

By Audience
- Therapist Toolbox
- Teacher Toolbox
- Parent Toolbox
- Explore All
By Category
- Organization
- Impulse Control
- When Executive Function Skills Impair Handwriting
- Executive Functioning in School
- Executive Functioning Skills- Teach Planning and Prioritization
- Adults With Executive Function Disorder
- How to Teach Foresight
- Bilateral Coordination
- Hand Strengthening Activities
- What is Finger Isolation?
- Occupational Therapy at Home
- Fine Motor Skills Needed at School
- What are Fine Motor Skills
- Fine Motor Activities to Improve Open Thumb Web Space
- Indoor Toddler Activities
- Outdoor Play
- Self-Dressing
- Best Shoe Tying Tips
- Potty Training
- Cooking With Kids
- Scissor Skills
- Line Awareness
- Spatial Awareness
- Size Awareness
- Pencil Control
- Pencil Grasp
- Letter Formation
- Proprioception
- How to Create a Sensory Diet
- Visual Perception
- Eye-Hand Coordination
- How Vision Problems Affect Learning
- Vision Activities for Kids
- What is Visual Attention?
- Activities to Improve Smooth Visual Pursuits
- What is Visual Scanning
- Classroom Accommodations for Visual Impairments
Visual Noise and Learning
- Free Resources
- Members Club
Executive Function
So, what exactly is executive function, explore popular topics.
What do all these words mean?
Executive Functioning Skills guide everything we do. From making decisions, to staying on track with an activity, to planning and prioritizing a task . The ability to make a decision, plan it out, and act on it without being distracted is what allows us to accomplish the most mundane of tasks to the more complicated and multi-step actions. Children with executive functioning issues will suffer in a multitude of ways. Some kids have many deficits in EF and others fall behind in several or all areas. Everyone needs to develop and build executive functions as they grow. Functional adults may still be struggling with aspects of executive functioning skills. Executive dysfunction can interfere with independence and the ability to perform activities. The cognitive skills are an interconnected web of processing that allows for self-regulation, planning, organization, and memory.
Executive Functioning Skills
As a related resource, try these self-reflection activities for kids .
What are executive functions?
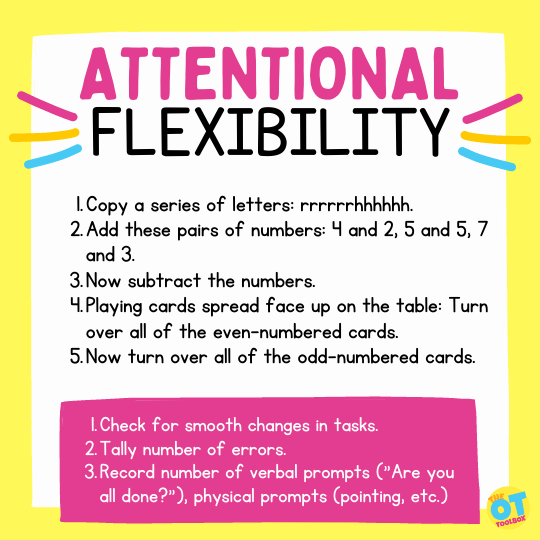
Executive functioning skills:, cognitive flexibility.
- Check for smooth changes in tasks.
- Tally number of errors.
- Record number of verbal prompts (“Are you all done?”), physical prompts (pointing, etc.)
Executive function and handwriting
How to build executive function skills:
Top executive function blog posts.

- Executive Functioning Skills , Free Resources
Tools to Stop to Think
- Attention , Executive Functioning Skills , Occupational Therapy Activities , Sensory
Self-Reflection Activities
- Executive Functioning Skills , Free Resources , Occupational Therapy
Drawing Mind Maps
- Executive Functioning Skills , Functional Skills , Occupational Therapy Activities
Executive Function Coaching
- Executive Functioning Skills , Free Resources , Mental Health , Occupational Therapy
The Power of Yet
Breaking Down Goals
- Attention , Executive Functioning Skills , Occupational Therapy
Executive Function Tests

- Attention , Development , Executive Functioning Skills , Occupational Therapy
Spring Activities for Executive Functioning
Executive function in products.

How-to Life Sequences Made Easy – Cut & Paste
Fix the Mistakes-Fun Themes Bundle

Task Completion Cards (5 Theme Bundle)
Play Dough Board Games-Full Year
Free Executive Function Resources
Coin Activities for Kids
How to Support Sensory Needs in the Cafeteria
What is Overstimulation Anxiety?

Sensory Tooth Brushing Tips for Brushing Teeth
Explore more tools, fine motor skills, functioning skills, handwriting, quick links, sign up for the ot toolbox newsletter.
Get the latest tools and resources sent right to your inbox!
Get Connected

- Want to read the website AD-FREE?
- Want to access all of our downloads in one place?
- Want done for you therapy tools and materials
Join The OT Toolbox Member’s Club!

Functional Cognition and OT: Our Time to Shine
One of things I love most about being an occupational therapist is the huge diversity in our scope of practice . Bridging the gap between physical therapy and speech pathology, occupational therapy practitioners truly get the best of both worlds. We are able to dip our hands into orthopedic conditions as well as cognitive impairments (via neuro rehab).
While we typically consider speech therapists the cognitive and language experts, occupational therapists do play a big part in cognitive therapy. Functional cognition relates to the cognitive skills required to complete those meaningful daily activities that we all know so well.
So What Do These Self-Care Tasks Include?
For OTs, these instrumental ADLs (or IADLs) include tasks such as online shopping or planning a weekly menu and grocery list. Treatment for functional cognition is truly a place for OTs to let our creativity shine. You probably have endless books with cognitive worksheets for patients to complete. But I would suggest ditching those for a bit, and bring it all back to our roots (aka: function ).
Think outside the box – I bet you can create some awesome activities or “worksheets” that are much more realistic and applicable to everyday life.
Everyday tasks don’t require just one cognitive component. We use memory, attention, problem solving, etc., cohesively to complete necessary tasks. So let’s think about the wide assortment of tasks we complete every day as adults.
Of course, some of these tasks will vary depending on the age range of your patients. Patients who are still working or have children will have different responsibilities, and thus a different set of IADLs, than those who are retired or are living in independent living/assisted living communities.
OTs are typically most attuned to two cognitively-related IADLs: paying bills and medication management. But adults obviously have so many more responsibilities, so why does our toolbox stop there?
As a parent, I can think about what I am responsible for and use that as a basis for forming challenging tasks for my patients.
- Make a weekly meal plan and coordinated grocery list
- Schedule my son’s before and after school sessions
- Make doctor’s appointments and write them on our family calendar
- Write checks to daycare
- Pay lunch money online
- Plan out a gift list for Christmas
- Manage the spending for each of my kids and nieces or nephews
- Figure out how long it will take me to get to various stores or offices using my phone map
- Plan vacations and date nights
The list goes on! We are all responsible for so many daily tasks.. And so are our patients. So get out there and find out what they personally need to do to help them live life to their fullest potential.
Functional Cognition and Mealtime
Planning a weekly meal schedule is such a common and necessary task, and one that can change each week since we typically don’t eat the same things over and over!
Have your patient write out a week’s worth of basic dinners, and under each item include the required ingredients. They can use that list as their shopping list, or combine ingredients if the meals match up well.

Prior to shopping for ingredients, have them look through a local grocery store’s ads to find items on sale that might correspond to their list. Did they choose ordering pizza one night? Locate the pizza restaurant of their choice on their phone and identify what they want to order.
If you are working with someone experiencing aphasia or even processing difficulties, consider simulating a call to the restaurant with you providing the prompts for ordering delivery, which includes asking for their phone number, what they would like to order, how they will pay, and their address.
Scheduling and Timing Appointments
We probably all have used calendar tasks with patients, having them organize a series of events onto specific calendar dates. But simply writing appointments down on a calendar does not cover the entire task requirement. We can work on functional math when determining when to leave home for appointments depending on how early we need to be there.
For example, if you made a doctor appointment for 1:15 pm and the office is 15 minutes away from your house, how early should you leave to arrive 10 minutes early? Rather than simply work on writing a patient’s name, address, and phone number correctly on a blank piece of paper, simulate this requirement in a real-life situation – have them fill out a doctor office new patient form.
Money Management
Managing money does not have to end at paying bills and balancing your checking accounts. As shopping online is so prevalent these days, it is a necessary addition to your intervention activities. Start with a designated task, such as planning a birthday party.
Involve all aspects of organizing the party, writing down whom to invite, food/snacks to be served, supplies needed, etc. Use the list to shop for supplies online and find a bakery that is close to their house (using their phone’s Map app) so that they can order a cake. Search for supplies on Amazon and write down the cost of each item.
Downgrade the task by providing a pre-fabricated list of supplies (rather than having them independently create one), and direct them to choose items that are most appropriate and required for a birthday party. Simulate a call to the bakery and take their cake order.
Have them calculate the total cost of the birthday party supplies and food (or separate these depending on how you grade the task).

You can use the same method for any entertainment activity and create varying challenges: going to the movies, planning a day out with a child or grandchild, or creating an estimated budget for a Christmas gift list.
Creating Your Own Scenarios
I seem to be making a case for task-specific simulation in intervention. We do this constantly with ADL practice, so why not up the ante on how we address functional cognition and use the same practice? With some spare time you can create your own scenarios, and you may enjoy doing it!
The University of Utah’s College of Health has a great resource for OT therapeutic activities that includes online bill paying (including utilities and credit cards) as well as a new online shopping activity – check this out to get you started.
Otherwise, have fun! Enjoy flexing your creative muscles and coming up with a product you can be proud of.
How do you like to incorporate functional cognition in your OT interventions? Please share your favorite functional cognition intervention tips and ideas in the comments below.
And for even more about working in neuro occupational therapy in general, you can also check out Renee’s Day in the Life as an Outpatient Neuro Occupational Therapist here .
This post was originally published on April 6, 2020 and last updated on February 26, 2024.
You may also like

Alternative Career Paths for Occupational Therapists

Top Occupational Therapy Volunteer Opportunities

Successfully Negotiate Your OT Job Offer
Leave a comment cancel reply.
Your comment *
This site uses Akismet to reduce spam. Learn how your comment data is processed .
Privacy Overview

