Pisay student tops essay writing tilt on COVID-19
A Grade 12 student of the Philippine Science High School-Western Visayas Campus (PSHS-WVC) emerged as Grand Prize winner in the Southeast Asian Ministers of Education Organization Tropical Medicine and Public Health (SEAMEO TROPMED) Network 55th Founding Anniversary Essay Contest.

Altair Mizar Emboltura bagged the Grand Prize after besting 210 entries in the Senior High School Category from the member-countries of the SEAMEO TROPMED, the PSHS said in a statement on Saturday, Oct. 16.
Emboltura’s winning piece is titled, “A Thief, A Tyrant, A Teacher”. In his essay, Emboltura, editor-in-chief of PSHS-WVC’s school paper Banaag, discussed how the COVID-19 pandemic significantly redefined aspects of life.
This year’s theme of the SEAMEO TROPMED essay writing contest is “What COVID-19 means to me”. It focused on the integration and inter-relation between Sustainable Development Goal (SDG) # 3 “Good Health and Well-being” and SDG # 4 “Quality Education”, according to the PSHS.
Among the objectives of the essay writing competition were to gather information related to COVID-19 effect on students; motivate students to write and discuss their perspectives about COVID-19; promote listening to students’ voices; and document these perspectives for further use in school programmes and policies.
Emboltura cited the crucial role of the youth in the country’s fight against COVID-19.
“I believe in the power of the proactive youth. Our role in winning the battle against COVID-19 includes inspiring, impacting, and speaking up not just for our fellow youth but for our whole community as well. However, all of our dedication, effort, and active participation would be put to waste if our leaders won’t listen to us,” he said.
“I call unto our leaders to not just hear us but also listen to us because our voice matters, especially in this unprecedented time,” he added.
The PSHS said the student leader is planning to pursue either biology, public health, or an accelerated medicine course in college, but his ultimate goal is to be a physician for the Filipino people.
Emboltura expressed hope that the healthcare workers will receive the necessary assistance from the government, including wage hike and hazard pay.
“Young people like me have been championing change in our fight against COVID-19 from the very beginning. As digital natives, social media became our biggest platform to speak up, to initiate and conduct countless community projects especially for the underprivileged and marginalized sectors of our society, and to advocate for noble causes such as the #NoStudentLeftBehind,” he said.
Emboltura was named as Young Achiever Awardee by the Municipality of Oton, and Outstanding Student of Iloilo Awardee 2020 by JCI Regatta.
He was also selected as one of the Ten Outstanding Junior High School Students of Iloilo for Academic Year 2019-2020 by The Outstanding Students Circle of Iloilo (OSCI).

Philippine Center for Investigative Journalism

Filipinos face the mental toll of the Covid-19 pandemic — a photo essay
Share this:.
- Click to share on Facebook (Opens in new window)
- Click to share on X (Opens in new window)

BY ORANGE OMENGAN
Depression, anxiety, and other mental health-related illnesses are on the rise among millennials as they face the pressure to be functional amidst pandemic fatigue. Omengan's photo essay shows three of the many stories of mental health battles, of struggling to stay afloat despite the inaccessibility of proper mental health services, which worsened due to the series of lockdowns in the Philippines.
“I was just starting with my new job, but the pandemic triggered much anxiety causing me to abandon my apartment in Pasig and move back to our family home in Mabalacat, Pampanga.”
This was Mano Dela Cruz's quick response to the initial round of lockdowns that swept the nation in March 2020.
Anxiety crept up on Mano, who was diagnosed with Bipolar Disorder Type II with Attention Deficit Hyperactivity Disorder and Obsessive-Compulsive Personality Disorder traits. The 30-year-old writer is just one of many Filipinos experiencing the mental health fallout of the pandemic.
Covid-19 infections in the Philippines have reached 1,149,925 cases as of May 17. The pandemic is unfolding simultaneously with the growing number of Filipinos suffering from mental health issues. At least 3.6 million Filipinos suffer from mental, neurological, and substance use disorders, according to Frances Prescila Cuevas, head of the National Mental Health Program under the Department of Health.
As the situation overwhelmed him, Mano had to let go of his full-time job. “At the start of the year, I thought I had my life all together, but this pandemic caused great mental stress on me, disrupting my routine and cutting my source of income,” he said.
Mano has also found it difficult to stay on track with his medications. “I don’t have insurance, and I do not save much due to my medical expenses and psychiatric consultations. On a monthly average, my meds cost about P2,800. With my PWD (person with disability) card, I get to avail myself of the 20% discount, but it's still expensive. On top of this, I pay for psychiatric consultations costing P1,500 per session. During the pandemic, the rate increased to P2,500 per session lasting only 30 minutes due to health and safety protocols.”
The pandemic has resulted in substantial job losses as some businesses shut down, while the rest of the workforce adjusted to the new norm of working from home.
Ryan Baldonado, 30, works as an assistant human resource manager in a business process outsourcing company. The pressure from work, coupled with stress and anxiety amid the community quarantine, took a toll on his mental health.
Before the pandemic, Ryan said he usually slept for 30 hours straight, often felt under the weather, and at times subjected himself to self-harm. “Although the symptoms of depression have been manifesting in me through the years, due to financial concerns, I haven't been clinically diagnosed. I've been trying my best to be functional since I'm the eldest, and a lot is expected from me,” he said.
As extended lockdowns put further strain on his mental health, Ryan mustered the courage to try his company's online employee counseling service. “The free online therapy with a psychologist lasted for six months, and it helped me address those issues interfering with my productivity at work,” he said.
He was often told by family or friends: “Ano ka ba? Dapat mas alam mo na ‘yan. Psych graduate ka pa man din!” (As a psych graduate, you should know better!)
Ryan said such comments pressured him to act normally. But having a degree in psychology did not make one mentally bulletproof, and he was reminded of this every time he engaged in self-harming behavior and suicidal thoughts, he said.
“Having a degree in psychology doesn't save you from depression,” he said.
Depression and anxiety are on the rise among millennials as they face the pressure to perform and be functional amid pandemic fatigue.
Karla Longjas, 27, is a freelance artist who was initially diagnosed with major depression in 2017. She could go a long time without eating, but not without smoking or drinking. At times, she would cut herself as a way to release suppressed emotions. Karla's mental health condition caused her to get hospitalized twice, and she was diagnosed with Borderline Personality Disorder in 2019.
“One of the essentials I had to secure during the onset of the lockdown was my medication, for fear of running out,” Karla shared.
With her family's support, Karla can afford mental health care.
She has been spending an average of P10,000 a month on medication and professional fees for a psychologist and a psychiatrist. “The frequency of therapy depends on one's needs, and, at times, it involves two to three sessions a month,” she added.
Amid the restrictions of the pandemic, Karla said her mental health was getting out of hand. “I feel like things are getting even crazier, and I still resort to online therapy with my psychiatrist,” she said.
“I've been under medication for almost four years now with various psychologists and psychiatrists. I'm already tired of constantly searching and learning about my condition. Knowing that this mental health illness doesn't get cured but only gets manageable is wearing me out,” she added. In the face of renewed lockdowns, rising cases of anxiety, depression, and suicide, among others, are only bound to spark increased demand for mental health services.
MANO DELA CRUZ

Writer Mano Dela Cruz, 30, is shown sharing stories of his manic episodes, describing the experience as being on ‘top of the world.’ Individuals diagnosed with Bipolar Disorder Type II suffer more often from episodes of depression than hypomania. Depressive periods, ‘the lows,’ translate to feelings of guilt, loss of pleasure, low energy, and thoughts of suicide.

Mano says the mess in his room indicates his disposition, whether he's in a manic or depressive state. “I know that I'm not stable when I look at my room and it's too cluttered. There are days when I don't have the energy to clean up and even take a bath,” he says.

Mano was diagnosed with Bipolar Disorder Type II in 2016, when he was in his mid-20s. His condition comes with Attention Deficit Hyperactivity Disorder and Obsessive-Compulsive Personality Disorder traits, requiring lifelong treatment with antipsychotics and mood stabilizers such as antidepressants.

Mano resorts to biking as a form of exercise and to release feel-good endorphins, which helps combat depression, according to his psychiatrist.

Mano waits for his psychiatric consultation at a hospital in Angeles, Pampanga.

