
Transforming the understanding and treatment of mental illnesses.
Información en español

Celebrating 75 Years! Learn More >>
- Health Topics
- Brochures and Fact Sheets
- Help for Mental Illnesses
- Clinical Trials
- Download PDF
- Order a free hardcopy
What is depression?
Everyone feels sad or low sometimes, but these feelings usually pass. Depression (also called major depression, major depressive disorder, or clinical depression) is different. It can cause severe symptoms that affect how a person feels, thinks, and handles daily activities, such as sleeping, eating, or working.
Depression can affect anyone regardless of age, gender, race or ethnicity, income, culture, or education. Research suggests that genetic, biological, environmental, and psychological factors play a role in the disorder.
Women are diagnosed with depression more often than men, but men can also be depressed. Because men may be less likely to recognize, talk about, and seek help for their negative feelings, they are at greater risk of their depression symptoms being undiagnosed and undertreated. Studies also show higher rates of depression and an increased risk for the disorder among members of the LGBTQI+ community.
In addition, depression can co-occur with other mental disorders or chronic illnesses, such as diabetes, cancer, heart disease, and chronic pain. Depression can make these conditions worse and vice versa. Sometimes, medications taken for an illness cause side effects that contribute to depression symptoms as well.
What are the different types of depression?
There are two common types of depression.
- Major depression includes symptoms of depressed mood or loss of interest, most of the time for at least 2 weeks, that interfere with daily activities.
- Persistent depressive disorder (also called dysthymia or dysthymic disorder) consists of less severe depression symptoms that last much longer, usually for at least 2 years.
Other types of depression include the following.
- Seasonal affective disorder comes and goes with the seasons, with symptoms typically starting in the late fall and early winter and going away during the spring and summer.
- Depression with symptoms of psychosis is a severe form of depression in which a person experiences psychosis symptoms, such as delusions or hallucinations.
- Bipolar disorder involves depressive episodes, as well as manic episodes (or less severe hypomanic episodes) with unusually elevated mood, greater irritability, or increased activity level.
Additional types of depression can occur at specific points in a woman’s life. Pregnancy, the postpartum period, the menstrual cycle, and menopause are associated with physical and hormonal changes that can bring on a depressive episode in some people.
- Premenstrual dysphoric disorder is a more severe form of premenstrual syndrome, or PMS, that occurs in the weeks before menstruation.
- Perinatal depression occurs during pregnancy or after childbirth. It is more than the “baby blues” many new moms experience after giving birth.
- Perimenopausal depression affects some women during the transition to menopause. Women may experience feelings of intense irritability, anxiety, sadness, or loss of enjoyment.
What are the signs and symptoms of depression?
Common signs and symptoms of depression include:
- Persistent sad, anxious, or “empty” mood
- Feelings of hopelessness or pessimism
- Feelings of irritability, frustration‚ or restlessness
- Feelings of guilt, worthlessness, or helplessness
- Loss of interest or pleasure in hobbies and activities
- Fatigue, lack of energy, or feeling slowed down
- Difficulty concentrating, remembering, or making decisions
- Difficulty sleeping, waking too early in the morning, or oversleeping
- Changes in appetite or unplanned weight changes
- Physical aches or pains, headaches, cramps, or digestive problems without a clear physical cause that do not go away with treatment
- Thoughts of death or suicide or suicide attempts
Depression can also involve other changes in mood or behavior that include:
- Increased anger or irritability
- Feeling restless or on edge
- Becoming withdrawn, negative, or detached
- Increased engagement in high-risk activities
- Greater impulsivity
- Increased use of alcohol or drugs
- Isolating from family and friends
- Inability to meet responsibilities or ignoring other important roles
- Problems with sexual desire and performance
Not everyone who is depressed shows all these symptoms. Some people experience only a few symptoms, while others experience many. Depression symptoms interfere with day-to-day functioning and cause significant distress for the person experiencing them.
If you show signs or symptoms of depression and they persist or do not go away, talk to a health care provider. If you see signs of depression in someone you know, encourage them to seek help from a mental health professional.
If you or someone you know is struggling or having thoughts of suicide, call or text the 988 Suicide and Crisis Lifeline at 988 or chat at 988lifeline.org . In life-threatening situations, call 911 .
How is depression diagnosed?
To be diagnosed with depression, a person must have symptoms most of the day, nearly every day, for at least 2 weeks. One of the symptoms must be a depressed mood or a loss of interest or pleasure in most activities. Children and adolescents may be irritable rather than sad.
Although several persistent symptoms, in addition to low mood, are required for a depression diagnosis, people with only a few symptoms may benefit from treatment. The severity and frequency of symptoms and how long they last vary depending on the person.
If you think you may have depression, talk to a health care provider, such as a primary care doctor, psychologist, or psychiatrist. During the visit, the provider may ask when your symptoms began, how long they have lasted, how often they occur, and if they keep you from going out or doing your usual activities. It may help to take some notes about your symptoms before the visit.
Certain medications and medical conditions, such as viruses or thyroid disorders, can cause the same symptoms as depression. A provider can rule out these possibilities by doing a physical exam, interview, and lab tests.
Does depression look the same in everyone?
Depression can affect people differently depending on their age.
- Children may be anxious or cranky, pretend to be sick, refuse to go to school, cling to a parent, or worry that a parent may die.
- Older children and teens may get into trouble at school, sulk, be easily frustrated‚ feel restless, or have low self-esteem. They may have other disorders, such as anxiety, an eating disorder, attention-deficit/hyperactivity disorder, or substance use disorder. Older children and teens are also more likely to experience excessive sleepiness (called hypersomnia) and increased appetite (called hyperphagia).
- Young adults are more likely to be irritable, complain of weight gain and hypersomnia, and have a negative view of life and the future. They often have other disorders, such as generalized anxiety disorder, social phobia, panic disorder, or substance use disorder.
- Middle-aged adults may have more depressive episodes, decreased libido, middle-of-the-night insomnia, or early morning waking. They often report stomach problems, such as diarrhea or constipation.
- Older adults often feel sadness, grief, or other less obvious symptoms. They may report a lack of emotions rather than a depressed mood. Older adults are also more likely to have other medical conditions or pain that can cause or contribute to depression. Memory and thinking problems (called pseudodementia) may be prominent in severe cases.
Depression can also look different in men versus women, such as the symptoms they show and the behaviors they use to cope with them. For instance, men (as well as women) may show symptoms other than sadness, instead seeming angry or irritable.
For some people, symptoms manifest as physical problems (for example, a racing heart, tightened chest, chronic headaches, or digestive issues). Many men are more likely to see a health care provider about these physical symptoms than their emotional ones. While increased use of alcohol or drugs can be a sign of depression in any person, men are also more likely to use these substances as a coping strategy.
How is depression treated?
Depression treatment typically involves psychotherapy (in person or virtual), medication, or both. If these treatments do not reduce symptoms sufficiently, brain stimulation therapy may be another option.
Choosing the right treatment plan is based on a person’s needs, preferences, and medical situation and in consultation with a mental health professional or a health care provider. Finding the best treatment may take trial and error.
For milder forms of depression, psychotherapy is often tried first, with medication added later if the therapy alone does not produce a good response. People with moderate or severe depression usually are prescribed medication as part of the initial treatment plan.
Psychotherapy
Psychotherapy (also called talk therapy or counseling) can help people with depression by teaching them new ways of thinking and behaving and helping them change habits that contribute to depression. Psychotherapy occurs under the care of a licensed, trained mental health professional in one-on-one sessions or with others in a group setting.
Psychotherapy can be effective when delivered in person or virtually via telehealth. A provider may support or supplement therapy using digital or mobile technology, like apps or other tools.
Evidence-based therapies to treat depression include cognitive behavioral therapy and interpersonal therapy. Using other forms of psychotherapy, such as psychodynamic therapy, for a limited time also may help some people with depression.
- Cognitive behavioral therapy (CBT) : With CBT, people learn to challenge and change unhelpful thoughts and behaviors to improve their depressive and anxious feelings. Recent advances in CBT include adding mindfulness principles and specializing the therapy to target specific symptoms like insomnia.
- Interpersonal therapy (IPT) : IPT focuses on interpersonal and life events that impact mood and vice versa. IPT aims to help people improve their communication skills within relationships, form social support networks, and develop realistic expectations to better deal with crises or other issues that may be contributing to or worsening their depression.
Learn more about psychotherapy .
Antidepressants are medications commonly used to treat depression. They work by changing how the brain produces or uses certain chemicals involved in mood or stress.
Antidepressants take time—usually 4−8 weeks—to work, and problems with sleep, appetite, and concentration often improve before mood lifts. Giving a medication a chance to work is important before deciding whether it is right for you.
Treatment-resistant depression occurs when a person doesn’t get better after trying at least two antidepressants. Esketamine is a medication approved by the U.S. Food and Drug Administration (FDA) for treatment-resistant depression. Delivered as a nasal spray in a doctor’s office, clinic, or hospital, the medication acts rapidly, typically within a couple of hours, to relieve depression symptoms. People will usually continue to take an antidepressant pill to maintain the improvement in their symptoms.
Another option for treatment-resistant depression is to combine an antidepressant with a different type of medication that may make it more effective, such as an antipsychotic or anticonvulsant medication.
All medications can have side effects. Talk to a health care provider before starting or stopping any medication. Learn more about antidepressants .
Note : In some cases, children, teenagers, and young adults under 25 years may experience an increase in suicidal thoughts or behavior when taking antidepressants, especially in the first few weeks after starting or when the dose is changed. The FDA advises that patients of all ages taking antidepressants be watched closely, especially during the first few weeks of treatment.
Information about medication changes frequently. Learn more about specific medications like esketamine, including the latest approvals, side effects, warnings, and patient information, on the FDA website .
Brain stimulation therapy
Brain stimulation therapy is an option when other depression treatments have not worked. The therapy involves activating or inhibiting the brain with electricity or magnetic waves.
Although brain stimulation therapy is less frequently used than psychotherapy and medication, it can play an important role in treating depression in people who have not responded to other treatments. The therapy generally is used only after a person has tried psychotherapy and medication, and those treatments usually continue. Brain stimulation therapy is sometimes used as an earlier treatment option when severe depression has become life-threatening, such as when a person has stopped eating or drinking or is at a high risk of suicide.
The FDA has approved several types of brain stimulation therapy. The most used are electroconvulsive therapy (ECT) and repetitive transcranial magnetic stimulation (rTMS). Other brain stimulation therapies are newer and, in some cases, still considered experimental. Learn more about brain stimulation therapies .
Natural products
The FDA has not approved any natural products for treating depression. Although research is ongoing and findings are inconsistent, some people report that natural products, including vitamin D and the herbal dietary supplement St. John’s wort, helped their depression symptoms. However, these products can come with risks, including, in some cases, interactions with prescription medications.
Do not use vitamin D, St. John’s wort, or other dietary supplements or natural products without first talking to a health care provider. Rigorous studies must test whether these and other natural products are safe and effective.
How can I take care of myself?
Most people with depression benefit from mental health treatment. Once you begin treatment, you should gradually start to feel better. Go easy on yourself during this time. Try to do things you used to enjoy. Even if you don’t feel like doing them, they can improve your mood.
Other things that may help:
- Try to get physical activity. Just 30 minutes a day of walking can boost your mood.
- Try to maintain a regular bedtime and wake-up time.
- Eat regular, healthy meals.
- Do what you can as you can. Decide what must get done and what can wait.
- Connect with people. Talk to people you trust about how you are feeling.
- Delay making important life decisions until you feel better. Discuss decisions with people who know you well.
- Avoid using alcohol, nicotine, or drugs, including medications not prescribed for you.
How can I find help for depression?
You can learn about ways to get help and find tips for talking with a health care provider on the NIMH website.
The Substance Abuse and Mental Health Services Administration (SAMHSA) also has an online tool to help you find mental health services in your area.
How can I help a loved one who is depressed?
If someone you know is depressed, help them see a health care provider or mental health professional. You also can:
- Offer support, understanding, patience, and encouragement.
- Invite them out for walks, outings, and other activities.
- Help them stick to their treatment plan, such as setting reminders to take prescribed medications.
- Make sure they have transportation or access to therapy appointments.
- Remind them that, with time and treatment, their depression can lift.
What are clinical trials and why are they important?
Clinical trials are research studies that look at ways to prevent, detect, or treat diseases and conditions. These studies help show whether a treatment is safe and effective in people. Some people join clinical trials to help doctors and researchers learn more about a disease and improve health care. Other people, such as those with health conditions, join to try treatments that aren’t widely available.
NIMH supports clinical trials across the United States. Talk to a health care provider about clinical trials and whether one is right for you. Learn more about participating in clinical trials .
For more information
Learn more about mental health disorders and topics . For information about various health topics, visit the National Library of Medicine’s MedlinePlus .
The information in this publication is in the public domain and may be reused or copied without permission. However, you may not reuse or copy images. Please cite the National Institute of Mental Health as the source. Read our copyright policy to learn more about our guidelines for reusing NIMH content.
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES National Institutes of Health NIH Publication No. 24-MH-8079 Revised 2024

New Research: Serotonin Does Have a Direct Role in Depression
Absence of evidence is not evidence of absence..
Posted November 5, 2022 | Reviewed by Vanessa Lancaster
- What Is Depression?
- Find a therapist to overcome depression
- There has been no direct evidence that serotonin plays a key role in depression until now.
- New research reported here uses a radioactive tracer and PET scans to show that serotonin activity is lower in people with clinical depression.
- While a small study, this work presents a new paradigm for directly assaying serotonin in psychiatry.
- Future research will seek to replicate or refute these findings and expand studies to larger and more diverse groups.
By Grant H. Brenner
Over the years, the serotonin hypothesis of depression , which suggests that low or impaired serotonin neurotransmission is related to the symptoms and possible causes of depression and related psychiatric disorders, has taken many hits.
Recently, a widely publicized review paper in Nature (Moncrieff et al., 2022) found no direct evidence that serotonin is involved in the pathophysiology of depression. This led to an explosion of reports and even attacks which reverberated across the internet about the serotonin hypothesis, the long-debunked “chemical imbalance” explanation, and, to an extent, psychiatry as a field.
The uproar is understandable–depression affects an estimated 20 million US citizens and nearly 300 million worldwide , and current treatments are only partially effective. There is a growing awareness that mental health problems are epidemic–a recent survey by the American Psychiatric Association found 79 percent of people see mental health as a public health emergency.
Moreover, rates of anxiety and depression are skyrocketing, especially among younger people , suicide has become a leading cause of death, and we are more aware every day of the hazardous effect of endemic stress and trauma on mental and physical health.
Despite various studies over the years and the recognition that antidepressant and psychedelic medications, 1 which improve depression, often increase serotonin levels and are associated with positive brain changes (such as increased neuronal complexity via "sprouting" and possible restoration of brain volume in areas like the hippocampus), there has been a startling lack of evidence showing a direct role for serotonin, perhaps because more sophisticated research methods have not been available.
Absence of Evidence Is Not Evidence of Absence
That is, until now. For the first time, study authors have found a clear association between altered serotonin activity and depression in a robust experimental design.
Researchers Erritzoe and colleagues (2022) report their findings in a recent paper in Biological Psychiatry entitled "Brain Serotonin Release Is Reduced in Patients With Depression." In this study, they compared two groups of people, 17 people with clinical depression (MDD group for major depressive disorder) rigorously diagnosed with depression and free from other conditions, not taking antidepressants at the time of the study (most never had, some had in the past), and 17 people without any mental illness (the HC or healthy control group).
The statistics analyzed clinical data and brain-imaging findings to determine if MDD and HC differed significantly in the serotonin neurotransmission, and if so, in what direction? If MDD showed lower serotonin, or 5HT, activity, this would directly support the serotonin hypothesis of depression.
Study participants were administered a mildly radioactive chemical developed to directly measure serotonin activity in the brain. Rather than the previous studies reviewed in the Nature article, which included indirect measures, using [11C]Cimbi-36 (a "radioligand") allows researchers to probe actual 5HT activity on PET (Positron Emission Tomography) and MRI (Magnetic Resonance Imaging) scan.
PET is an imaging approach more sophisticated than MRI. Unlike MRI, which produces a lower resolution scan indirectly estimating brain activity (often based on inferred blood flow), PET images positrons (a form of antimatter, antielectrons) to get a fine-grained, direct window into the brain's inner workings.
Why [11C]Cimbi-36? Prior PET studies have shown that when serotonin goes up, [11C]Cimbi-36 predictably and reliably goes down. It’s called a radioligand because the molecule contains a radioactive form of carbon that lights up on PET.
Study participants, in addition to careful clinical diagnosis, completed depression ratings and underwent PET-MRI imaging after being given a dose of d- amphetamine (a drug familiar for its use in treating ADHD and also for its abuse potential as a street drug and misused prescriptions).
Prior research has shown that if we give a dose of d-amphetamine to non-depressed individuals (HCs), [11C]Cimbi-36 levels drop significantly, reflecting an increase in 5HT activity. Is this response the same in people with depression? If not, it would lend new support to the serotonin hypothesis of depression.
The main study result was that in patients with depression, serotonin activity is indeed diminished compared with people without depression. Following d-amphetamine challenge, [11C]Cimbi-36 tracer binding across brain cortex (surface) areas was as expected for healthy individuals, consistent with prior experiments.

However, for depressed participants, a very different pattern emerged. When this group received d-amphetamine, [11C]Cimbi-36 binding was significantly lower than in the non-depressed group, reflecting underlying decreased serotonin activity in depressed patients compared with healthy controls. This activity was seen across many brain regions, reaching statistical significance in the temporal cortex (areas located on the sides of the brain, in rough proximity to the ears 2 ).
The effect was stronger in MDD participants who had never taken antidepressants (" medication naive") versus those who had but were not taking them during the study, but this finding is hard to interpret due to the small number of participants in the prior medication group.
Implications and Future Directions
Overall, this study found diminished serotonin activity in patients with diagnoses of clinical depression. This does not mean that depression is caused by serotonin deficiency or that medications that increase serotonin will treat depression. If only it were that easy.
The picture is much more complex than that, with an array of not only many different serotonin receptors and systems throughout the brain but also many other factors, including but not limited to an array of implicated non-serotonin neurotransmitters (norepinephrine, dopamine , glutamate, GABA, and others), the role of other biological factors and psychosocial factors, and the increasingly recognized role of supporting role of glial cells in brain function–cells which are not neurons but which support and modulate what neurons do. 3
This study is not the end of the discussion but rather a new beginning. It is the first study to show diminished serotonin activity in depression.
However, it is only one study with a relatively small number of participants, and as with any study requires replication to determine if it is really true and to build in more nuance to the study design to account for potential confounding factors (like time of day, clinical presentation in a more diverse population, the role of serotonin in disorders which overlap with depression, and so on).
In addition to the main finding that people with depression do have lower serotonin activity compared with those without depression, at least here, this work is important because it is proof of concept for a study approach to directly assess brain serotonin activity. This approach can and will be refined–for example, using challenges other than with d-amphetamine to perturb serotonin tracer activity.
Nevertheless, it is a powerful tool and one which, along with others under development such as computational tools to develop better ways of understanding psychiatric conditions (“ transdiagnostic approaches "), 4 will help to usher in a new era, with the expectation that growing understanding will enable more effective treatment and ultimate reduce the considerable suffering associated with mental illness.
Facebook image: Monkey Business Images/Shutterstock
1. Serotonin is also implicated in psychedelic medications, including psilocybin ("magic mushrooms") and LSD–however, the psychedelic effect may be different from the antidepressant effect (Kaplan et al., 2022), suggesting that aside from depression as a mental illness, culturally we may be looking for ways to break out of conventional, restrictive ways of thinking while folding this need into a medicalized view of human experience.
2. 3D Brain Online
3. A recent study found that astrocytes, a supporting cell in the brain, actually pull back part of their cell bodies ("leaflets") to expose the gap between neurons (the "synapse"), which in turn facilitates glutamate transmission involved in fear-based learning!
4. A recent paper discusses evolving diagnostic approaches in psychiatry: Identifying transdiagnostic mechanisms in mental health using computational factor modeling
Erritzoe D. CA, Searle G., Lewis Y., Passchier J., Azeem S., Beaver J., Nutt D., Knudsen G., Gunn R., Rabiner E. (2017): Serotonin release measured in the human brain: A PET study with [11C]Cimbi-36 and d-amphetamine challenge. BrainPET 2017. Berlin, Germany.
Erritzoe D., Godlewska B.R., Rizzo G., Searle G.E., Agnorelli C., Lewis Y., Ashok A.H., Colasanti A., Boura I., Farrell C., Parfit H., Howes O., Passchier J., Gunn R.N., Nutt D.J., Cowen P.J, Knudsen G. & Rabiner E.A., BRAIN SEROTONIN RELEASE IS REDUCED IN PATIENTS WITH DEPRESSION: A [11C]Cimbi-36 PET STUDY WITH A D-AMPHETAMINE CHALLENGE., Biological Psychiatry (2022), doi: https://doi.org/10.1016/j.biopsych.2022.10.012 .
Kaplan, A.L., Confair, D.N., Kim, K. et al. Bespoke library docking for 5-HT2A receptor agonists with antidepressant activity. Nature 610, 582–591 (2022). https://doi.org/10.1038/s41586-022-05258-z
Moncrieff, J., Cooper, R.E., Stockmann, T. et al. The serotonin theory of depression: a systematic umbrella review of the evidence. Mol Psychiatry (2022). https://doi.org/10.1038/s41380-022-01661-0
Obligatory Disclaimer: This Blog Post ("Our Blog Post") is not intended to be a substitute for professional advice. We will not be liable for any loss or damage caused by your reliance on information obtained through Our Blog Post. Please seek the advice of professionals, as appropriate, regarding the evaluation of any specific information, opinion, advice, or other content. We are not responsible and will not be held liable for third-party comments on Our Blog Post. Any user comment on Our Blog Post that in our sole discretion restricts or inhibits any other user from using or enjoying Our Blog Post is prohibited and may be reported to Sussex Publishers/Psychology Today. Grant H. Brenner/Neighborhood Psychiatry & Wellness/The Collective - Integrated Behavioral Health. All rights reserved.

