

Community Blog
Keep up-to-date on postgraduate related issues with our quick reads written by students, postdocs, professors and industry leaders.
Types of Research – Explained with Examples
- By DiscoverPhDs
- October 2, 2020

Types of Research
Research is about using established methods to investigate a problem or question in detail with the aim of generating new knowledge about it.
It is a vital tool for scientific advancement because it allows researchers to prove or refute hypotheses based on clearly defined parameters, environments and assumptions. Due to this, it enables us to confidently contribute to knowledge as it allows research to be verified and replicated.
Knowing the types of research and what each of them focuses on will allow you to better plan your project, utilises the most appropriate methodologies and techniques and better communicate your findings to other researchers and supervisors.
Classification of Types of Research
There are various types of research that are classified according to their objective, depth of study, analysed data, time required to study the phenomenon and other factors. It’s important to note that a research project will not be limited to one type of research, but will likely use several.
According to its Purpose
Theoretical research.
Theoretical research, also referred to as pure or basic research, focuses on generating knowledge , regardless of its practical application. Here, data collection is used to generate new general concepts for a better understanding of a particular field or to answer a theoretical research question.
Results of this kind are usually oriented towards the formulation of theories and are usually based on documentary analysis, the development of mathematical formulas and the reflection of high-level researchers.
Applied Research
Here, the goal is to find strategies that can be used to address a specific research problem. Applied research draws on theory to generate practical scientific knowledge, and its use is very common in STEM fields such as engineering, computer science and medicine.
This type of research is subdivided into two types:
- Technological applied research : looks towards improving efficiency in a particular productive sector through the improvement of processes or machinery related to said productive processes.
- Scientific applied research : has predictive purposes. Through this type of research design, we can measure certain variables to predict behaviours useful to the goods and services sector, such as consumption patterns and viability of commercial projects.

According to your Depth of Scope
Exploratory research.
Exploratory research is used for the preliminary investigation of a subject that is not yet well understood or sufficiently researched. It serves to establish a frame of reference and a hypothesis from which an in-depth study can be developed that will enable conclusive results to be generated.
Because exploratory research is based on the study of little-studied phenomena, it relies less on theory and more on the collection of data to identify patterns that explain these phenomena.
Descriptive Research
The primary objective of descriptive research is to define the characteristics of a particular phenomenon without necessarily investigating the causes that produce it.
In this type of research, the researcher must take particular care not to intervene in the observed object or phenomenon, as its behaviour may change if an external factor is involved.
Explanatory Research
Explanatory research is the most common type of research method and is responsible for establishing cause-and-effect relationships that allow generalisations to be extended to similar realities. It is closely related to descriptive research, although it provides additional information about the observed object and its interactions with the environment.
Correlational Research
The purpose of this type of scientific research is to identify the relationship between two or more variables. A correlational study aims to determine whether a variable changes, how much the other elements of the observed system change.
According to the Type of Data Used
Qualitative research.
Qualitative methods are often used in the social sciences to collect, compare and interpret information, has a linguistic-semiotic basis and is used in techniques such as discourse analysis, interviews, surveys, records and participant observations.
In order to use statistical methods to validate their results, the observations collected must be evaluated numerically. Qualitative research, however, tends to be subjective, since not all data can be fully controlled. Therefore, this type of research design is better suited to extracting meaning from an event or phenomenon (the ‘why’) than its cause (the ‘how’).
Quantitative Research
Quantitative research study delves into a phenomena through quantitative data collection and using mathematical, statistical and computer-aided tools to measure them . This allows generalised conclusions to be projected over time.

According to the Degree of Manipulation of Variables
Experimental research.
It is about designing or replicating a phenomenon whose variables are manipulated under strictly controlled conditions in order to identify or discover its effect on another independent variable or object. The phenomenon to be studied is measured through study and control groups, and according to the guidelines of the scientific method.
Non-Experimental Research
Also known as an observational study, it focuses on the analysis of a phenomenon in its natural context. As such, the researcher does not intervene directly, but limits their involvement to measuring the variables required for the study. Due to its observational nature, it is often used in descriptive research.
Quasi-Experimental Research
It controls only some variables of the phenomenon under investigation and is therefore not entirely experimental. In this case, the study and the focus group cannot be randomly selected, but are chosen from existing groups or populations . This is to ensure the collected data is relevant and that the knowledge, perspectives and opinions of the population can be incorporated into the study.
According to the Type of Inference
Deductive investigation.
In this type of research, reality is explained by general laws that point to certain conclusions; conclusions are expected to be part of the premise of the research problem and considered correct if the premise is valid and the inductive method is applied correctly.
Inductive Research
In this type of research, knowledge is generated from an observation to achieve a generalisation. It is based on the collection of specific data to develop new theories.
Hypothetical-Deductive Investigation
It is based on observing reality to make a hypothesis, then use deduction to obtain a conclusion and finally verify or reject it through experience.
According to the Time in Which it is Carried Out
Longitudinal study (also referred to as diachronic research).
It is the monitoring of the same event, individual or group over a defined period of time. It aims to track changes in a number of variables and see how they evolve over time. It is often used in medical, psychological and social areas .
Cross-Sectional Study (also referred to as Synchronous Research)
Cross-sectional research design is used to observe phenomena, an individual or a group of research subjects at a given time.
According to The Sources of Information
Primary research.
This fundamental research type is defined by the fact that the data is collected directly from the source, that is, it consists of primary, first-hand information.
Secondary research
Unlike primary research, secondary research is developed with information from secondary sources, which are generally based on scientific literature and other documents compiled by another researcher.

According to How the Data is Obtained
Documentary (cabinet).
Documentary research, or secondary sources, is based on a systematic review of existing sources of information on a particular subject. This type of scientific research is commonly used when undertaking literature reviews or producing a case study.
Field research study involves the direct collection of information at the location where the observed phenomenon occurs.
From Laboratory
Laboratory research is carried out in a controlled environment in order to isolate a dependent variable and establish its relationship with other variables through scientific methods.
Mixed-Method: Documentary, Field and/or Laboratory
Mixed research methodologies combine results from both secondary (documentary) sources and primary sources through field or laboratory research.

An academic transcript gives a breakdown of each module you studied for your degree and the mark that you were awarded.

An In Press article is a paper that has been accepted for publication and is being prepared for print.
A well written figure legend will explain exactly what a figure means without having to refer to the main text. Our guide explains how to write one.
Join thousands of other students and stay up to date with the latest PhD programmes, funding opportunities and advice.
Browse PhDs Now

PhD stress is real. Learn how to combat it with these 5 tips.

Statistical treatment of data is essential for all researchers, regardless of whether you’re a biologist, computer scientist or psychologist, but what exactly is it?

Dr Thirlaway gained his PhD in immunology from the University of Nottingham in 2018. He is now a Science Communicator at the Natural History Museum, London.

Amy recently entered her third and final year of her PhD at the University of Strathclyde. Her research has focussed on young people’s understanding of mental health stigma in Scotland.
Join Thousands of Students
- Skip to main content
- Skip to FDA Search
- Skip to in this section menu
- Skip to footer links

The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
U.S. Food and Drug Administration
- Search
- Menu
- For Patients
- Clinical Trials: What Patients Need to Know
Basics About Clinical Trials
What are clinical trials.
Clinical trials are research studies in which people volunteer to help find answers to specific health questions. When carefully conducted, they are the safest and fastest way to find new treatments and ways to improve health.
Clinical trials are conducted according to a plan, called a protocol, which describes:
- the types of patients who may enter the study
- the schedules of tests and procedures
- the drugs involved
- the dosages, or amount of the drug
- the length of the study
- what the researchers hope to learn from the study.
Volunteers who participate in the study must agree to the rules and terms outlined in the protocol. Similarly, researchers, doctors, and other health professionals who manage the clinical trials must follow strict rules set by the FDA. These rules make sure that those who agree to participate are treated as safely as possible.
Learn more about the basics of clinical trial participation, read first hand experiences from actual clinical trial volunteers, and see explanations from researchers at the NIH Clinical Research Trials and You Web site.
Why are clinical trials done?
Clinical trials are conducted for many reasons:
- to determine whether a new drug or device is safe and effective for people to use.
- to study different ways to use standard treatments or current, approved treatments so that they will be more effective, easier to use, or decrease certain side effects.
- to learn how to safely use a treatment in a population for which the treatment was not previously tested, such as children.
Who should consider clinical trials and why?
Some people participate in clinical trials because none of the standard (approved) treatment options have worked, or they are unable to tolerate certain side effects. Clinical trials provide another option when standard therapy has failed. Others participate in trials because they want to contribute to the advancement of medical knowledge.
Ensuring people from diverse backgrounds join clinical trials is key to advancing health equity. Participants in clinical trials should represent the patients that will use the medical products. This is often not the case—people from racial and ethnic minority and other diverse groups are underrepresented in clinical research. This is a concern because people of different ages, races, and ethnicities may react differently to certain medical products. Learn more about the clinical trial diversity initiative from the Office of Minority Health and Health Equity.
All clinical trials have guidelines, called eligibility criteria, about who can participate. The criteria are based on such factors as age, sex, type and stage of disease, previous treatment history, and other medical conditions. This helps to reduce the variation within the study and to ensure that the researchers will be able to answer the questions they plan to study. Therefore, not everyone who applies for a clinical trial will be accepted.
It is important to test drugs and medical products in the people they are meant to help. It is also important to conduct research in a variety of people, because different people may respond differently to treatments. FDA seeks to ensure that people of different ages, races, ethnic groups, and genders are included in clinical trials. Learn more about FDA’s efforts to increase diversity in clinical trials .
Where are clinical trials conducted?
Clinical trials can be sponsored by organizations (such as a pharmaceutical company), Federal offices and agencies (such as the National Institutes of Health or the U.S. Department of Veterans Affairs), or individuals (such as doctors or health care providers). The sponsor determines the location(s) of the trials, which are usually conducted at universities, medical centers, clinics, hospitals, and other Federally or industry-funded research sites.
Are clinical trials safe?
FDA works to protect participants in clinical trials and to ensure that people have reliable information before deciding whether to join a clinical trial. The Federal government has regulations and guidelines for clinical research to protect participants from unreasonable risks. Although efforts are made to control the risks to participants, some may be unavoidable because we are still learning more about the medical treatments in the study.
The government requires researchers to give prospective participants complete and accurate information about what will happen during the trial. Before joining a particular study, you will be given an informed consent document that describes your rights as a participant, as well as details about the study, including potential risks. Signing it indicates that you understand that the trial is research and that you may leave at any time. The informed consent is part of the process that makes sure you understand the known risks associated with the study.
What should I think about before joining a clinical trial?
Before joining a clinical trial, it is important to learn as much as possible. Discuss your questions and concerns with members of the health care team conducting the trial. Also, discuss the trial with your health care provider to determine whether or not the trial is a good option based on your current treatment. Be sure you understand:
- what happens during the trial
- the type of health care you will receive
- any related costs once you are enrolled in the trial
- the benefits and risks associated with participating.
What is FDA’s role in approving new drugs and medical treatments?
FDA makes sure medical treatments are safe and effective for people to use. We do not develop new therapies or conduct clinical trials. Rather, we oversee the people who do. FDA staff meet with researchers and perform inspections of clinical trial study sites to protect the rights of patients and to verify the quality and integrity of the data.
Learn more about the Drug Development Process .
Where can I find clinical trials?
One good way to find out if there are any clinical trials that might help you is to ask your doctor. Other sources of information include:
- FDA Clinical Trials Search. Search a database of Federally and privately supported studies available through clinicaltrials.gov. Learn about each trial’s purpose, who can participate, locations, and who to contact for more information.
- Clinicaltrials.gov. Conduct more advanced searches
- National Cancer Institute or call 1–800–4–CANCER (1–800–422–6237). Learn about clinical trials for people with cancer.
- AIDS Clinical Trials and Information Services (ACTIS) or call 1–800–TRIALS–A (1–800–874–2572). Locate clinical trials for people with HIV.
- AIDSinfo. Search a database of HIV/AIDS trials, sponsored by the National Institutes of Health’s National Library of Medicine.
What is a placebo and how is it related to clinical trials?
A placebo is a pill, liquid, or powder that has no treatment value. It is often called a sugar pill. In clinical trials, experimental drugs are often compared with placebos to evaluate the treatment’s effectiveness.
Is there a chance I might get a placebo?
In clinical trials that include placebos, quite often neither patients nor their doctors know who is receiving the placebo and how is being treated with the experimental drug. Many cancer clinical trials, as well as trials for other serious and life-threatening conditions, do not include placebo control groups. In these cases, all participants receive the experimental drug. Ask the trial coordinator whether there is a chance you may get a placebo rather than the experimental drug. Then, talk with your doctor about what is best for you.
How do I find out what Phase a drug is in as part of the clinical trial?
Talk to the clinical trial coordinator to find out which phase the clinical trial is in. Learn more about the different clinical trial phases and whether they are right for you.
What happens to drugs that don't make it out of clinical trials?
Most drugs that undergo preclinical (animal) research never even make it to human testing and review by the FDA. The drug developers go back to begin the development process using what they learned during with their preclinical research. Learn more about drug development .

