OJ, Stoffers-Winterling JM, Völlm BA, Kongerslev MT, Mattivi JT, Jørgensen MS, Faltinsen E, Todorovac A, Sales CP, Callesen HE, Lieb K, Simonsen E. Psychological therapies for people with borderline personality disorder. Cochrane Database Syst Rev. 2020;5(5):CD012955. https://doi.org/10.1002/14651858.CD012955.pub2 .
Van der Miesen, A. I., Hurley, H., & De Vries, A. L. Gender dysphoria and autism spectrum disorder: A narrative review. Gender Dysphoria and Gender Incongruence, 2018: 82-92.
van Schie, C. C., Lewis,K., Barr, K. R., Jewell, M., Malcolmson, N., Townsend, M. L., & Grenyer, B. F. S. Borderline personality disorder and stigma: Lived experience perspectives on helpful and hurtful language. Pers Mental Health, 2024: 1–11. https://doi.org/10.1002/pmh.1609 .
Woodbridge J, Townsend ML, Reis SL, Grenyer BSF. Patient perspectives on non-response to psychotherapy for borderline personality disorder: A qualitative study. Bord Personal Disord Emot Dysregul. 2023;10:13. https://doi.org/10.1186/s40479-023-00219-y .
Zahediabghari S, Boursiquot P, Links P. Impact of Psychotherapy on Psychosocial Functioning in Borderline Personality Disorder Patients. Int J Environ Res Public Health. 2020;17(12):4610. https://doi.org/10.3390/ijerph17124610 .
Download references
Acknowledgements
The authors would like to acknowledge the contributions by the participants of the president’s discussion of the ESSPD Borderline congress in 2022.
Open Access funding enabled and organized by Projekt DEAL. The work was not funded.
Author information
Authors and affiliations.
Department of Clinical Psychology and Psychotherapy, Freie Universität Berlin, Habelschwerdter Allee 45, 14195, Berlin, Germany
Babette Renneberg & Julia Sieg
German Center for Mental Health (DZPG), partner site Berlin, Berlin, Germany
Babette Renneberg
Department of Medical and Clinical Psychology, Tilburg School of Social and Behavioral Sciences, Tilburg University, Tilburg, The Netherlands
Joost Hutsebaut
Scientific Initiative of Neuropsychiatric and Psychopharmacological Studies (SINAPS), University Psychiatric Centre Duffel, Duffel, Belgium
Ann Berens & Mariana Mendoza Alvarez
Collaborative Antwerp Psychiatric Research Institute, Universiteit Antwerp, Antwerp, Belgium
Department of Medicine and Surgery, Unit of Neuroscience, University of Parma, Parma, Italy
Chiara De Panfilis
Department of Psychology, Julius-Maximilians-Universität Würzburg, Würzburg, Germany
Katja Bertsch
Department of Psychiatry, Kanta-Häme Central Hospital, Wellbeing Services County of Kanta-Häme, Hämeenlinna, Finland
Andres Kaera
Department of Psychiatry, Institute of Psychotherapy and General Psychiatry Service, Université de Lausanne, Lausanne, Switzerland
Ueli Kramer
Department of Psychosomatic Medicine, Medical Faculty Mannheim, Central Institute of Mental Health, Heidelberg University, Heidelberg, Germany
Christian Schmahl
German Center for Mental Health (DZPG), partner site Mannheim, Mannheim, Germany
North Wales Clinical Psychology Programme, Bangor University, Bangor, Wales
Michaela Swales
Institute for Psychosocial Prevention, Ruprecht-Karls-Universität Heidelberg, Heidelberg, Germany
Svenja Taubner
Faculty of Medicine and Health Sciences, Collaborative Antwerp Psychiatric Research Institute (CAPRI), University of Antwerp, Antwerp, Belgium
Mariana Mendoza Alvarez
You can also search for this author in PubMed Google Scholar
Contributions
The board members of the ESSPD (BR, CdP, ST, KB, AK, UK, JH, MS, CS) planned and designed the study. JH and AB contacted and talked with a group of experts from the Netherlands and Belgium to generate a first list of research topics and questions. This list was extended by additional experts with lived experience from further European countries. CdP, JH and BR edited this list. BR wrote the first draft of the manuscript, JS and MMA helped with the literature and further editing of the manuscript. All authors reviewed and edited the manuscript before submission.
Corresponding author
Correspondence to Babette Renneberg .
Ethics declarations
Ethics approval and consent to participate.
Human Ethics and Consent to Participate declarations: not applicable.
Consent for publication
All authors agree to submit the paper in its current form to BPDED. Please note that individuals with lived experiences from different European countries participated voluntarily and contributed anonymously.
Consent for publication individual person’s data: n.a.
Competing interests
All authors declare to have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Renneberg, B., Hutsebaut, J., Berens, A. et al. Towards an informed research agenda for the field of personality disorders by experts with lived and living experience and researchers. bord personal disord emot dysregul 11 , 14 (2024). https://doi.org/10.1186/s40479-024-00257-0
Download citation
Received : 07 February 2024
Accepted : 17 June 2024
Published : 08 July 2024
DOI : https://doi.org/10.1186/s40479-024-00257-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Public and patient involvement
- Experts with lived experience
- Personality disorder
Borderline Personality Disorder and Emotion Dysregulation
ISSN: 2051-6673
- General enquiries: [email protected]
- Skip to primary navigation
- Skip to main content
- Skip to primary sidebar
information for practice
news, new scholarship & more from around the world
- gary.holden@nyu.edu
- @ Info4Practice
Towards an informed research agenda for the field of personality disorders by experts with lived and living experience and researchers
We describe a collection of themes for a research agenda for personality disorders that was originally formulated for the ESSPD Borderline Congress in 2022.
Read the full article ›
Personality Disorders: Types, Causes and Impacts Essay
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment
Introduction
Defining personality disorders, types of personality disorders, origins of personality disorders, impacts of personality disorders.
The personality of an individual influence how he acts and it influences his perception of self and others. While people have different personalities, there are some common behaviors and patterns of thinking that are typical in a healthy personality. People who display deviant personality traits, often characterized by dysfunctional thinking patterns and uncontrolled emotions, are considered to have personality disorders (PD).
Personality disorders affect about 10% of the American population. This considerably high prevalence rate is of great concern since personality disorders are a significant source of psychiatric morbidity (Sperry, 2013). The disorders also lead to functional impairment affecting the everyday life of the individual.
To help increase our understanding of personality disorders, this paper will discuss the various types of disorders. It will highlight the causes and impacts of these disorders and proceed to explain treatments for personality disorders.
Personality disorder is the term used to refer to several different subtypes of maladaptive personality traits as identified by the Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV). Stricker and Widiger (2003) assert that personality disorders arise when “personality traits are inflexible and maladaptive and cause significant functional impairment or subjective distress to the individual” (p. 149).
Community based studies of personality disorders reveal that the prevalence rates of personality disorders in the US is between 6 and 10% (Samuels, 2011).
Tyrer (2007) states, “”it is still impossible to conclude with confidence that personality disorders are, or are not, mental illness” (p.1524). The reason for this is that there is an ambiguity in the definition of what personality disorders and at the present, basic information about this condition is still insufficient.
The DSM-IV outlines some general diagnostic criterion that can be used to identify personality disorder. To begin with, a person with this disorder will have demonstrated enduring patterns of inner experience and behavior that is contrary to the socially acceptable behavior.
This pattern of deviant behavior is manifested in how the person perceives and interprets himself and other people, the appropriateness of emotional response, and impulse control (Perry, Presniak & Olson, 2013). This enduring pattern is inflexible and evident in a wide range of a person’s social and personal life. It eventually leads to distress or impairment in a person’s social and professional life.
Personality disorders are recognizable through certain measurable phenomena including surface traits such as impulsiveness, specific behaviors such as self-mutilation, beliefs or cognitions such as an exaggerated feeling of self-importance, and self-reported feelings such as feelings of emptiness (Perry, et al., 2013).
An important consideration with a personality disorder is that it occurs over a long duration of time. In most cases, the condition can be traced back to a person’s adolescence or early adulthood years.
Demographic investigations reveal that personality disorder is associated with younger age with prevalence in the 16 to 39-year-old age group (Fairfax, 2011). The prevalence of personality disorders is influenced by the socioeconomic status of a person with a bias against individuals from lower socioeconomic backgrounds.
Paranoid personality disorder (PPD) is a disorder whose primary characteristic is an all-pervasive distrust and suspiciousness of another individual. Stricker and Widiger (2003) state that the person with PPD will show a tendency to read malevolent intentions in innocent or neutral situations. This inflated suspiciousness will make it hard for the individual with PPD to get along with others.
A person with PPD is likely to be overly argumentative and hostile towards others. The person will blame others for his own inadequacies and difficulties in life. This makes it hard for the person to work collaborate or closely with others. Since the individual with PPD tends to be rigid, controlling, critical, and prejudicial, he is hard and unpleasant to work with. PPD generally tends to afflict more men than women (Stricker & Widiger, 2003)
Schizotypal Personality Disorder (SPD) is characterized by introvertedness and the person suffering from this disorder will appear cold and distant. Perry et al. (2013) note that SPD results in disordered thinking and autistic fantasies.
Persons with STPD demonstrate extreme social anxiety due to their paranoid fears. A striking physical attribute of a person with STPD is that he will appear odd, eccentric and with peculiar behavior. Due to the eccentricity and the tendency to misinterpret or over personalize events, the individual will have difficulty being understood by others. If the person has friends outside of his immediate family, they are very few.
People with STPD drift towards fringe groups that support their unusual ideas such as believing in telepathy and clairvoyance. Individuals with STPD often make use of social isolation as a coping strategy.
This strategy is adopted since the defects in the person’s cognitive-perceptual evaluation lead to discomfort within social situations and misperceptions (Stricker & Widiger, 2003). In extreme cases, STPD might lead to psychotic episodes and a small proportion of persons with STPD end up developing the Axis 1 psychotic disorder, schizophrenia.
Antisocial personality disorder (APD) is a personality disorder distinguished by patterns of behavior that show a high disregard and violation of the rights of other people. The individual with ASPD will have character traits such as deceitfulness, irresponsibility, irritability and predisposition to acts of criminality (Stricker & Widiger, 2003). ASPD patients are also exploitative and lack the ability to empathize with others.
This combined with the impulsivity demonstrated by ASPD patients, makes them prone to committing reckless actions without considering the safety of others. Tyrer (2007) documents that people with ASPD lack remorse even when they have inflicted unnecessary harm on other people.
ASPD has a higher prevalence in men and there is a correlation between this condition and substance abuse. It is also common among those from lower socioeconomic classes.
Borderline personality disorder (BPD) is characterized by a pattern of impulsiveness and high instability in interpersonal relationship and self-image. The severity and chronicity of this disorder’s symptoms make it especially detrimental. A person diagnosed with BPD will have frequent and intense negative emotion.
BPD patients are unsure of their self-image and they have doubts concerning their personal views and even those of others. People diagnosed with BPD have exaggerated fears of being abandoned (Kernberg & Yeomans, 2013).
They may have paranoid ideations and are prone to engaging self-defeating behavior such as substance abuse and making bad decisions that destroy good relationships. BPD predisposes the individual to suicidal ideations and behaviors. The risk of suicide is significantly higher with research indicating that 10% of patients with borderline personality disorder commit suicide (Kernberg & Yeomans, 2013).
