This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search

Search menu
Effective decision-making: applying the theories to nursing practice.
Samantha Watkins
Emergency Department Staff Nurse, Frimley Health NHS Foundation Trust, Frimley
View articles · Email Samantha
Many theories have been proposed for the decision-making conducted by nurses across all practices and disciplines. These theories are fundamental to consider when reflecting on our decision-making processes to inform future practice. In this article three of these theories are juxtaposed with a case study of a patient presenting with an ST-segment elevation myocardial infarction (STEMI). These theories are descriptive, normative and prescriptive, and will be used to analyse and interpret the process of decision-making within the context of patient assessment.
Decision-making is a fundamental concept of nursing practice that conforms to a systematic trajectory involving the assessment, interpretation, evaluation and management of patient-specific situations ( Dougherty et al, 2015 ). Shared decision-making is vital to consider in terms of patient autonomy and professional duty of care as set out in the Nursing and Midwifery Council (NMC) (2018) Code, which underpins nursing practice. Consequently, the following assessment and decision-making processes were conducted within the remits of practice as a student nurse. Decision-making is a dynamic process in nursing practice, and the theories emphasise the importance of adaptability and reflective practice to identify factors that impact on patient care ( Pearson, 2013 ). Three decision-making theories will be explored within the context of a decision made in practice. To abide by confidentiality requirements, the pseudonym ‘Linda’ will be used throughout. Patient consent was obtained prior to writing.
Linda was a 71-year-old who had been admitted to the cardiac ward following an episode of unstable angina. She was on continuous cardiac monitoring as recommended by the National Institute for Health and Care Excellence (NICE) (2016) guideline for chest pain of recent onset. During her stay on the ward, the tracing on the cardiac monitor indicated possible ST-segment elevation ( Thygesen et al, 2018 ). It was initially hypothesised that she might be experiencing an ACS ( Box 1 ) and could be haemodynamically unstable.
Box 1. Acute coronary syndrome
- Acute coronary syndrome is an umbrella term that includes three cardiac conditions that result from a reduction of oxygenated blood through the coronary arteries, causing myocardial ischaemia. An ST-segment elevation myocardial infarction (STEMI) connotes the complete occlusion of one or more of the coronary arteries, which is demonstrated by patient symptoms and ST-segment elevation seen on an electrocardiogram (ECG)
- A non-ST-segment elevation myocardial infarction (NSTEMI) results from a partial occlusion of a coronary artery. Patient symptoms often present alongside dynamic ST-segment depression, T-wave inversion or a normal ECG
- Unstable angina is a result of a transient occlusion of the coronary arteries causing symptoms at rest or on minimal exertion, which may be eased/resolved with rest with or without glyceryl trinitrate (GTN)
- Signs and symptoms of ischaemia experienced by patient include: chest pain with or without radiation to jaw, neck, back, shoulders or arms, which is described as squeezing or crushing. Associated symptoms of lethargy, syncope, pre-syncopal episodes, diaphoresis, dyspnoea, nausea or vomiting, anxiety or a feeling of impending doom often also prevail
Source: Deen, 2018
The possibility that Linda was experiencing ST-segment elevation myocardial infarction (STEMI) meant that she needed rapid assessment of her condition. Stephens (2019) recommended the use of the ABCDE assessment as a timely and effective tool to identify physiological deterioration in patients with chest pain. The student nurse's ABCDE assessment of Linda is shown in Box 2 .
Box 2. ABCDE assessment * of ‘Linda’
- Airway: patent, no audible sounds of obstruction; however, unable to speak in full sentences due to dyspnoea
- Breathing: dyspnoeic, respiratory rate of 27, saturations of 85% on room air—with guidance from the senior charge nurse, 80% oxygen via non-rebreathe mask was administered ( O'Driscoll et al, 2017 )
- Circulation: tachycardia of 112 beats per minute, hypotensive at 92/50 mmHg, oliguric, diaphoretic, and with cool peripherals and a thready radial pulse
- Disability: She was alert on the AVPU scale, but anxious and feeling lethargic. Blood glucose was 5.7 mmol/litre
- Exposure: no erythema or wounds noted. She stated she had central chest pain, which was radiating to her jaw and back, described as ‘pressure’, and rated as a seven out of ten
* in line with Resuscitation Council (2015)
NICE (2016) recommends that the first investigation for patients with chest pain is to conduct an ECG as a rapid and non-invasive assessment for a cardiac cause of the pain. This was carried out and 2 mm ST-segment elevation in the precordial leads V1-V3 was noted, indicating a possible anterior STEMI ( Amsterdam et al, 2014 ). The student nurse had had basic ECG interpretation training as part of the nursing degree undertaken, but had also received informal teaching from registered nursing staff in cardiology. The ECG findings were confirmed by the senior charge nurse after they were alerted to Linda's condition, symptoms, and National Early Warning Score 2 (NEWS 2) ( Royal College of Physicians, 2017 ). The senior charge nurse escalated her care to the cardiology team. A diagnosis of STEMI was made by the cardiology team using the ECG findings and her physiological signs of deterioration from their assessment, within the context of her initial presentation to hospital for unstable angina. This diagnosis, coupled with the deterioration in her condition, meant that she required primary percutaneous coronary intervention (PCI). The NICE (2014) quality standard for acute coronary syndromes and the clinical guideline on STEMI ( NICE, 2013a ) recommend that primary PCI is initiated within 120 minutes to reperfuse the myocardium and prevent further myocardial cellular necrosis. This improves long-term patient outcomes ( Thygesen et al, 2018 ).
Decision-making theories
The recognition of an evolving STEMI on the cardiac monitor corresponds with the model of hypothetico-deductive reasoning ( Pearson, 2013 ) within the descriptive and normative theories ( Box 3 ). Thompson and Dowding (2009) highlighted that this model recognises that decision-making comprises four stages, beginning with cue acquisition. The specific pre-counter cues can be identified as the recognition of the abnormal tracing on the cardiac monitor ( Pearson, 2013 ), suggestive of ST-segment elevation, that indicated Linda might be experiencing haemodynamic deterioration with a cardiac cause. Subsequently, the decision to assess Linda formed the hypothesis generation phase of the decision and the recognition of the clinical signs as indicating STEMI ( Nickerson, 1998 ; Johansen and O'Brien, 2016 ). This hypothesis focused the assessment to identify and examine pertinent factors that supported this conjecture ( Pearson, 2013 ). However, the student nurse required more data to formulate a robust hypothesis thereby initiating the cue interpretation phase by conducting an ABCDE systematic assessment, including ECG. Lindsey (2013) argued that during cue interpretation, the health professional uses prescriptive guidelines to direct the assessment process and provide a rationale.
Box 3. Decision-making theories considered
- Descriptive theory: is concerned with each individuals’ moral beliefs regarding a particular decision
- Normative theory: connotes what decisions individuals should make logically
- Prescriptive theory: encompasses the policies that govern the remits of a decision within the evidence base that informs practice
Source: Pearson, 2013
Arguably, however, clinical knowledge of the pathophysiology of ACS is fundamental to effective cue interpretation, not simply the individual's knowledge of the NICE guidance ( NICE, 2013a ; 2013b ; 2014 ; 2016 ). The student nurse's existing knowledge of the symptoms of ACS supported the cue interpretation with assessing Linda's condition and possible diagnosis of ACS. This knowledge enriched the student nurse's understanding of the guidance, which could then effectively be applied as the central aspect of cue interpretation ( Deen, 2018 ).
Elstein and Schwartz (2002) conceded that the prescriptive theory knowledge synthesised for the decision must be accurate and evidence-based for hypothetico-deductive reasoning to be effective. Courtney and McCutcheon (2009) argued that reliance solely on clinical guidelines can limit decision-making and result in erroneous outcomes and should consequently be used in collaboration with the evidence base. By combining normative theory with prescriptive guidance, clinical decisions can be enriched and validated. Stevens (2013) highlighted that it is vital that the guidance used in corroboration with decision-making models is valid and reliable and therefore prescriptive theory must be critically evaluated against the evidence-base. The guidance published by NICE (2013a) is supported by the American College of Cardiology ( O'Gara et al, 2013 ), European Resuscitation Council ( Nikolaou et al, 2015 ), European Society of Cardiology ( Steg et al, 2012 ) and Cardiac Society of Australia and New Zealand ( Chew et al, 2016 ). Accordingly, these guidelines highlight the clinical signs of STEMI and the diagnostic investigations pertinent to this condition. Within the remits of practice as a student nurse, this evidence supported the decision to escalate Linda's condition.
Antithetically, during cue interpretation and the hypothesis generation phases, Pearson (2013) emphasised the importance of considering multiple hypotheses extrapolated from the clinical data, resulting in the selection of the most appropriate hypothesis when more data are obtained. Despite this, during the interpretation of the cues for the hypothesis, the student nurse failed to consider differential diagnoses, such as pneumothorax or pulmonary embolism, which have similar presentations to STEMI ( Deen, 2018 ). Consequently, this hypothesis generation had an element of uncertainty ( Bjørk and Hamilton, 2011 ), which could have impeded Linda's care by erroneously considering only one potential diagnosis and therefore focusing the assessment on that diagnosis. Student nurses can be considered ‘novice’ health professionals, demonstrating limitations in knowledge regarding differential diagnoses and therefore in potential hypotheses. Pearson (2013) argued that this is because student nurses lack the requisite experience to cluster information as effectively as an ‘expert’ health professional. Consequently, the presentation of one hypothesis is permissible within the remits of practice as a student nurse.
Assessment tools such as ABCDE ( Resuscitation Council UK, 2015 ) ensure that all factors indicative of deterioration are recognised. Consequently, by using a systematic assessment, any potential erroneous hypothesis can be precluded. Therefore, as Carayon and Wood (2010) state, the assessment tool was a barrier to active failure to recognise alternative diagnoses thus circumventing any serious consequences, highlighting the importance of comprehensive assessment to avoid error and safeguard the ethical principle of non-maleficence ( Beauchamp and Childress, 2013 ) fundamental to nursing. Antithetically, Benner et al (2008) argued that even the novice nurse should be able to consider multiple hypotheses within a situation, although they may not be able to reflect on these decisions within the moment. However, as Keller (2009) noted, the hypothetico-deductive model is based on presuppositions recognised by the health professional, such as the evolving cardiac tracing and history of pain, indicating that STEMI was the higher probable cause ( Deen, 2018 ). Consequently, a limitation of hypothetico-deductive reasoning is sufficient experience to aid in generating hypotheses.
Thereafter, in the hypothesis generation phase, the decision-making process evolved to include elements of pattern recognition theory ( Croskerry, 2002 ). The clinical decision that focuses on a single hypothesis can be compared to the use of pattern recognition ( Pearson, 2013 ) where existing knowledge is used to establish the hypothesis. Pearson (2013) commented that hypothetico-deductive reasoning is based on the synthesising and analysing of information whereas the formulation of one hypothesis is suggestive of pattern recognition, where the nurse uses previous experience to evaluate the situation. Consequently, the student nurse's previous experience of assessing a patient in acute STEMI may have guided practice to recognise ST-segment elevation on the telemetry, and then subsequently to conduct an ECG, and to recognise the associated clinical signs of STEMI and to gather a history of the pain using NICE (2013b) guidance on unstable angina, in line with Linda's initial presentation. Croskerry (2002) identified that health professionals who rely on pattern recognition initially recognise visual cues that are then supplemented with more in-depth data, often using assessment tools such as NEWS (and now NEWS 2) and ABCDE. Arguably, the recognition of similarities in clinical presentation, past medical history, and cardiac monitoring tracing of Linda's case to the previous case and use of ABCDE and NEWS 2 to further assess her condition and extrapolate data, identifies that previous experience can facilitate decision-making outcomes.
Finally, in the last phase of the decision-making in the hypothetico-deductive model, the student nurse evaluated the hypothesis and by using the merits from the cues ( Banning, 2008 ) established that STEMI was the most probable cause of Linda's deterioration and could escalate her care appropriately using the prescriptive theory tools described above.
Arguably, by using previous experience to guide practice, an element of confirmation bias may have affected the selection of data ( Thompson and Dowding, 2009 ) and consequently the student may have neglected other important data ( Croskerry, 2003 ). For instance, student nurses are inexperienced with chest auscultation and consequently could not have ruled out differential respiratory diagnoses. Stanovich et al (2013) acknowledged that confirmation bias can be circumvented when evidence is assimilated with hypothesis generation. The consideration that Linda may have been at an increased risk of myocardial infarction due to her age, history of smoking and admission to hospital for unstable angina ( Piepoli et al, 2016 ), indicated that the cause of her deterioration would most likely be cardiac. Thus, an evidence-based approach could inform practice and consequently, any limitations as a ‘novice’ would be minimised through rationalisation and critical thinking. Indeed, Stanovich et al (2013) argued that rationalising and critical thinking are markedly more important than existing knowledge. This is because even an ‘expert’ in a specific field does not have completely comprehensive knowledge, and therefore relies on a critical thought process to make rational decisions.
Conclusively, health professionals must be able to rationalise their decisions ( Johansen and O'Brien, 2016 ) and justify these decisions within the context of each presentation as a central concept of nursing ( NMC, 2018 ).
Communication is vital to establishing consent to treatment where the patient is regarded as having capacity under the Mental Capacity Act 2005. This is particularly significant when conducting investigations and escalating care to ensure that the patient's wishes are respected, and that the patient is empowered with knowledge regarding their condition and care ( Coultier and Collins, 2011 ). Linda was informed that her care required escalation to the appropriate clinical team, and then subsequently recommended to have PCI intervention as the most effective treatment for STEMI ( NICE, 2013a ; 2014 ). Presenting a default decision and using choice architecture can be construed as methods of liberal paternalism used to avoid impeded decision-making from choice overload ( Rosenbaum, 2015 ) or irrational decision bias ( Marewski and Gigerenzer, 2012 ). To escalate Linda's care within the recommended timeframe ( NICE, 2013a ; 2014 ), it was important to use elements of liberal paternalism ( Beauchamp and Childress, 2013 ) while preserving Linda's autonomy of choice ( Kemmerer et al, 2017 ). Linda had a right to make a decision against medical advice as per Re B (Adult, refusal of medical treatment) [2002] and these choices were presented to her by the cardiology team. As a health professional, a duty of care was owed to the patient to escalate concerns regarding her condition under the Code ( NMC, 2018 ).
Conclusively, all three theories of decision-making pertained to this patient's effective care. Nurses must be accountable for their decisions and act within the remits of the NMC (2018) Code. Patient care must consequently be effective, evidence-based and patient-centred. Accountability requires the health professional to act within the remits of their role to ensure safe care is delivered to the patient. This is a fundamental aspect of patient-centric care and principal to effective decision making. Demonstrably, the use of descriptive and normative theories can be interchangeable, however, the use of prescriptive theory is pivotal to validate clinical decision-making. The decision-making process can be further facilitated by use of structured assessment tools to reduce margin of error and improve outcome. Collaborative decision making is pivotal to advancing patient autonomy and empowerment but certain decisions require elements of paternalism to improve the process and uphold the ethical principles of beneficence and non-maleficence. Nevertheless, health professionals have a duty of care to adhere to decisions made by patients established to have capacity to give informed consent, irrespective of the personal beliefs of the professional.
- This article is a reflection on a case scenario where decisions were made in the care of a patient admitted for cardiac monitoring
- Nursing decision making is complex and involves a multitude of processes based on experience, knowledge and skill.
- Understanding the importance of decision-making theory and how these theories apply to practice can be effective in reflecting on practice, and the application of theory to practice can inform patient care
CPD reflective questions
- Consider the three different theories of decision making outlined here—which theory do you deem the most important to your practice? How does this affect your practice?
- Consider how reflecting on your own decision making can improve practice
- What can you do to enrich your own knowledge regarding patients with chest pain?
Fastest Nurse Insight Engine
- MEDICAL ASSISSTANT
- Abdominal Key
- Anesthesia Key
- Basicmedical Key
- Otolaryngology & Ophthalmology
- Musculoskeletal Key
- Obstetric, Gynecology and Pediatric
- Oncology & Hematology
- Plastic Surgery & Dermatology
- Clinical Dentistry
- Radiology Key
- Thoracic Key
- Veterinary Medicine
- Gold Membership
Making Decisions and Solving Problems
CHAPTER 6 Making Decisions and Solving Problems Rose Aguilar Welch This chapter describes the key concepts related to problem solving and decision making. The primary steps of the problem-solving and decision-making processes, as well as analytical tools used for these processes, are explored. Moreover, strategies for individual or group problem solving and decision making are presented. Objectives • Apply a decision-making format to list options to solve a problem, identify the pros and cons of each option, rank the options, and select the best option. • Evaluate the effect of faulty information gathering on a decision-making experience. • Analyze the decision-making style of a nurse leader/manager. • Critique resources on the Internet that focus on critical thinking, problem solving, and decision making. Terms to Know autocratic creativity critical thinking decision making democratic optimizing decision participative problem solving satisficing decision The Challenge Vickie Lemmon RN, MSN Director of Clinical Strategies and Operations, WellPoint, Inc., Ventura, California Healthcare managers today are faced with numerous and complex issues that pertain to providing quality services for patients within a resource-scarce environment. Stress levels among staff can escalate when problems are not resolved, leading to a decrease in morale, productivity, and quality service. This was the situation I encountered in my previous job as administrator for California Children Services (CCS). When I began my tenure as the new CCS administrator, staff expressed frustration and dissatisfaction with staffing, workload, and team communications. This was evidenced by high staff turnover, lack of teamwork, customer complaints, unmet deadlines for referral and enrollment cycle times, and poor documentation. The team was in crisis, characterized by in-fighting, blaming, lack of respectful communication, and lack of commitment to program goals and objectives. I had not worked as a case manager in this program. It was hard for me to determine how to address the problems the staff presented to me. I wanted to be fair but thought that I did not have enough information to make immediate changes. My challenge was to lead this team to greater compliance with state-mandated performance measures. What do you think you would do if you were this nurse? Introduction Problem solving and decision making are essential skills for effective nursing practice. Carol Huston (2008) identified “expert decision-making skills” as one of the eight vital leadership competencies for 2020. These processes not only are involved in managing and delivering care but also are essential for engaging in planned change. Myriad technologic, social, political, and economic changes have dramatically affected health care and nursing. Increased patient acuity, shorter hospital stays, shortage of healthcare providers, increased technology, greater emphasis on quality and patient safety, and the continuing shift from inpatient to ambulatory and home health care are some of the changes that require nurses to make rational and valid decisions. Moreover, increased diversity in patient populations, employment settings, and types of healthcare providers demands efficient and effective decision making and problem solving. More emphasis is now placed on involving patients in decision making and problem solving and using multidisciplinary teams to achieve results. Nurses must possess the basic knowledge and skills required for effective problem solving and decision making. These competencies are especially important for nurses with leadership and management responsibilities. Definitions Problem solving and decision making are not synonymous terms. However, the processes for engaging in both processes are similar. Both skills require critical thinking, which is a high-level cognitive process, and both can be improved with practice. Decision making is a purposeful and goal-directed effort that uses a systematic process to choose among options. Not all decision making begins with a problem situation. Instead, the hallmark of decision making is the identification and selection of options or alternatives. Problem solving, which includes a decision-making step, is focused on trying to solve an immediate problem, which can be viewed as a gap between “what is” and “what should be.” Effective problem solving and decision making are predicated on an individual’s ability to think critically. Although critical thinking has been defined in numerous ways, Scriven and Paul (2007) refer to it as “ the intellectually disciplined process of actively and skillfully conceptualizing, applying, analyzing, synthesizing, and/or evaluating information gathered from, or generated by, observation, experience, reflection, reasoning, or communication, as a guide to belief and action.” Effective critical thinkers are self-aware individuals who strive to improve their reasoning abilities by asking “why,” “what,” or “how.” A nurse who questions why a patient is restless is thinking critically. Compare the analytical abilities of a nurse who assumes a patient is restless because of anxiety related to an upcoming procedure with those of a nurse who asks if there could be another explanation and proceeds to investigate possible causes. It is important for nurse leaders and managers to assess staff members’ ability to think critically and enhance their knowledge and skills through staff-development programs, coaching, and role modeling. Establishing a positive and motivating work environment can enhance attitudes and dispositions to think critically. Creativity is essential for the generation of options or solutions. Creative individuals can conceptualize new and innovative approaches to a problem or issue by being more flexible and independent in their thinking. It takes just one person to plant a seed for new ideas to generate . The model depicted in Figure 6-1 demonstrates the relationship among related concepts such as professional judgment, decision making, problem solving, creativity, and critical thinking. Sound clinical judgment requires critical or reflective thinking. Critical thinking is the concept that interweaves and links the others. An individual, through the application of critical-thinking skills, engages in problem solving and decision making in an environment that can promote or inhibit these skills. It is the nurse leader’s and manager’s task to model these skills and promote them in others. FiGURE 6-1 Problem-solving and decision-making model. Decision Making This section presents an overview of concepts related to decision models, decision-making styles, factors affecting decision making, group decision making (advantages and challenges), and strategies and tools. The phases of the decision-making process include defining objectives, generating options, identifying advantages and disadvantages of each option, ranking the options, selecting the option most likely to achieve the predefined objectives, implementing the option, and evaluating the result. Box 6-1 contains a form that can be used to complete these steps. BOX 6-1 Decision-Making Format Objective: _____________________________________ Options Advantages Disadvantages Ranking Add more rows as necessary. Rank priority of options, with “1” being most preferred. Select the best option. Implementation plan: ______________________________________________________________________________ Evaluation plan: __________________________________________________________________________________ A poor-quality decision is likely if the objectives are not clearly identified or if they are inconsistent with the values of the individual or organization. Lewis Carroll illustrates the essential step of defining the goal, purpose, or objectives in the following excerpt from Alice’s Adventures in Wonderland: One day Alice came to a fork in the road and saw a Cheshire Cat in a tree. “Which road do I take?” she asked. His response was a question: “Where do you want to go?” “I don’t know,” Alice answered. “Then,” said the cat, “it doesn’t matter.” Decision Models The decision model that a nurse uses depends on the circumstances. Is the situation routine and predictable or complex and uncertain? Is the goal of the decision to make a decision conservatively that is just good enough or one that is optimal? If the situation is fairly routine, nurse leaders and managers can use a normative or prescriptive approach. Agency policy, standard procedures, and analytical tools can be applied to situations that are structured and in which options are known. If the situation is subjective, non-routine, and unstructured or if outcomes are unknown or unpredictable, the nurse leader and manager may need to take a different approach. In this case, a descriptive or behavioral approach is required. More information will need to be gathered to address the situation effectively. Creativity, experience, and group process are useful in dealing with the unknown. In the business world, Camillus described complex problems that are difficult to describe or resolve as “wicked” (as cited in Huston, 2008 ). This term is apt in describing the issues that nurse leaders face. In these situations, it is especially important for nurse leaders to seek expert opinion and involve key stakeholders. Another strategy is satisficing. In this approach, the decision maker selects the solution that minimally meets the objective or standard for a decision. It allows for quick decisions and may be the most appropriate when time is an issue. Optimizing is a decision style in which the decision maker selects the option that is best, based on an analysis of the pros and cons associated with each option. A better decision is more likely using this approach, although it does take longer to arrive at a decision. For example, a nursing student approaching graduation is contemplating seeking employment in one of three acute care hospitals located within a 40-mile radius of home. The choices are a medium-size, not-for-profit community hospital; a large, corporate-owned hospital; and a county facility. A satisficing decision might result if the student nurse picked the hospital that offered a decent salary and benefit packet or the one closest to home. However, an optimizing decision is more likely to occur if the student nurse lists the pros and cons of each acute care hospital being considered such as salary, benefits, opportunities for advancement, staff development, and mentorship programs. Decision-Making Styles The decision-making style of a nurse manager is similar to the leadership style that the manager is likely to use. A manager who leans toward an autocratic style may choose to make decisions independent of the input or participation of others. This has been referred to as the “decide and announce” approach, an authoritative style. On the other hand, a manager who uses a democratic or participative approach to management involves the appropriate personnel in the decision-making process. It is imperative for managers to involve nursing personnel in making decisions that affect patient care. One mechanism for doing so is by seeking nursing representation on various committees or task forces. Participative management has been shown to increase work performance and productivity, decrease employee turnover, and enhance employee satisfaction. Any decision style can be used appropriately or inappropriately. Like the tenets of situational leadership theory, the situation and circumstances should dictate which decision-making style is most appropriate. A Code Blue is not the time for managers to democratically solicit volunteers for chest compressions! The autocratic method results in more rapid decision making and is appropriate in crisis situations or when groups are likely to accept this type of decision style. However, followers are generally more supportive of consultative and group approaches. Although these approaches take more time, they are more appropriate when conflict is likely to occur, when the problem is unstructured, or when the manager does not have the knowledge or skills to solve the problem. Exercise 6-1 Interview colleagues about their most preferred decision-making model and style. What barriers or obstacles to effective decision making have your colleagues encountered? What strategies are used to increase the effectiveness of the decisions made? Based on your interview, is the style effective? Why or why not? Factors Affecting Decision Making Numerous factors affect individuals and groups in the decision-making process. Tanner (2006) conducted an extensive review of the literature to develop a Clinical Judgment Model. Out of the research, she concluded that five principle factors influence decision making. (See the Literature Perspective below.) Literature Perspective Resource: Tanner, C. A. (2006). Thinking like a nurse: A research-based model of clinical judgment in nursing. Journal of Nursing Education, 45 (6), 204-211. Tanner engaged in an extensive review of 200 studies focusing on clinical judgment and clinical decision making to derive a model of clinical judgment that can be used as a framework for instruction. The first review summarized 120 articles and was published in 1998. The 2006 article reviewed an additional 71 studies published since 1998. Based on an analysis of the entire set of articles, Tanner proposed five conclusions which are listed below. The reader is referred to the article for detailed explanation of each of the five conclusions. The author considers clinical judgment as a “problem-solving activity.” She notes that the terms “clinical judgment,” “problem solving,” “decision making,” and “critical thinking” are often used interchangeably. For the purpose of aiding in the development of the model, Tanner defined clinical judgment as actions taken based on the assessment of the patient’s needs. Clinical reasoning is the process by which nurses make their judgments (e.g., the decision-making process of selecting the most appropriate option) ( Tanner, 2006 , p. 204): 1. Clinical judgments are more influenced by what nurses bring to the situation than the objective data about the situation at hand. 2. Sound clinical judgment rests to some degree on knowing the patient and his or her typical pattern of responses, as well as an engagement with the patient and his or her concerns. 3. Clinical judgments are influenced by the context in which the situation occurs and the culture of the nursing care unit. 4. Nurses use a variety of reasoning patterns alone or in combination. 5. Reflection on practice is often triggered by a breakdown in clinical judgment and is critical for the development of clinical knowledge and improvement in clinical reasoning. The Clinical Judgment Model developed through the review of the literature involves four steps that are similar to problem-solving and decision-making steps described in this chapter. The model starts with a phase called “Noticing.” In this phase, the nurse comes to expect certain responses resulting from knowledge gleaned from similar patient situations, experiences, and knowledge. External factors influence nurses in this phase such as the complexity of the environment and values and typical practices within the unit culture. The second phase of the model is “Interpreting,” during which the nurse understands the situation that requires a response. The nurse employs various reasoning patterns to make sense of the issue and to derive an appropriate action plan. The third phase is “Responding,” during which the nurse decides on the best option for handling the situation. This is followed by the fourth phase, “Reflecting,” during which the nurse assesses the patient’s responses to the actions taken. Tanner emphasized that “reflection-in-action” and “reflection-on-action” are major processes required in the model. Reflection-in-action is real-time reflection on the patient’s responses to nursing action with modifications to the plan based on the ongoing assessment. On the other hand, reflection-on-action is a review of the experience, which promotes learning for future similar experiences. Nurse educators and managers can employ this model with new and experienced nurses to aid in understanding thought processes involved in decision making. As Tanner (2006) so eloquently concludes, “If we, as nurse educators, help our students understand and develop as moral agents, advance their clinical knowledge through expert guidance and coaching, and become habitual in reflection-on-practice, they will have learned to think like a nurse” ( p. 210 ). Implications for Practice Nurse educators and managers can employ this model with new and experienced nurses to aid in understanding thought processes involved in decision making. For example, students and practicing nurses can be encouraged to maintain reflective journals to record observations and impressions from clinical experiences. In clinical post-conferences or staff development meetings, the nurse educator and manager can engage them in applying to their lived experiences the five conclusions Tanner proposed. The ultimate goal of analyzing their decisions and decision-making processes is to improve clinical judgment, problem-solving, decision-making, and critical-thinking skills. Internal and external factors can influence how the situation is perceived. Internal factors include variables such as the decision maker’s physical and emotional state, personal philosophy, biases, values, interests, experience, knowledge, attitudes, and risk-seeking or risk-avoiding behaviors. External factors include environmental conditions, time, and resources. Decision-making options are externally limited when time is short or when the environment is characterized by a “we’ve always done it this way” attitude. Values affect all aspects of decision making, from the statement of the problem/issue through the evaluation. Values, determined by one’s cultural, social, and philosophical background, provide the foundation for one’s ethical stance. The steps for engaging in ethical decision making are similar to the steps described earlier; however, alternatives or options identified in the decision-making process are evaluated with the use of ethical resources. Resources that can facilitate ethical decision making include institutional policy; principles such as autonomy, nonmaleficence, beneficence, veracity, paternalism, respect, justice, and fidelity; personal judgment; trusted co-workers; institutional ethics committees; and legal precedent. Certain personality factors, such as self-esteem and self-confidence, affect whether one is willing to take risks in solving problems or making decisions. Keynes (2008) asserts that individuals may be influenced based on social pressures. For example, are you inclined to make decisions to satisfy people to whom you are accountable or from whom you feel social pressure? Characteristics of an effective decision maker include courage, a willingness to take risks, self-awareness, energy, creativity, sensitivity, and flexibility. Ask yourself, “Do I prefer to let others make the decisions? Am I more comfortable in the role of ‘follower’ than leader? If so, why?” Exercise 6-2 Identify a current or past situation that involved resource allocation, end-of-life issues, conflict among healthcare providers or patient/family/significant others, or some other ethical dilemma. Describe how the internal and external factors previously described influenced the decision options, the option selected, and the outcome. Group Decision Making There are two primary criteria for effective decision making. First, the decision must be of a high quality; that is, it achieves the predefined goals, objectives, and outcomes. Second, those who are responsible for its implementation must accept the decision. Higher-quality decisions are more likely to result if groups are involved in the problem-solving and decision-making process. In reality, with the increased focus on quality and safety, decisions cannot be made alone. When individuals are allowed input into the process, they tend to function more productively and the quality of the decision is generally superior. Taking ownership of the process and outcome provides a smoother transition. Multidisciplinary teams should be used in the decision-making process, especially if the issue, options, or outcome involves other disciplines. Research findings suggest that groups are more likely to be effective if members are actively involved, the group is cohesive, communication is encouraged, and members demonstrate some understanding of the group process. In deciding to use the group process for decision making, it is important to consider group size and composition. If the group is too small, a limited number of options will be generated and fewer points of view expressed. Conversely, if the group is too large, it may lack structure, and consensus becomes more difficult. Homogeneous groups may be more compatible; however, heterogeneous groups may be more successful in problem solving. Research has demonstrated that the most productive groups are those that are moderately cohesive. In other words, divergent thinking is useful to create the best decision. For groups to be able to work effectively, the group facilitator or leader should carefully select members on the basis of their knowledge and skills in decision making and problem solving. Individuals who are aggressive, are authoritarian, or manifest self-oriented behaviors tend to decrease the effectiveness of groups. The nurse leader or manager should provide a nonthreatening and positive environment in which group members are encouraged to participate actively. Using tact and diplomacy, the facilitator can control aggressive individuals who tend to monopolize the discussion and can encourage more passive individuals to contribute by asking direct, open-ended questions. Providing positive feedback such as “You raised a good point,” protecting members and their suggestions from attack, and keeping the group focused on the task are strategies that create an environment conducive to problem solving. Advantages of Group Decision Making The advantages of group decision making are numerous. The adage “two heads are better than one” illustrates that when individuals with different knowledge, skills, and resources collaborate to solve a problem or make a decision, the likelihood of a quality outcome is increased. More ideas can be generated by groups than by individuals functioning alone. In addition, when followers are directly involved in this process, they are more apt to accept the decision, because they have an increased sense of ownership or commitment to the decision. Implementing solutions becomes easier when individuals have been actively involved in the decision-making process. Involvement can be enhanced by making information readily available to the appropriate personnel, requesting input, establishing committees and task forces with broad representation, and using group decision-making techniques. The group leader must establish with the participants what decision rule will be followed. Will the group strive to achieve consensus, or will the majority rule? In determining which decision rule to use, the group leader should consider the necessity for quality and acceptance of the decision. Achieving both a high-quality and an acceptable decision is possible, but it requires more involvement and approval from individuals affected by the decision. Groups will be more committed to an idea if it is derived by consensus rather than as an outcome of individual decision making or majority rule. Consensus requires that all participants agree to go along with the decision. Although achieving consensus requires considerable time, it results in both high-quality and high-acceptance decisions and reduces the risk of sabotage. Majority rule can be used to compromise when 100% agreement cannot be achieved. This method saves time, but the solution may only partially achieve the goals of quality and acceptance. In addition, majority rule carries certain risks. First, if the informal group leaders happen to fall in the minority opinion, they may not support the decision of the majority. Certain members may go so far as to build coalitions to gain support for their position and block the majority choice. After all, the majority may represent only 51% of the group. In addition, group members may support the position of the formal leader, although they do not agree with the decision, because they fear reprisal or they wish to obtain the leader’s approval. In general, as the importance of the decision increases, so does the percentage of group members required to approve it. To secure the support of the group, the leader should maintain open communication with those affected by the decision and be honest about the advantages and disadvantages of the decision. The leader should also demonstrate how the advantages outweigh the disadvantages, suggest ways the unwanted outcomes can be minimized, and be available to assist when necessary.
Share this:
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
Related posts:
- Patient Safety
- Developing the Role of Manager
- Care Delivery Strategies
Stay updated, free articles. Join our Telegram channel
Comments are closed for this page.