An official website of the United States government
Here's how you know
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
What Are Clinical Trials and Studies?
On this page:
What is clinical research?
Why participate in a clinical trial, what happens in a clinical trial or study, what happens when a clinical trial or study ends, what are the different phases of clinical trials, questions to ask before participating in clinical research, how do researchers decide who will participate, clinical research needs participants with diverse backgrounds.
By participating in clinical research, you can help scientists develop new medications and other strategies to treat and prevent disease. Many effective treatments that are used today, such as chemotherapy, cholesterol-lowering drugs, vaccines, and cognitive-behavioral therapy, would not exist without research participants. Whether you’re healthy or have a medical condition, people of all ages and backgrounds can participate in clinical trials. This article can help you learn more about clinical research, why people choose to participate, and how to get involved in a study.
Mr. Jackson's story
Mr. Jackson is 73 years old and was just diagnosed with Alzheimer’s disease . He is worried about how it will affect his daily life. Will he forget to take his medicine? Will he forget his favorite memories, like the births of his children or hiking the Appalachian Trail? When Mr. Jackson talked to his doctor about his concerns, she told him about a clinical trial that is testing a possible new Alzheimer’s treatment. But Mr. Jackson has concerns about clinical trials. He does not want to feel like a lab rat or take the chance of getting a treatment that may not work or could make him feel worse. The doctor explained that there are both risks and benefits to being part of a clinical trial, and she talked with Mr. Jackson about research studies — what they are, how they work, and why they need volunteers. This information helped Mr. Jackson feel better about clinical trials. He plans to learn more about how to participate.
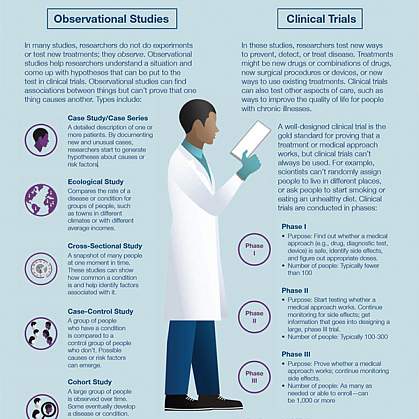
Clinical research is the study of health and illness in people. There are two main types of clinical research: observational studies and clinical trials.

Observational studies monitor people in normal settings. Researchers gather information from people and compare changes over time. For example, researchers may ask a group of older adults about their exercise habits and provide monthly memory tests for a year to learn how physical activity is associated with cognitive health . Observational studies do not test a medical intervention, such as a drug or device, but may help identify new treatments or prevention strategies to test in clinical trials.
Clinical trials are research studies that test a medical, surgical, or behavioral intervention in people. These trials are the primary way that researchers determine if a new form of treatment or prevention, such as a new drug, diet, or medical device (for example, a pacemaker), is safe and effective in people. Often, a clinical trial is designed to learn if a new treatment is more effective or has less harmful side effects than existing treatments.
Other aims of clinical research include:
- Testing ways to diagnose a disease early, sometimes before there are symptoms
- Finding approaches to prevent a health problem, including in people who are healthy but at increased risk of developing a disease
- Improving quality of life for people living with a life-threatening disease or chronic health problem
- Studying the role of caregivers or support groups
Learn more about clinical research from MedlinePlus and ClinicalTrials.gov .

People volunteer for clinical trials and studies for a variety of reasons, including:
- They want to contribute to discovering health information that may help others in the future.
- Participating in research helps them feel like they are playing a more active role in their health.
- The treatments they have tried for their health problem did not work or there is no treatment for their health problem.
Whatever the motivation, when you choose to participate in a clinical trial, you become a partner in scientific discovery. Participating in research can help future generations lead healthier lives. Major medical breakthroughs could not happen without the generosity of clinical trial participants — young and old, healthy, or diagnosed with a disease.
Where can I find a clinical trial?
Looking for clinical trials related to aging and age-related health conditions? Talk to your health care provider and use online resources to:
- Search for a clinical trial
- Look for clinical trials on Alzheimer's, other dementias, and caregiving
- Find a registry for a particular diagnosis or condition
- Explore clinical trials and studies supported by NIA
After you find one or more studies that you are interested in, the next step is for you or your doctor to contact the study research staff and ask questions. You can usually find contact information in the description of the study.
Let your health care provider know if you are thinking about joining a clinical trial. Your provider may want to talk to the research team to make sure the study is safe for you and to help coordinate your care.
Joining a clinical trial is a personal decision with potential benefits and some risks. Learn what happens in a clinical trial and how participant safety is protected . Read and listen to testimonials from people who decided to participate in research.
Here’s what typically happens in a clinical trial or study:
- Research staff explain the trial or study in detail, answer your questions, and gather more information about you.
- Once you agree to participate, you sign an informed consent form indicating your understanding about what to expect as a participant and the various outcomes that could occur.
- You are screened to make sure you qualify for the trial or study.
- If accepted into the trial, you schedule a first visit, which is called the “baseline” visit. The researchers conduct cognitive and/or physical tests during this visit.
- For some trials testing an intervention, you are assigned by chance (randomly) to a treatment group or a control group . The treatment group will get the intervention being tested, and the control group will not.
- You follow the trial procedures and report any issues or concerns to researchers.
- You may visit the research site at regularly scheduled times for new cognitive, physical, or other evaluations and discussions with staff. During these visits, the research team collects data and monitors your safety and well-being.
- You continue to see your regular physician(s) for usual health care throughout the study.
How do researchers decide which interventions are safe to test in people?
Before a clinical trial is designed and launched, scientists perform laboratory tests and often conduct studies in animals to test a potential intervention’s safety and effectiveness. If these studies show favorable results, the U.S. Food and Drug Administration (FDA) approves the intervention to be tested in humans. Learn more about how the safety of clinical trial participants is protected.
Once a clinical trial or study ends, the researchers analyze the data to determine what the findings mean and to plan the next steps. As a participant, you should be provided information before the study starts about how long it will last, whether you will continue receiving the treatment after the trial ends (if applicable), and how the results of the research will be shared. If you have specific questions about what will happen when the trial or study ends, ask the research coordinator or staff.
Clinical trials of drugs and medical devices advance through several phases to test safety, determine effectiveness, and identify any side effects. The FDA typically requires Phase 1, 2, and 3 trials to be conducted to determine if the drug or device can be approved for further use. If researchers find the intervention to be safe and effective after the first three phases, the FDA approves it for clinical use and continues to monitor its effects.
Each phase has a different purpose:
- A Phase 1 trial tests an experimental drug or device on a small group of people (around 20 to 80) to judge its safety, including any side effects, and to test the amount (dosage).
- A Phase 2 trial includes more people (around 100 to 300) to help determine whether a drug is effective. This phase aims to obtain preliminary data on whether the drug or device works in people who have a certain disease or condition. These trials also continue to examine safety, including short-term side effects.
- A Phase 3 trial gathers additional information from several hundred to a few thousand people about safety and effectiveness, studying different populations and different dosages, and comparing the intervention with other drugs or treatment approaches. If the FDA agrees that the trial results support the intervention’s use for a particular health condition, it will approve the experimental drug or device.
- A Phase 4 trial takes place after the FDA approves the drug or device. The treatment’s effectiveness and safety are monitored in large, diverse populations. Sometimes, side effects may not become clear until more people have used the drug or device over a longer period of time.
Clinical trials that test a behavior change, rather than a drug or medical device, advance through similar steps, but behavioral interventions are not regulated by the FDA. Learn more about clinical trials , including the types of trials and the four phases.
Choosing to participate in research is an important personal decision. If you are considering joining a trial or study, get answers to your questions and know your options before you decide. Here are questions you might ask the research team when thinking about participating.
- What is this study trying to find out?
- What treatment or tests will I have? Will they hurt? Will you provide me with the test or lab results?
- What are the chances I will be in the experimental group or the control group?
- If the study tests a treatment, what are the possible risks, side effects, and benefits compared with my current treatment?
- How long will the clinical trial last?
- Where will the study take place? Will I need to stay in the hospital?
- Will you provide a way for me to get to the study site if I need it, such as through a ride-share service?
- Will I need a trial or study partner (for example, a family member or friend who knows me well) to come with me to the research site visits? If so, how long will he or she need to participate?
- Can I participate in any part of the trial with my regular doctor or at a clinic closer to my home?
- How will the study affect my everyday life?
- What steps are being taken to ensure my privacy?
- How will you protect my health while I participate?
- What happens if my health problem gets worse during the trial or study?
- Can I take my regular medicines while participating?
- Who will be in charge of my care while I am in the trial or study? Will I be able to see my own doctors?
- How will you keep my doctor informed about my participation?
- If I withdraw from the trial or study, will this affect my normal care?
- Will it cost me anything to be in the trial or study? If so, will I be reimbursed for expenses, such as travel, parking, lodging, or meals?
- Will my insurance pay for costs not covered by the research, or must I pay out of pocket? If I don’t have insurance, am I still eligible to participate?
- Will my trial or study partner be compensated for his or her time?
- Will you follow up on my health after the end of the trial or study?
- Will I continue receiving the treatment after the trial or study ends?
- Will you tell me the results of the research?
- Whom do I contact if I have questions after the trial or study ends?

To be eligible to participate, you may need to have certain characteristics, called inclusion criteria. For example, a clinical trial may need participants to have a certain stage of disease, version of a gene, or family history. Some trials require that participants have a study partner who can accompany them to clinic visits.
Participants with certain characteristics may not be allowed to participate in some trials. These characteristics are called exclusion criteria. They include factors such as specific health conditions or medications that could interfere with the treatment being tested.
Many volunteers must be screened to find enough people who are eligible for a trial or study. Generally, you can participate in only one clinical trial at a time, although this is not necessarily the case for observational studies. Different trials have different criteria, so being excluded from one trial does not necessarily mean you will be excluded from another.

When research only includes people with similar backgrounds, the findings may not apply to or benefit a broader population. The results of clinical trials and studies with diverse participants may apply to more people. That’s why research benefits from having participants of different ages, sexes, races, and ethnicities.
Researchers need older adults to participate in clinical research so that scientists can learn more about how new drugs, tests, and other interventions will work for them. Many older adults have health needs that are different from those of younger people. For example, as people age, their bodies may react differently to certain drugs. Older adults may need different dosages of a drug to have the intended result. Also, some drugs may have different side effects in older people than in younger individuals. Having older adults enrolled in clinical trials and studies helps researchers get the information they need to develop the right treatments for this age group.
Researchers know that it may be challenging for some older adults to join a clinical trial or study. For example, if you have multiple health problems, can you participate in research that is looking at only one condition? If you are frail or have a disability, will you be strong enough to participate? If you no longer drive, how can you get to the research site? Talk to the research coordinator or staff about your concerns. The research team may have already thought about some of the potential obstacles and have a plan to make it easier for you to participate.
Read more about diversity in clinical trials .
You may also be interested in
- Learning more about the benefits, risks, and safety of clinical research
- Finding out about participating in Alzheimer's disease research
- Downloading or sharing an infographic with the benefits of participating in clinical research
Sign up for email updates on healthy aging
For more information about clinical trials.
Alzheimers.gov www.alzheimers.gov Explore the Alzheimers.gov website for information and resources on Alzheimer’s and related dementias from across the federal government.
Clinical Research Trials and You National Institutes of Health www.nih.gov/health-information/nih-clinical-research-trials-you
ClinicalTrials.gov www.clinicaltrials.gov
This content is provided by the NIH National Institute on Aging (NIA). NIA scientists and other experts review this content to ensure it is accurate and up to date.
Content reviewed: March 22, 2023
nia.nih.gov
An official website of the National Institutes of Health

Please consult the following sources for more information on these types of studies and terminology related to the studies.
- APA Style JARS Supplemental Glossary This webpage provides supplemental information on the terms used in APA Style JARS. This glossary is meant to supplement Chapter 3 of the Publication Manual of the American Psychological Association, Seventh Edition. It is not an exhaustive list of all terms employed in quantitative, qualitative, or mixed methods research, nor does it include all possible definitions for each term; definitions in addition to or different from those reported in this glossary may be found in other sources.
- APA Dictionary of Psychology More than 25,000 authoritative entries across 90 subfields of psychology.
- << Previous: Types of Scholarly Articles
- Next: Google Scholar >>
- Last Updated: Aug 19, 2024 2:23 PM
- URL: https://libguides.ggc.edu/research-101
Masks Strongly Recommended but Not Required in Maryland
Respiratory viruses continue to circulate in Maryland, so masking remains strongly recommended when you visit Johns Hopkins Medicine clinical locations in Maryland. To protect your loved one, please do not visit if you are sick or have a COVID-19 positive test result. Get more resources on masking and COVID-19 precautions .
- Vaccines
- Masking Guidelines
- Visitor Guidelines
Understanding Clinical Trials
Clinical research: what is it.

Your doctor may have said that you are eligible for a clinical trial, or you may have seen an ad for a clinical research study. What is clinical research, and is it right for you?
Clinical research is the comprehensive study of the safety and effectiveness of the most promising advances in patient care. Clinical research is different than laboratory research. It involves people who volunteer to help us better understand medicine and health. Lab research generally does not involve people — although it helps us learn which new ideas may help people.
Every drug, device, tool, diagnostic test, technique and technology used in medicine today was once tested in volunteers who took part in clinical research studies.
At Johns Hopkins Medicine, we believe that clinical research is key to improve care for people in our community and around the world. Once you understand more about clinical research, you may appreciate why it’s important to participate — for yourself and the community.
What Are the Types of Clinical Research?
There are two main kinds of clinical research:
Observational Studies
Observational studies are studies that aim to identify and analyze patterns in medical data or in biological samples, such as tissue or blood provided by study participants.
Clinical Trials
Clinical trials, which are also called interventional studies, test the safety and effectiveness of medical interventions — such as medications, procedures and tools — in living people.
Clinical research studies need people of every age, health status, race, gender, ethnicity and cultural background to participate. This will increase the chances that scientists and clinicians will develop treatments and procedures that are likely to be safe and work well in all people. Potential volunteers are carefully screened to ensure that they meet all of the requirements for any study before they begin. Most of the reasons people are not included in studies is because of concerns about safety.
Both healthy people and those with diagnosed medical conditions can take part in clinical research. Participation is always completely voluntary, and participants can leave a study at any time for any reason.
“The only way medical advancements can be made is if people volunteer to participate in clinical research. The research participant is just as necessary as the researcher in this partnership to advance health care.” Liz Martinez, Johns Hopkins Medicine Research Participant Advocate
Types of Research Studies
Within the two main kinds of clinical research, there are many types of studies. They vary based on the study goals, participants and other factors.
Biospecimen studies
Healthy volunteer studies.

