We have a new app!
Take the Access library with you wherever you go—easy access to books, videos, images, podcasts, personalized features, and more.
Download the Access App here: iOS and Android . Learn more here!
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs


Chapter 5: 10 Real Cases on Acute Heart Failure Syndrome: Diagnosis, Management, and Follow-Up
Swathi Roy; Gayathri Kamalakkannan
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Case review, case discussion.
- Full Chapter
- Supplementary Content
Case 1: Diagnosis and Management of New-Onset Heart Failure With Reduced Ejection Fraction
A 54-year-old woman presented to the telemetry floor with shortness of breath (SOB) for 4 months that progressed to an extent that she was unable to perform daily activities. She also used 3 pillows to sleep and often woke up from sleep due to difficulty catching her breath. Her medical history included hypertension, dyslipidemia, diabetes mellitus, and history of triple bypass surgery 4 years ago. Her current home medications included aspirin, atorvastatin, amlodipine, and metformin. No significant social or family history was noted. Her vital signs were stable. Physical examination showed bilateral diffuse crackles in lungs, elevated jugular venous pressure, and 2+ pitting lower extremity edema. ECG showed normal sinus rhythm with left ventricular hypertrophy. Chest x-ray showed vascular congestion. Laboratory results showed a pro-B-type natriuretic peptide (pro-BNP) level of 874 pg/mL and troponin level of 0.22 ng/mL. Thyroid panel was normal. An echocardiogram demonstrated systolic dysfunction, mild mitral regurgitation, a dilated left atrium, and an ejection fraction (EF) of 33%. How would you manage this case?
In this case, a patient with known history of coronary artery disease presented with worsening of shortness of breath with lower extremity edema and jugular venous distension along with crackles in the lung. The sign and symptoms along with labs and imaging findings point to diagnosis of heart failure with reduced EF (HFrEF). She should be treated with diuretics and guideline-directed medical therapy for congestive heart failure (CHF). Telemetry monitoring for arrythmia should be performed, especially with structural heart disease. Electrolyte and urine output monitoring should be continued.
In the initial evaluation of patients who present with signs and symptoms of heart failure, pro-BNP level measurement may be used as both a diagnostic and prognostic tool. Based on left ventricular EF (LVEF), heart failure is classified into heart failure with preserved EF (HFpEF) if LVEF is >50%, HFrEF if LVEF is <40%, and heart failure with mid-range EF (HFmEF) if LVEF is 40% to 50%. All patients with symptomatic heart failure should be started on an angiotensin-converting enzyme (ACE) inhibitor (or angiotensin receptor blocker if ACE inhibitor is not tolerated) and β-blocker, as appropriate. In addition, in patients with New York Heart Association functional classes II through IV, an aldosterone antagonist should be prescribed. In African American patients, hydralazine and nitrates should be added. Recent recommendations also recommend starting an angiotensin receptor-neprilysin inhibitor (ARNI) in patients who are symptomatic on ACE inhibitors.
Sign in or create a free Access profile below to access even more exclusive content.
With an Access profile, you can save and manage favorites from your personal dashboard, complete case quizzes, review Q&A, and take these feature on the go with our Access app.
Pop-up div Successfully Displayed
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait
We have a new app!
Take the Access library with you wherever you go—easy access to books, videos, images, podcasts, personalized features, and more.
Download the Access App here: iOS and Android . Learn more here!
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs

Chapter 4: 10 Real Cases on Valvular Heart Disease: Diagnosis, Management, and Follow-Up
Nikhitha Mantri; Puvanalingam Ayyadurai; Marin Nicu
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Case review, case discussion.
- Clinical Symptoms
- Full Chapter
- Supplementary Content
Case 1: Management of Patent Foramen Ovale
A 26-year-old woman presented to the emergency department (ED) with chest pain for 1 day. The chest pain started suddenly, was nonradiating, and was associated with arm movement. She did house cleaning 1 day prior to presentation. The pain was not relieved by taking over-the-counter medication. She denied palpitations, dizziness, shortness of breath, and trauma. Her family history and social history were unremarkable. On presentation to the ED, her vital signs were stable. On physical examination, she did not have any significant findings except chest wall tenderness. Her ECG showed first-degree atrioventricular block. Initial laboratory findings were unremarkable. She was given analgesics. The patient was transferred to the telemetry floor, where an echocardiogram was performed, which showed a normal left ventricular ejection fraction with no wall motion or valvular abnormality and a small patent foramen ovale (PFO). How would you manage this case?
This patient is a young asymptomatic woman who presented with musculoskeletal chest pain. Incidentally, she was noted to have a PFO, which is asymptomatic and does not require any treatment.
PFO is an opening in the atrial wall at the location of the fossa ovalis that remains open beyond 1 year of life. After birth, when the pulmonary circulation develops, the foramen ovale closes due to the increase in left atrial pressures, which takes up to 1 year.
PFO is usually asymptomatic and is often found incidentally. However, it carries a risk of paradoxical embolism in high-risk patients. Some patients present with systemic embolism causing organ infarcts and even myocardial infarction.
The diagnostic test of choice is echocardiography. PFO can be detected using color flow Doppler, contrast echocardiography, and transmitral Doppler.
Isolated PFO does not usually require any treatment unless it is associated with an unexplained neurologic event. Such conditions are treated with antiplatelet drugs and anticoagulation therapy. Percutaneous closure of the PFO is an option when there is contraindication to medical management and anticoagulant treatment, in the setting of paradoxical embolism or cryptogenic stroke. Surgical closure is indicated when the opening is >25 mm or when there is failure of a percutaneous device.
PFO is usually asymptomatic and is often found incidentally.
Isolated PFO does not usually require any treatment unless it is associated with an unexplained neurologic event.
Case 2: Management of Aortic Stenosis
Sign in or create a free Access profile below to access even more exclusive content.
With an Access profile, you can save and manage favorites from your personal dashboard, complete case quizzes, review Q&A, and take these feature on the go with our Access app.
Pop-up div Successfully Displayed
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Heart-Healthy Living
- High Blood Pressure
- Sickle Cell Disease
- Sleep Apnea
- Information & Resources on COVID-19
- The Heart Truth®
- Learn More Breathe Better®
- Blood Diseases and Disorders Education Program
- Publications and Resources
- Blood Disorders and Blood Safety
- Sleep Science and Sleep Disorders
- Lung Diseases
- Health Disparities and Inequities
- Heart and Vascular Diseases
- Precision Medicine Activities
- Obesity, Nutrition, and Physical Activity
- Population and Epidemiology Studies
- Women’s Health
- Research Topics
- Clinical Trials
- All Science A-Z
- Grants and Training Home
- Policies and Guidelines
- Funding Opportunities and Contacts
- Training and Career Development
- Email Alerts
- NHLBI in the Press
- Research Features
- Past Events
- Upcoming Events
- Mission and Strategic Vision
- Divisions, Offices and Centers
- Advisory Committees
- Budget and Legislative Information
- Jobs and Working at the NHLBI
- Contact and FAQs
- NIH Sleep Research Plan
- < Back To Research Topics
Coronary Heart Disease Research
Language switcher.
For almost 75 years, the NHLBI has been at the forefront of improving the nation’s health and reducing the burden of heart and vascular diseases . Heart disease, including coronary heart disease, remains the leading cause of death in the United States. However, the rate of heart disease deaths has declined by 70% over the past 50 years, thanks in part to NHLBI-funded research. Many current studies funded by the NHLBI focus on discovering genetic associations and finding new ways to prevent and treat the onset of coronary heart disease and associated medical conditions.
NHLBI research that really made a difference
The NHLBI supports a wide range of long-term studies to understand the risk factors of coronary heart disease. These ongoing studies, among others, have led to many discoveries that have increased our understanding of the causes of cardiovascular disease among different populations, helping to shape evidence-based clinical practice guidelines.
- Risk factors that can be changed: The NHLBI Framingham Heart Study (FHS) revealed that cardiovascular disease is caused by modifiable risk factors such as smoking, high blood pressure , obesity , high cholesterol levels, and physical inactivity. It is why, in routine physicals, healthcare providers check for high blood pressure, high cholesterol, unhealthy eating patterns, smoking, physical inactivity, and unhealthy weight. The FHS found that cigarette smoking increases the risk of heart disease. Researchers also showed that cardiovascular disease can affect people differently depending on sex or race, underscoring the need to address health disparities.
- Risk factors for Hispanic/Latino adults: The Hispanic Community Health Study/Study of Latinos (HCHS/SOL) found that heart disease risk factors are widespread among Hispanic/Latino adults in the United States , with 80% of men and 71% of women having at least one risk factor. Researchers also used HCHS/SOL genetic data to explore genes linked with central adiposity (the tendency to have excess body fat around the waist) in Hispanic/Latino adults. Before this study, genes linked with central adiposity, a risk factor for coronary heart disease, had been identified in people of European ancestry. These results showed that those genes also predict central adiposity for Hispanic/Latino communities. Some of the genes identified were more common among people with Mexican or Central/South American ancestry, while others were more common among people of Caribbean ancestry.
- Risk factors for African Americans: The Jackson Heart Study (JHS) began in 1997 and includes more than 5,300 African American men and women in Jackson, Mississippi. It has studied genetic and environmental factors that raise the risk of heart problems, especially high blood pressure, coronary heart disease, heart failure , stroke , and peripheral artery disease (PAD) . Researchers discovered a gene variant in African American individuals that doubles the risk of heart disease. They also found that even small spikes in blood pressure can lead to a higher risk of death. A community engagement component of the JHS is putting 20 years of the study’s findings into action by turning traditional gathering places, such as barbershops and churches, into health information hubs.
- Risk factors for American Indians: The NHLBI actively supports the Strong Heart Study , a long-term study that began in 1988 to examine cardiovascular disease and its risk factors among American Indian men and women. The Strong Heart Study is one of the largest epidemiological studies of American Indian people ever undertaken. It involves a partnership with 12 Tribal Nations and has followed more than 8,000 participants, many of whom live in low-income rural areas of Arizona, Oklahoma, and the Dakotas. Cardiovascular disease remains the leading cause of death for American Indian people. Yet the prevalence and severity of cardiovascular disease among American Indian people has been challenging to study because of the small sizes of the communities, as well as the relatively young age, cultural diversity, and wide geographic distribution of the population. In 2019, the NHLBI renewed its commitment to the Strong Heart Study with a new study phase that includes more funding for community-driven pilot projects and a continued emphasis on training and development. Read more about the goals and key findings of the Strong Heart Study.
Current research funded by the NHLBI
Within our Division of Cardiovascular Sciences , the Atherothrombosis and Coronary Artery Disease Branch of its Adult and Pediatric Cardiac Research Program and the Center for Translation Research and Implementation Science oversee much of our funded research on coronary heart disease.
Research funding
Find funding opportunities and program contacts for research on coronary heart disease.
Current research on preventing coronary heart disease
- Blood cholesterol and coronary heart disease: The NHLBI supports new research into lowering the risk of coronary heart disease by reducing levels of cholesterol in the blood. High levels of blood cholesterol, especially a type called low-density lipoprotein (LDL) cholesterol, raise the risk of coronary heart disease. However, even with medicine that lowers LDL cholesterol, there is still a risk of coronary heart disease due to other proteins, called triglyceride-rich ApoB-containing lipoproteins (ApoBCLs), that circulate in the blood. Researchers are working to find innovative ways to reduce the levels of ApoBCLs, which may help prevent coronary heart disease and other cardiovascular conditions.
- Pregnancy, preeclampsia, and coronary heart disease risk: NHLBI-supported researchers are investigating the link between developing preeclampsia during pregnancy and an increased risk for heart disease over the lifespan . This project uses “omics” data – such as genomics, proteomics, and other research areas – from three different cohorts of women to define and assess preeclampsia biomarkers associated with cardiovascular health outcomes. Researchers have determined that high blood pressure during pregnancy and low birth weight are predictors of atherosclerotic cardiovascular disease in women . Ultimately, these findings can inform new preventive strategies to lower the risk of coronary heart disease.
- Community-level efforts to lower heart disease risk among African American people: The NHLBI is funding initiatives to partner with churches in order to engage with African American communities and lower disparities in heart health . Studies have found that church-led interventions reduce risk factors for coronary heart disease and other cardiovascular conditions. NHLBI-supported researchers assessed data from more than 17,000 participants across multiple studies and determined that these community-based approaches are effective in lowering heart disease risk factors .
Find more NHLBI-funded studies on preventing coronary heart disease on the NIH RePORTER.

Learn about the impact of COVID-19 on your risk of coronary heart disease.
Current research on understanding the causes of coronary heart disease
- Pregnancy and long-term heart disease: NHLBI researchers are continuing the Nulliparous Pregnancy Outcomes Study: Monitoring Mothers-to-be (nuMoM2b) study to understand the relationship between pregnancy-related problems, such as gestational hypertension, and heart problems. The study also looks at how problems during pregnancy may increase risk factors for heart disease later in life. NuMoM2b launched in 2010, and long-term studies are ongoing, with the goal of collecting high-quality data and understanding how heart disease develops in women after pregnancy.
- How coronary artery disease affects heart attack risk: NHLBI-funded researchers are investigating why some people with coronary artery disease are more at risk for heart attacks than others. Researchers have found that people with coronary artery disease who have high-risk coronary plaques are more likely to have serious cardiac events, including heart attacks. However, we do not know why some people develop high-risk coronary plaques and others do not. Researchers hope that this study will help providers better identify which people are most at risk of heart attacks before they occur.
- Genetics of coronary heart disease: The NHLBI supports studies to identify genetic variants associated with coronary heart disease . Researchers are investigating how genes affect important molecular cascades involved in the development of coronary heart disease . This deeper understanding of the underlying causes for plaque buildup and damage to the blood vessels can inform prevention strategies and help healthcare providers develop personalized treatment for people with coronary heart disease caused by specific genetic mutations.
Find more NHLBI-funded studies on understanding the causes of coronary heart disease on the NIH RePORTER.

Recent findings suggest that cholesterol-lowering treatment can lower the risk of heart disease complications in people with HIV.
Current research on treatments for coronary heart disease
- Insight into new molecular targets for treatment: NHLBI-supported researchers are investigating the role of high-density lipoprotein (HDL) cholesterol in coronary heart disease and other medical conditions . Understanding how the molecular pathways of cholesterol affect the disease mechanism for atherosclerosis and plaque buildup in the blood vessels of the heart can lead to new therapeutic approaches for the treatment of coronary heart disease. Researchers have found evidence that treatments that boost HDL function can lower systemic inflammation and slow down plaque buildup . This mechanism could be targeted to develop a new treatment approach for coronary heart disease.
- Long-term studies of treatment effectiveness: The NHLBI is supporting the International Study of Comparative Health Effectiveness with Medical and Invasive Approaches (ISCHEMIA) trial EXTENDed Follow-up (EXTEND) , which compares the long-term outcomes of an initial invasive versus conservative strategy for more than 5,000 surviving participants of the original ISCHEMIA trial. Researchers have found no difference in mortality outcomes between invasive and conservative management strategies for patients with chronic coronary heart disease after more than 3 years. They will continue to follow up with participants for up to 10 years. Researchers are also assessing the impact of nonfatal events on long-term heart disease and mortality. A more accurate heart disease risk score will be constructed to help healthcare providers deliver more precise care for their patients.
- Evaluating a new therapy for protecting new mothers: The NHLBI is supporting the Randomized Evaluation of Bromocriptine In Myocardial Recovery Therapy for Peripartum Cardiomyopathy (REBIRTH) , for determining the role of bromocriptine as a treatment for peripartum cardiomyopathy (PPCM). Previous research suggests that prolactin, a hormone that stimulates the production of milk for breastfeeding, may contribute to the development of cardiomyopathy late in pregnancy or the first several months postpartum. Bromocriptine, once commonly used in the United States to stop milk production, has shown promising results in studies conducted in South Africa and Germany. Researchers will enroll approximately 200 women across North America who have been diagnosed with PPCM and assess their heart function after 6 months.
- Impact of mental health on response to treatment: NHLBI-supported researchers are investigating how mental health conditions can affect treatment effectiveness for people with coronary heart disease. Studies show that depression is linked to a higher risk for negative outcomes from coronary heart disease. Researchers found that having depression is associated with poor adherence to medical treatment for coronary heart disease . This means that people with depression are less likely to follow through with their heart disease treatment plans, possibly contributing to their chances of experiencing worse outcomes. Researchers are also studying new ways to treat depression in patients with coronary heart disease .
Find more NHLBI-funded studies on treating coronary heart disease on the NIH RePORTER.

Researchers have found no clear difference in patient survival or heart attack risk between managing heart disease through medication and lifestyle changes compared with invasive procedures.
Coronary heart disease research labs at the NHLBI
- Laboratory of Cardiac Physiology
- Laboratory of Cardiovascular Biology
- Minority Health and Health Disparities Population Laboratory
- Social Determinants of Obesity and Cardiovascular Risk Laboratory
- Laboratory for Cardiovascular Epidemiology and Genomics
- Laboratory for Hemostasis and Platelet Biology
Related coronary heart disease programs
- In 2002, the NHLBI launched The Heart Truth® , the first federally sponsored national health education program designed to raise awareness about heart disease as the leading cause of death in women. The NHLBI and The Heart Truth® supported the creation of the Red Dress® as the national symbol for awareness about women and heart disease, and also coordinate National Wear Red Day ® and American Heart Month each February.
- The Biologic Specimen and Data Repository Information Coordinating Center (BioLINCC) facilitates access to and maximizes the scientific value of NHLBI biospecimen and data collections. A main goal is to promote the use of these scientific resources by the broader research community. BioLINCC serves to coordinate searches across data and biospecimen collections and provide an electronic means for requesting additional information and submitting requests for collections. Researchers wanting to submit biospecimen collections to the NHLBI Biorepository to share with qualified investigators may also use the website to initiate the application process.
- Our Trans-Omics for Precision Medicine (TOPMed) Program studies the ways genetic information, along with information about health status, lifestyle, and the environment, can be used to predict the best ways to prevent and treat heart, lung, blood, and sleep disorders. TOPMed specifically supports NHLBI’s Precision Medicine Activities.
- NHLBI population and epidemiology studies in different groups of people, including the Atherosclerosis Risk in Communities (ARIC) Study , the Multi-Ethnic Study of Atherosclerosis (MESA) , and the Cardiovascular Health Study (CHS) , have made major contributions to understanding the causes and prevention of heart and vascular diseases, including coronary heart disease.
- The Cardiothoracic Surgical Trials Network (CTSN) is an international clinical research enterprise that studies heart valve disease , arrhythmias , heart failure, coronary heart disease, and surgical complications. The trials span all phases of development, from early translation to completion, and have more than 14,000 participants. The trials include six completed randomized clinical trials, three large observational studies, and many other smaller studies.