Full access? Get Clinical Tree

- Open access
- Published: 29 March 2022
A framework of evidence-based decision-making in health system management: a best-fit framework synthesis
- Tahereh Shafaghat 1 , 2 na1 ,
- Peivand Bastani ORCID: orcid.org/0000-0002-0412-0267 1 , 3 na1 ,
- Mohammad Hasan Imani Nasab 4 ,
- Mohammad Amin Bahrami 1 ,
- Mahsa Roozrokh Arshadi Montazer 5 ,
- Mohammad Kazem Rahimi Zarchi 2 &
- Sisira Edirippulige 6
Archives of Public Health volume 80 , Article number: 96 ( 2022 ) Cite this article
10k Accesses
5 Citations
6 Altmetric
Metrics details
Scientific evidence is the basis for improving public health; decision-making without sufficient attention to evidence may lead to unpleasant consequences. Despite efforts to create comprehensive guidelines and models for evidence-based decision-making (EBDM), there isn`t any to make the best decisions concerning scarce resources and unlimited needs . The present study aimed to develop a comprehensive applied framework for EBDM.
This was a Best-Fit Framework (BFF) synthesis conducted in 2020. A comprehensive systematic review was done via six main databases including PUBMED, Scopus, Web of Science, Science Direct, EMBASE, and ProQuest using related keywords. After the evidence quality appraisal, data were extracted and analyzed via thematic analysis. Results of the thematic analysis and the concepts generated by the research team were then synthesized to achieve the best-fit framework applying Carroll et al. (2013) approach.
Four thousand six hundred thirteen studies were retrieved, and due to the full-text screening of the studies, 17 final articles were selected for extracting the components and steps of EBDM in Health System Management (HSM). After collecting, synthesizing, and categorizing key information, the framework of EBDM in HSM was developed in the form of four general scopes. These comprised inquiring, inspecting, implementing, and integrating, which included 10 main steps and 47 sub-steps.
Conclusions
The present framework provided a comprehensive guideline that can be well adapted for implementing EBDM in health systems and related organizations especially in underdeveloped and developing countries where there is usually a lag in updating and applying evidence in their decision-making process. In addition, this framework by providing a complete, well-detailed, and the sequential process can be tested in the organizational decision-making process by developed countries to improve their EBDM cycle.
Peer Review reports
Globally, there is a growing interest in using the research evidence in public health policy-making [ 1 , 2 ]. Public health systems are diverse and complex, and health policymakers face many challenges in developing and implementing policies and programs that are required to be efficient [ 1 , 3 ]. The use of scientific evidence is considered to be an effective approach in the decision-making process [ 3 , 4 , 5 ]. Due to the lack of sufficient resources, evidence-based decision-making ( EBDM) is regarded as a way to optimize costs and prevent wastes [ 6 ]. At the same time, the direct consequence of ignoring evidence is poorer health for the community [ 7 ].
Evidence suggests that health systems often fail to exploit research evidence properly, leading to inefficiencies, death or reduced quality of citizens’ lives, and a decline in productivity [ 8 ]. Decision-making in the health sector without sufficient attention to evidence may lead to a lack of effectiveness, efficiency, and fairness in health systems [ 9 ]. Instead, the advantages of EBDM include adopting cost-effective interventions, making optimal use of limited resources, increasing customer satisfaction, minimizing harm to individuals and society, achieving better health outcomes for individuals and society [ 10 , 11 ], as well as increasing the effectiveness and efficiency of public health programs [ 12 ].
Using the evidence in health systems’ policymaking is a considerable challenging issue that many developed and developing countries are facing nowadays. This is particularly important in the latter, where their health systems are in a rapid transition [ 13 ]. For instance, although in 2012, a study in European Union countries showed that health policymakers rarely had necessary structures, processes, and tools to exploit research evidence in the policy cycle [ 14 ], the condition can be worse among the developing and the underdeveloped ones. For example, evidence-based policy-making in developing countries like those located in the Middle East can have more significant impacts [ 15 , 16 ]. In such countries resources are generally scarce, so the policymakers' awareness of research evidence becomes more important [ 17 ]. In general, low and middle-income countries have fewer resources to deal with health issues and need quality evidence for efficient use of these resources [ 7 ].
Since the use of EBDM is fraught with the dilemma of most pressing needs and having the least capacity for implementation especially in developing countries [ 16 ], efforts have been made to create more comprehensive guidelines for EBDM in healthcare settings, in recent years [ 18 ]. Stakeholders are significantly interested in supporting evidence-based projects that can quickly prioritize funding allocated to health sectors to ensure the effective use of their financial resources [ 19 , 20 , 21 ]. However, it is unlikely that the implementation of EBDM in Health System Management (HSM) will follow the evidence-based medicine model [ 10 , 22 ]. On the other hand, the capacity of organizations to facilitate evidence utilization is complex and not well understood [ 22 ], and the EBDM process is not usually institutionalized within the organizational processes [ 10 ]. A study in 2005 found that few organizations support the use of research evidence in health-related decisions, globally [ 23 ]. Weis et al. (2012) also reported there is insufficient information on EBDM in local health sectors [ 12 ]. In general, it can be emphasized that relatively few organizations hold themselves accountable for using research evidence in developing health policies [ 24 ]. To the best of our knowledge, there isn`t any comprehensive global and practical model developed for EBDM in health systems/organizations management. Accordingly, the present study aimed to develop a comprehensive framework for EBDM in health system management. It can shed the light on policymakers to access a detailed practical model and enable them to apply the model in actual conditions.
This was a Best Fit Framework (BFF) synthesis conducted in 2020 to develop a comprehensive framework for EBDM in HSM. Such a framework synthesis is achieved as a combination of the relevant framework, theory, or conceptual models and particularly is applied for developing a priori framework based on deductive reasoning [ 25 ]. The BFF approach is appropriate to create conceptual models to describe or express the decisions and behaviors of individuals and groups in a particular domain. This is distinct from other methods of evidence synthesis because it employs a systematic approach to create an initial framework for synthesis based on existing frameworks, models, or theories [ 25 ] for identifying and adapting theories systematically with the rapid synthesis of evidence [ 25 , 26 ]. The initial framework can be derived from a relatively well-known model in the target field, or be formed by the integration of several existing models. The initial framework is then reduced to its key components that have shaped its concepts [ 25 ]. Indeed, the initial framework considers as the basis and it can be rebuilt, extended, or reduced based on its dimensions [ 26 ]. New concepts also emerge based on the researchers' interpretation of the evidence and ongoing comparisons of these concepts across studies [ 25 ]. This approach of synthesis possesses both positivist and interpretative perspectives; it provides the simultaneous use of the well-known strengths of both framework and evidence synthesis [ 27 ].
In order to achieve this aim the following methodological steps were conducted as follows:
Searching and selection of studies
In this step, we aimed to look for the relevant models and frameworks related to evidence-based decision-making in health systems management. The main research question was “what is the best framework for EBDM in health systems?” after defining the research question, the researchers searched for published studies on EBDM in HSM in different scientific databases with relevant keywords and constraints as inclusion and exclusion criteria from 01.01.2000 to 12.31.2020 (Table 1 ).
Inclusion and exclusion criteria
Inclusion criteria were determined as the studies that identify the components or develop a model or framework of EBDM in health organization in the form of original or review articles or dissertations, which were published in English and had a full text. The studies like book reviews, opinion articles, and commentaries that lacked a specific framework for conducting our review were excluded. During the search phase of the study, we attempted as much as possible to access studies that were not included in the search process or gray literature by reviewing the references lists of the retrieved studies or by contacting the authors of the articles or experts and querying them, as well as manually searching the related sites (Fig. 1 ).
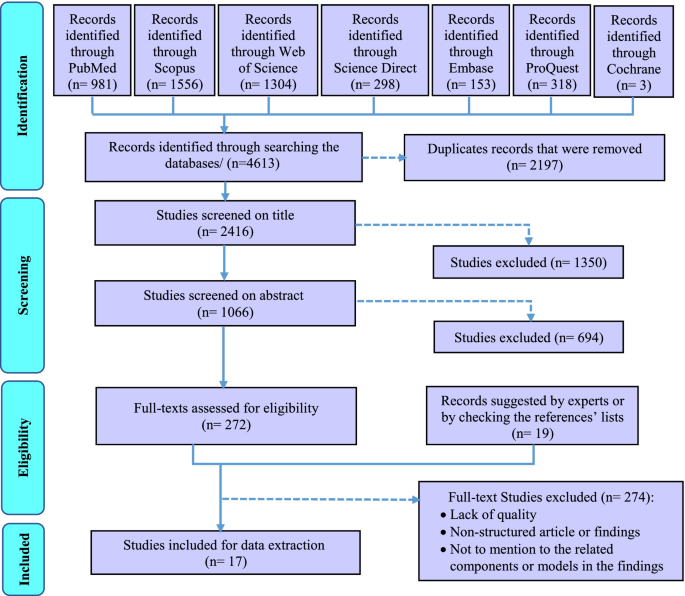
The PRISMA flowchart for selection of the studies in scoping review
Quality appraisal
The quality of the obtained studies was investigated using three tools for assessing the quality of various types of studies considering types and methods of the final include studies in systematic review. These tools were including Critical Appraisal Skills Program (CASP) for assessing the quality of qualitative researches [ 28 ], Scale for the Assessment of Narrative Review Articles (SANRA) [ 29 ], and The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers [ 30 ] (Table 3- Appendix ).
Data extraction
After searching the studies from all databases and removing duplicates, the studies were independently reviewed and screened by two members (TS and MRAM) of the research team in three phases by the title, abstract, and then the full text of the articles. At each stage of the study, the final decision to enter the study to the next stage was based on agreement and, in case of disagreement, the opinion of the third person from the research team was asked (PB). Mendeley reference manager software was used to systematically search and screen relevant studies. The data from the included studies were extracted based on the study questions and accordingly, a form of the studies’ profile including the author's name, publication year, country, study title, type of study, and its conditions were prepared in Microsoft Excel software (Table 4- Appendix ).
Synthesis and the conceptual model
In this step, a thematic analysis approach was applied to extract and analyze the data. For this purpose, first, the texts of the selected studies were read several times, and the initial qualitative codes or thematic concepts, according to the determined keywords and based on the research question, were found and labeled. Then these initial thematic codes were reviewed to achieve the final codes and they were integrated and categorized to achieve the final main themes and sub-themes, eventually. The main and the sub-themes are representative of the main and sub-steps of EBDM. At the last stage of the synthesis, the thematic analysis was finalized with 8 main themes and all the main and the sub-themes were tabulated (Table 5- Appendix ).
Creation of a new conceptual framework
For BFF synthesis in the present study, we compared the existing models and tried to find a model that fits the best. Three related models that appeared to be relatively well-suited to the purpose of this study to provide a complete, comprehensive, and practical EBDM model in HSM were found. According to the BFF instruction in Carroll et al. (2013) study [ 25 ], we decided to use all three models as the basis for the best fit because any of those models were not complete enough and we could give no one an advantage over others. Consequently, the initial model or the BFF basis was formed and the related thematic codes were classified according to the category of this basis as the main themes/steps of EBDM in HSM (Table 5- Appendix ). Then, the additional founded thematic codes were added and incorporated to this basis as the other main steps and the sub-steps of the EBDM in HSM according to the research team and some details in the form of sub-steps were added by the research team to complete the synthesized framework. Eventually, a comprehensive practical framework consisting of 10 main steps and 47 sub-steps was created with the potentiality of applying and implementing EDBM in HSM that we categorized them into four main phases (Table 6- Appendix ).
Testing the synthesis: comparison with the a priori models, dissonance and sensitivity
In order to assess the differences between the priori framework and the new conceptual framework, the authors tried to ask some experts’ opinions about the validity of the synthesized results. The group of experts has included eight specialists in the field of health system management or health policy-making. These experts have been chosen considering their previous research or experience in evidence-based decision/policy making performance/management (Table 2 ). This panel lasted in two three-hour sessions. The finalized themes and sub-themes (Table 6- Appendix ) and the new generated framework (Fig. 3 ) were provided to them before each session so that they could think and then in each meeting they discussed them. Finally, all the synthesized themes and sub-themes resulted were reviewed and confirmed by the experts.
Ethical considerations
To prevent bias, two individuals carried out all stages of the study such as screening, data extraction, and data analysis. The overall research project related to this manuscript was approved by the medical ethics conceal of the research deputy of Shiraz University of Medical Sciences with approval number IR.SUMS.REC.1396–01-07–14184, too.
The initial search across six electronic databases and the Cochrane library yielded 4613 studies. After removing duplicates, 2416 studies were assessed based on their titles. According to the abstract screening of the 1066 studies that remained after removing the irrelevant titles, 291 studies were selected and were entered into the full-text screening phase. Due to full-text screening of the studies, 17 final studies were selected for extracting the components and steps of EBDM in HSM (Fig. 1 ). The features of these studies were summarized in Table 4- Appendix (see supplementary data). Furthermore, according to the quality appraisal of the included studies, the majority of them had an acceptable level of quality. These results have been shown in Table 3- Appendix .
Results of the thematic analysis of the evidence (Table 5- Appendix ) along with the concepts proposed and added by the research team according to the focus-group discussion of the experts were shown in Table 6- Appendix . Accordingly, the main steps and related sub-steps of the EBDM process in HSM were defined and categorized.
After collecting, synthesizing, and categorizing thematic concepts, incorporating them with the initial models, and adding the additional main steps and sub-steps to the basic models, the final synthesized framework as a best-fit framework for EBDM in HSM was developed in the form of four general phases of inquiring, inspecting, implementing, and integrating and 10 main steps (Fig. 2 ). For better illustration, this framework with all the main steps and 47 sub-steps has been shown in Fig. 3 , completely.