Goals of Clinical Trials
Because every clinical trial is designed to answer one or more medical questions, different trials have different goals. Those goals include:
Treatment trials
Prevention trials, screening trials, phases of a clinical trial.
In general, a new drug needs to go through a series of four types of clinical trials. This helps researchers show that the medication is safe and effective. As a study moves through each phase, researchers learn more about a medication, including its risks and benefits.
Is the medication safe and what is the right dose? Phase one trials involve small numbers of participants, often normal volunteers.
Does the new medication work and what are the side effects? Phase two trials test the treatment or procedure on a larger number of participants. These participants usually have the condition or disease that the treatment is intended to remedy.
Is the new medication more effective than existing treatments? Phase three trials have even more people enrolled. Some may get a placebo (a substance that has no medical effect) or an already approved treatment, so that the new medication can be compared to that treatment.
Is the new medication effective and safe over the long term? Phase four happens after the treatment or procedure has been approved. Information about patients who are receiving the treatment is gathered and studied to see if any new information is seen when given to a large number of patients.
“Johns Hopkins has a comprehensive system overseeing research that is audited by the FDA and the Association for Accreditation of Human Research Protection Programs to make certain all research participants voluntarily agreed to join a study and their safety was maximized.” Gail Daumit, M.D., M.H.S., Vice Dean for Clinical Investigation, Johns Hopkins University School of Medicine
Is It Safe to Participate in Clinical Research?
There are several steps in place to protect volunteers who take part in clinical research studies. Clinical Research is regulated by the federal government. In addition, the institutional review board (IRB) and Human Subjects Research Protection Program at each study location have many safeguards built in to each study to protect the safety and privacy of participants.
Clinical researchers are required by law to follow the safety rules outlined by each study's protocol. A protocol is a detailed plan of what researchers will do in during the study.
In the U.S., every study site's IRB — which is made up of both medical experts and members of the general public — must approve all clinical research. IRB members also review plans for all clinical studies. And, they make sure that research participants are protected from as much risk as possible.
Earning Your Trust
This was not always the case. Many people of color are wary of joining clinical research because of previous poor treatment of underrepresented minorities throughout the U.S. This includes medical research performed on enslaved people without their consent, or not giving treatment to Black men who participated in the Tuskegee Study of Untreated Syphilis in the Negro Male. Since the 1970s, numerous regulations have been in place to protect the rights of study participants.
Many clinical research studies are also supervised by a data and safety monitoring committee. This is a group made up of experts in the area being studied. These biomedical professionals regularly monitor clinical studies as they progress. If they discover or suspect any problems with a study, they immediately stop the trial. In addition, Johns Hopkins Medicine’s Research Participant Advocacy Group focuses on improving the experience of people who participate in clinical research.
Clinical research participants with concerns about anything related to the study they are taking part in should contact Johns Hopkins Medicine’s IRB or our Research Participant Advocacy Group .
Learn More About Clinical Research at Johns Hopkins Medicine
For information about clinical trial opportunities at Johns Hopkins Medicine, visit our trials site.
Video Clinical Research for a Healthier Tomorrow: A Family Shares Their Story
Clinical Research for a Healthier Tomorrow: A Family Shares Their Story


Module 1: Introduction: What is Research?

Learning Objectives
By the end of this module, you will be able to:
- Explain how the scientific method is used to develop new knowledge
- Describe why it is important to follow a research plan
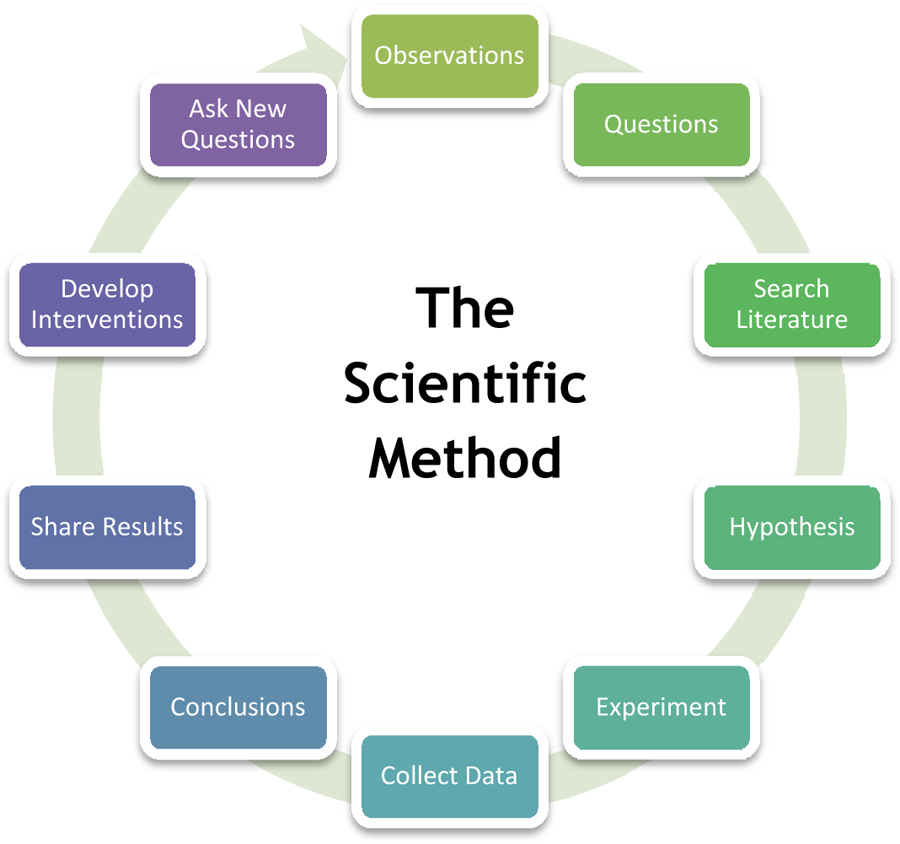
The Scientific Method consists of observing the world around you and creating a hypothesis about relationships in the world. A hypothesis is an informed and educated prediction or explanation about something. Part of the research process involves testing the hypothesis , and then examining the results of these tests as they relate to both the hypothesis and the world around you. When a researcher forms a hypothesis, this acts like a map through the research study. It tells the researcher which factors are important to study and how they might be related to each other or caused by a manipulation that the researcher introduces (e.g. a program, treatment or change in the environment). With this map, the researcher can interpret the information he/she collects and can make sound conclusions about the results.
Research can be done with human beings, animals, plants, other organisms and inorganic matter. When research is done with human beings and animals, it must follow specific rules about the treatment of humans and animals that have been created by the U.S. Federal Government. This ensures that humans and animals are treated with dignity and respect, and that the research causes minimal harm.
No matter what topic is being studied, the value of the research depends on how well it is designed and done. Therefore, one of the most important considerations in doing good research is to follow the design or plan that is developed by an experienced researcher who is called the Principal Investigator (PI). The PI is in charge of all aspects of the research and creates what is called a protocol (the research plan) that all people doing the research must follow. By doing so, the PI and the public can be sure that the results of the research are real and useful to other scientists.
Module 1: Discussion Questions
- How is a hypothesis like a road map?
- Who is ultimately responsible for the design and conduct of a research study?
- How does following the research protocol contribute to informing public health practices?
Email Updates
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
Nih clinical research trials and you.
The NIH Clinical Trials and You website is a resource for people who want to learn more about clinical trials. By expanding the below questions, you can read answers to common questions about taking part in a clinical trial.
What are clinical trials and why do people participate?
Clinical research is medical research that involves people like you. When you volunteer to take part in clinical research, you help doctors and researchers learn more about disease and improve health care for people in the future. Clinical research includes all research that involves people. Types of clinical research include:

- Epidemiology, which improves the understanding of a disease by studying patterns, causes, and effects of health and disease in specific groups.
- Behavioral, which improves the understanding of human behavior and how it relates to health and disease.
- Health services, which looks at how people access health care providers and health care services, how much care costs, and what happens to patients as a result of this care.
- Clinical trials, which evaluate the effects of an intervention on health outcomes.
What are clinical trials and why would I want to take part?
Clinical trials are part of clinical research and at the heart of all medical advances. Clinical trials look at new ways to prevent, detect, or treat disease. Clinical trials can study:
- New drugs or new combinations of drugs
- New ways of doing surgery
- New medical devices
- New ways to use existing treatments
- New ways to change behaviors to improve health
- New ways to improve the quality of life for people with acute or chronic illnesses.
The goal of clinical trials is to determine if these treatment, prevention, and behavior approaches are safe and effective. People take part in clinical trials for many reasons. Healthy volunteers say they take part to help others and to contribute to moving science forward. People with an illness or disease also take part to help others, but also to possibly receive the newest treatment and to have added (or extra) care and attention from the clinical trial staff. Clinical trials offer hope for many people and a chance to help researchers find better treatments for others in the future
Why is diversity and inclusion important in clinical trials?
People may experience the same disease differently. It’s essential that clinical trials include people with a variety of lived experiences and living conditions, as well as characteristics like race and ethnicity, age, sex, and sexual orientation, so that all communities benefit from scientific advances.
See Diversity & Inclusion in Clinical Trials for more information.
How does the research process work?
The idea for a clinical trial often starts in the lab. After researchers test new treatments or procedures in the lab and in animals, the most promising treatments are moved into clinical trials. As new treatments move through a series of steps called phases, more information is gained about the treatment, its risks, and its effectiveness.
What are clinical trial protocols?
Clinical trials follow a plan known as a protocol. The protocol is carefully designed to balance the potential benefits and risks to participants, and answer specific research questions. A protocol describes the following:
- The goal of the study
- Who is eligible to take part in the trial
- Protections against risks to participants
- Details about tests, procedures, and treatments
- How long the trial is expected to last
- What information will be gathered
A clinical trial is led by a principal investigator (PI). Members of the research team regularly monitor the participants’ health to determine the study’s safety and effectiveness.
What is an Institutional Review Board?
Most, but not all, clinical trials in the United States are approved and monitored by an Institutional Review Board (IRB) to ensure that the risks are reduced and are outweighed by potential benefits. IRBs are committees that are responsible for reviewing research in order to protect the rights and safety of people who take part in research, both before the research starts and as it proceeds. You should ask the sponsor or research coordinator whether the research you are thinking about joining was reviewed by an IRB.
What is a clinical trial sponsor?
Clinical trial sponsors may be people, institutions, companies, government agencies, or other organizations that are responsible for initiating, managing or financing the clinical trial, but do not conduct the research.
What is informed consent?
Informed consent is the process of providing you with key information about a research study before you decide whether to accept the offer to take part. The process of informed consent continues throughout the study. To help you decide whether to take part, members of the research team explain the details of the study. If you do not understand English, a translator or interpreter may be provided. The research team provides an informed consent document that includes details about the study, such as its purpose, how long it’s expected to last, tests or procedures that will be done as part of the research, and who to contact for further information. The informed consent document also explains risks and potential benefits. You can then decide whether to sign the document. Taking part in a clinical trial is voluntary and you can leave the study at any time.
What are the types of clinical trials?
There are different types of clinical trials.
- Prevention trials look for better ways to prevent a disease in people who have never had the disease or to prevent the disease from returning. Approaches may include medicines, vaccines, or lifestyle changes.
- Screening trials test new ways for detecting diseases or health conditions.
- Diagnostic trials study or compare tests or procedures for diagnosing a particular disease or condition.
- Treatment trials test new treatments, new combinations of drugs, or new approaches to surgery or radiation therapy.
- Behavioral trials evaluate or compare ways to promote behavioral changes designed to improve health.
- Quality of life trials (or supportive care trials) explore and measure ways to improve the comfort and quality of life of people with conditions or illnesses.
What are the phases of clinical trials?
Clinical trials are conducted in a series of steps called “phases.” Each phase has a different purpose and helps researchers answer different questions.
- Phase I trials : Researchers test a drug or treatment in a small group of people (20–80) for the first time. The purpose is to study the drug or treatment to learn about safety and identify side effects.
- Phase II trials : The new drug or treatment is given to a larger group of people (100–300) to determine its effectiveness and to further study its safety.
- Phase III trials : The new drug or treatment is given to large groups of people (1,000–3,000) to confirm its effectiveness, monitor side effects, compare it with standard or similar treatments, and collect information that will allow the new drug or treatment to be used safely.
- Phase IV trials : After a drug is approved by the FDA and made available to the public, researchers track its safety in the general population, seeking more information about a drug or treatment’s benefits, and optimal use.
What do the terms placebo, randomization, and blinded mean in clinical trials?
In clinical trials that compare a new product or therapy with another that already exists, researchers try to determine if the new one is as good, or better than, the existing one. In some studies, you may be assigned to receive a placebo (an inactive product that resembles the test product, but without its treatment value).
Comparing a new product with a placebo can be the fastest and most reliable way to show the new product’s effectiveness. However, placebos are not used if you would be put at risk — particularly in the study of treatments for serious illnesses — by not having effective therapy. You will be told if placebos are used in the study before entering a trial.
Randomization is the process by which treatments are assigned to participants by chance rather than by choice. This is done to avoid any bias in assigning volunteers to get one treatment or another. The effects of each treatment are compared at specific points during a trial. If one treatment is found superior, the trial is stopped so that the most volunteers receive the more beneficial treatment. This video helps explain randomization for all clinical trials .
" Blinded " (or " masked ") studies are designed to prevent members of the research team and study participants from influencing the results. Blinding allows the collection of scientifically accurate data. In single-blind (" single-masked ") studies, you are not told what is being given, but the research team knows. In a double-blind study, neither you nor the research team are told what you are given; only the pharmacist knows. Members of the research team are not told which participants are receiving which treatment, in order to reduce bias. If medically necessary, however, it is always possible to find out which treatment you are receiving.
Who takes part in clinical trials?
Many different types of people take part in clinical trials. Some are healthy, while others may have illnesses. Research procedures with healthy volunteers are designed to develop new knowledge, not to provide direct benefit to those taking part. Healthy volunteers have always played an important role in research.
Healthy volunteers are needed for several reasons. When developing a new technique, such as a blood test or imaging device, healthy volunteers help define the limits of "normal." These volunteers are the baseline against which patient groups are compared and are often matched to patients on factors such as age, gender, or family relationship. They receive the same tests, procedures, or drugs the patient group receives. Researchers learn about the disease process by comparing the patient group to the healthy volunteers.
Factors like how much of your time is needed, discomfort you may feel, or risk involved depends on the trial. While some require minimal amounts of time and effort, other studies may require a major commitment of your time and effort, and may involve some discomfort. The research procedure(s) may also carry some risk. The informed consent process for healthy volunteers includes a detailed discussion of the study's procedures and tests and their risks.
A patient volunteer has a known health problem and takes part in research to better understand, diagnose, or treat that disease or condition. Research with a patient volunteer helps develop new knowledge. Depending on the stage of knowledge about the disease or condition, these procedures may or may not benefit the study participants.
Patients may volunteer for studies similar to those in which healthy volunteers take part. These studies involve drugs, devices, or treatments designed to prevent,or treat disease. Although these studies may provide direct benefit to patient volunteers, the main aim is to prove, by scientific means, the effects and limitations of the experimental treatment. Therefore, some patient groups may serve as a baseline for comparison by not taking the test drug, or by receiving test doses of the drug large enough only to show that it is present, but not at a level that can treat the condition.
Researchers follow clinical trials guidelines when deciding who can participate, in a study. These guidelines are called Inclusion/Exclusion Criteria . Factors that allow you to take part in a clinical trial are called "inclusion criteria." Those that exclude or prevent participation are "exclusion criteria." These criteria are based on factors such as age, gender, the type and stage of a disease, treatment history, and other medical conditions. Before joining a clinical trial, you must provide information that allows the research team to determine whether or not you can take part in the study safely. Some research studies seek participants with illnesses or conditions to be studied in the clinical trial, while others need healthy volunteers. Inclusion and exclusion criteria are not used to reject people personally. Instead, the criteria are used to identify appropriate participants and keep them safe, and to help ensure that researchers can find new information they need.
What do I need to know if I am thinking about taking part in a clinical trial?