In addition to this, BPD is associated with acting out, passive-aggressive behavior and dissociation. There is an overrepresentation of BPD in psychiatric settings, with studies approximating that around 20% of psychiatric patients suffer from this condition (Fairfax, 2011). BPD is more often diagnosed in women with a 75% diagnostic bias in favor of females.
Histrionic personality disorder (HPD) is typified by excessive emotionality and attention-seeking by an individual. The person diagnosed with HPD will engage in behavior that is meant to be provocative or inappropriately intimate. According to Benjamin (2002), the person’s actions will either be flirtatious of focused on physical attractiveness.
In addition to this, the individual will demonstrate superficial emotional expression and tend to be melodramatic.
The HPD patient has a pathological need to be loved and desired and will use any means to be involved with others on an intimate basis (Benjamin, 2002). In most cases, the individual will wrongfully assume that a relationship is more intimate than it actually is since the person has an innate desire for romantic fantasy.
Avoidant personality disorder (AVPD) has extreme timidity and inhibition as the major characteristic. The person with AVPD feels inadequate and demonstrates hypersensitivity in social situations. Livesley (2003) states that the individual diagnosed with AVPD will have a strong belief that he is inept and inferior to that.
This leads to a low self-esteem and social phobia. Due to the high level of sensitivity, the individual is likely to develop mood disorders and anxiety disorders. AVPD is one of the most prevalent personality disorders since timidity, social insecurity, and shyness is common in the clinical setting and the general population.
The final common personality disorder is Obsessive-compulsive personality disorder (OCPD), which is typified by a preoccupation with perfectionism and control. Individuals diagnosed with this condition tend to be rigid and they are preoccupied with rules and details (Livesley, 2003).
Other people view them as inflexible and they are often described as control freaks. Due to the need for perfectionism, persons with OCPD are reluctant to delegate tasks and are often indecisive.
There is a strong relationship between sexual abuse and personality disorders. According to Livesley (2003), upwards of 70% of patients with borderline personality have a history of abuse. A study of patients with borderline personality disorder revealed that about one-third of these patients reported severe abuse involving an incestuous perpetrator, severe sexual acts and high frequency or duration (Livesley, 2003).
While sexual abuse does not necessarily cause personality disorder, these statistics demonstrate that abuse increases the probability of psychopathology. Abusive acts contribute to the development of personality disorders since they invalidate the recipient by ignoring personal boundaries, needs, and by violating expectations of autonomy, and freedom of choice.
Low socioeconomic conditions also increase the likelihood that a person will develop a personality disorder. Samuels (2011) reveals that individuals who have dropped out of high school are more likely to suffer from personality disorders than their peers who completed school.
This relationship might be because economic impoverishment contributes to the development of antisocial traits and this increases the likelihood of personality disorders occurring.
There is considerable support from twin and family studies that genetics contribute to the development of personality disorders. The genetic disposition is partly because personality traits are inheritable and these traits play a significant role in personality disorders (Livesley, 2003).
Genetic disposition for lack of mood and impulse control might increase the probability of developing personality disorders such as BPD, ASPD and PPD.
Some personality disorders cause physical damage to the individual suffering from the condition. Personality disorders such as BPD are accompanied by self-destructive behaviors by the patient. Kernberg and Yeomans (2013) document that a major prognostic issue in severe personality disorders is the presence of para-suicidal tendencies. The patient will engage in self-harming behaviors and also exhibit chronic suicidal tendencies.
The patient will have many repetitive suicidal attempts that are engaged in when he is feeling frustrated or angry. The anger and frustration that lead to the suicide attempt often appear without any trigger or apparent cause. Kernberg and Yeomans (2013) warn that without highly specialized psychotherapeutic treatment, the patient will end up succeeding in killing himself.
As evident from the definition, personality disorders lead to impairment in the individual’s occupation. The social competence of the person is distorted because of personality disorders.
For example, people with ASPD are unlikely to maintain steady employment due to their deceitfulness, aggressiveness and general irresponsibility and lack of regard for others (Livesley, 2003). Those suffering from PPD are difficult to get along with and uncooperative, which makes them unsuited for most work environments.
Personality disorders increase the risk of a person developing a psychotic disorder. While the third revision of the DSM (DSM III) officially recognized personality disorders as being different from psychosis, the relationship between the two is close. Most people with STPD develop major depression that might degenerate into a psychotic condition.
BPD was traditionally considered as a threshold psychotic disorder due to its adverse impacts and while this classification was changed, there is an overrepresentation of BPD in psychiatric settings (Sjastad, Grawe & Egeland, 2012).
Personality disorders increase the health care expenditure of a person leading to financial burdens. Individuals with personality disorders require medical attention to manage the condition. Studies indicate that personality disorders are not transient and a person will not outgrow the disease (Perry et al., 2013).
If a person fails to seek medical help, the condition will impair his social and occupational performance or even worse, lead to psychotic conditions.
A major complication in the treatment of personality disorders is that there is no single established screening or assessment tools and mental health care professionals often have to rely on self-rated questionnaires for personality disorder and structured interviews with the patient. The third revision of the DSM clearly distinguished personality disorders from other psychiatric disorders (Tyrer, 2007).
The DSM III officially recognized personality disorders as being different from psychosis and neurosis since while the condition is characterized by a sense of weak identity, the capacity to test reality is still intact in the individual.
There is a prevalent of biases and fears regarding the diagnosis of personality disorder. Clients and therapists agree that a personality disorder diagnosis can be derogatory and result in the discrimination of the patient due to the stigma attached to this disorder (Fairfax, 2011). Many patients, as well as families, find it hard to accept a diagnosis of personality disorder.
This denial leads to a postponement in the time when adequate treatment can be offered. This exposes patients who have severe personality disorders to additional risks. This greatly impedes on the ability of the disorder to be cured since personality disorder patients do better when the diagnosis is named and described.
Kernberg and Yeomans (2013) assert that in the case of personality disorders, “adequate diagnosis is the first step to an effective treatment” (p.9). Most personality disorders are under-diagnosed or misdiagnosed and this has a negative impact on the patient since effective diagnosis is necessary for appropriate treatment to be offered.
Before the mid-1950s, personality disorders were considered untreatable and clinicians expressed a sense of dread and hopelessness while dealing with these disorders. However, this changed in the late 1990s when research enabled clinicians to utilize effective and successful treatments (Dignfelder, 2004).
Since then personality disorders, including the most difficult, which is borderline personality disorder, are increasingly treatable. Dignfelder (2004) states that while the various personality disorders manifest in varied ways, they are similar in that for the vast majority of cases, these mental illnesses require professional intervention in order for remittance to occur.
There are a number of unique psychotherapies that can be used to treat personality disorders. Cognitive-behavioral therapy helps the patient to identify maladaptive behaviors or beliefs and make the necessary changes, therefore, reducing the negative moods and anxiety symptoms prevalent in some forms of PD.
It can also. Cognitive-behavioral treatment can help patients who have chronic suicidal tendencies due to their personality disorders. By using integrative cognitive cognitive-behavioral treatment, health care professionals can help to manage the condition (Livesley, 2003).
The second type of psychotherapy is dialectical behavior therapy, which helps the patient develop a healthy sense of mindfulness. Using this therapy, the individual diagnosed with PD is taught how to be aware of the current situation and to gain greater control of his emotions (Samuels, 2011). This reduces the extreme emotions that result in irritability or self-destructive behaviors among PD patients.
The final type of psychotherapy is Schema-focused therapy and it tries to change the way the individual views himself (Samuels, 2011). Since some personality disorders are caused by a dysfunctional self-image, it is possible that helping people to view themselves differently can alleviate the condition.
Health care professionals prescribe medications to personality disorder patients. Research indicates that medication does not cure personality disorders but it helps to reduce the symptoms.
Anti-anxiety medication can be used to overcome the physical symptoms that personality disorder patients suffering from excess anxiety have (Livesley, 2003). Since personality disorders predispose the person to get depressed, antidepressants can be used to manage depressive moods. Mood stabilizers can be used to reduce symptoms of aggression in the personality disorder patient.
Sperry (2013) asserts that the effectiveness of treatment outcomes is largely a function of how well treatment is suited for the particular disorder and the overall functioning of the patient. Personality disorders are characterized by pervasive patterns in psychosocial and character on the one hand and deficiencies in biological and temperamental tendencies.
Effective treatment for these disorders must, therefore, take into consideration these two unique perspectives. There is no single treatment approach to personality disorders. Instead, a combined and integrative approach that uses the various forms of therapy and medication management should be used.
Personality disorders are a major problem that might impede on the life of an individual. This paper has discussed the various types of personality disorders and some of their possible causes. It was then revealed the impacts that these disorders have. It has noted that personality disorders lead to high costs in terms of health care services utilization and cause immense human suffering.
The paper has shown that personality disorders can be managed or treated using psychotherapy and medications for symptoms of the specific disorder. However, the paper has acknowledged that personality disorders are difficult to diagnose correctly. With proper diagnosis, a patient can be treated successfully and this will enable him to live a normal life without the disabling personality disorder.
Benjamin, S.L. (2002). Interpersonal Diagnosis and Treatment of Personality Disorders. NJ: Guilford Press.
Dignfelder, S.F. (2004). Treatment for the ‘Untreatable’. Monitor Staff , 35(3), 46-47.
Fairfax , H. (2011). Re-conceiving personality disorders: Adaptations on a dimension? Counselling Psychology Quarterly , 24 (4), 313–322.
Kernberg, O., Yeomans, F.E. (2013). Borderline personality disorder, bipolar disorder, depression, attention deficit/hyperactivity disorder, and narcissistic personality disorder: Practical differential diagnosis. Bulletin of the Menninger Clinic . 77 (1), 1-22.
Livesley, J. (2003). Practical management of personality disorder . NJ: Guilford Press.
Perry, J.C., Presniak, M.D., & Olson, T. (2013). Defense Mechanisms in Schizotypal, Borderline, Antisocial, and Narcissistic Personality Disorders. Psychiatry, 76(1), 32-52.
Samuels, J. (2011). Personality disorders: Epidemiology and public health issues. International Review of Psychiatry , 23 (1), 223–233.
Sjastad, H.N. Grawe, R.W., & Egeland, J. (2012). Affective Disorders among Patients with Borderline Personality Disorder. PLoS ONE 7(12), 1-7.
Sperry, L. (2013). Handbook of Diagnosis and Treatment of DSM-IV Personality Disorders. NY: Routledge.
Stricker, G., & Widiger, T. (2003). Clinical Psychology . NY: John Wiley & Sons.
Tyrer, P. (2007). Personality diatheses: A superior explanation than disorder. Psychological Medicine , 37, 1521–1525.
- Anxiety Disorders: Definition, Causes, Impacts and Treatment
- Metacognition and Neuropsychology
- Borderline Personality Disorder
- Antisocial Personality Disorders in Women
- PPD Firm Organizational Culture
- Growth & Development: 5 to 12 Years
- Scaring Us Senseless
- Relationship Between Sleep and Depression in Adolescence
- Bullying and Suicide: The Correlation Between Bullying and Suicide
- Importance of Sense Organs
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2019, July 8). Personality Disorders: Types, Causes and Impacts. https://ivypanda.com/essays/personality-disorders/
"Personality Disorders: Types, Causes and Impacts." IvyPanda , 8 July 2019, ivypanda.com/essays/personality-disorders/.