Mano shares a laugh with his sister inside their home. “It took a while for my family to understand my mental health illness,” he says. It took the same time for him to accept his condition.
RYAN BALDONADO

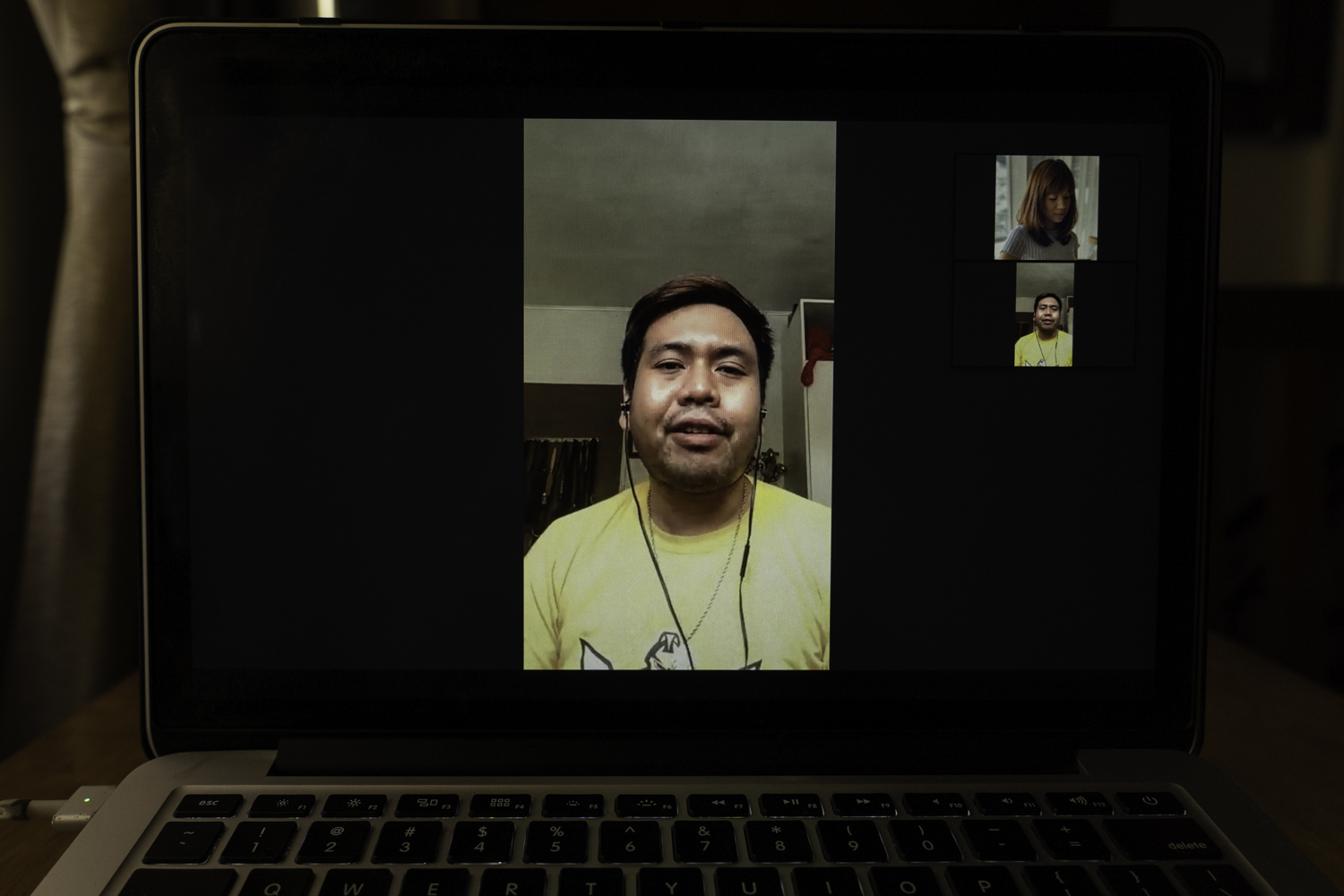
Ryan Baldonado, 30, shares his mental health condition in an online interview. Ryan is in quarantine after experiencing symptoms of Covid-19.
KARLA LONGJAS

Karla Longjas, 27, does a headstand during meditative yoga inside her room, which is filled with bottles of alcohol. Apart from her medications, she practices yoga to have mental clarity, calmness, and stress relief.

Karla shares that in some days, she has hallucinations and tries to sketch them.

In April 2019, Karla was inflicting harm on herself, leading to her two-week hospitalization as advised by her psychiatrist. In the same year, she was diagnosed with Borderline Personality Disorder. The stigma around her mental illness made her feel so uncomfortable that she had to use a fake name to hide her identity.

Karla buys her prescriptive medications in a drug store. Individuals clinically diagnosed with a psychosocial disability can avail themselves of the 20% discount for persons with disabilities.

Karla Longjas is photographed at her apartment in Makati. Individuals diagnosed with Borderline Personality Disorder (BPD) exhibit symptoms such as self-harm, unstable relationships, intense anger, and impulsive or self-destructive behavior. BPD is a dissociative disorder that is not commonly diagnosed in the Philippines.
This story is one of the twelve photo essays produced under the Capturing Human Rights fellowship program, a seminar and mentoring project
organized by the Philippine Center for Investigative Journalism and the Photojournalists' Center of the Philippines.
Check the other photo essays here.

Larry Monserate Piojo – “Terminal: The constant agony of commuting amid the pandemic”
Orange Omengan – “Filipinos face the mental toll of the Covid-19 pandemic”
Lauren Alimondo – “In loving memory”
Gerimara Manuel – “Pinagtatagpi-tagpi: Mother, daughter struggle between making a living and modular learning”
Pau Villanueva – “Hinubog ng panata: The vanishing spiritual traditions of Aetas of Capas, Tarlac”
Bernice Beltran – “Women's 'invisible work'”
Dada Grifon – “From the cause”
Bernadette Uy – “Enduring the current”
Mark Saludes – “Mission in peril”
EC Toledo – “From sea to shelf: The story before a can is sealed”
Ria Torrente – “HIV positive mother struggles through the Covid-19 pandemic”
Sharlene Festin – “Paradise lost”
PCIJ's investigative reports
THE SHRINKING GODS OF PADRE FAURA | READ .
7 MILLION HECTARES OF PHILIPPINE LAND IS FORESTED – AND THAT'S BAD NEWS | READ
FOLLOWING THE MONEY: PH MEDIA LESSONS FOR THE 2022 POLL | READ
DIGGING FOR PROFITS: WHO OWNS PH MINES? | READ
THE BULACAN TOWN WHERE CHICKENS ARE SLAUGHTERED AND THE RIVER IS DEAD | READ
Sákit Pighati and Pag-asa: A Pastoral Reflection on Suffering During the COVID-19 Pandemic in the Philippines
Affiliation.
- 1 Theology and Religious Education Department, De La Salle University, 2401 Taft Avenue, Manila, Philippines. [email protected].
- PMID: 33772688
- PMCID: PMC8000686
- DOI: 10.1007/s10943-021-01234-5
This article explores the concept of suffering as experienced by Filipinos during the COVID-19 pandemic. It draws inspiration from their narratives about how they faced, managed, and struggled during this tragic event. Their experiences were interpreted and analyzed concerning Filipino culture and tradition using a modified form of thematic analysis. Findings revealed three contextualized themes: sákit (pain), pighati (grief), and pag-asa (hope). These themes are then discussed in the light of John Paul II's Salvifici Doloris. A meaningful pastoral reflection on the basic realities of suffering is formulated to clarify our understanding of such a crisis.
Keywords: COVID-19; Filipino; Hope; Redemption; Suffering.
- Philippines

Coronavirus Disease 2019
Filipino responses to covid-19, research documents filipino panic responses to the global pandemic..
Posted April 30, 2020 | Reviewed by Kaja Perina
- What Is Anxiety?
- Find a therapist to overcome anxiety