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
7 Cognition Assessment and Intervention
Gabe Byars, OTR/L; Melanie Jacobs, OTAS; and Adrianne Monson, OTAS
Cognition is the process by which our sensory input is transformed, reduced, elaborated, stored, recorded, and used. It is our capacity to take in, organize, assimilate, and integrate new information with previous experience. Cognition allows us to adapt to environmental demands by using previously acquired information to plan and structure behavior to attain our goals. This chapter discusses how you the occupational therapist can make cognition assessments and design interventions.
In the Domain and Process and Physical Dysfunction Lecture, you learned about different cognition aspects. We discussed awareness, attention, memory, and executive function. The assessments that we talk about here are MoCA and Medi-Cog, which will help you tease out deficits in these different cognitive areas. Then, you will have an opportunity to practice designing interventions for individuals with different cognitive deficits.
This video discusses how to screen and treat clients with cognitive deficits.
Video is licensed under CC BY 4.0 .
Cognition Video Transcript
Cognitive Screenings Tips
The role of cognitive screenings is to gain a better understanding of your client’s cognitive strengths and deficits. We will practice two cognitive screenings: the Montreal Cognitive Assessment (MoCA) and the Medi-Cog. Also, you’ll find more functional cognitive assessments at https://multicontext.net/treatment-and-assessment-links-2 .
- MoCA is a screening tool designed to detect mild cognitive impairment.
- This screening tool uses 16 items that assess different cognitive domains: visuo-spatial, executive function, naming, memory, attention, language, abstraction and orientation.
- Scores range from 0-30. Scores lower than 26 indicate cognitive impairment concerns.
- https://www.mocatest.org/
- Medi-Cog is a screening tool designed to measure functional cognition.
- This screening tool uses a three-item recall, a clock drawing, and a medication transfer screening.
- There are 10 possible points in Medi-Cog. A score of 7 or lower indicates cognitive impairment concerns.
- https://www.pharmacy.umaryland.edu/media/SOP/medmanagementumarylandedu/MediCogPresentation.pdf
Cognitive Interventions Tips
Once a cognitive deficit is observed, the occupational therapy practitioner can treat with components, skills, and strategies
- Caution: There is limited evidence that treating components improves occupational performance.
- Example: Use memory games to treat components, such as Spot It.
- Example: Practice performing medication management repeatedly until the client can perform it successfully.
- Example: Teach the Goal-Plan-Do-Check problem solving strategy.
- Functional Cognition and OT: Our Time to Shine by Renee Leuschke, OTR/L
- Multicontext by Joan Toglia, Ph.D, OTR/L, FAOTA
Occupational Therapy Skills for Physical Dysfunction Copyright © 2023 by Gabe Byars, OTR/L; Melanie Jacobs, OTAS; and Adrianne Monson, OTAS is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License , except where otherwise noted.
Share This Book
Problem Solving: A Teaching and Therapeutic Tool for Older Adults and Their Families
- First Online: 26 November 2014
Cite this chapter
- Laura N. Gitlin 2
11k Accesses
Problem solving is integral to clinical reasoning and everyday occupational therapy practices. It can also be a systematic therapeutic modality for identifying client or family caregiver concerns and teaching new approaches to self-management. This chapter presents a systematic approach to help occupational therapists (OTs) identify target problem areas and potential modifiable contributing factors when working with older adults and families. The approach is applicable to a broad range of clinical problems associated with the consequences and management of chronic illness and provides therapists with an important tool for actively engaging clients in self-management.
The OT needs to have effective communication skills, respecting a family’s values and understanding where they’re coming from.… That’s critical, even more than knowing her intervention strategies.Family caregiver
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Bandura A (1986) Social foundations of thought and action: a social cognitive theory. Prentice-Hall, Englewood Cliffs
Google Scholar
Belle SH, Burgio L, Burns R et al (2006) Enhancing the quality of life of Hispanic/Latino, Black/African American, and White/Caucasian dementia caregivers: the REACH II randomized controlled trial. Ann Intern Med 145:727–738
Article PubMed Central PubMed Google Scholar
Bodenheimer T, Lorig K, Homan H, Grumbach K (2002) Patient self-management of chronic disease in primary care. JAMA 288:2469–2475
Article PubMed Google Scholar
Chee Y, Gitlin LN, Dennis MP, Hauck WW (2007) Predictors of caregiver adherence to a skill-building intervention among dementia caregivers. J Gerontol Med Sci 62(6):673–678
Article Google Scholar
Chodosh J, Morton SC, Mojica W et al (2005) Meta-analysis: chronic disease self-management programs for older adults. Ann Intern Med 143(6):427–438
Cuijpers P, van Straten A, Warmerdam L (2007) Problem solving therapies for depression: a meta-analysis. Eur Psychiatry 22:9–15
Farrell K, Wicks MN, Martin JC (2004) Chronic disease self-management improved with enhanced self-efficacy. Clin Nurs Res 13(4):289–308
Gellis ZD, Kenaley B (2008) Problem-solving therapy for depression in adults: a systematic review. Res Social Work Pract 18:117–131
Gitlin LN, Rose K (2013) Factors associated with caregiver readiness to use nonpharmacologic strategies to manage dementia-related behavioral symptoms. Int J Geriatr Psychiatry. Published online on May 7, 2013. doi:10.1002/gps.3979
Gitlin LN, Winter L, Corcoran M, Dennis M, Schinfeld S, Hauck W (2003) Effects of the home environmental skill-building program on the caregiver-care recipient dyad: six-month outcomes from the Philadelphia REACH initiative. Gerontologist 43(4):532–546
Gitlin LN, Winter L, Dennis M, Corcoran M, Schinfeld S, Hauck W (2006) A randomized trial of a multi-component home intervention to reduce functional difficulties in older adults. J Am Geriatr Soc 54:809–816
Gitlin LN, Chernett NL, Harris LF, Palmer D, Hopkins P, Dennis M (2008) Harvest health: translation of the chronic disease self-management program for older African Americans in a senior setting. Gerontol Pract Concepts 48:698–705
Gitlin LN, Winter L, Dennis MP, Hodgson N, Hauck W (2010) Targeting and managing behavioral symptoms in individuals with dementia: a randomized trial of a nonpharmacological intervention. J Am Geriatr Soc 58(6):1465–1474
Gitlin LN, Kales HC, Lyketsos CG (2012) Nonpharmacologic management of behavioral symptoms in dementia. JAMA 308(19):2020–2029
Article PubMed Central CAS PubMed Google Scholar
Hibbard JH, Stockard J, Mahoney ER, Tusler M (2004) Development of the patient activation measure (PAM): conceptualizing and measuring activation in patient and consumers. Health Serv Res 39:1005–1026
Kales HC, Gitlin LN, Lyketsos CG, for the Detroit Expert Panel on the Assessment and Management of the Neuropsychiatric Symptoms of Dementia (2014) Management of neuropsychiatric symptoms of dementia in clinical settings: recommendations from a multidisciplinary expert panel. J Am Geriatr Soc 62(4):762–769
Lorig KR, Sobel DS, Ritter PL, Laurent D, Hobbs M (2001) Effect of a self-management program on patients with chronic disease. Effect Clin Pract 4(6):256–262
CAS Google Scholar
Prochaska JO, Velicer WF (1997) The transtheoretical model of health behavior change. Am J Health Prom 12:38–48
Article CAS Google Scholar
Reuben DB (2007) Better care for older people with chronic diseases: an emerging vision. JAMA 298(22):2673–2674
Article CAS PubMed Google Scholar
Richards KC, Enderlin CA, Beck C, McSweeney JC, Jones TC, Roberson PK (2007) Tailored biobehavioral interventions: a literature review and synthesis. Res Theory Nurs Pract 21:271–285
Rose K, Gitlin LN, Dennis MP (2010) Readiness to use compensatory strategies among older adults with functional difficulties. Int Psychogeriatr, special issue on prevention. doi:10.1017/S1041610210001584
Schulz R, Burgio L, Burns R et al (2003) Resources for enhancing Alzheimer’s caregiver health (REACH): overview, site-specific outcomes, and future directions. Gerontologist 43(4):514–520
Szanton SL, Thorpe RJ, Boyd C, Tanner E/K, Leff B, Agree E, Xue Q, Allen JK, Seplaki C, Weiss C, Guralnik JM, Gitlin LN (2011) An innovative bio-behavioral intervention to improve functional status and quality of life of low-income disabled older adults: findings from the CAPABLE pilot study. J Am Geriatr Soc 59(12):2314–2320
Download references
Author information
Authors and affiliations.
Department of Community-Public Health, Center for Innovative Care in Aging, Johns Hopkins University, 525 N. Wolfe Street, Suite 316, Baltimore, MD, 21205, USA
Laura N. Gitlin
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Laura N. Gitlin .
Editor information
Editors and affiliations.
Karolinska Institute Associate Professor, Stockholm Sweden, Nacka, Sweden
Ingrid Söderback
The Case Study of Using Problem Solving for Marie, Living with Alzheimer’s Disease and her daughter Donna
Keywords: Behavioral symptoms, Caregiver burden, Caregiving, Problem solving
Introduction
The theme of this case study concerns family challenges associated with caring for a person with moderate stage dementia and the use of problem solving to identify discrete problem areas and potential solutions.
The students’ tasks include:
To determine strategies to help Donna manage her mother’s behavioral symptoms and to also be able to take better care of herself.
To work with Donna to identify underlying patterns and mutable factors that may be contributing to her mother’s behaviors.
To apply problem solving to come up with a set of strategies Donna agrees to try.
As a starting point, students should use the following references to gather background information.
Important references are:
Gitlin LN, Hodgson N (in press) Caregivers as therapeutic agents in dementia care: The evidence-base for interventions supporting their role. In: Gauglher J and Kane R (eds) Family Caregiving in the New Normal, Elsevier
Gitlin LN (2011) Problem solving in health and illness. In: Craft-Rosenberg M, Pehier S (eds) Encyclopedia of family health, Sage
Gitlin LN (in press) Problem solving: a teaching and therapeutic tool for older adults and family members. In: Söderback I (ed) International handbook of occupational therapy interventions, 2nd edn. Springer, New York, pp 205–216
Overview of the Content
Major goal of the actual interventions are to
Enable the caregiver to prevent, minimize, or reduce behavioral symptoms of her mother
Enhance the mother and the caregiver’s quality of life
Enable the caregiver to find time for herself
Learning Objectives
By the end of studying this chapter the learner will:
Understand how to apply problem solving with families caring for persons with dementia
Identify potential strategies (behavioral, environmental) that can minimize behavioral symptoms
Examine the interactions of persons with dementia, their care environment, and impact on families
The Background History of Mary and Her family
Personal information.
Marie is an 80-year-old female diagnosed with Alzheimer’s disease 4 years ago. She lives with her daughter, Donna, and her daughter’s husband and two teenage sons in a ranch house in a suburban area. Marie has her own bedroom, sitting room, bathroom, and kitchenette in an “in law” suite attached to the family home. Marie was a full-time wife and homemaker who never worked outside the home. Her husband passed away in 2000, and she came to live with Donna a year later as she was having difficulty keeping up with her finances, shopping, and other basic tasks of daily living.
Marie prided herself on her homemaking skills. She was a great cook and loved to bake. She enjoyed knitting and was an active community volunteer first with the children’s school and later (as they grew older) with her local church. She stopped driving her car right after her diagnosis, as she was afraid to drive.
Marie’s daughter reports that she appears to be easily agitated, highly anxious, and keeps repeating the same questions over and over with her (e.g., where are you going? When are we eating?). She has been resisting going out of the house for family dinners at the local restaurant or to attend church. She tends to become anxious and fearful when it is time to leave the house for anything (appointments, outings, etc.).
Donna is finding it increasingly difficult caring for her mother and attending to her other responsibilities including a part time job in her local school system, being there for her two sons and husband, attending to her household responsibilities, and taking care of herself. She is feeling very stretched and indicated she is having difficulty sleeping, feels very tired and alone, and feels very sad everyday to see her mom the way she is now. Donna wants help but is reluctant to ask anyone else to help her with her mom. She also can be a perfectionist and wants things done a certain way in her home.
Medical Diagnoses and Prognoses
Marie has dementia , most likely of the Alzheimer’s type. She is in the moderate stage of the disease, which is a progressively degenerative disease process. Her short-term memory is poor and she is having increasing difficulty initiating, planning, and organizing activities she used to do (e.g., cook a meal) demonstrating executive functional challenges. She continues to have some insight, although limited, of her cognitive changes. She is becoming increasingly agitated and confused as she loses her cognitive abilities. She is in relatively good physical condition with no other chronic conditions. Her vision is good with glasses but she is experiencing some hearing loss although she does not wear a hearing aid. While her ambulation in general is good, she did fall 6 months ago—she tripped over the carpet and fell to the ground. She was bruised but no bones were broken.
Reason for Seeking Occupational Therapy
Marie is experiencing behavioral symptoms, which prompted her physician to be concerned about her home safety and daily function. She suggested occupational therapy to assess Marie’s safety at home and to work with the caregiver to teach her behavioral management skills.

Occupational Performance Issues
Marie used to cook but is having difficulty knowing what to do in the kitchen. This frustrates her. She is also having increasing difficulty dressing and bathing herself, but she does not want any help from her daughter. She is starting to look a little raggedy which is not like her previous self.
The Student’s Report
The following guiding questions have been identified in developing possible solutions for Marie and Donna. These questions are generated from the available literature references and our clinical experiences:
What specific questions would you ask the caregiver to learn about her mother’s presenting behaviors?
What would you like to learn about Marie’s day?
What would you like to learn about the relationship of Donna and her mother?
What aspects of the physical and social environment would you want to learn about and/or for which you may have potential concerns?
Rights and permissions
Reprints and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Gitlin, L. (2015). Problem Solving: A Teaching and Therapeutic Tool for Older Adults and Their Families. In: Söderback, I. (eds) International Handbook of Occupational Therapy Interventions. Springer, Cham. https://doi.org/10.1007/978-3-319-08141-0_27
Download citation
DOI : https://doi.org/10.1007/978-3-319-08141-0_27
Published : 26 November 2014
Publisher Name : Springer, Cham
Print ISBN : 978-3-319-08140-3
Online ISBN : 978-3-319-08141-0
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Copyright © 2024 OccupationalTherapy.com - All Rights Reserved
Cognitive Interventions In The Home: A Practical Approach For OT Professionals
Krista covell-pierson, otr/l, bcb-pmd.
- Acute Care, Community and Home Health
- Cognition and Executive Function
- Gerontology and Aging
To earn CEUs for this article, become a member.
unlimit ed ceu access | $129/year
Editor's note: This text-based course is a transcript of the webinar, Cognitive Interventions In The Home: A Practical Approach For OT Professionals, presented by Krista Covell-Pierson, OTR/L, BCB-PMD.
Learning Outcomes
- Identify four ways an OT can integrate cognition into a treatment plan.
- List four assessments for cognition that are appropriate to use in the home setting.
- Recognize four types of memory impairments and distinguish between dementia and delirium.
Introduction
Today, we will delve into cognitive interventions in the home—a practical approach tailored for occupational therapy professionals. Our profession holds significant potential to profoundly impact individuals' lives, although, at times, it may seem challenging to grasp the full scope of our role. However, during our discussion, I aim to provide you with valuable insights that you can readily integrate into your practice.
I reside in Colorado and am the proprietor of Covell Care and Rehab, a private practice where we serve a diverse patient population. The majority of our patients contend with various cognitive impairments, an aspect of care that I find particularly rewarding. Our work extends to individuals coping with conditions such as dementia, brain injuries, mild cognitive impairment, and other cognitive-related issues.
In my 22-year career as an occupational therapist, I have come to believe that, as OTs, we can enhance our approach to addressing cognition. As we embark on a deeper exploration during this hour, I encourage you to consider how you can better assist patients facing cognitive challenges.
You might wonder why this topic is of utmost importance. Given your roles as OT practitioners, you likely recognize its significance and inherent value. However, I intend to equip you with the language and rationale to explain its importance to our patients, their families, our colleagues, supervisors, and third-party payers. Effective communication, both verbally and in written documentation, is crucial. Therefore, we will touch on various aspects of this skill.
Why Is This Important?
When defining cognition, it's essential to appreciate the multifaceted nature of the concept. Several skills interplay when we consider cognition. One definition I find particularly insightful is derived from the Dementias Platform in the United Kingdom, and it reads as follows: "Cognition is a term for the mental processes that take place in the brain, such as thinking, attention, language, learning, memory, and perception." The areas are listed below.
- Skill generalization and combination
- Functional cognition
We also know as OTs that these processes are not discrete abilities, like this gentleman in his raft (Figure 1).