IvyPanda . (2019) 'Personality Disorders: Types, Causes and Impacts'. 8 July.
IvyPanda . 2019. "Personality Disorders: Types, Causes and Impacts." July 8, 2019. https://ivypanda.com/essays/personality-disorders/.
1. IvyPanda . "Personality Disorders: Types, Causes and Impacts." July 8, 2019. https://ivypanda.com/essays/personality-disorders/.
Bibliography
IvyPanda . "Personality Disorders: Types, Causes and Impacts." July 8, 2019. https://ivypanda.com/essays/personality-disorders/.
Borderline Personality Disorder Research Paper

View borderline personality disorder research paper example. Browse psychology research paper topics for more inspiration. If you need a thorough research paper written according to all the academic standards, you can always turn to our experienced writers for help. This is how your paper can get an A! Feel free to contact our writing service for professional assistance. We offer high-quality assignments for reasonable rates.
Borderline personality disorder is a term that identifies a heterogenous group of patients with serious character pathology and behavioral disturbances. The main features of this disorder are behavior that is impulsive, dramatic, and often self-destructive; moods that are labile and reactive to life circumstances; interpersonal relationships that are stormy; and a sense of self-identity that is fragile and contradictory.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% off with 24start discount code, i. historical development of the concept of borderline personality disorder.
II. Borderline Personality Disorder Core Symptoms and Character Styles
III. Demographic and Data-Based Studies of Borderline Personality Disorder
Iv. etiology and relationship to other disorders, a. psychoanalytic hypotheses, b. bpd as an affective spectrum disorder, c. bpd as posttraumatic stress disorder secondary to childhood sexual and physical abuse, d. bpd as an impulse spectrum disorder, v. course of borderline personality disorder, vi. treatment of bpd.
More than one decade after the development and publication of DSM-III, borderline personality disorder (BPD) remains the most controversial category in the nomenclature. Disagreement persists regarding the term itself, the particular diagnostic criteria established for BPD by DSM-III and DSM-IV, the scope of applicability, and the extent of overlap with Axis I and other Axis II disorders. Ultimately, this degree and intensity of dispute reflect both the range of difficulties in identifying and working with those persons designated as borderline, as well as the more basic question of validity: whether the BPD construct describes a meaningful unitary syndrome that corresponds to an actually existing state of affairs. While this latter question can certainly be asked of any of the personality (Axis II) disorders, something about the borderline concept seems to have engendered the strongest controversy.
At least one major reason for the ongoing disputes is the fact that the very concept of borderline was born out of attempts to explain the clinical observation that certain patients seemed to do very poorly in psychodynamic psychotherapy. Thus, from the very first, this category was used to describe a disparate group of patients who had two things in common: they responded to psychotherapy by developing transient psychotic symptoms and they did not meet classical definitions of schizophrenia. It is not that they did not necessarily improve; many obsessional patients, for example, did not improve with psychotherapy. Rather, it is that these patients worsened in psychotherapy with a fairly specific pattern of acting out that showed up most dramatically in the development of severe transference problems. The difficulty confronting the predominantly psychoanalytic theoreticians and skilled therapists was how to fathom the nature of these patients who gave promise of being good psychotherapeutic cases, yet deteriorated during the course of a psychotherapy. Thus, the very origins of the borderline concept arose in the context of a clinical puzzle.
The solution to the puzzle, keeping in mind that American psychiatry held a much more encompassing concept of schizophrenia in the 1940s and 1950s than at present, was to conceptualize these patients who became worse in psychotherapy as having a schizophrenic core underlying the neurotic facade. This notion was given concrete expression in a paper by Hoch and Polatin in 1949 describing the new category of pseudoneurotic schizophrenia. The construct fit neatly into a psychoanalytic model that postulated a spectrum of psychopathology based upon increasing primitiveness of defense mechanisms, extending in an unbroken chain from mild neurotics at one end to deteriorated schizophrenics at the other. The pseudoneurotic patient served as the missing link, bridging neurosis and psychosis, and thus serving as visible proof of the continuity connecting mild and severe psychiatric disorders.
The problem with the pseudoneurotic schizophrenia construct was that the patients did not go on to develop the more classical symptoms of hallucinations and delusions nor the deteriorating course that is the usual outcome of schizophrenia. Nevertheless, the observation that there existed a group of patients who appeared neurotic, but worsened with intensive psychotherapy, was a valid finding that outlived the misleading label attached to it. The focus of what might be wrong with these difficult-to-treat patients shifted away from schizophrenia to consideration of severe character pathology, described as borderline states by Knight in 1953 and as the psychotic character by Frosch in 1964. In addition, the joint U.S.-U.K. diagnostic studies carried out in the mid-to-late 1960s demonstrated convincingly that many patients diagnosed as schizophrenic by American psychiatrists fit much better with manic-depressive and personality disorder symptoms and outcome. This diagnostic realignment tightened the diagnostic criteria for schizophrenia, thereby further emphasizing the differences between borderline conditions and schizophrenia.
In 1968, Grinker and colleagues published the results of their study of 58 hospitalized patients who fell into a broadly defined notion of borderline syndrome. These patients had difficulties in interpersonal relationships, transient losses of reality testing under stress, angry and depressive affects, and deficient self-identities. Cluster analyses of the data, primarily of measurements of ego functions, produced four major clusters. There was a “core” borderline group, two groups defined as bordering upon the psychoses and neuroses, and a fourth group embodying certain “as-if” features, most notably absence of a core self-identity. Grinker’s study, the first to utilize psychometric instruments and statistical analyses, moved the borderline concept away from the realm of schizophrenic spectrum disorders and provided the basis for future empirical studies that continued the attempt to define the still vague borderline syndrome.
It is instructive that in the next series of studies carried out by Gunderson and Singer in 1975, the primary diagnostic concern was still to demonstrate that borderlines were different than schizophrenics. At the same time that empirical studies were focusing on narrowing the construct of borderline, Kernberg developed a broader notion of borderline, based upon a fusion of ego psychology and object relations theory, to designate a form of personality organization that was characterized by the use of primitive ego defenses (denial, splitting, projective identification), intact reality testing (with transient regressions under stress), and identity diffusion. Kernberg’s construct of borderline personality organization includes the milder as well as the more severe forms of character pathology, and, in essence, encompasses most of the patients presently grouped under the Cluster B (dramatic, unstable)personality disorders: histrionic, narcissistic, borderline, and antisocial.
This was the state of affairs while the DSM-IV committee developed inclusion and exclusion criteria for the personality disorders. There were four competing and overlapping concepts of borderline, and the final result represented some degree of compromise between the various groups. Since ideological and economic considerations, in addition to empirical studies and clinical lore, influenced the final product, it is important to define these considerations in some detail. The four overlapping concepts of borderline were as follows: (1) A residual model based upon the schizophrenic spectrum concept, using the term borderline to designate those persons, usually relatives of schizophrenics, who displayed odd, eccentric thinking and schizoid interpersonal relationships; this group was given the term schizotypal personality disorder. (2) An affective disorder model, which considered BPD as an affective spectrum illness displaying prominent features of mood instability with a predominance of depression, anger, and preoccupations with suicide. (3) An empirically derived model based primarily on the research of Gunderson, with diagnostic symptoms placed into five major groupings: impulse/action patterns (including self-destructive behaviors); ego-dystonic, transient psychotic episodes; mood instability with primarily negative affects; disturbed but intense interpersonal relationships; and an unstable sense of self. (4) A psychoanalytic concept based primarily on the work of Kernberg, but encompassing theoretical formulations by Mahler relating to difficulties in the separation/individuation phase of child development.
The final configuration of BPD adopted was most influenced by Gunderson’s work, but nevertheless showed the strains inherent in a compromise between points of view that are ideologically very divergent. The results were the creation of several new personality disorders within Axis II, not based upon empirical studies, but with each reflecting to some extent components that were once loosely connected to the borderline concept. Essentially, in dividing the broad territory of the borderline syndrome, as this concept evolved during a 40-year span, the cognitive disturbances that had long been noticed were placed in the schizotypal personality disorder, the milder dramatic and attention-seeking traits were placed into the histrionic personality disorder, self-centeredness and entitlement became the core of the narcissistic personality disorder, and the affective symptoms of mood instability and negative affectivity (depression, anger, anxiety), along with impulsivity, were given prominence in the borderline personality disorder.
Borderline personality disorder was defined by DSM-III-R as a condition marked by a pervasive pattern of instability of mood, interpersonal relationships, and self-image, beginning by early adulthood and present in a variety of contexts, as indicated by at least five of the following:
- A pattern of unstable and intense interpersonal relationships characterized by alternating between extremes of overidealization and devaluation.
- Impulsiveness in at least two areas that are potentially self-damaging, e.g., spending, sex, substance use, shoplifting, reckless driving, binge eating.
- Affective instability: marked shifts from baseline mood to depression, irritability, or anxiety, usually lasting a few hours and only rarely more than a few days.
- Inappropriate, intense anger or lack of control of anger, e.g., frequent displays of temper, constant anger, physical fights.
- Recurrent suicidal threats, gestures, or behavior, or self-mutilating behavior.
- Marked and persistent identity disturbance manifested by uncertainty about at least two of the following: self-image, sexual orientation, long-term goals or career choice, type of friends desired, preferred values.
- Chronic feeling of emptiness or boredom.
- Frantic efforts to avoid real or imagined abandonment.
The revision of DSM-III-R into DSM-IV was completed by late 1993. Although the BPD construct did not undergo any major alterations, several changes were instituted which served to correct the overemphasis in DSM-III on the close relationship between BPD and the affective disorders and the omission of cognitive deficits. Criterion 3 (Criterion 6 in DSM-IV), which outlined the affective symptoms seen in BPD was changed to reflect reactivity of mood; this serves to emphasize the difference between the mood disturbances seen in BPD and the relatively situationindependent mood disturbances characteristic of the endogenous affective disorders (major depression and manic-depressive illnesses). Complementing this more accurate delineation of the type of mood disorder seen in BPD was the inclusion of a new criterion to reflect the specific cognitive disturbances of BPD. The DSM-IV calls for a ninth criterion as follows: Transient stress-related paranoid ideation or severe dissociative symptoms. There were a few additional changes to the original eight criteria, but these are relatively minor, either reflecting grammatical alterations in the interest of clarity or the result of low sensitivity/specificity ratings for a few items on further field testing. Thus, the description of the identity disturbance in Criterion 6 was reworded and the construct “boredom” was dropped from Criterion 7.
II. Borderline Personality Disorder Core Symptoms and Character Style
The clinical description of a psychiatric disorder does not correspond exactly to that disorder’s diagnostic criteria in DSM-III. The main reason for this is that a clinical description needs to be a full and rich portrayal of the condition under question, whereas the requirements for diagnostic criteria are vastly different. Diagnostic criteria must aim for those characteristics of an illness that capture a few of its core symptoms while avoiding overlap with neighboring conditions. For example, as indicated above, while boredom may very well be a characteristic mental state in BPD, it was also found in histrionic and narcissistic personality disorders and therefore was of little specific diagnostic value. It did not help discriminate between BPD and other Cluster B personality disorders. In addition, diagnostic criteria must have acceptable validity and reliability. The issue of validity of psychiatric disorders, especially of personality disorders, is a troublesome one, since there are not external validators. The construction of DSM-III had paid major attention, some would say excessively so, to reliability issues. For example, certain factors that most workers would agree are characteristic of a disorder, such as the psychological defense of splitting in BPD, were not included in the diagnostic criteria because of a preference for behavioral rather than psychological phenomena, presumably because assessment of behaviors permits greater agreement as to whether they are present or not as compared to psychological constructs.