SOL Mental Health is a practice of medical professionals, therapists, wellness experts, and administrative support staff dedicated to providing compassionate, conscientious care. We strive to constantly improve patient experience and raise the overall standard of what patients seeking mental health care receive.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Teletherapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience
Psychological Disorders
The biological basis of mood disorders, learning objectives.
- Describe genetic, biological, and psychological explanations of major depressive disorder

Figure 1 . Many medications designed to treat mood disorders work by altering neurotransmitter activity in the neural synapse.
Depression is linked to abnormal activity in several regions of the brain (Fitzgerald, Laird, Maller, & Daskalakis, 2008) including those important in assessing the emotional significance of stimuli and experiencing emotions (amygdala), and in regulating and controlling emotions (like the prefrontal cortex, or PFC) (LeMoult, Castonguay, Joormann, & McAleavey, 2013). Depressed individuals show elevated amygdala activity (Drevets, Bogers, & Raichle, 2002), especially when presented with negative emotional stimuli, such as photos of sad faces (Figure 2) (Surguladze et al., 2005). Interestingly, heightened amygdala activation to negative emotional stimuli among depressed persons occurs even when stimuli are presented outside of conscious awareness (Victor, Furey, Fromm, Öhman, & Drevets, 2010), and it persists even after the negative emotional stimuli are no longer present (Siegle, Thompson, Carter, Steinhauer, & Thase, 2007). Additionally, depressed individuals exhibit less activation in the prefrontal, particularly on the left side (Davidson, Pizzagalli, & Nitschke, 2009). Because the PFC can dampen amygdala activation, thereby enabling one to suppress negative emotions (Phan et al., 2005), decreased activation in certain regions of the PFC may inhibit its ability to override negative emotions that might then lead to more negative mood states (Davidson et al., 2009). These findings suggest that depressed persons are more prone to react to emotionally negative stimuli, yet have greater difficulty controlling these reactions.

Figure 2 . Depressed individuals react to negative emotional stimuli, such as sad faces, with greater amygdala activation than do non-depressed individuals. (credit: Ian Munroe)
Since the 1950s, researchers have noted that depressed individuals have abnormal levels of cortisol, a stress hormone released into the blood by the neuroendocrine system during times of stress (Mackin & Young, 2004). When cortisol is released, the body initiates a fight-or-flight response in reaction to a threat or danger. Many people with depression show elevated cortisol levels (Holsboer & Ising, 2010), especially those reporting a history of early life trauma such as the loss of a parent or abuse during childhood (Baes, Tofoli, Martins, & Juruena, 2012). Such findings raise the question of whether high cortisol levels are a cause or a consequence of depression. High levels of cortisol are a risk factor for future depression (Halligan, Herbert, Goodyer, & Murray, 2007), and cortisol activates activity in the amygdala while deactivating activity in the PFC (McEwen, 2005)—both brain disturbances are connected to depression. Thus, high cortisol levels may have a causal effect on depression, as well as on its brain function abnormalities (van Praag, 2005). Also, because stress results in increased cortisol release (Michaud, Matheson, Kelly, Anisman, 2008), it is equally reasonable to assume that stress may precipitate depression.
Diathesis-Stress Model and Major Depressive Disorders
Indeed, it has long been believed that stressful life events can trigger depression, and research has consistently supported this conclusion (Mazure, 1998). Stressful life events include significant losses, such as death of a loved one, divorce or separation, and serious health and money problems; life events such as these often precede the onset of depressive episodes (Brown & Harris, 1989). In particular, exit events—instances in which an important person departs (e.g., a death, divorce or separation, or a family member leaving home)—often occur prior to an episode (Paykel, 2003). Exit events are especially likely to trigger depression if these happenings occur in a way that humiliates or devalues the individual. For example, people who experience the breakup of a relationship initiated by the other person develop major depressive disorder at a rate more than 2 times that of people who experience the death of a loved one (Kendler, Hettema, Butera, Gardner, & Prescott, 2003).
Likewise, individuals who are exposed to traumatic stress during childhood—such as separation from a parent, family turmoil, and maltreatment (physical or sexual abuse)—are at a heightened risk of developing depression at any point in their lives (Kessler, 1997). A recent review of 16 studies involving over 23,000 subjects concluded that those who experience childhood maltreatment are more than 2 times as likely to develop recurring and persistent depression (Nanni, Uher, & Danese, 2012).
Of course, not everyone who experiences stressful life events or childhood adversities develops depression—indeed, most do not. Clearly, a diathesis-stress interpretation of major depressive disorder, in which certain predispositions or vulnerability factors influence one’s reaction to stress, would seem logical. If so, what might such predispositions be? A study by Caspi and others (2003) suggests that an alteration in a specific gene that regulates serotonin (the 5-HTTLPR gene) might be one culprit. These investigators found that people who experienced several stressful life events were significantly more likely to experience episodes of major depression if they carried one or two short versions of this gene than if they carried two long versions. Those who carried one or two short versions of the 5-HTTLPR gene were unlikely to experience an episode, however, if they had experienced few or no stressful life events. Numerous studies have replicated these findings, including studies of people who experienced maltreatment during childhood (Goodman & Brand, 2009). In a recent investigation conducted in the United Kingdom (Brown & Harris, 2013), researchers found that childhood maltreatment before age 9 elevated the risk of chronic adult depression (a depression episode lasting for at least 12 months) among those individuals having one (LS) or two (SS) short versions of the 5-HTTLPR gene (Figure 3). Childhood maltreatment did not increase the risk for chronic depression for those have two long (LL) versions of this gene. Thus, genetic vulnerability may be one mechanism through which stress potentially leads to depression.

Figure 3 . A study on gene-environment interaction in people experiencing chronic depression in adulthood suggests a much higher incidence in individuals with a short version of the gene in combination with childhood maltreatment (Brown & Harris, 2013).
Cognitive Theories of Depression
Cognitive theories of depression take the view that depression is triggered by negative thoughts, interpretations, self-evaluations, and expectations (Joormann, 2009). These diathesis-stress models propose that depression is triggered by a “cognitive vulnerability” (negative and maladaptive thinking) and by precipitating stressful life events (Gotlib & Joormann, 2010). Perhaps the most well-known cognitive theory of depression was developed in the 1960s by psychiatrist Aaron Beck, based on clinical observations and supported by research (Beck, 2008). Beck theorized that depression-prone people possess depressive schemas, or mental predispositions to think about most things in a negative way (Beck, 1976). Depressive schemas contain themes of loss, failure, rejection, worthlessness, and inadequacy, and may develop early in childhood in response to adverse experiences, then remain dormant until they are activated by stressful or negative life events. Depressive schemas prompt dysfunctional and pessimistic thoughts about the self, the world, and the future. Beck believed that this dysfunctional style of thinking is maintained by cognitive biases, or errors in how we process information about ourselves, which lead us to focus on negative aspects of experiences, interpret things negatively, and block positive memories (Beck, 2008). A person whose depressive schema consists of a theme of rejection might be overly attentive to social cues of rejection (more likely to notice another’s frown), and he might interpret this cue as a sign of rejection and automatically remember past incidents of rejection. Longitudinal studies have supported Beck’s theory, in showing that a preexisting tendency to engage in this negative, self-defeating style of thinking—when combined with life stress—over time predicts the onset of depression (Dozois & Beck, 2008). Cognitive therapies for depression, aimed at changing a depressed person’s negative thinking, were developed as an expansion of this theory (Beck, 1976).
Another cognitive theory of depression, hopelessness theory , postulates that a particular style of negative thinking leads to a sense of hopelessness, which then leads to depression (Abramson, Metalsky, & Alloy, 1989). According to this theory, hopelessness is an expectation that unpleasant outcomes will occur or that desired outcomes will not occur, and there is nothing one can do to prevent such outcomes. A key assumption of this theory is that hopelessness stems from a tendency to perceive negative life events as having stable (“It’s never going to change”) and global (“It’s going to affect my whole life”) causes, in contrast to unstable (“It’s fixable”) and specific (“It applies only to this particular situation”) causes, especially if these negative life events occur in important life realms, such as relationships, academic achievement, and the like. Suppose a student who wishes to go to law school does poorly on an admissions test. If the student infers negative life events as having stable and global causes, she may believe that her poor performance has a stable and global cause (“I lack intelligence, and it’s going to prevent me from ever finding a meaningful career”), as opposed to an unstable and specific cause (“I was sick the day of the exam, so my low score was a fluke”). Hopelessness theory predicts that people who exhibit this cognitive style in response to undesirable life events will view such events as having negative implications for their future and self-worth, thereby increasing the likelihood of hopelessness—the primary cause of depression (Abramson et al., 1989). One study testing hopelessness theory measured the tendency to make negative inferences for bad life effects in participants who were experiencing uncontrollable stressors. Over the ensuing six months, those with scores reflecting high cognitive vulnerability were 7 times more likely to develop depression compared to those with lower scores (Kleim, Gonzalo, & Ehlers, 2011).
A third cognitive theory of depression focuses on how people’s thoughts about their distressed moods—depressed symptoms in particular—can increase the risk and duration of depression. This theory, which focuses on rumination in the development of depression, was first described in the late 1980s to explain the higher rates of depression in women than in men (Nolen-Hoeksema, 1987). Rumination is the repetitive and passive focus on the fact that one is depressed and dwelling on depressed symptoms, rather that distracting one’s self from the symptoms or attempting to address them in an active, problem-solving manner (Nolen-Hoeksema, 1991). When people ruminate, they have thoughts such as “Why am I so unmotivated? I just can’t get going. I’m never going to get my work done feeling this way” (Nolen-Hoeksema & Hilt, 2009, p. 393). Women are more likely than men to ruminate when they are sad or depressed (Butler & Nolen-Hoeksema, 1994), and the tendency to ruminate is associated with increases in depression symptoms (Nolen-Hoeksema, Larson, & Grayson, 1999), heightened risk of major depressive episodes (Abela & Hankin, 2011), and chronicity of such episodes (Robinson & Alloy, 2003).
Contribute!
Improve this page Learn More
- Mood Disorders. Authored by : OpenStax College. Located at : https://openstax.org/books/psychology-2e/pages/15-7-mood-disorders . License : CC BY: Attribution . License Terms : Download for free at https://openstax.org/books/psychology-2e/pages/1-introduction

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Open access
- Published: 11 June 2018
Genetics of attention deficit hyperactivity disorder
- Stephen V. Faraone ORCID: orcid.org/0000-0002-9217-3982 1 &
- Henrik Larsson 2 , 3
Molecular Psychiatry volume 24 , pages 562–575 ( 2019 ) Cite this article
150k Accesses
528 Citations
318 Altmetric
Metrics details
- Neuroscience
Decades of research show that genes play an vital role in the etiology of attention deficit hyperactivity disorder (ADHD) and its comorbidity with other disorders. Family, twin, and adoption studies show that ADHD runs in families. ADHD’s high heritability of 74% motivated the search for ADHD susceptibility genes. Genetic linkage studies show that the effects of DNA risk variants on ADHD must, individually, be very small. Genome-wide association studies (GWAS) have implicated several genetic loci at the genome-wide level of statistical significance. These studies also show that about a third of ADHD’s heritability is due to a polygenic component comprising many common variants each having small effects. From studies of copy number variants we have also learned that the rare insertions or deletions account for part of ADHD’s heritability. These findings have implicated new biological pathways that may eventually have implications for treatment development.
Similar content being viewed by others
Polygenic profiles define aspects of clinical heterogeneity in attention deficit hyperactivity disorder

Differences in the genetic architecture of common and rare variants in childhood, persistent and late-diagnosed attention-deficit hyperactivity disorder
Shared genetic background between children and adults with attention deficit/hyperactivity disorder
Attention deficit hyperactivity disorder (ADHD) is a childhood-onset condition with impairing symptoms of inattention, impulsivity, and hyperactivity. Decades of research have documented and replicated key facts about the disorder (for a review, see ref. [ 1 ]). It occurs in about 5% of children with little geographic or cross-cultural variation in prevalence and often co-occurs with other conditions, including mood, anxiety, conduct, learning, and substance use disorders. Longitudinal studies show that two-thirds of ADHD youth will continue to have impairing symptoms of ADHD in adulthood. People with ADHD are at risk for a wide range of functional impairments: school failure, peer rejection, injuries due to accidents, criminal behavior, occupational failure, divorce, suicide, and premature death. Although many details of ADHD’s pathophysiology are unknown, neuropsychological and neuroimaging studies implicate brain circuits regulating executive functioning, reward processing, timing, and temporal information processing.
This article reviews data about the role that genes play in the etiology of ADHD from two perspectives. Family, twin, and adoption studies provide a firm foundation for asserting that genes are involved in the etiology of ADHD. The view from molecular genetics provides a basis for understanding mechanisms whereby genes affect biological pathways that lead to ADHD.
Family, twin and adoption studies of ADHD
Evidence for heritability from family, adoption, and twin studies.
A study of 894 ADHD probands and 1135 of their siblings aged 5–17 years old found a ninefold increased risk of ADHD in siblings of ADHD probands compared with siblings of controls [ 2 ]. Adoption studies suggest that the familial factors of ADHD are attributable to genetic factors rather than shared environmental factors [ 3 , 4 ] with the most recent one reporting rates of ADHD to be greater among biological relatives of non-adopted ADHD children than adoptive relatives of adopted ADHD children. The adoptive relatives had a risk for ADHD like the risk in relatives of control children [ 4 ].
Twin studies rely on the difference between the within-pair similarities of monozygotic (MZ) twin pairs, who are genetically identical, and dizygotic (DZ) twin pairs, who share, on average, 50% of their segregating genes. The mean heritability across 37 twin studies of ADHD or measures of inattentiveness and hyperactivity is 74% (Fig. 1 ). A similar heritability estimate of around 80% was seen in a study of MZ and DZ twins, full siblings, and maternal and paternal half-siblings [ 5 ]. The heritability is similar in males and females and for the inattentive and hyperactive-impulsive components of ADHD [ 6 , 7 , 8 ].
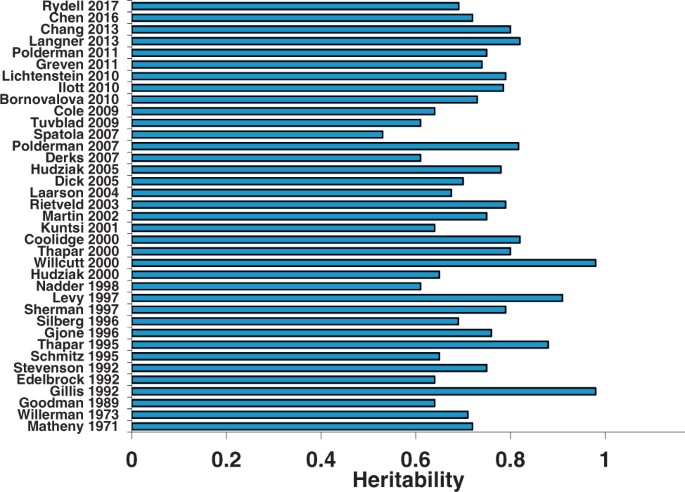
Heritability of ADHD from twin studies of ADHD diagnoses or symptom counts [ 153 , 154 , 155 , 156 , 157 , 158 , 159 , 160 , 161 , 162 , 163 , 164 , 165 , 166 , 167 , 168 , 169 , 170 , 171 , 172 , 173 ]
Only a few of the twin studies in Fig. 1 used categorical measures of ADHD [ 9 , 10 , 11 , 12 ]. Their heritability estimates range from 77 to 88%, which is consistent with the larger number of studies using symptom count measures of ADHD. Twin studies have explored whether ADHD is best viewed as a categorical disorder or as an extreme of a continuous trait. A study of 16,366 Swedish twins found a strong genetic link between the extreme and the sub-threshold variation of DSM-IV ADHD symptoms [ 13 ]. This study confirmed an early study of 583 same-sexed twin pairs using ADHD-III-R symptoms [ 14 ]. Both studies suggest that the diagnosis of ADHD is the extreme of a continuous distribution of ADHD symptoms in the population and that the etiologic factors involved in the disorder also account for the full range of symptoms. These data are consistent with clinical studies showing the clinical implications of subthreshold ADHD [ 15 ].
ADHD’s clinical features and course
Reporter effects.
Parent and teacher ratings of ADHD symptoms result in high heritability estimates (70–80%) [ 6 ]. In contrast, studies using self-ratings in adolescence and adulthood show lower heritabilities (<50%) [ 16 , 17 , 18 , 19 ]. Two twin studies examined these rater effects [ 20 , 21 ]. They showed that self-ratings, as well as different-parent and different-teacher ratings within twin pairs, were associated with lower heritability estimates (~30–40%) compared with heritabilities based on same-parent and same-teacher ratings (~70–80%) [ 20 , 21 , 22 ]. Low reliability of self-reports may explain why heritability estimates are lower in studies of self-rated ADHD symptoms. Using different informants for ADHD symptom ratings of each twin in a pair introduces rater effects (i.e., each rater experiences and reports different ADHD symptoms) or rater bias (i.e., a rater consistently over- or underestimates ADHD symptoms or similarities between twins). These effects could explain why heritability estimates are lower in studies relying on different informants for each twin in a pair compared with studies using the same raters [ 23 ].
Developmental effects
The first twin studies of ADHD in adults used self-reports and estimated heritability at 30–40% (Fig. 2) , (e.g. [ 24 ]), which is substantially lower than the heritability among children and adolescents. In contrast, one study estimated heritability to be 80% after combining self and parent ratings into a composite index of ADHD. Another study found the heritability of clinically diagnosed ADHD in adults to be 72% [ 25 ]. These findings (Fig. 2 ) suggest that the heritability of ADHD is stable during the transition from childhood into adulthood. They explain previous reports of low heritability for ADHD symptoms in adults as due to measurement error from rater effects. The higher heritabilities for clinically diagnosed adult ADHD confirm family studies suggesting that persistent ADHD is highly familial [ 5 , 26 , 27 ].
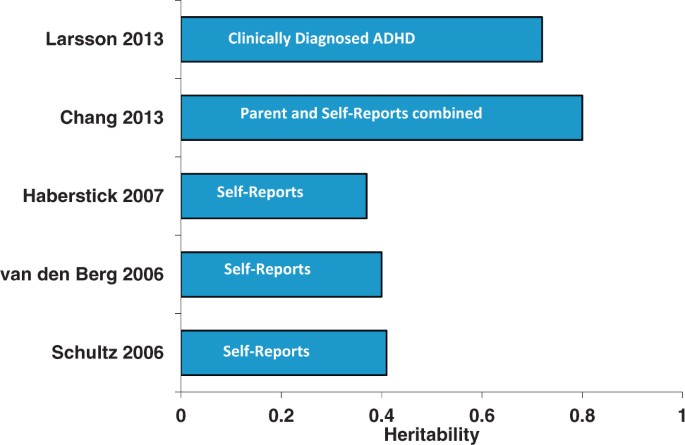
Heritability of ADHD in adults depends on method of diagnosis
Twin studies show that both stable and dynamic genetic risk factors influence ADHD over the course of the development from childhood to early adulthood [ 7 , 28 , 29 , 30 ]. These study findings explain the developmental structure of genetic risk factors for ADHD with both stable and dynamic processes. The stable component of the genetic risk suggests that persistent ADHD and its pediatric form are genetically linked. The dynamic component suggests that the set of genetic variants accounting for the onset of ADHD differs from those accounting for the persistence and remission of the disorder. For a review of the genetics of adult ADHD, see Franke et al. [ 26 ].
Psychiatric comorbidity
Multivariate twin and sibling studies have found a general genetic factor that influences ADHD and a broad spectrum of neuropsychiatric conditions [ 31 , 32 ]. These studies have shown that a latent shared genetic factor accounts for up to 45% of co-variance across childhood externalizing, internalizing, and phobia symptoms [ 31 , 33 ] and 31% of co-variance in childhood neurodevelopmental symptoms [ 34 ]. Similar results have been reported for register-based clinical diagnoses, with one study showing that a general genetic factor explained 10–36% of disorder liability across several psychiatric diagnoses [ 32 ]. Two studies have assessed the contribution of measured genetic variants for a general psychopathology dimension. One study estimated the SNP-heritability as 18% for maternal ratings of total problems on the Child Behavior Checklist, which measures internalizing, externalizing, and attention problems [ 35 ]. Similarly, another study estimated the SNP heritability as 38% for a general psychopathology factor derived from childhood psychopathology symptoms assessed by multiple raters [ 36 ]. These studies also support spectrum-specific genetic factors, such as genetic factors that load specifically on externalizing disorders [ 31 ]. The finding of externalizing-specific genetic factors for ADHD is consistent with a large number of twin and family studies demonstrating genetic overlaps of ADHD with oppositional-defiant disorder symptoms [ 37 ], conduct disorder [ 38 ], antisocial behavior [ 39 ], and substance use problems [ 40 , 41 , 42 ].