Figure 1. Man in a raft in the water.
Cognitive processes are intricately interconnected, akin to floating on a raft. Our objective is to equip our patients with diverse skills that harmoniously converge, enabling them to become proficient, functioning individuals, regardless of age. Therefore, when we clarify our purpose, we must emphasize that we are not solely focused on enhancing learning or memory.
Instead, our aim is for these improvements to translate into a higher quality of life. Effective communication plays a pivotal role here. While we often discuss these individual facets, it is equally essential to view the bigger picture and recognize the invaluable role that occupational therapists bring to the table.
Patients may have previously undergone neuropsychological evaluations, cognitive screenings with physicians, or worked with speech-language pathologists. Nevertheless, we can step in and comprehensively assess the array of skills listed here, aligning them with our patients' life goals. Thus, our presence within the cognitive team is highly practical.
The research underscores that when patients receive occupational therapy tailored to address functional cognition, it significantly reduces their risk of hospitalization or re-hospitalization. This outcome is compelling and resonates with various stakeholders, including third-party payers, administrators, supervisors, and, most importantly, our patients and their families. Keeping our loved ones out of the hospital is a shared priority for all.
Cognition Impacts ADLs
- Home management
- Financial management
- Community involvement
Moving beyond discussing cognition, let's look at how cognition profoundly influences our daily activities, our routines, and, ultimately, our quality of life. While it's not groundbreaking for us to acknowledge that cognitive skills impact daily living, what sets us apart is our ability to effectively communicate how we can enhance these activities.
The tasks I've outlined here serve as simple examples that can be seamlessly integrated into our therapeutic goals to demonstrate tangible improvements in function through enhanced cognition.
Is it truly impactful if someone can recall five random words when prompted? Not really, because it lacks functionality. What genuinely matters is if someone can remember five essential steps in operating their washing machine, enabling them to independently and efficiently do their laundry. The real victory lies in achieving practical, meaningful outcomes where individuals no longer require constant caregiver assistance.
Our approach involves identifying these personally significant tasks, aligning them with the cognitive processes that require improvement, and then guiding our patients through the journey of mastering these tasks. This approach benefits our patients and facilitates clearer communication in our notes and collaboration with our peers, which we will delve into further.
ADLs at Home
Figure 2 shows an infographic showing how the person, task, and environment are interconnected.
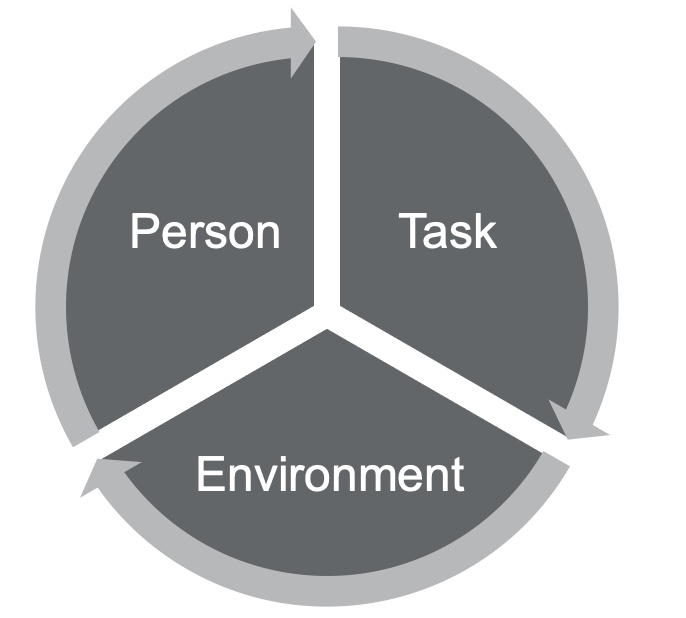
Figure 2. Person-task-environment diagram.
I frequently use diagrams like the one shown here because they align with the person-environment model, which emphasizes a holistic approach to assessing occupational performance. When working with our patients, conducting a comprehensive assessment is crucial. This assessment should encompass an examination of their skills, deficits, desires, mental and physical health, and medical needs. The goal is to develop a personal profile, recognizing that all these facets significantly impact an individual's functional cognition.
Next, we focus on identifying meaningful tasks, a process in which both the patient and their family members or caregivers play a vital role. Prioritizing tasks that resonate with the patient's motivations is imperative because intrinsic motivation is pivotal, especially when dealing with cognitive challenges. If a task isn't personally meaningful, it can be challenging to rationalize its importance, particularly for those already facing cognitive difficulties.
Additionally, it's crucial to assess how the patient perceives their skillset and compare it with our observations. Often, individuals with cognitive difficulties may overestimate their abilities. Input from loved ones and caregivers is equally valuable, as their perceptions might differ from our assessments.
A particularly rewarding aspect of our work is when we can engage with patients in their homes. This intimate setting allows us to witness their daily lives, which can be both dynamic and enlightening. Unlike a static therapy gym, homes vary, offering a unique and enjoyable challenge.
Here are two real-life examples that illustrate the diversity of environments we encounter. I had a patient who was living in a mother-in-law-type apartment above the garage. She had a huge family with members coming in and out all the time. It was distracting even for me during treatment, so I knew it was distracting for her, especially living with memory loss and cognitive fatigue related to chemotherapy treatments. I also had a patient who lived two minutes away in low-income housing. She had very limited resources and no social support system in town. Her family lived out of state, and she had no friends. She was dealing with crippling anxiety, memory loss, and decreased problem-solving skills related to years of alcohol and drug abuse. These are different people in two different environments. I can start by going into the home and looking for ideas and answers based on those environments. I can see what's meaningful to them. For example, I might see that they have a smartphone or notes next to the phone. I might see that they have their own cookbooks and like to cook. I can start using those things to make the tasks more meaningful when I'm in the environment. Working in the home setting requires flexibility and adaptability, but it's where the magic truly happens. Utilizing personal items like photographs, meaningful objects, or even the layout of their home can enhance memory recall and yield better results. Whether you're considering working in a home setting or already doing so, it's a personally rewarding endeavor. You'll find ample opportunities to connect with patients and significantly impact their lives.
Lastly, the American Occupational Therapy Association (AOTA) advocates for our role in the cognitive space. They define us as experts in measuring functional cognition, encompassing everyday task performance. Recognizing subtle cognitive impairments is crucial, as they often go untreated but can significantly impact an individual's functioning. As OTs, we treat cognitive impairments because they have the potential to compromise the safety and long-term well-being of our patients. By familiarizing yourself with AOTA's resources and language, you can strengthen your documentation and advocacy efforts, ensuring that OTs continue to play a vital role in addressing cognition and improving the lives of our patients. For additional information, refer to AOTA's resources on cognitive intervention.
Integrating Cognition Into a Treatment Plan
- Starts with chart review
- Education to patients/families of brain function as it relates to ADL at home
- Identification of areas of concern at home
- Administration of cognitive assessments at home
The integration of cognition into a treatment plan is a pivotal aspect of our occupational therapy practice. It's a process that begins with a thorough chart review, a step that some therapists may sometimes overlook in the midst of their busy daily routines. However, I want to emphasize the significance of this step. Neglecting it can potentially hinder the outcomes of your treatment plan.
A strong understanding of neuroanatomy is essential when reviewing medical records, especially in cases involving cognitive challenges. While most of us studied neuroanatomy in college, refreshing your knowledge may be a good idea, especially if it's been a while. Although we won't go into an in-depth neuroanatomy lesson, I'll touch on some key points to jog your memory. This knowledge will serve as a foundation for aligning the information you gather from chart reviews with your patient assessments. It also enables you to educate your patients, their families, and caregivers about what's happening in the brain.
You don't need to become a neurologist, but having a strategic understanding of the neurological aspects can significantly benefit your approach. For example, consider a patient who exhibits inappropriate behavior, like a previous client of mine. He would go out into public and act inappropriately, especially towards some of the women working at a local coffee shop. This gentleman was quite large, standing at 6'7", and that alone could be intimidating. Some of his inappropriate behaviors required occupational therapy intervention, but I also understood that trauma in his brain might have contributed to these behaviors. It's important to approach your work with a bit of strategy and understanding about what's going on neurologically. Knowing how specific areas of the brain might be contributing to certain behaviors can be incredibly valuable. It's all about bringing this understanding back to functional cognition.
If you find yourself without access to detailed medical records or relevant neurology reports, especially when dealing with a patient diagnosed with dementia but lacking associated medical documentation, consider requesting these records or making referrals to specialists. In some areas, neurology departments may have lengthy waitlists, so it's wise to get the process started early to ensure your patients receive timely support for their cognitive challenges.
Let's briefly review the critical regions of the brain. The frontal lobe, often referred to as our "mission control," plays a central role in cognitive functioning. It influences emotional expression, problem-solving, memory, judgment, and even sexual behaviors. Understanding this region can help us connect cognitive deficits with functional challenges. The temporal lobes are responsible for visual, olfactory, and auditory processing. These processes are vital for healthy thinking, emotional responses, and communication. The occipital lobes act as our visual hub, enabling us to interpret color, shapes, and object locations. In contrast, the insular cortex facilitates sensory processing, emotional expression, and some motor functions. The parietal lobe allows us to make sense of sensory experiences in the world, ensuring we can understand our surroundings and adapt our actions accordingly. There are also subcortical structures deep within the brain, including the diencephalon, pituitary gland, limbic structures, and basal ganglia. These structures can be likened to a "switchboard" or "mission control," simplifying complex medical concepts for our patients.
When educating patients and families about brain function in relation to activities of daily living (ADLs), consider using relatable examples and analogies. For instance, you could compare the brain to an avocado. This can make complex information more accessible and engaging.
Once you've conducted a chart review and gathered relevant information, it's an excellent time to begin educating your patients and their families about brain function and its implications for daily life. This step is crucial in building a strong foundation for your treatment plan. It helps your patients and their families understand the reasoning behind your interventions, making your approach transparent and empowering.
For instance, I once worked with an aide in an assisted living facility who had been caring for residents with different diagnoses for years but was unaware of the differences between these conditions and their effects on motor planning, cognition, and progression. Educating her about these differences transformed her perspective and improved her caregiving. Incorporate this education into your treatment plans and goals, and consider including caregiver-based goals when appropriate. By fostering understanding and collaboration, you can ensure that your interventions are effective and well-received.
Identifying areas of concern in the patient's home is the next crucial step. During evaluations, patients and their families may provide a wealth of information, but it's essential to sift through this data and prioritize. Given the pervasive influence of cognitive deficits, the list of concerns can be extensive. Start by identifying safety concerns, as these should always be addressed first.
Subsequently, focus on two to three areas that are particularly important to the patient and their family. This targeted approach allows for more manageable and effective interventions. Keep in mind that cognitive improvements in one area may have a positive ripple effect on other ADLs.
Treatment Planning Within the Home Environment
- Interpretation of results/Giving results meaning
- Identification of areas to work on
- Determining Functional Cognition!
Giving meaning to assessment scores is crucial. It's not enough to provide a number; we need to translate those scores into practical implications for the individual's daily life. This helps us pinpoint areas that require intervention and tailor our treatment plans to address specific functional challenges related to cognitive deficits.
Functional Cognition
- The cognitive ability to perform daily life tasks is conceptualized as incorporating metacognition, executive function, other domains of cognitive functioning, performance skills (e.g., motor skills that support action), and performance patterns.
- Making Functional Cognition a Professional Priority | The American Journal of Occupational Therapy | American Occupational Therapy Association (aota.org)
- Functional cognition should ONLY be evaluated in actual task performance. Home is ideal!
Functional cognition is a critical aspect of occupational therapy practice, and its definition has evolved over the years to provide a more comprehensive understanding of its role in daily life. The current definition emphasizes the integration of cognitive skills for performing activities of daily living (ADLs) and includes skills, strategies, and psychosocial elements. This updated definition acknowledges the impact of the environment, mental health, and physical health on an individual's cognitive abilities, making it a more robust framework for OTs to assess and address functional cognition in their clients.
Consideration for Functional Cognitive Treatment Planning
- Person focused
- Environment
- Emotional health
- Neurological and biological factors
In the realm of functional cognitive treatment planning, our focus naturally gravitates towards a person-centered approach. This inclination is hardly surprising, given that we, as occupational therapists, excel at catering to individual needs and aspirations. However, we may not always consider the profound impact of culture in our practice.
Culture, encompassing one's upbringing and early learning experiences, profoundly influences how individuals engage with their surroundings, perceive others, absorb and retain information, and form judgments. It's essential to recognize that these cultural nuances can vary significantly, especially when working with individuals from diverse backgrounds or those whose cultures we may not be intimately familiar with. A thoughtful exploration, whether through conversations with the patient or their family or through independent research, can unearth vital insights that should not be overlooked.
Cultural awareness aside, we must also cast our gaze upon the environmental factors that bear upon an individual's performance. Consider the case of a patient dwelling in a mother-in-law apartment, where chaos perpetually reigns. Amidst the constant juggling of pet care, from dogs to kittens and birthing cats, alongside the responsibility of caring for a boyfriend with brittle diabetes, distraction becomes a relentless companion, exhausting in its own right. Here, our task is to discern the nuances of such environments and strategize on managing their impact.
Emotional well-being is another facet deserving of our attention. A poignant quote aptly reminds us that "emotional function and cognitive function aren't unrelated to each other; they're completely intertwined." This truth is self-evident to anyone who has traversed the depths of grief, battled the shadows of depression, or grappled with the relentless grip of anxiety. When we encounter a patient navigating such emotional storms, we must acknowledge that their cognitive abilities may bear the brunt of these turbulent waters. A recently bereaved patient struggling to find equilibrium may exhibit signs of forgetfulness or cognitive struggle directly linked to their emotional state.
Lastly, we must not overlook the neurological and biological dimensions. Employing tools like brain scans and neuropsychological evaluations, we gain invaluable insights into the mind's inner workings. This knowledge becomes a cornerstone for crafting precise treatment plans and, where necessary, advocating for specialized care. Consider this parallel: just as you wouldn't prescribe the same medication for every patient with chest pain, so too should we be cautious of hastily offering psychiatric drugs without a comprehensive understanding of what's transpiring within the patient's brain. As occupational therapists, recognizing the significance of these assessments, our duty extends to educating our patients and championing their access to the expertise that can provide tailored solutions for their unique cognitive challenges.
Assessments to Use at Home
- Confusion Assessment Method: to identify patients with delirium: The_Confusion_Assessment_Method.pdf (va.gov)
- The Brief Interview for Mental Health Status
- Performance Assessment of Self-Care Skills
- Executive Function Performance Test
Let's now delve into the assessments that can be incorporated into our practice. Although some of these assessments may initially appear unconventional for occupational therapists, they offer valuable insights and are integral to comprehensive care.
The Confusion Assessment Method (CAM) and Brief Interview for Mental Health Status (BIMS) do not inherently align with traditional OT practices, but both have gained approval from Medicare for assessing cognition. CAM, for instance, aids in identifying delirium in patients. Delirium, which can range from subtle to severe, may not always be readily apparent. By conducting CAM, we ensure that cognitive assessments are appropriate, as addressing cognition when delirium is present can be counterproductive. Even if you are confident that delirium isn't a factor, utilizing CAM demonstrates a thorough approach, which can be crucial for third-party payer compliance. The Centers for Medicare and Medicaid Services (CMS) has integrated CAM into post-acute care assessments, which might already be a part of your healthcare team's protocol.
On the other hand, BIMS, another CMS-approved assessment, serves as a valuable tool for neuropsychological screening. For example, if you encounter a patient grappling with profound grief and depression, the BIMS can shed light on their mental state. It's essential to address mental health concerns before diving into cognitive evaluations. Collaborating with your healthcare team to determine who administers these assessments can streamline the process. Alternatively, you can administer them yourself; they are efficient and quick, providing a solid foundation for cognitive assessments.
Let's explore assessments that align more closely with traditional occupational therapy practices. The Performance Assessment of Self-Care Skills is a reliable, client-centered, performance-based assessment designed to measure occupational performance in daily life tasks. It can be effectively employed with adolescents, adults, and older adults, even in home settings. Comprising 26 core tasks, including mobility, basic ADLs, IADLs with a physical focus, and crucially, 14 IADL tasks related to cognition, the PASS provides a holistic view of a patient's abilities and how they navigate various tasks.
The Executive Function Performance Test examines a patient's capabilities in tasks like cooking, phone use, medication management, and bill payment within their home environment. It offers valuable insights into a patient's functional abilities and serves as an educational tool for families. Additionally, it's accessible as a free download, providing convenient access to a useful assessment tool.
Despite their initial differences from conventional OT practices, these assessments play an indispensable role in ensuring comprehensive care and tailored interventions for our patients.
Additional Assessments to Use at Home
- Fitness to Drive Screening Measure: Web-based to identify at-risk drivers
- Loewenstein Occupational Therapy Cognitive Assessment (LOTCA): Cognitive and visual perception skills in older adults are assessed
- Mini-Mental State Examination (MMSE): Measures orientation, recall, short-term memory, calculation, language, and constructability
- Cognitive-Performance Test (CPT): Explains and predicts capacity to function in various contexts and guide intervention plans
- Cognistat: Rapid testing for delirium, MCI, and dementia (can be used with teens to adults)
- Trail Making Tests A and B
Incorporating assessments into our home-based occupational therapy practice is essential for providing comprehensive care. One critical area that demands our attention is assessing a patient's fitness to drive. If you work in the community, be it outpatient, home care, or mobile outpatient services, addressing a patient's ability to drive is paramount, especially when cognitive issues are at play. However, determining whether a patient should drive requires specific skills and training. If you lack this expertise, it's crucial to connect with a Certified Driving Rehab Specialist (CDRS), often an occupational therapist or physical therapist with extensive training in driving assessments. Collaborating with CDRSs is vital, as it directly relates to public health, safety, and community well-being. The tragic example of a wrong-way driver causing a fatal accident highlights the significance of addressing driving concerns diligently.
Here are some assessments that you can integrate into your practice. The Loewenstein Occupational Therapy Cognitive Assessment, previously known as the LOTCA, assesses cognitive and visual perception skills. It aids in identifying various levels of cognitive difficulties and provides insights into a patient's learning potential and thinking strategies. This information significantly influences our treatment planning and intervention selection. Additionally, the LOTCA offers different versions tailored to different age groups, enhancing its versatility.