As indicated at the beginning of this research paper, there remains considerable controversy about the core characteristics and boundaries of BPD. Workers in the field have tended to bring to the evaluation of BPD their own theoretical and clinical perspectives in the evaluation of borderlines. In addition, some of the core characteristics of BPD, such as an increase in dissociative phenomena, appear to be changing in the past decade, a possibility that raises the question of the cultural influences and even faddish quality of some of the symptoms.
Most workers would agree that BPD is a relatively severe personality disorder, seen primarily in young adults, that presents with a characteristic cognitive style, mood disturbances, problematic interpersonal relationships, negative and deficient sense of self, and a variety of dramatic and impulsive behaviors usually of a self-injurious nature. These diagnostic features represent points distributed on a continuum of personality traits with somewhat arbitrary use of social norms to determine cut-off scores separating normal from pathological. Because of this, some workers in the field have advocated use of a dimensional rather than categorical model for the personality disorders, but a categorical model has always been adopted because it is easier to use in clinical work.
The cognitive style seen in borderline individuals encompasses three overlapping features. First, borderlines tend to have altered states of consciousness; these are usually referred to as dissociative states, and vary in intensity, density, and duration. They run the gamut from brief periods of self-absorption to fugue states lasting hours. The person may be partially or fully amnestic for some of the dissociative episodes. Second, borderlines tend to split their universe into good and bad, black and white. They have difficulty conceptualizing a person, including themselves, or an event, as encompassing positive and negative features. They tend to swing between the opposite poles of idealization and devaluation in their affections toward others. Third, borderlines tend to have impressionistic and global rather than precise and focused perceptions. They tend to be intolerant of unpleasant thoughts and images and to interrupt these processes with impulsive action, dissociation, and drug and alcohol use. There is a tendency toward imprecision and exaggeration, with a loss of salient detail. All of these disturbances are increased under conditions of stress.
The affective disturbances are characteristically mood instability or lability. Mood is typically reactive to environmental circumstances, but this must be taken to include the borderline’s own thought processes too. Negative affects, such as sadness, anger, and anxiety predominate the emotional landscape, but too literal adherence to this description would belie the positive affects and interpersonal warmth that borderlines can exhibit.
Problematic interpersonal relationships are a hallmark of borderlines. Their relationships are characteristically intense, stormy, and conflictual. Dependency needs, power struggles, and the idealization/devaluation swings described earlier tend to complicate most meaningful relationships. Victimization and entitlement themes in which the borderline alternates between being exploited by others and demanding reparations from others for damages incurred are frequent patterns seen in this disorder.
Borderline individuals tend to have a deficient sense of self, and what enduring image of themselves they may have is usually negative. A deficient sense of self refers to the absence of a stable sense of core identity, of knowing who you are. A certain degree of this is expected in adolescents and young adults in Western culture, but the borderline problem with identity, by definition, must go beyond the norm for this age group. Borderlines will take on different roles and personality characteristics, depending upon the dominant features of the group they are associating with. This has been referred to as the “as-if” personality, first described by Helene Deutsch in 1942. When not caught up in a persuasive group identity, borderlines tend to have very negative notions about themselves, ranging from dislike to contemptuous loathing.
Finally, borderlines characteristically are dramatic and impulsive in their actions. The patterns of impulsivity include directly self-injurious behaviors as well as an assortment of either ill-considered or risk-taking behaviors that also may be seen as self-destructive. Alcohol and drug abuse, bulimic eating disorders, promiscuity, and attraction to predatory partners are among the impusive actions seen in borderlines. As with the other core features of borderlines, the self-injurious behaviors range from infrequent and mild delicate cutting of the wrists to deep cutting of the limbs, torso, and genitals, as well as occasional ingenious use of cigarettes, lighters, caustic solutions, and hot irons to burn themselves. Suicide threats and attempts are also hallmarks of borderlines, most frequently but not exclusively with prescription as well as nonprescription medication overdoses. There are many more threats and gestures than serious attempts, leading to the use of the term “para-suicide” to describe these provocative actions of borderlines, but often the differentiation between manipulative and serious attempts is not at all clear.
There are no accurate measures of the prevalence of BPD in the community. Most estimates range from 0.5 to 1%, but may go higher as a broader concept of borderline, such as that used by Kernberg, is applied. The prevalence of the disorder in clinical settings is influenced by the type of clinical population under consideration. An average across studies indicates that the general prevalence of BPD is 10-15%, in inpatient settings about 20%, among outpatients with a personality disorder 30-35%, and among inpatients with a personality disorder 60-65%. Prevalence figures alone may be deceptive; it is possible that borderlines in an inpatient setting may have little similarity to outpatients who have never needed hospitalization. In most studies, excepting those done in VA and prison settings, 60-75 % of BPD are women.
Although DSM-III diagnostic rules do not permit differential weighting of the different criteria, most studies have demonstrated that several items contribute disproportionately to diagnostic efficiency. The presence of two, or at most three, specific criteria (impulsivity, unstable-intense interpersonal relationships, and self-injurious behaviors) predict most strongly the diagnosis of BPD, although once again, the type of clinical setting (inpatient or outpatient) will influence this finding.
There is considerable overlap (20-60%) between BPD and the other personality disorders, especially those of Cluster B, as well as schizotypal and dependent personality disorders. This finding continues to raise the question of whether personality disorders are discrete entities truly different from each other or reflect points on a continuum of serious character pathology. There are several Axis I disorders that have substantial overlap with BPD. These are alcohol and substance abuse disorders, bulimia, and the mood disorders, primarily dysthymia and major depression. To some extent, this finding reflects overlapping criteria (e.g., substance abuse is listed as a criterion for BPD), the heterogeneity of the BPD concept, and the fact that traits such as impulsivity and mood lability do express themselves in a wide array of behaviors.
Since it appears that BPD is not a unitary disorder, and since diagnostic threshold can be met in a polythetic system by fulfilling any five of eight (or nine, under DSM-IV) criteria, it is highly unlikely that a unitary etiology will be found for this or other Cluster B personality disorders. Theories about the etiology of BPD tend to follow major trends of interest in the behavioral sciences in general. Thus, the predominance of psychoanalytic constructs as explanatory hypotheses of human health and illness has given way to a variety of biological-genetic models in the past decade. Even the recent robust correlations between childhood sexual abuse and adult BPD symptoms are increasingly explained more in terms of long-lasting neurophysiological alterations of stress-response systems rather than in terms of psychodynamic mechanisms. The major theories of the etiology of BPD are as follow:
- Psychoanalytic model of stage-specific difficulties
- Deficit model (Masterson; Adler)
- Conflict model (Kernberg)
- BPD as an affective spectrum model
- BPD as post-traumatic stress disorder secondary to childhood sexual and physical abuse
- BPD as an impulse spectrum disorder
Based upon Mahler’s theories of the importance of successful resolution of the rapprochment subphase of the separation/individuation processes in toddlerhood (ages 15-30 months), several overlapping psychodynamic hypotheses were advanced to explain those BPD features that were thought to represent the consequences of rapprochment failure. These features were the mental operation and defense of splitting, identity diffusion, and deficiencies in object constancy and object relationships. Differences of opinion and emphasis exist between various psychodynamic theories: Masterson has suggested that the mother of the borderline is herself borderline and establishes emotionally impossible conditions for the toddler to achieve age-appropriate separation and individuation, thereby resulting in the development of a borderline personality in the child. Adler has emphasized the borderline child’s inability, under circumstances similar to those described by Masterson, to form internalized soothing, holding introjects, such that the borderline child (and adult) lacks basic ego functions such as frustration tolerance, stable self-object relationships, and methods for calming itself during periods of stress. Kernberg has postulated the likelihood of an excessive aggressive drive in the infant that interferes with the fusion of sexual and aggressive drives; Kernberg’s model therefore sees borderline pathogenesis as the result of a complex interaction between infant and caregiver rather than as unilaterally caused by a “not-good-enough” mother.
The basic problem with the psychoanalytic hypotheses regarding etiology of BPD is shared by psychodynamic explanations of behavior in general: first, difficulty in operationalizing and thereby in testing various theories and second, a lack of specificity whereby certain postulated mechanisms at best appear to be general risk factors (e.g., parental psychopathology) rather than the specific and inevitable cause of a particular outcome. This latter problem, of course, applies to all unitary theories of etiology. Finally, the nature of the psychodynamic hypotheses are such that supportive evidence comes primarily from retrospective rather than prospective studies, and from individual case studies in which the investigator testing the hypothesis is also the therapist commited to the hypothesis.
The observation that borderline patients are frequently depressed, and the prominence of mood instability in the symptom picture, have led to the hypothesis that an affective disorder underlies the borderline condition. Attempts to validate this hypothesis examined a variety of biological markers, familial patterns, follow-up data, and pharmacological responses. The initial findings, varying somewhat from study to study, were that from 20 to 60% of borderline patients met diagnostic criteria for an affective disorder, usually major depressive episode. This was not particularly surprising since the diagnostic criteria for BPD were slanted toward affective type symptoms. The studies have shown that patients with depression and borderline patients who were concurrently depressed resembled each other in regard to several biological markers of depression, such as the dexamethasone suppression test, REM latency time, and thyroid stimulating hormone response to thyrotropin, but the resemblances fell away with “pure” borderline patients, i.e., borderline patients who were not depressed.
Similar results were found in the family pedigrees of borderline patients. Borderline patients with concurrent depressions had a greater prevalence of relatives with affective disorders. However, this finding is true for most of the Axis II disorders, namely, that there is a higher prevalence of depressed persons in the families of patients with any personality disorder and depression. On the other hand, borderline patients without depression tend to have increased familial linkages to other disorders, namely, borderline and antisocial personality disorders, and alcoholism and drug abuse. Studies of pharmacological efficacy with borderlines have demonstrated minimal benefit from antidepressants, even with depressed borderlines, except for some amelioration of depressive symptoms. Lithium therapy has not proven valuable in treating BPD. There have been some indications that monoamine oxidase inhibitors are effective in reducing core borderline symptoms, thereby supporting the atypical depression model of BPD, but these findings have never been sufficiently replicated to be more than suggestive. Finally, the long-term follow-up studies have shown that most borderline patients do not go on to develop depressive syndromes, again arguing against a causal linkage between BPD and affective disorders.
Despite the fairly clear evidence that BPD is not a variant of affective disorders, most studies do show that a certain percentage of borderline patients have a recurrent affective disorder (either depressive or bipolar type II, i.e., depressions and hypomanias) and evolve into a typical affective disorder pattern after the dramatic borderline symptoms recede in the 30s. Thus, it seems likely that a subclass of borderlines has a primary affective disturbance.