Learn how heart disease may be different for women than for men.
Explore more NHLBI research on coronary heart disease
The sections above provide you with the highlights of NHLBI-supported research on coronary heart disease. You can explore the full list of NHLBI-funded studies on the NIH RePORTER .
To find more studies:
- Type your search words into the Quick Search box and press enter.
- Check Active Projects if you want current research.
- Select the Agencies arrow, then the NIH arrow, then check NHLBI .
If you want to sort the projects by budget size — from the biggest to the smallest — click on the FY Total Cost by IC column heading.
- Case report
- Open access
- Published: 09 February 2021
Clinical judgement in chest pain: a case report
- Mishita Goel ORCID: orcid.org/0000-0003-1540-2910 1 ,
- Shubhkarman Dhillon 1 ,
- Sarwan Kumar 1 &
- Vesna Tegeltija 1
Journal of Medical Case Reports volume 15 , Article number: 49 ( 2021 ) Cite this article
3880 Accesses
2 Altmetric
Metrics details
Cardiac stress testing is a validated diagnostic tool to assess symptomatic patients with intermediate pretest probability of coronary artery disease (CAD). However, in some cases, the cardiac stress test may provide inconclusive results and the decision for further workup typically depends on the clinical judgement of the physician. These decisions can greatly affect patient outcomes.
Case presentation
We present an interesting case of a 54-year-old Caucasian male with history of tobacco use and gastroesophageal reflux disease (GERD) who presented with atypical chest pain. He had an asymptomatic electrocardiogram (EKG) stress test with intermediate probability of ischemia. Further workup with coronary computed tomography angiography (CCTA) and cardiac catheterization revealed multivessel CAD requiring a bypass surgery. In this case, the patient only had a history of tobacco use but no other significant comorbidities. He was clinically stable during his hospital stay and his testing was anticipated to be negative. However to complete workup, cardiology recommended anatomical testing with CCTA given the indeterminate EKG stress test results but the results of significant stenosis were surprising with the patient eventually requiring coronary artery bypass grafting (CABG).
As a result of the availability of multiple noninvasive diagnostic tests with almost similar sensitivities for CAD, physicians often face this dilemma of choosing the right test for optimal evaluation of chest pain in patients with intermediate pretest probability of CAD. Optimal test selection requires an individualized patient approach. Our experience with this case emphasizes the role of history taking, clinical judgement, and the risk/benefit ratio in deciding further workup when faced with inconclusive stress test results. Physicians should have a lower threshold for further workup of patients with inconclusive or even negative stress test results because of the diagnostic limitations of the test. Instead, utilizing a different, anatomical test may be more valuable. Specifically, the case established the usefulness of CCTA in cases such as this where other CAD diagnostic testing is indeterminate.
Peer Review reports
Heart disease is one of the most commonly encountered medical conditions in the world. Individuals seeking medical help because of chest pain frequently require further testing for heart disease. Cardiac stress testing is a validated diagnostic tool commonly used to assess symptomatic patients with intermediate pretest probability of coronary artery disease (CAD). Baseline electrocardiogram (EKG) findings and ability to exercise are important factors to determine the most appropriate cardiac stress test. Exercise EKG stress test is preferred in patients who have normal baseline EKGs and are able to exercise. Patients found to have positive test results with chest pain usually undergo cardiac catheterization, while those with negative test results are usually considered to have non-cardiac chest pain. In some cases, the cardiac stress test may provide inconclusive results. The decision for further workup typically depends on the clinical judgement of the physician and the results may greatly affect patient outcomes. We present an interesting case of a healthy man who presented with chest pain and had an inconclusive EKG stress test, but further workup was performed and revealed multivessel CAD requiring a bypass surgery.
A 54-year-old, overweight (BMI 29), Caucasian man with a history of tobacco smoking and gastroesophageal reflux presented to the emergency department with chest pain. He described it as sudden in onset, while he was working on his laptop. Location was substernal, radiating to his left arm and jaw. Initially, the pain was 7/10 in intensity but it improved spontaneously even before he reached the hospital or received any medications. On further probing, he reported that he had experienced intermittent episodes of chest pain for the last 3 weeks but it was mostly exertional and was relieved with rest. The pain was not associated with shortness of breath, diaphoresis, or nausea/vomiting. He denied any fever, chills, cough, abdominal pain, urinary or bowel complaints. He did not have any family history of significant cardiac events.
On presentation, the patient was hemodynamically stable with a blood pressure of 139/85 mmHg and heart rate of 81 beats per minute. His EKG did not show any ischemic changes, no left ventricular hypertrophy, or left bundle branch block. Three sets of serial troponin enzyme were less than 0.010. Lipid panel showed total cholesterol of 235, triglycerides 408, HDL 26, and LDL could not be calculated. His pretest probability of CAD was intermediate on the basis of age and sex. Since the patient was chest pain free since admission and was able to exercise, an exercise treadmill EKG stress test was ordered. The patient achieved 95% of maximum predicted heart rate and 10 METs of exercise with normalization of slight T wave inversions that were seen in leads V2, V3, and V4 at rest. Thus, it was read as maximum asymptomatic stress test with intermediate probability of ischemia. Echocardiogram was obtained which showed normal left ventricular function and no significant valvular or wall motion abnormalities. At this point, cardiology was consulted to evaluate the patient and they recommended coronary computed tomography angiography (CCTA) for further risk stratification.
Diagnosis and management
CCTA results showed approximate 70% stenosis of the origin of the left anterior descending artery (LAD) secondary to noncalcified plaque extending over a length of approximately 4 mm (Fig. 1 ), approximate 40–50% stenosis of the proximal ramus intermedius branch secondary to mixed calcified and noncalcified plaque and scattered calcified and noncalcified plaque along the circumflex and obtuse marginal branches with 30–40% luminal diameter stenosis. Fractional flow reserve–computed tomography (FFR-CT) revealed a high likelihood of flow-limiting stenosis with a value of less than 0.5 secondary to the significant stenosis at the origin of the LAD and a low likelihood of flow-limiting stenosis in the left circumflex, ramus intermedius, and right coronary arteries.
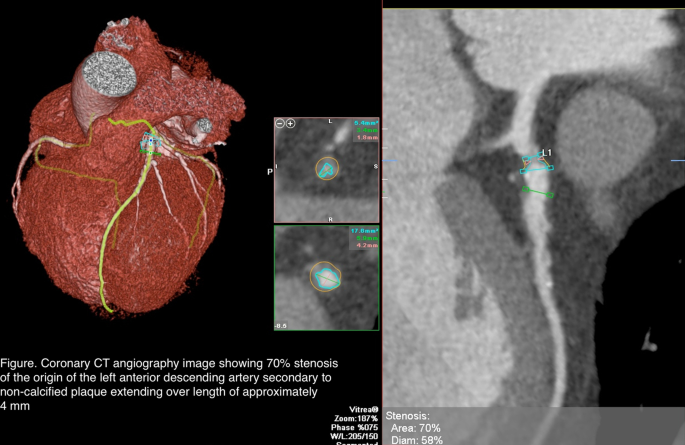
Coronary computed tomography angiography image showing 70% stenosis of the origin of the left anterior descending artery to secondary to non-calcified plaque extending over a length of approximately 4 mm
The patient was then taken for cardiac catheterization which showed a 95% stenotic lesion of LAD with partial perfusion (TIMI grade 2 flow) giving rise to diagonal 1, which has an ostial and proximal 70% stenosis; ramus intermedius with proximal 70% segmental stenosis; circumflex, nondominant vessel, which has mild disease in proximal distal segments, giving rise to obtuse marginal 1, which has proximal 70% stenosis. Cardiothoracic surgery was consulted and the patient underwent bypass graft surgery.
Outcome and follow-up
The patient did well after the surgery. He stayed in the hospital for 4 days post-op without any complaints and was discharged home in stable condition. A referral to home care was made to provide for monitoring of the patient's progress and detection of any complications during the immediate post-op period. Cardiac rehabilitation referral was also provided and the patient was instructed to follow up with a cardiologist and cardiothoracic surgeon.
Cardiac stress testing is usually performed for diagnosis of CAD in patients with intermediate pretest probability of CAD. Appropriate history, physical examination, and baseline EKG findings are crucial in determining the most appropriate and cost-effective stress test for these patients. According to the American College of Cardiology (ACC)/American Heart Association (AHA) guidelines, exercise stress EKG is recommended as an initial diagnostic test among patients at intermediate pretest risk who are able to exercise and who have an interpretable resting EKG [ 1 ]. In the presence of baseline EKG abnormalities, including ST depression greater than 1 mm, left ventricular hypertrophy, left bundle branch block, paced rhythm or pre-excitation, functional tests with imaging or anatomical tests including CCTA are preferred. Studies have shown that exercise EKG test is adequate for risk stratification of cardiac events which are found to be very low in patients with a negative EKG stress test [ 2 ].
Our case describes a commonly encountered scenario of a patient with few risk factors for CAD who presented to the hospital with chest pain and requires further diagnostic testing for CAD. Treadmill EKG is one of the most utilized CAD testing methods in our practice and the results guide further management of patients presenting with chest pain. A meta-analysis including 22 years of research revealed the pooled sensitivity of EKG stress test in detecting CAD to be 68% and specificity to be 77% [ 1 ]. Despite this, EKG stress tests continue to be one of the most commonly used and trusted tools in our clinical practice.
A cohort study comparing usefulness of dipyridamole echocardiography, dobutamine-atropine echocardiography, and exercise stress testing revealed similar sensitivity for diagnosis of CAD in patients presenting with chest pain [ 3 ]. In fact even in cases of multivessel CAD, studies have shown similar sensitivity of all three tests [ 4 ]. Studies have shown low prevalence of significant ischemia and CAD mortality in patients achieving more than 10 METs on exercise stress test [ 5 ]. In a 2014 randomized controlled trial, all cause mortality was found to be similar in patients with suspected CAD and normal resting EKG who underwent EKG stress test with imaging compared to those without imaging [ 6 ].
Physicians seldom see reports of indeterminate stress test results which is when they depend on expert opinion for further evaluation. In this case, the patient was an overweight 54-year-old man who had a history of tobacco use but no other significant comorbidities were known. He was clinically stable during his hospital stay. We anticipated his testing would be negative. To complete workup, cardiology recommended anatomical testing with CCTA given the indeterminate EKG stress test results and this was performed immediately. The results of significant stenosis were surprising to the care team. CCTA is a relatively newer non-invasive anatomical test that has a high diagnostic accuracy to identify the presence of coronary plaques and stenosis. Since it can also determine the extent of stenosis, it is being used for CAD risk stratification. In patients with low to intermediate probability of acute coronary syndrome (ACS), it can be used as an initial test to rule out ACS owing to its high negative predictive value. It is also being utilized as an alternative to invasive coronary angiography in patients with equivocal stress test results.
Our case demonstrates a situation where CCTA proved to be a more accurate diagnostic tool than EKG stress testing. The results significantly altered management as the patient concluded his hospital stay with coronary artery bypass grafting (CABG). Alternatively, if CCTA was not performed and the cardiologist deemed the indeterminate stress test results as negative, the patient may have been discharged and may have had a deleterious cardiac outcome. Recent guidelines from the National Institute of Health and Care Excellence recommend CCTA as the initial diagnostic test in patients with suspected CAD [ 7 ]. However, contrast-related side effects, availability of test, and cost are the main barriers to this recommendation at this time. CCTA has also been shown to have limited diagnostic accuracy in patients with intracoronary stents. The PROMISE trial showed no significant difference in clinical outcomes of patients with suspected CAD who underwent anatomical stress testing with CCTA compared to those who underwent functional stress testing [ 8 ]. However it may be worthwhile to utilize CCTA as the initial CAD diagnostic test if no contraindications are noted.
As a result of the availability of multiple noninvasive diagnostic tests with almost similar sensitivities for CAD, physicians often face this dilemma of choosing the right test for optimal evaluation of chest pain in patients with intermediate pretest probability of CAD. Optimal test selection requires an individualized patient approach. Our case describes a patient with intermediate probability of CAD presenting to the hospital with chest pain that resolved on admission and having a treadmill EKG stress test with indeterminate results. Decision to proceed with anatomical testing using CCTA was made and the patient was found to have significant CAD requiring CABG. Our experience with this case emphasizes the role of history taking, clinical judgement, and the risk/benefit ratio in deciding further workup when faced with inconclusive stress test results. Physicians should have a lower threshold for further workup of patients with inconclusive or even negative stress test results because of the diagnostic limitations of the test. Repeating the same test may result in uncertainty and indeterminate stress test should not be presumed as negative. Instead, utilizing a different, anatomical CAD test may be more valuable. Specifically, the case established the usefulness of CCTA in cases such as this where other CAD diagnostic testing is indeterminate.
Availability of supporting data
Data that supports this study have been referenced here.
Bourque JM, Beller GA. Value of exercise ECG for risk stratification in suspected or known CAD in the era of advanced imaging technologies. JACC Cardiovasc Imaging. 2015;8(11):1309–21.
Article Google Scholar
Christman MP, Bittencourt MS, Hulten E, et al . Yield of downstream tests after exercise treadmill testing. J Am Coll Cardiol. 2014;63(13):1264–74. https://doi.org/10.1016/j.jacc.2013.11.052 .
Article PubMed PubMed Central Google Scholar
Alberto J, Román S, Vilacosta I, et al . Dipyridamole and dobutamine-atropine stress echocardiography in the diagnosis of coronary artery disease: comparison with exercise stress test, analysis of agreement, and impact of antianginal treatment. Chest. 1996;110(5):1248–54.
Previtali M, Lanzarini L, Fetiveau R, et al . Comparison of dobutamine stress echocardiography, dipyridamole stress echocardiography and exercise stress testing for diagnosis of coronary artery disease. Am J Cardiol. 1993;72(12):865–70.
Article CAS Google Scholar
Bourque JM, Charlton GT, Holland BH, Belyea CM, Watson DD, Beller GA. Prognosis in patients achieving ≥10 METS on exercise stress testing: Was SPECT imaging useful? J Nucl Cardiol. 2011;18(2):230–7. https://doi.org/10.1007/s12350-010-9323-2 .
Article PubMed Google Scholar
Duvall WL, Lane Duvall W, Savino JA, et al . Prospective evaluation of a new protocol for the provisional use of perfusion imaging with exercise stress testing. Eur J Nucl Med Mol Imaging. 2015;42(2):305–16. https://doi.org/10.1007/s00259-014-2864-x .
Overview | Recent-onset chest pain of suspected cardiac origin: assessment and diagnosis | Guidance | NICE. https://www.nice.org.uk/guidance/cg95 . Accessed 18 Apr 2020.
Douglas PS, Hoffmann U, Patel MR, et al . Outcomes of anatomical versus functional testing for coronary artery disease. N Engl J Med. 2015;372(14):1291–300.
Download references
Acknowledgements
We would like to acknowledge contribution of Dr. Nishit Choksi and Dr. Nishtha Sareen, who were the cardiologists involved in care of this patient. All the above stated authors have contributed significantly in writing and editing the manuscript.
No funding received.
Author information
Authors and affiliations.
Department of Internal Medicine, Ascension Providence Rochester Hospital/Wayne State University School of Medicine, 1101 W University Drive, Rochester, MI, 48307, USA
Mishita Goel, Shubhkarman Dhillon, Sarwan Kumar & Vesna Tegeltija
You can also search for this author in PubMed Google Scholar
Contributions
We confirm that all authors have contributed in writing and drafting, obtaining images, editing and reviewing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Mishita Goel .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval or formal consent not required for this type of study.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
No competing interests to disclose.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Goel, M., Dhillon, S., Kumar, S. et al. Clinical judgement in chest pain: a case report . J Med Case Reports 15 , 49 (2021). https://doi.org/10.1186/s13256-021-02666-z
Download citation
Received : 20 November 2020
Accepted : 06 January 2021
Published : 09 February 2021
DOI : https://doi.org/10.1186/s13256-021-02666-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Stress test
- Coronary artery disease
Journal of Medical Case Reports
ISSN: 1752-1947
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Introduction
- Conclusions
- Article Information
The start of the early coronavirus disease 2019 (COVID-19) period (February 23, 2020) and later COVID-19 period (March 29, 2020), as defined by segmented regression analysis, are indicated by vertical lines. Dotted lines indicate the best-fit regression lines for the 3 periods (including the before COVID-19 period). Projected volumes with 95% CIs are displayed in gray. STEMI indicates ST-segment elevation myocardial infarction.
eTable 1. ICD-10 Codes
eTable 2. MS-DRG Codes Used in Treatment Approaches Analysis
eTable 3. Weekly Case Volumes in 2020
eFigure 1. Weekly Volumes by State
eFigure 2. Treatment Approaches
See More About
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
Gluckman TJ , Wilson MA , Chiu S, et al. Case Rates, Treatment Approaches, and Outcomes in Acute Myocardial Infarction During the Coronavirus Disease 2019 Pandemic. JAMA Cardiol. 2020;5(12):1419–1424. doi:10.1001/jamacardio.2020.3629
Manage citations:
© 2024
- Permissions
Case Rates, Treatment Approaches, and Outcomes in Acute Myocardial Infarction During the Coronavirus Disease 2019 Pandemic
- 1 Center for Cardiovascular Analytics, Research and Data Science (CARDS), Providence Heart Institute, Providence St Joseph Health, Portland, Oregon
- 2 Clinical Analytics, Providence St Joseph Health, Renton, Washington
- 3 Heart and Vascular Institute, Providence Regional Medical Center Everett, Everett, Washington
- 4 Providence Heart Institute, Providence St Peter Hospital, Olympia, Washington
Question How have case rates, treatment approaches, and in-hospital outcomes changed for patients with acute myocardial infarction (AMI) during the coronavirus disease 2019 (COVID-19) pandemic?
Findings In this cross-sectional study of 15 244 hospitalizations involving 14 724 patients with AMI, case rates began to decrease on February 23, 2020, followed by a modest recovery after 5 weeks. Although no statistically significant difference in treatment approaches was found, the risk-adjusted mortality rate among patients with ST-segment elevation myocardial infarction increased substantially.
Meaning The findings of this study show that changes in AMI hospitalizations and in-hospital outcomes occurred during the COVID-19 pandemic periods analyzed; additional research is warranted to explain the higher mortality rate among patients with ST-segment elevation myocardial infarction.
Importance The coronavirus disease 2019 (COVID-19) pandemic has changed health care delivery worldwide. Although decreases in hospitalization for acute myocardial infarction (AMI) have been reported during the pandemic, the implication for in-hospital outcomes is not well understood.
Objective To define changes in AMI case rates, patient demographics, cardiovascular comorbidities, treatment approaches, and in-hospital outcomes during the pandemic.
Design, Setting, and Participants This cross-sectional study retrospectively analyzed AMI hospitalizations that occurred between December 30, 2018, and May 16, 2020, in 1 of the 49 hospitals in the Providence St Joseph Health system located in 6 states (Alaska, Washington, Montana, Oregon, California, and Texas). The cohort included patients aged 18 years or older who had a principal discharge diagnosis of AMI (ST-segment elevation myocardial infarction [STEMI] or non–ST-segment elevation myocardial infarction [NSTEMI]). Segmented regression analysis was performed to assess changes in weekly case volumes. Cases were grouped into 1 of 3 periods: before COVID-19 (December 30, 2018, to February 22, 2020), early COVID-19 (February 23, 2020, to March 28, 2020), and later COVID-19 (March 29, 2020, to May 16, 2020). In-hospital mortality was risk-adjusted using an observed to expected (O/E) ratio and covariate-adjusted multivariable model.
Exposure Date of hospitalization.
Main Outcomes and Measures The primary outcome was the weekly rate of AMI (STEMI or NSTEMI) hospitalizations. The secondary outcomes were patient characteristics, treatment approaches, and in-hospital outcomes of this patient population.
Results The cohort included 15 244 AMI hospitalizations (of which 4955 were for STEMI [33%] and 10 289 for NSTEMI [67%]) involving 14 724 patients (mean [SD] age of 68 [13] years and 10 019 men [66%]). Beginning February 23, 2020, AMI-associated hospitalizations decreased at a rate of –19.0 (95% CI, –29.0 to –9.0) cases per week for 5 weeks (early COVID-19 period). Thereafter, AMI-associated hospitalizations increased at a rate of +10.5 (95% CI, +4.6 to +16.5) cases per week (later COVID-19 period). No appreciable differences in patient demographics, cardiovascular comorbidities, and treatment approaches were observed across periods. The O/E mortality ratio for AMI increased during the early period (1.27; 95% CI, 1.07-1.48), which was disproportionately associated with patients with STEMI (1.96; 95% CI, 1.22-2.70). Although the O/E mortality ratio for AMI was not statistically different during the later period (1.23; 95% CI, 0.98-1.47), increases in the O/E mortality ratio were noted for patients with STEMI (2.40; 95% CI, 1.65-3.16) and after risk adjustment (odds ratio, 1.52; 95% CI, 1.02-2.26).
Conclusions and Relevance This cross-sectional study found important changes in AMI hospitalization rates and worse outcomes during the early and later COVID-19 periods. Future studies are needed to identify contributors to the increased mortality rate among patients with STEMI.
The coronavirus disease 2019 (COVID-19) pandemic has profoundly changed health care delivery worldwide. Although early attention to COVID-19 was disproportionately focused on efforts to flatten the (pandemic) curve, recent studies have revealed a substantial decrease in hospitalization rates for acute myocardial infarction (AMI). Reports from Austria, 1 Italy, 2 and the US (California) 3 have noted lower admission rates for both ST-segment elevation myocardial infarction (STEMI) and non–ST-segment elevation myocardial infarction (NSTEMI). This decreased hospitalization rate likely reflects multiple factors. Most worrisome among these factors has been the reluctance of patients with AMI to seek medical attention out of fear that they may become infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). 4
We performed a retrospective, cross-sectional study of all AMI hospitalizations in a large multistate health care system. We sought to define changes in AMI case rates, patient demographics, cardiovascular comorbidities, treatment approaches, and in-hospital outcomes during the pandemic.
This study included patients aged 18 years or older with a principal discharge diagnosis of AMI who were admitted between December 30, 2018, and May 16, 2020, into 1 of 49 hospitals in the Providence St Joseph Health (PSJH) system located in 6 states (Alaska, Washington, Montana, Oregon, California, and Texas). We used International Statistical Classification of Diseases and Related Health Problems, Tenth Revision , codes to define the population (eTable 1 in the Supplement ). Individuals who were admitted as an outpatient were excluded. This study was approved by the PSJH Institutional Review Board, which waived the informed consent requirement because of the retrospective nature of the study.
The primary outcome was the weekly rate of AMI (STEMI or NSTEMI) hospitalizations before and after the pandemic onset. The secondary outcomes were patient characteristics, treatment approaches, and in-hospital outcomes (mortality, length of stay, and discharge disposition) of patients with STEMI or NSTEMI. Treatment approaches were defined by Medicare Severity-Diagnosis Related Groups (MS-DRGs) for percutaneous coronary intervention, coronary artery bypass graft surgery, and medical management of AMI (eTable 2 in the Supplement ).
Weekly volumes of AMI hospitalizations (categorized as STEMI or NSTEMI) are presented in the Figure as line graphs. Segmented regression analysis was used to ascertain volume changes over time. Using 2 identified break points (February 23, 2020 and March 29, 2020), we grouped cases into 1 of 3 periods for analysis: before COVID-19 (December 30, 2018, to February 22, 2020), early COVID-19 (February 23, 2020, to March 28, 2020), and later COVID-19 (March 29, 2020, to May 16, 2020). Segmented regression analysis was also used to identify the slope change in weekly hospitalizations during the 3 periods, with consideration of time dependence in the model.
Risk-adjusted in-hospital mortality was examined with 2 models. The first was the PSJH mortality risk model, which was a lookup table consisting of more than 5430 expected mortality rates. Such data were derived from the 3M All Patient Refined DRG, risk of mortality, and severity-of-illness grouper algorithm applied to a large inpatient database in the western US (eMethods in the Supplement ). The second was a multivariable logistic model, which considered all demographic variables listed in Table 1 . Results of the multivariable model were presented as adjusted odds ratio (OR) with 95% CI.
Patient demographics, cardiovascular comorbidities, treatment approaches, and in-hospital outcomes were summarized as descriptive statistics. Categorical data were presented as frequency (percentage). Numeric data were tested for normality and presented as mean (SD) or median (interquartile range [IQR]), as appropriate. Trends among the 3 COVID-19 periods were compared using univariate χ 2 , Fisher exact, or Kruskal-Wallis tests, as appropriate, for each variable. The level of statistical significance varied from P < .05 to P < .008, depending on Bonferroni adjustment for multiple comparisons (eMethods in the Supplement ).
The study cohort comprised 15 244 hospitalizations for AMI (4955 for STEMI [33%] and 10 289 for NSTEMI [67%]) involving 14 724 patients. Of those hospitalized, 5225 were women (34%) and 10 019 were men (66%), with a mean (SD) age of 68 (13) years ( Table 1 ). Before the COVID-19 period, the mean (SD) weekly case rate was 222 (17) patients for AMI, 72 (9) patients for STEMI, and 150 (13) patients for NSTEMI ( Figure and eTable 3 in the Supplement ). Beginning February 23, 2020, AMI hospitalizations decreased at a rate of –19.0 (95% CI, –29.0 to –9.0) cases per week for 5 weeks, marking the early COVID-19 period ( Figure ). Thereafter, AMI hospitalizations increased at a rate of +10.5 (95% CI, +4.6 to +16.5) cases per week, marking the later COVID-19 period. Weekly AMI hospitalization rates had not returned to baseline, however, by the last week evaluated (May 10, 2020; eTable 3 in the Supplement ). Similar trends in hospitalization for AMI, STEMI, and NSTEMI were observed in the PSJH system in all 6 states (eFigure 1 in the Supplement ).
Patients hospitalized for AMI in the early and later COVID-19 periods vs the before period were slightly younger (mean [SD] age, 67 [13] years vs 68 [13] years; P < .001) and more likely to be Asian (50 [6%] and 62 [6%] vs 667 [5%]; P = .01) or Native American individuals (20 [2%] and 21 [2%] vs 151 [1%]; P = .01) ( Table 1 ). Treatment approaches for patients with STEMI or NSTEMI were not statistically different across periods (eFigure 2 in the Supplement ). Median (IQR) length of stay for patients with AMI was shorter in the early COVID-19 period by 7 hours and in the later COVID-19 period by 6 hours compared with the before period (56 [41-115] hours and 57 [41-116] hours vs 63 [43-122] hours, respectively; P < .001) ( Table 2 ). Similar trends were observed for both types of AMI. A greater number of patients with AMI were discharged to home in the early and later COVID-19 periods vs the before COVID-19 period, with consistent findings among those with STEMI (235 [83%] and 284 [81%] vs 3402 [79%]; P = .02) and NSTEMI (465 [81%] and 587 [83%] vs 6976 [77%]; P = .006).
The observed (crude) in-hospital mortality rate was similar between periods for all groups ( Table 2 ). Compared with the before COVID-19 period, however, patients with STEMI had a statistically greater risk of mortality during the later COVID-19 period after adjusting for patient demographic characteristics and comorbidities (OR, 1.52; 95% CI, 1.02-2.26). Using the PSJH model, the observed to expected (O/E) hospital mortality ratio for patients with AMI was statistically increased in the early COVID-19 period (O/E ratio, 1.27; 95% CI, 1.07-1.48), with consistent findings in the later period as well (O/E ratio, 1.23; 95% CI, 0.98-1.47). These findings, however, were different for patients with STEMI vs those with NSTEMI. For patients with STEMI, the O/E mortality ratio was substantially higher in all 3 COVID-19 periods. These patients had a stepwise increase in the O/E mortality ratio from the before period (O/E ratio, 1.48; 95% CI, 1.34-1.62) to the early (O/E ratio, 1.96; 95% CI, 1.22-2.70) and later (O/E ratio, 2.40; 95% CI, 1.65-3.16) periods. The O/E mortality ratio for STEMI in the later period was statistically greater than the before period. In contrast, patients with NSTEMI had a consistently lower O/E mortality ratio for all 3 periods (before: O/E ratio, 0.80 [95% CI, 0.71-0.88]; early: O/E ratio, 0.91 [95% CI, 0.46-1.36]; later: O/E ratio, 0.71 [95% CI, 0.49-0.93]).
Consistent with previous reports, this study found a substantial decrease in AMI hospitalization rates in the early COVID-19 period. Beginning March 29, 2020, however, hospitalizations for AMI began to increase, albeit at a slower rate. Among the many factors likely associated with this rebound in cases was encouragement of patients with symptoms or signs of AMI to seek immediate medical attention, even amid the pandemic. 5 , 6
Although patient demographics and treatment approaches were fairly consistent across periods, patients with AMI hospitalized during the COVID-19 period were 1 to 3 years younger, had a shorter length of stay, and were more likely to be discharged to home. Possible explanations for these findings were greater reluctance by older patients to seek medical attention, hospital efforts to maintain bed availability, patient preference for early discharge, and concern about risk of contracting SARS-CoV-2 in post–acute care facilities.
Notable differences in risk-adjusted mortality were observed over the periods analyzed. Patients hospitalized for AMI during the early COVID-19 period had an increased O/E mortality ratio, associated disproportionately with patients with STEMI. In this population, the O/E ratio and risk-adjusted mortality rates were even greater during the later COVID-19 period. Given the time-sensitive nature of STEMI, any delay by patients, emergency medical services, the emergency department, or cardiac catheterization laboratory may have played a role. 7 , 8 Additional complications from delayed reperfusion (eg, conduction disturbances, heart failure, cardiogenic shock, and mechanical complications) 9 may have occurred in some patients. Further research is needed to identify factors associated with the higher mortality rate in patients with STEMI.
In the weeks and months to come, clinicians may see greater numbers of patients with more severe manifestations of AMI. With the uncertainty on timing of a COVID-19 vaccine, this study reinforces the need to address important care processes for patients with AMI to help mitigate further risk.
This study has several limitations. First, because the cohort was defined by coding data, it is possible that the primary reason for hospitalization was misclassified as an AMI. Second, the treatment analysis excluded outpatients and those with other MS-DRG codes. Although this group represented a small percentage of the total patient cohort (8% [1165]), treatment shifts may have been underappreciated. Third, the data set did not allow us to evaluate potential timing-related factors that may have contributed to higher in-hospital mortality (eg, time of symptom onset, first medical contact, and hospital arrival). Fourth, although the PSJH mortality risk model is not AMI-specific, we found consistent results with a multivariable model adjusted for patient demographic characteristics and comorbidities. Fifth, the COVID-19 status of patients included in the analysis was not available. As such, the higher observed rate of AMI mortality during the COVID-19 period could have been associated with concurrent SARS-CoV-2 infection.
Results of this cross-sectional study appear to validate previous concerns that large numbers of patients with AMI initially avoided hospitalization during the COVID-19 pandemic, likely out of fear of contracting SARS-CoV-2. Hospitalization rates for AMI have begun to increase but so has the risk of in-hospital mortality. Further research into factors associated with an increase in the STEMI mortality rate is warranted.
Accepted for Publication: July 10, 2020.
Corresponding Author: Ty J. Gluckman, MD, Center for Cardiovascular Analytics, Research and Data Science (CARDS), Providence Heart Institute, Providence St Joseph Health, 9427 SW Barnes Rd, Ste 594, Portland, OR 97225 ( [email protected] ).
Published Online: August 7, 2020. doi:10.1001/jamacardio.2020.3629
Author Contributions: Drs Gluckman and Chiu had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Gluckman, Chiu, Penny, Spinelli.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Gluckman, Chiu, Spinelli.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Chiu.
Administrative, technical, or material support: Gluckman, Wilson, Penny, Chepuri, Waggoner, Spinelli.
Supervision: Gluckman, Spinelli.
Conflict of Interest Disclosures: None reported.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- Search Menu
- Author videos
- ESC Content Collections
- Supplements
- Author Guidelines
- Submission Site
- Open Access Options
- Self-Archiving Policy
- About European Heart Journal Supplements
- About the European Society of Cardiology
- ESC Publications
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Terms and Conditions
- Journals on Oxford Academic
- Books on Oxford Academic
Article Contents
Introduction, case presentation.
- < Previous
Clinical case: heart failure and ischaemic heart disease
- Article contents
- Figures & tables
- Supplementary Data
Giuseppe M C Rosano, Clinical case: heart failure and ischaemic heart disease, European Heart Journal Supplements , Volume 21, Issue Supplement_C, April 2019, Pages C42–C44, https://doi.org/10.1093/eurheartj/suz046
- Permissions Icon Permissions
Patients with ischaemic heart disease that develop heart failure should be treated as per appropriate European Society of Cardiology/Heart Failure Association (ESC/HFA) guidelines.
Glucose control in diabetic patients with heart failure should be more lenient that in patients without cardiovascular disease.
Optimization of cardiac metabolism and control of heart rate should be a priority for the treatment of angina in patients with heart failure of ischaemic origin.
This clinical case refers to an 83-year-old man with moderate chronic obstructive pulmonary disease and shows that implementation of appropriate medical therapy according to the European Society of Cardiology/Heart Failure Association (ESC/HFA) guidelines improves symptoms and quality of life. 1 The case also illustrates that optimization of glucose metabolism with a more lenient glucose control was most probably important in improving the overall clinical status and functional capacity.
The patient has family history of coronary artery disease as his brother had suffered an acute myocardial infarction (AMI) at the age of 64 and his sister had received coronary artery by-pass. He also has a 14-year diagnosis of arterial hypertension, and he is diabetic on oral glucose-lowering agents since 12 years. He smokes 30 cigarettes per day since childhood.
In February 2009, after 2 weeks of angina for moderate efforts, he suffered an acute anterior myocardial infarction. He presented late (after 14 h since symptom onset) at the hospital where he had been treated conservatively and had been discharged on medical therapy: Atenolol 50 mg o.d., Amlodipine 2.5 mg o.d., Aspirin 100 mg o.d., Atorvastatin 20 mg o.d., Metformin 500 mg tds, Gliclazide 30 mg o.d., Salmeterol 50, and Fluticasone 500 mg oral inhalers.
Four weeks after discharge, he underwent a planned electrocardiogram (ECG) stress test that documented silent effort-induced ST-segment depression (1.5 mm in V4–V6) at 50 W.
He underwent a coronary angiography (June 2009) and left ventriculography that showed a not dilated left ventricle with apical dyskinesia, normal left ventricular ejection fraction (LVEF, 52%); occlusion of proximal LAD, 60% stenosis of circumflex (CX), and 60% stenosis of distal right coronary artery (RCA). An attempt to cross the occluded left anterior descending (LAD) was unsuccessful.
He was therefore discharged on medical therapy with: Atenolol 50 mg o.d., Atorvastatin 20 mg o.d., Amlodipine 2.5 mg o.d., Perindopril 4 mg o.d., oral isosorbide mono-nitrate (ISMN) 60 mg o.d., Aspirin 100 mg o.d., metformin 850 mg tds, Gliclazide 30 mg o.d., Salmeterol 50 mcg, and Fluticasone 500 mcg b.i.d. oral inhalers.
He had been well for a few months but in March 2010 he started to complain of retrosternal constriction associated to dyspnoea for moderate efforts (New York Heart Association (NYHA) II–III, Canadian Class II).
For this reason, he was prescribed a second coronary angiography that showed progression of atherosclerosis with 80% stenosis on the circumflex (after the I obtuse marginal branch) and distal RCA. The LAD was still occluded.
After consultation with the heart team, CABG was avoided because surgical the risk was deemed too high and the patient underwent palliative percutaneous coronary intervention (PCI) of CX and RCA. It was again attempted to cross the occlusion on the LAD. But this attempt was, again, unsuccessful. Collateral circulation from posterior interventricular artery (PDL) to the LAD was found. The pre-PCI echocardiogram documented moderate left ventricular dysfunction (EF 38%), the pre-discharge echocardiogram documented a LVEF of 34%. Because of the reduced LVEF, atenolol was changed for Bisoprolol (5 mg o.d.).
At follow-up visit in December 2012, the clinical status and the haemodynamic conditions had deteriorated. He complained of worsening effort-induced dyspnoea/angina that now occurred for less than a flight of stairs (NYHA III). On clinical examination clear signs of worsening heart failure were detected ( Table 1 ). His medical therapy was modified to: Bisoprolol 5 mg o.d., Atorvastatin 20 mg o.d., Amlodipine 2.5 mg o.d., Perindopil 5 mg o.d., ISMN 60 mg o.d., Aspirin 100 mg o.d., Metformin 500 mg tds, Furosemide 50 mg o.d., Gliclazide 30 mg o.d., Salmeterol 50 mcg oral inhaler, and Fluticasone 500 mcg oral inhaler. A stress perfusion cardiac scintigraphy was requested and revealed dilated ventricles with LVEF 19%, fixed apical perfusion defect and reversible perfusion defect of the antero-septal wall (ischaemic burden <10%, Figure 1 ). He was admitted, and an ICD was implanted.
Clinical parameters during follow-up visits
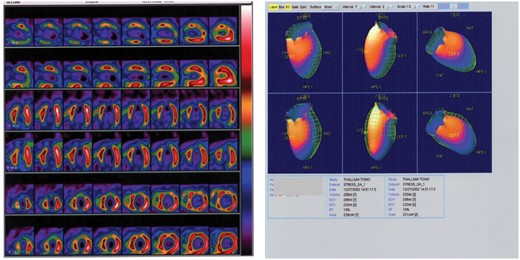
Myocardial perfusion scintigraphy and left ventriculography showing dilated left ventricle with left ventricular ejection fraction 19%. Reversible perfusion defects on the antero-septal wall and fixed apical perfusion defect.
In March 2013, he felt slightly better but still complained of effort-induced dyspnoea/angina (NYHA III, Table 1 ). Medical therapy was updated with bisoprolol changed with Nebivolol 5 mg o.d. and perindopril changed to Enalapril 10 mg b.i.d. The switch from bisoprolol to nebivolol was undertaken because of the better tolerability and outcome data with nebivolol in elderly patients with heart failure. Perindopril was switched to enalapril because the first one has no indication for the treatment of heart failure.
In September 2013, the clinical conditions were unchanged, he still complained of effort-induced dyspnoea/angina (NYHA III) and did not notice any change in his exercise capacity. His BNP was 1670. He was referred for a 3-month cycle of cardiac rehabilitation during which his medical therapy was changed to: Nebivolol 5 mg o.d., Ivabradine 5 mg b.i.d., uptitrated in October to 7.5 b.i.d., Trimetazidine 20 mg tds, Furosemide 50 mg, Metolazone 5 mg o.d., K-canrenoate 50 mg, Enalapril 10 mg b.i.d., Clopidogrel 75 mg o.d., Atorvastatin 40 mg o.d., Metformin 500 mg b.i.d., Salmeterol 50 mcg oral inhaler, and Fluticasone 500 mcg oral inhaler.
At the follow-up visit in January 2014, he felt much better and had symptomatically, he no longer complained of angina, nor dyspnoea (NYHA Class II, Table 1 ). Trimetazidine was added because of its benefits in heart failure patients of ischaemic origin and because of its effect on functional capacity. Ivabradine was added to reduce heart rate since it was felt that increasing nebivolol, that was already titrated to an effective dose, would have had led to hypotension.
He missed his follow-up visits in June and October 2014 because he was feeling well and he had decided to spend some time at his house in the south of Italy. In January and June 2015, he was well, asymptomatic (NYHA I–II) and able to attend his daily activities. He did not complain of angina nor dyspnoea and reported no limitations in his daily activities. Unfortunately, in November 2015 he was hit by a moped while on the zebra crossing in Rome and he later died in hospital as a consequence of the trauma.
This case highlights the need of optimizing both the heart failure and the anti-anginal medications in patients with heart failure of ischaemic origin. This patient has improved dramatically after the up-titration of diuretics, the control of heart rate with nebivolol and ivabradine and the additional use of trimetazidine. 1–3 All these drugs have contributed to improve the clinical status together with a more lenient control of glucose metabolism. 4 This is another crucial point to take into account in diabetic patients, especially if elderly, with heart failure in whom aggressive glucose control is detrimental for their functional capacity and long-term prognosis. 5
IRCCS San Raffaele - Ricerca corrente Ministero della Salute 2018.
Conflict of interest : none declared. The authors didn’t receive any financial support in terms of honorarium by Servier for the supplement articles.
Ponikowski P , Voors AA , Anker SD , Bueno H , Cleland JG , Coats AJ , Falk V , González-Juanatey JR , Harjola VP , Jankowska EA , Jessup M , Linde C , Nihoyannopoulos P , Parissis JT , Pieske B , Riley JP , Rosano GM , Ruilope LM , Ruschitzka F , Rutten FH , van der Meer P ; Authors/Task Force Members. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the Special Contribution of the Heart Failure Association (HFA) of the ESC . Eur J Heart Fail 2016 ; 18 : 891 – 975 .
Google Scholar
Rosano GM , Vitale C. Metabolic modulation of cardiac metabolism in heart failure . Card Fail Rev 2018 ; 4 : 99 – 103 .
Vitale C , Ilaria S , Rosano GM. Pharmacological interventions effective in improving exercise capacity in heart failure . Card Fail Rev 2018 ; 4 : 1 – 27 .
Seferović PM , Petrie MC , Filippatos GS , Anker SD , Rosano G , Bauersachs J , Paulus WJ , Komajda M , Cosentino F , de Boer RA , Farmakis D , Doehner W , Lambrinou E , Lopatin Y , Piepoli MF , Theodorakis MJ , Wiggers H , Lekakis J , Mebazaa A , Mamas MA , Tschöpe C , Hoes AW , Seferović JP , Logue J , McDonagh T , Riley JP , Milinković I , Polovina M , van Veldhuisen DJ , Lainscak M , Maggioni AP , Ruschitzka F , McMurray JJV. Type 2 diabetes mellitus and heart failure: a position statement from the Heart Failure Association of the European Society of Cardiology . Eur J Heart Fail 2018 ; 20 : 853 – 872 .
Vitale C , Spoletini I , Rosano GM. Frailty in heart failure: implications for management . Card Fail Rev 2018 ; 4 : 104 – 106 .
- myocardial ischemia
- cardiac rehabilitation
- heart failure
- older adult
Email alerts
More on this topic, related articles in pubmed, citing articles via.
- Recommend to Your Librarian
Affiliations
- Online ISSN 1554-2815
- Print ISSN 1520-765X
- Copyright © 2024 European Society of Cardiology
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.