Twin studies have tested for genetic overlap between ADHD and autism spectrum disorders (ASD) [ 43 , 44 ], which often co-occur [ 45 ]. Studies of community samples of youth, from the United States of America [ 46 ], the United Kingdom [ 47 ], and Sweden [ 11 , 48 ] show that genetic factors influence this comorbidity. Ronald et al. [ 47 ]. found genetic correlations between ADHD and ASD above 0.50. Similar results have been found in adult twin studies [ 49 ]. A register-based study in Sweden found that individuals with ASD and their relatives were at increased risk of ADHD. The pattern of association across relatives supported the existence of a genetic overlap between clinically ascertained ASD and ADHD [ 50 ]. Some features of ASD are differentially linked to either the inattentive or the hyperactive-impulsive components of ADHD [ 51 , 52 ]. For instance, Polderman et al. [ 51 ]. found that the symptoms reflecting the repetitive and restricted aspects of ASD showed the strongest genetic association with ADHD and a Swedish twin study found that the subcomponents of ADHD and ASD are influenced by specific genetic factors [ 48 ].
Fewer studies have explored how genetic factors contribute to the co-occurrence between ADHD and internalizing disorders. A large family study found an increased risk of attempted and completed suicide in first- and second-degree relatives of ADHD probands [ 53 ]. The pattern of familial risks across different levels of relatedness suggests that shared genetic factors are important for these associations [ 53 ]. Family studies that studied the association between ADHD and depression suggest that the co-occurrence is influenced by shared familial factors [ 54 , 55 ]. Twin studies of this issue suggest that shared genetic factors explain the overlap of ADHD with depression, anxiety, and internalizing symptoms [ 56 , 57 , 58 , 59 , 60 ]. For example, Cole et al. [ 59 ]. found that shared genetic factors explained most of the association between traits of ADHD and depression. Similar results were found by Spatola et al. [ 60 ]., who used a multivariate twin analysis to study the overlap between different subscales of the Child Behavior Check List (CBCL), such as affective problems, anxiety problems, and attention-deficit/hyperactivity problems.
In contrast to the wealth of information about the familial co-transmission of ADHD and many other disorders, very little is known about ADHD’s familial links to intellectual disability (ID). A meta-analysis reported that the intelligence quotient (IQ) of youth with ADHD is nine points lower than typically developing peers [ 61 ] and much evidence suggests it is valid to diagnose ADHD in the context of ID [ 62 ]. Faraone et al. [ 63 ] studied the genetic association of ADHD and ID in Swedish medical registry data. Individuals with ID were at increased risk for ADHD and relatives of ID cases had an increased risk for ADHD compared with relatives of those without ID. Model fitting analyses attributed 91% of the correlation between the liabilities of ADHD and ID to genetic factors. This work attributes nearly all the comorbidity between ADHD and ID to genetic factors. Only a few twin and family studies have explored how genetic factors contribute to non-psychiatric comorbidity. The literature suggests novel etiologic links with asthma [ 64 ], obesity [ 65 ], and epilepsy [ 66 ].
The search for common genetic variants
Genetic linkage studies.
Genetic linkage was the first genome-wide method applied to ADHD. This method searches the genome for evidence that a segment of DNA is transmitted with a disorder within families. A review of the linkage literature found substantial disagreement about which chromosomal regions are linked to ADHD [ 67 ]. Although there is some overlap in “suggestive” findings, no finding met genome-wide significance [ 68 ]. To make sense of these results, Zhou et al. [ 69 ] applied Genome Scan Meta-Analysis. They found genome-wide significant linkage for a region on chromosome 16 between 64 Mb and 83 Mb. Because the linkage method only detects genetic variants that have large effects, the paucity of significant findings for other loci suggests that common DNA variants having a large effect on ADHD are unlikely to exist. Nearly all ADHD linkage studies have selected either sibling pairs or small families from outbred populations. Another approach is to assess for linkage in multigenerational population isolates. Arcos-Burgos et al. [ 70 ] used this strategy to study 16 multi-generational families from Colombia. In some of these families, they found evidence supporting linkage to chromosomes 4q13.2, 5q33.3, 8q11.23, 11q22, and 17p11. one region implicated LPHN3 . For a review of supporting evidence, see ref. [ 71 ].
Candidate gene association studies
Early molecular genetic studies of ADHD sought to associate ADHD with genes that had some a priori plausibility as being involved in its etiology. Because the drugs that treat ADHD target dopaminergic or noradrenergic transmission, many studies examined “candidate genes” in these pathways. Results were frequently contradictory [ 26 , 67 ]. In the meta-analyses of Gizer et al. [ 72 ], eight candidate DNA variants showed a statistically significant association with ADHD across multiple studies. These variants implicated six genes: the serotonin transporter gene ( 5HTT ), the dopamine transporter gene ( DAT1 ), the D4 dopamine receptor gene ( DRD4 ), the D5 dopamine receptor gene ( DRD5 ), the serotonin 1B receptor gene ( HTR1B ) and a gene coding for a synaptic vesicle regulating protein known as SNAP25 . A meta-analysis covering all genetic association studies of adults with ADHD reported a significant association between adult ADHD and BAIAP2 (brain-specific angiogenesis inhibitor 1-associated protein 2). BAIAP2 is involved in neuronal proliferation, survival, and maturation and dendritic spine morphogenesis and may affect neuronal growth-cone guidance. These findings were significant even after Bonferroni correction [ 73 ]. For both the child and adult meta-analyses, the strength of each association, as measured by the odds ratio, is small, less than 1.5.
Many studies examined the dopamine transporter gene ( SLC6A3) , especially a 40-base pair variable number of tandem repeats regulatory polymorphism located in the 3′-untranslated region of the gene. This variant produces two common alleles with 9- and 10-repeats (9R and 10R). In humans, the 10R allele of this polymorphism has been associated with ADHD in youth [ 67 ] while the 9R allele is associated with ADHD in adults [ 74 ]. A meta-analysis showed that the 9R allele is associated with increased DAT activity in human adults as measured by positron emission tomography [ 75 ].
Genome-wide significant common variants
Genome-wide association studies (GWAS) scan the entire genome to detect common DNA variants having very small etiologic effects. By “common” we mean greater than 1% of the population. To do this, GWAS assay hundreds of thousands or even millions of single nucleotide polymorphisms (SNPs). Doing so has a statistical cost: to assert genome-wide statistical significance, an observed association must have a p value less than 0.00000005. This stringent p value needs very large samples.
The initial GWAS of ADHD [ 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 ] did not discover any DNA variants that achieved genome-wide significance, even when most of these samples were combined in meta-analysis having a sample size of 2064 trios (two parents and an ADHD child), 896 ADHD patients, and 2455 controls [ 87 ]. That study did find statistical significance for a group of candidate genes previously nominated by members of the International Multisite ADHD Genetics (IMAGE) project [ 88 ]. For a review of early GWAS studies, see Franke et al. [ 89 ]. Examination of the “molecular landscape” derived from the top findings from these initial GWAS studies along with other data concluded that genes regulating directed neurite outgrowth were strongly implicated in the etiology of ADHD [ 90 ]. Pathway and gene set analyses of GWAS data implicated pathways involved in the regulation of neurotransmitter release, neurite outgrowth and axon guidance as contributors to the etiology of ADHD [ 91 , 92 , 93 ].
A consortium of ADHD researchers completed a GWAS meta-analysis of 12 studies comprising 20,183 people with ADHD and 35,191 controls. For methodologic details about the studies contributing data to this meta-analysis, see Demontis et al. [ 94 ]. Twelve loci achieved genome-wide significance. None of the genome-wide significant SNPs showed significant heterogeneity between studies. Among the implicated genes, FOXP2 is especially notable because prior work had implicated it in adult ADHD (Ribases, 2012 #26445) and in speech and language disorders [ 95 ]. A FOXP2 knockout mouse study found that the gene regulates dopamine in ADHD-associated brain regions [ 96 ].
As described by Demontis et al. [ 94 ], other genes implicated by the genome-wide significant loci have relevant biological roles. DUSP6 regulates neurotransmitter homeostasis by affecting dopamine levels in the synapses. SEMA6D is expressed in the brain. It regulates neuronal wiring during embryonic development. ST3GAL3 harbors missense mutations associated with ID. LINC00461 is expressed in brain and includes variants associated with educational attainment. Another gene implicated at that locus is MEF2C , which has been associated with ID and several psychiatric disorders.
The consortium conducted several gene set analyses including three sets of genes regulated by FOXP2 : (1) genes enriched in wild-type versus control FOXP2 knockout mouse brains; (2) genes showing differential expression in wild-type versus FOXP2 knockout mouse brains; and (3) genes enriched in basal ganglia or inferior frontal cortex from human fetal brain samples. None of these sets were associated with ADHD. Also, non-significant was a set of candidate genes for ADHD previously proposed by a panel of ADHD experts [ 88 ]. Among these, only SLC9A9 showed a weak association with ADHD. No Gene Ontology gene sets attained statistical significance but a set of genes showing high intolerance to loss of function did associate with ADHD.
Common variant ADHD as a polygenic disorder
The GWAS analyses also showed that much of ADHD’s heritability is due to the polygenic effects of many common variants each having very small effects. The SNP heritability was 0.22, which is about one-third of ADHD’s heritability computed from twin studies [ 97 ]. The polygenic architecture for ADHD was confirmed by estimating polygenic risk scores in one subset of the sample and showing that it predicted ADHD, in a dose-dependent manner, in a validation subset. As seen for other psychiatric disorders [ 98 ], the variance explained by these risk scores was low (5.5%).
Further evidence for the validity of the ADHD’s polygenic background comes from analyses showing that the relevant SNPs were enriched for annotations implicating conserved regions of the genome (which are known to have biological significance) and for regulatory elements specific to the central nervous system. The discovery of a polygenic susceptibility to ADHD does not show which DNA variants comprise the susceptibility. It does, however, support the idea that more genome-wide significant variants will be discovered in larger samples.
Martin et al. [ 99 ] showed that ADHD’s polygenic liability derived from a clinical sample predicted ASD traits in a population sample, which confirms twin study data [ 48 , 51 ] and gene set analyses [ 100 ] showing genetic overlap between ADHD and ASDs. The polygenic liability score derived from Martin et al.’s ADHD case-control clinical sample also predicted both inattention and hyperactivity in the general population. This latter finding was replicated by Groen-Blokhuis et al. [ 101 ] who found that ADHD polygenic risk scores significantly predicted both parent and teacher ratings of attention in preschool- and school-aged children in the population. Likewise, Stergiakouli et al. [ 102 ] showed that the polygenic liability for ADHD traits in a population sample predicted ADHD clinical diagnoses in a case-control study. These results confirmed conclusions from twin studies that the liability for clinically defined ADHD is the extreme of a trait that varies continuously in the population [ 13 ].
Other polygenic score studies are confirming cross-disorder genetic associations previously predicted by family and twin studies. We have long known that ADHD co-occurs with conduct disorder. Both family and twin studies have implicated shared genes in this association [ 38 , 103 , 104 , 105 ]. Consistent with this prior work, Hamshere et al. [ 106 ] reported a high polygenic risk for ADHD among children with comorbid conduct problems. In a large population study, Larsson et al. [ 107 ] reported that the relatives of ADHD individuals had an increased risk for schizophrenia and bipolar disorder. Consistent with that report, the polygenic risk score derived from a large GWAS of schizophrenia significantly discriminated ADHD cases from controls [ 108 ]. This discrimination was strongest for alleles that were risk alleles for both adult schizophrenia and adult bipolar disorder, which confirms prior family and twin data suggesting a genetic link between ADHD and bipolar disorder [ 109 ]. Moreover, a joint GWAS of ADHD and bipolar disorder reported a significant correlation between the polygenic scores of ADHD and bipolar disorder and also identified genome-wide significant loci for the two disorders [ 110 ]. Similarly, prior reports of familial co-transmission of ADHD and depression [ 54 ] have been extended by showing shared SNP heritability between the two disorders [ 98 ]. Using a novel drug challenge paradigm, Hart et al. [ 111 ] found that the polygenic scores for both schizophrenia and ADHD were associated with the euphoric response to amphetamine, which suggests that the genetic association between these disorders may be due to variants in the neural systems regulating the euphoric response to amphetamine.
Using GWAS results from many studies, it is possible to compute genetic correlations that indicate the degree to which the polygenic architectures of two disorders or traits overlap. When Demontis et al. [ 94 ] correlated ADHD’s polygenic risk with 220 disorders and traits, many highly significant correlations emerged. Figure 3 shows some of the most significant of these correlations (each passing the Bonferroni significance threshold). Some of these genetic correlations fit with prior expectations (e.g., with neuroticism, depression and the cross disorder GWAS). Others are consistent with the clinical epidemiology of ADHD (e.g., with obesity, IQ, smoking and school achievement). In some cases, these significant correlations offer new directions for understanding comorbidity. For example, some have interpreted the comorbidity between ADHD and obesity, which has been confirmed via meta-analysis [ 112 ], as being caused by the impulsivity associated with ADHD. The genetic correlation data suggest that shared genetic risk factors, and an underlying shared pathophysiology, account for this comorbidity.
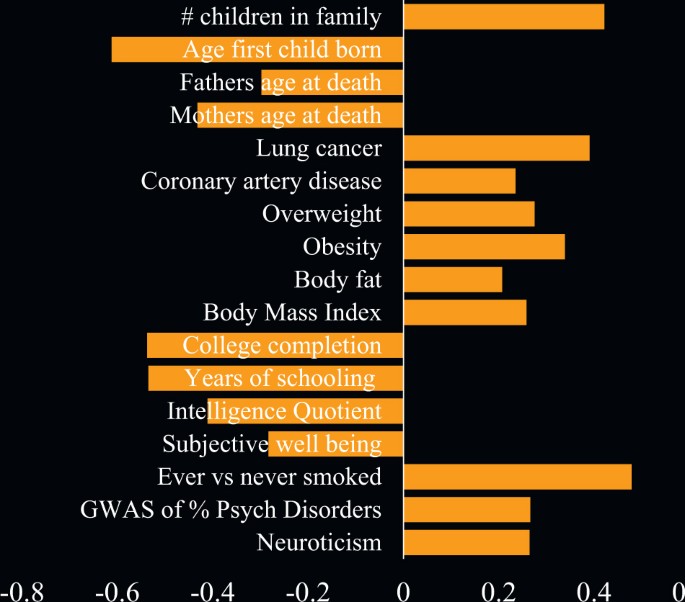
Genetic correlations of ADHD with other traits based on LD score regression
Some of the genetic correlations in Fig. 3 are entirely novel. These include ADHD’s genetic correlations with medical outcomes (lung cancer, coronary artery disease, parents’ age at death) and with demographics (number of children in the family, age first child born). There are, however, some consistent findings in the prior literature, which suggest that people with ADHD are more likely to have larger families [ 113 ] and more likely to die prematurely [ 114 ].
The search for rare genetic variants
Initially, information about rare DNA variants (<1% of the population) came from reports of syndromic chromosomal anomalies associated with multiple medical and psychiatric problems along with ADHD. Examples are velo-cardio facial syndrome fragile-X syndrome, Turner syndrome, tuberous sclerosis, neurofibromatosis, Klinefelter syndrome, and Williams syndrome (Fig. 4 ). In a single family, a peri-centric inversion of chromosome 3 co-segregating with ADHD symptoms [ 115 , 116 ] implicated SLC9A9 . Mutations of that gene lead to an animal model of ADHD [ 117 , 118 ] and have been associated with both autism [ 119 , 120 ] and ADHD [ 121 ].
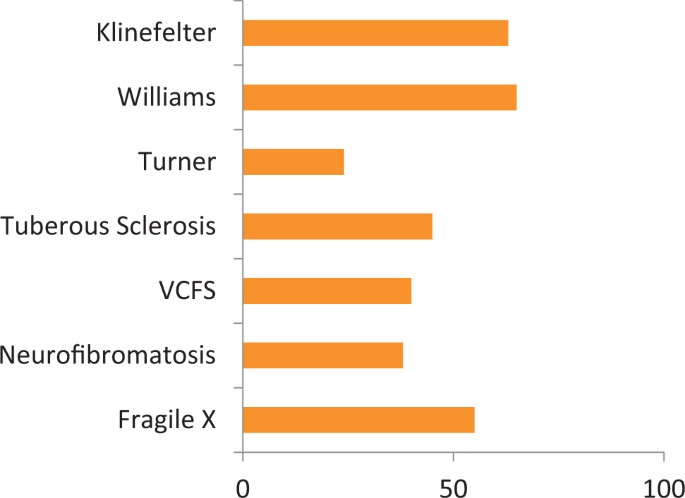
Prevalence of ADHD in rare genetic syndromes
The common variant genotyping arrays used in GWAS studies can detect large copy number variants (CNVs). Because CNVs often delete or duplicate a large genomic segment spanning part of a gene or even entire genes, they often have clear implications for gene functioning. Studies of CNVs in ADHD assessed ADHD youth and controls for the presence of large (>500 kb), rare CNVs [ 77 , 122 , 123 , 124 , 125 , 126 , 127 ]. Each study, except one, found an odds ratio greater than one, indicating a greater burden of large, rare CNVs among ADHD patients compared with controls. The discrepant study used a different definition of burden [ 125 ]. Only three studies found a statistically significant burden among ADHD patients for large CNVs (for a summary, see Thapar et al. [ 128 ]). As their review shows, deletions and duplications are equally over-represented in ADHD samples although statistical significance emerged only for duplications. Thapar et al. also found enrichment for duplications (but not deletions) previously implicated in schizophrenia and, to a lesser extent, ASDs. The top biological pathways implicated by these CNV studies were: respiratory electron transport, organonitrogen compound catabolic process, transmembrane transporter activity, carbohydrate derivative catabolic process, ligand-gated ion channel activity, methyltransferase activity, transmembrane transport and ion gated channel activity.
A study of 489 ADHD patients and 1285 controls found rare CNVs in the parkinson protein two gene ( PARK2 ) [ 123 ]. The result was significant after empirical correction for genome-wide testing. PARK2 regulates the cell’s ubiquitin-proteasome system which helps dispose damaged, misshapen, and excess proteins. Two other genes involved in this pathway ( FBXO33 and RNF122 ) had been implicated in other studies [ 84 , 129 ]. A study of adult ADHD did not find a significant effect for large CNVs, but did find a significant effect for small CNVs [ 126 ].
The CNV studies have implicated several biological pathways. Williams et al. [ 127 ] found that ADHD patients harbored duplications in the alpha-7 nicotinic acetylcholine receptor gene ( CHRNA7) and showed that the finding replicated in four independent cohorts from the United Kingdom, the United States, and Canada. Another replication was reported in an Italian sample [ 130 ]. The implication of the nicotinic system is particularly interesting given that nicotinic neurons modulate dopaminergic neurons, ADHD patients have a high rate of smoking [ 131 ] and nicotine administration reduces ADHD symptoms [ 132 ]. In a sample of 99 children and adolescents with severe ADHD. Lesch et al. [ 124 ] found several CNVs, including a 3 Mb duplication on chromosome 7p15.2-15.3 harboring neuropeptide Y ( NPY ). Investigation of other family members yielded an association of this duplication with increased NPY plasma concentrations and functional magnetic imaging assessed brain abnormalities.
Thapar et al. [ 128 ] reported biological pathway studies of ADHD CNV data pooled from five studies. These CNV data were enriched for genes previously implicated in schizophrenia, Fragile X intellectual disability and, to a lesser degree, autism. Several biological pathways were significantly enriched in the ADHD CNV findings, most notably ion channel pathways, which had been implicated in cross-disorder analyses of ADHD, autism, schizophrenia, bipolar disorder, and depression [ 133 ]. The CNV analyses also pointed to pathways regulating immune functioning and oxidative stress. These pathways had previously been implicated in ADHD by non-genetic studies, (e.g. refs. [ 134 , 135 , 136 ]).
Elia et al. [ 122 ] showed that CNVs impacting metabotropic glutamate receptor genes were significantly enriched across multiple cohorts of patients. Supporting evidence came from Akutagava-Martins et al. [ 137 ] who reported that CNVs in glutamatergic genes were associated with the cognitive and clinical impairments of ADHD. In a pharmacogenomics GWAS, an SNP in glutamate receptor gene GRM7 was one of the most significant findings [ 138 ]. Glutamatergic defects have been observed in a rat model of ADHD [ 139 , 140 ] and magnetic resonance spectroscopy in humans shows dysregulation of glutamate and glutamate/glutamine concentrations in ADHD patients(e.g. ref. [ 141 ]).
An exome sequencing study of ADHD [ 121 ] reported results for 123 adults with persistent ADHD and 82 healthy controls. Significantly more cases than controls had a rare missense or disruptive variant in a set of ADHD candidate genes. In an exome sequencing study of ADHD patients without a family history of ADHD, Kim et al. [ 142 ] reported six de novo missense SNVs in brain-expressed genes: TBC1D9, DAGLA, QARS, CSMD2, TRPM2 , and WDR83 . They also sequenced 26 genes implicated in ID and ASDs but found only one potentially deleterious variant. In an exome chip study, Zayats et al. [ 143 ] assayed a sample of 1846 cases and 7519 controls to search for rare genetic variants. They detected four study-wide significant loci that implicated four genes known to be expressed in the brain during prenatal stages of development: NT5DC1 , SEC23IP , PSD , and ZCCHC4 . Hawi et al. [ 144 ] found novel rare variants in the BDNF gene by sequencing 117 genes in 152 youth with ADHD and 188 controls.