There has been an increasing awareness of the frequency of childhood sexual abuse in the life history of many psychiatric patients. This awareness has paralleled a growing public consciousness of domestic violence of many types. The question remains unresolved as to whether child abuse and other forms of violence have indeed become more common recently, reaching epidemic proportions, or whether the social taboos that maintained silence over such assaults have been lifted, with the result of greater case-finding and reporting of such episodes. Among psychiatric patients, rates of childhood sexual abuse range between 25 and 80%, depending on the population surveyed and the survey methods. Surveys from such varied locations as state hospitals, community hospitals, outpatient clinics, and emergency rooms have been consistent in these findings. Reported rates are highest for borderline personality disorder, in the order of 50-80%. In the borderline population, there also appears to be a correlation between severity of certain types of symptoms, such as self-injurious behaviors and dissociative episodes, and the severity of the childhood sexual abuse experiences, as judged by age of first abuse, frequency and duration of abuse, degree of force and violence employed, and absence of ameliorative factors in the life of the child. The correlations between abuse and borderline symptomatology have been robust enough to lead several workers to hypothesize that most patients who have been diagnosed BPD are really suffering from PTSD and that this latter diagnosis makes better scientific and social sense, removing the stigma that has been attached to a BPD label. The case is strengthened by the logic of borderline symptoms, such as dissociation, as a learned response of the abused child to the horrors of the abuse experience, a response that was once adaptive, but has now become generalized as a response to all emotional flooding. In a similar way, self-injurious behavior seems to make sense as an expression of the self-hatred that the abuse victim directs inwardly.
There are several obvious problems to the linear causal chain that links childhood abuse to borderline symptomatology. The major problems relate to specificity between abuse and outcome. Patients with many psychiatric diagnoses, as well as many persons who do not have psychiatric symptoms have histories of childhood sexual abuse. Only a percentage of abused persons develop the BPD or PTSD picture. Conversely, not everyone with BPD has a history of childhood abuse. In addition, the abused child was most likely raised in a chaotic home with many other disturbing features, such that it is not valid to single out the experience of sexual abuse as the cause of adult problems. There are also considerable methodological problems related to the very sensitive nature of the topic and the fact that most of the research and clinical work are based upon retrospective reports of abuse in childhood. The methodological problems slice both ways; there are persons who have been abused and who deny it, and there are patients who may distort, exaggerate or invent abuse histories. There is no easy resolution to these issues, but, in general, the detailed reports by patients about their abuse appear to have credibility and are accepted by most researchers and health care workers. The particular diagnostic question discussed here about the overlap of BPD and PTSD, however, is less an issue of data than definition of causal relationships in human behavior. Thus, it appears that childhood sexual abuse and the disturbed environment in which the abuse occurred function as general risk factors predisposing to increased severity of many types of psychiatric and physical illnesses. Within the BPD population, there does appear to be a large subgroup whose symptoms and personality styles were profoundly affected by the experiences of childhood sexual abuse and whose symptoms can be understood as a form of PTSD. It needs to be kept in mind that PTSD is still a fairly vague concept encompassing many types of traumas and responses, and that most persons suffering from PTSD do not show borderline symptoms.
Although it sounds tautological to say that a syndrome characterized by impulsivity may be an impulse spectrum disorder, more is implied in the statement than meets the eye. Essentially, such a hypothesis raises the question of whether there is a group of disorders that share some common features in addition to impulsivity, such as familial linkage, associated psychiatric disorders, and underlying neurophysiological mechanisms. Family studies have shown an increased rate of alcoholism, substance abuse, and antisocial personality in the relatives of borderline personality. Other disorders considered related to problems with impulsivity include compulsive gambling, bulimia, intermittent explosive disorder, and the other Axis II personality disorders within Cluster B (histrionic and narcissistic). Studies are presently under way to investigate serotonergic and dopaminergic mechanisms that may have some linkage to impulsive behaviors.
It is well recognized that the notion of “impulsivity” is very vague, such that the various conditions being considered as impulse disorders may turn out to have very little in common beyond surface appearances. Conceptual clarification concerning what the terms “impulsive” and “compulsive” mean, and how these relate to the notion of “addiction,” will be necessary if the hypothesis regarding impulse spectrum disorder is to be of any practical use.
The initial delineation of borderlines as encompassing a group of difficult treatment cases combined with the finding of a poor outcome on short-term follow-up led to a fairly pessimistic outlook for patients with this diagnosis. Patients who were diagnosed in their late teens or early 20s as borderline were still doing poorly 2 to 5 years later, with ongoing self-injurious behavior and suicide attempts leading to multiple hospitalizations. It was not until the late 1980s that follow-up studies covered the 10- to 20-year period after initial hospitalization. Surprisingly, the outcome was much more favorable than the early studies indicated. In several independent studies from different parts of the country, it became clear that between 50 and 60% of BPD patients were doing fairly well as they moved into their 30s. Another 30-40% of patients showed varying levels of disability. Suicide rates ranged from 8 to 15 % on 10-year follow-up. The largest follow-up series of patients was reported by Stone, who traced 502 of 550 patients (of whom 193 met DSM-III criteria for BPD) who had been hospitalized on an intensive long-term psychotherapy ward at New York State Psychiatric Institute during the years 1963-1976. As judged by Global Outcome Scores (GAS), 63% of the BPD patients were in the good to recovered categories, another 16% had made a fair adjustment, 12% were doing poorly, and 9% suicided. Less favorable outcome was correlated with the presence of major affective disorder, antisocial personality, and a pattern of alcohol and drug abuse. Poor outcome was not correlated with self-mutilative behaviors in the early years of the illness. Patients with a history of childhood neglect or sexual abuse tended to do less well than patients without these histories. Finally, there was not a good overall correlation between outcome and psychiatric treatment; some patients with very good outcomes had minimal treatment following index hospitalization and some patients with extensive treatment had poor outcomes. It is possible that averaging the outcome data washes out a treatment effect, but this remains to be demonstrated.
Three has been as much controversy about the treatment of BPD as there has been about the diagnosis. To a large extent and with some overlap, treatment modalities have tended to follow etiological hypotheses. As one might expect with a condition that drew its initial delineation from a group of difficult-to-treat patients, no single modality has yet demonstrated clear-cut superiority or even effectiveness. Studies designed to evaluate treatment of BPD have been plagued by the usual problems of therapy outcome research: differing characteristics of the patient population, despite use of DSM-III criteria; difficulty in determining what constitutes evidence of improvement; difficulty in establishing control groups.
Psychodynamic psychotherapy has been the standard and accepted form of treatment of BPD, despite the many problems that arise in this form of treatment. In a sense, the BPD population, comprising primarily young verbal adults who are dysfunctional but nonpsychotic, have appeared to be the obvious if not ideal candidates for psychotherapy. Close to 50% of psychotherapy patients seen in private practice and at most outpatient clinics will have a diagnosis of BPD or a related Axis II Cluster B (narcissistic or histrionic) disorder. While there has been no canon defining a specific therapeutic protocol for BPD (or any other disorder), the work of Kernberg has been most influential in guiding the theory and practice of psychotherapy with borderlines. The therapy has tended to be a mix of supportive and exploratory work, with special attention paid to avoiding becoming enmeshed in ill-advised rescue attempts and other acting out features that are the hallmarks of borderline patients. The outcome results of the Menninger psychotherapy project reported by Wallerstein and Stone’s follow-up study suggest that it is impossible to predict, from patient characteristics alone, which patients would benefit most from supportive and which from exploratory psychotherapy, nor is there evidence that ultimate outcome is better with exploratory than supportive psychotherapy. A single study by Stevenson and Meares employing a 12-month psychotherapy regimen that utilized a written protocol based upon self-psychology demonstrated significant improvements across a broad range of measurements. Patients served as their own controls (pre- and post-treatment measures); a separate control group of patients was not used.
There has been increasing interest in cognitive-behavioral treatment (CBT) modalities for BPD. The essence of these modalities is a focus on recognizing and eliminating the factors that reinforce self-injurious behaviors, and learning and practicing new behaviors that will enhance the quality of life of the patient. Therapy is not directed toward underlying psychodynamic causes, since the assumption of CBT is that self-injurious behavior is a learned behavior that has become relatively independent of the specific causes that originally inspired it. CBT is done individually and in groups. Techniques that are taught and practiced include behavioral skill training, contingency management, cognitive restructuring, exposure to emotional cues, distress tolerance, interpersonal skills, and emotional regulation. Linehan and colleagues reported significant improvement in self-injurious and parasuicidal behaviors in a group of SIB borderlines in CBT compared to a group receiving treatment as usual. The improvements were not accompanied by changes in severity of reported depression, suicidal ideation, or reasons for living.
The relationship of BPD to PTSD in those borderlines who experienced sexual abuse in childhood suggests that a PTSD-oriented treatment program should be helpful. To date, this has not been the case, most likely because no overall effective program for the treatment of PTSD has been demonstrated. The treatment of PTSD usually includes group therapy, desensitization techniques, and pharmacological agents. There has been a proliferation of incest and sexual abuse treatment groups, some of which seem to be very helpful and some of which have a deleterious effect on some group members. No controlled studies have been reported. Pharmacological treatment of PTSD is in its infancy; different medications have been reported to be effective with particular components of PTSD, especially the sleep disturbance and depressions that accompany PTSD, but no agents appear to interrupt the flashbacks and intrusive imagery that form the hallmark of this disorder.
The pharmacological treatment of PBD is widely used, but relatively disappointing. Tricyclic antidepressants are effective only in alleviating depressive symptoms in those borderlines who are also depressed. Monoamine oxidase inhibitors have been reported to reduce the target symptom of rejection-sensitive dysphoria, but a controlled study is still wanting. There have not been controlled studies of the efficacy of the specific serotonin reuptake blockers to date. Lithium has not appeared to be of special benefit. There are mixed reports on the benzodiazepine anti-anxiety agents; there may be some benefit to the anti-anxiety properties, but several studies have reported a worsening of impulsive behaviors in BPDs taking these agents. In addition, long-term use of benzodiazepines would not be indicated in patients with significant alcohol or drug abuse histories. The single class of medications that has demonstrated significant short-term effectiveness in several key borderline symptoms has been low-dose anti-psychotics, but here the benefits must be weighed against the serious long-term side effects of these agents. A study of Soloff and associates in 1993 failed to replicate the positive findings of their earlier study reporting improvement in borderline patients with the use of antipsychotic medications.
There has been a recent trend away from long hospitalizations for borderline patients. While much of the driving force toward brief hospitalizations in all medical fields has been concern about rising medical costs, there has also been growing awareness of the deleterious rather than helpful effect of prolonged hospitalization of borderlines. Although there are undoubtedly some patients who benefit from a controlled hospital environment that prevents major self-destructiveness, the general experience has been that borderline patients continue their self-injurious behaviors in the hospital. This behavior sets up major conflicts with staff regarding proper responses to patients who challenge staff to prevent them from hurting themselves. Placing patients on one-to-one or constant observation has seemed to encourage rather than discourage self-injurious acts. The broad, but not unanimous consensus recently is that hospitalizations should be kept as brief as possible within the boundaries of responsible patient care, with the option of brief rehospitalizations seen as preferable to lengthy hospital stays.
Bibliography:
- Druck, A. (1989). “Four Therapeutic Approaches to the Borderline Patient.” Jason Aronson, Northvale, NJ.