Mini-Mental State Examination (MMSE) assesses orientation, recall, short-term memory, calculation, language, and constructive ability. While it's commonly administered in physician's offices, you can also use it in your home-based practice. There's a similar tool called the SLUMS (Saint Louis University Mental Screening), which is a free assessment option.
The Cognitive-Performance Test (CPT) is a performance-based assessment that explains and predicts a patient's capacity to function in various contexts. It employs the Allen Cognitive Levels for rating patients, which can be shared with their families to help them understand cognitive challenges better.
Although typically used in inpatient psychiatric facilities, the Cognistat can be adapted for home-based assessments. It's a rapid test that differentiates between delirium, mild cognitive impairment, and dementia and can be applied across various age groups.
The Trail Making Tests A and B evaluate general cognitive function, including working memory, visual processing, visual-spatial skills, selective and divided attention, processing speed, and psychomotor coordination. Trail Making Test B, in particular, has been linked to poor driving performance. If a patient performs poorly on this test and intends to drive, it's advisable to refer them to a CDRS or consider pursuing CDRS certification.
These assessments, though diverse in their applications and availability, expand our toolkit for home-based occupational therapy. Some may require purchase, while others can be downloaded. Discuss the possibility of integrating these assessments into your practice with your employer to enhance the quality of care you provide during home visits.
Clinical Observations
- Errors in math
- Frustration from the patient
- Distractibility
- Difficulty focusing
- Repeated phrases
- Requires redirection
- Unable to locate items
- Impulsivity
- Reduced reciprocity
- Reduced problem-solving skills
- Delayed or absent recall
- Changes in perception
- Poor insight
- Changes in personality
- Irritability
- Safety concerns
- Increased fatigue
- Decreased organization
It's essential to emphasize the value of your clinical observations and activity analyses in your documentation. These observations, rooted in your skilled assessment and honed through clinical experience, provide crucial insights into a patient's cognitive abilities and challenges.
For instance, consider an activity as straightforward as making a peanut butter and jelly sandwich, reminiscent of college days. While occasional difficulties in locating items or lapses in focus are common and may not necessarily indicate a cognitive issue, persistent patterns of such challenges warrant attention. If you consistently encounter these issues or receive complaints from families, it's an indication that cognitive assessment and intervention may be necessary, even if your initial focus was on a different aspect of care. Your ability to recognize these signs and adapt your approach is a testament to your clinical expertise and dedication to comprehensive patient care.
Home Strategies
- Visual cues
- Automatic timers
- Lighting alternatives
- DME for fall prevention
- Reduced clutter
- Alarm/alert systems
- Phones and computers
- Routine modifications
- Mental health support/activities
- Paper calendars
- Timers for time modulation
- Caregiver education
- Driving alternatives
- Dementia education and training
- Emergency preparedness
- “Just right challenge” tasks
- Safety training
- Stress management
Working in a patient's home setting can be an incredibly rewarding experience for occupational therapists. It provides a unique opportunity to tap into our innate creativity and adaptability as professionals. Here are some strategies and interventions that can be seamlessly integrated into home-based care:
Utilizing visual cues can be highly effective. For example, consider a patient who frequently snacks on unhealthy foods. To address this issue, you can clear a designated place on the kitchen counter, place a placemat there, and instruct caregivers to set out specific healthier snacks on the placemat. This visual cue prompts the patient to choose healthier options, promoting improved dietary habits.
While automatic timers can be useful, it's crucial that the patient understands their purpose. Many patients may become confused when timers go off without clear instructions. Therefore, ensuring the patient comprehends the intended use of timers and how to respond when they activate is essential.
In cases where certain areas lack adequate illumination, such as bathrooms, adjusting the lighting can reduce patient distress and confusion, particularly for those with cognitive impairments. Ensuring a well-lit environment can enhance their comfort and safety.
Managing a patient's energy levels throughout the day is vital. Cognitive issues, from dementia to brain injuries, can lead to increased fatigue. Therefore, helping patients modulate their activity levels and prevent excessive exhaustion is integral to care planning.
Smartphones, computers, and phones can be valuable tools for patients, provided they have a basic understanding of how to use them. Caregiver education in this regard can empower patients to leverage technology for various aspects of daily life.
Stress can significantly worsen cognitive function. Implementing stress management techniques and strategies can be beneficial for patients. This may include relaxation exercises, mindfulness practices, or simple stress-reduction activities.
Although not listed, exercise plays a crucial role in maintaining and improving cognitive function. Incorporating physical activity, even in modified forms, can engage the cerebellum and contribute to clearer thinking and improved cognitive abilities.
In summary, home-based occupational therapy allows us to be creative and tailor interventions to suit each patient's unique environment and needs. Utilizing visual cues, appropriate technology, and effective energy management can enhance our patients' quality of life and well-being while addressing cognitive challenges.
Adding Goals to Treatment Plans
- Client-based
- Assist level
When formulating goals for cognitive interventions, it's beneficial to employ the COAST framework, emphasizing client-centered, occupation-based, specific, and time-bound goals. These objectives should align with the principles of functional cognition and measure improvements in functional outcomes. Here are a few practical examples:
Medication Management Goal
For this goal, the focus is on the patient's ability to manage their medications effectively. In the COAST framework, the goal is tailored to a specific patient, the occupation in focus is the proper administration of daily medications, the patient will employ learned strategies to achieve this goal, the specific objective is for the patient to take all five of their daily medications using the strategies they've acquired, and the patient is expected to reach this goal within a timeframe of three consecutive days within two weeks.
Phone Management Goal
This goal centers around a patient's capability to manage medical appointments through phone calls. In the COAST framework, the goal is customized to meet the specific patient's needs, the occupation in focus is the efficient management of medical appointments via telephone, the patient is encouraged to strive for independent management using their contact list and iPhone, the specific aim is for the patient to make two phone calls with a flawless accuracy rate to manage medical appointments, and the patient is expected to reach this goal within the span of four treatment sessions.
Meal Preparation Goal
In this scenario, the goal is to enhance a patient's ability to prepare a meal, leveraging visual cues. In the COAST framework, the goal is tailored to meet the specific patient's needs, the occupation in focus is the independent preparation of a meal, visual cues will be used to assist the patient in achieving this goal, the specific aim is for the patient to prepare a simple meal while relying on visual cues placed within the kitchen, and the patient is expected to reach this goal within a specified timeframe.
In your documentation, it's crucial to be explicit about the cognitive strategies being employed. This guides the treatment approach and sets clear expectations regarding when the patient is anticipated to succeed. By adhering to the COAST framework and focusing on measurable functional improvements, your cognitive goals will effectively address each patient's unique needs and challenges.
Challenges With Documentation
- EMR useability
- Limited resources online or with employers
- Cognitive goals can require extra time to ensure quality
- Medically necessary required for billing
- Third-party payer authorizations can be more difficult to obtain
Documenting cognitive interventions can pose challenges, particularly within electronic medical records (EMRs) that may not be tailored to occupational therapists. It's not uncommon for EMRs to be more user-friendly for physical therapists, so OTs often need to get creative in how they use these systems. This might involve finding workarounds or advocating for the necessary resources and support from employers to ensure efficient documentation.
Cognitive goals and interventions may also require additional time compared to traditional physical therapy interventions. Justifying this extended timeframe in your treatment recommendations for third-party payers is crucial. Instead of merely stating that you're working on a specific task, such as transfer training, provide a clear rationale for the prolonged duration. For instance, if you're implementing errorless learning techniques or addressing specific cognitive challenges, explain why this additional time is medically necessary for the patient's benefit.
Navigating third-party payment authorizations can be more complex when dealing with cognitive disabilities. Advocacy becomes essential in such cases. You may encounter denials, but don't hesitate to appeal these decisions. Back your appeal with well-structured documentation that educates the payer about the intricacies of cognitive impairments and their impact on the patient's daily life. Emphasize the medical necessity of your interventions. This advocacy can lead to successful outcomes, as exemplified by a case where an appeal secured additional therapy sessions for a patient who ultimately achieved her academic and career goals despite cognitive challenges.
In summary, documenting cognitive interventions may require creativity within EMRs, justification for extended treatment times, and advocacy to secure the necessary authorizations. Through clear and informed documentation, you can effectively convey the medical necessity of your interventions and advocate for the best outcomes for your patients.
Billing for Cognition
- Therapeutic interventions that focus on cognitive function (e.g., attention, memory, reasoning, executive function, problem-solving, and/or pragmatic functioning) and compensatory strategies to manage the performance of an activity (e.g., managing time or schedules, initiating, organizing, and sequencing tasks), direct (one-on-one) patient contact.
- Therapeutic interventions that focus on cognitive function (e.g., attention, memory, reasoning, executive function, problem-solving and/or pragmatic functioning) and compensatory strategies to manage the performance of an activity (e.g., managing time or schedules, initiating, organizing, and sequencing tasks), direct (one-on-one) patient contact.
When it comes to billing for cognitive interventions in occupational therapy, there are specific Current Procedural Terminology (CPT) codes that you should use. These codes help you accurately document and bill for the services you provide. Here's a breakdown of the relevant codes:
The 97129 code is used for the initial 15 minutes of therapeutic interventions. It's important to note that this code is the same as 97130 in terms of definition. After the initial 15 minutes, you would use the 97130 code for each additional 15-minute increment of therapeutic interventions.
It's crucial to be precise in your documentation and use the language provided in the CPT code descriptions. This helps ensure that your third-party payer understands the nature of the interventions you're providing and approves the billing accordingly. For example, if your therapy session focused on executive function tasks, make sure to explicitly mention that in your documentation. By aligning your documentation with the CPT code definitions, you provide a clear and accurate account of the services you delivered.
To stay organized and informed, consider keeping a handy reference sheet of CPT codes and their definitions, even if you're experienced in your field. This can be a valuable tool for ensuring consistency and accuracy in your billing and documentation practices.
Types of Cognitive Impairments
As we wind down, I want to talk about delirium and dementia for a second.
Delirium Vs. Dementia
Delirium is a condition that, while more commonly associated with acute care settings, can also manifest in the community or during home care visits. As occupational therapists, it's essential to be knowledgeable about delirium because of its potential severity and impact on patients. You might be the primary healthcare provider present in these situations, so identifying delirium becomes crucial.
Delirium is characterized by a sudden onset and is primarily defined by disturbances in attention and awareness. Recognizing delirium is essential because it can lead to significant complications if left unaddressed. Being vigilant and informed about delirium ensures that you can provide appropriate care and support, especially when you're working in home care or outpatient settings where immediate access to medical personnel may not be readily available.
Delirium
- Disturbance in attention and awareness developing acutely tends to fluctuate in severity
- At least one additional disturbance in cognition
- Disturbances are not better explained by dementia
- Disturbances do not occur in the context of a coma
- Evidence of an underlying organic cause
Delirium is a condition characterized by its rapid onset and varying degrees of severity. It's marked by at least one noticeable disturbance in cognition, and it's important to note that this disturbance cannot be attributed to dementia. To help identify delirium quickly, you can utilize the delirium assessment we discussed earlier, which is a fast and efficient tool. If the assessment indicates delirium, seeking immediate medical attention is crucial. While it's rare to encounter someone in a coma during home visits, delirium can manifest in various ways and usually indicates an underlying cause.
Delirium can result from factors such as medication interactions, psychiatric issues, or infections. When you're in a home care setting and observe signs of delirium, it's essential to prioritize the person's safety and well-being by promptly getting them the necessary medical care.
- Significant cognitive decline in one or more cognitive domains.
- Cognitive impairment interferes with ADL.
- Cognitive impairment does not occur exclusively in the context of delirium.
- Cognitive decline is not better explained by other medical or psychiatric conditions.
Dementia is distinguished by significant cognitive decline in one or more cognitive domains, and this decline typically interferes with a person's ability to perform daily activities. It's important to note that delirium and dementia can coexist and are not mutually exclusive conditions. While someone with dementia can experience delirium, the two are distinct.
To diagnose dementia, a physician is required as it involves a comprehensive evaluation beyond the scope of occupational therapy. It's essential to remember that dementia is not a specific disease; rather, it is an umbrella term encompassing various conditions characterized by cognitive decline. Each type of dementia, such as Alzheimer's disease, vascular dementia, or Lewy body dementia, has its unique features and progression patterns. Thus, it's crucial to recognize that not all dementias are the same, and a proper diagnosis is necessary for appropriate management and care planning.
- Vascular dementia
- Dementia with Lewy bodies
- Frontotemporal dementia
- Alzheimer’s
- Mild cognitive impairment
- Encephalopathy
It's crucial to understand that dementia is a broad category encompassing various conditions, each with its unique characteristics and underlying causes. Dementia is not a single disease but rather a term used to describe a range of cognitive impairments. Here are some types of dementia and their distinguishing features:
Vascular dementia results from impaired blood flow to the brain, leading to problems with reasoning, planning, judgment, memory, and other cognitive functions. It is often characterized by cognitive deficits that can vary in severity, as if the brain's function has "holes" due to damage from inadequate blood flow.
Dementia with Lewy bodies is a progressive dementia characterized by a decline in thinking, reasoning, and independent function. Individuals with this type of dementia commonly experience sleep disturbances, visual hallucinations, and movement disorders, such as slow movements, tremors, and rigidity. It is closely related to Parkinson's disease.
Frontotemporal dementia refers to a group of disorders caused by nerve loss in the brain's frontal and temporal lobes. It can manifest as changes in behavior, empathy, judgment, foresight, and language abilities. The specific symptoms may vary depending on the regions of the brain most affected.
Alzheimer's disease is the most common type of dementia, accounting for 60-80% of dementia cases. It is characterized by progressive cognitive decline, including memory loss, language problems, and difficulties with daily activities. Plaques and tangles in the brain are hallmarks of Alzheimer's.
Mild Cognitive Impairment (MCI) represents cognitive impairments that are more significant than expected for an individual's age and education level but do not meet the criteria for dementia. While individuals with MCI are at increased risk of developing Alzheimer's disease, not everyone with MCI progresses to dementia.
Encephalopathy refers to a broad term for brain dysfunction. It can lead to a range of cognitive difficulties, including problems with concentration, suicidal thoughts, lethargy, vision issues, swallowing difficulties, seizures, dementia-like behaviors, and more.
Understanding the specific type of dementia is essential for appropriate care and interventions, as each type may require different management strategies and approaches. Additionally, dementia is a complex condition with various underlying causes, and research continues to uncover more about its mechanisms and risk factors.
- Stanley B. Prusiner
- Florence Clark, PhD, OTR/L, FAOTA
As we conclude this session, I'd like to share some valuable insights and practical tips for addressing cognition in occupational therapy. Remember, as occupational therapy practitioners, our role is to help people live life to the fullest, providing practical solutions for success in everyday living. We can assist individuals in maximizing their function, vitality, and productivity, regardless of their cognitive impairments.
It's crucial to advocate for our patients and for the occupational therapy profession's involvement in addressing cognition. Staying informed about neuroanatomy and emerging scientific findings allows us to develop creative and effective treatment plans tailored to each patient's needs, especially when working in a home-based setting.
One essential aspect to remember is that the brain plays a central role in all bodily functions. As Thomas Edison aptly put it, "The chief function of the body is to carry the brain around." Therefore, even when working on physical aspects with our patients, we must recognize the critical importance of cognitive function.
In documenting cognitive deficits influenced by psychosocial aspects during home visits, it's essential to provide specific examples. For instance, if a patient exhibits signs of depression that impact their daily life, you can document the patient's emotional state, any refusal to participate in activities, and your efforts to address their emotional well-being. While we cannot diagnose depression, we can highlight observable signs and symptoms and collaborate with other healthcare professionals for further evaluation and intervention.
Regarding the Allen Cognitive Levels, you can access resources and printouts online. There are books available, such as "Understanding the Allen Cognitive Levels," that can serve as valuable references. These levels can be instrumental in helping patients and their families better understand cognitive impairments and manage associated behaviors effectively.
In summary, occupational therapy practitioners play a vital role in addressing cognition, and we have the tools and knowledge to make a meaningful impact on our patients' lives. By advocating for our patients, staying informed, and using evidence-based approaches, we can help individuals with cognitive impairments lead more fulfilling and independent lives.
Thank you for joining this session.
Adamit, T., Shames, J., & Rand, D. (2021). Effectiveness of the Functional and Cognitive Occupational Therapy (FaC o T) intervention for improving daily functioning and participation of individuals with mild stroke: A randomized controlled trial. International journal of environmental research and public health , 18 (15), 7988. https://doi.org/10.3390/ijerph18157988
Cognition, Cognitive Rehabilitation, and Occupational Performance. (2019). AJOT , 73 (Supplement_2), 7312410010p1–7312410010p26. https://doi.org/10.5014/ajot.2019.73S201
Edwards, D. F., Wolf, T. J., Marks, T., Alter, S., Larkin, V., Padesky, B. L., Spiers, M., Al-Heizan, M. O., & Giles, G. M. (2019). Reliability and validity of a functional cognition screening tool to identify the need for occupational therapy. AJOT , 73 (2), 7302205050p1–7302205050p10. https://doi.org/10.5014/ajot.2019.028753
Manee, F. S., Nadar, M. S., Alotaibi, N. M., & Rassafiani, M. (2020). Cognitive assessments used in occupational therapy practice: A global perspective. Occupational Therapy International , 8914372. https://doi.org/10.1155/2020/8914372
Stigen, L., Bjørk, E., & Lund, A. (2022). Occupational therapy interventions for persons with cognitive impairments living in the community. Occupational therapy in health care , 1–20. Advance online publication. https://doi.org/10.1080/07380577.2022.2056777
Covell-Pierson, K. (2023). Cognitive interventions in the home: A practical approach for OT professionals. OccupationalTherapy.com , Article 5638. Available at www.occupationaltherapy.com