The final synthesized framework of evidence-based decision-making in health system management
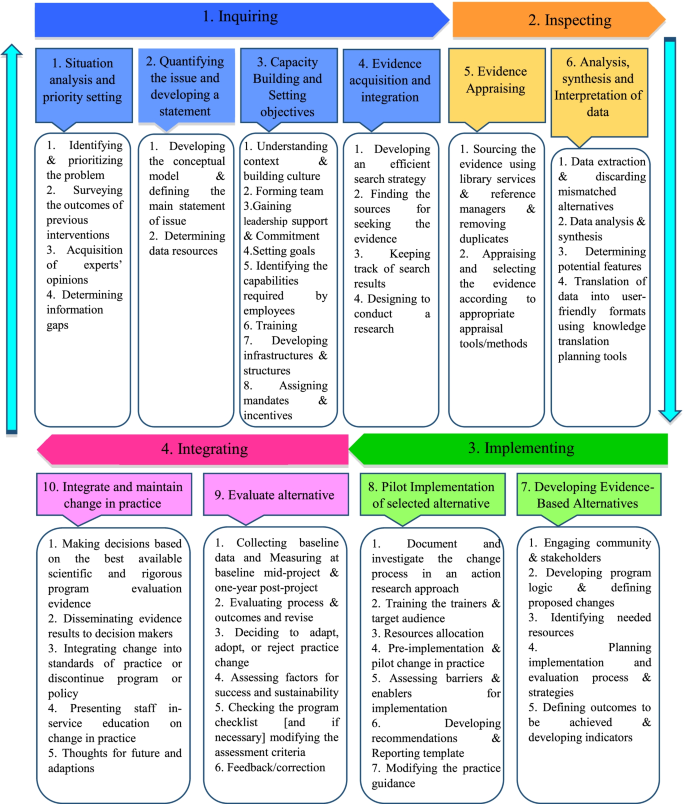
The main steps and sub-steps of the framework of EBDM in health system management
In the present study, a comprehensive framework for EBDM in HSM was developed. This model has different distinguishing characteristics than the formers. First of all, this is a comprehensive practical model that combined the strengths and the crucial components of the limited number of previous models; second, the model includes more details and complementary steps and sub-steps for full implementation of EBDM in health organizations and finally, the model is benefitted from a cyclic nature that has a priority than the linear models. Concerning the differences between the present framework and other previous models in this field, it must be said that most of the previous models related to EBDM were presented in the scope of medicine (that they were excluded from our SR according to the study objectives and exclusion criteria). A significant number of those models were proposed for the scope of public health and evidence-based practice, and only a limited number of them focused exactly on the scope of management and policy/decision making in health system organizations.
Given that the designed model is a comprehensive 10-step model, it can be used in some way at all levels of the health system and even in different countries. However, there will be a difference here, given that this framework provides a practical guide and a comprehensive guideline for applying evidence-based decision-making approach in health systems organizations, at each level of the health system in each country, this management approach can be applied depending on their existing infrastructure and the processes that are already underway (such as capacity building, planning, data collection, etc.), and at the same time, with a general guide, they can provide other infrastructure as well as the prerequisites and processes needed to make this approach much more possible and applicable.
It is true that evidence-based management is different from evidence-based medicine and even more challenging (due to lack of relevant data, greater sensitivity in data collection and their accuracy, lack of consistency and lack of transparency in the implementation of evidence-based decision-making in management rather than evidence-based medicine, etc.). Still, the general framework provided in this article can be used to help organizations that really want to act and move forward through this approach.
Furthermore, based on the findings, most of the previous studies only referred to some parts of the components and steps of the EBDM in health organizations and neglected the other parts or they were not sufficiently comprehensive [ 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 ]. Most of the previous models did not mention the necessary sub-steps, tools, and practical details for accurate and complete implementation of the EBDM, which causes the organizations that want to use these models, will be confused and cannot fully implement and complete the EBDM cycle. Among the studies that have provided a partly complete model than the other studies, were the studies by Brownson (2009), Yost (2014), and Janati (2018) [ 3 , 41 , 42 ]. Consequently, the combination of these three studies has been used as the initial framework for the best-fit synthesis in the present study.
Likewise, the models presented by Brownson (2009) and Janati (2018) were only limited to the six or seven key steps of the EBDM process, and they did not mention the details required for doing in each step, too [ 3 , 4 , 42 ]. Also, the model presented in the study of Janati (2018) was linear, and the relationships between the EBDM components were not well considered [ 42 , 43 ]; however, the model presented in this study was recursive. Also, in Yost's study (2014), despite the 7 main steps of EBDM and some details of each of the steps, the proposed process was not schematically drawn in the form of a framework and therefore the relationships between steps and sub-steps were not clear [ 41 ]. According to what was discussed, the best-fit framework makes the possibility of concentrating the fragmented models to a comprehensive one that can be fully applied and evaluated by the health systems policymakers and managers.
In the present study, the framework of EBDM in HSM was developed in the form of four general scopes of inquiring, inspecting, implementing, and integrating including 10 main steps and 47 sub-steps. These scopes were discussed as follows:
In the first step, “situation analysis and priority setting”, the most frequently cited sub-step was identifying and prioritizing the problem. Accordingly, Falzer (2009), emphasized the importance of identifying the decision-making conditions and the relevant institutions and determining their dependencies as the first steps of EBDM [ 44 ]. Aas (2012) has also cited the assessment of individuals and problem status and problem-finding as the first steps of EBDM [ 34 ]. Moreover, the necessity of identifying the existing situation and issues and prioritizing them has been emphasized as the initial steps in most management models such as environmental analysis in strategic planning [ 45 ].
Despite considering the opinions and experience of experts and managers as one of the important sources of evidence for decision-making [ 42 , 46 , 47 , 48 , 49 , 50 ], many studies did not mention this sub-step in the EBDM framework. Hence, the present authors added the acquisition of experts’ opinions as a sub-step of the first step because of its important role in achieving a comprehensive view of the overall situation.
In the second step, “quantifying the issue and developing a statement”, “Developing the conceptual model for the issue” was more addressed [ 37 , 41 , 47 ]. In addition, the authors to complete this step added the fourth sub-step, “Defining the main statement of issue”. This is because that most of the problems in health settings may have a similar value for managers and decision-makers and quantifying them can be used as a criterion for more attention or selecting the problem as the main issue to solve.
The third step, “Capacity building and setting objectives”, was not seen in many other included studies as a main step in EBDM, however, the present authors include this as a main step because without considering the appropriate objectives and preparing necessary capacities and infrastructures, entering to the next steps may become problematic. Moreover, in numerous studies, factors such as knowledge and skills of human resources, training, and the availability of the essential structures and infrastructures have been identified as facilitators of EBDM [ 51 , 52 , 53 , 54 , 55 ]. According to this justification, they are included in the present framework as sub-steps of the third step.
Considering the third step and based on the knowledge extracted from the previous studies, the three sub-steps of “understanding context and Building Culture” [ 56 , 57 ], “gaining the support and commitment of leaders” [ 39 , 57 , 58 ], and “identifying the capabilities required by employees and their skills weaknesses” [ 58 , 59 , 60 ] were the most important sub-steps in this step of EBDM framework. In this regard, Dobrow (2004) has also stated that the two essential components of any EBDM are the evidence and context of its use [ 32 ]. Furthermore, Isfeedvajani (2018) stated that to overcome barriers and persuade hospital managers and committees to apply evidence-based management and decision-making, first and foremost, creating and promoting a culture of "learning through research" was important [ 61 ].
The present findings showed that in the fourth main step, “evidence acquisition and integration”, the most important sub-step was “finding the sources for seeking the evidence” [ 39 , 40 , 41 , 60 , 62 , 63 ]. Concerning the sources for the use of evidence in decision-making in HSM, studies have cited numerous sources, most notably scientific and specialized evidence such as research, articles, academic reports, published texts, books, and clinical guidelines [ 39 , 64 , 65 ]. After scientific evidence, using the opinions and experiences of experts, colleagues, and managers [ 42 , 46 , 49 , 66 ] as well as the use of census and local level data [ 49 , 66 , 67 ], and other sources such as financial [ 67 ], political [ 42 , 49 ] and evaluations [ 49 , 68 ] data were cited.
The fifth step of the present framework, “evidence appraising”, was emphasized by previous literature; for instance, Pierson (2012) pointed to the use of library services in EBDM [ 69 ]. Appraising and selecting the evidence according to appropriate appraisal tools/methods was cited the most. International and local evidence is confirmed that ignoring these criteria can lead to serious faults in the process of decision and policy-making [ 70 , 71 ].
Furthermore, the sixth step, “analysis, synthesis, and interpretation of data”, was mentioned in many included studies [ 36 , 39 , 41 , 42 , 57 , 59 , 72 ]. This step emphasized the role of analysis and synthesis of data in the process of generation applied and useful information. It is obvious that the local interpretation according to different contexts may lead to achieving such kind of knowledge that can be used as a basis for local EBDM in HSM.
Implementing
The third scope consisted of the seventh and eighth steps of the EBDM process in HSM. In the seventh step, “developing evidence-based alternatives”, the issue of involving stakeholders in decision-making and subsequently, planning to design and implementation of the process and evaluation strategies had been focused by the previous studies [ 58 , 60 , 62 , 63 , 73 ]. Studies by Belay (2009) and Armstrong (2014) had also emphasized the need to use stakeholder and public opinion as well as local and demographic data in decision-making [ 49 , 67 ].
“Pilot-implementation of selected alternatives” was the eighth step of the framework. Some key sub-steps of this step were resources allocation [ 58 ], Pre-implementation and pilot change in practice and assessing barriers and enablers for implementation [ 40 ] that indicated the significance of testing the strategies in a pilot stage as a pre- requisition of implementing the whole alternatives. It is obvious that without attention to the pilot stage, adverse and unpleasant outcomes may occur that their correction process imposes many financial, organizational, and human costs on the originations. In addition, a study explained that one of the strategies of the decision-makers to measure the feasibility of the policy options was piloting them, which had a higher chance of being approved by the policymakers. Also, pilot implementation in smaller scales has been recommended in public health in cases of lack of sufficient evidence [ 74 ].
Integrating
This last scope consists of the ninth and tenth steps. The main sub-step of the ninth step, “evaluating alternatives”, was to evaluating process and outcomes and revise. After a successful implementation of the pilot, this step can be assured that the probable outcomes may be achieved and this evaluation will help the decision and policymakers to control the outcomes, effectively. Also, it impacts the whole target program and proposes some correcting plans through an accurate feedback process, too. Pagoto (2007) explained that a facilitator for EBDM would be an efficient and user-friendly system to assess utilization, outcomes, and perceived benefits [ 55 ].
Also, the tenth step, “integrating and maintaining change in practice”, was not considered as a major step in previous models, too, while it is important to maintain and sustain positive changes in organizational performance. In this regard, Ward (2011) also suggested several steps to maintain and sustain the widespread changes in the organization, including increasing the urgency and speed of action, forming a team, getting the right vision, negotiating for buy-in, empowerment, short-term success, not giving up and help to make a change stick [ 35 ]. Finally, the most important sub-steps that could be mentioned in this step were the dissemination of evidence results to decision-makers and the integration of changes made to existing standards and performance guidelines. Liang (2012) had also emphasized the importance of translating existing evidence into useful practices as well as disseminating them [ 47 ]. In addition, the final sub-step, “feedback and feedforward towards the EBDM framework”, was explained by the authors to complete the framework.
Some previous findings showed that about half and two-thirds of organizations do not regularly collect related data about the use of evidence, and they do not systematically evaluate the usefulness or impact of evidence use on interventions and decisions [ 75 ]. The results of a study conducted on healthcare managers at the various levels of an Iranian largest medical university showed that the status of EBDM is not appropriate. This problem was more evident among physicians who have been appointed as managers and who have less managerial and systemic attitudes [ 76 ]. Such studies, by concerning the shortcomings of current models for EBDM in HSM or even lack of a suitable and usable one, have confirmed the necessity of developing a comprehensive framework or model as a practical guide in this field. Consequently, existing and presenting such a framework can help to institutionalize the concept of EBDM in health organizations.
In contrast, results of Lavis study (2008) on organizations that supported the use of research evidence in decision-making reported that more than half of the organizations (especially institutions of health technology assessment agencies) may use the evidence in their process of decision-making [ 75 ], so applying the present framework for these organizations can be recommended, too.
Limitations
One of the limitations of the present study was the lack of access to some studies (especially gray literature) related to the subject in question that we tried to access them by manual searching and asking from some articles’ authors and experts. In addition, most of the existing studies on EBDM were limited to examining and presenting results on influencing, facilitating, or hindering factors or they only mentioned a few components in this area. Consequently, we tried to search for studies from various databases and carefully review and screen them to make sure that we did not lose any relevant data and thematic code. Also, instead of one model, we used four existing models as a basis in the BFF synthesis so that we can finally, by adding additional codes and themes obtained from other studies as well as expert opinions, provide a comprehensive model taking into account all the required steps and details. Also, the framework developed in this study is a complete conceptual model made by BFF synthesis; however, it may need some localization, according to the status and structure of each health system, for applying it.
The present framework provides a comprehensive guideline that can be well adapted for implementing EBDM in health systems and organizations especially in underdeveloped and developing countries where there is usually a lag in updating and applying evidence in their decision-making process. In addition, this framework by providing a complete, well-detailed, sequential and practical process including 10 steps and 56 sub-steps that did not exist in the incomplete related models, can be tested in the organizational decision-making process or managerial tasks by developed countries to improve their EBDM cycle, too.
Availability of data and materials
All data in a form of data extraction tables are available from the corresponding author on a reasonable request.
Abbreviations
- Evidence-based decision-making
Health System Management
Best-Fit Framework
Rychetnik L, Bauman A, Laws R, King L, Rissel C, Nutbeam D, et al. Translating research for evidence-based public health: Key concepts and future directions. J Epidemiol Community Health. 2012;66(12):1187–92.
Article Google Scholar
Nutbeam D, Boxall AM. What influences the transfer of research into health policy and practice? Observations from England and Australia. Public Health. 2008;122(8):747–53.
Brownson RC, Fielding JE, Maylahn CM. Evidence-Based Public Health: A Fundamental Concept for Public Health Practice. Annu Rev Public Health [Internet]. 2009;30(1):175–201. https://doi.org/10.1146/annurev.publhealth.031308.100134 .
Brownson RC, Gurney JG, Land GH. Evidence-based decision making in public health. J Public Heal Manag Pract [Internet]. 1999 [cited 2018 May 26];5(5):86–97. Available from: https://books.google.com/books?hl=en&lr=&id=yxRgAwAAQBAJ&oi=fnd&pg=PA133&dq=+criteria+OR+health+%22evidence+based+decision+making%22&ots=hiqVNQtF24&sig=jms9GsBfw6gz1cN2FQXzCBZvmMQ
McGinnis JM. ‘Does Proof Matter? Why Strong Evidence Sometimes Yields Weak Action.’ Am J Heal Promot. 2001;15(5):391–396. Available from: https://doi.org/10.4278/0890-1171-15.5.391 .
Majdzadeh R, Yazdizadeh B, Nedjat S, Gholami J, Ahghari S, R. M, et al. Strengthening evidence-based decision-making: Is it possible without improving health system stewardship? Health Policy Plan [Internet]. 2012 Sep 1 [cited 2018 May 15];27(6):499–504. Available from: https://doi.org/10.1093/heapol/czr072
WHO EIPNET. Using evidence and innovation to strengthen policy and practice. 2008.
Ellen ME, Léon G, Bouchard G, Lavis JN, Ouimet M, Grimshaw JM. What supports do health system organizations have in place to facilitate evidence-informed decision-making? A qualitative study. Implement Sci. 2013;8(1):84.
Oxman AD, Lavis JN, Lewin S, Fretheim A. What is evidence-informed policymaking? Health Res Policy Sys. 2009;7:1–7.
Armstrong R, Waters E, Dobbins M, Anderson L, Moore L, Petticrew M, et al. Knowledge translation strategies to improve the use of evidence in public health decision making in local government: Intervention design and implementation plan. Implement Sci [Internet]. 2013;8(1):1. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-84885076767&doi=10.1186%2F1748-5908-8-121&partnerID=40&md5=dddaf4029205c63877a3e6ecf28f7762
Waters E, Armstrong R, Swinburn B, Moore L, Dobbins M, Anderson L, et al. An exploratory cluster randomised controlled trial of knowledge translation strategies to support evidence-informed decision-making in local governments (The KT4LG study). BMC Public Health [Internet]. 2011;11(1):34. Available from: http://www.biomedcentral.com/1471-2458/11/34
Imani-Nasab MH, Yazdizadeh B, Salehi M, Seyedin H, Majdzadeh R. Validity and reliability of the Evidence Utilisation in Policymaking Measurement Tool (EUPMT). Heal Res Policy Syst. 2017;15(1):1–11.
El-Jardali F, Lavis JN, Ataya N, Jamal D, Ammar W, Raouf S. Use of health systems evidence by policymakers in eastern mediterranean countries: Views, practices, and contextual influences. BMC Health Serv Res. 2012;12(1):200.
Ettelt S, Mays N. Health services research in Europe and its use for informing policy. J Health Serv Res Policy [Internet]. 2011 Jul 29 [cited 2019 Jun 29];16(2_suppl):48–60. Available from: https://doi.org/10.1258/jhsrp.2011.011004
Sutcliffe S. Evidence-Based Policymaking: What is it? How does it work? What relevance for developing countries? 2005.
Campbell DM, Redman S, Jorm L, Cooke M, Zwi AB, Rychetnik L. Increasing the use of evidence in health policy: Practice and views of policy makers and researchers. Aust New Zealand Health Policy. 2009;6(1):1–11.
WHO. Supporting the Use of Research Evidence (SURE) for Policy in African Health Systems. 2007:1–72.
Health Public Accreditation Board. Public Health Accreditation Board STANDARDS : AN OVERVIEW. 2012.
Riley WJ, Bender K, Lownik E. Public health department accreditation implementation: Transforming public health department performance. Am J Public Health. 2012;102(2):237–42.
Liebman JB. Building on Recent Advances in Evidence-Based Policymaking. 2013:36. Available from: http://www.americaachieves.org/9F42769C-3A65-4CCB-8466-E7BFD835CFE7/FinalDownload/DownloadId-0AB31816953C7B8AFBD2D15DFD39D5A8/9F42769C-3A65-4CCB-8466-E7BFD835CFE7/docs/RFA/THP_Liebman.pdf
Jacobs J a, Jones E, Gabella B a, Spring B, Brownson C. Tools for Implementing an Evidence-Based Approach in Public Health Practice. Prev Chronic Dis [Internet]. 2012;9(1):1–9. Available from: https://doi.org/10.5888/pcd9.110324
Kothari A, Edwards N, Hamel N, Judd M. Is research working for you? validating a tool to examine the capacity of health organizations to use research. Implement Sci. 2009;4(1):1–9.
Oxman AD, Bjørndal A, Becerra-Posada F, Gibson M, Block MAG, Haines A, et al. A framework for mandatory impact evaluation to ensure well informed public policy decisions. Lancet. 2010;375(9712):427–31. Available from: https://doi.org/10.1016/S0140-6736(09)61251-4
Oxman AD, Vandvik PO, Lavis JN, Fretheim A, Lewin S. SUPPORT Tools for evidence-informed health Policymaking (STP) 2: Improving how your organisation support the use of research evidence to inform policymaking. Chinese J Evidence-Based Med. 2010;10(3):247–54.
Google Scholar
Carroll C, Booth A, Leaviss J, Rick J. “ Best fit ” framework synthesis : refining the method. BMC Med Res Methodol. 2013;13(1):1 Available from: BMC Medical Research Methodology.
Carroll C, Booth A, Cooper K. A worked example of “ best fit ” framework synthesis : A systematic review of views concerning the taking of some potential chemopreventive agents. BMC Med Res Methodol. 2011;11:29.
Barnett-page E, Thomas J. Methods for the synthesis of qualitative research : a critical review. BMC Med Res Methodol 9. 2009;59:1–26.
Public Health Resource Unit. Critical Appraisal Skills Programme (CASP) making sense of evidence;10 questions to help you make sense of qualitative research. Public Health. 2006.
Baethge C, Goldbeck-Wood S, Mertens S. SANRA—a scale for the quality assessment of narrative review articles. Res Integr Peer Rev. 2019;4(1):2–8.
Hong Q, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, et al. Mixed Methods Appraisal Tool (MMAT), Version 2018. User guide. McGill [Internet]. 2018;1–11. Available from: http://mixedmethodsappraisaltoolpublic.pbworks.com/w/file/fetch/127916259/MMAT_2018_criteria-manual_2018-08-01_ENG.pdf%0Ahttp://mixedmethodsappraisaltoolpublic.pbworks.com/
Titler MG. The Iowa Model of evidence-based practice to promote quality care. 2001.
Dobrow MJ, Goel V, Upshur REG. Evidence-based health policy: context and utilisation. Soc Sci Med [Internet]. 2004;58(1):207–17. Available from: http://www.sciencedirect.com/science/article/pii/S0277953603001667
Kohatsu ND, Robinson JG, Torner JC. Evidence-based public health: An evolving concept. Am J Prev Med. 2004;27(5):417–21.
PubMed Google Scholar
Aas RW, Alexanderson K. Challenging Evidence-based Decision-making: A Hypothetical Case Study about Return to Work. Occup Ther Int. 2012 [cited 2018 May 28];19(1):28–44. Available from: https://doi.org/10.1002/oti.326
Ward M. Evidence-informed decision making in a public health setting. Healthc Manag Forum. 2011;24(1 SUPPL):S8.
Champagne F, Lemieux-Charles L, Duranceau M-F, MacKean G, Reay T. Organizational impact of evidence-informed decision making training initiatives: A case study comparison of two approaches. Implement Sci [Internet]. 2014;9(1). Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-84900004312&doi=10.1186%2F1748-5908-9-53&partnerID=40&md5=df5573f17e19ef002d67cf669059aef4
Wright AL, Zammuto RF, Liesch PW, Middleton S, Hibbert P, Burke J, et al. Evidence-based Management in Practice: Opening up the Decision Process, Decision-maker and Context. Br J Manag. 2016;27(1):161–78. Available from: https://doi.org/10.1111/1467-8551.12123
Stamatakis KA, Ferreira Hino AA, Allen P, McQueen A, Jacob RR, Baker EA, et al. Results from a psychometric assessment of a new tool for measuring evidence-based decision making in public health organizations. Eval Program Plann [Internet]. 2017 Feb [cited 2018 May 16];60:17–23. Available from: http://linkinghub.elsevier.com/retrieve/pii/S014971891630009X
Harris C, Allen K, Waller C, Dyer T, Brooke V, Garrubba M, et al. Sustainability in Health care by Allocating Resources Effectively (SHARE) 7: supporting staff in evidence-based decision-making, implementation and evaluation in a local healthcare setting. BMC Health Serv Res [Internet]. 2017 Dec 21 [cited 2018 May 19];17(1):430. Available from: https://doi.org/10.1186/s12913-017-2388-8
Harris C, Garrubba M, Melder A, Voutier C, Waller C, King R, et al. Sustainability in Health care by Allocating Resources Effectively (SHARE) 8: Developing, implementing and evaluating an evidence dissemination service in a local healthcare setting. BMC Health Serv Res [Internet]. 2018;18(1). Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85042873576&doi=10.1186%2Fs12913-018-2932-1&partnerID=40&md5=2daa5bbd3ccddf299f7b9d527b6105af
Yost J, Dobbins M, Traynor R, DeCorby K, Workentine S, Greco L. Tools to support evidence-informed public health decision making. BMC Public Health [Internet]. 2014 Dec 18 [cited 2018 May 28];14(1):728. Available from: https://bmcpublichealth.biomedcentral.com/articles/ https://doi.org/10.1186/1471-2458-14-728
Janati A, Hasanpoor E, Hajebrahimi S, Sadeghi- H, Khezri A. An Evidence-Based Framework for Evidence-Based Management in Healthcare Organizations : A Delphi Study. Ethiop J Heal Sci. 2018;28(3):305–14.
Rosswurm MA, Larrabee JH. A Model for Change to Evidence-Based Practice. J Nurs Scholarsh. 1999;31(4):317–22.
Article CAS Google Scholar
Falzer PR, Garman MD. A conditional model of evidence-based decision making. J Eval Clin Pract [Internet]. 2009 Dec [cited 2018 May 19];15(6):1142–51. Available from: http://doi.wiley.com/ https://doi.org/10.1111/j.1365-2753.2009.01315.x
Ginter PM, Duncan WJ, Swayne LE. Strategic management of health care organizations. 8th Edition. Hoboken: John Wiley & Sons, Inc. 2018. p. 40.
Humphries S, Stafinski T, Mumtaz Z, Menon D. Barriers and facilitators to evidence-use in program management: a systematic review of the literature. BMC Health Serv Res [Internet]. 2014 Dec 14 [cited 2018 May 16];14(1):171. Available from: http://bmchealthservres.biomedcentral.com/articles/ https://doi.org/10.1186/1472-6963-14-171
Liang Z, Howard PF, Leggat SG, Murphy G. A framework to improve evidence-informed decision-making in health service management. Aust Heal Rev [Internet]. 2012;36(3):284–9. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-84865450745&doi=10.1071%2FAH11051&partnerID=40&md5=c42d56774cd486b8df8a5e4afec33a6a
Kohn MK, Berta W, Langley A, Davis D. Evidence-based decision making in health care settings: From theory to practice [Internet]. Vol. 11, Advances in Health Care Management. Emerald Group Publishing Ltd; 215–234 p. Available from: 2011. https://doi.org/10.1108/S1474-8231(2011)0000011012 .
Armstrong R, Waters E, Moore L, Dobbins M, Pettman T, Burns C, et al. Understanding evidence: a statewide survey to explore evidence-informed public health decision-making in a local government setting. Implement Sci [Internet]. 2014;9(1):188. Available from: http://implementationscience.biomedcentral.com/articles/ https://doi.org/10.1186/s13012-014-0188-7
McDiarmid M, Sandra K, Binns M. Evidence-based administrative decision making and the Ontario hospital CEO: information needs, seeking behaviour, and access to sources. JCHLA / JABSC [Internet]. 2007 [cited 2018 May 28];28:63–72. Available from: https://ejournals.library.ualberta.ca/index.php/jchla/article/viewFile/24060/17884
Brownson RC, Allen P, Duggan K, Stamatakis KA, Erwin PC. Fostering more-effective public health by identifying administrative evidence-based practices: A review of the literature. Am J Prev Med [Internet]. 2012;43(3):309–19. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-84865688888&doi=10.1016%2Fj.amepre.2012.06.006&partnerID=40&md5=a843f04e58b619ab9355a98bbfeef51a
Moussata CO. Evidence-Based Management and its Influence on the Practices of Senior Leaders of Hospitals in the Denver Metropolitan Area [Internet]. ProQuest Dissertations and Theses. [Ann Arbor]: Colorado Technical University; 2017 [cited 2018 May 19]. Available from: https://search.proquest.com/docview/1967189422?accountid=41313
Ward M, Mowat D. Creating an organizational culture for evidence-informed decision making. Healthc Manag Forum [Internet]. 2012;25(3):146–50. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-84867778644&doi=10.1016%2Fj.hcmf.2012.07.005&partnerID=40&md5=42f06b7236a4a1cd6a4739c7e1900764
Sosnowy CD, Weiss LJ, Maylahn CM, Pirani SJ, Katagiri NJ. Factors affecting evidence-based decision making in local health departments. Am J Prev Med [Internet]. 2013 Dec [cited 2018 May 19];45(6):763–8. Available from: http://dx.doi.org/ https://doi.org/10.1016/j.amepre.2013.08.004
Pagoto SL, Spring B, Coups EJ, Mulvaney S. Barriers and Facilitators of Evidence-Based Practice Perceived by Behavioral Science Health Professionals. 2007;63(7):695–705.
Weiss L, Sosnowy C, Maylahn C, Katagiri N, Pirani S. Evidence-Based Decision Making in Local Health Departments Evidence-Based Decision Making in Local Health Departments. Front Public Heal Serv Syst Res. 2012;1(3):1–7.
Lester L, Haby MM, Chapman E, Kuchenmüller T. Evaluation of the performance and achievements of the WHO Evidence-informed Policy Network (EVIPNet) Europe. Heal Res policy Syst. 2020;18(1):109.
Aas RW, Alexanderson K. Challenging evidence-based decision-making: A hypothetical case study about return to work. Occup Ther Int [Internet]. 2012 Mar [cited 2018 May 28];19(1):28–44. Available from: https://doi.org/10.1002/oti.326
Daouk-Öyry L, Sahakian T, van de Vijver F. Evidence-Based Management Competency Model for Managers in Hospital Settings. Br J Manag. 2020;00:1–20.
Isfeedvajani MS. Evidence-Based Management and its Application in the Hospital Management Process. Hosp Pract Res [Internet]. 2018 [cited 2018 May 28];3(2):35–6. Available from: http://jhpr.ir/article_60533_8313dd6afa580ef2afa689e6984c8844.pdf
Armstrong R, Waters E, Moore L, Dobbins M, Pettman T, Burns C, et al. Understanding evidence: a statewide survey to explore evidence-informed public health decision-making in a local government setting. Implement Sci [Internet]. 2014 Dec 14 [cited 2018 May 28];9(1):188. Available from: https://doi.org/10.1186/s13012-014-0188-7
Uneke CJ, Sombie I, Johnson E, Uneke BI, Okolo S. Promoting the use of evidence in health policymaking in the ECOWAS region: the development and contextualization of an evidence-based policymaking guidance. Global Health [Internet]. 2020;16(1):73. Available from: http://www.embase.com/search/results?subaction=viewrecord&id=L632558076&from=export
Janati A, Hasanpoor E, Hajebrahimi S, Sadeghi-Bazargani H. Health care managers’ perspectives on the sources of evidence in evidence-based hospital management: A qualitative study in Iran. Ethiop J Health Sci [Internet]. 2017;27(6):659–68. Available from: https://www.ajol.info/index.php/ejhs/article/view/162555
Spiri WC, Kurcgant P, Pereira MV. Perception Of Nursing Middle Managers About The Evidence-Based Management. Int Arch Med [Internet]. 2017;10(February):11. Available from: http://imedicalsociety.org/ojs/index.php/iam/article/view/2311
Harris C, Allen K, Waller C, Green S, King R, Ramsey W, et al. Sustainability in Health care by Allocating Resources Effectively (SHARE) 5: developing a model for evidence-driven resource allocation in a local healthcare setting. BMC Health Serv Res. 2017;17(1):1–18.
Belay T, Mbuya N, Rajan V. Data utilization and evidence-based decision making in the health sector: survey of three Indian states [Internet]. 2009 [cited 2018 May 26]. Available from: https://openknowledge.worldbank.org/handle/10986/3161
Niedzwiedzka BM. Barriers to evidence-based decision making among Polish healthcare managers. Heal Serv Manag Res [Internet]. 2003 May 21 [cited 2018 May 19];16(2):106–15. Available from: https://doi.org/10.1258/095148403321591429
Peirson L, Ciliska D, Dobbins M, Mowat D. Building capacity for evidence informed decision making in public health: A case study of organizational change. BMC Public Health [Internet]. 2012;12(1):137. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-84857132983&doi=10.1186%2F1471-2458-12-137&partnerID=40&md5=68e18844316881fb3f2662477825d441
Buffett C, Ciliska D, Thomas H. Can I Use This Evidence in my Program Decision? Assessing Applicability and Transferability of Evidence. National Collaborating Centre for Methods and Tools (NCCMT) School of Nursing, McMaster University. 2007:1–22.
Buffet C, Ciliska D, Thomas H. It worked there. Will it work here? A tool for assessing applicability and transferability of evidence (A: When considering starting a new program). National Collaborating Centre for Methods and Tools (NCCMT) School of Nursing, McMaster University. 2011;(905):1–2.
Dobbins M, Jack S, Thomas H, Kothari A. Public health decision-makers’ informational needs and preferences for receiving research evidence. Worldviews Evidence-Based Nurs. 2007;4(3):156–63.
Wright AL, Zammuto RF, Liesch PW, Middleton S, Hibbert P, Burke J, et al. Evidence-based Management in Practice: Opening up the Decision Process, Decision-maker and Context. Br J Manag [Internet]. 2016 Jan [cited 2018 May 28];27(1):161–78. Available from: https://doi.org/10.1111/1467-8551.12123
Imani-Nasab MH, Seyedin H, Yazdizadeh B, Majdzadeh R. A Qualitative Assessment of the Evidence Utilization for Health Policy-Making on the Basis of SUPPORT Tools in a Developing Country. Int J Heal Policy Manag. 2017;6(8):457–65.
Lavis JN, Paulsen EJ, Oxman AD, Moynihan R. Evidence-informed health policy 2-Survey of organizations that support the use of research evidence. Implement Sci. 2008;3:54.
Bastani P, Kavosi Z, Alipoori S, Imani-Nasab MH. Evidence- based Policy and Decision-Making among Health Managers: A Case of Shiraz Univer- sity of Medical Sciences. GMJ. 2017;6(1):30–8.
Greaves DE. Evidence-based management of Caribbean health systems: barriers and opportunities. Int J Health Governance. 2017;22(2):104–117.
Download references
Acknowledgements
This research, derived from Proposal No. 96-01-07-14184, was conducted by Mrs. Tahereh Shafaghat as part of the activities required for a Ph.D. degree in health care management at the Shiraz University of Medical Sciences. The authors wish to express their sincere gratitude to the research administration of Shiraz University of Medical Sciences for its financial and administrative support and to the English editorial board of Research Editor Institution for improving the native English language of this work.
As the overall study was an approved research project of Shiraz University of Medical Sciences and it was conducted by Mrs. Tahereh Shafaghat as part of the activities required for a Ph.D. degree in the health care management field, the Shiraz University of Medical Sciences supported this study. This study was sponsored by Shiraz University of Medical Sciences under code (96‑01‑07‑14184). The funding body was not involved in the design of the study, data collection, analysis, and interpretation, as well as in writing the manuscript.
Author information
Tahereh Shafaghat and Peivand Bastani have equal participation as first authors.
Authors and Affiliations
School of Management and Medical Informatics, Health Human Recourses Research Center, Shiraz University of Medical Sciences, Shiraz, Iran
Tahereh Shafaghat, Peivand Bastani & Mohammad Amin Bahrami
Department of Health Care Management, School of Public Health, Health Policy and Management Research Center, Shahid Saoughi University of Medical Sciences, Yazd, Iran
Tahereh Shafaghat & Mohammad Kazem Rahimi Zarchi
Faculty of Health and Behavioral Sciences, School of Dentistry, University of Queensland, QLD, 4072, Brisbane, Australia
Peivand Bastani
Social Determinants of Health Research Center, Lorestan University of Medical Sciences, Khorramabad, Iran
Mohammad Hasan Imani Nasab
Student Research Committee, School of Management and Medical Informatics, Shiraz University of Medical Sciences, Shiraz, Iran
Mahsa Roozrokh Arshadi Montazer
Faculty of Medicine, Center for Health Services Research, The University of Queensland, Brisbane, Australia
Sisira Edirippulige
You can also search for this author in PubMed Google Scholar
Contributions
PB and TSH designed the study and its overall methodology. BP also edited and finalized the article. TSH searched all the databases, with the help of MRAM retrieved the sources, scanned, and screened all the articles in 3 phases. TSH also prepared the draft of the article. MAB and MKRZ contributed to data analysis and synthesis. Also, the study was under consultation and supervision by ZK and MHIN as advisors. All the authors have read and approved the final manuscript.
Corresponding author
Correspondence to Peivand Bastani .
Ethics declarations
Ethics approval and consent to participate.
Since at this study a scoping review was conducted and then the best-fit framework synthesis was used for developing a comprehensive EBDM framework in HSM, there was no human or animal participant in this study. However, the overall research project related to this manuscript was approved by the medical ethics conceal of the research deputy of Shiraz University of Medical Sciences with approval number IR.SUMS.REC.1396–01-07–14184.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Tables 3 , 4 , 5 and 6 .
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Shafaghat, T., Bastani, P., Nasab, M.H.I. et al. A framework of evidence-based decision-making in health system management: a best-fit framework synthesis. Arch Public Health 80 , 96 (2022). https://doi.org/10.1186/s13690-022-00843-0
Download citation
Received : 30 October 2021
Accepted : 08 March 2022
Published : 29 March 2022
DOI : https://doi.org/10.1186/s13690-022-00843-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health system
- Best-fit framework synthesis
Archives of Public Health
ISSN: 2049-3258
- General enquiries: [email protected]
- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
When Health Care Providers Look at Problems from Multiple Perspectives, Patients Benefit
- Jemima A. Frimpong,
- Christopher G. Myers,
- Kathleen M. Sutcliffe,
- Yemeng Lu-Myers

Specialization has its limits.
Health care providers have vastly different ways of seeing and treating patients, as differences in profession, specialty, experience, or background lead them to pay attention to particular signals or cues, and influence how they approach problems. While diverse perspectives and approaches to care are important, if they are not managed appropriately, they can cause misunderstandings, bias decision-making, and get in the way of the best care. Two things can help health professionals get better at communicating with each other and adopting multiple perspectives themselves: 1) creating an environment that supports perspective sharing and effective communication among team members; and 2) building people’s capacity to adopt multiple perspectives.
Mr. Smith was ready to be discharged home after his laryngectomy, an extensive operation that removes a patient’s throat due to cancer. In the opinion of Dr. Lu-Myers, he was a capable man who had passed his physical and occupational therapy evaluations with flying colors. Mr. Smith had fulfilled the doctor’s list of clinical discharge criteria, and she was eager to send him home. She planned to entrust him and his family to manage his dressing changes, as well as his tracheostomy and drain care, with the support of frequent outpatient nursing visits — all very routine protocol, especially for someone who seemed alert and capable.
- Jemima A. Frimpong is an assistant professor at the Johns Hopkins University Carey Business School and Armstrong Institute for Patient Safety & Quality. Her research focuses on the adoption and sustainability of innovations, development and testing of organization-level interventions, and performance improvement, centered primarily on health care organizations.
- Christopher G. Myers is an assistant professor at Johns Hopkins University on the faculty of the Carey Business School, School of Medicine, and Armstrong Institute for Patient Safety & Quality. His research explores interpersonal processes of learning, development, and innovation in health care and other knowledge-intensive work environments. Follow him @ChrisGMyers .
- KS Kathleen M. Sutcliffe is a Bloomberg Distinguished Professor at Johns Hopkins University. Her research examines how organizations manage the unexpected and the dynamics of organizational reliability and resilience.
- Yemeng Lu-Myers is a resident surgeon specializing in otorhinolaryngology (ENT) at the University of Maryland Medical Center. Her research explores how patient demographics influence health outcomes and examines the effects of differential access to care.
Partner Center

An official website of the Department of Health & Human Services

- Search All AHRQ Sites
- Email Updates
- Contact DHR
Supporting Clinicians to Improve Decision Making and Patients’ Care
AHRQ’s Digital Healthcare Research Program funds research to support clinicians and other healthcare professionals in improving their ability to provide optimal health services to their patients. In 2020, a total of $65.3 million was invested in research projects to support technology-enabled decision making and reducing provider burden. Read more about how our research improves decision making in tandem with improving the experience of health professionals who use electronic health records (EHRs) and other digital healthcare technology.
Clinical Decision Making
Improving clinical decision making is dependent on clinicians’ ability to access the most relevant, accurate, and recent information to make evidence-based decisions regarding a patient’s healthcare. Integrating evidence-based clinical decision support (CDS) seamlessly into care helps clinicians by delivering the right information to the correct location and at the right time, so that clinicians can make the best care decisions. When well developed and implemented, CDS uses patient-specific data and relies on evidence-based findings to improve health and lead to the best possible outcomes.

Dr. Sheila Maria Gephart and a research-based team at the University of Arizona integrated a previously developed CDS into providers’ workflow in neonatal intensive care units to identify necrotizing enterocolitis (NEC) in premature infants. Researchers designed the NEC-Zero intervention to engage families and support team-based care and widespread adoption of evidence-based best practices for NEC prevention. The tool showed high rates of utilization and demonstrated potential for standardized clinical use, which the research team hopes will improve clinical care processes and neonatal outcomes.
EHRs have the potential to improve clinicians' diagnosis and treatment of obesity by providing tools such as CDS reminders. Yet, much of the CDS development, research, and funding focus has been on adult patient populations. Therefore, Dr. Mahnoos H. Sharifi and a Yale University-based research team are evaluating different tools within EHRs to assist pediatric care clinicians with providing higher-quality childhood obesity care to slow weight gain in children with obesity.
Social Determinants of Health (SDOH)
Social determinants of health (SDOH) are conditions in the environment where people are born, live, learn, work, play, and worship that affect a range of health and quality of life risks and outcomes. An integral part of healthcare delivery involves understanding these social and environmental factors of patients’ lives outside of the healthcare system. Addressing inequities in these conditions, supported in part through the access and use of contextual SDoH data, can help to eliminate health disparities and to improve individual and population health. However, collection and use of contextual SDoH data may not be feasible in a time-constrained visit. The use of integrated digital health IT tools can support the collection of SDoH data, including the following AHRQ-funded research:

Dr. Andrea Wallace and team at the University of Utah evaluated the integration of an electronic social needs screener into the emergency department (ED) workflow. This screener was designed to identify patients in need of referrals to non-emergency, community-based resources such as food, transportation, or housing assistance. The research team partnered with the United Way of Utah’s 211 service to facilitate referrals and found that the screener implementation did not pose significant technological, time, or cost barriers. Although only a small portion of patients with reported social needs ultimately received community-based services, the research highlights the feasibility and importance of integrating SDoH into ED discharge planning and its potential to reduce unnecessary ED use.
Read Dr. Wallace's Impact Story
Health Technology Design
Improving health technology design to support cognitive work and improve usability is a focus of AHRQ-funded research aimed at addressing EHR-related provider burden. The following research explored ways to improve technology design and use, including clinical workflow, communication, cognitive load, and user satisfaction to reduce provider burden:

Dr. Deborah Jill Cohen and team at the Oregon Health and Science University examined the informational needs of care teams to inform design principles for supporting health IT management and care coordination. The research team conducted a mixed methods study of community health center clinicians and clinical teams to identify a range of informational needs regarding patients’ SDoH. Based on these findings, the researchers defined a set of EHR design principles, which was then used to develop an SDoH data collection prototype. Usability testing of the prototype was promising, highlighting its potential to inform clinical decision making when caring for complex patients.
Dr. Christopher Harle and research team at Indiana University–Purdue University at Indianapolis developed two user-centered CDS prototypes, Chronic Pain OneSheet and Chronic Pain Treatment Tracker, to support guideline-based clinical decision making for chronic musculoskeletal pain management. The research team conducted a design workshop and usability testing with primary care providers to characterize information use and decision making patterns and found that information accessibility, organized tables, interactivity, and visual cues were imperative design factors. By characterizing common patterns in information availability, information use, and care planning primary care providers relied on during patient visits for chronic pain, the researchers created new EHR-based decision support tools to guide clinicians’ perceptions and judgments of noncancer pain. This led to increased use of guideline-based patient assessment and treatment.
Read Dr. Harle's Impact Story
Health IT systems must be designed to support healthcare providers’ cognitive work, workflow, and decision making needs, rather than requiring them to adapt their cognitive work and workflow to meet the system’s requirements. To address this, Dr. Aaron Zachary Hettinger of MedStar Health Research Institute performed a cognitive engineering analysis of ED clinicians’ cognitive needs and workflows to inform the design of health IT for use in complex healthcare environments. The research team conducted EHR data analyses, focus groups, interviews, and observations to identify gaps and challenges in existing health IT and to evaluate prototype usability in a clinical simulation center. The research team identified gaps and challenges related to existing health IT, as well as strategies to improve the methods for developing and testing before implementation.
Read Dr. Hettinger's Impact Story
Home healthcare (HHC) agencies have been slow to adopt EHRs and mobile technology. Therefore, transition into HHCs can be challenging because of the absence of, or limits to, an electronic information flow between hospitals and home care agencies. Dr. Paulina Sockolow of Drexel University developed and disseminated a set of IT and EHR design and implementation recommendations for use in HHC transitions. The research team examined nurses’ informational needs, decision making, and workflow during HHC admissions, finding that they often lacked the necessary information prior to entering a patient’s home and instead relied on prior experience to form plan-of-care decisions. This research highlights the need for standardized and interoperable health IT solutions for use in HHC settings.
Blood cultures are the only way to diagnose sepsis, a life-threatening bloodstream infection that can affect infants in the pediatric intensive care unit (PICU); however, overuse of blood cultures may result in unnecessary laboratory tests, unnecessary antibiotic use, prolonged hospitalization, and increased healthcare costs. To support clinician’s decision making, Dr. Anping Xie and team at the Johns Hopkins University developed, implemented, and evaluated an EHR-embedded CDS tool to support naturalistic decision making in blood culture utilization among PICU clinicians. The research team examined individual and team cognition and decision making associated with obtaining a blood culture and used those insights to develop the electronic CDS tool iteratively and found that unnecessary blood culture utilization was reduced. The process and architecture used in the development of the CDS tool may be applied to other conditions commonly seen in the PICU, such as venous thromboembolism and traumatic brain injury, and may potentially be generalizable to other healthcare settings.
Dr. Tosha Beth Wetterneck of University of Wisconsin–Madison designed and tested Tandem EHR, a prototype to support the cognitive work, such as information searching, situation assessment, problem identification, and problem solving, of primary care physicians and their teams. Through cognitive task analysis, the research team identified providers’ key situation awareness needs, which then informed the design of an EHR prototype. Usability testing of the EHR prototype showed positive results that underscore the need for technology to support the cognitive work of primary care providers and to improve teamwork, provider satisfaction, and quality of patient care.
- Director's Corner
- Current Priorities
- Executive Summary
- Research Spotlight
- Research Themes and Findings
- Research Dissemination
- Research Overview
- 2020 Year in Review
- 2019 Year in Review
- Engaging and Empowering Patients
- Optimizing Care Delivery for Clinicians
- Supporting Health Systems in Advancing Care Delivery
- Our Experts
- Search AHRQ-Funded Projects
- AHRQ-Funded Projects Map
- AHRQ Digital Healthcare Research Publications Database
- Health IT Survey Compendium
- Time and Motion Studies Database
- Health Information Security and Privacy Collaboration Toolkit
- Implementation in Independent Pharmacies
- Implementation in Physician Offices
- ePROs in Clinical Care
- Guide to Integrate Patient-Generated Digital Health Data into Electronic Health Records in Ambulatory Care Settings
- Children's Electronic Health Record (EHR) Format
- Project Resources Archives
- National Webinars
- Funding Opportunities
- Digital Healthcare Research Home
- 2018 Year in Review Home
- Research Summary
- Research Spotlights
- 2019 Year in Review Home
- Annual Report Home
The Value of Critical Thinking in Nursing