- Gunderson, J. G. (1984). “Borderline Personality Disorder.” American Psychiatric Press, Washington, DC.
- Herman, J. L. (1992). “Trauma and Recovery.” Basic Books, New York.
- Kernberg, O. (1984). “Severe Personality Disorders.” Yale University Press, New Haven, CT.
- Kroll, J. (1988). “The Challenge of the Borderline Patient.” WW Norton, New York.
- Kroll, J. (1993). “PTSD/Borderlines in Therapy: Finding the Balance,” Norton, New York.
- Linehan, M. M., Armstrong, H. E., Suarez, A., Allmon, D., and Heard, H. L. (1991 ). Cognitive-behavioral treatment of chronically parasuicidal borderline patients. Arch. Gen. Psychiatry 48, 1060-1064.
- Links, P. S. (1990). “Family Environment and Borderline Personality Disorder.” American Psychiatric Press, Washington, DC.
- Paris, J. (1992). “Borderline Personality Disorder: Etiology and Treatment.” American Psychiatric Press, Washington, DC.
- Soloff, P. H., Cornelius, J., George, A., Nathan, S., Perel, J. M., and Ulrich, R. F. (1993). Efficacy of phenelzine and haloperidol in borderline personality disorder. Arch. Gen. Psychiatry 50, 377-385.
- Stevenson, J., and Meares, R. (1992). An outcome study of psychotherapy for patients with borderline personality disorder. Am. J. Psychiatry 149, 358-362.
- Stone, M. (1990). “The Fate of Borderline Patients.” Guilford, New York.
- Wallerstein, R. S. (1986). “Forty-Two Lives in Treatment.” Guilford, New York.
ORDER HIGH QUALITY CUSTOM PAPER

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- World Psychiatry
- v.9(1); 2010 Feb
Personality disorder: a new global perspective
Peter tyrer.
1 WPA Section on Personality Disorders
2 Department of Psychological Medicine, Imperial College, London
ROGER MULDER
3 Department of Psychological Medicine, University of Otago, Christchurch, New Zealand
MIKE CRAWFORD
Giles newton-howes.
4 Hawkes Bay District Health Board, New Zealand
ERIK SIMONSEN
5 Institute of Personality Theory and Psychopathology (IPTP), Roskilde, Denmark
DAVID NDETEI
6 University of Nairobi, Kenya
NESTOR KOLDOBSKY
7 National University, La Plata, Argentina
ANDREA FOSSATI
8 San Raffaele Hospital, Milan, Italy
JOSEPH MBATIA
9 Ministry of Health, Dar es Salaam, Tanzania
BARBARA BARRETT
10 Centre for Economics of Mental Health, London
Personality disorder is now being accepted as an important condition in mainstream psychiatry across the world. Although it often remains unrecognized in ordinary practice, research studies have shown it is common, creates considerable morbidity, is associated with high costs to services and to society, and interferes, usually negatively, with progress in the treatment of other mental disorders. We now have evidence that personality disorder, as currently classified, affects around 6% of the world population, and the differences between countries show no consistent variation. We are also getting increasing evidence that some treatments, mainly psychological, are of value in this group of disorders. What is now needed is a new classification that is of greater value to clinicians, and the WPA Section on Personality Disorders is currently undertaking this task.
In the last 50 years, personality disorder has achieved a level of understanding and, indeed, respectability that now allows it to be considered as an equal partner with other mental disorders. Before the 1960s, personality disorder, with the possible exception of the antisocial group, was considered an unreliable and imprecise diagnosis with little or no clinical value. Since then, however, and particularly since the introduction of DSM-III in 1980, there has been increasing recognition that personality disorder, despite many imperfections in its classification, can be described and rated reliably. Personality disorder has been shown to have an important influence on the outcome of other mental disorders when present as a comorbid condition, and it may benefit from specific treatment. This article discusses these findings from a global perspective, as this has particular relevance to low-income countries in which personality disorder has until recently been seldom studied.
EPIDEMIOLOGY
Although national morbidity studies of mental illness have now become more frequent in developed countries, they do not often record personality disorder. One of the main reasons for this is the difficulty in conducting assessments of personality disorder, especially with lay interviewers. As a consequence, there are only a handful of such studies of the literature 1 - 3 . However, with the increasing use of short screening assessments for personality disorder 4 , 5 , it is possible to conduct such assessments with lay inter-viewers and provide valuable data.
Three major studies of the epidemiology of personality disorder have now been published in the last five years. The results are summarized in Table 1. By far the largest of these studies was conducted across 10 different countries, including six low- or middle-income countries. This study is particularly significant because it demonstrates that personality disorders are no less prevalent outside Europe, North America and Australia, where all previous data have been collected. The study is also important because it shows that problems in social functioning among people with personality disorder are clinically significant, even when the impact of other comorbid mental health problems has been controlled for 6 .
HOW COMORBID PERSONALITY DISORDER INFLUENCES OTHER MENTAL DISORDERS
As the identification of personality pathology has become increasingly robust, it has become possible to turn our attention to how this group of disorders affect other mental disorders, such as affective and psychotic disorders, more commonly identified and treated within mental health settings. Although the community prevalence of personality disorder appears to range from 3 to 10%, it is, as would be expected, much higher in secondary care settings 8 , 9 . As such, it would be expected to impact on psychopathology, outcome and service provision. The research undertaken to date, although limited in a similar fashion to the epidemiological data, would broadly support this view.
The best studied association is between depressive disorders and personality status. More than 60 studies have looked at the correlation between personality disorder and depression and, when combined using a meta-analytic approach, they confirm that people with a personality disorder are approximately twice as likely not to recover from a depressive episode as those with no personality disorder (unpublished data). This data is very similar to initial findings of poorer outcome in depression when personality pathology is present 10 . Studies do not make it clear whether this poorer outcome is due to the lack of treatments directed at the personality pathology or if personality disorder acts as a diathesis in these conditions 11 .
The findings in psychotic mental illness are far less clear. This field of research is less well developed and even the prevalence of personality pathology ranges from 4.5 to 100%. This huge variation appears to be related to the country of the study, the care provided and the tools used to measure personality 12 . It is not clear that personality measures in psychosis are reliable 13 . Outcomes in this group are also poorly studied 14 , although there are peripheral indicators that personality disorder in this group often shows itself in terms of violence 15 , crime 16 , and hospital readmission 17 .
Other research has examined the interactions of personality pathology and major mental illness within community and secondary care settings. This also supports the probability of poorer outcomes in personality disordered patients who are, by and large, treated for affective and psychotic disorders. Two-year outcomes in an Australian cohort showed the personality facet of neuroticism to be one of the few correlates predictive of poor outcome in those with mental illnesses 18 . Cross-sectional data has also suggested personality disorder, particularly its severity, to be associated with both higher social needs and greater social dysfunction in patients in a secondary care setting in England 19 .
Studies such as these suggest that personality dysfunction has a negative effect on function and outcome, but remains relatively undertreated. Why is this? The answer to this question is potentially multifaceted, although clinicians’ attitudes toward this difficult to manage group are important. For more than two decades, there has been the suggestion that mental health clinicians do not like patients with personality disorders 20 , and recent evidence suggests that clinicians perceive patients with personality disorders as more difficult, despite the objective evidence failing to support such a view 21 . These attitudes may adversely affect delivery of health care provision and as such make it more difficult for patients with personality disorder and comorbid mental disorders to access and receive appropriate management for either disorder.
It therefore appears that people with personality disorder and comorbid personality disorder have poorer outcomes, function less well in society and are stigmatized by clinicians in secondary services, reducing the odds they will receive optimum care. This is a combination which is potentially expensive when considering the delivery of health and social care services.
COST OF PERSONALITY DISORDER
As part of a recent report on the economic burden of mental health problems in England, the King’s Fund estimated the health and social care service costs of all people with personality disorder who are in contact with their general practitioners at £704 million per year 22 . When productivity losses were included, the cost rose to £7.9 billion per year. Soeteman et al 23 used a similar approach to calculate the cost of personality disorder by using data from health and social care contacts for people attending specialist personality disorder services. They calculated the total burden of personality disorder in the Netherlands to be £11,126 per patient.
These studies can be considered a useful starting point, but they do not provide an estimate of the total economic burden of personality disorder, because both of them used information on people who were in contact with services. Whilst service attenders provide useful opportunistic samples for research purposes, they are not representative of the personality disorder population as a whole. Indeed, we know that many of those with personality disorder are unknown to services 24 , reject treatment rather than seek it 25 , or are in contact with services but have a different primary diagnosis 26 . Thus, to date, the true cost of personality disorder remains unknown, but it is certainly substantial, falling to many service providing sectors (health, social services, criminal justice) as well as to the economy more widely (inability to work and premature death).
EVIDENCE OF TREATMENT EFFECTIVENESS
Most of the research conducted into the treatment of personality disorder has focused on those with borderline personality disorder. Systematic reviews of previously published randomized trials have concluded that too few studies have been conducted to draw clear conclusions about the treatment of this form of personality disorder, but they have highlighted the limited, if any, impact of pharmacological treatments and the promising, if still unclear, benefits of complex psychosocial interventions such as dialectical behaviour therapy 27 , 28 .
The treatment of people with borderline personality disorder has also been reviewed as part of the development of national guidelines. Following the publication of the American Psychiatric Association’s guidelines in 2001 29 (29), the National Institute for Clinical Excellence in England (NICE) published new treatment guidelines for borderline and antisocial personality disorder 30 , 31 . The evidence base led to three main conclusions: a) psychotropic drugs are of no proven value in the long term in these personality disorders, and their adverse effects normally preclude their use except for short periods and in crisis; b) if other treatments (mainly psychological) are to be given, they need to be administered using a structured team approach for borderline personality disorder and using cognitive therapeutic approaches (particularly group management) in antisocial personality disorder; c) in antisocial personality disorder, interventions that reward are better than those that punish.
Information on which to base treatment discussions for people with other forms of personality disorder is even more scant. Recent trials by Svartberg et al 32 and Emmelkamp et al 33 are noteworthy because they examined the impact of psychological treatments among people with cluster C personality disorders. Findings from these two trials disagree, with Emmelkamp et al demonstrating greater improvement among those offered 20 sessions of cognitive therapy compared to psychodynamic psychotherapy, while Svartberg et al found similar treatment outcomes among those receiving these two interventions.
For other forms of personality disorder in which the patients are treatment resisting (Type R) (i.e., they do not want their personalities to change), as opposed to treatment seeking (Type S) 25 , it may be better to try and adapt the environment to the personality and this can be done systematically in the form of nidotherapy 34 , 35 . This has received support in a recent randomized trial 36 .
Most of the putative successful treatments for personality disorder are time consuming and resource intensive, and need to be buttressed by a good theoretical base and therapeutic commitment. These conclusions match those of an expert panel on the management of people with personality disorder 37 , which also suggested that there is no “quick fix” in the treatment of these disorders, and that in most countries the resources are not likely to be available to treat them in this way.
While research for treatment of personality disorder that goes beyond the previous focus on borderline personality disorder is to be welcomed, findings from other studies show that in clinical practice people offered treatment usually meet diagnostic criteria for several categories of personality disorders 38 , 39 . Such findings add weight to the case for reclassifying personality disorder to ensure that the system used has clinical utility.