Occupational therapist and entrepreneur, Krista Covell-Pierson is the founder and owner of Covell Care and Rehabilitation, LLC. Krista created Covell Care and Rehabilitation to improve the quality of services available for clients of all ages living in the community through a one-of-a-kind mobile outpatient practice which aims to improve the lives of clients and clinicians alike. Krista attended Colorado State University receiving degrees in social work and occupational therapy. She has worked in various settings including hospitals, home health, rehabilitation centers and skilled nursing. Through her private practice, Krista created a model that she teaches other therapists looking to start their own business. She has extensive experience as a fieldwork educator and received the Fieldwork Educator of the Year Award from Colorado State University. Krista served as the President of the Occupational Therapy Association of Colorado for two years. She presents to groups of professionals and community members on a regular basis and has a heart to help others become the best version of themselves.
Related Courses
Course: #5963 level: introductory 1 hour, incontinence: practical tips for the occupational therapy practitioner (part 1), course: #3609 level: intermediate 1 hour, incontinence: practical tips for the occupational therapy practitioner (part 2), course: #3610 level: intermediate 1 hour, assessing and preventing falls at home: a practical approach for the ot, course: #5413 level: intermediate 2 hours, covid-19 with older adults: an update, course: #5494 level: introductory 2.5 hours.
Our site uses cookies to improve your experience. By using our site, you agree to our Privacy Policy .