Risks and potential benefits
Clinical trials may involve risk, as can routine medical care and the activities of daily living. When weighing the risks of research, you can think about these important factors:
- The possible harms that could result from taking part in the study
- The level of harm
- The chance of any harm occurring
Most clinical trials pose the risk of minor discomfort, which lasts only a short time. However, some study participants experience complications that require medical attention. In rare cases, participants have been seriously injured or have died of complications resulting from their participation in trials of experimental treatments. The specific risks associated with a research protocol are described in detail in the informed consent document, which participants are asked to consider and sign before participating in research. Also, a member of the research team will explain the study and answer any questions about the study. Before deciding to participate, carefully consider risks and possible benefits.
Potential benefits
Well-designed and well-executed clinical trials provide the best approach for you to:
- Help others by contributing to knowledge about new treatments or procedures.
- Gain access to new research treatments before they are widely available.
- Receive regular and careful medical attention from a research team that includes doctors and other health professionals.
Risks to taking part in clinical trials include the following:
- There may be unpleasant, serious, or even life-threatening effects of experimental treatment.
- The study may require more time and attention than standard treatment would, including visits to the study site, more blood tests, more procedures, hospital stays, or complex dosage schedules.
What questions should I ask if offered a clinical trial?
If you are thinking about taking part in a clinical trial, you should feel free to ask any questions or bring up any issues concerning the trial at any time. The following suggestions may give you some ideas as you think about your own questions.
- What is the purpose of the study?
- Why do researchers think the approach may be effective?
- Who will fund the study?
- Who has reviewed and approved the study?
- How are study results and safety of participants being monitored?
- How long will the study last?
- What will my responsibilities be if I take part?
- Who will tell me about the results of the study and how will I be informed?
Risks and possible benefits
- What are my possible short-term benefits?
- What are my possible long-term benefits?
- What are my short-term risks, and side effects?
- What are my long-term risks?
- What other options are available?
- How do the risks and possible benefits of this trial compare with those options?
Participation and care
- What kinds of therapies, procedures and/or tests will I have during the trial?
- Will they hurt, and if so, for how long?
- How do the tests in the study compare with those I would have outside of the trial?
- Will I be able to take my regular medications while taking part in the clinical trial?
- Where will I have my medical care?
- Who will be in charge of my care?
Personal issues
- How could being in this study affect my daily life?
- Can I talk to other people in the study?

Cost issues
- Will I have to pay for any part of the trial such as tests or the study drug?
- If so, what will the charges likely be?
- What is my health insurance likely to cover?
- Who can help answer any questions from my insurance company or health plan?
- Will there be any travel or child care costs that I need to consider while I am in the trial?
Tips for asking your doctor about trials
- Consider taking a family member or friend along for support and for help in asking questions or recording answers.
- Plan what to ask — but don't hesitate to ask any new questions.
- Write down questions in advance to remember them all.
- Write down the answers so that they’re available when needed.
- Ask about bringing a tape recorder to make a taped record of what's said (even if you write down answers).
This information courtesy of Cancer.gov.
How is my safety protected?

Ethical guidelines
The goal of clinical research is to develop knowledge that improves human health or increases understanding of human biology. People who take part in clinical research make it possible for this to occur. The path to finding out if a new drug is safe or effective is to test it on patients in clinical trials. The purpose of ethical guidelines is both to protect patients and healthy volunteers, and to preserve the integrity of the science.
Informed consent
Informed consent is the process of learning the key facts about a clinical trial before deciding whether to participate. The process of providing information to participants continues throughout the study. To help you decide whether to take part, members of the research team explain the study. The research team provides an informed consent document, which includes such details about the study as its purpose, duration, required procedures, and who to contact for various purposes. The informed consent document also explains risks and potential benefits.
If you decide to enroll in the trial, you will need to sign the informed consent document. You are free to withdraw from the study at any time.
Most, but not all, clinical trials in the United States are approved and monitored by an Institutional Review Board (IRB) to ensure that the risks are minimal when compared with potential benefits. An IRB is an independent committee that consists of physicians, statisticians, and members of the community who ensure that clinical trials are ethical and that the rights of participants are protected. You should ask the sponsor or research coordinator whether the research you are considering participating in was reviewed by an IRB.
Further reading
For more information about research protections, see:
- Office of Human Research Protection
- Children's Assent to Clinical Trial Participation
For more information on participants’ privacy and confidentiality, see:
- HIPAA Privacy Rule
- The Food and Drug Administration, FDA’s Drug Review Process: Ensuring Drugs Are Safe and Effective
For more information about research protections, see: About Research Participation
What happens after a clinical trial is completed?
After a clinical trial is completed, the researchers carefully examine information collected during the study before making decisions about the meaning of the findings and about the need for further testing. After a phase I or II trial, the researchers decide whether to move on to the next phase or to stop testing the treatment or procedure because it was unsafe or not effective. When a phase III trial is completed, the researchers examine the information and decide whether the results have medical importance.
Results from clinical trials are often published in peer-reviewed scientific journals. Peer review is a process by which experts review the report before it is published to ensure that the analysis and conclusions are sound. If the results are particularly important, they may be featured in the news, and discussed at scientific meetings and by patient advocacy groups before or after they are published in a scientific journal. Once a new approach has been proven safe and effective in a clinical trial, it may become a new standard of medical practice.
Ask the research team members if the study results have been or will be published. Published study results are also available by searching for the study's official name or Protocol ID number in the National Library of Medicine's PubMed® database .
How does clinical research make a difference to me and my family?