Create Free Account or
- Acute Coronary Syndromes
- Anticoagulation Management
- Arrhythmias and Clinical EP
- Cardiac Surgery
- Cardio-Oncology
- Cardiovascular Care Team
- Congenital Heart Disease and Pediatric Cardiology
- COVID-19 Hub
- Diabetes and Cardiometabolic Disease
- Dyslipidemia
- Geriatric Cardiology
- Heart Failure and Cardiomyopathies
- Invasive Cardiovascular Angiography and Intervention
- Noninvasive Imaging
- Pericardial Disease
- Pulmonary Hypertension and Venous Thromboembolism
- Sports and Exercise Cardiology
- Stable Ischemic Heart Disease
- Valvular Heart Disease
- Vascular Medicine
- Clinical Updates & Discoveries
- Advocacy & Policy
- Perspectives & Analysis
- Meeting Coverage
- ACC Member Publications
- ACC Podcasts
- View All Cardiology Updates
- Earn Credit
- View the Education Catalog
- ACC Anywhere: The Cardiology Video Library
- CardioSource Plus for Institutions and Practices
- ECG Drill and Practice
- Heart Songs
- Nuclear Cardiology
- Online Courses
- Collaborative Maintenance Pathway (CMP)
- Understanding MOC
- Image and Slide Gallery
- Annual Scientific Session and Related Events
- Chapter Meetings
- Live Meetings
- Live Meetings - International
- Webinars - Live
- Webinars - OnDemand
- Certificates and Certifications
- ACC Accreditation Services
- ACC Quality Improvement for Institutions Program
- CardioSmart
- National Cardiovascular Data Registry (NCDR)
- Advocacy at the ACC
- Cardiology as a Career Path
- Cardiology Careers
- Cardiovascular Buyers Guide
- Clinical Solutions
- Clinician Well-Being Portal
- Diversity and Inclusion
- Infographics
- Innovation Program
- Mobile and Web Apps
Heart Failure Center Patient Cases

HOME | HF CENTER HOME | FAQ | ABOUT
Heart Failure: Ask the Expert – Patient Cases
Welcome to the GCVI HF Center’s Ask the Expert – Patient Cases channel! On this channel you will have access to multiple heart failure patient cases published by leading ACC experts. We also encourage you to engage and consult with ACC global experts on cases specific to your practice. Ask the Expert through the online portal below!
Engage with ACC global experts!
Heart Failure Patient Case Quizzes
- Unrecognized HFpEF in a Type 2 DM Patient – Reducing CV and HF Risk
- Untreated HFrEF/Ischemic Cardiomyopathy in Type 2 DM – How to Optimize Medical Therapy to Improve Heart Failure Outcomes
- Restrictive Cardiomyopathies Series: Advanced HF Therapies in ATTR Cardiac Amyloidosis (Certified Patient Case Study)
- ECG of the Month: Variable QRS Morphologies in Heart Failure
- Untreated HFrEF/Ischemic Cardiomyopathy in Type 2 DM
- Unrecognized HFpEF in a Type 2 DM Patient
Regional Patient Case Quizzes Select your region to view available courses.

JACC Journals on ACC.org
- JACC: Advances
- JACC: Basic to Translational Science
- JACC: CardioOncology
- JACC: Cardiovascular Imaging
- JACC: Cardiovascular Interventions
- JACC: Case Reports
- JACC: Clinical Electrophysiology
- JACC: Heart Failure
- Current Members
- Campaign for the Future
- Become a Member
- Renew Your Membership
- Member Benefits and Resources
- Member Sections
- ACC Member Directory
- ACC Innovation Program
- Our Strategic Direction
- Our History
- Our Bylaws and Code of Ethics
- Leadership and Governance
- Annual Report
- Industry Relations
- Support the ACC
- Jobs at the ACC
- Press Releases
- Social Media
- Book Our Conference Center
Clinical Topics
- Chronic Angina
- Congenital Heart Disease and Pediatric Cardiology
- Diabetes and Cardiometabolic Disease
- Hypertriglyceridemia
- Invasive Cardiovascular Angiography and Intervention
- Pulmonary Hypertension and Venous Thromboembolism
Latest in Cardiology
Education and meetings.
- Online Learning Catalog
- Products and Resources
- Annual Scientific Session
Tools and Practice Support
- Quality Improvement for Institutions
- Accreditation Services
- Practice Solutions
Heart House
- 2400 N St. NW
- Washington , DC 20037
- Email: [email protected]
- Phone: 1-202-375-6000
- Toll Free: 1-800-253-4636
- Fax: 1-202-375-6842
- Media Center
- ACC.org Quick Start Guide
- Advertising & Sponsorship Policy
- Clinical Content Disclaimer
- Editorial Board
- Privacy Policy
- Registered User Agreement
- Terms of Service
- Cookie Policy
© 2024 American College of Cardiology Foundation. All rights reserved.
Case Study: Heart Failure Exacerbation Due to an Often Overlooked Cause
— shows importance of using wide differential when investigating hf.
by Kate Kneisel , Contributing Writer, MedPage Today