OT INTERVENTIONS
Play slideshow, occupational therapy interventions.

Occupational therapists help people participate in the things they want and need to do through the therapeutic use of everyday activities (occupations). At the core of occupational therapy is a belief in health through doing . "Doing" may range from participating in practical and leisure activities to more subtle activities such as cultivating empathy or identifying values. Psychosocial occupational therapy interventions seek to optimize human functioning using a holistic approach. Interventions may facilitate reaching a youth’s goals surrounding social skills, communication skills, decision-making, problem-solving, emotional regulation, coping strategies, healthy risk-taking, attention span and focus, intrinsic motivation, values identification, positive self-concept, time management, agency and self-efficacy. Interventions are customized to leverage a youth’s interests and strengths, facilitate optimal well-being, and to match a youth’s stage of development. OTTP occupational therapists practice client-centered, trauma-informed care. For a visual tour representing a small sampling of possible interventions, view our OT slideshow above.
Core Beliefs
• There is a positive relationship between occupation and health (physical/emotional) • ”All people need to...engage in the occupations of their need and choice , to grow through what they do, and to experience independence or interdependenc e , equality, participation, security, health and well being .” • Occupations structure daily life, are central to our identity and sense of competence, and have particular meaning and value to us. • Health and well being can be affected by environmental barriers to participation. American Occupational Therapy Association (2002). Occupational therapy practice framework: Domain and process. American Journal of Occupational Therapy, 56, 609-639.
Ot domain / scope of practice.
OT’s Established Body of Knowledge & Expertise
Areas of Occupation
Activities of daily living instrumental activities of daily living rest & sleep education work play leisure social participation, client factors, values, beliefs, spirituality body functions body structures , performance skills, sensory/perceptual motor & praxis emotion regulation cognitive communication / social , performance patterns, habits routines roles rituals , context & environment, cultural personal physical social temporal virtual , activity demands, objects/properties space social sequencing / timing required actions required body structures & function , american occupational therapy association (2002). occupational therapy practice framework: domain and process. american journal of occupational therapy, 56, 609-639..
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Beresford B, Clarke S, Maddison J. Therapy interventions for children with neurodisabilities: a qualitative scoping study. Southampton (UK): NIHR Journals Library; 2018 Jan. (Health Technology Assessment, No. 22.3.)