By Georgina Fairbrother
A recent study explored panic responses to COVID-19 in the Philippines. COVID-19 has been declared a global pandemic and has caused mass lockdowns and closures across the globe. An angle relatively unexplored amidst this global pandemic is the impact of COVID-19 on mental health. The survey conducted was a mixed-method study that gathered qualitative and quantitative data in order to better explore the different dimensions of panic responses.
The survey was conducted through convenience sampling by online forms due to government-mandated limitations of social contact and urgency. The online survey ran for three days and gathered 538 responses. The average age of a survey participant was 23.82, with participants ranging in ages from 13-67. 47% of those who completed the survey were working, 45.4% were students and 7.6% were not working. Of those who completed the survey, 1.3% had witnessed direct exposure to a COVID-19 patient, while 26% had witnessed exposure within their community, and 72.7% had not been exposed.
For purposes of the survey, the Health Anxiety Inventory (HAI) Short Week was adapted in order to test illness anxiety on COVID-19 amongst Filipinos. The HAI had four main sections used in this survey: 1) Symptoms of health anxiety (hypochondriasis), 2) Attitudes towards how awful it would be to develop COVID-19, 3) Avoidance, and 4) Reassurance. Responses to questions answered within these areas were scored on a 0-3 basis, compromising the quantitative portion of the study. To complete the qualitative section of the survey three open-ended questions were used. The open-ended questions used for qualitative purposes in this survey were:
“1. What came to your mind when you knew the existence of COVID-19? 2. How do you feel when you know the existence of COVID-19? 3. What actions have you done with the knowledge of existence of COVID-19?”
Upon completion of the survey, researchers were able to analyze data in regard to five different areas. First, researchers discovered that it was very evident that respondents were experiencing moderate illness anxiety in all four aspects listed by HAI. Secondly, by comparing locations, researchers also discovered that respondents residing in Metro Manilla exhibited less avoidance behavior compared to respondents residing outside Metro Manilla. While there is no definitive reason for this result, speculation looms around education , awareness, and proximity to COVID-19 cases. Thirdly, researchers looked at occupation, but determined illness anxiety was present regardless of occupation. Fourthly, researchers determined that respondents who had been in direct contact with those having COVID-19 were more likely to exhibit symptoms of hypochondriasis compared to respondents who had not witnessed or contacted anyone with COVID-19.
The fifth area that researchers explored upon completion of this survey was that of feeling, thinking, and behavior in response to COVID-19. Nineteen different themes were ranked by 100 experts based on their positivity and negativity. The themes included items such as the following: Health Consciousness, Optimism , Cautiousness, Protection, Compliance, Composure, Information Dissemination, Worry on self/family/others, Relating to Past Pandemics, Anxiety, Government Blaming, Shock, Transmission of Virus, Fear, Sadness, Paranoia , Nihilism, Annihilation, and Indifference. Upon completion of the survey, the highest-scoring themes amongst respondents included Fear, Social Distancing, Health Consciousness, and Information Dissemination. Meanwhile, the lowest-scoring themes included Indifference and Nihilism.
Overall, COVID-19 has become a global pandemic that is continuing to move and spread across the world. In the aftermath of this pandemic, it will be interesting to compare the panic responses of different countries. The Philippines approaches this study from a more socially collectivist perspective. With that being said, it was reported that the Philippines leaned towards more individualistic tendencies in times of fear. Another area to look deeper into would include how panic responses change from the initial shock of COVID-19 to lockdown phases to re-emergence phases.
Georgina Fairbrother is a current master’s student in the Humanitarian and Disaster Leadership program at Wheaton College. Prior to her master’s degree, she received a bachelor’s degree in Global Security and Intelligence studies from Embry-Riddle Aeronautical University.
Nicomedes, C. J., & Avila, R. (2020). An Analysis on the Panic of Filipinos During COVID-19 Pandemic in the Philippines. https://doi.org/10.13140/RG.2.2.17355.54565

Jamie Aten , Ph.D. , is the founder and executive director of the Humanitarian Disaster Institute at Wheaton College.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

At any moment, someone’s aggravating behavior or our own bad luck can set us off on an emotional spiral that threatens to derail our entire day. Here’s how we can face our triggers with less reactivity so that we can get on with our lives.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
- Subscribe Now
Filipinos face the mental toll of the COVID-19 pandemic
Already have Rappler+? Sign in to listen to groundbreaking journalism.
This is AI generated summarization, which may have errors. For context, always refer to the full article.

PRACTICE. Karla Longjas, 27, does a headstand during meditative yoga inside her room, which is filled with bottles of alcohol. Apart from her medications, she practices yoga to have mental clarity, calmness, and stress relief.
Orange Omengan
Omengan’s photo essay shows three of the many stories of mental health battles, of struggling to stay afloat despite the inaccessibility of proper mental health services, which worsened due to the series of lockdowns in the Philippines.
“I was just starting with my new job, but the pandemic triggered much anxiety, causing me to abandon my apartment in Pasig and move back to our family home in Mabalacat, Pampanga.”
This was Mano dela Cruz’s quick response to the initial round of lockdowns that swept the nation in March 2020.
Anxiety crept up on Mano, who was diagnosed with Bipolar Disorder Type II with Attention Deficit Hyperactivity Disorder and Obsessive-Compulsive Personality Disorder traits. The 30-year-old writer is just one of many Filipinos experiencing the mental health fallout of the pandemic.
COVID-19 infections in the Philippines have reached 1,149,925 cases as of May 17. The pandemic is unfolding simultaneously with the growing number of Filipinos suffering from mental health issues. At least 3.6 million Filipinos suffer from mental, neurological, and substance use disorders, according to Frances Prescila Cuevas, head of the National Mental Health Program under the Department of Health.
As the situation overwhelmed him, Mano had to let go of his full-time job. “At the start of the year, I thought I had my life all together, but this pandemic caused great mental stress on me, disrupting my routine and cutting my source of income,” he said.
Mano has also found it difficult to stay on track with his medications. “I don’t have insurance, and I do not save much due to my medical expenses and psychiatric consultations. On a monthly average, my meds cost about P2,800. With my PWD (person with disability) card, I get to avail myself of the 20% discount, but it’s still expensive. On top of this, I pay for psychiatric consultations costing P1,500 per session. During the pandemic, the rate increased to P2,500 per session lasting only 30 minutes due to health and safety protocols.”
The pandemic has resulted in substantial job losses as some businesses shut down, while the rest of the workforce adjusted to the new norm of working from home.
Ryan Baldonado, 30, works as an assistant human resource manager in a business process outsourcing company. The pressure from work, coupled with stress and anxiety amid the community quarantine, took a toll on his mental health.
Before the pandemic, Ryan said he usually slept for 30 hours straight, often felt under the weather, and at times subjected himself to self-harm. “Although the symptoms of depression have been manifesting in me through the years, due to financial concerns, I haven’t been clinically diagnosed. I’ve been trying my best to be functional since I’m the eldest, and a lot is expected from me,” he said.
As extended lockdowns put further strain on his mental health, Ryan mustered the courage to try his company’s online employee counseling service. “The free online therapy with a psychologist lasted for six months, and it helped me address those issues interfering with my productivity at work,” he said.
He was often told by family or friends: “Ano ka ba? Dapat mas alam mo na ‘yan. Psych graduate ka pa man din!” ( As a psych graduate, you should know better!)
Ryan said such comments pressured him to act normally. But having a degree in psychology did not make one mentally bulletproof, and he was reminded of this every time he engaged in self-harming behavior and suicidal thoughts, he said.
“Having a degree in psychology doesn’t save you from depression,” he said.
Depression and anxiety are on the rise among millennials as they face the pressure to perform and be functional amid pandemic fatigue.
Karla Longjas, 27, is a freelance artist who was initially diagnosed with major depression in 2017. She could go a long time without eating, but not without smoking or drinking. At times, she would cut herself as a way to release suppressed emotions. Karla’s mental health condition caused her to get hospitalized twice, and she was diagnosed with Borderline Personality Disorder in 2019.
“One of the essentials I had to secure during the onset of the lockdown was my medication, for fear of running out,” Karla shared.
With her family’s support, Karla can afford mental health care.
She has been spending an average of P10,000 a month on medication and professional fees for a psychologist and a psychiatrist. “The frequency of therapy depends on one’s needs, and, at times, it involves two to three sessions a month,” she added.
Amid the restrictions of the pandemic, Karla said her mental health was getting out of hand. “I feel like things are getting even crazier, and I still resort to online therapy with my psychiatrist,” she said.
“I’ve been under medication for almost four years now with various psychologists and psychiatrists. I’m already tired of constantly searching and learning about my condition. Knowing that this mental health illness doesn’t get cured but only gets manageable is wearing me out,” she added.
In the face of renewed lockdowns, rising cases of anxiety, depression, and suicide, among others, are only bound to spark increased demand for mental health services.
Mano dela Cruz

Ryan Baldonado
Karla Longjas

– Rappler.com
This piece is republished with permission from the Philippine Center for Investigative Journalism.
Add a comment
Please abide by Rappler's commenting guidelines .
There are no comments yet. Add your comment to start the conversation.
How does this make you feel?
Related Topics
Recommended stories, {{ item.sitename }}, {{ item.title }}, us fda to remove all posts warning public vs using ivermectin to treat covid-19.