NEED FOR A NEW CLASSIFICATION
If we accept the epidemiological figures, 3-10% of the adult inhabitants in the countries of the world have a personality disorder. However, only a minority of these (probably one in 20) has a severe personality disorder 40 and it is the people in this group who cause the most disruption to services and to society.
For the most severe personality disorders, the existing classification is unhelpful. It takes no account of severity and it generates the frequent comorbidity of several personality disorders across different clusters 41 , as well as the frequent use of the term “personality disorder not otherwise specified”, which, when often used more than any specific personality category, is a mark of dissatisfaction with the existing classification 42 .
The WPA Section on Personality Disorders is currently examining new ways of classifying personality disorder in ICD-11. As well as making suggestions over the classification of severity discussed above, the Section is considering revising the descriptions of the major personality disorder groupings. These would be fewer, overlap less and, we hope, possess greater clinical utility.
There is surprising consistency over the number and descriptions of the main dimensions of personality disorder in studies carried out with both psychiatric patients and normal populations. Three or four dimensions are uniformly reported 43 , 44 , 45 , 46 , in addition to the well-known five-factor model 47 that has been suggested for the core descriptions of DSM-V personality disorders 48 .
The first dimension is an externalizing potentially aggressive and hostile factor that incorporates borderline, antisocial, narcissistic, histrionic (cluster B in DSM-IV) and often paranoid personality disorder traits. Some studies report a separation of a factor incorporating callousness, lack of remorse and criminal behaviour (psychopathy), while others find a single broad factor. The second dimension is generally an internalizing factor consisting of neurotic, inhibited and avoidant, incorporating anxious, behaviour. This was once called asthenia, but is now best summarized as avoidant and dependent personality disorder traits (part of cluster C) in DSM-IV. The third dimension comprises schizoid symptoms: introversion and social indifference, aloofness and restricted expression of affect. In some studies these characteristics overlap with eccentric and odd behaviour and/or paranoid personality disorder symptoms, and an additional factor, peculiarity, has been suggested to make up a six-factor model 49 . The fourth factor comprises obsessionality, compulsivity and perfectionism and, although these are currently part of the cluster C grouping, the empirical data suggests they can be separated. In some studies this forms part of the internalizing factor, but most investigations report that obsessive compulsive personality disorder symptoms split off as a coherent and relatively independent set of behaviours.
While there is currently little evidence to support the validity of these factors, they almost certainly provide a better description of the range of personality abnormality than the current classifications. They can also be adapted to a developmental perspective that will allow personality disturbance to be identified long before the current cut-off age of 18 that is intrinsic to both DSM-IV and ICD-10 50 . Their importance will rest on whether they provide a more useful framework for organizing and explaining the complexity of clinical experience in personality disorders as well as predicting outcome and guiding decisions about treatment 51 . A new classification that does not improve clinical utility will be a failed classification.
There seems little to lose. A recent survey reported that three quarters of personality disorder experts thought the current DSM-IV system should be replaced 42 . Using four (or possibly more) overlapping factors seems preferable to continuing to act as though the ten current personality disorders are separate, when they have repeatedly been found not to be.
The next step will be to derive better structured clinical interviews that address these factors well, and this should generate competent research which can explore whether knowledge about aetiology, prognosis and treatment is enhanced by using the new classification.
The DSM-IV polythetic diagnoses describe poorly specified psychopathology and so it is natural that they fail to identify criteria that could correspond to the “core features” of each personality disorder diagnosis. The lack of clearly identified core features and a “vote-counting” approach to personality disorder diagnosis (i.e., list the number of symptoms that were met by a given subject, see if it is greater than a usually arbitrary cut-off value, and then make the diagnosis) prevented clinicians from making differential diagnoses within the axis II classification. The legacy is a diagnostic system that dissatisfies both the researcher and the clinician, being neither simple, accurate or useful. Thus, although it has promoted a huge, but widely scattered, amount of research on the aetiology, psychopathology, course and treatment of personality disorders, there are now good reasons to consider the DSM-IV approach completely out of date.
The WPA Section on Personality Disorders is currently considering revising the descriptions of the major personality disorder groupings in a way that not only makes good clinical sense but also enables separation from other disorders with which they are frequently confused, such as attention-deficit/hyperactivity disorder (ADHD) 52 . It will not be an easy task, and in reaching our conclusions we hope to have empirical evidence from as many field trials as possible, not just in highly developed countries, as a robust classification should travel well 53 , and to use these data rather than relying on the uncertain support of consensus committee opinion, as previous classifications have unfortunately been forced to do.
Table 1 Study methods and prevalence of personality disorder from recently published epidemiological studies
| Author, year (ref.) | Country | Method | Prevalence (%) | Screening instrument |
| Huang et al, 2009 (6) | Western Europe (WE), Colombia (C), | Household surveys Multiple imputation used to | WE: 2.4 | 33-item screening questions |
| Lebanon (L), | predict personality disorder | C: 7.9 | from the International | |
| Mexico (M), | scores using a three part | L: 6.2 | Personality Disorder | |
| Nigeria (N), | simulation procedure. Rates of | M: 6.1 | Examination (IPDE) | |
| People’s Republic of China (PRC), | personality disorder calculated as means of multiple | N: 2.7 | ||
| South Africa (SA), | imputation prevalence | PRC: 4.1 | ||
| United States (US) | estimates (n=21,162) | SA: 6.8 | ||
| US: 7.6 | ||||
| Coid et al, 2006 (3) | England, Wales, Scotland | Survey of a stratified sample | 4.4 | Screening questionnaire of |
| of 15,000 households (n=628) | SCID–II | |||
| Grant et al, 2004 (7) | United States of America | Random sample | 14.8 | Alcohol Use Disorder and |
| (National Epidemiologic Survey on Alcohol and | Associated Disabilities | |||
| Related Conditions) | Interview Schedule, DSM-IV | |||
| (n=43,093) | Version |
Home — Essay Samples — Law, Crime & Punishment — Jeffrey Dahmer — Borderline Personality Disorder: The Case of Jeffrey Dahmer
Borderline Personality Disorder: The Case of Jeffrey Dahmer
- Categories: Jeffrey Dahmer
About this sample

Words: 528 |
Published: Aug 1, 2024
Words: 528 | Page: 1 | 3 min read
Table of contents
The complexities of borderline personality disorder, the case of jeffrey dahmer, implications and further exploration.

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Verified writer
- Expert in: Law, Crime & Punishment

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
2 pages / 972 words
1 pages / 1647 words
4 pages / 1624 words
1 pages / 1357 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Jeffrey Dahmer
Jeffrey Dahmer, often referred to as the "Milwaukee Cannibal," is a name that strikes fear and disgust in the hearts of many. His gruesome crimes, which included the murder and dismemberment of 17 young men and boys, have [...]
When discussing infamous serial killers, two names that often come to mind are Ted Bundy and Jeffrey Dahmer. These two individuals have left a dark mark on history with their heinous crimes, but they also possess distinct [...]
Jeffrey Dahmer, also known as the Milwaukee Cannibal, was a notorious serial killer who committed heinous acts of murder and necrophilia. His influence on the practice of necrophilia is a chilling and disturbing topic that has [...]
Rule, A. (2019). The Stranger Beside Me: The Shocking Inside Story of Serial Killer Ted Bundy. Planet Ann Rule.Masters, B., & Masters, J. (1993). The Shrine of Jeffrey Dahmer. Hodder & Stoughton.Michaud, S., & Aynesworth, H. [...]
This essay explores the intricate aftermath of Dahmer's crimes, delving into the legal intricacies of his trial, the broad social and cultural impacts, and how his case influenced law enforcement, media portrayal of serial [...]
The name Jeffrey Dahmer sends shivers down the spines of those familiar with the horrors he committed. A notorious serial killer, Dahmer is remembered for the gruesome murders of seventeen young men and boys. However, beneath [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Health Topics
- Brochures and Fact Sheets
- Help for Mental Illnesses
- Clinical Trials
Substance Use and Co-Occurring Mental Disorders
What does it mean to have substance use and co-occurring mental disorders.
Substance use disorder (SUD) is a treatable mental disorder that affects a person’s brain and behavior, leading to their inability to control their use of substances like legal or illegal drugs, alcohol, or medications. Symptoms can be moderate to severe, with addiction being the most severe form of SUD.
People with a SUD may also have other mental health disorders, and people with mental health disorders may also struggle with substance use. These other mental health disorders can include anxiety disorders , depression , attention-deficit hyperactivity disorder (ADHD) , bipolar disorder , personality disorders , and schizophrenia , among others. For more information, please see the National Institute on Drug Abuse (NIDA) Common Comorbidities with Substance Use Disorders Research Report .
Though people might have both a SUD and a mental disorder, that does not mean that one caused the other. Research suggests three possibilities that could explain why SUDs and other mental disorders may occur together:
- Common risk factors can contribute to both SUDs and other mental disorders. Both SUDs and other mental disorders can run in families, meaning certain genes may be a risk factor. Environmental factors, such as stress or trauma, can cause genetic changes that are passed down through generations and may contribute to the development of a mental disorder or a substance use disorder.
- Mental disorders can contribute to substance use and SUDs. Studies found that people with a mental disorder, such as anxiety, depression, or post-traumatic stress disorder (PTSD) , may use drugs or alcohol as a form of self-medication. However, although some drugs may temporarily help with some symptoms of mental disorders, they may make the symptoms worse over time. Additionally, brain changes in people with mental disorders may enhance the rewarding effects of substances, making it more likely they will continue to use the substance.
- Substance use and SUDs can contribute to the development of other mental disorders. Substance use may trigger changes in brain structure and function that make a person more likely to develop a mental disorder.
How are substance use disorder and co-occurring mental disorders diagnosed and treated?
When someone has a SUD and another mental health disorder, it is usually better to treat them at the same time rather than separately. People who need help for a SUD and other mental disorders should see a health care provider for each disorder. It can be challenging to make an accurate diagnosis because some symptoms are the same for both disorders, so the provider should use comprehensive assessment tools to reduce the chance of a missed diagnosis and provide the right treatment.
It also is essential that the provider tailor treatment, which may include behavioral therapies and medications, to an individual’s specific combination of disorders and symptoms. It should also take into account the person’s age, the misused substance, and the specific mental disorder(s). Talk to your health care provider to determine what treatment may be best for you and give the treatment time to work.
Behavioral therapies
Research has found several behavioral therapies that have promise for treating individuals with co-occurring substance use and mental disorders. Health care providers may recommend behavioral therapies alone or in combination with medications.
Some examples of effective behavioral therapies for adults with SUDs and different co-occurring mental disorders include:
- Cognitive behavioral therapy (CBT) is a type of talk therapy aimed at helping people learn how to cope with difficult situations by challenging irrational thoughts and changing behaviors.
- Dialectical behavior therapy (DBT) uses concepts of mindfulness and acceptance or being aware of and attentive to the current situation and emotional state. DBT also teaches skills that can help control intense emotions, reduce self-destructive behaviors (such as suicide attempts, thoughts, or urges; self-harm; and drug use), and improve relationships.
- Assertive community treatment (ACT) is a form of community-based mental health care that emphasizes outreach to the community and an individualized treatment approach.
- Therapeutic communities (TC) are a common form of long-term residential treatment that focuses on helping people develop new and healthier values, attitudes, and behaviors.