Therapy interventions for children with neurodisabilities: a qualitative scoping study.
Chapter 4 therapy interventions: approaches and techniques.
- Introduction
An objective of this study was to describe current approaches and practices in the delivery of therapy interventions to children with non-progressive neurodisabilities. In this chapter, we present findings regarding this that have emerged from our interviews with professionals. We offer a broad view of the current situation placing this, when necessary, in the historical context of the development of physiotherapy, occupational therapy, and speech and language therapy. Parents’ reports of their experiences of therapy – for example the approaches and specific techniques – are presented in Chapter 5 .
- Understanding therapy interventions
Physiotherapy, occupational therapy and speech and language therapy can be described and understood at three levels:
- the overall approach a therapist brings to the assessment and management of a case
- the schools of thought that inform views regarding the appropriate way to manage a case
- the specific techniques, procedures, activities and equipment used.
There is some interaction, or interdependency, between these levels ( Figure 2 ). Certainly, the two higher levels influence what a therapist actually ‘does’ with a child. Equally, the overall approach will determine, at least to some extent, what are regarded as legitimate or acceptable schools of thought.
Therapy intervention constructs and their interconnections.
In this chapter, we report what our interviews with professionals reveal about these different ways of conceptualising or understanding therapy interventions. We also report how thinking on these matters is shifting and changing. We do not claim that this is the only way to understand and conceptualise therapy interventions, but is the clearest solution we found to presenting interviewees’ accounts.
- The overall approach
Four different, but interconnecting, facets appear to contribute to this concept of the ‘overall approach’:
- the objective of the intervention
- the role of the therapist
- the role of the child and family
- the place of the therapy in the life of the child.
The World Health Organization’s International Classification of Functioning, Disability and Health
Before moving on to describe each aspect of ‘overall therapy approach’ in turn, it is useful to offer a brief overview of the WHO’s ICF, published in 2002. This conceptual model was widely referred to in our interviews. It was clear that it not only offers a language and framework by which therapy interventions can be understood, but has also been a catalyst for change in the overall approach of therapies. It is a conceptual model that has been endorsed by all three profession, 20 – 22 with guidance issued to support its implementation (e.g. College of Occupational Therapists, 2004; Royal College of Speech and Language Therapists, 2005) as well as being integrated into the training of new therapists. 23
In 2002, WHO proposed a conceptual model of disability that sought to bring together elements of the pre-existing medical and social models of disability, and incorporate them into a biopsychosocial model of disability. 16 Figure 3 offers a representation of this model.
The ICF model of disability and health.
The meanings of the terms used in this model are as follows.
Body functions: physiological functions of body systems (including psychological functions). Body structures: anatomical parts of the body such as organs, limbs and their components. Impairments: problems in body function or structure such as a significant deviation or loss. Activity: the execution of a task or action by an individual. Activity limitations are difficulties an individual may have in executing activities. Participation: involvement in a life situation. Participation restrictions are problems an individual may experience in involvement in life situations. Environmental factors: these make up the physical, social and attitudinal environment in which people live and conduct their lives. p. 10. 16 Reprinted from Towards a Common Languages for Functioning, Disability and Health: International Classification Framework. World Health Organization, © 2002. URL: www.who.int/classifications/icf/icfbeginnersguide.pdf (last accessed 21 December 2017)
Overall approach: the objective of the intervention
In describing the overall objectives of a therapy intervention, interviewees framed this in terms of the ICF model. Three possibilities were described.
- First, the ‘ deficit model ’: here remedying physical/body dysfunction and distortion is seen as the end point, or objective, of therapy interventions or, as one interviewee described it, ‘fixing the child’ (OT-PB-01). This model can be regarded as the original starting point of all three professions.
- The second approach focuses on the achievement of specific activities, or occupations , that the child’s physical impairments have limited or rendered difficult, for example walking or articulating verbal speech. When interviewees offered a chronology of the emergence of these different models, this approach was described as emerging in the 1990s.
- The third approach is child/family focused, goals focused , in which the objectives of therapy are driven and guided by the child’s/family’s goals and desires. These goals should be expressed in terms of the child’s participation in everyday life, or life situations, that is relevant and meaningful for a child of that age (e.g. learning, self-care, communicating, moving about, friendships and being part of a family), rather than outcomes related to body structure/function or achievement of specific skills or activities. Within this approach, addressing dysfunction or impairment is no longer the key focus. This opens up alternative ways of intervening which may be as, or more, successful. One example is achieving independent mobility through the use of a wheelchair rather than through a lengthy and intensive physiotherapy programme. Another example is teaching a child to use augmentative and alternative communication systems and devices to communicate, or supplement verbal communication, rather than simply seeking to achieve verbal communication through speech and language therapy input:
The really complex ones, you can do as much therapy as you like, and it probably won’t make much difference – so let’s focus on the environment and the equipment and stuff . . . A1
A slightly different, or concurrent, conceptualisation emerged from interviews with occupational therapists. It had a more dichotomous stance: a ‘deficit-focused’ model versus a focus on achieving occupation, or participation, through modifications to the environment and/or providing equipment to facilitate the child’s engagement or participation.
The operationalisation of these approaches
A number of issues emerged during our discussions with interviewees regarding these three possible approaches to understanding the objectives of a therapy intervention.
First, there was clear evidence that all the approaches are being used by therapists. Furthermore, not all interviewees believed that the different approaches were incompatible. Thus, some viewed them as being necessarily connected, with achievements of particular skills or reducing pain, for example enabling higher-level outcomes (expressed in the goals identified by children or parents) to be achieved, even if not explicitly identified at the outset of the intervention:
[Let me give you this example] . . . A 7-year-old boy, with quite a severe impairment, was delighted that his newly acquired ‘pick-up and release skills’ meant he could now take a tissue out of a box and wipe his nose himself. He is now independently participating in his own personal care, and this gave him better self-esteem in the classroom. K1
Start with the child or impairment, working on the body structure and functions as a means to an end to achieving the desired occupation. Start with the occupation, looking both at the child and the environment to see what can be done to achieve the occupation. Both approaches are still occupational therapy. Yet the same situation can be looked at in different ways, involving different interventions, and with different people. That can be confusing and challenging . . . and it’s a sensitive topic within the profession. Some favour one, some the other, and others use a bit of both. N1
Second, a goals-focused approach was widely endorsed and, reportedly, operationalised. However, the implementation of participation-oriented, goals-focused approaches within the therapies was viewed by some as ‘under development’ as opposed to already achieved:
. . . in my service you can see a three-generation approach. The first generation used to do ‘body function/structure stuff’ working on things like fine motor skills, co-ordination, range of movement and postural stability. Then, about 12 years ago, with the second generation, it became much more about targeting an activity and participation. However, in reality it was more about targeting activity and the child’s skills than true participation. Now a third-generation model is needed, where [we] really target participation. [So my question is] . . . ‘What’s our third-generation approach going to be so that it actually targets participation head-on through the right hypothesis-change mechanism?’. L1
There’s been a bit of a shift in terms of whether body structure and function is meaningful in its own right, or whether it’s an intervention which enables children to participate in something. We’ve started on that shift, but we aren’t all the way. F1
This was also evidenced in some of our interviews when interviewees described goals that ranged across all of the ICF concepts. Thus, a goals-focused approach was being operationalised, but not necessarily within a framework of participation.
Third, it was not clear whether the shift to goals-focused approaches was simply a matter of the influence of new ‘ways of thinking’ informed by both ICF and family-centred practice, 24 or whether stringent cuts in funding had forced therapists and services into a position where intense work on body structure and function was no longer possible.
Fourth, there appeared to be a degree of confusion about the differences between the ICF concepts of ‘activities’ and ‘participation’, and the definitions offered for both varied considerably. Participation, as set out in the WHO report, was viewed by some as challenging in terms of its definition and measurement, in terms of both appropriate time points and the indicators of participation used. This is something we discuss in detail in Chapter 7 .
Finally, new ways of working, intervention programmes and practices have emerged or been developed in response to this shift in approach from deficit to activities or goals-focused approaches. Examples of these referred to by study participants included, for physiotherapy, the MOVE programme (www.move-international.org/) and for occupational therapy, goals-directed training. 25
Overall approach: the role of therapist
There was a consistent view that, over recent years, the role of therapists in the delivery of interventions to children with neurodisability has shifted. A number of interviewees – and across all therapies – referred to a ‘consultative model’ whereby the therapist assesses the child, develops an intervention programme and then trains, or ‘upskills’, others (assistant practitioners, parents, child, classroom assistant and/or teacher) to deliver it, with supervision and ongoing monitoring. This approach was regarded as more prevalent within community, rather than secondary care or acute, settings.
Two drivers for this change were presented by interviewees. First, many interviewees noted the reduction in funding for therapies for children with neurodisability, which had forced changes in the way therapists worked. The way NHS trusts have chosen to address resource constraints has, however, differed. In some trusts, specialty posts have been maintained – albeit operating in a consultative role – whereas in others, posts have been lost and/or downgraded. A second driver – attributed to the number of ‘influential leaders’ in the field – was the acknowledgement that, to be effective, therapy interventions cannot be restricted to what are relatively occasional sessions with a qualified therapist in a clinic setting:
. . . it’s an intelligent way of capacity building. Also, in schools it’s the staff who know the children better than the therapist does. The therapist will come in one or two times a term so it would be ludicrous to expect a change with that amount of contact. R2
There was a diversity of opinion as to whether or not this change is for the better. The dominant concern was that non-therapists may not be sufficiently skilled or competent to respond to changes in functioning or to evaluate the impact of the interventions and adjust the intervention accordingly:
There is something about the skill of the therapist in working with any one child with particularly complex needs, to be able to tune in to how the child is responding to what you are doing with them. . . . To make the kind of adjustment that you need to do to make the therapy work there and then, and to know whether you can push onto something more complex . . . O2
. . . I think intervention effectiveness is actually being diluted . . . by having less skilled staff. I can understand why they are doing it, but I think it’s short-sighted. Z1
A second concern was adherence to intervention programmes. This was typically spoken about in terms of the multiple demands on people’s time and/or a lack of understanding of the intervention programme and its objectives. Finally, this represented a very significant change in the day-to-day work of therapists that may be difficult to accept and assimilate:
Within practice there is a reluctance to change that [move to less hands-on and more activity-based therapy], particularly among those who have been trained in manual handling of patients and how to support and help them move. F2
Furthermore, it was noted that parents may struggle to accept the consultative approach. Many interviewees believed that seeking the input of private practitioners was often due to a desire for more intense input from a qualified therapist.
Overall approach: the role of the child and family
The goals-focused approach described earlier was often spoken about alongside descriptions of a change in the way children, and their families, are regarded within the context of a therapy intervention. The shift in thinking described was from regarding the child/family as passive recipients to viewing them as active participants in the therapy intervention. Some interviewees referred to this is a move from the ‘expert practitioner’ model to the ‘expert parent’ model:
We are looking for children and families to be active in the rehabilitation process. So, instead of a child coming into hospital and having all this therapy done to them, they are a real active participant in what they are doing and they’re actively involved in their rehabilitation process. L2
Occasionally, this shift was located, or attributed, within a wider change in the NHS to a focus on self-management. This was perceived to be driven by both an outcomes-focused approach and constrained resources.
Again, there was a sense that this study was being conducted at a time when thinking within each of the professions on such matters was in a state of change. Thus, we had interviewees who firmly advocated opposing approaches. Equally, there were interviewees who described the approach they were working towards, but had not yet attained:
I want us to get to the situation where we are working with families, giving them the right information – and doing that well and early enough – so that they can be empowered to . . . make decisions. A1
Therapists have always worked very closely with parents, and older children too, in terms of goal-setting and goal preferences. The idea of offering people informed choice is not there . . . at the moment. P2
With respect to the move to place children and families more centrally in decision-making and ‘condition management’ processes, a number of interviewees referred to ‘health-coaching’ models or programmes which were informing or influencing changes in their ways of working.
Overall approach: integrating therapy into everyday life
The final interconnecting strand within the concept of ‘therapy approaches’ is integrating therapy interventions into everyday life. Again, interviewees spoke of a shift in thinking: taking therapy out of clinic settings, and delivering in the settings and environments where the child spends his or her time. Linked to this were notions of integrating the therapy procedures into everyday activities and aiming to design the intervention to maximise engagement and motivation:
I say to families that it’s no good just doing things for a short time, so it’s better to incorporate activities into everyday life, or position their child so they can do something else as well. That way activities get embedded and done more often, and so more likely to make a difference. F1
Once more, the extent to which this approach was dominant in an individual therapist’s practice was dependent on the extent to which their practice reflective goals-focused, participative approaches.
A number of constraints to adopting such an approach – particularly around the settings in which therapists practised – was noted, particularly when, in the past, therapy was delivered in outpatient clinic settings. Here, commissioners could be reluctant to resource therapists working in the child’s everyday settings.
- Schools of thought
One of the topic areas NIHR wanted this study to investigate and report on was current ‘schools of thought’ within physiotherapy, occupational therapy, and speech and language therapy. This has proved difficult to elucidate.
However, it is possible to present three sets of ‘schools of thought’ revealed in our interviews with study participants:
- ‘traditional’ schools of thought
- emerging schools of thought
- early intervention.
We have conceived schools of thought as distinct from ‘overall approach’ that we reported in the previous section.
Traditional schools of thought
Different schools of thought advocate, or stipulate, different techniques or procedures to use with a child. Alternatively, they may posit different views on the mechanisms of change underlying technique or procedure. This notion of distinct schools of thought appears to be very similar to that observed in other specialisms. (For example, psychological interventions typically sit under different schools of thought, such as psychodynamic, gestalt and cognitive–behavioural.)
Although the notion of different specific schools of thought was referred to by interviewees across all three professions, it emerged most strongly in our interviews with physiotherapists. This was both in terms of the way they may act to firmly ground (or constrain) an individual therapist’s approach or, more typically, as an area of controversy or concern. In both respects, neurodevelopmental approaches (e.g. the Bobath approach), sensory integration theory and conductive education were the most frequently mentioned. Bobath and sensory integration theory also emerged as divisive schools of thought in our interviews with occupational therapists. A concern about, or active rejection of, these schools of thought was explained in terms of their basis being located within a ‘deficit model’ of intervention, and/or existing evidence on their impact/effectiveness.
As is a common theme through many of our data, there was a sense that these distinct, traditional schools of thought were, and would continue to become, less dominant. One of the key drivers for this appears to be the ongoing, higher-level reconstructions of what therapy is and what its objectives should be, which we described in the previous section.
Emerging schools of thought
The shifts in overall approach described earlier – from a deficit model to activity-based and now goals-focused/participation ways of working – appear, however, to have led to the emergence of new schools of thought within the professions. Of those described to us during the study, these typically drawing on principles or approaches developed within other specialisms. For example, cognitive–behavioural, problem-solving approaches, sometimes referred to as ‘coaching’, were reported as being used within occupational therapy. Global notions of ‘goals-focused approach’, family-centred practice and ‘evidence-based practice’ were referred to across all therapies as ‘schools of thought’ that the professions were adopting.
Early intervention
The final school of thought, applicable across all therapies, was the notion that early intervention is essential, and this should be the time when the intensity of the intervention is at its greatest. The rationale for early intervention is that it is likely to yield greater impact: supporting development and preventing permanent damage and/or deterioration. This argument is based on notions of neuroplasticity, physical and cognitive development.
Thus, it was also typically reported that the intensity of therapy interventions decreases as the child grows older (or in terms of time since brain injury). However, what was less clear was the rationale for tailing off therapy; indeed, it was a source of concern among some interviewees. Often this was expressed with respect to physical changes associated with puberty or to a child’s ongoing cognitive or communication development, and the implications this may have for the child’s needs for therapy input:
Younger children get more research and more therapy. Therapy is front-loaded so families get most at the preschool stage, some in primary school, rarely any in secondary school and none as adults. N2
- Techniques, procedures and equipment used by the different therapies
The purpose of this scoping study was not to provide an account of the enormous range of techniques, procedures and equipment currently being used by therapists in England. A different methodology would be required to generate such data. (We have, however, collated a list of all the techniques, procedures and equipment described to us by study participants. This can be found in Appendix 6 .)
Rather, what this study has achieved is an overview of the practice of physiotherapy, occupational therapy and speech and language therapy. We describe this in terms of a number of concepts:
- professional autonomy
- responsive practice
- managing prognostic uncertainty
- the role of protocols and care pathways
- working out of a tool box
- mode of delivery.
Professional autonomy
A first overarching principle of practice within therapies is the concept of professional autonomy. In many interviews, therapists were presented as working in an autonomous, individualistic way within their scope of practice (or qualification):
Assessment and hands-on work is probably more individualised, but we all sign up from the same baseline. F1
. . . certain institutions or individuals will have a favoured approach but ultimately it’s individual choice. Each physiotherapist is an autonomous practitioner . . . M2
This autonomy operated both in the choice of interventions and in the intensity, or dose, of the interventions. Despite this notion of autonomy, some interviewees noted that, within the NHS, practice has become more standardised over the past decade, driven by emerging evidence and the shift in overall approach to providing these therapies. The publication of protocols and the implementation of care pathways – both described below – also contributed to a standardisation of practice.
Responsive practice
The ability to make an ongoing assessment, even within the context of specific session, of the way a child is responding to an intervention and/or their ability or motivation to engage with an activity or procedure (sometimes on a moment-by-moment basis) was regarded as a core therapy skill. Responding to the child, and their response to an intervention, meant that therapists may be continually tailoring either their work with a child or the overall management of the case:
At the beginning of a session I may not have a definitive goal in mind, but will have an idea of what I’m hoping to achieve and structure the session accordingly. Over time, I may adapt and change the goals in order to make progress. So it’s a very fluid process and we need to be responsive and adaptive to get the best out of the child. M2
Managing prognostic uncertainty
With more complex cases, the issue of prognostic uncertainty and a lack of evidence of intervention effectiveness could lead therapists to trial a number of interventions, sometimes simultaneously, to establish a child’s potential capabilities and/or which technique suited the child best:
Parents with children with cerebral palsy always ask ‘[When] is my child going to talk, is spoken language going to be possible for them?’ And we can never answer that question because each child is so different. So it may be we set off on an eclectic approach, [thinking] . . . ‘let’s do some work on vocalisation or signing or symbols as well . . . V2
The role of protocols and care pathways
Participants used the term ‘protocol’ in two distinct ways. First, it was used to refer to the way in which a team or service managed a referral to their service. Here, both the terms ‘protocol’ and ‘care pathway’ were used. Thus, some study participants described the development, and early implementation, of a number of care pathways within their service, each specific to a particular presenting need or diagnosis. Typically, these were multidisciplinary, or integrated, pathways specifying who and when different professional groups should become involved with a child, and for how long.
Second, and more specifically, some techniques or presenting clinical needs were identified as having clear protocols in terms of assessment and/or management. For example, frequent references were made to NICE guidance on the management of spasticity. Interviewees drew attention to the fact that for many children with neurodisability, especially those with complex needs, there will be individualistic practice happening alongside protocol-informed practice(s).
Issues were raised of adherence to protocols, particularly when others were delivering the treatment, and the potential difficulties of implementing a protocol in an appropriate way for a particular child:
Protocols are anyway problematic because children vary and delivery is not always under their control. Children are at different ages and different stages and living in different families. . . . [And] to have protocols – good, evaluated ones – is one thing, but to implement them in families’ everyday life is another. M1
However, a much greater proportion of therapists’ work was reported as lacking any protocols. As a result, there could be great variation in the way in which a case was managed:
[There is] . . . huge variation in the interventions they receive. Not only in what they receive but in how often and from whom they receive it. N2
It’s been quite easy to write a pathway [protocol] for children with, say, hemiplegia receiving CMIT [constraint-induced movement therapy], or for those having Botox [botulinum toxin] injections as there’s quite a lot of evidence or guidance to draw on. Whereas all the others just get based on your clinical experience of managing other children . . . and what you see in the child. C1
Working out of a toolbox
Within the notion of professional autonomy described above, many interviewees described themselves as working out of a ‘toolbox’:
What you tend to find in practice is that most practitioners use an eclectic approach. It’s a little bit of this and a little bit of that. . . . it’s a little bit of what you’ve got in your toolbox. K2
We have a great big menu of interventions to choose from. P2
It’s about having that huge toolbox and choosing the right thing for the child, on the day almost. W2
Thus, in each case, a therapist brings a range of techniques, procedures, activities or items of equipment. There follows, through assessment of the child and the wider context, a process of clinical decision-making as to what particular ‘tools’ to choose, something that we report on in the following section.
Our analysis suggests that a number of factors influence the content of an individual therapist’s toolbox:
- the ‘overall therapy approach’ to which the individual therapist adheres
- their position, or beliefs, regarding schools of thought
- their training
- practices they have learnt from colleagues
- trends or ‘fads’
- team/clinical lead views
- the techniques, etc., that commissioners will fund
- clinical guidance (e.g. from NICE) or guidance or recommendations from professional bodies
There is a lot of individualistic work going on. We have very experienced therapists with strong beliefs based on their own clinical experience, which can be very powerful. P1
The notion of ‘embedded’ or ‘inherited practice’ was frequently mentioned. This was much more likely to be grounded in clinical consensus rather than in any evidence base:
There is a good level of consensus of opinion in what’s best in treatments and approaches to treatment which is cascaded down to therapists. . . . the team generates practice which then perpetuates down. I2
There is an awful lot of tacit knowledge that’s handed down through the profession . . . certain techniques, [and] ‘that is how you do it, [and] this is the right way to do it . . .’ F2
Embedded practice was also seen as a barrier to change in therapy approaches or to evidence suggesting that an intervention may not be effective:
. . . but a lot of therapists have done this [refers to a particular technique] for 30 years. [And] they can’t stop doing it if you don’t put anything in its place. F2
Trends or ‘fads’ in terms of particular techniques, procedures, activities or equipment were frequently mentioned by interviewees. Some were enthusiastic in their descriptions of, for example, a new technique that they or their team had started to use. Others were greatly concerned about the lack of an evidence-based rationale for adopting new techniques, equipment or practices. Furthermore, the commercial interests of manufacturers, or organisations, in promoting new techniques or equipment worried some interviewees. A further concern was that the successful use of a technique with a small number of children, or with respect to children of a particular developmental stage or diagnosis, could lead to wide-scale roll-out within a locality (or more broadly), which may not be appropriate:
There’s a massive growth in [name of technology] at the moment . . . and that’s very liberating for lots of young people . . . but it’s often being rolled out to children who are not ready yet . . . families and teams are spending an awful lot of money on technology that’s not being used effectively, and ultimately gets abandoned. O2
That said, there was an understanding of why therapists can be drawn to new (untested) practices and equipment. These are often presented, or marketed, with an anatomical or neuromuscular ‘rationale’ and some persuasive case studies. Furthermore, new techniques or practices may offer therapists a structure and process to their work. For example, a manual, an assessment pro forma and guidance on intervention intensity may be offered. Some interviewees believed that this could be very appealing to practitioners who were trained to be autonomous and work in a very individualistic way, but within a discipline where there is little sound evidence on which to base clinical decision-making:
You can book to go on your [name of course] or your [name of other course], and then you have your kit . . . [and then] . . . you know what you’re meant to be doing. S1
You’re taught in a staged way. It’s a clear, almost manualised, road map of what to do. It’s a qualification ‘in something’. It fills a gap. P1
Finally, the role of evidence in informing the content of a therapist’s ‘toolbox’ was typically regarded as very limited. However, included in our study sample were settings where sustained attempts were being made to use evidence, when possible, to specify intervention approaches. In these situations, evidence was (often) being drawn across from adult rehabilitation and/or other diagnostic groups.
Mode of delivery
A less common topic referred to in relation to therapy practice was mode of delivery. It appeared that, in the majority of interviews, study participants assumed that the research team already knew that they were referring to individually delivered interventions. However, a few interviewees reported using group-delivered interventions, and this typically appeared to be in relation to the management or treatment of non-complex issues.
- Factors affecting decision-making in the management of a case
One of the objectives of this study was to describe the factors that therapists reported as influencing their decision-making regarding the ‘therapeutic prescription’. We explored this in our individual interviews and focus groups with physiotherapists, occupational therapists and speech and language therapists.
The focus groups provided a useful opportunity to explore frontline practitioners’ views of the relative importance of factors brought to play in clinical decision-making in the management of a case. This exercise was conducted during six focus groups, with a total of 14 groups or subgroups completing this exercise. Participants were asked to rank the following factors:
- child’s and family’s characteristics and resources
- child’s presenting clinical/functioning needs
- clinical experiences managing similar children
- professional training
- research evidence on intervention effectiveness
- time and/or resources available to the therapist.
Table 12 sets out the results of that ranking exercise.
The relative influence of factors in clinical decision-making in the management of a case: therapists’ views ( n = 14)
Not unexpectedly, the dominant factor in decision-making was the therapist’s assessment of the child’s presenting clinical/functional needs , and it is important to note here that some groups explicitly stated that they had assumed this to also refer to the child’s, or parents’, goals. Only 3 of the 11 groups identified a different factor as the most important in informing clinical decision-making. In all cases, this factor was their professional training . A number of groups noted that the nature of other health interventions a child is receiving (e.g. other therapies, or medical/surgical interventions) may influence clinical decision-making and, in some cases, play a dominant role.
Clinical experience typically featured as a strong, but not the most important, influence on clinical decision-making. Here, many groups reported that they drew on not only their own clinical experience, but also that of colleagues. Discussing cases was an inherent part of their practice, and thus turning to others for input and advice was important and, possibly, more valuable or relevant than research evidence.
Views regarding the strength of influence of family characteristics and resources varied between therapists working in different settings. Those based in community teams viewed this as having a greater influence on decision-making than did those based in residential or school settings. Furthermore, the extent to which this factor was relevant to decision-making varied between families. Here, the key issue was the family’s capacity to take on a programme of therapy:
We know that some families will be able to take on therapy programmes and carry out a significant amount, but for others we know that we can’t possibly ask them to take this on as it would put an unbearable load on them and create an additional stress. G1
A further aspect of the role, or influence, of the family on clinical decision-making was revealed in our discussions with therapists. This concerned the pressure that therapists can feel parents place on them to ‘do something’ or try a particular approach.
A few interviewees developed this further, noting that a therapists’ implicit desire to help a child may influence their clinical decision-making:
. . . our own internal drivers to offer something positive into what can be quite catastrophic situations . . . G2
Therapists typically stated that resource issues should not influence their clinical decision-making. However, it was acknowledged that local directives can restrict the options open to a therapist. This can be at the team level; for example, clinical leads may adhere to particular approaches and practices. It may also operate at a trust level, with clinical decision-making affected by directives about whether specific procedures will be funded, the intensity of input (e.g. the frequency, number and duration of sessions) and/or the settings in which a therapist is permitted to work (e.g. clinic vs. home- or community-based work).
Research evidence was typically identified as having the least, if any, influence on clinical decision-making. The most frequent explanation for this was that there was a lack of evidence or that the existing evidence was not applicable to a particular diagnostic group:
Dysathria research does not include participants with learning disabilities, so that rules out most of our kids. G1
. . . it’s the same thing every time we try to do evidence-based guidelines: there is no evidence for use with children with ABI [acquired brain injury]. D1
Other explanations included scepticism about existing evidence, particularly if such evidence raised questions about a technique or approach that the therapist strongly believed, from their clinical experience, had positive impacts for children. In addition, therapists described coming to the decision that, for a particular child, existing evidence was not relevant or meaningful:
. . . research doesn’t necessarily work for everyone . . . it’s all about assessing it on a case-by-case basis. G1
A number of therapists referred to the difficulty accessing or ‘keeping up with’ evidence:
. . . there are so many diverse presentations among people we see that it’s hard to know all of the evidence. C1
Participants often reported looking to outputs from national professional bodies, or NICE, that summarised evidence and considered its implications. We also came across instances of services/teams or professional/clinical excellence networks seeking to collate and synthesise evidence in order to produce internal, or member, guidance:
It translates the evidence for you, and it’s really useful when it’s done like that. C1
We further discuss views on the perceived state of evidence in Chapter 8 .
- Cite this Page Beresford B, Clarke S, Maddison J. Therapy interventions for children with neurodisabilities: a qualitative scoping study. Southampton (UK): NIHR Journals Library; 2018 Jan. (Health Technology Assessment, No. 22.3.) Chapter 4, Therapy interventions: approaches and techniques.
- PDF version of this title (33M)
In this Page
Other titles in this collection.
- Health Technology Assessment
Recent Activity
- Therapy interventions: approaches and techniques - Therapy interventions for chi... Therapy interventions: approaches and techniques - Therapy interventions for children with neurodisabilities: a qualitative scoping study
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Interventions in the Scope of Occupational Therapy to Improve Psychosocial Well-Being in Older Adults with Low Vision and Mental Health Concerns: A Systematic Review
Affiliation.
- 1 Department of Occupational Therapy, Augusta University, Augusta, GA, USA.
- PMID: 34369234
- DOI: 10.1080/07380577.2021.1946733
Research has found that occupational therapy practitioners focus on functional and participation outcomes in the low vision population, but overlook corresponding psychosocial outcomes in rehabilitation. The purpose of this systematic review is to answer the PICO question: "What is the evidence to support interventions within the scope of occupational therapy for improving psychosocial well-being or quality of life in adults experiencing depression or anxiety as a result of low vision?" The team conducted a search of literature published between 2008 and 2020. Inclusion criteria consisted of interventions within the scope of occupational therapy for patients with low vision, and which measured mental health or quality of life factors. Eleven articles met inclusion criteria. The majority of the evidence consisted of 1B (45%) and 2B (36%) level randomized control trials. Two studies were 3B level evidence. Mental health outcomes were measured primarily using depression rating scales, although a number of studies also utilized vision-specific quality of life questionnaires. Established intervention themes included behavioral activation plus occupational therapy low vision rehabilitation, cognitive problem-solving approaches, usual care 'plus' skill-based training, and group service delivery approaches. Moderate evidence supports behavioral activation plus occupational therapy low vision rehabilitation, problem-solving approaches, and group service delivery approaches for improving mental health outcomes. There is moderate evidence that does not support usual treatment 'plus' skill-based training to improve mental health.
Keywords: Low vision; anxiety; depression; mental health; occupational therapy; rehabilitation.
Publication types
- Systematic Review
- Mental Health
- Occupational Therapy*
- Problem Solving
- Quality of Life
- Vision, Low*