"Medical Journeys" is a set of clinical resources reviewed by physicians, meant for the medical team as well as the patients they serve. Each episode of this journey through a disease state contains both a physician guide and a downloadable/printable patient resource. "Medical Journeys" chart a path each step of the way for physicians and patients and provide continual resources and support, as the caregiver team navigates the course of a disease.
This month: A noteworthy case study
Why has a 64-year-old man become increasingly short of breath over the past 2 weeks? That's what Sandra K. Rabat, DO, of A.T. Still University School of Osteopathic Medicine in Mesa, Arizona, and colleagues needed to determine, as they reported in Cureus .
The patient's medical history included a diagnosis of congestive heart failure and coronary artery disease in 2014, after stenting of his left anterior descending artery and right coronary artery. He also had high blood pressure and stage III chronic kidney disease (CKD) when he presented to the hospital for assessment after 2 weeks of worsening dyspnea.
The patient told clinicians he became winded even after a few steps, and that at night, he needed to prop himself up on three pillows to improve his breathing. He also had fluid retention in his lower legs, feet, and ankles that lasted all day, and continued to be worsening.
He said he was not aware of anything that might have exacerbated his shortness of breath, and that he did not use oxygen therapy or inhalers at home. He admitted that he was not consistent about taking his prescribed medications – carvedilol, lisinopril, furosemide, atorvastatin, and clopidogrel – and that that he sometimes forgot them entirely.
His family history was significant for premature coronary artery disease and the sudden cardiac death of his grandfather at age 49.
On questioning, he reported feeling that his heart beat was very rapid, but had no other observations. He said he did not use illicit drugs, smoke, or drink alcohol. Social determinants of the patient's health included experiencing homelessness, and he had very little social or family support.
Initial examination found that he was in a hypertensive emergency. His blood pressure was 220/110 mmHg and oxygen saturation was 84% oxygen on room air. Significant lab test findings included a creatinine level that was increased to 2.4 mg/dL from his baseline of 1.7 mg/dL. Troponins were 12,333 pg/ml and brain natriuretic peptide (BNP) was 1,431 pg/ml.
Clinicians noted the complexities of interpreting cardiac troponin levels and BNP in the setting of CKD. However, they said, "the magnitude of elevation of the troponins and BNP was very concerning for another process within the myocardium rather than being a false-positive elevation from CKD alone."
EKG findings included the following:
- Prolonged QTC interval
- Left-axis deviation
- Non-specific ST-T changes
- No ST-segment elevations
Chest x-ray showed that the patient had cardiomegaly with pulmonary edema. Given the high troponin levels and EKG results, the team ruled out ST-segment elevation myocardial infarction (STEMI) as a diagnosis in favor of non-ST-segment elevation myocardial infarction (NSTEMI).
In the emergency department, the patient was started on one dose of clonidine, nasal cannula oxygen, and heparin drip, and later also received hydralazine as needed for systolic blood pressure that exceeded 160 mmHg. In light of his elevated BNP levels and chest x-ray findings, the patient was admitted for acute exacerbation of congestive heart failure. Clinicians started the patient on aggressive diuresis with IV furosemide and accelerated his cardiac workup.
The workup for pulmonary embolus was unremarkable, given the patient's negative venous duplex and V/Q scan, the case authors noted. "Transthoracic echocardiogram revealed significant findings, including an estimated ejection fraction of 10% with moderate mitral regurgitation and moderate tricuspid regurgitation, a dilated right ventricle with severely impaired systolic function, and grade three diastolic dysfunction with restrictive filling."
The team noted that a previous echocardiogram performed about 2 years earlier showed that the patient's estimated ejection fraction had been 60% with preserved left ventricular systolic function. Because of the severity of his left ventricular dysfunction, and dilation of the left ventricle, the patient received a portable external cardiac defibrillator.
An ultrasound of his abdomen revealed bilateral renal atrophy with diffusely increased echogenicity bilaterally, which is indicative of CKD. Because he was in volume overload, clinicians continued his diuresis and closely monitored his creatinine levels.
After interval improvement of his kidney function, the patient underwent cardiac catheterization, which indicated "nonobstructive coronary artery disease and severe pulmonary hypertension."
Right heart hemodynamics revealed a mean pulmonary capillary wedge pressure of 40 mmHg, mean pulmonary artery pressure of 60 mmHg, and mean right atrial (RA) pressure of 32 mmHg, the case authors reported, noting that this ruled out nonischemic cardiomyopathy as a cause of the patient's acute decompensation.
Following the cardiac catheterization, the team discontinued diuretic treatment. The patient was started on dobutamine infusion at 5 mcg/kg/min, and the dose was titrated to achieve a minimum mean arterial pressure of 65 mmHg. He began taking isosorbide mononitrate and hydralazine, and continued with carvedilol.
Diuretic therapy with torsemide was reinstated. Treatment with an angiotensin-converting enzyme inhibitor or angiotensin receptor neprilysin inhibitor was contraindicated, due to the patient's medical status: acute kidney injury in the presence of CKD stage III and a glomerular filtration rate of less than 30 ml/min/1.73 m 2 .
Efforts to wean the patient off dobutamine, however, failed when his kidney function worsened to a creatinine level of 2.7 mg/dL, which the authors noted confirmed a need for inotropic support. When his kidney function improved, they started the patient on milrinone infusion with close monitoring, based on evidence of decompensated heart failure with low cardiac output and signs of end-organ hypoperfusion.
The objective was to combine milrinone infusion with standard heart failure therapy, including a beta-blocker, as tolerated. "The benefit of using milrinone over dobutamine in this patient's case is that milrinone, a phosphodiesterase inhibitor, will not antagonize a beta-blocker like dobutamine," the authors explained.
Because dobutamine's action is partly related to beta-1 and beta-2 adrenergic receptors, concomitant beta-blocker therapy would likely reduce the hemodynamic response to treatment, the team speculated. The patient was scheduled for a cardiac MRI, possibly to be followed by endomyocardial biopsy.
This proved to be unnecessary, however, when the test result came back as "positive for Coxsackie B viral antibody immunoglobulin G (IgG), indicating chronic viral infection," Rabat and co-authors said.
"This case highlights how viruses continue to be an underappreciated cause of heart failure. In fact, viral myocarditis is an underdiagnosed cause of acute heart failure and chronic dilated cardiomyopathy," as is iron deficiency anemia , the authors wrote.
Cardiomyopathy – which is associated with muscle or electrical dysfunction of the heart – is defined by the American Heart Association as a heterogeneous group of diseases of the myocardium, usually with inappropriate ventricular hypertrophy or dilatation.
Noting that viral myocarditis is often overlooked due to its varied presentation, Rabat and co-authors urged clinicians not to underestimate the substantial cardiovascular risks associated with a large spectrum of viral infections, some of which can lead to significant deterioration in decompensated patients.
"Coxsackie B virus is one of the most common causes of viral myocarditis and is responsible for 10-20% of all myocarditis and dilated cardiomyopathy cases," the case authors said. Parvovirus B19, adenovirus, Epstein-Barr virus, HIV, and COVID-19 have also been reported to cause myocarditis.
Viral myocarditis may go undiagnosed due to the wide variety of presentations, which can range from dyspnea to more aggressive symptoms suggestive of acute coronary syndrome. One review noted that among more than 3,000 patients with suspected acute or chronic myocarditis, dyspnea was found in 72%, chest pain in 32%, and arrhythmias in 18%.
"Myocarditis generally results from cardiotropic viral infection followed by active inflammatory destruction of the myocardium," the case authors stated. After the initial acute symptoms of viral myocarditis, the viral infection may either clear completely, persist, or "lead to a persistent auto-immune-mediated inflammatory process with long-term symptoms of heart failure."
A persistent viral infection of the myocardium can result in a progressive deterioration of left ventricular ejection fraction (LVEF), which likely explains the current patient's decline in LVEF from 60% to 10% over less than 2 years, Rabat and co-authors noted.
Despite being considered the diagnostic gold standard for acute or chronic inflammatory heart disease, endomyocardial biopsy is used infrequently because of the perception of associated risks and the absence of a widely accepted and sensitive histologic standard.
Endomyocardial biopsies may be complemented with use of liquid biopsy to monitor circulating biomarkers, including microRNAs (miRNAs), which have also demonstrated excellent diagnostic capability, the team noted. In fact, in a recent study , expression levels of miRNAs differentiated between patients with viral myocarditis, inflammatory cardiomyopathy, and healthy donors with a specificity of over 95%.
"However, further studies would be needed to elevate the routine use of miRNA-panel in addition to further guidelines to help optimize the management of this disease," the case authors wrote, noting that current guidelines advise optimal use of heart failure medications to manage symptoms.
Rabat and co-authors noted that the COVID-19 pandemic has brought to light a global sensitivity to viral infections. The pathogenesis of viral myocarditis in heart failure remains poorly understood and represents a significant global public health issue. The team urged clinicians investigating heart failure to maintain a wide index of suspicion and be aware "that even chronic Coxsackie B viral infection can cause an acute presentation of heart failure."
Read previous installments of this series:
Part 1: Heart Failure: A Look at Low Ejection Fraction
Part 2: Exploring Heart Failure With Preserved Ejection Fraction
Part 3: Heart Failure With Reduced Ejection Fraction: Diagnosis and Evaluation
Part 4: Case Study: Lightheadedness, Fatigue in Man With Hypertension
Part 5: Heart Failure With Preserved Ejection Fraction: Diagnosis and Evaluation
Part 6: Heart Failure Medical Management
Part 7: Managing Heart Failure Comorbidities
![case study for heart disease author['full_name']](https://clf1.medpagetoday.com/media/images/author/KKneisel_188.jpg)
Kate Kneisel is a freelance medical journalist based in Belleville, Ontario.
Disclosures
The authors reported no conflicts of interest.
Primary Source
Source Reference: Rabat S K, et al "A case report on an underappreciated cause of heart failure: Chronic viral myocarditis" Cureus 2022; DOI: 10.7759/cureus.27253.
Case Studies

The Starr Group: Supporting a Healthy Workplace
Company Background Industry: Insurance Location(s): Milwaukee, WI Number of employees: 36 The Starr Group is an insurance and risk-management agency that has been in business since 1956 and specializes in balancing insurance with alternative risk financing strategies while improving their customers’ total risk wellness. Products and services provided by the organization include commercial, group benefits,

The Dow Chemical Company – Total Worker Health
The Dow Chemical Company is a global Company with a diversified portfolio of specialty chemical, advanced materials, agro sciences and plastics businesses operating 300 sites in about 50 countries and with approximately 54,000 employees. At Dow, protecting people and the environment is part of everything we do and every decision we make. A commitment to safety, employee health and world-leading environmental performance is engrained in our Company and culture. Health is a strategic priority for Dow and is essential for our Sustainability.

Macy’s, Inc. Associate Well-Being & Disease Prevention
Macy’s, Inc. is one of America’s premier retailers. With fiscal 2014 sales of $28.1 billion, the company operates more than 880 stores in 45 states, the District of Columbia, Guam and Puerto Rico under the names Macy’s, Bloomingdale’s, Bloomingdale’s Outlet and Bluemercury, as well as the macys.com, bloomingdales.com and bluemercury.com websites. Macy’s diverse workforce includes approximately 166,900 employees, located across the country.

Deloitte: The Vitals of Well-being
Deloitte’s people are problem-solvers, creating change and making a difference in everything they do. And that’s not surprising: Innovation and problem-solving are in our organization’s DNA. Our founder William Welch Deloitte was the first person ever appointed as an independent auditor of a public company. That was in London in 1845. His company went international when he added a New York City office in 1880. Today, William Deloitte’s vision lives on through the nearly 200,000 partners, principals, and employees of the worldwide Deloitte Touche Tohmatsu Limited (“DTTL”) organization of member firms, providing services in audit, advisory, tax, and consulting. Today, Deloitte employs more than 70,000 U.S.-based professionals in over 100 offices across the country.

Johnson & Johnson’s Healthiest Workforce Commitment
“Caring for the world, one person at a time” has inspired Johnson & Johnson for over 125 years. With 128,000 employees in 60+ countries, Johnson & Johnson is the world’s largest, most diverse healthcare company, touching the lives of more than a billion people every day.

The American Heart Association’s Smoke-Free Meeting Policy
With more than 3,000 employees and 156 offices nationwide, the American Heart Association (AHA) is the nation’s oldest and largest voluntary organization dedicated to fighting heart disease and stroke. AHA’s mission is to build healthier lives, free of cardiovascular diseases and stroke. That single purpose drives all the association does, including funding innovative research, fighting for stronger public health policies and providing critical tools and information that save and improve lives.

Macy’s, Inc. Annual 5k Run/Walk

KKR’s First Aid Training
KKR is a leading global investment firm that manages investments across multiple asset classes. KKR aims to generate attractive investment returns by following a patient and disciplined investment approach, employing world-class people and driving growth and value creation at the asset level. Core to KKR’s values is the belief that thoughtful management of environment, social and governance issues is smart business and an essential part of long-term success.

Boston Scientific’s Worksite Wellness Pilot Program: Building a Culture of Health On-Site
Boston Scientific is dedicated to transforming lives through innovative medical solutions that improve the health of patients around the world. A leading creator of medical products and technologies, Boston Scientific has approximately 24,000 employees around the globe and more than 11,000 employees across the United States. As a global healthcare company, Boston Scientific’s commitment to improving patient health is clear. The company also believes there is an implied need to foster a culture of health and well-being for its own employees that allows them to work and perform at their personal best. For Boston Scientific, this concept of well-being reaches far beyond physical health, but focuses on a more holistic view of the work-life connection that ultimately can improve employee lives while elevating work productivity.

Humana’s Well-Being: Measuring, Motivating and Reporting Impact
Over the course of 54 years, Humana has transformed the ways it brings help and care to the people it serves. As a leader in the healthcare industry, Humana has evolved from a company with the episodic customer relationships of a traditional health insurer to a company dedicated to helping people improve their health and well-being, which has become part of the company’s culture. That shared enterprise purpose came into even sharper focus last spring when Humana publically announced a goal to improve the health of the communities it serves 20 percent by 2020, by making it easy for people to achieve their best health.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 14 December 2021
A case control study of occupation and cardiovascular disease risk in Japanese men and women
- Kota Fukai 1 ,
- Yuko Furuya 1 ,
- Shoko Nakazawa 1 ,
- Noriko Kojimahara 2 ,
- Keika Hoshi 3 , 4 ,
- Akihiro Toyota 5 &
- Masayuki Tatemichi nAff1
Scientific Reports volume 11 , Article number: 23983 ( 2021 ) Cite this article
5299 Accesses
10 Citations
6 Altmetric
Metrics details
- Epidemiology
- Occupational health
We aimed to investigate the risks of cardiovascular diseases associated with specific occupations, using a nation-wide, multicentre, hospital-based registry data from the Inpatient Clinico-Occupational Survey. The analysis included 539,110 controls (non-circulatory disease) and 23,792 cases (cerebral infarction, intracerebral/subarachnoid hemorrhage, acute myocardial infarction) aged ≥ 20 years who were initially hospitalized during 2005–2015. The participants’ occupational and clinical histories were collected by interviewers and medical doctors. Occupations were coded into 81 categories according to the Japanese standard occupation classification. Multivariable logistic regression analysis adjusted for age, admission year and hospital, smoking, alcohol consumption, hypertension, and shift-work was conducted by sex using general clerical workers as the reference. Increased risks of cerebral infarction, intracerebral hemorrhage, subarachnoid hemorrhage, and acute myocardial infarction, were observed in 15, 20, 25, and 1 occupation(s) in men, and 9, 2, 2, and 10 occupations in women. Motor vehicle drivers, food and drink preparatory workers, fishery workers, cargo workers, civil engineer workers, and other manual workers in men and other manual workers in women faced increased risks of all three stroke subtypes. Our findings demonstrate associations between specific occupations and the risk of cardiovascular disease incidence and suggest that the risk may vary by occupation.
Similar content being viewed by others


Chronic inflammation in the etiology of disease across the life span
David Furman, Judith Campisi, … George M. Slavich

Cardiovascular disease and cancer: shared risk factors and mechanisms
Nicholas S. Wilcox, Uri Amit, … Bonnie Ky