Filipinos’ happiness back to pre-pandemic levels – report

[Time Trowel] Evolution and the sneakiness of COVID
![about covid 19 pandemic essay tagalog [Time Trowel] Evolution and the sneakiness of COVID](https://www.rappler.com/tachyon/2024/02/tl-evolution-covid.jpg?resize=257%2C257&crop=455px%2C0px%2C1080px%2C1080px)
PUP’s first face-to-face entrance tests after 3 years draw over 20,000 examinees

WHO sees ‘incredibly low’ COVID, flu vaccination rates as cases surge

Checking your Rappler+ subscription...
Upgrade to Rappler+ for exclusive content and unlimited access.
Why is it important to subscribe? Learn more
You are subscribed to Rappler+

Search the United Nations
- Policy and Funding
- Recover Better
- Disability Inclusion
- Secretary-General
- Financing for Development
- ACT-Accelerator
- Member States
- Health and Wellbeing
- Policy and Guidance
- Vaccination
- COVID-19 Medevac
- i-Seek (requires login)
- Awake at Night podcast

COVID-19 photo essay: We’re all in this together
About the author, department of global communications.
The United Nations Department of Global Communications (DGC) promotes global awareness and understanding of the work of the United Nations.
23 June 2020 – The COVID-19 pandemic has demonstrated the interconnected nature of our world – and that no one is safe until everyone is safe. Only by acting in solidarity can communities save lives and overcome the devastating socio-economic impacts of the virus. In partnership with the United Nations, people around the world are showing acts of humanity, inspiring hope for a better future.
Everyone can do something

Rauf Salem, a volunteer, instructs children on the right way to wash their hands, in Sana'a, Yemen. Simple measures, such as maintaining physical distance, washing hands frequently and wearing a mask are imperative if the fight against COVID-19 is to be won. Photo: UNICEF/UNI341697
Creating hope

Venezuelan refugee Juan Batista Ramos, 69, plays guitar in front of a mural he painted at the Tancredo Neves temporary shelter in Boa Vista, Brazil to help lift COVID-19 quarantine blues. “Now, everywhere you look you will see a landscape to remind us that there is beauty in the world,” he says. Ramos is among the many artists around the world using the power of culture to inspire hope and solidarity during the pandemic. Photo: UNHCR/Allana Ferreira
Inclusive solutions

Wendy Schellemans, an education assistant at the Royal Woluwe Institute in Brussels, models a transparent face mask designed to help the hard of hearing. The United Nations and partners are working to ensure that responses to COVID-19 leave no one behind. Photo courtesy of Royal Woluwe Institute
Humanity at its best

Maryna, a community worker at the Arts Centre for Children and Youth in Chasiv Yar village, Ukraine, makes face masks on a sewing machine donated by the Office of the United Nations High Commissioner for Refugees (UNHCR) and civil society partner, Proliska. She is among the many people around the world who are voluntarily addressing the shortage of masks on the market. Photo: UNHCR/Artem Hetman
Keep future leaders learning

A mother helps her daughter Ange, 8, take classes on television at home in Man, Côte d'Ivoire. Since the COVID-19 pandemic began, caregivers and educators have responded in stride and have been instrumental in finding ways to keep children learning. In Côte d'Ivoire, the United Nations Children’s Fund (UNICEF) partnered with the Ministry of Education on a ‘school at home’ initiative, which includes taping lessons to be aired on national TV and radio. Ange says: “I like to study at home. My mum is a teacher and helps me a lot. Of course, I miss my friends, but I can sleep a bit longer in the morning. Later I want to become a lawyer or judge." Photo: UNICEF/UNI320749
Global solidarity

People in Nigeria’s Lagos State simulate sneezing into their elbows during a coronavirus prevention campaign. Many African countries do not have strong health care systems. “Global solidarity with Africa is an imperative – now and for recovering better,” said United Nations Secretary-General António Guterres. “Ending the pandemic in Africa is essential for ending it across the world.” Photo: UNICEF Nigeria/2020/Ojo
A new way of working

Henri Abued Manzano, a tour guide at the United Nations Information Service (UNIS) in Vienna, speaks from his apartment. COVID-19 upended the way people work, but they can be creative while in quarantine. “We quickly decided that if visitors can’t come to us, we will have to come to them,” says Johanna Kleinert, Chief of the UNIS Visitors Service in Vienna. Photo courtesy of Kevin Kühn
Life goes on

Hundreds of millions of babies are expected to be born during the COVID-19 pandemic. Fionn, son of Chloe O'Doherty and her husband Patrick, is among them. The couple says: “It's all over. We did it. Brought life into the world at a time when everything is so uncertain. The relief and love are palpable. Nothing else matters.” Photo: UNICEF/UNI321984/Bopape

Putting meals on the table

Sudanese refugee Halima, in Tripoli, Libya, says food assistance is making her life better. COVID-19 is exacerbating the existing hunger crisis. Globally, 6 million more people could be pushed into extreme poverty unless the international community acts now. United Nations aid agencies are appealing for more funding to reach vulnerable populations. Photo: UNHCR
Supporting the frontlines

The United Nations Air Service, run by the World Food Programme (WFP), distributes protective gear donated by the Jack Ma Foundation and Alibaba Group, in Somalia. The United Nations is using its supply chain capacity to rapidly move badly needed personal protective equipment, such as medical masks, gloves, gowns and face-shields to the frontline of the battle against COVID-19. Photo: WFP/Jama Hassan

S7-Episode 2: Bringing Health to the World
“You see, we're not doing this work to make ourselves feel better. That sort of conventional notion of what a do-gooder is. We're doing this work because we are totally convinced that it's not necessary in today's wealthy world for so many people to be experiencing discomfort, for so many people to be experiencing hardship, for so many people to have their lives and their livelihoods imperiled.”
Dr. David Nabarro has dedicated his life to global health. After a long career that’s taken him from the horrors of war torn Iraq, to the devastating aftermath of the Indian Ocean tsunami, he is still spurred to action by the tremendous inequalities in global access to medical care.
“The thing that keeps me awake most at night is the rampant inequities in our world…We see an awful lot of needless suffering.”
:: David Nabarro interviewed by Melissa Fleming

Brazilian ballet pirouettes during pandemic
Ballet Manguinhos, named for its favela in Rio de Janeiro, returns to the stage after a long absence during the COVID-19 pandemic. It counts 250 children and teenagers from the favela as its performers. The ballet group provides social support in a community where poverty, hunger and teen pregnancy are constant issues.