- Contingency management (CM) principles encourage healthy behaviors by offering vouchers or rewards for desired behaviors.
Behavioral therapies for children and adolescents
Some effective behavioral treatments for children and adolescents include:
- Brief strategic family therapy (BSFT) therapy targets family interactions thought to maintain or worsen adolescent SUDs and other co-occurring problem behaviors.
- Multidimensional family therapy (MDFT) works with the whole family to simultaneously address multiple and interacting adolescent problem behaviors, such as substance use, mental disorders, school problems, delinquency, and others.
- Multisystemic therapy (MST) targets key factors associated with serious antisocial behavior in children and adolescents with SUDs.
Medications
There are effective medications that treat opioid , alcohol , and nicotine addiction and lessen the symptoms of many other mental disorders. Some medications may be useful in treating multiple disorders. For more information on behavioral treatments and medications for SUDs, visit NIDA’s Drug Facts and Treatment webpages. For more information about treatment for mental disorders, visit NIMH's Health Topics webpages.
How can I find help for substance use and co-occurring mental disorders?
To find mental health treatment services in your area, call the Substance Abuse and Mental Health Services Administration (SAMHSA) National Helpline at 1-800-662-HELP (4357), visit the SAMHSA online treatment locator , or text your ZIP code to 435748.
For additional resources about finding help, visit:
NIMH's Help for Mental Illnesses page
National Cancer Institute’s Smokefree.gov website, or call their smoking quitline at 1-877-44U-QUIT (1-877-448-7848)
If you or someone you know is struggling or having thoughts of suicide, call or text the 988 Suicide & Crisis Lifeline at 988 or chat at 988lifeline.org . In life-threatening situations, call 911.
How can I find a clinical trial for substance use and co-occurring mental disorders?
Clinical trials are research studies that look at new ways to prevent, detect, or treat diseases and conditions. The goal of clinical trials is to determine if a new test or treatment works and is safe. Although individuals may benefit from being part of a clinical trial, participants should be aware that the primary purpose of a clinical trial is to gain new scientific knowledge so that others may be better helped in the future.
Researchers at NIMH and around the country conduct many studies with patients and healthy volunteers. We have new and better treatment options today because of what clinical trials uncovered years ago. Be part of tomorrow’s medical breakthroughs. Talk to your health care provider about clinical trials, their benefits and risks, and whether one is right for you.
To learn more or find a study, visit:
- NIMH’s Clinical Trials webpage : Information about participating in clinical trials related to mental disorders
- Clinicaltrials.gov: Current studies on mental illness and substance misuse : List of clinical trials funded by the National Institutes of Health (NIH) being conducted across the country
Where can I learn more about substance use and co-occurring disorders?
Brochures and other educational resources.
- National Institute on Alcohol Abuse and Alcoholism (NIAAA) Publications Order Form
- NIDA: Parents and Educators
- SAMHSA Publications and Digital Products
- Alcohol Use Disorder (also en español )
- Drug Use and Addiction (also en español )
- Mental Health and Behavior (also en español )
- Opioids and Opioid Use Disorder (also en español )
- Risks of tobacco (also en español )
- NIH Experts Discuss the Intersection of Suicide and Substance Use : Learn about common risk factors, populations at elevated risk, suicides by drug overdose, treatments, prevention, and resources for finding help.
- NIDA Common Physical and Mental Health Comorbidities with Substance Use Disorders Research Report
- NIDA Tobacco, Nicotine, and E-Cigarettes Research Report
- SAMHSA National Survey on Drug Use and Health
- Suicide Deaths Are a Major Component of the Opioid Crisis that Must Be Addressed
- NIMH and the NIH HEAL Initiative: Collaborating to address the opioid epidemic
- NIMH’s Role in the NIH HEAL Initiative
Last reviewed: March 2024
Unless otherwise specified, the information on our website and in our publications is in the public domain and may be reused or copied without permission. However, you may not reuse or copy images. Please cite the National Institute of Mental Health as the source. Read our copyright policy to learn more about our guidelines for reusing NIMH content.

COMMENTS
Personality disorders (PDs) can be described as the manifestation of extreme personality traits that interfere with everyday life and contribute to significant suffering, functional limitations, or both. They are common and are frequently encountered in virtually all forms of health care. PDs are associated with an inferior quality of life (QoL ...
In each issue of Personality Disorders: Theory, Research, and Treatment one accepted manuscript will be selected to serve as an "Editor's Choice" paper. Selection will follow discussion by the editor and associate editor and consider issues such as overall contribution, clinical implications, or the highlighting of important theoretical ...
Personality disorders constitute a major challenge for society, as well as psychiatry and psychotherapy. Specifically, in connection with emotionally unstable personality traits, large and rigorous studies [] emphasize the high costs for health and other services services.Recent research has featured different levels of personality functioning, that can be measured early in development and ...
Ten categories of disorders are described: paranoid, schizoid, schizotypal, antisocial, borderline, histrionic, narcissistic, avoidant, dependent, and obsessive-compulsive personality disorders ...
Review. Search methodology. The study aimed to conduct an exhaustive literature review on borderline personality disorder (BPD). The focus was placed on the disease's onset, diagnostic standards, signs, symptoms, treatment, and other aspects, focusing on its history, neurological foundations, and related comorbidities.
Personality disorders are highly prevalent in clinical practice. With the introduction of the Diagnostic Statistical Manual - 5th Edition (DSM-5) the multi-axial system of diagnosis for mental disorders has disappeared, which has led to an increase in research on personality disorders (e.g. Emmelkamp & Meyerbröker, 2020).In this Special Issues, several recent developments are discussed.
A major deviation from normal patterns of behavior. | Explore the latest full-text research PDFs, articles, conference papers, preprints and more on PERSONALITY DISORDERS. Find methods information ...
3.3 Most cited papers. The top 10 highly cited papers on BPD research were presented in Table 1.The most cited paper, by Marsha M. Linehan and colleagues, focus on the treatment of suicidal behavior in BPD ().The transition between suicidal and non-suicidal self-injurious behavior in individuals with BPD has attracted researchers's attention, mainly in cluster #4 "nonsuicidal self-injury ...
The most recent special issue of Personality Disorders: Theory, Research, and Treatment, titled "Methodological and Quantitative Issues in the Study of Personality Pathology," features the work of leading scholars on important methodological considerations for personality disorder research.Among the salient topics addressed in the special issue are registration (before, during, and after a ...
Personality disorders form a class of mental disorders that are characterized. by long-lasting rigid patterns of thought and behaviour which cause serious. problems with relationships and work ...
Disorders (DSM 5) classification of antisocial personality. disorder (A SPD) describe s individuals who engage in repeti-. tive irresponsible, delinquent, and criminal behavior. The. diagnosis is ...
Creativity and mental disorders are sometimes seen as intertwined, but research is still unclear on whether, how much, and why. Here we explore the potential role of shared genetic factors behind ...
List of Personality Topics. You can also come up with questions about your own about different topics in personality psychology. Some that you might explore include: Big 5 personality traits. The id, ego, and superego. Psychosocial development. Hierarchy of needs. Myers-Briggs Type Indicator. Personality disorders.
Topics of Psychology Research Related to Human Cognition. Some of the possible topics you might explore in this area include thinking, language, intelligence, and decision-making. Other ideas might include: Dreams. False memories. Attention. Perception.
General call for papers. Personality Disorders: Theory, Research, and Treatment ( PD:TRT ), the official journal of the North American Society for the Study of Personality Disorders, welcomes manuscripts from research psychologists, as well as researchers from other disciplines such as psychiatry, social work, and public health.
Background We describe a collection of themes for a research agenda for personality disorders that was originally formulated for the ESSPD Borderline Congress in 2022. Methods Experts with lived and living experience (EE), researchers and clinicians met virtually, exchanged ideas and discussed research topics for the field of personality disorders. The experts - patients, relatives ...
The present paper is the product of two consecutive editions (2019; 2021) of the European Society for the Study of Personality Disorders Summer School for early career researchers, which took place in Crêt-Bérard, Switzerland, with the support of the Department of Psychiatry, University of Lausanne (Switzerland), and the financial support of ...
Towards an informed research agenda for the field of personality disorders by experts with lived and living experience and researchers. We describe a collection of themes for a research agenda for personality disorders that was originally formulated for the ESSPD Borderline Congress in 2022.
Statistics: Personality Disorders: This webpage provides the statistics currently available on the prevalence of personality disorder among people in the United States. Multimedia. Experts Discuss Borderline Personality Disorder: Learn the signs, symptoms, diagnosis, treatments, and the latest research on borderline personality disorder.
A configuration of unsteady and acute relational associations characterized by oscillations between opposites of idealization and contraries of devaluation. Most commonly, the BPD patients might experience a life without sense of direction or meaning. Psychological Therapy: Borderline Personality Disorder.
Sample Personality Disorders Research Paper. Browse other research paper examples and check the list of research paper topics for more inspiration. iResearchNet offers academic assignment help for students all over the world: writing from scratch, editing, proofreading, problem solving, from essays to dissertations, from humanities to STEM. We offer full confidentiality, safe payment ...
Personality disorder is the term used to refer to several different subtypes of maladaptive personality traits as identified by the Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV). Stricker and Widiger (2003) assert that personality disorders arise when "personality traits are inflexible and maladaptive and cause significant ...
Borderline Personality Disorder - Science topic. Borderline personality disorder (BPD) (called emotionally unstable personality disorder, borderline type in the ICD-10) is a personality disorder ...
Abstract. Borderline personality disorder (BPD) is a chronic psychiatric disorder characterized by pervasive affective instability, self-image disturbances, impulsivity, marked suicidality, and unstable interpersonal relationships as the core dimensions of psychopathology underlying the disorder. Across a wide range of situations, BPD causes ...
Borderline personality disorder is a term that identifies a heterogenous group of patients with serious character pathology and behavioral disturbances. The main features of this disorder are behavior that is impulsive, dramatic, and often self-destructive; moods that are labile and reactive to life circumstances; interpersonal relationships ...
NIMH statistics pages include statistics on the prevalence, treatment, and costs of mental illness for the population of the United States, in addition to information about possible consequences of mental illnesses, such as suicide and disability.
Post-traumatic stress disorder (PTSD) is a disorder that develops in some people who have experienced a shocking, scary, or dangerous event. It is natural to feel afraid during and after a traumatic situation. Fear is a part of the body's "fight-or-flight" response, which helps us avoid or respond to potential danger.
Personality disorder is now being accepted as an important condition in mainstream psychiatry across the world. Although it often remains unrecognized in ordinary practice, research studies have shown it is common, creates considerable morbidity, is associated with high costs to services and to society, and interferes, usually negatively, with progress in the treatment of other mental disorders.
Conclusion. Borderline Personality Disorder is a complex mental illness that affects many individuals around the world. While it is essential to approach this topic with sensitivity, studying the case of Jeffrey Dahmer, who was diagnosed with BPD, can provide valuable insights into the disorder.
These other mental health disorders can include anxiety disorders, depression, attention-deficit hyperactivity disorder (ADHD), bipolar disorder, personality disorders, and schizophrenia, among others. For more information, please see the National Institute on Drug Abuse (NIDA) Common Comorbidities with Substance Use Disorders Research Report .