Pharmacogenetics of ADHD
Several studies have clarified the genetics of the metabolism of ADHD patients. Some patients are slow metbolizers of atomoxetine due to variants in the cytochrome P450 isoenzyme 2D6, which is regulated by the CYP2D6 gene. As a result, the half-life of atomoxetine ranges from 5.2 h in rapid metabolizers to 21.6 h in slow metabolizers [ 145 ]. Some work has looked into CES1 variants regarding the regulation of methylphenidate metabolism and CYP2D6/CYP3A4 variants and the metabolism of ADHD, but the evidence base has not generated consistent results for either children [ 146 ] or adults [ 73 ].
Myer et al. [ 147 ] used meta-analysis to evaluate pharmacogenetic studies of the efficacy response to methylphenidate for the treatment of ADHD. They found 36 studies comprising 3647 ADHD youth treated with methylphenidate. Statistically significant effects were found for: rs1800544 in ADRA2A (odds ratio (OR): 1.69; confidence interval (CI): 1.12−2.55), rs4680 COMT (OR: 1.40; CI: 1.04−1.87), rs5569 SLC6A2 (OR: 1.73; CI: 1.26−2.37), and rs28386840 SLC6A2 (OR: 2.93; CI: 1.76−4.90), and, repeat variants VNTR 4 DRD4 (OR: 1.66; CI: 1.16−2.37) and VNTR 10 SLC6A3 (OR: 0.74; CI: 0.60−0.90). The following variants did not reach statistical significance: rs1947274 LPHN3 (OR: 0.95; CI: 0.71−1.26), rs5661665 LPHN3 (OR: 1.07; CI: 0.84−1.37) and VNTR 7 DRD4 (OR: 0.68; confidence interval: 0.47−1.00). The significant findings were not due to publication biases. Although the odds ratios are small, these findings suggest that a personalized medicine approach to ADHD is a reasonable goal of future research.
Conclusions and future directions
There can be no doubt that DNA variants in genes or regulatory regions increase the risk for ADHD. In rare cases, a single genetic defect may lead to ADHD in the absence of other DNA variants. We do not know how many of these rare variants exist or if such variants require environmental triggers for ADHD to emerge. It is equally clear that no common DNA variants are necessary and sufficient causes of ADHD. Genome-wide association studies show that a genetic susceptibility to ADHD comprised of many common DNA variants accounts for about one-third of the twin study estimates of ADHD’s heritability. We do not know yet which variants or how many of them make up the polygenic component. The heritability that cannot be explained by main effects of rare or common variants is likely due to gene−gene interactions, gene−environment interactions or gene−environment correlations.
The convincing evidence for genes as risk factors for ADHD does not exclude the environment as a source of etiology. The fact that twin estimates of heritability are less than 100% asserts quite strongly that environmental factors must be involved. ADHD’s heritability is high, and that estimate encompasses gene by environment interaction. Thus, it is possible that such interactions will account for much of ADHD’s etiology. Environmental risk factors likely work through epigenetic mechanisms, which have barely been studied in ADHD [ 148 ]. The importance of the environment can also be seen in the fact that, as for other complex genetic disorders, much of ADHD’s heritability is explained by SNPs in regulatory regions rather than coding regions [ 149 ].
Another hypothesis for future research to explore is the possibility that ADHD is an omnigenic disorder. The omnigenic model of Boyle et al. [ 150 ] posits the existence of a small number of “core genes” having “biologically interpretable roles in disease” along with a much greater quantity of “peripheral genes” regulating the core genes. Because there are many more peripheral genes, they account for a greater proportion of the variability in heritability than do the core genes. Because core genes are more likely than peripheral genes to be relevant for developing biomarkers and treatment targets, separating these two classes from one another will require more research.
Gene discovery for ADHD has succeeded but has left us with unexpected results. None of the genome-wide significant findings had been predicted a priori and a set of ADHD candidate genes, implicated primarily by the disorder’s neuropharmacology, did not reach statistical significance. These findings challenge the idea that the core of ADHD’s pathophysiology rests within the machinery of catecholaminergic transmission. Instead, it is possible that the catecholaminergic dysregulation believed to underlie ADHD is a secondary compensation to ADHD’s primary etiology (see discussion by Hess et al. [ 151 ]).
In the years to come, we can expect breakthroughs in the genetics of ADHD to come from several fields of study. Our knowledge of rare variants should increase dramatically as we learn more about CNVs and as reports from exome, full genome and targeted sequencing studies unfold. With the discovery of genome-wide significant common variants, we look forward to studies that discover the functional variants responsible for these findings. With the discovery of these functional variants, we will learn more about the mechanisms whereby genetic risk variants increase the risk for ADHD.
Accumulating evidence from family, twin, and molecular genetic studies suggests that the disorder we know as ADHD is the extreme of a dimensional trait in the population. The dimensional nature of ADHD has wide-ranging implications. If we view ADHD as analogous to cholesterol levels, then diagnostic approaches should focus on defining the full continuum of “ADHD-traits” along with clinically meaningful thresholds for defining who does and does not need treatment and who has clinically subthreshold traits that call for careful monitoring. The dimensional nature of ADHD should also shift the debate about the increases in ADHD’s prevalence in recent years. Instead of assuming that misdiagnoses are the main explanation for the increased prevalence, perhaps researchers should explore to what extent the threshold for diagnosis has decreased over time and whether changes in the threshold are clinically sensible or not. A shift from categorical to dimensional constructs harmonizes with the Research Domain Criteria (RDoC) initiative of the National Institute of Mental Health [ 152 ]. RDoC seeks to define and validate dimensional constructs mediating psychopathology along with the neurobiological underpinnings of these constructs.
Unraveling the genetics of ADHD will be challenging. Technological advances are moving at a rapid pace. The next decade of work should give us more accurate measures of brain structure and function along with much more genomic, transcriptomic and epigenomic data. These advances will set the stage for breakthroughs in our understanding of the etiology of ADHD and in our ability to diagnose and treat the disorder.
Faraone SV, Asherson P, Banaschewski T, Biederman J, Buitelaar JK, Ramos-Quiroga JA, et al. Attention-deficit/hyperactivity disorder. Nat Rev Dis Prim. 2015;1:15020.
Article PubMed Google Scholar
Chen W, Zhou K, Sham P, Franke B, Kuntsi J, Campbell D, et al. DSM-IV combined type ADHD shows familial association with sibling trait scores: a sampling strategy for QTL linkage. Am J Med Genet B Neuropsychiatr Genet. 2008;147B:1450–60.
Article CAS PubMed Google Scholar
Alberts-Corush J, Firestone P, Goodman JT. Attention and impulsivity characteristics of the biological and adoptive parents of hyperactive and normal control children. Am J Orthopsychiatry. 1986;56:413–23.
Sprich S, Biederman J, Crawford MH, Mundy E, Faraone SV. Adoptive and biological families of children and adolescents with ADHD. J Am Acad Child Adolesc Psychiatry. 2000;39:1432–7.
Chen Q, Brikell I, Lichtenstein P, Serlachius E, Kuja-Halkola R, Sandin S, et al. Familial aggregation of attention-deficit/hyperactivity disorder. J Child Psychol Psychiatry. 2017;58:231–9.
Nikolas MA, Burt SA. Genetic and environmental influences on ADHD symptom dimensions of inattention and hyperactivity: a meta-analysis. J Abnorm Psychol. 2010;119:1–17.
Larsson H, Lichtenstein P, Larsson JO. Genetic contributions to the development of ADHD subtypes from childhood to adolescence. J Am Acad Child Adolesc Psychiatry. 2006;45:973–81.
McLoughlin G, Ronald A, Kuntsi J, Asherson P, Plomin R. Genetic support for the dual nature of attention deficit hyperactivity disorder: substantial genetic overlap between the inattentive and hyperactive-impulsive components. J Abnorm Child Psychol. 2007;35:999–1008.
Article PubMed PubMed Central Google Scholar
Sherman D, Iacono W, McGue M. Attention deficit hyperactivity disorder dimensions: a twin study of inattention and impulsivity hyperactivity. J Am Acad Child Adolesc Psychiatry. 1997;36:745–53.
Langner I, Garbe E, Banaschewski T, Mikolajczyk RT. Twin and sibling studies using health insurance data: the example of attention deficit/hyperactivity disorder (ADHD). PLoS ONE. 2013;8:e62177.
Article CAS PubMed PubMed Central Google Scholar
Lichtenstein P, Carlstrom E, Rastam M, Gillberg C, Anckarsater H. The genetics of autism spectrum disorders and related neuropsychiatric disorders in childhood. Am J Psychiatry. 2010;167:1357–63.
Thapar A, Harrington R, Ross K, McGuffin P. Does the definition of ADHD affect heritability? J Am Acad Child Adolesc Psychiatry. 2000;39:1528–36.
Larsson H, Anckarsater H, Rastam M, Chang Z, Lichtenstein P. Childhood attention-deficit hyperactivity disorder as an extreme of a continuous trait: a quantitative genetic study of 8,500 twin pairs. J Child Psychol Psychiatry. 2012;53:73–80.
Levy F, Hay D, McStephen M, Wood C, Waldman I. Attention-deficit hyperactivity disorder: a category or a continuum? Genetic analysis of a large-scale twin study. J Am Acad Child Adolesc Psychiatry. 1997;36:737–44.
Faraone SV, Biederman J, Spencer T, Mick E, Murray K, Petty C, et al. Diagnosing adult attention deficit hyperactivity disorder: are late onset and subthreshold diagnoses valid? Am J Psychiatry. 2006;163:1720–9. quiz 859
Haberstick BC, Timberlake D, Hopfer CJ, Lessem JM, Ehringer MA, Hewitt JK. Genetic and environmental contributions to retrospectively reported DSM-IV childhood attention deficit hyperactivity disorder. Psychol Med. 2008;38:1057–66.
Boomsma DI, Saviouk V, Hottenga JJ, Distel MA, de Moor MH, Vink JM, et al. Genetic epidemiology of attention deficit hyperactivity disorder (ADHD index) in adults. PLoS ONE. 2010;5:e10621.
Article PubMed PubMed Central CAS Google Scholar
Brikell I, Kuja-Halkola R, Larsson H. Heritability of attention-deficit hyperactivity disorder in adults. Am J Med Genet B Neuropsychiatr Genet. 2015;168:406–13.
Larsson H, Asherson P, Chang Z, Ljung T, Friedrichs B, Larsson JO, et al. Genetic and environmental influences on adult attention deficit hyperactivity disorder symptoms: a large Swedish population-based study of twins. Psychol Med. 2013;43:197–207.
Kan KJ, van Beijsterveldt CE, Bartels M, Boomsma DI. Assessing genetic influences on behavior: informant and context dependency as illustrated by the analysis of attention problems. Behav Genet. 2014;44:326–36.
Merwood A, Greven CU, Price TS, Rijsdijk F, Kuntsi J, McLoughlin G, et al. Different heritabilities but shared etiological influences for parent, teacher and self-ratings of ADHD symptoms: an adolescent twin study. Psychol Med. 2013;43:1973–84.
Kan KJ, Dolan CV, Nivard MG, Middeldorp CM, van Beijsterveldt CE, Willemsen G, et al. Genetic and environmental stability in attention problems across the lifespan: evidence from the Netherlands twin register. J Am Acad Child Adolesc Psychiatry. 2013;52:12–25.
Freitag CM, Rohde LA, Lempp T, Romanos M. Phenotypic and measurement influences on heritability estimates in childhood ADHD. Eur Child Adolesc Psychiatry. 2010;19:311–23.
Schultz MR, Rabi K, Faraone SV, Kremen W, Lyons MJ. Efficacy of retrospective recall of attention-deficit hyperactivity disorder symptoms: a twin study. Twin Res Hum Genet. 2006;9:220–32.
Larsson H, Chang Z, D'Onofrio BM, Lichtenstein P. The heritability of clinically diagnosed attention deficit hyperactivity disorder across the lifespan. Psychol Med. 2014;44:2223–9.
Franke B, Faraone SV, Asherson P, Buitelaar J, Bau CH, Ramos-Quiroga JA, et al. The genetics of attention deficit/hyperactivity disorder in adults, a review. Mol Psychiatry. 2011;17:960–87.
Faraone SV. Genetics of adult attention-deficit/hyperactivity disorder. Psychiatr Clin North Am. 2004;27:303–21.
Chang Z, Lichtenstein P, Asherson PJ, Larsson H. Developmental twin study of attention problems high heritabilities throughout development. JAMA Psychiatry. 2013;70:311–8.
Rietveld MJ, Hudziak JJ, Bartels M, van Beijsterveldt CE, Boomsma DI. Heritability of attention problems in children: longitudinal results from a study of twins, age 3 to 12. J Child Psychol Psychiatry. 2004;45:577–88.
Kuntsi J, Rijsdijk F, Ronald A, Asherson P, Plomin R. Genetic influences on the stability of attention-deficit/hyperactivity disorder symptoms from early to middle childhood. Biol Psychiatry. 2005;57:647–54.
Lahey BB, Van Hulle CA, Singh AL, Waldman ID, Rathouz PJ. Higher-order genetic and environmental structure of prevalent forms of child and adolescent psychopathology. Arch Gen Psychiatry. 2011;68:181–9.
Pettersson E, Larsson H, Lichtenstein P. Common psychiatric disorders share the same genetic origin: a multivariate sibling study of the Swedish population. Mol Psychiatry. 2016;21:717–21.
Waldman ID, Poore HE, van Hulle C, Rathouz PJ, Lahey BB. External validity of a hierarchical dimensional model of child and adolescent psychopathology: Tests using confirmatory factor analyses and multivariate behavior genetic analyses. J Abnorm Psychol. 2016;125:1053–66.
Pettersson E, Anckarsater H, Gillberg C, Lichtenstein P. Different neurodevelopmental symptoms have a common genetic etiology. J Child Psychol Psychiatry. 2013;54:1356–65.
Pappa I, Fedko IO, Mileva-Seitz VR, Hottenga JJ, Bakermans-Kranenburg MJ, Bartels M, et al. Single nucleotide polymorphism heritability of behavior problems in childhood: genome-wide complex trait analysis. J Am Acad Child Adolesc Psychiatry. 2015;54:737–44.
Neumann A, Pappa I, Lahey BB, Verhulst FC, Medina-Gomez C, Jaddoe VW, et al. Single nucleotide polymorphism heritability of a general psychopathology factor in children. J Am Acad Child Adolesc Psychiatry. 2016;55:1038–45 e4..
Nadder TS, Rutter M, Silberg J, Maes H, Eaves L. Genetic effects on the variatio and covariation of attention deficit-hyperactivity disorder (ADHD) and oppositional-defiant disorder/conduct disorder (ODD/CD) symptomatologies across informant and occasion of measurement. Psychol Med. 2002;32:39–53.
Faraone SV, Biederman J, Monuteaux MC. Attention-deficit disorder and conduct disorder in girls: evidence for a familial subtype. Biol Psychiatry. 2000;48:21–9.
Kuja-Halkola R, Lichtenstein P, D’Onofrio BM, Larsson H. Codevelopment of ADHD and externalizing behavior from childhood to adulthood. J Child Psychol Psychiatry. 2015;56:640–7.
Chang Z, Lichtenstein P, Larsson H. The effects of childhood ADHD symptoms on early-onset substance use: a Swedish twin study. J Abnorm Child Psychol. 2012;40:425–35.
Capusan AJ, Bendtsen P, Marteinsdottir I, Kuja-Halkola R, Larsson H. Genetic and environmental contributions to the association between attention deficit hyperactivity disorder and alcohol dependence in adulthood: a large population-based twin study. Am J Med Genet B Neuropsychiatr Genet. 2015;168:414–22.
Skoglund C, Chen Q, Franck J, Lichtenstein P, Larsson H. Attention-deficit/hyperactivity disorder and risk for substance use disorders in relatives. Biol Psychiatry. 2015;77:880–6.
Rommelse NN, Geurts HM, Franke B, Buitelaar JK, Hartman CA. A review on cognitive and brain endophenotypes that may be common in autism spectrum disorder and attention-deficit/hyperactivity disorder and facilitate the search for pleiotropic genes. Neurosci Biobehav Rev. 2011;35:1363–96.
Rommelse NN, Franke B, Geurts HM, Hartman CA, Buitelaar JK. Shared heritability of attention-deficit/hyperactivity disorder and autism spectrum disorder. Eur Child Adolesc Psychiatry. 2010;19:281–95.
Antshel KM, Zhang-James Y, Faraone SV. The comorbidity of ADHD and autism spectrum disorder. Expert Rev Neurother. 2013;13:1117–28.
Ronald A, Edelson LR, Asherson P, Saudino KJ. Exploring the relationship between autistic-like traits and ADHD behaviors in early childhood: findings from a community twin study of 2-year-olds. J Abnorm Child Psychol. 2010;38:185–96.
Ronald A, Simonoff E, Kuntsi J, Asherson P, Plomin R. Evidence for overlapping genetic influences on autistic and ADHD behaviours in a community twin sample. J Child Psychol Psychiatry. 2008;49:535–42.
Ronald A, Larsson H, Anckarsater H, Lichtenstein P. Symptoms of autism and ADHD: a Swedish twin study examining their overlap. J Abnorm Psychol. 2014;123:440–51.
Lundstrom S, Chang Z, Kerekes N, Gumpert CH, Rastam M, Gillberg C, et al. Autistic-like traits and their association with mental health problems in two nationwide twin cohorts of children and adults. Psychol Med. 2011;41:2423–33.
Ghirardi L, Brikell I, Kuja-Halkola R, Freitag CM, Franke B, Asherson P, et al. The familial co-aggregation of ASD and ADHD: a register-based cohort study. Mol Psychiatry. 2017;23:257–62.
Polderman TJ, Hoekstra RA, Posthuma D, Larsson H. The co-occurrence of autistic and ADHD dimensions in adults: an etiological study in 17,770 twins. Transl Psychiatry. 2014;4:e435.
Polderman TJ, Hoekstra RA, Vinkhuyzen AA, Sullivan PF, van der Sluis S, Posthuma D. Attentional switching forms a genetic link between attention problems and autistic traits in adults. Psychol Med. 2013;43:1985–96.
Ljung T, Chen Q, Lichtenstein P, Larsson H. Common etiological factors of attention-deficit/hyperactivity disorder and suicidal behavior: a population-based study in Sweden. JAMA Psychiatry. 2014;71:958–64.
Faraone SV, Biederman J. Do attention deficit hyperactivity disorder and major depression share familial risk factors? J Nerv Ment Dis. 1997;185:533–41.
Faraone SV, Biederman J. Depression: a family affair. Lancet. 1998;351:158.
Rydell M, Taylor MJ, Larsson H Genetic and environmental contributions to the association between ADHD and affective problems in early childhood-A Swedish population-based twin study. Am J Med Genet B Neuropsychiatr Genet. 2017;174:538–46.
Segenreich D, Paez MS, Regalla MA, Fortes D, Faraone SV, Sergeant J, et al. Multilevel analysis of ADHD, anxiety and depression symptoms aggregation in families. Eur Child Adolesc Psychiatry. 2015;24:525–36.
Chen TJ, Ji CY, Wang SS, Lichtenstein P, Larsson H, Chang Z. Genetic and environmental influences on the relationship between ADHD symptoms and internalizing problems: A Chinese twin study. Am J Med Genet B Neuropsychiatr Genet. 2016;171:931–7.
Cole J, Ball HA, Martin NC, Scourfield J, McGuffin P. Genetic overlap between measures of hyperactivity/inattention and mood in children and adolescents. J Am Acad Child Adolesc Psychiatry. 2009;48:1094–101.
Spatola CA, Fagnani C, Pesenti-Gritti P, Ogliari A, Stazi MA, Battaglia M. A general population twin study of the CBCL/6-18 DSM-oriented scales. J Am Acad Child Adolesc Psychiatry. 2007;46:619–27.
Frazier TW, Demaree HA, Youngstrom EA. Meta-analysis of intellectual and neuropsychological test performance in attention-deficit/hyperactivity disorder. Neuropsychology. 2004;18:543–55.
Antshel KM, Phillips MH, Gordon M, Barkley R, Faraone SV. Is ADHD a valid disorder in children with intellectual delays? Clin Psychol Rev. 2006;26:555–72.
Faraone SV, Ghirardi L, Kuja-Halkola R, Lichtenstein P, Larsson H. The familial co-aggregation of attention-deficit/hyperactivity disorder and intellectual disability: a register-based family study. J Am Acad Child Adolesc Psychiatry. 2017;56:167–74 e1.
Mogensen N, Larsson H, Lundholm C, Almqvist C. Association between childhood asthma and ADHD symptoms in adolescence—a prospective population-based twin study. Allergy. 2011;66:1224–30.
Chen Q, Kuja-Halkola R, Sjolander A, Serlachius E, Cortese S, Faraone SV, et al. Shared familial risk factors between attention-deficit/hyperactivity disorder and overweight/obesity—a population-based familial coaggregation study in Sweden. J Child Psychol Psychiatry. 2017;58:711–8.
Brikell I, Ghirardi L, D’Onofrio BM, Dunn DW, Almqvist C, Dalsgaard S, et al. Familial liability to epilepsy and attention-deficit/hyperactivity disorder: a nationwide cohort study. Biol Psychiatry. 2018;83:173–80.
Faraone SV, Mick E. Molecular genetics of attention deficit hyperactivity disorder. Psychiatr Clin North Am. 2010;33:159–80.
Lander E, Kruglyak L. Genetic dissection of complex traits: guidelines for interpreting and reporting linkage results. Nat Genet. 1995;11:241–7.
Zhou K, Dempfle A, Arcos-Burgos M, Bakker SC, Banaschewski T, Biederman J, et al. Meta-analysis of genome-wide linkage scans of attention deficit hyperactivity disorder. Am J Med Genet B Neuropsychiatr Genet. 2008;147B:1392–8.