- How Nurses Use Critical Thinking
- How to Improve Critical Thinking
- Common Mistakes

Some experts describe a person’s ability to question belief systems, test previously held assumptions, and recognize ambiguity as evidence of critical thinking. Others identify specific skills that demonstrate critical thinking, such as the ability to identify problems and biases, infer and draw conclusions, and determine the relevance of information to a situation.
Nicholas McGowan, BSN, RN, CCRN, has been a critical care nurse for 10 years in neurological trauma nursing and cardiovascular and surgical intensive care. He defines critical thinking as “necessary for problem-solving and decision-making by healthcare providers. It is a process where people use a logical process to gather information and take purposeful action based on their evaluation.”
“This cognitive process is vital for excellent patient outcomes because it requires that nurses make clinical decisions utilizing a variety of different lenses, such as fairness, ethics, and evidence-based practice,” he says.
How Do Nurses Use Critical Thinking?
Successful nurses think beyond their assigned tasks to deliver excellent care for their patients. For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood pressure and temperature and when those changes may require immediate medical intervention.
Nurses care for many patients during their shifts. Strong critical thinking skills are crucial when juggling various tasks so patient safety and care are not compromised.
Jenna Liphart Rhoads, Ph.D., RN, is a nurse educator with a clinical background in surgical-trauma adult critical care, where critical thinking and action were essential to the safety of her patients. She talks about examples of critical thinking in a healthcare environment, saying:
“Nurses must also critically think to determine which patient to see first, which medications to pass first, and the order in which to organize their day caring for patients. Patient conditions and environments are continually in flux, therefore nurses must constantly be evaluating and re-evaluating information they gather (assess) to keep their patients safe.”
The COVID-19 pandemic created hospital care situations where critical thinking was essential. It was expected of the nurses on the general floor and in intensive care units. Crystal Slaughter is an advanced practice nurse in the intensive care unit (ICU) and a nurse educator. She observed critical thinking throughout the pandemic as she watched intensive care nurses test the boundaries of previously held beliefs and master providing excellent care while preserving resources.
“Nurses are at the patient’s bedside and are often the first ones to detect issues. Then, the nurse needs to gather the appropriate subjective and objective data from the patient in order to frame a concise problem statement or question for the physician or advanced practice provider,” she explains.
Top 5 Ways Nurses Can Improve Critical Thinking Skills
We asked our experts for the top five strategies nurses can use to purposefully improve their critical thinking skills.
Case-Based Approach
Slaughter is a fan of the case-based approach to learning critical thinking skills.
In much the same way a detective would approach a mystery, she mentors her students to ask questions about the situation that help determine the information they have and the information they need. “What is going on? What information am I missing? Can I get that information? What does that information mean for the patient? How quickly do I need to act?”
Consider forming a group and working with a mentor who can guide you through case studies. This provides you with a learner-centered environment in which you can analyze data to reach conclusions and develop communication, analytical, and collaborative skills with your colleagues.
Practice Self-Reflection
Rhoads is an advocate for self-reflection. “Nurses should reflect upon what went well or did not go well in their workday and identify areas of improvement or situations in which they should have reached out for help.” Self-reflection is a form of personal analysis to observe and evaluate situations and how you responded.
This gives you the opportunity to discover mistakes you may have made and to establish new behavior patterns that may help you make better decisions. You likely already do this. For example, after a disagreement or contentious meeting, you may go over the conversation in your head and think about ways you could have responded.
It’s important to go through the decisions you made during your day and determine if you should have gotten more information before acting or if you could have asked better questions.
During self-reflection, you may try thinking about the problem in reverse. This may not give you an immediate answer, but can help you see the situation with fresh eyes and a new perspective. How would the outcome of the day be different if you planned the dressing change in reverse with the assumption you would find a wound infection? How does this information change your plan for the next dressing change?
Develop a Questioning Mind
McGowan has learned that “critical thinking is a self-driven process. It isn’t something that can simply be taught. Rather, it is something that you practice and cultivate with experience. To develop critical thinking skills, you have to be curious and inquisitive.”
To gain critical thinking skills, you must undergo a purposeful process of learning strategies and using them consistently so they become a habit. One of those strategies is developing a questioning mind. Meaningful questions lead to useful answers and are at the core of critical thinking .
However, learning to ask insightful questions is a skill you must develop. Faced with staff and nursing shortages , declining patient conditions, and a rising number of tasks to be completed, it may be difficult to do more than finish the task in front of you. Yet, questions drive active learning and train your brain to see the world differently and take nothing for granted.
It is easier to practice questioning in a non-stressful, quiet environment until it becomes a habit. Then, in the moment when your patient’s care depends on your ability to ask the right questions, you can be ready to rise to the occasion.
Practice Self-Awareness in the Moment
Critical thinking in nursing requires self-awareness and being present in the moment. During a hectic shift, it is easy to lose focus as you struggle to finish every task needed for your patients. Passing medication, changing dressings, and hanging intravenous lines all while trying to assess your patient’s mental and emotional status can affect your focus and how you manage stress as a nurse .
Staying present helps you to be proactive in your thinking and anticipate what might happen, such as bringing extra lubricant for a catheterization or extra gloves for a dressing change.
By staying present, you are also better able to practice active listening. This raises your assessment skills and gives you more information as a basis for your interventions and decisions.
Use a Process
As you are developing critical thinking skills, it can be helpful to use a process. For example:
- Ask questions.
- Gather information.
- Implement a strategy.
- Evaluate the results.
- Consider another point of view.
These are the fundamental steps of the nursing process (assess, diagnose, plan, implement, evaluate). The last step will help you overcome one of the common problems of critical thinking in nursing — personal bias.
Common Critical Thinking Pitfalls in Nursing
Your brain uses a set of processes to make inferences about what’s happening around you. In some cases, your unreliable biases can lead you down the wrong path. McGowan places personal biases at the top of his list of common pitfalls to critical thinking in nursing.
“We all form biases based on our own experiences. However, nurses have to learn to separate their own biases from each patient encounter to avoid making false assumptions that may interfere with their care,” he says. Successful critical thinkers accept they have personal biases and learn to look out for them. Awareness of your biases is the first step to understanding if your personal bias is contributing to the wrong decision.
New nurses may be overwhelmed by the transition from academics to clinical practice, leading to a task-oriented mindset and a common new nurse mistake ; this conflicts with critical thinking skills.
“Consider a patient whose blood pressure is low but who also needs to take a blood pressure medication at a scheduled time. A task-oriented nurse may provide the medication without regard for the patient’s blood pressure because medication administration is a task that must be completed,” Slaughter says. “A nurse employing critical thinking skills would address the low blood pressure, review the patient’s blood pressure history and trends, and potentially call the physician to discuss whether medication should be withheld.”
Fear and pride may also stand in the way of developing critical thinking skills. Your belief system and worldview provide comfort and guidance, but this can impede your judgment when you are faced with an individual whose belief system or cultural practices are not the same as yours. Fear or pride may prevent you from pursuing a line of questioning that would benefit the patient. Nurses with strong critical thinking skills exhibit:
- Learn from their mistakes and the mistakes of other nurses
- Look forward to integrating changes that improve patient care
- Treat each patient interaction as a part of a whole
- Evaluate new events based on past knowledge and adjust decision-making as needed
- Solve problems with their colleagues
- Are self-confident
- Acknowledge biases and seek to ensure these do not impact patient care
An Essential Skill for All Nurses
Critical thinking in nursing protects patient health and contributes to professional development and career advancement. Administrative and clinical nursing leaders are required to have strong critical thinking skills to be successful in their positions.
By using the strategies in this guide during your daily life and in your nursing role, you can intentionally improve your critical thinking abilities and be rewarded with better patient outcomes and potential career advancement.
Frequently Asked Questions About Critical Thinking in Nursing
How are critical thinking skills utilized in nursing practice.
Nursing practice utilizes critical thinking skills to provide the best care for patients. Often, the patient’s cause of pain or health issue is not immediately clear. Nursing professionals need to use their knowledge to determine what might be causing distress, collect vital information, and make quick decisions on how best to handle the situation.
How does nursing school develop critical thinking skills?
Nursing school gives students the knowledge professional nurses use to make important healthcare decisions for their patients. Students learn about diseases, anatomy, and physiology, and how to improve the patient’s overall well-being. Learners also participate in supervised clinical experiences, where they practice using their critical thinking skills to make decisions in professional settings.
Do only nurse managers use critical thinking?
Nurse managers certainly use critical thinking skills in their daily duties. But when working in a health setting, anyone giving care to patients uses their critical thinking skills. Everyone — including licensed practical nurses, registered nurses, and advanced nurse practitioners —needs to flex their critical thinking skills to make potentially life-saving decisions.
Meet Our Contributors

Crystal Slaughter, DNP, APRN, ACNS-BC, CNE
Crystal Slaughter is a core faculty member in Walden University’s RN-to-BSN program. She has worked as an advanced practice registered nurse with an intensivist/pulmonary service to provide care to hospitalized ICU patients and in inpatient palliative care. Slaughter’s clinical interests lie in nursing education and evidence-based practice initiatives to promote improving patient care.

Jenna Liphart Rhoads, Ph.D., RN
Jenna Liphart Rhoads is a nurse educator and freelance author and editor. She earned a BSN from Saint Francis Medical Center College of Nursing and an MS in nursing education from Northern Illinois University. Rhoads earned a Ph.D. in education with a concentration in nursing education from Capella University where she researched the moderation effects of emotional intelligence on the relationship of stress and GPA in military veteran nursing students. Her clinical background includes surgical-trauma adult critical care, interventional radiology procedures, and conscious sedation in adult and pediatric populations.

Nicholas McGowan, BSN, RN, CCRN
Nicholas McGowan is a critical care nurse with 10 years of experience in cardiovascular, surgical intensive care, and neurological trauma nursing. McGowan also has a background in education, leadership, and public speaking. He is an online learner who builds on his foundation of critical care nursing, which he uses directly at the bedside where he still practices. In addition, McGowan hosts an online course at Critical Care Academy where he helps nurses achieve critical care (CCRN) certification.
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Critical thinking in...
Critical thinking in healthcare and education
- Related content
- Peer review
- Jonathan M Sharples , professor 1 ,
- Andrew D Oxman , research director 2 ,
- Kamal R Mahtani , clinical lecturer 3 ,
- Iain Chalmers , coordinator 4 ,
- Sandy Oliver , professor 1 ,
- Kevan Collins , chief executive 5 ,
- Astrid Austvoll-Dahlgren , senior researcher 2 ,
- Tammy Hoffmann , professor 6
- 1 EPPI-Centre, UCL Department of Social Science, London, UK
- 2 Global Health Unit, Norwegian Institute of Public Health, Oslo, Norway
- 3 Centre for Evidence-Based Medicine, Oxford University, Oxford, UK
- 4 James Lind Initiative, Oxford, UK
- 5 Education Endowment Foundation, London, UK
- 6 Centre for Research in Evidence-Based Practice, Bond University, Gold Coast, Australia
- Correspondence to: J M Sharples Jonathan.Sharples{at}eefoundation.org.uk
Critical thinking is just one skill crucial to evidence based practice in healthcare and education, write Jonathan Sharples and colleagues , who see exciting opportunities for cross sector collaboration
Imagine you are a primary care doctor. A patient comes into your office with acute, atypical chest pain. Immediately you consider the patient’s sex and age, and you begin to think about what questions to ask and what diagnoses and diagnostic tests to consider. You will also need to think about what treatments to consider and how to communicate with the patient and potentially with the patient’s family and other healthcare providers. Some of what you do will be done reflexively, with little explicit thought, but caring for most patients also requires you to think critically about what you are going to do.
Critical thinking, the ability to think clearly and rationally about what to do or what to believe, is essential for the practice of medicine. Few doctors are likely to argue with this. Yet, until recently, the UK regulator the General Medical Council and similar bodies in North America did not mention “critical thinking” anywhere in their standards for licensing and accreditation, 1 and critical thinking is not explicitly taught or assessed in most education programmes for health professionals. 2
Moreover, although more than 2800 articles indexed by PubMed have “critical thinking” in the title or abstract, most are about nursing. We argue that it is important for clinicians and patients to learn to think critically and that the teaching and learning of these skills should be considered explicitly. Given the shared interest in critical thinking with broader education, we also highlight why healthcare and education professionals and researchers need to work together to enable people to think critically about the health choices they make throughout life.
Essential skills for doctors and patients
Critical thinking is not a new concept in education: at the beginning of the last century the US educational reformer John Dewey identified the need to help students “to think well.” 3 Critical thinking encompasses a broad set of skills and dispositions, including cognitive skills (such as analysis, inference, and self regulation); approaches to specific questions or problems (orderliness, diligence, and reasonableness); and approaches to life in general (inquisitiveness, concern with being well informed, and open mindedness). 4
An increasing body of evidence highlights that developing critical thinking skills can benefit academic outcomes as well as wider reasoning and problem solving capabilities. 5 For example, the Thinking, Doing, Talking Science programme trains teachers in a repertoire of strategies that encourage pupils to use critical thinking skills in primary school science lessons. An independently conducted randomised trial of this approach found that it had a positive impact on pupils’ science attainment, with signs that it was particularly beneficial for pupils from poorer families. 6
In medicine, increasing attention has been paid to “critical appraisal” in the past 40 years. Critical appraisal is a subset of critical thinking that focuses on how to use research evidence to inform health decisions. 7 8 9 The need for critical appraisal in medicine was recognised at least 75 years ago, 10 and critical appraisal has been recognised for some decades as an essential competency for healthcare professionals. 11 The General Medical Council’s Good Medical Practice guidance includes the need for doctors to be able to “provide effective treatments based on the best available evidence.” 12
If patients and the public are to make well informed health choices, they must also be able to assess the reliability of health claims and information. This is something that most people struggle to do, and it is becoming increasingly important because patients are taking on a bigger role in managing their health and making healthcare decisions, 13 while needing to cope with more and more health information, much of which is not reliable. 14 15 16 17
Teaching critical thinking
Although critical thinking skills are given limited explicit attention in standards for medical education, they are included as a key competency in most frameworks for national curriculums for primary and secondary schools in many countries. 18 Nonetheless, much health and science education, and education generally, still tends towards rote learning rather than the promotion of critical thinking. 19 20 This matters because the ability to think critically is an essential life skill relevant to decision making in many circumstances. The capacity to think critically is, like a lot of learning, developed in school and the home: parental influence creates advantage for pupils who live in homes where they are encouraged to think and talk about what they are doing. This, importantly, goes beyond simply completing tasks to creating deeper understanding of learning processes. As such, the “critical thinking gap” between children from disadvantaged communities and their more advantaged peers requires attention as early as possible.
Although it is possible to teach critical thinking to adults, it is likely to be more productive if the grounds for this have been laid down in an educational environment early in life, starting in primary school. Erroneous beliefs, attitudes, and behaviours developed during childhood may be difficult to change later. 21 22 This also applies to medical education and to health professionals. It becomes increasingly difficult to teach these skills without a foundation to build on and adequate time to learn them.
Strategies for teaching students to think critically have been evaluated in health and medical education; in science, technology, engineering, and maths; and in other subjects. 23 These studies suggest that critical thinking skills can be taught and that in the absence of explicit teaching of critical thinking, important deficiencies emerge in the abilities of students to make sound judgments. In healthcare studies, many medical students score poorly on tests that measure the ability to think critically , and the ability to think critically is correlated with academic success. 24 25
Evaluations of strategies for teaching critical thinking in medicine have focused primarily on critical appraisal skills as part of evidence based healthcare. An overview of systematic reviews of these studies suggests that improving evidence based healthcare competencies is likely to require multifaceted, clinically integrated approaches that include assessment. 26
Cross sector collaboration
Informed Health Choices, an international project aiming to improve decision making, shows the opportunities and benefits of cross sector collaboration between education and health. 27 This project has brought together people working in education and healthcare to develop a curriculum and learning resources for critical thinking about any action that is claimed to improve health. It aims to develop, identify, and promote the use of effective learning resources, beginning at primary school, to help people to make well informed choices as patients and health professionals, and well informed decisions as citizens and policy makers.
The project has drawn on several approaches used in education, including the development of a “spiral curriculum,” measurement tools, and the design of learning resources. A spiral curriculum begins with determining what people should know and be able to do, and outlines where they should begin and how they should progress to reach these goals. The basic ideas are revisited repeatedly, building on them until the student has grasped a deep understanding of the concepts. 28 29 The project has also drawn on educational research and methods to develop reliable and valid tools for measuring the extent to which those goals have been achieved. 30 31 32 The development of learning resources to teach these skills has been informed by educational research, including educational psychology, motivational psychology, and research and methods for developing learning games. 33 34 35 It has also built on the traditions of clinical epidemiology and evidence based medicine to identify the key concepts required to assess health claims. 29
It is difficult to teach critical thinking abstractly, so focusing on health may have advantages beyond the public health benefits of increasing health literacy. 36 Nearly everyone is interested in health, including children, making it easy to engage learners. It is also immediately relevant to students. As reported by one 10 year old in a school that piloted primary school resources, this is about “things we might actually use instead of things we might use when we are all grown up and by then we’ll forget.” Although the current evaluation of the project is focusing on outcomes relating to appraisal of treatment claims, if the intervention shows promise the next step could be to explore how these skills translate to wider educational contexts and outcomes.
Beyond critical thinking
Exciting opportunities for cross sector collaboration are emerging between healthcare and education. Although critical thinking is a useful example of this, other themes cross the education and healthcare domains, including nutrition, exercise, educational neuroscience, learning disabilities and special education needs, and mental health.
In addition to shared topics, several common methodological and conceptual issues also provide opportunities for sharing ideas and innovations and learning from mistakes and successes. For example, the Education Endowment Foundation is the UK government’s What Works Centre for education, aiming to improve evidence based decision making. Discussions hosted by the foundation are exploring how methods to develop guidelines in healthcare can be adapted and applied in education and other sectors.
Similarly, the foundation’s universal use of independent evaluation for teaching and learning interventions is an approach that should be explored, adapted, and applied in healthcare. Since the development and evaluation of educational interventions are separated, evaluators have no vested interested in the results of the assessment, all results are published, and bias and spin in how results are analysed and presented are reduced. By contrast, industry sponsorship of drug and device studies consistently produces results that favour the manufacturer. 37
Another example of joint working between educators and health is the Best Evidence Medical Education Collaboration, an international collaboration focused on improving education of health professionals. 38 And in the UK, the Centre for Evidence Based Medicine coordinates Evidence in School Teaching (Einstein), a project that supports introducing evidence based medicine as part of wider science activities in schools. 39 It aims to engage students, teachers, and the public in evidence based medicine and develop critical thinking to assess health claims and make better choices.
Collaboration has also been important in the development of the Critical Thinking and Appraisal Resource Library (CARL), 40 a set of resources designed to help people understand fair comparisons of treatments. An important aim of CARL is to promote evaluation of these critical thinking resources and interventions, some of which are currently under way at the Education Endowment Foundation. On 22 May 2017, the foundation is also cohosting an event with the Royal College of Paediatrics and Child Health that will focus on their shared interest in critical thinking and appraisal skills.
Education and healthcare have overlapping interests. Doctors, teachers, researchers, patients, learners, and the public can all benefit from working together to help people to think critically about the choices they make. Events such as the global evidence summit in September 2017 ( https://globalevidencesummit.org ) can help bring people together and build on current international experience.
Contributors and sources: This article reflects conclusions from discussions during 2016 among education and health service researchers exploring opportunities for cross sector collaboration and learning. This group includes people with a longstanding interest in evidence informed policy and practice, with expertise in evaluation design, reviewing methodology, knowledge mobilisation, and critical thinking and appraisal.
Competing interests: We have read and understood BMJ policy on declaration of interests and declare that we have no competing interests.
Provenance and peer review: Not commissioned; externally peer reviewed.
- ↵ Krupat E, Sprague JM, Wolpaw D, Haidet P, Hatem D, O’Brien B. Thinking critically about critical thinking: ability, disposition or both? Med Educ 2011 ; 357 : 625 - 35 . doi:10.1111/j.1365-2923.2010.03910.x pmid:21564200 . OpenUrl
- ↵ Huang GC, Newman LR, Schwartzstein RM. Critical thinking in health professions education: summary and consensus statements of the millennium conference 2011. Teach Learn Med 2014 ; 357 : 95 - 102 . doi:10.1080/10401334.2013.857335 pmid:24405353 . OpenUrl
- ↵ Dewey J. How we think. D C Heath, 1910 . https://archive.org/details/howwethink000838mbp doi:10.1037/10903-000 .
- ↵ Facione PA. Critical thinking: a statement of expert consensus for purposes of educational assessment and instruction. Research findings and recommendations. American Philosophical Association, 1990 , http://files.eric.ed.gov/fulltext/ED315423.pdf .
- ↵ Higgins S, Katsipataki M, Coleman R, et al. The Sutton Trust-Education Endowment Foundation Teaching and Learning Toolkit. Education Endowment Foundation, 2015 .
- ↵ Hanley P, Slavin RE, Elliot L. Thinking, doing, talking science. Evaluation report and executive summary. Education Endowment Foundation, 2015 , https://v1.educationendowmentfoundation.org.uk/uploads/pdf/Oxford_Science.pdf .
- ↵ Sackett DL. How to read clinical journals: I. why to read them and how to start reading them critically . Can Med Assoc J 1981 ; 357 : 555 - 8 . pmid:7471000 . OpenUrl
- ↵ Guyatt G, Cairns J, Churchill D, et al. Evidence-Based Medicine Working Group. Evidence-based medicine. A new approach to teaching the practice of medicine . JAMA 1992 ; 357 : 2420 - 5 . doi:10.1001/jama.1992.03490170092032 pmid:1404801 . OpenUrl
- ↵ Oxman AD, Sackett DL, Guyatt GH. The Evidence-Based Medicine Working Group. Users’ guides to the medical literature. I. How to get started . JAMA 1993 ; 357 : 2093 - 5 . doi:10.1001/jama.1993.03510170083036 pmid:8411577 . OpenUrl
- ↵ Rynearson EH. Endocrinology: a critical appraisal . Cal West Med 1940 ; 357 : 257 - 9 . pmid:18745588 . OpenUrl
- ↵ General Medical Council. Tomorrow's doctors. General Medical Council, 1993. http://www.gmc-uk.org/10a_annex_a.pdf_25398162.pdf
- ↵ General Medical Council. Good medical practice. General Medical Council, 2013. http://www.gmc-uk.org/static/documents/content/GMP_.pdf
- ↵ Edwards A, Elwyn G. Shared decision-making in health care: achieving evidence-based patient choice. 2nd ed . Oxford University Press, 2009 .
- ↵ Sumner P, Vivian-Griffiths S, Boivin J, et al. Exaggerations and caveats in press releases and health-related science news. PLoS One 2016 ; 357 : e0168217 . doi:10.1371/journal.pone.0168217 pmid:27978540 . OpenUrl
- ↵ Schwartz LM, Woloshin S, Andrews A, Stukel TA. Influence of medical journal press releases on the quality of associated newspaper coverage: retrospective cohort study. BMJ 2012 ; 357 : d8164 . doi:10.1136/bmj.d8164 . pmid:22286507 . OpenUrl
- ↵ Glenton C, Paulsen EJ, Oxman AD. Portals to Wonderland: health portals lead to confusing information about the effects of health care. BMC Med Inform Decis Mak 2005 ; 357 : 7 . doi:10.1186/1472-6947-5-7 pmid:15769291 . OpenUrl
- ↵ Moynihan R, Bero L, Ross-Degnan D, et al. Coverage by the news media of the benefits and risks of medications . N Engl J Med 2000 ; 357 : 1645 - 50 . doi:10.1056/NEJM200006013422206 pmid:10833211 . OpenUrl
- ↵ Voogt J, Roblin NP. A comparative analysis of international frameworks for 21st century competences: implications for national curriculum policies. J Curric Stud 2012 ; 357 : 299 - 321 doi:10.1080/00220272.2012.668938 . OpenUrl
- ↵ National Research Council. Taking science to school: learning and teaching science in grades K-8. National Academies Press, 2007 .
- ↵ Nordheim L, Pettersen KS, Flottorp S, Hjälmhult E. Critical appraisal of health claims: science teachers’ perceptions and practices . Health Educ J 2016 ; 357 : 449 - 66 doi:10.1108/HE-04-2015-0016 . OpenUrl
- ↵ Committee on Science Learning. Kindergarten through eighth grade. How children learn science. In: Duschl RA, Schweingruber A, Shouse AW, eds. Taking science to school: learning and teaching science in grades K-8. National Academies Press, 2007 .
- ↵ Vosniadou S. International handbook of research on conceptual change. 2nd ed . Routledge, 2013 .
- ↵ Abrami PC, Bernard RM, Borokhovski E, Waddington DI, Wade CA, Persson T. Strategies for teaching students to think critically a meta-analysis. Rev Educ Res 2015 ; 357 : 275 - 314 . OpenUrl
- ↵ Ross D, Schipper S, Westbury C, et al. Examining critical thinking skills in family medicine residents . Fam Med 2016 ; 357 : 121 - 6 . pmid:26950783 . OpenUrl
- ↵ Ross D, Loeffler K, Schipper S, Vandermeer B, Allan GM. Do scores on three commonly used measures of critical thinking correlate with academic success of health professions trainees? A systematic review and meta-analysis. Acad Med 2013 ; 357 : 724 - 34 . doi:10.1097/ACM.0b013e31828b0823 pmid:23524925 . OpenUrl
- ↵ Young T, Rohwer A, Volmink J, Clarke M. What are the effects of teaching evidence-based health care (EBHC)? Overview of systematic reviews. PLoS One 2014 ; 357 : e86706 . doi:10.1371/journal.pone.0086706 pmid:24489771 . OpenUrl
- ↵ Informed Health Choices Group. Informed health choices. www.informedhealthchoices.org
- ↵ Harden RM, Stamper N. What is a spiral curriculum? Med Teach 1999 ; 357 : 141 - 3 . doi:10.1080/01421599979752 pmid:21275727 . OpenUrl
- ↵ Austvoll-Dahlgren A, Oxman AD, Chalmers I, et al. Key concepts that people need to understand to assess claims about treatment effects. J Evid Based Med 2015 ; 357 : 112 - 25 . doi:10.1111/jebm.12160 pmid:26107552 . OpenUrl
- ↵ Austvoll-Dahlgren A, Nsangi A, Semakula D. Interventions and assessment tools addressing key concepts people need to know to appraise claims about treatment effects: a systematic mapping review. Syst Rev 2016 ; 357 : 215 . doi:10.1186/s13643-016-0389-z pmid:28034307 . OpenUrl
- ↵ Austvoll-Dahlgren A, Semakula D, Nsangi A, et al. The development of the “claim evaluation tools”: assessing critical thinking about effects. BMJ Open forthcoming .
- ↵ Austvoll-Dahlgren A, Guttersrud Ø, Semakula D, Nsangi A, Oxman AD. Measuring ability to assess claims about treatment effects: a latent trait analysis of the claim evaluation tools using Rasch modelling. BMJ Open [ forthcoming ].
- ↵ Sandoval WA, Sodian B, Koerber S, Wong J. Developing children’s early competencies to engage with science . Educ Psychol 2014 ; 357 : 139 - 52 doi:10.1080/00461520.2014.917589 . OpenUrl
- ↵ Pintrich PR. A motivational science perspective on the role of student motivation in learning and teaching contexts . J Educ Psychol 2003 ; 357 : 667 - 86 doi:10.1037/0022-0663.95.4.667 . OpenUrl
- ↵ Clark DB, Tanner-Smith EE, Killingsworth SS. Digital games, design, and learning: a systematic review and meta-analysis . Rev Educ Res 2016 ; 357 : 79 - 122 . doi:10.3102/0034654315582065 pmid:26937054 . OpenUrl
- ↵ Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review . Ann Intern Med 2011 ; 357 : 97 - 107 . doi:10.7326/0003-4819-155-2-201107190-00005 pmid:21768583 . OpenUrl
- ↵ Lundh A, Sismondo S, Lexchin J, Busuioc OA, Bero L. Industry sponsorship and research outcome. Cochrane Database Syst Rev 2012 ; 357 : MR000033 . pmid:23235689 . OpenUrl
- ↵ Thistlethwaite J, Hammick M, The Best Evidence Medical Education (BEME) Collaboration: into the next decade. Med Teach 2010 ; 357 : 880 - 2 . doi:10.3109/0142159X.2010.519068 pmid:21039096 . OpenUrl
- ↵ Centre for Evidence Based Medicine. Einstein—taking EBM to schools. http://www.cebm.net/taking-ebm-schools
- ↵ Castle JC, Chalmers I, Atkinson P, et al. Establishing a library of resources to help people understand key concepts in assessing treatment claims—the Critical Thinking and Appraisal Resource Library (CARL). PLoS One forthcoming .
- Search Menu
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Anglo-Saxon and Medieval Archaeology
- Archaeological Methodology and Techniques
- Archaeology by Region
- Archaeology of Religion
- Archaeology of Trade and Exchange
- Biblical Archaeology
- Contemporary and Public Archaeology
- Environmental Archaeology
- Historical Archaeology
- History and Theory of Archaeology
- Industrial Archaeology
- Landscape Archaeology
- Mortuary Archaeology
- Prehistoric Archaeology
- Underwater Archaeology
- Urban Archaeology
- Zooarchaeology
- Browse content in Architecture
- Architectural Structure and Design
- History of Architecture
- Residential and Domestic Buildings
- Theory of Architecture
- Browse content in Art
- Art Subjects and Themes
- History of Art
- Industrial and Commercial Art
- Theory of Art
- Biographical Studies
- Byzantine Studies
- Browse content in Classical Studies
- Classical History
- Classical Philosophy
- Classical Mythology
- Classical Literature
- Classical Reception
- Classical Art and Architecture
- Classical Oratory and Rhetoric
- Greek and Roman Papyrology
- Greek and Roman Epigraphy
- Greek and Roman Law
- Greek and Roman Archaeology
- Late Antiquity
- Religion in the Ancient World
- Digital Humanities
- Browse content in History
- Colonialism and Imperialism
- Diplomatic History
- Environmental History
- Genealogy, Heraldry, Names, and Honours
- Genocide and Ethnic Cleansing
- Historical Geography
- History by Period
- History of Emotions
- History of Agriculture
- History of Education
- History of Gender and Sexuality
- Industrial History
- Intellectual History
- International History
- Labour History
- Legal and Constitutional History
- Local and Family History
- Maritime History
- Military History
- National Liberation and Post-Colonialism
- Oral History
- Political History
- Public History
- Regional and National History
- Revolutions and Rebellions
- Slavery and Abolition of Slavery
- Social and Cultural History
- Theory, Methods, and Historiography
- Urban History
- World History
- Browse content in Language Teaching and Learning
- Language Learning (Specific Skills)
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Cognitive Linguistics
- Computational Linguistics
- Forensic Linguistics
- Grammar, Syntax and Morphology
- Historical and Diachronic Linguistics
- History of English
- Language Evolution
- Language Reference
- Language Acquisition
- Language Variation
- Language Families
- Lexicography
- Linguistic Anthropology
- Linguistic Theories
- Linguistic Typology
- Phonetics and Phonology
- Psycholinguistics
- Sociolinguistics
- Translation and Interpretation
- Writing Systems
- Browse content in Literature
- Bibliography
- Children's Literature Studies
- Literary Studies (Romanticism)
- Literary Studies (American)
- Literary Studies (Asian)
- Literary Studies (European)
- Literary Studies (Eco-criticism)
- Literary Studies (Modernism)
- Literary Studies - World
- Literary Studies (1500 to 1800)
- Literary Studies (19th Century)
- Literary Studies (20th Century onwards)
- Literary Studies (African American Literature)
- Literary Studies (British and Irish)
- Literary Studies (Early and Medieval)
- Literary Studies (Fiction, Novelists, and Prose Writers)
- Literary Studies (Gender Studies)
- Literary Studies (Graphic Novels)
- Literary Studies (History of the Book)
- Literary Studies (Plays and Playwrights)
- Literary Studies (Poetry and Poets)
- Literary Studies (Postcolonial Literature)
- Literary Studies (Queer Studies)
- Literary Studies (Science Fiction)
- Literary Studies (Travel Literature)
- Literary Studies (War Literature)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Mythology and Folklore
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Dance and Music
- Ethics in Music
- Ethnomusicology
- Gender and Sexuality in Music
- Medicine and Music
- Music Cultures
- Music and Media
- Music and Religion
- Music and Culture
- Music Education and Pedagogy
- Music Theory and Analysis
- Musical Scores, Lyrics, and Libretti
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Performance Practice and Studies
- Race and Ethnicity in Music
- Sound Studies
- Browse content in Performing Arts
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- Feminist Philosophy
- History of Western Philosophy
- Metaphysics
- Moral Philosophy
- Non-Western Philosophy
- Philosophy of Language
- Philosophy of Mind
- Philosophy of Perception
- Philosophy of Science
- Philosophy of Action
- Philosophy of Law
- Philosophy of Religion
- Philosophy of Mathematics and Logic
- Practical Ethics
- Social and Political Philosophy
- Browse content in Religion
- Biblical Studies
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Qumran Studies
- Religion and Education
- Religion and Health
- Religion and Politics
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Cookery, Food, and Drink
- Cultural Studies
- Customs and Traditions
- Ethical Issues and Debates
- Hobbies, Games, Arts and Crafts
- Lifestyle, Home, and Garden
- Natural world, Country Life, and Pets
- Popular Beliefs and Controversial Knowledge
- Sports and Outdoor Recreation
- Technology and Society
- Travel and Holiday
- Visual Culture
- Browse content in Law
- Arbitration
- Browse content in Company and Commercial Law
- Commercial Law
- Company Law
- Browse content in Comparative Law
- Systems of Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Government Powers
- Judicial Review
- Local Government Law
- Military and Defence Law
- Parliamentary and Legislative Practice
- Construction Law
- Contract Law
- Browse content in Criminal Law
- Criminal Procedure
- Criminal Evidence Law
- Sentencing and Punishment
- Employment and Labour Law
- Environment and Energy Law
- Browse content in Financial Law
- Banking Law
- Insolvency Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Politics
- Law and Society
- Browse content in Legal System and Practice
- Courts and Procedure
- Legal Skills and Practice
- Primary Sources of Law
- Regulation of Legal Profession
- Medical and Healthcare Law
- Browse content in Policing
- Criminal Investigation and Detection
- Police and Security Services
- Police Procedure and Law
- Police Regional Planning
- Browse content in Property Law
- Personal Property Law
- Study and Revision
- Terrorism and National Security Law
- Browse content in Trusts Law
- Wills and Probate or Succession
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Arts Therapies
- Clinical Science
- Dietetics and Nutrition
- Occupational Therapy
- Operating Department Practice
- Physiotherapy
- Radiography
- Speech and Language Therapy
- Browse content in Anaesthetics
- General Anaesthesia
- Neuroanaesthesia
- Clinical Neuroscience
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Genetics
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Genito-urinary Medicine
- Geriatric Medicine
- Infectious Diseases
- Medical Toxicology
- Medical Oncology
- Pain Medicine
- Palliative Medicine
- Rehabilitation Medicine
- Respiratory Medicine and Pulmonology
- Rheumatology
- Sleep Medicine
- Sports and Exercise Medicine
- Community Medical Services
- Critical Care
- Emergency Medicine
- Forensic Medicine
- Haematology
- History of Medicine
- Browse content in Medical Skills
- Clinical Skills
- Communication Skills
- Nursing Skills
- Surgical Skills
- Browse content in Medical Dentistry
- Oral and Maxillofacial Surgery
- Paediatric Dentistry
- Restorative Dentistry and Orthodontics
- Surgical Dentistry
- Medical Ethics
- Medical Statistics and Methodology
- Browse content in Neurology
- Clinical Neurophysiology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology (ENT)
- Browse content in Paediatrics
- Neonatology
- Browse content in Pathology
- Chemical Pathology
- Clinical Cytogenetics and Molecular Genetics
- Histopathology
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Popular Health
- Caring for Others
- Complementary and Alternative Medicine
- Self-help and Personal Development
- Browse content in Preclinical Medicine
- Cell Biology
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Addiction Medicine
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Learning Disabilities
- Old Age Psychiatry
- Psychotherapy
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Nuclear Medicine
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- General Surgery
- Neurosurgery
- Paediatric Surgery
- Peri-operative Care
- Plastic and Reconstructive Surgery
- Surgical Oncology
- Transplant Surgery
- Trauma and Orthopaedic Surgery
- Vascular Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Natural History
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Analytical Chemistry
- Computational Chemistry
- Crystallography
- Environmental Chemistry
- Industrial Chemistry
- Inorganic Chemistry
- Materials Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Organic Chemistry
- Physical Chemistry
- Polymer Chemistry
- Study and Communication Skills in Chemistry
- Theoretical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Game Studies
- Human-Computer Interaction
- Mathematical Theory of Computation
- Programming Languages
- Software Engineering
- Systems Analysis and Design
- Virtual Reality
- Browse content in Computing
- Business Applications
- Computer Security
- Computer Games
- Computer Networking and Communications
- Digital Lifestyle
- Graphical and Digital Media Applications
- Operating Systems
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Maps and Map-making
- Meteorology and Climatology
- Oceanography and Hydrology
- Palaeontology
- Physical Geography and Topography
- Regional Geography
- Soil Science
- Urban Geography
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Electronics and Communications Engineering
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- History of Engineering and Technology
- Mechanical Engineering and Materials
- Technology of Industrial Chemistry
- Transport Technology and Trades
- Browse content in Environmental Science
- Applied Ecology (Environmental Science)
- Conservation of the Environment (Environmental Science)
- Environmental Sustainability
- Environmentalist Thought and Ideology (Environmental Science)
- Management of Land and Natural Resources (Environmental Science)
- Natural Disasters (Environmental Science)
- Nuclear Issues (Environmental Science)
- Pollution and Threats to the Environment (Environmental Science)
- Social Impact of Environmental Issues (Environmental Science)
- History of Science and Technology
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Metals, Alloying, and Corrosion
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- History of Mathematics
- Mathematical Education
- Mathematical Finance
- Mathematical Analysis
- Numerical and Computational Mathematics
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Development of the Nervous System
- Disorders of the Nervous System
- History of Neuroscience
- Invertebrate Neurobiology
- Molecular and Cellular Systems
- Neuroendocrinology and Autonomic Nervous System
- Neuroscientific Techniques
- Sensory and Motor Systems
- Browse content in Physics
- Astronomy and Astrophysics
- Atomic, Molecular, and Optical Physics
- Biological and Medical Physics
- Classical Mechanics
- Computational Physics
- Condensed Matter Physics
- Electromagnetism, Optics, and Acoustics
- History of Physics
- Mathematical and Statistical Physics
- Measurement Science
- Nuclear Physics
- Particles and Fields
- Plasma Physics
- Quantum Physics
- Relativity and Gravitation
- Semiconductor and Mesoscopic Physics
- Browse content in Psychology
- Affective Sciences
- Clinical Psychology
- Cognitive Psychology
- Cognitive Neuroscience
- Criminal and Forensic Psychology
- Developmental Psychology
- Educational Psychology
- Evolutionary Psychology
- Health Psychology
- History and Systems in Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Psychological Assessment and Testing
- Psychology of Human-Technology Interaction
- Psychology Professional Development and Training
- Research Methods in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Human Evolution
- Medical Anthropology
- Physical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Theory and Practice of Anthropology
- Browse content in Business and Management
- Business Ethics
- Business Strategy
- Business History
- Business and Technology
- Business and Government
- Business and the Environment
- Comparative Management
- Corporate Governance
- Corporate Social Responsibility
- Entrepreneurship
- Health Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- International Business
- Knowledge Management
- Management and Management Techniques
- Operations Management
- Organizational Theory and Behaviour
- Pensions and Pension Management
- Public and Nonprofit Management
- Strategic Management
- Supply Chain Management
- Browse content in Criminology and Criminal Justice
- Criminal Justice
- Criminology
- Forms of Crime
- International and Comparative Criminology
- Youth Violence and Juvenile Justice
- Development Studies
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Asian Economics
- Behavioural Finance
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic History
- Economic Systems
- Economic Methodology
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- General Economics and Teaching
- Health, Education, and Welfare
- History of Economic Thought
- International Economics
- Labour and Demographic Economics
- Law and Economics
- Macroeconomics and Monetary Economics
- Microeconomics
- Public Economics
- Urban, Rural, and Regional Economics
- Welfare Economics
- Browse content in Education
- Adult Education and Continuous Learning
- Care and Counselling of Students
- Early Childhood and Elementary Education
- Educational Equipment and Technology
- Educational Strategies and Policy
- Higher and Further Education
- Organization and Management of Education
- Philosophy and Theory of Education
- Schools Studies
- Secondary Education
- Teaching of a Specific Subject
- Teaching of Specific Groups and Special Educational Needs
- Teaching Skills and Techniques
- Browse content in Environment
- Applied Ecology (Social Science)
- Climate Change
- Conservation of the Environment (Social Science)
- Environmentalist Thought and Ideology (Social Science)
- Natural Disasters (Environment)
- Social Impact of Environmental Issues (Social Science)
- Browse content in Human Geography
- Cultural Geography
- Economic Geography
- Political Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- African Politics
- Asian Politics
- Chinese Politics
- Comparative Politics
- Conflict Politics
- Elections and Electoral Studies
- Environmental Politics
- European Union
- Foreign Policy
- Gender and Politics
- Human Rights and Politics
- Indian Politics
- International Relations
- International Organization (Politics)
- International Political Economy
- Irish Politics
- Latin American Politics
- Middle Eastern Politics
- Political Behaviour
- Political Economy
- Political Institutions
- Political Methodology
- Political Communication
- Political Philosophy
- Political Sociology
- Political Theory
- Politics and Law
- Public Policy
- Public Administration
- Quantitative Political Methodology
- Regional Political Studies
- Russian Politics
- Security Studies
- State and Local Government
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- East Asian Studies
- Japanese Studies
- Latin American Studies
- Middle Eastern Studies
- Native American Studies
- Scottish Studies
- Browse content in Research and Information
- Research Methods
- Browse content in Social Work
- Addictions and Substance Misuse
- Adoption and Fostering
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Developmental and Physical Disabilities Social Work
- Direct Practice and Clinical Social Work
- Emergency Services
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Sport and Leisure
- Urban and Rural Studies
- Browse content in Warfare and Defence
- Defence Strategy, Planning, and Research
- Land Forces and Warfare
- Military Administration
- Military Life and Institutions
- Naval Forces and Warfare
- Other Warfare and Defence Issues
- Peace Studies and Conflict Resolution
- Weapons and Equipment