Only through clinical research can we gain insights and answers about the safety and effectiveness of treatments and procedures. Groundbreaking scientific advances in the present and the past were possible only because of participation of volunteers, both healthy and those with an illness, in clinical research. Clinical research requires complex and rigorous testing in collaboration with communities that are affected by the disease. As research opens new doors to finding ways to diagnose, prevent, treat, or cure disease and disability, clinical trial participation is essential to help us find the answers.
This page last reviewed on October 3, 2022
Connect with Us
- More Social Media from NIH
Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
Methodology
Research Methods | Definitions, Types, Examples
Research methods are specific procedures for collecting and analyzing data. Developing your research methods is an integral part of your research design . When planning your methods, there are two key decisions you will make.
First, decide how you will collect data . Your methods depend on what type of data you need to answer your research question :
- Qualitative vs. quantitative : Will your data take the form of words or numbers?
- Primary vs. secondary : Will you collect original data yourself, or will you use data that has already been collected by someone else?
- Descriptive vs. experimental : Will you take measurements of something as it is, or will you perform an experiment?
Second, decide how you will analyze the data .
- For quantitative data, you can use statistical analysis methods to test relationships between variables.
- For qualitative data, you can use methods such as thematic analysis to interpret patterns and meanings in the data.
Table of contents
Methods for collecting data, examples of data collection methods, methods for analyzing data, examples of data analysis methods, other interesting articles, frequently asked questions about research methods.
Data is the information that you collect for the purposes of answering your research question . The type of data you need depends on the aims of your research.
Qualitative vs. quantitative data
Your choice of qualitative or quantitative data collection depends on the type of knowledge you want to develop.
For questions about ideas, experiences and meanings, or to study something that can’t be described numerically, collect qualitative data .
If you want to develop a more mechanistic understanding of a topic, or your research involves hypothesis testing , collect quantitative data .
| Qualitative | to broader populations. . | |
|---|---|---|
| Quantitative | . |
You can also take a mixed methods approach , where you use both qualitative and quantitative research methods.
Primary vs. secondary research
Primary research is any original data that you collect yourself for the purposes of answering your research question (e.g. through surveys , observations and experiments ). Secondary research is data that has already been collected by other researchers (e.g. in a government census or previous scientific studies).
If you are exploring a novel research question, you’ll probably need to collect primary data . But if you want to synthesize existing knowledge, analyze historical trends, or identify patterns on a large scale, secondary data might be a better choice.
| Primary | . | methods. |
|---|---|---|
| Secondary |
Descriptive vs. experimental data
In descriptive research , you collect data about your study subject without intervening. The validity of your research will depend on your sampling method .
In experimental research , you systematically intervene in a process and measure the outcome. The validity of your research will depend on your experimental design .
To conduct an experiment, you need to be able to vary your independent variable , precisely measure your dependent variable, and control for confounding variables . If it’s practically and ethically possible, this method is the best choice for answering questions about cause and effect.
| Descriptive | . . | |
|---|---|---|
| Experimental |
Here's why students love Scribbr's proofreading services
Discover proofreading & editing
| Research method | Primary or secondary? | Qualitative or quantitative? | When to use |
|---|---|---|---|
| Primary | Quantitative | To test cause-and-effect relationships. | |
| Primary | Quantitative | To understand general characteristics of a population. | |
| Interview/focus group | Primary | Qualitative | To gain more in-depth understanding of a topic. |
| Observation | Primary | Either | To understand how something occurs in its natural setting. |
| Secondary | Either | To situate your research in an existing body of work, or to evaluate trends within a research topic. | |
| Either | Either | To gain an in-depth understanding of a specific group or context, or when you don’t have the resources for a large study. |
Your data analysis methods will depend on the type of data you collect and how you prepare it for analysis.
Data can often be analyzed both quantitatively and qualitatively. For example, survey responses could be analyzed qualitatively by studying the meanings of responses or quantitatively by studying the frequencies of responses.
Qualitative analysis methods
Qualitative analysis is used to understand words, ideas, and experiences. You can use it to interpret data that was collected:
- From open-ended surveys and interviews , literature reviews , case studies , ethnographies , and other sources that use text rather than numbers.
- Using non-probability sampling methods .
Qualitative analysis tends to be quite flexible and relies on the researcher’s judgement, so you have to reflect carefully on your choices and assumptions and be careful to avoid research bias .
Quantitative analysis methods
Quantitative analysis uses numbers and statistics to understand frequencies, averages and correlations (in descriptive studies) or cause-and-effect relationships (in experiments).
You can use quantitative analysis to interpret data that was collected either:
- During an experiment .
- Using probability sampling methods .
Because the data is collected and analyzed in a statistically valid way, the results of quantitative analysis can be easily standardized and shared among researchers.
| Research method | Qualitative or quantitative? | When to use |
|---|---|---|
| Quantitative | To analyze data collected in a statistically valid manner (e.g. from experiments, surveys, and observations). | |
| Meta-analysis | Quantitative | To statistically analyze the results of a large collection of studies. Can only be applied to studies that collected data in a statistically valid manner. |
| Qualitative | To analyze data collected from interviews, , or textual sources. To understand general themes in the data and how they are communicated. | |
| Either | To analyze large volumes of textual or visual data collected from surveys, literature reviews, or other sources. Can be quantitative (i.e. frequencies of words) or qualitative (i.e. meanings of words). |
If you want to know more about statistics , methodology , or research bias , make sure to check out some of our other articles with explanations and examples.
- Chi square test of independence
- Statistical power
- Descriptive statistics
- Degrees of freedom
- Pearson correlation
- Null hypothesis
- Double-blind study
- Case-control study
- Research ethics
- Data collection
- Hypothesis testing
- Structured interviews
Research bias
- Hawthorne effect
- Unconscious bias
- Recall bias
- Halo effect
- Self-serving bias
- Information bias
Quantitative research deals with numbers and statistics, while qualitative research deals with words and meanings.
Quantitative methods allow you to systematically measure variables and test hypotheses . Qualitative methods allow you to explore concepts and experiences in more detail.
In mixed methods research , you use both qualitative and quantitative data collection and analysis methods to answer your research question .
A sample is a subset of individuals from a larger population . Sampling means selecting the group that you will actually collect data from in your research. For example, if you are researching the opinions of students in your university, you could survey a sample of 100 students.
In statistics, sampling allows you to test a hypothesis about the characteristics of a population.
The research methods you use depend on the type of data you need to answer your research question .
- If you want to measure something or test a hypothesis , use quantitative methods . If you want to explore ideas, thoughts and meanings, use qualitative methods .
- If you want to analyze a large amount of readily-available data, use secondary data. If you want data specific to your purposes with control over how it is generated, collect primary data.
- If you want to establish cause-and-effect relationships between variables , use experimental methods. If you want to understand the characteristics of a research subject, use descriptive methods.
Methodology refers to the overarching strategy and rationale of your research project . It involves studying the methods used in your field and the theories or principles behind them, in order to develop an approach that matches your objectives.
Methods are the specific tools and procedures you use to collect and analyze data (for example, experiments, surveys , and statistical tests ).
In shorter scientific papers, where the aim is to report the findings of a specific study, you might simply describe what you did in a methods section .
In a longer or more complex research project, such as a thesis or dissertation , you will probably include a methodology section , where you explain your approach to answering the research questions and cite relevant sources to support your choice of methods.
Is this article helpful?
Other students also liked, writing strong research questions | criteria & examples.
- What Is a Research Design | Types, Guide & Examples
- Data Collection | Definition, Methods & Examples
More interesting articles
- Between-Subjects Design | Examples, Pros, & Cons
- Cluster Sampling | A Simple Step-by-Step Guide with Examples
- Confounding Variables | Definition, Examples & Controls
- Construct Validity | Definition, Types, & Examples
- Content Analysis | Guide, Methods & Examples
- Control Groups and Treatment Groups | Uses & Examples
- Control Variables | What Are They & Why Do They Matter?
- Correlation vs. Causation | Difference, Designs & Examples
- Correlational Research | When & How to Use
- Critical Discourse Analysis | Definition, Guide & Examples
- Cross-Sectional Study | Definition, Uses & Examples
- Descriptive Research | Definition, Types, Methods & Examples
- Ethical Considerations in Research | Types & Examples
- Explanatory and Response Variables | Definitions & Examples
- Explanatory Research | Definition, Guide, & Examples
- Exploratory Research | Definition, Guide, & Examples
- External Validity | Definition, Types, Threats & Examples
- Extraneous Variables | Examples, Types & Controls
- Guide to Experimental Design | Overview, Steps, & Examples
- How Do You Incorporate an Interview into a Dissertation? | Tips
- How to Do Thematic Analysis | Step-by-Step Guide & Examples
- How to Write a Literature Review | Guide, Examples, & Templates
- How to Write a Strong Hypothesis | Steps & Examples
- Inclusion and Exclusion Criteria | Examples & Definition
- Independent vs. Dependent Variables | Definition & Examples
- Inductive Reasoning | Types, Examples, Explanation
- Inductive vs. Deductive Research Approach | Steps & Examples
- Internal Validity in Research | Definition, Threats, & Examples
- Internal vs. External Validity | Understanding Differences & Threats
- Longitudinal Study | Definition, Approaches & Examples
- Mediator vs. Moderator Variables | Differences & Examples
- Mixed Methods Research | Definition, Guide & Examples
- Multistage Sampling | Introductory Guide & Examples
- Naturalistic Observation | Definition, Guide & Examples
- Operationalization | A Guide with Examples, Pros & Cons
- Population vs. Sample | Definitions, Differences & Examples
- Primary Research | Definition, Types, & Examples
- Qualitative vs. Quantitative Research | Differences, Examples & Methods
- Quasi-Experimental Design | Definition, Types & Examples
- Questionnaire Design | Methods, Question Types & Examples
- Random Assignment in Experiments | Introduction & Examples
- Random vs. Systematic Error | Definition & Examples
- Reliability vs. Validity in Research | Difference, Types and Examples
- Reproducibility vs Replicability | Difference & Examples
- Reproducibility vs. Replicability | Difference & Examples
- Sampling Methods | Types, Techniques & Examples
- Semi-Structured Interview | Definition, Guide & Examples
- Simple Random Sampling | Definition, Steps & Examples
- Single, Double, & Triple Blind Study | Definition & Examples
- Stratified Sampling | Definition, Guide & Examples
- Structured Interview | Definition, Guide & Examples
- Survey Research | Definition, Examples & Methods
- Systematic Review | Definition, Example, & Guide
- Systematic Sampling | A Step-by-Step Guide with Examples
- Textual Analysis | Guide, 3 Approaches & Examples
- The 4 Types of Reliability in Research | Definitions & Examples
- The 4 Types of Validity in Research | Definitions & Examples
- Transcribing an Interview | 5 Steps & Transcription Software
- Triangulation in Research | Guide, Types, Examples
- Types of Interviews in Research | Guide & Examples
- Types of Research Designs Compared | Guide & Examples
- Types of Variables in Research & Statistics | Examples
- Unstructured Interview | Definition, Guide & Examples
- What Is a Case Study? | Definition, Examples & Methods
- What Is a Case-Control Study? | Definition & Examples
- What Is a Cohort Study? | Definition & Examples
- What Is a Conceptual Framework? | Tips & Examples
- What Is a Controlled Experiment? | Definitions & Examples
- What Is a Double-Barreled Question?
- What Is a Focus Group? | Step-by-Step Guide & Examples
- What Is a Likert Scale? | Guide & Examples
- What Is a Prospective Cohort Study? | Definition & Examples
- What Is a Retrospective Cohort Study? | Definition & Examples
- What Is Action Research? | Definition & Examples
- What Is an Observational Study? | Guide & Examples
- What Is Concurrent Validity? | Definition & Examples
- What Is Content Validity? | Definition & Examples
- What Is Convenience Sampling? | Definition & Examples
- What Is Convergent Validity? | Definition & Examples
- What Is Criterion Validity? | Definition & Examples
- What Is Data Cleansing? | Definition, Guide & Examples
- What Is Deductive Reasoning? | Explanation & Examples
- What Is Discriminant Validity? | Definition & Example
- What Is Ecological Validity? | Definition & Examples
- What Is Ethnography? | Definition, Guide & Examples
- What Is Face Validity? | Guide, Definition & Examples
- What Is Non-Probability Sampling? | Types & Examples
- What Is Participant Observation? | Definition & Examples
- What Is Peer Review? | Types & Examples
- What Is Predictive Validity? | Examples & Definition
- What Is Probability Sampling? | Types & Examples
- What Is Purposive Sampling? | Definition & Examples
- What Is Qualitative Observation? | Definition & Examples
- What Is Qualitative Research? | Methods & Examples
- What Is Quantitative Observation? | Definition & Examples
- What Is Quantitative Research? | Definition, Uses & Methods
"I thought AI Proofreading was useless but.."
I've been using Scribbr for years now and I know it's a service that won't disappoint. It does a good job spotting mistakes”
Information for Research Subjects
Learn about becoming a research participant at the University of Rochester
True to the University of Rochester’s Mission Statement, ‘Learn, Discover, Heal, Create—and Make the World Ever Better’, research has been a long-standing tradition at the University of Rochester . Our researchers are among the nation’s leaders across a wide range of fields, including medicine, human behavior, education, politics, optics and economics.
Find an open research study
Faqs: participating in research.
Participating in research can be a fun and exciting way to give back to your community, but it doesn’t necessarily come without risk. Becoming a research participant is an important decision that should be taken seriously.
Background and overview
Research studies are done to discover new information or to answer a question about how we learn, behave, and function. Some studies might involve simple tasks like completing a survey, being observed among a group of people, or participating in a group discussion. Other studies, sometimes called clinical trials, involve more risky procedures like testing a new drug or medical device.
Each research study has its own set of criteria to determine who can participate. This depends on the research question being asked and may include restrictions based on age, behaviors, health status, or other traits.
Deciding to participate
Research is designed to benefit society. This might include learning how to live healthier lives, how to better treat conditions or diseases, why we do the things we do, or how we learn and develop. And while there are several reasons why people choose to participate in research, most people participate based on the possibility of helping themselves or others.
It’s important to understand that you may not directly benefit from participating in research. In fact, with a lot of research, you will not receive any benefit. For some types of research however, there may be a possibility that you could receive benefit, but there is no guarantee.
Most studies involve some risk, though the risks can range from very small to very serious. Some examples of risks include:
- side effects or reactions to experimental drugs, treatments, or procedures
- feeling anxious or uncomfortable
- breach in confidentiality or invasion of privacy.
Side effects or other risks you might experience may be temporary or go away with treatment, but in rare cases they may be permanent, cause disability, or be life threatening. There may also be risks in participating that we don’t know about.
To start, you will be given information about the study so that you can make an informed decision about whether or not to participate. You will also be given an opportunity to ask questions about the study. This process is called informed consent . Before you can start the study, you need to agree to participate (i.e., consent). Participation is always voluntary.
Once you provide consent, the specific procedures or activities you’ll be asked to complete can vary widely and depend on what is being studied. Regardless, all the activities you will be asked to complete will be described during the consent process.
Before you agree to be in the study, make sure you have a solid understanding of the following:
- the voluntary nature of the study
- why the study is being done
- who is doing the study
- the procedures, activities, tests, or treatments involved (including how long they will take, how often they have to be completed, and whether there are any other treatment options available rather than being in the study)
- potential risks, discomforts, or side effects
- potential benefits to participating, if any
- how your privacy will be protected
- how long your participation will last
- what will happen if you are injured while participating
- the costs to you, if any
- what to do if you change your mind about participating
- whom to contact with questions, concerns, or problems
Each study is different, so time requirements will vary. Some may require very little of your time, perhaps only 5–10 minutes, while others may require multiple visits over an extended period of time, sometimes up to several years. Your time commitment for a particular study will be described during the consent process.
informed consent
Informed consent is the process of telling interested individuals what is involved in taking part in a specific research study. Typically, this includes:
- reviewing written information
- giving the potential volunteer time to review this information while considering participation (taking it home to review with friends or family, if desired)
- discussing the information verbally
- answering any questions
Once all of the information is provided to you and your questions are answered, you will then be asked to decide whether or not to take part in the study.
All decisions are voluntary, and you must provide your agreement (i.e., consent) before any study activities can begin. Usually, this involves signing a consent form. Although, for some studies, verbally agreeing to participate may be sufficient.
Once you provide consent to be in the study, you will continue to receive important information about your participation throughout the study.
It’s important to understand what is involved in taking part in a research study and to carefully consider what that means for you. Research can pose risks to your health, safety, and welfare, so it’s important to understand exactly what those risks are.
It’s also important to understand that taking part in research is voluntary. You make the decision about whether or not to participate, and if you agree to take part, you can always change your mind later.
State law determines who can provide consent. In New York State, only individuals 18 years of age and older can provide consent. Minors, based on their age and ability, are usually asked for their agreement to participate in research, but their parent or legal guardian must also provide their permission to participate. Other special considerations are also made when a minor is a ward of the state or adults are unable to make decisions for themselves.
If you have questions about who can or cannot provide consent, be sure to ask the study team.
The following key points are most important about informed consent:
- Being in a study is voluntary—it is your choice.
- If you join a study, you can change your mind and stop at any time.
- If you have questions about anything that is not clear to you, you can ask them at any point of time before, during, or after the study.
- If you feel you need more time or information to make an informed decision about whether or not to take part in the study, do not hesitate to ask for it.
Subject Protections
Research studies involving humans must be approved and monitored by an Institutional Review Board (IRB). An IRB is a committee of individuals responsible for reviewing research to ensure adequate protections are in place to protect the people who take part.
For each study reviewed, the IRB checks to see that:
- there is a good reason to conduct the study
- the risks related to participating are the least possible
- the risks related to participating are reasonable given the knowledge that will be gained from conducting the study
- the plan for selecting subjects to participate is fair
- subjects will be provided enough information about the study
Protecting the information you provide to researchers is a high priority, particularly if you provide health-related or sensitive information.
As part of the IRB approval process described above, all researchers must provide a plan to adequately protect the information they plan to collect in order for the study to be approved. This might include assigning a code to the information collected instead of using your name or other identifiable information and storing the information in a secure manner.
You are free to withdraw from a research study at any time, for any reason. Your relationship with the hospital, clinic, academic institution, or employer will not be affected and you will not lose any benefits to which you are entitled.
Note that in some cases, a researcher may decide to end your participation in the study early. This may happen if the study is no longer in your best interest, if you can no longer complete study activities, or if the study ends early for some other reason.
Additional participant resources
Downloadable information.
- Participating in Research Overview
- Informed Consent
External resources
- About Research Participation (Department of Health & Human Service)
- Children & Clinical Studies (National Heart, Lung & Blood Institute)
- Clinical Research Trials and You (National Institutes of Health)
University research studies
- Search UR Health Research
- Join the UR Health Research Volunteer Registry to be contacted for future studies
- Follow UR Health Research on Facebook
- CenterWatch Clinical Trials Search
- ClinicalTrials.gov
- National Institutes of Health List of Registries
- ResearchMatch
share your thoughts
Report an issue, concern, or complaint
If you have participated in University of Rochester research and would like to report an issue, concern or complaint about the research you, or a family member, has participated in, please do so via our feedback form.
Share your feedback
What Are Cancer Research Studies?
What is cancer research and why is it important.
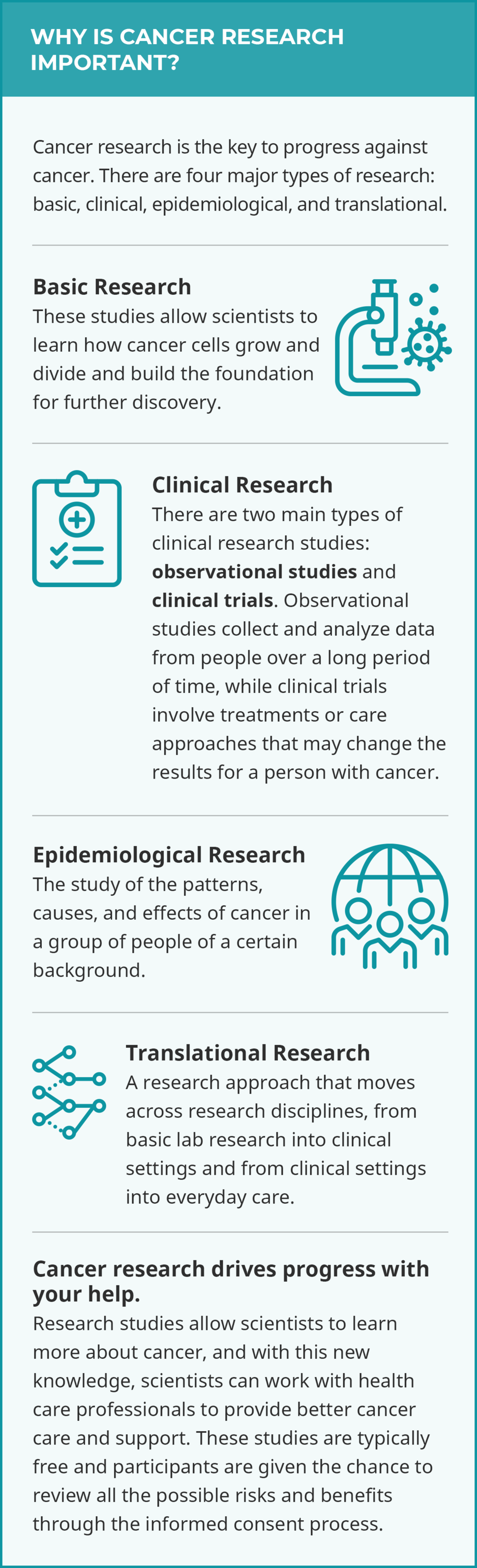
Research is the key to progress against cancer and is a complex process involving professionals from many fields. It is also thanks to the participation of people with cancer, cancer survivors, and healthy volunteers that any breakthroughs go on to improve treatment and care for those who need it.
Cancer research studies may lead to discoveries such as new drugs to treat cancer, new therapies to make symptoms less severe, or lifestyle changes to reduce the chances of getting cancer.
Cancer research may also address big picture questions like why cancer is more prevalent in certain populations or how doctors can make existing cancer detection tools more effective in health care settings.
These discoveries can help people with cancer and their caregivers live fuller lives.
Who should join cancer research studies?
When you choose to participate in a research study, you become a partner in scientific discovery. Your generous contribution can make a world of difference for people like you.
As scientists continue to conduct cancer research, anyone can consider joining a research study. The best research includes everyone, and everyone includes you.
Your unique experience with cancer is incredibly valuable and may help current and future generations lead healthier lives.
When more people of all different races, ethnicities, ages, genders, abilities, and backgrounds participate, more people benefit.
It is important for scientists to capture the full genetic diversity of human populations so that the lessons learned are applicable to everyone.
What are the types of cancer research studies?
See below for definitions on the four major types of research and their subtypes:
- basic research
- quality of life/supportive care
- natural history
- longitudinal
- population-based
- epidemiological research
- translational research
Basic Research
Basic cancer research studies explore the very laws of nature. Scientists learn how cancer cells grow and divide, for example, by growing and testing bacteria , viruses , fungi , animal cells, and human cells in a lab. Scientists also study, for example, the genes that make up tumors in mice and rats in the lab. These experiments help build the foundation for further discovery.