IMAGES
VIDEO
COMMENTS
Evidence-informed Interventions: Addressing Cognition for Adults with Traumatic Brain Injury. ... Describes the central concepts that ground occupational therapy practice and builds a common understanding of the basic tenets and vision of the profession. ... Teach the client how to use a problem-solving strategy (i.e., define problem ...
2. Add these pairs of numbers: 4 and 2, 5 and 5, 7 and 3. 3. Now subtract the numbers. 4. Playing cards spread face up on the table: Turn over all of the even-numbered cards. 5. Now turn over all of the odd-numbered cards. Check for smooth changes in tasks.
We are able to dip our hands into orthopedic conditions as well as cognitive impairments (via neuro rehab). While we typically consider speech therapists the cognitive and language experts, occupational therapists do play a big part in cognitive therapy. Functional cognition relates to the cognitive skills required to complete those meaningful ...
This screening tool uses 16 items that assess different cognitive domains: visuo-spatial, executive function, naming, memory, attention, language, abstraction and orientation. Scores range from 0-30. Scores lower than 26 indicate cognitive impairment concerns. Medi-Cog is a two-part brief cognition, literacy, and pillbox-skills assessment.
Problem solving is described as a series of steps including referral, data collection, assessment, problem identification, planning, intervention and evalua-tion, which is mirrored by the OT process. Additionally, there are consid-ered to be two stages (Robertson, 1996): identifying the problem (also called the occupational therapy diagnosis ...
Common interventions occupational therapy conducts through therapeutic care include: activity analysis, adaptive equipment, assistive technology, therapeutic exercise, education and training. OTAs use their creativity and problem-solving skills to design these interventions to be tailored to each client. They help their clients achieve greater ...
Abstract. Background: Evidence supports the role of occupational therapy (OT) for older adults, and therapeutic use of problem solving may provide a way to improve older adult's occupational performance. Aim: To assess the effectiveness and describe the contents of OT interventions aimed at improving older adults' occupational performance by strengthening their problem-solving skills.
Abstract. Problem solving is integral to clinical reasoning and everyday occupational therapy practices. It can also be a systematic therapeutic modality for identifying client or family caregiver concerns and teaching new approaches to self-management. This chapter presents a systematic approach to help occupational therapists (OTs) identify ...
Therapeutic interventions that focus on cognitive function (e.g., attention, memory, reasoning, executive function, problem-solving, and/or pragmatic functioning) and compensatory strategies to manage the performance of an activity (e.g., managing time or schedules, initiating, organizing, and sequencing tasks), direct (one-on-one) patient contact.
Psychosocial occupational therapy interventions seek to optimize human functioning using a holistic approach. Interventions may facilitate reaching a youth's goals surrounding social skills, communication skills, decision-making, problem-solving, emotional regulation, coping strategies, healthy risk-taking, attention span and focus, intrinsic ...
Problem-solving therapy teaching problem-solving skills in a structured way to enable participants to systematically identify problems, generate alternative solutions, select the best solution, develop and conduct a plan, and evaluate whether the problem is solved ... Occupational therapy interventions to improve performance of daily activities ...
The Canadian Occupational Performance Measure (COPM) was the most widely used assessment, where 56.7% of our respondents reported using the COPM. The wide use of this measure is consistent with earlier studies specific to cognitive impairments [ 11] as well as other general occupational therapy assessments [ 12 ].
The American Journal of Occupational Therapy, 57(5), 534-541. Bathing Bathing Reluctance to cooperate or delayed independence in bathing in young children with ASD can be due to a number of factors. It is important to explore the reasons behind this. Problem-solving considerations with bathing problems might include: Sensory sensitivities.
Problem-solving therapy (PST) is a cognitive-behavioral intervention developed by D'Zurilla and Goldfried to alleviate individuals' mental and physical problems and improve their ability to cope ...
Keywords: Activity performance, Breast Cancer, Occupational therapy, Problem solving, Rehabilitation, Quality of life Background Cancer is a serious and chronic disease, as well as being a disease-bearing uncertainty, bringing to one's mind death in great suffering and pains and leading to feelings of panic and anxiety [ 1 ] .
Background: Evidence supports the role of occupational therapy (OT) for older adults, and therapeutic use of problem solving may provide a way to improve older adult's occupational performance.Aim: To assess the effectiveness and describe the contents of OT interventions aimed at improving older adults' occupational performance by strengthening their problem-solving skills.
Summary This chapter contains sections titled: Introduction Strand One: The Theoretical Underpinning of Problem Solving Strand Two: The Relationship of Problem Solving to Other Models ... Clinical Reasoning in Occupational Therapy. Related; Information; Close Figure Viewer. Return to Figure. Previous Figure Next Figure. Caption. Additional ...
For example, cognitive-behavioural, problem-solving approaches, sometimes referred to as 'coaching', were reported as being used within occupational therapy. Global notions of 'goals-focused approach', family-centred practice and 'evidence-based practice' were referred to across all therapies as 'schools of thought' that the ...
Moderate evidence supports behavioral activation plus occupational therapy low vision rehabilitation, problem-solving approaches, and group service delivery approaches for improving mental health outcomes. There is moderate evidence that does not support usual treatment 'plus' skill-based training to improve mental health.