Radio journalist gives the facts on COVID-19 in Uzbekistan
The pandemic has put many people to the test, and journalists are no exception. Coronavirus has waged war not only against people's lives and well-being but has also spawned countless hoaxes and scientific falsehoods.
Featured Clinical Reviews
- Screening for Atrial Fibrillation: US Preventive Services Task Force Recommendation Statement JAMA Recommendation Statement January 25, 2022
- Evaluating the Patient With a Pulmonary Nodule: A Review JAMA Review January 18, 2022
Select Your Interests
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
A National Strategy for the “New Normal” of Life With COVID
- 1 Perelman School of Medicine and The Wharton School, University of Pennsylvania, Philadelphia
- 2 Center for Infectious Disease Research and Policy, University of Minnesota, Minneapolis
- 3 Grossman School of Medicine, New York University, New York, New York
- Viewpoint The First 2 Years of COVID-19—Lessons to Improve Preparedness for the Next Pandemic Jennifer B. Nuzzo, DrPH, SM; Lawrence O. Gostin, JD JAMA
- Viewpoint A National Strategy for COVID-19—Testing, Surveillance, and Mitigation Strategies David Michaels, PhD, MPH; Ezekiel J. Emanuel, MD, PhD; Rick A. Bright, PhD JAMA
- Viewpoint A National Strategy for COVID-19 Medical Countermeasures Luciana L. Borio, MD; Rick A. Bright, PhD; Ezekiel J. Emanuel, MD, PhD JAMA
- Viewpoint The Pandemic Preparedness Program Eli Y. Adashi, MD, MS; I. Glenn Cohen, JD JAMA
- Medical News & Perspectives Former Biden-Harris Transition Advisors Propose a New National Strategy for COVID-19 Jennifer Abbasi JAMA
- Comment & Response Strategy for the “New Normal” of Life With COVID—Reply Ezekiel J. Emanuel, MD, PhD; Michael Osterholm, PhD, MPH; Céline R. Gounder, MD, ScM JAMA
- Comment & Response Strategy for the “New Normal” of Life With COVID Afschin Gandjour, MD, PhD, MA JAMA
- Viewpoint COVID-19 Vaccination—Becoming Part of the New Normal Peter Marks, MD, PhD; Janet Woodcock, MD; Robert Califf, MD JAMA
As the Omicron variant of SARS-CoV-2 demonstrates, COVID-19 is here to stay. In January 2021, President Biden issued the “National Strategy for the COVID-19 Response and Pandemic Preparedness.” As the US moves from crisis to control, this national strategy needs to be updated. Policy makers need to specify the goals and strategies for the “new normal” of life with COVID-19 and communicate them clearly to the public.
SARS-CoV-2 continues to persist, evolve, and surprise. In July 2021, with vaccinations apace and infection rates plummeting, Biden proclaimed that “we’ve gained the upper hand against this virus,” and the Centers for Disease Control and Prevention (CDC) relaxed its guidance for mask wearing and socializing. 1 By September 2021, the Delta variant proved these steps to be premature, and by late November, the Omicron variant created concern about a perpetual state of emergency.
In delineating a national strategy, humility is essential. The precise duration of immunity to SARS-CoV-2 from vaccination or prior infection is unknown. Also unknown is whether SARS-CoV-2 will become a seasonal infection; whether antiviral therapies will prevent long COVID; or whether even more transmissible, immune-evading, or virulent variants will arise after Omicron.
Another part of this humility is recognizing that predictions are necessary but educated guesses, not mathematical certainty. The virus, host response, and data will evolve. Biomedical and public health tools will expand, along with better understanding of their limitations. The incidence of SARS-CoV-2, vaccination rates, hospital capacity, tolerance for risk, and willingness to implement different interventions will vary geographically, and national recommendations will need to be adapted locally.
It is imperative for public health, economic, and social functioning that US leaders establish and communicate specific goals for COVID-19 management, benchmarks for the imposition or relaxation of public health restrictions, investments and reforms needed to prepare for future SARS-CoV-2 variants and other novel viruses, and clear strategies to accomplish all of this.
Redefining the Appropriate National Risk Level
The goal for the “new normal” with COVID-19 does not include eradication or elimination, eg, the “zero COVID” strategy. 2 Neither COVID-19 vaccination nor infection appear to confer lifelong immunity. Current vaccines do not offer sterilizing immunity against SARS-CoV-2 infection. Infectious diseases cannot be eradicated when there is limited long-term immunity following infection or vaccination or nonhuman reservoirs of infection. The majority of SARS-CoV-2 infections are asymptomatic or mildly symptomatic, and the SARS-CoV-2 incubation period is short, preventing the use of targeted strategies like “ring vaccination.” Even “fully” vaccinated individuals are at risk for breakthrough SARS-CoV-2 infection. Consequently, a “new normal with COVID” in January 2022 is not living without COVID-19.
The “new normal” requires recognizing that SARS-CoV-2 is but one of several circulating respiratory viruses that include influenza, respiratory syncytial virus (RSV), and more. COVID-19 must now be considered among the risks posed by all respiratory viral illnesses combined. Many of the measures to reduce transmission of SARS-CoV-2 (eg, ventilation) will also reduce transmission of other respiratory viruses. Thus, policy makers should retire previous public health categorizations, including deaths from pneumonia and influenza or pneumonia, influenza, and COVID-19, and focus on a new category: the aggregate risk of all respiratory virus infections.
What should be the peak risk level for cumulative viral respiratory illnesses for a “normal” week? Even though seasonal influenza, RSV, and other respiratory viruses circulating before SARS-CoV-2 were harmful, the US has not considered them a sufficient threat to impose emergency measures in over a century. People have lived normally with the threats of these viruses, even though more could have been done to reduce their risks.
The appropriate risk threshold should reflect peak weekly deaths, hospitalizations, and community prevalence of viral respiratory illnesses during high-severity years, such as 2017-2018. 3 That year had approximately 41 million symptomatic cases of influenza, 710 000 hospitalizations and 52 000 deaths. 4 In addition, the CDC estimates that each year RSV leads to more than 235 000 hospitalizations and 15 000 deaths in the US. 3 This would translate into a risk threshold of approximately 35 000 hospitalizations and 3000 deaths (<1 death/100 000 population) in the worst week.
Today, the US is far from these thresholds. For the week of December 13, 2021, the CDC reported the US experienced more than 900 000 COVID-19 cases, more than 50 000 new hospitalizations for COVID-19, and more than 7000 deaths. 5 , 6 The tolerance for disease, hospitalization, and death varies widely among individuals and communities. What constitutes appropriate thresholds for hospitalizations and death, at what cost, and with what trade-offs remains undetermined.
This peak week risk threshold serves at least 2 fundamental functions. This risk threshold triggers policy recommendations for emergency implementation of mitigation and other measures. In addition, health systems could rely on this threshold for planning on the bed and workforce capacity they need normally, and when to institute surge measures.
Rebuilding Public Health
To cope with pandemic, and eventually, endemic SARS-CoV-2 and to respond to future public health threats requires deploying real-time information systems, a public health implementation workforce, flexible health systems, trust in government and public health institutions, and belief in the value of collective action for public good. 7 , 8
First, the US needs a comprehensive, digital, real-time, integrated data infrastructure for public health. As Omicron has reemphasized, the US is operating with imprecise estimates of disease spread, limited genomic surveillance, projections based on select reporting sites, and data from other countries that may not be generalizable. These shortcomings are threatening lives and societal function.
The US must establish a modern data infrastructure that includes real-time electronic collection of comprehensive information on respiratory viral infections, hospitalizations, deaths, disease-specific outcomes, and immunizations merged with sociodemographic and other relevant variables. The public health data infrastructure should integrate data from local, state, and national public health units, health care systems, public and commercial laboratories, and academic and research institutions. Using modern technology and analytics, it is also essential to merge nontraditional environmental (air, wastewater) surveillance data, including genomic data, with traditional clinical and epidemiological data to track outbreaks and target containment.
Second, the US needs a permanent public health implementation workforce that has the flexibility and surge capacity to manage persistent problems while simultaneously responding to emergencies. Data collection, analysis, and technical support are necessary, but it takes people to respond to crises. This implementation workforce should include a public health agency–based community health worker system and expanded school nurse system.
A system of community public health workers could augment the health care system by testing and vaccinating for SARS-CoV-2 and other respiratory infections; ensuring adherence to ongoing treatment for tuberculosis, HIV, diabetes, and other chronic conditions; providing health screening and support to pregnant individuals and new parents and their newborns; and delivering various other public health services to vulnerable or homebound populations.
School nurses need to be empowered to address the large unmet public health needs of children and adolescents. As polio vaccination campaigns showed, school health programs are an efficient and effective way to care for children, including preventing and treating mild asthma exacerbations (often caused by viral respiratory infections), ensuring vaccination as a condition for attendance, and addressing adolescents’ mental and sexual health needs. School clinics must be adequately staffed and funded as an essential component of the nation’s public health infrastructure.
Third, because respiratory infections ebb and flow, institutionalizing telemedicine waivers, licensure to practice and enable billing across state lines, and other measures that allow the flow of medical services to severely affected regions should be a priority.
Fourth, it is essential to rebuild trust in public health institutions and a belief in collective action in service of public health. 7 Communities with higher levels of trust and reciprocity, such as Denmark, have experienced lower rates of hospitalization and death from COVID-19. 7 Improving public health data systems and delivering a diverse public health workforce that can respond in real time in communities will be important steps toward building that trust more widely.
Conclusions
After previous infectious disease threats, the US quickly forgot and failed to institute necessary reforms. That pattern must change with the COVID-19 pandemic. Without a strategic plan for the “new normal” with endemic COVID-19, more people in the US will unnecessarily experience morbidity and mortality, health inequities will widen, and trillions will be lost from the US economy. This time, the nation must learn and prepare effectively for the future.
The resources necessary to build and sustain an effective public health infrastructure will be substantial. Policy makers should weigh not only the costs but also the benefits, including fewer deaths and lost productivity from COVID-19 and all viral respiratory illnesses. Indeed, after more than 800 000 deaths from COVID-19, and a projected loss of $8 trillion in gross domestic product through 2030, 8 these interventions will be immensely valuable.
Corresponding Author: Ezekiel J. Emanuel, MD, PhD, Medical Ethics and Health Policy, Perelman School of Medicine, University of Pennsylvania, 423 Guardian Dr, Blockley Hall, Philadelphia, PA 19104 ( [email protected] ).
Published Online: January 6, 2022. doi:10.1001/jama.2021.24282
Conflict of Interest Disclosures: Dr Emanuel reported personal fees, nonfinancial support, or both from companies, organizations, and professional health care meetings and being a venture partner at Oak HC/FT; a partner at Embedded Healthcare LLC, ReCovery Partners LLC, and COVID-19 Recovery Consulting; and an unpaid board member of Village MD and Oncology Analytics. Dr Emanuel owns no stock in pharmaceutical, medical device companies, or health insurers. No other disclosures were reported.
Additional Information: Drs Emanuel, Osterholm, and Gounder were members of the Biden-Harris Transition COVID-19 Advisory Board from November 2020 to January 2021.
See More About
Emanuel EJ , Osterholm M , Gounder CR. A National Strategy for the “New Normal” of Life With COVID. JAMA. 2022;327(3):211–212. doi:10.1001/jama.2021.24282
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Financing Firms in Hibernation during the COVID-19 Pandemic: Article Review Essay
Introduction, recommendations.
The COVID-19 pandemic affected the global economy just as much as the public health domain. However, most economies were able to recover significantly due to efficient policy responses. The article Financing Firms in Hibernation during the COVID-19 Pandemic by Didier, Huneerus, Larrain and Schmukler from 2021 discusses optimal policy choices for business security during the pandemic. The authors introduce the concept of firm hibernation , which refers to minimal spending required to sustain a firm for a period of mass lockdown. This idea is proposed in hopes of saving the relationships with the firms, allowing for a quicker economic rebound once the pandemic is resolved. Along with highlighting the importance of economic relationships, the authors also talk about the government’s function as a lender and last-resort loss absorber. The text poses certain implications regarding the preferable course of policy action during periods of external systemic shock.
Firstly, the unique features of the global pandemic, as opposed to other major economic crises, are covered. Global economic disruptions began in the financial sector before the COVID-19 crisis. Conversely, the coronavirus pandemic was an external system shock that occurred outside the economy. The virus can be distinguished from other disruptive factors by a high degree of uncertainty. The recovery from the initial disturbance in the economic sphere depends entirely on the virus’s elimination. Still, even if the disease is largely eliminated, the time required for the cultural rebound is also unknown. Additionally, there have been significant changes in consumer spending and investment patterns as a result of the COVID-19 crisis. Moreover, the virus’s activity may have long-lasting negative economic effects. All of the above suggests that in order to fight the fallout of the pandemic, policymakers must account for the uncertain nature of the situation and allocate resources with caution.
A potential response to the limitations of policy inaction during the pandemic is firm hibernation. The value of hibernation lies in the fact that it allows businesses to take on as little debt as possible to stay afloat during the pandemic and when the economy recovers and accrued loans need to be serviced. Furthermore, lending monetary resources can prevent long-term economic scarring by saving industry relationships and avoiding the emergence of zombie firms, groups that are out of business with existing outstanding debts.
Business relationships with other companies and customers are invaluable assets for economic sustainability. These connections deteriorate as a result of viable businesses being forced into bankruptcy, making recovery virtually impossible. A brief shock that irreparably damages a large number of relationships can have lasting negative effects on the economy and slow its recovery. The need for the aforementioned hibernation is stark in light of the severity of economic degradation.
In conclusion, the article discusses optimal responses to the COVID-19 economic crisis. Among the topics evaluated are the difficulties of dealing with exogenous health disruptions that affect the financial domain and the appropriate approaches to resource allocation in such instances. Judging by the findings of the authors, one can argue in favor of firm hibernation, a procedure that would sustain a business during reduced operation periods and prevent viable firms from going bankrupt. The efficacy of this approach is yet to be determined; however, the preliminary assessment of the virus’s nature, creditor functions, and relationship value predicts a solid solution to the economic crisis.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, May 8). Financing Firms in Hibernation during the COVID-19 Pandemic: Article Review. https://ivypanda.com/essays/financing-firms-in-hibernation-during-the-covid-19-pandemic-article-review/
"Financing Firms in Hibernation during the COVID-19 Pandemic: Article Review." IvyPanda , 8 May 2024, ivypanda.com/essays/financing-firms-in-hibernation-during-the-covid-19-pandemic-article-review/.
IvyPanda . (2024) 'Financing Firms in Hibernation during the COVID-19 Pandemic: Article Review'. 8 May.
IvyPanda . 2024. "Financing Firms in Hibernation during the COVID-19 Pandemic: Article Review." May 8, 2024. https://ivypanda.com/essays/financing-firms-in-hibernation-during-the-covid-19-pandemic-article-review/.
1. IvyPanda . "Financing Firms in Hibernation during the COVID-19 Pandemic: Article Review." May 8, 2024. https://ivypanda.com/essays/financing-firms-in-hibernation-during-the-covid-19-pandemic-article-review/.
Bibliography
IvyPanda . "Financing Firms in Hibernation during the COVID-19 Pandemic: Article Review." May 8, 2024. https://ivypanda.com/essays/financing-firms-in-hibernation-during-the-covid-19-pandemic-article-review/.
- Psychological Problems: Trauma and Lessons
- The Value of In-Person Human Interaction
- Facebook Advantages over MySpace
- The Great Financial Crisis and Its Causes
- Puerto Rico's Government and Economic Challenges
- Industrialization: Regional Science and Urban Economics
- Importing Substituting Industrialization in South Korea
- The City of Los Angeles and the 2008 Crisis
The Growing Epidemic of Elderly Abuse