Arcos-Burgos M, Castellanos FX, Pineda D, Lopera F, David Palacio J, Guillermo Palacio L, et al. Attention-deficit/hyperactivity disorder in a population isolate: linkage to Loci at 4q13.2, 5q33.3, 11q22, and 17p11. Am J Hum Genet. 2004;75:998–1014.
Arcos-Burgos M, Muenke M. Toward a better understanding of ADHD: LPHN3 gene variants and the susceptibility to develop ADHD. Atten Defic Hyperact Disord. 2010;2:139–47.
Gizer IR, Ficks C, Waldman ID. Candidate gene studies of ADHD: a meta-analytic review. Hum Genet. 2009;126:51–90.
Bonvicini C, Faraone SV, Scassellati C. Attention-deficit hyperactivity disorder in adults: a systematic review and meta-analysis of genetic, pharmacogenetic and biochemical studies. Mol Psychiatry. 2016;21:1643.
Franke B, Vasquez AA, Johansson S, Hoogman M, Romanos J, Boreatti-Hummer A, et al. Multicenter analysis of the SLC6A3/DAT1 VNTR haplotype in persistent ADHD suggests differential involvement of the gene in childhood and persistent ADHD. Neuropsychopharmacology. 2010;35:656–64.
Faraone SV, Spencer TJ, Madras BK, Zhang-James Y, Biederman J. Functional effects of dopamine transporter gene genotypes on in vivo dopamine transporter functioning: a meta-analysis. Mol Psychiatry. 2014;19:880–9.
Neale BM, Medland S, Ripke S, Anney RJ, Asherson P, Buitelaar J, et al. Case-control genome-wide association study of attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2010;49:906–20.
Yang L, Neale BM, Liu L, Lee SH, Wray NR, Ji N, et al. Polygenic transmission and complex neuro developmental network for attention deficit hyperactivity disorder: genome-wide association study of both common and rare variants. Am J Med Genet B Neuropsychiatr Genet. 2013;162:419–30.
Article CAS Google Scholar
Ebejer JL, Duffy DL, van der Werf J, Wright MJ, Montgomery G, Gillespie NA, et al. Genome-wide association study of inattention and hyperactivity-impulsivity measured as quantitative traits. Twin Res Hum Genet. 2013;16:560–74.
Fliers EA, Vasquez AA, Poelmans G, Rommelse N, Altink M, Buschgens C, et al. Genome-wide association study of motor coordination problems in ADHD identifies genes for brain and muscle function. World J Biol Psychiatry. 2012;13:211–22.
Hinney A, Scherag A, Jarick I, Albayrak O, Putter C, Pechlivanis S, et al. Genome-wide association study in German patients with attention deficit/hyperactivity disorder. Am J Med Genet B Neuropsychiatr Genet. 2011;156B:888–97.
Lasky-Su J, Anney RJ, Neale BM, Franke B, Zhou K, Maller JB, et al. Genome-wide association scan of the time to onset of attention deficit hyperactivity disorder. Am J Med Genet B Neuropsychiatr Genet. 2008;147B:1355–8.
Lasky-Su J, Neale BM, Franke B, Anney RJ, Zhou K, Maller JB, et al. Genome-wide association scan of quantitative traits for attention deficit hyperactivity disorder identifies novel associations and confirms candidate gene associations. Am J Med Genet B Neuropsychiatr Genet. 2008;147B:1345–54.
Mick E, Todorov A, Smalley S, Hu X, Loo S, Todd RD, et al. Family-based genome-wide association scan of attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2010;49:898–905 e3.
Sanchez-Mora C, Ramos-Quiroga JA, Bosch R, Corrales M, Garcia-Martinez I, Nogueira M, et al. Case-control genome-wide association study of persistent attention-deficit hyperactivity disorder identifies FBXO33 as a novel susceptibility gene for the disorder. Neuropsychopharmacology. 2015;40:915–26.
Lesch KP, Timmesfeld N, Renner TJ, Halperin R, Roser C, Nguyen TT, et al. Molecular genetics of adult ADHD: converging evidence from genome-wide association and extended pedigree linkage studies. J Neural Transm. 2008;115:1573–85.
Zayats T, Athanasiu L, Sonderby I, Djurovic S, Westlye LT, Tamnes CK, et al. Genome-wide analysis of attention deficit hyperactivity disorder in Norway. PLoS ONE. 2015;10:e0122501.
Neale BM, Medland SE, Ripke S, Asherson P, Franke B, Lesch KP, et al. Meta-analysis of genome-wide association studies of attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2010;49:884–97.
Brookes K, Xu X, Chen W, Zhou K, Neale B, Lowe N, et al. The analysis of 51 genes in DSM-IV combined type attention deficit hyperactivity disorder: association signals in DRD4, DAT1 and 16 other genes. Mol Psychiatry. 2006;11:934–53.
Franke B, Neale BM, Faraone SV. Genome-wide association studies in ADHD. Hum Genet. 2009;126:13–50.
Poelmans G, Pauls DL, Buitelaar JK, Franke B. Integrated genome-wide association study findings: identification of a neurodevelopmental network for attention deficit hyperactivity disorder. Am J Psychiatry. 2011;168:365–77.
Mooney MA, McWeeney SK, Faraone SV, Hinney A, Hebebrand J, Consortium I, et al. Pathway analysis in attention deficit hyperactivity disorder: an ensemble approach. Am J Med Genet B Neuropsychiatr Genet. 2016;171:815–26.
Aebi M, van Donkelaar MM, Poelmans G, Buitelaar JK, Sonuga-Barke EJ, Stringaris A, et al. Gene-set and multivariate genome-wide association analysis of oppositional defiant behavior subtypes in attention-deficit/hyperactivity disorder. Am J Med Genet B Neuropsychiatr Genet. 2016;171:573–88.
Groenman AP, Greven CU, van Donkelaar MM, Schellekens A, van Hulzen KJ, Rommelse N, et al. Dopamine and serotonin genetic risk scores predicting substance and nicotine use in attention deficit/hyperactivity disorder. Addict Biol. 2016;21:915–23.
Demontis D, Walters RK, Martin J, Mattheisen M, Als TD, Agerbo E, et al. Discovery of the first genome-wide significant risk loci for ADHD. Submitted for publication, bioRxiv. 2017;14558:1–43
Google Scholar
Lai CS, Gerrelli D, Monaco AP, Fisher SE, Copp AJ. FOXP2 expression during brain development coincides with adult sites of pathology in a severe speech and language disorder. Brain. 2003;126(Pt 11):2455–62.
Enard W, Gehre S, Hammerschmidt K, Holter SM, Blass T, Somel M, et al. A humanized version of Foxp2 affects cortico-basal ganglia circuits in mice. Cell . 2009;137:961–71.
Faraone SV, Perlis RH, Doyle AE, Smoller JW, Goralnick JJ, Holmgren MA, et al. Molecular genetics of attention-deficit/hyperactivity disorder. Biol Psychiatry. 2005;57:1313–23.
Lee SH, Ripke S, Neale BM, Faraone SV, Purcell SM, Perlis RH, et al. Genetic relationship between five psychiatric disorders estimated from genome-wide SNPs. Nat Genet. 2013;45:984–94.
Martin J, Hamshere ML, Stergiakouli E, O’Donovan MC, Thapar A. Genetic risk for attention-deficit/hyperactivity disorder contributes to neurodevelopmental traits in the general population. Biol Psychiatry. 2014;76:664–71.
Bralten J, van Hulzen KJ, Martens MB, Galesloot TE, Arias Vasquez A, Kiemeney LA, et al. Autism spectrum disorders and autistic traits share genetics and biology. Mol Psychiatry. 2017;00:1–8.
Groen-Blokhuis MM, Middeldorp CM, Kan KJ, Abdellaoui A, van Beijsterveldt CE, Ehli EA, et al. Attention-deficit/hyperactivity disorder polygenic risk scores predict attention problems in a population-based sample of children. J Am Acad Child Adolesc Psychiatry. 2014;53:1123–9 e6.
Stergiakouli E, Martin J, Hamshere ML, Langley K, Evans DM, St Pourcain B, et al. Shared genetic influences between attention-deficit/hyperactivity disorder (ADHD) traits in children and clinical ADHD. J Am Acad Child Adolesc Psychiatry. 2015;54:322–7.
Faraone S, Biederman J, Garcia Jetton J, Tsuang M. Attention deficit disorder and conduct disorder: longitudinal evidence for a familial subtype. Psychol Med. 1997;27:291–300.
Faraone SV, Biederman J, Keenan K, Tsuang MT. Separation of DSM-III attention deficit disorder and conduct disorder: evidence from a family-genetic study of American child psychiatric patients. Psychol Med. 1991;21:109–21.
Thapar A, Harrington R, McGuffin P. Examining the comorbidity of ADHD-related behaviours and conduct problems using a twin study design. Br J Psychiatry. 2001;179:224–9.
Hamshere ML, Langley K, Martin J, Agha SS, Stergiakouli E, Anney RJ, et al. High loading of polygenic risk for ADHD in children with comorbid aggression. Am J Psychiatry. 2013;170:909–16.
Larsson H, Ryden E, Boman M, Langstrom N, Lichtenstein P, Landen M. Risk of bipolar disorder and schizophrenia in relatives of people with attention-deficit hyperactivity disorder. Br J Psychiatry. 2013;203:103–6.
Hamshere ML, Stergiakouli E, Langley K, Martin J, Holmans P, Kent L, et al. Shared polygenic contribution between childhood attention-deficit hyperactivity disorder and adult schizophrenia. Br J Psychiatry. 2013;203:107–11.
Faraone SV, Biederman J, Wozniak J. Examining the comorbidity between attention deficit hyperactivity disorder and bipolar I disorder: a meta-analysis of family genetic studies. Am J Psychiatry. 2012;169:1256–66.
van Hulzen KJE, Scholz CJ, Franke B, Ripke S, Klein M, McQuillin A, et al. Genetic overlap between attention-deficit/hyperactivity disorder and bipolar disorder: evidence from genome-wide association study meta-analysis. Biol Psychiatry. 2017;82:634–41.
Hart AB, Gamazon ER, Engelhardt BE, Sklar P, Kahler AK, Hultman CM, et al. Genetic variation associated with euphorigenic effects of d-amphetamine is associated with diminished risk for schizophrenia and attention deficit hyperactivity disorder. Proc Natl Acad Sci USA. 2014;111:5968–73.
Cortese S, Moreira-Maia CR, St Fleur D, Morcillo-Penalver C, Rohde LA, Faraone SV. Association between ADHD and obesity: a systematic review and meta-analysis. Am J Psychiatry. 2015;173:34–43. appiajp201515020266
Barkley RA, Murphy KR, Fischer M. ADHD in Adults: What the Science Says. New York, NY: Guilford Press; 2010.
Dalsgaard S, Ostergaard SD, Leckman JF, Mortensen PB, Pedersen MG. Mortality in children, adolescents, and adults with attention deficit hyperactivity disorder: a nationwide cohort study. Lancet. 2015;385:2190–6.
Lo-Castro A, D’Agati E, Curatolo P. ADHD and genetic syndromes. Brain Dev. 2010;33:456–61.
de Silva MG, Elliott K, Dahl HH, Fitzpatrick E, Wilcox S, Delatycki M, et al. Disruption of a novel member of a sodium/hydrogen exchanger family and DOCK3 is associated with an attention deficit hyperactivity disorder-like phenotype. J Med Genet. 2003;40:733–40.
Zhang-James Y, Middleton FA, Sagvolden T, Faraone SV. Differential expression of SLC9A9 and interacting molecules in the hippocampus of rat models for attention deficit/hyperactivity disorder. Dev Neurosci. 2012;34:218–27.
Zhang-James Y, Dasbanerjee T, Sagvolden T, Middleton FA, Faraone SV. SLC9A9 mutations, gene expression, and protein−protein interactions in rat models of attention-deficit/hyperactivity disorder. Am J Med Genet B Neuropsychiatr Genet. 2011;156:835–43.
Article CAS PubMed Central Google Scholar
Patak J, Hess JL, Zhang-James Y, Glatt SJ, Faraone SV. SLC9A9 Co-expression modules in autism-associated brain regions. Autism Res. 2016;10:414–29
Patak J, Zhang-James Y, Faraone SV. Endosomal system genetics and autism spectrum disorders: a literature review. Neurosci Biobehav Rev. 2016;65:95–112.
Demontis D, Lescai F, Borglum A, Glerup S, Ostergaard SD, Mors O, et al. Whole-exome sequencing reveals increased burden of rare functional and disruptive variants in candidate risk genes in individuals with persistent attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2016;55:521–3.
Elia J, Glessner JT, Wang K, Takahashi N, Shtir CJ, Hadley D, et al. Genome-wide copy number variation study associates metabotropic glutamate receptor gene networks with attention deficit hyperactivity disorder. Nat Genet. 2012;44:78–84.
Jarick I, Volckmar AL, Putter C, Pechlivanis S, Nguyen TT, Dauvermann MR, et al. Genome-wide analysis of rare copy number variations reveals PARK2 as a candidate gene for attention-deficit/hyperactivity disorder. Mol Psychiatry. 2012;19:115–21.
Lesch KP, Selch S, Renner TJ, Jacob C, Nguyen TT, Hahn T, et al. Genome-wide copy number variation analysis in attention-deficit/hyperactivity disorder: association with neuropeptide Y gene dosage in an extended pedigree. Mol Psychiatry. 2011;16:491–503.
Lionel AC, Crosbie J, Barbosa N, Goodale T, Thiruvahindrapuram B, Rickaby J, et al. Rare copy number variation discovery and cross-disorder comparisons identify risk genes for ADHD. Sci Transl Med. 2011;3:95ra75.
Ramos-Quiroga JA, Sanchez-Mora C, Casas M, Garcia-Martinez I, Bosch R, Nogueira M, et al. Genome-wide copy number variation analysis in adult attention-deficit and hyperactivity disorder. J Psychiatr Res. 2014;49:60–7.
Williams NM, Franke B, Mick E, Anney RJ, Freitag CM, Gill M, et al. Genome-wide analysis of copy number variants in attention deficit/hyperactivity disorder confirms the role of rare variants and implicates duplications at 15q13.3. Am J Psychiatry. 2012;169:195–204.
Thapar A, Martin J, Mick E, Arias Vasquez A, Langley K, Scherer SW, et al. Psychiatric gene discoveries shape evidence on ADHD’s biology. Mol Psychiatry. 2015;21:1202–7.
Garcia-Martinez I, Sanchez-Mora C, Soler Artigas M, Rovira P, Pagerols M, Corrales M, et al. Gene-wide association study reveals RNF122 ubiquitin ligase as a novel susceptibility gene for attention deficit hyperactivity disorder. Sci Rep. 2017;7:5407.
Valbonesi S, Magri C, Traversa M, Faraone SV, Cattaneo A, Milanesi E, et al. Copy number variants in attention-deficit hyperactive disorder: identification of the 15q13 deletion and its functional role. Psychiatr Genet. 2015;25:59–70.
Kollins SH, McClernon FJ, Fuemmeler BF. Association between smoking and attention-deficit/hyperactivity disorder symptoms in a population-based sample of young adults. Arch Gen Psychiatry. 2005;62:1142–7.
Levin ED, Conners CK, Silva D, Hinton SC, Meck WH, March J, et al. Transdermal nicotine effects on attention. Psychopharmacol (Berl). 1998;140:135–41.
Cross-Disorder Group of the Psychiatric Genomics Consortium. Identification of risk loci with shared effects on five major psychiatric disorders: a genome-wide analysis. Lancet. 2013;381:1371–9.
Article PubMed Central CAS Google Scholar
Buske-Kirschbaum A, Schmitt J, Plessow F, Romanos M, Weidinger S, Roessner V. Psychoendocrine and psychoneuroimmunological mechanisms in the comorbidity of atopic eczema and attention deficit/hyperactivity disorder. Psychoneuroendocrinology. 2013;38:12–23.
Joseph N, Zhang-James Y, Perl A, Faraone SV. Oxidative stress and attention deficit hyperactivity disorder: a meta-analysis. J Atten Disord. 2015;19:915–24.
Chen MH, Su TP, Chen YS, Hsu JW, Huang KL, Chang WH, et al. Comorbidity of allergic and autoimmune diseases among patients with ADHD: a nationwide population-based study. J Atten Disord. 2013;21:219-27.
Article Google Scholar
Akutagava-Martins GC, Salatino-Oliveira A, Genro JP, Contini V, Polanczyk G, Zeni C, et al. Glutamatergic copy number variants and their role in attention-deficit/hyperactivity disorder. Am J Med Genet B Neuropsychiatr Genet. 2014;165:502–9.
Mick E, Neale B, Middleton FA, McGough JJ, Faraone SV. Genome-wide association study of response to methylphenidate in 187 children with attention-deficit/hyperactivity disorder. Am J Med Genet B Neuropsychiatr Genet. 2008;147B:1412–8.
Russell VA. Dopamine hypofunction possibly results from a defect in glutamate-stimulated release of dopamine in the nucleus accumbens shell of a rat model for attention deficit hyperactivity disorder--the spontaneously hypertensive rat. Neurosci Biobehav Rev. 2003;27:671–82.
Jensen V, Rinholm JE, Johansen TJ, Medin T, Storm-Mathisen J, Sagvolden T, et al. N -methyl- d -aspartate receptor subunit dysfunction at hippocampal glutamatergic synapses in an animal model of attention-deficit/hyperactivity disorder. Neuroscience. 2009;158:353–64.
Carrey NJ, MacMaster FP, Gaudet L, Schmidt MH. Striatal creatine and glutamate/glutamine in attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol. 2007;17:11–7.
Kim DS, Burt AA, Ranchalis JE, Wilmot B, Smith JD, Patterson KE, et al. Sequencing of sporadic Attention-Deficit Hyperactivity Disorder (ADHD) identifies novel and potentially pathogenic de novo variants and excludes overlap with genes associated with autism spectrum disorder. Am J Med Genet B Neuropsychiatr Genet. 2017;174:381–9.
Zayats T, Jacobsen KK, Kleppe R, Jacob CP, Kittel-Schneider S, Ribases M, et al. Exome chip analyses in adult attention deficit hyperactivity disorder. Transl Psychiatry. 2016;6:e923.
Hawi Z, Cummins TD, Tong J, Arcos-Burgos M, Zhao Q, Matthews N, et al. Rare DNA variants in the brain-derived neurotrophic factor gene increase risk for attention-deficit hyperactivity disorder: a next-generation sequencing study. Mol Psychiatry. 2017;22:580–4.
Trzepacz PT, Williams DW, Feldman PD, Wrishko RE, Witcher JW, Buitelaar JK. CYP2D6 metabolizer status and atomoxetine dosing in children and adolescents with ADHD. Eur Neuropsychopharmacol. 2008;18:79–86.
Froehlich TE, McGough JJ, Stein MA. Progress and promise of attention-deficit hyperactivity disorder pharmacogenetics. CNS Drugs. 2010;24:99–117.
Myer NM, Boland JR, Faraone SV. Pharmacogenetics predictors of methylphenidate efficacy in childhood ADHD. Mol Psychiatry. 2017;00:1–8.
Walton E, Pingault JB, Cecil CA, Gaunt TR, Relton CL, Mill J, et al. Epigenetic profiling of ADHD symptoms trajectories: a prospective, methylome-wide study. Mol Psychiatry. 2016;22:250–6.
Gusev A, Lee SH, Trynka G, Finucane H, Vilhjalmsson BJ, Xu H, et al. Partitioning heritability of regulatory and cell-type-specific variants across 11 common diseases. Am J Hum Genet. 2014;95:535–52.
Boyle EA, Li YI, Pritchard JK. An expanded view of complex traits: from polygenic to omnigenic. Cell . 2017;169:1177–86.
Hess JL, Akutagava-Martins GC, Patak JD, Glatt SJ, Faraone SV. Why is there selective subcortical vulnerability in ADHD? Clues from postmortem brain gene expression data. Molecular Psychiatry, 00:1–7.
Sanislow CA, Pine DS, Quinn KJ, Kozak MJ, Garvey MA, Heinssen RK, et al. Developing constructs for psychopathology research: research domain criteria. J Abnorm Psychol. 2010;119:631–9.
Chang Z, Lichtenstein P, Asherson PJ, Larsson H. Developmental twin study of attention problems: high heritabilities throughout development. JAMA Psychiatry. 2013;70:311–8.
Polderman TJ, Huizink AC, Verhulst FC, van Beijsterveldt CE, Boomsma DI, Bartels M. A genetic study on attention problems and academic skills: results of a longitudinal study in twins. J Can Acad Child Adolesc Psychiatry. 2011;20:22–34.
PubMed PubMed Central Google Scholar
Greven CU, Rijsdijk FV, Plomin R. A twin study of ADHD symptoms in early adolescence: hyperactivity-impulsivity and inattentiveness show substantial genetic overlap but also genetic specificity. J Abnorm Child Psychol. 2011;39:265–75.
Ilott N, Saudino KJ, Wood A, Asherson P. A genetic study of ADHD and activity level in infancy. Genes Brain Behav. 2010;9:296–304.
Bornovalova MA, Hicks BM, Iacono WG, McGue M. Familial transmission and heritability of childhood disruptive disorders. Am J Psychiatry. 2010;167:1066–74.
Tuvblad C, Zheng M, Raine A, Baker LA. A common genetic factor explains the covariation among ADHD ODD and CD symptoms in 9−10 year old boys and girls. J Abnorm Child Psychol. 2009;37:153–67.
Polderman TJ, Derks EM, Hudziak JJ, Verhulst FC, Posthuma D, Boomsma DI. Across the continuum of attention skills: a twin study of the SWAN ADHD rating scale. J Child Psychol Psychiatry. 2007;48:1080–7.