- < Previous chapter
- Next chapter >

9 Problem-Solving and Decision-Making Skills for Public Health Practice
- Published: October 2023
- Cite Icon Cite
- Permissions Icon Permissions
This chapter provides an initial definition of problem-solving and the components of the problem-solving process. It identifies common mistakes early in the process and their implications. It explains that the first step toward successful problem-solving is thoroughly and accurately defining the problem and acknowledging that multiple solutions must be considered. It explores multiple approaches to problem-solving, such as rational problem-solving and organic problem-solving, as well as a type of organic problem-solving called appreciative inquiry. The chapter also explores seven decision-making styles and elaborates on common mistakes made during the process, as well as how to overcome them.
Signed in as
Institutional accounts.
- Google Scholar Indexing
- GoogleCrawler [DO NOT DELETE]
Personal account
- Sign in with email/username & password
- Get email alerts
- Save searches
- Purchase content
- Activate your purchase/trial code
Institutional access
- Sign in with a library card Sign in with username/password Recommend to your librarian
- Institutional account management
- Get help with access
Access to content on Oxford Academic is often provided through institutional subscriptions and purchases. If you are a member of an institution with an active account, you may be able to access content in one of the following ways:
IP based access
Typically, access is provided across an institutional network to a range of IP addresses. This authentication occurs automatically, and it is not possible to sign out of an IP authenticated account.
Sign in through your institution
Choose this option to get remote access when outside your institution. Shibboleth/Open Athens technology is used to provide single sign-on between your institution’s website and Oxford Academic.
- Click Sign in through your institution.
- Select your institution from the list provided, which will take you to your institution's website to sign in.
- When on the institution site, please use the credentials provided by your institution. Do not use an Oxford Academic personal account.
- Following successful sign in, you will be returned to Oxford Academic.
If your institution is not listed or you cannot sign in to your institution’s website, please contact your librarian or administrator.
Sign in with a library card
Enter your library card number to sign in. If you cannot sign in, please contact your librarian.
Society Members
Society member access to a journal is achieved in one of the following ways:
Sign in through society site
Many societies offer single sign-on between the society website and Oxford Academic. If you see ‘Sign in through society site’ in the sign in pane within a journal:
- Click Sign in through society site.
- When on the society site, please use the credentials provided by that society. Do not use an Oxford Academic personal account.
If you do not have a society account or have forgotten your username or password, please contact your society.
Sign in using a personal account
Some societies use Oxford Academic personal accounts to provide access to their members. See below.
A personal account can be used to get email alerts, save searches, purchase content, and activate subscriptions.
Some societies use Oxford Academic personal accounts to provide access to their members.
Viewing your signed in accounts
Click the account icon in the top right to:
- View your signed in personal account and access account management features.
- View the institutional accounts that are providing access.
Signed in but can't access content
Oxford Academic is home to a wide variety of products. The institutional subscription may not cover the content that you are trying to access. If you believe you should have access to that content, please contact your librarian.
For librarians and administrators, your personal account also provides access to institutional account management. Here you will find options to view and activate subscriptions, manage institutional settings and access options, access usage statistics, and more.
Our books are available by subscription or purchase to libraries and institutions.
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Rights and permissions
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Research article
- Open access
- Published: 07 October 2020
Impact of social problem-solving training on critical thinking and decision making of nursing students
- Soleiman Ahmady 1 &
- Sara Shahbazi ORCID: orcid.org/0000-0001-8397-6233 2 , 3
BMC Nursing volume 19 , Article number: 94 ( 2020 ) Cite this article
28k Accesses
20 Citations
1 Altmetric
Metrics details
The complex health system and challenging patient care environment require experienced nurses, especially those with high cognitive skills such as problem-solving, decision- making and critical thinking. Therefore, this study investigated the impact of social problem-solving training on nursing students’ critical thinking and decision-making.
This study was quasi-experimental research and pre-test and post-test design and performed on 40 undergraduate/four-year students of nursing in Borujen Nursing School/Iran that was randomly divided into 2 groups; experimental ( n = 20) and control (n = 20). Then, a social problem-solving course was held for the experimental group. A demographic questionnaire, social problem-solving inventory-revised, California critical thinking test, and decision-making questionnaire was used to collect the information. The reliability and validity of all of them were confirmed. Data analysis was performed using SPSS software and independent sampled T-test, paired T-test, square chi, and Pearson correlation coefficient.
The finding indicated that the social problem-solving course positively affected the student’ social problem-solving and decision-making and critical thinking skills after the instructional course in the experimental group ( P < 0.05), but this result was not observed in the control group ( P > 0.05).
Conclusions
The results showed that structured social problem-solving training could improve cognitive problem-solving, critical thinking, and decision-making skills. Considering this result, nursing education should be presented using new strategies and creative and different ways from traditional education methods. Cognitive skills training should be integrated in the nursing curriculum. Therefore, training cognitive skills such as problem- solving to nursing students is recommended.
Peer Review reports
Continuous monitoring and providing high-quality care to patients is one of the main tasks of nurses. Nurses’ roles are diverse and include care, educational, supportive, and interventional roles when dealing with patients’ clinical problems [ 1 , 2 ].
Providing professional nursing services requires the cognitive skills such as problem-solving, decision-making and critical thinking, and information synthesis [ 3 ].
Problem-solving is an essential skill in nursing. Improving this skill is very important for nurses because it is an intellectual process which requires the reflection and creative thinking [ 4 ].
Problem-solving skill means acquiring knowledge to reach a solution, and a person’s ability to use this knowledge to find a solution requires critical thinking. The promotion of these skills is considered a necessary condition for nurses’ performance in the nursing profession [ 5 , 6 ].
Managing the complexities and challenges of health systems requires competent nurses with high levels of critical thinking skills. A nurse’s critical thinking skills can affect patient safety because it enables nurses to correctly diagnose the patient’s initial problem and take the right action for the right reason [ 4 , 7 , 8 ].
Problem-solving and decision-making are complex and difficult processes for nurses, because they have to care for multiple patients with different problems in complex and unpredictable treatment environments [ 9 , 10 ].
Clinical decision making is an important element of professional nursing care; nurses’ ability to form effective clinical decisions is the most significant issue affecting the care standard. Nurses build 2 kinds of choices associated with the practice: patient care decisions that affect direct patient care and occupational decisions that affect the work context or teams [ 11 , 12 , 13 , 14 , 15 , 16 ].
The utilization of nursing process guarantees the provision of professional and effective care. The nursing process provides nurses with the chance to learn problem-solving skills through teamwork, health management, and patient care. Problem-solving is at the heart of nursing process which is why this skill underlies all nursing practices. Therefore, proper training of this skill in an undergraduate nursing program is essential [ 17 ].
Nursing students face unique problems which are specific to the clinical and therapeutic environment, causing a lot of stresses during clinical education. This stress can affect their problem- solving skills [ 18 , 19 , 20 , 21 ]. They need to promote their problem-solving and critical thinking skills to meet the complex needs of current healthcare settings and should be able to respond to changing circumstances and apply knowledge and skills in different clinical situations [ 22 ]. Institutions should provide this important opportunity for them.
Despite, the results of studies in nursing students show the weakness of their problem-solving skills, while in complex health environments and exposure to emerging diseases, nurses need to diagnose problems and solve them rapidly accurately. The teaching of these skills should begin in college and continue in health care environments [ 5 , 23 , 24 ].
It should not be forgotten that in addition to the problems caused by the patients’ disease, a large proportion of the problems facing nurses are related to the procedures of the natural life of their patients and their families, the majority of nurses with the rest of health team and the various roles defined for nurses [ 25 ].
Therefore, in addition to above- mentioned issues, other ability is required to deal with common problems in the working environment for nurses, the skill is “social problem solving”, because the term social problem-solving includes a method of problem-solving in the “natural context” or the “real world” [ 26 , 27 ]. In reviewing the existing research literature on the competencies and skills required by nursing students, what attracts a lot of attention is the weakness of basic skills and the lack of formal and systematic training of these skills in the nursing curriculum, it indicates a gap in this area [ 5 , 24 , 25 ]. In this regard, the researchers tried to reduce this significant gap by holding a formal problem-solving skills training course, emphasizing the common social issues in the real world of work. Therefore, this study was conducted to investigate the impact of social problem-solving skills training on nursing students’ critical thinking and decision-making.
Setting and sample
This quasi-experimental study with pretest and post-test design was performed on 40 undergraduate/four-year nursing students in Borujen nursing school in Shahrekord University of Medical Sciences. The periods of data collection were 4 months.
According to the fact that senior students of nursing have passed clinical training and internship programs, they have more familiarity with wards and treatment areas, patients and issues in treatment areas and also they have faced the problems which the nurses have with other health team personnel and patients and their families, they have been chosen for this study. Therefore, this study’s sampling method was based on the purpose, and the sample size was equal to the total population. The whole of four-year nursing students participated in this study and the sample size was 40 members. Participants was randomly divided in 2 groups; experimental ( n = 20) and control (n = 20).
The inclusion criteria to take part in the present research were students’ willingness to take part, studying in the four-year nursing, not having the record of psychological sickness or using the related drugs (all based on their self-utterance).
Intervention
At the beginning of study, all students completed the demographic information’ questionnaire. The study’s intervening variables were controlled between the two groups [such as age, marital status, work experience, training courses, psychological illness, psychiatric medication use and improving cognitive skills courses (critical thinking, problem- solving, and decision making in the last 6 months)]. Both groups were homogeneous in terms of demographic variables ( P > 0.05). Decision making and critical thinking skills and social problem solving of participants in 2 groups was evaluated before and 1 month after the intervention.
All questionnaires were anonymous and had an identification code which carefully distributed by the researcher.
To control the transfer of information among the students of two groups, the classification list of students for internships, provided by the head of nursing department at the beginning of semester, was used.
Furthermore, the groups with the odd number of experimental group and the groups with the even number formed the control group and thus were less in contact with each other.
The importance of not transferring information among groups was fully described to the experimental group. They were asked not to provide any information about the course to the students of the control group.
Then, training a course of social problem-solving skills for the experimental group, given in a separate course and the period from the nursing curriculum and was held in 8 sessions during 2 months, using small group discussion, brainstorming, case-based discussion, and reaching the solution in small 4 member groups, taking results of the social problem-solving model as mentioned by D-zurilla and gold fried [ 26 ]. The instructor was an assistant professor of university and had a history of teaching problem-solving courses. This model’ stages are explained in Table 1 .
All training sessions were performed due to the model, and one step of the model was implemented in each session. In each session, the teacher stated the educational objectives and asked the students to share their experiences in dealing to various workplace problems, home and community due to the topic of session. Besides, in each session, a case-based scenario was presented and thoroughly analyzed, and students discussed it.
Instruments
In this study, the data were collected using demographic variables questionnaire and social problem- solving inventory – revised (SPSI-R) developed by D’zurilla and Nezu (2002) [ 26 ], California critical thinking skills test- form B (CCTST; 1994) [ 27 , 28 ] and decision-making questionnaire.
SPSI-R is a self - reporting tool with 52 questions ranging from a Likert scale (1: Absolutely not – 5: very much).
The minimum score maybe 25 and at a maximum of 125, therefore:
The score 25 and 50: weak social problem-solving skills.
The score 50–75: moderate social problem-solving skills.
The score higher of 75: strong social problem-solving skills.
The reliability assessed by repeated tests is between 0.68 and 0.91, and its alpha coefficient between 0.69 and 0.95 was reported [ 26 ]. The structural validity of questionnaire has also been confirmed. All validity analyses have confirmed SPSI as a social problem - solving scale.
In Iran, the alpha coefficient of 0.85 is measured for five factors, and the retest reliability coefficient was obtained 0.88. All of the narratives analyzes confirmed SPSI as a social problem- solving scale [ 29 ].
California critical thinking skills test- form B(CCTST; 1994): This test is a standard tool for assessing the basic skills of critical thinking at the high school and higher education levels (Facione & Facione, 1992, 1998) [ 27 ].
This tool has 34 multiple-choice questions which assessed analysis, inference, and argument evaluation. Facione and Facione (1993) reported that a KR-20 range of 0.65 to 0.75 for this tool is acceptable [ 27 ].
In Iran, the KR-20 for the total scale was 0.62. This coefficient is acceptable for questionnaires that measure the level of thinking ability of individuals.
After changing the English names of this questionnaire to Persian, its content validity was approved by the Board of Experts.
The subscale analysis of Persian version of CCTST showed a positive high level of correlation between total test score and the components (analysis, r = 0.61; evaluation, r = 0.71; inference, r = 0.88; inductive reasoning, r = 0.73; and deductive reasoning, r = 0.74) [ 28 ].
A decision-making questionnaire with 20 questions was used to measure decision-making skills. This questionnaire was made by a researcher and was prepared under the supervision of a professor with psychometric expertise. Five professors confirmed the face and content validity of this questionnaire. The reliability was obtained at 0.87 which confirmed for 30 students using the test-retest method at a time interval of 2 weeks. Each question had four levels and a score from 0.25 to 1. The minimum score of this questionnaire was 5, and the maximum score was 20 [ 30 ].
Statistical analysis
For analyzing the applied data, the SPSS Version 16, and descriptive statistics tests, independent sample T-test, paired T-test, Pearson correlation coefficient, and square chi were used. The significant level was taken P < 0.05.
The average age of students was 21.7 ± 1.34, and the academic average total score was 16.32 ± 2.83. Other demographic characteristics are presented in Table 2 .
None of the students had a history of psychiatric illness or psychiatric drug use. Findings obtained from the chi-square test showed that there is not any significant difference between the two groups statistically in terms of demographic variables.
The mean scores in social decision making, critical thinking, and decision-making in whole samples before intervention showed no significant difference between the two groups statistically ( P > 0.05), but showed a significant difference after the intervention ( P < 0.05) (Table 3 ).
Scores in Table 4 showed a significant positive difference before and after intervention in the “experimental” group ( P < 0.05), but this difference was not seen in the control group ( P > 0.05).
Among the demographic variables, only a positive relationship was seen between marital status and decision-making skills (r = 0.72, P < 0.05).
Also, the scores of critical thinking skill’ subgroups and social problem solving’ subgroups are presented in Tables 5 and 6 which showed a significant positive difference before and after intervention in the “experimental” group (P < 0.05), but this difference was not seen in the control group ( P > 0.05).
In the present study conducted by some studies, problem-solving and critical thinking and decision-making scores of nursing students are moderate [ 5 , 24 , 31 ].
The results showed that problem-solving skills, critical thinking, and decision-making in nursing students were promoted through a social problem-solving training course. Unfortunately, no study has examined the effect of teaching social problem-solving skills on nursing students’ critical thinking and decision-making skills.
Altun (2018) believes that if the values of truth and human dignity are promoted in students, it will help them acquire problem-solving skills. Free discussion between students and faculty on value topics can lead to the development of students’ information processing in values. Developing self-awareness increases students’ impartiality and problem-solving ability [ 5 ]. The results of this study are consistent to the results of present study.
Erozkan (2017), in his study, reported there is a significant relationship between social problem solving and social self-efficacy and the sub-dimensions of social problem solving [ 32 ]. In the present study, social problem -solving skills training has improved problem -solving skills and its subdivisions.
The results of study by Moshirabadi (2015) showed that the mean score of total problem-solving skills was 89.52 ± 21.58 and this average was lower in fourth-year students than other students. He explained that education should improve students’ problem-solving skills. Because nursing students with advanced problem-solving skills are vital to today’s evolving society [ 22 ]. In the present study, the results showed students’ weakness in the skills in question, and holding a social problem-solving skills training course could increase the level of these skills.
Çinar (2010) reported midwives and nurses are expected to use problem-solving strategies and effective decision-making in their work, using rich basic knowledge.
These skills should be developed throughout one’s profession. The results of this study showed that academic education could increase problem-solving skills of nursing and midwifery students, and final year students have higher skill levels [ 23 ].
Bayani (2012) reported that the ability to solve social problems has a determining role in mental health. Problem-solving training can lead to a level upgrade of mental health and quality of life [ 33 ]; These results agree with the results obtained in our study.
Conducted by this study, Kocoglu (2016) reported nurses’ understanding of their problem-solving skills is moderate. Receiving advice and support from qualified nursing managers and educators can enhance this skill and positively impact their behavior [ 31 ].
Kashaninia (2015), in her study, reported teaching critical thinking skills can promote critical thinking and the application of rational decision-making styles by nurses.
One of the main components of sound performance in nursing is nurses’ ability to process information and make good decisions; these abilities themselves require critical thinking. Therefore, universities should envisage educational and supportive programs emphasizing critical thinking to cultivate their students’ professional competencies, decision-making, problem-solving, and self-efficacy [ 34 ].
The study results of Kirmizi (2015) also showed a moderate positive relationship between critical thinking and problem-solving skills [ 35 ].
Hong (2015) reported that using continuing PBL training promotes reflection and critical thinking in clinical nurses. Applying brainstorming in PBL increases the motivation to participate collaboratively and encourages teamwork. Learners become familiar with different perspectives on patients’ problems and gain a more comprehensive understanding. Achieving these competencies is the basis of clinical decision-making in nursing. The dynamic and ongoing involvement of clinical staff can bridge the gap between theory and practice [ 36 ].
Ancel (2016) emphasizes that structured and managed problem-solving training can increase students’ confidence in applying problem-solving skills and help them achieve self-confidence. He reported that nursing students want to be taught in more innovative ways than traditional teaching methods which cognitive skills training should be included in their curriculum. To this end, university faculties and lecturers should believe in the importance of strategies used in teaching and the richness of educational content offered to students [ 17 ].
The results of these recent studies are adjusted with the finding of recent research and emphasize the importance of structured teaching cognitive skills to nurses and nursing students.
Based on the results of this study on improving critical thinking and decision-making skills in the intervention group, researchers guess the reasons to achieve the results of study in the following cases:
In nursing internationally, problem-solving skills (PS) have been introduced as a key strategy for better patient care [ 17 ]. Problem-solving can be defined as a self-oriented cognitive-behavioral process used to identify or discover effective solutions to a special problem in everyday life. In particular, the application of this cognitive-behavioral methodology identifies a wide range of possible effective solutions to a particular problem and enhancement the likelihood of selecting the most effective solution from among the various options [ 27 ].
In social problem-solving theory, there is a difference among the concepts of problem-solving and solution implementation, because the concepts of these two processes are different, and in practice, they require different skills.
In the problem-solving process, we seek to find solutions to specific problems, while in the implementation of solution, the process of implementing those solutions in the real problematic situation is considered [ 25 , 26 ].
The use of D’zurilla and Goldfride’s social problem-solving model was effective in achieving the study results because of its theoretical foundations and the usage of the principles of cognitive reinforcement skills. Social problem solving is considered an intellectual, logical, effort-based, and deliberate activity [ 26 , 32 ]; therefore, using this model can also affect other skills that need recognition.
In this study, problem-solving training from case studies and group discussion methods, brainstorming, and activity in small groups, was used.
There are significant educational achievements in using small- group learning strategies. The limited number of learners in each group increases the interaction between learners, instructors, and content. In this way, the teacher will be able to predict activities and apply techniques that will lead students to achieve high cognitive taxonomy levels. That is, confront students with assignments and activities that force them to use cognitive processes such as analysis, reasoning, evaluation, and criticism.
In small groups, students are given the opportunity to the enquiry, discuss differences of opinion, and come up with solutions. This method creates a comprehensive understanding of the subject for the student [ 36 ].
According to the results, social problem solving increases the nurses’ decision-making ability and critical thinking regarding identifying the patient’s needs and choosing the best nursing procedures. According to what was discussed, the implementation of this intervention in larger groups and in different levels of education by teaching other cognitive skills and examining their impact on other cognitive skills of nursing students, in the future, is recommended.
Social problem- solving training by affecting critical thinking skills and decision-making of nursing students increases patient safety. It improves the quality of care because patients’ needs are better identified and analyzed, and the best solutions are adopted to solve the problem.
In the end, the implementation of this intervention in larger groups in different levels of education by teaching other cognitive skills and examining their impact on other cognitive skills of nursing students in the future is recommended.