Why Participate in a Clinical Trial?
Get information on how to evaluate a clinical trial and what questions to ask.
Clinical Research
Clinical research involves the study of cancer in people. These cancer research studies are further broken down into two types: clinical trials and observational studies .
- Treatment trials test how safe and useful a new treatment or way of using existing treatments is for people with cancer. Test treatments may include drugs, approaches to surgery or radiation therapy , or combinations of treatments.
- Prevention trials are for people who do not have cancer but are at a high risk for developing cancer or for cancer coming back. Prevention clinical trials target lifestyle changes (doing something) or focus on certain nutrients or medicines (adding something).
- Screening trials test how effective screening tests are for healthy people. The goal of these trials is to discover screening tools or methods that reduce deaths from cancer by finding it earlier.
- Quality-of-life/supportive care tests aim to help people with cancer, as well as their family and loved ones, cope with side effects like pain, nutrition problems, nausea and vomiting , sleeping problems, and depression . These trials may involve drugs or activities like therapy and exercising.

Find Observational Studies
View a studies that are looking for people now.
- Natural history studies look at certain conditions in people with cancer or people who are at a high risk of developing cancer. Researchers often collect information about a person and their family medical history , as well as blood, saliva, and tumor samples. For example, a biomarker test may be used to get a genetic profile of a person’s cancer tissue. This may reveal how certain tumors change over the course of treatment .
- Longitudinal studies gather data on people or groups of people over time, often to see the result of a habit, treatment, or change. For example, two groups of people may be identified as those who smoke and those who do not. These two groups are compared over time to see whether one group is more likely to develop cancer than the other group.
- Population-based studies explore the causes of cancer, cancer trends, and factors that affect cancer care in specific populations. For example, a population-based study may explore the causes of a high cancer rate in a regional Native American population.
Epidemiological Research
Epidemiological research is the study of the patterns, causes, and effects of cancer in a group of people of a certain background. This research encompasses both observational population-based studies but also includes clinical epidemiological studies where the relationship between a population’s risk factors and treatments are tested.
Translational Research
Translational research is when cancer research moves across research disciplines, from basic lab research into clinical settings, and from clinical settings into everyday care. In turn, findings from clinical studies and population-based studies can inform basic cancer research. For example, data from the genetic profile of a tumor during an observational study may help scientists develop a clinical trial to test which drugs to prescribe to cancer patients with specific tumor genes.

Monica Bertagnolli, Director, NIH; former director, NCI; cancer survivor
Participation in Cancer Research Matters
I am so happy to have the opportunity to acknowledge the courage and generosity of an estimated 494,018 women who agreed to participate in randomized clinical trials with results reported between 1971 and 2018.
Their contributions showed that mammography can detect cancer at an early stage, that mastectomies and axillary lymph node dissections are not always necessary, that chemotherapy can benefit some people with early estrogen receptor–positive, progesterone receptor–positive, HER2-negative breast cancer but is not needed for all, and that hormonal therapy can prevent disease recurrence.
For just the key studies that produced these results, it took the strength and commitment of almost 500,000 women. I am the direct beneficiary of their contributions, and I am profoundly grateful.
The true number of brave souls contributing to this reduction in breast cancer mortality over the past 30 years? Many millions. These are our heroes.
— From NCI Director’s Remarks by then-NCI Director Monica M. Bertagnolli, M.D., at the American Society of Clinical Oncology Annual Meeting, June 3, 2023
Your Account
Manage your account, subscriptions and profile.
MyKomen Health
ShareForCures
In Your Community
In Your Community
View resources and events in your local community.
Change your location:

Susan G. Komen®
One moment can change everything.
Types of Research Studies
Epidemiology studies.
Epidemiology is the study of the patterns and causes of disease in people.
The goal of epidemiology studies is to give information that helps support or disprove an idea about a possible link between an exposure (such as alcohol use) and an outcome (such as breast cancer) in people.
The 2 main types of epidemiology studies are:
- Observational studies ( prospective cohort or case-control )
Randomized controlled trials
Though they have the same goal, observational studies and randomized controlled trials differ in:
- The way they are conducted
- The strengths of the conclusions they reach
Observational studies
In observational studies, the people in the study live their daily lives as they choose. They exercise when they want, eat what they like and take the medicines their doctors prescribe. They report these activities to researchers.
There are 2 types of observational studies:
Prospective cohort studies
Case-control studies.
A prospective cohort study follows a large group of people forward in time.
Some people will have a certain exposure (such as alcohol use) and others will not.
Researchers compare the different groups (for example, they might compare heavy drinkers, moderate drinkers, light drinkers and non-drinkers) to see which group is more likely to develop an outcome (such as breast cancer).
In a case-control study, researchers identify 2 groups: cases and controls.
- Cases are people who already have an outcome (such as breast cancer).
- Controls are people who do not have the outcome.
The researchers compare the 2 groups to see if any exposure (such as alcohol use) was more common in the history of one group compared to the other.
In randomized controlled trials (randomized clinical trials), researchers divide people into groups to compare different treatments or other interventions.
These studies are called randomized controlled trials because people are randomly assigned (as if by coin toss) to a certain treatment or behavior.
For example, in a randomized trial of a new drug therapy, half the people might be randomly assigned to a new drug and the other half to the standard treatment.
In a randomized controlled trial on exercise and breast cancer risk, half the participants might be randomly assigned to walk 10 minutes a day and the other half to walk 2 hours a day. The researchers would then see which group was more likely to develop breast cancer, those who walked 10 minutes a day or those who walked 2 hours a day.
Many behaviors, such as smoking or heavy alcohol drinking, can’t be tested in this way because it isn’t ethical to assign people to a behavior known to be harmful. In these cases, researchers must use observational studies.
Patient series
A patient series is a doctor’s observations of a group of patients who are given a certain treatment.
There is no comparison group in a patient series. All the patients are given a certain treatment and the outcomes of these patients are studied.
With no comparison group, it’s hard to draw firm conclusions about the effectiveness of a treatment.
For example, if 10 women with breast cancer are given a new treatment, and 2 of them respond, how do we know if the new treatment is better than standard treatment?
If we had a comparison group of 10 women with breast cancer who got standard treatment, we could compare their outcomes to those of the 10 women on the new treatment. If no women in the comparison group responded to standard treatment, then the 2 women who responded to the new treatment would represent a success of the new treatment. If, however, 2 of the 10 women in the standard treatment group also responded, then the new treatment is no better than the standard.
The lack of a comparison group makes it hard to draw conclusions from a patient series. However, data from a patient series can help form hypotheses that can be tested in other types of studies.
Strengths and weaknesses of different types of research studies
When reviewing scientific evidence, it’s helpful to understand the strengths and weaknesses of different types of research studies.
Case-control studies have some strengths:
- They are easy and fairly inexpensive to conduct.
- They are a good way for researchers to study rare diseases. If a disease is rare, you would need to follow a very large group of people forward in time to have many cases of the disease develop.
- They are a good way for researchers to study diseases that take a long time to develop. If a disease takes a long time to develop, you would have to follow a group of people for many years for cases of the disease to develop.
Case-control studies look at past exposures of people who already have a disease. This causes some concerns:
- It can be hard for people to remember details about the past, especially when it comes to things like diet.
- Memories can be biased (or influenced) because the information is gathered after an event, such as the diagnosis of breast cancer.
- When it comes to sensitive topics (such as abortion), the cases (the people with the disease) may be much more likely to give complete information about their history than the controls (the people without the disease). Such differences in reporting bias study results.
For these reasons, the accuracy of the results of case-control studies can be questionable.
Cohort studies
Prospective cohort studies avoid many of the problems of case-control studies because they gather information from people over time and before the events being studied happen.
However, compared to case-control studies, they are expensive to conduct.
Nested case-control studies
A nested case-control study is a case-control study within a prospective cohort study.
Nested case-control studies use the design of a case-control study. However, they use data gathered as part of a cohort study, so they are less prone to bias than standard case-control studies.
All things being equal, the strength of nested case-control data falls somewhere between that of standard case-control studies and cohort studies.
Randomized controlled trials are considered the gold standard for studying certain exposures, such as breast cancer treatment. Similar to cohort studies, they follow people over time and are expensive to do.
Because people in a randomized trial are randomly assigned to an intervention (such as a new chemotherapy drug) or standard treatment, these studies are more likely to show the true link between an intervention and a health outcome (such as survival).
Learn more about randomized clinical trials , including the types of clinical trials, benefits, and possible drawbacks.
Overall study quality
The overall quality of a study is important. For example, the results from a well-designed case-control study can be more reliable than those from a poorly-designed randomized trial.
Finding more information on research study design
If you’re interested in learning more about research study design, a basic epidemiology textbook from your local library may be a good place to start. The National Cancer Institute also has information on epidemiology studies and randomized controlled trials.
Animal studies
Animal studies add to our understanding of how and why some factors cause cancer in people.
However, there are many differences between animals and people, so it makes it hard to translate findings directly from one to the other.
Animal studies are also designed differently. They often look at exposures in larger doses and for shorter periods of time than are suitable for people.
While animal studies can lay the groundwork for research in people, we need human studies to draw conclusions for people.
All data presented within this section of the website come from studies done with people.
Joining a research study
Research is ongoing to improve all areas of breast cancer, from prevention to treatment.
Whether you’re newly diagnosed, finished breast cancer treatment many years ago, or even if you’ve never had breast cancer, there may be breast cancer research studies you can join.
If you have breast cancer, BreastCancerTrials.org in collaboration with Susan G. Komen® offers a custom matching service that can help find a studies that fit your needs. You can also visit the National Institutes of Health’s website to find a breast cancer treatment study.
If you’re interested in being part of other studies, talk with your health care provider. Your provider may know of studies in your area looking for volunteers.
Learn more about joining a research study .
Learn more about clinical trials .
Learn what Komen is doing to help people find and participate in clinical trials .
Updated 12/16/20
TOOLS & RESOURCES
In Your Own Words
How has having breast cancer changed your outlook?
Share Your Story or Read Others
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Perspect Clin Res
- v.9(4); Oct-Dec 2018
Study designs: Part 1 – An overview and classification
Priya ranganathan.
Department of Anaesthesiology, Tata Memorial Centre, Mumbai, Maharashtra, India
Rakesh Aggarwal
1 Department of Gastroenterology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, Uttar Pradesh, India
There are several types of research study designs, each with its inherent strengths and flaws. The study design used to answer a particular research question depends on the nature of the question and the availability of resources. In this article, which is the first part of a series on “study designs,” we provide an overview of research study designs and their classification. The subsequent articles will focus on individual designs.
INTRODUCTION
Research study design is a framework, or the set of methods and procedures used to collect and analyze data on variables specified in a particular research problem.
Research study designs are of many types, each with its advantages and limitations. The type of study design used to answer a particular research question is determined by the nature of question, the goal of research, and the availability of resources. Since the design of a study can affect the validity of its results, it is important to understand the different types of study designs and their strengths and limitations.
There are some terms that are used frequently while classifying study designs which are described in the following sections.
A variable represents a measurable attribute that varies across study units, for example, individual participants in a study, or at times even when measured in an individual person over time. Some examples of variables include age, sex, weight, height, health status, alive/dead, diseased/healthy, annual income, smoking yes/no, and treated/untreated.
Exposure (or intervention) and outcome variables
A large proportion of research studies assess the relationship between two variables. Here, the question is whether one variable is associated with or responsible for change in the value of the other variable. Exposure (or intervention) refers to the risk factor whose effect is being studied. It is also referred to as the independent or the predictor variable. The outcome (or predicted or dependent) variable develops as a consequence of the exposure (or intervention). Typically, the term “exposure” is used when the “causative” variable is naturally determined (as in observational studies – examples include age, sex, smoking, and educational status), and the term “intervention” is preferred where the researcher assigns some or all participants to receive a particular treatment for the purpose of the study (experimental studies – e.g., administration of a drug). If a drug had been started in some individuals but not in the others, before the study started, this counts as exposure, and not as intervention – since the drug was not started specifically for the study.
Observational versus interventional (or experimental) studies
Observational studies are those where the researcher is documenting a naturally occurring relationship between the exposure and the outcome that he/she is studying. The researcher does not do any active intervention in any individual, and the exposure has already been decided naturally or by some other factor. For example, looking at the incidence of lung cancer in smokers versus nonsmokers, or comparing the antenatal dietary habits of mothers with normal and low-birth babies. In these studies, the investigator did not play any role in determining the smoking or dietary habit in individuals.
For an exposure to determine the outcome, it must precede the latter. Any variable that occurs simultaneously with or following the outcome cannot be causative, and hence is not considered as an “exposure.”
Observational studies can be either descriptive (nonanalytical) or analytical (inferential) – this is discussed later in this article.
Interventional studies are experiments where the researcher actively performs an intervention in some or all members of a group of participants. This intervention could take many forms – for example, administration of a drug or vaccine, performance of a diagnostic or therapeutic procedure, and introduction of an educational tool. For example, a study could randomly assign persons to receive aspirin or placebo for a specific duration and assess the effect on the risk of developing cerebrovascular events.
Descriptive versus analytical studies
Descriptive (or nonanalytical) studies, as the name suggests, merely try to describe the data on one or more characteristics of a group of individuals. These do not try to answer questions or establish relationships between variables. Examples of descriptive studies include case reports, case series, and cross-sectional surveys (please note that cross-sectional surveys may be analytical studies as well – this will be discussed in the next article in this series). Examples of descriptive studies include a survey of dietary habits among pregnant women or a case series of patients with an unusual reaction to a drug.
Analytical studies attempt to test a hypothesis and establish causal relationships between variables. In these studies, the researcher assesses the effect of an exposure (or intervention) on an outcome. As described earlier, analytical studies can be observational (if the exposure is naturally determined) or interventional (if the researcher actively administers the intervention).
Directionality of study designs
Based on the direction of inquiry, study designs may be classified as forward-direction or backward-direction. In forward-direction studies, the researcher starts with determining the exposure to a risk factor and then assesses whether the outcome occurs at a future time point. This design is known as a cohort study. For example, a researcher can follow a group of smokers and a group of nonsmokers to determine the incidence of lung cancer in each. In backward-direction studies, the researcher begins by determining whether the outcome is present (cases vs. noncases [also called controls]) and then traces the presence of prior exposure to a risk factor. These are known as case–control studies. For example, a researcher identifies a group of normal-weight babies and a group of low-birth weight babies and then asks the mothers about their dietary habits during the index pregnancy.
Prospective versus retrospective study designs
The terms “prospective” and “retrospective” refer to the timing of the research in relation to the development of the outcome. In retrospective studies, the outcome of interest has already occurred (or not occurred – e.g., in controls) in each individual by the time s/he is enrolled, and the data are collected either from records or by asking participants to recall exposures. There is no follow-up of participants. By contrast, in prospective studies, the outcome (and sometimes even the exposure or intervention) has not occurred when the study starts and participants are followed up over a period of time to determine the occurrence of outcomes. Typically, most cohort studies are prospective studies (though there may be retrospective cohorts), whereas case–control studies are retrospective studies. An interventional study has to be, by definition, a prospective study since the investigator determines the exposure for each study participant and then follows them to observe outcomes.
The terms “prospective” versus “retrospective” studies can be confusing. Let us think of an investigator who starts a case–control study. To him/her, the process of enrolling cases and controls over a period of several months appears prospective. Hence, the use of these terms is best avoided. Or, at the very least, one must be clear that the terms relate to work flow for each individual study participant, and not to the study as a whole.
Classification of study designs
Figure 1 depicts a simple classification of research study designs. The Centre for Evidence-based Medicine has put forward a useful three-point algorithm which can help determine the design of a research study from its methods section:[ 1 ]