Derks EM, Dolan CV, Hudziak JJ, Neale MC, Boomsma DI. Assessment and etiology of attention deficit hyperactivity disorder and oppositional defiant disorder in boys and girls. Behav Genet. 2007;37:559–66.
Hudziak JJ, Derks EM, Althoff RR, Rettew DC, Boomsma DI. The genetic and environmental contributions to attention deficit hyperactivity disorder as measured by the conners’ rating scales—revised. Am J Psychiatry. 2005;162:1614–20.
Dick DM, Viken RJ, Kaprio J, Pulkkinen L, Rose RJ. Understanding the covariation among childhood externalizing symptoms: genetic and environmental influences on conduct disorder, attention deficit hyperactivity disorder, and oppositional defiant disorder symptoms. J Abnorm Child Psychol. 2005;33:219–29.
Larsson JO, Larsson H, Lichtenstein P. Genetic and environmental contributions to stability and change of ADHD symptoms between 8 and 13 years of age: a longitudinal twin study. J Am Acad Child Adolesc Psychiatry. 2004;43:1265–75.
Martin N, Scourfield J, McGuffin P. Observer effects and heritability of childhood attention-deficit hyperactivity disorder symptoms. Br J Psychiatry. 2002;180:260–5.
Kuntsi J, Stevenson J. Psychological mechanisms in hyperactivity: II The role of genetic factors. J Child Psychol Psychiatry. 2001;42:211–9.
Coolidge FL, Thede LL, Young SE. Heritability and the comorbidity of attention deficit hyperactivity disorder with behavioral disorders and executive function deficits: a preliminary investigation. Dev Neuropsychol. 2000;17:273–87.
Schmitz S, Fulker DW, Mrazek DA. Problem behavior in early and middle childhood: an initial behavior genetic analysis. J Child Psychol Psychiatry. 1995;36:1443–58.
Stevenson J. Evidence for a genetic etiology in hyperactivity in children. Behav Genet. 1992;22:337–44.
Edelbrock C, Rende R, Plomin R, Thompson LA. A twin study of competence and problem behavior in childhood and early adolescence. J Child Psychol Psychiat. 1995;36:775–85.
Gillis JJ, Gilger JW, Pennington BF, DeFries JC. Attention deficit disorder in reading-disabled twins: evidence for a genetic etiology. J Abnorm Child Psychol. 1992;20:303–15.
Goodman R. Genetic factors in hyperactivity: account for about half of the explainable variance. Br Med J. 1989;298:1407–8.
Willerman L. Activity level and hyperactivity in twins. Child Dev. 1973;44:288–93.
Matheny AP Jr., Brown AM. Activity, motor coordination and attention: individual differences in twins. Percept Mot Skills. 1971;32:151–8.
Download references
Acknowledgements
Dr. Faraone is supported by the K.G. Jebsen Centre for Research on Neuropsychiatric Disorders, University of Bergen, Bergen, Norway, the European Union’s Seventh Framework Programme for research, technological development and demonstration under grant agreement no. 602805, the European Union’s Horizon 2020 research and innovation programme under grant agreement no. 667302 and NIMH grant 5R01MH101519. Dr. Larsson is supported by the European Union’s Horizon 2020 research and innovation programme under grant agreement no. 667302 and the Swedish Research Council (2013-2280; 2014-3831).
Author information
Authors and affiliations.
Departments of Psychiatry and of Neuroscience and Physiology, SUNY Upstate Medical University, Syracuse, NY, 13210, USA
- Stephen V. Faraone
School of Medical Sciences, Örebro University, Örebro, Sweden
Henrik Larsson
Department of Medical Epidemiology and Biostatistics, Karolinska Institutet, Stockholm, Sweden
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Stephen V. Faraone .
Ethics declarations
Conflict of interest.
In the past year, SVF received income, potential income, travel expenses continuing education support and/or research support from Lundbeck, KenPharm, Rhodes, Arbor, Ironshore, Shire, Akili Interactive Labs, CogCubed, Alcobra, VAYA, Sunovion, Genomind, and NeuroLifeSciences. With his institution, he has US patent US20130217707 A1 for the use of sodium−hydrogen exchange inhibitors in the treatment of ADHD. HL has served as a speaker for Eli-Lilly and Shire and has received research grants from Shire.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Faraone, S.V., Larsson, H. Genetics of attention deficit hyperactivity disorder. Mol Psychiatry 24 , 562–575 (2019). https://doi.org/10.1038/s41380-018-0070-0
Download citation
Received : 29 August 2017
Revised : 31 January 2018
Accepted : 19 February 2018
Published : 11 June 2018
Issue Date : April 2019
DOI : https://doi.org/10.1038/s41380-018-0070-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Sex, hormones and cerebrovascular function: from development to disorder.
- Adeline Collignon
- Laurence Dion-Albert
- Vanessa Coelho-Santos
Fluids and Barriers of the CNS (2024)
The effectiveness of a dialogical family guidance intervention regarding child treatment response in families with a child with neurodevelopmental disorders
- Diana Cavonius-Rintahaka
- Anna Liisa Aho
BMC Psychology (2024)
Attention-deficit/hyperactivity disorder
- Mark A. Bellgrove
- Jan K. Buitelaar
Nature Reviews Disease Primers (2024)
Dissecting 16p11.2 hemi-deletion to study sex-specific striatal phenotypes of neurodevelopmental disorders
- Jaekyoon Kim
- Yann Vanrobaeys
Molecular Psychiatry (2024)
The Association between Threatened Miscarriage and Autism Spectrum Disorder and Attention-Deficit/Hyperactivity Disorder in Offspring by Age 14 Years
- Daire Buckley
- Ali S. Khashan
- Gillian M. Maher
Journal of Autism and Developmental Disorders (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Open Resources for Nursing (Open RN); Ernstmeyer K, Christman E, editors. Nursing: Mental Health and Community Concepts [Internet]. Eau Claire (WI): Chippewa Valley Technical College; 2022.
Nursing: Mental Health and Community Concepts [Internet].
- About Open RN

Chapter 7 Depressive Disorders
7.1. introduction, learning objectives.
- Apply the nursing process to clients with depressive disorders
- Describe nursing assessments related to depressive disorders
- Identify common nursing problems/diagnoses related to depressive disorders
- Establish a safe environment
- Apply evidence-based practice when planning and implementing nursing care
- Describe common treatments for depressive disorders
- Identify appropriate referrals to community resources
- Evaluate the effectiveness of interventions
- Provide patient education to clients and their family members
Depression is a common illness affecting an estimated 8% of adults in the United States annually. [ 1 ] Approximately 280 million people in the world have depression. [ 2 ] This chapter will discuss causes and types of depression, treatments for depression, and steps for applying the nursing process when caring for clients with depressive disorders.
7.2. CAUSES OF DEPRESSION
There are several possible causes of depression, including faulty mood regulation by the brain, genetic vulnerability, stressful life events, medications, and medical problems. Based on current research, it is believed that several of these forces interact to bring on depression. [ 1 ]
Certain areas of the brain help regulate mood, including the hippocampus, amygdala, and hypothalamus. See Figure 7.1 [ 2 ] for an image of these areas of the brain. Researchers believe that nerve cell connections, nerve cell growth, the functioning of nerve circuits, and levels of specific brain chemicals (called neurotransmitters) have a major impact on depression. [ 3 ]
Areas of the Brain Regulating Mood
The hippocampus is part of the limbic system in the brain that has a central role in processing long-term memory and recollection. For example, this part of the brain registers fear when you are confronted by a frightening situation, like an aggressive dog, and the memory of such an experience may make you wary of dogs you come across later in life. The hippocampus is smaller in some depressed people, and research suggests that ongoing exposure to the stress hormone impairs the growth of nerve cells in this part of the brain. [ 4 ]
The amygdala is also part of the limbic system and is a group of structures deep in the brain that are associated with emotions such as anger, pleasure, sorrow, fear, and sexual arousal. The amygdala is activated when a person experiences or recalls emotionally charged memories, such as a frightening situation, and sends signals to the hypothalamus to stimulate the sympathetic fight-or-flight response. Activity in the amygdala is higher when a person is sad or clinically depressed. This increased activity continues even after recovery from depression. [ 5 ]
The hypothalamus is involved in the stress response. The stress response starts with a signal from the hypothalamus. The hypothalamus, pituitary gland, and adrenal glands form the hypothalamic-pituitary-adrenal (HPA) axis, which governs a multitude of hormonal activities in the body and also plays a role in depression. When a physical or emotional threat looms, the hypothalamus secretes corticotropin-releasing hormone (CRH) that rouses the body. CRH follows a pathway to the pituitary gland, where it stimulates the secretion of adrenocorticotropic hormone (ACTH) into the bloodstream. When ACTH reaches the adrenal glands, it prompts the release of cortisol. The boost in cortisol readies the body to fight or flee by causing the heart to beat faster, the blood pressure to rise, and the respiratory rate to increase. CRH also affects the cerebral cortex, part of the amygdala, and the brain stem. It is thought to play a major role in coordinating one’s thoughts and behaviors, emotional reactions, and involuntary responses. Working along a variety of neural pathways, it influences the concentration of neurotransmitters throughout the brain. Disturbances in hormonal systems affect neurotransmitters and vice versa. [ 6 ]
Neurotransmitters
There are many types of neurotransmitters that play a role in depression [ 7 ]:
- Acetylcholine enhances memory and is involved in learning and recall. [ 8 ]
- Serotonin helps regulate sleep, appetite, and mood and inhibits pain. Research supports the idea that some depressed people have reduced serotonin transmission. Low levels of a serotonin by-product have been linked to a higher risk for suicide. [ 9 ]
- Norepinephrine constricts blood vessels, raising blood pressure. It may trigger anxiety and be involved in some types of depression. It also seems to help determine motivation and reward. [ 10 ]
- Dopamine is essential to movement. It also influences motivation and plays a role in how a person perceives reality. Problems in dopamine transmission have been associated with psychosis, a severe form of distorted thinking characterized by hallucinations or delusions. It’s also involved in the brain’s reward system, so it is thought to play a role in substance abuse. [ 11 ]
- Glutamate is a small molecule believed to act as an excitatory neurotransmitter and to play a role in bipolar disorder and schizophrenia. Animal research suggests that lithium stabilizes glutamate reuptake and smooths out the highs of mania and the lows of depression in the long-term. [ 12 ]
- Gamma-aminobutyric acid (GABA) is an amino acid that researchers believe acts as an inhibitory neurotransmitter. It is thought to help subdue anxiety. [ 13 ]
See Figure 7.2 [ 14 ] for an illustration of neurotransmitter communication between neurons at the synapse. Antidepressants immediately boost the concentration of chemical messengers in the brain (neurotransmitters), but people typically don’t begin to feel better for several weeks or longer. Experts have long wondered why people don’t improve as soon as the level of neurotransmitters increases. New theories explain that antidepressants spur the growth and enhanced branching of nerve cells in the hippocampus (a process called neurogenesis), and mood improves over several weeks as nerves grow and form new connections. [ 15 ]
Neurotransmitters at the Synapse Level
Every part of our body, including our brain, is controlled by our genes. Humans have almost 22,000 genes in their DNA within 46 chromosomes inside the nucleus of each cell. The sequence of nitrogen-containing bases within a strand of DNA forms the genes that act as a molecular code instructing cells in the assembly of amino acids into proteins. See Figure 7.3 [ 16 ] for an image of sequences of bases within a DNA strand that forms genes. Genes make proteins that are involved in biological processes. Throughout life, different genes turn on and off and make the right proteins at the right time. However, genes can alter biology in a way that results in a person’s mood becoming unstable. In a person who is genetically vulnerable to depression, any stress (such as a missed deadline at work or a medical illness) can then push this system off balance. [ 17 ]
Sequence of Bases Within DNA That Form Genes
It is well-known that depressive and bipolar disorders run in families. Mood is affected by dozens of genes, and as our genes differ, so does depression. As researchers pinpoint specific genes involved in mood disorders and better understand their functions, it is hoped that treatment for depressive disorders can become more individualized and more successful as patients receive targeted medication for their specific type of depression. [ 18 ]
Genetics provides one perspective on how resilient an individual is in the face of difficult life events. Temperament is determined by a person’s genetic inheritance and the experiences they have had in life. For example, one person may have the temperament of an introvert and tend to withdraw from social situations, whereas another person may have the temperament of an extrovert who seeks out social situations and feels energized by them. Cognitive psychologists believe that one’s view of the world and assumptions about how the world works influence how a person feels. Individuals develop their assumptions about life early and automatically fall back on them when loss, disappointment, or rejection occurs. For example, a person who was continually criticized as a child may have the genetic inheritance and temperament where they become so self-critical they can’t bear the slightest criticism from others, which can slow or block their career progress and make intimate relationships more difficult. Therapy and medications can shift thoughts and attitudes that have developed over time. [ 19 ]
Stressful Life Events
At some point, nearly everyone encounters stressful life events such as the death of a loved one, the loss of a job, the diagnosis of a severe illness, or the end of a significant relationship. Many individuals have also experienced traumatic childhood experiences that continue to affect their coping and functioning into adulthood. It is estimated that 61% of adults have experienced early adverse childhood experiences (ACEs) such as abuse, neglect, or growing up in a household with violence, mental illness, substance use, incarceration, or divorce. See Figure 7.4 [ 20 ] for an illustration of adverse childhood experiences. Toxic stress from ACEs can change brain development and affect how the body responds to stress. ACEs are linked to chronic health problems, mental illness, and substance misuse in adulthood. [ 21 ]
Adverse Childhood Experiences (ACEs)
Stress triggers a chain of chemical reactions and responses in the body. If the stress is short-lived, the body usually returns to normal. But when stress is chronic or the system gets stuck in overdrive, changes in the body and brain can be long-lasting. Every real or perceived threat to one’s body triggers a cascade of stress hormones that produces physiological changes called the stress response. Normally, a feedback loop allows the body to turn off “fight-or-flight” defenses when the threat passes. In some cases, though, the floodgates never close properly, and cortisol levels rise too often or simply stay high. These elevated cortisol levels can contribute to problems such as high blood pressure, immune suppression, asthma, and depression. Studies have also shown that people who have depressive disorders typically have increased levels of CRH. Antidepressants and electroconvulsive therapy are both known to reduce these high CRH levels. As CRH levels return to normal, depressive symptoms recede. Research also suggests that trauma during childhood can negatively affect the functioning of CRH and the HPA axis throughout life. [ 22 ]
Read the Adverse Childhood Experiences Prevention Strategy PDF.
Medical problems.
Certain medical problems are linked to up to 10% to 15% of all depressions. For example, hypothyroidism, a condition where the body produces too little thyroid hormone, often leads to exhaustion and depression, whereas hyperthyroidism (excess thyroid hormone) can trigger manic symptoms. Heart disease has also been linked to depression, with up to half of heart attack survivors reporting feeling blue and many having significant depression. Another example of depression linked to a medical condition is postpartum depression that occurs after pregnancy. [ 23 ]
The following medical conditions have also been associated with depression and other mood disorders [ 24 ]:
- Degenerative neurological conditions, such as multiple sclerosis, Parkinson’s disease, Alzheimer’s disease, and Huntington’s disease
- Cerebrovascular accidents (i.e., strokes)
- Some nutritional deficiencies, such as a lack of vitamin B12
- Endocrine disorders with the parathyroid or adrenal glands
- Immune system diseases, such as lupus
- Some viruses, such as mononucleosis, hepatitis, and HIV
- Erectile dysfunction in men
When considering the connection between health problems and depression, an important question to address is which came first, the medical condition or the mood changes. Stress of having certain illnesses can trigger depression, whereas in other cases, depression precedes the medical illness and may even contribute to it. If depression is caused by an underlying medical problem, the mood changes should disappear after the medical condition is treated. For example, after hypothyroidism is treated, lethargy and depression often lift. In many cases, however, the depression is an independent problem, which means that in order to be successful, treatment must address depression directly. [ 25 ]
Symptoms of depression can be a side effect of certain drugs, such as steroids or some types of blood pressure medication. A health care provider can help sort out whether a new medication, a change in dosage, or interactions with other drugs or substances might be affecting an individual’s mood. [ 26 ]
7.3. TYPES OF DEPRESSION
Depression is different from the usual mood fluctuations and short-lived emotional responses to everyday life stressors. When it is recurrent with moderate or severe intensity, depression can become a serious health condition that causes the affected person to suffer greatly and function poorly at work and school and can affect relationships with family and friends. At its worst, depression can lead to suicide. Over 700,000 people die every year due to suicide. Barriers to effective care for depression include a lack of resources, lack of trained health care providers, and social stigma associated with mental health disorders. [ 1 ] See Figure 7.5 [ 2 ] for an artistic depiction of an individual experiencing depression.
During a depressive episode , the person experiences a depressed mood (feeling sad, irritable, empty) or a loss of pleasure or interest in activities (anhedonia) for most of the day, nearly every day, for at least two weeks. Several other symptoms may also be present, which may include poor concentration, feelings of excessive guilt or low self-worth, hopelessness about the future, thoughts about dying or suicide, disrupted sleep, changes in appetite or weight, and feeling especially tired or low in energy. In some cultural contexts, some people may express their mood changes more readily in the form of bodily symptoms (such as pain, fatigue, or weakness) that are not due to another medical condition. During a depressive episode, the person experiences significant difficulty and/or impairment in important areas of personal, family, social, educational, and work functioning. [ 3 ]
A depressive episode is categorized by a provider as mild, moderate, or severe depending on the number and severity of symptoms, as well as the impact on the individual’s functioning. [ 4 ] Mild severity indicates the symptoms to make the diagnosis are present but result in minor impairment in social or occupational functioning. Moderate severity indicates symptoms and impairment are between mild and severe. Severe indicates the intensity is seriously distressing, unmanageable, and markedly interferes with social and occupational functioning. Read the full list of criteria for Major Depressive Disorder from the DSM-5 in the following box.
DSM-5 Criteria for Major Depressive Disorder [ 5 ]
Five or more of the following symptoms have been present during the same two-week period and represent a change from previous functioning; at least one of the symptoms is either (1) depressed mood or (2) loss of interest or pleasure.
- Depressed mood most of the day, nearly every day, as indicated by either subjective report (e.g., feels sad, empty, hopeless) or observation made by others (e.g., appears tearful). (Note: In children and adolescents, can be irritable mood.)
- Markedly diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day.
- Significant weight loss when not dieting or weight gain (i.e., a change of more than 5% of body weight in a month) or decrease or increase in appetite nearly every day. (Note: In children, consider failure to make expected weight gain.)
- Insomnia or hypersomnia nearly every day.
- Psychomotor agitation or retardation nearly every day (observable by others, not merely subjective feelings of restlessness or being slowed down).
- Fatigue or loss of energy nearly every day.
- Feelings of worthlessness or excessive or inappropriate guilt (which may be delusional) nearly every day (not merely self-reproach or guilt about being sick).
- Diminished ability to think or concentrate, or indecisiveness, nearly every day (either by subjective account or as observed by others).
- Recurrent thoughts of death (not just fear of dying), recurrent suicidal ideation without a specific plan, or a suicide attempt or a specific plan for committing suicide.
The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.
The episode is not attributable to the physiological effects of a substance or another medical condition.
According to the DSM-5 , the types of depressive disorders include the following [ 6 ]:
- With anxious distress (tense and/or restless)
- With mixed features (manic symptoms)
- With psychotic features (delusions and/or hallucinations)
- With peripartum onset (includes perinatal and postpartum depression)
- With a seasonal pattern (includes seasonal affective disorder)
- Persistent Depressive Disorder (Dysthymia): Depressed mood for most of the day for at least two years.
- Premenstrual Dysphoric Disorder: In the majority of menstrual cycles, at least five symptoms are present in the week before the onset of menses, start to improve after the onset of menses, and become minimal or absent in the week postmenses.
- Substance/Medication-Induced Depressive Disorder: A persistent disturbance in mood that develops during or soon after substance intoxication or during withdrawal from a substance.
- Depressive Disorder Due to Another Medical Condition: A persistent period of depressed mood that is the direct consequence of another medical condition.
Seasonal Affective Disorder
Seasonal affective disorder (SAD) is a type of major depressive disorder that affects about 5% of adults in the United States. People with SAD experience mood changes and symptoms similar to depression. The symptoms usually occur during the fall and winter months when there is less sunlight and usually improve with the arrival of spring. SAD is more than just “winter blues.” The symptoms can be distressing and overwhelming and can interfere with daily functioning. [ 7 ]
SAD has been linked to a biochemical imbalance in the brain prompted by shorter daylight hours and less sunlight in winter. As seasons change, people experience a shift in their biological internal clock or circadian rhythm that can cause them to be out of step with their daily schedule. SAD is more common in people living far from the equator where there are fewer daylight hours in the winter. [ 8 ]
SAD can be effectively treated with light therapy, antidepressant medications, cognitive behavioral therapy, or some combination of these. While symptoms will generally improve on their own with the change of season, symptoms can improve more quickly with treatment. Light therapy involves sitting in front of a light therapy box that emits a very bright light (and filters out harmful ultraviolet [UV] rays). It usually requires 20 minutes or more per day, typically first thing in the morning during the winter months. Most people see some improvements from light therapy within one or two weeks of beginning treatment. For some people, increased exposure to natural sunlight can help improve symptoms of SAD by spending time outside or arranging their home or office space to increase exposure to windows during daylight hours. General wellness activities such as performing regular exercise, eating healthfully, getting enough sleep, and staying active and connected (such as volunteering, participating in group activities and getting together with friends and family) can also help. [ 9 ]
Peripartum Depression
Pregnancy and the period after delivery can be a vulnerable time for women. Mothers can experience significant biological, emotional, financial, and social changes during this time. Up to 70 percent of new mothers experience the “baby blues,” a short-term condition that does not interfere with their daily activities and does not require medical attention. Symptoms include crying for no reason, irritability, restlessness, and anxiety. These symptoms generally last up to two weeks and resolve on their own. [ 10 ]
However, as many as 3 to 6% of women experience a type of major depressive disorder during pregnancy (called perinatal depression ) or after delivery (called postpartum depression). [ 11 ] See Figure 7.6 [ 12 ] for an illustration of perinatal depression from the National Institutes of Health.