The number of senior citizens is growing rapidly ; individuals aged 65 and older increased from 39.6 million in 2009 to 54.1 million in 2019 (a 36% increase) and is projected to reach 94.7 million by 2060. This has come about as a result of advances in modern medicine and improved living conditions.
However, over the last few years, reports not only in the U.S., but from around the world, have brought to light a major new pandemic that may reach deeply into the fabric and soul of our society: The usual respect and care of our aging population is decaying into a growing incidence of neglect and abuse. Increasing reports of horrific events that affect our aging population detailing prolonged suffering and premature death are now commonplace.
Frankly, elder abuse reflects a decay of basic human rights in a major segment of our society. This type of neglect has many faces which may include physical, sexual, emotional, and psychological abuse. Victims are also commonly subjected to financial abuse, often losing savings, assets, homes, and other material property. Individuals may also be exposed to abandonment and loss of contact with family and friends.
This form of neglect may impact the elderly the most, leading to emotional issues such as loss of dignity, self-worth, and respect. Such abuse may be a single event or a cycle of repeated acts. It can vary from subtle—such as not acting in a protective or loving manner in a relationship where there is an expectation of trust, but also within a family or in a senior care facility.
Read More: Why Americans Are Uniquely Afraid to Grow Old
Prior to the COVID-19, 1 in 10 elderly adults in the U.S. experienced elder abuse. A major review in 2017 of 52 studies from 28 nations reported that 15.7% of people over 60 were subjected to some form of abuse.
In 2020, this number doubled to 1 in 5—a nearly 84% increase. A study by the Administration for Aging stated that hundreds of thousands of seniors were abused, neglected and exploited by family and others. What is even more disturbing is that in 90% of cases, the abuser is a member of the family, based on findings in the study. In fact, two-thirds of the abusers were adult children or spouses. We, of course, find this to be a shocking statistic; since the dawn of recorded history the elderly have been given great respect and were cared for by both the family and the community as a whole.
Why did this natural relationship so greatly change in such a short period of time? We believe the root cause are shifts in family demographics: over time, adult children now live great distances from parents, but also may have stressful careers, leading to personal issues that distract from attention to parents.
The pandemic further aggravated this issue with a marked decline in visits and travel related to restrictions. Families were also unable to visit elderly relatives in senior care facilities in most states. This may have been a mechanism that loosened family bonds and connections that were never fully restored since the onset of the pandemic. Moreover, growing economic pressures brought on by the pandemic also impacted families. In most households, fewer individuals are free from the obligation to care for parents on a daily basis. The reason is that children must work in order to pay bills, rent, and buy food.
Read More: Why America Is Failing To Feed Its Aging
The pandemic also pressured families to care for elderly and frail family members at home because nursing homes were not accepting admissions. Caring for individuals with cognitive issues such as dementia and Alzheimer’s at home without help of course created many issues. This stressful home environment can trigger strong negative emotions in caregivers and lead to physical and verbal abuse. Use of alcohol and drugs also peaked during the pandemic and may also have played a key role in the rise of such abuse.
The escalating opioid crisis also led to an uptick in misuse and diversion of opioids by the elderly, which has transformed into an increase in pain and suffering of elderly persons with chronic pain. The increased prevalence of substance abuse has encouraged family members to raid the financial assets and valuables of elderly family members. Widespread layoffs and job loss during the pandemic are other factors underlying the exploitation of elderly parents by family members.
Social isolation, a byproduct of lock downs, further magnified these events in that typical family interactions abruptly ended, leading to a breakdown in families’ ability to spot early signs of decline in function or cognitive impairment.
Family members being unprepared or unable to take on the role of caregivers are an additional factor in the elderly being more susceptible to becoming victims of abuse and violence . Data indicates that it’s more likely for children to be raised without an extended family, devoid of exposure to elderly relatives living in the same household.
More From TIME
The pandemic also disrupted access to community centers, social workers, and support agencies that often aid families by offering staffing and education. Rising food and utility prices added further financial stress, ultimately leading to moral injury and burnout among care givers.
Technology has also played a role in the rise of financial abuse. It is now very easy to transfer financial assets electronically with a few key stokes from an elderly individual—often no signatures are necessary. Media reports are filled with stories of family raiding retirement accounts, selling assets, and taking homes away from the elderly. Elderly individuals may not be tech savvy and therefore vulnerable to financial abuse. They can also be easy targets for telemarketing schemes and internet fraud, placing them at risk for identity theft.
Many families may believe that placement of loved ones into a senior living facility may be representative of a loving and supportive “safety net.” However, this industry is also in crisis. Over 3.2 million adults are currently living in nursing homes and other long term care facilities in the US. As many as one-third of all adults will enter a nursing at point during their lives as the US population ages. Sadly, nursing homes are not a safe haven: abuse is increasing due to understaffing, improper training and staff burn out. The industry was greatly affected by the pandemic with loss of beds, lost income, and loss experienced caregivers. These factors have led staff members to take out their anger on they people they should be caring for. A shocking report by the World Health Organization reported that 66% of nursing home staff members admitted to abusing individuals under their care.
How can families and society deal with this pandemic of abuse? The most effective approach involves increased focus on education and community support. Families need access to home care services, including social workers, occupational therapists and physical therapists—team members who make important contributions to the comprehensive care of our loved ones. In some cases, this may also involve placement in a long-term care facility when the needs of a loved one are more complex in nature. Families should also be able to evaluate and monitor the care loved ones receive in long-term facilities. The need for transparency is essential, with “report cards” issued by government agencies available to the public.
At the very least, we should all attempt to reconnect with the elderly members in our lives. It can be transformative for both parents, children, and all members of an extended family and community—and can also address the nationwide epidemic of loneliness that so many elderly people suffer from.
More Must-Reads From TIME
- The 100 Most Influential People of 2024
- How Far Trump Would Go
- Why Maternity Care Is Underpaid
- Scenes From Pro-Palestinian Encampments Across U.S. Universities
- Saving Seconds Is Better Than Hours
- Why Your Breakfast Should Start with a Vegetable
- Welcome to the Golden Age of Ryan Gosling
- Want Weekly Recs on What to Watch, Read, and More? Sign Up for Worth Your Time
Contact us at [email protected]
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
- Public Health
Perspective
When pto stands for 'pretend time off': doctors struggle to take real breaks.
Mara Gordon