Classification of research study designs
- Does the study describe the characteristics of a sample or does it attempt to analyze (or draw inferences about) the relationship between two variables? – If no, then it is a descriptive study, and if yes, it is an analytical (inferential) study
- If analytical, did the investigator determine the exposure? – If no, it is an observational study, and if yes, it is an experimental study
- If observational, when was the outcome determined? – at the start of the study (case–control study), at the end of a period of follow-up (cohort study), or simultaneously (cross sectional).
In the next few pieces in the series, we will discuss various study designs in greater detail.
Financial support and sponsorship
Conflicts of interest.
There are no conflicts of interest.
The university of tulsa Online Blog
Trending topics in the tu online community
Nursing Research: What It Is and Why It Matters
When people think about medical research, they often think about cutting-edge surgical procedures and revolutionary new medications. As important as those advancements are, another type of research is just as vital: nursing research.
This type of research informs and improves nursing practice. In many cases, it’s focused on improving patient care. Experienced nurses who have advanced nursing degrees and training in research design typically conduct this research.
Nurse research can explore any number of topics, from symptomology to patient diet. However, no matter the focus of a research project, nurse research can improve health care in an impressive number of ways. As experts in their field, nurse researchers can pursue a wide range of unique career advancement opportunities .
Why Nursing Research Matters: Examples of Research in Action
Research drives innovation in every industry. Given that nurses are on the front line of the health care industry, the research they do can be particularly impactful for patient outcomes.
It Can Improve Patients’ Quality of Life
Patients diagnosed with life-threatening chronic diseases often undergo intense treatments with sometimes debilitating side effects. Nursing research is vital to helping such patients maintain a high quality of life.
For example, a 2018 study led by a nurse scientist explored why cancer patients undergoing chemotherapy frequently experience severe nausea. While the physical toll of chemotherapy contributes to nausea, the study found that patients who have factors such as children to take care of, high psychological stress, and trouble performing day-to-day tasks are often much more likely to experience nausea.
By identifying the root causes of nausea and which patients are more likely to experience it, this research allows health care professionals to develop evidence-based care practices . This can include prescribing anti-nausea medications and connecting patients to mental health professionals.
It’s Central to Making Health Care More Equitabl
A Gallup survey reports that about 38% of Americans put off seeking medical treatment due to costs. Unfortunately, cost is only one factor that prevents people from seeking treatment. Many Americans don’t live close to medical providers that can meet their needs, aren’t educated about health, or encounter discrimination.
As complex as this issue is, the National Institute of Nursing Research (NINR) asserts that the country’s nurse researchers can lead the charge in tackling it. In its strategic plan for 2022 to 2026, the institute highlights the following:
- Nursing has long been one of the most trusted professions in the country.
- Nurses often interact with patients, patients’ families, and communities more frequently than other health care professionals.
- The care that nurses provide must often take environmental and social factors into account.
These traits put nurses in the position to not only research health inequity but also put their research to work in their organizations. To help make that happen, NINR often funds nurse-led research projects focused on equity and social determinants of health. With that kind of backing, the field may become more transformative than ever.
It Can Strengthen the Health Care Workforce
While nursing research can be used to improve patient care, it can also be leveraged to solve issues health care professionals face daily. Research about the state of the health care workforce during the COVID-19 pandemic is a perfect illustration.
In 2022, a team of nurse researchers published a report called Nursing Crisis: Challenges and Opportunities for Our Profession After COVID-19 in the International Journal of Nursing Practice . In it, the authors provided concrete statistics about the following:
- Mental and physical health issues many nurses encountered
- Effects of increased workloads and decreased nurse-to-patient ratios
- How many nurses were planning to leave the profession altogether
As nurses themselves, the authors also offer actionable, evidence-based solutions to these issues, such as streamlining patient documentation systems and implementing employee wellness programs.
However, this type of research isn’t just important to solving workforce issues stemming from specific emergencies, such as the COVID-19 pandemic. By publishing quantifiable data about the challenges they face, nurse researchers empower other nurses and professional nursing organizations to advocate for themselves. This can help employers enact effective policies, support their nursing staff, and draw more talented people into the profession.
Career Opportunities in Nursing Research
Nurse researchers can work in any number of administrative, direct care, and academic roles. However, because nurse research often requires clinical care and data analysis skills, jobs in this field typically require an advanced degree, such as a Master of Science in Nursing (MSN).
While many more nurse research career opportunities exist, here are four career paths nurses with research experience and advanced degrees can explore.
Nurse Researcher
Nurse researchers identify issues related to nursing practice, collect data about them, and conduct research projects designed to inform practice and policy. While they often work in academic medical centers and universities, they can work for any type of health care provider as well as health care advocacy agencies.
In addition to conducting research, these professionals typically provide direct patient care. Many also write papers for peer-reviewed journals and make presentations about their work at conferences.
Clinical Research Nurse
Despite having a similar title to nurse researchers, clinical research nurses have slightly different responsibilities. These professionals are usually in charge of providing care to patients participating in medical research projects, including clinical trials and nursing research initiatives. They also typically collect data about patient progress, coordinate care between different team members, and contribute to academic papers.
Occupational Health Nurse
Also referred to as environmental health nurses, occupational health nurses serve specific communities, such as professionals in a particular industry or people who live in a particular area. They often educate their communities about relevant health risks, advocate for stronger health and safety regulations, and run wellness programs.
To carry out their duties, occupational and environmental health nurses must typically research health trends about the people they serve, including living and working conditions that put them at risk for illness or injury. They can work for private companies and government agencies.
Nurse Educator
Nurse educators prepare new nurses to enter the workforce or train experienced nurses in more advanced techniques. This can include teaching classes and providing on-the-job training. They often work for colleges, universities, and large health care providers.
While their duties don’t always include research, nurse educators must keep up with the health care industry’s needs and new patient care practices. This is so they can provide relevant education themselves and help their organizations design up-to-date curricula.
Make Nursing Research a Part of Your Journey
Conducting and implementing nurse research is a collaborative effort. It takes a team of informed leaders, skilled analysts, and creative educators to create effective, evidence-based policies. Those interested in pursuing nurse research should consider The University of Tulsa’s online MSN program , which can prepare you to fill any one of those roles and more.
All of TU’s MSN students take classes on research and evidence-based practices. However, the program’s specialty tracks allow students to take their studies in multiple research-oriented directions. For instance, if you’re interested in collecting and interpreting clinical data, you can choose the Informatics and Analysis track. If you have a passion for public health policy, the Public Health and Global Vision track includes classes on population health and epidemiology.
Delivered in a flexible online format, this program can be a great option for working nurses and nontraditional students alike. To find out more, read about TU’s admission policies and request more information today.
Recommended Readings
A Nurse Educator’s Role in the Future of Nursing
How Global Health Nursing Supports Population Health
What Can You Do With an MSN?
Gallup, “Record High in U.S. Put Off Medical Care Due to Cost in 2022”
International Journal of Nursing Practice, “Nursing Crisis: Challenges and Opportunities for Our Profession After COVID‐19”
Journal of Pain Symptom Management , “Risk Factors Associated With Chemotherapy-Induced Nausea in the Week Prior to the Next Cycle and Impact of Nausea on Quality of Life Outcomes”
Mayo Clinic, Nursing
National Institute of Nursing Research, Scientific Strategy: NINR’s Research Framework
National Institute of Nursing Research, The National Institute of Nursing Research 2022-2026 Strategic Plan
Recent Articles

How Leaders Drive Quality Improvement in Nursing
University of Tulsa
Aug 23, 2024