Perinatal Depression
Postpartum depression includes feelings of extreme sadness, anxiety, and exhaustion that may make it difficult for these new mothers to complete daily care activities for themselves and/or for their babies. Untreated peripartum depression is not only a problem for the mother’s health and quality of life but can also affect the well-being of the baby. Postpartum depression can cause bonding issues with the baby and also contribute to sleeping and feeding problems for the baby. In the long-term, children of mothers with peripartum depression are at greater risk for cognitive, emotional, developmental and verbal deficits, and impaired social skills. [ 13 ]
Severe postpartum depression can lead to postpartum psychosis, a medical emergency. Women who have postpartum psychosis may have delusions (thoughts or beliefs that are not true), hallucinations (seeing, hearing, or smelling things that are not there), mania (a high, elated mood that often seems out of touch with reality), paranoia, and confusion. Women who have postpartum psychosis are at risk for harming themselves or their child and should receive help as soon as possible by calling 911 or taking the mother to the nearest emergency room.
Read more information about perinatal depression on the National Institute of Mental Health’s Perinatal Depression webpage.
View the following youtube video on postpartum depression from the national institute of mental health [ 14 ]: postpartum depression, mixed features.
Depressive episodes can also be classified as “mixed,” meaning they alternate with periods of manic symptoms such as euphoria, irritability, increased activity, increased talkativeness, racing thoughts, increased self-esteem, decreased need for sleep, distractibility, and impulsive reckless behavior. [ 15 ] Characteristics and treatment of bipolar disorder are further discussed in the “ Bipolar Disorders ” chapter. See Figure 7.7 [ 16 ] for a comparison of the features of different types of mood disorders.
Mood Disorders. Used under Fair Use.
Read more information at the American Psychiatric Association’s What is Depression ? webpage.
Listen to the dark place podcast on the podbean website to hear personal perspectives on depression and other mental health topics., view the following youtube video of an advocate explaining her experiences with depression and her journey to recovery [ 17 ]:.

Depression Associated With Grief
People have difficulty coping with the death or loss of a loved one, job, or relationship. It is normal for feelings of sadness or grief to develop in response to such situations, but being sad is not the same as having depression. The grieving process is natural and unique to each individual and shares some of the same features of depression. Both grief and depression can involve intense sadness and withdrawal from usual activities with increased risk for suicide.
According to the American Psychiatric Association, grief and depression are different in these ways [ 18 ]:
- In grief, painful feelings come in waves, often intermixed with positive memories of the deceased. In major depression, mood and/or interest (pleasure) are decreased for most of two weeks.
- In grief, self-esteem is usually maintained. In major depression, feelings of worthlessness and self-loathing are common.
- In grief, thoughts of death may surface when thinking of or fantasizing about “joining” the deceased loved one. In major depression, thoughts are focused on ending one’s life due to feeling worthless or undeserving of living or being unable to cope with the pain of depression.
Grief and depression can coexist. When grief and depression occur together, the grief is more severe and lasts longer than grief without depression. Nurses must be able to distinguish between symptoms of grief and depression and assist people in getting the help, support, or treatment they need. [ 19 ]
Read more information about grief in the “ Grief and Loss ” chapter in Open RN Nursing Fundamentals.
7.4. treatments for depression.
Depression is one of the most treatable mental disorders. Between 80% and 90% percent of people with depression eventually respond well to treatment. Almost all patients gain some relief from their symptoms with effective treatment. Before a diagnosis is made or treatment planned, a mental health care provider should conduct a thorough diagnostic evaluation, including an interview, mental status examination, psychosocial assessment, and a physical examination performed by a primary care provider. In some cases, a blood test might be done to make sure the depression is not due to a medical condition like a thyroid problem or a vitamin deficiency. The evaluation also explores medical and family histories, cultural beliefs, and environmental factors as part of the psychosocial assessment with the goal of arriving at a diagnosis and planning a course of action. Treatments for depression include medications, psychotherapy, electroconvulsive therapy, transcranial magnetic stimulation, and encouraging self-care and effective coping strategies. Nurses should keep patient-centered care and client preferences in mind when implementing a client’s treatment plan. For example, the client should be educated about the possible adverse effects associated with antidepressant medication, and their ability to pay for and obtain transportation to treatments like psychotherapy should be considered. [ 1 ]
Antidepressant Medications
Brain chemistry may contribute to an individual’s depression and may factor into their treatment. Read more about the causes of depression in the “ Causes of Depression ” section of this chapter. For this reason, providers may prescribe antidepressants to help modify an individual’s brain chemistry.
Antidepressants are used to regulate and increase neurotransmitters in the brain to improve mood. There are several classes of antidepressants with different mechanisms of action and potential adverse side effects. Classes of antidepressants, their mechanism of action, and common side effects are outlined in Table 7.4 . [ 2 ] Common side effects are listed in this table by frequency of their occurrence. Some medications can cause QTc prolongation, which refers to delayed cardiac electrical conduction that can lead to dysrhythmias. Tricyclic antidepressants (TCAs) and monoamine oxidase inhibitors (MAOIs) often cause anticholingeric side effects (e.g., tachycardia, urinary retention, constipation, dry mouth, blurred vision, confusion, psychomotor slowing, sedation, and delirium). A specific medication class is typically initiated by the provider based on the individual’s symptoms, potential side effects, cost, and family history of success with certain medications.
Antidepressants
Review neurotransmitter actions and related central nervous system physiology in the “ Psychotropics Medications ” chapter.
Antidepressants may produce some improvement within the first week or two, but full benefits may not be seen for two to three months. If a patient feels little or no improvement after several weeks, the mental health care provider can alter the dose of the medication, add another medication, or substitute another antidepressant. In a similar manner, if a client develops ongoing bothersome side effects, the provider can switch them to a different medication. Nurses should encourage clients to contact their mental health care prescriber if a medication is not working within the expected time frame or if they are experiencing ongoing bothersome side effects. It is typically recommended that clients continue to take medication(s) for six or more months after the symptoms have improved. Long-term maintenance therapy may be suggested to decrease the risk of future episodes for people at high risk for recurrence. [ 3 ]
Black Box Warning
A Black Box Warning is a significant warning from the Food and Drug Administration (FDA) that alerts the public and health care providers to serious side effects, such as injury or death. Black Box Warnings are in place for all classes of antidepressants used with children, adolescents, and young adults due to a higher risk of suicide. All clients receiving antidepressants should be monitored for signs of worsening depression or changing behavior, especially when the medication is started or dosages changed.
Adverse/Side Effects
Nurses must monitor clients receiving antidepressants for side effects and report concerns to the prescribing provider. Clients should be instructed to immediately call their provider if they have any of the following symptoms, especially if they are new or worsening [ 4 ]:
- Thoughts about suicide or dying
- Attempts to commit suicide
- Worsening depression
- Agitation or restlessness
- Panic attacks
- Trouble sleeping (insomnia)
- Irritability
- Aggression, anger, or violence
- Dangerous impulses
- Increased activity and talking (i.e., signs of mania)
- Other unusual changes in behavior or mood
Serotonin Syndrome
High doses of antidepressants or a combination of medications that affect serotonin, such as antidepressants or triptans (used to treat migraine headaches) can cause a medical emergency called serotonin syndrome. The presentation of serotonin syndrome is extremely variable, ranging from mild symptoms to a life-threatening syndrome. It typically develops within 24 hours from the increased dosage or combination of medications and can be fatal.
Symptoms of serotonin syndrome can be classified into three categories [ 5 ],[ 6 ],[ 7 ]:
- Mental status changes: Agitation, restlessness, or delirium
- Autonomic hyperactivity: Tachycardia, hypertension, hyperthermia, diaphoresis, shivering, vomiting, or diarrhea
- Neuromuscular hyperactivity: Tremor, muscle hypertonia or rigidity, myoclonus, hyperreflexia, or clonus (including rapid, horizontal eye movements)
A mnemonic commonly used to remember the symptoms of serotonin syndrome is SHIVERS :
- S: Shivering: A neuromuscular symptom similar to tremors specific to serotonin syndrome
- H: Hyperreflexia (and myoclonus): Hyperactive reflexes most prominent in the lower extremities.
- I: Increased Temperature
- V: Vital Sign Abnormalities: Tachycardia, tachypnea, and labile blood pressure
- E: Encephalopathy: Mental status changes such as agitation, delirium, and confusion
- R: Restlessness
- S: Sweating
People may get slowly worse and can become severely ill if not quickly treated. Untreated, serotonin syndrome can be deadly. With treatment, symptoms usually go away within 24 hours, but permanent kidney damage may result even with treatment. Uncontrolled muscle spasms can cause severe muscle breakdown called rhabdomyolysis. Myoglobin is released into the blood with muscle breakdown and clogs renal filtrations, which can cause severe kidney damage if serotonin syndrome isn’t recognized promptly and treated.
Treatment of serotonin syndrome may include the following [ 8 ],[ 9 ]:
- Stopping all serotonergic medications.
- Providing supportive care to normalize vital signs such as IV fluids, cooling measures, and medications to control heart rate and blood pressure.
- Sedating with benzodiazepines, such as diazepam or lorazepam, to decrease agitation, seizure-like movements, and muscle stiffness.
- If symptoms persist, administering cyproheptadine to block serotonin production.
Serotonin syndrome, in its most severe form, can resemble neuroleptic malignant syndrome (NMS) caused by antipsychotic medications. However, NMS develops over a period of days to weeks.
Hypertensive Crisis
Hypertensive crisis can occur when clients taking monoamine oxidase inhibitors (MAOIs) also take medications containing pseudoephedrine or eat foods containing tyramine (aged foods; fermented foods; cured meats; alcoholic beverages such as beer or red wine; or overripe fruits such as raisins, prunes, or bananas). MAOIs inhibit the breakdown of tyramine, causing elevated tyramine levels in the body that can lead to hypertensive crisis. Hypertensive crisis is a medical emergency defined as severe hypertension (blood pressure over 180/120 mm Hg) with acute end-organ damage such as stroke, myocardial infarction, or acute kidney damage. Symptoms may include a severe headache accompanied with confusion and blurred vision. Tachycardia or bradycardia may be present and associated with constricting chest pain. Other symptoms include neck stiffness or soreness, nausea or vomiting, sweating, dilated pupils, photophobia, shortness of breath, severe anxiety, and unresponsiveness. Seizures may occur, as well as intracranial bleeding in association with the increased blood pressure. Hypertensive crisis is treated in the intensive care unit with intravenous medications that safely and quickly lower the blood pressure. [ 10 ],[ 11 ]
Patient Education Regarding Antidepressants
Clients should be instructed it may take 4 to 6 weeks for antidepressants to achieve their full effectiveness. They should not suddenly stop taking antidepressants or they may experience withdrawal symptoms. When it is time to stop the medication, the provider will slowly and safely decrease the dose. If clients stop taking the medication before the provider advises, the depression may return. They may not feel better with the first antidepressant they try, and they may need to try several different classes of medications to find one that works best for them.
Psychotherapy
Psychotherapy may be used alone for treatment of mild depression or in combination with antidepressant medications for moderate to severe depression. Psychotherapy may involve only the individual, but it can include others such as family members or couples therapy to help address issues within these close relationships. Depending on the severity of the depression, significant improvement can be made in 10 to 15 sessions. Group therapy brings people with similar disorders together in a supportive environment to learn how others cope in similar situations. [ 12 ]
Cognitive Behavioral Therapy
Cognitive behavioral therapy (CBT) is a form of psychotherapy that is effective for a range of problems including depression, anxiety disorders, alcohol and drug use problems, marital conflict, eating disorders, and severe mental illness. CBT helps a person to recognize distorted/negative thinking with the goal of changing thoughts and behaviors to respond to changes in a more positive manner. [ 13 ] Numerous research studies suggest that CBT leads to significant improvement in functioning and quality of life. Studies show that CBT has been demonstrated to be as effective as, or more effective than, other forms of psychological therapy or psychiatric medications. [ 14 ]
CBT is based on these core principles [ 15 ]:
- Psychological problems are based, in part, on faulty or unhelpful ways of thinking.
- Psychological problems are based, in part, on learned patterns of unhelpful behavior.
- People suffering from psychological problems can learn better ways of coping with them, thereby relieving their symptoms and increasing quality of life.
CBT treatment involves efforts to change thinking patterns. These strategies might include the following [ 16 ]:
- Learning to recognize one’s distortions in thinking that are creating problems, and then reevaluating them in light of reality.
- Gaining a better understanding of the behavior and motivation of others.
- Using problem-solving skills to cope with difficult situations.
- Learning to develop a greater sense of confidence in one’s own abilities.
CBT treatment also usually involves efforts to change behavioral patterns. These strategies might include facing one’s fears instead of avoiding them, using role-playing to prepare for potentially problematic interactions with others, and learning to calm one’s mind and relax one’s body.[ 17 ]
CBT aims to help clients develop skills to manage their feelings in healthy ways. Through in-session exercises and “homework” between sessions, clients develop coping skills, whereby they learn ways to change their own thinking and behavior, ultimately changing how they feel. CBT therapists focus on current situations, thought patterns, and behaviors rather than past events. A certain amount of information about one’s history is needed, but the focus is primarily on developing more effective ways of coping with life moving forward. [ 18 ]
Dialectic Behavior Therapy
Dialectical behavior therapy (DBT) is a type of cognitive behavioral therapy that provides clients with new skills to manage painful emotions and decrease conflict in relationships. It has been used successfully to treat people experiencing depression, bulimia, binge-eating, bipolar disorder, post-traumatic stress disorder, borderline personality disorder, and substance abuse. DBT focuses on providing therapeutic skills in four key areas [ 19 ]:
- Mindfulness focuses on improving an individual’s ability to accept and be present in the current moment.
- Distress tolerance is geared toward increasing a person’s tolerance of negative emotion, rather than trying to escape from it.
- Emotion regulation strategies are used to manage and change intense emotions that are causing problems in a person’s life.
- Interpersonal effectiveness techniques allow a person to communicate with others in a way that is assertive, maintains self-respect, and strengthens relationships.
Electroconvulsive Therapy
Electroconvulsive therapy (ECT) is a medical treatment reserved for patients with severe major depression who have not responded to medications, psychotherapy, or other treatments. It involves a brief electrical stimulation of the brain while the patient is under anesthesia. A client typically receives ECT two to three times a week for a total of 6 to 12 treatments. It is usually managed by a team of trained medical professionals, including a psychiatrist, an anesthesiologist, and a nurse. [ 20 ] See Figure 7.8 [ 21 ] for an image showing ECT electrode placement.
Nursing considerations regarding ECT include the following:
- Pre-procedure education
- Securement of informed consent
- Pre-procedure preparation
- Screening tools used pre- and post-ECT to evaluate side effects, including memory loss
- Medication administration
- Post-ECT care, such as monitoring vital signs and for changes in airway, breathing, and circulation, and implementing fall risk precautions post-anesthesia
A client must provide written informed consent before ECT is administered. In situations where a client is too ill to make decisions for themselves, the consent process is governed by state law (for example, a court-appointed guardian). [ 22 ]
Clients and their families should discuss all options for treatment with the psychiatrist before making a specific treatment decision. They should be provided with sufficient information to fully understand the procedure and the potential benefits, risks, and side effects of each treatment option before providing written consent. [ 23 ]
General anesthesia is provided during ECT, so presurgical preparation is provided with typical dietary restrictions before the procedure. Typically, this means no food or water after midnight and only a sip of water with morning medications. An intravenous line is inserted, and electrode pads are placed on the head.
A client typically receives ECT two or three times a week for a total of 6 to 12 treatments, depending on the severity of symptoms and the response to treatment. At the time of each treatment, a patient is given general anesthesia and a muscle relaxant, and electrodes are attached to the scalp at precise locations. The patient’s brain is stimulated with a brief controlled series of electrical pulses. This causes a seizure within the brain that lasts for approximately one minute. The patient is asleep for the procedure and awakens after 5-10 minutes, much as from minor surgery. [ 24 ]
ECT treatment has been associated with some risks such as short-term memory loss and difficulty learning. Some people have trouble remembering events that occurred in the weeks before the treatment or earlier. In most cases, memory problems improve within a couple of months. Some patients may experience longer-lasting problems, including permanent gaps in memory. [ 25 ]
Transcranial Magnetic Stimulation
Transcranial Magnetic Stimulation (TMS) is a noninvasive procedure that uses magnetic fields to stimulate nerve cells in the brain to improve symptoms of depression. TMS is typically used when other depression treatments haven’t been effective. It uses a magnet to activate the brain. Unlike electroconvulsive therapy (ECT), in which electrical stimulation is more generalized, TMS can be targeted to a specific site in the brain. A typical TMS session lasts 30 to 60 minutes and does not require anesthesia. During the procedure, an electromagnetic coil is held against the forehead near an area of the brain that is thought to be involved in mood regulation. Short electromagnetic pulses are administered through the coil. The magnetic pulses easily pass through the skull and cause small electrical currents that stimulate nerve cells in the targeted brain region. The magnetic field is about the same strength as that of a magnetic resonance imaging (MRI) scan. The person generally feels a slight knocking or tapping on the head as the pulses are administered. The muscles of the scalp, jaw, or face may contract or tingle during the procedure, and mild headaches or brief light-headedness may result after the procedure. It is also possible that the procedure could cause a seizure, although this adverse effect is uncommon. Because the treatment is relatively new, long-term side effects are unknown. [ 26 ]
Self-Care and Coping Strategies
Nurses can teach clients many coping strategies to reduce symptoms of depression. For example, regular exercise helps create positive feelings and improves mood. Getting enough quality sleep on a regular basis, eating a healthy diet, and avoiding alcohol (a depressant) can also reduce symptoms of depression. [ 27 ] Read more about coping strategies in the “ Stress, Coping, and Crisis Intervention ” chapter.
7.5. APPLYING THE NURSING PROCESS TO DEPRESSIVE DISORDERS
Assessing a client with a depressive disorder focuses on both verbal and nonverbal assessments. As the registered nurse conducts follow-up assessments, findings are compared to baseline admission assessments.
The role of the nurse in caring for clients with depression is related to primary nursing care, as well as collaboration with interprofessional team members. As a team member, the nurse may collaborate with psychiatrists, psychologists, licensed social workers, and other health care providers. The scope and practice of each team member is clearly defined within their professional licensure.
Psychiatric interview.
The registered nurse uses specific questions during the client’s admission process based on agency policy. It is also important to consider the impact of culture on a client’s perception of their illness. See suggested “ Cultural Formulation Interview Questions ” in the “Application of the Nursing Process in Mental Health Care” chapter.
Mental Status Examination
See Table 7.5a for common findings when assessing a client with a depressive disorder. (See expected findings for these components of a mental status examination in the “ Assessment ” section in Chapter 4.) Critical findings that require immediate notification of the provider are bolded with an asterisk.
Common Findings During Mental Status Examinations for Clients With Depressive Disorders
Psychosocial Assessment
As previously discussed in the “ Application of the Nursing Process in Mental Health Care ” chapter, psychosocial assessment obtains additional subjective data that detects risks and identifies treatment opportunities and resources. Agencies have specific forms used for psychosocial assessment that typically consist of these components [ 1 ],[ 2 ]:
- Cultural assessment
- Reason for seeking health care (i.e., “chief complaint”)
- Thoughts of self-harm or suicide (both current and historical)
- Current and past medical history
- Current medications
- History of previously diagnosed mental health disorders
- Previous hospitalizations
- Educational background
- Occupational background
- Family dynamics
- History of exposure to psychological trauma, violence, and domestic abuse
- Substance use (tobacco, alcohol, recreational drugs, misused prescription drugs)
- Family history of mental illness
- Coping mechanisms
- Functional ability/Activities of daily living
- Spiritual assessment
Screening Tools
Screening tools assess characteristics of specific mental health disorders. The screening tools listed below are examples of screenings, assessments, and question/answer prompts designed to address depressive disorders. These screening tools may be used on admission and at different times throughout the hospital or treatment stay. The findings may be used to compare and contrast client progress within the hospital stay, from a previous admission, or periodically on an outpatient basis. The registered nurse often conducts these tools as a collaborative member of the health care team.
Links to Common Screening Tools for Depressive Disorders
- Columbia-Suicide Severity Rating Scale (C-SSRS) PDF : A rating scale for suicidal ideation and behaviors that rates the degree of risk or intent of harm. It can be a self-assessment or administered by the health care professional.
- Patient Health Questionnaire-9 (PHQ-9) : A quick screening tool with nine criteria for assessing a client’s risk of depression.
- Beck Depression Inventory (BDI) : A 21-item self-assessment questionnaire that determines the severity of depression from none to severe.
- Hamilton Depression Scale (HDRS) PDF : A 17-item questionnaire used to rate the severity of one’s depression.
- Geriatric Depression Scale (GDS) PDF : A self-report of depressive symptoms for older adults; the new version is 15 questions.
- Edinburgh Postnatal Depression Scale (EPDS) : A self-report of ten statements by mothers to screen for postpartum depression.