A survey shows that doctors have trouble taking full vacations from their high-stress jobs. Even when they do, they often still do work on their time off. Wolfgang Kaehler/LightRocket via Getty Images hide caption
A survey shows that doctors have trouble taking full vacations from their high-stress jobs. Even when they do, they often still do work on their time off.
A few weeks ago, I took a vacation with my family. We went hiking in the national parks of southern Utah, and I was blissfully disconnected from work.
I'm a family physician, so taking a break from my job meant not seeing patients. It also meant not responding to patients' messages or checking my work email. For a full week, I was free.
Taking a real break — with no sneaky computer time to bang out a few prescription refill requests — left me feeling reenergized and ready to take care of my patients when I returned.
But apparently, being a doctor who doesn't work on vacation puts me squarely in the minority of U.S. physicians.
Research published in JAMA Network Open this year set out to quantify exactly how doctors use their vacation time — and what the implications might be for a health care workforce plagued by burnout, dissatisfaction and doctors who are thinking about leaving medicine.
"There is a strong business case for supporting taking real vacation," says Dr. Christine Sinsky , the lead author of the paper. "Burnout is incredibly expensive for organizations."

Shots - Health News
Health workers know what good care is. pandemic burnout is getting in the way.
Researchers surveyed 3,024 doctors, part of an American Medical Association cohort designed to represent the American physician workforce. They found that 59.6% of American physicians took 15 days of vacation or less per year. That's a little more than the average American: Most workers who have been at a job for a year or more get between 10 and 14 days of paid vacation time , according to the U.S. Bureau of Labor Statistics.
However, most doctors don't take real vacation. Over 70% of doctors surveyed said they worked on a typical vacation day.
"I have heard physicians refer to PTO as 'pretend time off,'" Sinsky says, referring to the acronym for "paid time off."
Sinsky and co-authors found that physicians who took more than three weeks of vacation a year had lower rates of burnout than those who took less, since vacation time is linked to well-being and job satisfaction .
And all those doctors toiling away on vacation, sitting poolside with their laptops? Sinsky argues it has serious consequences for health care.
Physician burnout is linked to high job turnover and excess health care costs , among other problems.
Still, it can be hard to change the culture of workaholism in medicine. Even the study authors confessed that they, too, worked on vacation.
"I remember when one of our first well-being papers was published," says Dr. Colin West , a co-author of the new study and a health care workforce researcher at the Mayo Clinic. "I responded to the revisions up at the family cabin in northern Minnesota on vacation."
Sinsky agreed. "I do not take all my vacation, which I recognize as a delicious irony of the whole thing," she says.
She's the American Medical Association's vice president of professional satisfaction. If she can't take a real vacation, is there any hope for the rest of us?
I interviewed a half dozen fellow physicians and chatted off the record with many friends and colleagues to get a sense of why it feels so hard to give ourselves a break. Here, I offer a few theories about why doctors are so terrible at taking time off.
We don't want to make more work for our colleagues
The authors of the study in JAMA Network Open didn't explore exactly what type of work doctors did on vacation, but the physicians I spoke to had some ideas.
"If I am not doing anything, I will triage my email a little bit," says Jocelyn Fitzgerald , a urogynecologist at the University of Pittsburgh who was not involved in the study. "I also find that certain high-priority virtual meetings sometimes find their way into my vacations."
Even if doctors aren't scheduled to see patients, there's almost always plenty of work to be done: dealing with emergencies, medication refills, paperwork. For many of us, the electronic medical record (EMR) is an unrelenting taskmaster , delivering a near-constant flow of bureaucratic to-dos.
When I go on vacation, my fellow primary care doctors handle that work for me, and I do the same for them.
But it can sometimes feel like a lot to ask, especially when colleagues are doing that work on top of their normal workload.
"You end up putting people in kind of a sticky situation, asking for favors, and they [feel they] need to pay it back," says Jay-Sheree Allen , a family physician and fellow in preventive medicine at the Mayo Clinic.
She says her practice has a "doctor of the day" who covers all urgent calls and messages, which helps reduce some of the guilt she feels about taking time off.
Still, non-urgent tasks are left for her to complete when she gets back. She says she usually logs in to the EMR when she's on vacation so the tasks don't pile up upon her return. If she doesn't, Allen estimates there will be about eight hours of paperwork awaiting her after a week or so of vacation.
"My strategy, I absolutely do not recommend," Allen says. But "I would prefer that than coming back to the total storm."
We have too little flexibility about when we take vacation
Lawren Wooten , a resident physician in pediatrics at the University of California San Francisco, says she takes 100% of her vacation time. But there are a lot of stipulations about exactly how she uses it.
She has to take it in two-week blocks — "that's a long time at once," she says — and it's hard to change the schedule once her chief residents assign her dates.
"Sometimes I wish I had vacation in the middle of two really emotionally challenging rotations like an ICU rotation and an oncology rotation," she says, referring to the intensive care unit. "We don't really get to control our schedules at this point in our careers."
Once Wooten finishes residency and becomes an attending physician, it's likely she'll have more autonomy over her vacation time — but not necessarily all that much more.
"We generally have to know when our vacations are far in advance because patients schedule with us far in advance," says Fitzgerald, the gynecologist.
Taking vacation means giving up potential pay
Many physicians are paid based on the number of patients they see or procedures they complete. If they take time off work, they make less money.
"Vacation is money off your table," says West, the physician well-being researcher. "People have a hard time stepping off of the treadmill."
A 2022 research brief from the American Medical Association estimated that over 55% of U.S. physicians were paid at least in part based on "productivity," as opposed to earning a flat amount regardless of patient volume. That means the more patients doctors cram into their schedules, the more money they make. Going on vacation could decrease their take-home pay.
But West says it's important to weigh the financial benefits of skipping vacation against the risk of burnout from working too much.
Physician burnout is linked not only to excess health care costs but also to higher rates of medical errors. In one large survey of American surgeons , for example, surgeons experiencing burnout were more likely to report being involved in a major medical error. (It's unclear to what extent the burnout caused the errors or the errors caused the burnout, however.)
Doctors think they're the only one who can do their jobs
When I go on vacation, my colleagues see my patients for me. I work in a small office, so I know the other doctors well and I trust that my patients are in good hands when I'm away.

Doctors have their own diagnosis: 'Moral distress' from an inhumane health system
But ceding that control to colleagues might be difficult for some doctors, especially when it comes to challenging patients or big research projects.
"I think we need to learn to be better at trusting our colleagues," says Adi Shah , an infectious disease doctor at the Mayo Clinic. "You don't have to micromanage every slide on the PowerPoint — it's OK."
West, the well-being researcher, says health care is moving toward a team-based model and away from a culture where an individual doctor is responsible for everything. Still, he adds, it can be hard for some doctors to accept help.
"You can be a neurosurgeon, you're supposed to go on vacation tomorrow and you operate on a patient. And there are complications or risk of complications, and you're the one who has the relationship with that family," West says. "It is really, really hard for us to say ... 'You're in great hands with the rest of my team.'"
What doctors need, says West, is "a little bit less of the God complex."
We don't have any interests other than medicine
Shah, the infectious disease doctor, frequently posts tongue-in-cheek memes on X (formerly known as Twitter) about the culture of medicine. Unplugging during vacation is one of his favorite topics, despite his struggles to follow his own advice.
His recommendation to doctors is to get a hobby, so we can find something better to do than work all the time.
"Stop taking yourself too seriously," he says. Shah argues that medical training is so busy that many physicians neglect to develop any interests other than medicine. When fully trained doctors are finally finished with their education, he says, they're at a loss for what to do with their newfound freedom.
Since completing his training a few years ago, Shah has committed himself to new hobbies, such as salsa dancing. He has plans to go to a kite festival next year.
Shah has also prioritized making the long trip from Minnesota to see his family in India at least twice a year — a journey that requires significant time off work. He has a trip there planned this month.
"This is the first time in 11 years I'm making it to India in summer so that I can have a mango in May," the peak season for the fruit, Shah says.
Wooten, the pediatrician, agrees. She works hard to develop a full life outside her career.
"Throughout our secondary and medical education, I believe we've really been indoctrinated into putting institutions above ourselves," Wooten adds. "It takes work to overcome that."
Mara Gordon is a family physician in Camden, N.J., and a contributor to NPR. She's on X as @MaraGordonMD .
- American Medical Association