The global epidemiology of hypertension
Katherine T. Mills, Andrei Stefanescu & Jiang He
Introduction
The incidence of cardiovascular disease (CVD), including stroke and coronary heart disease (CHD), has exhibited a decreasing trend in Japan since the late twentieth century 1 . However, CVD remains associated with a high disease burden and major concerns in workers.
Previously, socio-epidemiological studies suggested that the occupational grade or class, a known social determinant of health, may also be a risk factor for CVD 2 . In the Whitehall study, Marmot et al. classified 17,530 British civil servants into four occupational grades (administrator, professional and executive, clerical, and other) and reported that the 10-year CHD mortality rate was three times higher in the lowest grade (other) relative to the highest grade (administrator) 3 . In Japan, Zaitsu et al. recently reported the risks of CHD and stroke incidence associated with broad occupational categories (manager, professional, service, and blue-collar) in combination with industrial clusters (white-collar, service, and blue-collar) 4 . Compared to the study in Britain 3 , the study in Japan identified a stronger pattern of CHD risk in higher occupational classes 4 . Other studies have also reported an association between CVD and occupational classes 5 , 6 , however, the results have been inconsistent. Therefore, it is difficult for clinicians to apply the findings in actual practice, even if they collected past occupational histories.
We hypothesized that there might be hidden hazards in various subcategorized occupations that may contribute to the risk of developing CVD. This research background suggests a need to focus on the specific occupation as epidemiological evidence rather than as a feature that can be represented by occupational grades or classes 7 . Generally, occupational classification schemes are not sufficiently detailed to enable a fine-scale analysis of associations with health measures 8 . One recent study demonstrated that the use of a detailed classification of occupations more accurately predicted health measures than did a broader classification or various combinations of socio-economic factors 7 . This may also be due to unknown occupational-related potential factors besides the effects of individual health status factors such as hypertension, smoking, or alcohol consumption, which are risk factors for CVD. In other words, it is important to examine the association between an individual’s detailed occupation and the risk of CVD onset from the viewpoint of occupational medicine. Roles may be different between men and women in the same occupation. To the best of our knowledge, no previously published study has explored this relationship. Therefore, we aimed to examine whether the incidence of CVD differs depending on the specific occupation among adults who participated in a nation-wide large-scale inpatient registry in Japan.
Study design and participants
This is a nation-wide multi-hospital-based case–control study. The present study was conducted using data from the Inpatient Clinico-Occupational Survey, which has been conducted by the Rosai Hospital Group since 1984. The details of this survey have been described elsewhere 4 , 9 , 10 . Briefly, the Inpatient Clinico-Occupational Survey collects clinical and occupational history information for all inpatients older than 15 years who were admitted to facilities belonging to the nation-wide Rosai Hospital Group (> 13,000 beds in 34 hospitals as in the year 2015) and remained alive at 24 h after admission. The clinical history data of each patient were combined with a summary of inpatient treatment recorded by physicians. Definitive diagnoses for admission were coded using the International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10) 11 . Lifestyle habits (e.g., smoking and alcohol consumption) and history of hypertension were also included in the clinical history. All information was registered in the Inpatient Clinico-Occupational Database by the health information manager and a trained occupational history surveyor at each hospital. Data were collected at each admission for patients who were hospitalized multiple times during the study period. The clinical and occupational history registry rates were nearly 100% and 66%, respectively.
For the present study, we used data collected during 2005–2015, when the clinical and occupational data of 829,926 participants were subjected to analysis. For patients who were hospitalized multiple times, only the first hospitalization data were used. We excluded participants younger than 20 years (n = 18,094); those whose occupation were unclassifiable (n = 303); those for whom were unemployed as the longest-held occupation (n = 77,895), student (n = 18,993), homemaker (n = 118,973). Furthermore, we excluded those admitted for diseases of the circulatory system except CVD (n = 32,825). Finally, 562,902 participants remained for analysis.
This study was performed according to the tenets of the Declaration of Helsinki. Written informed consent was obtained from each patient prior to completion of all the questionnaires. Access to the dataset was provided under a research agreement between the study authors and the Japan Organization of Occupational Health and Safety. This study was approved by the Research Ethics Committees of Tokai University School of Medicine, Kanagawa, Japan (Protocol Number 18R-309) and the Japan Organization of Occupational Health and Safety (Protocol Number R1-006).
Cases and controls
CVD cases were defined as patients with a diagnosis at admission of cerebral infarction (ICD-10, I63; n = 12,826), intracerebral haemorrhage (ICD-10, I61; n = 4905), subarachnoid haemorrhage (ICD-10, I60; n = 1641), and acute myocardial infarction (ICD-10, I21; n = 4420). Consistent with the methodology used in previous studies 12 , the controls were defined as patients who were admitted at the same hospital and during the same period for reasons other than diseases of the circulatory system (ICD-10, I00 to I99 except for I21, I60, I61, I63; n = 65,591). The final analysis included 23,792 cases and 539,110 controls. The participant flowchart is outlined in S1 Fig.
Occupation assessment
The participants were interviewed regarding their current and three previous occupations, as well as the duration of each. Occupational history information was coded according to the Japan Standard Occupational Classification, which was published by the Japanese Ministry of Internal Affairs and Communications 13 by a trained occupational history surveyor. To accommodate the revision of the Japan Standard Occupational Classification which was published by the government during the survey, the Japan Organisation of Occupational Health and Safety created an original unified code of 81 occupations that would cover the revision. This unified classification is roughly compliant with the sub-major (two-digit codes, 43 groups) and minor (three-digit codes, 130 groups) categories of the International Standard Classification of Occupations 2008 (ISCO-08) 14 . For each participant, the longest-held of the four most recent occupations was adopted as the exposure variable. Information about shift-work history was also collected. The list of occupations and numbers of controls and cases in detail are presented in S1 Table.
Statistical analyses
The odds ratios (ORs) and 95% confidence intervals (95% CIs) of the incidence of CVD (cerebral infarction, intracerebral hemorrhage, subarachnoid hemorrhage, and acute myocardial infarction) were estimated using multivariable logistic regression analysis. We used general clerical workers as the reference group in all analyses because it was the most frequent category for both men and women and was considered to have less effect of various occupational hazards. Lifestyle habits (e.g., smoking and alcohol consumption) and history of hypertension were also included in the clinical history. Model 1 was the unadjusted model. Model 2 was created by adjusting for age (in years, continuous), admission date (in years, categorical), and admitting hospital (34 hospitals, categorical). We the adjusted admission date to explore potential heterogeneity introduced by changes in the environment within the occupation and by secular changes in diagnostic practices or treatment. Also, we adjusted the admission hospital to account for differences by region, despite the same occupation, such as rural and urban areas, since this database was nationwide database. Model 3 was further adjusted for smoking (never smoker, former smoker, current smoker), alcohol consumption (non-drinker, former drinker, current drinker), and hypertension (yes/no). In Japan, hypertension has a high prevalence and the outcome (CVD) is not only caused by the exposure (occupation). Since hypertension is both associated with occupation and CVD, we adjusted hypertension in model 3 as a potential cofounder. Model 4 was further adjusted for shift-work (yes/no). No missing values for confounders in the dataset for this analysis existed due to a standard protocol by trained interviewers.
While CVD is chronically affected by the cardiovascular system, it is a sudden-onset disease, and to account for acute effects, we conducted a sensitivity analysis using the current occupation as an exposure variable. A two-sided p value < 0.05 was considered statistically significant. All analyses were performed using the Statistical Analysis System (SAS) Software version 9.4 (SAS Institute, Cary, NC, USA).
The characteristics of the cases and controls are presented in Table 1 . Notably, the distributions of age and smoking status differed between these groups. Cases of subarachnoid hemorrhage included younger patients and tended to include large proportions of current smokers and alcohol drinkers.
Cerebral infarction accounted for the largest number of cases among both men and women, and the ORs of various occupations for the incidence of cerebral infarction were calculated using each model. The statistically significant results corresponding to occupations resulting from any of the four models are described in Fig. 1 a (men) and Fig. 1 b (women), and the full results are available in S2 Table. In the fully adjusted model (Model 4), high ORs of cerebral infarction were observed in 15 occupations among men (doctors, dentists, veterinarians, pharmacists; other health care workers; authors, journalists, editors; other managerial workers; merchandise sales workers; domestic hygiene service workers; food and drink preparatory workers; other service workers; fishery; motor vehicle drivers; other transport workers; electro-mechanic assembly workers; civil engineer workers; cargo workers; and other manual workers), as well as 9 occupations among women (other engineers; other managerial workers; customer service workers; residential facilities management personnel; agriculture; other mechanical assembly; food manufacturing; construction machinery operators; and other manual workers). Low ORs of cerebral infarction were observed in management staff of government officials and forestry among men, and none among women. The results of the unadjusted model (Model 1) differed somewhat from those of the other models. After adjusting for age (Model 2), however, the results remained consistent even with further adjustments (e.g., admission date, hospital, smoking, drinking, hypertension, and shift-work). The full results of cases of intracerebral hemorrhage, subarachnoid hemorrhage, and acute myocardial infarction are available in S3 – S5 Tables. These results were similar to those of cases of cerebral infarction, although smoking and alcohol consumption also appeared to affect the incidence of subarachnoid hemorrhage and acute myocardial infarction. Shift-work had no apparent effect on the associations of occupations with CVD.
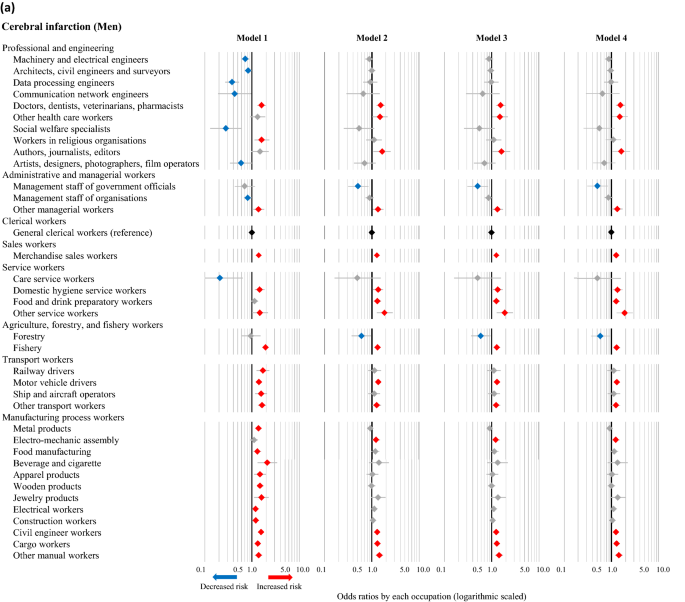
Odds ratios of cerebral infarction associated with occupations among men ( a ) and women ( b ) based on different models. The odds ratios (symbols) and 95% confidence intervals (bars) were estimated using univariate and multivariable logistic regression analyses, with general clerical workers as the reference. Red and blue symbols indicate statistically significant increases and decreases in risk, respectively. Model 1: Unadjusted. Model 2: Adjusted for age, admission date, and hospital. Model 3: Adjusted for the factors in Model 2 plus smoking, alcohol consumption, and hypertension. Model 4: Adjusted for the factors in Model 3 plus shift-work.
The fully adjusted ORs (Model 4) for cerebral infarction, intracerebral hemorrhage, subarachnoid hemorrhage, and acute myocardial infarction in association with various occupations were also calculated, using general clerical workers as the reference group. The statistically significant results corresponding to specific occupations in any of the four disease categories are presented in Fig. 2 a (men) and Fig. 2 b (women), while the full results are available in S2 – S5 Tables. The number of categories that were significantly associated with increased risks of cerebral infarction, intracerebral hemorrhage, subarachnoid hemorrhage, and acute myocardial infarction were, 15, 20, 25, and one occupation(s) among men, respectively, while two, zero, zero, and six occupations were associated with decreased risks of the respective conditions. Moreover, among men, increased risks of all three subtypes of stroke were observed in food and drink preparatory workers, fishery, motor vehicle drivers, civil engineer workers, cargo workers, and other manual workers. Among women, nine, two, two, and ten occupations were associated with a significantly increased risk of cerebral infarction, intracerebral hemorrhage, subarachnoid hemorrhage, and acute myocardial infarction, respectively, while one, zero, zero, and zero occupations were associated with decreased risks of the respective conditions. Moreover, female participants classified as other manual workers had increased risks of all three subtypes of stroke. Female food and drink preparatory workers also exhibited an increasing trend in the risk of all three subtypes of stroke, although these associations were not statistically significant.
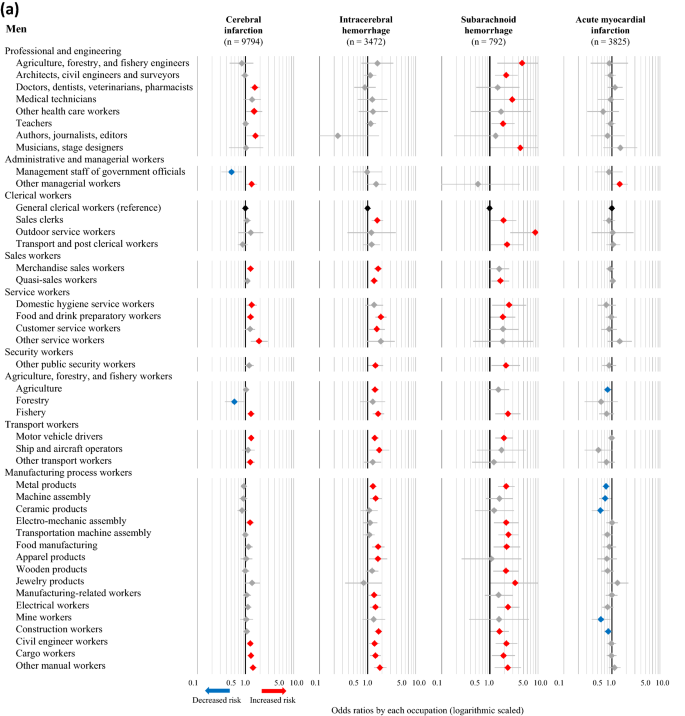
Odds ratios for CVD associated with occupations among men ( a ) and women ( b ). The odds ratios (symbols) and 95% confidence intervals (bars) were estimated using multivariable logistic regression analysis, with general clerical workers as the reference. The analysis was adjusted for age, admission date, hospital, smoking, alcohol consumption, hypertension, and shift-work. Red and blue symbols indicate statistically significant increases and decreases in risk, respectively.
The results of the sensitivity analysis, which included only participants whose current occupation was also the longest-held occupation, are presented in Fig. 3 a (men) and Fig. 3 b (women) as fully adjusted ORs (Model 4) of the incidence of CVD. Among men, two, 17, and 19 occupations were associated with an increased risk of cerebral infarction, intracerebral hemorrhage, and subarachnoid hemorrhage, respectively, to the same degree observed in the full population analysis, while two occupations were associated with a decreased risk. Consistent with the full analysis, male motor vehicle drivers continued to face increased risks of all three subtypes of stroke. Among women, two, one, and four occupations were associated with an increased risk of cerebral infarction, intracerebral hemorrhage, and acute myocardial infarction, respectively, to the same degree observed in the full population analysis.
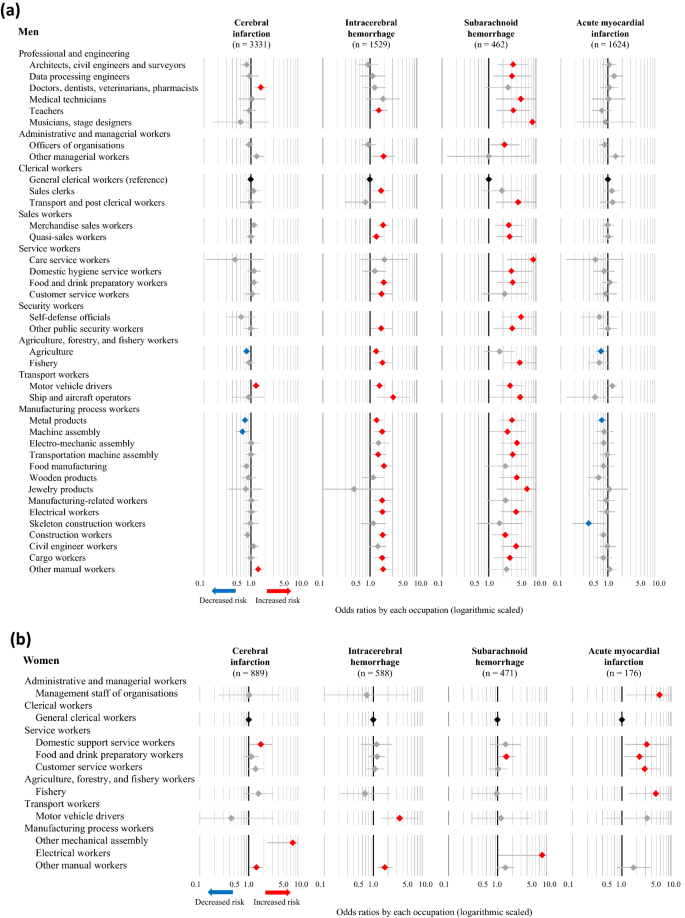
Odds ratios for CVD associated with occupations among men ( a ) and women ( b ) whose current occupation was also the longest-held occupation. The odds ratios (symbols) and 95% confidence intervals (bars) were estimated using multivariable logistic regression analysis, with general clerical workers as the reference. The analysis was adjusted for age, admission date, hospital, smoking, alcohol consumption, hypertension, and shift-work. Red and blue symbols indicate statistically significant increases and decreases in risk, respectively.
In this study, based on a data set from a nation-wide large-scale inpatient survey in Japan, we explored the potential associations between specific occupations and CVD. Although some previous studies have demonstrated associations between occupational classes or grades and CVD 3 , 4 , 15 , 16 , 17 , ours is one of the first to provide descriptive results associated with specific occupations. Interestingly, there were clear differences in the association of specific occupations with a risk for CVD between men and women, cerebral versus coronary, and between cerebral infarction and hemorrhage. There was one specific occupation that increased the risk for CHD in men, but ten occupations showed a significantly increased risk in women. On the other hand, men had many occupations that increased the risk for cerebrovascular diseases, but women had few.
Among men, only other management workers increased the risk for CHD. On the other hand, motor vehicle drivers, food and drink preparatory workers, and other manual workers exhibited a robust increase in the risk of all three subtypes of stroke when compared with the reference group of general clerical workers. However, in our sensitivity analysis (Fig. 3 a), only doctors, motor vehicle drivers, and other manual workers showed a slightly increased risk for cerebral infarction. While quasi-sales workers (i.e. other sales workers), food and drink preparatory workers, fishery workers, and manufacturing process workers (e.g., metal producers, skeleton construction workers, civil engineers, and cargo workers) faced increased risks of both intracerebral and subarachnoid hemorrhage, but not cerebral infarction. Hypertension plays a pivotal role in stroke, particularly hemorrhage 18 , although we conducted model-based adjustment for hypertension based on information of the present illness. We consider that these specific occupations with an increased risk for hemorrhage may temporarily and markedly elevate blood pressures in workers by mental or physical stresses. In addition, the ‘physical activity paradox’ is recently emphasized, and occupational physical activity (OPA) is considered to play an important role in CVD 19 . According to Steeves’s classifications 20 , the occupations that were found to be associated with intracerebral hemorrhage were classified as occupations with high OPA levels. The occupations with high odds ratios of intracerebral haemorrhage such as agriculture, forestry, and fishery engineers (OR = 4.72), outdoor service workers (OR = 8.86), communication workers (OR = 3.60) are considered to be high OPA level. Further investigation of OPA levels and CVD risk is needed.
In women, there were significant occupations associated with an increased risk of CHD, such as management staff of organizations, domestic support service workers, customer service workers, and fishery workers. These findings were different from those in men suggesting that it might be more mentally stressful for women than men, resulting in the development of coronary arterial atherosclerosis. However, the associations between specific occupations and cerebral hemorrhages were less clear. Three types of manufacturing process workers (food manufacturing, construction machinery operators, and other mechanical assembly workers) had a strongly increased risk of stroke. Orthostatic hypotension is an important risk factor for stroke 21 . Thus, among workers with these occupations, they stand all day, and chronic orthostatic hypotension might be a risk factor. Other engineers and other managerial workers also showed an increased risk for stroke. However, this classification was not clear, and the reason was unknown.
Motor vehicle drivers and food and drink preparatory workers exhibited a robust increase in the risk of all three subtypes of stroke. As for other possibilities, we may point out the risk of passive smoking. This is a major public health issue that is considered a risk factor for CVD 22 , 23 , 24 . In Japan, the Health Promotion Law enacted in 2003 obligated administrators of public facilities to make efforts to prevent passive smoking. However, restaurants and taxicabs were the least developed areas for passive smoking prevention. Until the late 2000s, Japanese taxi drivers were exposed to second-hand cigarette smoke due to passengers 25 . Many restaurants that employ food and drink preparatory workers do not impose restrictions on smoking, which was allowed in 95.9% of the customer areas and 85.0% of the employee work areas in restaurants in 2007 26 . According to the Japanese National Health and Nutrition Survey in 2013, 50.9% of people were exposed to second-hand smoke at restaurants 27 . The evidence suggests that second-hand smoke may have contributed to the increased risk of CVD among subjects employed in workplaces without smoking restrictions.
Although it is difficult to compare our findings with those of previous studies that focused on occupational classes or grades, our results generally appear to be consistent with those of earlier analyses. Particularly, socioeconomically advantaged groups tend to have a lower risk of CVD 6 , whereas so-called manual workers have a higher risk 16 , 28 . Our results demonstrate that several occupations in the categories of manufacturing process, service, and sales were associated with a high risk of CVD even after adjusting for age, smoking and alcohol consumption habits, hypertension, and shift work. Thus, our results indicate that information on the occupation of patients is important for physicians to prevent the onset of CVD.
One strength of this study is the use of an extensive set of detailed information about previous and current occupations which was collected by professionally trained investigators. An analysis of the relationships between occupations and CVD risk requires a large population for which specific occupation data are available. Although hypertension and smoking are the risk factors most strongly associated with CVD 29 , an assessment focused on the occupational histories of participants in a clinical population at risk of CVD is important from the viewpoint of occupational medicine. We noted that in our survey, the association between occupation and CVD remained even after other factors were adjusted, suggesting the involvement of hidden occupation-related factors.
Our study had limitations. First, the study may have been subject to selection bias regarding the controls (i.e., Berkson’s bias) 30 . The hospital admission probability is defined as the probability that the members of a community group will be admitted to the hospital 31 , and we selected controls from among patients admitted to the same hospitals as the cases. The distribution of the occupational profiles of our controls were nationally representative 4 , 9 . Yet, bias towards or away from null association may exist in the selection of hospital controls, who may be more biased toward risk factors for being hospitalized for any disease than the general population. Second, data regarding other clinical risk factors for CVD, such as blood pressure, total cholesterol, and glucose intolerance, were unavailable. However, we used self-reported data adjusted for a history of hypertension. Third, other socioeconomic covariates such as working hours or income which were examined in other relevant studies 6 , 32 were not assessed due to the lack of data. Employees who worked long hours had a higher risk of stroke than those working standard hours; the association with CHD was weaker 32 . Future studies should consider the effects of long working hours on the difference of onset of stroke and CHD. No strong association between the income level and CVD risk has been observed in Japan 6 . For available factors, we adjusted shift work as a work-related factor and achieved consistent results. Fourth, we considered only the longest-held occupation as the risk factor, and we did not consider the impact of a change nor sequence in employment. There is a possibility that they may have changed jobs or become unemployed depending on their health conditions. Further assessment is needed to address this variable.
In conclusion, the present study has clearly demonstrated the difference between long-held specific occupations and the risk of CVD. From the viewpoint of occupational medicine, our results may be valuable to investigate key factors among these potentially high-risk occupations in terms of the risk of CVD.
Data availability
The datasets are not publicly available due to restrictions used under the license for the current study. There are available on reasonable request from the corresponding author.