Laboratory Testing
For patients with depressive symptoms in the absence of general medical symptoms or findings on examination, the utility of screening laboratory tests has not been demonstrated. Commonly performed screening laboratory tests for new onset or severe depression include complete blood count, serum chemistry panels, urinalysis, thyroid stimulating hormone, rapid plasma reagin (RPR) for syphilis, human chorionic gonadotropin (HCG) for pregnancy, and toxicology screening for drugs of abuse. [ 3 ]
Routine laboratory monitoring is performed for some clients based on the medications they are taking, such as the following:
- May be impaired from medications the client is taking
- May be impaired from antidepressants
- Some medications require that drug levels be monitored to assess for toxicity and therapeutic ranges
Read more about laboratory monitoring required for specific medications in the “ Treatments for Depression ” section of this chapter.
Life span considerations.
Life span considerations influence how the client is assessed, as well as the selection of appropriate nursing interventions. Depressive disorders can be found across the life span from the very young to the very old. Read more about specific disorders in the “ Childhood and Adolescence Disorders ” chapter or the “ Vulnerable Populations ” chapter. It is important to individualize all interventions to the age and developmental level of the client. Review developmental stages in the “ Application of the Nursing Process in Mental Health Care ” chapter.
Depression Associated With Dementia
Individuals with dementia are susceptible to depression. Dementia refers to a group of symptoms that lead to a progressive, irreversible decline in mental function severe enough to disrupt daily life caused by a group of conditions including Alzheimer’s disease, vascular dementia, frontal-temporal dementia, and Lewy body disease. Alzheimer’s disease is one of the most common forms of dementia. Alzheimer’s disease causes impaired memory and the ability to learn, reason, make judgments, communicate, and carry out daily activities. An early symptom of Alzheimer’s disease can be subtle memory loss and personality changes that differ from normal age-related memory problems. They seem to tire or become upset or anxious more easily. They do not cope well with change. For example, they can follow familiar routes, but traveling to a new place confuses them, and they can easily become lost. In the early stages of the illness, people with Alzheimer’s disease are particularly susceptible to depression. [ 4 ]
While changes in the brain that cause dementia are permanent and worsen over time, thinking and memory problems can be aggravated by untreated depression. [ 5 ] Nurses should report new symptoms of depression in clients who have been diagnosed with dementia.
Read more about dementia at the Alzheimer’s Association’s webpage.
Reflective questions.
How does the nurse differentiate between depression, delirium, dementia, and psychosis
What are some common underlying medical conditions that could potentially mimic the symptoms of depression or mania in those who are elderly?
What other symptoms might a client who is a child/adolescent display that would indicate the need to assess for disorders other than depression?
Cultural Considerations
Review cultural considerations of care in the “ application of the nursing process in mental health care ” chapter., reflective questions:.
Reflect on how a client’s cultural values, beliefs, or preferences impact presenting symptoms, the nursing care plan, or treatment modalities. Consider the following components:
- Religious/Spiritual beliefs
- Language/Communication
- Nutritional preferences
- Potential drug-food interactions
- Rituals/Customs/Practices
- Gender dysphoria
Mental health disorders are diagnosed by mental health providers using the DSM-5 , similar to how medical conditions are diagnosed by trained medical professionals. Nurses create individualized nursing care plans based on the client’s response to mental health disorders. See common nursing diagnoses related to mental health disorders in the “ Diagnosis ” section of the “Application of the Nursing Process in Mental Health Care” chapter.
Risk for suicide is always evaluated for clients with depressive disorders because suicidal ideation is a symptom of depression. Other common nursing diagnoses and sample expected outcomes for clients with depressive disorders are discussed in the following section in Table 7.5b .
Table 7.5b.
Common Expected Outcomes for Nursing Diagnoses Related to Depressive Disorders [6]
Outcomes Identification
SMART outcomes are identified in relation to the established nursing diagnoses for each client. SMART is an acronym for Specific, Measurable, Attainable/Actionable, Relevant, and Timely.
Read more about outcomes identification in the “ Application of the Nursing Process in Mental Health Care ” chapter.
Planning interventions.
Interventions are planned based on the client’s nursing diagnoses, expected outcomes, and current status. Clients with depressive disorders are monitored closely for risk of suicide, and interventions are planned according to their level of risk. See interventions for clients at risk of suicide in the “ Application of the Nursing Process in Mental Health Care ” chapter.
Implementation
As discussed earlier in this chapter, a combination of pharmacological treatments and psychotherapies are often an effective approach to treating depressive disorders. There are three phases in treatment and recovery from major depression [ 10 ]:
- The active phase (6 to 12 weeks) is directed at reduction of depressive symptoms and restoration of psychosocial and work function. Hospitalization may be required, and medication and other biological treatments may be initiated.
- The continuation phase (4 to 9 months) is directed at prevention of relapse through pharmacotherapy, education, and depression-specific psychotherapy. This phase focuses on maintaining the client as a functional and contributing member of the community after recovery from the acute phase.
- The maintenance phase (1 year or more) is directed at preventing future episodes of depression. Medication may be phased out or continued.
Nurses target interventions based on the client’s current phase of treatment and recovery.
Interventions can be categorized based on the American Psychiatric Nurses Association (APNA) standard for Implementation that includes the Coordination of Care; Health Teaching and Health Promotion; Pharmacological, Biological, and Integrative Therapies; Milieu Therapy; and Therapeutic Relationship and Counseling . Read more about these subcategories in the “ Application of the Nursing Process in Mental Health Care ” chapter. See examples of interventions for each of these categories for clients with depressive disorders in Table 7.5c .
Examples of Nursing Interventions by APNA Subcategories
Nursing interventions are also planned that target common physiological signs of depression and associated self-care deficits. See common interventions for these conditions in Table 7.5d .
Nursing Interventions Targeting Physiological Signs of Depression and Self-Care Deficit [11]
Communication Tips
Some clients with depression are so withdrawn they are unwilling or unable to speak. Sitting with them in silence may feel like a waste of time, but nurses should be aware that providing therapeutic presence can be meaningful in supporting the client with depression. Helpful communication techniques for severely withdrawn clients and their rationale are described in the following box.
Guidelines for Communication With Severely Withdrawn Individuals [ 12 ]
- Rationale: Slowed thinking and difficulty concentrating impair comprehension and require time to formulate a response.
- Rationale: People often experience relief and decreased feelings of isolation when they share thoughts of suicide.
- Rationale: Platitudes minimize the individual’s feelings and can increase feelings of guilt or worthlessness because they cannot “snap out of it.”
- Rationale: When an individual is not ready to talk, direct questions can raise their anxiety levels. Pointing out objects in the environment draws the person into reality.
There are several guidelines for counseling individuals with depression, helping them identify current coping skills, and exploring new adaptive coping strategies:
- Encourage stress management techniques such as exercise, good sleep, and healthy food choices.
- Promote the formation of supportive relationships such as peer support and support groups to reduce social isolation and enable the individual to work on personal goals and relationship needs.
- Provide information about spiritual support as the individual defines it, such as chaplain or pastoral visits or spending time in nature; many people find strength and comfort in spiritual and/or religious activities.
- Help the client reconstruct a healthier and more hopeful attitude about the future (without providing false reassurance). [ 13 ]
Collaborative Mental Health Treatments
Nurses assist in implementing collaborative interventions based on the client’s treatment plan. Review collaborative mental health treatments and common medications used to treat depression in the “ Treatments for Depression ” section of this chapter.
Patient Education Regarding Antidepressant Medications
Nurses educate clients about their medications, including the manner in which they work, common side effects, and issues to report to their provider. Clients taking antidepressants should also be educated regarding the following considerations [ 14 ]:
- When taking antidepressants, it is important to follow the instructions on how much to take. Some people start to feel better a few days after starting the medication, but it can take four to eight weeks to feel the most benefit. Antidepressants work well and are safe for most people, but it is still important to talk with your mental health care provider if you have side effects such as sexual dysfunction, weight gain, dizziness, nausea, palpitations, drowsiness, insomnia, or anxiety. Side effects may go away as your body adjusts to the medication, but in some cases, switching to a different medication may be required.
- Don’t stop taking an antidepressant without first talking to your mental health care provider. Stopping your medicine suddenly can cause symptoms or worsen depression.
- Antidepressants cannot solve all of your problems. Antidepressants work best when combined with psychotherapy and healthy coping strategies. If you notice that your mood is getting worse or if you have thoughts about hurting yourself, it is important to call your provider right away.
- Some people who are depressed may think about hurting themselves or committing suicide (taking their own life). If you are having thoughts about committing suicide‚ please seek immediate help by calling your provider, 911, or 1−800−273−TALK to reach a 24−hour crisis center that provides free‚ confidential help to people in crisis.
- Some antidepressants may cause risks to the baby during pregnancy. Talk with your provider if you are pregnant or might be pregnant or if you are planning to become pregnant.
- For individuals who are very depressed or suicidal, it is important to provide close monitoring when the individual first starts taking an antidepressant medication. Often an individual may have increased energy to make a suicidal attempt when they first begin a medication, whereas previously they may have had suicidal thoughts but lacked the energy to make an attempt.
Supporting Family Members
It is important to support the family members and significant others who are living with an individual with a depressive disorder. Read tips on living with someone with depression in Figure 7.9 . [ 15 ]
Supporting Family Members and Significant Others
Evaluation of the client’s progress towards meeting expected outcomes occurs continuously throughout the treatment phase. Evaluation includes comparing results from screening tools, reviewing laboratory results, and monitoring the effectiveness of prescribed medications, treatments, and nursing interventions. Based on the evaluation findings, the nursing care plan may be modified, or new interventions or outcomes may be added.
7.6. SPOTLIGHT APPLICATION
Patient story: postpartum depression [ 1 ].
Maya is a healthy 32-year-old woman who has been married for over two years and is expecting her first child, a baby boy. She had a history of depression and generalized anxiety disorder.
She had been doing well with a combination of medication and cognitive behavioral therapy (CBT) for many years. Maya had decided in the months leading up to getting pregnant that she wanted to be off medication and worked with her psychiatrist to carefully accomplish this. She continued weekly therapy. She was mostly active, upbeat, and cheerful during her pregnancy. She gave birth to a healthy 7.3-pound baby boy. After the delivery, she started to feel sad, overwhelmed, and consistently tearful. She frequently felt irritable and on edge. This feeling persisted for the first ten weeks after the baby was born. She had limited support—her parents were divorced, and her mother was living in another state. Her in-laws were much older with numerous health complications and couldn’t help regularly.
Maya and her husband went to see her psychiatrist. She was quite tearful and felt she was a “failure as a mom.” Her baby cried incessantly, and she could barely get any sleep. Maya felt utterly incapable of soothing her baby and would get frustrated and tearful. She was so afraid of what she had learned about sudden infant death (SIDS) that she would barely allow herself to sleep. She felt that it was a constant race against the clock—with nursing, pumping, and changing. She was always cleaning bottles and diapers. She felt horrified with how she looked. She had expected to wear pre-pregnancy clothes immediately after childbirth. She hadn’t had a meal in peace or gotten her hair or nails done and couldn’t even think about having sex with her husband. He tried to be supportive, but also felt overwhelmed by it all. He felt she was inconsolable, and they both felt at a loss.
The psychiatrist talked about a variety of tools, including participating in cognitive behavioral therapy, incorporating 15-20 minutes of daily relaxation, practicing mindfulness skills, hiring help, getting her mom to stay with her for a few weeks, and seeking other support. Her husband understood the urgency of the situation and offered to take time off work and to do some of the overnight feedings. Maya decided to restart on her previous antidepressant and also joined a new moms’ support group and continued CBT weekly therapy.
Over the next few months, she was exercising more and getting more sleep and support and had significant improvement in mood and energy. She received some sleep training tips from her pediatrician as well. Maya and her husband shared with her psychiatrist that they were feeling significantly better. They were excited to share that they found a series of self-help parenting books to be particularly helpful and had gotten some helpful tips from others in the moms’ group.
“Wow, it really does take a village to raise a child, doesn’t it?” Maya commented to her psychiatrist. They spoke about how in previous generations new couples could rely on extended family support and how that support often doesn’t exist now. Also, inaccurate beliefs, such as babies are easy and infancy should be a happy time for parents, add to stress, conflict, and guilt. Being able to normalize the stress of adjusting to parenthood was extremely helpful for Maya and her husband.
What educational tips and strategies may have been of benefit to Maya as part of her prenatal care?
How have cultural and societal norms impacted families in relation to child rearing?
What support strategies and education might be offered to birth partners to help them anticipate challenges and recognize early signs of post-partum depression?
7.7. LEARNING ACTIVITIES
VII. GLOSSARY
A type of psychotherapy that helps a person recognize distorted/negative thinking with the goal of changing thought and behaviors to respond to changes in a more positive manner. [ 1 ]
An episode where the person experiences a depressed mood (feeling sad, irritable, empty) or a loss of pleasure or interest in activities for most of the day, nearly every day, for at least two weeks. Several other symptoms are also present, which may include poor concentration, feelings of excessive guilt or low self-worth, hopelessness about the future, thoughts about dying or suicide, disrupted sleep, changes in appetite or weight, and feeling especially tired or low in energy.
A medical treatment reserved for patients with severe major depression who have not responded to medications, psychotherapy, or other treatments. It involves a brief electrical stimulation of the brain while the patient is under anesthesia.
A type of psychotherapy that brings people with similar disorders together in a supportive environment to learn how others cope in similar situations. [ 2 ]
An acute rise and significantly elevated blood pressure, typically over 180/120 mm Hg, that causes acute end-organ damage such as stroke, myocardial infarction, or acute kidney damage. It can be caused by MAOIs, a class of antidepressants.
Therapy for seasonal affective disorder (SAD) that involves sitting in front of a light therapy box that emits a very bright light. It usually requires 20 minutes or more per day, typically first thing in the morning during the winter months. Most people see some improvements from light therapy within one or two weeks of beginning treatment.
Depressive disorder that occurs during pregnancy.
Feelings of extreme sadness, anxiety, and exhaustion that may make it difficult for mothers of newborns to complete daily care activities for themselves and/or for their babies. Severe postpartum depression can lead to postpartum psychosis.
Severe postpartum depression can cause delusions (thoughts or beliefs that are not true), hallucinations (seeing, hearing, or smelling things that are not there), mania (a high, elated mood that often seems out of touch with reality), paranoia, and confusion. Women who have postpartum psychosis are at risk for harming themselves or their child and should receive help as soon as possible by calling 911 or taking the mother to the emergency room.
A type of depression causing symptoms during the fall and winter months when there is less sunlight and usually improves with the arrival of spring. SAD is more than just “winter blues.” The symptoms can be distressing and overwhelming and can interfere with daily functioning. [ 3 ]
A medical emergency that can occur in clients taking medications that affect serotonin levels.
A noninvasive procedure that uses magnetic fields to stimulate nerve cells in the brain to improve symptoms of depression when other depression treatments haven’t been effective.
Licensed under a Creative Commons Attribution 4.0 International License. To view a copy of this license, visit https://creativecommons.org/licenses/by/4.0/ .
- Cite this Page Open Resources for Nursing (Open RN); Ernstmeyer K, Christman E, editors. Nursing: Mental Health and Community Concepts [Internet]. Eau Claire (WI): Chippewa Valley Technical College; 2022. Chapter 7 Depressive Disorders.
- PDF version of this title (53M)
In this Page
- INTRODUCTION
- CAUSES OF DEPRESSION
- TYPES OF DEPRESSION
- TREATMENTS FOR DEPRESSION
- APPLYING THE NURSING PROCESS TO DEPRESSIVE DISORDERS
- SPOTLIGHT APPLICATION
- LEARNING ACTIVITIES
Other titles in this collection
- Open RN OER Textbooks
Related Items in Bookshelf
- All Textbooks
Bulk Download
- Bulk download content from FTP
Recent Activity
- Chapter 7 Depressive Disorders - Nursing: Mental Health and Community Concepts Chapter 7 Depressive Disorders - Nursing: Mental Health and Community Concepts
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

COMMENTS
Study with Quizlet and memorize flashcards containing terms like Etiology, Biological Dimension, Role of Heredity and more. ... Depression tends to run in families and the same type of depressive disorder is often found among members of the same family. Studies of twins suggest that there is a higher concordance rate.
Biological explanations for MDD. Caspi et al and Kendler. Caspi et al (2003) Background information: - It is predicted that individuals' responses to stressful life events are dependent on genetic makeup. - The 5HTT gene has been suspected to be related to depression. - 5HTT is related to the reuptake of serotonin in the brain synapses.
Recent research on the etiology and genetics of major psychological disorders is revealing that there may be. Genetic Overlap. Study with Quizlet and memorize flashcards containing terms like Which statement best describes the medical model?, Etiology refers to, Bruno believes he is the king of Mesopotamia and demands complete obedience.
Another review by Danzer et al. suggests links between the inflammation-induced activation of indolamine 2,3-dioxegenase ... The etiology of depression is multifactorial, and it is worthwhile to examine the interaction between multiple factors, such as epigenetic, genetic, and environmental factors, in order to truly understand this mental ...
In addition to contributing to the etiology of depression, activation of proinflammatory signaling pathways occurs as a result of elevated OS. 140 Evidence suggests that MDD is associated with the ...
The purpose of this chapter is to review what is known or suspected about the causes of depression. Fundamentally, such depressive symptoms as sad mood, pessimism, and lethargy, are universal human experiences and are considered normal reactions to the struggles, disappointments, and losses of everyday life. However, for some individuals, the intensity and persistence of depressive symptoms ...
Depression (also called major depression, major depressive disorder, or clinical depression) is different. It can cause severe symptoms that affect how a person feels, thinks, and handles daily activities, such as sleeping, eating, or working. Depression can affect anyone regardless of age, gender, race or ethnicity, income, culture, or education.
Major depression is a common disorder, accounting for more disability than any other disorder worldwide. The rates of major depression in the United States rose markedly in the decade from 1991 to 2001, from 3.33% to 7.06%.1 This increase is of considerable consequence, because depression is associated with significant morbidity, disability, increased medical comorbidities, and mortality.2 It ...
Major depression is a common and potentially lethal condition. Early data suggest that the population-level burden of depression has been exacerbated by the COVID-19 pandemic. Prepandemic estimates of depression prevalence are required to quantify and comprehensively address the pandemic's impact on mental health in the U.S.
Depression also causes changes in the network of brain areas involved in processing physical pain, and the degree of hyperactivity in such areas as seen on brain scans correlates with the severity ...
Study with Quizlet and memorize flashcards containing terms like DSM, Editions of DSM, The Medical Model and more. ... Etiology of Depression: Genetic Factors ... Some studies suggest that BPII is more common in females than males. Course of Bipolar II Disorder. Average age of onset is mid-20s. Most often begins with MDE and is not recognized ...
Depression and anxiety have been identified as major causes of work absence due to sickness and long-term disability. Problem solving, stress reduction and cognitive behavioral therapeutic ...
By Grant H. Brenner. Over the years, the serotonin hypothesis of depression, which suggests that low or impaired serotonin neurotransmission is related to the symptoms and possible causes of ...
Major depression (MD) is a multifactorial disorder with a wide range of biological, psychological, and social risk factors. 1 It is a common psychiatric disorder and a leading cause of disability worldwide. 2 MD is characterized by persistent feelings of sadness and loss of interest or pleasure (anhedonia) for at least 2 weeks and is accompanied by additional symptoms such as changes in ...
the possible causes (of the depression) Etiologies of MDD. 9 groups of symptoms. - depressed mood. - diminished interest in daily activities. - significant weight change (loss or gain) 5% of body mass in one month. - insomnia or hypersomnia. - psychomotor agiation or retardation (slow or fast movement) - fatigue.
Depressive disorder (also known as depression) is a common mental disorder. It involves a depressed mood or loss of pleasure or interest in activities for long periods of time. Depression is different from regular mood changes and feelings about everyday life. It can affect all aspects of life, including relationships with family, friends and ...
Research suggests that the prevalence of children with major depressive disorder in Western cultures ranges from 1.9% to 3.4% among primary school children. ... Results such as these have led to the hypothesis that the biological causes of depression may in part be neurodevelopmental, with its biological underpinnings forming early on in brain ...
Psychology: Chapter 13. What is the medical model applied to abnormal behavior? It proposes that it is useful to think of abnormal behavior as a disease. It uses the terms mental illness, psychopathology, and psychological disorder. Some have critiqued the model- saying minds couldn't be sick.
The most common causes of depression are summarized in Fig. 1. ... and scientists and recent research in epigenetics suggest that these genes have a significant role in many diseases, such as cancer, autism, schizophrenia, obesity, diabetes, mental retardation, some neurological disorders, and even societal behavior, such as addiction: ...
Perhaps the most well-known cognitive theory of depression was developed in the 1960s by psychiatrist Aaron Beck, based on clinical observations and supported by research (Beck, 2008). Beck theorized that depression-prone people possess depressive schemas, or mental predispositions to think about most things in a negative way (Beck, 1976).
Decades of research show that genes play an vital role in the etiology of attention deficit hyperactivity disorder (ADHD) and its comorbidity with other disorders. Family, twin, and adoption ...
Child maltreatment, for example, is one of the most potent environmental stressors in the etiology and course of depression and other types of psychopathology. Extant studies suggest that childhood maltreatment at least doubles the risk for internalizing problems, including depression. 18,20,21,79,80
Depression is a common illness affecting an estimated 8% of adults in the United States annually. [ 1] Approximately 280 million people in the world have depression. [ 2 ] This chapter will discuss causes and types of depression, treatments for depression, and steps for applying the nursing process when caring for clients with depressive disorders.