IMAGES
VIDEO
COMMENTS
Ang sakit sa coronavirus 2019 o coronavirus disease 2019 (COVID-19) na dating kilala bilang 2019-nCoV acute respiratory disease, ay isang nakahahawang sakit dulot ng SARS-CoV-2, isang birus na may kaugnayan sa SARS-CoV. Naitala ang mga unang kaso nito sa Wuhan, kabisera ng lalawigan ng Hubei, sa Tsina noong Disyembre 2019, at mula noon ay kumalat sa buong mundo, na humantong sa nagpapatuloy na ...
Getting Through the COVID-19 Pandemic: Responses of Vendors, Drivers, and Residents of Pook Malinis, UP Diliman Alli eB. Bawagan, PhD Rose Angelie M. Hernandez Celeste F. Vallejos Abstrak Malinaw na ang epekto ng pandemya dala ng COVID-19 ay dama sa halos lahat ng bansa sa buong mundo, sa halos lahat ng sektor at pamayanan.
Pagsapit ng Abril 16, 2021, naiugnay ang kamatayan ng halos 2,990,000 [7] sa COVID-19. Sa Tsina, pagsapit ng ika-5 ng Pebrero, halos 80 porsiyento ng kamatayan ay naitala sa mga nakatatanda sa 60, at 75 porsiyento nito ay nagkaroon ng datihang kondisyon sa kalusugan na kinabibilangan ng mga sakit sa puso at diabetes. [365] Ang unang ...
Ang coronavirus disease (COVID-19) ay isang nakahahawang sakit na dulot ng bagong coronavirus. Karamihan sa mga taong magkakaroon ng impeksyon ay makararanas ng hindi malalang sintomas at gagaling. Ngunit ang iba ay makararanas ng malubhang sakit, lalo na sa mga matatanda at mga may dati nang karamdaman. Narito ang ilang mga simpleng hakbang na maaari mong gawin upang maprotektahan ang ...
Kinumpirma ang pagkalat ng pandemya ng COVID-19, isang bagong nakakahawang sakit na sanhi ng SARS-CoV-2 Theta variant, sa Pilipinas noong Enero 31, 2020, kung kailan nakumpirma ang unang kaso ng COVID-19 sa Kamaynilaan—isang Tsina na 38 taong gulang named na naipasok sa Ospital ng San Lazaro sa Maynila.Nakumpirma ang ikalawang kaso noong Pebrero 2, na isang 44 taong gulang na Tsino na ...
Kinumpirma ang pagkalat ng pandemya ng COVID-19, isang bagong nakakahawang sakit na sanhi ng SARS-CoV-2 Theta variant, sa Pilipinas noong Enero 31, 2020, kung kailan nakumpirma ang unang kaso ng COVID-19 sa Kamaynilaan—isang Tsina na 38 taong gulang named na naipasok sa Ospital ng San Lazaro sa Maynila. Nakumpirma ang ikalawang kaso noong Pebrero 2, na isang 44 taong gulang na Tsino na ...
Halimbawa: "Bago natin pag-usapan iyan, gusto kong talakayin ang tungkol sa kung ano ang sinabi mo sa virus na kasalanan ng ibang tao.". Magtanong: Tumutulong ang mga tanong sa pag-unawa. Ang pagtatanong sa mga tao kung bakit nila ginawa ang isang pahayag ay makatutulong sa iba na huminto upang hamunin ang mga ideyang nakasasama ng loob.
nagiging sanhi ng malalang sakit sa baga o paghinga/respiratoryo (SARS). Madalas maging sintomas. ng mga viral infections na ganito ang pagkakaroon ng mataas na init sa katawan, pagkakasakit ng. katawan, sore throat, malalang pagsipon at pagubo. Sa halos lahat ng kaso, tumatagal ito ng ilang.
Tindi ng sakit ng COVID-19. Karamihan sa mga taong may impeksyon ng COVID-19 ay magkakaranas lamang ng hindi malalang sintomas at ganap na gagaling. Ngunit may ilang tao na mas maapektuhan ng sakit. Lahat tayo ay may papel na ginagampanan upang maprotektahan ang ating sarili at ang iba. Alamin ang mga katotohanan tungkol sa COVID-19 at tulungan ...
Kung kailangan mo ng tulong sa pagkontak ng NDIS, mangyaring tawagan ang Translating and Interpreting Service (Serbisyo sa Pagsasalin at Pag-iinterpret) sa 131 450. Ang Coronavirus (COVID-19) at ang NDIS (PDF 115KB) Ang Coronavirus (COVID-19) at ang NDIS (DOCX 41KB) Ang "Mababang halagang Teknolohiyang Pantulong sa panahon ng COVID-19 ...
In this paper, I explore the intersections and particular forms of precarity, migration, and emotion, that are lived by overseas Filipino workers during the COVID-19 pandemic. Other scholars have also begun examining these intersections in light of the recent deluge of global-scale catastrophes. For example, Katharina Wuropulos (2020, p.
Emboltura's winning piece is titled, "A Thief, A Tyrant, A Teacher". In his essay, Emboltura, editor-in-chief of PSHS-WVC's school paper Banaag, discussed how the COVID-19 pandemic significantly redefined aspects of life. This year's theme of the SEAMEO TROPMED essay writing contest is "What COVID-19 means to me".
Covid-19 infections in the Philippines have reached 1,149,925 cases as of May 17. The pandemic is unfolding simultaneously with the growing number of Filipinos suffering from mental health issues. At least 3.6 million Filipinos suffer from mental, neurological, and substance use disorders, according to Frances Prescila Cuevas, head of the ...
Delta variant puts Philippine economy among most vulnerable in Asia. COVID-19 pandemic to cost PH P41.4 trillion over next 4 decades - NEDA. Philippine GDP growth slows but beats forecasts at 7. ...
This article explores the concept of suffering as experienced by Filipinos during the COVID-19 pandemic. It draws inspiration from their narratives about how they faced, managed, and struggled during this tragic event. Their experiences were interpreted and analyzed concerning Filipino culture and tradition using a modified form of thematic ...
Filipinos helping Fellow Filipinos. As COVID-19 strikes the Philippine nation, people rise together to counter it. At the forefront of the fight against the virus are our healthcare workers and various frontliners. Daily, they face the hazard of infection with their mantra: "We go to work for you.
Abstract. In this essay, we engage with the call for Extraordinary Issue: Coronavirus, Crisis and Communication. Situated in the Philippines, we reflect on how COVID-19 has made visible the often-overlooked relationship between journalism and public health. In covering the pandemic, journalists struggle with the shrinking space for press ...
Introduction. The World Health Organization (WHO) declared the Coronavirus 2019 (COVID-19) outbreak as a global pandemic, and the Philippines is one of the 213 countries affected by the disease [].To reduce the virus's transmission, the President imposed an enhanced community quarantine in Luzon, the country's northern and most populous island, on March 16, 2020.
First, it documents work attitudes during crisis situations (like the COVID-19 pandemic) in relation to a broad range of work-related issues such as how work is done (e.g., shifts to telecommuting, increased reliance on technology), job outcomes (e.g., feelings of stress), and employee coping behaviors.
Research documents Filipino panic responses to the global pandemic. A recent study explored panic responses to COVID-19 in the Philippines. COVID-19 has been declared a global pandemic and has ...
The 30-year-old writer is just one of many Filipinos experiencing the mental health fallout of the pandemic. COVID-19 infections in the Philippines have reached 1,149,925 cases as of May 17. The ...
Reading time: 3 min (864 words) The COVID-19 pandemic has led to a dramatic loss of human life worldwide and presents an unprecedented challenge to public health, food systems and the world of work. The economic and social disruption caused by the pandemic is devastating: tens of millions of people are at risk of falling into extreme poverty ...
Hundreds of millions of babies are expected to be born during the COVID-19 pandemic. Fionn, son of Chloe O'Doherty and her husband Patrick, is among them. The couple says: "It's all over. We did ...
In January 2021, President Biden issued the "National Strategy for the COVID-19 Response and Pandemic Preparedness." As the US moves from crisis to control, this national strategy needs to be updated. Policy makers need to specify the goals and strategies for the "new normal" of life with COVID-19 and communicate them clearly to the public.
Introduction. The COVID-19 pandemic affected the global economy just as much as the public health domain. However, most economies were able to recover significantly due to efficient policy responses.
Read More: Why Americans Are Uniquely Afraid to Grow Old Prior to the COVID-19, 1 in 10 elderly adults in the U.S. experienced elder abuse. A major review in 2017 of 52 studies from 28 nations ...
Pandemic burnout is getting in the way Researchers surveyed 3,024 doctors, part of an American Medical Association cohort designed to represent the American physician workforce.