Hata, J. et al. Secular trends in cardiovascular disease and its risk factors in Japanese: Half-century data from the Hisayama Study (1961–2009). Circulation 128 , 1198–1205. https://doi.org/10.1161/CIRCULATIONAHA.113.002424 (2013).
Article PubMed Google Scholar
Havranek, E. P. et al. Social determinants of risk and outcomes for cardiovascular disease: A scientific statement from the American Heart Association. Circulation 132 , 873–898. https://doi.org/10.1161/CIR.0000000000000228 (2015).
Marmot, M. G., Shipley, M. J. & Rose, G. Inequalities in death-specific explanations of a general pattern?. Lancet 323 , 1003–1006. https://doi.org/10.1016/S0140-6736(84)92337-7 (1984).
Article Google Scholar
Zaitsu, M. et al. Occupational class and risk of cardiovascular disease incidence in Japan: Nationwide, multicenter, hospital-based case-control study. J. Am. Heart Assoc. 8 , e011350–e011350. https://doi.org/10.1161/JAHA.118.011350 (2019).
Article PubMed PubMed Central Google Scholar
Chen, R., McKevitt, C., Rudd, A. G. & Wolfe, C. D. A. Socioeconomic deprivation and survival after stroke findings from the prospective south london stroke register of 1995 to 2011. Stroke 45 , 217–223. https://doi.org/10.1161/Strokeaha.113.003266 (2014).
Marshall, I. J. et al. The effects of socioeconomic status on stroke risk and outcomes. Lancet Neurol. 14 , 1206–1218. https://doi.org/10.1016/S1474-4422(15)00200-8 (2015).
Eyles, E., Manley, D. & Jones, K. Occupied with classification: Which occupational classification scheme better predicts health outcomes?. Soc. Sci. Med. 227 , 56–62. https://doi.org/10.1016/j.socscimed.2018.09.020 (2019).
Clougherty, J. E., Souza, K. & Cullen, M. R. Work and its role in shaping the social gradient in health. Ann. N. Y. Acad. Sci. 1186 , 102–124. https://doi.org/10.1111/j.1749-6632.2009.05338.x (2010).
Article ADS PubMed PubMed Central Google Scholar
Kaneko, R., Zaitsu, M., Sato, Y. & Kobayashi, Y. Risk of cancer and longest-held occupations in Japanese workers: A multicenter hospital-based case-control study. Cancer Med. 8 , 6139–6150. https://doi.org/10.1002/cam4.2499 (2019).
Fukai, K., Kojimahara, N., Hoshi, K., Toyota, A. & Tatemichi, M. Combined effects of occupational exposure to hazardous operations and lifestyle-related factors on cancer incidence. Cancer Sci. 111 , 4581–4593. https://doi.org/10.1111/cas.14663 (2020).
Article CAS PubMed PubMed Central Google Scholar
World Health Organization. ICD-10: International Statistical Classification of Diseases and Related Health Problems: 10th revision , 2nd ed. https://apps.who.int/iris/handle/10665/42980 (2004).
Wacholder, S., Silverman, D. T., McLaughlin, J. K. & Mandel, J. S. Selection of controls in case-control studies: II. Types of controls. Am. J. Epidemiol. 135 , 1029–1041. https://doi.org/10.1093/oxfordjournals.aje.a116397 (1992).
Article CAS PubMed Google Scholar
Japanese Ministry of Internal Affairs and Communications. Japan Standard Occupational Classification http://www.soumu.go.jp/english/dgpp_ss/seido/shokgyou/index-co.htm (2009).
International Labour Organization. International Standard Classification of Occupations . https://www.ilo.org/public/english/bureau/stat/isco/isco08/ (2016).
Marmot, M. G. & Shipley, M. J. Do socioeconomic differences in mortality persist after retirement? 25 year follow up of civil servants from the first Whitehall study. BMJ 313 , 1177–1180. https://doi.org/10.1136/bmj.313.7066.1177 (1996).
McFadden, E., Luben, R., Wareham, N., Bingham, S. & Khaw, K. T. Social class, risk factors, and stroke incidence in men and women a prospective study in the european prospective investigation into cancer in norfolk cohort. Stroke 40 , 1070–1077. https://doi.org/10.1161/STROKEAHA.108.533414 (2009).
Min, Y. I. et al. Cardiovascular disease burden and socioeconomic correlates: Findings from the Jackson Heart Study. J. Am. Heart Assoc. 6 , e004416–e004416. https://doi.org/10.1161/JAHA.116.004416 (2017).
Andalib, S. et al. Blood pressure variability: A new predicting factor for clinical outcomes of intracerebral hemorrhage. J. Stroke Cerebrovasc. Dis. 29 , 105340. https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.105340 (2020).
Holtermann, A., Schnohr, P., Nordestgaard, B. G. & Marott, J. L. The physical activity paradox in cardiovascular disease and all-cause mortality: The contemporary Copenhagen General Population Study with 104 046 adults. Eur. Heart J. 42 , 1499–1511. https://doi.org/10.1093/eurheartj/ehab087 (2021).
Steeves, J. A. et al. Daily physical activity by occupational classification in US adults: NHANES 2005–2006. J. Phys. Act Health https://doi.org/10.1123/jpah.2017-0465 (2018).
Min, M. et al. The association between orthostatic hypotension and cognition and stroke: A meta-analysis of prospective cohort studies. Blood Press. 29 , 3–12. https://doi.org/10.1080/08037051.2019.1689808 (2020).
Saito, J. et al. ‘Only Fathers Smoking’ contributes the most to socioeconomic inequalities: Changes in socioeconomic inequalities in infants’ exposure to second hand smoke over time in Japan. PLoS ONE 10 , e0139512–e0139512. https://doi.org/10.1371/journal.pone.0139512 (2015).
Öberg, M., Jaakkola, M. S., Woodward, A., Peruga, A. & Prüss-Ustün, A. Worldwide burden of disease from exposure to second-hand smoke: A retrospective analysis of data from 192 countries. Lancet 377 , 139–146. https://doi.org/10.1016/S0140-6736(10)61388-8 (2011).
Barnoya, J. & Glantz, S. A. Cardiovascular effects of secondhand smoke: Nearly as large as smoking. Circulation 111 , 2684–2698. https://doi.org/10.1161/CIRCULATIONAHA.104.492215 (2005).
Kobayashi, F. et al. Acute effects of cigarette smoking on the heart rate variability of taxi drivers during work. Scand. J. Work. Environ. Health 31 , 360–366. https://doi.org/10.2307/40967516 (2005).
Sakamoto, R. et al. Second-hand smoke in restaurants after enforcement of a health promotion law in Japan. J. Public Health Policy 28 , 156–161. https://doi.org/10.1057/palgrave.jphp.3200120 (2007).
Japanese Ministry of Health Labour and Welfare. The National Health and Nutrition Survey in Japan https://www.mhlw.go.jp/bunya/kenkou/eiyou/h25-houkoku.html (2013).
Novak, M. et al. Occupational status and incidences of ischemic and hemorrhagic stroke in Swedish men: A population-based 35-year prospective follow-up study. Eur. J. Epidemiol. 28 , 697–704. https://doi.org/10.1007/s10654-013-9833-8 (2013).
Ueshima, H. et al. Cardiovascular disease and risk factors in Asia: A selected review. Circulation 118 , 2702–2709. https://doi.org/10.1161/CIRCULATIONAHA.108.790048 (2008).
Schwartzbaum, J., Ahlbom, A. & Feychting, M. Berkson’s bias reviewed. Eur. J. Epidemiol. 18 , 1109–1112. https://doi.org/10.1023/B:EJEP.0000006552.89605.c8 (2003).
Berkson, J. Limitations of the application of fourfold table analysis to hospital data. Int. J. Epidemiol. 43 , 511–515. https://doi.org/10.1093/ije/dyu022 (2014).
Kivimäki, M. et al. Long working hours and risk of coronary heart disease and stroke: A systematic review and meta-analysis of published and unpublished data for 603 838 individuals. Lancet 386 , 1739–1746. https://doi.org/10.1016/S0140-6736(15)60295-1 (2015).
Download references
Acknowledgements
We would like to express gratitude to all the study staff in JOHAS for their commitment to data collection. We would like to thank Editage ( http://www.editage.com ) for editing and reviewing this manuscript for English language.
This work was supported by Research Project on Inpatient Clinico-Occupational Database of Rosai Hospital Group (2021).
Author information
- Masayuki Tatemichi
Present address: Department of Preventive Medicine, Tokai University School of Medicine, Isehara, Japan
Authors and Affiliations
Department of Preventive Medicine, Tokai University School of Medicine, Isehara, Japan
Kota Fukai, Yuko Furuya & Shoko Nakazawa
Department of Public Health, Shizuoka Graduate University of Public Health, Shizuoka, Japan
Noriko Kojimahara
Center for Public Health Informatics, National Institute of Public Health, Wako, Japan
Keika Hoshi
Department of Hygiene, School of Medicine, Kitasato University, Sagamihara, Japan
Chugoku Rosai Hospital Research Center for the Promotion of Health and Employment Support, Japan Organization of Occupational Health and Safety, Hiroshima, Japan
Akihiro Toyota
You can also search for this author in PubMed Google Scholar
Contributions
N.K., K.H., A.T., and M.T. received funding acquisition and collected data. Y.F., K.F., and S.N. designed this study and analysed the data. Y.F., K.F., and M.T. wrote the paper. K.F., N.K., K.H., A.T., and M.T. supervised this study and provided critical comments. All authors reviewed the manuscript.
Corresponding author
Correspondence to Masayuki Tatemichi .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary figure s1., supplementary table s1., supplementary table s2., supplementary table s3., supplementary table s4., supplementary table s5., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Fukai, K., Furuya, Y., Nakazawa, S. et al. A case control study of occupation and cardiovascular disease risk in Japanese men and women. Sci Rep 11 , 23983 (2021). https://doi.org/10.1038/s41598-021-03410-9
Download citation
Received : 15 June 2021
Accepted : 30 November 2021
Published : 14 December 2021
DOI : https://doi.org/10.1038/s41598-021-03410-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Incidence of coronary heart disease among remote workers: a nationwide web-based cohort study.
- Masayoshi Zaitsu
- Tomohiro Ishimaru
- Yoshihisa Fujino
Scientific Reports (2024)
Alcohol use patterns and risk of incident cataract surgery: a large scale case–control study in Japan
- Ryo Terauchi
Scientific Reports (2022)
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Open access
- Published: 15 June 2023
Case–control association study of congenital heart disease from a tertiary paediatric cardiac centre from North India
- Prachi Kukshal 1 ,
- Radha O Joshi 2 ,
- Ajay Kumar 1 ,
- Shadab Ahamad 1 ,
- Prabhatha Rashmi Murthy 3 ,
- Yogesh Sathe 4 ,
- Krishna Manohar 4 na1 ,
- Soma Guhathakurta 1 &
- Subramanian Chellappan 4
BMC Pediatrics volume 23 , Article number: 290 ( 2023 ) Cite this article
1100 Accesses
Metrics details
Congenital Heart diseases (CHDs) account for 1/3rd of all congenital birth defects. Etiopathogenesis of CHDs remain elusive despite extensive investigations globally. Phenotypic heterogeneity witnessed in this developmental disorder reiterate gene-environment interactions with periconceptional factors as risk conferring; and genetic analysis of both sporadic and familial forms of CHD suggest its multigenic basis. Significant association of de novo and inherited variants have been observed. Approximately 1/5th of CHDs are documented in the ethnically distinct Indian population but genetic insights have been very limited. This pilot case–control based association study was undertaken to investigate the status of Caucasian SNPs in a north Indian cohort.
A total of 306 CHD cases sub-classified into n = 198 acyanotic and n = 108 cyanotic types were recruited from a dedicated tertiary paediatric cardiac centre in Palwal, Haryana. 23 SNPs primarily prioritized from Genome-wide association studies (GWAS) on Caucasians were genotyped using Agena MassARRAY Technology and test of association was performed with adequately numbered controls.
Fifty percent of the studied SNPs were substantially associated in either allelic, genotypic or sub-phenotype categories validating their strong correlation with disease manifestation. Of note, strongest allelic association was observed for rs73118372 in CRELD1 ( p < 0.0001) on Chr3, rs28711516 in MYH6 ( p = 0.00083) and rs735712 in MYH7 ( p = 0.0009) both on Chr 14 and were also significantly associated with acyanotic, and cyanotic categories separately. rs28711516 ( p = 0.003) and rs735712 ( p = 0.002) also showed genotypic association. Strongest association was observed with rs735712( p = 0.003) in VSD and maximum association was observed for ASD sub-phenotypes.
Conclusions
Caucasian findings were partly replicated in the north Indian population. The findings suggest the contribution of genetic, environmental and sociodemographic factors, warranting continued investigations in this study population.
Peer Review reports
Congenital Heart Defect (CHD) is common structural abnormality occurring at the time of foetal development. Limited information is available on the exact mechanism of CHD pathogenesis. It affects 9 in 1000 live births globally [ 1 ]. This corresponds to 17% of the world CHD load from India [ 2 ], yet meagre genetic information available for the disease in the country. In early gestation, incidence is even higher as certain CHDs are complex and have been shown to result in foetal demise [ 3 ]. Septational abnormalities account for half of the cardiac congenital defects ranging from nonpathological to lethal [ 4 ]. Cardiac development is a complex process and requires intricate coordination of several molecular events for eventual normal structure and function of the heart. Any error/s in these steps result in pathogenic remodelling of heart [ 5 ]. Chromosomal aneuploidies like Trisomy 21, 18 and 13 are commonly associated with CHDs [ 6 , 7 ]. Though 80% CHDs are sporadic in origin [ 8 ], some familial cases of Atrial Septal Defect (ASD), Ventricular Septal Defect (VSD) and Hypoplastic Left Heart Syndrome (HLHS) are recorded but the inheritance patterns are complex [ 9 , 10 ]. The recurrence risk in off springs of CHD patients varies from 3- 20% depending on the lesion, with slightly higher recurrence in females [ 11 ]. Almost one half of the siblings with recurrent lesions in a family have a different lesion suggesting multifactorial etiology and illusive molecular mechanisms [ 8 , 9 , 12 ].
Technological advances now enable study of these developmental defects, thus closing the gap of knowledge between the morphology and genetics [ 6 ]. Novel techniques identify regions in the genome on which transcription factors act, driving their target genes and provide new knowledge on CHD development. The T-box transcription factors ( TBX5 ) gene is reported to interact with Nk2 Homeobox 5 ( NKX2.5) and GATA binding protein 4 ( GATA4 ) both transcriptional activator of Natriuretic peptide B, which positively regulates the developing heart. The involvement of several well-established cardiac transcription factors that are expressed in cardiogenic plates such as NKX2.5, GATA4, TBX5 , TBX20, Myosin heavy chain 6 (MYH6), Actin alpha cardiac muscle ( ACTC1 ) and Myocyte enhancer factor 2C ( MEF2C ) have been extensively studied in both human and animal experiments [ 13 , 14 , 15 , 16 , 17 ]. Role of Mutations in transcription factors have been studied for non-syndromic CHDs [ 18 ].
Point mutations of cardiac transcription factor genes, single nucleotide polymorphism (SNPs), aneuploidy, and chromosomal copy number variants (CNVs) are directly associated with CHDs. Association of single SNPs seldom lead to complex disease manifestation [ 19 ]. There are substantial genetic predispositions to inherited as well as de novo variants with variable effect sizes towards disease risk. Since mutations are rare it requires large numbers to be screened, also same mutations may not be present in all samples. Conventionally a multifactorial inheritance model has been proposed for CHD involving a multitude of susceptibility genes, with low-penetrant common variants or intermediate-penetrant rare variants, superposed on unfavourable environmental factors as causal [ 15 , 20 , 21 ]. Several ethnic or racial differences may also be observed [ 22 ]. It is important to investigate genotype–phenotype correlation to provide leads with an opportunity to predict the prognosis.
Limited genetic diagnosis is available for many of the CHDs. Therefore several commercial ventures to sequence genes have been undertaken [ 23 , 24 ]. These ventures discovered several de novo mutations in the known as well as new genes [ 6 , 12 ]. Genome wide association studies (GWAS) involve the comparison of genetic variants (known as well as unknown), which can be used to detect genetic risk factors of big and small effect to CHD manifestation [ 12 , 25 , 26 ]. So far more than 500 genes have been estimated with a potential role in the development of CHD [ 27 ]. Genetic studies on transcription factors like GATA4, NKX2.5, TBX1 and TBX20 have previously shown to identify new mutations in Indian population. [ 28 , 29 , 30 , 31 , 32 , 33 ]. Till date limited candidate gene studies have been done in India [ 34 ] and only one using exome sequencing [ 35 ].
Next generation sequencing (NGS) technologies meet a high standard of evidence and also afford correct predictions in novel datasets. In this study we select association findings from GWAS on CHDs and evaluate in a north Indian cohort. Screening for SNPs and not mutations may reflect better in an association study. Therefore, we chose to assess association of common variants primarily from previous GWAS or meta-analysis studies [ 26 , 36 , 36 , 37 , 38 , 39 ] in Caucasians and tested their replicability in our adequately powered study samples.
Methodology
Study samples.
The study was approved by Institutional Ethics Committee (IEC) at Sri Sathya Sai Sanjeevani Research Foundation (SSSSRF), Palwal, India. Samples were recruited from the Sai Sanjeevani biobank for Congenital Heart of SSSSRF from the period of September 2018 to September 2021. n = 306 CHD cases who underwent surgery or cath interventions at Sri Sathya Sai Sanjeevani International Centre for Child Heart Care & Research, Palwal, Haryana were recruited for this study. All methods were performed in accordance with the relevant guidelines and regulations laid down by Indian Council of Medical Research(ICMR). Samples from clinically identified known syndromes or showing distinct extracardiac features were excluded from the study. All the samples selected for the study were non-syndromic based on medical examination and the clinical phenotypes were segregated into cyanotic and acyanotic types. n = 108 cyanotic and n = 198 acyanotic CHD cases were included. Categorization of cases into 10 subphenotypes (ASD; VSD; TOF: Tetralogy of Fallot; VSD + PS:VSD + Pulmonary Stenosis; DCRV: Double Chamber Right Ventricle; TGA: Transposition of the Great Arteries; SV: Single Ventricle; AVSD: Atrioventricular Septal Defect; TAPVC: both Total and Partial Anomalous Pulmonary Venous Connection; Miscellaneous cases) was accomplished based on intervention procedure, ECHO findings and patient history. Sample distributions are given in Supplementary Table 1 .
Controls groups
Age matched control group of north India origin was an ideal control for this study but was unavailable and is a limitation of the study. Therefore, we compared it to adequately numbered adults of north Indian origin available in public database [ 40 ] ( http://asia.ensembl.org/Homo_sapiens/Variation ) and published literature [ 41 , 42 ]. The three groups described below were combined to get a substantial number of controls [ 43 ].
Control group1: n = 48 adults of north Indian origin unaffected for CHD based on clinical evaluation as well as an ECHO for confirmation were included in the study. Control group2: Since the inhouse control group was small, n = 489 open source 1000 Genomes South Asian data was also used as part of reference controls. Control group3: Comparable genotypes for 8 common markers from north India controls in a published study on Celiac Disease [ 41 , 42 ] was available for n = 1170 adults.
Marker selection
Assuming large hypothesis-free studies would reflect true associations with disease, most of the GWAS associations were tested in this study. In the absence of contemporary Indian data, associations from Caucasians who are closer to north Indians in ancestry [ 44 ], were tested for their contribution. Top 50 markers associated in GWAS catalogue for CHD phenotypes or through maternal influence were shortlisted but only 35 could be accommodated in the assay pool. SNPs having p > 10 –6 and a Minor Allele Frequency(MAF) > 0.001 were selected for inclusion. Priority was given to polymorphic SNPs having a functional implication on the gene product. The study samples had 80% power to detect associations for the SNPs having MAF > 0.1 and an Odds Ratio > 1.5.
Experimental method
Samples were isolated by the conventional phenol–chloroform phase separation method. The coded samples were blinded and genotyped through a commercial facility (Genes2Me: https://www.genes2me.com ) using Agena MassARRAY technology, which is based on matrix-assisted laser desorption/ionization—time of flight (MALDI-TOF) mass spectrometry. Genetic polymorphisms are distinguished by analysis of their individual mass, excluding the need for fluorescence or labelling. Control samples, duplicates, negatives and positives were used for quality control. Out of 35 SNPs, two failed in assay design and ten SNPs (rs6763159; rs11894932; rs365990; rs17189763; rs2010963; rs350916; rs436582; rs4366490; rs8061121; rs870142) gave ambiguous reads on QC and were removed from the analysis. Only 23 markers and samples which had > 80% genotype calls were retained in the study. A chi-square test was used for association measures and Fisher’s exact test was used, if the expected number was less than five. Statistical tools like SPSS version 21.0 and free online tools [ 45 ] ( https://vassarstats.net/ ) were used for analysis. Power was calculated using Quanto [ 46 ] ( http://biostats.usc.edu/Quanto.html ).
A total of n = 23 SNPs in Hardy Weinberg Equilibrium (stringent cut off: p > 0.001) were included in the analysis (Supplementary Table 2 ). Since two SNPs rs2046060 and rs12165908 were monomorphic hence they could not be utilised further for association study. No significant allelic association was seen among cyanotic and acyanotic cases groups. These were still analysed separately vs all controls.
Markers with allelic and genotypic associations are tabulated and presented in Table 1 and 2 for acyanotic, cyanotic and combined categories.
Allelic Association: rs73118372 on chr. 3, rs28711516 and rs735712 on chr. 14 exhibited association for all three categories (acyanotic, cyanotic and combined categories; Table 1 ). rs73118372 in CRELD1 (χ 2 = 15.7; p < 0.0001); rs28711516 in MYH6 (χ 2 = 11.18; p = 0.00083) and rs735712 in MYH7 (χ 2 = 10.98; p = 0.0009) showed strong allelic associations. Variant rs11874 in GOSR2 had nominal association (χ 2 = 3.81; p = 0.051) and rs185531658 an intergenic SNP on Chr 5 [ 39 ] showed association on Fisher’s test as allele counts were low ( p = 0.043) while rs659366 in UCP2 and rs2388896 intergenic SNP demonstrated a weak trend of association (Table 1 ).
All associations were mainly driven by similar association in the larger acyanotic group. For the SNP rs659366 the association strengthen (χ 2 = 5.74; p = 0.017) in the acyanotic group. The cyanotic association was established only for rs73118372, rs28711516 and rs735712.
Genotypic association
Similar trend was observed for genotypic associations as illustrated in Table 2 . rs1975649(χ2 = 5.74; p = 0.057) of SYNPR on Chr 3; rs28711516 (χ 2 = 11.75; p = 0.0028) and rs735712 (χ 2 = 13.03; p = 0.0015) on Chr 14 showed genotypic association. rs659366 demonstrated a trend on association (χ 2 = 5.46; p = 0.065).
Associations with CHD subtypes
Seven allelic associations with ASD; three with TOF; two with VSD + PS; one each with TGA and AVSD phenotypes were observed. rs735712 of MYH7 ( p = 0.0029) showed strongest association with VSD subtype amongst all associations observed. ASD, VSD and TOF categories were adequately numbered for association analysis. All subtypes except ASD, VSD and TOF were combined for analysis and showed association for rs73118372, rs28711516 and rs735712 (Table 3 ).
50% of tested SNPs were substantially associated in either allelic, genotypic or sub-phenotypes of north Indian CHD cohort validating their strong correlation with disease manifestation. Burden of CHD is overall heavy in India [ 2 ] and is prominent in north India. Several genetic determinants of this complex developmental disorder have been reported based on conventional candidate genes and contemporary GWAS but mostly in Caucasian populations. However it is very poorly investigated in the ethnically distinct Indian population. This study was an attempt to test the association of Caucasian findings prior to performing a hypothesis-free approach in the study cohort. Of the 23 SNPs which were successfully genotyped in the modest sized study cohort, 11 SNPs showing allelic or genotypic or association with the CHD sub-phenotypes (Table 1 , 2 , 3 ) in a trans ethnic population was noteworthy and reiterates the functional relevance of the associated genes/pathways in CHD pathogenesis.
Of the seven associations observed, four SNPs namely rs73118372 (missense variant) Chr 3; rs659366 (promoter region) on Chr 11; rs735712 (synonymous variant) and rs28711516 (missense variant) on Chr 14; are of functional relevance. Strongest allelic association was observed for rs73118372, rs28711516 and rs735712.