Study limitations
This study was performed on fourth-year nursing students, but the students of other levels should be studied during a cohort from the beginning to the end of course to monitor the cognitive skills improvement.
The promotion of high-level cognitive skills is one of the main goals of higher education. It is very necessary to adopt appropriate approaches to improve the level of thinking. According to this study results, the teachers and planners are expected to use effective approaches and models such as D’zurilla and Goldfride social problem solving to improve problem-solving, critical thinking, and decision-making skills. What has been confirmed in this study is that the routine training in the control group should, as it should, has not been able to improve the students’ critical thinking skills, and the traditional educational system needs to be transformed and reviewed to achieve this goal.
Availability of data and materials
The datasets used and analyzed during the present study are available from the corresponding author on reasonable request.
Abbreviations
California critical thinking skills test
Social problem-solving inventory – revised
Pesudovs L. Medical/surgical nursing in the home. Aust Nurs Midwifery J. 2014;22(3):24.
PubMed Google Scholar
Szeri C, et al. Problem solving skills of the nursing and midwifery students and influential factors. Revista Eletrônica de Enfermagem. 2010;12(4).
Friese CR, et al. Pod nursing on a medical/surgical unit: implementation and outcomes evaluation. J Nurs Adm. 2014;44(4):207–11.
Article Google Scholar
Lyneham J. A conceptual model for medical-surgical nursing: moving toward an international clinical specialty. Medsurg Nurs. 2013;22(4):215–20 263.
Altun I. The perceived problem solving ability and values of student nurses and midwives. Nurse Educ Today. 2003;23(8):575–84.
Deniz Kocoglu R, et al. Problem solving training for first line nurse managers. Int J Caring Sci. 2016;9(3):955.
Google Scholar
Mahoney C, et al. Implementing an 'arts in nursing' program on a medical-surgical unit. Medsurg Nurs. 2011;20(5):273–4.
Pardue SF. Decision-making skills and critical thinking ability among associate degree, diploma, baccalaureate, and master's-prepared nurses. J Nurs Educ. 1987;26(9):354–61.
Article CAS Google Scholar
Kozlowski D, et al. The role of emotion in clinical decision making: an integrative literature review. BMC Med Educ. 2017;17(1):255.
Kuiper RA, Pesut DJ. Promoting cognitive and metacognitive reflective reasoning skills in nursing practice: self-regulated learning theory. J Adv Nurs. 2004;45(4):381–91.
Huitzi-Egilegor JX, et al. Implementation of the nursing process in a health area: models and assessment structures used. Rev Lat Am Enfermagem. 2014;22(5):772–7.
Lauri S. Development of the nursing process through action research. J Adv Nurs. 1982;7(4):301–7.
Muller-Staub M, de Graaf-Waar H, Paans W. An internationally consented standard for nursing process-clinical decision support Systems in Electronic Health Records. Comput Inform Nurs. 2016;34(11):493–502.
Neville K, Roan N. Challenges in nursing practice: nurses' perceptions in caring for hospitalized medical-surgical patients with substance abuse/dependence. J Nurs Adm. 2014;44(6):339–46.
Rabelo-Silva ER, et al. Advanced nursing process quality: comparing the international classification for nursing practice (ICNP) with the NANDA-international (NANDA-I) and nursing interventions classification (NIC). J Clin Nurs. 2017;26(3–4):379–87.
Varcoe C. Disparagement of the nursing process: the new dogma? J Adv Nurs. 1996;23(1):120–5.
Ancel G. Problem-solving training: effects on the problem-solving skills and self-efficacy of nursing students. Eurasian J Educ Res. 2016;64:231–46.
Fang J, et al. Social problem-solving in Chinese baccalaureate nursing students. J Evid Based Med. 2016;9(4):181–7.
Kanbay Y, Okanli A. The effect of critical thinking education on nursing students' problem-solving skills. Contemp Nurse. 2017;53(3):313–21.
Lau Y. Factors affecting the social problem-solving ability of baccalaureate nursing students. Nurse Educ Today. 2014;34(1):121–6.
Terzioglu F. The perceived problem-solving ability of nurse managers. J Nurs Manag. 2006;14(5):340–7.
Moshirabadi, Z., et al., The perceived problem solving skill of Iranian nursing students . 2015.
Cinar N. Problem solving skills of the nursing and midwifery students and influential factors. Revista Eletrônica de Enfermagem. 2010;12(4):601–6.
Moattari M, et al. Clinical concept mapping: does it improve discipline-based critical thinking of nursing students? Iran J Nurs Midwifery Res. 2014;19(1):70–6.
PubMed PubMed Central Google Scholar
Elliott TR, Grant JS, Miller DM. Social Problem-Solving Abilities and Behavioral Health. In Chang EC, D'Zurilla TJ, Sanna LJ, editors. Social problem solving: Theory, research, and training. American Psychological Association; 2004. p. 117–33.
D'Zurilla TJ, Maydeu-Olivares A. Conceptual and methodological issues in social problem-solving assessment. Behav Ther. 1995;26(3):409–32.
Facione PA. The California Critical Thinking Skills Test--College Level. Technical Report# 1. Experimental Validation and Content Validity; 1990.
Khalili H, Zadeh MH. Investigation of reliability, validity and normality Persian version of the California Critical Thinking Skills Test; Form B (CCTST). J Med Educ. 2003;3(1).
Mokhberi A. Questionnaire, psychometrics, and standardization of indicators of social problem solving ability. Educ Measurement. 2011;1(4):1–21.
Heidari M, Shahbazi S. Effect of training problem-solving skill on decision-making and critical thinking of personnel at medical emergencies. Int J Crit Illn Inj Sci. 2016;6(4):182–7.
Kocoglu D, Duygulu S, Abaan S, Akin B. Problem Solving Training for First Line Nurse Managers. Int J Caring Sci. 2016;9(13):955–65.
Erozkan A. Analysis of social problem solving and social self-efficacy in prospective teachers. Educational Sciences: Theory and Practice. 2014;14(2):447–55.
Bayani AA, Ranjbar M, Bayani A. The study of relationship between social problem-solving and depression and social phobia among students. J Mazandaran Univ Med Sci. 2012;22(94):91–8.
Kashaninia Z, et al. The effect of teaching critical thinking skills on the decision making style of nursing managers. J Client-Centered Nurs Care. 2015;1(4):197–204.
Kirmizi FS, Saygi C, Yurdakal IH. Determine the relationship between the disposition of critical thinking and the perception about problem solving skills. Procedia Soc Behav Sci. 2015;191:657–61.
Hung CH, Lin CY. Using concept mapping to evaluate knowledge structure in problem-based learning. BMC Med Educ. 2015;15:212.
Download references
Acknowledgments
This article results from research project No. 980 approved by the Research and Technology Department of Shahrekord University of Medical Sciences. We would like to appreciate to all personnel and students of the Borujen Nursing School. The efforts of all those who assisted us throughout this research.
‘Not applicable.
Author information
Authors and affiliations.
Department of Medical Education, Virtual School of Medical Education and Management, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Soleiman Ahmady
Virtual School of Medical Education and management, Shahid Beheshty University of Medical Sciences, Tehran, Iran
Sara Shahbazi
Community-Oriented Nursing Midwifery Research Center, Shahrekord University of Medical Sciences, Shahrekord, Iran
You can also search for this author in PubMed Google Scholar
Contributions
SA and SSH conceptualized the study, developed the proposal, coordinated the project, completed initial data entry and analysis, and wrote the report. SSH conducted the statistical analyses. SA and SSH assisted in writing and editing the final report. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Sara Shahbazi .
Ethics declarations
Ethics approval and consent to participate.
This study was reviewed and given exempt status by the Institutional Review Board of the research and technology department of Shahrekord University of Medical Sciences (IRB No. 08–2017-109). Before the survey, students completed a research consent form and were assured that their information would remain confidential. After the end of the study, a training course for the control group students was held.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ahmady, S., Shahbazi, S. Impact of social problem-solving training on critical thinking and decision making of nursing students. BMC Nurs 19 , 94 (2020). https://doi.org/10.1186/s12912-020-00487-x
Download citation
Received : 11 March 2020
Accepted : 29 September 2020
Published : 07 October 2020
DOI : https://doi.org/10.1186/s12912-020-00487-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Social problem solving
- Decision making
- Critical thinking
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
EDITORIAL article
This article is part of the research topic.
Reviews in Healthcare Professions Education
Editorial: Reviews in Healthcare Professions Education Provisionally Accepted