Wellness Nurse: Career Definition and More

Types of Nursing Degrees
Aug 21, 2024
Learn more about the benefits of receiving your degree from The University of Tulsa
- Online Program Tuition
- AGACNP Certificate Online
- Online MSN Program
- Accelerated Online BSN
- RN to BSN Program
- RN to MSN Program
- MS in Cyber Security
- Meet the Team
- Nursing Student Practicum Requirements
- Disclosures for Professional Nursing Licensure
- On Campus Programs
Submission and Review
Submitting applications, irb applications.
All IRB applications are completed and submitted electronically through our online system OneAegis (IRBManager). OneAegis can be accessed through single-sign-on (SSO), or by clicking here .
The IRB application form is configured to support multiple types of submissions.
Initiate a new application for:
- New human subjects research projects
- Establishing a data repository or recruitment registry – a standalone recruitment registry or data/specimen repository. Registries and repositories require standalone protocols and cannot be embedded within an application for a larger project.
- A Preliminary IRB Determination – for a funded project that lacks definite plans for the involvement of human subjects because time is needed after funds are awarded to develop the final protocol and related study materials. A Preliminary IRB Determination is often requested to meet Just-In-Time requirements.
- Request to rely on an external (non-ISU) IRB — for studies involving collaboration between researchers at ISU and another institution, where the other Institution’s IRB will assume oversight responsibilities for both sites. If Iowa State will serve as reviewing IRB, please complete the relevant sections within a regular “Human Subjects Research Project” form.
An amendment is needed for the following actions associated with approved research:
- Modifications (guidance for non-exempt and exempt research )
- Continuing Review ( guidance )
- Closing the study ( guidance )
See OneAegis (IRBManager) How-To’s for instructional guidance for initiating various types of forms.
Exempt Review Wizard
The Exempt Review Wizard is an online form in the IRB’s online system (OneAegis, formerly IRBManager). The Wizard automates certification of exemption for certain types of research. Please review the following document’s information about eligibility, using the Wizard, and the automated review process.
Step-by-step instructions are available here .
Reporting Adverse Events or Unanticipated Problems
Serious adverse events or unanticipated problems involving risk to participants or others are reported through a form in OneAegis (IRBManager). See related IRB guidance for detailed reporting requirements and timelines.
Incidents that pose an immediate risk of serious harm to participants or others must be reported immediately to [email protected] or by phone ( staff directory ).
OneAegis (formerly called IRBManager)
OneAegis is the electronic system for IRB application submission and management of IRB-related study records. OneAegis was formerly called IRBManager—the system itself has not changed.
OneAegis supports an online IRB application and review process with conditioned questions, automated CITI training verification for study personnel, electronic signatures and routing, and email notifications for actions needed. It also allows for collaboration between researchers when completing the IRB application, as well as collaboration with the IRB office during IRB review. All IRB-related study materials and records are contained within the application and the online study record.

Entering Study Personnel
ISU-Affiliated personnel: Personnel are identified by their ISU email address. If an ISU-affiliated individual is not recognized when their email address is entered, they must log into OneAegis using their ISU credentials one time to establish themselves as a contact in the system. After this one-time log in, personnel can be added to the IRB application.
We strongly advise having all study personnel log into IRBManager before you complete the IRB application.
Non-ISU-Affiliated: Persons who do not have an ISU email address can be added using the form “Add Non-ISU Contact” in the Key Personnel section of the IRB application.
Signatures and Routing
IRB applications must be signed by the PI and Supervising Investigator (if applicable). Applications for new studies must also be reviewed and signed by the Chair of the Department overseeing the research. Individuals are notified by email when an IRB application needs review and signature. Signing the form involves entering username and password. After the form is signed, it will automatically route to the next stage in the submission or review process.
During the review process, IRB staff may send the form back with questions or revisions. Those who need to take action (e.g., submitter, PI, etc.) are notified via email.
OneAegis FAQ’s
The IRB application shows that my CITI training is “Missing.” What do I do?
OneAegis verifies CITI training completion by connecting with CITI databases overnight each day. Successful verification requires that the individual’s CITI account documents their affiliation with ISU and lists their ISU email address as the Primary Email Address in CITI.
If you have taken the training and your training is listed as “Missing” in the IRB application, please do the following:
- Check your CITI account and ensure you are affiliated with ISU and your ISU email address is listed as your primary email address.
- Check OneAegis the next day (after an overnight update).
If after the training still shows as “Missing” after both of the above steps are completed, please contact the IRB office ([email protected]).
The system does not find an ISU-affiliated individual when I enter their email address. What do I do?
If you see a message indicating contact not found after entering an ISU email address, that means the individual is not established as a contact in OneAegis.
All personnel must log into OneAegis using their ISU credentials (email address and password) one time to establish themselves as a contact in the system before they can be added to IRB applications. Individuals will be automatically established as a contact after logging into the system once—there are no additional forms to complete for ISU-affiliated persons.
We strongly advise having all study personnel log into IRBManager once, if they have not done so already, before you complete the IRB application.
OneAegis How-To’s
Review process & timelines.
IRB applications undergo a pre-review process to ensure that all materials and information needed for review are included and to determine the level of review necessary for the study (i.e., exempt review, expedited review, or review by the full committee). The terms exempt and expedited refer to categories of research that do not require review by the full committee. At ISU, expedited reviews are conducted by IRB Chair(s) or designated IRB members. Exempt reviews are conducted by qualified IRB staff.
Following IRB approval, the approved application, the IRB-stamped supporting documents, and the IRB approval letter are available to the PI and Supervising Investigator (SI) in OneAegis (IRBManager). PIs/SIs should read the approval letter carefully as it contains important information. Also, the IRB-stamped informed consent document should be used when enrolling study participants.
Review timelines depend on three primary factors:
- Review volume – IRB review load is typically highest mid-semester.
- Application quality – clear, complete, and internally consistent applications require much less communication between the PI and IRB staff, and therefore, less review time.
- Project complexity – complex, novel, or risky research typically requires more review time. In some instances, consultation with outside experts, legal counsel, or other campus departments is needed. Those processes take extra time.
PIs are advised to submit their applications well in advance of the proposed start date or the continuing review date of the study. Although a review often takes less time than shown in the table below, it’s wise to allow for the longer time frame, especially during peak periods such as the middle of fall and spring semesters.
| New protocol | 4-6 weeks |
| Modification | 3-4 weeks |
| Continuing review | 3-4 weeks |
IRB Meeting Schedule/Application Submission Deadlines
IRB meetings are normally held on the first and third Tuesdays of each month, including over the summer.* Completed applications must be submitted two full weeks in advance of the meeting. The two-week period is needed to prepare applications for the board and ensure IRB members have sufficient time for review.
Please note: The application due date applies only to applications to be reviewed by the convened IRB. Applications for exempt research or research that will be reviewed by a designated IRB member (i.e., “expedited review”) do not have submission deadlines; instead, these applications are placed in a queue for review in the order received.
| Virtual
| September 3, 2024 | August 20, 2024 |
| September 17, 2024 | September 3, 2024 | |
| October 1, 2024 | September 17, 2024 | |
| October 15, 2024 | October 1, 2024 | |
| November 5, 2024 | October 22, 2024 | |
| November 19, 2024 | November 5, 2024 | |
| December 3, 2024 | November 19, 2024 | |
| December 17, 2024 | December 3, 2024 |
*Changes in this schedule sometimes occur due to members’ absences, particularly during the summer and breaks or near University holidays.
IRB Approval Criteria
Federal regulations established the following criteria that must be satisfied for the IRB to approve non-exempt research. IRB application questions are designed to obtain the information reviewers need to assess whether project plans align with these criteria.
Risks to subjects are minimized – sound scientific design, no unnecessary procedures, adequate plans to prevent harm (when possible), researchers are qualified, etc.
Risks are reasonable in relation to anticipated benefits of the research – in other words, there must be adequate scientific justification for exposing research participants to any risks associated with the study.
Subject selection is equitable – participant selection should be justified by the research question(s); not solely due to ease of access (particularly if they may be vulnerable).
The research plan includes adequate provisions to protect the privacy of subjects and to maintain confidentiality of the data collected – the IRB considers both privacy and confidentiality at all parts of the study (recruitment, during data collection, security of the data, when reporting results or sharing data, etc.).
Informed consent will be obtained from each participant prior to their inclusion in the study and in accordance with regulatory requirements , unless waived by the IRB .
Informed consent will be documented (by handwritten or electronic signature), unless this requirement is waived by the IRB. If the documentation requirement is waived, the IRB may require written information to be provided to research participants.
When appropriate, additional safeguards are in place to protect the rights and welfare of subjects who may be vulnerable to coercion or undue influence (children, educationally or economically disadvantaged, individuals with impaired decision-making capacity, prisoners, students or employees—in some cases).
When appropriate (i.e., clinical trials, high risk research, etc.), the research plan includes adequate provisions for monitoring the data collected to ensure the safety of subjects.

IMAGES
VIDEO
COMMENTS
Here are six common types of research studies, along with examples that help explain the advantages and disadvantages of each: 1. Meta-analysis. A meta-analysis study helps researchers compile the quantitative data available from previous studies. It's an observational study in which the researchers don't manipulate variables.
There are various types of scientific studies such as experiments and comparative analyses, observational studies, surveys, or interviews. The choice of study type will mainly depend on the research question being asked. When making decisions, patients and doctors need reliable answers to a number of questions.
This type of research is subdivided into two types: Technological applied research: looks towards improving efficiency in a particular productive sector through the improvement of processes or machinery related to said productive processes. Scientific applied research: has predictive purposes. Through this type of research design, we can ...
The basis of a scientific research study follows a common pattern: Define the question. Gather information and resources. Form hypotheses. Perform an experiment and collect data. Analyze the data ...
Some studies use an inactive substance called a placebo. Multisite studies allow individuals from many different locations or health care centers to participate. Remuneration. If the consent form states remuneration is provided, you will be paid for your time and participation in the study. Costs. Some studies may involve additional cost.
Clinical trials are conducted for many reasons: to determine whether a new drug or device is safe and effective for people to use. to study different ways to use standard treatments or current ...
Clinical research is the study of health and illness in people. There are two main types of clinical research: observational studies and clinical trials. Read and share this infographic (PDF, 317K) to learn why researchers do different kinds of clinical studies. Observational studies monitor people in normal settings.
a form of inquiry in which qualitative research findings about a process or experience are aggregated or integrated across research studies. Aims can involve synthesizing qualitative findings across primary studies, generating new theoretical or conceptual models, identifying gaps in research, or generating new questions.
Other interesting articles. If you want to know more about statistics, methodology, or research bias, make sure to check out some of our other articles with explanations and examples. Statistics. Normal distribution. Skewness. Kurtosis. Degrees of freedom. Variance. Null hypothesis.
Placing research in the bigger context of its field and where it fits into the scientific process can help people better understand and interpret new findings as they emerge. A single study usually uncovers only a piece of a larger puzzle. Questions about how the world works are often investigated on many different levels.
Clinical research studies need people of every age, health status, race, gender, ethnicity and cultural background to participate. ... People with no known major health issues — also called normal volunteers — are needed for some studies. For new medications, it is safer and easier to start with healthy individuals. These studies look at ...
Introduction. In clinical research, our aim is to design a study, which would be able to derive a valid and meaningful scientific conclusion using appropriate statistical methods that can be translated to the "real world" setting. 1 Before choosing a study design, one must establish aims and objectives of the study, and choose an appropriate target population that is most representative of ...
The article is based on a selective literature research on study types in medical research, as well as the authors' own experience. ... organization, and money. So-called historical cohort studies represent a special case. In this case, all data on exposure and effect (illness) are already available at the start of the study and are analyzed ...
A meta-analysis is a type of systematic review that goes one step further, combining the data from multiple studies and using statistics to summarize it, as if creating a mega-study from many smaller studies.4. However, even systematic reviews and meta-analyses aren't the final word on scientific questions.
The National Academy of Sciences states that the object of research is to "extend human knowledge of the physical, biological, or social world beyond what is already known.". Research is different than other forms of discovering knowledge (like reading a book) because it uses a systematic process called the Scientific Method.
Clinical research includes all research that involves people. Types of clinical research include: Epidemiology, which improves the understanding of a disease by studying patterns, causes, and effects of health and disease in specific groups. Behavioral, which improves the understanding of human behavior and how it relates to health and disease.
Research methods are specific procedures for collecting and analyzing data. Developing your research methods is an integral part of your research design. When planning your methods, there are two key decisions you will make. First, decide how you will collect data. Your methods depend on what type of data you need to answer your research question:
Research studies are done to discover new information or to answer a question about how we learn, behave, and function. ... Other studies, sometimes called clinical trials, involve more risky procedures like testing a new drug or medical device. Who can participate? Each research study has its own set of criteria to determine who can ...
Research conducted for the purpose of contributing towards science by the systematic collection, interpretation and evaluation of data and that, too, in a planned manner is called scientific research: a researcher is the one who conducts this research. The results obtained from a small group through scientific studies are socialised, and new ...
One specific form of ethnographic research is called a case study. It is a detailed examination of a single group, individual, situation, or site. A meta-analysis is another specific form. It is a statistical method which accumulates experimental and correlational results across independent studies. It is an analysis of analyses.
Clinical Research. Clinical research involves the study of cancer in people. These cancer research studies are further broken down into two types: clinical trials and observational studies. Clinical trials are research studies that involve an intervention, which is a treatment or change that may affect the results of cancer.These can lead to new treatments, care, and improved results for ...
In observational studies, the people in the study live their daily lives as they choose. They exercise when they want, eat what they like and take the medicines their doctors prescribe. They report these activities to researchers. There are 2 types of observational studies: Prospective cohort studies. Case-control studies.
Research study design is a framework, or the set of methods and procedures used to collect and analyze data on variables specified in a particular research problem. Research study designs are of many types, each with its advantages and limitations. The type of study design used to answer a particular research question is determined by the ...
All of TU's MSN students take classes on research and evidence-based practices. However, the program's specialty tracks allow students to take their studies in multiple research-oriented directions. For instance, if you're interested in collecting and interpreting clinical data, you can choose the Informatics and Analysis track.
The research plan includes adequate provisions to protect the privacy of subjects and to maintain confidentiality of the data collected - the IRB considers both privacy and confidentiality at all parts of the study (recruitment, during data collection, security of the data, when reporting results or sharing data, etc.).