The variant rs73118372(c.1136 T > C) in Exon 9 of CRELD1 is associated with Downs syndrome [ 47 ]. CRELD1 is involved in the formation of atrioventricular cushion [ 48 ] and disrupts existing exon splicing, thus altering the protein configuration and making it unstable. It was associated for all cyanotic, acyanotic and combined categories, and with ASD and TOF sub-phenotypes. Intronic SNP rs1975649 ( SYNPR ; Intron2) also on Chr3 exhibited strong association both in allelic and genotypic categories and was also associated with ASD. Cardiac myosin is the molecular motor that powers heart contraction, a property essential for heart function. It also plays a pivotal role in muscle regulation, development, and mechanotransduction [ 49 ]. The α-MYHC ( MYH6 ) is expressed in atrial muscle and the β-MYHC ( MYH7 ) in skeletal slow-twitch muscle and have arisen through a tandem gene duplication event [ 50 ] on Chr. 14. The duplication event is not evident in the genomes of other vertebrates (e.g. birds, fish, amphibia) [ 51 ]. MYH6, MYH7 and MYH7B are associated with R amplitude [ 52 ]. Heterozygous pathogenic variants in MHY7 have been associated with septal defects or Ebstein anomaly [ 48 ] and of MYH6 with HLHS and cardiac conduction [ 53 , 54 ]. MYH6 is associated with non-syndromic coarctation of the aorta [ 38 , 50 ] and also presented in families of Shone complex [ 54 ]. Previous reports on MYH6 rs28711516 (c.166G > A; p.G56R) associations with atrial fibrillation [ 53 ] and sporadic dilated cardiomyopathy [ 55 ] and a GWAS study from south India [ 35 ] warrant further investigation of this gene. MYH7 mutations have been reported for Indian families [ 56 , 57 ]. Exon 12 variant rs735712 (c.1062C > T; p.G354G) has previously been reported in dilated cardiomyopathies in Indian population [ 58 ]. Previous linkage study using microarray identified rs1055061in HOMEZ, a ubiquitously expressed transcription factor on the same locus, in 83 consanguineous CHD families from India [ 59 ]. In present study, synonymous variant rs3746446 in MYH7B was associated only with ASD phenotype. This SNP showed strong association with congenital cardiovascular left-sided lesions [ 38 ]along with rs12045807, a SNP not associated in our study.
Allelic and genotypic association for combined as well as the acyanotic group for promoter variant rs659366 in UCP2 , having a role in reactive oxygen species (ROS) pathway [ 60 , 61 ] is already been reported to be associated with maternal diabetes in CHD offsprings [ 62 ] and with dietary factors in Asian populations [ 60 ]. It was also associated with ASD subtype. rs185531658, a SNP with the strongest association in 4034 patients of CHD [ 39 ], was nominally associated both with our combined data and in acyanotic group.
ELN rs2071307 showed mild association with AVSD and PKD1L2 rs55788414 with TGA subtype. GOSR2 rs11874, a promoter SNP, was detected in patients with anomalies of thoracic arteries and veins, and may affect the expression of GOSR2 [ 39 ]. It showed a marginal association in our population for combined and acyanotic categories. Missense variant rs35761929 in JAG1 , involved in Notch cell signalling was associated with ASD subtype in present study and was previously found in ten exome sequenced families from India [ 38 ]. During development, the notch pathway regulates embryonic cells destiny to be part of the heart, liver, eyes, ears, and spinal column. The Jagged-1 protein continues to play a role throughout life in the development of new blood cells. These four markers reported are too small in number to make a conclusive statement on its role based on the present results and warrant replication in larger sample set.
Findings in the study were predominantly from the coding region and a few from the intergenic region. The CRELD1, MYH6 and MYH7 interact with each other during development of the myosin filament, an active and essential component of the heart tissue. Only one of the strongly associated common variants per gene was tested in this study. There may be more rare and common variants associated from these genes and additional association studies are essential to estimate polygenic risk score to make a significant genotype- phenotype risk prediction for CHD.
This is a first study testing association of Caucasian GWAS SNPs in a north Indian population. All the SNPs studied have been previously shown to have a strong role in the development of CHD. 11 out of 21 SNPs were associated in the study cohort and highlighted the role of CRELD1, MYH6 and MYH7 in non-syndromic CHD. Strong association of markers from Chr3 and Chr14, and with ASD, VSD and TOF sub-phenotypes were notable in this study and warrant replication in independent CHD cohorts of north Indian origin. This may help uncover the mechanism of disease manifestation by a complex landscape of events influenced by variations in genetic, environmental and demographic patterns.
Availability of data and materials
The data used in this study are available from the corresponding author and could be requested by email. The data are not publicly available due them containing information that could compromise research participant privacy. All SNP information are available at the links: https://www.ncbi.nlm.nih.gov/snp/?term=rs12045807 , https://www.ebi.ac.uk/gwas/search?query=rs12045807 , https://www.ncbi.nlm.nih.gov/snp/?term=rs73118372 , https://www.ebi.ac.uk/gwas/search?query=rs73118372 , https://www.ncbi.nlm.nih.gov/snp/?term=rs1975649 , https://www.ebi.ac.uk/gwas/search?query=rs1975649 , https://www.ncbi.nlm.nih.gov/snp/?term=rs185531658 , https://www.ebi.ac.uk/gwas/search?query=rs185531658 , https://www.ncbi.nlm.nih.gov/snp/?term=rs2071307 , https://www.ncbi.nlm.nih.gov/snp/?term=rs3763592 , https://www.ncbi.nlm.nih.gov/snp/?term=rs2388896 , https://www.ebi.ac.uk/gwas/search?query=rs2388896 , https://www.ncbi.nlm.nih.gov/snp/?term=rs2228638 , https://www.ebi.ac.uk/gwas/search?query=rs2228638 , https://www.ncbi.nlm.nih.gov/snp/?term=rs659366 , https://www.ncbi.nlm.nih.gov/snp/?term=rs11065987 , https://www.ebi.ac.uk/gwas/search?query=rs11065987 , https://www.ncbi.nlm.nih.gov/snp/?term=rs11066320 , https://www.ebi.ac.uk/gwas/search?query=rs11066320 , https://www.ncbi.nlm.nih.gov/snp/?term=rs1497062 , https://www.ebi.ac.uk/gwas/search?query=rs1497062 , https://www.ncbi.nlm.nih.gov/snp/?term=rs28711516 , https://www.ncbi.nlm.nih.gov/snp/?term=rs735712 , https://www.ncbi.nlm.nih.gov/snp/?term=rs6495706 , https://www.ebi.ac.uk/gwas/search?query=rs6495706 , https://www.ncbi.nlm.nih.gov/snp/?term=rs3784481 , https://www.ncbi.nlm.nih.gov/snp/?term=rs6499100 , https://www.ebi.ac.uk/gwas/search?query=rs6499100 , https://www.ncbi.nlm.nih.gov/snp/?term=rs55788414 , https://www.ebi.ac.uk/gwas/search?query=rs55788414 , https://www.ncbi.nlm.nih.gov/snp/?term=rs11874 , https://www.ebi.ac.uk/gwas/search?query=rs11874 , https://www.ncbi.nlm.nih.gov/snp/?term=rs35761929 , https://www.ncbi.nlm.nih.gov/snp/?term=rs3746446 , https://www.ebi.ac.uk/gwas/search?query=rs3746446
Abbreviations
Actin alpha cardiac muscle
Atrial septal defect
Ataxin antisense RNA, BRCA 1 (Breast cancer gene1) associated protein
Atrioventricular septal defect
Coloboma, Heart defects, Atresia choanae, g rowth Retardation, Genital abnormalities, and Ear abnormalities
Congenital heart defect
Chromodomain helicase DNA binding protein 7
Chromosome number
Copy number variation
Cysteine rich with EGF like domains 1
Double chamber right ventricle
Endosulfine alpha
Growth arrest-specific 1
GATA binding protein 4
Golgi SNAP receptor complex member 2
Genome-wide association studies
Hypoplastic left heart syndrome
ISL1 transcription factor LIM/homeodomain
Jagged canonical Notch ligand 1
Long intergenic non-protein coding RNA 2252
Gap junction protein delta 2
Long intergenic non-protein coding RNA 2676
Myocyte enhancer factor 2c
Myosin light chains
Myosin heavy chain 6
Myosin heavy chain 7
Myosin heavy chain 7B
Nk2 homeobox 5
Neuropilin 1
Odd-skipped-related transcription factor 1
Proprotein convertase subtilisin/kexin type 6
Polycystin 1 like 2
Pulmonary stenosis
Tyrosine-protein phosphatase non-receptor type 11
SH2B (Src homology 2B) adaptor protein 3
Single nucleotide polymorphism
Single ventricle
Synaptoporin antisense RNA 1
Total anomalous pulmonary venous return
T-box transcription factors
Transposition of the great arteries
Uncoupling protein 1; VSD: Ventricular septal defect
Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol. 2002;39(12):1890–900.
Saxena A. Congenital Heart Disease in India: A Status Report. Indian Pediatr. 2018;55:1075–82.
Article PubMed Google Scholar
Bravo-valenzuela NJ, Peixoto AB, Araujo JE. Prenatal diagnosis of congenital heart disease: A review of current knowledge. Indian Heart J. 2018;70:150–64.
Buijtendijk MFJ, Barnett P, van den Hoff MJB. Development of the human heart. Am J Med Genet Part C Semin Med Genet. 2020;184:7–22.
Cohn JN, Ferrari R, Sharpe N. Cardiac remodeling-concepts and clinical implications: A consensus paper from an International Forum on Cardiac Remodeling. J Am Coll Cardiol. 2000;35:569–82.
Article CAS PubMed Google Scholar
Pierpont ME, Brueckner M, Chung WK, Garg V, Lacro RV, McGuire AL, et al. Genetic Basis for Congenital Heart Disease: Revisited: A Scientific Statement from the American Heart Association. Circulation. 2018;138:e653-711.
Article PubMed Central Google Scholar
Santoro SL, Steffensen EH. Congenital heart disease in Down syndrome – A review of temporal changes. J Congenit Cardiol. 2021;5:1–14.
Article CAS Google Scholar
Nees SN, Chung WK. Genetic basis of human congenital heart disease. Cold Spring Harb Perspect Biol. 2020;12(9):a036749.
Article Google Scholar
Øyen N, Poulsen G, Boyd HA, Wohlfahrt J, Jensen PKA, Melbye M. Recurrence of congenital heart defects in families. Circulation. 2009;120:295–301.
Ellesøe SG, Workman CT, Bouvagnet P, Loffredo CA, McBride KL, Hinton RB, et al. Familial co-occurrence of congenital heart defects follows distinct patterns. Eur Heart J. 2018;39:1015–22.
Burn J, Brennan P, Little J, Holloway S, Coffey R, Somerville J, et al. Recurrence risks in offspring of adults with major heart defects: results from first cohort of British collaborative study. Lancet. 1998;351:311–6.
Zaidi S, Brueckner M. Genetics and Genomics of Congenital Heart Disease. Circ Res. 2017;120:923–40.
Article CAS PubMed PubMed Central Google Scholar
Andersen TA, Troelsen KDLL, Larsen LA. Of mice and men: Molecular genetics of congenital heart disease. Cell Mol Life Sci. 2014;71:1327–52.
Bruneau BG. Signaling and transcriptional networks in heart development and regeneration. Cold Spring Harb Perspect Biol. 2013;5(3):a008292.
Wessels MW, Willems PJ. Genetic factors in non-syndromic congenital heart malformations. Clin Genet. 2010;78:103–23.
Xu H, Baldini A. Genetic pathways to mammalian heart development: Recent progress from manipulation of the mouse genome. Semin Cell Dev Biol. 2007;18(1):77–83.
Suluba E, Shuwei L, Xia Q, Mwanga A. Congenital heart diseases: genetics, non-inherited risk factors, and signaling pathways. Egypt J Med Hum Genet. 2020;21:1–12.
Kodo K, Nishizawa T, Furutani M, Arai S, Ishihara K, Oda M, et al. Genetic analysis of essential cardiac transcription factors in 256 patients with non-syndromic congenital heart defects. Circ J. 2012;76:1703–11.
Cerrone M, Remme CA, Tadros R, Bezzina CR, Delmar M. Beyond the one gene-one disease paradigm complex genetics and pleiotropy in inheritable cardiac disorders. Circulation. 2019;140:595–610.
Article PubMed PubMed Central Google Scholar
Zhang TN, Wu QJ, Liu YS, Lv J Le, Sun H, Chang Q, et al. Environmental risk factors and congenital heart disease: an umbrella review of 165 Systematic reviews and meta-analyses with more than 120 million participants. Front Cardiovasc Med. 2021;8:640729.
Spendlove SJ, Bondhus L, Lluri G, Sul JH, Arboleda VA. Polygenic risk scores of endo-phenotypes identify the effect of genetic background in congenital heart disease. Hum Genet Genomics Adv. 2022;3: 100112.
Knowles RL, Ridout D, Crowe S, Bull C, Wray J, Tregay J, et al. Ethnic and socioeconomic variation in incidence of congenital heart defects. Arch Dis Child. 2017;102:496–502.
Jerves T, Beaton A, Kruszka P. The genetic workup for structural congenital heart disease. Am J Med Genet Part C Semin Med Genet. 2020;184:178–86.
Paige SL, Saha P, Priest JR. Beyond Gene Panels: Whole Exome Sequencing for Diagnosis of Congenital Heart Disease. Circ Genom Precis Med. 2018;11:e002097.
Blue GM, Kirk EP, Giannoulatou E, Sholler GF, Dunwoodie SL, Harvey RP, et al. Advances in the Genetics of Congenital Heart Disease: A Clinician’s Guide. J Am Coll Cardiol. 2017;69:859–70.
Agopian AJ, Goldmuntz E, Hakonarson H, Sewda A, Taylor D, Mitchell LE. Genome-Wide Association Studies and Meta-Analyses for Congenital Heart Defects. Circ Cardiovasc Genet. 2017;10:1–9.
Jia Y, Louw JJ, Breckpot J, Callewaert B, Barrea C, Sznajer Y, et al. The diagnostic value of next generation sequencing in familial nonsyndromic congenital heart defects. Am J Med Genet Part A. 2015;167:1822–29.
Dixit R, Kumar A, Mohapatra B. Implication of GATA4 synonymous variants in congenital heart disease: A comprehensive in-silico approach. Mutat Res Mol Mech Mutagen. 2019;813:31–8.
Dixit R, Narasimhan C, Balekundri VI, Agrawal D, Kumar A, Mohapatra B. Functional analysis of novel genetic variants of NKX2-5 associated with nonsyndromic congenital heart disease. Am J Med Genet Part A. 2021;185:3644–63.
Bose D, Vaigundan D, Shetty M, Krishnappa J, Kutty AVM. Identification of intronic-splice site mutations in GATA4 gene in Indian patients with congenital heart disease. Mutat Res - Fundam Mol Mech Mutagen. 2017;803–8050:26–34.
Mattapally S, Singh M, Murthy KS, Asthana S, Banerjee SK. Computational modeling suggests impaired interactions between NKX2.5 and GATA4 in individuals carrying a novel pathogenic D16N NKX2.5 mutation. Oncotarget. 2018;9(17):13713–32.
Dinesh SM, Lingaiah K, Savitha MR, Krishnamurthy B, Narayanappa D, Ramachandra NB. GATA4 specific nonsynonymous single-nucleotide polymorphisms in congenital heart disease patients of Mysore. India Genet Test Mol Biomarkers. 2011;15:715–20.
Kusuma L, Dinesh SM, Savitha MR, Krishnamurthy B, Narayanappa D, Ramachandra NB. Mutations of TFAP2B in congenital heart disease patients in Mysore, south India. Indian J Med Res. 2011;134:621–26.
Raina JK, Panjaliya RK, Dogra V, Sharma S, Anupriya, Kumar P. “Association of MTHFR and MS/MTR gene polymorphisms with congenital heart defects in North Indian population (Jammu and Kashmir): a case–control study encompassing meta-analysis and trial sequential analysis”. BMC Pediatr. 2022;22(1):223.
Ramachandra NB. Nuclear co-repressor 1: a potential candidate gene in the manifestation of congenital heart diseases. Int J Hum Genet. 2020;20:55–65.
Cordell HJ, Töpf A, Mamasoula C, Postma AV, Bentham J, Zelenika D, et al. Genome-wide association study identifies loci on 12q24 and 13q32 associated with Tetralogy of Fallot. Hum Mol Genet. 2013;22:1473–81.
Mitchell LE, Agopian AJ, Bhalla A, Glessner JT, Kim CE, Swartz MD, et al. Genome-wide association study of maternal and inherited effects on left-sided cardiac malformations. Hum Mol Genet. 2015;24:265–73.
Hanchard NA, Swaminathan S, Bucasas K, Furthner D, Fernbach S, Azamian MS, et al. A genome-wide association study of congenital cardiovascular left-sided lesions shows association with a locus on chromosome 20. Hum Mol Genet. 2016;25:2331–41.
Lahm H, Jia M, Dreßen M, Wirth F, Puluca N, Gilsbach R, et al. Congenital heart disease risk loci identified by genome-wide association study in European patients. J Clin Invest. 2021;131(2):e141837.
Cunningham F, Allen JE, Allen J, et al. Ensembl 2022. Nucleic Acids Res. 2022;50(D1):D988–95.
Juyal RC, Negi S, Wakhode P, Bhat S, Bhat B, Thelma BK. Potential of ayurgenomics approach in complex trait research: leads from a pilot study on rheumatoid arthritis. PLoS One. 2012;7(9):e45752.
Negi S, Juyal G, Senapati S, Prasad P, Gupta A, Singh S, et al. A genome-wide association study reveals ARL15, a novel non-HLA susceptibility gene for rheumatoid arthritis in North Indians. Arthritis Rheum. 2013;65:3026–35.
Kang M, Choi S, Koh I. The effect of increasing control-to-case ratio on statistical power in a simulated case-control SNP association study. Genomics Inform. 2009;7(3):148–51.
Reich D, Thangaraj K, Patterson N, Price AL, Singh L. Reconstructing Indian population history. Nature. 2009;461:489–94.
Lowry R. VassarStats: Website for Statistical Computation. ( http://vassarstats.net/ ).
Gauderman WJ. Sample size requirements for association studies of gene-gene interaction. 2002;155(5):478–84.
Ghosh P, Bhaumik P, Ghosh S, Ozbek U, Feingold E, Maslen C, et al. Polymorphic haplotypes of CRELD1 differentially predispose down syndrome and euploids individuals to atrioventricular septal defect. Am J Med Genet Part A. 2012;158 A:2843–48.
Ritter A, Leonard J, Gray C, Izumi K, Levinson K, Nair DR, et al. MYH7 variants cause complex congenital heart disease. Am J Med Genet Part A. 2022;188:2772–6.
Barrick SK, Greenberg MJ. Cardiac myosin contraction and mechanotransduction in health and disease. J Biol Chem. 2021;297(5):101297.
Bjornsson T, Thorolfsdottir RB, Sveinbjornsson G, Sulem P, Norddahl GL, Helgadottir A, et al. A rare missense mutation in MYH6 associates with non-syndromic coarctation of the aorta. Eur Heart J. 2018;39:3243–9.
Desjardins CA, Naya FJ. The function of the mef2 family of transcription factors in cardiac development, cardiogenomics, and direct reprogramming. Journal of Cardiovascular Development and Disease. 2016;3(3):26.
Norland K, Sveinbjornsson G, Thorolfsdottir RB, Davidsson OB, Tragante V, Rajamani S, et al. Sequence variants with large effects on cardiac electrophysiology and disease. Nat Commun. 2019;10:1–10.
Ntalla I, Weng LC, Cartwright JH, Hall AW, Sveinbjornsson G, Tucker NR, et al. Multi-ancestry GWAS of the electrocardiographic PR interval identifies 202 loci underlying cardiac conduction. Nat Commun. 2020;11(1):2542.
Anfinson M, Fitts RH, Lough JW, James JM, Simpson PM, Handler SS, et al. Significance of α-Myosin Heavy Chain (MYH6) variants in hypoplastic left heart syndrome and related cardiovascular diseases. J Cardiovasc Dev Dis. 2022;9(5):144.
Shen C, Xu L, Sun X, Sun A, Ge J. Genetic variants in Chinese patients with sporadic dilated cardiomyopathy: a cross-sectional study. Ann Transl Med. 2022;10:129–129.
Basu R, Hazra S, Shanks M, Paterson DI, Oudit GY. Novel mutation in exon 14 of the sarcomere gene MYH7 in familial left ventricular noncompaction with bicuspid aortic valve. Circ Hear Fail. 2014;7:1059–62.
Alawani S, Paul A, Krishna M, Ahamed H. Familial left ventricular noncompaction cardiomyopathy due to a novel mutation in the MYH 7 gene. Ann Pediatr Cardiol. 2021;14:544–46.
Rani S, Masood S. Predicting congenital heart disease using machine learning techniques. J Discret Math Sci Cryptogr. 2020;23:293–303.
McGregor TL, Misri A, Bartlett J, Orabona G, Friedman RD, Sexton D, et al. Consanguinity mapping of congenital heart disease in a South Indian population. PLoS One. 2010;5(4):e10286.
Zhang S, Liu X, Wang T, Chen L, Yang T, Huang P, et al. Association and interaction effect of UCP2 gene polymorphisms and dietary factors with congenital heart diseases in Chinese Han population. Sci Rep. 2021;11:1–10.
Google Scholar
Tian XY, Ma S, Tse G, Wong WT, Huang Y. Uncoupling protein 2 in cardiovascular health and disease. Front Physiol. 2018;9:1060.
Luo L, Huang P, Wang TT, et al. Association of maternal diabetes mellitus and UCP2 gene polymorphisms with congenital heart disease in offspring: a case-control study. Chinese J Contemp Pediatr. 2020;22:1092–99.
Junco-Vicente A, Río-García Á Del, Martín M, Rodríguez I. Update in biomolecular and genetic bases of bicuspid aortopathy. Int J Mol Sci. 2021;22(11):5694.
Bilan F, Legendre M, Charraud V, Manière B, Couet D, Gilbert-Dussardier B, et al. Complete screening of 50 patients with CHARGE syndrome for anomalies in the CHD7 gene using a denaturing high-performance liquid chromatography-based protocol: New guidelines and a proposal for routine diagnosis. J Mol Diagnostics. 2012;14:46–55.
Bagheri M, Wang C, Shi M, Manouchehri A, Murray KT, Murphy MB, et al. The genetic architecture of plasma kynurenine includes cardiometabolic disease mechanisms associated with the SH2B3 gene. Sci Rep. 2021;11:1–10.
Ramachandran D, Zeng Z, Locke AE, Mulle JG, Bean LJH, Rosser TC, et al. Genome-wide association study of down syndrome-associated atrioventricular septal defects. G3 (Bethesda). 2015;5:1961–71.
Rani DS, Vijaya Kumar A, Nallari P, Sampathkumar K, Dhandapany PS, Narasimhan C, et al. Novel Mutations in β-MYH7 Gene in Indian Patients With Dilated Cardiomyopathy. CJC Open. 2022;4:1–11.
Gaspar HA, Breen G. Probabilistic ancestry maps: A method to assess and visualize population substructures in genetics. BMC Bioinformatics. 2019;20(1):116.
Li L, Dong J, Wang X, Guo H, Wang H, Zhao J, et al. JAG1 mutation spectrum and origin in Chinese children with clinical features of alagille syndrome. PLoS ONE. 2015;10:1–11.
Download references
Acknowledgements
The authors acknowledge the contribution of Cardiology and Surgery teams of Sri Sathya Sai Health and Education Trust for sharing the clinical findings and Sri Sathya Sai Sanjeevani Biobank for providing samples of the study respectively. The Authors thank ILS and Genes2Me for genotyping the samples. Authors acknowledge Dr. Thelma for sharing genotype information of samples used as part of controls in the study and Dr. Upasana Bhattacharya for technical suggestions.
The authors used institutional funding for this project.
Author information
Krishna Manohar is deceased.
Authors and Affiliations
Sri Sathya Sai Sanjeevani Research Foundation, NH-2, Delhi-Mathura Highway, Baghola, Haryana, District Palwal, Pin- 121102, India
Prachi Kukshal, Ajay Kumar, Shadab Ahamad & Soma Guhathakurta
Present address Sri Sathya Sai Sanjeevani Research Foundation, Kharghar, Navi Mumbai- 410210, Maharashtra, India
Radha O Joshi
Sri Sathya Sai Sanjeevani Centre for Child Heart Care and Training in Paediatric Cardiac Skills, Navi Mumbai Maharashtra, India
Prabhatha Rashmi Murthy
Sri Sathya Sai Sanjeevani International Centre for Child Heart Care & Research, NH-2, Delhi-Mathura Highway, Baghola, District Palwal, Haryana, Pin 121102, India
Yogesh Sathe, Krishna Manohar & Subramanian Chellappan
You can also search for this author in PubMed Google Scholar
Contributions
PK, ROJ and SC conceptualised the study and PK designed the experiments; PK, ROJ and AK isolated and quality checked the DNA samples. PK wrote the first draft of the paper and SA helped in data analysis and manuscript preparation; SG helped in clinical classification of samples and PRM, KM, YS and SC provided the study samples; AK collected the sample and patient history. SC and PK take the overall charge of the article. The author(s) read and approved the final manuscript.
Corresponding authors
Correspondence to Prachi Kukshal or Subramanian Chellappan .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval from Institutional Ethics Committee (IEC), Sri Sathya Sai Sanjeevani Research Foundation (SSSSRF) registered with National Ethics Committee Registry for Biomedical and Health Research, Department of Health Research (File no.: EC/NEW/INST/2022/2673) was granted under the number PSR00007/1/IEC/10/2019. Written informed consent was obtained for all participants and parents/ guardians and assent was provided by children above 8 years of age as per IEC, SSSSRF and ICMR guidelines. Involvement in the study was voluntary and there were no repercussions for non-participation. This study was performed in accordance with the declaration of Helsinki.
Consent for publication
Not Applicable.
Competing interests
The Authors have no potential competing interests to declare.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: supplementarytable 1..
Case and Control Sample distribution. Supplementary Table 2 . Details of Variants selected inthe study [ 63 , 64 , 65 , 66 , 67 , 68 , 69 ].
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kukshal, P., Joshi, R.O., Kumar, A. et al. Case–control association study of congenital heart disease from a tertiary paediatric cardiac centre from North India. BMC Pediatr 23 , 290 (2023). https://doi.org/10.1186/s12887-023-04095-x
Download citation
Received : 01 December 2022
Accepted : 27 May 2023
Published : 15 June 2023
DOI : https://doi.org/10.1186/s12887-023-04095-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Congenital Heart Disease
- North India
- GWAS variants
- Case–control association
BMC Pediatrics
ISSN: 1471-2431
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Featured Topics
Featured series.
A series of random questions answered by Harvard experts.
Explore the Gazette
Read the latest.