- 1 QU Health, Qatar University, Qatar
The final, formatted version of the article will be published soon.
The review articles encompass a wide range of topics, each offering unique perspectives on key aspects of healthcare. One article (Lyu & Li 2023) explores the challenges of translating evidence into practice and the role of clinical practice guidelines in guiding healthcare decisions. It emphasizes the importance of evidence-based practices in improving patient outcomes while highlighting the barriers and limitations in implementing these practices effectively. Another article (Keller, Ludwig, & Huber-Lang, 2023) focuses on the evolving patient-physician relationship, particularly in the context of technological advancements. It examines how technology influences communication between patients and healthcare providers, shaping the dynamics of care delivery and patient engagement. The article underscores the need for maintaining personalized, patient-centred care amidst the increasing reliance on digital health tools and telemedicine. Clinical reasoning, a fundamental aspect of healthcare practice, is explored in depth in another article (Vreugdenhil, Somra, & Ket, 2023). The review delves into the complexities of clinical reasoning processes among healthcare professionals, highlighting the differences between physicians and nurses in their approaches to problem-solving and decision-making. It emphasizes the importance of understanding these differences to foster effective collaboration and optimize patient care outcomes. Wrist arthroscopy, a specialized surgical technique for diagnosing and treating wrist injuries, is the focus of another review article by Shi, Lu, & Yu (2022). The review examines the advantages and challenges associated with wrist arthroscopy and explores evolving methodologies in training programs for surgeons. It highlights the importance of anatomical knowledge, operative skills, and innovative training methods in ensuring optimal surgical outcomes and patient safety. The review article by Ma, Zeng, & Wang (2022) investigates the application of the BOPPPS teaching strategy in medical education in China. It focuses on determining the effectiveness of the BOPPPS strategy in enhancing student engagement and learning outcomes compared to traditional lecture-based methods. This review underscores the potential of innovative teaching approaches in improving medical education delivery and preparing future healthcare professionals for clinical practice.Methodologically, each review article adopts a distinct methodological approach tailored to its research objectives and focus areas. For example, the article by Lyu & Li (2023) employs a systematic search methodology, spanning a ten-year period and incorporating grey literature to ensure comprehensive coverage of relevant studies. In contrast, Keller, Ludwig, & Huber-Lang (2023) utilize a narrative exploration approach, weaving together patient stories and clinical anecdotes to illustrate the nuances of the patient-physician relationship. Vreugdenhil, Somra, & Ket (2023) employ a structured analytical framework, the "onion model," to dissect clinical reasoning processes into layers, offering a comprehensive understanding of this complex phenomenon. The fourth article synthesizes existing research on wrist arthroscopy training, examining a wide range of methodologies and training programs to identify best practices in surgical education. Lastly, Ma, Zeng, & Wang (2022) utilize a meta-analysis and systematic review approach, adhering to established guidelines such as PRISMA and PICOS to evaluate the effectiveness of the BOPPPS teaching strategy. It conducts a rigorous analysis of available evidence, including the risk of bias assessment and statistical analysis, to draw meaningful conclusions regarding the impact of innovative teaching methods on medical education outcomes.Collectively, these review articles provide valuable insights into the multifaceted nature of healthcare and its implications for medical education and practice. They underscore the importance of evidence-based practices, personalized patient care, interdisciplinary collaboration, and innovative teaching methodologies in addressing the evolving challenges and demands of healthcare. Moving forward, further research is needed to explore the effectiveness of different educational strategies, the impact of technology on patient-provider relationships, and the optimization of clinical reasoning processes across healthcare professions. Additionally, ongoing evaluation and refinement of training methodologies, such as wrist arthroscopy training programs, are essential to ensure the continued advancement of surgical education and patient care.In summary, the review articles offer an exploration of various aspects of healthcare, from evidence translation and patient-physician relationships to clinical reasoning and surgical training. By examining these diverse topics through different methodological lenses, we gain valuable insights into the complexities and challenges of healthcare delivery and medical education. Moving forward, continued research and innovation are essential to address the evolving needs of patients, healthcare professionals, and healthcare systems worldwide.
Keywords: BOPPPS, Arthroscopy, Communication Skill, reviews, Health profession education
Received: 27 Dec 2023; Accepted: 26 Mar 2024.
Copyright: © 2024 Sethi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Mx. Ahsan Sethi, QU Health, Qatar University, Doha, Qatar
People also looked at
- Open access
- Published: 25 March 2024
Exploring the medical decision-making patterns and influencing factors among the general Chinese public: a binary logistic regression analysis
- Yuwen Lyu 1 ,
- Qian Xu 2 &
- Junrong Liu 1
BMC Public Health volume 24 , Article number: 887 ( 2024 ) Cite this article
227 Accesses
Metrics details
With the ongoing evolution of the healthcare system and shifts in cultural paradigms, there is a pressing need to delve into the medical decision-making behaviors of general Chinese public and understand their underlying motivations. This research seeks to elucidate the prevailing tendencies in these decision-making processes and to empirically validate the pivotal factors that shape their choices, offering valuable insights for healthcare policymakers and institutions.
A comprehensive survey was administered to 2,696 Chinese residents to examine their medical decision-making patterns. These patterns were classified into two primary categories: Unilateral Decision-making (Doctor-dominant, Family-centric, and Patient-driven subtypes) and Collaborative Decision-making (Doctor-led, Doctor-Patient, Patient-Family, and Doctor-Patient-Family subtypes). Binary logistic regression analysis was employed to empirically pinpoint the significant factors influencing these decision-making frameworks.
The study's analysis reveals distinct preferences in medical decision-making among Chinese residents. In the Collaborative Decision-making category, chosen by 70.81% of participants, the subtypes are as follows: Doctor-led (29.90%), Doctor-Patient (13.54%), Patient-Family (2.93%), and Doctor-Patient-Family (24.44%). The Unilateral Decision-making, preferred by 29.19%, includes Doctor-dominant (23.22%), Family-centric (1.74%), and Patient-driven (4.23%) models. The preference for Collaborative Decision-making is associated with higher educational levels, specific marital statuses (particularly married but childless), and choices of rural residents' basic medical insurance or occupational basic medical insurance. In contrast, Unilateral Decision-making correlates with males, individuals with religious beliefs, certain occupational roles (like civil servants), and holders of commercial or publicly funded medical insurance.
This study elucidates the complex interplay of socio-cultural and individual determinants shaping medical decision-making in China. The findings reveal a marked inclination towards collaborative models, closely linked to educational level, marital status, and specific insurance types, reflecting an evolving trend towards participatory healthcare. Simultaneously, the persistence of unilateral models, influenced by gender, religious beliefs, and occupational roles, highlights the heterogeneity within Chinese healthcare preferences. These insights are crucial for policymakers and healthcare practitioners, underscoring the need for adaptable, culturally attuned healthcare frameworks that cater to this diversity, thereby enhancing patient engagement and healthcare efficacy.
Peer Review reports
Introduction
Medical decision-making encompasses the deliberative process of choosing the most efficacious diagnostic and therapeutic options from a range of alternatives. Central to this process are stakeholders such as physicians, patients, and their families [ 41 ]. Given the disparate interests and value perspectives among these stakeholders, a spectrum of medical decision-making models has been delineated. Contemporary research posits that, based on the dynamics of communication and the power equilibrium between physicians and patients, these models can be broadly segmented into two primary paradigms: Unilateral Decision-making and Collaborative Decision-making [ 8 , 18 ].
Unilateral decision-making denotes a paradigm wherein a singular entity possesses the definitive authority in the medical decision-making process. This model can be further segmented into the doctor-dominant, family-centric, and patient-driven subtypes. In the doctor-dominant subtype, physicians, leveraging their expertise and experiential knowledge, independently chart the course of medical action. However, this approach often relegates patients and their families to subordinate roles, primarily involving them in information provision and adherence to prescribed treatment regimens. Such a paradigm can potentially undermine patient autonomy and hinder the advancement of informed consent processes, thereby risking suboptimal therapeutic outcomes [ 24 ]. In the family-centric subtype of medical decision-making, the patient's relatives, upon considering the physician's advice, make choices that align with their understanding of the patient's health and their core values. On the other hand, the patient-driven subtype is exemplified by patients independently directing their medical journey, guided by their personal values and preferences. Historically in Chinese medicine, the family has played a pivotal role in patient healthcare activities, exerting a significant authoritative influence in healthcare decision-making processes [ 12 ].
The traditional model of Unilateral decision-making is increasingly seen as inadequate in the context of contemporary medical practice, paving the way for the emergence of the collaborative decision-making model [ 49 ]. Collaborative Decision-making is a paradigm where multiple stakeholders actively participate and reach a consensus during the medical process. This model can be further delineated into the doctor-led, doctor-patient, patient-family, and doctor -patient-family [ 29 ]. In the doctor-led subtype, the physician, while considering the patient's input, primarily guides the treatment direction. However, the heart of Collaborative Decision-making lies in the doctor-patient model, a true embodiment of Shared Decision Making (SDM). Here, the physician and patient engage in an egalitarian dialogue, blending medical expertise with the patient's values to jointly formulate a treatment plan. This collaborative approach aligns with SDM frameworks like Elwyn et al.'s "three-talk model" and the Ottawa Decision Support Framework, which focus on structured decision-making phases and informed deliberation [ 10 , 42 ]. The significance of such collaborative models, especially SDM, is underscored by research from Pieterse AH et al. [ 16 , 38 ]. These studies highlight the crucial role of patient-physician collaboration and explore the challenges and facilitators encountered in implementing SDM across varied healthcare settings. The patient-family model adds another layer, involving both the patient and their family in decision-making, ensuring that treatment plans reflect both the patient's and family's values and perspectives. Lastly, the tripartite collaboration model, involving physicians, patients, and families, aligns with Chinese cultural values [ 11 ]. It emphasizes collective decision-making and respectful communication, reflecting the communal and family-oriented nature of Chinese society.
Each medical decision-making model possesses its inherent characteristics, underscoring the nuanced roles, power dynamics, and responsibilities of the involved stakeholders [ 35 , 50 ]. A conceptual framework, based on existing literature, classifies these models into two broad categories: Unilateral Decision-making and Collaborative Decision-making [ 29 ].
Unilateral Decision-making encompasses three subtypes:
Doctor-Dominant: The physician primarily makes decisions, often with limited patient or family input.
Family-Centric: Decision-making is led by family members, who consider the patient's needs and the physician's advice.
Patient-Driven: The patient independently makes decisions, possibly informed by their research or personal preferences.
Collaborative Decision-making, in contrast, involves multiple stakeholders and includes:
Doctor-Led: The physician guides the decision process but incorporates patient input.
Doctor-Patient: An egalitarian model where physician and patient jointly make decisions, embodying the essence of Shared Decision Making (SDM).
Patient-Family: Decisions are made collaboratively between the patient and family members.
Doctor-Patient-Family: This model integrates the physician, patient, and family in a tripartite decision-making process.
The choice of a model is influenced by factors related to both physicians and patients, such as demographics professional standing, health status, cultural background, and the doctor-patient relationship. Research across various cultures has provided insights into these dynamics [ 4 , 15 ]. In Italy, physicians' personal beliefs and specialties influence their decisions in early breast cancer treatment, underscoring the impact of individual professional judgment [ 28 ]. Simultaneously, the study found that Bengali patients received more supportive communication from Bengali doctors than ethnic minority patients, underscoring the importance of patient-centered communication for equitable healthcare across ethnicities [ 54 ]. Moreover, the study emphasized the complexity of patient values in decision-making, revealing that individuals with type 2 diabetes consider not just treatment-specific factors, but also life goals, philosophies, and personal and social backgrounds when deciding about insulin treatment, suggesting a need for a broader understanding of patient values in clinical decision-making [ 25 ].
In this context, a study from China contributes further by analyzing preferences in medical decision-making models among different demographics, revealing significant variations based on gender, age, and education level. This research indicates a general preference for physician-led decision-making, particularly the directive-collaborative model [ 29 ]. However, it primarily focuses on statistical preferences and correlations, pointing to a gap in the comprehensive understanding of specific factors influencing these preferences in the Chinese healthcare context. Building on previous research, this study is designed to address the scarcity of research in China on the diverse factors influencing medical decision-making, which has broader implications on a global scale. It aims to dissect public preferences and the array of factors impacting these choices in a Chinese context, providing insights that can be valuable not only within China but also for international comparisons. By systematically examining variables such as individual, familial, occupational, and regional characteristics, along with medical insurance types, it contributes to the global understanding of how these elements shape healthcare decision processes. It seeks to enhance global understanding of healthcare decision processes, thus advancing patient-centered medical practices in various cultural and healthcare systems.
Binary logistic regression
The binary logistic model, a specific variant of the broader multinomial logistic models, stands as a sophisticated statistical instrument adept at elucidating intricate interrelationships among observed variables, factoring in multifaceted interactions and influences. Its utility in the medical sphere is well-established. For instance, it has been leveraged to evaluate the interplay between individual attributes, such as age, gender, and genetic markers, and their association with risks tied to diverse chronic ailments [ 44 ]. Additionally, these models have been pivotal in shedding light on the nexus between environmental determinants, lifestyle choices, and other health-centric behaviors and a spectrum of health outcomes [ 39 ]. In the context of healthcare service consumption, multinomial logistic models have been tapped to dissect the factors underpinning patients' predilections for distinct medical services. For example, scholars have employed this paradigm to discern the influence of variables like household financial standing, health insurance coverage, and geographical positioning on patients' proclivities towards outpatient, inpatient, or emergency services [ 34 ]. Therefore, the deployment of the binary logistic model to analyze propensities in medical decision-making and their pertinent drivers can illuminate the inherent dynamics among these variables. Such insights can offer a profound understanding of the cognitive and behavioral tendencies individuals manifest when navigating medical decisions. This enriched perspective not only equips healthcare professionals to more adeptly cater to patients' aspirations and anticipations, thereby elevating healthcare service caliber but also enables patients to gain a nuanced grasp of their medical scenarios and treatment alternatives, promoting a more informed and engaged role in their healthcare decision-making process.
Binary Logistic Regression is primarily employed for a dependent variable with two categories. In this study, the dependent variable is specifically categorized into "Unilateral Decision-making" and "Collaborative Decision-making." Here, "Unilateral Decision-making" is designated as the dummy variable (with a value of 1), while "Collaborative Decision-making" serves as the reference category (assigned a value of 0). The form [ 23 ] of the model is:
Where \(p\) represents the probability of the event occurring, \({X}_{1},{X}_{2},\dots ,{X}_{k}\) is the independent variable, and \({\beta }_{0},{\beta }_{1},\dots ,{\beta }_{k}\) is the regression coefficient.
To assess the goodness of fit and explanatory power of the model, this study employs the McFadden R-squared statistical metric. This metric offers a quantified approach to gauge the extent to which the model fits the observed data, thereby ensuring the model's reliability and accuracy.
Variable selection and measurement
The sample data originates from a national-level research project completed by our research group in 2022, was collected from a broad spectrum of the general Chinese public. To ensure the quality and clarity of the survey, and to avoid ambiguity in responses, the concept of medical decision-making was clearly defined within the questionnaire. The survey was custom-designed to align with the research objectives and content and then integrated into the Questionnaire Star enterprise system. After a preliminary survey and consultations with experts in statistics and medical ethics, the questionnaire underwent three rounds of revisions, resulting in the final version that is detailed in Appendix 1 .
Participants in the sample ranged in age from 18 to over 75 years old, with educational backgrounds spanning from junior high school or below to undergraduate level and above. Additionally, data was collected on participants' occupational backgrounds, monthly family income, medical payment methods, religious beliefs, and family circumstances, among other relevant factors. A detailed description of the sample and variable definitions can be found in Table 1 .
Data collection and sampling
Survey methodology and quality assurance.
The data collection methodology for this study, utilized the Questionnaire Star system, a professional online survey tool, to ensure the accuracy and representativeness of the data gathered from participants. A stratified convenience sampling technique was employed to collect responses from a diverse sample of 2,696 individuals, spanning 31 provinces and cities across China, with the exclusion of Hong Kong, Macao, and Taiwan regions. To ensure the validity of the responses, the Questionnaire Star system was programmed with quality control measures such as quota rules for different occupational groups, time requirements to discourage incomplete responses, and anti-duplication measures like one-time entries per IP address, computer, or mobile device.
Sample size determination and statistical power
The survey was disseminated through WeChat, facilitating convenient access for participants and resulting in a substantial response rate of 48.54%, after the exclusion of 2,858 invalid responses through automated isolation techniques. The robustness of the sampling process was further ensured by a power analysis conducted using G*Power 3.1.9.7 [ 13 ], which determined that a sample size of 2040 was required to achieve a power of 0.95, given the medium effect size (OR = 1.2) and alpha level of 0.05. The actual power achieved post hoc was 0.9507, indicating that the study was sufficiently powered to detect the specified effect size. This comprehensive approach to data collection and sampling underscores the study's commitment to rigorous research standards and provides a strong foundation for the subsequent analysis of medical decision-making patterns among the general Chinese public.
Descriptive statistical analysis
To gain a comprehensive understanding of the demographic attributes of the sample population, an in-depth analysis was carried out. The sample encompasses a wide array of individuals, representing various ages, genders, educational backgrounds, occupations, income levels, family situations, living arrangements, and religious beliefs. This detailed demographic profiling is essential for contextualizing the research findings and assessing the representativeness of the sample. Presented below in Table 2 is a summary of these demographic and sociological characteristics.
This study conducted a detailed classification and statistical analysis of the medical decision-making models of 2,696 Chinese residents. The specific results can be found in Table 3 .
According to the survey results presented in Table 3 and Fig. 1 , only 29.19% of Chinese residents opt for the Unilateral decision-making model, while a staggering 70.81% prefer the collaborative decision-making model. This underscores the primary trend in China's medical decision-making, which is gradually shifting towards doctor-patient collaboration , rather than sole autonomous decision-making.
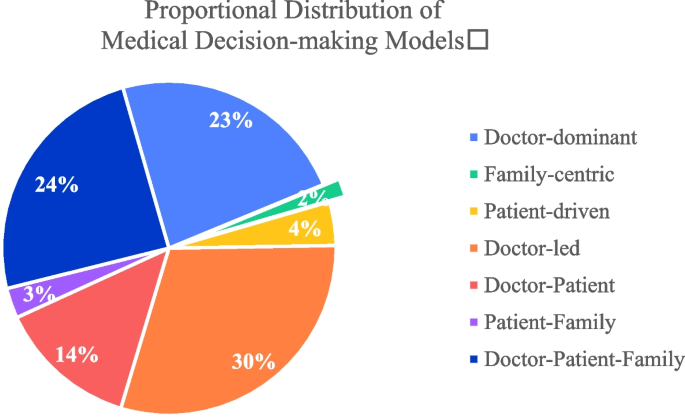
Distribution Pie Chart of Each Decision-making Model
First and foremost, within the realm of collaborative decision-making, the doctor-led collaborative model emerges as predominant, constituting 29.90% of the choices. This underscores the pivotal role physicians play in the decision-making trajectory, with patients actively engaging in the process, albeit under the physician's guidance. Additionally, the model where both the doctor-patient jointly partake in decision-making is also relatively prevalent, accounting for 13.54%. In the Chinese context, the decision-making model involving both the patient and their family members accounts for 2.93%, while the tripartite model encompassing the physician, patient, and family members constitutes 24.44%.
Secondly, within the realm of unilateral decision-making, the doctor-dominant model emerges as predominant, accounting for 23.22%. This reflects the elevated authoritative status bestowed upon doctors in medical settings due to their specialized knowledge and experience. However, the proportions of singular decision-making models led by family members and patients are relatively low, standing at 1.74% and 4.23% respectively. Under such decision-making paradigms, family members or patients are more inclined to make independent medical decisions without relying on the doctor's recommendations.
Binary logistic regression outcomes
This study employed a binary logistic regression model to empirically analyze the factors influencing the medical decision-making patterns (Unilateral Decision-making and Collaborative Decision-making) among Chinese residents. The detailed regression outcomes are presented in Table 3 .
Based on the results presented in Table 4 , the analysis revealed several significant predictors within the realms of individual characteristics, family characteristics, occupational characteristics, and medical insurance characteristics. Regarding individual characteristics, gender emerged as a significant factor, with males (β = 0.206, p < 0.05) more likely to engage in unilateral decision-making, as indicated by an odds ratio (OR) of 1.228. This suggests that gender plays a crucial role in decision-making styles. Additionally, education level was inversely related to unilateral decision-making (β = -0.113, p < 0.05), with an OR of 0.893, implying that higher education levels may foster a more collaborative approach. Furthermore, the presence of religious beliefs was positively associated with unilateral decision-making (β = 0.237, p < 0.05; OR = 1.267), suggesting that religious convictions might influence individual decision-making tendencies.
In the domain of family characteristics, the status labeled as Family Status_2.0 was significantly associated with unilateral decision-making (β = 0.307, p < 0.05; OR = 1.359), highlighting the influence of specific familial contexts on decision-making processes. Occupational characteristics also played a significant role, with certain occupations (Occupation_1.0, 3.0, 4.0, 5.0) demonstrating a higher propensity for unilateral decision-making compared to unemployment. This is evidenced by relatively high odds ratios (3.008, 2.027, 2.029, and 2.108, respectively), suggesting that occupational roles can significantly shape decision-making preferences. Medical insurance characteristics further influenced decision-making styles. Individuals with Rural Residents' Basic Medical Insurance or Occupational Basic Medical Insurance were less likely to engage in unilateral decision-making (ORs = 0.605 and 0.716, respectively), as opposed to those with Commercial Insurance or Publicly Funded Medical Care, who were more inclined towards unilateral decision-making (ORs = 1.299 and 1.266, respectively).
The model's intercept was significantly negative (β = -1.182, p < 0.01; OR = 0.307), indicating a generally low propensity for unilateral decision-making when all explanatory variables are at their reference levels. Notably, certain factors such as age, various family statuses, and regional characteristics (Central and Eastern) did not exhibit significant impacts on the decision-making category. This lack of significance suggests that these factors may not play a substantial role in determining decision-making styles within the context of this study.
The goodness-of-fit for the model, as indicated by McFadden's R-squared, was 0.065. Although this value might appear modest, it is within the acceptable range for logistic regression models in social science research, where perfect fit is rare due to the complexity of human behaviors and decision-making processes. The value of 0.065 suggests that while the model captured key aspects influencing medical decision-making, there are other unmeasured variables and inherent complexities in the data that are not fully explained by the model. This highlights the multifaceted nature of medical decision-making and the need for further research to explore additional influencing factors.
Distinctive trends in China's medical decision-making models within a cultural context
The study's analysis of decision-making patterns in China offers a unique perspective, contrasting notably with prevalent trends in Western healthcare systems. In unilateral decision-making, the prominent 'Doctor-dominant' model, accounting for 23.22% of responses, reflects a cultural preference for physician authority, diverging from Western emphasis on patient autonomy [ 43 , 47 ]. This inclination towards physician-led decisions aligns with traditional values of respecting authority figures, a theme recurrent in Chinese society [ 2 ].
In collaborative decision-making, the 'Doctor-Patient-Family' model, representing 24.44%, highlights the integral role of family in medical decisions. This triadic approach is deeply rooted in China's family-centric culture [ 20 ] and contrasts with the Western focus on individual patient autonomy in Shared Decision Making [ 6 ]. The 'Doctor-led' model's prevalence (29.90%) further emphasizes the deference to medical expertise, underscoring cultural differences in patient engagement and trust in healthcare professionals [ 29 , 31 ].
This research elucidates a paradigmatic shift in medical decision-making models, emphasizing the cultural congruence of a triadic model within the Chinese context. The prevalence of the 'Doctor-Patient-Family' model, as delineated in the findings, resonates with the collectivist ethos and entrenched family-centric values of Chinese society. This model diverges from the predominantly dyadic frameworks of patient-physician interaction that underpin Western healthcare models, which predominantly focus on individual autonomy as per SDM principles. The incorporation of family perspectives into the decision-making process aligns with the Confucian tenets of familial piety and collective welfare, deeply embedded in Chinese culture [ 3 , 51 ]. This triadic approach not only enhances the cultural appropriateness of healthcare interventions but also ensures that decision-making is reflective of a broader familial context, potentially leading to more harmonious and satisfactory healthcare outcomes. Consequently, this research contributes to a burgeoning dialogue in global health, challenging the universality of the SDM model, predominantly rooted in Western individualism. It posits that in societies like China, where familial dynamics play a pivotal role, healthcare decision-making models must evolve to incorporate these cultural specificities.
Key factors influencing medical decision-making patterns
According to the analysis results from Table 3 , different groups exhibit varied decision-making preferences when it comes to medical decision-making patterns. In terms of individual characteristics, factors such as gender, education level, and religious beliefs have a significant impact on the choice of medical decision-making models. Specifically, males and individuals with religious beliefs tend to lean more towards the unilateral decision-making model. This can be attributed to traditional cultural contexts where males or those with religious convictions often place a higher emphasis on individual decision-making autonomy [ 19 ]. Conversely, individuals with higher educational levels tend to favor the collaborative decision-making model. This inclination might stem from the belief that those with more advanced education place greater value on the collaborative relationship between doctors and patients, thinking that such collaboration can lead to better treatment outcomes [ 27 , 32 ].
In terms of family characteristics, marital status has a significant influence on the choice of medical decision-making patterns. Specifically, individuals who are married but childless tend to lean more towards the unilateral decision-making model compared to their unmarried counterparts. Firstly, this inclination may be related to the fact that those who are married but without children are in the process of family planning [ 5 ], and in certain medical decision-making scenarios, they prefer this model. Secondly, unmarried individuals might be more reliant on their family and social networks when making medical decisions [ 1 ], hence their inclination towards a collaborative.
In terms of occupational characteristics, certain job categories significantly influence the choice of medical decision-making patterns. Specifically, individuals in professions such as civil servants, corporate staff, enterprise workers, self-employed and migrant workers tend to favor the unilateral decision-making model. Civil servants, in particular, display the strongest inclination towards this model. This tendency might be attributed to the nature of their jobs and their social status, as they often prioritize efficiency [ 14 ]. On the other hand, corporate staff, enterprise workers, self-employed and migrant workers might be more concerned about medical expenses and have limited access to information [ 53 ], leading them to lean more towards unilateral decision-making approach.
Regarding the characteristics of medical insurance, certain insurance categories significantly influence the choice of medical decision-making patterns. Specifically, individuals who opt for commercial insurance and publicly funded medical care tend to lean towards the unilateral decision-making model. In contrast, those who choose the rural residents' basic medical insurance and the occupational basic medical insurance for employees are more inclined towards a collaborative decision-making approach. This divergence might be attributed to the differences in medical services and the range of choices provided by different types of insurance [ 7 ].
In terms of regional characteristics, residents from the central and eastern regions did not show significant differences in their medical decision-making patterns compared to those from the western regions. Firstly, despite regional disparities in economic development, education levels, and medical resources, the fundamental values and lifestyles of residents are profoundly influenced by Chinese culture [ 26 ]. Secondly, with the advancement of information technology [ 48 ], especially the internet and mobile communication technologies, the means and speed at which residents from different regions access medical information have greatly improved [ 17 ]. Therefore, even with disparities in economic and medical resources across regions, individuals did not exhibit significant differences in their choices of medical decision-making patterns.
Medical decision-making is a complex process, involving the balancing of various factors such as treatment outcomes, costs, and potential risks. Thus, even though certain groups may have clear inclinations in their medical decisions, these tendencies are not absolute.
Policy implications
In the Chinese medical environment, the choice of medical decision-making models is a multi-dimensional, multi-factorial complex process, closely related to individual characteristics, family background, occupational attributes, and types of medical insurance. This study provides empirical references for policymakers and medical institutions, helping to more precisely meet the medical needs of different groups. Based on the aforementioned research findings, this study proposes the following suggestions and countermeasures:
Firstly, Enhance Doctor-Patient Collaboration. Recognizing the critical role of the cooperative decision-making model, particularly the physician-led cooperative approach which aligns closely with the principles of Shared Decision Making, it becomes essential for medical institutions to prioritize training for doctors and healthcare professionals. This training should focus on the importance of effective communication with patients and their families, a cornerstone of SDM, thereby fostering a stronger partnership between doctors and patients [ 21 , 52 ]. Effective communication training, central to SDM, has been shown to significantly improve patient outcomes and satisfaction. It equips healthcare professionals with the essential skills to understand and address patient concerns more effectively, encouraging patient involvement in their own care [ 40 ]. Moreover, considering the pivotal role of the family in many cultural contexts, a balanced approach, integral to SDM, should be adopted to reconcile potential conflicts between individual autonomy and family-centered decision-making [ 36 ]. Training in SDM can also enhance the understanding of cultural nuances among healthcare providers, leading to more culturally sensitive and patient-centered care, a critical aspect of SDM [ 46 ].
Secondly, Enhance Targeted Health Literacy. The study indicates that individuals with higher levels of education tend to prefer the cooperative decision-making model. This suggests that individuals with higher educational levels are generally more receptive to health literacy education, facilitating their active participation in decision-making processes [ 22 ]. Enhanced health literacy enables patients to engage more effectively in discussions about their care [ 9 , 30 ]. Therefore, there is a need for increased opportunities in health education and training, particularly targeting patient groups with lower educational levels. Such focused interventions are crucial for improving collaborative decision-making in healthcare settings [ 33 ].
Thirdly, Pay Attention to Occupational and Social Role Factors. Different occupational groups have distinct preferences in medical decision-making models. Medical institutions should recognize the differentiated characteristics among various occupational groups, taking into account their social and cultural backgrounds, to offer more personalized medical services and decision support [ 45 ]. Fourthly, Refine the Medical Insurance System. The type of medical insurance has a significant impact on the choice of medical decision-making models. Policy makers should consider adjusting medical insurance policies to ensure that all types of medical insurance can provide reasonable, transparent, and efficient medical services to their beneficiaries [ 37 ].
In conclusion, medical decision-making is a complex process involving multiple factors. It requires the joint efforts of policy makers, medical institutions, and patients to ensure that patients can enjoy more humane and efficient medical services, thereby enhancing patient satisfaction.
Conclusions
This study delves deeply into the medical decision-making patterns of Chinese residents and their core influencing factors. The results reveal that the collaborative decision-making model predominates, especially the doctor-guided collaborative model and the joint decision-making model involving doctors, patients, and family members. This finding aligns with China's cultural background and family-centric values.
Furthermore, this research uncovers several key factors that significantly impact medical decision-making patterns, including religious beliefs, family status, occupation, and medical insurance. These factors not only reflect an individual's socio-economic status but are also closely related to culture, beliefs, and social structure. Therefore, medical decision-making is a complex phenomenon influenced by a myriad of factors. To better meet the medical needs of residents, policymakers and medical practitioners should consider these factors comprehensively and adopt corresponding strategies and measures. Simultaneously, as society evolves and transforms, medical decision-making patterns might change, necessitating continuous research and attention to consistently enhance the quality of medical services.
Nevertheless, the study, insightful in its examination of medical decision-making in China, presents two notable limitations. Initially, its constrained scope, focusing predominantly on a single cultural setting, may not encapsulate the vast array of challenges and dynamics prevalent in global healthcare systems, characterized by systemic inefficiencies, heightened costs, and persistent inequalities. Future endeavors will involve exploring and contrasting medical decision-making patterns across various global healthcare settings. This expansion will allow for a more comprehensive understanding of how cultural, economic, and systemic factors universally impact patient preferences and decision-making in healthcare, providing a more holistic view aligned with the dynamic nature of global healthcare challenges. Secondly, the study's reliance on binary logistic regression might not fully unravel the complex, multi-layered nature of healthcare decision-making. Moving forward, future research aims to incorporate more sophisticated models, such as nested logistic regression, to more effectively capture the hierarchical and diverse dimensions of healthcare decision-making, thereby enriching and broadening the study's applicability and relevance in the global healthcare context.
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Aral S, Walker D. Identifying influential and susceptible members of social networks. Science. 2012;337(6092):337–41.
Article CAS PubMed Google Scholar
Bennett K, Smith DH, Irwin H. Preferences for participation in medical decisions in China. Health Commun. 1999;11(3):261–84.
Article Google Scholar
Bian L. Medical individualism or medical familism? A critical analysis of China’s new guidelines for informed consent: the basic norms of the documentation of the medical record. J Med Philos. 2015;40(4):371–86.
Article PubMed Google Scholar
Bizouarn P, Fiat E, Folscheid D. Rational choice, prediction, and medical decision. Contribution of severity scores. Ann Fr Anesth Reanim. 2001;20(9):807–12.
Blair SL, Madigan TJ. Marriage and fertility preferences among young women in China: changes over time. J Fam Issues. 2021;42(10):2353–76.
Danner M, Geiger F, Wehkamp K, Rueffer JU, Kuch C, Sundmacher L, Scheibler F. Making shared decision-making (SDM) a reality: protocol of a large-scale long-term SDM implementation programme at a Northern German University Hospital. BMJ Open. 2020;10(10):e037575.
Dong K. Medical insurance system evolution in China. China Economic Review. 2009;20(4):591–7.
Edwards A & Elwyn G. Shared decision-making in health care: Achieving evidence-based patient choice. New York: Oxford University Press, USA; 2009.
Edwards M, Wood F, Davies M, Edwards A. The development of health literacy in patients with a long-term health condition: the health literacy pathway model. BMC Public Health. 2012;12(1):1–15.
Elwyn G, Frosch D, Thomson R, Joseph-Williams N, Lloyd A, Kinnersley P, Rollnick S. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27:1361–7.
Article PubMed PubMed Central Google Scholar
Fan R. Critical care ethics in Asia: global or local? J Med Philos. 1998;23(6):547–62.
Fan R. Contemporary Confucian Bioethics. China: Peking University Press; 2011.
Google Scholar
Faul F, Erdfelder E, Lang A-G, Buchner A. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175–91.
Fernández-Gutiérrez M, Van de Walle S. Equity or efficiency? Explaining public officials’ values. Public Adm Rev. 2019;79(1):25–34.
Frederick PD, Nelson HD, Carney PA, Brunye TT, Allison KH, Weaver DL, Elmore JG. The influence of disease severity of preceding clinical cases on pathologists’ medical decision making. Med Decis Mak. 2017;37(1):91–100.
Galletta M, Piazza MF, Meloni SL, Chessa E, Piras I, Arnetz JE, D’Aloja E. Patient Involvement in Shared Decision-Making: Do Patients Rate Physicians and Nurses Differently? Int J Environ Res Public Health. 2022;19(21):14229.
Haux R. Medical informatics: past, present, future. Int J Med Inform. 2010;79(9):599–610.
Ijäs-Kallio T, Ruusuvuori J, Peräkylä A. ’Unilateral’decision making and patient participation in primary care. Commun Med. 2011;8(2):145.
Inglehart R & Oyserman D. Individualism, autonomy, self-expression: The human development syndrome. In Comparing cultures (pp. 73-96). Leiden: Brill; 2004.
Jin P, Zhang X. Family refusal of emergency medical treatment in China: an investigation from legal, empirical and ethical perspectives. Bioethics. 2020;34(3):306–17.
Jordan Z, Tremblay C, Lipstein E, Jordan I, Boland L. Is sharing really caring? Viewpoints on shared decision-making in paediatrics. J Paediatr Child Health. 2020;56(5):672–4.
Kickbusch IS. Health literacy: addressing the health and education divide. Health Promot Int. 2001;16(3):289–97.
Hilbe JM. Logistic regression. Int encyclopedia Stat Sci. 2011;1:15–32.
King JS, Moulton BW. Rethinking informed consent: the case for shared medical decision-making. Am J Law Med. 2006;32(4):429–501.
Lee YK, Low WY, Ng CJ. Exploring patient values in medical decision making: a qualitative study. PloS One. 2013;8(11):e80051.
Leung K. Beliefs in Chinese culture. 2010.
Levinson W, Kao A, Kuby A, Thisted RA. Not all patients want to participate in decision making: a national study of public preferences. J Gen Internal Med. 2005;20(6):531–5.
Liberati A, Apolone G, Nicolucci A, Confalonieri C, Fossati R, Grilli R, Alexanian A. The role of attitudes, beliefs, and personal characteristics of Italian physicians in the surgical treatment of early breast cancer. Am J Public Health. 1991;81(1):38–42.
Article CAS PubMed PubMed Central Google Scholar
Liu J, Wu K, Xie H. Research on medical decision model and decision subject’s choice Tendency. Med Philos. 2018;39(10):14–20.
Lyttle DJ, Ryan A. Factors influencing older patients’ participation in care: a review of the literature. Int J Older People Nurs. 2010;5(4):274–82.
Lyu Y, Liu J. Construction of a shared decision-making model between doctor and patient in China based on selection preferences. Humanit Soc Sci Commun. 2023;10(1):1–7.
Matthias MS, Salyers MP, Frankel RM. Re-thinking shared decision-making: context matters. Patient Educ Counsel. 2013;91(2):176–9.
McCaffery KJ, Smith SK, Wolf M. The challenge of shared decision making among patients with lower literacy: a framework for research and development. Med Decis Mak. 2010;30(1):35–44.
Nguyen TA, Giang LT. Factors influencing the vietnamese older persons in choosing healthcare facilities. Health Serv Insights. 2021;14:11786329211017426.
PubMed PubMed Central Google Scholar
Odero A, Pongy M, Chauvel L, Voz B, Spitz E, Pétré B, Baumann M. Core values that influence the patient—healthcare professional power dynamic: steering interaction towards partnership. Int J Environ Res Public Health. 2020;17(22):8458.
Parish O, Williams D, Odd D, Joseph-Williams N. Barriers and facilitators to shared decision-making in neonatal medicine: a systematic review and thematic synthesis of parental perceptions. Patient Educ Counsel. 2022;105(5):1101–14.
Physicians*, A. C. o. Achieving a high-performance health care system with universal access: what the United States can learn from other countries. Ann Intern Med. 2008;148(1):55–75.
Pieterse AH, Finset A. Shared decision making-much studied, much still unknown. Patient Educ Counsel. 2019;102(11):1946–8.
Vrijheid M. The exposome: a new paradigm to study the impact of environment on health. Thorax. 2014;69(9):876–8.
Siebinga VY, Driever EM, Stiggelbout AM, Brand PL. Shared decision making, patient-centered communication and patient satisfaction–A cross-sectional analysis. Patient Educ Counsel. 2022;105(7):2145–50.
Sox HC, Higgins MC, Owens DK, Schmidler GS. Medical decision making. Hoboken: Wiley; 2024.
Stacey D, Legare F, Boland L, Lewis KB, Loiselle M-C, Hoefel L, O’Connor A. 20th anniversary Ottawa decision support framework: part 3 overview of systematic reviews and updated framework. Med Decis Mak. 2020;40(3):379–98.
Stammers T. The evolution of autonomy. N Bioeth. 2015;21(2):155–63.
Su G. Infections in Patients with Chronic Kidney Disease: Patterns, Outcomes and the Role of Vitamin D for Future Prevention. Stockholm: Karolinska Institutet (Sweden); 2019.
Suhonen R, Välimäki M, Katajisto J. Individualized care in a Finnish healthcare organization. J Clin Nurs. 2000;9(2):218–27.
Tan NQ, Maki KG, López-Olivo MA, Geng Y, Volk RJ. Cultural influences on shared decision-making among Asian Americans: a systematic review and meta-synthesis of qualitative studies. Patient Educ Counsel. 2023;106:17–30.
Tauber AI. Historical and philosophical reflections on patient autonomy. Health Care Analysis. 2001;9:299–319.
Tian S, Yang W, Le Grange JM, Wang P, Huang W, Ye Z. Smart healthcare: making medical care more intelligent. Global Health J. 2019;3(3):62–5.
Timmermans S. The engaged patient: The relevance of patient–physician communication for twenty-first-century health. J Health Soc Behav. 2020;61(3):259–73.
Tjia J, Clayton M, Chiriboga G, Staples B, Puerto G, Rappaport L, DeSanto-Madeya S. Stakeholder-engaged process for refining the design of a clinical trial in home hospice. BMC Med Res Methodol. 2021;21:1–9.
Yao X. Confucianism and its modern values: Confucian moral, educational and spiritual heritages revisited. J Beliefs Values. 1999;20(1):30–40.
Wahyudi A, Trihapsoro I, Yuwanto L, Indrawati R, Nazeli B. Patient and Family Engagement: The Secret Behind Quality Healthcare Services (Literature Review). East Asian J Multidiscipl Res. 2023;2(9):3645–64.
Wang WW, Fan CC. Migrant workers’ integration in urban China: Experiences in employment, social adaptation, and self-identity. Eurasian Geogr Econ. 2012;53(6):731–49.
Zakaria M, Karim R, Rahman M, Cheng F, Xu J. Disparity in physician-patient communication by ethnicity: Evidence from Bangladesh. Int J Equity Health. 2021;20(1):1–9.
Download references
Acknowledgements
Not applicable.
This research was funded by the National Social Science Fund Late-Funded Project, China (No. 22FZXB097) and the Social Science Key Laboratory of Guangdong Higher Education Institutes for Health Governance Based on Big Data Utilization, Guangzhou Medical University (Project No. 2023WSY007).
Author information
Authors and affiliations.
Institute of Humanities and Social Sciences, Guangzhou Medical University, Guangzhou, 511436, China
Yuwen Lyu & Junrong Liu
School of Health Management, Guangzhou Medical University, Guangzhou, 511436, China
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization, Yuwen Lyu and Junrong Liu; methodology, Yuwen Lyu; software, Yuwen Lyu; validation, Yuwen Lyu and Junrong Liu; formal analysis, Yuwen Lyu and Qian Xu; investigation, Junrong Liu; resources, Junrong Liu; data curation, Yuwen Lyu; writing—original draft preparation, Yuwen Lyu, Qian Xu and Junrong Liu; writing—review and editing, Junrong Liu; visualization, Yuwen Lyu; supervision, Junrong Liu; project administration, Junrong Liu; funding acquisition, Junrong Liu. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Correspondence to Junrong Liu .
Ethics declarations
Ethics approval and consent to participate.
All experimental protocols were approved by Guangdong Provencial Research Association of Medical Social Work. The approval reference number is GDYWSG2017-07-02. Informed consent was obtained from all subjects and/or their legal guardian(s).
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Lyu, Y., Xu, Q. & Liu, J. Exploring the medical decision-making patterns and influencing factors among the general Chinese public: a binary logistic regression analysis. BMC Public Health 24 , 887 (2024). https://doi.org/10.1186/s12889-024-18338-8
Download citation
Received : 18 September 2023
Accepted : 12 March 2024
Published : 25 March 2024
DOI : https://doi.org/10.1186/s12889-024-18338-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical decision
- Decision-making patterns
- Influencing factors
- Logistic regression
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]

Study: Monkeys are much smarter than we thought they were
I n a groundbreaking study published today in the journal Nature Neuroscience , researchers have discovered that monkeys, much like humans , are capable of complex deliberation and careful decision-making.
This new finding challenges the long-held belief that humans alone possess the ability to think deeply about a problem and consider multiple factors such as costs, consequences, and constraints in order to arrive at optimal outcomes.
"Humans are not the only animals capable of slow and thoughtful deliberation," said study senior author Dr. William Stauffer from the University of Pittsburgh School of Medicine. "Our work shows that monkeys have a rich mental state that renders them capable of intelligent thinking. It's a new paradigm for studying the neurophysiological basis for deliberative thought."
The study raises important questions about the nature of thought processes and decision-making in animals, and whether other species are also capable of engaging in the same level of complexity as humans. It also helps to shed light on the cognitive processes at work when we, as humans, make decisions about various aspects of our lives, such as who to spend time with or what to study in school.
Several decades ago, Dr. Daniel Kahneman, a Nobel Prize laureate, revolutionized the field of behavioral economics with his Prospect Theory. In his seminal book, "Thinking Fast and Slow," Dr. Kahneman posited that humans employ two distinct systems of thinking: one nearly instantaneous and automatic, and the other much slower and reliant on conscious logical reasoning that requires greater mental effort.
How the study was done
Dr. Kahneman referred to the first type of thinking as "slow" and the second as "fast." Slow, effortful thinking enables us to engage in complex activities such as writing music, developing scientific hypotheses, and balancing our checkbooks. Until now, it was believed that slow thinking was a uniquely human trait.
However, this latest research turns that notion on its head. By presenting monkeys with combinatorial optimization problems, which the researchers dubbed the "knapsack task," and rewarding the animals based on the value of their solutions, the study demonstrated that monkeys employed sophisticated mathematical reasoning and used efficient computational algorithms to tackle complex problems.
The scientists found that the animals' performance and speed of deliberation were dependent on the task's complexity, and that their solutions closely mirrored those generated by efficient computer algorithms specifically designed to solve the optimization problem.
"Results from this work will contribute neurophysiological evidence to enlighten centuries of discussions about dual process theories of the mind, the structure of thoughts, and the neurobiological basis of intuition and reasoning," wrote Stauffer in an accompanying research briefing.
Tao Hong of Carnegie Mellon University is the lead author of the paper. The study's findings not only provide valuable insights into the cognitive abilities of monkeys but also pave the way for a new paradigm in studying the neurophysiological basis for deliberative thought, with potential implications for better understanding the complex nature of decision-making across various species.
More about monkeys
Monkeys are a diverse group of primates that belong to the infraorder Simiiformes. They are divided into two major groups: New World monkeys, native to Central and South America, and Old World monkeys, native to Africa and Asia. Monkeys are known for their intelligence, social behavior, and adaptability to different environments.
Physical characteristics
Monkeys vary greatly in size and appearance, ranging from the tiny pygmy marmoset, which measures just 4.6-6.2 inches (12-16 cm) in length, to the large mandrill, which can reach up to 37 inches (94 cm) in length.
Monkeys typically have forward-facing eyes, flat faces, and dexterous hands with opposable thumbs. Some species also have prehensile tails, which they use to grasp and manipulate objects or to hang from branches.
Most monkeys are omnivores, eating a diverse diet that includes fruits, leaves, seeds, insects, and small animals. Some species, like the howler monkey, primarily consume leaves, while others, like the capuchin monkey, have a more varied diet.
Social behavior
Monkeys are highly social animals that usually live in groups called troops. These troops can range in size from just a few individuals to hundreds of members. Social hierarchies are common in monkey troops, with dominant individuals enjoying benefits like better access to food and mating opportunities. Monkeys communicate through vocalizations, body language, and facial expressions, and they often engage in grooming behaviors to maintain social bonds.
Intelligence and tool use
Monkeys are known for their cognitive abilities, problem-solving skills, and in some cases, their use of tools. Capuchin monkeys, for example, have been observed using rocks to crack open nuts, while some macaques have been seen using sticks to extract insects from tree bark.
Research has also shown that monkeys are capable of understanding basic arithmetic and recognizing themselves in mirrors, which is considered a sign of self-awareness.
Conservation
Many monkey species are threatened by habitat loss, hunting, and the illegal pet trade. Conservation efforts are underway to protect these primates and their habitats, including the establishment of protected areas, reintroduction programs, and education campaigns to raise awareness about the importance of monkey conservation.
In conclusion, monkeys are fascinating and intelligent creatures with complex social structures and diverse behaviors. As we continue to study these primates, we gain a greater understanding of their cognitive abilities and the evolutionary links between humans and other primates.
Other animals that demonstrate problem-solving ability
Yes, numerous animals demonstrate problem-solving abilities, indicating the presence of intelligence and cognitive skills across various species. Some examples of animals with notable problem-solving capabilities include:
Crows and other corvids
These birds are known for their exceptional problem-solving skills and have been observed using tools to access food. For instance, they can use sticks to extract insects from tree bark or crevices and even bend wires to create hooks for retrieving food from hard-to-reach places.
Elephants are highly intelligent animals capable of complex problem-solving. They have been observed using sticks and branches to swat flies or scratch hard-to-reach areas and can also recognize themselves in mirrors, suggesting self-awareness. Elephants have displayed the ability to cooperate and work together to solve problems, such as pulling a rope simultaneously to access food.
Dolphins are known for their intelligence and problem-solving abilities. They have been observed using tools like sponges to protect their snouts while foraging on the ocean floor. Dolphins can also learn and understand complex commands and have been shown to recognize themselves in mirrors, indicating self-awareness.
These highly intelligent invertebrates have demonstrated remarkable problem-solving skills. Octopuses have been observed opening jars, navigating mazes, and escaping from enclosures by manipulating objects and their environment. Their impressive learning and memory capabilities make them formidable problem solvers.
Domesticated dogs have evolved alongside humans and have developed a range of problem-solving skills. They can learn commands, understand gestures, and follow human cues to solve problems, such as locating hidden objects or navigating obstacles. Some breeds, like border collies and poodles, are especially known for their intelligence and problem-solving abilities.
Chimpanzees
As our closest living relatives, chimpanzees share many cognitive traits with humans. They have been observed using tools, such as sticks to extract termites from their mounds, and leaves as sponges to collect water. Chimpanzees also display complex social behaviors, such as cooperation and deception, which require problem-solving skills.
Rats are intelligent rodents that have shown the ability to solve problems and learn from their experiences. They can navigate complex mazes, recognize patterns, and demonstrate a rudimentary understanding of cause and effect. Rats have also been observed using tools and adapting their behavior based on previous experiences.
These examples illustrate that problem-solving abilities are not exclusive to humans and can be found across various animal species. Studying these animals and their cognitive skills can provide valuable insights into the evolution of intelligence and the diversity of problem-solving strategies in the animal kingdom.
Check us out on EarthSnap , a free app brought to you by Eric Ralls and Earth.com .

Learning to Stop Cut Generation for Efficient Mixed-Integer Linear Programming
- Haotian Ling University of Science and Technology of China
- Zhihai Wang University of Science and Technology of China
- Jie Wang University of Science and Technology of China
- Video/Poster
How to Cite
- Endnote/Zotero/Mendeley (RIS)
Information
- For Readers
- For Authors
- For Librarians
Developed By
Subscription.
Login to access subscriber-only resources.
Part of the PKP Publishing Services Network
Copyright © 2024, Association for the Advancement of Artificial Intelligence
Democracy relies on a free press.
MinnPost’s in-depth journalism is available paywall-free all year round.
Help keep it this way by making a donation today.

Nonprofit, independent journalism. Supported by readers.
Let’s not apply a statewide solution to a mostly metro problem
Share this:.
- Click to email a link to a friend (Opens in new window)
- Click to share on Facebook (Opens in new window)
- Click to share on Twitter (Opens in new window)
- Click to print (Opens in new window)

MinnPost’s Daily Newsletter
The latest on the politics and policy shaping Minnesota.
Delivered straight to your inbox.

Stay in the know.
MinnPost’s top stories delivered straight to your inbox Monday through Saturday.
Rare is there a city council meeting that has more than a few attendees; however, one issue brings constituents out like concert goers to see Taylor Swift: zoning and land use issues. These are among the most controversial and personal issues council members encounter as they serve the public. Decisions are made on a micro level down to one property adjoining the very next. This is done with scalpel precision in each community across the state. Zoning issues impact what are often individuals’ largest investments of their lives as they literally mortgage their future on a new home or business. Decisions on these delicate issues should not be made by legislators in St. Paul, but rather stay with local communities across Minnesota.
A cadre of legislators have advanced legislation (SF3964 or SF3980) that would vastly undermine local decisions and instead provide a statewide solution for what is largely a metro problem. In Greater Minnesota, a lack of development for decades provides more than enough justification to reject these proposals because there is already a vested interest to keep regulations to a bare minimum so as to promote construction. The one-size-fits-all approach being advanced threatens to undermine the very housing gains some of us have seen in rural parts of Minnesota.
For example, since the 1970s the City of Austin has allowed duplexes in single-family zoning areas (R1). We’ve found the duplexes blend nicely, but having St. Paul dictate that eight-plexes are allowed in R1 zones threatens homebuilders’ confidence to make an investment because they might suddenly have a multifamily unit next door that could significantly impact their property value. Cohesive and thoughtful planning has been the hallmark of communities for time immemorial. This is an obvious unintended consequence that could actually stymie production — the reverse of legislators’ goal.
Likewise, setting minimum lot sizes and dictating minimum square footage requirements from St. Paul continues the malignment of the good work done by municipalities. Requiring communities to accept a carte blanche tiny home approach forgets the other issues that can result when people have no place for their possessions and start accumulating them in their yard to more significant problems of dealing with infrastructure challenges caused by adding backyard small homes for density. Current water, sewer, electric or other infrastructure realities can’t suddenly accommodate a demand that hasn’t been planned for in the utility design. Determining long-term necessities, which are done in the local planning process, requires staff with intimate knowledge and elected officials at the local level to sort out these complex challenges.