How to realize immense promise of gene editing

Women rarely die from heart problems, right? Ask Paula.

When will patients see personalized cancer vaccines?
Exercise cuts heart disease risk in part by lowering stress, study finds.
Benefits nearly double for people with depression
MGH Communications

New research indicates that physical activity lowers cardiovascular disease risk in part by reducing stress-related signaling in the brain.
In the study, which was led by investigators at Massachusetts General Hospital and published in the Journal of the American College of Cardiology , people with stress-related conditions such as depression experienced the most cardiovascular benefits from physical activity.
To assess the mechanisms underlying the psychological and cardiovascular disease benefits of physical activity, Ahmed Tawakol , an investigator and cardiologist in the Cardiovascular Imaging Research Center at Massachusetts General Hospital, and his colleagues analyzed medical records and other information of 50,359 participants from the Mass General Brigham Biobank who completed a physical activity survey.
A subset of 774 participants also underwent brain imaging tests and measurements of stress-related brain activity.
Over a median follow-up of 10 years, 12.9 percent of participants developed cardiovascular disease. Participants who met physical activity recommendations had a 23 percent lower risk of developing cardiovascular disease compared with those not meeting these recommendations.
Individuals with higher levels of physical activity also tended to have lower stress-related brain activity. Notably, reductions in stress-associated brain activity were driven by gains in function in the prefrontal cortex, a part of the brain involved in executive function (i.e., decision-making, impulse control) and is known to restrain stress centers of the brain. Analyses accounted for other lifestyle variables and risk factors for coronary disease.
Moreover, reductions in stress-related brain signaling partially accounted for physical activity’s cardiovascular benefit.
As an extension of this finding, the researchers found in a cohort of 50,359 participants that the cardiovascular benefit of exercise was substantially greater among participants who would be expected to have higher stress-related brain activity, such as those with pre-existing depression.
“Physical activity was roughly twice as effective in lowering cardiovascular disease risk among those with depression. Effects on the brain’s stress-related activity may explain this novel observation,” says Tawakol, senior author of the study.
“Prospective studies are needed to identify potential mediators and to prove causality. In the meantime, clinicians could convey to patients that physical activity may have important brain effects, which may impart greater cardiovascular benefits among individuals with stress-related syndromes such as depression.”
This work was supported by the National Institutes of Health.
Share this article
You might like.
Nobel-winning CRISPR pioneer says approval of revolutionary sickle-cell therapy shows need for more efficient, less expensive process

New book traces how medical establishment’s sexism, focus on men over centuries continues to endanger women’s health, lives

Sooner than you may think, says researcher who recently won Sjöberg Prize for pioneering work in field
Harvard announces return to required testing
Leading researchers cite strong evidence that testing expands opportunity
Good genes are nice, but joy is better
Harvard study, almost 80 years old, has proved that embracing community helps us live longer, and be happier
Researchers developed new method for detecting heart failure with a smartphone
The new technology, which was created at the University of Turku and developed by the company CardioSignal, uses a smartphone to analyse heart movement and detect heart failure. The study involved five organisations from Finland and the United States.
Heart failure is a condition affecting tens of millions of people worldwide, in which the heart is unable to perform its normal function of pumping blood to the body. It is a serious condition that develops as a result of a number of cardiovascular diseases and its symptoms may require repeated hospitalisation.
Heart failure is challenging to diagnose because its symptoms, such as shortness of breath, abnormal fatigue on exertion, and swelling, can be caused by a number of conditions. There is no simple test available to detect it and diagnostics relies on an examination by a doctor, blood tests, and sophisticated imaging, such as an ultrasound scan of the heart.
Gyrocardiography is a non-invasive technique for measuring cardiac vibrations on the chest. The smartphone's built-in motion sensors can detect and record these vibrations, including those that doctors cannot hear with a stethoscope. The method has been developed over the last 10 years by researchers at the University of Turku and CardioSignal.
The researchers' latest study on using smartphone motion sensors to detect heart failure was carried out at the Turku and Helsinki University Hospitals in Finland and Stanford University Hospital in the US. Approximately 1,000 people took part in the study, of whom around 200 were patients suffering from heart failure. The study compared the data provided by the motion sensors in the heart failure patients and patients without heart disease.
"The results we obtained with this new method are promising and may in the future make it easier to detect heart failure," says Cardiologist Antti Saraste, one of the two main authors of the research article and the Professor of Cardiovascular Medicine at the University of Turku, Finland.
Precise detection uncovers heart failure
The researchers found that heart failure is associated with typical changes in the motion sensor data collected by a smartphone. On the basis of this data, the researchers were able to identify the majority of patients with heart failure.
The analysis of the movements detected by the gyroscope and accelerometer is so accurate that in the future it could provide healthcare professionals with a quick and easy way to detect heart failure.
"Primary healthcare has very limited tools for detecting heart failure. We can create completely new treatment options for remote monitoring of at-risk groups and for monitoring already diagnosed patients after hospitalisation," says CardioSignal's founding member and CEO, Cardiologist Juuso Blomster.
Consistent with several European countries, heart failure affects around 1-2% of the population in Finland, but it is much more common in older adults, affecting around one in ten people aged 70. Detecting heart failure is important as effective treatment can help to alleviate its symptoms. Accurate diagnosis and timely access to treatment can also reduce healthcare costs, which are driven up by emergency room visits and hospital stays, especially during exacerbations.
The joint research projects between CardioSignal and the University of Turku aim to promote people's health and reduce healthcare costs through innovation, improved disease diagnostics, and prevention of serious complications.
- Heart Disease
- Stroke Prevention
- Diseases and Conditions
- Neural Interfaces
- Information Technology
- Heart failure
- Artificial heart
- Coronary heart disease
- Ischaemic heart disease
- Heart valve
- Echocardiography
Story Source:
Materials provided by University of Turku . Note: Content may be edited for style and length.
Journal Reference :
- Francois Haddad, Antti Saraste, Kristiina M. Santalahti, Mikko Pänkäälä, Matti Kaisti, Riina Kandolin, Piia Simonen, Wail Nammas, Kamal Jafarian Dehkordi, Tero Koivisto, Juhani Knuuti, Kenneth W. Mahaffey, Juuso I. Blomster. Smartphone-Based Recognition of Heart Failure by Means of Microelectromechanical Sensors . JACC: Heart Failure , 2024; DOI: 10.1016/j.jchf.2024.01.022
Cite This Page :
Explore More
- Drain On Economy Due to Climate Change
- 'Tube Map' Around Planets and Moons
- 'Bizarre' Evolutionary Pattern: Homo Lineage
- Largest Known Marine Reptile
- Neolithic Humans Lived in Lava Tube Caves
- Imminent Carbon Release from the Tundra
- How Working Memory Reallly Works
- Substantial Global Cost of Climate Inaction
- Paradox of Extreme Cold Events in Warming World
- Plastic Pollution Kills Ocean Embryos
Trending Topics
Strange & offbeat.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Eur Heart J Case Rep
- v.4(6); 2020 Dec

A clinical and echocardiographic case report of carcinoid-related valvular heart disease
Ali j. ebrahimi.
1 Department of Cardiovascular disease, Northside Hospital/Tampa Bay Heart Institute, St. Petersburg, FL, USA
2 Division of Cardiology, University of Alabama Birmingham, Birmingham, AL, USA
Peter Marogil
3 Division of Cardiology, Franciscan Health, Chicago, IL, USA
Gregory Von Mering
Mustafa ahmed, associated data.
Carcinoid syndrome is a rare disease caused by malignant neuroendocrine neoplasms. When vasoactive substances enter the systemic circulation, the triad of cutaneous flushing, bronchospasm, and diarrhoea often characterize carcinoid syndrome. Rarely, carcinoid syndrome can progress to involve the cardiac system, a condition known as carcinoid heart disease, often affecting right-sided valvular structures.
Case summary
Here, we present a case of malignant carcinoid syndrome with associated carcinoid heart disease in a 63-year-old female. The diagnosis of her dual regurgitant and stenotic valvular disease is detailed, with accompanying two- and three-dimensional echocardiographic images demonstrating the patient’s complex tricuspid dysfunction.
Carcinoid heart disease encompasses a rare but important subset of valvular dysfunction caused by circulating vasoactive substances. Diagnosis utilizing serum studies, computed tomography scans, and echocardiography can help expedite the diagnosis and treatment of such rare conditions, and assist in the avoidance of complications. Despite its relatively well-recognized clinical presentation, carcinoid syndrome and its associated heart disease still remains a challenging condition to manage and treat, often requiring the input of several subspecialties to treat the condition appropriately.
Introduction
The carcinoid syndrome is a clinical condition defined by the symptomatic triad of bronchospasm, diarrhoea, and cutaneous flushing. The constellation of these symptoms can be ascribed to the circulation of vasoactive substances and their metabolites that can become deposited on or around intracardiac and valvular structures, contributing to the development of carcinoid heart disease. A rare cause of right-sided heart disease, only found in ∼20% the patients diagnosed with carcinoid syndrome, carcinoid heart disease, often affects right-sided structures such as the tricuspid or pulmonic valve, often causing regurgitation or, more rarely, stenosis of right-sided structures. 1 , 2 Identification and diagnosis of carcinoid heart disease is often with 2D or 3D echocardiographic evaluation. 3 Here we present an echocardiographic case of carcinoid heart disease displaying the less commonly encountered behaviour of being both regurgitant and stenotic due to structural changes caused by circulating hormones.

Case presentation
A 63-year-old female with a past medical history of hypertension who was undergoing treatment for a well-differentiated neuroendocrine carcinoma presented to our institution complaining of 3 months of progressive lower extremity oedema. Her physical exam was notable for basilar crackles bilaterally and a soft II/VI systolic murmur at the right mid sternal border accompanied by jugular venous distention. She was initially diagnosed with the neuroendocrine carcinoma 1 year previously. Six months previously, the patient presented to our hospital with complaints of chest pain that was ultimately diagnosed as stress-induced (Takotsubo’s) cardiomyopathy. Repeat transthoracic echocardiography (TTE) during the present evaluation revealed a recovered left ventricular ejection fraction (LVEF) (55–60%) compared with previous studies but, unexpectedly, the patient now displayed severe tricuspid regurgitation. A transoesophageal echocardiogram (TEE) was performed 1 week later to further define her valvular anatomy, and demonstrated a severely regurgitant tricuspid valve with fixed leaflets in a retracted position ( Figures 1 and and 2 ). 2 ). The valve leaflets, as well as the subvalvular apparatus including the chordae and papillary muscles, appeared markedly thickened ( Figure 3 ). The affected valve appeared to be stented open, displaying both regurgitant and stenotic behaviour. Paralleling her diagnostic workup by the patient’s internal medicine doctor and endocrinologist, a comprehensive evaluation was undertaken in the structural heart valve clinic including discussions with oncology and cardiothoracic surgery as to the potential and feasibility of repair options. Ultimately the patient was referred for surgical intervention of her dysfunctional tricuspid valve, and she underwent a surgical valve replacement with a 27 mm Epic porcine valve 1 month after TEE.

Transoesophageal echocardiogram demonstrating thickened and retracted leaflets.

3D TEE demonstrating thickened and retracted leaflets and subvalvular apparatus.

TEE with colour flow Doppler demonstrating severe tricuspid regurgitation.
Following surgery, our individual patient’s valve was sent to the pathology department, and the only significant finding was the demonstration of fibrous plaques, thought to be correlated with an underlying endocrine tumour. Unfortunately, 3 days into the post-operative period, and prior to discharge, our patient suffered an in-hospital cardiac arrest and expired due to an unstable arrythmia.
The term ‘carcinoid tumour’ refers to a heterogeneous group of neuroendocrine neoplasms most often found in either the gastrointestinal (GI) tract or lungs, and can exist as an isolated condition or part of a larger familial syndrome such as multiple endocrine neoplasia type I (MEN I). Neuroendocrine tumours (NETs) are rare; however, recent reports have suggested an increasing incidence from roughly 1 in every 100 000 to 5 per 100 000 people in the USA. 4 , 5 Within the GI tract, NETs are frequently located in the ileum, appendix, or rectum, and a certain subset can be extraluminal, involving pancreatic islet cells. 6
Many of the clinical manifestations of NETs are attributed to the production of vasoactive substances including serotonin, prostaglandins, tachykinins, and histamine. 7 , 8 These substances are typically metabolized by the liver, but, in the setting of hepatic metastases, they are able to enter the systemic circulation and result in the clinical findings associated with carcinoid syndrome. 9 The syndrome is classically characterized by the constellation of cutaneous flushing, diarrhoea, and bronchospasm.
Carcinoid heart disease, which is typically right sided, has been reported to occur in association with the syndrome; however, only ∼8% of NETs display this type of involvement, 10 , 11 although rates as high as 50% have been reported. 8 , 12 The pathology is mediated by plaque-like deposition of smooth muscle cells, myofibroblasts, and extracellular matrix substrates onto valves and endocardium, resulting in valvular dysfunction. 13 This process is thought to be primarily mediated through the release of serotonin and its analogues, which activate 5-hydroxytryptamine 2B (5-HT2B) receptors in the heart. 14 The tricuspid and pulmonic valves are the most commonly affected, and can demonstrate progressively worsening regurgitation and eventual stenosis as the severity of the disease progresses. 3 , 15 Frequently, the left side of the heart is spared due to the inactivation of vasoactive substances by the lungs, but reports of left-sided involvement have been documented in the presence of a right-to-left shunt or a bronchogenic carcinoid. 3
Carcinoid syndrome and its associated complications can be a challenging diagnosis for physicians to make. Most often the diagnosis is made utilizing the detection of serotonergic metabolites in a patient’s urine with the use of a 24-h HIAA (5-hydroxyindoleacetic acid) urine excretion level, often combined with serum studies investigating circulating levels of HIAA. In addition to metabolic studies, initial evaluation looking for the primary tumour can entail the utilization of transthoracic echo (TTE), cardiac magnetic resonance imaging (cMRI), computed tomography (CT), scintigraphy scanning, or positron emission tomography (PET). Unfortunately, these imaging modalities were not immediately available to our group in the treatment of this patient. Surgical tissue excision and biopsy are often needed to confirm the diagnosis, as well as possible definitive treatment involving surgically addressing the tumour. 10 , 15
Management of carcinoid syndrome can be challenging, but is often achieved through the use of somatostatin analogues, such as octreotide or other adjunct chemotherapies. 14 , 16 The treatment of carcinoid heart disease can be complex, and formal guidelines for management are lacking. There are limited data on ideal medical management for right-sided heart disease, but the mainstays of treatment include the use of (loop or thiazide) diuretics. Definitive therapy is achieved through surgical valve replacement; however, identifying the proper patients or the ideal timing has been shown to be challenging. 17–19 It is advised to take a multidisciplinary approach to these patients involving cardiologists, cardiothoracic surgeons, oncologists, and endocrinologists. Carcinoid heart disease imparts significant morbidity and mortality, and surgical intervention should be considered when symptomatic disease exists. During the peri-operative period, these patients are often at risk for developing a carcinoid crisis, manifested by the presence of hypotension, flushing, and bronchospasm. In order to avoid this complication, it has been recommended that an octreotide infusion be employed during the pre-operative period, prior to surgical intervention, and subsequently continued for 48 h post-operatively. 16 , 20
The recognition, diagnosis, and treatment of neuroendocrine tumours and their associated syndromes are a rare but important subset of malignancies capable of affecting the cardiovascular system. Rapid diagnosis utilizing serum studies, CT scans, and echocardiography can help expedite the diagnosis and treatment of such rare conditions, and assist in the avoidance of complications due to the effects of circulating vasoactive substances. Despite its relatively well-recognized clinical symptoms, carcinoid syndrome and its associated heart disease still remains a challenging condition to manage and treat, oftens requiring the input of several subspecialties to treat the condition appropriately.
Lead author biography

Ali Ebrahimi is currently a general cardiology fellow at Northside Hospital with a focus on interventional and structural cardiology. He is also an associate researcher in the echocardiography department at the University of Alabama at Birmingham.
Supplementary material
Supplementary material is available online at European Heart Journal - Case Reports online.
Slide sets : A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data .
Consent: The authors confirm that written consent for submission and publication of this case report including images and associated text has been obtained from the patient's next of kin in line with COPE guidance.
Conflict of interest: none declared.
Supplementary Material
Ytaa363_supplementary_data.

IMAGES
VIDEO
COMMENTS
On examination, the temperature was 36.4°C, the heart rate 103 beats per minute, the blood pressure 79/51 mm Hg, the respiratory rate 30 breaths per minute, and the oxygen saturation 99% while ...
A 67-year-old woman sought emergency medical care due to prolonged chest pain. In April 2009 the patient had prolonged chest pain and at that time she sought medical care. She was admitted at the hospital and diagnosed with myocardial infarction. The patient had hypertension, diabetes mellitus, dyslipidemia and was a smoker.
Presentation of Case. Dr. Jacqueline B. Henson (Medicine): A 54-year-old man was evaluated at this hospital after cardiac arrest associated with ventricular fibrillation. The patient had been in ...
Dr. Amy A. Sarma: A 54-year-old man was evaluated at this hospital because of new heart failure. One month before this evaluation, a nonproductive cough developed after the patient took a business ...
In this case, a patient with known history of coronary artery disease presented with worsening of shortness of breath with lower extremity edema and jugular venous distension along with crackles in the lung. The sign and symptoms along with labs and imaging findings point to diagnosis of heart failure with reduced EF (HFrEF).
Read chapter 4 of Patient Management in the Telemetry/Cardiac Step-Down Unit: A Case-Based Approach online now, exclusively on AccessCardiology. AccessCardiology is a subscription-based resource from McGraw Hill that features trusted medical content from the best minds in medicine.
However, to the best of our knowledge, no previous studies have investigated the role of traumatic experiences by means of a case-control design, comparing patients with heart disease and healthy people. This is also the first study adopting a psychodiagnostic tool, describing in detail the type and age of trauma.
Heart disease, including coronary heart disease, remains the leading cause of death in the United States. However, the rate of heart disease deaths has declined by 70% over the past 50 years, thanks in part to NHLBI-funded research. Many current studies funded by the NHLBI focus on discovering genetic associations and finding new ways to ...
Background Cardiac stress testing is a validated diagnostic tool to assess symptomatic patients with intermediate pretest probability of coronary artery disease (CAD). However, in some cases, the cardiac stress test may provide inconclusive results and the decision for further workup typically depends on the clinical judgement of the physician. These decisions can greatly affect patient ...
That risk was confirmed in a study with 2285 patients diagnosed with stable coronary artery disease and diabetes mellitus (female sex, 34.9%; age range, 55 to 68 years; mean age, 61 years), and followed up for five years 14. Cardiovascular death, non-fatal acute myocardial infarction or non-fatal stroke occurred in 12.9% (178/1388 patients) of ...
Key Points. Question How have case rates, treatment approaches, and in-hospital outcomes changed for patients with acute myocardial infarction (AMI) during the coronavirus disease 2019 (COVID-19) pandemic?. Findings In this cross-sectional study of 15 244 hospitalizations involving 14 724 patients with AMI, case rates began to decrease on February 23, 2020, followed by a modest recovery after ...
Introduction. This clinical case refers to an 83-year-old man with moderate chronic obstructive pulmonary disease and shows that implementation of appropriate medical therapy according to the European Society of Cardiology/Heart Failure Association (ESC/HFA) guidelines improves symptoms and quality of life. 1 The case also illustrates that optimization of glucose metabolism with a more lenient ...
The remaining lifetime risk of cardiovascular disease fell between 1960-1979 and 2000-2018 - from 36.3% to 26.5% in women, and from 52.5% to 30.1% in men. Researchers also found men and women in the 21st century were having their first cardiovascular disease events later in life. From 2000-2018, the average age of a first cardiovascular event ...
Welcome to the GCVI HF Center's Ask the Expert - Patient Cases channel! On this channel you will have access to multiple heart failure patient cases published by leading ACC experts. We also encourage you to engage and consult with ACC global experts on cases specific to your practice. Ask the Expert through the online portal below!
Discussion. "This case highlights how viruses continue to be an underappreciated cause of heart failure. In fact, viral myocarditis is an underdiagnosed cause of acute heart failure and chronic ...
The American Heart Association's Smoke-Free Meeting Policy. September 11, 2015. With more than 3,000 employees and 156 offices nationwide, the American Heart Association (AHA) is the nation's oldest and largest voluntary organization dedicated to fighting heart disease and stroke. AHA's mission is to build healthier lives, free of ...
The physical activity paradox in cardiovascular disease and all-cause mortality: The contemporary Copenhagen General Population Study with 104 046 adults. Eur. Heart J. 42 , 1499-1511.
Read international case studies of cardiovascular disease prevention in a joint report by the BHF and Public Health England. The UK has made progress on bringing down the premature death rate associated with cardiovascular disease (CVD) in recent years. But CVD still affects around seven million people in the UK, is responsible for one in five ...
Prevalence studies estimate that 23 million individuals worldwide have heart failure and that 2 million new cases are diagnosed annually. ... In this case, the presence of ... Tabbas R. Amyloid heart disease: new frontiesanda insights in pathophysiology, diagnosis, and management. . Tex Heart Inst J. 2005; 32 (2):178-184.
The questions raised in this chapter include queries regarding the Jonathan's risk factors for heart disease, main considerations of a cardio-protective diet, definition of troponin, the nutrition and dietetic diagnosis, and aim and implementation of the dietetic intervention.
Cardiac arrest is an electrical malfunction that causes the heart to stop beating suddenly. It can be caused by a heart attack, which is when blood flow to the heart muscle is blocked. Because most cardiac arrests occur at home, family members often are the initial rescuers. For them, witnessing a cardiac arrest is a life-altering moment.
Background Congenital Heart diseases (CHDs) account for 1/3rd of all congenital birth defects. Etiopathogenesis of CHDs remain elusive despite extensive investigations globally. Phenotypic heterogeneity witnessed in this developmental disorder reiterate gene-environment interactions with periconceptional factors as risk conferring; and genetic analysis of both sporadic and familial forms of ...
April 17, 2024 2 min read. New research indicates that physical activity lowers cardiovascular disease risk in part by reducing stress-related signaling in the brain. In the study, which was led by investigators at Massachusetts General Hospital and published in the Journal of the American College of Cardiology, people with stress-related ...
Approximately 1,000 people took part in the study, of whom around 200 were patients suffering from heart failure. The study compared the data provided by the motion sensors in the heart failure ...
In the present case report, the patient presented with prolonged chest pain, which does not rule out acute coronary syndrome (ACS), but raises the possibility of some condition associated with this coronary picture, such as pericarditis or mechanical complications. ... Sudden death risk in overt coronary heart disease: the Framingham Study. Am ...
The main results of this case-control study are the first to demonstrate that children with sickle cell disease show decreased heart rate variability at night compared with mainly obese children of similar ethnicity without SCD. They also show that children with SCD have lower diurnal pharyngeal compliance.
Case summary. Here, we present a case of malignant carcinoid syndrome with associated carcinoid heart disease in a 63-year-old female. The diagnosis of her dual regurgitant and stenotic valvular disease is detailed, with accompanying two- and three-dimensional echocardiographic images demonstrating the patient's complex tricuspid dysfunction.
1 INTRODUCTION. Congenital heart disease (CHD) is a prevalent type of congenital abnormality, occurring in 0.8% of live births globally. 1 Although the medical and surgical progress has improved both the survival rate and quality of life among CHD patients, some cases cannot benefit from the surgical treatment. Unfortunately, CHD remains a major cause of infant mortality linked to birth ...