Cities’ positions aren’t the municipal equivalent of Not in My Backyard (NIMBY). Local leaders are best equipped to handle these decisions and promote progress while balancing compromise and accommodating real concerns. We don’t need any of Taylor Swift’s “bad blood” that would come from an encroachment on local control. Instead, we encourage more assistance from the state to help cities accomplish our goal of encouraging more housing construction. Cities need a partnership, not a takeover.
Craig Clark is the city administrator for Austin.
Thanks to our major sponsors

We've recently sent you an authentication link. Please, check your inbox!
Sign in with a password below, or sign in using your email .
Get a code sent to your email to sign in, or sign in using a password .
Enter the code you received via email to sign in, or sign in using a password .
Subscribe to our newsletters:
- MinnPost e-mail newsletters
- Daily newsletter
- Sunday review
- Greater Minnesota newsletter
- And One with Britt Robson
- Events & member benefits
- Opportunities to give input/feedback
Sign in with your email
Lost your password?
Try a different email
Send another code
Sign in with a password
Privacy Policy
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health

Communication Skills, Problem-Solving Ability, Understanding of Patients’ Conditions, and Nurse’s Perception of Professionalism among Clinical Nurses: A Structural Equation Model Analysis
This study was intended to confirm the structural relationship between clinical nurse communication skills, problem-solving ability, understanding of patients’ conditions, and nurse’s perception of professionalism. Due to changes in the healthcare environment, it is becoming difficult to meet the needs of patients, and it is becoming very important to improve the ability to perform professional nursing jobs to meet expectations. In this study method, structural model analysis was applied to identify factors influencing the perception of professionalism in nurses. The subjects of this study were 171 nurses working at general hospitals in city of Se, Ga, and Geu. Data analysis included frequency analysis, identification factor analysis, reliability analysis, measurement model analysis, model fit, and intervention effects. In the results of the study, nurse’s perception of professionalism was influenced by factors of communication skills and understanding of the patient’s condition, but not by their ability to solve problems. Understanding of patient’s condition had a mediating effect on communication skills and nursing awareness. Communication skills and understanding of the patient’s condition greatly influenced the nurse’s perception of professionalism. To improve the professionalism of clinical nurses, nursing managers need to emphasize communication skills and understanding of the patient’s condition. The purpose of this study was to provide a rationale for developing a program to improve job skills by strengthening the awareness of professional positions of clinical nurses to develop nursing quality of community.
1. Introduction
Changes in the environment related to climate and pollution are causing health problems and various diseases such as respiratory and circulatory problems, metabolic disorders, and chronic diseases. Moreover, access to modern healthcare facilities has created greater expectations among patients receiving personalized healthcare and high-quality healthcare. As the difficulty of satisfying the demands of patients increases, enhancing nursing capabilities has become increasingly important [ 1 ]. To improve this, hospitals are making efforts to change the internal and external environments so as to increase the number of nurses, reduce the length of hospital stays, and enable efficient nursing practice. Despite these efforts, the workloads of nurses and the demand for clinical nurses are continuously increasing [ 2 , 3 ]. As a result, nurses are developing negative attitudes and prejudices toward patients, as well as negative perceptions of professionalism. To address this, the cultivation and strengthening of nursing professionals’ capabilities is essential.
Nurses’ perception of professionalism is an important element influencing their ability to perform independent nursing, and a good perception of their profession results in a positive approach to solving patients’ problems [ 4 , 5 ]. In addition, the characteristics and abilities of individual nurses can influence the level of care and enable them to understand patients, solve problems, and provide holistic care, which is the ultimate goal of the nursing process [ 6 , 7 ]. Thus, patients expect nurses to not only have medical knowledge of the disease but to also be able to comprehensively assess the patient’s problems and be independent and creative in nursing [ 8 ]. This attitude can have a major impact on the quality of nursing services and can inspire pride in the nursing occupation and professional achievement. These findings can also be used by nurses to prevent burnout and maintain professionalism [ 9 , 10 ].
To respond to the increasing demands for diverse qualitative and quantitative nursing services and to strengthen the capabilities of nursing professionals, efforts have been made to move nursing education toward scientific and creative education. However, in point-of-care environments, not only are nurses prevented from making independent decisions regarding nursing, but also the diverse personal capabilities necessary for such independent behavior are not sufficiently developed [ 11 ]. Therefore, it is important to enhance clinical nurses’ perceptions of the nursing profession; maintain a balance of nursing capabilities; provide novel, high-quality nursing services; and identify assistive nursing education methods and obstructive environmental factors [ 10 ].
Communication skills involve a person’s ability to accurately understand (through both verbal and non-verbal indications) another person, and sufficiently deliver what the person desires [ 12 , 13 ]. Good communication skills are a primary requirement for providing professional nursing services because they enable an in-depth understanding of patients, solving of complicated problems, and reasonable and logical analysis of situations [ 14 , 15 , 16 ]. When effective communication takes place, nurses’ problem-solving abilities and perceived professionalism strengthen [ 17 , 18 ].
According to Park [ 19 ], nurses have difficulties in interpersonal relationships when social tension and interaction skills are low and communication is poor. In addition, these factors are negatively affected not only in the work of the nurse but also in the perception of the profession. Communication skills are associated with both the formation of relationships with patients and the ability to perform holistic nursing [ 20 ]. In order to improve and develop the overall nursing function of a clinical nurse like this, it is important to complement the relevant integrated nursing abilities [ 21 , 22 ].
Previous studies have investigated the importance of communication skills for nurses, and the relationships between nurses’ problem-solving ability and their understanding of the patients’ conditions. Nonetheless, data that can comprehensively explain the structural relationships between these qualities and how they affect the job perception of nurses remains insufficient.
Therefore, the present study aims to identify the structural model for the relationships between nurses’ communication skills, problem-solving ability, understanding of patients’ conditions, and nurse’s perception of professionalism. Additionally, the study provides basic data necessary for developing programs for improving nursing abilities.
The purpose of this study is to construct a theoretical model that explains the structural relationships among nurses’ communication skills, problem-solving ability, understanding of patients’ conditions, and nurse’s perception of professionalism. In addition, the study aimed to verify this model using empirical data.
2. Materials and Methods
2.1. study design.
To create and analyze the structural model for clinical nurses’ communication skills, problem-solving ability, understanding of patients’ conditions, and nurse’s perception of professionalism, the theoretical relationships among the variables were developed based on related theories.
In this study, communication skills were set as the exogenous variables, whereas problem-solving ability, understanding of patients’ conditions, and perception of the nursing occupation were set as the endogenous variables. In addition, communication skills were set as the independent variables and nursing job perceptions as the dependent variable. This is because the ability of communication helps to maintain an intimate relationship with the patient and to assess the patient’s condition through each other’s relationship and to solve problems and develop correct understanding. Communication skills, problem-solving ability, and understanding of patients’ conditions were set as the parameters for determining causality. The research model is shown in Figure 1 .

Study model.
2.2. Study Participants
The structural equation model has less than 12 measurement variables. The sample size usually requires 200 to 400 participants [ 23 ]. A total of 250 participants were selected for the study. In line with ethical standards and practices, participants received a full explanation on the purpose of the study. They were briefed that the information collected would be used for research purposes only. Furthermore, they were informed that they could withdraw from the study at any time.
2.3. Data Collection Method
Data collection for this study was performed by two researchers unrelated to the hospital from April 20 to May 1, 2019. A questionnaire was used to collect data from clinical nurses working in five hospitals in Seoul, Gyeonggi, and Gangwon provinces. Of the 250 questionnaires disseminated, we received 225 completed returns. However, 54 were considered inaccurate, inconsistent, or unsatisfactory for coding purposes. Thus, 171 fully completed valid questionnaires comprised the final dataset for analysis.
2.4. Research Instruments
2.4.1. communication skills.
In this study, the communication skill instrument developed by Lee and Jang [ 24 ] was used. Its contents were modified and supplemented to clearly understand the communication skills of nurses. Our questionnaire comprised 20 questions with five questions each concerning “interpretation ability,” “self-reveal,” “leading communication,” and “understanding others’ perspectives.” The answers were rated on a five-point Likert scale ranging from 0 = “strongly disagree” to 4 = “strongly agree.” For this study, the Cronbach’s alpha value was 0.81.
2.4.2. Problem-Solving Ability
The tool developed by Lee [ 25 ] was used to measure the problem-solving ability of clinical nurses. The survey comprised 25 questions, with five questions each concerning “problem recognition,” “information-gathering,” “divergent thinking,” “planning power,” and “evaluation.” Items were scored on a five-point Likert scale ranging from 0 = “strongly disagree” to 4 = “strongly agree.” The internal consistency confidence value Cronbach’s alpha was 0.79.
2.4.3. Understanding Patients’ Condition
To measure nurses’ understanding of patients’ conditions, we developed 10 questions by revising and supplementing items from an existing understanding-measurement tool [ 26 ]. With a total of ten questions, we measured “diagnostic name,” “patient-treatment planning,” and “nursing intervention processes.” Items were scored using a five-point Likert scale ranging from 0 = “strongly disagree” to 4 = “strongly agree.” The internal consistency confidence value Cronbach’s alpha was 0.81.
2.4.4. Nurse’s Perception of Professionalism
Nurse’s perception of professionalism was measured using a tool developed by revising the 25 questions created by Kang et al. [ 1 ]. With a total of ten questions, we measured “vocation” and “autonomy.” Items were scored using a five-point Likert scale. The internal consistency confidence value Cronbach’s alpha was 0.81.
2.5. Data Analysis
To identify the relationships among the set variables, the data were computed statistically using the program included in IBM SPSS 24.0 and AMOS 23.0. (IBM Corp., Armonk, NY, USA). The analysis methods were as follows:
- Frequency analysis was conducted to identify the subjects’ demographic and general characteristics.
- The reliability of the questionnaire was verified using Cronbach’s α coefficients.
- Confirmatory factor analysis (CFA) was performed to verify the convergent validity of the selected measurement tool.
- The normality of the data was determined through analyzing the skewness and kurtosis of the measurement variables.
- The fitness of the model was verified using structural equation modeling (SEM).
- Bootstrapping was utilized to verify the mediating effect in the set study model, as well as the mediating effects of the nurses’ problem-solving ability and understanding of patients’ conditions.
3.1. Demographic Characteristics
The demographic and general characteristics of the study subjects are shown in Table 1 . Overall, 71 respondents were aged 25–29 years (41.5%), representing the most numerous age group. University graduates comprised 113 (66.1%) of the sample, while 50 (29.2%) held graduate degrees, with eight (4.7%) holding master’s degrees. Fifty-three respondents (31.0%) had over seven years of clinical experience, 43 (25.1%) had two to three years of experience, 42 (24.6%) had four to six years of experience, and 33 (19.3%) had less than two years of experience. Additionally, 121 respondents (70.8%) worked at secondary hospitals, while 50 (29.2%) worked at tertiary hospitals; 159 respondents (93.0%) reported that they were general nurses.
Participants’ general characteristics ( N = 171, %).
3.2. Technical Metrics of the Measurement Variables
The multivariate normality of the findings related to the factors of the latent variables was verified through standard deviations, skewness, and kurtosis. The present study meets the criteria for the skewness and kurtosis values mentioned by Hu and Bentler [ 27 ].
All sub-factors of the latent variables secured normality.
In this study, a normal distribution was obtained for each of the four sub-factors of communication skills, five sub-factors of problem-solving ability, three sub-factors for understanding the patient’s condition, and two sub-factors of the nurse’s perception of professionalism as shown in Table 2 .
Technical metrics of the measurement variables ( N = 171).
3.3. Correlations between the Measured Variables
The correlations between the measurement variables were analyzed using Pearson’s product–moment correlation coefficient analysis ( Table 3 ). The correlations among all individual measurement variables were found to show a positive correlation.
Correlations between the observed variables.
3.4. Confirmatory Factor Analysis of the Measurement Model
This study examined how well the measurement variables represented the latent variables in the measurement model. Each set path coefficient was evaluated using non-standardization factors, standardization factors, and standard errors. The path coefficients refer to the factor loadings in CFA. The standardization factors of the individual paths were shown to be at least 0.50 (except for vocation: 0.36), and the critical ratio (CR) was at least 1.96. This indicated that the measurement tool had good convergent validity ( Table 4 ).
Confirmatory factor analysis of the measurement model.
*** p < 0.001; CR: critical ratio.
3.5. Verification of the Structural Model
The structural model for relationships among clinical nurses’ communication skills, problem-solving ability, understanding of patients’ condition, and nurse’s perception of professionalism that would be suitable for predicting the influencing relationships was verified. Since the fitness index of the modified model was shown to be higher than that of the initial model, the final model for this study was set as shown in Figure 2 .

Final model. * χ 2 = 124.074 (df = 61, p <0.001), GFI(Goodness of Fit Index)= 0.90, RMSEA(Root Mean Square Error Approximation)=0.07, NFI(Normed Fit Index)=0.87, IFI(Incremental Fit Index)= 0.93, TLI(Tucker-Lewis Index)= 0.91, CFI(Comparative Fit Index)= 0.92.
3.6. Influencing Relationships between Variables of the Study Model
The standardization factors and CR values of the final model were examined to determine whether there were direct relationships between communication skills, problem-solving ability, understanding of patients’ conditions, and nurse’s perception of professionalism. The results are shown
For the relationship between communication ski in Table 5 .lls and problem-solving ability, the standardization factor was 0.85 and the CR value was 7.37; communication skills showed a statistically significant effect. Consequently. The relationship between communication skills and understanding of patients’ conditions also showed a statistically significant effect. Consequently, Hypothesis 1 was supported.
The relationships between the human effects of the measurement model.
* p < 0.05, *** p < 0.001; CR: critical ratio.
For the relationship between communication skills and nurse’s perception of professionalism, the standardization factor was 0.54, and the CR value was 2.02. Communication skills showed a statistically significant effect. Consequently. For the relationship between problem-solving ability and nurse’s perception of professionalism, the standardization factor was −0.056, and the CR value was −0.39. Problem-solving ability had no statistically significant effect. Consequently.
The relationship between nurses’ understanding of patients’ conditions and nurse’s perception of professionalism had a statistically significant effect. Consequently Figure 2 shows the influencing relationships between the study variables of the final study model, considering non-standardization and standardization factors of the relationships between the study variables.
3.7. Direct and Indirect Effects of the Variables
To grasp the significance of the mediating effect in the final study model, the direct and indirect effects of each variable were examined. To examine the mediating effect of the problem-solving ability and understanding of patients’ conditions variables, the bootstrapping method provided by the AMOS 23.0 program included in IBM was utilized. The results are shown in Table 6 .
Mediating effect analysis.
* p < 0.05, *** p < 0.001
The indirect effect of communication skills on nurse’s perception of professionalism through nurses’ understanding of patients’ conditions was statistically significant. That is, clinical nurses’ communication skills have an indirect positive effect on their nurse’s perception of professionalism, with nurses’ understanding of patients’ conditions acting as a parameter. We also found that the effect of communication skills on nurse’s perception of professionalism was statistically significant. Therefore, communication skills have a partially mediated effect on nurse’s perception of professionalism, with understanding of patients’ conditions acting as a parameter. However, communication skills were found to have no indirect positive effect on nurse’s perception of professionalism when problem-solving ability was set as a parameter.
4. Discussion
In this study, we developed and analyzed a hypothetical model regarding clinical nurses’ communication skills, problem-solving ability, and understanding of patients’ conditions, and how these factors influence their nurse’s perception of professionalism.
4.1. Effect of Communication Skills on Nurses’ Perception of Professionalism
Communication skills were found to have statistically significant effects on their relationship with nurses’ problem-solving ability, understanding of patients’ conditions, and nurse’s perception of professionalism. Nurses’ communication skills not only affected their problem-solving ability but also their understanding of patients’ conditions and nurse’s perception of professionalism. Good communication among nurses can reduce uncomfortable situations and improve interactions with patients, which can consequently enhance problem-solving [ 28 ]. Supporting our findings, Ancel [ 17 ] reported that communication skills afford the maintenance of amicable cooperative relationships with patients across diverse medical classes, thereby enhancing the efficiency of nursing-related problem-solving.
Nurses’ communication is also closely related to their understanding of patients’ conditions, particularly regarding the treatment processes. Nurses frequently experience difficulties as a result of poor communication with not only patients and their family members but also other medical personnel. Further, poor delivery of explanations and questions affects nurses’ understanding of patients’ situations and problems, and patients can also feel concern regarding whether nurses accurately understand their problems [ 29 ]. Nurses frequently experience psychological abuse when communicating with patients and develop stress or discomfort [ 30 ]; this can lead to distrustful relationships with and inhibited understanding of patients [ 31 , 32 ]. Vermeir et al. [ 18 ] reported that scientific approaches are required to understand patients in-depth. To accurately understand both oneself and others, the most important method is successful communication. Such findings support the present study’s indication that nurses’ communication is a basic means of solving nursing problems, with both actions being interrelated.
Our finding that nurses’ communication skills are structurally related to their nurse’s perception of professionalism supports the findings of many previous studies. Regarding nurse’s perception of professionalism, Adams et al. [ 33 ] as well as Lee and Kim [ 34 ] explained that a good perception leads to higher-level capabilities, fostering high-level nursing of patients and the development of autonomous vocation. The above studies reported that, since nurses’ communication skills are related to their nurse’s perception of professionalism, communication skills should be considered a predictor of success. Further, McGlynn et al. [ 35 ] recommended positively reinforcing communication skills to improve nurse’s perception of professionalism. This supports the findings of the present study, indicating that communication and nursing professional perception are interrelated.
Thus, communication skills are important for nursing patients. They enable nurses to accurately understand patients’ problems, serve (by forming patient trust) an important function in the process of administering nursing interventions, and positively affect nurses’ perception of their profession. As such, each concept is important. However, nurses working in the clinic are critically aware of their professionalism. In order to reinforce this, communication skills are required, and the emphasis is placed on strengthening the nurses’ ability to solve problems as well as assess and understand patients. As a result, communication skills play an important role in helping nurses understand patients’ problems accurately, build patient trust in nursing interventions, and create structural relationships that have a positive impact on the perception of nursing occupations. Therefore, efforts to improve nurses’ communication skills not only improve their problem-solving abilities and understanding of patients’ conditions but also improve their nurse’s perception of professionalism. To maintain the professionalism of nurses, “competency development programs” would be helpful, thereby emphasizing the need for their application in nursing colleges and clinical practice.
4.2. Relationship between Nurses’ Problem-Solving Ability and Nurse’s Perception of Professionalism
We found clinical nurses’ problem-solving ability to have no positive effect on their perception of professionalism. This contrasts with previous studies, which reported that problem-solving ability is helpful for such perception of professionalism [ 36 ]. We also found that problem-solving ability does not affect nursing professional perception through a mediating effect.
The present findings indicate that the distinctiveness of the fields of nursing should not be overlooked. In nursing organizations that have a culture of discouraging diversity, when negative results are obtained from attempts to solve nursing problems, confusion regarding the identity of nursing professionals means perception of the profession is not reinforced; in many cases, the opposite perception is formed. Furthermore, for those in lower-level positions, nurse’s perception of professionalism is thought to be low because they cannot voice their opinions and have difficulties such as excessive workloads. Although few previous studies have directly examined this, Vermeir et al. [ 18 ] explained that, as the role expectation for nurses increases, factors for job turnover increase as a result of a sense of confusion regarding the nurses’ role and increases in stress. These findings indicate that factors that degrade nurses’ problem-solving ability induce skepticism regarding nursing and possibly career change, thereby supporting the findings of this study.
However, in the present study, positive results with low levels of relevancy in the structural model but high correlations were found. It is expected that, if nurses’ environmental conditions are improved and their nursing capabilities are developed so that they can solve nursing problems with confidence, their nursing professional perception will improve.
4.3. Relationship between Nurses’ Understanding of Patients’ Conditions and Nurse’s Perception of Professionalism
Our findings indicated that the relationship between nurses’ understanding of patients’ conditions and nurse’s perception of professionalism was statistically significant. This supports Nilsson et al. [ 21 ] and Philip et al. [ 29 ], who reported that, in the fields of nursing, when patients accurately understand nurses’ instructions or explanations and health information, they can participate in, independently adjust, and engage in creative decision-making related to self-nursing.
McGlynn et al. [ 35 ] suggested that understanding patient problems is an important element in resolving negative situations; meanwhile, Heo and Lim [ 37 ] indicated that clinical nurses provide high-quality nursing services and develop self-efficacy when they apply professional knowledge and a desire to understand patients’ problems. These study findings accord with our own findings.
The aforementioned findings suggest that the development and application of programs that can enhance nurses’ understanding of patients’ conditions should be emphasized, and that studies of various patient types, the characteristics of patients by age group and hospital areas, as well as the introduction of simulation education programs to improve nurses’ understanding of patients’ conditions should be continuously implemented.
5. Conclusions
This study aimed to verify the structural relationships between clinical nurses’ communication skills and their problem-solving ability, understanding of patients’ conditions, and nurse’s perception of professionalism. We also aimed to identify, through a structural model, the mediating effects of nurses’ problem-solving ability and understanding of patients’ conditions in the relationship between communication skills and nurse’s perception of professionalism.
The findings of this study are as follows (all significance levels = 0.05). In the relationship between communication skills and problem-solving ability, the value of the standardization factor was 0.85 and the CR value was 7.37, indicating that communication skills had a statistically significant effect. In the relationship between nurses’ communication skills and understanding of patients’ conditions, the value of the standardization factor was 0.61 and the CR value was 6.35, indicating that communication skills had a statistically significant effect. In the relationship between communication skills and nurse’s perception of professionalism, the value of the standardization factor was 0.54 and the CR value was 2.02, indicating that communication skills had a statistically significant effect. However, in the relationship between problem-solving ability and nurse’s perception of professionalism, the value of the standardization factor was −0.05 and the CR value was −0.39, indicating that problem-solving ability has no statistically significant effect. Finally, in the relationship between nurses’ understanding of patients’ conditions and nurse’s perception of professionalism, the value of the standardization factor was 0.56, and the CR value was 2.14, indicating that nurses’ understanding of patients’ conditions has a statistically significant effect.
There are some limitations to this study. First, as we only examined nurses at secondary and tertiary university hospitals, our findings may not be generalizable to all clinical nurses. Replication studies examining a range of levels of medical institutions and associated workers are necessary. Second, the structural relationship between problem-solving ability and the nurse’s perception of professionalism turned out to be insignificant or mediated. Subsequent studies on the various approaches to revisit this structural relationship should be performed. Third, theories should be systematically developed to establish the values of the nursing profession, and additional studies are necessary to explore other variables.
Acknowledgments
We would like to thank the staff nurses who participated in the survey and took the time to complete the initial assessment.
Author Contributions
Conceptualization, A.Y.K. and I.O.S.; methodology, A.Y.K.; software, I.O.S.; validation, A.Y.K. and I.O.S.; formal analysis, A.Y.K. and I.O.S.; investigation, A.Y.K.; resources, A.Y.K.; data curation, A.Y.K.; writing—original draft preparation, A.Y.K.; writing—review and editing, A.Y.K. and I.O.S.; visualization, A.Y.K. and I.O.S.; supervision, I.O.S.; project administration, I.O.S. All authors have read and agreed to the published version of the manuscript.
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.

IMAGES
VIDEO
COMMENTS
Critical thinking is an essential element in decision-making, which involves choices, and problem-solving, which requires analysis. Decision-making A free flow of ideas is essential to problem-solving and decision-making because it helps prevent preconceived ideas from controlling the process. Many decisions in healthcare are arrived at by group or
Decision-making is essential to nursing practice ( Lauri & Salantera, 1998 ). Decision-making in acute care nursing practice is a complex process. Nurses must consider numerous, potentially competing factors when making decisions to meet patient and family needs ( Tanner, 2006 ). This process is further complicated by the fact that nurses may ...
Decision-making is a fundamental concept of nursing practice that conforms to a systematic trajectory involving the assessment, interpretation, evaluation and management of patient-specific situations (Dougherty et al, 2015).Shared decision-making is vital to consider in terms of patient autonomy and professional duty of care as set out in the Nursing and Midwifery Council (NMC) (2018)Code ...
Problems arise unexpectedly in the fast-paced health care environment. Nurses must be able to react using critical thinking and quick decision-making skills to implement practical solutions. By employing problem-solving strategies, nurse leaders and their staff can improve patient outcomes and refine their nursing skills.
An individual, through the application of critical-thinking skills, engages in problem solving and decision making in an environment that can promote or inhibit these skills. It is the nurse leader's and manager's task to model these skills and promote them in others. FiGURE 6-1 Problem-solving and decision-making model.
Globally, there is a growing interest in using the research evidence in public health policy-making [1, 2].Public health systems are diverse and complex, and health policymakers face many challenges in developing and implementing policies and programs that are required to be efficient [1, 3].The use of scientific evidence is considered to be an effective approach in the decision-making process ...
Informed decision making in clinical care. It is estimated that human knowledge doubles at a mind-boggling rate of every 12 hours. 1. Before development of the internet, information was accessed through books, journals, and peer exchange. Increasingly, with the advent of the internet, machine learning, and sheer computational power, much of ...
Healthcare decision-making has often been viewed as a complex multi-dimensional problem. • Multi-criteria decision-making techniques have been deployed for solving healthcare decision-making problems. • 140 articles published during 2013-2022 on multi-criteria decision-making applications in healthcare are reviewed. •
Learning to provide safe and quality health care requires technical expertise, the ability to think critically, experience, and clinical judgment. The high-performance expectation of nurses is dependent upon the nurses' continual learning, professional accountability, independent and interdependent decisionmaking, and creative problem-solving abilities.
Two things can help health professionals get better at communicating with each other and adopting multiple perspectives themselves: 1) creating an environment that supports perspective sharing and ...
Nurse leaders perceive their role as a problem-solver, which is a necessary step in advocacy. 27 Problem-solving is a process that contains the elements of decision-making and critical thinking. 28. The theory that emerged from the core categories explicitly focused on the central phenomenon of LHV in the nursing work environment.
Clinical decision-making (CDM) is a critical skill that each nurse should be equipped with. Nurses must have the ability to make firm clinical decisions in this new era of health care delivery. 7 For successful day-to-day patient care, nurses must be able to analyze a wide range of information, utilizing CDM expertise, to solve complicated problems that arise in clinical practice.
Figure 1. Three levels of decision making: strategic, tactic and operational (technical) ( 4) The significance of medical decision making, as mentioned previously, is huge. On a personal level, decisions can alter the lives of patients. But on a more broader scale, decisions can result in health care system changes.
AHRQ's Digital Healthcare Research Program funds research to support clinicians and other healthcare professionals in improving their ability to provide optimal health services to their patients. In 2020, a total of $65.3 million was invested in research projects to support technology-enabled decision making and reducing provider burden.
He defines critical thinking as "necessary for problem-solving and decision-making by healthcare providers. It is a process where people use a logical process to gather information and take purposeful action based on their evaluation." ... Nursing school gives students the knowledge professional nurses use to make important healthcare ...
Critical thinking is just one skill crucial to evidence based practice in healthcare and education, write Jonathan Sharples and colleagues , who see exciting opportunities for cross sector collaboration Imagine you are a primary care doctor. A patient comes into your office with acute, atypical chest pain. Immediately you consider the patient's sex and age, and you begin to think about what ...
It explores multiple approaches to problem-solving, such as rational problem-solving and organic problem-solving, as well as a type of organic problem-solving called appreciative inquiry. The chapter also explores seven decision-making styles and elaborates on common mistakes made during the process, as well as how to overcome them.
The complex health system and challenging patient care environment require experienced nurses, especially those with high cognitive skills such as problem-solving, decision- making and critical thinking. Therefore, this study investigated the impact of social problem-solving training on nursing students' critical thinking and decision-making.
the objectives, approach and methods of CHM. the importance of information in devising solutions to health problems. the role of data and its translation into indicators for defining the magnitude of health problems and the coverage of related services. the process of comprehensive analysis of health problems.
INTRODUCTION. Having strong coping skills to reduce stress and satisfaction on the decision-making process to be creative and also having problem-solving skill is necessary in life.[] In this way, learning should be defined "meaningful" and problem-solving skill is one of these ways.[]Unfortunately, traditional teaching method in universities transfers a mixture of information and concepts ...
The aim of this study is to identify the levels of decision making, problem solving, as well as to determine the interrelations and explain the differences in the decision-making and problem-solving skills according to socio-demographic and organizational characteristics. ... She teaches courses on management science, health care management ...
The synthesis of findings reveals limitations in strategic root cause analysis. In addition, the study introduces a supplementary decision-making frame of reference to aid the selection of appropriate methods across problem-solving, decision-making, and solution implementation stages.
The review articles encompass a wide range of topics, each offering unique perspectives on key aspects of healthcare. One article (Lyu & Li 2023) explores the challenges of translating evidence into practice and the role of clinical practice guidelines in guiding healthcare decisions. It emphasizes the importance of evidence-based practices in improving patient outcomes while highlighting the ...
With the ongoing evolution of the healthcare system and shifts in cultural paradigms, there is a pressing need to delve into the medical decision-making behaviors of general Chinese public and understand their underlying motivations. This research seeks to elucidate the prevailing tendencies in these decision-making processes and to empirically validate the pivotal factors that shape their ...
The abundance of data has transformed the world in every aspect. It has become the core element in decision making, problem solving, and innovation in almost all areas of life, including business, science, healthcare, education, and many others. Despite all these advances, privacy and security remain critical concerns of the healthcare industry. It is important to note that healthcare data can ...
Clinical reasoning concerns how to think and make the best decision-making process associated with the clinical practice ( 9 ). The core elements of clinical reasoning ( 10) can be summarized in: 1. Evidence-based skills, 2. Interpretation and use of diagnostic tests, 3. Understanding cognitive biases, 4.
Other animals that demonstrate problem-solving ability. Yes, numerous animals demonstrate problem-solving abilities, indicating the presence of intelligence and cognitive skills across various ...
Cutting planes (cuts) play an important role in solving mixed-integer linear programs (MILPs), as they significantly tighten the dual bounds and improve the solving performance. A key problem for cuts is when to stop cuts generation, which is important for the efficiency of solving MILPs. However, many modern MILP solvers employ hard-coded heuristics to tackle this problem, which tends to ...
A cadre of legislators have advanced legislation (SF3964 or SF3980) that would vastly undermine local decisions and instead provide a statewide solution for what is largely a metro problem.
Moreover, access to modern healthcare facilities has created greater expectations among patients receiving personalized healthcare and high-quality healthcare. ... and the CR value was −0.39. Problem-solving ability had no statistically significant effect. ... independently adjust, and engage in creative decision-making related to self ...